OCCUPATIONAL HEALTH
Item
- Title
- OCCUPATIONAL HEALTH
- extracted text
-
RF_OH_3_SUDHA
Checklist for Fire
and Explosion Risk
«
;
i
Are flammable materials present in smallest
possible amount ?
(2) Is any material liable to spontaneous combustion ?
Would spilled liquids run into other areas ?
Is waste material cleared up and removed regularly ?
Does any machine run hot ?
Is there anything to cause fire in risk area like spark,
flame, excessive heat ?
Can you get out quickly ?
Can all escape doors be opened from inside ?
Are all gangways, staircases, escapeways clean
and in good condition and open ?
H Has everyone been instructed in precaution about
flammable material in escape drill ?
Can you raise the alarm easily ?
ife Has the fire alarm been tested recently ?
Can you hear it everywhere, even in toilets ?
Is there a telephone near by ?
Are there enough fire extinguishers ?
Are extinguishers checked regularly and maintained ?
Are fire alarms working ?
ENVIRONMENTAL REVIEW OF INDUSTRIAL PROJECTS EVALUATED BY
DEVELOPING COUNTRIES
By Barry I. Castleman and Grace E. Ziem
Any developing country can require every foreign investor to submit as part
of the application to build industrial factories, mining operations, and other
industrial projects in the developing country, the necessary information on the
possi ble harm these projects m ay cause to the health ofdeveloping country workers
and people living in areas where the industrial projects would be built.
Another objective is to assure that these operations will achieve high
standards ofperformance; speci fically, the developing country government will be
provided with equipment to assure that workers’ exposure to health and safety
hazards does not exceed specified limits, and that releases of toxic substances into
air and water and onto land do not exceed limits specified in the
cooperative investment agreement between the developing country and the
foreign investor.
Leading global corporations, have issued policy statements on health, safety,
and the environment within the past year. One theme of these policy statements is
that the companies now say they will meet the same high standards worldwide that
they are required to achieve in their home countries in all new projects.
INFORMATION FROM FOREIGN INVESTORS FOR ENVIRONMENTAL REVIEW
A.
The foreign investor shall provide an Environmental Impact Analysis of the
proposed project,including:
3)
allegedly sustained by workers, including workers’ compensation claims;
explanation of all fines, penalties, citations, violations, regulatory agree
list of all raw materials, intermidiates, products, and wastes (with flow
ments, and civil damage claims involving environmental and occupational
1)
diagram);
2)
health and safety matters as well as hazards from or hann attributed to the
list of all occupational health and safety standards and environmental
standards (wastewater effluent releases, atmospheric emission rates for all
air pollutants, detailed description and rate of generation of solid wastes or
marketing and transport of the products of such enterprises;
4)
other wastes to be disposed of on land or by incineration);
3)
4)
equity partners and providers of technology;
plan for control of all accupational health and safety hazards in plant 5)
environmental and occupational health and safety for each plant location;
products, and wastes;
6)
copy of corporation guidelines of the foreign investor for conducting envi
subjectof controversy within the local community or with regulatory authori
manufacturer’s safety data sheets on all substances involved.
resolved in each case;
audits and reports by consultants;
8)
copies of safety reports, reports of hazard assessment, and risk analysis report
carried out with similar technology by the foreign investor and its consult
processes and products are used, including:
list of all applicable occupational health and safely standards and environ
mental standards, including both legal requirements (standards, laws, regu
copies, with summary, of all corporate occupational health and safety and
environmental audits and inspection reports forcach location, including such
and performance of existing plants and plants closed within the past 5 years
in which the foreign investor has partial or full ownership, where similar
explanation of cases where any plant’s environmental impact has been the
ties, including description of the practices criticized and how criticism was
7)
The foreign investor shal] provide complete information on locations, ages,
B.
1)
names and addresses of governmental authorities who regulate or oversee
operation, storage, and transport of potentially hazardous raw materials,
ronmental and occupational health arid safety impact analyses for new
projects;
5)
description of the foreign investor’s percentage of ownership and techonol-
ogy involvement in each plant location, and similar information for other
ants.
9)
copies of toxic release forms that have been submitted to governmental
bodies (e.g., the U.S. Environmental Protection Agency or similar agencies
lations) and corporate voluntary standards and practices forthe control of oc
in other countries) within the past 5 years, for all plant locations;
cupational and environmental hazards of all kinds;
any information considered relevant by lhe forcign investor.
2)
description of all cases of permanent and/or total disability sustained or 10)
AGREEMENTS ON POLICY
The foreign investor shall submit a statement of corporate policy on health,
C.
proposed project. The foreign investor shall agree that the proposed project
will pay the cost to the developing country' government for all medical and
safety, and environmental performance of worldwide operations. This must
exposure monitoring during the lifetime of the proposed project.
include the corporate policy on laws, regulations, standards, guidelines, and
practices for new industrial projects and production facilities. The foreign
G.
the staff responsible for carrying out this policy,
harmed as a result of lire project’s occupational hazards and
its authority and
responsibilities, and its position in the foreign investor corporate structure.
Such descriptions will also include the name, address, and telephone
H.
function. The foreign investor shall state whether it follows the same
standards worldwide for worker and environmental protection in all new
E.
F.
environmental
impacts, as determined by the government of the developing country.
The foreign investor shall follow marketing safeguards as restrictive as
those it applies anywhere in the world, to assure that workers and members
of the public arc not harmed as a result of the use of its products.
number of senior corporate management officials in charge of this staff
D.
The foreign investor shall agree that the proposed project will fully
compensate any person whose health, earning capacity, or property is
investor shall explain how its global policy is implemented by: describing
I.
projects; and if not, explain why not.
The foreign investor shall agree to provide the developing country immediate
If the foreign investor becomes awarcof asubstanital risk of injury to health
or the environment from a substance it manufactures or sells in the
access to the proposed industrial facility at any lime during its operation to
developing country, a risk not known and disclosed at the time of this
application, the foreign investor agrees to notify the environmental protection
conduct inspections, monitor exposure of workers to hazards, and sample
agency of the government of the developing country immediately of such
for pollution release.
The foreign investor shall agree to fully train all employees exposed to
J.
potential occupational hazards, including potential health effects of all
Substances Control Act of the U.S.A.)
The foreign investorshall provide the names, titles, address, phone, and fax
exposures and the most effective control measures.
The foreign investor shall agree to provide the developing country with
equipment to analyze workplace exposures and pollutant generation, including
but not limited to all limits specified in A.2) above, for the lifetime of the
risk. (This is similar to requirements under section 8c of the Toxic
numbers of its senior corporate officials charged with implementing envi
ronmental and occupational and safety and health policies including plant
design and operations, corporate inspections and reviews of plant perfonnance, and product stewardship.
REFERENCES
i.
2.
3.
1C1 announces corporate policy ol “uniform environmental standards lor all new plants worldwide and a comprehensive waste recycling policy”, (Chemical
Week. December 5. 1990)
Dow Chemical announces corporate policy to “ensure Dow facilities from Midland (Michigan. USA) to Malaysia operate under the same environmental
and safety standards... based on those of Dow’s U.S. operations", {chemical Week, October 17. 1990)
Castleman, B. “Corporate Standards Applied Internationally”. Global Development and Environment Crisis: Has humankind a Future? Asia-Pacific
People’s Environment Network, Penang. Malaysia, pp. 397-399, 1988.
Ref: Published in "NEW SOLUTIONS" Summer 1991 Page No. 75-76
•
'*
FrEH
NEWSLETTER
July-August, 1987
Vol. I
No. 5
Occupational Health: Some Issues
Vijay Kanhere
“ALMOST all the agents that have been recognised as be
ing carcinogenic in humans, have been identified as such
in the occupational setting”,—Encyclopaedia on occupa
tional health and safety by the ILO.
The greater the number of chemicals used in industries,
the greater are the number of affected persons. The ef
fects of chemicals in their acute form are obvious.
Thousands of persons affected due to MIC in Bhopal,
posed a grave problem to community health. And what
about the workers in the factory, who were slowly and
regularly being affected not only by MIC, but also by
other chemicals like phosgene? Are not the workers also
a part of the community?
Let us take the example of silicosis. It is usually treated
as tuberculosis. This has happened in Mandsaur in
Madhya Pradesh and Baroda in Gujarat. Workers in
Alembic Glass Works had to struggle for being treated
as patients of silicosis. What is the effect of these patients
on the community? Their lungs are affected, their
resistance to disease goes down and they readily contract
tuberculosis. This increases the occurrence of TB in their
families and the community.
Noise pollution in the community has been widely
discussed. It was a topic dealt with in a popular televi
sion serial as well. However, what is hardly ever mention
ed is that workers are day after day, for years attacked
by noise—in the textile mills, in engineering units, on
boilers, compressors... As the hearing capacity of
workers gets affected, apart from many serious possible
accidents, their irritability increases. Within the family,
it creates tensions. Everybody has to speak up so that the
affected worker.can understand. He/she too judges the
capacity of others from his/her or own and so starts talk
ing in a louder pitch, which irritates other family members
in turn.
There are carry-home diseases such as asbestosis.
Chemicals reach homes through overalls, clothes, un
washed body parts and they affect family members. One
ESIS doctor informed us that the majority of the cases
he treats are those of dermatitis, induced by exposure to
chemicals.
No longer can one think of occupational diseases as
an exclusively urban problem. In Punjab and
Maharashtra, there are areas where insecticides are sprayed
aerially by helicopters. These insecticides affect
agricultural workers and farmers. Chemicals used in
agriculture are increasing at a fast rate. In rural areas,
where residential areas and work-places are not sharply
differentiated, the effect of these hazardous substances
are going to be all the more.
The National Commission on Labour in its report in
1969 commented, “... the slow and agonising process of
an occupational disease may not stir the community as
much as it would in countries with chronic labour shor
tage, although to the near ones, it is a tragic occurrence.
Relief gets organised soon after the event, but prevention
gets side-tracked”.
However, in countries like India, relief too takes a very
long time. The Bhopal disaster made national and inter
national news. However, almost 7 months after the
gruesome event, conscious doctors had to move the
Supreme Court merely to get the supply of the proper
medicines. (Dr. Vohra Vs. the State, 1985). Even in a
metropolitan city like Bombay, relief has not been effec
tively organised even in cases of chlorine leakages.
In fact very often it is even difficult to get diagnosed.
as a victim of an occupational disease. Workers suffering
from asbestosis even in cities like Bombay, have to go
through a tiresome process merely for being diagnosed
properly as patients of asbestosis.
There are various reasons for this state of affairs".’ For
one thing, any talk about health and safety at the
workplace is seen as a direct threat to the profits as well
as to the power of the management. This also relates to
the lack of political will to take the health of the workers
seriously. This reflects in the content and approach of the
curriculum in medical colleges. Thus even the knowledge
about ‘notifiable diseases’ is absent with most doctors,
including those working in industrial areas.
This is glaringly brought forth in the fact that from the
year 1960 to 1980, there was not a single case reported
of 11 out of the 22 ‘notifiable diseases’. In this period only
30-32 cases of diseases have been reported per year, while,
with a much better technological set-up in the factories,
almost 20,000 cases of asbestosis are reported each year
in the US despite better preventive measures.
From this it is obvious that the doctors can and must
play greater role in learning about, diagnosing and repor
ting various industrial and occupational diseases. It is also
necessary to make this information available not only to
the industrialists and government agencies but more im
portant to the workers themselves, their relatives and the
public at large especially the poor who are most exposed
to these hazards. This is one important weapon to stop
the mindless and inhuman maiming of lives in this
country.
FOR PRIVATE CIRCULATION ONLY
To
The FRCH collective,
I acknowledge, with thanks, the receipt of the BiAnnual Report of your Foundation and the latest issue
of FRCH newsletter.
Both these publications bear your stamp and put forth
loudly and clearly the messages that need constant re
emphasis in our country.
I must confess that I cannot agree with all that is said.
Working, as I do, in a public hospital, full time, I see the
need for such hospitals and for specialities such as mine.
The poorest need excellent service no less than do the wellto-do and I feel that it is imperative that we keep our
public teaching hospitals in the forefront of patient care.
Unfortunately, these days it is the 5 star hospitals that are
in the forefront, whilst the public hospitals are starved
and downgraded.
Whilst there is no dispute regarding the need for effi
cient measures to improve public health, prevent disease,
educate the population at large and generally do all that
is possible to improve the economic status of the villagers
in particular and labourers in general, I see the ill effects
of these being pitted against development of the large
teaching hospitals. I feel that this is wrong. BOTH NEED
ATTENTION, DEVELOPMENT.
Sunil Pandya
Neurosurgeon
E.M.
K.
Hospital
Bombay
Notes from Medical Journals
Mukund Uplekar
Is our pursuit of a healthy body—a major threat to
health?
Ivan Illich, a long time critic of the medical establish
ment no longer views doctors as the major threat to
health. He has discovered a far more dangerous pathogen
the pursuit of a healthy body. Once again we have found
the enemy and once again he is us. Complacently we have
stood by while a multimillion'“health industry” has taken
over, offering advice and handholding to the fibre eating
health magazine readers whom the doctors are too busy
to see. These new pseudoscientist healers diagnose yeast
cells in the blood as a cause of your tiredness, and cure
it with a garlicky remedy that only they sell. They analyse
your hair to find out which mineral or vitamin you need
to buy from them. They measure your body fat by pin
ching you with calipers; determine your skin’s resistance
and electro-magnetic balance with galvanometers; and
perform stress tests, conveniently combined at health clubs
with a massage, a sauna, or the whirlpool. Various “Car
diovascular” exercises are carried out perched on a sta
tionary bicycle while hooked up to a pulse monitor that
lights up as you reach the top of an imaginary hill.
How harmful are these practices other than wasting
people’s money? Illich rails against these “sundry holistic
well-being programes” this “curious mixture of opionionated and detailed self care practices”. He thinks this
mumbo jumbo could cause even more harm than 100,000
patients being seriously injured each year by
hospitalisation.
Antibiotics in Antidiarrhoeals
In ‘Antibiotics: the wrong drugs for diarrhoea’ Health
Action International draws attention to the WHO state
ment that “antimicrobial drugs are not indicated for the
routine of acute diarrhoea”. Health Action International
claims that spending on antidiarrhoeals (nearly $ 150
million a year) diverts attention and resources from oral
rehydration which is a lifesaving treatment.
Products containing neomycin, streptomycin, chloram
phenicol and sulfonamides are singled out as being the
“worst of a bad lot”. For example, widespread and irra
tional use of streptomycin has led to the development of
bacterial resistance to the drugs for the treatment of tuber
culosis. And despite the well recognised risk of bone mar
row suppression, chloramphenical is present in 12
products.
Of the 12 regions surveyed, only Hong Kong has
stringent regulations to prevent the registration of an
tidiarrhoeals containing an antimicrobial. The report will.
be sent to health ministries, drug regulatory agencies and
medical schools around the world.
Interaction Between the Government, NGOs and the
Private Sector in Implementation of HFA
Abhay Bang
■ .Ideological basis of cooperation: The cooperation can the NGOs assume, especially if they want to increase
between the government and the NGOs in the health sec their impact by interacting with the government which
tor was always on the basis of common ideology and alone has the political responsibility and resources to pro
interests. Thus different categories of NGOs were col vide HFA?
The following roles may be posible
laborating at different times with the then ruling govern
1.
Research and Innovation
ments. Christian missions were actively cooperating with
2.
Demonstration
the British rulers with common imperial interests. The
3.
Training
Gandhian constructive institutions were active in col
4.
Evaluation
laboration with the Congress government with their com
5.
Building public opinion for changes in
mon roots in the freedom movement and ‘Congress’
government policies.
ideology. The gates were opened for the voluntary agen
While the last one is not cooperation with the govern
cies with closer links with the ‘opposition’ parties (when
these came into power under the name of Janata Party) ment in the narrow sense, this role is extremely impor
by allowing a major role to NGOs in the National Adult tant. The history of public health is studded with examples
Education Programme. Now with the free market ideology as to how this role has greatly improved the government
of the Rajiv Gandhi government, the private sector shall policies and programmes. The Sanitary Movement in
have more role. The talk of social marketing, of delegating Great Britain in the 19th century or the work of the en
the responsibility of advertisement of the national pro vironmentalists today are glaring examples. However, the
rest of the discussion in this paper does not include this
grammes to private agencies are a few examples.
Where do the NGOs in the health sector ideologically type of role.
stand today? Inspite of their tremendous diversity and dif 3. Issues in Government-NGO Interaction: In any work
ferent religious or economic roots, most of them explicitly ing together,compatibility on the following points is im
or implicitly believe in the welfare state with a mixed portant, and hence needs attention.
1. Ideology and Goal
economy. Obviously they do not find- any major
2.
Objectives (specific)
ideological problems in collaborating with the various
3.
Organisational structure and culture
governments in India. Even those who profess to have a
4.
Procedures and rules
radical ideology usually do not have problems in
5.
Personalities
cooperating with the government as long as they can con
6.
Finance
tinue to attack the system while retaining their safe posi
The ideology and the goal being similar, these don’t
tions in the urban universities and institutions. Many other
grass root workers or activists strive for limited reforms pose much problems in the actual working together. But
by opposing govern.ment policies; and yet in the long run the different emphasis due to the different objectives may
they too work with the government as their reforms are pose a problem. Down in the field, primary health care
seems to be reduced to fulfilling targets of a few vertical
accepted.
Thus most of the NGOs today have no major programme objectives. Family planning (FP) tops the list
ideological barriers for cooperating with the governments with immunisation and blindness control coming next.
Rest of the programmes or indicators like infant mortali
in India.
2 Role of the NGOs: Inspite of hundreds of failures of ty count little. The NGOs may have different or broader
implementation, the National Health Policy is more pro objectives and hence a tussle for priority may ensue. A
gressive than most of the NGOs. At least at the concep NGO may not be willing to go all out for the numerical
tual level, the Primary Health Care is oriented to preven targets of FP while for the government health officer, it
tion, outreach and use of paramedics, while most of the is a sacred cow.
There is a contradiction in the structure and function
NGOs are still curative oriented, running charitable
dispensaries or hospitals or diagnostic camps. Gone are of the Primary Health Care strategy. The National Health
the days of Albert Schweitzer or Father Demain when Policy has abandoned the unipurpose organisational
such individuals or NGOs outreached where no govern structure. Now we have buildings and a large number of
ment care reached. The most important outreach agen health workers so that an organisational basis is created
cies today are the government or the private practitioners. for continuous and comprehensive health care. And yet,
Thus in Gadchiroli district which is probably the most the health programmes are still conducted in the form of
difficult district in Maharashtra, there are 3 NGOs in campaigns which need a mobile structure and large scale
health, 34 PHCs, with 230 subcentres and 700 CHVs and propoganda rather than buildings and accessible workers.
about 300 General Practitioners (including Registered
In its relationship with the government organisation a
NGO is likely to face what may be called the ‘middle level
Medical Practitioners).
A recent study by FRCH on the NGOs in health in constraint’. At the top, the officers can take a broader view
Maharashtra concluded that the NGOs are concentrated about cooperation. The bottom level functionary may be
in the developed districts rather than the backward areas. happy to work with a.NGO because of more humane and
With the tremendous expansion of the government
health sector or the private practitioners, what new role
(continued on page 8)
Industrial Accidents: Whose Life, Whose Responsibility?
Sujata Gothoskar
are not really ‘accident’al at all) and this cause can be and
has to be pinpointed and removed. This process of pin
pointing and removing the cause of industrial accidents
and occupational diseases has important implications.
EVERY five minutes, one of the world’s workers is killed
and fourteen permanently disabled as a result of accidents
at work or occupational diseases, according to an estimate
by the International Labour Organisation (ILO). In In
dia, over the 30-year period from 1950-1980, 36,000
workers have been reported killed and 6.4 million injured
in accidents at work in the factories in the organised sec
tor, mines, ports, docks and railways alone. The number
of workers killed or maimed in the unorganised industry
can only be a guess. And over the years, statistics indicate
that injuries due to industrial accidents continue to
increase.
The number of fatal accidents has risen by 225 per cent
in the last 30 years, from 248 in 1950 to 806 in 1980. Nonfatal injuries, equally dangerous *, have been rising even
more rapidly, from 76,000 in 1951 to 355,000 in 1980—a
393 per cent increase.
Increase between the years 1950 and 1980
Increase in average daily employment
Increase in fatal injuries
Increase in non-fatal injuries
120 per cent
225 per cent
393 per cent
Number of fatal injuries per million human hours worked
Countries
number in
1979
1980
U.S.A.
U.K.
Japan
Yugoslavia
India
0.03
0.03
0.02
0.07
0.15
N.A.
0.03
0.01
0.08
0.15
To begin with, it puts a halt to deaths and mutilations
of more workers. Secondly, it asserts that workers have
a right to work without their lives or well-being being
jeopardised. Thirdly, it gives workers the right to know
and act in favour of their own safety according to the
knowledge they have gained about the work process. Four
thly, it makes a political statement about the primacy of
workers’ safety vis-a-vis either management prerogatives
or the blind profit motive.
An international comparison also indicates that acci
dent rates in India are exceptionally high. It is difficult
Theories of Accidents
to compare statistics for non-fatal accidents since criterion
The standard explanation for most accidents is that they
for reporting are different in different countries, but fatal
are due to either unsafe mechanical or physical conditions,
accidents can more easily be compared.
or unsafe actions, or both. However, the actual causes of
The figures for India are based on accident reports accidents cannot be attributed simplistically, but are much
received by the Factory Inspectorate, and therefore relate more complex, especially, if ‘unsafe actions’ are attributed,
only to ‘reportable’ accidents, i.e. those which lead to an as they usually are, to workers.
absence from work of two days or more.
For example, one could consider the accident at Union
Moreover, it is well known that even reportable ac
Carbide, Bhopal, in which Ashraf Khan was fatally in
cidents are very often not reported by employers, as they
jured. He was splashed with phosgene while opening a
wish to avoid paying compensation or getting prosecuted
pipe for maintenance work, panicked and removed his
for non-compliance with the law. And the law does not
safety mask before decontaminating himself, inhaled a
even cover construction workers or workplaces with power
fatal quantity of the toxic chemical and collapsed. The
employing less than 10 workers and workplaces without
management took the position that it was his unsafe
power having less than 20 workers (and most contractors
take care not to have more than 19 workers on any one action—removing his safety mask—which resulted in his
death. Yet the fact is that the pipeline was supposed to
site), so that soTne of the sections, which are subjected
have been properly evacuated and put under vacuum, ac
to most hazards—in small-scale industry, construction,
contract workers, etc,—are not included in accident cording to the company’s own laid-down procedures. The
pipe-line should have been empty. Ashraf had no reason
statistics at all.
Finally, these figures do not include the enormous to think he would be splashed with phosgene, and in the
number of people who are killed or disabled by oc circumstances, his panic was an entirely normal human
cupational diseases. Taking this into account, it appears reaction. Thus to say that this accident was due to both
that a significant proportion of the total working popula an unsafe action and an unsafe condition is really to
tion suffers from some form of injury, upto and including misrepresent its cause. If the design and processes can
fatal injury, due to occupational hazards. In short, the not pre-judge and plan according to entirely human
responses of the moment, clearly such designs and pro
situation is appalling, and it is getting even worse.
This points to the extreme urgency of monitoring ac cesses are at fault? As the safety manager at Siemens put
cidents. This is of course not an easy task. Nevertheless it, ‘the work place and work processes have to be not on
most accidents cause immense misery to workers and their ly full-proof, but also fool-proof. Even ‘deliberate ac
families and most accidents have a clear cause (i.e. they cidents’ should be planned against in the original scheme
itself. One did not even ask for that much in the Bhopal
case.
‘Every non-fatal accident has the potential to become a
Again, take the finding that contract workers have a
fatal one the next time it occurs.
higher incidence of accidents, especially fatal accidents.
For example, in a petroleum plant in Bombay, a contract
worker, working in a pool of liquid which he believed to
be water, threw a lighted match into it, it turned out to
be oil, however, and he was burnt to death. This would
be considered a clear case of an unsafe action but the
cause of the accident was ignorance on the part of the
worker. Thus to say that the cause of this accident was
an ‘unsafe action’ would be completely erroneous, because
to use untrained and uninstructed workers for work with
hazardous chemicals is to create an inherently unsafe
situation.
cident Prevention’ Industrial Safety, Health and Welfare Cen
tre, Central Labour Institute, Bombay)!’
If the accident proneness of a few individuals is not
responsible for most accidents, are there other factors
which are within the control of workers? Could there be,
for example, self-infliction of injuries in order to get timeoff from work? Or could a large number of accidents be
due to the carelessness of workers?
Of those interviewed, not even management represen
tatives thought that such causes could account for a
significant proportion of accidents. Nor does it seem likely
There are unlimited instances, indicating the fact that that workers would court death or mutilation if they could
it is absolutely necessary to go beyond the superficial avoid them. Most of the accidents are such that even if
the actual injury is minor, it could easily have been much
category of ‘unsafe action’ and investigate why the un
worse—and therefore to inflict it on oneself would involve
safe action took place.
incurring the risk of serious injury or disablement. Our
Another theory explaining the occurrence of accidents, investigation shows that where workers do take such risks,
attributes the majority to a few individuals who are it is for reasons beyond their control—e.g., because the
predisposed to have a high rate of mishaps. At three places work-situation itself forces them to do so, because they
out of twenty where we obtained interviews, one worker are ignorant of the dangers, because they are asked to do
was identified as a victim of repeated accidents, and in jobs for which they are insufficiently trained, and so forth.
a tyre factory and in the docks, there were a few such
On the other hand, the conditions and actions which
workers. But in most places, there were no such ‘repeaters’, routinely lead to accidents are within the control of
and even in cases, where a few workers repeatedly had ac management; and it is in recognition of this that most
cidents due to drunkenness and negligence, they were far modern health and safety legislation lays the responsibility
from accounting for even a significant proportion of the for providing a safe and healthy workplace on the
employer.
accidents.
This article is based on discussion and research work
Our findings were confirmed by other studies:
“Numerous studies carried out by research workers have fail done for the Accidents bulletin: No. 10, of the Union
Research
Group, Bombay and the several discussions with
ed to prove conclusively that any group of persons in a given
sample can be separated as accident-prone. Dr. Schulzinger, Rohini, Vijay, Ram and Jairus, and going through their
after careful study of 35,000 injury cases,... suggests that notes and jottings.
most accidents are due to the relatively frequent solitary ex
perience of a large numer of individuals. The total number
of accidents suffered by those who injure themselves year
after year... is relatively small... Professor Edwin E.
Ghiselli... advises that the term accident proneness should
never be used in studies of the causes of accidents and in
juries, as it is according to him “dangerous and misleading
and contributes nothing of practical value to our understan
ding of the causes of industrial accidents and injuries”. (‘Ac
References
R.R. Nair, Workplace accidents are increasing, Science Today, September.
1982.
K.C. Gupta, Challenges in the area of Occupational Safety and Health
in the coming decade, paper presented at International Congress on
Safety, Health and Environment, February, 1987.
H. Ganapathy, Prevention of accidents in building construction, Central
Labour Institute.
Ban EP Drugs: An Appeal to SC
Ravi Duggal
The hearing of the Public Enquiry commissioned by
the Supreme Court (SC) regarding banning of the
highdose Oestrogen Progesterone (HDEP) combination
was held on 14th July in Bombay. Like the earlier three
hearings in Madras, Delhi and Calcutta it was also a farce.
The very nature of the enquiry needs to be questioned.
The SC must look into this matter seriously because this
sort of an enquiry is the first of its kind and is going to
form a precedent. And a bad precedent would be both
unjust and dangerous.
First of all the Drug Controller (DC) cannot constitute
the authority to sit over such a hearing because it is par
ty to the decision-making process (in this case banning
or continuing the production and sale of HDEP). Given
the political economy of our country, aptly illustrated by
the Justice Lentin Commission’s exposure of the Drug Ad
ministration of Maharashtra, the impartiality of the DC
office cannot be assumed. The pharmaceutical industry
is too powerful a lobby and the DC authority is highly
influenced by the former. This was too obviously apparent
during the proceedings of the various hearings.
The SC should also question the manner in which the
concerned drug companies have gathered evidence in sup
port of HDEP, when internationally its hazards are well
recognised. It was amply evident during the hearings that
most gynaecologists and other medical and phar
macological experts who submitted in favour of the drug
companies did so for reasons other than their own belief,
practice and conviction. The written submissions given
by many gynaecologists and doctors are mere signatures
on standardised statements obviously circulated by the
drug companies.
to hunt around to gather proof for this. It is well known
and documented. The Lentin Commission has adequate
ly exposed the misdeeds of both the drug companies and
the Drug Administration. The dangerous and misleading
practices indulged by the medical profession in India to
make a fast buck are well known. General Practitioners
will administer injections, tonics, steroids and antibiotics
for ailments like headaches and colds or give an in
travenous drip of calcium gluconate to a patient complain
ing of tiredness. Gynaecologists will reconstruct hymens
to reassure virginity, conduct sex-determination tests, help
preselect sex of foetuses and do ceaserians and hysterec
tomies even when not required.
The prescription practices of an overwhelming majority
of doctors is largely unethical and irrational and this is
the danger that concerned people supporting the ban of
HDEP fear most because HDEP is being grossly misused
by doctors, like many other harmful and also relatively
harmless drugs. I will not go into the misuses and hazard
of HDEP because a lot has already been written and
documented about this.
What should the supreme court look into? First of all
it must scrutinise the adequacy and fairness of the enquiry.
The general experience of the hearings has been that the
fundamental basis of the enquiry was faulty and therefore
the enquiry invalid. More thought needs to go into for
mulating the structure and nature of the enquiry. The SC
must review this seriously because we don’t want a poor
and unjust enquiry to become a historical precedent. The
SC must assure impartiality and justice—a properly con
stituted unbiased enquiry commission, that seeks indepen
dent evidence and is not an interested party to the deci
sion, somewhat similar to the Justice Lentin Commission,
should do an adequate job.
Further, the entire focus of the public enquiry has been
The SC should also immediately put into effect the
on technical issues relating to HDEP and the clever use
of legal loop-holes. The DC and the drug companies, as earlier ban of HDEP that was made by the government
well as their supporters, have completely ignored social on the recommendation of the Indian Council of Medical
realities that are crucial in making decisions concerning Research, the premier medical research institution in In
human lives. The panel conducting the hearing compris dia. When many developed countries after bitter ex
ed only of “technical” persons from the DC’s office. No periences have already banned or withdrawn HDEP on
social scientist, lawyer, gynaecologist, or representative of grounds of well known health hazards, associated with
consumer and civil right groups were, there on the panel. the drug then why wait for further evidence to ban the
Worse still no woman was represented on the panel. Isn’t drug. Do we want another thalidomide type disaster? How
it ironical and unjust that the fate of a drug consumed can the SC and the government permit a known hazar
only by women is being decided by men who’ll never have dous drug to be produced, marketed and consumed free
to experience the hazards of the drug! Why does it always ly in the country? Even an iota of doubt about the harm
happen that any question that involves women’s rights, fulness of drug is sufficient reason to ban it, especially
security and health is treated with neglect, carelessness considering social realities of our country. It is indeed in
and apathy? These shortcomings in itself make the nature human to let loose a harmful drug on an uninformed and
of the enquiry questionable.
oppressed people.
The most important issue that should concern this en
quiry and has totally been overlooked is the nature of
medical practice in India. In general the type of private
medical practice prevailing in the country is grossly
unethical and irrational. The checks and control by the
Medical Council of India and the Drug control Ad
ministrations is virtually non-existent. One doesn’t have
Therefore it is important that the SC in reviewing this
public enquiry should reassess the basis of formulating
terms of reference and assure that social aspects of the
concerned issues are taken into account adequately. And
it is our fervent appeal to the Chief Justice of India to
ban HDEP with immediate effect in the larger public
interest.
PESTICIDE POISONING
Amar Jesani
Pesticide poisoning, including attempted suicide by in
gesting pesticide, is a significant health problem, par
ticularly in the third world countries. In our country
reliable statistics on pesticide poisoning are very difficult
to obtain, although there are some estimates and these
suggest an increase in the number of people suffering from
this problem. Of the third world countries, some studies
are available from Sri Lanka. A survey covering hospita
lised patients between the years 1975 and 1980 revealed
that 79,961 patients were admitted due to pesticide poison
ing, 6083 of whom died. Organophosphate compounds
accounted for 76 per cent of these poisonings. Further,
on analysing data for the year 1979 in this survey, it was
found that 73 per cent of these cases were due to attemp
ted suicide.
From the data of this Sri Lankan survey and others,
certain new and disturbing medical aspects of
organophosphate pesticide poisoning are emerging. The
most commonly seen, and known symptoms include
cholinergic crisis, with miosis, sweating, salivation, etc.
This is treated with high doses of the anticholinergic drug
atropine, cholinesterase reactivators (oximes) and pyridine.
In addition to this acute cholinergic-toxicity phase,
observed in all cases of organophosphorous pesticide
poisonings, some people suffer after two to five weeks of
exposure, from a delayed peripheral polyneuropathy in
volving the distal muscles of the extremities. This syn
drome is also known, though not properly documented
in our country.
Recently, in the March 26, 1987 - issue of the New
England Journal of Medicine, Senanayake and
Karalliedde have described another new syndrome of the
neurotoxic manifestation of the organophosphate poison
ing. They observed,in 10 out of 95 patients (in Sri Lanka),
muscle weakness after 24 to 96 hours after the cholinergic
illness, involving primarily the proximal limb muscles,
neck flexors, certain cranial motor nerves and the muscles
of respiration. The effect on respiratory muscles is indeed
very serious. Seven of these ten patients had difficulty in
breathing and three of them died of respiratory failure.
The authors have called it “an intermediate syndrome”
and the condition does not respond to atropine and
oximes.
This expansion in the clinical profile of the
organophosphorous poisoning has very serious medical
as well as public health implication, especialy in the third
world countries where these pesticides are liberally used,
carelessly packaged and dispensed and are the favourite
of those who want to commit suicide.
Jeyratnam, J de Alwis, Seneviratne R. S., Coppiestone
J. F., “Survey of pesticide poisoning in Sri Lanka” Bull.
WHO, 1982: 60: 615-9.
What is New?
40(5), 194-199, 1986.
Books
WHO Chronicle, “Maternal mortality: helping women off
Flavin Christopher,’ “Reassessing nuclear power: the
the road to death”.—WHO Chronicle, 40(5), 175-83,
fallout from Chernobyl”.—Washington: World Watch
1986.
Institute, 1987, pp.91.
British Medical Journal, “Measuring morbidity”.—BMJ,
Fukuoka Masanobu, “One—straw revolution: an in
294, 263, 31st January 1987.
troduction to natural farming”.—Rasulia: Friends rural Maria Mies, “Why do we need all this? a call against
centre, 1986, pp.181.
genetic engineering and reproductive technology”.—
UNICEF, “Learning together from the Sri Lankan ex
women’s studies Int. forum, 8(6), 553-560, 1985.
perience”.—Geneva: UNICEF, 1984, pp.112.
Robinson Jean C., “Of women and washing machines
Zaidi Akbar S„ “Issues in the health sector in
employment, house work, and the reproduction of
Pakistan”.—Islamabad: Pakistan institute of develop
motherhood in socialist China”.—China quarterly, 10,
ment economics, 1986, pp.20.
32-57, March 1985.
Mitra Ashok and Mukherji Shekhar, “Population, food
Prakash Padma, “Sexism in medicine” (paper for 3rd na
and land inequality in India: 1971”.—Bombay: Allied
tional conference on women studies, Chandigarh.—
publishers, 1980, pp.112.
pp.28, October 1986.
Eastman kodak company, “Information age
technology”.—Singapore: Addison—Wesley, 1986, Barreto Luis (Dr.), “Unemployment among doctors: its
roots in socio-economic development in India”.—MFC
pp.654.
meet, 10, January 78.
India, Government of, “Health information of India:
1986”—New Delhi: Directorate general of health ser Duggal Ravi and Gupte Manisha, “XYZ of sex”.—Indian
vices, 1986, pp.292.
post; 31st May 1987.
Ford Foundation, “Banwasi Sewa ashram (Anubhav: Ex
periences in community health)”.—New Delhi: Ford Awasthi Ramesh and Gupte Manisha, “Our destiny floats
with the clouds”.—Indian post, 14th June, 1987.
Foundation, 1987, pp.32.
Duggal Ravi, “Why population won’t fall”.—Indian post,
Reprints
13th June, 1987.
Fulop Tamas, “Health personnel for health for all”.progress or stagnation (part 1):—WHO Chronicle,
Duggal Ravi, “You can’t blame third world all the
time”.—Indian post, 30th May, 1987.
Books m Brief
Manish Mankad
Indian Council of Medical Research, “Medicinal plants
of India: Vol. 2”.—New Delhi: ICMR, J986, pp.600,
Rs.136/-.
The need for a systematic compilation of data on
medicinal plants in India has been felt by almost all
research workers engaged in the study of medicinal plants.
In 1976, Indian Council of Medical Research published
a first volume comprising of information on nearly 350
species of plants presented in alphabetical order (A to G).
The present 2nd volume extends the same (H.to P). It pro
vides in addition, separate indices for botanical names,
chemical constituents as well as names of plants in English
and regional languages of India. Further, classified lists
of plants according to their pharmacological activities are
furnished in one of the indices. This volume also contains
coloured plates of plants.
World Health Organization, “Concepts of health
behaviour research (Searo regional health papers no.13).
New Delhi: WHO; 1986.
The global strategy for Health for All by 2000 recognis
ed the need for health behaviour research (HBR). Despite
this good start, research efforts in relation to national
primary health care programmes were initially slow in
recognising the need for and committing resources for
social science research. HBR was needed to help reorient
the planning and implementation of primary health care.
(continued from' page 3)
liberal treatment. It is at the middle level where the pro
blem of rivalry and sharing of power arises and hence a
great resistance or even hostility may start.
A maze of procedures and inscrutable rules which are
characteristic of government functioning pose two types
of problems. NGOs often understand the intricacies of
these or can be easily trapped into immobility while
working with these. On the other hand the NGOs have
the advantage of autonomy and flexibility in their own
structure and their partnership with a government institu
tion or officer who is tied by the procedures may be like
a pair of unequal bullocks resulting in strain and
dissatisfaction to both.
Even in the seemingly faceless and impersonal govern
ment system, the success of cooperation may depend
heavily on personalities. A single person with vision and
openness for new things can make a world of difference.
Whether NGOs find a cooperative government officer or
an obstructive one in their path depends on their luck or
on political manoeuvering. How to match compatible per
sons- from two sides so that smooth working is possible
is a major issue.
Government money should be available to NGOs in
health if they too are working for HFA. And yet if NGOs
take money from the government, they are either subor
dinated by political weapons or they are trapped and im
mobilised by the endless restrictions and procedures which
This document defines the scope and future direction of
HBR within WHO/SEARO. HBR is viewed as part of
health systems research and an integral complement to
all primary health care components.
Feminist review, “Sexuality: a reader”.—London:
Virago, 1987.
The book includes discussion of issues relating to sexual
politics, the social construction of feminity and masculi
nity, psychoanalysis, lesbianism, pornography and
representation, sexual violence and adolescence, with each
article set in its time and context by a series of prefaces
especially written for this volume.
Fukuoka Masanobu, “One straw revolution: an introduc
tion to natural farming”.—Rasulia: Friends rural centre.
1986, pp.181.
The author describes the events that led to th'e develop
ment of his natural farming methods and the impact that
it has had on his land, himself, and the thousands of
people he has taught. He feels that natural farming pro
ceeds from the spiritual health of the individual. He con
siders the'healing of the land and the purification of the
human spirit to be the same process and proposes a way
of life and a way of farming in which this process can
take place. More than merely indicating methods, this
book aims at changing attitudes: about nature, farming,
food, human—physical and spiritual health.
necessarily accompany government grants. In both ways,
the NGO looses its qualities or autonomy and speed.
How can government money be made available to
NGOs and yet not have these side effects is an issue for
discussion.
CHV Experiment: A Case of NGO-Govemment
Interaction
When conceived, the CHV was to be a volunteer bring
ing with him/her the qualities of NGO, i.e. autonomy,
motivation, community participation, etc. And yet
during implementation he was converted into the lowest
category of government worker with little financial
remuneration. He was subordinated and internalised by
the government health structure.
A fate similar to that of CHV must be avoided by giv
ing attention to the various aspects of interaction discuss
ed above. And yet, this is a new area of organisational
research and innovation. Only through a process of trial
and error, experimenting and learning that a feasible
model will emerge. Respect for each other and openness
is an essential prerequisite on either side.
Abbreviations
NGO : Non-government organisation
HFA : Health for All
FP
: Family Planning
CHV : Community Health Volunteer
Edited by Sujata Gothoskar with the co-operation of Manish Manked and secretarial assistance from Anuradha Naik and Eleuterio Fernandes.
Produced by the Foundation for Research in Community Health, 84-A, R.G. Thadani Marg, Worli, Bombay 400 018. Telephone: 493 86 01. Printed
by Modern Ans and Industries, A-Z Industrial Estate, Lower Pare!, Bombay.
S OXFORD i
'J.ErX.T.ff.L l-ISff.l.Thl-J.N
/WDuSr^
Ref. No.
6 3 NN
Q
£r-j Tf) L. ■ !->^L th
Z7 -
P-ppl'/Cn
-~-V^
IJcrthf''
- Mcdfe^ O
D-r _
tsL-OfZ) <2s~>czLo
TJc
CO rc>)'rCcL
/3c^)K c
i.
h)&-p<.
2.
3.
r ooP Kajp
— C-O-r~>
iye.
/^C<.K>-> Cj
%>c\ Y )'^'T7c(j^
'IDE.PP.E&Stpr'S
i I ln^e-^3
&L<s7') r-L^olxJZ- c^L
4. /Az-zg^A^gU^k^^
hfajcAo
. erZe.
Ox^>
/■^c^e^i/i
c^n
sfeteJ-^cL ?
c^
cLCo ^.<s^<> <2
ctj’
hLe-aJ-Leck
g<s»z . e^ ^cet.cf
by
/~^CcH..
7br^~>
(. to yea^,
ElErt TflL.
HE-PL TH
PTZc>J3L£rlE>
HUMfW
T^Ac^oJ^
c^-)
. /-Ox-oZ"■ Pick
l=.XJcef)tan.s
_ fo - X-<a
P.k'...^ ./So. ..^2^<AC^
.P.-rt^c.
Jx^ro. >~>X.L\Ch
_______
—^■y'<s-LJ-p S------
2"crok'JacJ.L.
, J)
_ Scr"C-<'ca./.
-fi2- ~‘''J<~ fi a [s-T^Cj
7 ■/)■£_ ... 73 rcn^-m
—^r"?
___ LS&Jj'Cja^a.J
2.
p.rrcffo Le-tn-a
cZ>[
J-s-i c 'Li^z> /rt<xZ-
z.
FcX
-
A^7^/. /Xe^/ZA
Z<2
.5------ lx/■/
O ■ t^'Lejol^.L
fin
/-/-<£.<=<.O ■ /Y7.• I)
Pj^'cc^
<yz7A&//g->
ZTltfCX-cZA/1,
4>7 <-r<zke-/-y_Cje
- G-cfco-n
Z/- z
Z?.L>_ "?C Z?'l.c<Z7‘S-^'
C?2t<2.CX^^fC^iZak'
^ cS^T-xy^y^rec^ 4?
-
.
-
^Z77t.v//y7Z<" j .
J'a-y^> .. f) >cbLc^->.
Rei->c<hih'h^K<r^
df /reeled
Or
£>/<?.K<S>
ffircro/z
-C-i e~lc^^o
/• /'Wc
/v'fe-c=<< 'Co- K<oo
/T-T-e^c^^e^cj. tftc-
v^C’. /<-<-<£
ezcf L.^jrcn'k..
t>rjpe-^-pcn^c<l
Oceo/'ive.
/<e-ey-7uo
V'c:<~<z-c\-r->^
crr^>&o
'p-r-cxcHcejly
O-o
C^rS^yy<2->' Chirico-'
Coll<? c^cx-e-o
croj?- k)y
— Kke.^-n
raJ'hjzy'
crrCaoftecft ^iJuiaKcra
S
— Z!i_^a_cL^
^■C.jg Lcocj
.
c>/cX
o
jcd?
f^cr-olhLa. .
<2^ -TT_O cro
C^->oL
<S"oLt^ea. f7crr->
CZ>
^^crulcA.
b <?
co- cAaC-li^r l^p^pC'l
ohck be
Cnl'c Ccrr-wicbi-) after
Paints
Slough Works, has
st paint producing
>f the original buildings
nish making of Naylor
lay the site is a giant
Introduction
Slough Works situated in the Thames
Valley services the entire U.K. with
the decorative paints and industrial
finishes produced at Slough, from its
1,000,000 gallon capacity warehouse.
Paints Division also has its H.Q. and
Research and Development centre at
Slough. The operation starting with
patient research and development,
manufacture, marketing and
distribution is centred at Slough and
backed by the other paint producing
factories at Stowmarket and Glasgow,
the Hyde Works where plastic
sheeting and pvc coated fabrics are
made and the wallpaper manufacture
based at Oldham, plus the depots and
sales offices situated to keep pace
with the constant demand for ICI
Paints Division products.
The entire Dulux Gloss finish and
Emulsion ranges are manufactured at
Slough Works. Added to this are the
many industrial finishes for a variety
of markets and topcoats for the car
industry—paint in capacity from |
pint tins to a customer's 34,000
gallon tank filled continuously with
ICI Electrocoat primer. The 1,000
employees including skilled plant
operators, technicians and scientists
keep production over 10,000,000
gallons a year of finished products.
Other products including Dufix
adhesives and industrial varnishes are
made in the Resins section of the
Works which also make the main
constituent for all paints.
Paints Division stay ahead in the
highly competitive paint market to a
great extent because of the work of
the 500 personnel in Research and
Development Department. Winners
of the Queen's Award to Industry
in 1969 for research into polymer
dispersion, the department is
concerned with the invention of new
paints and coatings, the improvement
of manufacturing processes and
background research into the
properties of surface coatings.
Across the Wexham Road from the
Works and Research Department, is
the stylish Division H.Q. building,
housing the administrative force
which ensures the efficiency of the
Paints Division operation. The key
to this success is the new computer
centre which deals with the range of
services from accounts to paint
formulae.
ICI Paints Division is a worldwide
organisation with associate or
wholly owned factories in Australia,
Argentina, Canada, S. Africa, India,
Pakistan, Malaya, Portugal, Germany,
Trinidad and many more countries.
A liaison is kept with these
operations through the Overseas
at Slough.
From Slough the U.K. and overseas
markets are serviced with ICI paints
whether the order is for single tins
or tanker loads. The reputation of the
paint of being a top quality product
'backed by the technical resources
of ICI' is further ensured by the
Technical Service and Colour
Advisory Departments which offer a
service to all customers which helps
them to make the best use of the
wide range of ICI Paints Division's
products.
How Sheet
The popular misconception of paint
making is that the technique is just
a simple 'stick and bucket' process.
In recent years the paint industry
has seen a revolution in paint
manufacture with the introduction
of synthetic resins, complex
formulations and new machinery.
Even so, the basic constituents of
paint have not changed.
Paint is made from three components
—the pigment, which gives colour
and opacity, the resin or binder
which forms the film and the
thinner or solvent which makes it
possible to apply by brush, dip,
spray or other method. The
important steps in production are
first to make the binder—nowadays
almost wholly synthetic resin or
polymer and secondly to incorporate
the pigment into it using one of a
number of different machines.
e
Manufacture
It is from the Stores department at
Slough that the whole process of the
manufacture of paint begins.
Raw materials arrive here and vary
from a 24 ton load of pigment to a
5,000 gallon tanker of solvent. Raw
materials, are very diverse; with over
950 items from all over the world,
including the colouring and dyeing
pigments, some of which are very
costly items—(Monolite Fast Red
costs £5.10.0 a lb.). To the
decorator the Dulux tin is a well
known sight, and 50 million of these
tins are handled by the store each
year. The solvent tank farms
connected to the paints and resins
departments by a network of
overhead pipes are topped up by
a fleet of tankers to the tune of
150,000 gallons a week.
This covers the basic constitutents
of paint except resin which is
primarily manufactured on site in
We Resins Plant.
The manufacture of synthetic resins
has greatly improved the
Top: In the foreground one of the Solvent Farms,
with its network of overhead pipes feeding to the
Paint department. In the middle, is the oil farm which
services the Resins Plant.
Above: A row of 600 mixers, which are used in the
second stage of preparing a batch of paint. The vehicle,
thinner and drier is added to the concentrated paint
base ready for the final colour matching.
Left: The Alkyd Resins plant with its row of 'kettles',
which produce a wide range of resins used in products
manufactured by Paints Division.
Below: Speed and accuracy are essential in filling
'Dulux' into millions of cans of different sizes. Paints
Division engineers have designed ingenious machines
to do the job.
properties of durability, flow and
gloss retention in paint. The last
ten years has seen the introduction
of several new types, acrylics for
cars and industrial paints, P.V.A.
latex for emulsion paints and the
new Electrocoats for electro
deposition on metal surfaces. The
more traditional resins, alkyds for
air drying and stoving finishes and
urea and melamine resins are also
made on the plant.
The different types of resins are
made in separate buildings situated
at the far end of the site.
These products are made in reactors
commonly called kettles. Reaction
temperatures of up to 250 degrees
centigrade or higher are necessary
and the process lasts 12 hours or
more After the chemical process,
which calls for a high degree of skill
rom the plant operators, is
completed, the resin solutions are
tmnned, filter-pressed and pumped
to storage tanks' with a total capacity
of 350,000 gallons. Most of the resin
is supplied by pipeline to the paint
department for pigmentation, but
some is blended to produce clear
industrial insulating varnishes, beer
can lacquers and adhesives.
The Paint department is the hub of
the Works where the different
ingredients, the pigments from the
dry colour stores and the resins
meet to be dispersed into a base.
The pigments are dispersed in the
resins by a variety of machines; Ball
mills, large steel drums half full of
steel or porcelain balls, which
cascade as the drum revolves are
used to disperse the highly
concentrated pigment base for car
and industrial finishes. Fifty Ball mills
with capacity of 50 to 1,000 gallons
are housed in the Paint department.
Attritors and sand-mills use different
techniques to disperse the same
materials, the latter being used where
high quality Titanium pigments are
used as in Dulux White gloss paint.
High speed mixers have been
developed in the industry whereby
all operations are carried out on one
Manufacture
machine. The contents are both
mixed and ground by a blade shaped
like a circular saw two feet in
diameter, which transmits very high
dispersion power to the batch.
Emulsion paint is made by a similar
process except that the combination
of oil and resin is replaced by a
water based emulsion. The final
stage, is carried out in the mixing
section, where the base of the batch
of paint is transferred from the ball
mill, attritor etc. to a separate
finishing mixer, where carefully
weighed ingredients such as solvents,
dryers, anti-skinning agents, etc,
are added. It is at this stage that the
true colour of the paint is reached.
Tinters are added until the skilled
colour matcher has corresponded
the batch with the correct colour
standard. The various properties of
paint batch are then tested and
passed by the Control Laboratory.
The very large number of products
being manufactured at one time
necessitates that an accurate control
record is kept, not only of items
being manufactured, but also of
the stage which each has reached.
Decorative paint is strained into
portable containers and transferred
to another building to be filled into
tins. The paint is fed into the
machines by means of automatic
air controlled valves. Tins ranging in
size from | pint to 1 gallon are fed
into the machine, filled, capped and
passed along a conveyor belt for
packing. Half pint and 1 pint tins
are packed into cartons for easy
handling. These in turn are stacked
on pallets of uniform size into the
warehouse.
The warehouse, a four-storey
building, capable of holding over a
million gallons of paint, acts as a
store for finished products from
Slough and some products from
other factories in the Division, and
as a distribution centre to Paints
Division Depots and customers on
demand.
The paint is brought by fork lift
trucks and stored in bins or pallet
racks. Loading goes on day and
night onto long distance lorries and
local delivery vans. A proportion is
also for export. The entire works is in
full production day and night,
operating a three-shift system. The
smooth running operating includes
canteen facilities on site, a medical
centre, an efficient fire brigade
which is run by men on the works.
Training is given to all the plant
operators on joining the Company.
Much of the paint making history of
the last half-century has been
written here at Slough. The team
work, the technological skills and
the enthusiasm of all Paints
Division's personnel will ensure that
much of the future progress in paint
making will also take place here at
Slough.
Top right: Comparative hiding tests being carried out
in the Development department at Slough between
Dulux and other paints.
Above left: The latest development in the bulk
handling of pigments. The Titanium Dioxide silo holds
pigment used in the manufacture of Dulux Gloss paint
and Supercover Emulsion. The pigment is pumped
by compressed air from the 90 ton silo direct to the
high-speed mixers.
Centre right: Many hundreds of investigations are made
each year with the Electron Microscope, which can
magnify up to 50,000 times. It is used for examining
the shape and structure of pigments and extenders,
paint surface defects and for studying the internal
structure of paint films.
Above: Paint supplies are sent daily from Slough
Works Warehouse to Paints Division Depots
strategically placed throughout the country.
19 6 9
THE QUEEN'S AWARD TO INDUSTRY
ESSO
AT FAWLEY
Esso Petroleum Company, Limited is the U.K. affiliate of the
group parent company - the Standard Oil Company (New
Jersey). Founded in London in 1888, it is among the oldest and
largest of the oil companies in the United Kingdom. Its net assets
are over £300 million; with its affiliates it supplies more than a
quarter of the nation's oil products, and its annual turnover is over
£600 million. It collects more than £300 million each year in
Customs and Excise duties and the value of its total annual export
amounts to £20 million.
Esso Chemical Limited, founded in 1965, is the United Kingdom _
affiliate of the world-wide network of Esso Chemical Company i^J
which operates 64 manufacturing plants in 29 countries.
This leaflet provides a brief description of some of the refining and
chemical manufacturing processes of these Companies at their
Fawley complex; on the back page are listed some of the salient
facts and figures about Fawley.
Esso Petroleum Companymajor refining processes
Esso Chemical Limitedmajor manufacturing plants
1 Primary distillation
This is a process of fractional distillation. Crude oil is first heated
in a furnace and the vapours produced are then condensed in a
fractionating column to produce fractions of different boiling ranges.
These raw fractions are subsequently further refined or purified.
8
Steam cracking and ethylene recovery
Steam cracking is a high-temperature thermal cracking process to
produce olefins and diolefins as feedstocks for other chemical,
plastic and rubber manufacturing processes. The feedstock of
either naphtha or gas oil is vaporized, mixed with steam, and heated
to high temperatures. Under these conditions most of the high
molecular weight hydrocarbons in the feed are cracked to produce
a wide range of low molecular weight hydrocarbons including
ethylene, propylene, butenes and butadiene. These are separated
as saleable products or for further processing in other plants.
2 Catalytic cracking
Cracking breaks large oil molecules into smaller ones. One
application at Fawley is in cracking a heavy gas oil to form high
grade petrol and gas. The process used is known as 'fluid catalytic
cracking’ - 'fluid' because the catalyst (this helps the cracking
reaction without being changed itself) can be made to flow like a
liquid when it is blown with air or hydrocarbon vapour.
3^^/verforming
This process changes the configuration of atoms within molecules
rather than the size of the molecule. The Powerformer converts low
quality naphtha from primary distillation into a high-quality
petrol component.
4
Polymerization
Polymerization is the reverse of cracking; it builds up small
molecules into larger ones. Light gases, produced by the catalytic
cracker and chemical units, are combined to produce heavier
materials, such as heptenes and high-quality petrol.
9
Isobutylene extraction and recovery
This extraction process, using sulphuric acid as a solvent, separates
and recovers isobutylene from mixed butenes produced during the
catalytic and steam cracking processes. Isobutylene is one of the
feedstocks for the manufacture of butyl rubber.
10
Butadiene extraction
These units recover and purify butadiene from the raw
butadiene-containing streams produced by the steam cracking units.
Butadiene is fed to neighbouring International Synthetic Rubber
Company for the manufacture of the synthetic rubber - styrene
butadiene. End uses include car tyres.
11
Butyl rubber unit
This unit consists of a co-polymerization section where raw rubber
is made from purified feed streams of isobutylene and isoprene, and a
finishing section, where the raw rubber is dried, baled and
packaged. The unit has been recently expanded with facilities to
manufacture chlorobutyl rubber.
5
Treating processes
Almost all the fractions obtained by primary distillation need to be
further 'treated' to meet the very stringent specifications demanded.
One example is the removal of sulphur from such products as diesel
oil and white spirit. This is done by a Hydrofining process, where
sulphur compounds are converted to hydrogen sulphide. The H2S
is then fed to the Sulphur Recovery plant capable of producing up
to 60 tons/day of pure rock sulphur. Further examples of treating
are the Edeieanu process for the removal of aromatics from
kerosene and the copper sweetening process for converting corrosive
I^B ialodorous compoundsinto non-corrosive and inoffensive ones.
12
Aromatics extraction unit
Another extraction process, using a feedstock from the
Powerformer, rich in aromatics. This feedstock is subjected
to sulfolane extraction and subsequent fractionation to recover
toluene and benzene. These important intermediate chemicals are
used in making plastics, synthetic fibre, detergents, paints, dyes, etc.
6
Lubricating oil manufacture
Feedstocks for lubricating oil manufacture are prepared by vacuum
distillation of the residue from primary distillation of certain crude
oils. There are three further processes:
i
Phenol treating to remove undesirable aromatic compounds.
ii
Hydrofining to improve the colour and stability of the oil.
iii
Dewaxing to improve the 'pour' characteristics.
13
Methyl ethyl ketone unit
Butenes from steam cracking are extracted with sulphuric acid to
recover normal-butenes as secondary butyl alcohol. The crude
alcohol is purified by fractionation and dehydrogenated, by a
catalytic process, to methyl ethyl ketone (MEK) which is then
purified by further fractionation, mek is used as a solvent for
industrial and pharmaceutical applications.
7
Bitumens
On this unit the residue from vacuum distillation of Venezuelan
crude oil is blended with a diluent to produce a range of penetration
grade bitumens, some of which are subsequently air blown to produce
oxidized bitumens.
14
Paramins plant
A series of vessels in which various purchased and indigenous
chemicals are reacted or blended, in batch processes, to give a
wide range of additives, a number of which are used to improve
specific characteristics of lubricating, fuel and crude oils.
Some facts and figures about Fawley
The marine terminal
General
Small refinery commissioned in
deadweight tons (draught limitation 49 feet) turn a
24 hours. With over 18 million gallons of crude oil or ^ned
oroducts crossing the terminal each day, it handles more tonnag
foone°month than is handled by the Port of Southampton m a year.
Automation
Direct Digital Control (or D.D.C.) is the operational term which
describes the system of computer control installed in two areas ot
the refinery. The first of these was commissioned in 1968 and won
for Esso Petroleum Company the distinction of being the first oil
company to receive the Queen’s Award to Industry. In 1970 Esso
Chemical Limited were similarly honoured fortheir contribution to
the export market - the Company having increased its exports
from 16 per cent, to 33 per cent, on total sales over a three-year
period.
1921
First major expansion
1949-1951
Capacity of the refinery per year
19 million tons (13 mill/galI/
day)
Employees
about 2,200
Investment at Fawley
£140 million
Investment per employee
£63,000
Land area (includes undeveloped
foreshore)
3,300 acres (about 1,300 acres
developed)
Local rates per year
over £11 million
Local harbour dues, pilotage and
tugs per year
about £| million
Local wages, salaries, purchases
per year
£9 million
Utilities Required
Environmental control
Steam per hour
1| million lb.
Industrial development must always be at a certain cost in terms
of loss of amenities. Our aim at Fawley is to keep this cost down to
the minimum and have so far spent £3 million on eliminating or
minimizing nuisance that we might otherwise cause.
Noise control alone has cost about £500,000 and chimney stacks
have been constructed up to 450 feet above ground level to
facilitate rapid dispersion of flue gases. Extensive and stringent
precautions are taken to minimize the possibility of accidental
pollution of Southampton Water. Over 28,000 trees and shrubs have
been planted in a 2-miles-long belt to screen the refinery on the
landward side. More recently plans have been published on the
proposed landscaping of the refinery's foreshore.
Electricity per day
2i million units (more than
Southampton uses daily)
Electricity, peak load
107 megawatts
Water (fresh) per day
13 million gallons (cost £{
million)
Furnace fuel (oil and gas)
per day
850,000 gallons
Storage
Number of tanks and spheres
nearly 500
Standard Oil Company (New Jersey)
Largest tanks (two of largest
in world), capacity of each
over 21 million gallons
The parent company of the world-wide Esso group, owns in
whole or in part more than 300 affiliated companies employing
about 150,000 people.
Crude oil sources (1971)
At the beginning of 1972 Esso had interests in exploration and
production in 31 countries, refining in 37 countries and marketing in
more than 100.
y
Middle East
73 per cent.
Libya
22 per cent.
Venezuela
5 per cent.
During 1971 Esso affiliates completed a total of 834 wild-cat and
development wells, both off-shore and on-shore, in 20 countries
Product distribution (1971)
By sea
52 per cent.
Esso accounts for more than 15 per cent, of the free world's total
crude oil and natural gas production, 14 per cent of its
refining activity and 14 percent, of its petroleum productsales.
By pipeline
36 per cent.
<2 -COMMUNITY HEALTH Cat
./5r <47/1.(First Flbpr)St. Marks 3oi
BAN.,
.0 >E
By rail
9 per cent.
By road
3 per cent.
OCCOPAIIQNAL HEADTH SUH7EY.
In the final analysis
;‘J)
It is the Man that preduces
and NOT the machines
Hence it is richly rewarding to invest in preventive Mainte
nance of Human Component of Industry.
Your employeej be he a Shop Floor Hand, Supervisor or an
Executive, whatever be the motivation and rewards, cannot
contribute to your management by objective, if he is not
maintained in optimal health
*
What is not always obvious is thd employee in Sub-optimal
health is giving less than what he should, production.
To his gainful workj physiological and psychological demands
Of work, and work environments may be significant contributory
constraints.
Your organisation has an. .individual tty of its own,. diligently
developed for the climate of your enterprise. As a corollary,
your human needs are also special. Standard stereotyped pro
cedures may not be the best choice for you.
The" consultancy initially would consis of being in your plant
for’miflinium retired, number of d ays,, observing the working
of your men at work, workj work environment with your Doctor,
Safety Officer, Iridustriax Engineer, personnel officer on the
lines indicated earlier-, pre-parting an initial report, discuss
ing it individually with your officers, followed by group dis
cussion with yp.ur executives.- The report is then finalised
on this basite and presented to you for the phased implementation
The comprehensive offer is to:
I.’,-
Critically observe existing arrangements for curative
Medical care and preventive Health care in your
organisation to spot possible areas of better and.
effective utilisation.
2«
Observe ^Man-Machine systems” on the diop floor to
assay total long term effects on human component of
industry, particularly preventable ill-health, strain and
stresses, due to unscientific matching of man to machines.
3.
Study sickness absenteeism pattern investigate if this
is an occupational contribution to this and suggest remedi
cal measures.
4.
Study employment injuries and resultant lost time and
suggest methodology to scientifically investigate the
objective reduction of morbidity and financial waste.
.-...2
Eaivg-;.-,
5r*!i’doad
:2:
5.
Conduct a Safety Survey, -with particular emphasis on
human causes for Employment injuries.
6.
Medically interpret and utilise all previous survey
of Environment in planning men protection at places
' of employment in the context of environment.
7.
Plan for minimal additional work enviornment surveys
as indicated, such as Gaseous, Vapours, fumes, dusts
particles, heat, noise, vibration, lighting humidity
that could be the basis of work rationalisation and'
scientifically assist better and safe working.
Monitoring seeks to determine our total exposure to
pollutants. Accurate and reliable monitoring data are
essential in every step of pollution control (a) to
establish baselines from which changes ®n be measured
(b) to identify pollution problems, (c) to provide data
for defining standards (d) to evaluate pollution abate
ment results, (e) to provide evidence for enforcement
action, and If) to provide early warning of unforeseen
problems'1.
Occupational health monitoring programmes would have to
bo chosen and installed after clear and careful defining
of the sought objectives, since the difficulty of defin
ing in detail exactly that information is needed can be
surprisingly agonizing, at times. The inclusion of
specific physical, chemical and/or biological measure
ments and the specificity of responses expected therefrom
should be given due importance.
8»
To study the points raised by Factory Inspectorate that
have a Health basis and economically arrange to implement
them avoiding infructuous expenditure.
9,
List out possible hazardous occupations - statutory and
others and plan medical monitoring and remedical action.
*
.10
Mediecal aspects of environment pollution - Many diffi
cult Governmental rules and regulations arc in offing.
11.
Fatigue is the-basic cause of work imperfections and
.interruptions. Medical Sciences identify the multiple
causes of physical and mental fatigue and assist indus
trial Engineer and Personnel. Managers in making acceptable
decisions.
Initiate Medical and Industrial Engineering Personnel in
simple shop floor procedures to evaluate the physiological
cost of work which could koep_pf work study and job
< evaluation and wa!ge structural
.
*
*
S3
12.
On the basis of all this,, to suggest on integrated
working scheme for the medical and Safety services
in areas common objectives.
Your Medical services arc doing good work. But I an sure you
•will agree this can bo bettered by Occupational Health Orien
tation and result oriented reorganisation on the basis of
modern concepts of medical contribution to total professional
management.
All this has the objective of fully utilising the existing
Services to provide for preventive maintenance of human
component of industry to ensure the -work and productivity
of the employee docs improve
*
The additional funding, if any, -would be very minimal., but
benefit accrued would be substantial.
' '
You have all the elements that arc required. Wat I Qffx
offer-isdxpert neutral observer study, study of data and
findings delinking, linking, rcallignement and orientation
■with the final objective, that the employee benefits by all
interest and financial involvement your organisation has in
the postivo health of employees.
The total objective of the Occupational Survey is to offer
medical and para medical services for utilisation in man
potter conservation. This is not a sophistication of developed
countries, but is very relevant to developing countries
like ours, where well trained’man at machine- is a precious
asset of the organisation.. Abroad many agencies look after
him, but out hero, your mon conseravation is one of your
:
productive investmentsi
EPIDEMIOLOGY OF .tCCIDEMTS
Plan of Lecture
-
Introduction
1.
P-e.fln_i.tXon of
2.
Classification of Accidents
*
•Accidents
by site/situation/nature of external agent
nature of injury/severity
3.
Hartn.it.ude if the? orobl^n
A.
The Lpldefnioloolcal triad
Interaction of Agent, Host and Environmental factors
5.
Huron yr, Environment a X . fact orn
m
6.
a)
Traffic Accidents
b)
Domestic Accidents
c)
Industrial Accidents
?• P.cn.seauences- .and ..co,^,.Q.f, Accidents.
8.
Accident Prevention
a)
Primary (for each typo)
b)
Secondary - first Aid and emergency services
c)
Tertiary - Rehabilitation
COMMUNITY HEAItm ~
47/’> (First Fk or)St r‘ ‘L
9.
Rplanf Haalth/Safetv Education
10.
Role of legislation for standards
11.
Accident Pf^ynntion Pgoqifafnmo - Coordination of different organisations
12.
Areas of Renearch/iW-aemgea
INTRODUCTION
Soma ideas/facta
In ths time taken to read the special issue of World Health °n ^°od
accidents - Oct 1975 450 men,women and children would have bRGn killed
or injured on the world’s roads.
’Epidemic on wheels’ - ’Autosciorosis’
The energy crisis had a brighter side in Europe? Petrol prices and heavy
fines for exceeding new spaed limits l> ’ipse! to cut accidents by one-third.
Our attitude to accidents today is like that of our forefathers to
smallpox and cholera. We still think they are inevitable (side effect of
modern living)unpredictable. We now know that we are wrong.
Urbanisation, Industrialization and Growth of scientific technology is
making our hone, work site and general environment including our roads
more complex and in the absence of adequate action and education - more
possibilities of accidents in the future.
Definitions
(l)
a)’An unpramediated event resulting iB a roognisable injur$(WH0 1957)
’An occurence in a sequence of events which usually produces unintended
b)
injury, death or property damage (American National Safety Council)
Classiflc^UPh nf Accidents
(2)
By aite/aituation
a)
i)
Transport Accident
- Road Traffic
- Aircraft
- Watercraft
- Railway
h)
iii)
2s£M2atoialJlGSX£lsaL - industrial
— agricultural
- others
b) By. nature n^jj^-amil-agiaafc.
i)
ftiysical - Hoat/Radiation/Noise etc
11) Chemical - flaisons/corrooives etc
iii)
Mechanical - heavy objecta vehicles machinery ate
iv)
Biological - animalo
x 2 X
injury - cuts/bruiees/fraotures
i)
Physical
ii)
Bums/scalds
iii)
Asphyxi
iv)
Drowning
v)
Injury to special senses
vi)
Poisoning
Severity
d)
Ninor/Moderate/Severe
Fatal/Non Fatal
District Hgspjtai Profile. (10)
Accident cases
Kotor vehicles -19%
Burns
- 18%
Falls - 15.6%
Poisoning - 11.7%
Machinery - 8.4%
Fall of heavy object - 6.4%
Trains — 4.5%
Cycles - 4%
Draining - 0.77%
(3)
Maap^t.utfe of, .P.SP&LQP3.
Accidents in general
- Fourth leading cause of death at all ages
- Number one killer in 15-45 age group
- Epidemic in developed world.
In the west roles of infectious diseases and
accidents as causes of death have been reversed, 1946-infactious diseases
double of accidents 1951 - infectious diseases a accidents
1956 - Accidents double of infectious diseases
Raad Taaf.flfl
World - 7 million injured and 0.25 million killed every year (1?)
(west)
- 1 person killed every year per 1000 vehicles(e)
- 10% of hospital beds in some countries occupied by RT«s(l7)
BMMpiwdxta
» 3 J
- f or every person killed in a RTA, 10-15 are seriously injured and
30-40 receive minor injuries(17)
India. =
- 2 million motor vehicles on Indian roads in 1975 and its cities
suffer a road death toll 10-15 times greater than in UK or USA
(WIO 1975)
- Fatal accidents in Delhi is 1-2/day
— 6 persons killed every year per 1000 vehicles(e)
- Increase in population is 2,5% and increase in motor vehicles
is 15% per year.
Increase in RTA ia 15-20% per year
Hopp Accidents
Heat - Developed countries have 1 day disability per year for 5-10% of
the population
- USA - it is l/3rd of non-fatal and l/4th of fatal injuries
- UK - 35% of fatal injuries
- For every fatal domestic accident there are 150 significant non-fatal
and 3500 non significant, non fatal accidents
Ihdia - no- reliable statistics
- Estimated to be nearly half of all accidental deaths
indMatElal AcqAdenfra
UO£1J1 =
India- 3 million man days are lost annually in India due to industrial
accidents
- Rates vary for different occipaticns
Mines - 50/1000 workers
Docks/Rorta - 45/1000 workers
Railways 45/1000 workers
Factories 10/1000 workers
8 4 S
(4)
Agent -----. —
--■
. ..Host
For every type of accident
we
can determine Factors
that form part of the epidemiological or ecological triad
Environmsnt
a)
Aggnt
= vehicle
Host.
a» Road user
- pedest riant
- passenger
=■ driver
.En.viXQOac.ot
« Road and climatic and other environmental conditions
Domestic accident
b)
m Physical/chemical/FlQChanicai/Biological agents in home
AflgfeL
m Resident of home
qst
H.
Environment
4 Home environment
c) £S£!JQSy^2aLa£GAdgI&,
Agent,
s Rachine/Process/Materials
Hogt
=> Worker
Environment » Work environment
EflyaatiVS
(5)
in Accidents may be broadly divided into two
major catagoriee
a)
Hyman
- 00-85$ of accidents occur due to these factors
i)
Physical - defecte/dieabilitiae
ii)
PUxaiQlaalfial - Age/SBx-Fatigue
Hi) Psychological - intelligenco/accident pH)8900639
reaction time •* •aicohol/drugs
Etnot ional - Anger/Faar/Uorry/careleseness
iv)
Environmental. -
b)
These may be due to
i)
Physical factors — heat,light,■ noise
ii)
Chemical factors - poisonons, corrosives
iii)
Mechanical - fall of heavy object, impact etc
e.g.
— inadequate lighting
- slippery floors
- unguarded machinery
- defective vehicles
(6)
Epidemiological Factors in
A,
= Road Traffic Accidents
a)
IZflasi
Type
65.2% on straight roads
29.2% on intersect ion (7)
Design
Curative
Lighting S» 20% 06 accidents(6)
Skid resistance
Traffic signals
Separation of user typos
Usage and adequacy for traffic flow
b)
General
Environment,
Climate - rains etc
Visibility
Time of day
Maximum
9-1D A.M.
Day
c)
Vehicle
Maintenance of efficiency
**ights
Brakes
Steering
Tyres
Exhaust Asseably
Other parts
Ventilation
Interior design
Visual obstruction io
fl-5 P.M.(?)
-
night
: 6 i
.Road- uspx.Call .cat-HHOxles.) 96% of cases (17)
d)
Age
37% in 20-30
age group (7)
Sex
ill lea 5 times
more than females(7)
(17).
Physical defects
Rental defects
Education
47% illiterate (7)
T raining
Experience
•iJay of Life
*
concept
Fatigue
Visual efficiency I
n
,
I
Defective hearing j
4.8% had defect (7)
Reaction time
1% intoxicated drivoreC?)
Drugs/Alcohol
Accident prosseness
Ant icipaticn/Avoidanca
(defensive driving)
Category of
user — Pedestrians 41.1% of RTA(7)
B-Dopiest lc. .Ac.cldeP.ta. Cl)
a)
Cpfgmopeat-.t.vpga
Burra
Shocks
Accidental ingestion/poisoning
Falls
Cuts/injuries
Suffocation
Drowning
Liinb/halr in moving equipment
Poverty
Overcrowding
Poor housekeeping
Ill designed equipment
Lack of storage space
Open fires
Broken floors/stairs/walls
Absence of play space
bad electric connections
Easily accessible drugs/lnsectlcides - fuel agents
» 7 »
c)
Human factors
Children (Park 20)
Age
Crawling inquisitiveness
Sex
Experimentation/bravado
BiY8.ica.l
Poor health
Poor vision
Poor hearing
Qlri, people (Park 20)
Impairment of vision/hearing
Diminution of reflexes
Weakening of muscles
Physical disability
PsychoIonics1
Low intelligence
Fatigue
Accident prosseness
Drugs/Alcohol
Emotional
Anger
Fear
Worry
Stress
Carelessness
d)
Social Factors.
Ignorance
Children/aged people left at home
with inexperienced help or
no help at all
c « O.w,»afltAonal 'teldglta. - especially Industrial
a) Epy^nnM.
Poor house keeping
Temperature
Poor illumination
Humidity
Noise
Unsafe machines
Hazardous processes/materials
» 8 S
Hunan, factors
b)
same as in domestic accidents but also include other factors such as
experience
working hours
time of day or shift
inatt cntiveness
overconfidence
tnonot omy
lack of training
Social
c)
shop floor supervision
labour management relationship
social stress in industry
anri .<?»?&.af.Jl&qAtlfinftg,
(7)
Oeath
Pan
i’lorbidity
Suffering
Disability - temporary
- permanent - partial
— complete
Traumatic neurosis - fear, anxiety
loss of education
loss of productivity/job
sickness absenteeism
social consequences - unemployment, destitution etc.
Coat of Accidents is very difficult to determine because costing of many
of the consequences is difficult in practical terms
However costs would include
medical and
surgical treatment
cost of disability/death
loss of wages
reduced tax revenues
damage to property
legal compensation(to accident victims/family) and so on
administrative efforts - police 4 judicial investigation
Sweden 1970 - Population - 8 million
440 million sw.troness
loss due to accidents - 110 million dollars
8 9 8
(b)
Accident Prevention (17)
Accidents do not occur.
Accidents are caused.
In almost all kinds of
accidents over 90$ are due to somo error of a humabbeing.
Thus if the human
factor can be controlled over 90$ of the accidents can be prevented.
A s Primary prevention which
includes health promotion and specific
protection are therefore the most important components of accident prevention
programmes.
a)
Rqnd traffic,2'jR.Qtd.eotji,
Better design and maintenance of roads. Better design and maintenance
of vehicles legislation regarding standards.
Highway codes.
Road users — Education in road safrty
— Training for use/driving
- Licensing/Dpivirig
tests
Pre-license medical inspection/scresning for medical conditions
Screening for defective eyesight - colour blindness visual acuty etc.
Screening for alcohol/drugs -Breathalyser
Specific protection — safety belts/crash helmets
b)
Education of parents
Elimination of factors(Built in protection)
Regular repair and maintenance
Adequate and safe storage provisions
Regulation and enforcement of standards for housing/squipment/packinc/
labeling and warning regarding hazards
Social welfare measures
Mome help/child care/counselling
c)
Jjuiga.tjAp! A«icj,.rian&?,
Adequate preplacement examination
Adequate Job training
Continuing education
Adequate publicity/safety signals/postere
Establishing safety department under safety engines
Ensuring safe working environment with built in protection
Specific personal protection
Periodic survey to find out hazards
Careful reporting and maintenance of records
s 10
»
Thorough accident analysis system
B- Secondary Prevention i.e. early diagnosis and treatment
Screening for medical conditions/defoctive senses/screening for alcohol
a)
and drugs/psybhological screening are all measures to detect those utio
are accident prone or at risk of being involved in accidents.
Identification
of such individuals could come wider early diagnosis.
first
b)
Ajd at site of accident can be life saving
- Training of first aiders
in an important task
in prevention
of the
ill effects of accidents
- Provision and regular maintenance of first aid kits
- Refresher courses for first aiders(St Johns Ambulance and Red Cross)
Rrojd^xoilj^
c)
transport Facilities - to be used to take
accident victim to hospital or other expert medical attention
d)
Casualtv/Emernenev department of Hoaoitftl
well planned)
well equipped
well staffed
standardised regimes
24 hours availability of service
irompt medical/surgical treatment
S-r.e.rtiaEy PMMfifcttHl
Pleasures to limit disability and rehabilitation of accident victim
*
physically
(9)
mentally, socially and occupational
Rj?l^j.f_H.flalthi<SflFetV- - Education
Safety is basically a matter of individual adjustment.
the hazards of the immediate environment is essential.
Adaptation to
For ones physical
well being as well as for survival and this involves ability to anticipate
and recognise hazards.
It le therefore necessary to develop the attributes
essential to safe living!..
WBMaiMsxKkMKtiotdK
1) Safety knowledge
11) Safety attitudes
ill) Safety practices
* 11
Health and
Safety KAP should be inculcated in
all parent3, workera and
road users - in effect the whole community. For this every type of media
and every agency should be involved.
Ideally this should become part of
the general educational system.
(Demonstration of safety posters/pamphlcts/flip charts)
(1O)
Bole, of. Jj^lislatJjBID. -
Accident prevention needs the enforcement of
various standards/regulations/codes and the legislation for punitive measures
against those who do not follow these rules.
These include
Environmental legislation - safe roads
Safety factors in environmaital design
Housing standards
Built in protection in factories — statutory regulation
Threshold limit values
Packing standards
Labelling standards for drugs/chemicals/inaecticides/fuels
Statutory safety warnings etc.
(11)
A good accident prevention programme for a country/state/city will require
close and effective coordination in education and regulation of the
community by the following agencies
*
Health Department
Indust ties
Labour Department
Schools
Works & Hoaoing Department
Welfare agencies
Police Department
Trade unions
Education Department
Voluntary agencies
Law Department
Research institution
Accident
SmsnSlsa
Programme
s 12
(12)
Areas of, Research
1) Gathering of precise information about extent
type
characteristics
of different type of accidents at national/regional/district/city levels
ii)
Correlating accident experience with personal attributes and
environments in which accidents occur to determine predictable factors
ill) investigating newer and better methods of alterning human behaviour
iv)
Environmental and safesty engineering
v)
Better methods of personal protection
vi)
Evaluation of control measures
REFERENCES
1.
Accidents in childhood - '3H0 Tffil No 118 - Facts as a basis for prevention
2.
Accident prevention Ed Maxwell N Halsey, 1931 American Public Health
3,
Medical Aspects of Home Hazards Ed Alastair Nslsan Medical
Association
Commission
on Accident Prevention Royal College af Surgeons London, 1972
4.
The Epidemiology of Road Traffic Accidents WHO Regional Publications-
5.
Seminar on 'Accident Prevention' -
6.
Causes and Prevention of Road Traffic accidents - a study SP Mehta and
European Series No 2
SC Chawla Ind 3 prev
7.
brochure IA0H New Delhi, November 1977
& See Wed Vol 2 Sept 1970 P 32-5
An epidemiological study of Road Traffic nccidante in Neu Delhi
SP Mehta
Ind 3 Fled Research 56, 4 April 1968
B« Accident Problem in Comprehensive Health Care - RC Gupta Ind 3 of Public
Health Vol XV No 4 act 1971
9.
Management of Industrial and traffic accidents S
Roy Ind Fled 3 65
70-2 April 1977
10.
Accidents as a Public liealth
Vol XIII
11.
A study of Rural Residents in Rjndicherry S P Datta & PS Verma
Ind 3 of Public Health Vol
12.
Problem SAH Zaidi, Ind 3 of Public Health
No 1 3an 1969
XIII No 1 3n 1969
Papors on Accidents in Ind 3 of Occupational Health — issues
1963 - 3an to Sept
1965 - Feb War, 3une,3uly,Aug-Dec
1966 - Jan/'ar,'Apr
s 13 »
13.
14.
World Health October 1975
Road Traffic Accidents - Epidemiology
WHO Public Health ^apor Na 12
15.
Handout on ’Home *
Accidents
16.
Accidents p 5D5
-
control and Prevention
centre for Commimity Medicine»New Delhi
Text book of Preventioa and Social Medicine 3E
//////
Park - Sth Edition 1976
ACCIDENT ANALYSIS
High
Person
Initiating
Factors
---------- Accident
Susceptibility__ f
LOW
A PLAN (2)
IntermecJiate
Factors
Immediate
Special physical No
I
recognition
and Mental Factors;;
of Danger
i
'
Change in
Pattern of
Work.
Patterns of
operation
— Behaviour within
given environment
Increase in
Susceptibility
[Thin person
[This Day
[This activity
Point of l*o
Return
Takes a chance
continues usual
Patt ern
,
J
Increase in
Pot ent ia 1
Agent of Accident r J .
. ,
n
,
Environmental
Present
,
Factors
4-
J
?
Personal
Injury.
Unsaf o
. , . ,
Act ------ - Acc,ident
Increase Hazard
Makeshifts
High
Situation -------Home
Road
Work Site
'
No injury or
;----- . damage or
J,
negligible
Accident
Potential
Inter vention
LOU
Mitigating Factors
(Another person, Safety awareness
Accident Prevention (Safety efforts) up to this point. ^P^ic cut off)
Total Accident Situation.
£
Near
Accident
ERGONOMICS
ERGONOMICS:- Technology of Work Design.
ANATOM/:
---------------
(Anthropometry - body dimensions
(_.
^Biomechanics - force application
Work Physiology - Fnergy Expenditure
i
Environmental physical
environment
/ Skill Psychology
z
az
PSYCHOLOGY: '
“ decision making
Occupational Psychology,- Training
Effort
Individual differences.
1.
The effective practice of ergonomics involves the application
of principles of human anatomical, physiological and psychological
functions to work.
It I comprehends:
(1)
the total physical environment of the worker (heat, cold,
humidity, air speed, noise, lighting and decor);
(2)
the design of workplace, tools, machinery, furniture and
their layout;
(3)
(4)
(5)
energy requirements of work;
motor function requirements of the job;
the demand required of special senses (visual discri
mination, colour sense, hearing).
For convenience certain' aspects of ergonomics are dealt with
individually.
The visual requirements of work:
2.
Visual acuity. This may be described as the finest degree
of which the eye is capable of discriminating fine detail.
It is influenced by type- of detail, illumination, contrast
and surrounding brightness. For convenience it is measured
by the ability to read test charts of letters of graded sizes.
Normal vision is that when separations' of adjacent contours of
the letters subtending an angle of one minute of arc at the
eye can be made out.
3.
Binocular vision and depth perception. The co-ordinated
use- of the two eyc-s and the critical fusion of the two
images produce accurate stereo-scopic depth perception. With
monocular vision a degree of depth perception is possible
relating experience of relative sizes, change of shade with
distance- and motion parallax; this is inferior to binocular
vision and fails when lighting conditions■are poor.
.. 2 .
COMMUNITY HEALTH CELL
47/1,(First Floor)St. Marks Road
BANGALORE -560 001
'
2
4.
Colour vision. A variety of degrees of deficient colour
vision exist and tests may be addressed to the dark adapted
or daylight eye, transmitted or reflected light, sorting,
naming or matching. The dividing line between acceptable and
unacceptable varies according to the'requirements -of the...
job.
5.
Aids to vision.
ing headings: (1)
These maybe discussed under the. follow
... • . ..
.. ..
Illumination. A good standard of illumination is
the first aid to vision.
This implies an adequate -lighting intensity at the job,
adequate but not.excessive contract ■between the work piece
and its' immediate surround, the overall lighting of the
workplace and well designed lighting fittings. Adequacy
varies as the size of detail and the age of the worker.
The finer the.detail and the older the’worker the greater the
lighting intensity required. The ergonomic design of machinery
provides for the absence of specular reflection from metal
parts and layout of the workplace should avoid' problems
produced by natural lighting. The appropriate type of
light source (tungsten., varying phosphors in fluorescent tubes)
will determine case of colour.appreciation. Shadow may be
detrimental to certain visual tasks yet essential for others.
(2)
Spectacles. These may improve visual acuity to levels
suitable for the.work under consideration a.nd even-'Correct
minor stereoscopic defects. Where there is a major problem
in stereoscopy it may be possible by the use of appropriately
placed prisms to overcome lesser degrees of convergence defect
for the near point. An ophthalmic surgeon with experience
and‘interest in occupational problems ia an invaluable’help.
Orthoptic treatment .is of limited use.
(3)
Magnifying glasses. .These should be so. designed that
they do not obstruct work, interfere with binocular vision or by
colour fringes make vision tedious.
(4)
Einocular microscopes. These/have been used increasingly
to over-come resolution of fine work. Thcy'.may be of high
or low power, worn as spectacles or be conventional.- Binocular
‘enlargement may readily be obtained,- but the limit of human
manipulative- ability and physiological tremor may be- thelimiting factor.
6.
Job specification.
In analysing the■ suitability of a job
for- a worker, where visual function has been investigated,
the following questions must be asked;
(1)
What degree of visual acuity (near, middle and distant)
is required?
(2)
What degree of colour defect is acceptable?
(3)
Is stereoscopic vision (near, and distant) essential?
Detection of'visual defects;
7.
Testing vision. A variety of apparatus has been marketed
to permit rapid screening of workers for the various aspects of
vision under standardised conditions.
. .. 3
8. Although logically one should evaluate the job require
ments before determinino the fitness or otherwise of the appli
IQ,. unvcsticatiorr or complaints.. Irr analyst no a-job where
there are cnmpladirts of eye strain, conjun'ctivl is
■ - .
the fd.llow.Lng qtie-stions. must be asked.
(JL) Are- ail the visual requirement's of- the job met?
(Z) Arc the illumination' circumstances' defective?
(3j Arc there- other causes of' eye .Irritation present
(irritant volatile.-liquids and gases, ultr vi led
and infra-red, vernal-conjunctivitis, and related
conditions-, acne rosacea, etc.).
(4)
If the process is an ancient one and the physical
conditions constant' (for good or bad) for’years,
why has the complaint been made at this moment in
time? It may well- be that there arc provokino
factors of a social, personal or dcpartmental"’nature
forming facets of the whole problems
... 4
4
Complaints about heat, cold, humidity, stuffiness and draught:
11. Stuffiness.
This may be applied to the aroma of humanity,
tobacco or other aromatics notc-d on entering a room or to car ,
nose and throat discomfort. Alternatively it may be complainec
of when the effective temperature at head height exceeds that
at floor level by greater than 1.5"F.
12. Fraught. An air speed that produces disagreeable cooling
as distinct from that which produces comfort and freshness.
Even under severe conditions of radiant "and humidity discomfort
there is a limit to the air speed that is tolerable. Occasion
ally the ’cold radiation' effect of sitting hard by a single
glazed window in winter may be complained of as a draught.
13.
Heat. The combination of severe heat and physical effort
lays a considerable burden on the cardio-vascular system.
The effectiveness of protective, measures (physiological and
by shielding) experimentally is measured by the ability
to maintain the rectal temperature within safe limits and
to protect the heart from overload.
In practice monitoring
by pulse rate is effective.
It is unsafe for workers to
continue working when the pulse rate- exceeds 120 beats per
minute.
14.
Fitness for work implies both the ability of protective
measures to prevent overloading the heart and thermostatic
control and the fitness of the individual to work in protective
clothing.
15.
When conditions are severe it may be necessary to carry
out work that produces maximum permissible load in short
period. Under these circumstances the duration of rest
periods should permit return of the cardiovascular system
to' a gentle rate of wprking.
16.
Loss electrolyte and water by sweating requires appropriate
replacement. The nuisance of working at higher temperatures
should not be confused with the hazard of physical overload.
17i Cold. In- examining for fitness to work in extreme cold,
ordinary fitness is required (chronic bronchits, Reynaud
phenomena, peripheral arterial disease, myocardial ischaemia
and arthritis are contraindications). Truck driving docs not
make great physical demand but muscular fitness may be required
as for meat handlers. The solitude and the discomfort•• of
cold-room work are such that natural selection rapidly elimi
nates the.psychiatrically unsuitable. Acclimatization to cold
is a physiological adaptation that supplements the. adopting
of protective clothing.
18.
Thermal comfort. "This is concept that covers those
combinations of air temperature, radiant heat balance, air
speed and.humidity at which the majority feel comfortable.
Within this framework there are maxima and minima for these
features.
19.
In any large floor area, be it o'fficc or factory, there will
be microclimates developing resulting from architecture and
machinery. The clothing of workers will vary as will the amount
of physical effort.
.. 5
5
The following arc the statutory requirements:
The Factories Act, 1961 requires a minimum
temperature one hour after start of work oi
* F when a substantial proportion of the work
60
is carried out sitting and thermometers must be
displayed.
The Offices, Shops and Railway Premises Act,
1963, This requires after the same period a
temperature of 60.8’F (16‘C).
Action:
20.
Investigation of complaints of stuffiness. Fc-aling with
malodorous atmospheres is simple and the treatment is adequate
ventilation. Masking the aroma by scent prays or destroying the.
sense of smell by ozone is to be ceprccatc-d. IVherc the thermal
gradient appears to be at fault this requires to be measured
appropriately: thus if due to overhead radiant heating, c.g.
overhead steam pipes, ceiling panel space heating or lighting
fittings two black bulb (bolometer) not silver bulb thermo
meter reading arc indicated. The only remedy short of
redesigning the heating or lighting system is to increase air
speed at head level, checking results with the victim and
perhaps by means of a katahermometer. Where stuffiness is an
car nose and throat affect correction of humidity will be
required.
21.
Investigation of complaints about draughts.
In certain
situations draught is unavoidable : arthritics and bronchitics
arc well advised to keep clear of these jobs. The treatment
is to avoid draught generation, to protect the individual
or to increase the effective temperature.
22.
Investigation of complaints of excessive heat.
In
considering the fitness of an individual to work at high
temperatures apart from high motivation the following factors
should be considered:
(1)
Fitness of the cardio vascular system. Loss
of reserve due to myocardial ischaemia or
hypertension should be noted.
(2)
Fitness of skin. Most lesions do not do well
in a hot sweaty environment and any impairment of
sweating ability is inimical to temperature control.
(3)
Fitness of car, nose and throat to tolerate
dry or hot humid atmospheres.
Other aspects
such as dust, dirt, irritating fumes and
physical work.
23.
Patients with histories of renal calculus should avoid this
type of work with its hazards of urinary concentration.
24.
Heat shields to reflect radiant heat and the provision
of insulated cooled clothing are avai.lable to permit work near to
furnaces and in ovens. Their provision may to some extent
reduce requirements for fitness.
... 6
6
25,
Investigation of complaints about thermal discomfort.
In investigating complaints of thermal discomfort in a large area
it is not to be expected that one climate will suffice for the
lightly clad myxoedematous patient seated by a wintry window
and the thyrotoxic well clad male lifting heavy components
to a fiercely radiating machine. Studying the diagram that
precedes this section will suggest stratagems whereby both
workers may be assisted.
26.
Situations of environmental discomfort may arise that arc
not obviously amenable to solution. However the investigation
in itself may be- of benefit and the provision of facilities
for moderating the microclimates under the personal control
of the complaint (a window that may be opened; a small personal
fan or a radiant heater) though scientifically of low efficiency
may make the situation more tolerable for the worker.
27.
Complaints about climate, as about lighting and canteens,
while- justifiable may also indicate disease of departmental
and company morale that merits coincidental treatment if the
environmental treatment is to effect a permanent cure.
Seating and the Worker:
28.
Seating the healthy. The- chair and work bench or table
should bear relation to the floor and to each other so that:
The user's arms can work freely.' This deter
mines dimensions of chair arms.
(2)
The feet (allowing for shoe heels) can be
comfortably placed on the floor or a foot
rest. This determines seat height.
(3)
The knee can be kept at a rioht angle.
(4)
The seat should not compress the calf or
back of thighs (scat height, shape and-.uphol
stering).
(5)
The- back of the chair supports the lumbar
spine correctly (chair back).
(6)
Change of posture is permitted to the extent
of allowing the legs to be crossed without
altering the relation with the work surface
(height of desk and dimensions of knee hole).
(1)
29.
While the range of human dimensions is wide, a compromise
can be determined for fixed seats that will suit 80% of the
population. Adjustable scats and/or the provision of the
appropriate work surface height, of foot rests and additional
scat pads will- allow maximum comfort and a minimum, of fatigue.
30.
The desk or v/ork surface, should be such that too high
or low a reflectance is avoided to prevent harsh contrast
between work, its immediate surrounds and general room condi
tions. This stresses the.interdependence of different
facets of ergonomics.
31.
Seating the disabled. The worker in the wheel chair is
well catered for as. to seating as it is obvious to an-employer
that bench height requires adjustment.
For the worker with
degenerative joint disease affecting ankle,knee hip or lumbar
spine that is not ankylosed then not only is a chair matched
to floor and desk/bcnch height highly desirable, but there must
be facilities for .changing posture to prevent
'seizing up'
.. .7
7
to the extent of the work permitting intervals of standing
and walking. Where there is ankylosis, by trial and c-rror
suitable adjustment can be made to render the worker
tolerably comfortable.
Standing
Work:
32.
Work is often carried out standing because no thought has
been given to its being carried out sitting down. Nevertheless
it is rare to find bench or machine height suitable for standing
work. A machine operator may be poised :
(1)
with a foot on a pedal operating the machine
clutch producing a pelwice tilt and lumbar scoliosis;
(2)
gazing at what was hitherto head level to check
the rotating turret to sec- the correct tool is
presentee' ;
(3)
reaching to the left three feet away at knee
level to operate a wheel which turns turret
mechanism for a cutting tool;
(4^ reaching with the right hand to a distance at
waist level and to the right, four feet ahead;
(5)
gripping with four fingers of the right hand, the
thumb being used to operate a stud button.
33.
The structure of most machine tools consists of a power
unit, a cutting tool, a work, piece traversing mechanism, with
controls for operating and gauges for measuring, loosely knit
with sheet steel. The arrangements of controls and gauges on
a typical lathe were never designed for an able—bodied human
being to operate let alone a disabled person.
34.
The problem is more severe for the disabled who suffer
more rapidly than the normal worker. A machine operator may
also act as setter which involves lifting or in the absence
of a bench feeder he may be required to carry. materials and
completed parts.
Movements of the hands ;
35.
Gripping.
For an effective grip all four fingers and
thumb should He used <>nc' there is an optimum size of fist.
The grip is weakened when the thumb is separated'for■pressing
a button.
36.
In the hand tool^ shown in the figure, the remedy was to
use a lever not a button switch. Fifferent sized hands will be
able to grip at maximum force if the objects presented arc of
the- appropriate size. Unfortunately women will be provided, with
hand tools that arc too large for optimal grip. This combined
for example with the necessity to drive self tapping screws
forcibly (particularly where There arc. other factors such
as faulty components and imperfectly maintained apparatus)
predisposes to a high incidence of tenosynovitis. (Sec
'Ecat Conditions and Tenosynovitis.' - 5).
37.
The arthritic hand may grip better if the- diameter of the
'object oto be gripped is expanded but even then it is advisable
to avoid forceful repetitive gripping action. The weight of a
hand tool may also be- relieved by using a gantry for its support.
8
8
The operator-machine relationship:
38.
Much has been written of a philosophic nature on the
subject. Of interest are the observations that:
too much information militates against safe
and efficient working;
too little, information militates aoainst safe and
efficient working;
(3)
in the absence of high motivation, vigilance can
• only be, preserved for about half an hour.
(1)
(2)
39.
The first accounts for the. 'impossibility1 of driving
a train safely, the scconc' and third account for errejrs made in
such jobs as fault finding or radar scanning when points of
interest arc few ane’ far between and periods of inspection Jong.
40.
The grouping of controls on a machine should bear some rela
tionship to the parts of the system involvc-e1 and the- movements
should produce the anticipated result
41.
A difficult point is that of on-and-off toggle switches.
Standard practice in this country is down for 'oh ' whereas
elsewhere one switches up-wards for 'on'. Accidents occur
when in emergency the deeply ingrained response defeats the
appropriate resnonse.
42.
As’with grouping of controls so cials should bear some
relationship to function.
Many machines present more information
than is required by an operator. The'typical example is that
of the test equipment fit for laboratory use with twenty
switches and as many dials being used to test one function
only, particularly when a yes-no answer is required rather
than a reading on a scale (no matter how ergonomically designed
the scale).
43.
The choice- presentation of information by dial and
pointer or-digitally has rhyme and reason. Digital presentation '
gives rppid information but the pointcred dial indicates change
more readily.
44.
Motivation: Faults of lighting, heating, noise and physical.
design may be endured, where for reasons of prestige or money
the subject is highly motivated. .For this reason it is a mistake
to extrapolate from one situation to another and an objective
ergonomic improvement is doomed to failure unless the totality
of the exercise- is embarked on including, the participation of
the worker in the scheme.
4’5. The 'ergonomist'. . In practice, no one individual can be
expected to have a command of all the disciplines involved, namely
those of engineering, work study, psychology and biology. The
logical application of experience is the basis of ergonomics and
the final common pathway is the work study engineer, by which
is understbod a specialist in designing jobs and measuring
performance.
... 9
9
46.
Travel to work, risability may be- such that travel to
work is possible by public transport.
It may even be possible
to travel in the rush hour. Otherwise other employees may be
preparer’ regularly to provide transport in the absence of
personal transport.
47.
Travel at work.
In the vast factory site general parking
facilities may be well away from the work place; special
arrangements should be- made for the disabled. If the work
place is up or down staris, can the disabled person manage
there, or can suitable re-arrangements be made? The siting
of lavatory accommodation may be critical and access to
wheelchair must be determiner’.
48.
Sitting work.
Is the work surface adjustable to a wheel
chair? Are ergonomic aspects of seating, bench height and work
layout, compatible with disability? To what extent can they headjusted to suit?
In the- case of the arthritic, arc there facilities for
optional change of position to prevent joints 'seizing up'?
49.
Standing work. The energy expenditure of standing coupled
with the extraordinary postures demanded in operating machinery
are inimical to the well being of patients with arthritis of
spine and lower limbs. Varicose veins deteriorate with prolonge
standing stock still.
It may he possible- to modify processes
so that they may be readily carried out with greater efficiency
seated or again it may be possible to alternate between sitting
and standing.
50.
Pcdal-opcratc-d machinery. When the worker is seated and
no force is required, pedals may be a "'esirablc alternative to
hand-operated levers. Where carricc’ out standing even in the •
absence of force requires a drastic change is posture illtolerated by those with arthritis of the spine.
51.
Right and left hand work.
Forceful gripping work may
be precluded by disease or deformity of hand and'forearm.
Where there is functionally one hand only, careful thought
must be.given before exposing it to a severe hazard capablcof leaving the patient with no functioning hands. The
amount of force required may be reduced to non-hazardous
levels by change of tools and work study. Thus a hand tool
with slight modification may require- a less forceful grip
(ihcrcasing or reducing the diameter of the handle), and the
use of a well maintained specific tool such as a wire cutter
will use less.effort than an indifferent pair of pliers-cumcutters. Thought given to job design may allow for increased
physiological rest rendering it more suitable to the healthy
as well as the disabled.
Let handedness is rarely a demerit but may be founc’
to be so in certain assembly line work.
52.
Fine fingering and rapid movement.
It will be obvious
which neurological lesions and orthopaedic diseases precludethis type of work.
.. 10
10
53.
Lifting. Even where 'light sedentary work ' is specified.
it is well to enquire about lifting and carrying. The absence
of a bench feeder may necessitate the 'light sedentary worker'
carrying supplies of his raw materials and removing finished
work. Or again if required to act as a machine setter in
addition to 'sedentary machine operating', this may involve
forceful unlicking of chucks and lifting of parts of machine
and tool.
54.
Beinding and stretching. Where disability contra-indicates
this activity and even in the presence of health it is often
possible by job layout to restict all work parts and components
to within arm's readh: use of tiered trays and-the inclined
plane bring the work surface to hand. Bending to reach
controls may be obviated by resting the controls.
55.
Visual requirements. With further planning, it may be
possible to reduce the demand for acuity.
(Sec para 2). The
partially-sighted and the blind may be suited to work by
adaptation of apparatus. Organisations such as St. Fuhstans,
Royal National Institute for the Blind, Blind Persons resettle
ment Officers and Training Officers and Industrial Advisers to
the Blind Limited provide an advisory service to industry.
56.
Hearing.
Fe-w jobs demand perfect hearing ability; however,
there is rhe overall requirement in the- large' factory for
warning signals to be heard. These- may forewarn the appearance
of trucks or ladles of molten metal, the start up' of printing
presses, or the impending disaster. The deaf should not be
left at the mercy of the sound signal. They should be banned
from departments where sour/ signals arc life saving. As
for safety in the curtilage of the factory the weari-ng of an
arm band will warn truck drivers of the futility of giving
signal, of approach by the horn.
57.
Heat, cold, wet, and humid conditions. Too many sufferers
with bronchitis and asthma have become fatally ill, because
they have been urged to take job' in the fresh air, where a
more equable climate was really indicated. The relevant
conditions arc laic- down in this section, under the heading
of complaints about heat, cold, humidity, stuffiness and
draught.
58.
Skin irritants, sensitisers and degreasers. Normal people
should not be exposed to these hazards unprotected. Unfortuna
tely protective devices lapse or act as irritants or sensitisers.
Insofar as a skin lesion predisposes to injury from external
irritants and sensitisers, it is unwise to expose a patient
with active disease to known hazard. Care must be taken not
to exclude fit people from work by reasons of irrelevant
lesions. Ultraviolet light sensitive (iatrogenic or endogenous'}
workers can either avoid, ultraviolet light or wear barrier cream
on exposed parts.
59.
Lung and ear, nose.and throat irritants.
Patients with
otitis externa, otitis media, sinusitis, bronchitis and con-=junctivitis may suffer unduly from irritants such as butanol
and solvent naphtha, irritants to which the majority adapt.
. . Li
11
60.
Lung sensitisers.
The atopic patient becomes sensitized
readily to allergens and therefore should be advised to avoid
exposure to potent sensitizers, animal, vegetable and: mineral
as subsequent removal from exposure is no guarantee- of recovery.
61.
Fye hazards.
Patients suffering from monocular vision
and retinal, chorodial or lenticular disease, or receiving
therapy such as chloroquin should avaid exposure to further
hazard. This avoidance may be absqlute, as in eschewing work
with lasers or qualified as in the use of protective goggles
where there arc mechanical hazards ( See 'Fyes' - 25.).
62.
Hearing hazard. (See
'Noise' -42).
63.. Lung hazard, A worker who has succumbed to one dust
hazard should avoid another. Similarly a worker with
impaired lung function shoulc’ not risk further damage.
64.. Liver hazards. The patient convalescent from hepatitis,
the cirrhotic and the diabetic should avoid exposure to
range of chemicals with hcpatotoxic effects or requiring
detoxication by the liver.
65.
Kidney hazards. The worker with nephritis, gout or diabetes
shoulc’ avic’t exposure to such diverse materials as carbon
■tetrachloride, lead, mercury and certain nitro and amino com
pounds of bcnczcnc and phenol.
66.
Blood hazards. As a general principle patients with hyperac
tive bone marrow (chronic haemorrhage or haemolysis) should not
be exposer’ to ionizing radiation and possibly the same should
apply to benczenc exposure with a view to Icukacmogcncsis.
Patients with anaemia,. whether due to haemorrhage or haemolysis or
dyshacmopoicsis should avoid exposure to lead and chemicals
causing both methaemoglobinaemia one’ toxic anaemia.
67.
Central nervous system hazards. The epileptic should
avoid those factors;'that provoke attacks such as stroboscopic
effects of lights'arid machines. (See 'Org'ano Phosphorus' - 47
ane’ 'Methyl Bromide' - 38).
•68. Cardiac hazards.
Patients with evidence of myocardial
disease should avoid exposure to such substances as carbon
disulphide, trichlorcthylcne and causes of methaemoglobinaemia.
69. Flame, acid, glass, machinery, and heights. ’ The epileptic
and the patient unstable because of vertigo or leg weakness or
with weak grip, should not carry glassware or corrosives.
The
epileptic if uncontrolled is at risk from machinery and
ladders and a risk to others. However, care must be taken
not to penalise the balanced epileptic or the nocturnal epileptic.
70. Solitary work. Certain temperaments may fine' work in
isolation tolerable or even attractive but it may be equally
intolerable to others. The individual's preference should
be sought.
.. .12
cO/WMl'A/jtv
47/1'(HrstF(O0
CaL
bai\igai o ?Zf4ar,<s ‘^oaa
‘■'-ouOOOl
o? occur/;! 3S;,L rt
Saain-ir on • ■’
’iniv.-; H:-.tLT?. MAIN?
(r....-
Hi IHBUf.MX.iC
,X WC"-”KY IS &• IX
OSCWVi?L.:-NiL !f.Au7H I'd ?H !
Sr Ravi Marayan. «3K: 1HJPB SIH MB
Ross Institute Lecturer
St John's Medical College
Bangalore 560334
I n p o r t a n_e_®
o t
T o pi o
Vosij on the land is aan
«
*
olowt occupations. S ’*, eon 7U-75 S
of the Indian Labour Force is working in
agri cultural
-.• in
which we include Faming, the pl-wit iion;■ (organised agrlcul
forestry, livestock ;sn! .uiin.il husbar.•*.:>■
•. .i a host of hose b
cottage industries which are nalnly involved with the process!!
refining or Manufacture of food, clothia : and household goo-/
rhe
agricultural produce and/or its wiiatee.-. Jwr; though this eiscf?:
our
working force suiintaina literally all o'
work, their health «»?. especially th
*?
through it® r^gol’-..?, etrenoue
hjicar-.is of th-sir oecupatAosi haw not
received the attention and scientific r®f»srch they deserve. Ju addition
with the application of nodero technology to th® production c.' crepe one to
aniaal husbandry, the peasant today i« Kj!-:'- exposed to no.-xr hasar'u: of
which he has neither the requisite basic information or the ueo~«xperiencei
introduction of aechanisation, ch«sic.7.1 fert ills ere and a very l.-vrei ran,
*,
of pesticides are adding a new dissension to the health prohtat&e of the ,
unsuspecting agricultural population. Th ' tragedies of the Hanui<:odu Sy1
th® mystery diseases of Sagar in Shino'm. the endenic arthritis, of XalnJ
all events in recent Mstory which have brought to light only to '..all j
new problem and hanoe tha relevance of thin paper.
?o classify the agricultural occupations in India, for»
9
purpose
of scientific study, the following whose say bo usedj
,2
:2t
...gucmtuhal xhdbotet xa m (cla^-’icab® )
A.
PKOWCWM
1.
Unorganised aector - Cereals, pulaos, Oilseeds, Cotton, Ju~e,
Sugar cano, v-'-eiables, Fruit, Ha-r'er
2.
3.
4.
B.
Forestry
Lives tock/Aniaal
husbandry
- poultry, pi .'c-ry, Cattle anti gheap/coat keeping
5.
Fisheries
6.
Sericulture
i •>.1.
2.
C.
Organised sector
(Plantations)
~ Tea, Coffee, Uubber, Spices
\
- iv-< ■;
)?ood processing
- i. sorting, TJehuaking, Storage
ii.
Milling, rounding, ."rinding
iii.
Oil eanulnoture
iv.
’Gut* ^.:.:r<'lctui'«
v.
Distillations
vi.
Drying, ?iekling
Weaving
- Cotton, Wool, Jute, ^ilk
3.
Hope asking
- Jute, Heap, Kisa.1, Coir
4.
House hold item a
- Bns boo. Can.-, .Straw
5.
Faming imploanntB - Local asiith,v«, Carpenters
fttRAJ. .V^ISAJC.
1.
Masons/Brick kilno/Tile aanuJ’acture
2.
Pottery
3.
Leather work
4.
Handicrafts
5.
Metal saiths - Iron, brass, tin, gol -
6.
HlBCsllaneous
Si tuntlon
Analysis
1.
The Agricultural Worker
2.
The igricultural Work
3.
Ths agricultural Isploaents
4.
The Agricultural Cheaicala
5.
The Health Organisation
6.
Tfce Occupational DlHeaem
*
a) All those persona who are engaged in cultivating harvesting and treating
b)
c)
or processing .agricultural produce £«■;;, stock farcing an? brooding
is
In India More than 70^ of our labour fore/ in this category (1971 census)
He has no well defined status like ths industrial worker, because
i.
Ho in dlspsmed over all the- regions of the coun.xy -
aany quite inexcesaible
it. Be/sh» are usually unorganised
iii. Lack of general education and or vocational training
d)
Be/she belong to all age groups si . . ? agri culture is one industry
which employs, all sections of the population - each one u-. cording to
his capacities
e)
He/she has to support a larger depun-.ient population sine3 there is
usually a higher percentage of moz-;ii and children and old people
compared with the work force as a ’.diole
f)
Being part of a tradition-bound— Joint family *
set-up
ho it- by nature
sore superstitious caste-ridden, cul tin-ally bound and r uistant to
change and nen ideas
g)
With the process of rapid urban!.-: :':icn and industrial L-sii.ca and the
great attractions of the towns and cities the working population of
the villages are being gradually dr.»ined of nose of their nont
enterprising,' creative and intelli;?iit nections leading to an internal
brain-drain fron rural areas to eition which bon very Inportant
sociological and political implications.
h)
?h« agricultural worker nay be classified into three principal catagoriesi
i.
The share croppers - who work land owned by a p»re«» to whoe they
owe u pari oi th>4r harvest
ii.
The tenants
iii.
The wage earners
- who rent o.;. the land for a fa;, yoare at a tine
or landless
labourers
- work on a yc^rly/seaaonal baMs
iv. The bonded labour - special to the Indian situation
Precise Infomatlon of tho numbers and characteristics? of thes>.categorieB are lacking la our country.
.4
1) The agricultural worker includes men, wcnen and ovsn children
*
The latter work in agricultural rclsb-ad occupations virtually fros the
tine they boj<un to toddle around tlvrs house and this ia vith certain
detriment of their physical and intellectual devolopeant. This leads to
echool and. a high drop out rate.
a large percenta l of absonteedcn
This feature ic particularly iapo.'.'tant in the light of the f.ict that
1979 has been acclalned the International tear of the Child.
2.
’0?-K
ths
Agricultural walk consists primarily oi
i.
Production of food, stuff;: and seat natnrials for industry (thia
includes cultivation) barv-.sytiv and care of plants)
ii.
Breading and rearing cattle and other anlnala and birds
iii.
processing and conversion of produce of anisal and plant origin
The work has specific characteristics which dotemine tha typen of th®
environment and the typo of safety and health problems that thri •worker has
to face (HO Volutio 1)
(1) Work ia carried out in the open for nost of the time exposi g; the
agricultural worker to varying sliraut-x
*
and meteorological cocdittons
(heat, cold, 4< rain, storms etc)
(?) The seasonal and often pressing nature of the job which ■•taaaad
i.
long hours of work;
li. physical effort; and iii. sp-.:edy execution
(’5) The frequent changes in the type of work undertaken by the twao person
which provents
i.
demarcation of duties; and ii»
rotational eyeten of work and rest
vory difficult
(4)
The aanlfold contacts with animal anti plant world loading to dangers of
a.
Infectious or parasitic disoa es;
b.
a, t?n/stinfiB{
o. axpoeurs to duats containing fung'.U spores or allergy
producing substance;
d.
-ixpoeure to toxic or irritant VGjviable juices
Ko use of a wide range of agriavltural eh«ri.cals givrice to serious
(5)
risk of poisoning by skin absorption and or inhalation
1. Pentieidea;
(6)
ii.
Fe~tilii--rs;
iii.
Fungicides;
iv.
Herbicides;
v.
Seed dronoing
The considerable distances batwscsn home and work place especially for
jsovon ent of
flocks? over pasture lends leads to
a» considerable tise and arc-v in travelling;
b. increased risk of eosBuWig accident;
C. regular acai hours ani Sjc.’care uncertain
(7)
The living conditions of the woifs:: are often printtiv
.and unhygienic
the surrounding ijthor poor
and the cnviroswental sanitation
(8} The -jra'-at diversity of woriting r- •>.■■iuOdn
i.
Manual labour
ii.
Saall inplnuontB
iii.
Larger nochunical aethoSs
iv.
Agricultural Machinery
(9) The difficulty of proscribin.; fjnd applying standard'.' and. regulations
of safety and health in ssall
(10) The r-nploynent of Much casual
i.
any real occupational cuulifications;
ii.
ill Informed as to riuk.« find pr-i-vantive aeacur/a
iii.
3.
units, particularly in our country.
anal labour without
physiological unqualli’i d. for nature of won-:
(nothers and youn. children)
AG".mdr-Xim'W’UrJIJf
(Technology)
The technology in Agricultural fc us^ry can be broadly divided into two
«sjor groupe
A - Agricultural laolauents — tho'.’-s tools and inatruaants ahich are
operated annually or are worited by draft anlnala such aa ox«a, water
buffaloes or horeea.
Those ar? st-iinly used for
a. land clearance
b. seed bod preparation •» plou^ypu<Ml«r/cultlvatorc/harro
ia
*
*6i
planting - attachment to ploughs and cultivators
c.
d« intorcul tivation - hand hose-, spades, rates, forks, pick axes
e.
plant protection - spray© rr., tsioke *
generator
,
xl-tw throwers
soil injectors, funigators, bi.’f fcarero
harvesting and threshing - .:ii&las, scythes, cutlasses, rates,
f.
pitch ?.:>iko, Batchetes, fodder cutters or choppers,
winnower
crushera,
(sugaic
shellors
(corn)
(paddy rice)
I’.e^crtieators
(groundnut)
PoliaUers
(turarlc)
Miacellnneous
g.
- yoke of draft animals
- wheel bsrrown
- nhoarers/hand clippers
- water spraying devices
The nain hazards from agricultural isplenents are
a. Physical injuries from cutting edges of equipment
- small injuries hear serious (inadequate nadical 1’ncilities)
- seasonal pattern
- danger of tetanus
- lack of ara/hund/f ?ftt protection
b, Qu3ula"ive ill effect
*
to the- hi.dt'i of' the wositecx- over a ported
of time due to handlin. of
- poorly designod and heavy iaplemants
- in clinatea with extre-conditions
B - .yyricul tural Machinery
This is the machinery which is designed to Hunipulato soil and rondor
it aoro suitable for crop growin,;;, seed sowing, applyin;; ;!cultural
chemicals, plant protection, hnrv<?stliv; and storing crops
*
Ther
is an extremely wide varxoty or machine, but Lhes© are
essentially an arrangement of g“ara, chairs, belts, knives chatsre suspended
in a frame stationery or nobile which perlons the desired opo/ation while
aoving across the field
- The najor groups are
*
a. soil tillage machines
*
i. planting machines
c. cultivating Buchlnes
d. forage harvesting
e.
grair/fibre/vegetabl© harvesting
f. transport/eisvailng nashin s
•
*
B
agriculture chenical applicators
7
lit
h.
sortars/packerB
i.
power plants/elcciric ootoro
The machinery exposes the worker to throe Bain typos of hissaf'ds
1. I'rauaatic injuries such .-iO cuts, crushing, bums, fractures,
amputations
ii.
Organic injuries caused by noise and vibration free th®
Ba chine
iii.
Health, i»paiment caused by toxic substances sue};, aa agricultural
cheraiculn and engine exhaust fuaes
4. AC.ructarirkiL
chkhicals
One of the stoat significant developments in the agricultural
industry in India in the last 3 de>C:in the extensive introduction and
application of agricultural cheat cue to tackle various proWwe
1. pesticides
i. org-indchlcrino
ii. organophosphorous
2.
Fertilisers 1. nanoniu-a nl'.r-.te {. Nitrogenous
<< „
S phospha tic
U* urea
J potassium
3.
Fungicides - foliage, turf,
4.
Herbicides - arsenicals, borates, chlorates, Gu 304
Hi. others
fertilise re
J Trace element
e;o11,
seed dreaslK ■/, space fumigants
Anaoniuia sulphamates, dir.uat, cinitrocospounde,
5.
aodcntlcides
The toxicity and hazard of all these chemicals when used without
proper Information, precaution or prot ction la too well known to bear any
repetition,
5.
THS H ...LTH OdGASI ’VJI-sN
tocluding the agricultural voxkoa who are employed in the organised
plantation sector and who are ther-fore covered by the plantation labour
Uolfiie Act, all the other worka.s are not provided by any cpecific O.H.5.
except the ttsdical cover which is provided by the peripheral health service
infrastructure of Priaaiy KefLth Centres and sub-contras. Host of the
•edlcal personnel aro unaware and uninfomed of the occupational he ,1th
problean of the agricultural worke.3 and rural industries ..nu hence preventive
health uaiftt
and safety i;
college w radical professionals in
*
.-lect'id. Meitfr .«> :;’>j medieal
-y\il nor the .vericvitttral Colleges/
Universities? or the agrieultorsi cci. nstl&ts have hi&hll; ?
W.
*
undertaken research in thus
*
bo-in grossly nogl<:;fjt'xl»
one of the highest priority ar ’ ;’:
6.
ccGin-.n ;?y
••:
Bieeases principally ctmfc-; c»;'u.ocwaBlcaally
.questionably contrasted Through ->•
*
OccapatjU'as
as folio•.«
classified by
■OCCUPA?ic:id.L ''-S'.-.:’.'
■
;'/■■
„•
CA?Sg()1Y I
f^towlnally eontmoted t7u; ■. ■ g-> ;;?.-rloul turo
Viral
Viral enconhalitio
*
tick borne
Viral haesorrhagic fw?r, tick. l>orr.c!
BastoKUI
inthrax
Brucellosis
Leptospirosis
Tetanus
Tubercxiloaie, borine
Tularcnia
faraaitis
Ankylostcoiar.. b
©r have
.wl hence i.-hat should 3::>wa^ly have boon
and
t:nen
lirrul
fckies
Rdlteccsis
Viral enocrhtldtS.s, jnoeruit© ten®
Virrl hwtanfc^c ?bvor, noaquito 'erne
Eacrtartel
StabereEac-s i a, 'wm
SfctercvlerK -., r.vian
Hyioti-cgis
J^Usrla
3cna Tyrim
CAH-Xn
Vircl ■cvc'Yt tick lowse
Vf.3®l lever, oomtdte ' erne
Ceu rcz
Toot and :"cuth ••iseaae
kasJ,
I ctinaEyco-jia
Elx-staajDo:->. 9
’HsteiiLc.®303-i3
leiAx<nj..ii&i.s
CsjB^XXXKfClcsiS
HI
10
7.
Hazards
in
jricultuxal ralatorf incuatelf® hove been
dtwcrihnwi and « review of lltwr-iuro suggest-s the following
■' — t?Vantat icns
(uaneral)
- Inelemtjnt washer
1) ^iysical Hazards
Chemical Hazerde
ii)
~ Mjri>3ultural chumicnln
ili) t'ioto deal. Hazards
i) 1‘oek worm
11) ■'•nlwal & i'-naka nites
Ail) Infsotlue/pwtaito disoass
iv) FWhanical hazarda
hand injuria
:-.g.Ud.i>QP. fcu-fpated)
A) Too f-uat - Tea workers Aethmo
ii)
injuries and electric hazard of (frying
Coffee - trust i or
meet tines
«• Hum#
— 1’iru
* exclusion smzard
~ Allergic reactions of skin,, mucous membranes and respiratory
sysitm have bojen enctiuntcrod with persons handling groan coffee
possible aller->n ** £jlUl£Oiy£uafiiUi (finland -Jiortenya coffin
roastery workers)
exhaustion In coffee plants
•• haait or ’themal
*
~ Cofftwa uMsteo
( emission of odours
into water sources increasing
j -iolid
( its B 0 D
- tintrinsic; allorgic elrwolitto
H — ^wrlculturo
i)
Lemobitie of Iwnis - in workers reelin 5 raw silk
ii) Allergic skin raadttuns
Ail)
M> poisoning ~ Headache
*
*
vortiga
nausea vowit in-g in roaring
ro«««e Cecal fires unfid to k&cp it warm)
Av) Re<)iraftory disoa®« - Chpjnic
or allergic bwnehto
11
11
***
*»
Cult iwatian
1) H.nri injuries’; ciura to cutting trials
ii) mA a or on ras Luns frMn olant Cevdbnp into septic cores unl«m
treated properly
Hi) -‘ft’kag & poisnous insects
iv) Hdt bites
' ,r
d.
i) brake hazard
11) Incrvaesd risk of tetanus with alleula
ill) -kjslncntal caAa
iv) Skin puncfcurvn
I' ypertoratoxio of palm «.fing&rs ) handicraft workers
v)
£. £-v
i) ^n^co hazard **•
on»wxjs insects
ii) EiXs frota m kniuag
ill) Hypastaratoxla of palm and fingers
F.
A) *
aHo
whlla ulinbirttj
ii) Injuries Caused hy falling
nul>»
->n?jka tsitssa
iii)
£giir
i) Ukin infect lens dus to woskora standing in i>rucnAah water or
weftt ?ng or Boakin j ptN%‘s
ii) •>ulphurdioxidn in th« bleaching procsss
iii)
AcoieMnta frun un^uurrM nschinery
unora
i) Finaly ground capra duat r.»y form as tnqsloslva fixture dhich is
readily ignitable
11) Fires and a^jiloaiw-a due tu soiva&s used in oil extractions
iii)
-kin disorders duo tu cjnotant Imeralon in water (desnicatec coconut
iv)
lifting proolrne with hxw wfteks of capro ~ ?0—?5 kg.
factories)
v)’Ecipra itch’due to lnfast<atlxrf» with mitee
12
12
x.
twrynrr
1) ^M
**
8***
!.
cefomit iue. “ *l,23nU;;*
-li n'i position
- ^it lacww
— *
»calioxts/
lordosas
disorders — due to eyestrain
ii)
iil) Hafbl * finsar rfiaattfatMt ~ swullon finger Joints
*
arthritis, nevralgics
iv)
Hand trambung
v)
‘‘WianUil ixizards
vi)
Toxic hazards - dycstiffs - potassium or sodium bichroncile
•Amunie, str-.-ny adds, alkalies
vii)
-.r..!z infection f ran _rraj
3.
i) ttrau dust dwwaatitsss
ii) i^yug.jnic infections of skin
ill) •'hinltls pharyngitis/laryngitis/t racheobranchit ia
iv)
•llargic bronchial asthma
V)
^ubaonary Hycosiw
vi)
p'saCtivs inflararaatlxm of uye foreign hotiies in the eye
fratnatie injuries.
8. *■•
iafc
can he done to provide Pr<svwntlva Health *
fWntmantie
for this
high priority sodtor of workers
ft<wtCI fco hMftUqhb the importance of •’qrlcultural Medicine ««mJ health
hazards in ths agricultural arid lKM3»4Ma«N9l cotteyts induut rise in >111 forAtvt
dealing with aacypafcinrial and industrial health.
2) h.«Mj to CQjp.ncfc, all thn ! rfc-n r.p.i ^>Qjt..fchkLlia^ag^ AJPlMHfcJX
1) labour statistics
iii) !-istributbin by divisions
v) Traditional prucesseo used
ii) Xerographic data
iv) Knci/i health a!id safety probloms
in each
vi) HafceMsls vead
3) Hews to nlan <sut pilot tpida-lolugical research axStMr.-a
{,o 8tudy the
hazards and health prUsltuas of t ach of these groupa of workers
Already schemes to study the bldi warfcets, sericulture, coir workers,
tea nl-jntafcion wnifcoiB smd weavers are in rmigresa or iidhrj planned
by ft a H C
and •< U b ii-
13
i,;.q orj,>1 or/ifiRra
•
to th» pacts, iiiw.jl hmlth
pndilenn of the &»jricultural Markers .nd rur-il «,st lows wJ to train
the parent-deal twalth porsonnol to t»c!uctA«? ttw ptv'lo cn si'cle
Ctaavtary inuulw?Q© of these
stfid effective health »jtit} o.ifwtf nw-aauree
pssblms isui than prewtifli> rwt tie Induced in all training course’s.
coi;-; : ■■■'• *
« t*
®
5)
Ptudy
: i»’...;e •>. a•-.«> ha .».••.?» in of the • ■'i. efferent agricul
of ttscoWilnMl hudth
tural oceupatIona anri the intreivr/tvirtt of t;ir -eori-wlcu’.- •? s.-’icntlsta
W" • ?dc. . i.ur. J
wwi agrimdtur-il -n.^in.,.?
.-'.rs-'-rs in ths
Chinking of the h<? ;.ti» rjp iftc .-- ’■■• ;u-; or ft»w» j *or w- - dtion to the
hc-dth of th
*
plan? or animal ?«• the? jncr.Mdng of pk.-'?. rot Ion.
;:) .Ihvolwwant of tho
J'*
»
”■ ■
’■•’ .cA™,
in iopravlng ths
1) Packing — Isafe proof son- ■h'/ii c?:
ii) Mi-sllinrj “ aspstsijUy lr; tha :?®giunatl
ill) ‘’Earning of hajaarti
*
cu sxnii'-'itlan
iv)
Hse-Jisiun -.jf pg’ntrx.t ivc- r.v »«urr=:; isr
to
xn/Kouctii a
in ft; mat ion «i these.
illitsrula peasant ar Jant’ltsss latourer
ptoltti
Fix.;:) t?.:? :>ij.irtJs r-S in ths ifcis of tijase agricultural cii;inloalsi.
^QttCMltural tWle.Vio
iwst h. imps an integral ;;art c?' nut tasdisal .
adixcatton und cr ci
>a£inml
*
f;
*
botaosM
an integral part nf th
*
hs.ilth services far
farmmmt
ffijfflorBhana.iva hmlth csro prograrw of the
Artery :.u ilth tfsntrcr,,
®) ftwclvtnarfc of .’ill organiisatArntn/agmciias .:«nri govt.
dealing with
one r; ?iwra of ths jreufis Hwtitlonvd in the ela.-slficiAim tarlitr on <•
in the collodion of an inform^ion mao on -that particular or group
of ocn>4>akion
*
and aupportint^/aponsoring of rvst>art:h in
health and
safety prutdoHkJ of t?w uatksrs in that occipat ion.
9) lndlvi®a^?ig>up health tdoeation
aa part of the
£jdt«rmi»in tf the Kiosk 5;‘ovialopi’wr»t 'tgtmcia
*
tark .wd the ■''<usicultural
should toe undertaken the never
hazards due to nodemis.i&iijn in agriculture; .
10) Overall bodo-eoortMaic W
*VKiiot?|BC!nt
in <4
*idv
■ end ^anaral tyiy I'tfeicat.ion ,
Agricultural Medicine «hould fowa an integral pert.
3
4
OUR AIM
IMPORTANCE OF MAN-POWER
India is a developing country progressing towards a
better economy. The three potential factors for the econo
mic progress are (i) establishment of Industries, (ii) impro
ved agriculture and (iii) population control. The indices
of success are. better production in the industry and in the
field, and better health conditions of the labour.
Without human intervention, materials- money and
machine would be sterile instruments, indeed. Hence the
health of the industrial or agricultural workers is key to
satisfactory productivity. Health and Productivity are
reciprocatory and complementary.
Work upon which productivity depends has also its
hazards. Apart from accidents there are many conditions
which endanger health like, dust, noise, heat, toxic substan
ces, fatigue, etc. Most of the hazards can be controlled if
not eliminated by the joint effort of the labour, the manage
ment and the community-
HEALTH HAZARDS
Since independence in 1947, industrialization and
urbanisation in Mysore State have been phenominal. There
are 3,113 industries. The type of industries cover a wide
spectrum ranging from cottage/home industries like weav
ing, beedies, etc-, to larger ones, like steel, cement- paper,
NOISE is a part of modern life. It not only threatens
permanent deafness for certain workers but it also ha^^
textiles, chemicals, plastic, confectionary etc, etc.
close relationship with productivity.
MEN AND WOMEN AT WORK ESSENTIALLY ARE
MENT. THEIR HEALTH AND WELFARE IS IMPOR
TANT FOR PRODUCTION.
UNSATISFACTORY CLIMATE adversely affects pro
The total labour population is in the range of 4,95.454,
(industrial labour 2,35,561, labour in mines 26-393 planta
tion labour 77,068 and commercial labour 1,56,432).
The
labour population includes women as well as children
In
ductivity.
of our population is having agriculture as the main
occupation.
High temperature, humidity, poor lighting and
ventilation leads to lethargy and even accidents.
DANGEROUS
addition to the above labour section, a considerable segment
GASES
endanger health.
Carbon
monoxide from damp-furnaces, being colourless and
odourless, deceives the victim to disability and death. In
the manufacture of artificial fibres, workers run the risk of
contact with carbon disulphide, which when inhaled in
DEVELOPING INDIA IS LIKE A MAN RUNNING
THE CREATORS OF ALL PROGRESS AND DEVELOP
The factory is like a battlefield. Industrial workers
face many hazards depending upon the industrial process.
small quantities over long periods, can lead to depression,
personality changes and even insanity. Compounds efl
UPHILL—IT NEEDS ALL THE HEALTH AND WEL
cyanide have a wide use in electroplating and extraction of
FARE.
gold
These gases can kill a person in one or two minutes.
7
6
OCCUPATIONAL HEALTH—HEALTH EDUCATION
EMPLOYEES STATE INSURANCE SCHEME
DUST particularly in cotton textiles and fertilisers,
when inhaled over long periods result in a disease condition
A properly planned, Health and Health Education pro
gramme can deal with the hazards and promote health.
Occupational health work includes not only prevention of
illness and accidents but also the improvements of the
general health.
Employees State Insurance Scheme, is a part of the
National Welfare Scheme under operation in Mysore State.
It provides medical benefit to the insured persons and their
family members. The services include diagnosis, treat
ment, follow-up, sickness benefits, ambulance facilities, etc.
The scheme is now in force covering 50,000 employees and a
labour population of 1,85,000 in places like, BangaloreHubli, Dandeli, Mysore, Mangalore, Belgaum, Gulbarga,
Gokak, Davangere. Kollegal, T-Narasipur, Nanjangud, and
Harihar Under the scheme the Government have establi
shed a big hospital at Rajajinagar at Bangalore, created
specialists services and also started a number of dispen
saries with the personnel, for rendering the routine and
emergency services.
of lungs making the victims vulnerable to Tuberculosis.
Lead poisoning
Machine can be adapted to man rather than man to
machine- Fatigue can be diminished and monotony
avoided.
may result in mild complaints like abdominal pain (colic)
or even permanent disability like paralysis.
Routine periodical medical check up of the workers can
help in early detection, cure and prevention of many
conditions.
In addition to the above conditions specific to industry,
Noise and dust can be controlled if not completely elimi
nated by proper ventilation. Exposure to toxic substances
can be prevented.
METALS like lead cause poisoning among workers in
bdTtery factories and certain shipyards.
workers (agricultural as well as industrial) are amenable to
suffer from diseases common to the rest of the community,
like Malaria, Cholera, Diarrhoeas, Small-pox, Dysentrics.
Tuberculosis, Leprosy, Trachoma, etc.
They are also sus
ceptible and suffer from other conditions like mal-nutrition
and under-nutrition in addition to the disadvantages of
frequent pregnancy, delivery and large families.
DRAG OF ILLHEALTH ON THE ECONOMY IS
Modern science has provided effective weapons to
safeguard the health and welfare of the workers as well as
their families But what is required is the willing co
operation and practice of the measures by the workers, their
families, management and the society.
The State has also a net-work of 1,777 health and
medical institutions, Allopathic 1,342 and Indian Medicine
435, spread over the rural areas of the State to render pre
ventive and curative services to the community. These
institutions also provide routine health services to the
labour population (industrial as well as agricultural) except
those included in the Employees State Insurance Scheme.
Ignorance of the potential risks of the factory environ
ment can have tragic consequences. Education of the
managements labour and the community is basic to the
practice of all preventive and safety measures.
Simple
practice like proper and hygienic house keeping, which
often does not involve much expenditure is the fundamental
way to reduce the level of danger.
DOCTORS, NURSES, SOCIAL WORKERS. HEALTH
ENGINEERS AND ARCHITECTS CAN ALL CONTRIBUTE IN MAINTAINING PHYSIOLOGICAL AND
MENTAL WELFARE OF THE WORKERS AND THEIR
FAMILIES.
TREMENDOUS
JOB CAN BE ADAPTED TO THE HUMAN CAPA
CITIES—ANATOMICAL, PHYSIOLOGICAL AND PSY
CHOLOGICAL.
COMMUNITY HEALTH CELL
47/1, (First Ftoor)St, Marks Road
BANGALORE-660 001
ORGANISATION OF
HEALTH SERVICES IN
INDUSTRY
4.
INDUSTRIAL MEDICAL OFFICER
FUNCTIONS
DUTIES AND RESPONSIBILITIES
by
Dr. M. N. Gupta,
MB., B.S. (Pb), D.P.H. (Land), D.I.H. (Eng),
Qeputy Chief Adviser, Factories (Medl.),
^dinistry of Labour, Govt- of India-
1. THE INDUSTRIAL MEDICAL
OFFICER—FUNCTIONS
The problem of providing medical service for
the Public Health Service in the country instituted
such a programme for the niedical personnel.
Our shortage of trained medical men is appalling.
the industrial worker both in large and small
It is also sad to say that the medical men or the
plants is in the interest of the government,
“ doctor ” in our industries and factories has
employers, workers and all those interested in
not grown up with the Factories Act.
It must
promoting better standards of life to reduce the
also be realised that there is no substitute for days
losses sustained through sickness, accident and
and months lost because of disabling, sickness,
In a country as ours, such problems
and no substitute for the lives lost in accidents.
death.
assume wide proportion owing to both the climate,
The provision for industrial medical supervision
the poverty and the ignorance of the people which
is necessary, for, there are a large number of
has contributed widely to the existence of tropical
people in large industries and a larger number still
and other epidemic diseases.
in small factories.
Also such provision must be
In connection with the sickness among indus
provided step by step starting with factories and
trial workers, few employers know the rates of
industries with special toxic hazards or where work
Even in indus
is heavy or where there are a large number of
'sickness among their workers.
trial concerns where doctors have been employed
youngsters, women or
to provide medical relief, the incidence of diseases
must also be made to stimulate Works’ Commit
of occupation are totally unknown and the concept
tees to augment health and hospital facilities.
older workers.
It is, however,
The factors upon which
certain that a sickness and disease exact a heavy
supervision depends are :—
of such diseases is non-existent.
toll from the industrial population and has in
fluenced the efficiency and the earning capacity
of the worker to a marked extent.
While it is essential that a programme of
instructing the management in the advantages
of medical supervision be instituted by authori
ties concerned, it is of still greater necessity that
2
1.
industrial
Efforts
medical
Those relating to industry or factory.
(a) Place, housing, transport, hospitals,
climate, regionalisation.
(6)
Number of workers employed—single
or numerous units of small or large size.
(c)
Type
of
work—heavy,
dangerous,
toxic or shift or transport work.
COMMUNITY HEALTH CELL
(First Floor)St. Marks Hoad
BANGALORE • 660 001
1
Peoples Health
Type
(d)
of
worker—men,
women,
youngsters, active or sedantary.
The first contact with the medical department
should make the prospective employee realise
Buildings—Obsolete, modern, transi that here is a place where he can depend upon
(e)
In old and obsolete build
tion, and expanding.
genuine
help
Essentially,
and consideration.
ings where it is difficult to catch up with im
this scheme consists of dealing with job evaluation
provements in modem factory design.
and meet with the medical categorisation of the
(/) Contractors,
men
where
first-aid
arrangements for contract labour is necessary.
2.
worker.
laws of medical ethics, commands the trust of
Officer.
the employee and no confidential information
(a) Full-time—
Organisation with over 3,000regarding the medical state of the employee is
(i)
employees with nurses or first-aiders.
A set up
including a headquarter and subsidiary units
spread over the various production departments.
(ii)
A
regionalised
passed on to the management.
The Canadian
Army PULEMS
system^
is
type of
capable
number of
smaller
successfully placed in occupation.
A factory employing less than
3,000 people, with some special toxic hazards,
to one or two units, in the course how
as examining
surgeon
to
(5)
The functions of the Industrial
The Industrial Medical Officer must pay careful
attention to the following outstanding points:—
(6)
The occupational
selection of the employees is a problem of prime
be
in
his
to
indicate
safety
daily
to
work
Routine mass radiography is valuable
and cardiac pathological
The categories of workers should be
classified, as: fit for any work, no hazardous
machinery, no heavy lifting, work at ground
level, no extensive working, severe handicaps
such as blindness, and rejection.
Pre-placement examination of the worker
■ to assess his fitness for work.
should
conditions.
There is a difference of
Medical Officer remain the same.
be
performing
to detect pulmonary
In any case even with the above circumstances
basic principles for the provision of medical
can
while
anefficiently.
expanding factory.
degree only.
each
himself
ol ordinary general practice.
employed
The object
(4)
(6) Part-time—
service are the same.
Very few applicants are so unfit as to
(3)
be incapable of any class of work.
assistance and requiring lot of research work.
(ii)
Anything less than a full examination
(2)
is not fair to the worker or to the e mployer.
with nurses, first-aiders, pathological laboratory
(i)
any
unitsmination enables sub-standard persons to be
employing 50—250 people, with first-aiders.
(iv)
to
Only a careful pre-employment exa
(I)
A
adaptation
are:—
a group of factories.
(iii)
of
The essentials of a physical examination
administration works.
with assistant medical officers, nurses, etc., for
1.
The Industrial Medical Officer must
formulate his own scheme of categorisation in the
Those relating to the Industrial Medicalform of a code which, to comply with essential
(7)
At hazardous occupation, periodic exa
mination should be the rule.
(8)
The confidence of workers must be
importance and it is this aspect of the medical
gained, they must appreciate that medical super
officer’s work which if adequately carried out
vision is in their interests.
brings- the greatest applause and appreciation
of the management.
(9)
Employees returning after illness
some weeks absence should be re-examined.
of
Organisation of Health Services in Industry
Above all the industrial physician must THE WORKER
(10)
possess “ wisdom ” ; he must be the friend of
It is essential to note the following things when
considering the question of employment of people.
every one.’
Second important principle of industrial
2.
(I) Past history—especially the occupational
medical service is the organisation of emergency
history.
treatment and arrangements for swift clearance
must be made to elucidate the exact nature of his
It is not too much to impress
job and the raw material or the by-products that
of the acutely ill.
that this service helps to improve relations in
This is most essential. Careful enquiries
he handles.
factory between the workers and the manage
ment and many a life and limb are saved which
Age and physique—physical fitness for
(2)
the job he is about to handle or he is carrying out.
bring blessings in disguise from all concerned.
Deformities and diseases—a physical
(3)
Arrangements for periodic health examina handicap need not always be a bar to his employ
3.
tion of all workers, a systematic check up, especi-
ment.
The job must fit the worker, not the
, ally the examination of people about to be em
worker to fit in the job.
(4)
ployed in departments where toxic hazards exist.
Social background and family history.
Arrangements for examination of workers Most of the present day illnesses have in their
4.
background an unsound social fitting.
and report on their health state.
Statutory examinations of—
5.
(i)
(5)
all young people entering industry ;
If the worker is exposed to toxic hazards,
his periodic clinical examination should be directed
(ii)
periodic examination of these adole
(iii)
examination of people employed oncolour, skin and weight.
(a) General
scents ;
(6)
dangerous occupations.
6.
Provision for research.
(c)
The opportunities
bearing,
appearance,
Nose, mouth and eyes.
Lungs, liver, kidneys, bladder.
available for the investigation of industrial health
(d)
Muscular and skeletal system.
problems are innumerable and unequalled material
(e)
Nervous system.
is available to the keen, enthusiast and ambitious
(/) Special investigations:
Urine,
worker.
7.
Blood counts,
Education of the worker on health matters,
X-rays.
and providing advisory and consultation service
for every worker.
Keeping of medical records and their inter THE WORK
8.
While it is essential to have a knowledge of the
pretation to the management.
Provision of adequate, prompt and skilful physical capabilities of the worker, it is of still
9.
greater value to be able to have a conception of
first-aid.
10.
Provision of nursing and ancilliary services. the nature of the job that the man passed as
Industrial health supervision has three impor
tant aspects and it is the duty of the industrial
medical officer to devote his time and energy
to all thejthree aspects.
(i) The worker.
(ii) The work.
(iii)
The working environment.
>
medically or physically fit has to do.
Such factors
as the following about the work must be investi
gated :—
(a) Nature of Work—shift work, night
wdrk, work of arduous or monotonous nature.
(6) Demands of the work—demands upon
muscular and skeletal system in terms of gross
Peoples Health
or fine movements, weight lifting, standing,
chemicals is increasing and as such it is necessary
awkward positions, climbing, bending, kneeling.
for the industrial physician to have a knowledge
(c) Strain on sight, hearing.
of:—
(a) Toxic solids, liquids, gases, fumes and
(</) The need for protective appliances or
clothing, as in welding, chrome plating.
dust;
(e) The element of sudden danger or in
sidious hazard—danger from sudden explosions,
(A) Accidents of gassing, explosions, dust
hazards, insidious poisoning;
or slow absorption of lead fumes.
(c) Dangerous processes covered by regula
(/) Individual or team work.
tions ;
(g) Responsibility for the work or the safety
(d) Other processes carrying risk of indus
trial diseases.
of others.
(A) Working above or below ground level.
C.
(i) Mental demands.
BIOLOGICAL
Knowledge of epidemic
THE ENVIRONMENT
diseases and other.
diseases not specific to industry as Anthrax,
The industrial physician should have a work
Ankylosmostiasis, Weil’s disease.
ing knowledge of the industrial processes in
volved in the works in order to prevent occupa
tional disease.
It is incumbent on him to make
D.
PSYCHOLOGICAL
It is being increasingly realised that industrial
be
psychology is a subject, the knowledge of which
He should also possess
is very essential for the industrial physician.
a good knowledge of the clinical manifestations of
Such factors as monotony at work, anxiety,
frequent inspections of the work-rooms to
able to assess the hazards.
occupational diseases to which the workers under
his supervision may become exposed.
danger, fatigue, attitude of the worker towards
He should
the management and colleagues have psychologi
know the prodromal symptoms as well as symp
cal basis and their investigation is therefore neces
toms of disease when it is fully established.
sary.
The environment of
the worker
may
be
classified into 4 classes.
In the end, it is necessary to have an idea of the
work of the industrial physician.
His work is
divided into that performed—
A. PHYSICAL
It is the physical environment which is the
most difficult to control and also most important
for maintaining the physical fitness of the indivi
dual.
Such factors as ventilation, temperature,
(1) in the work’s surgery
or ambulance
room,
(2)
in the factory, offices, canteen, welfare
and safety department, etc.,
(3)
in his own office, laboratories, etc.
humidity, lighting, glare, noise, apparatus, machi
nery, work benches, seating arrangement, pro
tective measures and their provision, play an
important role on the health and well-being of the
work-people.
2. DUTY AND RESPONSIBILITY
OF INDUSTRIAL MEDICAL OFFICERS
Having such an interest in the health and the
welfare of the workmen in his medical charge as
has, been described above, it is necessary to have
B.
CHEMICAL
With the increasing use of a large variety of
chemicals in industry the risk from the use of
some knowledge of the. philosophy of industrial
health, supervision, as provided by the factory
doctor.
Organisation of Health Services in industry
The principle of humanitarian service
to
be prepared to accept rebuffs and criticism till he
labour is guided by certain standards of res
has blind faith of the two.
ponsibility expected of the industrial physician,
period that he has to be very careful and watch
which are grouped under the heading of “ Duties
movements.
of Industrial Medical Officers ”.
In every such
provision of health supervision, there must be
pronounced
magnificence
and
high
ranking
quality that will serve as a magnet to which all
support essential to the success of that provision
will
be attracted.
The composition of that
It is during this trial
He has to be alert, on. guard and
with an open mind make investigations.
He has
to be on the look-out to know each worker
individually in the earlier stages, and be able
to get the confidence of the two around him.
In the early stages he should act more as a colle
ague and not as a doctor.
He is working as a
support in our field embraces, employers of
member of a team and as such a high standard of
labour, the employees, the management, the
work and code of conduct is expected of him.
general medical practitioner, and a wide range of
In the disposal of the patients seen by him a
-others who directly or indirectly influence health
great amount of tact and diligence has to be
supervision, who are affected thereby, or who
used and for this he should be prepared to ask
have it within their power to aid in the prevention
of industrial maladies.
There must be a con
for cooperation from the management in order
that the interest of neither is jeopardised.
He
centration of purpose in the magnificence and
must arrange to guide the first-aider, the nurse,
■the quality of service, from which may be dis
the management and the patient in cases of
seminated the allocation of responsibility per
emergency illness.
taining to each interest involved.
Realising that
the team spirit be avoided, he should be guided
no matter how much planning goes into a subject
by the following duties and responsibilities of
its success depends entirely oh the spirit of those
In order that conflicts in
an industrial medical service :—
engaged in its operation, it is essential that the
1. He should carefully assess the suitability
industrial physician observed on his part the
of his own methods of examination, paying special
ethical rules which govern the professional rela
regard to the occupational history of the worker’s
tionships, between industrial physicians, their
illness.
colleagues in general practice, and the workers
and the staff under their professional care.
In this connection the management has a right
2. He should arrange for all emergency or
first-aid treatment at the place of employment of
the worker and should make proper entries of
to expect from the doctor—services that will be
the treatment offered and the instructions given
of use to all and which have a bearing on the
to the patient or other responsible person as
general improvement of the morale of the workers.
regards his disposal.
The worker also wants help and guidance and
3.
If it is necessary, in the interest of the
some one in whom he can put implicit faith when
patient, to continue treatment in the factory and
he feels like confiding his mental and physical
where such facilities exist, he should, in consulta
ailments in the doctor.
tion with the patient, arrange for such treatment.
The doctor has therefore two divergent kinds
4.
He should have knowledge of hazardous
In order that he can main
occupations and while examining persons employ
tain a happy mean between the two, he should
ed or about to be employed on such occupations
of people to please.
He is always
he should be able to advise the management on
faced with the difficulty of expression of opinion
the suitability of employment of such persons,
to both.
or their transfer or retirement,
be governed by these ethical rules.
Under such circumstances he has to
1
Peoples Health
5.
He should be prepared to advise upon the
He should supervise' the general sanita
16.
occupation of any worker, whose duties appear
tion of the works, and make necessary recommen
to be too heavy or otherwise unsuitable.
dations.
6.
He should possess expert knowledge of
17.
A large number of forms are always hated.
short-term illnesses in order to avoid confusion
There should be less codification on paper.
with illnesses of malingering.
legibly hand written note from the doctor can do
7.
18.
examination and those specially pertaining to the
industry in which he is employed.
8.
19.
engaged in medical services.
He should be prepared to collaborate with
the work and the working environment.
In case, where a worker is being treated
by another medical practitioner, and a report on
him is needed he should, with the consent of
his employer, place his special knowledge at the
disposal of the attending practitioner.
All medical records of workers are confi
dential documents and they must be treated as
such when in his custody.
All workers should be allowed free opport
unity to consult him.
No barriers to these con
sultations should be set up.
13.
He should be prepared to discuss health
problems of the family of the worker and these
should receive his adequate attention.
14.
He should be prepared to write health
memoranda for the education of the workers on
health problems.
15.
He should keep liaison with other people
and departments and agencies outside the factory
with such advice and data relating to the worker,
12.
Guard against
(6) the discipline of his staff.
(c) the professional duties of his staff.
11.
“ monuments ”.
(a) his own executive functions.
other departments in the factory and assist them
10.
Mistakes in diagnosis as well as in action
become
may
He should know his day-to-day responsibili these.
ties—
9.
A
He should know statutory requirements ofmuch.
He should pay special attention to people
suffering from tuberculosis and people in the
vulnerable group.
Local Hospital—
■ c
Casualty Officer.
X-Ray Department.
Skin Department.
General Practitioners.
Local Teaching Hospital or other HospitalDepartment of Medical Research.
Pathological, Bio-chemical and Bacte
riological Department.
Medical Officer of Health.
Certifying Surgeon for the District.
Indian Red-Cross or St. John Ambulance
Society.
Medical Inspector of Factories.
Tuberculosis institutions.
The Provincial Inspectorate of Factories,
Ministry of Labour.
Industrial
Health Advisory
Committee
of the Indian Research Fund Association
Industrial Health Research Unit, All India
Institute of Hygiene and Public Health.
The Indian Medical Association—Indus
trial Disease Committee.
The Chief Adviser of Factories, Ministry
of Labour.
OCCUPATIONAL HEALTH SERVICES—Training
*
**
A. F. HEREDIA
To a great extent every branch of medicine is becoming not only
specialised but superspecialised—namely it is becoming a matter of
team work rather than of individual responsibility. This is more so
in the field of occupational health, as I have already pointed out in
my address yesterday. It is obvious that a doctor cannot be an ex
pert in all phases of occupational health—he would require the
assistance of various other experts like engineers, chemists, physio
logists, psychologists, welfare officers, industrial health nurses etc.
However, in matters of health, the physician will have to take the
role of team leader and therefore he will have to be trained to take
his proper place. Though he will have to know what to expect from
each of his team mates, it is not necessary that an industrial physician
be an expert in all investigations involved. He must, however, be
a competent physician (which is his special line) and an expert in
diagnosis, treatment and prevention of diseases commonly met with
and of occupational diseases in particular. He should know the
principles of public health. He should establish good connections
with hospitals, private physicians and health authorities. He should
be conversant with the nature of work involved in various jobs in
his factory and of the risks to health in each.
Undergraduate Education: The qualifying doctor is being
trained as a general physician for practice in the community. A
large proportion of such doctors settle in towns (75%) or are em
ployed there. If one realises that almost half the population of
some towns is connected with industry, it would not be too much to
expect that such a doctor should have some knowledge of occu
pational medicine. Without overloading the curriculum or
placing undue emphasis on it, the following aspects of occupational
health may be taught. I am glad to say that I was fortunately on
the University sub-committee for advising on the syllabus in Pre
ventive and Social Medicine, and my suggestion for the inclusion of
occupational health in the teaching programme was accepted arid
has also now been recommended for inclusion in all the medical
colleges by the Medical Council of India.
Syllabus: The following may form the syllabus: The
development of the modern concept of occupational health.
Health aspects of the Factories Act and Rules.
Common occupational diseases, their diagnosis and prevention.
* Paper presented at the symposium held on 5th April, 1959 on “Occupational
Health Services,” during the 7th Annual Convention of the Bombay Branch of the
Society.
** Dept, of Preventive and Social Medicine, Grant Medical College Bombay 8.
Received for publication on 5-4-59.
174
INDIAN JOURNAL OF OCCUPATIONAL HEALTH
Principles of industrial hygiene and toxicology. The total time
taken will be 6 to 8 lecture periods and about 4 visits to factories.
(total 12 sessions).
Certificate course: For those doctors who wish to join an in
dustry or who are already employed in a plant, a special short course
may be offered. A more intensive study of occupational diseases,
industrial toxicology and of diagnosis, treatment and prevention will
be required, and also a more detailed knowledge of laws relating to
health in industry. Such a short course is most essential in order
to develop the longer and more intensive diploma course. Most
doctors will not be able to spare the time necessary for a long course;
also they may have no guarantee that they will be employed in in
dustry after the completion of such a long course. So the short
course will answer the needs of the greater number.
Post Graduate Diploma in Industrial Health: This should be
a course for the specialist in the branch. It should consist of two
parts and cover one full acdemic year. The first part will be largely
the general principles of public health. The second part will consist
of lectures on industrial law and labour relations, various aspects of
the industrial worker in India, social security, labour organisation,
industrial hazards, toxic agents and industrial dusts, methods of
examination and control, rehabilitation, industrial accidents and pre
vention, physiological hygiene, occupational diseases and industrial
medicine.
Paper read at' 27th •Annual Confergnug. pf.-Indian. Aa5.ociptj,on_p£
Occupational Hea 1th .in. February 1977 at Hhmgda.bad.
TEACHING AND SERVICE RESPONSIBILITIES OF A MEDICAL COLLEGE
IN THE FIELD OF OCCUPATIONAL HEALTH .
•
SX
Dr. Ravi Narayan
,MBBS
*
., DTPH (Lpnd),DIH (UK)
Ross Institute Lecturer
Dept, of Preventive & Social Madicine
St,Hohn's Hodical College,Bangalore 34
INTRODUCTION : ’
(l)
In 1971 the working population of India was about 1".?4 crores
or 32.9$ of the total population. Nearly 70$ of this population were
involved in agriculture as cultivators or labourers and the remaining
in plantations, mining and quarrying, manufacturing, processing and
repair industries, trade and commerce and the construction and
transport industry (refer Table 1)
TABLE I
.
DISTRIBUTION OF WORKING POPULATION. 1971
Iotal workers
in 1000
Categories
Percentage
1. Cultivators
78.176
43.34
2. Agricultural Labourer
47,499
26.33
3. Plantations,Livestock
forestry
4,296
2.38
922
0.51
of
4. Mining & quarrying
5. Manufacturing, processing
and repair
6,351
3.52
£? 0 0
b) Other than household 10,715
5.94
% $
6. Construction
2,215
1.23
7. Trade and Commerce
10,038"
5.57
8. Transport, storage
and communications
4,401
2.44
9. Other services
15,765
8.74
a) Household
(2)
Since independence the Government of India has through a system
of National Five Year Plans involving massive industrial and agricultural
development attempted to tackle the socio-economic problems of the country,.
During this process the working population more especially the non-agricult urn?.
occupations have been given higher priority in our social security system end
♦Now Postgraduate student at Centre for Community
f’lqtficine, An India Institute of Medical
Scientt's, New Delhi.
COMMUNITY HEALTH CELL
47/1,ri'--Koa
*
? 2 5
numerous schemes and acts have been created to provide adequate cover to
thd workers against
contingencies such as ill health and industrial
accidents (refer Table II and Table 1117. Many of these Acts lay down
provisions for basic health and first aid facilities fur the working
population in the form of a first aid centre, dispensary, part time
doctor or full time factory doctor or through the services of ESI
dispensaries and hospitals.
TABLE II
Social Security Schemes for Labour in India'
Employees State Insurance Scheme, 1948
Employees Provident Fund & Family Pension Fund Act, 1952
Payment of Gratuity Act, 1972
Death Relief Fund, 1964
Employees Family Pension Scheme, 1971
Coal Mines Family Pension Scheme, 1971
Coal Mines Provident Fund, Family Pension and Bonus
Schemes > Act, 1948
Workmen's Compensation Act, 1923
Maternity Benefits Act, 1961
TABLE III
Labour Welfare Acts in India
Factories Act, 1948
Contract Labour Act, 1970
Mines Act, 1952
Mine Workers Welfare Fund
Plantation Labour Act, 1951
Dock Workers Welfare Fund
Bidir & Cigar Workers Act 1966
Motor Transport Workers Act 1961
(3)
Rapid industrial and agricultural development since independence has
added a new dimension to the public health problems of the country since
increasing numbers of our working population both urban and rural are
being exposed to the physical, chemical, biological, mechanical and
psychological hazards of'their new working environments. In addition
environmental pollution due to industrial effluents is also becoming
a serious hazard to the urban populations. A recent study conducted by
the Central Labour Institute, Bombay,“has revealed the extent of some
5
3 5
of these hazards. To cite a few examples?"in the ceramic industry 10~?0%
of the workers have fallen victims to silicosis, bronchitis has affected 16%
of the textile workers in Bombay mills alone, one out of every three workers
in ferromanganese plants are suffering from ailments directly traceable to
their occupational environment" and so the list reads on.
In a country like India where communicable diseases and nutritional
deficiencies still take a heavy troll on the health of the population,
occupational health cannot be expected to have very high priority ip our
health planning. However the Government has taken.steos to study and
solve some of these problems by establishing important research and
teaching institutions in the country dealing with i.’nortant occupation ;!
heaIthaproblens (refer Table IV). The working population in the country
can be protected from the hazards of their working environment only if
a health service exists and the accumulated knowledge and research findings
of these institutions are applied through it. Medical teams working in
industries, plantations and other occupations either through ESI Scheme
or through provisions in existing legislation have'tended so far to provide
a purely curative-clinic oriented service and a certification facility.
However, a time has come when doctors working in industry and with other
occupational groups must begin to provide a much more comprehensive
occupational health service and the subject of this paper outlines certain
remedial measures with specific reference to the role of medical colleges
in the process of change. It must be added that- even today there are certain
public and private sector undertakings which do provide for a more
comprehensive occupational health service for their workers but these are
exceptions rather than the rule.
TABLE IV3
Occupational Health Institutes in India
Central Labour Institute, Bombay
Regional Labour Institutes, Kanpur, Calcutta and Madras
State Inspectorate of Factories
National Institute of Occupational Health, Ahmedabad
Central Mining & Research.Station, Dhanbad
Industrial-Toxicology Research Centro, Lucknow
National Environmental Engineering & Research Institute,
Nagpur
All India Institute of Hygiene and Public Health,Calcutta
Occupational Health Division, ICMR
0C6UPATI0NAL HEALTH SERVICE s Since the term ’comprehensive occupational health
service' will be used often in this paper, it is necessary that this is
explained at this juncture. Occupational health according to me is the
practice of Community Medicine is a setting where the working population
is considered as the community under care. A comprehensive health care
.... 4r
: 4 :
systeman industry/factory/occupational environment must includet
the followiig basis functions enumerated by Schilling, 1973.(5)
1.
Placing people in suitable work
2.
providing a treatment service
3.
controlling recognised hazards, secondary monitoring
4.
Identifying unrecognised hazards - primary monitoring
5.
Avoiding potential risks
6.
Screening for early evidence of non—occupational disease
7.
supervision of vulnerable groups
8.
counselling and health education
9.
surveillance of sanitary, catering and welfare amenities
10.
environmental
control outside the workplace
If occupational health is to become an important part of our health
services it is imperative that medical personnel of all categories must be
trained in the principles and practice of occupational health and in this
context the medical colleges of the country have an important role to play.
ROLE OF MEDICAL COLLEGES °
a) Pres ent in vo 1 vem ent 8
India has nearly 110 medical colleges with an annual output of over
13000 doctors. Many of them have joined and will be joining dispensaries,
health centres and hospitals dealing with working populations but few of
them would have had any preparation for it.
— The undergraduate curriculum in most colleges have if at all a few
lectures in occupational health and probably an afternoon visit to a factory.
- Very few medical colleges deal with occupational health problems, fewer have
occupational health units and only two offer postgraduate diplomas in Industrial
health. This state of non-involvement of medical colleges is particularly sig
nificant, since all the medical colleges with a few exceptions are located in
the large cities or towns where most of the post—independence industrial
development has taken place.
Medical Educationists and Health Administrators have rc.-.,.’.iced of late
that Medical Colleges must begin to get closely involved with tne existing
systems of health care delivery in the country and help to create a referral
services complex extending from the periphery all the way to the'teaching
hospital.2 Not only will this move help to strengthen the existing health
services by making available to it;the specialist services that medical college
departments can offer but will also help the medical college departments to
reorient their curricula and make it relevant to the actual health needs of
the country. This process will wean medical colleges away from the ’ivory
towered’ academic settings that they presently function in. In keeping with
.5
5 5 s
this philosophy, there is great scope for medical colleges to establish
links with health services in industries/plantations either directly or through
the ESI Scheme and whereever such services do not exist they can catalyse
their development.
These links can be of various typess
1. The Medical College through its department of Preventive and Social
Medicine and or occupational health can form links with ESI Hospitals
and dispensaries and attempt not only to strengthen their services but
also make them more comprehensive (Fig I).
2.
A Medical College could establish an occupational health unit which
could link up with the health services of a factory and help to make
it more comprehensive (Figure II). In factories which do not have a
service it could help in its development.
3.
A Medical College could help to establish a group occupational health
service for a number of factories and this group service could be a
separate unit if the factories are away from the Medical College, or
it could be situated in the college if the factories are around the
College (Figure III & IV).
4. A Medical College can through its existing rural and urban health centres
offer an occipational health service to selected groups of working
population or to neighbouring industrial units or factories (Figure V).
Figure I
Figure II ■
Medical College
P&SM / OH Unit
1 ■
ESI Hospitals
Medical College
P&SM/OH Unit
Factory Occupational
Health Service
1
Subcentros/Stations
4
ESI Dispensaries
First; Aid Posts
Figure II{ . j
Figure HI
Medical College ■
. Occupational-Health Dept
Medical College
P&SM / OH Unit
Group Occupational Health Service Factory- Factory
i
Factory
Centre
Factory
Centre
Factory
Centre
Factory
. Factory
Medical. College
PS fl / OH Unit
Urban Health Centre
Rural Health Centre
Selected
Occupational
Group
Selected
work
unit
■Selected
Occupational
Group
Small factories
industrial unit
Service Responsibilities
c)
Having developed different types of links described above, the medical
colleges can offer the following services!
1. It can undertake short-term or long term occupational health surveys
and epidemiological projects on specific occjpational health problems.
The interns, postgraduate students and faculties could be involved
in such projects.
2.
It can help to plan, organise and manage comprehensive occupational
health services in factories or for specific occupational groups.
3.
It can provide certain back-up facilities for doctors working in
indust ria1/occupational health services!
a) Specialist consultation
b) Specialist Services-
c)
Special laboratory investigations
d) Special examinations
e)
Information and advisory service
f) Library facilities
g) Statistical analysis services
for all these services the average medical collego can easily rely upon
its existing staff and facilities of various departments. It may have to
invest in a small industrial hygiene laboratory which should be capable of
measuring the important parameters of the working environment e.g. temperature!
humidity, noise, radiation, ventilation, lighting, gases and dusts.
d)
Teaching responsibilities
The main contribution that a medical college can make in strengthening
the existing occupational health services of the country is in the field of
training of medical personnel especially doctors.
1. All medical graduates should be given a good basic course in the
principles and practice of occupational health during their undergraduate
programme.
2.
Postings in well organised occupational health services should be introduced
as an option in the internship training programme in public health.
3.
For doctors interested in occupational health as a career, suitable
diploma courses should be established in occupational medicine and or
occupational hygiane.
,7
4.
For doctors and other medical personnel already working in factory
health services, the college can provide continuing education or
in service education through the organisation of short term adhoc
courses and seminars.
It is very important to stress at this stage that the teaching and
service responsibilities in occupational health taken up by a medical
college, should develop side by side so that teaching is backed by knowledge
gained in the field and service is based on sound academic principles. In
this endeavour medical colleges must establish close links with the ESI
Scheme, the local factory inspectorates and labour institutes and all other
institutions in the country dealing with occupational health problems.
e) Occupational Health Centre s All medical colleges in the-country have
been involved in recent years with the development of^'rural and urban field
practice areas and centres for providing students and interns training in
the principles and practice of community health. "Similarly for teaching
occupational health, a medical college can help to develop a comprehensive
occupational health centre in a factory and use this as a field practice
and demonstration centre. The advantages of organising a health service
within a relatively closed system such as a factory or plantation are
manifold? i) Systems of record keeping are complete, efficient and
comprehensive ii) Concept of. total health care can more easily be
practiced iii) Utilization of health services is greater iv) Dealing with
management and union is simpler than with community leadership v) With
management involvement preventive and promotive measures can be introduced
and their effects studied.
f)
Ross Institute Unit of Occupational Health, Bangalore
-Most of the ideas given in this paper are based on the experiences of
the Ross Institute Unit of Occupational Health which has been established, in
the Department of Preventive and Social Medicine, St.John’s Medical College,
Banoalore,
■ collaboration with the Ross Institute of Tropical Hygiene,
London School of Hygiene and Tropical Medicine. The objectives of the
Unit are!
1. To study the occupational health problems of workers in industry,
plantations and also non-industrial occupations.
2*.
To create an awareness and interest in the medical profession in the principles
and practice of occupational- health.
3.
To develop tho field of occupational health .in South India through teaching
' and research.
Over the last two years of its develSpment many ideas- are being
experimented within the field and Figure VI attempts ,to summarise this.
,8
s 8 :
Studies or. sericulture
workers, carpet weavers
and dairy workers
Rural Health Centre
Occupational Health Surveys
in Factories
a
I
'Information, Advisory 1 'Ross Institute Unit ofl
>and Laboratory Ser'|^-pccupational Health
I
Offices to Local Industry! i(P&SM Dept, SUFIC)
Plantations
Internship
Programme
Occupational
Health Studies
/Surveys
^Development of Occupational;Health Service for neigh—.
, bouring factories
Internship postings to
O.H.S. in Factories
Training' Courses
for Plantation
Medical Officers
SUMMARY'
industrial
1. Rapid/devolopment has added a new dimension to the public health problems
in the country-occupational health hazards and environmental pollution.
MBdical Colleges must begin to play increasing role in spreading the
concepts of occupational health.and developing comprehensive occupational
health services.
establish
3. Medical Colleges should/linkswith existing occupational health services., ■
It should undertake surveys, plan services and provide back-up services .
for industrial medical officers.
2.
4.
Medical colleges should strengthen undergraduates teaching in occupational
health organise suitable internship,- training programmes, establish.
diplomas and carry on in service training through adhoc courses and seminars.
ACKNOWLEDGEMENTS
I would like to acknowledge t he encouragement and guidance given
by; Maj Gen B Mahadevan (Professor & Head of the Dept, ofi Preventive and
Social Medicine), Dr.M.M.Mascarenhas and the Deans Dr.C.M.Francis and
Dr.L.Monteiro of St.John’s Medical College and Prof.L.J.Bruce Chwatt and
..9
Dr.Donald Mackay of Ross Institute, London, in the development of the
Occupational Health Unit in Bangalore and in the various experimental
activities carried out since its establishment in August 1974.
References s
1.
Govt, of India, 1976 - India 1975 •• a reference manual. Ministry of
Information and Broadcastsg, Publications Divisions
2.
Govt of India, 1975 - Health Servic:a and Medical Education^ ROPOrt
of the Group on Medical Education and Support Manpower, Pin.'stry of Health
and Family Pit nhir.g, N«a’‘i Delhi.
3»
Narayan, Ravi 1974 - Note oh Rose Institute Ur.it of Occupational Health,
.
Dept cf Preventive and Social Medicinn, St.John’s
Medical College, Bengajore (unpublished document)
4.
Narayan, Ravi 1973 — Trends in undo-graduate Medical Education im
India — Dissertation submitted for DTP?(unpublished)
5» Schilling R»SVF. 1973 - Occupational Health Practice, Butte)worths, London
Indian Express - 'Occupational Hazn-ds
*
7-
•
Editorial 26th January 1977.
Park J.E. Text Book of Preventive an 1 Social Medicine. 3rd Ed, Banarsidas
Bhanot, Jabalpur.
/////'7.7//////////
pc
461977
THE Ii£?-'.CT 0? INDUSTRIAL GHO .TH ON Hili.'.TH IN SOUTH-EAST ASIA
Professor W. 0. Phoon
M.B.,B.S.(ihlaya), P.R.C.P.(Glasgow), P.R.C.P.(Edin.), K.R.C.P.(London),
C.H.(England),
D.
D.I.H.(England), D.I.U.S.A.(London),
A.K.(S’pore), .P.P.C.H.(U.K.)
Head
Department of Social Medicine and Public Health
University of Singapore
COA.4P.4i :!'!!■]
4y/*,(
alth cell
War,lsRoad
•- — •‘-OnE- GfiO 001
ra, •>- '
INTRODUCTION
By "South-east Asia" i» usually meant the area comprising East Indies
and the Indo-chinese peninsula of continental Asia.
The term is usually
taken to include the countries of Indonesia, Philippines, Singapore,
Malaysia, Brunei, Burma, Thailand, Cambodia, Laos and Vietnam.
a population of approximately 250 million people.
It contains
Prom the sixteenth to
the first half of the twentieth century, all the constituent parts of the
region were colonies of Western powers, with the single exception of Thai
land.
By 1963, however, all parts of South-east Asia had gained their
independence except Portuguese Timor.
Brunei remained a British Protecto
rate.
The climate is predominantly tropical, with an annual rainfall
generally above 40 inches (1,000 mm.).
foods.
Rice and maize are the main staple
The region is very rich in natural resources, and produces rubber,
rice, sugar, teak, tin, pepper, bauxite, petroleum, palm oil, coconut oil,
etc.
The industrial development in the region, as a whole, is still at an
early stage.
However, it varies greatly, ranging from Singapore, which is
quite highly industrialized, with over 4,000 factories, to Laos, which has
virtually no major industry.
No matter at what stage of industrial development, all the govern
ments in the region do subscribe to a belief that industrialization is a
pre-requisite to progress and prosperity.
As has been aptly expressed,
though it ms in the context of south Asia and not South-east Asia,
"It is reasonable tint a discussion of economic development policies
in South Asia should begin with the ideology of industrialization.
A clamor
for industrialization is notable in all countries of the region: ./hen the
intellectually elite say their countries are underdeveloped, they mean, in
the first instance, that they have too little industry.
Thus spokesm n
for the South Asian Countries frequently use the terms ’pre-industrial1 or
’under-industrialized' as synonyms for ’poor’ or ’undeveloped’ " (ifyrdal
1968).
Mention of the commencement or the intensification of industrializa
tion is commonly made in national development plans.
The Second Five-
Year flan of the Federation of Malaya (now Malaysia) is a case in point.
Ye quote,
"For the future, the importance of manufacturing to the Federation's
long-run development and economic diversification pan hardly be over
emphasized" (Fed. of Italaya
1963).
The declared purpose of industrialization is usually to create more
financial resources in order to improve the standards of living for the
people.
More jobs would be available.
More money could be spent on commu
nity facilities such as schools, health clinics, and hospitals.
However,
economic reasons may sometimes take second place to emotional or political
ones:
",/hether or not there are sound economic reasons for the establish
ment of secondary industries in a primary producer country, the will and
desire to establish such industries usually increases as the country
progresses educationally and in political stature.
The fact that home
produced raw materials are exported, often thousands of miles, only to be
re-imported in a manufactured, or processed, and more expensive, form is
- 3 -
sufficient in itself to impel attempts to get up similar manufacturing
industries within the basic producer country” (l'ed. of Malaya
1957).
Most of the political leaders in South-slast Asia and the social
and other scientists who advise them fully realise that development does
not consist merely of industrial growth.
Bather, "development may be seen
as a process of improving the capability of a nation's institutions and
value system to meet increasing and different demands, whether they are
social, political, or economic” (Yeh 1971a.).
They are also cognizant of the fact that industrialization and the
concomitant process of urbanization nay result in undesirable by-products
as well as the desired products of more affluence and social amenities.
"With rapid industrialization, urbanization and physical re
development, new dimensions in health policy have to do with the Govern-:
ment's'concern for a more integrated approach towards the improvement of
the total ecological environment and therefore include attention and new
legislation with respect to industrial health, water and air pollution,
and other measures to promote mass participation in raising public health
standards” (Yeh.. 1971b).
THS COST in HUMAN SUFFERING
A common problem is to decide what is the acceptable price, in terms
of human suffering, which should be paid for development.
Another problem
is the difficulty of visualizing things which have not yet occurred and
persuading the decision-making bodies to divert funds from the primary
purpose of economic expansion to measures against pollution, adverse
social repercussions and ill-health which may result.
The social scientist may be "a voice in the wilderness” when he
argues that individual human beings are more precious than money or machines.
The industrialist does not own his workers, but he does his machines.
In
- 4 -
relatively socially-backward societies such as many of the South-east
Asian countries, there is usually an over-supply of unskilled labour.
The proprietor or manager usually gets off quite lightly financially if
workers in his factory are killed or injured.
Therefore the message, to be effective, has often to be directed
towards their pecuniary interests rather than towards their social
conscience:
"Xt is agreed that the primary objective of industry is to make
money, not to do charity.
However, let it be remembered that men are
the most important resources of any factory.
Any industrialist would be
considered a fool if he does not keep his machines properly lubricated
or regularly maintained, but only send them for repairs whenever they
break down.
Yet some industrialists permit managers, supervisors and
workmen to suffer from ill-health ... which must have telling, adverse
economic effects in terms of wrong decisions, poor morale and lowered
productivity" (Phoon
1971).
On the other hand, the community as a whole, may be more affected
by stories of human pathos rather than cold sets of facts and figures
usually presented by experts in Occupational Medicine and Safety.
Who
will not be moved by this true anecdote, describing a common yet very
tragic occurrence?
I once was in a factory and I met a little girl with three fingers
cut off.
This happened from an accident from a circulating saw.
'Then
I thought of her plight and I looked at the whole condition from the
beginning.
This girl was warded in the hospital for about three weeks,
was treated by doctors, res given medicine, then was given sickness
absence, of course, during the whole peiiod of time and at the end she
was given compensation and then I asked the manager of the plant, "How
much does it cost to have a guard on this circulating saw?"... I found
- 5 -
it was one-hundredth of the cost of the disabilities that had happened to
this poor girl" (El Batawi
1968).
Unfortunately, we are not told who paid for the hospital fees.
Probably the state, not the employer,
compensation.
lior are we told who paid for the
Probably the insurance company, not the employer directly.
'She employer perhapo
paid only the usual insurance premium, regardless
of whether the injury
had occurred or not.
So he probably still saved
money (his own) by not putting the guard!
Sometimes the occupational accidents and diseases which occur are
caused by the lack of technical education or orientation on the part of
the workers pouring into the thousands of factories newly set-up in recent
years;
"The rural education of the migrating youth frequently does not
Although technical
provide him -with the skill needed in urban areas.
education'' is more easily available in cities, the frequent preference for
white-collar jobs has resulted in only rudimentary provision of vocational
and technical education, even in cities.
Consequently, the urban youth is
also ill-prepared for industrial employment ...
Even when the migrating
youth is not exploited in factory employment, he has to adjust to the
fact of work dictated by the unfamiliar machine.
He is often puzzled
by the piece-meal nature of his work and disturbed by the impersonality
of industrial employment" (World Assembly of Youth
1967).
As so many hew factories spring up, there is a great shortage of
skilled nanagers and supervisors who can provide proper training and
supervision for the raw recruits.
This, in turn, leads to more mis’naps
in industry.
We do not need to apologize for concentrating our attention on
- 6 -
tjje worker, as he is the one exposed to the greatest concentrations of
noxious substances produced by industries as well as to tile physical
hazards of his working environment.
A recent seminar held in South-east
Asia stresses this:
"Ths majority of developing countries are today determined to start
with industrialization and to upgrade their overall economy as rapidly as
possible with a view to securing a higher standard of living.
A rapid
industrialization, however, produces far-reaching changes in society and
affects practically all of its strata.
A number of developing countries
are now passing through such a transition period and
are having to adjust
themselves to the requirements of modern society ...
"Radical changes in the way of living ... a completely changed type
of housing and social environment, and new working methods often lead to
a deterioration of mental and physical health.
The health problems resul
ting from the introduction of new industrial processes, and from urbani
sation and mechanization, are complex,in this context.
Of particular
importance, because of its contribution to the economic progress of any
nation, is the health of ths worker who is exposed not only to environ
mental and other community health hazards but also to a variety of physical
and chemical hazards in his work environment'' (-.HO
1971a).
THE JEFICCTS Of INDUSTRIALIZATION OCT TIE COrJWITY
I shall not go into a detailed discussion of the ill-effects of
industrialization on the general community.
In South-east Asia, as perhaps
the rest of the world, it is extremely difficult to separate the factors of
urbanization -nd the radical changes affecting traditional religions, cul
ture and customs from the factor of industrialization in the causation of
the dramatic transformation of most parts of the region during recent years.
It is also, perhaps, true to say that we cannot fully quantify all the ill-
- 7 -
effects directly resulting from urbanization.
As stated in a book devoted
to the subject,
"In the large cities ... it is not the quantitative gspects of public
health problems tliat are predominant.
The macro-hazards of epidemics have
given place to a complex of such micro-hazards as air and water pollution
and other unsolved issues of sanitation.
These, however, are not the only
factors of urbanization induced damages to health.
Others, as for instance,
urban noise, the increased risk of exposure to carcinogenic substances, or
the stressors of ci’ty life are all noxious effects endangering the health
of town dwellers.
In comparison with the mass destruction caused by epi
demics, the micro-hazards seem to be of minor importance; still, they are
by far not negligible if their chronic, often accumulative, effect is
considered" (Bakacs
1972).
The inevitable rural-urban migration has led to the equally inevitable
problems of overcrowding and the development of "shanty towns" with their
poor sanitation, object poverty and malnutrition.
Some of the capital
cities of South-east Asia have "shanty towns" accommodating a quarter or
more of their populations.
"The expanding industrialisation in traditional urban centres has
further exerted a special "pull" towards movement of people to cities ...
the result has been industrial expansion in already overcrowded urban
centres and the further migration of potential labour from rural to urban
areas in numbers surpassing employment opportunities, thus creating taro
serious problems of overcrowding and unemployment" (jegasothy
1957).
The problem of rural-urban migration is universally recognized but
effective solutions are not forthcoming.
Proposed solutions are many,
as exemplified by the following:
"How do we solve this problem?
Gan we say that let us stop indus
trialisation and let us go back to the villages?
i7e must industrialize
- 8 -
and do it rapidly.
Hie only solution, as I see it, is to industrialize
the villages instead of the cities,
Take the industries into the villages
rather than having the whole of village after village migrate into indus
trial complexes in the cities” (Reddy
.1967).
In Malaysia an attempt is being made to stem the tide of rural-urban
migration by paying more attention to the development of agriculture, so
that both jobs and productivity could be increased.
Moreover, agricultural
development is viewed as a necessary adjunct to industrial growth.
"In a very fundamental sense agricultural progress is a requirement
for industrial growth ... Planners still have much to learn about agri
culture '.s role in economic development.
But they are now in general agree
ment on the need to give high priority to both agriculture and industrial
development in national plans” (Robless
1968-).
THE DIt?gIC0Ifflld3 OB GXTRA.POLATIOH
SXEERMTCES 01' OTHER REGIONS
..e cannot merely extrapolate the experiences of Community Medicine or
Occupational Health, gained in the developed countries of the ..hst, to
another area of the world such as South-east Asia.
in the first instance, are very different.
The climatic conditions,
This is sometimes not suffi
ciently realised by experts cither domiciled in the region or visiting it;
"The basic hygienic evaluation of the impact of air-borne concentra
tions of chemicals in industrial atmospheres refers to temperate climatic
conditions.
Gros;, deviations of physical pressure,/ultraviolet and ionizing
radiation in the atmosphere of work sites may result in adverse effects from
these chemicals even if their concentration is permissible according to the
list of .Threshold Limit Values ...
"Human volunteers exposed to 2/o parathion dust at different ambient
temperatures have shown an increased absorption of para-nitro-phenol,
following their exposure to 28° - 46dC" (‘hssermann
1968).
- 9 -
Hot only is the physical environment in South-east Asia different.
from that in the Vest, but there are also inherent differences in the
population which my produce dissimilar reactions to toxic substances or
physical stresses,
■‘•'or instance, there are large numbers of people in
South-east Asia who are born with deficiency of the enzyme, 6-glucose-
phosphate dehydrogenase.
Since the first clinical case of this enzyme
deficiency in Singapore was described in 1959
(Vella and Pho on
1959),
it has been discovered that it is the commonest cause of kernicterus
(severe jaundice with affection of the brain in neonatal children) in
Singapore and that is quite a common cause of haemolytic anaemia, precipi
tated by chemicals and other substances.
OCCUPATIONAI. HE JiTK P20BMM3 IN 3OUTH-11A3T ASIA
■/e will now describe some of the occupational health problems which
exist in South-east Asian countries.
It must be stressed that the know
ledge about these problems is very scanty due to inadequate machinery for
the collection, processing and analysis of data in most parts of the region.
South Vietnam
By 1971, industries in Vietnam had been developing for twenty years.
There were 22,550 industrial enterprises which employed approximately
240,000 workers.
Industries included agriculture, forestry, mining,
construction and public utilities.
There are elaborate occupational health laws, including the provi
sion for the obligatory employment of a nurse for industries employing
less than 100 workers, and provision for nurses and part-time physicians
for industries employing more than 100 workers; and also yearly medical
examinations for all workers (Nguyen
1972).
these provisions arc not usually observed.
Unfortunately, however,
This sad state of affairs is
- 10 -
by no means unique to South Vietnam.
Some politicians seem to tend to
"solve” the problems of industrialization by merely "wishing them away"
by passing elaborate sets of legislation without providing for adequate
enforcement.
Thailand
320 cases of pesticide poisoning occurred in Rajburi Province in
5 years from 1966-1970, including 24 fatalities.
The province in 1971
contained a population of 3»789 comprising actual users and exposed persons
and was largely agricultural (Vongpanich et al. 1972).
30 cases of lead poisoning were described in small factories, making
or handling lead print-type or smelting and refining lead.
In 1969 lead poisoning cases occurred in children from families who
manufactured sugar from coconuts, during the process of which they used
the cases of worn-out storage batteries as fuel (Trishnananda and Attanatho
1971).
In 1965 the occurrence of manganese poisoning in a dry cell battery
plant was reported.
There were 44 cases of varying grades of paralysis in
employees working in the mixing and filling operation of the factory (..'HO 1971b
Indonesia
A survey among miners showed that
had silicosis.
Among carders
in the textile industry, an investigation on 20 revealed two cases of
bronchospasm associated with their job, one -case of repeated bronchitis
and two cases of chronic bronchitis.
poisoning have also occurred.
to be often unfavourable.
Occupational deaths from pesticide
The nutritional status of workers vas found
"The prevalence rates of such diseases, however,
appear to be relatively low due to the lack of reports, insufficient orien
tation of the physician to make the diagnosis, a high labour turnover ..."
(Suma'mur
1972).
"The most prevalent occupational diseases are pneumoconiosis and
- 11 -
dermatoses.
Occupational metal diseases, and some other industrial
poisonings, have been observed" (WHO
1971c).
The Philippines
Silicosis, lead poisoning, and intoxication from pesticides have
been described.
Cases of byssinosis have also occurred.
*
Burna
Apart from industries related to agriculture, the most important
industries were probably those related to oil refining and the wearing of
cotton and silk fabrics,
t/e do not possess inforintion on occupational
diseases in that country.
laos
There are small industries manufacturing cigarettes, matches, soft
drinks, rubber sandals and sawmills (United Nations
1966).
We do not
possess information on occupational diseases in that country.
Cambodia
Some agricultural and village industries exist.
..’e do not possess
information on occupational diseases in that country.
Ifelaysia
In a population of nine million in the Peninsular part of I&laysia,
there is a total work force of about 3.2 million.
Almost 50$ of workers
are engaged in agriculture, more than 9$ in manufacturing industries, 3
5$
*
in the construction industry,
cation, and 2.2$ in mining.
3.7$ in transport, storage and communi
Although there is a wide range of legislation,
certain sections of the working population are still unprotected.
ment problems exist (..HO
* Personal dommunication
1971d).
Enforce
- 12 -
Cases of poisoning from pesticides, lead poisoning, industrial
accidents in ihe construction and other industries, and occupational
dermatitis in the rubber and chemical industries, have been described.
*
A SIRG-Al-Oiffi CASS STUDY
Singapore
will bo discussed in greater depth, partly because the
author has better acquaintance with its problems and partly because it is
the most advanced industrially of all the countries in South-east Asia.
At first sight Singapore does not seem to have many things in common with
other countries in the region.
Its land area is, by far, the smallest
534.3 sq. kilometres or 225.6 sq. miles).
Its population is only approxi
mately 2,200,000. people of Chinese origin accounting for 76 per cent.
In
fact, many of the industrialized areas in the other South-east Asian coun
tries share the problems of Singapore.
.Moreover, at the rapid tempo of
development prevailing in the region, what exists in Singapore today will
probably exist in the neighbouring countries within a decade.
There is no doubt that industrialization has conferred immense
material benefits on the people of Singapore.
Partly because of indus
trialization, the average income per capita in Singapore is over U.S.#1,300
per annum, the second highest in Asia.
The contribution to the national
economy by industry is also rapidly increasing.
"Over the last decade, the manufacturing sector has grown considerably
whether measured in terms of output, value added or employment ...
The
manufacturing sector’s contribution to GPD at factor Cost lias risen from
9 per cent in I960 to 17 per oent in 1969" (huan
* Personal oommunication
1971).
it in interesting to recall that when the programme of rapid indus
trialization was commenced about fourteen years ago, that "The unemploy
ment problem appears to have overshadowed all other problems in Singapore
and lias become almost the exclusive reason for industrialization" (Goh
1969).
The number of jobs created by industrialization has meant that
the unemployment problem is no longer the only or even the most important
factor, as there is almost full employment and there are approximately
60,000 immigrant workers in Singapore now.
The immigrant workers are mostly
from I-hlaysia.
Very successful public housing programmes and the provision of better
community health facilities in the form of more doctors, nurses, clinics,
and hospitals have been made possible from the fruits of the industrializa
tion programme and have aide Singapore one of the cleanest and healthiest
countries in asia.
However, Singapore has not escaped the penalties of industrialization.
There are over 4,000 factories, employing an estimated total of
130,000 workers.
The most urgent health problem faced by factories is the
increasing trend of industrial accidents leading to deaths and injuries, as
shown by Table I.
The increasing trend is disproportionate to the increase of numbers
of workers and factories over the same period.
Table II shows the number of accidents reported for 1972 by industry
and number of factories where the total accidents exceeded 40.
figures
in brackets indicate fatalities.
Occupational diseases have also occurred.
It is not possible to give an exhaustive account.
Some examples,
perhaps, would suffice.
There are some 23 granite quarries employing about 1,500 workers
in Singapore ... In a 1965 survey, out of 1,183 workers X-IJayed, By had
- 14 -
TABES 1: EIDUiJlRIAL ACCIDENTS IR JINGABOIE:
Year
No. of
accidents reported
No.
fatal
No. perann:.htly
. .disabled
I960
1969
1970
1971
1972
3,147
8,714
9,682
10,197
10,675
109
132
1 c-. Q
147
186
703
731
886
1,072
1,474
TABIE 2 :
EJDUSTRIAI ACCIDENTS IN SINGAPORE
HI DETJUNT EUWoTRIES
No. of Accidents
(Incl . fatalities)
No. of
factories
1. Building and repairing of
ships, tankers and other
ocean-going vessels
645(3)
13
2. manufacturing of plywood
and veneer
319(2)
8
3. General building con
struction
295(22)
544
4. Civil engineering con
struction
117(3)
91
5. Stone Quarrying
103(2)
35
6. General enginneering works
73(1)
276
7. tanufacture and repair of
industrial and agricultural
machinery (including engines
and tubines)
68(1)
78
8. Spinning, weaving, printing
and finishing of yarns and
fabrics
66
14
9. Iron and steel rolling mills
62(1)
2
10. Building and repairing of
barges, lighters and boats
53
18
Industry
-15 -
definite silicosis and 24/» had suspected silicosis.
A similar survey,
concluded in 1971, found that 15?’ had definite silicosis and 17/? suspected
silicosis, out of 1,230 workers X-Rayed.
The other industries which have
a silica dust exposure are rubber powder factories, iron foundries,
pottery works, sand blasting operations and tombstone-making (phoon (1974).
Interesting cases dealt with by the Industrial Health Unit in 1972
included an outbreak of dermatitis in an electronic factory due to a liquid
soap which predisposed to photo-sensitivity and an outbreak of hysterical
attacks among female workers of a plastic toy factory.
"epidemic
This was the first
of hysteria ever reported in factory workers in Singapore (indus
trial Health Unit 1972).
Other occupational health problems in Singapore which have been reported
include lead poisoning, occupational dermatitis, decompression illness,
leptospirosis, heat stress and psychological problems due to ’-maladjustment
to jobs (Phoon (1973) and rockfish stings in fishermen (Phoon and Alfred 1965).
In a survey of 83 small factories, it was found that only 12 had
satisfactory standards of sanitation and safety.
These small factories,
have_very scanty financial resources, a high labour turnover, and often
very limited management and training skill - all factors which predis
pose to high rates of accidents (Phoon et al 1974).
The widespread practice by large firms of contracting out dirty or
dangerous work is also making enforcement of health and safety legislation
more difficult.
Employers sometimes inform Pactory Inspectors that the
hazards of lead-poisoning or silicosis "no longer exist" in their factories
because they have handed over the processes, involving such hazards, to
contractors!
■The situation, described below, exists in Singapore as it does in
Japan:
- 16 -
"One of the major problems of industrial health in today's Japan
is the hygiene problems of the "inner contract workers" who, though working
within u certain enterprise, .have no direct employment contracts with the
enterprise itself ... It has long been pointed out that the manufacturing
processes for which the inner subcontract workers are responsible are often
aangerous and unhealthy ones with a high incidence rate of labour accidents
and occupational hazards" (interxjat.'' Congr. Occup. Health 1969).
In 1969, the author listed some of the factors which impede the progresi
of occupational health in a developing country.
1.
The factors \x-re:-
Economic development usually get most of the money available.
Occupa
tional health measures do not usually receive sufficient government
funds, as it is argued that they can wait until the industries are fully
launched.
2.
t
The lack of sophistication by workers sometimes lead them to demand more
money to carry out dangerous jobs or increased compensation for permanent
disability rather than to demand that their working environment should be
rendered safe.
J.
Employers and workers may agree about the desirability of using safety
equipment, but disagree as to who should provide it.
4.
The characteristically hot and humid climate makes the regular usage
of personal protective equipment very uncomfortable.
5.
The polygot nature of many developing countries sometimes lead to
problems of communication between supervisors and workers, and these
in turn nay predispose to accidents.
6.
The lack of nnifonnity in health and safety standards in industries
established by multi-national companies in the developed countries
17 “
sometimes lead to confusion in the provision of health and safety measures
(fhoon ,1969).
In the opinion of the author, these factors have contributed to the
incidence of accidents and diseases in the industries in Singapore.
The ill-effects of industrialization on the general community are more
difficult to determine.
During the last few years, there has been more
congestion of traffic, more overcrowding, more pollution and increase in
the tempo of living.
occasions
During construction of factories, there have been
when mosquito breeding has increased due to the formation of
stagnant water.
In 1973, there were over 1,000 cases of Dengue haemorrhagic
fever in Singapore.
Some of them could be attributed to an increase in the
population of Aedes aegypti mosquitoes in construction sites.
Psychiatrists
have claimed that there is more mental ill-health in the community.
In the
report of a Committee on Crime and Delinquency, which vas set up by the
Government, it was stated that "crime among the young had increased at an
alarming rate over a five-year period from 1968 ... the cirmes by juveniles
against property with violence rose from 30 in I960 to 119 in 1972" (Straits
Times
1974).
Suicides do not seem, to have increased, though the mode of
suicide has changed.
Jumping from the upper storeys of high-rise apartments
has become the most popular method of committing suicide.
Could any or all
of these changes be justifiably attributed to industrialization?
what extent?
If so, to
If we ask ourselves the question, whether industrialization
has nude people happier or riot, we also run into the difficulty of defining
and quantifying what we mean by "happiness",
e lack a generally acceptable
"happiness" index or sufficiently sensitive indicators of social advancement.
Moreover, what may be accepted to be indicators of progress or prosperity
by some may be construed as pointers towards a sick society by others.
18 -
COiTCLUSIOIT
Perhaps the title "conclusion" is a misnomer, because the whole of
my paper is based on the ggemise than while we can see momentous changes
taking place in South-east Asia and the direct effects of industrialization
upon the health of workers, we are not yet in a position to evaluate
quantitatively either the benefit or harm of industrialization or to
balance the one against the other.
:b maintain, nonetheless, that oouth -east -isia offers an unique
opportunity to study the social and health effects of industrialization,
even though we may not know what they are exactly.
Some of the changer-;
which occurred during the hundred and fifty years of the Industrial
Revolution in the rfest are being re-enacted over decades in South-east
Asia.
BERMEO (South East Asia Ministers of Education Organization) has
set up a Tropical Medicine and Public Health programme, in an attempt
to pool the scanty training and research resources in the region.
Singa
pore has been selected as its centre for the study of Urban Health and
Occupational Medicine.
Hopefully, in the next few years or so, we may be able to gather
more knowledge and arrive at more concrete conclusions about the impact
of industrial growth on health in South-east Asia.
It may be, of course,
■chat we shall never have the whole picture, but it is surely a worthwhile
goal to advance the frontiers of knowledge about this most important
subject.
..’e can at least take consolation from the works of J. Bowlby,
"It must be remembered that evidence is never complete, that knowledge
of truth is always partial and that to see1.: certainty is to await eternity."
ACKHOWIiEDGBMBHTS
The author wishes to express his thanks to Dr. Ang Swee Chai for
helping in the preparation of this paper and to Miss Helen Chung for her
clerical assistance,
Bakacs, T. (1972) Urbanization and Human Health, Akademiai Kiado, Budapest,
ur,. 51-52
El Batawi, M. A. (1968) The Need for Developing Occupational Health and Safety
Brogrammes in Relation to Industirulisation in Asia & the ?3ar East.
Singapore Mod. J., 9, p. 220
Federation of inlqya (1957) Heport of the Industrial Development Dorking
Barty, p..4
Federation of Khlaya (1963) Second Five-Year Plan, quoted in Interim Review
of Development in lalaya under the Second I'ive-Year Plan, Malaya, p. 43
Goh, 0. T. (1969) Industrial Growth, 1>59-66,
Modern Singapore. Ooi, J. B.
and Chiang H. D, (ed.), Univ, of Singapore Press,
.p. 128
Huan, S. H. (1971) Ifeasures to promote Industrialization.
ine Singapore
You, P. 3. and lam, 0. Y. (ed.), Eastern Universities Press,
Economy.
p. 243
Singapore,
Internet. Congr. on Occup. Health (XVl) Tokyo (1969) Occup. Health in Japan
pp. 189-190
Industrial Health Unit (1972) Annual Report, Min. of labour, Singapore,
pp. 32-33
Jegasothy, S. J. (1967) The Social Impact of Urbanization.
Seminar on Urbanization, Singapore
-.hy Asian
p. 25
Jfyrdal, G. (1968) Asian Drama (vol II), Allen Dane the Penguin Press,
London,
p. 1150
Nguyen, Deng Due (1972) Occup. Health A Safety in Small Industries in
Vietnam.
•t'roc. of First Jymp. on Occup. Health in S.E. Asia, Singapore,
pp. 84-86
Phoon, W. 0. (1969) Factors Impeding the Progress of Occupational Health
in a Developing Country.
Proc. XVI Congr. Occup. Health, Tokyo, pp. 280-282
Ehoon,
& Safety it Work, Na: tonal Safety Mist Council
0. (1971)
of Singapore, Singapore,
Hioon,
p. 21
'. 0. (1973) Occup. Health Problems in Urban Singapore.
Proc.
Science and the Urban Environment in the Tropics, Singapore (2nd Congr.
of S’pcre Nat. Acad. Science), pp. 62-68
Pho on,
0. (1974), Safety & Health in Singapore.
Proc, of 7th Uorld Congr.
on Prevention of Occup. Accidents and Diseases, Dublin (in the press)
Phoon, W. 0. and Alfred, E, R. (1965) A Study of Stonefish (Synanceja)
Stings in Sin apove with a Review of the Venomous Pishes in Ihlaysia,
S’pore Med. J., 6, pp. 158-163
Pho on, W. 0., Chew, P.
*Jhn,
S. B., Hong, H. IC. C., and Phoon,
;. H. (1974)
A Survey of Health Conditions in Small factories in Singapore.
Proc, of
9th riilaysia-Singapore Congress of Medicine (in the press)
Reddy, K. V. (1967)’An Unfinished .'evolution.
..orld Assembly of Youth, Belgium,
Robless, C.
j.
Youth & Urbanisation in Asia,
p. 104
(1068) Lalaysian Agriculture & Economic Development.
Mission ox -agriculture, thluysian Centre for Development Studies,
The
p. 2
Straits Times (1974) Singapore, Aug, 28, pp. 1
Suma'mur, P. K. (1972) Occup. Health and Nat. Development Proc. first
Symp. on Occup. Health in S.E. Asia, Singapore, pp. 5-8
Trishnananda, M. and Attanatho, V. (1971) Some Observations on Lead Poisoning
in Thailand.
Proc, of first Synp. on Occup. Health in S.^. Asia, Singapore
pp. 182-134
United Nations (1966) Industrial Development, Hew York (vol III), pp. 14
Vella, ?. and Phoon,
0. (1959) A Clinical Case of 6-glucose-phosphate
dehydrogenase Deficiency. Med. J. Ihlaya, 13, pp. 309-312
- 21 -
Vfessermann, M. (1968) Problems of Toxicology in Industry and agriculture
in Developing Countries.
Proc, of Interna t. Seminar on Occup. Health
for Developing Countries, Ligos,
p. 129
U.iI.G. (1971a) Report of Liter-regional Seminar on Training and Services
in Occupational Health for Developing Countries, Indonesia,
•’.:I.O. (1971b) Ibid,
p. 28
J.H.O. (1971c) Ibid,
p. 16
W.H.O. (1971d) Ibid,
p. 23
.p. 3
".ongpanich, Id., Kritalugsana, 3. and Deema, P. (1972) Survey of pesticide
hazards in Agriculture.
Proc, of Pirst Symp. on Occup. Health in
S.IJ. Asia, Singapore pp. 185-188
World Assembly of Youth (1967) Youth & Urbanization in Asia, p. 132
Yeh, S. H. K. (1971a) Trends and Issues in Social Development.
The Singapoi
Economy, You, Ps S. an<? Dim, C. Y. (ed.), Eastern Universities Press,
Singapore, p. 266
Yeh, S. H. K. (1971b) Ibid, p. 272
']7''
HEALTH CELL
' ’ BAiur«»'k»Soaa
BAIVGAtORE-563 00J
OCCUPATIONAL HEALTH IN THE TROPICS
(A paper presented at the Symposium on Geographical Conditions and
Occupational Health at the XVIII International Congress on
Occupational Health, Brighton England, 14-19 September 1975)
by
W. Oo PHOON
A.M.(S’pore), M.B.,B.S.(Malaya), F.F.C.M.(U.K.), F.R.C.P.(Edin),
F.R.C.Po(Glasg.), M,R«C»P»(London), D»C.H«(England),
DoI.H.(England), D.I.H.S.A.(London)
Professor and Head, Department of Social Medicine and Public Health
University of Singapore, Outram Road, Singapore 3
Chairman, Committee on Occupational Medicine, School of Postgraduate
Medical Studies, University of Singapore
Member, Committee on Occupational Geographical Pathology, Permanent
Commission and International Association on Occupational Health
Member, W»H«O« Expert Advisory Committee on Occupational Health
Executive'Committee Member, Asian Association of Occupational Health
President, Society of Occupational Medicine, Singapore
OCCUPATIONAL HEALTH IN THE TROPICS
by Professor W. 0. PHOON
"You might be able to get two people to sleep in the same bed, but you
cannot get them to dream the same dream." Old Chinese proverb.
It is indeed a great and undeserved privilege,, for me to be
the opening speaker at this very distinguished international gathering.
May I claim your kind indulgence for what will be, perhaps, merely a
curtain-raiser (in the parlance theatrical circles) or a supporting bout
(in the language of pugilistic contests) to the Ibng series of erudite
papers which will follow mine.
For the purposes of my discussion, I
will adhere to the usual definition of "tropics", as meaning lands
lying between 23°285 north and south of the equator, although I do hope
that geographical pundits will forgive me if I .inadvertently stray from
these frontiers in my presentation.
For practical purposes, the tro
pical lands all fall into the category of developing countries, though
some are "more developing" than others!
In a sense, Occupational Health in the tropics is not new, if
by it is meant "the health of the gainfully employed."
Even before the
advent of the white man in the visage of traders, empire builders or
missionaries, witch-doctors, shamans and practitioners of the various
native..systems of medicine were looking after the health of the gainfully-
employed, be they warriors in the king’s army or peasants in the field.
With the establishment of Western colonies, mines and plantations were
developed, either by the colonial governments themselves or by multi
national companies.
As the Western-type of health care was virtually
non-existent, certainly in the rural areas where mines and plantations
usually are, it was deemed necessary to operate comprehensive health
2
services for both workers and. their families,' '
have existed to this day.
problems varied a great deal.
curative.
Many of such services
However, their emphasis on occupational health
Sometimes the services were predominantly
Sometimes they included a large preventive element as well,
mainly in general public health«Until recently, very few services paid
sufficient attention to the special risks of different forms of work to
the employee, and the' possible health consequences of such risks.
Let us now examine the thesis of whether there are in fact
significant differences between Occupational Health, as should be
practised in the tropics, and as practised in the non-tropical countries,
which are mostly developed ones.
Lot us also evaluate whether .‘these
differences are great enough to merit the establishment of a new dis
cipline or sub-discipline called, perhaps, Tropical Occupational Health.
After all, there is already a discipline in its own right by the name
of Tropical Medicine or Tropical Health, with chairs and institutes
situated, strangely enough, mainly in non-tropical countries!
There are
also centres, albeit fewer, specializing in "Tropical Paediatrics" or
"Tropical Child Health" awarding degrees for the subject, and other
institutions with emphasis on what they sail "Tropical Public Health".
THE IMPLICATIONS OF THE TROPICAL CLIMATE ON OCCUPATIONAL HEALTH
An obvious difference is that of climate, about which so much
has been studied and written that I need only to discuss it briefly.
There are certainly many occupational health problems arising from or
predisposed to by the tropical climate.
Heat problems tend to occur more
frequently, though I am somewhat surprised by their relative lack of fre
quency.
I have seen several cases of heat cramps and heat syncope among
3
European workers in the tropics, but very few among the indigenous popu
lation in such countries.
Dermatological conditions, which are related to or aggravated
by excessive sweating, tend to be more often seen, e.g. general pruritus
and miliaria rubra.
Severe forms of these conditions, of course, may
interfere with the performance of the duties or the health of the workers.
The hot, humid climate may also make it difficult to persuade
workers to use personal protection, e.g. respirators, aprons, etc.
“There are several reasons why the hazards associated with field appli
cation of insecticides are difficult to control in the tropics, namely,
Climate:- Protective clothing may be objectionable to workers in hot
humid countries.
In addition, high temperatures may increase the speed
of skin absorption of many chemicals.
This is dangerous,as often
washing facilities may not be adequate, in such circumstances.
Eating
(2)
immediately following spraying operations may be specially hazardous."'
In Occupational Hygiene, there are many problems affecting
instruments and measurements with them.
Rust and moulds are ever-pre
sent dangers, and the more delicate instruments require dehumidifiers
and air-conditioners as well as frequent inspection, as a'result J
The
high humidity of the atmosphere in many tropical countries may also
affect the results of some air-sampling instruments.
In Occupational Toxicology, our eminent chairman, Professor
Marcus Wassermann, has most ably summarized the differences in the tropics
"Hie basic hygienic evaluation of the impact of air-borne
concentrations of chemicals in industrial atmospheres refers to temperate
climatic conditions.
Gross deviations of physical pressure, ultraviolet
and ionizing radiations in the atmosphere of work sites may result in
adverse effects from these chemicals even if their concentration is
4
permissible according to the list of Threshold.Limit Values
“Pharmocological studies have drawn our attention to the fact
that during exposure to high temperatures, there is an increase in the
susceptibility and the rate of reaction to most drugs.
Experimental
studies have reported the increased susceptibility to chemicals like
D1JOC, parathion, cadmium, lead, benzene, carbon tetrachloride, benzene
vapours, gassing , carbon monoxide, hydrochloric acid, vapours and
nitrogen oxides ....
'■'Increased respiratory rate produced by a hot clima.te, a
modified rate of absorption, distribution and detoxification of the
chemicals and an altered level of the normal body functions due to the
work at high temperatures, are all factors which have to be considered
in recommending any implementation of hygienic work conditions."^)
There are, nevertheless, some advantages accruing from working
and living in the tropics, insofar as Occupational Health is concerned.
As there is no need to provide insulation against cold weather,
the factories tend to be constructed with open doors and high ceilings,
unless air-conditioning is installed.
general-ventilation.
There is therefore usually good
This is probably a reason why air-borne contaminants,-
such as inorganic lead dust, sometimes are not as high as expected in
storage battery factories, which have installed few or no environmental
health measures, such as exhaust ventilation.
Moreover, without being derogatory to the people from the
developed countries, it is probably generally true that workers in tro
pical countries bathe and wash themselves, more often than their counter
parts in the colder, developed countries.
This is mainly because of the great bodily discomfort which
5
arises from the heat, humidity'and sweat'in such climates.
From personal observation, it seems to me that Occupational
Dermatosis (or Occupational Dermatitis) is less frequent in tropical
workers than those in the West handling the same chemicals engaged in
This could be due to frequent bathing which should
the same processes.
at least reduce the amount of dermatitic agents in contact with the skin.
This has been postulated before by manyother authors.I am aware
that there are other possible explanations, such as the increased skin
thickness which occurs in coloured people.
There are somewhat different patterns of sickness Absenteeism
in tropical countries.
The absence of winter means that there is no
seasonal upsurge of respiratory illnesses, as there is often in the
temperate region.
The climatic conditions in the tropics do not favour
temperature inversion and the development of smogs.
It must be admitted,
however, that tropical countries have not yet reached the stage of such
intense industrial activity or concentration of motorised vehicles and
the gross atmospheric pollution resultant therefrom as those cities which
have suffered from severe smog episodes.
As we know, smogs produce an
increase in deaths and disability from cardiac and respiratory diseases.
I am not certain whether the incidence of rheumatism in the
tropics is different.
In colder countries we do know that the incidence
of rheumatic disorders is very high.
-‘Diseases of connective tissue are
responsible for much temporary or permanent disablement.
In the year
ended June 1967, just over one million spells of incapacity among the
insured population in Britain were due to ’rheumatic complaints' and
caused a loss of productivity of £190 million.
amounted to 35.19 million days.
Time lost from work
’Rheumatic complaints’ were second only
to accidents as regards the number of people affected and second only
6
to bronchitis for the number of days lost.'''3'
In temperate countries,
there is no question that chronic rheumatic diseases account for a
significant amount of sickness absenteeism, especially among the older
workers-
My own impression is that such diseases are less frequent in
the tropics.
THE DIFFERENT GENETIC INHERITANCE AND PHYSIQUE Of TROPICAL WORKERS
The workers in tropical climes are also endowed with different
genetic inheritance and physical constitution.
Admittedly, there are
probably as large differences among themselves as from .their fellows in
the non-tropical world.
In general, however, they are of smaller size
and more Slender build.
This has various Occupational Health implications
In terms of Applied Physiology, there are differences in heat metabolism
due to a comparatively greater skin surface for the same weight.
Ergonomics
It is unfortunately true that most vehicles and machines are
not designed for the anthropometric measurements of the indigenous wor
ker in most tropical areas.
The inappropriate indigenous location of
levers, gears and control panels are sometimes the cause for bodily or
mental fatigue. . For example, the size and design of the cabin of a heavy
lorry were such that the relatively puny worker in a certain tropical
country had to practise virtually both acrobatics and callisthenics to
operate the vehicle properly.
Hie dimensions and lay-out were, in fact,
designed for his much larger and heavier counterpart in the West!
This ergonomic problem, was commented upon several times in a
recent seminar in the. tropics:-
7
"We know that a great deal of research has already been carried
out especially in the field of physiology of work and that a large- number
of methods of investigation has been perfected, making it possible to
reach certain practical conclusions which are valid for all industries ....
However, one cannot ignore tha fact that most of this research has been
conducted in highly industrialized countries and on populations having
similar biotypic features, thus applied to individuals whose physiologi
cal, psychological and social adaptation to modern economic life has a
and
long historical process of progressive adaptation.
"Caution must be exercised lest Ergonomic principles, valid
in the West, are uncritically applied to developing countries."
(?)
EBzyme deficiency
The genetic make-up in the populations of different tropical
countries is too diverse for me to deal with in detail.
I would like,
however, to mention one genetic condition which is common and which may
be important in Occupational Health.
An inherited enzyme deficiency,
of 6—glucose—phosphate dehydrogenase, has now been reported in several
tropical countries, although it is also present in some countries of the
temperate zone as well, such as those of the vicinity of the Mediterranean.
In my country the first case was reported in 1959-
(8)
I am intrigued
to discover whether other researchers have evaluated how often such an
enzyme deficiency has led to haemolytic episodes in occupational circum
stances .
Skin pigmentation in differential diagnosis
I have already referred to skin pigmentation in respect to
occupational dermatitis.
There is also the problem of differential
8
diagnosis of Occupational Diseases, e.g. in heavy metal poisoning.
For
example, pigmentation on the gums and other parts of the oral cavity is
very common in dark races, and should not be mistaken for the lead line
of lead absorption.
Women and heavy work
In many countries of the tropics, there are many women engaged
in heavy labour.
The Chinese “Sarnsui" woman labourer with her red cap
and blue attire is a famous example, carrying heavy loads at construc
tion sites and in godowns.
In my opinion, it is necessary to sort out
the fiction from the truth about what occupations women should not dn on
health reasons.
Many of the existing taboos are related more probably
to body size than sex difference.
“First generation" workers and accidents
Some authorities in Accident Prevention have claimed that firstgeneration industrial workers are more prone to accidents than those with
fathers who had been employees in industry.
Apparently, some of the
familiarity in dealing with machines "rubs off" from sire to son.
I am
not sure about the truth of this hypothesis, but the rates of occupa
tional accidents are usually quite high in tropical countries with a sa
tisfactory notification and record system of such accidental
It is dif
ficult to extricate this "first generation" factor from the doncomitant
factor of poor education in the causation of accidents.
The lack of
literacy and sophistication, which is rampant in most tropical countries,
may be a great impediment to proper instruction in operating and safety
procedures.
To be fair, however, it may be the lack of linguistic talent
in the foreign "bwana" or "tuan" (employer) which may precipitate the
9
accident.
There is sometimes & tendency on the part of some expatriate
supervisors or employers to flatter themselves that they are masters of
a local language whereas, in fact, they are :tmurdering,! it.
This may
have disastrous consequences to Occupational Health or Safety.
Attitude towards authority
On the credit side of the :'halance sheet", it is perhaps still
true that the average worker in the tropics is still more respectful of
authority than his counterpart in non-tropical areas.
As a consequence,
he may comply more readily with instructions, necessary for good health
or safety at work.
Religious, cultural and social factors
Religious, cultural and social traditions all influence Occupa
tional Health practices.
In the Muslim World, employees fast during the
month-long "Ramadan" period, despite the fact that most of them are re
quired to work as usual.
They are forbidden by religion to eat or drink
from sunrise to sunset.
This has obvious implications concerning hydra
tion in hot conditions and energy expenditure in heavy work.
or
Workers in the tropics also tend to be more superstitious.
One electronics factory in Singapore almost closed down a short while
(9)
ago because several girl employees thought they saw a ghost there.K
Another company with which I was associated had to pay large sums of money
to exorcise an evil spirit in the work-site.
As the work-force was multi
racial, the company had to pay for three teams of exorcists,- Chinese,
Malay and Indian.
I also remember another instance wherein the expa
triate manager of a factory came to me in a panic, as some of his key
workers were threatening to resign, as they claimed to have seen headless
ghosts in their new quarters..
10
The Occupational Physician, Engineer or Nurse who scoffs at such beliefs
and practices may find himself ineffective in his role, no matter what
his own beliefs may be.
He must have a thorough appreciation of the re
ligious, cultural and social background of the people he serves so that
he could communicate effectively and recommend the most effective health
measures in a particular milieu.
THE DIFFERENCES IN ENVIRONMENT
■More biological hazards, including infections
There are more biological hazards in the tropics than in the
temperate zone.
Some fungal infections, e.g. tinea versicolor, abound.
Malaria alone accounts for far more deaths and'ill-health "in tropical
workers than metal poisoning, pulmonary dust dideases and occupational
cancers together.
Tuberculosis and other infectious diseases are common
causes of sickness absence.
Epidemics of cholera, typhoid, dysentery
and yellow fever, etc. have been known to devastate mines, lumber-camps
and plantations and even lead to their shut-down.
i°arasitic infestation
is often the real reason for the so-called "laziness" of tropical workers.
It is not easy to be well-motivated, hard-working and intelligent when
one has a haemoglobin value of seven g/l00ml. blood due to hookworm in
festation or a body temperature of 102°F„ due to malaria or is thinking
of a wife or child coughing blood as a result of pulmonary tuberculosis.
, Housing in shift work
There are also vast differences in the inanimate environment.
Shift work, for example, is a problem, because tropical workers tend to
have large families and crowded accommodation.
Many workers in industria
lizing tropical countries have had to give up lucrative jobs requiring
11
shift duties because they simply could not get enough sleep after a •
night's work.
■. s
Moreover, the architecture of workmens' quarters in'the
tropics is primarily designed to provide satisfactory lighting and
natural ventilation.
Noise is not kept out very much, unlike the work
ing class houses in the West where houses are designed to keep out the
cold, and as a by-product, noise is also kept out to a certain extent.
Environmental health problems
In the tropics, the conditions in the factory are often
radically different from those in the community from which the industrial
worker comes.
At work he may encounter wash-basins and flush toilets
whereas at home he may be inured to wells and bore-hole latrines.
He
cannot be really blamed, therefore, if he fouls up modern devices he is
unaccustomed to.
It is part of the duties of the Occupational Physician
or Nurse in the tropics, nonetheless, to give proper Health Education and
to devise effective measures to prevent the spread of contagious diseases
arising from such abuse.
DIFFERENCES IN OCCUPATION'
The occupations’.of most workers in the tropics will be mainly
agricultural within the foreseeable future.
Undoubtedly there will be
an increasing number of industrialized foci in the tropics, but I cannot
envisage extensive industrialization in most tropical countries for at
least one to two generations.
Therefore Occupational Health in the tro
pics must lay (.sufficient emphasis on the problems of those engaged in
agricultural, mining and other types of primary production.
In the follow
ing quotation, we can equate “developing countries" with "tropical
countries" quite legitimately:-
12
"The majority of the population in developing countries is
_employed,J.n. agriculture.
The most important risk to which the agri
cultural workers are exposed in these countries is snakebites.
In a
on "Nigeria’s experience in Occupational Health", G.O.
study made
Sofoluwe reports that in most plantations he visited, the most common
accidents registered were snake bites.
In the tropics, there are many trades and manufacturing
processes which have either not existedor disappeared-long ago from
the temperate zone.
The occupational hazards of these trades or pro
cesses are, as a consequence, not even mentioned in most Occupational
Health texbooks, as they are "exotic" to the Western authors, though
common place in their native setting.
Nature is still relatively rich and unspoilt in many parts of
the tropics.
Inroads are made, however, into the luxuriant jungles and
bush by development projects such as the construction of irrigation dams,
highways or airports.
These projects are necessary to improve the eco
nomy of the countries concerned, but those practising Occupational Health
must make sure that such schemes are accomplished with the minimum of
suffering by the workers and the least disturbance of the ecological
balance in the area.
A DIFFERENT TYPE OF OCCUPATIONAL HEALTH TEACHING
__________ SYLLABUS IS NEEDED IN THE TROPICS_______
I have already discussed what I think are the formidable and
extensive differences between Occupational Health in the tropics and non—
tropical areas.
If we accept that these differences exist, it stands
to reason that the training of Occupational Health personnel in the
tropics should be quite different from that in other areas of the world.
13
Obviously, the fundamentals of the subject may be the same but, in my
opinion, the syllabus in the tropics should have more emphasis on the
following aspects
(a)
Public Health.
One Professor from an institution which con
ducts an Occupational Health Course and is located in a developed
country recently observed, after visiting a tropical university, that
"Public Health is totally irrelevant to Occupational Health", thereby
(in my opinion) betraying his own total irrelevance to Occupational
Health in the tropics!
This is especially important, as there may be
very few Public Health experts around.
Family planning should be an
important part of the syllabus.
(b)
Infectious Diseases.
It is impossible for Occupational Health
personnel to protect the health of their work-force unless they know
sufficiently about the common infectious diseases in thetrppics.
(c)
Clinical Medicine.
In many areas of the tropics, it is easier
to avoid the artificial dichotomy between Preventive and Curative
Medicine, as prevails in many non-tropical countries.
Therefore, the
Occupational Physician must be trained in Clinical Medicine, as well as
minor general and Orthopaedic surgery, elementary f'T>hthalmology, Der
matology, to an even greater extent than in non-tropical areas.
"Generally speaking, however, training in internal medicine
and public health is essential as a background.
Internal medicine is
important since it. emphasizes the principles of diagnosis, which is
necessary if occupational diseases are to be recognized and differentiat
ed from those on non-occupational origin.
any preventive programme.
This must be a first step in
Public health training is important because
it orients the physician to think in terms of group phenomena of health
„ a(11)
and disease.1'
u
(d)
sight.
Occupational Hygiene.
This may seem a contradiction at first
It must be appreciated, however, that Occupational Hygienists
are even more rare in the tropics than in the temperate countries.
The
Occupational Physician, and perhaps even the Safety Engineer or the
Occupational Nurse, should have a sound working training in Occupational
Hygiene, otherwise there may be nobody to monitor the hazards of the
working environment.
The emphasis of such training should be in fairly
simple techniques using cheap, robust pieces of equipment which are
readily available and do not require much maintenance.
(e)
Nutrition.
The relationships between proper nutrition to
health and productivity should be taught.
Dietary advice and supplements
are often necessary for workers in the-tropics, unlike the situation in
other areas.
(f)
Behavioural Science.
The orientation should be towards those
aspects of behavioural science which are pertinent to societies evolving
from a tribal dr peasant community into modern ones.
(g)
''Occupational11 rather than merely 11 Industrial;1 Health.
AS
have been discussed above, industry may play only a minor role in the
lives and economy of most tropical countries for some time to come.
There
should, therefore, be adequate emphasis on all aspects of Occupational
Health rather than on mainly the industrial aspects, as is done in some
centres in non-tropical countries.
"The health problems of workers in developing countries are
more complex than those of industrialised nations because of the high
prevalence of epidemic and endemic diseases in most areas of the tropics.
Modern concepts of occupational health embrace all types of employment
including mercantile and commercial enterprises, service trades, utili
ties, forestry and agriculture.
The distinction between environmental,
15
occupational and industrial health is academic in the context of many
tropical families where the husband may work in the factory while the
wife and children cultivate a plot for food."^2)
THE LOCATION FOR SUCH A TEACHING- PROGRAW
V/here should an Occupational Health course for the Tropics be
taught?
Let me quote the words of two distinguished authorities on the
...
subject.
....
...........
"It is wrong for us to assume that the teaching programmes
planned for students from our countries will suit those from tropical
countries...so often in our country, we bemuse those men and women from
India and Africa with details of British industry and its health services..
"One of the most crucial long-term problems is where those who
will have the care of occupational groups in the tropics should be taught.
Ultimately, I believe that most of them should receive instruction in
their own countries with only the exceptional person who may himself be
come a teacher going to foreign universities."^^
"In my opinion there is need for greater regional co-operation,
including the provision of training facilities, than hitherto within this
part of the world.
In the past those seeking postgraduate experience
have gone to England or the United States.
Are the best results obtained this way?
Should this still be the case?
Alternatively should we not have
a closer look at what is available nearer home?
With few exceptions what
is needed is practical training, involving visits to many factories in
which the student carries out, for example, solvent, or dust, estimations
with the local occupational health specialist who is investigating im
plant or agricultural conditions which are currently the subject of com
plaint.
There is no effective substitute for real situations,
,(14)
16
I myself think that there is still a place for centres in the
developed world to train some■Occupational Health personnel from tropical
countries, but preferably the majority of the latter should be trained
in the tropics.
It is highly desirable that they should be trained in
conditions similar to those they will practise in.
AN ATTEMPT AT A TEACHING PROGRAMME IN OCCUPATIONAL
HEALTH FOR TROPICAL COUNTRIES
Permit me now to describe a new course in Occupational Health
conducted by the University of Singapore.
1973, with a class of four.
eight students.
The course was established in
In 1974, there were five and this year
They came from Indonesia, Philippines, Thailand,
Malaysia, Singapore, South Vietnam and Cambodia.
As far as Singapore
was concerned, there was a growing realisation and demand for Occupa
tional Health.
As far as the other countries in South-East Asia were
concerned, there was also a similar need.
It was felt by the South East
Asia Ministers of Education Organization (SEAMEO) that commonsense
dictated the pooling of scant resources and that it was far more econo
mical and useful to train people of the region in the region.
The cost of sending one person to distant centres overseas was equivalent
to the cost of training five or six persons in-situ. 'Besides, the train
ing acquired overseas may not be very relevant to the needs of South-East
Asia.
In pursuit of this objective, the course in Singapore has been
sponsored by and recognized by the Tropical Medicine (TROPMED) Division
of SEAMEO as the official course in the subject for the countries of South
East Asia, with a population of over 200 million people.course
is entirely financed by Singapore itself, but the majority of the fo_'■
■rn-ign students are awarded SEAMEO scholarships to attend.
The course leads
17
to the degree of Master in Science (Occupational Medicine) instead of
the Diploma in Industrial Health, as originally proposed.
There have
been considerable "teething” problems; but we are overcoming them gra
dually.
Problems included the lack of teaching staff, equipment, rele
vant books, selection of students and the drawing up of' a syllabus, de
signed especially for tropical countries.
The syllabi of
* Occupational
Health courses in developed countries were studied and modified consi
derably to suit our own requirements.
devised the perfect syllabus.
By no means do we claim to have
We still require to modify it annually
according to our experiences and the feed-back from the student's"which
is obtained regularly.
The details of the syllabus, entrance require
ments and examinations are contained in Appendices A and B.
They are
based on our philosophy about the needs of Occupational Health in the
tropics, as discussed in the earlier portion of this paper.
We are very
grateful to SE3ME0 TROPMED, China Medical Board, WHO and other bodies
for their valuable assistance and contributions in the form of consul
tants, equipment and books.
To ensure proper standards, we are inviting
international authorities to come to Singapore to serve as External Ex
aminers each year.
TROPICAL OCCUPATIONAL HEALTH OR OCCUPATIONAL
HEALTH IN THE TROPICS?
Should a new speciality of Tropical Occupational Health be
created?
On reflection, there seem to be many valid reasons for advocat
ing such a step.
Just as Tropical Medicine is part of Medicine, but a
special part thereof, and just as the terms Tropical Paediatrics or Tro
pical Public Health have been invented to fulfil a need, it is logical
to think of Tropical Occupational Health as a special segment of general
18
Occupational Health.
However, I rnyself prefer to stress the underlying
thread of unity running throughout the whole field of Occupational
Health, rather than the diversity which makes the field at once so
challenging and frustrating.
We must realise, nevertheless, that Occu
pational Health is not a monolith hut is more like a "coat of many colours"
We should Accept departures of teaching programmes designed to make the
subject more meaningful to the Tropics, not as a schism but as a wel
come extension of that discipline.
"There is a risk of teachers from
developing countries visiting centres in developed ones and coming back
filled with zest to introduce disciplines merely because these disci
plines are included in the curriculum of centres in the developed
countries.j would prefer to look on Occupational Health as appli
cable to both tropical and temperate zones, though the type of Occupa
tional Health teaching may need to be different in each zone, or perhaps
even from country to country.
We are living on one earth, and recent
developments on the international political and economic scenes have
made it even more imperative for us to learn from and help each other.
These words are as relevant concerning Occupational Medicine as General
Medicine
"Temperate zone medicine certainly owes
pical medicine.
a great deal to tro
Indeed, despite their interesting differences, it is
hard to separate tropical medicine from general me'dicine today...
“We have learned much from the tropics concerning the patho
physiology of disease..... We have much to learn there about the effects
of climate on health and efficiency...
(17)
Such, surely, is the spirit which motivated the creation of
the Committee on Occupational Geographical Pathology and which will un
doubtedly prevail in our deliberations at this symposium todpy.
19
Let us hope that all Occupational'Health Specialists at this
Seminar and. this Congress, both from the temperate and. tropical climes,
may not only share the same bed. but also dream the same dream - of
making the working lives of countless men and. women truly happy, healthy
and. productive.
SUMMARY
Tropical Medicine is generally acknowledged as a discipline in
its own right.
Could a case be ma.de out. for establishing Tropical
Occupational Health on a similar basis?
This paper deals with the problems of Occupational Health in
the tropics, particularly in South-east Asia.
It is largely based on
the experiences of the author and his colleagues.
Examples are given to
compare and contrast some striking differences between the prevalence
and epidemiology of occupational diseases in the tropics and those in
temperate countries.
They include heat stress, the greater importance
of biological hazards, the differences due to variation in genetic
constitution and in levels of education and sophistication, and the pre
ponderance of small-scale and traditional industries.
The study of such problems is complicated by the fact that
industrial populations in tropical countries are usually small and have
a large turnover.
Record-1inkage in most tropical countries is also
poorly developed.
Since the practice requirements of Occupational Health in the
tropical countries may differ greatly from those in the temperate ones
(in which most of the Occupational Health institutes and training centres
are located), it is contended that the training of occupational health
20
practitioners for the tropics should preferably be done in-situ,
The
traditional type of curriculum of Occupational Health training should
be modified also to fit the different needs of tropical countries.
There should be, moreover, a larger.content of community health
teaching, especially in subjects such as environment sanitation, micro
biology, nutrition, and family planning.
Finally, the author describes a newly-designed course in
Occupational Medicine at his centre, and discusses the successes and
difficulties regarding staff training, teaching,- curriculum development,
student recruitment and field practice during the last two years.
ACKNOHLEPGEMENTS
My grateful thanks are due to my many colleagues, both in
tropical and non-tropical areas, who have given mie as many useful ideas;
and to Mrs. E.H. Lee and Miss Helen Chung, who have managed to decipher
the tortuous contents of my manuscript and to transcribe it to legible
type so efficiently.
REFERENCES
(1)
Dar Es Salaam Group Occupational Health Service *(196$
)-,
Second
Report, p.6.
(2)
Singh, K.I. (1971)
Proc, of the First Symposium on Occup. Health
in South-East Asia, Singapore, p.175(3)
Wassermann,M. (1963). Proc. Lagos Internat. Seminar on Occup. Health
(4)
Lloyd-Davies, T.A. (1957)»
in developing countries, p.129.
The Practice of Industrial Medicine,
J. and A. Churchil, London, pp.223-224.
(5)
Davidson, S. and MacLeod, J. (1971 )•
The principles and practice
of Medicine, (10th Ed.),-pp.892-893.
Proc, of Seameo-Tropmed Seminar - Workshop on Ergonomics, Bangkok,
1972 Searoeo Tropmed D,-Bangkok, ppxii-xiii
0.(1972).
Ibid, p.7.
(7)
Phoon,
(8)
Vella, F. and Phoon, W.O. (1959)«
'A clinical case of 6-gluoose-
phosphate dehydrogenase deficiency.”
Med. J. of Malaya, Vol.13,
4, PP.309-312.
(9)
Kok, L.P. (1975)“
Epidemic hysteria (a psychiatric investigation)
Singapore Med. J., Vol.16, 1, pp.35-38.
(10)
Wassermann, M. (1968).
Proc. Lagos Internat. Seminar on Occup.
Health in developing countries, p.126.
(11)
Internat. Labour Org. (1967).
Organization of Occup. Health Ser
vices in developing countries, p.120.
(12)
Lucas, A.O. and Gilles, H.M. (1973).
tive Medicine for the Tropics.
Ltd. p«3O4
A short textbook of Preven
The English Universities Press
^/(13)
Schilling, R.S.F. (1961).
Teaching of Occup. Health, Industry
and Trop. Health: IV, Harvard School of Public Health, p.1?3»
(14)
Bell, A. (1971).
Proc, of the First Symposium on Occup. Health
in South East Asia, Singapore, p.2.
^15)
Phoon, W.O. (1972).
Proposal for the establishment of a regional
teaching course leading to the Diploma in Industrial Health at
the University of Singapore.
5th Annual Report, Central Co-ordi
nating Board for Trop. Med. and Pub. Health of SEAMEO, Bangkok,
P.27-31.
''/fl6)
Phoon, W.O. (1975)«
Teaching a new discipline.
Report of 6th
WHO Meeting -of Directors on Representatives of Schools of Pub.
Health, Hanila1 pp.89-90.
(17)
W.B. Castle (1963).
medicine.
Some contributions of the tropics to general
Industry and Trop. Health; V, Harvard School of Pub.
Health, p.57.
APPENDIX A
DEGREE OF MASTER OF SCIENCE
(OCCUPATIONAL MEDICINE)
(l)
A candidate for the degree of Master of Science (Occupational
Medicine) is required to pass an examination consisting of a
written section, practical section, a clinical.section and an
oral section.
(Il)
In order to be admitted to the examination, a candidate musts-
(a)
have held a medical qualification for at least three years;
and
(b)
have had one year of full-time experience in Occupational
and
(c)
have saticfaotoritycompleted the. course leading to the
medicine and/or Public Health;
degree of Master of Science (Occupational Medicine) pro
vided that this does not precede (b) above.
(ill) A candidate is required to submit a dissertation on a subject
approved by the
of the Department of Social Medicine and
Hoad
Public Health.
Form of Examination:
Written Examination
-
Practical Examination -
There shall be four papers.
Practical Examinations in Occupational
Hygiene and Clinical Laboratory tests with
particular reference to their application
to Occupational Medicine.
Clinical Examination
—
A clinical examination of patients with
particular reference to problems .of Oooupo-
tional Medicine.
An oral examination in any aspect of
Oral Examination
.....Occupational Medicine.
In the assessment of a candidate’s merit, the Board of Examiners shall ■
take into account the’candidate:s;dissertation and practical work during
the course.
— -•
‘
All sections must be taken at one and the same examination.
(IV)
The fee payable for admission or re-admission to the examination
is $150.
This sum is subject to alteration at any time.
Guide to the Examination:
(1)
General Preventive Medicine
Public Health including Communicable and Parasitic Disease
Control, Sanitation and Public Health Administration.
Epidemiology including epidemiology of non-communicable
diseases and especially OiQ.cupjxtional, disease.
Nutrition.
Biostatistics including Research Methodology and Evaluation
Techniques.
Social Sciences and Group Itynainics; including
social conditions of the community; social effects of illness;
social deviation.
Behaviour in relation to health and disease;
medical ethics in industry; the functions of management, trade
unions, personnel and welfare services.
Health Education including methods of educating management
and workers in the promotion and maintenance of health.
Family Planning.
(2)
Occupational Health
History of Occupational Health
Work Physiology including physical factors of the work
environment; general effects of work on health, ill-health
(4)
Practical Instruction
Teaching will include(a)
Sessions at Outpatient Clinics, Specialist Medical
Units and Industrial Health Unit and other Units
related to the study of inpury and disease caused
or adversely affected hy occupation
*
(b)
Visits to factories, other workplaces, laboratories
and research centres.
(c)
Field studies of. practical health problems in
factories and other work sites.
(d)
Practical work in a laboratory.
APPENDIX B
M.SC. COURSE . .
.
, . .
DISSERTATION
Regulations (XII):
Section 1:
"The course for the Mastership of Science-1i
..4i,ishall
*
>
comprise: .... (e) The‘preparation of a dissertation on
a subject approved by the head '<Sf'the Department- of-;
Social Iledicine and Public health.,,;a
"The dissertation shall be submitted not later than a
Section 3:
date, in the last term of the academic yehr,-toibeiide-^c)
cided by the Head of the Department of Social -Medicine
and Public Health."
Section. 5(b):
- ■
"...« In the assessment of a candidate's merit, the Board
of Examiners shall take into account the candidate's
dissertation...
The'following notes relating to th? Dissertation are issued
for the guidance of M.Sc. Course candidates.
A suitable Subject for dissertation should.fulfil the following
1.
■
criteria:
(a)
,
It should be in your field of special interest or experience.
It
may relate- to a project., in wh.icjh ,you.were personally associated.
(b)
It should be a subject on which.you.are in possession of adequate
basic-material or data to enable you to deal with it in a fairly
detailed manner.
If you app not already in possession, you should
be ensured, of the ready'availability and. accessibility of such
basic material or data.
(c)
It should be sufficiently limited in its field or scope to enable
you to pursue the matter fully and to arrive at some definite
evaluation or conclusion within the limited time available for
you to do so in the 1st and 2nd terms of the M.Sc. course.
(2)
Having initially satisfied yourself that the subject of your choice
fulfils the criteria above, you.ape advised to set out a very brief
outline of the proposed dissertation and to present this when
submitting the subject of dissertation for approval by the Head, of
the Department of Social Medieine and Public Health.
.
. ..
(3j .Each. of you will be assigned a member of -the Academic staff who will
advise you on the subject matter and writing of the dissertation.
You are, however, completely at liberty to consult any or all members
of the academic, staff, at any-wtually convenient time(s),.during: the.
writing of the dissertation.
(4)
The dissertation, is a means both for training and for assessing the
ability to pursue the study of a limited problem thoroughly,
objectively and critically, and to write a lucid and well-disciplined
report on such a study.
The quality of a dissertation, therefore,
does not depend on its length, but on the organization, manner of
presentation, and soundness of its contents.
(5)
Beware of the following which will impair the quality of a disserta
tion:
(a)
’*
Padding
with irrelevant material, however factual, interesting
or detailed this may be.
(b)
Making of loose or wild generalizations or statements which are
unsubstantiated or unjustified by available evidence.
(c)
Including only the ’pros’ "but omitting or forgetting the 'cons’
when pursuing a line of argument or when making recommendations.
(d)
. Failure to describe adequately the source(s) or nature of basic
material or data, or the methods by which they were obtained.
(e)
Making deductions from data without considering the limitations
imposed-by their nature or quality.
6.
Cognizance must be taken of other known sources of .information (books,
papers, reports,etc.) on the subject, and comparison, discussion,
reference, quotation and acknowledgement must be adequately made
where appropriate.
■(a)
For example:
If some other person has previously rep_orted_ op- a study of
similar nature, his findings..and conclusions must be mentioned
and, if relevant, compared with your own.
(b)
If a method, .technique, or procedure is used of which a .detailed
..............
.... ..jv J--l.L--1'-’'-'2
description is available elsewhere, reference must be made ±o the
literature concerned.
(c)
Where standard (conventional or otherwise) methods exist (say,
in classification, measurement, statistical indices, etc.)
these should be adhered to as far as possible, and adequate
reasons must be given for any deviation therefrom.
(d)
The sources of all information or opinion must be given, and the
references must be properly cited in accordance with a system
used by a respectable Medical Journal.
A list of references and
bibliography must be given at the end of your dissertation.
(References must include, where appropriate, unpublished or
personal communications in addition to published works.)
7.
There is no set pattern of presentation for dissertations - different
subjects require different treatment and presentation - but a useful
axiom might well be:
"Say what exactly you are going to do; do it;
and then say briefly what you have done.”
One point which needs to
be stressed is that whatever material or data are presented, they must
be carefully evaluated and discussed objectively.
8.
Do not spend too much time making the first draft of your dissertation.
Have this ready by the end of the first Term, so that the duration of
the second term will be available for redrafting and improving on it,
taking into consideration the queries and suggestions made by your
adviser.
Allow sufficient time for the dissertation to be type
written, proof-read, and bound, before the specified date for sub
mitting of dissertations.
The dissertation, when submitted, must be type-written (single face,
double spacing) and bound in stiff covers, with the title and author
clearly shown on the front cover.
9«
Free periods on the programme are intended to.be utilized for the
preparation of the dissertation.
Other, available free periods
resulting from cancellation of classes should also be so utilized.
N June last, some coal mines in Andhra
B
Pradesh, did not produce any coal as the
workers were forced to go on strike by
a section of the coalminers. It started because
a doctor at the collieries hospital would not
certify a worker as being unfit for duty. The
worker is reported to have tried to assault
the doctor and when the police whisked away
the worker, a splinter group forced a strike.
Thpmation was held to ransom and coal required
■ • by -many industries and railways could not
be produced'in adequate quantities. The coalmine
workers do not comeundertheEmployees State
. Insurance (ESI) scheme, but what happened
in the Bellampalli hospital is almost a daily
occurrence in many of the 89 ESI dispensaries
in the State, with workers swarming them to.
get certificates that they are suffering from
some illness or other.
Y. beseeching him to go on leave so that
he (X) could continue to work. Now. Y gets
sickness benefit and some "commission from
X for helping to get some wages During the
"sick leave" period, Y does not keep quiet
He either operates a cycle rickshaw or works
as a casual labourer elsewhere.
Indeed, many employers feel that sickness
certificates are being issued to workers very
liberally. They say that work is suffering because
of this. Absenteeism being on the high side.
production was going down They have often
complained that "sick" employees loiter in the
factory premises. Even the ESI Corporation
authorities seem to feel that the issue of sickness
certificates in Andhra Pradesh is on the high
side and have instructed that the practice be
curbed.
that the employees of an establishment that
engages more than 20 persons would be covered
by the scheme, beedi workers, those employed
in cinema houses, departmental stores and
such organisations are not covered. Since rice
mills and sugar factories are supposed to afford
only seasonal employment their employees
also do not come under the scheme. There
are about one lakh beedi workers in Nizamabad
and surrounding villages. If the ESI benefit
is extended to them. Nizamabad could have
a 400-bed ESI hospital The inspectors of the
Regional Directorate of the ESI Corporation
visit new areas to recommend the extension
of the scheme.
Dual control
Right from the day the ESI scheme was
implemented one has heard the complaint that
Leakages in benefi
Under the ESI scheme, a worker is entitled
to be compensated for loss of wages upto
91 days in a year when he is sick and does
not have any other leave to his credit. Where
a worker is having a chronic disease, he gets
wage benefit upto 309 days. If a worker suffers
injury during the course of work, the wage
benefit is doubled and there is no time limit.
He gets the wage benefits till he resumes
duty Unfortunately, according to the authorities.
many workers have been made to believe
that they are entitled to these wage benefits
as a matter of right, whether they are sick
or not.
But why do doctors give wrong
Certificates? A doctor answered by saying "when
la man comes to us saying he is having severe
stomachache and makes his condition appear
genuine, there is no method of finding out
that he is only a pretender." He pointed out
that invariably workers came complaining of
diard^a. "Sometimes we detain such persons
for groupie of hours under the pretext of
wanting to examine their stools. They either
run away or protest and try to attack us".
Weekly Edition —2
Sunday, October w, 1981 »
THE SfcSl HINDU
kwliaX Noddmal Meartpape/c
companies are reluctant to come under the
scheme as they feel that the managements
have made better arrangement for them One
labour leader commented that those who wanted
to increase productivity preferred to be outside
the ESI "which is meant only to help those
Hospitals under the Employees State Insurance scheme were
started to provide medical service to the workers. Many
malpractices are prevalent, resulting in dissatisfaction to all
the parties concerned — workers, doctors and employers.
P""M “
that the attention given to them was insufficient,
began to demonstrate They alleged that every
time a wound was dressed, the assistant wanted
money. The other complaints from the patients
were: The ward boy came in a drunken condition
and was habitually late by two or three hours.
There was no security in the wards and the
stainless steel tiffin boxes of the patients were
frequently being stolen, Dogs roamed about
freely even on the first floor of the hospital. •
taking away the bread supplied to the patients.
The cots and other furniture in the ward were
infested with thousands of cockroaches. Patients
As for the workers, they complain that
medicines are not easily available in the ESI
dispensaries and that the doctors do not examine
the patients properly. They feel sickness certifi
cates are not issued in deserving cases "while
it is given to undeserving cases quickly"
The ESI doctors have a different tale to
tell According to some of them, the patients
come and demand medicines which in their
(doctors') opinion the patients do not require.
Often, the workers bring prescriptions from
private doctors and without producing the pa
tients concerned, demand medicines. "Without
examining the patients we cannot certify that
they require certain medicines." Workers also
brought their neighbours' children or relatives
and tried to palm them off as their own demanding
treatment at the ESI dispensaries.
The
Directorate,
Insurance
Medical
Services. Andhra Pradesh, suggested to the
ESI Corporation that identity cards carrying
the photographs of the family members of
worker be introduced The Corporation did
not agree, as it felt that it was not feasible.
A growing child changed fast and looked.
after a period of months, different. Identification
marks were noted in the cards issued to the
workers but because of the rush of patients
it was not possible to check them. At the
ESI hospital in Hyderabad, a large number
of purdah-clad women turn up at the out-patient
department. It was difficult to verify their identity.
Doctors explained that workers complained
of shortage of medicines when they brought
prescriptions from private doctors who pre
scribed medicines with trade names Not all
medicines with trade names were under rate
contract. Therefore, the doctors made available
substitute medicines which were not acceptable
to the workers. One doctor pointed out that
the Indian Drugs and Pharmaceuticals Limited
gave raw materials to two other pharmaceutical
firms in the country who marketed the same
substance under different trade names. The
ESI made available the drug marketed by the
IDPL itself.. The workers seemed to think that
the doctors were deliberately not giving the
drugs marketed by the firms.
The doctors also said that if they insisted
that the patients be examined by an ESI doctor
or that the prescription should be from a specialist
to whom the patient was referred to by the
ESI the workers resented. The patients also
wanted medicines to be issued for a full month
"to avoid the inconvenience of coming to the
dispensary frequently" It was pointed out that
in Warangal town, tuberculosis patients were
given tablets and drugs for a period of one
month on the understanding that the patients
would take the injections regularly. But the
injectibles found their way to the market. The
patients’ conditions deteriorated Unmindful of
the loss of their health, they were interested
in making money in two ways — through
sickness benefit and by selling the drugs The
ESI doctors have begun to insist on the patients
coming once in three days. It has
helped in
medicines being administered to the patients
but also in regulating the dosage depending
on their condition
/ '
■
.
/
A doctor treating a patient at the ES I. hospital in Hyderabad
there are not sufficient number of doctors in
the ESI dispensaries and hospitals. There is
dual control over the ESI scheme. The ESI
Corporation is in charge of collection of the
employers' and employees' contributions,
disbursement of cash benefits and survey of
new areas for the extension of the scheme
The State Government is in charge of the
who want to be absent and yet get some
wages".
A charge against the ESI staff is that
they are not dedicated. A visit to the out-patient
department of the ESI hospital. Hyderabad
on October 12 showed the staff numbers were
not to be seen, as scores of patients had
reported an improvement in the situation for
some time, but with the "old cases" moving
out and new ones getting admitted there was
again deterioration in the services.
Insufficient space and staff are responsible
for the allegation that proper attention is not
being paid. The corridors of the OP department
••
1are very narrcy
run away or protest and try to attack us".
worker be introduced. The Corporation did
not agree, as it felt that it was not feasible.
A growing child changed fast and looked,
after a period of months, different. Identification
marks were noted in the cards issued to the
workers but because of the rush of patients
it was not possible to check them. At the
ESI hospital in Hyderabad, a large number
of purdah-clad women turn up at the out-patient
department. It was difficult to verify their identity.
Doctors explained that workers complained
of shortage of medicines when they brought
prescriptions from private doctors who pre
scribed medicines with trade names. Not all
medicines with trade names were under rate
contract. Therefore, the doctors made available
substitute medicines which were not acceptable
to the workers. One doctor pointed out that
the Indian Drugs and Pharmaceuticals Limited
gave raw materials to two other pharmaceutical
firms in the country who marketed the same
substance under different trade names. The
ESI made available the drug marketed by the
IDPL itself. The -workers seemed "to think that- the doctors were deliberately not giving the
drugs marketed by the firms.
The doctors also said that if they insisted
that the patients be examined by an ESI doctor
or that the prescription should be from a specialist
to whom the patient was referred to by the
ESI the workers resented. The patients also
V wanted medicines to be issued for a full month
Jt "to avoid the inconvenience of coming to the
". dispensary frequently". It was pointed out that
in Warangal town, tuberculosis patients were
given tablets and drugs for a period of one
month on the understanding that the patients
would take the injections regularly. But the
injectibles found their way to the market The
patients' conditions deteriorated. Unmindful of
the loss of their health, they were interested
in making money in two ways — through
sickness benefit and by selling the drugs. The
ESI doctors have begun to ihsist on the patients
coming once in three days. It has
helped in
medicines being administered to the patients
but also in regulating the dosage depending
on their condition.
At Nellimarla and Chittivalsa, tablets issued
to the "patients" were found strewn outside
the dispensaries some months ago. They were
thrown away by those who were more interested
in the "sickness certificates" than the medicines.
•'
Maternity ward
A man availing of sickness benefit
sometimes has a three-fold advantage. In one
town of Andhra Pradesh, a textile mill employs
“badli" workers when their regular workers
go on leave. If X were on relief duty and
were to know that the man he was subsituting
for was to return for duty, he would approach
The doctor is obliged not to give false
sickness certificates. Sometimes they arecoerced and some have said that inducements
too are held out to them. When workers do
not get leave in the normal course, they try
to get "sick'' so that they can then get "paid
leave". Workers wanting to go for harvest
or to be at home for festivals or marriages
resorted to this gimmick. Where the ailment
did not require hospitalisation, doctors have
started insisting on the patients turning up
at the dispensaries at frequent intervals
Not all workers in the State are covered
by the ESI scheme Though the ESI Act says
A doctor treating a patient at the E.S.I. hospital in Hyderabad.
there are not sufficient number of doctors in
the ESI dispensaries and hospitals. There is
dual control over the ESI scheme. The ESI
Corporation is in charge of collection of the
employers' and employees' contributions,
disbursement of cash benefits and survey of
new areas for the extension of the scheme.
The State Government is in charge of the
medical part of the programme, providing
doctors and nurses
Doctors posted to the ESI hospitals and
dispensaries are reluctant to join them. An
ESI doctor is not allowed to have private
practice and gets Rs. 200 per month as non
private practice allowance. Despite this, there
are doctors who have private practice.
In many specialities, there are no doctors
in the ESI hospital. For example, at Hyderabad,
the post of orthopaedic surgeon has been
vacant for over a year. There is no physiot
herapist. TB patients are referred to the hospital
for chest diseases where only. 25 beds are
reserved for workers.
Employees of organisations like the Bharat
Heavy Electricals Limited. Andhra Pradesh State
Road Transport Corporation and,some cement
who want to be absent and yet get some
wages".
A charge against the ESI staff is that
they are not dedicated. A visit to the out-patient
department of the ESI hospital, Hyderabad
on October 12 showed the staff numbers were
not to be seen, as scores of patients had
gathered at the counter. One patient who had
been brought from Uppal 20 kilometres away.
was neither able to sit nor stand and was
writhing with pain. Perhaps, it was a case
of appendicitis. For over half an hour, he
lay on the floor, contorting himself into all
positions before he was given an OP ticket
Earlier this year, there was an unusual
strike in the ESI hospital. Hyderabad. It was
not by the doctors or the nurses but by the
patients. The inpatients of a male ward, finding
Genuine
patfeots
suffer
HE ESI scheme, unfortunately seems to
have side-tracked from its main aim. It
is pointed out that some doctors attached
to the ESI. issue certificates to favour a section
of workers, and authorise the distribution of
medicine that often ends up in the black-market
This causes a temporary, scarcity of essential
drugs, apart from harming the cause of genuine
patients Other complaints are that comparatively
healthy people occupy beds which could have
been utilised by people suffering from acute
diseases, and that the quality and quantity
of food served in the hospitals leave much
to be desired.
T
It is interesting that participation of the
trade unions in the ESI scheme does not seem
to have done very much to check corruption.
Some employers are also known not to fulfill
*
the
commitments, and the Government draws
up a list of them every year Officially there
is also a free advisory service available to
anyone connected with the scheme However
there are not too mapy callers.
Initially when the LSI scheme was in
troduced m 1955. in W.Bengal. all' industrial
reported an improvement in the situation for
some time, but with the "old cases" moving
out and new ones getting admitted there was
again deterioration in the services.
Insufficient space and staff are responsible
for the allegation that proper attention is not
being paid. The corridors of the OP department
in the ESI hospital, Hyderabad, are very narro^^
and when patients crowd there, there is hard|^
space to move about. With more and more
industries being brought under the scheme,
there, is need to increase the staff and provide
more accommodation, those connected with
the scheme say.
Hyderabad Staff
Reporter
units using power and employing more than
20 persons were brought under its purview.
But later, in case of power using factories.
units employing between 10 to 19 workers
were also included. The scheme was also ex
tended to restaurants, cinemas, theatres, hotels
and road transport establishments. In the beginn
ing only those drawing less than Rs. 500 a
month were covered by its provisions. In 1975,
the range was raised to Rs 1,000 a month
group. At present, nearly 10.000 factories, head
offices, branch offices, sales offices etc. arfl
covered by the ESI scheme, serving directly
around 1.1 million employees in the State.
and indirectly over 3.5 million people are served.
Annually, around Rs. 10 crore are paid
to insured employees as cash benefit, the amount
increasing steadily over the years, the rate
of
permanent
disablement
benefit and
dependents' benefit were increased by 10 and
20 per cent respectively in 1977. Cash benefits
are also distributed through a network of 54
offices.
The bulk of the relief -is accounted for
by sickness benefit, amounting to nearly half
of the total official payments. Payments .are
made also for maternity, family planning, funerals
and on other heads.
On an average, well over 1,00.000 accidents
are reported annually. The ESI authorities have
made effective arrangements for procuring artific
ial limbs form a specialised centre in Pune.
The ESI authorities run eight general and
one tuberculosis hospitals in the State, while
they maintain a number of beds in other general '
hospitals Around 36.000 patients are treated
annually.
Painters exposed to
serious ailments
T
HREE years ago. in response
to an increasing number of
its members who were
reporting strange and debilitating
illnesses.- the International Brother
hood of Painters and Allied Trades
artG 4 running an "Ask the Doctor"
. in its journal. The letters
is
zd in.
"I told the foreman I was getting
numb around Jhs mouth and in
my hands." one painter wrote. "A
stationary object would move as
I dfced toward it." wrote another.
Araroccording to another. "I knew
the solvents must be bad because
when we came in to work each
day we had to haul dead rats
out of the rooms we had painted
the night before."
There are about 400.000 painters.
paint makers, sign painters, silk
screen printers and tile and carpet
layers in the U.S. who work with
coatings or adhesives made with
aromatic hydrocarbons and other
solvents, often in places that lack
adequate ventilation. Many of them
have complained for years of
feelings of dizziness or intoxication
while on the job.
recently, as paint maufacture^T have incorporated new
chemicals in their products and
as the toxicity of some,' such as
toluene and benzene, have become
more widely known, many industry
□Mka number of government and
officials have come to share
the conclusion of Mr. Frank Raftery.
the painters' union president, who
said:
"Toxic chemicals are a major
threat to painters that rivals or
exceeds the better-known health
threats to asbestos workers and
even to coal miners."
Dr. John Froinds, a government
toxicologist, who is acting Director
of the National Institute for Occupa
tional Safety and Health, agreed
that the chemical compounds in
paint presented "new and serious
problems."
"We are concerned about the
hazards of painting to such an
extent." he said, "that we are
conducting extensive research into
the carcinogenic and neurotoxic
effects in the workplace. Obviously, the United Automobile Workers an occupational safety official at
further research is needed to and the American Federation of the' painters’ union, the first
evaluate these problems."
Labour and Congress of Industrial symptom of neuropathy is de
Organisations have set up special pression.
and
"the
poisoned
Neurotoxins are poisons that de- departments to investigate the workers find it very hard to write
stray nerves or nervous tissue, problem.
us about It. much less to bring
resulting in neuropathy, ora dysfuncRelatively few negligence or pro- lawsuits."
tion of the way the nervous system duct liability cases have been
. usually works.
brought against the manufacturers
Among painters and others exof the chemicals, paints, lacquers, posed to solvents for long periods
Major segments of organised adhesives. and plastics that contain in poorly ventilated areas, the
labour have shown increased con- potentially neuurotoxic formulations symptoms • of toxicity often begin
cern about the effects that these with names like methyl-n-butyl with on-the-job dizziness, exhilaraand other toxic substances have ketone, toluene di-socyanate and tion. headache, blurred vision and
upon employees in the workplace, dimethylamino
proprionitrile. slurred speech. Sometimes they
In the last year the painters' union, According to Mr. Rodney Wolford, progress to hallucination and
permanent disorientation, paralysis
i
and other symptoms of injury to
the central nervous system.
A mortality study conducted for
thf- P lint - - union among workers
d their life expectancy to be i 1 years less than
the a .mirage American's.
.
In 1975 a pioneering medical
survey ol 1000 painters paint
makers tile and carpet layers and
wood finishers found that 71 per
1 b
i d reported some
to-"n reialed disorientation on the
J°b Ai Tariv as four Per cent
s'"ci 1
had 0" consci°usness
while working
' ■
•
X** -*-/
1
i
I ne study by Dr liming J Selikoff
°i Mount Sinai Medical School
1 tj'.'-rd that painters exposed to
soivonts were more likely to have
accidents such as falls from scaffoldings and trial they had potential'k dangerous difficulties driving
home from work
More recently a study of paint
hazards by the Johns Hopkins
University School of Public Health
found that there were minimally,
over 300 lox,c matG"a,s and 150
carcinogens potentially present in
J&TO1points Fifty seven per cent of the
$KT<,jgH!
I "t 1 al id'rttfAd m the study
rire -11
111 l,c Ri?Jist'.y p' Toxic
Substances
compiled
by
the
V "» S.1'
J X’**
' ’"''
°ccu| rational safety institute
More recently, a study of paint
hazards by the Johns Hopkins
University School of Public Health
found that there were “minimally.
over 300 toxic materials and 150
carcinogens potentially present in
paints." Fifty-seven per cent of the
paint solvents identified in the study
are listed in the Registry of Toxic
Substances compiled
by the
occupational safety institute.
One of the first acts of the Reagan
administration was to table a pro
posal for more explicit labelling
of all the hundreds of thousands
of products containing chemicals
that are known to cause symptoms
of toxicity in high concentrations.
The products are used by an
estimated 25 million American
workers, according to the Labour
Department's Occupational Safety
and Health Administration, which
developed the proposed regulations
in nearly five years of negotiation
with,the chemical industry.
Under the proposal, the labels
would have listed the products'
ingredients, given more specific
directions for their, use and de
scribed symptoms and treatment
of toxic reactions.
Since the proposed labelling
regulations have been tabled,
representatives of labour have been
moving on State Legislatures in
an effort to enact all or part of
the labelling rules on a state-by
state basis.
. But if states adopted conflicting
requirements for the labelling or
the use of potentially toxic sub
stances, one chemical trade associa
tion official said, "That would drive
the industry right up the wall, and
we might end up actually going
for some federal regulation." —New
York Times.
fiMUPAlWNALHEALIH
vooc
PRESIDENT’S
Members of the Delhi Branch of I.A.O.H. in
electing me as their President have laid a big
responsibility on me. Whereas I am grateful to
them for this expression of confidence in me, I am
very conscious of the responsibilities which I have
to shoulder during this period. This Branch being
so young has lot of teething problems which have
to be overcome.
My predecessor Dr. S.S.L. Verma with his
dynamic leadership infused life into this new
Branch of the Association and organised the
Branch with the help of so many of its active
Members snecially Dr. B.N. Bhattacharjee, Dr.
H.C. Govil, Dr. Gupta, Col. S.L. Chadha and Dr.
Pran Nath. The remarkable work done during
1976 in organising the All India Conference of this
Association is a standing proof of the capability in
organising, of the Members of this Branch.
Whereas we do not have to organise another All
India Conference of the nature done in January,
1976 in near future, there are lot of other activi
ties which we have to do to keep the Association
alive and kicking. For any Scientific Association
of this type with a narrow and limited scope like
Industrial and Occupational Health, it is essential
to my mind that we have a set of dedicated workers
to take the lead and keep on doing interesting and
useful activities throughout the period.
Personally I feel that for the Delhi Branch of
A.O.H. to be active, it is essential that its
I.
membership must increase to atleast three-fold of
what it is. Unless we have about 100 Members
we cannot expect in our Scientific Session, an
attendance of 30 to 40 every time because due to
other engagements and being out of station, a
number of Members cannot attend every meeting
inspite of their desire to do so. Every Member
therefore, and the Members of the Executive in
particular have to spread the message of this
Association amongst the Medical as well as non
medical officials in the Industry and different
occupations and try to enrol as many members as
possible. Whereas Dr. Pran Nath and few other
members have shown responsibility in this direc
tion efforts of others resulting in increased
membership is still awaited. For this we should
approach the Medical Colleges and specially
departments of Social & Preventive Medicine to
become members. This will not only increase
Dr. J. C. Mehta
M.D. (Med)., MRCP., M.D. (Hons), S.P.M.
Chief Medical Officer, Northern Railway
the Membership, but enrich the quality of scientific
work done by us. I am sure with a proper approach
most of the staff of departments of Social and
Preventive Medicine in the Medical Colleges would
like to join. Members from big Industrial Houses
should also be searched.
It is also essential that our Association holds
some Refresher Courses about Occupational
Health to prove its utility to the community. The
Scientific meetings have to be regularly organised
giving enough time for the participants to ensure
their attendance and fixing the venues in such a
way that it is convenient for most of them to
attend. Apart from the talks on useful and
interesting subjects, symposia and seminars should
be held at these Scientific meetings. For the
annual conference of the Association at Ahmedabad, we are sending some Members so that full
participation of this
Branch is ensured.
Suggestions from all doctors to infuse more life
in the Delhi Branch will be most welcome and
should be offered without hesitation.
I wish the very best for our Association and I
am sure with the help of all of you, we will be able
to improve this Branch further.
From Editor s Desk
Industry is the bulwark of any nation. No
industry can proceed at full speed unless its
individual human units remain healthy both phy
sically and mentally. The worker’s health is
really vital to the quantity, quality and continuity
of production. One skilled worker’s absence
because of preventable illness can greatly disturb
the smooth functioning of the production line and
cause losses out of all proportion to expectations
because of disruption of team work.
In addition to non-industrial causes of illness,
the industrial employees which include the
workers, supervisory and management personnel,
are particularly exposed to specific hazards which
are attributable to various industries and occupa
tions.
Administration of curative medicine and surgery
only, is not enough to keep them healthy. There
has been tremendous advances in industrial and
occupational health specialities with particular
stress on industrial hygiene and toxicology,
sanitation and health, conservation procedures,
role of nutrition, fatigue control, mental hygiene,
vital statistics and adaptation of the worker to the
job through job analysis aptitude and psychological
test. It is the application of these advances which
is a must to improve and maintain the health of the
workers. Remedies have to be found and provided
to prevent industrial accidents and occupational
diseases.
The efforts of those who have been identified
with the conservation of the health of the working
population must be intensified. Industrialists and
physician must contribute their share in the
responsibility for keeping the employed physically
and mentally fit, thus protecting the manpower
behind our industrial mobilisation which is rapidly
growing.
If we as members of this association become
thoroughly conscious of our responsibilities and
opportunities and to our scientific knowledge of
medical diagnosis, prevention and treatment we
add an equally thorough knowledge of the best
economical, political and social methods of
applying that knowledge to the good of both the
employers and employees alike, the public, the
Govt, and the employers will be willing to listen
to our suggestion and seek our advice.
DR. MAHESH CHAND GUPTA
Editor-in-Chief
We have done it.......
Hotel Hygiene Course
The hotel hygiene course was conducted for the
Indian Tourism Development Corporation, hotel
supervisory staff from 3rd to 5th August at the
Lodhi Hotel, New Delhi through lecture demons
tration and panel discussions and film shows and
by conducting this course, the Delhi Branch earned
Rs. 800/-. The lecture course was designed by Dr.
B.N. Bhaltacharjee, and Dr. R.K.. Sen Gupta.
Other courses were held in 1975 at the Ashoka
Hotel, Oberoi Intercontinental etc. and in 1975 the
Delhi Branch earned about Rs. 3000 from various
groups of hotels.
Consultancy Services.
The Delhi Branch designed consultancy services
for the small scale industries who have no resources
to look after the health of the workers as well as
in designing the safety measures for prevention of
accidents and environmental pollution etc. Dr.
Pran Nath, Certifying Surgeon, Haryana and Mr.
Jeeta Chandra, Chief Engineer, Gedorc Tools of
India who are very active members of the Delhi
Branch rendered this consultancy service at the
Faridabad Industrial Complex. It became quite
Popular and they have received requests from the
bigger industrial complex like Escorts, Modipon
etc. for rendering such consultancy service.
Technical meetings
Two technical meetings were held, one in the
Ncrthern Railway hospital, New Delhi where Dr.
J.C. Mehta, reviewed the strong and weak points
of the Delhi Branch activities in relation to holding
of the annual conference, as well as the summary
of the technical papers.
A second technical meeting was held at
Faridabad where Dr. Pran Nath read a paper ‘On
occupational Health hazards in engineering indus
try’ and Mr. Jeeta Chandra, Chief Engineer Gedore
read a technical paper on “Engineering central of
certain Occupational Health hazards in Engineering
Industry”.
Discussions with INTUC
Secretary, Delhi Branch took up the initiative
for motivating the INTUC for creating conditions
for improvement of the health of the industrial
workers, and as also for establishment of ‘Holiday
Homes’ for providing rest and recreation facilities
for the workers.
The Delhi Branch held its annual general meet
ing on 16th October, 1976 and the executive com
mittee was formed after due election. The branch
members conveyed their thanks to Dr. S.S. Verma,
Ex-President for his excellent leadership during his
tenure of presidentship.
Dr. J.C. Mehta, Chief Medical Officer, Nor
thern Railway, Baroda House, was elected as the
new President for the year 1977.
Future plans
During the last meeting of the year 1976 the
Delhi Branch drew up a programme for year 1977
as under:-
(a)
The Delhi Branch will publish a quarterly
newsbullitin from January, 1977 to keep all the
members informed about its activities and also for
facilitating exchange of views. This bulletin will
also threw some light on matters of importance in
the field of occupational health in India and other
parts of the world.
(b)
Membership campaign: The Executive Com
mittee decided that all the members of this com
mittee should make at least two new members
personally and contact various industries to send
their representatives as a member of this branch.
It will not be out of place to mention here that Dr.
Pran Nath, who is the Vice-President of the Delhi
Branch, had succeeded in enrolling 16 members
upto February, 1977.
(c)
Technical meeting: Delhi Branch has deci
ded this year to hold 6 technical meetings, one each
at Gaziabad, Faridabad, Modinagar, DCM factory
and two at the headquarters.
(d)
Production of a booklet on Indian Occupa
tional Health: The Delhi Branch has decided to
produce a small booklet for depicting the aims and
objectives of the IOH and distribute it to the indus
tries and trade unions as well as to others interested
in the field.
(e)
This branch has also mooted the idea for
establishing intimate contact with various ministers
connected with industry i.e., the Labour Minister,
the Health Ministry, Ministry of Petroleum and
Chemicals etc., Ministry of Railways etc. It also
proposed to make a liaison with Trade Union
Congress, ILO, WHO, UNICEF etc. so that the
image of the Delhi Branch of the Occupational
Health Association comes upto expected level. The
Branch has also proposed that it is ready to work as
a liaison office for the IOH headquarters at Delhi,
in order to raise its image in the eyes of the ad
ministrators of the country.
(f)
Workshop of occupational health : The
Branch has also decided to hold an annual multi
disciplinary workshop on occupational health in
the month of October, 1977. The details of the
workshops are under preparation.
(g)
The Branch also proposes to hold a National
Seminar in 197$ at Delhi, with the approval of
IOH. It is strongly felt that this seminar would
contribute greatly and provide the necessary plat
form for the exchange of newer knowledge and
experience in the field of occupational health bet
ween top-specialists of national and international
eminence.
GLIMPSES
OF
ANNUAL
CONFERENCE
Dr. Karan Singh
Union Health Minister
Inaugurates the
Conference
A view of Conference Delegates
The Delhi Branch hosted the 26th Annual
Conference from 10th to 12th January, 1976 at
Vigyan Bhavan, New Delhi. Dr. Karan Singh,
Union Minister of Health inaugurated the Confer
ence and Mr. Bal Govinda Verma, Deputy Minister
of Labour in his key-note address, highlighted the
role of the Indian Association of Occupational
Health in preventing accidents and promoting
safety of the health of the workers in the country.
High dignitaries like the Director General of
Health Services, representatives of W.H.O., l.L.O.
and Press Information Bureau were present in the
inauguration ceremony.
About 150 delegates from all over the country
attended the conference for three days continuously.
52 technical papers were read by the various spe
cialists in the field of occupational health. Dr. J.C.
Mehta, the Convenor of the Scientific Committee
accommodated every person to read their technical
papers even though it was presented in the last
moment. On 12th January a field visit was arranged
for all the participants to see the Faridabad
industrial complex in Haryana. They were served
with delicious lunch at the picturesque site on the
banks of the Bhadkal Lake After returning home
from Faridabad, the first Central Council meeting
was held at Delhi under the Chairmanship of the
new President, Dr. S.C. Chakrabarty.
Preparatory Committee
Meeting
Scientific Session in Progress
Dr. Karan Singh at
Occupational Health
Exhibition
Award giving Ceremony
Modern Trends in Future
Environmental Hygiene
Studies
By
Dr. B. N. Bhattacharjee
Introduction
Some Selected Problems
The old concept of health hazard to the workers
in the micro-environment is now fast changing
because the industrial workers are also exposed to
the pollution of macre-environment. It may be
very difficult to prove where the workers acquired
these health hazards, particularly, terratogenic,
mutagenic and carcinogenic conditions. In the past
many of the studies have proved that minerals and
heavy metals like lead mercury, zinc, manganese
etc. caused health hazards and diseases in the nticroenviionment of the industry. Emission of sulphur
dioxide, carbon monoxide and other gaseous sub
stances and dust in air as well as the industrial
effluents thrown in the water or land have been
important contributing factors for macro-pollution,
outside the industrial establishments. But the total
environmental pollution is now known to be caused
not only by industry but due to the increase in
population, disposal of untreated sewage, garbage
and other wastes by the local authorities in the
water or land, use of new chemicals, DDT & ferti
lizers etc. It cannot be denied that industrial growth
creates problems of effluent and waste in natural
environment, but the urbanisation of human settle
ments, supplies of basic requisites like water, hous
ing, transport, thermal power can all have adverse
effects on the enviroment in the absence of careful
planning. Some of the major environmental side
effects have known to accompany in varying
degrees, the process of development in agriculture,
transport and human settlements. Studies should
be taken up about the new pollution in the
micro-environment of the industry and its effect
on the worker as well as vertical studies on the
health of the worker at the macro-pollution level
wherein the workers are exposed to health hazards
for the second lime. Some points for future environ
ment hygiene studies in the industries has been
highlighted in this paper keeping in view the future
trends of environmental pollution to occur with the
growth of science and technology, affecting the
various aspects of human life.
It has now been proved in many countries that
by reducing the total quantity of pollution to which
one is exposed over a life time could greatly reduce
morbidities and deaths from several chronic diseases.
As such a study has to be developed for the workers,
taking into account all their social, psychological,
socio-economic life and living conditions. A valua
ble instruments in the activities of this kind should
be the utilisation of special work environment,
hygiene studies and laboratory examinations.
Current work operations can be critically examined
in some cases by building up essential segments of
operations, introducing modifications and then
testing them. The exploitation of the development
of new technology aimed at improving conditions
of different work places is a task deserving high
priority. But it is a task that must be pursued sys
tematically. Manufacturing firms, industries, safety
authorities and even trade unions and managerial
personnel must ststematically identify problem
areas, define sub-problems and by commissioning
experts, to tackle them, and explore some solution.
Public bodies entrusted with the responsibility for
research and development programmes in the
technology, medicine and the behavioural sciences
must support, initiate and coordinate all research
and educational projects in order to (1) lay a better
foundation for concrete solutions and (2) open
opportunities for new or alternative process which
promote equally good products to be made without
inflicting deletirious effects either on the worker’s
environment or on the external environment.
Of late many industrial countries have rapidly
increased interest in the problem of work environ
ment. Greater demands have been raised to abate
risk of accidents and to reduce the perils of health
of the working population. Thus the points of
consideration are mainly:1. Preventing occupational risks.
2.
Promotion of health.
3.
4.
Capacity for work.
Social security for workers.
To solve the above mentioned points microenvironmental assessment and its management
inside the industry should be planned. The points
for consideration with regard to protection of
health hazards caused to the industrial workers in
the macro-environment are (1) Public-laws, (2)
Technical cooperation, (3) funds, (4) public opinion
and (5) Trade Union movement.
Need for future environmental hygiene studies in
Industry
Much of the documents and data are available
in relation to micro-environment and its effect on
the health of the workers. But with the introduc
tion of new chemicals and synthetic materials in
the old industries unknown health hazards are
perhaps creeping in. An example may be cited in
this respect caused by poly Vinyl Chloride. PVC
was thought not to harm workers health until an
unusual condition affecting the bones of the fingers
of the workers was first reported in 1960’s. This
condition became known as acro-esteolysis (AOL).
In early 1974 reports appeared that liver cancers
are being found in experimental animals. This type
of cancer is known as angio-sarcoma. Now it has
been proved in U.K., Sweden, U.S.A., and USSR
that uncontrolled doses of this Poly-Vinyl Chloride
has caused angiosarcoma and consequent death of
industrial workers. Perhaps many more synthetic
materials and chemicals are producing unknown
insiduous diseases amongst the industrial workers
for which vertical studies are needed. Increase in
the incidence of cancer in the highly industrialised
countries has been linked up with the environment
al pollution but no exact identification has been
possible whether it was due to work in the micro
environment or due to pollution of the macro
environment. We are aware of many acute diseases
related or emanating from the industry, than about
the chronic effects. Little is known about sinergisitic effects of different circumstances or agents in
inter-action but now we know that they do occur.
More recently, support has been found for the
opinion that reducing the total quantity of pollu
tants to which one is exposed over a lifetime could
greatly reduce the morbidities and deaths from
several chronic diseases. If the liftime lead imposed
by polluted air in highly exposed areas were to be
cut in half, diseases of the respiratory tract would
decline sharply. To mention just one example
effect of Air pollutants both in the workplace and
outdoors may be cited. The best promise of achiev
ing substantial reductions is to tackle pollution
where the percentages are highest, that is at the
places where people work.
A close interplay obtains between the environ
ment of work and the external environment i.e.,
between microclimate and inacroclimate. It is the
strain imposed on man round the clock from all
sources that is counted. From now on, therefore,
every effort must be made to demolish the present
contrived barriers between work environment and
the surrounding environment.
A programme to improve the work environment
in line with the present of aspirations would definitly incur extra annual outlays. Hence the massive
effort of work environment cannot be implemented
without affecting on the wage levels, i.e. the way of
allocating wage costs into wages, social and health
services, preventive measures against occupational
hazards etc. International rules on aspects of
health upon work environment may contribute to
reduce these difficulties and will be of general value
to protect and promote the health of man at work.
Conclusion
By 2000 A.D. India’s population will be around
950 million and 35% of which would be engaged
in industry. Unless environmental hygiene studies
are undertaken seriously by them at the work place
as well as in the community, outside the manufac
turing units, new health hazards due to environ
mental pollution cannot be put to a halt.
Modern trend of environmental hygiene studies
is a team work. The various dimensions of the pro
blems has to be tackled by engineers, doctors,
chemists, plant managers and trade union who will
have to find out measures to prevent the dangers
of health hazards and risk of new diseases.
WITH BEST COMPLIMENTS FROM
INDUSTRIAL MEDICAL ENGINEERS
Safety Consultants & Manufacturers
Caxton House, 2E Rani Jhansi Road New Delhi-110055
Tel • 275228
Gram : Vaqupet
Distributors '■
JARDINE HENDERSON LTD.
4, Clive Row, Calcutta-700001
3
Providin'- treatment rcrvice-to maintain a safe
and healthy v-orkinc environment by providing prompt
one efficient initial treatment of lllnrroes and
injuric? at ■. ork. This also provides r r-idcmiological
evidence ai hazards.
1■
'•
■.
-'r •' h&al'. . .
rds„
■ 1lain,tin
•.h:
by ru-r-'.i-.ut.ion of the process or at least
:y rucce'T.fully c:or.< r oil ■' ng the ill-cf f< cts.
''•»
’..< search r.nd i.'e velop; • rd.- by Identifying the unrecognized
hazards. ?elective •.•■..
*:
in identifying health hazardsfrom tapparently trivial that interfere ■ 1th comfort
■. .ie ■ ney to " ■ ■ •
er life. .
; on
•.'■ays to control them.
Thir
p?nr r on v a distinct typer. of enquiry:
{a) The clinical observation of sick individuals who
seek. tr< atment.
(V) riel-’ rjr.-y rr.-’ or epidemiological methods.
r on 1 •:■■■■■ to further our medical benefits also.
■•
5 __
■ . ■
■-
the at Mention
-r peonies considering fatigue and
;j
■ "■ •"svcbo-t-oi.ial factors.
6.
. ning far
■1
early rvidi-nce of any disc-act "hat may fc ;-rtt.tnp inboth occu! ational
n?.-.~occur-utior-.l. In p.-.rtleu’ar,
occupational health service glvrc, unrivc?..u-d opportunity
for identifying; and dealing v.ith mental illness in its
very early stages.
7.
’ xecutive he alt’-
3.
Psychological pidoncc and councvliir-.
Jccu'at tonal
health here serves by i uo different tygef of courselingi
*
firs', at ,itter./a; er for treat™ nt and other routine
c:;amination!5-thir ranges iron simple advice about a
specific complaint to a
extensive counseling about
personal, social, emotional and even economic problemssccondly rhrn employees come voluntarily for advice
a! out a much broader problerc connected ■ itb their
ork or domestic life, Psychological guidance ,.jk?
counseling forms an important and useful function of
'.ccupationol Health Service.
9.
Health education •
individual
: rv'..r: ?y aducatingi
towards healthlr-r
r of living.
rvision.
1
™
10.
Cuprrvicion of • -elfare amenities especially
cant'm anr.: periodic checks of Kitchen.
•.preial periodic ry; na*ions of food handlers
and cantr ■■n staff,
Thue »>;r go on ....
triv.fr: , tinlrc'.ly, -stretching our arms and
xenir.:- health in all its aspects.
a)
b)
Addaptrd fron
;.r
-J
•
(: --owrnrr-T.T of India ifcdrrinkino)
Pich irerrun I'niVr T-lant
*
Tiruchiraram - 620 014.
Occupational Health practice, R.S.F. Schilling,
Butterworths, London 1973.
J
(Handout of Ross Institute Unit of Occupational Health
St. John s Medical College, Bangalore - 560 034. )
Ju- ■> <~tr!7y, thr
. • ■■
’
■
"
*. i"
■' R’. ly '••x'xrtful M
:orr. ■:
h» co.r-unity hr
—
'
-7;
1th st rvla htw
...._•„
• '
■;
?«• iS-' -hr
'*
•_
vl«u'! in the
|J ■
•; '
arc pmutf <r. isol^-’Jo.
acL;.V’-? If? oi' 'h<-
7rrz.»
s: rvicr? -.u
* i > < nrco i•.•-•.•••ulatio:scrc^.rurs of hi-al'l; cerv'ic':
b tots’
ai-JFft.
a
:-i -1V
' rlr.x.'"’-' h-71’
irntG.
77.;T;
.1.;
iv) If the villagers are willing to contribute their share
by:
1. Agreeing to pay a snail insurance charge
2. Agreeing to do Shramdan for some health projects
3. Agreeing to contribute volunteers that will help
run the health programme-.
v) If some date is already available about that area due
to previous or on-going survey etc., either in connec
tion with a health programme or as a.part of general
development activities.
2. Total Population Coverage:
The whole population must ' e covered.
Priorities :The weak and the. vulnerable: Children below 6
Fxpectant mothers
Nursing mothers
Promotion of health and prevention of disease.
Nutrition, Sanitation, Immunisations & Health Fducation
Adequate simple records.
3. "Health Insurance:
Fvcry body pays.
There may he a graded scale, depending upon the economic
status.
Advantages:Greater interest taken by the community.
Greater community participation.
People feel they own the programme-and it is their
(as indeed it always should be).
People who pay can also ask for good services, and
who can complain if the services are not good.
Keeping accounts develops the idea of accountability.
People do not value the treatment that is given free.
They may even throw away expensive drugs, thinking
them worthless.
Getting things free is not a good habit. It should
be discouraged.
Some people consider it ethically wrong to give sor
take things free.
There is ho such thing as FRFF. If the villagers are
not paying for it, somebody else must be paying for it.
4. The National Context and Constraints:
Ours is a poor country.
Cur health services should be affordable on a countrywide
basis, perhaps adding upto a few rupees per head per year,
It is no use creating an IFFAL or achieving "excellence
*
which cannot be copied on a large scale.
• • •Contd/3-
Instead, we should r-ncouracc local leadership, local
initiative and self reliance. At a practical level,
■ve should select suitable educated young men and women
from the vil lages themselves, and train them as health
workers. We should also involve the community in all
health work, right from the stage of planning onwards.
9. Community Participation;
A community should consider the health services as
their own. Community participation is the sine qua
non of any successful community programme. This is
one reason why the community must pay for its health kr
services partly, if not wholly.
The community must be involved in all stages of the
community health progra.me, including decision making.
Important areas of community articination;
Planning.
Financial contributions.
Selection of workers from the community.
Fvaluation of their work.
Village Health Conmitires can play a very useful role
here, as already mentioned.
10. Special Role of Health Education;
Health education is essential in a democratic set-up in
order to elicit the willing and enlightened cooperation of the people
It increases peoples competence to look after their own
he-1th, thus fostering self-reliance.
It helps people take greater interest Ln their health
services.
It helps people identify incompetent workers or incorr
ect measures.
FveryBody is interested in the working of his/her tody,
and in health. They will pay attention if health education is imagir
alively carried out, using for example puppet shows, one act plays,
practical demonstrations, mobile exhibitions, etc.
The following tonics should be covered:
First-aid
Simple nursing
Body knowledge
Contd/5-
..........5/Yoga
Personal hygiene
Palanccd diet
Some simple preventive measures etc,
11.
Phasing and filot projects:
We should start with a small area or start with only
a few services or both.
We should expand and multiply health services as wfe.
gain more:
insight
experience
confidence
acceptability
efficiency
12. Fsscntial Steps:
To Implement the Community Health Programme Objectives:
To create comprehensive integrated community health
services for the total population of defined rural areas,
with emphasised on vulnerable groups and on prevention.
Such a service should be made available on aregional basi
alongwith effective referral facilities.
Summary o f Stc ps:
1. A managing committee
Z_for the
Community Health Programme should t e
established, (if ooceo-sar;')
2. Constituting a ‘'Planning and Implementation’' Committee
for the Community Health Programme.
3. Selection of suitable area or areas of work. Selectio.
criteria already mentioned in the general approach.
4. To study the arca(s) to define its problems and assets.
Surveys:
This will involve planning and conduction of surveys cove;
ing the following variables:
Demographic
Socio-economic
Health - Existing problems
- Existing facilities
Contd/6-
6/5. Planning:
Preparation of preliminary plan
Piscussions
Readjustments
Finalization of the broad plan
6. Implcmentation:
Selection and training of workers
building and furnishing of hospitals, health
centres etc.,
Phaser’ beginning of health services
7. Records —
Should receive special attention.
8.
Evaluation of Community Health Services — both concurrent and
terminal. This should help bitter plannings:
Planning
Programming
Administration
Evaluation.
(Voluntary Health Cell)
Prepared by.Er.J.8.Gill
Asst.Prof.Centre
Community Afedictne
AIIMS New nelhi
2
XL-2XLJL L£_^rATin; r.L hfalth:
Occupational Ifcalth can he defined as the promotion
ane' maintenance of the physical and rental well-being of
workers with particular reference to the jobs they are
doing. This also includes the effort to achieve a psycho
physical balance between an employee and his job. Quite
a complete health-care procraiw-a comprehensive approach to
the total health needs of the employed population-starting
right from t’.c time of recruitment to extend throughout
an employee *t> working lift.
Herr is a service which goes to the workspot and
;wudics ■’’•it- man in action before hr nets into inaction.
Here is a service which aims at the well-being and
growth of an employe< as a total nan.
’’.hat cannot be cured .must be endured
*
of the past. It can be prevented,
is now a story
•■■?7T crxPkpPTtdAL :-;ahh r:;:- - Ilf ODiT'r.7:
An Occupational Health Services will donducts regular
medical examinations of its employe
re-right
*
from recruitment
onwards. Positive promotion of health, specific protection
against industrial health hazards and communicable diseases,
medical aid, supervision of work places- at intervals, health
education, psychological cuidance and the maintenance of health
statistics are all included in this service.
As a first step, it protects the employees * physical
and mental adjustment, in particular by the adaptation of vork
to man and each man to his job.
HQty OCOirmONAL HF/.LTH V.CSiKSs
1.
Placing people in suitable • ork. Through prr-placement
and periodic medical examinations and placing employees
in jobs that are suited to their physiological and
psychological equipment. ^replacement examination
also provides baseline data together with periodic
examinations. Periodic examination is a monitoring
procedure supplementary to environmental monitoring.
3
?rmii
(> i. o . . .-j vz.! .■... Aflarits Hoad
EAMGAX.03E - 5C0 00?
Industry in not just production
*
machines one’ their
. cintenancr
*
but a groupie special group of productive people
. work, their anxieties end *.orrirn, ’heir hopes and aspiraht - ■ I ral '. and happinr? :<> ’
■'// pro: motion
Of •'F-r'ititr !?;• .-.It ::r a ronn the employers with Special
reference to ■.>?'>; £.n
* : the psychophysical environment insidethe- factory is an absolute essential for letter output are'
1 li
■
„ .•■
:•••:'•-.'.■•
*
"■ thy
*
'
- ■ rJuct
?-.-€?■ t'...-,t can contribute to the national
.-of.-.
t'-ie all-rounr ck v« lop.'.xnt of th? nation.
Indeed,
nance £i.
important than Machine
COMMUNITY HEALTH CELL
rs. It depends on the
■'Sycholoe.icel. It depends
•-, on matters like nutrition, housing,
h; •'irr? in industry
*
industrial hygiene, personal hygiene
*
ere
i r.cortarit of all on a man’c -..ork
*
’.
Hou many of
arc averr o; the influence that work may have on health
and that’
• r son’s health may affect hir> or ’« r capacity
for v.ork? .• re:, so, our conception of health goes much,
much fati’.-f r; fa.-rchr? '.'-'.er i' io normally taken to Ic.
Farther than you c/n even inar.inc. The v;cll—l eine and growth
of cn employee as e total man - ’.A state of complete physical,
t ntal and social v./ l-’rcinn and not a mere absence of disease
“Health
'■ oners.
Conriderable •hou ,ht has Seen given to it and
a setming-ly rimplc fortaula has been chosen. It is ’adaptation
of rork to man are’ each man to his job’.
Simple?
Isn’t it??
Tut when the formula is
ilanded it opens up new vistas of healthful and happy living.
’Occupational Health Service
.
*
That’s it.
c I. lieve that
tappire e mployce s • chefms perfunctorily when they fall nick
*
and cor.e to the hospital is not enough. That’s why we
advocate an Occupational Health Service. Occupational Ifealth
deals rith healthy people at work everyday and orcs thatt
they remain healthy, that fit people become more adapted
to their »ork.
Occupational Health works while they work.
- Media
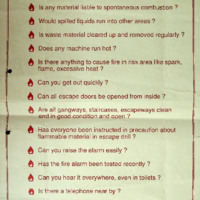 RF_OH_3_SUDHA.pdf
RF_OH_3_SUDHA.pdf
Position: 435 (27 views)
