[Untitled]
Item
- extracted text
-
RP-TB7,therculosis: Pathogenesis. Protection, and Control
'^'^^AmericarTsMiMy for Microbiology. Washington. DC 20005
Chapter 24
Immune Mechanisms of Protection
John Chan and Stefan H. E. Kaufmann
Acquired resistance against tuberculosis oping active disease. Any later imbalance
paradigmatically rests on cell-mediated of the immune system will promote micro
immunity, with the major factors being bial reemergence and ultimately result in
mononuclear phagocytes (MP) and T lym clinical disease. This chapter focuses on
phocytes. While the former cells act as the immune mechanisms involved in pro
the principal effectors, the latter ones tective immunity against tuberculosis,
serve as the predominant inducers of pro with the awareness that in most cases the
tection. At the same time, however, MP immune response activated during infec
provide the preferred biotype for the eti- tion with M. tuberculosis may be remarkologic agent "of tuberculosis, Mycobacte- ably powerful yet insufficient.
rium tuberculosis, and hence play a dual
role in tuberculosis, promoting not only
protection against the disease but also
survival of the pathogen. Similarly, T
cells not only are indispensable for pro
tective immunity but also contribute to
pathogenesis. A coordinated cross-talk
between MP and T cells, therefore, is
essential for optimum protection. Such
coordination is best achieved in the gran
ulomatous lesion, which provides the tis
sue site for defense against tuberculosis.
Even in the face of coordinated T-cell-MP
interactions, full eradication of the patho
gen is frequently not achieved, so that the
individual remains infected without devel-
John Chan • Department of Medicine, Montefiore
Medical Center, Albert Einstein College of Medicine,
Bronx, New York 10467.
Stefan H. E. Kauf
mann • Department of Immunology, University of
Ulm, Albert-Einstein-Allee 11, D-89070 Ulm, Ger
A HISTORICAL NOTE
In his epoch-making description of the
etiologic agent of tuberculosis in 1882, R.
Koch noted the intracellular location of
M. tuberculosis within giant cells (end
stage-differentiated MP) in granulomatous
lesions (Koch, 1882). In his endeavor to
develop an active vaccination
protocol for
.
"
’
’ t
treating tuberculosis, Koch jound
after administration of glycerin extracts of
M. tuberculosis culture supernatants, the
lesions of tuberculous guinea pigs became
heavily necrotized (Koch, 1890). In these
necrotic reactions, many microorganisms
died because of nutrient and oxygen defi
ciencies. Although Koch had already
noted that M. tuberculosis organisms can
be disseminated from such neciotizing
lesions to other tissue sites, he underrated
many.
389
390
f
I'
I
iL>r
IF
i
Mb
bF
Chan and Kaufmann
the detrimental
consequences of this effeet, which soon brought therapeutic vaccination with fubercultn to an end. E
Metchnikoff, a
contemporary but not a
close friend of Koch,
realize the importancewas
of the
MP first
i- to fully'
tenal immunity in general
i in
• antibacagainst tuberculosis in n t
i ‘n defense
nikoff, 1905) Thp
part,cular (Metch-
IN VITRO ACTIVATION OF
A
macrophage
antimycobacterial functions
Evidence has long existed tk .
ni urin,
■acteria
(Lurie
1969). Eartransferring strated that these cells'3 wh”*10"ics
68 dem°nprotection against tnv.r.
□ . ------ “*<
activated
.
b„.e. vitro by supernatants ’ twhen actlv
ated in
from immune animals stimulated lymphocytes f |‘mHmUnological|y
prompted numerous scientists
•
to attempt grees of antimycobacteri’ ,had. vanous dePassive vaccination L
agamst tuberculosis son and Youmans tin
(Pattera^e/tha'uch5:^-’ however ■----------re.’ Youmans, 1973^™
Klun and'
Youmans, 1973a, b;
Illh
,
.
—
197
^b;MuroakaetS
protection against t'-^ a'led ‘O transfer
- oumans,
access in this direction00 °S,SkThC firSt m a’” 1976)’ Soon’ hyc1976a, b; Turcotte
this directior —
hydrogen peroxide
1909 to 1910 by H Helmholtt °^ned in
One of the reactive c-~
- -• Helmholtz and O.
independently
succeed h °'Bai'' d'
(R0I) SCncra!ed -byoxygen
r- interme/ macrophages
tively transferring delaved
dr"1 ad°P‘ dUnn1f ‘he oxidati''e burst (Sbart
- — ra and KarS'tivity to tuberen
hypersen- n°vsky, 1959; Iyer et al ~
1961; Klebanoff,
(containing leukocytes^’111 Wh°,e b,°od 198?)’ WaS identified as the
.^“bacteriocidal effeas'of MP
Chase In 19« (aase7«!0MdL
E_ Suter independently found^hm nr
M'
'■ 1981). This finding
renting the significaVe "7 Ro?T h°n'
defense against
,
n host
gamma interferon (IF?/
°^s- Later,
the kev on 3
Was found to be
■rigged & TiVatin8 age"‘
-erSa-- r-d
1«3; Lune, 1964). AhhoCgh th^e sTuder'
I
f,
immune
contest Xnalive,n.VeSti8at°rS did no'
realized that "t
stra'cgies when they
lha'aXtion'oT
Macka"^ tolhow
rophag {u e"o°nfsa"'""^bacteria! mac
Phocytes (MaX aTd"^'^ by 'ymThat this activation is afftd a"!0"' 1967)'
murine macrophages^tlT't™1 effeC‘S °f
Hesch and Kaufmann ^7) 7 at\I986;
better-defined system (compie^oXs!
nlated lymp™esr^Obhain1,ed fr°m S,in”
'be antimycobacterial effects 'of6^™'”6
Phages. Recent remarkable advancesmacro3 made
ductionXut Characteriza(ion, and probinant DNA TecX0710^68 by recomsimilar in vitro exner 85, haVe facilita'ed
explore the potential oVih"0" deS'8ned '0
molecules in host Hof
hCSe ,nterest,ng
culosis. Thus tumo/1156 a8ainst M-
Chapter 24
TION OF
GE
L FUNCTIONS
ted that murine
'timycobacterial
systems (Lurie
ess, 1969). Earratories demonien activated in
mmunologically
ad various detetivity (Patter0; Klun and
and Youmans,
6a, b; Turcotte
ogen peroxide
xygen intermemacrophages
barra and Kar61; Klebanoff,
molecule that
effects of MP
• This finding
•h debate conROI in host
dosis. Later,
is found to be
ng agent that
al effects of
et al., 1986;
furnishing a
ed to one us
'd from stim1 to examine
• of macro
dances made
■n, and pros by recome facilitated
designed to
interesting
st M. tuberactor alpha
when used
to induce
ine macrovaufmann.
1990a). TNF-a also appears to play a criti
cal role in the control of BCG infection in
vivo, although its direct effect on the antimycobactcrial capacity of macrophages
has not been addressed in this model. Nev
ertheless, when TNF-a-specific monoclo
nal antibodies were used to probe the sig
nificance of this cytokine in defense against
mycobacteria, deficient TNF-a resulted in
poor granuloma formation and dissemi
nated BCG infection in mice (Kindler el al.,
1989). The significance of TNF-a in granu
loma formation has been demonstrated in
other infectious disease models (Chensue et
al., 1989; Amiri et al., 1992). More impor
tantly, preliminary studies suggest that anti-TNF-a antibodies markedly exacerbate
disease progression in murine experimental
tuberculosis (Flynn et al., personal commu
nication).
Other cytokines have been implicated in
macrophage defense against M. tuberculo
sis, although their roles are not as well
established as those of IFN-7 and TNF-a.
In vitro, interlcukin-4 (IL-4) and IL-6 have
the ability to induce macrophage antimycobacterial activity (Kaufmann et al., 1989;
Flesch and Kaufmann, 1990a, b) by mech
anisms presently undefined. Infection of
the human myelomonocytic cell line THP-1
with M. tuberculosis enhances production
of IL-6 (Friedland et al., 1993) compared to
that in cells infected with Toxoplasma gon
dii, an intracellular protozoan known to
elicit little inflammatory response even in
immunocompetent patients. In the murine
system, BCG or its subcellular components
are capable of inducing production of IL-6
by splenocytes (Huygcn et al., 1991). The
antimycobacterial effects of IL-4 and IL-6
(Flesch and Kaufmann, 1990a, b) in the in
vitro macrophage system are seen only
when these cytokines are added to macro
phage cultures after, but not before, the
establishment of BCG infection. This phe
nomenon sharply contrasts with the ability
of IFN-'y to induce antimycobacterial activ
ity in macrophages, which is markedly
Immune Mechanisms of Protection
391
blunted if it is given after initiation of infec
tion (Flesch and Kaufmann, 1990a). The
mechanism and the significance of this ob
servation are currently obscure, but it illus
trates well the complexity of the interaction
between macrophages, cytokines, and the
organisms as well as the limitations of ex
isting in vitro systems in dissecting the
likely complex cytokine network involved
during tuberculous infection. Thus, it is
known that THP-1 cells produce IL-8 in
response to M. tuberculosis infection in
vitro, but the role of this cytokine in host
defense in tuberculosis is completely un
known (Friedland et al., 1992, 1993). Nev
ertheless, it has been postulated that IL-8
plays a role in granuloma formation by
virtue of its ability to act as a chemotactic
agent for T cells (Larsen et al., 1989; Fried
land et al., 1992). IL-1 (Kobayashi et al.,
1985; Dunn et al., 1988; Kasahara et al.,
1988), IL-2 (Mathew et al., 1990; Cheever
et al., 1992), IL-4 (Mclnnes and Rennick,
1988; Chensue et al., 1992), and IFN-y
(Squires et al., 1989; Chensue et al., 1992)
may similarly contribute to resistance
against M. tuberculosis, since these cyto
kines have been implicated in granuloma
tous reactions in various in vitro systems,
including a murine schistosomiasis model.
Recently, IL-10 (Bermudez and Champsi,
1993) and transforming growth factor betal
(TGF-pi) (Denis and Ghadirian, 1991; Ber
mudez, 1993) have been shown to be asso
ciated with diminution of macrophage an
timycobacterial effect in vitro and with
disease exacerbation in mice infected with
M. avium. In contrast, preliminary studies
(Flynn and Bloom, personal communi
cation) indicate that administration of re
combinant IL-12, a recently characterized
heterodimeric glycoprotein produced by
various immune cells including macro
phages (D'Andrea et al., 1992; Schoenhaut
et al., 1992; Gazzinelli et al., 1993), may
confer resistance to tuberculosis in mice.
IL-12 has recently been shown to play an
important role in resistance to Leishmania
1
o
392
Chan and Kaufmann
^ajor, T. gondii, and Listeria monocytoge
nes (Gazzinclli ct al., 1993; Heinzel et al
1993; Locksley, 1993; Tripp et al., 1993)'
I he events triggered by IL-12 help identify
natural killer (NK) cells as a critical cellular
component in defense against M. tubercu
losis By virtue of their ability to produce
.’Ln response to ,L-12 (Kobayashi et
989; Wolf et al., 1991), NK cells can
rapidly activate macrophages to express
microbicidal functions during the early
nommmune” phase of tuberculous infec
tion, before the expansion and differentia
tion ol specific T lymphocytes. As cyto
kines are being examined in experimental
mycobacterial infection, it is becoming
antimycobacterial effector
clear that these molecules interact dynami I UNCTIONS
OF MACROPHAGES: HOW
cally to form a highly coordinated network
does m. tuberculosis survive?
that is configured by both host- and patho
The mononuclear phagocyte constitutes a
gen-specific factors, which together influ
ence disease outcome and progression.
potent antimicrobial component of cell-me
Compared to the murine system, much diated immunity. The precise mechanisms
ess is known about the activation of an- bV which these cells mediate killing or
timycobacterial activity in human macro inhibition of bacterial pathogens are, how
phages. While it is clear that IFN-7 has the ever,
€
not clearly understood. Nonetheless
capability to induce significant antimyco- m this section, some of the best-char
bactenal activity in murine macrophages, acterized antimicrobial effector functions
its role m the human system is unsettled.’ of macrophages—phagosome-lysosome fu
Thus, reports of the effect of IFN-7-treated sion, generation of ROI by the oxidative
human macrophages on the replication of burst, and production of reactive nitrogen
M. tuberculosis ranges from being inhibi intermediates (RN1) via the L-arginine-detory (Rook et al., 1986) to enhancing (Dou- pendent cytotoxic pathway—will be dis
vas et al., 1985). This inconsistency had cussed in the context of tuberculous infec
cast considerable doubts on the antimyco- tion together with the possible evasion
bactenal capability of human mononuclear mechanisms employed by the tubercle ba
phagocytes until the demonstration that cillus to escape killing by activated macro
1,25-dihydroxy vitamin D3 |1,25-(OH)1DJ, phages (Fig. 1).
alone or in combination with IFN--/and
TNF-ot, was able to activate macrophages
Phagosome-Lysosome Fusion
to inhibit and/or kill M. tuberculosis in the
The lysosome is a highly complex or
human system (Crowlc et al., 1987; Rook,
ganelle
containing numerous enzymes
1988; Denis, 1991b). Interestingly, IFN-7
within
its
own limiting membrane that are
stimulates human (Adams and Gacad, 1985capable
of
degrading a whole range of macKoetfler et al., 1985; Reichel et al., 1987)
romolecules
but not murine (Rook, J1990)
---- macrophages tiaux [1966], (reviewed in de Duve and WatBainton
and Kornfeld
to produce 1,25-(OH)2D3. probably via
To provide optimal conditions for
inducuon of 25(OH)D
3
-l
a
.hydroxyla
S
e
25( OH )D3-la-hydroxy la:
the functioning of these degradative en
the enzyme that converts 25(OH)D, to the
zymes, the intralysosomal milieu is main-
1
fl
4'
if
JI
I?
),
k
if
1,25(OH)2D3 to affect antimycobacterial ac
tivity in the murine system. This difference
m 1,25(OH)2D3 metabolism between mu
rine and human macrophages should serve
as a reminder that species variations exist
and a caution against the occasional readi
ness with which cross-species extrapola
tions of experimental results are made The
value of existing in vitro and in vivo murine
models in understanding tuberculosis must
however, not be understated.
Chapter 24
dihydroxylated
he inability of
'cobacterial acThis difference
between mus should serve
ariations exist
casional readiies extrapolaare made. The
n vivo murine
rculosis must,
XphI 0
Arginine
Op X
S? J/
NO
2FFECTOR
AGES: HOW
SURVIVE?
■ constitutes a
■nt of cell-memechanisms
te killing or
ns are, howNonetheless,
e best-charor functions
ysosome fuie oxidative
ive nitrogen
arginine-dewill be disulous infecble evasion
ubercle ba
ited macro
sion
implex orenzymes
ne that are
ge of maceand WatI Kornfeld
Jitions for
iative enJ is main-
nadph\
h2oJ
OH XSoq
Citrulline
—
\
7
J
NADP
NH®
®?tL /
10
tained at a relatively acidic state (pH ~5) by
an ATP-dependent proton pump (Ohkuma
and Poole, 1978; Ohkuma el al., 1982). It is
generally accepted that certain microorgan
isms, sequestered within the phagosome
upon ingestion by phagocytic cells includ
ing macrophages, are subject to degrada
tion by the various lysosomal digestive en
zymes transferred into this subceliular
compartment as a result of phagolysosomal
fusion (Cohn, 1963). This fusion process, a
highly regulated event, most likely consti
tutes a significant antimicrobial mechanism
of phagocytes. Examination of the interac
tion between isolopically labeled bacteria
and macrophages, using the generation of
acid-soluble radioactive materials as an in
dicator of degradation, suggests that certain
organisms are degraded extensively within
Immune Mechanisms of Protection
393
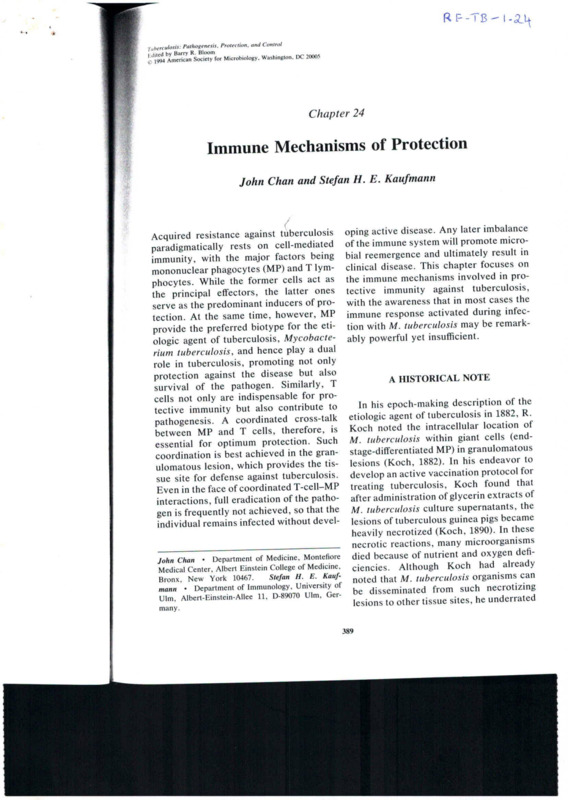
Figure 1. Antituberculous macrophage activities and
evasion mechanisms. Accumulating evidence suggests
that M. tuberculosis enters macrophages via specific
binding to cell surface molecules of phagocytes. It has
been reported that (he tubercle bacillus can bind
directly to the mannoase receptor via the cell wallassociated. mannosylated glycolipid LAM (1) or indi
rectly via complement receptors of the integrin family
(CR1, CR3) or Fc receptors (2). Phagocytosis (3),
triggered by engaging certain cell surface molecules
such as the Fc receptor, stimulates the production of
RO1 via activation of the oxidative burst (4). Experi
mental data indicate that M. tuberculosis can interfere
with the toxic effect of RO1 by various mechanisms.
First, various mycobacterial compounds including gly
colipids (GL). sulfatides (ST), and LAM can downregulatc the oxidative cytotoxic mechanism (5; see text
for details). Second, uptake via CR1 bypasses activa
tion of the respiratory burst. Cytokine-activated mac
rophages produce RNI that, at least in the mouse
system, mediate potent antimycobacterial activity (6).
The acidic condition of the phagolysosomal vacuole
can be conducive to the toxic effect of RNI (7).
However, NH/ production by M. tuberculosis may
attenuate the potency of the L-argininc-dependent
antimycobacterial mechanism and that of lysosomal
enzymes (8), which operate best at an acidic pH. In
addition, mycobacterial products such as sulfatides
and NH/ may interfere with phagolysosomal fusion
(9). Finally, the tubercle bacillus may evade the highly
toxic environment by escaping into the cytoplasm via
the production of hemolysin (10).
2 h after having been phagocytized (Cohn,
1963). Also, electron microscopic studies
indicate that the cell wall of Bacillus subtilis
is degraded extensively within 30 min after
phagocytosis by polymorphonuclear leuko
cytes (Cohn, 1963). How, then, does M.
tuberculosis survive the hostile environ
ment of phagolysosomes?
M. tuberculosis has the ability to produce
ammonia in abundance (Gordon ct al.,
1980). This volatile weak base accumulates
in M. tuberculosis culture filtrates in con
centrations of up to 20 mM and is thought to
be responsible for the inhibitory effect of
culture supernatants of virulent mycobac
teria on phagolysosome fusion (Gordon ct
al., 1980). In addition, ammonium chloride
(NH4CI) has been shown to affect the sal
tatory movement of lysosomes (D'Arcy
p
I
ii*
r
IIIlIll
i
394
Chan and Kaufmann
Hart et al., 1983) and to alkalinize the
fects of macrophages. This issue could perintralysosomal compartment (D’Arcy Hart
haps be addressed more rigorously and
et al., 1983). Thus, by virtue of its ability to
definitively by direct i
immunohistochemical
produce a significant amount of ammonia,
labeling of vacuolar membranes enclosthe tubercle bacillus can potentially evade
mg intracellular M. tuberculosis with
the toxic environment within the lysosomal
antibodies specific tto lysosomal glycoprovacuole by (i) inhibiting phagosome-lyso
teins (Joiner et al.,
' , ]1990) or by using the
some fusion and (ii) diminishing the po
"trap-resistant” ionic
---■j i._
impermeant fluors
tency of the intralysosomal enzymes via
(lucifer yellow, lissamine
alkalmization. This latter attribute of rais
Ir , ,
- rhodamine, and
sulforhodamine) as
as alternative
alternative lysosomal
lysosomal
ing intralysosomal pH might also be protec
(Goren et al.’, —
1987a, b). JFinally,
it
•
...
Hid
tive against the RNI cytotoxic mechanism markers
IS
likely
(hat
like
is
hkely
that
virulent
tubercle
bacilli
of macrophages (see below).
certain intracellular pathogens, including
Another
mycobacterial
i
.
*
UiUULIH
product
thought rickettsiae (Winkler,
^aVe.lhe abllity t0 inhibit phagolysosoa"d shi8cnac (Sansonetti
15 the
‘he sulfatides
SU'fatides (Goren et
« al
al.,
. 9Z.6b’’ dtr,vatives of multiacylated treha- et al., 1986), evade killing by escaping from
lose 2-sulfate,. a lysosomotropic polyan- phagocytic vacuoles into the cytoplasm (for
ionic
■ •■‘/Cw8lyCOhpid Produced by M. tuberculo- a review, see Falkow et al. [1992]). Hemo
lytic activities capable of lysing vacuolar
(Middlebrook et al., 1959; Goren eta?
membranes
are thought to be the common
1976a). Because of the ability of certain
virulent
determinant
that enables success
polyanionic compounds to entrap comful parasitization of the cytoplasm (Falkow
moniy used lysosomal markers
-------- 3 employed et al., 1992). Indeed, the translocation of
to •'
' phagolysosome
•
study
fusion, artifactual
"inhibition” of this process can occur and M. tuberculosis from within phagocytic
vacuoles into the cytoplasmic compartment
has spawned much
.---------- controversy (Goren et
has been reported (Myrvik et al 1984al., io«7
iy«/a, b). These entrapment phenomena could be secondary to the formation of McDonough et al., 1993). These observa
gelatinous, •sluggishly moving hydrocol- tions are reinforced by the presence of a
hemolytic activity in the tubercle bacillus
loids that physically retain lysosomalI mark
King et al., 1993). Also, the cytoplasmic
ers or to ionic interaction with cationic
location
made possible by this potential
makers such as acridine orange. Although
evasion
mechanism
could, in theory, facil
su fatides do not form hydrocolloids, the
itate
the
routing
of
mycobacterial compo
polyanionic nature of these glycolipids
nents into the major histocompatibility
poses questions concerning their ability to
±S„V (.^HC 1) !’athway of
presen
^a,‘bcXXX'of^V';1'-; “
,tatiOn’ ,hUS
“ - ------------------------- in part the
these ^-(ipidsXk ^
appears to be warranted. Regardless of the
chemical components of the tubercle bacil
lus that contribute to the inhibition of
Phagolysosomal fusion, this phenomenon
controversy notwithstanding) has been extensively studied (Armstrong and D’Arcv
Hart, 1971, 1975; Goren et al . W6b Myr
vik et al., 1984; D’Arcy Hart et al '1987)
and is certainly a mechanism bv which
y otoxic et
importance of MHC I molecules and CD8 +
1 cells in defense against M. tuberculosis
(Kaufmann, 1988; Flynn et al., 1992).
The Respiratory Burst
That ROI nlav « • n
defcn ‘ R01V s'8nificant ro|e in host
fied hv -h*8?1"' m'Cr°beS is best e“mPbl',a'cluent infectious complication
xperienced by chronic granulomatous dis-
[1988]), whose phagocytes cannot mount an
1
Chapter 24
issue could perngorously and
lohistochemical
branes encloslosis with anti0131 glycopror bV using the
-rmeant fluors
lodamine, and
,ve lysosomal
• b). Finally, it
le bacilli, like
ns, including
listeriae (Bieae (Sansonetti
escaping from
ytoplasm (for
992]). Hemo
sing vacuolar
the common
bles successasm (Falkow
islocation of
phagocytic
:ompartment
•t al., 1984;
-se observaesence of a
cle bacillus
-ytoplasmic
is potential
>eory, facilial compo>mpatibility
gen presen
in part the
and CD8 +
^berculosis
992).
»e in host
exempliiplication
itous disist et al.
mount an
oxidative burst (Sbarra and Karnovsky,
1959; Iyer et al., 1961; Klebanoff, 1980).
The significance of these toxic oxygen spe
cies in defense against M. tuberculosis,
however, remains controversial. Since the
report that H2O2 produced by lymphokineactivated murine macrophages kills M. mi
croti (Walker and Lowrie, 1981), much ef
fort has been focused on testing the role of
the oxygen radical-dependent killing mech
anism in defense against M. tuberculosis.
Such effort, however, provided evidence
indicating that oxygen radicals may not be
sufficient to inhibit and/or kill M. tubercu
losis (Flesch and Kaufmann, 1987, 1988;
Chan et al., 1992). The validity of these
findings has been reinforced by the demon
stration of evasion mechanisms employed
by the tubercle bacillus to elude the toxic
effect of ROI. Of these mechanisms, those
that are mediated by mycobacterial compo
nents lipoarabinomannan (LAM) and phe
nolicglycolipid I (PGL-1) are among the
best studied and characterized (for reviews,
see Brennan [1989] and Brennan et al.
[1990]).
LAM, a major cell wall-associated, phos
phatidylinositol-anchored complex lipo
polysaccharide, is produced by M. tubercu
losis in large amounts (15 mg/g of bacteria)
(Hunter et al., 1986; Hunter and Brennan,
1991). Immunogold staining has demon
strated that LAM exists in a capsular
sheath encasing M. tuberculosis (Hunter
and Brennan, 1991). This strategic location
places LAM at the frontline of attacks
directed by the various antimicrobial mech
anisms of macrophages. It has now been
shown that LAM can incapacitate the oxy
gen radical-dependent antimicrobial mech
anism at at least two levels: (i) studies using
electron spin resonance spectroscopy and
spin-trapping have shown that LAM is an
effective ROI scavenger (Chan et al., 1991);
and (ii) LAM can downregulatc the oxida
tive burst by inhibiting protein kinase C
(Chan et al., 1991), an enzyme that plays an
important role in activation of the oxidative
•
Immune Mechanisms of Protection
395
burst in phagocytic cells (Gennaro et al.,
1985; Pontyremoli et al., 1986; Wilson et
al., 1986; Gavioli et al., 1987). In addition,
since IFN-7 is a major factor for macro
phage activation (Hamilton et al., 1984;
Hamilton and Adams, 1987; Fan et al.,
1988) and has the ability to enhance ROI
production by phagocytic cells, it is possi
ble that LAM, by virtue of its ability to
inhibit transcriptional activation of IFN-7inducible genes (Chan et al., 1991), is able
to block the expression of an as yet uniden
tified factor(s) inducible by this cytokine
that is required for the oxidative burst.
These results are in keeping with the find
ings that mouse peritoneal macrophages
treated with LAM or infected with M. lep
rae (a LAM-producing pathogenic myco
bacterium) are not responsive to IFN-7
activation as assessed by microbicidal and
tumoricidal activities, O2- production, and
surface la antigen expression (Sibley et al.,
1988; Sibley and Krahenbuhl, 1988) and
may partially explain the inability of IFN7-stimulated macrophages from both hu
mans and mice to effectively kill M. tuber
culosis in vitro (Rook et al., 1986; Flesch
and Kaufmann, 1987).
Other mycobacterial components that in
terfere with the oxygen radical-dependent
antimicrobial mechanism of macrophages
arc PGL-I and the sulfatides. PGL-I is an
oligoglycosylphenolic phthiocerol diester
with its species-specific trisaccharide moi
ety glycosidically linked to a phenyl group
that in turn is attached to the branched
glycolic chain, phthiocerol; two hydroxyl
functions of the phthiocerol are estcrificd
by mcthyl-branched fatty acids (mycocerosates) (Hunter and Brennan, 1981; Hunter
et al., 1982). Although universally distrib
uted among M. leprae, the expression of
PGL-I in the various strains of M. tubercu
losis is much restricted (Daffe et al., 1987;
Brennan, 1989; Brennan et al., 1990). In
contrast, the sulfatides, derivatives of mul
tiacylated trehalose 2-sulfate (Middlebrook
et al., 1959; Goren et al., 1976a), are widely
396
Chan and Kaufmann
expressed among different strains of M
tuberculosis (Middlebrook et al
1959’
Goren et al., 1974, 1976a). Because of its
restricted distribution among tuberculous
isolates, the significance of PGL-1 in the
pathogenesis of tuberculosis remains to be
determined. Nonetheless, both PGL-1 and
the sulfatides have the capacity to down•egulate ROI production in in vitro macro-
the tubercle bacillus does not
disease
not equal
equal disease
the host must be equally sophisticated I,
evolvmg effective defensive strategic,
against this formidable invader. It follows
then that there must exist antimicrobial
mechanisms to which the bacillus suc
cumbs.
offTo^'p k SyStemS (Nci" and K,eba"-
Reactive Nitrogen Oxides
1
Ji
r
!
F
lK
e
f
!
Ct aL’ 1988; Vachu,a * a'-
The
L-arginine-dependent
cytotoxic
1989; Brozna et al., 1991), and PGL-I di
rectly scavenges oxygen radicals in a cell- pathway of activated macrophages consti
free system (Chan et al., 1989). Another tutes an important antimicrobial mecha
against intracellular parasites (for re
mechanism by which M. tuberculosis could nism
™
evade the toxicity of ROI is to avoid bind views, see Nathan and Hibbs (19911 I few
ing to macrophage cell surface compo and Cox [1991], and Nathan [1992]). The
nents such as Fc receptors, that would cytotoxic effect of this pathway is mediated
piovoke an oxidative burst. Instead, the through nitric oxide (NO) and related RN1
tubercle bacillus parasitizes MP via com generated from the substrate L-arginine via
plement receptors CR1 and CR3. molecules the action of the inducible form of the enw.h .'nle!rin family whose interaction Zy?CunuuC °Xide synthase («NOS) (Nathan
with na ligand
WIth
igand does not trigger ROI produc- and Hibbs, 1991; Nathan, 1992). Recent
tion (Wright and Silverstein, 1983), in rest studies have demonstrated an association
between the antimycobacterial effect of cy
ing macrophages (Schlesinger et al., 1990)
tokine-activated
murine macrophages and
I hus, as in other parasites (for reviews, see
the
activation
of
the L-arginine-dependent
sbeig [1991] and Falkow et al. [1992])
cytotoxic
pathway
(Denis, 1991b- Flesch
1a'|ClU1wm Bo^de'ella P^ssis (Reiman et
and Kaufmann, 1991; Chan et al 1992)
0), Histoplasma capsulatum (Buithus the capability of macrophages actilock and Wright, 1987), Legionella pneuva
cd by IFN-7 and Escherichia coli lipo
mophila (Payne and Horwitz, 1987), and
polysaccharide
or TNF-a to kill and/or
19R7/Z/p/,Z/?/nSPP’ (M°SSer and Edclson,
inhibit
the
virulent
Erdman strain of M
987, Russell and Wright, 1988; Talamastuberculosis
correlates
well with RNI proRohana et al., 1990), exploitation of integnn receptors may be a common scheme of ouclion. and nitrogen oxides generated by
acid'fication of nitrite are also mycobactclnvasion among pathogenic mycobacteria
Although these in vitro data provide sub- ncidal Chan et al., 1992). Deletion analy
mlpl,V?tbVldenCe tO SU8gest Path°genetic ses of the 5 flanking promoter sequence of
roles of the various mycobacterial glycolip murine iNOS indicate that IFN-y alone is
msufhcient for transcriptional activation of
ids, their in vivo significance is ppresently this gene
(Xii
' ,e el aI-’ 1993). The synergistic
undefmed and awaits rigorous genetic anal
effect of IFN-y and TNF-a in inducing
yses. Nonetheless, it is undeniable that
mactophage antimycobacterial function via
Mycobacterium spp. are extremely well
<NI production underscores the impor
adapted to the hostile environment of
tance
of these cytokines in defense against
Phagocytic cells, their deftness reflected by
M.
tuberculosis.
Indeed, IFN-y and IFN-y
the alarming morbidity and mortality
receptor
‘
-knockout
” mice that arc defi
caused by tuberculosis worldwide (Murray
cient
in
mounting
an
RNI response to infec
et al., 1990). However, since infection with
tion with the tubercle bacillus experience a
1
I
Chapter 24
report that the
to RNI varies
>93) further sigesistant myco■' such mutants
oecause of the
the mammalian
production,
on the precise
mediate antimyrgets that these
complexity of
1992). Nevcrrea of research
ificantly to the
^mistry in vivo
ns of virulent
■ly lead to new
>n of virulence
echanisms as
survival of M.
iy of iron meillus deserves
iship between
nown for dc1944; Weinset al., 1980),
i metabolism
tion are not
=nd characterng molecules
le variety of
(Nielands,
considerable
‘en reported
both in vitro
! in the pres:in hemogloences therecoli in a rat
ganisms are
icmoglobin.
>f this heme
ptaglobin, a
icmoglobin
rganic iron
t as hemo
I
I
globin, a direct connection of iron and infec
tion is made (Eaton et al., 1982). In human
diseases, the mortality rate of Vibrio vulnifi
cus is markedly increased in patients suf
fering from iron overload as a result of
conditions such as hemochromatosis and
alcoholism (Brennt et al., 1991; Bullen et al.,
1991). These experimental data thus suggest
a possible role of siderophores in bacterial
virulence.
Mycobactins, a group of iron-chelating
growth factors of mycobacteria, have been
considered a possible virulence factor of M.
tuberculosis (Snow, 1970). These hydroxamate derivatives chelate ferric ions with a
stability constant exceeding IO30 (Snow,
1970). Thus, mycobactins compete favor
ably for chelating Fe3+ with human ferritin
and transferrin, the major iron storage and
iron-transporting proteins, respectively.
The significance of these mycobacterial
iron-binding agents in the pathogenesis of
tuberculosis, however, remains to be estab
lished. Recently, the L-arginine-NO path
way has been reported to participate in
posttranscriptional regulation of the ex
pression of ferritin, transferrin receptor,
and 5-aminolevulinate synthase (a rate-lim
iting enzyme in erythroid heme synthesis)
in macrophages (Drapier et al., 1993; Weiss
et al., 1993). It is fascinating that the very
same pathway that produces potent antimycobacterial activities in macrophages par
ticipates also in the regulation of the metab
olism of iron, whose availability is essential
to the optimum growth of M. tuberculosis.
Dissecting this likely complex tangle may
uncover additional roles for the NO path
way in tuberculous infection and shed light
on the significance of iron in the pathoge
nicity of M. tuberculosis.
DOES M. TUBERCULOSIS INVADE
CELLS OTHER THAN PROFESSIONAL
PHAGOCYTES?
There is little doubt that M. tuberculosis
has the ability to establish infection in and
Immune Mechanisms of Protection
399
replicate inside of a wide variety of mam
malian cells in vitro (Sheppard, 1958). Yet
in infected tissues, the tubercle bacillus is
to be found only in polymorphonuclear
leukocytes and MP (Filley and Rook, 1991).
The findings by Filley and Rook that endo
thelial cells and fibroblasts infected by M.
tuberculosis exhibit increased sensitivity to
the cytolytic effect of TNF have led to the
hypothesis that this cytokine contributes
significantly to the immunopathology of tu
berculosis (Filley and Rook, 1991). The
enhanced susceptibility of nonphagocytic
cells to TNF upon mycobacterial infection
may also partially explain the difficulties
encountered in identifying such target cells
in vivo. It is also possible that these non
phagocytic cells serve as a reservoir for
bacterial multiplication and thus aid in dis
ease dissemination upon lysis by TNF. Re
search in these areas is just beginning to
draw attention and is likely to help provide
insight into the pathogenic strategies of M.
tuberculosis. Finally, unlike the processes
of other pathogenic bacteria such as the
enteric shigellae and salmonellae and the
gram-positive listeriae (for reviews sec Isberg 11991] and Falkow et al. [1992]), the
processes of adhesion and invasion by
which M. tuberculosis enters host cells are
just beginning to be understood. M. tuber
culosis gains entry into MP via cell surface
molecules, including the integrin family
CR1 and CR3 complement receptors (Schles
inger et al., 1990) and the mannose receptor
(Schlesinger, 1993). Recently, M. avium
has been shown to enter macrophages via
avp3, another molecule of the integrin fam
ily (Rao et al., 1993). Parasitization of
phagocytes via the CR1 and CR3 recep
tors by various pathogens avoids triggering
the oxidative burst (Wright and Silverstein,
1983). Whether the same advantage is
gained by engaging the mannose receptor
or the avp3 integrin is presently unclear.
Since the cytoplasmic domain of p subunit
of integrin is coupled to the cytoskeleton
(Albclda and Buck, 1990), it is possible that
■
400
Chan and Kaufmann
S-«8to‘Onit^theCp'
r~
don by the host cell (Isbe^w^)" D
^WbaGterial invasin
(Arruda et al.
—- ■
’ y93) b,nd also to
to integrin
integrin
receptors? Comprehensj'
Jension of these adhesion and invasion events
ln advancing our --"'s is very important
pathogenicity of M. understanding of the
tuberculosis.
CONTRIBUTION OF T CEILS To
wtichtsp" ^'eCU,CS- and C“
by the MHC class I / Pep,,des Present
bacte™m.spe^rc8DTPTr<t"ShM-
have been identified eon.-
’^Phocyt
« X“F"" “
acquired resistance
11
mann, unpublished data)
P Tcells
cells car.
further divided into CD4a/T
wh
ofXcerh'8en,Cpepddes'n <h ccont<
of protecdo^ TheyredobnSr°ry mCdialors
-ust interact wither Tehsonb0
mune system tn n uc s ° the imtance.
All
T-cell
nn
Opt,nium
cells, CDS Lb TP lPn'a,,OnS
(CD4 resisT
»
Conversely adonZ’ Pedrazz'ni « al.. 1987)
tuberculosis and BCC?'60!'011 a8a'nst "•
Ransfer of selecl^njT r,
contribute to protection Th^
T CeHs) Co,,ins
Collins.’^84;
1984; C
Orme 1987) c & (Orme and
these find
finding
T iytnphocytes has ^enlXl
'ngS' muta"‘”u : Consistent with
experiments showing that
P fi,cd b>' ?ency ■" the MHC classmice with a defimtce suffer more several.,
"" a"d scids devoid °f functionallv a.,’ H gene that are
lonally active CD4 T cells
tai M. i'«^3oXVearndy BCG6-Pferimen‘ r'h h BCG
ir control counterpart f“ daU) and M- and Kaufmann, unpubthan their
r <F'ynn C1
(Shcret al., al., unpublished
unpublished obseXaZr
oh«
^75, Jzzo and North
North, 1992)
conclusion, these exne
lnfect'°ns. In
Point to an essential role of^m
T-Cell Populations
T cells expressing an a/B-T-cell
constitute more f
P
;han 95% Of
cells in peripheral
contrast, 7/8 T ceUs organs and blood. In
are a minority at these
sites but they are more
A substantial role for CDX t
„ ■
prominent in mu
Protection against tnbrr iD8- f CC,,S ,n
cosal tissues such r •
asthejung. Forma! proof b7~ ^'"/^berculosi;
that a/p T cells are crucial r .
by several lines of ev
°S1S ’S ,ndicated
vMed3"06 against
a8ainS! ‘uberculosis0" acquired Depletion of CDS
CD8 T
T Pe
PC"
fr'menlal
mcnlal studies.
all a/p Tren's7 In 'th mUtanl m'Ce
coding the T-cell
m'Ce’ the 8ene en‘
been deleted by h"m .CePl°r P
had
(Mombaerts et al 1^?°S.^‘’'"bination
o/P-T-celi-deficient’ mice'm"’'1™8'’ these
sistant to sublethal R(-r fre a"vely reIhe first 4 weeks if r
eC"On duri"8
BCG rnartedry tc^as" :^"’
ultimately the a/P-T-cell-defidlT^’ and
CUmb t0
infection ILadel'^l^
~T'Xbodies ^SsT^
CDS T cells trarKf Jn.T,Ce- and se,ected
transfer
adoptive
against luberculo
8^(o
d°PtlVC proteclion
I’W; Muller et al 198^ o' and C
°"ins’
Collins,
drazzini et al., 1987)
°™e- 1987i peThese findings
have
becn further substantiated
■
--J recently by apnt mice in which the p2-
quiredforMHCcla it ^Se |32m is re'
‘
t mu
SUrfaCeexPression,
P2m-deficienl
mUtant m,ce are devoid of
Chapter 24
^3 T cells can be
} r cells, which
cs in the context
cs, and CD8 T
ptides presented
Products. Mycor lymphocytes
stently in experilosis (Kaufmann
off et al., 1988;
thermore, CD4
monoclonal annental infection
!osis and BCG
<ini et al., 1987).
ction against M.
ely depends on
-ells (Orme and
Consistent with
with a defiI gene that are
e CD4 T cells
fmann, unpublosis (Flynn et
) infections. In
ents strongly
2D4 T cells in
is. Consistent
-n as a result of
irus infection
uberculosis in
’8 T cells in
S is indicated
-ntal studies,
with specific
bates M. mand selected
e protection
»nd Collins,
e, 1987; Po
ndings have
‘ntly by apn'ch the 32een deleted
32m is re
expression,
devoid of
functionally active CD8 T cells. These mice
die rapidly from M. tuberculosis but not
from BCG infection. Impressive as these
studies are, it should be kept in mind that
p2m not only serves to stabilize MHC class
I surface expression but may also perform
other functions that could influence sur
vival of M. tuberculosis in p2m-deficient
mice. Furthermore, mycobacterium-spe
cific CD8 T cells have been isolated from
M. tuberculosis- and BCG-immune mice
(DeLibero et al., 1988). In contrast, such
mycobacterium-specific CD8 T cells were
rarely identified in patients suffering from
human tuberculosis (Rees cl al., 1988). CDS
T-cell lines derived from M. tuberculosisand BCG-immune mice arc MHC class I
restricted, thus raising the question of how
M. tuberculosis and BCG proteins gain
access to the MHC class I processing path
way (DeLibero et al., 1988). Although it is
generally assumed that M. tuberculosis re
mains in the cndosomal compartment, clear
evidence for escape of M. tuberculosis
from phagolysosomes into the cytoplasm
has been presented (Leake et al., 1984;
McDonough et al., 1993). Microbes resid
ing in the cytoplasm could then produce
proteins that contact MHC class I mole
cules, as has been clearly shown for Liste
ria monocytogenes. Alternatively, it can be
assumed that during persistent replication
within the phagosome, mycobacterial pro
teins or peptides are translocated into the
cytoplasm, where they contact the MHC
class I processing machinery. Recent evi
dence indicates that MHC class I process
ing can occur independently of microbial
egression into the cytoplasm (Pfeifer et al.,
1993).
Besides conventional MHC class I-rcstrictcd CDS T cells, T cells that arc appar
ently MHC class I nonrestricted have been
described (DeLibero et al., 1988). Similar T
cells have been identified in the listeriosis
system, where these T lymphocytes are
focused on peptides containing the Nformylmethionine (A-fMet) sequence pre-
•
Immune Mechanisms of Protection
401
sented by nonconventional MHC class lb
molecules (Kaufmann et al., 1988; Kurlander et al., 1992; Pamer et al., 1992). The
N-fMet sequence probably serves as a se
cretion signal in prokaryotic cells. In mam
mals, the 7V-fMet sequence is present only
in proteins encoded by the mitochondrial
genome (probably of prokaryotic origin).
Furthermore, nonconventional MHC class
lb gene products are highly conserved and
vary in only few mouse strains. Thus, it
appears that a subset of bacterium-specific
CD8 T cells is focused on (i) conserved
bacterial peptides and (ii) nonpolymorphic
presentation elements. If these observa
tions can be generalized to human tubercu
losis, important consequences for peptide
vaccination against bacteria with few pep
tides and independent of human lympho
cyte antigen polymorphism can be envis
aged.
A contribution of 7/8 T cells to protection
is suggested by indirect evidence. They
have been identified in reversal reactions of
leprosy patients and in tuberculous lymph
adenitis lesions (Falini et al., 1989; Modlin
et al., 1989). No evidence for increased 7/8
T cell numbers, however, has been ob
served in lymph node granulomas of tuber
culosis patients (Tazi et al., 1991). In mice,
7/8 T cells accumulate early at the site of
BCG replication, in draining lymph nodes
after immunization with complete Freund’s
adjuvant, and in the lung after aerosol im
munization with mycobacterial compo
nents (Augustin et al., 1989; Janis et al.,
1989; Inoue et al., 1991). Furthermore, the
progressive BCG infection in scid mice
compared to nulnu mice and mice depleted
of CD4 and CDS T cells has been taken as
evidence for a role of 7/8 T cells (Izzo and
North, 1992). Direct proof, however, has to
await experiments with mutant mice devoid
of 7/8 T cells. The 7/8 T cells from healthy
individuals proliferate vigorously in re
sponse to mycobacterial components (Kabelitz et al., 1990; Munk et al., 1990).
Although preferential 7/8-T-cell expansion
402
Chan and Kaufmann
by mycobacteria is caused to a large degree
by low-molecular-weight nonproteinaceous
components that act in a superantigen-like
fashion, 7/8 I cells also appear to be stim
ulated by M. tuberculosis antigens (Munk
et al., 1990; Pfeffer et al., 1990). Thus far,
the kind of antigens and presentation mol
ecules required for 7/8-T-cell stimulation
remain virtually unknown. Evidence from
other systems indicates that the relevant
peptides are presented by nonconventional
MHC molecules (Pamer et al., 1993). Per
haps the MHC class lb molecules involved
in CDS T-cell stimulation also participate in
7/8-T-cell stimulation.
J
*
cells appear sequentially in the following
order: PNG. NK cells, 7/8 T cells, a/B T
cells.
Evidence has been presented elsewhere
that T-cell lysis of BCG-infected macro
phages causes bacterial growth inhibition in
vitro (DeLibero et al., 1988). Perhaps target
cell lysis promotes discharge of toxic mac
rophage products that inhibit mycobacterial
growth. This in vitro observation may be
taken as evidence for a direct protective
effect afforded by cytolytic T cells. More
iimportantly, a coordinated interplay be
tween macrophage activation by IFN-7
(probably in conjunction with additional
mediators) and target cell lysis appears to
be required for optimum protection
T-Cell Functions
(Kaufmann, 1988). M. tuberculosis is ex
Various in vitro studies of the human and tremely resistant to macrophage killing.
mui inc systems show that mycobacterium- The persistence of M. tuberculosis in
reactive CD4 T cells are potent IFN-7 pro healthy individuals for years without caus
ducers (Emmrich et al., 1986; Kaufmann ing disease indicates that the immune sys
and Flesch, 1986). IFN-7 is also produced
tem generally fails to stcrilely eradicate this
by murine CDS T cells with mycobacterial pathogen and must rely on mycobacterial
specificity (DeLibero et al., 1988). As de containment and growth inhibition. Not
scribed above, this cytokine is the principal only prior to but also after IFN-7 stimula
mediator of antituberculous resistance. tion, macrophages are largely abused as
Mycobacterium-reactive CD4 T cells and habitat. Lysis of such macrophages pro
CD.8 7 ccl,s also exPress specific cytolytic motes bacillary release from a shelter. Proactivities; i.e., they lyse macrophages vided that the microorganisms
—.3 are taken up
primed with mycobacterial antigens or in- 'by more efficient phagocytes soon after
fected with BCG or M. tuberculosis (De their liberation, this mechanism should im
Libero et al., 1988; Ottenhoff et al., 1988).
prove host defense against tuberculosis.
It appears that these two functions not only Such an interplay between lysis and activa
are demonstrable in vitro but also contrib tion of MP would best be controlled in
ute to protection in vivo. Besides the well- productive granulomas (see below). At the
characterized a/p T cells, other cells also same time, target VV11
cell lysis causes tissue
produce IFN-7 and express cytolytic activ- damage, affect^organ functions
------- 3, and, in the
ities, suggesting their participation in acqui absence of phagocytosis, promotes micro
sition of resistance. In particular, both NK bial dissemination. Lysis of infected MP,
cells and 7/8 T cells produce IFN-7 and lyse therefore, i
• is a double-edged sword that,
mycobacterium-pulsed target cells (Munk depending on the general situation, has
a
et al., 1990; Bancroft et al., 1991; Follows beneficial or a detrimental outcome.
et al., 1992; Molloy et al., 1993). In ad
dition, polymorphonuclear granulocytes
T-Cell Antigens
(PNG) produce highly proteolytic enzymes
causing tissue liquefaction (Weiss, 1989).
At least two characteristics of M. tuber
At the site of M. tuberculosis growth, these culosis and BCG influence the type of anti-
Chapter 24
W. tuber'e of anti-
403
cines requires use of appropriate adjuvants
or viable carriers capable of targeting both
the MHC class I and the MHC class II
pathway. As long as MP fail to kill signifi
cant numbers of intracellular M. tuberculo
sis, secreted proteins and metabolically
produced peptides are the main, if not the
sole, source of antigens. Later, when M.
tuberculosis and M. bovis die in the acti
vated macrophage, somatic proteins be
come a major source of T-cell antigens. The
less metabolically active bacteria are, the
lower the relative proportion of secreted
protein antigens will be. Dormant tubercle
bacilli without significant metabolic activity
but resisting macrophage killing will be an
ineffectual source of any antigen. Both fea
©
tures may be relevant to the low effective
MHCH
MHCI \1
MHCII MHCI
ness of the only vaccine against tuberculo
sis available, BCG. First, BCG seems to
primarily activate CD4 T cells (Pedrazzini
et al., 1987). While this seems to be suffi
cient for protection against BCG, it appears
to be insufficient for effective vaccination
lAg|
somatic
against tuberculosis. Perhaps the shorter
secreted
intracellular survival of BCG together with
a deficiency in cytolysins restricts access of
BCG-derived proteins to the MHC class I
T (Months to years)
pathway. Second, owing to the shorter sur
Figure 2. Relationship between intracellular persis
vival time of BCG, somatic antigens will
tence of M. tuberculosis, antigen type, and 1-cell
predominate early after infection. Early
subset activation. (1) M. tuberculosis replicating in the
recognition of M. tuberculosis-infected
phagosome secretes proteins that are degraded into
macrophages, however, primarily depends
peptides and then translocated to the cell surface by
on T cells that recognize secreted proteins.
MHC class 11 molecules. (2) MHC class 1 molecules
capture M. tuberculosis peptides derived from se
Thus, the preponderance of CD4 T cells
creted proteins in the cytoplasm. Either the proteins or
and somatic antigens may explain, at least
peptides had been translocated from the endosomal
in part, the insufficient protection against
into the cytoplasmic compartment, or they were se
M. tuberculosis afforded by BCG vaccina
creted into the cytoplasm by M. tuberculosis after its
evasion of the phagosome. Later, M. tuberculosis is
tion.
gens that are recognized by protective T
cells. First, the intracellular location (phago
some versus cytosol) dictates processing
via the MHC class I or class II pathway.
Second, the intracellular viability of the
pathogen determines availability of poly
peptides for processing (Fig. 2). MHC class
1 versus MHC class II processing has been
discussed above. Because soluble protein
antigens are not introduced into the MHC
class I pathway, the design of subunit vac-
e lollowing
ells, a/p T
elsewhere
ed macronh bition in
haps target
toxic macycobacterial
'On may be
protective
ells. More
erplay beby IFN-7
additional
appears to
protection
-losis is exige killing.
rculosis in
■thout causimune sysadicate this
cobacterial
•ition. Not
-7 stimulaabused as
hages pro■iclter. Proe taken up
soon after
should im'erculosis.
id activairolled in
■v). At the
ses tissue
and, in the
■les micro“Cted MP,
•'ord that,
■on, has a
ne.
Immune Mechanisms of Protection
i
i y x I
(i) ^) (|) (j) (±)
I
killed and degraded, thus giving rise to somatic pro
teins. (3) Peptides derived from M. tuberculosis killed
in the phagosome contact MHC class II molecules. (4)
Peptides from somatic proteins present in the cyto
plasm are charged to MHC class 1 molecules. (5)
Neither the source of peptides nor the presentation
molecules involved in 7/8 T-cell stimulation are fully
understood. This sequence of events leads to a first
wave of T cells with specificity for secreted proteins
followed by a second wave of T cells with specificity
for somatic proteins. Ag. antigen.
THE IN VIVO SITUATION
In tuberculosis, the port of entry as well
as the major organ of disease is the lung.
After being inhaled, the pathogen is en
gulfed by alveolar macrophages that appear
to be insufficiently equipped tor microbial
404
II!
1
i
i
Chan and Kaufmann
killing. Probably these
alveolar macromay promote granuloma liquefaction
phages transport the pathogen ii
into the lung
and
rupture into the bronchoalveolar and
parenchyma and into P
’
vasdraining lymph
fecte'd’ mahere Hhe miCrObe rep,icates- In- ekv'X?S,hThe CellU,ar detritus
evalcd pO;, thus arising provide an excel
tec ed macrophages produce chemokines
at cause the extravasation of additional lent medium for M. tuberculosis that favors
ts uncontrolled multiplication. Rupture of
P agocytes (Oppenheim et al., 1991- Fried
lhe
granuloma promotes microbial disse
land et al., 1992). These inflammatory
msecreuy? 4™° and bl°Od mon^yfes) mation through the bronchoalveolar system
Crete significant amounts of proteolytic into the environment and through the vasenzymes generating an exudatfve tesfon
cular system to other tissue sites.
Activated MP also secrete TNF which
™ Wi®?1"0"'3 f°rma,io" (Kindler et
r
a .,1989 . Eventually, T cells activated in
draining lymph nodes as well as NK cells
tO ,he Site Of “flammation
Although NK cells and 7/8 T lymphocytes
seem to precede «/p T cells, the former two
WHY DO WE NEED MORE THAN ONE
T-cell population for
PROTECTION?
Given that in vitro CD4 T cells CD« t
ce ls, and 7/8 T cells are so ffighly “flar
are soon outnumbered by the last. The a/B
T cells and 7/8 T cells interact with MP that Wi ! respect to their functional competext^of m.yCObacterial Peptides in the con s“sCfor y, ° We need Several T-Ce" ^fl
text of adequate MHC molecules They sets for optimum protection to occur’ At
produce IFN-7, as do NK cells, which in the moment, this question cannot be fully
and^/S T fl'8' adVantage of CD8 T celll
act'vates tuberculostatic macrophage
and
7/8 T cells over CD4 T cells is their
high e'll '1 Produc,ive granuloma with a
restriction by MHC class I moleculeT
are confi11^ •tUrn°Ver develoPSi bacteria >
are confined in it, and their growth is re- which are expressed on virtually all host
e trictL 6 MHC C,aSS " “Passion is
t;™" ^.Although these granulomas effec
tively inhibit bacterial replication, they are Al hXh
Cexa'n h°S‘ Ce"S such as Mpgeaerally unable to sterilely eradicate the Although M. tuberculosis preferentially re
pathogens. In particular, the multinucle- sides m MP, a few parenchyma cells, typisXTb CeI1S warb°r M' ,ube™l°™ and These"1
ce1|l'e
become infected,
nese cells remain unnoticed by CD4 T
cXla
a™
t0 eradicate ,heir in‘racells and are identified only by CDS T cells
cellu|ar predators. Lysis of such cells
(and
perhaps 7/8 T cells). Second, the three
herefore, may contribute to protection by
allowing uptake by more efficient phagol vadoi Pk°PU at,ons ™y differ in their acti
vation kinetics, with 7/8 T cells probably
marbec3'6'’ ‘he productive granuloma
°f mycobacterial
wall anlT enCapsula,ed by a fibrotic growth8 Th' at
wall, and the center of the granuloma may growth. Thus, 7/8 T cells may perform
"n fibO
SeemS tO P'ay a nolafl|e role essential effector functions before a/p T
“fibrotic encapsulation and central necro- cells do. Although 7/8 T cells may be lesl
l’ ‘heir faS'er kinetics °f “obili^
sis (Vassal!., 1992). Encapsulation further tiol
contributes to microbial containment, and iron and activation may give them some
ow Partlal °2 pressure (pO.) in the mardX
H 'heSe T’Ce" poPula"'™»
necrotic center provides
undea
ln
.
“'°r functions lhas far
unfavorable
"Clear, e.g„ m their capacity to leave the
growth conditions for M ituberculosis.
’
Uncontrolled cell destruction•' Iby cytolytic T vascular bed or in their responsiveness to
cells, NK cells, activated MP, and/or'PW 1ndaTTryni8na,S' F°Urlh' a/P T ce“s
and 7/8 T cells vary remarkably in their
Chapter 24
‘Quefaction and
veolar and vasdetritus and the
ovide an exccllosis that favors
■ion. Rupture of
crobial dissemalveolar system
lrough the vassites.
!E THAN ONE
>N FOR
9
cells, CDS T
highly similar
ional compeal T-cell subto occur? At
mnot be fully
f CDS T cells
cells is their
I molecules,
'ally all host
xpression is
such as MP.
-rentially rea cells, typine infected.
by CD4 T
CDS T cells
■id, the three
1 their actils probably
cobacterial
iy perform
fore a/p T
lay be less
1 mobilizahem some
■opulations
s thus far
leave the
veness to
3 T cells
v in their
1
tissue distributions. In mucosal tissues, in
cluding the lung, as preferred port of entry
and site of disease manifestation in tuber
culosis, the percentage of 7/8 T cells is
markedly higher than in peripheral blood
and central lymphoid organs. Finally, reg
ulatory interactions between these T-cell
subsets may be required. In support of this
last possibility, evidence has been pre
sented that 7/8 T cells control activation of
a/p T cells not only in vitro but also in vivo
(Kaufmann et al., 1993). Most impres
sively, in the model of experimental listeri
osis of 7/8 T-cell-deficient mutant mice,
huge, abscess-like lesions develop that are
strikingly different from the granulomatous
lesions at the site of listerial implantation in
healthy controls (Mombaerts et al., 1993).
GENETIC DETERMINANTS FOR
SUSCEPTIBILITY AND RESISTANCE
IN TUBERCULOSIS
While there is little formal genetic evi
dence in humans, data obtained from epi
demiological investigations suggest that
susceptibility to many infectious diseases,
including tuberculosis, is under some ge
netic control (Motulsky, 1979; Skamene,
1986). The annual death rate from tubercu
losis reached 10% when the disease first
became prevalent in the Qu’appelle Valley
Indian Reservation in Canada, eliminating
half the Indian families in the first three
generations; yet 40 years later, the annual
death rate had dwindled to 0.2%, suggest
ing selection for host resistance (Goodman
and Motulsky, 1979). Clearly, it is conceiv
able that different genetic strains of the
same pathogen cause diseases in different
geographical regions, so that with contin
ued passage, as could be in the case of
tuberculosis in the Qu’appelle Valley, at
tenuated virulence and thus in a drastic
drop in death rate over time result. While
this confounding factor is difficult to rule
out, nonetheless, the higher degree of con-
•
Immune Mechanisms of Protection
405
cordance of tuberculosis among monozy
gotic than dizygotic twins (Comstock, 1978)
and the tragic incident of Lubeck in 1927
(Anonymous, 1935), in which infants inad
vertently immunized with a single viable
virulent M. tuberculosis strain displayed
marked differences in susceptibility ranging
from death to recovery, argue for a genetic
basis for resistance to mycobacterial dis
eases.
In contrast to work with the human sys
tem, experimental studies on the genetics
of resistance to an enormous variety of
infectious agents (salmonellae, ieishmaniae, mycobacteria, murine leukemia vi
ruses, rickettsiae, etc.) in inbred strains of
mice are abundant (Skamene, 1985). In the
case of resistance to Salmonella typhimurium, Leishmania donovani, and BCG,
compelling experimental evidence obtained
from backcross linkage analyses (Skamene
et al., 1982) suggests that resistance against
these three pathogens is under monogenic
control. This allele has been designated Ity,
Lsh, and Beg in the resistance models of 5.
typhimurium, Leishmania donovani, and
BCG, respectively. Through typing for re
sistance and susceptibility to BCG among
recombinant inbred mouse strains together
with linkage analyses and detailed dissec
tion of a 30-centimorgan segment on murine
chromosome 1, the cloning of the cDNA for
the Beg gene, designated Nramp (natural
resistance-associated macrophage protein),
has recently been achieved (Vidal et al.,
1993). Sequence analysis of the Nramp
cDNA reveals a 1,452-nucleotide open
reading frame that encodes a 484-aminoacid protein with structural homology to a
eukaryotic nitrate transporter. Analysis of
Nramp cDNAs from seven Bcgr and six
Bcgs mouse strains indicates that BCG sus
ceptibility is the result of a G-to-A transi
tion at position 783 associated with a non
conservative substitution of Asp-105 for
Gly-105 within a predicted transmembrane
domain of Nramp. Comparison of amino
acid sequences of the murine Nramp and a
406
i
Chan and Kaufmann
human homolog deduced from a partial
which dismutates to generate NO (Shank et
cDNA clone reveals 89% homology be
al., 1962) and other more reactive and per
tween the two species. Nucleic acid se
haps more toxic reactive nitrogen species
quence analysis indicates that Gly-105 of
such as the nitrogen dioxide radical. A
murine Nramp is conserved in the human
corollary of this possibility is that ammonia
sequence.
production by M. tuberculosis (Gordon et
While it is known that the BcgT gene
al., 1980) is a means by which generation of
confers resistance against mycobacteria by
toxic RNI could be intercepted via alkalinacting early during the nonimmune phase of
ization of the phagolysosomal content. The
infection in mice (in contrast to the MHC
existence of a human homolog of Nramp, at
genes, which appear to be associated with least by cDNA analyses (Vidal et al., 1993)
recovery after infection), the precise bio
together with the presence on human chro
chemical and molecular mechanisms of
how Nramp regulates resistance and sus mosome 2q of a region syntenic to the
30-centimorgan segment on murine chro
ceptibility to infection remain to be defined
(reviewed in Skamene (1986]). Experimen mosome 1 that contains the Beg allele
(Schurr et al., 1990) should presage opti
tal evidence strongly suggests that the
Nramp phenotype is mediated via macro mism in unraveling the genetic basis for
phages. It has been demonstrated that the resistance and susceptibility to mycobacte
rial diseases, at least at the early phase of
cell type expressing the Nramp phenotype
infection. It is hoped that the elucidation of
is derived from the bone marrow and is
relatively radioresistant. In addition, the one aspect of this difficult question will
form a firm springboard for understanding
phenotypic expression of Nramp can be
other as yet unknown genetic factors, e.g.,
inactivated by chronic exposure of mice to
the MHC molecules (Skamene, 1986), that
silica, a macrophage poison (Gros et al.,
aid in determining the outcome of myco
1983). Finally, Nramp mRNAs are prefer
bacterial infection.
entially expressed in the reticuloendothelial
system, particularly in macrophages. The
recent finding that RNI generated via the
CONCLUDING REMARKS
macrophage L-arginine-dependent cyto
Around the world, as many as 60 million
toxic mechanism is effectively antimycopeople
suffer from tuberculosis. This high
bacterial (Denis, 1991a; Flesch and Kauf
figure may lead to the false conclusion that
mann, 1991; Chan et al., 1992) and the
demonstration of marked structural resem protective immunity is totally insufficient
blance of Nramp protein to a eukaryotic for control of this disease. The figure, how
ever, is clearly qualified by the even higher
nitrate transporter (Vidal et al., 1993) lend
number of more than 1.7 billion infected
support to the hypothesis that regulation of
individuals, i.e., one-third of the world pop
RNI trafficking in macrophages might be
ulation, illustrating that in the vast majority
one way by which the resistance phenotype
of infected individuals, disease does not
of this gene is expressed. It is thus possible
develop in the face of an ongoing infection.
that Nramp participates in the L-argininedependent antimycobacterial pathway by Hence, protective immunity is extraordi
narily inefficient in terminating infection
transporting NO2", a relatively stable and
and, at the same time, highly efficacious in
nontoxic nitrogen oxide formed via the ox
idation of nitric oxide in the aqueous phase, preventing disease. Because the relation
ship between M. tuberculosis and host im
into the phagolysosomal compartment,
munity
underlying infection is a labile one,
whose acidic environment is requisite to
any
diminution
of protective immunity will
and allows the formation of nitrous acid.
cause progression into clinical disease.
I
Chapter 24
(Shank et
and pern species
adical. A
ammonia
3ordon et
deration of
ia alkalinntent. The
Nramp, at
al., 1993),
man chro
nic to the
rine chroBcg allele
■sage optibasis for
tycobactephase of
nidation of
-•stion will
erstanding
tors, e.g.,
L986), that
of myco-
<S
60 million
This high
■usion that
isufficient
ure, howen higher
i infected
orld popt majority
does not
infection.
:xtraordiinfection
acious in
relation
host imbile one,
inity will
jase.
•
Immune Mechanisms of Protection
407
human macrophages is associated with unrespon
siveness to IFN-7. J. Immunol. 150:1838-1845.
Bermudez, L. E., and J. Champsi. 1993. Infection
with Mycobacterium avium induces production of
interleukin-10 (IL-10), and administration of anti1L-10 antibody is associated with enhanced resis
REFERENCES
tance to infection in mice. Infect. Immun. 61:30933097.
Adams, J. S., and M. A. Gacad. 1985. Characterization
Bieiecki, J., P. Youngman, P. Connelly, and D. A.
of 1-alpha hydroxylation of vitamin D, sterols by
Portnoy. 1990. Bacillus subtilis expressing a haemol
cultured alveolar macrophages from patients with
ysin gene from Listeria monocytogenes can grow in
sarcoidosis. J. Exp. Med. 161:755-765.
mammalian cells. Nature (London) 345:175-176.
Albelda, S. M., and C. A. Buck. 1990. Integrins and
Bloom, B. R., and B. Bennett. 1966. Mechanism of a
other cell adhesion molecules. EASES J. 4:2868reaction in vitro associated with delayed-type hy
2880.
persensitivity. Science 153:80-82.
Amiri, P., R. M. Locksley, T. G. Parslow, M. Sadick,
Brennan, P. J. 1989. Structure of mycobacteria: recent
E. Rector, D. Ritter, and J. H. McKcrrow. 1992.
developments in defining cell wall carbohydrates
Tumor necrosis factor a restores granulomas and
and proteins. J. Infect. Dis. 11:S42O-S43O.
induces parasite egg-laying in schistosome-infected
Brennan,
P. J., S. W. Hunter, M. McNeil, D. Chatter
SCID mice. Nature (London) 356:604-607.
jee, and M. Daffe. 1990. Reappraisal of the chemis
Anonymous. 1935. Die Sauglingstuherkulose in
try of mycobacterial cell walls, with a view to
Lubeck. Julius Springer, Berlin.
understanding the roles of individual entities in
Armstrong. J. A., and P. D’Arcy Hart. 1971. Response
disease processes, p. 55-75. In E. M. Ayoub, G. H.
of cultured macrophages to Mycobacterium tuber
Cassell, W. C. Branche, Jr., and T. J. Henry (ed.).
culosis, with observations on fusion of lysosomes
Microbial Determinants of Virulence and Host Re
with phagosomes. J. Exp. Med. 134:713-740.
sponse. American Society for Microbiology, Wash
Armstrong, J. A., and P. D’Arcy Hart. 1975. Phago
ington, D.C.
some-lysosome interactions in cultured macro
Brennt, C. E., A. C. Wright, S. K. Dutta, and J. G.
phages infected with virulent tubercle bacilli. Rever
Morris, Jr. 1991. Growth of Vibrio vulnificus in
sal of the usual fusion pattern and observations on
serum from alcoholics: association with high trans
bacterial survival. J. Exp. Med. 142:1-16.
ferrin iron saturation. J. Infect. Dis. 164:1030-1032.
Arruda, S., G. Bomfim, R. Knights, T. Huima-Byron,
Brozna, J. P., M. Horan, J. M. Rademacher, K. A.
and L. W. Riley. 1993. Cloning of an M. tuberculosis
Pabst, and M. J. Pabst. 1991. Monocyte responses
DNA fragment associated with entry and survival
to sulfatide from Mycobacterium tuberculosis: inhi
inside cells. Science 261:1454-1457.
bition of priming for enhanced release of superox
Augustin, A., R. T. Kubo, and G.-K. Sim. 1989.
ide, associated with increased secretion of interleu
Resident pulmonary lymphocytes expressing the c/d
kin-1 and tumor necrosis factor alpha, and altered
T-cell receptor. Nature (London) 340:239-241.
protein phosphorylation. Infect. Immun. 59:2542Bail, O. 1910. Ubertragung der Tuberkulinempfindli2548.
chkeit. Z. Immunitaetsforsch. 4:470-485.
Bullen, J. J., P. B. Spalding, C. G. Ward, and J. M. C.
Bainton, D. F. 1981. The discovery of lysosomes. J.
Gutteridge. 1991. Hemochromatosis, iron, and sep
Cell Biol. 91:66S-76S.
ticemia caused by Vibrio vulnificus. Arch. Intern.
Bancroft, G. J., R. D. Schreiber, and E. R. Unanue.
Med. 151:1606-1609.
1991. Natural immunity: a T-cell-independenl path
Bullock, W. E., and S. D. Wright. 1987. Role of the
way of macrophage activation defined in the scid
adherence-promoting receptors, CR3, LFA-1, and
mouse. Immunol. Rev. 124:5-24.
pl50,95 in binding of Histoplasma capsulatum by
Barnes, P. F., S. D. Mistry, C. L. Cooper, C. Pirmez,
human macrophages. J. Exp. Med. 165:195-210.
T. H. Rea, and R. L. Modlin. 1989. Compartmental
Cahall, I). L., and C. P. Youmans. 1975a. Conditions
ization of a CD4+ T lymphocyte subpopulation in
for production, and some characteristics, of myco
tuberculous pleuritis. J. Immunol. 142:1114-1119.
bacterial growth inhibitory factor produced by
Beckman, J. S., T. W. Beckman, J. Chen, P. A.
spleen cells from mice immunized with viable cells
Marshall, and B. A. Freeman. 1990. Apparent hy
of the attenuated H37Ra strain of Mycobacterium
droxyl radical production by peroxynitrite: implica
tuberculosis. Infect. Immun. 12:833-840.
tions for endothelial injury from nitric oxide and
Cahall, D. L., and C. P. Youmans. 1975b. Molecular
superoxide. Proc. Natl. Acad. Sci. USA 87:1620weight and other characteristics of mycobacterial
1624.
growth inhibitory factor produced by spleen cells
Bermudez, L. E. 1993. Production of transforming
obtained from mice immunized with viable cells of
growth factor-p by Mycobacterium avmm-infected
Acknowledgments. S. H. E. Kaufmann acknowl
edges financial support from SFB 322, Landesschwerpunkt “Chronic Infectious Diseases," and from the
German Ministry of Science and Technology (BMFT).
408
*
If
II'
1
Chan and Kaufmann
the attenuated mycobacterial cells Infect. Inunun.
Cooper, A. M., I). K. Dalton, T. A. Stewart, J. P
12:841-850.
Griffin, D. G. Russell, and I. M. Orme. 1993 Dis
Chan, J., and B. R. Bloom. Unpublished observations.
semmated tuberculosis in interferon-y gene-dis
Chan J., X.-D. Fan. S. W. Hunter, P. J. Brennan, and
rupted
mice. J. Exp. Med. 178:2243-2247.
B. R. Bloom. 1991. Lipoarabinomannan, a possible
Crowle, A. J., E. J. Ross, and M. H. May. 1987
virulence factor involved in persistence of Myco
inhibition by l,25(OH)2-vitamin D, of the multipli
bacterium tuberculosis within macrophages Infect
cation of virulent tubercle bacilli in cultured human
hnmun. 59:1755-1761.
macrophages. Infect. Immun. 55:2945-2950.
Chan, J., T. Fujiwara, P. Brennan, M. McNeil, S. J.
( unha, F. Q., S. Moncada, and F. Y. Liew 199'>
urco, J.-C. Sibille, M. Snapper, P. Aisen, and B. R.
Interleukin-10 (IL-10) inhibits the induction of nitric
Bloom. 1989. Microbial glycolipids: possible viru
oxide synthase by interferon-gamma in murine maclence factors that scavenge oxygen radicals. Proc.
1'155^159 BiOChem' Bi°Phys- Res- Commun. 182:
Natl. Acad. Sci. USA 86:2453-2457.
Xinc’ R’ S' Mag,iozzo’ and B- R- Bloom.
D1CS’7M e C' LaCaVe’ M-A- Lanee,le’ and G- Laneelle.
1992. Ktllmg of virulent Mycobacterium tuberculo
Structure of the major triglycosyl phenolsis by reactive nitrogen intermediates produced by
phthiocerol of Mycobacterium tuberculosis (strain
activated murine macrophages. J. Exp. Med 175Canetti). Eur. J. Biochem. 167:144-160
1111-1122.
Dalton, D., S. Pitts-Meek, S. Keshav, I. S. Figari, A.
Chase, M. W. 1945. The cellular transfer of cutaneous
Bradley, and T. A. Stewart. 1993. Multiple defects of
hypersensitivity to tuberculin. Proc. Soc. Exp Biol
immune cell function in mice with disrupted interMed. 59:134-135.
feron-y genes. Science 259:1739-1742.
Chatterjee, I)., K. Lowell, B. Rivoire, M. R. McNeil
D'Andrea, A., M. Rengaraju, N. M. Valiente, J. Cheand P J. Brennan. 1992a. Lipoarabinomannan of
himi, M. Kubin, M. Aste, S. H. Chan, M. Kobayashi,
Mycobacterium tuberculosis. Capping with mannoD. Young, E. Nickbarg, R. Chizzonite, S. F. Wolf
In S°me Strains- J BioL Chem- 267:
and G. Trinchieri. 1992. Production of natural killed
6234-6239.
cell stimulatory factor (interleukin 12) by peripheral
Chatterjee. D„ A. D. Roberts, K. Lowell, P. J. Bren
P. J. Brcnblood mononuclear cells. J. Exp. Med. 176:1387nan, and I. M. Orme. 1992b. Structural1 basis
of
basis of
capacity of lipoarabinomannan to induce secretion of
“
P- M’ R' Y0,,"8’ A' H' G'>rd™. >”«
tumor necrosis factor. Infect. Immun. 60:1249-1253
K. H. Sullivan. 1987. Inhibition of phagosome-lyso
iT mA- '?•’ K D’ Finke,ma"’ P- Caspar, S. Heiny,
some fusion in macrophages by certain mycobacte
J. G Macedonia, and A. Sher. 1992. Treatment with
ria can be explained by inhibition of lysosomal
anti-IL-2 antibodies reduces hepatic pathology and
movements observed after phagocytosis. J. Exp
eosinophilia in Schistosoma mansoni-infcc^d mice
Med. 166:933-946.
while selectively inhibiting T cell IL-5 production J
D’Arcy Harl, p„
R Young M M
w
Immunol. 148:3244-3248.
Perkins, and M. J. Geisow. 1983. Chemical inhibi
Chensue, S. W., I. G. Otterness, G. I. Higashi, C. S.
tors of phagosome-lysosome fusion in cultured mac
Forsch, and S. L. Kunkel. 1989. Monokine produc
rophages also inhibit saltatory lysosomal move
tion by hypersensitivity (Schistosoma mansoni egg)
ments. A combined microscopic and computer
and foreign body (Sephadex bead)-tyPe granuloma
study. J. Exp. Med.
macrophages. Evidence for sequential production of
David, J. R. 1966. Delayed hypersensitivity in vitro: its
ottUm0r neCr°SiS faCtOr- JH2:
mediation by cell-free substances formed by lymIZol—Izod.
Ensues S W., P. D. Terebuh, K. S. Warmington,
S. D. Hershey, H. L. Evanoff, S. L. Kunkel, and G. I
Higashi. 1992. Role of IL-4 and IFN-y in Schisto
soma mansoni egg-induced hypersensitivity granu
loma formation. Orchestration, relative contribu
tion, and relationship to macrophage function J
Immunol. 148:900-906.
Cohn, Z. A. 1963. The fate of bacteria within phago
cytic cells. I. I he degradation of isotopically labeled
bacteria by polymorphonuclear leucocytes and mac
rophages. J. Exp. Med. 117:27-42
Comstock, G. W. 1978. Tuberculosis in twins: a reanalysis of the Prophit survey. Am. Rev. Respir
Dis. 117:621-624.
’
5"^.in,eraC,i°nle Duve, C., and R. Watdaux. 1966. Functions of
lysosomes. Annu. Rev. Physiol. 28:435-492.
D^B’t'ro, G., I. Flesch, and S. H. E. Kaufmann. 1988
Mycobacteria reactive Lyt2+ T cell lines. Eur J
Immunol. 18:59-66.
Denis. M 1991a. Killing of Myeobaccri^ lubercUlosis Within human monocytes: activation by cytoktnes and calcitriol. Clin. Exp. !m,84:2(l0_
zUO.
Dems, M. 1991b. Interferon-gamma-treated murine
macrophages inhibit growth of tubercle bacilli via
the generation of reactive nitrogen intermediates.
Cell. Immunol. 132:150-157.
Chapter 24
Stewart, J. i>_
me. 1993. Dison-y gene-dis-2247.
H. May. 1987.
of the multipli-ultured human
45-2950.
Y. Liew. 1992.
luction of nitric
in murine macCommun. 182:
nd G. Laneelle.
•cosyl phenoleulosis (strain
60.
■ S. Figari, A.
tiple defects of
dsrupted inter-
2.
diente, J. CheM. Kobayashi,
:e, S. F. Wolf,
•f natural killer
' by peripheral
'ed. 176:1387Gordon, and
igosome-lysom mycobacteof lysosomal
osis. J. Exp.
■Iordan, W. J.
emical inhibicultured mac■iomal moveid computer
ty in vitro: its
ned by lymNatl. Acad.
■'unctions of
-492.
mann. 1988.
nes. Ear. J.
n tuberculo>n by cytoiol. 84:200ted murine
bacilli via
ermediates.
Denis, M. 1991c. Tumor necrosis factor and granulo
cyte macrophage colony-stimulating factor stimu
late human macrophages to restrict growth of viru
lent Mycobacterium avium and to kill avirulent M.
avium: killing effector mechanism depends on the
generation of reactive nitrogen intermediates. J.
Leukocyte Biol. 49:380-387.
Denis, M., and E. Ghadirian. 1991. Transforming
growth factor (TGF-pi) plays a detrimental role in
the progression of experimental Mycobacterium
avium infection; in vivo and in vitro evidence.
Microb. Pathog. 11:367-372.
Doi, T., M. Ando, T. Akaike, M. Suga, K. Sato, and H.
Maeda. 1993. Resistance to nitric oxide in Mycobac
terium avium complex and its implication in patho
genesis. Infect. Immun. 61:1980-1989.
Douvas, G. S., D. L. Looker, A. E. Vatter, and A. J.
Crowle. 1985. Gamma interferon activates human
macrophages to become tumoricidal and leishmanicidal but enhances replication of macrophage-asso
ciated mycobacteria. Infect. Immun. 50:1-8.
Drapier, J.-C., IL Hiding, J. Wietzerbin, P. Kaldy,
and L. C. Kuhn. 1993. Biosynthesis of nitric oxide
activates iron regulatory factor in macrophages.
EMBO J. 12:3643-3649.
Dunn, C. J., M. M. Hardee, A. J. Gibbons, N. D.
Staite, and K. A. Richard. 1988. Interleukin-1 in
duces chronic granulomatous inflammation, p. 329334. In M. C. Powanda, J. J. Oppenheim, M. J.
Kluger, and C. A. Dinarello (ed.). Monokines and
Other Non-lymphocytic Cytokines. Alan R. Liss,
Inc., New York.
Eaton, J. W., P. Brandt, and J. R. Mahoney. 1982.
Haptoglobin: a natural bacteriostat. Science 215:
691-693.
Emmrich, F., J. Thole, J. D. A. Van Embden, and
S. H. E. Kaufmann. 1986. A recombinant 64 kilodal
ton protein of Mycobacterium bovis BCG specifi
cally stimulates human T4 clones reactive to myco
bacterial antigens. J. Exp. Med. 163:1024-1029.
Falini, B., L. Flenghi, S. Pileri, P. Pelicci, M. Fagioli,
M. F. Martelli, L. Moretta, and E. Ciccone. 1989.
Distribution of T cells bearing different forms of the
T cell receptor c/d in normal and pathological human
tissues. J. Immunol. 143:2480-2488.
Falkow, S., R. R. Isberg, and D. A. Portnoy. 1992. The
interaction of bacteria with mammalian cells. Annu.
Rev. Cell Biol. 8:333-363.
Fan, X.-D., M. Goldberg, and B. R. Bloom. 1988.
Interferon-gamma-induced transcriptional activa
tion is mediated by protein kinase C. Proc. Natl.
Acad. Sci. USA 85:5122-5125.
Filley, E. A., and G. A. W. Rook. 1991. Effect of
mycobacteria on sensitivity to the cytotoxic effects
of tumor necrosis factor. Infect. Immun. 59:2567-
2572.
Flesch, I. E. A., and S. IL E. Kaufmann. 1987. Myco-
Immune Mechanisms of Protection
409
bacterial growth inhibition by interferon-y-activated
bone marrow macrophages and differential suscep
tibility among strains of Mycobacterium tuberculo
sis. J. Immunol. 138:4408-4413.
Flesch, I. E. A., and S. H. E. Kaufmann. 1988. At
tempts to characterize the mechanisms involved in
mycobacterial growth inhibition by gamma-interfer
on-activated bone marrow macrophages. Infect. Im
mun. 56:1464.
Flesch, I. E. A., and S. H. E. Kaufmann. 1990a.
Activation of tuberculostatic macrophage functions
by gamma interferon, interleukin-4, and tumor ne
crosis factor. Infect. Immun. 58:2675-2677.
Flesch, I. E. A., and S. H. E. Kaufmann. 1990b.
Stimulation of antibacterial macrophage activities
by B-cell stimulatory factor 2 (interleukin-6), infect.
Immun. 58:269-271.
Flesch, I. E. A., and S. H. E. Kaufmann. 1991. Mech
anisms involved in mycobacterial growth inhibition
by gamma interferon-activated bone marrow macro
phages: role of reactive nitrogen intermediates. In
fect. Immun. 59:3213-3218.
Flynn, J. L., and B. R. Bloom. Personal communica
tion.
Flynn, J. L., J. Chan, K. J. Triebold, D. K. Dalton,
T. A. Stewart, and B. R. Bloom. 1993. An essential
role for IFN-y in resistance to Mycobacterium tu
berculosis infection. J. Exp. Med. 178:2249-2254.
Flynn, J. L., M. A. Goldstein, K. J. Treibold, B.
Koller, and B. R. Bloom. 1992. Major histocompat
ibility complex class I-restricted T cells are required
for resistance to Mycobacterium tuberculosis infec
tion. Proc. Natl. Acad. Sci. USA 89:12013-12017.
Flynn, J. L., I). Mathis, and B. R. Bloom. Unpublished
observations.
Flynn, J. L., R. Schreiber, and B. R. Bloom. Personal
communication.
Follows, G. A., M. E. Munk, A. J. Gatrill, P. Conradt,
and S. H. E. Kaufmann. 1992. Interferon-y and
interleukin 2 but no detectable interleukin 4 in y/8
T-cell cultures after activation with bacteria. Infect.
Immun. 60:1229-1231.
Forrest, C. B., J. R. Forehand, R. A. Axtell, R. L.
Roberts, and R. B. Johnston, Jr. 1988. Clinical
features and current management of chronic granu
lomatous disease. Hematol. Oncol. Clin. N. Am.
2:253-265.
Friedland, J. S., I). G. Remick, R. Shattock, and G. E.
Griffin. 1992. Secretion of interleukin-8 following
phagocytosis of Mycobacterium tuberculosis by hu
man monocyte cell lines. Eur. J. Immunol. 22:13731378.
Friedland, J. S., R. J. Shattock, J. D. Johnson, D. G.
Remick, R. E. Holliman, and G. E. Griffin. 1993.
Differential cytokine gene expression and secretion
after phagocytosis by a human monocytic cell line of
Toxoplasma gondii compared with Mycobacterium
410
1
Chan and Kaufmann
tuberculosis. Clin. Exp. Immunol. 91:282-286.
Hamilton, T. A., D. L. Becton, S. D. Somers, P. w
Gavioli, R„ S. Spisani, A. Giuliani, and S. Traniello.
Gray, and D. O. Adams. 1984. Interferon-y modu
1987. Protein kinase C mediates human neutrophil
lates protein kinase C activity in murine peritoneal
cytotoxicity. Biochem. Biophys. Res. Commun
macrophages. J. Biol. Chem. 260:1378-1381.
148:1290-1294.
Hemzel, F. P., D. S. Schoenhaut, R. M. Rerko, L E
Gazzinelli, R. T„ S. Hieny, T. A. Wynn, S. Wolf, and
Rosser, and M. K. Gately. 1993. Recombinant inter
A. Sher. 1993. Interleukin 12 is required for the
leukin 12 cures mice infected with Leishmania ma
Mymphocyte-independent induction of interferon y
jor. J. Exp. Med. 177:1505-1509
by an intracellular parasite and induces resistance in
Helmholz, H. F. 1909. Uber passive Ubertragung der
T-cell-deficient hosts. Proc. Natl. Acad. Sci. USA
Tuberkulin-Uberempfindlichkeit
bei
Meersch90:6115-6119.
weinchen.
Z.
Immunitaetsforsch.
3:371-375.
Gazzinelli, R. T., I. P. Oswald, S. L. James, and A.
Hibbs, J. B., C. Westenfelder, R. Taintor, Z. Vavrin,
Sher. 1992. IL-10 inhibits parasite killing and nitro
C. Kablitz, R. L. Baranowski, J. H. Ward, R. L.
gen oxide production by IFN-gamma-activated mac
Menlove,
M. P. McMurry, J. P. Kushner, and W E
rophages. J. Immunol. 148:1792-1796.
Samlowski. 1992. Evidence for cytokine-inducible
Gennaro, R., C. Florio, and D. Romeo. 1985. Activamtnc oxide synthesis from L-arginine in patients
tion of protein kinase C in neutrophil cytoplasts
receding interleukin-2 therapy. J. Clin. Invest. 89:
FEBS Lett. 180:185-190.
867-877.
Goodman, R. M., and A. G. Motulsky. 1979. Genetic
Hunter, S. W., and P. J. Brennan. 1981. A novel
Diseases among Askenazi Jews, p. 301 Raven
phenolic glycolipid from Mycobacterium leprae pos
Press, Inc., New York.
sibly involved in immunogenicity and pathogenicity
Gordon, A. H., P. D’Arcy Hart, and M. R. Young.
J. Bacterio!. 147:728-735.
1980. Ammonia inhibits phagosome-lysosome fu
Hunter,
S. W., and P. J. Brennan. 1991. Evidence for
sion in macrophages. Nature (London) 286:79-81
the presence of a phosphatidylinositol anchor on the
Goren, M. B., O. Brokl, P. Rol|er, H. M. Fales, and
hpoarabinomannan and lipomannan of Mycobacte
. C. Das. 1976a. Sulfatides of Mycobacterium
rium tuberculosis. J. Biol. Chem. 265:9272-9279.
tuberculosis; the structure of the principal sulfatide
Hunter, S. W., T. Fujiwara, and P. J. Brennan. 1982
(3L-1). Biochemistry 15:2728.
Structure and antigenicity of the major specific
Goren M. B., O. Brokl, and W. B. Schaeffer. 1974.
glycolipid antigen of Mycobacterium leprae. J Bio!
Lipids of putative relevance to virulence in Myco
Chem. 257:15072-15078.
bacterium tuberculosis; correlation of virulence
Hunter, S. W., H. Gaylord, and P. J. Brennan. 1986
with elaboration of sulfatides and strongly acidic
Structure and antigenicity of the phosphorylated
lipids. Infect. Immun. 9:142-149.
lipopolysaccharide antigens from the leprosy and
Goren, M. B., P. D’Arcy Hart, M. R. Young, and J. A.
tubercle bacilli. J. Biol. Chem. 261:12345-12351.
Armstrong. 1976b. Prevention of phagosome-lyso
Hwmn’.K” P’ Vandenbussd’G and H. Heremans.
some fusion in cultured macrophages by sulfatides
1991. lnterleukin-6 production in Mycobacterium
of Mycobacterium tuberculosis. Proc. Natl Acad
bovts BCG-infected mice. Cell. Immunol. 137:224Sci. USA 73:2510-2514.
Goren, M. B., A. E. Vatter, and J. Fiscus. 1987a.
olyanionic agents as inhibitors of phagosome-lyso
some fusion in cultured macrophages: evolution of
an alternative interpretation. J. Leukocyte Biol.
41:111—121.
Goren, M. B., A. E. Vatter, and J. Fiscus. 1987b.
Polyanionic agents do not inhibit phagosome-lyso4LP2 'in29UltUred niacr°Phages. J. Leukocyte
Griffiths, E., H. J. Rogers, and J. J. Bullen. 1980. Iron,
pkismids and infection. Nature (London) 284:508Gros, P., E. Skamene, and A. Forget. 1983. Cellular
mechanisms of genetically controlled host resis
tance to Mycobacterium bovis (BCG). J. Immunol.
131:1966-1973.
Hamilton, T. A., and D. O. Adams. 1987. Molecular
mechanisms of signal transduction in macrophages
Immunol. Today 8:151-158.
,nwo’1T‘AY; Yoshikai’ G- Matsuzaki, and K. Nomoto.
1991. Early appearing y/8-bearing T cells during
infection with Calmette Guerin bacillus. J. Immu
nol. 146:2754-2762.
Isberg, R. R. 1991. Discrimination between intracellu
lar uptake and surface adhesion of bacterial patho
gens. Science 252:934-938.
lyer, G. Y. N., M. F. Islam, and J. H. Quastel. 1961.
Biochemical aspects of phagocytosis. Nature (Lon
don) 192:535-541.
kzo, A A., and R. J. North. 1992. Evidence for an a/p
1 cell-independent mechanism of resistance to my
cobacteria. Bacillus-Calmctte-Gu^rin causes progressive infection in severe combined immunodefi
cient mice, but not in nude mice or in mice depleted
CD4+ and CD8+ T cells. J. Exp. Med. 176:581Jo6.
Jams, E. M„ S. H. E. Kaufmann, R. H. Schwartz, and
A. M. Pardoll. 1989. Activation of y/8 T cells in the
Chapter 24
’» S. D. Somers, P. yy.
■84- Interferon-y moduy in murine peritoneal
260:1378-1381.
L R. M. Rerko, L. E.
'3. Recombinant interwith Leishmania ma09.
sive Ubertragung der
-it
bei
Meerschch. 3:371-375.
• Taintor, Z. Vavrin,
« J. H. Ward, R. L.
Kushner, and W. E.
cytokine-inducible
‘fginine in patients
J- Clin. Invest. 89:
■an- 1981. A novel
icteriuni leprae posY and pathogenicity.
1991. Evidence for
asitol anchor on the
nan of Mycobacte■ 265:9272-9279.
J- Brennan. 1982.
he major specific
um leprae. J. Biol.
J- Brennan. 1986.
e Phosphorylated
the leprosy and
:12345-12351.
1 H. Heremans.
Mycobacterium
tmunol. 137:224and K. Nomoto.
I T ceils during
cillus. J. Immuween intracellubacterial patho• Quastel. 1961.
i. Nature (Lon-
ence for an a/p
istance to my> causes proJ immunodefimice depleted
Wed. 176:581-
Schwartz, and
T cells in the
•
Immune Mechanisms of Protection
411
primary immune response to Mycobacterium tuber
Klun, C. L., and G. P. Youmans. 1973a. The effect of
culosis. Science 244:713-717.
lymphocyte supernatant fluids on the intracellular
Joiner, K. A., S. A. Fuhrman, H. M. Miettinen, L. H.
growth of virulent tubercle bacilli. J. ReticuloendoKasper, and I. Mellman. 1990. Toxoplasma gondii:
thel. Soc. 13:263-274.
fusion competence of parasitophorous vacuoles in
Klun, C. L., and G. P. Youmans. 1973b. The induction
Fc receptor-transfected fibroblasts. Science 249:
by Listeria monocytogenes and plant mitogens of
641-646.
lymphocyte supernatant fluids which inhibit the
Kabelitz, D., A. Bender, S. Schondelmaier, B. Schoel,
growth of Mycobacterium tuberculosis within mac
and S. H. E. Kaufmann. 1990. A large fraction of
rophages in vitro. J. Reticuloendothel. Soc. 13:275human peripheral blood y/8+ T cells is activated by
285.
Mycobacterium tuberculosis but not by its 65-kD
Kobayashi, K., C. Allred, S. Cohen, and T. Yoshida.
heat shock protein. J. Exp. Med. 171:667-679.
1985. Role of interleukin 1 in experimental granu
Kamijo, R., J. Le, D. Shapiro, E. A. Havell, S. Huang,
loma in mice. J. Immunol. 134:358-364.
M. Aguet, M. Bosland, and J. Vilcek. 1993. Mice that
Kobayashi, M., L. Fitz, M. Ryan, R. M. Hewick, S. C.
lack the interferon-y receptor have profoundly al
Clark, S. Chan, R. Loudon, F. Sherman, B. Perussia,
tered responses to infection with Bacillus Calmetteand G. Trinchieri. 1989. Identification and purifica
Guerin and subsequent challenge with lipopolysac
tion of natural killer cell stimulatory factor (NKSF),
charide. J. Exp. Med. 178:1435-1440.
a cytokine with multiple biologic effects on human
Kasahara, K., K. Kobayashi, Y. Shikama, I. Yoneya,
lymphocytes. J. Exp. Med. 170:827.
K. Soezima, H. Ide, and T. Takahashi. 1988. Direct
Koch, R. 1882. Die Atiologie der Tuberkulose. Ber
evidence for granuloma-inducing activity of interliner Klin. Wochenschr. 19:221-230.
leukin-1. Induction of experimental pulmonary gran
Koch, R. 1890. Weitere Mitteilungen liber ein Heiluloma formation in mice by interleukin-l-coupled
mittel gegen Tuberkulose. Dtsch. Med. Wochen
beads. Am. J. Pathol. 130:629-638.
schr. 16:1029-1032.
Kaufmann, S. H. E. 1988. CD8H T lymphocytes in
Koeffler, H. P., H. Reichel, J. E. Bishop, and A. W.
intracellular microbial infections. Immunol. Today
Norman. 1985. Gamma interferon stimulates pro
9:168-174.
duction of 1,25-dihydroxyvitamin D3 by normal hu
Kaufmann, S. H. E., C. Blum, and S. Yamamoto. 1993.
man macrophages. Biochem. Biophys. Res. CornCrosstalk between a/p T cells and y/8 T cells in
mun. 127:596-603.
vivo: activation of a/p T cell responses after -y/8 T
Kornfeld, S. 1987. Trafficking of lysosomal enzymes.
cell modulation with the monoclonal antibody GL3.
FASEBJ. 1:462—468.
Proc. Natl. Acad. Sci. USA 90:9620-9624.
Kurlander, R. J., S. M. Shawar, M. L. Brown, and
Kaufmann, S. H. E., and I. Flesch. 1986. Function and
R. R. Rich. 1992. Specialized role for a murine class
antigen recognition pattern of L3T4+ T cell clones
I-b MHC molecule in prokaryotic host defenses.
from Mycobacterium tuberculosis-immune mice. In
Science 257:678-679.
fect. Immun. 54:291-296.
Kwon, N. S., C. F. Nathan, and D. J. Stuehr. 1989.
Kaufmann, S. H. E., M. E. Munk, T. Koga, et al. 1989.
Reduced biopterin as a cofactor in the generation of
Effector T cells in bacterial infections, p. 963-970.
nitrogen oxides by murine macrophages. J. Biol.
In F. Melchers (ed.), Progress in Immunology.
Chem. 264:2049^20501.
Spring Verlag, Stuttgart, Germany.
Ladel, C., and S. H. E. Kaufmann. Unpublished data.
Kaufmann, S. H. E., H. R. Rodewald, E. Hug, and G.
Larsen, C. A., A. O. Anderson, E. Apella, J. J.
DeLibero. 1988. Cloned Listeria monocytogenes
Oppenheim, and K. Matsushima. 1989. The neutro
specific non-MHC-restricted Lyt2+ T cells with
phil-activating protein (NAP-1) is also chemotactic
cytolytic and protective activity. J. Immunol. 140:
for T lymphocytes. Science 243:1464.
3173-3179.
Leake, E. S., Q. N. Myrvik, and M. J. Wright. 1984.
Kindler, V., A.-P. Sappino, G. E. Gran, P.-F. Piquet,
Phagosomal membranes of Mycobacterium bovis
and P. Vassalli. 1989. The inducing role of tumor
BCG-immune alveolar macrophages are resistant to
necrosis factor in the development of bactericidal
disruption by Mycobacterium tuberculosis. Infect.
granulomas during BCG infection. Cell 56:731-740.
Immun. 45:443-446.
King, C., M. Sathish, J. T. Crawford, and T. M.
Li, Y., A. Severn, M. V. Rogers, R. M. J. Palmer, S.
Shinnick. 1993. Expression of contact-dependent
Moncada, and F. Y. Liew. 1992. Catalase inhibits
cytolytic activity of Mycobacterium tuberculosis
nitric oxide synthesis and the killing of intracellular
and isolation of the locus encoding the activity.
Leishmania major in murine macrophages. Ear. J.
Infect. Immun. 61:2708-2712.
Immunol. 22:441-446.
Klebanoff, S. J. 1980. In R. Van Furth (ed.). Mononu
Liew, F. Y., and F. E. G. Cox. 1991. Nonspecific
clear Phagocytes, Functional Aspects, part 2, p.
defence mechanism: the role of nitric oxide. Immu
1105-1141. Nijhoff, Boston.
nol. Today 12A:17-21.
412
I
i,
fl
Chan and Kaufmann
Liew, F. ¥., Y. Li, A. Severn, S. Millott, J. Schmidt,
different stages. Nature (London) 360:225-231
M. Salter, and S. Moncada. 1991. A possible novel
Mosser, D. M„ and P. J. Edelson. 1987. The third
pathway of regulation by murine T helper type-2
component of complement (C3) is responsible for
( Hi2) cells of a Thl cell activity via the modulation
the intracellular survival of Leishrnania major Na
of the induction of nitric oxide synthase on macro
ture (London) 327:329-331.
phages. J. Immunol. 21:2489-2494
Motulsky, A. G. 1979. Human Genetics. Raven Press
Locksley. R. M. 1993. Interleukin 12 in host defense
Inc., New York.
against microbial pathogens. Proc. Natl. Acad Sci
Muller, I„ S. P. Cobbold. H. Waldmann, and S. H. E.
USA 90:5879-5880.
Kaufmann. 1987. Impaired resistance against Myco
Lune, M. B. 1942. Studies on the mechanism of
bacterium tuberculosis infection after selective inimmunity in tuberculosis. The fate of tubercle bacilli
vivo depletion of L3T4* and Lyt2+ T cells. Infect
ingested by mononuclear phagocytes derived from
Immun. 55:2037-2041.
normal and immunized animals. J. Exp. Med. 75:
Munk. M. E., A. Gatrill, and S. H. E. Kaufmann. 1990
247.
Antigen-specific target cell lysis and interleukin-2
Lurie, M. B. 1964. Resistance to Tuberculosis. Har
secretion
by Mycobacterium tuberculosis-aclNdled
vard University Press, Cambridge, Mass
y/6 I cells. J. Immunol. 145:2434-2439.
Mackaness, G. B. 1969. The influence of immunologi
Muroaka, S., K. Takeya, and K. Nomoto. 1976a. In
cally committed lynphoid cells on macrophage acti
vitro studies on the mechanism of acquired resis
vation in vivo. J. Exp. Med. 129:973.
tance
to tuberculous infection. I. The relationship
Mackaness, G. B.. and R. V. Blanden. 1967. Cellular
between
lymphocytes and macrophages in cellular
immunity. Prog. Allergy 11:89-140.
immunity to tuberculous infection. Jpn. J Micro
Mathew, R. C., S. Ragheb, and D. L. Boros. 1990.
biol. 20:115-122.
Recombinant IL-2 therapy reverses diminished
Muroaka, S., K. Takeya, and K. Nomoto. 1976b. In
granulomatous responsiveness in anti-L3T4-treated,
vitro studies on the mechanism of acquired resis
Schistosoma manjom-infected mice. J. Immunol
tance to tuberculous infection. IL The effects of the
144:4356-4361.
culture supernatants of specifically-sensitized lym
McDonough, K. A., Y. Kress, and B. R. Bloom. 1993
phocytes on the growth of tubercle bacilli within
Pathogenesis of tuberculosis: interaction of Myco
macrophages.
Jpn. J. Microbiol. 20:365-373.
bacterium tuberculosis with macrophages. Infect
Murray, C. J. L., K. Styblo, and A. Rouillon. 1990.
Immun. 61:2763-2773.
Tuberculosis in developing countries: burden, inter
Mclnnes, A., and D. M. Rennick. 1988. Interleukin 4
vention, and cost. Bull. Int. Union Tuherc. 65:2.
induces cultured monocytes/macrophages to form
Myrvik, Q. N., E. S. Leake, and M. J. Wright. 1984.
giant multinucleated cells. J. Exp. Med. 167:598Disruption of phagosomal membranes of normal
611.
alveolar
macrophages by the H37Rv strain of My
Metchmkoff, E. 1905. Immunity to Infectious Dis
cobacterium tuberculosis. Am. Rev. Respir Dis
eases. Cambridge University Press, London.
129:322-328.
Middlebrook, G., C. M. Coleman, and W. B. Schaeffer.
Nathan,
C. 1992. Nitric oxide as a secretory product of
1959. Sulfolipid from virulent tubercle bacilli. Proc.
mammahan
cells. FASEB J. 6:3051-3064.
Natl. Acad. Sci. USA 45:1801-1804.
Nathan, C. F., and J. B. Hibbs, Jr. 1991. Role of nitric
Modlin. R. L., C. Pirmez, F. M. Hofmann. V. Torigian,
oxide synthesis in macrophage antimicrobial activ
K. Uyemura, T. H. Rea, B. R. Bloom, and M. B.
ity. Carr. Opin. Immunol. 3:65.
Brenner. 1989. Lymphocytes bearing antigen-spe
Neilands, J. B. 1981. Microbial iron compounds. Annu
cific c/d 7-cell receptors accumulate in human infec
Rev. Biochem. 50:715-731.
tious disease lesions. Nature (London) 339:544-548
Neill, M. A., and S. J. Klebanoff. 1988. The effect of
P- A- Meyn> K- D' Sml,h. “"<1 C- Kaplan.
phenolic glycolipid-I from Mycobacterium leprae on
1993. Recognition and destruction of bacillus CalI ic antimicrobial activity of human macrophages J
mette-Gudrin-infected human monocytes J Exo
Exp. Med. 167:30-42.
Med. 177:1691-1698.
Mombaerts, P., J. Arnold!, F. Russ, S. lonegawa. and
S. H. E. Kaufmann. 1993. Differential roles of a/(3
and y/8 I cells in immunity against an intracellular
bacterial pathogen. Nature (London) 365:53-56
Mombaerts, P„ A. R. Clarke, M. A. Rudnicki’ J.
lacomini, S. Itohara, J. J. Lafaille, L. Wang Y
Ichikawa, R. Jaenisch, M. L. Hooper, and S. Tonegawa. 1992. Mutations in T-cell antigen r~;receptor
genes a and b block thymocyte development
t at
Nelson, B. J., P. Ralph, S. j. Green and c A
1991. Differential susceptibility of activated macro
phage cytotoxic effector reactions to the suppres
sive effects of transforming growth factor-Bl J
Immunol. 146:1849-1857.
Neu, H. C. 1992. The crisis in antibiotic resistance.
Science 257:1064-1073.
Nussler, A., M. Di Silvio, T. R. Billiar, R. A. Hoffman,
D. A. Geller, R. Selby, J. Madariaga, and R. L.
Simmons. 1992. Stimulation of nitric oxide synthase
1
Chapter 24
60:225-231.
^987. The third
responsible for
nia major. Nav. Raven Press,
m, and S. H. E.
: against Mycoer selective inT cells. Infect.
ufmann. 1990.
1 interleukin-2
/ons-activated
<9.
oto. 1976a. In
cquired resis■e relationship
ges in cellular
'pn. J. Micro-
oto. 1976b. In
cquired resis
effects of the
insitized lymbacilli within
55-373.
ouillon. 1990.
'burden, inter
fere. 65:2.
Wright. 1984.
-s of normal
strain of MyRespir. Dis.
ry product of
■64.
Role of nitric
robial activ■unds. Anna.
fhe effect of
<m leprae on
rophages. J.
C. A. Nacy.
ited macroie suppres-tor-pl. J.
resistance.
. Hoffman,
and R. L.
e synthase
I
pathway in human hepatocytes by cytokines and
endotoxin. J. Exp. Med. 176:261-266.
Ochoa, J. B., B. Curti, A. B. Peitzman, R. L. Simmons,
T. R- Billiar, R. Hoffman, R. Rault, I). L. Longo,
W. J. Urba, and A. C. Ochoa. 1992. Increased
circulating nitrogen oxides after human tumor im
munotherapy: correlation with toxic hemodynamic
changes. J. Natl. Cancer Inst. 84:864-867.
Ochoa, J. B., A. O. Udekwu, T. R. Billiar, R. D.
Curran, F. B. Cerra, R. L. Simmons, and A. B.
Peitzman. 1991. Nitrogen oxide levels in patients after
trauma and during sepsis. Ann. Surg. 214:621-626.
Ohkuma, S., Y. Moriyama, and T. Takano. 1982.
Identification and characterization of a proton pump
on lysosomes by fluorescein isothiocyanate-dextran
fluorescence. Proc. Natl. Acad. Sci. USA 79:27582762.
Ohkuma, S., and B. Poole. 1978. Fluorescence probe
measurement of the intralysosomal pH in living cells
and the perturbation of pH by various agents. Proc.
Natl. Acad. Sci. USA 75:3327-3331.
Oppenheim, J. J., C. O. C. Zachariae, N. Mukaida,
and K. Matsushima. 1991. Properties of the novel
proinflammatory supergene "intercrine” cytokine
family. Anna. Rev. Immunol. 9:617-648.
Orme, I. M. 1987. The kinetics of emergence and loss
of mediator T lymphocytes acquired in response to
infection with Mycobacterium tuberculosis. J. Im
munol. 138:293-298.
Orme, I. M., and F. M. Collins. 1984. Adoptive
protection of the Mycobacterium tuberculosis-in
fected lung. Dissociation between cells that pas
sively transfer protective immunity and those that
transfer delayed type hypersensitivity to tuberculin.
Cell. Immunol. 84:113-120.
Oswald, I. P., R. T. Gazzinelli, A. Sher, and S. L.
James. 1992. IL-10 synergizes with IL-4 and trans
forming growth factor-beta to inhibit macrophage
cytotoxic activity. J. Immunol. 148:3578-3582.
Ottenhoff, T. H. M., A. B. Kale, J. D. A. Van Embden,
J. E. R. Thole, and R. Kiessling. 1988. The recom
binant 65 kD heat shock protein of Mycobacterium
bovis BCG/M. tuberculosis is a target molecule for
CD4+ cytotoxic T lymphocytes that lyse human
monocytes. J. Exp. Med. 168:1947-1952.
Pabst, M. J., J. M. Gross, J. P. Prozna, and M. B.
Goren. 1988. Inhibition of macrophage priming by
sulfatide from Mycobacterium tuberculosis. J. Im
munol. 140:634-640.
Pamer, E. G., M. J. Bevan, and K. Fischer Lindahl.
1993. Do nonclassical, class lb MHC molecules
present bacterial antigens to T cells? Trends Micro
biol. 1:35-38.
Pamer, E. G., C.-R. Wang, L. Flaherty, K. Fischer
Lindahl, and M. J. Bevan. 1992. H-2M3 presents a
Listeria monocytogenes peptide to cytotoxic T lym
phocytes. Cell 70:215-223.
•
Immune Mechanisms of Protection
413
Patterson. R. J., and G. P. Youmans. 1970. Demon
stration in tissue culture of lymphocyte-mediated
immunity to tuberculosis. Infect. Immun. 1:600603.
Payne, N. R., and M. A. Horwitz. 1987. Phagocytosis
of Legionella pneumophila is mediated by human
monocyte complement receptors. J. Exp. Med. 166:
1377-1389.
Pedrazzini, T., K. Hug, and J. A. Louis. 1987. Impor
tance of L3T4+ and Lyt-2+ cells in the immuno
logic control of infection with Mycobacterium bovis
strain bacillus Calmette-Gudrin in mice. Assessment
by elimination of T cell subsets in vivo. J. Immunol.
139:2032-2037.
Pfeffer, K., B. Schoel, H. Guile, S. H. E. Kaufmann,
and H. Wagner. 1990. Primary responses of human
T cells to mycobacteria: a frequent set of 7/8 T cells
are stimulated by protease-resistant ligands. Ear. J.
Immunol. 20:1175-1179.
Pfeifer, J. D., M. J. Wick, R. L. Robert, K. Findlay,
S. J. Normark, and C. V. Harding. 1993. Phagocytic
processing of bacterial antigens for class I MHC
presentation to T cells. Nature (London) 361:359362.
Pontyremoli, S., E. Mellon!, F. Salamino, B. Sparatore,
M. Michetti, O. Sacco, and B. L. Horecker. 1986.
Activation of NADPH oxidase and phosphorylation
of membrane proteins in human neutrophils: coor
dinate inhibition by a surface antigen-directed
monoclonal. Biochem. Biophys. Res. Common. 140:
1121-1126.
Rao. S. P., K. Ogata, and A. Catanzaro. 1993. Myco
bacterium avium-M. intracellulare binds to the integrin receptor aJJ, on human monocytes and
monocyte-derived macrophages. Infect. Immun. 61:
663-670.
Rees, A. D. M., A. Scoging, A. Mehlert, D. B. Young,
and J. Ivanyi. 1988. Specificity of proliferative re
sponse of human CD8 clones to mycobacterial anti
gens. Eur. J. Immunol. 18:1881-1887.
Reichel, H., H. P. Koefller, and A. W. Norman. 1987.
Synthesis in vitro of 1,25-dihydroxyvitamin D, and
24,25-dihydroxyvitamin D, by interferon-7-stimulated normal human bone marrow and alveolar
macrophages. J. Biol. Chem. 262:10931-10987.
Reiman, D., E. Yuomanen, S. Falkow, D. T. Golenbock, K. Saukkonen, and S. D. Wright. 1990. Rec
ognition of a bacterial adhesin by an integrin:
macrophage CR3 (aM32> CDllb/CD18) binds fila
mentous hemagglutinin of Bordetella pertussis. Cell
61:1375-1382.
Rook, G. A. W. 1988. The role of vitamin D in
tuberculosis. Am. Rev. Respir. Dis. 138:768-770.
Rook, G. A. W. 1990. The role of activated macro
phages in protection and immunopathology in tuber
culosis. Res. Microbiol. 141:253-256.
Rook, G. A. W., J. Steele, M. Ainsworth, and B. R.
414
Chan and Kaufmann
Champion 1986. Activation of macrophages to inhtbH proliferation of Mycobacterium tuberculouscomparison of the effects of recombinant gamma
interferon on human monocytes and murine perito
neal macrophages. Immunology 59:333-338.
Russell, D. G., and S. D. Wright. 1988. Complement
receptor type 3 (CR3) binds to an Arg-Gly-Sapcontaimng region of the major surface glycoprotein,
gp63, of Leishmania promastigotes. J. Exp. Med
168:279-292.
Sa^neta P. J., A. Ryer, P. Ckrc, A. T. MaurelH, and
J. Mourner. 1986. Mulliplication of Shigella ftexneri
w«hm HeLa cells: lysis of the phagocytic vacuole
and plasmid-mediated contact hemolysis. Infect
Irnmun. 51:461—469.
Sbarra, A. J., and M. L. Karnovsky. 1959. The bio
chemical basis of phagocytosis. I. Metabolic
changes during the ingestion of particles by poly
morphonuclear leukocytes. J. Biol. Chem. 234:
1355—1362.
Schade, A. L., and L. Caroline. 1944. Raw hen egg
Xhl,e,/an<? thC rOle Of iron in grow,h inhibition of
ugella dysentenae. Staphylococcus aureus, EschlOO-lZTs'' and SaCC,iaromyces ^evisiae. Science
Schlesinger L. S. 1993. Macrophage phagocytosis of
virulent but not attenuated strains of Mycobacte
rium tuberculosis is mediated by mannose receptors
in50l292^2n93O0.COmP'ement reCeP'OrS-
Med. 107:237-245.
Sher, N. A., S. D. Chaparas, L. F. Greenberg, E. M
Merchant, and J. H. Vickers. 1975. Response of
congenitally athymic (nude) mice to infection with
v"(strain
BCG,‘J'Natl'Cancer
Sibley L D„ S. W. Hunter, P. J. Brennan, and J. L
Krehenbuhl. 1988. Mycobacterial lipoarabinomannan inhibits gamma interferon-mediated activation
of macrophages. Infect. Irnmun. 56:1232-1236.
Sibley, L. D., and J. L. Krahenbuhl. 1988. Induction of
unresponsiveness to gamma interferon in macro
phages mfected with Mycobacterium leprae Infect
Irnmun. 56:1912-1919.
Skamene, E. 1985. Genetic control of host resistance
^in-li0" and mallgnanCy- Prof!- Le'^ocyte Biol.
Skamene, E. 1986. Genetic control of resistance to
mycobacterial infection. Curr. Top. Microbiol. Im
munol. 124:49-66.
P- Gr0S’ A- F<’r8Ct P- A- L- K»nBSh»v„,
C. St. Charles, and B. A. Taylor. 1982. Genetic
regulabon of resistance to intracellular pathogens
Nature (London) 297:506-509.
Snow G. A. 1970. Mycobactins: iron-chelating growth
factors from mycobacteria. Bacterio!. Rev. 34:99-
S<l“,r“, K. E., R. D. Schreiber, M. J. McElrath, B. Y.
Rubin, S. L. Anderson, and H. W. Murray. 1989.
Experimental visceral leishmaniasis: role of endog
Schlesinger, L. S., C. G. Bellinger-Kawahara, N. R.
enous IFN-7 in host defense and tissue granuloma
Payne and M. A. Horwitz. 1990. Phagocytosis of
tous response. J. Immunol. 143:4244-4249.
Mytobactenum tuberculosis is mediated by human
Stamler. J. S., D. J. Singel, and J. Loscalzo. 1992.
monocyte complement receptors and complement
lochemistry of nitric oxide and its redox-activated
component C3. J. Immunol. 144:2771-2780.
forms. Science 258:1898-1902.
Schoendon, G., J. Troppmair, A. Fontana, C. Huber,
Suter E. 1952. The multiplication of tubercle bacilli
H.-C. Curtis, and A. Neiderwieser. 1987. Biosynthe
within normal phagocytes in tissue cultures J Exn
sis and metabolism of pterins in peripheral blood
Med. 96:137.
’
'
mononuclear cells and leukemia lines of man and
Suter, E. 1953. Multiplication of tubercle bacilli within
mouse. Eur. J. Biochem. 166:303-310
mononuclear phagocytes in tissue cultures derived
Schoenhaut, D. S., A. O. Chua, A. G. Wolitzky, P. M.
from normal animals and animals vaccinated with
DWyCr’ W- McMomas> P- C. FamilBCG. J. Exp. Med. 97:235.
letti, M. K. Gately, and U. Guhler. 1992. Cloning and
Tatamas-Rohana, P„ S. D. Wright, M. R. Lennart,,
expression of murine IL-12. J. Immunol. 148:3433and D G. RnSSell. 1990. Lipophosphoglycan (LPG)
3440.
from Leishmania mexicana promastigotes binds to
Schurr, E., E. Skemene, K. Morgan, M.-L. Chu, and
members of the CR3. P150,95 and LFA-1 family of
P. Gros. 1990. Mapping of Coldal and Col6a3 to
eukocyte integnns. J. Immunol. 144:4817^1824.
proximal murine chromosome 1 identifies conserved
layeh, M. A., and M. A. Marietta. 1989. Macrophage
inkage of structural protein genes between murine
oxidation of L-arginine to nitric oxide, nitrite and
chromosome 1 and human chromosome 2q. Genom
nitrate. letrahydrobiopterin is required as a cofac
ics 8:477-486.
tor. J. Biol. Chem. 264:19654-19658
Shank, J. L., J. H. Silliker, and R. H. Harper. 1962.
Tazi A I. Fajac, P. Soler, D. Valeyre, J. P. Battesti,
The effect of nitric oxide on bacteria. Appl. Micro
and A. J. Hance. 1991. Gamma/delta T lymphocytes
biol. 10:185.
are not increased in number in granulomatous le
Sheppard, C. C. 1958. A comparison of the growth of
sions of patients with tuberculosis or sarcoidosis.
selected mycobacteria in HeLa, monkey kidney,
Am. Rev. Respir. Dis. 144:1373-1375.
and human amnion cells in tissue culture. J. Exp
Tripp, C. S., S. F. Wolf, and E.
- ------- --- R. Unanue. 1993.
L
Chapter 24
. Greenberg, E. M.
1975. Response of
e to infection with
j). J. Natl. Cancer
Brennan, and J. L.
il lipoarabinomanicdiated activation
56:1232-1236.
. 1988. Induction of
terferon in macrorium leprae. Infect.
'•til’d
'I of host resistance
>g. Leukocyte Biol.
ol of resistance to
op. Microbiol. Irn. A. L. Kongshavn,
lor. 1982. Genetic
:ellular pathogens.
n-chelating growth
•eriol. Rev. 34:99J. McElrath, B. Y.
W. Murray. 1989.
sis: role of endogtissue granuloma244-4249.
J. Loscalzo. 1992.
ts redox-activated
of tubercle bacilli
: cultures. J. Exp.
ircle bacilli within
: cultures derived
i vaccinated with
M. R. Lennartz,
phoglycan (LPG)
-tstigotes binds to
LFA-1 family of
44:4817-1824.
989. Macrophage
•xide, nitrite and
uired as a cofac8.
J. P. Battesti,
a T lymphocytes
anulomatous leor sarcoidosis.
75.
Unanue. 1993.
1
Interleukin 12 and tumor necrosis factor a are
costimulators of interferon y production by natural
killer cells in severe combined immunodeficiency
mice with listeriosis, and IL-10 is a physiologic
antagonist. Proc. Natl. Acad. Sci. USA 90:37253729.
Turcotte, R., Y. Des Ormeaus. and A. F. Borduas.
1976. Partial characterization of a factor extracted
from sensitized lymphocytes that inhibits the growth
of Mycobacterium tuberculosis within macrophages
in vitro. Infect. Immun. 14:337-344.
Vachula, M., T. J. Holzer, and B. R. Anderson. 1989.
Suppression of monocyte oxidative response by
phenolic glycolipid I of Mycobacterium leprae. J.
Immunol. 142:1696-1701.
Vassalli, P. 1992. The pathophysiology of tumor necro
sis factors. Annu. Rev. Immunol. 10:411-452.
Vidal, S. M., D. Malo, K. Vogan, E. Skamene, and P.
Gros. 1993. Natural resistance to infection with
intracellular parasites: isolation of a candidate for
Beg. Cell 73:469-485.
Walker, L., and D. B. Lowrie. 1981. Killing of Myco
bacterium microti by immunologically activated
macrophages. Nature (London) 293:69-70.
Weinberg, E. D. 1974. Iron and susceptibility to infec
tious disease. Science 184:952-956.
Weinberg, E. D. 1978. Iron and infection. Microbiol.
Rev. 42:45-66.
Weinberg, E. D. 1992. Iron depletion: a defense
against intracellular infection and neoplasia. Life
Sci. 50:1289-1297.
Weiss, G., B. Goossen, W. Doppler, D. Fuchs, K.
Pantopoulos, G. Werner-Felmayer, H. Wachter, and
M. W. Hentze. 1993. Translational regulation via
iron-responsive elements by the nitric oxide/NO-
•
Immune Mechanisms of Protection
415
synthase pathway. EMBO J. 12:3651-3657.
Weiss, S. J. 1989. Tissue destruction by neutrophils.
N. Engl. J. Med. 320:365-376.
Werner, E. R., G. Verner-Felmayer, D. Fuchs, A.
Hausen, G. Reibnegger, and H. Wachter. 1989. Par
allel induction of tetrahydrobiopterin biosynthesis
and indoleamine 2,3-dioxygenase activity in human
cells and cell lines by interferon--y. Biochem. J.
262:861-866.
Wilson, E., M. C. Olcott. R. M. Bell. A. H. Merrill, Jr.,
and J. D. Lambeth. 1986. Inhibition of the oxidative
burst in human neutrophils by sphingoid long-chain
bases. J. Biol. Chem. 261:12616-12623.
Winkler, H. H. 1990. Rickettsia species (as organ
isms). Annu. Rev. Microbiol. 44:131-153.
Wolf, S. F., P. A. Temple, M. Kobayashi, D. Young,
M. Dicig, L. Lowe, R. Dzialo, L. Fitz, C. Ferenz,
R. M. Hewick, K. Kelleher, S. H. Herrmann, S. C.
Clark, L. Azzoni, S. H. Chan, G. Trinchieri, and B.
Perussia. 1991. Cloning of cDNA for natural killer
cell stimulatory factor, a heterodimeric cytokine
with multiple biologic effects on T and natural killer
ceils. J. Immunol. 146:3074-3081.
Wright, S. D., and S. C. Silverstein. 1983. Receptors
for C3b and C3bi promote phagocytosis but not the
release of toxic oxygen from human phagocytes. J.
Exp. Med. 158:2016-2023.
Xie, Q. W., R. Whisnant, and C. Nathan. 1993. Pro
moter of the mouse gene encoding calcium-indepen
dent nitric oxide synthase confers inducibility by
interferon gamma and bacterial lipopolysaccharide.
J. Exp. Med. 177:1779-1784.
Zhu, L., C. Gunn, and J. S. Beckman. 1992. Bacteri
cidal activity of peroxynitrite. Arch. Biochem. Biophys. 298:452-^57.
- Media
 RF-TB-1.24.pdf
RF-TB-1.24.pdf
Position: 6252 (1 views)