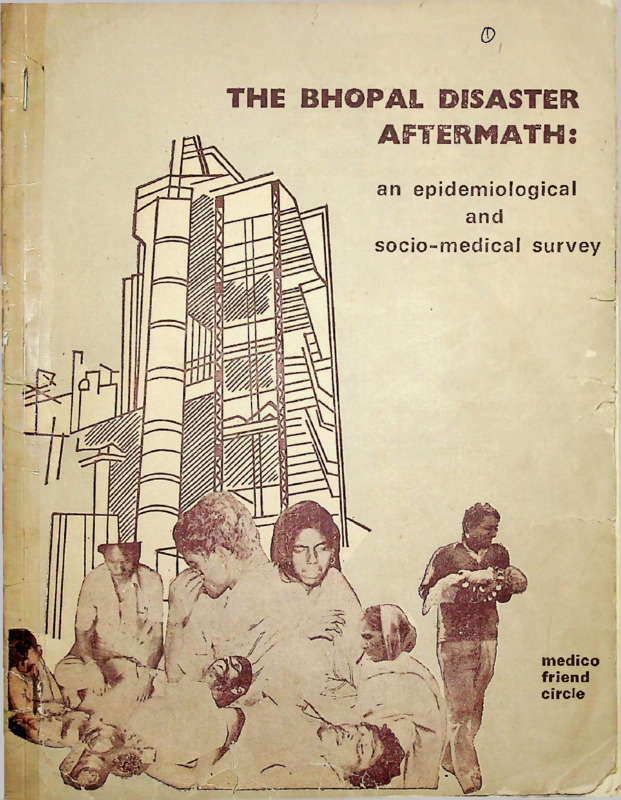
The Bhopal Disaster Aftermath: an epidemiological and socio-medical survey
Media
- Title
- The Bhopal Disaster Aftermath: an epidemiological and socio-medical survey
- extracted text
-
fl)
THE BM0PA1 DISASTER
AFTERMATH:
• .
an epidemiological
and
’1
socio-medical survey
r ■
V
■ p
I
i
i
~T|
medico
friend
circle
/13d7]
Dedicated to the thousands
who died or were disabled
by the Bhopal Gas Disaster
--the worst industrial
accident in recorded history.
With a resolve
to prevent
medical research
from becoming an instrument of
exploitation of human
suffering.
With a determination
to make
medical research
an expression of
human concern.
(
I
rice Rs. 8
-
-MUMI-- HrAfTH
THE
CFf (
BHOPAL DISASTER
AFTERMATH
an epidemiological and socio-medical study
15 - 25 March 1985
medico friend circle
r
i
ACKNOWLEDGEMENTS
i
To,
The people of Jaya Prakash Nagar and Anna Nagar for their warm and
welcoming attitude which greatly helped our study.
Rukmini Bahen and friends of SEWA and Ramachandra Bhargava
and colleagues of Gandhi Bhavan for their hospitality in BhopalThe Preventive and Social Medicine Department of Baroda Medical
College fortheir technical cooperation.
Friends of the Gujarat Sangharsh Vahini (Rashmi, Ambarish, Trupti,
Rajesh and Kaumudi) for their help in tabulating and analysing data.
Jan Vigyan Samiti, Kanpur and all our generous friends and members
for their donations, big and small.
A large circle of mfc friends and contacts for their support and
encouragement, and for their critical comments on the draft manu
script of this report.
1
i
•
COMMUNITY HEALTH CELL
47/1, (First F>r > 3t. Marks Hoad
BANGALO.iE-5u0 0Q1
ii
J
ERRATA
Page
Line
1
3
'where' should read 'were'
6
34
'except' should read 'accept'
6
40
'polo' should read 'pool'
13
19
'weight (ii)' should read '(ii) weight'
43
24
'rigorouly' should read 'rigorously'
46
14
'Hindu' should read 'The Hindu'
52
16
'Gag' should read 'gas'
56
16
'muscie aches' should read 'muscle aches'
62
36
'paramteers' should read 'parameters'
63
31
'on' should read 'of'
65
7
'victims' should read 'victims'
TABLES
Page
18
Table No.
1C
'Others' in Anna Nagar 13.36 should
read '1 3.86'
24
3A
Blurred vision/photophobia
J P Nagar 77.02 (144) should read
'77.02 (114)'
A. Nagar 33.40 (53) should read 38.40 (53)
32
60
After J P Nagar468 should read (46.8)
35
7
15-44 Female FEV (Lit) in A.N. 2.25 (2.42)
should read '2.25 (0.42)'
■ .1
J
AT A H H 3
A,
oniJ
ses9
S'
c
f
I
'Jqeoos' bsai biuoris ‘jqaoxe’
AS
0
Mooq' bsoi bluorte %oloq‘
OA
8
‘tcigiew (iif bssi bluorte ‘(ii) idpiew*
er
sr
■ v‘ bf ci hi *
vleuoioeir bsei bluoris 'vluoiooii1
:
SA
ubni I sriT' Jssi b’uorls ‘c ?n:H‘
r- -
‘asQ' beoi bluorla 'ob£
er
£8
‘?9(kr '•Heurn' bsei bluoris 'aodo- 9i .cjr.c
dr
uU
?6iBq'bssi bluorle'siosjfns\ sq*
d£
So
'to' bssi /Jucru no*
re
v
co
'amiror/' bsei bloods 'emi.:?;.
i
I
83
S
3 ? J S AT
d
■oM ©IdBT
i. n - -
or
8F
AS
A£
bluotfg 8dA ,cn:.;1 9 L i: ;A
03
££
(Ji J) V33 916G1S" A-8 F
V
5S
’38.£ F‘ bsei
Gidodqotortq.noiaiv bsnulS
bid bluorie (AM) £0AV ibqbH S L
‘(MT) 20 VV
(£8 . GA.3g b69i bluorie (£•:•) '
(8.8;)
(£A.£) g2.£ .H.
Sc sr-.-'; .-
'(-‘•.0} c£.£ bs^> h.’uort^
■
.
i
THE STUDY TEAM
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
Ashvin Patel (Baroda)
Co-ordinators
Anil Patel (Mangrol)
J
Daxa Patel (Mangrol)
Nimitta Bhatt (Baroda)
Manisha Gupte (Bombay)
Padma Prakash (Bombay)
Mira Sadgopal (Hoshangabad)
Marie D'Souza (Nandurbar)
Shirish Datar (Karjat)
Anant Phadke (Pune)
C. Sathyamala (New Delhi)
and three volunteers from Baroda Medical College
1.
2.
3.
Ramesh Durvasula
Hemant Vithalani
Bipin Patel
iii
I
PREFACE
The Bhopal disaster has been an unprecedented occupational and environ
mental accident. Equally unprecedented have been the imperatives for relief, re
habilitation and research in the aftermath of the disaster.
The local situation has been extremely complicated and dynamic. While
health service providers and researchers have had to face many medical challenges,
government and voluntary agencies involved in relief and rehabilitation have had to
face many logistical and organizational challenges.
For the medico friend circle too, in its intervention in research and
continuing education strategies in support primarily of voluntary agencies, it has
been both a challenge and a thought provoking learning experience. The experience
of planning, organising, analysing and communicating our research findings based
on a modest study has brought us further in touch with the apathy, vested interests
and status quo factors which obstruct action in favour of the disadvantaged in society.
Having seen the intensity of health problems of the disaster victims and the
inadequacies in the strategies employed to ameliorate them we cannot but help raise
critical comments on all components of the social medical system who are there to
handle such problems.
Our objective, however, is more than critical analysis. Through this
epidemiological study we have tried to make our own small contribution to a better
understanding of the health problems that prevail in the aftermath of the disaster.
We have also made suggestions for a more comprehensive relief and rehabilitation
strategy.
A word of caution here—most of our observations are of the situation as it
existed at the end of March 1985. Six months have passed in the process of ana
lysis, consensus seeking and understanding our findings. During these six months,
many further developments--both positive and negative--have taken place in Bhopal
at the governmental and the non-governmental initiative.
We hope that this report will atleast help to highlight to our readers among
other matters that—
(i)
what people say and feel is as important evidence as what we can discover
through our over-mystified medical technological approach;
(ii)
in the absence of a community oriented epidemiological perspective,
decision making about relief efforts, following a disaster can be adhoc and
often irrelevant; and
(iii)
for research to be relevant to the lives of the people, the findings
and inferences drawn must be communicated to the health service pro-'
viders and the patients themselves through an effective communication
stiategy.
Finally we hope that through this report, we shall stimulate debate, dialogue
and a commitment to a deeper understanding of the problem, leading to more relevant
and meaningful interventions.
Ravi Narayan
Convenor
Bangalore
2 Oct 1985
iv
CONTENTS
Page
Acknowledgements
ii
Study team
iii
Preface
iv
1.
INTRODUCTION
1
2.
OBJECTIVES OF THE STUDY
3
3.
BACKGROUND : TWO MEDICAL THEORIES
6
3.1 Pulmonary Fibrosis Theory
6
3.2 Enlarged Cyanogen Pool Theory
8
MATERIALS AND METHODS
12
4.1 Sample population
12
4.2 Methods
12
4.3 Building rapport with the people
14
4.4 Plan of Analysis
15
OBSERVATIONS AND RESULTS
16
5.1 Non-responders—some observations
16
5.2 Comparison of samples
17
5.3 Socio-economic profile in the Bastis
18
5.4 Morbidity analysis
21
DISCUSSION
33
6.1 Role of Chronic Diseases and Smoking
38
6.2 Pulmonary Theory : An assessment
39
6.3 Enlarged Cyanogen Pool Theory : An assessment
41
6.4 Magnitude of the Problem : An issue of Damage/Compensation
44
6.5 Thiosulfate controversy
45
6.6 Implication for research
47
4.
5.
6.
v
r
7.
RECOMMENDATIONS
49
7.1 Community based Epidemiological Research
49
7.2 Mass Relief Programme
50
7.3 Listing of the victims; claims for compensation
50
7.4 Health Committees
51
7.5 A communication strategy on health related issues
51
APPENDICES
52
I
Proforma (6 sections)
52
II
English translation of Handout
61
III
ICMR minutes of 14.2.1985
62
IV Study of Medical Relief
65
V
67
People's Perception
REFERENCES
69
ADDITIONAL READING
71
vi
I
CHAPTER 1
INTRODUCTION
Many months after the Bhopal gas tragedy, conflicting reports kept coming
in from Bhopal. There ware reports that the gas victims continued to present at the
out patients departments with serious physical symptoms and they where getting
very little relief by the standard package of treatment which included antibiotics,
steroids, antacids, cough mixtures, eye drops and bronchodilators.
Doubts were being raised that the disaster victims were developing a sense
of dependence and were exaggerating their symptoms in order to draw more and
more benefits. It was also felt that the first wave of mortality and morbidity
had receded and that there was no significant residual damage and morbidity. The
feeling of ''all was well" was becoming stronger.
In February 1985, another dimension of the human suffering in Bhopal
came to light. The Indian Council of Medical Research (ICMR) came out with a
finding that the gas affected population of Bhooal was probably suffering from a
chronic cyanide like poisoning and that the use of an antidote - sodium thiosulfate—
could improve their condition. The situation was, however, further compounded by
a total clamp down of information by local state health authorities.
The medico friend circle (mfc) had decided at the annual meeting in
Bangalore, end of January 1985, to respond to a series of appeals from various
non-governmental groups and to undertake an epidemiological and medico social
investigation with the primary purpose of supporting disaster victims, citizens'
groups and voluntary agencies in their struggle for meaningful relief, rehabilitation,
justice, and for information.
However, at that point the collective knowledge of mfc was too inadequate
(cyanide poisoning was still in the future) for a meaningful formulation of the
pioblem in Bhopal. Naturally the formulation of concrete objectives for the study
was not possible either. This evolved as the study progressed in stages. It was
however felt that the mfc should collect its own field data and get first hand
information about the health status of the disaster victims.
A few mfc members had visited Bhopal in mid-February and had identified
certain urgent areas for action (1).
The team for this epidemiological study was in Bhopal from 15 to25 March
1985. It consisted of a voluntary group of clinicians, doctors working in community
health projects and health activists from different parts of India. During the stay and
subsequently as the collected data was being analysed, it was realised that two
medical theories to explain the continuing symptoms were competing to gain
supremacy :
i) The 'pulmonary' theory which believed that in view of the available
information about the effects of MIC, only extensive lung damage
(leading to diffused pulmonary fibrosis) and direct injury to corneas
of eyes could be expected.
ii) The 'enlarged cyanogen pool' theory which believed that the effect of the
released gases on the patients was to increase the cyanogenic pool inside
their bodies leading to chronic cyanide-like poisoning.
I
Both these theories are explained further in the text. It is important to
realise, however, that this was not a purely academic controversy but a very serious
problem having a direct and immediate bearing on the lives of the people. The
controversy had resulted in the adherents of the pulmonary fibrosis theory (who
dominate the medical establishment in Bhopal) steadfastly refusing to treat the gas
victims on a mass-scale with sodium thiosulfate which had been advanced as an
antidote by the ICMR on the basis of its research findings. Tne net outcome of this
unseemly controversy was that the suffering of the people was continuing without
any relief in sight.
A study undertaken in a situation where two proponents of opposing
theories are busy in a controversy cannot ignore th°se theories. We did not. in
fact we consciously kept this controversy in mind and analysed our findings
accordingly. Needless to add that the study does not and cannot aim to provide
decisive arguments to resolve the controversy fully.
However the critical analysis does not remain narrowly confined to the
merits and demerits of the contending theories only. It goes much beyond that.
The inherent force of the logic of the criticism impinges upon the much wider issues
of weaknesses in methodology, perspective, orientation and setting of objectives of
medical research as it has been carried on in Bhopal. The serious gaps in the very
fabric of research efforts have direct and vital connection not only with the
urgent issue of relief from suffering, damages and compensation to the victims of
the poison gas, but also wiih the issjeof fixing the responsibilities on ell those
who have perpetuated the suffering of thousands of people of Bhopal.
We outline a series of conclusions and recommendations for urgent consi
deration by all concerned.
A summary of this report is also being releasedin English for wider circula
tion and a lay version in Hindi for the gas affected people in Bhopal.
If, through this modest effort we have moved towards the establishment of
a 'people oriented science' and endorsed the peoole's 'right to know', we would
have felt that our efforts were more than worthwhile.
- medico friend circle
Justice is but truth in action and we cannot hope
to attain justice until we have the proper respect
for truth.
—Anon
2
CHAPTER
2
OBJECTIVES OF THE STUDY
The Indian Council of Medical Research (ICMR) has initiated over 22
ressearch projects to study the sub-acute, chronic and late effects of the Bhopal gas
disaster. The objectives of the medico friend circle (mfc) intervention in Bhopal
jvaas not to duplicate the efforts of ICMR. We neither have the resources nor me
^c»cess to technical supports that are required for such efforts;nor for that matter the
maandate. We believe that the primary role of organising research linked to relief
anid rehabilitation efforts lies with the governmental and national institutions that
have been established with the tax payers' money.
In January 1985 when we first decided to undertake this study, there was
•isardly any official information available on the health situation of the gas victims of
Blihopal. The clamp down on information was unmistakable. From whatever little
imformation we could obtain, it was clear that people in large numbers were reporting
sy/mptoms like shortness of breath, cough, excess lacrimation, fatigue, headache, loss
off appetite, etc. This was a list of symptoms. Only symptoms, apparently uncon
nected to one another by underlying patho-physiological mechanisms, dominated the
sccene.
Naturally at a meeting in Bombay we first set the following series of
objectives.
(i) Assessing current health status and medico-social problems (ii) Prioritizimg in terms of magnitude and implication for rehabilitation (iii) Identifying health
problems that required health education efforts (iv) Studying existing plan of relief,
reesearch and rehabilitation services and (v) Studying people's perception of these
sservices.
Later on, when the study was in progress in Bhopal, we came across
more substantial
information.
The conflict of two medical theories came
before us in sharp focus and the far reaching implications of this conflict for
relief, rehabilitation, compensation etc. were tentatively grasped in those days.
TThe objective was slowly evolving and finally came to be a thorough-going critique
oof the two medical theories and the implications flowing from them.
Our initial
sact finding, appraisal of information and situation analysis, led us to identify a
sseries of issues of concern: (i) secrecy on any type of data/information on the
(disaster; (ii) secrecy of ICMR research study plans; (iii) absence of open scientific
idebate on research findings, (iv) the vertical, clinical and organ centred nature of
(research projects; (v) the absence of encouragement to non governmental initiatives;
(vi) the adhoc and populist approach to relief and rehabilitation; (vii) the absence
of authentic scientific and research based information for the medical teams
providing services; (viii) the absence of demystified but authentic information to
the disaster victims for their evolving mevament/struggle for a more relevant relief
and rehabilitation programme.
These concerns led to a reassessment of the Bombay objectives and a
series of new objectives emerged to best meet the emerging situation. These were( i) To assess the current health status and related problems of the people
on a sound epidemiological/ community basis;
( ii) To assess the findings in the light of the medical controversy between
'exclusive pulmonary pathology' vs. an 'enlarged cyanogenic pool'
leading/ to a chronic cyanide like poisoning;
3
I
i
(iii) To evolve a critique of the ongoing
programme;
research
and
medical
relief
(iv) To identify factors that have important implications for the relief,
rehabilitation strategy (including claims for compensation);
(v) To assess the people's perception of the ongoing health care services;
(vi) To make suggestions for a more meaningful relief/research/rehabilitation policy.
The health problem situation as it evolved in Bhopal which helped give a
final shape to the objective, has another interesting aspect which bears on metho
dology of the study.
V
During and after the study many have commented that our reliance on>
symptoms is somewhat unsatisfactory, that they are subjective and therefore we are
on shaky ground and that more objective data like bio-chemical measurements,
X-rays etc. as were done by other groups (e.g. the Nagrik study) is missing in our
study, rendering it less solid. This faith and attachment to laboratory tests. X-rays
and other types of 'objective' tests is interesting but difficult to understand.
When predominance of a broad range of symptoms was the only important
fact known and even after the fact of 'enlarged cyanogen pool' came to be known,
what could be the biochemical-pathological tests that could be done in a sample
population so as to make our study more objective and less shaky? The only bio
chemical tests of real value, suggested by the 'cyanogen pool' theory are augmented
output of urinary thiocyanate following intravenous sodium thiosulfate and study of
blood gases. Both these tests were of course, beyond our reach. However, that
should not mean that studies at less sophisticated levels like ours, have no objecti
vity about them.
With regard to X-rays, it should be noted that the place of chest-radiography
is extremely limited. Its only legitimate use is in the detailed follow-up of those
whose pulmonary function studies have shown very significant lung diseases (19).
Furthermore X-ray findings sometimes bear little relation to the patient’s disability,
loss of function or severity of other symptoms (10)
The other test which is of real
value Is pulmonary function tests. The forced vital capacity (F V.C.) and the forced
expiratory volume in the first second (F.EV. 1) are the simplest, most repeatable,
valid and among the more discriminating tests reflecting mechanics of breathing.
They have had most extensive trials during the past 25 years and regression equa
tions for predicted normal performance are better documented than for any other
respiratory test (10,19). We have in our study undertaken these tests.
Biochemical parameters, which are routinely studied in clinical settings
where the problem situation is much more settled and clear-cut, cannot be easily
and automatically used with a view to improve objectivity, in a situation like the
Bhopal gas disaster. This is completely new and unknown territory in so far as
little is known about MIC's effect on the body. To use such parameters would be
like shooting in the dark. These 'solid' 'objective' tests themselves do not
necessarily lend objectivity to any study in such an inherently difficult and ill-defined
problem situation. In doing so we are only reinforcing and perpetuating the popu
lar, mythical notions about scientific objectivity. To study symptoms is not
necessarily to be subjective—but about this later.
4
L
in
*
^4
I
J)
<
Ul
d
>
a
□
t-
(0
CHAPTER 3
BACKGROUND : TWO MEDICAL THEORIES
The disaster that took place in Bhopal on the night of 2/3 December 1984
has been universally accepted as the worst man-made industrial and environmental
accident in recorded history. Forty tonnes of stored methyl■ isocyanate (MIC)
escaped into the atmosphere killing over 2500 people and over three thousand cattle
and affecting over two lakh people according to official estimates. These shocking
statistics do not adequately express the actual enormity of the human tragedy—of the
lives lost, the families disrupted, the people disabled and ill and the thousands
impoverished.
The relief efforts that were initiated soon after were handicapped by the
absence of authoritative information on the released gases; the unwillingness of the
Union Carbide company to part with authentic information; the absence of meaning
ful information among the relevant sanctioning, licensing and inspecting authorities
in the State and the Centre; the lack of preparedness of the local bodies and govern
mental health authorities to handle the unprecedented consequences of such a
disaster and the absence of technical or toxicological expertise on MIC among our
scientific community (1).
In the early hours of 3rd December 1984 when hundreds were pouring in to
Hamidia Hospital seeking medical relief, the beginnings of two medical theories
which would later on compete with each other to occupy the central position were
clearly discernible.
They are going to be the main focus of our report,
try to elaborate on these two medical theories.
In this chapter we will
They are (3.1) Exclusively Pulmonary Pathology Theory, which has
been referred to as 'Pulmonary theory' throughout this report. It is so called be
cause it claims that all the mortality and the prevalent morbidity in the gas hit
population of Bhopal is exclusively due to direct injury to lung tissues which over
a period will lead to diffuse pulmonary fibrosis.
I
((3.2) Enlarged Cyanogen Pool Theory, which for the sake of brevity is referred
to as 'Cyanogen pool' theory' throughout the report. This theory postulates chronic
cyanide poisoning of the victims due to enlarged cyanogen pool, in addition to
direct lung/eye damage.
It must be stated clearly and unambiguously at the very beginning that the
Indian Council of Medical Research (ICMR) which is the main protagonist of 'cyano
gen pool' theory does except the fact that lungs have been damaged by MIC gas and
a proportion of the morbidity may be due to that. It is, in fact, therefore the pro
ponent of mixed pathology, but for the sake of discussion and convenience, it is
called the protagonist of'cyanogen pool'theory. Supporters of pulmonary theory
include a dominant faction in Gandhi Medical College, Bhopal and has strong
support in the health department of MP Government. They are adamantly refusing
to accept any other theory, but their own theory. Naturally they are totally opposed
to cyanogen polo theory.
3.1 Pulmonary Theory
According to this theory, isocyanates, of which MIC is one member, are
6
toxic, irritant gases that directly damage the tissues they come in contact with-lungs
and corneas of eyes. The acute and long lasting pathological effects therefore are
to be seen only in lungs and eyes, and the effects of hypoxia secondary to lung
damage.
A small proportion of (about 5-10%) persons exposed to these substances
also develop sensitization (2,5).
The effects of isocyanates even in high doses on the gastrointestinal tract is
minimal (4).
It can induce blindness or visual impairment depending on the degree and
location of scarring (2,3).
Among the isocyanates toluene di-isocyanate (TDI) has been shown to
produce Central Nervous System (CNS) damage, manifested as loss of memory,
diminished mental capacity, persistent headache, personality changes, irritability,
depression etc (6)
But any such effect by MIC on CNS has been dismissed as
anecdotal "because MIC is such a severe primary irritant it would be apt to produce
such a severe degree of irritation that death would occur before sufficient absorption
of the compound could occur to produce systemic effects" (6).
This brings us to the central point of the theory, which is to explain why
MIC exoosure must produce damage to only lungs and corneas excluding all other
organ systems. Wny for instance MIC, an isocyanate, cannot have long lasting
CNS effects whereas another isocyanate, TDI, can have long lasting effect on brain
function?
Among the three isocyanates used in industry MIC is much more reactive
than the other two e.g. TDI and MDI (Methyl Di-isocyanate). It has been argued
that 'MIC is so readily decomposed by water, the chances are "very very remote"
that this iso-cvanate could enter the blood stream, be whisked to internal organs
and produce damage there, by reacting with target proteins'. It is further argued that
'for the same reason MIC lacks the hardiness to be a carcinogen. Molecules of the
compound would have to penetrate the cell wall and reach the DNA to do their ge
netic dirty work. It is virtually unthinkable that molecules of MIC could survive
such a cellular journey' (2,9).
This is the point : the high reactivity of MIC molecule renders it nonspe
cific and therefore it is bound to damage only those organs which come into
direct contact with it — lungs, eyes and skn. The skin may however escape because
MIC fumes may not penetrate the skin (3). The logical corollary of it is that long
term problems in survivors can be due to extensive lung damage and corneal damage
only.
Mr. W. Anderson, Chairman of Union Carbide Corporation, U. S. felt so
confident that in a letter of 3rd January 1985 (exactly one month after the disaster)
he wrote to an activist group which is monitoring the Bhopal Disaster to say that
'those injured by Methyl Isocyanate (MIC) are rapidly recovering and display little
lasting effects
for example, no case of blindness' (11).
The pulmonary theory therefore, must reject any other explanation for the
presence of wide ranging symptoms in the community and also the treatment based
on alternative explanations.
7
For the same reason some U. S. Scientists have characterised such
reports of Cyanide Poisoning of the exposed population 'highly questionable'
and 'probably spurious'. They have further argued that there is no known
metabolic pathway that converts isocyanate into cyanide (2).
The clash of theories extends to the whole range of health problems in
Bhopal.
i
Thus according to the ‘pulmonary theory' the large number of deaths in the
early hours of the morning of 3rd December 1984 were due to carbon monoxide
poisoning and to others the deaths were due to cyanide poisoning. We have no
definite information regarding the nature and quantity of dangerous gases that were
□resent in the atmosphere after the massive gas leak. However it is known that the
thermal decomposition of methyl Isocyanate can lead to the oroduction of a variety
of toxic substances including Carbon monoxide (CO) and Hydrogen Cyanide (4).
Tne temperature of toxic fumes gushing out of the tank was at least 1 20 degrees
centigrade (12).
An investigation was undartaken by the ICMR at a very early stage to sort
out this controversy. Particular attention was paid to find out clear evidence of
carbon monoxide and/or cyanide. A large number of control blood samoles and
also samples of blood already preserved in the deep freeze in the Medico Legal
Institute and fresh samples from cases who subsequently died were examined for
evidence of carbon monoxide poisoning (carboxyhaemoglobin) or cyanide poisoning
(cyanomethemoglobin) by spectrophotometric analysis (14). In none of the samples
was there evidence of either.
In contrast to this, a study of 113 MIC affected people who themselves
reported to K.E.M. Hospital, Bombay showed carboxyhaemoglobin (COHb) at a
concentration of more than 2% in 93% of cases. (The normal levels of COHb in
blood are 0.5 - 0.8 %. In smokers the levels could be as high as 1 5%, the average
being biing 5%) (13). This sample however is not a representative sample and the
control is lacking. Moreover aop/sex structure and smoking status are not given
(8). Bes;des, the effects of COHb levels less then 5% are controversial. COHb
levels of 20%, decrease tissue oxygenation and affect performance (10).
3.2
■ .
Enlarged Cyanogen Pool Theory
v
One of the most important developments of the complex findings among
Bhopal disaster victims has been the evidence favouring what may be termed an
'Enlarged Cyanogen Pool' theory. Professor H. Chandra of Medico Legal Institute
of Gandhi Medical College, Bhopal noticed in the early hours of 3rd December when
the first autopsies were being performed that even the venous blood of dead bodies
was cherry red in colour (so called arterialization of venous blood). All the internal
organs, lungs, intestines, kidneys, brain, muscles, etc. were bright red in colour.
This led him to suspect that victims could have succumbed to cyanide poisoning
(14,15).
A visiting German clinical toxicologist Dr. Max Daunderer is reported to
have detected cyanide in the affected patients (14,15,1 7) Unfortunately his findings
could not be repeated because of technical and methodological problems (14,15).
ICMR set out to 'identify the presence of either the original products'. The objec
tive was to obtain a better understanding of the probable detoxification mechanisms
which would help in the prompt use of an antidote to remove toxic substance still
circulating in the body (14).
8
As has been pointed out in 3.1 above, attempts to establish the presence
of either carboxyhaemoglobin or cyanomethemoglobin in the blood failed. However
all the samples of all victims showed twin bands of oxyhaemoglobin( 14) which is
an indication of a change in the nature of the haemoglobin molecule.
Special note must be taken here that from as early as the first week of the'
disaster, the ICMR approach to the problem pointedly ignored the theoretical notion
of the MIC molecule being too reactive to reach the blood stream and causing
damage to the internal organs.
Following a rapid study of available literature by Dr. Sriramachari it was
felt that the mechanisms of conjugation of isocyanate should be investigated
vigorously. The equivocal results in the increase of blood urea in fresh autopsy
tissue samples as well as qualitative reports of the presence of cyanide in tissue led
to the hypothesis that either due to inhalation of hydrogen cyanide from the conta
minant or cyanide radicals released by the breakdown of MIC within the body, there
was every likelihood of either acute cyanide or chronic cyanide poison operating
(14). This idea was reinforced by literature scan where in there is a reference to
the cyanide pool and its major excretory pathway through urinary thio
cyanate (14)
5 CYANOGEN
POOL
Major palb
CN“
Minor
pefh.
minor
2- iminoihiazolidine4- carboxylic acid. .
HC bJ
in expired air
CNS“ -
u
C M" poo I
Excretion.
Cyawocoba la win.
v
metabolism of
one carbon
compounds.
HCNO
HCOOM
CO2
some excreted
in urine.
L
9
As shown in the diagram above, there is a cyanogen pool in the body
which normally generates extremely small amounts of cyanide radicals in the course
of normal metabolic processes of the body. These cyanide radicals are easily
removed from the body by a process of detoxification which converts the cyanide
radicals into relatively harmless thiocyanates which are excreted as urinary thiocya
nates. This detoxification process is controlled by the enzyme called rhodanase in
the liver.
I
The process of detoxification by the rhodanase system can be accelerated
bv sodium thiosulfate if given in large amounts- This provides the rationale for
injection of sodium thiosulfate for the treatment of cyanide poisoning.
Also the amount of urinary thiocyanate excreted in the urine following
injection sodium thiosulfate gives an indirect clue of the size of cyanogen
pool in the body
And this provides the rationale for sodium thiosulfate as
an epidemiological tool of investigation of the hypothesis of 'enlarged
cyanogen pool' in the MIC exposed population of Bhopal to which we will
return in the Chapter 6.
p
} I
This pool of cyanogen is proposed to have been enlarged in the MIC
exposed population of Bhopal. According to the theory small quantities of cyanide,
but much larger than that which would be normally produced in the body, is con
tinuously contributed to the cyanogen pool of the gas victims from MIC molecules
which are attached to alia chains of haemoglobin molecules - a process that is called
carbamylation of haemoglobin. Cyanide blocks the activity of a large number of
enzymes but the most important from the point of view of its effects is the enzyme
called cytochrome oxidase in all toe cells w lich controls the oxygen utilisation of
theceils. This leads to under-utilisation or non-utilisation of oxygen at the cellular
level producing chronic hypoxia which is responsible for the whole range of
symptoms. At the same time carbon dioxide transport is also reduced. The study of
gases like oxygen and carbon dioxide in the blood may provide clues to disturbance
of gas utilisation and transport at the cellular level. The ICMR continued to pursue
its inquiry further to explore the idea of the cyanogen pool and its major excretory
pathway through urinary thiocyanate.
It decided to undertake a double blind clinical trial to find out the useful
ness of sodium thiosulfate injections on 30 patients. 10 out of 19 who were given
sodium thiosulfate showed marked clinical improvement and had an 8 to 10 fold
increase in the excretion of urinary thiocyante, whereas 1 out of 15 who got
injection glucose showed such increase (14). The full details of this most crucial
trial have not been made public and the findings have been contested by those who
uphold the 'pulmonary theory'. Tnis controversy has been further discussed in
Chapter 6. The opoonents of 'cyanogen pool' theory claim to have conducted their
own study with sodium thiosulfate and the results were according to them, dis
couraging. However it is known that it was not a double blind clinical trial like
ICMR's and that full details of this trial have not been made public either !
Alongside this investigation, studies of arterial and venous blood oxygen
and carbon dioxide levels were undertaken. This was to understand the state of
oxygen utilisation al tissue level and carbondioxide removal from the tissues.
Following are the salient findings of the investigation.
a) Level of oxygen in arterial blood was lower than normal (14)
b) Similarly level of carbon dioxide in the arterial
than normal (14)
10
I
blood was also lower
c) Inspite of raised haemoglobin levels its oxygen carrying capacity was
lowered. There is a probability of some compensatory mechanism,
operating such as indicated by elevated levels of 2-3 Diphosphoglycerate
(2-3 DPG) in the blood which is one of the mechanisms to improve the
oxygen utilisation by the tissues (14)
d) Following the treatment with sodium thiosulfate the carbon dioxide
level in venous blood increased, with improved clinical condition. This
preliminary observation tends to indicate that following administration
of sodium thiosulfate, patients appear to better utilise the oxygen. The
higher levels of carbon dioxide in the venous blood probably means that
venous carbon dioxide is being carried in solution. This could be du?
to some alteration in the haemoglobin molecule, possibly by mechanisms
such as carbamylation of end-terminal amino groups (14) .
All these findings such as increased haemoglobin concentration, twin
bands of oxyhaemoglobin, more than doubled normal values of 2-3 DPG in the blood
and clinical improvement, augmented output of urinary thiocyanate and rise in carbon
dioxide level in venous blood following sodium thiosulfate injections are unexpected
but highly suggestive.
These findings strongly suggested that tissue utilisation of oxygen in gas
victims is problematic. This is not a simple function of reduced diffusion —perfu
sion ratio leading to anoxia as one would expect in exclusive pulmonary damage.
The pathology is not only in the lungs, probably it is at a cellular level in
all the vital organs. Logically speaking it is not imoerative for the theory to chase
only MIC molecule in the cellular processes. There may be other molecules deri
ved from MIC or other toxic gases which contribute to the cyanogen pool. The
cyanogen pool theory may stand or fall the critical tests but these findings if true
are in need of explanation.
11
I Z’P /
COMMUNITY HEALTH CELL
47/1, (First Floor) 3c. .Marks Soad
BANGAtO3£ - 5u0 001
CHAPTER 4
MATERIALS AND METHODS
4.1
Sample Population
I
Two bastis (slum areas) were selected for the study: ( i ) JP Nagar. which
was the worst affected, is situated right in front of the U tion Cirbide factory;
(ii) Anna Nagar, which is about 1 0 km. south of the factory was selected as a control
(see mao)
It is important to clarify here that no area in Bnopal which has similar
bastis was unexposed to MIC at the time of the disaster and hence Anna Nagar was
also exposed. However, it was one of the least affected areas. In the absence of
any available information regarding the quantum of gas exposure of various com
munities differences in postexposure mortality can be taken as a criterion of difference
in gas exposure. Our assumption, therefore, in selecting Anna Nagar as the least
affected was based on the available mortality rates from the Department of Infor
mation and Publicity, Government of Madhya Pradesh - JP Naoar 2 34% and Anna
Nagar 0 32%
This assumption was further corroborated by our study-finding of a
difference in mortality between JP Nagar (36.6/1000) and Anna Nagar (7.9/1000),
in the three month p°riod between MIC gas exposure and our study. Another
significant finding which justified this selection of samples was the fact that 45
persons (30%) out of our sample in JP Nagar had been hospitalised after the gas
exposure whereas the figure for Anna Nagar was one person (J.72%), a clear indi
cation of the differential exposure.
L
1
Both these bastis were more or less comparable with respect to housing,
sanitation and economic characteristics though there were some socio-cultural
differences among the two areas, in that the inhabitants of Anna Nagar were predo
minantly migrant labour from the south who were, however, resident in Bhopal for
many years.
We decided on a sample size of about 180 persons of both sexes of more
than 10 years age for each basti (This was based on the assumotion that
significant morbidity would be atleast 15% in JP Nagar and 5% in Anna Nagar.
We wished to have a 90% chance of finding this difference with significance level
of 5% in a two tailed tes* i. e. 2a = 5% and B = 90%). It needs to be emphasised here
that the assumptions on which the sample size was computed, are quite stringent. For
our ouroose sample siz^ is more than adequate. Since random selection of indivi
dual persons was noi possible, we decided to select at random 60 families from each
basti to yield the desired number of persons. Random selection of families in both
bastis was fortunately possible because the ICMR had already provided a numbar
plate for each household. This provided the much needed sampling frame from
which random sampling of families was done with the help of random number tables.
Children below 10 years were excluded from our sample because of the
fact that their reporting of symptoms and pulmonary function tests would be
unreliable.
4.2 Methods
As will be noted by the readers, history-taking has been our most important
method of study. Methodological issues arising in respect of this method have been
discussed in Chapter 2—'Objectives of the study* 'and below in the section of
'Morbidity Analysis*. The following were undertaken during the study.
12
4.2.1 History-taking and physical examination of each individual
A detailed proforma was designed for the study which was to be administred to each eligible member of the selected families (Appendixl). It included
the following sections.
Section I : This included the following information about each household:
family composition; deaths or missing members since the gas leak; occupation;
income; history of smoking or chronic respiratory diseases (TB, asthma and chronic
bronchitis) of each member. Details of loans taken by the family and compensation
received were also elicited.
Section II : This was to be filled for each individual in the household
included in the sample. It included details of occupation and income; change in
income due to i11n ess/disabiI ity following gas leak; certain details about exposure
and safety measures attempted; whether hospitalised after exposure and history of
smoking and chronic respiratory illnesses (TB, asthma and chronic bronchitis).
Section III : Every individual included in the sample was subjected to a
systematic enquiry of 26 symptoms. The patients own description of these
symptoms were listened to avoiding much direct questioning.
A general physical examination was also done including (i) height and
weight (ii) and (iii) pulse and respiratory rates for full one minute in resting posi
tion after lapse of considerable time to ensure relaxation (iv) eye examination
including cornea, lens, pupillary reflexes, distant vision and near vision (v) general
signs like oedema, jaundice, cyanosis (vi) examination of skin; (vi.) respiratory
system; (viii) cardiovascular system; (ix) central nervous system; (x) alimentary
system.
The parameters for each system are shown in Appendix I.
Section IV : This was for each woman belonging to the reproductive age
group included in the sample. It included menstrual history; history of gynaecolo
gical complaints before and after gas leak; pregnancy and its outcome; if a nursing
mother then details of lactation before and after exposure.
4 2. 2 Pulmonary Function Tests (PFTs) which included Forced Expiratory
Volume in 1st second (FEVI) and Forced Vital Capacity (FVC) for each individual.
PFTs were recorded by Morgan's electronic spirometer set as BTPS. Three readings
were recorded and the highest reading was taken for analysis.
For the interpretation of PFTs, height of each individual was measured by a
straight aluminium rod on which a metal measuring tape was fixed. Weight was
measured by standardised bathroom scales. The sample size of PFTs was further
extended by additional observations on other families selected at random in both
bastis. PFTs were performed by a doctor who had adequate experience of using the
spirometer under field conditions.
4.2.3 Haemoglobin estimation using Sahli's haemoglobinometer was done on a
random sample of the two bastis.
4.2.3
An enquiry into the people's perceptions of the existing services was done
13
by administering a questionnaire (section vi) to one member of each family jn.
eluded in the sample. These included questions recording availability and accessi
bility of services, quality of service, type of treatment given, attitude of examining
doctor, cost of treatment, and nature of doctor-patient communication.
4.3
Building rapport with the people
The mfc team arrived in Bhopal to undertake the study in the third week
of March 1985 (15th - 25th) . three and a half months after the tragedy. Numerous
teams of investigators and relief workers both governmental and non-governmental
had visited the selected bastis, made enquiries, offered or promised relief, raised
expectations about compensation and assistance.
For the mfc team to ensure, therefore, that it would still be able to get
reliable, authentic and relevant information it was necessary to counter this pre*
conditioning of the basti dwellers and establish a meaningful rapport, free of sus
picion, of false expectations and a sense of dependency. We therefore, employed the
following strategy :
(a) Two days before the study, while selecting the samples the Coordinator
and a team member visited the selected bastis and had informal discussions with
some of the people explaining the objective of our study and the possible outcome;
►
(b) A hand-out prepared in Hindi was freely distributed among the basti
dwellers. It clarified the role of the mfc, explained about the need for a sample
and mentioned the possible follow up action. It specifically clarified that we were
not providers of service but were facilitating a more relevant plan of serivces
(Appendix II).
(c) During the actual survey, time was $.
spent with each family answering
their numerous enquiries and listening patiently to their stories.. C
Occasionally
when non-sample individuals/families approached the team members they were also
listened to and occasionally given an examination;
(d) A summary of findings was made and handed over to each person in
the sample; because we believed that it was a right of the people to get a record of
.the findings.
(e) In all our contacts with the people, it was very clearly stated that
though the team was a medical one, it was not going to provide any treatment nor
be involved with compensation claims. However, wherever it was necessary a
prescription was given though this was rather occasional;
I ’
(f) A commitment was also made that the salient findings of the study and
our recommendations would be made available to the people of the affected bastis to
help them demand their rights to meaningful health services.
This methodology of informal, frank and participatory communication had
its own rich dividends. The basti dwellers in both Anna Nagar and JP Nagar wel
comed us into their homes warmly and took us into confidence. They appreciated
our 'listening' attitude and this generated a lot of cooperation and support to our
efforts. A major point of frustration for many of them was that though they had
received treatment from government and other services, they had felt that the doctors
were not taking them seriously and were summary in their approach. This affected
the credibility of the existing services.
14
Our decision to concentrate very consciously on rapport building ensured
that there was not one refusal among those who were present at the time of our
visits. Moreover although several health surveys are supposed to have been done
in these bastis, we found that in hardly any family, we had selected in our sample
was there any health survey done. There was, therefore, no question of families
being flooded witn same types of questions and getting conditioned, consciously or
unconsciously, to answer in a particular way or pattern.
4.4
Plan of Analysis
Ths plan of analysis of the data collected by us was as follows:
(i) All parameters in history, symptomatology and findings of clinical
examination and lung function tests have been quantified and the
percentage in each of the two bastis have been compared;
(ii) Relevant statistical tests have been applied to determine whether the
differences, if any, are statistically significant;
(iii) Both the theories in the current medical controversy i.e. the pulmonary
fibrosis theory and the 'cyanogen pool' theory have been kept in mindz
consciously during the analysis to raise critical questions about both
these theories from our findings;
(iv) Basically the important problem areas have been identified. There has
been no attempt to group symptoms into specific diagnostic categories
and both signs and symptoms have been taken into account in the
analysis.
He is unwise who acts without investigation-
—Charaka Samhita
15
CHAPTER 5
OBSERVATIONS AND RESULTS
I
5.1 Non-responders: some observations
ii
In JP Nagar in the 60 families selected there were 203 eligible persons
whereas in Anna Nagar, the corresponding figure was 163.
In JP Nagar, 60 out of 208 individuals could not be interviewed and
examined, giving a non-response rate of 29%. The corresponding figure for Anna
Nagar is 15% (25 out of 163).
■
Several home visits were made by the survey teams in both
reduce non-response rates.
the bastis to
We feel that the given non-response rate in JP Nagar and Anna Nagar
will not have a significant effect in the differences in rates of serious morbidities.
Because, first, the age and sex structure of both responders and non-responders in
both bastis is more or less similar. Secondly there was not one case where a
person was at home but refused to cooperate. Had there been many such refusals
amongst non-responders "the results would have been biased in unpredictable
manner".
i
In JP Nagar majority of non-responders (about 60%) were out of town
mainly for the reasons of treatment or fear of another gas leak. Twenty five per cent
of them were out for work. At Anna Nagar about 50% were out of town for the
purpose of social visits whereas 25% were out for work.
There have been large epidemiological studies where non-responders have
been as large as 30%. This did not necessarily vitiate its results (22).
In the case of non-responders, if we are blind with respect to both exposure
and outcome then the difficulty increases (22). In JP Nagar we have no information
about the outcome in non-responders but we have recorded information that about
50% of them (28/60) were exposed to gas on 3rd December, in the remaining half
many may have been exposed but we have failed to record definite information. No
one among the non-responders in Anna Nagar was heavily exposed to MlC gas.
Thus with regard to exposure status we are not completely blind.
I
If we make an assumption (though it is unlikely in view of available
history of exposure in at least 50% of non-responders) that all the non-responders
in JP Nager and Anna Nagar were normal, this will have an effect of narrowing
down the differences in rates of morbidities between the two bastis. Even then the
difference in rates of all serious symptoms between JP Nagar and Anna Nagar
except for dry cough, lacrimation, breathlessness at rest and impotence remain
statistically highly significant.
‘
•
The reduction In sample size due to non-response rate has also not effected
the outcome at all, because much greater differences in the rates of morbidity than
had been expected (or assumed) between the two communities meant that our pur
pose of finding significant differences (if there was any) would have been served
well even by much smaller size of the sample than the ones we studied.
16
5. 2
Comparison of samples of J P Nagar and Anna Nagar
Tables 1-A and 1-B show that both these sample populations are compara
ble with reference to age, sex structure, history of smoking habits and chronic disea
ses. Table 1-C shows that occupations’and income levels are also comparable
though the J P Nagar population was probably socio-economically better off than
the Anna Nagar population. This income difference cannot however affect the
observed differences in morbidities between the two samples. Table 2 shows that
body surface areas (M2) calculated from height and weight records are also compa
rable in the two samples. This is particularly relevant in the context of pulmonary
function tests.
Comparisons of some of the important characteristics of J P Nagar and
Anna Nagar populations (study/control populations)
Table 1 A
Age-Sex Structure
Age
J P Nagar
%
n = 148
Sex
Anna Nagar
%
n = 138
11-15 years
M
F
8.10
9.46
10.14
4.35
16-45 years
M
F
35.81
33.78
34.78
31.88
M
F
6.63
10.14
6.75
8.70
46 +
Table 1 B
History of smoking and chronic diseases
Smoking (a)
+
J P Nagar
Anna Nagar
%(n= 148)
% (n= 138)
77.24
25.0
75.0
9 58
90.41
89.62
22.75
Chronic
diseases (b)
10.37
(a) a smoker is one who has smoked at least one cigarette per day for at least one
year in a life time.
(b) chronic diseases specifically included asthma, chronic bronchitis, tuberculosis
and others.
17
Table 1 C
Occupation and income levels
J P Nagar
Anna Nagar
%
n = 148
%
n = 138
Unskilled
18.91
27.73
Skilled
7.43
8.73
Self-employed
13.51
15.32
Service
14.18
10.21
House work
29.72
24.08
Others
16.21
13.36
Occupation
Per capita income per
month before gas exposure
Less than Rs. 50.00
4.68
4.58
Rs. 51-75
10.93
22.93
Rs. 76-100
16.40
21.10
Rs. 101-125
14.84
13.76
Rs. 126 and above
53.12
37.61
5.3 Socio-economic profile in the bastis
5.3.1 Occupational structure
The residents of both JP Nagar and Anna Nagar were long term residents of
these bastis. Residents of JP Nagar were predominantly Muslims and Harijans with
a wide range of occupations that included daily wage labour, construction workers,
beedi rollers, cobblers, railway and factory employees, self employed artisans and.
others. Almost 1 /5th (19%) of the working population in JP Nagar was unskilled.
18
Residents of. Anna Nagar were, predominantly.Tamila and-Maharashtrians
and had a similar range of occupatian apart from a large number of potters. The
percentage of unskilled workers was 28%.
The percentage of skilled persons in both samples was less than 10%. The
category 'others' in the table is mainly represented by students.
5.3.2
Income levels and change in income since gas exposure
The income levels of both the samples are shown in Table 1-C. JP Nagar
residents are generally of higher income levels as compared to Anna Nagar, e.g. before
the disaster 68% of the families in JP Nagar had an income more than Rs. 100.00/
capita/month whereas the corresponding figure in Anna Nagar was 51%.
After the disaster, in JP Nagar 65% (42 out of 64) of the working persons
experienced a drop in income ranging from 20% to 100% with a median of 50%
drop in income (Fig. 1)
In contrast, in Anna Nagar only 9% (6 out of 64) reported a drop in income
after the disaster. The extent of the drop in income was in the range of 20% to 55%
(Fig.1).
Two individuals in JP Nagar showed an increased income after the gas
disaster being exceptions rather than the rule.
(a) one person who was a loco-daily wage earner and got a job in the
loco-loading department after the event with an increased scale of pay;
(b) one woman (housewife) who started brick loading after the'disaster as her
husband was not able to work after the disaster. Since our focus was on
individual income rather than family income such an instance of increase
is misleading. In actual fact with the husband being unable to work the
family income had not been increased.
5.3.3
Compensation received and loans taken
During the acute phase of the crisis the only source of inconTe if at all was •
the compensation received by families (only those who had deaths in the family)
and loans taken from money lenders and others locally.
Some of our findings were:
In J P Nagar
Compensation of Rs.10,000.00 was given to 8 persons (out of 26 reported
deaths). One non-respondent family had 5 deaths and 1 child survivor of 8 years in
an orphanage. We could not elicit compensation details in this case.
Compensation was also given to other families who did not have a death.
In our sample 2 persons got below Rs. 500.00; 3 persons between Rs. 500-1000,
4 persons between Rs.1000-2000 and 1 person between Rs. 2000-3000.
13
F
I
o
o
CN
o
co
O
O
in
o
co
o
6
co
6
o
o
CD
6
co
o
o
°?
o
O
OOfrl0081"
u
VI
□
0CZL-.
V)
O
CL
X
®
w
Q
D)
oooi-
co
.2
®
’E
□
E
E
o
o
Q.
Ui
®
CD
Q.
□
o
o
<
z
<
z
z
<
ooz.-:
oo9-: :
oo9-:
00fr-
JC
X)
<
O
s.
c 006-:
o
<5 008a
♦-
Ct
£0014o
E
E
o
o
c
008003-
v>
75
5
001-
’■5
l
ift'
c
OOVL-
o
008
®
E
I •
. I
o
u
c
c
©
ex
c
x:
o
©
c
0011-
a> ooo t-*
a
c
o 006w
©
CL
a
z
CL
Q.
00
'u>
®
0
CL
oo9-: .
a.
□
£
5
a>
E
o
o
c
£
<
<
K_
©
®
Ct
008-
ex
c
u
u.
11
5 0031-*
«
009-•
oov008- ♦
003-•
* « * ♦
00 L-
6
OOO
CN
CO
6
in
o
o
% Uj 0UJO3UI Ul eSB9J08Q
i
Twenty families in which there were no deaths and to whom no compen
sation was given had to take loans for medical treatment and for the migration during
'operation faith'. Many of them put their ornaments, vessels etc. on mortgage.
In Anna Nagar
Seventeen families who did not have a death in the family had to take loans.
Most of them specifically mentioned that this was during 'operation faith' when they
went outside Bhopal for a while.
5.4 Morbidity Analysis
5.4.1 General comments
Before presenting the analysis of morbidity, two issues must be sorted out.
One, it must be stressed again that there is no population which matches
JP Nagar socio-economically or in respect to housing and sanitation which
was not exposed to the toxic gases on 3rd December, 1984. A control population
selected like Anna Nagar is not strictly speaking a 'non-exposed' population as it
should be but serves as a control population by virtue of being minimally exposed
in comparison to JP Nagar. This also implies that even in our control pooulation
one would expect to observe some of the disabilities or debilitating morbidities in a
higher proportion of the population than would be the case in an unexposed control
area. Actually this is what we did observe and the Anna Nagar sample had dafinitely a larger number of serious symptoms in a sizeable proportion of persons stu
died (Tables 3-A to 3-C)
This is something which is quite unexpected and in fact narrows down the
differences in rates of symptoms observed between the two populations. The health
impact of the toxic gases on the exposed population is, therefore, much greater than
what our study reveals.
Seen in this background alone can one appreciate the devastating impact
on the health of highly exposed populations. Because in spite of the dampening
effect on the differences in rates explained earlier, the rates of many serious symp
toms (indicating widespread underlying damage to the physical and mental health of
the victims of the gas disaster) in JP Nagar are higher than Anna Nagar with an
extremely high level of significance (Table-3-A and 3-B).
Two, the dependence of the study on symptoms may be felt to be proble
matic by many, since it is 'subjective' and therefore less dependable. As discussed
in Chapter 2 the problem situation as it was unfolding was such that one had few clues
as to the pathophysiological disturbances taking place in the bodies of the gas victims.
The only loud and clear clue was the people complaining of symptoms. What
biochemical pathological parameters could be included in the study to enhance the
objectivity of the study? None, except one as we have tried to argue above.
We acknowledge freely the problems of relyingion symptoms reported by
the individuals. We would, however, like to draw attention to the fact that even
in more understood problem situations like epidemiological studies of chronic bronc
hitis, emphysema, angina pectoris also, the most reliable tool of epidemiological
study is recognised to be the questionnaire. Of course, these tools as developed
by Medical Research Council (U.K.) and American Thoracic Society (U.S.A.) have
been standardised to varying extents. Similarly, the epidemiological too! in the
21
COMMUNITY HEALTH CELL
47/1. (First Floors, Marks noad
BANGAlO^- •560 001
study of psychiatric disorders is also a questionnaire. It is not necessarily true that
since symptoms are reported by the individuals, they are subjective and hence less
reliable than biochemical measurements. The point is not whether we are using
so called subjective or objective measurements, the point is whether we are employ
ing appropriate methods and tools to answer clearly the critical questions we are
raising in a given problem situation.
■
True, an important limitation of this study is non-standardization of the
questionnaire i.e. ability of the questions to elicit the same answers on two or more
occasions (reliability) and the ability of the questions to measure what was intended
(validity). Due to limitations of time this was not possible.
r
..
However the varied symptomatology presented by the subjects of the study
were not mentioned by them casually but given in graphic detail; words and' exam
ples used by the patients while describing their symptoms clearly showed the gra
vity of the symptom as well as its effect on the person's day to day work. The
different manner in which the symptom was described also showed that the person
was informing us of a problem based on his/her own experience and not just vague
hearsay expressions. This is particularly important since in the absence of signs in
the same proportion as symptoms, doctors attending on these people in busy
government clinics were often passing off the symptoms reported, as compensation
'malingering' or'not of clinical significance'. We have every reason to believe that
these symptoms were real expressions of physical and mental ill health and many
should be accorded the same significance as the use of patterns of cough with or
without expectoration in the diagnosis of chronic bronchitis or the use of anginal
history in the diagnosis of Ischaemic Heart Disease.
The commonest symptom reported was breathlessness on usual exertion and
the specific descriptions recorded were: (1) while excessive talking; (2) on brisk,
walking; (3) doing house-hold work in a hurry; (4) fetching water and firewood;
(5) cannot go till the market; (6) little walking - say 100 yards; (7) while coughing;
(8) while riding a bicycle etc.
5.4,2 Symptomatology and signs - a comparison
Tables 3-A - 3-C show the difference in rates of the 26 symptoms that had
been enquired into in both the sample populations. It must be emphasised that a
symptom was recorded as positive only if it was present at the time of the study.
Five symptoms were not significantly different. These were blood in sputum, fever,
jaundice, blood in vomit, stool or malena and vomiting.
Six symptoms were significantly different. These were dry cough, breath
lessness at rest, lacrimation, skin problems, bleeding tendency and impotence.
Fifteen symptoms were highly significantly different. These were cough
with expectoration, breathlessness on usual exertion, chest pain/tightness, blurred
vision/photophobia, headache, weakness in extremities, muscleache, fatigue, loss of
memory, tingling/numbness, nausea, abdominal pain, flatulence and anxiety/depression. Moreover critical symptoms like breathlessness on usual exertion, lacri
mation, pain/tightness in chest, blurred vision, weakness in extremities, fatigue,
loss of memory, tingling/numbness, anorexia, nausea, flatulence and anxiety/depression were not reported in a monosyllable 'yes' but described in such graphic
detail that their presence could not be doubted.
22
5.4,3
Clustering
It was obvious from the study findings that most of the persons in JP Nagar
had more than one symptom present. To further study the pattern of clustering of
symptoms, we grouped the symptoms according to the system they naturally belong
to. Some overlap in such grouping is inevitable but it does reveal the overall pattern
e.g. an important symptom like breathlessness on usual exertion which is reported
with highest frequency does not squarely belong to one system like cardiovascular
or respiratory system alone. Both these systemscan with equal legitimacy lay claim
to this most frequent and crucial symptom and this is particularly important
since we are examining critically two dominant medical theories in this study-'cyanogen pool' theory and 'pulmonary theory/
All the symptoms were grouped together system wise as follows :
(a) Pulmonary system (P)
The grouping of symptoms suggesting diffuse pulmonary fibrosis is based
on Harrison's Principles of Internal Medicine 10th edition, 1983 (Chapter
280, P.1567).
They include breathlassness at rest and on accustomed
exertion, dry cough and cough with expectoration, weakness in extremities
and pain/tightness in the chest. To be included in this group the combi
nation of symptoms had to have cough with or without expectoration and
dyspnoea at rest or usual exertion.
(b) Gastro-intestinal system (Gl)
They included anorexia, nausea, vomiting, abdominal pain and flatulence.
Table 2
Comparison between body surface area ( M2) in JP Nagar and Anna Nagar
according to age-sex (figures in brackets show S .D)
Body surface area
(mean)
in Sq M2
n= 136
n = 137
1.23
(0.14)
1.22
(0.19)
F
1.22
(0.12)
1.15
(0.13)
M
1.49
(0.09)
1.51
(0.12)
F
1.37
(0.11)
1.35
(0.12)
M
1.50
(0.14)
1.53
(0.09)
F
• 1.37
(0.09)
1.41
(0.22)
M
1.35
(0.04)
1.38
(0.15)
F
1.32
(0.06)
1.28
(0.05)
15-45 years
61 4-years
Anna Nagar
M
11-15 years
45-60 years
J P Nagar
Note: The differences in mean BSA's were tested by't* test — all
were statistically non-significant fNS)
23
the
differences
Table : 3 A
Comparison of Symptoms reported by individuals in J.P. Nagar and Anna
Nagar. (Expressed in percentage. Numbers of cases are shown in brackets.)
bl
No.
Symptoms
J.P. Nagar %
A. Nagar %
P. Value*
P
(a)
1.
Dry Cougn
27.70 (41)
14 49 (20)
2.
Cough with Expectoration
47.29 (70)
23.91 (33)
< 0.001
3.
Breathlessness at rest
10.13 (15)
2.89
(04)
< 0.025
4.
breathlessness on
usual exertion
87.16 (I29)
35 50 (49)
< < 0.001
5.
Chest pain/tightness
50.0
(74)
26.08 (36)
< < 0.001
6.
Weakness in Extremities
65.54 (97)
36’95 (51)
< < 0.001
7.
Fatigue
81.08 (120)
39.85 (55)
< < 0.001
8.
Anorexia
66.2.1 (98)
28 26 (39)
< < 0.001
9.
Nausea
58.10 (86)
16.66 (23)
< < 0.001
10.
Abdominal pain
53.37 (79)
25.39 (35)
< < 0.001
11.
Flatulence
68.91
(102)
25.36 (35)
< < 0.001
12.
Lacrimation
58.78 (87)
42.62 (58)
<< 0. 01
13.
Blurred vision/photophobia 77.02 (141)
33.10 (53)
< < 0.001
14.
Loss of memory for
recent events
45.27 (67)
11.59 (16)
< < 0.001
15.
Tingling/numbness
5*1.72
20.28 (28)
< < 0.001
(81)
*(a) P Values were calculated by X2 method.
24
<
0.01
Table : 3 B
Comparison of Symptoms reported by individuals in J.P.Nagar and Anna
Nagar. (Expressed in percentage. Numbers of cases are shown in brackets.)
(Symptoms significantly different but not analysed further)
SI.
No.
Symptoms
J. P. Nagar %
A. Naga'%
P. Value
•(a)
1.
Skin problems
29.05 (43)
11.59 (16)
<
2.
Bleeding tendency
9.45 (14)
2.89 (04)
< 0 025
3.
Headache
66.89 (99)
42.02 (58)
< < 0.001
4.
Muscle ache
72.97 (103)
36.23 (50)
< < 0 001
5.
Impotence
8.10 (12)
0.72 (01)
< .05
6.
Anxiety/Depression
43.92 (65)
10.14 (14)
< < 0.001
0 01
Table : 3 C
Comparison of Symptoms reported by individuals in J P Nagar and Anna
Nagar
(Expressed in percentage. Numbers of cases are sho wn in brackets.)
(Symptoms - Non-significant)
Si.
No.
Symptoms
J. P. Nagar %
A. Nagar %
P. value*
1.
Blood in Sputum
10.13 (15)
7.24 (10)
N.S.
2.
Fever
27.70 (4’1)
• 28.98 (40)
N.S.
3.
Jaundice
0 67 (01)
00
N.S.
4.
Blood in vomii/stcol/malena
12.16 (18)
10.14 (14)
N.S.
5.
Vomiting
11.48 (17)
5.79 (C8)
N.S.
“”2
*(a) P Values were calculated by X method.
25
(a)
r
(c) Eye Symptoms
They included blurring of vision and or lacrimation.
(d) Central Nervous System (CNS)
Disturbance or loss of memory and tingling and numbness.
The foliovying symptoms were not included in this classification: impotence,
anxiety/depression,’headache, muscleache, bleeding tendency, skin problems.
Table 3-D shows the incidence of the combination of these symptom complexes.
Some very interesting facts emerge.
As large as 63.5% (94/148) persons reported all the important symptoms.
Only 2.7% (4/148) have symptoms which are exclusively pulmonary.
Atleast
35.14% of persons do not have any pulmonary symptoms.
Table 3-E further explores the group of patients without pulmonary symptoms and
we found the following significant facts:
About 21% persons have Gl symptoms without pulmonary symptoms.
About 22% persons have eye symptoms without pulmonary symptoms.
I
About 15% personshave CNS symptoms without pulmonary symptoms.
i
In the last three categories symptoms of other systems may or may not
have been present.
An important further point of comparison between JP
Nagar and Anna
Nagar with reference to this grouping of svmotoms is that every person in JP
Nagar reported atleast one serious symptom but quite a few in Anna Nagar
did not report any serious symptom.
!
Table: 3 D
Symptoms
Symptom groups
■ 11
No /Total
%
P + G. I. + Eye + CNS
92/148
62.16
P (Pulmonary only)
4/148
2.7
P - NIL (ie G.I./CNS/Eye)
52/148
35.14
(For
. symptoms
included in
grouping
26
V
please
refer
4.4.3)
Table : 3 E
Symptom Complexes excluding Pulmonary System
Symptom Groups
No./Total
%
GJ. (with or without eye/CNS)
31/148
20.94
Eye (with or without GI/CNS)
32/148
21.62
CNS (with or without Gl/Eye)
23/148
15.54
Table : 4
Patterns of disturbance of vision in 10 — 45 yrs of population in J.P. Nagar
and A. Nagar (Figures in brackets indicate actual number )
J.P. Nagar %
Anna Nagar %
(D
74.24 (98/132)
(a)
28.57
(34/117)
Abnormal distant vision
(2)
42.0
(65/141)
(a)
21.88
(21/96)
Abnormal near vision
(3)
17.55 (20/114)
(b)
8.74
(9/103)
Corneal Opacity
(4)
( 7/148)
2.8
(4/138)
Blurring of vision
•
4.7
(b)
NOTE
1.
2.
Includes Photophobia.
Normal vision 6/9 — Distant Vision tested
by means of Snellen's chart
3. By means of near vision chart
4. In J.P. Nagar and Anna Nagar each there
are two central opacities.
(a) tested by X^d.f.l
P <0.001
(b) tested by X2d.f.l
P - Non-significant
27
f.
I
5.4.4
Disturbances of vision
Table 4 shows percentage disturbance of vision of the age group 10-45 years
of population in both communities. Persons above 45 years of age have been
excluded because of the higher rates of cataract in this population which would
contribute to disturbance in vision.
Significantly higher percentage of individuals complained of blurring of
vision in JP Nagar rather than in Anna Nagar. As large as 42% in JP Nagar had
abnormal distant vision compared to 22% in Anna Nagar. The difference is highly
significant statistically. As to the abnormalities in near vision the differences
between the two populations are of some significance (but this difference misses 5%
level of significance very narrowly : X2 d.f.1 3.62).
t
The difference in the rate of corneal opacities between the two communities
irrespective of their position on the cornea is not significant statistically (see Note 4
to table 4). However individual case histories had recorded that new corneal opa
cities had emerged after the gas leak in both JP Nagar and Anna Nagar.
Abnormalities of distan tvision, although large, cannot fully explain the
extent of blurring of vision in JP Nagar. Moreover significantly larger proportion
of abnormal distant vision in JP Nagar is itself in need of explanation. It is relevant
at this stage to point out that examination of eyes by trained ophthalmologists un
dertaken by other teams have so far failed to identify abnormalities in the anterior
and posterior chambers of the eyes to any significant extent ( 14 ).
The combination of these findings is unexpected but significant. The
experts had predicted that there will be no problems of vision of such magnitude and
whatever residual problems of vision there would be, that would be because of
corneal opacities.
5.4.5 Pulse/Respiration Rate/Hemoglobin Concentration
Tables 5-A, 5-B and 5-C show the comparisons of resting mean pulse rates,
resting mean respiratory rates and meag hemoglobin concentrations, respectively
between the two samples and in both sexes.
j*
• 11 i
Mean pulse rates and mean respiratory rates in both sexes in both JP Nagar
and Anna Nagar are not different statistically. However, mean hemoglobin concen
tration in both males and females is significantly higher in JP Nagar than in Anna
Nagar.
A
The higher concentration of hemoglobin is probably masking resting tachy
cardia and resting tachypnoea in JP Nagar but the degree of tachypnoea and tachy
cardia masked is not likely to be very high.
5.4.6 Other clinical findings
Clinical examination of all individuals in the sample showed the following:
(i) 9.4% (14/148) individuals in JP Nagar had rales and rhonchi in the chest
as against 2.1% (3/148) in Anna Nagar. The difference is significant stati
stically (P < 0.025). Significantly higher rates of rales-rhonchi in JP Nagar
may well be due to increased sensitization of the bronchial tree following
28
■ 1.
It
MIC exposure, but the rate is too small to account for the much higher rate
of breathlessness on exertion;
(ii) We identified no case of cyanosis, a significant negative finding in view of
the fact that 87% of the individuals in JP Nagar have breathlessness on
exertion, have increased concentration of hemoglobin and that extensive
pulmonary damage is expected to have occurred.
(iii) There was one case of oedema of leg, one case of
history) and one case of palpable hepatomegaly.
hemiplegia (longterm
(iv) There was one case of jaundice and no spfenomegaly;
(v)
No significant findings in cardio-vascular system or central nervous system.
5.4.7 Effects on the Reproductive System Of Women
5.4.7.1 Gynaecological problems
The comparisons of symptomatology in this group of symptoms has been
done in two stages :
Ci
(i) comparison between symptoms in women of JP Nagar before and after
the gas leak (in the same women);
(ii) comparison between symptoms in women of JP Nagar and Anna Nagar
after the gas leak (between samples).
Tables 6-A, 6-B, 6-C, 6-D and 6-E show the comparison of mean mens
trual cycle lengths, percentage distribution of flow types, percentage distribution of
colour and percentage distribution of dysmenorrhoea and leucorrhoea.
The salient findings are that women of reproductive age group in JP Nagar
have significantly shortened length of menstrual cycles after the exposure to the
gas compared to the lengths of cycles in the same group of women before the gas
leak and lengths of cycles of women in Anna Nagar after the gas leak. Significan
tly more number of women in JP Nagar also had abnormalities of menstrual flow—
scanty, or heavy and blackish discharge (Tables 6-A - 6-C), dysmenorrhoea (Table
6-D), and leucorrhoea (Table 6-E), after the gas exposure when compared to the
internal/external control mentioned above.
It may be argued that increased rates of leucorrhoea in JP Nagar after the gas
exposure may be because of break-down in sanitary conditions due to the disaster.
The disaster obviously did not lead to physical destruction of the housings and
whatever sanitation that there was, people did not flee to refugee camps where
sanitory breakdown may be nearly total. Therefore this argument of sanitation is not
really applicable to the study.
5.4.7.2 Pregnancies and their outcome
Four women in JP Nagar and five women in Anna Nagar were pregnant at
the time of our study. There was one abortion in Anna Nagar and none in J P Nagar.
There was no instance of still birth. The numbers in the sample are too small to
29
i
■ I1
Table . 5 A
Mean pulse rate/minute (S.D.) in males & females of J.P. Nagar and Ann*
Nagar. •
I '
J.P. NAGAR
ANNA NAGAR
Male
77.13 (11.28)
n = 67
77.94 (10.68)
n = 73
Female
85.73 (13.21)
n = 78
85 05 (11.20)
n =59
Total
81.70
80.4
(13.20)
n = 145
• All the differences in mean pulse rates were
found to be non-significant.
(13.0)
n =132
tested stasticall/ by *t* test and
Table : 5 B
Mean Respiration
Nagar and Anna Nagar.*
K>
I;
11
■
Rate/minute (S D.) in males & females of J. P
J.P.NAGAR
ANNA NAGAR
Male
21.73
(3.98)
n = 69
21.21
(3.84)
n = 74
Female
21.84
(4.93)
n—70
20.92
(3.70)
n = 56
Total
21.87
(4.51)
n-139
21.09
(3.77)
n = 130
• All thedifferences in mean respiration rates were tested stastically by 'f test and
found to be non-significant.
30
i
Table : 5 C
(The figures
Mean blood Haemoglobin in gm.% in J.P. Nagar & Anna Nagar.
in brackets are S.Ds of means, n = sample size.)
J.P. NAGAR
ANNA NAGAR
Male
14.68 (1.79)
n = 11
(a)
12.70 (1.35)
n = 17
Female
12.7 (1.46)
n = 20
(b)
10.79 (1.34)
n = 18
xd.f26 = 3.18
xd.f36 = 4.20
(a)
(b)
P
P
j
<0 01
< 0.001
Table : 6 A
Mean Menstrual cycle length in days in J.P. Nagar and Anna Nagar after
and before gas exposure. (Figures in brackets indicate S.D. in days.)
J.P. NAGAR
ANNA NAGAR
Before
After
Before
After
32.32
25.59
35.41
36.10
(13.51)
(12.04)
(20.09)
(19.89)
n = 31
n = 31
n «= 29
n = 29
tj= 2.06
d.f. 60
P. < 0.05
ta = 0.131
d.f. - 56
P> 0.8
rj.a.
j.a.
differences in mean menstrual cycles length in days between J. P. Nagar and
Anna Nagar after the gas exposure.
!J.a
’
d.f.
P < 0.05
2.46
58
31
/
‘
I
.
F
Table ; 6 B
I
Percentage distribution of Flow in J.P. Nagar & Anna Nagar before and
after the gas exposure. (Figures in brackets are number of cases)
NAGAR
ANNA
NAGAR
J. P.
Scanty
Excess
Total
Scanty
Excess
Total
5.5
11
100
2.6
18.4
100
(2)
(4)
(36)
d)
(7)
(38)
25.7
31.4
100
5.8
20.7
100
(9)
(11)
(35)
(2)
(7)
(34)
Before
After
X2 = 11.96
d f. = 2.
P < 0.01
X2
< 1
d.f. = 2.
P > 0.50
After the gas exoosure
J. P. Nagar & Anna Nagar
X2 = 7.8?
d. f. = 2.
P<0025
Table : 6 C
Percentage distribution of colour of menstrual flow in J P. Nagar and
Anna Nagar before and after the gas exposure, (Figures in brackets are No,
of cases)
J. P.
NAGAR
Black
Total
Black
Total
Before
5.8
(2)
100
(34)
0
(0)
100
(37)
After
46 8
(15)
1C0
(32)
8 8
(3)
100
(34)
ANNA
NAGAR
X2 = 14.46
X2 = 3.41
d.f = 1
d.f. = 1
P< 0.001
P - N.S.
After the gas exposure J.P. Nagar & Anna Nagar
X2 => 12.03
d.f. = 1
P <0.001
32
it
I
Table : 6 D
Percentage distribution of Dysmenorrhoea in J. P.Nagar and Anna Nagar
before and after the gas exposure. (Figures in brackets are number of cases.)
ANNA NAGAR
J. P. NAGAR
Before
After
+ ve
Total
+ ve
Tota I
28.5
(10)
100
(35)
48.7
(19)
100
(39)
65.6
(21)
100
(32)
39
(14)
(36)
X2 = 9.21
d.f. = 1
P < 0.01
100
X = 0.71
d.f. = 1
P - N.S.
After the gas exposure
J. P. Nagar & Anna Nagar
X2 = 4.89
d.f. - 1
P < 0 05
Table : 6 E
Percentage distribution of Leucorrhoea in J. P. Nagar and Anna Nagar—
before and after the gas exposure
(Figures in brackets are number of cases.)
ANNA NAGAR
J. P. NAGAR
Before
After
NonSpecific
Leu.
Specific
Leu.
Total
15.5
(7)
22.2
(10)
0
(0)
35.5
(16)
100
(45)
100
(45)
X2 = 22.5
d.f. - 2.
P < 0.001
NonSpecific
Leu.
16.6
(7)
14.6
(6)
X2 = 1
d.f. = 2
P-N.S.
After the gas exposure
J. P. Nagar & Anna Nagar
X2 = 7.455
d.f. = 2.
P < 0.025.
33
Specific
Leu.
Total
14.3
(6)
14.6
(6)
100
(42)
100
(41)
reveal any significant changes. Moreover the foetuses which are likely to have
been damaged about three months ago at the time of the gas leak are now in the
second trimester and therefore, it will be a few mcwe weeks before the adverse impact
on pregnancies will be correctly estimatable.
5.4.7.3
Lactation
I
I
50% of nursing mothers in JP Nagar reported lactation failure or decrease
in output as compared to 11 % (1/9) of mothers in Anna Nagar.
5.4.8
Effects on Reproductive System : Of men
Impotence: Table 3-B shows that the percentage of men reporting symptoms
of impotence was 8.1% (12/148) in JP Nagar and 0.72% (1/138) in Anna Nagar
(significance of difference P<0.05).
5.4.9
Pulmonary Function Tests
Table 7 shows the comparison between the sampled subjects of JP Nagar
and Anna Nagar on two parameters of lung function measured in the study - Forced
Expiratory Volume in the 1st second (FEV1) and Forced Expiratory Capacity (FVC).
The difference between JP Nagar and Anna Nagar are statistically signrficant in bothisexes in the age groups of 15-45 and 46-60 years, The difference in
other age/sex categories are however, not statistically significant, This may be due
to smaller number of observations in these categories. The mean values in all these
categories and the FEV1/FVC ratio in all categories are diminished in JP Nagar in
comparison to Anna Nagar.
The pattern in the age groups 15.-44 and 45-60 shows a restrictive type of
pulmonary function, while in the over 61 's the pattern is mainly obstructive.
5.4.10
Anxiety/Depression
From our field level interviews in which we spent much time listening to the
people's experiences we identified syndromes of anxiety and or depression in 43.92%
of the subjects (65/148) in JP Nagar and 10.14% of subjects (14/138) in Anna Nagar.
This difference is statistically significant.
From the sharing of experiences we gathered that there was much fear,
apprehension, anxiety symptoms, gas-phobia, fear of the restarting of the factory
operations and frank depression. In some cases there was some degree of mental
confusion.
5.4.11
I npairment of Memory
Many people described a definite change in their memory for recent events.
They narrated different examples of situations in which their memory seemed to fail
causing them much worry: e. g. (i) forgetting where something has been kept;
(ii) forgetting whether a meal has been taken or not; (u’i) forgetting whether salt has
baen added to the 'dal' or not; (iv) forgetting the names of the children; (v) forgetting
the day or time; (vi) after coming out of the house forgetting for what purpose one
came out; (vii) students complained that they could not remember lessons or poems
learnt before the episode.
34
Table : 7
Distribution of Mean values of Body Surface Area (M2), FEV (Litre.), FVC
(Litre)
FEV/FVC% in different age-sex groups, in J. P. Nagar and Anna
Nagar. (a) * (Figures in brackets are S.Ds) n = number of persons in each
cell. P = p value.
BSA (M2)
Age-Sex
in yrs.
J.P
A.N.
FEV (Lit )
FVC (Lit.)
J.P
J.P.
A.N.
J.P.
1.72
(0.77)
P = N.S.
2.20
(0.51)
87.05
87.8
2.07
(0 88)
P = N.S.
2.10
(0.40)
84.3
84.2
A.N.
FEV,/FVC
%
A.N
10-14
1.23
(0.14)
n =4
1.22
(0.19)
n=4
1.59
(0.74)
P=NS
1.93
(0.48)
1.22
(0.12)
n =3
1.15
(0.13)
n=6
1.76
(0.84)
P = NS
1.77
(0.33)
1.49
(0.09)
n = 45
1.51
(0.12)
n = 55
2.04
(0.47)
2.66
(0.51)
P <).001
2.39
(0.47)
P <0.001
2.99
(0.55)
79.1
88.9
M
1.37
(0.11)
n = 56
1.35
(0.12)
n = 52
2.2'5
1.64
(2.42)
(0-44)
P <0.001
1.97
(0.38)
P <0.001
2.54
(0.43)
76.3
88.6
F
1.50
(0.14)
n = 12
1.53
(0.09)
n=6
1.88
(0.53)
P <0.05
2.26
(0.19)
2.20
(0.43)
P <0.05
2.54
(0.24)
85.3
88.9
M
1.37
(0.09)
n = 11
1.41
(0.22)
n=7
1.51
2.13
(0.18)
2.48
(0.21)
85.9
P <0.01
1.86
0.58)
(P <0.01
79.8
F
1.35
(0.04)
n =2
1 38
(0.15)
n =4
1.91
0.94
(0.39)
(0.15)
P <0:02)
1.83
(0.35)
P = N.S.
2.17
(0.16)
61.8
88.0
M
1.32
(0.06)
n =3
1.28
(0.05)
1,39
(0.31)
P <0.05
1.90
(0.07)
1.96
(0.31)
P = N.S.
2.13
(0.15)
63.4
86.2
F
M
F
.
15-44
45-60
(0 48)
6 I -F
(a)*
n =3
All the differences in Mean Values between J.P.
each age-sex category were tested by't'iast.
35
Nagar & Anna Nagar in
p
;l ■'
!
I
Table : 8
Exposure History and safety Measures
»*•
Anna Nagar
J P Nagar
Where at
the
time of leak
Wet
towel
In the Basti
5
Out of home
(in Bhopal)
1
Blanket
Ran
out
Nil
Wet
towel
Blanket
Ran
out
Nil
7
124
8
9
6
64
52
1
2
2
5
Out of Bhopal
11
10
Total No. 158
Total No. 148
Note: Nil means remained in the house without safety measure.
Table : 9
p'
Number of attacks (respiratory infections) in one month preceding the
study
Anna Nagar
JP Nagar
Age
One attack Often
Nil
One attack Often
Nil
10-15 yrs
3
13
15
4
1
16
16-45
15
46
35
24
7
68
46 +
3
14
4
4
_n_
21
73
4
54
32
12
95
In statistical terms 67/148 subjects in JP Nagar (45.27%) and 16/138
subjects in Anna Nagar (11.59%) complained of this symptom. The difference is
highly significant.
Miscellaneous observations
5.4.12 School Performance of Children
A discussion with one of the school teachers in the affected area revealed
that the school attendance had fallen because many families had moved away, many
pupils had died or become too ill to continue. Of those who returned to school,
the teachers felt that there appears to be no visible physical effect but they are not as
'active'as they used to be. They do not go out to play that often. They are not rest
less when they have to sit for long periods in class as they used to be. Some of
them have developed a disinterest in school work. Even though all had not lost their
immediate kith and kin, many had seen their friends and cousins die and were affec
ted by this.
36
Many members of the team themselves observed this general listlessness or
apathy of the children, and many were dyspnoeic as well. The visual impressions
of these problems between JP Nagar and Anna Nagar was distinctly different, the
impression in Anna Nagar being similar to what one expects in an average slum
area - lots of children playing around, inquisitive, running about, active.
5.4.13 Effect on immunity/resistanoe
We enquired about the experiense of respiratory infections In the study and
control population in terms of number of attacks in the one month preceding the study.
Table 9 shows this finding. 73/148 in JP Nagar had many attacks of respiratory
infections while only 12/138 in Anna Nagar gave this history. In JP Nagar this was
often described as a continuous respiratory problem. This is an important suppor
tive finding but cannot be taken directly to mean a state of lowered resistance to
infection resulting in frequent upper respiratory infections but is strongly indicative
of it.
5.4.14
Enquiry into exposure and safety measures employed
Table 8 shows where the people in our sample were at the time of the
incident and whether they employed any safety measures (wet towel, blanket, run
ning out) to protect themselves against the gas leak.
The fact that many ran out and few used a wet towel is a good indication
of the lack of awareness or safety education of the residents of the bastis. Most of
them had no idea about the hazardous nature of the plantoperation nor about measures
to protect oneself in the event of a gas leak. Even those who used a wet towel used
it by instinct rather than due to an awareness of precautionary messages.
Concern for man himself and his safety must always form the
chief interest of all technical endeavours. Never forget this in
the midst of your diagrams and equations.
Albert Einstein
37
■
CHAPTER 6
c?
DISCUSSION
I
The present study is a community based, case/control study in randomly
selected samples of families. It provides a much more authentic picture of the
state of health of the gas affected communities than one can get from studies
conducted on inpatient/outpatient populations of the hospital, which is the chief
characteristic of the studies undertaken by the protagonists of the two medical
theories. Self selection in hospital based studies necessarily occurs which distorts
the community perspective. These effort may give some understanding of the
quality of the problem, but give little information on the actual pattern and quantum
of morbidities prevalent in the.community. There is no substitute for community
based epidemiological studies. Our study has the merit of shifting the focus from
the health problems of hospital based patients to the health problems in the com
munity outside the hospital and dispensaries.
It is not too difficult to understand why the health establishment of
Bhopal including the dominant faction in the medical college of Bhopal did not
attempt such community based epidemiological studies.
However it is not easy to understand why the ICMR after having broken
fresh ground and hit upon a potent and fertile hypothesis of 'enlarged cyanogen
pool’ theory did not go all out for community based epidemiological studies to ex
ploit its full potentials.
But before we go into such intriguing and intricate problems let us first
examine the role of chronic diseasesand smoking in producing the morbidity and
mortality in the Bhopal gas victims, and then critically assess the claims of
'pulmonary theory’ in the light of our findings and available information.
6.1
Role of chronic diseases and smoking
Many have argued that a significant proportion of the mortality and residual
morbidity is reflective of the base line ill health including a higher prevalence of
chronic diseases like tuberculosis and higher smoking rates.
Our findings do not lend support to such speculation. Out of 26 persons
who died in our sample study of JP Nager after the gas exposure, one was reported
to have been a smoker and none to have had any chronic diseases.
i he age/sex breakdown of the dead in JP Nagar are as follows
Age in
years
'
0-1
2-5
6-15
16-45
M ale
1
4
2
5
Female
2
3
2
5
45 4-
I
Among these only one 45 year old male was a smoker.
Women in JP
Nagar generally didn't smoke. Among the dead there were 13 women, 7 males
under 15 and 4 males between 16-45 who did not smoke.
38
The findings of the morbidity survey are also significant. A quarter of the
sample in both the communities — JP Nagar and Anna Nagar—were smokers
and yet most of the serious symptoms are significantly higher in JP Nagar than in
Anna Nagar. Moreover the given smoking rates in JP Nagar cannot fully explain
the mici hg ier symptom rates in JP Nagar. A similar argument would apply
to the chronic diseases as well which in our survey specifically included history
or tuberculosis, bronchitis and asthma. This was found to be around 10 oercent
in both communities and is much too small to explain the high rate of symptoms.
The question therefore we now come to is : How much do our study
findings support or question either of the theories? or to put it differently, how much
of our study findings can be explained by either of the theories.
6.2 Pulmonary theory : an assessment
Pulmonary theory's greatest strength is in its simplicity and plausibility..
The theory has a formidable backing of a range of western experts.
The adverse effects of isocyanates other than MIC, which are widely used
in industry, have been extensively studied. These effects are mainly confined to
lungs. Changes in the blood have never been implicated.
The probability of the MIC molecule's ability to enter the blood stream and
reach other organs, thanks to its supposed high reactivity, has been rated extremely
low indeed. Furthermore it has been argued that 'there is no known metabolic path
way that converts isocyanate into cyanide' (14).
Autopsy findings have consistently shown damage to the lung tissue, of
course damage to the other organs has been shown too. Pulmonary function tests
have consistently shown impairment of ventilatory functions. In so far as MIC causes
direct damage to the corneas, impairment of vision is an expected finding.
The difference among the believers has been with regard to the type, extent
and duration of damage.
Thus the American Public Health specialists maintain that eyes and lungs
of a considerable proportion of the population will be greatly damaged. Sooner or
later many victims will succumb to suffocating onslaughts of emphysema, asthma
and pneumonia. Sizeable number of people could develop permanent blindness
due to damage to the corneas. The damaged lung tissue of victims makes them
much more vulnerable to common respiratory infections which could become fatal (9).
Then there are others who are much more optimistic about the extent and
duration of damage. Thus as we have already quoted. Mr. W. Anderson, Chairman
of Union Carbide, U. S. made a confident prediction as early as 3rd January 1985
that victims are rapidly recovering (11) .
These arguments favouring the 'pulmonary theory' are however general
without specific reference to the actual situation in Bhopal where massive exposure
to MIC gas has occured.
Let us now see how the 'pulmonary theory' stands up to critical exami
nation in the light of facts brought out in Bhopal.
39
►
6. 2.1
Deaths
The believers of the pulmonary theory have tenaciously held on tg the idea
that the very high death rate following the gas leak was due to Carbon Monoxide
poisoning and not because of cyanide poisoning (besides pulmonary oedema).
As we have seen earlier, the ICMR studies have shown that blood samples
of the dead stored in deep freeze and the blood samples of critically ill patients
who subsequently died, showed no evidence of carboxy haemoglobin (carbon mono
xide combined with haemoglobin) (14). The K.E.M. Hospital study on 113 self repor
ting MIC exposed persons cannot lend support to the theory of carbon monoxide
poisoning either because of the reasons we have discussed in para 3.1, Chapter 3.
According to the theory one expects at least some of the post exposure
deaths to be due to lung infections. In our study out of 26 deaths in JP Nagar 52
occured within 5 days of the gas leak because of the direct toxic effect of the gas.
6.2.2
Diseases - Disabilities
It is here however that the theory runs most into deep trouble. The pulmo
nary theory cannot explain the high rates of symptomatology even 3 months after
exposure in a population which is not hospital bound. For instance it cannot explain
fatigue(81 %), blurring of vision (77%), muscle ache (73%), flatulence (68%), head
ache (67%), anorexia (66%), nausea (58%), excessive lacrimation (58%), tingling
and numbness (54%), loss of memory (45%); and anxiety depression(43%). Even
the most common and disturbing symptom like breathlessness on usual exertion (87%)
cannot be fully explained by this. (Table 3A)
The simultaneous presence of all serious symptoms suggesting
involvement of not only lungs but gastro-intestinal tract, brain and vision in
as large as 62% of the sample population in JP Nagar cannot be explained by
the pulmonary theory. (Table 3D). It is not the point whether all the above symp
toms are part of the symptomatology of extensive pulmonary damage; the point is, are
they all present simultaneously in such a large proportion of individuals who are not
so ill as to be in the hospital? True, ventilatory capacities are diminished in JP
Nagar significantly which supports the pulmonary theory, but even here the reduction
is not large enough to explain such a high rate of breathlessness on exertion, weakness
and fatigue. It obviously cannot explain exclusively non pulmonary symptoms
in as high as 15 to 21% (Table 3E). Even if we grant that there is extensive lung
damage in a large proportion of cases there should be commensurate clinical findings
in those individuals. One naturally would expect high rates of respiration and pulse
and cyanosis. None of these are found in our study (Table 5A and 5B).
This is an odd finding. One can of course argue that tachycardia and
tachypnoea in JP Nagar is masked by rise in haemoglobin (Table 5-C) which is a
result of hypoxia produced by extensive pulmonary fibrosis. But surely where
extensive lung damage is supposed to have occured because of MIC exposure one
expects'suffocating onslaughts of emphysema, bronchitis, asthma', etc. (9) with
attendant compromised gas exchange at alveolar level. This must lead to not only
hypoxia (low oxygen level in the blood) but also to retention of carbon dioxide in
the blood which in turn must lead to increased ventilatory efforts to wash out excess
build up of carbon dioxide.
Besides, 'cyanogen pool' theory can explain haemoglobin rise without
having to account for not much increase ki pulse rate or respiratory rate.
40
Looking at visual disturbances also we see an interesting set of facts.
The pulmonary theory explains and predicts visual impairments solely by virtue of
direct injury to corneas which may result in opacities producing visual impairment
(2,3). In JP Nagar only 7 out of 148 individuals have corneal opacities, of these
only 2 are central opacities which matter. The rate in JP Nagar (4.7%) is not
statistically significant when compared to the rate in Anna Nagar (2.8%). This ex
tremely low rate of opacities can obviously not explain 74% of blurring of vision in
JP Nagar which is statistically significantly higher than in Anna Nagar (Table 4).
Carboxy haemoglobin levels of more than 5% in large numbers of individuals can
explain this but there is no such evidence. The pulmonary theory cannot explain
either the high abnormal rates of distant vision in JP Nagar (42%) which is highly
significantly higher than that in Anna Nagar (22%) (Table 4). Finally the evidence
from the effects seen on the reproductive system is significant. A significantly
shortened menstrual cycle (Table 6-A), increased rate of dysmenorrhoea (Table 6-D),
increased leucorrhoea after the disaster in the women (Table 6-E) and increased
percentage of impotence in men of JP Nagar (Table 3 BJ as compared to Anna Nagar
cannot be explained by the pulmonary theory.
Very high rates of symptoms implicating all the important systems in the
body call for a theory which can explain disturbances in all the systems by postu
lating a mechanism which must be operating in all the systems. 'Pulmonary theory'
clearly lacks the theoretical mechanism with an integrative power to account for the
wide range of symptoms in JP Nagar. 'Cyanogen pool theory' precisely achieves
this at least tentatively.
6.3
'Enlarged cyanogen pool' theory : an assessment
By postulating chronic poisoning by cyanide which is slowly released from
haemoglobin bound MIC, it suggests that at the cellular level in practically all the
organs oxygen utilisation has been impaired. The bewildering and apparently
unconnected wide range of symptoms can be explained with the help of this theory.
Our findings per se pose no serious problems to this theory.
This is very interesting but then excess cyanide radicals in the body fluids
have not been demonstrated. Its presence is inferred from increased levels of
urinary thiocyanate following injection of sodium thiosulfate. This however is not
its main handicap. Nor is the 'cyanogen pool' theory suffering from the handicap
of uncompromising dogmatism which characterises 'the pulmonary theory'. From
the very beginning, until now unlike 'the pulmonary theory' it doesnot claim to be
the only theory whicn can explain everything in Bhopal. It readily accepts that at
least a part of the human suffering may well be because of direct damage to the
lung tissue and eyes by MIC gas. Its main problem lies in a different area.
Events postulated and substantiated very tenuously to be taking place at the
cellular level cannot be directly connected to events occuring (symptoms) in a large
proportion of individuals in the community- The chain of links that connects the
two must be demonstrated at least tentatively. This has not been done. We
therefore now turn to a critique of the 'cyanogen pool' theory.
There are two kinds ®f evidence both indirect, to suggest chronic cyanide
poisoning, (1) Inadequate utilisation of oxygen and removal of carbon dioxide indi
cates a metabolic block at cellular level. There is also some evidence that carbon
dioxide removal from tissues is increased after injection of sodium thiosulfate,
(2) The clear rise in the urine output of thiocyanate following injection of sodium
thiosulfate perhaps indicates an enlarged cyanogen pool.
41
However the data available on botfi the types of studies (changes in the
blood gases and urinary thiocyanate following sodium thiosulfate) is very scanty and
fragmentary, which makes informed and in depth examination of these studies almost
impossible. Furthermore these studies are done on hospitalised patients. To
extend the findings and lessons of these studies to home based ambulatory persons
as ICMR does is not acceptable on methodological grounds.
We find ourselves not equipped enough to appraise more critically the
meaning and interpretation of blood gas studies but we do offer our criticism of
the way a potent tool of epidemiological research such as sodium thiosulfate has
been used so far resulting in non-illumination of many critical areas of tox ic effects
on the human population.
In the double blind clinical trials carried out by ICMR and others on 30
hospitalised patients in Jan.-Feb.1985 two outcomes were observed, one, clinical
improvement and two, urinary thiocyanate levels following sodium thiosulfate or
glucose as placebo (14). The released information so far does not say clearly as to
what was observed in the clinical outcome. However if we go by clinical criteria
used in subsequent studies (not double blind trial) which are made public, we can
make a reasonable guess as to what was probably observed, i.e. (i) weakness and
breathlessness at rest and (ii) increase even after mild exertion (14). From our point
of view these are only pulmonary symptoms constituting only a small proportion of
all symptoms. They do not include non pulmonary symptoms like blurring of vision,
nausea, anorexia, flatulence, fatigue, weakness, headache, etc. And yet the minutes
of the ICMR meeting of 14-2-1985 (16) contained detailed guidelines for categories
of patients to be given injection sodium thiosulfate which included patients suffering
from acute and/or chronic symptoms relating to respiratory, gastrointestinal and
neuromuscular systems following MIC gas exposure.
This is clearlv far from satisfactory. There is no published evidence by
ICMR which says that a significant proportion of non pulmonary symptoms are re
lieved also. We are therefore, bound to question the explanatory power of the
'cyanogen pool* theory to account for high rates of non pulmonary symptoms. Also
ICMR data related to hospitalised patients, cannot say much about the community
where large numbers of persons have wide ranging symptoms. Based on such a few
and limited studies how can the cyanogen theory explain these symptoms in the
community ?
Have there been community based trials focussing on the whole range of
symptoms so that, even if indirect, evidence for existence of an enlarged cyanogen
pool and its extent in the community may be established ? No.
This is not all. Significantly increased urinary output of thiocyanate in
patients who are given sodium thiosulfate compared to those who are given only
glucose is not a finding which is non problematic. This is so, because we do not
know the effect of sodium thiosulfate on the urinary output of thiocyanate in a heal
thy population.
Going by whatever evidence ICMR has published so far, it is not adequate
enough to explain the wide range of symptoms in a high proportion of the
ambulatory population as revealed by our study.
f-J
I’ki
!1 ■
This criticism clearly leads one to suggest that ICMR does not have adequate
evidence to substantiate the 'Cyanogen pool* theory or if it has got it for some
unknown reasons it has not made public full details 5 months after the disaster.
42
ICMR cannot make a claim that necessary information is being generated,
for how can it then issue two press releases giving details of guidelines for thio
sulfate therapy for the symptoms including non pulmonary symptoms ?
To summarise our arguments :
On the night of 3rd December, between
100, 000 to 200, 000 persons in Bhopal got severely
exposed to MIC gas
(14,18,12). A vast majority of them are still complaining of serious, debilitating
symptoms indicating involvement of many systems.
According to the cyanogen pool theory each of these exposed persons has
an enlarged cyanogen pool in his/her body leading to chronic cyanide poisoning.
This whole population may be made up of different categories of people from the
point of view of the state of the cyanogen pool in their bodies and its manifestations
in the form of various symptoms.
There may be some who have been ill enough to be hospitalised, those who
have attended OPD only and those who belong to neither group, but have serious
symptoms nevertheless. Of course there may be various degrees of overlap here.
Similarly there may be various categories of symptom complexes in each of the above
described groups.
The idea is not to workout all possible permutations and combinations!
But along the two axes of symptom complexes and degree of seriousness of symptoms
a limited number of concrete epidemiological groupings/profiles may be present
which can be and must be identified.
The whole point of our criticism is that out of all such existing epidemio
logical groupings who together make the total population of gas victims, the ICMR
has chosen to study rigorouly only one tiny group: a seriously ill patients (hospitali
sed), whose pulmonary symptoms have been kept in focus. The rest have been
ignored. They remain unidentified, unknown and the existence or otherwise of an
enlarged cyanogen pool in these groups remain untested, although such a potent tool
of epidemiological investigation as sodium thiosulfate is available all through out!
Our arguments must not be understood to mean that our aim is to reject
the 'cyanogen pool' theory. The theory is to be rejected only when the arguments
advanced in its support are found wanting, untenable. Here we are not criticising
and rejecting the arguments which have been advanced in support of cyanogen pool
theory. On the contrary we are complaining, bitterly, that the possible, sensible
and comprehensive arguments in support of 'cyanogen pool' theory have not been
advanced because they have not been develooed. Without these arguments the
cyanogen theory remains untested and weak. And this is because ICMR has not
bothered to develop this theory and to build up the arguments by following relevant
lines of research so clearly suggested by the theory and the nature of problem facing
us.
This is the criticism of methodology, perspective, orientation and objectives
of research strategy. This has helped more than anything else to put the theory
under the shade before it was given a fair and rigorous trial. This is not a criticism
of the theory per se. Many have expressed fears that by this criticism we might be
forced to oppose the mass treatment of sodium thiosulfate. Far from it.
This fear arises in part from the fact that if gaps in evidence are highlighted
then the theory may suffer and with that sodium thiosulfate therapy might be
rejected and condemned. We do not agree. As we have tried to argue above, the
43
I
gaps in the evidence because of lack of efforts to build up evidence is not the same
as negative evidence. The theory cannot be rejected before it is properly tested.
The whole point is that the evidence can be and must be built up if the theory is
sound and is to be properly tested.
There may be some hesitation on account of the fear—again not really sound
that further trials may mean further delay in treatment and that it may not be ethical
to carry out such trials.
Taking the second point first : It is not ethical not to give benefit of treat
ment to the remaining groups. It is perfectly ethical to give them treatment especially
when we know that on the one hand there is a disturbing possibility of chronic cya
nide poisoning in such a vast number of people, and on the other hand sodium thio
sulfate is such a harmless drug.
Coming to the first point : Used as we are to a division and distance between
research and action, we may not be quick enough to grasp that this division and
distance is artificial and has no connection with the real world where efforts to
understand and solve the problems almost simultaneously is possible I
The science of clinical trials has advanced so much that with the help of
well established statistical methods like Sequential Analysis, a series of quick, short
duration, rigorous trials in the relevant epidemiological groups described above can
be easily mounted. From a minimum of data, reliable and valuable conclusions can
be drawn. We do not have to wait for a long time for the results of clinical research
to come through before the treatment is initiated.
It is also possible to initiate mass treatment on the one hand, since no
ethical problems are involved and launch well planned, comprehensive programmes
of research in the chosen epidemiological groups on the other hand so that the whole
scientific case to support 'cyanogen pool' theory may be built up and the treatment
is based on rational, scientific, foundations. Specific care should be taken that all
who are getting treatment should have proper records showing identity of person,
precise clinical description and outcomes.
These strange and inexplicable lapses of ICMR have other implications and
far reaching consequences not only for establishing the case for the 'cyanogen pool'
theory, and treatment and relief as we have seen above but also for compensation
damages for the gas victims and for continuing relevant research programmes.
6.4 Magnitude of the problem : an issue of damage/compensation
We undertook this small and modest study within the severe limitations
imposed by man, material and time constraints. The purpose of the study was to
bring into focus the real issues of health that seemed to be out of focus.
To design and implement a much larger and more compiehensive series of
epidemiological studies (i) to elucidate and substantiate the 'cyanogen pool'theory
(ii) to help the suffering gas victims of Bhopal byway of medical relief (iii) to help
them put up claims for damages and compensation against the Union Carbide, can
not be undertaken by us.
The issue of compensation/damages for Bhopal gas victims is now before
the American courts. The crucial question is : How can medical evidence for tens
of thousands of gas victims be presented in the court? Fortunately American courts
44
<
accept epidemiological evidence in such cases as the Bnopal disaster. A represen
tative case from each of the relevant epidemiological groupings may be presented
before the jury. Once the jury is satisfied, it canthen be given statistics of other
similar cases, based on proper epidemiological studies. The damage for all the
identified victims may then be awarded (20).
I
A detailed working out of epidemiological profilesand listing of the gas
affected population assigning each to one of the profiles is thus crucial to claim
damages from Union Carbide.
Easily between 50 to 70% of the ambulatory population in the severely
affected areas of Bhopal are still complaining of one or more serious symptoms
implicating different body systems like the respiratory/gastro intestinal/ ocular and
neuromuscular systems.
It has been estimated that about 100,000 to 200,000 people of Bhopal
suffered serious exposure to MIC gas (14, 18, 21). Since we have excluded chil
dren below 10 years from our study who constitute about 30% of the total population
we can give an estimate of suffering in 70,000 to 140,000 population. By most
conservative estimates the number of persons still suffering is between 30,000 to
60,000 at the lower end. We stress again that even the upper estimate is a severely
conservative estimate especially since it excludes children below 1 0 years who are
suffering also. Practically nothing has been thought about them let alone anything
being done for them thanks to the exclusive focus on the hospital population. ,
6.5 Thiosulfate controversy
It is obvious that differences in theory can also lead to difference in the
treatment. But in Bhopal the differences about treatment have clearly gone beyond
academic differences.
The believers in the pulmonary theory in the beginning treated the gas
victims with bronchodilators, steroids, antibiotics, oxygen etc. This was the most
obvious line of treatment at first. However, the symptoms continued unabated
inspite of treatment.
Later it was known that cyanide poisoning was astrong possibility and
many including doctors themselves availed of thiosulfate injections to obtain relief.
ICMR issued guidelines for such treatment by 14th February 1985 based on the
findings of a double blind clinical trial which is accepted as one of the most rigorous
scientific methods of study.
Inspite of all this the medical establishment of Bhopal held back the
treatment from the gas victims and continued to put obstacles in the way of
implementation of this recommendation. Why ?
The minutes of the ICMR meeting of 14th February (16, Appendix-Ill)
specifically mentions that all participants (which included members of the opposing
medical lobby as wellj agreed finally to the guidelines and a decision to convey the
same to the health authorities in Bhopal as well as the Ministry of Health at the
Centre (to ensure adequate supplies of sodium thiosulfate) was also recorded. These
minutes were circulated to all the staff of the medical college recommending
necessary action on 18th February 1985. Nothing came of it. Sodium thiosulfate
is still not being given on a mass-scale to the gas victims. Besides this, a bogey of
45
I
F
supposed ill effects of treatment is being raised. The evidence produced is worse
than flimsy (2 out of 200 patients treated with sodium thiosulfate developed rash
and nausea-vomiting and 2 patients severely moribund died after sodium thiosulfate
treatment!).
At a symposium on pulmonary function held in the Medical College at
Bhopal on 24th March 1985, when a senior Professor was asked by the mfc team
why sodium thiosulfate was not being more widely used, when seniors like him had
given their consent to it earlier (Ref. appendix-ill ICMR minutes - 14-2-85), the
matter was brushed aside by a denunciation of ICMR and questioning the validity of
the double blind study. This reaction was indeed strange since if he had not been
satisfied with the results or methods of the trial, the dissent or objections should have
been raised and minuted in the proceedings of the meeting and ICMR should have
been required to release further details of the controversial trial.
On 3rd April 1985, Hindu, Madras carried a news report. Another senior
Professor Emeritus of the Medical College, Bhopal was asked by press reporters why
victims of the gas exposure were still not being given injection sodium thiosulfate.
The reply recorded was even more surprising. 'How do you expect me to administer
sodium thiosulfate to gas affected persons when I am not convinced about the need
for it - simply because someone however eminent he is, has said it and patients are
asking for it ?'
Strange argument this! In invoking the doctors'right to choose the treat
ment one should not forget that this right is not arbitrary. The doctor is under
obligation to take cognisance of well tested scientific facts. In this case it is not
the opinion of the eminent person that is the issue. The issue is whether the
opinion is based on a rigorous scientific trial and whether there exists equally strong
arguments which contradicts the outcome of the trial. In the name of 'the doctors
right to choose the treatment' a doctor cannot ignore existing scientific evidence.
What is conveniently also glossed over is the fact that only a few months earlier
most doctors had accepted meekly the dictates of the health department banning the
use of sodium thiosulfate.
This is pathetic. Is there no one to pull up these 'eminent' people whose
behaviour is both unethical and unscientific?
In our country we have a body of health professionals - the Indian Medical
Association (I.M.A.). I.M.A. considers itself fo be a custodian of health of the
people. To fulfill this role it has also taken up thecause of merit in medical educa
tion. Thus not long ago it launched a tirade against introduction of village health
workers in the health services in rural areas. 'How can these illiterate villagers be
entrusted with such a sensitive and responsible task as diagnosis and treatment of
ill persons?’, it argued vehemently. Again, when it was a case of reserving a few
seats in medice I colleges for Scheduled Castes and Tribes, it promptly jumped into
acton raising a hue and cry, to defend the cause of merit, supporting the anti-reser
vation agitation which raised such untruthful slogans as 'people's health is in danger',
save lives, abolish reservations':
(!
Now here in Bhopal, months after the disaster, months after the establishment
of sodium thiosulfate as effective therapy, months later when thousands of gas vic
tims are still complaining of debilitating symptoms forcing them to stay at home
without jobs, without income, what is I.M.A. doing to reprimand the medical
estabishment in Bhopal which simply refuses to give a vital drug to the thousands?
Nothing. Just looking the other way. A body which is so concerned about heatlh
46
and lives of people should have decided a clear policy on the thiosulfate issue long
ago. It did nothing of the sort.
Emboldened by such tacit approval the medical establishment in Bhopal
continues to behave in a strange and arbitrary fashion throwing all pretences of
being scientific overboard and continues to deny a vital drug to gas disaster victims.
Strangely the ICMR too has chosen not to release the details of the study
and to allow this important trial to be subjected to wider and open scientific scru
tiny especially when its scientific worth ps being questioned.
Does it realise that
by not releasing this crucial information and critical data which could have helped
solve the controversy it has become partly responsible for the continuing suffering
of countless unknown, unfortunate gas disaster victims whose health may have been
further damaged — damaged even irreversibly ?
6.6
Implications for research
Because of ICMR's ambivalence and lack of openness even 5 months after
the disaster and even after being in possession of a potent tool (sodium thiosulfate)
not only to treat but also to investigate further the disease pattern, ICMR has
apparently made no progress in this vital area ol research which demands our maxi
mum attention. Whatever information ICMR has released (ICMR update 10-3-85)
so far on the research it has sponsored is scanty and fragmentary.
It is a sad commentary on these research efforts that 5 months after the
disaster with a mass of population continuing to complain of serious symptoms, no
comprehensive picture of morbidity pattern in the community is put together either
by ICMR or the medical establishment of Bhopal.
A very large proportion of the exposed population have more than one
system's involvement. Intrinsic connections to all those disturbances must be clearly
understood. Based on this insight, a community based, integrated comprehensive
research programme should be mounted. Only this will reveal the true extent of
suffering and its pattern and probable causes. Quite a few research studies
sponsored by iCMR lack this integrated approach (Ref. ICMR update JOth March
1985 - Part II)
The approach of examining say 200 eyes, or 200 lungs and so on indepen
dent of one another lacks this integration. Strange as it may sound, but it seems to
derive its rationale—unconsciously—from the pulmonary theory model, wherein the
toxic gas directly hits the target organ (lung, eye etc.) to produce damage without
any intrinsic connections—which is at the heart of the 'cyanogen pool' model!
The focus of research should become suffering in the community (and not
only hospital based patients). Only when this happens, ICMR will mount well de
signed, clinical trials in the community using the potent tool of sodium thiosulfate,
to work out epidemiological profiles existing in the gas affected community:
i)
to find out who among the affected are relieved by it and who are not
relieved and to what extent.
ii)
to find out the pattern of improvement and extent of improvement
various groups of symptoms
Hi)
to find out what is the natural history of the range of serious symptoms
47
in
iv)
and to work out patterns and degrees of disabilities
A small sub-sample of persons from each epidemiological category may be
selected to study the blood gases. We stress again that a series of such studies
must be done on the ambulatory populaton among which there may be 85,000 who
carry a serious morbidity load.
Using the potent tool of sodium thiosulfate in this way ICMR will be
able to establish not only the 'cyanogen pool'theory but also treatment schedules
for the suffering population.
Only from such studies we will have detailed epidemiological profiles of
those wno are going to recover with sodium thiosulfate and those who are not.
We would then need a mass survey to identify all such persons so that proper and
just damages may be claimed from the Union Carbide. It is obviously not enough
that Union Carbide be asked to pay damages for those who are dead. It must also
ba made to pay those who have been disabled - physically, mentally and
socially. Mr. W. Anderson, Chairman of Union Carbide should not get away with
statements that 'all is well'with Bhopal.
Industrialisation is creating a high-risk environment for everyone. But
experience shows that it is the poor who face the highest risks and dangersThey get the dirtiest, most hazardous of jobs and poverty forces them to
live in the dirtiest environments. Yet few people pay any attention to their
plight, and even fewer are prepared to do anything about it.
The state of India's Environment
— a citizen's report
Centre for Science and Environment
48
CHAPTER 7
RECOMMENDATIONS
Around 90,000 gas affected persons in Bhopal continue to suffer from such
debilitating symptoms as breathlessness on exertion, fatigue, headache, disturbed
vision, loss of memory, loss of appetite and more.
The physical and mental disability has meant loss of jobs and consequent
loss of income for the survivors (Fig. 1). 65% of working persons in JP Nagar have
reported a drop in income as against 9% in Anna Nagar. In atleast half of the working
population the rate in drop of income has been 50% or more. This is by any stand
ard a picture of massive socio-economic disruption. The suffering - atleast part of it
continues not because there is no remedy for it. Many, if not all, might have been
relieved if prompt and adequate treatment with sodium thiosulfate - an antidote
to cyanide poisoning was given to them.
This was not done, and it is still being withheld from them. We have tried
to make a case in the last chapter that the problem of medical relief, rehabilitation
and damage to the thousands of victims has been turned into a tangle due to the un
seemly conflict between the two medical theories.
Although outwardly the conflict is theoretical, it has little to do with scien
tific rigor and debate. The supporters of the pulmonary theory have dogmatically
stuck to their lame and indefensible theory and have successfully stalled mass treat
ment by sodium thiosulfate, thanks to the support they have in decision making and
power centres.
The supporters of cyanogen pool theory on the other hand after having made
a brilliant and bold breakthrough have chosen to lapse into a kind of inaction not
following up the theory to its logical end by undertaking relevant epidemiological
research, allowing the theory to remain vulnerable to attack.
Indian Medical Association, 'the custodian of peoples' health', is of course
looking the other way and lending indirect, if not direct, support to the pulmonary
theory.
The right atmosphere to make relevant, comprehensive and people oriented
recommendations is of course not there. Even then we would like to make recom
mendations based on our understanding of the problem situation so that, individuals,
groups, organisations and the gas victims may be helped, even if in a small measure
in their struggle to get justice and a better deal from the Union Carbide and from the
Government of M.P.
Of all recommendations we believe the most decisive and central is the
research-cum-action programme which is in a way linked to all the major issues of
medical relief, rehabilitation and compensation for damages.
The whole scheme of recommendations follows logically from it.
7.1
Community Based Epidemiological Research
7.1.1. The research endeavour must shift its focus from the present hospital or
dispensary based seriously ill patient orientation to a family and community based
49
ambulatory patient orientation so that the quantity and quality of the problem can be
clearly demarcated. Epidemiological profiles of ill health and disability in the
community need to be urgently built up. Well designed clinical trials using sodium
thiosulfate not only as a therapeutic tool but a potent epidemiological tool as well
need to be initiated on ambulatory patients in the community - to find out who is
and who is not relieved, extent of improvement and natural history of the range of
serious symptoms (e.g. breathlessness on exertion, disturbed vision, fatigue etc.)
This will enable it to test and substantiate the 'enlarged cyanogen pool' theory, to
help it establish mass therapy with sodium thiosulfate on a firmer scientific base
than is the case today and to help refine, modify and consolidate profiles of signi
ficant epidemiological groupings so that classification of the entire gas affected
population becomes possible.
7.1.2 Since the possibility of chronic cyanide poisoning in Bhopal is very high
an ongoing surveillance programme covering the total affected population should
assess the risk to the unborn and newborn babies.
7.1.3 Health problems related to women's reproductive system should be conti
nually monitored.
7.1.4 Quite a high proportion of gas victims are suffering from psycho-social stress.
They must be properly rehabilitated.
7.1.5 In view of the possibility of lung damage it is necessary to have monitoring
of pulmonary functions for a much longer time since the process of lung fibrosis is
insidious and takes a long time to develop fully. Special care must be taken for
those whose pulmonary symptoms show no improvement after sodium thiosulfate
treatment. Similarly a special watch must be kept on visual disturbances since it
is closely related to work performance.
7.1.6. An important but neglected dimension of the existing research endeavour is
the lack of informed consent. This is a minimum medical ethic which even in the
unprecedented situation of Bhopal is reasonable, relevant and possible. People
must be informed about the test being done, their rationale and their informal/
formal consent be taken. This is their right and is the only way that medical
research becomes an instrument of human welfare and does not degenerate into an
instrument of exploitation of human suffering for esoteric research and career
advancement.
6.2
Mass Relief Programme
As we have discussed in Chapter 5, while the epidemiological studies are
underway, mass treatment with sodium thiosulfate can begin.
Special care must betaken to maintain medical records of each individual
containing a record of his/her symptoms, amount of sodium thiosulfate given and
outcome recorded in terms of improvemant/no improvement of symptoms and urinary
thiocyanate excretion if measured. The records system must be modified in the
light of new information emerging. A copy of the essential contents of the record
must be given to each individual.
7.3 Listing of the victims : claims for compensation
A list of all gas victims, each assigned to one of the epidemiological
groupings must be prepared. This is of vital importance for the claims of compen
sation for all the gas victims.
50
1A
i
Health committees
The tasks described in 6.2 and 6.3 are huge ones. The Government machi
nery however big cannot accomplish these tasks. Involvement of voluntary groups
working amongst people must become an integral part of the health service structure
if these tasks have to be accomplished properly and in time. This will also ensure
the people’s right to know.
7.5
A communication strategy on health related issues
There is need to evolve urgently and immediately a continuing education
strategy for medical personnel and a health education strategy for people exposed to
the toxic gas as part of an overall community health approach to the disaster aftermath.
A multi-pronged approach using different groups of people should be developed.
The aim should be to translate existing knowledge and new knowledge derived from
ongoing research effort into supportive intervention in the lives of the people. This
will not only meet the people's need but also satisfy their right to information about
their own health.
7.5.1 We recommend that all health personnel involved in relief/rehabilitation ser
vices should be continuously educated and kept informed through news letters,
informal group meetings at regular intervals and other means and kept updated with
latest research results and guidelines emerging out of these. For a start the content
of this continuing education for health personnel must include
ICMR guidelines for sodium thiosulfate therapy and the scientific rationale
for this line of treatment.
ii) Disaster induced psycho-social stress and methods of management
counselling and supportive psycho and chemotherapv.
iii) Possible risk to unborn foetus, need for surveillance of pregnant women,
counselling about risk and helping couples with the decision to continue
or to take the option for MTP.
iv) Family planning advice and need for contraception till detoxification is
completed.
v) Role of Respiratory Physiotherapy.
vi) Low cost nutritious recipes for mothers whose babies have had to be weaned
due to effects on lactation.
vii) Caution against overdrugging particularly steroids and antibiotics - their
side effects and rationale for use.
viii) Need for open-minded surveillance of affected population especially highrisk groups to identify emerging chronic and long term effects.
ix) Importance of family based records and improving doctor-patient communi
cation of findings and treatment.
i)
7. 5. 2 We recommend that a dynamic, creative, non-formal health education of the
affected community must also be initiated including open group meetings, posters and
pamphlets with demystified health messages and audio-visuals. The health messa
ges must be built around the life style, culture and the existing socio-economic
situation of the people to have any impact or relevance. These should include
most of the areas outlined in 7.5.1 (above) This is particularly relevant since the
disaster aftermath has led to a socio-economic crisis in the life of the victims.
51
APPENDIX I
■
I
1
BHOPAL STUDY PROFORMA
i
Medico-friends circle, 17-25 March, 1385
SECTION I : INFORMATION REGARDING HOUSEHOLD
1.
2.
3.
4.
5.
House Number
Area/Basti
Head of household
Religion
Type of cooking fuel used
i) Firewood
ii) Cowdung cake
iii) Saw-dust
iv) Coal
6.
Composition of family;
11
I ;
No.
(tick whatever is used)
(v) Kerosene
(vi) LPG Gas
(vii) Other
(specify)
(start with household head - Do not
include members who are dead or
missing since Gag leak)
Age
Name
I
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Before
Loan
Compensation
52
After
Sex
CD
JZ
CO
CO
§
a
CD
c£
CO
CD CD £ x co
_ CD Z3 co
V) CLX: TD O)
CD C
o ®
,52 co
co .—
-Q co
i.
CO CD
c5 .£ £ £
co
CD
CN
CO
CD
«—■
co
co
>»
o
2
co
° CD
a2„
x O CO —
CD
CO
.£
C
!<
CN
•— c O
CD — ’
co
2 “CO
S —o c7
O 3 -5 a 2 CO
_£Z
o
I
£
co
CO
co
O)
.£ CO
co
23
o
E cd CO
CD
■o
CD
CO
C
CD
•O
_ZD
co
Q.
ZD
o c
o
c
CD
E
co
Z
O5
-X
CO
CD
CD
co
co
CD
CD
O
C
co
CD
.£
co
co
E
o
■U
(O
CD
•u
CO
ZD
co
o
*
£P
£
cc
CD
C
co
co
cb
M- CD I.’ —
Q
o ■£> o
E
CD
~
CD
.E
8^
e-S
ii B
X
CD
CO
CO
o
JD
E
E
a
CD
C
U>
CD
CD
<
CO
E
o
E
•U
co
JO
<D
■u
CD
c
'"U
co
CD
CD
CD
<D
E
co
£
CD
-£Z
$
c
o
E
o
c
o
CD
CL
cn
o
2
I 'I ^1
co
I
in
<6 |
co
Q
(r
{ I
SECTION II : FOR INDIVIDUAL MEMBERS OF HOUSEHOLD
1.
2.
3.
!
4.
House No.
Area/Basti
Head of household
Name of individual
Staying in this basti
since when (month & year)
II
5.
i
6.
a) Occupation/job/
vocation
(Before gas leak)
b) Since when
(years, months)
c) Has gas leak affected
your job? (specify)
d) What is your present
occupation
7.
Income data :
1 .
Per day
Regular/
irregular
Per month
Before gas leak
II
After gas leak
8.
Where were you during the
gas leak
9.
Did you use any safety measures? How did you protect yourself? (water
towel, direction of running with respect to UCIL, doors closed, open, etc.)
10.
Smoking status;
Current
11.
lr j ■
Past
Nonsmoker
Hospitalization for gas effect?
When?
For how long?
54
12.
Chronic illnesses?
Parti
culars
Yes/No
Chronic
illness
other than
respiratory
Chronic respiratory illnesses
Asthma
TB
Bronchi- Lung
tis
cancer
Other
(specify)
!
Duration
13.
Number of episodes of the following in the past 3 months:
Disease
1.
Common cold
2.
Cough
3.
Fever
No. of attacks
Duration
Name of Investigator: —,
Date
55
I
r
SECTION 111 : : EXAMINATION DETAILS
• I
i
I
1.
House No.
2.
Area/basti
Head of household
3.
4. Name of individual
5. Examination details:
Symptoms
1.
Dry cough
2.
Cough with expectoration
3.
Blood in sputum (haemop:ysis)
4.
Breathlessness at rest
5.
Breathlessness on accustomed
exertion
6.
Lacrimation
7.
Fever
8.
Chest pain or tightness
9.
Skin problems (itching,
burning, infection)
10.
Jaundice and its symptoms
11.
Blood in stool or vomit/malena
12.
Bleeding tendency
13.
Blurred vision and photophobia
14.
Headache
15.
Weakness in extremities
16.
Muscie aches
17.
Fatigue
18.
Lossof memory (amnesia) recent
19.
Tingling, numbness
20.
Anorexia
21.
Nausea
22.
Vomiting
23.
Pain in abdomen/burning
24.
Flatulence/heaviness
25.
Impotence
Age:
Yes
(Specify)
No.
i
If yes,
duration
6.
7.
General examination:
i. Height
ii. Weight
iii. Pulse rate
iv. Respiratory rate
cms
kgs
Eye examination:
i. Cornea
ii. Acuity of vision
iii. Pupillary reflexes
iv. Lens
Distant vision
R
L
Pin hole
Near vision
N8 — R
PR
NR
8. Jaundice (sclera)
9. Cyanosis
10. Skin examination
11.
12.
Oedema
Respiratory system:
i. shift of mediastinum
ii. air entry
iii. foreign sounds
CVS
13.
14.
CNS
i. Muscle power
ii. Wasting
iii. Plantar
v. Knee
C
S
K
A
15.
Alimentary system:
16.
17.
18.
Anxiety/depression
Diagnosis
Remarks
i.
Liver
Name of investigator:
Date:
57
ii.
Spleen
iii.
Ascites
SECTION IV : LUNG FUNCTION TESTS
1.
House No.
2.
Area/Basti
3.
Head of household
4.
Name of individual
5.
i) Height :
cms
ii) Weight :
kgs
iii) Surface area:
'J I
6.
Lung function:
Recording
FEV-j
r '■
1
2
3
Name of Investigator :
hI Ii, .
Date
58
FVC
SECTION V : ADDITIONAL PROFORMA FOR WOMEN
1.
House No.
2.
Area/basti
3.
Head of household
4.
Name of individual
5.
Marital status
6.
Menstrual history:
Age:
Past (since wfnn)
Details
1.
Occurrence
2.
Dysmenorrhoea
3.
Flow
4.
Peculiarities
5.
Leucorrhoea
6.
Itching
7.
Burning sensation with urination
(cycle per month)
Doctors seen
7.
Yes/No
a.
Whether pregnant during gas leak?
b.
If yes, exposure during which month of pregnancy?
c.
Outcome of pregnancy:
1.
Spontaneous abortion
2.
MTP
3.
Still birth
4.
Premature delivery/live
5.
Full term
6.
Still pregnant (whether
foetal movements normal)
Lactation
(milk output)
Yes/No
Remarks (when, how, any peculiarities?)
Details
8.
Present (after
gas leak)
Supressed
(significant)
Name of investigator:
Date:
Normal
PATIENT'S PERCEPTION ABOUT AVAILABLE HEALTH
FACILITIES
L;
SECTION VI :
'r
2,
Can you walk down to the government hospital/dispensary?
34
How long do you have to wait in the dispensary in the queue for your turn to
come?
1. Where do you go for medical treatment?
a.
.
i
•i 'I
I
a.
examination
b.
getting medicines
Private doctor
b.
Government dispensary
c.
Self-medication
4.
How many days of medicines are given at a time?
5.
a.
Do you get all the medicines from the government dispensary? Yes/No
b.
If not, do you have to buy any medicines from the market?
• ■
A few medicines/all the medicines
i
:
(specify)
6.
Were the medicines useful?
7.
How was the behaviour of the government doctor?
■
a.
8.
enquiry
b.
c.
examination
Were.you referred to the hospital anytime during this illness?
advice
Yes/No
If yes, how was the experience at the hospital?
9.
Did you go to a private doctor?
Yes/No
If yes, did he tell you anything different about your illness?
\
I-
How much did you spend for private treatment?
a.
10.
Doctor's fees:
b.
Drugs
Has any doctor told you so far anything about the nature of your disease or has
given any advice?
Yes/No
It yes, what was the advice?
60
APPENDIX II
An English translation of a Handout in Hindi distributed among the
people of the bastis selected for the study.
To our brothers and sisters affected by the gas leak tragedy in Bhopal.
We are a team of socially-conscious doctors and health workers belonging
to a group called the medico friend circle. As an expression of our concern for you
all we have come to try and help you in our own small way. We have come to
assess and find out whether there are any ways in which the medical relief and
advice that is being given to you can be improved.
Soon after the disaster some of our members came to Bhopal and were
involved in relief work. They also made suggestions to the government about
medical relief work based on their own experiences. These suggestions are also
available in Hindi. We have now come to investigate in detail what are the
health problems you still have three months after the disaster and to try and find
out what can be done for them. From these investigations and from an assessment
of the treatment services being given to you, we hope to make suggestions to the
government and to all those involved in health work of improvements that can be
made.
All of you have been affected by the gas leak. To find out the health
effects of this exposure it is not necessary to examine everyone of you. To find
out the main effects on your health it would be adequate to do a complete survey
on every tenth or twentieth house in the basti. From this survey it will become
evident as to how many of you are suffering from the different illnesses caused by
the gas exposure.
Whatever we find out on examination of each of you will be written out
concisely in a note, a copy of which will be given to you. Apart from this we shall
also send you a copy of whatever other general recommendations we have about
improving your health status.
We shall explain to you what has been the effect of the gas on each and
every part of your body and what you should do to tackle this situation. Which
drugs are useful ? Which drugs are not useful ?
With your cooperation we shall try to decide whether there will be any
improvement in your lungs by the use of respiratory exercises. We shall teach you
these respiratory exercises. These exercises will also help to prevent further damage
to your lungs.
Brothers and Sisters - We are not working for government or any other
official agency. We have come here through the support of collections made from
many others who have contributed as an expression of their concern for you. We
are doing what we can through this low-cost venture and have come here volun
tarily. We are confident that you will give us your whole-hearted cooperation in
this work.
Yours
Bhopal Study Team,
medico friend circle
6f ’
I ■■■
lf7
i !1
■
APPENDIX III
I I#
INDIAN COUNCIL OF MEDICAL RESEARCH
MINUTES OF THE MEETING ON THIOSULPHATE THERAPY IN MIC
EXPOSED POPULATION HELD ON 14TH FEBRUARY, 1985 AT HEAD
QUARTERS NEW DELHI.
■
1.0
■
'
r
3 !
Participants
ICMR Representatives
Dr. J.S. Guleria
Dr. N.P. Mishra
Dr. P.S. Narayanan
Dr. P.N. Pande
Dr. K. Ramachandian
Dr. A. Ramaiah
Dr. H.H. Siddiqui
Dr. S. Sriramachari (Chairman)
Dr. C.R. Ramachandran
Dr. A.K. Prabhakar (Rapporteur)
Dr. R. Parhee
(Rapporteur)
2.0 The Chairman, Dr. S. Sriramachari, Additional Director General, ICMR, wel
comed the members on behalf of Prof. V. Ramalingaswami, Director-General, and on
his own. He explained that the purpose of the meeting was to discuss the different
aspects of use of Sodium Thio Sulphate (NTS) in MIC exposed population. He
also reiterated that the preliminary results of the double blind study conducted at
the 30 bedded community hospital at Bhopal had indicated the presence of
"cyanogen pool" in the exposed persons. He pointed out the several physiological
parameters and optimal time for urinary excretion of thiocyanate had since been
worked out and the method of monitoring could thus be standardised. He informed
that since the utility of NTS had been established, the criteria of selection and con
traindications, if any of cases, details of dosage, duration of administration should be
urgently worked out. Apart from the continuation of the Controlled Studies with
Thiosulphate Therapy, the questions relating to the extension of the therapeutic
measures to all patients with clinical symptoms should be decided.
4 ’
On the basis of the double-blind trial conducted by Dr. Narayanan and
Dr. A. Ramaiah at Bhopal Dr. Guleria and other members of the group emphasised
that Sodium Thio Sulphate should not be withheld from affected victims and should
be made available to all patients with clinical symptoms. However, he cautioned
that strict criteria for use need to be laid down. This should include specific
criteria for selection of patients based on
symptoms and severity of
exposure; as well as guidelines for maintenance of records; investigations; moni■ toring for adverse reactions; and clinical and laboratory investigative follow up
paramteers. In addition, contraindication for use should be clearly spelled out.
He also mentioned that the final decision for use and/or stoppage of treatment
with Sodium Thiosulphate should be left to the judgement of the clinician.
i: ■
i
I
r
Dr. N.P. Mishra, presented, in brief, his earlier as well as recent observations
on the use of NTS at Gandhi Medical Coll age, Bhopal. He mentioned that he had
observed adverse reactions in 2 persons among 200 individuals who had received one
• injection of NTS. Severe gastro intestinal symptoms of vomiting and nausea, with
fever was observed within 10-20 minutes of injection. Dr. Mishra stressed that this
drug should be administered to hospitalised patients. In this connection, Dr. P.S.
Narayanan presented his experience with 322 injections of NTS administered to 76
patients. The only mild advers^/e'actfon observed in 2 patients was feverishness
experienced several hours after receiving the injection which was relieved with
aspirin in one case. In view of this, the members of the group felt that NTS in
jections should be given to patients at hospitals, clinics and dispensaries under
“62
medical supervision, with strict monitoring for adverse reactions. As it may not be
possible to admit all patients while they are under therapy, it was considered advis
able to keep the patients under medical observation for at least one hour after admi
nistering the injection.
Dr. Mishra informed that the predominant symptoms observed in patients
suffering from effects of MIC relate to the respiratory, gastro intestinal and neuro
muscular systems. In addition, patients with psychological symptoms are seen.
Dr. Narayanan emphasised that some patients present themselves with relapse or
recurrence of symptoms after having obtained almost complete relief from the acute
phase.
After considerable discussion, it was agreed that NTS injections should be
given to all patients with the following criteria;
1.
Patients suffering from acute and/or chronic symptoms relating to the respira
tory, gastrointestinal, and neuromuscular symptoms, The symptoms should be
causally related to possible exposure to MIC gas;
2.
Patients presenting with recurrence of symptoms after having obtained some
measure of relief from the acute phase;
3.
Recorded cases of acute pulmonary oedema and/or coma, that occured imme
diately following the episode, and who are currently symptomatic;
4.
Patients who have a history of death in their family, and also those who reside
within 2 km of the factory in the direction of the wind on the day of the tragedy
or in the vicinity of the factory.
It was emphasised that baseline clinical and laboratory data should be
obtained for all recorded cases. With regard to old cases, where records may
be available fresh baseline data should be obtained.
Detailed discussion was held regarding dose and duration of treatment. It is
generally understood that in acute or severe cyanide poisoning, 12.5 to 25 gm of NTS
can be administered as a single dose intravenously. However in the preliminary
trials, clinical improvement had been observed with I gm of NTS given as a single
dose, or in 3 successive doses. Giving allowance for the lime lag in the build up of
the cyanogen pool after its first depletion, it was felt that the subsequent injections
could be given after larger intervals. It was finally suggested that two regimens on
administration of NTS should be followed, viz:-
NTS,
NTS,
A.
Day
Day
1
2 to 6
2
1
gm
grn
B.
Day
Day
Day
1
3
5
1
1
1
gm NTS,
gm NTS,
gm NTS,
intravenous
- do - do - do - do -
‘ weight,
* ’ . Urine
Children should receive lower do?3S appropriate to the body
should
be
monitored
initially
prior
to
the
injection,
and then
levels of thiocyanate i------------- ------w t. .
‘ ‘ . Whenever possible, 24 hour
daily, 3 hours after administration of the ‘injection,
Ikaline Diuretic with sodium chloride
urine output should be monitored. Mixture Alkaline
-33
‘ .
J
should be administered to the patient to facilitate excretion of thiocyanate, for the
duration of therapy. Therapy may be terminated if thiocyanate excretion reaches or
remains at normal levels. The members of the group agreed that the drug should
not be administered routinely to pregnant women. The decision for use will depend
upon the severity of the symptoms. Pulse rate, respiratory rate, response to exercise,
and level of physical activity should be recorded during therapy and afterwards in orderto evaluate the progress of improvement. Adverse reactions, if any, should be brought
to the notice of the local senior physicians and health authorities including the ICMR.
I
It was also recommended that urine estimation of sodium thiocyanate should
be standardised at all centres undertaking this investigation. For this purpose,
Dr.A. Ramaiah was requested to help instandardising the procedure at the labora
tory, of the Medico Legal Institute at Gandhi Medical College, Bhopal. For quality
control periodical crosschecking between the two laboratories should be worked out.
Ii 'ii
Finally, it was recommended that Dr. A. Ramaiah should prepare a detailed
protocol on the laboratory monitoring of thiosulphate therapy in MIC affected
population. This would be circulated to all members of the group at the earliest.
All the participants including Dr. N. P. Mishra and Dr. P. S. Narayanan
agreed to the above recommendations. It was decided that the above information
should be conveyed to the concerned health authority in Bhopal as well as Min. of
Health so as to ensure adequacy of supply of NTS. The next meeting of the group
would be held after 3-4 weeks to review the progress of the studies.
The meeting ended with a vote of thanks to the chair.
****
I
• h
c
I
?»
6"4
APPENDIX IV
STUDY OF MEDICAL RELIEF TO GAS VICTIMS
Some members of
( the team visited various medical centres near JP Nagar—
the basti selected for our study. These included:
i)
a government polyclinic
ii)
the DIG Hospital—a 30 bedded hospital specially established for care of
disaster victims
iii) three non-governmental private clinics in the adjoining area.
From these visits and interviews with the doctors, some understanding of
the dynamics of medical relief services emerged. The points specifically noted were
staff pattern, timing, availability of drugs, standard guidelines if any and doctors'
perceptions of the health problems etc.
Government Services
i)
The polyclinic was kept open 24 hours of the day. It was an ordinary
dispensary and did not consist of specialists from different branches as the
name suggests.
ii)
The DIG hospital was, however, staffed by specialists in medicine,
obstetrics, ophthalmology, paediatrics, EXIT and surgery. It had 14 doctors
and a smaller number of paramedics. The out-patients department
was open from 9.00 a.m. to 1.00 p.m. and for one hour in the evenings.
About 600-800 patients were seen per day, resulting in long queues.
There seemed to be no problem of drugs - these being available in adequate
range and quantity.
There were no standard guidelines for investigating, diagnosing and treating
gas victims. The doctors used their own lines of treatment-. Most of the
doctors interviewed had no definite knowledge about the role of sodium
thiosulfate nor had seriously reviewed the problem of danger to the foetus
and the option of MTP for pregnant women. There were no definite criteria
for referring patients to bigger hospitals. Facilities for routine biochemical
and microscopic investigations were available.
The DIG Hospital was also being used for the double blind clinical trial of
ICMR on the rationale/ efficacy of sodium thiosulfate. It had facilities for
blood gas analysis and measurement of urinary thiocyanate levels by
spectrophotometry. These were being carried out on all patients being
selected for a course of sodium thiosulfate injections.
iii)
Our interviews with doctors about the range of symptomatology and clinical
syndromes tney were seeing each day in the OPD'S revealed that even
though they thought that many patients were ill, they felt that many were
exaggerating and implicating the gas in all types of complaints. The
quality of reporting/recording these symptoms and findings of examination
were poor and would therefore, not be of much use in any type of
retrospective research studies.
65
I
1/
r
’
On the whole though a medical service had been established and medical
teams were available to the gas disaster victims, we felt that these had not been
adequately oriented to meet the demands of the situation; there were no standardised
guidelines for investigation or management; and no continuing education or on
going communication of research and other information to the treating doctors to
support rational management. The doctors' attitudes were somewhat biased
against the phenomena of multisystemic symptomatology with many of them
perceiving this as malingering or compensation neurosis.
By and large due to inadequate planning the dispensaries were understaffed
and the doctors overworked. This was particularly true of the DIG hospital.
Non-government clinics
Three such centres were available near the basti. One of them was a free
clinic specially set up after the gas disaster with the help of a Muslim Charitable
group. The therapist was using mainly homeopathic medicines but also had
ayurvedic and allopathic medicines in his armamentarium. He used these 'depen
ding on the case’. He made tall claims of cure for gas related diseases as well as
other problems. Our intensive but informal talks with the basti people for three
days did not reveal any cases of substantial relief with his treatment schedules.
Another general practitioner had a clinic about 1 km. from the basti. He
was not an MBBS doctor but his clinic was overcrowded. He seemed courteous
and soft spoken to his patients but hardly examined anybody in detail. Injections,
antibiotics and prednisolone were liberally used. In his discussion with us he shared
that antibiotics, antacids, bronchodilators and steroids had been used by him to treat
the patients without much result. He did not know about the details of the use of
Inj. sodium thiosulfate or the medical controversy about it. However, he thought
that the advice given by a forensic expert (doctor of the dead as he described him)
regarding cyanide poisoning should be taken with ’a pinch of salt'. He also felt
that some of his patients who had been given injection sodium thiosulfate had not
benefited. He also shared with us that he himself had been exposed to the gas and
suffers from symptoms even now. Recently he had started taking an ayurvedic
preparation with 'gratifying results'.
The third practitioner was a lady doctor working near the basti. She had
closed down her clinic after the disaster for two months and could not tell us much.
She had used antacids, cough mixture and antibiotics without much results. Most
patients, she said, did not come back the next day in spite of their continued illness
since "they were too poor to pay fees every day". When asked specifically about
the problems of women, she felt that there had been an increased incidence of
gynaecological problems but since she did not undertake gynaecological exami
nations, she could not give further details. Most of these cases were referred to her
sister who was a trained gynaecologist. None of these practitioners had received
any communication or guidelines from the government health service doctors or
medical college and there was no coordination between them and the government
polyclinics or dispensaries.
p
66
APPENDIX V
PEOPLE’S PERCEPTION ABOUT AVAILABLE MEDICAL FACILITIES
Forty out of the sixty families selected in our study of JP Nagar were
included in the survey of people's perceptions of the available medical services.
One person from each of the families was interviewed and the questions asked are
given in Appendix I (study proforma. Section 6). The main findings of this survey
were :
(i) Choice of treatment : Seventy percent had gone to government dispen
saries and 82 5 percent had gone to private practitioners and only one was
on self-medication. Ten persons had not gone to any government dispen
sary and five persons had not gone to any private practitioner. Many had
decided to go to private practitioners because they were dissatisfied with
the experience in the government hospitals.
The distances were not too much and most people said they could walk
down to the government hospital or dispensaries
(ii)
Time at dispensary/hospital : Six persons said they had to wait 1-2
hours for their turn in the hospital, 8 persons - 2-4 hours and 13 persons
more than 4 hours. The delays were probably due to thase service units
being understaffed and to overcrowded.
(iii)
Medication : Medicines were given mostly for 1-3 days in 70 percent of
the cases whereas 6 respondents said they had received medication for more
than three days. (This is inclusive of the practice in the private-clinics).
Medicines were received free in the government dispensary by 70 percent of
the respondents. 5 persons mentioned they had to buy a few medicines
from the market.
Twenty five percent had no relief from the medication, 52.5 percent got
some symptomatic relief while one respondent mentioned that he got
substantial relief.
Interestingly the only therapy that was being given was drugs which were
being prescribed faithfully by the doctors in large doses and repeatedly with
no thought of over-medication. Many patients showed us platefuls of
coloured capsules and tablets which they had received from different
doctors in the same centres and in different centres. These were not very
effective but were continuously being prescribed in a sort of routine condi
tioned reflex!
■
(iv)
Attitude of doctors and quality of care : Forty percent said that the
doctors hardly made any enquiries, whereas 42. 5% mentioned that the
enquiries were sympathetic. 15 percent said that no examinations were
done, 37. 5% had cursory examinations and 25 percent had proper
physical examinations. 75 percent were given no advice other than
instructions for medication. One received some reassurance and only
one could recall being given sorrte dieta’ry advice.
(v)
Referrals to Hospital : Nineteen respondents were referred to hospitals
during the last few weeks. 9 felt the same after hospitalisation, 5 felt
worse and 3 got better.
67
I
(vi)
Experience with private practitioners : The experience with private
practitioners, whom over 82.5 percent had consulted/ was not very
different except that the doctor-patient relationship was somewhat more
satisfying. All of them got a medication but no other advice.
Ten respondents had spent upto Rs. 100.00 on treatment, 10 between
Rs. 100. 00 and Rs. 500.00 and 13 had spent more than Rs.500.00. No
doubt this was adding to the economic burden of the families and would
be reflected in the loans taken by many families. One family had spent
more than Rs. 3500/- on treatment.
(vii)
Health education : Thirty seven of forty respondents had been given no
inkling about the nature of the illness or any other supportive advise, e.g.
no smoking for those with lung complaints, special advise to women
who were pregnant, breathing exercises, psychological reassurance or
counselling. One mentioned that he had been told 'it was a recurring
illness'.
r
68
REFERENCES
1.
Bang, Abhay. et al
Medical Relief and Research in Bhooal - the realities and recommendations
medico friend circle report Feb. 1985
2.
Dagani Ron 1 985
Data on MIC's toxicity are scant, leave much to be learned
Bhopal Report, C & EN Fab. 11, 1985.
3.
Anon
Methyl Isocyanate, Toxicology profile
4.
Rye, A.W. ( 1983 )
Human responses to Isocyanate exposure
J of Occup. Med, Vol. 15, No.3,March 1983
5.
NIOSH ( 1979 )
A recommended standard for occupational exposure to Diisocyanates.
US Dept, of Health Education & Welfare Publication No. 78 - 125, April 1979
6.
Axford, A.T. et al ( 1976 )
Accidental exposure to Isocyanate fumes in a group of firemen
British J. of Indust Med. 1976. 33, 65 - 71
7.
Procter. N. H. and Hughes. J. P. (Ed)
Methyl Isocyanate
From Chemical Hazards of the work place J.B. Lippencote, Philadelphia, 1978
8.
Praful Bidwai ( 1985 )
Bhopal's unending tragedy - Times of India, 25th - 27th March 1985.
9.
Eklavya ( 1 985 )
Bhopal City of Death A people's views of death - their right to know and live
Eklavya report, Bhopal.
10.
Bouhuys, A (1974)
Breathing—physiology. Environment and Lung Disease
Grune L. Stratton, N Y. London 1974.
11.
Anderson, W.M., Letter to the Peoples Research Institute and Environment,
Japan dated January 3, 1985, Consumer Interpol Memo No. 2/85(5),
19 February, 1985.
12.
Diamond, Stuart
New Strait Times, 15 February 1985
13.
Petersdrof, Robert K. et al (Ed.)
Harrison's Principles of Internal Medicine,
Mc-Graw-Hill, New York, tenth edition^ 1983.
14.
I.C.M.R. (1935)
j
Health effects of exposure to toxic gas at Bhopal—an update on I.C.M.R.
sponsored researches, 10th March 1985
69
15.
Sriramachari. S. (1985)
Pathology and clinical toxicology of the Bhopal disaster.
I.C.M.R. handout, New Delhi.
16.
I.C.M.R. (1985)
Thiosulfate therapy in MIC exposed
Minutes of the meeting in I.C.M.R., 14th Feb. 1985
17.
Daunderer. M. (1985)
Methyl Isocyanate
Mimeograph
18.
I.C.M.R. (1985)
The Bhopal disaster - current status (the first nine
research.-
I
i
days) and programme of
19.
Cduv, Florey and Leeder, S.R. (1982)
Methods for cohort studies of chronic Air-flow Limitation.
W.H.O. Geneva.
20.
Fera, Ivan
Will Justice be done? Illustrated Weekly of India, 31st March 1985
21.
Gopalakrishnan, K & Ganguly, T. (1984)
The way the killer works from Gassed-Bhopal's Night of Horror - Cover Story
of The Week - 16-22nd Dec. 1984 Malayala Manorama Publication.
22.
Mac Mohan B and Pugh T.F.
Epidemiology, Principles and Methods
Boston 1970
I
I
' 70
ADDITIONAL READING MATERIAL
1. I.C.M.R. (1985)
Projectization of I.C.M.R. supported research.
2.
Ramalingaswami, V. (1985)
Medical Research Problems in Bhopal
I.C.M.R. handout, New Delhi.
3.
I.C.M.R. (1985)
Medical Research on Bhopal Gas Tragedy
Press release - 31st Jan 1985
4.
I.C.M.R. ibid, press release, 12th Feb. 1985
5.
I.C.M.R. ibidz press release, 27th Feb. 1985
6.
I.C.M.R. (1985)
Guidelines for treatment of Bhopal Gas Victims
Press release, 4th April 1985
Non-Governmental Sources
7.
Delhi Science Forum (1985)
Bhopal Gas Tragedy - a report
8.
Bang, Abhay (1985)
Learning from the relief work - a report from Bhopal
medico friend circle bulletin - 109, Jan. 1985
9.
mfc (1985)
Medical Research in Bhopal - are we forgetting the people,
medico friend circle bulletin - 112, April 1985
10.
Bang, Rani & Sadgopal, Mira (1985)
Effects of the Bhopal disaster on women's health - an epidemic of gynaecolo
gical diseases- (Part - I) Mimeograph
11.
Bang, Rani (1 985)
Effects of the Bhopal disaster on women's health - an epidemic of gynaecolo
gical diseases (Part II) Mimeograph
12.
mfc (1985)
The mfc Bhopal Study - a press release
medico friend circle bulletin - 112, April 1985
13.
Banerji, D & Lakhan Singh
Bhopal Gas Tragedy - an epidemiological and sociological study
J N U News, April 1985
14.
Citizens Committee for Relief and Rehabilitation (1985)
Medical survey on Bhopal Gas victims bbtweer?104 to 109 days after exposure
to MIC gas
-report of a joint study in collaboration with Voluntary Health Association of
India, New Delhi.
71 ’
MIC and Isocyanates
%
1
i
I
r
15.
Singh, Sarabjeet (1985)
Chemistry, fate, pharmacology and effects of methyl isocyanate.
Drug information desk handout,
Department of pharmacology, Gandhi Medical College, Bhopal.
16.
Patel Chest Institute (1985)
Adverse effects of MIC and related compounds (Phosgene, Hydrocyanic acid,
Carbaryl, Carbon monoxide) Mimeograph
17.
Cohen, S & Oppenheimer, E.
Biological formation and reaction of Cyanates, Chapter 20.
18.
Worthy. W. (1985)
Methyl Isocyanate : The Cnemistry of a Hazard
C & EN,11th Feb. 1985
19.
Lancet (1966)
Hazards of Diisocyanates
Editorial, Jan. 1, 1966
20.
Lancet (1984)
Calamity at Bhopal
Editorial, 15th Dec. 1984
21.
Kimmerle, G & Eben A. (1964)
Toxicity of Methyl Isocyanate and its quantitative determination in the air.
Archiv Fuer Toxicologic Vol 20 p. 235-241, 1964 (German)
22.
Pozzani, U.C. & Kinkead, E.R. (1966)
Animal and Human response to methyl isocyanate
Presented to American Indust Hygiene Assoc. May 1966
23.
Smyth, H et al,
Range Finding Toxicity data - List 7
American Indust Hygiene Assoc. Journal 30 Sept - Oct. 1969 p. 470-76
24.
Melon Institute (1970)
Methyl isocyanate - acute inhalation toxicity, human
response to low concentration, guinea pig sensitization and
cross sensitization to other isocyanates special report—33-19
Chemical Hygiene fellowship - Carnegie Melon University
25.
Melon Institute (1963)
Range finding tests on Methyl Isocyanate
Confidential report 26-75
26.
Longley, E.O. (1964) k
Methyl - di-isocyanate - a respiratory hazard
Archives of Environ Health, Vol. 8. p. 898, 1964
Australia.
72
II
■
27.
Le Quesne, P.M. et al (1976)
Neurological complications after a single severe
exposure to T.D.I.
British’U. of lndust ,Med 1976 33, 72-78
28.
Bernstein, L. (1982)
Isocyanate - induced pulmonary diseases—a current perspective
J. Allergy Clin. Immunol. July 1982, Vol. 70
No- 1, p. 24-31
29.
Dewair, M.A. & Baur X.J. (1982)
Studies on antigens useful for detection of Ig E
antibodies in isocyanate sensitised workers.
J. Clin Chem Clin Biochem. Vol. 20,1982, p. 337 - 340
30.
Baur X. et al (1984)
Acute airway obstruction followed by hyper-sensitivity
pneumonitis in isocyanate workers (MDl)
Journal of Occup. Med. Vol. 26, No. 4 April 1 984
31.
Munn. A. (1965)
Hazards of Isocyanates
Ann. Occup Hyg 8 : 163, 1965
32.
Brooks S.M. (1977)
Bronchial Asthma of occupational origin
Scand. J. Work Environ Health, 3:53, 1977
33.
Union Carbide (1976)
Methyl Isocyanate
Product Information manual.
34.
Union Carbide (1985)
Telegram from Union Carbide Corporation, USA
on treatment of MIC pulmonary complications.
35.
Union Carbide (1985)
Bhopal Methyl Isocyanate - Investigation report
UCC, USA.
36.
Union Carbide (1982)
Operation Safety Survey of CO/MIC/Sevin units of
Union Carbide India Ltd. Bhopal Plant
May 1982 Report, UCC, USA.
37.
OSHA, (1978)
Occupational Health Guidelines for MIC
OSHA, US Dept of Labour.
Others
Miscellaneous
38.
Doherty, P.A. et al (1982)
•
>
Congenital Malformations induced by infusion of
Sodium Cyanide in the Golden Hamster
Toxicol Appl. Pharmacol 64, 456-464
• 73
39.
Loeser, E (1983)
Long term toxicity and carcinogenecity studies with 2,4/2,6
TDI (80/20) in Rats and Mice
Toxicology Letters 15 (1983) 71-81, Eiserier Biomedical Press
40.
Ministry of Health, Mozambique (1984)
Mantakassa : an epidemic of spastic paraparesis associated
with chronic cyanide intoxication in a cassava staple area
I
1. Epidemiology and clinical and laboratory findings in patients
2. Nutritional factors and hydrocyanic acid content of
cassava products
Bulletin of W.H.O. 62 (3) 477-492 (1934)
i
41.
Durham, W.F.
Toxicology
From Dangerous properties of Industrial materials
Ed. Van Nostrand and Reinhold
42.
Bhar, B (1985)
Bhopal Tragedy
Annual conference souvenir - 1985
of Indian Associaton of Occupational Health.
43.
Ramachandran R. (1985)
Bhopal elusive answers
Frontline, Jan. 26-Feb. 8, 1985
44.
Eklavya (1985)
Bhopal— the state of the environment
A preliminary report on the 100th day after the gas disaster
Eklavya. Bhopal.
45.
Eklavya (1985)
Bhopal gas tragedy—Questions of a people's science
Exhibition booklet (Hindi)
Eklavya, Bhopal.
I
I
8
46.
Goswami, H.K. et al (1984)
Genetic assessment of Union Carbide Gas tragedy in Bhopal.
I —Effects on Somatic chromosomes and hemoglobin
Bionature, Vol. 4, No. 2, December 1984.
47.
Varma. V.S. (1985)
Review of Literature on Cyanide Poisoning and treatment
Mimeograph
48.
Swamy B. (1985)
Antidote to MIC poisoning
Hitavada, 3rd May 1985
I
?
j
74’
I
1
3
49.
Kinston, W. and Rosser R. (1974)
Disaster : Effects on Mental and Physical State
Journal of Psychosom. Research. 18 : 437
50.
Cobb. S and Lindemann. E (1943)
Neuropsychiatric Observations during the coconut grove fire
Am. Surgery. 117:814
51.
Lindemann. E (1944)
Symptomatology and management of acute grief
Am. J. Psychiatry 101 : 141
52.
Lifton. R and Olson. E (1976)
The human meaning of total disaster
Psychiatry 39 : 1.
53.
Titchner. J.L. and Kapp F.T. (1976)
Family and character change at Buffalo creek
Am. J. Psychiatry 133 : 295
54.
Stern. G. (1976)
From chaos to responsibility
Am. J. Psychiatry. 133 : 300
55.
Erikson. K. (1976)
Loss of Community at Buffalo creek
Am. J, Psychiatry 133 : 302
56.
Newman. C.J. (1976)
Children of disaster : Clinical Observation at Buffalo creek
Am. J. Psychiatry 133 : 306
57.
Rangell, L. (1976)
Discussion of the Buffalo Creek Disaster : The
course of Psychic trauma
Am. J. Psychiatry 133 : 313
58.
Murthy, R.S. et al (1985)
Mental Health Care Manual for Medical Officers. - Bhopal, April 1985
NIMHANS, Bangalore.
59.
ICMR (1985»
Minutes of Third meeting of the working group
on thiosulphate therapy of the MIC exposed population
held on 4th April 1985 at ICMR headquarters.
60.
ICMR (1985)
Press release of 5th May 1985 on Review meeting of
ICMR projects held in Bhopal on 3rd I 4th May 1985
n
61.
B
Directorate of Information and Publicity, M.P.
Govt. (1985) Important toxicological findings
regarding MIC exposure. Review meeting of ICMR projects
Khabar, 5th May 1985
75
62.
Ibid
Report on Thiocyanate level in Bhopal water
News Item • 17th May 1985
63.
Narayan, T. 1985
Personal communication from Bhopal - 25th May 1985
64.
Peters, C G. et al (1985)
Acute cyanide poisoning.
Anaesthesia.
1982,
Vol. 37, p. 582 - 586
i
65.
Bowler, R.E. (1944)
The Determination of Thiocyanate in Blood serum
Biochem : J 38 1944 p. 385 - 388
66.
Densen, P.M. et al (1967)
A chemical test for smoking exposure
Arch. Environ Health - Vol. 14, June 1967
67.
Waldholz. M. (1985)
Bhopal Death Toll, survivor problems still being debated.
The Wall Steert Journal, Thursday, March 21, 1985.
Available from mfc office
326 V Main I Block
Koramangala
Bangalore 560034
1.
Medical Relief and Research in Bhopal-the realities and recommendations (Feb 1985)
Rs. 2.00
An Epidemic of Gynaecological Diseases:
effects of Bhopal disaster on Women's Health
--Rani Bang
Rs. 2 00
Review of available literature on MIC
and details of ICMR and other studies
Rs .2.0C
Rationale for the use of sodium
thiosulphate as an antidote in the
treatment of the victims of the Bhopal
gas disaster - a review
Rs. 2.00
5.
The Bhopal Disaster--mfc bulletin 109
Rs. 2.00
6.
Medical Research in Bhopal--are we
forgetting the people--m;c bulletin 112
Rs. 2.00
7.
The Challenge of Bhopal—mfc bulletin 114
Rs. 2.00
8.
The need for a Communication Strategy
Rs. 2.00
2.
3.
4.
76
4
r
t
medico friend circle
The medico friend circle (mfc) is a circle of friends with medicai/nonmedical backgrounds who share the common conviction that the present system of
health services and medical education is lopsided in the interest of the privileged
few and must be changed to serve the interests of the large majority, the poor, mfc
fosters a 'thought current' upholding human values, people and community
orientation of health care and medical education, demystification of medical science
and a commitment to the guidance of medical interventions by peoples' needsand
not commercial interests.
mfc offers a forum for dlalogue/debate, sharing of experience and
experiments with the aim of realising the goals outlined above, and for taking up
issues of common concern for action.
For further details regarding mfc BHOPAL STUDY, contactAshvin Patel
ARCH
21 Nirman Society
Alkapuri
Vadodara 390005
OR
Anil Patel
ARCH
Mangrol (At & PO)
Via Rajpipla
Dist. Bharuch
Gujarat 393150
1
I
Position: 347 (20 views)