Acute Respiratory Infections and Child Survival - Problem and the Possibilities
Item
- Title
- Acute Respiratory Infections and Child Survival - Problem and the Possibilities
- Creator
- Abhay Bang
- Date
- 1988
- extracted text
-
)
*7J
MIC,.
XIV ANNUAL MEET
Acute xes~ir~:tory xnfections and child Survival
Prcblem and_the _Posibilitres
- Abb ay Bang -
u
As public health Improves ir. the developing countries and
other infections are better controlled..
it can be expected that
the respiratory infections will emerge from their present obscurity11
A. Monro and Johnson,(1968)
(1)
The prophetic words of Monto and Johnson have become a reality
with the emergence of Acute Respiratory Infections (AEl) control
programme initiated by WHO.
Surprisingly the attention to acute
respiratory infections in children -was redrawn by a relatively -w••.ox
study which was a by product of Narangwal studies.
McCord and
Kielmann published in 1978 their experiences titled "
successful
programme cf medical auxiliaries treating childhood diarrhoea., arid
•Pneumonia" ' (2) in which they reported that the village level
Family Health Workers (similar to ANMs) in Narancwal Project were
given training to identify pneumonia in children and treat with
injection penicillin.
The case fatality rate of childhood pnevmor: La
in community dropped from 105 per 1000 episodes to 22 ( P<’0..02).
Today efforts are being made to develop National ARI control progr
ammes in various developing countries including India, ano. this is
being expectantly locked at as a major -cool to reduce childhood,
rnort-a lity.
This paper shell try to review the ep.,demiologic end Operatio
nal rationale of this programme and try to identify certain problems
which the croup at MFC annual meet can discuss..
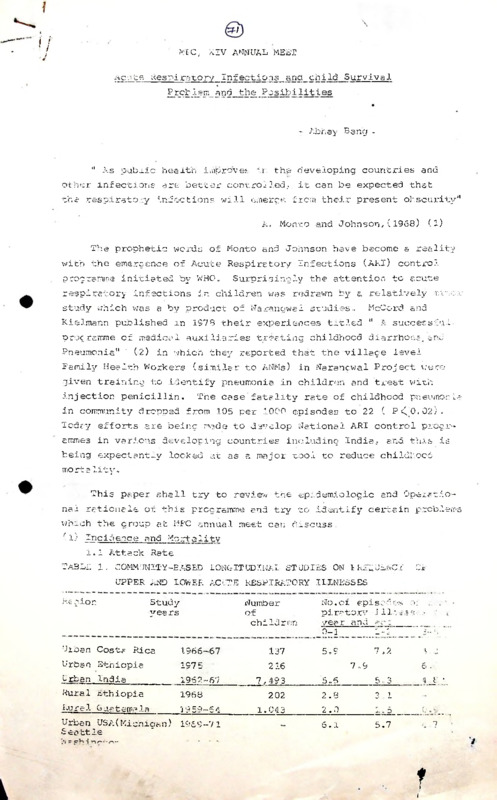
(1) -ncidence and Mortality
1.1 Attack Rate
TABLE 1. COMMUNITY-EASED LONGITUDINAL STUDIES ON LRiEJENCY
OF
UPPER AND LOWER ACUTE RESPIRATORY ILLNESSES
Re gion
Studyyea rs
Number
of
children
Urban Costa Rica
1566-67
137
Urban Ethiopia
197 5
216
urban India
1952-6'7
Rural Ethiopia
1968
Aural. Guatemala_______ 1959-54
Urban USA(Michigan)
Seattle
1959-71
No. of episodes ;■>:
piratorv illo-sse- •
year and
___
0-1
" 1>.....................,
7,2
5.9
■i.
5 .
7 .9
7,493
5..6
5,3
202
2.8
3 1
1.04 3
2.0
5.1
J'. 1.
__
C
5.7
f
I
i
■2
Table 2 - Frequency of ARI In urban and rural areas
Urban
New Delhi
Vellore
Seattle, USA
Rura 1
Pun jab
Bangladesh
Source
No. of epi sodes/yr
No, of
children
Study
years
Area
Infants
1962-67
7 493
5.6
1969-72
4.5
5.3
4.8
6.2
4.8
5.0
2.5(0-14 years)
12 0
1975-76
1978-79
3-5
7.3
135
390
1965-67
1-2
2.3
197
2.5
2.3
(4)
The frequency of attacks of ARI per child per year is similar
in the developed and the developing countries.
It is more in Urban
as compared to rural area in develooing countries. This pattern
succests thet socio-economic development is not a major determinant
of rhe frequency of ARIs.
But it is an important determinant of the
Severity of infection and the resultant mortality.
Table 3. Amu? 2 incidoncc
Place.
f pneumonia in children
Year of
Study
No. of pneumonie./1000
children
Infants
Seattle, USA
Nev/ Mexico & Arizona, USA
1972-73
(Red Indians)
Punjab, India
197 0-7 3
1966-73
291.4
1-4 yr
0-5
36.0
30.0
39.9
91.2
94.1
Source (4)
1.2 Childhood mortalitv due to ARI
TliBLE 4. MORTALITY FROM INFLUENZA AND PNEUMONIA IN CHILDREN UNDE.-.
FIVE IN FOUR COUNTRIES OF THE WESTERN PACIFIC,(RATES PEA
1000, 1974-75)
Country
V
Australia(1974)
Uaper. .197 5?
Siji(1975)
Philippines ■' 19"4)
ARI Mortality rates per 1000 ch lid re ■.
Infants
2r£_Z£.-:..£g
0.04
0.66
0.85
0.07
4.67
0.5
yr
c.
3
~ Twenty four times higher than Australia rete
2
Seventy-three times higher then Australia rate
Source: (3)'
Different studies have reported different rates of mortality
due to ARI in India, ranging from 15% to 25% of the total childhood
deaths, (4). The opinion and experience differs as to which causes
more deaths in children - diarrhoea or ARI. One estimate based
on SRS data was that ARI was responsible for 5 lakhs to 7 lakhs
childhood deaths in an year in India. (5).
Globally, ARI causes
4 million childhood deaths annually i.e. about 27% of all child
hood deaths. (10)
75% of ARI deaths ere due to pneumonia.
ratio-
The case fatality
in the cases of pneumonia--in-rural Punjab
and 6% in toddlers.
was 12% in infants
A study in Papua New Guinea (1980-81) reported
that if untreated, the case fatality in the cases of Pneumonia
was 25% in under five (6).
1.3) Studies after studies have shown that ARI forms the major
load on health care.
20 to 40% of outpatient and 12 - 35% of
childhood hospital admissions were due to ARI (4)
One really wonders as to how could such major problem
remain neglected by the public health persons till very recently.
2) Aetiology:
Aetiologically ARI is even more diverse than
diarrhoea, and except for whoooing cough or diphtheria which
have specific organisms and Characteristic clinical pictures,
most of the clinical entities are caused by variety of organisms.
To determine the causative organisms in acute lower respiratory
infections (ALR’J) is difficult because children don't bring
out sputum aad because many organisms ere common commensals
in the upper respiratory tract. Only reliable method to get
uncontaminated specimen is lung puncture and aspiration in the
cases of Pneumonia. This is risky procedure and hence can be
justified only in seriously ill children thus making the sample
very selective. A seriese of such studies in developing coun
tries showed that in 60% of such cases, a bacteria could be
grown from the lung aspirate and the commest were S. Pneumoniae
end H. influenzae. This was in contrast to developed countries
where viruses and mycoplasma were the major organisms.
.. 4
4
Table 5. Results of bacteriological studies on lung aspirates
in children with pneumonia who had no previous
antimicrobial treatment.
ZARIA
NIGERIA
NUMBER
AGE
RECIFE,
BRAZIL
60
88
3 months
to 8 years
SAG PAULO,
BRAZIL
37
GOKOKA,
NEWARK,
PNG
N.JERSEY
(U.S.A.)
78
27
2 months
15 years
3 months
to 4 years
2 months
to 7 years
0-12
(+) CULTURES^
61.3
60.0
54.1
57 .7
22.2
STR. PNEUMONIAE
H. INFLUENZAE
57.4
16.6
UNKNOWN
58.3
25.0
75.0
15.0
13.3
35.5
50.0
STR.PNEUMONIAE
+ H.INFLUENZAE
STAPH. AUREUS
OTHERS
14.8
37.0
33.3
11.1
5.6
5.0
5.0
2.2
15.7
50.0
The lung aspirate studies implicating these 2 bacteria as the
commonest cause of childhood pneumonia wd the report from Narangwel
thst treating these children with penicillin by FHWs resulted in
the dramatic reduction in the mortality led to what is called the
case management approach of ARI control.
3)
Epidemiologic features of ARI pose 2 major problems making
them particularly resistant to primary prevention.
i) The transmission is airborne and breaking this transmission
is practically impossible
ii) The large variety of causative organisms mean that
immunisation by one single vaccine is not possible.
Thus there is no one magic remedy which will rid human kind
off ALIs. But there are many possible approaches, each making
some dent on the problem.
3 • (1) Reduction in crowding;
- Rural areas have lower frequency of ARI
- Communities in the presettlement phases of civilisation
5
5
have very low rates of airborne transmission of ARIs because
the oroenisms can not survive in the absence of a large size
of human community in constant interaction with each other.
Thus to reduce the incidence of ARI, population density needs
to be brought down - something which people won't be willing to do
for the sake
reducing ARI.
- Better and spacious housing does not seem to make change as
long as population interaction is dense.
This is obvious
from the fact that the incidence of ARI in urban areas of
developed countries is same as that of developing countries.
3.(2) Nutrition:
A recent study in Manila reflects our state of understanding.
(7) The incidence of ARI per child per year was seven and there
was no difference in attack rate between the malnourished as compared
to well nourished children. But the outcome of lower respiratory
infection was grossly influ .enced by the nutritional state. The
case fatality ratio were
Welnourished children
Mild malnutrition
Severe Malnutrition
6/1000 episodes
23/1000
77/1000
Similarly, case fatality ratio in low birth weight neonate is
60% as compared to 20% in the normal birth weight neonates.
Incidence of Lower respiratory infections is significantly less in
breast fed infants as compared to bottle fed infants.
3.(3) Smoke
Both, the domestic smoke and the smoking habits of
parents increase the incidence of Ar.I in children. Antitobacco
campaign and the smokeless chulhas have something to offer
here.
3.(4) Vit A deficiency - Studies in Indonesia suggest that there
is higher mortality from ARI in children who had eyesigns of
Vit A deficiency.(7)
3.(5) Immunisation: WHO estimates (8) that 5 million children die
of ARI every year -(2 million children die of measles and its
complications of which 1/3 due to complication of pneumonia,
i.e. about 7 Lakhs ARI related de?ths. 4.5 Lakhs children
die of immunisable respiratory diseases like Diphtheria,
Whooping cough, TB,1
Thus immunisation can prevent about 25% of
the total mortality due to ARIs.
NATIONAL HEALTH POLICY; EXPECTED
IMMUNIZATION STATUS FROM
1980-2000 IN RELATION TO ARI.(9)
1980
1985
1990
1995
2000
DPT
25
70
85
85
85
BCG
65
70
70
85
85
85
85
85
85
85
85
Beneficiaries
Vaccine
Infants
Measles
Schoo1 chile ren
5-6
DT
20
80
During the next five years, over 82 million infants and
expectant mothers' ere planned to be covered under the programme.
It is a difficult task and involves administration of over 840 mil
lion doses of different type of vaccines.
Current status of vaccination coverage in relation to ARI
( in million)
Year
Vaccine
198-1-85
1985-86
DPT
BCG
Target
14.00
14.5
Achievement
12.18
12.31
Target
14.04
14.04
Achievement
13.34
12.89
Measles.
" From the above table, it is clear that we ere far behind
the targets and need a lot of strengthening. Moreover, measles
vaccine has been included in 1985 and yet to achieve its peak.
In
1986-87, 5.6 percent of targets set for measles were achieved
though percentage achievement as per set tercets for DPT a.nd BCG
was higher i.e. 77.7 and 75.1 respectively." (9)
The two other major killer bacteria are pneumocous and H.
influenzae
which cause pneumonia.
The vaccines against both of
these-have been developed but suffer from the problems of inadeguate immunogenicity, leek of universal efficacy and high
. . .7
cost,
( A)
7
: I
►
Respiratory syncytial virus and para influenza virus ere
known to be important causes of bronchiolitis in children leading
to death. Effective vaccines against these 2 viruses are yet to
be developed.
New research in the vaccine related techniques is very fast
and it may not be very long before vaccines against these 4 import
ant organisms are also developed. Most of the ARI related deaths
then would become preventable.
2(S’)""Case Management Approach:
It is a secondary prevention
approach based on the- assumptions that
- Majority of the acute lower respiratory infections (ALRI)
ere caused by bacteria and hence are amenable to
antibiotics.
- It is possible to develop simplified standard guidelines
for eerly diagnosis and treatment of ARIs and prevent
deaths by training auxiliary health workers.
WHO has strongly recommended use of this approach and has'
( 14)
0-r
O
r
suggested following classification of ARI for decisions] management
1) Child with cough but respiratory rate less than 50 per'minute
Mild ARI----------- No antibiotic necessary
2) Child with cough-----
with respiratory rate more than 50/
minute but no chest indrawing
- Moderate ARI Needs antibiotic but can be treated in
OPD or at home
3,' Child with cough with indrawtng of chest or inability to drink
O<.
.4x1 .
feeds hospitalisation
The choice of respiratory rate 50 per minute to single out
ohncren who need antibiotics was based on a study in Papua New
r .
(11)
Cumea
which/extensively quoted bellow
Table 6. Mean respiratory rate in 200 paediatric outpatients with
cough
Age
12 months
12 months
All ages
Mean_respiratory_rate_(.breaths/min) _in
Children with
Children without
Midpoint
crepitations.
between means)
Crepitations
(breeths/min)
62 ,6(n=44)
44.9(n=62)
54.0(n=23)
59.7(n=67)
37.4(n=71)
40,9(n=132)
53.8(n=10$)
46.7(n=94)
50.3(n=200)
a
a
Table 7. Clinical signs in 200 paediatric outpatients presenting
with'couch, with or without crepitations
n_
With' crepitation(n=67) Without_crepitations133
No.with this
clinical sign
present=
true positive
Clinical sign
No.with this No.with
clinical sign this
absent=
clinical
false'negative sign
present=
false
positive
No .with
this
clinics 1
sign
absent
true
negative
Respirations 40/min
60(90)
7(10)
55(41)
78(59)
Respirations 50/min
48(72)
19(26)
25(19)
108(81)
Rapid respiration **
52(78)
15(22)
36(27)
97(73)
Breathless(as stated
by the mother)
43(64)
24(36)
31(23)
102(77)
Respirations 50 or
breathless
62(93)
5(7)
49(37)
84(63)
Temperature 37.5%
35(52)
32(40)
52(39)
81(61)
* Figures
in parentheses are percentages
Under 12 months old = respiration 50/min.
Aged 12 months or
more= respiration 40/min.
" Since the midpoint between the mean respiratory rates in
children with and without crepitations was 50.3 breaths per
minute (Table B) this respiratory rate is likely to give the lowest
number of false positive plus false negative results in predicting
the presence or absence of crepitations- Table 6 shows that the
child age had little effect on the respiratory rate the>best predieted the presence or absence of crepitations. <1
11 In both these age groups, the children with cough and no
crepitations had similar respiratory rates to those with no cough."
" Our findings are supported by a recent prospective study in
American children which showed that tachypnoea was the clinical
sign that best predicted the presence of an infiltrate on chest
X-ray.
A history of rapid breathing reported by the mothers was
almost as good an indicator as the physical finding of tachypnoea.
Tachypnoea was a better sign than the presence of crepitations,
(11)
fever, nasal flaring, pallor or grunting."
The choice of antibiotic at first level and at referral level
should be based on
- Activity against pneumococi and H. influenzae
- ease of administration
9
Following ere the possible candidates with their advantages
and disadvantages.
WHO recommendations on antibiotics for oup.vtients with moderate
.ARI
Activity against
the ■bacteria. .
causing
pneumonia
Toxicty
PROCAINE
PENICILLIN
AMOXYCILLIN
AMPICILLIN
COTRIMOXZOLE
Good, but the
Good, but the
Good.
number of
number of
resistant bacteria
resistent bacteria
is increasing
is increasing.
1/500"15
Diarrhoea and
Fatal bone
marrowtorash common.
1/250,000 get fatal Fatal anaphylaxis xicty
and fetal
anaphylaxis. Skin
in less than
minute madness"
testing is NOT
Administration
1/250,000
necessary
skin rash
occur
routinely
rarely-
Intramuscular
Oral.
50,000 u/kg once
Amoxycillin 10
a day
mg/kg 3 times a
day.AmpiciIlin
Grain
Trimethoprim
4 mg/kg
2
times a day
15 mg/kg 4 times
a day
Cqst for 5 days,
for a 10 kg child
comments
US $0.20
US $0.40
US $0.08
Usually effective,
Usually effective
Effective
long acting,but
but mild side
and cheep,
intramuscular
effects common
but may
cause
administration
required.
serious
side eff
ects (rare) .
. . 10
10
Antibiotics for the Treatment of Acute Respiratory Infections
in Hospitalised Patients
CHLORAM
PHENICOL
OXACILLIN
GENTaMI
CIN
AMPICI BENZY
LI IN
I PENICIL1 IN
Good
PATHOGEN SENSITIVITY
Haemophilus influenzae
verygood
poor
Fair
Streptococcus
pneumoniae
Good
Fair
Poor
verygood verygood
Staphylococcus aureus
Fair
Fair
Good
Poor
Poor
Group A
Streptococcus
Good
Good
verygood
verygood
Chlamydia
Poor
Resistant
Resistant Resistant Resist
ant
Gram-negetive enteric
bacteria
Good
Resistant
verygood
Fair
Fair
Good
Resistant
USAGE OF SECOND LINE ANTIBIOTICS
Hospitalised cases of Pneumonia
Benzylpenicillin 50,000 units/kg
IM every 6 hours
Neonatal pneumonia(age 6 weeks)
Benzylpenicillin 50,000 units/kg
IM every 6 hours plus
Gentamicin 2.5 mg every 8-12 hours
(Kenamycin 10 mg/kg IM every 8-12
hours when Gentamicin is unavai
lable)
Very severe cases of Pneumonia
Severe malnutrition
'(cyanosis, uneble to drink)
Chloramphenicol 25 mg/kg IM every
6 hours (maximum 1 gram per dosee)
Suspected staphulococcal
pneumonia,(empyema, abscess,
pneumatocele)
Oxacillin 50 mg/kg IM every 6
hours plus Gentamicin 2.5 mg/kg
IM every 8-12 hours
or
chloramphenicol 25 mg/kg IM
every 6 hours (maximum 1 gm/dose)
Source-(12)
Two special recommendations are
- Not to use penicillin V as it does not provide protection
against H. influenzae
- Not to use combinations of procaine with Benzathene pen'
i -•
11
as the low levels produced by the later do not kill common
bacteria causing pneumonia.(12)
Operation research and demonstration projects were started
in many countries in early eighties following reports of successful
results from Na.rangwal and Papua New Guinea. Some underdeveloped
countries are now at the verge of launching National ARI control
programmes following initiatives of WHO.
(4) QUESTIONS FOR DISCUSSION
Many areas remain gray.
following questions.
-Some of these are expressed in the
Participants can contribute their information
from literature or experience to discuss these question.
1)
The reported studies estimate annual incidence of Z.RI( including
J upper respiratory infections) in rural children to be 2.5.
In the experience of participants, is this a true picture x
A prospective study in West Bencal(13) by a paediatrician who
actually lived in the study village reported that the noses
of children were running on an average 43 weeks each year.
Actually often it was difficult to differentiate as to when
the
earlier attack of U R I was over and the next started.
2)
Immunisation, is one of the-powerful strategy to reduce, .
incidence end mortality due to ARIs. What do the participants
feel about the .present coverage of DPT and measles immunisationx
What are the problems with Measles end DPT immunisation ? Does
cluster*-" immunisation solve some of the'se. problems x'. What
other methods can b,e used to improve,.the coverage and- efficacy x
3')
The case management approach may reduce the mortality of
pneumonia but does, not cut d'6wh_.the transmission of bacteria,
like Chemotherapy of TB, leprosy or Malaria does. Should
one use case management approach x ’ Is there a more radical
end, effective solution to' the problem of ARI mortality
4)
Nature 1.history of pneumonia is not fully understood. Of
all the pneumonias in community, how many ere caused by
bacteria .? Do hospital- lung puncture' studies represent the
microbiology of pneumonia in community x How many of comm
unity acquired pneumonia are viral where an antibiotic•Is
unnecessary x
In the absence, of answers to these questions the case mana
gement approach■ may, result in large scale over, use of
antibiotics in viral pneumonias. Should antibiotics be used
in such state of knowledge x (
5)
Are the Diagnostic criteria of Respiratory rate 50 and
difficulty in breathing used, to make the management decision-’
sound enough •
Can you suggest better-ones x
. - 12
12
■'?
■
.
"■
.
-.r
' h'
■
';N
'b-'N
c.rp
V- + -/'. ■
h :
-E. •;
.Nt..; i
'
6) Presence of. -crepitations . in; chest <iis;; commonly- used ^|s'
criteria. for diagnosing ' ALRI.\ Should/ stetrioscopic ce.-p-.-
(r
introduced at the level of ANMs and presence of -crepitations
be mad.e the diagnostic. : criteria:?, for giving ■a'ntLbiptfcs/'^
instead of -relying''bn 'respiratory-rate...alone
7) What is the necessity of X1ray facility in. ARI control
programme ? Should it be introduce ,and., jafb wha-t; level .<?■
•
- -■
Eder- -cc- .1 ' ■'
■'l1/
8) ' Should the antibiotics 'be .given in .the h-endsj bfi nori-doctors
-like VHWs-or ANMs.? Which antibiotic -is'1 appropriate' with
what type of worker ? Should the ANM be. allowed to give
injection penicillin in the field ?
-.9) Otitis . media and. streptococcal' pharyngitis' are hot'
treated with antibiotics in the.plan of case managementsuggested by WHO. Should these be.treated with antibiotics ?
10) Should the-national 7\RI control, programmes be. planned and
implemented using case.management approach at the present
level of knowledge and experience F
REFERENCES
1. Monto, A. and Johnson, K. .:' Am.j' Trop.Med.Hyc. 19.68, 17 :867-74
2. McCord,C. end Kielmann,AsTropice 1 Doctor' 197?',. 8:220-225
3. World Health Organisetion: Research on acute respiratory
infections Document No ACMR 24/82.13
4. Narein, J.P. :Epide.mi.l.oogy of acute respiratory, infections'.
Indian Paediatrics 1967 :54:153-160.'
\ '
' ' ;
5. Steinhof f, M.C i end. John, T, J. :Acute - respiratory inf ections in
. Children in India. Proceedings of workshop on ARI held at
North Carolina May 18-19, 1983.
6. Pio, A, Leowski, J. and ten Dam, H.G.: The problem of ARI in
Children in developing countries, WHO Document RSD/83..11
7. ARI News issue No.4, April 1986.
.
.
3. ARI News issue No 2 'August .1985.
9) Sehgal, P-N. and Khare,' S.Immunisation Programme and control
of vaccine preventable ARI Diseases: Paper presented in
workshop on ARI at NICD, New Delhi April 1987.
10. Leowski.J.:World Health Statistical Quarterly 1986 Vol.39,13844
11. Shann.F, Hart,K.and Thomas, D.:Bulletin of World.Health
Organisation (1984)62(5) 749-53
12. ARI News, issue No 5, August 1986
13. Sinha,D,P.,Children of Ichag,Thesis submitted for the'decree
of Doctor at of Public Hee 1th,The Johns Hopkins University
Baltimore
.
■ ■
' ' *■ ' .
14. WHO/UNICEF:(1986) Basic principles for control of ARI in
ri,..
;v, j _
pr,
•
,
;j -
Position: 889 (15 views)