RF_DR_30_SUDHA.pdf
Media
- extracted text
-
RF_DR_30_SUDHA
3<M
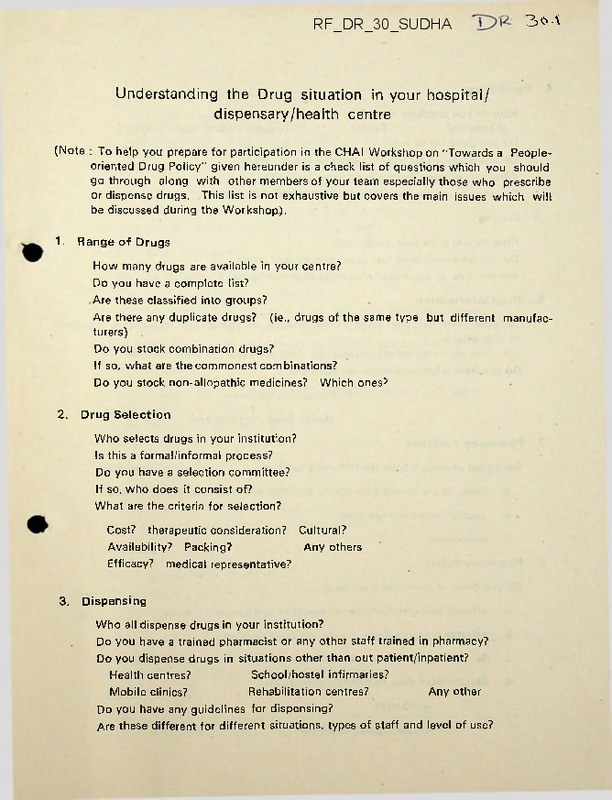
Understanding the Drug situation in your hospital/
dispensary/health centre
(Note : To help you prepare for participation in the CHAI Workshop on "Towards a Peopleoriented Drug Policy" given hereunder is a check list of questions which you should
gothrough along with other members of your team especially those who prescribe
or dispense drugs. This list is not exhaustive but covers the main issues which will
be discussed during the Workshop).
1.
Range of Drugs
How many drugs are available in your centre?
Do you have a complete list?
Are these classified into groups?
Are there any duplicate drugs? (ie., drugs of the same type but different manufac
turers)
Do you stock combination drugs?
If so, what are the commonest combinations?
Do you stock non-allopathic medicines? Which ones?
2.
Drug Selection
Who selects drugs in your institution?
Is this a formal/informal process?
Do you have a selection committee?
If so, who does it consist of?
What are the criteria for selection?
Cost? therapeutic consideration? Cultural?
Availability? Packing?
Any others
Efficacy? medical representative?
3.
Dispensing
Who all dispense drugs in your institution?
Do you have a trained pharmacist or any other staff trained in pharmacy?
Do you dispense drugs in situations other than out patient/inpatient?
Health centres?
School/hostel infirmaries?
Mobile clinics?
Rehabilitation centres?
Any other
Do you have any guidelines for dispensing?
Are these different for different situations, types of staff and level of use?
4.
Purchasing
How do you purchase drugs?
Wholesale?
Retail?
Through medical representative?
Do you purchase in bulk?
Do you purchase by generic names or brand names?
What sort of trade discounts do you allow/accept?
Do you prepare any medicines in the hospital/dispensary?
5
Pricing
How do you price your medicines?
Do you give medicines free or at concessional rates?
Are the 'free' or purchased medicines of the same type?
6.
Drug Information
Do your staff get any kinds of information on therapeutic indications, dosages
or side effects
Are these from medical representatives, drug companies or other sources?
Do you have a locally written—a) formulary
b) therapeutic manual
c) standardised drug regimes?
7.
Pharmacy Facilities
Does your pharmacy have the following facilities?
a.
8.
basic library of reference books, bulletins and information filing system
b.
special locked storage space
c.
refrigerator
Pharmacy Policy
Do you have an institutional policy on
a.
storage and administration of narcotics and dangerous drugs?
b.
adverse drug reaction—monitoring and reporting
c.
Ref Dealing with persuasive pressure tactics of sales representatives
d.
Standardised drug distribution policies for
—ward stock
—prepackaged prescription
—protected drugs
—free drugs
e.
9.
standing orders for department/pharmacy
Expiry Dates
Do you have any policy about use of expired drugs?
If you use some beyond the expiry date, which are these?
For how long beyond expiry date do you use them?
10-
Foreign Drug Donations
Do you get drugs donated from abroad?
Do you have a list of drugs?
Sources?
Do they have instructions for use in a language your staff can understand?
If not, how do you get the information translated?
Do you have any in large quantities/or types which you cannot use?
11.
Banned Drugs
Are you aware of the drugs banned by the government in July 1983?
Do you have a banned brand list?
Are your staff aware of the ban?
Have you weeded these drugs out of your practice.
12.
Problem Drugs
Look at the list of problem drugs (p.)
Do you stock any of these in your pharmacy?
Which are the brands? What are the indications?
13.
Placebos
Do you use any drugs as placebos?
Which are the commonest? and for what situation?
14.
Initiatives
Have you taken any initiatives in recent years to rationalise your prescription/dispensing practices, in your institution?
What are they? How successful have they been?
15.
Other information
Is there any other information about your pharmacy/dispensary or about drugs used
in your centre which is relevant but is not covered by 1 to 14?
Ethics of Drug Prescription
Fr. George Lobo,
S.J.
Use of drugs to be regulated by the principles of t»s totality
(overall good of the patient) and of doiible effect
(the good e-ffete-t
effect overriding any hramful effect). Unfortunate situation of
srers overpricing, overprescribing and misprescribing of drugs-^ften
untried and dangerous drugs are prescribed.
Reasons ;
technological model of health care leading to the mani
pulation of the patient,
to the neglect of preventive health, herbal
medicine and to the transgressing of legitimate bounds of human
experimentation; desire for instantaneous relief of symptoms;
creation
of air of magic by the use of exotic drugs with esoteric names;
capitalist system with an overemphasis on the profit motive; deep
rooted cultural alienation,
effect of neocolonialism,
leading to the
Ksxprxdgpsustinn depreciation of all that is indigenous and uncritical
acceptance of all that- is foreign; dependent status of developing
countries allowing undue pressure
from multinationals; drug pres
cription and medical research directed by the pharamceutical industry;
bourgeois captialist values leading to the
'get rich quickly' nut
mentality on the part of physcians.
Reraedie s: development of a person-centred and holistic approach
to health care;
physicians regaining true autonomy and ideals of the
medical profession;
countering capitalism,
cultural alienation and the
interference of foreign powers; massive movement against this ncxix
manipulation by drug companies;
supporting well intentioned efforts
of the government to check abuses in the production, distribution
and use of drugs;
reducing the list of pharacopia in hospitals;
developing ethical values and understanding of right norms among all
concerned.
DRUGS FOR PRIMARY HEALTH CARE
What is primary health care?
Primary health care is essential health care made available to
individuals and families in the community and has to be
(l)
accessible, assuring equitable access to all,
(2)
acceptable, based on the life pattern of the people,
(5) effective, in providing an adequate level of care, and
(4) affordable, without the imposition of excessive burden on the individual,
family or community.
It is the first contact care, where most of the usual, everyday health care
needs can be met.
Primary health care is an approach which integrates at
the community level all the elements which are necessary to improve the
health of the people.
It is a response to the fundamental human need of
being assisted in the actions needed to live a healthy life and when illness
comes, get relief from pain or suffering and restoration of health.
Primary health care includes promotion of health, prevention of
disease, cure of disease where possible, care and rehabilitation.
Among the
important factors in promotive and preventive measures are health education
to lead a normal healthy life, avoiding risk factors, good nutrition, safe
drinking water and sanitation.
Food production in the country is adequate
but it distribution is bad, due to poverty, unemployment and lack of education.
Water supply is not safe, especially in the villages.
There are still lakhs
of villages which are classified as problem villages (those which do not have
an assured source of drinking water within a distance of 1.6 km).
Disposal
of excreta lags far behind; only 2% of the rural population has been covered
by satisfactory disposal, while a neighbouring country like Sri Lanka has had
a remarkable progress in this area.
India, a signatory to the Declaration of the Alma Ata International
Conference on Primary Health Care is committed to provide an acceptable level
of health for all by the year 2000 AD.
Primary health care has to be defined
in terms of function and the scope and quality of care under each function.
It is also necessary to decide what proporgtion of the GNP should be alloted
to health care and what part of it to primary health care, though this can
present problems^. An integral part of this commitment is the provision of
all essential drugs to all those who need them, in adequate quantity and
quality, and at affordable prices, wherever the person is.
The ability to
2
meet the cost or to reach the place should not be considerations in providing
the essential drugs.
Drug production
The production of pharmaceutical products in India is estimated to
be Rs.18,000 million in 1983,
If we compare our production with the production
in affluent countries or even with the average world figures, it is extremely
low.
The world consumption of pharmaceutical products was estimated in the
year 1981 to amount to Rs.763 billion.
India's share comes to about one in
five hundred while her population is about one in six.
Even this limited amount is wasted in the production, distribution
and consumption of non-essential and useless drugs, a large proportion being
vitamin combinations and tonics.
Often they are spurious.
25,000 formulations made by over 5000 production units.
There are over
This compares with
something like 3000 formulations in the Scandinavian countries.
What are the drugs required?
Drugs are required for prevention, cure and symptomatic relief. The
2
World Health Organization has, in 1983, listed about 250 drugs as essential .
This'is a large scale modification of the list prepared in 1977 and revised and
updated in 1979.
The objective of WHO action programme on essential drugs and
vaccines is to ensure the regular supply to all people of safe and effective
drugs and vaccines of acceptable quality at lowest possible cost in support of
3
primary health care .
They have also given a list of 22 drugs for primary
health care.
These drugs "can be used effectively and safely by responsible
individuals with little formal medical knowledge".
The report also states
"highly trained workers might use a wider range of drugs appropriate to their
diagnostic skills" and advocated that where there is no scarcity of medical
manpower, many potent drugs could be used.
Primary health care is the involve-
ment of the practitioner(doctor, nurse, medical assistant, auxiliary, or primary
health worker), to whom a person first turns, when ill or seeking advice.
varies from country to country and even within the country.
This
The W.H.O. expert
committee observed "...-the preparation of a drug list of uniform, general
applicability and acceptability is not feasible or possible".
equally true for a vast country like India.
The same is
In India, there is a reasonable
ratio of trained doctors to population in the majority of places; in many
situations, they will be the persons for primary contact; in others, these will
be trained nurses, community health workers or others.
the health care in the first contact
Depending on who provides
situation, the use of drugs will vary.
I shall take the situation where a qualified physician is available; in other
- 3 -
situations, the list of drugs may have to be drastically curtailed, being
nearer the twentytwo drugs listed by the expert committee of W.H.O.
Choice of drugs
The drugs for primary health care must be well-chosen.
The choice
has to be based on a survey of the mobidity pattern in the area or region.
To ensure optimal benefits, the definition and determined implementation ot
clear national policies are required .
The steps to success in the choice
4
and supply of essential drugs have been listed .
They are
(1)
A comprehensive National Drug Policy
(2)
Selection of essential drugs
(3)
Drug production and procurement
(4)
Logistics of supply
(5)
Proper use of drugs
(6)
Quality control
(7)
Training of personnel.
National Drug Policy:
There is an imperative need to have a comprehensive
National Policy, based upon the socioeconomic, political and other options
and the practical implication of that policy.
There is need for a clear
decision as to what diseases and symptom complexes come within the purview of
primary health care.
A purposefully determined regimen of treatment should
be worked out for each disease and symptom complex, leaving the rarer treat
ment regimes to the specialists att the
referral care. In declaring the bold
5
New Drug Policy of June 1982, Bangladesh followed 6 precepts .
(1)
Elimination of harmful and useless drugs.
were banned.
As follow-up, 1,700 such drugs
(Similarly, in Philippines, about 6,000 out of an estimated
15,000 drugs in the country would be phased out during this year.
In Mexico,
over 10,000 drugs have been closely evaluated and many duplications, obsolete
products and those with limited or doubtful benefits &ave been eliminated,
reducing the number of drugs available to 329, in 583 combinations).
(2)
Increased domestic production of essential drugs.
(3)
Public distribution system of essential drugs.
(4)
Bulk importation of pharmaceutical materials from different sources at
competitive prices (Many countries have been able to do this, achieving
economy.
Tetracycline which used to be imported at 102 U.S.dollars per
before the Policy was imported at U.S.S 27 per kg.).
(?)
Use of generic names.
(6)
Encouragement of locally organised applied drug research.
Selection of drugs
should be based on the prevalence of morbidity in the
kg.
4
community.
The list should be drawn up by a regional committee of doctors,
pharmacists and others interested and involved in primary health care.
and yet comprehensive drug information should accompany the
list.
Concise
The common
diseases in our country are infectious diseases, parasitic infestations, acute
diarrhoeal diseases and malnutrition.
India, in common with other less affluent
countries, has a young population with about 42%
under 15 years of age.
Hence
the diseases common among children have preponderance; drugs required for their
care must have priority.
Periodic revisions must be made to meet the changing
needs or based on better assessment of the needs and the availability of more
cost-effective drugs.
It is better to have only one preparation for each
indication, avoiding unnecessary duplication.
The drugs, where possible, are
better supplied in tablet form for ease of administration; they should also
have keeping qualities under the existing and often exacting
temperature and humidity.
conditions of
The packing must be efficient but not expensive.
The choice of the drug should be based on
((l) proven efficacy; well tried drugs should be preferred to newer
drugs whose efficacy, side-effects and adverse reactions have
not been fully established.
(2) low cost, commensurate with efficacy; the cost of the whole
treatment should be considered and not merely of single dose.
(5) safety in the hands of the user.
Drug production and procurement:
The country should as far as possible
become self-sufficient in the production of drugs for primary health care.
Where imports are necessary, they should be obtained on the basis of bulk
purchases on global tenders and selection with due regard to quality and cost.
Considerable savings can be effected.
Even affluent countries have taken measures to contain the costs .
The nine countries in the European ^aaun^rio^~ took steps to reduce the cost
of drugs.
Among them are
(1) Fixing of prices or limiting profits of pharmaceutical companies
(2) Limiting sales promotion activity
(3)
Regulation of retail margins
(4)
Circulation of information to doctors to encourage economical prescribing,
Logistics of supply:
An adequate supply of the essential drugs must be
ensured at all times, in all places and in suitable dosage forms including
paediatric dosages.
The challenge is to devise systems that will provide
essential drugs where they are needed, matching the supply to the health
care needs.
It often happens that the essential drugs are not available at
- 5 all times, leading to shortages.
This has happened often to the large
scale treatment of tuberculosis, leprosy and other diseases.
Sometimes
it has happened because manufactures debiberately did not produce them or
retailers refused to stock and dispense them, all clamouring for a larger
margin of profit.
Villages and regions may be cut off in certain seasons
for a variety of reasons.
duality control:
It is most important that quality, stability and bio
availability are assured, through proper monitoring at different points in
supply and use.
Social and economic damage is caused by the
7
indiscriminate advertising and marketing activities . We do not have well-
Regulating the drug trade:
organised and effective agencies like the Food and Drug Administration of
USA. Even in advanced countries, promotional activities go far beyond what
is reasonable, eg., the Benoxaprofen affair or the Opren scandal®:
"A combination
of an unscrupulous pharmaceutical firm, feeble watchddgsgw and gullible doctors
had been responsible for the use of an unnecessary and unsafe drug .................. key
figures were extravagantly entertained at sponsored conferences in attractive
venues".
Drugs for immunization:
primary health care.
High priority must be given for immunization in
The commonly preventable diseases must be prevented.
This is high technology and highly cost-effective.
Everyone knows of the
success story of small-pox eradication; it is estimated that about a billion
dollars have been saved by giving up compulsory vaccination.
Infectious
diseases take a big toll in our country, especially of infants and children.
The cost for treating the patients with these infectious diseases and the
complications and sequelae are very high.
Among the common infectious diseases
which can be effectively prevented today are
diptheria,
poliomyelitis,
measles,
whooping cough,
tetanus.
Newer effective vaccines may be added, depending on the cost - benefit.
Drugs for cure:
Some of the more essential drugs are listed; a few more
will be needed, based on regional requirements and other factors.
Antimicrobials:
Infectious diseases being the commonest, priority
should be given for drugs to fight them.
The proportion of the pharmaceutical
6
budget spent on antibiotics and antiparasitic drugs was 24% in India,
compared to 4% in the Federal Republic of Germany and 15% in Britain9.
Well - tried, cost-effective antimicrobials from among the many available,
This would necessarily include the penicillins (crystalline,
should be selected.
procaine and oral) and ampicillin; one or two potent and safer sulphonamides
could be included.
be useful.
Drugs like chloramphenicol and tetracyclines will also
The misuse of antimicrobials is fraught with danger, especially the
development of resistance.
threat.
Antimalarials:
Malaria is again becoming a major
From an all-time low annual incidence of 100,000 in 1965, it has
risen to -ataay millions.
Chloroquine is a good drug.
Unfortunately, resistant
strains have developed especially in the northeast and are spreading to other
parts of the country.
also included.
Primaquine may be provided for radical cure; quinine is
Dapsone can still be the basis of treatment,
Antileprosy:
though multidrug treatment with rifampicin, clofazimine and/or ethionamide
is common now and probably cost-effective.
Antituberculous:
It is estimated
that there are about 9 million people in India suffering from tuberculosis
with about one-fourth of them being infective.
from pulmonary tuberculosis.
About 50,000 die per year
The drugs required for standard therapy such
as INH plus streptomycin plus PAS/Thiacetazone/ethambutal or the short course
including rifampicin must be..available.
Antiamoeb/ic:metronidazole; Antihelmi
nthic: Mebendazole.
Antianaemic : Ferrous sulphate; folic acid.
almic - Vitamin A.
Antifilarial:diethylcarbamazine.
Antizerophth-
Antifungalgriseofulvin;
Antikala-azar (in regions where kala-azar is present).
Drugs for symptomatic relief
Analgesic and antipyretic: aeetylsalicylic acid; paracetamol; morphine in
special situations.
Inflammation:Glycerine and mag. sulph.; ibuprofen.
Cough: Noscapine; pheniramine maleate.
magnesium sulphate; senna.
Diarrhoea:rehydration salt. Constipation:
Vomiting: promethazine.
Allergy: Chlorpheneramine.
Asthma:ephedrine, aminophylline and salbutamol; adrenaline injections for an
acute attack or status asthmaticus.
Angina:glyceryl trinitrate; propranolol.
Hypertension and congestive heart failure:hydrochlorothiazide; digoxin.
and convulsive disorders:phenobarbitone; phenytoin.
Epilepsy
Sedatives and hypnotics:
diazepam.
Poisoning:atropine sulphate injections; activated charcoal; syrup
of ipecac.
Antacid:aluminium hydroxide.
Colicky pain: Oxyphenonium bromide.
Diabetes mellitus:an oral hypoglycaemic like gliben-
clamide or metformin; insulin.
Uterine bleeding:ergometrine; Oxytocin.
Urinary
tract infections:Cotrimoxazole..Ear infections: Choramphemicol/gentamicin drops
(Other requirements for ear,
nose and throat conditions will have to be met).
Skin conditions: Disinfectant: chlorhexidine; gentian violet; iodine.
Soothing
- 7 -
agent:calamine lotion.
Ringworm and other fungi^Whitfields ointment
(benezoic acid plus salicylic acid).
Scabies and liceibenzyl benzoate.
Topical antibiotics:chloramphenicol - 1% ointment; tetra
Eye conditions:
cyclines - 0.5% ointment (other materials, including spectacles will have
to be provided).
Psychiatric conditions:
Amitriptyline, chlorpromazine, fluphenazine.
In addition to the drugs mentioned, there is need for intravenous solutions
like normal saline and 5% dextrose, surgical dressings, suture materials and
a local anaesthetic.
Malnutrition:
The most important health - threatening condition in our
country is malnutrition, mostly protein - calorise malnutrition, though
specific deficiencies are also present.
Adequate food intake is the solution.
While there are many factors like lack of unjust distribution, poverty and
lack of education, primary health care should ensure adequate intake of balanced
food, with easily available foodstuffs.
Tobacco:
care.
The smoking epidemic should be of great concern in primary health
While cigarette consumption is declining in many affluent countries,
it is increasing in our country.
The tragic effect is increase in lung
cancer and cardiovascular and other diseases related to smoking.
A campaign
must be mounted as part of primary health care against smoking.
Alcohol:
The alcohol problem is a growing threat to health.
and 1980, alcohol consumption increased by 500% in Asia.
Between I960
Alcohol - related
problems affect not only the individual drinkers but also their families and
the general community and can be physical, mental or social in nature.
Chemicals in the environment:
A class of substances are being added to the
environment; these are synthetic chemicals.
Many of them can be toxic and
need to be dealt^in the same way as poisons and infections.
Among them are
pesticides and insecticides (example: highly toxic organo-phosphorus compounds);
their metabolites; industrial effluents (an example is disease produced in
people who ate fish rendered toxic by the presence of methyl mercury); herbicides
(Aguset Orange); Fungicides.
All these call for prevention, recognition and
management. There are an estimated 575,000 cases of human poisonings by
pesticides in developing countries every year with some 10,000 deaths^.
Lack
of protein in the food of rural workers is an additional factor that makes
these chemicals even more dangerous.
Agricultural spraying (including aerial)
is common in the countryside but its effects are not always known.
India is
proud to be the largest manufacturer of pesticidal chemicals in the whole of
- 8 South Asia and Africa, with a licensed capacity of 78,000 tornes^ .
Search for new drugs
Affluent countries are spending vast sums of money on the search
for new products to counter diseases met commonly in those countries and
which often do not have relevance to the morbidity and mortality in our
country.
Because the pharmaceutical firms do not have a ready market for
some of the drugs required in our country, these transnational firms do not
develop them.
The large transnationals are not interested in the problems
of a poor country.
We must also catch up on the newer of natural products
These drugs could be manufactured with the level of technology
12
available in our country ,; we have traditionally been producing these plants
of "biodrugs".
and their products and we should not have to import the finished products
from the affluent countries.
It is necessary that we develop a research base.
The Government must
actively undertake and stimulate and encourage research into pharmaceutical
preparations, essential to combat the diseases most important to our country.
They should give sizeable grants to the Indian firms engaged in research and
also make it obligatory for all pharmaceutical firms in the country to set
apart and utilize a proportion of their sales turnover for research and
development of new products, relevant for primary health care.
The Government
should also give sizeable grants to Universities, Medical Colleges and research
institutions for search for new products and technology.
Production of all
essential drugs must be taken up by the Government, with the collaboration of
voluntary nonprofit organizations; so also the distribution and supply of these
drugs.
There should be no scope for profiteering.
The pricing policy should
be such that the burden on the public is eased; there should be no excise and
other similar duties on essential drugs or the raw materials.
There is no
need for high pressure salesmanship, with very large numbers of salesmen, free
samples, gifts and free travel in the country and abroad for conferences or
pleasure for those doctors who push the products.
also advertisements in media for the public.
These should be banned as
All essential drugs should be
free of patents and be known only by the generic name; at the same time the
profession and the public should be assured of quality.
This starts with good
manufacturing practices and subsequent monitoring of quality through to
utilization.
Drug information
Every drug is a poison.
benefit than harm.
Drugs are prescribed because they give more
One must be careful of the adverse reactions and be especially
- 9 -
watchful in infants and children (particularly small-for-date babies,
protein-calorie malnutrition, infections), elderly patients and pregnant
women.
Adequate information should be given to the patient about the drug.
These would include
What is the dose; frequency of use; route; relation to meals?
Does it cure or give symptomatic relief?
What to do if the drug is not working? Is there a lag period?
How long to take? When to discontinue?
What are the side-effects? adverse reactions?
What are the precautions during work in the field or the factory?
How is it to be stored?
Evaluation
It is necessary to make periodical evaluation of the efficacy of
primary health care including drugs.
Measurements of health, morbidity and
mortality, immunization, improvements in water supply and sanitation, consumer
satisfaction and community invlovement will all form part of it.
Changes must
be made periodically in the drugs as needed for better health care.
References
1. Boland, R and Young, M: Putting a price on primary health care, World
health forum, 1983,4(2):131-134
2. The use of essential drugs.
Technical Report series, 685, W.H.O. Geneva,
1983 (WHO 4 technical report series 615, 1977 and 641, 1979).
3• diagnostic, therapeutic and rehabilitative technology - The work of WHO,
, Geneva, 1984.
4.
Seven steps to success in essential drugs supply - World Health, Geneva
July 1984.
World Health, Geneva, July 1984.
5.
Mostafa, A.B.M.Ghulam. The nettlegrasped.
6.
Sharing the costs of health care; conclusions of an International seminar
held at Wolfsberg, Switzerland; World Health Forum, 1981,2:85-95.
7.
Jayasuriya, D.C. Regulating the drug trade in the third world World Health
Forum, 1981, 2:423 -426.
8.
9.
10.
Opren Scandal, The Xancet (Editorial) 1983, II: 219-220.
Drug use in the third world, Stancet, Editorial, 1980, 11:1231.
Mercier, M and Draper, M.Chemical Safety: the international outlook, World
Health, Geneva, Aug -Sept., 1984.
11.
Krishnamurti, C.R. India's boom in chemicals, World Health, Geneva,
Aug - Sept., 1984.
12.
Lozoya, X. Biodrugs are coming, World Health June 1983, p.7., quoted in
World Health Forum, 1983, 4(2): 171.
.'Du
IN SEARCH CF AnpRfTRTATC fTEf’CTNE-1
COUGH 1TXTHRES
Oough sedatives and expectorant mixtures are probably the most
commonly prescribed preparations along with tonics, and the sale of these
forms the butter on the bread of quite a few pharmaceutical firms. This
study was nrcmpted by our need for a cheap and effective anti—tussive.
INDICATIONS for CfflGH gTjpn ppg cants
Oough is a protective reflex which helps to expel irritant
matter from the respiratory tract. Indiscriminate arrest of cough is
not desirable. If the cough is due to centre being too hvpersensitive to
reflex irritation from the upper respirator'’' tract (larynx and above) and
where cough is of unproductive nature central depressants like opiates
are indicated. Tn children sedation at night is more effective.
HTTJITY’ OF ROHGH EXPECTORANT’S
Expectorants are used in the treatment of cough due to irritation
of the respiratory mucosa below the epiglottis and respiratory conditions in
which the secretion is thick and viscid needing liquifaction. Commonly
used expectorants (Ammonium chloride,-, iodide, Tnecacurha, are supposed to
stimulate outnut of resniratorv tract fluid refl.exly through irritation of
gastric mucosa, for this, simple steam inhalation 'id’ much-better, effective
and reliable therapy.
It must be remembered that except for dextromethorphan and codeine
(eentrally-acting cough suppressants) experimental nroof of effectivity of
other drugs used in cough mixtures is totally lacking and rationale for their
use can be debated.
With these facts in mind, we evaluated most of the cough mixtures
available in the market today and found out some interesting facts.
1) Most of the proprietary preparations available as cough
remedies generally contain a central cough suppressant, an expectorant, an
antihistaminic and a brochodilator in nleasartly flavoured syrupy base.
Combining the therapeutically incompatible ceugh suppressants and expectorants
cannot be justified except for the fact that it enablas the pharmacy to sale
their product with a good margin of profit (cough sedative is costly due to
condeine content), when sold in market as a cough remedy. It is -interesting
to find that a num cough expectorant is not cheaper than a pure cough
sedative or cough sedative-expectorant mixture. It is also interesting to
find that the cough mixtures available in bulk (5 litre Jar) are only cough
expectorants and these are the preparations dispensed bv a private practitioner
as a cough remedy in’all cases of cough irrespective of their site of
irritation (even if the site is above glottis)
?,) The average daily cost of taking a cough remedy is:
Cough sedative-expectorant - 1.50 to 2.25 Rs./day (40 ml., syrup)
Pure cough sedative
- about 1.10 Rs./day
Pure cough expectorant
- 1 .25 to 2.25 ps./day (.40 ml. syrun)
Mote:- The cost of cough mixtures with same ingredients varies as
much as 50$.
1*7
...2
: 2 :
3) Many available commercial preparations contain drugs in either
quite inadequate or excessive doses and some of them contain drugs which
are out dated and no longer recommended.
These observations prompted us to evolve a sedative mixture and
an expectorant mixture containing only the required, drugs in adequate dose in
a palatable base and'which would.be reasonable priced. As we have no
access to the "required drug's in their nowder 'orm which are available only in
bulk, wn arrived at approximate cost by using- tablets available in the
market, so that cost computed by us is necessarily higher than it would be
tor the drug companies who buy the dru^s in bulk in their coder form.
Stoll-a difference can be. made out between the market nrico of commercial
preparations and the cost, of the mixtures as ’irenared by us using tablets
bought in..retail.
HCM o’O PREPARE COUCH MIXTITE ;
1) Cough sedative
Crush and make into nowder
a) 10 tablets of codeine nhosnhat'(100 ml.)
(10 mg.-6 paise each 1
+b) 5 tablets of ephedrine HOT
... ■ -•
(30 mg.-1.5 paise each)
+c) 5 tablets, of chi ornhenorarine
maleate (4 mg-2 naise each)
ii)
Dissolve the powder in warn water and filter
iii)
Tissolve 6 heaped teasooonsful of sugar (66 gms. 20 paise)
in £ cup of boiling water and add 1 drop of pineapple flavour.
iv)
Add 0.5 gm (flat teaspoonful) of Na bemoate as preservative to
the filtrate and mix well with sugar solution to make it 100- cc.
total. (1 teaspoonful flat = 2.2 gms.)
i)
Dose : 10 ml/6 hrly for adult
5 ml/6hrly for children
Cost
55 naise ner day.
2) Cough Expectorant (1OO ml.)
i)
ii)
iii)
iv)
Crush and make into powder.
a) 5 tablets of chlorpheniramine maleate (4mg.-2paise each) ..
b) 5 tablets of ephedrine HC1 (30 mg-1.5 naise each)
e) less than one flat teaspoon+'4l of anrioniuin chloride (3gms.-3 paise)
•(1 TSE flat= 4 gms)
Dissolve in hot water and filter.
Dissolve 6 heaped toaspoonful of sugar (60 gms-20 naise) . in
cup
of boiling water to which 2 drops of p-’.neannle flavour are to be
added.
Add- 500 mg (l/8 toaspoonful flat) of Na benzoate as preservative to the
filtrate and mix it with sugar solutio? to make 100 cc
Dose." 10 ml/6hrly/day adult
costt 16 paise per day.
Remefnber Na benzoate is added to avoj d fungus overgrowth.
Those who wish .to utilise the drug idthin 48 hours, need not add the
preservative. Please preserve in clean container to avoid fungus overgrowth.
S- njiv■Chugh
Medico friends Circle
S-!vagram
■
‘H- h 2>-v£-(
Hcc^.^ i^J'J
Vn
T) p- 3o. S'"
J- c4 t%^7n o /
5 Ob &i
c/ Ob Gj
tCrul-n
NitX
We.U.
Vl (3 U, [
e.-7H^CL7v
16,
dissolve.
co^?
vn
vn
I enJ hl) co i i h CoXn^n [\JejTs-
£-Lictyv<
*4
IA VI r)
.■Dissolve.
MlWjL.
S UxJtjusn
Ifrl
L<^r
Do
CUCC«TO llyIf?
(CTC-rvl
Co<
2>e?cLi ^3v> Q,VU/d >1 &U.
r
vS v-L
j)A C-L.lb'vt"
VAjf UTt
Wesfe-.
D(> 'n ‘b'jl fee n-VjOodjL.
W(aoC
£ ■JOVA. * /=> I jC <j i n <j
ViodA
9&o ex-
fSejo^oo-kr
)3>em£^
^1
(oooc.
q, S
VJexc/k
'^oeaScote,
UwC. ,
c
xooiA^-
klvX’
\-ycd^y
Heed’
rndtM. “Tetkt
viaoc
I
& VVOl
/3 €.3ls >j cc\_Lt
CwU
> Cxa\A (rCa"
fe-
A U.O p £
VaY\^x|
C.ooj
/§ 6i
W C-X,oi.
rwat-j)
[ZA-v
CX C.Cvtb^'jkj
I Xu law kr
cvjej
^Cufo7
(X bnttV
AUjDXJO
^nr\_4
Um.
2—-
tuwL
c\'(j
(
y
Lc~
Ccixoi
,Xte/
LthjUl cool. "TM/^
CA_
^-0'0
.b X^ Ja iu
ikortu
%kuJ£L
-^-o v
kr
'
"jX
3 Oi'O G\ Ly CQjXjJvi
PoNokr
BoraoC ^Yl
^7 6y
/-^uLh bu.'/^'"(" XA
€0ilin (AUjCfix-P^ f l-4-e-Ajt I^jl ^■vuX-luh'L LbvjtiJ Ckl
ebsselves .
U<se the
£— vviho-J—, TcL/<i_ CLaX-C
’■hoe-fr Over- 7^2^/-.
4iZb./(Q
£ C-kdA
.So<Vo Uoin
Cr
CxtyXxc/-
<N o t~ 6Lveci GxG-Lc ,
LxJ'YTtx CO /i tiLrO<_cj
(yi'Yvl'iVXiL/Vx/
i - -^o< C^'U.^'n
r
i oV
rzh '.x.U.u<
Milk
cnxo c>Li
Varvuruo cAlGjcti-rxJ
i OY\<£xir)tY.
f' ■ <r o cjl ok c-vq
v
|V)£<0y^-yOK.
V
c^Uave^'v
T)
'So. 6
APPENDIX - 2
LIST OF ALLOPATHIC iEDICIDES USED AT SLBCEUTFE LEVEL
2.1
MEDICINES TO EE CAP.LIED BY HEALTH WORKER (HALE)
For Internal Use :
1.
Aspirin, Hienacctin and Caffeine (APC) tablets
2.
Belladonna and phenobarbitone tablets
3.
Cliloroquine tablets
4.
Dried aluminiun bhdroxide tablets
5.
Ergot tablets
6.
Iron and folic acid tablets
7.
Magnesium hydroxide tablets
8.
iagnesiun sulphate
9.
-'opyratiine (Antihistamine tablets)
10.
List bismuth kaolin
11.
Ehthalvl suphathiazole tablets
12.
Hperazine citrate tablets
13• Rehydration powder
14« Tincture codeine co.
15.
Triple-sulpha tablets
16.
Vitamin A solution
For External Use;
17.
Antiseptic lotion
18.
Benzoic salicylic ointment
19.
Benzyl benzoate emulsion
20.
C-entian biolet 2 per cent
21 • I'ercurochrome 2 per cent
22.
Methyl salicylate liniment
23.
Potassium permanganate crystals
24.
Silver nitrate eye drops
25.
Sulpha cetariide eye and ear drops 10 per cent
26.
Sulphanilamide skin ointment
27.
Sulphonamide dusting povder
28.
Tetracycline eye ointment
29.
White vaseline
2.2 MEDICINES TO 33 KE RE AT SUBGEiiTFE
For Internal Use
1.
Bipheniun hydroxy-naphthoate granules
2.
Liquid paraffin
3.
list, alkaline
4« list, carminative
.Contd/2-
: 2 :
5.
Mist. sedative expectorant
6.
Multi vitamin tablets (A, B, C,D)
7.
Syrup ferric anmonium citrate
For External Use
B. Boric acid powder
9.
Calamine lotion
10.
Methylated spirit
11.
Tincturd benzoin co.
12.
Tincture iodine
13.
Zinc boric dusting powder
DP- 30.3-
ESSENTIAL DRUGS LIST FOR PRIMARY HEALTH *
CARE LEVEL.
1.
Aluminium Hydroxide + Magnesium Hydroxide
(Tab/Liquid, Antacid)
2.
Antihaemorrhoidal oint.
3.
Aspirin Tablet (Acetylsalicylic acid) for adults only
4.
Benzoic acid + salicyclic acid ointment
(Unguantum of Whitefield).
5.
Benzly benzoate lotion
6.
Calamine lotion
7.
Charcoal Activated
8 Chloroquine Tablet
9 Chlorpheneramine maleate
10.
Tablet
Citremide + Chlorhexidine
llo Ethinylestradiol + Levonorgestral Tablet
(low dose)
**
12. Ferrous sulphate + folic acid Tablet
13.
Folic acid
14.
Gentian violet solution
15.
Glycerine suppository
16.
Iodised salt
17.
Lysol/Cresol solution
18.
Magnesium sulphate
19.
Mebendazole Tablet
20.
Oral Rehydration Salts
2
*
The above drugs can be used by Auxiliary Nurse, Midwives,
Public Health Nurses and adequately trained and supervised
village workers.
** Proper training to be imparted to Family Planning workers to
dispense contraceptive pills and follow-up.
2
21.
Paracetamol Tablet and Syrup
22.
Phenoxymethylpencillin Tablet
23.
Simple cough linctus
24.
Tetracycline eye ointment
25.
Vitamin A Capsules and Tablet
26.
Vitamin-C Tablet.
Source:
INTERNATIONAL CONSULTATION ON
RATIONAL SELECTION
OF
DRUGS
17th-21st July 1986
New Delhi
VOLUNTARY HEALTH ASSOCIATION OF INDIA
T) p. "50/-
hTIAI DRUGS H.-'T FOR IKIK'-RY H -LIU *
CARE LEV'LL,
1.
Aluminium Hydroxide r Magnesium Hydroxide
(Tab/Liquid, Antacid)
:?<> Antihaernorrhoiual oint,
3,
Aspirin Tablet (Acetylsalicylic acid) for adults only
4.
Renzoic acid * sJicyclic acid ointment
(Unguantum of Whitefield),
S.
ssenzly benzoate lotion
6,
Calamine lotion
7o Charcoal Activated
8
Chloroquine Tablet
9
Chlorphenerarinc maleate
10.
Citremide
11,
c-thinylestradiol
(low dose)
**
12.
fc'errous sulphate + folic acid Tablet
13,
14,
Folic acid
Gentian violet solution
IS.
Glycerine suppository
16.
Iodised salt
17.
Lysol/Cresol solution
18.
Magnesium sulphate
19.
Mebendazole
Tablet
I
20,
Oral Rehydration Salts
Tablet
Chlorhexidine
Levcnorgestral Tablet
2
The above drugs can be used by Auxiliary Nurse, Midwives,
Public Health Nurses and adequately trained and supervised
village workers,
** sroper training to he imparted to Family Planning workers to
disense contraceptive pills and follow-up.
*
2
21.
Paracetamol 'Tablet and Syrup
22.
Phenoxymthylpencillin Tablet
23.
Simple cough linefeus
24.
Tetracycline eye ointment
25.
Vitamin A Capsules end Tablet
26.
Vitamin-C Tablet.
Sources
TNT5. ’ IGATICMAL CCK5UI.TATICH OH
RATICUAT. SELEC IIGN
OF
DRUGS
17th-21st July 1986
new belhi
VOLUNTARY he-.ltk association of ikpia
n>pi
BAN INJECTABLE CONTRACEPTIVES -
INDIZiN WOMEN DESERVE A' BETTER DEAL
A c-.rapaign group has been formed in Bombay to protest
against the Drug-controller of India approving NET-EN as a
contraceptive. Two companies - UNTCHEM and GERMAN
REMEDIES -- have boon given licences to manufacture this
drug.
Today's protest demonstration in front of Oberoi Towers,
where tho Family planning dissociation is holding a closed
door conference of 'experts' on NET-EN. Ue plan to continue
with the campaign and expand it to include all longacting contraceptives.
What are' Injectable Contraceptives? Injectable Contracept
ives C I C~J prevent pregnancy more or less in the same way
as oral contraceptives. But they are administered by
inj oction and are long-acting. The best-known ones are
Depo-provera and NET-EN
Depo needs only one injection
every 3 months and nET-EN, one every 2 months.
Population control enthusiasts consider injeatables
tho 'ideal form of contraception for women in the thirdworld because of the ease with which tnex can bu administered
on a mass -scale and the low failure rate. To those who
look at women in the third world as nothing but faceloss
factors to be considered in any strategx of population
control thex cook up, the benefits seem overwhelming and
the 'risks' in terms of women's, health negligible. There
has been a concerted campaign lately to 'soli' the idea
of 1 Cs through the media and elsewhere. The conference
organised by tho Family Planning tsrociation on 28th and '29tk
December 1984.at Oberoi, is part of this 'marketing
strategy'.
Dcpo-proyora and ..NET-EN -the controversial ccntracoptives. . .
Depo-provera has been the centre of a fight between
Wealth groups and women's groups on the one side and'
pharmaceutical companies on the other since the sixties,
.when the Upjohn Co. of USA sought approval .for it in the
sixties. Upjohn has fought a hard and long battle in tho
U 3 unsuccessfully. They desparately wanted approval
before their exclusive rights on the drug expired. The
campaign in the U S and elsewhere brought Depo-provera a
'bad name'. Zuoproval for its manufacture has not been given
by the Drug-controller of India. But neither has any
explanation been iven to 'the_ public or _to interested
orpup.s_ about why it has not been approved,.
Meanwhile,
ITET-EIT ■ another 1 C about which not much is known has been
approved in India and licence .to manufacture it has been
granted to two companies - Unichon and German Remedies.
Both Depo-provera and NET-EN have been used in India
for several years now for research purposes. This research
has been carried out maily cn poor women by voluntary
agencies who conduct community health programmes, under the
supervision of the Indian Council of Medical Research.
The
reports of tho studies have not been published till today
2
and ICMN has refused to make is available to anyone,
.ill
interested parties are supposed to tako their word for it
that while Depo is not so good, NET—BN is just fine. Past
experience with contraceptives and other drugs does not
inspire in us any such trust or confidence. We believe
that we have a right to know the details of the research
studies, to make our own investigations and tc come to our
c;/n conclusions,
We do not consider the masses of women
mere pawns in population control strategics to whom cont
raceptives are ’sold1 on the basis of incentives without
prior information.
What we do know about ICs is quite disturbing. Upjohn
Co,, conducted two animal safety studies in the sixties a seven year one on. beagle dogs and a ten year one on
monkeys. Within three and a half years of the dog study,
all dogs on high doses and half on low doses were dead due
to inflomation of uterine lining.
(The two on low doses
who survived had their uteruses removed.) All control
dogs and survived except one which died of bite wounds
and four which were sacrificed by the researchers. The
dogs also developed cancer of the breasts, drug-induced
diabetes and various other problems.
At this point, Upjohn
declared that beagle dogs were not the ideal animals to
judge risks to human females. Later even the monkey
studies in which cancer of the uterus occured were said to
be 'irrelevant to human experience'. The history of this
controversy has been marked with disinformation and a
desparate desire on the part of the company to maximise
profits without making sure first that the drug is safe.
Breast cancer, two types of uterine cancer, serious
menstrual disturbances; and masculinisation of female foetuses
are some of the serious effects of Depo-provera,
Others are
depression, decroased libido, nausea, dissines's, (weight
gain without any increase in nutrition)etc.
The W H 0 report on I Cs (1982) says that the
majority of women on I Cs have their menstrual cycle dis
rupted. The extent of disruption is stunning.
"less than
one third of women on Depo report having any normal
menstrual cycle during the first year of usage' and
'approximately half tho users ( of NET-EN) reported at:
least one normal construal cycle during the first year'.
Both the above quotes from the WHO report are examples of
the concerted attempt tc underplay.the dangers of I Cs. In
fact, a significant number of women stop having their
periods only to have severe bleeding after injections are
withdrawn while others bleed every day of tho month while
on the drug. But everyone concerned seems to feel that
it is a minor side-effect.
For Indian women who hold the
world record for anemia, it is a very very significant
side effect.
There is far lotft information available about NET-EN
on human metabolism, on infants exposed to them through
breast-milk or about their carcinogenic properties. No
one seems tc know why the majority of women on those
drugs suffer from construal chaos. No do they know why
these women put on weight without more nutrition or why
they are depressed.
3
Yet the advocates of 1 Cs, including the U H C, consider
them an. ideal form of contraception. Their favourite
phrase is risk-benefit ratio,
According to tnem if the
benefit outweighs risk, the- drug should ba used.
BUt the risks are taken only by women.. The benefits are
majh_fcylfor~ the pharmaceutical companies, the population
control experts and the Governments of third world countries.
There is a lot that is wrong, with our family planning
polici.es.
Its always our families and their plans, A
beginm'ng must be made somewhere to correct theip, Lets
start with the newest strategy which is about to be imposed
on the masses of Indian -women.
Lets struggle against the
inundation of this country with ICG,
CU< DBTL’.ITBS;
j) Ban all long-acting contraceptives and
withdraw approval for NET-EN,
2)
Make public all studies in India an Repo and NET-BIT.
immediatoly.
3)
Stop experimenting on third world women with hazardous
drugs and contraceptives.
4)
• Institute a public enquiry on the controversial
injectable and implanted contraceptives,
JOIN US III OUR STRUGGLE FOR A SETTER DEAL FOR CUR WOMEN.
Group against long-acting contraceptives,
1«
Forum Against Oppression Of Women,
2)
Women's Centre, Bombay,
3)
Medico-friends' Circle.
Strce Mukti Sanghatna
5)
Sangharsh Vahini,
References
1.
Kroente Kurt : "Polypharmacy - causes, consequences
and cure", Ammmerical Journal of Medicine,Aug.85.p
2.
Harvey S.C.: Gastric Antacids and p Digestants from
Goodman and Gilman's. The pharmacological basis of
therapeutics, MacMillan Publishing Co. New York
Sixth Edition, page 988.
3.
McGuigan J.E.s Peptic ulcer from Harrison's Principles
of Internal Medicine edited by Isselbacher K.J. et al,
McGraw Hill, Kogakusha Ltd, Tokyo, Ninth Edition 1980
page 1371
4.
Stenson W.F.: Gastrointestinal Diseases from Manual
of Medical Therapeutics edited by Campbell and Frisse,
Little Brown and Company, Boston,24th Edition, 1983
page 249.
5.
Satoskar R.S. Bfrandarkar S.D. : Pharmacotherapy of
peptic ulcer from Pharmacology and Pharmacotherapeutics,
Popular Prakashan, Bombay, 7th Edition, 1980. page 478.
6.
Lam S.K. et al s Randomised Crossover trial of tripotassium dicitrate bismuthate versus high dose
cimetidine for duodenal ulcer resistant to standard
dose of cimetidine. Gut 1984, 25 : 7036.
*
7.
Lee F.I. et al : Comparison of Tripotassium dicitrate
bismuthate tablets with Ranitidine in healing and
relapse of duodenal ulcers. Lancet Sth June 85 :(i) p1.
*
1299-13
8.
Martin D.F. et al : Differences in relapse rates of
D^uodenal ulcer healing with cimetidine or tripotassium
dicitrate bismuthate. Lancet 81, Is p.7-10
9.
Richardson C.T.; Peptic ulcer disease from Stein's
textbook of Internal Medicine edited by Stein J.H.
Little Brown and Company, Boston, 1st edition, 1983
page 93-104.
10.
Peterson W.L. et al :
Healing of Duodenal ulcer with an antacid regimen.
The New England Journal of Medicine 1
77,
*
297 p.341-345
11.
12.
Gulhati C.M.s Antacids s MIMS India, 1982, 2.10- p.-13
Hetzel D.J.s Cimetidine treatment of Duodenal ulceration
Gastjftoentrelogy 1978, 74 p.389-392
13.
Feldman M.: Inhibition of gastric acid secretion by
selective and non selective Anticholinergics.
Gastroentrology 1984, 86 p.361-366.
McManus J.P.s Gastroentrology 1984, 86 p-205-1
*
comment to article of Heppell J. et al on 'Not anther
*
ulcer
Ann. Surg 1983 (198(1)s1-4(July).
14.
15.
16.
17.
Hollander D. et al s Antacids Vs. Placebos in peptic
ulcer therapy, a controlled double blind investigation.
JAMA 1973, 226 p.1181-1185
Editorial article: Cimetidine resistant p Duodenal
ulcers Lancet 1985, (i) p-23-24(of Jan.5, 1985)
Ippolite AF et al : cimetidine versus Intensive Antacid
therapy for duodenal glcer Gastroentrelogy 1978,
74 p.393-395
cont1d
References (cent’dj
IS.
Mendelo F.F. A. I.: Wh~t has been happening to
duodenal ulcer ? Gastroentrology 1974, 67 p.
1020-1022.
19.
Sussor M et al : Civilisation and peptic ulcer,
Lancet 1962, 1 p.115-119
Sonnenberg A et al ; Changing mortality of peptic
ulcer disease in Germany. Gastroentrology 1983,
84 p-1553, 1557.
Sonnenberg A ; Occurance of Cohort phenomenon in
peptic ulcer mortality from Switzerland,.Gastro
entrology 1984, 86 p.398-491.
20.
21.
22.
Chaltane C.S.s Epidemiology of Peptic ulcer in
India, from Progress in sJiax clinical medicine in
India edited by Ahuja M.M.S., Arnold-Heinemann
Publishers, New Delhi, Third Series 1979p.207-227
23.
Beckus H.L. : The therapy of peptic ulcer from
Textbook of G'stroentrology edited by Bockus H.L.
et al, W.B. Squanders Company, Philadelphia,
Vol. 1, Third Edition, 1974. p.697.
T)R- '50^1
A SURVEY OF COUGH SYRUPS
Objective ;
To study the various cough syrups and similar products used
in the treatment of cough, to find out the rationality of their
usage in therapy for cough, by doing a detailed analysis of the
various ingradients of the mixtures and also finding out the cost/
day's treatment.
MethcKioloay :
(June ,85)
Eighty products listed by MIMS India,/classified as expecto
rants, cough suppressants, mucolytics and decongestents were
included in the survey.
They were analysed according to the rationality from thera
peutic point of view under various categories A,B,C...... as laid
down in the summary part.
To judge the effectiveness of a particular cough mixture
following criteria should be considered.
As far. as possible it should have a single ingredient which
is proven to have the desired effect, e.g., (a) if the unproduc
tive, dry cough is to be suppressed it may contain noscapine,
codeine, etc., as single constituent.
(b) If the sputum is to be expectorated (brought out) it may
contain an expectorant like Potassium Iodide as single consti
tuent. However, steam is the best expectorant and administration
of other compounds is not proven to be more efficacious for the
expectorant action.
(c) In patients of asthma or chronic bronchitis where aim is to
dilate the airways and hel; clear them of excess secretions
it could contain bronchodilators like Salbutamol, ephedrine, etc.,
as single constitutent ingredients.
Whatever the ingredients are present, they should be in suffi
cient doses which would be therapeutically efficacious.
For therapeutic effects tablets are ^referred over liquid
preparations most of the times. However when a soothing effect
on the pharyngeal mucosa (inside of throat) is desired, one could
opt for alternatives like drinking hot fluids or simple sugar
syrups or sucking a sugar cube, etc.
In case of multiple ingredients it is necessary to see that
the ingredients do not antagonise each other's actions in any
form.
e.g, A cough expectorant should hot be combined with a cough
sup^re ;sant or an antihistamine; a bronchodilator with an anti
histamine or a cough suppressant., etc.
The cost of therapy with a particular formulation advised
should be reasonable, i.e, as low as possible for the desired
action - the therapeutic benefit.
In any case, one has to make sure that the cough syrup or
whatever formulation is being used has the capacity to produce
the action for which it is being marketed.
Summary of the survey findings
The formulations are categorised as explained below :
Category
A
-
Only Antitussive (can suppress the cough reflet)
B
-
C
-
Only expectorant (which help in bringing out the \
sputum)
Only mucolytics (which is supposed - to liquify
the sputum)
contd............... 2/-
Category
D
-
Only bronchodilator (which dilates the bronchi)
E
F
-
Only Antihistamine, (anti-allergic compounds)
Expectorant + xntitussive
Expectorant t Bronchodilator
G
-
H
-
Expectorant •!■ Mucolytics
I
-
Expectorant :■ Antihistamines
Having more than 2 of the A,B/C,D/E.
J
-
K
-
Bronchodilator
Antihistamine
L
-
Bronchodilator
Mucolytics
Table - 1
Break up of Categories
Total No. of formulations i 80
Category
Rational
Formulation
Irrational
Formulation
A
B
C
5
2
-
4
D
2
-
-
6
-
E
-
F
G
2
-
H
-
I
J
K
__
-
7
'47
-
3
11 (13.75%)
69 (86.25%)
__
Table - 2
Type of formulation
Tablets/capsules
19
Liguids/Syrups
56
23.75%
70.00%
5
80
100 %
Other forms
TOTAL
6.25%
con'td...... 3/-
Table - 3
No. of
Formulations
No. of
Ingredients
1
2
3
%
9
11.25
11
20
13.75
25.00
4
11
13.75
5
13
6
7
7
2
16.25
8.75
8
5
9
10
1
0
0
11
12
1
2.50
6.25
1.25
-
1.25
100.00
Cos t/day for an
Adult
No. of
Formulations
Below Re. 0.50
1
Re. 0.50 - below 0.95
5
23
Re. 1.00 - Rs. 1.95
Rs. 2. 00 and above
TOTAL
%
: 1. 36
6.84
31.50
44
60.27
73
99.97
Conefusion :
The findings of this survey are left open to the
people for discussion. But we would like to raise the basic
issues such as the uselessness of the mixtures in cough
therapy, especially the liquid preparations when compared to
the medical benefits they are liekly to have.
■,i
ho;
0 001 .
08'i”!
ANTACIDS
Prepared by:
Dr.J.D. Lakhani
Asstt.Prof.in Medicine &
Neurology
Medical College
BARODA
1.
Introduction
2.
General Information
a)
b)
c)
Uses of Antacids
Classification
Individual Antacids : (1) Aluminium hydroxide
(2) Aluminium phosphate (3) Other Aluminium
compounds (4) Calcium carbonate (5) Magnesium
hydroxide and oxide (6) Magnesium trisillicate
(7) Magnesium carbonate (8) Magaldrate
(9) Sodium bicarbonate (10) Sodium citrate
(11) Tripotassium dicitratS bismuthate
(12) Miscellaneous gastric antacids (13) Antacid
combinations.
d)
Gastrointestinal Protectives and Abdosbents :
(1) Simethicone (2) Kaolin (3) Activated charcoal
(4) Pectin (5) Magnesium triscillicate.
3r
Comparison of Antacids
4.
Choice of Antacid
5.
Dosages of Antacid
6.
Evaluation of available preparations
7.
Review of promotional literature
8.
Practices and malpractices followed by G.P.s
9.
10.
11.
Other antiulcer drugs and surgery
Role of gastric antacid in management of Peptic ulcer.
Dangers of antacids
12.
13.
Epidemiological aspects of peptic ulcer
Clinical aspects
14.
Preventive aspects
15.
16.
Issues - Hyperacidity - Antacid pru
Action Plan
17.
Conclusions
18.
References
"The desire to take medicine is perhaps the greatest
feature which distinguishes man from animals"
- Sir William Osler.
The human desire 'to take medicine' carries, however
a price tag . A desire to take Antacids in any 'dyspepsia',
'flatulance', 'gas', 'belching
.
*
'Bosborygms'
has made
them one of the most abused drugs. Because of irresponsible
advertising it has become misused drugs and public has
started believing that man is constantly fighting a battle
against acidity and every little belch or upper gastro
intestinal upset calls for an antacid.Who is responsible
for such misuse of Antacids ? The answer is four 'P's ;
(1) Power of Placebo :'Mahy studies have revealed
substantial incidence of placebo responsiveness of individuals
with minor gastrointestinal upset.
£
.
(2) Physicians; The first weapon used by a physician
for any abdominal discomfort is 'Antacid'.
(3) Pharmaceuticals: Irresponsible advertising has
misguided physicians and public. In profit maximisation and
adoption of management principle like 'foot-in-the
door-phenomenon' has made antacids most abused drug. The
drug proved^effective for healing ulcer is promoted for
indigestion’*1.
(4) Public: They have started believing that they have
to pay penalty in form of ulcer for their stressful life.
general Information of Gastric Antacids
Gastric antacids are agents that neutralises or remove
acid from the gastric contents. They are indicated in
following conditions :
(1) Peptic ulcer : Administration of antacids has been
the major accepted form of treatment for peptic ulcerJ.
(2) Reflux Oseophagitis : Reflux of gastric contents
through an incompetent lower oesophageal sphincter
can
lead to oesophageal inflammation and cause heart burn.
Hiatal hernias can be seen on radiogrpphs of patient with
reflux oesophagitis. The medical therapy of patients with
reflux is mainly aimed at reducing the quantity and acidity
of the gastric contents available for reflux which is done
by Antacids.
(3) Use as prophylaxis for GI bleeding - The patients
who are seriously ill especially admitted in intensive
care unit are having risk of development of upper GI
haemmorhage. Many of these patient^ have been treated
prophylactically with either antaiids or cimetidine to
prevent haemmorhage. Studies have shown that antacids are
more effective than placebo or cimetidine for this purpose
(N.Engl.J. Med.302:426, 1980) Surg.Gynecol.Obstet.153:214,1981).
(4) Erosive gastritis which is also known as
haemorrhagic gastritis or multiple gastric erosions is an
important cause of upper GI bleeding. Once bleeding stops, a
regimen of hourly antacids or cimetidine is the line of
management.
2
Though these are the scientific usages of antacids,
in practice, it is used in wide variety of conditions.
Lay people use them as self medicament in almost any
GI condition.
Classification^
Antacids are commonly divided into :
1) Nonsystemic antacids
2) Systemic antacids.
Nonsystemic antacids includes aluminium hydroxide,
magnesium hydroxide, magnesium oxide, magnesium trisilicate,
calcium carbonate, bismuth carbonate and calcium phosphate.
These drugs are water insoluble, generally unabsorbable
and are called nonsystemic because they do hot produce
systemic alkalosis.
Systemic antacids include compounds like sodium
bicarbonate and sodium citrate which are absorbed into the
systemic circulation and may cause metabolic alkalosis.
2
Individual Antacids
(1) Aluminium Hydroxide s It is a weak antacid and
generally is marketed with other antacids. Although it is
considered to be nonsystemic, some absorption from the
gastrointestinal fract occurs. The acid neutralizing
capacity has been found to differ according to the process
of manufacture, age of the product and it is varying from
batch to batch in the case of given product. Pepsin activity
is not significantly inhibited. Particles of wet aluminium
hydroxide are somewhat adhesive and the compound is demulcent.
The role that the demulcent action plays in the treatment
of peptic ulcer is controversial.
Adverse reaction s Constipation, hypophosphaemia
interfere with absorption of drugs like tetracyclines, iron
salts, antich/olinergic drugs digoxin and PAS. Aluminium
hydroxide may prevent the absorption of phosphate from
the intestine which would result in hypophosphatemias and
osteomalcia giving use to proximal myopathy. Encephalepathv
. might result in patients undergoing hemodialysia.
Other uses ? It can be used to reduce intestinal
absorption of phsophate ine case with phosphatic renal
calculi and in chronic renal failure.
(2) Aluminium phosphate ; It is sometimes prefered to
aluminium hydroxide as it does not interfere with phosphate
absorption. It has however no special advantages and it is an
ineffective antacic^.
(3) Other aluminium compounds ? Basic Aluminium carbonate
has its pharmacological property same as Aluminium hydroxide.
However its capacity for neutralisation is greater.
Amongst the aluminium containing Antacids it is best for
the management of phosphatic nephrolithiasis.
Dihydroxyaluminium sodium carbonate combines in a
single chemical entity, properties of both sodium bicarbonate
and aluminium hydroxide. The drug is partially systemic
antacid. It is claimed better than aluminium hydroxide
however lacks the confirmatory data.
3
Dihydroxyaluminium aminoacetate is a basic salt of
aluminium and glycene. Claims that the substance is less
constipating than aluminium hydroxide are not objective,
but there is less aluminium per chemical equivalent.
The capacity for neutralisation is low.
(4) Calcium carbonate s It occurs as a white, odourless
powder with a chalky taste. It was the first gastric antacid
to be used. It has remained popular for a century and a
half. Its antacid effects are rapid in onset and relatively
prolonged in duration CaCO3 has a high capacity for
neutralising acid in vivo. It is inexpensive. It was
m considered to be the most effective antacid for many years.
However today, CaCO3 is used much le$s frequently.
Adverse reactions s CaC03 has long been considered to be
a nonsystemic antacid. However enough is absorbed to cause
systemic and renal effects in certain circumstances. A
slight to moderate alkalosis occurs. Hyper calamia may
result in patients having uremia.
It may cause acid rebound,
might be because of ■.'actionof Ca++ on the small intestine
to stimulate release of gastrin.
It has tendency to produce
constipation and fecal concretions. The administration of
CaC03 promotes positive phosphate balance and lead to
hyperphosphatemia especially in patients who have developed
milk alkali syndrome. Disturbance resulting from the
liberation of carbondioxide may lead to belching in some
individuals. Nausea is also an occasional complaint.
Hypercaleiuria and alkalgria predispose to nephrolithiasis.
(5) Magnesium hydroxide and oxide s Magnesium oxide, a
on contact with water is converted to magnesium hydroxide and
then acts. Magnesium oxide is available as a light colourless
powder insoluble in water, while Magnesium hydroxide
is
available as milk of magnesia containing 7 to 8.5% of magnesium
hydroxide.
It is quick acting antacid and the action is prolonged.
Mg(OH)
as milk of Magnesia has long been popular among the
laity
as an antacid and a
cathartic. Acid rebound
occurs. However it is insignificant.
Adverse reactions ? It has mild cathartic action. It is
contraindicated in patients having impaired renal function or
it might cause hypermagnesimia. Although Mg(OH)3 is
classified as nonsystemic antacids, 5 to' 10 % of the
magnesium can be absorbed.
(6) Magnesium trisilicate ; It has too slow rate of reaction
with acid, to be useful for the management of peptic
ulcer. Even in a normal person it. rarely elevates the
intragastric pH above 2.7. As it becomes gelatinous in
consistency it provides a protective coating to the ulcer
crater.
*
Adverse reactions - laxation by high doses. Approximately
5% is absorbed any hypermagnesemia can occur in patients with
renal insufficiency. Approximately 7% of silica may be
absorbed which may lead to siliceous nephroliths. Intestinal
concretions also occur. It is good absorbent which may
interfere with absorption of dietary proteins and number
of other drugs. It adsorbs pepsin also.
4
(7) Magnesium carbonate ; This antacid has properties
similar to those of magnesium hydroxide except that
carbondioxide is liberated which may cause belching. It has
been shown to be an excellent antacid in clinical practice.
(8) Magaldrate ? It is complex hydro>ymagnesium aluminate
which reacts with acid in stages. The aydroxymagnesium is
relatively rapidly converted to magnesiim in and the
aluminate to hydrated aluminium hydroxide. The aluminium
hydroxide then reacts slowly to give a Sustained antacid
effect. Magaldrate more consistently buffers the gastric
contents than do th® mixtures. The PH is usually maintained
between 3.5 to 4.
*
Its systemic effects are those of
Mg(OH)2.
(9) Sodium Bicarbonate sit exerts immediate and rapid antacid
action in the stomach because of its solubility, however it
has short duration of action. It is a systemic antacid.
Eructation of the carbon dioxide liberated during the process
of acid neutralisation often gives the patient a sense of
relief from abdominal discomfort. This is the basis of its
reputed carminative action.
Adverse reactions ; Chronic use of NaHCOc alone as an
antacid (taking with milk) can cause milk alkali syndrome.
Because of its sodium content it might lead to weight gain,
volume expansion, increase in BP and may promote oedema.
It may be hazardous in renal insufficiency, incipient or active
hypertensives and in CCF patients. Continuous maintenance
of raised pH by NaHC03 in stomach may lead to stimulation
of gastrin and rebound '
acidity.
Other uses s (1) In metabolic acidosis
(2) In urinary tract infection to mkke
urine alkaline and to prevent precipitation of
substance like sulfonamide and uric acid, it is used.
(3) For topical application it is usede
as an antipruritic lotion, as an eyewash, motith wash,
douch to loosen wax
in the ear and in enemata.
(10) Sodium citrate s Sodium citrate has properties, similar
to those of sodiumbicarbonate except that there is no
liberation of carbondioxide. Effervescent preparation that
'fizz' consist of sodium bicarbonate and citric acid which
react in solution producing cerbondioxide and sodium citrate.
(11) Tripotassium dicitrate bismuthate (de-nol) ; A
colloidal bismuth preparation accelerates healing of gastric
and duodenal ulcer. In a crossover trial, Lam et al found
that colloidal bismuth subcitrate headed 85% cimetidine
resistant ulcers whereas high dose of cimetidine headed only
4*%
. Similar comparison was done with ranitidine and
healing. Relapse of duodenal ulcer was compared. Though
there was no statistical difference in healing at 4 wks and
8 wks with both these drugs there was difference in relapse
rates. 74% and 84% of ranitidine beated patients developed
relapse of duodenal ulcer after 4 months and 8 months
respectively. In contrast to this,^41% and 55% of the patient.
treated with TDB develdpedgrelapse'. Similar results have
been obtained by Martin DF .
5
Agvarss reaction : It causes black discoloration of
stools . Liquid preparation is less acceptable to the
patient because of its odoijr. However TDB tablets can be
given which arc effective and acceptable'.
(12) Miscellaneous gastric o.ntstcids : Gaviscon is mixture
af containing small amounts of NaHCO3, -.I(0H)3, Mg2Si308
and Alginic acid. It makes foam (raft) which floats on top
of gastric juice. It is intended that in gastro oesophageal
reflux, the floating mixture is. the first material to make
contact with the oesophagus. However it has negligible effect
on gastric acid below the raft.
The mineral hydrotalate (MggAI^ (OH)
)
*
CO.J.4H2
has
an acid neutralising capacity 84% of that of Mg(OH)2.
Milk as antacid has very little effect.
(13) Antacid combinations s Antacids are combined for a
variety of reasons and probably'such combinations can be
considered rational. Laxative and constipating compound can
correct the disadvantage of each other, a fast acting
ingredient can be combined with a slow acting ingredient to
increase the total buffering time, the daily dose of a
single entity can be decreased to reduce the risk of toxicity,
patient compliance can be improved by combining agents,
rather than by giving multiple sep-arate preparations.
The most common mixture of antacids are those of
/\I (OH) 3 and Mg (OH) 3 in gravimetric ratio of 2s 1 or Isl.
Gastrointestinal Protectives and Adsorbents ; These are
discussed here because they are used in combination with
Antacids.
1. Simethicone s It is a common ingredient in the
antacid combinations. It is included to defoam the gastric
juice in order to decrease the tendency towards gastrooesophageal reflux.
It is light'gray, translucent liquid of greasy
consistency. It is a mixture of liquid demethylpolyolloxanes
with antifoaming and water repellent properties. It is
promoted as an adjunct in the treatment of conditions
in which gas is a problem, such as flatulence, functional
gastric bloating and a postoperative gaseous destension.
It has also been used to reduce gas shadows in radiography
of the bowel to improve visualisation in gastroscopy
clinical studies in support of these recommendations are
not convincing. Simethicone is used in combination with
antacids, antispasmodics, sedatives- and digestants.
2. Kaolin is a native hydrated aluminium silicate
powdered and freed from gritty particles by elutrication.
It is used internally and externally for its adsorbent
properties.
6
3. /Activated charcoal ; It is an odourless, tasteless
fine black powder which is residue from the destructive
distillation of various organic materials, treated to
increase its '' adsorptive power. The adsorptive capacity
of various brands of activated charcoal differs enormously.
It has broad speetal adsorptive activity and is rapid in
action. It is used in emergency to treatment of oral drug
poisoning.
4. Pectin s It is a purified carbohydrate product
obtained from fruits and chemically consists of chiefly
polygalacturonic acid. It is claimed to be an adsorbent and
demulcent.
■/. I
■ 5. Magtrisilicate s It is an effective gastrointestinal
adsorbent but a weak antacid, discussed earlier.
Comparisons of
various Antacids
o
The ideal antacid should have following characteristics 5
1. It should be potent in neutralising
acid
2. Inexpens ive
3. Should not be adsorbed from the gastrointestinal tract.
4. Should contain negligible amount of sodium
5Sufficiently palatable.
6. Readily tolerated and
.free from side effects.
Although the ideal antacid is yet to be developed, a
number of preparations are available which can be used for
the treatment of patients with duodenal ulcer.
One of the 'ways by which we can compare the antacids
is by comparing the buffering capacity of individual antacids.
This buffering capacity is expressed in form of mulliequivalent
of acid neutralised per gram or per ml. of antacid. Western
literatures of various proprietary brands of antacid
suspension and tablets and their buffering capacity is
available. However such data is leading for Indian brands of
antacids. Following chart of western brand antacid is given
to give an idea of their buffering cppacities according to
their ingredients.
Buffering capacity
meq/15 ml.
Sodium content
meq/15 ml.
l.AI (OH)3
*Amphogel
20
0.9
2.Al(OH)3+Mg(0H)2
Maalox Therapeutic
concentrate
95
0.11 '
Antacid
Maalox plus
40
(containing simethicone)
• .18
3.CaCO3
Turns tablet
19.5 per 2 tab.
• .125
4.Al (OH)3+Mg(0H)2+CaCO3
Carnalox
54
• 133
(Chart from Manual of Medical Therapeutics - 24th Edition
p. 251).
7
It is evident that maximum buffering capacity is of
Antacids containing Mg(0H)2.
Choice of Antacid
1.
In general.liqgid antacids are more effective th?n tablets4.
Tablet preparation of magnesium hydroxide and/or aluminium hydroxide
possess little acid neutralising capacity and are not recommended in
the treatment of duodenal ulcer3.
2.
Magnesium hydroxide is a potent antacid but large, frequent dose
can cause severe diarrhoea. For this reason it is combined with
Al(0H)3. In most popular preparation, this antacid howevet would be
contraindicated in patients with severe renal disease.
3.
Aluminium hydroxide has moderate buffering activity and is
hardly used alone as an antacid.
4.
Calcium carbonate though effective in expensive and well tolerated
antacid, it produces a genuine acid rebound. Again it might lead
to hypercalcemia, hypercalciuria and milk alkali syndrome and
that is why not preferred.
5.
Magnesium trisallicate which is xRdMssd included in various
antacid mixtures is a slow acting and weak antacid.
Dosage of antacids
Antacid'-dosage should be based on multiequivalents of
g
neutralising capacity rather than on volume or number of tablets . An
80-100 mEq dose of. antacid is usually prescribed for patients with
ulcer disease. This dosage varies from 30 ml. of magnesium and
aluminium hydroxide containing antacid to 45 ml. of an aluminium
hydroxide contqining antacid. As in India the neutralising capacity
of various proprietary brands of antacids is not available,
scientific recommendation about the dosage is difficult to mkke.
In Western set up where three meals per day is taken,
recommended dose of antacid is 80 - 100 mEq of liquid antacid. 1 and
3 hours after meal and at bed time 4,9,10. This means a person
has to take antacid 7 times in a day. If the most potent antacid
is used it means that person has to drink 210 ml. of liquid antacid.
If the stomach is empty, antacids must be taken frequently. In
treating fasting patients, for example, patients in intensive
care units it may be necessarijt to give antacids every 30 to 60
min. to achieve adequate reduction of acidity.
In adai Indian set up we take meals twice in a day. Thus 5
dosages logically may be sufficient. However this needs confirmation.
Evaluation of available preparations
I have triad to analyse the
MIMS-. India (Vol. 2 November 10)
conclusions.
intacid preparations listed by
and have come to following
1 . 34 brands of antacids is listed.
2. Of these 34 brands 15 are marketed in the form of liquid,
and tablets both. 15 are marketed only in tablet form and 4 are marke
ted only in liquid form.
In view of less rationality of tablet preparation, to have
30 brand out of 34 in tablet form of which is 15 are marketed in
tablet forms only seems concernable.
8
3. I have tried to designate a commercial preparation
'pure antacids' for preparation having a single and/or combined
ingredient in form of antacid without having combination of
gastrointestinal adsorbents or anticholinergics, for the
evaluation purpose,
out of 34 listed
1 pure antacids (as defined earlier)
5
preparation
2 having added simethicone
(dimethyl polysiloxar.es)
23 preparations.
Thus if I want to prescribe an antacid for a patient of
Duodenal ulcer and I do not want simethicone to be given to him
I would have only choice of these 5 antacid preparations.
5. If we analyse still further these 5 antacid preparation
none is suitable for my patient of duodenal ulcer. Demerits of
those 5 antacids are as below -
1.
Aiucinol - is basically aluminium containing antacid
and thus would be a weak antacid,
2.
Alludrox - contains only Al(0H)3. The alludrox Md contains
Al(0H)3:Mg(0H)3 in ratio of 3:1 - ideal ration being 1:1.
3.
Eugastrid - 4 antacids are combined of which 3 are weak
antacids.
.4.
Gclusil - Magtrisillicate and aluminium hydroxide - both
are weak antacids.
5.
Magsil - 4 antacids combined.
6.
Gelusil in India contains Magtrisillicate and aluminium
hydroxide while in United States of America Gelusil-1 contains
Al (0H)3 and Mg(0H)3.
7.
Most liquid preparations arc available in very small packing
e.g. Almagel in 175 ml, Allugel in 210 ml, Dlgene Gel in 210 ml,
Diovol in 175 ml, Gelusil in 175 ml. This would be hardly sufficient
for (1 ) day! This itself suggests that most antacid are working
as placeto rather than antacids.
8. If a liquid preparation is prescribed 40 ml x 7 times in a
day for 6 wks, a person may require 12600 ml. of antacid moaning
that he has to buy 60 bottles of 210 ml packing.
9.
If antacid containing methylpolysiloxane is prescribed
for CDU than a person would be taking and paying fur 63000 mgm of
methylpolysiloxane extra, h person taking 3/4 kilo of methylpoly
siloxane without any benefit (antacid contains average 25 mgm/5 ml
and if requirement is 12600 ml f antacid it would came to 63000 mgm).
Review of Promotional literature
As I mentioned in the starting of this paper (quoting the
standard textbook of pharmacology) that because of irresponsible
advertising, antacids are
most abused drugs. This state of
affairs is not present only in India but all over the world.
'Rennie' one of the most popular brand of antacid available on
the counter in UK writes 'Digestif Rennie - for on the spot
relief' . This tablet contains 680 mgm of calcium carbonate and
80 mgm of light magnesium carbonate. The other caption which is
written on the package is 'Digestif Ronnie reliev@s acid indigestion,
heart burn, nervous indigestion, acidity, flatulence upset stomach
and dyspepsia'.
- 9 As it is with this Ronnie tablets most of the antacids are
promoted as the drug for antiflatulence. No where it is written
that antacid relieves the flatulence on the contrary antacids like
NaHCO3, MgCO3 liberate CO2 which might produce belching.
The other common finding is almost all antacid preparations
are. promoted for variety of conditions.
However scientific indications of antacids are few and specific.
Many a times it is promoted for indigestion. How are the antacids
going to improve the digestion , As mentioned by Kurt Kroenke in his
article on polypharmacy that pharmaceuticals adopt foot in the door
policy. The drag like antacids was marketed and accepted by the
medical science as antiulcer drug had a foot inside and thus it is
now promoted for indigestion.
Practices and Malpractices followed bv the GP
Physicians are not less responsible for misusing the antacids.
Most.of the times it is prescribed to give placebo effect, When a
patient comes to a doctor for pain in abdomen, something has to be
prescribed and that is in form of antacids.
In the indicated
patients it is prewcribod in smaller doses. Many a times because
of lack of time knowledge and diagnostic skill antacids are
prescribed which is moreso by the unscientific doctors. Again there
is a belief that anta.qids are harmless and thus they are prescribed
for a very long tin. . Such belief is common among the doctor
and also in public. Many Indian patients are fussy about their
habit of passing stools every day in the morning. They find
magnesium containing antacids useful for their bavel habits. This
feeling is reinforced by the doctor by saying that 'you are passing stool
because you get bettor digestion with help of the pills,'.
Other antiulcer drugs and, surgery in the management of peptic ulcer
H2 receptor antagonist cimetidine is now widely used in the
treatment of duodenal ulcer.^4 % patients develops nealing in th®
ulcer by cimothidine therapy . The other H2 receptor antagonists
like ranitidine and Omeprezol have also been tried in the management
of duodenal ulcer,
Anticholinergics have been used for many years to decrease
gastric acid secretion. Because of their side effects and advent of
H2 receptor antagonists they are used much less frequently as antisecretory agents. Recently a selective antirnuscgrinic type of
anticholinergic PIERENZEPIN has been developed .
Surcalfale (carafate) a drug that coats ulcer crater them
from acid and pepsin is also been used. Prostaglandin E2 is also under
experimental stage.
Current medical treatment of duodenal ulcer,'be it with
cimetidine, ranitidine, sucralfate, deNol, prostaglanotin or
antacids is successful in not more than 75-^ %’of patients and
thus surgery would be required in the rest
. '
Role of Gastric antacid in the management of peptic ulcer
What share antacid has today in the management of peptic
ulcer , Today we have so many new drugs especially H2 rc-cepter
blocker drugs. The Goodman-Gillman's text book writes 'The
status of antacid is presently in a stage of evolution. The use
of cimetidine will^undoubtodly decrease but will not abolish the
need for antacids' ,
10
I have an opinion that antacid has a very little role today in
the management of peptic ulcer. Treatment with cimetidine is
much more convenient, is advantageous in that bavel function is
not altered and is no more expensive .
Hollander and Harlan did not find any significant difference
betwe^g antacids and placebo in its effectiveness in a double blind
trial . In contrast to this another double blind clinical trial
showed that large dose antacid renimer. had statistically significant
better ulcer healing rates in comparison with placebo^ulcer
healing occurs^ in 45% receiving placebo while in 78% treated
with antacid) .
Though antacid efficacy is proved by this study
and is accepted by most text books also the question is that if
ulcer healing is occurs in 45% of patient with placebo why to give
antacid , Again the same article has proved that ANTACID WAS NOT
MORE EFFECTIVE than PLACEBO IN RELIEVING ULCER SYMPTOM.
Antacid therapy can be useful in paiient who has cimetidine
resistant duodenal ulcer. Most studies show tnat H2 receptor
antagonists -t heal about 85% of duodenal ulcer after 2^gonths, but
relapse rates on withdrawal of the drugs are very high . A
multicentric trial of cimetidine versus intensive antacid therapy
for duodenal ulcer showed similar rates of heading with both the form
of therapy. 80% of cimetidine beatod patients became asymptomatic
by week 4, as did 63% of antacid treated patients (p
0.1) . In
pregnant patients antacid is preferred to cimetidine therapy.
Dangers of Antacids
2
The presence bf an antacid in the gastric contents increases the
volume of gastric juice secreted and the output of HC1. An elevated
pH induces the pyloric antrum to release gastrin. In patients with
duodenal ulcer this is more marked. Acid rebound is known to occui
with many antacids like CaC03, Mg(0H)2, NaHC03. Gastric alkalinization
may lead to increased susceptibility to various acid sensitive
microbial pathogens such as Brucella abortus,. Antacids like Mg(0B)2
and CaC03 can cause significant elevation ..of urinary pH and
predispose to UTI and urolithiasis, antaci-d .interact with other
drugs by pH related and other mechanisms.
Epidomidoqical aspects of peptic ul cer
The absolute prevalence is not known. For duodenal ulcer,
estimates have ranged from 6 to 15 per cent. This variation may be
related to the population examined, differences in study design,
diagnostic method and perhaps to actual changes in frequency of
duodenal ulcer disease. It is suggested that 10% of the population
has a clinical evidence of duodenal ulcer at sometime in their life time.
18
It seems that duodenal ulcers are declining . Susser and Stein
reported decline in^death rates in England and Wales after 1950
due to peptic ulcer . Similar finding is from Germany . The same
fact was observed by Sonnerborg in Switzerland. He compiled
mortality figures as follows^ .
Country
G.U.
Population
D.U.
D.U.
G.U.
Population
male
_____ femal£ ___________
England and
35.3
29.1
25,186,100
Wales
52.1
35.5
23,881,300
West Germany 59.3
29.6
29,348,400
34.0
11.8
36.8
28.1
3,074,700
35.0
16.6
Switzerland
32,205,000
■
3,228,100
The figures refer to the averages of the period 1971-80. The
death rate, of gastric ulcer and duodenal ulcer are expressed
per million living men or women per year.
11
As far as epidemiology of peptic ulcer in India is
concerned following differences are notedz .
1.
Peptic ulcer affects maximum subjects a decade
earlier than west.
2.
Duodenal ulcer is more prevalent than gastric ulcer.
Significant difference is noted in the incidence of
peptic ulcer in southern and northern parts of India and
is believed by some th t the incidence is more in sogth
in comparison with north. Many studies have correlated this
difference with food habits and customs. However ng
conclusive ]6roof is evident. In India pepti^ulcer also
affects those in poor socio economic strata .
Brief clinical aspects of Peptic Ulceft
Epigastric pain of burning or gnawing character is th
most frequent symptom which occurs from 90 mm to 3 hour af
eating which is relieved by food and antacids. Change in
the character of pain often indicate the presence of
combinations. The complications of peptic ulcer includes
bleeding, gastric outlet obstruction perforation,
penetration and lutractability.
<+ Q
Peptic ulcer is a term used to refer a group of
ulcerative disorders of upper gastrointestinal tract, which
appear to have in common participation of acid pepsin in
their pathogenesis. The Zollinger Ellison syndrome
(gastrinoma) may be considered a form of peptic ulcer.
New studies have demonstrated following facts which
have important bearings in the management of peptic ulcer.
They are s
1.
Ulcer symptoms may resolve even though the ulcer is not
healed.
2.
Many patients with active disease have no ulcer
symptoms and may present with complications.
3.
Many patients with ulcer like symptoms may have no
evidence of an ulcer even after careful readiographic
and endoscopic examination.
Preventive aspects
23
1.
The prevalance of duxodenal ulcer disease is higher
in aggregate smokers than in non smokers. The frequency of
the anodation apparently increases in proportion to the
amount of smoking.
2.
Alcohol, a gastric secretons stimulant should be
avoided. It .damages the gastric mucosal barrier.
3.
High dose of aspirin ingestion is anociated with
an increased incidence of gastritis and gastric ulcer and
should be avoided in patients with an active or healed pep
tic ulcer. Other drugs, such as respine, indomethacin
or phynylbutazone may cause epigastrine distresg but there
js no evidence that they cause peptic ulceration^.
12
4.
Coffee, tea and meat extractives are to be avoided
for the same reason ,
5.
There is no evidence that Bland diets are beneficial
in beating ulcer disease. Therefore regular diet should be
prescribed. Milk is a poor buffer and its protein and
calcium content promotes acid secretion.
6.
Reduction of stress some patients have undue stress
at work or at home and sometimes modification of the work
or home situation cum reduce anxiety .
Issues ? I could bring out five issues from this paper,
they are ;
1.
What is role of antacids in todays management of peptic
ulcer disease when we have their better drugs available ?
2.
Which is the best antacid ?
3.
What should be dosage of antacid in Indians situation
where we take meals twice in a day
4.
What is hyperacidity
5.
What is role of pris
antacids
The first three issues I have discussed earlier and
I have presented my view. The last two are discussed below.
What is HYPERACIDITY
'This is very common diagnosis made by general
practitioner and a physician, however a question would
arise whether such condition really exist ? Textbook of
medicine and journals mentions about peptic ulcer but no
where the clinical entity like hyperacidity exists. Many a
times Hyperacidity is taken as synonyms for Peptic ulcer.
Againa any patient having upper abdominal discomfort
is stamped having hyperacidity and then he is loaded
with antacids. Does Hyperacidity exists without an
ulcer ? Many pharmaceuticals literature writes in indications
of antacid therapy peptic ulcer and hyperacidity
separately.
It is described by the workers that many patient with
ulcer like symptoms may have no evidence of Ulcer even
after careful radiographic and endoscopic examination.
A dilemma exists especially for the Indian situation
where diagnostic facility of endoscopy and radiology
is available to an average middle class Indian patient,
is so small that confirmation of diagnosis by endoscopy or
radiology and then starting management would be
impracticable and costly. Nevertheless healing patient
under broad umbrella of hyperacidity means we are misusing
antiulcer drugs especially antacids.
- 13
Role of pru Antacids
In USA antacids are taken in pru form. This
means when patient has pain they woqld take antacids.
Such practice is .also observed in India. However
there is no evidence on the effectiveness of
antacid prn to prevent ulcer recurrence.
The other question is does antacid relieve the pain
of peptic ulcer ? In a multicentric double blind
while accepted clinical trial it was shown that
antacid regimen was not more effective in relieving ulcer
symptoms and pain so I feel that placebo can do same
job as what antacids are doing.
Action plan suggested to LOCQST
1.
Education of lay public, general practitioners and
physicians to give correct idea of antacid therapy. They
should be informed that ANTACIDS ARE NOT FREE FROM
DANGERS AND IT HAS NOTHING TO DO with DIGESTION.
2.
Counter sale of antacids should be discouraged.
3.
If LjCOST desires to manufacture antacids it
should be liquid preparation of Mg(0H)2 and Al(0H)3 in
ratio of 1:1 (without adding simethicone) which would
have high neutrilising capacity. The preparation should
be like isMqalox which is very popular in west.
4.
To find out neutralising capacity of various
antacid brands available in India.
5.
To find out whether adding of simethicone increasing
toxicity decreases the effectiv eness and increases the
cost of available antacids in India.
CONCLUSION
On concluding this paper I feel that antacids
are more misused than used moreso in Indian situation.
Again we are lacking in many scientific details.
Regarding present paper I have shown my- personal view
which may be biased and I am open to correction.
- Dr.J.D.Lakhani.
DK 30.11
L
0
C
OST
GPO Box 134
BARODA-390001 .
By :
Dr.Sagun Desai
DRUGS IN PULMONARY TUBERCULOSIS
The treatment of pulmonary tuberculosis presents a
fascinating challenge to the respiratory physician since
modern chemotherapeutic agents offer the near certairity of
cure, provided that a proven regimen cf treatment is applied
assiduously for a sufficient length of time. The difficulty
lies in maintaining treatment with a combination of potenti
ally toxic drugs for a long time, since the regimens which
embody "standard" chemotherapy require sustained treatment
for 9 to 18 months, although the efficacy of shorter regimens
lasting 4 to 6 months is being investigated.
'
Objectives of combination chemotherapy (essential in
TB) ;
1.
to prevent emergence of resistance
2.
to eradicate the infection in the shortest possible
time
3»
to reduce the incidence of ADR.
IMP : 1 .
To keep the no; of drugs to minimum which can achieve
above objectives.
2.
For successful anti TB R^, regular surveillance
throughout the course of treatment by an experienced
health care team so as to reduce the total dosage
or duration of Rx.
Anti - TB drugs
-------- _1
" Fir ^t-line" drugs
INH
Most
Rifam,
effective
Etham
Least
SM
Toxic,
Pyrazinamide
" Sec ond-Lihe
drugs
Used in’Rx of
infection resistant to the first line drugs.
PAS
Thiac eta zone
Ethionamide
Cydoserine
Capreomycin
Viomycin
Kanamicin
bacteriostatic for "resting" bacilli but bactericidal
for rapidly dividing micro.
Tuberculostatic cone : 0.025 to 0,05
8/m.
Penetrates cells easily effective against intra
cellular org.
2
FIRST-LINE DRUGS ;
1 .
Isonicotinic acid hydrazine, Isoniazid.
INH :
.
Highly effective, primary drug for chemo of TB.
.
bactericidal
anti TB agent, mainstay of anti-TB Rx,
included in all current chemotherapeutic regimens
against susceptible mycobacteria.
History ;
Observation that nicotinamide was tuberculo
static, Fortuitous discover (1945) - Chorine.
Chemistry;
fs/
‘
;
)
-
Hydrazide of isonicotinic acid
-
Iproniazid - Lsoprgpyl
derivatives of isonicotinic
acid - to<5z toxic for use
in TB, used as MA 01,
/
”.
* Mechanism to spedrum of Action ;
actively
,
effective against /
growing mycobacteria but
less so against resting organisms.
.
mode of action precisely not known.
Possibly inhibits synthesis of mycolic acids which
are components of mycobacterial cell walls..
.
Selective toxicity against myco.
only because of
the above mech. since mycotic acid is not present
in mammalian cells or other micro-organisms.
.
Spectrum of mech, - .only myco.
mycobacteria an resistant.
.
If used alone myco. develop resistance against it
very rapidly C’- never used alone (except for
preventive’Rx xp in certain specific situations).
Always used with one more agent atleast,
: 1
Rt:,.-;:
'
■
.
Some atypical
.- .
Clinical Pharmacology
.
readily absorbed from the GIT - nearly always.
administered by the oral route
,
Aluminium containing antacids - interfere with
absorption.
*
There is no conclusive evidence of a difference in
therapeutic efficacy or in the incidence of toxicity
related to rate of acetylation of INH in Pts receiving
the drug every day.
3
.
a large oral dose —> peak serum level of 10—15
ywg/ml in 1-2 hr (GG - 3-5yUg/ml _n 1-2 hr).
.
widely distributed in all body tissues including
pleural effusion and CSF.
.
penetrates caseous tissue and macrophages, thus
effective against intracellular organisms.
.
t|
•
Meta.
INH
-
rapid inactivators
-
slow inactivators
-
0.5 - 1.0 hr.O GG
070 min
2-4 hrs.
( 3 hr,
In liver.
N-acetyltransferase
—-—-------- —-------- —3 Acetyl isoniazid —>
acetylation
excreted largely in the urine,, small amount
excreted unchanged.
Imp : In pts with severe renal failure (creatinine
clearance
lOml/min.) and slow inactivators
dosage
modification necessary, monitor
Plasma levels of
INH.
It is not clear whether dosage adjustment is
necessary in Pts with impaired hepatic function, although
there is some evidence that serum isoniazid levels are
increased in chronic liver disease.
*
Importance of Genetic (Acetylator status).
In vitro - myco. exposed to inhibitory concentrations
of INH for 10 h or morelose viability. But ifbthe
inhibition is short-lived they slowly recover the
capacity to synthesise mycotic acid. This observation
may explain the loss of therapeutic effectiveness of
INH in pts, who are rapid in activators and who are
R-xeti by intermittent dosage regimens. If the doses are
spaced too far apart i.e, less often than twice weekly.
In contrast, the neurotoxic effects of INH are
more likely to occur in slow inactivators who have
a greater tendency to accumulate the drug, particularly
those treated by high dosage intermittent regimens,
and some authorities advocate the administration of
prophylactic pyridoxine to all patients receiving
INH therapy in order to prevent possible neuropathic
side-effects;
It has been suggested that hepatotoxic meta
bolites are more likely to accumulate in rapid
inactivators who would therefore be more liable to
isoniazid induced hepatic neo ?osis, but measurements
have
shown that the actual exposure of rapid
inactivators to the relevant compound, acetylhydrazine,
is no greater than that of slow inactivators, and
clinical studies confirm that there is no increased
risk of hepatic toxicity among rapid inactivators of
INH whether treated with INH alone or with a combi
nation of INH and rifampicin.
A dminist rat i on & Dosage :
Normally administered by mouth, either as tablets or as a
syrup/elixir. Also IM ./ those who are vomitting or /inj. for
unable to take oral Rx.
i
Dose in adults
:
5 mg/kg - max, 300 mg as a single daily
dose,
Children (since tolerate higher doses) 10-15 mg/kg.
For pts on twice weekly regimen :
15 mg/kg.
“(give 10 mg/g pyridoxine to all pts taking INH in order
to avoid possibility of neuro-toxic side effects. R.B. Cole) - personal view.
This precaution is particularly important in adults
receiving large doses of 10 mg/kg or more of INH/d or
in those who may be predisposed to peripheral neuropathies
by other conditions such as alcoholism or malnutrition.
£
Slow release INH preparations (matrix INH) have
been studied in an attempt to provide an effective onceweek'ly intermittent regimen, but these have proved unsatis
factory'.' the blood cone, achieved in rapid INH inacti
vators are’ inadequate except with doses which would be
likely to cause toxicity in slow inactivators.
Toxic Effects :
Neurotoxic effects - dose related, more likely to occur
in slew than in rapid inactivators.
.
Peripheral neuropathy - due to pyridoxine def,
of
excessive excretion of pyridoxine in pts receiving INH
-respond to pyridoxine Rx - tingling in legs/feet and
occasionally in hands.
CNS effects - dizziness(related to high dose), insomnia,
restlessness and memory loss (at ordinary dose), may ppt
fits in previously stable epileptics, excessive overdusagc—> acute psychosis, convulsions and coma,
Occ - muscle
pains, arthropathy, and "frozen shoulder".
Hypersensitivity reactions - not common - occasionally
fever or skin rashes. It is one of the drugs which can
induce the syndrome of SLE - though this is rare, anti
nuclear antibodies can be found in a substantial proportion
of pts —■> vasculitis.
*
Pyridoxine (15-50 mg/d) - especially in malnourished,
predisposed to neuropathy, (i,e, elderly,, pregnant
women, diabetics, alcoholic. and uremics) - G.G.
A
Other toxic effects
Haematological reactions
(agranulccy^csis, "ecsihcphilla, thrombccytopesia,
metha ine-. -glcbinemia, tinnitus, urir. xy retertion (G.Gj
Most important reaction is hepatctcxicty usually
occurs as a reversible asymptomatic elevation of serum
transaminase, occasionally manifests as clinicdL
jaundice proceeded by git symptoms, rarely leading to
massive hepatic necrosis. Hepatotoxicity may occur at
any time during the cause of INH therapy in approximately
20% of individuals who receive the drug and in about
5% it has to be withdrawn
of developing hepatoce
llular damage. In the great majority of pts the
abnormalities subside without any alteration in the INH
regimen, and it is usual to persist with treatment unless
the serum glutamic oxalacetic transaminase (SGOT) value
exceeds 5 times the upper limit of normal or if symptoms
and signs of hepatitis develop.
The development of INH hepatotoxicity does not
correlate with the plasma drug concentration and is
probably unrelated to be due to an allergic phenomenon
for which the exact mechanism is at present undefined,
INH is commonly administered concurrently with other
hepatotoxic antitubercular drugs, especially rifampicin,
and most evidences suggest that rifampin hepatotoxicity
is enhanced by INH, particularly in slow inactivators
who have higher INH serum levels.
Drug Interactions ;
Concurrent administration of INH inhibits the
metabolism of DPH—-?.<■ e^sed serum levels —>CNS toxicity
(disorientation, drowsiness, lethargy, ataxia, nystagmus,
psychotic behaviour and coma) INH interferes with the
parahydroxylation of DPH which is the raxe-limiting step
in DPH metabolism, exact mech. is not known. Slow acetyl* r'rs are more at risk, but not invariably so :
laIn practice, dosage reduction of DPH from 300 to
100-200 mg daily is indicated if clinical signs of toxicity
are encduntered, and if facilities are available for
measuring serum DPH cone, it is advisable to avoid
levels y 20 jig/ml.
Clinical Use ;
*
Most widely used of the anti-TB agents
.
effectiveness
.
cheapness and
.
relative lack of toxicity
of its
It is part of most regimens for TB,
Use in prevention :
Used as a single agent in the preventive
of~‘rffi~"( sometimes called "disease prophylaxis"),
in which chemotherapy is given to individuals who show
evidence of infection although there is no sign of disease
at that time. The use of INH alone for chemoprophylaxis
has only very rarely led to the emergence of resistant
strains of M. tuberculosis. Eased on the code of practice
6
recommended, by the American TF°racic Society and the U.S.
Public Health Service Centre for Disease Control joint
statement
' ■The indications for preventive therapy with INH can be
categorised as follows :
1.
Household contacts of an active case of TB,
2.
Radiological evidence of apparently inactive TB,
3.
Positive tuberculin reactors : either recently converted
from negative to positive within the past two years or
with increased susceptibility to the disease •,« of
complicating factors such as long term corticosteroid
or immunosuppressive therapy, D.M. or silicoses, or
below the age of 35 years who have not received BCG
vaccine.
The reason for giving preventive INH therapy to
positive reactors below the age of 35 years is based on the
argument that these individuals have a relatively high risk
of developing active disease but little likelihood of
suffering INH hepatotoxicity, which occurs mainly in older
age groups.
Single chemotherapy with INH also has a place in
the Rx of progressive BCG infection, which rarely compli
cates BCG vaccination. Such cases are usually characterised
by regional lympl ol< nitis and localised abscesses.
Treatment with INH in the usual dosage for 3 months is
sufficient to control the infection.
2• Rifampin (Rifampicin)
•
Semi- synthetic derivative of the antibiotic rifamycin B.,
which was isolated from streptomyces mediterrance.
.
Of established importance in anti TB chemotherapy.
of its effectiveness in short-c©urse treatment
.
One
.
Besides TB, also useful in Rx of a wide range of
bacterial infections and some systemic mycoses,
k
of the. main drawbacks - high cost.
Mechanism of actionj
.
bactericidal
acts by inhibiting the activity of DNA-de pendent
RNA polymerase, which is the enzyme responsible
for catalysing the polymerisation of certain
ribonucleotides into RNA molecules, a step which
transfers genetic data from CNA to RNA. The
selective toxicity of rifampin depends » upon the
relative insensitivity of mammalian RNA polymerase
to the drug.
7
Bactericidal for both intracellular and extracellular
org.
.
* Spectrum of action ;
.
.
Highly active against M, Tuberculosis and M.Leprae.
active against gram positive cocci including peni
cillin and methicillin-resistant S. aureus and
against Neisseria species.
,
lower degree of activity against gram negative bacilli.
.
potential synergistic action with trimethoprim
against gram negative pathogens and with amphotericin
B against fungi (under investigation).
Primary resistance to rifampicin is low but resi
stance develops rapidly during therapy among most micro
organisms which are initially sensitive, usually resulting
from a single, large-step mutation which alters the confor
mation of DNA-dependent RNA polymerases and prevents
rifampin binding. In the therapy of TB, it is therefore
always used in combination with other drugs,
*
Pharmacology ;
.
readily absorbed from the G.I.T., but the presence of
food diminishes absorption and rifampin is therefore
usually administered on an empty stomach.
.
A normal oral dose of 600 mg — -> peak blood level of
about 7 Ug/ml after 1.5-3 hours and effective therapeu
tic levels are maintained for 12-24 hours,
.
The drug is widely distributed in all body tissues
including CSF and pleural exudate, and because it is
1i_pid soluble it penetrates cells and k'i'lIs intracellular
microorganisms. About 85% is protein bound
.
t 1/2 - 1.5 - 5 hrs, increased in presence of h jpatic
damage. Decreasedin pts receiving INH concurrently
who are slow inactivators progressive decreased t
in
first 14 days due to induction of hepatic enzyme.
.
partly deacetylated in the liver and is excreted in the
bile in both the deacetylated form' and as the unaltered
drug. The latter is reabsorbed and recirculates through
the liver, but the metabolite is very largely excreted
in the feces. Eventually about 60% of the drug is
excreted in this way. Slight accumulation may occur in
patients with hepatic dysfunction due to cirrhosis,
suggesting that care should be exercised in the use of
rifampin in the presence of liver disease.
,
Rifampin induces hepatic metabolising enzymes, includ
ing those responsible for its own metabolism, leading
to a gradual reduction in the serum half-life during
the first week of therapy, but this is insufficient
to alter the therapeutic effectiveness of the drug
and no dosage adjustment is necessary.
.
Rifampin and its deacetylated metabolite are also
excreted to a lesser extent in the urine, but it does
not accumulate in patients with impaired renal function
and no reduction in dose is indicated.
—s 8
* Administrat ion and Dosage _£
.
Normally h given by mouth in a single daily dose in the
early morning 1 hr before breakfast.
.
Usual dose in adults is approximately 10 mg/kg body wt.,
often standardised to 450 mg/day in those weighing^
/ 50 kg and 600 mg/day for the remainder. In children
the recommended dose is 10-20 mg/kg upto a maximum of
600 mg/d.
.
also used in intermittent twice weekly anti TB regimens
using doses of 600 mg or 900 mg twice weekly.
Toxicit’
Although rifampin can cause a wide range of adverse
effects, they are relatively infrequent, and only rarely do
they necessiate the withdrawal. They includethe following:1.
G.I. disturbances = nausea, abdominal distension,
epigastric discomfort and diarrhoea which seldom require
a change of therapy.
2.
Drug-induced hepatitis, difficult to attribute specifi
cally to rifamp-n; • the drug is commonly used in combi
nation with other hepatotoxic agents, notably INH,
transient elevation in liver enzymes during early weeks
or Rx, subsides spontaneously whether Rx is cont. or
not.
Ccc. increase in serum bilirubin or clinical jaundice,sign for immediate withdrawal.
Jaundice more likely to occur in elderly, in alcoholics
or those with pre-existing liver damage, but the risk of
hepatitis in patients with normal liver function appears
to be slight.
3.
Hypersensitivity reactions
rare. Rashes,
urticania
itching of skin., redness and watering of eye, may occ.
require witndrawal. Anaphylatic shock can also occur.
4
Neurological symptosm = headache, drowsiness, dizziness,
and ataxia - occ. rarely - acute psychosis.
Several other imp. adverse reactions are largely
but not entirely confined to patients Rxed with high bLsskz
dosage intermittent regimens or who take their Rx irregularly
with long intervals between doses.
These effects include the following :5.
An influenza-like reaction ('Flu syndrome"), characterised
by fever, chills, muscle aching,nausea and vomitting,
may come on several weeks or months after the commence
ment of Rx, usually, ppted 1 or 2 hrs after the ingestion
of a dose. It subsides spontaneously after a few hours
but recurs with subsequent doses and is much more common
in patients on once weekly regimens who are taking higher
doses, i.,e,. 1200 mg cr more. It is attributed to an
9 :-
immunological reaction, preventable by cent. Rx which is
thought to result iha in neutralisation of rifampin
antibodies. This can be avoided by reverting to daily
a dmini st rat i on.
6.
Thrombocytopenia—-—?bleeding■(with high-dose intermittent
Rx, appears to have an immunological basis. Contra-indicated
if thrombocytopenia observed,
7.
Renal failure with intermittent Rx or when resumed after
an interval. Usually due to acute tubular necrosis which
may have an immunological basis, since high titres of anti
bodies to rifam have been observed. Withdrawal of rifam
—>recovery of renal function, but further use of rifam
is contra-indicated,
teratogenicity
Potential- _ ' 'U
-unknown, best to avoid the use of
Rifam during pregnancy. It crosses placenta.
8,
*
9.
Other biological effects£
(Which are of interest but which do not appear to
affect the clinical use of the drug. )
.
Immunosuppressive effects on both humoral and cellmediated immunity, readily reversed after R-x is
disc ontinued.
.
Associated with light chain proteinuria in the
majority of patients.
.
Harmless reddish discoloration d£ the urine and faeces,
sometimes also affecting tears, saliva and sweat
(due to both active drug and metabolites) - warn the
pt., in order to allay unnecessary anxiety,
* OTPS Interactions :
(appears after 5-8 days of admin.
and persists fcr 5-7 days after
stopped)
Rifam----- ■* induction of hepatic microsomal enzymes
responsible for drug metabolism------ —=» increased rate of
elimination of several important drugs if administered
concurrently with them. They are -
1 .•
Warfarin, leading.to the need for an unusually high
dose to maintain effective anticoagulation
2.
Tolbutamide, digitoxin, quinidine, propranolol,
metoprolol, clifibrate, ketocanazole
3.
Corticosteroids.
4.
Oestrogens----- -^menstrual irregularity and unwanted
pregnancy in pts taking OC agents.
absorption
Concurrent admn. of PAS impairs the
?
car ful spacing required (8-12 hrs).
5.
* Suppresses T cell function and cutaneous hypersensitivity
tuberculin. Immunosuppresseht observed in animals but not
delitarious effect in humers.
10
* Clinical Uses :
3.
.
Primary role in Rx of mycobacterial infections in
combination with other chemotherapeutic agents.
.
rifampicin - INH combination - essential element in
most of the successful short-course regimens.
.
Used in Rx of pts who did notreceive the drug during
initial therapy, in Rx of extra-pulmonary TB i.e.
IBM, Rx of Ii.f, due to atypica mycobacteria like
M. Kansasii.
.
Not used in Rx of pulmonary infections due to
strepto/staph though effective . . of availability
of o t'nereffective antibiotics, •. its use can —>
delay in
of underlying TB or---- >> development
of resistant bacteria.
.
Legionnaire's dis. that fails to respond to erythro
mycin or tetracycline since Legionella pheumcphilia
is highly susceptible.
.
multiple-resistant pneumococcal pheumonia
.
resistant staphylococcal endocarditis
.
preventive Rx of nasopharyngeal carriers of meningOy
cocci,
.
Leprosy.
Ethambut ol /
.
The value of ethambutol in the initial treatment of
TB is wall established and the drug is used in most
of the current standard regimens.
,
Synthetic, tuberculostatic agent, discovered in 1961
.
Adv : relatively cheap, low toxicity, effective
by oral administration,
»
M/A - uncertain, thought to inhibit RNA synthesis
by mycobacteria.
* Spectrum of Activity :
.
limited to my-cobacteria only
,
primary resistance of M, tuberculosis to Etham
is low, but increased when used alone, /.used in
combination with one or more other effective anti-TB
agents.
" Clinical Pharmacology :
about^ 80% absorption orally, remainder excreted unchanged
in feces.
.
P.O. 25 mg/kg—> max. serum cone, of 2-6 ug/ml after
2-4 h —0»4 ug/ml at 10 hr. elimination naif-time 4 h, in pt with normal renal function.
11
70% of ingested, dose excreted unchanged by the kidneys
and upto 15% metabolised to inactive compounds
excreted in urine.
Widely distributed in body tissues but therapeutic cone.
achieved in CSF only in presence of meningeal inflammation
Mammalian cone, in RBC 1-2 times more than in plasma,
thus RBC serve as a depot ' for Etham.
preferentially, concentrated in RBC and about 20-30%
protein bound.
Administration and Dosage :
Administered by mouth in a single daily dose of 15-25
mg/kg body weight in adults and children
10 years
< 10 years —35 mg/kg in order to achieve peak
serum ccnc. of y 2 pg/ml, (Note: in tils dose the risk
of ccular toxicity and the difficulty of recognising it
in small children must be remembered).
Commonly used in the first an 2 months of combined
anti-TB Rx in a dose of 25 mg/kg body weight and is then
either stopped or in seme regimens maintained at a lower
dose of 15 mg/kg throughout the continuation phase of
Rx in order to decrease the risk of ocular toxicity
which is dose related. Still to be on safer side, use
15 mg/kg dose even during initial therapy, since it has
provdd to be clinically effective (R.B. cole).
.
Modification of dosage essential in pts with renal
failure
elimination is largely dependent upon
renal function.
.
This can be achieved by giving the usual dose of 25 mg/kg
at interval of
-
36-48 h when creatine clearance 10-50 ml/min.
48 h or large if creatine clearance <10 ml/min.
estimation of serum ethambutol ccnc. desirable as a
guide to dosage - aim at obtaining (max. not > 5 pg/ml at
2 h, declining to 0.5 |ig/ml before the next dose.
.
Clearance increased by peritoneal and haemodialysis
dosage supplementation necessary.
* Toxic Effects ;.
M IMP .adverse effect -
Retrobulbar Neuritis.
•—> progressive loss cf peripheral vision cr impaired
visual acuity, particularly to green,—
central scotoma
12
Optic neuritis - incidence 1% when d^cse is 25 mg/kg initially
for 2 months and then 15 mg/kg or maintenance (custemary
regimen), 5% when higher dose continued for 6 months.
changes usually but net always reversible on withdrawal
of the drug
Guod to carry out a comprehensive optholmomolo.gical
examination periodic check up and monitoring of vision,
reporting of any visual disturbance promptly.
.
Other complications - rare
peripheral neuropathy independent of INH Rx.
nephrotoxicity, reversed on withdrawal.
Hyperuricemia - quite common .'. of decreased renal
clearance of uric acid —^occ. pptn. of ac. gout.
-
allergic skin reactions.
* Clinical Uses ;
.
important component of combination Rx, especially in
the initial phase of therapy in standard xf 9 month
regimen.
.
If does not contribute significantly to 6-month short
course chemotherapy, and in this role it is less
effective than pyrazinamide in preventing relapse.
.
effective in twice--weekly interminent chemotherapy
when combined with INH after a 2 or 3 month initial
phase of daily triple therapy.
.
usually INH alone is used for chemoprophylaxis, but
some clinicians prefer to use a combination of INH and
Ethambutcl, especially in pts from a community in which
prevalence of INH resistance is high i.e. Asians.
In the chemoprophylaxis of contacts of patients with
INH-resistant TB it has been suggested that ethambutcl
may be used as an alternative preventive agent.
,
Ethambutcl is effective in Rx of TB infections resist
ant to other chemotherapeutic agents and is used
successfully in treating some atypical mycobacterial
infections, such as those due tc M. Kansasii.
Pyrazinamide"
* sythetic pyrazine derivative of nicotinamide.
,
bactericidal in vitro
.
though bactericstatic activity of Pyrazinamide was
recognised as long age as 1952, until recently its use
has largely been confined tc the Rx of infections
resistant tc the standard drugs,
of its low in
vitro activity and significant record of hepatotoxicity.
But in the last few years there has been increasing
clinical evidence to suggest that pyrazinamide can make
an effective contribution tc 6-mc-nth regimens possibly
by using it only during the first two months of
**
Other toxicity ; pruritus, joint pain, GIT upset, abdominal
pain, malaise, headache, dizziness, mental confusion,
disorientation, ha lire in'th on„
at a slightly acidic. 'pH.
13
combined Rx, The role of PZ therefore is undergoing
reappraisal, and it appears that the risk of hepatitis
from the use of PZ in these short-course regimens is
much lower than was suggested by earlier studies, in
which larger doses were used for longer periods,
.
PZ - a synthetic derivative of nicotinamide.
.
No antimycobacterial activity at neutral pH, but it is
effective against phagocytosed living tubercle bacilli,
presumably due to the acid pH within macrophages.
.
effective only against M. tuberculosis which rapidly
develops resistance to PZ unless the drug is used in
combination with other effective anti-TB agents.
Clinical Pharmacology ;
.
readily and nearly completely absorbed rrom
.
single oral dose of 20 mg/kg---------- C max of 65 ug/ml
within 2 hours. (45 mg/ml at 2 h, 10 ug/ml at 15 h) - GG.
*
2
=
GIT.
6 h,
.
penetrates into liver, kidneys, lungs, therapeutic levels
in CSF in ,TBM.
.
active drug and meta (pyrazinoic and 5~hydroxypyrazinoic
acid) filtered by glameruli, Nearly all of the unchanged
drug reabsorbed from renal but' tubules while meta
excreted in the urine. Urinary cone. 50-100 ug/ml for
several h. after a
.
pyrazinoic acid decreases tubular secretion of uric acid
which leads to hyperuricemia „.d occ. to clinical gout.
.
accumulates in jaundiced pt, suggesting that it is
metabolised in liver.
Administration and Dosage ;
.
Early trials - daily dose of 40-50 mg/kg——
Unacceptably high incidence of hepatitis—> clinicians
discarded it as a first, line drug.
.
more recent assessment ---- > revision of view.
Risk of hepatic toxicity is small when lower doses are
used in 6-month regimens of combined chemotherapy
(Hong-Kong trials).
,
Now adult daily dose 20-55 mg/kg. in 2-3 divided doses,
0.5 gm tablets available, commonly 1 g. bd or
0.5 g tds.
,
In intermittent regimens, 40-60 mg/kg 2-3 times a week
or even 90 mg/kg once a week without serious incidence of
side effects.
Toxicity ;
:
MIMP adverse effect of PZ is its tendency to cause hepa
titis. Effect-dose related u. Symptoms of hepatitis,
£iver enlargement and rarely death due to hepatic necrosis
-: 1 4
-
in pts Rxed for 3-6 months with PZ in the dose of 40-50
mg/kg/d i.e. 3 g/d.
.
Incidence of hepatitis decreased with dose of 2O~35^mg/kg
although an increase in hepatic enzyme levels in upuo
9% pts.
.
If is sensible to avoid use of PZ in people with impaired hepatic function
withdrawal the drug if SCOT increase very much
during the course of Rx,
advise pt to report prompty all S/S suggestive of
he pat ic t ox ic ity.
,
Arthralgia - mainly of shoulders,knees, fingers - common.
i Increase serum uric acid in patients on daily therapy.
Usually improves spontaneously after a few weeks, aspirin
appears to be more effective, than allopurinol
in Rxing
it symptomatically.
.
Concurrent PZ and probenceid
affects tubular excrericn
of uric acid and may enhance urate retention.
Others; anorexia, nausea, vomiting, dysuria, malaise,
fever.
* Clinical Uses ;
.
Use of PZ in primary Rx of TB witji modern short-course
chemo, regimens throughout the world both with daily
and intermittent Rx, highly encouraging and the incidence
of troublesome or serious toxicity has been small with
dosage used now.
.
More evidence on the drug's toxicity is needed to show
whether PZ has a place in routine anti-TB regimens.
.
At present PZ is occ. used in the technically advanced
countries for the Rx of TB infections resistant to more
a effective and less toxic agents. In developing
countries where drug-re sistqnt TB is more common,
satisfactory results have been obtained in Rx regimens
using PZ in various drug combinations with ethionamide
and cycloserine and with PAS and streptomycin.
*
5 • St re pt ocyc in
Until the introduction of rifam. and etham. into routine
anti TB and Rx within the last few years, SM with INH and
PAS provided a standard chemotherapeutic regimen which
was reliable and highly effective.
First clinically effective drug to become available
for Rx' of Mist. TB - from 1947-52 - only effective
agent available to Rx TBr
15
Usual course tas all 3 for initial 2-4 months,
stop SM at this stage, cont. remaining 2 ' until a total
duration of 18-24 months.
Now Rifam + INH + Etham.
But SM still used -
1.
When oral drugs cannot be administered
2.
In Rx of infections resistant to other drugs but
sensitive to SM,
3,
In Rxing large pulmonary lesions with cavity,
4.
In some short-course regimens.
5.
In some completely supervised twice-weekly regimens
especially when the administration of the injection
provides an excuse or supervision of concurrent oral
therapy in out-patients who cannot .be relied upon to
take medication.
Need for IM inj
toxicity
0 Sufficiently serious drawbacks of SM
(’ to discourage its use for Rxing
pulm TB when the other drugs arereadily available, but
amongst poorer population and in developing countries
where cost is a highly important consideration in the
choice of Rx, SM still appears to play a useful and
relatively inexpensive part in short course and supervised
intermittent regimens.
6• Thiacetazone ; ’
Although more’ toxic and rather less effective than the
others, TZ currently has a place among the first-line
anti TB drugs in developing countries
of its
cheapness.
*
,
A thiosemicarbazene, fairly active against M,.tuber,
.
Toxicity - considerable variation in different communities
- due to differing standards of observation or
interpretation,
.
Resistance emerges during course of Rx. unless TZ is
used in conjunction with atleast one other effective
anti TB agent.
,
Well absorbed from the gut.
150 mg P.O.
Cmax of
2
1pg/ml in 4-6 h, 20% excreted unchanged in the
urine.
Administration and Dosage ;
.
adult dose - 150 mg as single daily dcse, administered
with INH (300 rag) as a single tab. Twice weekly
(intermittent regimen) dose = 450 mg TZ + INH 15 mg/kg
twice a week.
16
*
.
Incidence of toxicity low in above doses.
.
Commonest side effects - aiorexia, nausea, vomitting
and occ, diarrhoea.
Ototoxicity
dizzness and rarely
to ataxia. BM depresion
agranulocytosis & anaemia.
Allergic slrin reactions (not usually serious) but occ,
Steven -J h ison syndrome & e foliative dermatitis which
necessiate withdrawal of drug. Hepatitis also reported
but may be due to companian drug i.e. INH.
Clinical Uses £
,
The only indication for using TZ in the primary Rx of
pulm TB is in developing countries where cost is the
predominant factor in determining the choice of TB Rx
programme.
,
Widely used in Africa and Asia, usually combined with
INH in a daily oral regimen lasting 18 months with SM
for the first 4-8 weeks. / 90% success with this regimen
in East Africa, but less effective in Singapore, and
more toxic.
/greater
than
TZ has a possible role in twice weekly interminent Rx
of pulm TB, but e ineffective in short course regimen.
SECOND LINE DRUGS ;
.
More toxic and generally less effective than the firstline drugs .'. use largely confined to the Rx of
infections which are resistant to the usual anti TB drug.
,
As with the other drugs, resistance is likely to emerge
during Rx unless atleast one other effective drug is
used concurrently.
1•
Para-aminosa licy lie Acid (PAS) :
.
Until recently PAS was an essential component of the
"classical" antituberculosis regimen, which also
included SM and INH, but it has now been displaced
from standard chemotherapy in the developed countries
by Etham and Rifam, which produce fewer side effects
and fewer interruptions of Rx.
,
bacteriostatic, effective only against M, tuber, and
occ. strain of M. Kansas!!, MTC - 1 ug/ml,
.
m/a - competitive antagonism with PABA—> inhibition
of synthesis of microbial folate---- -> inhibition of myco
bacterial growth, (similar to sulfonamides) specific for myco.
.
Well absorbed from gut, widely distributed in the
body including the pleural fluid and caseous tissue.
.
tj^ - 0,75 h
4g- — -^75 ug/ml in 1.5 - 2 h.
acetylated in liver, excreted in urine.
17
■t ”l/2
increased in presence of impaired renal function,
avoid in severe renal failure.
Usual daily dosage in adults
doses, often combined with INH.
*
-Side.
.
12 g given in 2 divided
feet s_y_
Major - GIT irritation - ' anorexia, nausta, vomitting,
abdominal pain, diarrhoea in 25-40% cf cases, decreased
when taken with food, this effect -•
>do.creased
pt compliance.
Others :
generalised malaise, joint pains, sore threat,
skin eruptions cf various types, leucopenia
agranulocytosis, eosinophilia, lymphocytesis,
thrombc-cytopesia, ac. haemolytic anaemia.
lymphadenc-
.
Hypersensitivity reactions - Fever, r-a$hs>s .
pathy, eosinophilia, in 5% pts.
.
Hepatitis
.
Others - BM depression, hypokalemia, (secondary to GIT
disturbances) and goitre.
hepatic necrosis may occur.
2 • Cycloserine ;
.
an antibiotic with a bacteriostatic effect against
mycobacteria and some other organisms i.e, E.Coli.
.
m/a - inhibition of bacterial cell wall synthesis.
.
Well Htezer absorbed from gut, widely distributed
through out the body tissues, including CSF.
.
Excreted in the urine - 2/^^d as unchanged ana
.
Accumulates in pts with impaired renal Fn. needing
dosage adjustment if necessary.
.
Usual dosage in adults - 250 mg bd, increased to 500 mg
bd in seriously ill pts - but higher dose may not be
tolerated due to nephrotoxicity.
as■ unidentified metabolites.
Toxicity can decreased by adjusting the dose to give
plasma levels not / 30 pg/ml.
-greater than
.
MIMP AIR ; on CNS - headache, insommia, trnntois,
convulsions, various psychotic disturbances, incidence
of mental/neurological toxicity - 16% in pts receiving
500 mg/d. (Hong-Kong study). Rarely peripheral
neuropathy.
.
Contraindicated in epileptic pts, use cautiously in those
with mental disturbances such as depression or anxiety.
Toxic symptoms resolve when cycloserine is discontinued.
18
*
3, Ethionamide ;
•
,
derivative of isonicotinic acid
.
bacteriostatic against mycob, tuber but little activity
against other mycobacteria.
.
well absorbed after oral administration and widely distri
buted in tissues, reaching significant cone, in CSF.
metabolished
largely
in liver,
1% excreted unchanged in urine.
.
.
*
available as tabs of 125 & 250 mg. Usual adult dose
250 mg bd, which may be increased to a maximum of
1.0 g/d. depending on the pt's ability to tolerate the
GIT side effects. This can be minimised by taking with
means or as a single bedtime dose.
Others :
Severe postural hypotension.
,
Most common - anorexia, nausea and vomiting, metallic
taste,
,
depression, psychological disturbances - quite common.
.
Neurological symptoms - headache, restlessness, visual
and olfactory disturbances, tremors, convulsions, and
peripheral neuropathy have been reported.
.
Allergic skin reactions, gynaecomastia, alopecia,
.
hepatitis - particularly in diabetics.
.
teratogenic in animals .1 avoid during pregnancy.
C max - 20 p.g/ml in 3 hr. after 1.00 g P.O.
Propionamide - n-propyl derivative of ethio, with
similar anti TB activity and equivalent toxicity,
no advantage over ethiaonamide,
»
Capreomycin ;
,
polypeptide antibiotic derived from streptomyces
ca pre olus.
.
bacteriostatic action against M. tuber with some in vitro
activity against uhx other mycobacteria.
.
effective against organisms resistant to the more
commonly used anti TB drugs.
.
cross resistance between capteomycin and viamycin
is the rule
, and it frequently occurs between
capreomycin and kanamycin.
.
oral absorption unsatisfactory,
I M inj,
.
Adult dose of 1 gm------ >
administered by
Cmax of 30 ug/ml in 2 hrs.
•
50% excreted unchanged in the urine - remainder meta
but mode 2 site of inactivation unknown.
*
daily dose - 15 mg/kg (adult 1 g) by a single IM inj.,
usually for a period of 4-6.months;
.
dosage reduction advisable in pts with renal dysfn.
•
*
5.
*
.
rather similar to those of SI4
.
Nephrotoxicity - protein, casts and cells in urine,
uremia and renal K+ loss
hypokalemia.
.
.totoxicity - vertigom tinnitus, deafness.
likely to occur in the elderly.
.
allergic reactions - eosinophilia, fever, rashes.
More
Viomycin
.
bacteriostatic against M. tuberculosis which is
1/4M — 1/2 that of Streptomycin,
.
obtained from stepto. puniceus.
.
effective against SM - resistant organisms,
exhibits cross resistance with capreo. and Kana.
.
nose : by im
, daily dose of 1-2 g, for a period of
3
2weeks and thereafter in doses of 1-2g,2 or 3 times
per week.
A ER ;
.
vesticular disturbances, deafness,
.
nephrotoxicity
.
allergic reactions.
\ -
Noteavoid the use of viomycin in conjunction with other
ototoxic, or nephrotoxic drugs, such as kanamycin and
capreomycin, although it has been used successfully with SM.
.
Therapeutic efficacy of viomycin appears to be low.
TREATMENT OF PULMONARY TUBERCULOSIS :
,
Before the availability of Etham-and Rifam, the "Classical”
regimen of chemotherapy for TB included - SM, INH & PAS.
SM - daily by inj for 2-3 months with INH & PAS.
then INH + PAS in twice daily regimen for period
upto 18 months, for 12 months in mild infections
and 2 years in case of severe cavitary disease.
This type of therapy provided (l)
guard against chance resistance of organisms
against one of the drug.
20
2)
conformed with the concept of two phases in
chemotherapy - an initial period of
intensive drug therapy when the bacillary population
is large, followed by a less intense phase of
continuation therapy when the number of organism
has substantially decreased.
,
This regimen was highly successful when properly super
vised and it has been the standard against which modern
regimens have been measured.
•
Disadvantages ?
Ill M in j, of SM
lengthy dependence on pt compliance and
significant toxicities of PAS & SM
.
In developing countries - similar regimen was used where
150 mg of TZ substituted PAS as a comparion drug to
INH
of its relative cheapness.
,
Benefits of Etham, & Rifam,
-
greater efficacy
J
permitted introduction
of shorter and less
toxic, regimens.
S
Also led to the introduction of a wider variety of
regimens of Rx which allow greater flexibility in
circumventing adverse effects, improving supervision by
means of intermittent administration and shortening the
duration of therapy.
.
Cardinal rules of therapy - unchanged i.e.
requiring careful attention to detail in the
application of an approved regimen and
skilled supervision' throughout the duration of
therapy to ensure that drugs are taken as prescribed.
*
Standard Chemotherapy ;
In U.S.A , daily oral INH + Etham for 18 months + daily
IM of SM fcr first 3 months in the case of extensive
cavitary lesions or if the pt comes from an area wks.se
where drug resistant infection is prevalent.
Accepted modifications
1.
For extensive dis. - oral rifampin & INH may be used
throughout instead of the 3 drug regimen.
2.
If parenteral therapy is necessary during the early
stage of Rx, a combination of SM and INH may be used
for the first 3 months (Streptc-erbazide).
3.
PAS is preferable to etham as a companion drug to INH
in young children », * of the difficulty of recognising
visual toxic symptoms, in this age group.
21
:-
4,
INH with Etham is the preferred combination for the
Rx °f TB in pregnancy,
of possible teratogenic
effects of Rifampin,
*
In Australia : a rather similar regimen, ini.tial.tydaily
drug
3therapy with INH & Rifam + either SM or
Etham, given for 2-4 months, followed by continuation
Rx with INH and Rifam to complete 18 months.
'
In Britain :
9-month short-course regimen.
(see below)
* Intermittent Chemotherapy
.
The main indication for intermittent chemo is in the Rx
of individuals who cannot be relied on to take daily
Rx unsupervised but who can be interviewed once or twice
weekly and watched while they take their drugs,
,
generally speaking intermittent regimens are less toxic
than daily ones; and they can be combined with short
course chemotherapy (see below) to produce regimens
which are highly effective in urban populations where
every dose is supervised.
.
Intermittent chemo can be successful, if given through
out the course of Rx, even in short-course regimens of
only 9 months, but at present most authoritaesfavour an
initial phase of intensive daily therapy followed by a
twice-weekly continuation regimens.
.
some drugs, such as INH, are unsuitable for once weekly
administration, and twice-weekly regimens are currently
considered safer and more effective. The advantage of
three-weekly schedules have yet to be defined.
.
Recommended intermittent regimen in USA ;
daily conventional Rx for 1-4 months, followed by
twice weekly INH 15 mg/kg orally + 25-30 mg/kg
IM or INH 15 mg/kg + Etham 50 mg/kg - both orally
- maintained for 18 months.
*
.
Recent reoorts show that prolongation of intermittent
regimen beyond 1 yr is unnecessary when fully supervised.
.
The twice weekly combination of INH 15 mg/kg + Rifam
600 mg with or without an initial phase of daily Rx,
has produced good results with a low level of adverse
effects, although intermittent rifampin in higher dosage
is more likely to cause systemic reactions,
Short,-Course, Chemotherapy ;
Advantages (Fox & Mite hi son)
,
reduction in cost of Rx
,
reduction in chronic drug toxicity
of drug used is less.
,
improvement in patient cooperation
,
improvement in surveillance of Rx
,
diminished likelihood of relapse if pts default early from
the Rx.
total quantity
22 :-
Various experimental studies to determine and compare
the frequency of bacteriological relapse in chemothera
peutic regimens ranging from 4-12 months.
Rec ommendat iQii :
INH 300 mg
0
(adopted in UK)
Rifam 450-600 mg
Q
daily for 9 months
Etham 15-25 mg/kg or $
Strepto
(
daily for 1 st
2 months
Note; - The use of streptc instead of ehham for the initial
phase"of Rx is equally effective but leads to a greater
incidence of s ide-f f feet s.
Shorter f treatment regimens lasting 6 or 4 months
have shown considerable promise and are particularly
relevant in developing countries where the problem of
cost and the difficulties of lengthy supervision are
overriding c cnsiderat ions.
Streptomycin + INH + Rifam + Pz
daily for first 2 months,
followed by a continuation phase
of daily INH + Rifam for 4 months
$
J
0
Q
Q
Singapore trial,
highly successful,
When cont. phase reduced to 2 months, relapse
rate 8-24%,
Most recent development - in order co decrease the costs
inconvenience and toxicity of anti TB chemo has been
the trial of 3-month and 2-mcnth regimens of daily
SM
INH + Rifam + PZ for the Rx of pts for whom the
.diagnosis of pulm TB seems likely on clinical and
radiological grounds but for whom microscopy
sputum reveals no AFB. Observations after 1 year of
follow-up suggest that those with negative cultures
show a very low incidence of subsequent relapse if Rx is
stopped after 2 or 3 months, but in those with
positive cultures the incidence of relapse was at a
level which would generally be regarded as unacceptable.
The potential of these observations lies in the
possibility of safely • stopping Rx at 3 months if
the initial cultures have proved negative, but a
longer period of observation will be needed before
reliable conclusions can be drawn.
Combination of iritermitent Rx with short-course chemo
provides an alternative choice of regimen which
minimises the total drug load and permits full
supervision of every dose.
A high level of effectiveiiess has been . obtained
by giving SM + INH + Rifam + PZ daily for an initial
phase of 1-2 months followed by a continuation phase
consisting of twice weekly SM + INH + PZ to a total
Rx duration of 6-8 months.
USA trial - unsupervised
INH 300 mg
Rifam 600 mg
followed by
daily orally for 1 month
23
INH 900 mg
Rifam 600 mg
0
J twice weeklY for a further 8 months.
Further work necessary to demonstrate the
superiority of this type ,pf regimen over others.
* Management :
.
of Pulm TB
Objective eradication of infection in every person
with active disease by administering a therapeutic
regimen of proven efficacy for its full duration.
The objective should be to achieve success with the
least possible disturbance in the normal life of the
pt or his family.
Major management problems to be considered are •
*
(1 )
Choice of regimen
(2)
Selection of patients for hospital Rx
(3)
Supervision of therapy and
(4)
Retreatment chemotherapy.
Choice of Regimen :
In the routine management of pulm TB the initial
regimen is customarily a standard schedule of Rx which
has been shown by trial and experience to be effective in
that population. Preliminary assessment is necessary to
identify any factors which may give rise to modification
of the standard regimen.
Such common factors
Modifying factors
.
Modification recommended
Previous anti TB chemo
Retreatment regimen, if pssx
possible with-hold Rx
until sensitivities of the
infecting micro ascertained.
Pt originates from an
area where resistant
organisms common.
Always use 3 drugs in the
initial phase of therapy,
or until sensitivities
ascertained.
Unstable social background . consider fully supervised
due to psychiatric domestic interminent chemo regimen.
or financial difficulties
,
Pregnancy
Avoid rifampin during the
first trimester.
,
Serious disturbance of
vision young children,
and the aged.
Avoid ethambutol.
24
,
Impaired, renal function
Modify dosage of SM,
Etham. & PAS, or
avoid use,
.
a-Eipaired hepatic function
Avoid rifam or monitor
hepatic enzyme cone.
Once the decision is made the patient should be fully
informed of the nature and duration of the therapeutic
regimen to which he is submitting himself, including
the possibility and character of adverse effects,
so that he can adjust to the constraints which will be
placed on hem and learn the importance of strict
adherence to the Rx schedule.
*
Selection of patients for Hospital Treatment ;
Hospital admission at the start of therapy is not
necessary for the routine management of pulm TB,
but certain categories of patients are best treated
in hospital initially. They include the following :
Very ill patients requiring supportive therapy
and nursing care
2)
Uncooperative patients - with unfavourable
social or domestic circumstances, h/o poor
cooperation, mental disturbance, alcoholism, or
drug addiction. Hospital admission is usually
necessary for the duration of the intensive
initial phase of Rx which preceedes a fully
supervised out-patient intermittent continuation
phase.
3)
Patients with drug resistant disease who require
Rx with second-line drugs of high toxicity.
4)
Infections patients with highly susceptible
domestic contacts such as tuberculin-negative
children or family members with impaired immuno
logical defence mechanisms.
Imp, :
There is strong evidence to show that the risk of
infection to contacts is minimal once the index case
has started Rx.
The choice between hospital and out-patient therapy
must depend on the individual circumstances of the
patient and the facilities which are available in the
E& location for safe and efficient ambulatory case.
*
Surveillance of Therapy ;
Imp ;
The aims of treatment supervision be clear -
1.
To ensure adherence to the recommended regimens.
2.
To detect evidence of adverse effects as early as
possible;, and take corrective steps if indicated.
25
3.
To monitor recovery by regular examination, smear,
and culture examination of sputum, including
sensitivity testing if compliance is suspect, and
radiographic examination of chest.
4,
To terminate Rx as soon as the approved regimen
has been completed.
.
Most physicians with experience, develop their own
schemes for treating pulm TB for achieving these
objectives which suit local circumstances.
.
Follow-up of the patients is a must, because the
maintenance of an unbroken therapeutic regimen becomes
increasingly important as treatment schedules are
shortened and the total number of doses is progressivelyreduced.
.
If is probably safe to discharge the patient from
further follow-up, once an approved regimen of Rx is
completed, provided that the physician is satisfied
that compliance has been good and there is adequate
bacteriological, clinical and radiological evidence
of successful treatment.
.
Only patients who are known or thought to have had
irregular chemotherapy or an inadequate duration of Rx
should be followed for a limited period, but routine
chest radiography, or sputum cultures rarely lead to
the detection of reactivation disease, almost all
cases presenting with symptoms. The discharged
patient must therefore be. encouraged to return to the
clinic promptly if he develops symptoms that might
indicate a relapse.
Retreatment Chemotherapy ;
Recurrence of infection during or after a course of
anti TB •
chemotherapy calls for a careful reassessment
to determine the reasons for treatment failure.
Causes of Treatment
Failure in Pulm TB
Failure
.
.
Cause
Infection with resistant
micro-organisms
.
Choice of an inadequate
regimen
.
-
previous ineffectual Rx
primary resistance,
most common in develop
ing countries.
-
Single drug therapy
One or more drugs given
in insufficient dosage
Inadequate duration
of Rx,
26
Failure of adherence
to the prescribed
regimen
Inadequate explanation
and/or supervision of
therapy.
Intolerable side effects.
Therapeutic errors such as single drug Fix, insufficient
dosage, or inadequate duration of therapy are common
in developing countries and have led to a substantial
pool of resistant organisms in some countries.
Primary resistance to one or more anti-TB drugs
occurs overall in / 1 0% of infections in the highly ^less thai
developed countries but the rate is considerably higher
in developing countries and immigrant populations from
such countries.
A much more important reason for treatment failure is
lack of cooperation with the recommended regimen, and
the great majority of failures is found among individuals
of low intelligence, vagrants, alcoholics, and drug
addicts.
In planning the retreatment of patients who have had
previous chemotherapy it is therefore necessary to take
account of the ethnic and geographical origins' of the
individual, the social background, and the precise
nature and duration cf earlier treatment. The current
sensitivities of sputum cultures should be obtained
to enable the. optimal drug regimen xo be determined,
and in general no Rx should be given until the results
of reliable resistance tests are available.
The following principles provide a guide to
the successful chemotherapy of patients with resistant
infection :
i.
Patients should be assessed prior to Rx for
possible increased risk of hepatic or renal
toxicity, and close men iter ing for adverse
effects should be maintained throughout, including
measurements of plasma drug levels where necessary.
2.
Treatment should begin with atleast 3 drugs to
which the organisms are known to be sensitive,
using the most effective of the available drugs
and taking into consideration their potential
for toxicity in any given patient.
3.
Drugs should be administered under strict super
vision, initially in hospital. A parenteral drug
is useful when patients progress to outpatient
therapy since it provides an apportunity for
supervising pill swallow.ing when the patient
attends for injections.
27
4,
5.
Frequent tests of sputum microscoj.y culture and
drug susceptibilities be made during Rx.
more than
Prolonged therapy for / 18 months may be required
and adjunctive surgery is occasionally indicated.
Since most patients vi.th drug-resistant disease have
acquired it •,- of failure to adhere to previously
recommended Rx, the success of Rx depends to a very large
extent upon the establishment of a sympathetic
relationship between doctor and patient.
(Paper prepared for Rational Therapy Cell of LCCOST)
Dp- 30-.D—
n 7?
41st ANNUAL CONVENTION
CATHOLIC HOSPITAL ASSOCIATION OF IND^A
23-26 NOVEMBER 1984
WORKSHOP THEME
'Eternal vigilance is re.wired to
ensure that the health system
does not get medicalised, that the
doctor-drug producer axis does
not- exploit the people and that
the abundance of drugs does not
become a vested interest in ill-health'.
----- ICMR/ICSSR Health for All Report.
Venue: ST JOHN’S MEDICAL COLLEGE, BANGALORE 560034
SIGNIFICANCE OF THE THEME
2
THE Workshop is to help participants understand the
issues relevant to drug prescribing, drug distribution
and pharmacy policy in our institutions in the context
of the ICMR/ICSSR warning and to challenge them to
participate in the growing national response to
the problem.
WHAT does the ’abundance of drugs' mean to the millions
of the poor in our country who struggle in life to
make both ends meet? Can they ever have access to the
modern health care system which has become a business
today, rather than remaining at the service of humanity
at large? Do they have essential and life saving drugs
at their reach within a price range they can afford?
IS our drug policy today more profession-oriented, drug
industry-oriented rather than patient-oriented? Whose
interests are we serving in our institutions?
HOW can we move towards a more people and patient-oriented
drug policy?
THESE are some of the QUESTIONS which we shall respond to
in our Workshop.
ooooooooooooooooooooooooooooooooooo
"Community Health is a process
of enabling people to exercise
collectively their responsibi
lities to maintain their health
and to demand health as their
right. Thus it is beyond mere
distribution of medicines,
prevention of sickness, and
income generating programmes".
—CHAI new vision
OOOOOOOOOOOOOOOOOCOO ooooooocooooooo
OBJECTIVES
1.
3
TO CREATE AN AWARENESS 0?ti
the health situation in India, the role of drugs
in health care, the pattern of drug production
in India vis-a-vis the people's health needs, the
dynamics of the drug industry, the pattern of drug
distribution and availability in the health system,
the national drug policies and laws.
2.
TO CREATE AN AWARENESS OFsirrational use, over use and misuse of drugs by
health personnel.
3.
TO DISCOVER
the social, economic, political, cultural and
. other factors responsible for this problem.
4.
TO DISCOVER
how all of us are part of the problem at a
personal level.
5.
TO CONSIDER
the various responses at national/regional levels
in the areas of s— consumer awareness and people's
movements; continuing professional education;
pressure group on policy makers; search for low cost
alternatives; individual/group action; institutional
policy changes.
6.
TS DISCOVER
ways and means by which we can respond to this
situation at individual, institutional and
regional/nati.onal levels.
4
PROGRAMME HIGHLIGHTS
^Sessions on:
Understanding the problem
Drugs and the healing ministry
Towards rational therapeutics
What to do to tackle the problem
Some initiatives in the country
The people 1s medicine
:iGroup discussions on:
What/why the problem in our health institutions?
What can we do to tackle this problem?
niLiturcry
Reflecting on our calling and the faith dimension
of our response
i;^Exhibition on
Socio-political dimensions of Health and Drugs
Rational Drug Therapy
Home remedies and Herbal medicines
\;^Studies ons
Drugs for a Community Health Center'
Understanding the injection/tonic culture
Use/misuse of drugs in surgery
Drug situation in small rural hospitals
Cost of treatment
^Cultural Programme
Understanding the problem from the poor man's
point of view.
5
SYNOPSIS OF PAPERS
Drugs for Primary Health Care (c M Francis)
An integral part of our commitment to primary health care is
the provision of essential drugs to all those who need
them, in adequate quantity and quality and at affordable
prices wherever the person is. The various aspects of
the drug problem needing our attention include production,
what drugs are required, choice of drugs, National Drug
Policy, selection of drugs, drug production and procurement,
logistics of supply, quality control, regulating the drug
trade, drugs for immunization, drugs for cure, drugs for
symptomatic relief, search for new -drugs, drug information
and the need for evaluation of the efficacy of primary
health care including drugs.
The Ten Commandments of the Drug Industry (Augustine Veliath)
1. Thou shalt have tens of thousands of drugs
2.
Thou shalt not question the price of a drug
3.
Thou shalt not tamper with nature's garden
4.
Thou shalt respect they doctor more than thyself
5.
Thou shalt betray thy people and thy nation for petty rewards
6.
Thou shalt not covet, court, or subscribe to any other
system of medicine
7.
Thou shalt never reveal company secrets
8.
Thou shall first seek remedies for fashionable ailments
9.
Thou shalt be a dumping ground for banned drugs
10.Thou shalt be a guinea pig for new and untried drugs.
6
The Ethics of Prescribing (George Lobo, sj)
Discusses reasons for the unfortunate situation related to
drugs prevalent today, viz., technological model of
health care leading to manipulation of the patient,
search and demand for instantaneous cure of symptoms,
mystification of medicine, profit motive and 'free
enterprise1 of the pharmaceutical industry, a deep
rooted cultural alienation from the people, exploitation
of dependent developing countries, decreasing emphasis
being given to preventive medicine and other systems
of medicine.
The use of drugs should be regulated by the principles of
totality (overall good of the patient) and of double
effect (the good effect overriding any harmful effect).
It suggests remedies for the development of a personcentred and holistic approach to health care.
Professionals in the Church - an introspection (George Joseph)
Serious questions have been raised about the institutional
witness of the church in India, particularly its
relevance in the social context of today. In the case of
the Healing Ministry there is urgent need to critically
look at our priorities and commitment and our style of
functioning in the light of the gospel. The role of the
professionals have to be reassessed as part of an
overall effort to bring back the true spirit of 'Diakonia'
into this ministry.
The whole issue regarding the need for evolving a 1 rational
drug policy' has to be seen in this perspective.
7
What is Rational Drug Therapy? (Mira Shiva)
Rational drug therapy means practice of socially
conscious, relevant, concerned and yet scientifically
sound medicine. It recognizes the non-role of drugs
in certain conditions, the role of alternative systems
of medicine and recognizes the limitations of Western
Medicine ;» our social context.
It emphasises selective use of drugs based on essentiality,
efficacy, safety, easy availability, easy administration,
quality drugs preferably of indigenous production.
Rational Drug Therapy recognizes the concept of essential
drugs and the concept of graded' essential drug lists for
different levels of health personnel. It recognizes the
right of health personnel and consumers to drug information
and its effective communication„
It is taking of a conscious decision to boycott certain
drugs and use others only when needed. ~t means
prescription with awareness, to avoid as far as possible
— iatrogenesis (drug induced problems, drug interactions,
adverse drug reactions and emerging drug resistance).
It is understanding the role of drugs and rational drug
therapy in the emerging health movement.
What can be done at a pharmacy level (Alan Cranmer)
(a) Management of Pharmacy Services include involving the
users of the service; the Pharmacy Committee - its
constitution and functions, viz., implementation of
hospital policy, selection of medicines, sources of
medicines, cost versus quality, basic drugs and formula
tions, medicines banned In India and abroad, medicines
from other systems; stock control; prescribing
discipline and pharmacy discipline;
Good dispensing services involve need for good
professional service to patients, proper presentation
of patient's medicines, preparation of medicines in
the pharmacy compared to purchase, medicines in the
pharmacy and at clinic level.
contd..
8
(c)
Relationships with suppliers, ie., with representatives
in the pharmacy and an assessment of products offered
and their sources.
(d)
Educational requirements - basic courses, legal
requirements, course content, continuing education for
pharmacists.
(e)
Relationships with hospital colleagues.
INITIATIVES IN THE COUNTRY
(1)
Arogya Dakshata Mandal, Pune has been raising awareness
about drug related issues among medical professionals
and the lay public since the past 8 years. They publish
a monthly—''Pune Journal of Continuing Health Education' —
on drug issues and are also bringing out a book >
'Rational Drug Therapy' in December 1984.
They launched a movement called 'Operation Medicine’ in
1977 against irrational prescription cf vitamins, tonics
and tinned foods.
(2)
All India Drug Action Networks A number of groups have
been working in the field of drug related issues at
various levels during the past 3-4 years. They have
been in contact with each other and have been working
informally together sharing information, putting forward
a memorandum (demanding a Rational Drug Policy),
participating in campaigns, lobbying with government etc.
In August 1984, they felt the need to have a more organized
base and have formed the All India Drug Action Network.
CHAI is also a member of the Network.
(3)
Lok Vigyan Sanghatana, Maharashtra, or the People's Science
Movement have launched campaigns about anaemia and
irrational anti-anaemia drug preparations and also about
over the counter drugs. They organize jathas, hold district/
town seminars, write in the mass media etc.
(4)
Kerala Sastra Sahitya vanished is a voluntary non-government
organization consisting of scientists, doctors, engineers,
social scientists, teachers, students, workers, peasants,
technicians who arc committed to popularising science and
channelising it for social revolution. The KSSP has recently
decided to take up the Drug issue and Initiate a big campaign
to expose the anti-people and exploitative tactics of the
Multinational Drug Companies. The questions of essential
versus non-essential and dangerous drugs, the inadequacy
of drug safety control measures, the rising prices cf
life saving drugs and the non-implementation of the Hathi
Committee recommendations are the highlights of the
programme.
10
(5)
LOCOST or Low Cost Standard Therapeutics is a collective
voluntary enterprise for rational therapeutics. LOCOST
aims to promote low cost, scientifically tested medicine
under generic names. LOCOST is a response to a growing
demand and challenge of the voluntary health sector to
meet the needs of the deprived sectors of the society
for not only low priced but also good quality medicine.
LOCOST includes procurement, quality testing and control,
distribution and educational efforts, and is located in Gujara
(6)
Bangarapet Mission Tablet Industry in Karnataka is a
successful small scale venture providing low cost, good
quality formulations to some mission hospitals in the
country.
(7)
Low Cost drugs and Rational Therapeutics Cell of the
Voluntary Health Association of India, New Delhi, has
been instrumental in bringing together various groups in
India on the issue of drugs. They have been providing
informational backing to these groups-, organizing meetings,
informally coordinating some actions etc.
(8)
medico friends circle is a group of socially conscious
individuals, interested, in the health problems of our
people. Through their monthly bulletin-, they discuss
drug issues among others. They have formed a Rational
Drug Policy Cell and have launched a campaign on antidiarrhoeals.
(9)
The Kurji Holy Family Hospital Formulary is the result
of the accumulated experience of the hospital over the
last 10 years. It gives a comprehensive, list of drugs
to treat 98% of the hospital admissions. It also gives the
generic name, dosage, indications, contra-indications
and side effects of these drugs. Information about
comparative cost of treatment is also provided.
11
(10)
State Forums; During the past year drug action forums
have been active in Andhra Pradesh and West Bengal.
Drug Action forums are also being initiated in Gujarat
and Orissa.
(11)
The Pharmacology Department.of__thc Post-Graduate Institute
of Medical Education and. Research, Chandigarh, provide
unbiased technical information on drugs and therapeutic
through a monthly publication 'The Drugs Bulletin'.
(12)
Others; The following organizations have also been
involved in drug related issues and are part of the
All India Drug Action Network;
Consumer guidance Society of India, Bombay
Consumer Education Research Centre, Ahmedabad
Federation of Medical Representatives
Association of India
Health Services Association, Calcutta
Delhi Science Forum, New Delhi
People's Participation in Science and Technology,
Madras/Bangalore
Centre for Science and Environment, Delhi
Centre of Social Medicine and Community Health,
J N University, New Delhi
W hat
we
can
do ?
— Support them
— Join them
— Keep them informed about what you arc doing
12
RESOURCE MATERIALS
Hi People, Pills and Prescriptions, column in MEDICAL
SERVICE since May-June 1984.
iii Objectives of the Workshop, a handout.
iii Understand. ng the Drug situation in our Hospitals,
a check list.
iii Towards a People-Oriented Drug Policy, Special
Convention Issue of MEDICAL SERVICE (October-November
1984) and a supplement to this issue will be
distributed during the Workshop.
iii Druos awareness and Action, mfc BULLETIN Special Issue
No.107 November 1984.
iii DECCAN HERALD Supplement on the Workshop.
'What people really need, first
and foremost is clean drinking
water, latrines,
school and
land, not urban hospitals with
their wonder drugs".
— Planning Commission
COOOOOOOOOOOOOOQOOOOOO'‘OOOOOCOOOOOGOOOO
AN INSPIRATION
13
Reading
The story of the sickman
at the pool of Bethsaida
John 5: 1-9
Reflection
The action of Jesus in bypassing the pool is an
Invitation to us to look more critically at
our own h<iilth care system. Thanks to our
emphasis on curative health care, we have grown
accustomed to thinking solely in terms of the
health needs of the- individual rather than addressing
ourselves to the community as a whole. While
concentrating on the symptoms, we have failed
to take into account the environment and other
social factors. Poor sanitation, polluted water
supply, the superstitious beliefs and taboos
of the community are also related to sickness and
disease.
Further, the miraculous pool in its ineffectiveness is
a symbol of our own ineffective health care system
despite the highly qualified doctors and nurses,
well equipped private and public hospitals, medical
research centres and multinational drug industry.
The dooi man in tho gospel story lived very close to
the pool, yet he was helpless because of his
poverty. In like manner the poor in our midst
remain helpless in the shadow of an expensive,
curative health care system that is geared
exclusively to the service of the rich.
Sources The Bible; Aspirin or Dynamite
by Cedric Rebello s.j.
PGIS
LocosT
a voluntary effort
for the use of the correct
medicine
PRESCRIPTION GUIDANCE AND INFORMATION SERVICE
Low Cost Standard Therapeutics (LOCOST) was founded with the goal of
promoting rational drug therapy. We seek to promote this by two major
activities : (a) supply of good quality essential drugs under generic names
and (b) educational efforts.
The Prescription Guidance and Information Services (PGIS) of LOCOST is
an educational effort to promote awareness about the correct use of
medicines. PGIS is therefore for the benefit of both prescribers as well
as patients.
WHY THIS SERVICE ?
The average patient suffers from a lack of information. In addition he,'she
perceives the doctor as a high priest of a magic cult. The patient also has
almost unquestioning faith in the power of drugs, tonics and injections. The
doctor on the other hand, has his/her own compulsions and limitations,
compulsions which make doctors yield to social/peer pressures and current
fads of prescribing certain types of drugs. Quite often even senior doctors
from reputed institutions are Known to respond : “ Dr. X gives this drug to
his patients. I know it is irrational but if I do not do the same, I will
lose my patients ". A scientific attitude to healing is thus sacrificed and
that too at the expense of the patient.
An added [imitation is that doctors quite often do not have the time to
update their madical and pharmacological knowledge. A major source of
drug disinformation are the drug companies. Through various subtle and
not so subtle means, they use medical representatives/agents to persuade
doctors to prescribe quite often, irrational brand name combinations. Again
the patient as the end user is the one who suffers by way of irrational
( and sometimes harmful ) prescriptions. PGIS is an attempt to restore this
gross imbalance in the healing process, a process in which the patient is
more an active than a passive participant.
Two main aspects of PGIS being proposed are :
(1) Information dissemination to doctors who write prescriptions, and
(2) Guidance to the patients regarding the correctness and use of medicines
prescribed in a particular condition.
LtHIOST
THE PGIS CELL
1st Floor, Premanand
Sahitya Sabha Hall,
Opp. Lakadi Pool,
Dandia Bazar,
LOCOST has identified a number of expert doctors' in the Baroda Medical
College and a few from outside also. At least two experts in each of the
common specialities have been included in this cell. They will respond to
the various requests .through LOCOST.
BARODA-300 001
PRESCRIPTION INFORMATION
the medicines does not have
It is often found that the person who is prescribing
enough access to the latest information regarding the disease and related drugs. The
PGIS cell will respond to requests for information relating to the use of a particular
drug. In all such cases, it will be assumed that the diagnosis made by the prescriber
is correct, unless the prescriber specifically requests for assistance in diagnosis also.
THE APPROACH TO PRESCRIPTION INFORMATION
The individual requests should be routed through
LOCOST office. Only in cases of
emergency, the Coordinator. PGIS, may be contacted directly. Attempt should be made
to send the requests in writing to LOCOST. The PGIS Coordinator and the experts
concerned will be in turn consulted by LOCOST. The names of the persons concerned
i.
e. the doctor who sends the request and the experts who give the advice will be
kept completely confidential, if required.
An attempt will also be made to approach the doctors working
in
institutions.
Prescriptions from such doctors, if requested, will be discussed in person or at group
meetings organised by the institution. One or more experts from the
PGIS cell will
attend these meetings and the pros and cons of a particular prescription will be
discussed in detail. In such cases we would prefer, if.the prescriptions to be discussed
along with other related information is given well in advance. (In case a group meeting
is being held, LOCOST will require a notice in advance )
♦
PRESCRIPTION GUIDANCE
The objective here, is to help the patient, the end user of medicines to know the
correctness of the medicines prescribed. The PGIS will give comments on following
aspects of the prescription : correct medicine for a particular diagnosis, adequacy of
the trea'ment, the uselessness or harmful effects of
any medicine, the. side effects of the medicines
required, the dosage, alternatives available both in
terms of cost, quality and nature of medicines, etc.
Whereever possible, other aspects of the therapy
will also be explained.
This will help the patient by developing an under
standing regarding the treatment given to him/her.
This will also equip the patient and relatives or
friends to questionand to ask for more information
from prescribers in future. Thus the ultimate aim is to build up consumer awareness
and initiative to bring about a change towards more rational therapy.
THE APPROACH TO PRESCRIPTION GUIDANCE
1.
The patient (or the relative/friend) sends the prescription with relevant details
to LOCOST. ( See Box below ).
2.
The prescription will be critically studied by LOCOST's PGIS cell. The PGIS
cell consists of a group of expert doctors who are conscious of rational
therapy practices.
3.
The PGIS Cell will send its comments on the prescription to the prescriber
for his/her reactions Modificatons if necessary, will be made based on the
prescriber's reactions. If no response from the prescriber is received within 10
days of sending comments, then the comments will be passed on to the
patient.
4.
The copy of the final comments will also be sent to the prescriber. (Note :
Suitable modifications of the above procedure wiil be made as and when.
For instance, if the patient does not want the comments and his/her identity
revealed to the doctor the PGIS Cell may defer the comments to the doctor
by say one to two months However, requests by patients that the doctor
be not informed at all, will not normally be acceded.)
INFORMATION NEEDED FOR PRESCRIPTION GUIDANCE
While sending the request to LOCOST the patient would be required to give
the following information :
(a)
Name and address of the patient;
(b)
Name and address of the prescriber to whom a copy has to be sent;
(c)
Age, sex, history of the patient and symptoms at the time of consultation
of the doctor;
(d)
Diagnosis (preferably written on the prescription in the doctor's own hand);
(e)
List of medicines with dosage taken before the current prescription (past
six months);
(f)
Details of iabora’ory tests, x-ray tests, special procedures and medicines
prescribed by the current prescriber, those taken by the patient and results
of the same;
(g)
Any other relevant detail/document (copy to be enclosed);
(h)
Original prescription or photostat copy.
(i)
Present condition of the patient.
A COLLECTIVE EDUCATION
In conclusion, PGIS is a person-to-person service that would hopefully lead to
collective awareness about the correct use of medicine. The collective awareness
could then result in collective action and programmes in many other areas of drug
policy and other issues in health.
LOCOST is aware of the limitations of PGIS : Personal examination of the patient
may not be feasible, the scope of PGIS may not cover all diagnostic situations
as also the fact that a large number of 'successful' treatments may not be touched,
and so on and so forth. The service may not be useful for the patient as it will take
at least 10-15 days to give a balanced view on
the prescription. However, queries by doctors for
information can be attended to faster. In cases
of exceptional emergency, the PGIS coordinator
will decide about the mode of response and
communication depending on the merits of
each case
LOCOST is keen on not encouraging legal battles
between the pat'ent and the doctor. PGIS is a
beginning, a collective effort to facilitate
awareness, education and action. Action towards more rational therapy and towards
conserving scarce resources of patients as well as that of the community.
AN INVITATION
LOCOST is also prepared to facilitate prescription/medical audits of hospitals, dispensaries
and community health projects, if so requested. You may be a like minded doctor, a
patient or a person simply interested in social change. We seek your cooperation
and collaboration. Please spread this idea. Put patients ard doctors in need in
touch with us. Write to us with your views.
Contact us at : Prescription Guidance and Information Sei nice (PGIS)
LOCOST
1st Floor, Premanand Sahilya Sahha Hall
Opp. Lalcadi Pool, Dandia Bazar
Baroda-390 001.
LOCOST is a non-profit trust
Other ntnjor programmes of LOCOST include : (a) Supply of generic
drugs to voluntary groups, (b) Promotion of quality awareness among preseribers and users.
(c) Research on issues in community pharmacology, (d) Documentation and dissemination of infor
mation on community health issues.
Product Information Sheet
LoeosT
LOW COST STANDARD THERAPEUTICS
G. P. O. Post Box No. 134, Vadodara-390 001.
Generic Name :
Mebendazole.
Some Brand Names :
Presentation :
Wormin, Idibend, Mebex, etc.
Tablets of 100 mg.
Pharmacological action : Broad spectrum anthelminthic drug effective against most of
the common worm infestations. Acts by inhibiting glucose uptake irreversibly in worms.
It does not alter the glucose level in host.
Therapeutic indications : Single or mixed worm infestation with round worm, hook-worm,
thread worm and whipworm. For hydatid cyst with prolonged treatment.
Dose in adults : In roundworm, hookworm and whipworm infestations : 1 tablet two
times a day for 3 days continuously. It may be repeated after 3 weeks if necessary.
For threadworms, 1 tablet once only.
Dose in children :
To be repeated after 2 weeks.
Remains same as above.
Use in pregnancy :
Should not be used in first 3-4 months of pregnancy.
Use in lactation :
Quite safe.
Use in Hydatid cyst :
Precautions :
400-500 mg. 3 times a day for 21-30 days.
Should not be used in patients allergic to Mebendazole.
Contraindications :
None.
Adverse reaction : No systemic toxicity. Transient
diarrhoea may occur with massive infestations.
abdominal
pain,
nausea
and
Instructions to patients : No fasting or purging is necessary before or after treatment.
Personal hygiene instructions must be given.
Note :
All possible contacts may also be treated for worms.
Overdose :
No overdose toxicity.
Significant interactions :
None.
References :
1,
Goodman, Alfred Gilman et al : The Pharmacological Basis of Therapeutics, Macmillan
Co. Inc. New York. 1980, Sixth Edition.
Publishing
2. Lawrence, D. R. : Clinical Pharmacology, 1980, Fifth Edition.
3.
Satoskar, R. S. et al : Pharmacology and Pharmacotherapeutics, Popular Prakashan, Bombay 1983,
Eighth Edition.
This medicine has been tested for quality by LOCOST in
laboratory.
a
reliable and independent
V>jl. 3o.it,
I
L.
(COVER STORY)
HE. .LTH ACTION
RATIONAL, DRUG USE
The Probler_
Drugs arc the hallmark o£ Modern Medicine. The
'healing professions' throughout the aces have
always used 'natural’ or ’synthetic’ products
for their medicinal value, to treat various
common ailments of people. Drugs, however, have
never in the past dominated the medical scene
as they have done in the second half of this
century. Today, the ’rill for every ill
*
culture is well established. It has ensured
that we are probably the most 'drugged
generation’ of all times. Not a very healthy
thoughtJ
Throughout the centuries, philosophers, social
activists and concerned doctots have warned
against the dangers and problems of overuse,
of misuse^of drugs by doctors and the people.
"The physician who sets about to treat
a disease without knowing anything
about it is to be punished even if he is
a qualified physician; if he does not
give proper treatment, he is to be
punished more severely; and if by his
treatment the vital functions of the
patient are impaired, he must be
punished most severely."
—Koutilya Arthashastra
"Physicians prescribe medicine of which
they know little, to cure diseases of which
they knot? less in human beings of which
they know nothing."
—Voltaire, 18th century
"The incidence of disease cannot be
manipulated and so increased sales
volume must depend at least in part
on the use of drugs unrelated to
their utility or need or in other
words improperly prescribed. Human
frailty can be manipulated and
exploited and this; is fertile
ground for anyone who wishes to
increase profits."
—Kefautfer Committee Hearing
on Drugs, USA
"I believe that Modern Medicine
treatments for disease are seldom
effective and they are often more
dangerous than the diseases they are
designed to treat.
I believe that modern medicine has
gone too far by using in everyday
situations extreme treatments designed
for critical conditions.
I believe that more than ninety
percent of modern medicine could
disappear from the face of the
earth—doctors, hospitals, drugs—
and the effect on our health woulu be
immediate and beneficial.
—Dr Mendelsohn, Confessions
of a Medical Heretic, 1980
“There are two types of physicians—
those who promote life and attack
diseases; those who promote diseases
and attack life.
—Charaka Samhita
THE INDIAN SITUATION
The Indian Council o£ Medical Research and the
Indian Council of Social Sciences Research set
up a joint study group to study the health
situation in India and evolve an alternative
strategy for our commitment to ’Health for All
by 2000 AD."
This high powered expert committee
had some very interesting things to say about the
present situation of drugs and prescribing
practices, in their Report published in 1981.(1 )
*
"There is now an over-production
of drugs (often very costly) meant
for the rich and well-to-do while
the drugs needed by the poor people
(and these must be cheap) are not
adequately available. This skewed
pattern of drug production Is in
keeping with our inequitous social
structure which stresses the
production of luxury goods for the
rich at the cost of the basic needs
of the poor......
* One of the most distressing aspects
of the present health situation in
India is the habit of doctors to over
prescribe glamorous and costly drugs
with limited. medical potential. It is
also unfortunate that the drug producers
alv.’ays try to push doctors into using
their products by all means—fair or
foul. These basic facts are mor
*
responsible for distortions in drug
production and consumption than anything
else.
*
Eternal vigilance is required to
ensure that the health care system does not
get me'Realised, that the doctor-drug
producer axis does not exploit the people
and that the abundance of drugs does not
become a vested interest in ill-health."
These warnings are a serious indictment of the medical
profession and the drug industry in the country. It
confirms the growing evidence that drugs are being
pushed on an unsuspecting public by devious
methods which masquerade as 'sales promotion
*
of drug companies and ‘professional prescribing
practice’ by doctors and health workers. All
of us who are committed to 'Health
*
need to be
concerned about this situation. The promotion
of a 'Rational Drug Use1 by the medical
profession and health -..orkezs and ultimately
by the consumers—the patient community and
the public is an Important item on the agenda
of HEALTH ACTION.
Irrational Drug Use—seme dimensions
To understand the principles of Rational Drug
Use, one needs to first identify and appreciate
the elements of irrationality in the present
situationA spate of reports appearing in our
newspapers and periodicals highlight these
elements.
Of all of them, however, the
report of the recent ’Lenten Commission' and
its shocking findings are the most telling.
Irrationality in drug use arises out of three sets
of factors
*
A.
Irrationality in drug production, marketing
and availability
Bo
Irrationality in prescribing practices of
doctors and health workers
C.
Irrationality in drug use by the consumer public
All these taken together result in the' situation we
find ourselves today.
A.
Irrationality in drug production, marketing
and availability
* Industrial policy
Drug policy continues to be part of the industrial
policy and not part of the health policy. Industrial
growth and profit margins determine the policy and
not health needs of the people.
*
abundance
There is a plethora of drugs produced in the
country. The Hath! Committee recommended 116 as
essential and. the WHO says 200 are necessary.
At present there are over 45000 formulations in
the country.
* Quality of drugs
Twenty percent of the drugs available in the
country are substandard and spurious. Many are
adulterated. Many are old and being sold after
the expiry dates are over.
Turmeric powder in tetracycline capsules and
poor quality intravenous fluids have been
reported. The substandard glycerol
*
in J J Hospital
highlighted by the Lenten report is another
example.
* Unwanted Drugs
The formulations available include the followings
i.
Banned drugss Drugs which have been
banned in many countries such as Lomotil
and Clioquinol.
ii.
Irrational combinations; Formulations
which have combinations that are
antagonistic or irrational. The Hath!
Committee had suggested weeding out of
atleast 23 such groups of preparations.
These ’..ere finally banned by a gazette
notification in July 1983 but continue
to be available.
(See Dangerous drug list—page
iii.
Hazardous or Bannable drugs»^Without
)
noi' be c<vtx.ic, bit
prescription or adequate medical supervision ..
preparations containing analgin, oxyphenbutazone
and cortico-steroids are the commonest example
(Refer A to Z of Drug use - page
iv.
)
Dru ,s promoted for indications that are
not clinically proven or are potentially
dangerous, eg. Promotion of EP Forte
combinations for pregnancy testing and
induction of abortion even when there
is well documented evidence that risk
of foetal deformity is increased by the
use of these preparations.
v„ Costly Drugs;
Drugs which are inflated
in cost by inclusion of costly., additional,
often unnecessary ingredients or by
cosmetic embellishments in manufacture and
packaging. Tonics and high protein foods
especially baby foods are good examples.
* Wrong Priorities
There is over-production of unimportant drugs or
drugs for the rich while drugs for some common
health problems are in short supply.
Tonics,
vitamins, hormone preparations and high protein
substitutes are being produced in wasteful
abundance while drugs for leprosy and tuberculosis
(two major public Health problems) are
produced at one third and one fourth of
actual requirements. Similarly Vitamin A and
many vaccines urgently required for child
care programmes art? frequently in short supply.
* Over-trie-counter s- les
Sale of drugs over the counter without doctor's
prescriptions or the necessary statutory checks
are not at all uncommon. This results from
inadequate drug legislation and even more
inadequate drug controls. Over-the-counter
unauthorised sales of prescription drugs,
which now-a—days do not even have the
precautionary product information make the situation
even more hazardous.
* Escalating Prices
Price control policies have been both inadequate
and ineffective and hence the cost of drugs has
been constantly escalating. Withyliberalization
policies of the present government ,this is
bound to increase further. The purchasing power
of majority of our patients is limited. With
increasing prices, patients are forced to buy
only part of a prescription or go in for substandard
alternatives promoted by the drug shops.
Bo
Irrational Drug Prescribing
Doctors, nurses and he ilth workers often prescribe
or administer drugs irrationally.
The types of irrational drug prescribing has been
classified
follows: (Sj
Type of irrational
drug use
1. Extravagant
prescribing
Occurs if a drug
prescribed when:
is
- a less expensive drug
would provide comparable
efficacy an-- safety
-- symptomatic treatment of
mild conditions divert
funds from treating serious
illness
— a brand name is used where
less expensive e uivalents
are available.
2. Over-prescribing
— the drug is not needed
- the cose is too large
- the treatment period is too
long
- the quantity dispensed is
too great for the current
course of treatment
3& Incorrect pr<ascribing
- the drug is given for an
incorrect diagnosis
~ the wrong drug is selected
for the indication
- the prescription is
prepared improperly
- adjustments are not
made for co-existing
medical, genetic,
enviremental or other
factors.
4O Multiple
prescribing
- two or mor-- medications are
used when one or two would
achieve virtually the same
effect.
- several related conditions
are treated when treatment
of the primary condition
will improve or cure the
other conditions
5o Under prescribing
needed medications are not
prescribed
- dosage is inadequate
- length of treatment is
too brief.
|J|...... _______ .________ (Li
Taken, from Managing Drug Supply, Management Sciences
for Kehlth, Boston/xliassachusetbs, USA
\
How docs such prescribing take- place?
There arc many background factors which lead to such
prescribing practices.
a.
trair.ir.<-,
Doctors, nurses, pharmacists and health workers
may be inadequately trained in the use of drugs.
The training may be theoretical and not geared
to the practice of prescribing in the real life
situation. Technical minutiae may be stressed
at the cost of information on cost, social
context and hazard,
b.
Inadequate continuing education
The doctor,pharmacist,nurse or health workers
in field practice are inadequately supported
by s process of continuing education by their
professional associations and training institutions.
Once graduation is over, there is little opportunity
to refresh one’s kr.o;■ledge of drugs and medical
matters through unbiased sources of information.
* c• Unethical madias! .advertising
Medical advertising of drugs has more often than
not found to be full of unproven clsimb of efficacy.
In addition.promotional literature all over the world
by the 3<sne company for thw same "rug has been found
to be vastly different. Facts are withheld or modified
Statistics are u-'.ec' in a blare’. m-nn
* :r. Drug company
sponsored misl:- formation’ is not uncommon.
Drugs Tetracycline (antibiotic used against various
infections; Lederle Laboratories)
Caution against use
U.S.A.
Adverse reaction
publicized
By infants, children;
Vomiting, diarrhoea
during pregnancy; liver
nausea, stomach
or kidney impairement
upset, rashes.
(latter can be fatal)
kidney poisoning;
or if overly
can poison fetus.
sensitive to light.
Mexico
Caution against use
Adverse reactions
publicised
By infants, children?
vomiting, diarrhoea,
during pregnancy or
nausea, stomach
if overly sensitive
upset.
to light.
Brasil
Argentina
By infants, children,
vomiting, nausea,
du ring pr c gmancy
stomach upset, rashes
None
None
Courtesy; Mother Jones, USA
d.
Prescribing for prestia.e/po'wer
Doctors especially often prescribe extravagantly as
r. sign of'prestige
*
and ’power
.
*
In India people
often consider - a good doctor to be one who gives
a long, costly prescription, in keeping with his
list of degrees. Many doctors succumb to this
cultural status symbol. A vicious cycle is maintained
thereby.
Patient, why do you take so many drugs?
I take ■ them since the doctor has prescribed it.
Doctor, why do you prescribe so many
different, similar and -expensive dings?
I proscribe. them kecau'se the patients
expect them..
e. Busy outpatients
Many or our institutions axe understaffed especially
those run by the government. The queues at the
out-patient clinic are long and there is a heavy
rush. Lack of time to make a.good clinical
judgment often results in an irrational
prescription including drugs for all eventualities.
f. Inducements by medical companies
Mif-information is not the only method by which
doctors are made to prescribe irrationally by
medical companies. Sales promotion includes a host
of practices such as unethical trade discounts,
bribes, gifts, sponsorship for conferences and
travel. The commercial proposition induces many
doctors to prescribe unethically.
Unauthorised nrescril.ln.,
Health workers and practitioners of other
non-al].opathic systems ox meficine arc often
by virtue of their training unauthorised to
prescribe all the drugs in the medical
armsiinentariurn. Health'worker may be trained to
prescribe only a few drugs. Too often they get a
larger number or drugs and dispense them to get
the; community’s approval and get greater prestige.
Many traditional medicine-practitioners, dispense
allopathic drugs with little background training
or knowledge.
Drugs as a substitute for caring
Drugs have become a symbol of the new medical
culture, where treatment is primarily drug oriented
and all other aspects of 1 caring
*
and nursing
of the patient are relegated to the background.
When simple home remedies like hot water gargles and
nursing procedures can provide relief to many symptoms
of the patients, doctor'.- prefer to prescribe
symptomatic drugs instead, thus increasing drug
consumption irrationally.
i.
-Cmtnercialization of the medical profession
There was a time not so lone, ago ..!'■• n the doctors’
profession kss.8 vocation. Aspirants to the profession
saw service to the sick and ailing .as more important
than the financial rewards they would ger., if at all
from their grateful patients. Today the situation has
chanced..drastically, Parents are willing to pay lakhs
to get their children Into me leal school. Wo such
investment would be snare if the returns were not
equally •rewarding.’ Aspirants today therefore see
.medicine as a business investment. Ir such a social
ethos 'irrational prescribing' for pecuniary benefits
■f
would not at all be pawned upon. In fact it may even
be seen as a steppinstone to success.
C.
Drug use by Consumer Public - irrational dimensions
i.
d/? 1 f-medleation; Medication by patients themselves
is net an uncommon problems. Either they are too
poor to consult doctors or because of the easy
availability of drugs they medicate themselves,
encouraged by the pharmacists, advertisements,
peer group information or advise of family members.
A..survey conducted 1 ./ the Rational Institute of
Nutrition in the twin cities of Hyderabad and
Secunderabad covering 10 percent of the 330 retail
pharmaceutical shops showed that self-medication
rate was an al ermine 46 percent.
1 i.Use ..of ur.u111 i ze<5 . drnos
It is a very common habit among the consumer public
to take a medicine, not ns the doctor has directed
but just enough to £ el better. This is often the
case with antibiotics an-' particularly for children.
Unused medicine is kept in the home pharmacy and given
to one or other of the children or family member who gets
the same symptoms, next. Unused or unutilized portion
of prescribed medicine is eft er. kepibeyond expiry date.
If proper storage precautions are not taken, it may also
get denatured. Use of such medicines is a major cause
of untoward reactions.
iii.
Inade-.-y.at-a lah<-liin.c or storage of. medicine
Medicines pr-scribed by doctors are often inadequately
'labelled by the dispensing pharmacist. Storage instructions are
are ■. not very clearly explained to the patient. The
medicine cupboard is'often a source of irrational drug
use. Children inay.hdve ac- css to it and this may lead to
accidental poisoning.
. Poor-croup exchange
iv.
Consumers of drugs often advise relatives, friends
and neighbours about the benefits a particular
prescribed drug has given them. They are
advised to take these drugs for what is
thought to be a similar complaint or disease.
This peer group exchange is often the cause
of much irrational drug use by the lay public.
v.
Status-symbol drugs
b |OJ S-ClKc-x? S
ck
Ko-u'cS Axxvfi A?^.ce-rn <2-
status symbol drugs. They are thought to be more
effective and also being costlier are considered to be
of greater prestige value. Patients often demand or
pressurise their doctors to prescribe one or more
of these and doctors often comply with the request
to r tain the patient and family in their practice.
vi.
Multiple consultations
Patients often go to many doctors seeking quick
relief of their symptoms. The doctors are not often
aware that consultation with them is one of many such
concurrent events. Generalists and Specialists may both
be consulted. Practitioners of different systems may be
consulted simultaneously. Different medicines given
by different doctors are then consumed with the hope
of getting relief. When relief does occur it is not
easy to decide which medicine brought it about.
Multiple prescriptions then become a way of
life when symptoms reccur. Many drugs may potentiate
one another,. Others may work at cross purposes. When
the consultation is of plural systems the confusion is worse
vii.Inadequate Consumer Awareness
Probably one of the key factors for irrational
drug use by consumers is the absence of awareness
of drug use, misuse and the effects of overuse.
Consumer education is next to absent in India. Due
to loopholes in the existing laws, precautionary
product information is not supplied with the medical
products. The media, the medical proles ion, the
educational system and the social welfare agencies
concentrate on the misuse of psychotropic substances
and drug abuse. Misuse, overuse or abuse of commonly
prescribed drugs is not considered to be an
adequately serious problem for consumer education.
The problem is further compounded by a large illiterate
population and for the need of such efforts to be in
multiple languages when they do get organised.
RATIONAL DRUG USE - PRINCIPLES
The irrationalities and predisposing factors promoting
unsafe drug use in our country have been described. The
challenge that faces all of us today is How to counter
this phenomena?
Health for All by 2000 AD would be an
empty slogan if we did not join and participate actively
in a consumer and professional movement to tackle
the ’irrational drug use’ problem. In the absence
of prompt efforts in thirdirection, we would probably
arrive at a situation--overabundant drugs and ill-health
for all by 2000 AD. What could be our prescription for
action?
A thorough understanding of the situation would
lead us to appreciate the following principles.(J3)
Rational Drug Use
* means practice of socially conscious, relevant
and scientifically sound medicine
* emphasises the selective use of drugs based on
-essentiality
- efficacy
- safety
- easily availability
— low cost
- ease of administration
- adequate quality
- preferably of indigenous production
recognises the concept of essential drugs and the
concept of graded lists for different levels
of health personnel
recognises the non-role of drugs in certain conditions,
the role of alternative systems of medicine in some other
conditions and recognises the overall limitations of
allopathic medicine in our economic, social and cultural
context.
accepts a conscious decision to boycott certain drugs
which arc hazardous or bannable or banned and use all
others only when they are really needed.
means prescription with awareness, to avoid as far as possible
iatrogenesis which includes—
- drug induced problems
- drug interactions
- adverse drug reactions
- emerging drug resistance
* recognises the rights of health personnel and
consumers to unbiased drug information and its
effective communication.
* understands the role of drugs in the emerging
health movement.
______________________________________ _o_
;"DB~G<ax--iiaMenal--Prug Use, Mira Shiva, CHAI Workshop
For all of us concerned about the increasing medicalisinq
of health action and the 'over abundance of drugs8 becoming
E 'vested interest in ill health* there is a phenomenal
challenge in making the above principles of Rational
Drug use barista- common knowledge
- common practice
- common commitment.
In conclusion, drugs have allayed pain and suffering over the
centuries. They have helped many live,more comfortable,
productive and meaningful lives. All or us committed to the
health movement must ensure that drugs should continue to
to play their limited but useful role in the medical
service. However, the use of drugs knowingly and
unknowingly, to make profit out of human health must stop.
And it will only if
Governments?
drug industrya/j j
planners;
he 1th professionals;
medical colleges;
pharmacy colleges;
nursing colleges;
drug controllers;
pharmacists;
journalists and medica persons;
teachers and educators;
social development activists;
consumer groups;
and
the public
commit themselves to promoting a Rational Drug Use.
References
1.
ICMR/ICSSR (1981)
Health for All—An alternative Strategy.
2.
VHAI (1986)
Banned and Bannable drugs
3.
Shiva Mira (1985)
Rational Drug Therapy
Medical Service, Vol. 42, No.l, January 1985.
4.
Management Sciences for Health (1982)
Managing Drug Supply
Boston, Masachusetts, USA
5.
Narayan Ravi (1984)
Consumer Alert—Consumer Action
Medical Service, Vol 41, No.9, October-November 1984
6.
Werner David & Bower Bill (1982)
Helping Health Worker’s Learn
Hesperian Foundation, USA.
All India Drug Action
Network (AIDAN)
All India Drug Action Network
(AIDAN) is a coordinating body of
Voluntary Health, Consumer, Science
Organizations and individuals actively
tolved in this field, from different
rts of India; set up to :
i
Work towards a Rational, Propeople Drug Policy in India and to
ii
Exchange ideas, experiences about
different aspects of alternative
practices at grass root level
pertaining to the production,
distribution, use etc. of Rational
Drugs.
PERSPECTIVE
AIDAN realizes that the health of
people depends primarily on nutrition,
sanitation, living and working
conditions, social culture..etc and that
availability of health services especially
of drugs, has only a secondary role to
play. But at the same time, in India,
where infectious diseases predominate,
>gs can save large-number of lives
and remarkably reduce sufferings. The
Rational Drug Policy, can therefore,
play an important role as part of a
Rational Health Policy. However,
during the last thirty years, along with
a rapid increase in the range and
volume of drug-production, there has
been a more rapid rise in the
irrationalities at all levels of the drug
policy (i.e. Research, Production,
Distribution, Marketing, Education
and Use) due to a lack of scientific
approach coupled with the profiteer
ing by the drug industry. Secondly
even 39 years after independence, the
«
multinational drug companies con
tinue to dominate the drug scene in
India; self-reliance continues to be a
dream. As a result, essential drugs are
in short supply, out of the reach of the
majority of the people who need them;
whereas there has been a plethora of
high-cost, useless, hazardous drugs in
the market.
There is, therefore, a dire need to
work for a Rational Drug Policy
which should have the following
objectives:
A Assessing the real drug-needs
1
To identify the real drug needs in
consonance with the health need of
the people, particularly those
required for primary health-care; to
prepare a graded essential and
priority list of drugs for different
levels of health-expertise in keeping
with actual health needs of the
people.
2
To eliminate irrational, useless and
hazardous drugs. (This has become
one of the most important problems
today).
B Production, Price and Quality
control
1
To produce and make rational
drugs available at low prices to the
people, particularly the essential
and priority drugs. Adequate
supply of free drugs to the poor
people through the state health
system.
2
To ensure strict quality control of
all drugs.
C Drug Distribution
To establish a national corporation
for the distribution of drugs;
retailing of drugs through appro
priate channels and government’s
health infrastructures.
D Drug Information & Ethical
Marketing
1
To ensure a drug information
system for health personnel and
consumers.
2
To ensure ethical marketing
3
To abolish brand names and
introduce generic names of all
(drugs)
E Self-reliance
1 To develop self-reliance in drug
technology.
2
To foster and encourage the growth
of the Indian Sector and to provide
a leadership role to the public
sector.
3
To aim at quick self-sufficiency in
the output of drugs with a view to
reducing the quantum of imports.
F Research and Development
1 To promote research and develop
ment for self-reliance and to meet
the real health needs of the Indian
people.
2 To evolve strictly ethical mode of
medical research.
G Legislation and Administration
1 To provide comprehensive drug
legislation
and
administrative
support to deal effectively with and
implement all the above aims and
objectives.
2 To ensure smooth Centre-State
relations and inter-departmental
coordinations for effective drug
production, drug control and drug
supply.
H Human Power Development
To fulfill the needs for the above
Rational Drug Policy, different
types of technical personnel (e.g.
druggists, paramedics technicians
etc) need to be adequately and
appropriately trained in adequate
numbers.
Some elaboration of these
objectives ( A to H) has been
published in the form of a 16 page
pamphlet “Rational Drug State
ment” of AIDAN and is available
for Rs. 1-50 from Dr. Mira Shiva,
Coordinator, AIDAN. A substan
tial document “A Rational Drug
Policy” (see at the end) give^fc
much more detailed account.
EVOLUTION & ACTIVITIES
Some groups and individuals
concerned with misuse of drugs came
together in 1981 and launched a
campaign against the high dose
combination of estrogen and proges
terone. The campaign proved to be
effective and the Government had to
ban this combination. Encouraged by
this success, attempts were made to
rouse public opinion against irrational
and hazardous drugs. Through the
interaction during these campaign, it
was felt that there was a need for a
regular network to co-ordinate this
work; to lobby for a rational drug
policy as a whole and not only about
hazardous drugs. A loose c^
ordinating network was formed
*
1983. A series of prolonged and
intense discussions were held amongst
those who had been consistently active
in this collective work during those
couple of years and a Rational Drug
Policy Statement (RDP Statement)
was prepared outlining our basic
common
understanding
briefly
elaborating the points enumerated
above.
Within the perspective of this RDP
Statement, member organisations &
individuals have tried to create public
awareness through various means
(articles in periodicals, pamphlets,
meetings..etc.) On different aspects of
the drug policy, particularly the
relationship between plethora of
irrational drug combinations and the
paucity of essential drugs and that
between high prices of drugs and the
domination of multinational drug
companies. (At the end, a list of
publications in English on the drugs
issue by member organisations has
been given.)
From 1984, a new drug policy by
jbj Government was quite in the air
rd hence AIDAN as a collective
focussed its attention on this new
policy. A detailed critique of the report
of the steering committee of the new
National Drugs and Pharmaceutical
Development Council (NDPDC) was
submitted to the Government; a spate
of newspaper articles were written,
concerned parliamentarians were
appraised of our perspective and
demands by providing substantial
material. A signature campaign
amongst doctors enlisting medical
demands about new drug policy was
carried out in different parts of the
country.
After the announcement of the New
Drug Policy on 18-12-86, its antiawjple, pro-industry, irrational charac* yis being exposed in the eyes of the
f
public.
Apart from lobbying about the
policy issues at the National level,
some member organizations of
AIDAN have been active in educating
doctors, paramedics and the lay people
about Rational drug use in their
practice. For example:
★ “Drugs Diseases Doctors” by Drug
Action Forum, West Bengal, is a
periodical for doctors which is
almost exclusively devoted to
rational use of drugs and .to
highlight misuse of drugs.
☆ Voluntary Health Association of
India has been training their
paramedics in rational drug use and
has published health related
booklets.
☆ LOCOST has been trying to evolve
a method of supplying good quality
generic name drugs at cheaper rates,
to the voluntary sector and
promoting rational use of drugs.
WHAT YOU CAN DO FOR
AIDAN
1 To become an active member of
AIDAN please write to the cooridnator on the following address.
Dr. Mira Shiva C-4/14, S.D.A.
New Delhi 110 016.
2 To study the substantial material
published during last few years by
AIDAN members or by other
fraternal groups; and to write in
various periodicals with the help of
this material.
Please do not forget to send a
copy of the cuttings of published
material to the AIDAN Co
ordinator.
A list of such publications is
given at the end of this brochure.
3
To sell this material to appropriate
groups, socially conscious doctors,
activists, Journalists...etc.
4
To foster Rational Drug Policy
Cells in your area or within already
existing appropriate organizations
to carry out the above work of
lobbying as well as to promote
rational knowledge and use of
drugs in your area. For example, a
local group can launch a campaign
amongst doctors as to why they
should not accept any drug samples
from any drug company, or why
they should not use hazardous
drugs like E.P. forte, Analgin,
Butazones, Anabolic Steroids,
Clioquinol, Combination ofstrepto-
mycin with chloramphenicol or
with penicillin...etc.
Campaign amongst the people
about primary importance of oral
Rehydration in diarrhoea; and try
to start “diarrhoea-treatment cent
res” by paramedics under the
guidance of a doctor and about the
wastage of money involved in the
use of most of the highly advertised
over-the-counter drugs and the
alternative to these brands.
Lobby with the Government on
the basis of awareness amongst the
people about★ The urgent need to make
available measles vaccine on a
priority basis in the Government
centres or to shelve the plans to
give NET-EN injections to
women.
Lobby with the professional
bodies like in Indian Academy of
Paediatrics, IMA to
★ promote rational use of medi
cines amongst its members; to
conduct seminar on the new
drug policy;
★ to pressurize the Government to
immediately make available the
measles vaccine in its pro
gramme.
★ to prepare and distribute healtheducational material for parents
on child-health and about do’s
and don’ts about drugs.
Only a couple of illustrative
examples have been given above
about some of the types of activities
that you can take up. Many such
instances and also other types of
activities are possible depending
upon resources.
5
If you are interested and are in a
position to do academic work; this
will also be helpful. If you are a
doctor, you can contribute to the
above mentioned periodicals or you
can prepare a study of various
formulations belonging to any one
of the groups of drugs (cough
mixtures, haematinics, antacids., etc)
that are available in the market to
assess their rationality. Studies
conducted by the Medico Friend
Circle (see at the end) offer such
examples and have proved to be
very useful in re-education of
doctors.
If you are an economist
sociologist, you may study from that
angle, various aspects of a rational
drug policy-for example, the real needs
of the Indian people about different
drugs for example, how much of
isonex-the antitubercular drug-would
be required to treat all the TB-patients
in India?
How much money is
wasted, concretely speaking, on
irrational drugs? What is the impact of
the new drug policy on the ex-FERA
companies, Indian monopoly drug
companies, medium size companies?...
etc. If you are an artist, you can draw
posters, cartoons, prepare songs, make
a slide show...!
This is a movement and different
types of people with different skills can
make valuable contributions. Let us alWx
together work towards a ‘Rational Drug Policy”.
LITERATURE ON DRUGS IN
ENGLISH PUBLISHED BY
AIDAN MEMBERS
I AIDAN Materials:
i
Rational Drug Policy statement:
pp 16, Rs. 1.50, VHAI (see below)
ii
A Rational Drug Policy; pp.162,
2nd edition 1986, Rs. 20.00 (This
book and C1 - see below-are very
substantial resource books on
different aspects of Drug Policy)
Published by Voluntary Health
Association of India for AIDAN
40, Institutional Area, South of
I.I.T. New Delhi-110 016.
iii
Critique of the New Drug Policy,
April 1987 (under preparation)
available at VHAI and CED).
iv
Drug Alert-Hazardous Drugs, pp
52, Rs. 6/II Material Published by AIDAN
Members:
A Arogya Mitra Mandal 2117,
Sadashiv Peth, Pune 411 030 —
Our Health, Our Medicines,
Rs. 10/-
Catholic Hospital Association
of India (CHAI) PB 2126,
157/26 Staff Road, Secunderabad
500 003
1
•
Health Action — a monthly
published by Health Accessories
for All (HAFA) propagates
Rational Drug Therapy and
Critical approach on Health Care
delivery.
Subscription Rate:
Life Membership
: Rs. 1000/Annual — Individual
: Rs. 60/Annual — Institutional : Rs. 80/Foreign-Annual
: USS 50/Foreign-Life
: USS 500/Single copy
: Rs.
7/Themes covered by past issues in
1988 include Immunization, Infec
tious diseases, Tuberculosis, Nutri
tional Anaemia, Diarrhoea, Acute
Respiratory Infections, Antenatal
Care, Rational Drug Therapy,
Nutrition, Leprosy, Addictions and
Blindness.
1989 — Sports and Health,
Growing Child, Hypertension,
Mental Health, Accidents and
Poisoning, Diabetes, Community
Health, Allergies, Dental Health,
Universal
Immunization
Pro
gramme, Cancer and Shelter
(Housing).
2 Buyer’s Guide —
A purchase guide to Health Care
products and services — useful for
Hospitals and Dispensaries.
Price Rs. 175/3
Herbal and Home Remedies —
Loose Leaf format. Photographs
and sketches of herbs used
commonly as home remedies.
Price Rs: 40/4
Mini-manuals in Hindi (set of 10
titles) — Illustrated guide to deal
with common health problems in a
simple and rational way, giving
both allopathic and home remedies.
Topics covered are Scabies,
Pneumonia, Tuberculosis, Polio,
Care of Eyes, Ears and Teeth.
Price: Rs. 15/- for whole set.
C Centre for Education &
Documentation, 3 Suleman
Chambers, 4 Battery Street,
Behind Regal Cinema, Bombay400 039
i
Aspects of Drug Industry in India,
M Bhagat, pp. 130, 1982. Rs. 19
ii
Brief List of the Literature on
Drugs and Drug-related issues
available at C.E.D. with facility
for xeroxing and sending by post.
Most of the literature in this list is
available for sale with C.E.D. and
V.H.A.I.
iii
Injecting NET-EN into India,
Mira Sa vara, June 86 Rs. 5.
D Delhi Science Forum, B-l, Ilnd
floor, ‘J’ Block, Saket, New Delhi110017
i
Drug Industry and the Indian
people, Dr. Amit Sen Gupta,
(ED.)
co-publisher-F.M.R.A.I.
Patna, pp 333, 1986, Rs. 40-00,
Harbdound Rs. 100-00
E Drug Action Forum West
Bengal
i
Drug Disease Doctor (Quarterly);
Ed. Dr. P.K. Sarkar, P. 254,
Block-B, Lake Town, Calcutta-
700 089. Annual Subscription
Rs. 12-00.
Poster: Drugs for the people or
People for the Drugs, Rs. 3/F Kerala Shashtra Sahitya Parishad (KSSP) Parishad Bhavan,
Marvencheri Lane, Trichur 680
002.
i A decade after Health Committee,
Ed. Dr. B. Ekbal, Rs. 35/ii
Drug Alert-Hazardous Drugs
(AIDAN) pp. 52, Rs. 6/iii
National policy for Universal salt
lodization-A critique. Dr. K.P.
Arvindan, Rs. 3/G Medico Friend Circle
Rational DrugPolicy Cell,50, LIC
quarters, University Road, Pune411 016.
i “Tonics how much an economic
waste ?” by Dr. Kamala Jaya Rao,
xeroxed 6 page article from MFC
Bulletin: Rs. 5-00 (available free
of charge with V.H.A.I)
ii “Scientific Scrutiny of some overthe-counter-drugs” by Dr. A.R.
Phadke, xeroxed copy of the
reprinted article in “Medical
service” Oct-Nov. 1985, 7 pages:
Rs. 6-00
Sahib Street, II Lane, Madras 600
012, pp 56; revised edition,
Februrary 1987 Rs. 10-00
ii
“Multinationals in the Indian
Drug Industry” by Dr. A.R.
Phadke, xeroxed copy of the 5
page article from MFC bulletin,
Rs. 4-00 iv) Dipyrone, Hoechst
and the Boston Study, Wilbert
Bannenberg, reprint from MFC
Bulletin No 123, December 1986,
4
pp. Rs. 2-00
v
Drug Alert-Hazardous Drugs,
pp 52, Rs. 6/H Pondicherry Science Forum
i Issues involved in drug policy. (A
brief account of some of the issues
discussed in I,II and Di published
by Chennai Books; 6, Thayar
iii
I
i
ii
iii
iv
Voluntary Health Association
of India (VHAI) 40, Institutional
Area, south of IIT, New Delhi110016
Banned and Bannable Drugs, pp.
67, Rs. 15-00
Drug Information pack; Rs. 15-00
The use of Essential Drugs
(reprint from WHO) Rs. 10-00
(for other books, see T in^p"
beginning)
“Do you really need all these”, a
leaflet, Rs. 2-00
Reprints from: “Where there is no
Doctor”, Right and wrong uses of
modern
medicine: Re.
1/Instructions and precautions for
Injections: Re. 1/-. The uses,
dosage and precautions of
common medicines, Rs. 2-50
vi
Leaflets of Rs. 0-50 each: The
declaration
of Alma Ata,
Drugging of Asia, WHO essential
drugs, Bangladesh drug policy.
Hazardous bannable and dumped
drugs, Our concern about drugs,
Essential drugs, The Courageous
Bangladesh.
vii
Posters: Murder in the name0
v
medicine, profits before the people
Rs.
5-00 each ‘Can you
understand the small print’, Ban
Bannable drugs, Drugs can be
dangerous too. Don’t judge a
medicine by its packaging, Rs.
3-00 each.
For a list of other publisher’s books
on drugs available at VHAI, please
write to the publication officer, VHAI.
For mode of payment, postage., etc,
please write to individual publishers
listed above.
Dp.
DRUG ACTON—FACT SHEET
WHO - Essential Drugs
Policies for providing essential drugs
The selection of essential drugs. Technical Report Series 615.
WHO, 1977. Excerpt.
“While drugs alone are not sufficient to provide health care,
they do play' an important role in protecting, maintaining and
restoring the health of people. In recent years, there has been a
tremendous number of pharmaceutical products marketed;
however, there has not been a proportionate improvement in
health.
Many pharmaceutical products are marketed with little con
cern for the differing health needs and priorities of individual
countries. Promotional activities of the manufacturers have
created a demand greater than actual needs. Since up to 40% of
the total health care budget in developing countries may be
spent on drugs, the result has been an increase in the cost of
health care or a reduction in funds available for other health
services. The cost has affected even the affluent nations, and
their governments are increasingly worried by the rising ex
penditure on pharmaceutical products. In developing countries,
the problem is magnified by limited economic resources, short
age of trained health personnel, and lack of organised drug
policies. In the least developed countries, where communicable
diseases and lack of elementary health care are the major medi
cal concerns, large segments of the population are in urgent
need of essential drugs.
It is clear that for the optimal use of limited financial re
sources the available drugs must be restricted to those proven to
be therapeutically effective, to have acceptable safety and to
satisfy the health needs of the population. The selected drugs
are here called ‘essential’ drugs, indicating that they are of the
utmost importance, and are basic, indispensable and necessary
for the health needs of the population.
Drugs included in such a list would differ from country to
country depending on many conditions, such as the pattern of
prevalent diseases, the type of health personnel available,
financial resources, and genetic, demographic and environ
mental factors.
Because of the great differences between countries, the prep
aration of a drug list of uniform, general applicability and
acceptability is not feasible or possible. Therefore, each country
has the direct responsibility of evaluating and adopting a list
of essential drugs, according to its own policy in the field of
health.
The list of essential drugs based on the guidelines put for
ward in this report is a model which can furnish a basis for coun
tries to identify their own priorities and to make their own
selection.
The notion that the number of necessary drugs is relatively
small is supported by experience. Several developing countries
that have adopted limited drugs lists report good aceptance, as
well as favourable medical and economic results. Lists and for
mularies with a limited number of drugs are also successfully
used in many developed countries.
A limited list may not provide for the needs of every' person but
certainly should meet those of the vast majority. Whether or not
drugs or pharmaceutical products outside the list are available
in the private sector should be a local decision.
Limited drug lists have several advantages:
1.
Reduction in the number of pharmaceutical products to
be purchased, stored, analysed, and distributed;
2.
Improvement in the quality of drug utilisation, manage
ment, information, and monitoring;
3.
Stimulation of local pharmaceutical industries;
4.
Assistance to the least developed countries in urgent
need of high-priority drug programmes to solve their primary
health care problems.
An effective programme of drug selection coupled with
2
appropriate information and education may help to improve
attitudes regarding the role of drugs in health and disease.”
General principles for establishing a list of essential drugs
The following principles were considered by the Expert Com
mittee to be a foundation on which to establish a list of essential
drugs:
1.
Adoption of a list of essential drugs is part of a national
health policy. This implies that priority is given to achieving
the widest possible coverage of the pop-ulation with drugs of
proven efficacy and safety, in order to meet the needs for
prevention and treatment of the most prevalent diseases.
2.
Only those drugs for which adequate scientific data are
available from controlled studies should be selected.
3.
Each selected pharmaceutical product must meet adequ
ate standards of quality, including when necessary bioavaila
bility.
4.
Concise, accurate and comprehensive drug information
drawn from unbiased sources should accompany each list of
essential drugs.
Reprinted By : VHAI - New Delhi
3
'DP- 50 4 2
VOLUNTARY HEALTH ASfOCI^FW, KA^HAT AKA
Seminar on Iff.? CW DW'" AM) DW. POLTCY
5EE25Z
(i)
ZE£22hl£
*ftie following letter went out to nil the Members of
VBA (K) in early September.
"The V.H.A.T. goal has been and will always be a 'He'? thy
Community’. We seek ’to promote social Justice in the
provision and distribution of health care’. With the
incrers’ng emphasis on "Primory Health Care” ue are all
in an increasingly irmo-t”nt quest for priori ties.
He arc seeking clean water before antibiotics, food
before vitamin pills, vaccination before kidney machines,
mother’s milk before powdered baby foods mixed with
dirty wa+er, and health for villages °nd slums before
more hospitals for the affluent suburbs of c”ni
sl
*
citle«, The dilemma before many of our members is how
to shift priorities from our commitment to hospital
systems to our increasing commitment to community
health care systems.
Che of the big problems we are facing in our hosrlt'ls
is the increasing cost, of drug bills. Drugs are becoming
the mainstay and main cause of expenditure tn our
hosnltel system. Any shift of priority can only result
from a concerted notion on our part to look ®t drug
policy and drug costs and see whether we, os a group
of voluntary health workers, can do anything to reduce
the drug bills
a fi^st step towards shifting
priorities. Can i/c change our nr-scrlbing policies?
C°n we stock low cost drugs? Can we produce Iw cost
drugs?
The TCMH/iCSSH study on "Health for all - an alternative
Strategy" warns us that eternal vigilance Is renuired
to ensure that the health care system does not get
medic”llsed, that the doctor-drug-producer axis does
not exploit the people nnd that the abundance of drugs
does not become a vested interest in ill health."
Can we V.H.A. ifanbers do anything about.Jt>,
individual! >• and collectively?
To find an answer to this growing problem we have
organised a seminar for ”11 members on October 3rd,
at ft John's Medical College, Bangalore.
Join us to discuss the following issues !
- The pattern of drug production should be oriented
to the disease pattern in indie, with an emphasis
on the production of essential «nd basic drugs.
If we agree, what can we do about it?
.2
s2:
- We cry for drugs needed by poor nnd underprivileged
groups which should be produced in adequate
quantl+ies and sold at cheapest possible prices.
How may we bring about this?
- CSie of the most distressing aspects of the health
service today is the habit of doctors to overprescribe
or to prescribe glamorous and costly drugs with
limited medical potential. Can the medical profession
in our hosnitals be made more discriminating in
prescribing habits?
- The small scale drug industry needs to be encouraged
and expanded subject to strict duality control. Can we
produce low cost alternatives in our hospitals, health
illags communities?
- Fifteen thousand branded drugs are on sale in Didia.
But a Government Committee on Drugs and Pharmaceuticals
industry (1375) believes that health needs can be met
by only 116 drugs. Can we agree to a simple standardised
low cost pharmneopia for the Voluntary Health Sector?
- A Government Committee looking at drug costs has
recommended acceptance of
- A basic drug list
- Generic Prescribing practice
- Bulk purchasing
- Local formulations
- Use of indigenous drugs
Taken separately, each policy is a powerful weapon for
change; taken together, they build into an integrated
strategy. Can we consider these and accept them to
change the drug scene in our hosnitals?
These are many of the issues we will discuss
together in the workshops.. Please send representatives
from your hospital/health centre institution to share
with us your experiences and ideas. The Seminar is open
to all Health .Administrators, Doctors, NUrses, Pharmacists
Paramedical Workers and Voluntary Workers associated
with Voluntary Health Care Agencies.®
(2)
E £ Z. 1 1 J? i p a t i o n
Over
Members and
local Invitees registered on
3rd October 81 for this ssninar. Important among the local
participants were the Deputy Director (Pharmacy), Directorate
of Health and Family Welfare and the Deputy Drug Controller and
represenative of the Drugs Testing Laboratory of the Government
of Karnataka.
(3)
H E S 0 U P C F.
P E p2 0 W2
Mr Alan Crnnmer, Consultant Pharmacist CMAI based in
Holdsworth Memorial Hospital, Ifysore and Dr Havi Narayan, Asst.
Professor of Community Medicine, St John’s Medical College,
RcnfT',lo’*e, were the key resource persons. Dr Thang’m’ Joseph,
Professor of Pharmacology, St John's Medical College, Dr
”rmn Pa©,
Profess©’* of Community Medicine, qt John's Medic
*'I
College,
Dr Prennnando chetty (Dy Dfrec+or, Pharmacy), Dr Dara S Amar,
Assoc Prof of Community Medicine, St John's Medic®! College,
Dr Manohar, Physician of St Philomena's Hbsplt.nl, Bangalore,
Dr Sylvia Bnhu, Paediatrician, Baptist Mission Hdsnlt>»l, Bnnralore,
were additions! resource persons who chaired the ne-nfons and
group discussions
*
Dr K F Peters and D- P " Bal were guest speskern
on 'Homeopathy1 and 'Ayurveda. • respectively during a session on
the Pole o" these two systems in Health C®re.
H 1.? 21
(4)
iS h ~ —
9.00 am
Registration
9,30 rm
Introduction to Seminar
s Dr Sylvia Dabu
Self-introduction by participants
9.50 am
reunion T
- chairmen» Dr Th®ngcm Joseph
Feynoto ©Tier T
- low Cost Drugs and
Drug Policy (an overview)
: Dr Ravi Narayan
grvnote n®n<r Tf
— fibs©!'al Phar®acy
Policy for io-,j Cost
(Drugs
(some perspre
iven)
*
: Mr Alan Cmnner
DMCirOTON
11.15 am
COFFEE
11.30 am
Qn'D? DT-; '•re cto v
Group A-l
(Npom fb.119)
Group 0-1
('bom Eb. 117)
Outlining a Prescribing
Policy
—do-
: ChairmanJ Dr Manohar
Croup B-l
(Ttoom ?b»119)
Outlining a Pharmacy
Policy
: Chrtrmeni Dr K Premananda Shc'ty
12.30 pm
i Chairmen» Prof
Bmn® ”ao
LUNCH
4
t4:
l.so m
QrofT nr‘9”''''TCM TT
Grow 0—2
(’bom lb. 117)
Cnre Study on Menngen'nt t Ch^lrmcni Prof r*', ’
of Diarrhoea
tbo
Grouo >2
(nonm ro.ns)
-do-
s Ch«1.rmnni Dr Pylvln B
*hu
Grown B-2
(room lb. 119)
Drrvlnp up list of
baslc/essentlal drugs
t Ch^lmens Dr Dara S Anar
2,?P om
Session TT
I’fcle of Ayurveda
end Honeopsthy
» Chairman t Prof S7 Rama Rno
1. Homeopathy
— Dr K E Peters
2. Ayurveda
— Dr P a rpf
3* ’0
TEA
3.45 nm
Sepglon TTT
- Ch«lwinnt Dr ThongTn Joseph
rjcT! ??7 td»7
Group renorts by
^pporteurs of Groups "-I ft 2, 0-1 ft 2 "nd HL ft B»2
^ccnT-rrr- •'7To,y!
Vote of tbonks
(5)
Ma 1 n
(a)
221212
s Fr Bern’WI Morns
*
Hon
Secretary, VHA (F)
2 £ . JJ 2 Z 2 2 12
i1 2 2 3 2 2 2
IQ'’ Cont Drugs end Pruy Pol icy
An overvie-..’ of the issue concerned with the '’emlnar theme was
presented by Dr •writ Wsrnyan taking four publications ar, resource
material, these were i
1.
11.
Hi.
iv.
the Hothi Ccrrnittoe ’teport (1075)}
the Earthsern publication, Bru,?-- and the Third World,
by Anil Apparwal
+he IGf-'r/TCS -” study on Health fbr All - nn sltfy?rM.vr
Strrtegy
Henlth for the Mill tons, April-June 1981 issue on
Vfcdlefnes
If neonle rrtte-ed
Re n"«gon
*<
‘d *om© foots on the Ftur industry in Jhdla
Mftillflhtinp the following poln+st
1* Too wany b''”,ndrd ppppcrfttlons.
sSt
Too many companies'—mostly private with a strong
profit laotlve;
tit. Tewed consumption of drugs betw'-en urh"n/rur«>l areaju.
lv, Overproduction of drugs Bc’nt for illnesses of rich;
v. Drug colonialism; and
vi. absence of clem cut government poller
*
ii.
He then highlighted the ebometerlotfeg of the nrrscrtMnr nolley
/A e. CA-«-> Pc-r Ki^s-> c\^' e
of the medical profession stressing on,tonic and Injection practice
of dootoT, irrational combinations, high pressure advertising tmtics,
including those of monetary end materiel inducements, drug misuse
md over mf under prescription
*
He also stressed the problem of improper
medical ’mining and near absent continuing education.
Among the many alternatives recommended by ’■'«??.0. and National
Committees, hr outlined the nros and eons of !
a. essential drug list;
b, generic prescribing;
c. indigenous medicine;
d, non-drug ther-’nics.
Finally hr set out oomnonente of m alternative policy for
group discussion.
(b)
&emit. * 1 Phrnraiseypolicy *fo
.Doot Drugs
* Alm Crmmrr shared his perspectives gained over yprrs of
M
consultancies for CHAT and CD! group of hospitals.
H? outlined the needs for a lov cost ohnrmncy policy for drug supplies
to the Health Core Delivery Systems at 3 levels otjtiers
*
1st tier; Mcdleinrs. '"or .Community Health "orberq which should be
cheap, effective symptoraatlcnjly, r^sy dosage regimens,
without problems of side effects or drug resistance
*
A list of 1R had been recommended by the TCMH study
*
Pnd .tiert
Medicines for the Primary Hc-lth Centre
In addition to those used by Community Hmlth Workers,
medicines at thio tl^r would include long term thrmples
Hire TH and Leprosy, Anti—biotins, emergency drugs and
related !E»-teri.els for preventive services like v^rciner
etc, Facilities for refrigeration would be cn-'Ontial
*
Jfeslth Education md family Welfare Counselling would
be additional priorities.
r> t
Jto jtho .Kris^LtlL.Bh.Z2ӣSlZ
Hr str- ssed the need for « Phe’-i«oy Corraitte©
outlining f’s objectives. Ik- giaour' rd the importance
of proper invent:«ry procedures, storage facilities,
ncngonal stocking and group purchnnlng. He- also dealt
on the possible hospital baaed crug production Including
v. solutions, rehydrntion nowderg, inlection solutions
l.
skin preparations nnd so on. Efe then went on to
ord line questions which should be consider-d while
evolving a Pharmacy Policy.
(") G r o n o T 1 2 c v n s i o n
The participants were divided J into three groups for
grail group disourstons. Groups-A f- 0 disowned components of a
org-eriMrg policy and l«tcr discussed +he treatment pf
as s c^-e study. Group B discussed ecmnonrnts of n Hosuitol pharmacy
policy and l«ter discussed the criteria nocesTry in evolving an
Essentlal/pasio drug list. For the assistance of the groups the
following four sets of questlonB/guldlines were drawn up and
circulated.
Outlining a Preraribin? Policy
Row many oc the following components of ^n
alternative PHr^OPlPTTlC POLICY c^n '.re acoep
*
as "■ group
committed to ’Health for All •?
IP yes, why?
If no, why not?
(1) Accepting an EG''.E?TTAT/B^TC IWG LFT for our practice
(2) Accepting GENERIC PFEfCRTBTHG
(S) Accepting CO,'T as an important criteria for selection
of a remedy in addition to safety, efficacy and ruality.
(4) Discouraging prescriptions of drugs whose only additional
advertised value are:
a) Cometlo enibellishmentsj
b) Klog'snt. pack IngJ
c) Jnnd'ruate evidence of greater v^luej
/?) Irrational combinations)
e) Tnitative drug
.7
(5) Hbt accepting phyefclan’s gomnles find other
monetary or mete’*
!
inducement which corrupts
us to promote » companies product le., we prescribe
a product which we thick is best suited for a
condition, not. becmse the company grvo us the maximum
materiel advantage,
C>) Other component which should be includedi
a)
Indigenous medicine?
b)
Kbn-drug therapies?
e) Continuing Education of the Health Profession?
2.
d)
Promoting Primary Health Centre Priorities? and
e)
Bsre-foot pharmacy
Outlining a Pharmacy Policy
OiiosMons to bo pondered about J
(1) Can a Hospital devise p formulary of good quality, low
cost medicines?
Can this be common “or nil Voluntary Hosni tele?
(2) How con preseribers• compliance be ensured or is
freedom of prescribing likely to make this impossible?
Can we ensure Health Workers’ compliance with their
formulary (medicine list)?
Will doctors also prescribe from this list?
Ts it possible to prevent prescriptions to medical
shops being given?
(3)
Where simple low cost drugs will not be sufficient,
how do we subsidise to all or those who need help most?
Should all patients contx-ibute to the cost of medicines?
If so, how?
(4)
Wil1 a Pharmacy Committee, Including Doctors, Administrators
and Pharmacists holo in Iraniwanting cost control or
ovality control policy? (In most Hosni tale medicines arc the
second largest item of expenditureJ)
(5)
Have we asked our pharmacists to research coats? If so,
does he know how to do so?
Have we provided tools for the job? If so, what tools?
(n) Are bulk drugs purchases possible on a group of
Hosnftals-br.se? What methods e°n we devise for obtaining
low cost drugs either for one or many Hosnifsls?
(7)
Do we consider proper stock control, record keeping and
auditing of medicines, purchase and distribution?
a) unnecessary expenditure?
b) essential?
What are our reasons for our attitudes?
»e i
(8)
It) many Hospitnlg the Pharmacy Is an iirportnnt
Income producing section. Will a witch to low cost
drugs raise cost or make it instead a burden on the
That itutlon?
(9)
Is the production of medicines in the Pharmacy i
a) too time consuming
b)
too costly in terms of personnel or equipment
c)
uneconomic?
(Broadly thinking of two typest ncn-sterlle
prescriptions and sterile prescriptions) How would you
advise your Hosoital Management?
S. Case Study on Management of Diarrhoea
Diarrhoea ranks hlghsuaong the morbidity and mortality
figures for this country. Hie etiologic agents are most often food «nd
water borne microbes and viruses. Mortality In this illness is most
often due to loss of body fluids as a secondary effect of the diarrhoea.
Developed nations In contrnst, hwe s relatively low
prevalence of such infectious diarrhoea-—proncr sanitation and
protected water supply accounting for decreased prevalence and not
better drvgr? to treat the infection.
Th the past, when the markets were not flooded with
Innumerable drug" and drugs combinations, simple home remedies were
used to contain diarrhoea.
Listed belo’j are some of these st mole home remedies and
their basic ingredients.
(1) Dietary restriction to easily assimilate
carbohydrates, rice, arrow-root, sago etc.
(?) Cords - lactobacilli
(g) Ten - Tannin
(4) Pomegranate — Tannin
(5) Popny seeds - Cpintrs
((?) Tender coconut water - Hydration
(7) Bananas - Pectin
Scientific knowledge? tod«y supports the symptomatic
treatment of diarrhoea with particular attention to maintaining hydration
While there is a definite nlaer for use of 4PPW"T
*TK
^TTBODTF^
In the treatment of diarrhoea, the most, common occurrence today is
tnnppronriete use of multiple antibiotics, further complicating
the diarrhoea by severe alteration of normal gastro—intestinnl flora.
Discuss some of the onuses for this occurrence and suggest
feasible solutions.
,9
»9s
4. Drawing -in
15,003 br-ndcd drugs firs an trie In Indio.. But th©
Gorexnmnnb Cocnitte© on Drugs nnd lha.•••mc-ubic'.l industiy telinres
that health needs would te met by on,y 116 t'ra^s.
Could tro Hot out tho CBIT!?HIA which aanbsrs of
TEA could us© in formulating a Hot of eorentiril/
basic t’ngo to to used in their am institutions
fox’ hospital and health cure?
(7) ■Ls.-Xl^uLoji si
S, y. ,s. t p rxs.
q?
To widen the parnp'ctivns of tho participants n spacial
Bossion o : the rol© of H<xxo0p'xthv and Ayurveda. in
was
osg niro". ’■ ’o-bBSOr hatja Tho md© pi©' toinniy Introductory remrl's
cn the irwrt'’noe of tr’diticna’’ medicine particularly in the light
of those ’oi rr an Integra1 wart of our culture.' and historic ’1 traditions.
Dr Paters outlined the history of Hcenopathy and mnticned
ha? Dr Hahnom■®i accidently noticed tho symptoms that cinchona. bark
produosc in a healthy person and ©touch upon tho idea that ’like is
cured by Hiro
*
- sintja ©imijibuB currentuf. Ife then out'in!
*
the
min inportnc© of this system of medicine. In rawer to a '’.uesticn
ho added that among th© many cases that were being referred to hin
\
ty Allopaths new-a-days tho most inportant for which Hcmopathy had
gool cures were planter warts, hydrocele and hemin especially in
Child-hoof, migraine, cervical spondylitic, hyperacidity, hjiysrtensicn
and heart disease.
Dr Pf ’tai outlined the philosophy and main princi los of
Ayursedn., Ho too, in answer to n euesbicn, mentioned the conditions
of Jam-Hao, loueorihooa, Rieunatism, Asthm and lfype-tonrd.cn o-s tho
main dironros which wore being raferrod to thorn by Allopaths "n’ uheroin tho
Ayurw'ic ryston had good cures.
Sw ftr:nlSK?88 anti humility of both sponfcers were '"-.y impro-rivo
on-’ xkj liooc mmbors of V5IAT wll1 bo roro open to those iyotems in
their future work.
£0 H C T. U D I H G
SgSSIOH
e--> el m * 1
Iha participants of the WA (K) Seminar on LCW COST P’lJG
/•DA DTvJG
reccranended that through n process of eentinous
dialogue .n’ dircuflcicn eatSh winter hospital, dispone-' ry orhca’th
centre thro: h ite radical and ph-ir^-cy staff should—
a. appoint a THER.-PEOTICS or FTARJftCY C(Xr TTT’ll
consisting of doctors, phans'-oistn and other
no: -ters of a hocpit^l or health centre toaa invcOLwd with
..K)
»10:
adrdnistreticn of drugs.
b) yornul'^ta a list of Baefo/teeential drugs (Foxsiulaiy)
i.
The JEiO drug lint could bo ta-’en ar a basic
docurnnt to work an. The list wo Id bo prepared
ce?. the b' slfl of disses® groups and Include
diagnostic agents, vaccines ote., within this
group th® "rremgesrnt wil" bo alphabetical.
ii. 3io listing should bo generic ns tSiic clearly
indicates tho drug boing administered, ®iis
nny also contribute to ro using costs.
lit. ~r. c rxi bio i.wllabi'’ity is a probion, either
n p••tint name wty be included or tho manufacturer®
nr’.-n ~ivon. As bioavailability studies are not
av'liable for noct dru-s in India, this will bo
an tho basis of clinical jutlgoraent.
iv. Sio '’let of approved suppliers for drugs in
th© foroulary must be sot out by the Hicmacy
Con ittoe. Shis will ensure ounlity and
continuity of supply.
v.
Strength of injections and other medicines to be
et ’tod algo minimum and taajcimum dooes and
noo■■'i-’.tric foeosK, »
vi.
Tro -uronts of toxic reactions, poisoning and
other emeigendos to be cot out.
vid.. Pro cribing policy and rules to bo included in
the front of thn formulary, tliore specific dr:.go
don nd special prescription, this is to be
in ’icntod by tho iton coioemcd.
viii.
c)
To whom should th® fomilaiy be given - doctors,
nurres, nursing stations. Amendmnts sen bo
iesuod for these en’y to the holders who are
rotnoasibln for adding to their copies.
^vclve a consensus among ’prescribing staff’ tar r’s
the followingpolleles in prescribing*
i. Generic prescribing;
ii. national drug thorepy which emphasises
officiant, safe, eaey to administer, Tgi cost, drug
.11
:11:
ill, 'irccr’.r ging prescription of '’rugs whoso
only ed ’itionnl rr’ver'tipo'’ v
luo •'■to *
- coamtio oratoV’iehBrsnts;
- ■ ■•ttreetlw^lng -nt pact ring;
- in ^oquato evidence of gre'ter vPiioj
- irrational combination;
- irritative or ne-too drug
d)
StouLv?
ecnsonaue asnang ’prescribing st'1 *
ff
■ nrl’pti rmey st' ff’ about tho unethical nature
of tho sr.torin'’ an/’ sonotniy inrhiconents provided
ty nodical canpanioo including free rhyricsan
sfreplcs especially if these are modifying or
decidl”" our proscribing policy—ant! deci e on
action to cuntor the high peer a/’rertieing
presf-ure t’cties of nedieni companies,
e)
coopt port n-r an import' nt critori”- in selecting
a drug Cor proscription. This is in addition to safety f
offtc'ic;- n-> r^iabl'-ity.
f)
Sitro'•.:clr" proper stoat- control, record knnping,
•"-’ittn- of mficincs, pu ch^so ."Jr! distribttbicn
bee upe
think those -'ro oerentinl enr? not
imnocor: 177 eapenditure,
g)
Cairi-’er the pro-liction of sinpln phamnoeutic l
prop r tions in the honpito pharrT-cy on a co.et“',ff' otiv!
b 'sic tobring down drug costs for the patients. Those
eotik? inclut’e mixtures» ointnrantn, rohytlroticn pcedor,
iv fluids ana nepy paediatric preparations.
h)
Prcnoto c greater openness and urr’orstnnriing of th®
in’ig nciUc ncn»rHcpathic tr'diticns of nodicino
Ulfs Ajrj;rzr'ki nntf H®e opethy nnd nou-o’rug thor’-plon
likfl '-*cg'. , Haturopnthy and Acupuncture so that their
ueo rn.-’ offteaoy can bo farther retr’aiehed and they
could to used in oar future progr-nron in an into.gr tel
tff’y.
1) Protaot'- the priori b loc in Prim-ry Hpolth Caro in
all our progr'mos sano of which am -
- olo n u tor before antibiotics;
- foo’ tefom vit^nin pills;
- vneein.ifcicn before Jdr’ney machines;
- mother
s
*
'.nllk tofoio powdered trly focy’s;
- ho- 1th for villagers and alum dwallnrs before
noip hospitnis for affluent suburbs of
* capital
cities and so on.
j) In addition to all the above (a) to (i) t all Wl (I)
nonb>rr- should be involved in a caitincus dialogue tete’oen
aootorr ana ■rhansacists and to an active participant
in continuing education on all tho above issues to
doctors, nurros, pars-aedleal perscnnol, patients,
stiK’onts of ray'ietil prof'seiem, interns, junior
'’octcm an
* ’ all the isombers of th© ocmunity.
!:) .Th this tr o'
* Which we eat for ourselves wo raqusot
our
ticn, tho V?IA(K) to teop uo infoirsl of all
o.sp?ctr- o'.’ this fioloiuo on drugs through cur nsudr-thor
and eny other mens available to it lite neotings/eonin'rs
otc.
1) ^21
b? p" not rmeh uso. tiTVwp .rro
o^Jh. ^V-rsr-vicas and nrtre Control Ihpartwnt inraiLgvl
gags. ■••"AV.
gi£lQg»_w.i^, the, f^nto Government Ife-dth Atrthorftias.
and holp to. evolve n policy v.’bpmtv both G<yvnmmnt---^Vol^.b
>To: J.th Agencies can work in a nannintrful
p?rtncr&r» to achiova -fee noil.t Hoalth for All, tez 2<XX1 AD.
Ro source Cos
*
th o
o n i n ft r
on
LOW COS? nR-JGS A HD DRUG POLICY
1t Drugs
the
Public'ticn.
World. - Anil Agarwal—cn E’Arthsnrin
a. Has1th for All - An Aitornnttvo 9tr->togy — ZClIR/teSTR
Joint Ronort 1920.
3.
rfelicinon ns if Poonln l-httnrod—Honlth for the MUHcns
WIAI, April-June 119
*.
4.
Report of the Cerr ittoo on Drugs f,nfi Rnnjncoutieal
Ih<’urtiy (fhthi Car-it tea), April 1975.
5.
SJASOT HUD, Doe. 1 ''X)
6.
With for All by 2000 AIL-Resource r^'ty Dr CW Francis,
Do-;n, Ct John’s iir’ical College (IJ3’A Ccnfterence, 19^0).
7.
Bia-r.nc',utic',ls, Drug Policy nnri Health Cn.re.
Bibile Ibnorinl. Icnt-nr? iy Dr WR Ounerfitne, Fob. 1979.
(>. -Thporb o? Techno"’ o ■'/ r'nd its impact on DeWlonraont—
Report of 'hniri-'r’ o.'1 Bolhi Ccienco Fomw, Ifay 1979.
9.
Hie rhr,:xr'.c‘*
utic'lyhiotry ~ Drug Pricing Policy "nd
Production ■— n study : K Jayarma
*
Economic Timse,
10th Iby - Juno ">, 1576.
10.
I-yth awl Ro-.11 y o? -'rug Industry, Booklet (.^tending
Ccnnitbee of the i’iticnal Carxmtlcn cn Eccncmic
Sidepore’enoo - nd Rr -r-peetiTO of Drug Jh 'Ustxy).
4
-wig
THE SUNDAY TIMES OF INDIA
UF you've
graduated
from the AFMC and have set up
practice as a G.P. and are young
and full of energy and enthusi
asm, the world is a wonderful
place to live in. Now all you
have to do is sit by and rake it in
as your practice begins to flou
rish while you try your hand at
playing god — right?
Wrong — at least if you happ
en to be Manik Hiranandani. “I
became disenchanted with the
traditional methods of allopathic
medicine early on in my practi
ce." says Dr Hiranandani. "I
found its limitations crippling.
Allopathy has no really effective
treatment for anything other than
acute bacterial infections or
accidents."
So Dr Hiranandani systemati
cally set about acquiring skills in
various fields of alternative medi
cine. This involved attending
annual conferences abroad, seek
ing out experts and learning
from them by observing their
methods of treatment.
Confidence began to develop
when
his
first
case,
an
87-year-old arthritic woman.
made a remarkable recovery —
and since then there has been no
looking back. Today, the doctor
has a vast practice and thousands
of satisfied patients whom he
has treated , using methods as
diverse and strange-sounding as
acupuncture, iridology and cra
niosacral osteopathy. Many of
these have been people in acute
suffering, "given up" by end
less successions of practitioners.
Dr Hiranandani's resurrcctive
powers have certainly brought
him fame — but interestingly,
he is widely known in many
other quarters as well.
A prominent activist of the
consumer movement, he posses
ses the distinction of having tak
en the FDA to court — and won:
for having singlehandedly mana
ged to get many harmful and
unnecessary drugs off the mar
ket. "We all complain about the
state of things. Wc all say that
somebody ought to do some
thing. So I did!” he smiles. "I
have no liabilities so it wasn’t dif
ficult for me to stick my neck
out and see that I won!”
Practical enough to identify a
vacuum and move in with an ori
ginal contribution. Dr Hiranandani’s book on non-invasive acu
puncture. the only one of its
kind, is used as a text book all
over the world. "Many patients
dislike the thought of being pier
ced," he explains, "and today it
is possible to dispense with
needles using laser and ultra
sound for acupuncture. When I
first started using these tech
niques their inception was so rec
ent that other doctors were
unaware of how they worked
and there was not even any litera
ture to leant from. A book,
explaining things, was needed
desperately — so 1 wrote it!"
In keeping with his preoccupa
tion with the consumer move
ment, a forthcoming book, A
Consumer's Guide To Good
Health, brings to the common
man vital information, often inac
cessible or neglected, such as
how to choose a good doctor, the
rights of a patient, home remed
ies- for common ailments and
many others.
26 JANUARY 1992
impressive. His patients are. to
coin
a
phrase,
walking
advertisements.
Roland Madeira, an Air India
purser, is a classic example.
Immobile for five weeks after
suffering a slipped disc, Mr
Mcdeira was hospitalised and an
operation was imminent. "But I
came to see Dr Hiranandani,” he
says, "and was restored suffi
ciently to be able to walk out of
the clinic. Two more sessions
and the pain was gone.” Now, a
total convert, he has directed
many colleagues — for whom
backache and slipped discs are
routine occupational hazards —
/i,
propagate the practice of integrat
ed medicine ■— treating patients
with techniques from .arious
schools as per their requirement
— and spread it to other parts of
the world.
Sceptics abound, "1 started
off that way too." confesses the
doctor, “but when I discover
something that works, no matter
how unconventional. I adopt it. I
have learned a lot by just being
receptive to seemingly --.range
ideas. People sometimes chal
lenge me and that is perfectly
natural, but 1 have no inclination
to prove anything to them. They
have the choice of being convinc
SINGLED OUT
SAAZ KOTHARE
Dr Manik Hiranandani: An acupuncturist, a consumer activist,
a writer and a cook to boot.
Another book in the pipeline
is to consist of a collection of his
own recipes. As it turns out. Dr
Hiranandani is an excellent cook
— preoccupied not just with
taste but health and food value
as well. This consuming passion
extends to shopping for the best
and freshest of ingredients for
each dish.
Widely travelled, he looks
after his health by going on regu
lar holidays — sometimes skiing
or sailing, or simply retreating to
an ashram. For one who lives a
life so suffused with leisure and
variety, the quantum of his tangi
ble achievements at work is
to Dr Hiranandani who has set
them right again.
The v/ord • of these miracle
cures has spread far and wide
and today Dr Hiranandani splits
his practice between two clinics
in south Bombay where he lives
for half the year. The other half
he spends in Hong Kong as medi
cal director of the Vital Life Cen
tre, a centre where he intends to
ed by my results if they wish
to.”
Retired businessman N. R.
Kamani. for instance, reluctantly
decided to try out acupuncture
when he was struck with excruci
ating toothache and his dentist
was away. Today. Mr Kamani
has his own acupuncture machi
ne and when affected by a minor
ailment, just phones in to Dr
Hiranandani for instructions.
“The idea.” the doctor
explains, “is not just to cure pati
ents and relieve them of their
pain, but to ensure that they staycured, become self-sufficient.
and don't keep coming back to
me.”
For one who lives a
life so suffused with
leisure and variety,
the quantum of his
tangibie
achievements at
work is impressive.
Patients who come for treat
ment are not just treated — they
arc also given some background
and understanding of the proce
dure to which they are subjected.
Logical explanations .arc provid
ed whenever asked for. And for
those that scoff at his unortho
dox methods. Dr Hiranandani
has merely a sympathetic Smile.
“You can argue with thousands
of my satisfied patients,” it
seems to say.
<>
'Dp. .30.2.0
Voluntary Health Association of India
C-14, Community Centre
Safdarjung Development Area.
New Delhi-110016
Telegrams': VOLHEALTH
New Delhi-110016
, u
668071
Telephones : 668Q72
‘5/4/85'
After throrou^i and careful reoxamiaatian tf all past and
presently available •evj.deace on. the therapeutic vain
*
aid
medical use of BUT42DLIHN (dienylbdtazone) aid T&DSRIL
(oxyphenbutazone) CLba-Geigy Pharma has taken the following
decisions :
1.
X
w
The indications for BUTA.20LIQEN -will be farther restricted
to the treatment of only four classical frame
rheumatic diseases
-
active ankylosing spondylitis
-
acute gouty arthritis
-
active rheumatoid arthitis
-
ute
*
a
attacks »f osteoarthritis
2.
He medida.use if BUTaZDUHN in these feur indications
will be recanmended only for cases where ether therapeutic
measure, including ether non-steroidal, anti- inflammatory
drugs, have been tried aid found unsatisfactory. BUTA2DLIJZN
will thus become a drug of second choice,
3-
Sales of T4JDTRIL will be discontinued world -wide.
The implementation of these decisions will begin immediately and will
be completed in the third quarter of 1965. National health authorities
have been informed. Physicians and pharmacists are .again reoiested
not to exceed our specific recommendations concerning the use of both
oroducts. There is no imminent health hazard to patients under treatment.
It has to be remembered that both drugs have ¥cen standard medications in
long and widely accepted medical use for decades.
Early in 1984, on the basis of a comprehensive benefitrisk evaluation
conducted on its own ini.tiati ve, CLba-Geigy Pharma had already severly
curtailed the use of BUTA33UIILN and T'£LD2RJL. ■■■- • •
cont' d .. 2
.
2
■.it- reeaEiended time Unites f»r usa, eaw±ien«d.■=J
ee-«ripti«n
*
for certain patients and stoc-ycd sales of pediatric forms
and combination products altogether. He restricted field
of indi cations was in line with clinical evidence demonstrating
the .efficacy'and safety of both nroducts .under just those
limited conditions. This step was supported later on by
■carreaponding decisions of most national health, authorities .
A sharp decline of sales resulted during 19&7> on a worldwide
scale, as had' to be expected .
*
Sp.bsecuently
Ci.bai-Geigy Pharma carefully surveyed the
usage of both drugs. It -turned cut that the limiting
fonditians set forth for the use of BUT.A2DI.inr.liJ have been
res.-fteted to considerable degree. This was- far less the
case with TAlID7f.IL, following traditional patterns of use.
In »rder tb ensure ding safety to. the best possible extent,.
we have therefore decided to still further 1 ~imi t the
recommended Usafe of BLT-ZDLI DL'I and to .discontinue offering
T-dDSlIL in «ur product range. In many individual cases a
specific need for the treatment of patients with BUTiZDLIDIN
which have not responded,to other therapies in the limited
range of its indications, still, exists. Responding to such
need by a eontinued^offcriTig--^,. Bill AZOLI DIN for proper medical
use is thus in the best interest of battents^bjiffering from
serious rheumatic disease. Ciba-Geigy Pharma will 'further.
monitor BUTp./DLIHi'I in order to assure it's appropriate use.
In its search f&r
*
todayd s b?op®r mcdicaj;.-aj.ee of BUT-2DI.T .Hi.;
.-.nd TA-iDDREL,. G’.ba-Goigy p-f^ffea had al so. dismiss cd its position
with consumer representatives'; ’ - Together witfi- opinions of
medical experts expressed in'scientific literature their
arguments have .been token into due account , if. th *
ur
decisions of today we: intend to m.cke again a major contribution
tq drug safety btftft in industrialized and developing countries.
IDENTITY OF PRODUCT OR SUBST. NCR
1J
' -A-’
Use »f the product
:
Generic .erDaemon .name
:
Brand(s)
'
•
'
*
Non-steroidal
.
,
- ;(i) phenylbutazone
,
b
anti-inflammatory drug
(i) Butazolidin \
(ii) Oxyphenbutarone
,£li) Tanderil
Manufacturer/Di. stri tutors -Giba-Geigy
(There are also <ther brands of phenylbutazone and oxyjhenbutazone
Containing drugs manufactured by Ciba-Geigy and othe companies .
This Alert refers sct-cddcally to Butazolidin and Tanderil).
15 P. 30. '2_|
British Journal of
Supplement 70
Vol 44 i\lo 8
August 1990
Pg. 22-25
linical
Practice
LJ
A symposium supplement
A review of childhood pyrexia
and the therapeutic options
for the 1990s
A MEDICAL TRIBUNE
UK LTD PUBLICATION
\\ arwick Castle
2 April 1990-
A double-blind comparison off itaproffen and
paracetamol m juiveimMe pyrexia
J SIDLER, B FREY
*.
Lucerne, Switzerland
K BAERLOCHER, Ostschweizerisches Kinderspital, St Gallen, ’Kinderklinik,
Introduction
The pyrexia which frequently accompanies childhood illnes
ses is thought by some clinicians to be a relatively innocuous
component of the body’s defence against disease. However,
parental and medical concern increases with the extent of
the rise in body temperature and the length of time over
which a grossly abnormal temperature is sustained, and it
has been demonstrated that these factors increase the likeli
hood of complications such as febrile convulsions. During a
febrile illness the child’s status is dull and his/her catabolism
is increased.
The catabolic effects of infectious illness which are largely .
attributed to fever are reduced when fever is lowered, and
there is an advantage in maintaining a near normal body
temperature during an infection in that the patient feels'bet
ter and eats better.
Fever is the result of many stimuli, either of an endogen
ous or an exogenous nature. Bacteria, virus, fungi, anti
body-antigen reactions and various drugs can induce it. It is
thought that it may be due to the production by leucocytes
of an endogenous pyrogen, a low molecular weight protein
nature, which probably acts on the thermosensitive
neurones in the pre-optic hypothalamic region. Although
not totally explained, the action of the endogenous pyrogens
seems to be connected to the release of mediators such as
serotonin and the prostaglandins E, and E2, which are con
sidered to be the central mediators or modulators of the
onset of fever. That is why the inhibitors of prostaglandin
synthesis are antipyretic.
In this study a double-blind comparison was undertaken
of ibuprofen syrup and paracetamol syrup in the treatment
of juvenile pyrexia.
Ibuprofen and paracetamol are both analgesic antipyretic
drugs, ibuprofen being a propionic derivative ^jnd
paracetamol a para-aminophenol derivative. With rega'®L>
indications, ibuprofen has been traditionally used as an amiinflammatory and analgesic and paracetamol as an antipyre
tic, although recently ibuprofen has also been used as an an
tipyretic. This fact is due among other things to:
o Pharmacological evidence of its antipyretic properties.
Already in 1970, Adams had shown the antipyre^ activity of ibuprofen to be 20 times greater than that. oRicetylsalicylic acid in rats with fever induced byvjgRs.
• Better knowledge of the pathology Q^^|B?5the impli
cation of prostaglandins in its ongiH^^msubstances with
similar pharmacokinetics the one which shows a greater
capacity for inhibiting prostaglandin synthesis has the
most potent antipyretic effect.
• The good tolerability of ibuprofen proved by controlled
trials and confirmed by the wide use of the
an
anti-inflammatory and analgesic, particularl^he/Ht 1tas
become available in some countries without need of a
doctor’s prescription.
Aims
This study was designed to extend investigations with ibup
rofen in children admitted urgently to hospital for the treat
ment of a variety of fever-producing conditions and had the
following aims:
o To compare the antipyretic efficacy of ibuprofen (at two
different strengths) and paracetamol.
■.,.
o To compare the incidence and severity of side effects.
Study details
The study, a double-blind, parallel group, multipledose
trial, was conducted at two centres in Switzerland.
Suitable patients for the study were children of either sex
in an age range of five months to 13 years, weighing bet
ween 7 and 36 kg and having a rectal temperature of 38.5°C
or more.
Details of the study were explained to the parent or legal
guardian before informed consent was obtained for the child
to take part in the study.
Children with severe systemic diseases including a bleed
ing disorder, a history of peptic ulceration, chronic dyspep
sia or chronic gastrointestinal bleeding, or a history of
asthma were excluded from the study. Also excluded were
those receiving immunosuppressive treatment, those receiv
ing treatment likely to interact with the study medication,
those considered by the investigator to be unsuitable for
entry, those allergic to the study medication or related com
pounds, those suffering from hepatic, renal or cardiac diseasc
tolerate a rectal probe.
Ninety suitable hospital pa^rats were allocated to one of
the following treatments by random distribution in blocks of
three such that there were initially the same number of pa
tients in each group:
° A single dose of ibuprofen syrup at 7 mg/kg body weight
(formulation 20 mg/ml).
° A single dose of ibuprofen syrup at 10 mg/kg body weight
(formulation 30 mg/ml).
° A single dose of paracetamol syrup at 10 mg/kg body
weight (formulation 30 mg/ml).
Patients received the first dose of study medication at
baseline (Hour 0), providing medication likely to affect the
assessments had not been taken in the preceding four hours.
A second or third dose of the medication could be adminis
tered only at eight-hour intervals, and only in cases where
the rectal temperature was 38.2°C or more.
Demographic data recorded at entry to the study com
prised age, sex, body weight, presumptive diagnosis and
concomitant drug therapy.
Data recorded
Withdrawals
Patient body temperatures were recorded at 10 minute inter
vals for a minimum of 12 hours and a maximum of 24 hours
after the first dose of study medication using a rectal sound
connected to automatic data logging equipment. Additional
written records of body temperatures were provided at
Hours 0, 0.25, 0.5, 1,2, 3, 6, 8, 12, 16, 20, and 24. Changes
in the clinical condition of the patients were recorded on a
five-point scale (1 = much worse to 5 = much improved) at
Hours 3, 6, 8, 12, 16, 20 and 24.
Details of withdrawals, side effects and any changes in
concomitant drug therapy were rcorded.
Of the 90 patients recruited to the study, one patient was
excluded from the efficacy analysis (prescribed Ponstan on
the day prior to entering the study).
Eighteen (20%) of the 89 eligible patients withdrew from
the study-three taking the 7 mg/kg ibuprofen medication,
four the 10 mg/kg medication and 11 the paracetamol medi
cation. The main reason for withdrawal was lack of response
(Table 1).
Table 2. Summary of side effects.
Treatment group
Ibuprofen Ibuprofen Paracetamol
10 mg/kg
7 mg/kg
10 mg/kg
Quality of data
The timing of a number of assessments was not at the
scheduled time. In such cases assessments were taken to the
nearest scheduled time. If as a result two or more assess
ments represented the same scheduled time, the assessment
nearest to the scheduled time was used in the analysis and
the other assessments were disregarded.
Vomiting
Abdominal pain
Rash on forearms
Got cold at 35.5°C
Total number of
side effects
Analysis otdata
Side effects
' ■'y~~~-—■
* --------------------- ■
1
1
1
—
—
1
2
—
—
—
3
1
2
Six patients suffered side effects: three in the 7 mg/kg ibup
rofen group, one in the 10 mg/kg ibuprofen group and two
in the paracetamol 10 mg/kg group (Table 2).
The treatment groups were assessed for comparability with
respect to baseline information. Clinically significant differ
ences were allowed for in the subsequent analysis.
Reasons for and times of withdrawal/drop-out were re
ported and the frequency of complaints reported on each
treatment were tabulated.
The principal measures of efficacy were the reduction of
body temperatures three hours after dosing. The measures
were analysed using a paired t-test and 95 per cent confi
dence intervals were calculated for the mean differences.
The body temperature three hours after dosing was also
analysed by analysis of covariance with the pre-treatment
value as covariate. Differences between treatment groups in
the proportion of patients with a drop in body temperature
of 1°C or more at three hours were compared using a chisquared test.
Reduction in temperature
The reduction in temperature at three hours was significant
for all three treatment groups: ibuprofen 7 mg/kg, —1.64°C;
ibuprofen 10 mg/kg, —2.09°C; paracetamol, ■—1.29°C.
Twenty-six (90%) patients in the ibuprofen 10 mg/kg
group had a decrease in temperature of 1°C or more. The
corresponding numbers of patients in the ibuprofen 7 mg/kg
and paracetamol groups were 23 (79%) and 20 (74%) re
spectively. There were no statistically significant differences
between treatment groups in the proportion of patients with
a decrease of 1°C or more.
Patients in the ibuprofen group had a significantly lower
mean temperature (Fig 1) than patients in the paracetamol
groSfp (pjgO.05 for the 7 mg/kg group, p==0.01 for the 10 mg/
kg group). The covariate age had no effect on the temper
ature at three hours, the ibuprofen being more effective ac
ross the whole age range of 5 months to 13 years.
Results
At this stage the results for the automatic data logging are
not available. The data presented here are those recorded
by hand.
Table 1. Summary of withdrawals.
Ibuprofen
7 mg/kg
Treatment group
Ibuprofen
10 mg/kg
3
27
4
25
Withdrawals
Yes
No
Complete recovery
Lack of response
Patient vomited
Second dose of medication not taken
Squirrel temperature defect
Unknown
Total number of patients
2
4
—
1
— ■
30
——
—
—
29
Paracetamol
10 mg/kg
Overall
11
19
2
5
1
18
71
2
11
1
1
1
2
89
—
2
30
T)p_ SO- 'i-T
Fig 1. Mean temperature up to three hours
by treatment group.
The analysis of temperature over time (Fig 2) showed
that there were significant differences between the treat
ment groups, with the overall mean temperature for the two
ibuprofen groups significantly lower than for the
paracetamol group. There was a significant treatment group
by time interaction, suggesting the magnitude of the differ
ences between the ibuprofen and paracetamol groups varied
over time. The paracetamol temperature curve only came
down to the ibuprofen 7 mg/kg curve at 12 hours after 59%
of patients in the former group received a second dose of
paracetamol at eight hours (Fig 2). The differences were
greatest between three and eight hours and 16 and 24 hours.
Analysis of clinical condition at three hours and over time
showed there were no significant differences between the
treatment groups. Less than half the children required a sec
ond dose to control fever in the iouprofen groups. (38% in
the 7mg/kg group, 44% in the lOmg/kg group), whilst just
over half the children (59%) required a second dose in the
paracetamol group.
Conclusions
Fig 2. Mean temperature over time by treatment group
(adjusted for age and baseline temperature).
• Treatments were efficacious. All three treatment groups
showed a significant reduction in temperature from
baseline to three hours and the temperature remained
lower over the 24 hours of the study.
• Temperature reduction was greater in the ibuprofen
groups. There was a significantly greater reduction in
temperature at three hours in the ibuprofen groups than
in the paracetamol group, with a larger number of pa
tients showing a decrease of 1°C or more.
® Temperature reduction was fastest in the ibuprofen 10 mgl
kg group. Patients in the ibuprofen 10 mg/kg group had
a significantly lower mean temperature at three hours
than patients in the paracetamol (10 mg/kg) group.
• Mean temperatures for ibuprofen groups were lower than
for paracetamol group. The overall mean temperatures
for the two ibuprofen groups were significantly lower
than the corresponding paracetamol group mean. The
magnitude of the differences varied significantly over
time.
o Clinical condition improved more rapidly for ibuprofen
groups. Whilst there was no significant difference in over
all clinical condition between the treatment groups, the
rates of improvemat were greater at three hours in the
ibuprofen groups^
® Good tolerab;ii:--^^Kf^Kadoses of study medication
were well tolerated, with only six patients reporting side
effects.
R^prmte^witnpermisson from British Journal ol Clinical Practice, Hong Kong. Published by Medical News Tribune. l8/20J<^ubast^arg™
Bombay-400 023.
-Z7oloC tet
pi^-2-
C
<i<5>vvO
L /^yc^iYC^-io /&(
_Z7
Sr
r
c „ 3V
3-
( OJ p C<O_ X <3
oJL p kc^Lxi Lczv- cj
Axn:
a.<T|a ^1
Xox_>~/
1
3
:, A-f<si^<o_ o-
.La
;
~Pfa
>
c
-e_£\
/\J S a} i D
CiZL?L(; /CT _J_(
■>
tU'-O-C'Xc!.,
-t //-( OlCdLftx
a
■
C.(L-vtS-Ksa-M
P O. Se^x . 4fe ooz
£c>=_<o fe,
i 7 HCctcLUi:
Px^-^',
QQ
^>^cL\<k q_
K<=lfeoJ-
^_U
(LgcuJlCl^o '^tXS^l^CC^Sj?
deJU. Q^pL>| (Xi-^^/cy
/7C^
■i- 20 b
Ils I 2S'".
T)
io * X3
0-7
PPST NEWSLETTER
Vol.L, No.l
February 198'+
Concern about health care, drugs policy and suitability
of modern medicine in developing countries has been expressed
in various forms.
Exploitation by multinational drug compa
nies, aided by the 'ignorance' of the medical profession and
apathy of the governments have made medical care expensive
and ineffective.
The lack of adequate nutrition has made the
’je of powerful drugs dangerous.
In this newsletter we present an interview with Dr.
Zafrullah Chowdhury, one of the founders of the Gonoshasthya
Kendra, Bangladesh, during his visit to Madras in December
1983.
The Gonoshasthya Kendra (People's Health Center)
was set up'to provide adequate health service in the rural
areas of Savartharna , increase the independence and bar
gaining power of women and to bring about a change in the
infrastructure and thereby allow for the economic and
social development of poor villagers, i.e. 90^ of the popu
lation of Bangladesh' .
The main activity of the Kendra
is a health programme involving training in rural health
care, curative care through rural centers, preventive care,
family planning, a health, insurance scheme, a pharmaceutical
plant and publication and distribution of literature to
assist medical practitioners in rural areas.
In addition
vocational training and classes in literacy and 'conscience
raising' are given to villagers.
The Kendra was also actively involved in the formulation
of the Bangladesh Drug policy which has resulted in the
banning of over I7OO drugs.
As a result, tremendous pressure
has been put upon the Bangladesh Government by various Western
countries including USA, UK, Holland, etc.
In view of the relevance of these issues to the situation
in our country, we are reproducing here the interview con
tributed by Madras Group.
Dr. Chaudhury started by presenting a brief account of
the People's Health Centre;
In 1971> a group of doctors from England came to
Bangladesh during the War of liberation and worked in the
liberation army.
At that time we got a new perspective
on health.
All of us went back to England after the war,
but some of us came back to Bangladesh in 197^-•
We started
a primary.health centre.
We realised that poverty and
malnutrition cannot be tackled just by doctors alone but
Contact Address:
c/o J.K.Suresh, 6^A, Shop Street
Basavanagudi, Bangalore $6 0 004-.
2
a doctor could be a leader for a team of health workers
who tackle major issues.
We selected women from villages
who had had 5-10 years of schooling and trained them as
health workers.
They give curative care, do all family
planning, including operations, like abortions and steri
lization, do pathological investigation (with slides, urine,
etc.).
One or two are trained to take ECG.
They have
high technical competence and have been checked by experts
f-om WHO, Harvard, Johns Hopkins, etc.
Women were also
trained in handicrafts and other crafts such as welding,
carpentry, etc. - functional education was given to provide
a source of income.
Education is very important: Kerala
has a good health system due to education and a good public
distribution system.
School children can in fact act as
teachers.
Our lessons on oral rehydration for diarrhoea are
very effectively taken home by school children.
Recently we have gone into the production of drugs.
Our drugs are 1/3 to 2/3 cheaper.
All our health services
are paid for.
We have a Health Insurance Scheme under
which the poor people get all the care for $0 P.
Middle
class patients pay 10 Takas/year and 2 Takas/visit in addi
tion to charges for pathological examination etc.
The
rich pay 25 Takas/year and 5 Takas/visit.
This leaves us
with a deficit of 50/ in our budget, which we meet by local
and foreign donations.
Our pharmaceutical unit wild, break
even this year and from next year we will make profits.
We intend to use a part of this money to increase production
and a part to support research and services.
In our center we train medical students in a brief twoweek course.
We talk about nutritional status of Bangladesh
and several relevant social and economic factors that the
regular medical course does not touch upon.
We also train
traditional birth attendants.
PPST :
What is the strength of your group?
We are a trust with 4- local health centres.
We have
500 full time and 500 part-time workers.
PPST ' How does the medical community react to you?
ZC 3
ZC :
Generally the profession is angry with us for our role
in the drug policy and several other things.
When
we started the two-week course for medical students
some medical college staff protested.
But students
who have gone through our course support us.
They
also dislike our training of paramedics for operations
etc.
We find that the present medical education is
irrelevant to Bangladesh.
We are trying to make it
in Bengalee.
This is also opposed.
We are branded
as communists.
3
At present Bangladesh has about 15-,000 doctors.
Oyer
5,000 of them are abroad.
We have nine medical colleges
producing 1^00 doctors every year.
In rural areas
the-'e is only one doctor for every 5^,000 people though
the government claims that there is one for every 7,000
people.
6000 of our doctors are in the major cities.
In addition, villages have several unqualified 'quacks'
(over 30-,U0,000).
There are about 17,000 pharmacies
and over <0,000 unregistered pharmacists.
PPST :
What are the government health facilities available
to the people?
ZC 1 Government hospitals are like in India.
There is
a primary health centre for every 150 - 350,000 people
which are given 30,000 taka/year for drugs.
Over half
of this is sold outside.
They are very ineffective and
what they offer is mostly curative care.
We have all
our four centres in rural areas.
We are also thinking of
covering urban slums.
PPST I What is the present status of the drug policy?
ZC
There is great pressure from USA to revise it.
The
'review committee' has made some concessions.
The
major concession is that third party licensing continues
till present licence runs out, i.o., a company can sell
a right to produce a brand name drug to another.
Two
American companies have, a contract till 1985.
The government is not insisting that the 5-5 drugs sold
in PHC's should be sold by generic names alone.
The
medical profession often says that brand names are used
in India, after all they are also scientific etc.
The
fundamentalists also oppose us since 65^ of all our
health workers are women and they ride bicycles etc.
Some of the drugs banned here are coming in through India.
Several countries have tried such bans earlier and failed.
Sri Lanka wanted to rationalize its drug policy and failed
under pressure from US government and companies.
Bhutto
tried it in Pakistan but hud to withdraw the order since
over 90^ of their drugs are made by multinationals.
In our case, when the government asked us to formulate
the drug policy, I did not think a military government
could do it.
We explained to Gen. Ershad the problems
faced by Sri Hinka etc.
There was no ’popular pressure'
as such, but the government had some backing since we had
commenced production of some vital drugs.
We were also
backed up very well by other countries, voluntary organi
sations , and social organisations.
There has been
tremendous pressure on the government.
In India an 'aura' has been built up about drugs.
India is among the top ten drug producers.
Here the
national bourgeosie has joined hands with the inter
national bourgeosie.
Jr’ori'c-.jve".
tn
....... < —
PPST I Why is the drug industry'reaping such huge profits?
Tobacco, arms and drugs are making the highest profits.
There are many reasons for the profitability of drugs.
firstly the doctor is ignorant - our curriculum is not
preparing us well.
We assume that multinationals
produce quality drugs.
In fact they are terrible.
I saw the Glaxo factory in Bombay.
I think it should
be closed.
The 'paying client is different from the
doctor who prescribes.
Consumer awareness is also
poor.
In countries that have National Health Service
like Britain, the patient is not the buyer.
When
Margaret Thatcher asked the NHS to buy generic drugs,
immediately the- prices came down by 7 - >4-2%.
ZC
Our own pharmaceutical company is run by a trust.
There are no share holders who stand to gain by increased
profits.
As per our charter our profits cannot exceed
We encourage people to visit our quality control
department.
PPST :
ZC ;
What are your relations with the government?
Do
you also advertise? How do you counter the propaganda
of drug companies?
Multinationals bribe our government heavily,
which
our company does not - so many are unhappy.
Initially
we wanted to supply only to the government.
We had
to popularise our drugs and wo did it through local
language.
We do-have medical representatives.
All
our literature is in Bengalee so that the public would
read it.
There was a hue and cry over this.
We
promote our drugs only by generic names.
The passage
of time is helping us.
Doctors are learning to live
without Novalgin and once a burcacracy siezes upon a
government decision to act, it is not an easy task tc
change it.
We also write articles in major national dailies to
counter the propaganda of major drug companies.
We have not yet started any alternate schools.
We
have not supported the revival of 3-year trained
doctors since it would create a feeling of being
second class doctors.
5
PPST :
What is your attitude to traditional health systems?
JC I
In our new curriculum we are integrating traditional
health system.
We have examined (i.e. a panel has)
over 80,000 ayurvedic drugs.
Only about PJ,000 have
been retained.
For example, for pneumonia we accept
3 ayurvedic drugs.
There are about 3->+,000 ayurvedic
physicians though ’they' claim over 4-0,000.
Also
about 3,000 Unani physicians.
Most of the village
doctors are quacks.
PPST ;
JC :
What is your approach to family planning?
It is to be linked to the whole issue of development
and women's emancipation.
We sterilize only if a
couple has at least three children (with youngest
at least k years) and with P kids if both husband and
wife consent.
The government has over 4-0,000 workers for family
planning.
Tubectomy gets priority.
The use of
Depo Provera has not been stopped.
In 1971*- I was
responsible for getting Ifepo Provera into Bangladesh.
We were naive at that time and got taken for a ride.
The government is pushing sterilization with gifts etc.
PPST ;
Can paramedics degenerate into quacks?
ZC ;
In isolation they cannot do much curative work.
People
like paramedics better - they are more concerned.
PPST :
Do you think of traditional systems of medicine
purely as a drug alternative?
They might offer an
entirely new perspective on health.
For example,
what should be taken as indicators for health?
Rather than infant morality, etc. , should we not aim
for increased awareness, interest and participation
in our health?
ZC Z
Yes.
We have to give increased knowledge about
health.
We encourage familities to improve their
own health.
We have translated Werner's book ('Where
there is no Doctor' by David Werner) into Bengali.
The last part of the meeting was a general discussion on
the attitude towards traditional health systems (specifically
Ayurveda).
It was suggested to Dr. Chowdhury that different
health systems have their own criteria to understand and
expalin drug action.
Hence it may not be correct to
'evaluate' ayurvedic drugs, but they have to be observed
in operation.
This view however was not accepted by Dr.
Chowdhury who felt that the criteria of modern medical system
could indeed be used to check the efficacy of and 'standard
ize' all the drugs.
5
PPST :
What is your attitude to traditional health systems?
JC :
In our new curriculum we arc integrating traditional
health system.
We have examined (i.v. a panel has)
over 80,000 ayurvedic drugs.
Only about ^5,000 have
been retained.
For example, for pneumonia we accept
3 ayurvedic drugs.
There are about 3-4-, 000 ayurvedic
physicians though 'they' claim over 4-0,000,
Also
about 3,000 Unani physicians.
Most of the village
doctors are quacks.
PPST :
JC :
What is your approach to family planning?
It is to be linked to the whole issue of development
and women's emancipation.
We sterilize only if a
couple has at least three children (with youngest
at least < years) and with Z. kids if both husband and
wife consent.
The government has over 4-0,000 workers for family
planning.
Tubectomy gets priority.
The use of
Depo Provera has not been stopped.
In 197
*+
I was
responsible for getting Eepo Provera into Bangladesh.
We were naive at that time ana got taken for a ride.
The government is pushing sterilization with gifts etc.
PPST *
Can paramedics degenerate into quacks?
ZC .'
In isolation they cannot do much curative work.
People
like paramedics better - they are more concerned.
PPST :
Do you think of traditional systems of medicine
purely as a drug alternative?
They might offer an
entirely new perspective on health.
For example,
what should be taken as indicators for health?
Rather than infant morality, etc. , should we not aim
for increased awareness, interest and participation
in our health?
ZC
Yes.
We have to give increased knowledge about
health.
We encourage familities to improve their
own health.
We have translated Werner's book ('Where
there is no Doctor1 by David Werner) into Bengali.
The last part of the meeting was a general discussion on
the attitude towards traditional health systems (specifically
Ayurveda).
It was suggested to Dr. Chowdhury that different
health systems have their own criteria to understand and
expalin drug action.
Hence it may not be correct to
'evaluate1 ayurvedic drugs, but they have to be observed
in operation.
This view however was not accepted by Dr.
Chowdhury who felt that the criteria of modern medical system
could indeed be used to check the efficacy of and 'standard
ize' all the drugs.
COMMUNITY HEALTH CELL
326, V Main, 1 Block
Koramengaia
,
Bangalore-560034 - '
India
DETAILS REQUIRED TO BE FURNISHED ON NEV/) DRUGS
If any pant of the information is in a foreign language, an
accurate and complete translation shall be appended to such part
(together with the originals).
For the purpose of this w ostionnaire, the term ’New Drug’
shall have the meaning as specified in the Explanation under Rule 30-
A/69-B/75-B of the Drugs and > 'on .etics Rules and would also include :(a) A drug which has been approved for use under certain conditions and
for administration in a specific manner and which is now proposed to
be indicated for new conditions or in a different manner; (b) a
combination of two or more drugs even though each may have been
approved separately.
1.
(a) The chemical description of the drug and a declaration of
the internationally or nationally accepted generic name if any (name
of the country or the name of the pharmacopoeia in which this has
been accepted as the generic name may be mentioned) or if it has no
proper name, the name under which it is proposed to be sold;
(b) If the chemical composition of the drug is not known, such
other details as are known.
2.
The description of the pharmaceutical form/forms in which it is
proposed to be marketed and the route of administration, the proposed
dosage and the claims to be made for such a drug.
3.
A detailed statement of the composition of the drug giving the
amount of each ingredient whether active or not, contained in a
stated quantity of the drug as for example per tablet per millilitre
etc.
4.
Details of the method of manufacture; the details should include
the raw-materials used in various stages in (a) the synthesis of the
pure drug if it is synthesized; (b) process of preparation if it is
obtained from natural resources such as plants, animal tissues, or by
growth of micro-organisms etc.; (c) the manufacture of the finished
products containing the new drug(s) as the active ingredient(s),
the precautions taken to see f at these raw-materials’intermediates,
2
etc., are not present .as impurities in the final product may be rive
In the case of inert ingredients the specifications for acceptance for
the manufacture of the finished product may also bo stated.
5.
Analytical specifications o'. the new drug and its preparations
containing the drug. The details should include the tests for proper
identity, purity, quality and the ...ethod for assay.
In the case of a preparation containing only one active ingredi
ent, the analytical methods suggested should be capable of assuring
its identity and determining its strength within a reasonable degree o
accuracy either in presence of or after’ removal of other inert ingredi
ts. In the case of a combination containing 2 or more active ingredi-{
ents, the analytical methods should be capable of identifying and
determining wherever possible the strength of all the active ingredi
ents individually. The specifications should also include limits for
impurities. The information may preferably be in the form of a mono
graph in a pharmacopoeia.
6„
Details of the stability studies, the date of expiry proposed
to be assigned to the drug or its formulations and special storage
precautions to be observed, if
7.
,
Details of investigations thai^iave been made to shw whether or (
not the drug is safe and effective for use :- If possible data as to
how the new drug compares, under identical experimental conditions in
respect of efficacy and safety, with other drugs known to be used for
same indications may also please be given,
(a)
Efficacy; Full reports of adequate irx _vitro and in vivo studies
by at least two methods reasonably applicable to the type of drug
under investigation for assessing its efficacy;
(b)
Pharmacological studies: Details of pre-clinical investigations
including studies made on laboratory animals in which methods used and
the results obtained are clearly set forth. The animal studies may not
be considered adequate unless they give proper attention to the
conditions of use recommended in the proposed lebelling for the drug
3
or to the conditions of clinical trials planned with the drug. The
information should also .include pharmacodyanamic studies on important
physiological system, such as cardiovascular system, respiratory system
central nervous system, the urinary system and antonomic nervous
system.
(c)
Bipchemical Studies : Detail.' of biochemical studies showing the
absorption and wherever possible the distribution, metabolism and
excretion of the drug. The infer ation whether any metabolites were
identified, if so, their excretion and whether they have any effect on
the activity or toxicity of the drug may also be given if techniques
are available for these studies.
(d)’
Toxicological Studies: Toxicity should be studied in several
species, two or more in both acute experiments and long term investi
gations. One of the species should be non-rodent. Both sexes should, he
studied. Animals used should be of healthy stock and adequate precau
tions taken during study to avoid extraneous infections. Adequate
numbers should be used at each dose level. In atleast one of the speci
selected, the drug should, if possible, have an activity related to th
expected therapeutic effect. Studies should include administration by
those routes recommended for use or for clinical trials. At least one
should bo systemic. The details should cover acute, sub-acute and
chronic toxicity studies. Adequate control groups administered all
constituents of the drug other than the active substance should be
included in all these studies. The over-all toxicological data should
fully rofZtet the nature of now drug such as for example whether the
drug is for short or
longer administration or whether it is to be
used in infants, children, pregnant women or menopausal women etc.
In case, some of the observed changes are considered to be
unrelated to the drug, the basis on which such a conclusion is drawn
be clearly explained.
4
(i)
Acute ‘toxicity : Two or more
routes of administration, one <■.'
which should at least be systemic if the drug is intended for systemic
use, should be used in atleast two or more species mentioned above.
Several dose levels should be used. LD—50 value with limits of error
should also be included.
(ii)
Sup-acute and chronic toxicity;
Two or more species should
be taken for long term studies and both sexes should be selected, v/henever possible the species chosen should be used and at least one experi
mental group should receive a dose that is toxic to sone animals.
The details and duration see table laid down in Appendix I,
. Chronic toxicity;- Duration of toxicity studies pending on the
nature of the drug and species of the animal used should conform to the
requirements laid down in Appendix I.
The parameters studied should cover changes in appearances and
behaviour, rate of weight
gain or loss, urine stool and blood analysis
including hematology, liver and kidney functions tests. Detailed post
mortem studies should include weights and microscopic comprehensive
histological examination of all important organs. Local response of the
tissues at the site of drug administration should also be recorded.
(iii)
Where the mtiire of the drug indicates such a possibility
special studies for as essing carcinogenicity and drug dependence should
be conducted.
(iv)
Teratogenic studies; Should lie carried out if the drug is to
be studied in women of child bearing age. These should be in atleast two
species of animals, rats oi' mice and another species in which the in
cidence of spontaneous abnormalities in reproductive physiology are
reasonably well known and in which there is a placental transfer of the
drug. The
studies covering single generation be conducted to evaluate
the effect of the drug on fertility, implantation of the ova, develop
ment of the embryo and fetus, resorption, abortion, delivery, number of
live births, size of litters, teratogenesis, viability of the new born,
growth of the young, etc.
Any deformities or abnormalities observed
5
-5should be clearly stated. These studies should be carried out at a
dose level which will not be toxic to the mother,
O’
-1- case the application is for clinical trials, details of the
nature of the trials planned may be indicated.
Phase, I: Studies should be carried out in healthy volunteers or
patients with mild degree of disease who volunteer for this study. Phase
I trials start when the 'New Drug1 is first introduced into man and only
animal and in vitro data are available. This investigation is carried
out with the purpose of determining human toxicity and pharmacological
action including any untoward effects, preferred route of administratio:
and safe dosage range.
Phase II and would extend to initial trials on a limited number
of patients for specific disease control or prophylactic purposes. This
study shall also include mode of absorption and excretion and where
possible distribution of the drug.
Clinical trial or phase III trial- is for assessment of the drug's
safety and effectiveness and optimum dosage schedule in the diagnosis,'
treatment, or prophylaxis of groups of subjects involving a given disease
or conditions.
In all the above cases, a reasonable protocol formulated on the
basis of facts accumulated in the earlier studies belonging to the plan
of investigation shall be submitted. The plan of investigation should
indicate the number of patients to be treated with the drug, the number
to be employed as controls, if any, clinical uses to be investigated;
route of administration of the drug; proposed dosage; the kind of clini
cal observation and laboratory tests to be undertaken prior to, during and
after administration of the drug, the estimated duration of the investi
gation; whether any other drug is also intended to be given alongvith
the new drug under investigation and copy of report forms to be used to
maintain an adequate record of the observations and the tests and
results obtained. If it is a comparative trial, what other drugs are
intended to be used for comparison, their dosage, route of administra
tion etc.
.6
-69•
Combinntion of drugs:'
The combination of drugs should generally fall into four broad
groups,
1.
The first group of combinations are those vzhere ope of the active
components is a new compound.
(a).
Clinical trials.
(b).
Marketing permission,
x
treated on the same lines as
$
2.
This group of combinations should
any new drug, and the data which
«
needs to be the same as described
$
under guidelines for new drugs.
The second group of combinations would be vzhere individually
fl
marketed drugs are combined for the first time and where the individu .1
drugs have potent pharmacodynamic actions on vital organs.
( a)
Cliriical Trials:
In such cases an adequate summary of pre-existing information fro
pre-clinical and clinical investigations with, the individual active
components, results of clinical studies of the combination if carried
out in other countries pertinent reports on side effects, contra
indications and limitations of the components, rationale of combining the
drugs in the stated proportion, toxicity (acute toxicity with LD 50
a
values of the individual components and the combination under identical
experimental conditions) and pertinent pharmacological studies should
be submitted to obtain permission to carry out clinical trials.
(b)
Marketing permission
Results of clinical trials in India and if available from abroad,
should be submitted before a marketing permission can be granted.
5.
In the third group would fall already marketed combinations
wherein only modifications in proportion of individual ingredients is
considered, or vzhere new claims are made.
(a)
Clinical trials;
For such combinations appropriate rationale should be submitted to
obtain clinical trial permission.
.7
-7(b)
Marketing permission:
Results of human studies should be submitted for marketing
permission.
4.
The fourth group of combinations including drugs whose individual
active components have been widely used for several years and where the
manufacturers do not claim any extra advantage other than those of a
physical combination and convenient administration. Some of the examples
in this group are (a) Vitamins,(b) minerals,(c) digestive enzymes,
(d) nutritional products,(e) antacids,(f) non-specific anti-diarrhoeals,
(g) laxatives, (h) analgesics,(i) certain topical preparations other
than those containing steroids.
For this group of drugs no animal or human data is required and
marketing permission may be granted straight away.
10.
Copies of published or unpublished reports of clinical trials
pertinent to an evaluation of the safety and effectiveness of the drug.
11.
Certificate of approval or free sale certificate issued by the
Health authorities
in the country of manufacture and the names of the
countries where this drug is being marketed.
12.
Drafts or specimens of label, package, literature etc, proposed
to be adopted for marketing this drug in this country.
13.
Information in the package insert, literature etc. must not contain
incorrect statements, half-truths or unverifiable assertions about the
contents, effects (therapeutic as well as toxic) or indications of the
drug.
In describing the literature for medical profession, stress should
be laid down on rendering factual data, general statements should be
supported by adequate and acceptable scientific evidence. Promotional
material should not be exaggerated or misleading.
A full description based on current scientific knowledge should
include nature and content of the active ingredients with generic na... .■
per dose; action and uses; dosage; form of administration, mode of
application, if any; side effects and adverse reactions; precautions
.8
and contraindications; tre:at ’.ent in case of poison!•:<' and references
io
14.
the scientific or professional literature.
'."aether the drug is cporoved by the . ’ood <?-. .drug Administration
U.S.A, or by t. e j)unlop Committee, U,. . if so, whether any restrictions
are imposed on sole, way of labelling etc. ( a copy of the literature
including, if any, side effects, contraindications, precautions,
warning etc., us approved by these authorities nay be sent).
-9X^^Clinical J?han?..'; CT=_ Clinical trials : I4P= Marketing )
Category
Duration of Human
Phase
chronic toxicity.
Administration.
Oral
I* or
Subacute or
Upto 2 weeks.
C.P. , 0. j.. > 2 species; 2 weeks.
1-I.P.
r* id
2 species; upto 4 weeks
Upto 3 months.
C.T., M.P.
C.P.
C.T.
Several Days
Parenteral
’ species ; upto 6 mont'
11.P.
5 months to
2 species; upto 3 weeks
2 species; 4 weeks.
2 species; 3 months.
C.T., M.P.
2 species; 6 months.
unlimited.
Inhalation
-• ' •?
4 species; 5 days
M.P.
(General
( 3 hrs./day)
II.
Anesthetics)
Dermal
1 species; single 24 hr
C.P.
Short“term
exposure followed by
application.
2 week observation.
III.
C.T,, M.P.
1 species; 20-day repea
exposure (intact c;
abraded skin).
Long-term
C.P., C
1 species; number of
M.P.
applications and dura
tion commensurate with
the preparation and th'
duration of use. The
.
occlusive irritant te;
may be sufficient
-101V.‘ ’ OphthTaTmic'
5ingTe~'“~~
Otic
application
Nas.al
Multiple
application
“
""TrriTatibn~'€eV^“gya3e‘d'
*
1 species; 3 weeks daily
C.P., C,T.
applications, as in
clinical use,
K.P. '
1 species; duration
commensurate with period of
drug administration
*
V.
Vaginal
or
Rectal
C.P., C.T., 1 species, duration &
■
number of applications
determine by proposed use.
Animal. toxicity requirements for different phases of evaluation
"
■
= Clinical Pharmacology; C.T., = Clinical Trials;
(C.F
hi. P. = Marketing)
Category
Subacute
or chronic
Duration of
human
administration.
Phase
Several days
upto 2 weeks.
C.P., C .T., M.P. 2 Species ; 2 vzeeks.
Oral
toxicity
C.P.
2 species;- 4 weeks.
2 species ;-3 vzeeks.
2 species ; 4 vzeeks.
C. T., i'l .P.
or
parenteral
upto 3 months
6 months to
unlimited.
Dermal
C.T.
2 species;
3 months
M.P.
C.T., M .P.
2 species;
6 months.
2 species;
6 months.
C.P.
1 species; single 24 hrs.
Short term
exposure followed by 2
application
week observation
Long term
C.T., C .P., M.P.
1 species; no, of applications and duration comme
nsurate with the prepara
tion and the duration of
use. The occlusive irri
tant test may be suffi
cient.
Inhalation
(General
anesthetics)
C.P., c,»1 • J II. P.
species;
5 days
(3 hrs./day).
Ophthalmic Single
Otic
application
Nasal
4
Irritation tests
graded doses
multiple
application.
1 species; 3 vzeeks
c»p., p C«
daily applications,
as in clinical use.
M.P.
1 species; duration
commensurate with uerioc.
of drug administration..
Vaginal
C.P., C.T
1 Species; duration
I i.P.
and number of
Rectal
appli cations determined
.
by proposed use_._ __
:O)2 30.,
"
) •fArn.o«<iA
H
OBJECTIVES
!•
To enable the voluntary health projects/private dispensaries and hospitals to draw their own essential drug lists,
suitable to their own requirements and thus suggest a policy for
their availability to the patients.
2.
To ascertain and draw a list of the minimum drugs required
and give an idea of minimum level of competence and facilities that
may be required to deal with the illness at a given health set up.
3.
malting
To provide a reference list of drugs to ■the doctor for
a rational choice of drugs in the given condition.
4.
To provide a prioritised reference list for stepwise avail
ability of essential drugs in a given health set up.
THE LISTS
List - A r List of drugs required at a health set up equi
valent to "L primary health centre. It may be a small community
health project with not enough diagnostic facilities.
List - B ; In addition to the drugs in List-A, List B
drugs are required au secondary heal tn organisations which has at
least a qualified Medical Officer with some diagnostic facilities
such as a small pathological laboratory. This may be a referal
centre at town or taluka level.
List- C : In addition to the List A and List B, drugs1', jzhese
drugs are required to be used at a tertiary level health set/up i.e.
a district level hospital, medical college"and teaching.
1/
List - D : These drugs can be handled by the para mpdical
workers with adequate training.
uist - E ; All the deviations from the Essential Drugs
list of WHO, as published vide their Technical Report series No.722
are included here alongwith the reasons for the deviation, in case
of each of them.
PRIORITIES
The drugs in every list are divided into two Priority I
drugs and Priority II drugs. This is from the view point that if
the priority I drugs are made available at each setup, then they
will meet the need for drugs most of rhe conditions. The priority II
drugs serve as supplementary to the priority I list. It alsqo
indicates the priority for usage e.g. Aspirin & Paracetamol/claffiified as Priority I drugs at primary health organisation as A
analgesic and antiinflammatory drugs. - meaning thereby that in
majority of the cases these -two drugs should be able to take
care of the need. Only a few cases ma y need Ibuprofen.
FORMULATIONS
An attempt is also made to suggest the strengths and forms
of each drug to avoid the dilemma of choosing from hundreds of
formulations for each drug.,
LIMITATIONS OF THE LIST
1.
The list does not suggest all alternative rational drugs
which may be used in given condition. This implies that the drugs
outside this list are not necessarily "non-essential" or
"irrational." This list gives only the list of minimum priority
drugs which have to be made available at particular health set up.
2
2.
It is possible that it may be necessary to use the drugs
outside this list in individual patients. A proper record of
such cases may be kept. It should contain the detailed history,
reasons why the present drugs cannot take care of the condition
and what is the additional advantage of the other drug being
chosen. Such a record will help in the improvisation of the list
after proper review.
APPLICABILITY OF THE LIST
1.
You may be a general practitioner or at a village level
dispensary or in a hospital. These lists will give you a reference
guide to examine the utility of the many drugs being stored or
used at your institution.
2.
Some institutions are faced with a situation where donors
supply a big chunk of drugs, and the physician in charge is under
pressure to use them even if he/she thinks such drugs as
unnecessary. These lists can be used to act as a reference for
both the donors and the administrators.
3.
A LARGE NUMBER OF DOCTORS BELIEVE' THAT THE LIMITED DRUG
LIST WILL HARM THE PATIENTS' BEST INTERESTS. THESE LISTS CAN BE
A STARTING POINT FOR CONCRETE EXPERIMENTATION IN THIS REGARD. A
FEW CATEGORIES OF DRUGS CAN BE SELECTED AND AN ATTEMPT BE MADE
TO PRESCRIBE THE DRUGS IN THESE CATEGORIES FROM THIS LIST. THE
EXPERIENCES MAY BE RECORDED SYSTEMATICALLY AND OVER A PERIOD OF
TIME - SAY ONE YEAR - A REVIEW CAN BE DONE WITH THE TEACHERS IN
PHARMACOLOGY, COMMUNITY PHYSICIANS AND EXPERTS IN VARIOUS
DISCIPLINE. THE RESULTS OF SUCH A REVIEW BE GIVEN WIDE PUBLICITY
TO START HEALTH AND DRUG ACTION BY SO MANY CONCERNED INDIVIDUALS
AND INSTITUTIONS.
4.
The Govt, and a large number of public & private sector
companies are giving health benefits to their employees. This
list can serve as a guiding list to them and will help them
to formulate their rational drug policy and other health benefits.
LIST
A
DRUGS REQUIRED AT PRIMARY HEALTH CARE ORGANISATION
Name of Medicines
Priority 1
.'Priority 2
Category
No.
Sr.
No.
1.
Anaesthetics
1.1
General Anaesthetics and Oxygen
1.
Oxygen
1.2
Local Anaesthetics
2.
Analgesics, Antipyretics, Non
steroidal Anti Inflamatory Drugs
and Drugs to treat Gout.
2.1
Non Opioids
Formulation
Inhalation (Gas)
2.
Acetylsalicylic
acid.
Tab. 300 mg.
3.
Paracetamol
Tab.
Syp.
Tab.
Tab.
4.
Ibuprofen
2.2
Ooioids analgesies
3.
Antiallergics
5.
6
‘Codeine
Chlorpheniramine
Maleate.
500 mg.
125 mg/5 ml.
200 mg
400 mg.
Tab. 30 mg.
Tab. 4 mg.
SyP. 4 mg./5ml
Inj. 10 mg /ml
4.
Antidotes and other sub stance soused in poisoning
4.1
General
7.
4.2
50 gm sachets
powder.
Specific
g
5.
Activated Charcoal
Atropine
Inj. 0.5 mg/ml.
A;; tiepileptJ.es
9.
Phenobarbital
6.
Anti infective Drugs :
6.1
Anthelminthic Drugs
Ip.IL.
Mebendazole
Tab. 30 mg.
Tab. 60 mg.
Tab. 100 mg.
Pyrantel Pamoate-. Tab. 500 mg.
Suspension 50 mg/ml.
... 2
2 :s
List A Contd,
Cate
gory
No.
Sr.
No.
6. 2
Antiamoebic Drugs
Name of Medicines
Priority 2
Priority 1
12,
Metronidazole
Tab. 200 mg./ 400 mg,
Susp. 200 mg/5 ml.
13.
Chloroquine Phosphate
Tab. 150 mg/Base
Syp.
50 mg/5 mil base
6.3
Antibacterial Drugs
6. 3.1
Penicillins
14;
Inj. 10 lac IU(Sodium
Ini. 50 lac IU POttasium)
Inj.
3 lac IU
Benzyl Penicillin
Procaine benzyl
pencillin.
16,
Benzathine benzyl Inj. 12 lac IU
Penicillin
Other antibacterial drugs
* sterate or Ethyl
succinate^
15:.
6.3.2
6.3.3
17.
Erythromycin
18.
19..
*
20
Sulphadimidine
Sulphamethoxazole j
+ Trimethoprim
'Tetracycline
21.
Doxycycline
22.
Amoxyciline
Rifampicin
Dapsone
Clofazimine
24.-.
25
Tab.
400 mg +
80 mg.
Cap. 250 mg(hydrochloride).
Cap. 100 mg(as .hydro
chloride)
250 mg (as trihydrate)
125 mg- /5 ml ~ powder
for oral susp.
Cap. 150 mg, 300 mg.
Tabs. 50 mg, 100 mg.
Cap.
50 mg, 100 mg.
Anti tuberculosis Drugs
26.
Ethambutol
27.
Isoniazid
Thiacetazone + )
Isoniazid
5
Antifilarial Drugs
28.
6.4
Tab. _ 250 mg. (as
Oral susp. 125 mg/
5 ml.
Tab. 500 mg
An'tileprosy Drugs
22.
6.3.4
Formulation
29.
Diethyl Carbamazine
Tab. 200 mg, 400 mg
800 mg.
Liquid 100 mg /5 ml.
Tab. 100 mg, 300 mg.
Tab. 150 mg + 300 mg
Oral Liquid = 50 mg./
5 ml.
Tab. 50 mg, 100 mgm.
' 'citrate)
... 3
:s 3
List *A' Contd.
Cate
gory
No.
Sr.
No.
6. 5
Antifungal Drug
30.
Name of Medicines
Priority 1
'Priority 2
Anti leishmaniasis Drugs
6.7
Antimalarial Drugs
31.
Pessary of One lakh
unit.
Nystatin
6. 6
Tab. (Ph ospha te,
Sulphate) 150 mg
(Base) .
Syp. (phosphate.
Sulphate) 50 mg/5 ml.
Chloroquine
Primaquine
32..
Formulation
6.8
Anti schistosomal Drugs
6.9
Antipanosomal Drugs
7.
Antimigraine Drugs
8.
Antineoplastic & Immunosuppressive drugs
9. .
Antiparkinsonism Drugs
10.
Blood Drugs Affecting the
10.1
Anti Anaemia Drugs
Tab. (as Phosphate)
7.5 mg.
33.
34.
Ferrous Sulphate
Folic acid
Tab. 200 mg
Tab. 1 mg.
35.
Ferrous sulphate +
Folic Acid.
Tab. 200 mg + 200
micrograms.
10,2
Anticoagulants and Antagonists
11.
Blood products and Blood Sub
stitutes.
11.1
Plasma substitute
11.2
Plasma Fractions _for Specific uses.
12.
Cardiovascular Drugs
12.1
Antianginal Drugs
12.2
Antidysrhythmic Drugs
12.3
Antihypertensive Drugs
12.4
12.5
Cardiac Glycosides
Drugs used in Shock - Anaphylaxis
3 6-
Epinephrine
Inj. 1 mg/ml (hydro
chloride)
4
:s 4
List 'A' contd.
Cate
gory
No.
Sr.
No.
13.
Dermatological Drugs
13.1
An•'dfungal Drugs
37.
12.2
Name of Medicines
Priority 1
Priority 2
3 8-.
Nystatin
39.
Miconazole
Oint./Cream, 1 lac
IU/gm
Oint/Cream, 2%
Anti Infective Drugs
Neomycin +
Bacitracin
Oint. 5 mg neomycin
sulphate + 500 IU
bacitracin zinc/gm.
Anti inflammatory and
Antipruritic Drugs
.4:1,
Calamine lotion
Lotion
42-
Hydrocortisone
°int./Cream 1%
- (acetate)
43-,
Betamethosone
Oint./Cream
(Valerate) 0,1%.
13.4
Astringent Drugs
13.5
Keratonlastic and Keratolytic agents.
44-
13.6
Formulation
°int./Cream 6% + 3%
Benzoic Acid +
Salicylic Acid
40.
13.3
,
Coal tar
-
Topical Soln. 20%
Scabicides and Pediculicides
45.. Benzyl Benzoate
-46- ‘ Lindane (BHC)
14.
Diagnostic Agents.
15.
Disinfectants
47.
Chlorhexidine
Iodine
Gentian Violet
16.
Diuretics
17.
Gastrointestinal Drugs
17.1
Antacids and other antiulcer
Drugs.
*
'S©
Aluminium Hydroxide +
Magnesium (Trisilicate
Lotion, 25%
Lotion, 1%
Solution, 5%
Tincture,2% and 7%
Topical Solution, 1%
Tab. 250 mg.+ 125 mg
Oral Susp. 320 mg/
5 ml.
Oral suspension
equivalent 550 mg
of MgO/10 ml.
5
»
Cat.
No.
SrNo.
17.2
Antiemetic Drugs
51,
17. 3
.
Formulation
Tab. 10 mg, 25 mg.
Promethazine
Antihaemorrhoidal Drugs
Local anaesthetic,
astringent and
anti inflammatory
drug combination.
Ointment.
Anti spasmodic drugs
53,
17. 5
5
p . Name of Medicines
----Priority 1
Priority 2
52.
17.4
5
Tab. 1 mg.
Atropine
Cathartic Drugs
54.
Bisecodyl
17.6
Diarrhoea
17.6.1
Antidiarrhoeal (Symptomatic) Drugs
17.6.2
Fluid Replacement Solution
55,
56,
Loperamide
Oral Rehydration
Salt
Tab. 5.0 mg.
Tab. 1 or 2 mg.
Sodium Chloride 3.5 gm
+ Trisodium citrate
dihydrate 2.9 gm
+ Potassium chloride
1.5 gm
4- Glucose 20 gm for
1 litre solution.
18.1
Hormones
Adrenal Hormones and synthetic substitutes;
18.2
Androgens
18.3
Contraceptives
18i
*
57
°ral Contraceptive
pills,
18.4
Estrogens
18.5
Insulins and other Anti Diabetic Agents
18.6
Ovulation Inducers
18.7
Progestogens.
18.8
Thyroid Hormones and Antithyroid Drugs.
19.
Immunologicals
Ethyl Estradiol +
Norethasterale 30 microgram + 1 mgm.
-
.
6
:i 6 ::
List '.A1 c ontd.
Cat.
No.
Sr.
No.
19.1
Diagnostic Agents
19.2
Sera and Immunoglobulins
19.3
Vaccines
19.3.1
For Universal Immunisation.
Name of Medicines
Priority 1
Priority 2
Formulation
58-
BCG Vaccine
Inj.
59,
60.
DPT Vaccine
DT Vaccine
Inj.
Inj.
Inj.
Measels Vaccine
Solution
62. Poliomyelitis Vaccine
Inj.
63.Tetanus Vaccine
NOTE ; All vaccines should comply with
WHO. requirements for biological
substances.
61..
19.3.2
For specific groups of Individuals.
20.
Muscle Relaxants and Cholinesterase Inhibitors
21.
Ophthalmological Preparations
21.1
Antiinfective Agents.
64.
65.
21.2
Antiinflammatory Agents
21.3'
Local Anaesthetics
66.
Drops 10%
Eye Oint. 1%
Sulfacetamide ■
Te tracycline
Solution 0.5%
Tetracaine
21.4
Miotics and Antiglaucoma Drugs
21.5
Mydriatics
22.
Oxytoe ics
67.
Ergometrine
23.
Peritoneal Dialysis Solution
24.
Psychotherapeutic Drugs
68.
25.
Diazepam
Tab. 0,2 mg
(Maleate)
Tab. 5 mg.
Respiratory Tract/ Drugs Acting on the
7
: 7 ::
List 'A' Contd.
Cat.
No.
Sr,
No,
25.1
Anti Asthmatic Drugs
25.2
Name of Medicines
_
Priority 1
Priority 2
Formulation
€9,
Aminophylline
Tab. 100 mg
70.
Ephedrine
Tab.
71.
Salbutamol
Tab. 2rag, ,4 r.g
Liquid 2 mg /5 ml.
72,
Adrenaline
Inj. 1 mg/ml.
30 mg.
Antitussives
73,.
Tab. 10 mg.
Codeine
26.
Solutions Correcting water Electrolyte, and acid base distarbancer,~ .
__ _ _____ ,
26.1
Oral
2 6.2
Parenteral
26.3
Miscellaneous
74.
27.
Water for injection
in 2 ml, 5 ml, 10 ml.
ampoules.
Vitamins and Minerals
75.
76.
76.
Tab/Cap. 50000 IU
Cap./Tab. 25,000 In
Oral Soln. 1 lakh/ml.
Ergocalciferol
Retinol (Vit. A)
Ascorbic acid
Tab. 50 mg.
LIST - B
DRUGS REQUIRED AT SECONDARY HEALTH CARE ORGANISATION
(The drugs in List - A should also be available).
Name of Medicine
Priority 1
Priority 2
Cate
gory
No.
Sr.
No.
1
Anaesthetics
1.1
General Anaesthatics and Oxygen
Thiopental
1,
1.2
Lidocaine
•
2.
2.1
Analgesics, Antipyretics, Non-'steroidal Anti inflamatory
- _urug's and drugs to treat Gout.
Non Opioids
Allopurinol
Indomethacin
3.
4.
2.2
e
3.
Powder for Inj. Of 5
gm, 1.0 gm in amp.
Inj. 1%, 2% in vial
of 30 ml
*
Inj. 1% 2% + Epine
phrine 1:1 lac in
vial, topical forms
2-4% (hydrochloride) .
Local Anaesthetics
2.
Formulation
Tab. 100 mg.
Cap. 25 mg.
Opioids
5.
Morphine
Inj. 100 mg/ml.
6.
Pethidine
Inj. 50 mg/ml.
Antiallergies
7.
Dexamethasone
Tab. 0.5 mg, 4 mg.'
Inj. 4 mg (Sodium
Phosphate) in 1 ml.
ampoule.
8.
Epinephrine
Inj. 1 mg. (hydochloride) in 1 ml.
ampoule.
9.
Prednisolone
Tab. 5 mg.
4.
Antidotes and other substances
used in Poisoning.
4.1
General
4.2
Specific
Sodium thiosulfate
10.
11,
12.
Atropine
Pralidoxime
(PAM)
Inj. 250 mg/ml in
50 ml amp.
Inj. 1 mg/ml.
10 ml amp/vial.
Inj. 1 gm. powder.
2 :;
List 'B' Contd.
Cate
gory
No.
Sr.
No.
5.
Antiepileptics
Name of Medicine
Priority 1 Priority 2
13.
Diazepam
Inj. 5 mg/ml.
2 ml. Amp.
14.
Phenytoin
Cap. 25 mg/ 100 mg.
Syp. 100 mg/5 ml.
15.
16.
Ethosuximide
Carbamazepine
17.
Valproic Acid
6.
Antiinfective Drugs
6.1
Anthelminthic Drugs
6.2
• ..
18.
6.3.1
Penicillins
19.
Cap . 250 mg.
Syp. 125 mg/5 ml.
Inj. 1 gm powder/vial
Chloramphenicol
Gentamicin
20.
Inj. 10 mg, 40 mg/ml.
2 ml. vial.
21.
Phenoxy Methyl
Pencillin
Susp. 12.5 mg/5 ml.
Tab. 250 mg.
22.
Ampicillin
Cap. 250 mg, 500 mg.
Powder for susp.
12 5 mg/5 ml.
Inj. 500 mg/vial.
Other antibacterial Dru^s
23.
6.3.4
250 mg.
200 mg.
200 mg.
200 mg/5ml.
Tab. 500 mg.
Dilcxanide Furoate
Antibacterial Drugs
6.3.3
Cap.
Tab.
Tab.
Syp.
Antiamoebic Drugs
•
6.-3
6. 3.2
Formulation
Tab. 100 mg.
Syp. 25 mg/5 ml.
Nitrofurantoin
Antileprosy Drugs
24.
Ethionamide
Tab. 125 mg, 250 mg.
25.
Protionamide
Tab. 125 mg.
Pyrazinamide
Streptomycin
Tab. 500 mg.
Powder for inj.
0.75 gm and
1 gm/vial.
Antituberculosis Drugs
26.
27.
3
s s 3 •°
List 1B‘ contd.
Name of medicines
Priority 1
Priority 2
Cat,
No.
Sr.
No.
6.4
Antifilarial Drugs
6. 5
Antifungal Drugs
28.
29,
Tab. 125 mg, 250 mg.
Griseofulvin
Nystatin
6. 6
Antileishmaniasis Drugs
6.7
Antimalarial Drugs
30.
6.8
Antischistosomal Drugs
6,9
Antipanosomal Drugs
7.
Antimigraine Drugs
Chloroquine
Sulphadoxine )
Pyrimethamine )
Inj. 200 mg/5ml.
Ergotamine
Tab. 2 mg (as tar
trate) .
33.
8.
Antineoplastic and Immunosuppressive Drugs.
9.
Antiparkinsonism Drugs,
10.
Blood, Drugs affecting the
10. 1
Anti anaemia Drugs
Inj. equivalent to
50 mg. iron/ml.
2 ml. inj. or 10 ml.
amp.
Hydroxocobalamine Inji 1 mg/ml. amp.
35.
10.2
Anticaogulants and Antagonists
11.
Blood products and Blood substitutes.
11.1
Plasma Substitutes
11.2
Plasma fractions for specific uses.
12.
Cardiovascular Drugs
12.1
Antianqinal Drugs
39.
Tab. 500 mg + 25 mg.
Iron Dextran
34.
36.
37.
38.
Tab. 5 lac IU
Tab. 300 mg.
Quinine
31.
32.
Formulation
Propranolol
Glyceryl Trinitrate
Isosorbide dinitrate
Verapamil
Tab. 10 mg, 40 mg.
Tab. 0.5 mg.
Tab. 5 mglsublingual)
Tab. 40 mg/ 80 mq.
... 4
:: 4
List J3' Contd.
Cat.
No.
Sr.
No.
12.2
Antidvsrhythmic Drugs
Name of .Medicines
40
4-f ,
Tab. 10 mg, 40 mg.
Tab. 10 mg, 15 mg.
Procainamide
Quinidine
Tab. 250 mg, 500 mg.
Tab. 200 mg.
Antihypertensive Drugs
45 ,
Reserpine
Tab. 40 mg, 80 mg
(Hydrochloride)
Tab. 0.1 mg, 0.25 mg.
46..
Clonidine
Tab. 100 microgram
47 .
43,.
49
Methyldopa
Hydralazine
Hydrochlorothiazide
Tab. 250 mg.
Tab. 50 mg.
Tab. 50 mg.
44 .
12.4
Formulation
Isoprenaline
Propranolol
4 2<»
43 .
12.3
-----Priority 2
priority 1
Propranolol
Cardiac Glycosides
Tab. 0.25 mg.
Oral Soln. 0.05 mg/ml
Digoxin
SO'.
12.5
Drugs used in Shock - Anaphylaxis
13.
Dermatological Drugs
13.1
Antifungal Drugs
13,2
Antiinfective Drugs
13.3
Anti inflammatory and antipruritic drug S ’
13. 4
Astringent Drugs
13.5
Keratoplastic and Keratolvtic Agents
.
Podophylline
Solution 10-25%
13.6
Scabicides and Pediculicides
14
Diagnostic Agents
15.
Disinfectants
16.
Diuretics
52,
Hydrochlorthiazide
Tab. 50 mg.
535
54.
Furosemide
Tab. 40 mg.
Tab. 25 mg.
Chlortalidone
*
17
Gastrointestinal Drugs
17.1
Antacids and other antiulcer Drugs
55, Ranitidine
Tab. 150 mg.
5
List '3' Contd.
Name of Medicines
Priority 1
Priority 2
Cat,
*
No
Sr,
No,
17.2
Antiemetic Drugs
5(2,
573.
Promethazine
Metoclopramide
Formulation
Tab.' 10 mg, 25 mg
Inj. 25 mg/ml 12 in
2 .ml amp.
Oral liquid 5 mg/5 ml
Tab. 10 mg.
Inj. 5 mg. /ml in
2 ml amp.
17.3
Antihaemorrhoidal Drugs
17.4
Anti
5
*
17
Cathartic Drugs
17. 6
Diarrhoea s
spasmodic Drugs
Antidiarrhoeals (Symptomatic Drucrs)
17.7
Fluid Replacement Solution
18.
Hormones
18.1
Adrenal Hormones and Synthetic
585
59 ;
60 *
_
Substitutes
Dexamethasone
Prednisolone
Hydrocortisone
6’1'
*
18.2
Androgens
18.3
Contraceptives
Dexamethasone
4 mg/ml.
Norethisterone.
Tab, 0,35 mg.
18;4
Estrogens.
18.5
Insulins and other Anti Diabetic agents
6? -
Tab. 0.5 mg.
Tab. 5 mg
Powder for Inj.
100 mg/vial.
Leute Insulin
Inj. 40 lU/ml in 10 ml
64.
Insulin Soluble
Inj. 40 lU/ml in
10 ml.
6 5.
Glibenclamide
Tab s. 5 mg.
18.6
Thyroid Hormones and Anti- Thyroid drugs
•——
■-
19.
Immunologicals
19.1
19.2
Diagnostic Agents.
Sera and Immunoglobulins
6
:: 6 :;
List 1B' Contd.
Cat.
NO.
*
Sr
No.
Name of Medicines
Priority 2
Priority 1
Tetanus Antitoxin Inj. 50,000 IU in
vial.
(Human)
Inj. 500 lU/vial.
Inj. 10,000 IU
Diphtheria
" 20,000 IU in
Anti tokin
vial.
Inj. 1000 IU in 5 ml
Anti Rabies
hyperimmune serum
665-
67,.
63 .
69,
76 c
19.3
Formulation
Anti Snake Venom
Anti-D Immunoglobulin (Human)
Inj.
Inj. 0.25 mg/ml.
Vaccines
19.3.1
For Universal Immunisation ;
19.3.2
For specific groups of Individuals :
Inj.
71. Typhoid Vaccine
Inj.
72 . Rabies Vaccine
Note ; Ail vaqcines should comply with WHO requirements of
Biological substances.
Muscle Relaxant and Cholinesterase inhibitors
20.
21.
Ophthalmological Preparations
21
1
*
21.2
Anti.infective Agents.
Antiinflammatory Agents.
*7 o
. Hydrocortisone
21.3
Local Anaesthetics
21.4
Miotics and Anti-glucoma Drugs
21.5
Mvdriatics.
22.
Oxytocics
V.
Inj, 0.2 mg/ml
(Maleate) in 1 ml
ampoule.
Ergometrine
23.
Peritoneal
24.
Psychotherapeutic Drugs.
75 .
Eye oint. 1%
Dialysis Solution.
Chlorpromazine
Tab. 50 mg, 100 mg
Syp. 25 mg/5 ml.
(as hydrochloride).
7
7
List ' B> Contd.
Cat.
No.
Sr.
no.
25.
Respiratory Tract, Drugs acting on the
25.1
Anti Asthmatic Drugs
76-;
Name of Medicines
Priority 1
Priority 2
Formulation
Inj. 25 mg/ml.
Aminophylline
77,
Cromoglycic acid
(Cromolyn)
Oral Inhalation
(Cartridges)
20 mg/dose (Sodium
salt) .
7&
Bad ome tna s one
Oral Inhalation
0,05 mg/dose.
Inj, 1 mg/ml in 1 ml
ampoule (as hydro
chloride) ,
7/4)1
Epinephrine
25.2
-1 Antitussives
26.
Solutions correcting water Electrolyte and acid base
di sturbance s
26.1
Oral
26. 2
Parenteral
80.
Potassium Chloride
Oral Soln. 05 C.m/5ml
81.
Glucose
82.
Glucose +
Chloride
Inj. Solution 5%
Isotonic.
500 ml, 1000 ml.
50% in 25 ml amp.
Inj. Soln. 4% +
0.18%.
. ,)
83,
Sodium Chloride
Sod.
26.3
Miscellaneous
27.
Vitamins and Minerals
Inj. Soln. 0,9%
isotonics.
84.
Pyridoxine
8$8&.
Riboflavin
Tab. 25 mg.
Tab, 5 mg.-
Thamine
*
Tab
*
ST
Calcium Gluconate Inj, 100 mg/ml.
in 10 ml. amp.
50 mg.
LIST
C
DRUGS REQUIRED AT TERTIARY HEALTH CARE ORGANISATION
(The Drugs in List 'A' and List 'B' should also be available).
Cate
gory
No.
1.
1.1
Name of medicines
Priority 2
Priority 1
Sr.
No.
Anaesthetics
General Anaesthetics and Oxygen.
1.
2.
3. .
1.2
Formulation
Anesthetic Ether
Halothane
Nitrous Oxide
Inhalation (gas)
Bupivacaine
Inj. 0.25% and 0.5%
in 10 ml amp.
II
II
II
II
Local Anaesthetics
4.
•
2.
Analgesicsy Antipyre tics, Non steroidal
Anti Inflamatory Drugs and drugs to
treat Gout,__________________________________
2.1
Non Opioids
5.
Colchicine
Tab. 0.5 mg.
6.
Probenecid
Tab. 500 mg.
2.2
Opioids-
3.
Antiallergics
4.
Antidotes and other substances
used in Poisoning.
4.1
General
4.2
Specific
.• -
7.
Sodium Nitrate
Inj. 30 mg/ml in
10 ml. amp.
8.
Sodium Thiosulfate
Inj. 250 mg/ml
in 50 ml amp.
9.
Deferoxamine
Inj. 500 mg in vial.
10.
Dimercaprol
Inj. 50 mg/ml in
oil, 2 ml amp.
11.
12.
mg/ml.
Protamine Sulphate Inj. 10
Inj. 200 mg/ml.
Sodium Calcium
5 ml/amp.
Edetate
13.
14.
D-Pencillamine
Nalexone
5.
Antiepileptics
6.
Antiinfective Drugs - Anthelmintic Drugs
15.
16.
Cap. 250 mg.
Inj, 0.4 mg/ml.
Tiabendazole
Chewable Tab,500 mg.
Niclosamide
Tab. 500 mg.
2 ::
List C Contd.
Cat.
No.
Si?.
No.
6.2
Antiamoebic Drugs
Name of Medicines
Dr ionty I
Priority 2 .
IS.
Antibacterial Drugs
6.3.1
Penicillins
6.3.2
Inj. 60 mg in 1 ml
amp.
Inj. 500 mg in 100 rrl
Metronidazo'-e
6.3
T9.
—.
Dehydro emetine
17.
Formulation
Cap. 500 mg.
Inj. 500 mg in vial
Syp. 125 mg/5ml
Cioxacillin
Other antibacterial drugs
20.
Salazosulphapyridine
21.
Erythromycin or
Lactobionate
Cephalosporin
22.
Tab. 500 mg.
Inj. 500 mg in vial
Syp. 125 mg/5ml.
Cap. 250, 500 mg.
6.3.3
6.3.4
6.4
Antileprosy Drags.
Antituberculosis Drugs.
Antifilarial Drugs
6.5
Antifungal Drugs
23.
Flucytosine
Cap. 2 50 mg, Infusion
2.5 g in 250 ml.
24
Amphotericin-B
Inj. 50 mg in vial.
Quinine
Inj. 300 mg/ml
in 2 ml amps.
6.6
Antileishmaniasis
Drugs.
6.7
Antimalarial Drugs
25
6.8
6.9
Antischistosomal Drugs
Antipanosomal Drugs
7.
Antimigraine Drugs
8.
An tineoplastic and Immunosuppressive Drugs
8.1
Immunosuppressive drugs
25.
8.2
Azathioprine
Tab. 500 mg.
Inj. 100 mg as
sodium salt in vial.
Cytotoxic Drugs
27.
Bleomycin
Inj.15 mg as sulph
in vial.
28.
Busulfan.
Tab. 2 mg .
3 ::
List C Contd.
Cat.
No,
9.
Sr,
No.
Name of Medicines
Priority 1
Priority 2
29.
Calcium folinate.
3'0.
31.
Chlorambucil
Cyclophosphamide
32.
Cytarabine
33.
Doxorubicin
3'4.
Fluorouracil
3 5-
Methotrexate
3 6.
Procarbazine
3 7.
Vincristine
Tab. 15 mg.
Inj. 3 mg/ml in
10 ml amp.
Tab. 2 mg- .
Tab. 25 mg.
Inj, 500 mg. in via.’
Inj. 100 mg in vial.
; .
Inj. 10 mg and
50 mg in (as hydro
chloride) vial.
Inj. 50 mg/ml. in
5 ml amp.
Tab. 2.5 mg.
Inj. 50 mg as sodium
in vial.
Cap. 50 mg (as
hydrochloride).
Inj. 1 mg and 5 mg
in vial.
Antiparkinsonism Drugs
3 8.
39.
Levodopa
Levodapa +
Carbidopa
Th rihexyph enydy1
40.
10.
Blooc3, Drugs affecting the
10.1
Anti
10.2
Anticoagulants and Antiaqonists
Tab. 250 mg.
Tab. 150 mg + 10 mg.
Tab. 250 mg + 25 mg.
2 mg. tabs.
Anaemia Drugs
41.
Warfarin
Tab. 5 Mg.(Sodium
salt)
42.
Phytomenadione
Inj. 10 mg/ml
1 & 5 ml amp.
43.
Heparin
44
Protamine
Inj. 1000 IU )
5000 IU 1 ml
20000 IU )
amp.
Inj. 10 mg/ml in
5 ml amp.
Sulfate
11.
Blooc1 Products and Blood Substitutes.
11.1
Plasma Substitute
4 5.
11.2
Formulation
Dextran
Plasma Fractions for
Specific uses.
4 S'
Albumin, human.
Inj. 6%, 500 ml.
Inj. solution, 25%
(dried) .
:t 4 ::
List C contd.
Cat.
No,
Sr.
No.
acts of Medicine
...
Priority Priority 2
Factor VIII
Concentrate
Factor IX
complex
(Coagulation
factors II,VII,
IX, X) concentrate
(dried)
12.
Cardiovascular
12.1
Antianqinal Drugs
47;
4g.
12.2
Propranolol
Verapamil
12.4
Ini. 1-mg in 1 ml arm..
(as HC1) . t
Inj. 2,5 mg/ml m
2 ml Amp.
4g.Propranolol
Inj. 1 mg in 1 ml
ampoule.
5 0.
Inj. 20 mg/ml in
5 ml Amp.
Lidocaine
I’nj. 100 mg/ml in
10 ml amp,
antihypertensive Drugs
52
Propranolol
53.
Sodium Nitroprusside
Inj. 1 mg in 1 ml
Ampoule.
Inj. 50 mg in Amp.
Cardiac Glycosides
5/..
12.5
All plasma fractions
should comply with
WHO Requirements of
collection processing
and Quality control
of human blood and
blood products.
Antidysrhythmic Drugs
Procainamide
12.3
Formulation
Digoxin
Inj. 0.25 mg/ml in
2 ml amp.
Drugs used in Shock - Anaphylaxis.
55.
Dopamine
13.
13.1
Dermatological Drugs
Antifungal Drugs
13.2
13.3
Anti infective Drugs
Antiinflammatorv and Antipruritic Drugs
'13.4
Astringent Drugs
13.5
Keratoplastic and Keratolytic Agents
13.6
Scabicides and Pediculicides
Inj. (as hydrochlo
ride) 40 mg/ml in
5 ml vial.
:: 5 ::
List C Contd.
______Name of Medicine
Priority 1
Pariority 2
Cat,
No.
Sr.
No.
14.
Diagonistic Agents
14.1
Ophthalmic Drugs
Flurescein
14.2
Eye drops 1%
(Sodium salt)
Radio Contrast Media
Meglumine Amido trizoate
Sodium amidotrizoate
Barium Sulphate
lopanoic Acid
Propyliodone
lotroxate
Disinfectants
16.
Diuretics
Inj. 60% in 20 ml
ampoule.
"
50% in 20 ml.
amp.
Powder.
Tab, 500 mg.
Inj. 600 gm/1 in 20
ml. ampoule.
lohexol
15.
Formulation
Inj. 300 mg in 5 or
10 ml ampoule.
Solution 8 gm (as
iodine) in 100-250
ml.
57.
Spironolactone
Inj. 10 mg/ml in
2 ml amp.
Tab. 25 mg.
58-
Mannitol
Inj. 10% & 20%
59.
Triamterene
Tab. 50 mg.
56.
Furosemide
17.
Gastrointestinal Drugs
17.1
Antacids and other Antiulcer drugs
60.
Cimetidine.
17. 2
Antiemetic Drugs
17.3
Antihaemorrhoidal Drugs
17.4
Anti spasmodic Drugs
17. 5
Cathartic Drugs
17.6
Diarrhoea
Inj. 100 mg/ml in
2 ml amp.
17.6. 1 Antidiarrhoeals (symptomatic) Drugs
17.6.2 Fluid Replacement Solution
... 6
6
List C Contd..
Cat.
No.
Sr.
No,
18.
Hormones
18.1
Adrenal Hormones and Synthetic Substitutes.
18.2
_ ___ Lams of medicine--------------------Priority 1
Priority 2
Fludrocortisone
Tab. 0,1 mg
(acetate)
Testosterone
Inj. 200 mg (as
enantate) iri 1 ml
amp. and 25 mg (as
propionate) in 1 ml
amp.
Androgens
62.
18.3
C ontreceyfives
53.
Depot Medroxy Pro
gesterone acetate.
Norethisterone
Enantate.
Estrogens
64.
18.4
Ethinylestradiol
65
18.5
xnnvJ.ins and other Antidiabetic Agents.
18.6
Ovulation Inducers
66
Clomifene
18.7
Progestogens
18.8
.Th-yjroid Hormones and Antithyroid drugs.
Inj. 150 mg in 3 ml
vial.
Inj. 200 mg in vial.
Tab. 0.05 mgG
Tab. 50 mg (citrate)
67
Levothyroxine
68
Potassium Iodide
Tab. 0.05 mg, 1 mg
( sodium salt)
Tab. 60 mg.
69.
Propylthiouracil
Tab. 50 mg.
19.
Immunologicals
19.1
Diagnostic Agents
70
19.2
Formulation
Tuberculin purified
Protein derivative (PPD)
Injection
Sera and Immunoglobulins
71
72
Anti-D immunoglobulin (human)
Immunoglobulin.- human
normal.
19.3
Vaccines
19.3.1
19.3.2
For universal Immunisation
For specific groups of individuals.
Inj. 0.25 mg/ml.
Injection.
7
:: 7 s :
List C contd,
Name of Medicine
Priority 2
Priority 1
Cat.
No.
Sr.
No,
20.
Muscle Relaxants end Choline steraseb Inhibitors
Neostigmine
7-1,
Gallamine
Inj. 20 mgm/ml.
75.
Suxamethonium
Inj. 50mg/ml in2ml
Amp. (Chloride)
7 6.
Pyridostigmine
Tab, (bromide) 60 mg.
Inj. (bromide) 1 mg.
1 ml. amp.
Ophthalmological Preparations
21.1
Antiinfective Agents
21.2
Antiinflammatory Agents
21.3
Local Anaesthetics
21.4
Miotics and Antiglaucoma Drugs
Acetazolamide
77.
78.
Homatropine
Solution (hydrobromide)
2%
Inj. 10 IU in 1 ml
amp.
Oxytocin
Peritoneal Dialysis Solution
Intraperitoneal
dialysis solution
8124
Solution (hydrochlo
ride or nitrate) .
2%, 4%
Pilocarpine
Oxytocics
SO.
23
Tab. 250 mg.
Mydriatics
70.
22
Tab. 15 mg Bromide
Inj. 0.5, mg (MetilsuIfate in 1 ml amp.)
73.
21
21.5
Formulation
Parenteral solution.
Psychotherapeutic Drugs
82.
Ami tryptiline
Tab. 25 mg. (Hydro
chloride) .
83.
Haloperidol
Tab. 2 mg.
Inj. 5 mg in 1 ml amp.
84.--
Imipramine
Tab 10 mg7 25 mg.
(hydrochloride)
89.
876
Lithium carbonate
Chlorpromazine
(hydrochloride)
Cap. or Tab 300 mg.
Inj. 25 mg/ml in
2 ml amp. -
78
5? 8
List C contd.
Cat.
No.
2
5.
Sr.
No,.
______Name of Medicine
Priority. 1
Priority 2
87.
Fluphenazine
Respire tow Tract, Drugs
Formulation
Inj. 2 5 me :/ml amp.
(decanoate or enantate) ,
acting on the
25.1
Anti Asthamatic Drugs
25.2
Antitussives
26.
Solutions correcting water electrolyte acid base
disturbances.
26.1
Oral
26.2
Parenteral
88.
Sodium bicarbonate
26.3
Miscellaneous
27.
Vitamins
and Minerals
Inj. solution, 1.4%
isotonic.
(Na+ 167 mmol/1
• HCO^ 167 mmol/1)
LIST D
Lis- of Drugs which can be used by the Village Level
Workers with adequate training.
Formulations
Drugs
1.
Acetylsalicylic Acid
Tab 300 mg,
2.
3.
.Activated Charcoal
Antacid
(Aluminium Hydroxide +
Magnesium Hydroxide).
Po’.der 50 gm. sachets.
4.
5.
6.
An Antihaemerrhoidal drug.
Atropine
Aminophylline
Tab. 1 mg (as Sulfate)
Tab, 100 mg.
7.
8.
9.
Benzoic Acid + Salicylic Acid
Betamethasone
Benzyl Benzoate
Oint. (Benzoic Acid 6%v
Solacylic Acid 3%)
Oint.0.1%
Lotion., 25%
10.
Bisecodyl
11.
12.
Calamine
Chlorhexidine
*
Tab
, 5 mg
Lotion.1% (Acetate)
Solution, 5% (diqluconate
,
for dilution)
Tab.
250 mg
Tab 125 mg.
13.
Chloroquine
14.
15.
Chlorpheniramine Maleate
Clofazimine *
16;
17.
18.
Coal Tar
Codeine (As antitussive)
Dapsone *
19.
20.
21.
Diethyl Carbamezine *
Diazepam
Ephedrine
22-
Ergometrine (for post partum
Haemorrhage)
23.
Ethyabutol *
Tab, 200 mg/400 mg/800mg
24.
25.
26.
Folic Acid
Gentian Violet
Glycerine Suppository
- Tab 5 mg
Solution!y
27;
28;
Iodine
Iron
Solution? 2.5%
29;
Iron + Folic Acid
30.
31.
32.
Isoniazid
Isoniazid + Thiacetazone
Lindane
33.
34.
Loperamide
Mebendazole
35;
Metronidazole
36.
Myconazole
Phosphate
Tab., 4 mg.
Caps, 50 mg, 100 mg.
Solution, Topical 20%
Tab. 15 mg., syp. 12 mg/ml
Syp. 12 mg/ml.
Tab.50 mg( citrate)
Tab. 2 mg.
Tab. 30 mg.
Tab. 0.2 mg(Maleate)
Solution
Tab;,200 mg. (as sulphate)
Tab.
Tab., 200 mg + 0.2 mg.
Tab.100 mg, 300 mg.
Lotion 75 mg + 150 mg,
150 mg + 300 mg.
Tab.2 mg.
’
Tab, 100 mg;
Tab. 200 mg.
Oint. or cream 2%
(Nitrate) .
s 3 2r *
List D continued.
Formulations
Drugs
Ointment 5 mg neomycin
sulphate + 500 IU
bacitracin Zinc/gm.
37.
Neomycin + Bacitracin
38.
Nystatin *
Pessary 1 lac I.U.
39.
Oral Rehydration Salt
Oral contraceptive pills
W.H.O. Formula.
Tab. 0.03 mg + 0.15 mg.
40.
(Ethynylestradiol +
Levonorgestrel )
Tab.
Syp.
Tab.
Syp.
500 mg.
x
125 mg/5 ml.
25 mg (hydrochloride)
5 mg/5 ml ( -do)
41.
Paracetamol
42.
Promethazine
43.
44.
Cap-150 mg, 300 mg.
Tab. 4 mg.
45.
Rifampicin +
Salbutamol
Sulphacetamide
46.
Tetracycline
Eye Oint. 1% (Hydrochlo
ride)
47.
48.
Vitamin A
Capsule 2 lac I.U.
Vaccines +
Note
Eye drops 10% (sodium
salt) .
These drugs could be given under supervision
and periodic monitoring by the doctor.
They should be easily accessible all round
the year either at the centre or in the
village.
VARIATIONS FROM WHO E.D. LIST
Sr.
no.
1
Category No.
4.2
Locost
list
C
2
Name of Drug
Reasons for inclusion/
exclusion
Protamine Sulphate
Included because this
is a specific antidote
for heparin which is
widely used at Tertiary
health care level
eg. heart surgery.
Methylthianinium
Chloride
3
6.1
Piperazine
Excluded because broader
coverage as an anthel
mintic drug can be had
by use of Mebendazole
and Pyrantel Pamoate
4
"
Praziquental
Excluded because this
drug is used against
Schistosomiasis which
does not occur in our
country at present
*
5
6.3.2
Spec tinomycin
Excluded because this
is useful for gonorrhoea
in multiple resistant
cases which are still
not common in India.
6.
6.4
Suramin Sodium
Excluded because the
specific parasite is
not reported to be
occuring in India.
7
6.6
Pentamidine
Sodium Stiboglu
conate,
Excluded because
Leishmaniasis does not
occur in India.
8
6.7
Amodiaquine
Excluded because
Amodiaquine and
Chloroquine belong to
the same category of
chemical group
*
sharing
same actions
*
adverse
effects, etc.
9
9
Thrihexyphenydyl
Included because it is
more easily available
in India.
Biperidin
Excluded because W.H.O.
has suggested Biperi
dine or any substitute
drug of same group.
Thrihexyphenydyl is
suggested in this list.
C
2
Variation from WHO E.D. List Contd.
Sr.
no.
Category No.
-
Locost
list
Name of Drug
Reasons for inclusion/
exclusion
Clonidine
Included because it is
easily available in
India and cheap anti
hypertensive drug - a
substitute for Methyld'v
opa.
12.4
Digitoxin
Excluded because not
available in India.
12.
13.4
Aluminium Acetate
13.
13.5
Salicylic Acid
14.
14
C
Edrophonium
15.
16
C
Triamterene
Included as a substi
tute for Amiloride,
Amiloride
Triamterene as its
substitute included.
Calcium Carbonate
Excluded because other
agents are available,
and possibility of its
adverse effects.
10.
12.3
11.
B
Excluded because the
combination- of Benxoic
acid and salicylic acid
will suffice the use.
16.
17.1
17.
17.1
A
Ranitidine
Included because of its
advantages such as less
incidence of adverse
reaction and less dos
age frequency, there
fore seitec ted as a
substitute for
cimetidine.
18.
17.6.1
A
Loperamide Tab.
Included because of
its symptomatic use
in emergency situa
tion for adults.
19.
19.3.2
Influenza vaccine
Meningococcal
vaccine.
Yellow fever
vaccine
Excluded because of
their non-feasibility
in Indian context.
20.
21.1
Silver Nitrate
Solution.
Excluded from Locost
List because better
antibacterials are
available.
Dvt So xt.
REPORT OK THE PUBLIC BOARD OF INQUIRY ON DEP0-P2DVERA
17 OCTOBER, 1984
findings CF FACT
I.
DATA AVAILABLE ON TEE LONG-TERM RISKS OF DMPA
ARE INSUFFICIENT AND INADEQUATE TO PROVIDE A
BASIS FOR A DECISION WHETHER THE BENEFITS OF
TEE DRUG AS A CONTRACEPTIVE OUTWEIGH ITS DIS
ADVANTAGES UNDER CONDITIONS OF GENERAL MARKET_
---- ING IN THE USA
There are adequate data to assess the efficacy and
benefits of DMPA as a contraceptive,
There is also
sufficient information on its short tern side effects and
risks.
The drug is clearly a highly effective contraceptive ;
with certjin specific advantages, and it doos'not appear to
pose any immediate irreversible serious side effects.
However, the facts relating to the long tern consequences of
the use of the drug are inadequate and insufficient to
provide a basis for risk assessment.
This is a serious
deficiency in light of the specific questions that have been
raised that the drug may have major adverse effects following
its long term use or that may become evident only after a
latent period. Most important among these has been the
concern over the drug’s carcinogenic potential.
The long term consequences of he use of DMPA on
neoplasias, in particular of the breast and uterus, as well
as osteoporosis and atherosclerosis are of particular rele
vance for any risk/benefit assessment of the drug's use in
the United States because of the susceptibility cf the
population in this countjyy to these diseases.
In the absence of adequate data on the long term
consequences of tho drug it is not possible to arrive at any
scientifically defensible conclusion whether or not tho
benefits of the drug, when used as a contraceptive, outweigh
its risks..for the average healthy individual in the United
States.
'Lt also makes it impossible to compare the risk/
benefit ratio x of DMPA with that of other drugs available
for contraception.
II.
Data from the STUDIES CF RHESUS MONKEYS and beagle
DOGS CAN NOT BE DISMISSED AS IRRELEVANT TO THE HUMAN
WITHOUT CONCLUSIVE EVIDENCE TO THE CONTRARY.
SUCH
EVIDENCE IS NOT AVAILABLE AT THIS TIME. THEREFORE, TEE
FACT THAT MALI GRANT NEOPLASIAS DEVELOPED IN TWO
SPECIES IN TARGET ORGANS CF SEX STEROIDS MUST BE
CONSIDERED AS AN INDICATION OF A POTENTIAL OF
PROGESTOGENS,' INCLUDING DMPA, TC PROMOTE THE DEVELOP
MENT CF MALIGNANCIES IN TARGET ORGANS
The findings from animal tests implicate DMPA as a
potential promoter of neoplasias because;
1)
Chronic administration of DMPA Was associated with the
development of malignant neoplasias in two mammalian species.
5.
Data arc also inadequate to establish effect of MPA on
bone and on the profile of plasma lipoproteins, inform
ation needed to evaluate whether the long term use of
the drug will or will not predispose the individual to
osteoporosis or to atherosclerosis. Cur conclusions of
Law do not rely on this finding.
I
'
V -
..j-t
.->•■- ■•■; v;Sjf. -v?
•
2
-
2)
The neoplasias developed in target organs of sex
steroids «
3)
There is good evidence tc support the conclusion that
in both species the malignancies were drug related.
-i4)
There is no evidence to support the conclusion that
the effect of the drug is to be attributed only to the
administration of excessively high doses and that the effect
of lower doses would differ qualitatively from those of
higher doses.
Therefore, DMPA in these experiments exhibited the
characteristics of a potential carcinogen according to
generally accepted criteria. Under the circumstances, to
dismiss the findings as irrelevant to the human would require
conclusive experimental evidence of fundamental differences
among the species in the basic mechanisms of action of the
hormone or in the responses of target cells. There is as
yet no such evidence at hand.
Specifically, there are no
data on the histogenesis of the neoplasias nor on the
mechanism of action of progestogens on the presumed cells of
origin of the neoplasias in the teat animals. Therefore,
there is no evidence to support the claim that the
malignancies developed either in c ell types unique to the
species or as a result of a species specific response of
target cells to progestogens.
Conversely, data on women who
have been exposed for prolonged periods to the relatively
unopposed action of progestogens are inadequate to warrant
the conclusion that their response to this hormonal state in
terms of neoplasias would differ in some fundamental way
from the two species of test animals.
III.
THE DATA CH THE HUMAN ARE INSUFFICIENT AND INADEQUATE
TO EITHER CONFIRM OR REFUTE THE IMPLICATION OF THE
ANIMAL DATA THAT DMPA MAE INCREASE THE RISK OF CANCER
IN NOMEN USING DMPA AS A CONTRACEPTIVE,
I
The available data on the human can not provide a basis
for conclusing whether DMPA, used as a contraceptive, does
or does not influence the incidence of carcinomas in general
or of the accessory organs of reproduction in particular,
because;
4)
They fail to provide information on an adequate number
of long term users of DMPA, or on ex-users who have been
followed for a long enough period of time. There are only
minimal data on subjects that have
used DMPA for 5
years or longer with most of the data reported having boon
obtained from women who have used the drug for 2 years or loss
2)
In the majority of the studios tliore were no controls
followed in parallel with those using DMPA. In many
studios from developing countries there is not even informat
ion on the background incidence of the diseases being
studied in DMPA users that could serve as a basis for
comparison.
3)
In a number of the retrospective studies there is
reason to question tho adequacy of the record keeping on
subjects receiving DMPA and, therefore, of the possibility
3
of retrieving the data subsequently for any valid analysis.
To obtain the direct evidence needed to resolve the
issue would have required purposeful, systematic collection
and recording of data on users of DMPA and appropriate
controls with consideration of the natural history of the
diseases being monitored. Not until recently have subh
studios been initiated. Until they are completed and full
reports of them available their value as evidence is limited.
IV.
IN CASE CP CONTRACEPTIVE FAILURE UITE DMPA, THE RISK
CF A MOTHER GIVING BIRTH TO A MALFORMED CHILD IS
UNLIKELY TO BE MEASURABLY GREATER THAN THAT POSED BY
THE ORAL CONTRA CEILIVES J The chaHCE IN EACH CASE CAN
BE ESTIMATED TO BE SMALL ENOUGH NOT TO POSE AN OBSTACLE
TO THE USE CF THE DRUG AS A CONTRACEPTIVE UnEN OTKERUISE
INDICATED.
Data have not been systematically collected on offspring
that have been inadvertently exposed to DMPA in utero.
Conclusions, therefore, can only be based on the body of
epidemiological data obtained on the effects of a variety of
sox steroids, including progostogons, on the developing human
fetus.
In those cases, tho drugs had been administered for a
variety of indications and at various times during pregnancy,
This is clearly a less than ideal data base. Nonetheless it
can provide some general estimate of tho magnitude of the risk
According to these data tho risk of various malformat
ions attributable to protestogens for the various malformat
ions implicated is low. The rate of contraceptive failure
with DMPA when used appropriately is also low.
Consequently,
the chance of a mother bearing a malformed child following
contraceptive failure can be estimated to be small. However,
because DMPA is a long acting depot preparation, tho
exposure of any susceptible fotus to tho drug is likely to
bo more prolonged than with oral contraceptives.
Consequent
ly, tho range of critical and vulnerable events that may come ■
under tho drug's influence may also be expected to be greater
than with oral contraceptives.
,t should bg possible to
counter balance this disadvantage of DMPA by ensuring that
contraceptive failure is kept at a minimum ’and taking the
necessary stops to avoid inuocting women already pregnant.
As with oral contraceptives this risk should not, in itself,
constitute a reasonffor not using the drug if otherwise
indicated,
There have been no 'direct determinations of tho concent
rations of MPA in the- blood of breast fed infants of
mothers receiving DMPA as a contraceptive nor if tho amount
of the drug transferred passed onto tho infant is sufficient
to have a biological effect. This information is needed
before advocating the use of DMPA as a contraceptive to
lactating mothers in the postnatal period and before it is
possible to conclude that tho drug doos not poso any risk
of functional teratogenicity.
With the increasing
use—and abuse—of
antibiotics, bacteria are
learning to fight back against
the deadly drugs
It is unfair to
□lame the GP
alone for
increasing
antibiotic
resistance.
Patients
should be
educated
against selfmedication
9ld yOU
\ \ / 7ou have the sniffles, you are running a
\ S' / temperature and your headache won't
\ / let you think. Your doctor sympathises
with your desire to be back to normal
L_.J
for tomorrow’s crucial event and pre
scribes an antibiotic. You wince at the price, but the
next day. there is good news because you are
already feeling fine. Good doctor, you think indul
gently and spread the word to your friends.
Now for the bad news: the antibiotic could mil
have made you better. An antibiotic takes more than
a day io even begin to effectively cure you — at
least for most common infections.
Perhaps you didn't need the antibiotic anyway as
you probably had a viral infection. And though doc
tors never bother to explain this to patients, antibio
tics have no effect on viruses.
The truth is that antibiotics arc among the most
used and most abused of drugs today. By some esti
mates. more than ten percent of all drugs prescribed
in India arc antibiotics. And because they
arc
expensive, they account for almost ha:'
the value of all drugs sold in the market
So what, you shrug, perhaps I took th ■
wrong medicine. But I got better, didu t
I?
Maybe you did. But maybe you also
Some little-known facts about antibiotics
The beginning
And now...
Mass production of the
first antibiotics began
during World War II,
when penicillin was
found to have reduced a
great number of
amputations and
casualties.
Take a look at these
figures. Incredible as it
may sound, today, the
Indian drug market has
70.000 formulations
available to doctors and
patients — even though
the World Health
Organisation lists only
250 essential drugs.
With so many
antibiotics in the inarkc
today with so many
Then, since it was
relatively cheap
the use of antibiotics
spread like wildfire.
resistaraee
The more you take, the less it works
helped create more antibiotic resistant
.terms (pathogens) within your body.
That could mean that someday, when
your body really needs an antibiotic
drug to fight a serious illness, the drug
won’t have the desired effect.
Cn tha market: more ehats
variations, this leads
to tite dangerous abuse
of drugs by an
unsuspecting public.
T11 goes back a little to the days when Alexander FlcLlming discovered penicillin, which led finally to
the use of the first antibiotics in the Forties. Mass
production of the first antibiotics, penicillin and
streptomycin, began during World War II. Penicil
lin opened the flood gates to a variety of antibiotics
that worked very effectively against disease
causing bacteria.
Since it was relatively cheap and easy to admi
nister. and since they worked miraculously on the
then life-threatening diseases like tuberculosis,
typhoid and venereal disease, the use of antibiotics
spread like wild fire.
Even today, newer antibacterials (for the pur
poses of this article, antibacterials and antibiotics
are being used synonymously in terms of their
getion, i.e, inhibiting bacteria) are being created
regularly by drug designers with a little tinkering of
the organic chains of older drugs, or with other che
mical jugglery. The potential for new' drugs seems
limitless.
Except for one thing. Even five decades after the
first antibiotics were introduced, bacterial diseases
remain a major cause of illness, and even death.
Bacteria
evolve much
faster than
human beings.
The only way
out against
them is to keep
one step ahead
through
technical
innovation
Suffer the little ones
prescribed antibiotics
provide no cure.
The overuse of
antibiotics is
particularly shocking
when it is extended to
children, who can
develop resistant strains
of bacteria in their
systems which they pass
on io other children.
These children can then
develop diseases for
which commonly
Good news for the
manufacturer
J The vulnerable ones: not
5 ati pediatricians core
The economic problem
has not stopped
pharmaceutical
companies from
pumping a lot of money
into the antibiotics
research market.
Cynics would say it is
with good reason. The
53
jzjszlehswia.: j."'
son. The spiralling prices of newer
drugs that arc entering the market each
day also mean better bottom lines for the
drug industry. And the obsolcsence of
older, cheaper antibiotics is only good
news for pharmaceutical companies. As
doctors prefer to, or are forced to use
higher order antibiotics to kill simple ail
ments. the bills that go up are the
patients'.
Take a look at lhese figures. The Indi
an drug market has 70.000 formulations
available to doctors and patients when
WHO lists only 250 essential drugs and
even the Hathi committee which went
into the issue found only 116 drugs
ksenlial for India. The mind-boggling
Wgurc of 70.000 preparations includes
many unessential and sometimes danger
ous drugs that arc .in fact banned in many
other countries.
antibiotics. Millions of dollars arc spent
to research, produce and market each
new-generation antibiotic drug. And the
pharmaceutical companies have to pass
on the cost to the consumer. Which they
do. IT at is why a newer antibiotic, such
as Ceftum (which is a new antibiotic
drug called ccfuroximc) from Ailcnhury’s costs around Rs 41 for one 500 mg
tablet, whereas the middle-range anti
microbials like cephalexin costs Rs 9.50
for a 500 mg tablet. Compare that to sulphonomides, or cotrimoxazoles like
Scplran, which costs between 75 paise
to Rs 1.50 per tablet depending on its
strength.
And these arc only the more common
antibiotics. Some of the higher-order
injectable antibiotics can cost upto Rs
350 per dose, whereas the higher-order
tablets can reach upto Rs 90 per tablet.
•/ -
At what price?
The hill that goes up is the
patient ’.s'
'TPlie problem with overusing antibio11 lies of course, is quite special, due to
the resistance factor. Bui there are other
related problems as well. Price becomes
a big factor in the introduction of newer
56
One of the ways of
tackling resistance is
to develop missiles
that penetrate the
■ shields that bacteria
develop around
them
And if the Dunkel draft agreement goes
through, you can expect drug prices to
go through the roof.
It is not just the price factor, however.
There is also the question of side effects. ■
While they have undoubtedly played a
crucially important role in human health
in the last 50 years, antibiotics have also
been guilty of generating problematic
side effects, most of which arc common
ly known, but some of which can even .
be deadly. For instance, the known side
effects of the relatively new antibiotic. '
gentamicin, (available only as an injecta
ble) arc nephrotoxicity (which can lead
to kidney damage) and ototoxicity. I
(which can cause deafness).
The rapid obsolcsence of old drugs :
and the corresponding manufacture of
new drugs also brings a sort of consumer
culture into the drug inr1" ,ry It only
increases the misuse of medicine. Dr S.
P. Tekur, an active member of the Drug
Action Forum and of the Bangalore
based Community Health Cell, who him- i
sell runs a child health clinic, is very dis- ■
turbed about the widespread irrational \
use of drugs.
There arc so many antibiotics in the
market today, with so many variations
in side effects, half life and site
effectiveness that it is understandable
that doctors themselves are confused. .
But sometimes, this leads to the danger
ous abuse of drugs on an unsuspecting.
ill-informed and apathetic public. Doc- ■
lor Tekur cites the instance of Nor
floxacin and Ciprofloxacin, which
belong to the family of the recently intro
duced quinolones. "The recommended
dosage per day is 400 mgs twice a day."
he says. "They are not meant for •
children."
Quinolones are contra-indicated for ,
children under 14 because they have
been reported to cause damage to die ;
joints of immature animals. And yet."
says Dr Tekur. "this antibiotic is availa
ble in 100 mg tablets, which tempt pedi
atricians to try them on children ”
Shocking instances of antibiotic
abuse like this expose the complete lack |
of coordination and implementation of I
the government’s drug policy. But con
sumer awareness is the only really effee- ,
live means to stop the misuse of drugs. j
and especially antibiotics. Because the ,
vested interests of the manufacturer, the I
prescriber and the dispenser combine to I
perpetuate this misuse. And it is left to i
each individual to say, IT’S MY BODY. ’
AFTER ALL. °
Rohini Nilekani/Bangalore
SUNDAY 7—13Novcmt».’
ALL INDIA DRUG ACTION NETWORK
-
_______________——----------
RATIONAL DRUG POLICY
^‘;7
$■ ays :^^r- »>
SC1_Z7- odv/R,
CT< cx-uS
yoo C> £ </
SP (D ^>0 •■ 2-g.
AIDAN
All India Drug Action Network (AIDAN), the
co-ordinating body of the individuals and organisations
l-a o-to.FL. 4vu»kM. concerned with and engaged in the problems of health &
a
lj
\
drug, works towards the adoption and implementation of
a Rational Drug Policy in India and sets out the following outline for the Drug Policy.
/
Health
Policy &
Drugs
Vu
Majority of the Indians suffer from the/diseases qf
poverty and ignorance, i.e., communicable diseases,
' .
*
■
diseases due to undernutrition etc. Industrialisation, \
Modernisation and Urbanisation have led to, spread of
\
consequential diseases. Most of these illriesses are
preventable and curable. What we need theri, is adequate
nutrition, safe water, universal sanitation, environmental
protection and a primary medical service, available to
all.
Role of
Drugs
Drug is the most important element in medical care
which, though constitute only a small part of the overall
health care as stated above, is the most urgent, unavoid
able, essential and priority need in the country where
incidence of death and disability from diseases is high.
So long the basic elements of health care is not made
available universally, medical care will continue to be
the priority service to reduce death and disability and
in this context, drugs understandably assume a vital and
priority role.
Present
situation
Out this life-saving function of drugs has been
exploited by the drug industry in such a manner that the
developing health culture heralds more harm.than good.
To the people, doctors and non-doctors alike, drugs
appear as panacea for all ills. Health is still regarded
as an individual or personal responsibility and it is
believed that freedom from disease could be obtained by
better & better and more & more drugs. Such a belief
among educated and illiterate alike has led to a universal
craze for drugs and this DRUG CULTURE has come to dominate
the society. In this situation, drugs appear to be the
best commodity for unlimited profit-making by the drug
industry, since hardly any consumer ask for the necessity,
utility, rationality, price-justifiability & harmful
effects of a drug. It is not even asked whether a
substance sold as Drug is actually a Drug at all. As a
result, 60% of the drugs in the market are unscientific
or harmful or substandard; a large
contd
2
2
E>>Z.
Humber of them are not actually drugs; many drugs
are consumed by those who do not need it; people die
or are disabled from the effects of harmful drugs;
drugs are sold at fantastically high prices; and
most serious of all, life-saving and essential drugs
are not available to those who need them most.
Objectives
of Rational
Drug Policy
Broad objectives of the rational drug policy
should therefore be:
A. To authorise manufacture and marketing of
only those drugs which are accepted or endorsed as
drugs by the standard medical text books, eliminating
all so-called drugs without scientific basis, from
the drug market.
B. To ensure availability of safe, essential
and quality drugs to all the needy - particularly who
lack purchasing power.
C. To ensure drugs are sold at rational prices
providing reasonable and known profit margin.
D. To attain self-sufficiency or self-reliance
in priority drugs needed to combat dominating diseases
afflicting majority of the population.
E. To ensure dissemination of all relevant
informations regarding production, pricing, trade
practices, efficacy, scientificity, limitations and
adverse effects of drugs to the medical profession,
health personnel and people at large.
F. To eliminate abuse of drugs at all levels.
G. To organise and build up *
peoples movement
in order to realise the above objectives.
In order to achieve the above objectives the
following measures are necessary and in the process of
phase-wise implementation, certain measures should be
accorded priority.
For objective A.
1.
National Drug Authority (Ref. Hath! Committee):
Overall executive authority for National Formulary,
Drug Registration, Drug Licensing, Drug information,
Ethical Control, Quality control, Import & Export
Policy, under the control of the Ministry of Health.
This permanent body shall be composed of representstives of Health Ministry, Parliament, State Health
Ministries, Medical profession. Trade Union, Industry,
Trade, Pharmacists, Social Action groups on drug &
health.
2.
National Formulary shall be drawn up providing
contd. ••• 3
= 3 =
up-to-date pharmacological & therapeutic information.
3.
Drug Registrations A separate body will ensure
registration of only drugs having scientific basis and
acceptance, thereby eliminating all so-called drugs
having no pharmacological basis, from the Formulary.
4.
Quality Control: A separate body to ensure
quality functioning at all levels, e.g. production,
distribution & consumption, and monitoring adverse
reaction.
5.
Legislation & Enforcements NDA will recommend
to the Ministry of Health for necessary legislation
from time to time and supervise & monitor enforcement
of those laws & regulations. The relevant fields are Registration of drugs, labelling & advertisement,
price-control, prescription control & sale of toxic/
poisonous/habit forming/dangerous drugs, deterrant
penalty for violation of law, technology transfer,
Import & Export, Drug Control Authority, Prosecution,
etc.
6.
All single ingredient drugs shall be regis
tered & marketed in International Non-proprietory
Names or suitable generic names.
7.
R & D : Separate body to approve, guide and
monitor all R & D activities on drugs on the basis of
the actual need of Indian People. No R & D be allowed
without prior registration and contious monitoring.
8.
All these separate bodies, viz. 3, 4, 6 & 7
shall function at the state level, subordinate and
accountable to NDA.
For objective B
1.
Priority Drugs: An expert body under NDA
shall identify, after studying & monitoring prevailing
disease pattern, the priority drugs on the basis of
greater mortality, greater morbidity, severe sequelae,
national health programmes; select such drugs on the
basis of efficacy, high therapeutic index, low cost,
shelf-life & storage requirements, self-reliance,
ease of administration, potential for misuse and
bioavailability. It should also prepare graded essen
tial drug lists required for different levels of
medical care. This will be a continuing function
according to changing needs & priorities, and ongoing
scientific development.
2.
Distribution: This is the most crucial
problem of the drug policy.
contd
4
Voluntary Health Association of India
40, Institutional Area,
(Near Qutab Hotel), South ofllT,
New Delhi-110016
ED-4 (3)
Telegrams: VOLHEALTH
New Delhi-110016
Phones:668071,668072
April 18,1988
Dear friends,
Since VHAI is venturing into some new areas of work,
I felt you might like to get some orientation of these
issues. Enclosed notes prepared by Dr.A.T.Dudani
(Consultant VHAI), will give you some clear ideas on
these issues.
Sincerely yours,
Alok Mukhopadhyay
Executive Director
Encl; as above
PESTICIDE PROBLEM IN IMDIA
Pesticides are used in Agriculture to control various kinds of
pests. In public health these highly poisonous organic
chemicals are use to control disease carrying insects such as
mosquitoes for Malaria.
Since pesticides are highly dangerous and harmful to human
health it is necessary to know about their uses and also how
to handle these with minimum danger to all concerned which
includes the factory and farm workers. To add to this problem,
pesticides get into the food through grains, fruits vegetables
and even water. Once again through the feeds and fodder they
get into milk both of animals and humans as also in the meat
poultry etc thereby creating a vicious cycle through which
these circulate.
The sprayers in the farms quite often get nausea, vomiting,
headache a rash or other symptoms. The long term effects
may be death from acute poisonings or leukemia or cancer
for which well documented evidence exists.
By and large the pesticides use should be avoided by resort
to good agricultural practices but where this is not possible
careful use is the answer. Likewise the world is now turning
to biological control of these insects. This involves use of
pests which prey on the pests that are harmful to man. This
is also being called Integrated Pest Management which is
becoming popular world wide.
Unfortunately there are very powerful interests which thrive
on manufacture and sale of these harmful chemicals irrespective
of serious threat to ecology, environment and human health.
There is very little or nill information in the country on the
illnesses caused by the pesticides, many of which are sold
in bags and paper envelopes without labels or loose. Data
collection of cases of pesticide poisonings will help a great
deal as also education for farm and factory workers and their
families and highlighting the problem and working towards
reduction and correct use of pesticides till these are can
be totally eliminated through alternate methods of disease
(plant and human) control.
PROBLEMS CREATED BY JUNK FOODS AND RADIOACTIVITY IN FOODS
THROUGH ENVIRONMENT
JUNK Foods briefly are foods of low or "poor nutritional value
which are finding an important place in the market.
An important factor of these is the attractive and expensive
packaging in which these are sold at prices which have no
relevance to their food value. Woven into the products which
have flooded the market is aggresive advertising on the T.V.
Junk foods are thus objectionable as these appeal to the
vulnerable groups specially children.
In our context these
also divert the attention of the economically weaker sections
or the have nots who like to imitate the well off.
The Junk foods are characterised by high saturated'fat, high
salt and sugar and limited nutritional value- such as candy,
soft drinks, flavoured . ices, french fries, and several
other fancy products that are on the market. Some cereal
foods fall in this category also.
Instead there is need
to promote the use of natural foods. In the USA Govt, have
put curbs on Junk foods as these were replacing the natural
foods in the school feeding.programmes for which US Govt.
was spending some 3 billion dollars annually, to promote
nutritious meals.
Many of the Junk foods need to be got analysed by our
Laboratories and public educated vis-vis merits of nutritious
foods and high prices.
Instead there isjaeed to promote
consumption of fruits and vegetables. A ’^art of the programme
should be ban on advertising and price control of packaged
products with seme relation to nutritional quality as is being
done in USA.
A new danger has come to notice in this country from the
recent disclosures about radioactivity in butteroil and milk
powder imported as Gifts from EEC after Chrnobyl disaster.
Now the Govt.is embarking upon a programme of food
irradiation which involves use of radioactive Cobalt 60
and Cesium 137. Results from exposure to radioactivity
of Hiroshima and Nagasaki survivors and their off springs
gives conclusive evidence of harmful effects of radiation
even after 30-40 years in the form of genetic disease,
leukemia and cancer. A close study, education and
campaigning is needed in case of both the above problems
which are assuming serious dimensions.
Informing, Advocacy and Influencing policy makers and decision
makers for support programmes of common public interest throug.i
'
Parliament and Press
In the context of our democratic set up, we have access to the
decision makers and policy makers either direct or through
the parliament and the media.
Considering the high demands and limited public resources and
heavy pressures that exist, for ensuring that the legitimate
public interest causes such as those in the neglected health
sector do not suffer clue to lack of essential financial
resources, it is necessary to use the accepted democratic
norms as above.
Approach to highest level, the Minister/Prime Minister.
This can be done either through writing or when possible
and necessary through .personal meetings or through delega
tions. In some cases it may also be possible to draw
attention through arranging conventions/seminars/conferences
and ensuring that the concerned Minister is the Guest of
Honour.
However the procedure outlined at 1 above may not always
be easy or convenient or applicable as the issues involved
may not be of such vast magnitude or importance.
In
such a case we could influence policies and programmes
and financial support by enlisting the help of M.Ps(or the
M.L.A.s or Parishad members as the case may be' to raise
the issue through questions in Parliament/State Assemblies/
Zila Parishad etc., as the case may be.
This means active and close ccntrats with M.P.s who are
willing and interested in raising the issues through
questions or dur:ig Budget sessions or through other
channels such as calling Attention and half hour discussions.
It is also possible to raise issues through Supplementary
questions even if the question has been raised by any
other member but on a related issue.
All this requires advance action and planning. Quite often
it is advantageous if a news report can be arranged which
draw attention to the problem in any place or community.
Based on such a news report, it is easier to frame a
question and have this put through the M.P.(etc).
Framing the question is itself an art and a science
but this can be learnt through practice. A look at
the list of questions admitted in the Parliament would
help in this direction. A question has to be put in some
22 days in advance for the date fixed by the Speaker for
that particular Ministry , in case of starred questions for
the Lok Sabha for which discussion is possible through
supplementaries. For a written reply, 11 days are
required. For Rajya Sabha 11 days are required ) oth for
starred and written replies.
3.
The M.P.needs to be briefed and contacted if full advantage
is to be obtained. After the reply is given, it is
important that a copy of the reply is obtained on the same
day and released to the helpful press for coverage.
Based on the replies in the Parliament, followup should be
made by writing letter to the concerned Minister/Pm through
an M.P. Once again copies of this letter may be released
to the Press in c?der to build up public pressure and
opinion. In short this is an unending cycle to the
pursued till objective is attained.
LOW COST DRUGS AND RATIONAL THERAPEUTICS
Workshops
Organised National Drug Policy, Trichy
May 1987
Drug and Health Policy, Panchgani
CDMU Workshops in Siliguri
Feb.1937
June, 1987
National Drug Policy Seminar
Indian Medical Association
* "Drugs and Cosmetics Act"
Indian Association of Public Health, Maulana Azad
* "Implications of the New Drug Policy in Primary Health Care"
National Campaign Committee for Rational Drug Policy
National Drug Policy Seminar
* "Hazardous Drugs"
Rational Drug Use in Paediatrics - AIIMS and WHO
* "Consumers Views on Drug Policy and Economics"
LEGAL
Banned Drugs Case appearance in Court of Justice Rangannth
Mishra with Dr. Vincent Panikulangara in the Supreme Court.
EP Case - Appearance in the Public Hearings
Delhi Public Hearing
(150 page submission made)
10th April 1987
Calcutta Public Hearing
10th July 1987
Bombay Public Hearing .
14th July 1987
NATIONAL DRUG POLICY
Drug Price Control Order with the Kelkar Committee for
formulation of Category II drugs
ALL INDIA DRUG ACTION NETWORK RELATED
AIDAN Annual Meet, Bombay
Launching of WIDAN, Bombay
Feb. 1987
Jan. 1987
Drug Action Network, Karnataka
Preparatory and Review meeting, Bangalore
Drug Action Forum, West Bengal
meeting on Drugs, Calcutta
August, 1987
Dec., 1987
Jan. 1988
..2..
session taken
?2?
SCHOOL HEALTH RELATED
Teacher Orientation Programme on School Health, Nangloi
School Health Teachers Training Programme, Lajpat Bhawan
PRIMARY HEALTH C/aRE
VHAI orientation programme on "Primary Health Care" -
August 1987, Jamkhed for programme staff and Executive
Secretaries.
MISCELLANEOUS
1. MFC meeting, 1987 (Population Control) Jan.‘88 (Child Survival)
2. People's Science Movement (Bhopal)
3. Gram Niyojan Kendra (Non health groups)
4.
Role of Voluntary Organisation in Primary Health Care?
National Institute of PHC - September 1987
5. Role of NGO's in Health Care, FRCH„
DRUG CAMPAIGN AT INTERNATIONAL FORUMS
World Consumer Congress, Madrid Sept. 87
Theme; Consumer Solidarity
* "Rational Drug Policy Dealing with the Critics"
-International Conference, Bielefeld, Oct. 87
Theme?Less Drugs Better Therapy
* 'Drug Issue Chaos and Crisis - views of the Third World"
Workshop - Need for International Controls
Action for Rational Drugs in Asia
Theme; "Drug Patents"
*"The Indian Patent Policy"
Consultation on Biotechnology and the Third world and its
Socio economic impact on Health & Agriculture, Bogue, 87.
^session taken
;3;
Plans for 1988
ONGOING WORK
1. Follow up of the EP case
2. Follow up of the Drug Policy; specially in area of;
i. Essential Drug List and the formulation of
Category I & II drugs list.
ii. Drug Pricing - Resist further rise in drug prices
in area of Trade Commission, Excise Duty and Chemist fees
Withdrawal of Hazardous drugs - 7 combination drugs
recommended for being weeded out by DCC.
Besides the above work in the following areas will go on:
- Monitoring and control of unethical drug marketing practices■
- Ensuring availability of unbiased drug information to doctors
by way of updated National Drug Formulary on lines of
British National Formulary.
- Demand for consumer caution and warnings for potentially
hazardous drugs in regional language e.g. drugs contraindicated
in pregnancy.
Proper measures and clear dosage guidelines for paediatric
medicines specially antibiotics.
- Drug Legislation reform and action against the violations
of Drugs and Cosmetics Act eg. action on Lentin Commission
report.
- Ensuring effective quality control and drug control.
The above will require formal informal meetings acquiring of
information not easily available senling of consumer alerts
use of the press and need to respond to crisis from time to
time.
Workshops Planned
Rational Drug Use in Medical Education in collaboration with
Kanpur Medical College - second half of 1988.
Rational Diarrhoea Care Western & Traditional concepts.
Four workshops on Rational Drug Use (responding to requests)
Consultation in workshops, seminars, discussions, dialogues, con
sultations and training programme on drugs will continue with
. .4..
; 4;
other like minded organisations, social action groups
etc.
- special focus of drug work will be Rational Drug Use
in Children, Rational Drug Use in National Health Programmes,
Women and Pharmaceuticals.
Preparation cf material
Compilition of the update of -
- Banned Bannable drug List
- Rational Selection of Drugs
- Taste of Tears.
Summary of the Lentin Commission Report
The EP campaign and its outcome - summary report
Status report of the Drug situation in India for
State of India's report.
Dr. Mira Shiva MD
Coordinator
Low Cost Drugs &
Rational Therapeutics
jg/22.4.1988
DOSAGE SCHEDULE FOR AHTIMALARIAL
,
DRUGS
Radical Treatment for P V & P M
4 AQ
(chloro
quine )
8 AQ (Primaquine)
Age
Presumptive
treatment
4 AQ (chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150 mgm
150 mgm
+ 2 .5 mg for 5 days
nil
Radical treatment for P.f. cases
4 AQ chloroquine
75 mgm
150 mgm )
)
4-8 years
300, mgm
8-14 years
400 mfpn
14ft aboi’e
600 mgm
•
30'0 mgm
+ 5 mgm for 5 days
300 mgm )
450 mgm
+10 mgm for 5 days
450 mgm )■
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR J®?imaquine
+ 12-5 mgm
(■q- tablet)
+ 25 mgm
(1 tablet)
nil
50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
Sexual
stage
P.T.
Phase
Clinical
Suppressors
4 AQ
+++
++
for al 1 nv. & pm.
=
++
8 AQ
+++
4--K+
-
Pvrimetha
mine (Daraprim)
Quinine
Sulphate
Progaunil
+++
+++
+
Casual
Pronhyloxis
+
Sprontocidal
++
OR 7.5 mgm for 1 day
-doOR 15 mgm
OR 30 mgm
-do-
OR 45 mgm
-do-
DOSAGE SCBSDULE FOR ANTIIULARIAL
DRUGS
_^ndica1_ treatment f<DT PV.&PM.
Pre sump tive
treatment
4'AQ (chloro
quine)
4 AQ
(chlord
quine)
8 AQ (Priinaquine)
0-1 year
75 mg si
75 mgni
+
1-4 years
150.mg ip.
150'nigra
Age
4-8 years
WO ngra-
3OC mgm
8-.14 yoffjrs;
450 r.gm
IS & stove
600 Elgin
450 mgm
600 ngn
Asexual
stage
4 AQ
£^ 4.
Radical treatment for — P.f.
cases
— — — — — —— _ — —
——————— ——— ——— ——— ————————
4 AQ chloroquine
nil '
75 Bigm
2.5 mg for 5 days
150 ngm )
)
5 mgri
+ 10 mgm
+ 15 Kgn
Sexual
stage
ail P v. & rm.
for 5 days
300 mgr. )
for 5 days
450 ngm )
for 5 days
600 Elgin
+ Damprim
+ 12. 5 mgm
H tablet)
+ 25 mem
(1 tablet)
+ 50 mgm
(S__ia blots)
Action of Antimalarian Dturs
Clini
P.T.
Casual
prophycal suprePhase
s so r s
loxis
=
++
-
Sprontocidal
-
+++
+++
-
+
++
++
++
-
+
+
+++
+++
+++
-
+
-
-
+
+
+
S'AQ
Fyri.~ - tha
mine ( Da rap rim)
Quinine Sulphate
progannil
++
++
OR
~------- - —
'----- ----
-
Primaquine
nil
OR 7.5 mgm for i oay
OR 15 mgm
-doOR 30 Eigm
OR 45 ngn
-do-
-do-
.
DOSAGE SCHEDULE FOR AUTIMALARIAL
DRUGS
Radical Treatment for P V & p M
8 AQ (Primaquine)
Presumptive
treatment
4 AQ (chloro
quine )
4 AQ
(chloro
quine)
0-1 year
75 mgn
75 mgm
+
1-4 years
150
150 mgm
+ 2-5 mg for 5 days
Age
nil
Radical_treatment for P.f. cases
4 AQ chloroquine
75 mgm
150 mgm )
)
+ Daraprim
OR primaquine
+ 12.5 mgm
(■^ tablet)
+ 25 mgm
(1 tablet)
nil
OR 7.5 mgm for 1 day
OR 1 5 mgm
-d 0-
0R 30 mgm
-do-
0R 45 mgm
-do-
4-8 years
300 PlgD
300 mgm
+ 5 mgm for 5 days
300 mgm )
8-14 years
400
Z50 mgm
+10 mgm for 5 days
450 mgm )
14ft above
600
600 mgm
+15 mgm for 5 days
600 mgm
+ 50 mgm
Casual
Pronhyloxis
Sprontocidal
Action of Antimalarial Drugs
Asexual
stage
Sexual
stage
ft pm
Pvriraetha
mine (Da ran rim)
Quinine
Su In hate
Progaunil
P.T.
Phase
Clinical
Suppressors
DOSAGE SCHEDULE FOR AUTIMALARIAL
DRUGS
Radical Treatment for P V & P M
8 AQ (Primaquine)
Presumntive
treatment
4 AQ ( chloroquine)
4 A0
(chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150
150 mgm
+ 2.5 mg for 5 days
Age
nil
Radical treatment forP.f. cases
4 AQ chloroquine
75 mgm
1 50 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgm for 5 days
300 mgm )
8-14 years
400 mgm
450 mgm
+10 mgm for 5 days
450 mgm )
1 4 & abo^e
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR primaquine
+ 12.5 mgm
(■^ tablet)
+ 25 mgm
(1 tablet)
nil
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
Sexual
stage
P.T.
Phase
Clinical
suppressors
0
4 AQ
8 AQ
+++
++
for all nv. ft pm.
■ -
Pvrimetha
mine (Daranrim)
Quinine
SuInhate ■
P rogaunil
+++
Casual
Prophyloxis
Snrontocidal
=
++
—
—
+++
-
+
++
OR 7.5 mgm for 1 day
OR 1 5 mgm
-d 0-
OR 30 mgm
-do-
OR 45 mgm
-do-
DOSAGK SCHRDIHE FOR AWIMALARIAL
PRTJGS
Radical Treatment for P V & P M
8 AQ (Primaquine)
Presumntive
treatment
4 AO ( chloroquine)
4 AO
(chloro
quine)
0-1 year
75 mgn
75 mgm
+
1 - 4 years
150 mTiTi
150 mgm
+ 2.5 mg for 5 days
Age
nil
Radical treatment for P.f. cases
4 AO chloroquine
75 mgm
1 50 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgn for 5 days
300 mgm )
8-14 years
400 mgm
450 ngm
+10 mgm for 5 days
450 mgm )
14^ aboire
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR primaquine
+ 12.5 mgm
(-J- tablet)
+ 25 mgm
(1 tablet)
nil
+ .50 mgm
(2 tablets)
Action of Antimalarial Drugs
4 AQ
Asexual
stage
Sexual
stage
+4-4-
++
P.T.
Phase
Clinical
Suppressors
Casual
Prophyloxi s
Sprontocidal
=
4+
+++.
—
+
++
Pvrimetha
mine (Dara nrim) ++++-+
+
+++
+
+
for all nv. & pm.
8 AQ
+++
—
Quinine
Guin hate
+++
Progaunil
-H-
"
+++
-
+
+4-
—
+
OR 7.5 mgm for 1 day
-doOR 15 mgm
OR 30 mgm
-do-
OR 45 mgm
-do-
FOR ANTIMALARIAL
DOSAGE
DRUGS
Radical Treatment for P V & P M
Presumptive
treatment
4 AG ( chloroquine)
4 AO,
(chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150 mgm
150 mgm
+ 2-5 mg for 5 days
Age
8 AQ (Primaquine)
nil
Radical treatment forP.f. cases
4 AQ chloroquine
75 mgm
150 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgm for 5 days
8-14 years
400 mgn
Z50 mgm
+10 mgm for 5 days
450 mgm )
14 & aboire
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR Primaquine
+ 12.5 mgm
(-§■ tablet)
+ 25 mgm
(1 tablet)
nil
300 mgm )
+ -50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
4 AQ
+++
++
for al 1 nv . ft pm.
8 AQ
Pvriinetha
mine (Daranrim)
Quinine
Sulphate
Progaunil
Sexual
stage
-
+++
P.T.
Phase
=
■4—r+
Clinical
Suppressors
++
OR 7.5 mgm for 1 day
OR 1 5 mgm
-d 0-
Casual
Prophyloxis
Sprontocidal
—
+
++
OR 30 mgm
-do-
OR 45 mgm
-do-
DOSAGE SCHEDUIE FOR AJJTDIALARIAL
DRUGS
Radical Treatment for P V &_P M
Presumptive
treatment
4 AQ (chloro
quine)
Age
4 AO
(chloro
quine)
0 - 1 year
75 mgm
75 mgm
1 - 4 years
150 mgm
150 mgm
8 AQ (Primaquine)
+
nil
Radical treatment for P.f. cases
4 AQ chloroquine
75 mgm
+ 2.5 mg for 5 days
150 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgn.for 5 days
300 mgm )
8-14 years
400 mgm
450 mgm
+10 mgm for 5 days
450 mgm )
14 & £iboire
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR primaquine
+ 12.5 mgm
(-g- tablet)
+ 25 mgm
(1 tablet)
nil
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
4 tO
8 AQ
Sexual
stage
+ •!—J4—ffor all nv. & pm.
-
+++
Pvrimetha
mine (Daraprim) ++■
++
Quinine
Sulnhate
+++
Progaunil
+++
P.T.
Phase
Clinical
Suppressors
Casual
Prcohyloxis
Snrontocidal
OR 7.5 mgm for 1 day
OR 1 5 mgm
-d 0-
0R 30 mgm
-do-
0R 45 mgm
-do-
DOSAGE SCHEDULE FOR AJ^DfALARIAL
DRUGS
Radical Treatment for P V & P M
Age
Presurmtive
treatment
4 AQ (chloro
quine)
4 AQ
(chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150 mgm
150 mgm
+ 2.5 ng for 5 days
Radical treatment for P.f. cases
8 AQ (Primaquine)
nil
4 AQ chloroquine
‘
75 mgm
150 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgm for 5 days
300 mgm )
8-14 years
‘400 mgm
Z50 mgm
+10 mgm for 5 days
450 mgm )
14 & abo^e
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
hk Daraprim
OR primaquine
+ 12.5 mgm
(-g- tablet)
+25 mgm
(1 tablet)
nil
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
4 AO
8 AQ
Sexual
stage
+++
++
for all nv. ’ft pm.
-
+++
P.T.
Phase
Clinical
Suppressors
++
=
+
+++
PTrinetha
mine (Daranrim) ++++-+
Quinine
Sulnhate
Progaunil
+++
+++
-
Casual
Prophyloxis
■
+
+
Snrontocidal
' OR 7.5 mgm for 1 day
OR 15 mgm
-d o—
OR 30 mgm
-do-
OR 45 mgm
-do-
DOSAGE SCI PCD UDE FOR AI-TOIALARIAL
DRUGS
Radical Treatment for P V & P M
8 AQ (Primaquine)
Presumptive
treatment
4 AQ (chloro
quine)
4 AQ
(chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
■ 150 mgm’
150 mgm
+ 2.5 ng for 5 days
Age
Radical treatment for P.f. cases
4 AQ chloroquine
+ Daraprim
<
nil
75 mgm
150 mgm )
)
4-8 years
300 mgm
30'0 mgm
+ 5 mgm for 5 days
300 mgm )
8-14 years
400 nigra
Z50 ragm
+10 mgm for 5 days
450 mgm )
1 4 ft aboi>e
600 mgm
600 mgm
.+15 mgm for 5 days
600 mgm
+ 12.5 mgm
(-g- tablet)
+25 mgm
(1 tablet)
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
4 AO
+++
for all nv,. ft pm.
8 AQ
Perinetha
mine (Daranrim)
Quinine
Sulnhate
P rogaunil
Sexual
stage
-
+++
OR primaquine
P.T.
Phase
Clinical
Suppressors
Casual
Prophyloxis
Snrontoeidal
=
++
-
-
+-r+
—
+
++
nil
OR 7.5 mgm for 1 day
OR 15 mgm
-do-
OR 30 mgm
-do-
OR 45 ngm
-do-
r
DOSAGE SCHEDULE FOR ANTIMALARIAL
DRUGS
Radical Treatment for P V & p M
Presunntive
treatment
4 AO. ( chloro
quine)
Age
4 AO
(chloro
quine)
8 AQ (Primaquine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150
150 mgm
+ 2.5 mg for 5 days
nil
Radical treatment for P.f. cases
4 AQ chloroquine
75 mgm
150 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgn for 5 days
300 mgm )
8-14 years
400 mgm
Z50 mgm
+10 mgm for 5 days
450 mgm )
14 & abo^e
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR primaquine
+ 12.5 mgm
(•^ tablet)
+25 mgm
(1 tablet)
nil
OR 30 mgm
+ 50 mgm
(2 tablets)
Action of Antinalarial Drugs
■ Asexual
stage
4 AQ
Quinine
Sulnhate
Progaunil
Sexual
stage
+++
++
for all nv. ft pm.
P.T.
Phase
=
Clinical
Suppressors
4-r
Casual
Pronhyloxis
-
OR 7.5 mgm for 1 day
OR 15 mgm
Snrontocidal
OR 45 mgm
DOSAGB SCHTTTIE FOR ANTIMALARIAL
DRUGS
Radical Treatment for P V & P M
Age
Presumptive
treatment
4 AO (chloro
quine)
4 AO
(chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150 m.gm
150 mgm
+ 2.5 mg for 5’ days
'8 W (Primaquine)
Radical treatment forP.f. cases
4 AQ chloroquine
75 mgm
nil
150 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgm for 5 days
300 mgm )
8-14 years
400 ingm
750 mgm
+10 mgm for 5 days
450 mgm )
14 & aboi^e
600 ngm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
+ 12.5 mgm
(•J- tablet)
+25 mgm
(1 tablet)
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
4 AO
8 AQ
Sexual
stage
+++
++
for all nv. ft pm. .
-
+++
Pvrimetha
mine (Daraprim) ++
++
Quinine
Sulphate
+++
+++
Progaunil
++
++
P.T.
Phase
Clinical
Suppressors
Casual
Pronhyloxis
Snrontocidal
nil
OR 7.5 mgm for 1 day
OR 1 5 mgm
-d o-
■0R 30 mgm
-do-
0R 45 mgm
-do-
DOSAGE .SCHWUIE FOR AOTIMALARIAL
DRUGS
Radical Treatment for P V & P M
4 AO
(chloroquine)
year
75 mgm
75 mgm
+
- 4 years
150 mgm
150 mgm
+ 2-5 mg for 5 days
Age
0
8 AQ (Primaquine)
Presumntive
treatment
4 AO (chloro
quine )
nil
Radical treatment for P.f. cases
4 AQ chloroquine
75 mgm
1 50 mgm )
)
4 - 8 years
300 mgm
300 mgm
+ 5 mgm for 5 days
300 mgm )
8 - 14 years
400 mgm
A50 mgm
+10 mgm for 5 days
450 mgm )
14^ above
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR primaquine
+ 12.5 mgm
(•7 tablet)
+ 25 mgm
(1 tablet)
nil
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
Sexual
stage
4 An
for all nv. ft pm.
Pvrimetha
mine (Daranrim)
Quinine
Sulnhate
Progaunil
P.T.
Phase
Clinical
Suppressors
Casual
Prophyloxis
Snrontocidal
OR 7.5 mgm for 1 day
OR 1 5 mgm
-d 0-
0R 30 mgm
-do-
OR 45 mgm
-do-
DOSAGE SCHEDULE FOR ANTIMALARIAL
DRUGS
Radical Treatment for P V & P M
Age
Presumntive
treatment
4 Ao ( chloroquine)
0-1 year
75 mgm
75 mgm
+
1-4 years
150 Flerm
1 50 mgm
+ 2.5 mg for 5 days
4 AQ
(chloro
quine)
8 AQ (Primaquine)
nil
Radical treatment forP.f. cases
4 AQ chloroquine
75 mgm
1 50 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgii for 5 days
300 mgm )
8-14 years
400 mgm
Z50 mgm
+10 mgm for 5 days
450 mgm )
14 & abora
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
+ Daraprim
OR primaquine
+ 12.• 5 mgm
(i tablet)
+ 25 mgm
(l tablet)
nil
50 mgm
(2 tablets)
OR 7.5 mgm for 1 day
-d oOR 15 mgm
OR 30 mgm
-do-
OR 45 mgm
-do-
Action of Antimalarial Drugs
Asexual
stage
Sexual
stage
4 AQ
for all nv. ft pm.
8 AQ
Pvrimetha
mine (Daranrim)
Quinine
Sulnhate
P rogaunil
P.T.
Plia.se
Clinical
Suppressors
Casual
Pronhyloxis
Snrontocidal
a
DOSAGF SCPUDULTI FOR AFTIMAIARIAL
DRUGS
Radical Treatment for P V & P M
Presurrotive
treatment
4 AQ (chloro
quine )
4 AQ
(chloro
quine)
0-1 year
75 mgm
75 mgm
+
1-4 years
. 150 m<<m
150 mgm
+ 2.5 mg for 5 days
Age
8 AQ (Primaquine)
nil
Radical treatment for P.f. cases
4 AQ chloroquine
75 mgm
150 mgm )
)
4-8 years
300 mgm
300 mgm
+ 5 mgm for 5 days
300 mgm )
8-14 years
400 mgm
Z50 mgm
+10 mgm for 5 days
450 mgm )
14 & above
600 mgm
600 mgm
+15 mgm for 5 days
600 mgm
dk Daraprim
OR primaquine
+ 12.5 mgm
(y tablet)
+25 mgm
(1 tablet)
nil
+ 50 mgm
(2 tablets)
Action of Antimalarial Drugs
Asexual
stage
Sexual
stage
Clinical
Suppressors
P.T.
Phase
4 AQ
+++
++
for all tjv. & pm.
=
8 AQ
+++
+++
+++
-
'
Progaunil
+++
Snrontocidal
++
+
P^rimetha
mine (Daranrim) ++
Quinine
Sulnhate
Casual
Pronhyloxi s
+
++
OR 7.5 mgm for 1 day
-dcOR 15 mgm
OR 30 mgm
-do-
OR 45 mgm
-d.o-
CMNTRN m RUR-U, TIALTH AI-ID SOCIAL EDUCATION
At-1
1 Ashok PAigaTV Tirupattur 635 601
WTNOLg. Dauoc ,QAg£OI.
Readers may have noticed that this year we stopped using a
number of drugs that are still being freely sold in the
chemists' shops.
We do not feel that it is sufficient to add
and subtract medicines from our armamentarium.
People
concerned should know why this is being done.
This education campaign was conducted at three levels.
At
first our staff read up on the use of these drugs and their
side effects. Papers were presented during staff seminars and
a pharmacology textbook in Tamil was bought. The seminar
papers were cyclostyled and have been distributed to over 60
interested organisations and individuals around Tamilnadu.
The next step was to carry the message to our VLWs at their
refresher courses and to the general public during
street plays and public meetings.
The Tamil monthly magazine
'Aakkam' has also carried one of our staff's articles on the
danger of ANALGIN.
We also went one step further and carried the debate to the
portals of the academic institutions.
We asked specialists
from the medical colleges the opinions on some of the
controversial drugs.
Nine teachers from Vellore, Chingleput
and Madras Medical Colleges replied and their views have been
compiled. We are also planning to. translate their comments
into Tamil.
We are cooperating with a consortium of five non-governmental
organisations in Chingleput District who are arranging meetings
on this issue in their area.
Similarly we have supported a
group of Ayurvedic and Allopathic medicos in Coimbatore who
published information brochures and held meetings about
bannable drugs.
There are also a few individuals in Madras
who are in contact with us on this issue.
What follows is a summary of the views of the experts on
some of these drugs;
33(7, T?« fU,.
^°C'S
- * "B^’G^oAe- Ss-o 03^
Fixed dose combinations of Chloramphenicol .and Streptomycin,
~~C?or oral" use}:
This is not recommended
- Pharmacology Professor, MMC.
"These combination medications have been stopped from being used
by many advanced countries. Wonder why our country still continues
to manufacture them".
- Pediatrics Professor 1, Vellore.
General Medicine
Pediatrics
Pharmacology
Surgery
Other
For
Against
1
3
2
1
1
1
6
Fixed dose combinations of Penicillin and Streptomycin:
"(Found useful) in an animal model of staphylococcal endocorditis.
Even here simultaneous administration of the two drugs in requisite
dose is preferred to a fixed dose combination".
- Pharmacology Professor, MMC.
"Manufacturing licence should be withdrawn"
- Pediatrics Professor 2, Vellore
For
Against
General Medicine
1
3
Pediatrics
2
—
Pharmacology
1
Surgery
1
Other
1
_2_
_7_
Anabolic Steroids:
"Fracture in debilitated individuals; where improvement in
debilitating.disease is not satisfactory with other treatment".
- Medicine Professor, Chingleput
" To what extent they are beneficial is a moot question. Should
not be used in Pediatric age group”,
- Pharmacology Professor, MMC
"Should be used by only qualified Paediatric and adult endocrino
logists" .
- Pediatrics Professor 2, Vellore.
" Where there is excess protein breakdown in limited situations".,
- Medicine Professor, Vellore.
"Can be used with reservation".- Medicine Asst. Prof, Chingleput.
Specific
Conditions
Against
—
1
1
3
1
1
—
—
1
1
—
—
—
■M.M. MV
WWMVM
MVM.-M
2
———
_5
2
For
General Medicine
Pediatrics
Pharmacology
Surgery
Other
—
Oxyphenbutazone & Phenylbutaz;one:
"Only in ankylosing spondylitis where it is sometimes the only
effective drug".
- Medicine Professor, Chingleput.
"Should be discontinued forthwith".
- Pediatrics Professor2, Vellore.
"Have to be used only be qualified physicians under medical
supervision".
- Pharmacology Professor, MMC.
"For ankylosing spondilytis
rheumatoid arthritis"
For
General Medicine
Pediatrics
Pharmacology
Surgery
Other
—
M.
—
1
—
and acute phlebitis and rarely in
- Medicine Professor, Vellore.
Specific
Conditions
2
•
—
1
—
—
Against
2
2
—
1
M.MVW.
mvvmvm
MV MV MV
1
3
_5_
Kaolin:
"Not necessary - I never use it"
- Medicine Professor, Chingleput
"Has little actual benefit. Can be used as a non-specific antidiarrhoeal agent.
It is not a toxic drug".
- Pharmocology Professor, Madras.
"Is of no benefit whatsoever"
For
General Medicine
Pediatrics
Pharmacology
Surgery
Other
2
- Pediatrics Professor 2, Vellore.
Against
2
2
1
1
_4_
.4
Diphenoxylate:
"Useful in adults only where there is moderately severe diarrhoea.
I use only 1 tablet dose in 6 hours",
- Medicine Professor, Chingleput.
''Contraindications: Allergy; Jaundice; Children below 2 years.
Physiological and psychological dependence can occur if used in
large doses over extended period because it is a member of the
pethidine group".
,
F
- Pharmacology Proiessor, Madras.
"Useful when used with antibiotics in adults".
- Medicine Asst. Prof., Chingleput.
Specific
For
No Comment
Against
Conditions
—
General Medicine
1
2
1
—
Pediatrics
2
—
—
Pharmacology
1
—.
—
—
Surgery
1
—
Other
—
—
1
———
•Cm*
•MM.
2
1
3
3
Loperamide:
"Not essential"
~ Medicine 'Professor, Chingleput.
"Of use only in specific situations and hence should be decided
by qualified gastroenterologists only".
- - -Pediatrics Professor'_2,' Vellore.
"Fatal Paralytic Ileus and CITS manifestations (may result from
its use in children)".
- Pediatrics Professor 1, Vellore.
"Neurogenic & Functional Diarpoheas".
- Medicine Asst. ProfChingleput.
"Used in Diarrhoea".
General Medicine
Pediatrics
Pharmacology
Surgery
Other
- Pharmacology Professor, Madras.
For
Specific
Conditions
No Comment
Against
1
1
1
—
1
1
—
—
—
1
—
—
—
—
1
1
—
—
1
_3_
_2_
_1_
„3_
Hvdroxyq uinolines:
"As it is potentially dangerous it should not be used as chronic
amoebiasis in India is sometimes a life long disease".
- Medicine Professor, Chingleput.
"Some types of intestinal
amoebasis and diarrohea".
- Pharmacology Professor, Madras.
"Orally for amoebic colitis"
General Medicine
Pediatrics
Pharmacology
Surgery
Other
- Medicine Professor, Vellore
For
Specific
Conditions
No Comments
Against
1
—
1
—
1
—
1
—
—
—
1
—
—
2
1 ■
—
—
1
2
2
1
4
Analgin:
"Parenteral use is adviae.able"~ - Surgery Asst. Proff., Chingleput
- Medicine Professor, Chingleput.
"Can be sparingly used."
"Its use as a routine analgesic is not recommended"
- Pharmacology Professor, MMC.
- Medicine Professor, Vellore.
"Never"
"Could cause renal failure, aplastic anemia"
- Pediatric Profe ssorl, Vellore.
For
Rarely
Against
1
2
1
2
1
General Medicine
Pediatrics
Pharmacology
Surgery
Other
1
1
i
i
I
I
tni
H
I
I
I
2
Drug
For
Specific
Conditions
Rarely
Against
CHLOROSTREP
3
-
6
No
STREPTOPEN
2
-
7
No
ANABOLIC STEROIDS
2
5
2
Restrict
ANALGIN
3
2
4
Restrict or Ban
OXYPHEN +
PHENYL BUTAZONE
1
3
5
No
KAOLIN
4
-
4
May Be
DIPHENOXYLATE
2
1
j
May Be
LOPERAMIDE
3
2
3
May Be
HYDROXY QUINOLINES
2
2
4
Restrict or Ban
Conclusion
CENTRE TOR PJ.KAI. HEALTH AND SOCIAL EDUCATION
A—11 Ashok Nagur Tirupattur 635 501
DETAILS 0? SOME COMMENTS DY PHARMACOLOGY PROFESSOR - M-4C
1. 1'2 xed dose combinations of Chloramphenicol °< Streptomycin (for oral use)
This is not recomended. Chloramphenicol is reserved for typhoid and has to
be used with caution because of the danger of bone marrow depression. There
are-i-nstance&awlierej it has produced diarrhoea. In intractable bacillary
dysentery, the two nay be.used independently. There is no added advantage
or a firm basis for such a combination.
2. Fixed dose combinations of Penicillin & Streptomycin.
Synergism invitro by a combination of Penicillin and Streptomycin has been
demonstrated with staphylococcus aureus. Eradication of microorganism from
infected vegetations was found to be more rapid in an animal model of staphyloccal endocarditis treated with this combination. Penicillin altera the
structure of the cell wall end can markedly increase the entrance of aminogly
cosides into these bacteria; this’is the only condition where this combination
is used. Even-here simultaneous administration of the two drugs in the
requisite dose in preferred to a fixed dose combination.
3. Analgin (Metamizcle Sodium),
Preparations: (Dipyrone, Analgin, Uovalqin) 500 mg
or I.V.
tab
tds
used orally l.M
It is closely related, to aininopyrine and is documented for its ability to
cause agranulocytosis. Hence, its uso as a routine analgesic is not recommended.
'Shock' lias also been reported, after the parenteral use of this drug.
4. Oxyphenbutazone and Phenylbutazone.
Oxyphenbutazone; (Tanderil, Suganril)100-200 mg tab tds
Phenylbutazone; (Butazolidine, Zolandin)’ 100 , 200 mg tab tds
3oth are anti-inflammatory agents and have to be used only by qualified
physicians under medical supervision. Phenylbutazone has been banned in many
countries. Oxyphenbutazone is the active metabolite of phenyl butazone. They
have a number of adverse effects and are contra-indicated in blood, bone marrow
diseases, allergy, peptic ulcer, hypertension end congestive cardiac failure.
Reference;
The Pharmacological basis of Theraneuticsed.
7th ed. 1985, Macmilan publishing Company.
Alfred Goodman Gilman et’al
Essentials of Medical Pharmacology X.D. Tripathi, 1935.
Jaypee brothers, New Delhi.
FURTHER COMMENTS DY PEDIATRIC PROFESSOR 2: VELLORE:
1. With regard to Anabolic steroids, my comments that it should be used only
by qualified Paediatric and Adult Endocrinologists applys only to such
preparations as oxnndrolone. As you are aware there are many anabolic
steroids available in the market and I wouldn't use any of them for any
indications in endocrinology even. Oxandrolone is fairly specific for
growth disorders and Oxy.metholone is used for treatment for aplastic anaemia.
Apart from these two drugs, I will not .-ecorunend any other anabolic steroids.
I thought I must make my stand clear in this regard.
2. With regard to Loperamide, once again I would like to make it very
explicit that the indications will be only in secretory diarrhoea whore an
infective aetiology is totally ruled out. And also only in cases of
intractable chronic diarrhoea in children.
Position: 263 (20 views)