Vanitha.pdf
Media
- extracted text
-
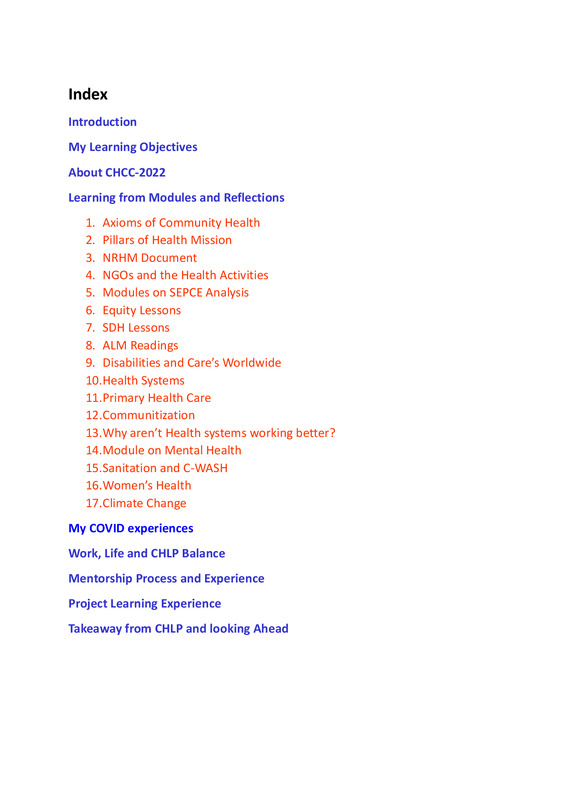
Index
Introduction
My Learning Objectives
About CHCC-2022
Learning from Modules and Reflections
1. Axioms of Community Health
2. Pillars of Health Mission
3. NRHM Document
4. NGOs and the Health Activities
5. Modules on SEPCE Analysis
6. Equity Lessons
7. SDH Lessons
8. ALM Readings
9. Disabilities and Care’s Worldwide
10.Health Systems
11.Primary Health Care
12.Communitization
13.Why aren’t Health systems working better?
14.Module on Mental Health
15.Sanitation and C-WASH
16.Women’s Health
17.Climate Change
My COVID experiences
Work, Life and CHLP Balance
Mentorship Process and Experience
Project Learning Experience
Takeaway from CHLP and looking Ahead
Introduction
My Community Health journey must have started around 1988 when
I was barely 13 years of age. I was brought up in a city and used to
visit our village house which my father bought and my relatives lived
there. My playmate in the village was our domestic help’s daughter, a
brilliant girl. She was not interested in studies. I used to encourage
her to study saying she would have a better future than her parents.
She said I will make a living as a weed remover. It was around that
period of time I must have made up my mind to pursue medical
education in college and practice in the same village in future even
though I didn’t return till date.
To work with the poor and needy was always in thoughts. I chose
Traditional Indian Medicine -Siddha in college and did my PG also. My
dreams chased me and found myself working with a group of Siddha
doctors who formed an NGO in 2015. I was suggested to do this
course with SOCHARA by my senior and adviser Dr. G. Sivaraman,
Member, Tamilnadu State Planning Commission.
My Learning Objectives
1.To help achieve Integration of traditional Indian medicine in Public Health
2.To learn more about community health through experience of others.
3. Learn through more readings when I am accountable to a curriculum.
4.Anticipated to learn to write impressive project proposals which will help in
increasing funding.
These were my expectations from this course.
Today I am happy to know that my expectations from this course were fulfilled
and most importantly I am left with a worldwide web of friends and
acquaintances who are ever-ready to help each other.
ABOUT CHCC-2022
I came to Bangalore with no idea about what this meet holds for. I was open to
what the five days would unfold for me. I would say that I rediscovered the
15-year old Vanitha in me,at the end of the confluence meet. I always felt I was
more matured at 15 years when I passed my High school than at any age of my
life. Here are my key takeaways and rejuvenating reflections from the
CHCC-2022.
Sangamithra Project, Dr. A. K. Anthony’ s Kerala Story of Covid Pandemic,
SOCHARA’s Health Policy Research and Action, People’s Health Manifesto by
JSA, Health for ALL-People’s Resource Book were the books recommended to
read on the inauguration of CHCC.
In the inaugural meet Dr. Prityush, President, SOCHARA introduced SOCHARA
as a Resource library, open and flexible learning, Networking and its Synergistic
Outcomes, How we can learn from others and respect each other. His speech
and body language itself was a glimpse of what he conveyed. My learnings
gained momentum from here once again.
Dr. Ravi Narayan’s insightful lecture-Health is well-being. We are always doing
outside learning. We should do inside learning. Once a month sit and think
what am I? These insights opened some windows of my heart. Hey these
people are doing a noble service through education for HUMANS irrespective
of their age, backgrounds and positions in society. This was the thought felt.
Rani gave me an insight into Plurality and how to come out of it and CELEBRATE
DIVERSITY.
INSIGHTS Learning CONCEPTS slowly opened the different chambers of my
pre-occupied mind-set.
CHLP in 6 lines,
Go to the People
Live among them
Love them
Learn from them
Start with what they know
Build with on what they have
There cannot be as simple an effective project as this.
It was an enthusiastic day to learn the success of TIA, Mallur and ACCORD
activities in detail. Very inspiring and awe struck by the commitment of
founders and community.
Presentations of Senior fellows of CHLP 2021
Umetha and Seigel Tambhat’s Community life and career is interesting
challenging.
Stories of Assam floods, hilly terrain, cut-off roads, seasonal variations, early
harvest, monsoon and floods with multiple communities. The paper reading
about North-East was very less for me. I didn’t know much about the
communities there. Have met a Manipuri during my college and knew only
what she said in our discussions. The developing India in my Mind crumbled to
pieces after the stories from NE.
Epigenetics used for positive approach in the Child and Youth Well Being
Program of Dr.Shilpa Terrance. This acquaintance has blossomed into a
friendship. My husband Dr.Rajashankar has joined their Adolescent and Mental
Health course starting January 2023.
Abirami and Aravindan -another couple of CH inspiration. How Dr. Ravi changed
the course of DoctornetIndia to HealthnetIndia is another point to relish in
their journey. Aravindan wanted to take this Monsoon Simulation games to
Urban schools, the thought I harbour too. He said it is equal to a two - year
Developmental studies PG course.
Suresh’s lecture on the activities of CH work in Tamilnadu made me proud
momentarily. I began to understand the role of politics in health positively for
the first time. He briefed on the activities of SOCHARA in awareness, action
plan, training, networking and building Solidarity, Communitisation part within
Health and its role in NRHM in Tamilnadu.
MAYA Bazaar visit
Breathing an urban slum for the first time. Seen many in documentaries and
films. Lack of common toilets-Sanitation is a major issue. Waste segregation
chart -Monitoring was educating. Life goes on even in these packed housing
with all its happiness and woes. The community work by SOCHARA team was
explicit from the reception we got. Many lanes were well maintained and
community partnership was evident. Barriers to acting on the SDH.
Disapproved to build toilets. Casteism is an important component in Sanitation.
Cultural aspects like temple behind, toilets next to their house. Painting walls
and Kalakendra are Positive approaches to enter and build rapport with
community. SOCHARA not only teaches it SHOWED how to achieve Community
Health.
Communication Skills
Dr. Magimai’ s Communication and Inter-personal Relationship, Rapport
building session was interesting, informative, proactive.
One has to be flexible to be Happy.
Do not easily overlap or develop a conflict free life.
The success of communication is the feedback from your receiver.
Sharpen our senses to be more effective for communication skills.
Values are how much importance you give to your belief system.
Knowing or unknowingly I am deleting information from the person before me.
At any point of time our eyes are capable of taking 20 lakhs info. That’s why
automatic deletion happens. We should be aware of this at any time.
He gave an exercise to do at the end of Six months.
Map is NOT the Territory
My Map is Subjective (Partial from my eyes-Biased)
My Map is important to Me.
Your Map is important to You.
Let’s make an attempt to look at the person’s Map from His point of View.
In the next 6 months I have ask myself and others on these questions.
Learning from Modules and Reflections
1.Axioms of Community Health -vast yet deep.
Community Health axioms revealed that Siddha Medicine is a Community
Medicine as it is relevant to the axioms. The Key takeaways from this module
are,
Rights and Responsibilities to achieve Health For ALL.
Different Community health approaches to solving public health issues.
“The primary determinants of disease are mainly economic and social and
therefore its remedies must also be economic and social”-Prof Geoffrey
Ross,1992
2.Pillars of Health Mission
A. Community involvement
B. Monitor against agreed milestones
C. Human Resource Management
In due course of time, I shifted from community medicine learnings of Siddha
to Public Health like focus. These learnings gives more clarity and helps
understand causes of my shift in focus.
3.NRHM Document.
Health Plan for each village through Panchayat Raj institutions.
Equity principle to bring equality
Equity also means focus on where more need, more representations required
viz., Dalit subcastes, differently abled, chronic patients.
Health should be achieved by all of us. Both PHS and community are equally
responsible.
The learnings from this document helped me understand about the network of
community sensitive people, doctors, social persons who come together and
made suggestions from prior learnings and results to bring a renaissance in
Public Health.
4.NGO s and their Health oriented Activities
I am impressed and awestruck after reading the contribution to community
health of Bangladesh and Jamkhed India Case studies by Chowdhury and Perry
On the unique scheme of income generating through its own social enterprise
BRAC-Bangladesh.
When someone perceives a need, an NGO is likely to follow-FOX,1987 I am 100
percent with this statement with the experience of the start and functioning of
our NGO.
Village Committee and Public Health people have equal rights and are equal
stakeholders - Power shifting. Program should form from ground level to
materialize. What’s happening is actually the reverse.
Learnings from Videos:
Bloom’s Taxonomy
Ameer explained the dimensions (knowledge, understanding, skill, analysis,
synthesis, evaluation, creativity) and their position in community illustratively
on a triangle. Actually, the ladder of dimensions must be reversed.
Only through democratic way Health can be achieved. Vaccine production and
democratic distribution issues is a good example of implementation challenges.
Tribal people had a holistic approach to health for generations. Nature is God
for them. We have to be sensitive to their needs.
6-7 villages make one Panchayat of 5000 population. There are very few health
workers to handle such a large population in each panchayat.
Gender inequality in rations is a revelation of health problem which I had not
thought of before.
My understanding of COVID issues changed after Amir’s VL. I could see the
other side of the coin on the many factors involved in COVID spread when the
government claimed it as a social irresponsibility.
I have started spreading this message to the community. Demand Health as a
Right-only awareness can achieve Health. Health is a political struggle. We need
evidential representation to policy implementation.
I want to work in this phase of community health.
At this stage I understood the abbreviation SOCHARA-Society for Community
Health Awareness Research and Action and the founders and office bearer’s
actions for more than five decades.
Apart from providing health care we have to address many other problems and
have policies in all sectors.
I got acquainted to various movements and bodies working on the Political
Struggle for Health.
RVHSA-challenge- Women empowerment in their activities due to gender
inequality in society
AWARE- Action for welfare and awakening in Rural environment
SOCHARA-Society for Community Health Awareness Research and Action
JAMKHED INDIA and Bangladesh Case studies by Chowderie and Perry mention
in detail about the Unique scheme of income generating through its own social
enterprises.
Mukhta Bai Pol of JAMKHED said “I can also be the next one to light another
lamp of better health”.
MIYCN- Home Fortification Program and BRAC, Bangladesh are my greatest
Inspirations.
5. Module on SEPCE Analysis
The live sessions only helped me grasp the dept of this module. I could relate
few sensitive readings which helped me understand SEPCE analysis of a
context.
Covid crisis and migrant workers document is an in-depth study which will find
way to improve health of migrant workers in the long run. It can give inputs to
the Public Health to work keeping SEPCE factors during treatment.
Kerala State DISHA is a most needed and good sustainable health program.
Health is a dynamic fact. It helped to think about disparities within a
mentioned sector of people. Taught us to create opportunities despite
inequality removing barriers viz. Equity.
Intersectoral issues in community were discussed in ALMs.
Eutopia and Solidarity were two new relevant, positive words and prerequisites
learnt for CH journey.
In the live sessions on this module, we learnt SEPCE Analysis will help us take
one step forward to implementation.
6. Equity lessons from Prasanna
The following takeaways helped me understand the meaning and
necessity of Equity for Health.
❖ UNEQUAL TREATMENT FOR UNEQUAL CONDITIONS TO MOVE IN THE
PATH OF FAIRNESS AND JUSTICE IS EQUITY
❖ Inverse Care Law -Tudo Hart: The one who needs the most gets the
least.
❖ The dream of Public Health is of minimizing preventable death and
disability which is also the dream of Social Justice.
❖ POLITICS AS POWER-SEEKING JUSTICE IS ULTIMATE POLITICS
❖ Medicine is a Social Science and Politics is nothing but medicine on a
grand scale.
❖ A WAY OF DOING JUSTICE IS COMMUNITY HEALTH.
❖ Rights are always claimed not given.
❖ Freedom of Speech -Article 19
❖ Right to Health Act 2005
❖ Awareness is a Market Phrase
❖ FOR ANY RIGHT TO BE IMPLEMENTED THE DUTY BEARERS ARE THE
CONSTITUTION, ACTS OF PARLIAMENT, GOVERNMENT, POLICY,
BUREAUCRATS
❖ Life expectancy of different sub-groups.SC 5-6 years less than other
castes.
❖ Data is actually facilitating Rights. If you have data you can claim Rights
❖ Nirman Bhavan in New Delhi and White Hall in London are places
where Civil Servants are located. Michael Marriot did a study on the
Civil servant Social gradient in Health. Where you position yourselves
in Society decides your life expectancy. We have to actually move
people in the ladder of hierarchy.
❖ Primitive Tribals of Orissa affected by Sickle Cell Anemia and Malaria.
❖ The staple food of Uraus and Mundas is Mahua which is rich in iron
content, then why these are endemic to these diseases
❖ DUAL LOYALTY-FOR HEALTH WORKER ACCOUNTABILITY IS TO
EMPLOYER BUT LOYALTIES SHOULD BE WITH PATIENTS. THAT IS WHY
HEALTH RIGHTS MATTER TO OVERCOME LACK OF LOYALTY.
7.SDH Lessons from Janelle
Though in the first instant, it seemed Greek and Latin, the structure and its
importance was understood on drawing the structure for every health issue
in the community. The following steps has to be followed, it is that simple.
A. Take one determinant and see how it impact the other determinants
and what can be done.
B. What are the ways to bring people forward in that particular context
C. SDH framework helps us place the determinant we are looking at
D. Power further decreases as we go down in the SDH analysis
E. All change that happens in community level is due to social cohesion
and social capital.
F. Identify structural determinants and intermediary determinants
G. From individual to global level there is a roadmap-the framework
H. We should know where we are located in the framework, our position,
what we can do, how we can network to bring the change
I. When doing this we should not isolate other groups. Others should be
given awareness and involve them
8.METHODOLOGY
SEPCE is learning in progress. We should try to apply, tools, principles, axioms,
community health approaches in single case studies and real - life situations
frameworks.
Take one determinant and see how it impacts the other determinants and what
can be done. What are the ways to bring people forward in that particular
context.
1.We have to build an evidence-based influence in change in policy
2.Collect data of population
3.Identify the barrier to SDH
Experential evidence building context with the community
Building background reading
Role of health system in community
Looking at intermediary factors
Building evidence is most important
Have SEPCE and CSDH reflection on all we read
Always look for strengths that lie in the community as well
Lot of mind mapping
Pictorial representation is important
9.CORE Values for Action on SDH
SDH- the conditions in which people are born, grow, work, live and age and the
wider set of forces and systems shaping the conditions of daily life
Ex: childhood experiences, housing, education, social support, family income,
employment, communities, access to healthcare etc.
CORE Values:
1. HEALTH EQUITY: “the absence of unfair and avoidable or remedial
differences in health among population groups defined socially,
economically, demographically or geographically and forms the ethical
foundation for the CSDH framework and action on SDH
Health inequities impact<Individual Functional Capabilities
Agency impacts <Individual Freedom
Rights impact <Health
2. HUMAN RIGHTS FRAMEWORK: Everyone has the right to a standard of
living adequate for the health and well - being of himself and his
family, including food, clothing, housing and medical care and
necessary Social Services Art25-1948 Universal Declaration of Human
Rights (UDHR). Primary responsibilities for protecting health equity
rests with governments (asserted by WHO’s Constitution.1978 Alma –
Ata Declaration, Ottawa Charter on Health Promotion,1986 and Rio
Political Declaration,2011)
Rights Concepts helps:
● Diffused social demands into focused, legal and political
claims
● Evaluate the performance of political authorities in terms
of equitable distribution
3. DISTRIBUTION OF POWER: Empowerment is the locus of decision
making about health shifts to the people whose health status is at
issue.
Human Right to Health based Empowerment: The Empowerment of
deprived communities to exercise the greatest possible control over
the factors that determine their health
“Power corresponds to the human ability not just to act, but to act in
concert. Power is never the property of an individual, It belongs to a
group and remains in existence only so long as the group keeps
together”-Hannah Arenett
Action to reduce Health Inequities involves changing the distribution of power
within society to the benefit of disadvantaged group-1986, Ottawa Charter
9.ALM REFLECTIONS
The whole history of Cholera in India
Transformation of food and farming in Rayagada Orissa, Sitapur Dt, UP and
Chintamani in Karnataka by Suda
The Attapadi Story by Mathew Sunil George-How can my milk which gives life
become the poison that killed my child?
These helped me understand Actions on SDH in a much better way.
Rio Political Declaration-SDH,2011
All for Equity and Health for ALL-global action. Health Equity is a shared
responsibility
Action on determinants for both vulnerable groups and entire population is
essential to create inclusive, equitable, economically productive and healthy
societies. Positioning human health and well-being constitutes a successful,
inclusive and fair society in 21st century.
Global Goals
Eradicate hunger and poverty
Ensure food and nutritional security
Access to safe drinking water and sanitation
Employment, decent work and social protection
Protecting environments
Delivering equitable economic growth
Address Social Determinants-contribute-achievement of Millenium
Development Goals
Assignment given in online sessions motivated Experiential
Learning
Visited a Wellness Centre -at Ilavelangaal within a Sub centre in Keelakottai in
Tuticorin Dt. It is under PHC control. NCD prevention is assisted by MLHP- Mid
level Health Provider (Asst. VHN). They are trained in Yoga. The centre has
Emergency Management Drugs and the staff is trained in using them also. I
could see IEC materials like charts and drugs with labels. Tamilnadu is really
doing well in implementing most of the Health schemes and is a forerunner.
The literature study in2008 of Global Structure Research Circle, reflects 2013
Ayushman Bharat,2018 NHM, 1988 Jan Swasthya Program (all male) that each
program had some disadvantages. Therefore, Community Health Work is
Village Council’s work. It has to be Comprehensive and Preventive. Causes
existing locally and approach has to be people centric. No single model fits all.
Local capacity building. Not only a biomedical paradigm shift but empowering
community is the key.
10.Reflections and Understanding on Dr. Nicholas,Asson for
Disabilities
Disabled Person’s Organisations must ensure …
Education, Empowerment and Social Inclusion for the Challenged people.
Involving normal children with disable children to give a sustainability.
Spreading awareness, distributing food stuffs.
Home based rehabs. Teaching the individual as much of self-care they can do.
Medications to mentally challenged people. Specific programs to be
undertaken for this group.
Awareness to community around the disabled people through home visits,
transmitting knowledge.
Conduct Adolescent Girl’s groups-sessions including disabled girls.
Govt. teachers need to know sign language and Braille.
Can contact Organisation for Rare Disease, Indira Gandhi Hospital, Bangalore.
CARER’S WORLDWIDE
Emotional support groups for Carers
Simple cost-effective model
92 % carers are participating
400 carers are trained in bare foot councelling
71% are having mental health issues
Carer’s Co-operative has a financial initiative part also
11.HEALTH SYSTEMS-Dr. Devadasan
System introduced by Engineering Sciences, picked up by managerial sciences
and two decades ago taken by Health sciences
All the activities whose primary purpose is to promote, restore and maintain
health
Elements of Health Systems-Food, Organs, Individual, Community, Hospital,
Government Health Policies, WHO, Other governments and Nations
Health Care Services
TB Control, Institutes, Hospitals
Health Staff
Doctors, Nurses, Lab, Admin, VHN, ASHA
Finances
Govt. Taxes, Insurance, Patient’s Money
Community
Level of Coverage, Involvement etc.
Pharmaceuticals
Adequate Medicines
Infrastructure
Hospitals, Private Clinics, Equipments
Information
Statistics included or excluded,expenses etc.
Policies
Health for All,NHM
Values
Based on Equity,solidarity,financial affordability
Context
May do well in one context,poor in other context
Governance
Appropriate policies, implementation,
guidelines,accountability
Kerala-Demographic accessibility
People are aware of Rights
Public Health Governance is Better
Health Outputs
Health Goals
Financial
Increased access to Quality Care
Improved health, Response to Community,Social and
● Describe and Analyse a Health Problem
● An Intervention-Financial-Bonus for Doctors,Human Resources Element is
affected
Reflections
Use the health systems framework to understand a health problem.There are
atleast 10 elements to consider.Remember they are interconnected. These are
not linear interactive it may produce expected or unexpected outcomes
12.PRIMARY Health Care
Promotive, Preventive, Curative, Palliative
Include Traditional Medical Systems
Comprehensive,Computed and Interdisciplinary staff
Continuous Information system, Referral system
Patient Centric-Should be accessible
South-Asian
Countries Srilanka
and Malaysia
Maximum5000/PHC
Comprehensive Continuous Care to all kinds of people
Very operational Referral hospital service-Good
rapport within the system
PHC supervision from Central,State or National
level,linked with ICDS,Education,Civil
supplies,Government team trained and updated
regularly
Europe
3000-5000/PHC
In UK a GP responsible for 500 families
Average 1500,Referral to County Hospital
District Health Team monitors the team and
community feedbacks.They give added service of
Community Nurse
GP can refer baby to social service in case of drunkard
father
GP in UK is 3 year specialization have to renew every 3
years.Robust training updates.
Primary Care specialists not responsible for the people
They undergo rigid training,for every years
re-registration
30000/PHC,our Urban PHC in Palayankottai caters
50,000
Decentralising by Health and Wellness Centre for
5000-No competency yet
Referral services not formal-weak
PHC are supervised to some extent
No robust training updates.Registered for life.Patient
has to pay fees for facilities
Like US not responsible for the patient who comes
No supervision or relationship from any sector
US
India-Govt
India- Private
Healthcare
Patient seek auto-referral
Spend a lot of money for all health cares
13.Community Participation- Changing health services - to needs of
community
Reflections
Health service is a key output of a health system. Health Services should have
primary and secondary service.Must be more accessible and affordable.
Communitization-Dr.Thelma Narayan
Community Action on Health initiated by NRHM 2005-2008
Sokhey Committee-1937 Community work-9 months Program carried out 5
years in full fledge
Bhore Committee-Result Nagaland Community People are decision makers
there
Green Manual of Community Health Workers
USHA-In MP even before NRHM
Globally in USSR -FELDSHERS,China BAREFOOT DOCTORS,Iran BEHRVAZ,Central
and South America,Africa etc as a promotion by Alma Ata ‘s Health for ALL goal
and Comprehensive Primary Health Care strategy 1978
Reflections
Social health activists must increase.In 1990s SOCHARA gave an effective
recommendation that ASHAs must be women.
Community Action for Health is ONE Path.Community should emerge as
active subjects.
There is no single set of best practices.
Some characterisitcs are common for better performance.
Procurement and distribution systems tha t actually deliver interventions are
fine.Sufficient health workers with right skills and motivation group need to
be created.
Fair, inclusive sustainable financing systems required
Governments should try to improve on their goals every year.Coverage goals
have to improve.
Common concerns of all nations
Ageing Population
Provision of Chronic care or Social security Reforms
New epidemics
Avian or Human Pandemics Influenza,COVID
Difference faced among countries-there is a relative severity of challenges
faced,the way the health systems have evoleved, economic,social,political
context,determines the nature and effectiveness of response.
14.Why arent health systems working better?
Services must be effective, assured quality,safe,health providers must be
responsive to patient’s demands
Funding for Health--● Tax based funding
❖ Social Health Insurance
❖ Community or micro insurance
❖ Micro credit
❖ Even conditional cash transfers
Intersectoral Determinants---Health Outcomes
❖ Working with finance ministries to justify budget demands in tne context of
macroeconomic planning, poverty reduction strategies, medium term
expenditure frameworks work with ministries of labour,education and civil
service on pay
Conditions,health worker training,retention,working with trade and
industry around access to drugs and other supplies
❖ Attention to health determinants must be maintained as investments in
education, housing,transport,waterand sanitation,improved governance or
environmental policy can all benefit health.
❖ Health System Agenda is not Static.
❖ Pattern of disease,care and treatment are charging
❖ 80% NCD deaths in low and mid income countries
Thailand Model of Reducing Health Inequities
Health Insurance Schemes
Waive user charges for low income families
Subsidized voluntary health insurance
Extension of Government welfare scheme to all children under
12.elderly and disabled from 1990
Universal Coverage from 2001
Sealing up infrastructure from 1970s
Reflections
Thailand’s Health System systematically for over 3 decades-NHP has a
Universal Health Care.
Cuba is having better health policy compared to US where 16% of gdp
US spends on healthcare. So, it is not necessary to have BIG money to
provide UHC is my understanding.
15.MODULE ON MENTAL HEALTH
Reflections
To have good mental health,we need to do creative work especially in
leisure
Well-being is a person’s ability to understand one’s own capacity,
manage regular stress of life, work productively and contribute to the
community.
Impact of mental and nervous diseases burden is 10% more than
other diseases like Cancer, DM and heart diseases.
Mental health is necessary for all our collective good health
All mental problems start at 14 years
15-19 age group suicide is 4th leading cause of death
Mental health depends on
biological,genetical,psychological,environment,family tolerance and
previous history
In India budget for Mental health is low
Tamilnadu government has recently started a pilot study on adolescent
mental health for children in government schools in 9 districts to begin
with.This shows the gravity felt by all sectors.
In 2022 so many factors affecting mental health viz. gadgets,media,
films and COVID
Stress is NOT BAD at all times
Positive Stress
Tolerable
Stress
Toxic Stress
First time to
school,Interview
etc.
Loss of
family
member
Childhood abuse,Neglect,
Household Dysfunction,Mother
treated violently,Substance
abuse, Divorce
How to prevent Toxic Stress
Protective environment
Improve Resilience-7Cs to improve resilience
Competence Help them know their unique abilities and skills
Confidence
Help them develop self confidence
Connections Understand individual’s connection to
family,environment
Character
Right and wrong in thought,word and deed
Contribute
Give them oppurtunity to participate in community
work
Coping
Teach them how to manage the situation
Control
Help them or allow them to decide on controlling
themselves on this life’s decision
16.SANITATION AND C-WASH
Reflections
Communitisation-Confronting existing superstition,Planning,
Monitoring,Implementation
It was practically demonstrated by SOCHARA during Maya Bazaar visit
New vision of Health and Health package beyond the professional package
of actions-CHLP,RGIPH,APU
Understanding SEPCE determinants/ Impact-Effort to build a system in
which Health for All becomes a reality.
Toilets
Needs based assessment with stakeholders
Sensitize them first
Needs and budget follows
Prepare Modules
Principle of Appropriate Technology
Eco-Toilet Models-Less water consumed and can be built above ground
17.Women’s Health
Reflections
This session threw open the need for women’s health monitoring and the
methods. The online discussions sent a supportive message of being cared
by atleast some part of the society as a woman to me and highlighted the
importance my responsibilities to this community of mothers.
Life Course approach to Women’s
Health-Reduce disease in late part of life
Important to focus on early interventions
Focusses on a healthy start and aims to target all the critical and
potentially risked periods in the lifetime
Long term vision-addresses the cause of ill health and not the
consequences
This product helps to strengthen Health Care Systems horizontally as
Vertical is taken care by Public Health.
18.Climate Change
Reflections
This module unearthed many problems faced due to climate change which
could have been reversed ,now the same problems seem inevitable.
In recent years, extreme weather events have become increasingly common.
This has a great impact on the community in terms of injury, death, damages,
and loss. The health system should be at the centre of the community and be
able to provide essential medical services in case of emergencies. However,
there is a growing concern over how prepared our health. The importance of
ensuring that healthcare facilities and hospitals are safe, able to minimize the
risks to human life and infrastructure, and are better prepared in advance of,
during, and after catastrophic events to meet the immediate medical
requirements of the affected community. By making a hospital more resilient
to these climatic events, a community is also made more resilient. Therefore,
it is essential to have a multi-stakeholder approach in place, effective
interventions, and stringent laws and policies to make hospitals resilient and
safe. It is imperative that the safety of hospitals becomes a topic of national
concern so that advocacy, education, and awareness campaigns can be
targeted to create a culture of safety throughout the healthcare sector.
My COVID EXPERIENCES
I lost 6 kilos weight inspite of being at home safe and secured and
having good food and rest in the first wave
That showed my anxiety over the migrant workers,mentally
ill,single parents,no income agony thrown open by COVID
Second wave shattered my courageous oust as a doctor
Academically was seeing myself giving lectures online which I
could not do before due to family and professional commitments
We as an NGO conducted 100 day Kabasurakudineer
camps,supplied Rations to LGBT community, treated
mild,moderate and severe cases of COVID with Siddha medicines
Co-Directed our first documentary film ,”Prevention of Third
Wave” highlighting immune boosting foods and diets for children
that was of help in many cases of COVID during first and second
waves in India
WORK -LIFE-CHLP BALANCE
⮚ Work,life and CHLP is equally important to me
⮚ In the first trimester,I was able to do all assignments,reading
ALMs,attend online sessions regularly.
⮚ Second Trimester- By this time I understood my position in
community building,my privileges and responsibilities.
⮚ My family commitment (Palliative care)increased,work commitments
were being postponed,my ALM readings could not be completed on a
regular basis. Anyhow, 90 percent of online sessions I attended kept
me within the course network always.
⮚ In the third trimester,family responsibilities doubled,work
commitments increased and my project work did not get started as
there was no response to my request for permission to work in
Srilankan Rehabilitation Camp from the government.
⮚ A peer pressure was slightly building when fellows shared the
completion or process of their projects.
⮚ The encouragement and suggestions of facilitator
Karthikeyan,founders,mentors of SOCHARA eased the pressure
⮚ SOCHARA has eased many pressures regarding WORK,LIFE AND
COMMUNITY RESPONSIBILITY
⮚ I am a spiritual person. SOCHARA has helped me to move another
step forward in my spiritual journey as well.
Mentorship Process and Reflections
⮚ It’s the first time I am introduced to mentors of high stature and
experience
⮚ I am grateful for choosing a very senior person with lots of
experience in folk-lore traditional knowledge and community
medicine for me
⮚ I didn’t converse with my mentor regularly for no reason
⮚ From the few conversations we had he helped me to work in depth
and focussed
⮚ Travel with my mentor is an excellent experience and going to be a
life-long one
Project Learning Experiences
⮚ I came to know of my neighbourhood,a Srilankan refugee community
⮚ During CHLP only I thought of knowing more about my neighbours
⮚ I entered the community and befriended few women
⮚ The leader of the community informed me that I have to sought
permission from the government to enter into the community.
⮚ Till date not received any nod for implementing my project in the
community
⮚ I come to know that it is not easy to get permissions from
government to work in sensitive communities like Srilankan refugees
in Tamilnadu
⮚ I learn from facilitators and mentors that it is the reality in ground
⮚ Before CHLP my project plan and work would be wider ,including
more people.
⮚ After CHLP I view the same work in depth, identifying
issues,chalking out determinants of Health, planning to communitise
and empower the foremost stakeholders-the community
Takeaways from CHLP and looking ahead
⮚ A new chapter of life has opened after CHLP
⮚ My future community work is to focus on objectives and work in-depth
⮚ Health is a political struggle and I have fallen into its waters
⮚ I foresee to swim in the waters till the GDP on Health triples or till I
breathe my last
Part B
Background
Malnutrition is a serious global burden affecting the growth and development of
young children. Nearly half of the mortalities in children under the age of five
years are attributed to under nutrition(UNICEF,2021),predominantly seen in low
and middle-income countries. Childhood overweight and obesity are also rising
in these countries (WHO,2021). According to World Health Organisation
(WHO,2021) malnutrition is referred to as deficiencies or excess intake of
nutrients, imbalance of essential nutrients or impaired uptake of nutrients.
Undernutrition is manifested by (low weight for height), stunting (low height
for age), underweight (low weight for age) and micronutrient deficiencies
(WHO,2021). United Nations Children’s Fund (UNICEF) estimated the
prevalence rate of wasting was 45.5 million(6.7%), stunting was 149.2
million(22%),and overweight/obesity was 38.9 million(5.7%) worldwide
(UNICEF,2021)
The growth, development and survival of young children are threatened by the
triple burden of malnutrition, which includes under nutrition, hidden hunger and
overweight. The consequence of poor nutritional status in children is profound
and associated with impaired cognitive ability, poor school attendance and work
performance in the later stage of life (WHO 2021, UNICEF 2021). India is one
of the lower middle- income countries and stands at the 107 position on the
Global Hunger Index 2022. According to a recent National Multi- dimensional
Poverty Index (NMPI) reports (2022) proportion of population suffering with
poverty is higher in rural areas (32.7%) compared to urban areas (8.8%) in
India. In rural Tamilnadu, about 29.3% of households with inadequate access to
th
food,65.3% of homes lack sanitation facilities, 10% of people without access to
potable water, and 7.4% families with poor maternal health. Tirunelveli is one
of the top 15 districts in Tamilnadu with the inadequate access to food. Rural
households in the district alone accounts for 30.8% of inadequate nutrition,
61.8% of unimproved sanitation facilities, 10.4% of poor access to safe drinking
water, and 7.9% of deprived maternal health (NMPI,2022)
Goals towards the development of social and economy cannot be accomplished
without addressing the problems of malnutrition. The multidimensional
approaches of the sustainable development goals 2 by the United Nations aims
to end hunger, no poverty, achieve food security, improved nutrition, quality
education, gender equality, access to clean drinking water, improved sanitation
and promoting sustainable agriculture by 2030, which are directly influenced on
the nutritional outcomes. By 2025, SDG 2.2 targets are to end all forms of
malnutrition in the nations.
Government of India in line with state governments has implemented various
programs such as (Integrated Child Development Services (ICDS),
Reproductive Child Health, National Rural Health Mission, Janani Suraksha
Yojana, Rajiv Gandhi National Creche Scheme, Total Sanitation Campaign and
National Rural Drinking Water Program) address malnutrition and related
problems in the country (Poshan Abhyan). Despite numerous initiatives, rate of
progression is still quite gradual. India is home for children with 35.5% stunted,
19.3% with wasting, and 32% with malnourished. In Tamilnadu, the proportion
of stunting, wasting and malnourished were 25%, 14.6% and 22%.
Recently, UNICEF restructured its 1990s conceptual framework on maternal
and child nutrition to achieve specific targets of SDG 2. The framework outlines
the basic, immediate, underlying and enabling determinants of malnutrition.
These determinants are multifaceted and intertwined with each other. The
immediate and underlying determinants of malnutrition are greatly influenced
by inadequate intake of food, poor maternal child feeding practices, household
food insecurity, lack of access to potable water, and poor sanitation and
unhygienic living environment such as open defecation. In turn, these
determinants are influenced and enabled by economic, political, social cultural
norms, environmental conditions, national and global contexts, capacity,
resources and governance. Therefore, identifying determinants and bridging
gaps that are impeding the progress is need of the hour to address the root
cause. The project aims to bridge the gaps through interventions suiting the
local needs. Thus, the awareness sessions and intervention with Amukkura
churanam is observed to bring an impact in reducing malnutrition and anaemia
incidence in children and adolescents in the rural and urban parts of Tirunelveli
district in the southernmost part of India.
Rationale
Child’s health is the foundation of all growth and development, which include
physical growth, cognitive (learning and thinking) development, social and
emotional growth, and mental health. Children are vulnerable beings, more at
risk to illness and health complications. When children are spared from disease,
they can grow into healthy adults, and in this way, contribute to the
development of dynamic and productive societies. Protecting and improving the
health of children is of fundamental importance.
The world is facing a double mandate. More than half of deaths are due to
conditions that could be easily prevented or treated given access to health care
and improvements to their quality of life. A great deal of work remains to
further improve the health outcomes of children.
Children must also be given a stable environment in which to thrive, including
good health and nutrition, protection from threats and access to opportunities to
learn and grow. There is expanding need among the children living in shelter
homes. They majorly need added attention to maintain good health. Investing in
these children is one of the most important things to build a better future for
them.
The immune system is the body’s defence against invading microbes and
harmful substances by recognizing and responding to antigens. Common child
health issues mainly related to immunity include allergies, colds, conjunctivitis,
gastritis, hand, foot and mouth disease, impetigo, lice and worms. These are
mainly attribute to immunity. Nutrition is an important determinant of immune
responses in children and nutritional deficiencies alter their immune responses
increasing risk of infection. Optimal nutritional status – the state of the body
with respect to each nutrient and overall body weight and condition-is a
powerful factor in promoting health and preventing and treating diseases. Good
nutrition for children is essential to achieve their full developmental potential,
physical, cognitive growth and development.
Malnutrition leads to failure in early physical growth, delayed motor skills,
cognitive and behavioural development: it diminishes immunity and increases
morbidity and mortality (1) Balanced nutrition and supplements help children to
keep away from infections.
It is clear from previous research that many facets of children’s daytime
functioning, including emotional health, interpersonal relationships, and
academic performance, are negatively affected by poor sleep (2)
Keeping the above as contexts for the present project, there is a need for
ready-to-use supplementary and therapeutic foods and create awareness on
traditional and available food sources for the physical development, cognition
and specifically to improve the immunity of the children.
Compared to modern supplementary and therapeutic foods and medicine,
AYUSH medicine is perceived to be more affordable, accessible and acceptable
to the communities in which it operates (Oyebode et al,2016)
The World Health Organization, in recognition of the role of AYUSH medicine
especially in resource-constrained settings, has called for preservation and
acknowledgement of its use in cases where such use has been scientifically
validated ( Global Action Plan for the Prevention and Control of NonCommunicable Diseases, 2013-2020)
AYUSH and Siddha Culinary medicine can play an important role in realizing
the dream of “New India’ by providing quality healthcare and medical care for
its citizens. At present we are witnessing a highly receptive environment where
the value of AYUSH systems in healthcare is widely recognised (3) Among
several interventions aimed at immunity building and malnutrition,
Aswagandhadhi (Amukurra) Churna, an Ayurveda (and Siddha) Rasayana drug
is known to improve immunity and combat malnourishment.
Aswagandhadi or Amukura Churnam has been indicated for the conditions like
Pandu (Anemia), Aruci (anorexia), Ajirnam (indigestion), kshaya (weakness)
and Kirumi (worms). These symptoms are commonly seeni in children suffering
from malnutrition and therefore widely prescribed by Ayurveda practitioners for
malnutrition (Wankhede et al,2015). In a study conducted among children in
shelterhomes, ashwagandhadi administered with milk significantly improved
the nutritional status of the children (Sangeetha et al,2020)
A Chennai based NGO,Vaishnavi Welfare and Charitable Trust is providing
milk with Aswagandhadi churna, under the Jeevani Milk Program, to around
560 children since four years to improve the nutritional status of the children.
The results are very encouraging specific to physical development and enhanced
nutritional status of the children (Sangeetha et al,2020)
A sizeable portion of Indian children suffer from low food intake induced
under-nutrition potentially resulting from poverty, ignorance etc(3,4). Over
one-fifth of Indian population comprises children aged 5-14 years, that is, the
group covering primary and secondary education. Research studies indicate that
nutritional deficiencies and poor health in primary school age children are
important causes of low school enrolment, high absenteeism, early dropout, and
poor classroom performance (5)
Only thing that is needed is a scientific research and documentation of these
drugs and procedures, quantification of their effects and standardisation of their
quality, so that the literature instils confidence among consumers and
practitioners.
Therefore, the present observational study assessed the effect of Amukura
churnam on the overall development of the children between the age group of 6
to 12 years residing in shelter homes and children of low socio-economic group
attending SEED Trust hospital OPD.
Methodology
Interventions to achieve impact has two outcome measures and two different
group of activities.
Outcome A:
The Government of India officially recognises formalised systems of medicine
like Ayurveda, Unani, Siddha, Yoga, Naturopathy and Homeopathy. The
non-formalised systems like tribal medicine, herbal and home remedies which
have provided the basis, sustenance and rejuvenation avenues to these systems
remains unrecognised because of their inherent amorphous nature.
Activities:
The focus of nutrition programs for Indian children has largely been post-birth ,
with child and feeding-centred interventions. It is known that 50 percent of the
growth failure that gets accrued by two years of age occurs in the womb owing
to poor nutrition of its mother both during pregnancy and before pregnancy
(UNICEF/ for every child)
1.Awareness sessions on Ante-natal care using Simple home remedies
(Presentations attached)
2.Traditional food practices demonstrations and screening relevant videos to
reduce incidence of anemia and malnourishment in children(Video links
attached)
Outcome Measures: Improve quantity and nutrient level of food consumed in
household, preventing micronutrient deficiencies and anaemia, increasing
women’s access to basic nutrition and health services, improving access to
water, sanitation education and facilities, Empowering women to prevent
pregnancies too early, too often and too close together.
Presentation covers 15 cost effective traditional food sources and their nutritive
values, incorporation techniques.
Outcome B:
WHO defines Traditional Medicine as “the sum-total of all the knowledge and
practices whether explicable or not, used in diagnosis, prevention and
elimination of physical, mental or social imbalance and relying exclusively on
practical experience and observation, handed down from generation to
generation, whether verbally or in writing.
Activities:
1.To identify the children with poor nutritional status and cognitive abilities
based
2. Supplementation of Amukura Churanam with milk/honey to children in a
shelter home in Tirunelveli Dt. and to children visiting SEED Trust hospital
Outcome Measures
Improved survival, health, physical growth, cognitive development, school
readiness and school performance in children and adolescents
Inclusion criteria
● Children residing in shelter home
● Children visiting SEED Trust Hospital
● Aged 6 to 12 year
● Willing to freely give Informed consent (through
themselves/parents/ guardian /head of institution
Exclusion criteria
● Currently receiving any form of supplement
● Too unwell to participate in the study
● Any serious ailments
● Mental health problems
ASSESSMENT
Nutritional Assessment
A.
A.
B.
C.
Anthropometry
Biochemical methods
Clinical Methods
Dietary methods
Cognitive Assessment
Sleep Pattern
Duration of Observation: Three months (Sept 18-Dec 18,2022)
Screening observations before intervention with Amukura Churanam in 111
subjects
Symptoms
Pallor
Recurrent upper respiratory infection
Weakness
Fatigue/tiredness
Cramps in calf muscle
Bodyache
Pain in legs
Loss of appetite
Male
7
6
12
10
13
7
13
16
Female
5
6
2
4
2
3
5
Data Entry
The data is entered in Epicollect5. Epicollect5 is a free and easy-to-use mobile
data-gathering platform developed by the CGPS Team of Oxford BDI and
publicly available at https://fiveepicollect.net. It provides both the web and
mobile application for the generation of forms(questionnaires) and freely hosted
project websites for data collection.
All the field investigators and the study team will be trained on epicollect5. The
data will be generated in excel and then converted into a SPSS Version 21 for
appropriate statistical analysis.
Results and Discussion
The data collected from the children will not be disclosed and their personal
identity will not be known.
From the follow-up screening done at the end of three months intervention with
Amukura churanam. The following findings noted.
1. There is no marked improvement in reduction of pallor.
2. Appetite has improved in almost all subjects.
3. Recurrent upper respiratory infections reduced in many barring few.
4. Cramps in legs in both sexes reduced remarkably.
5. Bodyache is reduced in all subjects.
6. Pain in legs reduced in half of the subjects.
7. Weakness reduced in all subjects.
This study is an observational study involving four service organisations.
The children are visited regularly for medical consultations at the request of the
head of the shelter home even before the study. They are still visited by a
Siddha doctor.
How we scale up from here?
Literature evidences of Amukkura Churnam and the clinical experience of
AYUSH practitioners on their recommendations,dosage, side-effects if any were
collected.
Nutritional supplementation with traditional foods like Ragi, sesame, Moringa,
Curry leaves, groundnuts need to be supplemented to increase availability of
nutritional calories.
A multi-centric study involving National Institute of Nutrition, Hyderabad is the
next step ahead in this direction. The findings will help governments to include
Aswagandhadi Churna as a Nutritional supplement which improves digestion
and supports nourishment in children. The supplementation can bring down the
stunting,wasting and anemia prevalence very much.
This will increase government postings for non-allopathy doctors and
practitioners throughout the country.
Will pave way for Integrative Medicine to be the mainstream medical model of
India.
Axioms of Community Health followed in this project
● Integration of health and development activities
● Preventive, promotive and rehabilitative actions
● Applying with low cost, effective, appropriate technology in
health care, health communications and recording systems
● Recognition of local, indigenous, health resources like herbal
medicines and time-tested home remedies
● Confronting the biomedical model with new attitudes, skills and
approaches
● Confronting the existing super structure of medical/health care to be more
people and community oriented
● An effort to build a system in which Health for ALL can become a reality.
Acknowledgements
This study was possible due to an empathetic group of intellectuals or persons
willing to work for a cause.
Vaishnavi Trust ,Chennai
Siddha Evergreen Eighty Seven Doctors Trust, Tirunelveli
VMSS Valliyoor
Fenivi Solutions, Kavalkinaru
Athimaduram Media Activities
I am grateful to my Mentors Prof.Dr.Hariramamurthy sir and Dr.Karthikeyan for
mentorship
I am thankful to the SOCHARA team of facilitators,founders and fellows for the
everlasting supports
My students, teachers and our trust doctors.
https://youtu.be/uh6UIQCBWMk
https://youtu.be/u5_zW-Nyb2U
https://youtu.be/d-ELk77uuIg
https://youtu.be/yM7hDxgXT7w
https://youtu.be/zdpaFBadqmA
https://youtu.be/f3QT7KCNb1A
Position: 549 (12 views)