Umachaitanya - Final report.pdf
Media
- extracted text
-
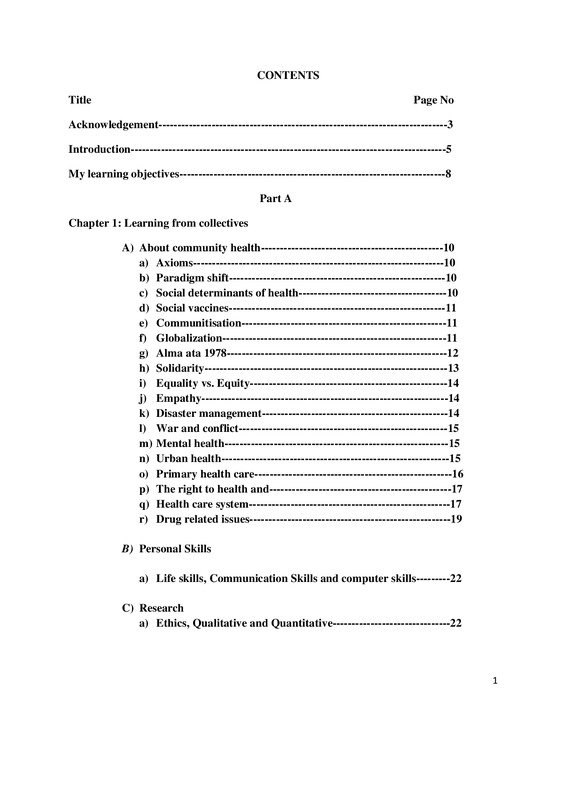
CONTENTS
Title
Page No
Acknowledgement----------------------------------------------------------------------------3
Introduction-----------------------------------------------------------------------------------5
My learning objectives----------------------------------------------------------------------8
Part A
Chapter 1: Learning from collectives
A) About community health------------------------------------------------10
a) Axioms------------------------------------------------------------------10
b) Paradigm shift---------------------------------------------------------10
c) Social determinants of health---------------------------------------10
d) Social vaccines---------------------------------------------------------11
e) Communitisation------------------------------------------------------11
f) Globalization-----------------------------------------------------------11
g) Alma ata 1978----------------------------------------------------------12
h) Solidarity----------------------------------------------------------------13
i) Equality vs. Equity----------------------------------------------------14
j) Empathy-----------------------------------------------------------------14
k) Disaster management-------------------------------------------------14
l) War and conflict-------------------------------------------------------15
m) Mental health-----------------------------------------------------------15
n) Urban health------------------------------------------------------------15
o) Primary health care----------------------------------------------------16
p) The right to health and------------------------------------------------17
q) Health care system-----------------------------------------------------17
r) Drug related issues-----------------------------------------------------19
B) Personal Skills
a) Life skills, Communication Skills and computer skills---------22
C) Research
a) Ethics, Qualitative and Quantitative-------------------------------22
1
Chapter 2: Learning through other activities
a) Learning from Books--------------------------------------------------------------23
b) Learning from Organisational visits--------------------------------------------27
c) Learning from Workshops--------------------------------------------------------28
d) Learning from Journal club------------------------------------------------------28
e) Learning from Documentaries---------------------------------------------------28
f) Learning from Films---------------------------------------------------------------32
g) Learning from Presentations-----------------------------------------------------32
h) Learning from Games--------------------------------------------------------------32
i) Learning from SOCHARA team and field mentors and friends---------32
Part B
Chapter 3: Observations and Learning from field placements
A) First field placement observations------------------------------------33
B) Second field placement observations---------------------------------49
C) Third field placement observations-----------------------------------60
D) Learning from three field placements--------------------------------63
Chapter 4: Research studies----------------------------------------------------------------64
A) Study 1-----------------------------------------------------------------------64
B) Study 2-----------------------------------------------------------------------73
-
References-------------------------------------------------------------------------85
-
Annexure I------------------------------------------------------------------------87
-
Annexure II-----------------------------------------------------------------------89
-
Annexure III----------------------------------------------------------------------91
Points for in depth interview-------------------------------------------------------93
Chapter 5: Pictures---------------------------------------------------------------------------94
2
Acknowledgement
I thank the Almighty God for leading me to these better circumstances with His extended promises
and being with me and loving me in all circumstances.
I would love to express my gratitude to all the generations who made this day possible by passing
on and sharing the information, their experience, learning’s, challenges, valuable suggestions and
feedback.
Special thanks to Dr. Thelma Narayan and the entire SOCHARA team, staff, my field mentors and
my co-fellows with whom I had a unique community health experience which has enriched my
learning’s with a great degree of sensitisation towards social issues and helped me overcome my
shortcomings as well as challenges to emerge out of the cocoon to fly with colourful wings.
I would like to extend my gratitude to the people, the professionals in the health department and
other fields, social workers and individuals whom I met during this period of my fellowship, who
have dedicated their work and lives for the betterment of the people by contributing a lot; by adding
a drop to the ocean
3
WITH LOVE TO MOM, DAD AND TO MY SIBLINGS
4
Introduction
I did my studies in different parts of Andhra Pradesh. Some years of my education were in the
village, some years in town and some years in cities. I am a traditional and timid girl. All the
experience I had whether through education or through being in different places didn’t make any
difference and without my knowledge I used to get offended while reading books or newsletters
regarding issues related to dalit and women. Even watching films used to make me uncomfortable;
in old and new films, the moral of the story is how women always should be a submissive. I never
understood how to express my feelings, nor did I ever channelise my thoughts and always found
myself to be caught in fear to speak up. On the other hand my parents work in NGO sector at grass
root levels. Their primary concern has been to give us academic education. My parents strongly
believe education makes a difference and always used to encourage reading books on different
social issues and used to involve us in different protests, programmes and would encourage us to
interact with people. My parents tried to make us understand things but to be honest I didn’t pay
much attention to them though I had some degree of sensitisation.
The problems like caste, gender, class were structurally deep rooted in the society and I never
understood how to solve the problems though I tried to read and analyse a bit on my own. This is
because I had my own understanding and attitude towards solving problems. I always used to think
I will get a good job and will try to help people; like looking after orphans, old age people, helping
the marginalised and women etc..,
Only Sochara helped me to understand my parent’s ideology better; about being a catalyst and
enabling people to fight for their rights. I admit I didn’t understand their holistic approach. Now
my love and respect towards them has increased.
I got a chance to do a six-month training course; each month two days on patriarchy, child
marriages and rights of the girl child, held from March to August 2013, where I got to know new
problems. For the first time I got to know about domestic violence and exploitation of the single
women, widows in traditional families and children.
For the first time I got to know about the exploitation ladder. Children are the most vulnerable
and exploited group.
5
Minorities
Physically challenged people
People with mental illness
Transgender
Dalits and Adivasi’s
Women
children
Minorities
Physically challenged people
People with mental illness
Transgender
Dalits and Adivasi’s
Women
children
Through newspapers I got to know about foreign direct investment (FDI) though it seemed to be
good in the eyes of government, at that time I became scared and concerned for the farmers and
wondered what if the farmers were not left with choice and forced to sell their products only to
these shops established in that area and in the long run their autonomy may be lost.
6
Trafficking is also a major problem where young girls and women are forced to do sex work,
exploited and taken as a sex slaves. They live all their lives in dark and there is no way to come
out of that. This is very painful when this exploitation occurs in the name of religion. E.g.
Devadasis and there are instances where because of conversions or during riots women become
the target group
Poverty and many other problems were a concern but never had I realised this from the point of
view of health e.g. how poverty impacts health and vice versa; I always looked at it from a
biomedical lens.
When I applied to the Community Health Learning Programme (CHLP) fellowship and even when
I joined Sochara I didn’t have any clue of what the fellowship was about; but only had a vague
idea that it is all about learning by sharing, in an NGO environment and that it is about community
health (the only word I could relate to was “health” which is related to my subject). My mother
encouraged me saying that it was a good opportunity to learn which would be useful to me as well
as to the country in the long run. My primary objective was to know more about the NGO sector.
After my interview I was asked to write my area of interest and learning objectives and I didn’t
have any clue about what to write, except the interview part where I had been asked about my
village demographics, health situation and the other circumstances. Thelma Ma’am suggested I
opt for drug related issues as I have a background of Masters in Pharmacy. With the help of
Chander and Janelle I wrote my learning objectives for the Community Health Learning
Programme. As I started to adapt I extended my objectives and by the end of the year I was able
to learn and have knowledge about all the objectives.
My education and being in different places is not at all waste, but in fact an asset which helped me
to enhance my learning skills in this one year and I could relate to different concepts, , improve
my understanding and adapt to the environment in a better way.
Now, for the first time I see things and analyse things through the lens of Social Economical
Political Ecological Cultural view point.
“They cannot make history who forgets history”- by Dr. B. R. Ambedkar. Fortunately this
fellowship helped me to read the history of the Country on various issues.
From the bottom of my heart I thank the Almighty God for his love, my parents for their support
and Sochara for giving me this opportunity.
7
My learning objectives
Following are my learning objectives that I noted at the beginning of my fellowship:
● To learn how to prevent the irrational use of drugs
● To learn how to be an Activist
● To learn skills related to
- Research
- Action oriented work [field]
- Report writing
- Computer skills
- Drawing
My parents are social activists and are working with dalits, women and children. Learning from
them to work with the people who are vulnerable and are poor to encourage them to be educated,
maintain hygienic conditions, to know about their rights at work place and in society, has
empowered me to contribute to the country through my work.
I hope the CHLP Community Health Learning Programme will help me understand the
circumstances related to health issues especially in relation to the poor and the marginalised
I am interested in social work, that’s how I wrote about my experience with the people during
holidays and about my participation in some protests and meetings on different issues.
8
As I started reading I got to know new things and I emphasised the objectives in terms of
drug related issues as follows:
● To sensitise, enable, motivate the community regarding rational drug usage
● To promote the rational usage of drugs, rational prescription by doctors and rational
dispensing by chemists
● To promote the manufacture of essential drugs, vaccines etc., to meet the national needs as
the pharma sector failed to meet the needs of nation in production of vaccines, anti venoms
and essential life saving drugs; but there is raise in production of nutraceuticals,
combination drugs and adding of vitamin to the existing molecules, being marketed as new
products and there are drug induced problems, drug interactions and adverse effects
(adverse drug reactions).
As my learning continued, I further evolved my objectives in the second collective, and these
are as follows;
1. To understand public health in depth.
2. Drug related issues
● To promote the rational drug usage.
● To know more about rational drug policy and to find the possible ways in implementing
the policy.
● To be part in people's health movement.
3. To have knowledge about disaster management.
4. To learn to gather in-depth information (evidence) and document evidence on different sociohealth issues.
5. Project proposals
6. Report writing
7. Field exposure.
As I started learning about community health I also thought to learn about public health system
and found out that public health is
● The science and art of preventing disease, prolonging life and promoting health and
efficiency through organised community effort – C.E.A. Winslow in 1920
● Community health is adopting a community approach for public health
9
PART A
Chapter 1: Learning from collectives
A) About community health
a) Axioms
1) Rights and responsibilities
2) Autonomy over health
3) Integration of health and development activities
4) Building decentralised democracy at community and team level
5) Building equity and empowering community beyond social conflicts
6) Promoting and enhancing the sense of community
7) Confronting the biomedical model with new attitudes skills and approaches
8) Confronting the existing superstructure of medical/ health care to be more people and
community oriented
9) A new vision of health and health care and not a professional package of actions
10) An effort to build a system in which health for all can become a reality.
It is about how to build the strong “countervailing power” in order to achieve the Health as the
fundamental non- negotiable right. To bring public into public health and to give a platform for
the community to exercise “axioms”
10
b) Paradigm shift
- Bio- medical approach to socio-community model
- A shift from individual to community focus
- People as patients to equal participants
- Providing to enabling and empowering
- Drug and technology to education and social processes
- Physical and pathological to broader psychosocial, cultural, economic, political and
ecological dimensions
- Professional control to demystification and social control
- Preventing, promoting, curing at primary level
- The community back into primary health care
- The public back into the health policy discourse and policy process
The importance of the paradigm shift is to achieve the “goal” Health For ALL by bottom top
approach rather than the top down approach were the programmes were just imposed on
community without considering the interests of the community. To be the “tap turners off but not
the floor moppers” to treat the root cause of the disease or illness. E.g. in a place where the malaria
is prevalent, government through the health workers tried to eradicate by providing the bed nets to
people and failed. When they try analysing causes for the failure found out that people were unable
to sleep in the nets, some used for fishing, some as pillow and some to cover themselves from cold.
c) Social determinants of health
- Social (should beat Caste, Gender, class)
- Economic (developing sustainable process rather than eg: taking steps to develop
horizontal approach than vertical approach to tackle the diseases)
- Political (Countervailing power)
- Cultural (Each community have their own set of beliefs and accordingly the reaction
towards a particular issue depends and it is important to address these issues. It is also
important to promoting acceptance and tolerance above the religion, class, caste, race and
language ) and
- Ecological (Promoting sustainable environment, hygiene, sanitation)
When I reflect on the “social determinants of health” I was able to understand the several factors
which influence the ill health structure. In society certain groups are most vulnerable to the ill
health (children, women, sex workers and transgender etc..,). Economically poverty in the country
leads to lack of basic amenities and food resulting in poor immunity which further results the
community to be susceptible for the diseases. Politically on large the policies influence the
economy of the nation. Culturally should respect the people values, beliefs and try to deal with
assumptions, perceptions so as to involve them to participate and be accountable for their rights
and responsibilities.
11
According to WHO the definition of health is:
“Health is a state of complete physical, mental and social well-being and not merely an absence
of disease or infirmity”
Reference: Health For All, NOW! The people’s health sourcebook, pg 62
Health is further dependent on how the individual, family, community, government and private
sector and global factors influence health of the individual
Individual
Family
Community
Government and
private sectors
Global
d) Social vaccine
Vaccines are for prevention of disease and the term social vaccine is to develop the vaccine from
the point of addressing the social determinants of health; social, economical, political, ecological
and cultural aspects to understand and act to bring about health equity worldwide.
e) Communitisation
Communitisation is all about bringing community into community health where the community is
enabled and empowered to exercise their rights and responsibilities in implementing the
programme by participating in the planning, organising and in monitoring and evolution.
f) Globalisation
Neo- liberalisation and the idea of a world without walls, world as one family has brought many
changes in the inter-relationships among countries. Globalisation has brought free market
economy into timeline. The rich are becoming richer and poor becoming poorer. It is increasing
12
the inequalities among the countries. Budget cuts on health, education and increasing subsidies for
the MNC’s. Shifting to cash crops is resulting in environmental and economic imbalance in the
country. Showing government as inefficient to meet the challenges and making the role of private
sector strong through a policy process.
Reference: Health For All, NOW! The people’s health sourcebook, (chapter 1)
g) Alma Ata Conference 1978 by WHO and UNICEF
From the class I could understand the Alma Ata in a way which is very simple to
remember:
➢ Principles of Alma Ata:
● Health for all
● Health as a human right
● Equity
● Social justice
➢ Logic of Alma Ata:
● To strengthen the primary health care
● Promote peace
● Spend more budgets for the health needs
● To fill the gaps between developed and developing countries
➢ Strategies of Alma Ata:
● People’s participation
● Intersectorial co-ordination
● Appropriate technology
➢ Approaches of Alma Ata:
● 4 A’s and Q
● Availability, accessibility, affordability, acceptability and quality
● Prevention, promotion, curative and rehabilitative
Health for All can be achieved not only by providing bio-medical model and addressing the health
needs of the nations just by providing the medicine, but taking measures to provide the basic
amenities and addressing the socio-economic conditions of people in all the nations.
From the class I could even understand the difference between social and technical approach to
attain health for all. Technical approach is a top down approach (vertical) which doesn’t involve
people’s participation and compel them to follow guidelines of the programme whereas social
approach considers the culture, believes, environmental factors which influence a particular
condition and tries to bring changes
13
▪ Nutrition
▪ Education
▪ Water and sanitation
▪ Mother and child care
▪ Prevention of common endemic diseases
▪ Immunisation
▪ Treatment of diseases
▪ Essential drugs
When I reflect on this I could relate with the Rakku’s story and Radha’s story where there is so
much inequity in the world especially in our country where there are barriers of caste system which
was much prevalent in those days and of course in these days India has its own challenges
including the challenges of those days. Directly this Declaration even brings these challenges into
consideration and stresses on the sustainable social and economic development of the people as a
contribution for the better quality of life and to world peace. It is very surprising to know that the
goals were still not achieved and adding to that privatisation of the health system lead to the worst
situation where irrational practices including irrational diagnostic and therapeutic practices were
being a challenge these days. From my field I could observe that the patient’s voice is not heard
and could really see the knowledge difference/gap (no sharing of information) between the Doctor
and the Patient, which is making health for all impossible.
All the committees’ right from Bhore committee 1946 to Alma Ata in 1978, highlight some points,
India has come up with the National Health Policy of 1983 to strengthen primary health care. The
second National Health Policy 2002 has a different approach
h) Solidarity:
Solidarity helps to work towards social justice and overcome inequalities and problems. Through
networking and by collective action we can see the impact at larger levels. I learned that Being
accountable and Participating actively brings solidarity.
“A sphere of ideas, values, institutions, organizations, networks and individuals located between
the family, the state and the market, and operating beyond the confines of the national societies,
polities and economies”.
Source: OUP- Global Change and Health, 2005
i) Equality vs. Equity
In the beginning I was told to go around Sochara to see and observe things where I found one
cartoon poster of a woman and a man and cloth. Each person needs cloth with different length to
cover. This gave me immense hope that there are many ways to express the views of a person in
an effective manner. I understood the concept of Equality vs. Equity and by myself am able to
14
explain to others as back in my college days I failed to explain the need of equity in society.
Importance of extending the hand to the people who are in need and here is another picture that
explains the equity concept
Source: Internet
j) Empathy
Here in Sochara we are given time to reflect and share our thoughts before the session starts and
that’s how I got to know how different people view a problem differently. To try and fit into
another’s shoe and view things from their point, Empathy helps in not only accepting other points
of view but also helps one to be tolerant.
k) Disaster management
I never thought of disasters; being one of the refugees of a cyclone in my childhood, the orientation
classes and readings about disaster management gave a broader picture of what should be done
and what should not be done during disasters and that good will alone is not enough. The disasters
can be caused during floods, droughts, cyclones, earthquakes, communal violence, war/conflicts
and refugee migration, displacement due to development, fire, hooch tragedy, industrial gas/
pollution, road/rail accident, air accident, internet related panic. During these disasters I came to
know that the concern should be, to provide security with dignity, shelter, displacement, water,
sanitation, food as epidemic can burst out therefore proper surveillance should be there and can be
able to provide medical services either emergency or primary or home based care. Apart from
medical care there is a need for community information awareness, psycho social care, women
friendly centres, child friendly centres, disability issues and human rights issues. The most
important aspect is to have networking and coordination, community mobilization partnership,
needs assessment and advocacy skills
15
The person should be well equipped with the skills to volunteer during disasters
Chennai floods: the discrimination that has taken place during Chennai floods among the CRPF
(central reserve police force) and sanitation workers shows how the government and people’s
behaviour towards the sanitation workers without whom the city will not be clean in such a short
duration
L) War and conflict
Alma Ata -1978 speaks about the peace between the nations and to decrease the budget spending
on the defence and use it for the promotion of health that every individual irrespective of their
race, religion, caste, should be able to have access to primary health care.
The main cause of the war is insecurity, fear, greed, aggressiveness and power, it is also the interest
of the army forces/ arm manufactures creating the conflict environment. Also discussed about the
consequences of war like property loss, destruction, refugee crisis, economic disability, shortage
of food, water and other amenities, kills civilians/ causes disability.
M) Mental health:
Discussions on mental health in sessions, workshops, articles, panel discussion in alumni meeting
and through documentaries and films helped me learn about mental health from the perspective of
community which is otherwise impossible. As a medical person I know mental illness is due to
chemical imbalance, but for the first time I came to know about the gravity of the issue in the
society that there is lot of stigma attached to it. Unfolding the mental health issue itself is vast. The
workshop which I attended for the first time that involved every one’s participation is Reshma’s.
I learned how important it is to let go of things. In the second workshop at Alternative Law Forum
I heard the struggle of the people suffering from emotional disturbance and their point of view to
deal with the illness. E.g. It is like any other disease if a person gets fever no one will question the
person why did you get fever, but to the person who is having the mental illness is being questioned
as to why did the person is going through emotional imbalance when everything seems to be fine.
It is not a thing which is developed deliberately.
About the LGBTQ community from the interaction with the activist and through reading I got to
know that the sexual orientation is not a constructed identity or a disease to deal with or a mental
disorder as such but for this the community has to undergo through lot of struggle to negotiate
about the issue. There is no platform for them to share or discuss but discussions were killed, As
the community is very small and there are lot of assumptions, theories, research papers but were
oriented towards the biomedical model and went through lot of trial and error and finally the
community is now able to negotiate the issue. As we the mainstream people don’t have the
constructed sexual orientation so also the LGBTQ community.
N) Urban health:
16
From the class I came to know that it is estimated that by the year 2050 half of the population will
be urbanized and as the urban populations are rapidly increasing, the smaller cities and the cities
where the rapid growth is taking place and these cities has to provide the basic amenities to the
population. People mostly migrate to the cities in search of jobs and daily wage work. There will
be a raise in the informal settings and slums where poverty is prevalent and urbanisation itself is a
health determinant
● Urban settings will face different problems if not properly planned
● Addressing social determinants of health
In the urban setting the most common problems faced by the dwellers are lack of water and
sanitation, proper drainage maintenance, women and child care, adolescent health care, mental
health, elderly people, not friendly environment for disabled people, urban violence and substance
abuse, urban poverty, communicable diseases, non communicable diseases. In the long run it is
important to maintain the city in such a way that it reduces pollution by improving transportation
facilities, traffic safety, controlling air pollution and livelihood increasing activities.
➢ After the session I just reflected as how the urban health policy should be with respect to
field experience. Along with strengthening the public health system (considering all the
health problems including women and child care, adolescent health, elderly care,
communicable and non-communicable diseases, mental health and health accessibility for
the disabled people), education system (empowering women along with adolescent girl and
boys) coordinating with the other departments which work for the development of the city
and the life of citizen. Strengthening the municipal corporation for proper maintenance of
the city by building proper drainage system (it helps in disaster management and reduces
extent of exposure for the sanitation workers dealing with the hazardous work), supply of
safe drinking water, improving the living conditions and providing basic amenities to the
slums, taking steps to reduce pollution, providing identity cards to the migrants to have
access to different health and other schemes provided by Government, building barrier
free settings for the disable people, increasing livelihood opportunities, taking steps to
reducing hazardous occupations.
s) Primary health care, the right to health and health care and the health
system
The Academic curriculum is structured and emphasizes more on understanding the diseases but
doesn’t equip student to work in a particular geographical area. Understanding the community
from the point of Social Determinants of Health is not a primary motive as the colleges have to
follow the guidelines set by Medical council of India. In India health is a state subject and public
health looks at the whole of India and counts in terms of similar conditions but fails to understand
the particular community and environmental conditions.
Due to lack of human resources there is a burden on doctors. Doctors can only repair the damage
but he/she can’t provide the nourishment needed for the family to keep good health in the first
17
place.. It will be very difficult to try and understand the background of the person and the
conditions which are leading to a particular clinical condition. When we speak about ‘Public
Health’ we are addressing the health of the people from a broader perspective addressing their
primary needs and the 5 A’s: Availability, Accessibility, Affordability, Acceptability,
Appropriateness and Quality as well. Health and its determinants should also be addressed in terms
of preventive, promotive, curative and rehabilitative. Above all should look at Public health in
terms of accessibility towards the essential drugs and rational medication.
The right to health:
According to my understanding Health is nonnegotiable fundamental human right.
Health care and the health system:
Through sessions I came to know about the three tier health care system primary health centre,
secondary and tertiary health centre. From the gross root level where ASHA’s work to ensure that
the primary health needs are met in a particular area with particular number of households and
from sub-center during emergency refers to Primary health center. It makes every state responsible
for raising the level of nutrition and standard of living of its people.
During my field placements through visit to Upper Primary health centre in Railway Kodur I have
seen that there are no facilities to give primary care, where health care mostly depends on referrals
to the tertiary center in Tirupati, lack of infrastructure, lack of human resources etc.., lead to the
situation where people look at private clinics in the town. There are several factors influencing the
health system; there is a rise in number of caesareans in Andhra Pradesh and it became a burden
to common people but on the other hand the tertiary health centre is unable to provide its service
to all who come to the hospital as number of persons per bed almost five times more. It clearly
shows the lack of infrastructure and human resources. Country should try and work towards
providing the infrastructure and should strive to be self sufficient.
18
Drug related issues
Community health as earlier mentioned is to deal with the Social determinants (SEPEC), 5 A’s
and quality. On the other hand in order to prevent the irrational use of the drugs; to prevent
consequence which are leading to resistance of the strains; promotion of rational medication
becomes as important as all the earlier mentioned concepts.
DRUG:
According to DRUGS AND COSMETICS ACT 1940 The term drug includes.., All the
medicines for internal or external use of human beings or animals and all substance intended to
be used for or in the diagnosis, treatment, mitigation or of any prevention of disease or disorder
in human beings or animals, including preparations applied on human body for the purpose of
repelling insects like mosquitoes.
19
A generic drug- is a chemically equivalent, lower-cost version of a brand-name drug,
costing 30-80% less! A brand-name drug and its generic version must have the same
active ingredient, dosage, safety, strength, usage directions, quality, performance and
intended use.
A rational drug is one that is mentioned in the standard textbooks of pharmacology and
medicine and which is accepted worldwide.
Essential drugs –Those drugs which satisfy the health care needs of the majority of the
population.
WHO definition: “Rational use of drugs requires that patients receive medications
appropriate to their clinical needs, in doses that meet their own individual requirements
for an adequate period of time, at the lowest cost to them and their community”
Access to essential medicines is a core component of comprehensive primary health care
(WHO, 1978)
They are selected on the basis of prevalence of disease, efficiency, safety and cost
Rational drug emphasize the selective use of drugs based on
Essentiality, Efficacy, Safety, Easy availability, Low cost, Ease of administration, adequate
quality, preferably of indigenous production
India’s initiative
The Indian patent act 1970, ensured the growth of the indigenous pharmaceutical sector and the
drug price order protected the consumer from irrational drug policy.
Shift
Essential drug policy has been shifted to pharmaceutical policy of India
There is knowledge asymmetry
Stake holder will be the power controllers.
Rational medication and Advantages of Essential drug list:
Medical advantage:
•
•
•
It is medically, therapeutically and scientifically sound and it ensures use of drugs
It limits the use of irrational and hazardous drugs and decrease the risk of iatrogenesis
(drug and doctor induced disease)
It improves the possibility of monitoring adverse drug reactions in patients
20
Social advantage
•
•
•
It responds to the real health needs of the people
Facilitators the dissemination of correct information about the drugs to health personnel,
medical practitioners and consumers in general
Priorities the most urgent needs of the people for essential health care
Economic advantage:
•
•
•
•
Prevents wastage of scarce resources on non-essential drug
Economics sale achieved by priority drugs brings down their prices
It curtails the aggressive marketing of non-essentials
Economically benefits patient prevent wastage on irrational and non-essential drugs
Administrative advantage:
Makes quality control easier because of facilitates the streamlining of production, storage and
distribution.
Need for pharmaceutical industries
There will be always a need for the pharmaceutical industries.
As the shift from essential drug policy to pharmaceutical policy of India; there is a need
for
people’s
science
movement
health
science
movement
people’s drug
policy
In which way pharmaceutical industries can strengthen the primary health care system
Self sufficient, self reliant, Bringing down the prices, production of high quality life
saving drugs (vaccines, anti venoms)
21
-source: from various books on drug related issues- Sochara library (find from references
and books I read).
B) Personal skills
a) Life skills, Communication skills and Computer skills
During this fellowship I have even learned about life skills, communication and computer skills. I
learned about Critical thinking, creative thinking, self awareness, decision making and problem
solving skills.
Communication skills:
Communication: is sharing of information ideas, opinions, attitude, experience between two
individuals/ two communities. I got to know about the importance of having good communication
skills especially when we are working with the people. A community health person should build
good rapport with the people, should not be like a saviour but should be like a servant and a
catalyst. Health worker should not have pre-conceived notions about people, but try and
understand the different viewpoints of the problem. We should not jump to conclusions as each
view point is valid. Listening is an important skill so as to not miss any important point in the
discussion. During Dr. Magimai Pragasam communication sessions I learned
SOLER: listen by
S- Sit straight
O- Openness
L- Lean forward
E- Empathy
R- Relax
Computer skills:
I learned and improved the computer skills in searching articles, analysing research data using Epi
info and other software for preparing PPT presentations. In the sessions we are also thought how
to use social media to strengthen the professional skills and relationships and to make use of social
media to spread awareness about appropriate technology.
Research
a) Ethics, Qualitative research and Quantitative research
22
Research is the systematic investigation into and study of materials and sources in order to
establish facts and reach new conclusions; as there has been a steady growth of research in the
social sciences and in social science research in health in India. National committee for ethics in
social science research in health (NCESSRH) brought THE ETHICAL GUIDELINES FOR
SOCIAL SCIENCE RESEARCH IN HEALTH by CEHAT; where it gave 10 ethical principles
for research, rights and responsibilities of researchers and institutions, how the rights of
participants should be taken care by a researcher and it also gave the rights and responsibilities of
peer reviewers/ referees, rights and responsibilities of editors and publishers, rights and
responsibilities of funders and sponsors and organisational mechanism for ethics.
I learned the complete process of doing research by following all the ethical guidelines.
I am able to learn Qualitative research, quantitative research and the mixed method by doing two
studies during my fellowship.
Chapter 2: Learning from other sources
Books read during fellowship
1) Title: “Taking Sides - The choices before the health worker” By Dr. C Sathyamala,
Nirmala Sundharam, Nalini Bhanot
In order to come out of the assumptions understanding community is very important and this book
gives a detailed view of community and constraints faced by health workers.
● Throughout history, all human populations have lived with the need for treatment of
disease and sickness.
● Every society evolved its own ways of dealing with this reality.
● Society has potent tools to actively intervene in the disease process and it seemed just a
matter of time before suffering and pain could be vanished from human consciousness
forever.
● Debate about the effectiveness of modern medicines and need to find alternatives.
● It is true that at present there are alternate model of health care an adequately address the
issues involved.
● Such a model would have to evolve out of day to day experience of both the health worker
as well as people from whom health services are intended.
● Health services of our country rest on the work being done by middle level worker- nurses,
ANM, and paramedicals. It is these workers who confront the social and economic reality
of the people they work with.
● These workers are expected to follow the orders and not really take part in decision
making. Even if they involve in decision making their training doesn’t prepare them to
translate practical experiences into conceptional thought and vice versa.
● Bhore committee, Mudaliar committee, Shrivastav committee
23
2) Endless filth -The saga of Bhangis by Mari Marcel The kaekara (Stan) Subramanham,
Gudalur, Tamil nadu
The book gives the picture of manual scavengers and sanitation workers in INDIA
3) Rakku’s story: structure of ill health and the source of change -by Sheila Zurbrigg
4) Health for all, now! – The people’s health sourcebook
What globalization does to people’s health!
Confronting commercialisation of health care
5) Title: The revised - A lay persons guide to medicines
What is in them and what is behind them – LOCOST, Vadodara. 2006
6) Title: The health objectives of the drug policy government of Karnataka standard
treatment guidelines. 2005
I read this book to understand the essential drugs concept. It says that;
• Effective health care requires a judicious balance of prevention and curative services is an
adequate supply of appropriate medicines.
• To ensure the availability and accessibility of essential drugs to all citizens.
• To ensure safety, efficacy and quality of drugs.
• To ensure good prescribing and dispensing practice.
• To promote the rational use of drugs by prescribers, dispensers and patients through
provision of the necessary training, education and information.
• To promote the concept of individual responsibilities for health, preventive care and
informed decision making.
• It also says achieving these objectives requires a comprehensive strategy that not only
includes improved supply and distribution, but also appropriate and extensive human
resource development.
• When treating patients the final responsibility for the well being of the individual patient
remains with the physician. Prescribers must take steps to ensure that they are competent
to manage the common conditions presenting at their practice and familiarize themselves
particularly with those aspects of the treatment guidelines relating to those aspects of the
treatment guidelines relating to those conditions.
7) Title: A decade after Hathi committee
Hathi committee has given the suggestions and recommendations to the government in order to
24
Develop self
reliance in
drug
technology
Keep careful
watch on the
quality of the
drugs
produced
Provide
leadership
role to the
public sector
Hathi
committee
Ensure drugs
available
abundance in
reasonable
prices
Aim at quick
self sufficiency
Foster and
encourage the
growth of the
Indian sector
8) Title: Under the Lens
Health and Medicine (Medico friends circle) - edited by Kamala. S, Jaya Rao, Ashvin J Patel,
Published in MFC Bulletin, Issue Number 53-95
9) The politics of essential drugs
This book discusses the about the initiative of Gonoshasthaya pharmaceuticals in order to
manufacture low cost essential drugs of the highest quality. The book documents the effort of
grassroots health initiative to create a space in which the people’s means truthful information and
rational prescription decisions prevail over corporate greed, intrigue, skulduggery, bribery and
outright profiteering
10) Title: Towards a critical medical practice
Reflections and dilemmas of medical culture today- Edited by Anand Zachariah, R.
Srivatsan and Susie Tharu on behalf of the CMC Vellore- Anveshi collective
25
Women
11) Title: Toward a new psychology of women –by Dr. Jean Baker Miller
Dr. Jean Baker Miller is a psychoanalyst and through her experience and her insight as a women,
expresses with clarity and compassion her ideas as women and their future in the world
The book says that a woman has the enormous strength of having the qualities such as tenderness,
cooperativeness, unselfishness but has been devalued as characteristics of a subordinate sex and
women have endorsed this attitude
This book speaks about:The temporary and permanent inequalities in the world, structure of the dominant and subordinate
psychology and about the psychology of both the sexes with clarity
It is interesting to know about the temporary and permanent inequalities
1) Between parents and children, teachers and students, therapists and clients
2) The birth defines oneself: race, sex, class, nationality, religion etc..,
The difference between temporary and permanent inequalities is that:
1) There is no notion that superiors are present primarily to help inferiors
2) No goal to end the unequal relationship
3) There is a great deal of disagreement and confusion
Dominants label subordinates a defective or substandard and subordinates doesn’t believe in their
own ability to fulfil the wider or more valued roles and any questioning of normal situation as
threatening tries to suppress conflict
The chain of exploitation is at different levels such as the subordinates try to imitate dominates
within each subordinate group, anything done to overcome this chain results in psychological or
social conflicts.
Reflection:
This book has given me a broader understanding of the gender issue
History
12) Title: The destruction of Hyderabad by A.G.Noorani
This book speaks how the Hyderabad in 1949 was invaded and how the Muslim families were
looted (about 10 crores), destroyed and men in the families were killed and jailed and the most
vulnerable groups like women being raped and were taken away and kept in the houses for days,
incidents of looting the property, forceful conversions of women and children took place.
26
Gives an opinion that minorities were always under threat no matter the countries importance of
sensitising people to live in harmony, peace and love
Autobiography
13) Title: Autobiography of Yamini Krishnamurthi
This book is about a very well known classical dancer; she is from Chidambaram which means
small temple and how she developed the passion for classical dance and her role in promoting all
the Indian classical dances.
Reflection:
I just wanted to understand her thought process, as a woman and as a classical dancer her
understanding about various social issues. She mainly focuses on her experience, passion for
classical dance and her role in promoting the classical dance
14) Title: RESHMA fallen down by Reshma Valliappans
Suffering from Schizophrenia Reshma shares her life experience and the way she has dealt with
the circumstances she has been through in her life
15) Title: Indian doctor in jail, the story of Binayak Sen
Medical education is imparted largely through state-owned/funded institutions at highly subsidized
costs. There are 195 recognized allopathic medical colleges in the country producing over 20,000
medical graduates every year 75 per cent of whom are from public institutions. (These figures have
changed with recent rapid increase in the number of medical colleges). However, the outturn from
these institutions does not benefit the public health services because 80 per cent of them outturn
from public medical schools either joins the private sector or migrates abroad.
Reading about Dr. Binayak sen is like understanding politics and authority, working for Human
rights issues resulted in him being in custody and industrialisation is the main starting point where
the land grabbing resulted in the forceful eviction of the people resulting in violating the human
rights
16) Title: God, faith and health – “Exploring the spirituality –healing connection”
By Jeff Levin, PH.D, Foreword by Larry Dossey, M.D
In Sochara we are taught to go to the people to live with the people to love the people and Learn
from people
As per the WHO the Definition for the Health – “It is a state of complete physical, mental and
social well being and not merely the absence of disease or infirmity”, and India suggested to add
spirituality as mind body and spirit go together and without spiritual wellbeing the health will be
incomplete.
27
The book has been written based on the evidence that it explored the religious practises like
meditation, yoga by studying the physical (chemical) changes while practising and praying.
Observations and results are just as any other clinical trials for pharmaceutical drug.
Some critique about the book
Just as any other drug exploring spirituality in the patients may also have negative impact that may
become a constraint to seek medication and the sensitive issue like developing guilt within oneself.
It says that along with the medication physicians can practise to explore the spirituality in the
patients that can bring out positive effects of the healing quickly. And the physician should be
sensitive enough to explore or deal the situation. Religious affiliation may present the opportunity
for potentially long term benefits to your health and well being above and beyond the more obvious
benefit to your soul. Cohen has noted, health means restoring the body, mind spirit to balance and
wholeness.
In each tradition; spiritual teachings and medical wisdom go hand in hand.
Eg: - the Hindu and yogic traditions produced ayurvedic medicine; Buddhism from Tibet produced
Tibetan medicine; traditional Chinese medicine grew from the spiritual heritage of China and the
Unani medical system has flourished in the Muslim world of south Asia. Healing related insights
of Jewish mystics, Dr. Epstein identified key features of the Hebraic medical tradition. Central to
this philosophy is the body mind unity”. Dr. Julius Preuss’s biblical and Talmudic medicine, reads
like a comprehensive medical text book, its six hundred plus pages filled with details on anatomy,
physiology, pathology and treatment for every bodily system. Torah, Tanakh, Talmud and other
Jewish sacred writings those are coherent and fleshed out as any other religiously based healing
system. In this way physical, mental or emotional and spiritual factors worker in tandem to
promote health and well being. “A drop of sunshine” documentary has shown how Reshma
Valliappan has overcome the schizophrenia by looking at the other ways of dealing with the health
situation including yoga, counselling and faith.
17) Camps of wrong: A fact finding report on sterilisation deaths in Bilaspur 16-18 November
2014
Sama resource group for women and health, Jan Swasthya Abhiyan, National alliance for maternal
health and human rights.
The tragic deaths of the 13 women all in their 20’s or 30’s and the critical condition of the 70 other
women, following procedures of laparoscopic sterilization in bilaspur district, Chhattisgarh. The
surgeries were performed by Dr. R. K. gupta, a surgeon, who was assisted by a team of fellow
medical professionals. The women having fallen ill after consuming ciprofloxacin tablets that were
provided to them following the surgeries at the camp It was also suspected that ciprofloxacin was
contaminated with Zinc Phosphide, a rat poison. This books gives the fact findings of the incident
28
Reflections: In the name of controlling population growth the central government
Organisational visits
The world is full of inequalities and as I have already mentioned about the ladder of exploitation
Visits gave hope that there are different organisations working with different exploited groups and
supporting them at every level, encouraging, enabling, empowering and showing empathy to the
exploited groups
Reflections on workshops attended:
1) Panel discussion about mental health:
This was at the SOCHARA CHLP Dissemination meeting in December 2015 in Bengaluru.
It had a good beginning by Sri. Keshav Desiraju, IAS (Retd.), who addressed the keynote and as a
former Principal Secretary, Ministry of Health and Family Welfare, Govt. of India had a wide
range of knowledge about the functioning of the Government of India. From him the interesting
quote is that, “Government doesn’t lack in having ideas but the will to implement the ideas”.
My learning’s are:
➢ Sri. Keshav Desiraju addressed almost all the health issues and tried to analyse why it is
unable to address the health needs of the nation.
➢ The lack of human resources, proper facilities in the public health system.
➢ RTE: explained how the private schools were collapsed and still having the nonfunctioning government schools and expressed alarm of preventing privatisation of the
health.
➢ I am really surprised to listen about the thoughts of RMP’s integration and how it failed,
which I heard from my first field when I spoke to RMP’s.
➢ I felt happy when Sri. Keshav Desiraju addressed that the alcoholism, domestic violence
and mental health go together because I used to think about the women who were in that
particular situation and the affect of these problems on the women. The mental pressure,
the pain and the negligence and disrespect everything contributes to the disturbance of
mental health of the women. Which in turn affects adults and their contribution
(productivity) to the country? And particularly the health of the poor women and their
ability to deal with the situations.
➢ It shows that it is not a new problem and the importance of addressing it. This is thought
provoking and led as a means to the panel discussion.
● Panel discussion: Integrating mental health with primary health care. Given wide range of
inputs to think over from the discussion of panellists Dr.Mathew Verghese, Prof. of
Psychiatry, NIMHANS, Dr. Mani Kaliath, director, basic needs of India, Dr. Ramakrishna
Goud, additional professor, Dept. of Community Health, St. Johns Medical College.
29
➢ I remembered the short films which we have been watched in Sochara earlier and
could relate to the seminar better.
➢ As all of them have a lot of experience in this respective area and could analyse the
gaps in meeting the mental health needs of the people and integrating mental health
with primary health care.
Some important points which were brought up were related to basic ethics like reflecting back
about the chain of exploitation (any one can be a part of it, at one point of time without realising
it), being ethical is related to one’s own behaviour based on day to day basis, preach want you do
and learning process is from living together in the harmony with the people.
The assessment of looking back, looking around, and looking forward and critical analysis of what
we are doing to know where we are now, what we want to be, what we should be.
On the whole the Sochara has done an enormous work for the community health directly and
indirectly by influencing and moulding the fellows to work for the community health. The meeting
was arranged in a very structured manner and even helped me to realise my internal growth of
screening the things. I realised and felt that how important to know, how to emphasise and express
my views regarding any topic. It really gives the optimistic outlook seeing the great spirits come
together and sharing their experience.
Journal club
Sharing and presenting the books and discussing the issue gave more insight into the topic. Camps
of Wrong, MFC bulletin on Urban Health, ICMR Ethical guidelines; THE ETHICAL
GUIDELINES FOR SOCIAL SCIENCE RESEARCH IN HEALTH by CEHAT, Malur story.
Documentaries
1) Merit interrupted
This documentary discussed the issue of social welfare hostels (SWH), budget cuts: pumping in
lesser and lesser money to maintain the social welfare hostels, what is the scenario in 80’s and the
situation in current days, how it is affecting the dalit students, the impact as a whole
It gives a clear picture of how the social welfare hostels run and the difficulties faced by the dalit
students and the reasons for huge no. of dropouts in unprofessional education. To be out of the
poverty cycle that is being faced in the village and with lot of hopes to study; many of them step
into the city and face a very new cycle but which is pretty much similar to the slavery their parents
were under back in the villages for ages making their hopes upside down and the document says
there are still many who don’t have even this opportunity to study
In order to pay the fees, buy books and to eat food (no mess facility in the SWH’s) students go for
part time jobs like catering, donating blood, driving Autos and the other part time jobs for the basic
30
needs, for the sustainability to continue studies, working as part time and full time for the political
parties of which they are paid very less and going for clinical trials of which many of them lost
life and without realising many students lost the track of their main goal “studies”.
Do dalit students really misuse the reservations? Do they really not know the value of
scholarships? Do they simply dropout in the middle of the studies? Are they really not serious with
the studies? Why only gets enough marks to pass the examinations etc.., for all these questions this
documentary shows/gives the ground reality of the difficulties/ struggles faced by them; the actual
reasons and how they are under a new form of exploitation.
This reminded me about reading articles in the new papers about the SWH not only in cities but
also in the adivasi and rural areas. SWH’s for the high school students, under graduate students
and graduate students has to fetch water from the nearby BC SWH’s and with roofs leaking with
clear distinguishment between the SC/ST SWH’s and BC SWH’s, where the facilities will be very
worse to stay there but the aspirations as well as poverty of the dalit students make them stay in
the SWH’s for pursuing the higher studies.
It also speaks about the politicians how they play politics which results in suppressing the
aspirations of dalits, also speaks about the multinational pharmaceutical companies who target this
group of people who are lonely, healthy and really in need of money, doesn’t question what it is
really meant/ results. It is very heart breaking to know that they will be paid 2000-3000/- for the
clinical trials.
One of my friends rightly articulated about the Dalit students first giving up their mind (giving up
studies), than body (their energy to the political parties) and finally soul (clinical trials).
2) Banglored in Bangalore
The documentary shows how the metropolitan city became a cosmopolitan city and how it is been
concretised and the greenness is lost and how increase in pollution causing health problems in
children. The documentary also talks about different social and environmental issues.
Films:
1) Out in the dark
31
The film is about the love between two men from different countries Israel and Palestine
Homosexuality is seen as a sin, lot of stigma attached to it and honour killing is widely spread.
Main motive of the film is to spread awareness and sensitise people about the issue.
2) Bombay talkies
The film has four strong stories about the different social issues.
The story about a kid where he starts identifying his sexual orientation but due to his father and
society for the time being he wants to hide his desire and on the other hand his sister doesn’t get
much encouragement from her parents for her dreams.
It touches sensitive line, very important point to understanding how people are forced to think
straight and how the mainstream is dominant over these people.
LEARNING FROM PRESENTATIONS
Sochara, MFC, Silver jubilee
After each presentation I could analyse how I presented and where I went wrong and try and
understand the ways to express in a right manner.
LEARNING FROM GAMES
By playing monsoon game I came to know the hardships of the farmers as cultivating agriculture
depends on weather and one cannot predict the circumstances like no rains, good rains or moderate
rains and whether something affects the crops output which alters the living conditions of the
farmers and the family. It also gave clear picture of how Dalits and Adivasi’s face discrimination
and a complete cut-off from the entire village as they forced to live outside the city and even if
they has access also they might not turn up to avail it as to avoid facing discrimination and being
suppressed again and again.
LEARNING FROM SOCHARA TEAM, STAFF, FIELD MENTORS AND FRIENDS
It is an excellent opportunity to be a part of SOCHARA as I learned every skill needed to run an
organisation from administration to office work, maintaining library, accounts everything has been
oriented in the sessions, taking part in cleaning outside the Sochara to maintain the surrounding
clean everything is being a part of accountability to work. Sochara team, staff and co-fellows
support and sharing helped me to enhance my knowledge and ability to think practically.
CHAPTER 3: OBSERVATIONS AND LEARNING FROM FIELD PLACEMENTS
Field placements:
1. Railway Kodur, Andhra Pradesh
32
Dr. Samuel memorial trust
2. Bapu nagar, Madhya Pradesh
CPHE Bhopal
3. Hyderabad, Telangana
Anveshi resource centre for women
A) First field placement observations
Introduction
A) Understanding the field placement organisation, their projects and observations:
Dr. T. M. Samuel memorial medical and dental center
The Dr. T. M. Samuel memorial medical and dental center is a clinic. Within the premises of the
clinic along with the medical and dental centre there are diagnostic laboratory centre and Thomas
medicals. There is no organization as such but providing the health service through a bio-medical
model.
History:
The founder of this Dr. T. M. Samuel memorial medical and dental center is
Dr. T. M. Samuel.
In 1938 Dr. T. M. Samuel after completion of MLP profession from Stanley medical
college worked in KLM hospital in Renugunta for some time and joined in Lutheran mission
hospital for leprosy people, which is 1 ½ KM away from Kodur. In 1939 started his own practice
and had a dispensary for inpatients and outpatients in R. S. Road, Kodur.
He voluntarily went to the villages and used to cover the radius of 15 KM of Kodur, to
treat people who are seriously ill and to attend delivery cases. For inpatients that come from longer
distance, he provided shed (shelter), food and water for free. In 1972 June Dr. M. S. Thomas his
son took charge of the hospital after the death of Dr. T. M. Samuel the hospital was shifted to the
present premises and inpatients service is closed.
Dr. M. S. Thomas completed his M.B.B.S in 1966 from Kurnool medical college and did
his internship in anaesthesia from CMC Vellore for about 1 ½ years. After completion of internship
worked in Christian fellowship hospital in Oddanchatrram in Madurai district Tamilnadu for 3 ½
years, later worked in CSI Nagiri for 10 months.
In 2008 Dr. Abraham Thomas has started the dental hospital.
OBSERVATION:
33
● People from all the surrounding villages and all the castes come to this clinic. Those people
who come here were satisfied by the treatment provided to them. Doctor takes time,
examines carefully provides appropriate treatment, very particular to mention about the
course completion. Never uses generic always prescribes branded drugs only. Mostly the
cases of diabetic, B.P, fever (malaria), general fever, cold, cough, allergies etc.., for serious
problems refers to Government Tirupathi tertiary health centre or to the specialists.
● Dr. Thomas because of his age there is a limitation in the number of patients he is
examining. Therefore the people looking for the other possibilities.
● Daily labours finding it difficult to spend the whole day for getting treated therefore people
were seeking RMP’s. Due to the limited treatment, people who are suffering from fungal
infections, wounds with secretions were consulting RMP’s. Self medication for body pains
(pain killers) is commonly found among sanitation workers.
Understanding and describing a community:
Obanepalli panchayat:
Obanepalli panchayat is divided into 7 villages
34
Obanepalli
Voddi palli
Bayanapallii
Obanepalli
panchayat
Gandhavari
palli
Yerramitta
Singirivari
palli
Kotha palli
General information about the Obanepalli panchayat:
● Number of households :
➢ In Yerramitta village
100 households:
➢ In Obanepalli village
Harijanawada: 200 households
Arundathiwada: 264 households
➢ Bayanapalle:
35
600 households
➢ Singirivari palli:
114 households
➢ Gandhavari palli:
23 households (ST-10, BC-7, OC-6)
➢ Voddi palli: Didn’t visit
➢ Kotha palli. Didn’t visit
Caste system:
● People were very friendly and I was received warmly in all the villages, school teachers,
Anganwadi teachers, helpers, people were very sweet open and shared their opinions,
experiences wholeheartedly.
● These villages were geographically placed according to the caste system. The formal or
informal leaders were not seen in any village I went. In the higher caste people there is
togetherness which can’t be seen in the lower caste people. There is no unity and had fear.
Caste difference as such won’t be spoken openly but till now the power is in the hands of
landlords and even if case there are any leaders from the lower caste will have support from
the landlords therefore everything will be in favour to them. More than 60% of the lower
caste people were not having favourable conditions to grow socially and economically.
● Source of income:- Cultivation of papaya, banana, mango, citrus, Mosambi (nursery only
for export), sesame seeds etc.., Because of the bore system, cultivation of any plant or crop
is possible but people here show interest to cultivate only cash crops like papaya, banana,
mango etc..,
● Water supply system and sanitation system:
Recently the CM of A.P inaugurated the N.T.R water plant in Bayanapalli.
The underground water is contaminated with the calcium (they say so) people find
accumulation of white sheet like calcium at the top of water when stored over night.
● Education:
As a whole in SC and ST’s there are people who completed degree, B.tech, M.tech, M.sc
due to the huge competition many of them are not having jobs and they go for agricultural
labour, driving and private jobs in small scale sector for wages. Some of them even work
in the small shops as workers.
About panchayat office:
● Obanepalli panchayat is opened only once in the month where people can come up with
their problems. During other days they will go to the main office in Kodur.
Gandhamvaripalli:
● In this village the difference were clearly seen between the dalits and non-dalits. The nondalits live in the constructed buildings and the dalits in the poor huts without any electricity
connections and were living there for 30 years in the same place and they don’t even own
the land of their hut. Many times the MRO’s assured them to give the documents of the
ownership of the land but nothing has happened so long and this is due to some politics
36
where the landlords don’t get the labourers if there is an improvement in the lives of dalits.
Those who can afford rents were moved out of the village, but some still struggle for the
livelihood and for the basic needs.
G.P.Colony
History:
Before 1930, 10 families From Nellore come and settled in Kodur
Visit to Grama panchayat colony and panchayat office in Kodur.
From panchayat office collected some information.
No hamlets for this panchayat
This covers 60 sq. Km of the Kodur.
According to the panchayat records:
Total population:
MPTC: -
Population
Total
Males
Females
Altogether
32,725
16,561
16,164
SC:
4112
2061
2051
ST:
1620
831
790
OC+BC:
26993
13,679
13,314
8 members
This year it is SC reservation and surpunch is Sri Tippana krishnnaya.
37
There are 11 wards and 20 ward members
Ward members
Males
Females
OC-10
5
5
SC-3
2
1
BC-6
3
3
ST-1
-
1
WHSR:-4
Over head water tanks
Direct pumping motors: 30
The works this panchayat carry out water, sanitation, and lighting.
➢ Protected water supply, any repairs and on/off.
19 contracted workers.
➢ Street lights.
3 workers: for on/off and replacing the lights.
Total
1414
lights- MV-15
SV-249
Tube
1150
lights-
➢ Sanitation workers:
43 contracted workers.
For every 90 days one official leave
38
5 regular workers
1 sanitary maestri
1 sanitary Inspector
➢ Once in every 15 days :chlorination
Weekly: introduction of waste oil into the pools where there is stagnant water.
➢ Meetings:
Three types:
1. Regular or general meeting: For every 90 days and it is mandatory to inform the
staff before 5 days.
2. Emergency meetings: mandatory to inform the staff before 24 hour.
3. Special meetings: there will be no chance of conducting such meetings.
➢ Schemes:
Panchayat office gets budget through house tax and water tax and allots these funds
according to the priority for the needs after general meeting with all the panchayat
members. Panchayat even receives support from the central government through funds for
the development (14th finance).
➢ Maintenance :
Births and deaths register:
● Within 21 days
Pension register:
● For Senior citizens- old age pensions
● Widow
● PHC- both for physically handicapped candidates and mental illness people.
● Pension is based on the infirmity:✓ If the infirmity is above 90% 1500 rupees only
✓ If the infirmity is below 90% 1000 rupees only
39
➢ From the G.P.Colony, The boys were not at all interested in the studies they were ready to
work hard rather than studying. This involves social, cultural and economical factors,
which are influencing them to draw a circle around them from mingling with the others in
the society.
Medical facilities available to the people in and around Kodur
Government hospital U.P.H.C Kodur
● This is upgraded primary centre but when it comes to the access from the point of people,
it is inferior even to the sub centre and it is a 30 bedded hospital, poor facilities, no
reliability, even for normal deliveries they are referring to the tertiary hospital, from the
people i came to know that the PHC is far better than before and one can image how worst
it is in functioning before.
RUYA and Women and child maternity hospital Tirupathi:
● This is the government tertiary hospital; there is a separate wing for women and child
maternity hospital within the premises. the staffs were rejecting admission of the pregnant
women especially for the patients where the PHC is available near to them, since the
tertiary hospital is overcrowded with the inpatients, for which deliveries takes even outside
the hospital, 2 delivered women were given a single bed and despite it had good name for
the hospitality and also for the maintenance of clean and hygienic hospital and even the
premises. The staff of the hospital has to work restlessly and has to satisfy a larger crowd.
The only drawback for this hospital is overcrowding which is clearly the failure of the
maintenance of the PHC’s in their functioning and treating the patients. The hospital is
thronged by pregnant women from different parts in Rayalaseema Andhra Pradesh and
even from Tamil Nadu.
SVIMS: Sri Venkateswara Institute of Medical Sciences:
This is the institution in Tirupati run by the Tirupati Devasthanams which is a tertiary care referral
centre. People get subsidy for the treatment. Half of the amount will be recovered from the tirumala
tirupati devasthanams and balance should be paid by the benefits. SVIMS is implementing this
through the NTR Vaidya Seva Scheme of Govt. of Andhra Pradesh and the Sri Venkateswara
Pranadana scheme of the TTD. People were satisfied with the treatment they provide.
BIRRDS:
Balaji Institute of Surgery, Research and Rehabilitation for the Disabled (BIRRD) is a medical
hospital established in 1985 by Tirumala Tirupati Devasthanam to treat patients suffering from
poliomyelitis, cerebral palsy, congenital anomalies, spinal injuries, and the orthopaedically
40
handicapped. When I asked about any school for the physically and mentally challenged children,
people shared about BIRRDS.
Kadapa AYUSH:
Government medical hospital:
Some families from G.P.Colony receive homeopathy treatment from Ayush department, kadapa.
RIMS:
Rajiv Gandhi Institute of Medical Sciences also RIMS is a medical institute located in Kadapa.
Most of the people also go to this hospital.
Puttur:
● People from Andhra Pradesh and Telangana go to Puttur for bone settings. It is a
Traditional bone setting practice and is known as puttur kattu.
● Manohar raju is a permanent worker as a driver in the sanitation department in panchayat,
because of surface subsidence at the dumping once the tractor reversed and along with the
tractor he fell down and his right leg and hand were affected he went to Putttoor for
treatment but didn’t take rest for the intended days and the swelling remained the same
even after years.
● Women from the G.P.Colony went to orthopedician when her hand was broken but she is
not comfortable with the treatment so she went to Putttoor for getting treated, she is
satisfied with the treatment in Putttoor.
Observation in Obanepalli panchayat and G.P.Colony
Health care providers and medical pluralism:
● In this area there are no Traditional birth attendants (TBA’s) or Dias they used to
be before 15 years in Obanepalli.
Local healers:
● People in this area are having superstitious and blind beliefs almost every child is
having thread (black, yellow) with different metal models around their neck.
● People from here go to chittor district, kanipakam village to Ganapati temple to treat
their family member or relative against black magic.
41
● In Obanepalli village people go to two women (fortune teller) who reside in that
village if people fall sick. And this process is also associated with the rituals and
pooja’s.
● 5th class student from Obanepalli shared her experience when she fall sick out of
fear when she saw something in the air coming to her and later one of the women
after offering prayers got healed.
Bone settings:
● For minor bone settings people from the surrounding area will go to Anantarajpeta (3 km).
● For major bone settings people from the surrounding area will go to Puttoor which is (100
km) from this area.
● These days there is a slight change in treatment given but still people prefer to go to Puttoor.
● Snake bite and other insects bites : Gaddhalarevupalli
● Jaundice: Gumddluru (Ayurvedic) treatment.
Practitioners of Alternative system of medicine in India and practitioners of Allopathy:
● In this area we can find access to allopathic Medicine. Once in a month ANM will visit the
village and provide medicine to the community and even in Anganwadi centres.
● People from village access medicine for fever, cold, cough, stomach pain and other
common sickness from the local shop in the village.
● To whom ever I interacted with the people in village of Obanepalli they said that they were
not interested to go to government hospital due to timings and not sure about the service
they provide in the government hospitals, and even the rush and should wait for their tern
(time) and during emergency, according to some people they are used to go to private
hospital.
● Home remedies: there is no idea about home remedies for every ill they were used to take
pills.
● The people from Obanepalli panchayat, chemists and RMP’s all were satisfied with the
ambulance 108, and mobile clinic 104, that they have noticed a huge difference before and
after introduction of 108 and 104.
● People from OC villages expressed a deep gratitude for this opportunity and even
complained that there is break off from 3 months.
● The G.P.Colony people don’t have the access to this mobile clinic and they all desired for
this opportunity.
Person’s with Mental illness:
1. Female, 18 years.
42
Due to weakness, she developed mental illness during childhood, has above 90% infirmity.
In her childhood parents admitted her in Renugunta School for mentally retarded children
but her condition became worse. Now she is at home. When she was 15 years old her father
applied to join in a school for mentally retarded children but was rejected because of her
age. And when he went again then also got rejected saying that she has completed her 18
years.
Her father is working in a private clinic and earns Rs. 6000 per month and her mother is a
housewife. Has taken to many hospitals and she is not cured. They have even given
ayurvedic medication for thrice but medicine made her situation even worse. Now her
mother is looking after her.
2. Male, 22 years,
The person was diagnosed with Schizophrenia. Before 5 years chikungunya attacked him
after recovery he stayed in the house and slowly started behaving abnormal, started
rejecting food and water thinking it might be a poison and many more, family members
thought it was evil spirit so took him to swami’s, one of the swami said that it might be
problem in his brain with is word his mother took him to vizag mental hospital. Now he is
recovering slowly.
3. Female, 40 years,
The person was married and had no children, taking advantage of this, her husband got
married again. She is staying alone with her mother and very depressed.
Physically handicapped persons:
From G.P.Colony
➢ Male, 29 years, the person is been attacked with polio and his two legs got affected.
Working as an electrician, wants to work in grama panchayat for electric department
(lighting) but no vacancies, Even there is a bias due to polio panchayat member were afraid
to take him because it is difficult for him to do the job.
➢ Blindness and visual impairment:
● The sanitation workers migrated from the Nellore district, No importance for the
girl child education is seen among the people and even some girls were not
interested in higher studies, when it comes to marriage parents were not interested
to marry them outside the Kodur therefore preferring first cousin marriages /
conseguenous marriages such that the girl will be along with them and it is safe for
43
the girl. This is resulting in genetic problems like visual impairment and physical
problems.
● 4 boys and 1 girl are having visual impairment among sanitation worker families.
● Two boys were having visual impairment above 95%. One boy was studying in the
school for blind children in Nellore and all the others were staying at home.
● Hearing impairment is also common among the sanitation workers.
Interaction with the people other than sanitation workers in the G.P.Colony:
● There were 80 families in the G.P.Colony; all the others apart from the sanitation workers
were also facing the same problems of infrastructure in the colony. People from different
districts migrated to Kodur in search of livelihood; it is a typical slum and there are fruit
sellers, daily wage workers, seasonal workers, woodcutters, agricultural labourers, and
even works instead of sanitation workers when the sanitation workers fall sick. For the
livelihood all the people in the slum toil the day doing different works and when they go
instead of the sanitation worker they even face the same problems.
● Always people from villages they seek slums for the livelihood and interacted with the
young lady of 24 years who got married recently and not even having rented house and
staying in the relatives house there is no space to adjust everyone inside so they sleep
outside and if it rains they have to sit under the roof outside.
● Before 6-8 years back, girls used to get married at very young age where now they were
below 25 years with kids and has to take all the responsibilities. Eg:- Dandu lakshmi 24
years of age lost her husband and got 4 children, she has not undergone any basic education
and now she has all the responsibilities to rear her children and don’t know any other work
except sanitation work. While going for work her eldest girl child has to look after her
siblings and her childhood, education and everything is question mark?
● In this colony there were giving least preference to the girl’s education which is out of their
ignorance and even social factors were associated. When it comes to boys other than studies
they prefer to work hard, they are ready to toil the whole day.
● If the sanitation workers were moved out the others in the colony don’t know where to go.
Only very few have property documents so the others will be sent out without being
replaced.
44
Interaction with Arundathi Wada member:
Venkata lachamma lives in arundathi wada. She comes to G.P.Colony to sell fruits, from her and
even from the G.P.Colony members I came to know about the situation of their colony. Arundathi
wada is a colony where the SC caste people reside and there is no proper infrastructure like proper
housing, electricity connection, street lights, street roads, water supply, there is shabbiness and dirt
all over the colony and there are threat of snakes and other insects. Open defecation is common
and women in that colony were facing inconvenience and facing treat snakes while going out for
defecation.
● Venkata lachamma’s daughter Sirisha is 25 years old and she had three children
Mounika (6 years), Kiran Kumar (4 years), Kumar Krishna (11 months). During
delivery Lachamma took Sirisha to U.P.H.C in Kodur but doctor referred to Tirupati
saying that it is risk to deliver in U.P.H.C, when they went to tirupati women and
child maternity hospital it is normal and safe delivery, the staff in tirupati says not to
come to the hospital since they have U.P.H.C in Kodur, so the people were in great
dilemma not knowing where to seek health facilities.
● Similar findings were found when interacted with the postnatal mothers about the
U.P.H.C function, No one is willing for the institutional delivery because of the staff
behaviour, facilities and lack of reliability.
● In spite of the high cost people who can get debts, preferred to go to private clinic for
Deliveries which is leading to increased debts and people who can’t afford were
seeking traditional birth attenders or the people working in the hospitals.
Visit to Bayanapalli village and interacted with Rama Krishna (traditional healer for snake
bite).
From the villagers I come to know about the traditional healer of snake bite and interacted with
him about the treatment he give, all the fortune tellers and the traditional healers follows rituals.
Muneshwarudu temple it is 12 km inside the forest and people from all these villages go on foot
to the temple for offering prayers, he is very particular to says that he gained this knowledge from
his master who is an adivasi belongs to Yerramitta village.
The traditional healer follows some rituals, offers prayers on particular days, collects the medicine
from the forest and gives free treatment to the people; he says that no one is willing to learn and
practice the treatment procedure since this is associated with rituals.
Visit to other NGO (Sneha Seva Sadhan).
45
The president of this NGO is Partha Saradhi, his father and brothers were sanitation workers in
panchayat and his wife is Anganwadi teacher in the G.P.Colony, he started this NGO in memorial
of his friend, gave free tailoring coaching to the 1000 people. Conducting programmes for
promoting the government schemes/programmes like RTE, child line, NREGS etc.., that people
might be benefited. Educate people, children, youth, and women and giving support to the
handicapped persons by collaborating with government. In G.P.Colony he conducted a
programme, to make the colony members realise and prioritise problems and colony members for
one problem they were least interested, and it is girl child education and started to give excuses
that there is no safety outside for girls in terms of teasing, rapes etc, but came to know that girls
are having problems even from the boys within the colony. When a boy missed from the colony
helped in finding him (boy’s family member shared). And in the G.P colony there are 6-8 family
heads and there are some disputes within descendents that there no unity.
Kanchamma colony
Visited Kanchamma colony, interacted with one woman and her family, from her I came to about
the condition of that village there is no transport facilities, no roads, no proper houses, no
Anganwadi centre. All the children are playing sometimes they will go for work along with their
parents, as far as they can maintain the hygienic conditions they were maintaining but recently
water tank was build and the level of the water supplying lines were equal to the level of soil where
the water mixes with mud and there is all over shabbiness it is impossible for them to fill their pots
in a hygienic conditions. Recently government is making arrangements to provide Anganwadi
.There is no unity between the village members, because of the lack of the knowledge, and the
innocence of the village members some people of higher caste always suppress and frightens these
people. In this village if these people need money they take dept from them so they are like bonded
labours to them and due to these they have to work for their so called masters even if they fall ill,
and have to make sure about their presence whenever their masters needed them. And the people
here have a lot of faith in their masters. If anyone violates or disobeys or neglects the rules of the
higher caste people they will beat up and work will be questionable. As Kodur is surrounded by
the mountains, there are many villages which don’t have any facilities where mostly the tribals
live.
Interaction with the chemists in Kodur, learning and reflection:
● There is a mixed opinion about the generic and branded drugs. Some chemists were very
proud that they were selling the branded drugs which have good therapeutic value and had
an opinion that doctors because of greed are prescribing the generic drugs. And in some
cases it is true where it will be case only when the doctor is not having his own pharmacy
within the premises/ partnership with the medical store.
● Some chemists were up to date and know about generics, but the profit margin and the
stoke once received can’t be returned to the manufacturer this is reverse in case of branded
46
drugs the leftover drugs were taken back (can be returned) to the pharmaceutical industry,
therefore no loss in case of branded drugs, if it is with the generics the loss has to be borne
by the chemist himself.
● In the pharmacy stores the chemist were aware of the generics, the effectiveness of the
generic drugs, but people insist or take only the drugs prescribed by the doctor or the
company they are familiar with/ only the drugs which has effectively worked, for Eg. If a
person comes to buy the drug if he studies or sees the familiar company name in the drug
store insists to give that drug only/ which they know from the advertisements. And from
the chemist point of view he doesn’t want to lose the customer.
●
I have never seen the chemist giving bill to the people, in two months field only one man
asked for the bill, people were so busy that they were unable to spare even a little time and
which is resulting the income lose to the government, there is huge demand for the fast
relief medicines, usage/ demand for the high is commonly seen.
● When I spoke to them about the common health problems in Kodur, mostly people was
facing respiratory problems due to dust. There is also a rise in non communicable diseases
like diabeties and blood pressure. Fevers like malaria, dengue and typhoid were commonly
seen.
● The government of Andhra Pradesh is supporting the entrepreneurs by giving loans to
establish generic shops.
● These generic medical shops will be helpful to the full extent only when the public health
system is strengthened and gets full support from officials, the working staff, and people.
Until and unless people own the system and make the government worker accountable for
their work.
● As the mobile units were going to the villages and checking for the non-communicable
diseases (lifestyle diseases) then and there and giving/ supplying free medication. Later on
if there is any problem in reaching this mobile unit to the village, people go to chemists
with the strips in order to continue the medication which is very difficult to get in the
medical stores as drugs are available only with different branded names, but people insist
for the same medicine. People can afford this generic medication and that’s how there is a
need for the shift to generic medication essential. As government is taking steps to
implement the schemes even the society and the people should support and encourage the
good schemes which are people friendly.
Pharmacy association president:
47
● Kodur medical shops/chemists have an association. Where there is president and vicepresident and the association looks after the problems faced by the chemists, including
applying for new licence and the renewal of the license at times.
● Almost except 2 or 3 all the other chemists from the different backgrounds and having the
experience of 25-30 years mostly in running the medical shop.
● But when I see to this process I felt it making business out of people’s health which is the
obstruction and very far from the aspiration of health for all.
RMP association president:
● There are 25 RMP practitioners in Kodur and some of them were practising since 30 years.
I have seen a long queue in front of the RMP practitioners. The people who normally come
to RMP’s belong to SC, ST and minority communities.
● There are several factors (social, political, economical and cultural) which influence/make
people seek the RMP’s.
● Daily labourers, because of not having the job security can’t skip the work for the day,
according to the people going to a general M.B.B.S doctor is time consuming and the
consultation fee is high. Those who come for the treatment will give some amount as they
wish, Sometimes people don’t even give anything. If someone in the house is seriously ill
calling an M.B.B.S Doctor is costly (have to provide even charge for his/her travel), but
RMP’s (registered medical practitioners) charge less. Before the Aarogya Sri Health
insurance programme of the Govt. Of Andhra Pradesh they used to follow a referral system
but now people were directly going to the tertiary hospitals.
● Poor people were benefitted from the Aarogya Sri for life saving conditions especially for
heart surgeries etc..,
● RMP’s have right to give only limited medication:
➢ Only first aid (any cleaning).
➢ Prescribe only fewer medicines.
➢ Should not give injection.
➢ Rarely can give IV fluids.
● But it is reverse where prescribing high doses, giving injections.
48
● Newer licence for RMP’s was no longer allowed to practise since there is a need for the
legal practitioners.
The association had got the new method having membership in the RMP association has opened
doors for the new RMP practitioners through which they can get the license and can practise.
2ND FIELD PLACEMENT:
Second Field placement experience and learning in Bapunagar, Bhopal, MP:
Visit to Bapunagar and Rajivnagar:
Interaction with the Anganwadi, Balwadi and community:
When I visited Bapunagar and Rajivnagar for the first time I saw very pathetic situations, where
people were very close to soil and there is no place to stand or sit there is all over shabbiness and
dirt and it is sad to know people were living there for decades and government hasn’t taken any
steps to improve their situation. No proper drainage system and along with that people were facing
many other problems of social issues like domestic violence and alcoholism. Especially in
Rajivnagar men don’t work and women and children go for rag picking in the early hours and the
men usually take away the little money they have, for drinking alcohol.
Visited the Anganwadi and Balwadi in Bapunagar:
The staff of Sochara introduced me to the Anganwadi teacher and to the worker, and said that I
will be here for 2 months, to learn and to work along with them for the improvement and to
understand the communities in Bapunagar. From the Anganwadi we got the information about the
people living in that community. Many of them were shifted to the multistorey buildings by paying
1, 20,000 Rupees. In the Bapunagar slum the children from the Jharra community were not willing
to go to Anganwadi very less number were wishing to go. From the Anganwadi Everyday enrolled
children get milk and supplementary food. The staff of Sochara even introduced us to Priyanka
one of the MUSKAAN staff works as balwadi teacher. MUSKAAN an NGO in Bhopal mainly
focuses on educating the children of the lower socioeconomic community and after experiencing
the situation got to know how important it to be having balwadi to develop confidence in the
children of the slum.
49
Details of community:
•
Population: 900
•
Many of them shifted to multi-storey buildings and even the Anganwadi teacher is new
therefore there is a lot of confusion about the no. Of families left to multi-storey buildings.
•
Three main problems associated with shifting are:
-
•
Joint families. (Parents shifted to the apartments and nuclear families stayed back.)
Those who can afford shifted to multi-storey buildings, has given their houses for
rent in slum.
- Those who can’t afford have given the apartment for rent to others and they stayed
back in the slum.
As per the records now there are 211 households in which 50 households belongs to Jharra
community (a migrant adivasi group).
According to Anganwadi teacher Jharra people were Members don’t come to Anganwadi usually
but if they want to come they prefer to come in groups for taking supplementary food.
Observations:
➢ Wasting water
➢ Maintenance of sanitation and hygienic conditions
➢ Malnutrition
➢ Alcoholism
➢ Domestic violence
➢ Flow of migration hasn’t stopped.
➢ People were still seeking slum for shelter.
Visit to Bapunagar, interaction with the Vishwakarma community:
People from different parts of M.P especially from villages where there are no basic amenities
migrate to Bhopal for the livelihood. When I spoke to the community members they said that
alcoholism is very common and men won’t stop until health of that person is spoiled. And they
said that 3 men died due to alcoholism. When it comes to work women don’t work. They rear
goats and sell the goats when goats become old and it is the additional income. I interacted with
Archana Yadaav, 19 year girl staying with her brothers and want to learn tailoring for the
50
livelihood purpose. And to Anju Thakurs who is a pregnant woman and had baby girl in her first
delivery and newly shifted to slum.
Formal and informal leaders:
Before there used to be one but after his death no one cared about the slum and no one is
representing the community members.
The other communities include Pandits, Thakurs and Muslims:
● People who can afford, at least meeting their basic amenities; trying to maintain hygienic
conditions.
● Different community people do different works eg:- Jharra- loha (work with iron)
- Vishwakarma- lakdi, majdoori (work with wood)
- Yadaav- mistri (involved with construction work)
- Mohammadians- sweepers etc..,
● Regarding the health facilities they can access from the Bapunagar.
- Sarada hospital (private which is near to the slum.)
- Government hospital at 1250 bus stop which is 3 KMs.
- Hamilia hospital which is 5 KMs.
- Kushi lal hospital 1 km.
Visit to Bapunagar, interaction with the Jhara community:
● There are informal representatives of the Jharra community who solve problems in the
community or they go to the panchayat about the different problems in the community.
Jharra: Men over here work on daily basis and labourers, welding, sieves making, women usually
don’t prefer to work but sometimes (if the economic condition is worse) prefers to work as
agricultural labour; like grass cutting, soya bean fields, etc.., The place where the lower community
stays is very narrow but the place where the others live is quite spacious there is wastage of water
everywhere in the slum when there is a supply and no valves to turn off the tap. We did a
community walk in the slum the houses were katcha and made out of sheets and the slum has very
narrow streets to walk and the drainage system was open and it is flowing right beside the houses
and the tap were near to the drainage and the pumps were paved along with drainage. The effect
of engagements at very young age can be seen eg: - Sitha (name changed), 14 years, divorced (boy
just left her). Tried to speak with the women in the community I felt that they feel shy to speak up
and was lacking confidence which usually find in the lower community. A group of women from
Jharra community said they were born and brought up in Bapunagar. They were from the age of
23 to 45 year old. I spoke to them about the basic amenities and they say that, they were enough
51
and pure water and no problem with power. According to their ability they eat all kinds of curries
along with roti’s. According to them, in village it will be more difficult because here at least they
are getting water for drinking.
Difference between lanes of Jharra community and other Communities
The basic elements which government has neglected in Bapunagar:
•
Basic sanitation.
•
Women, Children and adolescent care
•
Health Education and Promotion
•
Health education and promotion to Kishore
balika's.
•
In anganwadi’s every Saturday there will be a
meeting for kishore balika’s but they need more
attention.
Balwadi in Jharra community
Findings:
•
Engagements in childhood.
•
Jharra community doesn’t support girl child education.
•
Girls not interested in studies.
•
These days who are in their 20’s-30’s were interested to
school.(women)
send their children to
52
•
Government hospital: People were complaining about the sterilisation that without their
concern/ knowledge sterilisations were being conducted.
•
Health seeking behaviour: - people go to hospital and if not cured, then they go to the
temple and offer animals.
Migration:
•
Realised the importance of
•
➢ Mobilising, enabling and empowering.
Multi buildings (apartments) won’t alone help to
become smarter or slum free India.
✓ There is a need to
• Strengthen the villages.
•
Provide Alternative livelihoods in the villages itself.
Anganwadi in Vishwakarma area
VISIT TO TAMIA:
Exposure visit to the rural health system of a tribal area in Madhya Pradesh:
1.
2.
3.
4.
5.
6.
District hospital
Civil hospital
Community health centre
Primary health centre
Sub health centre
Grama Arogya Kendra (village health centre).
We visited Anganwadi (Which also hosts the Grama Arogya Kendra), Health Sub Centre
(HSC) and Community Health Centre (CHC). PHC is closed due to festival Dussera.
In the public sector, a Health Sub-Centre is the important and first point of contact between
the primary health care system and the community. A Sub-centre provides interface with
the community at the grass-root level, providing all the primary health care services. It is
the lowest rung of a referral pyramid of health facilities consisting of the Sub-centres,
Primary Health Centres, Community Health Centres, Sub-Divisional/Sub-District
Hospitals and District Hospitals. The purpose of the Health Sub-centre is largely preventive
and promotive, but it also provides a basic level of curative care. Grama Arogya Kendra is
newly introduced programme which is at a lower level to sub-centre and according to the
53
mandatory there should be 16 drugs which can meet the needs of the people, Anganwadi
teacher is the in charge of the Grama Arogya Kendra. Pregnant women come to the
Anganwadi for the supplementary food and educated on the ANC checkups.
● Dr.Vijay Singh is the Mandal Health Officer and he explained us about the
functioning of the public health system in rural area.
Visit to PHC: Started our journey to visit PHC and Bharia tribe, but the PHC was closed due to
daussera so we couldn’t visit PHC but we met Anganwadi of the village chindi who is working
from 2006 and we interacted with her on her role and duties. She is friendly and as per her
knowledge she even explained about the people she is dealing with. From there she took us to the
Anganwadi centre where grama arogya Kendra is functioning. She showed us the medical kit.
There should be 16 essential drugs as mandatory at the grama arogya Kendra level.
Nutritional rehabilitation centre: The children from Anganwadi who are severely malnourished
were sent to the NRC. Where the mother and child gets therapeutic supplementary food for 14
days and even medicine to the child if needed in case of diarrhoea(ORS) or any other severe
condition due to malnutrition.
NRC in Tamia: As I haven’t visited any NRC before, it gave a good impression regarding the
maintenance of the centre. NRC’s main intention is to eradicate severe malnutrition in children
below 5 years. The children should be enrolled in the Anganwadi and if the child is severely
malnourished the Anganwadi refers to the NRC. Along with the food, in NRC the mothers were
educated on the issues of health, Family planning, Counselling, Knowledge on malnutrition and
Hygiene (personal). There is the follow up for 4 times, where the mother and child were called to
the centre. If there is no response they will inform Anganwadi regarding follow up. Repetition of
the severely malnourished child is at most twice, Health education CDS through mamta, Abhiyan
are played at NRC; approximately there is 40% malnutrition in the block. There are 10 beds and
all were provided with the mosquito nets. When we reached there, the mothers were watching T.V.
● NRC does get the feedback from the mothers about the NRC.
● Some Mothers will be unwilling to stay for 14 days in the centre.
Delivery ward:
● After the visit to NRC we visited delivery ward which is opposite to NRC. It is an 8 bedded
ward, where only the normal delivery takes place and the caesarean deliveries were referred
to district hospital. Delivery ward was hygienic. There is one staff nurse Sunanda who is
on duty when we went there.
54
Functioning of the ward: In the ward there are 4 delivered women. We met two mothers in the
ward. Spoke to them about the age and the weight of the child when born.
About sterilisation: Only bleaching powder is used, Mostly use and throw disposals were used
during deliveries.
Waste management: as per the rules there were four dust bins of different colours for the waste
separation and disposal.
As explained to us it is not up to mark but basic needs were met as we are with the officials we
can’t talk to people about the facilities and their actual opinion about the services.
Visit to Community health centre, Tamia, chhindwara:
This CHC is covering about 90% tribal population.
● Dr.vijay singh is the Mandal officer
● Mr. Gyan dass is the BCM
● Mr. Chet ram is the supervisor.
Under this CHC there are 4 PHC’s:- Dela khari, chindi, chawalpani, gaildubba (not functioning.)
Mandatory Essential list should be: for CHC -142, PHC-116, SHC-32, Grama panchayat-16.
CHC services:● 108, JSY, X-ray but it is not in a working condition.
● Laboratory facilities, HIV/AIDS, Dengue, Haemoglobin, Mobile unit, First aid, Medicine,
Spot diagnosis, Spot treatment, Lab technician, Doctor, ANM, pharmacist, lab, Male
doctor, pharmacist, ANM and in the other female doctor, pharmacist, ANM, availability of
Free drugs.
● Programmes under PHC: mother and child development, nutritional health programmesJSY, malaria, T.B.
● 5-10 sub centres are compiled under PHC, All the reports from the sub-centre were send
to PHC’s. And PHC is under block level and the population will be 25-35 lakes. Lower
health unit is sub health centre. For every 5-7 villages, in tribal area there will be either
ANM or MHW (male health worker) but in urban there will be both female and male
workers. For every village there should be ASHA and it is under Block community
mobilise who monitors work of 200 ASHA’s.
Cidholi Bharia:
It is 15 km from Tamia, we met a family in the village who explained us about the Bharia tribe
and their practises interacted with the women who explained about the custom usually followed in
55
the village. Whenever someone dies in the tribe they made sculpts on the wood and place it at
place in the village in their memory of the families/persons. The Bharia tribe is the most primitive
tribe but the people were educated that after 2 kids they were going for the sterilization. If
something happens to the children they regret for being sterilised. Even i have noticed many
dispensaries run by the unauthorised persons.
● Usually the Bharia tribe people go to the trees and pray to their God’s but the Gond tribe
brings leaves to the house and follows the rituals. And according to my observation these
people respect nature and don’t even harm the plants even by plucking the leaves.
● Bharia tribe people were less in number (primitive) and are very friendly and welcoming.
● They speak Dravidian language.
Visit to Dhawani sub centre:
Interacted with Tuldas- ANM, Narmada ASHA (dosra bani)
5 villages under this
1 ASHA/village and it varies according to population in the village
For 1000 members/ 1 ASHA and the sub centre has the Population of 5550.
Functioning of the sub centre:
●
●
●
●
●
●
●
●
●
●
●
Mother and child,
ANC,
PNC,
Immunisation,
Identification high risk cases and referred to nearest PHC/CHC.
ANM will prepare the slide for T.B and sends to CHC from where they get results.
On Tuesday’s – tours i.e., village immunization, scabies, fungal infections,
common URI, general cold, pneumonia.
Common diseases - malaria, seasonal viral flu, T.B.
People here are well educated in terms of having number of children.
Usually after two children parents usually the mother goes for sterilisation, if
something happens and if they lose a child they regret for getting sterilised.
The sub centre was well maintained in terms of cleanliness. Due to daussera people
were not there. ANM and ASHA’s (2) were there and we interacted with them.
Adarsha Anganwadi:
56
The functioning is similar to all the other Anganwadi’s except that this Anganwadi gets extra funds
to have all facilities which an Anganwadi should have.
For the appearance the Anganwadi is with proper building, beautifully decorated with colourful
paintings and has lot of toys for kids to play and sink for washing hands etc..,
About its services:
Total number of children registered was 98. Those who come regularly were 38 children. Children
here get basic education, supplementary food, and monthly weigh checkups.
●
●
●
●
●
Pregnancy- registration, weight, mid arm circumference., HB- ANM, IFA,
Immunisation- BCG, T.T
supplementary food
Severely malnourished children were sent to NRC.
kishore balika’s ((11-18) 15 girls) were educated about the Changes in the body,
menstruation, AIO’s, white discharge, hygiene, violence against women and about help
line no.
Reflection: Adarsha Anganwadi should be a model not only in terms of facilities but also in terms
of attendance of the children and all the children should be well nourished.
About Tamia Literacy rate is low, socio-economic status is of this people is low. People go to
unauthorised persons for treatment. Most of the people follow home remedies. For Snake bite and
pneumonia they don’t take proper care. There is a delay taking proper health care.
Patalkot view:
We visited patalkot view on our way to Bharia tribe. It is a beautiful view which is suitable for the
excursion. For the nature lovers it will be a best place to visit. Rafi sir explained us that people
used to think that it is formed after the explosion of the volcano that is why it is under prohibition
for a longer period of time and no one is allowed to enter. A part from our official visits we have
a great time enjoying nature, and getting to know the tribal people, good food in nidhi’s house and
had great time with her kid ruma.
Interaction with the kishore balika’s:
In Bapunagar slum in balwadi, along with Nidhi mam interacted with the kishore balika’s on
education, hygiene and sanitation, marriage and health problems.
57
● In the discussion Sonu of 13 years, anjali of 13 years, manisha of 16 years, shoba of 14
years were participated.
● The main aim is to analyse their views on above mentioned issues.
Regarding education:
Generally girls will not study after 5th standard there is only one girl who completed 10th, even
boys don’t study after 10-12th standard, sometimes due to the attitude of teachers the children drop
out the schools thou there is a government school nearby. Parents try to send them to school but
some drop out because of lacking interest studies. Some regret dropping out the studies. There is
no proper guidance to the youth in the Bapunagar. Parents are willing to educate their children but
there is no proper guidance and motivation to the children regarding education.
Reflection: There should be proper guidance regarding education and future plans. Good that
balwadi is there but the facilities were not up to mark. According to my observation From the Jhara
community children preferred to go to balwadi than to go to Anganwadi. In Anganwadi thou they
don’t find anything wrong when it comes to the attitude of the teacher they were not convenient.
Children were getting informal education and even sometimes supplementary food i find it is not
enough. There should be much more done to the slum children regarding leading them in the
correct path. Letting them know about the importance of education and enhancing the capabilities
of the adolescents and the youth.
Regarding hygiene and sanitation:
There is proper supply of water to Bapunagar, there are separate toilets for each house, some were
educated in washing hands before eating and also washing hands after using the toilet, drinking
water is covered with the lids. They mentioned that they were taking bath everyday and washes
cloths. Personal hygiene: some uses sanitary pads some uses cloth and changes twice a day during
menstrual cycle. When it comes to outer appearance they look unclean when compared to the
others in the slum.
Marriage● All are engaged before 6-8 years of age, no choice, married after 18 years of age, domestic
violence is prevalent, men often beat up their wives and alcoholism is common. Dowry is
given based on whatever they can afford to give.
● Girls don’t even remember their engagement. Parents will tell them about the person to
whom they got engaged to. Girls don’t have any option to take decision about the partner.
● Once they grown up if the boy doesn’t like to get married to the girl he engaged to, the
engagement will be cancelled. The girl who has been rejected will not face any problem in
terms of stigma she will get married to another one.
● But if that happens to a girl they won’t allow girl to break the engagement.
● If someone runs away they will find and bring them and beat them up.
58
● For the problems within the jharra community they have informal leaders. They facilitate
the panchayat.
● At times people of Jhara community in the city from different slums meet in a place.
Health problems:
Usually these adolescents share the problems with their parents. If not with their friends. Primarily
they consult doctor for the treatment. If they find no difference they offer prayers by sacrificing
the hen or goat in the temple.
Work:
Women from this community don’t prefer to work. If there is a situation to work they prefer to
work in the fields (agricultural labour). From this they go to cut grass in the parks, soya bean fields
etc..,
Reflection:
In Babunagar as per my observation, the Jharra community people were living very close the
soil/mud. No proper drainage system and the water pumps were equal to level of soil so the pump
and the drainage are at the same level; the level of the house is very low where the water from the
drainage can easily flood into the houses. No proper streets to walk with in the community. The
houses were very closely built in a very little space. All the houses were katcha. People were very
poor that can’t even afford to buy cloths. The children were wearing the torn cloths after taking
bath.
When it is to compare the Jhara with the other communities within the slum it is very clear that
jharra is a lower community and we can easily make it out the years of exploitation they faced.
They have to adjust within the small area where there is no proper drainage system and place where
they live is little lower to the level of the soil, but in non jharra community the taps were built
much higher to the level of soil and it is cemented.
3RD FIELD PLACEMENT
Research Centre for Women’s Studies
➢ The Centre is located in Hyderabad, India.
59
The main activities:
➢ Research,
➢ Critical reflection and
➢ Analysing the different issues, literature and have individuals working with different
groups.
➢ Education, Dalits, minorities and LGBTQ
➢ Health and healthcare systems, development studies, law and critical legal studies, and the
public domain.
➢ Draws fellows of interdisciplinary scholars and activists from many fields.
● Current project: City and Sexuality - A Study with Youth Living and Working in
Hyderabad City.
Foremost I would love to thank Sochara for giving me the wonderful opportunity to have field
exposure during my fellowship I was placed in 3 different areas and being to three different places
enriched my learning abilities as well as my attitude towards society. Through this one year
fellowship for the first time in my life I focussed my thoughts on social issues and Health from the
Community perspective. Being Anveshi made my desire come true without which my primary
motive (to know about different social issues) of coming to Sochara might not be fulfilled. As
Sochara is keen in community health Anveshi is into literature and keen in various areas like
women, dalits, minorities, LGBTQ, health, education research and critical reflection. Anveshi is a
research centre for women studies and have fellows who work with different groups in the society
and analysing the different issues is a part of their work. Draws fellows of interdisciplinary scholars
and activists from many fields, as Anveshi is also mentoring the short term fellows. The current
project is city and sexuality; A Study with Youth Living and Working in Hyderabad City. As far
as I understood this project is looking into the way urbanization and migration to cities is changing
the shape of Women’s aspirations; Changed hopes, desires and affections with respect to
opportunities, work, marriages, personal relationships, public conduct and experience. Sexuality;
refers to the concrete way of these desires, hopes and affections are mapped on to their bodies,
relationships with others, objects and modes of work. I had an opportunity to go to field along with
the Project fellows and got to see the conditions of the social welfare hostels and the aspirations
of the students and even this gave the glimpse of the circumstances of the villages the students
came from. The students are with open mind to accept the new students who come to stay and even
adjust as they see themselves in the other person.
60
Interaction with Navdeep had made my thoughts clear on the LGBTQ issues and watching the
films Bombay talkies, out in the dark Come to know how the issue has been medicalised and tried
to develop different theories and as the group is very minor the problems faced by them
People, the main stream think straight they are several social norms which influence the decision
making capability of the people. Acceptance and tolerance of the other person when the ideology
of the other person is different or when they differ in their opinion.
Interaction with Suneetha the senior fellow has given wider understanding about gender as her
area of interest is gender and minorities. Being the upper caste women how she looks at the gender
issue and her experience in Anveshi has given her the space to exercise the flexibility which has
given better results in creating the environment of the work place and work.
➢ Through discussions about the project: Rethinking of urban development by vinita pandey,
the history of sexuality vol. I by Michel Foucault
Through the discussions I could understand the international aspects and how globalisation
influences different social issues.
Interaction which Gogu Shyamala author and poet in Telugu has given the glimpse picture of the
politics behind the caste and several factors influencing some people to move towards the
Naxalism the darkness and how the lack of education, suppression of women and other social
norms leading to another kind of darkness in women of lower caste.
As I stepped in Anveshi the first thing which attracted me is the library, due to enthusiasm I pulled
out many books kept a side to read. I thought I have enough time to read and absorb more things
though I am placed to do research for 45 days. I thought with in no time I will finish my research
study but slowly I realised through my pilot study that finding doctors is tough and interaction
with them is much more tough and taking consent to interact with his patients is impossible I tried
for one week in all the possible ways but couldn’t find a doctor who can be a part of my study. As
doctors primary objective is to see patients and everything comes secondary. There are many
barriers from the timings of the practitioners, their busy schedule and number of hospitals in the
area. Doctor’s reluctance towards the study is a big barrier as they don’t even want listen or give
their opinion and finding excuses to not to be a part of study.
When I approached a nursing home which has medical shop with the setting as soon as I introduced
myself “Doctor said why you want me to participate in the study there are many other small
hospitals in this area and you can do your study with those doctors”. The other doctor said “yes,
you can ask me your questions and I said that he should sign the consent form as a part of the study
he immediately reacted that I am not interested and I don’t want to give my opinion. When I
approached another doctor said “It is almost noon and it is late so try me some other time if I have
enough time I will participate in the study”. I went to him again this time there are no patients and
61
it is around mid morning Doctor welcomed and said to sit but I found he is hesitating to participate
in the study he is not willingly giving the answers so I didn’t force him to give answers.
Later I have taken some contact details and spoke to them on phone and went to physicians and
completed my study through some changes in the initial study. R. Srivatsan Guidance helped a lot
in approaching Doctors and People from different backgrounds which lead to better results of
research as well as my understanding towards the realities of the health system. Under the guidance
of Srivatsan I even learned how to understand the author’s point of view and his/ her ideology
towards the issue and how the author is analysing the issue in a particular situation under the
influence of several factors during a particular period. To try and understand whether it is true or
his perception. This helped me to understand the way to read books, analyse the book and
understand the topic better.
62
D) Learning from the three field placements and understanding through the
community health perspective:
My field learning objectives
1) To understand the community
2) To understand the community priorities
3) To understand the field placement organisation and their projects
4) To understand the role of the pharmacy and pharmacist in health
5) What are the regulatory systems and how the systems function?
6) How about the access to essential medicine in that area
My second and third field learning objectives
1) Learning by reflection
2) To find the activities and involve
3) Contribution/ intervention
4) Reflection
5) Research
Comparing the collective sessions the knowledge obtained through books with the field
realities:
People have their own set of understanding the circumstances and the real situation of their lives
and social factors. People are struggling for the basic amenities. Work, food and shelter are the
main priorities and health becomes secondary. In order to improve the health situation in India
have to work at the larger aspects and that’s what SOCHARA is doing. Equipping the fellow to
get familiarise with the concepts and realities and try and apply the skills the fellows acquired
during the fellowship in to the work they do. Networking and working along with the authorities
and influencing the policy makers for the betterment of the Country.
63
Part B
Research
STUDY: 1
Acknowledgement:
This pilot study was conducted as a part of organisational analysis by the joint effort of SOCHARA
and Dr. T. M. Samuel memorial medical and dental center. I am grateful to Dr. Abraham Thomas
and Ms. Sheeba Simon for helping and supporting me to initiate this study and to all the workers
who willingly took part in this study.
To assess the living and working conditions of the Panchayat
sanitation workers of railway Kodur, Andhra Pradesh, INDIA
By Vipparthi Uma chaitanya, SOCHARA, CHLP fellow, Batch 12, 2015-2016
ABSTRACT
Aim: The present study aims to assess the living and working conditions of the panchayat
sanitation workers of railway Kodur; with a focus on work related health issues; with the objective
of providing a framework for the best practices in town waste management, inculcating
occupational safety and dignity of work, with public awareness and participation.
Introduction:
This study was conducted among the sanitation workers of Kodur panchayat.
Kodur panchayat has an area of 60 sq km with 32,725 Population (2011 census). Study was
conducted among sanitation workers, total workers (48: - 23 men and 25 women) were included
in the study of which 48 (100%) participated. Disposal of waste includes 6 tractor loads per day,
including street sweepings, waste from households, shops, hotels, panchayat dust bins. Data were
collected by direct interview using a structured questionnaire which included questions about
housing and sanitation, working conditions, health, socio-economic conditions, awareness,
problems and solutions.
Objective of the study is to assess and analyse the living and working conditions of sanitation
workers; with a focus on their work-related health issues; and provide evidence for policy
recommendations towards occupational health safeguards and a dignified working environment;
64
in an effort to create a proper town waste management plan through policy implementation and
public sensitisation.
Subject and methods:
The study was conducted among all the sanitation workers (48) of Kodur panchayat of
which 43 were contract based workers and have no job security/PF even though some of them had
10 to 20 years of experience. Only 5 of them were permanent workers. The work includes sweeping
streets and roads, collecting and transferring waste into tractor, collecting waste from households,
clearing the clogged drains, clearing pools filled with stagnant water and waste, using
disinfectants. They work 8 hours a day in 2 shifts; 5 to 10 AM and 2 to 5 PM.
Data were collected by direct interview using a structured questionnaire which included
questions about education, housing and sanitation, working conditions, with a focus on health
hazards, socio-economic conditions and awareness. Problems and solutions were discussed in
detail and participant observations were analysed, tabulated and recorded.
Findings:
i.
Work is carried out without any protective gear, even during rains; Sweeping,
collecting, and transferring waste without any safety measures; Stepping into
clogged drains bare foot for cleaning; soon after clearing the block people again
throw waste in drainages. Clearing pools filled with stagnant water and waste.
Carrying dust bins to the vehicles for dumping and loading containers manually.
ii.
There is no segregation of waste; Infectious medical waste is not segregated from
the domestic waste and injuries with needles were observed commonly.
iii.
Work related health issues were prevalent; Exposure to exhaust fumes resulted in
eye diseases. Carrying loads resulted in excessive exertion resulting in increased
incidence of musculoskeletal problem. Frequent handling of bleaching powder is
leading to skin infections.
iv.
No protective measures were taken; workers were not vaccinated for tetanus,
hepatitis A, hepatitis B, polio or typhoid. There is no regular health monitoring
/checkups. Working on empty stomach resulted in higher risk of gastrointestinal
disorders. Burn injuries have occurred while burning the waste in the open places.
65
v.
Poor housing, hygienic practices and sanitation; A side effect of solid waste handling
is that the filthy nature of the work demotivates people about self hygiene. Women
reported preparing meals immediately after returning home from work without
changing clothes. Alcoholism and chewing pan along with tobacco was found to be
high; many of them developed this habit exclusively after joining the work.
vi.
Poor socio-economic conditions; Very poor awareness about girl child education.
Between 17 to 20 years of age, boys were discontinuing their studies. Not able to
provide nutritious food to their children. Many of them had incurred debts for
medical expenses (71.42%). These people face discrimination in the society because
of this work.
vii.
Per day 6 tractor loads of garbage were dumped. Deaths before retirement were
found to be 7. These people were not ready to access government health care system
due to lack of reliability/credibility, proper equipments, services and lack of
accountability in the hospital staff.
Table 1
66
Prevalence of reported Occupational Morbidities:
S.NO
Morbidities
Number
%
1
Accidents & Falls
9
18.75
2
Injury from sharp objects
18
37.5
3
Animal bites + Fire burns
4
8.33
4
Water
borne
11
22.91
Musculoskeletal morbidities (all
42
87.5
and
vector
diseases#
5
body parts) @
6
Head ache
13
27.08
7
Respiratory
3
9.09
17
51.51
Nail
12
25
GIT problems (upper and lower
10
28.57
(Infections/allergies)
8
Eye problems*
9
Skin
problems
and
infection$
10
stomach).
● #Typhoid, jaundice, Dengue, malaria. @neck, shoulder, back pain, lower back, and knee.
*eye irritation, redness, watering. $bacterial and fungal, fingers and toes.
Results:
67
The reported prevalence of occupational morbidities were as shown in Table 1 falls &
accidents (18.75%), injuries with sharp objects like needles and glass pieces (37.5%), head
ache ( 27.08%), water & vector borne disease (22.91%), animal bites & fire burns (8.33%
) were high, The current prevalence of body and joint pains (87.5%), eye problems
(51.51%), dermatological problems & nail infections (25%), respiratory diseases (allergy)
(9.09%) and GIT problems (28.57%) are also found.
Table 2
Living conditions of all the 35 families:
S.NO
Amenities & facilities
Number
%
1
Permanent house
26
74.28
2
Proper roofing
16 (out of 26 houses)
61.53
3
Running water
11
31.42
4
Toilets
8
22.85
5
Electricity
14
40
6
Mobile phone
21
60
7
Aarogya sri health card
35
100
8
Medica
9
25.71
26
74.28
Government
l care
Private
68
Table 3
Socio-economic conditions of all the 35 families:
S.N
Socio-economic factors
Number
%
Education
Government
27
67.5
Private
13
32.5
Anganwadi
4 (below 5 years)
100
O
1
(Till
14
years)
2
Nutritious food and diet
24
68.57
3
Habits
Alcoholism
14
60.86
Chewing pan
22
45.83
Medical
25
71.42
Others
35
100
Maintaining Hygienic living conditions
35
100
4
5
Debts
69
Results:
Table 2 and 3 shows that workers were facing lack of amenities like toilets, proper roofing to the
houses, running water, electricity, permanent houses and health care. But they strive to provide
nutritious diet, education and maintain hygienic living conditions. 71.42 % had incurred debts for
medical expenses and had habits like alcoholism (60.86%) and chewing pan (45.83%) along with tobacco.
Discussion and Recommendations:
● All Hazardous wastes including hospital waste were commonly dumped in the panchayat
dustbins. Workers handle these medical wastes without any safety devices or protective
gear. There should be strict implementation of segregation of hospital wastes from general
wastes. Equipments like needle burners should be compulsorily used in hospitals.
● A good protective gear should be provided for the prevention of spread of diseases through
waste.
● Conduct regular medical checkups of these workers. Vaccinate solid waste workers for
hepatitis A and B, tetanus, diphtheria, polio, typhoid and rabies vaccination.
● In order to At households, commercial establishments and institutional buildings,
implement source segregation of non-hazardous recyclable wastes, so that the emission of
exhaust fumes into the environment is reduced at disposal sites while burning the waste.
● Collection workers who transfer and load waste in the vehicle were doing it manually;
hence they should be provided with gloves, masks and slip-resistance shoes. Riding steps
on solid waste collection vehicles should be self-cleaning and slip-resistant since injuries
from falls were common. Jumping on and off from the riding step should be prohibited.
● Provide solid waste workers and waste pickers with a place to wash with soap before eating
or going home after work. Provide training on the value of good hygiene in disease
prevention, including clean bandaging over any skin discontinuities during work. Ideally,
all workers should be given working clothes/bodysuits.
● Develop training on occupational and environmental health and injury issues relating to
solid waste management for staff at all levels Provide health and safety plans for all staff
70
at all levels, including operational procedures for safe waste handling, accident response
procedures and first aid.
● Provide solid waste workers and waste pickers with clean drinking water, sanitation
facilities, proper housing, roofing and drainages.
● Especially during rains functional and useful gear which as easy to use and suitable for
maintaining hygiene, should be strictly provided. Solid waste workers should wear highly
visible colours to help collection vehicle, visually locate workers’ positions during
reversing and loading and other drivers to avoid traffic accidents.
● Development indicates that cost-effective investment in sanitation requires hygiene
promotion and education to achieve successful reduction in mortality and morbidity rates.
Results:
The reported prevalence of occupation related morbidities as shown in Table 1, like falls &
accidents (18.75%), injuries with sharp objects like needles and glass pieces (37.5%), head ache (
27.08%), water & vector borne disease (22.91%), animal bites & fire burns (8.33% ) were high,
The current prevalence of body and joint pains (87.5%), eye problems (51.51%), dermatological
problems & nail infections (25%), respiratory diseases (allergy) (9.09%), GIT problems (28.57%).
Habits: alcoholism in men (60.86%), chewing pan along with tobacco in men and women
(45.83%).
Conclusion:
The work related health-problems among sanitation workers were reported to be high. The
prevalence of injuries with sharp objects, Musculoskeletal pains, eye problems, dermatological
and Respiratory problems were reported to be high. Measures are needed to improve the work
environment of these workers by ensuring availability of protective gear based on ergonomic
principles, clean drinking water and washing and sanitation facilities, during working hours. The
extent of occupational injuries among panchayat workers is present in a level that needs immediate
public health action. Implementation of basic occupational health and safety services including
training on occupational health and safety, ensuring the provision and use of personal protective
devices are highly advisable. Workers were facing lack of amenities like toilets, proper roofing to
the houses, running water, electricity, permanent houses and access to an affordable and
appropriate health care system, Government should strive to provide all these basic amenities
71
including regular health monitoring to improve their living and health conditions. There should be
awareness among the public about segregation of waste at source and usage of dust bins. People
should develop sensitivity towards the life and dignity of sanitation workers.
With increasing consumerism, the amount of garbage being produced has increased
manifold. Sanitation workers are indispensable to a healthy society. They work in very unsafe
conditions without any proper safeguards, irrespective of sun and rain, and constantly exposed to
obnoxious odours and harmful substances, to maintain public health and safety. But society
stigmatises them as lower castes doing unclean work. As citizens of this country, sanitation
workers should enjoy the right to a dignified life as provided by the Constitution of India. This
study throws light on the gravity of the issue with an aim to create a proper policy framework
ensuring the occupational safety and dignity of sanitation workers, who toil daily to keep our public
spaces clean.
STUDY: 2
72
Acknowledgement:
This Research study was conducted as a part of CHLP fellowship. I am grateful to Dr. Thelma
Narayan and Dr. R Srivatsan mentors Sochara team and SISEC members for supporting me to do
this study and to all the Doctors and people who willingly took part in this study.
Aim: A study on Pharmacy Practices of general practitioner/ polyclinic owned pharmacies in
Durgabai Deshmukh colony, Amberpet, Hyderabad
The study title has been change since enough clinics (minor group in the city area) were not found
in the D. D colony the area of the study is extended to the surrounding areas of shivam road, vidhya
nagar, RTC cross roads, ashok nagar, jawahar nagar colony, padma shali colony, thalla basti, ranga
nagar, begum pet and tarnaka
Objective of the study:
1) To study the use of rational therapeutics and whether the practitioners (poly clinic GP’s)
follow the WHO essential drug list (EDL)/ National List of Essential Medicines (NLEM)
2) To study standard regulations and prescription auditing for my understanding
3) To study whether patients are prescribed rational drugs with generic names or branded
drugs
4) To study whether patients knew about brand drugs vs. generic drugs
5) To understand the positive and negative impacts of these pharmacy practises on the patients
Introduction:
Though before and after independence there are many committees from Bhore committee
to NHM which emphasizes the importance of strengthening the primary health care system
still people look upon PHC’s only for immunization and sterilisation (family planning)
because of many reasons like focusing more on the family planning and allotting budget
and higher pressure to meet the targets and the behaviour of the staff etc.., and for the other
ailments people mostly seek private sector. [1,2] As the new NLEM included only with
384 medicines [3] the market is flooded with more than 80,000 formulations and
unnecessary combinational drugs [4] which has high potential risk to the patients and GP’s
owned pharmacy who are most likely to be driven by the profit motive and facing
commercial competition may likely prescribe branded drugs or drugs of their own interest
which may lead to irrational drug practices [5,6,7] and as we know there is a drug resistance
associated with these issues. According to the estimated data 70 per cent of allopathic
doctors are in the private sector and about 80 per cent are individual practitioners. People
usually utilise these services especially the general practitioners. [1,2,8,9]
73
Purpose of the study:
In my first community posting as a participatory observant for two months and through
interaction with the chemists and RMP’s in a small pocket of Andhra Pradesh I came to
know that the practice of owning pharmacy by GP’s is prevalent and it is reportedly a
common practice. As the previous studies says there is a lack of prescribing generic drugs
and there are very few studies on GP owns pharmacy hence I find it relevant to do this
study. Research is for the social change to explore the ways to bring positive change in
society, Given short duration of time it will be an exploratory study, for the benefit of the
people results will be used for Reports, Journal article; organizational publications if any,
for personal learning about research and research ethics, for professional sharing of the
knowledge with the co-CHLP fellows.
Methods used:
➢ Study Methodology:● Study Design – Mixed method; Qualitative method quantitative method
● Study Population- General Practitioners/ poly clinics having own pharmacy and patients
who consult these clinics but as per the challenges there is a slight change in the study
population, doctors and patients. Sample is taken according to convenience (who agree to
participate in the study) and patients were interviewed at their residence
● Sampling-
●
◦
Sampling Method- non probabilistic sampling
◦
Sample Size- the actual number is 10 clinics, 10 doctors but 12 doctors were
interviewed and 20 patients.
Inclusion criteria- only the General practitioners/ polyclinics having own pharmacy but
has interviewed general practitioners and even specialists some doctors didn’t own
pharmacy and initially thought to interview the patients who consult these clinics but
interviewed at their residence as patients felt inconvenient at hospital due to sickness.
● Exclusion criteria- below 18 and after 60 year aged people will be excluded, doctors and
patients not interested to participate in the research. Even the patients above 60 years were
included who agreed to participate in the study willingly
74
Finding the Doctors without any contacts: Initially I find it difficult to interact with the Doctors
finding ways to interact with the doctors on parallel I interacted with the Doctors through contacts
despite of their busy schedule and different timings some Doctors agreed to speak willingly
Prescription study: Patients who agree to the study allowed me to look at the prescriptions
Interaction with chemists: Medical shops which are connected to the clinics, some hospitals have
medical shops inside the hospital, some medical shops are independent. Some of the independent
chemist agreed for the discussion. I didn’t interact with the chemist having medical shops inside
hospitals as I have to go through the Doctors, therefore I couldn’t interact
Interviewed patients: Went to the slums and colonies to find people who are willing to participate
in the study and interviewed them (taken their opinion regarding the private clinics and generic
medicine and government hospitals)
Findings:
Private health care system:
Though they are measures taken to strengthen the public health care system in India most of the
people in the community make use of private health care system as the timings and distance of the
private clinics is in favour to the community. Though Doctors have the motive to serve people;
most of them were unaware about the generics since they have the idea of good medicine
(effective) and bad medicine (not so effective), the concept of generics has not gone into the public
(doctors and patients), even after years of experience recently some Doctors have the Idea of
generics but there is a issue of accessibility of the generics. (Respondent 5). Patients instead of
travelling are willing to take medicine in nearby shops. Branded drugs are available and are easily
accessible. Though there should be one generic shop with in half kilometre they were not
recognised or preferred due to lack of awareness (both Doctors and Patients fall under this
category). “Single ingredient drugs and effective drugs are being eliminated due to less market and
profit and were brought as combinational drug”. (Respondent 5). Doctors and chemists say to ban
the Branded drugs so as to prescribe the Generics. Only in government hospitals NLEM is followed
and there is no force to follow NLEM in private clinics and doctors were unaware of NLEM and
only follow clinical establishment guidelines. “I don’t follow NLEM; I prescribe according to the
clinical needs of the person”. (Respondent 7). The source of knowing about different Brands is
very simple as the CIMS and NIMS books of medicines. Once the doctor starts practising the
information regarding drugs will be known from CIMS (current index of medical specialities) or
NIMS. “I don’t know about generics I know that generics are not 100% effective. I prescribe only
branded drugs. I don’t know about NLEM. I prescribe combinational drugs as female patients are
happy to take single drug than single ingredient drug compliance is more”. (Respondent 8) The
information of different brands of a molecule their price, dosage, indications, side effects, contra
indications etc.., were known. Medical representatives will come and introduce about different
75
drugs and benefits of the drug but there is a lack of authentic information and mostly the medical
representatives gives biased and half of the information about a particular drug. “50% of the
information given in the CIMS is not authentic as the indications for some drugs were given wrong
which might cause doctors to prescribe for wrong indications”. (Respondent 11). Doctors know
about single ingredient drugs but then indulge in the practices of prescribing combinational drugs.
“Only single ingredient drugs are effective but since compliance is more use of combinational drug
are more”. (Respondent 3) Prescription auditing is not possible and lack of committed people and
infrastructure and resources leading to weak regulations “Due to Lack of human resources it is
difficult to do prescription auditing”. (Respondent 6). In government sector doctors prescribe
according to the NLEM. “I am thought about generic drugs in my academics so I prescribe only
generics”. (Respondent 10). There is a difficulty in the availability and accessibility of generic
drugs “It is not good to make people run for a drug to the other end of the city so I use and prescribe
locally available drugs” (Respondent 12). Unnecessarily more drugs were prescribed in the
corporate hospital “The clinical needs of the each person differs and treatment depends according
to the situation of the person, due to high usage of antibiotics in corporate hospitals sometimes the
condition of the patient becomes serious and will not respond to any treatment and every time
careful examination and treatment should be given during that time the alternative medicine will
help” (Respondent 12). Medical representatives (MRs) play a role in given the information about
the new drugs or different company products. “Those who come to us give the information about
the drugs under price control only” (Respondent 8). Mostly MRs will try to influence Doctors to
try the drug to know about results. “I don’t want to try the effect of new drug on my patients it is
not my duty; it is responsibility of the drug inspector to check on the efficiency of the drug. There
are other drugs which work effectively. During my practise I have seen the generic drugs, branded
equivalent drugs and drug with less price also work effectively and it is not my due to bother
whether they are effective or not; drug inspector should see that only efficient drug were in the
market”. (Respondent 11) some doctors tried to justify the prescription practises “Let government
ban branded drugs then I will prescribe generic drugs”. (Respondent 7). Some doctors were taking
advantage of recent treatment guidelines. “These days’ doctors are prescribing more and more tests
and it is a burden to the patients doctors are lacking the skill to identify the disease without test
and it is due to the recent guidelines for evidence based treatment but it is also misused ”
(Respondent 2).
Findings:
Interviews with people:
1) Out of 21 people interviewed 5 are below 30 years of age and 12 are between 30 to 50 years and
4 are above 50 years of age (Table 1). 3 are not having any educational background, 13 have
76
completed pre university education and 5 members are graduates. (Table 2). 14 of them are
females and 7 of them are males. (Table 3). 4 of them know about generics in a way that they get
medicine with discount from some shops and usually they only but the drugs for chronic non
communicable diseases like diabetics and hypertension and 17 of them had no idea of drugs
(branded or generic). (Table 4). Mostly the persons I interacted doesn’t go to hospital for head
ache and other issues unless it is serious, they get medicine from medical shop. In case of children
they don’t take choice but go to doctor. 19 of them don’t opt for self medication by seeing
advertisements or by knowing from other sources like family and friends and 2 of them go by
advertisement and use self medication but take assistance of chemist (Table 5). Though there is
an issue getting half of the prescription due to economic constraints they are satisfied with the
treatment they are getting from the private doctors due to distance, timings, kind of approach
they receive. (Table 6). Out of 21 no one is educated about the side effects of the drug. (Table 7).
Out of 21 no one wants shift to generics unless the doctor encourages. (Table 8). Out of 21 no one
is informed about alternatives. (Table 9). 18 brought half of the prescription most of the time and
1 person. (Table 10)
Table- 1
Age of the participants
77
Age
Below 30
30-50
50-70
Total
Frequency
5
12
4
21
Table- 2
Qualification of the participants
Qualification
Till pre degree
Degree
Pg
No education
Total
Frequency
13
2
3
3
21
Table- 3
GENDER
Gender
Female
Male
Total
Frequency
14
7
21
Table- 4
Generic drugs usage
Generic drugs usage
Frequency
78
Yes
No
Total
4
17
21
Table- 5
Self medication
Self medication
Yes
No
Total
Frequency
2
19
21
Table- 6
Satisfaction of the treatment
Satisfied with the treatment
Yes
No
Total
Frequency
20
1
21
Table-7
Education about side effects
Educated about Side effects
No
Total
Frequency
21
21
Table- 8
Shift to generic drugs
Shift to generic drugs
Frequency
79
No
Total
21
21
Table- 9
Informed about alternatives
Informed about alternatives
No
Total
Frequency
21
21
Table- 10
Instances of bringing half of the prescription
Instances of bringing half of the prescription
Yes
No
I wish Namaste and bring medicine
Total
Frequency
18
2
1
21
Discussions:
1) The first objective – To study the use of rational therapeutics and whether the practitioners
(poly clinic GP’s) follow the WHO essential drug list (EDL)/ National List of Essential
Medicines (NLEM)
- Private practitioners are not forced to follow NLEM list.
- Most of the doctors were not prescribing according to NLEM list
● Doctors view point: Let Government ban Branded drugs then we will prescribe generics
and there is no pressure to follow NLEM. (Interviewee 7)
● Chemists view point: why should government allow to manufacture such drugs (FDC’s:
fixed dose combinations) and tell us not to sell
● Patients view point: if only doctor advices patients are likely to shift to generic drugs In
order to save time and money sometimes patients go and get medication from the medical
shop, use of painkillers are common
● Experts(who works for drug related issues) view point: Misuse of drugs results in the drug
resistance hence proper monitoring should be done
80
2) For the second objective – To study standard regulations and prescription auditing for my
understanding
-
●
●
●
●
No standard regulations and prescription auditing but in order to run a clinic should
follow clinical establishment guidelines and clinics are following these guidelines
Doctors view point: Only clinical establishment guidelines were followed and no time to
educate or to create awareness among people. (Respondent 4)
Chemists view point: experience is the qualification and these chemists as well are with
good intention that customer should be relieved from sickness with in a due time, has the
idea of costly drug works effectively and such drugs are good.
Patient's view point: they are least bothered about the standard regulations if the doctor
gives concession he/ she is a good doctor
Experts(who works for drug related issues) view point: creating awareness by Health
education [such as proper intake of nutritious food , importance of completing the course,
maintaining hygienic (drinking water and sanitation) conditions, following good
prescription practises, avoiding sub prescription, over prescription and extravagant
prescription] is as important as treating a patient.
3) For the third objective – To study whether patients are prescribed rational drugs with
generic names or branded drugs
-
●
●
●
●
No patient is prescribed with generics
Doctors have mixed opinion about generics some think that if the cost of the drug is
high the drug works effectively, some think that drugs manufactured by small
companies are not effective but recent ban on the drugs showed that even the
established pharmaceutical company products were also sometimes substandard
Doctors view point: For the combinational drugs the compliance is more and patients are
satisfied. (Interviewee 3 and 8)
Chemists view point: branded ( costly) drugs work effectively
Patient's point of view: even if patients know drugs where they get for cheap we don't trust
those drugs because only costly drugs and only doctor prescribed drugs are effective
Experts(who works for drug related issues) point of view: generics and branded equivalent
generics are as effective as branded drugs
Doctors view point:
-
Doctors say that compliance is more for combinational drugs and are little cheap than
the single ingredient drugs
81
-
Patients feel compliance since they are getting less no of drugs.
Awareness should come from the drug using sections if they ask for the generics
change may be possible
- The Government, Doctors, Pharmaceutical companies and the Patients all are
responsible for the failure of the health system.
- Involvement of the politicians, rich people and pharma lobbying is altogether the
result of present situation in the country
- Doctors are not favouring the Public as they have money divisions among the chemist,
labs etc.., eg:- if a patient is encouraged to get test if he finds out a lab where it cost
150/- when he comes with result to the doctor says it is not authentic since it is a fake
lab and orders him to go to lab from where he/ she has money division
4) For the fourth objective – To study whether patients knew about brand drugs vs. generic
drugs
99% of Patients don’t know about generics
Have immense faith in Doctors
98% of them even they knew about the cheaper drugs they don’t go for it unless the
Doctor encourages them
● Doctors view point: generics should be promoted but it not good to make them run here
and there in a city for a particular drug.
● Chemists view point: If the name of the drug once established it is very easy to market it
as there will be demand for the particular drug. e.g. no one will come and ask for dippers
for kids but specifies to give pampers as the brand is so popular and the same applies to
drugs
● Patient's view point: As prescribed by the doctor same brand and dosage is used by the
patients
-
5) For the fifth objective
-
To understand the positive and negative impacts of these pharmacy practises on the
patient's.
Patients does not have any benefit from this kind of practice (Respondent 5)
It is just that patients get prescribed drugs at one place (Respondent 12)
82
-
On a long run no one knows the side effects caused by the FDC but were easily
available as the industries want to market them. Mr. Sam Son George, The Drug
Information (Pharmacist Karnataka State Pharmacy Council).
With doctors:
S.No
Respondent 1
Respondent 2
Respondent 3
Respondent 4
Respondent 5
Respondent 6
Respondent 7
Respondent 8
Respondent 9
Respondent 10
Respondent 11
Respondent 12
Area of interview
RTC cross roads, Hyderabad
Tarnaka, Secunderabad
Tarnaka, Secunderabad
Begum pet, Hyderabad
Ashok nagar, Hyderabad
Gunrock
enclave,
Secunderabad
Shivam road, Hyderabad
Balanagar, Hyderabad
Balanagar, Hyderabad
Balanagar, Hyderabad
Yeshwanthpur, Bangalore
Jaya nagar, Bangalore
Gender
Male
Male
Male
Male
Male
Male
Male
Female
Male
Male
Male
Male
Recommendations of doctors:
-
-
Patients have immense faith in doctors hence doctors should be educated about
generic medication and single ingredient drugs
Lack of awareness among the doctors itself is causing the problem
As government is promoting polio vaccine with film stars; promotion of generic drugs
should also be done.
There should be awareness creation should be done at every corner as effective as
vaccine promotions
Most of the doctors have the intention to serve people therefore government should
encourage them to promote generic medication by creating awareness since most of
the doctors and chemist have no idea about the generic Vs branded drugs, most of
them think if the drug is high cost it is more effective. There is misuse of supremacy
of the private Doctors which is mainly because of the money division among the
druggist, labs, Doctors. (Interviewee 5)
Eg: - Apollo hospital promotes its services through free camps about the orthopaedics
branch where patients come to know about Apollo likewise concept of generics and
adverse effects of combinational drugs should be promoted.
83
-
-
There is a treat where single ingredient drugs are slowly eliminating from the market
and hence government should take initiative to protect the lives of its people.
Government, Doctors, patients, chemists and pharmaceutical companies all these
sections are responsible to strengthen good health situation in the country
Drop in box should be arranged in order to prevent wastage of medication as chemist
won’t accept the remaining drugs and this can be distributed to the patients who can’t
afford
In academics curriculum should include NLEM and about the Communitisation
processes as once the students complete their education and come out into the
community they are not having any clue and have to start learning from beginning as
curriculum is not updated -drug information pharmacist.
Other factors influenced the study:
For this study I interviewed doctors from different backgrounds some work in government sector
and some private sector ranging from single physician clinics (small clinics) to multi speciality
hospitals and doctors who are interested in the public. Therefore there is a lot of contradiction
within the results and each doctor’s understanding differed to the issue of NLEM, clinical
regulations, prescription audit, Branded and Generic Drugs, selection of the drug and the positive
and negative impacts of the health system. Though I wanted to study about the factors influencing
pharmacy practises I also ended up finding the challenges faced by doctors at different levels.
Results:
Some of the Doctors were justifying prescribing branded drugs by saying “Let Government ban
Branded drugs then we will prescribe generics and there is no pressure to follow NLEM”.
(Respondent 7) regarding the clinical establishment guidelines and prescription auditing some said
that there is a lack of human resources. “Only clinical establishment guidelines were followed and
no time to educate or to create awareness among people”. (Respondent 4) about combinational
drug prescribing practises doctors were justifying by “For the combinational drugs the compliance
is more and patients are satisfied”. (Respondent 3 and 8) when it comes to the consumers part
99% of Patients don’t know about generics. Have immense faith in Doctors. 98% of them even
they knew about the cheaper drugs they don’t go for it unless the Doctor encourages them. Patients
do not have any benefit from this kind of practice (Respondent 5). It is just that patients get
prescribed drugs at one place (Respondent 12). On a long run no one knows the side effects caused
by the FDC but were easily available as the industries want to market them. Mr. Sam Son George,
Drug Information Pharmacist (Karnataka State Pharmacy Council).
References:
84
1. C. Sathyamala, Nirmala Sundharam, Nalini Bhanot. Taking Sides. ANITRA. June 1986.
2. Zurbrigg Sheila. Rakku's Story: Structures of ill- health and the source of change.
Bangalore: George Joseph; 1984. (chapter 3)
3. Report of core committee for revision of national list of essential medicines Nov 2015.
[cited on 2016 Jan 4] Available from http://cdsco.nic.in/WriteReadData/NLEM2015/Recommendations.pdf
4. National coordination committee. Health for all now: the people’s health source book.
Second edition, Chennai: AID- India. January 2004. pp. 263-360
5. LOCOST. The revised A lay person’s guide to medicines what is in them and what is behind
them. Vadodara. India. 2006. pp. 129-153
6. Patel V, Vaidya R, Naik D, Borker P. Irrational drug use in India: A Prescription survey
from Goa. J Postgrad med[serial online]2005[cited 2015 Dec 11]; 51:9-12. Available from:
http://www.jgmonline.com/text.asp?2005/51/1/9/14015.
7. Gudadappa s. kasabi, Thilakavathi Subramanian, ramesh reddy allam, chitra A. grace,
shivanna reddy, and manoj v murhekar. Prescription practices & use of essential medicines
in the primary health care system, Shimoga district, Karnataka, India. Indian J Med Res.
2015 Aug; 142(2): 216–219.[Cited on 2016 Jan 14] available from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4613444/
8. Lawton Robert burns, bhuvan srinivasan and mandar Vaidya. india’s health care industry:
innovation in delivery, financing and manufacturing. India’s hospital sector: a journey from
public to private health care delivery. cambridge university press; 2014 [2015 Jan 14]
Available from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400322/ pp. 156.
9. Madhav G. Deo. Doctor population ratio for India- the reality. Indian J Med Res. 2013
Apr;
137(4):
632–635.[cited
on
2016
Jan
17]
available
from:http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3724242/
10. Task force on health and family welfare. Govt. Of Karnataka. Karnataka towards equity.
quality and integrity in health. Final report of the task force on health and family welfare.
Bangalore. Government of Karnataka. April 2001. pp. 342-360
11. Health and family welfare services. Government of Karnataka Standard treatment
guidelines. Karnataka state drugs logistics and warehousing society(R). Bangalore. 2005.
12. ICMR. Ethical guidelines for Biomedical research on human subjects. New Delhi. 2006
13. NCESSRH. Ethical guidelines for social science research in health. CEHAT. Centre for
enquiry into health and allied themes. Mumbai/ Pune. January 2004
85
14. Ramana k v. Patient safety: a developing world perspective. Research gate,
DOI:10.5455/amr.20150501120912; May 2015 [cited on 2015 Dec 18]. Available from:
http://www.researchgate.net/publication/275886426.
15. High Level Expert Group Report on Universal Health Coverage for India Planning
Commission of India New Delhi, November, 2011. [Cited on 2016 January 18]. Available
from: http://planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf.
ANNEXURE-I
Consent Form for Participation in a Research Study
Title of Study
A study on Pharmacy practices of general practitioner / polyclinic owned
pharmacies Durgabai deshmukh colony, Amberpet, Hyderabad.
SOCHARA is an independent organization situated at Bangalore facilitates a Community Health
Learning Program through SCHOOL OF PUBLIC HEALTH EQUITY AND ACTION
86
(SOPHEA). In this learning program fellows learn “community based” approach for community
health awareness and action.
Principal Investigator Uma chaitanya Vipparthi is a fellow of community health learning program
and as a part of her fellowship learning purpose she is expected to conduct a field study. She has
chosen to conduct a study on Pharmacy practices of general practitioner / polyclinic owned
pharmacies. Durgabai deshmukh colony, Amberpet, Hyderabad under the assistance of Dr.
Srivatsan R, ANVESHI, Hyderabad and convener, medico friend circle, the purpose of this study
is for learning as well as for initiating action wherever necessary.
You may inform to persons whose contact details are given below for any adverse effect in
connection with the study.
S J Chander
Programme Officer
SCHOOL OF PUBLIC HEALTH EQUITY AND ACTION (SOPHEA)
No.
359,
1st
Main,
1st
Block,
Koramangala,
Bengaluru – 560 034 Karnataka, India
Email: chc@sochara.org
Phone: +91-80-25531518, 25525372
Web: www.sochara.org
ANNEXURE-II
Participant Information Sheet
My name is uma chaitanya Vipparthi. I am a student of the Community Health Learning Programme
(CHLP) in an NGO called SOCHARA (Society for Community Health Awareness Research and Action)
in Bangalore. As a part of this programme, I am conducting a research study along with ANVESHI in order
to understand more about the rational drug therapeutics, pharmacy practices. I would like to kindly request
your permission to participate in this study.
87
This note provides an explanation of the nature of the research. This sheet may contain words that you do
not understand. If there is anything you need clarity on, please feel free to ask me. At the end of this
information sheet you will find my contact details
A study on pharmacy practices of general practitioners/ polyclinics owned pharmacies will help in
understanding the use of rational therapeutics and whether the practitioners (poly clinic GP’s) follow the
essential drug list, whether patients are prescribed rational drugs with generic names or branded drugs,
whether patients knew about generic drugs effectiveness, sources where they can access generic drugs, the
positive and negative impacts of this system on the patients, to get an idea about standard regulations and
prescription auditing to be followed by general practitioners, prescription study by comparing with the
NLEM / essential drug list of the state/ area. Research is for the social change to explore the ways to bring
positive change in society, Given short duration of time it will be an exploratory study, for the benefit of
the people results will be used for Reports, Journal article; organizational publications if any, for personal
learning about research and research ethics, for professional sharing of the knowledge with the co-CHLP
fellows. Your answers through in-depth interview will be very important in helping us to understand the
underlying factors that impact overall health of the nation.
Some of the questions are very personal and if you do not feel comfortable to answer you can refuse them.
Your participation in this study is voluntary and you can withdraw at any time you do not need to give any
reasons for not answering the question.
The interview will be around 20-30 minutes along with your permission; I will also record the whole
interview. If you are not comfortable with this, please let me know I will write instead of recording and
with your consent your words will be copied exact for the purpose of creating a report. I assure you that
everything will be confidential and your identity will be protected. All confidential data will be handling
only by me.
All the information is used only for research purpose.
You will not receive any resource of benefits for participating in this study but the information that you
provide might help us to use for the benefit of the nation.
88
For more information or clarification:
S J Chander
Programme Officer
School Of Public Health Equity And Action (SOPHEA)
No.
359,
1st
Main,
1st
Block,
Bengaluru – 560 034 Karnataka, India
Email: chc@sochara.org; Web: www.sochara.org
Phone: +91-80-25531518, 25525372
Koramangala,
Thank you for your time. This sheet is for you.
89
ANNEXURE-III
Participant Consent Form
Title: A study on Pharmacy practices of general practitioner/ polyclinics owned pharmacies in Durga bai
deshmukh colony, Amberpet Hyderabad.
I have read and understand the participation information sheet (or it has been read to me). I understand that
it includes me for taking part in an interview. I have been explained the purpose and the way of the study.
I have been informed that this study includes prescription survey to compare with the NLEM and Essential
drug list of the state / area, to understand the standard regularities and prescription auditing of the clinic and
the pharmacy practices of the clinic will be studied. I have been informed that there will be no direct benefits
for me. I understand that the information I will provide is confidential and will not be disclosed to any other
party or in any reports that could lead to my identification. I also have been informed that the data from
study can be used for preparing reports and the reports will not contain my name or identification
characteristics. I have been provided with the name and contact details to whom I can contact. All my
questions have been answered to my satisfaction. I had enough time to decide whether I am going to
participate or not. I know that I am participating as a volunteer and I can step out of the programme
whenever I want and it is not necessary to give an explanation. I know that research team will see my
details. I give consent for my details to be used for the research purposes mentioned in this form. All
information regarding consent and purpose of the study has been explained to me in the language I
understand. I provide consent to the following:
90
Yes
No
Participation in the in-depth interview
Audio-recording of the in-depth interview
Publishing of words/sentences spoken in interview
verbatim
Name of participant: ______________________________________
Date: ________________________________________________
Place: ________________________________________________
_______________________
Withdrawal of consent
I hereby wish to WITHDRAW my consent to participate in the study described above and understand that
such withdrawal WILL NOT endanger my relationship with the Institute of Public Health
Name of participant: ______________________________________
Date: ________________________________________________
Place: ________________________________________________
91
Points for in depth interview:
●
To study the use of rational therapeutics and whether the practitioners (poly clinic GP’s) follow
the WHO essential drug list (EDL)/ National List of Essential Medicines (NLEM)
➢ To study whether the prescribing practices are associated with Single active ingredient drug
(pharmacologically effective)
➢ Choosing drugs which are relatively safe
➢ Choosing cheaper alternatives
●
➢ Core components of primary health care
To study whether patients are prescribed rational drugs (National list of essential medicine) with
generic names or branded drugs
➢ Method of selection of drugs (brand/generic)
●
➢ If generics which company? Why?
To study whether patients knew about generic drugs effectiveness, sources where they can access
generic drugs
➢ Have they ever asked for the cheaper alternative (generic) drugs to the doctors
➢ Do they have any idea of the cheaper alternatives work as effective as costly drugs
➢ Do they knew about the shops where they can access the cheaper alternatives drugs
➢ Have they ever took half of the prescription due to economic constraints
●
To understand the positive and negative impacts of this system on the patients
➢ How much time do GP’s spend in educating the patients about the disease, drugs and side
effects
➢ Treating patients without prescription whenever necessary
➢ To understand patients point of view regarding this system/ difference between public and
private sector
➢ To study whether patients were treated cost effectively
●
➢ Whether patients were given the informed choice regarding the drug usage
To study standard regularities and prescription auditing
➢ To understand it from the point of community health
➢ To study the standard regularities which are to be followed by the GP’s
➢ To study the process of prescription auditing
➢ What are the drugs identifying storage methods
➢ How do you maintain the expiry date drugs
92
Collective session’s pictures:
Life skills
FRLHT
Medico Friends Circle
Alumni Meeting
Alumni Meeting
Communication Skills
93
APD visit
Work shop on Mental Health
Field pictures
Book readings
RMP attached with Medical shop
94
Sanitation workers
Adolescents working instead of parents
Water pumps paved along with open drainage
working in an unfriendly environment
This fellowship has fulfilled the quotation in my life “Cultivation of mind should be the ultimate
aim of human existence” of Dr. B. R. Ambedkar and Set a way forward to “be educated, be
organised and be agitated”.
95
Position: 623 (11 views)