Rajeev_B_R - Final report.pdf
Media
- extracted text
-
Rajeev B R | CHLP Fellowship | February 2015-April 2016
Community Health Learning
Programme Report
SOCIETY FOR COMMUNITY HEALTH AWARENESS AND RESEARCH
ACTION
Contents
Prologue- How I landed at SOCHARA ...................................................................................................................... 5
Learning Objectives.................................................................................................................................................... 8
Community Orientation and Preparation ............................................................................................................... 9
Building Blocks for Fellowship......................................................................................................................... 9
Understanding Community, Society, Development and Health ............................................................ 16
Understanding Community Health and Public Health.............................................................................24
Health system in India ...................................................................................................................................... 27
Social Determinants, Equity and Public Health ......................................................................................... 32
Health Systems and Policy ............................................................................................................................... 34
Environment, Sanitation and Health ............................................................................................................. 37
Local Health Traditions .................................................................................................................................... 41
Field experiences ...................................................................................................................................................... 44
My field area ........................................................................................................................................................ 44
Organisation ........................................................................................................................................................45
Community Health programme ...................................................................................................................... 52
Health Status........................................................................................................................................................56
Religion and Cultural aspects ..........................................................................................................................62
Physical Infrastructure ...................................................................................................................................... 63
Agriculture and food production ....................................................................................................................65
Education ............................................................................................................................................................. 66
Environment ........................................................................................................................................................67
Field Research ............................................................................................................................................................70
Abstract .................................................................................................................................................................70
Background .......................................................................................................................................................... 71
Methods ................................................................................................................................................................ 73
Results: ..................................................................................................................................................................74
Understanding Oral Health ..........................................................................................................................74
Conditions or Symptom Complexes ............................................................................................................ 77
Local Health Traditions.................................................................................................................................78
Social Issues and Challenges ........................................................................................................................ 81
Discussion ............................................................................................................................................................ 81
Conclusion ........................................................................................................................................................... 84
Reflections ............................................................................................................................................................85
Social, Economic, Political, Cultural and Environmental Analysis ......................................................................87
Development Parameters (Axioms) of ACCORD .................................................................................................. 88
Pedalling forward the Community Health Journey .............................................................................................. 89
1
Oral Health in Action ............................................................................................................................................... 94
Oral Health Policy: rational basis .................................................................................................................. 94
Gudalur experience ........................................................................................................................................... 94
London Charter .................................................................................................................................................. 94
Forum for Oral Health Action in India ..........................................................................................................95
Reflections of the Community Health learning Programme ............................................................................... 96
References .............................................................................................................. Error! Bookmark not defined.
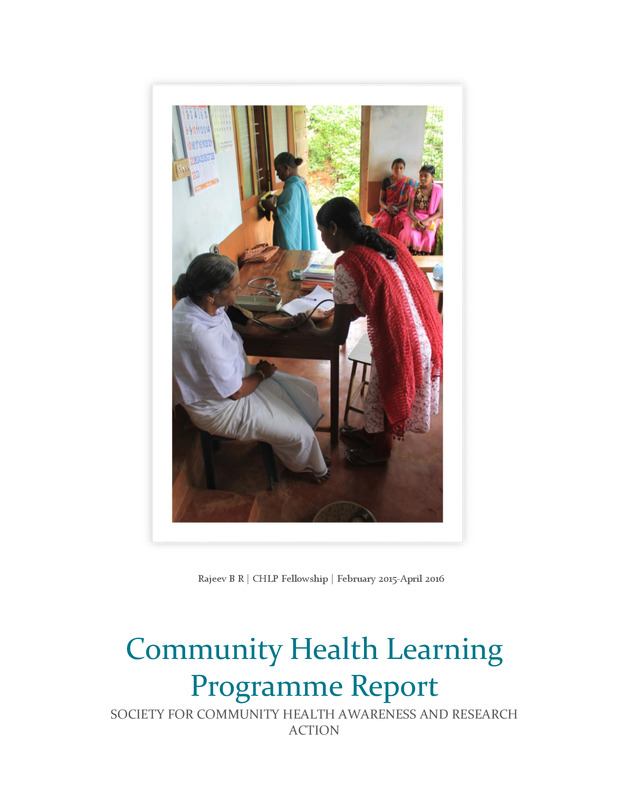
Cover Page photo: Adivasi health worker checking blood pressure of an elderly Mullukurumba
woman at ACCROD’s area centre in Ayyankolli village in the Nilgiris district.
2
I cannot express enough thanks and I am in debt forever to everyone in this journey. This journey
would have not been possible without Samantha and Dr Eugenio at first place. Ravi and Thelma
have been parent figures to me guiding, patting, cheering me every time I found myself in difficult
situations.
SOCHARA is wonderful place with beautiful people with beautiful hearts. Friendly smiling faces
always welcome people here. Mohammed’s immense knowledge on demographics and public
health, Chander’s anti-tobacco and Kumar’s social work experience with various organisations
have been a source of inspiration and joyful learning.
Adithya’s climate change sessions were eye openers, Rahul’s google head was always welcoming
us to discuss, Prasanna’s proverbs and polyglot skills were much appreciated, Janelle’s friendly
and caring attitude, Krishna’s communication techniques, Chandran’s virtual skills and Prahlad’s
santitation sensitivity techniques were not just inspiring but moving. The smooth functioning of
SOCHARA wouldn’t have been possible without Hari Bhaiya, Tulsi Bhaiya, Joseph, Vijayamma,
Kamalamma, Maria, Mathew, Vinay and Victor. They manage logistics efficiently. Special thanks
to the librarian, Swamy who has well maintained this treasure trove. All these made the learning,
a fun filled experience and I want to thank everyone.
At Gudalur, ACCORD and ASHWINI were very supportive. I would like to thank the Adivasi
community for their love and support. My heartfelt thanks to Stan, Mari, Shyla, NK, Rahul,
Ankur, Srikanth, Anna, Bhuvana and Vinoth who made Gudalur experience, a wonderful time.
Special thanks to Mahantu who mentored and guided me. It would not be fun without Royson,
Viraj, Mahesh, Jyothi and all the school children and teachers. I wish to thank Durga, who helped
me writing the consent and information sheet in Tamil and also helped me in transcribing
interviews. Gudalur stay will remain as a special memory.
This journey wouldn’t have been a pleasant one without my co fellows. Finally, I want to thank
my ever supportive family and friends.
3
ACCORD- Action for Community Organisation, Rehabilitation and Development
AMS- Adivasi Munnetra Sangam
ANM- Auxiliary Nurse and Midwife
AMF- Adivasi Mutual Fund
ASHA- Accredited Social Health Activist
ASHWINI- Association for Health Welfare In the Nilagiris
ATLM- Adivasi Tea Leaf Marketing
AYUSH- Ayurveda, Yoga, Unani, Siddha and Homoeopathy
CHESS- Community Health Environment Survey Skill-share
CHLP- Community health learning programme
EAG- Empowered action group states
FRA-Forest Rights Act
HIV/AIDS- Human Immune Deficiency Virus/ Acquired Immune Deficiency Syndrome
IMR- Infant mortality rate
JAAK- Jana Arogya Andholana Karnataka
JSA- Jan Swasthya Abhiyan
LGBT- Lesbian, Gay, Bisexual and Transgender
LHT- Local Health Traditions
LMIC- Low and Middle Income Countries
NRHM- National Rural Health Mission
NHRC- National Human Rights Council
MSS- Mahan Sangharsh Samiti
PHC- Primary Health Centre/care
SOCHARA- Society for Community Health Awareness Research Action
SDH- Social Determinants of Health
TFR- Total Fertility Rate
UHC- Universal Health Coverage
VHSNC- Village Health, Sanitation and Nutrition Committees
VBVT- Vishwa Bharathi Vidyodaya Trust
WHO- World Health Organisation
4
During my training in Dental Public Health, there was lack of contextual understanding of the
entire public health. The course was for three years and I had hardly visited any PHC’s. The only
exposure was when there was dental outreach camp organised in a PHC. I had never met a health
worker or even an ANM. My understanding of villages and their problems were from books,
newspapers and scientific journals. I knew, I lacked the humanness in the training. I studied
5
about the national health programs of India, but didn’t have a solid understanding on their
implications at grass roots. There was a void in my training and When I heard about the
programme modules from both Samantha and Dr Ravi Narayan, it was something I was looking
for.
Besides, my staff at college were not friendly. Their understanding of social determinants was very
poor and didn’t encourage me either. Some of them were rude and hostile too. I would long for a
mentor or guide who is friendly and non-hierarchical. During my training, I undertook an online
offering course of “Health for All” by Johns Hopkins University. The course oriented me to
community health. It was the first exposure to primary health care. The case studies which were
used to explain in the course were success stories on how to bring about change in health status
of a community. Jamkhed1 and Gadchiroli2 projects were used as case studies (Arolle & Arolle,
1974). I understood about a health worker and how they can be agents of change. Since then, I
knew, I wanted that kind of exposure to real life situations and understand for the perspectives of
the people living in affected areas. When I met Dr Ravi Narayan, he was talking about what all I
wanted. I was presented with a training module which exactly what I was looking for.
My interest in humanities goes back to my childhood days. There are few incidents and
experiences during my growing years which had profound influence on my leaning towards
humanities. I was very much interested in Archaeology and History during my school days. I
always took part in social project competitions where I would prepare models and charts on
Egyptian, Roman civilisations and many others. I also won several prizes which further boosted
my interest. It was in one of those times, I came across books on humanities in my school and
public library. I read a lot about how cultures and beliefs in different societies and their influences
on economics, political scene, etc. I had decided that I would study sociology then, but my family
opposed this. They believed that, arts and humanity disciplines would not earn enough bread. My
interest in humanities remained hard, but I chose dentistry as a career out of compulsion.
It was in my third year under graduation, when I was introduced to Preventive and Social
Medicine, my childhood interests were revoked. I showed more interest in the social component
of medicine. It gave a new dimension to my understanding of how health and development go
hand in hand. For ex, the Great sanitary reforms of England which took place in the 18th century
had influenced the public health movement across the western hemisphere and decreased the
prevalence of communicable diseases (Park, 2014). Contrarily, communicable diseases still exist in
India because the structural and socio-cultural determinants are not addressed adequately.
Indigenous cultures exist across the globe and they form a unique ecology. Their behaviours are
in harmony with the environment they live in. The concept of self-sustaining and use of locally
available materials make them more adaptable and amenable to the laws of survival. In such a
context, they place health in the hands of their age old traditions which are yet to be explored.
This is where my interest in public health grew much stronger.
My interest in culture goes back to my roots. My forefathers are from a small village called
Molkalmuru in Chitradurga. It is well known for handloom industry. My forefathers weaved silk
1 Jamkhed is a small town in Ahmednagar district of Maharashtra. Jamkhed project is a Comprehensive Rural Health
Programme started by Drs Mable and Raj Arolle in 1970.
2 Gadchiroli is a district in central India. SEARCH (Society for Education, Action and Research in Community Health)
started by Drs Abhay and Rani Bang in 1985 at Gadchiroli.
6
sarees. Here, Swakulasali, Pattasali and Padmashalis and many other weaving communities have
engaged themselves in the handloom profession for generations. All weaving communities
belonged to the shudhra group of social stratification3. Shudra means one who is skilled in an art.
The artisan strata include wide variety of occupations based on skilled handwork. Thus the
artisans were the suppliers of basic essentials and products for the smooth functioning of society.
From clothes to jewellery, iron to pottery; Shudras were the economical drivers and key
contributors of industry and machinery during the pre-independent India. This class included
tantuvai (weavers), swarnakara (goldsmith), vaidyas (healers) etc.
Molkalmuru silk sarees have a distinct style. Contrast colours of body and border, silver reinforced
gold zari, bird figures such as peacock, swan, parrot, floral pattern, and mango and temple images
are very unique to Molkalmuru style. There is rich history and culture represented in the sarees.
Today, the saree industry is dying. With this, the salubrious culture will also be lost and all will be
a thing of past. The motifs in the sarees not just had an attractive feature and also told a story. For
ex, peacocks and mangos are very common here. It is with no doubt, the flora and fauna also were
a part of daily life and thus adorned the sarees too. The craftsmanship means skills which are
learnt hard way. It represents civilisation and a learned activity which is socially accepted. Sadly,
with sarees gone and not much peacocks left, these all will be forgotten soon. It was not just
about which figure showed up on the saree. It is about how the weaving community understood
the nature around and expressing it in the form of art.
I also want to narrate another incident. This was when I was doing my Master's. My senior
researched on “Comparative Assessment of Knowledge, Attitude and Beliefs on oral health in Siddi
tribals, Tibetan refugees and Local population”. I had doubts about the reliability and validity of
the results of the thesis. His methodology was fairly simple. He visited them only once and
interviewed using a pre designed questionnaire. What puzzled me the most, was, how would one
reveal any personal information to a total stranger? I believe, one has to understand the social
dynamics of a community in all angles to win the confidence and then proceed to ask sensitive
questions.
Through Samantha’s experience at Kalahandi in Orissa, I got a clear picture of how the fellowship
works. Field work would give me an opportunity to live with the community and observe them
closely. Besides, joining CHLP was a calculated risk. The uncertainty of job and the stipend
offered for CHLP was just enough for sustaining and meeting monthly expenses. I took a while to
decide about it. I considered other options of either work or studying further. After much thought, I
decided to apply for this fellowship. I appeared for the interview and later was selected and that's
how I ended up at SOCHARA.
3 Shudra is the fourth varna, whose mythological origins are described in the Purusha Sukta of the Rig veda, one of the
sacred texts of Hinduism, and later explained in the Manusmṛti.
7
General
1.
2.
3.
4.
5.
Learn community action from a community point of view
Understand community health in action
Learn the health system in India- principles, delivery, etc.
Understand the social determinants of health in India
Understand the cultural factors influencing health in India determined by knowledge,
attitudes and behaviour.
6. Learn the quantitative and qualitative tools of measuring the health burden.
7. Understand the intricate networks through which community health functions
Research
1.
Learn conducting a community mapping, ethnographic methods, focussed groups
discussions, key informant interview method.
2. Understand health through anthropological view- human development, interactions and
existence in harmony with environment.
3. Observe and learn the indigenous way of life.
Personal
1.
2.
3.
4.
5.
Working in a team
Understand different cultures of fellow participants
Inculcate more good habits, learn from my mistakes, and become more integral.
Networking with various people from all areas
Learn new languages
8
BUILDING BLOCKS FOR FELLOWSHIP
The batch of 2015-16 consisted a diverse set of people from different backgrounds. There were full
time and flexi (part time) fellows. Most of them were from social sciences background such as
social work, anthropology, law and psychology. Few of them from bio- medical background such
as medicine, dentistry and pharmacy. There were with journalism, textiles and management
background too. People from different parts of India representing north east, north, central, south
and western India were there too with one exception from United Kingdom. This mix of
education, language, culture, etc was unique but posed many challenges in terms of
understanding the subject, language barrier, culture shock to name a few. It was important to
understand others and self at the same time to have a harmonious and cordial relationship with
all the fellows and the facilitators of the programme. The need to learn intra and inter personal
skills became imperative to understand oneself better.
Johari window was first conceptualised by Joseph Luft and Harrington Ingham in 1955 to help
people better understand their relationship with themselves as well as others (Luft & Ingham,
1955). It is a framework to categorise our levels of knowing a person. The arena block represents
traits of a person which are known by that person and others. The Facade block representing
information about a person which their peers are unaware of.
Figure 1: Johari Window
The blind spot represents information that the person is not aware of, but others are and
Unknown representing the person’s character that are not recognized by anyone including the
person. Johari region is what is known about a person by others in the group, but is unknown by
the person him/herself. It is the quadrant 2 - 'blind self' or 'blind area' or 'blind spot'. here are two
key ideas behind the tool: to build trust with others by disclosing information about oneself and
with the help of feedback from others, one can learn about oneself and come to terms with
personal issues. By explaining the idea of the Johari Window, one can help team members to
understand the value of self-disclosure, and you can encourage them to give, and accept,
9
constructive feedback. This can help people build better, more trusting relationships with one
another, solve issues, and work more effectively as a team. The ultimate goal of the Johari
Window is to enlarge the Open Area, without disclosing information that is too personal. The
Open Area is the most important quadrant, as, generally, the more people know about each other,
the more productive, cooperative, and effective will be when working together.
At the end of the Johari class, we were given a sheet of paper to write one good quality about each
other. This exercise was to make the fellows think positively and reflect upon some good qualities
observed in the fellows only within a few days of interaction. It was a test to examine the
observation skills and also about knowing a person much more.
Communication skills were introduced during the first collective session. The two-day
workshop on communications skills was an eye opener and team building and team work
exercise. It opened up every fellow from their inhibitions, timidity, language barrier and
inferiority complex to certain extent. Nearly 90% of the exercise was non-verbal and action
oriented. There were improvisation exercises such as voice modulation, imitation, mime shows
and role plays.
Figure 2: Communication skill workshop in progress
10
The sessions were modelled to train fellows to cope up with challenges that one might face in
field. There were sessions related to role plays to communicate the message effectively with
minimal props. Fellows were divided into two groups to come up with a health issue and conduct
a role play highlighting a health issue and also capturing the nitty grits of daily life. Our group
decided to showcase childhood morbidity and the effective role played by ASHA worker. We used
common diarrhoea as a highlight to draw attention. It was a tedious job to have a consensus on
what we do as a group and, to manage it effectively without falling apart with the group, was the
lesson learnt. Some of the group members were difficult to convince and tried to subjugate other
weak voices. Soft skills expose the dynamics of a group and, more over this exercise was apt at
that time. We were preparing for the field and this exercise helped us in understanding the
management of the community members with whom we have to work.
Figure 3: Fellows in imitation session during the communication workshop
Social skills like interpersonal skills are very vital for anyone who interact and work with people
on a day to day basis. People skills is the ability to communicate effectively with people in a
friendly way. It involves, understanding ourselves and moderating our responses, talking
effectively and empathizing accurately and building relationships of trust, respect and productive
interactions. Soft skills enable those qualities and attributes needed to succeed in community
dialogue. They encompass an individual’s ability to listen well, to communicate effectively, to be
positive, to manage conflict, accept responsibility, show respect, build trust, work well with
11
others, manage time effectively, accept criticism, work under pressure, and demonstrate
discipline.
In one of Dr Ravi Narayan’s class, we were asked the names of our support staff- Mr Tulsi Heera
Adhikari and Mr Hari Ojha or Tulsi bhaiya and Hari Bhaiya as we call them with affection. Dr Ravi
tested us, whether we were good at soft skills. Also, we were subjected to another test. Hari
bhaiya or Tulsi Bhaiya would get us tea twice daily, once at 10 30 am and at 3 pm. We were
observed, whether we helped to serve each other or not. This was also, to check if we had
hierarchical attitude. It was also to know how caste and class biased we were.
During field visits, this was an important people skill to bear in mind. People in the community
would only entertain us when equality is established after the acquaintance stages of relationship
are over. Being unbiased and displaying behaviour of trust, respect, equality is as vital to develop
cordial relationship in order to bring behavioural changes in the community. The tea test, as what
I love to call it, is crucial to establish the initial communication. During my field visits, I was
offered black tea with copious amount of sugar which I detested whole heartedly, was offered at
every house visited and any meeting that I attended. With very less chance to deny the adivasis’
love and hospitality, I would drink it. Dr Ravi would tell us that, it was their way of judging a
person if he or she is discriminator.
Our gender sensitivity was also checked by how many men cared to lift up the flappers in the
toilet.
Our
cleanliness
quotient was also checked if
we cared about flushing
toilets after use, dustbins
used well, cared to keep the
surroundings clean. All
these exercises were to
prepare for any challenges
in field or in future. All of us
got together and cleaned up
the premises of SOCHARA
twice.
We
called
it
Shramadhan4. Shramadan
was popularised during the
freedom movement by M K
Gandhi. It is an altruistic act
of gift of labour or in simple
terms
doing
voluntary
contribution of work for
public
cause.
It
was
Gandhiji’s call to the nation
to do shramdhana at every level to uplift the self and others. Gandhiji wrote in Indian Opinion,
that intellectuals should contribute to upliftment of their fellow labourers by earning a living
through physical labour: “Last but not least, it seems to us that, after all, nature has intended man
Figure 4: Fellows doing Shramadan
4
Shramadana means the giving of your time, energy and skills for the benefit of others without any personal gain or
benefit.
12
to earn his bread by manual labour-'by the sweat of his brow”. (Gandhi, 1910 ). Shramadan today
has become an annual event on October 2nd celebrated as Gandhi Jayanthi, the birthday
celebration of M K Gandhi. People exhibit sycophantic gestures to pose for cameras and media
attention. It is sad to witness the actual shramadan is lost.
We all gloved our hands, picked up brooms to clean up the pile of garbage dumped by passers-by
in front of SOCHARA. The place was a nuisance to eyes and nose. It was a painstaking labour
subjected to heavy duty, stench of the garbage, directly exposed to micro-organisms and insects,
potential danger of infections, etc. The act made us realise how difficult it would be for hundreds
of Pourakarmikas5 who clean up the city every day. The health concerns are many. The detritus
also had sharp objects such as broken glass pieces, needles, blades and severed ends of metals. Dr
Thelma Narayan had provoked us about having civic responsibility of knowing people around us.
She asked if anyone us ever bothered to find out about their lives, or even their names. This
shramadana did stir up interest about the municipal sweepers. Shwetha Gupta, co fellow who
resided in the next building of SOCHARA found out the name of the pourakarmika of her lane.
Her name was Ramulamma who came from neighbouring state of Andhra Pradesh and has been
working for several years. Ramulamma complained that, they don’t get paid on time. The
contract labour laws are often criticised as anti pourakarmikas. (DNA, 2012) They prevent diseases
in cities. Yet they have minimal job security measures. They contract communicable diseases
quite often and do not have free access to medical care. They are underpaid and work involves
manual segregation of waste without self- protection. The occupational safety and health
measures are completely violated. The pourakarmikas put across their demand and held a strike
too. (Ramani, 2015)
Figure 5: Newspaper column showing the demands made by Pourakarmikas
In another session, we were all given three green colour cards and were asked to write about our
personal, professional and expectations of CHLP. I scribbled few thoughts into the paper.
Although, in hindsight, when introspected, some goals and expectations have been met. While
some of them have been re looked. Particularly, professional goals. I wanted to join the CHLP as a
flexi and leave if I got admission for doctoral studies. But, I decided to finish the course, because
the course provided a solid community exposure which I didn’t want to jeopardise.
5 Pourakarmika is a Kannada term referred to labourers who clean the roads and drainage in Bangalore city.
13
Values such as Equity, rights, social justice, inclusiveness, respect for local health cultures,
solidarity and secularism were facilitated at different stages of collective. 2015 was of particular
relevant to the values discussed. The political scene in India and also across the world was
turbulent and many events were testimonies for violating these values. These values are
intertwined and are moral characters which are practised at an individual, family, community,
national and global level in an egalitarian world. All religions advocate theses values. They are
integrated in a person as one grows. Values are decided by the society and evolve over time. These
values conflict with greed, ego and selfishness. These values have been used as a weapon to
influence critical mass in social movements. Dr R Srivatsan, a political theorist who was the
convenor of medico friends circle6, mentioned about Gandhiji’s Ramarajya7 concept as a utopian
political independence thought. (Gandhi, 1937) Gandhiji adopted seva8 for Harijans9, Mitratva10
for Muslims and Satyagraha11 against the British.
Values relate to the norms of a culture, but they are more global and abstract than norms. Norms
provide rules for behaviour in specific situations, while values identify what should be judged
as good or evil. While norms are standards, patterns, rules and guides of expected behaviour,
values are abstract concepts of what is important and worthwhile. A silent prayer offered for the
victims of Chennai cyclones during the National Dissemination meeting was a norm but reflects
solidarity. Values are generally received through cultural means, especially transmission from
parents to children. Parents in different cultures have different values. For example, parents in
a hunter–gatherer society or surviving through subsistence agriculture value practical survival
skills from a young age. The adivasis12 of Gudalur where I did my field observations showed
immense community bonding and sharing. Mari Marcel Thekaekara, co-founder of ACCORD and
a regular columnist at New Internationalist shares her views about sharing and caring among the
adivasis of Gudalur. She mentions how a young Adivasi girl shared a biscuit with her siblings
given to her (Thekaekara, 2015). Values such as these are a part of their lives and they don’t seem
to be puzzled by these gestures.
All these values are to be taught and learnt by self or through others at home, school, college,
university, work place, etc. Community health learning begins with recognizing these values as an
important part of our lives. Important to us is rights. Right to health is a fundamental right to
attain highest possible standard of health. Community health emphasizes rights and entitlements
as one of the axioms.
Secularism was by far the most argued topic in the past one year in print and social media. New
terms such as “Sicklularists” have sprung up. In my opinion, secularism means to treat everyone
and everything equal. Indian constitution upholds secularism. Accordingly, all religions,
languages, people and cultures are equal. Secularism in India, thus, does not mean separation of
religion from state. Instead, secularism in India means a state that is neutral to all religious
6 medico friends circle is a think tank founded in 1974 by a group of people inspired by socialism and left movements.
The founders were followers of freedom fighter, Jayaprakash Narayan.
7 Ramarajya- Gandhian idea of political independence, i.e., sovereignty of the people based on pure moral authority
8 Seva is a selfless service offered to anyone in need.
9 Harijans is a word coined by Gandhiji referred to Dalits who were considered untouchables.
10 Mitratva is Sanskrit term for friendship.
11 Sathyagraha means “insistence for truth”. It was a non-violent resistance which Gandhi used in his campaigns in
South Africa and India.
12 Adivasis or original inhabitants. I prefer to use the term instead of tribal. Adivasis also means indigenous.
14
groups. Romila Thapar, noted historian shares her views on secularism. “A secular society and
polity does not mean abandoning religion. It means the religious identity of an Indian has to give
way to the primary identity of a citizen. And the state has to guarantee the rights that come with
this identity, as the rights of citizenship”. (Thapar, 2015)
Denial of Right to Health is the most argued case in almost all LMIC. A national level public
hearing on denial of right to health in public and private sector was organised by NHRC in
association with SOCHARA, JSA, JAAK and other civil society organisations13. The meetings were
held at four different places in India. The southern regional meeting was convened in Chennai
and was to be held on December 14 and 15th, 2015. The deluge at Chennai forced NHRC to cancel
the meeting.
According to WHO, “The right to the highest attainable standard of
health” requires a set of social criteria that is conducive to the health
of all people, including the availability of health services, safe
working conditions, adequate housing and nutritious foods.
Achieving the right to health is closely related to that of other
human rights, including the right to food, housing, work, education,
non-discrimination, access to information, and participation.
The right to health includes both freedoms and entitlements.
Freedoms include the right to control one’s health and body
(sexual and reproductive rights) and to be free from interference
(free from torture and from non-consensual medical treatment
and experimentation). Entitlements include the right to a system
of health protection that gives everyone an equal opportunity to
enjoy the highest attainable level of health.
Vulnerable and marginalized groups in societies are often less likely
to enjoy the right to health. Three of the world’s most fatal
communicable diseases - malaria, HIV/AIDS and tuberculosis disproportionately affect the world’s poorest populations, placing a
tremendous burden on the economies of developing countries.
Conversely the burden of non-communicable disease – most often perceived as affecting highincome countries is now increasing disproportionately among lower income countries and
populations. Violations or lack of attention to human rights can have serious health
consequences. Overt or implicit discrimination in the delivery of health services violates
fundamental human rights. Many people with mental disorders are kept in mental institutions
against their will, despite having the capacity to make decisions regarding their future. On the
other hand, when there are shortages of hospital beds, it is often members of this population that
are discharged prematurely, which can lead to high readmission rates and sometimes even death,
and also constitutes a violation of their right to receive treatment.
Figure 6: Newspaper
advertisement on NHRC
meeting
The goal of a human rights-based approach is that all health policies, strategies and programmes
are designed with the objective of progressively improving the enjoyment of all people to the right
13 The word ‘Civil Society Organisation’ is deliberately used for substituting Non-Governmental Organisations.
15
to health. Interventions to reach this objective adhere to rigorous principles and standards,
including: Non Discrimination, Availability, Accessibility, Quality, Acceptability, Accountability
and Universality. (WHO Committee on Economic, 2009)
UNDERSTANDING COMMUNITY, SOCIETY, DEVELOPMENT AND HEALTH
Understanding a community is an arduous task. It involves careful observation of everything
without making a value based judgment and reporting honest picture devoid of preconceptions. It
is a hard assignment to be non- prejudiced. Our upbringing is always modelled on the basis of
questioning and critiquing. The very essence of science is based on the strong foundations of
questioning the way it is, and understanding things the way they function means getting down to
a level where one sheds his or her hierarchical attitude and looks through the eye of the
observant.
The concept of community is a sociological construct. It is a set of interactions, human
behaviours that have meaning and expectations between its members. Not just action, but actions
based on shared expectations, values, beliefs and meanings between individuals. Observation is
the key here. It involves careful watch of the functioning of a system. Observation is the
foundation of descriptive studying. The cognitive senses have to be working at their best to be
accurate. Reporting as it is, is not as easy as it seems so. The observant should have an eye for it
and write whatever appeared to the eyes, which means that, it is a skilful job
and highly competent work. A thorough knowledge of what has to be done. Even while
everything works well, acknowledging the grey areas in between apparent black and white is the
real challenge. My understanding of the community is still in a nascent level and I think, I have
made an attempt at understanding little bit of the black and white areas, although some of the
grey areas were understood in due course with help.
Community is defined as “a group of people with diverse characteristics who are linked by social
ties, share common perspectives, and engage in joint action in geographical locations or settings”.
(Kathleen M. MacQueen, 2001 ) According to a research, community has five core elements—
locus, sharing, joint action, social ties, and diversity which were was cited by 20% or more of
respondents. (Kathleen M. MacQueen, 2001 )
Community largely encompasses animate and inanimate objects. There is an objectification of
characters such as our people, my place, etc. and that determines the identity of a person or a
group of people. Society is a web of social relationships. It includes every relationship which
established among the people. This social relationship may be direct or India organised or
unorganized, conscious or unconscious. But community consists group of individuals. A definite
geographical area is not necessary for society. It is universal and pervasive; but, a definite
geographical area is essential for a community.
Community sentiment or a sense of "we feeling" is not essential in a society; community
sentiment is indispensable for a community. There can be no community in the absence of
community sentiment. Society is wider; there can be more than one community in a society.
Community is smaller than society. There cannot be more than one society in a community.
Society is abstract. It is a network of social relationships which cannot see or touched. On the
16
other hand, community is concrete. It is a group of people living in a particular area. We can see
this group and locate its existence.
A collective is a group of entities that share or are motivated by at least one common issue or
interest, or work together to achieve a common objective. Collectives differ from cooperatives in
that they are not necessarily focused upon an economic benefit or saving, but can be that as well.
Class and Caste have differences have existed in India and elsewhere since time immemorial. Dr.
Ketkar defines caste as "a social group having two characteristics: (i) membership is confined to
those who are born of members and includes all persons so born; (ii) the members are forbidden
by an inexorable social law to marry outside the group." Baba Saheb Ambedkar, the architect of
Indian Constitution, argues that caste existed long before Manu14. (Ambedkar, 1979) He was an
upholder of it and therefore philosophised about it, but certainly he did not and could not ordain
the present order of Hindu Society. His work ended with the codification of existing caste rules
and the preaching of Caste Dharma. At the outset that the Hindu society, in common with other
societies, was composed of classes and the earliest known are (1) the Brahmins or the priestly
class; (2) the Kshatriya, or the military class; (3) the Vaishya, or the merchant class; and (4) the
Shudra, or the artisan and menial class. He further argues that, particular attention has to be paid
to the fact that this was essentially a class system, in which individuals, when qualified, could
change their class, and therefore classes did change their personnel. His thesis revolves around
proving that some castes were formed by imitation, the best way, it seems to me, is to find out
whether or not the vital conditions for the formation of castes by imitation exist in the Hindu
Society.
This process of imitation is coined as “Sanskritisation”15 by eminent Sociologist and Anthropolgist,
M N Srinivas. (Srinivas M. , 1952) In today’s times, there is a myth that caste and class practices
are predominantly observed in rural areas, which is often the reason quoted for migration after
job opportunities. Dr Ravi Narayan mentions that, class and caste practices are more obvious in
urban educational centers. (Collective notes) The unfortunate death of Mr Rohit Vemula, a Dalit
doctoral scholar is a typical example of urban caste practices. The 26-year-old PhD student killed
himself inside the campus of Hyderabad Central University. Rohit was a member of the
Ambedkar Students' Association, which fights for the rights of Dalit (formerly known as
untouchable) students on the campus. He was one of five Dalit students who were protesting
against their expulsion from the university's housing facility. The five faced allegations that they
attacked a member of the Akhil Bharatiya Vidyarthi Parishad - the student wing of India's ruling
Bharatiya Janata Party. They all denied the charge and the university cleared them in an initial
inquiry, but reversed its decision in December, 2015. Rohit in his suicide note, he writes, (Vemula,
2016)
14
Manu is the name accorded to the progenitor of humanity, He is ascribed to the Sanskrit text, Manusmriti which is
considered by some Hindus to be the law laid down for humans.
15
Sanskritisation may be briefly defines as the process by which a ‘low caste’ or tribe or other group takes over the
customs, ritual, beliefs, ideology and style of life of high and in particular, the twice born (dwija) caste.
17
“The oppressive attitude of bureaucracy and brahminical mindsets of a few… The value of a man was
reduced to his immediate identity and nearest possibility. To a vote. To a number. To a thing. Never
was a man treated as a mind. As a glorious thing made up of star dust. In very field, in studies, in
streets, in politics, and in dying and living"
Swami Vivekananda said: "Caste is an imperfect institution, no doubt. But if it had not been for
caste, you would have had no Sanskrit books to study. This caste made walls, around which all
sorts of invasions rolled and surged but found it impossible to break through." The newly created
Telangana state’s movement started off as a Dalit movement and politically motivated campaign.
Policy towards Dalits is often criticised as appeasement and vote bank politics rather than
genuine desire for uplift of the backward classes. Despite the commonly held belief that casteism
and untouchability are prevalent only in rural India with few traces of this practice in
cosmopolitan cities, a report reveals notions of impurity and inferiority that still dictate the
occupations and livelihoods of Dalits, particularly in the city of Hyderabad. (Mehta, 2015) Swami
Vivekananda’s words are true in this case. Caste has made an impregnable walls and these provide
platform for vote bank politics.
Today’s, class discrimination is not caste based, but it is the urban elite education based; opines
Dr Ravi Narayan. (Collective notes) Rohit’s suicide created a stir in nation. Politicking of his caste
status also picked up instantaneously. Caste based reservations continue in government and
educational institutions. There is a hidden discrimination of the scheduled castes and tribe
students in educational institutions. It is much more obvious in government offices. Government
jobs are called based on reservations. The Maharaja of Mysore, Shri Krishnaraja Wodeyar IV and
his Diwan, Sir Mokshagundam Vishweshwaraih argued on caste based reservations. Sir M V had
opposed caste based reservations. He stated in his memoirs, “My idea was that by spreading
education rapidly and adopting precision methods in production and industry, the State and its
entire population would progress faster. By ignoring merit and capacity, I feared production would
be hampered and the efficiency of the administration” (Vishweshwaraih, 1951)
The new class of educated middle class urban elite have bought about a new dimension to caste
and class issues. There is a feeling of threaten among a lot of educated mass. The identity crisis
which is a result of heavy competition has led to class distinction. The most affected are the
scheduled tribes, especially the adivasis. Their primitive traits, geographic isolation, shyness with
the community at large have made them vulnerable to exploitation.
Social exclusion in today’s times is no more related to caste oppression and women exploitation.
The structural determinants which enable a person or group of people to go below the line of
social mobility is a recognised fact. LGBT, minorities, debt ridden farmers, SC and ST, adivasis,
migrant labourers, urban slum dwellers, people with mental and physical disabilities, drug
addicts, delinquent etc. face discrimination and marginalisation at many levels.
According to the WHO’s Social Exclusion Knowledge Network, Exclusion consists of dynamic,
multi-dimensional processes driven by unequal power relationships interacting across four main
dimensions - economic, political, social and cultural - and at different levels including individual,
household, group, community, country and global levels. It results in a continuum of
inclusion/exclusion characterised by unequal access to resources, capabilities and rights which
leads to health inequalities. (Jennie Popay, 2008)
18
Social exclusion will have direct consequences on the health inequalities. Both of them have
underlying social and structural determinants governing the relationship. The WHO Commission
on Social Determinants of Health (CSDH, 2006) framework for action on health inequalities
highlighted the socioeconomic and political context and including: the labour market; the
educational system; religion and other cultural systems; and political institutions. These give rise
to patterns of social stratification based on differential access to economic status, power and
prestige. Income levels, education, occupation status, gender, race/ethnicity and other factors are
used as proxy indicators of these differential social positions. Based on socioeconomic position
individuals and groups experience differences in exposure and vulnerability to healthcompromising conditions. Socioeconomic position determines the level or frequency of exposures
and the level of vulnerability (intermediary factors through which social inequalities generate
health inequalities). The fundamental driving force for social inequalities and thus for health
inequalities within the CSDH framework is ‘power’ embedded in social relationships and
exercised through the formal and informal institutions and organizations making up the
socioeconomic and political contexts.
Figure 7: WHO framework of Health inequalities and social determinants
Power dynamics play a major role in health. Underneath questions of injustice and inequality is
the question of power. Power is the degree of control over material, human, intellectual and
financial resources, exercised by different sections of society. (Miller, 2006) Empowerment of
women, oppressed, weaker sections is the common talk by sociologists, activists and social
workers.
Empowerment is a strong social process involving power dynamics. When we say, women
empowerment, it means giving equal power to women in all situations. It is a social, economic
19
and politically ascribed status delivered to women. At a family level, woman empowerment means
the husband or the men in the family give equal status. It is the same at community level too.
Community empowerment is a dynamic process where the oppressed or the weak are able to
access entitlements and exercise rights.
It is a complex situation where the stronger section of the society is ready to accord the equality
and equity position to the weaker. It is often mistaken and implied that, empowerment is
enabling the powerless to become aware of their rights. But, it is forgotten and misled by civil
society organisations, media and politicians. For ex, the 33% reservation for women in the Indian
Parliament is perceived as instrument to gain equal status as men. In my opinion, empowering
only happens when the men are ready to share the platform along with women, rich are ready to
help poor, government is ready to structurally elevate poverty, etc. Nevertheless, women have
achieved incredible success as change agents. Majority of the health workers are women. Had
they not actively participated in the health care delivery, women and children related diseases
would still have been in an upsurge motion.
Dr Ravi Narayan narrated a story about community empowerment which he was part of, Mallur
Health Cooperative: In Mallur village in Karnataka, a health cooperative attached to a milk
cooperative was set up way back in 1973. Encouraged by the success of the milk cooperative, the
members persuaded doctors of the St. John Medical College to start a health care centre, which
would be self-sustained, financed and managed by the community. The health cooperative
provides services to nearby villages. During the first two years, members contributed at the rate of
one-two paise per litre of milk sold by them. Subsequently, five percent of the profits from milk
sale were given to the health centre. (ICMR, 1976)
Community empowerment is also a process where the community is aware of the issues around
them and take right informed decisions to deal the issues. It encompasses the principles of health
promotion. Health promotion is the process of enabling people to increase control over, and to
improve, their health. It moves beyond a focus on individual behaviour towards a wide range of
social and environmental interventions. (Promotion, 1986.) The Lalonde report16 from the
Government of Canada, which contained a health promotion strategy "aimed at informing,
influencing and assisting both individuals and organizations so that they will accept more
responsibility and be more active in matters affecting mental and physical health".
Another example for community empowerment is the adivasis of Gudalur. ACCORD started
working in 1984 with land rights movement. Within two years of their work, ACCORD with AMS
was able to reclaim about two thousand acres of land from local land lords. The Adivasi
community realized that they had poor access to health care despite presence of primary health
care centres. The PHC staff discriminated them and ill-treated most often. They realized that they
wanted a health care and, thus they demanded for health services to ACCORD. It was at that
time, Dr Devadasan and Dr Roopa started the community health programme. The community
health programme was able to reduce communicable diseases to a great extent. But, the acute
conditions, emergencies couldn’t be handled and mortality still continued. The adivasis realized
16
Marc Lalonde, who was the Canadian Minister of National Health and Welfare in 1974, proposed a new "health field"
concept, as distinct from medical care. The new concept "envisage[d] that the health field can be broken up into four
broad elements: Human biology, Environment, Lifestyle, and Health care organization;" that is, determinants
of health existed outside of the health care systems. It was one of the first documents which drew global attention
towards social determinants of health.
20
that they need a hospital to handle emergencies. Thus, a adivasi community owned hospital came
into existence. The Adivasi ownership changed the power dynamics in Gudalur. The hospital was
open to non-adivasi too, but they had to get permission from the local sangha17 to avail treatment.
Until then, the adivasis were dependent on non-indigenous people for many things. With quality
care provided at the hospital, non-indigenous people began to realise that they were dependent
on adivasis for health. The power was now vested in adivasis or it was hard earned and also
importantly shared by non-indigenous people.
Even 67 years after Independence, the problems of Adivasi communities are about access to
basic needs. These include, but are not restricted to, elementary education, community
healthcare, sustainable livelihood support, the public distribution system, food security, drinking
water and sanitation, debt, and infrastructure. For them, equality of opportunity remains largely
unfulfilled. In this context, it is important to stress that the values of adivasi18 culture are
transmitted in a manner that protects the right of the bearers of knowledge to determine the
terms of the transmission without exploitation or commodification. Nor can the Adivasis’
unhindered access to land and forests, especially in scheduled areas, be understated. Indigenous
communities have, over the decades, witnessed the fragmentation of their habitats and
homelands and the disruption of their cultures through predatory tourism. All this has left them
shattered and impoverished. Entire communities across states have been dispossessed
systematically through state action, and have been reduced from owners of resources and wellknit, largely self-sufficient communities to wage earners in agriculture and urban agglomerates
with uncertain futures. Yet, we can scarcely forget that the rights of adivasi communities in India
are protected by the Constitution and special legislations.
Indigenous communities across the world face extinction, social exclusion, exploitation,
marginalization, main streaming, acculturation, etc. Scores of these largely self-sustaining
traditional communities continue to this day in remote jungles, forests, mountains, deserts, and
in the icy regions of the north. A few remain completely isolated from modern society. Their
home is under threat. Most forests where the indigenous communities dwell are source of
minerals such as coal, timber and other resources. These attract industries and apathy by
governments cause conflicts. Some of them even give way to extremist activities and have resulted
in naxal and maoist movements. The identity crisis particularly of culture, environment, religious,
etc have led to the present conflicts.
The people of Mahan19are facing the threat of wipe out. Giant corporations like Essar and
Hindalco are after the coal reserves below these forests. Over 14,190 lives and livelihoods were
dependent on the Mahan forests, Madhya Pradesh. Their culture, community and lives are
intertwined with the forests that the corporations threaten to destroy. Displacement from their
natural habitat was devastating for the indigenous community.
17 AMS- Adivasi Munnetra Sangam (www.adivasi.net) is a conglomerate of village level groups called sanghas containing
members from the indigenous communities.
18 The term has vernacular and local synonyms such as Girijanalu (Hill inhabitants) in Andhrapradesh, Kaadu
Manushyaru (forest dwellers) in Karnataka, Malaivasi (Hill inhabitant) in Tamil Nadu, Adibasi (same as adivasi) in
Orissa, Chattisgarh and Jharkand.
19
Mahan in Madhya Pradesh is one of the oldest Sal forests of Asia
21
Hindalco and Essar want to mine for coal in Mahan. The coal mining companies pose a threat to
destroy the lives of the indigenous people of Mahan. The people of Mahan have come together to
reclaim what is theirs. The MSS was formed in March 2013 to protect the forests and land from
coal mining. Since then, the MSS has expanded to 11 villages. They have also organised rallies and
public meetings to raise awareness of their rights in the region. The Forests Rights Act20 (2006)
entitles communities to decide for themselves. It recognises forest dwellers’ rights and makes
conservation more accountable. In Mahan, the people are fighting for their right to ensure this
law is implemented and their rights are respected. With the help and support of Greenpeace
international and other environmental activists, MSS was able to get a stay from the court on the
mining activities. (Greenpeace, 2013)
Another success story of Adivasi struggle is Niyamgiri in Odisha21. State-owned Orissa Mining
Corporation, which was granted mining rights for 30 years in 2004. It was granted a right to mine
in the Niyamgiri forest area which is rich in bauxite deposit, to supply ore to Vedanta Resources.
In 2013, a dozen villages in southern Odisha invoked their right to worship the Niyamgiri hilltop,
warding off government plans to open a bauxite mine in their neighbourhood. The struggle ended
up in the court. The Supreme Court passed a historic and exceptional referendum order in
January,2014, to refuse final forest clearance to the proposed mine. Environmentalists world over
celebrated the victory of the Dongariah and Jarnia Kondhs primitive tribal groups from one of
least developed corners of the country. But the state government has gone back to the court to
revoke the case. (MOHANTY, 2015)
Legally and constitutionally, Clause 5 of Article 19, specifically is concerned with protection of
interests of scheduled tribes as distinct from other marginalised groups through limitations on
right to freedom of movement [sub-cause 1(d)] and right to freedom of residence [sub-clause
1(d)]. This, with existing protections offers a core and express fundamental right protection to
adivasis (as distinct from legal/ statutory protection) from a range of state and non-state
intrusions in scheduled areas as well as from the perennial threat of eviction of adivasis from their
homelands. (Kannabiran, 2015)
Stephany reports about Eco Village. Traditional indigenous communities offer the best example of
sustainability. Worth mentioning is Eco villages. Ecovillages aren’t about technology. They are
locally owned, socially conscious communities using participatory ways to enhance the spiritual,
social, ecological and economic aspects of life. Findhorn Ecovillage in the United Kingdom is one
of the best known and has half the ecological footprint of the UK national average. It includes 100
ecologically-benign buildings, supplies energy from four wind turbines, and features solar water
heating, a biological Living Machine waste water treatment system and a car-sharing club that
includes electric vehicles and more. (Leahy, 2015)
Traditional knowledge and a holistic culture is a key part of the longevity of many indigenous
peoples. The march of progress means that efforts are being made both to extract the resources
on which these communities rely and to ‘mainstream’ indigenous groups by introducing Western
medical, educational and economic systems into traditional ways of life. The traditional medicine
20 The Scheduled Tribes and Other Traditional Forest Dwellers Act better known as Forest Rights Act passed in 2006
upholds the rights of forest dwellers across India's forest areas for democracy, livelihood and dignity.
21 Odisha, previously called Orissa is a state in the eastern side.
22
practiced by the indigenous communities relies entirely on the forest for herbs and medicinal
plant sources. It is well documented that, some of the modern medicines are derived from the
traditional indigenous medicine knowledge.
It is important to preserve these biodiversity cultures and practices, especially local health
traditions. The Karnataka knowledge commission was set up in 2000 to focus on the key
components of the public health system in Karnataka state. The knowledge commission charted
an actionable plan to revitalise local health traditions by state patronage and encouraging LHT’s
based home remedies and recognising LHP to strengthen local health traditions in primary health
care through state and university accreditation mechanisms. (Karnataka Knowledge Commission,
2012)
Agrarian distress is another important social issue that is plaguing the country. There is an
increase in the number of farmer suicides across India. Inflation, loans and debts, failure of
rainfall, pesticide and insecticide issues, increase in the price of fertilisers and falling prices of
crops, political treaties, etc are among the many reasons for this social issue.
The agrarian distress can be traced back to Green revolution22 . The introduction of genetically
modified seeds which yielded high production of crops. This genetically modified seeds also
require heavy feed of fertilisers and pesticides. Heavy use of chemicals and continued high
production of crops at a massive scale have rendered the lands untenable. Climate change and
less rainfall have pushed farmers to edge.
With the liberalization of the economy in 1991, more banks started giving loans to farmers to buy
heavy machinery including tractors and to dig tube wells. More agriculture based industries like
Monsanto came in. The underlying agrarian crisis is a result of marginalization of agrarian
economy in national policy since the economic reforms of 1991. The increasing growth of
multinational companies’ influence in the changing global political economy is apparent. This
coincides with the quiescence of farmers’ movement as compared to 90’s which is reflected in the
changing rural society and their attitudes. (Posaani, 2009)
Many activists and civil society organisations have been fighting against the lobbying of
developed countries and supranational companies in imposing treaties and sanctions on
developing countries. The commonly debated topic is the price fixing on crops based on the
international trade as against the free trade. Vandhana Shiva, a noted activist has been in the fore
front of agitation against Monsanto and other agriculture based companies who are trying to
monopolise the agricultural market. Control over seed is the first link in the food chain because
seed is the source of life. When a corporation controls seed, it controls life, especially the life of
farmers.
22 Green Revolution in India was a period when agriculture in India increased its yields due to improved agronomic
technology. The introduction of high-yielding varieties of seeds (hybrid seeds) and the increased use of
chemical fertilizers and irrigation led to the increase in production needed to make the country self-sufficient in food
grains, thus improving agriculture in India. The methods adopted included the use of high-yielding varieties of seeds
with modern farming methods. Measures adopted were the use of high yielding varieties of seeds or hybrid seeds,
expansion of irrigation infrastructure, use of insecticides and pesticides, consolidation of holdings, land reforms,
improved rural infrastructure, supply of agricultural credit, use of chemical or synthetic fertilizers, use
of sprinklers or drip irrigation, use of advanced machinery and the use of vector quantity.
23
The Agreement on Agriculture, negotiated during the Uruguay Round of the General Agreement
on Tariffs and Trade, which determines the price of crops is criticised for
reducing tariff protections for small farmers, a key source of income in developing countries,
while simultaneously allowing rich countries to continue subsidizing agriculture at home.
In July 2015, as many as 90 farmers committed suicide in Mandya and Mysore districts of
Karnataka. The relatives of deceased reported that lack of institutional credit as major problem.
(The Hindu, 2015) This issue was also riased in the legislative sessions. Activists and the media
rightly question loopholes in the National Crime Records Bureau data, pointing out that several
state governments often report no farm suicides, contrary to local media reports. Suicides of
farmers represent only the tip of the iceberg. Farm suicides, whether owing to purely agricultural
reasons like crop failure, or the complex pressures on an Indian farmer, must be tackled seriously
on the basis of a comprehensive examination of the causative factors, and the context.
UNDERSTANDING COMMUNITY HEALTH AND PUBLIC HEALTH
Community health is a process of enabling people to exercise collectively their responsibility for
their own health and to demand health as their right. It involves the increasing of the individual,
family and community autonomy over health and over organisations, means, opportunities,
knowledge, skills and supportive structures that make health possible. (CHC Team, 1989)
Public health is more technical field. It involves epidemiological investigations to produce
evidence based information. The social influences on public health include the current paradigm
of individual responsibility and independence, as opposed to community-based values.
Community health deals with translating the information obtained into a meaningful action.
Meaningful action means, the information of the community, by the community and for the
community. Community is involved in the decision making right from the conception of the
problem. It is a political stand taken to emphasise the democratic values. Community is
empowered to make their informed decisions.
Public health also works towards translatory reseach and action. For example, in case of Malaria,
the preventive strategy is to provide insecticide treated nets. This is based on evidence based
research results. One of the preventive startegies for HIV/AIDS is use of condoms by men. In both
these cases, the preventive strategies are accepted methods of disease transimission. But, in
reality, this strategy has met with many challenges and is proved to be partially successful. Use of
condoms has many psychosocial factors associated with it. Some people might object to the use of
latex or some aren’t comfirtable using it.
In case of Malaria, particularly among the indigenous communities of Madhya Pradesh, it was
observed that Malaria still continued to be prevalent despite governement providing insecticide
treated nets. After careful observations, it was seen that the Bharia and other indigenous
communities didn’t use the nets. Most of these people were engaged in collecting Mahua 23. They
would go into the forest during April and stay there coinciding with the blossoming of Mahua
flower. During these times, it was observed they wouldn’t use the nets or some would use them to
cover the trees to collect the flowers into the net. Malaria incidence peaked during April and was
23 Mahua- Madhuca indica, a flower found in the forests of central India. It is used for making liquor.
24
mainly seen in those who ventured into forests to collect flowers. (Collective notes, 2015). It was
clear about the causative relationship between Malaria peaking during April and the activites of
the people. This discovery was possible bacause, there was an effort to understand the causality
from the community point of view. This falls in the room 4 of Johari window. It was unknown to
both people and the investigators why nets failed to prevent Malaria.
Community health focusses on this aspect of why certain thing fails and certain things work. It
involves careful observation of the community from a sociological and anthropological lens to
understand the community dynamics. It is that effort to make the community to feel that health
is a fundamental right and they are entitled to basic primary care. It is a medium in which health
is advocated by the community theemselves. The community is placed at the cetre of an issue and
helped to solve the problem through action that is locally relevant with an ultimate aim of ‘Health
for all’. Community health recognises that health is not just biomedical construct, but the cause of
health issues are rooted outside the framework of medical personnel and infrastructure. It weighs
heavily on the social and structural determinants of health.
Individuals recognised for their social skills are identfied from the community and are used as
change agents. Dais24, health workers, community leaders such as local health healers, village
heads and indigenous community chiefs are engaged continuosly to communitise health. There is
collective dimension and consensus building within the community to analyse the situationa and
prioritise issues. Community health action emerges from contect of wider sociao-economic,
cultural process of change and aims at an integrated approach to reduce duplication of the work,
and establishes interactive communication to disseminate community health perspectives into
masss education. A dialogue is established with key governement planners, policy makers and
community members and feedback is valued to continuosly modify the strategies. Community
health is a movement overviewing community empowerment especially marginalised groups,
sharing of resources, networking, socio-epidemiological approach to priority setting to solves
issues and linking with other social movements to garner support and stand in solidarity.
(Community Health Cell-Red book, 2011)
Axioms of Community Health was facilitated by Mr Prasanna Kumar Saligrama and Mr
Chander S J. The axioms or principles of Community Health is a summary of axioms derived from
the reflection of SOCHARA team. The axioms are a result of analysis built on grounded theory to
evolve alternative approach to understand and practice community health. The alternative
approach to community health that emerged became known as ‘social paradigm of health’ and
was rooted in the framework of rights and responsibilities. (Cell, 2011)
1.
Rights and Responsibilities: In Gudalur, the adivasis demanded for health care and as a
result of it, they have an excellent model of community health programme. (Fieldnotes,
2015) It is embodied in the Health Promotion concept. ‘The process of enabling people, to
exercise collectively their responsibility, to their own health and demand health as a right’.
2. Autonomy over Health: Manikantan, who was a health worker and now working as lab
technician at ASHWINI mentioned that, in his childhood, they had come across many
deaths. Once he became a health worker, he realised it was easy to prevent many deaths
through simple measures and vaccinations. He along with other highly motivated young
adivasis worked at villages to improve the health status. When they realised that some
24 Dai is the traditional midwife
25
deaths weren’t preventable with the existing infrastructure and added discrimination at
public health care facilities, they realised the need to have a hospital for themselves. This
autonomy for self-care and taking health matters into their hands is what community
health aims at. The community members explored the opportunities, used their existing
knowledge and took support from others to make health possible. (Fieldnotes, 2015)
3. Integration of Health and development activities: Community health approach includes
attempt to integrate health with development activities including education, agricultural
extension and income generation programmes. Gudalur is a typical example of
community development integrated with health activities. It all started as land rights
movement and community health came later. ACCORD felt the need for a school based
on alternative model and value based education, tea was grown in the land reclaimed,
soap making and honey processing and selling in fair trade market. All these development
activities complimented health. The health programme was a comprehensive approach
oriented at preventive and curative services. The local indigenous healers are encouraged
to be a part of the health system. Some of the dais were trained to be health workers.
Community based health insurance was implemented to sustain health programme. (N
Devadasan, 2004) Adivasis are organized into groups at village level to form sanghas for
increased involvement and participation of the community through formal organization
(AMS), health team, finance team, education team, etc. (Fieldnotes, 2015)
4. Decentralised democracy at community level: This value system pervades the interaction
between the community and health action initiators. A non-hierarchical, participatory,
people centred, team building and empowering ethos built in the system is the
community health approach.
5. Equity and Empowering community beyond social conflicts: The system should be
inclusive and equitable. It should reach out to the marginalized. The Kaattunayakans
consider Bettakurumbas and Panniya25 group as inferior, but the community health
programme at ASHWINI is impartial and involves all sections of the society even the nonindigenous group. ACCORD, AMS and ASHWINI recognizes the cultural differences
between the indigenous groups and have a sensitive approach to community health.
Figure 8: Adivasi team members meeting at ACCORD
25
Kaattunayakans, Mullukurumba, Bettakurumbas and Panniya are the four indigenous groups present in Gudalur and
Pandalur taluqs of Nilagiris.
26
6. Promoting and enhancing the sense of community: The efforts to imbibe the concept and
spirit of community, to improve group dynamics and group inter-relationships are
preliminary to evolve community actions.
7. Confronting biomedical model with new attitudes skills and approaches: Gudalur model
works on the primary health care model. Although an effort to counter the
compartmentalization of professional activities is carried out, it faces many hurdles. The
non-hierarchical and participatory decision making systems allows people of the
community to discuss and express their views.
8. Confronting the existing super structure of medical/health care to be more people and
community oriented:
9. New vision of health and health care and not a professional package of actions:
10. Effort to build a system in which health for all can become a reality:
Figure 9: Panniya traditional dance at Putheri festival. The dance and music bring communities
together and enhance sense of community
HEALTH SYSTEM IN INDIA
Health disparities in India. Inequalities are a part of all societies. Disparities exist across all
aspects of life. Without the object of difference, monotony will take a pedestal. But where do we
need disparities and where not, is an objective thought that reflects the values of any society. AS
Humans, we are different in almost all aspects. We speak different languages, wear different
clothes and eat varieties, like different movies and the endless list spirals. But there are few
sectors where all of us unanimously agree to have no disparity and the one that takes utmost
priority is Health.
27
Health inequalities or disparities have been existing since the first man and woman set their foot
on this earth. We find disparity at all levels ranging from global to family. The most accepted
reason for these differences are individual and community immunity governed by genetic makeup
which are influenced by environmental factors like social, political, economic and cultural,
behavioural factors.
In India, health disparities are universal. The main focus is always on the Empowered Action
Group states and Assam. The health indicators of these states influence the national values and
present a skewed picture. Therefore, this essay attempts at presenting the national and state level
statistics in a disaggregated form.
India has a low sex ratio of 943 females per 1000 males which has shown slight improvement
compared to the last decade (933/1000). The highest sex ratio is seen in Kerala with 1084 and least
seen in Haryana with 879 females per 1000 males. Among the union territories, Puducherry has
the highest ratio of 1037 and Diu and Daman has the least ratio of 618females per 1000 males
(CBHI, National Health Profile, 2013). Among the EAG and Assam; Madhya Pradesh (920),
Rajasthan (932), Uttar Pradesh (943) and Uttarakhand (997), Odisha (996), Chhattisgarh (974)
are two extremes of the spectrum. The rural-urban divide is highest in Uttarakhand, rural sex
ratio is 1032 compared to 919 in urban. The lowest ratio is seen in Morena district of Madhya
Pradesh (833) and highest ratio is seen in Tehri Garhwal in Uttarakhand (1224). (AHS, 2013)
The birth rate of India in 2013 is 21.4 (21.2-21.6). The state with the lowest birth rate was seen in
Goa (13.0) and the highest is seen in Bihar (27.6). The rural (22.9)-urban (17.3) divide is quite
evident. (SRSBulletin, 2013) Whereas according to AHS; Uttarakhand (18), Odisha (19.6), Assam
(21.2) and Bihar (26.1), Uttar Pradesh (24.8), Madhya Pradesh (24.5) continue to remain two
extremes of the spectrum in all the three rounds. The rural-urban divide is highest in Uttar
Pradesh and Madhya Pradesh. i.e. for Uttar Pradesh 26.4 rural & 19.6 Urban & in Madhya Pradesh
26.7 & 19.8 respectively. (AHS, 2013)
IMR has declined considerably to 42/1000 live births (2012) from 47 (2010). However, there is huge
gap in rural (46) and urban (28). (CBHI, National Health Profile, 2013) IMR has further reduced to
40/1000 live births in 2013. Little improvement is seen in the gap in rural (44) and urban (27).
Among the states, Assam and Madhya Pradesh show highest IMR of 54, whereas Goa shows the
least at 9/1000 live births. The gender gap in IMR is not wide with 39 in males and 42 in females.
A similar fashion is observed in rural-urban region. IMR in females (46) is more than males (43) in
rural as well as in urban (Females: 28, males: 26). (SRSBulletin, 2013) Whereas according to AHS;
Jharkhand (36), Uttarakhand (40), Chhattisgarh (46) and Uttar Pradesh (68) Madhya Pradesh
(62), Odisha (56) continue to remain two extremes of the spectrum in all the three rounds.
Jharkhand records the lowest IMR while UP records the highest. IMR in rural area remains
significantly higher than that of urban area across AHS States. The rural-urban divide is highest in
Assam, rural IMR is 59 compared to 31 in urban. More female infants die as compared to males. In
Rajasthan, female IMR is 60 compared to 51 for males, the difference is the highest. In Baseline
also, Rajasthan recorded maximum difference with female IMR as 65 compared to 55 for males.
(AHS, 2013)
Health situation in India has recorded several gains in health since the new millennium. Life
expectancy at birth has risen from 62·5 years in 2000, to 66 years in 2013. In 2013, the infant
mortality rate was 40 per 1000 livebirths—down by a third since 2003 Between 2001 and 2013, the
28
maternal mortality ratio fell from 301 per 100 000 livebirths to 167 per 100 000 livebirths. The
spread of HIV/AIDS has been contained, and, in March, 2014, WHO officially declared India polio
free. In August, 2015, WHO declared India free of maternal and neonatal tetanus. Yet, 2014 ended
with the tragedy of sterilisation deaths in the Indian state of Chhattisgarh and inflicted blindness
through botched cataract operations in Punjab. 2015 saw similar tragedies as more than 100
people died in Mumbai from consumption of illicit liquor, and the number of dengue cases
increased throughout the country, as compared to the previous year stark reminders of
inadequate accountability, poor infrastructure, and low-quality health services in India’s healthcare sector. (Vikram Patel, 2015)
The new NFHS-4 data for 15 states shows that 37 per cent of children under the age of five in these
states is stunted, a fall of just five percentage points in a decade. Bihar and Madhya Pradesh are
the worst off, with 48 and 42 per cent respectively of children stunted. The proportion of
underweight children has reduced equally slowly, from 39 per cent to 34 per cent, with Bihar and
Madhya Pradesh the worst off again. The one success has been in the area of child wasting (low
weight for height). The states for which data is available have more than halved their proportion
of wasted children in the last decade, from 48 per cent to 22 per cent. The proportions of adult
men and women with below normal Body Mass Index have also declined. (NFHS-4, 2015)
Aligning with the NFHS data, a survey conducted in Gudalur showed undernutrition is a serious
problem for all the communities except the Mullukurumbas (Overall undernutrition prevalence
[BMI <18.5] 41.54%; individual tribe prevalence: Paniya 56.22%, Bettakurumba 40.54%,
Kattunayakan 60.00% and Mullukurumba 19.34%). (Srivatsan and Zachariah, 2015)
Figure 10: Newspaper article showing NFHS-4 results on Nutrition status in India
29
Data also shows that anaemia in women has increased in many states. In Meghalaya, the
percentage of anaemic women in productive age has gone up from 46.2% during NFHS-3 to 56.2%
in NFHS-4. Haryana follows a similar trend—from 56.1% to 62.7%. Awareness regarding
HIV/AIDS among women has also dropped marginally in some states. The total fertility rate in
Urban MP, urban Uttarakhand, urban Haryana now have below replacement level TFR. Rural
Karnataka, rural West Bengal, rural Uttarakhand, are also below replacement, and all three states
overall as well. Of the 13 states for which these factsheets have been released, only 3 states have
above replacement level TFR: Bihar, MP, and Meghalaya. (NFHS-4, 2015)
The health situation looks bleak and gloomy. The Economic survey of 2015-16 shows certain loop
holes. As per NFHS-4, the percentage of children fully immunized in the age group (12-23
months) is above 80 per cent in Sikkim and West Bengal. All the 12 states have more than 50 per
cent children fully immunized. India ranks 143 among 190 countries in terms of per capita
expenditure on health ($146 PPP in 2011). It has 157th position according to per capita government
spending on health which is just about $44 purchasing power parity. India’s performance on the
indicator on treatment of diarrhoea needs improvement in terms of enhancing the coverage.
(Economic Survey, 2016) Although, Diarrhea is the third leading cause of childhood mortality in
India, and is responsible for 13% of all deaths/year in children under 5 years of age (Subitha
Lakshminarayanan and Ramakrishnan Jayalakshmy, 2015), priorities are given to those diseases
which can be prevented by immunization. This reflects on the political priority based on
capitalistic attitude.
NRHM was launched in 2005 as the flagship programme of the Government of India to provide
effective healthcare to the rural population of the country, undertaking architectural corrections
of the health system, and improving access to equitable, affordable, accountable and effective
primary health care. The Framework of Implementation detailing the vision, mission and
strategies of the programme defined communitisation of the health system as one of the five
pillars of NRHM.
A major challenge in most developing countries relates to providing basic amenities (such as
education, health, water supply, roads, electricity, etc.) to their citizens, especially the poor and
the rural populations. It is in this setting that Communitisation, which is a third way of
governance offers an alternative approach in governance, one that proposes to improve public
delivery systems at the grassroots. It calls for a ‘paradigm shift’ in the governance system: a shift
to empower, harness, and strengthen the ‘social capital’ of communities at the grassroots.
Communitisation argues that when the option to streamline the government system has failed
and privatization is seen as an unviable alternative, ‘then, there is a third way to leverage the
funds, the expertise and the regulatory powers of the government with the social capital of the
user community and combine the best of the public and the private sector system’. (Pandey, 2010)
Communitisation is a contract between the government and the community. In this contract, the
community becomes the owner of the government institutions and assets and is granted powers
and resources to manage the employees and maintain institutions. In other words, it is
privatization of government-owned public institutions in the hands of the user community. It is
‘empowerment, delegation, decentralisation and privatisation at the same time. Here, the
government actively engages itself as active partner, assister, monitor and supervisor of the
community. It follows the three T principle: Trust, Train and Transfer the power to the
community.
30
Communitisation includes community involvement and active participation. Alma Ata
declaration on PHC also emphasises on this aspect. The definition of PHC also mentions that
"essential health care" that is based on scientifically sound and socially acceptable methods and
technology, which make universal health care universally accessible to individuals and families in
a community. It is through their full participation and at a cost that the community and the
country can afford to maintain at every stage of their development in the spirit of self-reliance
and self-determination"
Communitisation is a new word introduced in the NRHM in 2005. The community action for
health within the NHRM has many strategies for communitisation. The two key instruments
towards communitisation under the NRHM were – the implementation of a Community Health
Worker (ASHA) programme, and the institutionalization of community action through the
formation of VHSNC and Rogi Kalyan Samiti26. Communitisation is an effort to bring people's
health in people's hands. Community empowerment, accountability and responsibility are
underlined within this concept of governance. Since health is a fundamental right, demand for
quality health care has to be exercised by everyone. Communitisation aims at motivating
community for fair health care.
Communitisation process involving community participation and active involvement can happen
only when there is a supportive environment. For example, if the polices and laws are not
socialistic and rather capitalistic, there is minimal chance for any sort of scope to improvement.
The Ottawa charter27 for Health promotion has rightly upholds the supportive environment
which influences pyscho-social behaviour of the entire communities.
The trigger or stimulus for active participation comes often in situations of disaster at one end or
when there is a mass provocation. Chennai deluge in December 2015 was definitely manmade
disaster. Government's apathy and incompetence at many levels has resulted in such a
catastrophe. But, the Chennai people themselves showed an extraordinary solidarity and have
stood the challenge of selfishness, hate or any negative emotions. They came forward to help their
own citizens. People of Chennai showed active community participation to find solutions in their
immediate vicinity. Youth making makeshift boats using those materials which would float,
helping people to get out of their homes, arranging food supply is nothing but taking
responsibility on their shoulders.
Prime Minister, Mr Narendra Modi's signature campaign on cleanliness and sanitation- "Swach
Bharat Abhiyan"28 got a massive response from the community. Although, short lived, it generated
a lot of noise and made people think about it. Leadership roles are crucial in bringing
communities together. In one addressing, Modi asked the packed crowd, whether he need to tell
everyone to keep their surroundings clean, reminding that responsibilities are not given, but
actively assumed.
The above examples also touch a difficult issue of sustainability. Any programme to last long,
needs a sustainable thought process, thinking, meticulous planning, flexible and more
26 Rogi Kalyan Samiti is a decentralised democratically formed group at village level for the welfare of patients.
27 Ottawa charter on Health Promotion is an international agreement signed at the First International Conference on
Health Promotion in 1986 to achieve Health for All by 2000.
28 Swacch Bharath Abhiyan or Clean India Mission is a national campaign by Modi’s government to clean roads and
develop infrastructure.
31
importantly adaptable to ever changing demands and environments. Timely reflections and
reinvigorations are necessary to reflect upon failures and success.
Community is a group of people and with it comes a diversity of various kinds. And keeping all of
them together on one path to reach a goal is not just an uphill task but most
challenging. Community dynamics are certainly complex in a country such as ours. In such a
situation, local self-governance plays a major role. It is a sad state that the present government
has cut down the budget to Panchayat Raj and thus weakening the foundations of a very strong
attribute of our Democracy. Ideally, the village panchayat system is itself a community
empowerment process and a strong political institution. The VHSC will also be able to deliver the
work if the system is supportive and encouraging. And, this support is provided by the village
panchayat provided the system is integral, sensitive and responsive.
Communitisation was an effort to 'scale up' simple community health strategies of having
community health workers, health activists and village health committees to the entire rural
population of 750 million in 2005. These strategies worked very well at micro level through NGOs
where there was presence of committed leadership and support systems. The scale up process was
needed as all citizens have a right to better health and access to health care and therefore
mechanisms were created to enable this. It was ambitious in scope and met with several
challenges.
Some of the key challenges facing NHM are the incentive based work of ASHA. Complete
commitment to the job is not reported since there is no job security. Also, the coordination
between ANM and ASHA is crucial. Often times, ANM look down towards ASHA as subordinates.
One brutal incident where an ASHA was gang raped during her routine home visits show the
systems inadequacy in management and providing security. (Gangotri, et al., 2015)The crux of the
success is dependent on the strengthening the overall health system. Financial constraints always
slow down the process. The recent union budget allocation to health has proven this fact. Only
0.21% (Rupees 938 Crore) of the total infrastructure investments in India is in the health sector.
(Saha, 2016)
Social Determinants, Equity and Public Health
Social determinants of Health are the conditions in which people are born, grow, live, work
and age. These circumstances are shaped by the distribution of money, power and resources at
global, national and local levels. (WHO-CSDH, 2008) The social determinants of health are
mostly responsible for health inequities - the unfair and avoidable differences in health status
seen within and between countries.
Health equity and social determinants are acknowledged as a critical component of the post2015 sustainable development global agenda and of the push towards progressive achievement
of UHC. If health inequities are to be reduced, both SDH and UHC need to be addressed in an
integrated and systematic manner.
32
Figure 11: Social determinants of Health
Social Model of Health (Dahlgren and Whitehead, 1991) talk of the layers of influence on
health. It describes the social ecological theory to health. The attempt to map the relationship
between the individual, their environment and disease is explained. Individuals are at the
centre with a set of fixed genes. Surrounding them are influences on health that can be
modified. The first layer is personal behaviour and ways of living that can promote or damage
health. –ex, choice to smoke or not. Individuals are affected by friendship patterns and the
norms of their community. The next layer is social and community influences, which provide
mutual support for members of the community in unfavourable conditions. But they can also
provide no support or have a negative effect. The third layer includes structural factors:
housing, working conditions, access to services and provision of essential facilities.
Dahlgren and Whitehead's model highlights a causal relationship between individual lifestyle
'choices', social networks, working and living conditions and economic, political and
environmental factors, globally, nationally and locally. While the configuration of these different
layers and factors can have both positive and protective influences on our lives, they can also
undermine health and wellbeing, both for individuals and communities. For example, adverse
economic conditions have implications for employment and training opportunities, public
services such as health, social care, education, the wide range of services provided by local
authorities, as well as the funding they provide to support local voluntary sector services. Where
adverse conditions persist, they can have a significant and negative impact on: social attitudes,
social cohesion and social mobility.
Social determinants were well established in academic circles and have been the subject of
considerable study, but it was quickly discovered that the concept didn’t work on the ground. The
grantees—most of whom were dealing with real challenges at the community level, didn’t
necessarily resonate with this frame. For some it was so patently obvious that it became a truism.
33
A study was conducted to gain a deep understanding of people’s thoughts and feelings about
health differences across populations in the United States. The research was to find proxy word
that could replace “the social determinants of health” as the leading descriptor for this area of
work. While the testing showed that this phrase doesn’t work for audiences, there is still not a
neat replacement. But the research found a list of phrases that in context helped people
understand the concept more clearly. These are the precise phrases that were tested and that
scored well. The proxy statements use colloquial, values-driven language and relatable lifestyle
references that engage audiences. These statements all focus on the solution versus the problem.
Some of the statements implicitly acknowledge the notion of personal responsibility. (Robert
Wood Johnson Foundation, 2010)
Figure 12: Proxy statements for Social Determinants of Health
SDH in India over the past two decades, five issues emerge as the most urgent to address: air
pollution (both indoor and outdoor), child undernutrition, unimproved sanitation, employment
conditions, and gender inequality. These priorities coincide with the major risk factors
contributing to lost years of healthy life in India, as identified in disease burden analyses.
Household surveys reveal the striking proportion of the Indian population exposed to indoor air
pollution, which is particularly significant for women and young children who typically spend
more time inside near stoves. Child undernutrition continues to affect a significant proportion of
households in more and less developed states alike, and has failed to significantly decline despite
national economic growth. Unimproved sanitation facilities also remain too common in India,
most significantly in rural areas. India has made progress in reducing child labour, but many
other aspects of employment conditions continue to be problematic – a lack of job security,
insufficient safety measures, and inadequate compensation. Gender-based inequities persist in
employment and governance, limiting women’s power in households, businesses, and private and
public decision-making. Caste-based inequities are also significant, with members of scheduled
castes and scheduled tribes consistently worst off. (Krycia Cowling, 2014, )
HEALTH SYSTEMS
The world is witnessing an unprecedented change in this century, more than any other time in
the recorded history of humankind. While the cost of living has become more affordable for
people with middle and lower incomes, we are also confronted with challenges such as climate
change, wars, pandemics, and, more importantly, a gap between rich and poor that is growing
34
unabatedly. Despite these serious threats to human life, the human development index has
increased globally from 0.597 to 0.711 from 1990 to 2014. (UNDP, 2016) Indicators of
development depend on many determinants such as economic, environmental, cultural, social,
and political factors. Development and health status are not mutually exclusive; each has a
complementary role in the process of human development.
Understanding health as a synergistic relationship between the physical, social, psychological, and
spiritual elements that contribute to the well-being of individuals and/or groups in their physical
and social environments and applying this into building health system is necessary. The role of
responsive health systems is imperative in this phenomenon. In recent times, events which have
drawn international concern such as the Zika virus pandemic; Ebola crisis; cyclones in Chennai
and Western Pacific; Earth-quakes in Nepal, Indonesia, and elsewhere; and many other
emergencies have rallied the world behind a new global thinking and sense of solidarity. At the
outset of all these calamities lies a health system, because of which the events have been either
successfully managed or the reasons why it occurred at first place have been analysed and suitable
solutions are explored.
Two aspects of a health system that contribute fundamentally to its effectiveness include
resilience and responsiveness. Responsiveness is the ability of a health system to be inclusive,
whereas, resilience in the ability to withstand a shock. Resilience is a strong element of the health
system, while responsiveness is more to do with ethos and values of the larger society. It is widely
recognised that a country’s health status is a direct result of the extent to which its health system
addresses a range of diseases and serves all sections of society, with equitable distribution of
services and social justice as underlying core principles. Weak health systems are characterised by
lacking core capacity in governance, financing, health workforce, or information systems.
(Margaret E Kruk, 2015)Some of the key features of a resilient and responsive health system are
discussed here.
Any health system should have a sound information system. They are regularly updated about
demographic, social, geographic, and meteorological indicators. A strong epidemiological
surveillance system can itself predict impending threats. Systems thinking in public health will
help predict such emergencies. It will prepare to quickly identify a medical emergency, try to
isolate it locally, and coordinate with other sectors to direct resources of all kinds towards it.
Natural disasters and wars offer salient examples of this need for responsiveness. The war in Syria
and terrorism in parts of Africa, for example, have caused millions of people to migrate, a large
number of whom require supportive health services. In addition to exacerbating fragile health
conditions, this exodus has resulted in many deaths, especially among children. Such emergencies
inflict catastrophic damage on both people and the environment and frequently result in disease
epidemics. Being prepared for such untoward consequences makes a robust and resilient system,
where there is little or no disruption of other essential services and investments in the social
sector.
Health systems should be diverse and multifunctional in operations. The variety of diseases which
often present in a community requires a platform, where a multitude of workers and facilities
alike offer first point of contact to provide primary health care. This system must be optimally
functional at all times, having constant interaction with, as well as winning trust and confidence
from, the community it serves. Such a health system also provides care related to all diseases
ranging from oral health to mental health.
35
A responsive, self-regulating health system must also be able to respond to health emergencies as
well as continue providing services undisturbed in unaffected areas. Response to a crisis, be it a
disease outbreak or other disruption resulting in a surge of demand for health care, requires both
a vigorous public health mobilisation and a highly proactive and functioning health-care delivery
system. The recent union budget in India is a bitter example of how political priorities are often
made at the expense of such social investments, including education, health, water, and
sanitation. India is one of the countries that spends the least on the healthcare sector, with public
spending on health care at around 1% of GDP as compared to 3% in China and 8% in the UK. This
reflects a low prioritisation of health by the government, as well as the potential for inadequate
responsiveness of the national health system.
Human rights is also an important consideration in responsive and resilient health systems.
Corruption, discrimination, and abuse of various forms by the staff of a health care system are the
most commonly cited reasons for why people chose private over public services. Better
governance which provides for a voice for all people, inclusive decision-making processes, and
accountability are essential for people-centred systems. Political action is needed to ensure the
above and a strong countervailing civil society is also required.
A functional and responsive health system is driven by an integrated network of actors and
institutions in various sectors, including policy-makers, activists, community representatives,
administrators, researchers, and educators, all of whom must be brought together in a
collaborative effort to construct and maintain such a system. Enabling an eco-structure
containing a triumvirate of technocrats, politicians, and civic leaders will help to come up with
solutions that are locally relevant and which also will be resilient. Ecostructure is the set of
expectations and norms about what everybody thinks policymakers are doing. Ecostructure
determines how policymakers, citizens, and technocrats view themselves. Technocrats who
become engaged in model building are building more than models – they are building shared
expectations and a new eco-structure that fosters new engagement between politicians and civic
leaders. Social mobilization and inter-sectoral action are essential for re-orienting health systems
to be more people-centred.
Communitisation, a strategy used in National Health Mission in India, is an effort to 'scale up'
simple community health strategies of having community health workers, health activists, and
village health committees to the entire rural population of 750 million in 2005. These strategies
worked very well at a micro level through non-governmental organisations, where there was a
strong presence of committed leadership and support systems. The scale up process was needed
as all citizens have a right to better health and access to health care and therefore mechanisms
were created to enable this. By contrast, Indigenous people are a resilient community. They have
a lot of sharing and caring exhibited by community bonding. These inherent features are often
overseen. Particularly, their traditional healing is dependent on herbs which are easily available
and locally relevant. Failure to recognise the local traditional health systems is not only
unfortunate but also irresponsive and selective.
Research can evaluate and suggest new ways in which health systems and inter-sectoral
collaborations can better respond to people’s emerging health needs, be directly accountable to
communities, and ensure the rights and dignity of all people who use and provide health care
services. Participatory action research in particular can directly enable people to voice their
36
concerns and provide ideas for better health systems. In the case of the Zika crisis and the many
uncertainties we are facing related to this emergency, we need collaborative research to
understand disease transmission and thereby to find effective solutions. This situation, so far has
no clear solution besides increased mosquito control and advice women not to become pregnant
in the next two years – hardly a solution to a challenge with such serious effects. (David L.
Heymann, 2016)
These crises also shed light on holes in our international health system. For example, one of the
reasons why the Ebola crisis became a catastrophe was the lack of responsiveness of the global
health system, supported by inadequate local and regional systems. The Ebola epidemic has
illustrated that several preconditions for resilience were lacking. The first of these preconditions is
recognition of the global nature of severe health crises and clarity about the roles of actors at all
levels of the global health system. An important point here is that some of these disasters showed
us shortcomings in the system and thus demonstrated the importance of more resilient and
responsive systems worldwide.
Health-care systems are complex adaptive systems that must be able to respond to unexpected
developments and demonstrate the capacity to adapt in normal times. A resilient and responsive
health system should have a strong information system and at its foundation be diverse, selfregulating, integrated, and adaptive. Applying systems thinking in public health can help predict
and respond effectively to unseen developments and strengthen a system’s resilience to
emergencies and unexpected strain. The importance of resilience and responsiveness to the
challenges one open’s the piece with, and how in order to meet these challenges, we must all
work collaboratively toward systems that have these qualities.
ENVIRONMENT, SANITATION AND HEALTH
Environment Health is a trans-disciplinary branch of public health which aims at assessing and
protecting against harmful external physical, chemical and biological factors to prevent disease
and create health supportive environment at the personal, family, occupational, community and
global level, and working towards the wellbeing of people and communities by enabling them to
manage and improve their own community environment through an eco-sensitive perspective,
and empowering them to demand eco-justice through action directed by evidence based on sociopolitical-economic cultural analysis with an equity, rights and social determinants perspective.
(Pradhyumna and Narayan, 2012)
Environemntal health has been a public health concern since the times of Industrial revolution.
Disasters such as volacanoes, forest fires and the man made disasters like Chernobyl and
Fukushima nuclear disasters, Bhopal gas tragedy, etc have opened a new arena within the public
heath. It predicts the overacrhing climate change along with deforestation, increase use of fossil
fuels, wars, etc. It opens the truth of the unpreparedness of the health system to which these
environmental disasters throw us at. The Bhopal gas tragedy is a testimony of irresponsive health
system. There was limited knowledge of the health effects of the chemical exposure that occurred
in Bhopal. The identity of the released chemicals itself was a subject of debate. Medical personnel
also found themselves unable to handle this unusual situation, pointing towards the inadequate
training and preparation for industrial disasters. The economically disadvantaged communities
bore a double burden of disease – malnutrition and exposure to hazards of industrialization.
37
Therefore, there was an urgent need for a toxicological investigation to aid rational therapeutic
care (treatment and rehabilitation) of the victims. The symptoms and signs of exposure in victims,
pathological findings in organ systems during examination and autopsy, and analysis of chemical
agents provided clues to answer the above questions. (Naryan, 1990)
In recent times, climate change has proven its tremendous impact and the torrential rains that
created a havoc across the south eastern coast of India is one among the chain of events which
was not just detrimental but devastating too and many more such events to come in our way.
COP21 stands for the 21st Conference of the Parties to the United Nations Framework Convention
on Climate Change held at Paris in December 2015. The key aim was the "stabilisation of
greenhouse gases in the atmosphere at a level that would prevent dangerous anthropogenic
interference with the climate system". The final destination is a world where temperatures rise
not much more than 2°C above the level they were in 1850-1899 period. With the COP21 summit
on climate change; global leaders, scientists, activists and the entire world focused their attention
on this historic event. The decisions made here will predict earth’s future. Many governments
have pledged to reduce the green-house gases to reduce the impact on environment.
The implications of climate change for a global population of 9 billion people threatens to
undermine the last half century of gains in development and global health. The direct effects of
climate change include increased heat stress, floods, drought, and increased frequency of intense
storms, with the indirect threatening population health through adverse changes in air pollution,
the spread of disease vectors, food insecurity and under-nutrition, displacement, and mental ill
health. The Lancet commission on Health and Climate change recommended policy changes to
protect public health. The Commission recommends that over the next 5 years, governments:
(Watts N et al, 2015)
1. Invest in climate change and public health research, monitoring, and surveillance to
ensure a better understanding of the adaptation needs and the potential health cobenefits of climate mitigation at the local and national level.
2. Scale-up financing for climate resilient health systems world-wide.
3. Protect cardiovascular and respiratory health by ensuring a rapid phase out of coal from
the global energy mix.
4. Encourage a transition to cities that support and promote lifestyles that are healthy for
the individual and for the planet.
5. Establish the framework for a strong, predictable, and international carbon pricing
mechanism.
6. Rapidly expand access to renewable energy in low income and middle-income countries,
thus providing reliable electricity for communities and health facilities; unlocking
substantial economic gains; and promoting health equity.
7. Support accurate quantification of the avoided burden of disease, reduced health-care
costs, and enhanced economic productivity associated with climate change mitigation.
38
Figure 13: An overview of the links between greenhouse gas emissions, climate change, and health
A workshop on Energy and Health organised by CHESS facilitated interactions with coal impacted
community in sharing of knowledge and skills of basic documentation of impacts on health and
environment. Skills of health documentation through symptom survey skills; lung function tests,
basic skills of environmental monitoring, dust samplings, etc. was shared to enable the
communities to record health and environmental impacts. An overview of the policy, planning
and governance surrounding energy and electricity in India major threw light on the energy
challenges faced by India, namely - Huge Energy Poverty, Limited availability of natural resources
and Ecological impacts of conventional energy use. Coal Bearing Act was explained by Mrs Sudha
Bharadwaj, a legal activist from Chattisgarh Mukti Morcha. She explained how this act was more
dangerous that the land acquisition act. She further spelled out that for mining, companies need
to apply for a mining license, but if the company does not own the land, they are required to get
consent from the owner to mine that area. The mining lease is not about acquiring the land, but
about simply giving consent and collecting compensation. Hence, people do not realize that they
are letting go of their rights over that land while giving consent. (Collectivenotes, 2015)
Environmental Sanitation and Public Health have been interrelated. The history of public
health begins with the Great Sanitary reforms of England in the 19th century. Providing safe
drinking water and sanitation have been the priorities of health committees, Alma- Ata
declaration, Millennium and Sustainable Development goals. Environmental sanitation has two
major problems- waste management and open defection besides many other water and vector
borne diseases which are a result of inadequate safe water supply and sanitation.
39
The Garbage issue is becoming a universal problem. It is more accentuated in developing
countries where waste management disposal is under strengthened. Bangalore’s famed sobriquet
as Garden city is tarnished with its piling garbage. The city generates 4000 tonnes of waste a day
and now the BBMP is looking at a ban on plastic to reduce some of the burden. Since the garbage
is being sent to landfill sites instead of the seven designated waste collecting centres, the city’s
garbage woes are unending. Gundur village, one of the waste collecting centre has seen
unprecedented flow of garbage and resulting nuisance. The villagers staged several protests, but
all in vain. The muck spilled out of dustbins on to city streets and festered in stinking piles in
landfill villages, provoking protest after protest.
Recently, another opportunity was lost. On an invitation from Sweden, a team of officials headed
by the then additional chief secretary Ratna Prabha visited the country to study its solid waste
management system. Sweden is so efficient that it even imports waste from other European
countries. It has 32 waste-to-energy plants, where 99% of garbage is incinerated to produce steam,
which runs generator turbines, public transport and generates electricity, while only 1% ends up
in landfill. These plants run in the heart of the city with zero pollution. The team recommended
adopting Swedish technology to use the converted fuel for public transport buses and minimize
burden on landfills. But after two rounds of discussions with Swedish counterparts, the ideas were
dropped citing high cost. (Aiyappa, 2014)
Mobilising the citizens to demand the right for clean city is vital. The Residents Welfare
Association in Koramangala 29have mobilised and organised citizens to monitor the progress of
their newly introduced ‘no plastic’ in their neighbourhood. Learning from others experiences,
they encourage composting degradable waste within the households to minimise waste input to
waste management system. The Karnataka High Court’s decision on segregating waste at
household itself is laudable. (Natraj, 2015) The waste management will definitely reduce a
plethora of problems such as stray dog menace, dengue, malaria risk reduction, and many more.
In this case, there is a strong community action for health observed. The residents action as well
as the collective action by many civil society organisations’ work which resulted in the legal
framework has resulted in brought civic responsibility.
VHSNCs have been set up at the village/gram Panchayat level under the leadership of the
Sarpanch (village leader) and the health worker in the village for carrying out activities leading to
improvements in health, sanitation, and nutrition of the villagers. Each month, the workers of
Ministry of Women and Child Development and the Ministry of Health and Family Welfare
jointly hold a Village Health and Nutrition Day in the village. VHSNCs and Village Health and
Nutrition Days provide an institutional platform for fostering convergence and addressing the
social determinants of health at ground level. The VHSNCs set up at the village level under the
NRHM have been known to carry out activities, such as sanitation drives, filling of pot holes,
drives to control spread of vector-borne diseases, provision of nutritional support for
malnourished children, purchase and installation of water purifiers at the Anganwadi centers30.
One significant and internationally unique source of early life disease in India is open defecation,
especially in rural India. open defecation in India is much more common than in even much
poorer countries. India has the largest rural open defecation rate in South Asia by a very large
29 Koramangala is a suburban neighbourhood where SOCHARA is located.
30 Anganwadi centre means "courtyard shelter" in Indian languages. They were started by the Indian government in 1975
as part of the Integrated Child Development Services program to combat child hunger and malnutrition.
40
margin. According to WHO and UNICEF Joint Monitoring Programme estimates, 61% of rural
Indians defecate in the open in 2015, compared with only 32 % of rural people in sub-Saharan
Africa. Research suggests that rural Indian households reject the types of latrines promoted by the
World Health Organization and the Indian government partly because their pits needed to be
emptied every few years. Latrine pit emptying, which is routine in other countries, is substantially
complicated by rural India's history of untouchability- work of disposing of human faeces is
associated with severe forms of social exclusion and oppression.
Open defecation spreads germs into the environment, and therefore makes growing children sick.
One form of this sickness is diarrhoea, which robs growing children of the food that they eat.
Another resulting disease could be environmental enteropathy, a chronic inflammatory response
of the intestines to repeated exposure to the germs spread by open defecation; it reduces the
ability of children’s intestines from absorbing nutrition. the consequences of open defecation for
Indian children may be worsened by high population density and the problem of child stunting is
worse in villages where a higher percentage defecate in the open. (EconomicSurvey, 2016)
The social and economic impact of sanitation issue in India is ignored and not considered on the
policy process. The Swacch Bharath Abhiyan, which is the new name given to the older Nirmal
Bharath Abhiyan, aims at building toilets. The government claims to have built over 80 lakh
toilets in 2015 alone has failed to show the social impact of the issue. Poor access to sanitation also
has mental health impact particularly on women. (Ganesh, 2014).
Community led total sanitation drive aims at recognising and acknowledging open sanitation as a
public health issue by the community members. The walk of shame helps the community
members to realise and practically understand the problem which in turn is expected to motivate
the community for increased use of toilets. The problems often noticed is either with construction
of toilets and maintenance of the toilets which means periodical emptying of pits. The use of
appropriate technology to construct low cost toilets have overcome the first problem, but
emptying the pits periodically is usually carried out by the safaaikarmacharis31-oppressed class.
The behavioural and emotional factors hinder the successful use of toilets. There are efforts to
convert the human waste into organic manure and its social acceptability has to be time tested.
(Prahlad, 2015)
LOCAL HEALTH TRADITIONS
Local health traditions have been there since time immemorial. The dawn of medicine is traced
back to the origins of humankind. But the question of when did it turn into an organised system
of research, testing, conversion into practise, acceptability by the people and finally migration of
knowledge to far off regions are all intriguing. If we have to agree that, there were local practised
health traditions across the world, when did they evolve into an organised system with written
records and thus maintaining the continuity? When did this system evolve into modern
medicine? Another question is how did these local health traditions remain locally within the
adivasis or other groups while others evolved and became popular.
31 Safaaikarmacharis are a group of people, socially stratified, whose traditional occupation is manual scavenging of
human waste.
41
Wendy Doniger, popular American Indologist argues that many traditions have evolved and
polished over time including languages. Prakrit and other vernaculars came first and Sanskrit
evolved from it as a polished form. She introduces interesting terms, ‘Laukification’ and
‘Deshification’. (Doniger, 2015)These terms are opposite to ‘Sanskritisation’, used to describe the
way that Vedic social values, vedic ritual forms, and Sanskrit learning seep into local popular
traditions of ritual and ideology (in part through people who hope to be upwardly mobile, to rise
by imitating the manners and habits, particularly food taboos, of Brahmins and in particular
avoiding violence to animals). (Srinivas M. , 1952)
‘The process by which the sanskritik tradition simultaneously absorbs and transforms those same
popular traditions, is equally important, and that process is called oralisation or popularisation, or
Deshification32 or Laukification33. Cross fertilisation between the sanskritik and laukika traditions,
have followed many areas and health has not escaped this transformation. What started as
lokaparampara34 in health also witnessed such sanskritik metamorphosis. And, as a result, we
have Ayurveda which also must have evolved in a similar fashion when the elite sanskritik
brahminical ideas seeped into local health traditions. The amalgamation of such another local
health tradition is the Persian, Mongolian and Arab over centuries with the Hindu traditions was
Unani. The distinctive feature of these local health traditions with that of what is claimed to be
classical forms is that, lack of written texts. All these LHT have been passed since generations
orally. There are no debates and discussions over texts and theories. These traditions are followed
as told by their forerunners. It is interesting to note that local health traditions are popular among
the Adivasi communities and others is because the materials used were locally available and easily
affordable. Hence they became Laukified or remained as a Lokaparampara. Ayurveda involved
rigorous training and the materials used were expensive like oils, mineral salts, etc. which were
often procured from far places. The elite could afford it and there was also a Brahmin whose
superior position commanded authority. Hence, it might have become a classical tradition.
The traditional medicine into classified into loka (oral folk form) and sastra (codified classical
form). (Shankar, 2001) This distinction of LHT and the classical health traditions into Prakritik
and Sanskritik is again a dominant world view. The classification itself is systematic and based on
the availability of texts, evaluation of backgrounds such as familial or ethnic, etc. The worldview
of this classification is an elitist, brahminical and colonially influenced. The distinction between
the loka and sastra are widely acknowledged and this classical view is viewed as a complementary
relation, and over time, is replaced by mutual exclusivity. The historical analysis of how this
distinction is necessary to understand the present political context surrounding LHT’s
legitimisation issue. (Unnikrishnan & Hari Ramamurthy, 2012)
Ausadhir nama rupabhyam
janatehjyapa vane avipascaiva
gopasca ye canye vanacarina35
32 From the ‘local’ or ‘deshi’
33 ‘Laukika’-of the people (loka)
34 Lokaparampara means Local tradition
35
Charaka Samhita, Sushruthana, Chapter 1, verse 120
42
Charaka mentions that ‘shepherds, cowherds and those living in the forest are knowledgeable
about medicinal materials both by name and form’. This implies that forests are rich repositories
of health knowledge. There was constant interaction between the two forms and over time the
distinction grew big. The legislations passed post-independence gave rise to institutionalisation of
medical system and legitimising only the registered and the class room trained practitioners
leaving behind indigenous health systems. (Unnikrishnan & Hari Ramamurthy, 2012) This comes
in the wake of arguing the scientific basis of the indigenous as well as the classical health systems
against the western biomedicine. The western medicine in its modern phase is the paradigm for a
scientific knowledge system which is based upon the various viewpoints such as sociology,
epistemology, empirical analysis, etc. There is an argument that this view point is unlikely to be
found in the Indian systems of medicine unless an unbiased criterion is established to call a
knowledge system as scientific. (Balasubramanian & Radhika, 1989)
At a global level, WHO in its stewardship role has cleared the ambiguity between traditional, folk
and indigenous medicines. It acknowledges that traditional knowledge eludes precise definition
and description, containing as it does diverse and sometimes conflicting characteristics and
viewpoints. Who defines Traditional medicine as ‘including diverse health practices, approaches,
knowledge and beliefs incorporating plant, animal, and/or mineral based medicines, spiritual
therapies, manual techniques and exercises applied singularly or in combination to maintain wellbeing, as well as to treat, diagnose or prevent illness’. (WHO, 2002) The support in the form of
acknowledgment to legitimise LHT is necessary to push forward the agenda to revitalise LHT at
national levels. The term local traditional healer was first mentioned in the draft National Health
Policy on Indian Systems of Medicine in 2002. There have been few attempts to recognise LHT at
both national and state levels. NRHM seeks to revitalize local health traditions to strengthen the
public health system. A mission group on public health was set up by the Karnataka Knowledge
Commission and it recommended an actionable plan to revitalise local health traditions by state
patronage and encouraging LHT’s based home remedies and recognising LHT to strengthen local
health traditions in primary health care through state and university accreditation mechanisms.
(Karnataka Knowledge Commission , 2012)
On other hand, there are attempts to comprehensively document and assess local health
traditions with the objective of promoting best local health traditions. (Hafeel & Suma, 2007) The
documentation of indigenous medicine by individuals and civil society organisations are an effort
to preserve the biodiversity of these traditions. The way forward is to recognise these traditions
and provide a legitimate platform. This is seen as one of the reason for erosion on LHT
(Unnikrishnan & Hari Ramamurthy, 2012). Use of the LHT at primary health care level is
beneficial particularly to treat common diseases, for mother and child care and also to treat snake
bites. Manual for health workers are prepared by WHO and NRHM are helpful in delivering care
to the marginalised and the economically weaker sections.
43
MY FIELD AREA
It all began when I was briefed during the orientation sessions about field areas that we have to
choose to work for six months. We had to intern at a civil society organisation working towards
community development and health. During these sessions we were also given assignments to
read about various organisations involved in community health movements across India.
Voluntary Health Association of India has published a series of books called Anubhav both in
Hindi and English about such organisations. Each fellow had to pick up one book and read about
it and present it to the fellows followed by discussion on the discussed organisation. This exercise
gave us an idea about the community health movement in India and the challenges it faced.
Most importantly, it oriented towards the kind of work involved and idea about community
health in various settings was instilled. I had picked up Vivekananda Girijana Kalyana Kendra36.
My interest in adivasis grew much strong. Initially, I had decided to go to this organisation, but
the logistics didn’t work out. Dr Mahesh Matpathi, was working with the ACCORD as the
community health programme coordinator and I had known him through Samantha. With more
reading on ACCORD and consulting Dr Thelma Narayan, Dr Mahesh Matpathi and Samantha, I
decided to go to ACCORD. Although practical reasons preceded over other reasons. It was easily
connected to Mysore and Bangalore by road. The weather was pleasant and the nature
surrounding it gave me a perfect getaway from the scorching heat and pollution of Bangalore. The
Shola Trust37, related to ACCORD was working with nature conservation and wildlife, which was
also my interest. Thus, the primary area of interest- adivasis, and next wildlife and nature
conservation, besides other practical reasons, I chose Gudalur as my field area.
Gudalur is a small town located in the lower Nilagiri 38hills. It is located at a strategic meeting
point of three southern states of India. The name suggests of Koodal which means Joining
in Tamil and Ooru means village or place and thus Koodaluru could have evolved to Gudalur. It is
a municipality town within The Nilagiris district of Tamil Nadu state. Tea industry dominates the
region. The first tea plantations in India came up in this region. It is surrounded by protected
sanctuaries- Mudumalai Tiger reserve and Mukurthi National Park.
According to 2011 census, Gudalur had a population of 49,535 with a sex-ratio of 1,032 females for
every 1,000 males, much above the national average of 929. A total of 5,359 were under the age of
six, constituting 2,719 males and 2,640 females. Scheduled Castes and Scheduled Tribes accounted
for 27.66% and 3.65% of the population respectively. The average literacy of the town was 79.48%,
compared to the national average of 72.99%. The town had a total of 12101 households. There were
a total of 18,807 workers, comprising 551 cultivators, 1,759 main agricultural labourers, 206 in
house hold industries, 14,488 other workers, 1,803 marginal workers, 90 marginal cultivators, 278
marginal agricultural labourers, 119 marginal workers in household industries and 1,316 other
marginal workers. Gudalur has a heterogeneous community. It has a mix of people from various
36 Vivekananda Girijana Kalyana Kendra (VGKK) was started by Dr H Sudharshan.
VGKK is working in the areas of
education, health and sustainable livelihood of the Soliga indigenous group in Biligiri Ranga Hills of Chamaraj Nagara
district in Karnataka.
37 http://www.thesholatrust.org/
38 Nilagiri refers to Blue Mountains.
44
backgrounds. Hindus form the majority (59.83%), while Muslims (26.01%) were the second largest
religious There are 14.1% Christians, 0.01% Sikhs, 0.05% following other religions and 0.01%
following no religion or did not indicate any religious preference. (Census, 2011).
ORGANISATION
The story of ACCORD is nothing, but the story of the innocent indigenous people. It is a perfect
example of community empowerment. ACCORD has been the reason for the success of the
community empowerment. ACCORD,39 a civil society organisation was founded in November
1985. It is the brain child of Mr Stan Thekaekara and his wife Mrs Marie Marcel Thekaekara and a
young 19-year-old Mullukurumba Adivasi called Mr K T Subramanyam. The main objective of
ACCORD is to fight against the unjust alienation of the adivasi lands and other human rights
violations by organising them as a strong group.
ACCORD was born in November 1985 to support the adivasi community in Gudalur valley to
organise themselves and assert their rights - especially land rights. Since the adivasis are a small
minority here in Gudalur, ACCORD's core aim has been to support the adivasi community “enter
mainstream society as equal partners and on their own terms in dignity and pride”. The scope of
work covers community organisation, economic empowerment, health, education, legal support,
cultural revitalisation and advocacy with state and central governments. (Thekaekara, Mari
Marcel, 1994)
Figure 14: Organogram of ACCORD
39 http://www.adivasi.net/index.html
45
The organogram above describes the position of ACCORD in the functioning of the work at the
Gudalur valley. Unlike the other civil society organisations, ACCORD doesn't hold a superior
position dictating terms and conditions. Rather, it plays a role of a supportive and guiding force
for all the activities happening under the aegis of Adivasi Munnetra Sangam.
ACCORD'S history is an interesting tale. Stan and Marie were once travelling in the bus passing
by Gudalur. An indigenous woman was ill-treated, her fellow passengers accused her of brave act
of getting into a bus and sitting on a seat. Untouchability and social segregation was a common
norm practised over the indigenous people. Moved by the shocking way of treating their fellow
passenger, the couple decided to know more about problems of the indigenous
people. Coincidently, Subramanyam, was also provoked by the treatment he and his community
received, met Stan and thus the three musketeers set out to work with the community. During
the 60's and 70's, there was heavy influx of migrants from neighbouring Kerala, settling as tea,
coffee and pepper growers. The Chettan community were money mongers and started to exploit
the indigenous people. They would lend money and if a person couldn't pay back, they would take
over the lands of indigenous people. Thus, a large number of people lost their lands and other
property to wealthy landlords resulting in the rampant alienation of adivasis from their lands and
their human rights were grossly violated.
ACCORD's work is based on community led analysis, planning, implementation and evaluation. It
mainly focused on community led institutions, thus avoiding hierarchical structure.
Also, coordinated activities in fields such as community organization, health, education and
economic development.
ACCORD's work can be phased at four levels. The phase I was mainly involved with human rights
interventions (1986- 87) and saw the birth of ACCORD, AMS, land reclamation, prevention of
atrocities. During the phase II, it focused around development intervention (1988- 94) like
economic development of the adivasis, community health, building of hospital (ASHWINI). The
third phase saw the development of community institutions (1995 to date) such as the Mahasabha
leading to formation of VBVT, ATLM, Madhuvana Estate, AMF, initiating Just Change. Finally,
now it is in the phase IV- forging ahead and ensuring sustainability.
ACCORD has right from its inception, always had two arms. The professionals or support team
whose role is that of a catalyst and the adivasi team being trained to take the community into the
challenges of the 21st century. ACCORD’s task is to make the process of change continuous and
irreversible. ACCORD began, by first supporting the creation of strong village level organisations
called sangams which have been federated to form the AMS. Today the AMS, which is recognised
by the State Government as the representative body of the adivasis of the area, consists of 312
village sangams clustered into 8 areas and covers a population of nearly 25000 people.
However, when the community felt the scope of the health work should be expanded to include
curative care by the setting up a community owned hospital, they decided to create a separate
organisation. ASHWINI40 was set up in 1990 to provide curative services through the 40 bedded
Gudalur Adivasi Hospital. Today ASHWINI through the AMS provides a 3 tier health care service.
In 1995, based on the success of ASHWINI it was decided to institutionalise all their development
40
www.ashwini.org
46
interventions. ASHWINI also provides midwife training under the National Social Service
Scheme. It is recognised by the state government and the university grants commission.
The Vishwa Bharathi Vidyodaya Trust41 runs the Vidyodaya School along with a residential school
for dropouts under the government's Sarva Shiksha Abhiyan42 programme. It also conducts a twoyear teacher training course and has a large outreach programme. The Adivasi Tea Leaf Marketing
Society (ATLM) is the collective that markets the tea leaves of the adivasis while another informal
society has been set up to market the wild honey collected by the Kattunayakans under the brand
called BEE WILD. The Madhuvana Plantation, a common property resource, is a 176-acre tea and
coffee plantation meant to generate income for the various development interventions. All these
work under the umbrella of the AMS and the board members are predominantly adivasis selected
by the AMS. ACCORD is a community focussed movement, which is also led by the community.
In today's interrelated world, a holistic approach is essential. This also includes conservation and
maintaining the community's symbiotic relationship with their ecosystem and environment. The
recognition of the enactment of The Scheduled Tribes and Other Traditional Forest Dwellers
(Recognition of Forest Rights) Act, 2006, popularly called the Forest Rights Act, as a significant
and landmark legislation which had huge challenges and implications both for the community
and for conservation. ACCORD played an active role in supporting the community to ensure a
proper implementation of the Act. 31 special Gram Sabhas43 have been constituted in Gudalur and
Pandalur Taluks in accordance with the Act. These councils are increasingly being recognised by
the government as a vehicle not only for the implementation of the Act, but also for development
programmes of the government. AMS is working actively to strengthen the capability of the Gram
Sabhas to take on these challenges. Coupled with this, is the work on cultural revitalisation. Part
of the price that the adivasis may end up paying to enter mainstream society is a loss of their
cultural identity. In order to prevent this from happening ACCORD works with young people to
ensure that traditional knowledge values and cultural practices are passed on to the next
generation.
Ecoscape is a community based eco-tourism initiative started to empower the indigenous
communities. The social entrepreneurship model allows local communities to self-sustain and
also protect environment. It is located within the Madhuvana estate. Just Change is a fair trade
enterprise linking communities and business. The tea and other produce like honey, coffee,
pepper are traded with fishing communities and self-help groups in exchange of goods at a fair
price. AMF is the process of setting up a community bank as well as a series of community
enterprises.
Understanding the community
The focus of my observations were the indigenous communities. The predominant groups in
Gudalur and Pandalur taluq are the Panniya, Kaattunayakans, Bettakurumba and Mullukurumba.
These people live away from the rest of the society. They live in a small hamlets located deep in
the forests or tea plantations. Social seclusion is quite evident with the indigenous communities.
The trend of mingling and mainstreaming is evident. Many of the elderly and adults whom I
41 www.vidyodaya.org
42 Sarva Shiksha Abhiyan is the Government of India's flagship programme for achievement of Universalization of
Elementary Education
43 Gram Sabhas means Tribal Village Councils
47
interacted have all confided about shyness to talk to strangers and have expressed fear of nonindigenous people in the 70’s and 80’s. Some of the people whom I visited in the villages, shied
away from talking to me. The indigenous groups are classified as semi primitive, hunter-gatherers.
They are spread across Gudalur, Pandalur and the neighboring Wayanad district of Kerala. The
anthropometric features of these people are distinct and they can be clearly distinguished from
the non-indigenous groups.
Panniya, the majority population among the indigenous groups were traditionally bondage
labourers. They were enslaved by the landlords in their farms and plantations. Now most of them
are engaged in manual labor. Although, the bondage labour continues sporadically, but is usually
not prominent. They speak a dialect of Malayalam. The term Paniyan originates from the
Malayalam word pani meaning work; pannikkar means worker or labourer. The term paniyan is
used to address males, whereas the females are referred to as panichi.
Figure 15: Panniya (left) and Mullukurumba (right) woman
Kurumbas : They are the pre-Dravidian ancient inhabitants of the Nilagiris. Kurumba is not the
name of a single tribe. Rather it indicates a common name applied to different ethnic
communities in and around the Nilagiri area in Tamil Nadu, Karnataka and Kerala. In the Mysore
plains they are considered as a shepherd caste. Their name probably originates from their early
occupation of tending sheep (kuru) as a pastoral people. Five different groups called Kurumbas
have been identified in the Nilagiris—each of them being a distinct ethnic group differing from
the others in language, religion, traditional occupations and other cultural features.2 They also
inhabit different parts of the Nilagiris. The Alu or Palu Kurumbas live in the higher ranges, the
48
Betta Kurumbas (also called Kadu Kurumbas) and Jenu Kurumbas (also called Kattunayakans) in
the lower heavily forested areas, and the Mullu and Urali Kurumbas in the lower ranges and
foothills. Only the latter two groups of Kurumbas live in Pandalur taluk and in Wayanad district
of Kerala.
Mullukurumba are settled agriculturists. They are economically better off compared to the other
groups. They speak a dialect of Malayalam. The word mullu means arrow or thorn, but can also be
related to the word mula (bamboo), which grows profusely in this area and is an intrinsic part of
their culture and occupation. The Mullu Kurumbas are bow-men and hunters. Traditionally, the
Mullu Kurumbas were a forest people dependent on food gathering, hunting of small game,
extensive fishing carried out mostly by women, and slash and burn agriculture. Today they have
become settled agriculturists cultivating either their own land or work as labourers for big
landowners and coffee and tea plantation owners. As marginal farmers they cultivate both dry and
wet lands. In dry fields they raise spices such as pepper and ginger and crops like coffee and
plantains. They cultivate paddy in the swampy wetlands.
The Mullu Kurumbas speak a Kannada dialect called Kurumba bhasha with an admixture of Tamil
and Malayalam words. They live in uni-ethnic settlements in the Wayanad district of Kerala, and
there are 10 settlements of theirs in Pandalur taluk with 8-12 households in each settlement. Their
houses are neat, clean and aesthetic with a colour wash to the walls and designs. They are
arranged in a planned manner around one or more quadrangles at the centre of which is a temple
house, called deiva perai or koil veedu (god’s house). This is of the same design as the other houses
and its walls are decorated with various designs drawn and inscribed by the men at the time of its
construction. A separate shed for husking harvested grains is also put up near the temple.
Figure 16: Mullukurumba women sowing paddy
Figure 17: Mullukurumba women sowing paddy
49
Bettakurumba were traditionally elephant trainers. Some of them are employed by the forest
department to herd elephants.
Kaattunayakan44 are the most primitive among the four groups. They live near the borders of the
forest. Traditionally, they were hunters and gatherers. They are known for their honey collection
skills. They speak Kannada corrupted with Malayalam. They were also involved in shifting
cultivation.
The adivasis of Gudalur have lived in these hills for time immemorial. The Edkal inscriptions at
Wayanad provide a valuable evidence that the adivasis were here since 3000 BC. Mullukurumba
group were skilled warriors and hunters. They had helped Pazhassi Raja of Waynad in many of his
war campaigns. Mullukurumbas supposedly helped the British to build the road between Sri
Rangapatna and Calicut passing through Sulthanbatteri and hence were given lands to cultivate as
a pay for their service.
The adivasis in the Gudalur valley have been exploited by the British officials, local landlords,
forest department and by the government staff too. Large-scale migration of non-adivasis into
Gudalur can be traced back to the mid-19th century. At that time, much of the area was under the
control of the Nilambur Kovilagam, a royal family from neighbouring Kerala, who leased out land
for the establishment of first coffee and tea plantations primarily to the British. The emergence of
this plantation economy required labour from the plains. The next significant wave of migration
was in the 1950s when the post-independence state launched the “grow more food” campaign to
contain the effects of famine. During this time, smallholders from the neighbouring state of
Kerala were encouraged to cultivate food crops and develop the agricultural economy of
independent India. The last major wave of migration into Gudalur was after the Sirimavo–Shastri
Pact in 1964, a pact that resulted in the repatriation of over five lakh Tamils from the plantations
of Sri Lanka to various parts of South India. (Karthik & Menon, 2016).
Along with this, the nationalisation of the forests and the resultant driving out the indigenous
and non-indigenous communities out of the forest alienated the people in their own homeland.
The indigenous community which is less than 10% of the population faces economic and social
challenges. All these have further driven them to poverty and displacement. The atrocities against
the adivasis were more commonly acted by the local landlords. They would occupy the lands
belonging to the adivasis, fence it and claim it as theirs.
In one such incident, land belonging to the adivasis which had a sacred grove was occupied by a
landlord. Group of men including young K T Subramanyam, a Mullukurumba youth approached
Mr Stan Thekaekara for help. Stan and the group of men removed the fence and built huts in the
land reclaiming their position. The landlord later set fire on the huts and sought police action
against them, resulting in jailing of the men. They were later released on bail, but the struggle
continued.
There were gross human right violations on the adivasis. They were already economically and
socially exploited, but now, there was final extermination from the society and stripped of their
44 Kaattunayakan means master of the forest
50
basic human rights and values. The adivasis realised that they were unorganised and dependant
on the landlords. They lacked unity and a collective spirit to fight.
Figure 18: Panniya family standing in front of their demolished hut
The land rights movement started with organising the village members as sanghas. It is a three
tier structure organised at village, area and taluq level. This came to be known as the Adivasi
Munnetra Sangam. In 1988, these sangams federated to form a registered society- AMS, a peoples’
movement bringing all the five tribes together. Today the AMS covers close to 20,000 adivasis in
over 200 hamlets. The interventions helped many families to reclaim land and today nearly a 1000
families own small plots ranging from half an acre to two acres. On December 5th of 1988, all the
adivasis marched in Gudalur town. An unprecedented display of solidarity and unity was seen. It
was for the first time; the outside world got to know about the sheer numbers of the adivasis.
Until then, it was acknowledged as few people of adivasis. This historic day is celebrated every
year as Adivasi day. (Fieldnotes, 2015)
Figure 19: One of the Sangam meetings
51
Figure 20: Demonstration on the court road in Gudalur on 5th December 1988
COMMUNITY HEALTH PROGRAMME
At another level, the health of the adivasis was alarming. Malnutrition was rampant; many women
died in childbirth; children as well as adults died of preventable diseases like dysentery and
tuberculosis. People preferred to stoically await death at home, rather than go to an unfriendly,
alien hospital far away.
There were a series of catastrophic incidents in Theppakad, where three maternal deaths occurred
in a single village, which were all preventable. The adivasis by now were all an organised group
realised the need for health care. The provocation came, because the existing health systems
wasn’t accommodative to them. They were ill-treated in PHC’s and widespread discrimination
existed even within the health care providers. The adivasis were sensitised to the health issue and
asked ACCORD for health care services.
Two young doctors, Dr Devadasan N and Dr Roopa, joined ACCORD to fight the health battle.
With patience, they trained a cadre of adivasi village women as “health workers”.
Chemban Manikantan who began working as a helper in the mobile clinic as a part of health outreach programme of ACCORD. He along with Parashu Shridharan and others underwent health
guide training under Dr Roopa and Dr Deva. With the help of AMS and ACCORD, an area centre
in Devala, where health related work was carried out. His initial work was limited to identifying
Anaemia cases and giving the patients few Iron capsules. He remembers, carrying a small box
containing essential medicines and distributing it in the community. His duty was to refill the
health kit from the cupboard. He then underwent more training to diagnose and treat common
ailments. He would also maintain growth chart of children, immunisation schedule in every
community. Manikantan added,
52
“The health condition very was poor, there were no check-ups for pregnant women, no one got
vaccinated, TB was high, Pregnant mothers would die often and many were weak and also had
Anaemia”.
He remembers about three maternal deaths within a month in Theppakkad. When enquired, it
was found that, the Bettakurumbas were fearful of visiting health facilities coupled with besides
poor access to health care.
The severe and serious cases in the community had to be taken to distant either
Sulthan Batthery, Mysore, Coimbatore or Bangalore. The adivasis felt it was very stressful and
taxing on their pocket. A The young doctor couple trained young adivasis to become health
workers.
The focus of the work in the villages was the health of the most vulnerable group – namely
pregnant women and under five children. A weekly mobile clinic would visit the villages covered
by the health worker to cater to more serious patients and also to upgrade the skills and
knowledge of the health worker. An important step had been taken towards the objective of
encouraging people to access health services.
Figure 21: The first health worker team
After almost three years of gruelling, often frustrating effort, the tide slowly turned. Infant and
maternal deaths were no longer accepted as commonplace and inevitable. And patients seeking
curative care began pouring in. The problem now was that there seemed nowhere to treat the
more serious cases. The government hospital was overcrowded and impersonal, private hospitals
prohibitively expensive.
Fortunately, in 1990, another doctor couple joined the team. Dr Nandakumar Menon, a surgeon,
and his wife Dr Shylaja Menon, a gynaecologist had just returned after 10 years in the United
States, wanting to start a hospital for the poor in rural India. They joined ACCORD. ASHWINI,
another society, was started to cater to the health needs of the community. They started a clinic
53
within the ACCORD office. Youngsters from the different adivasi tribes with some schooling were
trained as nurses, accountants and other support staff. Manikantan recalls, the initial trainees
were, Ambika, Sita, Janu, Uma, Meenakshi, Janaki and Padmini.
Dr Deva and Dr Roopa were against duplicating the work of government, i.e. starting a hospital
and providing institutional care. Dr Shylaja adds,
"It was a lesson learnt that, health care lies in a spectrum and there is no demarcation between
community services and organisational care"
They decided to jump into action and started their work at Gudalur. They started a modest
hospital at a rented building. So modest, that the operation theatre was just 6*6 feet. They would
spend most of the time at field raising awareness about health and hygiene. She narrates,
"there was a man who would stand outside the hospital all day and they got suspicious and when
they enquired about his presence, he was a patient waiting to see a doctor, but was scared to go in".
This was the situation and they realised they had to deal with more complex issues. They also had
a condition to start the hospital. They also want to treat non indigenous people, because it was
about helping poor people irrespective of their caste and creed. AMS agreed to it, but had its
doubts in the beginning. She adds,
“community participation can be demanding sometimes because they would ask for what they are
informed. The logistics, man power, finance would be a challenging task to manage and hence they
stressed to include the no- indigenous people to be included for availing the services. Also, the nurses
realised that it was important to show others about their achievement. It was a matter of selfesteem”
Figure 22: Doctors and health workers on their field visits
54
The 20-bedded Gudalur Adivasi Hospital was set up to complement the community health work.
The secondary care hospital is efficiently managed by the adivasi team with the help of a few
professionals. Soon afterwards, a process of active decentralization was set up, with the
establishment of 8 area centres each covering between 20 and 60 adivasi villages, so as to bring
health care to the door step of the villagers. Also the health care expanded. The eight area centres
(Devala, Ayyankoyil, Devarshola, Erumad, Paattavayal, Sri Madurai, Ponnani and Gudulur) which
were already functioning as administrative centres of AMS were supported with health centres.
Volunteers from the community enrolled for the health workers training. They would receive
training of 15 days in the field and at hospital for a day. They were taught to identify symptoms of
Anemia and fevers, ANC measures and first aid techniques. The senior health workers now
supervise these area centres.
The area centres are run by trained adivasi nurses called “Health Animators”, who are more
skilled in curative care than the health workers were. People come to the sub-centre for all their
basic health needs. What the Health Animators cannot handle at the area-centre is referred to the
Gudalur Adivasi Hospital. The health animators also visit each village on a regular basis. They
treat minor illnesses, take health education classes, and continue, in collaboration with the old
health workers, to monitor pregnant women, children under five years of age, and persons with
chronic diseases like TB, asthma, etc
Figure 23: Cheeru, a healthworker carrying essential medicines and other supplies in her backpack
and visiting a hamlet close to Gudalur
55
Figure 24: Omana, a health worker at Devala area centre in a conversation with Gudalur Adivasi
Hospital team regarding a screening outreach programme
HEALTH STATUS
The health trends in the Gudalur Adivasi population is quite inspiring in some conditions and
rather displeasing in other cases. Everyone agrees to the fact that, communicable and preventable
deaths related diseases with commonly prevalent in the 80’s when ASHWINI started. The
common diseases were TB, Malaria, Anaemia, Diarrhoea, Pneumonia, etc. In 1986, the situation
was comparatively worse than the national averages. Deaths from Anaemia, Tetanus and
Diarrhoea were common. There was high incidence of Eclampsia. Antenatal check-ups were less
than 2%. Primary Immunisation was less than 5%. High incidence of Maternal and Infant
mortality was seen because of the above reasons. The cultural and social factors played a major
role besides economic and political determinants.
Table 1; Comparison of death rates between Gudalur Adivasis and the National data
National
data (2005)
Scheduled tribes
(2005-06)
Gudalur
Adivasis(2009)
U5MR 42.1
95.7
55.1
IMR
36.1
62.1
45.9
MMR
16.3
NA
1
With the communitisation of the primary health care and the development activities
complementing the health care, health indicators such as IMR, MMR, etc. have shown remarkable
improvement. Graph 1 and Graph 2 shows the trend in the mortality rates. MMR has been
considerably low compared to the national average and ST data. (SRS, 2011)
56
Sickle Cell Anaemia is another common disease observed in the adivasis. Dr Shylaja opines that, it
is because of inbreeding. When asked about counselling the indigenous people about it, she adds,
"It is not difficult to change the attitudes and cultures of the people. One of the health animators
knowing the consequences, married her cousin and had a baby with sickle cell disease". Manikantan
observes that, the Panniya and the Kaattunayaka group are more vulnerable to sickle cell disease
than others because of increased practice of consanguinity. Sickle cell disease is also seen in the
Chettys45 and Badagas46.
While the other disease prevalence and incidence decreased, Hypertension, Diabetes Mellitus,
Cardiovascular stroke, Mental illness, etc increased. These diseases are also attributed to
developmental activities. A recent study was conducted with a goal of understanding the risk
factors of common diseases among the Gudalur adivasis in relation with development. I was
found that development stress may be affecting the tribes differentially causing differences in illhealth. Among the Mullukurumbas this may be due to access to better food, changes in physical
activity, overweight and alcohol leading to diabetes and hypertension combined with smoking
leading to one pattern of cardiovascular risk leading to more heart attacks. Among the Panniyas,
Bettakurumbas and Kattunayakans, development may be leading to lack of or access to poorer
foods and alcohol leading to hypertension and undernutrition that be leading to another pattern
of cardiovascular risk profile with increased risk of strokes. (Zachariah & Srivatsan, 2015)
Trend in the IMR among the
Gudalur Adivasis
IMR/1000 live births
300
250
250
200
150
105
100
50
0
1985
48
1990
1995
2000
2005
45.9
2010
28.1
2015
2020
Year
Graph 1: IMR trend in the Gudalur Adivasis
45 Chetty’s are the local landlords
46 Badagas are an indigenous group living in the higher Nilagiris hills
57
MMR/1,00,000 live births
Trend is the Maternal mortality rate among
the Gudalur Adivasis
5
4
4.5
3
3
2
1
1
0
1998
0
2004
2010
2015
Year
Graph 2: MMR trends in the Gudalur Adivasis
Sickle cell anemia is another cause of concern among the adivasis. The prevalence is 14%.
(ASHWINI, 2015)ASHWINI has been implementing a well-designed and comprehensive Sickle
Cell control programme for more than ten years among the adivasi and Chetty population of
about 30,000 in the Gudalur valley, Nilagiris district, Tamilnadu. It is managing the Sickle Cell
Disease Center for the Nilagiris district and has done lot of work to begin addressing this issue on
a local and national level. ASHWINI's strategy of controlling the disease with a combination of
clinical and community-based team members to implement a successful management system for
adivasi populations is worth documenting and sharing with other organisations working with
adivasis.
Malnutrition is another area of concern. Anecdotal reports of malnutrition are misleading.
Chemban from Ponnani village in a meeting mentioned that, although the quantity of food the
adivasis ate was less few decades back, but they were healthy in contrast to the present situation
where quantity has increased but quality has reduced. While, Madha of Ayyankolli village told
that the situation was bad. They didn’t have enough food to eat previously, but the government
fair price shop provides them enough grains now. A study on the malnutrition of the under 5
children conducted among the community have shown around 104 children under “Severe”, 462
children under “Moderate” and 668 children under “Normal &G1”. (Klatz, 2015)
The current adults remember that in their childhood they had a wide food basket which was
primarily obtained from the land and forest. This included range of cereals, millets, tubers, leaves
and fruits from the forest, a variety of hunted meat and fish from the streams. Although there
were periods of starvation, the food quality was better. Today their primary food source is rice
given through the public distribution system. Most of the food is bought with scanty amounts of
vegetables and fruits, minimal protein and fat. Although physical activity has reduced from their
childhood, the most members interviewed are still very active.
Zachariah recently surveyed the risk factors for non-communicable diseases and found the
influence of development and health status i.e., the development of small towns in the vicinity
and the entry of urban concepts, processes and organizations like health care, education, wage
58
labour, and development/community health groups have all led to changing health profiles
among the adivasis. (Zachariah, Anand, 2015)
The Mullukurumba tribe which is socioeconomically better off has higher rates of diabetes,
obesity and hypertension. All the other three tribes have almost non-existent diabetes, moderate
rates of hypertension and high rates of low BMI (chronic energy deficiency). The villages which
were more developed had higher rates of diabetes, hypertension and obesity. The villages which
were less well developed had higher rates of hypertension and low BMI. From this, it can be
inferred that the, villages and tribes have different cardiovascular risk profiles based on their
development parameters. Review of community mortality statistics showed that the foremost
cause of death in the community was heart attacks and strokes. The overall rates of deaths due to
strokes and heart attacks are equal to urban Kerala. (ASHWINI, 2015) In Mullukurumbas, the
main cause of death was heart attacks probably secondary to obesity, diabetes, hypertension and
less physical activity. In the other three tribes the chief cause of death was stroke probably due to
wide-spread hypertension.
To bridge the gap in provision and accessibility of the health services, a community based health
insurance scheme is followed at ASHWINI. The AMS members pay Rs 22 per year per person a
premium. This has resulted in increased utilisation of services and mobilise resources within the
adivasis. The geographic reach and the total number of subscribers are challenging, but it has
made the health care services affordable to the Gudalur adivasis. (N Devadasan, 2004)
Mental Illness is on a rise in the Gudalur Adivasis in the last decade. An analysis of the mortality
rates was conducted in 2004 and revealed that suicides were the second most common deaths
after cancer. A baseline survey was conducted. This was done to assess the burden of the disease
in the community and to start discussions about the topic. Village leaders, health workers and
youth groups were involved in the discussions. 184 villages were covered in the survey. Meetings
were held in each of these villages and a survey form was used to collect data regarding number of
people with abnormal behaviour, mental retardation, alcoholism, substance abuse and suicides.
Peoples’ attitude to the causation and treatment of mental illness was also studied.
More than 60% of the surveyed were completely or partially ignorant about issues concerning the
mental health of the community. About 12% of the people had strong misconceptions and wrong
beliefs about mental illness. This fact is more striking, when we consider that the survey was
conducted only in sangam villages. Adivasi members in sangam villages are expected to have
comparatively more exposure to health issues than the non-sangam villages, due to continuous
interaction of ASHWINI’s health team with them.
The most important result of this base line study was that it triggered lots of discussions in the
villages on mental health. The community members came together to discuss various new issues
like mental health, suicides, depression, alcoholism, epilepsy etc. 67 new patients were identified
during the course of this base line study and people felt that they need to be followed up or some
sort of treatment should be started. (ASHWINI, 2009)
The spread of addiction to alcohol and ganja47 during the course was highlighted in many
occasions of the community mental health programme.
47
Ganja is the local name for Tetra hydro Cannabis
59
Figure 25: All team meeting in which alcohol de-addiction was discussed
Mental illness, in Stan’s opinion is caused by the erosion of the values and ethos at family and
community level. Indigenous communities who are known have high community bonding and
sharing attitudes are also facing mental issues is because of losing these value systems. Therefore,
the community based approach to treat these illnesses would be an appropriate measure.
Alcoholism is the newest health issue which has a mental, social and economic impact on both
the individual and the family. The government outlets where liquor is easily available have made a
huge impact. The exploitation of the adivasis by luring them to alcohol for cheap labour is also
reported. The government policy on producing alcohol is, at first place, the cause of alcoholism.
There is a political stand and the vested interest of the industry.
Figure 26: Mental health care provided by missionary hospital
The health infrastructure in Gudalur and Pandalur are adequate. There is a mix of both public and
private health care centres. Primary health centres are located for every ten thousand populations.
The government schemes such as Muthulakshmi Reddy scheme for mother and child health
attract people. With the availability of better public health care facilities and the monetary
benefits given through the government schemes, institutional deliveries have increased. There is
60
still a tendency for home deliveries among the adivasis, although the numbers have reduced.
There were 45 home deliveries among the adivasis in 2014 (Fieldnotes, 2015). The NRHM has
introduced a new health worker in hilly and Adivasi region called ‘tribal coordinator’ who job is to
convince the adivasis to avail more services at PHC.
In one of the discussion with a facilitator, who claimed that ASHWINI’s work is not
supplementing, but duplicating the work. (Collectivenotes, 2015) The records of health indicators
at ASHWINI are used by the health officials to add up the numbers to show an upward health
status. But undermining the actual situation. This is refutable. The claims are observatory and
from the field experience, the health records are used by the officials to actually note the health
indicator status. The district health survey found out that 0.6 women in 2013 had home deliveries.
(DLHS, 2013)When the number of the home deliveries among the adivasis of Gudalur is
extrapolated to the entire district population and compared to the district survey, the numbers
are comparable.
Several civil society organisations are carrying out health care in this region. The Nilagiris
Waynad Tribal welfare society hospital is located in Ambalamoola in Pandalur taluk of Nilagiris
district in Tamil Nadu. It is a private non-profit hospital. The hospital was functioning on the
model of PHC with selective primary health care. It was also the district monitoring center for TB.
Besides, numerous for profit private hospitals, Christian missionary hospitals also are providing
services.
One of the Christian mission hospital was exclusively rendering mental health services in the
region. It was run by the Catholic health association of India, a charitable catholic missionary
hospital located in Pattavayal in Pandalur taluk. Selective secondary care was provided by
ASHWINI and few other hospitals. The nearest tertiary care
centres were located in Calicut and Mysore. Crossing the forest to
reach Mysore during night times is prohibited and hence, most of
the times, patients are referred to Calicut Medical College.
The Integrated Child and Development Care is provided by
Anganwadis, better known as Balawadi. A visit to a Balawadi in
Erumad village in Pandalur taluq to check the number of Adivasi
children availing the services revealed a good picture. But
according to Mrs Cheeru, an Adivasi health animator at ACCORD
mentioned that, it wasn’t feasible with the young nuclear Adivasi
families because of their work schedule. Most parent are labourers
at estates and the timings are not compatible with the Balawadi
timings. Hence most parents take their children along with them
to the work site. The occupational health needs to be explored in
this region.
Figure 27: Demographic details
in a PHC
61
RELIGION AND CULTURAL ASPECTS
Cultural aspects of the Gudalur adivasis are unique. Many cultural facets describe the way of life
of the adivasis at Gudalur. Each of the indigenous group have their unique dressing style. Men,
irrespective of all groups, wore a piece of white cloth tied around their waist. Panniya women tied
a white cloth about a meter or two, around their chest covering their breasts. They also tied a
small piece of cloth around their waist to secure the bigger cloth creating a big pocket. They
wrapped their upper body with another piece of cloth. Blouse are a recent addition. So are sarees.
The women have curly hair greased with coconut oil. Most women cut their hair at shoulder level.
Marriage is often consanguineous, but it is fast eroding. The inbreeding explains the reason
behind high prevalence of Sickle cell anemia among the adivasis. Marriage between groups is not
permitted, although cases of such union have taken place. Mr Velan, education animator at
Ponnani once told me that, they resent such activities and who ever goes against the norm are
excommunicated. Madhavi, a Kaattunayanaka health guide mentioned that, they go to
Mullukurumba houses, but wouldn’t go to a Bettakurumba and Panniya house. The latter are
considered low. She said that they wouldn’t have marriage alliances with any other adiavsi groups.
When probed further, she mentioned that Panniya women don’t follow the monthly menstrual
rituals and this is absolutely unacceptable to them.
Panniya religion is animist. Ancestal spirits and male and female deities are worshipped. The
spirits are invoked for good actions by their shaman called ‘Attali’. Their chief goddess is Katta
Bhavathi (goddess of the forest). Devil worship is also prevalent. Most of the Panniya songs invoke
their ancestral spirits and deities. Panniya stories depict the relationship between Panniyans and
their non-Adivasi masters, the problems with their wives over affairs in their master’s household,
and their relationship with animals around them. Sanskritisation is also happening to some
degree where Hindu gods and goddesses are worshipped together with other castes and tribes,
which implies an acceptance of the Hindu caste system with its hierarchies.
The Kattunayakans worship nature in the form of animals, birds, the sun, the moon, even shelter
and the shade. They still worship rocks, hills, snakes and animals claiming their origin from them.
They have implicit faith in charms, sorcery and black magic. Deities are Mari, Mastideiva (male)
Hethappan and Mala Deivom and they also worship Siva by the name of Bairava. They celebrate
festivals like Onam and Vishu. Their oral tradition flows through music and dance along with
songs and tales about forest trees, wild life, famous temples and about acceptable behaviour in
kinship relationships. Musical instruments used are the thambattai, kuzhal, pipi, kulalu, mard,
parai, tempte, pukiri, kadimai and tavai. Their council, headed by the muttam (headman), is called
Nyaya. Every settlement also has a headman called karanvar or modale.
Parvathi, education coordinator once told me while walking to a village to meet a healer, that
they didn’t worship any Hindu deities like Ganesha or Shiva. They only worshipped Kaavu48.
Kaavu is a sacred grove worshipped by the adivasis. It consists of tree or a group of trees. The
surrounding area is maintained neatly and sometimes smeared with cow dung. It has been well
documented that sacred groves often play a key role in biodiversity conservation, especially in
48
Sacred grove
62
highly modified landscapes. They maintain some habitat heterogeneity, sometimes acting as
‘stepping stones’ for long range dispersal of numerous species. This is especially true for a region
like Gudalur, where communities have lost a considerable part of their ancestral domain to both
the state (in the creation of forest plantations, particularly the Tantea corporation) and
immigrants into the area who have appropriated their lands and converted it into monoculture
plantations.
Velan said that, usually a white liquid seeping plant or tree is revered in the Kaavu. Over the
years, there has been increased identification with Hinduism or sanskritisation has seeped into
their names, folk traditions, celebrations and also marriages. The Brahmin priest is invited to
conduct a marriage of late which was not followed in the earlier days. There have been increasing
number of religious conversions mainly to Evangelical order. Vishnu, a school teacher at VBVT
told me that, people who never understood their own religion go into others.
Figure 28: Sacred grove at Naduvattam village
PHYSICAL INFRASTRUCTURE
In terms of physical infrastructure, the situation is fair. Topographically, the lay of the land is mix
of hills, valleys, rivulets. The scene is dominated with tea plantations. The condition of roads here
ranges from below average to good. The roads connecting between major towns and villages and
those particularly the interstate roads are asphalted and maintained well. But those connecting
small villages are average, and are not maintained well. The local public transport is fairly good
considering its price. There are few buses in a day connecting hamlets and villages. There are
numerous private jeeps and auto rickshaws operating between short distances. These are often
overcrowded and suffocating to travel. They ply between all villages and hamlets every few
minutes at a price higher than public transport service. There are few bus shelters. People stand at
a designated point on the side of the road. The plight is pitiable during monsoons.
63
Electricity supply is fairly good in all areas except in section 17 land, but the government has
provided solar lamps. Section 17 land is a litigated land which was earlier leased to the British by
the Nilambur Kovilagam royal family. After the land reforms in 1970’s, the land fell into petty
hands and the presently in court. The area is now termed section 17 by the revenue department
and is devoid of basic services since it is under litigation. Tele-connectivity of mobile phone
services is good and land line telephones are decreasing. The broadband services and the internet
connectivity are above average.
Figure 29: Thatched bus shelter near Gudalur
Adivasis live alongside the non adivasis. But most live separately in groups. Their houses are of
substandard quality, although the hill area development board of the state government are
constructing house of fair quality.
Figure 30: Kaattunayaka hut
64
AGRICULTURE AND FOOD PRODUCTION
Gudalur adivasis are historically hunters and gatherers. Kaattunayakans engaged in shifting
cultivation, while the Mullukurumbas grew paddy and millets. Full-fledged agriculture only began
with civil societies involvement in land reforms in 70’s and 80’s. Tea was encouraged to grow,
because it was onetime investment and economically sustainable.
Traditionally adivasis depended were self-sufficient for food. The forest gave them a lot - a wide
range of fruits, tubers (roots), leaves, wild vegetables and of course meat. They also grew a range
of traditional vegetables – like different kinds of greens, yams, pumpkins, beans etc. But over the
years as they became more and more part of the mainstream society and less dependent on
forests they have slowly shifted from a highly nutritious and varied traditional diet to a less
nutritious diet – with rice as the staple. And as they became more and more dependent on cash
they increasingly spent less time on growing their own food and instead buying from the shops.
Thereby shifting from a varied and protein rich diet to a carbohydrate rich diet. A recent survey
found that the food basket has shrunk. (Zachariah, Anand, 2015)Today their primary food source
is PDS rice. Most of the food is bought with scanty amounts of vegetables and fruits, minimal
protein and fat.
Similar trend was recorded by Dr Denis Burkitt, the popular epidemiologist from Ireland who did
primary work in Africa. He noticed that diet in Uganda was rich in fibre based vegetables and
tubers as compared to the diet back at home in UK. This research laid the foundation to our
understanding of diet based diseases and the usefulness of diet. (Collectivenotes, 2015)
Figure 31: A Public distribution system shop displaying the picture of rice sold at the outlet in
Ayyankolli village
65
EDUCATION
According to Planning Commission, the school drop-out rate among STs in Tamil Nadu between
classes 1-8 is 71.60%. (Planning Commission, 2000) In the Nilagiri district, it is about 74% between
the 8th and 10th standards. This was higher than that recorded in Karnataka and Kerala. In the
Nilagiri district the drop-out rate of the tribal girl child is much higher than among the STs of
other districts. The literacy level among the Adivasi communities in Pandalur taluk is the lowest
in the district with high drop-out rates at the upper primary and high school levels. In Gudalur
block there are 9 Government Tribal Schools, 21 government primary schools, 15 government
middle and higher secondary schools, and 10 Christian missionary schools from the primary to the
higher educational levels. The fees charged by the private schools are on the high side with the
tuition fee being more than Rs 5000 per year. Additional expenditure on the uniform, transport
costs, books could be further taxing. The accessibility is another issue. The percentage of Adivasi
students passing the 10th standard exam is also very low. One of the important reasons for low
enrolment of girls in the Adivasi areas is the lack of relevance of formal education for their roles
and responsibilities in their own culture.
VBVT is providing value based alternative education to the adivasis and non adivasis. The school
is modelled on alternative pedagogy. The education system here stresses on cooperation and
group work, creating a possibility for children to work at their own pace, co-curricular activities
are given equal importance and firm value-base is inculcated. Rahul, the English teacher at
Vidyodaya school has successfully organised many camps for the children. The main aim was to
expose the children to different cultures, activities, problems, etc. in a place they have no access
or opportunity to go. Variety of activities like sports, village walk, chat with village elders, talk by
senior AMS members, discussion and debate about social topics and reflection about it through tshirt painting, etc. are organised. These camps also include sports activities which encourage
team spirit. Stress was laid on Frisbee. This activity garnered enthusiasm and was used to grab the
children’s attention towards education.
Figure 32: Children on a transect walk in the forest during the camp
66
ENVIRONMENT
Gudalur’s dense malarial forests were opened up in the late 19th century with colonial zest, as
mentioned above, first for coffee, then tea plantations, when the Nilambur Kovilagam leased out
large tracts of land to wealthy British planters. An enormous labour force was required to clear
these forests and transform them gradually into the uniform rows of well-pruned tea bushes
interspersed with silver oak trees that still dominate the landscape. The repatriation of Sri Lankan
Tamils during the late 60’s and 70’s resulted in converting nearly 27,000 acres of forest to tea
plantations to provide employment and livelihood.
With the forest cut for agricultural purposes, the green cover declined drastically. Further, the last
remaining forest was declared Mudumalai Wildlife sanctuary. With further encroaching the forest
cover above 1500msl, the sholas too were not spared. This caused much more ecological
imbalance. The Sholas are a mosaic of mountain evergreen forests and grasslands. They are found
only in high altitude (>1500 metres asl) regions within the tropics, and are limited to the southern
part of the Western Ghats. They are characterised by undulating grassland patches, interspersed
with thickets of stunted evergreen tree species, and are home to a host of endemic and
endangered plants and animals. They are also vitally important in keeping water cycles alive. They
retain most of the rain they get over the monsoons, and release it slowly through the year via a
network of streams and rivers, that eventually serve the needs of a huge number of human
settlements across south India.
With sholas encroached, the water table has reduced further. The remaining rivulets also began to
dry with inadvertent planting of Eucalyptus trees along the rivulets. These trees are known to
suck the underground water leaving behind a dry top layer of sand. This resulted in decrease in
fauna because of shortage of water. Villagers recall witnessing herds of deer decades back near the
water bodies.
Figure 33: Encroaching Shola grasslands
67
The government policies such as ban on the use of hydraulic excavators and tube well diggers are
implemented well but selectively carried out to benefit the government work. River Ponnaniyer
meandering through the Nilagiri forests passes through the Ponnani village. Recently, the village
municipality used a hydraulic excavator to clear the weeds along the river. With it, rich biome and
invaluable water plants also were removed. Worse, the fish depending upon the algae were not
spotted. Fish from the river was an important source of protein for the indigenous people here.
Unscientific practices not only harm the environment but also affects the people depending on it.
Reckless environmental destruction and its consequences are detrimental to humans and affects
health directly and indirectly.
Figure 34: River Ponnaniyer now flowing lifeless
Indigenous communities across the world have played a significant role in conserving their
natural world. Their lifestyles, cultural practices and spiritual belief systems, intentionally or
otherwise, have resulted in a relatively harmonious balance and stability through centuries. The
hunting traditions among the Adivasi are rooted in ecologically conscience. They have rules
governing hunting.
They wouldn’t hunt cats, domesticated animals, pregnant and younger ones also spared. Dog
usually accompanies the hunting team and to help them find the catch. The hunting is carried at
special occasions and a strict calendar based on the reproductive season of animals is followed to
avoid the animals which cannot be hunted. There are more lessons to be learn from them. (AMS,
2013)
Another concern across the world is the human animal interaction which is heading towards
conflict is basically due to the encroachment of the forests. Wildlife trespass into human
settlements often in search of food. This either results in killing of animals or wildlife preying on
68
domesticated animals and sometimes on humans. Reports of human-animal conflict appear
regularly in newspapers.
Figure 35: Adivasis going on a hunt (ACCORD Archives)
Figure 36: Co-existing with Animals-Leopard pug marks spotted during a village visit
69
Exploring perspectives of local traditional healers on oral health among the indigenous
population, South India: Reflections on qualitative research orientation and
communitisation of this initiative.
ABSTRACT
Background: The indigenous concept of health and disease is based on holistic approach where
illness, wellbeing, culture, environment, etc are intertwined. Rural India faces roadblock to oral
health care in terms of Accessibility, Availability, Acceptability and Affordability (4A’s) especially
in the indigenous areas where health seeking behaviour among the indigenous communities is
driven by cultural ethos and influenced by local beliefs. The health system operates on biomedical
model which causes cross cultural conflicts that may mediate with 4A’s.
A preliminary study was conducted as a brief project of community health learning programme to
understand the perspectives of local traditional healers on oral health and explore the
convergence and divergence with the current dentistry framework to support further integration
of health systems.
Methods: This study involved participant observation for six months focusing on the
determinants of oral health in the indigenous groups in Gudalur, South India. Observations in
homes, community facilities, within the region were supplemented by in-depth interviews and
focussed group discussions with ten local traditional healers. The transcripts of the discussion
revealed overlapping symptom conditions and were categorised into themes-culture, health
conditions, local health traditions, social position and relations, difference with western
biomedicine, access to herbs, etc. Grounded theory helped analyse observations and interviews.
Reflections: While the results are still analysed, this paper focusses on two challenges that the
researcher faced in this evolving study. Researcher is a dentist with a training emphasised on
biomedical, evidence based, epidemiological western framework who is trying to learn qualitative
participant observation research. The research is focussing on communitisating the research with
the support of local organisation to bring about participant action.
Results: Cultural practices such as prayers, rituals and offerings along with herbal therapies play
a major role in healing. Changing social, economic, political, cultural and environmental
determinants have increased the prevalence of oral diseases. Some of the causes, diagnosis and
treatment for common oral conditions are both contradictory and some supportive to western
biomedical framework. Those supporting factors support integration by complementing or
supplementing the health system.
Conclusions: Researcher is undergoing a paradigm shift from patient to person centred health
care, subject to participant research and biomedical to social care. Community based health
systems inclusive of local health traditions make a responsive people centred health systems.
70
BACKGROUND
Oral health is an integral part of general health. (WHO, The World Oral Health Report 2003.
Continuous improvement of oral health in the 21st century-the approach of the WHO Global Oral
Health Programme. , 2003) Oral health, like the rest of the body parts and their functions,
contributes to the overall quality of life of an individual. Oral diseases affect majority of the
Indian population. 83% of 6-19 year olds are affected with dental caries. (FDI, 2009)Prevalence of
Edentulousness is 19% in the age group of 65-74 years and the age standardized incidence of oral
cancer is 12.6 in India. (WHO, The World Oral Health Report 2003. Continuous improvement of
oral health in the 21st century-the approach of the WHO Global Oral Health Programme. , 2003)
Oral health delivery system is still following the inverse square law in India. (AIIMS, 2001)Rural
India faces roadblock to oral health care in terms of accessibility, availability, acceptability and
affordability. According to Central Bureau of Health Intelligence statistics, India has 5278 dentists
working at Government hospitals. (CBHI, 2013) There is no data available on the number of dental
surgeons working in rural area. The Dentist-Population ratio is 1:10,120.85 and the only 59% of
Indian population is served by Dentists. (CBHI, 2013)
The NRHM seeks to revitalize local health traditions and mainstream AYUSH including
manpower and drugs, to strengthen the Public Health System at all levels. However, there is no
mention about local health traditions in the joint Government of India and WHO workshop draft
on effective utilization of manpower. (Prakash, Duggal, & Mathur, 1999)Although, the draft
acknowledges AYUSH as a part of oral health care delivery system in India. Deprofessionalisation
of medicine is a recognized modality of delivering health services for effective primary health care
practice. Besides, medical doctor, the role played by multitude of social workers, accredited social
health activists, practitioners of Indigenous medicine, etc. is indispensable.
Local health traditions have been catering to health needs of the people since time immemorial.
Particularly worth mentioning is their role in lives of Adivasis’ or indigenous people. Tribal
concept of disease and treatment, life and death is culturally varied. (Gupta, Shrama, & Sharma,
2014) Traditional system of medicine also includes the local health traditions and sometimes
referred to as folk medicine. This system depends upon remedies found in nature, otherwise
available locally. Local health healers form an important part of the health care system within the
indigenous communities. World Bank recognizes their significant role in a health system.
Traditional Healers are usually informal, unrecognized by the government, and do not interact
with the rest of the health system. Yet they can be a formal part of a system. (World bank, 2013)
WHO notes that Traditional Healers are especially significant in developing countries because
they are more accessible and affordable. In addition, they are more socially accepted as compared
to formally trained health workers from the urban areas. (WHO, 2003)
The adivasis living in the Gudalur region belongs to different groups, each one with their own
identity, culture and occupation. The four adivasi groups – Mullukurumba, Bettakurumba,
Panniya and Kaattunayaka make the major adivasi population in Gudalur. Development activities
and exploitation over decades have caused much trouble to this minority group. However,
government and other civil society groups are working for their betterment in many areas
including health. One of the civil society organization working for adivasis is ACCORD. ACCORD
is actively working for the past three decades for adivasis’ land rights, education, health, and
housing and cultures all of them revolving around community empowerment. ASHWINI was
71
born out of such demand from the community to meet the increasing needs of the health.
ACCORD began realizing that the input of the medical systems is making traditional healing
practices slowly disappear. ACCORD has engaged in mobilizing the traditional healers in adivasi
communities to a forum where in they can share their experiences between themselves. Health
seeking behaviour among the adivasis is driven by cultural ethos and influenced by local beliefs.
The utilization of institutional healthcare services is sought after the alternatives of traditional
healing/ black magic/ sorcery are exhausted. (Gandhi, Verma, & Dash, 2015)One study has
documented the high prevalence of Periodontitis (gum diseases). (Philip, Chithresan, &
Vijayalakshmi, 2013) Another study reported that, Panniyas might have favourable compliance for
oral health promotional programs. (Vivek, Jain, Sequeira, Battur, & Tikare, 2012)
However, no qualitative studies have been done concerning their beliefs and illness behaviour
related to oral problems. Gandhi noted in her observation that many Adivasis would visit to
health institutions only after visiting a local traditional healer. (Gandhi, Verma, & Dash, 2015)
Therefore, some ethnographic knowledge is needed to understand how and why modern health
services are perceived and used in a society. This data is lacking in oral health especially in the
Gudalur adivasi community. Thus the aim of this study was to describe the beliefs and illness
behaviour related to oral health problems in the Gudalur Adivasi community from the perspective
of their traditional healer.
Aim and Objectives:
Aim: To describe the beliefs and illness behaviour related to oral health problems in the Gudalur
adivasi community from the perspective of their traditional healer.
Objectives:
1.
To document the understanding of the oral health conditions and the views of oral health by
local traditional healers.
2. To document the information about causes, prevention and treatment of the most common
oral conditions from the perspective of the local traditional healers.
3. To understand the perspectives of the causes of the oral health problems.
4. To explore the convergence and divergence with the current dentistry framework to support
further integration of health systems by the host NGO.
Review of Literature
A report on stakeholder’s workshop on “AYUSH Interventions in Public Health” documents the
work carried by ACCORD and ASHWINI hospital in Gudalur. ACCORD began realizing that the
input of the medical systems is making traditional healing practices slowly disappear. Hence they
are currently documenting the local health traditions. Accordingly, the region houses different
specialists of traditional healers who are traditional bone setters, etc. Efforts to mobilize the
traditional healers in adivasi communities to a forum where they share their experiences between
themselves. The need to document the existing practices and also take up an initiative in
traditional medicine in the existing institutional community health programme like, training
community health workers from the community itself, to identify and prevent illnesses like
diarrhoea, to provide immunization and nutrition to pregnant women and children, to improve
health awareness among the adivasi community. (FRLHT, 2008)
72
A study exploring the health seeking behavior of the adivasis’ belonging to the Panniya,
Kattunayakan and Bettakurumbas is examined. The pattern and determinants of access and
utilization of healthcare services amongst these tribal and the determinants of the out of pocket
expenditure were analysed. Despite public provision of healthcare services, healthcare seeking
behavior was predominantly driven by ethos and belief system. The utilization of institutional
healthcare services was sought after the alternatives of traditional healing/ black magic/ sorcery
were exhausted. The probability of utilization of public health services among Panniyas and
Kattunayakans was less as compared to the Bettakurumbas due to trust wedge emanating from
historical psychological trauma inflicted upon Panniyas. Similarly, for Kattunayakans their
culture which is embedded in ethnomedicine and symbiotic relationship with forests explains the
trends. Also, the penetration of NGO’s providing culturally compatible health services to
indigenous people was exacerbating the underutilization of public facilities. The preference for
traditional healers over qualified health personnel was not explained by differential in
expenditure but due to cultural factors. (Gandhi, Verma, & Dash, 2015)
Methods
The study involved ethnographic observation for six months focusing on the determinants of oral
health in the indigenous groups in Gudalur, South India. Purposive representative sample with
an effort to get at least one from each adivasi group. The participants were selected using
convenient or snowball sampling method drawing mostly from the healers known to ACCORD
through their outreach.
Persons who identify themselves as local traditional healers. Traditional healers are defined
according to World Bank as “Traditional healer services refer to the application of knowledge,
skills, and practices based on the experiences indigenous to different cultures. These services are
directed towards the maintenance of health, as well as the prevention, diagnosis, and
improvement of physical and mental illness. Examples of traditional health service providers
include herbalists, faith healers, etc. (WHO, Report on WHO Traditional Medicine Strategy, 2003)
Other inclusion criteria were, persons who are living and practicing local traditional
medicine/folk medicine for substantial time period49, local traditional healers who belong to any
of the Gudalur adivasis- Mullukurumba, Bettakurumba, Panniya and Kaattunayakan and local
traditional healers know to ACCORD through their outreach.
Ethical clearance was from the SOCHARA Institution, Scientific and Ethical committee,
Bangalore and permission was obtained from the AMS.
The data was collected between October 2015 and November 2015. Observations in homes,
community facilities, within the region were supplemented by in-depth interviews and focussed
group discussions with local traditional healers. Local traditional healers were identified through
networking and snowball sampling method. Oral or written informed consent was taken after
explaining the intention of the study in local language50. Local traditional healers were
interviewed in depth based on the themes (Annexure 1). Few local traditional healers were invited
for a focused group discussion to examine both internal consistency of the information provided
49 This was fixed for about 10 years
50 Tamil was used as local language here. The adivasis were fluent in Tamil, although it was not their mother tongue.
73
by the interviewees and understand the new dimension of their understanding of health
institutions and the process of referral to ASHWINI or any other health institution. The
interviews and discussions were tape recorded for ease of interviewing and later transcribed and
analysed.
The emerging themes were analysed using deductive inductive methods to identify perspectives
of oral health by the local health healers. Data collected was thematically analysed to
understand the oral health and illness behaviour, causes, diagnosis, treatment patterns
through local health healer’s perspective and also to explore the convergence and divergence
with current dentistry framework to support integration of health systems. Grounded theory
helped analyse observations and interviews.
RESULTS:
Ten local health healers took part in the interview. The age ranged between thirty-two and sixty.
There were two females and eight male participants.
Table 2: Demographic details of the interviewees
SL
NO
1
AGE
SEX
PLACE
Male
INDIGENOUS
GROUP
Panniya
NA
2
3
4
5
6
7
NA
32
46
60
48
49
Male
Male
Female
Male
Female
Male
Panniya
Bettakurumba
Panniya
Kaattunayaka
Kaattunayaka
Bettakurumba
Ponnani
Kummamoola
Thondiyalam
Ayyankolli
Ayyankolli
Theppakadu
8
9
10
NA
52
50
Male
Male
Male
Kaattunayaka
Bettakurumba
Kaattunayaka
Chembakolli
Theppakadu
Chembakolli
Thondiyalam
OCCUPATION
(S)
Agriculture,
AMS member
Health guide
Agriculture
Housemaker
NA
Traditional Dai
Daily wage
labourer
Agriculture
NA
NA
The transcripts of the discussion revealed overlapping symptom conditions and were categorised
into themes-understanding oral health, health conditions, local health traditions, social position
and relations, difference with western biomedicine, access to herbs, etc.
Understanding Oral Health
The local understanding of the anatomy and physiology of oral structures are elusive and
extraneous. Nevertheless, in the colloquial, terms such as mouth, teeth, tongue, jaws, bone, etc.
are used with reference to oral health. Vaayi is the term used for mouth, pallu for teeth, naakku
for tongue, elumbu for bone are used in the local dialect of Tamil. The vernacular terms are given
more importance here, because they express the emotion and the proper meaning attached to
disease or condition or even a structure.
74
Oral Hygiene
Oral hygiene refers to cleaning and maintaining of the teeth only. The cleaning and brushing of
teeth is a daily routine and is carried out in the morning everyday by all. Tooth paste and tooth
brush have come into their lives only recently. Until then, aduppu kari (charcoal) from a variety of
trees other materials was used. Some of the adivasis still follow it.
When I was a small boy, I brushed my teeth with nellu ummi (paddy husk) M1
Others spoke of using kari from Nilagiri (Eucalyptus), Thega (Teak wood), Silver oak, Maanga
Maram (Mango tree), Saathu, Kaathaadi maram, eeti maram, Idala maram and mixing it with salt
and stored in a box. Karimathi (), Nugge maram are not used because it will cause vaayipunnu
(mouth ulcers).
The detailing of the ingredients of the dentifrice is given importance and followed. For ex, salt is
used along with charcoal. The following quote illustrates the reason behind why salt is added.
What we should think is, what should be used when. Why we use salt is because, if there is a germ in
the tooth, then that will be gone. That is why we use salt. Even in paddy husk, we use salt along with
it. M1
While everyone acknowledged the use of toothpowder and toothpaste by the members of the
community. Toothpaste is equated to Colgate and is vernacularly used by most people. There is a
transition from the use of homemade charcoal to commercially available dentifrices.
Earlier, there was no toothpowder or Colgate. Only in the last 40 years, our Adivasi people have
started using Colgate heavily. Most people now don’t use charcoal. M4
Adverse Habits
The use of vetthalai pak (betel quid)51 is traditionally accepted as a norm in the adivasis. Some
people consume it only after meals to ward off the smell of the breath. Most of the elderly folk
chew regularly and continuously. Tobacco is also chewed along with the quid. This habit is now a
thing of older adults and of the elderly, while the younger ones prefer commercially available
tobacco sachets. The habit is simply learnt by doing. Children pick it up by observing their elders.
People chew a lot of beetel and tobacco leaves here… They have got into the habit. Even the children
do it. M4
If parents were educated, and if the children were chewing, “You shouldn’t chew it” No one tells
them. They say, “It’s a child only” and would praise them…whatever parents do, children also learn.
F2
The relation between chewing beetel quid and oral hygiene is illustrated by the following quote
51 Beetel quid – Areca nuts are placed and lime paste is smeared on the Beetel leaf folded neatly into a quid.
75
……. Some people chew vetthalai pak nicely, its pashe (paste) will stick to the teeth. If we use
charcoal and brush it properly, then there won’t be any problem. M1
The awareness about the effects of adverse habits is there. The knowledge about diseases and
their causation is aware.
They say people using Hans52 will get vaayi cancer (oral cancer).M7
Alcoholism is also recent development. Adivasis drank locally made naati saara (country liquor).
Although, occasionally53 consuming alcohol is a cultural norm, many interviewees revealed that,
many adivasis consume alcohol heavily. Increase in capital and earning potential are believed to
be one of the reason.
If one has hundred rupees, then he will immediately buy a quarter. Today, 95% of people drink
alcohol. This wasn’t there before. M1
Nutrition
There is a general consensus that the quality of food was better then, although the quantity was
less. Food security was an issue then and often adivasis starved. The access to forest, meant that
they hunted and dug Kelangu (tubers).
we ate kelangu,… there were five to six varieties of kelangu available. ..we call it kaattukelangu
(forest tubers). M1
Whoever ate Noorkelasu54 in those days, they lived for 100 years. In Kannada, it is said that,
noorekelasu tindavarige nooraysu anta (who ever ate Noorkelasu lived for 100 years)…if we have any
worries and we eat kavalekelasu55, all worries will go. In those days, they were named for a reason.
Bendikelasu, a tuber named so is also there. We roast the tuber and eat it. M4& F2
Also, everyone complained about the use of Vazham/Eruvu56 which has caused a compromise in
the quality of the crops. The eating habits were distinct. Food was cooked in earthen pots as
compared to the use of Aluminium and stainless steel used in today’s times. Food was consumed
on a plantain leaf or naakele57
Diet during illness was followed. The self-control over food and strict diet to be followed during
illness is additional therapy by itself. One healer said,
Suppose, If I have sorangu (rashes) and if it isn’t going, I shouldn’t be eating katharikaayi (Bitter
gourd) and karuvadu (dry fish). If I eat them, it will aggravate. If I don’t’ eat them I will be fine. We
should be knowing what to eat and what not to eat. M1
52 commercially available chewable tobacco
53 during Putheri (harvest festivals) or when someone passed away to forget the pain of death.
54 Noorukelasu is a root tuber consisting of numerous long slender tubers attached to one common stalk. The numbers
give an impression of one stalk containing a hundred tubers, hence the name. (Nooru= hundred in Kannada)
55 Kavalekelasu; kavale in Tamil means worry and kelasu means tuber
56 Vazham in Tamil and Eruvu in Kannada is the same as chemical fertilisers, pesticides and insecticides
57 Naakele (Naak=tongue, ele=leaf) is a broad tongue shaped leaf used to eat food over it.
76
Conditions or Symptom Complexes
Pallu Vali (Tooth pain)
Tooth ache is the most common complaint with which people presented to the healers. Dental
Caries is also understood as the reason behind the Tooth ache. Karumolagu (Black pepper) and
Nelli Pattam (Gooseberry bark) and Lavangam (Clove) are used to reduce the pain in the teeth by
most healers.
Vaai Kola (Mouth swelling)
Swelling in the oral cavity is also a common complaint told to the healers. Healers explained the
associated symptoms as trismus and inability to chew. Two healers mentioned that the swelling is
commonly seen during the winter season.
…vaai kola (swelling), pallu vali (tooth pain),.. in January, when it is cold M2
Sothu Pallu (Tooth Decay)
Dental caries is not seen in all, but healers notice a rise in dental caries among the children,
compared to their childhood times. They identify it as a black discolouration on the tooth. It
progresses to a level, what they describe it as, ‘eating away the entire tooth’ The reason for dental
caries is observed as eating sweets. M5
Some people chew beetel quid even while sleeping. This way teeth will turn black and disappear soon
M3
While another healer describes the cause of dental caries as
.. in some people, there will be gap in between teeth. There will be Sali (calculus) in the gap which
causes sothu (decay)…. But, in some people, there could be some problem in the elumbu itself, or if
there is less raktham (blood), if there is less koluppu (fat) which can lead to many diseases.M1
Loosu Pallu (Shaky teeth)
Weakening of gingiva and periodontal tissues are considered as the result of improper hygiene.
The awareness of brushing teeth twice daily was noticed in one healer.
That is because of eating vetthalai pak, and also not brushing teeth properly, and not brushing
before sleep. People only brush their teeth in the morning M3
Vaayi punnu (Mouth Ulcers)
Ulcers in the mouth occur because of using charcoal of few trees.
77
Vaayi Cancer (Mouth Cancer)
Cancer of oral cavity is seen commonly among women and noticed often. They reported,
It begins as Vaayi punnu and grows to become a cancer and complain of inability to eat. The reason
for its occurrence is chewing a lot of vettalai pak, smoking cigarette and beedi58 M4 & F2
Cancer is also seen in those who don’t eat vetthalai pak or drink saara. In this case, it could be
because of raktham sambandham pattadhu (Blood related).M4
Pallu edukkuradu (Removing tooth)
When it came to extracting teeth, there was apprehension and fear associated with extraction of
teeth. This fear let them to leave the tooth in the mouth and wait until fell off. This belief has
evolved to getting the teeth extracted because of the belief that rotten teeth will spread to others
teeth.
..no one was taking the tooth out…..When it becomes bad it would fall on its own. Scared to take
out. Now they have started doing it and feel if they don't take out the bad one it will spread. M5
Mobile teeth were removed off by themselves and was seen as a pain reliever.
If there was loose tooth, they will only make it much more loose and remove it out. If they knew how
to remove it, they will grab it and remove it slowly. Then there will be a little relief. M4 & F2
Local Health Traditions
The local health traditions are presented with respect to the healers’ perspective of their position
in the society, acquiring the knowledge, practise methods, elements of preaching and rituals,
future and continuity of the tradition, people’s attitudes, differences between western
biomedicine and their system and how they see other traditional systems.
Social Position
The vaidyar (healer), didn’t just treat diseases. He/she was given importance within the and
commanded moraippu (respect) and the position claimed obeisance not only in the family, but
also in the paadi (village) and the confines of the village boundaries.
Vaidyar had his own moraippu (respect)….in the paadi (tribal village), he is like an elder… as the
times changed, those kattupaadu (rules) are no more. M1
The social position is localised to the area. This meant that, his or her position was also relatively
higher than other adivasis and also other community members. The position also was applicable
58 Beedi is Indian cigarette filled with tobacco flake and wrapped in a Tendu (Piliostigma racemosum) leaf tied with a
string at one end.
78
to other communities like those of Chettis. The vaidyar also sometimes was a karnavar59 and
would be invited by Chettis for both happy and mourning ceremonies to perform rituals.
People respect a lot. In ours, even the chetti community also, respect the karnavar. We have a
temple in Ponnani.. Vishnu temple. The Chettis also have a share in the temple. We also take part in
theirs. M2
Learning
Medicine part of the healing was learnt by observation and this tradition is practised for
generations. It is often familial and passed on from Paattan-paattan (ancestors) time. However,
there has been no written records. All the healers learnt it from their parents or grandparents
since their childhood, except one healer who started learning few years back although his parents
and their parents were practising it.
Practise
Practise of medicine is similar to that of modern doctor. They usually don’t go to a different place
and treat. Whoever comes to them are treated. The assurance of healing is not offered, although
the confidence in the healers by the community members cannot be validated. There is a mutual
understanding between the healer and the patient and the relationship is personal.
if someone like that comes to asking for me, I will give them some medicines. Then I will say, “If it
doesn’t cure, then come again! If it doesn’t heal, come for the second time.” And if it doesn’t heal by
then, I will ask them to see another person…there are chances that, they will get well and some
people no matter who gives, there won’t be any healing. M1
When it comes to paying for the services, it is more of a personal offering and above the service
provider and consumer relationship. The patients would offer whatever they can and there is no
compulsion. Often, the service is returned in kind. The vital part here is the custom followed. Like
in the case of this healer, the
“Nanga,…Hoovu kaayi, ondu kottevu. Kottadu, hecchi hetthana ninga kottaadadhu ninga kaanalu
bandide. Ee koosu ulla kaala ganta, iduvulla guna kododu neene, hecchi hetteva”60
With our treatment, they have a child, we ask them to bring the child to us and offer the child to
god. Once they offer, they can give whatever they feel like. We keep the child in front of the God and
ask them to pray, “because of your medicine, that is herbal medicine, we have a child now”
If they wish they can keep kaanike (offering) or something at that time. Some people give sari to my
wife and a shirt and a tundu (dothi) to tie around for me, and some people give us nelavelakku (lamp
stand) and keep it over the ground. But we won’t take it in our hands directly from their hands. It is
kept over the ground and we take. M4
59 Karnavar is a religious head in the Adivasi community
60 Kaattunayaka language
79
Prayers and elements of preaching
Prayers are an integral part of the healing with the healers. The rituals and timing of the prayers
varies from one healer to other. Some offer prayers to their daivam (god) in their house before
heading out to get herbs, while some offer in the forest before cutting the herbs. Two healers
advise the patients also to visit a temple except one healer who doesn’t pray.
I don’t offer any particular prayers, but I think of the god and pray in my mind that this medicine
should work. Personally I don’t do anything openly like offering prayers to kavu (sacred grove), but I
just pray in my mind. M3
There are no particular days to give or not give medicine. But the timing of the taking medicine
was important. One healer said,
there are no restrictions to give medicine on new moon or some days like that. but you must take
before the sun rises. It is a practice. M5
Future of LHT
The tradition is passed to the next generation. Not many youngsters show interest, only few have
picked up. The practise is taught to their children. The learning is mostly by observation and
following the instructions. There is a belief that it is an ancestral property and a common
consensus about not letting it go off. Secrecy is maintained by some healers about disclosing the
information about herbs and preparation.
when the medicine is being prepared none should see it. If they see it, they will also give it. That’s the
reason many wont teach.M5
People’s attitude towards LHT
Healers think that although adivasis acknowledge LHT, the usage has come down after the
hospitals have started providing good care. Deliveries are more at hospitals these days because
the government schemes and monetary benefits. Sometimes, adivasis come to the healers after
the hospital care wasn’t satisfactory.
Differences with western biomedicine
There healers differ with western medicine. They believe that, western biomedicine’s effect is
short lived while traditional medicine takes time to show its effect but it provides a long lasting
effect. There is also a consensus about going to hospital for few ailments. They would only ask the
patients to see a doctor. There is a concern about the inadvertent use of western medicine even
for small illness which can be treated at household level.
In our community people are aware that they should go to the hospital. Herbal medicine is also
important. But now for everything people go to the hospital. We have many herbal medicine. First
they have to use this and then go for that. M5
80
Social Issues and Challenges
Right to denial of Health
Discrimination and ill treatment towards adivasis at PHC’s and other government hospitals was
one of the reason why they hardly visited them. The doctors wouldn’t see them or are made to
wait for long time.
the doctors wouldn’t even see an Adivasi patient. They would ignore us since we were adivasis’. M1
Social situation
The situation has changed. There is a consensus that their lives have changed after ACCORD’s
intervention. The awareness about their rights, education, health has improved. The shyness to
talk to others outside their community has reduced. Many believe that their culture has also
changed. The knowledge on basic arithmetic while dealing with finance and commerce has also
improved. They have realised their entitlements. But there is a concern that development
activities have also bought other issues such as ill health, alcoholism, etc.
there used to be no dress. But now we have lots of food and lots of materials like oil, soap. It is not
like the old times. We have food. But no health. F2
Access to herbs
By far the, biggest challenge faced by healers is the availability of herbs. Access to herbs is
challenging with the given situation. Restricted entry to the forest, abuse by the forest officials,
loss of forest cover and subsequent rise in tea plantations, use of chemicals in the plantations,
lack of space to grow herbs are some of the reasons quoted by the healers.
We don’t grow the herbs. When we need medicine we get it from forest. we have to go without being
seen. Now it is difficult. M6
Health guide experience
Some of the healers have also worked as health workers. The healing experience with health
worker training is additive and has brought positive developments. It becomes an important
mechanism to deliver health services because a vaidyar or a karnavar held a high position.
When I was here (as a health guide), lot of people used to come here with their problems, even if it
was their family problems like marital problems. They would come and ask, “there is a problem,
please do something”. I go and perform rituals. Then they will feel better.M2
DISCUSSION
In the course of understanding the cultural and social construct of oral health among adivasis
from the perspectives of local health healers, Positionality of the investigator should take
precedence. When interpreting, the investigator’s positionality that of urban, middle class,
western biomedical trained, evidence seeking, different cultural background can and will have an
impact on the interpretations. The interpretations are often, a subjective attempt to objectively
81
describe the situation. Personal is political. Personal descriptions and statements are political. It
states a person’s stand on an issue.
The concept of health and quality of life is abstract and difficult to define. It becomes even more
complex to translate it into an action, particularly for those who look for solutions to the
problems. Health refers to a multidimensional complex and it is well acknowledged as having no
defined boundaries. This is in contrast to the existing health care delivery system which is
reductionist and compartmentalised. Health, however can be defines as “an individual’s subjective
experience of his/her functional, social and subjective wellbeing”. Consequently, it refers to our
experience of our bodies and ourselves and the consequences of that experience for the conduct
of daily life. As such, it is a sociological and psychological concept which applies to people and the
populations. It belongs to the socioenvironmental paradigm and commits us to the development
of ways of measuring perceptions, feelings and behaviours.
Kalachaaram61 is the ‘explicit and implicit collection of ways, both general and specific,
established by humankind, of thinking, feeling, and acting, more or less differentiated in groups
integrated by each of the other groups, somehow distinguishable in time and space and internally
between them’. (Turin & Satriani, 1978) In such socio environmental paradigm, it is important to
consider the cultural influences of health. Particularly that of local health traditions which are a
cultural construct in the adivasis. The lack of primary health care services and environmental and
sanitation strategies that take into account the cultural differences of the adivasis in our country
is evident. This could be because of the insufficient organised health system within the
indigenous communities and also because of limited financial support and lack of definite
strategy that is culturally defined. (Eder & Garcia Pu, 2003) At the outset, indigenous health
systems are resilient and responsive. They are inclusive, locally relevant, and use naturally
available materials. The concept of well-being among the adivasis is limited to basic essentials of
life and being content with that. Health forms an integral part of all the dimensions of well-being
and not considered as separate entity.
The practitioners of healing among the adivasis are everyone in the community. Although, there
are few people who spend more quality time on learning, practising and disseminating it to the
next generation, the harbingers of this tradition are everyone. Mothers at homes, men at field,
elderly through their experiential learning, etc, all of them practise it. The vaidyar is a sanskritised
term referred to the healer, they are known as pacchamarandukarar62. The healers are mostly seen
as possessing a technical or practical capacity, But, at the same time, some of their knowledge is
linked to belief and directly related to the natural settings around them. As, Kleinman termed
them as "non-professional specialist or expert who offer some form of alternative or non-orthodox
therapy" to their respective village community. Hence they may be few in numbers but their
influence affects every villager in the close knit isolated community. (Klienman, 1985)
Oral health in indigenous groups are studied less. The beliefs and illness behaviour related to oral
health problems were studied in the Orang Asli indigenous group in Malaysia. The traditional
healer who is called Tok Halaq’s role in prevention and health promotion was crucial. (Saub &
Jaafar, 200 I)
61
62
Kalachaaram is the Tamil and Malayalam equivalent of culture
Pachamarandu is herbal medicine and the practioner is called Pachamarandukarar
82
To understand this phenomenon of health culture among the adivasis, a grounded theory is
essential. Going into the field with a pre-set of questions to find answers for, defined aims and
objectives wouldn’t work to understand health traditions which are intertwined in a complex
process which result in the well-being of the group rather than an individual. The treatment is
aimed at an individual, but the diagnosis and prognosis is from the collective analysis of the
community in which the individual lives. The environment in which a community lives, the
structural and social determinants are given importance in the entire process of understanding
the disease to curing it.
The earlier health concept was holistic and comprehensive. There was no reductionism. Oral
health is not distinctly seen from the rest of the body health. At delivery level, the indigenous
communities, marginalised, people in hilly regions are inadequately reached to the health system.
Local health traditions form the fourth tier in the health system. People often seek healers help
for common diseases. Our initial aim was to find out how much importance was given to oral
health through a key informant interviews. There was an attempt to understand the oral health
conditions and the views of oral health by local traditional healers. This preliminary analysis also
aimed at understanding the convergence and divergence with the current dentistry framework to
support further integration of health system.
It was anticipated that it would be difficult to gain their cooperation since they are generally shy
and secretive towards outsiders. While few were very easy to approach. Hence, a lot of time and
patience was taken to build their trust and confidence. This took a couple of visits over several
weeks to be establish a good rapport. Taking the help of the local Adivasi coordinator from
ACCORD as a guide and interpreter ensured that our intention was well explained. As a result,
full cooperation from the community as well as the healers was obtained without reservations.
They shared their experiences and views willingly without restraint.
Scambler noted that symptoms that present in a "striking" way (such as toothache in this study)
are more likely to be interpreted as illness and more likely to receive prompt attention than those
which present less dramatically. However, given the quantity of symptoms and illness
experienced by people it is apparent that most are treated by self-medication. Most families have
some knowledge of how to treat common illnesses. This also applies in treating toothache in the
adivasi community. (Scambler, 1991) Dental caries, tooth pain and swelling in the oral cavity were
the commonly noticed symptom complexes. One possible reason could be due to the fact that
dental caries and toothache was the most easily recognized and can significantly disrupt one's life
routine.
As far as dental caries was concerned, although their belief on how the tooth become rotten was
remote from the scientific explanation, nevertheless its rationale may be related to the
maintenance of environmental cleanliness and hygiene in general. This may be considered as a
Positive belief that is quite harmless to oral health. However, there is a need to try to relate this
belief to include personal hygiene in addition to the established belief of caring for the
environment. This could be used as the basis of health education messages for health promoters
to reach the adivasi community.
For periodontal disease, anecdotal reports on its high prevalence among the adults has to be
explored. Although, there is knowledge about improper oral hygiene and it causes, the proper
knowledge about prevention and promotion is lacking. This could be due to the low impact of
83
periodontal disease on their routine life as compared to toothache due to caries. This is also
coupled with the availability and affordability of oral hygiene aids such as tooth paste and
toothbrush. There is an increase in the use of these aids, but the availability is still out of reach for
the entire community. From the healer’s perspective, the use of herbal twigs to clean teeth is still
prevalent and this has to be explored further.
The oral hygiene is only limited to cleaning teeth. There was no mention of other hygiene
measures such as gargling, tongue scraping, etc. The extensive use of beetel quid and tobacco is
another cause of poor oral hygiene. It is not surprising that oral cancer is commonly encountered
in this community with the common habit of betel quid chewing laced with tobacco, lime and
betel nut. These are known risk factors for oral cancer and pre cancer lesions. Since betel quid
chewing was extensively practiced in this community. The awareness of oral cancer is important.
Self-examination on how to detect early signs of oral cancer should be taught to the healer and
the community in general. It is recommended that a survey of oral cancer/pre-cancerous lesions
be carried out in this community to ascertain its incidence.
In a community where modern health facilities including dental treatment are not easily
accessible, alternative care should be made available, especially in cases of emergency pain relief.
The healer could play a role in primary oral health care. They could be involved in promoting
healthier oral self-care practices. Some form of basic health education and training could be
organized in the community.
Finally, the health promotion strategy should turn to improving the environment in which they
live to enable them to practice a healthier lifestyle. For instance, to get water to clean themselves
up more often was difficult enough, let alone to brush their teeth several times a day and before
sleeping. There were other more pressing basic needs to be fulfilled such as getting adequate food,
clothes and a better housing condition. Buying toothbrushes and toothpaste must be very low in
their order of priority. Hence the relevant agencies need to improve the overall economic,
educational and social needs of the Gudalur adivasis. These will definitely lead to a better health
and hence their overall quality of life in the long-term.
CONCLUSION
Researcher is undergoing a paradigm shift from patient to person centred health care, subject to
participant research and biomedical to social care. Community based health systems inclusive of
local health traditions make a responsive people centred health systems.
84
REFLECTIONS
To understand the local health traditions in an open mind requires plenty of unlearning. This
process could be bit more frustrating and compelling oneself to not be judgemental. Nevertheless,
complete unlearning is not possible because of the strong attitudes, though process and the world
view with which an investigator starts the study.
During the course of this exercise, I faced several challenges. First and foremost, obtaining the
permission to conduct the research from the community members was taxing. They had to be
briefed about the objectives and purpose of the study. Meanwhile, the ACCORD has asked me to
assist the community members in forming a research committee to look into the ethical
considerations. With the help of Dr Ravi Narayan, I used the guidelines for social science research
(CEHAT, 2000) to form a committee that looks into giving permissions for conducting research
on adivasis of Gudalur. I charted out the guidelines in the Tamil and to make the process simpler,
the colloquial was used to explain them about the process of questioning and reasoning.
After the preparation, the first application to the committee was this present research. I had to sit
through three such meetings to get the final approval. I had to explain the committee members
how this research is going to help my understanding of local health traditions and the overall
culture of the adivasis. I explained them painstakingly, in simple terms how the knowledge
generated from this study can be utilised to engage the healers within the existing health system.
The final approval came after I promised that the data in the form of audio tapes and also a report
of the study will be submitted back to ACCORD and ASHWINI. Although this process was hard,
it involved the community to decide if they wanted the study or not. The Cuenca declaration on
‘Research for People’s Health’ envisages active community participation.
“Research should bring about social action by the mobilization of people and communities as
participants and collaborators. Biomedical research should be integrated with social research.”
“Research should involve dialogue between investigators and representatives of communities as well
as the people directly” (Research for People's Health , 2005)
One of the challenges was meeting the healers. My idea of healer was influenced by movies where
the healer would be grinding some leaves and always busy collecting herbs from forests. However,
this false imagination was deleted from my mind, after I started visiting villages in Gudalur.
Healers are people with other duties or occupations. Pacchamarandu is only given when asked.
Rest of the time, they are busy in their daily chores. Finding suitable time to meet them with the
help of animators63 at ACCORD was a little hurdle. The animators had to be free and take me to
the healers. Once, I had to meet a healer at one of ACCORD’s area centre. He used to work as a
health animator earlier, but relinquished to become a diviner. One of the animator at the area
centre didn’t get along with this healer. The healer wasn’t very comfortable talking to me during
the interview process because of the presence of other animator.
The ethical issues of getting the permission was one learning experience, but other ethical issues
were further challenging. Getting to healer’s house and meeting them was one step success, but
convincing them to talk about LHT was another practical challenge. One of the healer was very
63
Animator is a term used in ACCORD office for the Adivasi coordinators working in different fields. There
are health animators, finance and education animators likewise.
85
timid and hesitant to talk to me. Her husband goaded her, but was futile. With much convincing,
I managed to talk to her, she showed signs of disinterest, uneasiness and was lackadaisical. I had
to stop interviewing her against her will.
There were fruitful outcomes of the study as well. In one of the group discussions, a healer was
curious about my next plan after data collection. He suggested, that I should talk to the school
authorities at VBVT and convince them to organise children’s camp with healers. They should be
taken on forest transect walk to identify the herbs and explain the use of it too. His went on to
say, “we should teach our children and make sure they also know it (herbal medicine)”
While the results are still analysed, this study focusses on two challenges that were faced in this
evolving study. The positionality as researcher, dentist, training emphasised on biomedical,
evidence based, epidemiological western framework who is trying to learn qualitative participant
observation research were disturbing in terms of making value based judgements. The research is
focussing on communitising the research with the support of local organisation to bring about
participant action. Many questions of how to mobilise the community to turn towards locally
available and relevant health tradition will be a daunting task.
86
Access
Standard of
living
Equity
Access to
rights and
Entitlements
Local
health
traditions
Less
rainfall
Loss of
forest
Social
Justice
Agriculture
and other
livelihood
activities
Social
Economic
Political
Cultural
Environmental
Social
Economic
Political
Cultural
Environmental
FRA
Education
AMS
Community
bonding
Animal
conflict
Well Being
Well Being
87
Access to
Rights
Economic
Independe
nce
Entitlemen
ts
Leadership
Education
Parameters
Cultural
values and
Identity
Health
Unity
Self
Governanc
e
88
In October 2015, I pedalled for a social cause on a fund raising venture. The funds were collected
for the Gudalur Adivasi development activities. The week long ride64 was more than a fun or
leisure ride, it was a great learning experience. We stopped over at organisations involved in some
sort of community development. What was supposed to be an adventure filled joy ride, turned
out to be a moving experience. I learnt a great deal of community health more than I ever did in
the last few months of classes and field work at SOCHARA and at ACCORD respectively. Every
place I visited had an interesting tale to narrate. Everyone, I met had a story to tell. Every event
that unfolded, bewildered me and awakened to the reality.
I cycled nearly 400kms from Bangalore to Gudalur in Lower Nilagiris on my mountain terrain
bike. The ride would start off early morning by 6 am passing through the countryside, enjoying
the green waves made by the wind as it cuddled the blades of paddy, ragi and sugarcane and the
forests of rural Karnataka and Tamil Nadu. The ride would finish for the day by noon at a school
or at a not for profit organisation involved in activities such as rural employment, youth
development, revival of traditional economies, alternative education, community health
programme, tribal development, women empowerment, etc. The cycle ride was unique in many
ways. First of all, it was not a race and participants could cycle at their pace. If it was difficult, one
could load the bike on the truck behind and relax in it. The ride was a fund raising event. All the
money raised would go into various development activities of Gudalur adivasis. Most importantly,
the ride passed through the beautiful countryside of South India and offered a chance to meet
interesting people and know about their inspiring work.
On the first day, as we biked past Bangalore's deafening motor vehicle traffic and chaos on
Mysore road, the overwhelming stench of drainage was strong enough to clip my nose tightly with
my fingers and I rode as quickly as possible to avoid any more assault on my olfactory sense. The
huge stream of Bangalore city's drain used to be once upon a time a river, called River
Vrishabhavathi, and only now the water is replaced with nitrate and phosphate rich sewage. What
was once a life supporting river is now dead and carries the litter of urban civilisation. It reflects
poor governance and passive participation of the civil society. I felt helpless held myself
responsible too for being the passive part of governance. We passed through the first green patch
as we moved away from the city. The board read "Kumbalgodu forest". I couldn't see any variety
of flora. Neither shady humongous trees nor wet forest floor! It was a perfect parade of an infantry
of eucalyptus trees planted under the afforestation scheme. What a disappointment! I felt angry at
what mankind has done to the nature which has given us surplus and yet the greed doesn't
subside. The rest of the ride was through the scrub and arid deciduous forest of Saavanadurga
with its huge monolith hill and ruined fort on top in the backdrop.
We met young architects of a rural architectural firm called Andagere architects. They were
reviving traditional rural economies like blacksmithery, country tile making and using the
products in their work thus creating livelihood.
We stayed at Hosa Jeevana Haadi (New path in life) in Melukote on the second day. It was
founded by Sri Surendra Koulagi and Smt. Girija Koulagi, a couple inspired by Mahatma Gandhi
64 www.madcycletours.in
89
and Jayaprakash Narayan. The Trust has been striving to create a non-violent and egalitarian
order of society. Its core area of work is welfare, education, rural industry, environment and
agriculture. Surendra Koulagi, now a nonagenarian, whose age doesn't seem to mellow down his
zeal. We met his son, Suresh Koulagi, a pleasant looking man who manages the activities of the
trust. Mr Suresh's spoke about his life journey that took many interesting turns. He said, "I once
read One Straw Revolution by Masanobu Fukuoka after graduating as engineer. That book changed
my life. I decided to come back to my village and work here".
Figure 37: Participants riding through Bandipur forest
According to him, the greatest problem the country is facing today is, youth of the nation are
feeling disempowered and diffident and the haughty misconception that urban area provides
more happiness. His tone expressed apprehension about today's education system leading to
individualism. He added, "Youth want to earn more money by quick means without much effort.
Most of them want a comfortable air conditioned rooms, but none want to till the land, sow grains,
reap yield. The capitalistic market based economy is luring away the creative minds of the country.
Very few are interested in handicraft skilled work like sericulture, carpentry, weaving".
The next day we were heading towards Mysore- the cultural capital city of Karnataka. A small
stretch of the route, about 10 kms, was on the mound of the left canal of Krishna Raja Sagara
Dam. It was by far the most picturesque landscape. Quietly flowing water on one side and bright
green carpet made up of paddy fields on the other side. The air smelt of the water filled with algae
and fresh foggy soil. Few small and yet quaint villages dotted the otherwise emerald fields. The
scene was very romantic, reminding me of poems of the Kannada poets Kuvempu, Da Ra Bendre
and English poet Wordsworth, etc. This lustful decor has to be enjoyed and words fall short of
describing the countryside grace.
90
A grand welcome at Mysore by the Green Hotel staff just added merry to the wonderful day.
Garlands, lemon drizzle cake, samosa, tender coconuts kept coming in. Green Hotel at Mysore is
one of the best social business initiatives. The Green hotel initiative is on the model of sustainable
tourism was started by Dame Hilary Blume. The profits of the hotel are used for economic and
environmental issues in and around Mysore. Their pragmatic solutions have helped thousands of
people through their eco-friendly business- charity model. That evening we visited Dhwani, a
slum dweller's women federation. The women self-help groups have made a tremendous progress
in housing, community development, education and health. One-woman in her forties trained as
a midwife told us that she has delivered more than 250 babies successfully. Each one has been
through their own ordeals and their cheerful smiling faces gave me hope. Their success story
narration was filled with emotions, hardships, toil and sweat.
After a day’s break and relaxing, we visited another organisation outside Mysore called Rural
Health and Literacy Programme. We celebrated Dasara with the children of Ashadeepa and
Ashakirana. These two home for children for both boys and girls respectively, are alternative
schools aiming at providing vocational training alongside education. Children sang, danced and
shared their innovative experiences on recycling garbage from the kitchen. The guava fruits from
the farm grown by the children were sweet and toothsome.
We were already four days past and deeply involved in the journey. The ride got more absorbing.
We passed by meadows, hills, shrub forests, dried lakes, canals, ruins, etc. Train of milkmen
carrying churns on their motorcycle backs, migratory birds enjoying the tropical heat, perplexed
villagers’ faces became our norm. Dawns were chilling with roosters crowing almost everywhere.
Men hurrying into their fields, women folk sweeping muddy floors and the perfect protein and
carbohydrate diet breakfasts were a big hit. As the day faded, gloaming golden sky was idyllic. The
Indian countryside is diverse and offers more than one can imagine.
On the way to Sargur, we broke for breakfast under a tamarind tree at Puttegowda’s farm.
Puttegowda was growing Okra, Tomatoes, and Avarekaayi (Hyacinth beans) in only two acres of
his four-acre plot. He complained about water shortage and hence couldn’t grow in the rest of the
farm. This was shocking to me as we passed through Krishna Raja Sagara reservoir which was
about 30 kms away. What was supposed to be an irrigational project hasn’t served its purpose and
that fact baffled me. With rainfall, less than the average this year, agrarian distress escalated. As
predicted, the monsoons failed and resulted in heavy economic loss which had its repercussions
felt long afterwards too. Farmers committed suicide and this caused an uproar in the state
legislative sessions. Agrarian distress can be devastating on the families and it is rightly called,
“Indian agriculture is a gamble with monsoons” and that made sense to me. Sympathising with
Puttegowda’s plight, I felt heavyhearted.
It was a joy ride from Sargur to Chikkayalchatti. The first half was around the Berambadi state
forest and later half through the plains before we entered the Bandipur Tiger Reseve. As we were
passing the last village and the patches of fields along the kutcha road, I spotted women standing
still in the fields with an expression of disgust, nervousness and anxiety. My involuntary smiling
face wasn’t received well. I sensed some discomfort from these women because of our presence. A
little away about 10 metres, a woman in her early 20’s stood up quickly in shock. She was near the
edge of the field. I also spotted a pitcher next to her and that was the clue. All these women were
attending to their nature’s call. I felt embarrassed. Their loathing faces were strongly repulsive. It
must be awful to them. Open defecation, sanitation and safe drinking water is a big public health
91
problem in India. I recalled Mr Prahlad’s view, an environmentalist working on sanitation at
SOCHARA. He opines that, women go out to defecate because many do not have toilets at their
houses, but also because it is the only time they get to venture out their fortified houses, gossip on
mundane things with the other women folk. The kutcha road turned into a terrain soon afterward
and my focus shifted to the safety while balancing the bike on the gravel road. The distant Nilagiri
hills were visible. The blue hue of the mountains created a mirage. The day was welcoming the
dusk with warmth. The eerie silence, green meadows, chirping birds, blue mountains and the
early night sky was like taking a short ride into a beautiful medieval painting.
Chikkayalchetti is a small charming village of only five houses. The village headman, also the
priest at the only temple in the middle of the village around which houses are located, hosted us
and his family cooked the Mysore style food. Ragi balls with coconut chutney, rice with sambar
was served while we sat in rows on the floor. The villagers were very warm and kind. The bon fire
under a huge Banyan tree was perfect for the chilly night. All of us sat around the fire and the
topic of the chit chat became horror stories. David’s horror comedy jittered everyone and all of us
laughed at ourselves. I retired to the sleeping bag around the fire and stared at the starry sky. I
hadn’t seen a starry twinkling night sky in years and was trying to recall the last time I was
amazed to such an incredible wonder. I slowly passed into slumber.
Next day was to the final destination- Gudalur. The entire stretch was in the forest. First,
Bandipur and then Mudumalai. It was complete uphill and total highway ride. We had to be extra
cautious of the reckless motorcycle and car drivers. The forest road was laid with tarmac with few
potholes the size of a small crater at frequent intervals. At one point, I spotted two forest officials
on either side of the road handpicking plastic litter and loading it into their sacks hanging from
their waists. They looked like tea pickers on the higher hills. I couldn’t stop admiring them and
applauding their effort. Environmental pollution has become universal in India even in protected
areas. Swach Bharath Abhiyan doesn’t seem to have any effect so far. We further passed though
Bamboo forests and finally made it to Gudalur after seven days of cycling through Indian
countryside.
Thighs aching, joints biting, spirit dying, alas, I made it to the final destination. It seemed
impossible in the beginning but the team spirit and the wonderful support team helped me reach
my goal. Most importantly, the people we met made a remarkable impact. Learning from
everyone’s experiences and listening to their tales brought goose bumps over my skin.
Community health is the outcome of every action done towards wellbeing of an individual, family
and the community. The farmers complained about the lake which was dried, and they say, they
have never seen the lake bed in their lifetime. Climate change is here for sure. How will the
farmer be happy when there is no water to grow crops? The mental agony of the elderly when all
their younger ones want the comforts of the urban space. How do we address the problem of open
defecation when the problem is not with the ability to afford toilets but rather the complex social
construct driven by paternalism and oppression of the weak?
Hive of activities always engage the village folk throughout the year. Women, young, old,
everyone is involved. Men fight over lands and their heads held high egotistically. There are all
sorts of things happening. There is much more bonding and community relations are stronger.
India lives in her villages. As I start to think seriously, I understand the concept of rural selfgovernance without any unequivocal note. Mahatma Gandhi talks about village life in Harijan,
92
"My idea of village Swaraj is that it is a complete republic, independent of its neighbours for its own
vital wants, and yet interdependent for many others in which dependence is a necessity" (Gandhi, M
K, 1942) I agree on Mahatma Gandhi’s statement without ambiguity. The village life contradicts
capitalism and sadly the market economy has invaded rural life and has shaken the foundations of
Figure 38: Visiting a Khadi weaving centre in Melkote
the solidarity.
On a travel note, this has been my favourite travel journey so far in my life. I have been asked
quite often about my favourite destination and now I proudly announce it as rural India. I want to
visit again and again to know more. The whole ride was organised with great care. Responsible
tourism is what I believe in and this ride truly lives by it. Before the ride, I was a cocky
nonchalant person with ‘know it all’ attitude. I admit now, I know little as much as a tiny shred of
a cotton fibre of a warp in the vast textile that is made rich with intertwined weft weaved by, of
and for mankind.
There sprouts a wisdom once in a lifetime or perhaps twice to get out of the self-made cocoon and
to see the world as it is. To see it without prejudice and premonition. In that journey, everything
appears natural with no fancy sparkling notions attached. The world is a stark truth. Things that
we often tend to oversee because of ignorance becomes apparent. People and places appear more
connected and that wisdom helps us to see the reality of what they are made up of and what it
takes to be there.
93
Oral health is one of the health areas which have considerably received little attention in India
and elsewhere. Oral health in India is a neglected public health problem. The exact burden of oral
diseases and its effect on body is not known in the Indian context
ORAL HEALTH POLICY: RATIONAL BASIS
Oral health is integral and essential to general health. Oral health is necessary for well-being of an
individual. Quality of life of an individual is determined by oral health. The ability to perform
essential functions such as chewing, speech, smiling, etc. is very much determined by optimally
functioning oral cavity and related structures. The inter-relationship between oral and general
health is backed by vast body of evidence. Periodontal diseases are the sixth complication of
Diabetes Mellitus. A number of common risk factors affect non communicable diseases including
oral health. Many systemic diseases manifest orally before the actual symptoms show up. Thus
early detection of oral signs and symptoms of systemic diseases such as microbial infections,
immune disorders, etc. is crucial for reducing premature mortality. The need for oral health policy
is imperative. The whole role of knowledge translation into a policy process and therefore the
decision making authority, is a socio-political issue which is complex and challenging. The need
to collect data about the prevalence of diseases and its risk factors should be the first priority.
GUDALUR EXPERIENCE
Dr Pramila Nair, a senior paediatrician was convinced about oral health neglect and its
detrimental effect on general health. I spoke to her about the evidence between Pregnancy related
Periodontal diseases and Pre term low birth weight and miscarriages. She conveyed the message
to Dr Shylaja. Dr Shylaja decided to have a compulsory oral health check-up included in ANC for
all pregnant women among the Adivasi people. Although, this is a small step in preventing
morbidity and mortality, it is still a major advancement. If health policies work at organisation
level, I'm optimistic that can work at national level too. This demonstration can prove the
relationship between oral health and general health.
Once I was talking about oral hygiene practices to children at VBVT. One boy from the group
shooted a question at me, "we cannot afford toothbrush, yet you are asking me to brush our teeth
using toothbrush and toothpaste". It was a slapping question. It also made me re question the
approach towards finding solutions to the bigger problem. Healthcare should be acceptable,
available and most importantly affordable. The health education modality is always routinely
focussed on brushing techniques, oral hygiene measures, and diet. It has never focussed on
grabbing the attention of the public to sensitise on this issue.
LONDON CHARTER
In May 2015, I attended the International Centre for Oral Health Inequalities research and policy
meeting at London. The meeting had a series of talks about social inequalities in oral health,
94
evidence based actions and policy implications. The attendees were asked to contribute to the
London charter based on their personal experiences. The London Charter addresses the social
determinants of oral health primarily and also calls for action. (Watt, Sheiham, Listl, & Peres,
2015) I suggested addition to the agenda, on Community involvement which is outlined in the
principles of Primary health care. There was emphasis on “Communitisation” which involves
community empowerment, community action and active participation. The success of National
health mission in India can be attributed to the concept of communitisation. The use of health
workers (professionals complimentary to dentists) can be a useful tool in reaching out to the
community can be used to scale up the services. The shift in the paradigm even in dentistry is
now gearing up to the oral health shift and the discovery of social determinants of oral health has
contributed to our understanding of oral health from social justice view point.
FORUM FOR ORAL HEALTH ACTION IN INDIA
A network of likeminded community dentists was formed and named it Forum for Oral Health
Action in India. medico friends circle was an inspiration for the initiation for this network. There
are three members and expects to have more members on this network. This first work
undertaken by this network was collecting evidence for denial of right to oral health in public and
private care. A draft of ‘Oral Health Equity in India’ was also prepared. This evidence was to be
presented at the National Human Rights Commission meeting at Chennai, but was cancelled due
to the deluge.
The next work undertaken by the forum was filing a Right to Information application on the
irregularities in conducting National Oral Health survey. Our complaint is based on the
newspaper article titled “Rs 3.5 crore dental health report rejected over 'flaws' after seven years of
work” covered in UK’s leading newspaper Daily Mail on 23rd November 2015. (SHARMA, 2015) The
article reports a huge corruption scandal on the conduct of the National Oral Health Survey. It
also acknowledges that the report would be a guiding document for the oral health policy in
India. In summary, Ministry of Health and Family Welfare sanctioned 4 crores to the Dental
Council of India to conduct the survey called, called “National Survey on Availability of Dental
Health Manpower and Disease Prevalence in Urban and Rural India”. DCI in turn to a private
agency to conduct the survey. After much delay, the private firm submitted the report and DCI
found irregularities in the validity of the report.
95
Everything that happens, happens for a reason
Community Health Learning Programme happened for a good reason. I am not sure, if coming to
SOCHARA was serendipitous or coincidental. I was looking for a guru, also a mentor, friend,
guide and who will help sort out my confusions and help me in choosing the right path. I
remember the road outside Fireflies intercultural centre, when we were there for CHESS meeting.
The road was curvy, lined with trees with shedding leaves. It was dusty, rugged and less travelled
road. I realised that moment that, I had chosen a less travelled road. I knew, I would find my way
out. I trusted SOCHARA.
The environment at SOCHARA is very friendly and non-hierarchical. People, here are highly
motivated and very dedicated. Their experiences speak about them. Some of their stories inspire
to take risks and move a step ahead of peers. Truth is told in a subtle yet blatantly. The message is
delivered clearly. Speaking of truth, we were also made to analyse any given information in all
viewpoints and then understand the truth in a logical manner. This realisation of truth, made me
think with an intellectual mind to minimalise the grey areas and to see as much black and white
areas as possible. SOCHARA’s work reinforced the belief that things can work and good work will
be recognised. It is a luxury to be here. The space created to experiment and voice out opinions
and views, loudly, was radical compared to my previous learning centres. This is a parallel world
with lots of good people. In fact, SOCHARA is called as ‘University without walls’.
Community health journey is a hard one. It aims at building an egalitarian society with just and
equity as core principles. Capitalism is encountered at every milestone. Market based economy is
challenged to overcome inequalities. The role of rights and responsibilities of both community
and individual are emphasised. The life skills required to manage intra and interpersonal skills
which in turn are important aspects of community health are taught with simulation exercises.
Outreach concept to reach the much bigger community which is the core value of public health is
the objective to reach ‘Health for All’ goal. To reach this goal, one cannot work in vacuum and
therefore networking becomes necessary. SOCHARA with its vast network of organisations in
India and abroad and also with the government has demonstrated a way to solve health issues
governed primarily by social problems. It gives the required strength and belief in the system and
reinforces the fact that, it is possible to get things worked. During the course, we met inspiring
people and had chance to know their work. They were all engaging public in the political process.
Most of them were ‘Scholar activists’ who have an excellent combination of skills, competencies
and activism.
Reflecting on the readings and observing the current scenarios then, I understood that
sanskritisation has taken a political stand. It has given way to turmoil. The whole beef fiasco,
lynching of Muslims, Hindu reconversions, the suicide case of the Dalit scholar, targeting
university students across India, anti-nationalism debate and many other disturbing events reveal
an authoritarian process of exercising power. The political stand one can take is particularly
debated and accused. The neglected health issues such as alcoholism, mental health and oral
health have deep rooted invisible political relations. Mr Keshav Desiraju, former union health
secretary, during the annual dissemination meeting said, “to be a woman, destitute and diseased is
96
a deadly combination in India”. When we try to look at this statement carefully, one can easily
notice that, health is a political process and needs strong political commitment.
If at all there is any learning that happened, I must confess, unlearning happened to a great
extent. There were unlearning of dominant attitudes and ignorant behaviour. Sharing and caring
with fellows made me more gender, language and community sensitive. An important and crucial
habit that, I am still developing is ‘value based judgement’. I learnt this as part of ethnographic
understanding of adivasis, which later, I started implementing in my life too. To remain neutral in
understanding a process or culture or an individual reflects on how we perceive things. It is the
most difficult exercise. Getting into others shoes and see the world through their eyes makes one
see the entire situation so different to that of the former understanding.
The community experience at Gudalur was powerful and had a tremendous influence on me.
Learning from the community, their lifestyle, attitudes, worldview left a mark on myself. They
have solutions to everything and considering that in problem solving is crucial. Lao Tsu, the
Chinese scholar said,
Go to the people
Live among them
Learn from them
Love them
Start with what they know
Build on what they have:
But of the best leaders
When their task is done
The people will remark
“We have done it ourselves.”
It left a sound advice for practising in my field work. I learnt a vast amount of knowledge,
particularly working knowledge. I used many opportunities to speak up. The words were carefully
used to express the views and concerns emphasising sensitivity in practise. Being political or
apolitical is a conscious decision made on an everyday basis and I have come to terms in my
political stand which is basically centrist based on Gandhian, Marxist, Socialist, and a little bit of
Capitalist ideas. I could have been more organised, should have taken notes regularly and should
have written my reports on time, which I regret. Nevertheless, better late than never. I will try to
improvise. My reading and writing has improved, but still needs more precision and less word
mongering.
On a philosophical note, there was a lot of reflection and reinvigoration into my thought process.
Community health is based on facilitating and fulfilling basic essentials of life. It is to lead a
simple life, yet not to forget to celebrate the journey of life. When you also leave selflessness,
there is self -realisation and the higher power acquired makes happier and shows direction to a
meaningful life.
Years ahead, I would like to work closely with marginalised communities. I also want to learn
more about health systems, health policies and engage in participatory action research to make
health available, acceptable, affordable and adaptable.
97
Academically, discerning between public and community health was possible. Public health is
technical knowledge based completely on sound epidemiological and statistical theories that are
logic and scientific. To a great extent, it doesn’t consider the social part of the issue. The
boundaries in which it works provide a solution that is often deduced in an arithmetic fashion.
For ex, providing condoms to prevent HIV/AIDS. Community based clinical trials based on
epidemiological principles have proved the effectiveness of condoms in preventing the spread of
HIV/AIDS, but this knowledge doesn’t throw light on how successfully it is compliable with the
users. The cultural and social factors affecting the human behaviour are not given much
importance in public health. Community health attempts at this lacuna. Community health is a
process of enabling people to exercise collectively their responsibility for their own health and to
demand health as their right. In case of HIV/AIDS, the community affected by the disease is also
considered to solve the issue. The affected persons are also consulted to find solutions at all levels
of prevention. They will be an important part of the entire process from identifying the problem
Public
Health
Health
System
Community
Health
Figure 39: Relation between Community Health and Public Health
to finding the solution. Health systems is at the outset having both these arms of approaches to
solve health issues. It bridges these with a community oriented policy. The NRHM is modelled on
this Communitisation process of enabling the people through highly motivated people from the
community to advance towards health for all goal. It is now adopted as a policy. The roots of this
approach was by various demonstrations across India to show community health’s success by a
cadre of personnel ranging from technical (medical, nursing, public health) personnel to nontechnical (health workers, health activists, teachers, anganwadi workers, dais, socialists,
anthropologists, policy makers, bureaucrats, politicians). Health policy is the tool to implement
the strategy which is effective and also for the benefit of the community. Community health is a
social process dealing with the larger social determinants that are the actual causes of health
issues. It is a political struggle for a better society.
98
AHS. (2013). Annual Health Survey. New Delhi: Ministry of Demography and Statistics.
AIIMS. (2001). National Oral Health Care Programme Implementation Strategies. New Delhi: All India
Institute of Medical Sciences,.
Aiyappa, M. (2014, COtober 13). TOI. Retrieved from www.timesofindia.com:
http://timesofindia.indiatimes.com/city/bengaluru/Why-is-the-garbage-problem-all-muckedup/articleshow/44795079.cms
al, W. N. (2015). Health and climate change: policy responses to protect public health. Lancet, 1-60.
Ambedkar, B. R. (1979). CASTES IN INDIA: Their Mechanism, Genesis and Development. In B. R.
Ambedkar, Dr. Babasaheb Ambedkar: Writings and Speeches Vol 1 (pp. pp. 3-22). Bombay :
Education Department, Government of Maharashtra.
AMS. (2013). The food book of the adivasis of the Gudalur. Gudalur, Tamil Nadu, India: Adivasi Munnetra
Sangam.
Arolle, M., & Arolle, R. (1974). Comprehensive Rural Health Project.
ASHWINI. (2009). Addressing the hidden mental illness in the community: ASHWINI Mental Health report.
Gudalur: ASHWINI.
ASHWINI. (2015, December 15). ASHWINI. Retrieved from http://www.ashwini.org:
http://www.ashwini.org/sicklecell.php
Balasubramanian , A., & Radhika, M. (1989). Local Health Traditions: an Introduction. Chennai: Lok
Swasthya Parampara Samvardhan Samithi.
CBHI. (2013). Central Bureau of Health intelligence. Retrieved from www.cbhidghs.nic.in:
http://www.cbhidghs.nic.in/writereaddata/mainlinkFile/Human%20Resources%20in%20Health%2
0Sector-2013.pdf
CBHI. (2013). National Health Profile. New Delhi: Ministry of Health and Family Welfare.
CEHAT. (2000). ETHICAL GUIDELINES FOR SOCIAL SCIENCE RESEARCH IN HEALTH. Mumbai: Centre
for Enquiry into Health and Allied Themes.
Cell, C. H. (2011). Community Health- In Search of Alternate Processes. A report of study- reflection-actionexperiment. Bangalore: SOCHARA.
Census. (2011). "Population By Religious Community - Tamil Nadu" (XLS). New Delhi: Commissioner, Office
of The Registrar General and Census; Ministry of Home Affairs, Government of India.
Charaka. (n.d.). Sushruthana Chapter 1, verse 120.
Collectivenotes. (2015).
CSDH. (2006). Closing the Gap in a Generation. Geneva: WHO.
Dahlgren G, a. W. (1991). Policies and Strategies to Promote Social Equity in Health. Stockholm: Institute for
Futures Studies.
David L. Heymann, J. L. (2016). Partnerships, Not Parachutists, for Zika Research. The New England Journal
of Medicine, 2.
Devadasan, S. M. (2004). ACCORD Community Health Insurance Increasing access to hospital care.
Economic and Political Weekly, 3819-3825.
DLHS. (2013). Nilgiris District Level Household and Facility Survey-4. New Delhi: Governement of India.
DNA. (2012, November 20). Retrieved from http://www.dnaindia.com/:
http://www.dnaindia.com/bangalore/report-new-garbage-contract-is-anti-pourakarmika-1767079
Doniger, W. (2015). The Hindus an alternative history. New Delhi: Speaking Tiger.
EconomicSurvey. (2016). The Economic Survey of India 2015-16. New Delhi: Ministry of Finacne.
Eder, K., & Garcia Pu, M. M. (2003). Model of Indigenous Maya Medicine in Guatemala. Chimatenango:
ASECSA.
FDI. (2009). The Oral Health Atlas- Mapping a neglected global health issue. . Cointrin: FDI World Dental
Federation.
Fieldnotes. (2015).
99
Foundation, R. W. (2010). A new way to talk about Social Determinants of Health. New York: Robert Wood
Johnson Foundation.
FRLHT. (2008). Initiatives for Promotion of AYUSH intervention in the Public Health Systems of the country.
A Report on Stakeholders Workshop on “AYUSH Interventions in Public Health” . Bangalore:
Foundation for Revitalization of Local Health Traditions.
Gandhi, M K. (1942, July 26). Harijan, pp. 308-9.
Gandhi, M. K. (1910 ). In Indian Opinion .
Gandhi, M. K. (1937, January 2). Ramarajya. Harijan, p. 374.
Gandhi, S., Verma, V. R., & Dash, U. (2015, July 15). International Health Economics Association. Retrieved
from /www.healtheconomics.org: https://ihea2015.abstractsubmit.org/presentations/14318/
Ganesh, C. K. (2014). Poor access to Sanitation: A determinant of Mental Health. Dimentions, 4-5.
Gangotri, Pritisha, Bhargava, R., Abid, R., Velankar, J., & Dasgupta, J. (2015). Report of independent factfinding into the incident of gang-rape and death of an ASHA worker Somwati Tyagi, in Muzaffarnagar
District Uttar Pradesh, India. New Delhi: NATIONAL ALLIANCE FOR MATERNAL HEALTH AND
HUMAN RIGHTS & HEALTHWATCH FORUM UTTAR PRADESH.
Greenpeace. (2013). Greenpeace. Retrieved from www.greenpeace.org:
http://www.greenpeace.org/india/en/What-We-Do/Quit-Coal/save-mahan/
Gupta, p., Shrama, V., & Sharma, S. (2014). Healing Traditions of the Northwestern Himalayas. In Briefs in
Environmental Science (p. 149). Springer.
Hafeel, & Suma. (2007). Report of Rapid Assessment of LHT in Tamil nadu. Bangalore: FRLHT.
Health, M. g. ( 2012). Towards a community oriented public health system development in Karnataka.
Bangalore: Karnataka Knowledge Commission, Government of Karnataka.
Hindu, T. (2015, July 29). Agrarian distress and suicides. The Hindu.
ICMR. (1976). Alternative Approaches To Health Care. New Delhi: ICMR.
Jennie Popay, S. E. (2008). Understanding and Tackling Social Exclusion. Geneva: WHO.
Kannabiran, K. (2015, July 24). Constitutional conversations on Adivasi rights. The Hindu.
Karnataka Knowledge Commission . (2012). Towards a community oriented public health system devlopment
in Karnataka. Bangalore: Government of Karnataka.
Karthik, M., & Menon, A. (2016). Blurred Boundaries: Identity and Rights in the Forested Landscapes of
Gudalur, Tamil Nadu. Economic and Political Weekly, 43-51.
Kathleen M. MacQueen, E. M. (2001 ). What Is Community? An Evidence-Based Definition for Participatory
Public Health. Am J Public Health, December; 91(12): 1929–1938.
Klatz, H. (2015). Prevalance of Malnutrition among the under 5 children among the Gudalur Adivasis.
Gudalur: ACCORD.
Klienman, A. (1985). Indigenous systems of healing: question for professional, popular and folk care. In S. J,
Alternative medicine: Popular and policy perspectives. London: Tavistock.
Krycia Cowling, R. D. ( 2014, ). Social determinants of health in India: progress across states. International
Journal for Equity in Health8, 13:8.
Leahy, S. (2015, May 8). Inter Press Service News Agency. Retrieved from http://www.ipsnews.net/:
http://www.ipsnews.net/2015/05/living-the-indigenous-way-from-the-jungles-to-the-mountains/
Luft, J., & Ingham, H. (1955). The Johari window, a graphic model of interpersonal awareness. In Proceedings
of the western training laboratory in group development. Los Angeles: University of California.
Margaret E Kruk, M. M. (2015). What is a resilient health system? Lessons from Ebola. The Lancet, 1910–12.
Mehta, V. (2015). Caste, Urban Spaces and the State: Dalits in Telangana. Chennai: The Hindu Centre for
Politics & Public Policy.
Miller, L. V. (2006). Dynamics of Power inclusion and exclusion. Non profit online news journal, 38-56.
MOHANTY, M. (2015, September 22). OMC writes to environment ministry seeking guidance on Niyamgiri
bauxite deposit. Economic Times.
Narayan, A. P. (2012). EXAMINING ENVIRONMENT AND HEALTH INTERACTIONS: Responding with
communities to the challenges of our times. Bangalore: SOCHARA-SOPHEA.
Naryan, T. (1990). Health impact of Bhopal disaster – an epidemiological perspective. Economic and
Political Weekly, 1905–14.
100
Natraj, P. (2015, December 17). Deccan Herald. Retrieved from www.deccanherald.com:
http://www.deccanherald.com/content/518175/karnataka-hc-orders-two-bins.html
NFHS-4. (2015, January 18). National Family Health Survey, India. Retrieved from http://rchiips.org/:
http://rchiips.org/NFHS/factsheet_NFHS-4.shtml
Pandey, R. S. (2010). Communitisation: Third way of Governance. New Delhi: Concept Publishing company.
Park. (2014). Preventive and Social Medicine.
Philip, B., Chithresan, K., & Vijayalakshmi, S. V. (2013). Prevalence of periodontal diseases among the adult
tribal population in Nilgiris- an epidemiological study. Intnl J Pub Heal Dent., 8-12.
Planning Commission. (2000). Report of the planning Commission. New Delhi: Government of India.
Posaani, B. (2009). Crisis in the countryside: Farmer suicides and the political economy of the agrarian
distress in India. London: London School of Economics.
Prahlad, I. (2015). Enviornmental Sanitation-Reflections from Practise. Bangalore: SOCHARA-SOPHEA.
Prakash, H., Duggal, R., & Mathur, V. (1999). Guidelines for Meaningful and Effective Utilization of Available
Manpower at Dental Colleges for Primary Prevention of Oro-dental Problems in the Country” A GOIWHO Collaborative Programme. New Delhi: AIIMS.
Promotion, O. C. (1986.). First International Conference on Health Promotion. Ottawa.
Rajeev, B. R. (n.d.). Collective notes. Fellow. Bangalore, Karnataka, India.
Ramani, C. V. (2015, December 2). The Hindu. Retrieved from http://www.thehindu.com/:
http://www.thehindu.com/news/cities/bangalore/pourakarmikas-cant-take-itanymore/article7938740.ece
(2005). Research for People's Health . Bangalore: People's Health Movement (Global Secretariat),
SOCHARA.
Saha, D. (2016, March` 2). The News Minute . Retrieved from www.thenewsminute.com:
http://www.thenewsminute.com/article/why-health-sector-allocation-budget-2016-simply-notenough-39697
Saub, R., & Jaafar, N. (200 I). ADental-Anthropological Study of Health and Illness Behaviour Among Orang
Asli of the Semai Tribe: The Perspective of Traditional Healers. Med J Malaysia , 401-408.
Scambler, G. (1991). Health and Illness behavior. In S. G, Sociology applied to medicine (pp. 33-46). London:
Bailliere TindalL.
Shankar, D. (2001). Agenda for Revitalisation of local Health Traditions. New Delhi: Voluntary Health
Asscoaition of India.
SHARMA, N. C. (2015, November 23). Daily Mail. Retrieved from http://www.dailymail.co.uk/:
http://www.dailymail.co.uk/indiahome/indianews/article-3330963/Rs-3-5-crore-dental-healthreport-rejected-flaws-seven-years-work.html.
Srinivas, M. (1952). Religion and Society of the Coorg.
Srinivas, M. N. (1989). The Cohesive Role of Sanskritisation and other Essays. Oxford: Oxford University
Press.
SRS. (2011). Sample Registration System MMR Bulletin. New Delhi: Government of India.
SRSBulletin. (2013). Sample Registration Survey. New Delhi: Ministry of Demography and Statistics.
Subitha Lakshminarayanan and Ramakrishnan Jayalakshmy. (2015). Diarrheal diseases among children in
India: Current scenario and future perspectives. J Nat Sci Biol Med. Jan-Jun; 6(1), 24–28.
Team, C. H. (1989). Community Health in India. Health Action.
Thapar, R. (2015, October 18). What Secularism is and Where It Needs to Be Headed. Retrieved from
http://thewire.in/: http://thewire.in/2015/10/18/what-secularism-is-and-where-it-needs-to-beheaded-12539/
Thekaekara, M. M. (2015, December 11). New Internationalist Blog. Retrieved from http://newint.org/:
http://newint.org/blog/majority/2015/12/11/indigenous-sustainable-example/
Thekaekara, Mari Marcel. (1994). Anubhav series- ACCORD. New Delhi: VHAI.
Turin, R. p., & Satriani, L. L. (1978). Appropriation and destruction of the culture of the subaltern classes.
Mexico.
UNDP. (2016, March 12). United Nations Development Program. Retrieved from www.hdr.undp.org:
hdr.undp.org/en/data
101
Unnikrishnan, P., & Hari Ramamurthy, G. (2012). Local Health practioners in India. In V. S. Abraham,
Medical Pluralism in Contemporary India (pp. 279-304). New Delhi: Oriental Blackswan.
Vemula, R. (2016, January 18). What did Rohith Vemula, PhD scholar who committed suicide, say before his
death? India Today.
Vikram Patel, R. P. (2015). Assuring health coverage for all in India. LANCET, 2422–35.
Vishweshwaraih, S. M. (1951). Memoirs of working life. Bombay: Caxton Press.
Vivek, S., Jain, J., Sequeira, P. S., Battur, H., & Tikare, S. &. (2012). Understanding oral health beliefs and
behavior among Paniyan tribals in Kerala, India. . JIOH.
Watt, R. G., Sheiham, A., Listl, S., & Peres, M. A. (2015). London charter on Oral Health Inequalities. Journal
of Dental Research, 1-3.
WHO. (2002). WHO Traditional Medicine Strategy. Geneva: WHO.
WHO. (2003). Report on WHO Traditional Medicine Strategy. Geneva: World Health Organization.
WHO. (2003). The World Oral Health Report 2003. Continuous improvement of oral health in the 21st
century-the approach of the WHO Global Oral Health Programme. . Geneva: World Health
Organisation.
WHO Committee on Economic, S. a. (2009). Non-discrimination in economic, social and cultural rights,
General comment No. 20. Geneva: WHO.
WHO-CSDH. (2008). World Health Organisation. Retrieved from www.who.org:
http://www.who.int/social_determinants/sdh_definition/en/
World bank. (2013). Retrieved from http://web.worldbank.org:
http://web.worldbank.org/WBSITE/EXTERNAL/TOPICS/EXTHEALTHNUTRITIONANDPOPULA
TION/EXTHSD/0,,contentMDK:20190826~menuPK:438812~pagePK:148956~piPK:216618~theSitePK
:376793,00.html
Zachariah, A., & Srivatsan, R. (2015, December). Anveshi. Retrieved from http://www.anveshi.org.in/:
http://www.anveshi.org.in/home/
Zachariah, Anand. (2015). Urbanisation and Cardiovascular risk: moving from framingham. mfc bulletin, 6.
102
Position: 185 (24 views)