RF_DR_2_SUDHA.pdf
Media
- extracted text
-
RF_DR_2_SUDHA
THE LANCET, FEBRUARY 20. 1982
435
ESSENTIAL DRUGS FOR PRIMARY-HEALTHCARE STANDARD PACKAGES
standardised treatment schedules. The impetus for this work
was provided by the involvement of one of us (S.P.S.) in the
health care of refugees and the provision of emergency drug
supplies. However, the methods used for that particular
situation have more general applicability.
METHODS
Stephanie P. Slmmonds
Godfrey J. A. Walker
Zurffruf/ n£_Tny»>^/
hwfHmr firhml uf-Hygirwttrui
MUCH has been written about the usefulness of a standard
limited number of drugs for primary health care in
developing countries,1"4 and recommendations have been
made for standard treatment and management of common
conditions.M The World Health Organisation lists 200
essential drugs.9 There are, however, several steps between
deciding which preparations should be available for a
primary-health-care worker and estimating how much of each
drug will be needed to cover the majority of disease episodes
that such a worker will be likely to encounter in a given period
in a given population. We have assessed these requirements
from the predicted “incidence” of various diseases and
We considered a standard population of 10 000 having age
structure similar to that found in many developing countries—i.e.,
half were aged less than 15 years. It was estimated, on the basis of
repons of outpatient clinics from several countries, that the likely
average number of “curative” contacts between individuals and the
primary-health-care worker would be of the order of 4 per year.1<>l2
This would give a figure of around 10 000 patient-contacts in a
3-month period.
It was further assumed that the type of conditions with which
children and adults would present can be generalised and predicted.
For these broad disease categories, decisions about treatment
regimens (tables I and n) were made after wide consultations. By
consideration of the likely contacts, prevalence of symptoms, and
standard treatment regimens, estimates of the probable basic drug
requirements for a specific population were prepared (table m). The
number of preparations listed has been deliberately restricted, bur a
more extensn e list was prepared for a more senior health person (a
doctor or nurse) who could be supporting and supervising the
primary-health-care worker.
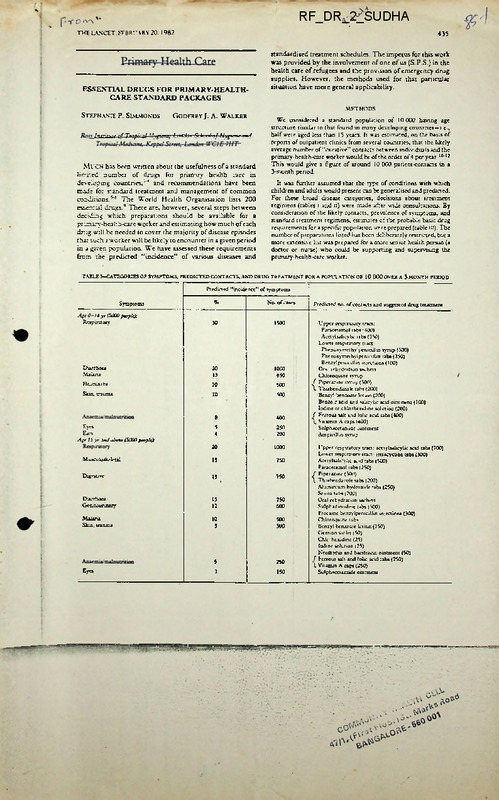
TABLE I—CATEGORIES OF SYMPTOMS, PREDICTED CONTACTS, AND DRUG TREATMENT FOR A POPULATION OF 10 000 OVER A 3-MONTH PERIOD
Predicted "incidence" of symptoms
%
No. of cases
0-14 yr (5000petyleji
Respiratory
30
1500
Symptoms
Diarrhoea
Malaria
20
13
1000
650
Helminth*
10
500
Skin, trauma
10
500
8
400
5
4
250
200
Eye*
Ears
Agr 15 yr okJ aboct (5000pevpk):
20
1000
M ttsculcikdctal
15
750
Digestive
15
750
D-jrrhoea
Gemtcurmarv
15
12
750
600
Mai*na
Skm, trauma
10
5
500
300
5
250
3
150
Eye*
Predicted no. of contacts and suggested drug treatment
Upper respiratory tract:
Paracetamol tabs *400)
Acetylsalicylic tabs (350)
Lower respiratory tract
Phenoxymethylpemcilltn syrup (300)
PhenoxymcthylpenicilUn tabs (350)
Benzylpenicillin inject ions (100)
Oral rebvdrstion sachets
Chloroquine syrup
/ Piperazine syrup (500)
\ Thiabendazole tabs (200)
Benzyl benzoate lotion (200)
Benzox acid and *abcybc acid ointment (100)
Iodine or chlorhcxidine solution (200)
( Ferrous salt and folic acid tabs (400)
< V namin A caps (400)
Sulphacetamide ointment
Ampicilhn syrup
Upper respiratory tract: acetylsalicylic acid tabs (700)
Lower respiratory tract, tetiacycbne tabs (300)
Acetvlsalicviic acid tabs (500)
Paracetamol tabs (250)
f Piperazine (300)
\ Thiabendazole tabs (200)
Aluminium hydroxide tabs (250)
Senna tabs (200)
Oral rchvdration sachets
Sulphadimidinc tabs (300)
Procaine benzylpenicillin injections (300)
Chloroquine tabs
Benzyl benzoate let ion (150)
Gentian violet (50)
Chk hcxidine (25)
Iodine solution (25)
Neomycin and bacitracin ointment (50)
f Ferrous salt and folic acid tabs (250)
I Vitamin A caps (250)
Sulphacetanudc ointment
■ ■■ '
THE LANCET, FEBRUARY 20,1982
436
TABLE 11—SUGGESTED STANDARDISED TREATMENT SCHEDULE
TABLE III—BASIC DRUG REQUIREMENTS FOR A POPULATION OF 10 000
FOR 3 MONTHS
Drug
DISCUSSION
The success of primary-health-care workers depends to a
substantial extent on the amount of support and supervision
they receive. To be successful in their important promotive
and preventive roles they need to be seen to be providing
credible first-line curative services. A pan of this is the
continuing provision of essential drug supplies.
A method is suggested here of how the range and quantities
of a limited number of essential drugs for a specific
population and time period might be estimated.
The particular listing and quantities will obviously vary
according to such factors as: the actual age structure of the
population; the particular local disease patterns (we have
included malaria as being “typical”, but this will not be so in
many areas); the diagnostic capability of the primary-health
care workers; and national prescribing policies.
Pharmaceutical form
and strength
Analgetics (2):
Tab 300 mg
Acetylsalicylic acid
T ab 500 mg
Paracetamol
Antihelminthie (7'2):
Tab 500 mg
Piperazine
Svrup 500 mg/5 ml
Pip.-razme
Tab 500 mg
Thiabendazole
Antibacterial (7'3):
Syrup 125 mg'5 ml
Ampicillin
Injection 0-6(1 million IU)
Benzylpenicillin
Phenoxvmethvlpenicillin Tab 250 mg
Phenoxvmethvlpenicillin Svrup 250 mg/5 ml
Procaine benzylpenicillin Injection 3-0 g (3 million IU)
Tab 500 mg
Sulphadimidme
Tab 250 mg
Tetracycline
Antimalanal (7'6)Tab 150 mg'base
Chloroquine
Syrup 50 mg 5 ml base
Chloroquine
A ntianaem ta: (11'1)
Ferrous salt and folic acn. Tab 60 mg iron with
0-25 mg folic acid
Dermatological (14)'
Ointment 25 g rube
Benzoic acid and
salicylic acid
Benzyl benzoate
Lotion 25%
Crystals
Gentian violet
Neomycin and bacitracin Ointment 25 g
Antacid (17'1):
Tab 500 mg
Aluminium hydroxide
Cathartic (17-5):
Tab 7-5 mg
Diarrhoea (17-6'2):
Sachet 27 • 5 g/litre
Oral rchydration salts
Anti-infcctive (21 ■ 1):
Ointment 10%, 5 g tube
Sulphacet amide
(ophthalmological)
Solutions (26):
2 ml
Water for injection
10 ml
Water for imcction
Surgical disinfectants (27):
Solution 5%
Chlorhcxidine
Solution 2-5%
Vitamins (28)'
Caps 200 000 IU
Retinol
REFERENCES
1THO
1977. JI: 404-07.
This work nas formed the basis for W.H.O./U.N.H.C.R.
recommended emergency health kits for refugee
populations.! 1 The use of these kits will be evaluated over the
next year.
Correspondence should be addressed to S. P. S.
17 000 tabs
5000 tabs
2500 tabs
10 litres
3500 tabs
400 battles
500 vials
5000 tabs
300 bottles
300 vials
6000 tab*
9000 tabs
2000 tabs
10 litres
9000 tabs
100 rubes
200 g (8 boules)
50 tubes
5000 tabs
500 tabs
5500 sachets
400 tubes
500 amps
500 amps
10 litres
5 lares
1000 caps
Figures in parentheses refer to VI' H.O classification.*
• Amounts rounded up to the nearest 500 for tablets and sachets.
It is important that adequate supplies are regularly
provided, and to assist with this a simple drug reordering
form has also been devised.
Copies of the additional Using of drugs for health personnel supporting
pnrnary-b-Ahh-care workers and the drug reordering forms referred to in the
terr art available from Emergency Relief Operations, World Health
Organisation. Geneva.
Total required
for 3 mo*
service. J PwN Hlth Pohn 1980; 1: 2S8-79,
10 000 refugees for J month*. Geneva. W H.O. 1981
■
Hiairacoutxcals for Primry Health Caro
Che cf the reccmncndaticns of the Alma Ata Conference has been with
respect to the production, import, distribution and utilization of drugs
and pharmaceuticals to jnsuro the availability of essential drags at
feasible costs.
Thcucl sone advances have been made by the pharmaceutical industry
in the countsy, India is V :; ;ing far behind in the provision of pharma
ceuticals for the people. The amount that is utilised for the purchase
of drags and pharmaceuticals by a person in Lidia is extremely small
ccraparcd to what is used in the developed countries and even in sone of
the doreloping countries. Miilo increase in expenditure of drugs is
not an indicator of h alth it is necessary that a certain minimum amount
is available for the purchase of drugs and pharmaceuticals to care for
the sick. A look at the amounts spent by some countries is revealing.
Bstimatoc1 purchase of human nharnaccuticals (1975)
Per capita
Average
West Germany
USf 53.35
Japan
38.45
U.S.A.
35.05 .
U. K.
19.50
India
0*75
Not only is the consumption of pharmaceuticals low in Lidia but oven
for the lew consumption, the production of pharmaceuticals is not enough.
The financial requirements for the manufacture of bulk drugs have boon
estimated to bo Bi.720 crores for 1983-84, with a production of formulation
of ?s.2>160 crores. The investment in the public and private sectors is
of the order cf Rs.150 crores and Rs.400 crores, leaving a gap of Rs.1,610
crores. Wo arc still dependent almost entirely on other developed countries
for those products. In the International trade in medicinal products
there is
wide disparity between the developed countries and the devel
oping countries.
International trade in medicinal products 1969-1974
Imports
Exports
1969
1974
1969
1974
Developed market economy countries 62.4
67.1
94.2
92.8
Developing countries
32.9
5.8
7.2
37.6
'
COMMUNITY r2 CEUL
47/1.(F:-stF«oo r)3t. Marks Read
... 56C G01
Ton c" :: ri.'s in -i ' world accounted for 86.8% of all the exports in
1969 and 84.4% in 1974. Those countries are therefore in a position to
control the pr eduction of drugs as regards the nature of the products,
the priorities and the final prices. Modern drugs are mostly chemical
substances dorived from potro-chemical or fermentation industries. The
German chemical industry was the only major international supplier'
before World War I. 7 ter other developed countries joined t- r.., espec
ially when it was found that the Germans witdrew their supply -'f
of
the more important drugs from the international market; th®. countries in
volved also put large duties on the imports discouraging the report? of
these drugs and thereby helping the indigenous production of th? drugs.
The State acted as a facilitator in the growth of the ph'ame lov.tico
industries in the countries and was mediator between interests of the
industry , the nodical profession and the consuming public.
largo capitals, modern technology, expertise and extensive- promotion
activities are necessary in the highly sophisticated pharmaceutical trade
and there is a 'concentration of these industries in the enveloped world.
The Pharmaceutical industries are often a part of the activities of the
firm which is mainly a chemical industry. Hoechst which rented 2nd in
world Wide drugs was one of the 8 largest companies in the w~-rlJ of
overall not sales in 1976. Bayers which was among the top 15 trans
national companies in total drug sales was one of the most successful
firms in the world, in regard to the overall not sales in 1976. Most of
the loading transnational companies dealing with pharmaceuticals have
widely diversified interests, A country lite- India has little chance to
compote.
Research and Dcvolo-cnont: Research and Develoment are often geared’
to the needs of the more developed countries (because of the greater pur
chasing power) and carried out in the technologically forward countries.
The developed countries have different prevalent disease p'ttcms from
those in the- under-developed countries. There is a change from communic
able and parasitical illnesses to chronic and degenerative such as heart
disease, cancer and various stress-related diseases. This would mean
that linos of research which could have yielded beneficial results in
tackling health problems of countries like India by development of cheaper
andcfficacious drugs may not bo followed up.
There is a possibility of a geographic redistribution of industry
based research. This is evident in some of the countries like Mexico and
Honkang. It is because (l) certain development costs particularly for
research personnel are lower in developed countries, (2) the requirements
for testing human subjects are less formidable and (3) delays in-rogis-'
traticn of new products are shorter. Nevertheless this change in alloc
ation of part of production and development of drugs has not affected the
industrialised countries' disease orientation of the Transnationals,
Patent: The great majority of patents registered in tire developed
countries are in the chemical sector .and among them a great majority con
cern drug .products, but the nationals within the group of developing
countries am only 6% of the-total number of patents; a 11 the remainder
were by other countries. Very few of the patents registered by foreigners
are actually worked in the developed countries. The Patent holders very
often decide not to use then and therefore do not develop them and also
prevent others from developing the -product; tho patent has worked adversely
in providing the consumer with cheaper, effective drugs.
Piancticr.: Many of these drugs arc given intor-so promotion by various
advertising- moons when doctors became used to recommendin' the drug by its
brand nane, and not by tho generic name. Che drug nay be In own by a voiy
large number of different brand names and’ depending upon the capacity to
advertise and exploit, the- sane drug marketed by different firms may bo
sold at different levels iu ■ .iffe rent countries. There are certain countries
which arc not'.' insi:'-'.'ng
purchases being made by generic names. S< ne of
the developed combr-.es l.’.k Norway have national formularies and nrchnsos
had to bo restricted t- tho drugs found in the formulary
Th. total
number of drugs in the Korwogian -formulary comes to about two thousand
whereas in India there are over 15,000 products in the market/most of them
being duplicate products. It lias been estimated that marketing expenses
wore equivalent to 15 - 35- of tho sales and represent rotaghly 3 times the
expenditure an research -u.d development.
Pricing and Rrofitalxilitys Only a small proportion of the selling
price of the drugs represents direct cost of production. Evon where- the
substance has boon produced by the same manufacturer, costs vary greatly"
between the various distributors. The firms often get monopolies by var
ious methods and therefore are able to fix the price. Hie US Trade Comm
ission found that tho first company to patent Tetracycline, Messrs. Pfizer,
was directly responsible for "procurement by misrepresentation" of monopoly
control over tetracycline. It was found that Pfizer and Cynamid had con
cluded a secret agreement by which Cyno-.raid withdrew its application for
patent for tetracycline after accepting an offer from Pfizer to divide up
the market for tho drug.
P-ricin; pattern is often higher in the developing countries.
100 tablets of 10 mg librium tho cost was
U.K.
-
0.83 US’'
Mexico
-
4.42
Costa
Rica
-
7.03
For
The transnational companies have charged whatever the national market
would bear.
One of the ways in which 'the prices are n-Aipulated is loy transfer
pricing. The prices of intermediate chemicals which are produced only by
a few firms are fixed at different levels and supplied at different costs to
imports by subsidiaries or joint operations in developing countries.
U.K. has a system of negotiating profits with pharmaceutical firms.
Hoffman la-Roche, the biggest manufacturer of drugs in the world , included
the costs of active ingredient of Librium at £4.37/- per kilogram. When
operations and overhead costs in the United Kingdom were computed the
prices were set at a level that showed & profit of less then 5^. However
the Monopolies Commission found that the cost of the active ingredient
listed elsewhere in Lurcpo- was £9/- per kilo for librium. Roche was
using a much higher transfer price. After negotiations, Roche agreed to
repay £3.75 million in excess profits and also agreed to fix tho prices
of the drug at half the earlier price. Transnationals declare prices in
various countries at different levels, depending upon the tax situation,
restrictions on repatriation of profits and regional req-uiroments.
With a situation like this, India one of the poorest countries, can
not depend cn these transnational companies for our.req-uirements of
essential drugs(which would really number less than 200) and wo should
see that they are made available to the people. This could, bring about
substantial savings in the health expenditure.
CHRISTIAN MEDICAL ASSOCIATION OF INDIA
PHARMACY WORKSHOP PAPER
PREPARATION OF INTRAVENOUS FLUIDS
Introduction The preparation of intravenous fluids has been
'.'ndertaken in Christian Hospitals for many years with a varying
degree of competence and exellence of product. In recent years due to
accidents both in India and other countries more and more emphasis is
being placed on the construction of the accommodation, equipment and
chhemicals used in the manufacturing process.
Ibis paper discusses the standards for which the Pharmacist should aim
Many of these standards are the result of scientific observation and
experiment and a few based on personal opinion.
?ar;t I
The Construction Standards f
fncse vary with the type of work to
follows?
)epartment
ne and can be outlined as
1) Wash-up .Room This is the area where the containers are received
and washed and also where the rubber liners and caps will be prepared
for use. This room needs to comply with go<d standards of hospital
construction. In it will be located sinks for soaking and washing of
the bottles and a good water supply is essential.
2) Mixing Room In this re
the chemicals will be weighed or'
measured and the mixing of jhe solution um ertaken.
3) Filling Room This v; 1?. be connected directly with the Mixing Room
so that the solution ca1 be taken into it. Also this room will have a
connection with th? Was.-Lr.g-up Room so tha the bottles can be trans
ferred easily. In the Filling Room the solution will be filtered into
the final containers.
i
The construction of the Mixing Room and Ft ling Room will have to
comply with high standards so that contamination of the fluid is
reduced to the absolute minimum. Hie following are guidelines?
a) The floors and walls must be smooth and without cracks or joins
This can be best achieved by using mosaic laid in a continuous form
and not tiles which inevitable have to be joined with cement which in
time breaks down leaving cracks which can accumulate dirt. The same
material can be used for the benches unless formica is preferred.
b) All ledges and gaps in construction must be eliminated including
windowsills.
o) All services such as water and e..
outside the room, and where possibl
situated beneath the bench.
-city should have the conduit
.itches should be outside or
d) Ultraviolet light should be installed to help eliminate bacteria
from the air. It must be remembered that UV light is of limited value
and thorough cleaning methods are still essential.
e) The entrances and exits to these rooms should have an 'airlock' to
reduce the entrance of unfiltered air
f) These rooms will need to be airconditioned. By this means clean
air is admitted under slightly positive pressure which prevents the
entry of unfiltored air through any appertures ,or~when doors are opened.
Z;.) Autoclave/still Room Next to the Filling Room should be a room
where the autoclave is installed and also the stills because it is a
help to have all the heat generating equipment in one placo. The
distillate can usually be piped through the wall and if possible the
waste hot water can be piped to the Wash-up Room to be used in the
bottle washing work. The Autoclavu/still Room can be of normal hospital
hospital construction with the addition of efficient extractor fans .
47/1,(.~irs- - ‘
r,';ALT';’1 CE<-L
•••OnE - Quo qqi
-1
j
4
?
j
2
Fart I
The Construction Standards of the Department (contd)
J-j Quality Control Section
following tests:
Intravenous Fluids are subjected to the
Chemical, analysis
■>) Bacteriological Tests
o)' Pyrogen Tests
In each case a separate room will be required of normal hospital
building standards- For the pyrogen testing the room where the test is
carried out will need to be airconditib’ -d or have facilities for
keeping the rabbits for 18 hours befc"
’.est is carried out- In
addition an animal house will be nee!
6) Store Room A store will be esse.
for keeping a supply of
bottles and other stock required in the preparation of the fluids and
also one for the storage of the finished product with facilities for
k.-oping batches separate until the result of the tests are known until
which time issues cannot be made.
Part II
Equipment
The choice of equipment is not an easy matter with so many companys
manufacturing Pharmaceutical equipment. Quality should be the first
consideration. Buying cheap equipment frequently leads to problems
with servicing and as the makers insist on payment at the time of
delivery if they default in any way it is almost impossible to get
redress.
1
The following items are required-,
1) Stills There are two typos available in India, namely, the
Barmstead type and the Kilburn type. The forner is to be preferred
although it is more expensive. The main pro!lem with the Kilburn type
is that any leaking of raw water is very likely to enter the distillate
and leaking does appear to be a problem.
The principle ot the still is simple and that is -that there is a boiling
chamber from which the steam is led to a condenser cooled with cold
water which having absorbed some of the heat from the condenser
passes into the boiling chamber. Genera11 ■ ’for every litre of
distillate there- is 1 litres of coolir
r wasted.
A reliable company for this equipmen
Steel. There is a choice
of capacities but one producing not 1 . that 10 litres per hour is
recommended. It is an advantage to have two stills so that if ono is
out of order the other will allow soma production to continue.
2) Collecting Vessels For the collecting of distilled water stainless
steel vessels should be used. The size will depend on the amount of
intravenous fluid to be prepared. The vessels should be straight sided
to enable thorough cleaning to be carried out. When purchasing care
should be taken to ensure that any welded joints are smooth and free
from pitting which will permit the collection of dirt.- ■'
- The storage of distilled water for more than 3 to 4 hours is not
recommended but this can be extended to about 7 hours by the use of a
heated tank. Much longer storage is possible in tanks vri-th Ultra
violet lamps but this is not practicable for most hospitals.
Mixing can usually be undertaken in one of the collecting vessels
especially where small batches are prepared.
3) Balance^ One balance for weighing up to say, 2 Kgs will be required
for the weighing of dextrose and other bulk chemicals and another
two pan chemical balance for the weighing of small quantities of salts
especially where electrolyte solutions are prepared.
zvorys prepare satisfactory coarse balances but care should be taken
to specify stainless steel pans as the plated type may soon become spoiled.
Part II
3qyj.pm-.eni (conic )
'..inqr Wquiprnent 3tc.i-J.css
41 apatui-.; eh-.j.d "ba provided and glass
mea-ures. The measures should be of goor-c-.uaTit;- a?'d ■ those from
Corning Glass Ltd are io be recommence: .l-st'-ibuteci. by Borosil). If
possible obtain class A measurewhich ha 3 c oe .-b? ficate of accuracy.
Never use. plastic measures. Glass stirring r. ds will also be needed.
zl) Pilfers Generally sintered glass filters are used although
sintered steel are available from ove ’he type preferred is
the pipeline type which enables fi?
v'ect into the final
containers. The filter required s’
apable of removing
particles visible io the eye from
tion but not bacteria as
this type filter very slowly. The g.
required is Porosity 3
(sometimes called PG 3)« Bacterial filter- are porosity 5 OT 5 on 3.
After each use the filters must be thoroughly rinsed with distilled
water. Occasionally, say once a week, the filter should be washed
chemically and the manufacturers instructions should be followed.
In the absence of instructions the following may be used;
a)
Allow to drip through under gravity concentrated
sulphuric acid with 1% sodium nitrite at about 80°C.
b)
Allow to drip through under gravity a chromic acid
solution prepared as follows?
Potassium Bichromate
Acid Sulphuric Concentrat'd
Distilled Water to
80 grammes
120 mis
1000 mis
I-’ethod a) is much to be preferred because with thorough rinsing
all traces of the chemical are removed. C’ comic acid is very toxic
and this solution should be k<»pt for very dirty or contaminated
filters. Large volumes c-’ distilled water will be required for
rinsing.
Sintered glass filters are available fre5) Vacuum Pump The system generally
pressure and for this a. vacuum pump i;
manufactured by Pharma-Lftb--ladiirda.
Corning Glass (Borosil)
;cd is filtering under negative
ceded. Suitable pumps are
ay.
_. ... ^
6) Autoclave It is much to be ptor the Pharmacy to have
its own autoclave. A shared autc-x
jents problems- for
supervision in operation rs. well
. .. semes .it vfl'll be available.
It is essential that the autocl avu car. gir o a .terepevature of 121.5 0
(15 lbs/sq in press :re)• and a thermometer and pressure gague must be
fitted. If possible- a record of the mrdntenance of temperature
throughout the cycle should be attached. The capacity of the autoclave
will relate to the production of the fluids but very small ones
should not bo purchased.
Satisfactory autoclaves are produced by NatSteel.
7) Clarity Checking Light All fluids must'be checked after autoclaving
and this can be done with a light source in a box with a back panel
of white (to shot; up black particles) and black (to show up white
particles). This box. can be constructed locally.
5) Capping Machine Generally screw caps will bo used on the bottles
and these must be covered with a paper cap prepared by hand or a
machine applied aluminium foil cap. The latter is to be preferred as
this gives a professional finish. This cap indicates that a bottle
has not been opened when it is in place thus providing a useful
safeguard.
4
>a^t iii
Staff Arrangements
The following staff will he needed;
1) Pharmacists The work of the department must be under the direct
supervision, of a registered Pharmacists and should posess either the
Degree or Diploma in Pharmacy. Some states insist that a degree
Pharmacist should control this work. However’ the guiding principle
must be competence and experience. The number of Pharmacists needed
will depend on the work load.
2) Aides It will be a great time saver if an aide is trained to do
i-.uch work as washing bottles, preparing rubber bungs and caps and
Iceping the department tidy. It must be remembered that his work is
important and that he should have his responsibility explained to
If the work of pyrogen testing is undertaken another aide will be
required to look after the rabbit house.
lling rooms thestaff must
ile dress as follows;
3) Dress When working in the mixing ar
cover their ow.i clothing with provides
a)
b)
c)
d)
Cap covering the hair
Mask covering the mouth and nose
A gown which covers the outdoor clothing.
If possible shoes should be provided and failing this the outdoor
footwear should be removed.
This dress should not be worn outside the sterile work area. This
clothing is similar to that worn inside the operating theatre and
the Pharnacists should dress similarly to avoid contamination of the
fluids which could have serious results.
<) Personal Health and Hygene This must be of the highest order.
Staff suffereing from infections such as colds and coughs must not
enter the area.
Part IV
Theory and Practice of Intravenous Fluid Preparation
1) General Cleanliness The whole section must be kept very clean and
thera should be not accumulation of rubbish or r<. -.ely used items. The
Pharmacist in charge must carefully supervise cleaning procedures.
which should be written down.
Cleaning staff who work in the wards should not be admitted to the
mixing and filling rooms. These rooms should be cleaned with an
antiseptic solution and the walls and benches with alcohol 'fCP/o if this
is available.
Hater ‘for'In,lection Quality ~This is fr'
in a still which can produce pyrogen f
immediately.
'
distilled water prepared
.iter and then autoclaved
When water boils there is a tuburlent action on its surface which
throws up droplets of raw water into the steam and are there'fore
carried over into the condenser and become part of the distillate.
To. prevent this carryover (technically entrainment) of water droplets
baffles are introduced which allow only steam to enter the condenser.
.■’aw water may contain bacteria and therefore almost certainly pyrogens.
P’-vogens are produced chiefly ba Gram-negative bacteria and are
lipidpolysaccharides the lipid part being the pyrogenic agent the
action of which is enhanced by the polysaccharide. They have a. .
molecular weight of about 1 million and are about the size of a small
virus. It has been shown that even a small amount of pyrogen is injected
a reaction results.
1
Dart 17 Theory and Practice of Intravenous Fluid, Preparation (contd)
_2) Water for Injection Quality (contd)
~lic presence of pyrogens is most serious in large volume injections
because
a; a large volume injection will contain a correspondingly large
r.rioont of pyrogen
b) Large volume injections are normally given intravenously and the
pyrogens will act quickly.
> Patients receiving these injections are often seriously ill.
The pyrogen reaction is rather like a chill and the most serious symptom
is a rise in body temperature which may 1 'patal for a patiient
already feverish.
The preparation of pyrogen free solui
nature of the pyrogens which are?
b)
c)
,s complicated by the
Tot Los .Toyed by the temperature at which solutions are autoclaved.
Water soluble and cannot therefore be removed by filtration
They are unaffected by the common bactericides
However they are non volatile and so the method of distilling water
described eliminates them.
The Pharmacopoeias direct that the distilled water collected must be
sterilised immediately. This is because on storage the water will.
become contaminated by bacteria leading to the formation of pyrogens.
This instruction is generally taken to mean that distilled water may
be kept for about 3 hours. To keep contamination to a minimum the
vessel containing the water should be carefully covered. Some
authorities state that distilled water may be kept about 6 to 8 hours
in a vessel hop; at 70 -• 80°C but this should be avoided if possible.
Water must never be stored overnight.
Distilled -,-atcr muat be free from dissolved salts and a well constructed
still should .ensure that this is so.
3)-Preparation..of Intravenous Fluid Bottles This is a very important
job usually given to an ride. Poor work in this connection can result
in the loss of a batch of fluids.
7:11 bottles, both new and reused ones, must be examined carefully for
cracks and other flaws and those so damaged must be rojected. The
bottles arc then put to soak in a deter'
such as Iteol or Teepol.
Soap must not be used as this leaves on the glass which may be
detatched during the autoclaving. Pre
.ons such as Vim and Surf
should not be used as these tend to su-esch the glass.
.After soaking the bottles must be scrubbed either mechanically or by
hand using a good quality brush which must be in good condition. The
detergent solution is then washed away with plenty of tap water, allowed
to drain for a short time and then rinse.j with distilled water and
drained. The final rinsing before filling must be with freshly
distilled water.
In some hospitals the bottles are dried in a hot air oven after rinsing
with distilled water as this reduces the possibility of pyrogens
forming. In either case the bottles should be used as soon as possible
after the cle aning procedure.
4) Weighings and Measurings Those must be done with great care on a
balance of suitable capacity and liquids measured in glass measures of
suitable capacity. All weighings and measurings must be checked by
another pharmacist and in doing so he must check not only the weights
but also the source of the material on the balance pan. Even very
experienced pharmacists have been known to make mistakes and in this
workr such mistakes are not only waateful but also may bo fatal to
patients.
6
Part IV
Theory and. Practice of Ir.tv
. buid, Pro car at ion (oontd)
5) Filtering Before filtering the •?.
al?, .tubing and filter
head must be rinsed through with fre53.1 istilled water. The first 100
to 200 mis of the filtrate of the solution should be rejected, because
this tri.ll have been diluted by water remaining in the filter from the
rinsing. After the filtering of the batch is finished the filter,
tubing, etc., must be rinsed again with fresh distilled ’water.
u) Closures, for the Intyayenous fluid Bottles Rubber closuers should
be obtained from reliable manufacturers because poor quality rubber
can impart chemical impurities to the solution on autoclaving.
The liners will need cleaning before use and the following procedure
is suggested;
Boil for 15 minutes in a solution of 2% Sodium carbonateand 0.1%
detergent.
b) Rinse thoroughly
c) Boil in fresh distilled water for 15 minutes
d,’ Rinse in fresh distilled water.
a)
The liners are then ready for use. Only enough for immediate use should
be prepared.
Opinions about this cleaning procedure vary but the less violent the
cleaning procedure the better because this in itself will tend to
release further chemicals from the rubber.
The aluminium caps should be washed thoroughly and boiled in I.
distilled water and finally rinsed in fre-h distilled water.
7) Sterilisation As soon as the bott
. filled they should be
packed in the autoclave for sterilise
Do not overfill the autoclave
as this tends to hinder the penetration of he load by the steam.
Delaying of sterilisation will greatly increase the danger of pyrogen
reactions and ouch delays must not be allowed to occur.
On closing the autoclave door steam is allowod to enter the chamber
and as soon as the temperature reaches 121.5 C the cycle timing is
begun. This temperature must be. maintained for 30 minutes when
sterilising 5^0 ml bottles.
At the end of the cyclo the steam is turned off and the chamber pressure
allowed to reach zero. Thon the door can be opened cautiously a few
centimetres to allow the bottles to start cooling. The door can then
be opened fully after about 20 minutes. This procedure helps to
rodveue the charing of dextrose solutions. The bottles must not be
removed from the autoclave for at-wt an hour otherwise bottles may
explode duo to sudden temperature clange’.: and such explosions are very
dangerous as '.glass fragments and nearly boiling solution are blown
across the room.
\
^/Examination. of botules for Clarity Wren the bottles are cool they
should be examined using the light box anfl. any with particulate matter
present should be rejected.
S') Capping and Labelling Alumunium foil or paper caps should be applied
■•Ihofe foil caps are used it is best to have one colour for all
solutions. Different colours tend to encourage staff to identify bottles
by colour rather than by reading the label.
Printed labels should be attached and +
details
?.) Volume of the Injection
o, 'Tamo of Injection and source
of formula, e.g. BP
c) Strength where applicable
d) llilliequivalents where
applicable
should bear the following
e) Sterility statement
£) Batch number ot date
g) Name of Hospital
h) Clarity warning
Part V The_Quality £ontr ol. Te.sting^cf..Intravenous Flu- da
1) Clarity testing This is referred, to in Part IV 8). above.
2) Chemi.-'.- 1 Analysis After- the sterilising of the solution (and.
bef.*L<? xf possible J 'the contents, of the solution should be analysed
bo- .’ qualitatively and quantitatively and other tests carriedn out
aso.rding to the Pharmacopoeia! monographs.
3'1 Bacteriological Testing The absence of aerobic and anaerobic
basierxa must be established by inijod'cing samples into suitable
media and controls should be set up. Tnese tests require 7 days
incubation. befora the results are known. Similar tests may be done
for fungi.
Pvrogor T-stir.g This test is designed to establish the absence
of pyrogens xn the solution. Unfortunaxely there is no reliable
chemical test so a tv st based on rabbits is used. The principle of
the test is to observe if there is any temperature rise on giving
tie fluid intravenously such solutions being rejected.
The details of the test is set out in the Pharmacopoeia. The test
demands that three rabbits each weighing not less than IKg are used.
They must not have been used for a pyrogen test in the previous
three days and within the last 3 weeks if a pyror-en- response was
observed in a test. At least one day before the test they are
checked with pyrogen free sodium chloride injection and if the body
temperature rises significantly that animal should not be .used.
For the test the animals are kept in a room which is within 3°C of
their living quarters or failing this th.y must be kept in the
test room for 18 hours. Pood ic withheld from the rabbits overnight
and water during the vest. The materiel under test ■i-i_i*-.jooted into
the ea. vi'-u and the temperature-s--record?! at 30 minute in terva.1 5
for 3 hours. The-temperature is determined by rectal thermometer.
The interpretation of the results is that the summed response of the
■group of three rabbits does not exceed that of the first column in
the table the solution passes the test. If this lies between the two
figures then the test is repeated on a further group of three rabbits
if necessary up to a total of four groups being used. If at any stage
the summed response exceeds the figure in the third column of the
table- the solution fails the test.
Tic results of all the above tests should be 'iiown before the
.intravenous fluid is released for use.
These tests are expensive to undertake, especially the pyrogen test,
e
it may be more economical to send the test material to a
laboratory specialising in this service.
Table for Pyrogen Test Results
Number of
Rabbits
3
6
9
12
Material Passes if
summed response
does not exceed
1.15
2.80°
4.45°
6.60°
Material fails if
summed response
exceeds
2.65 o
o
4.30
o
5.95 o
6.60
A.Cranmer, MPS
Consultant Pharmacist.
Group Discussion on Prescribing Policy - Groups 81 & DI
Questions to be pondered about
1.
Can a Hospital devise a formulary of good quality,
cost medicines?
lou
Can this be common for all Voluntary Hospitals?
2.
How can prescribers ' compliance be ensured or is freedom
of prescribing likely to make this impossible?
Can we ensure Health Workers' compliance with their
formulary, (medicine list)?
Will doctors also prescribe from this list?
Is it possible to prevent prescriptions to medical shops
being given?
3.
Where simple lou cost drugs will not be sufficient, how do i_
we subsidise to all or those who need help most?
-•
Should all patients contribute to the cost of medicines?
—I f-so, how?
4.
Will a Pharmacy Committee,
including Doctors,
Administrators
and Pharmacists help in implementing cost control or
quality control policy? (in most Hospitals medicines are
the second largest item of expenditure1.)
5.
Have we asked our pharmacists to research costs?
does he know how to do so?
Have we provided tools for the job?
If so,
If so,
what tools?
6.
Are bulk drugs purchases possible on a group of Hospitals-base?
What methods can we devise for obtaining lou cost drugs
either for one or many Hospitals?
7.
Do ue consider proper stock control, record keeping and
auditing of medicines, purchase and distribution:
a)
unnecessary expenditure
b) essential?
What are our reasons for our attitudes?
8.
In many Hospitals the Pharmacy is an important income
producing section.
Will a suitch to lou cost drugs raise
cost or make it instead a burden on the Institution?
9,
Is the production of medicines in the Pharmacy :
a)
too time consuming
b)
too costly in terms of personnel or equipment
c)
uneconomic?
(Broadly thinking of tuo types: non sterile prescriptions
and sterile prescriptions)
Hou would you advise your
Hospital Management?
r;roic i. ■■■~.:ooi no;: oy ioi/.
PH.tRIiACY WORKSHOP PAPJtR
P.'iZRKACY DESICi: AMD OROAi.'ISATIOIT
The number of people seeking medical help will "be large in many
Christian Hospitals. From the patients attending outpatient department
admissions will be made and bookings taken for confinements and
surgery.
From the O.P.D. the patient, after seeing the doctor, will proceed
to the Laboratory, Pharmacy, dressing room, etc., for further health
care. Therefore the siting of these service departments is important.
In the smaller hospitals there will be one Pharmacy only and this
should be sited centrally and if possible at •_he junction of the
Outpatient and Inpatient departments. In larger institutions there
will probably be an inpatient Pharmacy and one for out patients sited
in that department.
Make sure that it is easy for patients to find the Pharmacy. Direction
boards should be written in the Regional Language and English and in
Hindi where this’is appropriate^. Remember not all patients can read
so a colour and a symbol for the Pharmacy is helpful.
Design of the Pharmacy
In a medium sized hospital the department may be as followss
a)
b)
c)
d)
e)
Dispensing Section
Sterile Products manufacture which will be principally I.V. fluids.
Non sterile products manufacture -- mixtures, ointments, etc..
Store
Office for the Chief Pharmacist
a) Diepensing Section If possible make the window arrangements for
patients to collect their medicines so that at least two may bo
dispensed for at one time. In some areas it is an advantage to have
one window for men and one for women. An arrangement whereby the
nursing staff can obtain medicines quickly is appreciated by them.
Try to make the queue system work by having barriers so that only
one patient at a time can get to a particular window. It is very
distracting to have patients waving prescriptions at you whilst
dispensing.
Each Pharmacist should have reasonable working space. The benches
must be high enough to work at without bending over ana. stools of the
correct height should be provided so that a Pharmacist may sit and
work. The bench tops should be of polished stone or Formica bvt
remember chemicals such as silver nitrate and. acriflavine stain
these materials and so any spliiage must be wiped up immediately.
Stocks of medicines for dispensing should be closes at hand. Much
walking is time consuming and tiring. Tabl?ts of much demanded
tablets can be stored on either side of the dispensing window in
small compartments.
b) Sterilu Products This section requires a washing up room for the
bottle cleaning, a mixing and filling room and an autoclave room.
In addition facilities for assay and'pyrogen tests on the final
product. (Further details are given in the Pharmacy Workshop Paper
'Preparation of Intravenous Fluids')
c) non-storilo Products Ono room till probably be sufficient. It
must be fitted with easy clean benches, water supply and good lighting
A high ssikndard of cleanliness is essential because it has been
■established that many pathogenic organisms can be transmitted through
these preparations.
r
HEALTH CELL
Lcsif-i of the Pharmacy (contd)
&) ,§i£E2 This must be of a size adequate for the work load, of tic
Pharmacy. Adjustable steel shelving is the best but is expensive.
Do not have the shelves too wide apart as this can waste much space.
The store should be cool even in the hottest weather. A refrigerator
must oe available for heat sensitive medicines such as vaccines,
oxytocin and insulin.
Offioafor -cho Chief Pharmacist An office should be available
for the Chief Pharmacist and here the various clerical work and
stock records can be maintained. Reference books and journals should
be- available, for the staff and could be kept in the Office.
Day to Day work in the Pharmacy
Try to organise the work lead so that it is spread evenly throughout
the day. Tn many hospitals the ward baskets come to the Pharmacy
when it opens and this work is cleared before the ward and C.P.D.
prescriptions are likely to be receivnl.
flake sure that all the Pharmacists know what is required of them in
their allocated duty and a written job description often helps to
prevent misunderstandings. All. Pharmacists, especially in smaller
hospitals should undertake all the types of work so that during
periods of sickness or annual leave the work will not be seriously
interrupted. All duty ciiangoo nbonia ’h-*.
in wr»i+ir5 ■Hw.vip.
the departmental notice board. The Pharmacist who is to attend, to
calls during the hours when the Pharmacy is closed should not leave
the hospital compound and should inform the Doctor on call and the
duty sister of his whereabouts if this is different from his quarter s.
Weekend and Sunday duties will also have to be. arranged and some
compensatory off duty time should be allowed.
Training Programmes Where the Pharntcy is well developed it should
be possible for the senior members of the staff to give lectures to
the more recently qualified Pharmacists. Juniors should, also be
encouraged to prepare papers and to listen to the constructive
criticism of their seniors.
The postgraduate training for the Diploma in Pharmacy is 750 hours
practical training. Well developed Pharmacy facilities are urgently
needed for this purpose and the Drugs Controller for the State
can give the necessary information on gaining recognition.
Dispensing of Medicines When taking the proscription from the patient
make sure that it is written by one of the Hospital doctors. Read it
through and if there should be any error do not show the patient by
your expression or speech that there is anything wrong but chock
quietly with the pfusoriber. Do not do anything which might destroy
the confidence of the patient.
Dispensing should bo carried out as quickly as possible but without
haste or omission of any chocking, packing and laoelling. Packing
of medicines should be carried out in a professional manner. Nover,
never pack tablets in pages torn from old journals or newspapers,
and never pack ointments in papers. Plastic bags and containers are
available quite cheaply and proper pricing of medicines will cover
the cost of these materials. It is bettor not to use medicine
bottles brought by patients which may wall be d'.rty and thus
contaminate clean medicines. Provide oottlos icr the patients for
which a small charge may bo made.
Labelling should bo clear and nc at. It :.s preferable to use printed
labels in suitable languages. Taka time to explain the directions to
the natient. It has boon definitely established that patients do not
remember what the doctor lias told them and this is an important task
for the Pharmacist. Never, never stick one label over another. This
is potentially a very dangerous h®it.
Propackin,? of medicines Much time can be saved by the prepacking of
medicines. This may be done in commonly used sizes for mixtures,
ointments and tablets. faoh packet should be- labelled with the name
of the contents and on dispensing a label must be attached giving the
patient's name and directions.
Staff Matters
Provision should be made for hand washing in the Pharmacy and if at
all possible with running water. It is surprising how many pharmacies
are deficient in this respect.
Uniforms should be worn by all. They will normally be provided by
the Hospital or an allowance made towards their provision. Uniforms
help to identify staff, protect personal, clothing, and protect the
work being done from contamination bound to be brought in from
outside’
Remember when tne patient leaves the Pharmacy, which is usually the
last department he visits, he takes away two things with him his medicines neatly packed and labelled and his impression of the
Pharmacist which should be one of a helpful,cheerful person.
A.Cranmer, KPS
Consultant Pharmacist’
Christian Medical Association
Ct
CHRISTIAN MEDICAL ASSOCIATION OF INDIA
.
GENERAL ADMINISTRATION OF THE PHARMACY
o
- o--/
WORKSHOP-PAPER
“PHARMACY
-- —------//£
Control of the Pharmacy Service.
All hospital departments come under the control of the Medical
Superintendent but in all but the smallest hospitals he will delegate
his authority to a head of deparitaent lor day to day control of its
working.
General policy will be laid down for the administration of the
Pharmacy but unfortunately this is rarely done in writing.
Pharmacy Sub-committee This Sub-committee will give guidance in thd
running of the Pharmacy and should have the following members;
a) Medical Superintendent (Chairman)
b) Medical Specialist (Vice chairman)
c) Chief Pharmacist (Secretary)
d) Administrative Officer
•■?•) Another Specialist urobably a pediatrician
Ether members o.’ the Hospital staff can be called to meetings where
matters concerning them are to be discussed.
The functions of the sub-committee should be set out in broad terms
as followsa) To help in the general administration of the Pharmacy
b) To publish a formulary
c) To set out general purchasing policy
d) To examine requests for medicines to be added to the formulary
e) Disciplinary matters such as professional misconduct. This will
not interfere with the general discipline for dealing with serious
misconduct which is in the hands of the Administration.
f) To deal with complaints and s.-ggesticns about the Pharmacy Service.
Meetings should be held about once a month and if possible the interval
between meetings should be regular. Do not make the Subcommittee too
large or it will be difficult to choose a time when most members can
be present.
Pharmacy Budget In smaller Hospitals the Pharmacy will not have its
own budget but medicines will appear a. income and expenditure item
with other hospital expenditure and income. Larger Hospitals will
sot dotn the expenditure as follows:
a) Staff salaries
b) Electricity ad water charges
c) Depreciation on equinment
d) Depreciation on buildings
e) Purchase of new equipment
f) Purchase of medicines
3) Write off of spoiled medicines
. .--.net this will be set income
grants.
erived from medicines plus any special
.hen arriving at the amount to be budgeted for medicines the following
must bo remembered;
r.) The average expenditure over the last three yea^s is calculated
e) The number of inpatient days and outpatients over the last throe
years is noted. The trend of increase or decrease is calculated as a
percentage and this taken as the incr?ase/decroaso to the figure
arrived at from a).
c 1 iLTtf anticipated increase in the prices of medicines and whether
the trend is for the doctors to pre serf
more expensive items.
£
Pharmacy Bud.gut (conid.)
d) The budgeted receipts for medicines and Pharmacy Services will
reflect the sank percentage above expenditure as in previous years.
.''ho Pharmacy Sub-committee will be able to discuss this and offer
suggestions for modification to the Kanagement.
Some Hospitals donot stock medicines cccauso of the very considerable
outlay needed. However failing to keep adequate stocks had the
following adverse effects:
a) Christian Hospitals are generally in need of all the income which
can be generated and failure to keep stock puts money into the pockets
of local business mon.
b; The Hospital Pharmacy staff and equipment are not being put to
full use. The waste of a Pharmacist's skills is a loss to the Hospital.
c; If patients bills are carefully prepared and presented on time
money is collected quickly and company bills can be paid by the due
rilling of Patients
'."he billing of inpatients for medicines at the time of dispensing
has been discussed in the Pharmacy Workshop Paper 1 Distribution of
icdicincs io Patient Areas'. How ver a few additional procedures have
to be considered.
Private, Patients Patients who are paying high ward rent will probably
not want ~o pay for their medici'es at the time of dispensing. One of
the fclloiing will avoid this wh-lst making sure that an accurate
record is kept:
a) A cost sheet is added to the Patients chart. This is sent to the
Pharmacy with the normal patient's special medicine requisition and
when th; Pharmacist prices this he also adds the details to the cost
sheet, It the end of the period, probably one week, the office will
total tie value of medicines supplied and add the amount to the bill,
b) Thu proscription is written in duplicate one copy for the Pharmacy
and one whan priced for the office who will keep these to add to the
p-'.t’.orcs bill.
ilethx a) is simple and savos a good deal of office time and takes
very little Pharmacy time.
8j>\oial_Fvnd I atients These patnients treated free from some of the
Hosplt?’ Special Funds such as the Leprosy and Village Community Health
Funds.
Li.-r.oy Medicines When medicines arc used from the Emergency Tray
:f
saving medicines kept on the wards they are replaced cither
in. nurse ‘.raking out an indent form in the usual way, asking the
t:"...-t to pay and then replacing the item on the Tray. In the case
c nth c.r discharge or death this cost is added to the final bill
?c ’ ' ■ nurse must show the Pharmacist that the medicines have been
c_d fir L...fo‘. . they can be replaced.
v. ■ --.us Drupe and Ward Stock ModicinuS
c? in one of the following ways:
Stock medicines can bo paid
daily Charge. Throughout the wards over a period of at least six
ninths the value of medicines issued as stock is calculated at the
ojtient charge rate. From the record office the total number of
ir.patiunt days (not inpatients) is obtained, which is divided into the
vtlue of medicines issued giving the amount spent per patient per day.
Ci discharge the patient is charged the number od days of his stay
niltidied by i? ■ daily charge. This method is quick and easy to
administer and allows a collection to be made against expensive
antiseptics and disinfectants often overlooked in charging patients.
3
.-yangerous Drugs and. Ward Stock Medicines (oontd)
c) I.edicines Listed from Chart- This method requires the sister to .
prepare a list of ward stock medicines given to the patient at the time
of discharge- This is then priced by the office and added to the bill.
This method suffers from two disadvantages, firstly the making of
lists is often inaccurate and secondly it takes a good deal of nursing
and office time.
■ i,;ht_ .fmergencv Cupboard Medicines. Payment for these is either raised
by the Pharmacist reporting to the ward sister the medicines used and
an indent being raised for the replacement in the usual way or the
amounts used, which will be fairly small, are added to the patients
final bill.
Cutpatients In a few cases outpatients will not pay for their medicines
at the time of dispensing. These will have to be billed and this can be
•done by the Pharmacy, h copy of a till book page is attached. This
bill must be sent to the Office for the official account to be made.
This book can also be used for staff purchases if the Pharmacy Offers
such items as baby foods and tonics. These amounts will normally be
collected from the salaries so the bills must reach the office well
before pay day.
O\tpatients_ Free Medicines When medicines are supplied free the Pharmacy
account must be credited and this can be done by one of the following
methods;
a) Charity receipt book. This is an ordinary receipt book for which
no cash is taken but the amount is credited daily to the Pharmacy
b) Pharmacy keeps a record bock in which all free medicines are listed
and valued, and the amount added to the Pharmacy account at the end of
a suitable period.
Refunds On occasions patients will be advised to stop taking medicines
already prescribed and purchased from the hospital. In this case
-Ithough it is not obligatory it is a help if the Pharmacy takes the
.■■.•Heines again and arranges for a cash refund. This is done as followss
The patient takes the medicines tc the Pharmacy together with his
-.ash receipt and the Pharmacist completes a form for the Office stating
the medicines r -ceived and the value ail receipt number.
. i The patient goes to the office and s'.gns for the refund.
■’ The Pharmacist replaces the medicines in stock making the necessary
:::: series in the records.
It is normal practice not to accept parts o? bottles of liquid or loose
Gablets end in any case the value of these. will probably be low.
Pricing of Medicines
.-di.oines Purchased and Dispensed Unchanged Th..s is a very important
,-.otter because it involves the contribution the Pharmacy can make to
th-: income of the institution and also some le.gat obligations. For the
oast few years the Government authorities have sei the maximum retail
urioe ’or the medicines of all companies which is printed on the
container together with the statement :Local Taxes Lxtra’. These taxes
oje Seles Tax end octroi. The method o:‘ calculating the price- is given
in the following example;
Rs 12.00
Piaximum Retail Price
96
Sales Tax at Ofc
Octroi at 2%
Price to patient
12.96
26
Rs 13.22
.. or oon’xnience- the. price is normally rounded to the nearest flye paise
ir. this case J si3.20.
4
.is Pirctiascd and. dispensed Unchanged, (contd)
i'his pricing -.ri.ll allow a margin of income over expenditure of about
12;7 , and from this departmental costs have to be covered. The icome
may be increased where special contracts are arranged. It is
•^urmissable to charge lower prices when- desired.
1,'cn Sterile Preparations These are items prepared m the Pharmacy and
include such items as mixtures, ointments and lotions. The price of
those is calculated in much the same way as that for intravenous fluids
out below. At least 12/% above cost should be charged and reasonably
■-.ore because professional skills are involved.
St'. rile Pre pay at i ons The biggest part of this will. be intravenous
fluids and the following example will give an idea of how to calculate
cost and the. amount to be charged.
Salaries (estimated at 4/5 Bpharm
Pharmacist and /■ aide)
742.00
Chemicals (based on 5% Dextrose
solution = 25.35 Kg <? Rsl4/- x Kg)
390.00
Labels, celophane, rubber bands
at 2 p per bottlo
23.00
Rubber liners
190.00
Blectricity
1000.00
Water
10.00
Depreciation on equipment (10% per annum)
100,00
Depreciation on buildings (2/% per annum)
44.00
Bottles at Rs4/~ each (used average of
six times)
759.00
+ 10% rejects
3268.00
327.00
Rs
3595.00
This is the total cost for a monthly average production of
1154 bottles.
Bach bottle costs to produce
Rs ?-.12
Cuggostd mice to the patients
Rs 6.50 per bottle
The suggested price may seem high compared with. the cost but it must
to remembered that at least 12g% is added and also that quite a number
of bottles will probably be given free to patients. Also in the near
future it will probably be obligatory to have the bottles assayed and
pyrogen tests carried out. The retail mice of manufacturers’ bottles
is not less than Rs?.50 at present.
A.Orarmor, MPS,
Consultant Pharmacist
Christian Medical Association
CHRISTI A?1 MEDICAL AOSOUI‘•TIOI: Cl-'. INDIA
p,-.45fAC-'' v? y.cs.ur ?.<•?&•:
; epicures - PRQCUBEri; t a: id sir ok control
Purchase of' iiedj cines
Sources The cheapest sources are not always the best. The major Indian
a_;:l International companies have quality control and research
laboratories to ensure that th. products are of a high standard. Their
prices may oe a little higher than some but there is the assurance of
good quality.
v?ij>ei’ia IOV F'C CC-iicto— LLfL'llf-S©
cmPO »
a,- Good quality. This can be decided by
i") Quality Control tests carried out in the Hospital but these .
will not be possible for roost institutions
The
ii)
Pharmacists experience in selecting companies
iii)
By listening to the comments made by your doctors
iv)
General reading and comments by other Pharmacists
b) Continuity of Supply This is not easy to ensure but the Pharmacist’s
general experience will be a help*
c)
Company Dispatching Orders QuicldLy
d)
Company giving maximum discount
obtaining discounts
There are several methods of
i> Bulk orders - see below
ii) By negotiation of terms. Sometimes a local distributor will forgo
some of his profit to gain business or he may agree t?- pay some of
the taxes such as Octroi. It is important to ensure that the correct
com any rates are charged.
iii; Seeking quotations from company offices. This may be done
through a representative. As competition gro-ws with more companies
making the same medicines the larger firms can often he persuaded to
give some special discount.
Hsthods of Purchasing Bearing in mind what has been said above the
following arc possible;
a) From the Manufacturer. This ensures the correct rate being
charged as well as availability of stock and is the best method for
all large purchases. Do not change companies frequently but rather
■try to build a good business relationship with those you chouse.
Many of them are sympathetic to the needs of Christian Hospitals.
b) Bulk Purchasing This will normally be from the manufacturer who
is often ready to give discount for a guaranteed purchase- of an item
during a year. Usually it x-ri.ll be agreed that the goods can be
delivered an paid for in anything up to 12 deliveries a year.
It must be remembered that when such a contract is entered in to
the Hospital must take the agreed quantities to get the concession
T 3, uG e
When taking contracts be careful about the amount of money required
for each payment. Remember that money tied up in stock is not earning
any return. The discount given must at least equal the interest which
could be earned by placing the money in the bank.
2
Placing of* Orders
This must he the job of the Pharmacist who will
know the company details outlined above, /ill Pharmacists must make
sure that they are competent in this respect.
The Indian Pharmaceutical Guide is a help in selection of companies
out it is only a list and is not necessarily a guide to -uality.
Vihesi orders are writton the Medical Superintendentor Chief Pharmacist
may sign them. In many hospitals it is the former as he likes to know
the amount of bills likely to be received in the near future.
It is an advantage to have a printed order book rather that to have to
write letters. It should be in duplicate so that the Pharmacist can
keep the carbon copy. (More copies can be made if other Hospital
departments require them) On the order form the following details
should appear:
1)
2)
3)
4)
5)
6)
7)
8)
Hospital name and address including the pin code
The Railway Station
Order number
Conditions under which the order is placed
Quotation number
Space for name and address of company
Items, size and quantity required
Signature
It is not wise to use company order forms because these are of
varying size, require filing, and have no Hospital order number.
Company Representatives Many companies employ representatives to
detail their products to doctors and pharmacists. Representatives are
trained with impressive sales talk and great care must be taken not
to over order the items they are pressing you to purchase. Do not be
taken in by, 'If you purchase this I will see that the doctors
prescribe it'. It is best to make it a rule not to place orders with
representatives bu rather send them direct to the company which gives
you time to think. Similarly doctors should not so place orders. 411
orders must go through the Pharmacy order book.
Representatives can take a lot of your time and vary rarely do they
have a new, important medicine to tell you about. It will help you to
keep control of the situation if you see them at certain days and times
in. the week. It is fairly easy to end an interview by standing up and
saying, 'Thank you for coining'.
Special Orders These arc orders for Narcotic Drugs and for Spirit.
Make sure that you know the procedure for obtaining the transport
passes and for the renewal of the licences in your State. Do not
forget to start the renewal in plenty of time and at least 2 months
before expiry.
Payment of Dills This is not norm?illy the responsibility of the
Pharmacist. However, watch when payments fall due and if necessary ask
the office to pay on the due date. The Hospital's relationship with
the companies is greatly influenced by this matter and a good name
once lost is hard to recover.
Part II
Receipt of Good:
Receipt, of Documents The company will usually send the documents
that is the carrier's way bill and invoice by one of the following
methods?
a) Through the Bank. The documents are sent to the Bank and the
Hospital's representative has to go to the bank and pay the invoice
amount plus a fee for their release. They are then taken to the
carrier's godown where the goods can be collected. Where there is
an octroi charge the octroi office rekease the good only after
Payment of this tax.-
b) Direct. In this case the Company sends the Way Bill and invoice
direct to the Hospital whose representative ban go direct to the
carrier's or octroi office as in a)
Method b is obviously to the advantage of the Hospital because the
goods are received on credit and Ijj to 30 days is allowed for
payment. Method a is used by a few companies for all customers and
by most companies when customers delay payment beyond the duo date
Payment for Transport Charges Almost all companies will pay the
cost of transport when the invoice amount is above a certain figure
often Rs300/-. The amount will be set down in the Company's terms
of business and it is a good policy to read these. If a way bill
is received 'Froight to Pay' make sure that the amount is deducted
from the invoice.
Taking Delivery of the Goods At the carrier's office all boxes and
other packages must be carefully examined for damage cr signs of
pilferage. The suspect boxes must be weighed and compared with the
weight recorded on the way bill. If the weights differ or their is
any doubt whatever take 'Open Delivery'. This means that bn opening
you reserve the right to complain and call the carrier to see the
damage as you may wish to make a claim on him. Otherwise the
signature of acceptance implies that you are satisfied and release
him of responsibility.
Unp asking the Go ods On arrival at the Hospital the goods are
unpacked either in the Pharmacy or at a central receiving point.
The idea of a central, receiving point for all types of hospital
purchases is a good one provided that it is efficiently run and at
the same time it is remembered that staff have to be provided for
it. In practice because of the special nature of the medicines it
is usual for the Pharmacist to have opened the parcels and then
these are placed on a bench and carefully counted. The items with
pack siao and quantity should be listed in the Goods Received Book.
under the company's name. This book should have numbered pages so
that reference can be made to it on the invoice and stock card.
The goods are then placed in the store.
Part III
Store
The Store should be neatly in one of the following ways?
1) Alphabetically under generic (official) names so that all the
items of one medicament are together, e.g. Under tetracyclines the
items on the shelf would be - capsules, intramuscular injection,
intravenous injection, ointment, vaginal tablets.
2) Alphabetically as in 1) but the store divided into sections for
Chemicals, Injections Tablets, Ointments., etc.
3) Pharmacological groups. This method isdifficult to organise
satisfactorily so is rarely used in store keeping.
There will probably hate to be a separate section for bulk items
such as disinfectants and some chemicals.
Pay/_±1I_
Stores (con.id.)
When placing new supplies in the store the new stock oust always be
put behind the older stock to ensure strict rotation of use. Make
sure that the store is always clean and tidy.
Invoices These will be received at the same time or shortly after
the goods. The- details of the quantity received must be written on
the stock cards (see below). The invoice is checked against the
Goods Received Book and the book entry number written on the invoice.
The invoice number is written on the Goods Received book entry.
The invoice is then signed and sent to the office for payment. It is
useful to have a Pharmacy seal for the invoices and a suitable design
is given below.
Rec by
Bate
Rec
Hospital Name
Entered on Price
checked
cards
GRB No
Order
checked
Passed for
payment
Bate passed
for payment
PART IV
STOCK RPGQRBS
Stock Cards These are the centre of Pharmacy stock control and
must be kept carefully especially with regard to keeping up to date
with issue and receipt entries. Stock cards are preferable to bound
ledgers because of the ease with which they are operated and economy
in space. Separate cards for receipts and issues is an advantage for
the same reason. To ensure se_ curity each new card can be numbered
and signed by a senior officer. The following are the details needed
on the cards:
Receipt Card
1) Name of medicine (generic)
2) Pack size
3) Card folio number
4) Manufacturer's name
5) Suppliers names
6) Bate of Order
7) Order number
8) Ifantity ordered
In addition the card may show
9) Bate of receipt
10) Order number
11) Goods received book number
12} Suppliers number
13) Invoice number
14) Qi 1 anti ty r e ce i ve d
15) Total cost including Sa .es Tax16) Expiry date
I?) ".'nit rate
18) Monthly consumption rate
19) Lead time
20) Buffer stock
21) Reorder level
Issues Card
1)
2)
3)
Bate
Amount issued
Stock balance
and in addition may show
4) Amount received
5) Issued to (dept name)
It is useful to have a bin card in the stores for each item so that
as quantities are removed an immediate record is made. This is a
check on the stock cards. Tor this purpose an- issues card can be used
1NDIA is still in the early
stages of the industrial revo
lution with 80 per cent of the
people living in rural areas. As
industrialisation grows, urbani
sation will make supply of medi
cal care easier in respect of
distance from health care centres
and provision of facilities for a
larger percentage of people.
At present urban areas have
many advantages in medical care
facilities. Both Government and
voluntary agencies provide clinics
and hospitals, sometimes of a
highly sophisticated
nature.
However, the majority of people
who want to obtain even simple
care are put to great expense over
travel and loss of working time
to utilise them. A real problem
is getting medicines to the people
where they are, rather than
forcing them to come to towns.
For the urban poor the problems
are similar but distances less;
medicines need to be taken to
where they live, often in the
most unattractive localities.
problem has been tackled and
different answers tried in differ
ent places. A three-tier structure
consisting of a basic health
worker, a health centre, and a
referral hospital is the most
likely to succeed in giving an
adequate medical service.
Basic Health Worker: The basic
health worker, who in some areas
is exposed to other disciplines
such as simple agriculture, sani
tation, etc. is being trained to
provide health care treating a
5. Diarrhoea : kaolin powder,
a simple tablet.
6. Worm treatment: piperazine
tablets for round and thread
worms. A treatment for hook
worm, very often the cause of
severe anaemia.
7. Iron tablets : Ferrous sul
phate. Ferrous fumerate. (The
latter said to be less of an
irritant to the stomach).
8. Vitamin tablets : Vitamin B
Complex and multivitamins.
Medicines for Low Income Groups
ALAN CRANMER, m.p.s.
high percentage of patients who
do not need more highly trained
help. Such workers are best
selected from the community
they are to serve and could be
teachers or post office officials for
example.
9. Antiseptic : perhaps dilute
savlon for wound cleansing.
10. Eye lotion : either boric
acid lotion or a locally prepared
normal saline solution.
11. Salt solution : a mixtuie
of sodium chloride with some
other salts, in dry form, to be
mixed in water to save dehydra
tion, especially in children with
diarrhoea.
Patients naturally want their
prescriptions dispensed as soon
as possible. However, persuad
ing pharmacists to set up in
Following training in simple
villages is very difficult. Like diagnosis and the medicines to
all health service personnel they be used, a medicine kit is
want to live at the standard to supplied consisting of simple
which they are accustomed,
medicines to treat common
Cheap to Maintain
educate their children, and see a
illnesses. Such a list might be:
reasonable return on the invest
Such
medicines would be
I. Malaria : quinine, chloro
ment in their own education,
cheap to maintain and could be
pharmacy facilities and stock. It quine.
given either free or at low cost
is doubtful if many places would
2. Colds : aspirin, paraceta
to patients. It is better to make
be able to support a medical shop. mol, a decongestant.
a charge because frequently free
Its viability is even more doubtful
3. Coughs : a cough tablet medicines arc not much valued
whilst the majority of doctors, for
or perhaps a simple mixture, by the recipient. These medicines
similar reasons, practice in urban
although supplies of the latter would be supplied to the health
areas. How then can the provision
are more difficult to get.
worker from the nearest health
of medicines be made possible?
4. Fevers : aspirin, paraceta centre. He would
have a
The complex nature of this mol.
working relationship with the
July-August 1980
LTH ctVV
.. p. a
■ 1_
Niar'.<s Aoao
59
centre because it would be to
these that he would refer patients
needing to be examined by the
doctor and this doctor would
also be responsible for supervis
ing the basic health workers.
Additionally, the health worker
would arrange for clinics for
immunisation of children, and
give advice on family planning.
This medicine list has the
advantage that ail the medicines
may be handled by unqualified
persons and do not need a
doctor’s prescription. One pro
blem with staff trained at this
level is that they often want to
have more medicines as their
knowledge and experience grows.
This must be firmly resisted
because they have neither the
diagnostic skills nor the facilities
to observe patient reactions to
the treatments or to'dea! with
them. This trend in the past
has led. to compounders and
nurses setting up as doctors in
rural areas with many attendant
problems such as the incorrect
use of antibiotics, leading to the
development of resistant strains
of bacteria, etc.
Health Centre : A wider range
of medicines will be needed at
the next level of medical care so
that serious conditions such as
tuberculosis, hypertension, etc.,
can be treated on a long-term
basis with some monitoring of
the patient’s response to treat
ment. Records and treatment
for leprosy patients can also be
maintained. At this level will be
found health centres serving a
number of villages but not more
than about eight kms from any
one of them. There would
preferably be a resident doctor,
nurse, and para-medical worker.
If it is not possible to maintain a
60
doctor in residence then regular
and frequent clinics should be
available. During his absence it
would act in a manner similar
to that of the basic health worker
and the availability of medicines
would be the same.
registered Pharmacist goes with
him. It has to be clearly under
stood that nurses and para-medi
cal workers are not permitted to
dispense nor to undertake dis
pensing under the supervision of
a pharmacist.
A number of medicines would
be necessary for use by the
■doctor and some decision has to
be made about the type of cases
to be treated at health centres.
Specific guidelines for medicines
are difficult to describe briefly;
but the items would not include
any which are not found in the
World Health Organisation’s
1979 List of Essential Medicines1.
This List gives proven medicines
for many illnesses but avoids
expensive and doubtful remedies.
The stock available would need
to be revised from time to time
in the light of experience. Pay
ment by patients will probably be
necessary for medicines, so the
simpler these are the better.
Most treatments will be more
expensive than at the health
worker level so it may be neces
sary to subsidise medicine costs.
Referral Hospital: The referral
hospital will have a proper
pharnacy service with the widest
range of medicines; but again,
those to be stocked should be
based on the 1979 WHO List
of Essential Medicines. The
policy of the hospital should be
to hold in stock enough medicines
to provide at least 90 per cent
of the medicines prescribed.
At health centre level the pro
vision of medicines on the pres
cription of a doctor comes under
the provisions of the Pharmacy
Act. One important Section of
the Act (Section 42) states that
“any person who is not a regis
tered Pharmacist shall compound,
prepare, mix or dispense any
medicine only on the prescription
of a medical practitioner”. The
one exception to this rule is that
a doctor may dispense his own
prescriptions and is exempt from
registration under the Act. This
is almost certain to cause staffing
problems at health centre level;
so if a doctor travels to various
clinics it will be helpful if a
Provision of Medicines
In considering the problem of
obtaining and prescribing medi
cines, it is necessary to look at
their availability, prescribing
habits and the expressed needs
of patients. Each of these factors
has a considerable influence on
what is promised or prepared in
the hospital pharmacy. Inevita
bly the major demand will be for
solid dosage forms such as tablets
and capsules as these have simple
storage requirements and need
no skilled person for administra
tion.
There is a growing number of
pharmaceutical companies
in
India producing thousands of
items which are mainly combina
tions of several medicaments
in solid dosage forms. Many of
the formulations produced by
different companies are almost
identical and it is rarely that a
new drug is introduced. Products
are generally promoted by high
pressure salesmanship by both
Indian and multinational com
panies. These methods
on
occasion include the offer of
Voluntary Action
discounts on purchases of a
certain number of units or total
value which require careful scru
tiny to ensure that the products
are really required and that the
discount will in fact be helpful
and not involve the purchase of
unprofitable quantities resulting
in overstocking and possibility of
time-expired drugs being left on
the pharmacy shelves. Some
inducements to purchase arc
intended unduly to influence
officers with powers of ordering
and these include personal gifts
of saris and suit lengths of mate
rial, or refrigerators and fans,
and should not be permitted by
the rules of the purchasing orga
nisation. Usually these offers are
made in connection with the pur
chase of multidrug formulations
which, as suggested, will not
feature largely in purchasing
policy.
Types of Medicines
Medicines available on the
market are of two types and the
value of each needs considera
tion.
Basic drugs are usually
preparations of single drugs and
include analgesics and antipyre
tics, antihypertensives, antibio
tics, diuretics, etc. From such
preparations the majority of
patients can be treated economi
cally. There are however also
multidrug formulation':.
The advantages and disadvan
tages of including more than one
drug in a dosage form should be
considered ’•
Advantages :
— A few combinations are
synergistic, e.g. co-trimoxazole
in certain illnesses.
— Reduced side-effects, c.g.
July-August 1980
release formulations are available
on the market at many times
— Compliance with treatment.
the price with no significant
A patient may understand and
advantage to the patient.
remember how and when to take
Tonics are very often part of
a single, medicine whereas he
may default on a number of the drug companies listed pro
different ones. (This also raises ducts and profit margins are high.
the question of how many condi These are normally based in a
tions to attempt to treat at one malt or aqueous alcohol base
which makes them pleasant to take.
time).
In almost all cases a balanced,
Disadvantages :
not expensive diet will provide
— In multidrug formulations sufficient minerals and vitamins
the dosage ratio is fixed and of the types included in tonics.
does not permit the physician to Some tonics include the glycero
adjust dosages.
phosphates which have been
— Adverse reaction to any of incorporated presumably because
the ingredients cannot be identi lecithin contains phosphorus in
the form of the glycerophosphates
fied.
radical and therefore would be
— Inappropriate combinations
more easily assimilated by the
are found e.g. anti-inflammatory
tissues. There is no evidence to
drugs with prednisolone; simple
support this assumption3, and
analgesics with diazepam.
therefore to pay for such ingre
— Ignorance. Prescribers are dients is wasteful. Except in
frequently unaware of the con cases of severe illness, when
stituent drugs. A Montreal swallowing is difficult, the pres
survey2 showed that the most cribing of tonics is economically
frequently prescribed of 23 com unsound.
binations was correctly identified
Nutrition is an essential part of
by only two-thirds of the physici
ans and for seven of the 23 not a reducing dependence on tonics
single prescriber answered cor and other food products. As
rectly. Hospital pharmacists did stated earlier, this need not mean
an expensive diet. Health work
slightly better.
ers can and are being trained
Cost is probably a variable in teaching the selection of locally
factor but, not infrequently, available foods so that adequate
combination drugs arc more quantities of minerals, vitamins,
expensive partly because they carbohydrates, fats and proteins
include drugs not required by are included in the diet, especi
the patient’s condition.
ally for children. Food habits
and taboos die slowly and teach
Costly Formulations and
ing requires a sensitive and
Food Products
patient approach by all levels of
staff. Health workers in the
Some simple medicines are community must set the example
available in more costly formu themselves, and here dedicated
lations which are not significantly women workers with children can
more active. For
example, achieve great improvements.
ferrous sulphate tablets cost a
Baby foods prepared artificially
few paise each but some sustained
Isoniazid with pyridoxone.
61
have often been condemned and will cure all conditions rapidly.
are not to be recommended, The problems of maintaining
except in exceptional circum sterility of syringes is consider
stances, because of the problem of able in busy clinics; so injections
preparation and administration. should be prescribed only where
Often the mother does not under there is a problem of patient
stand the mixing technique and, compliance with treatment or
for economic reasons, over-dilutes the oral route is unsuitable.
the food with serious conse
— Quick results are expected or
quences for the baby.
Bottle desired by all and the prescriber
cleaning and sterilisation present should resist changing treatments
problems in rural areas. Teaching for this reason. The treatment
about weaning and weaning of tuberculosis and leprosy
foods would prevent many of arc particularly difficult in this
the malnutrition cases seen at respect and patience is required
clinics and hospitals.
in explaining the need for taking
Various Pressures
The prescriber is subject to
great sales pressure from the
industry which, like other indus
tries, survives, develops, and
satisfies its shareholders by
maintaining and increasing sales.
The prescriber is the one who will
ultimately shape the pharmaceuti
cal industry, and education for
doctors in prescribing and resist
ing pressures is essential They
need orientation in prescribing
essential, proven treatments for
sufficient periods and basing
such prescriptions on such lists
as that provided by WHO, there
by avoiding the costly items so
often promoted. Working closely
with an experienced pharmacist
can help to minimise the stocking
of unsuitable
medicines; but
efforts by both doctor and
pharmacist are required.
medicines regularly.
— Costly formulations appear
attractive in multi-coloured cap
sules or specially shaped tonic
bottles. So these should be kept
out of sight of patients even if
they are part of the stock.
— Education is an essential
part of the programme so that
all from the doctor to technicians
and health workers will not
themselves expect such treatment
and thus guide patients into a
more reasonable acceptance of
simpler medicines.
Pricing and Selection
of Drugs
Prices charged for medicines
have to be calculated in accord
ance with Drug Price Centrol
Orders by the manufacturers and
submitted to Government for
approval. The approved price
is that printed on the container
and to that sales tax and any
The prescriber is also subject other local taxes may be added.
to pressure from patients who, There is therefore reasonable
with very little knowledge, often uniformity in prices. The retail
try and dictate the medicine they pharmacist must keep to this
want to have. This pressure price structure and is forbidden
includes:
to add anything to it for his
— Demands for injections. services. The purchaser has every
Patients assume that an injection right to a receipt for his pay
62
ment on which must be written
the name and quantity and
price of the medicine supplied.
The patients most likely to suffer
from
deliberate
over-charge
are the illiterates; so for them a
receipt is even more important as
evidence to show what they have
purchased.
Any
over-charge
should be brought to the notice
of the pharmacist and if he re
fuses to correct the situation, a
complaint to the Drug Control
authorities in the State is in
order, and an investigation will
be ordered if evidence can
be supplied to support the
complaint.
In the matter of selection of
suppliers of medicines,' quality
should be the first consideration.
Here, the knowledge and experi
ence of the doctors and pharma
cists are very important. It is
wise in the case of each durg to
list the names of, say, two manu
facturers who have shown relia
bility, in terms of quality, pricing
and supply and to keep to those.
It is possible to find in certain
markets antibiotics and other
drugs at much below the average
price. Generally they are un
branded and there is the risk that
they may contain adulterated or
spurious drugs and so should be
avoided.
The supply of medicines to
rural and urban low income
groups needs careful thought and
systematic action to ensure that
patients get the medicines really
needed and at prices which they
can afford. The prescriber has
a very important role to play in
moulding manufacturing policy
and public opinion.
Almost all medicines are pro(Contd. on page 76)
Voluntary Action
STOCK ANALYSIS AMD.ORDERING SYSTEMS
Deciding on the amount of stock to be kept and the amount and time
to order are very important if over and under stocking are to be
avoided. The first step is to find out the pattern of investment.
A
C Analysis
followed,’
For this analysis the following steps have to be
The cost of each item is multiplied by the number used during
the year giving the total expenditure,
2) The items are listed in descending order of total expenditure.
3) The percentage of the cash investment for the first 10% of items
is established. This -..ill be found to be about 70% (a items)
4) The percentage of cash investment for the next 20% of items is
established. This will ba found to be above 20% (3 items)
5) The remaining 70% of items will be found to take the remaining
10% of the investment (C items)
1)
The method of 'Stock Control in the Pharmacy Dispensing area as well
as stock levels can be derived from this Analysis as shown in the
table below.
Category of Item
A
r
Dumber of items as
% os the inventory
10%
20%
70%
Value of items
expressed as a,
percentage of the whole
70%
20%
10%
Stock
minimum
medium
large
Buffer Stock
small
medium
large
f ast
medium
TTUtWT.'Ih ‘
or slow
i ndivid.ua!
record
individual
o?eraTal
general
record
Tv V LIO VGT
Admin. Control in
Dispensing Area
From this table it ’.-rill be seen that the items where the most money
is invested should be held in ccmparitively small amounts (a). A small
amount of excess stock will tie up large sums of money. Items in
C category will bo held in large quantities because the investment is
small. Orders for A items will be placed frequently ana. for C items
much less often.
The use of ell items will be carefully recorded in the store but in
the Dispensing Area only on category A and some B items individual
records will be required. This is fully dealt with in the paper
'Distribution of Medicines from the Pharmacy to Patient Areas'
Following this analysis the next step is to decide on the ordering
method which will be one or a combination of the following methods?
■Q7c-i.c.rl Ordering System This is a time based system which usually
involves an annual review of the stock level of all items and the
requirement for the following year is calculated taking into account
the amount used in the previous year and th? stock in hand. From
this information the orders arc placed either annually of up to four
times a year regardless of the stock position. There are certain
disadvantages in the use of this system, namely
6
Cyclical Ordering System (contd)
1) Unforsecable fluctuations in demand cannot be controlled
;>) Advantage cannot be taken of special contracts' except at the
revue time
3) Placing of orders is concentrated at a few periods of the year
Fixed Quantity Ordering System This system is based on the quantity
of stock of the items held. A point is fixed below which the stock is
not allowed to fall. The advantage of this system is that the stock
level is the guide for ordering and that orders arc spread out in
tine. However if the lead time and usage fluctuate too much a new
re-order level has to be fixed*
To operate this system the following must he understood;
1) Lead_Time This is the time taken expressed in weeks between
the Pharmacy writing the order and the goods being received in the
store .
2) Buffer Stock This is the stock kept to cover fluctuations in
demand. For example, there is often a season of Typhoid when more
than usual chloramphenicol is prescribed. It is difficult to decide
exactly when that season will begin so extra stock must be held to
cover such emergency situations.
The buffer stock is calculated by multiplying the difference bet.ioen
the- maximum and average issue rate by the lead time (all expressed
in weeks);
Buffer stock
(max demand - aver demand) x lead time
=
Example;
Maximum demand
Average demand
Lead time
=
=
=
20 vials/week
14 vials/week
2 weeks
Buffer Stock
=
=
(20 - 14) x 2
12 vials
lte~ord ur Level This is the level at which the new order has to be
3)
placed. It is not the same as the Buffer Stock because no account is
taken of the useage during the load time. The Reorder Level is
calculated by the addition of the buffer Stock to the expected demand
during the Lead Time
Re-order Level
=
Average Demand x Lead Time + Buffer Stock
Example from above;
Re-order Level
4) ■•'aximurq Stock Level
Re-order Level.
=
14 x 2 + 12
—
4 0 vi d s
This is generally taken to be tw. ee the
It is obvious that one of the two systems alone will probably not
be satisfactory for all items in the store although the Fixed Quantity
Ordering System will be the most used but if rigidly applied would
not permit the taking up of contracts. These systems need to be applied
.r.tb. common sense so that the best use c.-.n be made of them to ensure
adequate but not excessive stock le-’dc.
A.Cranmer
Consultant Pharmacist
Christian Medical Association
11
1.
the dispensing and supply of drugs shall be
carried out by c ? under the supervision of
a qualified person.
2.
the premises where drugs are supplied or
stocked shall be open to inspection by an
inspector appointed under the Drugs and
Cosmetics Act who can, if necessary, take
samples for test.
3.
The drugs shall be stored under proper con
ditions.
The key word here is SALE
In the Act and Rules we have
a license to sell, stock or exhibit for sale
required of retailers and wholesalers - defined
and governed.
-
a license to repack for sale - defined and
governed.
a license to manufacture for sale - defined
and governed.
The exemption in Schedule K in effect, if not in intent,
negates the whole of the Pharmacy Acts and xRules in
regard to the hospital pharmacy.
The hospital pharmacy
does not sell, nor manufacture for sale - it compounds
and dispenses. NO Sale - therefore, NO LICENSE.
The definition of 'manufacturing' in the Act is ambiguous.
Manufacturing in relation to any drug or cosmetic includes
any process, or part of a process for making, altering,
ornamenting, finishing, packing, labelling, breaking up or
otherwise treating or adopting any drug or cosmetic with
a view to it's sale (there's that word again) and distri
bution - but excludes the compounding or dispensing of
any drug, or the packing of any drug or cosmetic in the
ordinary course of retail business, and to 'manufacture
shall be construed accordingly'.
The word SALE excludes
the hospital from the role of a manufacturer.
Hospital pharmacy has no legal definition at this time
in India. The hospital pharmacists are seeking a defini
tion and subsequent control. Until that time we have to
act reaponsibly, ruled by norms and behaviour accepted
by all who are dealing with human.
-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-oOo-
Renu/
5.1.1978
-y
PHARMACY
COMMUNITY HEALTH CELL
introduction:
‘ ;-'“ 3
■ \ ; r/iarksRoad
,L 51)0 001
"that profession which is concerned with the art
and science of preparing from natural and synthe
tic sources suitable and convenient materials for
distribution and use in the treatment and preven
tion of disease.
It embraces a knowledge of the
identification, selection, pharmacologic action,
preservation, combination, analysis, and standardi
zation of drugs and medicines.
It also includes
their proper and safe distribution and use whether
dispensed on the prescription of a licensed physician,
dentist, or veterinarian, or in those instance where
it may be legally done, dispensed or sold directly
to the consumer."
HOSPITAD PHARMACY AND ITS IMPORTANCE:
The practice of pharmacy in a hospital setting:
In the
average hospital, the pharmacy will fill thousands of pre
scriptions and disperse as many ward orders’ and requisitions
in a single year Purchase of drugs and the value, of the.
annual inventory run into many thousands of rupees.
A fairly
high percentage of the total annual expenditures of the hos
pital go for pharmaceutical services.
This emphasizes the
need for very careful attention to the effect that pharma
ceutical services have on the efficiency of both clinical
and administrative services in every size hospital.
The idea of the hospital pharmacy with a well qualified phar
macist in charge has been accepted by the larger hospitals
as a necessity. .Small hospitals have not taken this position
largely because of the fear of increasing their operating
deficits hospitals which fail to employ a pharmacist with
proper training, experience,, and talent are seriously lower
ing the efficiency of their services and operations. A well
organized pharmacy will function effectively in its own sight
and also contribute to the whole integrated hospital organi
sation.
In hospitals where pharmaceutical services do.not appear to
be of sufficient volume fully to utilize the time of a compe
tent registered pharmacist, several alternatives are employed
to maintain good services without undue cost.
It has been
traditional to assign- to the pharmacist other duties, Parti
cularly those relating to general administration, such as
purchasing. Most pharmacists, by experience, are well quali
fied in this regard.
Recently there has..been a movement to
retain the pharmacist in professional medical fields.
Examples of division of time between limited pharmacy duties
and others include laboratory or x-ray functions, or super
vision of ■ central sterilizing and supply services.
Another
alternative which probably will gain in favor in coordinated.
hospital prograins is the employment of a qualified pharmacist
on a part-time basis by two or’more small hospitals where
travel time is not too great-
The Pharmacist incharge, with the approval and cooperation
of the director of the hospital should initiate and develop
rules & regulations pertaining to the administrative policies
of the department.
The professional policies of the depart
ment should be formulated by the pharmacist and the Pharmacy &
Therapeutic Committee and approved by the administration.
2 :-
RESPONSIBILITIES OF THE PHARMACIST;
The pharmacist in charge shall be responsible for:
(a) the
preparation and sterilization of injectible medication when
manufactured in the hospital, (b) the manufacture of pharma
ceuticals, (c)
the dispensing of drugs, chemicals and- pharma
ceutical preparations, (d) the filling and labeling of all
drug containers issued to services from which medication'is
to be administered, (e) necessary inspection of all pharma
ceutical supplies on all services, (f) the maintenance of an
approved stock of antidotes and other emergency drugs, (g) the
dispensing of all narcotic drugs and alcohol and the mainte
nance of a perpetual inventory of them, (h) specifications both
as to quality and source for purchase of all drugs, chemicals,
antibiotics, biologicis, and pharmaceutical preparations used
in the treatment of patients, (i) furnishing information con
cerning medications to physicians, interns and nurses,
(j) establishment and maintenance, in cooperation with the
accounting department, of a satisfactory system of records and
book-keeping in accordance with the policies of the hospital
for (1) charging patients for drugs and pharmaceutical sup
plies, (2) maintaining adequate control over the requisition
ing and dispensing of all drugs and pharmaceutical supplies,
(k) planning, organizing and directing pharmacy policies and
procedures in accordance with the established policies of the
hospital, (!)• maintenance of the facilities of the department
(m) cooperation in teaching courses to students in the school
of nursing and in the medical, intern training program,
(n)
implementing the decisions of the Pharmacy and Thera
peutics Committee, (o) the preparation of periodic reports on
the progress of th§ department for submission to the adminis
trator of the hospital.
EDUCATION OF THE PHARMACIST:
-
’
Diploma in. Pharmacy Course
One year basic sciences - Chemistry, Physics,
Anatomy, Physiology, Hygiene, English, Biology.
One year professional - General Pharmacy, Dispen
sing Pharmacy, Pharmaceutical Chemistry, Pharma
cognosy, Pharmacology, Forensic Pharmacy.
Internship - 750 bourse in an institution approved
by the Pharmacy Council of India.
-
Bachelor in Pharmacy Degree
I
year - English, Mathematics, Physics, Biology,
Chemistry.
II
year - Mathematics, physiology, Pharmaceutical
Chemistry I and II.
Ill
year - Pharmacognosy, Pharmacology and Toxico
logy, Pharmacy Administration and Industiral Business Management, Pharmaceutical
Engineering, Pharmaceutical Chemistry III,
Pharmaceutics I.
IV
year - Pharmaceutical Chemistry. Ill and-IV,'
Pharmaceutics II and III, -Pharmaceutical
Engineering, Forensic Pharmacy.
Internship - 750 hours in an approved institution
(only if registration is sought)
FACILITIES:
Adequate pharmaceutical and administrative facilities should
be provided for the pharmacy department.
In addition to the
equipment needed for the compounding dispensing, and manufaeturing of pharmaceuticals, these facilities should also in
clude (i) an adequate library and filing equipment to make
information concerning drugs readily available to both phar
macists and physicians,
(ii)
special locked storage space
to meet the legal requirements for storage of narcotics,
alcohol and other drugs, (iii) a refrigerator for the sto
rage of thermolab.ile products (iv)
adequate floor space for
all pharmacy operations and the storage of pharmaceuticals
at a satisfactory location provided with proper lighting and
ventilation.
PERSONNEL:
The number of pharmacists required for any particular hos
pital varies with the program/ policies,. responsibilities,
services and their utilization for inpatients, outpatients,
employees and the public.
The workload consists of both measurable activities and those
which do not easily lend themselves to quantification.
In
general each category requires about one-half of the time of
the pharmacist. More readily measured items include filling
of prescriptions, issues to patient care areas, including
outpatients, compounding, and pre-packaging.
v
■ ■ ■
•
THE PHARMACY AND THERAPEUTIC COMMITTEE
an advisory group of the medical staff which serves
as the organizational line of communication or liaison
between the medical staff and the pharmacy department.
This committee is composed primarily of physicians and
the pharmacist and is selected under the guidance of
the medical staff.
It also is a policy recommending
body to the medical staff and to the administration of
the hospital on all matters related to the use of drugs.
Functions and scope
1.
To develop a formulary of accepted drugs for
use in the hospital.
2.
Advise an all matters pertaining to the use
of drugs.
3.
Advise on selection or choice of drugs.
4.
Evaluate clinical data on new drugs.
5.
Prevent unnecessary duplication of drugs.
6.
Recommend additions and deletions of drugs
from list accepted for use.
7.
Develop a basic drug list and provide for
its constant revision.
8.
Recommend policies regarding safe use of
drugs in the hospital.
/-
4 :-
9.
Study problems relative to dispensing and
administration of drugs.
10.
Review Adverse Reaction Reports.
11.
Evaluate periodically medical records in
terms of drug therapy.
THE HOSPITAL FORMULARY
a continually revised compilation of pharmaceuticals
which reflects the current clinical judgement of the
medical staff.
-
A system whereby the medical staff of a hospital,
working through a Pharmacy and Therapeutic Committee
evaluates, appraises, and selects from among numerous
available medicinal agents and dosage forms those that
are considered most useful in patient care,'
Purpose of the Formulary:
The Pharmacy or Therapeutics Committee should develop or
adopt a suitable formulary of selected medications.
This
sarves two main purposes: it promotes rational therapeutic,
and it prevents unnecessary duplication, waste, and confu
sion, and thus promotes economy to both the patient and the
hospital.
There is a loss to the patient and the hospitaj.
when many brands of the same drug are stocked and prescribed.
Economy in medication does not mean the use of inferior
remedies.
A formulary must be sold to the medical staff on
its merits—, sound therapeutics and quickly obtained qua
lity drugs for every condition or disease entity.
The eco
nomy of. a formulary is a corollary or result of this system
in effect.
The use of a formulary has many advantages, but should not
be so inflexible as to restrict the physician.
Its content
and pharmacy procedures should be reviewed periodically by
the above ccmmiZtee.
Guiding Principles
1.
The hospital formulary system shall be sponsored
by the medical staff based upon the recommendations
of the Pharmacy and Therapeutic Committee.
2.
The medical staff shall adopt written policies and
procedures governing the hospital' formulary system
as developed by the Pharmacy .and Therapeutic Com
mittee.
These policies and procedures shall afford
guidance in the evaluation or appraisal, selection,
procurement, storage, distribution, use, safety pro
cedures, and other matters relating to drugs in the
ho sp it al.
3,
The Pharmacist, with the advice apd guidance of the
Pharmacy and Therapeutics Committee, shall be res
ponsible for specifications as to quality, quantity,
and source of supply of all drugs and chemicals, biologicals and pharmaceutical preparations used in the
diagnosis and treatment of patients, and for assuring
that quality is not compromised for economic conside
rations.
-: 5
4.
Prior agreement by the prescriber must be obtained
to permit the pharmac.st to dispense upon prescrip
tions and medication orders, formulary drugs with
out reference to brand identity.
Recently the HATHI COMMISSION has recommended to the
Government that all life saving drugs be sold by generic
name at a reduced price rather than by brand name.
PURCHASE ABB INVENTORY CONTROL
Drug stocks in nursing units should be standardized and be
kept at a useful minimum and should be inspected by the phar
macist, accompanied by the nursing supervisor, at least
monthly.
The pharmacist's principal function in purchasing is to es
tablish standards and specifications for medication and equip
ment. He alone is responsible for sub-standard or dangerous
items reaching the patient.
The pharmacist is familiar with
the pharmaceutical and chemical manufacturers, their distri
bution system and discounts.
He is also familiar with firms
which furnish other professional supplies.
It is his duty
to have in stock at all times an adequate supply of the
proper quality.
A sound purchasing and control system is
e ssential.
A purchase record card on each item stocked in the pharmacy
is necessary.
The purchase when recorded with the date,
quantity and. price, will reveal when reordering the product
the need for obtaining larger or smaller quantities. Quan
tity discounts may be taken advantage of, dependent on busi
ness conditions, and over-stocking is prefented.
Control of
prices to be charged is easily effected, cost changes are
noted and the selling price adjusted at the same time.
Purchase of drugs and pharmaceuticals should be on a bid
basis where practicable.
CONSIDERATIONS:
R.O.L.
-
'reorder level' - the minimal holding, or
stock, of an item that has been determined
from a study of tiem required to obtain
that item from the source of supply.
E.O.Q.
-
'the economic order quantity' - the optimum
quantity of an item to be ordered at any one
time taking into consideration the following'
factors: normal flow rate, the cost of order
ing, the cost.of holding, relative avail
ability.
Three methods of establishing E.0.Q. in
ascending order of efficiency.
1.
Replenishment System - the purchase is
made on fixed ordering times rather
than quantities.
Inventory is reviewed
at periodic intervals, an order is
placed to replenish the withdrawals.
6 :-
2.
The Fixed Order Quantity System - the
R.O.L. is established and an order is
placed when the stock reaches this
level.
The E.O.Q. is fixed on an
annual turnover basis.
3.
The Exponential Smoothing Technique a sophisticated scientific approach to
determine the E.O.Q. so as to achieve
maximum economy.
ABC Analysis - a computation of the annual rate of consumption
of items, by value, and arranging a list in descending order.
The items which contribute 70/ of the consumption is classi
fied as A, the next 20% as B, and the remaining 10/ as C.
Rigid control of the A items is a decided economic advantage,
minimal control of B items narrows the task, and negligible
control of the C items would result in an efficient operation.
Manufacturer or Supplier Ledger - an individual ledger main
tained on each manufacturer, or supplier, that permits a per
manent register of all transactions with same.
Purchase order — a triplicate, preferably, order form used
to requisition drugs, or chemicsils from the manufacturer
and/or supplier.
G.R.N. - 'gools received note', in duplicate recording the
receipt of all drugs and chemicals ordered on the purchase
order.
Invoice - do cument usually sent separately by post for the
drugs of the.micals supplied by the manufacturer, and/or sup
plier indicating amounts sent and values attached.
Stock' register - a perpetual inventory maintained on all
items by means of individual 'stock cards', and suitable stock
ledger.
Indents - fin indenting form used to requisition drugs or
chemicals from the pharmacy stores.
Record of .Bated Pharmaceuticals - R of D.Ph. - in every
pharmacy there will be drugs remaining in stores which will
soon Ijecom.e useless in the near future because of the expiring
date.
The pharmacist should list these drugs and inform the
medical st.aff so that they can prescribe the same.
A practical! application of the above is possible in all hos
pitals regardless of size.
The main prerequisite is a sepa
rate store; room, that is, separate from the dispensing opera
tion.
Drug stociv in nursing units should be standardized .and be
kept at a useful minimum & should be inspected by the pharma
cist, accompanied by the nureiing supervisor, atleast monthly.
DRUG DISTRIBUTION
GENERAL CONSIDERATION
Prescription. - the term refers either to an order for medica
tion or to Vhe medication dispensed by the pharmacist as a
result of tile order.
A prescription order issued by a
7 :-
physician is specific in character in that it designates a
particular medication for a particular individual at a
particular time.
The Label - assures the specificity of the prescription for
a particular patient by a physician.
It indicates the
directions for utilization of the prescription.
Pre-packaged prescriptions - prescriptions packaged at a
prior time in anticipation of dispensing.
Ward Stock - drugs that are kept at the nursing station issued
to the patient as directed on the medication order written
in the patient's chart.
Dangerous Drugs - Opium and its derivatives, natural or
synthetic; pethidine, cocaine, methadine require special
attention to record their distribution, accountable to the
government authorities.
Protected drugs - those drugs that are kept in reserve to
combat organisms resistant to ordinary therapeutic agents.
Emergency drugs - drugs kept ready for immediate use on patient
in extreme distress.
Free drugs - those drugs which may, at the discretion of the
clinician, be given free to an indigent patient.
Prescription charge - prescriptions are dispensed and not sold.
The dispensing charge recovers the cost of the drug plus a
service charge for handling plus a contribution to the main
tenance of the institution.
PROCEDURES FOR DISTRIBUTION
In order to systematize his work, the pharmacist's daily work
schedule is coordinated with the activities of the other
departments of the hospital.
The systematic collection and
delivery of floor baskets to the nursing units each morning
saves nurses' time by reducing•requisitioning to a minimum,
making frequent trips to the pharmacy unnecessary, and by
avoiding delays in the daily nursing program with prompt
deliveries.
A requisition system is essential in saving the time of all
departments served by the pharmacy.
The. requisition for
special medication should contain all needed information
whether written by a physician, intern or supervisor.
This
includes date, floor and room number, patient's initials;
whether medication is for oral or hypodermic use when both
are available size of dose and frequency of administration.
Methods of distribution Out-patient
-
on a doctor's prescription, from a
pharmacy dispensing unit.
In-patient
-
1.
Ward stock
Advantages:
Ready access.
Disadvantages: Duplicate inventory,
little control, responsibility on
nursing staff detracting from their
time for patient care.
8 :-
2.
Main dispensing unit
Advantages:
Maximum control of
drug flow, one inventory, dispen
sing by licensed pharmacists.
Disadvantages:
Time lag due to
distance in large hospitals.
Combination ward stock and dispen
sing unit.
3.
Advantages:
Adequate control of drug
flow, dispensing primarily by licensed pharmacists, minimizes ward drug
holdings, bulk supply of common
drugs reduces 'handling' expenses,
minimizes time disadvantage of (2),
minimizes duplication of inventory.
/
/
!
'
'
Observations:
1.
It is false economy to insist that the patient supply
his own prescription container. He must purchase it
somewhere, why not from you? The containers brought
by the patients are not clean, usually uncapped, cracked,
etc.
Few drugs can withstand contamination, exposure
to the atmosphere and still maintain their integrity.
2,
In the United States of America where the literacy
rate is probably 99% plus, the incidence of patient
error in reading label directions is in the neighbour
hood of 12%. Think of the patient error in this
country with prescriptions dispensed without labels.
LABEL ALL PRESCRIPTIONS IN THE VERNACULAR AND INSIST
at the point of delivery that the directions be ex
plained in detail to the patient.
j
/
Drug Pricing
Hospital Pharmacy Dispensing is an income producing depart
ment.
The medication cost per patient day is reduced by
proper management.
The charges for medication to patients
is established on a business like basis, usually above cost.
It must maintain the pharmacy department as a whole as well
as return an amount to the institution which will help off
set the administrative costs and extend its charity to the
community. An exception to this may be made on the ordinary
drugs- stocked in the floor medicine cupboards which are
often dispensened without charge to the patient.
This avoids
irritating and time consuming accounting of charges.
To do this an adequate price schedule must be
derived -
Three basic types 1.
Straight percentage - Cost of Goods sold plus a
fixed percentage
Disadvantage
-
Low cost drugs do not carry their
proportion of costs. High costs
drugs carry too much - puts too
great a burden on the patient.
/-
9 :-
The written policies should specifically cover the
writing of prescriptions and charges for drugs to
hospital employees.
The pharmacy must co-ordinate
its services with the business office in pricing &
promptly submitting all charges & credits.
Partly-Used Dru; e
A definite policy is needed in relation to unused
portions of prescriptions, particularly for discharged
patients.
Approval of the attending physician, with
adequate instructions for continuing use by the patient,
should be provided in situations where the remaining
portions of a prescribed drug are to be taken home upon
discharge.
All other unused portions of specific pre
scriptions should be returned to the pharmacy for
‘appropriate disposition, usually destroyed.
Modifica
tion of charges, if indicated, should be reported to
the business office.
2.
Graduated percentage - Low cost drugs - higher percent
age Mark-up
High cost drugs - low percentage
Mark-up
3.
Professional fee + Cost of goods sold
Consideration:
1.
Government Price Order
2.
Needs cf the Institution
3.
The competition
4.
Own expectations
LEGAL ASPECTS OF HOSPITAL PHARMACY
A.
Legislations of Government of India:
Some of the Acts promulgated by the Government of India
are :
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
The Drugs Act of 1940
The Drugs Control Act of 1950
The Drugs Rules of 1945
The Drugs and Cosmetics (Amendment) Act of 1965
The Pharmacy Act of 1948
The Drugs and Magic Remedies (Objectionable
Advertisements) Act of 1954
The Dangerous Drugs Act of 1930
The Dangerous Drugs (Import, Export and Tran
shipment) Rule of 1957
Opium Act of 1878
The Poisons Act of 1919
The Medicinal and Toilet Preparation (Excise
Duties) Act of 1955
The Medicinal and Toilet Preparation (Excise
Duties) Act of 1956
Drug Price Control Order 1970
10 :-
B.
Narco tics:
The Dangerous Drug Act, 1930, of the Government of India
defines dangerous drugs and delegates powers to the
State to make rules permitting and regulating-import, ex
port, transport, possession and sale of "manufactured
drugs" that are under this act.
Therefore, each hospital
should familiarize itself with rules and regulations
governing the handling of dangerous drugs in its own
State (for example, the Madras Manufactured Drugs Rules,
1932 for Tamil Nadu).
Permits must be obtained for purchasing and dispensing
of narcotics, dangerous drugs and alcohol.
These permits
are to be renewed annually. Narcotics and dangerous
drugs must be kept in a separate locked cubboard.
C.
Daily Control:
An absolute perpetual inventory must be maintained by the
pharmacy department for the receipt and issuance of each
narcotic.
This is accomplished by maintaining a narcotic
stock register which will have a separate sheet in the
register for each item.
To complete the record for doses administered on the ward,
a record of narcotics must be maintained.
In all cases,
issues at the ward level should be approved only .after
the ward supervisor has satisfied herself that the ward
record has been compiled and completed in all details for
former issues.
This Record of Narcotics must be kept by every ward the
OPD, operating and delivery rooms and returned to the
pharmacy at regular intervals for checking.
If the hospital pharmacy has an -analytical section, records
of analytical reports about I.V. & raw materials purchased
must be- maintained.
The Drugs controller checks these
reports at intervals.
D.
Spirits
A perpetual inventory must be maintained also for receipts
and issues from the storeroom for rectified and methylated
spirits.
This inventory will be checked annually by the
local excise and taxation officers before another permit
is granted.
All the above records must be kept on file for a minimum
of five years and are subject to government inspection
at any time.
E.
Legal implications of Hospital Phayoagy
Section 123 of the drug rules (The Drugs and Cosmetics
Rules, 1945) states that the hospitals are exempt from the
provisions of Chapter IV of the Drugs and Cosmetic Act,
1940, to the extent and subject to the conditions specified
in the Schedule K. Schedule K, paragraph 5A, gives the
exemptions as the provisions of Chapter IV of the Act -and
the Rules thereunder which require them to be'covered by
a sale license, subject to the following conditions,
....... /-
[RUG rU-rHE!'S On HEALLRE?
"The greatest danger to Health in India is the over
mer’icalising of our Health Care System. Eternal vigilance
is required that the Doctor-drug producer axis does not
exploit the people and that the 'abundance ' of drugs does
not become a vested interest in health".
- ICM1/ICSSR study on 'Health for All '
-an alternative strategy
The- problem of Drug Policy and low cost drugs encompasses
a very v/ide spectrum of issues-multinationalism, industrial
policy, medical advertising, research, drug production,
medical education, price control and so on. The recent
upsurge in interest in this important area of health policy
has led to the publication of numerous reports, books and
papers and many seminars and workshops have and sre being
organised. In the final analysis any collective action in
the form of policy, analysis, research or education can only
result from an individual understanding of the related issues
translated into a prescribing policy to be accepted volunta
rily by doctors, nurses, para-professionals and others in
their attempt to contribute to a solution of the problem.
Readers of this bulletin arc requested to think over
the following facts, observations, conclusions taken from
’HO, ICiTl, ICSSR, Earthscan, VHAI, Govt, of India and other
sources of information. Can we collectively accept as many
of these 9 -points as possible?
(1) 15090 branded drugs are on sale in India but a
Government Committee believes that Health needs would be
met by only 116 drugs.2,3
There is now an overproduction of drugs (often very
costly) meant for the- rich and well to do, while the drugs
needed by the poor people (and these must be cheap) are not
adequately available*
'AHO in its report on selection of essential drugs has
prepared a list of 200 drugs, needed for health care.^
The real purpose of an essential drug list must be seen
as taking drugs to £hose who need them most, not as reduc
ing the drugs bill.^
Could we accept an essential drug list for our
practice in which cost would be an important criteria in
selection in addition to efficacy, safety and quality?
(2) All UN agencies and governments involved in pre
paring a list of essential drugs are convinced that pres
criptions should be through the generic names of drugs
only.6
Generic name is not chemical name but official,
international, non-proprictary name e.g., not
Acetylsalicylic acid but Aspirin.2
Branded named products cost higher because they
include promotional costs and cost of claims of additional
ingredients in formulation e.g., Librium by Roche is
available for Rs. 16/- per 190 tablets but generic equi
valents are available for Rs. 1.50.°
A study of UNCTAD has shown that bio-availability
argument for branded drugs i.e., therapeutic difference
COMMUNITY HEALTH CELL
47/1.(First Floor) St. Marks fioac
BANGALOaE-560 0»>
based on formulation is not very valid for most drugs.°
Could we accept Generic prescribing? i.e., By Aspirin
not riusprin, >isprin, etc.
(3) In India 60 firms with Foreign shares accounted
for 70% of the country's total drug sales in 1973-74. The
remaining 307$ was shared by 116 large and 2,500 small manu
facturing companies.2
Drug industry in India is an offshoot of development
of the industry in the Western World
is in private
hands which produces mainly for profit.
ICIF./ICSSH and the- Hathi Commission have recommended
that Lhe small, scale sector, cooperative sector should be
encouraged. Hospital and dispensary based formulations
should be promo led.
Can we prescribe drugs which are Indian rather than
foreign, Government rather than private industry, small
scale and cooperative sector rather than large sector?
(4) One of the most distressing aspects of the present
health situation in India is the habit of doctors to pres
cribe glamorous and costly drugs with limited medical
potential•
The drugs required by the poor are not produced on thcmain grounds that there is no profitable market end adequate
demand for them, while the country continues to be flooded
by plethora of costly and wasteful drugs meant for the
minor illnesses of the rich and well to do.'
Multiple drug combinations often containing drugs in
amounts far in excess of what is required are presently
marketed in India. There is a collosal national wastage
of drugs because of such combinations.3
Packaging increases the cost of drugs very greatly
because the trend is to make it attractive and highly ele
gant and to a:’r cvn-etic embellishments to promote sales.'
The drugs Consultative Committee examined 34 categories
of fixed dose combinations and concluded that in the case
of 23 categories of there formulations there was no therapeutic rationale for their marketing.6
Could we stop prescribing drugs whose only additional
advertised values are a ) cosfeetic embe11i s hment
b ) Elegant packing
c ) Irrational combination
c! ) Imitative drugs
e) Inadequate evidence of greater value?
(5) 25/. of a total production of th.700 crores in
1976 as analysed by ,? Task force of the Planning Commission
was on vitamins, tonics, health restoratives and digestive
enzymes.'
An IC?41/ICSSR study observed that production of INH
and Dapsome arc a third end a quarter respectively, of the
3
-3-
minimal requirements of the country. On the other hand,
tonics and vitamins ’hich are -ostly alcoholic preparation
and spin money arc- produced in wasteful abundance .'I
A M." study on tonics has shown that most of the high
potency or ’forte ' preparations of multi-vitamins are a
sheer economic waste.4 These are not only a drain on the
patients 1 nurse but also help only to vitaminise our sewage
Can we stop this ’tonic ' practice?
(5) A :'HO report, notes that drug advertising and con
tacts '■•n th representatives of pharmaceutical firms are
often the main sources of information for a physician on
drugs and sometimes the only one. Such information is
largely influencer by commercial interest.6
Drugs are often being prescribed l;y doctors not
because they think a particular one is best suited for the
situation but because the company which produced it gives
the maximum monetary and material advantages and inducements
to them. These range from free samples (often sold in
practice), pens, calendars, diaries, teas, lunches, travel
and conference attendance costs.f,6
Medical training in Colleges docs not train future
physicians to judge a preparation critically .............. nor
coos it include conscious immunization against the half
truths of persuasive industrial advertising.°
Can we stop accepting physicians samples and other
forms of inducements from Medical Companies?
(7) Many medicinal herbs and roots that arc- used by
grandmothers, local dais and village- medicine men have
been scientifically tested aiK researched and known to have
therapeutic value. Their descriptions in journals collect
dust in reference libraries.2.6
Herbal medicines and home remedies are not only low
cost and easily available but their popularisation will
help in breaking the doctor-drug producer axis for over
39% of the common minor ailments which are now being over
treated .
China hac integrated over 50 herbal medicine and home
remedies in their armamentariums not only as a drug policy „
but as an expression of local participation in health carc.‘:»6
Can we propogate simple home remedies and locally
available herbal medicine alter studying their efficacy?
(3) A very large number of techniques of healing are
leing researched today in which diseases are tackled and
cured without drugs. bion-drug therapies include Yoga,
Pranayama, Meditation, Accupuncture, Acupressure and
Chiropractice among others. Traditional systems of Medicine
such as Ayurveda, tJnani, Homeopathy which use drugs but of
a different sort arc- being researched in various places and
the therapeutic effectiveness of many of their products are
being discovered and documented.
Can we adopt a more open policy of enquiry and use of
traditional medicine and non-drug therapies?
4,
-4—
(9) Health Care is recoining increasingly a quest for
priorities. ’Clean water before antibiotics, food before
vitamin pills, vaccination before kidney machines, mothers
milk before powdered baby foods mixed with dirty water,
health for villagers and slums before more hospitals for the
affluent suburbs of capital cities’.2
Inspite of our preoccupation with Drug Prescribing
policy could we commit ourselves to other more important
Health Care Priorities?
- ravi narayan
Inferences :
1
• Health for All - as al ter
ICi7F/ICSSP Deport (1980)
2.
Drugs and the third ’..'orld, Anil Aggarwal
Earthscan publication, 10 Percy Street,
Lo nd on WIF01! ■ (1978)
3.
Hathi Committee :F.e-port of the Committee on Drugs
air' Pharmaceutical Industry, Ministry of Petroleum
and Chemicals, Govt*, of India (1975)
4.
In Search of a Diagnosis MFC book containing
reprints from bulletin
5.
The Selection of Essential Drugs. '-'HO Expert Committee,
’AHO TRS No.61511977) and 641(1979)
6.
Medicines as if people mattered - Health for the
.Millions (VHAI bimonthly ) Vol.VII No.283, April-June 1981.
strategy
D-10/344
MS :k: 27/2/84
MISUSE OF DRUGS AND
OUR ROLE AS SOCIALLY CONSCIOUS HEALTH PERSONNEL
Aspects of the drug problem requiring our attention and
unde rs tanding*
Health needs and medical care
Principles of Rational Drugs Therapy, and Medical Education:
* Drug Policies which encourage misuse of
Drugs in medical care
* Number of drugs
-
Confusion propounded by 30,000
* Kinds of drugs - Combination drug
- Substandard
- Hazardous and irrational
* Drug Control - How ineffective
* Drug prices - trends - medical care - health institution
* Impact of Drug prices on Voluntary health institutions
* Disease patterns and the drug needs and actual drug
production patterns
* Shortages of essential and life saving drugs - the case
of anit-TB drugs
* Drug information, the lacunae
*. Adverse reaction
How and Why misuse of drugs occurs?'
Commonly misused drugs
Principles of Rational Drug Therapy
Role of Socially conscious health personnel
Recommended readirgfcr self education.
Health Needs and Medical Care
/better
Today there is/understanding of HEALTH as well as the recogni
tion of the implicit relationship of disease with UNMET BASIC
NEEDS OF FOOD, CLEAN AND ADEQUATE DRINKING WATER,__ CLEAN EN
VIRONMENT.
All that goes on in the name of ’Medic-al
Services’ at constantly increasing costs, is being increasing!’
questioned by more and^ more people today.
For approximately 60-70% of Indians below or around poverty
line no amount of medicines ’modern1 or ‘traditional’ can deal
effectively with most of their health problems having their
roots directly or indirectly in poverty.
coMJcraN'TT
oat
47/1, (ri. u > fiao;) -■
•• k- <»oacf
BAWGALO.UL-56O001
h-10/344_____
MS:k:27/2/84
(The well off can afford adequate care for themselves and
don't real’v need us.)
r
We, the health personnel realize the limitations of our role
even as 'deliverers of curative and medical care', We are
unable to help with,"and en'sure consistent supply of adequate
nutrition even after wehave made -an accurate diagnosis of
second or third degree malnutrition with multiple vitamin
def iciencies>■ -•-Even;while we. go., on. diagnos ing and dealing
with serious and fatal diarrhoes, (the childhood killer
number 1,) we somehow cannot ensure adequate supply of clean
water.
/found
that
On looking back we realize that we were never trained to be
"facilitators of health." in the real sense of the word.
Actually sane of us sincerely believed in the importance of
health education, in prevention of dise.ase. Unfortunately we_
much of the health education 'given' in all good faith does
not necessarily result in changes in 'attitudes or behaviour.'
The subtle but crucial difference between "giving of health
education" and ''being able to communicate,
. be listened
to,
be 'heard' and understood, was painfully realized
only with experience in the field.
Realization of this, as well as realization
- The pressing health needs of the people who needed
us mos t
- The limitation of our training which does not equip
us to deal with their problems effectively
- The expected and traditionally accepted role of voluntar.
health institutions
-
The obvious need for the changing role of health insti
tutions, towards more relevant functioning, leaves many oi
the more sensitive and socially conscious health per
sonnel from service oriented health institutions facing
a moral crisis and dilemma.
For the time being let us accept, that voluntary health
institutions (like others) are geared only to "deliver medic-.
care" and they do so with commitment and sincerity. Medical
care as it exists today is based mainly on 'use of drugs, '
whether it's in a big teaching hospital, health centre or
even in most community health programmes.
/are
made
When accusations/that health personnel all over misuse drugs,
and are "pawns in the hands of the drug industry" and "part of
an exploitative medical industry complex" - the allegations
are very serious and cannot be rejected without as analysing
them.
Principles of Rational Drug Use in our medical education
It is a very well recognized (but an unfortunate) fact that
our medical education has not equipped us adequately to deal
effectively with the. problems as they exist in the field.
Our teaching of pharmacology and Therapeutics is from Ivory
towers for Ivory towers. Principles of 'Rational therapeutics'
are not taught keeping in mind the conditions under which the
0/34 4
vMS:k : 27/2/84
: 3 :
health personnel will have to be functioning in the field - ie.
- With limitation of diagnostic facilities and of
supportive staff
- With heavy workload and pressure of time & diversity
of function
- With financial constraints with ever increasing deficits
- Shortages of drugs
- Little or no referral facilities or help in consultation
- Long distances and hopeless transports facilitiee Involved
which make revisits by patients for reports and follrwup
difficult
To deal effectively with all these constraints calls for con
concern and2 co.hunt
stant innovativeness initiative,
______skills,
*
________________
ment. It is a fact that those "undrained brains" meeting all
these challenges in the field to the best of their ability are
worthy of deep respect.
Unfortunately in many cases as the different constraints
increase, the situation deteriorates in the absence of authen
tic need based drug information with no facilities for meaning
ful ongoing medical education to certain lacunae begin to
occur - unwittingly. Our medical education nevei geared us
for dealing with these lacunae.
/with
Insptite of the encylopedic knowledge of pharmacology we
acquired, we find ourselves totally foxed when confronted with
hundreds of unheard of drugs. We are unable to critic ally
evaluate,f rem amongst the hundred of brands of the same pro
duct,,- the most rational product to stock our pharmacies/and
to prescribe.
Our entire medical educ ation is based on the use of generic
named drugs and that too mostly single ingredient, drugs. The
medical journals also use non-proprietary generic,, names
and then we walk into the world of Brand names - of which
there are 30,000 in India. Many health personnel don't see
the unreasonableness of the brand names - till confronted by
a critically sick patient with numerous prescription slips
full of unfamiliar brand names" The realization that most of
these are combination drugs with varying contents of ingredients
makes it all the more complicated to figure out what was
prescribed and actually consumed.
Out education does not equip us with a thorough understanding
of:
- our country's health & drug policies
- our people's health needs & health priorities
- the rationale behind generic drugs over brand names
- the existing drug control mechanism and its ineffective
ness
- concept of essential drug list and its relevance for a
deve1jping country like ours
- irrationality of most combination drugs
D-10/344
MS:k:27/2/84
4:
- the various hazardous drugs banned in various countries
- which should not be allowed to be manufactured, marketed
and prescribed
-
- the half truths and biased drug information fed by the
drug industry on which the health personnel tend to
depend
in the absence of EASY ACCESS TO UNBIASED
MEDICAL „RUG INFORMATION.
- ■
According to the working qr >up on Rational Drug Therapy of
WHO, gut of 17 ways in which doctors misuse drugs, the common
est is overuse.
Over use of Drugs means:
- too large., a quantity of drug
- for too long
- prescribing of an unnecess iry drug
. /•
- prescribing of many drugs adding no additional benefit
fur the' same purpose
Factors leading to overprescribing
1.
2.
3.
4.
5.
"
Inadequacy of time and facilities for diagnosis.
Lack of knowledge of drugs and prescribing principles
(over prescribing to avoid risk of underprescribing)
Pressures exerted by patients
Heavy"and'uoften unethical practices, marketing by drug
companies and distribution of samples.
Desire to retain patients good will."
Another problem f or Failure on part of the patient in taking
drugs pr.tiperlT-;' ie. right drug given to the right patient
with INADEQUATE or NO appr.pri ite drug information may not
be taken properly. Reasons being -
1.
/which
rtay have
been
2.
3.
/Stoping
Failure to understand and follow.the prascribers instructjons/giyen too vaguely or not at all.
Treatment by more th .an one doctor often of more than
■1 system of medicine.
Self medication’ by patient.
41"'/Premature cessation of drug is due tc financial reason,
fear of harmful effects _.(most allopathic drugs are con
sidered hot), and because. >f "s ome unacceptable' mild side
effect.
5.
Drug substitution at the chemists.
6.
Illegible prescription.
7.
Chemists own vested interest.
Principles of Rational Drug Therapy is based on"Rational pres
cribing - the right drug for the right patient at the right
time at .thd right..amo.uiLts and with due consideration to rela-'
five costs." (Dept. :-f Health Education Welfare, 19691 .
£>-10/344
MS:k:27/2/84
:5:
Rational Therapeutics is based /’n
a)
-
As accurate a diagnosis as possible under the constraints
of diagnostic facilities and supportive staff and costs.
(Relative contributions of history taking, physical exami
nation and lab investigation tp diagnosis and management
of medical outpatients, B.M.J. 2, 486-89).
(In 83% new hospital outpatients the final diagnosis was
reached on history and referring doctor's note. Only 5%
diagnosis was reached after investigations).
Hamptom, J.R., Harrison, MJG,, Mitchell, JRA,
Pritchard, J.S* and Seymore C. (1975).
b)
Appropriate use of Drugs
Drugs available should be:
1) Eff ective
2) Safe .
3) Economical
4) Essential
5) Easily available.
6) Acceptable (culturally and socially to the patient^
7) With little, scope for misuse
8) Easily administered
(See article on Rational Drug Therapy - Drug Issue - April ••
June 1982 - HfM). Therapeutic Guidelines, Upanda, J.
Yudkin, G Brown, AMREF.
c)
Effective Communication to the patient about usa^
drugs
Various studies have shown that between 10% to 90%
patients with an average of 50% do not take prescribed
treatment, they forget or reject their doctor's advice.
(Ref. Psychological studies of doctor-patient communica
tion in contributions to medical psychology Ed Rachmann,
■Oxford Pergamon Press, Page 9-42). Dr. George J Caranasos
et al in the Journal of the American Medical Association
(JAMA))talking about lack of communication between Doctor
and patient says:
"Patients also cannot identify correctly 60% of
their medicines. Forty percent of patients receive
drugs prescribed by 2 or more physicians, increas
ing the possibility of drug interactions. Twelve
percent of patients take drugs prescribed for some
one else and 60% of the patients consider their
drugs completely safe."
Coranasos, George J et al, Drug Induced Illness Reading to
Hospitalization, JAMA, 228 - 713-717, 1974.
Dr. Hulka an epidemiologist at the University of North
Carolina and others revealed that 58% of the total number of
patient^tudied made mistakes in the way they took their medica
tion - they .took either too much, not enough or at the wrong
time,
D-10/344
MS:k:27/2/84
' iv*
.......
In our Indian context, eff ecf/communication. with illiterate,
often ignorant patients, for whom what we consider supersti
tions is a reality, requires special skill and on this d°pe^ds
whether the drug will be taken
\
- at the times suggested
- in correct amounts
- in a correct way
- for the correct duration and that-the patient would be
able to report back any serious adverse reaction and
not consider it worsening of the disease or consider the
diagnosis to be wrong.
Most of our rural patients who are used to home remedies,
traditional systems of medicine - western medicine is alien even though it is often associated with the "awe" and "mystery"
accorded to white man's medicine. The dangers of these medi
cines and the importance of taking it properly is often under
estimated. In this social context our responsibility as
effective communicators, and educators obviously increases. The
need to shoulder, and appropriately delegate some of these
responsibilities to other trained staff is very pivotal in
rational drug therapy.
What Encourages Drug Misuse?
/their
1. Drug Policies which allow;haz.ardous and irrational drugs
to flood the market;,, .which allow their heavy promotion and
creation of false needs are very much to'blajne. Even concern
ed Health Personnel have so far never felt'the need to express
their coinion in all this
x'h p war f the drug industry is
obvious from some of the following examples:
Eg. Lifting of price restriction on category III drugs by the
Govt, in return of dissolving of the foreign equity shares by
certain multi-national from 70% to 40% and having/demand met.
Finding more and more unessential but profitable drugs flood
ing the market is but a natural outcome. (For categorize
of Drugs & Drug Price Control Order .see Drug Situation
in
India.)
Another example is the enability of the Govt, to ban the
2 3 irrational combination drugs which the Drug Consultative
Committee recommended for withdrawal, because of vested
interest ( list available with VHAI) .
The drug companies getting a stay order:
- on Govt, decision to allow sales of 5 single ingredient
drugs only under generic names
.- on Go’t.'s decision to ban high dose estrogen-progesterone.
combinations involved in the hormonal pregnancy test
scandal (the tests were officially banned since 1976).
/but
’ The f act-that Bangladesh heavily dependent ..on foreign drug
imports/could manage to ban 1707 hazardous and irrational drucrmakes our indifference and apathy all the more' pathetic.
D-10^334
MS<k:27/2/84
Number of Drugs
2.
There are 30,000 drugs in the market. Hathi Commission
recommends 116 essential drugs while WHO recommends about 200
essential drugs to deal-with 90% of the problems in most hos
pitals. Studies based on information recall showed that it
was not possible to remember important information of more
than 100 drugs - this being the highest estimate. Most of us
can remember much less.
' ■
.... .
A survey of 92 hospitals conducted by a Chruch Agency indicat
ed that 25 drugs were adequate to take care of most of the
problems according to WHO working group on Rational Drug
Therapy.
WHAT
/ARE THE DECIDING FACTORS GUIDING THE CHOICE OF THE DRUGS THAT
WE PRESCRIBE?
Many times it's not the principles of rational drug therapy,
but the subtle influence of the drug representatives and
their biased medical literature.Wien confronted with too many
diverse unfamiliar drugs, with each drug being sold under 50
to 200 different names - confusion and misuse is the expected
end result.
3
.
Combination Drugs
Kinds of drugs with expected misuse potential are Combination
Drugs. 60-70% of the brand products in the market are not
single ingredient drugs but combinations of 2 or more. Less
than '5% of drugs in the WHO's Essential Drug List are combina
tion drugs. In combination drugs many of the. most importanc
ingredients are in sub-therapeutic doses or the combinations
a re totally irrational and non-sens ic al.-
- the cost of combination drugs is any day more than cost
of single ingredient drugs.
.
t 1
- what is probably worst is the potential for adverse
re actions it is known that chances of drug interactions
increase with the increase in number of drugs prescribed.
The chances of drug interaction increases by 40% when 6
or more drugs are prescribed. The fact that 2 or 3 combi
nation drugs may easily contain 6 or more known or unknown
ingredients is often overlooked.
ADVERSE DRUG REACTIONS
Problem of adverse reactions with too many drugs another
serious concern. In States adverse drug reactions kill more
victims than does cancer.of the breast - They rank among top
10 causes of hospitalization alone, they are held accountable
for as many as 50 million hospital patient days a year. They
may interfere with diagnostic tests, causing a missed or
errouneous diagnosis.
They may spare a patient's life but leave him blind or deaf,
afflicted with kidney liver or brain damage, bone necrosis,
uIteration of the bowel, intestinal haemorrhage, skin scars,
: 8:
extreme sensitivity to sunlight or other disabilities that
may last fof'mohths or years ••'(•Ref-.—Dale -G. .Friend - Adverse
Reactions to Drugs Clinical Pharmacology and ...Therapeutics 5
257/ 1964) (AMA Drug Evaluations 1971).
"Dnly during the past 10 years have we begun to recognize the
magnitude, seriousness and complexity of the problem. Today
it is only too obvious that adverse drug reactions represent
a major oublic health menace of alarming proportion" (Pills
Profits and Politics - Milton Silverman and Philip R Lee).
Adverse Drug Reactions are not a rarity. In States where the
Drug Control Authority is very strict, where drugs are not
prescribed-by RMP's and untrained personnel or freely avail
able over the counter without prescription, Uhe extend of
adverse drug reaction- is-fairly significant. The following
reports shogld act as a timely warning for us - ..as we set out
to find new drug markets in our villages - in the name of
development of medical services with little or no .-controls
and checks.
According to Dr. Louis Sherwood and Dr. Edith Pauis in
New England Journal of Medicine "18-30% of all hospitalized
patients end up with drug reaction which often double their
stay in hospital." (Preventable Drug ReactionsCauses and
Cures, NEJM 284: 1361-1368, 1971). ‘
Dr. Herschel Jick of Boston Collaborative Drug Surveillance
Programme one of the most comprehensive drug monitoring
organizations of . the-world-. Say, "We have reported that in
30% of hospitalized medical patients atleast one adverse drug
reaction develops during hospitalization and using the estimaJa
that about one third of the approximately. 30 million people
admitted to the OS general hospitals per year are admitted to
general medical services, we may estimate that about 3,000,000
hospital patients suffer an adverse'drug reaction in medical
units each year".
"Dru9 ~ Remarkably nontoxic, NEJM, 291- 824-829
1974). , bemeUS hospitals have reported that as many as 20%
of their patients were admitted because of drucr induced —~
disease .
--------------------——:----- - ——
Miller, L.C. "How Good are our Drugs?"
' .
Distinguished lecture delivered December 30, 1-969 before t-hrAmerican Association for Advancement of Science, Boston, Mass
Am J Hospital Pharm. 27: 367-374, 1970.
"Serious drug reactions anywhere • from 15% to a hirrb a nw
been reported in hospitalised patientsGotti Eh?°^53ve
Drug Reaction and the AatopsyArch.' Mtho! 90
Over the counter drugs which don't require a nresor-i r+.-i
considered safe by most people. A studv entii-ho
are Illness leading t- Hospitalisation" reported that
Induc£cl
implicated in 32 out of 177 (i.e. 18.1% admissions"
UgS
ranasos, George J et al. Drug Induced Illness
■
Hospitalization, JAMA 288: 713-717, 1974)
leading to
The drug adverse reaction reportina svstem
k-s u i U?
m India. Recognition of adverse drug reaction coly/d®velopeG
Wible if the he 11th personnel are aware of ?he
?
crations of interaction^
“ toxic it v -'nd
various asso*
toxicity and sick effects of drugs
D-10/344
MS f k : 27/
:9:
The tendency to underplay side effect & toxicity of drugs by
/cogni'- drug companies has led to underestimation & almost total dere-/
tion.
Our attempts at finding out about the understanding and
This
awareness of the clioquinol (Mexaform & enterovioform) induced
was ob- toxicity ----- the SMON syndrome. The story of the clioquinol
vious
controversy has been hitting the headlines. The crippling of
in
more than 11000 Japanese with these drugs being the biggest
drug scandal of the century — as bad as the Thalidomide dis
aster. We found that very rarely was the history of engestion
of hydroxyquinolines was taken, when dealing with a patient
with neurological problems. Since there are more than 90
brands, a doctor could hardly be expected to remember them,
or the patient recall the name, specially if it had been taken
over the counter. 'Scientific"conclusions of the medical
establishment — there is no SMON in India,is therefore
unacceptable.
Substandard and Spurious Drugs and Drug Control.
(52% of the drugs in the Indian market are assessed to be
substandard'I- Anil Aggarwal in Drugs & the Third World) .
The accepted official figures are 30%. According to the
Estimates Committee Report Nov. '83 only about 20%. We have
controlled drugs - is just as wrong.
Why have the health personnel not raised their voice against
this and demanded better quality control. Mechanism, when
it is so crucial for quality of health care? The bigger and
better known drug companies taking advantage of the situation
have been able to successful push their products because of the
aci>14gedvbetter quality control. Unfortunately most of the
spurious and imitation drugs are imitations of precisely these
expensive popular brands. Ensuring that all the drugs in the
market meet a certain standard and arc quality controlled is
the responsibility of the Govt, and the Drug Industry. Putting
this added responsibility on the shoulders of the prescribing
doctor is incorrect and the prescribing by health personnel
of expensive brand drugs, to their poor 5>©tients to deal with
the problem is equally incorrect & unjustified. A coordinated
and coherent demand for adequate and effective drug control
mechanisms, adequjzlate numbers of efficiently functioning qua
lity control labs and drug inspectors should be made by all
socially conscious health institutions. An unhealthy depend
ence on the multinationals to as a solution, is actually not
the most appropriate solution.
Hazardous and Irrational Drugs
Our last Drug Workshop in Jaipur focussed precisely on this.
There is absolutely no reason why any sensible health institu
tion should continue to stock any of the hazardous or irra
tional drugs. The list of 23 combination drugs recommended
for weeding out by our own Drug Consultative Committee.
Bangladesh's list of 1707 banned drugs ‘as well as the 16 Cri
teria for withdrawl which are entirely in keeping with WHO's
recommendations for Rational Drug Therapy,are available.
All health personnel believing in Rational TherapeutiCs should
voluntarily BOYCOTT dangerous and useless drugs - the above
2 to start with. The 'Govt, ban on these drugs may come too
late, and because of the pressure and vested interest never
come- at all. The Gazette notification by Drug Controller of
India banning 22 categories of drugs on 23rd July 1983 is
either not known, nor implemented. Outrageously sales of these
products containing Phenacetin, Amidopyrine, Paediatirc
Letracyclin continue.
D-10/344
MS:k:27/2/84
:10:
The boycott by 3000 doctors and veterinary doctors led by
Dr. Olle Hansson in Sweden against all Ciba Geegy products
i
was because Ciba Geigy continued to produce and sell c ' /
clinoquinals (mexaform and Enteroviagorm) in the third world,
inspite of the fact that 11000 cases of SMON (Sub acute MyeioOptic Neuropathy) had been identified in Japan and reports from
all over the world have been coming 43 cases of SMON have been
identified in Sweden itself from where subsequently Clinoquinok
like in most other countries is banned. The boycott was
because of continued sales in the 3rd world countries like India
and not in Sweden, where it was already banned.
What are we, the health personnel from the 3rd world doing
about sales of hazardous products to our people?
Some of the problem drugs are:
- Hormonal Pregnancy tests
- Anabolic Steroids
- Amidopyrines, Phenacetin
- Butazalidine
- Diethylstilbaestrol and hormones in pregnancy
- Lomotil in infants
- Paediatric Tetracyclines
- Ancolcxin in Pregnancy for Nausea
- Clinoquinols
- Steroids being used indiscrimenately
- Antibiotics being used indiscrimenately for viral infec
tions .in wrong doses etc. & incomplete courses
- 2nd line anti TB drugs
- anti hypertensive, ant idi abet?03
- Tranquillizers
. ...
Drug Information - The-Lacunae
Charles Medawar in "Drug Disinformation" compared the drug
information given in MIMS (Monthly Index of Medical Specialities)
from UK and in Ireland. Discrepancies in the drug information
given by the same drug companies in the 2 different countries
showed their double standards. Comparing MIMS (UK) with MIMS
(India) would make our hair stand on end - and demonstrates the
triple standards followed by the drug companies.
- How come Anecoloxin durg company, an antinausea drug is
specifically indicated for morning sickhess when it is contra
indicated in pregnancy in States?
- How ccme we have so many more indications and such few contra
indications and side effects for anabolic steroids, for drug''
like the butazoledines .
- How come dosages of lomotil for children and Syp. Lomotil arc
still available when they are banned for use in kids due to
associated respiratory arrest paralytic illness and toxemia?
D -<10/344
, MS? :2 //2/H4
- How come drugs containing amidopyrines were allowed to be
produced and marketed without giving all the information
which led to their being banned in most countries. (vAile
attempting to compile information on it, we found hardly
a paragraph devoted to it in Goodman Gillman in the Pharmaccdology Text Book because in most countries it had become
obsolete)i Cibalgin and Ergopyrin have known high popularityall amidopyrines sales have been officially BANNED from
31st October 1982 prescribing and selling them is illegal
Talking about Drug Information it is a well recognized fact
that the Drug Industry spends a lot on doctors. Dr. Yudkin in
his study in Tanzania 1978 calculated that "£1000 per year is
spent on providing information to a single doctor - a very cal
culated investment which has always paid well.
/I
In UK which consumes much more drugs than us there is one drug
representative for 30 doctors while in developing countries
like Tanzania there is one drug representative for 4 doctors.
In Phillipines there is/drug representative for 2 doctors.
In the absence of' any alternative source of unbiased informa
tion the prescribing practices of most doctors are highly
influenced by these interactions. I am not mentioning the
inticing role of samples, cut backs and other incentives. This
lack of unbiased and authentic drug information is one of the
most important causes of drug misuse. Since we believe that
health personnel in the voluntary- health sector are above all
this .
Drug list and Drug Prices
Drug prices are increasing and going to increase. With increas
ing drug doctor dependency and heavy marketing of nonsensical
and inessential drugs - drug use is going to increase. With
our training of VHW's - we have ensured inadvertantly that the
pills reach the remotest corners.
Eventhough an average Indian spends much less on health care
than his counterparts in the West, he SPENDS A MUCH LARGER
PERCENTAGE OF HIS -ANNUAL INCOME. A study done by Health Work
ers in Piaxtala, Mexico showed that people spent 40 - 60% of
their annual income on medicines. The cost of drugs in many
third world countries is increasing between 30-50% each year
(Yudkin 1978; Pichard 1980). The impact on Voluntary Health
Institutions of these increasing drug prices is going to be
twofold:
- they will either incur higher and higher deficits
- or become unreasonably high priced and out of reach for
the majority they set out to serve. It will be a ques
tion of 'service without survival1 or 'survival without
service 1.
Tradiitional selection, purchase, stocking and prescribing of drugs
are needed by the health institution with the patients and
their own present and future in mind. Rational selection of
drugs is good economics.
~ ~’
D-10/344
MS:k:27/2/84
The Health'Status, Health Needs and Drug Needs of our People
For a country with such a large medical manpower and medical
technological know how in terms of drug production* the health
status of our people specially the women and children - is
disappointingly poor.
(.*We are the biggest producers of Drugs in the third
world)
The-most, important health parameter reflecting the develop
ment of a society as a whole is the Infant Mortality Rate i.e.
number of children who die before they reach one year of age
per 1000 live births.
' ■ .
Our figures are 120/1000 while Sri Lanka, our little neighbour
has managed to achieve 45/1000. 50% of the Indian children
get
the calories they require. 60% of the children under 6
suffer from severe anemia and protein calorie deficiency.
40,000 children become blind each year because of Vit. A defi
ciency and about 3 million children suffer from other forms
of Vit. A deficiency i.e. nigh blindness, dry eyes and dry
skin. 24% of all deaths are due to non-immunization for dis
eases like such TB, whooping cough, diphtheria, measles,
polio. 48% of the children below 5 years suffer from moderate
to severe forms of malnutrition.
W omen
Where women are concerned their worsening health status is
reflected in the declining sex ratio
1946
950 Females/1000 males ~
1971
930 Females/1000 males
Our maternal mortality figures are 163/1000 delivery. 50%
of the pregnant mothers are found to be anemid. 14% of all
deaths are related to pregnancy, childbirth and early infancy
though in terms of %--they constitute only 4% of all diseases.
5 6% of all deaths ate preventible.
Where' some of the major health problems' for the country are
concerned. About 2% of all the Indians have T.B. and lOmillion
ie.
of the worlds 20 million TB patients are Indians.
2.5 million of these being infectious and 1/3 of. th6 worlds
10 million leprosy patients are also---------- here. Diarrhoeal
diseases kill 1,5 million Indians mainly children each year.
1.2 million e.e. 40% of the 3 million new malaria cases each
year die because of it. Waterborne diseases like malaria
(including infection with plasmodium, falciparum (cerebral
malaria), Filaria, polio, kalazar, Japanese B Enephalitis has
shown an increasing trend.
Basic needs of water and sanitation have to be met.
1/3 of the 5.8- lakh villages covering a population of 160million
(out of 680 million) still have no access to potable water.
1/3 of the 40 million households night soil is still collected
and disposed off manually (Gandhi had seen not merely decreased
chances of pollution of water source and food but also the
emancipation of the sweeper - the Bhangi). The health
D-10/344
F$ :k: 27/2/84
:13:
personnel as well as the policy makers know that with improveci
water supply and sanitation programmes 80-85% of all illnesses
specially the water borne ones CAN BE PREVENTED.
*56% of all deaths are preventable.
- Mukararam Bhagat
in Aspects of Drug Industry.
Source: Centre for Monitoring Indian
Economy CMIE Bombay
Most of these are diseases of poverty and therefore realiza
tion that 60% of the Indians liive below (or on the margin of
the poverty level is very significant (poverty level - as
assessed in relation to average calorie requirement ONLY a level which does not take clothing, housing, schooling,
medical expenses into account).
If fulfilling of -their basic minimal needs of food, water,
sanitory living — is not given a priority, by the health
services - we would atleast expect to see the curative care
services for the majority to be functional and appropriate.
It is the LOPSIDEDNESS in even this, which apparently forms
the basis of our health care services that makes it all the
more painful.
75% .of the Indians have no access to even essential life
.saving drugs. So 20% or so basic drugs are available and it
is only to 5% of the economically well off that all modern
drugs are available. Production"of drugs is NOT in relation
to the health needs and people 's health priorities-, .
Of the 636.9 crores worth of drugs sold in 1980 '
19% were antibiotics
10.21% vitamins
4.41%.tonics '
4.24% antianaemic preparations
4.71% cough. & cold (the increase in growth
within last 5 years has been i.e. 137 crore
worth of vitamins 70-items sold in 1980.
Source:
Br. A. Patwardhan as quoted in
VHAI’s Drug-Situation in
India, Jan. '82.
Our National Formulary has over 60,000 drugs and chemicals
ie. about 15-20,000 brand drugs, out of these 68% are obsolete
and unessential only about 5000 are useful and 2500 of marginal
use.
In 1979-80, only Rs. 350 crores worth of drugs out of Rs.1260
crores worth manufactured were essential and life.saving the
rest were tonics, digestive, enzymes, formulations of medicnes
with marginal benefit. Many vital bulk drugs in huge quanti
ties have been wasted which could have been utilized for manu
facture of essential drugs.
Source:
J.S. Mazumdar in Drugs Industry Instru
ments of Policy.
Since the Government Health Authorities and the Drug Industry
has failed to ensure provision of atleast the basic essential
life saving’drugs -to the people who need them - the time has
£--10/344
MS :k: 27/2/84
: 14 :
now come for the people to ensure that the National H®^lth
and Drug Policies are made in accordance to their heaitn
and not according to the dictates of the drug industry.
Things would have been different if 80% of our medical mannow;
was not concentrated in the urban areas and serving mere 2Cw
of the ponulatioh; if their western model training and the.
unfortunate present reliance on the drug industry and.sophisti
cited medicine had not ensured that they lose touch with the
socio-economic reality of the 80% of the Indian population
living in rural areas, and urban slums.
Some of the glaring examples of the contradictions existing
in the care of our priority health problems are dealt with
below:
Malnutrition and Anaemia: We are taught their ideal manage
ment, but very few know of what nutritional advice and treat
ment to give to a pregnant woman whose husband gets less than
/family minimum wages which feeds a/f ive,. iric luding underfives, and
sick aged parent. Why is it difficult to obtain single ingre
of
dient Ferrous sulfate. Folic Acid Thiamine or B12 which
patients need and can'' afford. On the contrary there is a gay
abundance of expensive Vitamin Fortes often in ridiculous
combinationg^nd tonics. An article "Tonics - an economic
waste?" by Kamla Jayrao of M.F.C. deals very appropriately
with this subject.
Diarrhoea: We are taught about antidiarrhoeaIs, but very few
can very accurately and easily prepare GST, nor confidently
prescribe only oral rehydration therapy without feeling a
compulsion to prescribe anti-diarrhoeals. The fact that many
of the Commercial ORS packets are not even in the keeping of
WHO recommendations seems to be of little concern. According
to WHO most of the popular antidiarrhoeaIs have little or m
role (HfM - Special issue on Diarrhoe,
Dec. ’83).
Shortages of .essential and life;snving drugs reflect that it
Shortages.of anti TB is a perfect example of
a r>rnfnhealtJe A1"
takin3'on the decision making role whiK t’health personnel of the .country passively witch on th 1
mg of the health and drug situation - where the rA
worsenmajority are concerned.
th P or and the
Shortages of Essential and Life saving drugs ea TR n
Some of the painful facts about the
dru9s
is LB, a major killer.. We
L of world's TB patients i c
We have
have A
Patients, cf
of which 2.2 million are highly inLrti^
dna g Lakhs die annually
because of TB.
llv he.™,
m.n
A survey report Iron
Bombay recently indicated a 4 fold incr
ise in infectious cases
of TB within 1 year.
NTI Bangalore and TB Centre Delhi which have beer,
longitudinal studies of TB in areas
areas'with'much^etterVH1Ve?
: P
1-—o do not indicate Sy chIncf^n
^B
structure than most
places
incidences. This is
‘ xnspite
'
of the drugs,
“
medical advances.
D-10/344
MS:k:27/2/84
:15:
The only thing that is deceasing steadily is the production
of anti TB drugs inspite of the increase in total numbers of
TB patients* One would think that the health personnel a...over .would be up in arms and atleast demand
to know the
reason of this downward trend and shortages* This is when man j
of them have felt the shortages in their areas themselves.
TB authorities refuse to admit there are short sges of anti TB
drugs.
The answer to our requests to our member institution'.
to let us know if they have faced anti TB drug shortages for
proof, has been - evidence mainly silence.
Talking of TB it is known that 92% of the infections TB cases
are AWARE OF THEIR SYMPTOMS and 52% seek medical help on their
own. 90% of these come away with cough syrups and topics. The
fact that our case finding and case holding is as hopeless as
it is, makes the whole story of rational TB care - a tragic one.
Misuse of 2nd line drugs and steroids does occur, with increas ing numbers of infectious TB cases, emerging resistance and
known limitations of BCG - TB picture is bound to get gloomier.
TB patients continue in the meantime to consume gallons of
different types of tonics cough syrups, gulp down different
coloured vitamin pills, steroids or semething to improve appe
tite or bring down fever.
The fact that the medical establishment has failed to deal
effectively with a problem like TB could mean that without
realizing
- we are beginning to lose touch with the actual health
needs of the people.
- with our silence we‘ve allowed the Drug industry to
subtly control our prescription practices and our deci
sion making
Story of leprosy care is not too different while 1/3 of world's
leprosy patients live or should we say struggle for survival
in India, our drug industry produces 3g of the minimal require
ment of Dapsone. While some health personnel in remote areas
treating leprosy patients cry themselves hoarse about the short
ages of this cheapest antileprosy drug — the medical community
comes up with a better way of treating leprosy patients —
the multi drug regimen.
Ensuring, that adequate essential drugs are produced and made
availabe is the responsibility of the socially conscious health
personnel — soecially those in the voluntary sector.
If we could realize that production of unessential nonsensical
drugs is at the cost of production of essential and life
saving'drugs - we'd be more aggressive in getting the former
thrown out and no longer extend the tolerance which we have
done in the past.
There has been enough talk about issues related to drugs, but
does drug misuse still continue? those misusing drugs fall
into one of the following 3 categories:
why
<$'4
flate \
D-10/344
FiS~\< 27/2/84
:16:
Category 1:
Those that misuse them, and do so knowingly
for vested interest and couldn't care less.
Category 2:
'
Those misusing them, but do so out of iqnorancbecause of inadequate or biased information
available to them.
Category 3:
Those that are aware about the true nature of
drugs and would not like to prescribe them,
' but find themselves prescribing these drugs
for various reasons. The most common reason
being 'patient demand'.
Unfortunately after graduation we have the licence to practice
as we please, with no checks, no controls, "and sometimes in
some cases with no sense of medical ethics. Till malpractices
and misuse of drugs remain unchallenged by medical cdleagues
consumer groups, peoples organizations and the patients them
selves - they will continue and increase.
Where category 2 and 3'are concerned what is needed is creatic
and development of alternate channels of information. It is
true that socially conscious health personnel from institution
in the field, could easily teach the medical graduates and
doctors in the more privileged medical institutions what
Rational Drug ■‘■’herapy in the field, with all its constraints is
all about. Specially when supported with authentic need based
information and their own experience and that of others in the
field.
Some of the important roles of the health personnel in the
field are:
1.
Deliverer of rational health care to the patients.
2,
Facilitator for the people in their obtaining the necessi
ties for their health needs eg. water, work, wages etc.
3.
Educator in the real sense of the word,where colleagues,
and patients, are concerned.
Participator in analyzing major policy decisions at macro
level which has an impact on peoples health, and'always
attempting to ensure that health and drug policies are
Socially just and that they enhance health and not
jeopordize it.
5. Researcher - creating alternatives based on observations,
c 1 in ic al studies, atleast identifying areas requiring
. exploration and research.
4.
The pioneering effort towards Rational Drug use and towards
changing role of health personnel will necessarily have to cor.
and will come from the voluntary health sector. We offer our
support and solidarity to such courageous pioneers. We extend
them a warm welcome, to the drug action network. .Constituting
socially conscious individuals and organisations.
(Dr. Mira Shiva, MD)
Coordinator
Low Cost Drugs and Ration -.1 Therapeutic
(Prepared specially for Andhra Pradesh VHA & West Ben^-''
General Body Meetings on Rational Drug Use)
CENTRE FOR SCIENCE AND ENVIRONMENT
807 Vishal Bhawan,
95 Nehru Place,
New Delhi-110019
INFORMATION SERVICE ON
Science and Society-Related
Issues
TOWARDS HEALTH AND FAMILY WELFARE FOR ALL VII
PRESCRIPTIONS AND THEIR PRESCRIBERS
Everytime a patient goes to a dqctor he '.’ants a
prescription. But do doctors always prescribe right ?
Do they sometimes overprescribe ?
The enclosed article
analyses two common prescriptions.
COMMUNITY HEALTH CELL
47/1, (First Floor)3c. Marks Road
BANGALORE - 560 001
Author Dr Ulhas Jajoo is a Reader with the department of
medicine in the Mahatma Gandhi Institute of Medical Sciences
at Sevagram.
The Centre for Science and Environment Is a non-profit, non-governmental, quasi-academic research organisation that has been set up
to increase public awareness of the role of science and technology in national development. The Information service Issues news
and feature items in six languages—English, Hindi, Marathi, Bengali, Malayalam and Punjabi—prepared by a research team consisting of
professionals qualified in science and technology.
Director : P- Dasgupta
Director of Research : Anil Kumar Agarwal
PRESCRIPT IONS AND THEIR PRESCRIBERS
By Dr. Ulhas Jajoo
Everytime a patient goes to a doctor, he goes with an element
of faith.
He expects two things from the doctor : one, the
doctor will diagnose the cause of the problems; and, two he
will prescribe some medicines to get rid of the cause.
But do doctors always prescribe right ?
Do they sometimes
overprescribe ?
Let us study a few prescriptions usually given by qualified
doctors.
The following are actual prescriptions for two common
problems for which ’ie often visit doctors.
Case I : The disease is acute diarrhoea.
The history of
illness is loose motions 3-4 times a day from first day; no fever,
no abdominal pain and no vomiting; and, passed urine five times
in last 12 hours.
The treatment given is Lomomycin syrup two
teaspoonful six hourly; Lomotil tablet one with each stool;
Pecto-Kab two traspoonful six hourly; Baralgan twice a day;
Flagyl syrup two teaspoonful three times a day; and Pentaimine
one tablet twice a day for three days.
Let us analyse this prescription.
diarrhoeas are self-limiting.
(Lomomycin).
Firstly, most acute
They do not require antibiotics
Secondly, Lomotil is a drug of the morphine group
which may reduce the frectuency of motions but hides the fluid
loss which continues within the cjut.
In the false security
of diarrhoea being controlled, the child may land up with severe
dehydration.
Thirdly,Bismuth Kaolin (Pecto-Kab) has no role in
treatment of diarrhoea.
It creates a false impression of
/more...
CSE/2
diarrhoea being controlled as it solidifies stool.
Fourth, unless
pain is severe, Baralgnn like drugs do not have any use.
They
should never be given in twice a day dose but only as a single
Fifth, Flagyl is a drug
dose, when required, to relieve pain.
used for amoebiasis and giardiasis.
Unless stool examination
reveals these organisms, addition of this drug to a prescription
of bacterial diarrhoea (antibiotics are being given already)
is not ethically justified.
Sixth, Pentalmine is a drug used
against worms. It is the costliest wormicide available in market.
Rationale of 'V''''-tngyi this drug to the prescription, cannot be
explained without carrying out a stool examination.
The Conclusion is : this is a 'shot-gun' therapy. All the
drugs against the common causes of diarrhoea have been prescribed.
Some drugs are not ethically justified.
The most important
part of the treatment of diarrhoea is oral rehydration (to avoid
the dehydration) is totally missing. One glass full of water
with a pinch of salt, sodium bicarbonate and two teasooonful
of sugar is all that is required which is available with everybody
at home.
Most diarrhoeas of this type are self-limiting and
Get cured by the third day.
The cost of such a minor ailment
has been alarmingly raised by visiting a doctor.
Case-2 : The disease is common cold.
is running nose for two days; cough f°r
The history of illness
one day; throat pain,
one '’ay; and, mild fever one day.
The treatment given is tablet septran twice a day for seven
days; otrivin nasal drops thrice a day for seven days; tablet
Cosavil, one tablet thrice a day for seven days; tablet Crocin
one tablet twice a day for seven days; Benedryl cough syrup,
one teaspoonful three times a day; Injection B-rcomolex; throat
lozenges; and, syrup B-complex one teaspoonful twice a day.
/more...
CSE/3
Common cold is a self-limiting viral infection which responds
within seven days if treated and takes a week if not treated.
Role of a potent antibiotic like 'Septran' which can sometimes
harm the patient cannot be justified.
nasal drops to dry nose.
the market.
Otrivin contains ephedrine
It is the costliest preparation in
Cosavil contains aspirin and an antihistaminic
drug which also helps in drying the nose.
Combination of Crocin - a
pain and fever relieving drug - when aspirin is already being
given is not justified.
To sunpress the irritating cough of
common cold, one does not need a Benadryl syrup (which has
antihistaminic drug as an ingredient), but codein syrup or tablet.
Addition of ben-^dryl syrup to the drug list only helps in
increasing the cost of the prescription.
Use of injection
B-complex and Syrup B-complex is unwarranted except to help
pharmaceutical firms or the doctor to fetch money out of an
injection. Throat lozenges are costly. They help only to
suppress the cough by their local action. The age old remedies
like "Harada", "Jesthamadh" or throat paint application are
better.
The simple conclusion is : the prescription is mainly to
provide "bread and butter" to the nrescriber and to the drug
industry.
The real therapy — repeated saline gargles or steam
inhalation - is totally forgotten.
The repetition of the same
drug in different forms has increased the cost of treatment.
There can be innumerable such examples.
The observations
f^om the prescription can be summarised as follows:
1.
Unscientific prescribing: Many nrescrijpitiam reveal combination
of incompatible drugs. Many times the doses of the drugs
prescribed are inadequate. This reflects poverty of the
knowledge of the prescriber.
/more
CSE/4
2.
The prescription is aimed Rt„early relief of symntore even
if it is likely to harm the patient in the long run.
For
examole : doctors have a shotgun therapy thcirprescription
which covers all possible causer for a particular clinical
symptom so as to avoid efforts required for a careful diagnosis
This tendency exnoses a patient unnecessarily to many drugs
and their side effects.
It reflects the inferiority on the
part of a doctor to properly diagnose the cause of illness.
Secondly, potent drugs have been used when they should
normally be preserved for desperate situations.
For example:
(i) use of broad spectrum potent antibiotics even for an
illness which docs not require them, exposes the population
to the problem of d v L~~fnr r• r. ist^.nchnr against these drugs.
(ii) Corticosteroid preparations like Betnelan, Wymisone,
etc, though good drugs are like double edged sword.
If not
used at a proper time and in proper conditions they can harm
the patient in the long run.
3.
Many prescriptions are aimed at earning money.
Most
illnesses that a private practitioner deals with are self
limiting. Once a patient has come to a doctor, he feels it
obligatory to prescribe some drugs even if not necessary.
Most doctors do not charge consulting fees separately.
They
dispense drugs from their dispensary at an exorbitant cost,
which includes their consulting ch-rge.
The charge depends
on the paying capacity of the person.
The name of the drug
dispensed is never told to the patient because if the patient
knows it,
he may try to compare the cost
the market
rate,
m?rethe number of drugs prescribed/bic ger is the
profit.
The big list of drugs, thus, is a mechanism to earn
money without the patient being aware.
Doctors have conditioned the minds of the people to drugs
so much that now if a doctor does not prescribe, for instance,
an injection, the patient starts demanding it.
CSE/5
ur-
The
a poet
is on the patient’s pocket — in India, usually
person — who spends all that he has in blind faith.
It
is not the doctor alone who earns in this business, but also
the pharmaceutical industry.
A doctor's knowledge is enriched
from time to time by pharmaceutical agents, who try to convince
him that his company’s product is the best available.
A heap
of physician’s samples is usually enough to convince- those who
are hesitant.
The free samples arc then sold.
to see a doctor whotefuses
patient.
this bribe.
It is unusual
The sufferer is the
The doctor hardly ever knows anything about that the
ingredients in the brand drug that he is prescribing, nor does
he have knowledge
of other similar brand drugs which may be
cheaper.
Why is all this happening in a noble profession that is
concerned with human suffering ?
The root of the malady lies in our value s ystein.
profession has unfortunately been commercialised.
The medical
If this goes
on too long, the faith in the healer may cease to exist.
ir
Phenyl butazone - oxyphenbutazone
hazardous drugs
Prepared for:
Drug Action Network core
group meeting at Sevagram
30 •- 31 July 1984
Dr. Mira Shiva, VHAI
U, K,:
On 6th March 1984, U K banned Phenylbutazone.
On 3rd April.' 1984. Ciba Geigy withdrew Oxyphenbutazone, a
breakdown product of phenylbutazone from U K market.
In Germany 65 such drugs have been banned, and. use cf another
206 severely restricted.
In Finland, manufacturers have been asked to withdraw these
drugs.
In U 3 the Public Citizen Health Research Group has asked the
department of Health and Human Services for an imminent danger
Japan
has severely restricted the use of these drugs.
IOCU has sent world wide consumer alerts.
Norway, Federal
Republic of Germany, Italy, Australia, Sweden, Finland and
Bangladesh have severely restricted their sales.
It is not that, we have not bean concerned about the misuse of
these antiinflammatory agents and their irrational combinat
ions, prior to the knowledge of these bans. We feel that after
receiving unbiased authentic information about the extent of
the adverse effects related to these drugs, it is our respon
sibility to alert others. The public needs to be informed of
their dangers realizing that a significant number of patients
to buy the drug- over the counter’ unwarned and unijjf ormed.
We are using this as yet another case where, double standards
have existed in the drug information given to doctors in the
West and to our own doctors.
The total .annual turn-over of the two products of phenyls
butazone and Oxyphenbutazone (BUT'AZOLIDIN & TANDRIL of Ciba
Geigy's) fetch 200 million Swiss-Francs ie. £ 65 million ie.
ite 1170 million and these drugs have been in the market since
1952 and i960 respectively and are well known). It is very
unlikely that, Ciba Geigy will withdraw these products from
the third world, specially after having already stated their
decision to withdraw liexaform(Clioquinol) and Dianabol(Anabolic
Steroid) from the world market. Withdrawing Butazolidin and
Tandril at this point would lead to a financial set-back. It is
unlikely that Ciba Geigy will give in very easily toconsumer
pressure- a stand already made clear by the makers of Eutazolidin and Tandril.
What are these drugs
for?
Phenylbutazone and Oxyphenbutazcne are non-steroidal
antiinflammatory drug's which also have mild anti-pyretic and
analgesic properties. They give only SYMPTOMATIC RELIEF and
COMMUNITY II4ALTH CELL
47/1, (First Floor)St. Marks Road
BANG '* 1.0 IE - FRO 001
, . .2
in no way ALTER the course of the illness. In the U.S. the
labelling indicates the drug for "acute gouty arthritis",
"active rheumatoid arthritis", "active ankylosing spondylitis",
"short term treatment of acute attacks of degenerative, joint
disease of the hips and knees, and not responsive to other
treatment and painful shoulders". Ciba Geigy warns that Tandtil
should not be given to children below 14 years(The Physician
Desk Reference, U S A).
Similarly, warning for elderly patients is given, that
every effort to discontinue the use of these drugs after a
period of 7 days should be made as there is "exceedingly high
risk of severe fatsi toxic reactions".
In Malaysia, dose packages for children as small as 12
months carry inserts. Ciba Geigy states, that in elderly pat
ients as also in long term therapy, smaller maintenance doses
are indicated.
In.West Germany, the use of the 2 drugs is severely res-"
trictcd to:
1) ankylosing spondylitis; and
2) gout for the maximum of 7 days.
(In a personal communication from Dr Olle tlanasen, January
6, 1984).
In the third world it is indicated for minor ailments
including joint stiffness of muscles and joints lumbago, head
ache, viral infection and fever and for long term treatment.
Phenylbutazone was introduced into India in 1349 strictly
for treatment of rheumatoid arthritis and. allied disorders.
The drug is more of an OTC product in India being freely
consumed by public, often without prescription, for aches,
pains and fever.
Phenylbutazone with its equally potent relative oxyphen-^l
butazone needs to be taken more seriously. IT IS A BAD BET TCi
G:J5BLE WITH IT IN NON-RHEUMATIC DISORDERS.
" Io India, oxyphenbutazons is being used for treatment of
fractures, post operatively, in dental practice;' ordinary~
common joint pains; bodyaches and backaches" according to Pune
Journal of Continuing Health Education, June 1981.
/in the
Dr W V Rane of Arogya Dakshata Mandal talking about oxy
phenbutazone has pointed out that it is being promoted for
quicker post operative healing. Not only is this unethical but
it is also unscientific and irrational. More painful is the
fact according to him that a study was conducted by ♦’
Professor of an Orthopaedic Department for bone healing and
that too on • Paediatric patient. The paper was presented to
an August gathering and most probably, received its quota of
applause and mutual back scratching from the Conference
sponsors. No one in that scientific gathering questioned the
rationale and ethics of conducting the study on children, when £n
the U.S/ Medical Pharmacology books the use of these drugs in
those below 14 is contraindicated.Probably the drug company
sponsoring the study preferred• not to give tnis dismissable
bit of information.
...3. ..
.
■ "Phenylbutazone' and' oxyphenbdtnzone should nut be Used unless the uriner'had been examined fifr" protein and a blood
examination and had shown that white cells and platelet counts
were within the normal range. B K Ansell, Prescribers Journal,
1969, 8, 120 in 14 art in dale- the e xtrapharmacopia, 23th
oition, 1982. a routine urin'e and blood test prior to usage of
the drug is recommended. In view of the additonal costs this
may not always be possible forthe poorer patients. An extra
caution and restrain in the utilization of. t hese A rugs is there
fore, indicated.
In India the drugs have been recommended by certain ma
facturers for minor problems and feeble conditions. Gifford.
1973 has been quoted in MIMS editorial, November 1982 that
according to Pharmacology books "Phenylbutazone as an antioyretic and an analgesic is relatively inferior to aspirin?
Phenlb__________________________________________________
utazone as an antiinflammatory
effective, but
serious toxicity limits its use in long term therapy. - In
rheumatoid .arthritis, phenylbutazone has a limited, x-o.e and
should be used primarily for acute exac~frat ions not relieved
WI2J ARE THE DAIGER3 ASSOCIATED WITH THE USE OF PHENYLBUTAZONE
OXYDHENBUT AZ ONE?
Bone Marrow Toxicity:
aplastic anaemia or pancytopenia ie. tot.nl bone marrow
shut down which is fatal in over 50% cases. Agranulocytosis,
which is a severe depression of white blood (granulocyte cell
production - fatal in about 35% cases). Leukaemia which is a
cancer of bone marrow; Gastro intestinal bleeding or peptic
ulceration - fatal in about 20% cases.
Other risks are liver damage Hepatitis in less than .1%
cases access to liver. It is mainly hepatic-cellular necrosis.
Hepatitis usually starts within 4 weeks of starting treatment
but in 20% cases can bo started upto or even after 1 year.
Cholestatic Jaundice occurs in less than 3% cases. Servin
sickness type of hyper-sensitivity, ulcerative stomatitis,
nephritis(kidney failure) thrombocytopenia(depletion of plate
let count) are other serious side effects, tnough some of these
are much rarer. (Ref: Phenylbutazone and hepatitis-Fowler P D
Woolfe D, Alexander 3 Rheum Rehabilitation, 14, 17, 1975).
MI14S editorial adds that "because of its sodium and
chloride retention properties, phenylbutazone can increase
plasma volume by as much as 50%, thus straining cardiac funct
ions and occassionally causing acute pulmonary edema. Since,
toxic effects are more pronounced in the senior citizens, the
drug is contraindicated for use in geriatic patients.
The seriousness of the Problem:
A STUDY IN SWEDEN OF DRUG INDUCED BLOOD DYSCR13IAS ATTRI
BUTED PHENYLBUTAZONE AS THE DOMINANT CAUSE. (Drug induced
dyscrasias in Sweden Battinger L E & Westerholm N, Brutish
Medical Journal, 3 339 1973).
Incidence of bone’marrow aplasi due to-phenylbutazone
and cxyphenbutazone is assessed as 1 in 33000 to 1 in 990,00.
Aplusie" anaemia or agranulocytosis were quoted as underlying
or contributing causes of death. In 376 death certificates
in the year October 1974 to September 1975? the mortality rate
was estimated as 2.2 per. 100,000 cases.
The study 'of fatal bone marrow depression with special
reference to phenylbutazone and oxyphenbutazone- Inman W H W,
British Medical Journal 1-1500 (1977). The effect of bone
marrow depression is serious..Drug induced agranulocytocisphenylbut.azone. Pisciotta A V Drugs 15 132 (1978) Drug induced
bone carrow depression by phenylbutazone, British Medical
Journal 4, 490 (1973).
Ciba Geigy's adverse effects department at its head office
in Basle in one its internal memos in February 1983, gave its
findings of 1182 reported deaths from these drugs
2724
detailed patient reports of other adverse effects. Well^k
ever 1/2 of these deaths were from bone narrow toxicity inclu^F1
ding leukemia, gastro-intestinal'bleeding or perforated ulcers.
Of the 6716 cases of undesirable side effects reported on the
drug, 777 persons have known to have died with Butazolidin
between 1952 and 1081. Of 4165 cases of side effects reported
with Tandril, 405 persons are reported to have died. 199 cases
of serious undesirable effects and 18 deaths have been reported
in Japan.
After 12 years, the receipt of the first report of adverse
reaction to Butazolidin from Great Britain, came from West
Germany indicating that identification of adverse reactions
come along only with experience and a high degree of alertness
and suspicion about possible adverse reactions. In third
world countries, adverse reaction reporting is.depressingly
inefficient, as are the controls on potentially hazardous drugs.
Double standards in giving the drug information to tie health
personnel makes matters worse.
•
Phenylbutazone and oxyphentubazone is poorly tolerated by
many patients. Even if diarrhowa, nausea, nervousness, insomnia
are associated with the drug, it is ignored that the potential
fatality cannot be overlooked. Some type of side effect is
noted in 10 to 45 °/° of patients and medication may have to be
discontinued in their cases. Its use should be limited to
short term therapy of not more than a week during any one trea
tment period. Even then, the incidence of disturbing the Side
effects is about 10%. Phenylbutazone has a limited role in the
therapy of rheumatoid arthritis. It is primarily used for
relief of acute exacubations of the disorder that are not
relieved by the other measures.
Goldman Gillman; 5th Eiditicn
Chapter- 17.
According to Martindale : ^Although phenylbutazone is
efxoctive,in almost all rheumatic disorders including ankylo
sing spondylitis, osteo arthritis, rheumatoid arthritis and
reitusdeseas, it is GENERALLY RESERVED FOR USE IN TUB TREAT+
ME® OF RHEUMATIC DISORDERS where less toxic drugs have failed.
- Martindale' ; 28th IXlidion
...5...
In 1975, a study was done in U.K. to determine the true
incidence as opposed to the reported incidence of deaths due
to .aplastic anaemia, and agranulocytosis in people using
phenylbutazone or oxyphenbutazone. In U.K. even where all death
certificated mentioning a. drug have to be reported to the
Government Drug Authority, only 1 out of 4 deaths duo to drugs
were found to have been reported. It was only because of the
study, that the relationship of tho drugs and death could be
found. According to Oliver Gillie, medical correspondent,
Sunday Times, states "In Britain whore the 2 drugs have been
used cemparitively cautiously, 512 deaths associated withihem
have been recorded between 1964 and 1980. But, the- real total
is probably at least double that world-wide^ as reported in
the Ciba Geigy internal report (Ref: Dr Hanssen) which records
1132 deaths associated with the drug upto 1982.
Since it is impossible that almost half of these deaths
secured in Britain alone, many deaths must have gene unrecorded
in other countries and the actual figures would certainly run
into many thousands, giving Butazolidin and Tandril amongst thcr
highest death total for any drug*.
Scrip. ITo. 854; December 12, 1983;
pg.18.
In U.K. the death rates were found to be 22 deaths per
million users of phenylbutazone, and 38 deaths per .million
users of oxyphenbutazon. Dr Sidney Wolfe uses the companies
own estimates of patient exposure world-wide ie.75 million
users of phenylbutazone, 66 million users of oxyphenbutazon to
estimate the number of patients that must have been affected.
Using the U.K. study result and their mortality rate due to
these drugs as the basis, he estimates the following;
with phenylbutazone, about 75 .million people exposed
by 22 deaths per million ie. about 1650 deaths.
with oxyphenbutazone, about 60 million people expo
sed by 38 deaths per million ie. 2280 deaths. Total=
3930 deaths(ie. 1650+2230)
World wid-e from aplastic anaemia and agranulucytisis; 3930
deaths musfc have secured many of which went unreported. The
internal document shows that aplastic anaemia and agranulo
cytosis constituted 37.8% of the deaths. If 3930 deaths consti
tutes only 37.8% of total deaths, then the total number of the
deaths duo to these drugs would be approximately 10,400 ie.
10,400 deaths world-wide merely due to'use of 2 drugs. If we
try to extend this to other brands
are ■* available in the
market, then there would definitely be more deaths. By mid
1982, 311 deaths in U.S. were reported. It is known that only
one in ten deaths due to those drugs got reported. In other
words total deaths would be over 3100.
According to Dr Olio Hanssen .another Ciba Geigy's internal
memo has stated in light of the ’dancers of the"dtijg-’"the
presence of many newer equally effective non-steroidal anti
inflammatory drugs now available in the market with comparati
vely less toxicity, that it is reasonable and necessary that
the risk and benefit ratio . of Butazolidin and Tandril should
be carefully reassessed for tho indications of all forms of
inflammatory and degenerative arthritis as promoted, to see if
such promotions are justified".
6
»Sslay~isia;
Consumer association of Penang report 'based on discussions
with University Hospitals, Pharmacologists reports that
phenylbutazone and oxyphenbutazone are amongst the__5_ob'ugs
accounting for the majority of the adverse drug reactions
suffered, by patients, admitted into the hospital • 0 o ns urn o r
Association of Penang has demanded an immediate recall of
the drug from the market for the safety-and health of the
Malayasian Consumer.
Japan:
Mainichi Daily News which is a Japanese newspaper deuicatod to International understanding covered the news in its
headlines on 9th February, 1984. Ciba Geigy's antiinflammator
pain killing drugs killed 1182 in the world.
INTERNAL DOCUMENTS OBTAINED
BAN IS CALLED FOR
The newspaper covered the issue daily in its morning ar
well as in the evening issue, including a strong editorial,
The headlines on February 11, stated that the Government igy'o..
findings of courts in drug poisonings. Apparently,two litiga
tions took place .about 10 years ago. Investigations should bar
been done. About 15 deaths in Japan due to those drugs have a
so far been recorded. *'
. pharmaceuticals Co. stocking;
preparations of Ciba Geigy's declared withdrawal according to
Mainichi, February 10. February 12th- Mainich;,. "Documents of
side effects ordered severe restrictions being decided am1 ’....
is possible for all drugs containing these drug".
India;
Pune Journal of on-going Education : In this issue no. of
57, Juno 81, in a letter to the Managing Director of Ciba
Geigy, the Journal had raised strong objection .against their A
new product parazolnndin (parasolandin being a combination of
paracetamol and phenylbutazone) for indicating it for conditions
like fever.
C E R C:
CERC prepared a document on irrational and hazardous a. '■ ' ■
inflammatory agents, including phenylbutazone and ■ oxyphencnzcAO
combination with amidopyrines. They had submitted this to uh..
Drug Control Authorities and demanded their ban. It is imp oct
ant for us to be constantly aware that the situation in Ind.:. ?.
is more serious than the countries mentioned earler.
1k
2.
5.
We have these d rugs av.ailable over the counters in any
dosage for any duration of time with our (falsely con';i.’ui J
to believe in the sanctity .and magic of western medicine^ .
Patients are rarely given any warnings by their doctors
and if.they buy the drugs overthe counter they can ramely
make head or tail of the medical literature inserts..
Phenylbutazone and oxyphenbutazone' have been available often
dendly combinations with amidopyrine, analgin, paraceta
mol, diazepan, Vitamin B, dextrapropoxyphone acetomir.ophe
which makes the combination.
Phenyl butazone and oxyphenbutazone are dangerous drugs.
CONSOLIDATED list of products whose CONSUMPTION and/or
HAVE DEEN BANNED. WITHDRAWN. SEVERELY RESTRICTED
OR NOT APPROVED DY GOVERNMENTS
First
sale
Issue
PHARMACEUTICALS
I
|
PRODUCT NAME
IDENTIFIER
1
|
RANGAlOnE-560 001
COMMUNITY HEALTH CELL
47/1, (F irst Floor)S t. Marks Hoad
LEGISLATIVE OR REGULATIVE ACTION
Country
1
1
I
HORMONAL PREGNANCY TESTS
ef f ec t i ve
Date
|
:
in view of their apparent association with birth defects.
AUT
1978
Withdrawn
1978
Withdrawn from the market following consideration of
their use with birth defects.
GBR
1977
Owing to evidence of congenital
the manufacturer.
GRC
1980
All preparations containing estrogens and progestogens
testing were withdrawn.
ITA
NOR
197%
1970
Withdrawn from
abnormalities,
SAU
In view of their association with birth defects,
preparations are not recommended for use.
1978
Banned for
intended for pregnancy
the market.
NZL
April
the evidence associating
these products were withdrawn by
Voluntarily withdrawn from the market.
SGP
|
Description of Action Taken/Grounds for Decision
BEL
VEN
CAS NUMBER
all
such estrogen/progestogen
importation.
Not approved for use and/or sale.
K
CONSOLIDATED LIST OF PRODUCTS WHOSE CONSUMPTION AND/OR SALE
HAUE BEEN DAMNED, WITHDRAWN. SEVERELY RESTRICTED
OR NOT APPROVED BY GOVERNMENTS
First
I ssue
PHARMACEUTICALS
I
|
PRODUCT NAME
IDENTIFIER
I
|
TETRACYCLI ME(PED I ATRIC)
LEGISLATIVE OR REGULATIVE ACTION
|
Country
CAS NUMBER
|
60-54-8
:
Description of Action Taken/Grounds for Decision
effect ive
Date
BGD
Under the provisions of the Drugs(Contro1) Ordinance, tetracycline syrups have
been banned as they are harmful to children and pregnant mothers ; they disturb
bony growth of children up to 12 years of age and discolor teeth
DNK
Products currently available on the market.
IND
Liquid oral dosage preparations have been prohibited for manufacture and sal.e—
for reasons of health risks associated with use and/or questionable therapeutic
va1ue.
1975
Preparations for rectal use-C
withdrawn from the market owing to their
non-constant absorption. Since 1979. labels of concentrated liquid preparations
have warned about possible dischromic effects on tooth enamel.
1973
The Ministry of Health withdrew syrup formulations of tetracyclines (mixtures,
suspension or drops) particularly intended for pediatric use on the grounds
that tetracyclines interfere with the growth of bones and teeth in infants.
PER
1974
The package insert and/or label for this product requires a warning that its
use may be dangerous in nursing infants, children under 3 years of age and
pregnant women, due to the drug's well known effects on bone formation.
PHL
1978
Preparations containing ch 1 ortetracyc1 ine. oxytetracyc1 ine, tetracyc1ine.
demec1ocyc1ine, ro1itetracyc1 ine, methacyc11ne, dexycycline, minocycline, and
other tetracycline derivatives in the form of syrup (mixture or suspension) or
drops particularly intended for pediatric use are no longer acceptable by
Administrative Order No.342.
JOR
NZL
Pediatric preparations have been voluntarily withdrawn
1
f 87
CONSOLIDATED LIST OF PRODUCTS WHOSE CONSUMPTION AND/OR SALE
HAVE BEEN BANNED, WITHDRAWN. SEVERELY RESTRICTED
OR NOT APPROVED BY GOVERNMENTS
First
i ssue
PHARMACEUTICALS
I
I
PRODUCT NAME
IDENTIFIER
I
| ESTROGEN-PROGESTOGEN PREPARATIONS FOR SECONDARY AMENORRHEA
|
| CAS NUMBER
LEGISLATIVE OR REGULATIVE ACTION :
Country
1
|
effective
Da te
DEU
DNK
Oct.
|
Description of Action Taken/Grounds for Decision
1980
The Federal Health Office has withdrawn from the market relatively high-dosage
combination products containing estrogens and progestogens indicated for the
treatment of secondary amenorrhoea.
An expert committee had emphasized the
need to exclude pregnancy before such products are used, having regard to their
propensity to induce abortion.
1974
Use of high-dosage products has been cancelled.
SAU
The Drug Committee has advised using these combination products only after
pregnancy has been ruled out. Relative!/ - ■ ■
• «-ge products are restricted
for use.
VEN
Combinations for this
indication are not approved for use and/or sale.
•
-
70
Voluntary Health Association of India
-7Q(b_l
C-14, Community Centre
/ ~/ 1 6.7$aJdarjung Development Area
New Delhi-110016
G-psdsd }£sscrrt isil
Telegrams : VOLHEALTH
New Delhi-110016
,
u
668071
Telephones : 668Q72
Ijisis
3 X£lgJ-AiPXt-nPte ?
These are the guidelines to help Community health progra
mmes and health institutions draw up their own essential drug
list.
This is a compilation of various drug lists and it empha
sises the concept of Essential drugs. For those believing in
and for those involved in alternative health care, the concept
of Essential drugs is an integral part of health work.
The format used for this compiled list is based on WHO's
Essential drugs list , Technical Report Series 685. An outline
of it is given. It should^be noted that certain drugs are
repeated as they are used more than one disease entity.
The various drug lisi£ as they appear in the compiled form
are as follows:
BANGAlO-iE 560 301
Those drugs included in the Hath! Committee have been
uxiderlined. This drug list is meant to-be a guideline to help
health care institutions in the voluntary health sector to
select their own essential drug list. It is up to us to show
it to the government ajd Our medical colleagues who believe in
commercialisation of medical care that good health care does
not necessarily depend upon the length and variety ■-'f the
drugs used.
COWSHiONITY HEALTH CELL
Category I - for village level workers
Category II - for Primary Health Cure.up to Thana complex lev<:.
CMC Christian Medical Council list - Contact do.6'3,August
1981, "Getting Essential Drugs to the People"- Stuart
Locost: - Low cost standard therapeutics a collective vo'turWai'y
enterprise for rational therapeutics
C/0 Amr.l, G P 0 Box No. 7, Vadodara 390001.
ZJlsx
Essential drug list drawn up by sub-group dealing with'.
this at VHAI's Pune Workshop "The Drugs Issues seeking feasible alternatives".
PS I; - Formulary of Post Graduate Institute of Medical
Education and Research.
SL:~
Sri Lanka graded Drug list included here is list of
drugs recommended for doctors incharge of Peripheral
health centre.
Gambia restricted drug list based on their national
formulary.
E<?ho
An English NGO supply equipment and drugs to Charity
Hospitals overseas.
Action Mede or.
Our 4^rible., recommend at ions
A >
ror trained village Health worker level
B
)
for trained Paramedic or middle level workers
c
)
for doctors involved in primary health care
47/1, (F irst F loor)!-:. Morks Road
EMRO(Eastern iiedit eranean Regional Office)- WHO
List A - for Sth class passed
List B - for that are class 10 passed and have had training
It is extremely difficult to go against thecurrent created
by the market forces. It is a true test of our conviction and
our capability to convince others.
* - Alternative substitute from the same therapeutic group
can be selected based on comparative lost and availability of
equivalent products, eg. Hydrochlorothiazide: any other thia
zide type diuretic currently in broad clinical use.
Lumbers in the Paren thesis following the drug
names indicat
1) Drugs subject to international control under the Single
Convention on Narcotic Drugs(1961) and the Convention on
Psychotropic substances(-1971)
2) Specific expertise, diagnostic precision or special equip
ment required for proper use
5) Greater potency
4) In renal insufficiency, contraindicated ord'osage adjust
ments necessary.
5) To improve compliance
6) Special pharmacokinetic properties for purpose
7) Adverse effects diminisn benefit/risk ratio
8) Limited indications or narrow spectrum of activity
9) For epidural anaesthesia
Letters in the. parentheses following the drug names indi
cated the reasons for the inclusion of compelementary drug;
When
A.
drugs in the main list cannot be made available
When
B.
drugs in the main list are known to be ineffective or
inappropriate for a given individual
For
C.
use in rare disorders or in exceptional circumstances.
The criteria of selection of essential drugs,
Steps to be taken to implement such a programme. Provisi on of
information on essential drugs as recommended by WHO have been
dealt with earlier. In the text of the paper the format of the
drug list is as follows:
Revised model list of Essential Drugs - a WHO Expert Committee
Report - Technical Report Series
635
1.
anaesthetics
1.1 general anaesthetics and oxygen
1.2 Local anaesthetics
2.
Analgesics, antipyretics, nonsteroidal antiinflammatory
drugs and drugs used' to treat Gout.
2. 1 non - opioids
2.2 Opioid analgesics and antagonists
3. Antiallergics.
4. Antidotes and other substances used in poisonings
4.1 general
4.2 specific
5.
Antiepileptics
6.
Antiinfective drugs 6.1 anthelmintic drugs
6.2 antiamoebic drugs
6.3 antibacterial drugs
6.3.1 penicillins
6.3.2 other antibacterial drugs
6.3.3 antileprosy drugs
6.3.4 antituberculosis drugs
6.4 antifilarial drugs
6.5 antifungal drugs
6.6 antileishmaniasis drugs
6.7 antimalarial drugs
6.8 antischist os omal drugs
6.9 antitrypanosomal drugs.
...iii..
Antimigraine drugs
Antine©plastic and immunosup pressive drugs
Antiparkinsonism drugs
Blood,drugs affecting the
10. 1 antianaemia drugs
10.2 anticoagulants and antagonists
11. Blood products and blood sub stitutes
plasma substitute
1 1 °2 plasma fractions for specific
1 1.3 plasma substitute.
uses.
12. Cardiovascular drugs
12.1 antianginal drugs
12. 1 entiarrhythmic drugs
12.3 antihypertensive drugs
12.4 cardiac glycosides
12.5 drugs used in shock or anaphyl13. Dermatological drugs
13.1 antifungal drugs
axis.
13.2 antiinfective drugs
13.3 antiinflammatory and antipruri. ■
■ i
tic drugs
13.4 astringent drugs
13.5 kerat©plastic and keratolytic
13.6 scabicid.es and pedi- ' ’’.drugs.
culicides
14. Diagnostic agents
14.1 ophthalmic drugs
14.2 radiocontrast media
1p. Disinfectants
16. Diuretics
17. Gastrointestinal drugs 17.1 anacids and other antiulcer
drugs
17.2 antiemetic drugs
17.3 antihaemorrhoidal drugs
17.4 antispasmodic drugs
17.5 cathartic drugs
17.6 diarrhoea, drugs used in
17.6 1 ant id iarrhoeal(symptomatic
17.6 2 replacement solution, drugs.
18. Horraones
13.1 adrenal hormones and synthetic
18.2 androgens.
substitutes
18.3 estrogens
insulins
and
other
antidiabetic
18.4
agents
18.5 oral contraceptives.
18.6 ovulation inducers
18.7 progestogens
18.8 thyroid hormones and antithyi&fl.
19. Immunol ogicals
19.1 Sera and immunoglobulins
19.2 vaccines
1V9.2 1 for universal immunization
19-2 2 for specific groups 01 indivi20. Muscle relaxants(peripheral: _y acting) and choline- duals.
st erase inhibitors.
21. Ophthalmological preparations. 21.1 anti infective agents
21.2 a nt i inflammatcry ag e nt s
21.3 local anaesthetics
21.4 miot ic 3
21.5 mydriatic s
21.6 systemic preparations
22. Oxytocics
23. Peritoneal dialysis solution
24. Psychotherapeutic drugs
25. Respiratory tract,drugs acting on the 25.1 antiasthmatic C
drugs
25.2 antitusqives
26. Solutions correcting water electrolyte and ac id-base di st n
26.1 oral
b anc e
parenteral
27. Vitamins and minerals.
a i<-
7.
8.
9.
10.
■sential Drug List
Rout e of admin 1st rat i on d osa;
jL^s^L^st
PG]
:mc?
o
I Emij
.forms
.and strengths
C
Anaesthetics.
1.1 General anaesthetics and Oxygen
inhalation
ether,anaesthetic(2)
powder for injection,0.5g,1.Og
th iopental (2)
(Sodium salt) in ampoule
1 • 2_ Local anaesthetics
.5% inj, 1,2(hydrochloride)in vial
inj.1%, 2% + epinephrine 1:100000
topical forms 2-4 (hydrochloride^ I"
*Lid ocaine
2. Analgesics,antipyretics, Nonsteroidal antiinflammatory
P
A'-G/ _dr u-c’ s used to treat Gout.
2_. 1 Ron-opioids
. ac gty Isali.c^rlic
tablet 100-500mg, suppository,
50-150mg poed Aspirin
“ibuprofen
tablet 200mg
ind omet acin
capsule or tablet 25 mg
tablet 100-5OOmg,suppository 100mg
+ syp
paracetamol
2.2 Opioid analgesic antagonists
(PhenylbutazOne)/ Oxyphenbutasone
morphine(1)
inj 10mg(sulfate or hydrochloride)
in 1 ml ampoule
;
p ethidine.Hcl 5ml/ml
2_. Ant i al 1 e rg i c s
*chlorphenamine
episjephrine
tablet 4mg(maleate)
inj 10mg in 1ml ampoule
inj 1mg(as hydrochloride in 1ml I
ampoule
I
jA
’A
?iain List
Complementary List
.___________ _______
Route ofiadministration dosage
forms and strengths
Lie &is iCMC iLov,pui GT.” SL G| E -AM
A B
jCos t
1
En ro
1
chareoal,activated
i
i
—
i
4. Antidotes and other substances used in poisonings
4.1 General
.....
—
I’
Powder
4.2 specific
atropine
inj 1 mg(sulfate)in 1ml ampoule
diazepam
inj 5mg/ml in 2ml ampoule
5._ Antiepileptics
phenobarb it al( 1)
B
tablet 50mg,1OOmg,syp 15mg/5ml
capsule or tablet 25mg,1OOmg(sodium.
inj 50mg(sodium salt/ml in 5ml v?a± )
B
■
phenyt .in
in j... Earalg.efedg £Hat hi)
6. Antiinfective drugs
6.1 Anthelmintic drugs
mebendazole
tablet 100mg
6.2 _Antiamoffi ic drugs
chloroquine
diloxand.de
metronidazole
A
B
1
tablet 200-500mg
dehyro emetine(B)k1,7) inj 60mg(hydrochloride)in 1ml ampot Le
furazolid ine
.
to 500mg hydrate/5ml
,
tablet 200mg(as phosphate or sulfate
tablet 5OOmg(furoate)
inj 60mg
B
B
B
pthalyl s alb hat h i a z ole
1
1
i
C
C
a
piperazine
tablet 500mg(citrate or adipate)
senna tablet Ilevamisol)!! tablet elexir.
Elexir or syp(as citrate)equivalent I
t et r-achl or el'~.yl in e (Hat hi)
•
-
Route of administration dosage
forms and stretgths
6,3.1 Be.
*ampicillin(4)
■.ListCMC! Loir
»
;
.
LPU PG-HSL
cost
j Emro•> B
$
-4-
Capsule or tablet 25Omg,5OOmg
(annydrous)I
powder for oral suspension 1 25mg
(anhydrous)/5ml
powder for inj 500mg(as sodium
salt) I in vial
B
benzathine b enzylpenicillin(5
inj 1.44mg benzylpencillin
B
fortified benzyl penicillin
procaine benzyl penicillin 30000
u/ml + benzyl
pencillin 10000 u/ml
powder for inj 0.6g
B
enzvlpenicilli:
B
Imllion IU) 3.Og(=5millionIU0>(as
sodium or potassium salt)in vial
phenoxymethyl penicilli
tablet 250mg(as potassium salt)I
powder for oral suspension 250mg
(as potassium salt)/5ml
B
procaine benzyl penicillin(7)
powder for inj 1g(=1million IU)
3g(=3 million IU)
B
6.3.2 other antibacterial drugs
capsule 250mg
powder for inj 1g(as sodium succa nat
in vial
capsule ortablet 250mg(as lacto
erythromycin
bi onate)/5ml
powder for inj 500mg(as lactobionate) in vial
inj 10mg,40mg(as sulfate )/ml in
*g ent amjc in (4)
2ml vial
tablot 200-500mg
*chloramphenicol(7)
B
B
C
B
Main list
Compl ementary list
ns.(4) (sulphadiazine)
. *sulfamethoj1 azole+tricethoprim(4 )
Route of administration dosage
forms and strengths
List
A
B
SI G E .41*1 C I
TJ.S1 CMC j Low!
!
( ost |pu|gi.
Em: ’0
inj 500mg in 100ml
Suppository 500mg, 1g
tablet 500mg,oral suspension nOOmg
/
x
5ml
inj 1g(sodium salt Jin 3ml ampoule
tablet 100rag+20mg,400mg+80mg
1
A
. B
*t et racy'clin e(4.)
doxycyline(S)(5,6)
capsule or tablet 250mg(hydrochior id e)
capsule or tablet 100mg(as hydroch:
loride)
inj 100mg(as hydrqchloride)/5ml in
nitrodurant oil-’: A.B)(4.7) tablet 100mg
ampoule
Hydroxy cuinc
. jEUXaa olj=£ in?
clofazimine
dap sone
1
I
’
100mg tablet
6• 3»3 Antilepr wsy_c rugs
capsule 100mg
tablet 50mg;,100mg
rifampicin
6
et haimfrmit ol
t ab1et 100-JOOmg
pyrazinami'd e
tablet 5009g
rifampicin
B
1
■
; c
. c
•
B
capsule or tablet 15Orag,JOOmg
. streptomycin _-(4)
.
t h i o.ac et az on e^isoniazid
powder for inj 1g(as sulfateJinviaL
. B
i
i
j
i
tablet 50mg+100Eg,15Omg+3OOmg
Thiacetazone
di.Qj.llvl£.2£ba.
•
•
capsule or tablet 150mg,300mg
. 4 Ant it ub ere ul os is drugs
tablet 100-500mg(hydrochloride)
isoniazid
I
!
!
6*.4 ..-.ntifilarial, drugs
tablet 5O'-ig(citrate)
6.5 Aj it if tin al d_rug
I
JI
■
'■
I
I
1
ll
i.
I
!
i
! °
1
*
i
!
1
1
1
|
!C i
L :
1
1
»
!
j
*
ent ary li
6.6 Ant ileishcianiasis '
•odiun stibogluconate................... ~
p:entanidi ne
6.7. A
*chloroquine
.arial drugs
,J-’ '
q o o5• •o
Rout e~oT acTnnist"rat’'.”on~dosage
forms and strengths
i stlii st iHciow
Cos t.
A™
! B
Eafro
'PU?GI SL G
-■
•
inj 53^ equivalent of 10% antimony
in 30nl
powder for inj 200ng in vial .
B
( C
C
tablet 150ng(as phosphate or
syrup 50cg(as phosphate or sulfate
tablet 7?5ag ((SSi^’heSphStej
tablet 500ng(as bisulfate or
inj JOOng(as diHyJrScSloride)/
al in 2al ampoule
.quinc
jquinine
pyran: et he ine
sulfadoxine+pyrimethamine(B) tablet 500ag+25mg
' • Ant is igraine drugs
.. •
tablet 2..".g(as tartrate)
B
B
B
B
affecting the blood
10j Bl Q.OC. _ _ runs
_____________
10.1 Zn-uianaer-ia drugs
tablet equivalent to 6Ocig iron
ferrous salt .1
(as sulfate or fumarate)
oral solution equivalent'to 15ag
iroh(as sulfate) in 0.6r.l
tablet 1ng
folic acid(2)
inj log(as sodium- salt) in 1ml aajoul
*hydroxoc obalamin( 2)
tran(B)(5)
A/'
inj 1r.g in 1nl ampoule
inj equivalent to 50mg iron/al
in 2ml ampoule
s scular drugs
12^
_____________________
12’. 1 iJitianginal drugs
_•
tablet (sublingual)0.5ng
C
1 P
7
M'.in list
Co iplonentary list
Route of administration dosage
forms and strengths
—
1 ist
F7
PG I SI G E /JX[ 3
C
CMC. jOW
ost.
Emrc
—
t et racycline .ointment
c hloranphenicol
13.3 antiinf lam...atory ..and antipruritic drugs
*betameth?,zone(3)
ointment or cream 0.1%(as valen ite)
*cala.mine lotion
^hydrocortisone
B
lotion
ointment or cream 1%(acetate)
B
B
•
13.5 Kerat aplastic and k er at olyt.ic_.agents
salicylic acid
solution topical 5/6
•
B
1 3« 5 Scab ic ides and -p.d iculicid es
b enzyl b enzoat e
1 ot i on 257°
14 • Diagnostic agents
tub ereulin, purified' pf ot’ien
derivative (PPD)
"
injection
fluroescein
eye drops 1/( sodium salt)
*chlorhexidine
*iodine
^furos em1.de
14.1 Ophthalmic drugs
”15 ■ Disinfect nub f?
1Diuretics
- - -
*hyd rochlorhtniazide
B
C
tablet 4Ong
inj 10ng/nl in 1ml ampoule
tablet 5 Ong
•
B
B
•
oral suspension equivalent to
550mg magnesium oxidu/10s 1
t ab. ant ac ijXuat hi )
*pror?ethazine(^) 17.2”^tiemetic"?’rigs tablet 10mg,25mg(hydrochloride)t fel.
chlojr^.-"'S’i’Zin(i
'
.
solution 5%(gloonate)for dilutii >n.
solution 2.5^
17X Gastrointestinal drugs
alur.iniiu':. hydroxide!.;^
tablet 500mg
oral suspension 320ng/5ml
magnesium hydroxide
A
elixir or syrup 5mg (hydrochloric e)
/5ml
•
•
A
I
....7.....
Main list
Complementary list-
Route of administration dosage
forms and strengths
ow I !
List cmc: ostkpqpGi
SI G E
!
Erurc
!
t et racyc line .ointment
c h 1 o ranp h enic ol
15.5 .Ant i inflam-, at cry _and _ antip r ur i t ic drug s
*betanethasone(5)
ointment or cream 0.1%(as valer; ite)
*calanine lotion
^hydrocortisone
B
-
B
15.5„_Keratoplaetic and kerat oly.t..ic„agents
salicylic acid
..............
‘soKfion topical 5%
B
15<o Scabicides and p:diculicides
benzyl benzoate
lotion 25'7°
1 -r , U J- Il 0 S bic
*furoRenide
15. Disinfectants
16. Diuretics
’
'*hyd r ochl grot hiaz id e
•
■
injection
eye drops 1%(sodiun salt)
solution 5%(glconate)for dilutii in.
solution 2.5^
B
tablet 40ng
inj 10ng/ml in 1nl ampoule
tablet 5 Ong
B
•
B
•
oral suspension equivalent to
5 5 Ong magnesium oxide/10r 1
tab. antacid(nuthi)
*pro;?ethazine(£) 17.2 -xtiemetic drugs tablet 10mg,25r.ig(hydrochioride)?
Ghloi;-.-)-,r--.--.^ine
■—
•*
B
C
17j, Gastrointestinal drugs
aluniniiu- hydroxide (fl)
~~
tablet 500ng
oral suspension 520ng/5ml
r.iagh<esium hydroxide
A
ll"t s
tuberculin, purified pfStiea'”
derivative (BPD)
fluroescein
14.1 Ophthalmic drugs
*chlorhe-xidine
*iodine
I
C
B
lotion
ointment or cream 1%(acetate)
'
i
elixir or syrup 5rag (hydrochloric e)
/5„i
1
•
I •
I
•
i
JMC Low
"pg" .SL
list
Conpleicentary last
Route of administration dosj^e ililst Last
B
; ost p
___________ ____________________ .____________ f ora s a nd. sire ng t h s___________
__
.. -Bq C.G.
3
...
•
oral rehyd ration 17.2j6._2 Repl ace.a ent solution
salts(for glucose-sait solution)
ip e c a c uan&a
ant i flat ul er t
activated charcoal
•
solution
’ 18. Hormones
18.1 -firenal hcemoi es and synthetic substitutes
*d exam ethos on a
Jr-.
,•
tablet 0.5ng, 4ng
inj 4ng(sodiua phosphate)in 1ml
ampoule
♦prednisolonetablet 5mg
♦ethinyl estradiol 18.3 _3strogcns
tablet 0.05ng
♦glibenclamide
0
•
C
13.4 Ins_ulin_s and_,other antidabetic agents
' .. ..................
tablet" 5 mg............. ...
c
.V
T ol ub at arid c_
injection
c
Cnlorproparjide
1'3.5 Oral, c ont x-p,copt ives
* st hi hyl := st r.~.d 1 cl
*1 even.ergor'trol
'
tablet 0.03mg+15ng+0. 25ng
—
■.
C
1
1
I
I
i
1
!
.
insulin
J
.... ---- 3
inj 1mg(sulfate in 1d1 ampoule
17.6.1 IntidjjriAogaJ.( sympto iptic)drugs
tablet 3 Orc (phosphate)
gamma benzene hexacliloride(.l)
___________________________________
17.3 hntilaeavrtahoidgl drugs
♦local- anaesthetic, astringent
and ant iinila;.. .acry drug
ointment or suppository
Oxyphenonium bromide
♦atropin c (Rat hi) 17.4 Antispasmodic drugs tablet ,1i>g( sulfate)
■'codeine(l)
II
.1'1
. ..9
Main list
Complementary list
18.8 Thyro.
levothyroxine
Route of administration dssage
forms and strengths.
lis'fTist' CMC |Ld'w
A I B
■ Cost: PU?GI SL
......
one; and a nt i h yd r o id d rug s
tablet 0.05mg,0.1mg(sodium salt)
iC
potassium iodide
*propyit hie urac il
tablet 60ng
tablet 5 Ong
0
ant iv eno
Ual^‘Jplasma fractions should
comply with WHO requirements
in j for the collection,processirand quality control of human
blood and blood products
inj 10000 IU
20000 IU in vial
inj 50000 IU in vial
c
d iptherii
t tig- nus ant it oxi:
1.9•
1 .for. universal kuunizati_on_
BCG- vac cine (dried )
inj )all vaccines should comply
d qphjtxie Kia._P..antu&i.s-t et anug_eg co n.e. in j ) the WHO requirements for
biological substances.
diphtheria-tetanus vaccine
inj)
measles vaccine
inj)
•p.oliQ-.yelitis vacc.ine(liveattenuatec )inj/oral solution
i
ith
t etanus vacciae(WHO,Hath!)
i&g
19.2.2 cholera TABC,small pox
.
21x Opthalmologfcal preparations
silver nitrate. 21.1 antiinfectivo agents solution(eye drops) 1%
eye ointment 10%(sodium salt)
sulfacetamide
21.2 lilt iin.
hydros ori
' solution(eye drops) 10% sod iura saJ _t
eye ointment 1% (hydrochloride)
tory agents
!B
iB
; Bi
I ;
I i
’ b|
: I
i
10
Main list
Compl.
Route of administration dosage
forms and strengths.
lis^CMC'Low]
I
°
|cosiPU|PGI SLG
2J....4. nipt ic
solution(eye drops)2'%,4^(hydroclcride or nitrate)
21.5_x'.yd
physi ost igcinp~Qp,
solution( eye drops) 2-%(hydrobrodid
• h£riat ropinef 1)
22. p-rvt
tat>let 0.2mg(maleate), n
*ergomet:
mj 0.2mg(maleate)m 1ml ampoule
oxyt ucin
iinj 10 IU in 1nl ampoule
24 . Paychothera?eut ic- drugs
t ab 1 et 1OOag (hyd r oc hl or id e)
dchlorpz omazine
syrup 25-ig(hyd rochloride)/5al
inj 25ag(hydrochloride)nl in 2 ml
tablet 5 mg
ampoule
25. Respiratory tract, drugs acting on
pilocarpine
25/1 antiasthmatic "Slugs’
'
'
tablets 200ng
inj 25mg/ml in 10ml ampoule
inj 1rag(as hydrochloride)in 1mloi;Le
tablet 4mg(sulfate)
oral inhalation(aerosol)0.1mg
d oee
syrup 2mg(sulfate)/5nl
*salbutamol
arate maliate in 1000
.rd 5 ng, ephedrine 10ng,
■line 125 2 (Hat hi)
nos c ap ine(c op
tablet 50ng(as hydrochloride)
0 I
i'lain list
Complementary list
l^stiCMC
ro ;
Route of administration dosage
forms and strengths.
26. Solutions con ecting water, electrolyte and acid-base
disturbance; _
■oral rehydration'^feal'vs^ror o'Iucoe e-salt solution) (for compositon see
17.6.2 replacement solution)
potassium chloride
oral solution
glucose'(dextroso)26.2 Pnrentoral
injectable solution5% isotonic, 50%
hypert onic
glucose with s odium chi or id t.
injectable solution 4% glucose 0.18
s odi urn chiorid e
(Ka+0anpl/1) (01-30 mnol/1)
injectable solution
potassium chloride
sod ium bicarb onato
Sodium chloride (cholera fluid)
"
" 1.4% isonic(Na+167 lie ol/1!)
(HCO'3-167 nnol/1)
injectable solution 0.9% isotonic (
(Na*154 mmol/1) (01-154 n.ol/1)
in 2ml,5ml,10~l ampoules
calcium carbonate gluconate
water for injection
27. Vitonins and j inerals
ascorbic acid
~
.....
----- tablet 5Ong
♦ergocalciferol
capsule or tablet 1.25:ag(5OOOO IU)
oral solution .25ng/ml(10000 IU)
*nic ot in a" a id e
tablet 5Ong
pyridoxine
tablet 25cg(hydrochloride)
r et ino 1
capsule or tablet 7.5ng(25OOO IU),
60sg( 20000 IU0>
.
rib oflavin
oral solution 15mg/ml(5OOO IU)tab.5mj
tablet 0.5mg(as fludride)
s od iur f 1 uivd a (8)
vitamin
& D
vit E c-tudax (Prophylactic ITS11 therapeutic NFI with Vit C+ folic acid)
tablet + injection)
c,y r.ac obrJ-
i
|
;
i
j
t
•
Voluntary Health Association of India
Telegrams : VOLHEALTH
New Delhi-110016
C-14, Community Centre
Safdarjung Development Area.
New Delhi-110016
Telephones :
668071
668072
“July 17, iV'BZt
ESSENTIAL DRUGS
A DEMAND FOR PRIORITIZATION
Prepared for
V H A I members,
Drug Action Networkers
and all those who believe
in the concept
and implementation
of Rational Drug and Health Policy
Background paper
for
Drug Action Network
Core Group Meeting
K'xdha
30 - 31st JULY 19^4.
Dr. Mira Shiva
Coordinator
Low Cost Drugs
and Rational Therapeutics
V.H.A.I.
CtgrtMUNITY HEALTH CELL
W/1, (First. HoorJSt. Marks Hoa<j
BAA!GALORE - 560 001
E~4/37S(c) LCD & RT
7ih'I:pt: '19.7. '34 ~
SSSENTIAL DRUGS -- A DEMAND FOR PRIORITIZATION
- Dr. Mira Shiva, VH/I.
Content Out!ine
I.
Essential Drugs - An Introduction
II.
Courageous Efforts - Brief Review
Chile
Srilanka
Pakistan
Mozambique
Bangladesh
W H 0
India.
Ill.
Our Efforts in the area of essential drugs
.The. Selection of essential drugs and the essential drug programme
- W H 0 Recommendations.
V.
The Rationale of Essentia?. Drugs
Drug List?
or Why do we need an Essential
A.
Existing low priority to essential drugs*needed for the
priority health needs; and the deteriorating trends in output.
B.
DPCO The Drug Price Control Order and its regative impact on
Production of Essential, and life saving drugs i.e. Category I
and II drugs.
C.
Poor performance of multinationals in production of essential drugs.
D.
Dilution of PERA companies - an invitation to more formulations.
E.
The need for rational use of scarce resources. Controlling Cost
by:
1. preventing wastage of scarce foreign, a' cchangs oy net
importing excess inessentials.
2.
ensuring preventive health measures before promoting
inessential drugs.
3.
ensuring placing essential dru^s before inessential drugs
4.
increasing production of essential drugs, decreasing
drug costs through economy of scale.
5.
ensuring bulk purchase of selected essential drugs and
thus cutting costs.
3-V37S(o) LCD & RT
VH.'I:ptl9.7. '8'4
'71 o
2
F.
Subsidizing costs of essential drugs
G.
Need for j^lui.n^;ng_ nsrlcct demand and thus the drug
production pattern in favour of essential drugs
H.
Need to decrease drug misuse and overuse
I.
Need for efforts in preventing Iatrogenesis
J.
Need for ensuring unbiased drug information for health
personnel and consumers.
K.
Need for ensuring better quality control
L.
Need for ensuring generic prescribing
Graded Essential Drug List
1•
ESSENTIAL DRUGS
INTRODUCTION
The concept of essential drugs is the focal point of the drtigs
issue and of the rational drug policy.
Our focussing on essential, drugs does not mean that by ensuring
production and supply of essential drugs., tho health care status of
our people will dramatically improve. Wc are focussing on it to high
light the fact that majority of our pcoplo are net merely deprived of
health care facilities, but whatever they are given by way of health
care does not necessarily have their interest in mind. Tho kind of
health care facilities, medical technologies and drugs being promoted
under the garb of "sciontificity" and "modern advances" and as "latest
break through" usually serve the interest of tho "mpdical industry" i.c.
tho drug industry and tho medical establishment. Some of these modern
myths and superstitions have to be demolished. Eg. Myth I - medicine
is a noble profession brimming with selflessness, putting patients
interest and welfare, above self interest.
Myth II - Tho drug industry
produces 'pills for every ill' and is fighting an unselfish battle
against death and disease. If it wasn’t for them, lots of us would bo
sick and suffering if not dead. Myth III - India is a welfare state,
signatory of the Alma Ata Charter giving priority to Primary Health Care,
and that our health policies are people oriented and are guided by reco
mmendations of Committees like the Shore Committee, 194b, Hathi Committee
1975- Alternative strategy Health for All "ICMR-ICSSR Report 1981"and
even the last year-,the National Health Policy Statement all of which
emphasise that the health needs of the majority, have to take priority
over sophisticated,centralised,costly,high technology medical services
meant for the minority with the purchasing power.
....3/
-4/37S(o) LOU & RT
K/l:pt:19.7.’84
3
The concept of essential dr tigs, questions the health personnel
who arc supposed to safeguard the health of the people; it questions why
their prescriptions include irrational, iriossontial, costly combinations
and often hazardous •drugs. It questions the medical establishment for
not demanding’ bans on bannablo drugs, nor attempting to ensure and
implement such bans. It focusses th attention on the present day mcdica
services- private and government; the proscription patterns; the grocs
lack of accountability to the public or to any medical council. The
doctors bask in the prestige that comes, with the practice of ’white
man's’ medicine.
It is the public that pats them on-a pedestal (not
far bolow'tho one mount for tho Almighty). In reality, they, like the
drug manufacturers and their representatives are no better than salesmen;
and medical care is debased into a ’commercial service'and it sells,
even if the people needing it have to bog, borrow, or steal.
If tho prescription patterns have to be based unmodified
blindly, unchallenged on the.medical text book Written by and for the
West - then we should also ensure that their controls go with them.
There should be registration with the medical council, need to pass
board exams after certain years of practice, medical audit and withdrawal
of modical license for unethical.medical practice. If our state mechanism
is meant to ensure anything, it is to ensure total safeguard against
those who in the name of medicine, believe in making quick money, and
use their medical license, to exploit the people.
Not merely are such
medical practitioners whoso number is fast increasing an insult to
medical practice, but they sot examples for others, so that medicine
has become a "Dhanda" (business) for many. Youngsters bribe, fudge
mark sheets, pay lakhs of capitation fees to get admission in medical
colleges to join their ranks - while Primary Health Centres lie unstaffed,
unequipped and disfunctional. Rarely do the prestigious medical establish
ments raise a hue and cry over the ever increasing modical swindles;
against the decreasing health budget of tho 5 year plans; against
the drug bans that never come or are never implemented; against health
and drug policies that ere not in the interest of the people.
l&thjl ~ The drug industry is there not to serve, but safeguard its
own interests. The performance of multinationals in decreasing product
ion of essential and life saving drugs, and the double dualing in giving
biased drug information; thcer ensuring tho purchase of drug .prescript
ions for ones company by gratifying doctors with samples, gifts and
sponsored medical conferences. i-Jith Loan licensing, products of many
of the big narno companies arc produced by small scale drug outfits
with as much quality control as most other small scale drug companies.
All commercial enterprises serve a purpose, but a few like
drug industry start sharing the role of a healer, server, educator,
benefactor, having touched the dizzy heights of highly technical
mystified science.
Myth III - The third myth of course is that our health policy is
geared to fulfil the health needs of the majority.
The health budget has steadily decreased. It may have been
broken up under different heads but with increasing population and
increased need for health services, health budget should be going up
much more rapidly.
....... V
IAI:pt:l9.7.'S4
How has tho money boon spent? What are thodisparities existing?
'what has been the role of the policy makers? i.nat has happened to the
various recommendations mentioned earlier? The perspective should have
been set when wo attained independence. The direction being pursued now
hasn’t changed very much from the pro-independence period.
The public
has had no soy ip deciding the kind of doctors it wants trained with its
money and what kind of health facilities and drugs it needs. Such an
intervention by the consumers remained impossible. inspite of the numbers
because sc far they have remained unorganized and fragmented.
Focussing public attention on the issue of essential drugs, provides
a platform for organizing the consumers for focussing attention on our
health care services, on our legislations, policies, education and
legal systems.
It is to focus on tho role tho experts, the committees and policy
makers have played in tho past (many of whom are known to have been
bought and sold), It focusses on tho role of consumers and on thoir
demand for participation in decision making as a majority, for the benefit
of tho majority.
Demand for essential and life saving drugs as a priofity is an
exercise in demystifying medicine; it is an exercise in public education,
an exercise in ensuring that public needs guide and influence decision
making. This demand is also an exercise in learning to boycott drug
decisions and policies which are thrust down peoples throats against
their will and against the interest of tho majority.
It is part of a slowly emerging consumer movement, peoples science
movemeitt and also peoples health movement. It is an integral part of a
larger process and not a piece-meal demand of a minor rectification.
The politics of health at the concrete level can only be based on
peoples action. As Fritjof Capra points out in tho Schumacher Lectures
'Refusal to take oven a single pill is such a political act'. On this
political philosopjay is based tho mobilization for essential and life
saving drugs as a priority.
Just as manufacture, sale and proscriptions of hazardous and irrational
drugs is a oppressive political act, refusal to become victims of this
oppression is a political response.
II.
COURAGEOUS EFFORTS - A Brief Review
Ths concept of essential drugs list is nothing new nor did it have
its origins in WHO’S Technical Report Series No. 615 (1977) as many believe
Many efforts had been made prior to this. We just mention few.
CHILE:
As far back as 1973, the Chilian Medical Commission comprising of
Dr. Salvador Allende had believed in limiting tho drugs to those that had
demonstrable therapeutic value and thus 'scale down the pharmacopoa'.
Allondo during his short tenure as President quite successfully compelled
ths medical profession to serve "basic" rather than profitable needs.
He proposed to ban drugs not proscribed for clients in North America
or Europe.
5/
L-4/375(-) LCD & RT
VfLrl:pt:19.7.'S4
dithin one wook after the taking over of the military junta on
11th September 1973 the Chilian doctors who participated ir. this
rcvclutionization of medicine, these outspoken proponents of Chiltm
medicine based on community action rather than on drug imports and
drug consumption were assassinated. Plan with much" courageous ideas
even though they arc for the benefit of the people, are seldom
appreciated.
SRI L/jiKA:
In 1971 under the guidance of Sencka Bibile, Sri Lanka had formed
the State Pharmaceutical Committee to launch its people oriented now
Drug Policy. The number of drugs in the market were slashed down "from
2100 to 600 and made available mostly under generic names and obtained
by calling international tenders. Within 6 months there were savings
of about
in relation to expenditure incurred earlier.
It is absolutely essential for those of us involved in drug work,
to know how the resistance from multinationals, their governments, wit!
support from Sri Lanka’s own medical establishment forced the Sri Lanka
government, to give into vested interests and revert some of itsown
bravo and correct decisions.
PAKISTAN:
Pakistan’s attempts at restricting the drug list to essentials,
with rejection of unessontials met with similar resistance from the
2 most powerful lobbies in the medical industry 'the drug industry
and the medical establishment'.
INDIA:
In 1975, the Hathi Committee in India recommended a restricted
essential drug list of 116 drugs which were to bo sold under their
generic names. There was no dramatic opposition to the recommenda
tions. They wore just very effectively ignored. So much so that
today for interested health and consumer groups no copies of the
Hathi Committee recommendations are available,, from the health ministry
Those recommendations are shrouded in cob-webs. The difference between
the Indian experience with essential drugs and that of others is that
the demand for them did not emerge from enlightened medical profess
ionals arid has till recently remained an official exercise. It was
not from people like Dr. Scnoka Bibile of Sri Lanka, Dr. z.afrullah.
Chowdhry and Dr. Nurul Islam of Bangladesh, Dr. Salvador Allende oi
Chilo.
MOZAMBIQUE:
After its liberation from Portuguese rule in 1975 the Mozambique
government took some drastic decisions regarding its health and drug
policy. Health was nationalized and private practice banned within
one month of independence.
The number of drugs were decreased from
to 430 medicines in 1977. Essential.drug list was revised
in 1980 and contained only 343 drugs. ONLY THESE DRUGS COULD BE
PRESCRIBED.
. .
^aZ3?S(o) LCD & RT
VHAI: p t; 19.7, 184
The result cf streamlined contracts -was that the drug prices of many
essential drugs camo _dp'Mloriginal prices. The essential
drugs became available, to more people in remote areas, not just to the
privileged few. This could be done with the drug import costs the sama
as they were.10 years ago because the selection was more sensible.
W H 0:
The WH) Expert Corarittee on essential drugs in Technical Report Series
615 gave the criteria for selection of essential drugs and a model of
such a list. Another report, in 1979 was- followed by the Technical Report
Series 6o5 which dealt with the ’use of Essential Drugs' and gave the
essential drug list for emergency situations and primary health care.
BANGLADESH;
In June 1982 Bangladesh's Military regime under General Ershad,
promulgated a Drug Policy based on WHO ‘recommendations. 17Z>^2 drugs
were banned because of their hazardous and irrational nature. This
of course had been prccodod by educational campaigns about rational
drug use by some of the individuals involved in pushing the National
Drug Policy. The January 1982 international conference on Health and
Pharmaceutical Policies was one such attempt organized by Gonosliasthya
Kendra. Through its monthly magaz ino "G ones hast hya Patrika" dealt
with this and other issues systematically. Dr. Zafrullah Chowdhury
admits that the Hathi Committee and its recommendations hold great
inspiration for evolving and for implementation of the Bangladesh drug
policy.
In Bangladesh the rcs^Lctod drug list constitutes of 150
drugs. The grading of 150 selected essential drugs has also boon done
based on location of utilization and level of potential users.
I
II
Ill
12 Essential drugs have been selected for village level health
workers.
- Additional 33 essential drugs for Primary Health Care up to
Thana Health complox level.
- Additional 105 essential drugs for use up to tertiary level.
-
There is also a list of 76 supplementary drugs for rcsti-ictcd use which
after discussion wn 11 bo compiled to 100.
The heavy pressure being applied to dilute or just scrap this
courageous pro people drug policy, which is ironically very much based
on tic WED guidelines for Rational Drug use - has come from the multi
national drug lobby and the medical lobby. The loudest voice being
from the US based multinationals and from B M A (Bangladesh Medical
Association). It is openly stated by the latter that if India can
allow unrestricted sales of drugs banned in Bangladesh, the drugs must
bo safe and wonderful. After all Indian Medical Establishment with
all its brains and advanced technology can't be wrong - (any way -wo
al 1 nw continued manufacture and sales of drugs banned by our Drug
Controller of India and recommended for withdrawal by our expert
committees.)
Efforts to gather support for Bangladesh's bravo drug policy had
been made by us right from the beginning and our efforts continue;
since survival of Bangladesh drug policy is crucial for the people of
Bangladesh and other third world countries including India.
............... ?/
3-4/378(o) LCD & RT
VHAI: pt:19>7.'#4
Zimbabwe's Government has selected 376 essential drugs to bo
used in the public health system. Government will not make foreign
exchange available for importing drugs outside this list.
■■'/hy is this concept of essential drugs seen as such a big threat by
medical establishment and the drug lobby? The reason is~vcry obvious.
It interferes with the drug companies profit making oven though in
reality it benefits more people.
Ill.
OUR INITIATIVES IM PROMOTING AWARENESS OF
ESSENTIAL DRUGS'
By the end of 1980, the drug is sue, t lie rational use of drugs and
the role of non-drug therapy and of systems of medicine etc. had become
an important component of our training programmes; whether it was up
grading of diagnostic and therapeutic si-dlls of middle level health
workers, holistic health workshops, community health or health care
management training programmes.
By January 1980 a clearly defined strategy of drug work was drawn
up. Tliis was lator presented to VHAI's general body for ensuring organi
zational support. This work strategy figures in the special issue of
Health for the Millions - April-June 1981 and indicates the various
levels at which it was felt that intervention was required. (Right from
village hospital to health personnel and their trainers; policy makers,
drug companies, multinationals and international drug and health action
groups).
In April-Juno 1981 issue of our bi-monthly wo informed our VHAI
members and HEM readers of the concept of essential drugs and gave the
essential drug list meant for Primary Health Caro. The list of irra
tional and'hazardous drugs wliich was at that time recommended for being
weeded out, was also disseminated to warn the health personnel and
health institutions about them.
By 1981 end a serious attempt to draw up an essential drug list
of 50 drugs and recommended management of 10 commonest health problems
was made, based on the invited view's and opinions of selected academi
cians, health personnel in the field or hospitals and pharmacologists
etc. (There wore too many disparities in the responses and effort
to compile a very unanimous and coherent result based on these responses
was abandoned. It was found that most health personnel were not
fam-ili,nr with ths concept of essential drugs and WHO'S essential drug list)
In January 1982, the first drugs workshop 'Drugs Issues and
Feasible Alternatives’ -was'organized in Pune to bring socially
conscious health personnel, consumer group activ ..sts 'or drug action
together. The Hathi Committee and WHO essential drug lists were
made available to the participants of the first Drug Workshop in Pune
as well to the participants of various training workshops and organi
zation Development (0D) seminars etc. conducted by VHAI and dissemina
ted amongst various levels of health and non-health personnel.
A sub group constituted of doctors and pharmacologists mot during
the course of the workshop to compile a mutually acceptable essential
drug list. (The Pune workshop list - in the comparative drug list
was an outcome of this effort). See Annexuro I.
8/
VHAIzpt; 19.7.'84
8
:
By August 1982 it was fully realized that an essential drug list
drawn up by us even as a group would not necessarily be acceptable to
health personnel, /aid if while attempts to influence government autho
rities wont cn side by side in the voluntary health sector, the accept
ance and implementation of this had to bo ensured.
The exercise to draw up a comparative essential drug list was
undertaken for 3 reasons:
1.
To demonstrate that any rational drug policy formulated
had a lot in common, no matter from which country.
2.
That it was not a handful of concerned persons but expert
committees that had drawn up those lists. The fact that
these exports believed in the concept of essential drugs,
we folt would have greater convincing and educational value.
3.
The rationale in making the comparative drug list available
to the individuals in ths field and solicit a response from
those informed individuals was to give a better guidelineas well as to involve them in the evolution of a process,
The comparative essential drug list prepared incorporated the
following drug lists:
-
WD
-
Hathi Committee
PGI (Test Graduate Institute list) Dr. V.S. Mafahur
Pune Workshop list
Sri Lanka list
Restricted lists used by ECHO UK and Action Kedeor (both
agencies are. involved in bull-: purchase of essential drugs for
third world countries).
It was obvious that those essential drug lists would provide guide
lines for drug selection for larger nodical institutions. But for smaller
health programmes with which I was mainly involved in the course of ny
work, there was a need for a graded essential drug list,- based on the
experience, qualifications of the health personnel
- the availability or non availability of other health .fnr.i 1 -it-ies
specially referrals
- availability of supervision, consultation and on going education
- the gamut of health problems dealt with and the workload
- resources available in terms of finances, manpower, diagnostic
facilities, transport etc.
Effort to obtain graded essential drug lists from Bangladesh,
Sri Lanlfi, Mozambique and EMRO have been made.
Dealing with Resistance:
The- most vccal argument against the concept c-f essential drug list
by the drug lobby and its supporters is that it is relevant only for
the extremely poor countries and not for developed countries nor a
country like India with the most developed pharmaceutical industry in
the third world. This is far from true since drug lists of many developed
countries are highly rationalized and limited. Prolification of nonessential drugs is no indicator of development.
••••?/
a-4/37S(o) LCD & RT
VH/I:pt: 19.7.'84
:
9
:
In 1982 a request to the Editor MIMS was made tc:
1) delate the drugs that wore recommended forbeing weeded out by
the Drug Consultative Committee
2) indicate clearly the drugs included in WHO essential drug list,
so as to give a guideline for the readers to help them in their
selection process - by underlining or writing these drugs in capitals
or italics.
This evoked besides a personal response, an editorial in KIMS
where the relevance of the essential drug list only for ties struggling
poor countries was emphasised. Dr. Halfden Mahler, Secretary General
WHO was quoted as saying "that a consignment of antimalarials was
received in a certain country with as much celebration and gaity as
demonstrated at that country's independence". This was an attempt to
show that the concept of essential drug list is meant only for extremely
poverty stricken and net countries like ours.
This is totally untrue.
Developed countries have made more serious efforts to restrict drugs.
In UK, the 6500 preparations is considered too many by the Rational
Health Campaigners and^&harles Mcdawar of Social Audit in his latest
book 'The Wrong Kind of Medicine’. Norway has about 1900 preparations.
The Norwegian authorities have licensed a total of 730 active ingredients.
An attempt to have less of irrational and non-sensical drugs is not
limited to the third world countries but developed countries themselves.
How long in the name of ’free enterprise1 and so called ’clinical freedom’
will irrational and hazardous drugs continue to be inflicted upon the
people specially when they are ill affordable by them at the cost of
their actual health care needs being met?
Today the question is not whether to include or delete a particular
drug, but for health personnel and people alike to bo exposed to and
to internalize the concept of essential drugs, so tint they can make an
informed choice about.essential and unessential drugs.
"The benefits of our huge drugs list are essentially to do with
trade, not health. The advantages of a restricted drug list include
having fewer bad drugs and a reduction in drug induced disease, and
better information about drug use and loss confusion about which drugs
tc use". (Charles Mcdawar ’The Wrong Kind of Medicine’ page 15).
Dr. John Yudkin who has long boon concerned about third world
drug policies says 'the drug companies must not bo permitted to beconss
a hazard to health in the underdeveloped world by failing tc provide
information or by drawing scarce resources, away from more effective
projects'.
10/
^~4/378(o) LCD w RT
' VHAI:pt:19.7.'S4 '
10
IV.
SgSCTIOH OF SSaSNTIAL DRUGS ARD STEPS FOR
r-Asgst?n:;g an esssntial drugs iwgram®’
WID RBCXWBNDATIONS
In order to ensure that an essential drugs programme is adequately
instituted at the National level, several steps arc advised:
1. Establishment of a list of essential drugs, based on recommenda
tions of a local committee- constituted of individuals competent in the
fields of medicine, pharmacology, and pharmacy as well as peripheral
health workers.
2. The international non-proprietary (generic) names for drugs
or pharmaceutical substances should bo used whenever possible and
prescribcrs should be used whenever possible and prescribers should be
provided with a cross index on noproprietary and proprietary names.
3. Concise, accurate, and comprehensive drug information should
be prepared to accompany the list of essential drugs.
1. Quality, including stability and bio-availability should
be assured through testing or regulation.
5. The success of the programme is dependent on efficient
administration of supply, storage and distribution at every poinb from
the manufacturer to the end user.
Government intervention may be
necessary to ensure the availability of some drugs in the formulations
listed,.and special arrangements may need to be instituted for the
storage and distribution of drugs that have a short shelf life or
require refrigeration.
6. Efficient management of stocks is necessary. To eliminate
waste and to ensure continuity of supplies, a Procurement Policy should
bo based upon detailed records of turnover. In some instances drug
utilization studies may contribute to a batter understanding of true
r equirements,
7. Need for both clinical and pharmaceutical research under
local conditions.
Criteria for selection of essential drugs;
ESSENTIAL DRUGS ARE THOSE THAT SATISFY THE
HLLTH CARE NEEDS' OF THS MAJORITY OF Tffi
PEOPLE. THEY SHOULD THEREFORE, BE AVAILABLE
AT ALL TILES IN ADEQUATE AMOUNTS AND IN THE
APPROPRIATE DOS ACE FORMS.
Only those drugs should be selected for which sound and adequate
data on efficacy and safety are available. Ard from adequate clinical
studies and for which evidence of performance in general use in a variety
of medical settings has been obtained.
3-4/373(o) L® & RT
VH.'Z:pt:19.7.'84
Each selected drug must bo available in a form in which adequate
quality, including bio-availability can bo assured. Its stability under
tho anticipated conditions of storage and use must bo ostaMifthfid,
The choice between 2 or mono drugs which are similar in all the
above respects, should be based on. careful evaluation of their relative
efficacy, safety, quality, price (of tho cost of taking a full course
and not merely tho unit cost) and availability.
Other criteria to be kept in mind are pharmacokinetic properties
and availability of facilities for manufacture or storage.
Formulations should be single ingredient drugs. Fixed dose
combinations should be acceptable only when a combination provides a
proven advantage over single compounds administered separately in
therapeutic effect, safety or compliance.
Selecticn of Dosage forms:
Tablets are usually loss expensive than capsules, but while
the cost factor should be token into account, tho selection should also
be boned on a consideration of pharmacokinetics, bioavailability,
stability under ambient climatic conditions, availability of excipients
arid established local profeian.ee.
- A range of dosage strengths is provided from which suitable
strengths should be selected on the basis of local availability and need.
- The use of scored tablets is recommended as a simple method
of making dosage more flexible.
- There is a need to periodically revise and update the list.
But' frequent and extensive clianges arc clearly undesirable since they
result in disruption of channels of procurement and distribution and may
have implications for the training of health personnel.
Provision of information or. essential drugs:
’Concise, accurate .nd comprehensive information on the uso of
essential drugs should be available to all proscribcrs in a format that
is appropriate to their responsibilities and levels of training.1
Drug information sheets for tho doctors by WID’s Export Committee
on tho selection of essential drugs has boon compiled in tho following
format:
1. International Nonproprictary Narae(IKl'l) of each active
substance, and recommended dosage form.
2, Pharmacological information: brief description of pharma
cologiccZ effects and mechanism of action.
3.
Clinical information:
3.1
3.2
Indications: whenever it is thought appropriate, simple
diagnostic criteria should bo provided.
Dosago regimen and relevant pharmacokinetic data:
12/
LCD &_RT
VF4I:pt:19.7.'S4
12
:
,-.vcragc dosage and range fcr adults and children
Dosing interval
Average duration of treatment
Special situations, eg. renal, hepatic, cardiac
or nutritional insufficiencies which require either
upward or downward dosage adjustments.
3.3
Contraindications
3.4
Precautions (reference to pregnancy, lactation etc.)
3.5
Adverse effects (quantitate by category, if possible,
3.6
Drug interactions (to bo mentioned only if
clinically relevant: drugs used for self-medication
should be included)
3.7
Overdosage:
3.7.1 Brief clinical description of symptoms
3.7.2 Non drug treatment and supportive therapy
3.7.3 Specific antidotes
3.2.1
3.2,2
3.2.3
3.2.4
4.
V.
Pharmaceutical information.
THE RATIONALE OF ESSENTIAL DRUGS
The concept of essential drugs is the backbone of any Rational
Drug Policy. The repercussions of acceptance and non-acceptance of an
essential drug list are too many. If there is one unanimous demand which
has to come from us people it has to bo the selection of an essential
drugs list based on the health needs of majority, for priority to bo,
given to
- ensuring their production
- ensuring their officiant distribution
— ensuring appropriate stocking of pharmacies with these drugs
- ensuring appropriate drug prescription and practices to be
based on those accepted drugs.
Since 46% of the drugs marketed are obtained ever the counter without
a prescription (according to WIN Drug Utilization study) it is obvious that
altered or improved 'prescription practices' alone cannot alter the drug
consumption patterns. With the degree of self prescription of drugs,
selection of essential over unessential drugs can have a groat impact.
Specially if this is associated with a total boycott by the consumers
and health personnel, of highly irrational and hazardous drugs' as was
done by Swedish doctors.
The boycott led by Dr. 011c Eansson, Paediatric
Neurologist in the international campaign against clioquinol, moxaform
related drugs was later joined by doctors of Norway, Denmark - total 1y
by over 3000 doctors and veterans. The implementation of essential
drugs list needs to be done urgently and the reason why it is so crucial
arc given bclowi
A.
Existing low priority to essential drugs needed for the priority
hcalth needs and the deteriorating trend:
~~~
The myth of 'pill for every ill' detracts from the real health
issues being dealt appropriately. The majority of drugs manufactured
are unessential and not based on the health needs of our people. Of the
1260 crores worth of drugs manufactured in India in 1979-' 80, onl$-Rs. 350
crores worth of drugs were'essential and life saving drugs, the rest were
mainly non-essential drugs.
13/
3-4/378(e) LCD & P.T
VEH: pt: 19.7.’34
The following figures speak for themselves;
Table
1978.
Category
I
1950
4.5%
3.62
II
16.72
13.22?
III
67.1%
68.62
IV
11.7%
1 Zp.62
Source:
FMRAI News
July 1984.
The production of category I drugs i.e. essential and life
saving drugs and Category II drugs (essential drugs) is showing a
dealining trend according to Ministry of Petroleum and Chemicals and
Fertilizers.
Production of antimalarial, anti-TB, antifilarial and anti
leprosy drugs have been trailing far behind the estimated demand and
while demand has increased the actual production has been falling.
In fact, production of the antimalarial Chloroquin, and the anti tuber
culosis PAS, INH and thiacctazone fell short of estimated demand by
about 34, 50, 44 and 70? respectively in 1979-'30, except for a small
increase in INH production for al 1 those drugs decreased further in
19SO-'81 .
Estimated demand Production in tonns MT Estimated Production
1979-80
79-80
80-81
81-82
82-83
Antimalarial
Chloro quin
Amodiaquin
250
40
35.-6
38.49
34.62
23.15
58.96
26.02
70.00
33.00
Antitub orcular
PAS & Salts
INH
Thiacctazone
Streptomycin
600
200
40
300
481.74
112.43
12.55
220.16
405.46
129.20
S.Z>4
227.33
261.97
110.40
13.98
255.45
290.00
128.00
25.00
266.00
Antifilarial
DSC
30
21.57
18.99
16.43
13.00
Antileprosy
DDS
28
16,20
21.05
25.61
30.00
Ref:
Dr. W.Y. Rano - Why don't our drugs match our diseases Science Today - October 1982,
...14/
S-4/378(e) LCD & RT
VHAI:pb:1?.7.'84
Demand Projection :Cor Bulk drugs for the period 1979-80 to '&/4-'35
E st imat ed R c quir ement
Base year
79-80
80-31
81-32
82-83
83-84
84-85
Antimalarial
Chloroquin
Amdiaquin
250
40
275
46
300
53
335
61
365
70
400
80
Anti Tubercular
PAS
INH
Thiacctasono
Streptomycin
600
200
40
300
630
240
42
330
660
290
44
363
700
360
46
400
730
415
4-8
440
770
500
50
485
Antifilarial
DSC
30
33
36
40
45
50
Anti lopresy
DDS
28
32
37
45
50
56
Ref:
The Indian Pharmaceutical Industry Problems and Prospects
P.L. Narayan, NCAER Study National. Council of APplied_gconomxc
Research - January 1984.
- ICMR and ICSSR study on Alternative Strategy had indicated the
grossly inadequate drug production for IB and. leprosy which happen
to bo our priority health problems.
With half of the TB patients
of the world in India our production of IN® was loss than 1 /3 of the
minimum, requirement.
- Tha Malaria- deaths in Rajasthan-wore not merely duo to drug
resistance and cerebral malaria, but duo to non-availability of
chloroquin even at certain government PHCs. The estimated require
ment and the actual production are getting further apart and reliance
on imports is resulting for drugs that are so routinely needed.
Chlcroquin imports in tons
1979-'80
1980 - '81
1981 - '82
Production
Imports
Production
Imports
Production
Imports
35.2
52.8
34.6
71.8
59
166.3
Rof:'- HC/ER Report - The Indian Pharmaceutical Industry.
National Council of Applied Economic Research.
/
15/
g-4/37S(o) LCD & RT
Vk'l:pt:19.7.'S4
- There are an estimated 60 m-i~l 1 ion iodine deficiency cases
of goitre in India. It is known that children of' iodine
deficient mothers are known to bo born as cretins, deaf,
mutes and mental subnormality.
I ho simple technology of product: .on of iodized salt is known.
Merely 50 paisa worth of iodized salt can make all the difference
between a child being normal and subnormal.
We still produce only 20/ of the iodized salt required.
Required amount of iodized salt : ,s - 7 lakh tons
- 2 lakh tons
Amount produced
- 1 lakh tons
Amount sent to Nepal
Amount left for utilization for
- 1 lakh tons
the 60 ini Ilion goitre cases
When adequate production of an essential low cost item like
iodized salt for a National Goitre Programme cannot be assured,what
happens to production cf the essential drugs for non priority national
programmes can very well be imagined.
In Kenya, in a pilot project funded by DANIDA and SID A, »supplies
of drug kits containing 39 drugs in 15 rural districts has increased the
accessibility of essential medicines for the rural population from
1 QI to l-i&o.
B.
DPCO and its negative impact on Production of Category I and II drugs:.
Under DPOO (Drug Price Control Order) the mark up on Category I
drugs is limited to 40/ ajd that on Category II is 60/. Producing category
IV drugs because of the high mark up allowed arc therefore definitely most
profitable.
For the decreasing priority being given to essential and life saving
drugs DPOO is therefore blamed. With the decontrol of prices of 75/ of
the drugs as is being r ccommendcd by the drug lobby and its supports, a
further switch to production of more profitable unessential drugs is
imminent. If government is serious about ensuring that essential drugs
are sold at a reasonable price - this can be done by doing away with taxes.
C•
Poor porforma: ,ce of multinationals in production of essential drugs;
The outright, calculated neglect of the priority drug needs of
the majority is trail known. The following table speaks volumes. (Sec
Annoxure II - Production of Essential Drugs by Multinationals and Organised
Sector)
D.
Dilut on of I- jRA Companies - an invitation to more formula|j^ons;
With the d:‘J.ution of •'.’orcign equity shares to 40/? various
comnssir>ns are bonne granted to the FER.A companies so that bulk to
foiumJ’jons r -: : wi'" tr increased from 1:5 to 1:10. With the drug
production pattern as it iSj we can look forward to more formulations
and more unessont ial drugs irrelevant to our peoples health need.
Bulk production ’jy foreign sector for 1982-'S3 was Rs. 55 crores worth;
the formulation turnover according to 1:5 ratio should not have exceeded
Rs. 275 crores, however, Rs. 515 crores worth'd formulations wore
produced i.e. cure than 1:10 ratio when only 1:5 was allowed.
16/
3-4/37S(o) LCD A- AT
VFJiX: pt: 19.7.134
:
E•
16
:
National use of scarce resources:
i) Wastage of scarce foreign exchange: • India with its level of
indebtedness to IMF World Bank, IDA etc,, can hardly afford to sqandor
its scarce foreign exchange for importing inessential drugs.
ii) Inessential vs basic health needs: Worse still is the
enforced wastage of scarce resources of the poor on useless nonsensical
drugs, when they can hardly afford adequate food and clctiring and bare
essentials. When the percentage of people, below or around the poverty
line happen to be around 60 - 7Ga of a country's population - the very
production and heavy promotion. of costly irrational and hazardous drugs
is criminal.
A strong public opinion alone can ensure withdrawal of
such drugs, with priority being given to essential and life saving drugs.
iii) Inessential vs essential drugs: Often inessential drugs
are bought at the cost of specifically needed essential drugs. For the
ignorant majority, the difference between the therapeutic value of a
costly tonic, vitamin, digestive ensymes, antipyretic and much needed
specific drug eg. antiasthmatic, antibiotics etc.
all written in the
same proscription - does not exist. This was shown by Vocna Shatrughana's
study of Prescription writing and drug consumption. By ensuring
priority availabiility and prescription of essential drugs, wo would bo
contributing to preventing the wastage.
iv) Economics of scale increased: If essential drugs wore given
priority in production, through sheer economics of scale, the production
cost would decrease for the manufacturer and thus the consumer.
v) bulk purchase; An essential drug list can ensure bulk purchase
of selected essential drugs, which can cut down drug costs.
F•
Influencing market demand end thus the Drug Production pattern in
favour of essential drugs:
~
If the concept of essential drug list was widely propagated, accepted
by choice cr by legislation, this would necessarily influence the
prescription pattern and hence the drug demand in tie market. This would
definitely alter the drug production pattern towards essential drugs.
G.
Decrease drug misuse and over use:
This can bo done with identification of- drugs which are - thera
peutically effective, safe, easy to administer, and of appropriate cost
preferably single ingredient well tried drugs. The use of drugs w’hich
arc of doubtful value, costly, irrational and hazardous drugs should bo
avoided. Majority of the drugs available are combination drugs. This
increases costs as these drugs are often in subtherapeutic and irrational
dosages. According to Halfden Mailer, 9C$ of drugs in the developing
countries are non essential.
Preventing Iatrogenesis JD ^ugs induced health hazard):
As long as potentially hazardous drugs with very high risk
(compared to) benefits ratio, are misused and overused, unwarranted high
incidence.of iatrogenesis is bound to occur.
17/
■E—47378(c) LCD _&_RT
VH11: pt: 19~.7?84’~'
17
:
In US?, where the drug control and the proscription practices
arc much better controlled, the incidence of iatrogenesis is vary high.
One in 5 hospital admissions are known to be duo to iatrogenesis. In
India we have such a high degree of self prescription, prescription
writing by unqualified health personnel and by qualified personnel who
are made highly biased by drug representatives. Tills along with poor
drug controls ensures drug misuse, overuse and iatrogenesis. Most
cases of iatrogenesis ore not diagnosed in India. This of course doos
not imply that they don't exist.
Most of the combination .rugs have 2 or more ingredients. It is
known that with consumption of over 6 drugs compared to 2, chances of
drug interaction increase by 4<# as compared to 5'/ ■
I.
Dripj; Information for health personnel and consumers possible:
‘with 30,000 drugs in the market it is impossible not to be
confused about thorn,. 4 doctor may bo familiar with the drugs ho or she
uses routinely. Unfortunately ho or she cannot be so with the various
brands used by others. Their prescriptions are often taken from one doctor
to another by critically oi' chronically sick patients.
Confusion abounds, since majority of the health personnel have no
access to pharmaceutical index to figuro out what drug has been given.
Majority of the drugs in the market, are combination drugs. Lack of
familiarity with the contents and their dosages makes matters worse.
If proscription practices for the majority of the health problems could
be based on essential drugs? Relevant drug information about their
relative cost, dosages, indications, contraindications, side effects and
toxicity could be made available to health personnel and consumer
caution be ensured?
Studies also indicate that it is impossible to remember details
of even 1C0 drugs in routine practice. Ensuring that these prescribed
drugs are the ones that people need and not what are roost heavily pushed
by tlx drug companies because of their profitability, is our responsibility.
Focussing on all aspects of essential drugs and rational drug use in
medical education would ensure their bettor use which would bo bettor
for .the nation and the patients.
J.
Ensuring better quality control:
There are 30,000 formulations in tho market. Most of them are
combination drugs and one in 5 drugs in the market is substandard. With
a lesser number of drugs in the market which are single ii.gy^cient drugs
quality control can bo better streamlined.
Making profits by promoting
unessential drugs is crazy, but 'o make inadequate number of essential
drugs available, with even these being substandard, is really unacceptable.
K•
Ensuring generic proscribing:
Generic prescribing is recommended by WK) itself as it cuts down
drug costs.
Pharmacology input during medical education, nomenclature used
in medical literature and medical journals is based entirely on generic
names.
18/
VHAIzpt: 19.7.'84
:
1S
:
With a restricted essential drug list generic prescribing can
definitely be ensured. The pharmaceutical industry and government drug
control authorities would have to take greater responsibility to ensure
quality control AT ALL L3VBLS. Brand name prescribing is*no solution
for substandard drugs. Brand names do not prevent spurious drugs enter
ing the market as most spurious drugs arc imitations of well known
brands. Name of the specific drug house can be written if it is felt
absolutely necessary. Generic proscribing is possible with single ingre
dient essential drugs which arc quality controlled.
Subsidizing costs of essential drugs:
With restricted list of drugs meant for the health needs of
the majority, subsidizing is possible by removing sales tax, excise duty
and octroi for those, /my loss in the taxes can be compensated by
increasing taxes on cigarettes, alcohol and other such anti-health
products or more so on luxury items meant for the rich. In conclusion,
demanding an essential drug programme is aimed at focussing attention
and giving priority to health needs of the majority.
GONCLUSION/Sbi-IK/RY
Demanding priority production and distribution for essential
drugs is accompanied by demand for a just health care delivery system.
Wo know that a just health care delivery system cannot exist in isolat
ion in a socially unjust system.
Demand for essential'drugs before un
essential drugs is accompanied by demand for employment, fair wages,
f,ood, water, sanitation and all that goes to ensure good health. Our
fight for essential drugs and health care as a fundamental right of
every Indian, specially the deprived sections is a fight against the
unjustice of the present socio-political system, which in reality
accepts this deprivation of health and basic health care as a normal
phenomenon.
E-4/378(o) LCD.&IT
VH;iI:pt:19.7.,S4
Annexuro III
PRODI CTIOII OF ESSENTIAL DRUGS BY MULTINATIONALS AND ORGANIZED SECTOR
Name of the firms
PAS
T HI ACIT AZONE
ETHAMBUTOL
RIFAMPICIN
STREPTOMYCIN
Abbott
Mil
Nil
Nil
Nil
Nil
Nil
Nil
ACCT
Nil
Nil
Nil
Hoechst
Nil
Nil
Nil
Nil
Nil
S.K. & F.
Nil
Nil
Nil
Nil
Nil
Searle
Nil
Nil'
Nil
Nil
Nil
Sandoz
Nil
Nil
Nil
Nil
Nil
Hoche
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Mil
Sarabhai
Nil
Yes
Yes
Nil
Yes
Boehringer Knoll
Nil
Nil
Nil
Nil
Nil
Glaxo
Nil
Nil
Nil
Nil
Yes
E, Merck
Nil
Nil
Nil
Nil
Nil
Ciba-Giegy
Nil
Nil
Nil
Nil
Nil
Pfizer
Yes
Yes
Nil
Nil
Yes
Warner
Nil
Nil
Nil
Nil
Nil
Burrough Wellcome
Nil
Nil
Nil
Nil
Nil
German Remedies
Cynamid
Ethnor
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Yes
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Parke-Davis
Disease in Indir
h" T .c. "
■: -ruparod for the Drug 'Workshop in Jaipur, organized
For sharing this endeavour, we are grateful to the following
for their help and moral support in compiling the Essential
Drug List
->
.
-f -Prof-.-M M S Ahu-ja,:Hepd Department, of Medicine, ..A-L T M 3
(Temporally-jAd visor)- The use oi Essential Drugs /Technical
Report Series 685, WHO.
Dr v S Mathur,PG-I Chandigarh, Editor Drug Bulletin
for
i) providing the graded EMRO list for which he was
a consultant
ii) for providing the PGI drug formulary
iii) for being wi+' us at Pune Workshop -January 1982
where Pune Drug List was finalized.
Er Qasem of Gonosasthya Kendra, for having kindly complied
to our request to send the graded Bangladesh drug list.
Dr Joel Fernando, Medical School, Sri Lanka for providing
the Sri Lanka drug list.
Friends in Echo and Action Medeor who sent their lists.
Late Mr John Agacy, Secretary Low
t Drugs and Rational
Therapeutics, who tediously typed the first draft of the
Comparative Essential Drug list in alphabetical order.
Alphonse our Secretary of Low Cost Drugs and Rational
Therapeutics for typing this comparative drug list based
on WHO format.
Voluntary Health Association of India
1Q/54O(b)
^2575784
C-14, Community Centre
Safdarjung Development Area.
New Delhi-110016
Telegrams : VOLHEALTH
New Delhi-110016
Telephones
668071
668072
Rationality in Banning Fixed Dose Combinations
M C Bindal, Ri'S Saxena(Mrs), Suman Lata(Mrs) &'B F Jaju
Dept of Pharmacy & Pharmacology,
LLRM Medical College, Meerut.
Hathi Committee (1975) appointed by Government of India
pointed out that the medicinal needs of the people in India
can be met by only 116 drugs. However, over 25,000 drug formu
lations continue to be sold and prescribed in India. Many of
th®= formulations are unnecessary variations of identical basic
drugs sold under different brand names or without any proven
therapeutic effect or they are too toxic for human consumption.
Unless there is a clear cut proven therapeutic superiority or
a fixed dose combination, such combinations not only put finan
cial hardship to poor patients but also expose the patients to
the undesirable effects of the unnecessary medicament(s) of
such formulations. Dr H Mahler, The Director General of WHO
feels that 98 % of the drugs available in the developing world
aE not essentials hence not required. The Drug Technical Advi
sory Board (DTAB) of India has recently (1982) recommended the
weeding out of the following fixed dose combinations with an
uniform cut off date of March 51, 1985.
1. Fixed dose combination of amidopyrine.
2. Fixed dose combinations of vitamins w th antiinflammatory
agents and tranquilizers.
5. Fixed combinations of atropine with analgesics and antipyret ics.
4. Fixed dose combinations of strychinine and caffeine in tonicj
5. Fixed dose combinations of yohimbine strychnine and testo
sterone and vitamins.
6. Fixed dose combinations of iron with strychnine and arsenic
and yohimbine.
7. Fixed dose combinations of sodium bromide/chloral hydrate
with other drugs.
8. EL xed dose combinations of ayurvedic, unani drugs with
;
modern drugs.
jj ,
9. Fl® d dose combinations of phenacetin.
1
10.Fixed dose combinations of antihistaminics with ant id iarr-=
hoeals.
< „
11.Fixed dose combinations of penicillins with sulphonamides. II S
12.Fixed dose combinations of vitamins with analgesics.
> <
15.Fixed dose combinations of tetracycline with vitamins C.
I
14.Fixed dose combinations of hydroxyquinoline group of drugs§ “
except preparations which are'usud’for ths treatment of
diarhhoofe addadysentery.
gf
j| ii
15.Fixed dose combinations of steroids for internal use except ..
combinations of steroids with other drugs for the treatment ?
of asthma.
16.Fixed dose combinations of chloramphenicol except with
strept omyciri.
17.Fixed dose combinations of ergot except combinations of its
a Ikaloid ergotamine with caffeine.
18.Fixed dose combinations of prophylactic vitamins with antiTB drugs except combinations of INH with vitamin Bg
The rational for the undesirability of the above said fixed
dose combinations can be based on the forthcoming arguments
and facts.:
COWMUMJTY t.TALTH CELL
1.Fixed Dose Combinations of Amidopyrine:
Fixed dose combinations of amidopyrine(ami&opyrine) are
irntional because amidopyrine is an outdated and obsolete drug
as it causes bone marrow depression leading to agranulocytosis
which may be fatal(Beavei' 1965). Even though it has marked
antipyretic and analgesic properties, its "over the counter"
sal: in the united States had been prohibited since 1938(Moodbuiy 1970). In view of the recent development of newer and
safe? antipyretic analgesics, it is in public interest to drop
out amidopyrine altogether from physicians armamentarium.
2. Fixed Dose Combinations of Vitamins with Antiinflammatory Agents
and Tranquilisers:
The addition of vitamins to antiinflammatory agents and
tranquillisers in fixed dose combinations does not yield any
proven increases in the therapeutic effects of these combina
tions. In a way they are just like placesbos but certainly en
hance the cost of formulations. In most of the patients requir
ing either antiinflammatory or antipsychotic therapy, vitamin
deficiency is not an usual associated feature even in our coun
try where malnutrition is so prevalent. Hence vitamin supple
mentation with these drugs is both a wat-te of vitamins as well
an unnecessary financial burden f-r.. the patients.
3.Fixed Dose Combinations of Atropine with Analgesics and Anti
pyretics:
Analgesics and antipyretics reduce the raised body temp
erature to normal(antipyresis).But Atropine is known to cause
hyperpyrexia (ie. it may raise the body temperature). Hence
such combinations is therapeutically antagonistic and is there
fore irrational. Furthermore, even in cases of visceral pain
(eg. colics), where atropine may be advised with the idea of
its antispasmodic property, simultaneous administration of an
antipyretic analgesic, which is ineffective against visceral
pain has hardly any therapeutic advantage. All the more such
combinations unnecessarily expose the patients to the potential
toxicity of antipyretic analgesics.
4.Fixed dose Combinations of Strychnine and Caffeine in Tonics:
Fixed dose combinations of strychnine and caffeine in tonics
areundesirable because strychnine (formerly used as an appetiser)
is now an obsolete drug and its.enthusiastic use in tonics may
even ind&ce convulsions particularly in susceptible individuals.
Similarly caffeine though, has a mild CNS stimulant effect
leading to little temporary mood elevation and relief from fat
igue, has no tonic effect on the body. Furthermore caffeine
products mild physical dependence and habitual use of this drug
in tonics may-cause psychological and physical dependence for
such formulations.
Fixid
5.
Combinations of Yohimbine, Strychnine with Testosterone
and Vitamins:
Fixed dose combinations of yohimbine and strychnine with
testosterone and vitamins are irrational because yohimbine is
no longer regarded as therapeutically useful aphrodiasiac in
man even when mixed with methyltestosterone(Laurance,1980).
Fuifehermore, yohimbine should not be used therapeutically beca
use of its side effects viz Central excitation,'raised blood
pressure, increased heart rate. Strychnine is also -how an
obsolete. Vitamins do not play any therapeutic role(except in
deficiency diseases) and simply act as placebo, of course, giving
the psychological boost to the patient.
.. .3..
6.Fixed dose Combinations of Iron with Strychnine, Arnica and
Yohimbine:
Strychnine, arnica and yohimbine combinations are used as
stimulant appetizers. In most of'the patients (except women)
generally there is no deficiency of iron because iron is adeq
uately stored in the liver. However, in very specific anaemic
cases supplemental iron therapy may be given separately. To
add iron in these formulations is irrational and may be just
for the purpose of increasing the price of the formulation or
to seek patient rights for the formulations.
7.Fixed cose combinations of Sodium Bromide/Ohloral Hydrate with
other drugs:
Fixed dose combinations of sodium bromid/chloralhydrate
with other drugs can now be considered irrational because both
these drugs are now obsolete due to their toxic manifestations!
Bromides on prolonged administration replace the chloride ions
of the body. Because of the slow onset of action, cumulative
poisoning, manifesting as conjunctivitis, GIT symptoms, derma
titis and mental disturbances is likely to occur. Further their
exeeding slow onset of action and low potency make these
bromides unreliable hypnotics.
Chloral hydrate, being an irritant of the ijucous membranes,
causes gastritis leading to a variety of GIT symptoms eg.nausea
vomitting flatulence and epigastric distress. Chloral hydrate
can even cause hepatic and or renal damagel In view of the
recent and more safer hypnotics there is now no justification
of prescribing chloral hydrate to patients.
8.Fixed dose combinations of Ayurvedic and Unani drugs with
Modern drugs:
The modern (Allopathic) drugs are well, standardised and
their standardization methods are official. In case of ayurvedic
and unani drugs, official standardization methods are not
available at present. Therefore, it does not argue well to have
a combination of ayurvedic and/or unani drugs with modern drugs
bevause of the standardization problems of the resulting for
mulations. In view of the lack of authentic repeatable research
data on the efficacy of fixed dose combinations of ayurvedic
and unani drugs with modern drugs, there is no justification
of such formulations to be sold for use by the general public.
9.Fixed dose combinations of Phenacetin:
Phaiacetin is gradually loosing its importance because it
causes kidney damage when used in large amounts or for long
periods. Hence it has no place in routine analgesic, antipyretic
and antiinflammatory therapy. Therefore, fixed dose combinations
of phenacetin are outdated and hazardous. Formulations contain
ing aspirin with phenacetin and often with caffeine' are promoted
with claims that they provide greater analgesic effect and/or
cause fewwer side effects than does aspirin alone. In most con
trolled clinical trials such claims have not been found correct.
10.Fixed dose combination of Antihistaminics with Antidaarrhoeals:
The fixed dose combinations of antihistaminics with anti'■
diarrhoeals is rational, only in certain specific cases where
the diarrhoea is due to allergy(like protein allergy). In these
specific cases, the antihistaminics may be prescribed separately
so that such combinations are not irrationally used in the tre
atment of all other types of diarrhoea. Routine use of these
I
.. .4...
c.ombinations is not only a waste of ant ihi st aminic drugs but
also it exposes the patients to the undsirable effects of this
class of compounds.
11.Fixed dose combinations of Sulphonamides with Penicillins:
Even though sulphonamides and penicillins individually
de have important role in the therapy of infections. The com
bination of penidillin with sulphonamides is undesirable. This
is because the antagonism of the antibacterial effect may result
when bacteriostatic (Sulphonamides) and bactericidal(Penicillin)'
agents are given concurrently,(Jawetz and Gunnison, 1953). In
addition oral combinations may even induce penicillin sensi
tivity.
12.Fixed dose combinations of Vitamins and Analgesics:
In the fixed dose combinations of vitamins with analgesics,
the vitamins do not play any therapeutically beneficial role
and rather act as placebo. Therefore, such combinations are
therapeutically irrational. Since such formulations are likely
to be misused by the patients and if administered for long'
periods because of their vitamin contents, such combinations
are likely to expose the society to.a veriety of undesirable
effects of analgesics.
13.Fixed dose combinations of Tetracyclines with Vitamin C:
There is no specific therapeutic indication of giving
tetracylines and vitamin C together because tetracyclines -'t
does not cause any specific vitamin G deficiency. Therefore,
this combination is of no therapeutic superiority and may be
produced by drug companies just for enhancing the cost of their
product. Further, in inffective conditions where tetracyclines
are indicated, vitamin G deficiency is not an usual associated
feature, such formulations should not be routinely employed.
14.Fixed dose combination of Hydroxyquinolines group of Drugs
except preparation which are used for the treatment of Diarr
hoea and Dysentery:
Halogenaled hydroxyquinolines are indicated only in inte
stinal infection like amoebiasis. So the combination of hydro
xyquinoline with some other antidiarrhoeal and antidysentery
drugs like enzymes for the treatment of dyspepsia is undesirable
because hydroxyquinolines may induce Subacute Myelooptic
neuropathy(SMON). Due to this toxic manifestation the use on
this drug in clinical practice has been abandoned in many ad
vanced countries. The clinical use of these formulations for
such simple conditions like dyspepsia exposes these patients
to the risk of SMON. and hence should not be employed.
15.Fixed dose combinations of Steroids for Internal use except
combinations of steroids with other drugs forthe treatment of
Asthma:
In view of the acute onset of the benefical effect of
steroids in a large number of clinical conditions, their use
has tremendously increased in recent years. However, fixed
dose combinations of steroids with other drugs are objection
able as it is extremely important to adjust the steroid dose
to the minimum that produced the desired effect and the dose
of the other drug if altered, not on the patients need for it
(other drug) but on his need for steroid. In view of the
widespread use of such combinations, the patients are exposed
to toxic cumulative effects of these drugs. However, in case
...5...
of asthma, since immumological factors play an important role
and adrenal steroids cause nonspecific reducation of the res
ponse to the antigen antibody reactions, the fixed dose combi
nations of steroids with other drugs in the treatment of
asthma is therapeutically rational and justified.
16;Fixed dosecombinations of Chloramphenicol except with Strepto
mycin;'
Chloramphenicol is a drug of cnoice only in the treatment
of enteric fever and gastroenteritis. Its combination with
streptomycin in the treatment of gastroenteritis is therapeuti
cally justified because this combination has been found thera
peutically superior to either of these drugs alone in the
treatment of mixed infections of the gastrointestinal tract.
But combination of chloramphenicol with other drugs(like tetra
cycline) is irrational because both the drugs have almost the
same antimicrobial spectrum and also because chloramphenicol
is more toxic as it may cause aplastic anaemia.
17.Fixed dose combinations of ergot except combinations of its
Alkaloid Ergotamine with Caffeine:
Ergot alkaloid, ergotamine is effective in the treatment
of migrains because it is a vasoconstrictor agent and p: events
the rhythmic distension of extracranial arteries.
Caffeine may be allowed in combination also because of its
vasoconstrictor effect on intracranial vessels. However the
combination of ergotamine with other drugs(like paracetamol,
prochlorperazine etc) have no therapeutic advantage and hence
irrational.
18.Fixed dose combination of Prophylactic vitamins with antitubercular’drugs except combinations of I N H with vitamin Bgq
Fixed anti tubercular drus (except INH) are irrational
becuase in these combinations, the vitamines have on therapeu
tic role to play (of course unless there is a vitamins defi
ciency) and they simply act as placebo and might give some
psychological boost to the patient. However, because INH causes
vitamin B6 deficiency, its combination with vitamin B6 is
rational and therapeutically justified.
Another drug combination which has been recently banned
in this country after a much hue and cry from the medical
experts is that of Estrogen Progesterone (E P combinations).
These combinations were used for test for pregnancy. The use
of E P hormonal preparations were banned in USA by the Food
and Drug Administration (EDA) in 1975 because these p.eparaticns were found to seriously damage the foetus.
It is often alleged that drug companies levy a heavy burde
on the common man by charging more and more through their
dubious multiple drug formulations which are their £ari-nted
products. For ex-ample, the real pain killer in most ofthe
analgesic tablets is .aspirin, the market is flooded with a
number of costlier pain killers containing in addition salicy
lamide, caffeine and quinine sulphate, which have no proven
synergistic efficacy. Similarly, amongst anti-cold ointments,
only menthol is said to be of any real therapeutic value. Here
too, other ingredients of dubious value like camphor, turpen
tine and thymol are often aided in order just to put in market
a new formulation and thus increase the price of such a
pat ented formulation.
...6
In our opinion such anti-social problems must be tackeled
at nil levels. The responsible persons of the society in the
medical’and health field, like doctors and pharmacists should
keep a close watch on the dru^s banned inthe developed countries
and also on the drugs which on clinical trials have not been
found safe and effective. These responsible men should convey
all the cli’nical information on such drugs or their combinations
to the appropriate .authorities of the Government of India-Though
the Drug Technical advisory Board (DTiB) ,Drug Consultative
Committee(DCC) and Director General of Health Services(DGHS)
have been entrusted with this job by the Government of India
but other responsible men in the medical field will also have
to keep a vigil so that there is no oversight on the part of
the official machinery and the harmful and obsolete drugs from
developed countries are not dumped in t>ur country any longer.
The World Health Organization(VliO) should also play an effective
role inthis regard and ensure that only safe ®d effective ■' •
drugs are sold to member countries. In addition, the government
must adopt the recommendations of WHO on essential generic
preparations. In a developing country like ours, the goal must
be to ensure availability of essential drugs to patients and
health education to all about safe water, sanitation and finally
sufficient nutritious food.
However, the major problem lies in the fact that a large
number of drug formulations in India have not been adequately
evaluated for their safety and this again emphasises the need
to exercise strict quality control . This becomes much more
significant in the light of the recent statement by the Gover
nment in Rajya Sabha that 17.5% of the drug manufactured and
sold in the country in tne last three years were found to be
sub standard.
Over all, if employment of such fixed dose combinations
aids the busy physician and does not significantly represent
a lessoning of his individualized orientation to his patient
and are rational from the therapeutic point of view, they ar
a boon to therapeutics otherwise a curse to the patient and
the society.
REFERENCES:
Woodbury, D M (1970) inalgesics-Antipyretics, antiinflammatory
agents and inhibitors of uric acid synthesis in The Pharmacolo
gical basis of therapeutics by Goodman, L S and Gilman,IV
Edition, The Macmillan Company, London,pp 314-347.
Beaver, W T(1965) Mild analgesics: A review of their clinical
P. armacology. Am J Med. Sci 250, 577.604.
Jawetz E and Gunnision J B (1955) Antibiotic synergism and
antagonism: an assessment ofthe problem .Pharmacol Rev.5,175-192
Laurance, D R(1980) Clinical Pharmacology, Ed fifth, E L B S
Publication, Churchill Livingstons, pp 331, 536,552,617,848
Source: The Eastern Pharmacist-June '83.
Circulated by the Voluntary Health Association of India
for Drug Action Net Workers for infoiwbion
and necessary action.
• Voluntary Health Association of India
10/310(
C-14, Community Centre
?'g^fdarjong Development Area.
New Delhi-110016
Telegrams : VOLHEALTH
New Delhi-110016
T , ,
668071
Telephones : 668072
HAZARDOUS, banned, BA1WJ3LB AND DUMPED DRUGS
(Prepared for Drug Action Core Group meet at Wardha 30-51 st
July '84 as a Background paper for discussion)
The issue of dumped drugs for past few years has been
much in the news. The multinationals involved in manufacture
and sales of such drugs have received their dure share of
condemnation; Foreign government policies which provided the
scope for exports of such hazardous products have been condem
ned by many-of us eg. the Clayton Me nd me nt Act and the U.S.
Resolut ion.
It is well known that sales of medical technologies and
drugs is a commercial enterprise, the motivation is'profit
making and not 'service' or 'welfare work'.
Realizing all this the question arises as to how much as
citizens of India, can we expect our drug control authorities
to safe guard our interests. The pressure from the drug indu
stry is immense. It is not merely money power but political
connect ionsjk influence over the medical lobby. Many of the so
called medical experts are in their pay roll, many others are
conducting 'scientific studies' sponsored by the companies,
attending conferences' sponsored by the companies, receiving
gifts and samples from the companies. This affiliation is not
unexpected. Inspite-of knowing this our expectations from our
drug control authorities is high. After all our pharmaceutical
industry is the most developed in the third world, ( ie accord
ing to UNIDO it belongs to Category 5,~ developed enough to be
self sufficient).
We have demanded that our imports, production and sales
sh°tf£ give priority to essential, life saving drugs over irra
tional and hazardous drugs. This being along with WHO's guide
lines for Essential drugs programme. The drug industry and its
supporters allege that concept of essential drugs is only for
struggling, least developed third world countries and not for
a country like India, with its-well developed industry and
high and advanced level of medical expertise .However, this
same lobby puts India in the category of less developed
countries when it comes to the issue of banning drugs and drug
control, claiming that c onsid
of hazards over efficacy
are luxuries which we cannot afford!
However, consumers anywhere in the world have a right to expeoit
that irrational hazardous drugs are not issued licences and
that licenses of such banned drugs should be withdrawn as soon
as possible, bans implemented, and that all drugs in the market
are quality controlled. We have 20% substandard drugs ieJin 5
will not be effective With increasing number of spurious drugs
floating in the market, the problem is beginning to take danger
ous proportion.
Since 1980 we've been concerned about this issue of dumped
and hazardous drugs. We widely circulated the list of combinat
ion drugs recommended for being weeded out and printed it in
our special issue of HEM on Drugs April-June 1981. Since then
the story of the drug ban has got more and more convoluted and
fascinating. Our earlier belief is only reconfirmed that the
government is not serious about controlling the sale of
...2...
hazardous drugs. The budget allocation for ensuring this, the
expertise, technical personnel, quality control labs, qualified
drug inspectors, mechanism to keep the health personnel and
the public informed about these drugs has remained depressingly
inadequate. Inspite of all the hue and cry raised by health
and the consumer groups, nothing very much has happened.
The health of the nation seems to be relatively unimport
ant, as indicated by decreasing health budget. The Central
Drug Contrl authorities allege that they have no real powers
where implementation is concerned .as this depends entirely on
the state drug control authorities. They argue that they have
inadequate budget and infrastructure.
Expenditure on Health as a percentage of total plan
Programme
Health sub
total to plan
FYP VI
FYP I FYP II FYP III FYP IV FYP V
1951-56 1956-61 1961-66 1969-74 1974-79 1980-85
3.83
3.04
2.79
2.74
1.73
1.87
One glance at what is happening to the health budget is enough
to indicate the priorities health care is receiving in our
welfare state.
We have 600 drug inspectors in the country (Hath! Committee
has recommended). The required number is one for
drug
units and
chemist shops. Only Maharashtra, Gujarat and
Kerala have the stipulated number of drug inspectors and an
adequate drug control mechanism.
In this p.aper we will not touch upon the extent of the
problem of substandard and spurious drugs and the name-sake
action being taken against those involved in their produce
and sales.
Our focus will be on what has happened to the drugs reco
mmended for being weeded out in 1980. In 1980 the Drug
Consultative Committee a statutary body consisting of medical
experts under Section 7 of the Drugs and Cosmetics Act (Central
act 23 of 1940) nominated a subspecial committee to go into
the rationality of 34 categories of fixed dose combination
drugs. They were to study whether these drugs should be with
drawn or allowed to be manufactured and sold.
The criteria Used by the Committee is very sensible andf§Jrg^I±
A Sub Committee of the Drugs Consultative Committee, com
prising state drug controllers, has laid down well thought
out and rational yardsticks to determine the desirability
of combinations of drugs. As per these norms, combinations
of drugs should only be allowed in the following cases:
a)
b)
c)
If there is synergistic action
Where there is corrective action
When two or more drugs are normally prescribed toge
ther and taken by .the patient simultaneously.
d) When the dosage of each of the drugs need not be
i nd ivid uali z ed.
e) Where a fixed dose combination would ensure better
. . .5
patient compliance due to convenience of admini
stration.
f) Where two or more drugs, prescribed separately,
may lead to non ingestion of one of the drugs,
thus adversely affecting the health of the patient.
Conversely, fixed dose combinations of drugs should
hot be permitted under the following circumstances:
Where adverse interactions may occur
When one of the combined drugs becomes toxic'on ■
prolonged use
c) When abrupt withdrawal of one of the drugs caused
wi thd rawal sympt om s
d) If sub therapeutic doses are used in the absence
of clinically demonstrable synergism
e) When pharmacokinetic behaviour of the individual
agents is grossly different.
a)
b)
Thee riteria used by Bangladesh for banning 1742 drugs is
given in the appendix 1.
We' 3-1 just look at what was involved in attempts to ban
a few drugs eg. Amidopyrines, High dose E P drugs, Paediatric
tetracyclin. steroid combinations are dealt with later under
ambiguity is the name of the game.
The sub committee submitted its report, recommended a ban
of 25 combination drugs and giving their reasons for recommend
ing the ban. 16 categories of these drugs were recommended for
immediate, weeding and 7 of the categories to be weeded over.
a specified time. Over 500 brand drugs "would "thus be affected
(This list of 25 combinations and the reasons are attached in
the appendix);.' This report was presented to the DCC at a
special meeting on 10.10.^i^d later to DTAB and Ministry of
Health and Family Welfare accepted it in 1981. The DT AB (Drug
Technical Advisory Board) a Statutary body under section 5..of
the Drugs, and_Cosmetics Act Central Act 25 of 1940 recommended
banning' ofTS' fixed dTose" c'omt)i'nati6n('list" affdehed as appendix
2)
Under section 25 P of the Drugs and Cosmetics act 1940
the Central government has had the powers to issue such
directions to the State governments as required to execute
the Drug act. Under section 18 of the act the state government
has had the power to 'prohibit manufacture,distribution and
sale of drugs by a gazette notification.
These drugs were randomly selected from the Pharmaceuti
cal Guide. Out, _of these 550 brands 44 brands were marketed by
foreign, sect or, '8.'by)p.ublTc... sector ancT S^Bi^l^'riyat'e ..'sector.
A point t~o~"hote is that most of these drugs were being produ
ced by private Indian companies and not multinationals. This
was to be : -'-H phased l_discont,inuat_i_on. According to the
authorit ies"the purpose "was 't’o give "time limit to firms who
may have already purchased the bulk drugs for manufacturing
the formulations". What compassion and consideration'shown
to the drug companies?
. ..4. ..
.J-1ID0PYRINE
The Drug Controller of India(DCI) by DO No.1273/77 DC
directed the State Drug Controller to ban the fixed dose, comb
ination of amidopyrine on effect from 3.2.82. Orders were
issued to stop manufacture from 1st July '82 and sale by
October 31st '82. This ban was later extended further to 31.3.83.
The DCI-through his DO No. 19013/8/81D dated 22.4.82
directed the State Drug Controllers to ban the manufacture of
fixed dose combinations from 30.9.82 and their sales from
31'.3.83. Sequal to V^S'.vn’e panel report government decision to
withdraw 350 unnecessary drugs was taken.
When Maharashtra 14DA did. ban amidopyrines, the multina
tional most affected managed to get a stay order on the grounds
that the drug' was allowed' to be marketed in other states by
their state FDA's. In J9’8O'3_3 fbrm'ulatibhs of amidopyrine pro
duced by 20 sb manufactures were in the market. Multinationals
and other big drug houses highly trusted by the public such
as SuhriiGeigy, Sandoz, Suhudgeigy, Unichem, Ethnor, Thorns,
f
Ind on were involved. Most of these drugs were being sold with
out adequate warning.
As Praful Bidwai on 19th August 1980 stated in the
Financial Times Harmful drugs production still not stopped,''reluctant to lose their market share, these companies have
merely continued to produce and market amidopyrine and are
continuing to sell their preparations without even an additi
onal warning about the drugs side effects.
Mukaram Bhagat Centre^ for .Education’and Documentation,' .•
'in ’Aspects bf'Drug Industry in’India' gives the example of
Tamilnadu government medical list for government hospitals in
which drugs like amidopyrine, phenacetin and analgin are very
much included even when they wore considered harmful and been
disallowed.
PHENACETIN AND HOLOGBNATED HYPROXYQUINCLINE:
Ban of (fixed dose combinations of phenacetin and hologenated and hydroxyquinoline was to be effective from 1.11.82.
The date of the ban of fixed dose combination of amidopyrine,
phenacetin and halogenerated hydroxyquinolines was extended
to 31.3.83 through DO No. X19013/8/81-D dated 13.8.82.
In 1979 January the Drug Controller of India had issued
an order to gradually phase out amidopyrine as always 'phased
discontinuation' process was not meant to be implemented as
there were no specific DEADLINES.
HIGH DOSE QE E P DRUGS:
Through another DO No. 12-48/79-DC dated 26.6.82 the DCI
directed the State Drug Controllers to ban the manufacture
of high dose estrogen and progestorone combination from
31.3.83 and their sales from 30.6.83.
M/S Unichem Labs Bombay (OP 2927/82 of writ petition
2928/82), 14/S Nicholas Labs Bombay and 11/S Organon (now known
as Infar (India)Ltd Calcutta filed writ petitions in Bombay
and Calcutta high courts against the DCI's instructions to
ban these drugs, their contention
that Central government
has no powers to ban the drugs. The high court of Bombay and
Calcutta have' granted stay orders and these products continue
to be available in the market.
Even though section 10A and 26A of the am ed ned D r ug a nd
Cosmetics Act (April '82) empower the Central Government to
prohibit import, manufacture and sale of any drugs considered
ha'rmful/t oxic or irrational etc. Since the matter regarding
high dose E P drugs was in the court, these drugs have EQT beer.
included in the gazette notification of the DCI issued, on
25.7.85 banning 22 fixed dose combinations.
What is. absolutely objectionable is the fact that(this is
inspite of the act of the Drug Controller of India's earlier
instruction dated 26.6.82 banning the production and sales of
high dose E P drugs from 51.3.85 and 50.6.83) M/S Organon
(INDIA) Ltd have managed to obtain extention of licences to
manufacture these products foi’ another 2 years.
A sample of high dose E P drugs from Calcutta with manu
facturing date 31.12.83 indicates that the ban is not merelybeing flaunted by Organon but by other drug companies manufa
cturing these products.
The misuse of these drugs for hormonal pregnancy tests
and for attempting to induce abortions continues massively.
PAEDIATRIC TETRACYCLIN
Manufacture of .Paediatric tetracyclin drops was to be
banned from 1.5.82, no date was then given for marketing.
Paediatric tetracyclin have since been banned on paper. They
are still available, OTC, without warning.
Paediatric tetracy&lin ban too does not figure in the
gazette notification of July 23rd 1983.
On April '82 the Drugs and Cosmetics Act was amended
whereby the Central Government and the Central Drug Control
Authorities were given specific powers to 'ban the import,
manufacture and sale of drugs in public interest'. (This was
mentioned in the drug Action Network Newsletter October '83).
Section 3(b)(1) was substituted and section 10A and 26a
were inserted in the act. This came into effect from 1.2.83.
This means that had our Central Drug Control authorities wanted
it, gazette notifications banning the manufacture and sale of
these drugs could have been undertaken immediately under the
powers invested in it under section 26A of the act exercised.
The implications of this delay have been that certain
drug companies have challenged th,e drug Controller of India's
authority to ban these drugs. Some of them have even got stay
order against specific bans, making these bans ineffectual and
the whole drug control authority of our nation a laughing stock.
The drug control authorities see their role as mainly advisory
and hence don't feel particularly perturbed. Actually to come
to think of it no one in the Health Ministry at Centre or State
level seems to be particularly perturbed.
Allowing this extended time period, during which imports
manufacture and sales have continued amounts to 'arbitoriness
and discrimination' under article 14 of Constitution of India
6.
according to Vincent Panikulangara since these drugs would.be
dumped in the market, substitutes withheld. With our efficiency
of drug control mechanism, products in the chemists shops wil..
continue to be sold and never withdrawn.
According to Section 261 of the Drugs and Cosmetics
Act 1940 •
"Without prejudice to any other provisions cont
ained in this chapter, if the central government
is satisfied that the use' of any drug or cosmetic
is likely to involve .any risk to human beings or
animals or that o.ny drug docs not have the thera
peutic value claimed or purported to be claimed
for it or contains ingredients and in such quant
ity for which there is no therapeutic justification
and that in the public interest it is necessary or
expedient so to do, then that government may, by
notification in official gazette prohibit the manu
facture, sale or distribution of such drug or
Cosmetic".
.
"
Under section 10?. of Drugs and Cosmetics Act of 1940 also
there is a mandate that following a gazette notification
imports of injurious drugs can be banned.
.Article 47 of the Constitution of India lays down
that
"The State shall regard the raising of the level
of nutrition and standard of living, of its people
and the improvement of public health as among its
primary duties and in particular the state shall
endeavour to bring about prohibition of the con
sumption except for medical purposes of intoxica
ting driinks and of drugs which are injurious to
health".
Under section 53 P the DCI directed the State Drug Control
Ilers tolban the 20 fixed-dose combinations. The State Drug
Controllers under section 18 of the act could exercise their
power and prohibit their manufacture and sales by issuing a
gazette notification, According to Vincent Panikulangara, the
State Drug Control authorities are guilty of not exercising
their power and taking responsibility. They have thus violated
section 18 and 33 of the Drugs and Cosmetics Act and violated
the fundamento.1 right of the public citizens to health and life
under section 21 of the Constitution of India. Article 14 of
the Constitution is also violated by their having acted in a
arbitrary and discriminatory manner contrary to public interest,
in favour of the Drug companies. '■
Kerala High Court Judge Mr Potti's judgement on Vincent
Panikulangara1s writ petition speaks for itself.
"As. between the. live_s_.of the_ citizens of this
country on the _one ha.nd_. and loss that may result to
the manufactures and traders by the immediate “ban
on the.manufacture’and. sales on the otherj 'the'’
government had chosen_to view, the latter as o'f
m'ore.“cdhcern"J “It is the'duty' of t he " stat e to
protect its citizens from injury and harm especially
...7...
when the injury is not inevitable".
Acting Chief Justice
P Subramanian Potti and
Justice Paripuran
Kerala High Court, in their dire
ctive to the Union of India to release
the list of brand names of banned drugs.
In October 1982 M/S Nicholas(India)Ltd Bombay filed a
writ petition in Bombay High Court against the decision to ban
the fixed dose combination of aspirin and vitamin C. The
Bombay high court after the hearing of the respondent ruled
that State Drug Control authorities has no power under Section
18 of the Drugs and Cosmetics Act to stop the manufacture and
sale of these products. (The high court ruled that it would be
open to the respondents as and when the law has been enacted
to pass any fresh order as it is considered necessary in accord
ance with the law after following procedures prescribed by the
government) .
Subsequent to the Drug_Amendment Act coming into force on
1.2.85 the manufacturers have again gone to court challenging
the central government and sections 2bA and 10A of on grounds
of "LACK OF OBJECTIVE CRITERION for such ban".(A special hand
out on Rationale of the ban is available with us).
The Commissioner of FDA Maharashtra State(which is suppo
sed to be having the best drug control mechanism) had informed
the DC I that in the light of the ruling_given by the Bombay
High Court "it would not'be possible for him to take any action
to stop the manufacture and sale of any of the fixed dose
combinations in quest ion".(Letter dated 9 June 1984 by Drug
Controller of India to us).
It was probably the above as well ns Vincent's writ
petition against the state and central drug control authorities
for not having used their power that forced DCI to issue the
gazette notification. .1 point to note is that drugs banned earlier and at different types make the brand banned list. E P
drugs arc not’included ift-the’gazette notification. ■L' .
..
The ambiguidty of the wording of the gazette notification
hit us early, when we attempted to compile the banned brand
list. It was not clear whether for eg. in Category 4 include
- any drug containing yohimbine or strychnine would be banned
(as neither of the two were considered to have therapeutic
value and infact could lead to s’erious side effects as stated
even by the DCC).
- or the ban was applicable to drugs containing both yohimbine
and strychnine.
- or to yohimbine and strychnine with testosterone or vitamins
- or ONLY to drugs which contained all 4 ie. yohimbine,
strychnine, testosterone and vitamins.
Another doubt was regarding criteria 12 ie. whether it
could effectively deal with steroid and antihistamines combi
nation which could be indicated for allergy as well as asthma.
First of all DCC had recommended a ban, of all steroid combin.ations. Making this exception would obviously encourage misuse.
After all. doesn't the microscopic print in the medical litera
ture for high dose E P drugs (now-a-days say only.secondary
amenorrhea and isn't it true that ft is mostly used for pregn
ancy testing and attempting abortion', "changing the indication
...8...
on paper of a hazardous drug won't alter its use. Similarly
allowing steroid combination for asthma won't present their
misused for other conditions
The DCC had recommended banning of all fixed dose steroid
combination, DTAB decided to prohibit manufacture of fixed
d °se Combination of bronchodilators, antihistnminics a nd tran
quillizers with corticosteroids as early as October 4, 1980.
Dr B Shankaranand, the then DGHS, chairing a meeting had
said "The current medical practice in all the developed count
ties is to give corticosteroids separately and fixed dose
combinations of corticosteroids with other drugs are bein.a
discouraged".
Prof. Harkishan, Singh of tho Department of Pharmaceutical.
Sciences Punjab University stated, ..that there existed "published
evidence to show that cortico steroids taken in small doses
over longer periods are more harmful than if taken in larger
doses over shorter time".
The Drug Consultative Committee comprising of all state
Drtig Controllers entrusted the responsibility of evaluating
54 categories of fixed dose combination, on basis of their
rationality to a sub-committee. The sub committee comprising
of some distinguished medical experts recommended a ban on
steroid combinations. The Committee warned against compulsory
intake of steroid because the "fixed dose combinations of
steroids for internal use can produce serious side effects viz
fluid and electrolyte disturbances, hyperglyceria glycosuria,
increased suscesptibility to infection including TB, peptic
ulcers, osteoporosis, steroid myopathy, cushings syndrome and
Hersutism, combination with bronchodilators etc.".
Dn December 51 , 1981 , the Drug Technical Advisory Board
constituting of exactly the same .members reversed its own
earlier decision. It felt that there was a need for getting
wider medical opinion and further details and allowed the sales
of these products.
(
Dr Gulati MIMS Editor in his editorial MIMS India Vol.2
Mo. 5 February 1982 writing about the "somersault on steroids"
says "they must have had very extraordinary "reasonit 6
a) reverse their own earlier decision
b) ignore the advise of DCC
c) consider the opinion of tho whole battery of eminent and
distinguished medical specialists from research institutions
v
as inadequate so as to ask further details and wider medianl
opinion".
It would be interesting to find out how and why this
change in their stand on fixed dose combinations of steroids
took place. We would very enthusiastically have undertaken this
exercise, had obtaining information such as this, been a less
teilious, less time energy consuming and less frustrating affair
The Kerala High Court judgement, in response to Vincent
Panikulangara's writ petition Op 8459/1982 had directed the
Central and State Drug control authorities "tojpublish the
list of tra.de/brand names and the names of the manufacturers
of' these drugs/This 'was in 1982. Repeated requests for the
s'-une have' been made to the"Central Drug Controllers office.
Some of the' Drug Action networkers have been requested to do
the same at the State level.
...9...
Excuses ware made that the drugs have been licenced anc.
registered with State health authorities and the centre alleg
edly has no clue about the various femulations and brands
involved. The drug control mechanism is so inef+’■’^ient that
even to obtain just the list of, these products has taken more
than one year’" To '‘ensure their ban“6r 1 quality control' would
definitely take a century.
It should be noted that the drug ban will be applicable
for lesser drugs than what we had anticipated. Tnspite of the
presence of irrat'ional and hazardous ingredients only these
drugs will be banned that contain all the ingredients mention.,’
in the various categories eg. under category 5 -only those
drugs containing all the following io. yohimbine + strychnine +
Test esterone + Vitamins will be affected.
According to Dr Das Gupta, Asst.Drug Controller the
banned brand list will be ready in about 3 months. We had pre
pared our own black lists of banned or bannable drugs as far
hack as 1982 which have been circulated amongst the health
care institutions in the voluntary sector and drug action
networkers. These black lists have been for
1 ) Clioquinols, hydroxyquinolines ie. mexaform and Co
2) .'mid onyrines - abalgen Ergopyrine
3) Paedintric t etracy clin
4) Diphenoxylate - lomotil etc.
5) Anabolic steroids
5) Penicillin and streptomycin
)
T T,nn
„
7) Chloramphenicol and streptomycin
n
u rec
1 n°
8) High dose E P drugs
9) Antiinf 1 acimatory agents and steroids etc.
(Background papers based on the above underlined drugs had
been prepared and are available).
2-3 attempts nt compiling the banned brand list ..based on
drug banned by the gazette notification have been made. Three
things have prevented us from widely circulating them.
i) Our expectat ions ..from. qur_ drug, control authorities_t o jnnke
thjp available at least after the Kerala. High Court judgement
’Couff writ' ■pciit'iqn) ~
........
ii) The difficulty" in''oBt?ining' the drug list of. formulations
f r om Jihe State Drug Control' authorit ies.
iii-)The process of reforraulation" of various drugs taking place
’
with our 'not h'avi'ng'"any'in’f’o'rmatidh''a.s'to'
a) which drugs were being formulated and sold as reformu
lating? ’
b) Which drugs were being reformulated but their banned
formulations under the same BRAi© existed ..'.were sold
unscrupulously in the market?
c) Which were the hazardous banned drugs still being manu
factured and sold as such?
Our health and drug control-.authorities get extremely upset
when we mention the achievements of Bangladesh in their attempts
towards ?. Rational Drug Policy. Inforced to mention Bangaldesh
again. It should be noted that .after the issuing of the
Promulgation banning 1742 drugs in June 1982 the time period
given to the drug companies of 3, or 6 or 9 months was given
to withdraw these products from the market, to destroy these
products even their export to other countries was strictly
prohibited. We, on the other hand have failed to implement ,a
recommended bah by our own government committees and banned
by cur ’.own drug controller. The drugs banned were more few
hundred, not over a 1000. The time period given was for the
. . .10...
drug companies to complete the manufacture of their formulati
and sell off their stocks. The stocks surprisingly like Med us
head never seem to finish off.
Nepal, Pakistan, Malaysia, Sri Lanka, and Bangladesh feel
that clioguinoT (hydroxy’quindline') formulations.have no signi
ficant t her ap e ut’ic' value ,and can have_ma j or s id e effect s, They
have' <1 ecid’ed' to’ban 'these d rugs. C.iba Geigy makers,_p_f..m oxa, form
have announced their plans, to withdraw .the drug. frpm_int_errntional,marker. We continue to allow them to be sold and pro
moted under more than 90 brands (including those produced by
our public sector.)
The Drug campaigners from Bangladesh, Sri Lanka have
complained about the outrageous smuggling in of these banned
products from India. Our continuing to allow.the manufacture
and sales of these hazardous and irrational products is not
merely hazardous to the health of our people, it also cr^rtes problems for our littler neighbours who are attempting to rat
ionalize their drug- policies, in the interest of their people^
If our government authorities cannot jnake all that goes
wit hjeiisuring 'good .Health, 'available ~~f o Its“'7U0_jiiIIi‘5n.people
it "has no "business* to’ allow irrational -and, hag a rd o us d rugs to
b’e~in'flicfecr"up’d’ii~t'hem.
................... ”
We will compile our own banned brand list and while the
game playing goes on between the health, drug- control authori
ties of centre and state . „1 the-irug industry and the high
courts we will ensure that all these drtigs are BOYCOTT IS'by
health personnel as well as consumers.
The DC I had in one of his meetings last year pointed out
that unhygienic conditions in the public hospitals, lack of
clean water, sanitation quackery and unethical practices by
medical personnel were greater problems than continuing sales
of few hazardous drugs.
We want to make it clear that the issue here is not
4
m erely _of _b arming a few hazardous 'and irrational drugs but it’
£ s t o ' f de us on’ '(what ' is((g'oi'ng“'‘u'n "iiTt he name ~oT’"he.aTE h "cire’''
It is t o~ high ~light' ~t'H,at _when causes of ill ”heaTtfi’'"lie"~els’ewhere” in primarily~~1e’al•
h®1 alone)' wiTl'Tfiore come
ab'qut "a" ’signi'ficant’ c’EangoEin (fffS’lieal't’h status axil "quality of
liXQ. _olC.o?urlpeople?’ There" are no effective pTITs against
poverty and the diseases of poverty. To deny people their
right to health care is bad enough, but to let loose 'garbage
and trash in the name of medical care is is inexcusable
’
inflaunting and totally unacceptable.
Dr Mira Shiva
Coordinator
Low Cost Drugs & Rational Therapeutics.
-MM
./ 1 6.7.84
Grad ed Bssential Prug.List
These are the guidelines to help Community health progra
mmes and health institutions draw up their own essential drug
list.
This is a compilation of various drug lists and it empha
sises the concept of Essential drugs. For those believing in
and for those involved in alternative health care, the concept
of Essential drugs is an integral part of health work.
The format used for this compiled list is based on WHO's
Essential drugs list , Technical Report Series 685.. An outline
of it is given. It should^be noted that certain drugs arc
repeated as they are used more than one disease entity.
The various drug listens they appear in the compiled form
are as follows:
EMRO(Eastern Mediteranean Regional Office)- WHO
List A - for 8th class passed
List B - for that are class 10 passed and have had training
SL;~
G•-
E^ho
AM " v
A '
B
)
c
)
Formulary of Post Graduate Institute of Medical
Education and Research.
Sri Lanka graded Drug list included here is list of
drugs recommended for doctors incharge of Peripheral
health centre.
Gambia restricted drug list based on their national
f ormulary.
An English NGO supply equipment and drugs to Charity
Hospitals overseas.
Action Mede or.
Qur humble recommendations
for trained village~liealth worker Level
for trained Paramedic or middle level workers
for doctors involved in primary health care
Those drugs included in the Hath,! Committee have been
utiderlined. This drug list is meant fo.’be a guideline to help
health care institutions in the voluntary health sector to
select their own essential drug list. It is up to us to show
it to the government ajd Our medical colleagues who believe in
commercialisation of medical care that good health care does
not necessarily depend upon the length and variety of the
drugs used.
<
PG I;-
COMMUNITY HEALTH CELL
47/1, irs t F Io o r)S t. M arks Hoad
u A N G A lO ae -560 001
Bangladesh drug list:
Category I - for village level workers
Category II - for Primary Health Cr.re.up to Thana complex levef.
CMC Christian Medical Council list - Contact No. 63,August
1981, "Getting Essential Drugs to the People"- Stuart
Locost ■. - Low cost standard therapeutics a collective volun^a?/
enterprise for rational therapeutics
C/0 Aror.l, G P 0 Box No. 7, Vadodara 390001.
PC:Essential drug list drawn up by sub-group dealing with'.
this at VHAI's Pune Workshop "The Drugs Issues seeking feasible alternatives".
It is extremely difficult to go against the current created
by the market forces. It.is a true test of our'conviction and
our capability to ponvijnce others.
* - Alternative substitute from the same therapeutic group
can be select'd based on comparative Jest and availability of
equivalent products, eg. Hydrochlorothiazide: any other thia
zide type diuretic currently in broad clinical use.
numbers in the Paren thesis following the drug
names indicat
1) Drugs subject to international control under the Single
Convention on Narcotic Drugs(1961) and the Convention on
Psychotropic subs.tances( 1971)
2) Specific, expertise, diagnostic precision or special equip
ment required for proper use
3) Greater potency
4) In renal insufficiency, contraindicated or dosage adjust
ments' necessary.
5) To improve compliance
6) Special pharmacokinetic properties for purpose
7) Adverse effects diminish benefit/risk ratio
8) Limited indications or narrow spectrum of activity
91 For epidural anaesthesia
Letters in the parentheses following the drug names indi
cated the reasons for the inclusion of compelementary drug
When
A.
drugs in the main list cannot be made available
When
B.
drugs in the main list are known to be ineffective or
inappropriate for a given individual
For
C.
use in rare disorders or in exceptional circumstances.
The criteria of selection of essential drugs,
Steps to be taken bo-implement such a programme. Provisi on of
information on essential drugs as recommended by WHO have beer
dealt with earlier. In the text of the paper the format of the
drug list is as follows:
Reprised model list of :Essential Drugs - a WHO Expert Committee
Report - Technical Report Series
635
1.
anaesthetics
1.1 general anaesthetics and oxygen
1.2 Local anaesthetics
2.
Analgesics, antipyretics, nonsteroidal antiinflammatory
drugs and drugs used to treat Gout.
2.1.non - opioids
2.2 Opioid analgesics and antagonists
J.
Antiallergics .
4. Antidotes and other substances used in poisonings
4.1 general
4.2 specific
5. Antiepileptics
6. Antiinfective drugs 6.. 1 anthelmintic drugs
6.2-.antiamoebic drugs
6.3 antibacterial drugs
6.J.1 penicillins
6.3.2, other antibacterial drugs
6.3.3 antileprosy drugs
6.3.4 ant it ub orc ul os is drugs
. .
6.4 antifilarial drugs
6.5 antifungal drugs
6.6 antileishmaniasis drugs
6.7 antimalarial drugs
6.8 antisc hist os omal drugs
6.9 antitrypanosomal drugs.
Antimigraine drugs
Antineoplastic and immunosuppressive drugs
Antiparkinsonism drugs
Blood,drugs affecting the
10.1 antianaemia drugs
10.2 anticoagulants and antagonists
11. Blood products and blood substitutes •
11.1 plasma substitute
11.2 plasma fractions for specific
11.3 plasma substitute.
uses.
12.1 antianginal drugs
12. Cardiovascular drugs
12.1 antiarrhythmic drugs
12.3 ant ihypert e ns ive d r ug s
12.4 cardiac glycosides
12.5 drugs used in shock or anaphyl13.1 antifungal drugs
axis.
13. Dermat ological drugs
13.2 antiinfect ive drugs
13.3 antiinflammatory and antipruri.~ .
, .
. ,
tic drugs
13.4 astringent drugs
°
13.5 keratoplastic and keratolytic
13.6 scabicides and pedir- ' '’-drugs.
culicides
14.1 ophthalmic drugs
14. Diagnostic agents
14.2 radiocontrast media
1 5 - Dis inf ect ants
16. Diuret ics
17. Gastrointestinal drugs 17.1 anacids and other antiulcer
17.2 anti emetic drugs
17.3 antihaemorrhoidal drugs
17.4 antispasmodic drugs
17.5 c at ha rt i c d rug s
17.6 diarrhoea,, drugs
_ used
_ .
in
17.6.1 antidiarrhoeal(symptomatic
17.6.2 replacement solution drugs.
18.1 adrenal
'
~ hormones
■
18. Hormones
and synthetic
18.2 androgens.
substitutes
18-.-3 estrogens
'
18.4 insulins and other antidiabetic
18.5 oral contraceptives.
agents
18.6 ovulation inducers
progest
ogens
18.7
18.8 thyroid hormones and antithyitfid13. Immunologicals
19.1 Sera and immunoglobulins
7.
6.
9.
10.
20.
21.
22.
23.
24.
25.
26.
27.
1V9.2.1 for universal immunization
19.2.2 for specific groups of indiviMuscle relaxants(peripherally acting) and choline- duals.
st erase inhibitors.
Ophthalmological preparations. 21.1 anti infective agents
21.2 antiinflammatory agents
21.3 local anaesthetics
21.4 mi ot ic s
21.5 myd ri atic s
Oxytocics
21.6 systemic preparations
Peritoneal dialysis solution
Psychotherapeutic drugs
Respiratory tract,drugs acting on the 25.1 antiasthmatic
25.2 antitussives
drugs
Solutions correcting water electrolyte and acid-base distui26.1 oral
bonces.
Vitamins and minerals. 26’2 Parenteral
Z>$HC
Hn8mS(6P)
cuP'
Pm>' L
PT ESCFIPIN3 DRUGS
Questions to be answerer before writing a prescription :
I 1.
Is this drug really necessary ?
Exactly what is to be accomplished by the drug therapy ?
Do I have the requisite experience and knowledge about this
drug ?
f~4. Have I weighed the potential toxic effects of the drug
I
against the benefit which is expected ?
|_ 5. Have I checked for possible allergic risks, idiosyncratic
tendencies, and the patient's drug diet which might interact
with the new agent ?
6. Have I selected the best agent available for this particular
purpose ?
7. What is the best route of administration and form of the drug ?
8. What dose regimen will be most appropriate for the pruposes
of this therapy ?
9. For what period of time, days, weeks, months, will it be
advisable to continue this therapy ?
10. What precautions shall I follow to ensure .<? r ■ continuation
of this therapy (appearance of signs and symptoms, blood
counts, prothrombin time, etc.) ?
11. Is the patient reliable for this type of therapy ? .Will be
have proper supervision from his attendants ?
12. Have I given the necessary instructions to the patient or to
the responsible relative ?
2.
3.
7
$
While these factors in drug therapy appear obvious,
it is also evident that some physicians routinely neglect them.
Toxic reactions to drugs arc not completely avoidable, but they
can be kept to the irreducible minimum by exertion of care and
precautions. The development of an automatic reflex of checking
the above points would ensure the proper degree of conservatism
necessary to use drugs safely. So important are these points in
modern drug therapy that some advanced clinics and hospitals have
trained clinical pharmacists to advise and check and if necessary
„correct the physician's prescribed regimen.
Now what about the G.P.
The practicing physician receives a lot of advertising
material from drug companies. Many physicians confide that they
consign this material unread to> the waste container. Nevertheless,
the fact that this' expensive advertising method is continued
means that it must be effective. On the other hand, it is_only
fair to state that this is one of the few means that drug companies
have to communicate directly with the physician. Much of the
material is informative. Some- of it is extremely valuable. It should
be understood that drug companies are requirecrTo^Tend—packaging
inserts (the slip of directions and precautions with each unit
package) to each physician before a new medicine becomes generally
marketed. In many instances this wilT'be the only opportunity a
physician will have to see this valuable information. He should not
. . .2
: 2
:
only carefully rear' these packaging slips but also keep them
on file. They are a bc-tter review of a drug than any other
source short of a scientific article or text
They contain
information about the exact chemical s.ruc’ur.
nxicit
pharmacology, its clinical use, contraindications and toxicities,
and recommended dosage schedules. Often they give references co
sicientific and clinical literature.
In many instances, drug companies will also write.to
each physician informing him of a recently discovered toxicity
or precaution in the use of their products.
This may be in advance.
of published information or governmental warning. Therefore, the
’physician who does not read the drug company literature is negli
gent and is denying himself the benefit of oriyileted. communiy
cations It does not takemany moments to scan- through and distinouish between the valuable and the exaggerated claim.
The many drug samples which also arrive in the mail serve
the purpose of acquainting the physician with the actual appearance
of a particular product. They arc, of course, an excellent indu
cement for the physician to try them on himself, his family, or
patients. For the most part, the physician should refrain from
succumbing to this inducement. After examination of the actual
product, it should be disposed of with certainty, not simply
dropped in the '"aste container. Many a case of poisoning has
occurred because the victim learned that the garbage can in back
oT~the physician's house was a ready source of medication. Also,
some unprincipled persons make a practice of collecting paysi ranc
samples for black-market sale.
The second common source of information is the detail
man. Some large companies employ as many as 4QO or 500 of these
_gentlemen. They are generally pharmacists or college- graduates-"
wRo~’are quite personable and have a flair for conversation. They
are assigned territories with the task of regular visits to
physicians, clinics, and hospitals to indoctrinate the profession
with their drug products. For the most part, they have'received
some instruction about drugs in the home office", given by~Ehe~
scientific and medical staff of the company. /-. few have medical
jj backgrounds of.an incomplete nature. Thus, it should be under
stood that their sole function is to describe their product and
it purported virtues and advantages over existing products. Th<~'>
are in no position to instruct the- physician in what to prescrib^^^®
and how to treat disease. The physician who learns his pharma
cology and therapeutics from a detail man has descended to the
level of quackery and should be-"retired. By contrast, many busy
and competent physicians go as far as to refuse to see a detail
man. This is undoubtedly to puritan a view. Most detail “men ar"
upright and conscientious personjand they do have information to"
offer. Perhaps the best doctrin to follow is "let the buyer
beware". Neverprescribe a new product until you have yourself
checked reliable sources of information and are sure you are
acquainted with all the facts and background of the drug °
de^X-fflanjs plug may legitimately be cut short by simpld renues+i3•
sTip‘
Tt is often amusing to compare advertising
with the cold information of the critically reviewed packaging irv
PHARMACOTHERAPY VIS A VIS PLACEBOS
V. ISWARIAH. BA., MB., F. R. C. F.
.Izxfe Professor Emeritus, St. John’s Medical College, Bangalore.
Scientists who assemble in conferences
periodically have often to digest a mass of
factual details garmered from the corners
of institutional laboratories far and near,
that well nigh their heads will be blood
with the bludgeoning of heavy data.
These lines therefore are not intended to
rummage the depths of the ‘scientific mind’
but rather to be a salve to the grey matter
for a little recreating thinking.
The word ‘Placebo’ is of Latin origin
with an eccliastical and medical significance.
Eccliastically, it refers to the introductory
response to vespers to the dead. Tn medicine
the word ’Placebo’ or ‘I shall please’ has
come to signify a drug having no really
curative power other than psychological.
Antiquity and Scope of Placebos
Placebos
date
back
to beyond
Hippocrates and they were known as such.
The Pharos of Egypt were treated by rare
medicinal agents like bile of corcodile from
the Nile, milk of tiger, fat of viper, horns
of unicooss (a mythological animal)
gallstones of wild boar, the rarity of these
agents subserving the placebo element. The
enormous success of homeopathy in the
18th century where drugs were prepared
spectacularly and given in great dilution
that they could not possibly have exerted
any pharmacological action, is another
example of placebo.
But why go to history ? Doesnot every
prescription carry with it the placebo
element? A prayer to Jupiter (Rx super
scription or Superstition??) starts the
prescription, it is written on an elegant
letter head with the doctor’s merits and
signed by him, it has to be taken to a drug
house, that the patient has to pay for it,
that it has often a bad taste.are not all
these placebo elements? The more they
pay for it ’or subject themselves to sacrifice,
the more efficient is the treatment and is
not there an element that contributes to
treatment apart from pharmacotherapy ?
Variety of Placebos
Placebos have been classified into two
main groups i.e., the True and the False.
f.J- *.
cC^
Ml
’
, - jV3
Swift, “ no patient will ever care to be
handled or treated by a personality for
whom he has no respect or veneration,
even if he happened to be an eminent
doctor.”
The first or the true placebo is a lactose
tablet bread pill, caramel mixture, more
effective if coloured, mottled or scored and
with a riot of taste- The pure placebo
relieves the patient and tranquillises the
recepient. The doctor intends this. It
may be styled psychotherapy practised by a
general practitioner with an innocuous
agent. One cannot say if the benefit
conferred is dependent on the low
intelligence of the patient. Perhaps a
costly placebo may be needed for the
sophisticated rich. The giving of the
med'cine is a symbol of "I will take care of
you”. A whole body of knowledge, wisdom
and experience is epitomised in the medica
ment. The medicament also fulfills the
patient's need to feel dependent. A bitter
or nauseating agent fills the need for punish
ment which many feel that they need at
some time or other. The riot of smells and
tastes is very effective in creating an illusion
of an efficacious medicine. Valerian and
Asafoetida were once popular ‘Specifics’
for hysteria and hypochondria. Valerian
by the way enjoyed a further advantage.
Its utility is not likely to be disturbed by
information which the patient may obtain
from the dispenser. If the pharmacist
looks up its action in his old Materia
Medica book, he is sure to find a very long
list of conditions for which it is recom.
mended without a vestige of reality. No
one
denies that
when a genuine
therapeutic agent is used, the element of
suggestion is also there; the element of
optimism that the physician conveys to the
patient is there to reinforce the specific
action of the drug. One has here to
remember the old observation of Jonathan
The Second or the False placebo or
adulterated placebo or bastard placebo
is in a different category. If in the true
placebo the doctor plays a pardonable
hoax or deception with the intent of
pleasing the patient or tranquillising
him or relieve his symptoms, in the latter
or false placebo the doctor
gives
something that he thinks will help the
patient and in so doing relieves his own
symptoms, tranquillises his own self, applies
the balm of flattering function to his own
self, in other words he practises deception
on himself. When one uses an agent of
questionable pharmacological activity, a
new arrival on the market or in amounts
that can by no possibility exercise phar
macological action, there is the real danger
of deceiving two-the patient and himself.
To this category belong many hormonal
products, multivitamins, haemato. nervine
tonics, polyantibiotic, steroidal umbrellas.
The doctor tells the patient with a gusto
of conviction that the patient is going to
be cured by it, but it deceives the doctor
despite the patient improving in a self
limiting ailment.
Range of Placebos
The extent of this type of placebo
action has only been recently appreci
ated. In reviews of New York Hospital
Pharmacopeias every 25 years since 1816,
amongst a list of 160 drugs, every subsequent
review recommended deletion of a third
30
of the exiting list, not because better substi
tutes were available but the old ones were
declared inert. This means that all the
cases treated with those discarded ones
(if alive) were cured not by pharmacology
but by placebo. Who knows the fate of
I. P. 1966 in A. D. 2000?
Again, the extent of placebo action has
been appreciated by controlled study of
new drugs. Till some years ago, we
thought we were making a big advance in
rational treatment when we began a study
of a drug by comparing, say a 100 cases
treated with the drug with 100 cases not
treated at all. We now realise that we
have to assess a new drug by comparing it
with a group not treated with any drug
and a group treated with a placebo.
Dr. Wolff of Cornell University found in
his study that sucrose tablet and some
innocuous injections had about the same
effect in preventing sea-sickness as
barbiturates and hyoscine. Seidel and
Abraham found that hypodermic injections
of saline were just as effective as vaccines
in rheumatoid arthritis.
Frantic claims were made not so long
ago for antihistaminics as cure for common
cold. Controlled study with placebos
revealed that cases treated with many of
the antihistaminics were no better than
controls in the incidence, severity of
symptoms or duration of colds. The
old adage “Treated cold lasts one week ;
untreated cold lasts SEVEN DAYS ”
still stands.
belief that many medications are on the
border line between pharmacology and
placebo and there is always the chance of
hitting'on some effective remedy in a jum
ble. This is the attitude to which rational
pharmacotherapy is opposed, the result
deceiving the doctor as the action of medi
caments. Baneful drug interactions in poly
pharmacy are dangerously revealing them
selves. In a very extensive study by
Morreli H. F. and Kenneth L. (California
Medicine 109 : 380, 1968 ) Dangerous
reaction by drug combination in
many directions are pointed out. The
development of rational therapeutics will
continue to lag in this country as long as
we encourage the use of preparations with
some potent agents in a jumble of several
other deceptives. To validate a pure
placebo by a useless amount of some potent
material is a substandard practice or hyposcientific procedure. The path of thera
peutic advance is strewn with the bones and
bottles of those who failed to make a con
trolled study. The doctor who has best
results with a set of drugs in which he beli
eves highly, is the one who is least fitted to
evaluate results critically. The author
knows a physician who never fails to pres
cribe Becozyme for any ailment; the com.
pound has obviously upset his proportions.
Apparatus, Tests, Injections,
Placebos
X.rays al
Mass not to speak of class has sufficiently
progressed ‘in civilisation' as to;want an
’Injection’ in preference to oral medication.
Every house surgeon on night duty should
have had expereince of injecting 0.5 ml of
distilled
water
to tranquillise
a
Physicians who indulge in polypharmacy
or lengthy prescriptions are actuated by a
ai
patient who had had a taste of morphine.
To such a kind of a patient, the specific
kind of treatment is a conditioned reflex.
Dogs that are given morphine frequently in
large dosts invariably vomit. If this is
done regularlay for 2 to 3 weeks and then
sterile saline substituted, the dogs will also
vomit. The needle and the injection, set
off the pharmacological response to
morphine.
Lay dabblers in medicine who exemplify
■the old adage “Little knowledge is dange
rous ; drink deep or caste not the Pierian
spring ’ have great faith in biochemical tests,
repeated blood taking preferably simultan.
eously with urine test, blood pressure
apparatus to cause cramps, an elegant typed
report —these then are the symbol of
‘I will take care of you’ or the placebo
element in treament.
Dr. Lipkin of Cornell college describes
a series of cases of Raynaud’s disease
treated with mecholyl iontophoresis In a
control series, saline was applied instead of
mecholyl and sometime did not turn on
the current but only clicked the dial. Some
improvement was noticed in every case of
control and in 6 out of 25 cases, the results
were excellent. In one case the patient was
so treated three times a week by the nurses
without the doctor’s knowledge with very
satisfactory results. Previously this patient
had been unable to go out in the cold
weather without suffering spasms. Another
patient was unable to work for the first
hour after she reached office as the
touch of the typewriter key would throw
her finger into spasm. She was given saline
iontophoresis weekly and a saline intra.
muscular injection twice
remarkable improvement.
weekly
with
Surgical Placebos
That placebo role is not exclusive.y in the
physician’s realm has to be remembered.
How many tonsils, appendices, gallbladder,
and healthy teeth have been sacrificed to
provide placebo treatment. It is said that
in America a category of women of the
leisured class who carry in their handbags
not only cosmetics but also results of
several lab tests, who with a relish and gusto
talk of their ailment, and who are fond of
the company of physicians as they are the
only persons with whom one dared to talk
continuously of one’s self without interrup
tion, contradiction or censure, these are the
types that court surgical placebos. Each
partial evisceration tranquillises them for a
brief period till they allow themselves to be
practically eviscerated by some one or
more surgeon (D.M. Dunlop). How many
elderly spinsters have been frightened to
surrender their infructuous uterus on
the slightest symptom of menopause,
as they knew ‘ too much' about cancer ?.
Placebos and Changing Concepts in
Therapeutics
As in sartorial realm so in medicine we
are victims of changing consent in treat
ment. Focal sepsis, intestinal intoxication,
allergy, avitaminosis, adapatation syndrome
and today peihaps genetically determined
disorders, have all had their day. We have
had diets for Bright's disease, ketogenic diet
for urinary infection, step ladder diet of
alarming complexity for diabetes, diet for
hypertension, heart disease (poor sodium)
bewildering number of diets for peptic
ulcer. Some of these are not only unplea
sant to the patient, but often positively
detrimental to him as in Sippy’s diet that
often ended in scurvy and anaemia.
Haematemesis often precluded solid diet
for several days ; today pulped meat is pre
sented hardly the blood had darkened the
oral region. What a heavy toll did focal
sepsis receive ! Langdon Browne recalls an
incident of his colleague Prof. Leycock
Says he,“......... he an eminent physician
when on a ward round drew attention of
students to a patient’s teeth pointing out
to them that such teeth indicated that the
patient was of what was then called “Rheu
matoid diathesis”. Thereupon the patient
much to the amusement of the students
took out the dentures and handed to the
Professor asking him if he would like to
look at them near at hand”. Tonsils, gall
bladder, appendix came in this group,
while for some time the colon was deemed
the nigger in the woodpilex of health.
And how about allergy ? Any undiagno
sed disease made the medical hunter go in
quest of an allergen in the woods. Story
is told of an asthmatic Edinburugh busi
nessman who had only two nights of free
dom each month from his affliction, when
he journyed to and from London for his
monthly meetings. In the train he slept
like a child. It occurred to the physician
in attendance that the pillows in the sleep
ing car were stuffed with some composite
material and not feathers and that he
might be allergic to feathers : his skin test
was suggestive. And so every pillow and
cushion in his Edinburugh house was rip
ped open, the feathers removed and the
composite material installed. But, the
asthma at home was as bad as ever. The
physician had later realised that it was
there in his nuptial couch but not in the
sleeping berth to which he was far more
allergic, than to feathers. If we stick to
the allergy concept, the wife was the alien.
gen I
Placebo Drugs :
About three decades ago, much doubt
was raised in the minds of pharmacologists
if the so called expectorants used in cough
like Ipecac, Scilla, Ammonia carb, Iodide
work by faith or by pharmacology. Am
monium chloride is sometimes prescribed
in cough mixture in 5 gr. doses, but when
given in 30 gr. doses to make the urine
acid, does one ever see patients spending
their time coughing up sputum ? Pota
ssium iodide is undoubtedly excreted by
the salivary, bronchial, lachrymal and nasal
glands. There is no reason to believe
however that they will run at their bronchi
alone when we wish it and not at the nose
and eyes, and if they do we call it iodism.
When we administer atropine or belladona,
we do so hoping that it will have its action
just where we want it to act; if it is to reduce
bronchial secretion, we think it won’t
affect other secretions or the eye. If it is
to be given in fairly large doses to reduce
spasm, we expect no other action but just
antispasmodic action.
Pharmacologists
have been teaching that emetics in sub
emetic closes cause expectorant action.
Some recent findings seem to suggest that
emetics in * supraemetic doses alone have
33
expectorant action. If these are esta
blished,' have' not all the expectorants so
far had exerted placebo action and not
pharmacological one ?
But it has to be said that in rejecting
a patient’s request for a tonic or declining
to offer medication when none is of value,
a doctor may fail to make effective use of
considerable body of scientific evidence on
the placebo effect. A report quoted in an
Editorial in B.M.J. ( 11:437, 1979.23rd
May) says that a third of health
service prescription falls into the placebo
category. But the Editor asks *.......... Are
they used in a systematic way ? The
“ Pharmacology " of inert placebos include
dose effects, time related effects and even
drug dependence'.
Intelligence
and
Suggestion
in
Placebo
Therapy
As noticed, it is sometimes assumed that
the element of suggestion as applied to
placebo therapy is present in lower degree
of intelligence. Often then there is not
much relationship between the state of
intelligence and the responsiveness to
placebos. Sometimes one comes across a
highly sceptical patient in whom
even genuine therapeutic agents do not
work.
Medical men who had to treat
other medical men should have encoun
tered difficulties in the use of drugs, which
otherwise give no trouble in the case of
non.medical patients. On the other hand
those who are eager to be told about the
details of treatment and be warned
about possible side-effects may be the
34
first to complain of side effects even
before minimum therapeutic dose had
been administered.
Harry Gold gives an instance of
his
encountering
another physician.
Says Gold, “I noticed him breathing very
heavily when we walked upstairs and when
asked replied that for many years he had
heart failure with auricular fibrillation and
showed me his legs that were almost twice
their normal size, He carried a bottle of
Tr. Digitalis in his back pocket and took a
few drops now and then. When I asked
him why he did not take more and' that
regularly, he said that he was very sensitive
to digitalis He had also become some
what addicted to heroin to control his
nocturnal cough and dyspnoea. Here was
a very intelligent scientist in advanced
heart failure virtually without treatment
with the only drug he needed. On
condition that I would treat him without
his wanting to know the details, I made up
a bottle of medicine containing a teaspoon
ful of Tr. Digitalis with a tablespoon ful of
Tr. Valerian. The taste as well as the large
quantity per dose threw him off the track
completely. He took a daily dose contain
ing about 3-4 ml. During the first few
days he carried on almost without a
moment of sleep because he was too busy
passing urine. He lost about 40 pounds
and all symptoms of failure subsided.
When he knew that he was receiving few
drops of digitalis, it made him so sick to
his stomach, but when he was kept' in the
drark he took more than a teaspoonful.
The efficiency of a placebo bears little rela
tion to the intelligence of the patient”.
Conclusion
It goes without saying that the selection
of patients for placebo therapy is as impor
tant as the selection of patients for any
other form of therapy.
As we grow old we come to realise that
all knowledge is provisional. Controls with
drugs reveal wide ramification of the ele
ment of placebo in drugs or even non-drug
therapy. Actions and results once attribu
ted to many drugs are not there ; but ins
tead something new and perhaps pleasant
appears. Havelock Ellis reiterates in his
writings how he was like Saul, the son of
Kish who went out to seek his father’s
missing asses but found a kingdom. He
had searched for truth but had not found
it : instead he found beauty. When we
search for truth we often encounter beauty
and stop to say “Behold the Truth".
Some may ask if in an ideal community,
educated public, abundant doctors with
adequate time and energy and wherewithal,
whether it would be necessary for this form
of therapeutic device or placebo. Is it the
best device if the doctor patient relationship
■s of the optimum or ideal kind ? One is
inclined to answer that when it has lived
from the time of the Pharos of Egypt to
the Americas of 20th century, placebo or
chemical device for psychotherapy will re
main for all time-
It is more important to look ahead, than backwards
That is why our eyes were placed in front
You cannot
escape the responsibility of tomorrow
by evading
to - day
«
Words are
—
Abraham
*
the voice
of the mouth
are the voice of the heart
35
Lincoln
«
Kind deeds
Kipp and Zonen C C Oximeter
Direct oxygen saturation measurement of
blood during heart catheterization. The use
of CC Oximeter for the recording of dye
dilution curves is an application of utmost
importance. The instrument represents a new
application of reflex oximetry.
Very short time lag ( 15-20 seconds ) enables the
instantaneous observation of the local oxygen
saturation
LEITZ Large Field Microscope:
ORTHOPLAN
with
Projection
Trinocular body for wide field eye
Attachment.
pieces of 30 mm diameter.
The field of view 28 mm dia of the ortho, plan is upto more
than twice as that of a conventional microscope.
B. B R A U N
CONTINUOUS
INFUSION
EQUIPMENT
The apparata have been used since long in Pharmoco.
logy and Physiology where it is essential to inject small
quntities of liquids at a constant accurately reproducible
rate. These instruments have been recognized as essential
requirement not only in this field but even more so
in human medicine
For further details of these Instruments, please write to:
Sole Distributors
THE SCIENTIFIC INSTRUMENT COMPANY LIMITED
Allahabad
Bombay
Head Office:
Calcutta
Madras
New Delhi
6, Tej Bahadur Sapru Road
Allahabad.
nt ial Drug List
ementary List
Route of administration dosage
Lis^As^MdL
Emro
J ‘P
PG] sl'g 3 ■ AM
I II !
£orms. .and. strengths
1 . Anaesthetics
1.1 General anaesthetics and Oxygen
ether,anaesthetic(2)
inhalation
powier for injection,0.5g,1.Og
(Sodium salt) in ampoule
thiopental/2)
1 » 2 .Local anaesthetics
.5% inj, 1,2(hydrochioride)in vial
inj.1%, 2% + epinephrine 1:10000C
topical forms 2-4(hydrochloi'ide)a'L
*Lid ocaine
2
isics,antipyretics, Nonsteroidal antiinflammatory
and drugs used to treat Gout.
2. 1 Non- op i o id s
. ag.ety Isalicylic
tablet 100-500mg, suppository,
5O-15Omg poed Aspirin
* ibuprofen
tablet 200mg
ind ometacin
capsule or tablet 25 mg
tablet 100-500mg,suppository 100mg
+ syp
A
A
2. 2. Ooioid .analgesics and antagonists
A
(P h eny lb ut a z on e)/ 0 xyp henb ut a z on e
morphine(1)
inj 10mg(sulfate or hydrochloride
in 1 ml ampoule
pethidine He 1. 5ml/ml
2_. Ant iallergic s
*chl orphenamine
epinephrine
I
tablet 4mg(maleate)
inj 10mg in 1ml ampoule
inj 1mg(as hydrochloride in 1ml
ampoule
[a
I
>A
4.2 specific
*
atropine.
,di?azppam
■
inj 1 mg (sulfate) in 1ml ampoule
inj 5mg/ml in 2ml ampoule
. 5. 'Ant i ep ileot ic s
•■phenobarbital! 1)
;
j . ■
tablet 5Omg,1OOmg,syp 15mg/5ml
capsule or tablet 25mg,1OOmg(sodium^ )
inj 50mg(sodium salt/ml in 5ml vial
phenyl .in .
ir4_p3iiild.^iixdfi.( Ha t hi)
;
6. Antiinfective drugs
6.1 An’bhelmixTtiic drugs
inelendazole
tablet 100mg
tablet 500mg(citrate or adipate)
piperazine
senna tablet llevamisbl)II tablet elexir,
. ,
.
, T
Elexir or syp(as citrate)equivalent!
t.et rac hl or el'nyl in e (Hat hi)
chloroquinediloxand.de
to 5 OOmg hydrate/5 ml
6.2 Aritiamos) ic drugs
«
~
'
tablet 200mg(as phosphate or sulfate
tablet 500mg(furoate)
metronidazole
tablet 2OO-5OOmg
... . - (jekyr0 emetine(B) K1 ,7) inj 60mg(hydrochloride)in 1ml ampov le
furazolidine
pt h alyl; ship hat h iazole <mfr*]
inj 60mg
En ro
pui Gi SL G E AI4
—■
> >
4. Antidotes and other substances^ us ed in poisonings
4(. 1 Ere neral
charcoal,activated
Powder
1CMC
tri tri >
> tri
OO
tri
tri >r.
>
1Ctrl >
|
_______________________________________________________ ______________________ 4
Lis
tri
Ho^srofiadministration dosage
forms and strengths
_____________
>
Complementary List
/lain List
II
•
5
Main list
Complementary list
6.3 .Ant ib ?.ct.eriald rugs
6,3.1 Penicillins
*ampicilli'n(4)
’
■
■
- Route of administration dosage
forms ana strengths
----fjist L^st CMC Loi
PU PG I SL G
| Emr >___
cos'
E AM
4..
Capsule or tablet 25Omg,5OOmg
(annydrous)I
powder for oral suspension 1 25mg
(anhydrous)/5 ml
powder for ini 5'00mg(as sodium
salt) I in vial
B
benzathine benzylp0nicillin(5;
inj 1,44mg benzyipencillin
B
fortified benzyl penicillin
• ’ ■
procaine benzyl penicillin 30000
u/ml + benzyl
pencillin 10000 u/ml
powder for inj 0.6g
ImiLlion IU) 3.0g(=5millionIUO>(as
sodium or potassium salt)in vial
B
.benzylpenicillin
.
phenoxymethyl penicillin
~
'
B
tablet 250mg(as potassium salt)I
powder for oral suspension 250mg
(as potassium salt)/5ml
prbeaihe benzyl oenicillin(7)
powd'er for inj 1g(=1million IU)
,
’
3g(=3 million IU)
6. :Antiinfactive drugs
6.3.2 other antibacterial drugs
*chloramphenic01(7)
capsule 250mg
powder for inj 1g(as sodium sued nati 0
in vial
erythromycin
■ .
■
capsule ortablet 250mg(as lacto
bi onate )/5ml
powder for inj 500mg(as lactobionate) in vial
*gentair,icin(4)
inj 10mg,40mg(as sulfate)/ml in
2ral vial
met ronidazolo
tablet 200—500mg
B
B
•
B
B
C
■
I
.... 4.. .
Complementary list
Main list
Routs' of administration dosage
forms and strengths
List Lisi CMC L OW
B
ost ■ pu:
'Bm: -o
*SjiLfajLu'ii±ilx.e(4) (sulphadiazine)
inj 500mg in 100ml
Suppository 500mg, 1g
tablet 500mg,oral suspension |OJmg '
*sulfamethoxazole+tricethoprim(4)
inj 1g(sodium salt)in Jml ampoule
tablet 100mg+20mg,400mg+80mg
' ‘
'
B
SI G E AM C I
II
■
B
*.t. ,et ran vc1ine(4)
" , '
■ doxyeyline(B)(5;6)
'■
capsule or tablet 250mg(hydrochior .de)
capsule or tablet l00mg(as hydroch
lpride)
inj -100mg(as hydrochioride)/5ml in
nit rod urant o'ii_ > A. B) (4.7) tablet 100mg
ampoule
Hydroxy quinolines
. PurAzolidine
100mg tablet
6. 3.3 Antilepr^sy crugs
clofazimine
capsule 1OOmg
dapsone
;
?
tablet 50rag,100mg
•
B
C
capsule or tablet 150mg,300mg
6.5.4 Antituberculosis drugs
■
■
tablet 100-500mg(hydrochloride)
rifampicin
’
etham>>ut’ol
isoniazid
pyrazinamide
■
... tablet 100-300mg
'
•
•
C
B
•
■ tablet 500ipg
rifampicin
capsule or tablet 150mg,300mg
0
0
streptomycin ,(4)
thiuacetazone^isoniazid
powder for inj 1g(as sulfat e) invia^
tablet 50mg+100mg?150mg+300mg
B
B
i
n
I
I
T hiacetazone
6 j.4 ..^nt if ilarj ai d rug s
d i st hyl c a rb an a zine '
'
tablet 50ng(citrate)
'6.5 Ant if gn,;. al drugs
nystatin
'
................. ’
' tablet 500000 IU
; •
■
•
c
J
Rout e of aatrn. nisTrat ion dos’ag'e
forms and strengths
ai
sod ite
6.6 Antileishmaniasis
it ib ogluc onat e
pentamidi .1
ListjList :MClow i
A_ 1 B
CosCPU?GI
inj 33% equivalent of 10% antimony
in 30ml
powder for inj 200cg in vial
SL G
B I II
( G
0
6.7 Antir.alarial drugs
^chloroquine
tablet 150mg(as phosphate or
syrup 50mg(as phosphate or sulfate
/5 ml
tablet ??5BgHl5m§(g^ho§ph5te^
tablet 300mg(as bisulfate or
inj 300mg(as diHyif^cfiloride)/
ml in 2.'.;1 ampoule
'primaquine
:_q uinjne'
i,ul:
:ine+pyrimetha-~ine(B) tablet 5OOng+25mg
graine drugs
tablet 2.3g(as tartrate)
B
B
drugs affecting the blood
10- Blood_______________
10.1 Anm i ana emi a d rug s
tablet equivalent to 60ng iron
ferrous salt
(as sulfate or fumarate)
oral solution equivalent to 15ng
iron(as sulfate)in 0.6ml
tablet 1mg
folic: acid(2) .
inj 1mg(as sodium salt)in 1ml anpoul
*hydroxoc obal. •in(2)
ertran(B)(5)
i.uv ..secular drugs
12.1 Anti.unginal drugs
inj 1mg in 1ml ampoule
in j equivalent to 50mg iron/ml
.in ,2ml ampoule
C
tablet ( sublingual)0.5-ug
G
Complementary list
. Route of administration dosage
forms and strengths
.1st 'Li st CMC.low’-gB
(Cos'..PU’GI SB G p '
Eel
t ablet(s ublingual)5ng
tablet 10ng,40ng(hydrochioride)
inj 1mg(hydrochloride)in 1ul ampoule
tablet 40ng,80ng(hydrochloride)
inj 2.5ag/c.l(hydrochloride)in_ ;2.g^ „
propranolol
ipaail
thaj c_ drugs
-------Hrablet 250ng,500ng(hydrochloride)
inj 100ng(hydrochloride)/ill in
10ral amp oule
ve drugs
TOTlot 5 Ong(hud r ochlorid e)11
tablet 50ng
12.5
*hyd
*pj*ppTtens>lol
rpine(/i).(7)
epinephrine-
0
C
B
;c
12.4 Cardiac , ,?vcosides
—•--------- tablet 0.0625 rig,O.25ng.
•
. .
oral solution 0.25 r.g/ml
inj O.25ng/nl in 1r.il ampoule
in s hock or anaphylaxis
inj 1:.:g(as hydrochloride) in 1clamp >ule
inj .'..epheritermine sulphate
15mg/cl
in j nor/ac en al in (Hat hi)
■1cg/El
- ' . • ~" 1 5_._'liermatdomical drugs
2ehsoia - u
'■ -p ■.nurigal
acid + salicylic acid - ’ ■
Whitfield o~i.4Vmei t (i.athi)
15.2 4_ntiinfe'etive drugs
■ <’O'-vcin-i-bacitracin
ointment 5m5 neomycin sulfate+50011
3
C
tu w '
digaxin(4)
tablet 4Ong,80ng(hydrochloride)
t ab 1 et 0.1mg,0.25 mg
inj 1ng in 1nl ampoule
C
Main list
Co ip lame nt ary -List
Route of administration dosage
forms and strengths
1
ist
CMC.
Enrc
'ostPPl PG I SI G E .AM
1
f oto,-J
.... 7....,
,
tetracycline ointment
. chloramphenicol
15.5, .-Pat j. inflam^at pry ~and _ antip r or it io d r ug s
♦betamethazonef?)
ointment or cream 0.1%(as valer; ite)
-
♦calamine lotion ■
♦hydrocortisone
salicylic acid
1'3.5 Keratoplaetic and keratoJLyt..lc_agents
" "solution topical 5$
benzyl benz ease
13.6'Scabicidea and p.diculicides
lotion 25%
.
,
14, Diagnostic agents
tub erculin, purified’ p'foti'en
derivative■(PPD) "
*
'fluroescein
♦chlorhexidine
♦iodine
14.1■Ophthalmic drugs
15- Disinfectants
B
lotion
ointment or cream 1%(acetate)
B
•
B
•
B
A
•
injection
B
eye drops 1%(sodium salt)
C
solution 5%(gloonate)for dilutic m.-'
solution 2.5$
B
16,' Diuretics
♦furosemide
■
♦hydroohloratniazide
'
tablet 40mg
inj 10mg/ml in 1ml ampoule
tablet 5Ong
•
•
•
B
B
17A Gastrointestinal drugs
aluminiium hydroxide (.PT
tablet 500ng
oral suspension J20ng/5ml
41A
oral suspension equivalent to
550ng magnesium oxide/10r 1
,t ab. ant ac id (u.At hi)
,
n .
♦proriethazine(^)'l7.2 hntie2eFic''drtgs tablet . 10ng,25mg(hydrochloride)? e.l.
chlOTcn.-.-o■•'T.-inn
’
elixir or syrup 5ng(hydrochloric e)
..... ■
/5ral
A
•magnesium hydroxide
I II
8
PU 'PG SL
Route of administration dosage "listLi stOMCr
__forns
and ------strengths
- .nopj.
Kiir, list
< iB
tmrv
17.3. Antil aemcrfchoid^l drugs.
local anaesthetic, astringent
. . .ointment or suppository
f^do^e^a^hi) 17.4. Antispasmodic drugs, tablet ,1i?g( sulfate)
;.
„
j , s
*CQderne(1)
’
, ‘
, inJ 1ag.(sulfate in 1nl ampoule
17.0.1 -cnt.i(i ;i..r i n_g^a. i aympt omaiic )d rugs
tablet 30h. '(phosphate)
3
Qral dehydration-ITjS.^ ReplaceAeih__ solution
saltsQfor'glucose-salt solution)
jpec’acuanh?.
antiflat ultjrt
activated charcoal
■
j
■ gamna benzene he^achloride(.1) ‘
18.
„GS
*prednisolone
'glib enclanid e
solution
es and synthetic substitutes
tablet O.5ihg,4og
inj 4ng(sodium phosphatc)in 1ml
ampoule
tablet 5mg
.
.
tg.blet 0.05ng
11.4 Insulins and other antidabetic agents
.
.
tablet” 5ag ''
^Tplubut.-gide^ f
C.il orp roparaid e:
injection
?
c
C
C
C
C
rrd. icl
tablet O.O5r;g+15ng+O. 25.
N-.iin li-'t
Co'-.-;lementary list
-
2 evot hyr oxine
.
Route of administration dasage
_ jforms and strengths.
'
lisfTi^E'jCMU
' j
......
18.8 Thyroid hormongg and antihydroid drugs
ly o.b lot 0 • 05mg 5 0 • 1 nig ( s od ium salt)
potassium iodide
tablet 60mg
*propylthieuracil
tablet 5Ong
1fi^unologicals
antivenom
corp
19.
1
Sera
and.
ai^moncglQbulins
_
.
-> .
mf-X-—n -x-im-A-e.
■
inj) all plasma fractions should
) comply with WHO requirements
diptheria antitoxin
inj) for the collection,processir
) and quality control of humar
) blood and blood products
inj)10000 IU
20000 IU in vial
tetanus..ant itoxin
inj 50000 IU in vial
—
19.2 Vaccines
19-2*1. ,<for. .universal _ifn:i.unizat_i_ori_
BCG vaccine(dried)
inj )all vaccines should comply i ith
diphtheria ner-tusis-tetanus cocaine .in j ) the WHO requirements for
diphtheria-oetanus vaccine
mj;
'measles vaccine
inj)
;polio? ye3.itis vaccine(liveattenuatec )inj/oral solution
tetanus vaccine(WHO,Hathi)
ipij
19.2.2 cholera T^BC,email pox
211. Opthalmologieal_preparations
silver nitrate. 21.1 antiinfectivo agents solution(eye drops) 1%
sulfacetamide
eye ointment 10%(sodiu.i salt)
*tetr?.cyclinec.chlora.mphenicol
golution(eye drops) 10% sodium sa..t
eye ointment 1% (hydrochloride) ; .
Main list
Route- of administration dosage. IisTf
A
I
forms and strengths.
Bnrfc
ary
Miotic s
pilocarpine
£1
CMC Low
cosi PU !PGI SBG E
solution(eye drops)2%,4%(hydroclcride or nit rat e)
?1 • 5 MydrtAitii
phy s i ost i-gmine -O aj i-s.)
solution(eye drops)2%(hyd robrodid e)
hbrnatropinelir '
22. Ozytocics
^ergometrine
'
ISj S^K^teatoTln' 1ml ampoule
oxytocin
imj 10 IU in 1ml ampoule
24 Paychotherap a at ic drugs
^chlorpromaziae
tablet 100mg(nydrocnloiide)
syrup 25mg(hydrochloride)/5ml
in j 25 mg (hydrochi or ide) ml in 2 ml
*diaz.epam
tablet 5 mg
ampoule
25. Respiratory tract, drugs acting on
*aminoPhyllineS-ri'antiastitiatTc'd 1-ugsiets'200ng
B
inj 25mg/ml in 10ml ampoule
epinephrine
inj 1mg(as hydrochloride)in ^louLe
*salbutamol
tablet 4mg( sulfate)
oral inhalation(aerosol)0-1cg pci
syrup 2mg(sulfate)/5ml
dose
C
adrenalin tartarate maliate in 1000
C
PET- phep^ioard 5tg, ;cphi.dr.Jne 10ng,
" *'*”
tn.eOphyline 1_252(Hathi)
B
noscapin‘e(cough suppressant)
ephedrine (A)
3
tablet 30mg(as hydrochloride)
i I]
coMtvufc! ■'/
h cell
47/1,(.-irst F
3c. Marks Road
BAWG<-.~O.iE - 560 001
Oonplenentary list
Main list
Route of administration dosage
forms and strengths.
Objecting water,electrolyte and acid-bast
disturbance;
■oral rehydration°feal?§fior.mlucoe e-salt solution) (for comp os it on see
17.6.2 replacement solution)
p ot a s ff i un c hiprid e
oral solution
glucose-' (dextrose)26. 2 Parenteral •: injectable solution5% isotonic, 50%
hypertonic
glucose, with s odium chloridu
injectable solution 4% glucose 0.18
sodium chloride
(Na+Onnpl/1) (01-50 mmol/1)
potassium^ chi pride ,,
’ injectable Solution
s od iun ■ b fcarbonat e
Sodiumi chloride (cholera fluid)
calcium carbonate gluconate
water for injection
ascorbic acid
*ergocalciferol
*nicctinapide
pyridoxine
retinol
,
"
" 1.4% isonic(Na+167 mm
(HCO5-167 ramol/1)
injectable solution 0.9% isotonic(
(Na*154 mmol/1 ) (01-154 mmol/1)
in 2ml,5ml)10ml ampoules
27, Vitamins a "nd r in er a Is
afflet 5Ong
capsule or tablet 1.25mg(50000 IU)
oral.solution .25ng/ml(10000 IU)
.
tablet 5 Ong
'
tablet 25ng(hydrochloride)
riboflavin'
sodium flui‘»da(8)
yit ami n _ & D :
.capsule or tablet 7.5mg(25000 IU),
60mg( 20000 IU0>
oral solution 15ng/m.l(5OOO IU)tab.5mg
tablet 0.5ng(as fludride)
(Prophylactic iTFI therapeutic ini’I with Vit 0+ folic acid)
tablet +' injection)
cynacob:'J.aj..in_B 1 2(.Iathi)
"hvu hixoe
-iU
vAt.
nit i
Lt T-
r:
Learning to use antibiotics wisely
First guidelines
1.
Use' an antibiotic that kills bacteria rather than one that
just slows them down. This usually gives quicker results,
and prevents the infection from becoming resistant to treatment
2.
Use an antibiotic that causes fewer side effects and is less
risky. For example, if the person is not allergic, it is
safer to use penicillin or ampicillin rather than an
antibiotic like erythromycin that can cause poisoning.
3.
When possible, use a narrow-range antibiotic that attacks
the specific infection rather than one that attacks many
kinds of bacteria. Broad-range antibiotics cause more
i
o
h
problems—especially darrhea and thrust—because they attack
good bacteria along with the bad. ■‘■'he good bacteria
prevent the growth of harmful things like moniliasis
(funguijs that can cause diarrhoea, thrush, etc.)
4.
Use a broad-range antibiotic only when no other will work,
or when several kinds of bacteria may be causing the infection
(as with infections of the gut, peritonitis, appendicitis,
some urinary infections, etc.)
Additional guidelines f^itefuKtha-^ba^gninq
5.
Use antibiotics only for bacterial infections. Do not use
them for viral infections, because antibiotics do nothing
against viruses (common cold, measles, chicken pox etc.)
2
6.
Be careful never to give more than the recommended dose of a toxic
(poisonous) antibiotic. However, it is usually not dangerous
to give higher doses of an antibiotic that is not poisonous
(penicillin or ampicillin). For example, it is all right to
use penicillin for months or even years afterjit has expired,
and to increase the dose to allow for any loss of strength. (But
tetracycline becomes more poisonous when old. It should never
be used beyond the expiration date or in more than the recommended
dose.)
7.
Do not use an antibiotic that slows down bacteria together with
an antibiotic that kills them. 'rhe combination is often less
effective than one alone. (Once the bacteria are captured or
slowed, they stay hidden where the other antibiotics cannot
kill them.)
For example, never use tetracycline in combination with
chloramphenicol.
8.
Whenever possible, avoid using a toxic medicine for a person
with diarrhoea or dehydration. A dehydrated person's body
cannot get rid of poisons as quickly in the urine. Even normal
doses of a toxic medicine may build up and poison the person.
o
(Sulfas are especially riskly for treating diarrhea. Unless
the person is making a lot of xfurine, sulfa can form crystals
in the kidneys and cause damage.)
9.
Do not use toxic medicines during pregnancy—especially during the
first three months.. Some medicines can cause severe birth defects.
10.Use a medicine the family can afford. When choosing between
medicines, always consider the relative cost, and weigh# this with
other advantages and disadvantages.
—Helping Health Workers Learn
David Werner and Bill Bower
*
P)ekoL piKeA
,) P).
ZTAi4<x- /‘ilQ
PRESCRIBING
DRUGS
Questions to ask yourself before writing a prescription.
: Is this drug really necessary ?
: Is it being given to make the patient feel
that something is being done ?
: What aim is to be achieved by this drug ?
What disorder of function is to be corrected ?
What symptom/s have to be relieved ?
: What is the-approved or generic name ?
What class does it belong to ?
What are its characteristics ?
Do I have the requisite experience or know
ledge to use ir ?
Have I weighed the potential toxic effects
against -the benefit ?
By what route, in what dose and at what inter
vals is the drug to be given and why ? In
what form/s does the drug come ?
1.
"•
Need
2.
Aim
3.
‘
Knowledge
4.
Route and
Dosage
5.
Alternatives
Have I selected the best agent available for
this particular purpose ?
What other remedies might have been chosen ?
How do these compare in effecacy, safety, cost ?
6.
Duration
: For what pc-riod of time, days weeks or months
will it be advisableto continue therapy ?
When and how could a decision be made to stop ?
7.
Observations : What observations can be made to judge whether
the aim has been achieved ?
When should they be made and by whom ?
What laboratory investigation if any would
help in this assessment ?
8.
Elimination
: How is the drug eliminated ?
Will the patients illness change the usual
pattern of distribution, effects or elimination
of the- drug ?
9.
Unwanted
effects
: What are the side effects or toxic effects of
the drug ?
Are they acceptable ?
How frequent are they ?
How can they be modified/managed ?
'
: Have I checked for the following :
a. Possible allergic risks
b. Possible idiosyncratic reactions
c. Patients drug diet which may interfere
with the drug
What precautions can I take to ensure conti
nuation of therapy.
2
11. Contraindications
: Are there any conditions in which this drug
is contraindicated ?
Are these 'absolute' or 'relative' ?
Are there any drugs which should be avoided
when the patient takes this treatment ?
Which and why ?
12. Patient point: What docs the patient believe about the drug ?
of view
What has he been told about it ?
And what has he remembered ?
Does he need additional information ?
13. Patient
reliability
: Does his relative need additional information ?
Is the patient reliable for this thpe of
Therapy ?
Will he ne.ed/get proper supervision by
relatives or attendants ?
14. Cost
; Is the drug the cheapest drug of that type ? £
If not could a cheaper drug do the job
as well ?
15. Finally is there anything else I need to know about this
drug ?
Adapted from 7
i.
A Herxheimer : The Lancet II 1186-1187, 27th Nov 1976
ii.
Formulary and Therapeutic guide-Kurji Holy Family
Hospital
iii.
Prescribing drugs - MNAMS Handout, Dept of Pharmaco
logy, St.John's Medical College, Bangalore.
(general Laws)
Medical practioners must know and thoroughly understand tire
basic provisions in law that provide them protection.
Relevant provisions in the Indian Penal Code are detailed hi the
following.
(Section: 52,80,88,89,90,9293,269)
The Doctrine of Good Faith
act done for the benefit of a person with due
competence, care and caution.
Deficiency in medical service
failure to follow due norms.
Free and informed consent
Consent without coercion or inducement and after
full information to the patient.
Negligence - its essential ingredients
/
act done without due care and caution.
Negligence - legal requirements to prove negligence
Duty to care
Deficiency in service
Damage
Direct correlation between deficiency and damage.
I
GOOD FAITH
IPC-52. Nothing is said to be done or believed in “good faith”
which is done or beheved without due care and attention.
The term rashly implies an indifference to obvious consequences
to the safety of others.
ACT MOT SMTEMDED TO CAUSE DEATH,
DOME BY CONSENT IN GOOD FAITH FOR
PERSON'S BENEFIT
PC. 88. Nothing, which is hot intended to cause death, is an
offence by reason ofany harm which it may cause, or be intended
by the doer to cause, or be known by the doer to be likely to
cause, to any person for whose benefit it is done in good faith,
and who has given a consent, whether express or implied, to
suffer that harm, or to take the risk of that harm.
Explanation -
Mere pecuniary benefit is not
benefit within the meaning of
sections 88,89, and 92.
QlHEFOUR Ds J
1.
Duty to care (Duty to care arises only when a doctor accepts
or agrees to treat a patient. The acceptance or the agreement
can be express or implied, against payment or free)
2.
Dereliction of that duty or deficiency
3.
Damage to the patient
4.
Direct correlation between the deficiency and damage (The
damage must be a direct result of the deficiency alleged)
(liability )
A.
Personal
B.
for act of subordinate, agent or
employee
C.
ofhospital
Respondent Superior “let the master
answer”.
The captain of the ship doctrine
Vicarious (substitute) liability' or
Tortuous Liability
DEFENCE AGA0NST NEGLIGENCE
1.
Denial Defence Actual denial of negligence having taken
place.
2.
Affirmative defence by providing new factual information
to show that the plaintiffs condition has a cause other than
the doctor’s negligence.
3.
Delegation of duty to a subordinate
4.
Contributory negligence by the patient.
5.
Assumption of risk by the patient.
6.
Emergency of the situation.
7.
Release of tort feasor.
8.
Res judicata
9.
Statutes of limitation
10.
Immunity to charitable and government institutions.
Cnus of proof
- Generally . the onus to prove negligence is of the complainant.
However, later it may be shifted to the defendant as the
complainant does to posses the necessary details to prove his
allegations, the defendant then is required to prove the absence
of negligence.
Exception
Res Ipsa Loquitur, "the thing speaks for itself"
"Common sense dictated that the accident could happen only if
someone - a doctor or a nurse - was negligent."
" The doctor had direct control over the apparent cause of that
injury but failed".
Gross negligence".
W'
Spiralling drug prices, and less than ethical trade
practices by pharmaceutical companies,
endanger the wide eyed Indian consumer’s
physical and financial health.
BY JANAKI VENKATARAMAN
een to your comer drug store
lately? One of my friends did,
and he’s never been the same
again. "Do you know what I had to pay
fur the antibiotics my medical specialist
B
prescribed me?" he asked dazedly and,
without waiting for an answer, went on,
"For just four capsules 1 paid Rs 107!
And I have to lake eight in all. Rs 214
for one course of antibiotics — I am
going to be wiped out!" he moaned.
"That must be a third generation an
tibiotic," 1 murmured sympathetically.
"Why the devil is my doctor prescrib
ing me third generation drugs? I was
happy with my first generation Rs 3-acapsulc treatment," the man wailed, ad
ding, "The pharmacist tells me that if I
had got the antibiotic last year, I would
have paid only Rs 90.25. At this rate, 1
imagine we’U have to choose to fall ill
only when the drug prices arc just right.
And that’s not all. The doc prescribed
me a course of Vitamin C which costs
around Rs 15 per sheet now. He also
prescribed a ‘vitaliscr’ because I told
him I was feeling none too perky — that
course set me back by Rs 50. I have
spent Rs 300 on just one visit to the drug
store — this is apart from my doc’s fees,
which he has hiked recently. You know
what I think? If the disease doesn’t kill
you, your medical bill definitely will."
"That’s an observation as old as the
hills," 1 told him unkindly and the con
versation ended right there.
My friend, of course, was not the only
one to complain about the rising drug
prices. Over the last six months, despite
the fact that the Union government has
been dithering over the new drug policy
(which is likely to lake a great many
drugs off the price control list) the prices
of
many
medicines
(barring
paracctamols and a few such very basic
drugs) have been rising steadily and, ac
cording to most consumers, alarmingly.
There has been an increase of a mini
mum of Rs 2 per ten capsules or tablets
of even basic vitamins. While drug
manufacturers point out, not without
truth, that drug prices are still the
cheapest in the world in India, lhere is
ASIOE
really no point in talking about open
market prices in pharmaceuticals here as
long as the per capita income and buying
power of the average Indian remain what
they are today. As it is, only 25 percent
of Indians are said to be able to afford
allopathic medicines on a regular basis,
and these are concentrated in the urban
areas. The vast majority of rural Indians
manage on home remedies, cheap and
spurious allopathic drugs, or no drugs at
all.
here is a very strange situation
T
prevailing in the Indian phar
maceutical industry today. While India
has perhaps the largest concentration of
drug manufacturers in any country in the
world — some 4000 regular manufac
turers, apart from countless small units
and loan licensees (who use the facilities
of a registered pharmaceutical unit on a
lease basis) who do not come under any
form of stringent drug quality or price
control. There is still a shortage of many
essential drugs which Indians require.
Every country has its own pharmaceuti
cal needs and the governmental drug
contro( authorities are expected to make
sure that these
arc available to
the
ordinary
citizen
without
failure in supply,
in good quality
and at reasonably
affordable prices.
Consider
the
drugs that are
used to treat a
few diseases that
Indians
seem
prone to. Half the
world’s
lubcrculosis patients
live in India, one
third
of
the
world’s leprosy
patients are In
dian; 1.5 million
Indian children
die of prevent
able and easily
treatable
diar
rhoea; 40,000 children become blind an
nually for lack of Vitamin A. Epidemic
breakouts of typhoid, jaundice and
cholera arc common, and yet each time
the epidemic breaks out, it is found that
there is a shortage of supply of the
medicines meant to treat these diseases.
Take just two instances of our lopsided
pharmaceutical development. A study by
the All India Drug Action Network
shows that at least 10 million Indians
suffer from TB, 2.5 millions of these arc
infectious and 5 lakhs die from the dis
ease every year. The BCG vaccine has
been found to be largely ineffective in
preventing the disease, so the answer to
the question of controlling the disease
clearly lies in treating it, early and ef
fectively. Yet the traditional drugs used
for fighting the disease arc in perennial
short supply — India produces only one
third of its requirement of anti TB drugs.
The latest and most effective drugs for
fighting the disease are too pricey to be
dispensed free to patients under the na
tional TB control programme. It is not
that Indian pharmaceutical concerns do
not have the capacity to meet these
needs — it has been found that their
$
f si-4
11
capacity is very under utilised in the
production of traditional anti-TB drugs
like Streptomycin. At the same time
Streptomycin is being manufactured in
hazardous combinations with other drugs
to be indiscriminately used in treating
fevers, other infections, even diarrhoea.
Injection ampoules of Streptomycin in
combination with penicillin are found in
plenty. It has been pointed out time and
again that such irrational use of Strep
tomycin (where it is totally unwarranted)
can lead to patients resisting the drug
when it is used on them for treating TB.
ake the case of an even more basic
T
drug — Vitamin A. Deficiency in
JLiis vitamin is causing blindness in
thousands of Indian children, it also
leads to higher infant mortality, a greater
incidence of diarrhoea and measles
among little children. The long term and
real solution is for all Indian children to
be given a nutritious, balanced diet
which contains adequate quantities of
foods rich in Vitamin A. All round in
flation is, however, making this more
difficult for families to provide. The only
viable alternative is to supplement the
children’s diet with Vitamin A in drug
form. Yet the production of Vitamin A
has not only not increased in the country,
it has actually decreased. At the same
time, while the vitamin is becoming in
creasingly scarce for children it is being
added to cattle and poultry feed and
edible oil — this docs not really benefit
the children who suffer from Vitamin A
deficiency, as their families are hardly
likely to be able to afford vitamin en
riched cooking oil.
The above arc just two instances of our
lopsided pharmaceutical production. It is
so lopsided as to appear mad. Yet, as
everyone knows, there is always some
reason and method behind every mad
ness. The reason is the drug price control
order of the government. And the
method is to circumvent it by culling
down on the production of drugs con
trolled by it and increasing the produc
tion of new formulations/variations,
which arc not covered by the drug price
control.
Very frequently essential medicines
vanish from the shelves of the phar
macists as manufacturers create an artifi
cial short supply and eventually manage
to hike up the price of the concerned
drug just a little. "Time and again my
patients complain that one or another of
the drugs I prescribe for them arc not
available even after they have searched
12
in four or five shops,” says Dr S Jagad- panics and multinationals, they began to
hecsan, a GP. "Keeping drugs in short diversify."
Many multinationals did this by
supply is obviously just a marketing
branching off into the production of so
strategy," he says.
"The real problem is the government's called health foods like high protein
totally unrealistic price control policy," beverages, and also into the manufacture
says Jayanth Asher of Asher Phar of pesticides and other chemicals. Both
maceuticals, a Madras based drug con they and the bigger Indian companies
cern. He merely echoes the sentiments did one other thing to escape the
of drug manufacturers all over India. stranglehold of the drug price control
"Since the government brought in the order — they began concocting new for
drug price control order in the early mulations of old drugs, and also inessen
1970s, the prices of almost all inputs in tial drugs and tonics, which they pushed
the pharmaceutical industry — raw for all they were worth by suitably
materials, packaging material, transpor ‘persuading’ doctors. As all indigenous
tation, electricity charges, everything — ly manufactured new formulations are
have gone up. Yet we were made to ar exempt from the DPC order for a few
tificially hold down the line on our sell years after their launch, the drug com
ing price. At one point doing this panies began making a killing on these
became non-viable. Many small units products. Consequently
the Indian
began to fall sick. As for the bigger com- market is now flooded with drug for
mulations and inessential health tonics
and tablets which arc useless at best and
hazardous at their worst.
A
JLhe
Indian market is
now flooded with inessential
and spurious formulations
and tonics which are useless
at best and hazardous at
worst, due to drug
manufacturers trying to
escape the grip of the drug
price control order.
s far as one can see the drug com
panies have displayed no com
punction about pushing these wasteful
and expensive products to a wide eyed
and largely ignorant public through the
medium they trust most — the medical
practitioner.
As R Srinivasan, Secretary, Phar
maceutical Distributors Association, puls
it, in a little trade journal he edits, "We
have to admit the fact that ethical
promotion, the values that were prevail
ing about 10 to 15 years ago, have vir
tually disappeared... Manufacturers have
to survive in the present competitive
market. The name of the manufacturers
or their reputation, arc no longer the fac
tors that influence the medical profes
sion..." So what docs?
Well, as both pharmaceutical manufac
turers and several doctors we met
agreed, doctors arc definitely being per
suaded to prescribe new formulations by
drug company representatives, with cost
ly gifts, extravagant launch parties, and
attractive ‘commissions’ in the form of
airconditioners, refrigerators and the
like, if they prescribe a desirable amount
of the drug concerned. Many drug
manufacturers arc said to sponsor con
tests and schemes to encourage doctors
to push their brands, as if they were sell
ing cosmetics. Even the public sector
IDPL is said to have recently offered a
deluxe Maruti car to doctors in a contest
to promote awareness of one of its
brands. Further, almost all medical semi
nars, study tours abroad for medical
teams etc, seem to be sponsored by one
ASIDE
drug company or the other. In such an publish, there’s hardly any unbiased in rchydration therapy, a pinch of salt and
of
atmosphere, it seems difficult to imagine formation about drugs available for the a scoop of sugar in a tumblerful
boiled water is enough to bring com
a doctor prescribing a drug totally im consumer to go by.
partially. Many arc not averse even to
Consider some of the drugs which have mon forms of diarrhoea under control!
Similarly the over-the-counter pain
pushing inessential but expensive for been banned worldwide because of their
mulations on their unsuspecting patients, observed hazardous effects on patients, killer, Analgin, has been banned in
even though they know that the formula but arc still sold in India, one way or the many countries around the world, as it
tion is not likely to help them in any other. In 1971, after evidence from can cause a blood disease which could
significant way. One senior member of Japan, USA, Canada, France, India and be fatal. For pain and inflammation, for
the Drug Manufacturers Association a host of other countries piled up to which it is usually recommended, ordi
candidly admitted that many of the ex prove that Clioquinol, the drug used to nary Aspirin would be just as effective
pensive haemoionic syrups prescribed by treat diarrhoea (and popularly marketed and far less dangerous. But Analgin is
forms in
doctors for ‘improving the general as Mcxaform and Enterovioform by a sold commonly in various
health’ of their patients, are nothing but multinational drug company) had very India.
Oxyphenbutazone,
prescribed
for
blood collected from slaughter houses serious side effects, including damage of
various
muscular
(the cattle, although
pains,
aches
and
they arc supposed to
sprains,
is another
be tested by vets who
drug
which
was
have to certify that
withdrawn from the
their meal is safe for
world
market,
by
consumption, hardly
the
very
company
ever arc), to which
which first manufac
anti-coagulants, pre
servatives,
alcohol,
tured it, because of its
serious side effects,
sugar and Vitamin
leading to fatalities,
B12 are added. "It’s
bottled and sold as the
but is marketed in
thing for anaemia and
India to this day. More
a
host
of
other
often than one likes to
deficiencies. In fact,
remember, the ques
the Drug Regulatory
tion of why a drug
Body has said quite
banned elsewhere in
clearly
that
such
the world was being
syrups
have
no
sold in India, when
therapeutic value, but
raised in Parliament,
they have not been
has been answered
thics seem to have vanished from pharmaceutical
banned, all the same.
with bland ignorance
Worse, as the blood is
from the health mini
salesmanship. Doctors are often said to be ‘persuaded’
not treated for any
ster
concerned
with lavish gifts to push products, which are irrational,
bacteria it may con
("Banned? Is that so?
tain,
there is
no
No
side
effects
have
often useless, but always expensive, on their
guarantee that it may
been reported from
unsuspecting patients.
not spread some infec
anywhere
in
our
tions from cattle to
country,” is the stand
humans," he said, ad
ard response). One
ding, "What is the
doctor with whom we
point of pushing such
discussed this issue
a product on the unwary customer except the central nervous system and blind came up with an amazing explanation.
the profit of the manufacturing com ness, the drug was banned worldwide. It "Not every drug banned in Western
took more than another ten years for countries needs to be banned here," he
pany?"
But then, all this is only to be expected the government of India to ban the drug said. "What harms them may not harm
in a country in which hazardous drugs, in this country. But, despite the ban in us, as we are racially different from
banned in very many countries in the 1982, Clioquinol continues to be sold them."
rest of the world, are still sold freely. In here. Here’s how. A little after the ban,
"How come the hazardous drugs are al
a rather frightening booklet the Volun another government gazette notification ways banned in the
developed
tary Health Association of India warns excluded all preparations for treating countries but marketed in the develop
diarrhoea
from
the
ban
and
those
in
that no official list of drugs, banned by
ing nations?
the Drug Controller of India, has so far tended for external use (Clioquinol is
That has nothing to do with race!"
been publicised, so that the general safe as an external medicine). Therefore
"But don't you sec? The Western na
countless
people
continued
to
lake
the
public or even medical practitioners arc
tions are also the developed nations and
totally unaware of them. Except for the drug long after it was banned else the Asian and African countries just hap
pamphlets which the dntg companies where. The sad truth is that most forms pen to be developing," countered the
themselves provide along with the drugs of common diarrhoea, for which it is doctor. He did fall silent, however, when
and promotional literature, which they used, arc easily treated by the oral it was pointed out to him that many of
la—J
ASIDE
13
the banned drugs sold in India still, have Naicken street in George Town,” one
been strictly banned in Bangladesh (ra doctor advised me. "There arc wholesale
cially akin to us) which has. suprising- dealers of common drugs there who
ly, a very enlightened and strict drug could sell you the tablets at a fraction of
policy.
the cost compared to those from reputed
oluntary agencies have been fight companies. But no one can vouch for
the quality or efficacy of those drugs.”
ing a losing battle against inessen
But who buys and uses these drugs?
tial, hazardous and irrational drugs. The
"Cross Madras city limits and the dis
last mentioned are usually combination pensaries stock all manners of drugs
drugs in which one of the components from small lime manufacturers. In
is cither entirely useless for treating the Madras itself, doctors who dispense their
condition of the patient or, sometimes, own prescriptions stock them. These are
dangerous. Tonics and diet substitute doctors who usually charge around Rs 5
crowd the chemists’ shelves whereas a per patient and try to keep their drug
sensible diet would help patients more. costs within that limit. As you go deeper
Food substitutes like glucose drinks are south, many of the multinational and
sold at high rates whereas these nutrients major Indian drug companies often do
V
manufacturers complain about being ex
cluded from all economic benefits by
the government. "The present economic
liberalisation should apply to-the phar
maceutical industry too,"
they say.
"While this could make the costs of
drugs spiral upwards for a while, there
is no question that market competition
will bring down the price."
One wishes this were true. But we all
know that the price of any commodity,
once it goes up, never comes down, atleast not substantially. And if India
were to agree to the Dunkel Proposal for
Drug Patents (how long it can resist
that, one doesn’t really know) that
whopping cost will definitely be passed
on to the consumer. The only good thing
million Indians suffer from
tuberculosis, atleast 5 lakh die annually
from the disease. 40,000 Indian children go
blind every year from Vitamin 4 deficiency.
Yet there is perennial short supply of both
anti-TB drugs and Vitamin A, not because
the Indian drug industry does not have the
capacity to produce them, but because it is
not profitable for it to do so.
can be easily got from a good diet and
sunlight. Combinations of pain killers
with sedatives, which' arc extremely
habit forming and could easily be fatal
when taken in excess, arc sold across
the counter. Many pain killers arc com
bined with vitamins and a higher price
charged for this, while there is no ration
ale for combining the two. The best
way to sell and buy essential drugs is in
their individual form, marketed under
their generic names. The profusion of
brand names merely confuses doctors
and patients alike.
The extent to which spurious drugs
abound in the market is hardly ever ex
posed in urban areas. "Go to Nainiappa
14
not feature in the local drug shops,
which stock only the
medicines
produced by small pharmaceutical units
in the region. Such units do not come
under the drug price control order (but
their prices are naturally limited by
competition) and often they are hardly
ever subject to rigorous quality control,"
said our informant.
The pharmaceutical
industry alone
cannot, of course, be blamed for the
sorry state of affairs. The fact remains
that government drug controlling bodies
arc lax, often ignorant and have a ten
dency to interact too closely with the
pharmaceutical companies.
As for the other side of the story, drug
about removing price curbs on the phar
maceutical industry is that it might en
courage the mass production, and
therefore easy availability, of essential
drugs. But that in itself might mean
nothing if the consumer cannot afford to
buy them.
"If liberalisation doesn’t take place and
drugs are not removed from the grip of
price control, you can be sure that in the
next few years, the pharmaceutical in
dustry will be unable to produce essen
tial drugs and then the country will have
to import them — the cost will be much
more,"
warned
a
pharmaceutical
manufacturer. "What we arc now facing
is an unbearable burden. The cost of
ASIDE
every input has gone up, we are taxed
at the raw material level and at the
product level and then we pay sales tax.
The industry will simply crumble at this
rate."
ill it, really? Critics of the drug
industry point out that even as
things
are, it’s in a very profitable
shape. S Pushpavanam, consumer ac
tivist and secretary of the Constuner
Protection Council, Tiruchi, points out
that even under the mark up set up by
the DPCO, 1979, a wide profit margin
was given to drug manufacturers. This
was further increased tn 1987. Now the
industry is demanding a 100% to 120%
mark up. "None of the pharmaceutical
companies have suffered a loss in the
last decade. None of them have gone
sick... the investing public arc enjoying
the boom in the pnee of their shares,"
he points out.
id you know that
some oft prescribed
haemotonic syrups are
nothing but the blood of
cattle collected from
unhygienic slaughter houses
(and untreated for bacteria) to
which preservatives and
Vitamin B 12 have been
added? Such tonics are sold
even after the Drug
Regulatory Body has certified
that they have no
therapeutic value."
ASIDE
Sane Medicine
Tips on what to look for when buying drugs.
"•
harmaceuticals, and medicine in
general,
have
always
been
shrouded in mystery for the common
man. Besides, the patient is always
anxious not to question his doctor
about the line of treatment or
medicines prescribed by him, for fear
of causing offence. In other words
most of us, when prescribed something
by a doctor, accept it without question.
Perhaps it would be better to have a
little more awareness of what exactly
we are consuming by way of drugs,
enquire about their side effects and
learn to read the fine print on the
tablet foils. The Voluntary Health As
sociation of India offers a few tips to
consumers about how to get the best
out of drugs without letting them
cause us bodily or financial harm.
* When your doctor prescribes a
drug do ask him
about its side ef
fects, especially if you have health
problems which could be aggravated
by the intake of such drugs. Ask him
for how long you should take the drug
and then follow his instructions im
plicitly. Ask him also about the diet
and other precautions you should take
while you arc on the drug.
* Do not buy irrational or hazardous
drugs — a well balanced diet is far bet
ter for your health than expensive diet
supplements or tonics. If vitamins have
to be taken they should be taken for a
specific deficiency, not at random.
* Try to get information about
banned drugs from the state drug con
troller’s office — do not use them.
-J
* If you find banned drugs being
sold, buy a supply, get a bill from the
chemist and submit both to the state
Drug Controller, the Drug Controller
of India and the All India Drug Action
Network (AIDAN).
* Encourage use of home remedies
for minor ailments.
* Encourage a clean environment
which can prevent many diseases.
* Encourage your local doctors to
prescribe only essential, single, ap
propriate drugs — avoid taking fixed
combinations of drugs unless specifi
cally asked to do so by your doctor.
* Study the contents of popular, overthe-counter painkillers etc, and find out
if they contain hazardous chemicals.
Do not buy them if they do.
* Do not allow strong anti-diarrhoeal
drugs to be given, especially to
children, without trying oral rchydration therapy first. It often stops all
ordinary forms of diarrhoea.
* If given a very long prescription,
find out which are the essential drugs
and which are merely tonics. A lot of
food can be bought for the price of
those tonics, which usually have little
value. Many patients in India have
only enough money to buy the essen
tial drugs. If pressurised to buy the
tonics as well they might buy only a
short supply of the essential drugs,
which will not help them get well al
all.
* Drugs without printed information
about them in their packages should be
reported to the state Drug Controller.
15
reasonable prices? The first solution
that comes to mind is that the govern
ment take up the manufacture of essen
tial drugs and flood the market with
them. But this is easier said than done.
Almost all the public sector drug in
dustries, including the giant, IDPL,
face heavy losses and the threat of
closure owing to sheer inefficiency,
corruption and unrealistic overheads.
small wonder then, that drug prices arc
shooting up!"
TT
I j t is the same get-wcll-fast syndrome
_lk.of the patients that is responsible for
doctors prescribing them the latest third
generation antibiotics. These, apart from
being phenomenally expensive (owing to
the research and development efforts that
have gone into them) arc not really
necessary in many cases. They arc, in
fact, dangerous, in the sense that by in
discriminate use, the patient might easily
develop a resistance to them and later,
when he really needs them, they might
not work for him. As far as expense
goes, however, newly developed drugs
do become less expensive a few years
after their introduction. There are two
reasons for this — one is that they are
| not covered by the drug price control
’ order for a few years after their intro
duction, so drug companies hike up the
price of these drugs to the maximum
during this time. The other is that the
price of a newly introduced drug stays
high until competition from other drug
companies bring it down. One doctor
showed us identical strips of a recently
introduced antibiotic. The strip from an
earlier batch cost Rs 175 for ten, while
the price of the later batch was Rs 115
for ten — obviously between the two
batches, the competition had come up
with the same drug, al a lower price!
Even at Rs 115, the drug was obvious
ly being sold al a profit, so consider the
profit margin of the earlier batches!
Small wonder, then, that consumer ac
tivists point out that "the profit margin
in the pharmaceutical industry can be as
high as between 100 percent to 400 per
cent!"
What may then be done to ensure easy
availability of essential drugs al
Vv
ery
many drugs,
banned elsewhere in the world
because they are hazardous to
human health, continue to be
sold freely in India. Even
when a drug is banned, the
government gazette couches
the ban in such ambiguous
language that drug
manufacturers easily find
loop-holes in it to continue
manufacture and sale of the
banned drug.
The story of IDPL sounds, in fact, hor
rific. "Its losses are ten limes its capital,
pilferage of drugs (and replacement with
spurious capsules or tablets) is rife, the
labour arc heavily unionised and ineffi
cient — n’s simply becoming non-viablc," said one doctor in the know. "It
certainly hasn’t built up any confidence
in
the
consumer
regarding
the
government’s ability to keep up a steady
supply of essential drugs."
Over the years, alleast two committees
have been set up by the government to
bring in a newer and more rational drug
policy — the Haathi
Committee of
1975 and the Kclkar Committee. Both
have made a number of recommenda
tions, not one of which has been imple
mented. In fact, it is said
that
Bangladesh, when it formulated its drug
policy took
suggestions from
the
Haathi Committee report!
India has a teeming drug manufactur
ing industry, with almost Rs 4,800 crore
worth of formulations. With the govern
ment slowly liberalising the economy,
these formulations arc expected to touch
the Rs 16,000 crore mark within a year
or so. Whatever its profitability, almost
no pharmaceutical concern engages in
original research and development. R
& D wings being engaged merely in
duplicating (sometimes 'as early as
within six months) formulations dis
covered abroad. As no patent cost is paid
‘at the moment, in the ease of Indian drug
companies, this amounts to cheap copy
ing. As a result drugs arc, when all is
said and done, far more affordable in
India than elsewhere in the world. But
for how much longer? Caught between
the swiftly spiralling prices of drugs on
the one hand and the rising costs of
hospitalisation on the other, and pres
surised into buying diet supplements
and inessential and hazardous medicines
from all sides,.the Indian consumer is
likely to be exploited to the full — as
long as he doesn’t pul his foot down
and develop an awareness about his
health needs. Otherwise, as a wag once
put it, ‘You spend the first half of your
life spending your health
to gather
wealth and the rest of it spending your
wealth to get back your health’! The
way drug prices arc skyrocketing now
that should perhaps read, ‘Spending your
wealth, even as you earn it, on recover
ing your health.’
With reports from:
Sudha G Tilak
Indira Krishnan
Elizabeth Cherian
ASIDE
TFWllS
Some doctors place the blame for the
consumer
having to pay more for his
medicines squarely at his own door. Dr
Sumanth
Raman
points out, "The
patient always seems to want instant
relief and even though all he might
need is a paracetamol tablet, he doesn’t
feel satisfied until he is given something
much stronger. The doctor is forced to
oblige,
otherwise the patient merely
moves on to the next doctor who can put
him back on his feel faster! Also,
patients seem to believe that the more
they spend on the treatment, the more
effective it is likely to be. When one
brand of the same medicine is cheaper,
l^oth doctors and patients automatically
^pSsume that it has sacrificed quality —
CLARIFICATION: In the article
Steroids at play on sports fields, on
May 22, 1995, in the sixth para it
should have read as: "These drugs
are used with a hope to overcome
I the phobia”; and "In fact, ampheta
mine takers almost always 'think'
they are performing better than
they actually do.”
sray
July 9, ]994
Irrational Prescription
HE government's contortions on the drug policy woulo have
been amusing if it were not for the fact that they crucially affect
the current and future health status of all sections of the population.
However, the recent spun of ministerial blether on the 'forthcoming'
drug policy, increasingly irresolute and uninformative, appears to
indicate that a decidedly pro-industry policy is all packaged and
ready, awaiting a politically appropriate moment.
The policy has been a long time in the making because the
government finds itself in something of a bind. It cannot openly
succumb to the pressures of the politically influential pharmaceutical
industry in the face of the persistent challenge, nationally and
internationally, from the consumer movement to introduce a
semblance of rationality in the ‘therapeutic jungle’, proliferating in
India. And yet, the logic of its initiatives on the economic front is
pushing the government towards a more liberal environment with
fewer controls on pharmaceutical products. All this has meant that
over the last year or so, discussions on the tjrug policy have focused
on such issues as the size of the price control basket, mechanisms
for determining prices, decontrol, export benefits, etc. The entire
debate on the quality of essential drugs and the rationality, efficacy
or the necessity of the thousands of products which strew the drug
market has been mislaid.
According to reports the new ‘drug policy’ will recommend that
the price control basket shrink further to include as few as 30 drugs
from its present 143 under two categories. And this spread is to be
determined not by such criteria as the country’s requirement, the
efficacy of the drug, etc; but by such factors as the turnover limit.
This is hardly surprising given that the government has never
attempted to assess requirements of drugs on the basis of actual
need, nor perhaps developed the expertise needed to conduct such
an exercise. Requirements are estimated, when necessary, generally
on the basis of the previous year’s sales. This has led to distortions
such as the almost perennial shortage of drugs for tuberculosis or
vitamin A supplement for the blindness control programme, while
a wide range of combination analgesics, combination antibiotics'
and irrational dosage formulations are widely available making up
|he Rs 6,000 crore market. Nor is it surprising that the price control
basket is to shrink yet again. The industry has painstakingly
T
endeavoured to show how difficult it is for the government to
implement price control norms for a large number of drugs,
especially given the industry's own propensity for embroiling the
authority concerned in long drawn out disputes over price fixation.
That the solution lies not in limiting price control but in limiting the
number of products in the market, a point repeatedly made by the
WHO now being echoed by the World Bank, is unacceptable
because itimpinges on such sensitive issues as the stale's interference
with the market.
Another component of the policy is to be the constitution of a
national drug control authority (NDA). Such an authority was
mooted in the 1986 policy, but the manner in which it is taking
shape now is perturbing. Its main task appears to be to facilitate
price fixation, and the ministries of industry and chemicals and
fertilisers are reportedly in disagreement over who should have
Economic and Political Weekly
July 9, 1994
authority over such a body. Meanwhile there are reports that the
NDA will effectively override the authority of the drug controllers,
whose links are with the health ministry, in the states and the centre.
This would mean in effect, that the role of the health ministry in
evolving the drug policy, already small, will be further curtailed.
India, incidentally, is perhaps the only country where the major
responsibility for formulating and implementing a policy en the
pattern, pricing and availability of drugs does not lie with the health
ministry. It is hardly surprising then, that issues such as an essential
drugs programme are unheard of in connection with the process of
evolving a new drug policy.
Thirdly, the policy reportedly emphasises the need to encourage
R and D and proposes several steps towards achieving this end. This
clearly is the government's instant response to the drug MNCs
reported hesitation in expanding their R and D operations without
adequate assurances from the government. But what kind of
research will this be? Even if the investments were to be in
developing new products, it is pertinent to note that only three out
of the ten new drugs developed offer superior therapeutic value. In
the absence of controls on the type of products to be introduced in
the market, this move will, if it produces anything at all, only add
to the profusion of the ‘therapeutic jungle'.
Essentially then, the new drug policy, it would appear, will
drop all pretence of treating drugs differently from other
merchandise. That this can only lead to distortions because the
prescribing and use of drugs are influenced by solely commercial
promotional methods, especially in countries with little or no
continuing education programmes for doctors and no statesponsored or other alternative therapeutic information, has been
widely accepted today. The disastrous state of India’s national
formulary and the absence of uniform prescription guidelines has,
for instance, further aggravated the prevailing confusion in the
drug market. A recent prescription audit in one district of
Maharashtra of over 3,000 prescriptions from private and public
institutions using internationally accepted indicators has shown
that over 45 per cent were grossly irrational. More than 55 per cent
of the doctors were found to prescribe morin than three drugs
usually unnecessarily. The realisation that drugs must be treated as
an integral component of health care has prompted a growing
number of countries, including Bangladesh, Pakistan, Bhutan,
Sri Lanka in the neighbourhood, the Andean countries, Nicaragua,
Australia and several African, west Asian and European countries
"to take steps towards introducing an essential drugs programme.
Interestingly, the World Health Assembly held in May last has
passed a firm resolution on the need for promoting the concept of
an essential ’drugs programme and implementing controls on
unethical promotion and marketing of drugs. But this would
necessarily mean the availability of a comprehensive graded drug
list which would automatically weed out the unnecessary, unethical
and of course, hazardous formulations—in other words, a drug
policy with an essential drugs programme as its central focus. This,
unfortunately, is not what the central government and industry
mean by a drug policy.
1695
mfc ms
TOWARDS RATIONAL THERAPEUTICS
Extracts of a letter from a young doctor in a small rural
hospital in Madhya Pradesh.
Dear Friend,
......About drug prescribing practices in our hospital—
in the first few months of my work I had ordered many new drugs.
Later I realised mainly because of financial conditions of the
patients that only important essential drugs and a minimum
possible list should be adopted.
Antibiotics
We use commonly Procaine Penicillin and Penidure.
They used to use a lot of Streptopen, which I don't. I mainly
use procaine penicillin. Then I use a lot of septran when
there is double pathology, like respiratory tract infection
with urinary tract infection or otitis media. We use tetracyclines
very rarely. Injection Terramycin I don't use at all. So also
Chloromycetin. I never use chloramphenicol. If I doubt enteric
fever, I start with septran. Then we have streptomycin only for
TB patients. Crystalline penicillin I use only in new borns.
At present I feel very confident regarding the usage of antibiotics
and I don't use two drug combinations,so I have stopped using
chlorostrep.
Diarrhoea
This is usually controlled with rehydration salts and plenty
of oral fluids.....Slowly discontinuing lomotil and other drugs.
■ 7/
D ’ WlSv. -J.- HEALTH CELL
' Fir- - - ’cor'jSt. Marks Road
BAMGAkDRE- 560 001
2
Cough syrups/Tonics
When I joined there were lots of varieties of cough syrups,
cough/cold tablets and also lots of variety of tonics. It took me
nearly a year to cut down many brands. We had 11 brands of cough
syrup and 10 brands of tonics.
Now we make cough mixture in the hospital for free patients
and we have 3 other brands of cough syrup
About tonics—it takes a lot of patience to convince patients—
they don't need tonics—they can get the same benefit with proper
food and milk/eggs. Now-a-days very few people ask for "Thakath
ka sissi"
and we have only two types of tonics....
I have kept multivite tablets, fersolate and calcium tablets.
Not a single brand of costly vitamin capsules or tablets are
stocked. They used to use a lot of varieties. Slowly I stopped
even B-complex injections...
For TB patients we have pyridoxin. For children we have
Vit A & D and multivite drops. Vit C.
I hardly use—nor do I
use calcium injections except in tetany.
Antacids
We had lots of brands before. Now we use Belladinal and two
brands of antacids only.
One thing I have succeeded in proving here is that you
can run a small hospital and treat patients successfully with only a
handful of drugs which are cheap and good quality. Why do we insist
on each doctor or specialist having his own petty brand of drugs
in our large hospitals and even the medical college hospitals?
Yours sincerely.
L.M.
World Health Organization
Organisation mondiale de la Sante
FORTY-SEVENTH WORLD HEALTH ASSEMBLY
Provisional agenda item 19
A47/7
21 March 1994
WHO ethical criteria for medicinal
drug promotion
Report by the Director-General
In resolution WHA45.30 the Forty-fifth World Health Assembly urged Member States "to
intensify efforts to involve government agencies including drug regulatory authorities, as well
as pharmaceutical manufacturers, distributors and the promotion industry, health personnel
involved in the prescription, dispensing, supply and distribution of drugs, universities and
other teaching institutions, professional associations, patient and consumer groups, and the
professional and general media (including publishers and editors of medical journals and
related publications), in the implementation of the principles embodied in the WHO ethical
criteria on medicinal drug promotion."
The same resolution requested the Director-General:
(1)
to request the Council for International Organizations of Medical Sciences
(CIOMS) to convene a meeting of interested parties in collaboration with WHO to
discuss possible approaches to further advancing the principles embodied in WHO’s
ethical criteria for medicinal drug promotion;
(2)
to consider other approaches and mechanisms in the Member States to improve
the implementation of WHO’s ethical criteria for medicinal drug promotion;
(3)
to report the outcome of the meeting of interested parties and other actions of
the Organization relevant to this issue to the Forty-seventh World Health Assembly
through the Executive Board.
The report of the resulting consultation (Geneva, 5-7 April 1993), as prepared by the
Chairman in agreement with all participants, is attached.
Following consideration of this subject by the Executive Board at its ninety-third session,
when it noted the Director-General’s report of which this is the updated version, the
attention of the Health Assembly is in turn drawn to the progress made and to the
recommendations of the CIOMS/WHO consultation (Annex).
A47/7
CONTENTS
Page
Introduction
3
Future activities
3
Matters for particular attention of the Health Assembly
4
Annex. CIOMS/WHO Consultation on WHO Ethical Criteria for Medicinal Drug
Promotion (reflections and recommendations)
5
2
M7/7
INTRODUCTION
1.
The meeting requested in resolution WHA45.30 was jointly organized by WHO and CIOMS, and held
in Geneva, 5-7 April 1993. Each of the interested parties, as defined in the resolution, was represented at
the consultation.
2.
Background papers were prepared by WHO. Further papers describing the results of relevant studies
or giving views on key issues were prepared by participants representing, in particular, industry, regulatory
and academic bodies and consumers. A report of a preliminary meeting on the complementary issue of
the provision and dissemination of "independent" drug information was also brought to the attention of
participants. The full proceedings will become available during 1994.
3.
The report of the consultation (Annex) reflects the spirit of the debate. It was prepared on the basis
of contributions made during the meeting and further comments during the drafting process. It is
constructive and forward-looking. It focuses primarily on the application of the criteria in developing
countries. It does not dwell on the deficiencies of the past. It sets out a commitment as agreed between
the parties and outlines tasks for the future. It also defines an overriding ethical precept: the right to be
informed.
FUTURE ACTIVITIES
4.
The 19 recommendations of the consultation are broad in scope. They relate to education and
communication; the interface between promotion and regulation; the development of national policies;
and international collaboration. It appears that all the interested parties accept the validity of the WHO
ethical criteria and are prepared to work collaboratively to further their implementation.
5.
it was generally appreciated that challenging problems will continue to emerge; that the policies and
programmes of the interested parties will also change; and that the ethical criteria themselves will need
to be adapted to changing circumstances. It was recognized that if collaborative efforts to promote the use
of the criteria are to succeed they must not only be concerted: they must be responsive to change, and they
must be given time.
6.
There was recognition throughout the consultation. that progress will be dependent upon the
leadership provided by WHO. It was recognized that the Organization is particularly well-placed to
appreciate the needs and circumstances of national drug regulatory authorities as part of national drug
policies and to further develop dialogue on how control of advertising can best be integrated into the
process of drug registration. It must be achieved without limiting the capacity to meet other vital objectives
of the registration process, including the need to assure quality and to prevent trade in substandard,
spurious and counterfeit products.
7.
WHO is already promoting implementation of the ethical criteria from the regulatory perspective
through:
- promulgation of its Guiding principles for small national drug regulatory authorities,' and preparation
of model legislation and model software package for drug registration, which provides a means of
controlling drug promotion through the establishment of an approved scientific data sheet;
- development of its Model prescribing information, its system of information exchange on national
regulatory decisions, and its contribution to the United Nations Consolidated List of Products
1 WHO Technical Report Scries. No. 7'X) (1990), Annex <>.
3
A47/7
whose Consumption and/or Sale have been Banned, Withdrawn, Severely Restricted or not
Approved by Governments;
- field-testing of recently prepared guidelines for use of the Certification Scheme on the Quality of
Pharmaceutical Products moving in International Commerce, which now contains provision for
exchange of drug data sheets and for approved labelling.
8.
WHO remains concerned, however, about the paucity of "independent" factual and authoritative
information directed to prescribers and to patients and other users of drug products in many countries.
9.
WHO is also providing information to Member States on national initiatives to compare labelling of
locally-manufactured drug products that are produced for the domestic market and for export to developing
countries, respectively.
10. The following statement, issued following the consultation by the International Committee of Medical
Journal Editors’ meeting in Chicago in August 1993, is encouraging:
Most medical journals carry advertising, and advertising generates income for owners of journals, but
advertising must not be allowed to influence editorial decisions. Editors must have full responsibility for
advertising policy, and readers should be able to distinguish readily between advertising and editorial
matter. Juxtaposition of editorial and advertising material on the same product or subject should be
avoided wherever possible. Finally, editors should consider for publication all criticisms of advertisements.
11. Further discussion of these activities and on progress achieved in implementing the recommendations
contained in the report of the WHO/C1OMS meeting on the ethical criteria will be contained in the
Director-General’s progress reports on WHO’s revised drug strategy.
MATTERS FOR PARTICULAR ATTENTION OF THE HEALTH ASSEMBLY
12. Delegates at the Forty-seventh World Health Assembly are invited to note the progress in advancing
the principles and improving the implementation of WHO’s ethical criteria for medicinal drug promotion,
and attention is drawn in particular to the recommendations contained in the report on the C1OMS/WHO
consultation.
M7/7
ANNEX
CIOMS/WHO CONSULTATION
WHO ETHICAL CRITERIA FOR MEDICINAL DRUG PROMOTION
Geneva, 5-7 April, 1993
BACKGROUND
The CIOMS/WHO Consultation on WHO’s Ethical Criteria for Medicinal Drug Promotion was held
in Geneva, 5-7 April, 1993. The meeting was attended by representatives of national drug regulatory
agencies, the pharmaceutical industry, health professionals, consumer advocates, editors of scientific
journals, and the Secretariats of WHO and CIOMS.
The meeting was held in response to a resolution of the Forty-fifth World Health Assembly in May
1992, that called upon WHO, in collaboration with CIOMS, to convene a meeting of interested parties to
discuss possible approaches to advancing the principles embodied in WHO’s Ethical Criteria for Medicinal
Drug Promotion.
In his opening remarks to the Consultation, the Director-General of WHO, Dr Hiroshi Nakajima,
called for the participants to build their contributions on "dialogue" and "consensus". He said that an
important opportunity would be lost if the participants insisted on dwelling on the symptoms of the
problems posed by drug promotion, rather than on the causes that underlie them. Only if these causes were
fully analysed, and appropriate solutions identified, would the outcome of this consultation be of lasting
value.
Dr Bryant, Chairman of the Consultation, pointed out the major tasks of the consultation to the
participants:
• to examine the problems that surround inappropriate promotional practices as they conflict with
the Ethical Criteria for Medicinal Drug Promotion, with special reference to developing countries;
• to consider what further steps are required to more fully understand the nature of those problems,
keeping in mind the ways in which the problems vary' according to a country’s social, economic,
commercial and health development;
• to explore what concrete actions might be undertaken to remedy those problems, keeping in mind
that short, medium and long-term strategies would be required, both taking into account the
limitations of developing countries, and being aware of the particular strengths of those countries;
• to forward to the Director-General a report of the deliberations for his consideration for further
action.
PREAMBLE
WHO’s Ethical Criteria for Medicinal Drug Promotion are built on health care imperatives that
themselves have an ethical base. Equity is the fundamental value underlying the development of public
health services, according to which there should be universal coverage and care according to need.
5
Annex
A47/7
An essential part of such services is that physicians and patients should have knowledge about and
access to therapies that are appropriate to their needs. Two further concerns bear on the natureof these
services:
• the regulation of medicinal drugs must ensure the quality of drugs and information relating to
them;
• the promotion of medicinal drugs must be consistent with their rational use.
The World Health Assembly, in its resolution WHA41.17 (1988) that established the Ethical Criteria,
urged Member States "(1) to take account of these ethical criteria in developing their own appropriate
measures to ensure that medicinal drug promotion supports the aim of improving health care through the
rational use of drugs"; and "(2) to monitor and enforce, where appropriate, the implementation of the
measures they have developed."
In 1992, a further resolution was adopted by the Assembly stressing the lack of progress in this area
and requesting that further action be taken to implement the Ethical Criteria. The challenge to the
Consultation, therefore, was to define impediments to implementation of the Ethical Criteria. Several
aspects of this challenge were identified as:
• inappropriate promotion of medicinal drugs;
• limitations in the capacities of developing countries to establish drug regulatory and monitoring
systems; and
• inadequate communication of the existence, meaning and purposes of the Ethical Criteria.
A further challenge involved exploring the potential for more constructive interactions among the
relevant parties: (1) to support efforts of countries to ensure that medicinal drug promotion does not
conflict with the rational use of drugs; and (2) to adopt measures based on the WHO Ethical Criteria as
appropriate, and to monitor and enforce such measures.
A critical reference point with respect to the Ethical Criteria is that they should be integral to a
comprehensive national drug policy as defined and recommended by WHO:
"To ensure an adequate supply of safe and effective drugs of good quality, every country should have
a national drug policy as an integral part of its health policy. Appropriate legislation and regulations
will be needed to help implement such a policy." (Guidelines for Developing National Drug Policies,
World Health Organization, Geneva)
Such a national drug policy would include provisions to control drug promotion, disseminate reliable
independent information, and ensure the quality of available drugs.
Rights to information emerged as an issue of fundamental importance. The participants concurred
that an ethical precept inherent in the Ethical Criteria is that patients and prescribers have a right to
information about medicinal drugs that is factual and supportable, and that provides specific directions for
appropriate drug use and monitoring of therapy. Positive claims for a product must always be balanced by
information concerning important side-effects, contraindications, warnings, etc. The information should be
provided in such a way as to allow patients to decide whether they wish to receive the therapy. This right
to information should be emphasized and preserved.
The right to objective and balanced information is an essential element of national drug (and health)
policy, and is ensured through the establishment of a national regulatory capacity, preferably as part of an
6
Annex
A47/7
RECOMMENDATIONS
Given the critical importance of education and communications about the Ethical Criteria, we
recommend:
• that relevant educational materials be developed and disseminated both nationally and
internationally by WHO, universities and other interested parties;
• that WHO alert Member States to the importance of this role for universities and other
educational institutions and assist them in educational programme development;
• that WHO take a leading role in promoting the provision of therapeutic guidelines for prescribers,
including information that is independent and comparative, and includes explanations of the Ethical
Criteria;
• that WHO, member state regulatory authorities, the International Federation of Pharmaceutical
Manufacturers’ Associations (IFPMA), the World Federation of Proprietary Medicine
Manufacturers (WFPMM), the International Organization of Consumer Unions (IOCU), Health
Action International (HAI), and other interested parties explore ways in which clearing house
functions relating to WHO’s Ethical Criteria and medicinal drug promotion can be established,
identifying specific areas in which interested parties can fulfill these functions. WHO, for example,
could act as a clearing house for regulatory and legal information.
II.
STUDIES IN RELATION TO THE ETHICAL CRITERIA AND DRUG REGULATION AND
PROMOTION
While many of the problems associated with inappropriate promotion are well known, the
understanding of others would be assisted by further studies. Studies on the implementation and
monitoring of the WHO Ethical Criteria for Promotion of Medicinal Drugs would also be beneficial.
Implementation and Monitoring in relation to the Ethical Criteria. Resolution WHA41.17, calls for
Member States to take the Ethical Criteria into account as they develop measures to ensure that medicinal
drug promotion supports the rational use of drugs, and to monitor and enforce the measures they have
developed. WHO and its Member States have also been concerned about the limited awareness and use
of the Ethical Criteria. Thus, at issue are both the monitoring of the quality of promotion, and the
monitoring of the implementation of WHO’s Ethical Criteria.
5.
Periodic review of the Ethical Criteria. The Ethical Criteria should be reviewed periodically and
modified as appropriate. Such review and modification should be undertaken judiciously, after careful study
of the Ethical Criteria and their effectiveness internationally and at country level, and of how changes might
impact on related policies of WHO, governments and other interested parties.
6.
Study of the content, flow and use of information relating to medicinal drugs. There are often
dysfunctional relationships between the quality of information related to medicinal drugs and those who
would stand to benefit from it. People need accurate, independent and comparative drug information. At
times, however, the information is inappropriate, whatever its distribution. At other times, the information
is appropriate, but it doesn’t reach those who could use it. At still other times, the potential user may not
have the capacity to absorb and benefit from the information. These problems suggest the usefulness of
a study of the flow, content and uses of drug related information.
7.
8.
Formulate a typology of countries with respect to their current capacities for appropriate drug
regulation and control of promotion. Developing countries vary greatly in their capacities for drug
regulation and for controlling drug promotion.
8
The development of a typology that identifies the
A47/7
Annex
integrated drug policy, as proposed in WHO’s Guiding Principles for Small National Drug Regulatory
Authorities.
Another issue of serious concern in the drug field is the production, promotion and distribution of
spurious and counterfeit drugs. The participants urged that WHO continue its work with Member States
and other parties to combat this problem as a follow-up to the "Joint IFPMA/WHO Workshop on
Counterfeit Drugs", held in Geneva, 1-3 April, 1992.
The spirit and proceedings of the Consultation reflected a common commitment to enhance the
positive contributions of medicinal drugs to the well being of people in all countries, with special concern
for those of the developing world, and ensuring that this contribution is not impeded by inappropriate drug
promotion.
TOPICS RECOMMENDED FOR FURTHER ACTION
I.
EDUCATION AND COMMUNICATION
The Ethical Criteria should be widely disseminated, well understood, and function in support of the
improvement of health care through the rational use of drugs. Education and communication about the
Ethical Criteria are essential.
1.
Materials for the education of health personnel and other appropriate parties. Educational materials
relating to the Rational Use of Drugs and the WHO Ethical Criteria are currently limited in both
appropriateness and availability for the varied audiences who need to be reached, including health
personnel, the general public, marketing managers, sales representatives and the media.
2.
Roles of universities and other educational institutions in furthering the use and effectiveness of the
Ethical Criteria. Universities are in a critical position to contribute to greater understanding of the Ethical
Criteria by health personnel. Thus, promoting an awareness of problems associated with drug promotion,
and developing critical appraisal skills concerning pharmaceutical promotion and other sources of
information about drugs, should be an integral component of undergraduate and continuing education for
health personnel. Universities can also undertake research on relevant issues, such as how well drug
promotion complies with WHO’s Ethical Criteria.
Guidance for prescribers. Health personnel with responsibilities for prescribing medicinal drugs often
lack up-to-date knowledge of drugs and their rational use. An international collaborative approach can be
taken to develop and provide guidance to prescribers, such as assisting in the production of therapeutic
guidelines that provide information that is independent and comparative, and includes explanations of the
Ethical Criteria and their applications to prescribers and other parties.
3.
4.
Clearinghouse functions for materials relating to WHO’s Ethical Criteria and to medicinal drug
promotion. Several kinds of materials could be helpful to countries and organizations working toward more
effective approaches to the implementation of WHO’s Ethical Criteria for the promotion of medicinal
drugs: existing legislation relating to medicinal drug promotion; national and organizational codes relating
to ethics and medicinal drug promotion; materials available from drug regulatory agencies; and
educational programs that promote the WHO Ethical Criteria and develop critical appraisal skills.
Additionally, information concerning regulatory actions taken by national authorities could be of use both
to other regulatory authorities and national and international organizations. These materials are often
widely dispersed and difficult to access.
7
A47{7
Annex
characteristics of countries at different stages of this process, as well as the sequence of developmental steps
required to increase competence in this field, would provide an analytical method for increasing
understanding of these problems.
RECOMMENDATIONS
To promote and carry out studies appropriate to the effective implementation of the Ethical Criteria
for the Promotion of Medicinal Drugs we recommend:
• that WHO, in consultation with concerned parties, determines how to proceed with monitoring of
the implementation of the Ethical Criteria, continues its work to develop performance indicators
in this area, and considers what remedial measures should be taken when there is non-compliance
with the content of the Ethical Criteria;
• that WHO. in consultation with interested parties, periodically review the Ethical Criteria;
• that WHO, in consultation with interested parties, explore the possibilities of initiating studies of
the content, flow and use of information relating to medicinal drugs;
• that WHO take the lead in developing a typology of the current capacities of countries for
appropriate drug regulation and for controlling promotion and in using the typology for studying
capacity building in this field.
III.
NATIONAL POLICIES AND ACTIONS
Each country must have its own national drug policy, which has the purpose of ensuring an adequate
supply of safe and effective drugs of good quality, an integral part of which will be legal and procedural
arrangements for ensuring the appropriate uses and promotion of medicinal drugs. These arrangements
will involve interactions with other interested parties, including pharmaceutical companies and their
associations, distributors, health professionals, consumer groups and universities.
Drug regulation, drug quality, drug promotion. The central features of a national drug policy
encompass responsible approaches to drug regulation, drug quality, the quality of information, the rational
use of drugs, the provision of affordable drugs, and drug promotion. A vital element of national policy and
legislation is the capacity to regulate and control drug labelling and drug promotion through a product
licensing system. Additional crucial components of national drug policy include: the provision of
independent information and education about drugs; the development of critical appraisal skills in health
professionals and consumers; monitoring of ethical standards of pharmaceutical promotion, and auditing
the quality of medicinal drug use. Thus, the Ethical Criteria become an integral part of such national drug
policies.
9.
10. The establishment of national drug policy committees. A national drug policy committee can
strengthen capacities for formulating policies, procedures and programmes that will lead to responsible
national pharmaceutical programs. Such committees may begin as ad hoc arrangements and devolve
specific major responsibilities to legally established bodies. They should involve all interested parties:
government, manufacturers, health professionals and consumers. Other structural approaches to the
development of drug policies also need to be explored.
11.
The establishment and strengthening of national pharmaceutical industry associations. Corporate
practices consistent with the Ethical Criteria should be promoted by national pharmaceutical industry
associations.
9
Annex
A4717
12. Medical representatives, symposia and other meetings. The Ethical Criteria lay down explicit
guidelines for acceptable training and conduct of medical representatives and for the conduct of symposia
and other meetings to ensure that they are educational rather than promotional.
13. The complementarity of self regulation and national regulation. Self-regulatory codes with
appropriate sanctions rigorously applied can assist in the implementation of the Ethical Criteria. An
interactive combination of seif-regulation by companies and national regulation by governmental authorities
is often a constructive arrangement. One functioning without the other can be sub-optimal. The value of
autonomous bodies to set ethical standards, review and/or clear promotional material, and adjudicate
complaints is recognized.
RECOMMENDATIONS
In view of the importance of national actions relating to the Ethical Criteria for the Promotion of
Medicinal Drugs, we recommend:
• that WHO and all interested parties emphasize the importance of the Ethical Criteria being
incorporated in and supported by national drug policies;
• that governments consider the establishment of National Drug Policy Committees;
• that National Industry Associations be set up and that international industry associations help to
establish such associations;
• that WHO, in concert with Member States, consumers, IFPMA and other associations
representative of pharmaceutical companies, and national medical associations formulate
approaches to problems associated with medical representatives and symposia, including further
development and adoption of codes of training and conduct of medical representatives and conduct
of symposia, in ways that are consistent with the Ethical Criteria.
IV.
INTERNATIONAL COLLABORATION
While national level regulations, procedures and other arrangements for promoting the rational use
of drugs are essential, critical contributions are needed from the international level. Important questions
arise on how international organizations and interested parties can interact in ways that are supportive of
national activities in furthering these important efforts.
14. Roles of WHO. WHO has a central role in assisting Member States in establishing and strengthening
their programmes for ensuring the quality and rational use of drugs. The Ethical Criteria for the Promotion
of Medicinal Drugs represents additional potential support for national drug policies. The further
development by WHO of performance indicators, monitoring procedures, and educational modules would
assist in the implementation of the Ethical Criteria.
15. Editorial policies. The peer-reviewed journals have played a pivotal role in ensuring the scientific
integrity of materials they publish. Editors of professional journals can contribute further to rational health
care not only by publishing good scientific work on medicinal drugs but also by ensuring that all drug
advertisements in their journals accord with the WHO Ethical Criteria.
16.
Relationships of international and national associations.
The IFPMA, WFPMM, and bodies
representing generic manufacturers, are key partners in the international effort to ensure responsible
promotion of medicinal drugs in accordance with the Ethical Criteria.
10
A47/7
Annex
17.
Codes of international and national associations and local companies.
Codes that govern the
promotion of medicinal drugs in ways that are consistent with and supportive of the Ethical Criteria
represent an important contribution. Consultation among the involved parties is required to establish,
maintain and update such codes so they achieve their intended purposes.
18. International, national and local consumer groups. Consumer groups have key roles to play in this
field by, inter alia, promoting the existence of the Ethical Criteria, encouraging their use, developing
training and educational materials, and doing studies to monitor promotion. International and local
consumer groups can be mutually supportive in these efforts taking account of possibilities to collaborate
with all concerned parties.
19.
National and international coalitions of concerned parties. In recent years there has been greater
collaboration among the various parties concerned with improving health care through the rational use of
drugs. Now the challenge is to further cooperation among these parties so as to strengthen understanding
of and compliance with the Ethical Criteria.
RECOMMENDATIONS
Important contributions can be made at the international level to arrangements for the promotion
of medicinal drugs and the implementation of the Ethical Criteria. Accordingly we recommend:
• that WHO continue its constructive role in this important field;
• that scientific journals develop advertising guidelines similar to the guidance they provide to
authors, to ensure compliance with the Ethical Criteria;
• that the IFPMA and WFPMM and other bodies exert their further efforts and positive influence
on the formation and activities of national associations of pharmaceutical companies in their
respective areas;
• that the IFPMA, WFPMM, national associations and local companies continue to develop their
own codes relating to the promotion of medicinal drugs in ways that are consistent with the Ethical
Criteria;
• that international, national and local consumer groups continue the key roles they are playing in
working with governments and industry toward constructive actions relating to the Ethical Criteria
for the Promotion of Medicinal Drugs, particularly pursuing studies of promotion, monitoring
compliance with the Ethical Criteria, and working to create a critical awareness among consumers.
• that WHO, CIOMS and other interested parties, including donor organizations, consider how these
national and international interests and resources can be brought into more effective interaction
in relation to the Ethical Criteria, including, as one possibility, the convening of regional meetings
to consider these issues.
REFLECTIONS ON THE CONSULTATION
The World Health Assembly established the Ethical Criteria for Medicinal Drug Promotion in the
expectation that they would strengthen national and international capacities for controlling inappropriate
drug promotion and support the rational use of drugs.
However, WHO and relevant parties have been concerned that the Ethical Criteria have not been
widely disseminated and implemented, and that their role in controlling inappropriate drug promotion has
11
A47/7
Annex
been less than had been anticipated. Accordingly, the Assembly requested WHO, in collaboration with
CIOMS, to convene a consultation in order to explore further steps that might be taken to advance the
principles embodied in the Ethical Criteria
While the Consultation focused primarily on the problems developing countries have in responding
to the Ethical Criteria, the Consultation was also concerned with the ways in which these issues apply to
developed countries.
An underlying reality of this field has to do with tensions existing between industry, governmental
regulators and consumer advocates on a variety of matters including drug promotion. Such tensions can
have positive effects in that all parlies have a common commitment to the well-being of the public, though
their perspectives and approaches are often different.
One of the challenges to this consultation was to capitalize on the common commitments and
substantial strengths of the interested parties and to identify the areas in which agreement and collaboration
could proceed.
The consultation was considered by all who attended to have been a success in bringing participants
into substantial agreement on a number of issues and actions to be taken. One overriding ethical precept
(that of rights to information) and nineteen Recommendations for Further Action form the core of the
Report of the Consultation. The Recommendations have a wide range - Education and Communication
in Relation to the Ethical Criteria; Studies in Relation to the Ethical Criteria and Drug Regulation and
Promotion; National Policies and Actions; and International Collaboration.
This Report has been carefully constructed on the basis of contributions during the Consultation and
the further commentary of participants during the drafting and finalizing of this document.
It should be clear, however, that the larger part of the work in this field still lies ahead. The
Recommendations of the Consultation set the stage. The Executive Board of WHO and the World Health
Assembly can take the policy decisions necessary to carry the Recommendations, modified as they see
appropriate, toward implementation, including the important step of encouraging Member States to act in
full support of the Recommendations.
It is apparent that the relevant parties - national drug regulators, industry, consumers, health
professionals, international organizations, professional and general media - are prepared to work
collaboratively toward greater effectiveness in this field. But such collaboration will not follow
automatically. Challenging problems will continue to emerge. The Ethical Criteria will not be static, nor
will the policies and programmes of the interested parties. Effective collaboration will require concerted
attention, persistence in pursuing key issues (such as identification of measures and procedures for
monitoring, and related research), and continued openness to concerted action.
These steps and relationships will build on the growing realization that all parties have a common
responsibility, built on fundamental ethical principles, for the well being of patients individually, and of the
public collectively.
12
WORLD HEALTH ORGANIZATION
A45/13
18 March 1992
ORGANISATION MONDIALE DE LA SANTE
FORTY-FIFTH WORLD HEALTH ASSEMBLY
Provisional agenda item 19.2
IMPLEMENTATION OF WHO’S REVISED DRUG STRATEGY
SAFETY AND EFFICACY OF PHARMACEUTICAL PRODUCTS
Progress report by the Director-General
In resolution WHA43.20 the Forty-third World Health Assembly requested the
Director-General, inter alia, "to report to the Executive Board and the Forty-fifth
World Health Assembly on the use of the ethical criteria for drug promotion
endorsed by resolution WHA41.17, and on progress made and problems encountered
in implementing the revised drug strategy, the report to cover drug supply,
prescribing practices, development of human resources, training of relevant health
personnel on the rational use of drugs, quality assurance and drug information". In
addition, at its meeting in January 1988 the (then Ad Hoc) Committee on Drug
Policies of the Executive Board requested a report on the outcome of a review of
the WHO International Drug Monitoring Programme and on guidelines for the
implementation of the WHO Certification Scheme on the Quality of Pharmaceutical
Products Moving in International Commerce.
The present report was reviewed during the eighty-ninth session of the
Executive Board by the Committee on Drug Policies. It provides background
information relevant to resolutions EB89.R2 (WHO ethical criteria for medicinal
drug promotion) and EB89.R3 (WHO Certification Scheme). The Board concurred
with the Committee’s recommendation that this report should be reproduced in full
as a progress report by the Director-General to the Forty-fifth World Health
Assembly.
CONTENTS
Page
I.
RELATIONSHIPS WITH NATIONAL DRUG REGULATORY AUTHORITIES
..................................
2
II.
WHO ETHICAL CRITERIA FOR MEDICINAL DRUG PROMOTION ....................................................
10
III.
THE WHO CERTIFICATION SCHEME ON THE QUALITY OF PHARMACEUTICAL
PRODUCTS MOVING IN INTERNATIONAL COMMERCE ...................................................................
17
WHO INTERNATIONAL DRUG MONITORING PROGRAMME
29
IV.
...........................................................
A45/13
page 2
I.
RELATIONSHIPS WITH NATIONAL DRUG REGULATORY AUTHORITIES
CONTENTS
Page
1.
INTRODUCTION ...................................................................................................................................................
2
2.
HARMONIZATION OF REQUIREMENTS FOR DRUG REGISTRATION
..........................................
3
3.
EXCHANGE OF INFORMATION ON NATIONAL REGULATORY DECISIONS ................................
4
4.
WHO INTERNATIONAL DRUG MONITORING PROGRAMME
............................................................
4
5.
WHO MODEL UST OF ESSENTIAL DRUGS .............................................................................................
4
6.
WHO MODEL PRESCRIBING INFORMATION ..........................................................................................
5
7.
WHO CERTIFICATION SCHEME ON THE QUALITY OF PHARMACEUTICAL PRODUCTS
MOVING IN INTERNATIONAL COMMERCE .............................................................................................
5
8.
WHO GUIDING PRINCIPLES FOR SMALL NATIONAL DRUG REGULATORY
AUTHORITIES ......................................................................................................................................................
6
9.
A MODEL COMPUTER APPLICATION TO SUPPORT THE DRUG REGISTRATION
PROCESS .............................................................................................................................................................
6
10.
ENFORCEMENT OF LICENSING DECISIONS .........................................................................................
6
11.
THE INTERNATIONAL PHARMACOPOEIA ..............................................................................................
7
12.
BASIC TESTS FOR PHARMACEUTICAL SUBSTANCES AND DOSAGE FORMS
....................
7
13.
STABILITY OF PHARMACEUTICAL SUBSTANCES AND DOSAGE FORMS
14.
QUALITY ASSURANCE: IMPLEMENTATION AND TRAINING ASPECTS
15.
INTERNATIONAL NONPROPRIETARY NAMES
1.
INTRODUCTION
..............................
7
...................................
8
........................... .. ......................................................
9
“
1.1
WHO’s revised drug strategy devolves from the Conference of Experts on the Rational Use of Drugs
(Nairobi 1985), which brought together representatives of governments, pharmaceutical industries, and
patients’ and consumers’ organizations to discuss ways of ensuring the rational use of drugs, in particular
through improved knowledge and flow of information, and the role of marketing practices in this respect,
especially in developing countries. In 1986 a report on this meeting and the revised drug strategy12was
presented to the Thirty-ninth World Health Assembly, which endorsed the strategy in resolution WHA39.27.
1.2
Subsequently, the Director-General reported to the Health Assembly on two specific components of the
strategy. In 1988 proposals to extend the use of the WHO Certification Scheme on the Quality of
Pharmaceutical Products Moving in International Commerce2 and ethical criteria for medicinal drug
1 Document WHA39/1986/REC/1, p. 93.
2 Document WHA41/1988/REC/1, p. 53.
A45/13
page 9
Pharmaceutiques (Dakar, February 1991); a symposium on quality management in drug procurement was
organized jointly by the West African Pharmaceutical Federation, the International Pharmaceutical Federation
and WHO (Accra, February 1991); and an international workshop of authorities on computer-based drug
regulation was held with funding from the Italian Government (Windhoek, July 1991).
15.
INTERNATIONAL NONPROPRIETARY NAMES
15.1 A call to assign International Nonproprietary Names (INN) to the rapidly increasing array of products
produced by recombinant technology indicates the need for seeking extrabudgetary resources to supplement
those available to WHO. There are indications, for instance, that some 400 monoclonal antibodies alone are
under development. Also in contention is a wide range of other peptide regulatory factors including cytokines
(interferons, interleukins, colony-stimulating factors), erythropoietins, plasminogen activators, growth hormones
and other growth factors. The WHO Committee on International Nonproprietary Names for Pharmaceutical
Substances faces an inevitable linguistic challenge in its attempts to extend the INN nomenclature in a
reasonably systematic manner in the face of such demands.
15.2 The challenge is aggravated when manufacturers seek to promote these products using brand names that
are derived from INNs or use stems selected from INNs. Since, with few if any exceptions, no two products
that are manufactured independently by these methods can be accepted to be totally identical, and may
con, . quently not be clinically interchangeable, there is a consensus among national nomenclature commissions
and ate WHO Committee that every such product that is independently produced should be assigned a
distinctive INN (unless absolute proof of identity with another product is provided). The assignation of trade
names is unlikely to hold significant commercial advantage in these circumstances, but WHO undertakes to
consult interested national drug regulatory authorities and IFPMA before exercising any initiative in this
regard.
15.3 In the meantime, national authorities are invited to reconsider a recommendation made by the WHO
Expert Committee on Nonproprietary Names for Pharmaceutical Substances in I9751 that the inclusion in
brand names of generic stems selected by the Committee should be discouraged and, as far as is practicable,
disallowed.
1 WHO Technical Report Series, No. 581, 1975.
A45/13
page 10
II.
WHO ETHICAL CRITERIA FOR MEDICINAL DRUG PROMOTION
Resolution WHA43.20 requests the Director General, inter alia, "to report to
the Executive Board and the Forty-fifth World Health Assembly on the use of the
ethical criteria for drug promotion endorsed by resolution WHA41.17
In this
resolution, Member States were urged to take account of these criteria when
developing measures to ensure that medicinal drug promotion supported the aim of
improving health care through the rational use of drugs. It also appealed to those
involved in the prescription, dispensing, supply and distribution of medicinal drugs to
use the criteria appropriately, to adopt the measures developed and to enforce the
standards thereby proposed.
__________ I
CONTENTS
Page
1.
INTRODUCTION....................................................................................................................................................
10
2.
USE OF THE CRITERIA BY GOVERNMENTS ............................................................................................
11
3.
USE OF THE CRITERIA BY MANUFACTURERS OF PRESCRIPTION DRUGS.............................
11
4.
USE OF THE CRITERIA BY MANUFACTURERS OF NON-PRESCRIPTION DRUGS
................
12
5.
USE OF THE CRITERIA BY TEACHERS AND OTHER HEALTH PROFESSIONALS
..................
13
6.
THE ISSUES
.........................................................................................................................................................
14
1.
INTRODUCTION
l.l
The WHO ethical criteria are based on a draft prepared by an international group of experts comprising
drug regulatory officials, representatives of pharmaceutical manufacturers, prescribers, consumer advocates,
lawyers and medical journalists. They "constitute a frame of reference for proper behaviour in the promotion
of medicinal drugs", but "do not constitute legal obligations; rather they set out general principles which could
be adapted by governments to national circumstances". Member States are urged "to take them into account in
developing measures to ensure that medicinal drug promotion supports the aim of improving health care
through the rational use of drugs".'
1.2
An appeal is addressed to the public and all interested parties, including pharmaceutical manufacturers,
teachers and editors of medical journals to use them as appropriate to their spheres of competence, activity
and responsibility. Both governments and nongovernmental organizations are requested to monitor and
enforce relevant standards and other measures that they develop.
1.3
Promotion is defined within this context as "all information and persuasive activities by manufacturers
and distributors, the effect of which is to induce the prescription, supply, purchase and/or use of medicinal
products". Specifically discussed are all forms of advertisements addressed to physicians, health-related
professionals and the general public; the training and responsibilities of medical representatives; the offer of
free samples of drugs for promotional purposes either to prescribers or, in the case of non-prescription drugs,
to the general public; sponsorship of symposia; post-marketing scientific studies, surveillance and
' Ethical criteria for medicinal dntg promotion. Geneva, World Health Organization, 1988, back-cover text.
A45/13
page 11
dissemination of information; packaging and labelling; information for patients, package inserts and booklets;
and promotion of exported drugs.
2.
USE OF THE CRITERIA BY GOVERNMENTS
2.1 The responses to an enquiry circulated by WHO to all national drug regulatory authorities in September
1990 show that, in general, those countries with highly evolved drug regulatory mechanisms have already
enacted provisions largely comparable in their general intention with the criteria. Several, none the less, have
expressed an intention either to include the criteria, or to adapt them for inclusion, in legal instruments. Thus
far, the Ministry of Health of Turkey has used them as the basis for updating regulations on promotion of
medicinal drug products for human use, and the Media Council of Australia has incorporated them in its
Therapeutic Goods Advertising Code which is binding upon virtually all print, radio, television, outdoor and
cinema media throughout the country.
2.2 The criteria have also served to draw to the attention of governments various particulars on which there
is no consensus among Member States. Some of these differences reflect differing national conditions, but
others reflect divergencies on matters of principle. For instance, some countries, but not others, permit within defined limits - advertising of prescription products directly to the general public. Some permit
comparative advertising, others do not. Different national positions also prevail, for example, on the
admissibility of short (or "reminder") advertisements, the use of radio and television and other non-print
media, and the use of product samples for promotional purposes.
2.3 One fundamental point that is evident from the replies received, and from the review of relevant
legislation in the International Digest of Health Legislation, is that effective oversight and control of promotion
is possible only when a comprehensive national drug licensing system is in place. Control of promotion implies
the existence of standards. In so far as these standards control precise promotional claims, they are
product-specific and they can be determined only by an approved scientific "data sheet" that is incorporated
into the product licence. Countries that have yet to develop a product licensing system are able to promulgate
and enforce general provisions intended to control promotional practices, but they lack the means to check
claims on a product-specific basis.
2.4 Even those countries with rigorous product licensing requirements face a daunting task in verifying the
compliance of all written advertising material with the approved data sheet. Few countries possess regulatory
authorities with the human resources to proactively screen all advertising copy. Some have set up autonomous,
multidisciplinary committees to assume this screening function and to review or adjudicate on specific
complaints about promotional practices. Some have introduced collateral measures that require the product
licence holder to refrain from promoting or distributing a new product until a copy of the approved data sheet
has been issued to every registered practitioner. Some have resorted to exemplary prosecution of companies
and responsible employees for wilful breach of regulations. All depend, however, on a high level of compliance
and self-regulation within the industry to enable them to root out inadmissible practices with reasonable
efficiency.
3.
USE OF THE CRITERIA BY MANUFACTURERS OF PRESCRIPTION DRUGS
3.1 The International Federation of Pharmaceutical Manufacturers Associations (IFPMA) - which has 45
member national associations representing manufacturers of approximately 80%, by value, of the world’s
prescription medicines - first adopted a Code of Pharmaceutical Marketing Practices in 1981. This sets out
"minimum standards" to be adopted by companies wherever their products are marketed. Many national
pharmaceutical manufacturers associations have drawn up more detailed codes through which they exercise
varying measures of self-discipline. This control is effected by national adjudicating committees which include
members who are independent of the industry. Their work is carried out in an essentially reactive manner by
hearing complaints from third parties and sometimes from other companies. The sanctions imposed are
administrative: publication of the names of offending companies and, in extreme circumstances, exclusion from
membership of the national association for stipulated periods of time. None of this has any impact on other
companies, often established in countries without highly evolved regulatory authorities, that are not affiliated to
IFPMA. Indeed, these may operate without any tangible external control or oversight.
A45/13
page 12
3.2 Complaints concerning activities of multinational companies in countries that possess no national
disciplinary body can be transmitted directly to IFPMA, which is responsible for administering its international
code. In this case, each complaint is referred for consideration to the member association in the country in
which the headquarters of the accused company is based, although the final opinion communicated to the
complainant is formulated by an IFPMA committee which incorporates independent assessors. Given the scale
on which the industry operates and the intensity of its promotional activities, the number of cases referred to
IFPMA is small: a total of 70 complaints, relating to 912 cases, has been filed over the past 10 years and the
annual returns demonstrate a falling trend in the number of cases notified over the past four years.
3.3 IFPMA has informed WHO that it considers systematic monitoring of company marketing activities as
quite impracticable and that monitoring could therefore be conducted only on a very limited and arbitrary
basis. In commenting on the operation of its Code, IFPMA emphasizes that details of complaints processed
between 1983 and 1989 have been published in 10 status reports, and states: "... strenuous efforts have been
made to make the existence of the Code known as widely as possible and also to encourage use of the
complaints procedure. Although the text of the Code has remained unchanged since its original definition,
explanatory material has been added, most recently in January 1989, and many thousands of copies in
three-language versions have been distributed throughout the world both within and outside the industry.
Additionally the Code has featured in several numbers of the [IFPMA] periodical 'Health Horizons’, most
recently in May 1989. This publication has a circulation of about 10 000, mainly within the developing world”.
IFPMA also notes that, in several instances, complaints have challenged the justification of the product, rather
than the manner in which it is promoted. The Code reflects the view that, provided the product has been duly
authorized for marketing by a competent regulatory authority, it is not for IFPMA to question the judgement
of that authority.
3.4 IFPMA has never formally adopted the WHO ethical criteria for medicinal drug promotion. However, it
has stated: ”... the criteria have been examined closely in comparison with the [IFPMA] Code, which had
already been in existence for seven years when they were defined. The conclusion was reached that, in so far
as they related to the prescription medicine sector of the industry, there was full congruence between the two,
even though certain provisions elaborated in some detail in one document were covered in a more general
requirement of the other and vice versa. Since the IFPMA Code is an obligation on its members, the formal
adoption of the wording of certain recommendations of the criteria in the Code text would result in conflict
between existing regulations in some countries and the requirements of the Code”. It sees, in this connection,
an important distinction between the binding nature of its Code and the broader advisory purview of the WHO
ethical criteria which constitute "an appeal to concerned parties for adoption to the extent considered
appropriate to their field of competence”. Notwithstanding this distinction, IFPMA contends that "the two
documents are fully consonant one with the other and that the industry represented by IFPMA is responding
in a practical and effective way to the appeals of the World Health Assembly”.
4.
USE OF THE CRITERIA BY MANUFACTURERS OF NON-PRESCRIPTION DRUGS
4.1 The World Federation of Proprietary Medicine Manufacturers (WFPMM) comprises 50 member
national associations representing manufacturers of medicinal products that are identified by and sold under a
trade mark, trade name, brand or other trade symbol, and that are sold or offered for sale to the general
public mainly for use in self-medication. It has developed a statement of policy on advertising to the public,
and it issues guidelines for voluntary codes of advertising practice which take into consideration the WHO
ethical criteria.
4.2 WFPMM does not, itself, promulgate a code on the grounds that "varying conditions ... relating to
distribution differences, advanced or less advanced state health services, differing climatic conditions affecting
the prevalence of particular minor ailments, legislative differences, etc., will call for differences in the content
of such Codes". It believes that "a combination of national laws, voluntary industry codes on a national level,
and responsible individual company action are effective in maintaining high standards of advertising among the
various nations - taking into account the vital matter of local conditions". It also considers, having regard to
lack of pharmacy retail outlets in many areas, even within some developed countries, that "it would be quite
improper and not in the public interest to attempt to harmonize retail distribution controls on an international
basis".
A45/13
page 13
4.3
In commenting on the WHO ethical criteria, WFPMM considers that, in several particulars, the
recommendations do not distinguish clearly between prescription and non-prescription medicines, or between
"patients" and "consumers". The requirements of the latter for information, it is pointed out, differ in that
patients are under the supervision of a prescriber, while consumers take their own decisions on self-care. It
also believes that advertisements of non-prescription products - particularly having regard to the wide range of
media employed - cannot be used effectively to convey detailed basic information on medicines; they can only
create awareness of a product, and indicate its approved uses. Advertisements, it contends, are not the place
to indicate the limitations on the use of a non-prescription medicine other than to specify the category of
people who should use it. In a statement of policy on consumer information it identifies labelling as the
vehicle for conveying precise and detailed information to the consumer, both at the time the product is
purchased and when it is used. However, the statement provides no insight on the extent to which products
are actually selected by purchasers on the basis of their labelling rather than on impulse or recollection of a
superficial advertising claim.
5.
USE OF THE CRITERIA BY TEACHERS AND OTHER HEALTH PROFESSIONALS
5.1 In adopting the criteria, the Forty-first World Health Assembly, by resolution WHA41.17, urged Member
States to take them into account in developing measures to ensure that medicinal drug promotion supports the
aim of improving health care through the rational use of drugs. None the less, since advertising is inherently
promotional in character, there is a need for complementary objective, independent information that is
directed both to the health professions and to the public at large. Within the medical establishment, the
challenge lies primarily with clinical pharmacologists to promote the changes of attitude implicit in the rational
use of drugs; but internists, specialist clinicians and pharmacists each have a vital contribution to offer.
5.2 Doctors will always stalwartly defend their professional freedom to prescribe as their judgement dictates.
However, enough has been learned from the introduction of institutional formularies, antibiotics policies and
therapeutics committees in recent years to show that peer review of prescribing practices, when undertaken
with competence and sensitivity to the need for consultation and feedback of information, can be not only
tolerated but welcomed by the profession at large.
5.3
The delivery of medical services is engulfed by an unprecedented cost crisis. The divide between what is
possible and what is practicable has passed the stage at which it might be bridged simply by increased charges
on patients and public funds. Inevitably, the options are most limited where the need is greatest, but
everywhere it is becoming necessary to set priorities and to ensure that they are respected. In varying degree,
governments have become directly engaged in cost saving - most notably by promoting generic prescribing, by
excluding specific products from reimbursement schemes, by issuing advice to doctors on good prescribing
practices and, in some instances, by imposing limits on their drug budgets. Critics argue that prescribing
regulation may lead to false economies that neither save money in health care provision overall nor maintain
standards of patient care, and that may well neglect the improved quality of life that drug treatments can offer.
These differing viewpoints will be resolved only when the generality of prescribers is persuaded, by training or
otherwise, routinely to consider costs when weighing the relative advantages and shortcomings of treatment
options.
5.4 To this end, WHO is collaborating with the International Union of Pharmacology to depict clinical
pharmacology as a specialty of relevance to the socioeconomic aspects of health care. Two exploratory projects
have been initiated with this objective in view. One is directed to collating and reviewing information on the
teaching of therapeutics in medical schools around the world. The other seeks to compare and to evaluate
approaches to the treatment of commonly occurring diseases,in a wide variety of medical settings. Preliminary
discussions have also been held with a view to updating, within this perspective, the WHO report on clinical
pharmacology: scope, organization and training, which was issued in 1970.'
5.5
Within WHO, many programme activities are currently directed to rationalization of therapeutic
management, particularly in relation to infectious and transmissible diseases. The biennial updating of the
WHO Model List of Essential Drugs and the production of the complementary Model Prescribing Information
series has become a highly coordinated activity, involving not only many technical programmes but also their
1 WHO Technical Report Series, No. 446, 1970.
A45/13
page 14
expert advisory panels. WHO Drug Information, now in its fifth year as a subscription periodical, is firmly
established as a journal that reflects WHO policies and activities from both the socioeconomic and the
technical standpoints in relation to drug use. In future, a higher profile will also be accorded to the
pharmaceuticals section of the United Nations Consolidated list of products whose consumption and/or sale have
been banned, withdrawn, severely restricted or not approved by governments. With the agreement of the United
Nations secretariat this will be produced on an annual basis, initially in English, as a service to national drug
regulatory authorities.
6.
THE ISSUES
6.1 The basic issues to be confronted are not new, although they constantly acquire new dimensions. Some
problems, given good will by all concerned parties, are open to solution. Progress with regard to the others will
be dependent upon the availability of necessary human and material resources.
6.2 Health Action International, a public interest group represented in 60 countries, that actively promotes a
more rational use of drugs, has recently produced a valuable annotated bibliography to illustrate the panoply of
problems that developing countries, in particular, face in their efforts to achieve rational and economic drug
use? It cites, inter alia, three targets for urgent action that have direct relevance to the WHO ethical criteria:
more objective information on the rational use of drugs; more direct access by consumers to such information;
and stricter controls on advertising. The directness of the appeal belies the complexity of the issues.
6.3 Many independent publications, directed to personnel at every level within the health care system, are
currently available on the properties and uses of medicinal products. Virtually all, however, are produced
commercially with a view to maximizing sales, and they are concerned with medicine as it is practised in highly
developed countries. Even among these, very few, as yet, discuss cost-effectiveness or other socioeconomic
aspects of drug use.
6.4 WHO is perhaps alone in the extent to which it caters, in its printed outputs, for the needs of developing
countries. It faces two perennial problems, however: its outputs are restricted to the working languages of the
Organization, and lack of exchangeable currency in the target countries frustrates effective penetration into
their markets. The distribution of free copies of its publications is necessarily limited and, even at reduced
prices, booklets intended primarily for use in developing countries, such as the volume dealing with drugs for
parasitic disease in the WHO Model Prescribing Information series, are unlikely to generate sales of more than
a few thousand copies. Reprinting of material locally by arrangement, either in the original or in the national
language, is welcomed. In selected cases, this has dramatically increased the number of printed copies, but in
general it does no more than partially solve the underlying difficulty.
6.5 It is encouraging, none the less, that many countries are using material generated within WHO in the
compilation of their own national drug formularies. However, doctors also need regularly to update
information on the contemporary therapeutic issues that are discussed in the quarterly bulletin WHO Drug
Information. Two other approaches, one at each end of the technology spectrum, offer promise in alleviating
this difficulty. One relies upon local initiatives by doctors and pharmacists, usually in university departments of
medicine or pharmacology, to produce independent drug bulletins that are circulated to networks of subscribing
doctors. Given encouragement and modest financial support in local currency from official sources, some such
initiatives are already exerting a demonstrable influence on local prescribing patterns. The second approach
looks to the future. Technology in data transmission has now developed to the extent that it will become
cost-effective and practicable within the next few years for virtually all countries to receive information from
WHO on diskette not only for reading but - by arrangement with WHO - for low-cost local printing and
reproduction. A preliminary inquiry among national drug regulatory authorities has shown that a large
majority are already able to handle - and would indeed welcome - information in this form.
6.6 At the present time, however, it is apparent that the resources of pharmaceutical companies to produce
information regarding the use of their products surpass those of governments and the health-related
professions. Ostensibly, highly evolved regulatory authorities already possess the statutory powers and
' Hardon, A. et al., eds. The provision and use of dmgs in developing countries. Amsterdam, Health Action International,
1991.
A45/13
page 15
regulations to exercise the controls required over advertising and other forms of promotion of products.
However, the situation that confronts regulators is never static. Pharmaceutical companies have developed in
recent years into major sponsors of postgraduate medical education and scientific debate, and their advertising
revenues sustain the production of all but the most prestigious medical journals. Much of this activity brings
undisputed benefits. This gain could not now be cast aside without gross disruption. None the less,
sponsorship of education and research inevitably provides a vehicle for bias and an opportunity for veiled
promotion. The problem now in developed countries is not simply the imbalance in the availability of objective
information and promotional material but the difficulty of distinguishing the one from the other.
<5.7 Specific industry-sponsored approaches currently under scrutiny by the United States Food and Drug
Administration1 include press releases and press conferences; company or privately-funded journals, journal
articles, letters and reports and special supplements to journals; lecture tours by scientists or experts that
promote one company’s product or disparage a competitor’s; company-financed scientific and educational
seminars, symposia, conferences, programmes and meetings; celebrity endorsements of products;
advertisements that feature questionable, unsubstantiated, or selected research particularly if it is funded by the
company; and distribution of videos and computer disks of promotional material disguised as news and
educational information.
6.8 Two key areas of research that are particularly vulnerable to the bias of sponsorship are post-marketing
studies and cost-effectiveness analyses of newly approved products. Post-marketing studies are intended to
provide information on the performance of new drugs under conditions of routine use, but opportunity exists
to build a promotional dimension into the design. Cost-effectiveness studies are of value to health planners
concerned with the delivery of health care. They are also helpful to pharmaceutical companies, which sponsor
much research of this type, both for promotional purposes and for strategic planning. Formal evidence of
ambiguity in the objectives of such studies is wanting, but it has been claimed from the vantage-point of
experience that "review of manuscripts before publication is usual, attempts to fund only positive studies are
the rule, and incentives for investigators to make favourable assumptions are ever present".2
6.9 In countries where market potential is low, this type of sponsorship bias holds little attraction. But
advertising inevitably assumes importance to a local manager who is otherwise unable to maintain sales
sufficient to ensure a secure profit margin. Where regulatory oversight is limited, this is too often reflected in
journal advertisements containing vague, unqualified claims as well as technical details that are sometimes cast
in a typeface too small to be legible. The consequences of this can be profound. Where microbiological
facilities are not available, concern about hypothetical antibiotic resistance can be exploited in such
advertisements to provide a justification to propose reserve antibiotics for indiscriminate routine use. In a
recent extreme case, promotion of potentially dangerous drugs for infantile diarrhoea in developing countries
was curbed by some internationally based companies only when evidence associating one of these products with
fatal paralytic ileus was publicized internationally. Some of these shortcomings constitute manifest breeches
not only of codes but, in some cases, of regulations and statutes.
6.10 With such lapses in mind, the President of IFPMA issued an open letter to the leadership of the world
pharmaceutical industry in July 1991 stating, inter alia:
For the future, it is clearly imperative that, in the public interest as well as the long-term interests of our
industry, all possible steps are taken to maintain scrupulous respect for the principles of the Code. As an
international industry we claim with justification to observe internationally consistent standards and we
must be seen to do so, whether it be for product quality, marketing practices or any other aspect of our
business. When different norms between countries have to be observed the differences must be seen to
be for valid reasons and companies should be prepared to give convincing and vigorous responses to any
challenges in this regard.
' Kessler, DA. Drug promotion and scientific exchange: the role of the clinical investigator. New England Journal of
Medicine, 325: 201-203 (1991).
2 Hillman, A., Eisenberg, J., Pauly, M. et al. Avoiding bias in the conduct and reporting of cost-effectiveness research
sponsored by pharmaceutical companies. New England Journal of Medicine, 324: 1362-1365 (1991).
A45/13
page 16
I would urge you to ensure that your staff members are continually reminded of the need to follow
well-defined guidelines for marketing activities and to maintain consistent operating standards in all
countries. Furthermore, observance of these standards should be required of your licencees and agents
as a condition of the relationship.
6.11 From the governmental perspective, consideration is bound to turn to the need for stricter controls.
Supplementary legislation will be of value only to the extent that it can be effectively enforced. Evidence of
frailty in enforcement capability is evident in relation not only to substandard advertising, but to a disquieting
prevalence of counterfeit, spurious and substandard products on many national markets. Effective enforcement
becomes possible only where there is a credible drug inspectorate complemented by an efficient drug licensing
system. Prosecutions cannot be brought to bear in many instances under typical national drug laws until the
legitimate market has been defined through formal licensing of products, manufacturers and wholesalers.
6.12 The administrative requirement of formal licensing can be realized initially by issuing "licences of right"
which simply define and provisionally legitimize each medicinal product notified by the responsible person as
having been available on the market prior to the day on which licensing requirements were introduced. No
assessment is implied in the issuance of a provisional licence. Technical reviews can be undertaken and
definitive licences issued subsequently at a speed consonant with the resources of the licensing authority.
However, provisional licensing confers two immediate advantages: unlicensed products are identifiable,
de facto, as illegal; and the licences of products that are adjudged, on specific criteria, to be unsafe or
inefficacious can immediately be either withdrawn or modified by administrative action. Since the product
licence includes a description of the approved indications for the product together with information on
contraindications, precautions and adverse effects, it also provides an immediate control both of product
labelling and of advertising claims.
6.13 The administrative exercise involved in setting up such a licensing scheme is not necessarily labour
intensive even if traditional filing methods are used; but if data entry and retrieval are computerized, the
compilation and subsequent use of the system for enforcement purposes is greatly facilitated. A readily
adaptable software package which - with sufficient harmonization of licence applications - could readily allow
controlled automated entry of licence details into the data base, is currently being developed by WHO with
funds received from the governments of Germany and Italy. The intention is to offer it, free of charge and
copyright, to every interested national drug regulatory authority.
6.14 Even when such licensing systems have become standard administrative tools within regulatory
authorities, effective pre-screening of all proposed advertising copy will be beyond the capability of small
regulatory authorities. An exemplary level of self-discipline will still be required from manufacturers and other
product licence holders if expected standards are to be met, and their representative national associations will
still need to exercise meaningful oversight in their implementation.
6.15 Self-discipline and self-regulation are prerogatives that create an expectation for accountability of action
and a willingness to subject norms and standards, whether actual or enjoined, to debate. IFPMA accepts this
thesis and has reacted favourably to a proposal that a forum to enable these issues to be debated by interested
parties should be created within the Council for International Organizations of Medical Sciences (CIOMS) - an
international organization established jointly by WHO and UNESCO in 1949 that serves the scientific interests
of the international biomedical community in general and has a long tradition of involvement in bioethical
matters.
THE POLITICS OF HEALTH SECTOR REFORM
IN DEVELOPING COUNTRIES:
THREE CASES GF PHARMACEUTICAL POLICY
By
Michael R. Reich
Harvard School of Public Health
665 Huntington Avenue
Boston, MA 02115
! |
Prepared for the Conference on
Health Sector Reform in Developing Countries: Issues for the 1990’s
New England Center, Durham, NH
10-13 September 1993
THE POLITICS OF HEALTH SECTOR REFORM
IN DEVELOPING COUNTRIES:
THREE CASES OF PHARMACEUTICAL POLICY
By Michael R. Reich
INTRODUCTION
Policy reform is a profoundly political process. Politics affects the origins, the
formulation, and the implementation of public policy, especially when significant changes are
involved. For the health sector as well, policy reform requires political skill, as President
and Hillary Clinton have discovered (Figure 1) (Peterson, 1993). Yet these political
dimensions are seldom analyzed systematically for health sector reform in developing
countries. The tendency, especially in public health, is to portray policy reform as a
technocratic or economic process. Both economists and health policy analysts tend to
provide detailed prescriptions on what should be done, but without clear instructions on how
to do it and without good explanations of why things go wrong. A similar pattern has been
observed for economic policy-making. As noted by Robert H. Bates, ’Politics is rarely
placed at the center of economic research’ (1991:272). Decision makers in most instances
are left to rely on their intuition in managing the politics of reform.
The 1993 World Development Report (WDR), on "investing for health," exemplifies
the downplay of politics. The report provided seven chapters on what countries should do to
improve the allocative efficiency of health expenditures in poor countries, but only five
paragraphs on the process of health sector reform, under the heading of "directions and
prospects for reform’ (1993:164-165). And these paragraphs provided few concrete or
specific ideas about how to manage what the report called the "continuous and complex
struggle" of health sector reform. A similar pattern exists for the more general efforts to
promote structural reform in poor countries. Miles Kahler identified a tendency on the part
of external agencies (such as the World Bank and the International Monetary Fund) to avoid
an explicit analysis of politics, even for major economic policies, and even when political
factors were recognized as critical to success; instead, these agencies engaged in implicit or
ad hoc political analysis (Kahler, 1989:157-158).
The 1993 WDR seems to rely on a model of policy reform that assumes right action
will naturally follow from rational analysis. In presenting its conclusions, the WDR
(1993:15) cautioned, "At first glance, it might appear that adoption of this Report’s major
recommendations will be easy" (although the report did not suggest why one might believe
that the proposed policy changes would be easy to achieve). The report then continued to
say that "in reality, change will be difficult, since an array of interest groups may stand to
lose — from suppliers of medical services to rich beneficiaries of public subsidies to protected
drug companies." But the report still discussed policy reform according to a simple model of
political economy: "Broad reforms in the health sector are possible when there is sufficient
political will and when changes to the health sector are designed and implemented by capable
planners and managers’ (1993:15).
represents a value-laden choice of political philosophy, even when (or especially when) the
choice is presented as a technical decision. Three broad value systems, reflecting
fundamentally different visions of the good society, are commonly called into play to provide
the philosophical foundations for policy reform.
Perhaps the most common value system today for policy reform is the utilitarian
perspective. This approach employs a consequentialist calculation and comparison of policies
to determine which option will achieve the most results for the least inputs. As Kymlicka
observed, consequentialism “seems to provide a straightforward method for resolving moral
questions. Finding the morally right answer becomes a matter of measuring changes in
human welfare, not of consulting spiritual leaders, or relying on obscure traditions"
(1990:11). To carry out this calculation for health sector reform, the WDR adopted the
metric of cost-effectiveness, using Disability Adjusted Life Years. While this metric may not
be the only standard used by the WDR, it certainly stands head and shoulders above all
others. The report is titled “investing in health" and the dominant concern is how to obtain
ie most “health gain per dollar spent.” The WDR’s recommendations are driven primarily
y cost-effectiveness considerations, and they generally assume that if an action is costeffective, then it should be done.
<
A second value system is the communitarian perspective, which emphasizes an
empirical social contract (whether explicit or implicit) that exists within some actual
community. This philosophical approach can provide a community-based notion of the
common good, to justify and guide the redistribution of resources through health sector
reform. The international movement toward primary health care can be viewed as a
communitarian argument to provide health care resources for rural residents of poor
countries. The movement for "community-oriented primary care," which seeks to improve
primary care in poor communities, is similarly based on principles of grounding health policy
and health services "in communities, for communities, and with communities" (Geiger,
1993:946). A communitarian approach to allocating health resources would not necessarily
be concerned about the cost-effectiveness of maximizing health within a particular society; it
would instead seek to improve health within a particular segment of the society, as part of a
community-based vision of the common good, regardless of whether those actions were the
{Jtiiost cost-effective. The emphasis on community participation with the PHC movement also
corresponds to a communitarian emphasis on a communal political search for the good life
(Kymlicka, 1990:226).
To some extent, the WDR proposed a double metric for health sector reform, seeking
to increase efficiency and increase equity at the same time. The report, however, did not
make clear whether both must increase in order to be acceptable, or how the relative
importance of the two objectives should be weighted in deciding what to do first, or what to
do when cost-effectiveness and equity are in conflict. In addition to these conceptual
ambiguities, efforts to combine efficiency and equity can be polio..ally hazardous. Joan
Nelson warned, "While efficiency and social justice argue for targeting benefits to the poor,
political incentives point toward broader targeting that reaches some of the more politically
Reich: The Politics of Health Sector Reform
3
In short, political analysis by economists tends to underspecify the political conditions
under which health reform is likely to succeed. The WDR, for example, did not provide any
evidence to support the assertion that "sufficient political will" is a necessary condition for
health reform; nor did the report define the concept of political will in a succinct or explicit
manner — a pattern I have criticized elsewhere (Reich, 1993). It might have been helpful, at
least for some readers, if the report had included this political concept in the introductory
section on "definitions and data notes," along with explanations of such economic concepts as
cost-effectiveness, allocative efficiency, and disability-adjusted life year (1993:x-xii). Other
economists, in their analyses of health sector reform, have recognized more directly the ways
in which the current problems and policies in the health sector are "the outcome of a political
process" and concluded that significant policy reform is only likely to occur "if there is a
corresponding change in the distribution of political power" (Birdsall and James, 1992:25).
But they similarly provided few indications of how power should be redistributed (either the
proposed reconfiguration or the preferred process) in order to achieve the desired policy
reform.
This paper examines the politics of health sector reform in poor countries in four
steps. First, I review some of the main reasons why policy reform is political. Next, I
briefly describe three political economic models of the policy reform process. Third, I
present three successful cases of pharmaceutical policy reform in developing countries, in
order to explore the political conditions under which health sector reform is likely to
succeed. Finally, I draw some conclusions about the politics of health sector reform, and
indicate practical implications for policy makers and international agencies. The paper
argues that for reform to succeed, policy makers must develop methods to understand,
analyze, and then manipulate the political conditions in favor of policy reform. The paper
suggests that the method of political mapping can help policy-makers [ini analyzing and
managing key aspects of health sector reform.
WHY IS POLICY REFORM POLITICAL?
Policy reform is inevitably political because it seeks to change who gets valued goods
in society. Five specific reasons can be proposed to explain the political dimensions of
policy reform: 1) reform represents a selection of values that express a particular view of
the good society; 2) reform has distinct distributional consequences in the allocation of both
benefits and harms; 3) reform promotes competition among groups that seek to influence the
distributional consequences; 4) the enactment or non-enactment of reform is often associated
with regular political events or with political crises; and 5) reform can have significant
consequences for a regime’s political stability or longevity. Each of these reasons is briefly
explored below, to provide an approach to thinking about policy reform in general, which
can then be applied to reform efforts in the health sector.
Values'. No single definition of the substance of policy reform is universally accepted
in the health sector, or in other sectors either. Indeed, the substance of policy reform
Reich: The Politics of Health Sector Reform
2
influential middle deciles. Tight targeting of more than compensatory benefits may be a
realistic option only for governments that do not need political support" (Nelson, 1989:110).
The WDR recognized this point briefly, in a paragraph (1993:165) that suggested a gradual
shift in resources rather than sudden changes, in order to maintain the support of middle
classes and urban groups. In short, the report briefly recognized the potential dangers of 1
making policy recommendations in a political vacuum. But the report left unexplored the '
implications of compromising the principles of cost-effectiveness and equity in order to create
political feasibility for policy reform.
The third main value system used to guide policy reform is the libertarian perspective.
This approach emphasizes the principle of individual liberty, that one is entitled to use one’s
natural endowments to make whatever deals and choices one can, as long as the action does
not infringe on the life and liberty of others. The state’s role, in this perspective, is limited
to the protection of individuals against unjust appropriation, in what Robert Nozick called the
’minimalist state" (1974). This theory is non-consequentialist, based on the belief that
liberty alone will produce a moral society, without any efforts by the state to redistribute
goods in society. The libertarian approach enshrines the market, with its free exchange of
j^ds and labor, as the key to policy reform.
Libertarian values, and the role of the market, provided the foundation for many
policy reform efforts in poor countries in the 1980s, especially for economic policy. (Some
market-oriented reforms, however, were more consequentialist and utilitarian in emphasizing
the greater effectiveness of the market compared to state intervention). These reforms
typically sought to reduce the degree of state intervention in the economy, privatize stateowned industries, improve the efficiency of government services throiijgh competitive
mechanisms, remove government regulatory structures that promoted tent-seeking behavior
and obstructed private enterprise, and limit government expenditures and subsidies.
Adjustment programs usually included specific measures on: 1) exchange rate reform
(currency devaluation), 2) import liberalization (removal of government controls over
imports); 3) abolishment of price controls in the domestic market; and 4) fiscal reform to
reduce government subsidies. In the 1980s, a major international debate arose over the
health and nutrition consequences of structural adjustment policies, with UNICEF in
particular calling for efforts to protect the poor and vulnerable groups in poor countries and
to place "the human dimension" at the core of economic policy reforms (Jolly, 1988:101).
.^►tly in response to these criticisms, the international architects of economic reforms moved
away from a libertarian position and sought to strengthen the state’s capacity to protect social
welfare, thereby adopting a more utilitarian view.
The choice of a value system to explain and justify a major policy reform represents a
political choice, not only because of the philosophical ambiguities about how to defend one
system over another, but also because the choice has real consequences for the distribution of
resources among different groups in society.
Reich: The Politics of Health Sector Reform
4
Distributional consequences: Policy reform can produce predictable patterns of
distributional consequences across different social groups; indeed, reform is often intended to
produce a particular redistribution. Reform can redirect benefits from urban to rural, or
from rich to poor, or from organized to nonorganized, or from one ethnic group to another,
depending in part on the philosophical assumptions of the reform. In short, policy reform is
political, because it seeks to affect who gets what and, as discussed below, it affects group
competition in society over who gets what.
The distributional consequences of policy reform can have a significant impact on the
ease of implementation. For example, according to Nelson, "The political difficulty of pro
poor measures increases to the extent that the resource transfer from privileged groups is
obvious, long-term, and large (relative to the incomes of these same privileged groups)"
(1989:100). Experience with economic reform suggests that targeting the poor encounters
significant political obstacles, as noted above. Nelson reported that "the poor usually benefit
to the extent that their priority concerns overlap with those of the somewhat better'off. If
their interests diverge, the poor are not likely to gain much, and they may even lose ground"
(Nelson, 1989:99).
On the other hand, policy reform that promises to benefit more powerful groups in
society, or that is perceived as regressive in placing additional burdens on the poor, can elicit
protest from domestic groups as well as international agencies. The distributional
consequences of structural adjustment reforms, in the economic sector, resulted in street
protests in some countries (especially when subsidies were abruptly Amoved from specific
commodities) and also produced a campaign from UNICEF to alter the adjustment policies
(Jolly, 1988), even though some economists continued to question to strength of the evidence
on health and nutritional consequences (Behrman, 1988). And, indeed, the call for
"adjustment with a human face" did result in revised efforts by multilateral banks to protect
the more vulnerable groups in poor countries from adverse consequences of economic policy
reforms. Distributional consequences thus can affect the politics of international agencies,
and thereby produce changes in reform strategies.
The tendency for policy reform to have potentially regressive consequences is
reinforced by a classic problem of collective action: that concentrated effects on more
powerful groups in society tend to have more influence on government decisions than
dispersed effects on more powerless groups (Olson). For example, policy makers may be
more willing to take the risk of offending the relatively powerless poor, because of dispersed
costs, lack of strong social organization, physical distance from the national capital, and low
voting turnout, rather than offending the relatively powerful middle class, because of more
concentrated costs, availability of strong social organization, physical proximity to the seat of
government, and high voting turnout - even when the aggregate costs are likely to be higher
for the poor than for the middle class.
'
A key political question for policy reform is when and how this problem of collective
action can be overcome. What are the political conditions under which reform can have
Reich: The Politics of Hea’th Sector Reform
5
distributional consequences that do not simply reinforce the existing skewed distribution of
economic and political power? Two provisional answers are provided by the literature on
economic reforms: through political alliances, and compensatory benefits. Nelson reported
that in many situations where governments give higher priority to the needs of poor people,
"Political salience increases where the poor are actually or potentially allied with groups in a
position to threaten the government’s security" (Nelson, 1989:97). Second, progressive
distributional consequences are more likely to be politically feasible when other groups also
receive some benefits, or as noted above, when the interests of the poor overlap with the
interests of the more powerful. How much inefficiency is needed, in order to make pro-poor
policies politically palatable, will depend on other political circumstances, including the
existing patterns of group competition.
Group competition: Policy reform affects the interests of groups in society,
including interest groups, bureaucratic agencies, and political parties. Simple-minded
pluralism would postulate that different groups will compete to protect their interests, and
that the "stronger" group will win out and thereby affect the substance and implementation of
the policy adopted. The pluralist predictions do not always work out in practice, however,
due to political biases that affect the relative power of groups, the transaction costs of
gating new groups, and the dilemmas of collective action associated with the dispersion and
concentration of costs and benefits.
Political leaders are particularly concerned about the differential impacts on groups in
the government coalition. Every regime has its allies and partners, arranged in various types
of coalitions, to provide support for the government and its policies. As John Waterbury
wrote, "Coalitions vary from country to country and over time, but at any point in the
reform process, some coalition members stand to lose or gain more thiart others. The crucial
challenge for political leadership is to avoid injuring the interests of all coalition members
simultaneously" (Waterbury, 1989:39). Similarly, "political leaders must gauge when
injuring the interests of specific groups will trigger a disruptive response" (Waterbury,
1989:46). The strength of the governing coalition, and the confidence of leaders in their
ability to control different groups in the coalition, affect the willingness of leaders to assume
the political risks of reform (Nelson, 1990a:328). Weak and divided governments are most
likely to procrastinate about reform, even when confronted with the sticks and carrots
wielded by international agencies (330).
"
For economic policy, Waterbury argues that it is possible and highly desirable to
construct the reform agenda in phases in order to spread the burdens of adjustment across
coalition members and avoid harming all allies simultaneously (1989:52). The timing of the
reform process, as discussed below, thus can affect group competition and regime stability.
Waterbury warns that "only under the most dire circumstances" should all elements of
economic reform be introduced at once. While a large literature exists on the questions of
appropriate sequencing of economic reform policies (cited by Waterbury), little exists for
health sector reform.
Reich: The Politics of Health Sector Reform
6
In managing the reform process, political leaders are advised to use both
compensation and obfuscation: ’Compensatory payments may help to mitigate the impact of
adjustment and to sequence the distribution of pain among coalition members and large
segments of the population. Forthright declarations of policy intent, the laying out of
timetables, and the public targeting of specific interests may well leave leaders without room
to maneuver and lead to the defection and opposition of groups vital to regime maintenance"
(Waterbury, 1989:55). Outside agencies that require strict accounting, accountability, and
transparency may contribute to undermining the success of policy reform. Political leaders
need to control group competition in policy reform through a two-table bargaining game
(Putnam, 1988). The bargains reached with external actors, including international agencies
and multinational corporations, must be politically acceptable and sustainable in the domestic
political game. Putnam (1988:434) described the two-game politics of international
negotiations as follows:
At the national level, domestic groups pursue their interests by pressuring the
government to adopt favorable policies, and politicians seek power by constructing
coalitions among those groups. At the international level, national governments seek
to maximize their own ability to satisfy domestic pressures, while minimizing the
adverse consequences of foreign developments. Neither of the two games can be
ignored by central decision-makers, so long as their countries remain interdependent,
yet sovereign.
! I
Managing the politics of group competition in policy reform requires a good
understanding of who is for the reform, who is against it, and who is not mobilized in one
direction or the other. A political strategy for policy reform needs to consider the interests
or objectives of key stakeholders, and how important those interests are in the group’s
priorities. The direction of causation between groups and policies, however, may not always
be clear. In some cases, a new policy creates an organized interest group out of the
beneficiaries — a pattern observed in both rich and poor countries (Horowitz, 1989:207). In
other cases, enactment of a new policy requires an existing interest group that is both well
organized and highly mobilized. A policy maker’s ability to mobilize quiescent groups and
to quell activated groups can affect the political success of policy reform (Edelman, 1971).
As Nelson observed, "If benefits of structural changes are often delayed and accrue to
individuals and groups who are not politically organized and may not even recognize their
potential gains when the policy is launched, prospects for coalitions in support of the reforms
are poor" (1990:359). Managing these processes of group competition must include
consideration of timing.
Timing: The opportunity to achieve policy reform is often affected by external
events. Reform is usually more feasible at the beginning of a regime than at the end of a
regime (although some political leaders at the end of their time in power may introduce
reforms to prolong their power or reap some last-minute benefits). Major concurrent events
(either real or symbolic) can open up political windows for reform, in democratic as well as
non-democratic systems. Disasters, both natural and human-created, provide policy
Reich: The Politics of Health Sector Reform
7
entrepreneurs with an occasion to push for long-desired ideas. An ability to recognize and
exploit those transitions that open windows for reform — before the windows slam shut —
thus can affect whether reform is achieved.
Horowitz argued that timing is an important explanation for when policy change
occurs and how it occurs, in both positive and negative senses. "Fortuitous timing — in the
sense of simultaneity of events — can open up the policy process. But timing is also an
important constraint. Events and conditions accidentally synchronized can turn that decision
in a direction different from the one it might otherwise have taken" (1989:204). Because of
the many constraints that affect policy making in poor countries, Horowitz stated that "a
disproportionate number of policies are adopted at exceptional times — times of crisis, times
when there is a strong demand for change, times when unusual events have immobilized
obstacles to new policy or drastically changed the composition of decision making bodies.
At such times, organized interests are frequently ineffective. Ideas for policy become
important forces, and elites have a good deal of freedom to put their ideas into operation"
(1989:205).
Moments of regime transition provide an important opportunity for policy reform.
♦e transitions are generally accompanied by a delegitimization of the previous
government, which makes it easier to dismantle existing policies and structures, and an
increased executive autonomy or legitimacy for new government in the "honeymoon" period,
which makes it easier to introduce new policies and structures (Haggard and Kaufman,
1989:75). Keeler showed a similar pattern for major policy reforms in a study of established
democratic polities (Britain, France, and the United States), demonstrating that the size of a
government’s mandate (measured by a mandate index), along with the severity of the crisis
confronted, are good predictors of the size of the window for reform aha the scope of
legislative achievement. Waterbury noted two different electoral strategies of political timing
for democratic regimes: pushing through an adjustment package just after receiving a popular
mandate in an election; or starting to implement the adjustment package and then calling an
election, hoping that beneficiaries will support the government in the election (1989:52-53).
Nelson concluded in her review of economic reforms in 13 countries under 19 governments,
"It is hardly news that political leaders are reluctant to take austerity measures shortly before
elections" (1990:328).
gfc
Regime transitions are critical for non-democratic as well as democratic governments,
{^overcoming the forces opposed to reform. Waterbury wrote, "Only in rare
circumstances — for example, when a new regime comes to power through a coup or the
ballot box - is the leadership likely to be supported by a consensus sufficient to allow it to
lay out policy goals and to stick by them without jeopardizing the cohesion of the regime
itself" (1989:55). Of course, the importance of timing depends in part on the substance of
the reform. Radical changes require careful consideration of timing, while minor
incremental changes are not as dependent on timing. Moreover, the nature of the reform
may depend on the nature of concurrent events; natural disasters may create opportunities for
certain types of reform, but not for others. Efforts to enact sudden changes in policy,
Reich: The Politics of Health Sector Reform
8
without propitious concurrent events, can challenge the legitimacy of governments, including
authoritarian regimes.
Regime stability: Finally, policy reform is political because it can pose significant
political risks and can provide significant political benefits for regimes in power (and for
opposition groups out of power). In some cases, efforts to enact policy reform can affect the
stability and longevity of governments. One prominent example in health is Mrs. Indira
Gandhi’s aggressive family planning policy in India in 1976-77, which created coercion and
chaos, and in 1977 contributed to her resounding electoral defeat (Gwatkin, 1979). Most
political leaders have a strong sense of self-interest and a strong instinct of survival;
consequently, they are reluctant to carry out reforms that have a high probability of
disrupting the government and ending their rule.
Whether policy reform affects regime stability, in turn, is influenced by various
factors. The country’s broader political economy provides the context within which policy
reform occurs and thereby shapes its political consequences for the regime. Relevant factors
include the regime type, especially the degree of democracy or state control over society, as
reflected in factors that affect public participation, such as literacy, freedom of association
and speech, social activism, and income differentials. If a policy reform can be symbolically
connected to an ongoing political struggle within a country, then it can become threatening to
regime stability. In extraordinary situations, efforts to push through policy reform can
contribute to a government’s downfall, especially when opposition] ayises from previously
quiescent sectors or from former allies.
I.
Regime transitions to democracy provide opportunities for policy reform, and indeed
often require policy reform. But these systemic changes also create vulnerabilities due to the
emergence of new political competition (Haggard and Kaufman, 1989). Expanded pluralism
can produce a form of policy gridlock, in which decisions are blocked through democratic
processes. And in extreme situations, as in some of the new countries of Eastern Europe,
political liberalization can unleash ethnic hostilities that obstruct efforts at policy reform and
undermine regime stability.
This review of why policy reform is political remains incomplete, but I hope that the
main point is persuasive. This point, which is gaining wider acceptance, stresses the
importance of a political economic perspective in assessing the prospects for policy reform
and in explaining the successes and failures of the reform process (Grindle and Thomas,
1991; Nelson, 1989; Reich, 1993). As Alberto Alesina wrote about economic policy, "In
most cases the crucial ingredients of policy reforms are very simple. The real difficulties are
political; for instance, how to share the burden of adjustment, how to implement the program
without creating social unrest, and so on. Political issues are much more difficult than
technical issues of how to design the ’perfect’ program, from the point of view of economic
theory" (1992:5). Perhaps better political models could persuade skeptics (should they still
exist) about the unavoidable importance of politics in the policy reform process.
Reich: The Politics of Health Sector Reform
concept of political will (Reich, 1993a), and sought to give it substantive content and utility.
These three mechanisms, I believe, represent three clusters of political conditions under
which policy reform can occur.
The political will model assumes that decisions by political leaders are both necessary
and sufficient for major policy change. This model resembles the benevolent dictator in a
Platonic state, similar to the traditional public administration view of how policy is made.
The model posits a technocratic approach with a rational actor model of decision-making,
and assumes a strong state, good institutional capacity, and adequate political capital. On the
other hand, the model tends to ignore the political constraints to policy reform, and can be
politically naive. This model is what Alesina (1992) called the 'social planner* model, in
which rational analysis is used and implemented by politicians to make the "right* choices, to
enhance the public interest of society, regardless of the consequences for particular
constituencies or for political futures.’ In this model, decision makers seek to maximize (or
^gt least increase) the public interest. Empirically, this model may operate under certain
•political circumstances, such as a strong mandate, strong state, narrow coalition, and strong
leadership. The model also shows striking similarities to the concept of the developmental
state, which is seen as underlying the successes of the East Asian countries (Oni?, 1991).
According to this model, policy reform occurs when political leaders exercise their ’will" to
further the public interest.
The political factions model assumes that politicians seek to | serve the desires of
different groups, including interest groups, bureaucratic agencies, and political parties. This
model subsumes the interest group approach to policy making, with its emphasis on the
political competition of groups and ideas, and also the bureaucratic politics approach, with its
emphasis on how government organizations seek to protect and promote their narrow
sectarian interests. In this model, rational analysis serves mainly as a means to promote and
serve organizational interests. This model resembles what Alesina called the ’partisan*
model in the economic literature, in which aggregate policies (such as fiscal and monetary
measures) are used to achieve significant redistribution of income and wealth, in order to
reward specific constituent groups. In this model, decision makers seek to serve the interests
gbf their constituencies and can redistribute goods to fit with ideological principles. Some
versions of the model assume pluralist principles about the free competition of groups to
determine policy. According to this model, reform occurs when it corresponds to the
preferred distribution of benefits to specific constituent groups of government leaders.
The political survival model assumes government officials seek to protect individual
interests, as power-holders, whether elected or non-elected, in order to maintain or expand .
their existing control over resources. This model incorporates many of the principles of the
public choice school, arguing that politicians operate on a logic of "opportunistic* politics
(Alesina, 1992). In this model, decision makers manipulate fiscal and monetary policies, for
example, in order to achieve an expansionary economic period just before elections in hopes
of increasing the probability of political survival. Under non-democratic regimes, the logic
of opportunistic politics would lead politicians to drain the public purse for personal gain,
Reich: The Politics of Health Sector Reform
11
POLITICAL MODELS OF POLICY REFORM
For the purposes of this paper, policy reform is defined more in terms of the degree
of change rather than the direction of change. I have sought to avoid assessing the contents
of policy reforms, and have focused more on the process than the outcome. The concept of
policy reform can also be approached through the degree of anticipated difficulty of
implementation. Policy reform usually involves a complex package of significant changes,
while incremental changes in policy involve fewer and simpler alterations. The distinction
made by Peter S. Cleaves (1980) between 'less problematic" and "more problematic"
changes in policy provides a good description of the characteristics of policy reform (Figure
2). All policy changes that fit on the "more problematic" side may not be reforms, but it
seems likely that all reforms would fit on the "more problematic" side.
In searching for good political models of policy making processes in developing
countries, one soon discovers that the literature is rather sparse. "Comparative public policy
is a young field, even younger than the systematic study of politics in the developing
countries of Asia, Africa, and Latin America. The hybrid of these two fields — comparative
public policy in developing countries — is younger still" (Horowitz, 1989:197). The
comparative analysis of health policy processes in developing countries is even more
underdeveloped. Many studies exist of health policy from epidemiologic and economic
perspectives; but few address the political aspects of health policy in developing countries.
The literature on the political economy of policy reform, on the other hand, mostly examines
economic policies, especially in the stabilization and trade arenas. Various models are
proposed, including political as well as economic variables, and involving different
assumptions about how and why policy reform works (or does not) in popr countries.
This section represents a brief foray into the field of comparative health policy in
poor countries, to suggest clusters of political conditions when reform is possible. When can
political leaders overcome the constraints of group competition and the demands of political
survival and introduce significant reforms in policy? In addition, what can leaders do to
shape political circumstances to enhance the probability of significant change? Even when
analysts try to explain the factors leading to success or failure of reform, they often fail to
address the possibilities of changing the balance of power or managing the politics of policymaking processes in order to improve the probability of success. The literature provides
little practical advice on how to identify opportunities for change, or how to assess the
positive and negative factors that cannot be changed, in order to determine whether success is
likely.
I propose three political mechanisms for consideration: political will, political
factions, and political survival. These three categories may seem, to some, rather odd
choices for policy-making models. They correspond roughly to three models described by
Alberto Alesina (1992) in his review of political models of macroeconomic policy and fiscal
reform — but with new names. I have chosen these names to emphasize the political
dimensions of reform. In doing so, I have retreated from my previous critique of the
Reich: The Politics of Health Sector Reform
10
especially if it seemed their time in office might be coming to an end. According to this
model, reform occurs when it serves the personal political survival or the personal pecuniary
interests of political leaders.
A full elaboration of these models of policy reform is beyond the scope of this paper.
It is worth noting, however, that the three models are not necessarily mutually exclusive, and
that all three forms of decision-making may coexist in some countries. On the other hand,
some nations may be characterized by a particular political model of policy reform, at least
for a limited period of time, which would then have distinct consequences for the likelihood
of policy reform. (One could, for example, operationalize the three models and assign
countries to the specific categories, in order to determine the degree to which the success of
reform is explained by these clusters of political conditions. This methodological approach is
not adopted here. For this type of analysis, which seeks to explain different choices in
economic policy adjustment and implementation, in 13 nations, using fives set of political
economic factors, see Nelson, 1990b.)
These three models, as with all models, have both advantages and disadvantages. On
the one hand, these models simplify reality into neat packages that do not easily correspond
t£eal world situations. Indeed, models are intended to simplify the real world, in order to
test hypotheses, provoke debate, and encourage people to rethink their assumptions. The
models thus present ideal types, which rarely exist in such pure form. On the other hand,
the models reflect conventional wisdom about how the world works. From this perspective,
the models of political will, political factions, and political survival may be useful in
articulating common assumptions about policy reform. Nelson, for example, proposed
variations on a political will model and a political factions model as "two extreme positions
[that] mark the outer bounds of debate" on stabilization and adjustment programs; she also
noted that these positions nonetheless arise in international financial circles and in political
analyses in efforts to explain failed reforms (1990b:24). Similarly, the three models
proposed above may be useful in analyzing the attitudes of both governments and
international agencies regarding health sector reform processes.
PHARMACEUTICAL POLICY REFORM
The reform of pharmaceutical policy in poor countries represents one of the most
t
portant areas of health sector reform, as well as one of the most contested. Remarkably,
pharmaceutical policy represents one of the few areas in the health sector for which both the
World Bank and the World Health Organization agree that major restructuring is needed.
Their agreement, however, emerges from different value orientations. The WDR, for
example, cited the pharmaceutical sector as an important target for reform, with "substantial
scope for reduction of waste and inefficiency in government health programs," and "the most
promising area for efficiency gains in the short run" (1993:159). The Bank called for
improvements in the selection and quantification of drug requirements, the use of essential
national drug lists, and competitive purchasing of drugs. The Bank thus stressed the
Reich: The Politics of Health Seaor Reform
12
utilitarian basis for improved pharmaceutical policies, in seeking to achieve maximal utility
from limited resources, reflecting its traditional emphasis on the cost-effective use of health
sector resources (Hall, 1986). The World Health Organization has called for similar policy
reforms, for the past decade, through its Action Program on Essential Drugs. But the WHO
has justified its reforms to the pharmaceutical sector on the basis of achieving greater equity,
through improved accessibility and affordability of basic drugs to poor people, and with
hardly a mention of improved efficiency (Reich, 1987).
Pharmaceutical policy provides a good area to explore health sector reform for several
other reasons as well. First, pharmaceutical expenditures in poor countries typically account
for between 10 and 30 percent of total recurrent costs of public sector health expenditures,
ranking second after salaries (World Bank, 1993:146). In many countries, pharmaceutical
purchases account for an even higher proportion of private expenditures. These high
expenditures make drugs a high priority issue for policy makers. Second, pharmaceutical
policy usually involves both the public and private sectors, as well as domestic and"
international actors, in various patterns of collaboration, competition, and conflict. It thus
serves as a good example for other areas of health sector reform, such as the introduction of
user fees and the promotion of private sector activities, which also involve multiple actors in
complex patterns of interaction (but are not considered in this paper). Third, discussion of
pharmaceutical policy often elicits a debate about basic social values, including the roles of
the market and the state, and the relative importance of efficiency and equity.
! I
For these reasons, an analysis of pharmaceutical policy reform promises to hold
important lessons that are relevant for other areas of health sector reform (including efforts
to reduce government inefficiencies as well as those intended to increase government
revenues). On the other hand, pharmaceutical policy reform may not be representative of all
types of health sector reform (such as the expansion of primary health care, or the promotion
of immunization). To the extent that the patterns of pharmaceutical reform are not
representative of other health areas, the analysis below will be limited in its generalizability.
I will return to this question in the paper’s conclusion.
Three cases were selected for analysis of pharmaceutical policy reform: Sri Tanka,
Bangladesh, and the Philippines. These three cases represent major policy reforms,
including many of the characteristics shown in Figure 2, and they stand prominently among
the successful instances of pharmaceutical reforms of the 1970s and 1980s. The three cases
embody key elements of reforms recommended by both the World Bank and the WHO for
the pharmaceutical sector, although they also involved more government intervention in
market activities than considered desirable by the World Bank. The three cases also
generated substantial controversy, at both domestic and international levels, concerning the
passage and implementation of the reform packages. Below, I present the substance of
pharmaceutical reform in the three countries, and then compare the three experiences, in
search of common patterns in the political feasibility of policy reform.
Reich: The Politics of Health Sector Reform
13
Sri Lanka: Pharmaceutical reform in Sri Lanka followed the landslide election in
1970 of the Sri Lanka Freedom Party (SLFP) and the inauguration of a strong coalition
government consisting of the SLFP and two Marxist parties. Mrs. Bandaranaike returned to
power (following her previous stint from 1960 to 1965) as the head of a coalition government
that, according to one observer, "exhibited greater ideological coherence and sense of
purpose than any previous such alliance. It also dominated Parliament more completely and
was forcefully reminded that there was a constituency for thorough radicalism by the 1971
Insurgency [by the JVP, a radical Sinhalese party and unemployed rural youths]" (Moore,
1990:349-50). These conditions spawned a transformation of the Sri Lankan economy, with
a wave of nationalizations, expansion of the public corporate sector, and enlargement of the
state’s control of economic activities. Sri Lanka’s pharmaceutical sector reforms occurred
within this broad shift in government and political economy.
Following the inauguration of the new government, the Prime Minister set up a twomember committee, including a prominent university-based pharmacologist and a member of
Parliament, to prepare a report on measures to rationalize the pharmaceutical sector in Sri
Lanka. Their report, issued in 1971, provided the basis for pharmaceutical reform
ickremasinghe and Bibile, 1971). The main recommendations of the report, and their
ectives, were as follows (Lail and Bibile, 1978; Jayasuriya and Wijesinghe, 1991):
S
1. Channel all imports and distribution of final pharmaceutical products and
pharmaceutical chemicals through a state trading corporation, in order to reduce the
import bill and reduce retail prices.
2. Reduce the number of drugs permitted, replace brand nam^s by generic names,
and replace private advertising of drugs with information provided instead by the
state, in order to improve health, through the use of drugs with high therapeutic
properties and through better prescribing practices.
3. Remove the protection of process and product patents, in order to obtain newer
drugs from the least expensive sources.
4. Provide state imported pharmaceutical chemicals to local manufacturers, in order
to promote local production, with distribution and promotion carried out by the state.
5. Expand quality control facilities in the Ministry of Health’s laboratory, in order to
assure high quality of imported and locally produced drugs.
In 1971, the Sri Lankan government established the State Pharmaceutical Corporation
(SPC) to implement the reforms of the Wickremasinghe and Bibile report, under the Ministry
of Industries and Scientific Affairs, instead of the MOH. The SPC soon began replacing the
134 private importers of pharmaceuticals, and by mid-1973 had become the sole importer.
An international tendering system, with quality control requirements, was used to purchase
low-cost generic products when available, to seek non-patent observing sources for newer
Reich: The Politics of Health Sector Reform
14
patented products, and to bargain with transnational sources for patented products that were
not available elsewhere. In addition, the government initiated the National Formulary
Committee to reform the list of drugs for the private sector, using similar principles as
applied to the public sector since 1959. Brand names were almost entirely eliminated, with
the total number of drugs reduced from 2100 to 600. Patent protection laws were not
amended in Sri Lanka, but purchases from non-patent-observing sources were actively
pursued. Overall, implementation was most successful in the areas of import, distribution,
drug list reduction, and promotion, with little progress in amendment of patent law,
promotion of local production, and improvement of local quality control facilities. The
reforms thus contained some libertarian values (using the competitive international market for
procurement), some utilitarian values (emphasizing cost-effective purchases of a limited list
of generic products, ignoring certain property rights), and some communitarian values
(emphasizing redistribution to poorer members of the community in order to support the
common good).
Opposition to Sri Lanka’s pharmaceutical reform came from both foreign and
domestic sources. On 10 May 1973, Joseph Stetler, the President of the U.S.
Pharmaceutical Manufacturers Association, wrote an aggressive and threatening letter
addressed to Sri Lanka’s Prime Minister (Lail and Bibile, 1978:310). The letter vigorously
attacked all of the major provisions of the country’s pharmaceutical reform and argued that
the policy would have counterproductive consequences — inhibiting the growth of local
industry, discouraging high-quality companies from participation in the tenders, encouraging
the purchase of low-quality products with poor health consequences, (discouraging
international companies from participation in the Sri Lankan market by reduced patent
protection, reducing the therapeutic efficacy of drugs by relying on generics with problems in
bioequivalence, and reducing the information available to pharmacists and physicians due to
restrictions on promotion. Stetler backed up the PMA’s complaints about the reform with a
broader economic threat, stating that 'the action calls into question the Government’s
position with respect to all foreign investment in Sri Lanka."
Within Sri Lanka, opposition to the reform emerged from private medical
practitioners and from local representatives of the international pharmaceutical industry (Lail
and Bibile, 1978:311). The domestically based opposition focused on criticism of the quality
of SPC purchased drugs, alleging that the lower-cost generic products and the products
procured from non-patent observing sources were therapeutically ineffective. The medical
profession resisted the change from brand to generic names, due to qualms about the quality
of generics and to habit of using brand names. In addition, some patients preferred wellknown brand name drugs. According to Lail and Bibile (1978:319, 13n), "The SPC
managed, by means of the gradual pace of change and some compromise, to avoid an all-out
battle with local firms."
These reforms were achieved in the early years of Mrs. Bandaranaike’s government,
when the coalition was strongly united in its goals. During these years, the United Front
government (as it was known) instituted a ceiling on land-holdings and houses, and imposed
Reich: The Politics of Health Sector Reform
15
severe import restrictions. The pharmaceutical reforms thus fit with the redistributive,
socialist, and statist strategies of the regime in power. The substantive elements of the
pharmaceutical reform depended on strong support from progressive academic elites,
characterized by Professor S. Bibile, who recognized the socialist government as an
opportunity to implement long-desired reforms. (Similar academic entries into government
efforts at policy reform occurred in other sectors as well.) The threat of the 1971 Insurgency
provided a political impetus to reform, by demonstrating the existence of a radical sentiment
in rural areas and justifying transformative policies that might coopt the potential for broad
based revolt. The severe economic conditions existing in Sri Lanka in the early 1970s
provided an economic rationale for policy reforms that promised to reduce government
expenditures while purchasing larger quantities and achieving greater health impacts.
As domestic political circumstances changed in Sri Lanka, pharmaceutical reform
slowed down and was partially reversed. In 1975, the most radical party in the coalition, the
Lanka Sama Samaj Party (LSSP), quit the government, and the Prime Minister "moved
distinctly to the right" (Lail and Bibile, 1978:305), showing less enthusiasm for
pharmaceutical reform. The shift in governmental position was accompanied by more vocal
criticism of pharmaceutical policy by vested interests, including doctors and local
r^esentatives of multinational drug companies, resulting in some concessions by the SPC
on the retention of brand name drugs (309). In early 1977, the Sri Lanka Communist Party
quit the coalition government, followed by the resignation of the Minister of Industries, in
protest of the Prime Minister’s "right-wing policies," including the refusal to nationalize
multinational drug companies in Sri Lanka (326). In July 1977, after the SLFP government
fell, elections were held, resulting in a resounding defeat for the SLFP and no seats in
Parliament for the Marxists (the first time since the introduction of universal suffrage)
(Moore, 1990:350).
I
The new government that assumed power in 1977 was based on the United National
Party, with over 80 percent of the seats in Parliament. This party won with campaign
promises of economic liberalization, market-oriented policies, and pro-Western geopolitics.
The UNP regime reversed some crucial elements of Mrs. Bandaranaike’s pharmaceutical
reform - as its own reform policy. In particular the State Pharmaceutical Corporation lost
its monopoly on imports and distribution outside of state institutions, as the private sector
was allowed to reenter the pharmaceutical market. The partial privatization reportedly
Induced price competition between the SPC and the private sector, contributing to a marketonented control over drug prices through SPC decisions to import and distribute products
that were considered to have excessive profit margins in the private sector (Jayasuriya and
Wijesinghe, 1991:22). In general, the UNP government criticized the reported achievements
of the previous regime’s pharmaceutical policy and sought to improve the policy in areas of
quality control, advertising, and efficiency of the SPC. Indeed, rather than a total reversal,
the UNP policy retained and extended some important aspects, such as the concept of
essential drugs in registration (Weerasuriya, 1993) and the role of the centralized state
purchasing in the pharmaceutical system (for public institutions), but had little success in
promoting domestic production, reflecting broader problems of economy policy?
Reich: The Politics of Health Sector Reform
16
Bangladesh*: On 24 March 1982, Lieutenant-General and Army Chief of Staff H.M.
Ershad overthrew the Bangladesh government and seized power, declaring martial law later
that day. To explain his actions, Ershad declared that "economic life has come to a position
of collapse, the civil administration has become unable to effectively function, wanton
corruption at all levels has become a permissible part of life. . . [the] law and order situation
has deteriorated to an alarming state. . . [and there has been] bickering for power among the
members of the ruling party" (Bergman, 1991).
Among the new government’s top items for reform was pharmaceutical policy.
Within about four weeks of taking over, Ershad had convened an eight-member expert
committee to transform government policy on drugs, and two weeks later, on 11 May, the
committee presented its report. The committee unanimously recommended 16 criteria as
guidelines to reorganize the country’s pharmaceutical sector. While "keeping in view the
health needs of the country," the report stated its overall objective as follows: "Consistent
with the declared guidelines of Government to provide basic needs of life to the majority of
the people through austerity and to improve the economy of the country, wastage of foreign
exchange through the production and/or importation of unnecessary drugs or drugs of
marginal value have to be stopped" (Report of Expen Committee for Drugs, 1982). The
report appended a list of drugs to be removed from the market, based on the committee’s
evaluation of all the registered and licensed pharmaceutical products manufactured and
imported in Bangladesh. The report thus articulated utilitarian values (in maximizing the
health benefits of drug purchases) and communitarian values (in seeding to improve the
common good), and became the basis of the new national policy. :
The Bangladesh Drug (Control) Ordinance of 1982 was issued soon thereafter, on 12
June 1982, as a declaration by Chief Martial Law Administrator Ershad. The policy applied
the concept of essential drugs to both the private and public sectors for pharmaceuticals in
Bangladesh (an essential drugs list had been used since 1978 for procurement by the
government’s Central Medical Stores). The policy’s basic strategy was to exclude all nonessential drugs from the country, rather than to promote essential drugs in the public sector
while allowing the coexistence of a broader private market. The policy created a restricted
national formulary of 150 essential drugs and 100 specialist drugs, with 12 at the health post
level, 45 for primary health care, and the full list at tertiary hospitals. The act banned about
1,700 drugs from production or sale in three categories: 299 harmful drugs that were to be
destroyed within three months; 127 drugs that required reformulation within one year, due to
unnecessary, unscientific, or harmful ingredients; and 1,240 drugs that did not conform to
the 16 basic principles and had to be withdrawn within 18 months (Government of
Bangladesh, 1985). The ordinance also included measures to promote local manufacture and
to restrict the operations of foreign firms within Bangladesh. For instance, if products were
produced by local firms, multinationals were not allowed to import similar drugs. The
policy also imposed restrictions on transfer prices, requiring that they be similar to
international competitive prices.
Reich: The Politics of Health Sector Reform
17
Ershad’s rise to power had created favorable political conditions and incentives for
pharmaceutical reform. First, the policy embodied a populist strategy of basic needs
(reduced prices of essential drugs) to appeal to Bangladesh’s rural poor, who continued to be
bypassed by development efforts, despite nearly $13 billion of aid funds committed in the
country in the first decade after independence in 1971 (Sobhan, 1982:16). Second, the Drug
Policy created a political alliance with one sector of local industry and also with a number of
prominent left intellectuals, symbolized by Dr. Zafrullah Chowdhury (a key architect of the
new drug policy) as a development activist and a freedom fighter. Third, the policy
articulated a vision of self-reliance and priority provision of basic national needs and an
attitude of proud defiance against the multinationals — a stance of economic nationalism.
Finally, the policy generated international legitimacy through its support by international
agencies and nongovernmental development organizations.
The new drug policy received an immediate and hostile response from the
pharmaceutical industry. Domestic firms in the Bangladesh pharmaceutical industry
association (Bangladesh Aushad Shilpa Samity, or BASS) purchased full-page advertisements
in the Bangladesh press to oppose the drug policy. International firms did the same, arguing
t^ the new policy would discourage foreign investors, would result in more harm than good
fWpublic health, and would not achieve the goals of increased availability of medicines.
Ultimately, the international industry argued, the policy would result in decisions by
companies to halt all pharmaceutical production, including that of essential drugs, and to
leave Bangladesh. Attacks on the drug policy continued from The Pulse, a medical
newspaper in Bangladesh, which denounced the policy as ’unimaginative, ill-conceived and
hasty,* releasing "evil forces" in the market, putting additional burdens on the common man,
"delaying recovery from diseases," and "prolonging suffering of the patients’ (Anon., 1984).
Pressure on Ershad’s government came also from foreign governments, which
asserted that the policy would discourage private investors from entering or staying in
Bangladesh. Ambassadors from the United States, West Germany, the United Kingdom, and
the Netherlands individually visited the Health Minister and the Chief Martial Law
Administrator to express their displeasure (Chetley, 1990:99-100). In addition, the U.S.
ambassador helped to arrange for a visit of experts from the Pharmaceutical Manufacturers
Association and from companies in July 1982. Given the importance of foreign aid in |
Bangladesh, the official complaints could not easily be ignored by the new government.
The Bangladesh Medical Association (BMA) also quickly emerged as a vocal
opponent to the new drug policy. The BMA reportedly agreed with the policy’s ultimate
objectives but not with its formulation process, criticizing the committee’s lack of
consultation with the BMA (Chetley, 1986). The BMA criticized the methods used to review
all drugs on the market in a two-week period and also attacked the involvement of foreigners
from NGOs in design of the drug policy. Although one person in Ershad’s expert committee
on drugs (K.M.A. Humayun Hye) was also a member of the BMA’s pharmaceutical
subcommittee, and the other subcommittee member was consulted in the formulation process,
the General Secretary of the BMA was not officially consulted because of his connections
Reich: The Politics of Health Sector Reform
18
with a multinational pharmaceutical company (Chowdhury, 1992). Because of these
conflicts, the BMA refused to discuss the policy’s implementation after its announcement in
June 1992.
The World Health Organization and international consumer organizations, on the
other hand, praised the drug policy. WHO Director-General Halfdan Mahler visited Dhaka
in September 1982 and stated, "I take this opportunity of congratulating our host country on
its courage in starting to put its drug house in order along the lines recently endorsed by the
World Health Assembly" (Patel, 1983). In 1986, the International Organization of
Consumers Unions published a document that commended the drug policy and the
government leader who supported it, stating "General Ershad of Bangladesh is one of the few
leaders to have acted on this international consensus of health experts" (Tiranti, 1986).
Praise came as well from international medical journals, especially Tropical Doctor and the
Lancet.
While the Bangladesh government persisted with the main thrust of its drug policy,
some changes were introduced in response to complaints and pressure from industry and
foreign governments. Soon after adopting the policy, the government established a Review
Committee of six military doctors who submitted their report in August 1982. Although
never made public, the report apparently criticized several aspects of the drug policy (Anon.,
1984). Subsequently, the government made a number of concessipns to industry in formal
amendments to the policy, which included: permitting some banned products back on the
market, extending the time periods for implementation, introducing an appeals process
(Jayasuriya, 1985:13-16), and altering the list of allowed products. With these compromises,
the policy survived opposition from the international pharmaceutical industry, the Bangladesh
Medical Association, and Western governments.
Ershad achieved several domestic political objectives with his pharmaceutical reform.
His goals included populist political objectives (providing lower prices on some common
drugs for the poor), economic political objectives (winning support from the domestic
pharmaceutical industry), symbolic political objectives (creating the symbol of an external
enemy), and broader legitimacy (gaining domestic and international recognition for his
innovative policy). The policy’s continuity, however, depended on creating an additional
constituency for the policy out of previous opponents. As the policy’s benefits of increased
local production became clear, the policy transformed the local industry’s initial opposition
into support. By 1986, the Bangladesh pharmaceutical industry association had reversed its
initial opposition to the policy and had become a vocal and public supporter of the drug
policy.
The fate of Bangladesh’s 1982 pharmaceutical reform, however, remains to be
determined in the post-Ershad political era. In early December 1990, senior army personnel
in Bangladesh forced Ershad to resign, after several months of rising protests against the
government. His fall from power resulted from a combination of economic distress, political
instability, and increasing interest group mobilization, which persuaded the military to
Reich: The Politics of Health Sector Reform
19
withdraw its support from Ershad. An important element in the political equation was
increasing opposition from the Bangladesh Medical Association, in protest to Ershad’s
proposed health reform policy that was announced in July 1990. Following parliamentary
elections in February 1991, a new government took office and announced that the drug
policy would be reviewed and revised, responding to both domestic and international
pressures. The nature of the revision, however, remains undecided in 1993.
The political contrasts between the implemented pharmaceutical reform and the failed
health reform are striking and instructive (Reich, 1994). The pharmaceutical reform
strengthened the international legitimacy of the Ershad regime and withstood international
corporate opposition while reversing domestic corporate opposition; the health reform, on the
other hand, strengthened domestic opposition to the government and mobilized the physicians
association into active protest. The pharmaceutical reform occurred at the start of Ershad’s
rule, when hopes were strong that he might bring order to Bangladesh and promote
development; the health reform attempt, by contrast, occurred eight years into Ershad’s
government amidst unstable political circumstances, when he was struggling to control a
rising tide of protest from various social sectors. The pharmaceutical reform was rapidly
enacted and actively implemented for eight years, with important changes in the production,
>ort and sales systems for drugs in Bangladesh (with problems remaining on the demand
side, including persistent problems in prescribing patterns, smuggled products, and poor
distribution); the health policy, on the other hand, suffered a rapid withdrawal from public
debate following Ershad’s removal from office. The pharmaceutical reform occurred under
highly favorable political circumstances; the health reform confronted highly unfavorable
political conditions, with obvious results.
Philippines: In February 1986, the Philippines underwent a drhrAatic political
reversal and renewal, as the "People Power" movement ended the 16-year regime of
Ferdinand Marcos in a revolutionary atmosphere and installed a new government under the
leadership of Corazon Aquino. In March of that year, Dr. Alfredo Bengzon, a neurosurgeon
with a Masters in Business Administration, assumed the helm of the Health Ministry, with a
strong commitment to reform the country’s health system. In addition, Bengzon was
fortunate to have a good political relationship with President Aquino, because of his role
(along with others) in helping to persuade her to challenge Marcos in the election (Kintanar
and Robles, 1992:33). The mood of revolutionary fervor that accompanied Aquino’s
umption of power created fertile conditions for systemic change in many sectors in the
lippines; while some reforms materialized (as in pharmaceutical policy), others remained
unfulfilled promises (such as land reform).
S
According to Bengzon, he arrived at the issue of pharmaceutical reform "by
serendipity" (Bengzon, 1991:6). In April 1986, one month after taking over responsibility as
Secretary of Health, he "became aware" that pharmaceutical expenditures accounted for 18 to
20 percent of his Department’s annual budget. He responded by seeking to improve the cost
effectiveness of procurement, to use the Department's purchasing power to obtain better
terms and volume discounts, and thereby expand the government’s supply of drugs. In
Reich: The Politics of Health Sector Reform
20
exploring the existing system, he discovered that the Philippines did not have a national
pharmaceutical policy and that decisions on pharmaceutical production, trade, and
information were dictated by the groups involved, heavily influenced by their own interests.
He concluded, "In effect then, there was no policy or program standing up for the Filipino as
patient and consumer" (1991:6). Bengzon resolved to correct this situation, to improve the
procurement problems in his agency, and to improve the availability of drugs to the
(populace. In presenting the policy, he subsequently emphasized the libertarian principle of
providing consumers with greater choice.
To prepare a draft national drug policy, Bengzon followed a consultative and iterative
process that involved all the interested parties, in both public and private sectors (Figure 3).
The Department’s top management (the secretary and two undersecretaries) served as the
"initiators and task masters" of the process (Kintanar and Robles, 1992:35). They created a
task force to provide background information on pharmaceutical issues and to frame the rules
and timing of the consultation process. Different social sectors were then requested to
review the terms of reference for the policy and submit position papers, leading to the
identification of seven key issues. Face-to-face meetings followed with 61 organizations and
99 individuals. The policy was then created during a live-in retreat by the Department’s
Executive Committee with "appropriate consultants," and was presented to President Aquino
for review in early April 1987. She announced the new policy at the end of the month, just
over a year after the Department started work on pharmaceutical reform (Bengzon, 1991:67).
‘ '
To provide a solid legal foundation for pharmaceutical reform, the proponents sought
specific constitutional and legislative goals. The new Constitution of 1987 gave a strong
mandate to cost-effectiveness, equitable distribution, and government regulation of
pharmaceuticals. Article 13, Sections 11 and 12, stated, "The State shall adopt an integrated
and comprehensive approach to health development which shall endeavor to make essential
goods, health and other social services available to all people at affordable cost. . . the State
shall establish and maintain an effective food and drug regulatory system." Following the
announcement of the new drug policy, the Congress unanimously passed the Philippine
Generics Act in September 1988, giving the Department of Health the necessary authority
and sanctions to implement key measures of the PNDP. The Generics Law included the
following key provisions (Bengzon, 1991:9):
1. The use of generic name in labelling and advertising, prescribing and dispensing.
2. Development of an Essential Drugs List with a core list of 297 drugs and a
complementary list of 263 drugs.
3. Information, education, and communication campaigns to various social sectors
and to the public at large.
Reich: The Politics of Health Sector Reform
21
4. Provision for penalty, which ranges from reprimand for the first conviction to
fines and suspensions of licence to practice for repeated violations.
5.
Contingency authority empowering the Secretary of Health to do the following:
a. issue rules and regulations to drug manufacturing companies to produce,
distribute and make available to the public, medicines in the form of generic
drugs, and
b. import raw materials when there is a shortage, for the use of Filipino
owned or controlled drug establishments, to be marketed and sold exclusively
under generic nomenclature.
Opposition to pharmaceutical reform crystallized around the Generics Law, emerging
from sources both domestic and foreign, especially from US organizations. Kintanar and
Robles (1992:42) described the adversaries and their complaints:
_ The Philippine Medical Association filed a suit questioning the Generics Law; some
W multinationals also brought the issue of generic labelling guidelines to court; the
president of the Drug Association of the Philippines — the organization of
multinational firms — called the Essential Drugs List "extremely dangerous"; the head
of the American Chamber of Commerce in the Philippines, Gordon Westley,
expressed deep concern "over proposals to use government power to closely control,
widely prohibit and minutely redirect private activities in the health sector"; two
American senators (Allan Cranston and Richard Lugar) warned President Aquino to
"look carefully at plans. . . to implement a National Drug Policy because. . . the task
of stimulating new US investments may become more difficult"; lastly, the US State
Department was supposed to have floated a document saying that "to avoid serious
damage to the Philippine reputation as a place to invest, we urge. . . the government
of the Philippines to implement the Generics Law in as non-discriminatory and noncompulsory manner as possible."
In addition, a small group in the Philippine Medical Association attacked the Generics
Law as a violation of their human rights because of legal sanctions for physicians who
d^tgard regulations on generic prescribing. A small number of newspaper columnists also
criticized the Generics Law (1992:51-52).
Supporters of pharmaceutical reform employed various strategies to contain the
opposition, including: continued political support from President Aquino; constituency
building and alliances with the church, the media, academia, and health professionals; court
decisions against the plaintiffs and in favor of the policy; public protests by "people’s
organizations" and consumer groups against the firms that filed court suits; public
demonstrations in support of President Aquino and the Generics Law; and social marketing
of the policy through the mass media to the public and health professionals (Kintanar and
Reich: The Politics of Health Sector Reform
22
Robles, 1992:42-43). The initiators of pharmaceutical reform anticipated opposition and
prepared for it, collecting substantive documentation for court challenges and designing
political strategies to mobilize domestic and international support. They also implemented
the policy in "relatively easier areas" first, in order to produce visible successes, and agreed
to some compromises in implementation, in order to receive cooperation from key
organizations such as the Philippine Medical Association (1992:48).
Advocates of pharmaceutical reform in the Philippines recognized the importance of
political timing, in passing and implementing the reform; they also recognized that new
political circumstances could permit a reversal of the policy. The potential for reversal arose
after changes in the executive and legislative branches of government, following the election
of Fidel Ramos as the new President in May 1992, who appointed a new Secretary of
Health, along with the election of a new Congress. The head of the Philippine National
Drug Policy Programme, writing with a journalist, concluded in 1992, "Undoubtedly,
opponents of the PNDP are awaiting a propitious moment, one that will give them the
opportunity to turn back the clock. . . . The problem this spells out is clear: a programme
such as the PNDP is not simply something that can be started, no matter how profound that
start is, and then left alone to its own devices. It has to be watched, monitored, supported":
It also has to press forward to sustain the pace and institutionalize its accomplishments"
(Kintanar and Robles, 1992:53). Their conclusion reflects a basic principle, that reform is
constructed and sustained through politics, and its corollary, that Reform is also dismembered
and reversed through politics.
i,
DISCUSSION
The three case studies share a number of conditions that contributed to making policy
reform politically feasible. Below I review and compare these conditions, to identify key
political variables that affect the feasibility of pharmaceutical reform, and to explore
principles that may be generalized to other areas of health sector reform. Figure 4 provides
a summary of the political dimensions of pharmaceutical reform in Sri Lanka, Bangladesh,
and the Philippines.
It goes without saying, almost, that three case studies do not constitute proof in social
science. At best, three cases can provide the basis for a persuasive argument (and three
cases are certainly better than one or two). The limitations of this method are well known,
and do not merit repetition here. But it may be worth noting ways in which the analysis
could be strengthened. The number of cases could be expanded, and statistical methods
could be used to analyze correlations between the political conditions in a society and the
political feasibility of a reform. Another approach is to include cases where pharmaceutical
reform failed, as in Nigeria and Peru, to seek differences between feasibility and failure. A
third alternative is to explore other successful cases of health sector reform, outside the
pharmaceutical field, to seek commonalities. Due to the limitations of this essay, the
Reich: The Politics of Health Sector Reform
23
concluding remarks below should be considered exploratory and tentative, for additional
research if considered worthwhile.
Values: The three cases all relied on multiple values in justifying and explaining the
policy reform. In each case, the reform involved a complicated package of policy measures,
which included different philosophical principles. All three cases promised more costeffective results, invoking utilitarian values, as well as increased attention to the poor and
vulnerable groups in society, suggesting communitarian principles. The reform in the
Philippines was defended as improving patient choice, a libertarian objective, but it also was
criticized for restricting physician choice at the same time. The reform in Sri Lanka relied
upon a vigorous use of the international market to obtain the best products at the lowest
price. This mixture of principles, often vaguely articulated, appeared in all three cases, and
suggests that policy reform probably does not involve a one-to-one correspondence to a
single philosophical axiom. Indeed, if reform is based on a single dominant value, which is
explicitly stated and rigorously applied, it could have adverse consequences, making the
reform more vulnerable and inflexible, and thereby more susceptible to opposition. A
striking commonality is that political leaders in all three cases used the realm of values to
digwiguish the new regime sharply from the old and to appeal to specific constituencies (in
th" cases, the majority poor in each society).
Distributional consequences: In these three cases of pharmaceutical reform, the new
policies were intended to have similar distributional consequences, as shown in Figure 4.
Benefits would accrue in the short term to the poorer groups of society, through improved
access to lower priced drugs, with additional benefits emerging over time to local
manufacturers that could replace imports. Costs, on the other hand, wbu|d be borne by
multinational corporations that would lose markets or market share for Specific products, and
also by some patients who preferred or depended on products that were no longer allowed
(including, for example, members of the urban elite who used certain brand-name products).
Physicians would lose some degree of choice, through restricted lists of essential drugs, and
could lose some income through sales of pharmaceutical products, but would gain through
greater availability of basic products and improved efficiency in drug management. In all
three cases, two groups of cost-bearers for the reform (multinational corporations, and
physicians) were better organized than the presumed benefit bearers (poorer populations of
the society), and political leaders needed to design strategies to cope with the political aspects
dBmese distributional consequences, as discussed next.
Group Competition: The three cases showed distinctly similar forms of group
competition, with different strategies adopted by the political leaders involved. For this
particular reform, a predictable pattern of opposition emerged, with similar groups making
similar arguments in each case. In all three countries, the national physicians association and
various US private organizations (the Pharmaceutical Manufacturers Association or the
Chamber of Commerce) became mobilized in opposition to the reform. The governing
coalitions, in all three cases, were sufficiently strong to resist the pressures mounted by both
internal and external groups, although they adopted different approaches. In Sri Tanka, the
Reich: The Politics of Health Sector Reform
24
government relied heavily on appeals to national interest and common good, bolstered by
powerful inputs of technical expertise from national authorities. In Bangladesh, the policy
reform occurred through an unusually rapid change, using the coercive power of government
to squash some opposition, revisions in the policy as concessions to meet other complaints,
and rewards to local manufacturers to transform their initial opposition into public support
for the reform. In the Philippines, group competition was managed through a consensus
building process engineered by advocates in the Ministry of Health, along with efforts to
persuade the physicians association to support the reform and to mobilize social pressure
against the opposition from presumed beneficiaries of the policy among the general
population.
The three cases illustrate the two-table political bargaining described by Putnam
(1988), and confirm his point that the domestic political variables often count more than the
foreign political variables of MNCs and international banks. Even market domination by
foreign firms (at 75-80% of the domestic market) could not obstruct pharmaceutical reform
in these three countries. In short, for these cases, the economic structure of the market was
less important than political circumstances in determining the feasibility of reform.
Timing: The three cases confirm the general principle that opportunities for major
reform have a better chance of success in the early periods of new regimes, in both
democratic and non-democratic states. In all three countries, the pharmaceutical reforms
occurred in the first years, when political leaders still enjoyed extia political "capital" not yet
expended, when coalitions were strong and supportive, when social problems could be
blamed on the errors of the previous regime, and when the general public mood still looked
optimistically on future prospects. The failure of the health policy in Bangladesh, which was
introduced in 1990 after eight years of Ershad’s rule, shows how the accumulation of
political problems toward the end of a regime can frustrate policy reform. The three cases
suggest that the political will model may have some limited applicability at the start of a new
regime, but not in a pure sense. Even Ershad, despite his power as a military dictator,
needed to negotiate with different groups and provide concessions in order to gain support or
non-interference (as suggested by the political factions model). And the political leaders in
Sri Lanka and the Philippines similarly became involved in negotiations with different groups
to assure the reform’s acceptance. The cases suggest that the political factions model is
closer to reality, and that the political skill of leaders and the timing of reform critically
affect the probability of success.
The three cases also reflect the general principle that policy entrepreneurs seek
opportune moments to push their pet ideas (Kingdon, 1984). In Sri Lanka, Dr. Bibile had
long sought to achieve a comprehensive pharmaceutical reform, and enthusiastically pursued
the chance offered by Mrs. Bandaranaike’s government. In Bangladesh, Dr. Zafrullah had
attempted to persuade previous governments to enact a pharmaceutical reform, without
success, and had a major role in convincing Ershad to launch the reform process. In the
Philippines, Dr. Bengzon became the internal initiator of pharmaceutical reform, even though
he had not previously advocated this reform, but a number of consumer groups outside the
Reich: The Politics of Health Sector Reform
25
Figure 1
Politics of Health Sector Reform in the United States
Source: The News & Observer (Raleigh, N.C.) 23 August 1993: 10A.
government strongly supported and pushed for the policy change. A similar pattern can be
found in the United States, where the Jackson Hole group had plotted and planned for a
number of years, with a special commitment from Dr. Enthoven, for an opportunity to get its
proposal for "managed competition" on the agenda for health sector reform — and they
succeeded with Clinton.
Political stability: In these three cases of pharmaceutical reform, the governments
successfully resisted strong opposition from domestic and foreign pressure groups. In short,
the political leaders managed the policy reforms in ways that protected the regime’s stability.
The challenge, however, is not only to protect the regime’s stability from being undermined
by policy reform, but also to protect the reform’s continuity from being undermined by
subsequent political change. As I noted above, political processes provide the means to
achieve policy reform, but they also provide the means to unravel previous reforms. A
policy reform is especially vulnerable to political reversal when it redistributes resources to
relatively powerless and unorganized groups in society. A reform can be protected against
full reversal if constituencies are created both inside and outside government, as has
happened in Sri Lanka since 1977. The degrees of reversal for Bangladesh and the
Philippines are still uncertain. A reform can also be protected if the marginal groups can
become better organized and develop into an effective constituency for the redistributed
system, or if they can ally themselves with more powerful groups in society (Reich, 1991);
this is not easy to achieve in pharmaceutical reform, because of the collective action
dilemmas, that is, the transaction costs that mitigate against organizing the unorganized.
Implications for health sector reform: Which lessons of pharmaceutical reform are
relevant for other substantive areas of health sector reform? While I do Aot present evidence
for the following assertions, I would suggest several broad conclusions that apply to the
politics of other health sector reforms. First, the three cases reflect the spatial role of
physicians as an organized interest group in health sector reform. Any effort to reform the
health sector must take into account the physicians association, and must design strategies to
coopt, neutralize, or mobilize this group. Second, while health is often a relatively low
national priority compared to the productive sectors of the economy, the three cases show
that it is possible to catapult health sector reform onto the national political"agendaT~Third,
the cases suggest that the political conditions for policy reform can be manipulated by skilled
political leaders, to create reforms that are both politically feasible and politically sustainable.
A systematic assessment of the opportunities and probabilities for enacting health sector
reform can be carried out through political mapping (Reich, 1993), to assist decision makers
in managing the politics of policy reform.
Reich: The Politics of Health Sector Reform
26
Figure 2
Characteristics of Policy Affecting its Implementation
Less Problematic
More Problematic
Simple technical features
Complex technical features
Marginal change from status quo
Comprehensive change from status quo
One-actor target
Multi-actor target
One-goal objective
Multi-goal objective
Clearly stated goals
Ambiguous or unclear goals
Short duration
Long duration
Source: Cleaves, 1980:287.
ENDNOTES
1. As Bates (1991:265) noted, Kenneth Arrow in his book on Social Choice and Individual
Values long ago dispelled the notion of a state that adopts policies to maximize some social
welfare function, unless there is a dictator who can make the appropriate decisions without
compromise and despite opposition. And, as Bates emphasized, the world’s experience with
dictators on both the right and the left shows otherwise. The policies adopted by these
governments (and others) "do not represent the preferences of some single actor. They
represent the outcome of a political struggle, in which competing interests with rival visions
of the social good seek the power to impose policies that are consonant with their preferences
upon the collectivity" (1991:265).
2. More generally, the post-1977 economic reforms by the United National Party did not
promote exports very effectively, due to a substantial continuation of import contrdls
(Navaratne, 1991), and did not involve a vigorous privatization program, consisting mainly
of a slowdown in the creation of new state-owned enterprises, with only two sales completed
by mid-1990 (Adam et al., 1992:312-313). An analysis of Sri Lanka’s post-1977 economic
reforms, and its divergence from a "classic" structural adjustment and stabilization program,
however, is a separate story from the main thrust of this paper.
3.
This section on the Bangladesh pharmaceutical policy draws on Reich, 1994.
Reich: The Politics of HeaLh Sector Reform
27
Figure 3
Consultation and Consensus-Building Process
Followed for the Philippines National Drug Policy
Source: Bengzon, 1991:7.
Figure 4
The Politics of
Pharmaceutical Policy Reform in Three Countries
Reform
Politics
Sri Lanka
•
Bangladesh
' L
Philippines
Values
- democratic election,
socialist values,
redistributive
- for common good (C)
- use inti market (L)
- cost effective (U)
- military coup,
populist, anti
corruption
- basic needs for
common good (C)
- reduced usage of
unnecessary drugs (U)
- democratic election,
people's power
revolution,
- social equity (C)
- efficient
procurement (U)
- patient choice (L)
Distributional
consequences
- pro-poor
- anti-MNC
- reduced benefits to
urban elite
- potential benefits to
local firms
- improved efficiency
- pro-poor
- anti-MNC
- reduced benefits to
urban elite
- potential benefits to
local firms
|
- improved efficiency *
- pro-poor
- anti-MNC
- reduced benefits to
urban elite
- potential benefits to
local firms
- improved efficiency
Group
competition
- policy change based
on local academics &
official report
- persuasive power of
common good
- opposed by med
assoc & USPMA
- sudden change with
little consultation
- coercive power of
govt plus concessions
- opposed by med
assoc & USPMA &
local firms
- consensus-building
process through
MOH, with
mobilization of social
groups
- opposed by med
assoc & USPMA
Timing
- post-election, party
switch, strong socialist
mandate
- economic difficulties
- start of coalition govt
- post-military coup, as
one of first govt
actions by Ershad
- seeking natl and inti
legitimacy
- post-election in
democratic
revolutionary spirit
- near start of Aquino
govt
Political
Stability
- coalition govt, when'
govt weakened due to
divisions, policy
weakened
- partial reversal when
new govt elected in
1977
- able to withstand
strong challenge by
MNCs and western
govts
- head of state involved
- concessions offered
and opponents coopted
- able to withstand
strong challenge by
MNCs and western
govts
- President involved
- strong Minister of
Health
abbreviations: C = communitarian; L = libertarian; U = utilitarian; MNC = multinational
corporation; USPMA = US Pharmaceutical Manufacturers Association
BIBLIOGRAPHY
Adam, Christopher, William Cavendish, and Percy S. Mistry. 1992. Adjusting Privatization:
Case Studies from Developing Countries. London: James Currey Ltd., pp. 299-322.
Alesina, Alberto. 1992. "Political Models of Macroeconomic Policy and Fiscal Reform,"
World Bank Policy Research Working Papers, WPS 970, September.
Anon. 1984. "Bangladesh: Government's Drug Policy Assailed Again," Lancet 14 January:
97.
Bates, Robert H. 1991. "A Critique by Political Scientists," in Gerald M. Meier, ed., Politics
and Policy Making in Developing Countries: Perspectives on the New Political Economy. San
Francisco: International Center for Economic Growth, pp. 261-272.
Behrman, Jere R. 1988. "The Impact of Economic Adjustment Policies," in David E. Bell
a^hMichael R. Reich, eds., Health, Nutrition, and Economic Crises: Approaches to Policy in
the Third World. Dover, MA: Auburn House, pp. 103-144.
Bengzon, Alfredo. 1991. "National Drug Policy: International Perspectives,’ Australian
Prescriber 14 (suppl/1):6-11.
Bergman, D. 1991. "Bangladesh's Opening for a New Beginning. Economic and Political
Weekly, 16 February: 382-6.
I
Birdsall, Nancy, and Estelle James. 1992. "Health, Government and the Poor: The Case for
the Private Sector," World Bank Policy Research Working Papers, WPS 938, July.
Chetley, A. 1986. "Bangladesh: New Measures to Improve Provision of Pharmaceuticals,"
Lancet 1 November: 1029-30.
Chetley, A. 1990. A Healthy Business? World Health and the Pharmaceutical Industry.
I^pdon: Zed Books.
Chowdhury, Zafrullah. 1992. Personal Communication.
Cleaves, Peter S. 1980. "Implementation Amidst Scarcity and Apathy: Political Power and
Policy Design," in Merilee S. Grindle, Politics and Policy Implementation in the Third
World, Princeton: Princeton University Press, pp. 281-303.
Edelman, Murray. 1971. Politics as Symbolic Action: Mass Arousal and Quiescence. New
York: Academic Press.
Geiger, H. Jack. 1993. ’Community-Oriented Primary Care: The Legacy of Sidney Kark,"
American Journal of Public Health 83:947-947.
Government of Bangladesh. 1985. ’Drug Control and Distribution in Bangladesh,* in WHO,
The Rational Use of Drugs, Report of the Conference of Experts, Nairobi, 25-29 November.
Geneva: World Health Organization: 215-222.
Grindle, M. S., and J. W. Thomas. 1991. Public Choices and Policy Change: The Political
Economy of Reform in Developing Countries. Baltimore: Johns Hopkins University Press.
Gwatkin, D. R. "Political Will and Family Planning: The Implications of India's Emergency
Experience," Population and Development Review 5:29-60, 1979.
Haggard, Stephan, and Robert R. Kaufman. 1989. "Economic Adjustment in New
Democracies," in Joan M. Nelson, ed. Fragile Coalitions: The Politics of Economic
Adjustment. New Brunswick: Transaction Books, pp. 57-77.
Hall, Karen Lashman. 1986. Pharmaceuticals in the Third World: An Overview. Population,
Health and Nutrition Department of The World Bank, PHN Technical Note 86-31,
November.
Horowitz, Donald L. 1989. "Is There a Third-World Policy Proiess?" Policy Sciences 22:
197-212.
Jayasuriya, D.C. 1985. The Public Health and Economic Dimensions of the New Drug Policy
of Bangladesh. Washington, D.C.: Pharmaceutical Manufacturers Association.
Jayasuriya, D.C., and F.D.C. Wijesinghe. 1991. Essential Drugs in Sri Lanka: Regulatory
and Economic Aspects. Nawala, Sri Lanka: Institute of Comparative Health Policy and Law.
Jolly, Richard. 1988. "A UNICEF Perspective on the Effects of Economic Crises and What
Can Be Done," in David E. Bell and Michael R. Reich, eds., Health, Nutrition, and
Economic Crises: Approaches to Policy in the Third World. Dover, MA: Auburn House, pp.
81-102.
Kahler, Miles. 1989. "International Financial Institutions and the Politics of Adjustment," in
Joan M. Nelson, ed. Fragile Coalitions: The Politics of Economic Adjustment. New
Brunswick: Transaction Books, pp. 139-159.
Keeler, John T.S. 1993. "Opening the Window for Reform: Mandates, Crises, and
Extraordinary Policy-Making," Comparative Policy Studies 25:433-486.
Kingdon, John W. 1984. Agendas, Alternatives, and Public Policies. Boston: Little, Brown.
Kintanar, Quintin L., and Alan C. Robles. 1992. "Making Policy: Focus on the Philippines,"
in Alan Robles, Malou Mangahas, Sheila S. Coronel, and Eric Gamalinda, eds., Prescription
for Change: National Drug Policies, Social Transformation and the Media. Manila: Philippine
Center for Investigative Journalism, and Stockholm- Dag Hammarskjold Foundation, pp. 3253.
Kymlicka, Will. 1990. Contemporary Political Philosophy: An Introduction. New York:
Oxford University Press.
Lail, Sanyaja, and Senaka Bibile. 1978. "The Political Economy of Controlling
Transnationals: The Pharmaceutical Industry in Sri Lanka, 1972-1976," International Journal
of Health Services 8:299-328.
Moore, Mick. 1990. "Economic Liberalization versus Political Pluralism in Sri Lanka?
Modem Asian Studies 24:341-383.
Navaratne, N.M.C. 1991. "Who Bears the Incidence of Import Protection? Evidence from Sri
Lanka," World Development 19:1409-1419.
N^on, Joan M. 1990a. "Conclusions," in Joan M. Nelson, ed., Economic Crisis and Policy
Cn^ce: The Politics of Adjustment in the Third World. Princeton: Princeton University Press,
pp. 321-361.
Nelson, Joan M. 1990b. "Introduction: The Politics of Economic Adjustment in Developing
Nations," in Joan M. Nelson, ed., Economic Crisis and Policy Choice: The Politics of
Adjustment in the Third World. Princeton: Princeton University Press, pp. 3-32.
! I
Nelson, Joan M., ed. 1989. Fragile Coalitions: The Politics of Economic Adjustment. New
Brunswick: Transaction Books.
Nelson, Joan M. 1989. "The Politics of Pro-Poor Adjustment," in Joan M. Nelson, ed.
Fragile Coalitions: The Politics of Economic Adjustment. New Brunswick: Transaction Books,
pp.95-113.
Nozick, Robert. 1974. Anarchy, State, and Utopia.'New York: Basic Books.
Mancur, Jr. 1965. The Logic of Collective Action: Public Goods and the Theory of
Groups. Cambridge: Harvard University Press.
Oni§, Ziya. 1991. "The Logic of the Developmental State," Comparative Politics 24:109126.
Patel, S.J. 1983. "Editor's Note," World Development 11:251-252.
Peterson, Mark A. 1993. “Political Influence in the 1990s: From Iron Triangles to Policy
Networks," Journal of Health Policy, Politics and Law
Putnam, Robert. 1988. ’Diplomacy and Domestic Politics: The Logic of Two-Level Games,"
International Organization 42:427-360.
Reich, Michael R. 1987. "Essential Drugs: Economics and Politics in International Health,"
Health Policy 8:39-57.
Reich, Michael R. 1991. Toxic Politics: Responding to Chemical Disasters. Ithaca: Cornell
University Press.
Reich, Michael R. 1993a. "The Political Economy of Health Transitions in the Third World,"
in Lincoln C. Chen, Arthur Kleinman, and Norma Ware, eds., Health and Social Change:
International Perspectives. Boston: Harvard University Press.
Reich, Michael R. 1993b. Political Mapping of Health Policy: Draft Guidelines. Boston:
Harvard School of Public Health.
Reich, Michael R. 1994. "Bangladesh Pharmaceutical Policy and Politics," Health Policy and
Planning, in press.
Report of Expert Committee for Drugs. 1982. Mimeo from N. Islam, Chairman of
Committee. Dhaka. 11 May.
I |
Sobhan, R. 1982. The Crisis of External Dependence: The Politictd Economy of Foreign Aid
to Bangladesh. London: Zed Press.
Tiranti, D.J. 1986. Essential Drugs: The Bangladesh Example Four Years On. Oxford:
International Organization of Consumers' Unions, New Internationalist Publications, and War
on Want.
Waterbury, John. 1989. "The Political Management of Economic Adjustment and Reform,"
in Joan M. Nelson, ed. Fragile Coalitions: The Politics of Economic Adjustment. New
Brunswick: Transaction Books, pp. 39-56.
Weerasuriya, K. 1993. "Essential Drugs and the Registration of Pharmaceuticals: The Sri
T ankan Experience," Bulletin of the "World Health Organization 7:229-235.
Wickremasinghe, S.A., and S. Bibile. 1971. The Management of Pharmaceuticals in Ceylon.
Colombo: Industrial Development Board of Ceylon.
World Bank. 1993. "World Development Report 1993. New York: Oxford University Press.
P R- ~ X .
GOVERNMENT OF INDIA
H^HI UltilPl'fl
Dr. A. Rama Mohan Rao .
State Informatics Officer &
Technical Director
MINISTRY OF INFORMATION TECHNOLOGY
<1^1 <4
- PlqlH
National Informatics Centre
(Karnataka State Unit)
FR ts
rRT, W W,
6th & 7th Floor, Mini Tower
ST. SiUj-seK 4WT, chisik - F£.o “k
Dr. AmbedkarVeedhi, Bangalore - 560 001
Phone : 286 3790,286 3218
Fax
:286 3382
Grams : NICNET
E-mail : root@nicksu.kar.nic.in
Website : http://kar.nic.in
No.
rq. C 33 ) I 9 k —
l~>J 0 / ' “33
(tkiai
Dated
03-10-2000
Sir,
As per the request of the Directorate of Health and Family Welfare Services, we
have prepared the draft study report for the computerisation of "Drugs Procurement and
Distribution System" after having the extensive discussion with the officers of your
department. I am enclosing the same for your approval.
NIC is ready to take up immediately the development of the web site to update the
drugs stock position of GMS on daily basis so as to know the drugs position of GMS
throughout the state on click of mouse. This web site may be temporarily hosted on the
NIC server till the GMS comes up with its network.
Yours Sincerely,
(A.Rama Mohan Rao
Shri. Sanjay Kaul, l.A.S.
Commissioner
Directorate of Health and Family Welfare Services
Ananda Rao Circle
Bangalore
TDY REPORT
ON
COMPUTERISATION
OF
DRUGS PROCUREMENT AND DISTRIBUTION SYSTEM
OF
DIRECTORATE OF HEALTH AND FAMILY WELFARE
SERVICES,BANGALORE
SEPTEMBER,2000
BY
NATIONAL INFORMATICS CENTRE, BANGALORE
Computerisation ofDrugs Procurement & Distribution System. DIRHFW, Bangalore
COMMITTEE TO STUDY THE PROCUREMENT AND DISTRIBUTION OF
DRUGS IN THE HOPSITALS
The Government of Karnataka in the Order number: HFW 145 HPC 99,
Bangalore dated 01-01-2000 has constituted a committee to study the procurement and
distribution of drugs in the hospitals.
1.
Dr.K.B.Makapur, Director, State Health Institute
Chairman
ofHealth and Family Welfare Services, Bangalore
2.
Shri. Anandrajashekar, Drugs Controller,
Member
Bangalore
3.
Shri.K.R.Shrinivas, CAO, KHSDP, Bangalore
Member
4.
Dr. A.Rama Mohan Rao, Technical Director and
Member
State Informatics Officer, NIC, Bangalore
5.
Dr.M.B. Karakannavar, Additional Director,
Member
KFW, Gulbarga
6.
7.
Dr. Sulochana, KHSDP, Bangalore
Member
Dr.V.R.Satish, Resident Medical Officer,
Member
NIMHANS, Bangalore
8.
Shri. Sai Vilvananthan, CAO-cum-FA, DIRHFW,
Member
Bangalore
9.
Shri. P.S. Bhagwan, Deputy Director, DIRHFW,
Member
Bangalore
The objectives of the committee were to study the existing set-up and functions
of the Government Medical stores and present the specific recommendations to the
Government of Karnataka in respect to the following.
1.
Quantification of drug requirements (including the basis on which the
quantities are to be studied.)
Prepared by NIC, Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIRHFW,Bangalore
2.
Procurement and Inventory Monitoring including the records to be kept
computerised of inventory control, scheduling of purchasing and minimum
and maximum stock limits to be maintained in respect of each drug.
3.
Establishment of drug stores at the district/divisional level (including whether
the sub stores and distribution centre and present system of centralised
procurement should continue or whether the sub-stores should directly
procure the drugs from R.C. holders as per the local requirements and settle
the bills on the basis of funds released by the Directorate.)
4.
Distribution of drugs to the districts (including whether the delivery system/
collection system to be followed and in case of the former , whether such
delivery is to be done by the G.M.S or R.C. holders)
5.
Storage requirement with reference to legal or licensing conditions and the
estimated cost.
6.
Staffing pattern and training requirements (Financial implications should be
assessed in case additional staff is proposed.)
7.
Stock and issue registers to be maintained in the hospitals / centres/
institutions and how the public is to be kept informed about the drugs
availability in the stock.
8.
Whether the financial limits to supply of drugs to the various institutions need
to be enhanced and if so to suggest the essential financial limits together with
the additional requirement of funds.
9.
Any other matter incidental to arising from any of the above terms.
In the proceedings of the meeting, the committee requested NIC to prepare a
report on Drugs Inventory System in the Government Medical Stores and sub stores.
As per the directions by the committee, NIC has prepared this report covering the
objectives of computerisation, proposed computerised system, System requirement,
infrastructure requirement, cost estimation, training and manpower requirement.
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIRHFIV,Bangalore
1.0. INTRODUCTION:
1.0.1. Background
The Government Medical Stores, Bangalore under the Directorate of Health and
Family Welfare Services, Bangalore performs the following functions :
«
Forecasting the departmental requirements of the drugs/medicines/chemicals
based on the average consumption of drugs for past one or two years, balance on
hand and the indents.
»
Preparation and issue of Purchase Orders to the Primary Manufacturers identified
in the Rate Contract Book by the High Power Committee.
o
o
Collecting penalty in case of belated supply of drug items.
Supplying the drugs purchased from various sources to the indenting Health
institutions as per their indents and Budget provision.
®
Storing the Drugs items safely in separate stores within the Government Medical
Stores.
•
Monitoring the movement of drugs
o
Monitoring the Stock availability
1.0.2. Drawbacks
The existing system has the following drawbacks.
- In the prevailing manual management system there was no comprehensive
information collection and retrieval mechanism available .
- The data is not in ready to use form and hence considerable time and energy is
being wasted for compilation processes.
- Laborious procedures in certain tasks like stock availability listing
- Preparation of MIS reports is laborious
- Delay in official communication
- Search and retrieval of information is laborious
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIPIIFW,Bangalore
1.0.3 The requirements of the health institutions
There is a need to make the system more effective in handling the distribution of
drugs related activities by the department. The institutions want the system to should be
capable of providing qualitative services. Hence the necessity for
A transparent system in availability of drugs
A transparent system of distribution of drugs
-
Faster processing of indent/request for drugs
-
Projection of the future requirement of drugs in a better way
Avoiding delay in official communication
1.0.4. Need of the Sub stores
Institution wise monitoring of utilisation of drugs
avoiding delay in distribution by bringing the stores near the institutions
Avoiding delay in official communication
-
Projection of the future requirement of drugs in a better way
-
Monitoring of drugs being lifted by hospitals/institutions
1.0.5. Need of the Government Medical Stores
-
Institution wise monitoring of utilisation of drugs
-
Improvement in procurement and accounting system
Analysis of movement of drugs by scientific methods
1.0.6. The Guidelines
The guidelines set for the new system is as follows
-
to bring transparency in distribution of drugs
-
to reduce the time for distribution management
-
to improve the distribution facilities by using modem techniques
Prepared by NIC, Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIRHFW,Bangalore
to establish a wider reach for interaction with public
1.0.7. Objectives
Automate the issue of drugs to the indentors with necessary validations
Automate submission of indent details
-
Facilitate monitoring the movement of drugs
Facilitate the checking of drugs availability position at the sub stores
Generation of statistical reports dynamically
Keep track of the defaulters who fail to furnish stock details
-
Easy and wide access/ restricted access of information related to drugs , medical
stores and the suppliers.
Keep track of the expiring/banned/prohibited/non-standard drugs and raise alerts.
Analysis of the drugs movement in a scientific method.
-
To project the future requirement of the drugs in a scientific way.
1.0.8. Purpose
The purpose of this document is to discuss about an information system for the
Government Medical Stores, Bangalore and the proposed sub stores at the district level,
which is expected to lead to the development of a Drugs Monitoring and Information
System. The requirements discussed have been derived from the discussions between the
Officers of the Directorate, Health and Family Welfare Services, Bangalore, Government
Medical Stores , Bangalore and NIC. This document attempts to satisfy the functional
and administrative requirement of central stores and sub stores in a detailed manner.
Prepared by NIC, Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIRHFW,Bangalore
1.0.9. Scope
The scope of this document is to outline the necessity of an information system and
various modules for GMS, Bangalore and Sub stores. It covers the following modules.
1.
State level Drug Inventory System
2.
Sub Store level Drug Inventory System
3.
System for Purchasing drugs
4.
System for monitoring distribution of drugs
5.
System for monitoring consumption of drugs at various levels/stores
1.0.10. Abbreviations followed in this document:
DIRHFW
Directorate of health and Family Welfare Services
GMS
Government Medical Stores
MIS
Management Information System
SRS
Software Requirement Specification
NIC
National Informatics Centre
NICSI
National Informatics Centre Services Incorporated
TAC
Technical Advisory Committee
HPC
High Power Committee
LL
Leased Line
VSAT
Very Small Aperture Terminal
RF
Radio Frequency
FAQ
Frequently Asked Questions
DHO
District Health Officer
Prepared by NIC.Bangalore
Computerisation ofDrugs Procurement & Distribution System, DJRHFIP, Bangalore
2.0. Functional Description
2.0.1. Organisation Chart:
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIRHFIV,Bangalore
2.0.2.Existing system
2.0.2.1. at the directorate:
Directorate
GMS
Hospital
PHC.PHU.CHC
Prepared by NIC, Bangalore
Computerisation ofDrugs Procurement & Distribution System, DIBHFIV,Bangalore
2.O.2.2. at the districts:
Zilla
Parishat
DHO
PHC.PHU,
CHC
Prepared by NIC, Bangalore
Computerisation of Drugs Procurement <& Distribution System, DIRHFII', Bangalore
2.0.3. Proposed Set-up
It is proposed to have one Server at the GMS to take care of the computerisation
of all the activities of the GMS and sub stores. The server will be used to maintain the
database of GMS activities and will carry out the networking and e-mail services of all
the sub stores.
The GMS will be linked to web via NICNET with RF link connectivity/ LL/
VSAT which give 64 kbps 12 Mbps data transfer.
It is also proposed to provide 5 nodes in GMS by giving one Pentium client
system to each section to have access to carry out their functions on the computer.
All sub stores shall be provided with one Pentium system with printer and
modem to do their work on computer in their office itself. All district sub stores will be
connected with GMS through NICNET.
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement & Distribution System, DIRHFIV, Bangalore
2.O.3.I. Inventory Monitoring System
Approve/Print Order of indent
approval
Browse the
Sub store details and drugs
details
Sub store
Public
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement <?• Distribution System,D/RHFH',Bangalore
-
Easy monitoring of consumption of drugs
Storing and retrieval of historic data
Compilation of drug-wise, supplier-wise data by the computer
-
Facilitates data mining
Easier analysis of drug movement providing necessary information for
decision making and planning the purchase of drugs
Quick communication in case specific drug control and management.
-
An access to communicate complaints from clinics.
Prepared by NIC, Bangalore
Computerisation of Drugs Procurement & Distribution System.DIRIIFW,Bangalore
2.0.3.2. Internet and E-mail Services
One of the computer systems acting as a server will be configured to handle the
internet and e-mail services of GMS and all the district sub stores. It will maintain the
e-mail addresses and mailboxes of GMS and all the district su6 stores. Thus it helps
building up faster and easy communication.
The sections of GMS and district sub stores can use effectively e-mail service so
that the information/circulars/letters can reach fast and reliably to the destination.
It will also be able to take care the transfer of data between GMS and district sub
stores. All the district sub stores can access the internet also.
The networking of the district sub stores with the GMS will be done using dial up
mode of operation through the N1CNET.
2.0.3.3. Web based information
A Web site will be hosted by NIC for Government Medical Stores at its head
office. This web site will contain the drugs availability position in sub-stores. The
institutions can access this site.
Web based applications will be provided to the offices/officials of the department
to query the information and compare their stocks with others or any other related
information.
Benefits :
Some of the benefits of the proposed system are :
Availability of the information centrally
On-line generation of statistical reports.
-
Easy monitoring of stock position of drugs
Prepared by NIC.Bangalore
Computerisation of Drugs Procurement & Distribution System,DIRHFJV,Bangalore
SuDolies
2.0.3.4. Drugs Inventory at the sub stores:
Prepared by NIC,Bangalore
Computerisation of Drugs Procurement & Distribution System, DIRHFW, Bangalore
2.0.3.5. Purchase system at the Directorate
Directorate
GMS
Sub-stores
Hospitals
PHCs.PHUs,
CHCs
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement & Distribution System, DIRHFW, Bangalore
2.0.3.6. Purchase System at the districts
Zilla Parishat
DHO
Sub-store
PHC.PHU,
CHC
Prepared by NIC,Bangalore
Computerisation ofDrugs Procurement & Distribution System, DIRHFIV, Bangalore
2.0.3.7. Distribution System at the Sub stores
GMS
Zilla
Parishat
Sub store
Hospital
PHC,
PHU.CHC
The sub stores maintain the stock received from both ZP and GMS separately and
distribute the same to the health institutions according to the terms and conditions laid
down for distribution.
Prepared by NIC, Bangalore
Computerisation ofDrugs Procurement & Distribution System,DIRHPW,Bangalore
3.0. Project Execution Scenario
3.0.1. Infrastructure Requirement
The department has to provide the following infrastructure requirements to the
computer centre at the GMS as well as sub stores.
The site specifications for the GMS computer centre is are follows:
-
Vinyl flooring for the computer
If the room height is beyond 12 feet, false ceiling has to be provided.
Two 1.5 Ton Air Conditioners with stabilizers are to be fixed for clean
environment and to maintain temperature.
Single phase KEB input power to be provided with circuit breaker on 15/5
Amp. Universal sockets 2 Nos to connect UPS.
UPS outlets having 4 Nos. Of 5 AMP 3 pin socket with switch to be provided
with each distribution box at computer room and for clients. 3 distribution
boxes in computer room and one each for clients proposed.
Separate computer graded clean earth should be made with a pit and the
grounding to be transmitted to the power sockets ofKEB inlets for UPS.
Voltage between ground and neutral should be less than 3 volts.
Preferably a separate phase should be drawn for AC unit. The power outlet
should be terminated with the circuit breaker of the 20 Amps capacity and
heavy duty 15 Amps socket.
The district substore should provide clean, dust free room/place to install the
Computers. It should provide separate proper grounding to computer.
The computer table, chair, printer table and pedestal fan have to be provided
to every client computer at the GMS. Two steel almirahs are required at the computer
centre to keep computer related items.
One telephone connection has to be provided to the district computer centre to
establish the networking connection with local NIC office.
Prepared by NIC, Bangalore
Computerisation ofDrugs Procurement cJ- Distribution System, DIRHFW,Bangalore
One telephone connection has to be provided to the district computer centre to
establish the networking connection with local NIC office.
3.0.2. Manpower
1.
It is necessary to identify/ nominate one senior officer as a nodal officer at the
GMS. The nodal officer will take care the implementation of the software by
coordinating and pursuing with the other officers and staff. He will organise activities at
the computer centre. Fie will assist the Joint Director at the Government Medical Stores
in the computerisation work. Fie will interact with the institutions and the Directorate
office in respect of computerisation activities.
2.
The department may recruit/hire one
technical person to take care of the
maintenance of systems at the GMS, implementation of the software. The technical
person will also help the department in conducting the training programs. And also three
data entry operators may be taken for initial one year to handle the data entry.
3.
The department may also recruit/hire one data entry operator for each of the
sub stores on contract basis for the first year to take care of the maintenance of systems
at the sub stores, implementation of the software. After one year, the staff at the sub
stores are expected to use the systems themselves.
The minimum educational qualification required for the technical person is
B.Sc. with 3 years experience in the computer field
Or
B.Sc., PGDCA
Or
M.Sc. With computer Knowledge
Prepared by NIC,Bangalore
Computerisation of Drugs Procurement & Distribution System.DIR.IIF1V,Bangalore
The GMS may work out to post two clerks/typists at the computer center and put
them exclusively on the computer related activities. Subsequently the concerned section's
staff can be asked to do their work on the computer. The selected typists/ clerks will
assist other staff in their computer related work.
It is proposed to use the existing staff to handle the regular operations of the
Government Medical Stores computerization with proper training after one year.
Prepared by NIC. Bangalore
Computerisation of Drugs Procurement cC- Distribution System, DIRI-lBW,Bangalore
3.0.3. Training
For the effective utilization of the computers and proper implementation of
the computer packages, it is essential to create awareness in the officers and staff of the
department. To achieve this it is necessary to train the officers and staff on the
computers. This may be done in phases.
The department may organise the computer training program by sending the
officers and staff to private training agencies on the following topics for 6-7 days. ■
i.
Fundamentals of Computer
ii.
Windows 2000
iii.
MS - Office 2000
iv.
E-Mail Services
NIC will take care of training on the application software developed for the
department.
Prepared by NIC,Bangalore
Computerisation of Drugs Procurement & Distribution System,D/RIIFII',Bangalore
3.0.4, Cost estimate :
The following estimates show the cost of computer hardware, software and other
items.
For the GMS office
Items
Quantity
Approximate
Cost in Rs.
Lakhs
SERVER - Pentium III, 600 MHz or above,
256 MB RAM, 2x9 GB HDD (SCSI), CD-ROM,
DAT Drive, 1.44 MB FDD, 4/8 GB DAT
CLIENTS- Pentium 111,667 MHz or above , 10 GB
Hard disk (IDE)
64 MB RAM, 1.44 NIB FDD, CD ROM
1
1.50
5
2.50
High Speed Laser Printer
Dot Matrix Printer
Inkjet Printers
1
5
1
1.40
0.75
0.07
Scanner
1
0.30
CD writer
1
0.20
7.5 KVA online UPS with 30 minutes backup
1 KVA online UPS with 30 minutes backup
1
1
1.75
0.40
Modem - 56.6 KBPS, External
2
0.12
Printers -
UPS
Software
MS - Windows NT Server Enterprise (25 Users
license)
MS- SQL Server 7.0 Enterprise (25 Users license)
MS Office 2000 Professional
MS Visual Studio 6.0 Enterprise edition
C-DAC ISM Soft Kannada software
Mdeamon (50 Users license)
MS Proxy
1
0.96
1
6
1
5
1
1
1.82
0.90
0.40
0.10
0.23
0.22
High speed connectivity
1
8.00
RF/LL/VSAT - IP Advantage ( any one of them)
Total:
LL - Leased Line through DOT
Prepared by NIC, Bangalore
21.62
Computerisation of Drugs Procurement & Distribution System. D/RI IHI', Bangalore
At district sub stores:
Items
Quantity
Approximate
Cost in Rs.
Lakhs
COMPUTER-Pentium III, 667 MHz or
above, 64 MB RAM, 10 GB Hard disk
(IDE), 1.44 MB FDD, CD ROM
Dot Matrix Printer 132 cols, 24 pin,
240 cps
UPS 1 KVA online with 30 minutes
backup
Modem 56 Kbps, External
27
13.50
27
4.05
27
10.80
27
1.62
27
27
27
4.05
0.54
0.81
SOFTWARE
MS - Office 2000 Standard
ISM -Soft Kannada
Internet Connection
35.37
Total :
The following estimate will show the cost of infrastructure and manpower.
For the GMS office
Items
Approximate
Cost in Rs.
Lakhs
Site preparation, furniture, Telephone etc
2.00
Man Power
2.50
One Programming Assistant and three Data Entry Operators from
man power agency for an initial period of one year
Total :
Prepared by NIC.Bangalore
4.50
Computerisation ofDrugs Procurement c£- Distribution System,DIRHFW,Bangalore
At the sub stores :
Items
Quantity
Approximate
Cost in Rs.
Lakhs
Site preparation, furniture, Telephone etc
27
13.50
27
13.50
Man Power
One Data Entry Operator from man power agency
for an initial period of one year
Total:
27.00
Total cost of Hardware, software. Infrastructure & Manpower :
(GMS and Sub Stores)
10% handling charges for NICSI for the items to be supplied by :
NICSI
Transportation charges on software to be supplied by NICSI
10 % sales tax on the software to be supplied by NICSI
(or 4% sales tax with form D)
10 % Post budget increment on hardware cost
:
Rs. 0.84 Lakhs
Rs.4.74 Lakhs
Grand Total
Rs. 100.13 Lakhs
Rs 88.49 Lakhs
Rs.4.96 Lakhs
Rs. 1.10 Lakhs
Recurring Charges
AMC on hardware
: 7 % of cost of Hardware
Satellite connectivity Charges
: Rs.2.00 Lakhs per annum
AMC for the VSAT will be taken up by NIC. All other AMCs for the equipments i.e, the
hardware, operating system support and RF link/ Leased Line (as the case may be) to be
directly handled by the department with the vendor.
Prepared by NIC, Bangalore
A prescription that worked
HERE used to be a time when no tem. Medicines were
fampicin (450 mg) that
the Delhi hospitals
news was good news. As we prepare being procured a cou
j bought this year, they
for the next millennium, media ple of months before
saved Rs 6.30, which
gatekeepers have turned this bit of re their expiry dates so
meant they had Rs 2.8
ceived wisdom on its head — today, good that they could be
lakh more in their kitty
news is no news, unless it’s a no-news day. junked and the endless
tq get more of - this
One such piece ofgood news that never got flow of orders to manu
chronically scarce med
reported has got the World Health : facturers maintained;
icine. One can keep list
Organisation excited like never before. expensive alternatives
ing examples, but the
The Delhi Model, in fact, is the new buzz were invariably pre
point of this good news
word in Geneva, apart, of course, in ferred and prescribed;
isthatittakesjustacouChandigarh, Chennai and Calcutta. What non-essential drugs we
pie of people with clear
is this Delhi Model all about, and why is re being stocked up in
intentions and a clear
it going to be replicated in Thailand. numbers that had no
head to make a differ
Myanmar. Vietnam. Daos and Kam basis in the demand for
ence to a system we
puchea? Well, simply because it is a com them; traditional medi
Sourish Bhattacharyya
keep writing off.
mon-sense solution to a chronic malady of cines were being bought
But how did this become possible? It
just because the government had said so
our healthcare delivery system.
took
just
one
public-spirited
medical ad
and
not
because
doctors
were
prescribing
Just one out of five people going to
government-run hospitals for treatment them; and reputed firms were being dis- ministrator, Ranjit Roy Chaudhury,
get the free medicines that is due to them. com-aged because clerks sat over bills to Emeritus Scientist at ■ the National
It really doesn’t matter, then, if the state extract their cuts. Public money, in other Institute of Immunology, New Delhi,
provides them free treatment, for lite words, was being despatched down the who doubles as health adviser to.the
money they spend on drugsand what hos tubes — the same money that could be Delhi government, to make it happen.
pitals call consumables (which can be a spent buying drugs that never seem to be Teaming up with C. R. Vaidyanathan, a
former Union Health Secretary, and R.
syringe or a stent) is enough to drive around at hospital stores.
Today, the Delhi government saves 30 Parameswar, former Deputy Comptro
them back to the clutches of their villa ge
fatcat or factory foreman. No wondler percent of its budget for medicines and ller and Auditor General, he set in mo
each cycle of illness pushes the unseen, this money is ploughed back into procur tion a system that cut waste and struck
unheard majority farther into the ing more medicines. Translated into at the vested interests that allowed it to
morass of poverty. Even in Delhi, before money, it means a budget of Rs 40 crore fester. All that this troika did was pre
1992, though 30-35 percent of the national getting you medicines worth Rs 50 crore, pare a list of 250 essential drugs good
capital territory’s health budget was be something unimaginable in a govern enough for 90 percent of the ailments
ing spent on medicines to be distribute d ment set-up. In people terms, it means that treated at public hospitals; shortlist
free, chronic shortages were forcing pa the money saved on the purchase of250 mg companies for the supply of these medi
amoxycillin capsules enabling govern cines (any firm with a turnover of less
tients to make theirown arrangements.
The system of hospital-based procure ment hospitals to procure nine million than Rs 8 crore, the mohalla manufac
ment of medicines, in fact, was riddled chloroquin tablets for their malaria con turer, in other words, was kept out of the
with all the flaws that are present at all lev- trol programmes. Similarly, for every ten bidding process); fix rates for the drugs
els of the public health-care delivery sys tablets of the anti-tubercular drug ri to be purchased; and encourage doctors
T
4p8
to prescribe only these medicines so that
they were easily available to the in
tended beneficiaries.
The new system had two implica- ■
tions. One, it was easier for the govern- J
ment to flex its bargaining muscle be- >
cause now the companies were talking '
bulk orders. Two, drug purchases from |
now on were to be both need-based and ’
people-oriented, and not governed by
whimsical circulars or corrupt clerks. 1
Tlie list was transparent and the rules ;
were clear, which is why the Delhi high ■
court refused to entertain a petition >
moved by aggrieved manufacturers '
thriving in the old system. And the con- ■
fidence the system created among top •
drug companies was evident in their par- j
ticipation in the centralised bidding ;
process, encouraged by the new rule
making it mandatory for hospitals to ■
clear their bills within a month.
An exercise by the Delhi government •
to assess the new system’s success has ■
exposed some shocking examples of i
waste that need reiteration. The study,
conducted by an independent agency, ;
revealed startling differences in prices •
at which drugs had been purchased by
the Delhi government and the Central J
government respectively — for atnoxy- •
cillin syrup, for instance, the price dif- I
ferential was Rs 3.95, and it shot up to Rs J
15.60 when a comparison was made with ;
the government-owned Super Bazar. '
It's a pity, really, that in four years the !
Delhi Model has found more takers j
abroad than in India. Maybe even the ;
Health Ministry believes good news is •
no news.
/
0 BROADCASTING
The cable conundrum
Even as the conditional access system for cable television viewing is all set to be made a statutory
requirement, the potential impact of the proposed changes on the industry and on consumers is the
subject of an intense debate.
view them would receive a basic tier of Free
To Air (FTA) channels at a reduced price.
In order to protect public access to major
entertainment and information content,
B Mumbai
the government plans to include a ‘mustcarry’ clause in the FTA category. This
OVING from the back alleys to the means a genre-wise breakup, ensuring that
corridors of Parliament, cable wars people who opr to settle for the basic tier
are now being fought in the national arena.
are not deprived of a staple diet including
This battle is likely to change the face of general entertainment, news, film, music
channels and the like.
the cable and satellite TV industry in
Satellite broadcasters who now offer a
India.
The Lok Sabha unanimously passed bouquet of channels - some FTA and
the
Cable
Television
Networks some pay - have reportedly been working
behind the scenes to stall the Bill in
(Regulation) Amendment Bill in May.
Parliament. They fear that they will lose
Burby the time the Bill reached the Rajya
Sabha, it was enveloped in an intense
advertising revenue with the introduction
debate on its viability and its potential of CAS. Less popular channels, which are
impact on the industry and consumers.
now aired with other pay channels, may
With the debate yet to be resolved, the get less advertising support. They may
proposed law may now be introduced even have to transform themselves into
through an ordinance. While it is strong
FTA to remain relevant, making them
ly resisted
by broadcasters,
the even more dependent on advertising.
Information and Broadcasting Ministry
Anil Baijal, a senior official at the I&B
s^Atfhe amendment as being vital to
Ministry who was involved in drafting the
b™fng transparency and regulation to
Bill, says that the CAS will put people in
rhe chaotic Indian cable television mar control: “They can pay minimal rates for
ket. This piece of legislation introduces,
the FTA basic tier, and select pay channels
for the first time, a Conditional Access depending on their interest." Also, set-top
System (CAS) that enables consumers to
boxes would bring in far greater trans
buy their cable channels a la carte, rather parency. They would provide a real pic
than having to pay for the entire slew ture of media consumption habits, and
foisted on them by cable operators.
eliminate problems such as under-report
Large cable distributors like the ing of the number of subscribers by cable
Hindujas’ Incable have been lobbying operators and inflated ratings by broad
hard and long to get the Bill passed. If casters. The system will also help rhe gov
passed, subscribers to cable television ernment plan for entertainment tax
would only be able to view pay channels accruals in a realistic Fashion. Cable oper
through special set-top boxes. They would ators are required to announce the prices
be billed on the basis of die number of pay of FTA and pay channels.
channels they select, rather than being held
The pricing and regulation of the basic
tier and the cost of the new technology, as
liable for a monthly lump sum in accor
dance with the cable operators’ own choice well as the practical issues involved in
implementing CAS, have been thrashed
of channels.
The consumers’ right to choose is the out by a consultative process involving the
logic put forward by the Union Ministry government, broadcasters, cable associa
of Information and Broadcasdng in intro tions and consumer groups. A Task Force
ducing the law. Pay channels are trans was set up in July 2001 to identify ways to
implement addressable cable systems, and
mitted in an encrypted or scrambled form,
and with CAS, those who do not wish to evolve standards for the new technology
AMULYA GOPALAKRISHNAN
mNew Delhi
DIONNE BUNSHA
M
84
required. According to the latest NRS
(National Readership Survey) figures,
there are around 45 million cabled homes
in India. Of these, set-top box manufac
turers estimate, about 10 per cent would
choose pay channels. They calculate an
average cost of Rs. 1,500 to Rs.2,000 for
an analog set-top box and about Rs 5,000
for a digital one, says the Ministry.
Some ofthe fiercest opposition to CAS
has come from the usual suspects - Star,
Sony and Zee, the three big broadcasters
whose audiences will now be splintered. If
they remain pay-channels, their subscrip
tion as well as advertising revenue could
take a beating if people do not take to the
new technology’. Also, with the ratings
game becoming more transparent, their
advertisement earnings will be direcdy
affected. This means that special interest
channels cannot ride piggyback on the
popularity of other channels in the same
bouquet. Someone in rural India, for
instance, could choose thewidely-watched
Star Plus without having to pay for Star
World, which remains popular only with
urban upper-class audiences.
Naturally, this could radically disrupt
the marketing strategy of broadcasters,
who stand ro lose both advertising and dis
tribution revenues ifpeople do not opt for
set-top boxes. Broadcast networks now
have ro decide whether to rely more on
advertising or subscription for their rev
enue, and cannot straddle both as they
have been doing all this while. Analysts feel
that this may put pressure on many cur
rent pay-channels to go FTA, in order to
maintain their reach and ratings.
However, Shanronu Aditya, who
heads Sony Entertainment, denied this
possibility. “We believe that the One
Alliance bouquet consisting of SET,
MAX, AXN, Discovery, CNBC and
Animal Planet is a robust bouquet and all
rhe channels have dedicated viewers and
each channel can stand by itself as well.
There is no question of going Free to Air."
CAS has definitely ensured a more
competitive era for big broadcasters,
FRONTLINE. SEPTEMBER
of human lifespan over which the drug is dogs for certain drugs.”
likely to be administered therapeutical
Clearly, the company cannot have it
ly...etc. etc."
both ways. If it was known that sponta
According to a fact sheet on NN622
neous rat tumours are likely, the species
issued by Novo Nordisk on July 26, all should not have been used at all. If not,
genotoxic tests on the compound were neg ethics demanded that the cause of rat
ative, indicating that the drug in all likeli tumours be established - determine
hood does nor have any genotoxic whether they were indeed spontaneous
carcinogenicity potential. A genotoxic tumours-before continuing with the tri
compound affects the genetic material. A als.
non-genotoxic carcinogen requires a long
More fundamentally, the company
exposure period, and when a drug is meant would seem to have not fulfilled even the
for chronic use, its potential non-genotox basic requirement for conducting Phase III
ic carcinogenicity' needs to be ruled our.
trials under Schedule Y. The Schedule says:
The long-term carcinogenicity' studies on “If the drug is a new drug substance dis
NN622 were being carried out from this covered in India and not marketed in any
perspective. In the Indian context, the very other country, Phase III data should be
fact that such studies were being conduct obtained on at least 500 persons distrib
ed means that they should conform to
uted over 10 to 15 centres.” By choosing
Article 3.5 of Schedule Y.
to have only 130 patients, distributed
Novo Nordisk has violated this across eight centres. Novo Nordisk violat
requirement on two counts. One involves ed this regulation.
the choice of rat as one of the species, when
Legally Novo Nordisk cannot be ques
according to the company’s own state
tioned because it had obtained the DCGI’s
ments, spontaneous tumours are known to
Break up of patients in Phase III
arise in rats with many ofthe cu trendy mar
trials of NN622 in country-groups:
keted drugs. Also, in response to the
Frontline questionnaire, Kapur stated that
• United States/Canada - 650
a similar drug that has been marketed had
• Latin America - 200 •
resulted in tumours in rats. Given this sit
• Austraiia/New Zealand - 100
uation, conforming to Schedule Y would
• European Union countries
call for the choice of a species other than
(Scandinavia, United Kingdom,
rats. Two, the average life-span of bred
France, Italy, Belgium, Austria,
mice is about two to three years. Assuming
Germany, Ireland, The
that the average period over which a Type
Netherlands) - 800
2 diabetes drug will be administered would
• Non-E.U. European countries
be half the human lifespan, the carcino
(Estonia, Switzerland, Hungary,
genicity data needed for permission for
Poland. Slovenia) — 250
clinical trials should span at least a year, and
• Asia (India, Hong Kong, Malaysia,
not six months as in the case of the data
Singapore, Philippines, Taiwan,
submitted by the company.
Thailand) - 550; (130 in India
The company has claimed that the
alone spread over eight centres.)
tumours occurred after the mice were
exposed for a period of time equivalent to
between half and full life expectancy. The clearance for its clinical trials. The DCGI
patients, on the other hand, were exposed has, however, refused to answer Frondine’s
questionson thesubject. ICMRsourcessay
to a maximum of six to seven months,
equivalent to about 0.5-1 per cent of that when the council asked the DCGI why
human life-span. In the Indian case, since the application was not referred to the
the Phase III trials had begun only in
ICMR and under what circumstances the
March, the period of exposure was only approval was given, the DCGI stated that
four months. Therefore, according to the the clearance was given since this was an
company, the risks for the human subjects international study and involved multi
of trials are minimal.
country trials. In particular, the DCGI
The issue is not so much the risk of would have to explain why trials were
exposure but the ethics of conducting allowed even after it was informed of rat
trials by' the company. “You cannot pro tumours in February.
According to Novo Nordisk, the risk
ceed with a general assumption that
tumours seen in rats are spontaneous," ofexposure to humans participating in tri
points out Bal. “Spontaneous tumours als was negligible on two counts. First, the
are dependent on the class of drugs being duration of exposure was much less than
tested, dosage and several other factors.
the period over which the animals were
exposed. Second, the tumours may be
We have seen spontaneous tumours in
FRONTLINE. SEPTEMBER 27. 2002
rodent-specific. Novo Nordisk has argued
that rodent urine is significandy different
in composition from human urine and it
is possible that tumours were caused by a
mechanism leading to the formation of
crystals in the rodent urine. The formation
of such macro- or micro-crystals might
eventually be found to be the cause of the
carcinogenicity findings in the urinary tract
system in the rodent, in which case, the
mechanism would be of no relevance to
humans, the company has stated.
In any case, the company’s fact sheet
has stated that all patients will be called for
an end-of-trial visit. The company has sug
gested that patients have a urine sample^
taken a year after the drug trials in orcl^H
to document any adverse drug reaction
(ADR). However, in response to an e-mail
question, the company refused to provide
details of the in-built liability clause in the
Patient Consent Form and whether the
company would bear the costs of treat
ment if any ADR linked to NN622 were
to be detected. It merely said: “Novo
Nordisk will work according to the liabil
ity clauses valid in the individual protocols
and patient consent forms.”
* HE Swiss company Novartis Pharma
JL AG had entered into an agreement
' 1
with Novo Nordisk in July 2001 for
obtaining commercial rights over
NN622 in the United States, Canada and
Mexico against some milestone payments
to the latter. However, Novartis termi
nated the agreement in October 2001.
There has been speculation in phAna
business circles that perhaps Novarflrod
some inkling early on of the problems
relating to animal tests.
The DRL-Novo Nordisk licensing
agreement was the first instance of an
Indian drug discovery being licensed to a
foreign multinational for the international
market. It was hailed as an indication of the
emerging Indian R&D potential in the
ongoing globalisation in the pharma sec
tor. The setback may dent that image some
what but does not lower that potential.
What the issue has brought to light is how
ethics are sidestepped in favour of overrid
ing commercial interests and how the reg
ulatory mechanisms of the country are
becoming weaker even as MNCs enter the
Indian market in a big way. In this context,
i twould be unwise to implement the recent
recommendation of the
Planning
Commission Working Group to ease reg
ulations on clinical trials and revise
Schedule Y accordingly without a thor
ough revamping of the functioning of the
DCGI itself. ■
Ill trials. (See box)
Refuting allegations of illegal and
unethical clinical trials, the company stat
ed that the Phase III trials had received
approval in all countries in accordance with
internationally accepted as well as domes
tic laws and guidelines governing such tri
als. “Adequate short-term as well as
long-term animal toxicity studies as
required including those under Schedule Y
of the Indian Drags and Cosmetics Act, at
the current stage of rhe development of the
drug, were provided when die trials were
approved,” it said.
However, statements made by Novo
Nordisk with regard to the nature of these
fciimal trials have been contradictory.
while suspending the Phase III trials, the
company had described the animal studies
as “preclinical” ones, which, by definition,
should mean studies conducted before all
phases of human trials. “Preclinical car
cinogenicity studies,” the July 22 release
said, “are an integral part of the develop
ment of new drags for chronic use. The
purpose of doing preclinical carcinogenic
ity studies in animals is to investigate if a
newdrughas potential for causing tumours
after long exposure in animals. Due to com
plexity of conducting state-of-the-art pre
clinical carcinogenicity studies data from
such studies do not usually become avail
able until very late in Phase III clinical
development.” The last sentence would
seem self-contradictory.
However, an August 14 company
release, issued in response to news reports
iujj^e Indian media, stated that rhe
rnBRe that had developed tumour had
been treated with ragaglitazar for almost
rwo years. Given that Phase II trials had
begun in September 2000, it is clear that
the animal tests could not have been “pre
clinical”, even assuming that the term is
meant to indicate only the starting date,
as Phase I trials should have lasted at least
six to eight months. So in all likelihood,
the long-term carcinogenicity studies (in
rats and mice) were initiated well after the
human trials had started. (The company
did not provide dates and other details of
Phase 1 and Phase II trials that were
sought through an e-mail query.)
The apparent contradiction may
seem somewhat academic because, in any
case, the results of animal trials were not
available before the human trials. But
therein lies the crux of the matter, an issue
of ethics - whether human trials should
be initiated before results of animal trials
relating to long-term carcinogenicity
become available.
Countering criticism that the animal
82
trials were not initiated well in advance, the
release further said: “Some types of animal
studies must be performed before starting
human trials... These studies show whether
the new medication has any unwarranted
side effects which develop in less than six
months of treatment. Safety data from sixmonth toxicity studies on two animal
species (rat and dog) were made available
to rhe authorities as required by law, before
the human studies were initiated...The car
cinogenicity studies must be performed on
compounds that are developed where treat
ment ofpatients is expected to exceed more
than six months. According to interna
tional guidelines, these types of long-term
carcinogenicity studies need not be con
ducted prior to entering Phase III devel
opment. The study data is only required at
the time of (marketing) approval of the
medicine.”
Said Bhargava: “I do not care about
laws and regulations. It is simply unethical
to begin human trials before animal tests
are over. I can understand (this argument)
in the caseofHIV or cancer where there is
no treatment available and it is in human
interest to reach a new potential drug
quickly to the people. But diabetes is not
incurable and there are a whole lot of
drugs.”
“The existing system of guidelines for
clinical trials and long-term carcinogenic
ity' studies do not address the case of drag
development for chronic use adequately.
Even the guidelines of the Indian Counc'd
of Medical Research (ICMR) lack clarity
in this respect,” points out Vineeta Bal of
the National Institute of Immunology
(Nil), New Delhi, who has been concerned
with ethical issues in biomedical research.
Vineeta Bal added: “It is precisely for
drugs meant for chronic use that long-term
carcinogenicity results should be known
before you begin clinical trials. Generally,
such animal studies will take about three to
four years. Companies are not willing to
wait chat long. So they carry out such stud
ies in parallel widr clinical trials, which is
not ethical. There could be some flexibili
ty in the case ofa disease like HIV. But this
flexibility has to be made more specific
instead of the existing vagueness, which
companies exploit to their advantage.”
Said Vasantha Muthuswamy of the
ICMR: “We insist on animal test results as
per the requirements of the Schedule Y of
the Indian Drags and Cosmetics Act to be
available before clinical trials can be
approved whenever a drug is referred to us.
While die referral process is meant to be
mandatory, some cases are sent to us and
some are not. This particular case did not
come to us.” However, there is inherent
vagueness and an apparent inconsistency
in Schedule Y with regard to carcinogenic
ity studies. As a result, it is open to inter
pretation and it may be argued - as indeed
Novo Nordisk has—that the company had
complied with the requirements under
Schedule Y.
CLOSER reading of the Schedule
shows that Novo Nordisk has not
complied with other aspects of the regula
tions as well. In Schedule Y, under Animal
Toxicity (Appendix I, Item 4), a clear dis
tinct ion has been made between long-term
animal toxicity'data and mutagenicity/carcinogenicity data that are required to be
submitted for obtaining clearance for clin
ical trials (Article 1.2). Long-term toxicity'
studies are required to be carried out in at
least rwo mammalian species, one ofwhich
should be non-rodent. The Schedule also
specifies (Appendix III) that for drags to be
administered (orally, parenterally or transdermally) to humans for a period longer
than 3 months, animal test data (in the two
species) over a period of six months are
required to be submitted if the clearance
required is for Phase III and/or marketing
permission (MP).
,4s the press release of August 14 has
stated, it is this 6-month data (in rat and
dog) that rhe company had supplied to
the Drug Controller General of India
(DCGI) in order to get approval for clin
ical trials under the Indian law. The
response of Anil Kapur, Managing
Director ofNovo Nordisk India Pvt. Ltd,
to Frontlines e-mail questionnaire makes
it clear that the term long-term toxicity
has been interpreted to include carcino
genicity as well. If it was a question of
semantics alone, it could be argued that
carcinogenicity is a facet of long-term
toxicity and, therefore, requirements
under Schedule Yhave been met. But the
requirements of mutagenicity/carcinogenicity studies data are different and
have been specified in Article 3.5 of
Schedule Y. It states: “These studies are
required to be carried our if the drug or
its metabolite is related to a known car
cinogen or when the nature and action of
the drug is such as to suggest a carcinogenic/mutagenic potential. For carcino
genicity studies, ar least two species
should be used. These species should not
have a high incidence of spontaneous
tumours and should preferably be known
to metabolise the drug in the same man
ner as humans... The drug should be
administered 7 days a week for a fraction
of the lifespan comparable ro the fraction
A
FRONTLINE, SEPTEMBER
2002
El CONTROVERSY
Drug trials and questions
The suspension of clinical trials of a promising new anti-diabetes drug in humans following reports of
drug-induced tumours in laboratory mice raises a host of ethical issues.
R. RAMACHANDRAN
THICS and commercial interests
often do not go together. One indus
trial sector where this conflict is perhaps
most evident is pharmaceuticals. It is not
uncommon for pharmaceutical companies
to tend to exploit regulatory loopholes in a
bid to enter the market quickly when the
perceived commercial potential for a
promising novel drug is big. A case in point
is the recent controversial worldwide clin
ical trials by a multinational company of a
new anti-diabetes drug discovered in India.
After several months of Phase III clin
ical trials of the drug ragaglitazar in 2,550
individuals across 32 countries, the Danish
pharmaceutical
multinational
Novo
Nordisk suspended the trials on July 22
after the discovery of urinary bladder
tumour in mice on July 8. The drug, codenamed NN622 by the company, was dis
covered by the Hyderabad-based drug
company Dr. Reddy’s Laboratories (DRL)
and was licensed out to Novo Nordisk in
August 1998. Before licensing, the drug
was called DRF-2725 by the Indian com
pany and, according to the DRL
spokesman, had undergone “preclinical
and some preliminary toxicology studies”.
The objective of any Phase III trials is
to obtain sufficient data about the efficacy
and safety of the drug in a large number of
patients of both sexes in multiple centres
usually in comparison with a standard drug
and/or placebo if a standard drug does not
exist. On successful completion of Phase
III trials, permission is granted to market
the drug. In the present case, of die 2,550
persons, about 1,100 had received NN622
while the rest had received another drug,
or a placebo, according to a company state
ment.
Ragaglitazar (NN622/DRF-2725) is a
dual-action insulin sensitiser for the treat
ment of Type 2 diabetes. Insulin sensitis
ers are substances that stimulate the body’s
ability to utilise insulin. It is characterised
as a “dual-action" drug because of its abil
ity to regulate both sugar and fat levels in
blood. In medical jargon, the drug is a
“PPAR (peroxisome proliferator-activated
E
ERONTLINE, SEPTEMBER 27. 2002
receptor) alpha and gamma agonist”. It is
stated to be chemically and pharmacolog
ically different from currently marketed
“PPAR agonist” anti-diabetic drugs and
constitutes a new class of insulin sensitis
ers.
According to media reports, Phase II
trials of the drug began in September 2000
and were completed in September 2001,
when the company announced that the tri
als had provided clinical proof of the con
cept for NN622 and said that it had
decided to initiate Phase III trials. Novo
Nordisk claimed that in pre-clinical animal
tests and Phase I and Phase II human tri
als, NN622 had demonstrated “significant
potential to regulate blood glucose and dia
betic dyslipidaemia (or abnormal blood
lipid levels)”. Phase III trials began in
November 2001.
The company claimed that the com
pound would be among the first to reach
the market from a new generation of dual
action sensitisers under development.
According to market sources, the nearest
competitor to NN622 was Glaxo
SmithKline’s Farglitazar (GI262570),
which was also withdrawn recently owing
to a different kind of adverse reaction.
Apparently, the Glaxo drug was ahead of
Novo Nordisk in the development cycle.
Therefore, NN622 would have been the
first to hit the market had Phase III trials
reached completion.
The company release of July 22 said:
“Novo Nordisk’s decision was taken in
response to findings of urine bladder
tumours in one mouse and a number of
rats treated with ragaglitazar. All current
clinical trials involving ragaglitazar have
been stopped and all planned new clinical
trials have been postponed, while prelimi
nary data from studies in rats and mice are
being investigated.”
Apparently, tumours had been seen in
a number of rats in February itself.
However, clinical trials were continued
because, according to the company, many
drugs currently available in the market have
been shown to cause tumours in rats and
so the findings were not considered to be
alarming. A Novo Nordisk release added:
“It is a known fact that the development of
such tumours in rats is species-specific and
does not have any implications for humans.
Nevertheless, this data was immediately
shared by Novo Nordisk with the regula
tory authorities and the trial continu^
with the knowledge and consent ofthe reg
ulatory authorities concerned.”
According to the company, all the
patients were asked to reassess their con
tinued participation in clinical trials, and
sign a new Patient Informed Consent
Form, which included information about
the tumours found in rats. “(Considering)
the fact that tumours have now been
reported in two species, it was not ethical
to continue trials in humans until it can be
documented that the mechanism by which
these tumours develop is specific to
rodents,” the release said.
However, the company refrained from
disclosing the names of the countries and
the centres where the trials had been going
on. Details about Indian subjects partici
pating in the trials would perhaps not have
come to light but for the fact that, through
a PH story ofAugust 13, Pushpa Bhatia,
the eminent biologist and former diSBr
of the Centre for Cellular and Molecular
Biology (CCMB), Hyderabad, questioned
the ethics of carrying out human trials
before the animal trials were completed.
As a member of the institutional
ethics committee of the Nizam Institute
of
Medical
Sciences
(NIMS),
Hyderabad, Bhargava had reasons to be
concerned as the NIMS was one of the
Indian centres participating in the Phase
III trials of NN622. According to Novo
Nordisk, which responded immediately
with a press release, 130 persons from
India were part of the suspended NN622
trials and half of them would have
received doses of NN622. In response to
an
e-mailed
questionnaire
from
Frontline, Novo Nordisk provided a par
tial break-up of the number of patients
participating in Phase III trials in coun
try groups rather than individual coun
tries. It also refused to give any more
information beyond stating that eight
Indian centres were involved in the Phase
81
GOVERNMENT OF KARNA TAKA
DRUGS CONTROL DEPARTMENT
PALACE ROAD, BANGALORE-560001.
WORLD BANK ASSISTANCE
- CAPACITY BUILDING OF
DRUGS TESTING LABORATORY
WORLD BANK ASSISTANCE - CAPACITY BUILDING OF DRUGS TESTING
LABORATORY, DRUGS CONTROL DEPARTMENT, GOVERNMENT oF~
KARNATAKA.
PROPOSAL AT A GLANCE
Expenditure in Lakhs
Head
a) Precision instruments/equipment
b) Technical Staff
c) Construction of additional space
for laboratory.
d) Infrastructure for the laboratory
e) Furniture
f) Operating cost (consumables and
service charges)
g) Training of Analysts
h) Library and References Section
(a) Establishment of “NICNET"
(b) Journals & Reference Books.
i) Maintenance of equipment’. '
j) Providing transport facilities
(including maintenance & staff)
k) Computerisation
I) I EC activity to be kept at the
disposal Government of India.
m) Sampling and Travel expenses.
Total:
One time
capital
expenditure.
230.00’
—
Per annum
recurring
expenditure.
—
Total recurr-ing expendi-ture for 5 years.
—
48.80
244.00
—
—
—
—
20.00
2.00
100.00
10.00
—
5.00
**
10.00
6.00
25.00
30.00**
30.00
50.00
***15.00
10.00
- -
50.00***
—
20.00
100.00
489.00
250.00
20.00
20.00
—
5.00
600.00
*To be purchased in a phased manner in 3 years. (25% is added due to foreign
exchange fluctuations to the original proposal)
To be spent at the rate of
1st year
- 2.00 lakhs
llnd year
- 4.00 lakhs
llrd year
- 6.00 lakhs
IVth year
- 8.00 lakhs
Vth year
- 10.00 lakhs
TOTAL ASSISTANCE SOUGHT
IN LAKHS
A. CAPITAL EXPENDITURE
B. ONE TIME EXPENDITURE INCLUDING HI-TECH
EQUIPMENT .
C. RECURRING EXPENDITURE FOR 5 YEARS.
Total:
TOTAL:
Rs.1089.00 lakhs.
LABORATORY
250.00
350.00
489.00
1089.00
ABSTRACT OF EXPENDITURE
I.
ONETIME EXPENDITURE - Rs.479.00 Lakhs
HEAD
1) Instruments
2) Construction
3) Infrastructure
4) Furniture
5) Establishment of'Nicnet"
6) Transport facility7) Computerisation
8) I.E.c.Activity
TOTAL
- II. RECURRING EXPENDITURE -
Rs.in lakhs
230.00
250.00
20.00
20.00
5.00
10.00
50.00
15.00
600.00
RS. 489.00 LAKHS
STAFF
Head
Drugs Testing
Laboratory Technical Staff
OTHERS
Per annum
Per 5
Years
48.80
244.00
48.80
TOTAL
244.00
Head
a) Journals and
periodicals.
b) Operating cost.
c) Maintenance of
instruments.
d) Training of Analysts.
e) Maintenance of vehicle
including salary of
drivers
f) Computerisation
TOTAL
Per annum
Per 5 •
years
5.00
20.00
6.00
(average)
2.00
25.00
100.00
30.00
6.00
10.00
30.00
50.00
49.00
245.00
10.00
Grand Total: Rs.600.00 + Rs.489.00 = Rs.1,089.00 Lakhs
SUMMARY OF POSTS TO BE CREATED UNDER WORLD BANK ASSISTANCE SCHEME
DRUGS TESTING LABORATORY
1.
2.
3.
4.
r 5.
--Resignation
■
•• ■•■•<•'« ^o.of posts
Technical Officer
1
Senior Chemist
5
Junior Chemist
20
Laboratory Supervisor
10
Laboratory Attender
_________
• 10
3
c
WORLD BANK ASSISTANCE - CAPACITY BUILDING EXPANSION OF DRUGS
fESTINGTABORATORY OF DRUGS CONTROL DEPARTMENT, GOVERNMENT OF
KARNATAKA.
The Drugs Control Department, Government of Karnataka has been
entrusted
with the responsibility of overseeing the quality of Drugs and Cosmetics. Drugs Industry
in the recent years has recorded Phinomenal growth
and the turnover of drug
formulations and bulk drugs is in the order of more than 10,000 crores per annum in the
country.
India being a vast country and regulation mechanism over the manufacture
rests with the concerned State Drugs Controllers there has been an increased need to
exercise stricter vigilance over the quality of the drugs.
The Drugs Control Department has been functioning in Karnataka State since
1965.
The department has three wings namely, Enforcement Wing, Drugs Testing
Laboratory
and
Pharmacy
Education
Government College 'of Pharmacy).
(i.e.,
Board
of
Examining
Authority
and
As a result it has not been possible to increase
the capacity of the laboratory to take up analysis of increased number of samples and to
update with modern sophisticated instruments.
After careful consideration and examination of all aspects, this proposal has been
prepared involving a total expenditure of
(a) Capital expenditure Rs.250.00 lakhs for
providing additional space for laboratory (b) One time expenditure of Rs.350.00 lakhs
for purchase Hi-tech equipments including developing infrastructure and (c) a recurring
expenditure of Rs.489.00 lakhs at the rate of Rs.97.80 lakhs per annum. A brief note
under each head is given to illustrate the proposal.
(a) Instruments and equipment,
(b) Technical Staff,
(c ) Construction of Additional Space for laboratory,
(d) Infrastructure,
le) F u mfture for laboratories,
(f) Operating costs,
(g) Training of Analysts,
_(h) Library and reference Section,
(j) Maintenance of equipment.
(J) Providing transport facility
IkLComputerisation
(I) lEC activity to be kept at the disposal of
-Government of India.
LIT) Sampling and Travel expenses.
4
Karnataka State has been a model state despite various limitations. The aim of
the department is to provide an excellent facility particularly in the field of Test and
Analysis
so that every kind of drug can be analysed without any delay.
Present
capacity of the laboratory in terms of number of samples which can be analysed is
around 2,000 - 2,500 which is inadequate and as such the capacity has to be increased
so that the field officers
duties.
can draw more samples in the course of discharge of their
Inspite of efforts there is delay in the test and analysis of samples resulting in
backlog of samples.
The department is confident of overcoming the delay if the
proposals contained herein are implemented.
| (a)INSTRUMENTS AND EQUIPMENT]
It is proposed to equip the laboratory with modern and sophisticated instruments
for precise, quick and accurate analysis.
The total expenditure (one time capital
expenditure) is estimated to be around Rs.230.00 lakhs. The expenditure is proposed
to be incurred in a phased manner in three years. This step will increase the efficiency
of the laboratory in terms of capacity. The list of instruments proposed to be procured
are shown in ANNEXURE-I.
| (b) TECHNICAL STAFF"]
While equipping the laboratories as proposed above and thereby increasing the
capacity it is essential to provide adequate technical staff.
Hence, the department
proposes to create additional technical staff of the following cadres.
Name of the Cadre
1) Technical Officer (Instruments maintenance)
_2) Senior Chemists
3) Junior Chemists
4) Laboratory Supervisors
■5)-Laboratory. Attendees
Post/s
1
5
20
10
JjO
The anticipated expenditure towards additional technical staff is around Rs.
48.80 lakhs per annum which comes to Rs. 244.00 lakhs for 5 years - details shown in
ANNEXURF-li
5
|~(c) CONSTRUCTION OF ADDITIONAL SPACE FOR THE LABORATORY |
In view of the proposal to acquire additional sophisticated instruments as well as
to recruit additional technical staff, there is need to provide additional space to house
the equipment and to allot work space. Hence, it is proposed to construct an additional
2 730 sq. mts. on the existing building complex.
The department has its own land and building. There is enough scope to take up
additional construction so that another 2,730 sq. mts. area can be built.
The construction cost works out to approximately Rs.250.00 lakh.
| (d) INFRASTRUCTURE FOR NEW SECTIONS"]
In order to provide necessary infrastructure such as partitions, gas, electricity,
sanitary connections, air-conditioning and generators a one time capital expenditure of
Rs.20.00. lakhs is expected to be incurred.
|
The
(e) FURNITURE FOR LABORATORY~|
Laboratories
needs
necessary
furniture
and
works
benches
etc.
Expenditure towards providing furniture to the laboratory on one time basis is estimated
to be around Rs.20.00 lakhs.
|
(f) OPERATING COSTS
|
In the day to day analytical work, consumables such as Glass wares, Chemicals
and Solvents are essential.
In addition expenses towards service facilities such as
Electricity and Gas have to be met with.
Laboratory needs to procure reference
standards from authentic sources which is an essential requirement in drug analysis.
An estimated annual expenditure of Rs.20.00 lakhs under this head is expected to be
Incurred wTi'ich comes^o'Rs.TOG.WteTiTsTorTve-yea?s.
[ (g) TRAINING OF ANALYSTS/TECHNICAL STAFF |
is essential that analysts and other technical staff working in the laboratory are
sent for refresher course/training
periodically
to
update
their knowledge.
An
expenditure of Rs.2.00 lakhs per annum is expected to be incurred which comes to
Rs-10.00 lakhs for five years.
6
|
(h) LIBRARY AND REFERENCE SECTION
|
For any laboratory to funcfioin, the library and reference facilities are of utmost
importance.
It is proposed to modernise the library by linking with “NICNET” facililty
and to subscribe to various journals (National and International) on various aspects of
analysis of Drugs and Cosmetics.
The anticipated expenditure towards this head is
around Rs.30.00 lakhs (Rs.5.00 lakhs towards one time„.expenditure to establish
"NICNET” and Rs.25.00 lakhs towards recurring expenditure for 5 years for subscribing
to Journals and Books).
0) MAINTENANCE OF INSTRUMENTS AND EQUIPMENT |
Periodical servicing and replacement of parts whenever required for instruments
forms annual maintenance feature. A total expenditure of Rs.30.00 lakhs for 5 years is
earmarked at the rate of:
YEAR
RS.IN LAKHS
1st
2.00
2nd
4.00
3rd
6.00
4th
8.00
5th
10.00
0) PROVIDING TRANSPORT FACILITY
With a view to exercise stringent quality control over drugs it is necessary that
amples are collected even from remote areas at the quickest possible time. It will be
Tactically difficult for the inspectorate .staff .to .depend jjponjsublic transport of wide
average.
Therefore it is proposed to purchase two transport vehicles for sampling
Jrpose at one time expenditure of Rs.10.00 lakhs. A recurring expenditure of a sum of
s.30.00 lakhs at the rate of Rs.6.00 lakhs per annum towards maintenance cost fuel
id driver salary has been earmarked.
7
(k) COMPUTERISATION
From the point of convenience as well as axes to information, it has become
necessary a computerized the entire activity of Drugs Testing Laboratory.
This will
result in increased efficiency it has been proposed to computerized the laboratory at a
one time expenditure of Rs.50.00 lakhs and a recurring expenditure of Rs.50.00 lakhs at
the rate of Rs. 10.00 lakhs per annum is anticipated for this purpose.
IEC ACTIVITY TO BE KEPT AT THE DISPOSAL OF GOVERNMENT OF INDIA
A sum of Rs.20.00 lakhs (one time expenditure) is proposed to be kept at the
disposal of Government of India for IEC activity."
(m) SAMPLING AND TRAVELLING EXPENSES
Since the Drugs Testing laboratory, Karnataka ia a statutory laboratory, analysis
)f legal samples are carried out. As per the Drugs and Cosmetics Act only the Drugs
nspectors have to draw samples and while drawing samples fair price for the samples
lave to be tendered. As it is proposed to increase the sampling a recurring expenditure
. >f Rs.100.00 lakhs at the rate of Rs.20.00 lakhs per annum has been earmarked
wards cost of sampling and travel expenses towards drawing of samples.
(R.An^NDARAJASHEKAR)
DRUGS CONTROLLER FOR THE
STATE OF KARNATAKA, BANGALORE.
ANNEXURE-I
IJst of Analytical Instruments proposed to modernise Drugs Testing Laboratory.
Government of Karnataka, Bangalore,
3.
Instrument
UV Spectrophotometer with
Library (1)
■HPLC (1)
HPLC Columns (10)
Computer and Printer for HPLC
HPLC Filtration Kit
Computer based Integrators for
HPLC and GC
Distilled water plant with Frac
tionating Columns(2)
Tablet Dissolution Tester(2)
3
Tensile Testing Machine
SI.No.
1.
2.
3
4.
5.
5.
7
0.
Autotitrator (1)
1.
I.T.I.R. with Library
2.
Polarimeter
3.
4.
5
6.
Centrifuge
B.O.D.Incubator(2)
Laminar Flow Bench
Top Loading Balances(2) with
diaital orinter.
Tele Thermo meter.
Elisaprinter with reader
Refrigerator with deep
freezer(2)
Refractor (1)
Gas ChromatographColumns for Gas Chromatograph
Travelling Microscope
Water Purification system
Reverse Osmosis System
7.
3.
9,
9.
L
t.
----- —.
Utility
Identification and Quantification of
drugs
-doAccessory to HPLC
-doAccessory to HPLC •
Accessory for the above.
Preparation of distilled water.
For carrying out dissolution test of
tablets and capsules.
Measurement of Tensile strength of
Adhesive
Tapes,
Candoms,
Switches etc.
Required for K Titrations & Potentio
metri.
Identification & Quantification of
drugs.
Testing
of
Optically
active
compounds.
Analysis of Blood & Blood Products.
Sterililty test.
Micro-biological testing of drugs.
Precision weighing.
Pyrogen testing.
Testing of Blood & Blood Products
Storage of reference standards and
for routine work.
Refractive Index of certain drugs.
Quantitative estimation of drugs.
Accessory for the above.
Medical devices testing
To prepare HPLC grade water.
Preparation of water of distilled
water.
h
9
r26.
28.
Automic Absorption Spectrophoto
meter.
Particle sizer
N.M.R.
Laboratory information and
management systems software.
Un-interruptible power supplies
30.
(20 KVA)
Spectroflouro photometer
"rF
. ~3Z Z Polygraph with Operating table.
■ '29-^
Trace elements analysis.
Measurement of articles in IV fluids
For confirming purity & structure of
drugs.
Useful for Automatic data Acqui
sition & instrument control.
To get continuous power supply.
Flouroseoence Analysis.
Pharmacological testing of drugs.
10
ANNEXURE-II
Statement indicating the total expenditure that would be incurred for the creation of
proposed additional posts on the basis of salary and other allowances at the entry
stage under capacity building of the Drugs Testing Laboratory
No.of
posts
regui
-red
Pay
scale
2
3
4
Technical Officer
1
?
Senior Chemist _
5
j
Junior Chemist
20
.
Lab.Supervisor
10
Lab. Attender
10
SI.
Name of the post
No
r
TOTAL
Rs.
Salary and allowances per month per post
calculated on the basis of mean basic pay for
promotional posts and minimum basic pay for
direct recruitment posts.
Rs.
Rs.
Rs.
Rs.
Rs.
8
9
5
6
7
H.R.A C.C.A
Total
Basic
D.A.
Pay
800010,720
13440
63008,762
11840
55755,575
10620 '
45756,572
8400
27753,790
4950
Total per
annum
per post
Rs.
Total for
five
years
Rs.
1.0
11
3,960
1,179
200
16,065
1,92,780
9,63^
3,242
964
200
7,90,080
39,50,400
2,063
613
200
20,28,240
1,01.,41,200
2,432
723
150
11,85,240
59,26,200
1,402
417
90
13,168
x5
8,451
x20
9,877 x
10
5,699
x'10
6,83,880 j 34,19,400
48,80,220 ] 2,44,01,100
ANNEXURE-IJJ
;
■
ESTIMATE for proposed construction of additional ACCOMODATION
EnR~~LABORATORY AND RESEARCH AND DEVAIoF^MENT WING AT DRUGS
TESTING LABORATORY, PALACE ROAD, BANGALORE?
LinP Estirnate
T
Construction of building at rear side of the main building
rear side quardrangle.
A. BLOCK:
(GF, FF, SF & TF) 4 x 34.0 x 9.00
1,224.00 sq.mt.
El BLOCK: '
(GF. FF, SF & TF) 4 x 19.0 x 9.00
684.00 sq.mt.
C BLOCK : For construction of
existing animal house for
SF&TF 2 x24.60 x 16.00
787.20 sq.mt.
D, BLOCK:
Ramp to connect the
main building and animal
house and lift room. 2 x 8.30 x 2.10 34.86 sq.mt.
Total
2,730.06
sq.mt.
at Rs.6,000/- sq.mt.
Rs.1,63,80,360
Rounded to
Rs.164.00 lakhs
2.
Providing wall panelling with accuostic arrangement, false
Rs. 12.00 lakhs
Ceiling, Veniyel flooring etc. in the existing auditorium.
for 264 sq.mt
3
Rs. 15.00 lakhs
Providing Dias in Auditorium including sitting
arrangements
4.
Rs. 15.00 lakhs
Providing additional lift arrangements for'D'Block
5.
Rs. 12.00 lakhs
Providing A.C. arrangements
6.
Rs. 15.00 lakhs
Electrification charges LS
7.
Rs. 15.00 lakhs
Providing water supply and sanitary arrangements LS
8.
Rs. 2.00 lakhs
Miscellaneous and rounding off including escalation of
—___ rates LS
r
TOTAL
! Rs.250.00 lakhs
ls/revwb-ll/131299
or
The GPHFMinilab®
Protection Against Counter
feits and Substandard Drug
Products
Simple Test Methods for
the Quality Assurance of
Pharmaceuticals
Medical Mission Institute
Co u nut© ir feat and Substandard
Pharmaceuticals
Counterfeiting of phar
maceuticals and the proli
feration of substandard
drugs constitute a serious
health risk for the popu
lation around the world.
Experts assume that as
many as seven percent of
the world's total sale of
drugs is already being
counterfeited. Most hit
are the people living in
developing countries for
whom high quality and
inexpensive drugs are not
readily available and
where the means for an
effective drug quality
control system are not yet
fully in place.
Based on this situation, the German Pharma
Health Fund e.V. (GPHF). a non profit making
organization established by research based phar
maceutical companies in Germany, has developed
some easy-to-use test methods that are designed
to protect the people in developing countries
against the, frequently fatal, consequences of
taking counterfeited or substandard pharmaceuti
cal drug products. This developing work has been
done in close cooperation with Prof. Peter Pachaly.
School of Pharmacy at University of Bonn and
Prof. Klaus Fleischer.
Department of Tropical
Medicine at the Medical
Mission Institute in Wurz
burg. Germany.
The Objectove:
Provision of Easy-to-use and
Versatile Test Methods
’ The objective of the
GPHF-funded project is
the provision of simple
test methods which
makes it possible to idenc
tify substandard or coun• k—
£>■
terfeited pharmaceuticals
under the specific conditions encountered in deve
loping countries. The
method in question should be inexpensive, trans
portable, versatile and used reliably even by less
experienced local personnel in developing coun
tries.
r
ft
After several years of development, the GPHFMinilab® was subjected to lengthy field testing in
Kenya, Tanzania. Ghana and on the Philippines
between 1997 and 1998. These tests have shown
that the Minilab is a practical and effective tool
for the identification and quality assurance of
pharmaceutical drug products.
The trials have confirmed also that all procedures
employed by the Minilab can be performed with
out any problems in primary health care stations.
hospitals and pharmacies even when based in
rural areas. Furthermore, all methods in use are
also suited for customs officials based at har
bours, airports or any other port of entries. Thus.
the GPHF-Minilab® is a very helpful and impor
tant tool for all government authorities, profes
sional bodies and non-governmental organisati
ons working in public health care and being res
ponsible for a constant supply of high quality
drugs in developing countries.
Verifying ©irag Quailatty:
Four Simple Tests Are
Required Only
Attention Focussed
on Counterfeit Drugs
The Minilab's test scheme employs a set of four
physical and chemical tests in order to decide on
the quality of a given drug product:
. Sophisticated visual inspection scheme on solid
dosage forms including the associated packa
ging material for a timely rejection of rough
counterfeits.
. Simple tablet and capsule disintegration tests
for a preliminary assessment of deficiencies
related to drug solubility and availibility.
3. Simplified colour reactions for a quick check of
any drug present, thus ensuring the drug's iden
tity.
4. Easy-to use thin layer chromatographic assays
for a quick check of any quantities of drug pre
sent. thus ensuring the drug's potency.
Based on the Essential Drug List of the World
Health Organization (WHO) and prevailing prac
tice, fifteen of the most used drugs have been sel
ected which are also known to be liable for fre
quent counterfeiting. The short list of the GPHFMinilab® does include many essential antibiotics
and antiparasitics as well as some analgetic and
anti-inflammatory' drugs many of which are
instantly life-threatened if diluted down to
nothing:
• acetylsalicylic acid
• amoxicillin
• ampicillin
° chloramphenicol
• chloroquine
° cioxacillin
• co-trimoxazole
• erythromycin
• mebendazole
» metamizole
• metronidazole
• paracetamol
• penicillin V
• prednisolone
• tetracycline
A Complete Laboratory
Assembled in Two Cases
The GPHF-Minilab® has been designed in such a
way that all the labware required fits into two
mobile units each having the size of a standard
suitcase and weighing about 10 kg when fully loa
ded. The GPHF-Minilab® can be operated with
out an external power supply if required. Both.
the low weight and independence from power
makes the GPHF-Minilab® a truly mobile system
and fit for use tn the field.
The GPHF-Minilab® is equipped with a full set of
secondary standards for reference purposes and
contains all the necessary laboratory accessories
in order to perform all tests on the spot without
any restrictions. The equipment includes, for exam
ple. caliper rules, test-tubes including rack, pipet
tes. precoaled TLC plates, developing chambers,
all glass containers and vials in different sizes for mix
ing and battery-powered UV handlamps of various
preset wavelengths for an easy detection of drugs.
The GPHF-Minilab® comes with two manuals
written in plain English and lull of descriptive pic
tures and illustrations (about 130) explaining all
analytical methods and operation procedures
taking the form of a step by step guide (Volume I
'Colour Reactions'. Volume II 'Thin Layer Chro
matography'). All procedures are also provided
in a summarized version on laminated sheets resi
stant to spillage for routine bench work.
Alongside the GPHF-Minilab® are travelling
about 40 kg of reagents and solvents as a
!1 start-up package such completing the stanI I
dard version of a GPHF-Minilab® when
>
ordered first time. Finally, a reliable labora
tory management will be facilitated using
the reporting, stock record and order forms
supplied.
Drug QuaDoty ComtroD
Low Cost
The overall priority
during the GPHF-Mini
lab® development was to
present reliable lest
methods employing a
simple and versatile tech
nology which would
make the GPHFMinilab® affordable to
everybody. After inten
sive development work and product sourcing the
entire test system of the GPHF-Minilab® can be
offered at a bought-in price of 2.570 USS (2,260
EURO) excluding any taxes, shipping costs and
customs fees.
The quantities of reagents and solvents supplied
in the start-up package are sufficient to support at
least 3.000 colour reactions in order to verify the
drugs' identity and 1.000 TLC runs in order to
verify their potency thus ensuring that the costs
for one quality check are about 1.3 USS or 1.0
EURO only. Replacement of consumables is
required from time to time, maintenance, howe
ver. not. All analytical reagents and the equip
ment arc carefully selected so to ensure that they
are locally available and that the GPHF-Minilab
is permanently fit for use.
The GPHF-Minilab® will be supplied to all inte
rested parties willing to undertake permanent
efforts to monitor their drug supplies consistently.
It is primarily dedicated to people who are wor
king in the public health care system of develo
ping countries and are directly responsible for a
constant supply of high quality drugs.
Minilab Training:
Well Advised and
Recommended
Special efforts were made to keep all operation
procedures of the GPHF-Minilab® as simple as
possible. However, the German Pharma Health
Fund (GPHF) and the Medical Mission Institute
recommend an introductory training course
regarding the proper use of the Minilab's analyti
cal techniques especially for less experienced
local staff involved in day-to-day drug analysis.
Continuous training at relatively low costs will be
offered
o at the training centre of the Medical Mission
Institute in Wurzburg. Germany. (Duration:
1 to 5 days depending on the actual background
knowledge of the trainees)
o at training centres of the Medical Mission Insti
tute or any other GPHF partner organization in
developing countries (Duration: 5 to 10 days
depending on the actual background know
ledge of the trainees)
o on request by the GPHF-Minilab® Project
Manager.
For further details on the GPHF-Minilab”
contact:
German Pharma Health Fund e.V. (GPHF)
P.O.Box 150 123*60061 Frankfurt/Main-Germans
Tel/Fax: Im. ++49-69-63153257
Internet: http://www.gphf.org
Missionsiirztliches Institut Wurzburg (.M1W)
- Appro lech Lehrlabor Hermann Schell-Str. 7
97074 Wurzburg ■ Germans
Tel/Fax: Int. ++49-931-80485-15/-25
or
Technologic Transfer Marburg (TTM)
in die Dritte Welt e.V.
Aui'der Ktipferschmiede I
35091 Colbe-Germany
Tel/Fax: Int. ++49-6421-87373-0/-73
who is a licensed distributor of the
GPHF-Minilab .
Published by: German Pharma Health Fund e.V. (GPI IF)
Concept/Edilor: Christian von Berg (MS&L)
Design: Christopher Wahrenberg
1st edition. August 1998
from:
sanajorc renu ana cnmu <sanajbrc@icener.net>
To:
"Dr Dabade" <drdabade@sancharnet.in>: "Sudarshan H" <vqkk@vsnl.com>: "Shvamala
Rhaskaran" <vani3@hotmail.com>; <shyamanarang@hotmail.com>’ <esparun@bgl vsnl.net.in>:
<:soch?.r?@vsp!.com>: <’v?.n@Ysri!.corn:>‘ <pr?.s?.nn?i
nC?r?rn’j.n!ty
Gc.
'Ancnji.il riiaukt/" ^aniui>jj(§/.vsiii.cui‘ii>t <nubsroy@vsni.net>, <jss_9at1iyari@rediffir1aii.corn>
Subject*
Re- ISRGFNT- Find Col Gnoinath
I uesdav. August 19, 2UU3 9:20 AM
Sent:
5 ?
b 11iyi
rrjrrv£
vpp
News
New "Delhi
F
5 J 2 <2 T’:T
■—
J
lor nrics rovjsjcn
n w.vApie&&pu<um<wuiav.iviwxvG3v32v/iui uinuiix.siimu
&-3 i-
-y
A.
TTr 0^7^^
r:.!,
_
_ . __
r'5'2 tp1 tf* 2"?
n O S'® * *Cn ? tT? *
CrO1
£- - - _ _----- ----- -o -- ----- —o-
PhnT-nci Tr.-.ijnr G1nx<'Srni!hr<Tr1(.
,vhhV G1e<! •■•
leave petition f9T P) in
nicuivum iiuiuieu uy ilic guvcimiieni wuuiu apply lu ail baivlivs oi lucviivuics, old and ilcvv, widi die leian dispeiisei,
irrespective or wnen they were released to the market, the He order, which caught the entire pharma industry unaware,
can he of serious conscmiencc if the government decides to strictlv implement it and defend the high court in the SC.
Pharma industry bodies iDma anc OPPi have already approached rhe government for a friendly resolution of the issue.
The industry is hocetiil that the government had not favoured the HC order, which was based on the writ petition tiled bv
GGK as coercive action was taken against the company by local dn.19 authorities in Varanasi for violating the notified
rncs£ Joi Lo.-hcc ofins^ciiisc *s*s2ssd prior to ths govermneiit ords..
iicaiiiiViif
sanajcrc renu ano cninu <sanaiorcig)icenet.ner>
abade@sancharnet in>: "Sudarshan H" <vgkk@vsnl.com>: "Shvamala
hvamanaranai?i)hotiTiail com>’ <esoarun(®bol vsnl net.in:
implement tne policy tin a list of essential ana iires-aving drugs is prepared
brouoht into the basket of essential drugs
inn dru
f Health ana ramiiv welfare to
into consideration
a division oencn consisting of Chief justice im k jam ana jus-tice V <□
iuhcui wmcn was niqmv detrimental to tne puouc interest,
ine petitioners
which was mentioned ii he nevi
vv'as promulgated
Pago 2
rar enquiries an
cuv-if USeiHClKb 01
aiyueu uiat me puncy was iiameu Keepmy hi miiiu me vv t G ayi eemeiits
ana qionaiisation or economy.
ui me cenue. He iiau aisu suumitteu mat me yuvei 1111 lei it was yet to cuine
out with ths dhco while stating that the Government would not Give awav
its power on drug nririnn
Vviiiiiiy uie juuyemeiil iui trie Dencii, Chief Justice Jam ruled, "the price
control mechanism adopted in tne policy to deter-mine drugs under price
control
arhitrAry as it defeats the entire purpose of enuitAble
dributiori v.r.d 3VQiiab«Mty o« ccscntiMi drugs st u tUn price.
P:top 1 rrf 1
Main identity
From:
To:
"Pineite Lechlak" <On5443@in-box.net>
<sue.spence@pacificnet.net>
Sent:
Sunday. August 24 2003 8:52 AM
Subject:
We Offer The Lowest Prices On The Internet
i
i
discount Prescription iDraas Are Hare!
Visit Our Website And See How Much You Can Save?
We are proud to provide affordable health care!
We understand that the high cost of pharmaceuticals can
prevent you from obtaining the medications you need,
negatively impacting your standard of living and quality of life
Wever Pay High Prices On Prescription Drugs Again!
No more future mailing here
r8AWP15LNcvBLI36JSQ4HYm
Australian Prcscriber Vol. 20 No. 4 199/
.
■iiiliiiii in
Medicinal mishaps
Aspirin and non-steroidal
anti-inflammatory drugs
PreparedbyJ. Dowden, Editor, and A. Rohan. Secretary,
Adverse Drug Reactions Advisory Committee, Canberra
Aspirin has been available without prescription for many
years. Although it is readily available, it is not free of adverse
effects. Some patients have reactions to aspirin which may
have presenting symptoms ranging from a skin reaction to
angioedema and shock.
Hypersensitivity to aspirin is more frequent in patients with
asthma. An analysis of spontaneous reports received by the
Adverse Drug Reactions Advisory Committee indicates that, of
the 47 cases of bronchospasm associated with ingestion of aspirin.
30 patients had a history of asthma. Furthermore. 16 of these
30 asthmatic individuals were known to be allergic to aspirin.
While health professionals will generally be aware of the risks
associated with this class of drug, patients may not have this
knowledge. Patients with aspirin hypersensitivity, particularly
if they are asthmatic, should be aware that aspirin can trigger
90
bronchospasm. Patients (and even some health care workers)
may also not realise that other non-steroidal anti-inflammatory
drugs (NSAIDs) are pharmacologically related to aspirin and
can cause the same adverse reactions, especially in those who
have had a previous allergy to aspirin.
A recent case highlights the issue of cross-reactivity:
A 49-year-old man with asthma and known hypersensitivity
to aspirin was given a single indomethacin 100 mg
suppository for back pain. This suppository' was given
while he was a hospital inpatient. He experienced acute
respiratory distress with laboured breathing and
hypercapnia. He lapsed into semi-consciousness and
required urgent respiratory support involving intubation
and assisted ventilation in intensive care. He subsequently'
recovered from the episode.
With the increased availability of NSAIDs over the counter,
there is an increased potential for adverse reactions. While
consumer product information may help to warn about cross
sensitivity, health professionals can also alert patients they
know to be hypersensitive.
$Y\OG\
RATIONAL DRUG BULLETIN j|
% * S f
Fluoroquinolones—Tendinitis Alert
-Avijit Hazra
The fluoroquinolones are a recently synthesized group
of fluorinated antimicrobial drugs that have followed from
the earlier quinolones like nalidixic acid and cinoxacin.
Unlike the older generation quinolones, the
fluoroquinolones have much broader antibacterial
spectrum and more favourable action profiles. In addition
to rapidly killing most common Gram-positive and Gram
negative bacteria, they can inhibit various intracellular ■
pathogens such as Brucella, Chlamydia, Legionella,
Mycobacterium spp. Ciprofloxacin, ofloxacin, pefloxacin
and sparfloxacin have good activity against staphylococci,
including methicillin resistant stains. They are also active
against Pseudomonas aeruginosa and enterococci.
Ofloxacin and pefloxacin are under evaluation for the
treatment of leprosy. The potent antibacterial activity of
fluoroquinolones owes considerably to their unique mode
of action. However except for sparfloxacin,
fluoroquinolones are not active against anaerobes and
are less effective against pneumococci.
As a group the fluoroquinolones are relatively safe drugs.
The known adverse drug reaction (ADRs) are summarised
in Table 1. Their potency, broad spectrum and relative
safety have led to wide clinical use in diverse contitions
like gonorrhoea, chlamydial genital tract'infections,
urinary tract infections, shigellosis, respiratory tract
infections (less effective in community acquired
pneumonia), infections of bones, joints and soft tissues
and atypical mycobacterial infections. They are also used
for antibacterial prophylaxis in neutropenic patients. In
the US, in a single year (1995), retail pharmacists filled
14.4 million prescriptions for this group of antibiotics
alone. In India, exact figures are not available, but going
by the proliferation of brands, their use is already
widespread. The fluoroquinolones currently available in
the Indian market are ciprofloxacin, lomefloxacin,
norfloxacin, ofloxacin, pefloxacin and sparfloxacin.
:ln the context of expanding use and vigorous promotion
of fluroquinolones it is important to note that a new and
potentially serious ADR attributed to these, drugs has
come to fight, namely tendinitis and tendon rupture. The
salient features are as follows :
O Tendinitis following the use of fluoroquinolones has
been reported from a number of countries including
Australia, Belgium. France, UK and USA
G
The Achiles tendon is most commonly involved and
the involvement is often bilateral. Other affected
tendons include the rotator cuff of the shoulder, the
long tendon of the biceps, the long extensor of the
thumb and various small tendons of the hand.
®
Reports so far have implicated most of the available
fluoroquinolones including ciprofloxacin, enoxacin,
lomefloxacin, norfloxacin, ofloxacin and pefloxacin.
It remains to be seen whether the latest introduction,
sparfloxacin shares this drawback.
• The risk of tendinitis appears to be greater with old
age, concomitant use of corticosteroid drugs and
renal dysfunction
• The time to onset of inflammation is variable, ranging
from a day to several months after the initiation of
therapy. In a large proportion of cases tendinitis has
developed within a week.
• The reaction has occured at usual therapeutic doses
and also at higher doses. Clear dobe dependence is
yet to be seen.
• Tendinitis has resulted in tendon rupture. Rupture of
the Achilles tendon is a serious complication that
disables the patient for a long time and often
requires hospitalisation.
•
Even without rupture, the inflammation may take
long to settle, which it eventually does. Treatment
is mostly conservative, through bed rest and
physiotherapy. A ruptured Achilles tendon may
require immobilization in a cast.
• To avoid serious complications it has been
recommended that the offending drug should be
withdrawn at the first sign of inflammation.
RATIONAL DRUG BULLETIN
The reported incidence of tendinitis is low compared to the volume of
fluoroquinolone usage. However most criteria of causality appear to
be fulfilled and the consequences can be serious. Prescribers need
to be aware of this possibility. We expect that Indian manufacturers
will take cognizance of the fact and voluntarily include a warning in
the patient package inserts for the benefit of the users.
Table 1 : Adverse drug reactions and special precautions in the
use of fluoroquinolones
•
Common reactions : Anorexia, nausea, gastrointestinal upset,
headache, dizziness, skin rashes
•
Less common and rare reactions : Photosensitivity reaction,
serious hypersensitivity reaction like anaphylaxis, central nervous
system (CNS) manifestations such as hallucinations, delirium
or seizures, asymptomatic rise of blood urea nitrogen, creatinine,
and liver enzymes, jaundice, leukopenia, thrombocytopenia and
other blood dyscrasias.
•
Concomitant use of asprin like drugs may potentiate the CNS
stimulant effect of flouroquinolones leading to seizures.
•
Flouroquinolones such as ciprofloxacin and enoxacin impair
theophylline clearance. Toxicity may appear on concurrent use.
•
May potentiate the toxicity of cyclosporin, digoxin and warfarin.
•
History of epilepsy, severe hepatic disease or renal insufficiency
requires cautions use
•
Flouroquinolones are not recommended for use in children under
15yrs. because of the tendency to produce arthropathy in this
age group
•
In general their use is not recommended during pregnancy and
lactation because they have shown genotoxicity in animals and
are excreted in breast milk. Experience of use in these conditions
is limited.
•
New adverse drug reaction; Tendintions and tendon rupture.
PEFLOXACiN
• CATEGORY: A fluoroquinolone with broad spectrum
of activity.
• ACTION : Bactericidal activity against Gram
negative and Gram-positive organisms. Methicillin
sensitive Staph aureus susceptible. Mycobacteria
show moderate susceptibility. Not avctive against
anaerobic organisms.
Action by inhibition of bacterial DNA gyrase and
prevention of supercoiling of DNA.
• PHARMACOKINETICS : Rapid and complete oral
absorption Time to reach peak levels 1-1.5 hours
Food slows absorption. Widely distributed into
tissues and body fluids. Effective diffusion into CSF.
Plasma protein binding 20-30%. Extensively (90%)
metabolised and one of the metabolites is norfloxacin.
Renal clearance low Half-life is 6.0 to 13 hours.
Liver disease increases plasma levels but renal
impairment has no effect.
• INDICATIONS : Intraabdominal and gynaecological
infections, Bacteraemia, severe systemic infections,
gonorrhoea.
• DOSAGE: Adults 400 mg 2 or 3 times a day orally or
IV. In severe infections a loading dose of 800 mg can
be given. Dose reduction in severe liver disease.
• CONTRAINDICATIONS
:
Quinolone
hypersensitivity, pregnancy and lactation, children
under 15 and G6PD deficiency.
• ADVERSE REACTIONS: Usually mild and transient
nausea, vomiting, gastric pain, skin reactions, CNS
effects, photosensitisation.
• CAUTION : In patients with history of epilepsy, CNS
damage and severe cerebrovascular disease, liver
disease. Hypersensitivity reastions may occur.
• INTERACTION : Alterations in theiphylline kinetics.
increase in oral anticoagulant effect. Rifampicin
reduces and cimetidine increases half-life of
pelloxacin. Convulsions may occur when NSAIDs
are used concomitantly
Food especially milk and yogurt may reduce
absorption
Information on a fluoroquinolone in :
CIMS Drug Profiles 1993;2 (4) : 21
References:
1.
The Achilles heel of fluoroquinolones. Australion Adverse Drug Reactions Bulletin 1997; 16 (2): 7.
2.
Sasich LD, Wolfe SM. Petition by Public Citizen's Health Research Group to US FDA to require a warning on
all fluoroquinolone antibiotics. Public Citizen 1996; August 1.
3.
Huston KA. Letter : Achilles Tendinitis and tendon rupture due to fluoroquinolone antibiotics. New England
Journal of Medicine 1994; 331: 748.
4.
Pierfitte C, Gillet P, Royer RJ. Letter: More on fluoroquinolone antibiotics and tendon rupture. New England
Journal of Medicine '1995; 332: 193.
5.
Szarfman A, Chen M, Blum MD. Letter: More on fluoroquinolone antibiotics and tendon rupture. New England
Journal of Medicine 1995; 332: 193.
(no C3.
RATIONAL DRUG Bll I I Illi
Zinc Supplementation : Side-stepping the Real Problem
Avijit Hazra
Zinc is an essential micrountrient that occurs in all tissues
of the body and subserves diverse functions. It is a
constituent of various enzyme systems and is essential to
normal cellular metabolism, cell division, sexual
development, intestinal function, immune function and
perhaps also taste and vision.
The average adult human body contains around 3 g zinc
but there is no substantial store. A daily dietary supply is
therefore essential. Red meat, liver, fish, egg and sea foods
are rich in readily absorbable zinc. Plant foods, including
cereals, are frugal sources. Moreover the phytates and lignin
in vegetable matter impede the absorption of zinc.
Phosphates, calcium and copper can also interfere with
zinc absorption. Overall only small proportion of dietary
zinc is absorbed. Body zinc is 99% intracellular and plasma
zinc level averages 100 pg/dl (15 pmol/l). Excretion is mostly
in faeces with only traces appearing in urine The US
recommended daily dietary allowance for zinc is 5 mg for
infants, 10 mg for children, 15 mg for adult men and 12 mg
for adult woman (+ 3 mg during pregnancy; + 7 mg during
the first 6 months of lactation and + 4 mg during the next 6
months). The UK reference nutrient intake is somewhat
lower at 9.5 mg and 7 mg per day for adult men and woman
respectively.
A spectrun of zinc deficiency signs and symptoms have
been reported over the past 3 decades. These include
anorexia, stunted growth, delayed sexual development,
hypogonadism, hypospermia, disorders of keratimzation,
hair loss, impaired immune function, chronic diarrhoea,
impaired wound healing, night blindness and reduced taste
sensation. Biochemical abnormalities include reduction of
plasma zinc, alkaline phosphatase and testosterone levels;
impaired T-cell function and reduced RNA polymerase
activity in various tissues. The point to note here is that
most of these manifestations are of well established zinc
deficiency correlating wth significantly lowered plasma zinc
levels. Mild deficiency is difficult to diagnose, whether
clinically or through laboratory tests.
Certain individuals are at high risk of zinc deficiency :
• Persons with acrodermatitis enteropathica — a genetic
disorder in which zinc absorption is grossly reduced.
• Pregnant women on marginal diet, though a clearcut
zinc deficiency is yet to be demonstrated during
pregnancy.
• Poorly fed infants, particularly at the time of weaning.
• Children with protein-energy malnutrition
• Children with diarrhoea A vicious cycle of chronic
diarrhoea and zinc loss may be set up since diarrhoea
can be both cause and effect of zinc deficiency. Moreover
the associated defect in cellular immunity may
predispose to diarrhoeal infections.
o Adolescents with the habit of eating soil and dirt
(geophagia — an unusual cause of zinc deficiency which
can however be very severe).
• Chronic alcoholics.
e Patients on total parenteral nutrition (TPN).
o Patients on long-term penicillamine therapy.
Other chronic infections, strict vegetarianism and old age
are regarded as potential risk factors for zinc deficiency.
Zinc supplementation is necessary when a clear-cut zinc
deficiency exists. Such supplementation has restored
plasma concentrations in children receiving intensive
hospital treatment of kwashiorkor Zinc supplementation
may also reduce the intensity and duration of acute
diarrhoeal episodes in children. In acrodermatitis
enteropathica, large oral doses of zinc (30 - 45 mg/day)
may bypass the mucosal absorption block. However excess
zinc is not without toxicity. Doses in excess of 200 mg/day
are emetic and around 1 g/day may be fatal It has been
recommended that chronic supplementation in excess of
15 mg/day should only be under careful medical
supervision. Impairment of copper status has been reported
in healthy volunteers receiving modest doses and patients
given 150 - 300 mg/day have developed frank
hypocupraemia, microcytosis and neutropenia.
The practice of routine zinc supplementation is however
bereft of sound therapeutic rationale. Clear-cut zinc
deficiency is relatively uncommon. Marginal deficiency is
almost impossible to diagnose without plasma level
determination, which facility is not readily available in our
situation. Although zinc contributes to protective immunity
in diarrhoea, it is not recommended for routine treatment or
prophylaxis. The precise mode of action and status of zinc
are unknown and other trace elements may well contribute
to the integrity of a physiological system as complex as the
intestinal mucosa. As already mentioned, unequivocal zinc
deficiency has not been documented during pregnancy. The
risk in the elderly is modest. More studies are needed.
Unfortunately the practice of zinc supplementation has
'caught-on' in India and is tending towards ridiculous
proportions, particularly in urban practice. Table 1 presents
zinc preparations currently available in the India market.
Some facts immediately become obvious :
1. The sheer number of brands is amazing and the list is
far from exhaustive.
2. The zinc content per unit dose varies widely.
RATIONAL DRUG BULLETIN
Table 1 : Zinc containing formulations in the Indian market
Brand
Zinc content per unit dose
HIFI SOFTULES
Zinc sulfate (anhydrous)
15 mg / capsule
OSIFORT
Zinc sulfate
20 mg / capsule
NEUROGARD
Zinc sulfate
100 mg / tablet
BECOZINC
Zinc sulfate monohydrate
54.93 mg / capsule
SUPRADYN
Zinc sulfate
2.2 mg 1 tablet
B-COLENZ
Elemental zinc
22.5 mg 1 capsule
Z&B
Zinc sulfate monohydrate = Elemental zinc
15 mg / capsule
FEFOL-Z
Zinc sulfate monohydrate
61.8 mg / capsule
XENEXFORTE
Elemental zinc
20 mg / capsule
ALPROVIT
Zinc sulfate
3 mg /15 ml
KINETONE LIQUID
Elemental zinc
9.23 mg / 14 ml
BECOZINC SYRUP
Zinc gluconate = Elemental zinc
15 mg / 15 ml
GLOBAC LIQUID
Zinc sulfate
30 mg / 15 ml
AQUAMIN LIQUID
Elemental zinc
1.5 mg / 15 ml
ANTOXID
Zinc sulfate monohydrate
27.45 mg / capsule
HI-FE SYRUP
Zinc sulfate
7 mg / 15 mil
GLOBIRON SYRUP
Zinc sulfate
7 mg /15 ml
GRD BIX granules
Elemental zinc
22.5 mg / 20 g
RIDAGE
Zinc sulfate monohydrate
27.45 mg 1 tablet
PRAMILAC power
Elemental zinc
5.6 mg /15 g
REVITAL
0.5 mg / capsule
Zinc sulfate
SYU GRANULES
Zinc sulfate monohydrate = Elemental zinc
7.5 mg /15 g
REVITAL LIQUID
■0.5 mg / 10 ml
Zinc sulfate
ECOPROT PLUS
Elemental zinc
15 mg/20 g
granules
Data source : Current Index of Medical Specialities (CIMS), Vol 20, No. 2 (May-Aug), 1997
Per unit cost
Rs. 1.20
Rs. 1.20
Rs. 1.21
Rs. 1.25
Rs. 1,29
Rs. 1.30
Rs. 1.38
Rs. 1.39
Rs. 1.60
Rs. 2.36
Rs 2.45
Rs. 2.48
Rs. 2 51
Rs 2.78
Rs. 2.80
Rs. 2.88
Rs. 2.99
Rs 3.69
Rs. 4.00
Rs 4 58
Rs. 4 95
Rs. 4.25
Rs. 5.43
Rs. 8.30
3. Price range is also wide. Tablets and
capsules cost the least per unit dose,
liquids (other than paediatric drops) are
•IRON
To prevent and treat pregnancy anaemia
more expensive while granules and
•ZINC
powders generally cost the most.
To ensure proper foetal development
All of these brands are compound
•FOLIC ACID, VITAMINS & MINERALS
formulations containing, in addition to
To meet the incremental demand during pregnancy
zinc, iron, other minerals,vitamins, amino
ft
acids, proteins or other ingredients. Many
are intended for anaemia or nutritional
Capsules
supplementation with the zinc
Iron and Zinc pair for Total Pregnancy Care
component being vigorously promoted
Fat further details please contact:
as bonus for growing children, expectant
or nursing mothers, the elderly and the
convalescent. Some are punched
together as antioxidants and some as
general stress relievers. Curiously there
of a tonic
Zii
is not one single-ingredient preparation for the prescriber who diagnoses a clear-cut case of zinc deficiency. To provide 20
mg of elemental zinc (a dose considered minimum for supplementation in adults) many of these brands will require more
than one unit dose per day. Obviously, if these drugs were used specifically for zinc supplementation, the cost of one day's
treatment would cover the cost of 1 egg or 30 g of animal food with most, and 2 eggs or 60 g of animal food with many
Food supplementation might therefore be more rational and more economical than drugs unless a clear-cut zinc deficiency
is documented. In the latter case, with few exceptions like TPN or acrodermatitis, short-term supplmentation would
probably suffice while the nutritional status is improved.
provide
R.B.TONE
iHNMHMHI
RATIONAL DRUG BULLETIN
In the final analysis therefore, the money that is spent on supplemental drugs might be better utilized in improving the
nutritional status with food. A determined commitment to fundamentals, effective use of oral rehydration, encouragement
of breast feeding, improvement of hygiene and nutrition education comprise a better and more long-lasting solution to the
problem of zinc deficiency most of the time and in the majority of patients.
References :
1. Olson RE, Berdanier CD. Microminerals. In : Munson PL, Mueller RA, Breese GR, eds. Principles of
Pharmacology : Basic Concepts & Clinical Applications. New York : Chapman & Hall, 1995 : 997-1023.
2.
Falchuk KH. Disturbances in trace element metabolism Isselbacher KJ, Braunwald E, Wilson JD, Martin JB,
Fauci AS, Kasper DL. Harrison's Principles of Internal Medicine. 13th ed. Vol 1. New York . McGraw-Hill Inc.,
1994 : 481-4.
3.
Childhood morbidity, immunity and micronutrients. WHO Drug Information 1996 ; 10 (1) : 12-6
■£. Sazawal S, Black R, Bhan M, et al. Zinc supplementation in young children with acute diarrhea in India. New
r England Journal of Medicine 1995 ; 33 : 869-74
Using drugs in gastritis and peptic ulcer disease
The advent of potent antiulcer drugs has greatly reduced the prevalence and the morbidity from peptic ulcer disease
(PUD). Nevertheless, the problem has not disappeared and is likely to stay with us in the foreseeable future. The
incidence of gastritis is probably greater than frank endoscopically confirmed ulceration. Both gastritis and PUD may be
iatrogenic in origin, resulting from the use of ulcerogenic agents, most notably the non-steroidal anti-inflammatory drugs
(NSAIDs). Phenylbutazone, oxyphenbutazone and azapropazone carry the maximum risk, paracetamol and ibuprofen are
relatively safe while naproxen, ketoprofen, flurbiprofen, diclofenac, piroxicam and indomethacin pose mtermadiate risk.
Some of the newer NSAIDs, namely nabumetone and nimesulide, may also be safe in this respect but experience with
them is still limited. The following table lists drugs which should be used with extra care or avoided altogether in
suspected gastritis or PUD. Some of these drugs are ulcerogenic by themselves, some aggravate existing disease while
the anticoagulants and thrombolytics pose the danger of serious bleeding. Corticosteroids can cause silent perforation
of ulcers. It should be noted that, apart from drugs, excess of smoking, alcohol and caffeinated beverages may also
predispose to ulceration.
Table : Status of drugs in peptic ulcer disease
Contraindicated
Acipimox
Amantadine
Anticoagulants, oral e.g. Warfarin
Baclofen
Corticosteroids
Dipyridamole
Estramustine
Heparin
NSAIDs
Reserpine
Thrombolytic agents e.g. Alteplase, Streptokinase
To be used with caution
Anticholinesterases e g. Neostigmine, Pyridostigmine
Betahistine
Diethylpropion
Mazindol
Methysergide
Nicotine, transdermal
Nicotinic acid
Phentermine
Potassium chloride
Probenecid
Sulfinpyrazone
Subscription for next issue onwards (eight pages each Bulletin) annually inclusive of postage :
IndiaStudents : Rs. 30.00 Professionals/lndividuals : Rs. 50.00 Institutions and Organisations : Rs. 70.00
Foreign- U.S. $5.00
EDITORIAL BOARD |
Dr. Santanu Tripathi
Dr. N. C. Banerjee
Dr. Amitava Nandi
Dr. Satrujit Dasgupta
Dr. Bijoy Jacob
Dr. B. N. Nag
Dr. Suwit Wibulpolprasert
Dr. K. Balasubramaniam
Ms. Margaretha Helling Borda
Mr. AmitavaGuha
Mr. M. Sarkar
PUBLISHED BY: Community Development Medicinal Unit, 47/1B Garcha Road|Calcutta-700 019.
Phone : (033) 474 8553, Fax: (033) 475 5668, Printed at: PRINTMATIX, 71 Elliot Road|Calcutla-16, Ph.: 29 5484
1 of 2
Community rteuiiri Ceii
from:
jo <jvargnese(g>cmai.org>
To:
"oha" <oha-ncc<aiyahoogrouDs.com>
Sect*:
■v’ertda” Aor:! 05 2004 7.29 PM
ipr>a-i'iCCj i~v»: c.ssv.i~>ucu orug cist ixamataKa »or luiormaLiori
4/12/04
Aii Karnataka yuvi hospitals, FriCs io ioiiow ED iisi submitted by State Pharmacy Councii
rxamalaka yuvciiiiiicfii has accepted aii uoseiiuai diuy list lecuiiiiheud by iiie State riiaunaCy Council, in a inajui
initiative by the Statu government, aii government hospitals ano tire 2,565 primary ireaitir centers nave to put into use
me essentia, orug list wim immediate etrect.
Although the recommendations for the essential drua list was made by the Karnataka Pharmacy Council, a major
initiative was taken in this recard bv the members cf an NGO of medical soecialists. Drua Action Forum fDAF).
Karnataka
' i ne situation is dangerous anti a majoi cause for concern as combination drugs are mostiy a shotgun therapy where
in me event of a side effect it wouid be difficult to pin point which drug is the cause of the reaction. Often ingredients in
me comomation orug are not recaliea Dy me aoctors. I nere nave Deen several representations maoe Dy UAF,
Karnataka against tne sale of non-essentiai drugs to tne Drugs Controller General or India and former drugs controller
Anand Ra,ashekar on various occasions," informed Dr. Prakash Rao.
The main reasons for increased sales of non-essential drugs are attributed to the nexus between pharmaceutical
companies and medical practitioners, poor vigilance of the state drugs control departments end lack of initiative by the
nQwarrirnonf rooirifc: O’jf OAF Kc,mafnkc’
Con ibinaiiuno like EiviFLAis Pius which Contains ibuprofen 4uuing and Faiacciuiiiui 325 mg (bum pain kiiieis) aiu
useless and cannot double the effect of pain reiiei. Such combinations oniy add io me cost of therapy and incteases
me sioe errects, pomtea out ur. Hrakasn mao
Any doctor would be in a better position to combine two different drugs to the patient. Hence available combination
drugs now available in the market are useless. Doctors prescribe combination drugs because cf aggressive promotion
by the pharma sector There is low therapeutic awareness among doctors who are at the mercv of the dnio comnanles
for ths details of the rlnins end their effirarv he averred
(.Antibiotics)
(Antispasmodics), i linicaim Pius, Sedyi, riexidoi and ‘vespereX (Anti psychiatric), AsmapoX, Asriiatelie, GliiiiiCiuS Bfvi,
Cadiphyiiate Sixer, Seuonai, Tedrai (Anti respiratory), Digene Gei, ivioticare iviro, Logascid and Heiibaci (Anti uicer).
Dr. Praxasn Rao also brought tortn tne issue of anemia in pregnant women wnere tne most popular drug in single
ingredient form is ferrous sulphate and folic acid. However, numerous expensive and Ineffective ferrous salts.
formulations of iron oolvmaltose and carbonyl iron are marketed.
DaspitA the British Pharmacopeia excluding hemoglobin as a drug for human use world wide. In indie, it is sold under
brand namas: Giobiron Hemfast and Heppforte. Hemon!obin in combination of vitamins minerals and proteins:
/Coe/wril i-ieorwvin W«*/»e*f**l ikrsrz\l DDTaioo
Arnt
i|ac IJItirof*
Hi
ilesc
i o control me situation, uer. KarnataKa recommends a muiti-prongea approacn in association witn tne drugs control
department, medical practitioners and consumers where regular and frequent education and awareness programmes
are organized in every district. It calls for a strict vigilance bv the state drugs control department on the sale of drugs
and to increase the number of Adverse Drug Reaction cells in the country. Another suggestion Is to include Rational
Dnig Use as a subject in medical colleges to educate doctors on the dangerous reactions of non-essential dnigs
s To visit your group on the web, go to:
htto://ground.vahoo.com/droun/oha-ncc/
T?/2- •
MEDICINE
The healing paradox
There is a need to develop and refine the magic of the physician-patient relationship that
complements the precise pharmacologic interventions that may be prescribed.
ABRAHAM VERGHESE
S a practicing physician, I confess
that I learn about the latest medical
breakthroughs while reading my morning
paper. When my office mail eventually
brings me the original study, my pleasure
in the journal’s pristine cover and untou
ched pages has been diminished because
the tidings arrived before the messenger.
But here is why I cannot complain: the
science reported in my newspaper is gen
uinely newsworthy, deserving its place
alongside matters of state and economy.
For example, two weeks ago we learned of
a promising approach to the prevention
of cervical cancer - a vaccine against one
type of papilloma virus that is an antece
dent to this malignancy. Imagine that. A
vaccine for cancer! On the same day as
that announcement came the first report
of a vaccine that might prevent genital
I herpes. And then there’s the ongoing
news of the unravelling of the human ge
nome in all its amazing complexity. His
tory will draw a line here: Before Genome
and After Genome. The Rosetta stone has
been found and applied to the sacred
scroll, and it promises important break
fast reading for years to come.
But my morning paper, laden with
science, also carries evidence of our dis
trust of science and our search for another
kind of healing. You’ve seen it: a full-page
advertisement for a product that you
know is too good to be true. The text has
large type, a before-and-after picture, no
listing of the contents of the product and
a blizzard of endorsements from “scien
tists” and “patients” that rake the place of
data. These products are life extenders,
fat fighters, growth-hormone releasers,
relievers of limb pains, rebuilders of mus
cle and bone and sometimes all of the
■)ove together. I think of them as quark
drugs, phantoms that if they could be
studied in careful trials would soon lose
the “r” for a “c” and be revealed for what
they are.
But rhe market for such remedies is
huge. Indeed, estimates are that nearly
half of all adult Americans use some sort
of dietary supplement, and the sales of
A
FRONTLINE. FEBRUARY 14, 2003
these products in 2000 amounted to
more than Si5 billion! I plead guilty:
echinacea and ginkgo have made appear
ances in my medicine cabinet, as I reac
hed for magic for some ailment or other. I
had no guidance, no data of the son a
scientist should accept, no package insert.
I tried them on faith. Alas, they did
nothing.
The good news is that many such
treatments are being systematically and
carefully studied through the aegis of the
National Institutes of Health; what we
know thus far is that few products live up
to their claims, many have the potential
for toxicity and the quality control on this
stuff is awful. Here is the bad news: 70
per cent of us would take these products
anyway, even if they were shown to be no
better than snake oil. Even as science
measurably changes our life and extends
our life spans, as a society we are suspi
cious of science.
I am not a crusader against alternative
medicines or its practitioners. 1 am all for
things that make us feel better and that
don’t hurt us. But I do wonder ar the
paradox of even the most rational of us
being drawn to these bottles with pictures
of ugly tubers and weed-like plants on
them. Why do we become dreamy-eyed
hearing the songs of the New Age pied
pipers whose melodies interweave quan
tum physics and the workings of the co
lon in beautiful but completely fictional
ways? Like revivalist preachers, they invite
our faith, our willingness to search for
magic in ancient, undecipherable Orien
tal practices (as opposed to the new, quire
decipherable. Western practices). In re
turn they offer nostrums, tonics, tapes,
books, diets, retreats, mantras, votive can
dles and cruises; they bring colour, fra
grance and incense to an illness
experience that otherwise plays out in
black and white.
In this golden age of science, disease
and treatment have become demystified.
If you went to a doctor clutching your
stomach in days of old. rhe doctor, after a
good bit of probing and hemming and
hawing, would retreat to the dispensary
and with great ceremony compound a
mistura carminative^ vividly coloured in
a medicinal bottle. Short of surgery or an
autopsy, no one would be precisely cer
tain what you had. But come clutching
your stomach to a medical doctor these
days, and after a careful history and exam,
the doctor can “see” your gallbladder,
measure the distress of your pancreas, ex
amine the lining of your colon and much,
much more if need be and then institute
the precise cure.
Therein lies the rub: we are perhaps
in search of something more than a curecall it healing. If you were robbed one
day, and if by the next day the robber was
caught and all your goods returned to
you, you would only feel partly restored;
you would be “cured” but not “healed”;
your sense of psychic violation would re
main. Similarly with illness, a cure is
good, but we want the healing as well, we
want the magic that good physicians pro
vide with their personality, their empathy
and their reassurance. Perhaps these were
qualities that existed in abundance in the
pre-penicillin days when there was little
else to do. But in these days of gene ther
apy, increasing specialisation, managed
care and major time constraints, there is a
tendency to focus on the illness, the cure,
the magic of saving a life.
Science needs to be more cognisant of
the other magic, the healing if you will,
even as we reach for the proven cures. We
need to develop and refine that magic of
rhe physician-patient relationship that
complements the precise pharmacologic
interventions we may prescribe: we need
to ensure the wholeness of our encounter
with patients; we need to not lose sight of
rhe word “caring” in our care, of the pa
tient. And doggedly, in this fashion, one
patient at a time, we can restore faith in
the fantastic advances of science we are
privileged to witness.
Abraham Vcrghese is a professor if medicine and
director of she Centre for Medical Humanities
and Ethics ar the University of Texas Health
Sciences Centre, San Antonio. His latest book £.
1 he Tennis Partner.
York Times Service
□
SCIENCE
Collective instincts
New studies suggest that many animals practise democracy, going
by their propensity to make group rather than individual decisions.
JAMES GORMAN
HEN red deer stand up and hon
eybees dance, they are not simply
stretching their legs or indicating where
the nectar is, according to a new study. As
bizarre as it may seem, they are voting on
whether to move to greener pastures or
richer flowers. The process is uncon
scious, the researchers say. No deer counts
votes or checks ballots; bees do not know
the difference between a dimple and a
chad. But no one deer or bee or buffalo
decides when the group moves. If democ
racy means that actions are taken based
not on a ruler’s preference, but the prefer
ences of a majority, then animals have
democracy.
Not surprisingly, decisions based on
majority preferences tend to fit in with
what most individuals in the group want.
But, the researchers say, this is not a mere
tautology. An analysis based on some hef
ty mathematical models that they devel
oped shows that democracy in groups of
animals can have a tangible survival edge
over despotism.
Dr. Tim Roper of the University of
Sussex in Brighton, United Kingdom, did
the research with Dr. Larissa Conradt and
reported it in the current issue of Nature.
“There are human cases of decision
making to which our model would be
relevant,” Roper said, like “small groups
making rather simple decisions.” But the
question - how rhe decision gets made - is
the same. And although human groups,
and individual animals, have been well
studied, little attention has been paid to
decision-making by groups of animals.
Dr. Thomas D. Seeley of Cornell,
whose research on bees was cited in the
paper, said that most of the study on ani
mal decision-making had been at the indi
vidual level, and although there seemed to
be groups that decided, en masse., to act,
“there’s really been no theory about why
you would expect the decision-making to
be democratic, or distributed.” Seeley said
that die paper was “a good first step” that
could lead to other research.
Conradt and Roper did their research
in two parts. First they reviewed earlier
W
research to determine whether various
group decisions were being directed by
one individual or seemed to come from
the group as a whole. For example, obser
vations of group behaviour showed that
red deer moved when more than 60 per
cent of adults stood up - that is, voted
with-their feet. In African buffalo, he said,
adult females made the decisions, voting
with the direction of their gaze. Whooper
swans voted with head movements. They
would move when a large number made
low-intensity movements, or when a
smaller number made high-intensity
movements.
Somehow, unconsciously, the animals
sense when enough of them get the urge
to go. It is certainly a decision by a major
ity, but what to call it is another question.
The more complicated aspect of the
research involved mathematical models
that Conradt and Roper developed to
analyse the benefits to animal groups, of
different ways of decision-making that
they described as democratic or despotic.
In essence rhe models compared costs to
individuals in the event of not getting to
do things when they wanted to. Having to
wait or hurry up was considered a cost,
and the presumption was that for animals
as for people, time is money or food or
something important to survival.
These are abstract models, and not
ways to process the previous research. And
what they show is that when majorities
decide, more individuals get what they
want, and that should translate into better
survival. There could, of course, be sit
uations with incredibly smart or sensitive
despots that maximise the benefit to the
group, but Conradt and Roper did not
come up with them. Roper said the re
search was meant to suggest a new way of
looking at decision-making and a new ar
ea for research. The models apply only to
animals that make group decisions.
It may be that some animals, like do
mestic cats, for instance, do not vote, do
not care to vote and have no interest in
any sort of group activity. They were not,
however, a subject of the paper. Roper
and Conradt modelled democracy and
despotism. They did not consider anar
chy. ■
New York Times Service*
in the village of Odem in the
Israeli-occupied territory of Golan
Heights. Observations of group
behaviour among red deer showed
that they moved when more than 60
per cent cf adults stood up - that is,
voted with their feet.
FRONTI INt. H HR I’ARY bi. .’003
-pi'J—9orld Trade Organization finally agrees cheap dru%s deal
Fiona Fleck Geneva
A long awaited trade deal to give poor nations access to cheap lifesaving drugs for diseases such as AIDS,
malaria, and tuberculosis was agreed on 30 August after eight months of stalling—which was mainly due to US
objections.
Negotiators from the 146 member nations of the'World Trade Organization (WTO) who hammered out the deal
hailed it as a major breakthrough.
"All people of good will and good conscience will be very happy today with the decision that the WTO members
have made," said .Amina Chawahir Mohamed, Kenya's ambassador to the Geneva based body. "It's especially
good news for the people of Africa, who desperately need access to affordable medicine."
Some aid organisations criticised the deal. M&lecins Sans Frontteres said it "threw up new legal, economic, and
political obstacles" to poor countries wanting to import cheap generic copies of patented drugs and that it was
"designed to offer comfort to the US and the Western phannaceutical industry."
Until now. under a WTO system known as the compulsory licence, patents for lifesaving drugs could be waived
only for countries that could produce cheap generic drugs themselves.
The deal is a breakthrough because trade rules have now been altered to allow' poor countries—most of which do
not have their own drugs industry—to issue a compulsory licence to a third country', such as India or Brazil, to
pr^^ce cheap generic drugs and to import these to address a public health crisis.
WTO member nations had originally agreed to give poor countries better access to cheap drugs at the WTO
ministerial meeting in Doha, Qatar, in November 2001 (B.W 2091 ;323: 1146[Free Full Text]). But because of
difficult negotiations in trying to balance humanitarian concerns and business interests, the deal has only just been
concluded in time for trade ministers to give it their blessing at their next biennial meeting, on 10-14 September in
Cancun, Mexico.
The breakthrough agreement came after a plea from .African nations in the form of a joint statement to negotiators
saying that nearly 2.2 million Africans had died from AIDS and other major diseases since talks became
deadlocked on 16 December
"For us, the request by the African countries was a decisive factor. All of us couldn't fail to be touched by that,"
said Luis Felipe de Seixas Correa, Brazil's ambassador to the WTO.
Washington had opposed the original deal hammered out in December, fearing that cheap drags intended for poor
countries could be diverted back to developing countries and undermine the drugs industry, even though most
countries agree that such a scenario is unlikely.
But trade negotiators addressed US concerns with a statement saying that rules allowing countries to override
patents "should be used in good faith to protect public health... [and] not be an instrument to pursue industrial or
commercial policy objectives."
The statement also calls for special measures to prevent drugs being smuggled into rich countries, including
special packaging or differently coloured tablets.
186, 217
' P'V A f
jMews
Drugs could still be costlv under World Trade Organization deal
Fiona Fleck
Geneva
A landmark deal that allows poor countries without any manufacturing capability of their own to waive
international trade rules and import cheap copies of patented drugs is likey to be a complex procedure that may not
reduce prices enough, experts say.
LIN secretary’ general Kofi Annan issued a statement to the World Trade Organization meeting in Cancun,
Mexico, last week, after the deal was clinched in Geneva, saying that it was a "moral imperative" for each of the
organisation’s 146 member countries to implement the agreement without delay.
Although the organisation’s meeting in Cancun ended in disarray when members could not agree on the reduction
of subsidies to farmers in the developed world and representatives of African countries walked out, the agreement
regarding cheaper drugs for developing countries was unaffected.
Campaigners for cheaper drugs welcomed the fact that the agreement had been reached (6 September, p 517) and
that it applied to ail drugs but warned that the new procedure could be time consuming and bureaucratic and that
the drugs may still be too expensive.
Dr^nathan Quick, director of essential drugs and medicines at the World Health Organization in Geneva, said
thMRal was only part of the solution to the problem of getting affordable drugs to the people that need them, such
as people with AIDS and HIV in the poorest African countries. Other issues included distribution and a lack of
qualified staff.
"Now we have the deal. It’s the start we have and we're looking ahead," Dr Quick said. He added: "The point is to
implement it, monitor it, see if it works, and adjust it if it doesn't.”
Campaigners fear that poor countries in Africa, Asia, and Latin America that could benefit from the deal may
have to go through unnecessary’ red tape to prove that they have no manufacturing capability of their own.
Also, generic drug manufacturers rear that they may’ get tangled up in red tape, which could be a disincentive to
manufacture the drugs and could slow’ down the process. Campaigners say it is unrealistic to require
manufacturers to declare that they are producing drugs tor humanitarian not business purposes, but they hope that
this requirement will be treated as a formality.
Campaigners also fear that rules on making the drugs’ packaging distinctive, so that cheap copies of patented
dn^s cannot be mistaken for the originals and diverted to developed countries, could push up costs.
However, even when these problems have been dealt with the price of the drugs might be too high for some of the
world’s poorest countries.
it is now' imperative ibr countries to put the agreement to the test by taking full advantage of all the flexibilities
contained in the agreement to increase access to medicines for their populations," the charity Medecins Sans
Frontieres, which has lobbied hard for better access to drugs, said in a statement.
For example, small African countries could group together and place a joint order with a manufacturer of generic
drugs to make it a viable business proposition for the company.
a
>
r ci lA ’
0
'J
BMJ 2003;327 (20 September)
Editor’s choice
A bad week for drug companies?
The United States is hugely important for drug companies. Tire pharmaceutical market is worth more
than SI 50bn, and annual spending has been rising by almost 20% a year (p 642). Prices are not regulated
in the way they are in many other countries, and companies are allowed to advertise directly to
consumers—so boosting consumption. But now the cost of drugs has become an important political
’(V
issue, and a bill has been introduced into Congress that would require government agencies to gather
evidence "comparing effectiveness [and] cost effectiveness" of the most commonly prescribed drugs
■(,i
"relative to other drugs or treatments ibr the same disease."
.
Tllftill aims to reduce costs, but it could also improve quality. The proposal is to conduct many more
head to head trials of common treatments—trials like the ALLHAT (antihypertensive and lipid lowering
to prevent heart attack trial), which showed that diuretics are just as good as much more expensive drags
for treating hypertension. The whole world stands to benefit from such trials.
The industry is lobbying against the bill, but its problems are much deeper than congressional irritations, i
lv ; '"I
Companies are failing to produce enough new drugs, and the investment bank Dresdner Kleinwort
j ■
Af.c.
Wasserstein thinks that the industry is operatinga business model that is unsustainable (Guardian 12
:
'•
'
September 2003). Companies have on average been producing three "new molecular entities" a year, but
the bank predicts tliis will decrease to 0.3 per company. The industry has been increasing sales by 12%15% for 30 years, with half of the increase coming from raised prices. Now globalisation and political
endeavours are making such price increases impossible.
The answer, the bank suggests, is further mergers —only mergers with a difference. Companies should
now concentrate on particular' therapeutic areas—cardiovascular, cancer, etc. This could give them
"dominance" (which sounds like a polite word for a monopoly) in those areas. The result could be just a
h.^iul of companies.
The bill before Congress stops short of proposing that a drag would have to be shown to be better than
other drugs before being given a licence. Europe doesn't require such a demonstration either, but the ,
National Institute for Clinical Excellence (NICE) in England and Wales looks for evidence that a
j ,
treatment is appreciably better titan what is already available before advocating its use in the NHS,
I
which is most of the market in Britain. NICE has just been independently evaluated by the World Health
Organization, and an important recommendation is that it "break its close links with the drag industry
and make its processes more transparent" (p 637). The institute has set new standards of transparency,
but drag companies have insisted on some of their material being confidential. The material should be
made publicly available.
Richard Smith, editor
c ’'"
BMJ 2003;32/:642 (20 September'
News
VS politicians want federal funding to discover cost effectiveness of new drugs-
Ray Moynihan
Washington, DC
A bill before the US Congress calls on health authorities to investigate whether expensive new drugs
offer value for money, by comparing their risks and benefits with other treatments and older drugs.
I
■ <
'
'pi \\
-zv £
\-A P- b • '"
Currently new drugs are approved on the basis of their superiority over a placebo, with no requirement
to show an advantage over existing treatments or cheaper generic pills.
If passed, the new legislation would see US taxpayers spending $75m (£47m; €67m) in 2004 to fund
studies of the cost effectiveness of the nation's most expensive classes of drugs—something done
routinely in other countries but a move that is bitterly opposed by the drug industry in the United States.
Ar^iai spending on prescription drugs is rising by almost 20% a year in the United States, where it is
now in excess of SI 50bn. The cost of drugs is one of the fastest growing components of overall
healthcar e costs, which are also rapidly rising and becoming a key political issue in the race for the
White House.
A group of Democrat and Republican politicians introduced the latest bill into the House of
Representatives in June. Specifically the bill requires that the federally funded National Institutes of
Health and the Agency for Healthcare Quality and Research gather scientific evidence "comparing
effectiveness, cost-effectiveness, and, where appropriate, comparative safety" of the costliest and most
commonly used prescription drugs "relative to oilier drugs or treatments for the same disease or
condition."
The bill, known as HR 2356, does not call for a change in the way new drugs are approved by me r 66u
and Dwg Administration, but it does demand more information on whether a new drug is worth its price
once it is on the market, particularly when compared with other available treatments.
O^of the bill's sponsors, Jo Ann Emerson, a Missouri Republican, said that the studies would provide
0 Coyi’-’V ' - •
basic information to doctorsand their patients about which drugs were best for them. The results could
BtuUl/kfi.
also be used to inform decisions on coverage by private and public insurers, including Medicare, which |, vjv-„ c,,
yog/,provides health care to people aged over 65. "I believe we have to do everything possible to use the
principles of market competition to get prices of drugs down. This is one way to do that," Ms Emerson
said.
Jeff Trewhitt, a spokesman for the industry group Pharmaceutical Research and Manufacturers of
America, said the studies being proposed in the new bill were highly subjective and that people
"advocating cost effectiveness studies are often advocates of spending less." When asked about the
industry’s lobbying efforts to undermine the bill, he said, "We are watching it."
Ms Emerson, who has sponsored other bills to reduce drug costs, said that although the industry was
quietly lobbying to kill her latest bill there was a good chance that some version of the plan for cost
effectiveness studies would be passed by both the House of Representatives and the Senate and be sent
to the president for approval later this year.
Australia has had laws for almost a decade requiring studies of the cost effectiveness of any new drug by
comparing it with existing treatments before the drug can be listed on the publicly funded
pharmaceutical benefits scheme.
Australia's system, which has been the target of sustained attack by elements within the drugs industry',
has become something of a global model for how to obtain value for money in prescription drugs.
Compared with other countries Australia pays a low price for "me too” drugs while paying closer to the
average for truly innovative drugs, and across all categories of drug it pays less than half the price paid in
the United States.
In the United Kingdom the National Institute for Clinical Excellence now regularly bases its decisions
regarding new drugs on evidence based evaluation of their effectiveness and cost effectiveness,
comparing their costs, risks, and benefits with other treatments. An example is the recent guidance on
glitazones for type 2 diabetes, which used cost effectiveness analysis to recommend against using the
expensive new drags as a second line treatment incomhmaiion with metformin or a sulphonylurea,
except in certain restricted circumstances.
h-^fitish Columbia similar evidence based comparisons underpin the reference pricing programme used
io price some classes of prescription drags. In this programme several drags in a class are compared: if
they are essentially similar the subsidy offered to the public is based on the cheapest price in the class,
and consumers pay for any difference if their doctor chooses a dearer drag.
Like the systems in Australia and the United Kingdom and the proposed plan in the United States,
British Columbia's programme has been heavily attacked by the drug industiy.
The studies used in the Canadian progranune are provided by an organisation based at the University' of
British Columbia called the Therapeutics Initiative, and its managing director, Dr Tim Wright, says that
what is really needed is "head to head" trials that compare different drugs, rather than studies that simply
compare a drag with a placebo.
Like other experts around the world, Dr Wright argues that such head to head studies should be
mandatory after a new drag has been approved. "Il's essential to know the benefits and harms of newer
therapies, compared to the best available existing treatment," he said, giving as a good example a recent
tr^ the antihypertensive and lipid lowering to prevent heart attack trial (ALLHAT) of different
ammypertensive drugs (JAMA 2002; 288: 2981-97j Abstract/Free Full Text]). Recent analysis of
ALLHAT results indicate that the United States could save more than 8430m a year if doctors favoured
tire older- and cheaper thiazide drags.
Mr Trewhitt said that .ALLHAT had already been contradicted by a subsequent trial and that head to
head studies would slow down the delivery of drugs io new patients.
News
MCE is told to break its close links with drug industry
Zosia Kmietowicz
London
The National Institute for Clinical Excellence (NICE) has been advised by an independent review to
break its close links with the drug industry and to make its processes more transparent.
Experts from the World Health Organization who carried out the review have advised NICE that, to
avoid any possible bias, pharmaceutical physicians should not be members of committees that make
judgments on particular drugs or devices.
Kees de Joncheere, regional adviser for health technology and pharmaceuticals at WHO, said that
although he understood thatphaimaceutical physicians could offer useful input about how and why trials
were conducted, a physician from one company on a committee that is appraising another company's
product cannot always be independent. Instead manufacturers' views should be represented through the
consultation process, he said.
Moreover, if it wished to be truly transparent NICE needed to examine whether it could continue to
include confidential materials in its appraisals process, said the review.
"We recognise that NICE has set new standards in the consideration of stakeholder inputs and
transparency, including provision of documents and Information, via the NICE website. However, to
gain access to key information NICE also accepts material designated as confidential. In the main this
comes from the pharmaceutical industry," said Mr de Joncheere.
"Whilst we welcome the steps they have taken to push these boundaries with the industiy, NICE should
reconcile this inherent contradiction," he said.
NICE, which has been recommending drugs and devices to the NHS in England and Wales since 1999,
invited WHO to conduct an independent review of its work after advice from the House of Commons
Health Select Committee last year.
.-g^gether the review team made 28 recommendations on all aspects of how NICE is tun, from its
dWning principles to its selection of topics and appeals process.
Michael Rawlins, NICE'S chairman, said the findings from the WHO team would feed into a review' of
methods and appraisals currently being conducted by the institute. The board was also considering
making three key documents that were currently kept confidential open to the public, he said. These are
the overview of each drug or device appraised, comments received on draft overviews, and the contents
of appeals.
However, disclosing confidential materials from drug companies might be more difficult, as it might
JSOJAUMlsv any rijuuc puvuuuuuu, mc sam.
The WHO report, Technology Appraisal Programme of the National Institute for Clinical Excellence is
accessible at www.nice.org.uk
> ,■
I '
Prescripfiioini Drag C©m|0®ra(iov@ Effi®©dw®mi®®s AeS ©? 2@©3
m Hoics®)
HR 2356 IH
108th CONGRESS
1st Session
H. R. 23S®
To require the National Institutes of Health to conduct research, and the Agency for Healthcare
Research and Quality to conduct studies, on the comparative effectiveness and cost
effectiveness of prescription drugs that account for high levels of expenditures or use by
individuals in federally funded health programs, and for other purposes.
UN THE HOUSE ©F REPRESENTATIVES
Jun® 5, 2@©3
Mr. ALLEN (for himself, Mrs. EMERSON, Mr. BERRY, Mr. BEREUTER, Mr. WAXMAN, Mr.
YTTM ; of O.c:=.:'.o, Mr. MTHT of Florida, Mr. SUTKNECHT, Mr. SNYDER, Mrs. BONO, Mr.
COOPER, and Mr. WAMP) introduced the following bill; which was referred to the Committee on
Energy and Commerce
A BOLL
To require the National Institutes of Health to conduct research, and the Agency for Healthcare
Research and Quality to conduct studies, on the comparative effectiveness and cost
effectiveness of prescription drugs that account for high levels of expenditures or use by
individuals in federally funded health programs, and for other purposes.
Be it enacted by the Senate and House of Representatives of the United States of
America in Congress assembled,
SECTION U. SHORT TITLE.
This Act may be cited as the 'Prescription Drug Comparative Effectiveness Act of 2003’.
SEC. 2. NIH RESEARCH AND AHRQ STUDY ON EFFECTIVENESS OF CERTAIN
PRESCRIPTION DRUGS.
(a)
IN GENERAL
CI) RESEARCH BY NIH- The Director of the National Institutes of Health, in
coordination with the Director of the Agency for Healthcare Research and
Quality, shall conduct research, which rnay include clinical research, to develop
valid scientific evidence regarding the comparative effectiveness, cost
effectiveness, and, where appropriate, comparative safety of covered
prescription drugs relative to other drugs and treatments for the same disease or
condition.
(2)
ANALYSIS BY AHRQ(A) IN GENERAL- The Director of the Agency for Healthcare Research
and Quality, taking into consideration the research of the National
Institutes of Health under this section, shall use evidence-based practice
centers to conduct studies or other analyses of the comparative
effectiveness, cost-effectiveness, and, where appropriate, comparative
safety of covered prescription drugs relative to other drugs and
treatments for the same disease or condition.
(B) SAFETY- In any analysis of comparative effectiveness or cost
effectiveness under this subparagraph, the Director of the Agency for
Healthcare Research and Quality shall include a discussion of available
information on relative safety.
(3)
STANDARDS- The Director of the Agency for Healthcare Research and
Quality, in consultation with the Commissioner of Food and Drugs, the Director of
the National Institutes of Health, and stakeholders, shall develop standards for
the design and conduct of cost-effectiveness studies under this subsection.
(b)
COVERED PRESCRIPTION DRUGS- For purposes of this section, the term
'covered prescription drugs' means prescription drugs that, as determined by the
Director of the Agency for Healthcare Research and Quality in consultation with the
Administrator of the Centers for Medicare & Medicaid Services, account for high levels of
expenditures or use by individuals in federally funded health programs, including
Medicare and Medicaid.
(c)
ANNUAL REPORT- Each year the Director of the Agency for Healthcare Research
and Quality shall prepare a report on the results of the research, studies, and analyses
conducted by the National institutes of Health and the Agency for Healthcare Research
and Quality under this section and submit the report to the following:
(1)
The Congress.
(2)
The Secretary of Defense.
(3)
The Secretary of Health and Human Services.
(4)
The Secretary of Veterans Affairs.
(5)
The Administrator of the Centers for Medicare & Medicaid Services.
(6)
The Director of the Indian Health Service.
(7)
The Director of the National Institutes of Health.
(8)
The Director of the Office of Personnel Management.
(d)
REPORTS FOR PRACTITIONERS- As soon as possible, but not later than a year
after the completion of any study pursuant to subsection (a)(2), the Director of the
Agency for Healthcare Research and Quality shall—
(1) prepare a report on the results of such study for the purpose of informing
health care practitioners; and
(2) transmit the report to the Director of the National institutes of Health.
(e) NIH INTERNET SITE- The Director of the National Institutes of Health shall publish
on the institutes' Internet site, and through other means that will facilitate access by
practitioners, each report prepared under subsection (c) or (d) by the Director of the
Agency for Healthcare Research and Quality.
(f)
EVIDENCE- In carrying out this section, the Directors of the National Institutes of
Health and the Agency for Healthcare Research and Quality shall consider only
methodologically sound studies, giving preference to studies for which the Directors
have access to sufficient underlying data and analysis to address any significant
concerns about methodology or the reliability of data.
(g)
AUTHORIZATIONS OF APPROPRIATIONS(1) NIH- There are authorized to be appropriated to the National Institutes of
Health to carry out this section $50,000,000 for fiscal year 2004, and such sums
as may be necessary for fiscal years thereafter.
(2) AHRQ- There are authorized to be appropriated to the Agency for Healthcare
Research and Quality to carry out this section $25,000,000 for fiscal year 2004,
and such sums as may be necessary for fiscal years thereafter.
SYNOPSIS
1.
Petitioners are leading non-profit NGOs working in the field of public health.
2.
They noticed SLP (C) No 3668/2003 filed by Union of India against the order of the
Karnataka High Court restraining the U.O.I. from giving effect to the Pharmaceutical
Policy (PP) 2002 on the grounds that from the list of 74 drugs found in the 1995 price
control order some are likely to be omitted when the fresh list is prepared in
accordance with the PP 2002.
3.
They also noticed SLPs (c) 6652 of 2003 and 6638/2003 filed by the Indian Drug
Manufacturers Association and the Organisation of Pharmaceuticals Producers of
India respectively seeking to impugn the High Court order. Permission has been
granted to file the SLPs and notice has been issued.
4.
All these petitions proceed on the erroneous footing that the DPCO order of 1995 is
sacrosanct, not informing the Hon’ble court that both the World Health Organisation
and the Union of India have in 2003 released their lists of Essential Medicines
(AnnexuresPl and .P2).
5.
WHO Guidelines for National Drug Policies, the National Health Policy 2002 and the
Union of India Pharmaceutical Policy 2002 have the aim of ensuring the availability
of essential medicines at affordable prices to the population, and in particular, to the
poor.
6.
It is the petitioners’ case that this entire list of essential medicines ought to be under
price control for reasons set out in the petition. Unfortunately a vast range of
essential drugs is just not available at affordable prices and rampant profiteering
exists.
7.
There is a public health crisis in India. India accounts for 30% of the world’s TB
cases, has the second highest of HIV infected cases, one third of the world’s leprosy
cases, 19 crore illness episodes of diarrhea per year in the under-five population
(which cause one third of the mortality of under-fives), and a steep rise in noncommunicable diseases like diabetes, hypertension, heart disease and cancer.
Hypertension and diabetes affected people in India together account for more than 6
crores, larger than the population of many European nations. Medical expenses is the
second largest cause of rural indebtedness. India has one of the lowest rates in the
world for access to affordable essential drugs.
8.
This crisis was recognized in the National Health Policy 2002 document which noted
that “the availability of essential dr.gs is minimal, the public health services
dysfunctional, the supply of drugs grossly inadequate, and patients purchase drugs
privately.”
9.
Public health investment declined from 1.3% of GDP in 1990 to 0.9% (1999) India’s
public expenditure on health is one of the lowest in the world.
10.
On the other hand the country' has been flooded with over 60,000 drugs and
formulations by 20,000 manufacturers. Most developed countries have a much smaller
list of approved drugs and formulations. The WHO Model Lisi of Essential Medicines
2003 contains only 325 drugs, which are considered adequate to meet the priority
health care needs of populations.
11.
Petitioners share the concern of the citizens of India regarding widespread sales of
spurious, substandard and drugs beyond expiry' dale and point out the uncontrolled
number of formulations add to the complexity of the problem mid urgent action in tins
area is required.
! 2.
The fault lies in the fact that it is not the Ministry of Health and Family Welfare but
the Ministry of Chemicals and Fertilisers, which has from the Drug Price Control
Order (1979 to 1987 to 1995) reduced the number of drugs under DPCO from 347 to
142 to 76 respectively. This has adversely affected access to safe, affordable and
essential drugs for the public and has had grave economic and health consequences for
the poor.
13.
Petitioners have pointed out that for many public health problems the drugs required
though in the essential list of medicines are not under price control.
14
Petitioners have pointed out that no criteria of scientific pharmacology has been used
in deciding drugs for drugs in price control m the DPCO 1995 - many of which are
non-essential, outdated, and even hazardous.
15.
That essential drugs such as oral dehydration solution (for diarrhea), drugs for anemia
(which is a major public health problem especially in women in children), vaccines
for important infectious diseases like rabies, hepatitis B, drugs for HIV disease noncommunicable diseases like heart disease, cancer, are not in the DPCO list of 1995.
That the drugs for TB, malaria, leprosy, hypertension are poorly represented in the
DPCO list of 1995.
16.
Even drugs under price control have flouted the orders and have widely varying
prices.
17.
Elsewhere, and specifically, Canada has had its Patented Medicines Prices Review
Board, France has its Transparency Commission and Economic Committee on
Medicines, Egypt has all drugs under price control, Italy has restricted wholesale
margins, German}' has its reference pricing system, and some system of price
monitoring and price regulation prevails in Japan, Netherlands, China, Indonesia,
Colombia and so on. In some of these countries drug pricing is tied with national
health system reimbursements and or insurance schemes. In the absence of either in
India, the havoc on the majority of the population can well be imagined. Petitioners
have pointed out that establishment of National Drug Authority as envisaged by the
Hathi Committee and later reiterated by the 1986 and 1994 policies is imperative.
18.
The government in its previous policy documents has accepted the responsibility of
keeping a check on the price of all drugs and formulations. However in reality apart
from the list of price-controlled drugs, there is virtually no control over rhe price of
other drugs and formulations. Even in the case of price controlled drugs which
number only 76, violations of price control occur. We urge the court to take
cognizance of the marked variation in the prices of the drugs both under price control
and outside it, which clearly points to profiteering at the cost of people, and direct the
authorities to take action.
19.
The Indian pharmaceutical market with over 20,000 producers,
100,000
formulations, a poorly developed quality control infrastructure and an ineffective and
apathetic drug regulatory syotom is virtually unregulated in many of ita activities.
20.
The pharmaceutical sector being a critical sector dealing with the lives of people
needs regulation not only in pricing, but also in the area of rationality, safety, efficacy
and quality of the products it manufactures.
that this Hon’ble Court direct the government to control the
formulations. These waste the meagre resources of a poor population.
22.
The pharmaceutical sector needs stricter regulation with regard to drug quality,
availability of hazardous drugs and banned drugs.
23.
Petitioners have pointed out that there is a good case for abolishing all excise duties,
sales tax and other local taxes in manufacture and sale of essential drugs.
Dates
1973
1977
1978
rlathi Committee releases its report With a list of 116 essential drugs.
WHO releases its Model List of Essential Drugs
Alma-Ata Charter on Comprehensive Primary Health Care of which access to
Essential Drugs was one of the eight components of Primary Health Care declaration signed by 134 Governments including India.
1979
The Drug Price Control Order (DPCO) list of drugs under price control contains
347 drugs.
1987
The DPCO list is pruned to 142 drugs by the Ministry of Chemicals and Fertilisers.
2
1995
The DPCO list is further pruned to 76 drugs.
1996
The U.O.I releases the first National Essential Drugs List.
2002
The Ministry of Chemicals and Fertilisers releases the Pharmaceutical Policy 2002
document.
12.11.02 Karnataka High Court makes an order in W.P. 21618 of 2002 staying the
pharmaceutical policy 2002.
2003
WHO releases its “ WHO Model List of Essential Medicines 2003”
2003
U.O.I. releases its “National List of Essential Medicines 2003”.
10.3.03 SLP(C) 3668/2003 is filed by U.O.I. impugning the order of the Karnataka High
Court dated 12.11.02. Notice is issued.
1.8.03
SLPs 6652/2003 and 6638/2003 are filed by the Indian Drug Manufacturers
Association and the Organisation of Pharmaceutical Producers of India
respectively. Permission is granted to file SLPs. Notice is issued.
1.9.03 The present writ petition is filed.
WHO/EDM/QSM/99.4
MedacaS
products
SiracO the
Internet
A guide to finding reliable information
WHO/EDM/QSM/99.4
Original: English
Distribution: General
Medical products
and the Internet
A guide to finding reliable information
Regulatory Support Series, No. 8
©World Health Organization (1999)
This document is not a formal publication of the World Health Organization (WHO).
All rights are reserved by WHO. The document may. however, by freely reviewed, abstracted,
reproduced or translated, in part or in whole, but not for sale or use in conjunction with
commercial purposes.
The views expressed in this document by named authors
are solely the responsibility of those authors.
World Health Organization
Geneva 1999
Introduction
Summary of key points
The Fifty-first World Health Assembly (Resolution WHA51.9, May 1998)
O If used properly, the Internet allows quick and easy access to
requested the Director-General of WHO to develop a guide on medical
health information. It provides useful information on such topics as
products and the lnternet.The guide was intended to serve as a model for
diseases, conditions, therapies, medical products, and health and medical
Member States to adapt into locally meaningful advice for Internet users in
organizations and institutions (see Point I).
order to help them to obtain reliable, independent and comparable
information on medicinal products.The guide in this booklet has been
fthc information you obtain from the Internet can be helpful when you
prepared to meet the Health Assembly request. It has been developed in
consult your doctor or other health care provider about your disease or
consultation with drug regulatory authorities, drug information experts,
condition. But the guidance from the Internet should not replace
consumer organizations, and the pharmaceutical industry. It is a model
consultation with your health care provider (see Point 2).
guide, designed to be translated into national languages and modified as the
local situation may require.
WHO would be grateful to receive any comments on experience gained
O Although it is often difficult to determine, you still need to verify the
source of information available on the Internet (see Point 2).
from the practical use of the guide which would help in developing it
further. Contact information appears below.
Department of Essential Drugs and Other Medicines (EDM)
O Information that sounds too good to be true, in particular, requires
verification and careful assessment (see Point 3).
World Health Organization
1211 Geneva 27, Switzerland
email: reggiv@who.ch
O Be cautious about buying medical products via the Internet. In many
countries, selling or buying medical products via the Internet may at
^^sent be an illegal activity. You are strongly advised to obtain your
Finally, national health authorities - such as drug regulatory agencies -
and WHO are working together to address the illegal advertising and sale
medical products through legitimate distribution channels such as
pharmacies (see Point 4).
of medical products through the Internet. It is important that Internet
users report suspected illegal activities and problem cases to their national
health authorities.
O Consult your doctor or other health care professional before you
decide to treat yourself (see Point 5).
------- POI NT
The Internet is a valuable
source of information, but
be sure you know and] trust
the source
Finding reliable health
and medical information
*n the Internet
Reliable sources of health and medical
information are available on the
Internet.This information can be
The Internet is a valuable source of health
information on topics such as diseases,
conditions, therapies, medical
products, and health and medical
organizations. When used properly, it
allows quick and easy access to such
helpful when you consult your health
care provider about your disease or
condition, though it should not
replace such consultation (see Point
V).As you search for and evaluate
information, however, keep these
information from on-line medical libraries,
considerations in mind:
universities, health associations and government
agencies. However, the quality of health and
medical product information on the Internet
It may be difficult to determine the
source of the information you find on a
Looking at a web site?
Check the following:
1 Is there clear indication
K
of the name and contact
address of the web site owner?
■ Is it clear which organization(s)
contribute funding, services, or
other support to the web site?
• If advertising or sponsorship is
a source of funding, is this
clearly stated?
• Is this a site for consumers,
health professionals, or some
other audience?
• When was the information
displayed last updated?
varies, and it is often difficult for the Internet
■h site and to verify that source. If you
ore not familiar with the source of information, you may be able to find out more
user to identify the true source of the
about it from health care professionals or reliable organizations with which you
information and to determine whether it is
are familiar. Your own reliable sources may be able to give you help to evaluate
reliable, complete and up to date.
the reliability and quality of the web site information.
There are many health and medical sites on the
Internet which do provide good information that may
not be easily available from other media.They may be
designed for health professionals or for consumers.
However, even information from reliable sources may
require special training in order to evaluate it properly
and to determine whether the information applies to
your disease or condition.The information provided by
these web sites covers such topics as:
O Research being conducted on a particular disease or
Health authorities and organizations in each country can provide a list of
a condition - including rare diseases - and related clinical trials;
sites with links to reliable sources of health and medical information.
Additionally, several private organizations are actively searching for ways to
O New product approvals by health authorities in your country for a
ensure the quality of information on the Internet. Internet users may be
specific disease or condition;
interested in following or participating in these discussions and reading
what others have to say on this topic.The following box lists two examples
• General information about diseases or conditions, such as high blood
of organizations that are conducting such activities. National authorities
pressure, arthritis or obesity;
I
• Support groups for people with certain diseases and conditions, such as
>ld identify and list additional organizations and reliable web sites
known to them.
HIV/AIDS or cancer;
Health on the Net Foundation: http:Wwww.hon.ch
• Lists of international, national and local organizations that provide
support and information for a disease or condition.
Internet Healthcare Coalition: http:Wwww.ihc.net
POINT
headlines
Finding ireUiialbDe medkail
product information
on the internet
Claims that the product is available from only one source, for
a limited time
Testimonials from “famous” medical experts
. Claims of
“no risk” or lack of any risk information - remember: no product or
treatment is completely risk-free
^^Claims that a product is "scientifically proven" and "absolutely safe”
|r
The Internet also offers information on medical
O Products with the same name may contain different ingredients in
products. As you search for and evaluate
different countries. Therefore, when searching for information you should
look at the International Nonproprietary Name (INN) of the active
product information, however, keep
these considerations in mind:
y
ingredients and not just the product name (brand name, trade name).
&
O If information sounds
too good to be true, it
probably is.The following lists some warning signs that medical product
O Product information should be as complete as possible, and it should
information may not be truthful: • Advertisements or information that
include at least the elements outlined in the following box:
use phrases such as "scientific breakthrough","miraculous cure”, “exclusive
product", “secret formula", "ancient ingredient”, "without risk”, "anti-ageing",
"improve sexual performance", and "all natural"
O Case histories from “cured” customers claiming amazing results.Whe^
you see a testimonial, ask for proof of its “typical” nature;
G A list of symptoms and diseases it is claimed the product cures - for
example, claims that one product can cure or treat HIV/AIDS, cancer.
arthritis, Alzheimer’s disease, wrinkles, weight problems, memory loss, and
so on • Advertisements that tout the latest trendy ingredient in the news
Looking at product information?
A reliable web site will provide the following information:
^croduct name
^Fctive ingredient(s)
• name of other ingredients
known to cause problems
to some people
• what to use the product for
• when not to use the product (for
example, in pregnancy, allergies,
interations with other medicines
or foods)
• how to use the product
• possible undesired effects
• how to store the product
° manufacturer’s name and
contact information
• last update of the information
the laws and regulations of your country.There is no assurance of safety
and effectiveness for such unauthorized products. As an Internet user,you
Be cautious about
buying medkail products
on the [Internet
may find it difficult to distinguish between products that have met the
requirements of your government and those that have not.
Information about medical products being developed and tested in
*
ntanans is available on the Internet If you have a disease or condition for
which there is currently no treatment or cure, you may have searched for
Medical products are often offered for sale on the Internet. Offering for
information about your disease or condition and read about these new
sale and selling medical products or buying medical products from another
products on the Internet. Although new products are often not available for
country via the Internet may be illegal.Therefore, before buying a product,
prescription, sometimes a health care professional may prescribe a
you should find out if it is legal to do so. If you are considering buying
medication for you before approval, or discuss enrolling you in a clinical
medical products through the Internet, be cautious, because you may risk
trial to study the product. It is important to understand that there may be
your health and waste your money. Consult your health care professional
additional risks to using such a product before approval, because the
before self-treatment.
possible adverse effects (which may be serious or life-threatening) and the
There are many reasons why medical products bought through the
effectiveness and proper dosage schedule may not be known. In some
Internet could represent a danger to you, or at the least cause
cases, a prescription product may be unavailable in your country but
inconvenience or loss of money.Ten of these reasons are discussed here.
approved for use in another. In such a case, your country may have special
I
Safety and efficacy assurance may be lacking - In many countries,
legal procedures allowing you to import prescribed medicines from abroad.
could be done with the help of your health care professional, through
before medical products are approved, licensed or authorized for salef
the companies that develop and market them must conduct research and
legitimate distribution channels.
demonstrate to a drug regulatory authority that the products are safe,
2
effective and of good quality for human use. Although these authorized
Instructions for use may be inadequate -To be used properly
and safely, medical products need to be accompanied by precise
medical products may be available through the Internet, there may also be
instructions. There is no assurance that a product obtained via the Internet
products for sale that have not been studied and evaluated according to
will have the correct instructions for use, dosage and precautions. In
----- POINT
8
Products bought across borders may not be allowed in
See your health care
professional before you decide
treat yourself or change
your medication
your country - Countries have different laws about what medical
products can be sold and shipped across national borders.This means that
it is possible that products that are not approved for marketing in your
country or products that have been identified as a hazard to public healthy
may not be allowed into your country if they are identified at entry. If yoe
have already paid for the product, you may not be able to receive it or have
its cost reimbursed. In addition, the prescription status of medical products
Even after finding reliable, truthful health or medical information on the
varies from country to country. For instance, products that are available
Internet, it is important to go to your health care provider to discuss your
only on prescription in one country may be sold without prescription, or
disease or condition and the information you have found before you take
may even be unregulated, in another.
9
steps to treat yourself.This is important for several reasons:
Products with the same name may be different in different
O Not all diseases and symptoms need medical treatment. You may be
countries - Internet users need to be aware that products with the
taking medicines or using medical products unnecessarily and exposing
same name may contain different ingredients in different countries.
yourself to an unnecessary risk O Many medications or other medical
Therefore, you may be taking the wrong product. In addition, countries may
products may cause harm if they are used improperly. It is important to be
have different standards for the quality of medical products and their
manufacture. Products purchased across borders might not be exactly the
under the care of a health care
same product or quality as in your own country.
professional when using such products
I ZAYour personal information may not remain confidential
'
^Appropriate medication or appropriate
I \y Many web sites require you to disclose personal medical data. Users
medical treatment for your disease or
must be aware that there is no assurance that this information will be kept
symptoms is important to your health.
confidential. Users who feel uncomfortable with the potential use of their
Not every medication is appropriate for
personal data should purchase their medical products through
everyone. For example, some individuals
conventional, legitimate distribution channels.
may be allergic to certain medications.
A health care professional can help you to determine the best medicine or
treatment for your disease or condition.
O A health care professional can provide guidance on how best to take
your medication safely. For example, the effectiveness of some medications
may be influenced by other products, such as other medications, alcohol or.
certain foods. Mixing your medication with these other products could
strengthen or weaken the effect of the medication or cause an adverse
reaction.This could be dangerous to your health or, at the very least,
interfere with your timely recovery O Patients with particular
characteristics , such as pregnant or breast-feeding women, the elderly and
children, have special concerns, needs and considerations when taking
medication or using medical products. In particular, a number of
medications are specifically known to cause harm to unborn children.
Pregnant women should therefore be sure to consult a health care
professional before self-treatment O Any time you take medication or use
a medical product it is important to inform your health care professional of
any side-effects you may experience when using the product. By going
through your health care professional for treatment, you can make sure
that he or she will be better prepared to advise you or change the
0
treatment if you do have an adverse reaction to a product O By ordering
medical products through the Internet you may deprive yourself of the
opportunity for personal, professional care and advice from your doctor,
pharmacist or other health care professional.
Other titles in the Regulatory Support Series:
• Report of a Training Workshop for Drug Regulatory Officials
on the Assessment of Applications for Marketing Authorizations.
Nicosia, 14-18 December 1997 (WHO/DMP/RGS/98.1)
• How to Implement Computer-assisted Drug Registration.
(WHO/DMP/RGS/98.2)
• SIAMED: Model System for Computer-assisted Drug Registration.
User manual. (WHO/DMP/RGS/98.3)
• QCL: Model System for Handling Sample Information in a Quality
Control Laboratory. User manual. (WHO/DMP/RGS/98.4)
• Marketing Authorization of Pharmaceutical Products with Special
Reference to Multisource (Generic) Products: A Manual for a Drug
Regulatory Authority. (WHO/DMP/RGS/98.5)
■ Practical Guide to the Use of the WHO Certification Scheme on
the Quality of Pharmaceutical Products Moving in the International
Commerce. (WHO/DMP/RGS/98.6) in preparation
SIAMED: Model System for Computer-assisted Drug Registration.
Introduction and Brief Description of Functions and Facilities.
(WHO/DMP/RGS/98.7)
® World Health Organization 2002
AU rights reserved. Publications of the World Health Organization can bg
obtained from Marketing and Dissemination, World Health Organization,
20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax:
+41 22 791 4857; email: bookorders@who.int). Requests for permission
to reproduce or translate WHO publications - whether for sale or for
noncommercial distribution - should be addressed to Publications, at the
above address (fax: +41 22 791 4806; email: permissions@who.int).
The designations employed and the presentation of the material in this
publication do not imply the expression of any opinion whatsoever on
the part of the World Health Organization concerning the legal status of
any country, territory, city or area or of its authorities, or concerning the
delimitation of its frontiers or boundaries. Dotted lines on maps represent
approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers' products
does not imply that they are endorsed or recommended by the World
Health Organization in preference to others of a similar nature that are
not mentioned. Errors and omissions excepted, the names of proprietary
products are distinguished by initial capital letters.
The World Health Organization does not warrant that the information
contained in this publication is complete and correct and shall not be
liable for any damages incurred as a result of its use.
^Safety of Medicines
A guide to detecting and reporting
adverse drug reactions
Why health professionals need to take action
Introduction
Glossary
The purpose of this Guide is to help health professionals to participate
in the very important process of continuous surveillance of safety and
efficacy of the pharmaceutical products which are used in their clinical
practice. Continuous evaluation of their benefit and harm will help to
achieve the ultimate goal to make safer and more effective treatment
available to patients.
The terms are from "Safety Monitoring of Medicinal Products'1
1. An adverse drug reaction (ADR) is 'a response to a medicine which is
noxious and unintended, and which occurs at doses normally used in
man'.
In this description it is of importance that it concerns the response
of a patient, in which individual factors may play an important role,
and that the phenomenon is noxious (an unexpected therapeutic
response, for example, may be a side effect but not an adverse reac
tion).
______________________________I)
The objectives of the Guide are to raise awareness of
the magnitude of the drug safety problem and to convince
health professionals that reporting of adverse reactions is
their moral and professional obligation.
The ultimate goal of the Guide is to reduce drug morbidity
and drug mortality by early detection of drug safety prob
lems in patients and improving selection and rational use of
drugs by health professionals.
2. An unexpected adverse reaction is 'an adverse reaction, the nature or
severity of which is not consistent with domestic labelling or market
authorisation, or expected from characteristics of the drug'.
3.
A drug or medicine is'a pharmaceutical product, used in or on the hu
man body for the prevention, diagnosis or treatment of disease, or for
the modification of physiological function'.
4.
A side effect is 'any unintended effect of a pharmaceutical product
occurring at doses normally used by a patient which is related to the
pharmacological properties of the drug'.
It is a model guide which can be translated into national languages
and modified as the local situation may require.
WHO would be grateful to receive any comments on experience
gained from the practical use of the Guide which would help in devel
oping it further. Please contact the Department of Essential Drugs and
Medicines Policy (EDM) with your comments:
(
Dr Mary Couper
Department of Essential Drugs and Medicines Policy (EDM)
World Health Organization
1211 Geneva 27, Switzerland
email: couperm@who.int fax: + 41 22 791 4761
Essential elements in this definition are the pharmacological nature
of the effect, that the phenomenon is unintended, and that there is no
deliberate overdose.
5.
An adverse event or experience is defined as 'any untoward medical
occurrence that may present during treatment with a medicine but
which does not necessarily have a causal relationship with this treat
ment'.
The basic point here is the coincidence in time without any suspicion
of a causal relationship.
6.
A serious adverse event is any event that:
❖ Is fatal
❖ Is life-threatening
❖ Is permanently/significantly disabling
❖ Requires or prolongs hospitalization
❖ Causes a congenital anomaly
❖ Requires intervention to prevent permanent impairment or dam-(
age
7.
A signal refers to 'reported information on a possible causal relation
ship between an adverse event and a drug, the relationship being
unknown or incompletely documented previously'.
Usually more than a single report is required to generate a signal,
depending upon the seriousness of the event and the quality of the
information.
The magnitude of the problem
During the last decades it has been demonstrated by a number of
studies that medicine morbidity and mortality is one of the major health
problems which is beginning to be recognized by health professionals
and the public. It has been estimated that such adverse drug reactions
(ADRs) are the 4lh to 6,h largest cause for mortality in the USA,2. They
result in the death of several thousands of patients each year, and many
}more suffer from ADRs. The percentage of hospital admissions due to ad
verse drug reactions in some countries is about or more than 10%3,4,5.
Norway
11.5%
France
13.0%
UK
16.0%
In addition suitable services to treat ADRs impose a high financial
burden on health care due to the hospital care of patients with drug
related problems. Some countries spend up to 15-20% of their hospital
budget dealing with drug complications6.
Beside ADRs, medicine-related problems include also - drug abuse,
misuse, poisoning, therapeutic failure and medication errors.
There is very limited information available on ADRs in developing
countries and countries in transition. However, one may expect that the
situation is worse rather than better. This problem is also caused by a
lack, in some countries, of legislation and proper drug regulations, in
cluding ADR reporting, a large number of substandard and counterfeit
products circulating in their markets, a lack of independent information
and the irrational use ol drugs.
'. ?
Why postmarketing surveillance and
reporting ADR is needed
Why pharmacovigilance is needed in
every country
The information collected during the pre-marketing phase of drug
development is inevitably incomplete with regard to possible ADRs. This
is mainly because:
There are differences among countries (and even regions within
countries) in the occurrence of ADRs and other drug-related prob
lems. This may be due to differences in e.g.:
Tests in animals are insufficient to predict human safety;
Patients used in clinical trials are selected and limited in number, tht^''
conditions of use differ from those in clinical practice and the dura
tion of trials is limited;
By the time of licensing exposure of less than 5000 human subjects to
a drug allows only the more common ADR to be detected;
e 8A
drug manufacturing processes used which influence pharma
ceutical quality and composition;
the use of traditional and complementary drugs (e.g. herbal
remedies) which may pose specific toxicological problems,
when used alone or in combination with other drugs.
❖ Information about rare but serious adverse reactions, chronic toxic
ity, use in special groups (such as children, the elderly or pregnant
women) or drug interactions is often incomplete or not available;
Therefore health professionals worldwide should report on ADRs as it
can save lives of their patients and others.
genetics, diet, traditions of the people;
drug distribution and use including indications, dose and
availability;
At least 30,000 people need to be treated with a drug to be sure that
you do not miss at least one patient with an ADR which has an inci
dence of 1 in 10,000 exposed individuals7;
Thus, post-marketing surveillance is important to permit detection of
less common, but sometimes very serious ADRs.
diseases and prescribing practices;
c
Data derived from within the country or region may have great
er relevance and educational value and may encourage national
regulatory' decision-making. Information obtained in one country'
(e.g. the country of origin of the drug) may not be relevant to other
parts of the world, where circumstances may differ.
Therefore, drug monitoring is of tremendous value as a tool for
detecting ADRs and specifically in relation to counterfeit and sub
standard quality products. ADR monitoring is to help ensure that
patients obtain safe and efficacious products.
The results of ADR monitoring have also a very important edu
cational value.
How voluntary reporting on ADRs can
prevent new medicine tragedies from
developing
It took many decades before the deleterious effects of aspirin on the
gastro-intestinal tract became apparent and almost as long before it was
recognised that the protracted abuse of phenacetin could produce renal
papillary necrosis; 35 years elapsed before it became clear that amydopy^.
rine could cause agranulocytosis; and several years before the associa
tion of phocomelia with thalidomide became obvious8.
Withdrawals from the market as a result of spontaneous reporting
INN
Reason for
Year of
Year of
(brand name)
withdrawal
marketing
withdrawal
bromfenac (Duract ®)
serious hepatotoxic effect
1997
1998
encainide (Enkaid ®)
excessive mortality
1987
1991
flosequinan (Manoplax ®)
excessive mortality
1992
1993
temafloxadn (Omniflox®)
haemolytic anemia
1992
1992
benoxaprofen (Oraflex ®)
liver necrosis
1982
1982
mibefradil (Posicor ®)
multiple drug interaction
1997
1998
terfenadine (Seldane®)
fatal cardiac arrythmias
1985
1998
After the "thalidomide tragedy'' many countries have established^
drug monitoring systems for early detection and prevention of possible
drug-related morbidity and mortality. Their success depends on the
cooperation of the medical profession in reporting suspected ADRs,
especially to new drugs.
10 '
Some examples demonstrate how very astute, alert and observant
medical doctors have been helped to prevent the development of drug
morbidity and drug mortality by reporting on suspected ADRs which
resulted in the withdrawal of dangerous drugs from the market or in
restriction of their use.
How voluntary reporting on ADRs can
influence labelling
Why health professionals are in the best
position to detect and report on ADRs
There are many examples of the importance of ADRs reporting in the
improvement of information in labelling ofmany effective pharmaceuti
cal products (new possible ADRs, contraindications, dosage etc.).
Cyclophosphamide has been on the market for several years in many
countries. In January 2001 there were some new reactions included ii’|’’
the labels: Stevens Johnson syndrome and toxic epidermal necrolysis;
they were not included in the Physician Desk Reference (PDR) 1995.
For example:
EPIDERMAL NECROLYSIS
STEVENS JOHNSON SYNDROME
Losartan was marketed in the USA since 1995. Some of the new reac
tions that have been discovered after launch and included in the PDR are:
VASCULITIS
PURPURA ALLERGIC
Report suspected adverse
drug reactions.
(incl. HENOCH-SCHOENLEIN PURPURA)
ANAPHYLACTIC SHOCK
Leuojloxacin was launched in the USA in 1997. In February 2000 the
label torsade de pointes was included.
All healthcare providers (physicians, pharmacists, nurses, den
tists and others) should report ADRs as part of their professional
responsibility, even if they are doubtful about the precise relation
ship with the given medication.
You can reduce the suffering
and save thousands
of patients lives by doing
one thing:
ERYTHEMA MULTIFORME
ANAPHYLACTOID REACTION
The effectiveness of a national postmarketing surveillance pro
gramme is directly dependent on the active participation of health
professionals. Health professionals are in the best position to re
port on suspected ADRs observed in their every day patient care.
f
How to recognize ADRs
Since ADRs may act through the same physiological and patho
logical pathways as different diseases, they are difficult and some
times impossible to distinguish. However, the following step-wise
approach may be helpful in assessing possible drug-related ADRs:
1.
Ensure that the medicine ordered is the medicine received and
actually taken by the patient at the dose advised;
2.
Verify that the onset of the suspected ADR was after the drug
was taken, not before and discuss carefully the observation
made by the patient;
3.
Determine the time interval between the beginning of drug
treatment and the onset of the event;
4.
Evaluate the suspected ADR after discontinuing the drugs or
reducing the dose and monitor the patient's status. If appropri
ate, restart the drug treatment and monitor recurrence of any
adverse events.
5.
Analyse the alternative causes (other than the drug) that could
on their own have caused the reaction;
6.
Use relevant up-to-date literature and personal experience as a
health professional on drugs and their ADRs and verify if there
are previous conclusive reports on this reaction. The National
Pharmacovigilance Centre and Drug Information Centres are
very important resources for obtaining information on ADR.
The manufacturer of the drug can also be a resource to consult;
7.
' 14
Report any suspected ADR to the person nominated for ADR re
porting in the hospital or directly to the National ADR Centre.
What should be reported?
For "new" drugs - report all suspected reactions, including mi
nor ones. (In many countries drugs are still considered “new"
up to five years after marketing authorization);
For established or well-known drugs - report all serious or un
expected (unusual) suspected ADRs;
Report if an increased frequency of a given reaction is ob
served;
* Report all suspected ADRs associated with drug-drug, drug
food or drug-food supplements (including herbal and comple
mentary products) interactions;
Report ADRs in special fields of interest such as drug abuse and
drug use in pregnancy and during lactation;
Report when suspected ADRs are associated with drug with
drawals;
❖ Report ADRs occurring from overdose or medication error;
Report when there is a lack of efficacy or when suspected phar
maceutical defects are observed.
Thus, report all suspected
adverse reactions that
you consider of clinical
importance as soon as
possible!
Acknowledgements
References
1 Safety Monitoring of Medicinal Products. Guidelines for setting up
and running a Pharmacovigilance Centre. Uppsala Monitoring Cen
tre - WHO Collaborating Centre for International Drug Monitoring,
EQUUS, London, 2000.
2
Lazarou J. et al., 1998. Incidence of ADR in hospitalized patients: a
meta-analysis of prospective studies. JAMA, 1998, 279 (15) 1000-5.
3
Moore N et al. Frequency and cost of serious adverse drug reactions irF
a department of general medicine. Br J Clin Pharmacol 1998, 45(3),
301-308.
Imbs JL et al. Latrogenic medication: estimation of its prevalence in
French public hospitals. Therapie, 1999, 54(1) 21-27.
5
Griffin GP. The evaluation of human medicines control from a na
tional to an international perspective. Ad Drug React Toxico Rev.,
1998, 17(1), 19-50.
6
White T et al. Counting the cost of drug-related adverse events. Phar
macoeconomics, 1999, 15(5). 445-458.
7
Strom BL. Pharmacoepidemiology. 2nd ed. Chichester: John Wiley,
1994.
8
Venulet J. The Drug Monitoring Programme. In: Drug Surveillance,
Geneva 1994, 13-21.
Useful Websites
WHO
www.who.int/medicines/
Section: Quality Assurance and Safety: Medicines
WHO Collaborating Centre for International Drtig Monitoring (Uppsala
Monitoring Centre)
www.who-umc.org
2S3
The document was prepared by Dr V.K. Lepakhin, Senior Clinical
Adviser, Essential Drugs and Medicines Policy, WHO. The kind
assistance and contributions are acknowledged from Dr M. Couper,
Dr M. Everard, and Dr L. Rago, WHO, Geneva, Switzerland; Professor
R.H. Karim Al-Saudi, Jordan University of Science & Technology,
Jordan; Ms Niamh Arthur, Irish Medicines Board, Dublin, Ireland;
gr A. Astakhova, Federal ADR Centre, Moscow, Russia; Dr I.R. Edwards
* Dr S. Olsson, WHO Collaborating Centre for International Drug
Monitoring, Uppsala, Sweden; Dr Kenneth Hartigan-Go, Bureau of
Food & Drugs, Department of Health, Manila, Philippines; Dr P. Honig,
Center for Drug Evaulation and Research, FDA, USA; DrN.A. Kshirsagar,
King Edward VII Memorial Hospital, Bombay, India; Professor Dr R.
Meyboom, LAREB Foundation, Netherlands; Professor Sang Guo-Wei,
State Drug Administration, Beijing, China; Dr R. Santos, European
Agency for Evaulation of Medical Products, UK; Dr Rachida SoulaymaniBencheikh, Institut National d'Hygiene, Rabat, Morocco.
1
Coordination of document- Caroline Mullen, QSM/WHO
Design: Marilyn Langfekl
Photo copyright: PhotoDisc
Position: 800 (9 views)