Ankit - CHLP report .pdf
Media
- extracted text
-
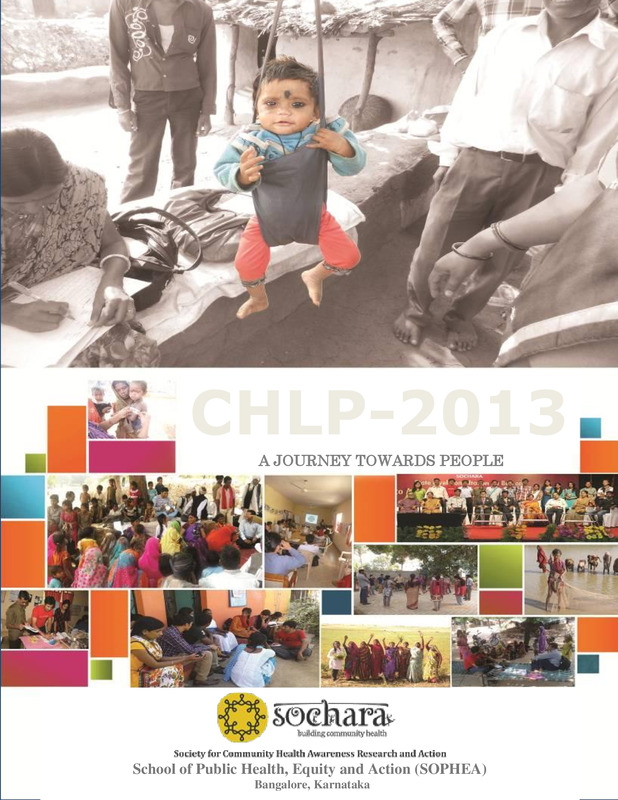
CHLP-2013
A JOURNEY TOWARDS PEOPLE
1
School of Public Health, Equity
and Action (SOPHEA)
CommunityBangalore,
Health Learning
Program-2013
Karnataka
Community Health Learning
Program
2013
Annual Report
ANKIT VASHISHTHA
FELLOW, SOPHEA
School of Public Health, Equity and Action (SOPHEA)
Bangalore, Karnataka
2
Community Health Learning Program-2013
Contents
Topic
Page no.
2
Title Page
3
Contents
Few words from my soul
4-5
6-7
Why “CHLP”
My Learning Objectives
Learning from collective teaching sessions and field visits
Learning from field work [ Case Studies / Reflections]
Research Study Report
Overall Learning / Conclusions.
3
Community Health Learning Program-2013
8
Few words from my soul
It will be injustice with my feeling which i shared through my limited account of word
because whatever I got, I learnt, I felt and I did throughout this fellowship, will always
remain with me as a great memory of my time. It is said that people remembers all the
good moment at the end of life stage, I am sure this journey will be a part of those
gathering of memory. It is not only the fellowship program; it is a parallel life which
walks with fellow. Despite my absolute inexperience in the field of community health
and social issue, I am thankful for the interview committee to bring me here and made a
part of journey of community health. Therefore I am thankful to Dr. Thelma and Dr.
Ravi with deep sense of gratitude for considering me worthy for this program.
For me, Dr. Thelma and Dr. Ravi should not be taken separately, God made them
for each other. It seems that God had to make a humanistic and healthy environment; they
sent two people on earth with same sense of understanding. They met, married together
and discover SOCHARA to fulfill the plan of GOD. They both are calm, kind, cool,
intelligent and proactive. They always supports fellows with compassion, never ever
discourage for any off beam deeds, provide constant moral inspiration, all sort of comfort
and support for learning actively to progress throughout fellowship as well as in future.
I was keen to understand people, society and moreover peep into inside me. With
the inner learning, I got the chance to understand me. This is the additional beauty of this
program that we were taught to see the social context with spiritual view.
In the succession of sharing my gratitude, I would do it for all Aadiwasi
brothers and sisters who became part of my study and without whom the study was not
possible. Due to their leading cooperation, CNRC could manage and regulate effectively
at their habitat.
It‘s an honor to express my regards to my beloved teacher and technical guide
Mr. As Mohammad for his encouragement, constant guidance and support, he is very
kind and delightful personality. They love fellows equally and provide all guidance
which fellow want to learn.
4
Community Health Learning Program-2013
I feel happy thanking to Dr. Vijay Gupta, Hon. Secretary, CID organization for
all the help he has done in shaping this work and supporting me throughout the study. He
took interest in my study and provided me all the required resources for field experience.
Because of his constant support my research objective became feasible and could achieve
successfully.
I express my sincere thanks to all the team members of SOCHARA and CID
organization, for their constant support. They cared, encouraged, taught and facilitated
me throughout my seasonal classes and field work. They were only the person who made
extraordinary environment for learning and brought idealism of the fellowship and social
work into reality.
I thanks to my all of co-learner for making my time and life wonderful and
memorable. Because of their dedication, I learnt few essential lessons for future progress.
I wish them all the best for their future and request them to keep in touch.
Last but not a least, because it is very important for me, I would convey my
heartily gratitude to my respected and lovable father Mr. Umesh Vashishtha, for his
constant guidance for my active learning and in research activities throughout my field
work. My mamma and chhotu (my younger brother) missed me a lot and I missed them
too without whose emotional sacrifice, enthusiasm for my growth and admirable support,
this fellowship would not have been possible.
5
Community Health Learning Program-2013
Why “CHLP”
As I took myself, I am committed to serve for social sector and keen to put effective
action. Being affective from spiritualism in life, I always want to do for people around
me and serve some beneficiary step for them. I belong from social allied background and
the circle which is active professionally with social sector that‘s how I remain connected
with health concern challenging issue in a major part life. I want to take this whole as my
carrier. When I heard about this fellowship and knew its benefit for my carrier, I thought
that my god is giving me this opportunity which I was always seeking for.
Through this Community Health Learning Program, I would be able to serve my
duty for public and community health concern issue and would get splendid opportunity
for research and build my own knowledge bank and gain my capacity for serving as a real
social worker in my near future. With this program, I would be able to research
independently and share my effort to support and participate in the process, campaigns
and movements to make ―Health for all‖. I would be able to gain critical knowledge
regarding public health and would get an opportunity to participate in the various
community health initiatives, quality and person centric approach and opportunity to be
guided by various experienced resource person so it would help me to get knowledge
skills and attitudes to begin a career in public health / community health. Because of this
Community Health Learning Program is a teaching learning program in community
health, public health education and regarding with health policy. It direct to learn a new
public health paradigm focused on health equity, social justice, underlying social
determinants of health including gender, community participation, inclusive and open
health systems and health policy development.
6
Community Health Learning Program-2013
My Learning Objectives
Key-learning Objective: To study comprehensively onthe Primitive Tribal Group named Sahariya by multidimension analysis through different aspects (socio-economical, socio-cultural and
socio-environmental causes, source of livelihood, etc)
Study the prevalence of malnutrition among Sahariya tribal community.
Understand the community based rehabilitation model in health.
Develop the concept of Community based Nutrition Management System through
Community-NRC.
Other Objective: Conceptual study on the science of Nutrition in Public Health.
Understand the epidemiological research concept and framework.
Develop effective skill on information and evidence based communication for
progressive and collective action among civil and govt. authorities.
To build knowledge on various social toolsto work effectively in future.
Research Objective: Conduct the study to assess the impact of Community-NRC among children aged 5
of Sahariya tribal community.
Inside Learning Objective: Learn to live with people with unity and humanity and work with people applying equity.
Bringing effective transparency into my personality.
7
Community Health Learning Program-2013
My Journey towards People
First of all remembering my Guru Shri Saibaba ji, I would start my journey towards people which
my Guru did throughout his life by spiritual concepts and they brought many changes in life of people of
Shirdi during his life.
The people who lives in different corner of the world and belongs from any segment of society are
struggling to achieve something to make them-selves happy, healthy and wealthy. This competition to
remain happy, healthy and wealthy brought few sharp minded peoples ahead and many people remain
back loosing this race of wealth and development.
The class theory says, People in this world can be categorized in three segments of classes.... Poor,
Middle and Upper class. Poor class who has nothing and struggle day and night to sustain their life.
Practically these people have a very low economy, social wealth, identity, power and other sources of
life establishment. Many scholar activists raise their voice for social and economical justice for these
people so that they can access equal chance to grow upwards.
One of the unknown sources says the 90/10 gap in inequity based take hold of socio-economical
and resources in this world. It means 10% of reaches, wealthy and powerful people of the world has hold
of 90% of resources and vast section of people which is around 90 % of world population are bound to
use only rest of 10% of resources. Therefore unfortunately this sort of inequity based distribution has
become deep rooted cause of poverty of large amount of population of the world.
Well, Let us discuss about main aspect which directly affects millions of the people‘s lives and no
one can live Satisfactory, Feel Peacefully, Physically, Mentally, Socially and Spiritually life in
absence of that aspect. Guess what...... Ok I give you choice.... Money! Yes for large extent it affects
human life but many of the riches people does not fulfilled the above mentioned red marked underlined
qualities, So therefore absolutely Money cannot be that aspect.
Now let‘s think about the word “HEALTH”. This word of 6 letters keeps important deep in human
life. This is only a word which has the capacity to give anyone a Satisfactory, Feel Peacefully,
Physically, Mentally, Socially and Spiritually life. One of my great faculty in SOCHARA always used
to says ―For many so called scholars, HEALTH is not everything but for real scholars Without
HEALTH, everything is nothing.‖ According to WHO, ―Health is a complete state of physical, mental
and social well-being, and not merely the absence of disease or infirmity.‖
Now if we thinks HEALTH for Aadiwasi community, they were proactive for their health because
of their dependency on nature. It means all of the above qualities were exist among aadiwasi community
from ancient ages but gradually it were snatched by systematic approaches of development, means the
nature which upon they were dependent are being destroyed. Therefore straight away it can be
concluded that all the determinants of health for aadiwasi community like land, forest, food chain etc are
8
Community Health Learning Program-2013
legally ban for them after independence. They cannot pluck on forest land, wood and other resources are
not legally available for the ancient community of around their own habitat, Therefore n be said, the
systematic so called developmental approaches are making them deprived from their entire basic
determinant of livelihood or we can say HEALTH is ban for them.
But, Who will initiate the effort for their rights to health? We- the people from civil society, Aam aadmi,
Government, or they only themselves. This is the question always jumps into brain. Do we think they
are not capable enough to take or fights for their right to health? The answer is Yes, they are capable but
seeking systematic and technological information from us. There is a need of their effort to get their
rights of health, education, better livelihood, food and etc. This is the point where the terminology
COMMUNITY HEALTH is needed.
COMMUNITY HEALTH is the process to enable community to take collective action for their
health and the allied determinant so that they could take health as their fundamental rights, They
can ask to govt to provide health facility, job, food, shelter, their habitat and allied environment. They
also can take what they thinks best for them, not what govt thinks good for them because they live in the
surrounding.
It requires equity based approaches with social justice for marginalized community and decentralized
approaches which can make them enable to take decision for their own growth.
Here my area of study to bring community health among Sahariya tribal community of MP.
DATA HIGHLIGHTS: THE SCHEDULED TRIBES (Focused Sahariya)
The Scheduled Tribe (ST) population of the State of Madhya Pradesh is 12,233,474 as per 2011
census. This constitutes 20.3 per cent of the total population (60,348,023) of the State. Madhya
Pradesh holds 1st rank among all the States/UTs in terms of ST population and 12 th rank in respect of
the proportion of ST population to total population. The growth of the ST population during 2001-2011
has been 26.4 per cent, which is 2.1 per cent higher than the overall growth of total population (24.3
per cent). The State has a total of forty six (46) Scheduled Tribes, and all of them have been
enumerated in 2011 census.
The Scheduled Tribe population in the State is overwhelmingly rural, with 93.6 per cent residing in
rural areas. At district level, STs have returned the highest proportion in Jhabua district (86.8 per cent)
followed by Barwani (67 per cent), Dindori (64.5 per cent) and Mandla (57.2 percent) districts. Bhind
district preceded by Morena and Datia has the lowest proportion of STs (0.5 per cent).
9
Community Health Learning Program-2013
Nutritional Status– A Primitive Tribe of MP and Rajasthan
ABSTRACT The Saharia is reported to be one of the most backward tribes of MP and Rajasthan.
Recently the media reported incidents of starvation deaths among Saharia tribal community in
Kishanganj blocks of Baran, Shyopur and Shivpuri. Therefore, a rapid survey was carried out to assess
the diet and nutritional status of the Saharia tribal population. Many villages, where Saharia tribal
population is concentrated were selected in consultation with the district officials. The study revealed
that a majority of the households surveyed were nuclear families. About 81% of the male head of the
households and 96% of their female counterparts were illiterate. The major occupation of the head of
the household was either agricultural labour or other labour (82%). Only about 42% of the HHs
surveyed the possessed varying extent of land. In general at household level, the consumption of all
the foods except cereals and millets were below the suggested levels. The intake of protein, calcium,
iron, thiamin and niacin were comparable to the recommended allowances, while the intake of other
nutrients such as total fat, energy, vitamin A, riboflavin, vitamin C and free folic acid were below the
recommended levels. On clinical examination, the prevalence of Bitot spots among preschool children
was found to be higher (8.3%) indicating that vitamin A deficiency is a major public health problem in
the tribal population. The prevalence of under nutrition (weight for age <Median –2SD) among 1-5
years children were significantly higher (72%) than that reported for the State of Rajasthan (48%)
(DWCD,1998).Breast-feeding practices revealed that majority of the mothers initiated breast-feeding
on the third day of the delivery. About 85% of the mothers discarded colostrum, mostly because of the
traditional practice. The observations highlight the need for strengthening health and nutrition
programmes in this area.
Nutritional status of the population largely depends on the consumption of food in relation to their
needs, which in turn is influenced by the availability of food and purchasing power. The socio-economic
conditions like agricultural pattern and occupation profile are different among different tribes and are
determined by the eco- system they live in. Several studies have shown a close relationship between
the tribal eco-system and their nutritional status. The tribal populations are ‘at risk’ of undernutrition
because of their dependence on primitive agricultural practices, and uncertainty of food supply. There
is a broad understanding of the nutrition problems of population living in urban and rural areas, while
such information on tribal population is meagre. Earlier studies indicated that the nutritional status of
tribal people is very poor compared to their rural counterparts. Recently, starvation deaths were
reported among Sahariain many districtby the media, due to prevailing severe drought conditions.
Study carried out earlier in the State of MP and Rajasthan revealed that recurrent droughts had
adversely affected household food.
10
Community Health Learning Program-2013
Population - Size & Distribution
Out of forty six (46) STs, Bhil is the most populous tribe having a number of 4,618,068, constituting
37.7 per cent of the total ST population. Gond is the second largest tribe, with a population of
4,357,918 constituting 35.6 per cent. Four other STs in the descending order are Kol, Korku, Sahariya
and Baiga. Along with Bhil and Gond, the six tribes constitute 92.2 per cent of the total ST population
of the State. Pardhan, Saur and BhariaBhumia have a population ranging from 105,692 to 152,472;
together, they form 3.2 per cent. Four tribes, namely, Majhi, Khairwar, Mawasi and Panika having
population in the range of 47,806 to 81,335 account for another 2.2 per cent of the ST population;
remaining thirty three tribes along with the generic tribes constitute the residual 2.5 per cent of total
ST population. Tribes having below 1000 population are twelve in number. Of them, five tribes,
namely, Mina, Andh, Birhul, Parja and Nagesia each have less than 500 populations.
Bhils have the highest population in Jhabua district followed by Dhar, Barwani and West Nimar
districts. Gonds have major concentration in Chhindwara, Mandla, Betul, Seoni and Shahdol districts.
Other four major groups Kol, Korku, Sahariya and Baiga have registered the highest population in
Rewa, East Nimar, Shivpuri and Shahdol districts respectively.
Sex Ratio
The overall sex ratio of the ST population in Madhya Pradesh is 975 females per 1000 males which is
lower than the national average of 978 for all STs. At the individual level, Gond and Baiga have over all
sex ratio higher than that of the national average. Sahariya have shown the lowest overall sex ratio.
The sex ratio among the STs, in the age group 0-6 years (979) is higher than that of all STs at the
national level. Except Korku, Kol and Sahariya, the three major tribes have higher child sex ratio than
that of the national average.
Age group
All ages
0-6 years
All ST’s India
978
973
All ST’s MP
975
979
Sahariya
938
969
Literacy & Educational Level
The overall literacy rate of the STs has increased from 18.4 per cent at 1991 census to 41.2 per cent at
2011 census. Despite this increase, the literacy rate among the tribes of Madhya Pradesh is lower if
compared with that of all STs at the national level (47.1 per cent). Male and female literacy rates among
the tribes (53.5 per cent & 28.4 per cent) are also lower in comparison to those at the national level (59.2
per cent & 34.8 per cent).
11
Community Health Learning Program-2013
Litracy rate
Persons
Females
All ST’s (State)
41.2
28.4
Sahariya’s
28.7
15.9
Marital Status
The data show that 51.9 per cent of the ST population is ‗never married‘ whereas ‗married‘ persons
constitute 43.9 per cent. ‗Widowed‘ persons form 3.9 per cent while less than half per cent are (0.4 per
cent) ‗divorced and separated‘.
Marriages of girls and boys below the legal age for each are in practice among the tribes of Madhya
Pradesh. Married girls below 18 years and married boys below 21 years constitute 2.5 per cent and 4.6
per cent respectively. These proportions are higher than those recorded for all STs at the national level
(2.1 per cent and 2.8 per cent). The STs namely, Kol, Sahariya and Baiga have registered the proportions
of such marriages higher than the State average.
The mean number of children ever born per ever married ST woman (45 – 49 yrs.)is 5 which is higher
than the total STs at national level (4).
Religion
Hinduism is the predominant religion (91.1 per cent) of the State. As many as 96.1 per cent STs are
Hindus.Tribes following ‗other religions and persuasions‘ account for 3.2 per cent. Christian and
Muslim tribes constitute 0.5 per cent and 0.1 per cent respectively.
Learning community-Sahariya tribe
Sahariya, the only primitive tribe of the MP, Rajasthan and UP state. They are mostly under privileged
group. They are basically 'Bhel'. There are some differences with the 'bhel' tribe like the main arms of
'Bhel' is 'Dhanush-ban' and Sahariya's is ‗Kulhada'. The name Sahariya is said to be derived from the
Arabian word 'Sehara' or 'wilderness'. The Muslim rulers found them residing in jungle, gave them their
present name 'Sahr' which means 'Jungle' and accordingly they came to be called 'Sahariya' meaning
residents of jungle. Even in the absence of genuine historical account it may be stated that the Sahariyas
have been one of the earliest settlers in Rajasthan. Rajasthan Government has announced this area as a
Sahariya region. Sahariya live in infrastructural weak and remote areas, not well connected through
road/bridge network even now. Lack of exposure to modern life and historic exploitation by landlords
who paid them less wages, has left Sahariya extremely primitive and backward. In the last one decade
there has been some interest and efforts towards 'Sahariyas' development. After the emergency period,
states government has constituted 'Sahariya Innovative Project'.
12
Community Health Learning Program-2013
Social Life
Sahariyas generally reside in separate basti in the village which is called Saharana. The religious
practice by these tribals is Hinduism and they speak a dialect influenced by Hadoti. The Sahariyas
maintained ecological equilibrium with their
environment for ages, despite low level of technology. Mostly they were engaged as gatherers of minor
forest produce and agriculture labourers. The main business are gathering & selling of forest wood,
Gum, Tendu leaf, Honey, fruits and vegetables. Though Sahariyas, in general are primitive, but all of
them are not so. Some of them are settled cultivators. Others are landless labourers and forest produce
gatherers. They live in small families. The elder sons live separately after marriage and younger son bear
the responsibilities of the parents and unmarried brothers-sisters. Marriages are performed after attaining
the age of 15 years. There are some arranged marriages and some in the ceremony in the fairs.
Gautra
Gautra are very significant in Sahariya's marriages. The main gautra of the Sahariya's are 'Sohara',
'Gorchia', 'Dotiya', 'Chauhan', 'Seliya', 'Bakhudiya', 'Parodiya', 'Gogaiya', 'Kalkhoriya', 'Somliya',
'Khelra', 'Nugapan', 'Sagruliya',
'Bandwal', 'Babuliya', 'Jeswariya', 'Baraliya', 'Pagdiya', 'Kanwar', 'Kasriya', 'Susiyar', 'Navoliya',
'Churawat', 'Dewriya', 'Badhiya', 'Parani', 'Matvehi', 'Semriya', 'Devriyan','Bhagya', 'Silwar', 'Pawar',
'Girwar'.
Festivals
They worship public Goddess 'Tejaji', 'Dhakar Baba', 'Durga', 'Hanumaan', 'Lalbai', 'Bejasan'. They
mainly celebrate festivals like 'MakarSakranti', 'SavniAmavasya', 'Janmashtmi', 'RakshaBandhan',
'Deepawali', 'Holi' and 'TejaDashmi'
Food Habits
Sehariya takes seasonal 'Kandmul' fruits and vegetables found in forests. Vegetables leafs of 'Senjna',
'Phang', 'Bichotiya', 'Kanna', 'Bansi', 'Charetha', 'Churangli', 'Barsak', 'Lahaylai', 'Chaurai', 'Totam',
'Chani', 'Bajar', 'Rajan' etc. are very commonly taken by Sahariyas in their foods. Crushed dry 'ber' with
salt is also eaten with interest. They are non-vegetarian also. They eat Hen, fish, sheep, goat, egg,
pigeon, rabbit and other forest found animals.
13
Community Health Learning Program-2013
Sama
'Sama' is the seeds of the special grass found in the jungle. Sahariyas made delicious foods from the
seeds of this grass. The seeds of the ‗Sama‘ grass are crushed to flour and chapatis are made. The sama
flour are also used to make 'kheer', 'Rabri' etc. The sama seeds flour is a nutritive value which is also
used by
the urban people in their fast (Upwas).
Source of livelihood
Since from inception Aadiwasis were depends on Nature. Forest, river, pond and all sort of natural
amenities were part of their life. Gradually need of capital become enhance and they started selling
natural amenities to sustain their livelihood. Wood and Tenduis generally being used among Sahariya
tribal. Now Sahariya switches their places in search of jobs. This migration is developing various
problematic issue among of them.
14
Community Health Learning Program-2013
Briefly description of problem analysed:•
•
•
•
•
•
•
•
•
•
•
•
•
Land availability
People‘s awareness and education.
Irregularity in ICDS policy implementation.
Government is granting in NRHM but not implementing.
Systematic lack of Medical Rehabilitation.
Parent mostly time living apart from child for livelihood.
Migration.
Alcoholic habit.
Morel education because community is insensible for child protection.
Source of livelihood.
Land availability.
Job opportunity.
Rain falling.
REFERENCES
Census 2001-2011.
CID and Action Aid.
Department of Women and Child Development: India Nutrition Profile. DWCD. Ministry of
Human Resource Development (1998).
15
Community Health Learning Program-2013
Session reflection during collective session at Bangalore and
field visit.
Plastic Cow:KARUNA Trust organized a discussion on plastic management in Bangalore city and all over the India.
Basically we can see anywhere in India that one of the most striking images is the cow wandering on the
road. In cities, towns and villages numerous cows and bulls sit or wander peacefully, settling down to
chew the cud. It gives the impression of a society living together peacefully with animals. The holy cow,
the Mother of India is revered by all and, in most states, is not allowed to be slaughtered. India has an
open garbage system, which means open garbage bins on the roads overflowing with stinking waste.
Dogs, monkeys, pigs, rats and cows eat whatever they can find to survive. In cities and towns, large
numbers of cows on the roads eat from garbage bins, foraging for fruit and vegetable leftovers, anything
edible and smelling like food.
Since plastic bags have invaded our lives, almost all garbage and food waste is disposed in plastic bags.
These bags spill out either on the road or from municipality dustbins. Since the plastic bags are knotted
at the mouth, cows, unable to undo the knot, eat food leftovers including the plastic. Slowly, over time,
they build up a huge amount of plastic inside their stomachs. It gets entangled with different materials
and it becomes hard like cement inside their rumens, which is the first belly of the cow.
The Plastic Cow Documentary projection were organized at spot which is made by Kunal Vohra
from Altair films with scholar inputs from various environmental activists, toxicologists, government
authorities, householders, students, journalists, etc.
The Green Foundation - The farmer’s friend and traditional boon for
agriculture
We visited Green Foundation to look on a splendid community led initiative to preserve agricultural
environment using bio fertilizer and promoting seed bank method.
The GREEN Foundation began its work in 1997 with a handful of women in the small village of Thalli,
South India, driven by the aim of helping small scale and marginal farmers of the country.
With over 50% of India's workforce finding employment in the agricultural sector, the country's poverty
issues cannot be addressed without considering the plight of the Indian farmer. Foundation work to
strengthen the food and economic security of these farmers through a multi-pronged approach
16
Community Health Learning Program-2013
Empower communities to use bio-fertilizers and preserve rear spicies of seed with mutual
effort
Preserve the ecology through community seed bank
Empower women in agriculture by SHGs
Lobby for political change
Preserve indigenous knowledge related seeds,
Basic Need India – A genuine place to know Community Mental Health
Community Mental Health is one of the innovative concept on which BNI working for many years. The
Basic Needs India aims to concentrate on the social, economic and development needs of people with
mental illness and their families through new initiatives to contribute in the reduction of poverty. Basic
Needs India - Works with established development organisations particularly in the rural areas, to enable
them to adapt their programmes so as to take into account the needs of people with mental illness.
Encourages the formation of self-help groups of people with mental illness and their families. They
are supported to provide for themselves through appropriately developed and managed schemes.
Trains and supports people with mental illness and their family members to become contributing
members by developing appropriate income generation programmes
Develops partnership with existing organisations to help them include poverty alleviation work in
their own communities.
State level consultation on Ban on Tobacco Advertising, Promotion and
Sponsorship.
SOCHARA organized a state level consultation on TAPS with the partial collaboration with
Karnataka Government and R.G.U.H.S. As a prior preparation, team SOCHARA visited public
places to collect sample of evidence which reveal the contravention of COTPA-2003 in Bangalore
city.
Tobacco industry has been instrumental in spreading the tobacco epidemic globally through
aggressive marketing campaigns. It is the only industry that kills its 5.4 million loyal customers every
year. In 2005, the WHO Framework Convention on Tobacco Control (WHO FCTC), the first treaty
negotiated under the auspices of the WHO, came into force. Article 13 of FCTC suggests a
comprehensive advertising ban, within five years of entry into force of FCTC for each party.
Currently, only 19 countries of the world (representing 6% of the global population) are covered by
17
Community Health Learning Program-2013
comprehensive ban on tobacco advertising, promotion and sponsorship (TAPS), with 101 countries
imposing partial bans and 74 countries having no ban at all. This is a matter of public health concern..
Despite existing TAPS prohibition laws, tobacco industry circumvents the laws to promote their
products by employing innovative and at times, covert marketing strategies. Indirect or surrogate
tobacco advertising such as dark advertising, brand stretching, corporate social responsibility (CSR)
activities, promotion through films and new media such as internet, discounts or free-gift offers,
distribution of free samples, sale of tobacco products in the form of children's sweets/toys, etc. gained
momentum with increasing pressure on tobacco industry . Guidelines for implementing Article 13 of
FCTC, describe comprehensive TAPS ban to apply to all form of commercial communication,
recommendation or action and all forms of contribution to any event, activity or individual with the
aim, effect or likely effect of promoting a tobacco product or tobacco use either directly or indirectly.
In 2003, India passed COTP Act in parliament to comprehensively ban on tobacco product under
some mentioned guidelines. Comprehensive TAPS ban would lead to reduction in initiation and
continuation of tobacco use; as such a policy measure would have large population level impact,
thereby reducing demand for tobacco.
FRLHT (Foundation of revitalization of local
health tradition) I-AIM (Institute of Ayurveda and Integrated
Medicine) IHST (Institute of transdiciplinary health
sciences and technology)
We stayed for two days at FRLHT to study the way to conserve traditional knowledge related to
AYUSSH. This place was really a wonder for our country. The multi-disciplinary track record of
FRLHT – I-AIM- IHST over the period 1993- 2013, demonstrates out of the box thinking. Its growth
in the last 20 years is evidence of dedication, hard work, perseverance and efficiency.
In 1993, FRLHT embarked on an ambitious program for Insitute. Conservation of wild
populations of medicinal plants. Today this program has grown into the largest medicinal plants
conservation network of 108 forest parks in the entire tropical world. FRLHT is also a pioneer in
18
Community Health Learning Program-2013
Threat assessments of wild populations. FRLHT are basically acting on few themes which are given
below: Conservation of natural medicinal resources
Information technology and traditional knowledge
Bridge between traditional knowledge and science
Scientific repositories of natural resources
Revitalisation of folk healing systems
Research hospital
A herbal public ltd company owned by rural women and small farmers
Botanical repository
Rural health security
Scientific research
Rural livelihoods
Clinical services
Literary research
Educational Innovation.
The Association of People with Disability (APD) – The place which
believes ability in disability
APD was the great innovation of Hema mam who is the strongest lady, I have ever seen. She believes
the hidden ability in disable people and She take out all the able feature of any disable people. For the
last 52 years, APD has worked on the comprehensive rehabilitation of economically marginalized
people with disabilities. Through grassroots rural and urban community programmes that include
therapeutic services, mobility aids, integrated education, advocacy and livelihood training; APD has
been able to transform the lives of over 28000 persons with disability. With an estimated 70 million
persons with disability in India, APD is among organizations that are at the forefront of the urgent,
nationwide movement to overcome the growing challenge to support, rehabilitate and include people
with disability into mainstream economy and social life.
APD are running mentioned program.
Education
Training and Employment
Therapeutic services
Horticulture Units
People‘s Organizations and Advocacy
Resource Support to Organizations (RSO)
District Disability Programme
19
Community Health Learning Program-2013
Transaction Analysis
In the series of learning, we attended a two day workshop on Transactional analysis at Seva Sadan.
During this session, we were given information on psychopathological method of human behaiviour.
Accordingly, Transactional Analysis is one of the most accessible theories of modern psychology.
Transactional Analysis was founded by Eric Berne, and the famous 'PARENT ADULT CHILD'
theory is still being developed today. Transactional Analysis has wide applications in clinical,
therapeutic, organizational and personal development, encompassing communications, management,
personality, relationships and behaviour. Whether you're in business, a parent, a social worker or
interested in personal development, Eric Berne's Transactional Analysis theories, and those of his
followers, will enrich your dealings with people, and your understanding of yourself. This section
covers the background to Transactional Analysis, and Transactional Analysis underpinning theory.
Transactional Analysis is a theory which operates as each of the following:
a theory of personality
a model of communication
a study of repetitive patterns of behavior
There are three main Ego state are exist in any human personality which is,
Parent
Parent is now commonly represented as a circle with four quadrants:
Nurturing - Nurturing (positive) and Spoiling (negative).
Controlling - Structuring (positive) and Critical (negative).
Adult
Adult remains as a single entity, representing an 'accounting' function or mode, which can draw on
the resources of both Parent and Child.
Child
Child is now commonly represented as circle with four quadrants:
Adapted - Co-operative (positive) and Compliant/Resistant (negative).
Free - Spontaneous (positive) and Immature (negative).
20
Community Health Learning Program-2013
KARUNASHRAY - Centre for Palliative care
Karunashraya is a hope zone for those who are seeking care at their last moment of life. This is running
by Bangalore Hospice Trust,
Palliative Care
The diagnosis and treatment of cancer is a threat to survival and to the self. It threatens not only the
patient’s physical health but also their psychological well being. The process from diagnosis to
treatment to terminal phase has profound psychological impact to the patient.
As the cancer advances and there is no scope for further curative treatment, the treatment becomes
palliative. The word palliation is derived from the latin word ‘pallium’ meaning ‘cloak or cover’. In
palliative care, distressing symptoms are covered with treatment whose primary aim is to make patient
comfortable. (Source- wikipedia).
What is Palliative Care
The Indian Association of Palliative Care (IAPC) defines Palliative Care as the active total care
applicable from the time of diagnosis, aimed at improving the quality of life of patients and their
families facing serious life-limiting illness, through the prevention and relief of suffering from
pain and other physical symptoms as well as psychological, social and spiritual distress. A
holistic and multi disciplinary approach, Palliative Care’s primary goal is to achieve the best
possible quality of life for patients and their families. It also involves care and support for
caregivers. Palliative Care helps family members and caregivers to manage the patient’s illness
and cope better during bereavement.
Need for Palliative Care
A multi-disciplinary approach, Palliative Care requires integrated intervention from doctors, nurses,
physiotherapists, occupational therapists, counselors and even spiritual guides.
Drug administration: Patients undergo pain assessment twice a day and receive medication based
on the pain level. Drugs are administered at optimum levels.
Physiotherapy improves blood circulation.
21
Community Health Learning Program-2013
Counseling: With a direct co-relation between the state of mind and pain, counselors play a key
role in helping patients maintain a high sense of dignity, self worth and a positive outlook. They:
Identify and tackle concerns by counseling patients and families
Discuss the best approach and interventions required before rendering them
Play the role of mediators and wish fulfillers
Diversional therapy alleviates pain to a great extent. Karunashraya volunteers work with patients
on craft activities or entertain them. Patients are also encouraged to take care of each other as this
strengthens bonds between them besides offering psychological support.
Prayer: Some patients find relief in visiting the prayer and meditation rooms.
Fulfilling wishes: Karunashraya focuses on granting the wishes of patients to the extent possible –- from
providing meals of their choice to reuniting them with family members to helping them watch their
favorite movies and even arranging for meetings with celebrities like Aamir Khan, Shiv Raj Kumar,
Chiranjeevi etc.
ROSHNI- A light of hope
ROSHNI is one of the active organization which
is working for mentally challenged children.
ROSHNI was founded in 1998 in Gwalior,
Madhya Pradesh with the objective of providing
direct services for persons with neurological and
other impairments, raise awareness about
disability, build capacities to increase the
numbers and strengthen the knowledge and skills
of the lay and the professional, family and
community, to enable the inclusion of persons
with disability into the community. Swami
Swarupanandaji encouraged and supported the
advent of specialist services for persons with
disability and provided space and administrative support at the Ramakrishna Ashrama, with ROSHNI
required to fund its operations through its own resources. ROSHNI was perhaps the first specialist
rehabilitation service provider for the disabled to appear within the State, and certainly so within the
district of Gwalior. Sadly, despite the numbers of persons affected directly and indirectly by disability,
22
Community Health Learning Program-2013
rehabilitation services outside the so-called Metros – and to a marginal extent a few state capitals – are
largely non-existent. The Ashrama offers the environment of a vibrant community complete in all
respects, with a value system that inspires and empowers the people at ROSHNI—those working for the
persons with disability and the persons with disabilities, their families and, indeed, all other stakeholders
including the volunteers, donors, supporters. ROSHNI has been growing and expanding in terms of the
extent and range of services, impact, skills and knowledge and support base.
ROSHNI extends the entire gamut of specialist services to persons with disability and their families,
despite the severe constraints imposed by limitations in availability of professionals. Gwalior does not
have professionals, and few from the cities are willing to come to such small towns – especially as
therapists, social workers, special educators etc. command much higher salaries in the cities than can be
matched with the limited resources what ROSHNI have. It is a tribute to the commitment and sense of
service of the professionals at ROSHNI that they are able to meet the various rehabilitation needs of
persons with disability in the region.
ROSHNI is a day care centre, especially focussing
on mentally retired person of each age group. They
made categorisation into three age groups keeping
concentrate on a type of person‘s stage.
1. Early Intervention (0-5 years)- Assign the
degree of retireness.
2. Primary Intervention (6-15 years) - Initiate
rehabilitation through various method .
3. Vocational (16-53 years) - Provide
vocational training to make them selfreliant.
The key intervention is done by ROSHNI
during these long span of time:Assessment by special educators and
therapists, in all areas and detailed individual programmes.
Family support and training in techniques of practical care for Home–Based Children / Adults.
Special education-group & individual sessions.
Speech & communication assessment and programming.
Medical, hearing, vision and dental clinics.
Mobility, postural & orthotic aids provided for use at the centre and at home.
Individual therapy sessions.
Pre-vocational Training.
Vocational assessment and skill development.
Support to Students in Mainstream Schools-Therapy & Special Education.
Advocacy & Awareness Raising.
23
Community Health Learning Program-2013
Training of parents / teachers / professionals / community workers.
Outreach - Urban and Rural.
Expert Opinion
“Ms. Rakhi Ashthana”
(Principal, ROSHNI and EX-coordinator,CBR)
Ms Ashthana is aexperienced worker in community based rehabilitation in disability. She has
dedicated her life for person with mental retardation and has been working for mental disability
for a long while.Shecooperated very much and made my visit successful. While discussing
about ROSHNI, I built my understanding on the basis of a few informal queries….
Q:- How society treats people with mental distorted ?
Society is made up of all of us, what we think society thinks. Almost every person considers them
abnormal. In other words, they do not have a same behaviour quality which is found in so called normal
person. Thereforesociety shows sympathised behaviour towards people with mentalretardation or people
with mental illness.
Q:- How do you define the role of community or society towards the welfare of these
people?
I feel, society need not to show any different with these people, they are the equal part of the society.
Society can support by helping these people through various way. Many times children refuse to go back
to home due to domestic violence or rude behaviour of neighbour. I observed, almost every time, these
so called normal people behave like psychological sick. These children never harmed anyone,but I scare
with so called normal person. Society is problematic itself so society have to change themself.
Q: -If you were the policy maker, What step are taken by you?
As I told you, these people are a part of society therefore it is no any need to make different law for
them but there condition should not be ignored. They need collective support and rehabilitationsservices
must be regular and approachable. These people need special care. Policy maker should think over
24
Community Health Learning Program-2013
collective rehabilitation methodology. Policy maker are flowing money behind many unnecessary
promotion instead of to put their focus on these issue. Society should be regularly aware through
advertisement, IEC and campaign.
KARGERICON-2013
The 4th Annual Conference of The Karnataka Chapter of the Indian Academy of Geriatrics
25
Community Health Learning Program-2013
Critical corner
Ejipura bulldozed
A Story of
Justice Vs Humanity
There are a disaster came in Bangalore but this time disaster made by
human to destroy the life of curtain section of people. A cruel
demolition at Ejipura occurred driven by BBMP (Brihut Bangalore
Maha-nagarPalika). They are only vaguely aware of the politics
behind the demolition drive (homes demolished to make way for a
mall to be built by Maverick holdings). They are here because it
would
be
inhuman
not
to
react.
Of the 2,000 odd families and overall 6000 people that once lived
here, less than a few families are still around. These are the people
who have nowhere else to go, no any curtain amount to pay in terms
of home rent and not even a few hundred rupees to pay a luggage
truck to shift their few belongings. The only relief has been given by
a few individuals who have volunteered to help them.
However, these volunteers too have met with certain forms of
resistance. Even, an old woman of 60-year age died
apparently due to trauma. Min cause is to stay without roof
overnight in slum and main thing is, We could not resist
against of this cruel action. It was ordered by the High Court
and high court refused to hearing against this demolition....
1. The people of this large slum spent their fourth
consecutive night only under the sky.
2. At least 2,000 families were deprived even from a
single roof after a three-day demolition drive last
week.
3. Rosemary, an old woman, who was evicted along with
her family, died allegedly due to trauma.
4. Residents of Ezipura continuously demanding their
shelter but now their constitution and law and order
26
Community Health Learning Program-2013
still became a huge barrier for them. High court refused to consider any case against of this cruel
demolition until it accomplish.
5. A group of 40 women went to demand their roof but instead of listening them, police started
striking them. All of them were became victim of that cruelty.
6. Now this incident divided human society in two sections, one belongs from elite and powerful
background and another refer venerable and weaker section.
7. After this cruel demolition, Call for help was happening from every side…. People were
screaming to support them, a few of people support them, most of people were watching the
drama.
How was it happening?
It is not happen suddenly, this entire game was under execution from so many years; we
watched only the outcome now. When we observed situation minutely, so many things come out.
People itself were divided in two part even it was justice according to law and order, For the name of
poverty remove movement, A few of Government official, politician and elite section executed poor
remove movement under the safeguard of court‘s order. Whichever the fact was, people had to
suffer. That fight initiated between Human‘s Greed verses Humanity and now fight became…….
Justice verses Humanity
Ankit Vashishtha
Reference:
1/25/13- The Hindu : Cities / Bangalore : Police stall Ejipura residents protests outside CM residence.
Photo courtesy :- The Hindu.
Mental health and mental health act, 1987
A critical discussion after Guru bhaiya‟s session on Mental Health
Mental Health is considered as one of the most complicated structure of Health of human in society. It
is considered ―Health is not everything but everything without health is nothing and absolutely there is
no health without mental health‖.According to World Health Organization, mental health as "a state of
well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of
life, can work productively and fruitfully, and is able to make a contribution to his or her community". It
27
Community Health Learning Program-2013
means a normal and healthy person can deal with problem and situation of life and able to take decision.
He can communicate effectively and contribute the society with their custom, traditions, and other
events and also can love and harmony with every individual and society. Mental wellness is generally
viewed as a positive attribute, such that a person can reach enhanced levels of mental health, even if the
person does not have any diagnosed mental health condition. This definition of mental health highlights
emotional well-being, the capacity to live a full and creative life, and the flexibility to deal with life's
inevitable challenges.
MENTAL HEALTH ACT, 1987
(For care and rehabilitation of mentally ill person)
The Mental Health Act 1987 repeals Indian Lunacy Act 1912 and Lunacy Act, 1977 (Jammu &
Kashmir) and extends to whole of India. Under this Act 1987, a "Mentally ill person" means a person
who is in need of treatment by reason of any mental disorder other than mental retardation.
My Comments,
1. The Mental Health Act is one of the good legislations. It came into force in 1993 however it is
enacted in 1987 which shows that the Act was given low priority.
2. Mental Health Authorities are formed as a watchdog bodies to assure the quality of services. Govt.
and private psychiatric hospitals need to get license from these authorities. Practicing psychiatrists have
raised objection for this because other branch of medicine do not have similar regulatory bodies to
access the quality of care. At the same time psychiatric hospital may be one which is providing "total
care" or general hospital may be providing specialised psychiatric care.
3. Role of judiciary in admission and discharge of psychiatric patients give an impression of criminal
flavour (Dutta 1995).
4. There is a need of big investment in development of infrastructure and provision of basic facilities in
mental hospital which is still largely ignored.
5. The Act excluded mental retardation, dementia etc. which cannot be treated. But very fact is that these
conditions need gentle mental care and excluding may be against human rights of these patients.
6. Power and duties of police officers in respect to certain mentally ill persons have been laid down in
Chapter 4 part B (Sect 23), of the Act. But we can see many mentally ill patients wandering in public
places in conditions of total neglect and squalor. This indeed is testimony to the fact that the way section
23 is presently put to use has failed to achieve the objectives of the Act.
28
Community Health Learning Program-2013
7. "Voluntary admission" not always real voluntary rather misused. This need to be more specific and
must have experts opinion on the subject.
References:
Antony JT. A Decade with the Mental Health Act 1987. Ind J Psychiatry 2000: 42(4): 345-355.
Govt. of India. The Persons with Disability (Equal Opportunities, Protection of Rights and Full
Participation) Act, 1995.
Dutta AB. Medicolegal problems of psychiatrists in private practice. Journal of clinical
psychiatry 1995.
The Gazette of India. The Mental Health Act 1987. Govt, of India
Direct Benefits Transfer (DBT) Scheme
A Magical Stick or Slow Poison
The Union Government of India has launched the Direct Benefits Transfer (DBT) programme to give
benefits like scholarships, pensions, NREGA wages, LPG, PDS etc. directly to the bank or post office
accounts of beneficiaries. There are also talks of direct transfer of subsidies for food, fertilizer and
kerosene at a later stage. It is an anti-poverty program launched by Government of India on 1 January
2013. This program aims to transfer subsidies directly to the people living below poverty line.
In this scheme, Money transfer can be a good way of helping the poor in many circumstances. Indeed,
many schemes that are not directly cash transfer schemes also work mainly through cash transfer, such
as the National Rural Employment Guarantee programme, which certainly has helped the poor through
creating jobs and generating cash income for a great many poor people in rural India. Cash is easy to
handle and can be, in many cases, easily monitored. It cannot be sensible to be generically against cash
transfer schemes, in a country with a lot of poverty and a commitment to use public money to make the
very poor a bit less poor.
Although, The Direct Benefits Transfer (DBT) programme is a particular scheme of cash transfer, and
we have to ask what it may be displacing and whether the losers will not be rushed into more poverty. It
is not the modality of cash transfer that is the only issue, but also how much, and for whom, and also,
instead of what. If, for example, it is instead of subsidised food, we have to make sure that the people
who depend on cheaper food will have enough cash to buy the unsubsidised food. There is also another
complication is that of the distributional effects of different kinds of benefits within the family. If the
cash transfer is not additional to food subsidies, and is given ―instead of‖ food subsidies, it would be
important to make sure that the money given would be used for nutritional purposes and, equally
29
Community Health Learning Program-2013
importantly, that it would be divided within the family in a way that addresses the manifest problems of
undernourishment and deprivation of young girls.
Another biggest complication is availability of bank and post office at very close distance and to become
beneficiary under this scheme, bank account must be log in with Aadhar. There are around 70%
population is bound to survive below poverty line and many of them do not have any account and
Aadhar. Even if it is made sure about these difficulties,there may still be a serious problem of transition,
especially if there is a time lag in opening an account in a bank, or in a post office, to receive the cash
transferred. If, meanwhile, the subsidised food disappears, the poor who fail to open an account
adequately fast, for one reason or another, will lose doubly through not having the cash yet, and through
the fact that others will have the cash to buy food which would keep the food prices high. The transition
problem need not be impossible to handle, but attention will have to be paid to that, bearing in mind that
many of the poorer Indians lead a life of hand-to-mouth existence, and any delay in the period of
transition may plunge some people into extreme hardship. All this is in addition to the long-run
problems of the modality of cash transfer, including distributional issues, as well as the adequacy of the
amounts of cash transferred.
Conclusion :- Cash transfer can be a very useful system to supplement other ways of making India a
less unequal society, but it is not a magic stick, and its merit and demerit have to be assessed and
examined with an open mind.
Reference:
Study Material on Cash transfer published by VikasSamvad and written by Sachin Jain.
Article of Sandeep Joshi in January edition of the Hindu.
http://en.wikipedia.org/wiki/Direct_Benefit_Transfer
http://www.thehindubusinessline.com/features/taxation-and-accounts/direct-benefittransfer/article4276770.ece
PANCHAYATS EXTENSION TO SCHEDULED AREAS
(PESA) ACT, 1996
Plot, forces and processes that led to the enactment of PESA Act
In the series of lawful change for most marginalized and deprived section like tribes, the 73rd
constitutional amendment Act came into force in 1993, which transferred certain decision-making
powers to the three tiered Panchayati Raj Institutions (PRIs) and made this process of devolution of
power constitutional and mandatory. The States of Indian Union were directed to make suitable
amendments to their respective Gram Panchayat (GP) Acts to translate the central amendments into a
concrete reality. However, these amendments did not cover the scheduled areas of the country, which
30
Community Health Learning Program-2013
enjoy a special status under the 5th Schedule of the Indian Constitution. But there was a provision as per
part IX in the constitution for these amendment acts to be extended to scheduled areas of the country,
which suggested that ‗ parliament may, by law, extend the provision of this part to the scheduled areas
and tribal areas referred to in clause (I) subject to such exceptions and modifications as may be specified
in such law.‘ As per legal activist Mr.JayantVerma, It is a most effective gram sabha initiative rights in
5th schedule in Indian Constitution but not effective in non-5th schedule areas.
The Indian government took more then three years to bring about another law for extending the
provisions of the 73rd and 74th Constitutional amendment acts to the scheduled areas of the country.
The States, while making amendments to their respective GP Acts also did not take the suggestion of the
central amendment seriously and rather interpreted the suggestion to their advantage as there was no
directives to prohibit the States to have their own laws for the scheduled areas. Finally, a new law was
enacted by the Indian Parliament on the 19th of December 1996 that was preceded by a few important
developments.
• Firstly, some tribal outfits and a number of organisations working for the tribal launched a movement
for ―Tribal Self- Rule‖ in Scheduled Areas, which gained momentum with major part of the Scheduled
Areas across the States jumping into the movement.
• Secondly, because of a verdict of the AP High Court delivered on the 23rd of March, 1995 which held
that the application of the AP Panchayati Raj Act, 1994 to the Scheduled Areas of Andhra Pradesh (AP)
was unconstitutional. The Indian government by then had formed a committee of MPs and experts under
the Chairmanship of sitting MP Dr.Dilip Singh Bhuria and with Dr. B. D. Sharma (former
Commissioner of SC & ST Commission, Govt. of India) a leader of the Tribal self-rule movement as
one of the members. The committee was given a mandate to:
(i)
(ii)
prepare the salient features of the law which may be taken up for enactment by the union
parliament for extending provisions of Panchayati raj to the Scheduled Areas of the country
and,
suggest the variations and modifications to be brought about in other relevant acts under the
Vth Schedule to further strengthen the system of self-governance in the Scheduled Areas.
The committee submitted its report on the 17th of January 1995 and the parliament enacted
the new law on the 19th of December 1996 which came to be known as the Central Act 40 or
the PESA (Provisions of Panchayats Extension to Scheduled Areas) Act of 1996. It may be
noted here for a greater understanding later on that this act was approved in the parliament
without any debate or discussion on it. And those who said ―Yes‖ to it hardly knew what was
there in the bill.
The committee under Dr.Bhuria rather had much more
and detailed deliberations on the proposed enactment, which
was missing when PESA was enacted in the union parliament.
This has far reaching implications in the sense, later on there
31
Community Health Learning Program-2013
was none to own the new act (PESA) and to defend it when it ran into rough weather or to protest
against any violation of the act. Infect it was Dr. B. D. Sharma who drafted the act and Dr.Bhuria who
presided over the meeting who were the only people going round the country to defend the act wherever
its violation was reported.
The Salient Features of PESA in Brief
• First of all, PESA has extended the provisions of Part IX of the Indian Constitution relating to
Panchayati Raj to Scheduled Areas of the country with necessary exceptions and modifications.
• Secondly, PESA has elaborated on those exceptions and modification which are to be kept in mind
when a State legislature makes a law or act covering the Scheduled Areas of the State.
• Thirdly, PESA has directed the States which have got areas to make an Act on the basis of PESA
within a year of the enactment of PESA.
• Fourthly, PESA is directive for the States and not a law by itself.
• Finally, PESA has asked the State
legislatures to make laws for the Scheduled
Areas ―which shall be in consonance with the
customary law, social and religious practices
and traditional management practices of
community resources‖.
One of the highlighting features of PESA is its
suggestion that, ―every Gram Sabha shall be
competent to safeguard and preserve the
traditions and customs of the people, their
cultural identity, community resources and the
customary mode of dispute resolution‖. In
addition to this, the Central Act of 1996 provides extensive powers to Gram Sabha in the Scheduled
Areas in the following sectors:
i)
ii)
iii)
Approval of plans, programmes and projects for social and economic development prior to their
implementation,
Identification of beneficiaries of anti-poverty programmes,
Certify utilisation of fund spent by the Panchayat.
PESA after giving the above exclusive powers to the lowest unit of grass root democracy has
further provided that the Gram Sabha or Panchayats at appropriate level shall have the following
powers:
i.
To be consulted on matters of land acquisition and resettlement.
32
Community Health Learning Program-2013
ii.
iii.
iv.
v.
vi.
vii.
viii.
ix.
x.
Grant prospecting licence for mining lease for minor minerals and concessions for such
activities.
Planning and management of minor water bodies.
The power to enforce prohibition or to regulate or restrict the sale and consumption of any
intoxicant.
The ownership of minor forest produces.
The power to prevent alienation of land and to restore any unlawfully alienated land of a
scheduled tribe.
The power to manage village markets.
The power to exercise control over money lending to scheduled tribes.
The power to exercise controls over institutions and functionaries in all social sectors.
The power to control local plans and resources.
While prescribing such wide ranging powers to ―Gram Sabhas or Panchayats at appropriate level‖,
PESA has further warned that, ―the State legislation that may endow Panchayats with powers and
authority as may be necessary to enable them to function as institutions of self-government. It also
contains safeguards to ensure that Panchayats at higher level do not assume the powers and authority of
any panchayats at the lower level or the Gram Sabha‖.
FOREST RIGHTS ACT (2006)
After harsh public debate for more than a year since tabling in the parliament on 13 December 2005, the
Scheduled Tribes (Recognition of Forest Rights) Bill, 2005 which was re-christened as ―The Scheduled
Tribes and Other Traditional Forest Dwellers (Recognition of Forest Rights) Act, 2006‖ was passed in
the parliament, lower house of Indian parliament, on 13 December 2006. President of India assented to
the Bill on 29 December 2006 and the Act came into force. However, the debate since the tabling of the
initial bill in December 2005 to the passage of the
Act in the LokSabha have brought the age-old
prejudices against the tribal peoples to the fore
and further eroded their rights.
The Draft Scheduled Tribes (Recognition of
Forest Rights) Bill, 2005 faced stiff opposition
from two quarters.
First, a few environmentalists advocated
management of forest, wildlife and other biodiversity with complete exclusion of tribal
people, local communities or forest dwellers
contrary to the Rio Declaration, decisions of the
33
Community Health Learning Program-2013
Conference of Parties of the Convention on Biological Diversity and recommendations of the
United Nations Forum on Forest.
Second, the Ministry of Environment and Forest had opposed the Bill on the ground that
implementation of the bill will result in the depletion of the country's forest cover by 16 per cent.
This is despite the fact that over 60% of the country's forest cover is found in 187 tribal districts
where less than 8% of national population lives. This reflects the culture of the tribal peoples to
conserve forest.
Under the forest right act, those villages which
were not being beneficiary under schedule 5 of
constitution will be given genuine right to take and
capture land of the forest with prior consultation of
forest official even this act provide right to grab the
land if gram sabha grant permission to capture
against forest department.
PESA and FRA both of the act can be effective if
and only if community and gram sabha is ready to
initiate to take lead to take land right to improve
their source of livelihood. Land is also considered the basic amenities for remote communities to
sustain their livelihood. Therefore, There is absolutely no doubt that it is basic determinant to sustain
livelihood, stop migration and control death from hunger and surely put down rate of malnutrition in
these community of tribes.
Discussion in Medico Friends Circle on Guddi bai sting
operation at PHC -Lukwasa
Narrative minutes with scholars on Guddi bai case ………
(Source :- Minutes of the Mid Annual Meet of the Medico Friend’s Circle, 4th - 5th August, 2013, Bhopal available
at www.mfcindia.org )
“After tea, Ankit showed his short documentary – „Why Systemic Murder‟. Ankit is a CPHE fellow
from Sochara, Bangalore. This film was shot on his mobile, in Kolaras is block in district Shivpuri in
MP. This is in a particular PHC where lots of deaths has happened. The team have a good rapport
with the community and had asked the people to inform them if certain issues come up in the PHC.
The film showed a woman who had recently delivered a dead child, lying on the floor of a PHC room,
34
Community Health Learning Program-2013
which had empty beds. The placenta was there close to the woman and hadn‟t been removed. The
doctor on duty was an eye specialist as the other doctor had gone for some other duty. According to
Ankit, the other staff were not willing to touch the woman or her placenta who was a dalit. So even
after about an hour delivery, she was lying in the grounds next to a pool of blood and placenta. The
family members wanted to take her to a higher facility.
Abhijeet said that this is the norm in MP. Many of these kinds of cases are happening. Lots of powerful
evidence can be generated if these kinds of films can be taken of other cases as well. There has been lots
of activities in MP since the last few months on maternal and infant deaths. In 2010, MP had said that
they have 90% institutional deliveries but they give the most fraud and fudged figures. Emergency
obstetric care is important but institutional delivery is not important.
Sunil- we had supported institutional delivery when NRHM was brought in as we had seen that the TBA
training and other efforts hadn‘t worked. But now after 5-7 years of NRHM, we don‘t see much changes
in the health infrastructure, and therefore institutional delivery is not helping.
Jasodhara- there are three things, one is the presence of one doctor and his/her going off duty, the
second is the health system‘s attitude towards the poor and tribal women, how she is delivered on the
ground and no one touches her. The third is that people have been debating about institutional delivery
because poor are not treated well in public hospitals. The dai also cannot provide EMOC services as she
does not have the back up or the referral services. So the question is about the policy, health systems and
institutional delivery process.
Sarojini – we need to follow certain ethics when we present, the strategies are different for sting
operation and research. We need to think about what are the safeguards for these people.
Syed- we don‘t support institutional delivery but then what is the remedy in cases of emergency? The
woman stays 25-30 km far away from the PHC which has no roads and no transport, so what is the
solution.
Subhankar- there has been maternal death investigation by UNICEF in Purulia. These findings can be
of help.
Abhijeet- Video documentaries are needed but not any kind of sensationalisation. Process is also
important, but we do not want bad politics to happen. We had suspended the critical thinking when we
said okay to institutional deliveries. We did not study the deliveries, what were the problems, the
interpretation of report will be different for different people. NHSRC‘s JSY report has got the findings
what we also say but the recommendations go in a different track. It says we need to give more time but
the findings show something different. This paying of money to the ASHA for bringing women for
institutional delivery is also a kind of coercion. ASHA‘s income is dependent on that so she will
35
Community Health Learning Program-2013
encourage women to go to institutions. But no one is questioning this. When we change organizational
hats, do we also suspend our critical insights?
Srivats- these issues should be politicized. There is an organic connection between political parties and
people which can be used to put pressure, whether good or bad politics, doesn‘t matter as this is one way
of putting pressure.
Raju- what is the response for this case and what is the solution. He had done similar string operations
in civil hospital where a baby was sold off to another couple because the parents could not pay 15,000
rs. He got the story, told all the media personnel that it is their responsibility and they took it for 15 days
and after that the health secretary filled an FIR against the doctors and nurses. Now there is no
corruption in this particular civil hospital.
Srivats- the person who is undergoing that should know that they have certain rights, it should be their
voice.
Ankit- the reality is quite different. We have been trying for their voice. For example there was a case
where the forest department fired bullets and one person died during a patta demand. So people don‘t do
anything after that.
Ajay- we have been seeing these kind of cases. In one CHC, some 40km from Barwani, in the middle of
the process of delivery, when the child‘s head was out, the staff said that they won‘t be able to handle it.
Ajay was present, he himself went ahead of the ambulance in a bike and had informed the district
hospital in advance. Here they were there and the community knew them, they were able to save the
mother and child. The government is like a rubber ball, if you pressurize it, then it works, when you
leave it, then it goes back to its shape.
Junaid- in case of migration how do we pressurize the system
Sunil narrated the case of a DM who managed to get money from other funds for hospital beds. The
beds were procured but once when he went there, he saw the patients lying on the floor. On questioning,
the staff said that the patients will spoil the bed! No formula is there, different formula have to be tried
out for a better solution.
Sathyu – we do not think about the migrant worker population. 90% are unorganized and migrant
workers work does the most dangerous work. We need to think about them and give special focus
otherwise we are leaving out a huge chunk of population.
Raju- need to work on absorptive social norms. Policies are there but the societies need to absorb it.
36
Community Health Learning Program-2013
Abhijeet- mobilizing is difficult for the people who are somehow on the brink of survival. VHSC is not
the mobilization. There seems to be an overall change and there is a serious disjunct from expectations
from large scale programmes and the community.
The term „Going Against the Current‟ was coined as the theme for the 40th annual meet. Jasodhrara
said that in the last seven years people have gone in direct implementation others have gone to
institutions- so are we going against the current or we are going along with the sail.
Suneetha said that when we say that the community is not thinking, there is no public which is thought
to be universal or accessible; for too long, the dalits, adivasis and obcs have been denied access to these
spaces and even punished for venturing into this spaces. They functioned as private spaces of the
privileged classes and castes. How will a dalit or tribal community think it is theirs? They are alienated.
Ankit- the discussion was good but there is no direct solution. Community mobilization, systems
approach is needed. But when will things finally work? How long?
Abhijeet- it is not complete black and white, there will be lots of reasons behind any death. There has
been a slow change, we are the mediums of change. Need to retain the anger, so as to channelise it
”
Discussion and suggestion on CAH project at Tamil nadu
About CAH (Community action for Health)
(Source :- http://cahtn.in/about.php)
CAH project essentially consisted of the formation of committees at various levels. While
broadly based on the concept of the pilot phase, where the major activities were the formation of Village
Health Water and Sanitation Committees, their orientation, training in the use of tools, the use of these
tools to monitor the health care services of the village, the collation of these results in village health
report cards and their feedback to both the village community as well as to the public health system.
Committees at the higher level were to aggregated data from the individual committees at the lower
levels. Once the data was collected and aggregated a series of public hearings were facilitated where the
district level health officials were invited to have a face to face dialogue with the people. The next phase
has some important differences. These include:
Expansion of the area of coverage from 200 villages to 450 panchayats in the same 5 pilot phase
districts. The processes will be covering whole blocks (3 per district).
The modification of the tool in light of the experience and feedback of the pilot phase.
37
Community Health Learning Program-2013
The evolution / activation of committees above the village level to ensure feedback at various levels.
The evolution of institutional feedback mechanisms to ensure regular interaction between
communities and the public health system.
Sensitization of the public health staff.
Sensitization of the panchayati raj institutions and members.
The creation of village level action plans for health based on the findings of the village health report
cards.
My suggestion on Project:
The CAH project is a good way to promote communitization aspect of NHM, The initial success of
this project indicates the need of form this project in other BMAROU states. This would be great
step to promote PPP positively in all over the nation.
In the way of completion of the CAH project, The community leading in all aspects and determinant
of health and withdrawal of civil society must be insured as a part of the programatic logical
framework.
The genuine PRI system must be insured by the state government and district government should not
be given authority to influence the work of PRI.
Though, there is a very less ASHA in TN and pilot area of the project. There should be a demand as
of community health monitor cum activist (not as a part of the state health system).
There should be some legal power (parallel power at least to panchayat secretary ) must be given to
this community health monitor cum activist calling an amendment in the Tamilnadu Panchayat act,
1994.
There should be a separate module for community health monitor cum activist insuring an ideal role
of ASHA in the pilot area.
The training of social analysis, monitoring and activism should be given by selecting well civil
society.
Proper and regular channel of incentive and salary must be insured for this community health
monitor cum activist.
Guideline for training module and incentive should be designed by members of civil society,
selected leader of various PRI and AGCA.
The AGCA should immediately increase this demand for community health monitor cum activist.
38
Community Health Learning Program-2013
Understanding Malnutrition
WHAT IS MALNUTRITION?
Malnutrition is:
poor nutrition due to an insufficient, poorly balanced diet, faulty digestion or poor utilization of
foods. (This can result in the inability to absorb foods.)
Malnutrition is not only insufficient intake of nutrients. It can occur when an individual is getting
excessive nutrients as well.
WHAT CAUSES MALNUTRITION?
Human beings need a wide variety of nutrients to supply essential energy. The main nutrition what we need
most…..
protein
vitamins
minerals
If any one of these nutrients is deficient in a person's diet, he/she may suffer from malnutrition
Malnutrition also occurs when there is an imbalance of energy and protein in an individual’s diet. The body
may become unable to absorb the nutrients it requires to function properly.
*For example, if a child is suffering from energy and protein malnutrition, they will most likely have deficiencies
in iron, calcium, and other vitamins and minerals.
39
Community Health Learning Program-2013
WHO IS AFFECTED BY MALNUTRITION?
Individuals who are dependent on others for their nourishment. (infants, children, the elderly, prisoners)
Mentally disabled or ill because they are not aware of what to eat.
People who are suffering from tuberculosis, eating disorders, HIV/AIDS, cancer, or who have undergone
surgical procedures are susceptible to interferences with appetite or food uptake which can lead to
malnutrition.
Well malnutrition can be taken place by so many reason but generally using common sense main cause
behind most of the causes is hunger and a person cannot afford food only and only due to poverty. Nearly
3 billion people in the world are living on less than $1 a day. Even planning commission of India considers
Rs. 33 as minimum amount. They have little access to their basic needs, including adequate nutrition to
help their bodies stay in balance. Poverty may also prevent individuals from accessing education, which can
lead to misinformation about adequate nutrition.
Effects of malnutrition
Nutritional deficiencies can contribute to various diseases which can be found everywhere, but most often
go without cures/treatment in Less Developed Countries (LDCs). A few effected diseases is given below:-
Kwashiorkor/Marasmus
Kwashiorkor, which means “disease of the displaced child” in the language of Ghana is a protein deficiency
which results is characterized by inability to gain weight, diarrhoea, lethargy and a swollen belly.
Kwashiorkor can lead to comatose as well as death.
Similarly, Marasmus is a disease resulting from protein deficiency which affects children early in life
(typically in the 1st year) slowing growth, decreasing weight and hindering proper development.
Nutrition supplements, rehydration and education all can all serve to cure and prevent these diseases.
Beriberi
Beriberi is a thiamine (vitamin B1) deficiency which is common in South East Asia where many diets consist
solely of white rice.
Beriberi affects the proper functioning of the nervous system as well as the circulatory system and heart.
Pregnancy, breast feeding mothers and those who are ill with fever may have a heightened dependency on
thiamine and may develop a deficiency.
Thiamine is best acquired through foods such as pork, beef and whole grain (unrefined) breads and grains.
40
Community Health Learning Program-2013
Pellagra
Pellagra ”rough skin” is a niacin (or Tryptophan) deficiency which often results in the “3 Ds”; diarrhoea,
dementia and dermatitis.
The large scale consumption of corn has resulted in many cases of pellagra because corn is poorly absorbed in
the body. The best sources of Niacin are broccoli, eggs, dates, beef, salmon, seeds and peanuts.
Scurvy
Scurvy is a disease which is born of Vitamin C deficiency. It is characterized by bleeding around hair follicles,
anemia and gingivitis.
Scurvy may occur in those who consume large amounts of junk foods, smokers (as smoking depletes
Vitamin C) and those who don’t have proper access to sources of vitamin C. Namely, the poor.
Rickets
Vitamin D deficiencies may result in “Rickets” which is a lack of proper calcium characterized by poorly
developed and deformed bones.
Vitamin D can be best found especially cow milk but is very low in breast milk. Thus, women in developing
countries are contributing to this disease if their baby’s sole source of nourishment is breast milk.
Measuring Malnutrition
Height for age (H/A), is an indicator of chronic malnutrition. A child exposed to
inadequate nutrition for a long period of time will have a reduced growth and
therefore a lower height compared to other children of the same age (stunting).
Weight for age (W/A), is a composite indicator of both long-term malnutrition
(deficit in height/"stunting") and current malnutrition (deficit in weight/ "wasting").
Weight for height (W/H), is an indicator of acute malnutrition that tells us if a child is
too thin for a given height (wasting).
For all 3 indicators (W/H, W/A, H/A), we compare individual measurements to international
reference values for a healthy population.
Middle upper arm circumference (MUAC), is another anthropometric indicator.
MUAC is simple, fast and is a good predictor of immediate risk of death, and can be
41
Community Health Learning Program-2013
used to measure acute malnutrition from 6-59 months (although it overestimates
rates in the 6-12 month age groups).
SAM <110mm
However, the risk of measurement error is very high, therefore MUAC is only used for quick
screening.
The World Health Organization (WHO) defines malnutrition as the cellular imbalance
between the supply of nutrients and energy and the body’s demand for them to ensure
growth, maintenance, and specific functions.
Classification of malnourished status
Classification
Definition
Grading
Gomez
Weight below %
median WFA
Mild (grade 1)
Moderate (grade
2)
Severe (grade 3)
75%–90% WFA
60%–74% WFA
<60% WFA
Waterlow
z-scores (SD)
below
median WFH
Mild
Moderate
Severe
80%–90% WFH
70%–80% WFH
<70% WFH
WHO
(wasting)
z-scores (SD)
below
median WFH
Moderate
Severe
-3%</= z-score < -2
z-score < -3
WHO
(stunting)
z-scores (SD)
below
median HFA
Moderate
Severe
-3%</= z-score < -2
z-score < -3
Kanawati
MUAC divided by
occipitofrontal
head
circumference
Mild
Moderate
Severe
<0.31
<0.28
<0.25
Cole
z-scores of BMI for
age
Grade 1
Grade 2
Grade 3
BMI for age z-score < 1
BMI for age z-score < 2
BMI for age z-score < 3
Abbreviations:
42
Community Health Learning Program-2013
BMI ( body mass index), HFA (height for age), MUAC (mid-upper arm circumference), SD
(standard deviation), WFA (weight for age), WFH (weight for height), WHO (World Health
Organization).
Gomez Classification: The child's weight is compared to that of a normal child (50th
percentile) of the same age. It is useful for population screening and public health
evaluations.
Percent of reference weight for age = [(patient weight) / (weight of normal child of
same age)] * 100
Waterlow Classification: Chronic malnutrition results in stunting. Malnutrition also
affects the child's body proportions eventually resulting in body wastage.
Percent weight for height = [(weight of patient) / (weight of a normal child of the
same height)] * 100
Percent height for age = [(height of patient) / (height of a normal child of the same
age)] * 100
Classification of Malnutrition in Children
Mild
Malnutrition
Moderate
Malnutrition
Severe
Malnutrition
Percent Ideal Body Weight
80-90%
70-79%
< 70%
Percent of Usual Body
Weight
90-95%
80-89%
< 80%
Albumin (g/dL)
2.8-3.4
2.1-2.7
< 2.1
Transferrin (mg/dL)
150 - 200
100 - 149
< 100
Total Lymphocyte Count
(per µL)
1200 - 2000
800 - 1199
< 800
Wellcome Classification: evaluates the child for edema and with the Gomez classification system.
Weight for Age (Gomez)
With Edema
Without Edema
60-80%
kwashiorkor
Undernutrition
< 60%
marasmic-kwashiorkor
marasmus
43
Community Health Learning Program-2013
References:
Growth Monitor Manual- NIPCCD
To build understanding about the technical aspect of measuring Nutrition status, Tabled
data has been derived from various web sites.
Causes of Protein Energy Malnutrition (PEM)
(Most critical in rural and tribal area)
Protein energy malnutrition (PEM) is one of the most important public health problems in many developing
countries. It is a wide-spread deficiency disease among children of low socio-economic groups generally
people from rural and tribal area. In many areas nearly half the children do not survive to the age of five
years by protein calorie malnutrition and those who survive may suffer from impaired growth and perhaps
mental retardation.
Protein energy malnutrition is characteristic of children under five years whenever the diet is poor in protein
and calories, though no age is immune. The effect of protein deficiency in adults may show itself in the form
of loss of weight, reduced subcutaneous fat, anaemia, great susceptibility to infection, inability to do
sustained hard work, delay in healing of wounds and oedema.
The acute form of protein energy malnutrition is often precipitated due to inability on the part of the mother
to supply proper nutrients to the foetus and later inability on her part to lactate. Marasmus is most common
in infants found in twins; whereas kwashiorkor occurs most often among children beyond this age.
The degree of severity of protein calorie malnutrition is related to the extent of growth failure. It is expressed
by the weight loss per age as compared to the weight of normal children. Loss of weight by 11-25% is
classified as Grade I, weight loss by 26-40% as Grade II and weight loss by more than 40% as Grade III in
protein-calorie malnutrition.
Causes of Protein Energy Malnutrition
The following are the most important factors responsible:
Inadequate diet:Inadequacy of dietary intake may be due to several reasons such as:
Low purchasing power; inappropriate choice of foods; non-availability of foods.
Prolonged breastfeeding, late introduction of supplementary foods.
Diarrhoea and intestinal parasitism in children due to unhygienic feeding habits.
44
Community Health Learning Program-2013
Shortening the period of breastfeeding without satisfactory supplements.
Lack of knowledge:Ignorance of the requirements of a growing child and the improper use of available resources.
Traditions, Customs-and-Beliefs:Culture is often responsible for certain food habits. Even child-rearing practices in the rural and
tribal areas (ignorant older girls in the family are given charge of looking after the young infant) are
responsible for this deficiency.
Nutrition Rehabilitation Centre (NRC)
The Nutrition Rehabilitation Center (NRC) is a unit for rehabilitation of
undernourished children plus supportive care and capacity building of mothers and/or
other cares. A mother is provided with accommodation, food and emotional support as
her child is nursed back to health. It is launched under collaborative scheme of UNICEF
and Govt. of India. It is a unit for restoring severely acutely malnourished (SAM) children
to good health while educating their mothers about nutrition and child care. The mother
is provided with accommodation, food and emotional support as her child is nursed
back to health. When mother and child return to their village, the mother shares her
new knowledge with her family and neighbours.
Objectives/ Services
1. Treatment &Patient management.
2. Nutritional support to inmates. Nutrition education to his/her family members.
3. Other counseling services viz. Family planning, Better hygiene practices, Psychosocial care & development.
45
Community Health Learning Program-2013
4. Capacity building of the primary care givers on Preparation of low cost nutritious
diet from locally available food ingredients,
5. Developing Feeding habits & time management in mothers, imparting knowledge of
developing kitchen garden etc.
6. Follow up Services.
Strength:
Mother or local guardian (Primary care giver) will be accepted with the client.
In case of orphan child, care giver may be hired for supporting the baby for the
entire period of stay in the Nutritional Rehabilitation Centre.
In above case honorarium may be paid from RKS ( RogiKalyanSamiti) to the Care
giver.
Period of Stay :
As recommended by treating Physician & Nutritionist-cum Counselor.
Usually it is of 14 days. But may be extend up to 28 days.
Community Based Nutrition Management
System-An Evolution
As it may guess by title that It is a conceptual framework to develop community effort to
decrease the level of malnutrition especially in those areas where people are most
vulnerable and public health system of government is not able to reach and rehabilitate by
providing basic amenities of primary health care. It is community led management
system in which nutritive facility will be carried by the community and to the
community. An evolution of community based nutrition management system was first
observed in 1985 (Accordingly ―Urban MCH working paper‖) to establish the
effectiveness in treating malnourished children by the support of local people. Gradually
it has been adopted by many social managers but could not be able to succeed this model
46
Community Health Learning Program-2013
due to affected by external policy intervention. Therefore it began to consider that
community has to take control of management, execution and will have to be responsible
for outcome and eventually not supported any external input. It may call a whole system
in which community will be having ownership and decision making power with
responsibility of execution.
Community based nutrition rehabilitation centre (From the site):Community based nutrition rehabilitation centre is a community based approach
towards the management nutritive support to children and to decrease the prevalence of
disease or health event occurred by malnutrition.
Case study:Village:-Bhati
Distance:- 32 KM from Block Kolaras and 60 KM from District Shivpuri.
Socio-economics status:- 100% People of BPL.
Number of Household (Sahariya):- 44
Population:- 160 Sahariyas
Bhati is a village where the concept of CNMS is running under developing mode. There are several cast
exists in this village. Sahrana (Locality of Sahariya) is situated a little far from village. Recently
Villagers of Bahti got a new aanganwari centre in village but at other hand another center is under
construction in Saharana. People of poor socio-economic status are living there in which status of child
looks quite miserable. They are absolutely not getting any running support by the administration.
Several child deaths have occurred due to hunger. Having seen this situation, Organization and Sahariya
Jan Gathbandhan (SAJAG, An community based organization of Sahariya) organize a survey. Through
this, 63 children were measured weight and Through IPC it were concluded that due to long distance and
labour work women is not able to admit her children and themselves in NRC at Kolaras. This was the
central cause of establishment of CNRC. SAJAG develop a plan for this concept and it is initiated from
1st November 2012. In which SAJAG and a few active people from community took responsibility to
execute CNRC. In this series of changing, A campaign for hygiene has taken place and community
collected nutritive food by contribution and distributed to children. SAJAG made a list of local available
food and arranged by the community. The weight and height is being taken at every Thursday and found
that children are coming out from severity. Now all SAM children have driven out from nutrition
deficiency and to fulfil the protin requirement, women from community initiated fishing from the
nearest pond. It is a trial based initiation which accomplished successfully and still providing the
services.
47
Community Health Learning Program-2013
Marking Method of Malnourished Status of
children in family by CNRC
48
Community Health Learning Program-2013
Here as it is shown that a flower pot with
yellow leaf in which pot represents a family and
number of leaves represents number of children
in this family. Yellow colour of leaf indicates
the
initial
nutritive
status
(medium
malnourished) of child before intervention of
CNRC and green spot (well nourished)
indicated the present status of child. The child
name is Rajendra which is written beside the
leaf unit.
Similarly here, Rani and Lovekushis two
children in a family. Initially Lovekush was
categorized as SAM and Rani was
categorized as medium malnourished but
after intervention both of them has come out
from their initial status, and at present both
of them are out of malnourished status.
Growth Monitor Chart (As per WHO standard)
(Weight for age)
49
Community Health Learning Program-2013
Understanding on diseases and its prevention under public
health system
D
isease: -“A disease is an abnormal condition that affects the body of an organism”or in other
words “A condition of the body or some part of the body or organ of the body in which its functions are
disrupted or disarranged”. It is often construed as a medical condition associated with specific symptoms
and signs. It may be caused by factors originally from an external source, such as infectious disease, or it
may be caused by internal dysfunctions, such as autoimmune diseases.
In humans, "disease" is often used more broadly to refer to any condition that causes pain, dysfunction,
distress, social problems, or death to the person afflicted, or similar problems for those in contact with the
person. In this broader sense, it sometimes includes injuries, disabilities, disorders, syndromes, infections,
isolated symptoms, deviant behaviors and atypical variations of structure and function, while in other
contexts and for other purposes these may be considered distinguishable categories. Diseases usually affect
people not only physically, but also emotionally, as contracting and living with many diseases can alter one's
perspective on life and their personality.
Types
There are many ways in which disease can be categorized, but in essence, Disease can be
categorized in two ways: Communicable diseases
Non communicable diseases
Communicable Disease:Communicable diseases are those that are transmissible from one person, or animal, to another. The disease
may be spread directly, via another species (vector) or via the environment. Illness will arise when the
infectious agent enters the host, or sometimes as a result of toxins produced by bacteria in food. The spread
of disease through a population is determined by environmental and social conditions which favour the
infectious agent, and the relative immunity of the population. An understanding of the disease and the
measures necessary for its containment and management is therefore important.
Types of communicable disease: Respiratory Infection:-Tuberculosis, SARS, Diphtheria, measles, pneumonia, Polio, Cough etc.
Intestine infection:-Cholera, diarrhoea, Viral Hepatitis, poliomyelitis, Typhoid, Hook Warm,
Amoebiasisetc.
Arthropod Disease:-Malaria, Dengue, Filariasis, Chikungunyaetc.
50
Community Health Learning Program-2013
Zoonosis:-kfd, rabies, yellow fever, J.E. etc.
Surface Infection:-trachoma, tetanus, Leprosy, STD.
Infectious agents and examples of diseases
The organisms that cause disease vary in size from viruses, which are too small to be seen by a light
microscope to intestinal worms which may be over a metre long. The groups of infectious agents are listed
with examples of diseases they cause.
Bacteria:-Pneumonia, tuberculosis, enteric fever, gonorrhoea.
Viruses:-Measles, varicella, influenza, colds, rabies
Fungi:-Ringworm
Protozoa:-Malaria, giardia.
Metazoa:-Tapeworm, filariasis, onchcerciasis (river blindness), hookworm
Prions:-Kuru, Creutzfeld-Jacob disease, Bovine spongiform encephalopathy (BSE)
Modes of transmission
Direct transmission
Direct contact with the infected person as in touching or sexual intercourse.
Droplet spread through coughing sneezing, talking or explosive diarrhoea.
Faecal-oral spread when infected faeces is transferred to the mouth of a non-infected person, usually
by hand.
Indirect transmission
Indirect transmission of infectious organisms involves vehicles and vectors which carry disease agents from
the source to the host.
Vehicles are inanimate or non-living means of transmission of infectious organisms. They include:
Water, If polluted, specifically by contaminated sewage. Water is the vehicle for such enteric (intestinal)
diseases as typhoid, cholera, and amoebic and bacillary dysentery.
Food is the vehicle for salmonella infections (which include enteric fever), amoebic dysentery, and other
diarrhoeal diseases, and poisoning. Any food can act as a vehicle for infection especially if it is raw or
inadequately cooked, or improperly refrigerated after cooking, as well as having been in contact with an
infected source. The source may be another infected food, hands, water or air.
51
Community Health Learning Program-2013
Sometime, Milk is the vehicle for diseases of cattle transmissible to man, including bovine tuberculosis,
brucellosis. Milk also serves as a growth medium for some agents of bacterial diseases such as
campylobacter, a common cause of diarrhoea.
Air is the vehicle for the common cold, pneumonia, tuberculosis, influenza, whooping cough. measles. and
chickenpox. Discharges from the mouth, nose, throat, or lungs take the form of droplets which remain
suspended in the air, from which they may be inhaled.
Soil can be the vehicle for tetanus, anthrax, hookworm. and some wound infections.
Fomites, This term includes all inanimate objects, other than water, milk, food, air, and soil, that might play a
role in the transmission of disease. Fomites include bedding, clothing and the surfaces of objects.
Vectors are animate or living vehicles which transmit infections in the following ways:
Mechanical transfer. The contaminated mouth-parts or feet of some insect vectors mechanically transfer
the infectious organisms to a bite-wound or to food. For example, flies may transmit bacillary dysentery,
typhoid, or other intestinal infections by walking over the infected faeces and later leaving the diseaseproducing germs on food.
Intestinal harbourage.Certain insects harbour pathogenic (disease causing) organisms in their intestinal
tracts. The organisms are passed in the faeces or are regurgitated by the vector and the bite-wounds or food
are contaminated. (Ex. plague, typhus.)
Biological transmission.This term refers to multiplication of the infectious agent during its stay in the
body of the vector. The vector takes in the organism along with a blood meal but is not able to transmit
infection until after a definite period, during which the pathogen changes. The parasite that causes malaria is
an example of an organism that completes the sexual stages of its life cycle within its vector, the mosquito.
The virus of yellow fever also multiplies in the bodies of mosquitoes.
Non Communicable Disease
A non-communicable diseaseis a health event or disease which is non-infectious and non-transmissible
among people. NCDs may be chronic diseases of long duration and slow progression, or they may result
in more rapid death such as some types of sudden stroke. They include autoimmune diseases, heart
disease, stroke, many cancers, asthma, diabetes, chronic kidney disease, osteoporosis, Alzheimer's
disease, cataracts, and more. NCDs are distinguished only by their non-infectious cause, not necessarily
by their duration. Some chronic diseases of long duration, such as HIV/AIDS, are caused by
transmissible infections. Chronic diseases require chronic care management as do all diseases that are
slow to develop and of long duration.
Types of Non communicable Disease:-
52
Community Health Learning Program-2013
Cardio vascular Disease:- Stroke
Coronary Heart Disease:- Hypertension
Renal Heart Disease:-Night Blindness, Obesity.
Rheumatic Heart Disease:Chronic KEDNEY Disease:Cancer:Chronic obstructive pulmonary disease (COPD)
Stages of Diseases:
Acute disease
o An acute disease is a short-lived disease, like the common cold.
Chronic disease
o A chronic disease is one that lasts for a long time, usually at least six months. During that
time, it may be constantly present, or it may go into remission and periodically relapse. A
chronic disease may be stable (does not get any worse) or it may be progressive (gets
worse over time). Some chronic diseases can be permanently cured. Most chronic
diseases can be beneficially treated, even if they cannot be permanently cured.
Refractory disease
o A refractory disease is a disease that resists treatment, especially an individual case that
resists treatment more than is normal for the specific disease in question.
Progressive disease
Progressive disease is a disease whose typical natural course is the worsening of the disease until death,
serious debility, or organ failure occurs. Slowly progressive diseases are alsochronic diseases; many are
also degenerative diseases. The opposite of progressive disease is stable disease or static disease: a
medical condition that exists, but does not get better or worse.
Scope of Diseases
Localized disease
53
Community Health Learning Program-2013
A localized disease is one that affects only one part of the body, such as athlete's foot or an eye
infection.
Disseminated disease
A disseminated disease has spread to other parts; with cancer, this is usually called metastatic disease.
Systemic disease
A systemic disease is a disease that affects the entire body, such as influenza or high blood pressure
Reference: Class Notes.
http://en.wikipedia.org/wiki/Disease
THE SHIP CAPTAIN‘S MEDICAL GUIDE for Communicable disease.
http://en.wikipedia.org/wiki/Non-communicable_disease
Tuberculosis
Type of Infection:- Respiratory Infection
Agent:- Mycobacterium tuberculosis
Authorised Program:- RNTCP (India)
Suggested Treatment:- DOTS (Directly Observed Treatment- Short course)
Tuberculosisis a common, and in many cases lethal, infectious disease caused by various strains of
mycobacteriaex. Mycobacterium tuberculosis. Tuberculosis typically attacks the lungs, but can also
affect other parts of the body. It is spread through the air when people who have an active TB infection
cough, sneeze, or otherwise transmit respiratory fluids through the air.Therefore it can easily describe
that Tuberculosis is "A specific disease caused by infection with Mycobacterium tuberculosis, the
tubercle bacillus, which can affect almost any tissue or organ of the body, the most common site of the
disease being the lungs."
Symptoms:The classic symptoms of active TB infection are a chronic cough with blood-tinged sputum, fever, night
sweats, and weight loss (the latter giving rise to the formerly prevalent term "consumption"). Infection
of other organs causes a wide range of symptoms.
Diagnosis:-
54
Community Health Learning Program-2013
Diagnosis of active TB relies on radiology (commonly chest X-rays), as well as microscopic
examination and microbiological culture of body fluids. Initially sputum smear test examine is been
convene and treatment or further test suggested by doctor according to result. Some precaution is
necessary like history of disease, classification of disease whether it is pulmonary or extra-pulmonary.
Treatment:Treatment is difficult and requires administration of multiple antibiotics over a long period of time (Ex.
DOTS). Social contacts are also screened and treated if necessary. Antibiotic resistance is a growing
problem in multiple drug-resistant tuberculosis (MDR-TB) infections. Prevention relies on screening
programs and vaccination with the bacillus Calmette–Guerin (BCG) vaccine.
The objective of TB treatment are:- (As normed by RNTCP)
To decrease mortality and morbidity by ensuring cure, minimizing relapses and preventing
development of drug resistance.
To decrease the infection and brake the chain of transmission of infection.
To achieve above whilst minimize side effect of drugs.
Who gets tuberculosis?
Tuberculosis is spread from person to person through tiny droplets of infected sputum that travel
through the air. If an infected person coughs, sneezes, shouts, or spits, bacteria can enter the air and
come into contact with uninfected people who breathe the bacteria into their lungs.
Although anyone can become infected with TB, some people are at a higher risk, such as:
Those who live with others who have active TB infections
Poor or homeless people
Foreign-born people who come from countries with endemic TB
Older people, nursing home residents, and prison inmates
Alcoholics and intravenous drug users
Those who suffer from malnutrition
Diabetics, cancer patients, and those with HIV/AIDS or other immune system problems
Health-care workers
Workers in refugee camps or shelters.
Revised National Tuberculosis Control Programme (RNTCP)
Objective
The objective of Revised National Tuberculosis Control Programme (RNTCP) is to
provide free and domiciliary treatment to the patients detected through “Universal
55
Community Health Learning Program-2013
Access” under passive case finding method. Directly Observed Treatment Short Course
Chemotherapy (DOTS) is the strategy of RNTCP.
Responsible authority :1. Ministry of Health and Family Welfare.
2. State Health Ministry.
3. State TB Officer at Health Directorate.
4. District TB Officer at all District Head Quarters.
5. Designated Medical Officer at Sub‐district level TB Unit.
6. Medical Officer at Designated Microscopy Centre.
7. DOTS Centre.
TB TREATMENT ORGANOGRAME (Normed by RNTCP)
56
Community Health Learning Program-2013
DOTS
DOTS is Directly Observed Treatment Short Course. The most important component of DOTS is
DOT. Under this, the medicines are administered to the TB patient under direct observation of a trained
DOT Provider thus ensuring successful treatment completion. The DOT Provider may be health
workers, community volunteers, ASHA, Anganwadi Workers etc except family member who is
acceptable and accessible to the patient and accountable to the health system.
The article reviews the elements of the DOTS strategy to control the tuberculosis epidemic WHO
declared TB" a global emergency" in 1993. A DOT (directly-observed treatment, short-course) is an
intermittent, supervised system of drug-intake by patient, which eliminates drug-default. It has been
described by WHO as "the most important public health breakthrough of the decade in terms of lives
saved"
More than doubles the accuracy of TB diagnosis.
Its success rate is up to 95%.
It prevents the spread of tuberculosis by prioritizing sputum positive patients for diagnosis and
treatment, thus reducing the incidence and prevalence of TB.
It helps in alleviating poverty by saving lives, reducing the duration of illness and preventing
new infectious cases.
It improves the quality of care and removes stigma.
It prevents treatment failure and the emergence of MDR‐TB by ensuring patient adherence to
treatment and uninterrupted supply of anti ‐TB drugs.
It lends credence to TB control efforts and the health system.
The 5 major components of DOTS are:i)
Political will.
ii)
High-quality sputum microscopy.
iii)
Uninterrupted supply of short-course chemotherapy drugs.
iv)
Directly-observed chemotherapy as treatment.
v)
Systemic monitoring or accountability.
57
Community Health Learning Program-2013
Medical Entomology:A study of the arthropods of medical importance is known as medical entomology or
can be described as study of insects.
Vactor born or Arthropod born disease
"Vector-borne disease" is the term commonly used to describe an illness caused by an
infectious insects that is transmitted to people by blood-sucking arthropods. The arthropods
(insects or arachnids) that most commonly serve as vectors include:
1.) blood sucking insects such as mosquitoes, fleas, lice, biting flies and bugs
2.) blood sucking arachnids such as mites and ticks.
The term ―vector‖ refers to any arthropod that transmits a disease through feeding activity.
Vectors typically become infected by a disease agent while feeding on infected vertebrates (e.g.,
58
Community Health Learning Program-2013
birds, rodents, other larger animals, or humans), and then pass on the microbe to a susceptible
person or other animal. In almost all cases, an infectious microbe must infect and multiply
inside the arthropod before the arthropod is able to transmit the disease through its salivary
glands. The most common vector-borne diseases are carried by mosquitoes and flies. Some
diseases caused by vector are: Malaria- Annual morbidity of 4-5 million cases.
Filaria -estimated 236 million people.
Scabies.
Typhoid.
Dengue, hemorrhagic fever, Japanese encephalitis and KFD in India.
The prevalence rates for trachoma in India vary from 0.5 per cent in West Bengal to
79 per cent in Punjab and Haryana.
Mosquito
Mosquitoes constitute the most important single
family of insects from the standpoint of human
health.
The four important groups of mosquitoes and
disease in India.
o Anopheles (Malaria)
o Culex (Filaria, J.E., Encephalitis)
o Aedes(Dengue, Chikungunya)
o Mansonia.
Malaria
Type of Disease:-Vector born Infection
Agent:-Malarial Parasite (Plasmodium falciparum)
Environmental Agent:-Mosquito ( Female Anophylize )
Authorised Program:-National Anti-Malaria Program under National Vector Borne
Disease Control Programme (NVBDCP)
59
Community Health Learning Program-2013
Malaria is a mosquito-borne infectious disease of
humans and other animals caused by a parasite
named Plasmodium. It begins with a bite from an
infected female Anopheles mosquito, which
introduces the protists through saliva into the
circulatory system. In the blood, the protists travel
to the liver to mature and reproduce.
Symptoms:Malaria causes symptoms that typically include fever and headache, which in severe cases can progress
to coma or death. The early stages, malaria symptoms are sometimes similar to those of many other
infections caused by bacteria, viruses, or parasites. Symptoms may include:
Fever.
Chills.
Headache.
Sweats.
Fatigue.
Nausea and vomiting.
Symptoms may appear in cycles and may come and go at different intensities and for different lengths of
time. But, especially at the beginning of the illness, the symptoms may not follow this typical pattern.
The cyclic pattern of malaria symptoms is due to the life cycle of malaria parasites as they develop,
reproduce, and are released from the red blood cells and liver cells in the human body. This cycle of
symptoms is also one of the major indicators that you are infected with malaria.
Diagnosis:Malaria is usually diagnosed by the microscopic examination of blood films or by antigen-based
rapid diagnostic tests (RDT). Microscopy is the most commonly used method to detect the
malarial parasite. Despite its widespread usage, diagnosis by microscopy suffers from two main
drawbacks:
Many areas (especially rural) are not equipped to perform the test.
The accuracy of the results depends on both the skill of the person examining the blood
film and the levels of the parasite in the blood.
60
Community Health Learning Program-2013
Prevention and Treatment:Several drugs, most of which are used for treatment of malaria, can be taken to prevent
contracting the disease during travel to endemic areas. Though we have some prophylaxis as
Chloroquine may be used where the parasite is still sensitive. However, due to resistance one of
three medications—mefloquine (Lariam), doxycycline (available generically), or the
combination of atovaquone and proguanil hydrochloride (Malarone)—is frequently needed.
There is some complication of prophylaxis. The prophylactic effect does not begin immediately
upon starting the drugs, so people temporarily visiting malaria-endemic areas usually begin
taking the drugs one to two weeks before arriving and should continue taking them for four
weeks after leaving. Use of prophylactic drugs is seldom practical for full-time residents of
malaria-endemic areas, and their use is usually restricted to short-term visitors and travellers to
malarial regions. This is due to the cost of purchasing the drugs, negative adverse effects from
long-term use, and because some effective anti-malarial drugs are difficult to obtain outside of
wealthy nations. The use of prophylactic drugs where malaria-bearing mosquitoes are present
may encourage the development of partial immunity.
Thereforemethods used to prevent malaria include medications, mosquito elimination and the
prevention of bites. The presence of malaria in an area requires a combination of high human
population density, high mosquito population density and high rates of transmission from
humans to mosquitoes and from mosquitoes to humans. If any of these is lowered sufficiently,
the parasite will eventually disappear from that area.
Epidemiological Triad of Malaria
Mosquito
Plasmodium
Human
“Yes, some precaution and prevention can eradicate Malaria”
61
Community Health Learning Program-2013
But how
The major step can be taken to eradicate malaria by breaking chain of one or more side of above
triad. The parasite of malaria only can be spread from diseased human to mosquito and mosquito
to another human. Therefore environmental, host and agent factor is necessarily to understand
cause of disease.
Leprosy
Type of Disease:-Communicable Surface Infection
Agent:-Mycobacterium Laprae
Environmental Agent:-All patient with active Leprosy
Authorised Program:- National Leprosy Eradication Program(NLEP), 1983.
Leprosy, also known as Hansen's disease (HD), is a chronic disease caused by the bacteria
Mycobacterium leprae.Leprosy can be progressive, causing permanent damage to the skin,
nerves, limbs and eyes. Contrary to folklore, leprosy does not cause body parts to fall off,
62
Community Health Learning Program-2013
although they can become numb or diseased as a result of secondary infections. These occur as a
result of the body's defences being compromised by the primary disease. Secondary infections, in
turn, can result in tissue loss causing fingers and toes to become shortened and deformed. There
is attack rate 4.4%- 12% within 5 yearsin Lepromatous leprosy contacts. The Incubation period
of leprocy is 6 month to 40 year but Generally incubation period is 5-7 years to develop this
diseas. Leprosy is a leading cause of permanent physical disability. Timely diagnosis and
treatment of cases, before nerve damage occurred, is the most effective way of preventing
disability due to leprosy.
History:•
•
•
•
•
The first known written mention of leprosy is dated 600 BC.
In 'SusruthSamhita' and treatment with 'Choulmoogra oil'
Leprosy was referred to as 'Kusht' in the Vedic writing.
Initially Leprosy patients were isolated and segregated.
In India 'The Lepers Act 1898' was enacted, which discriminated against the Leprosy patients
and segregated them socially.
Type of Leprosy and symptoms:
Paucibacillary:-It is characterized by one or more hypopigmented skin macules and patches,
where skin sensations are lost because of damaged peripheral nerves that have been attacked by
the human host's immune cells.
Multibacillary:-It is characterized bymore hypopigmented skin at various part of body.Large
patches may affect a whole limb, and peripheral nerve involvement with weakness and loss of
sensation is common.
A few type of leprosy are:• Indeterminate leprosy (IL)
• Tuberculoid leprosy (TT)
• Borderline tuberculoid leprosy (BT)
• Borderline borderline leprosy (BB)
• Borderline lepromatous leprosy (BL)
• Lepromatous leprosy (LL)
Diagnosis:Leprosy is diagnosed by finding at least one of the following cardinal signs:
63
Community Health Learning Program-2013
Definite loss of sensation in a pale ( hypopigmented) or reddish skin patch
A thickened or enlarged peripheral nerve, with loss of sensation and/or weakness of the muscles
supplied by that nerve
The presence of acid-fast bacilli in a slit skin smear.
Tissue smear testing
Skin biopsy
Sensory testing
Lepromin testing
Polymerase chain reaction (PCR) analysis
Treatment:MDT (Multi Drug Therapy):It is a combination of drugs that is very safe and effective in treating leprosy & to prevent the emergence
of drug resistance. MDT is provided in convenient blister packs covering four weeks of treatment. MDT
is safe for women and their babies during pregnancy and breast-feeding. MDT can be given to HIV
positive patients, that on anti-retroviral treatment and to patients on treatment for tuberculosis (TB). This
treatment,
Are accessible to all who need them.
– Coverage: MDT treatment can be provided at all health units.
– No geographical, economic or gender barriers.
Are patient-centred and observe patient‘s rights, including the rights to timely and appropriate
treatment and to privacy and confidentiality.
Address each aspect of case management
– Diagnosis is timely and accurate, with supportive counseling.
– Treatment with MDT is timely, free-of-charge and user-friendly.
– Prevention of disability interventions are carried out appropriately.
– Referral for complications and rehabilitation is done as needed.
– Maintain simple records and encourage review and evaluation.
64
Community Health Learning Program-2013
Epidemiological Triad of Leprosy
Contact with patient of Leprosy and other environment factor.
Mycobacterium Laprae
Human
Social Stigma:Leprosy stigma is a kind of social stigma, a strong feeling that a leprosy patient is shameful and is not
accepted normally in society. Those affected by the disease continue to face social stigma and
discrimination. There can be a treatment for disease but absolutely any stigma has no treatment until
society analyse itself. Therefore it is dire needed to treat the patient rather than to reject their existence.
The patient of leprosy need treatment, care and love.
Environment and Health
Environment:The surroundings or conditions in which a person, animal, or plant lives or operates or
All the external factors present around man.
Components:
Physical
Biological
Social
Cultural
A famous quote says that ―If you want to study disease, study the health and Environment.‖
Environment has direct relation with health of human. Better accommodation, access to natural
resources at adequate level. Not only this, environment is by product of human and social nature and
65
Community Health Learning Program-2013
their beliefs.We need fresh air, well housed, and drinkable water and other resources to fulfil the daily
requirement of himself.
Water is a basic amenities of human. We need clean, safe and wholesome water to servive. Safe water
is,
• Free from pathogenic agents
• Free from harmful chemical substances
• Pleasant to taste, free from colour and odour
• Usable for domestic purposes.
There are 71 % area is covered by water out of which 2.86% of water is drinkable and 0.014 % is being
used. Even then unequal distribution of water, natural activities and geographical condition is creating
crises among people.
There are many diseases caused by water, it is categorized by two ways…
Water related Disease.
Water Born Disease.
Those caused by the presence of an infective agent:
(a) Viral: Viral hepatitis A, hepatitis E, polio myelitis, rotavirus diarrhea in infants
(b) Bacterial: typhoid and paratyphoid fever, bacillary dysentery, Escherichia coli diarrhea, cholera
(c) Protozoal: amoebiasis, glardiasis
(d) Helminthi: roundworm, threadworm, hydatid disease.
(e) Leptospiral: weil‘s disease
Those due to the presence of on aquatic host:
(a) Snail :Schistosomiasis
(b) Cyclops: fish tape worm
There for water has to be clean by applying a few purification methods, but it also depend on quantity of
water and its requirement for the population.
66
Community Health Learning Program-2013
Position: 549 (12 views)