RF_WH_2_SUDHA.pdf
Media
- extracted text
-
RF_WH_2_SUDHA
ARTICLES
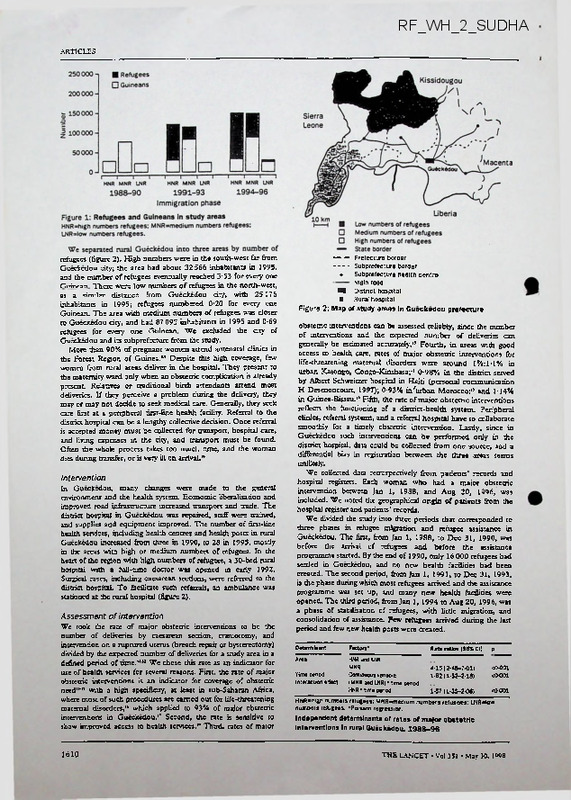
refugees (figure 2). High numbers were in the south-west far from
Gueckedou dry, the area had about 32 566 inhabitants in 1995,
and the number of refugees eventually reached 3-53 for every one
Guinean There were low numbers of refugees in the north-west,
at a similar distance from Gueckedou dty, with 25176
inhabitants in 1995; refugees numbered 0'20 for every one
Guinean. The area with medium numbers of refugees was closer
to Gueckedou dty, and had 87 095 inhabitants in 1995 and 0*69
refugees for every one Gninran We excluded the dty of
Gueckedou and its subprefecture from the study.
More than 90% of pregnant women attend antenatal clinics in
the Forest Region of Guinea.” Despite this high coverage, few
women from rural areas deliver in rhe hospital. They present to
the maternity ward only when an obstetric complication is already
present. Relatives or traditional birth attendants attend most
deliveries. If ±ey peredve a problem during the delivery, they
may or may not dedde to seek medical care. Generally, they seek
care first at a peripheral first-line health facility. Referral to the
district hospital can be a lengthy collective decision. Once referral
is accepted money must be collected for transport, hospital care,
and living expenses in the dty, and transport must be found.
Often the whole process takes too much time, and the woman
dies during transfer, or is very ill on arrival. '•
Intervention
In Gueckedou, many changes were made to the genera!
environment and the health system. Economic liberalisation and
improved road infrastructure increased transport and trade. The
district hospital in Gueckedou was repaired, staff were trained,
and supplies and equipment improved. The number of first-line
health services, induding health centres and health posts in rural
Gueckedou increased from three in 1990, to 28 in 1995, mosdy
in the areas with high or medium numbers of refugees. In the
heart of the region with high numbers of refugees, a 30-bed rural
hospital with a full-time doctor was opened in early 1992.
Surgical cases, including caesarean sections, were referred to the
district hospital. To facilitate such referrals, an ambulance was
stadoned at the rural hospital (figure 2).
Assessment of intervention
We took the rate of major obstetric interventions to be the
number of deliveries by caesarean section, craniotomy, and
intervendon on a ruptured uterus (breach repair or hysterectomy)
divided by the expected number of deliveries for a study area in a
defined period of time."” We chose this rate as an indicator for
use of health services for several reasons. First, the rate of major
obstetric intervendons is an indicator for coverage of obstetric
need”"’ with a high specificity, at least in sub-Saharan Africa,
where most of such procedures are carried out for life-threatening
maternal disorders,•• which applied to 93% of major obstetric
interventions in Gueckedou." Second, the rate is sensitive to
show improved access to health services.’’ Third, rates of major
1610
------ Prefecture border
------ Subprefecture border
•
Subprefecture health centre
1
Main road
■I District hospital
■ Rural hospital
Figure 2: Map of study areas In Gueckedou prefecture
obstetric interventions can be assessed reliably, since the number
of interventions and the expected number of deliveries can
generally be estimated accurately.'’ Fourth, in areas with good
access to health care, rates of major obstetric interventions for
life-threatening maternal disorders were around 1%:1-1% in
urban Kasongo, Congo-Kinshasa;" 0-98% in the district served
by Albert Schweitzer hospital in Haiti (personal communication
H Desenoncourt, 1997); 0-93% in'urban Morocco;” and 1-14%
in Guinea-Bissau.” Fifth, the rate of major obstetric interventions
reflects the functioning of a district-health system. Peripheral
clinics, referral systems, and a referral hospital have to collaborate
smoothly for a timely obstetric intervention. Lastly, since in
Gueckedou such interventions can be performed only in the
district hospital, data could be collected from one source, and a
differential bias in registration between the three areas seems
unlikely.
We collected data retrospectively from patients’ records and
hospital registers. Each woman who had a major obstetric
intervention between Jan 1, 1988, and Aug 20, 1996, was
included. We noted the geographical origin of patients from the
hospital register and patients ’ records.
We divided the study into three periods that corresponded to
three phases in refugee migration and refugee assistance in
Gueckedou. The first, from Jan 1, 1988, to Dec 31, 1990, was
before the arrival of refugees and before the assistance
programme started. By the end of 1990, only 16 000 refugees had
settled in Gueckedou, and no new health facilities had been
created. The second period, from Jan 1, 1991, to Dec 31, 1993,
is the phase during which most refugees arrived and the assistance
programme was set up, and many new health facilities were
opened. The third period, from Jan 1, 1994 to Aug 20, 1996, was
a phase of stabilisation of refugees, with little migration, and
consolidation of assistance. Few refugees arrived during the last
period and few new health posts were created.
D®t®rmln«nt
Factors’
Rat® ratios (95% Cl)
P____
Area
HNR ano LNR
MNR
Continuous variable
(MNR ano LNR)* time period
HNR" time oenod
4-15 (2-46-7-01)
1-82(1-52-2-18)
<0-C01
<0-001
Tim® period
interaction effect
<0001
1-67 (1-35-2-06)
HNR»high numbers refugees: MNR-medium numbers refugees: LNR« low
numbers refugees. •Poisson regression.
Independent detennlnants of rates of major obstetric
Interventions In rural Gueckedou. 198S-96
THE LANCET • Vol 351 • May 30. I»«8
ARTICLES
with medium numbers of refugees had initially higher
rates of major obstetric interventions than the areas with
low and high numbers, the presence of refugees and the
refugee-assistance programme were associated with a
significantly greater increase in intervention rates in the
area with high numbers of refugees compared with rhe
two areas with lower numbers of refugees.
Discussion
M*°r
I
36
2
oostetrie
interventions (01
Exoected 3904 10442 3018
deliveries (n)
13
48
5
4143 11081 3203
41
95
8
3852 10303 2978
Immigration phase
Figure 3: Rates (95% Cl) of major obstetric Interventions by
study area and period
HNRshigh numoers refugees: MNR=madium numbers refugees:
LNRsHow numbers refugees.
Statistical analyses
Since major obstetric interventions can be assumed to be
distributed as a Poisson event, we calculated Poisson confidence
intervals (95%) for rates, and used Poisson regression analysis to
estimate the trend over time in each area. We estimated rate
ratios for the three areas, comparing each time-period with the
previous one. To test the hypothesis of the equality over time in
the different areas, we included the main effects of time and area
in the model, together with an interaction term (time' area).
Results
During the study period, 981 major obstetric interventions
were performed in Gueckedou hospital. Interventions on
464 urban residents, 249 refugees, and 19 women from
outside the prefecture were excluded from analysis. For
1994-96, rates of major obstetric interventions for
refugees in rural areas of Gueckedou were estimated at
0-83%. These were not further analysed.
We analysed 249 major obstetric interventions carried
out on Guinean women living in rural Gueckedou (figure
3). During 1988-90, before the arrival of the refugees,
intervention rates were very low in all rural areas. After the
refugees arrived, the rates of major obstetric interventions
.rose from 0-03% (95% CI 0-0-09) to 1-06% (0-74-1-38)
’in the area with high numbers of refugees, from 0-34%
(0-22-0-45) to 0-92% (0-74-1-11) in the area with
medium numbers, and from 0-07% (0-0-17) to 0-27%
(0-08-0-46) in the area with low numbers. The estimated
rate ratios over time were 4-35 (2-64-7-15) for the area
with high numbers of refugees, 1-94 (0-97-3-87) for the
area with low numbers, and 1-70 (1-40-2-07) for the area
with medium numbers of refugees.
In a Poisson regression analysis (table), a model that
included time and the area with medium numbers of
refugees as main effects and a term for the interaction
between time and area (high numbers vs medium and low
numbers) provided the best fit (goodness of fit x:=7-22 for
five degrees of freedom). The area with medium numbers
had an independent effect on intervention rate, and there
was an overall time trend. Most importantly, there was a
significant interaction with time for areas with low and
medium numbers compared with the area with high
numbers, in which the effect on the rate of major obstetric
interventions over time was significantly greater than the
base rate (rate ratio 167 [1-35-2-06]). Although the area
THE LANCET - Vol 351 • May 30, 1998
Our data show that the use of referral health services by
the rural population of Gueckedou increased substantially
over time. The only obvious difference between the areas
with high and low numbers of refugees was ±e impact of
the refugees and the refugee assistance programme.
It seems unlikely that bias could explain the differences
we found. We tried to avoid misclassification of refugees
as Guineans, although some Guineans may have
registered falsely as refiigees to obtain free medical care.
Such misclassification, if it occurred, was, however, more
likely in the area with many refugees than in areas with
lower numbers of refugees. False refugees would thus
lower the observed increase in intervention rates for
Guineans in the area with many refugees.
During the study period, independent of the refugees
and the refugee-assistance programme, important changes
took place in the Gueckedou health system and in the
general environment. These changes decreased certain
obstacles to timely obstetric care. The Guinean Ministry
of Health and the German Development Cooperation
have improved the quality of care and the financial
accessibility at the hospital of Gueckedou, and have
developed a network of first-line health services in the
prefecture.
During
the
same
period,
economic
liberalisation resulted in more access to money and higher
availability of transport. These changes could have
improved the access to the hospital, and may explain why
the rate of major obstetric interventions increased in all
study areas, including the area with low numbers of
refugees in which the impact of the refugee-assistance
programme was weak.
The presence of many refugees in certain areas of
Gueckedou has, however, led to additional social and
economic changes. First, economic changes have been
more important in the refugee-affected areas. The
presence of and assistance to refugees has transformed the
economy in remote rural areas. The presence of freely
settled refugees meant cheap labour and increased
exploitation of agricultural resources. Relief food was
sometimes resold’, which substandally increased trade and
circulation of money in the area. Some Guineans
registered as refugees and obtained free food, and,
therefore, economic assets. Agencies assisting the refugees
employed hundreds of staff, which introduced more
money into the local economy. These changes may have
enabled better access to cash for the Guinean rural
population of the refugee-affected areas. Patients
commonly mention lack of access to money as the main
constraint when seeking emergency medical care.
Second, transport infrastructure was substantially
improved. Roads and bridges were repaired, mainly to
allow food aid to be transported to the refugee
settlements. Consequently, many more cars arrived in the
area. The ambulance permanently stationed at the rural
hospital in the area with many refugees undoubtedly
facilitated referral to the district hospital in Gueckedou
1611
ARncu-s
and decreased the need for money. The ambulance was
free of charge for refugees and Guineans. Since the
ambulance started operating in 1992, it transported most
of the obstetric emergencies to the district hospital. Efforts
to improve the road infrastructure were also made in the
area with low numbers of refugees, but much less was
achieved than in the area with high numbers.
Third, there was probably a “refugee-induced demand”
for health care. Before the war, health services in Liberia
and Sierra Leone were better and more advanced than in
Guinea, and the population used them more often. When
confronted with a serious disorder, therefore, refugees
living in close contact with the Guineans may have
encouraged them to use the health services.
Lastly, more health services were developed in the areas
into which refugees moved. When the first refugees
arrived, serious efforts to upgrade first-line and secondline health services, were underway in Guinea, based on
cost-recovery schemes.” Between 1988 and 1995, a health
centre was opened in most sub-prefectures of Guinea. In
the refugee-affected areas this process was faster and more
widespread. Full coverage with health centres was already
achieved in 1992, and many additional health posts'were
created.
Rates of major obstetric interventions in the area with
high numbers of refugees were still low in 1991-93, and
die changes took several years to become effective. This
delay probably shows that there is an important time lag
between the introduction of improvements in the health
system, and increased use by people living in remote rural
villages.
The greater increase in rates of major obstetric
interventions in the area with many refugees than in the
other two areas is probably because of the more intensive
refugee assistance programme and the presence of
refugees. We could not identify fully, however, what part
each of these factors played, nor whether we identified all
important factors. The combination of factors probably
contributed to the increased use of referral health services
by the host population. The changes that were introduced,
however, decreased only partly the obstacles to timely
obstetric care. Rural people still face important financial,
logistic, and cultural barriers to such care. Efforts are
being made in Gueckedou prefecture to set up small-scale
health-insurance schemes to overcome these barriers.
None of the changes made in the refugee-affected areas
was specific for obstetric interventions. All health services
were general and the ambulance transported any patient
referred to the hospital. Therefore, access probably
improved for all disorders, not only for obstetric care.
The approach to refugees in Guinea made this positive
effect on the host population possible. Refugee assistance
followed the refugees to where they settled and supported
the refugees* own coping mechanisms. Several factors
were favourable to such a non-directive approach to
refugee settlement and assistance. The refugees arrived
gradually, in several waves, and were spread over a large
area. The administrative and health authorities were not
therefore, overwhelmed by the influx. Moreover, many
refugees were culturally related to the host population in
Guinea, with whom they had had contacts before arrival.
This cultural proximity facilitated assistance by the host
population. With between 15 and 20 inhabitants per km3
the Forest Region of Guinea is not densely populated and
has a relative abundance of underused agricultural
resources. The population is generally positive towards
1612
strangers, who are perceived as an economic asset for
villages.” The refugee-affected areas were also far from the
capital, Conakry, and the refugees were not thought to be
a threat to national security by the government of Guinea.
At the time of the refugees’ arrival the conditions
prevailing in the health system were favourable to an
integrated approach to refugee assistance. In most districts
the Ministry of Health had launched new integrated
health centres and was upgrading the hospital. With stocks
of drugs and medical equipment readily available locally,
new health facilities modelled on the national health policy
could be created overnight. Medecins Sans Frontieres was
assisting the Ministry of Health in this development of
health facilities in the Forest Region before the arrival of
the refugees. The two organisations were, therefore, able
to put a refugee-assistance programme together, which
may have contributed to the local and national impression
of control of the influx. Indeed, all medical refugee
assistance was organised by the Ministry of Health and
Medecins Sans Frontieres, in collaboration with the other
foreign health agencies already working in the Region. No
new health agencies brought relief during the first years of
the refugee influx. During the first months, the
operational role of UNHCR was limiter! The agencies
present agreed that medical assistance to refugees should
respect the overall policy of the Ministry of Health to
avoid negative impact on the changing and still fragile
national health system. Resources that became available
through the refugee-assistance programme were partly
invested to reinforce the overall health system.
The situation of the refugees in Guinea was, therefore
different from that for many refugees, who generally arrive
more quickly in larger numbers.” During such acute
refugee emergencies, most attention is focused on
decreasing the burden of the acute health crisis faced by
the refugees. The scope of the crisis and the urgency of
the necessary measures commonly mean that parallel
refugee health services are organised by foreign relief
agencies to deliver a standard package of emergency-relief
measures. The relief is generally well managed by relief
agencies” and has probably decreased death rates,” but
logistic and military constraints might prevent timely
implementation. Unfortunately, this relief approach is
commonly perpetuated beyond the acute rmergmry,
especially when refugees have been housed in rampo 7 The
effects on the health services of the host country, which
does not have enough resources to cope, are often
negative’ and all relief resources are used exclusively by
the refugee health services. Relief organisations often
recruit medical staff from the host country, which can
hamper the functioning of the health services in countries
with scarcity of such staff? The health authorities that are
supposed to coordinate relief measures in their area can be
overwhelmed by new relief actors, further weakening the
local health services. The host population may not be able
to use the refugee health services, even if they are better
staffed, equipped, and supplied than those of the host
country. The quality of care available to the host
population may, therefore, decrease as a consequence of
the assistance to refugees.
In other countries, conditions for an integrated
approach to refugee assistance may be less favourable.
However, the positive effects for the host population
documented in Guinea show that it might be worthwhile
for host governments to consider such an approach
whenever possible. Relief agencies involved should adapt
THE LANCET • Vol 351 • May 30, 1W8
ARTICLES
intervention methods accordingly. An integrated approach
to refugee assistance is probably also more cost-effective.
In Guinea, the overall yearly cost of medical assistance to
refugees was estimated at US$4 per refugee.7 This cost is
much lower than the yearly cost of medical services in
refugee camps—often USS20 per refugee.
The improved access to health care for the host
population in our study should not give the impression
that the refugee influx and the way it was dealt with was
always beneficial to the host population. The refugees and
the refugee-assistance programme in Guinea caused
substantial social and economic changes. The absorption
of such a large population increase in a rural area may also
have had important consequences on the ecological
equilibrium. These changes may jeopardise the long-term
livelihoods of certain strata of the population. The poorest
of the host population may be the worst affected by
changes to the economy.24 Labour opportunities may be
lost because of the presence of cheap refugee labour, and
increases in market prices and increased monetarisation of
the economy may decrease their purchasing power.
Although there are no data to support this hypothesis in
Guinea, the benefits of better access to necessary hospital
^mre may have favoured only Guineans who also benefited
Wm economic change.
A non-directive approach to refugees has the potential
to avoid the negative impact of emergency refugee relief
on the health services of the host country, and to improve
access to health care for the host population. Which
conditions enable such approach and appropriate
intervention methods should be studied in other refugeeaffected areas.
Contributors
AU investigators contributed to the study design, data analysis, and revision
of the manuscript. Vincent De Brouwere and Wim Van Lerberghe had
previous experience of the methods. Wim Van Damme collected data in
Guinea as part ofhis doctorate study on refugee health care in sub-Saharan
Africa.
A cknowledgments
We thank M L Yansane, D Fassa, K Marah, and D Diallo of the Ministry
of Health in Gueckedou, Guinea, and B Verbruggen and G Mirhanx of
Midedns Sans Fronderes in Guinea for their collaboration during the field
work; C Ronsmans and P Van der Scuyft for assistance with the Poisson
analysis, R Ecckels for useful comments on previous drafts. The study was
supported by a research grant from the Fund for Scientific Research,
Flanders, Belgium (FWO-S 2/5-KV-E95), and from the European Union
(IC18-CT96-0113).
1 Toole MJ, Waldman RJ. Prevention of excess mortality in refugee and
displaced populations in developing countries. JAMA 1990; 263:
3296-302.
2 Toole MJ, Waldman RJ. Refugees and displaced persons. War, hunger,
and public health. JAMA 1993; 270: 600-05.
THE LANCET • Vol 351 • May 30, 1998
Porignon D, Notennan JP, Hennan P, Tonglet R, Soron'gane EM,
Lokombc TE. The role of the Zairian health services in the Rwandan
refugee crisis. Disasters 1995; 19: 356-60.
Collins S. Ignoring the host: the impact of recent refugee crises on
health infrastructure in Ngara district, Tanzania. Amsterdam:
Medecins Sans Frontieres 1996: 1-89.
5
Goyens P, Porignon D, Soron’gane EM, Tonglet R, Herman P,
Vis HL. Humanitarian aid and health services in Eastern Kivu, Zaire:
collaboration or competition? J Refugee Stud 1996; 9: 268-80.
6
Van Damme W, Drame ML, Yansane ML, Boelaert M,
Van Hauwaert W, Verbruggen B. Le role des services de same du pays
d’accueil dans la prise en charge des refugjes: 1’experience de la Guinee.
Dev Same 1997; 127:23-27.
7
Van Damme W. Do refugees belong in camps? Experiences from
Goma and Guinea. Lancet 1995; 346: 360-62.
8
Yansane ML. Comite technique prefectoral de same. Gueckedou:
Ministere de Same Publique, 1996: 1-89.
9
Drame ML, Lynen L, Vandemoortele E. Rapport annuel 1991.
Direction Prefecxorale de la Same. Guinea: Ministere.de Same
Publique, 1992:1-9.
10
Thaddeus S, Maine D. Too far to walk: maternal mortality in context.
Soc Sei Med 1994; 38: 1091-110.
11
Van Lerberghe W, Pangu KA, Van den Brock N. Obstetrical
interventions and health centre coverage: a spatial analysis of routine
data for evaluation. Health Policy Ptam 1988; 3: 308-14.
12
Van Lerberhe W, Pangu KA. Comprehensive can be effective: the
influence of coverage with a health centre network on the
hospitalisation patterns in the rural area of Kasongo, Zaire. Soc Sd Med
1988; 26: 949-55.
13
De Brouwere V, Laabid A, Van Lerberghe W. Quels besoins en
interventions obstetricales? Une approche fbndee sur 1’analyse spatiale
des deficits au Maroc. Rev Epidemiol Sami Publique 1996; 44: 111-24.
14
Nordberg EM. Incidence and estimated need of caesarean section,
inguinal hernia repair, and operation for strangulated hernia in rural
Africa. BMJ 1984; 289: 92-93.
15
De Brouwere V. Les besoins obstetricaux non converts: la prise de
conscience de la problematique de la santc matemelle au Maroc.
Louvain: Universite Catholique de Louvain, 1997: 1-225.
16
Van den Broek N, Van Lerberghe W, Pangu KA. Cesarean sections for
maternal indications in Kasongo (Zaire). Im J Gynecol Obstet 1989; 28:
337-42.
17
Kourouma K, Conde S, Gody M. Analyse des taux de cesarienne en
Guinee. Conakry Minivrrr de Same Publique, and Gesellschaft fur
Teghnkehe Zusammenarbeit, 1997: 1-18.
18 Nordberg EM, Mwobodia I, Muniu E. Hospital catchment area and
surgery in Meru district, Kenya. East Afr Med J 1995; 72: 127-29.
19 Menezes d'Alva FR. Analyse du programme de reduction de la
mortalitc matemelle dans le district sanitaire de Gabon. Antwerp:
Institute of Tropical Medicine, 1997: 1-59.
20 McPake B, Hanson K, Mills A. Community financing of health care in
Africa: an evaluation of the Bamako Initiative. Soc Sei Med 1993; 36:
1383-95.
21 McGovern M. Identities and the negotiation of displacement in
Southeastern Guinea. Oxford: Refugee Studies Programme, 1996:
1-19.
22 Goma Epidemiology Group. Public health impact of Rwandan refugee
crisis: what happened in Goma, Zaire, in July, 1994? Lancet 1995; 345:
339-44.
23 Toole MJ. Vulnerability in emergency situations. Lancet 1996; 348:
840.
24 Chambers R. Hidden losers? The impact of rural refugees and refugee
programs on poorer hosts. Ini Migrat Rev 1986; 20: 245-63.
1613
Draft outline, May 24,1993
CHAPTER 6: EMPOWERMENT AND FERTILITY
by
Simeen Mahmud
A.
Historical overview
1.
Traditional transition theory
Traditional demographic transition theory maintains that
aggregate economic development and modernisitation in a society
will ultimately lead to declines in aggregate fertility levels
(Coale,1973).
While
different
societies
will
follow
this
generalised path at different paces depending upon specific
contexts, the completion of transition will be characterised by
declines in mortality levels followed by declines in fertility
levels that tend to stabilise at levels significantly below pre
transition levels. It is assumed that improvements in overall
health and hygiene including the control of epidemics with modern
technology, a rise in literacy levels, and increases in income and
consumption levels will produce appropriate responses in fertility
behaviour patterns of populations experiencing transition. Implicit
in these assumptions is that economic development and modernisation
will effect all segments of the population including women, so that
there should also be visible improvement in the level of female
education and increase in female participation in modern sector
employment which will then motivate couples to limit fertility.
While these theories have recognised that modernising changes
in the economy may influence the motivation of couples to limit
fertility, they have not paid much attention to the dynamics of the
decision making process about reproduction at the individual or
couple level. There is no recognition about how these changes could
affect women's power and autonomy from male domination and their
implications for the fertility decisions of couples and women. Not
surprisingly, they have been unable to explain fertility patterns
in many parts of the developing world where power balances favour
men, and where a range of fertility regimes have been found to
occur in diverse socio-economic contexts, a reality most recently
confirmed by the World Fertility Surveys
(WFS:
Cleland and
Hobcraft, 1985). In attempting to explain "deviant" fertility
patterns in the developing world a macro concept of "women's
status" (measured by aggregate indicators like female literacy and
school enrollment rates or labour force participation rates) was
introduced
as
a
"catch-all"
variable
but
there
was
poor
understanding about both the concept as well as the linkages to
fertility (Mauldin and Berelson, 1978).
2.
Micro vs macro influences
Embedded in the traditional transition theory is the maternal
role incompatibility hypothesis which stipulates that women in
modern sector employment have lower fertility due to role conflicts
between "mothering" and "working". However, this conflict is not
elaborated in terms of its implications for women's domestic power
or role in fertility decision making, but rather more in terms of
a
lack
of
complementarity
between
women's
time
use
in
childbearing/childcare and work outside the home. A reappraisal of
the hypothesis has led to the conclusion that micro rather than
macro structural changes may better explain the relationship
between women's work and
fertility.
Examining the working
environment of women in Malaysia, Mason and Palam concluded that it
was the "household's opportunity structure" through which it
accumulates status and resources which shaped this relationship
(Mason and Palam,1985).
The need to look more carefully at micro-level relationships
that may influence in important ways the fertility decision making
process and how these relationships may vary by social and cultural
contexts was clearly indicated. One of these relationships was
identified as that between men and women in the society, and the
important implications of women's status on their domestic power
and on demographic outcomes was recognised even quite early on
(Mason,1984).
3.
Women's status and fertility theories
More recent demographic theories of fertility decline in the
developing world have invoked the concept of relative female status
as an explanatory variable. Demographers, most notably Caldwell and
Cain, have theorised about the linkages between some concept of
women's status in patriarchal societies and their fertility
behaviour patterns (Caldwell, 1976, 1981; Cain, 1979, 1981). The
essence of these theories is that an improvement in women's status
relative to men will lead to fertility decline.
The argument is that changes in the socio-economic structure
which affect aggregate indicators such as mass and female education
and women's access to or participation in gainful employment will
lead to a significant reduction in the subordination of women by
men (in the first case because of the emotional and material
nucleation of families, and in the second case because of the
reduction of women's economic dependence on men). It is further
argued that this is sufficient to bring about declines in existing
fertility levels since reductions in female subordination will lead
to an increase in the costs of children due to a reversal in the
"wealth flows" and/or a reduction in the "risk-insurance value" of
children to parents. Cain describes the situation of women in
patriarchal societies of South Asia while Caldwell draws his
conclusions from family experiences in the patriarchal Yoruba
community in Nigeria.
However, given that fertility decision making, if at all done
consciously, ultimately takes place within a household context,
there are no explanations about the mechanism through which reduced
subordination of women at the household level can be translated
into a greater role in fertility decisions in situations where this
is empirically observed. Nor do they provide plausible explanations
in situations where these predictions are not valid.
B.
Empirical evidence of the status-fertility relationship
1.
Female education and fertility
One of the first empirical linkages between women's status and
fertility was evidenced in the strong and consistent relationship
between female education and fertility levels. A comprehensive
review of evidence across the developing world revealed that female
education and fertility was inversely related in 11 out of 20
cases, the higher the literacy rate of a country, the more likely
there was to be an inverse relationship, and that female education
was more likely to be inversely related to fertility than male
education (Cochrane,1982). The effect of education on fertility is
hypothesised to be indirect through its impact on certain
"intervening variables". Thus, the effect of education on fertility
depends on how education effects the demand for children, the
supply of children and the use of fertility regulation to limit
births.
Although much of the attention on how female education affects
fertility is focussed on its impact on the costs and benefits of
children, some studies have looked at variables that could provide
insights into women's roles in the fertility decision making
process. It was found, for instance, that education increased the
wife's age at marriage,
husband-wife communication and the
knowledge, attitude and access to birth control all of which were
negatively related to fertility adjusted for age. These factors
could potentially exert a positive impact on women's participation
in fertility decision making but more research is needed to
establish these pathways under different contexts.
(Box on these cross-national correlations ?)
In discussing the complex mechanism through which improved
maternal education raises child survival in rural Punjab, Dasgupta
concludes that education raises skills and self-confidence,
increases exposure to information and alters the way in which
others respond to them (Dasgupta, 1990). Caldwell, too, examining
Nigerian data suggests that women who have been to school are more
likely to elicit behaviour from others like mother-in-law, husband
or health worker that are favourable to child survival (Caldwell,
1979) . These could very well be the same mechanisms through which
education could impact on women's autonomy with regard to
childbearing decisions.
2.
Women's work and fertility
The other source of empirical evidence drawn upon to
illuminate the relationship between women's status and fertility
are studies that examine the effect of women's work and fertility.
However, as Youssef (1982) concludes "Research to date has failed
to provide a clear and consistent explanation of the relationship
between women's employment and fertility, and has not confirmed the
causality". What is recognised, nevertheless, is that both women's
work and fertility emerge from "a family decision making process
that encompasses a number of goals . . . reacting in response to a
common set of social and economic forces as well as to unfolding
events over the life cycle" (Lloyd, 1985).
Empirical observations about the impact of women's work on
fertility and child care can be differentiated along the lines of
type and magnitude of remuneration, work place, type of activity,
and occupation. There are even situations where maternal employment
has been associated with higher infant/child mortality and
undernutrition, reflecting a negative impact on child care, as well
as larger completed families, reflecting a positive impact on
fertility, suggesting that the effect of employment may be more
context specific than that of education. Also, causality is less
easy to establish since most women may work at various points in
their reproductive years,
so that fertility and employment
decisions affect one another.
The important distinction to be made when trying to establish
a relationship between women's work and fertility is that between
earning an income and controlling it. Work which does not alter the
existing gender pattern of control over productive resources and
women's labour is not likely to have any impact on women's decision
making power with regard to fertility. Although it has been
established that women who leave their home for work have the
lowest fertility in most societies, the explanation most commonly
forwarded is that of role conflict. It could very well be that
going out of the home, especially in traditional societies, could
provide women with an enhanced self esteem, greater independence,
access to information and services, peer support and so on that
increase women's self confidence in independent decision making,
e.
i.
their autonomy.
Studies of poor women in South Asia involved in subsistence
income earning work have concluded that these women have a less
subordinate position to men in the household relative to women who
depend entirely on their husband's incomes. These women appear to
have a certain degree of autonomy in their behaviour including in
the use of contraceptives and exhibit significantly lower fertility
levels (N. Nelson; Mahmud,1993). However, evidence is limited and
more work needs to be done to identify pathways of impact on
women's autonomy.
3.
Linkages to women's decision making power
Empirically,
the
education-fertility
(as
well
as
the
education-infant/child mortality)
relationship has been more
consistent than the employment-fertility relationship. This seems
quite understandable since education, being in a sense more
instrumental in terms of influencing learned perceptions should
have a stronger and more consistent impact on women in the form of
enhancing capabilities needed to "gain some control over one's own
life and over the resources needed for survival".
However, it is not yet sufficiently clear what type of
education has the greatest potential for impact on women's decision
making power,
and under what specific contextual conditions
strategies for "empowering education" may be sustained. For
example, aggregate indicators of education are all based on the
Western model of education (as emphasised by Caldwell), but many
would argue that this type of formal schooling with a certain
number of years spent at school, while assisting women to behave in
a more modern way with regard to acceptance of new technology
(birth control, ORS, child vaccination, hygeinic habits), was
totally irrelevant to enhancing capabilities of poor rural women in
traditional situations. Also, it is argued that it tends to
reinforce traditional gender inequalities rather than to question
them. On the other hand, the case can be made for a more informal
and strategic type of education with empowering for women's
practical
and
strategic needs
(cross
reference
chapter on
empowermrnt) . Questions regarding mechanisms of influence as well
as contexts under which these are feasible still remain to be
answered and provide the directions for future research.
The case for the effect of employment on women's decision
making power is more difficult to establish since there is a
diverse range of the type of work that women engage in and the
conditions under which these are undertaken. Empirically, it has
been the experience that both the type of work and the context of
work has significant and varying influence on women's perceptions
about identity and wellbeing and on "enhancing capabilities" for
increasing that wellbeing. The evidence, not surprisingly, has been
mixed,
especially since the effect of employment is often
confounded with the education effect
(eg.
in the case of
professional or non-traditional occupations).
In any case, whatever the direction of causality, there is
sufficient reason to believe that causality is in both directions
since decisions about women's work and fertility are not once for
all decisions and evolve in response to one another and to other
events and decisions. The significance for women's empowerment
strategies lies in identifying the work environment that leads to
an enhancement of women's autonomy and decision making power and
the pathways of influence under situations of varying male control
over women's labour. In this regard, too, much work needs to be
done to answer questions about the viability and sustainability of
these straregies.
C.
Conceptualising pathways of influence
1.
The concept of female status
As the concept of the status of women has entered mainstream
demography, its complexity has led to the use of alternative
definitions and synonyms (female autonomy, women's rights, men's
situational advantage). Mason (1984) reviews these definitions and
concludes that beyond the common focus on gender inequality
"demographers have more than one thing in mind when they discuss
women's status". The three basic dimensions of gender inequality
focussed most commonly were (1)
inequality in prestige,
(2)
inequality in power and (3) inequality in access to or control over
resources.
The complexity derives from the fact that women's status is a
multi-dimensional concept: that there is more than one dimension on
which it is possible for men and women to be unequal, although in
reality a higher status in one dimension,
e.g.
control of
productive resources, may mean a higher status in other dimensions;
that women may be "powerful" in one area such as in domestic
matters but may be completely powerless in another area such as in
the control of productive resources. Superimposed on this is the
fact that gender inequality may vary by location such as the social
unit (family, neighbourhood, community, state) and by stage in the
life cycle (unmarried daughter, young bride, young mother, older
mother of many surviving children, woman with no children, motherin-law, widow, old woman with no assets, and so on).
There is a need to recognise that the different dimensional
and locational components of women's status as used in the
literature may not necessarily respond to structural changes in a
nicely consistent manner. For example, do women who are able to
access productive resources including market opportunuties for
income generation have a higher status because of their freedom
from seclusion (purdah) or have a lower status because they have to
give up the social status associated with purdah (Youssef, 1982).
Alternately, poor women who have to engage in income earning
employment or even educated women in professions may appear to be
less dependent on or subordinate to men in the household but may in
fact have very little autonomy in decisions regarding their incomes
(Safilios-Rothschild, 1980).
2.
How status influences fertility decision making
Drawing conclusions from anthropological studies in developing
countries Epstein (1982) defines women's role as "the way she is
expected to behave in certain situations" and her status as "the
esteem in which she is held by different individuals and groups who
come in contact with her". As a woman proceeds through the
different phases of her life cycle she assumes different roles and
is "awarded different prestige ranking by different people within
her social range". These rankings are in most part hierarchical and
is also closely correlated to the various roles assumed by a woman
within her "social range" which includes the household, the
neighbourhood, the community and the state, generally in the
chronological order of life cycle events. All of these status
rankings in this highly structured system are primarily determined
by
the
woman's
reproductive
outcomes,
being
significantly
influenced by the gender, the number and the timing of her births
(Cain, 1981 in comparing regions in South Asia). However, in
certain situations where women traditionally have access to
independent productive resources these status rankings may also
depend upon women's productive outcomes (Boserup, 1970; Cain, 1981;
Adams and Castle chapter).
Hence, within the existing societal power structure women are
able to ascend to status levels with higher rankings that are
associated with visibly higher levels of "power" with regard to her
relationships within the household (such as control over the labour
of younger household members and domestic labourers, decision
making power in domestic matters and so on) and to a limited extent
with regard to the broader community (such as the prestige awarded
to the elderly) . This type of "power" is however limited or
circumscribed to the extent that it is derived from men and
relationships with men (Safilios-Rothschild, 1982) and does not
significantly increase women's decision making power relative to
men with regard to either their labour or their reproduction.
Given these structural constraints to women's independent
decision making, the mechanisms by which women's status as achieved
through their traditional roles can influence fertility may be
conceptualised as follows:
(Box with diagramme representing these linkages based on Mason,
1984.)
Existing economic and social (including kinship) institutions
determine the low status of women in society. The low status of
women is characterised by gender based inequalities in prestige or
esteem, in the control over productive resources and in decision
making power. These inequalities determine the economic dependence
of women on men and their lack of autonomy from male control, both
of which are instrumental in controling women's labour and
fertility. Women's economic dependence and lack of autonomy dictate
their fertility behaviour and outcome rather than considerations of
their own wellbeing. With changes in the economic and social
structures of communities that are favourable to women (such as
those leading to higher female education or increased female
employment in gainful activities)
it is expected, but with
considerable lag, that women's status will improve reducing the
gender based inequalities. These improvements will eventually
reduce women's economic dependence on men and their lack of
autonomy, so that some concerns for women's own wellbeing may be
reflected in fertility outcomes.
3.
The concept of autonomy/freedom from male domination
Upto now discussions of women's status have primarily focussed
on gender inequality as an outcome but not on decision making power
or women's autonomy as they effect these outcomes. Even when
demographers have used the concept of female autonomy,
its
implication for women's freedom of control from others has been
restricted to personal matters. Dyson and Moore (1983) explain the
equality of autonomy between men and women as implying "equal
decision making ability with regard to personal affairs", but do
not extend their definition of female autonomy to include decision
making power beyond personal affairs. This is misleading because
fertility decision making, while very much a personal concern for
women, is also significantly influenced by family and often
community situations to the extent that childbearing determines
women's status in those social locations.
There is also no discussion about how gender perceptions of
identity and wellbeing, often utilised to maintain existing
inequalities in status (Sen,1990; Papanek, 1990) can be shaped by
power relations between men and women or about how these
perceptions may determine women's autonomy in decision making
affecting their lives.
Clearly,
the concept of
female
autonomy needs to be
distinguished from that of women's status since the question of
power relations between men and women and how they affect decision
making is very central to it. Even though women may rise to higher
status levels through their traditional roles, both as producers
and reproducers of labour, their subordination to men is not
necessarily reduced. Thus, although women may gain some power over
the lives of younger women and some younger men in the household,
they still have very little power and autonomy about decisions
affecting their own lives (Safilios-Rothschild, 1982). In fact,
women's greatest subordination occurs at a time when they are being
initiated into fertility behaviour patterns that are not geared
towards their own wellbeing but towards that of their families.
Even when women are earning incomes they are often unable to
translate these into decision making power if men control the
income and the conditions under which women can work.
The
traditional gender balance of power is such that male dominance
over women at all dimensions and locations takes the form of
variously controlling women's labour and fertility, and the
consequences of their fertility, by restricting their power and
ability to make independent decisions about their labour and their
reproduction.
It may be hypothesised that the major constraints to
increasing women's wellbeing in a male dominated environment has
been their lack of autonomy from men in decision making which
affects their wellbeing, including reproduction, and the fact that
women are resigned to accept the "legitimacy of the established
order". Sen (1990) has argued that women's perception (or the lack
of them) of their own wellbeing and self-worth can be an important
factor in the perpetuation of existing gender imbalances in power,
but that these are not necessarily resistant to change or
alteration through conscious social policy.
4.
Empowerment and its linkages to fertility decision making
The previous discussion would imply that one way of increasing
women's autonomy and decision making power would be to provide them
with an alternative power base that was independent of the
domination of men. Even in societies characterised by highly skewed
gender balance of power and control of productive resources, women
may gain access to power from certain kinds of empowering
experiences
like the process of politicization
for gender
awareness,
processes
of
economic
change
or
processes
of
mobilisation for economic, social or psychological support.
(These processes are described in the chapter on Conceptualising
Empowerment. That chapter will also try to define empowerment in
terms of a process rather than an end or even a means to an end,
and that it is a process that the process of gaining power "begins
in the mind with self image and confidence, with understanding the
environment, with ability to turn weaknesses into strengths ...)
The mechanism by which such empowering processes may impact on
women's autonomy and fertility decision making is conceptualised
below:
(Box showing how the mechanism of impact of women's status on
fertility is modified by introducing the notion of increased
decision making power and autonomy which accompanies women's
empowerment strategies)
The pathways of influence of women's empowerment on their
fertility behaviour may be both indirect and direct. Empowering
experiences impact on women's perceptions of selfworth and
wellbeing and through them on their economic dependence on men and
their lack of autonomy in decision making. These impacts flow back
into
the
hierarchical
social
structure
through
women's
relationships with men and other "powerful" women to exert
influence in changing the established gender inequalities in
prestige, control over resources and decision making power, i.e.
the components of women's low status. Changes in women's status
then affect fertility behaviour through the traditional channels as
described in the previous box. This is the indirect effect of
empowering experiences on fertility. The direct impact on fertility
is through the formation of new relationships within the different
social locations (household, community, state, market) which
embodies self confidence, access to independent information, peer
support, physical mobility and so on, in such a way that women's
own wellbeing (family size preferences, health needs, birth control
preferences, employment alternatives, healthy children) as well as
that of their children and other vulnerable groups dictates
fertility behaviour and outcomes. Also, since the empowering
experience is conceptualised as a process rather than an end,
impacts on fertility behaviour is also expected to be an on-going
flow responding to external forces and life cycle events as they
unfold.
5.
Power sharing and responsibility
Obviously, if fertility decision making has to be a conscious
one by both men and women in response to structural changes that
effect them differently, then the mechanism by which these changes
influence decision making has to do with the balance of power
between women and men in all the different social locations like
the household, community and the state within which they interact.
In other words, there must be a reallocation of power in favour of
women at all different dimensional and locational contexts,
allowing them to alter their reproductive behaviour for their own
wellbeing. This may entail some "negative externalities" in terms
of men feeling threatened or the established order being questioned
by more "powerful" women.
So far women have had to bear the burden of reproduction at
the cost of their own wellbeing (economic independence, education,
health, healthy offspring, mobility), while men have been enjoying
the benefits. Thus, the underlying assumption of empowering
strategies for women has been that altering reproductive behaviour
is primarily a woman-specific concern, perhaps even a concern with
opposing gender interests.
Increasingly, it is clear that the concern needs to be not
only gender neutral but also a societal concern, i.e. women's
empowerment strategies need to incoroporate a greater role and
responsibility even accountability of men and the broader societal
institutions. The empowering process must be able to elicit a more
caring and responsible attitude and behaviour from the other actors
in this decision making scene. In other words, it must be ensured
that the empowering process does not burden women with additional
segregated
responsibility.
The persistence
of gender based
allocative inequalities in a society is not only determined by
power relations but also rationalised by the implicit priorities
and generalised notions of distributive justice that have emerged
over many years. It should be remembered that these relations and
notions are not likely to vanish automatically with the process of
women's empowerment.
Other existing political structures such as the lack of a
democratic state structure, the presense of a communist or a
socialist state structure, the presense strong patron-client
relationships, the emergence of religious fundamentalism will
significantly influence the operationalisation and impact of
strategies for women's empowerment.
REFERENCES
A.J.Coale (1973). Will be provided.
W.P.Mauldin and B.Berelson (1978) "Conditions of fertility decline
in developing countries,
1965-1975",
Studies in Family
Planning, 9(5), 139-41.
K.O.Mason and V.T.Palam (1981) "Female employment and fertility in
Peninsular Malaysia: The maternal role incompatibility
hypothesis reconsidered", Demography, 18, 549-575.
J.Caldwell (1976) "Towards a restatement of demographic transition
theory", Population and Development Review, 2, 321-366.
(1979) "Education as a factor in mortality decline: An
examination of Nigerian data", Population Studies, 33(3), 395413.
(1981)
Will be provided.
M.Cain and S.Nahar (1979) "Class, patriarchy and women's work in
Bangladesh", Population and Development Review, 5, 405-438.
M.Cain (1981) "Risk and insurance: Perspectives on fertility and
agrarian change in Bangladesh and India", Population and
Development Review, 7, 435-474.
K.O.Mason (1984) The Status of Women: A Review of its Relationships
to Fertility and Mortality, The Rockefeller Foundation, New
York.
N.H.Youssef (1982) "The interrelationship between the division of
labour in the household, women's roles and their impact on
fertility",
in R.Anker, M.Buvinic and N.H.Youssef (eds)
Women's Roles and Population Trends in the Third World, Croom
Helm, London and Sydney.
C.Safilios-Rothschild (1980)
Will be provided.
(1982)
"Female
power,
autonomy
and
demographic change in the Third World", in R.Anker, M.Buvinic
and N.H.Youssef (eds) Women's Roles and Population Trends in
the Third World, Croom
Helm, London and Sydney.
T.Scarlett Epstein (1982) "A social anthropological approach to
women's roles and status in developing countries: The domestic
cycle", in R.Anker, M.Buvinic and N.H.Youssef (eds) Women's
Roles and Population Trends in the Third World, Croom Helm,
London and Sydney.
E.Boserup (1970) Women's Role in Economic Development, St.Martins
Press, New York.
M.Dasgupta (1990) "Death clustering, mother's education and the
determinants of child mortality in rural Punjab, India",
Population Studies, 44, 489-505.
C.Lloyd (1991) "The contribution of the World Fertility Surveys to
an understanding of the relationship between women's work and
fertility", Studies in Family Planning, 22(3), 144-161
S.Singh and J.Casterline (1985) "The socio-economic determinants of
fertility", in J.Cleland and J.Hobcraft (eds) Reproductive
Change in Developing Countries: Insights from_ the__World
Fertility Survey, Oxford University Press, New York.
N.Nelson (19 ) Why Has Development Neglected Rural Women: A Review
of the Literature from South Asia, Pergamon Press,
S.Mahmud (1993) "Female power: A key variable in understanding the
relationship between women's work and fertility', (unpublished
manuscript), Bangladesh Institute of Development Studies,
11
12
Dhaka.
A.K.Sen (1990) "Gender and cooperative conflicts", in Irene Tinker
(ed) Persistent Inequalities: Women and World Development,
Oxford University Press, New York and Oxford.
H.Papanek (1990) "To each less than she needs, from each more than
she can do: Allocations, entitlements, and values", in Irene
Tinker
(ed)
Persistent
Inequalities:
Women
and
World
Development, Oxford University Press, New York and Oxford.
T.Dyson and M.Moore (1983) " On kinship structure, female autonomy,
and demographic behaviour", Population and Development Review,
9, 35-60.
S.Cochrane (1982) "Education and fertility: An expanded examination
of the evidence" in G.P.Kelly and C.M.Elliot (eds) Women's
Education in the Third World: Comparitive Perspectives, SUNY
Press, Albany.
(Draft for discussion-Feb, 2001)
Health Task Force
Women's Health
Why the need to look at Women's Health as a separate agenda• Consequences of poor health of women, as against those of men, are far greater since their poor
health translates into poor health of families, particularly the children who represent the future
generation. A mother’s death has twice the impact of afather’s death on child survival. "Women Days- Lost' due to ill health therefore includes many hidden but critical factors which impact on
the family and in the larger context on the health of the community and the nation.
• Also, gender related factors impact negatively on all issues related to women, including health.
Health status of women in Karnataka:
The overall health and developmental status of women and children in Karnataka has improved over
the past several decades.
But, as can be seen by the health indicators and developmental indices, the improvement does not
compare favourably with that of States like Kerala, Tamil Nadu, Andhra Pradesh, Maharashtra etc.
There is a considerable disparity between Rural & Urban Karnataka, between males & females and
regional disparities with the districts of Raichur, Koppal, Gulbarga, Bidar, Bellary, Bijapur and
Bagalpur characterized as category C due to poor health and other developmental indicators.
Health Indicators of Karnataka:
Infant Mortality Rate (IMR)
The IMR is 51.5 according to NFHS-2, and 58 according to SRS 1998.
IMR is 70 for Rural and 25 for Urban areas and varies from 29 in Dakshina Kannada to 79 in Bellary.
The Maternal Mortality Rate (MMR) according to UNESCO is 450. But recent estimates by SRS
(1998) places it at 195 per 100,000 live births.
Life Expectancy at Birth (LEB)
The International Conference on Population Development had resolved to target an LEB of 70 by 2005
and 75 by 2015. Karnataka has only reached 62.
LEB of women was higher than that of men throughout the State, but the difference ranged from the
highest of 9 in Kolar and Hassan and only 0.62 in Bangalore (Urban).
LEB was highest in Dakshina Kannada with 68.82 and lowest in Bellary with 57.12years.
Crude Birth Rate
The SRS estimate of CBR in 1998 was 22 per 1000 population; 23.1 in rural as against 19.3 in urban
areas. CBR has been fluctuating widely rather in Karnataka and the regional disparity is similar to
other indices.
Crude Death Rate (CDR)
CDR as estimated by SRS (1998) was 7.9 per 1,000 population; 8.6 in rural as against 6.9 in urban
areas.
CDR varied from a low of 7 in Dakshina Kannada & Shimoga, to a high of 10.5 in Gulbarga.
Developmental Indices of Karnataka- HDI4 GDI
The Gender-related Development Index (GDI) measures the overall achievements of women and men
in the three dimensions of the Human Development Index (HDI) -life expectancy, educational
attainment and adjusted real income-and takes note of inequalities in development of the two sexes.
The methodology used imposes a penalty for inequality such that the GDI fells when the achievement
levels of both men and women in a country go down or when disparity between their achievements
increases. The GDI is therefore the HDI discounted for gender inequality.
Though the GDI and HDI are not comprehensive and do not cover all aspects of human development
they serve to high light disparities within the State as well as Ae consequences of gender
discrimination.
According to the 1991 census the Gender Ratio is 960 women for 1,000 men. This is worse than in
Kerala, Andhra Pradesh, Orissa and Tamil Nadu. But more disturbing is the fact that it has worsened
between 1981 & 1982.
The Gender Ratio is unfavourable to women in most districts except in Dakshina Kannada & Hassan
The IMR for females is 72, and highest in Dharwad Bellary & Bidar.
Age specific mortality rates indicate that 26% of deaths of women occoured between 15 - 34years of
age as against 15% among mea
Reasons for the poor health status of women in Karnataka:
The efforts taken to address women’s issues have been inadequate, distorted, vertical, top-down and
have rarely emerged out of women's priority concerns. Gender disaggregated data is often not
collected on women’s morbidity, suffering and paia
• Health seeking behavior of women: The ingrained gender insensitiveness in society has led to
women themselves relegating their own physical and mental health, emotional and social needs as
their last priority, if at all.
' • The health needs of women are addressed by the RCH programs, which are restricted to the
reproductive phase. Very little systematized attention is being paid to their other health needs and
much less to their emotional needs.
Factors for consideration:
The Gender Concept
Gender
Gender is the different meanings and roles that societies and culture assign to people, based on whether
a person is male or female. It is a strong, but often unacknowledged, part of what we learn as we grow
up, for example, how we treat each other and ourselves.
" This means that men are expected to behave in a particular manner, women in a different manner and
transgendered persons in another manner.
These divisions and roles are not equal between men and women and women are usually given less
powerfill and restricted roles to perform. This also means that the impacts of social phenomena are
different on the different genders.
These roles change with changing times as well as within communities from time to time due to factors
like improved literacy, higher economic status etc.
Gender Diicrimination
From the time of conception the girl child is discriminated against all her life. This includes being
subjected to foeticide & infanticide and sexual abuse; being weaned from breast feeds earlier than male
babies; her nutritional, health, emotional and other needs being given the last priority, having
restricted access to education- either not sent to school at all or if sent, not allowed to complete her
education in order to look after siblings or do household & other work; and are often married off
during adolescence.
The woman is required to meet the needs of her family before her own needs and acquires recognition
as » family member only after she bears a child, and more specifically a male child.
She has very little decision-making power and issues concerning her are marginalized.
When gender discrimination has been socialised and internalised, it is no longer visible to the gender
insensitive. Unfortunately, religion, health care, education the legal system, employment and the
media, reflect and promote gender discrimination.
Men continue to control decision-making, limited family resources, women's sexuality, freedom of
movement, access to the world outside the home, etc.
So women need a supportive environment to ensure that they are fed adequately, are educated and can
make decisions regarding their life and their children.
Gender sensitivity
Gender sensitivity is an understanding and consideration of different needs of women and men arising
from their unequal social relations and that a policy or programme can thus benefit women and men
differently.
Gender sensitive indicators
Gender sensitive indicators are required to measure the integration of gender sensitivity into any given
programme. They will point out changes in the status and roles of women and men over time, and
therefore measure whether gender equity is being achieved.
Gender issues related to health care
Even when available, health care services are underutilized by women because:
• They are occupied all day with work related to childcare & household tasks, and work outside the
house, and often neglect illnesses in the early stages.
• Health services available are insensitive to women’s needs. They are staffed with male workers;
privacy is ignored; the timing is inconvenient and long waiting periods result in lost wages.
• .Access to health care facilities is inadequate. These include factors like long distances; lack of
transport and even when available an inability to pay for it; a lack ofindependence that prevents
them from leaving their homes alone and restricts them from using their own income or savings;
the expenditure incurred even in the supposedly free health care facilities etc. This is especially
critical when emergency care is required and is a major factor resulting in high maternal and
neonatal mortality.
• The health needs other than those associated with their reproductive capacity are neglected.
• Their awareness of available facilities tends to be lower than that of men.
• They are also not aware of their rights and often do not think they have any.
Poverty & illiteracy
40 % of people in Karnataka are below Poverty Line. Poverty coupled with Gender bias and poor
social and economic status of girls and women limits their access to education, good nutrition as well
as money to pay for health care and family planning services.
Though the enrolment in primary schools exceeds 8.2 million; percentage of children in age group 614 attending schools is 65.3(rural) & 82.4 (urban) and drops out rates have declined from 69% in 1950
to 16.5% , still 2.6 million children (28%) in 6-14 age group are out of school.
Girls participation has gone up from 44.5 in 1980 to 48 in classes Ito 4 and from 39 to 45 in classes 1
to 7and the drops out rates has declined from 73% to 17%. But still there is need for improvement
Literacy programmes are not sustained despite good work in the early years. So the literacy rate is 56%
for Karnataka but rural female literacy in Raichur is a dismal 16.48%
3
Low levels of Female Literacy is a major factor resulting in high rates of maternal & infant mortality,
female foeticide, skewed sex ratio & dowry deaths.
Some reasons for girls not being sent to school are- to care for younger siblings, housework etc., for
economic reasons, fear of sexual harassment and sexual abuse, far off locations, an overwhelming
number of male students and a fear of not being able to get a groom with higher educational
qualification than the daughter.
Women & Work
Wage earning empowers women in decision making. Non -wage earners do not have this advantage
and their contribution is not even recognized. The down-side to this is the fact that very often women
do not have control over their earnings. Also, work outside the home places an additional demand on
the women who are already burdened with household work; reproduction and child rearing; and family
demands- both physical and mental.
1 Girls start working earlier than boys, work longer and harder throughout their lives. The energy
consumption in mere survival tasks of fetching fuel, water, fodder, care of animals; washing; cleaningwhich are exclusively women’s responsibility, results in negative nutritional balance and calorie
deficit The situation worsens when women also have to perform hard labour for wages. Walk long
distances to fetch water and fuel, especially in hilly areas; take care of large extended families, caring
of children, elderly, sick husband and animals is done by women alone with little or no help.
All the above domestic work is unpaid work and is cbnsidered unproductive work. Even when
women work outside the home, they domot get equal.wages for equal work and are made to perform
unskilled jobs which are poorly paid, more hazardous and demanding. They face various occupational
health hazards. Rural women cooking in poorly ventilated huts using wood and cow dung cakes as
fuel, are exposed to 100 times the acceptable level of smoke particles. This is equivalent to smoking 20
packs of cigarettes a day and can cause Chronic Obstructive Pulmonary disease. Women forced to earn
their living as commercial sex workers are prone to infections like STDs, HTV, etc. from their male
clients.
Nutrition
Malnutrition
Though the incidence of severe malnutrition has declined to negligible levels, problems due to milder
levels of protein -calorie malnutrition, and deficiency of iron, iodine and vitamin A deficiency are seen
among a majority of women & children in India.
The Women & Child Departmen and not the department of H&FW is responsible for ensuring the
nutrition of the people. The ICDS projects have not been able to ensure adequate nutritional coverage
for children.
Denial of adequate food to girls, partly due to non-availability and partly due to discrimination, results
in the lower nutritional status of women. Height for age is a sensitive indicator of adequacy of
nutrition. This data shows that girls are more malnourished than boys today in Karnataka
An inadequate diet has life-long consequences for girls and their growth and development is
jeopardised. The nutritional needs of girls especially of iron, vitamin A, calcium and iodine, increases
with the growth spurt associated with puberty and onset of menstruation Early marriage and early
pregnancy further deplete their inadequate reserves.
The woman herself is partly responsible for this. She considers her nutritional and health needs as the
last priority and does not know the importance of her own health as a contributing factor in ensuring
the health of her children
Rising food prices, limitations of the public distribution system and shift to non-edible cash crops, will
undoubtedly worsen the existing nutritional status of women.
Other than the direct ill health caused, malnutrition in women directly contributes to mortality &
morbidity in infants and children.
A child's physical & mental potentials are formed during the period from conception to 3years of age
ofwhich rapid development takes place in the first 18months. So the nutritional status of women
during pregnancy and lactation and of young children is of paramount importance for later
development
Likewise, the nutritional status of adolescent girls shapes the nutritional status of women during
pregnancy and lactation.
• 20% of maternal mortality is directly related to anaemia.
The prevalence of Anaemia among women in Karnataka:
Age in years
Mild%
10.0-10.9gm/dl-children,
pregnant women
10.0-11.9gm/dl-nonpregnant women
Moderate%
7.0-9.9gm/dl
Severe%
< 7.0gm/dl
15-24
29.3
16.4
1.7
47.4
25-34
25.4
12.5
2.4
40.2
35-49
25.8
12.2
2.7
40.7
Any
form%
Source :NFHS D, 1999
N.B.: at least one additional case of sub-clinical iron deficiency occurs for each case of iron deficiency
anaemia, when prevalence rates are <50%.
- It must be noted that 10% prevalence is the cut off point, triggering the need for public health
action.
• Severe Iodine deficiency in utero can cause cretinism in the baby, but milder deficiencies also
cause lower levels of mental retardation.
• Amongst the causes of infant deaths which includes respiratory infection (14.7%), dianfiea (7.3%)
and umbilical cord infections (5.7%), the major cause is prematurely (48.2%), which has a direct
relation to women’s health.
• Inadequate food intake during pregnancy is responsible, in 15-20% of women, for inadequate
weight gain, which in turn increases their vulnerability to infection; and increased maternal and
infant mortality as well as morbidity.
• Inadequate weight gain during pregnancy results in low birthweight babies, which in turn results in
lower IQ by an average of 5 points below that for babies within the normal range of birthweight
Post-Menopamal problems
Age-related and hormone related problems in women aged around 45 years or above, range from
bleeding / prolapse / Uro-genital problems /cancer / Cardiovascular risk / Alzhimers / depression / etc.
5
• Also included is Osteoporosis, leading to fractures and resulting problems like life long immobility
following hip fractures for instance. It is silent and is caused by trivial injuries and even minor physical
efforts like coughing, sneezing, lifting buckets etc but it is preventable
Bone Mineral Density test or Densitometry is a scan which provides a quick, painless and accurate
measurement of bone density, but is accessible by very few.
Tuberculosis:
TB kills more women annually than all causes of maternal mortality combined. It is the leading cause
of healthy years lost among women of reproductive age group [8.7 Million DALYs lost 2.5 Million
(STD) 3.6 Million (HIV)]. This loss added to the cost of treatment, perpetuates poverty.
And now, HIV and drug resistance is increasing the burden of TB especially in productive years.
Although the prevalence of pulmonary tuberculosis is lower in women, the progression from infection
to disease is higher because of the delay in access to medical care. This is due to underlying problems
of ill health, malnutrition, repeated childbirth; burden of work & childcare; fear & stigma etc.
Children are more likely to be infected if their mother has TB than if their father has TB
Thus, not only does TB affect women more, women with TB have a greater negative impact on
society.
RTI/STI
W Three types of RTFs need to be addressed appropriately.
•. Sexually transmitted diseases, for example, Gonorrhea, Syphilis, Trichomonas Chlamydia,
HIV/AIDS.
• Endogenous, due to overgrowth of existing bacteria, for example, Candidiasis during pregnancy.
• Infections caused by instrumentation, for example, following a pelvic examination, septic abortion,
etc.
RTFs can cause pain, dysmenorrhea, discharge, infertility, ectopic pregnancy following pelvic
inflammatory diseases, etc. A large percentage of women are asymptomatic and therefore are unaware
of the presence of any infection.
Women are more prone to infections than men because of a larger mucosal surface available for entry
of infecting organisms. Young girls are more vulnerable to RTFs specially’STD, as are older
menopausal women.
Women infected by partners with HIV pass it on to their unborn child.
RUs/STIs are supposedly dealt with through the RCH program. But the ineffective implementation of
this component, biological vulnerability to these diseases, the lack of power to negotiate responsible
0 behavior from their sexual partners and the non-availability of lady medical officers in adequate
numbers, all contribute to increasing incidence of these eminently preventable diseases amongst
women.
HIV/AIDS:
Incidence & Prevalence:
India has the largest number of people living with HIV/AIDS in the world. Latest reports from NACO
estimates the prevalence of HIV/AIDS in India at anywhere between 3.5 to 4 million cases. The
numbers per se may not be seen as large compared to other health-related problems. What is alarming
is the steady rise in incidence, with estimates that the numbers are doubling every three years.
From the first HIV sero positive individual detected in 1988 in Karnataka the numbers have risen
dramatically and is estimated to be upwards of 0.15 millioa Six districts viz. Bangalore Urban,
Mangalore, Udipi, Dharwad, Bellari and Mandiya contribute to 73.3% of HIV positive cases in this
6
State. It is also no longer confined to the so-called "high risk behavior" groups. The infection is
spreading rapidly to the general population or the so-called "low risk" population of women and youth.
HIV/ADDS control activities, initiated in 1992 is carried out by State AIDS Control & Prevention
Society (KSAPS) include Surveillance, Blood Safety, Awareness and targeted interventions
programmes and Medical management, care & support of People Living With HTV/AIDS (PLWHAs).
The various factors that impact negatively on the implementation of the programme are:
The vertical mode & therefore a lack of integration with the Department of Health & Family Welfare.
Biological (physiological), gender inequalities, social, cultural and economic factors make women
more vulnerable to STDs & HTV/AIDS and have to be factored into the programmes.
Addressing AIDS will be far more difficult in a country like India, where leucorrhea and gonorrhea,
which can be prevented and treated, have not yet been successfully addressed.
Gender & HIV/AIDS
Lack of responsible sexual behaviour in men is clearly due to the gender roles. Women have fewer
choices and little or no decision-making power, both within the private and public spheres. For many
women, questioning the extra-marital sexual behaviour of their husbands, negotiating condom use or
asking them to get contraceptive pills, means inviting violence.
• The culture of silence around sexuality in general and women’s sexuality in particular implies that
women have inadequate knowledge about their body, sex and sexuality, reproductive health, STDs
HTV/AIDS etc. infectioa This often leads women to underestimate the risk of HIV infection.
• In the absence of clear laws and policies pertaining to the manner in which partner notification is to
be ensured, men (also women) may or may not disclose their HIV status to their sexual partners.
• Even if a women is aware of her partner's HIV status, she may not be in position to choose or insist
on safer sexual practices.
• Health care services, including counseling care and treatment are often inaccessible to women.
• Studies have found that in cases where the woman's infected status become known first, she is
either chased away, beaten up or forced to commit suicide.
• Fear of violence has also interfered with women's ability to take a course of AZT to reduce risks of
transmission to the foetus.
Other Gynaecological problems:
Abortions
20% of maternal mortality is due to abortion-related causes. Medical Termination ofPregnancy (MTP)
has been legalised under the MTP Act of 1971, under certain conditions, i.e. only prior to 12 weeks; it
is not allowed after 20 weeks, unless it is a life-saving measure and is performed after consulting two
doctors.
Hie spiralling number of abortions(legal and otherwise) and abortion deaths reflect the increase
in the number of inflicted, unwanted pregnancies which women have to bear. Women also have to bear
the consequences of the abortion, be it death due to bleeding and sepsis following abortion, or a sense
of shame and guilt, specially when it involves young unmarried mothers. The majority of abortions are
almost a substitute for family planning, as they are sought by married women, some being
multigravida. Some are related to prenatal sex determination & foeticide.
A number of "illegal abortions" are also being conducted by untrained people, using methods that are
not medically approved leading to a high incidence of morbidity and mortality.
Infertility
Infertility is a medical as well as major social problem. There is a need to change public opinion and
attitudes towards childlessness ofwomen. Even if the problem is structurally or functionally in the
male partner, it is the women who is labelled and not treated in society with empathy and acceptance.
Uterine Prolapse
Heavy work at construction sites, walking long distances on steep hills in search of water or fuel, or
climbing 2-3 storeys up a narrow staircase with buckets of water. Certain childbirth practices, such as
pressing the abdomen during labour to hasten delivery also leads to prolapse of the uterus, especially if
this is associated with a poor perineal muscular tone due to frequent pregnancies and malnutrition.
Cancer
Magnitude of cancer problem in Karnataka
Magnitude and patterns of cancer in Karnataka are well documented by both Population Based Cancer
Registry and Hospital Based Cancer Registry of Kidwai Memorial Institute of Oncology (KIMIO).
About 35,000 new cancers are estimated to occur in Karnataka The average annual age adjusted
incidence rate of cancer from 1982 -1991 was 113 per 100,000 in males and 138 per 100,000 in
females. Hie higher incidence of cancer in females is due to the greater proportion of cancer of the
cervix and breast PBCR data shows these two sites of cancer constitute over 40 percent of all cancers
in women, accounting for over 11,000 cancers in Karnataka in 1994.
It is estimated that by year 2000, there will be 5447 new tobacco related cancer in Karnataka among
males & 3507 among females.
Factors leading to this high incidence include changing life-styles; high incidence of risk behavior both sexual as well as substance abuse; lack of personal and reproductive hygiene etc. Lack of clean
water, poverty, gender inequality etc. are other indirect factors.
In terms of prevention of cancer, whether by primary or secondary prevention, over 60 percent of all
cancers in males and nearly 40 percent of cancers among females fall into this category.
But, as per the HCR about 85% male patients and 90% of female patients present when the disease has
(spread beyond the site of.origin. It is difficult to give ope single reason for this phenomenon.
A combination of factors like lack of awareness, economic conditions, inadequate access to proper
diagnostic facilities, fear of the disease and poor knowledge of the outcome of treatment could possibly
contribute to the advanced stage of presentation.
Cancer Cervix:
It is estimated that by year 2000, there will be 5503 new cervical cancer cases in Karnataka.
The study conducted between 1980 and 1986 by the Department of Oncology, Kidwai Memorial
Institute of Oncology found that, cancer cervix formed 40% of female malignances and 88.47% of all
gynecological malignances. About 84% of these women were between the ages of 35 & 64 years; only
32% of cases presented for treatment at stage 0 and in the majority (97.1%), cancer had spread
0.
beyond the cervix at the time of diagnosis.
Reasons for delay in seeking treatment were: lack of awareness of the symptoms of cervical cancer
(57.6%) and inadequate advice by medical personnel to whom they had reported their symptoms
(33.7%)
8
Early Diagnosis of Ca Cervix
Since treatment of pre-invasive cases markedly reduces cervical cancer mortality and prognosis
declines considerably as the stage of the disease advances, the primary goal of public health efforts
should be to promote early detection through screening programme.
Cytology-based screening in India is not feasible due to the scale on which it is required (and the
concomitant level ofresources), and the lack of quality control. An ICMR study in 1986 estimated that
even with a 12-fold increase in cytology services only 25% of
women at risk could be covered by the year 2000 AD.
But screening by visual inspection of the cervix " downstaging cancer cervix” if used can detect early
stage disease in about 50% of cases compared with the current 5%.
A number of women below the age of 35 years have cervical dysplasia, but only a very small
proportion will develop a malignancy. Thus, for a cost-effective screening programme, screening
should have a high coverage of women above 35 years, and should have a low frequency.
Breait Cancer
It is estimated that by year 2000, there will be 2949 new breast cancer cases in Karnataka, many of
them presenting at late stages for treatment
A study conducted in Bombay points to an increasing incidence of breast cancer among the urban
women, especially among the elite due to factors such as increased age at first pregnancy, fewer
children, decreased lactation etc. This is in contrast to the incidence of cancer cervix, which is seen
more among the rural as well as urban poor due to poor reproductive hygiene; higher incidence of
STDs, numerous pregnancies etc. Infection with the Human Papilloma Virus (HPV) is also implicated
as a causal factor.
Early detection of these cases can be implemented by awareness about self- examination of the breast
by women as well as annual examination by a medical officer. Mammography is also recommended
but is not affordable by the majority of women.
Violence against Women
Violence against women covers the whole gamut of domestic violence, sexual violence, sexual
harassment, rape and sexual abuse, marital rape, forced prostitution; dowry related violence; abuse of
children, neglect of widows and elderly women, etc. It has been recognized as a major public health
and women’s health problem, and occupational health hazard.
Despite ahistory of law reforms and increasing visibility around sexual violence, violence against
women has continued unabated in India.
A first-ever study in India conducted by the International Centre for Research on Women found that
45% of the women interviewed were victims of domestic violence. These figures are an
underestimation according to researchers, as women were not willing to talk about it
According to a research carried out in 1997-98 by RAHI, a support centre for women survivors of
incest, 76% of 600 women interviewed had been sexually abused in childhood or adolescence.
80% of rapes are perpetuated by relatives or men known to the women; 24% of rapes involve young
girls, less than 16 years of age.
Domestic Torture constituted 30.4% of the total crimes committed against women in 1996 in 1996,
rape formed 12.8% of the total reported crimes against women in India Humiliation through verbal
abuse and forcing women to work like servants are extremely common.
9
A study conducted by Sakshi, an NGO working on women’s issues, in March 1996 revealed that 72%
of women respondents had heard or encountered sexual harassment at the workplace.
The number of "missing women per 1,000 men" is an indicator of the increasing violence against
women. This according to Census of India 1991 is 73 for the country, 89 IN Bihar, 36 in Kerala, 26 in
Tamil Nadu and 40 in Karnataka
Violence against girls and women is prevalent among alLiocial classes and castes in India, touching
women at every stage of life & linked to their low social status within a patriarchal society. Violence
has its roots in the way men have been socialised to exert social and economic control over their wives
and other females in the household. Control over women’s sexuality is an integral component of this
process, where men believe they have the right to have sex with their wives regardless of whether or
not their wives consented and justified wife beating as appropriate discipline when their wives refused
sex In a discussion be researchers with men in a Tamil Nadu village, the justification for violence was
"A cow will not be obedient without beatings".
When couples are unable to produce children, it is the woman who is blamed, ostracized and abused,
regardless of which partner is infertile or the cause of infertility.
Violence has a strong bearing on some of the most intractable reproductive health issues - unwanted
pregnancies, forced abortion, HIV and other sexually transmitted infections and other complications of
pregnancy.
Clearly then; its implications on policies on issues like ADDS prevention, population control and
ensuring reproductive health rights are immense.
Gender based violence leads not just to physical injuries, but to psychological problems including
depression and suicidal tendency. Mental cruelty by men with low self worth especially against women
who perform better than themselves at work, jealousy towards wives are examples of violence.
Alcohol related Violence
Several studies show that that there is astrong co-relation between substance abuse and domestic
violence. It is also seen that violence during relapse is only during drinking. Failure to address
domestic violence issues among substance abusers interferes with treatment effectiveness and
" contributes to relapse.
Woman’s response to violence is limited by the choices available to her.
Women prefer to suffer silently and believe that men are justified in beating them; a way to survive in
the marriage and protect her children and herself
Though women with better education reported less violence, their economic independence does not
seam to matter much when it comes to resistance.
The very nature and functioning of the present system of redressal is such that women would not want
to approach it for succor till the situation seems to threaten their lives or more importantly, that of their
children.
For the majority of women, there is no safety valve at all. Though some pick up courage to register
complaints with police, the latter refuse to accept, dubbing them as "domestic problems which ought
to be settled within the family itself’. They are directed by the police to undergo a medico-legal
examination/ report Even when there are obvious injuries, in the absence of a fracture these are
10
recorded as only 'simple injuries' in which case minimal action will be taken. This kind of
minimalization leads to a lack of clarity regarding the violence suffered as well as of their rights.
In 1989 the Supreme Court of India passed a judgement in which it used the moral character and
conduct of a minor victim to reduce the sentence of two policemen who were convicted of gang rape.
Expressions describing the minor as "lewd and lascivious"; criticism that she had taken seven days to
report the crime; reflected in the judgement
Despite India's constitutional promise ofgender equality, judgements like this demonstrated how
gender bias, stereotypes and myths in dealing with the phenomenon of violence against women, impact
on judicial decision making.
The need of the hour is changing the irrational prejudices in society and myths and stereotypes that
impact on the mechanisms of redressal available. There is a vital need for gender-sensitizing the
police, lawyers and judges through an interactive educational forum to enable them to understand
violence as women experience it
Laws pertaining to women like laws related to rape, sexual abuse, sexual harassment, divorce, marital
rape, domestic and other violence etc. have to be changed to empower women. This should also
include changes in the legal procedures and processes to enable the women to have easy access to
justice.
Child sexual abuse
Sexual Abuse is - Being tricked or forced, into any form of penetrative or non-penetrative sexual act
Child sexual abuse is sexual abuse of a person under 16 years of age.
Sexual Abuse is not confined to ‘rape’. Any form of abusive behaviour expressed through language
(sexual comments), body exposure and / or body contact that may be accompanied by other forms of
abuse falls into this category.
Often the offense starts as an innocuous, affectionate gesture, which is acceptable in the society. Most
often the abuser is a person very close to the child whom he-/ she trusts, loves and respects. Easy
accessibility to the child, opportunities to be alone and intimate with the child and a close relationship
between the abuser and victim play a major part in the initiation and continuation of child sexual
abuse. Disclosure is usually met with disbelief and dismissal.
Sexual gratification is seen as a normal need in males, but not so for females; is associated with a
“Macho image”; an aggressiveness that is acceptable. Therefore most sexual acts by men, whether
normal or deviant, and whether within legal and ethical boundaries or not is accepted and is forgiven.
These are some reasons why in India, statistically more girl children are abused than boys.
With such emphasis on virtue and virginity in girls in our culture, sexual abuse in any degree is all that
more traumatic.
Long term effects include behavioral problems, the victims are maladjusted, prone to extreme feelings
of guilt, shame and depression, unable to cope with ordinary everyday situations and relationships even
as adults, long after the abuse has stopped.
Female feticide & infanticide
Biologically, 105 boys are bom for every 100 girls. In the first year of life, through higher death rates
among boys, these figures even out Logically, there should be 1000 women for 1000 men.
But Indian population statistics reveal a consistent and alarming decline in the population of women
and, more importantly, girls right through the century.
In 1991 in Karnataka the sex ratio was 960 females for every 1,000 males.
This decline in female ratio is the result offemale foeticide/infanticide, due to deep-rooted gender bias
in all sections of our society.
The reason for this is that daughters are perceived as an economic and social burden on the family
because of the dowry system, their dependency on males and therefore a lower status of women and of
course the son obsession in our patriarchal society. Most women feel that it is better for a female to die
in the womb than to be ill-treated later. On the other hand, the son perceived as an asset, a
breadwinner, capable of supporting himself and the rest of the family, a person who will continue the
family lineage, perform funeral rights and support parents in the old age.
If unchecked, foeticide and infanticide will permanently damage the demographic balance in India
This will lead to an increase in sexual crimes against girls and women.
Prenatal Sex Determination
Prenatal tests like Chorionic villous biopsy, Amniocentesis and Ultrasonography which should be used
for detection of abnormalities in the foetus, are widely misused for sex determination by doctors.
Ultrasonography, a non-invasive method done during 14-16 weeks of pregnancy, is presently the most
sought-after, and has a success rate of 96%.
Moreover, doctors have been promoting female foeticide at the cost of woman’s health through life
threatening second trimester abortions.
The use of pre-pregnancy sex selection by X-Y Separation is also increasing.
The Abortion bme
The subject of selective female abortion is a highly complex issue raising many ethical and moral
questions. The justification for liberal abortion laws in India is for health and humanitarian reasons
and individual entitlement to an abortion by a w'omea The government gave licenses to only trained
doctors, some hospitals and nursing homes to conduct abortions on four humanitarian grounds under
aseptic conditions. It certainly did not give a license to kill at random and by no means on gender bias-
Legal aspects
The first law in India banning infanticide was enacted in 1870 during British rule. The Central
government has begun to regulate prenatal diagnostic techniques.
But the nexus between some doctors and private ultrasound clinics that help determine the sex of the
foetus have led to a virtual epidemic offemale foeticide, even though the real culprits form only a
minority amongst the medical fraternity.
Enacting laws regulating the conduct of the medical and paramedical fraternity alone will not check
this deep-rooted social evil which originates from gender bias. Awareness about its dangerous
consequences will help catalyse the evolution of abroad social movement against foeticide and
.infanticide.
Adolescent population
There is an increasing adolescent population with specific needs, which are not met by the present
health and social structures.
India's adolescents (10-19 years) population is estimated at 21.8%, and married adolescents at 20 per
1000 population. 6% urban and 21% rural woman aged 15 to 19 years married before the age of 15
years.
A majority of adolescent girls have nutritional inadequacies including under nutrition; stunting; iron
deficiency and aneamia; deficiencies of other micro-nutrients like iodine vitamin A; calcium, zinc and
folate; and obesity. This results in malnutrition during pregnancy and therefore to maternal and infant
mortality and morbidity.
12
Adolescent fertility is estimated at 17% and contraceptive practice is very low. Unmarried adolescents
(who constitute a sizable proportion of abortion seekers), often delay their abortions until dangerously
late because of ignorance or fear of social stigmatization.
Sexual behavior patterns which set in during adolescence can lead to sexual and reproductive health
problems; RTIs & STIs; HIV/AIDS; the majority of new infections occuring in the age group of 1424years.
Other issues related to adolescents are sexual abuse, prostitution, street children, violence, suicide and
substance abuse. It has been found that in the six major cities of India, 15% of prostitutes are below 15
years and 24% between 16-18 years of age.
Adolescents are capable of responsible behaviour and can take the right decisions if empowered with
information and the freedom to do so.
Empowerment
The management and monitoring of the basic health services that a community is entitled to by the
community itself would go a long way to ensuring availability, accessibility and quality. The
community should be capable of determining their basic health needs, evaluating the local health
situation and the services that exist and improving upon them. In other words, to ensure that the
peoples health is the people's hands.
Empowerment of the community, especially women, adolescents, the poor and the marginalized to
make informed choices in issues relating to their health, amongst other important decision-making
issues is the single most important factor that needs to be addressed if the health status of the
community has to improve.
Empowerment will enable them to demand and get the services they are entitled to. A strong and active
Panchayat will be able to help achieve this empowerment
Health education
While the provision of primary health care services (like immunisation; control ofdiarrhoeal diseases,
acute respiratory infections, malaria, tuberculosis; and provision of antenatal and postnatal care) are
important in the short run, interventions that focus on the underlying causes of ill-health are much
more significant in the long-term. Continued emphasis on the curative approach had led to the neglect
of the preventive, promotive and public health aspects of health care.
Health E ducation will form part of the empowerment process and therefore will have to be addressed
as a long-term, separate, planned activity.
Recommendations:
Recommendations to tackle gender inequality:
A department to implement "Genderization of Health" headed by an Additional Director should
be set up/ identified to ensure the priority and importance that this program warrants. Needless to say
the head should have a thorough understanding of gender issues. This department can implement the
following recommendations and also co-ordinate inter- sectoral participation.
1. All Health -care personnel should be sensitized on issues relating to gender inequalities. The
curriculum for Medical Education and for training programs for health care personnel should
include gender perspectives.
13
» 2. Gender disaggregated data should be collected and gander sensitive indicators to evaluate gender
equity should be integrated in all plans & programs. Examples of gender disaggregated data would
include birth and death details, admissions & attendance at schools, hospital in-patient & out
patient records, immunization details, salary patterns for the same jobs and so oil
3. This department should support research on women’s health needs.
Inter-Sectoral participation
1.
Government departments and programmes:
• Gender sensitization of all government functionaries of all departments should be ensured, and
institutionalized within government training systems at the entry and in-service levels.
• Women's issues and perspectives must be part of every sectoral plan/programme and not be
limited only to the department of women and child development
• Every department should prepare a women focused action plan. Gender analysis and gender audit
of all plans, programs and policies both before and after should be made compulsory. Institutional
capacity should be created within all ministries to ensure implementation and independent
mechanisms which include participation of women activists for monitoring this.
• Laws pertaining to Inheritance and ownership of land and other assets need to be changed to give
fair and equal rights to the women.
• There should be advocacy for equal wages for men & women.
The Gender Empowerment Measure (GEM) looks at the level of participation of women in the
economic and political life in comparison with men through four indicators- the percentage of
women in Parliament, as administrators and managers, as professionals and technical workers and
the share of women in national income. The GEM and other gender indicators should be used as
the basis for improving interventions and programmes to achieve Gender equity.
Recommendations to improve Nutrition of women and children:
1.
Weight gains of less than 4.3kg by 14 weeks of pregnancy approximately doubled the risk of
"small for gestational age newborns" as well as incidence of preterm delivery regardless of total
weight gain.
Therefore strategies aimed at improving the nutritional status ofpregnant women, who are usually seen
only after 14 to 16 weeks under RCH now has to look at pre-pregnancy nutritional status and
correction of Iron & other micro-nutrients deficiencies.
• The ICDS / School Health programme should include adolescents especially, girls and
nutritional inadequacies (Height-weight comparisons, Hb levels) identified and corrected with
A IFA, mid-day meals etc.
• The health worker should educate adolescent girls & women about nutrition and the additional
nutritional requirements during puberty, pregnancy & lactation; the quantity and kinds of food that
they have to consume during these times; anemia, its cause, iron rich foods and importance of
taking IFS despite any side effects that may occour, and emphasize the influence of the mother’s
nutritional status as a factor influencing the health of their unborn and breast-fed child.
• Periodic checks will have to be kept on the pregnant women's Hb and weight The reasons for .
continued low Hb & / or low weight gain should be ascertained and corrected.
Example: Have the women actually consumed the complete course of IFA tablets, and for those who
did not complete it and what were the underlying reasons for it
Have the pregnant women actually consumed the food supplied to them through the RCH /
Anganwadi program.
14
2. Awareness regarding Osteoporosis; the importance of taking food rich in calcium like Ragi, milk
products etc.should be given. Pregnant women can be told to get the elders at home for a review and,
give them Calcium rich food to prevent life-long problems.
Recommendations for improved STD & HIV/AIDS programmes:
The Department of Health & Family Welfare should be fully involved, with KSAPS as the prime
mover and should include the following:
Access to clean menstrual cloth, adequate water, privacy while bathing, toilet facilities, etc. should be
ensured.
It is equally important to ensure responsible behaviour by male sexual partners. The strategy must be
sensitive to gender factors. The 'men make a difference' campaign, attempting to make men more
responsible in the control of the epidemic is an example of this.
Awareness about STDs & HIV/AIDS by ANMs and other health workers for the community. This
should include risk reduction, behaviour change and condom promotion as well as efforts to minimize
stigmatization.
Early diagnosis, treatment and counselling of STDs patients and their sexual partners.
Early diagnosis and treatment of TB patients. For the tuberculosis programme to be effective, it should
address these gender related barriers to TB diagnosis and treatment; Women should be educated about
how TB in the mother will affect the children.
Voluntary testing and counselling support
Early diagnosis and treatment of opportunistic infections in PLHWAs.
Care and support of PLHAs.
Anti-Retroviral Therapy (ART) for pregnant women and newborns for prevention of vertical
transmission.
Ensuring blood safety by increasing voluntary donations, rational & optimal blood use and ensuring
quality of screening for Transfusion Transmissible Diseases (TTD).
Ensuring bio-safety in health care institutions & safe disposal of hospital wastes.
Availability of laboratory services for diagnosis of STDs even at the PHC level; & diagnosis of HIV at
District Hospitals.
Drugs for ART; effective treatment of STDs, Opportunistic infections, TB etc.
Specifically:
1. Improve diagnostic, medical and counselling services for STI & HIV/AIDS for the patient as well
as the sexual partner.
2. Train PHC MOs on detection & treatment of STI/RTIs, both syndromic as well as Lab-diagnosis
based.
3. Train PHC technicians on laboratory tests that are required to be performed. Ensure that QC is an
integral part of the testing.
4. The "Family Health Awareness Week" programmes.have been very successful. Explore the
possibility of conducting these more often & at regular intervals; strengthen the "pre-programme"
awareness component; provide table-top laboratory diagnosis; and adequate supply of drugs on the
spot
5. Another avenue that can be explored is to have a "Medical-care" stall at shanties (market days).
6. Train PHC MOs to ask women leading questions regarding problems related to the reproductive
system, make a provisional diagnosis and refer to FRUs if necessary. Most women do not
volunteer this information due to lack of awareness, lack of or presence of mild symptoms only
which they tend to ignore, shyness in the presence of male MOs, lack of privacy etc.
15
Recommendations for Cancer control among women:
Health Education, early detection and management of Cancer Breast, Cervix and Oral Cancers by
trained health personnel should be taken up as an integrated programme. In addition, women can be
taught to conduct sc!f-e;samination of the breast
Women health personnel (both health workers and lady medical officers) should be trained to
perform visual inspection of the cervix and triaging its appearance into normal, abnormal and
suspicious of malignancy; and making appropriate referrals
2.
Health education programmes regarding commonly occouring cancers, their aetiological & risk
factors, especially tobacco, & alcohol and importance of early diagnosis should be undertaken.
Health education programmes to disseminate information about Cancer Cervix should target both
women and men & be a part of a broader public health programme on reproductive health. It should
give information regarding the role of early marriage, repeated childbirth, poor hygiene of male
partners and repeated infections, unsafe sexual practices, reproductive hygiene and smoking in the
etiology of cervical cancer & use of condoms as a preventive measure. It is particularly important that
cervical cancer initiatives do not become obsessed with the issue of number of sexual partners or
"promiscuity" is not as straightforward as counting the number of partners; it is often a value
judgement
3.
HE should facilitate safe hygiene practice, promote safe sex practice and also encourage women to
demand visual inspection from the trained health workers.
4.
Prior to the launching of public health efforts to prevent and downstage cervical cancer, it is critical
to ensure the availability and accessibility of therapeutic services- early detection, treatment,
referral networks, and palliative care. Ifs no use empowering women, if diagnosis, referral and
treatment are not guaranteed.
5.
Early detection programmes should be effected by ensuring the following:
- promote early detection and down-staging through appropriate .screening methods.
- Target women 35-64 years of age groups.
- Do not link with other unrelated programmes like RCH as the target age group is different
- Maintain registry
- Referral & Follow up
- All health personnel should be responsible for and given training for doing visual inspection &
procedure to sterilise the gloves and specula. They should be provided with a torch, sufficient
specula & gloves, and those performing cytology with slides, a slide box, a glass marking pencil
and fixative solution. The screening can be performed at the PHC, Primary Health Unit, and the
village school or at the homes of the women.
|6. For further investigations samples required (Cervical smear / FNACs, etc) can be drawn at the PHC
&
sent to District Laboratories for investigations. Surgeries and chemotherapy can be performed at
FRUs. Only cases requiring Radiation need referral to specialized centers.
7.
Palliative care can ensure that unacceptable, unnecessary suffering can be avoided. Nearly 80-90
per cent of pain can be managed using drugs, which cost less than aspirin. Early stage disease can
be successfully treated by either surgery or radiation therapy, but in the advanced stages, only
radiation therapy and palliation are useful.
8.
The treatment lasts for four to six weeks and will entail travel to one of the metropolitan cities
where cancer treatment is available and considerable economic and emotional sufferings.
9.
Treatment of early'stage cancer is not less expensive (or less technology intensive) than late stage
disease; however, it is more effective because of higher rates of survival and cure. Bleeding and
foul-smelling discharges which occour in late stages can be avoided.
1.
16
Public-private partnerships in all these areas is essential. Eg. Specialists to augment serving of
Government doctors; Radiation therapy totally free or at minimal costs by using their facilities at
night time or during other lean periods / holidays...
11.
Anti- tobacco legislation should be enforced at the earliest Efforts to ensure social boycott of
tobacco is also essential.
.
10.
Recommendation! for improved services for adolescents:
Adolescents need health information and services particularly with regard to nutrition, sexuality and
reproduction. There is need to promote reproductive health among adolescents. Right to factual
information to maintain good health must be met, because in reality, peers and parents often give
misinformation, pass on dangerous beliefs and practices or transmit a dis-empo'wering mind-set
regarding sex and sexuality.
1. Health education activities targeting especially adolescents should receive a considerable boost It
should include apart from other health issues nutrition; sanitation; reproductive system,
reproductive rights & responsibilities; population issues; human sexuality, sexual rights &
responsibilities; RTI/STI; HIV/AIDS; substance abuse; values & life skills; gender issues; their
rights and their responsibilities to themselves, their families as well as to society etc.
This is best provided with the help of trained, teachers, self-help groups & other NGOs as well as the
IMHWs & JFHWs, anganwadi teachers, peers etc. and by the use of media
2.
This should be supported by Health services - A lab-diagnosis based treatment & counseling for
RTI/STI
3.
Alternate, vocational-training based programs could be made available for school dropouts. This
will provide access to them to implement adolescence education.
4.
Provide access for teenagers to health service delivery points such as PHCs, subcentres and CHCs,
ensuring privacy and confidentiality.
5.
Strengthen existing facilities and provide safe MTP services to all married/unmarried adolescent
girls irrespective of age.
6.
Advocate for policy changes at all levels to promote reproductive health services, including
contraception to both unmarried and married teenagers.
7.
Legislation for reproductive health and sex education in the formal school system^
Recommendations to address Violence against women and girls
Violence against women and girls at societal and household levels to be eliminated through
strengthening of institutional capacity, involvement of women, and review of certain existing legal
provisions.
1. Health Sector:
• Guidelines for addressing domestic violence should be incorporated into the national health
policies.
• Diagnostic and treatment guidelines for domestic violence and emergency room policies and
procedures for dealing with abuse victims should be developed.
• Privacy is essential when interviewing clients about domestic violence and this should be ensured.
• Health personnel should be trained adequately and sensitively to recognize signs of violence, to do
early medical check-ups for trauma & give legal advice and counseling,
The health care giver should be trained to actively look for physical injuries, especially patterns of
untreated injuries to the face, neck, throat, and breasts.
Other indicators may include inconsistent explanations for injuries and evasive answers, complications
in pregnancy, stress related symptoms such as headache, backache, chronic pain gastrointestinal
17
distress, sleep disorders, eating disorders and fatigue; anxiety, palpitations, hyperventilation, panic
attacks; sad, depressed affect; or talk of suicide.
The interviewer should be trained use concrete examples and hypothetical situations when asking
about violence rather than vague, conceptual questions.
They must also be familiar with common excuses used. For example- 'T only pushed her," " She made
me so angry, I didn't know what I was doing." " pressure of work”....
• Substance abuse treatment programs and domestic violence programs should be linked and should
include specialized counseling; a relapse prevention plan etc.
All substance abusers should be screened for current and past domestic violence, including childhood
physical and sexual abuse.
It is extremely important to convey to the survivor that there is no justification for the battering; that
substance abuse is not the real reason for the violence though it is often used as an excuse.
Families have to be counselled to break the cycle of “violence - honey mooning - violence” that the
abuser inflicts on the family.
2.
Social support:
Mechanisms to help women and children in immediate danger from a batterer, including referral to
women's shelters should be available.
"For long-term support rehabilitation centres, community linkages, professional services including
counseling, legal aid, social security and skill training in income generating skills, a directory of
information on available support services are also necessary.
The above services if provided by NGOs should have the active support of the Government
Mechanisms to make men accept personal responsibility for their behaviour and to change their
behaviour should be developed.
■ 3. Legal and judicial issues:
• Police, lawyers and judges should be gender sensitised through workshops and training sessions,
which would make them aware of the nature of violence against women, in particular domestic
violence, sexual violence (including child sexual abuse) and dowry offences.
• The language employed in official court correspondence, decisions and oral communication when
referring to women litigants, witnesses and lawyers should be gender sensitive and not derogatory
to women, perpetuating traditional myths about women's roles.
• An advisory body ofjudges, legal activists and women's rights/human rights organizations should
be constituted under the auspices of an autonomous body like the National Judicial Academy to
review past judgements to highlight cases of gender bias, as a starting point of gender equality
education
• Certain existing legal provisions and laws may need to be reviewed and changed.
Recommendations to reduce the incidence of female foeticide and infanticide.
1. Implementation of the 1994 law:
The Karnataka government was most active in the first two years in implementation of the law.
Thereafter the Appropriate Authority has lost interest and has not even met since 1998.
They have refused to register ultrasound machines because of opposition from ultrasonologists.
Urgent steps should be undertaken to correct the above to implement the law both in letter as well as in
spirit
• To effectively implement the law18
4
Avoid criminal isati on of female infanticide. Do not victimize victims
Otherwise will not be able to reach out to these backward social groups
2.
Unless we actively look for female infanticide, we will not find it
• Gender disaggregated data on children bom, as well as percentage of female foetuses aborted
should be gathered and studied for trends which can specifically point to particular doctors /
hospitals / nursing homes / ultrasonography clinics where female foeticide is being practiced.
• Information should be collected to estimate the incidence as well as to understand some of the
causes. Female foeticide is seen almost exclusively amongst Hindus. Religious leaders could be
urged to spread awareness about gender issues, violence against women and the evil nature &
consequences of female foeticide & infanticide.
3.
IMA and Medical fraternity should:
• Disseminate information about Prenatal Diagnostic Techniques Act,1994 among doctors on a war
footing.
• Sensitize doctors on the gravity of the situation caused by selective female foeticide.
• Socially boycott known offenders.
4.
To change attitudes and behaviour of men:
Engage in IEC activities with men, women, girls and boys, in relation to violence and sexuality
so that they value women’s roles and responsibilities, engage only in consensual sex between partners,
arrive at peaceful settlements of conflict within the family and participate equally with their spouse in
decisions and practices relating to contraception and to enable women to exert greater control over
their own security and sexuality through gender awareness.
5.
To provide timely referral of women to health problems derived from male violence against
women.
Train the health staff in gender issues related to violence and sexuality to enable them to raise
-awareness in the community about such issues, and in diagnosing health problems that derive from
•violence such that they can effectively refer clients to appropriate services.
Recommendations to deal with Child Sexual Abuse:
The Health Education Programmes should include facts about Child Sexual Abuse, through including
the fact that this is a crime punishable by law.
Parents, teachers and health personnel should be trained teach children about body parts that are
private to them, how to avoid “bad touch” and to report any misbehaviour at once to them.
They should be trained to recognize signs of abuse which can include psychiatric problems, abnormal
or inappropriate sexual behaviour, physical signs like genital / anal injuries / bleeding, staining of
underwear, pain while passing urine or stools; sores / ulcers in and around genitals, anus or mouth,
STDs etc.
Long term psychological support for sexually abused children of a trained counsellor / psychologict /
psycho-social worker / psychiatrist should be identified within the Health system.
Legal, social and rehabilitative support for children abused by a close relative should be ensured
through W&C department
Recommendations for Empowerment of women:
1. Income- generation schemes:
19
•
•
•
•
Income- generation schemes amongst women strengthen sustainable health programmes as well
and should be encouraged. These should be supported by capacity building in managerial,
accounting and banking skills for women's groups.
General information about opportunities, threats and options; technology etc. as well as
government schemes for the benefit of rural women related to income generation, welfare, health
and education should be made available through local women’s groups and panchayat Information
on land rights of women and instruments of local governance should also be available.
The ground reality around the micro-credit and other development schemes for women should be
analysed by gender and development experts.
Occupational health and safety measures and if possible additional measures such as provision of
creates at the work place and staggered work-timings to suit the convenience of women will
improve the overall productivity of women workers.
2. Role of Panchayat:
• Panchayat members at all levels especially at the village level should be sensitized on gender issues
and oriented with regard to their responsibilities, entitlements and duties to the community.
• More women should be encouraged to become Panchayat members.
• They should be trained in and encouraged to participate in activities and programmes pertaining to
9
empowerment of women, health, RCH, I CDS, school health, literacy etc. They should also ensure
involvement of local youth and women's associations.
• The panchayat system should ensure empowerment by first creating awareness and later, through
community involvement and active participation of the people, to prepare village health action
plans to meet specific local needs.
• It should also ensure inter sectoral coordination with related programs such as sanitation and water
supply, Health Promotion, Literacy etc.
•• It should ensure genderization of all functionaries, plans and programmes at the grass roots level.
• It should ensure that the community recognizes and acknowledges all facets ofwomen’s role in
society. Men and women should be aware of the cost of the "unpaid work” done by the average
woman at home & outside.
• Measures should be taken to make people aware of services available and the “cost of services” by
displaying these details on notice boards in hospitals and by issuing bills for services rendered
indicating full or part subsidy given, depending on user fee charged. This should include the
detailed list of free services, drugs etc. available.
^3. Empowerment training:
Empowerment training of women, women’s groups and Panchayat women members should be
implemented. Apart from information on Health, gender issues, available services etc. it should include
components of skills building, enhancement of self esteem, life skills, communication skills and their
rights and responsibilities.
A pilot training programme for women’s empowerment was tested in Bangalore rural, Bidar, Bellary,
Chamrajnagar and Koppal in 1999-2000. This GOI supported programme provided training kits and
manuals (which were translated into Kannada). Mahila Samakhya and NGOs were involved in its
implementation. This should be evaluated, improved upon and implemented in all districts, especially
Northern districts with poor HDL
4. Health Education:
20
Health Education for the community, especially women, adolescents, the poor and the mai^inalized
will form part of the empowerment process to help them make informed choices in issues relating to
their health. It will have to be addressed as a long-term, separate, planned activity.
Aggressive health education programmes should be integrated with health and medical care
programmes, with emphasis on;
Environmental health
Personal hygiene
Nutrition education
Healthy habits.
21
515
Section on Underdevelopment and Health
THE UNTOLD STORY:
HOW THE HEALTH CARE SYSTEMS IN
DEVELOPING COUNTRIES CONTRIBUTE
TO MATERNAL MORTALITY
T. K. Sundari
This article attempts to put together evidence from maternal mortality studies in
developing countries of how an inadequate health care system characterized by
misplaced priorities contributes to high maternal mortality rates. Inaccessibility of
essential health information to the women most affected, and the physical as well as
economic and sociocultural distance separating health services from the vast
majority of women, are only part of the problem. Even when the woman reaches a
health facility, there are a number of obstacles to her receiving adequate and
appropriate care. These arc a result of failures in the health services delivery system:
the lack of minimal life-saving equipment at the first referral level; the lack of
equipment, personnel, and know-how even in referral hospitals; and worst of all,
faulty patient management. Prevention of maternal deaths requires fundamental
changes not only in resource allocation, but in the very structures of health services
delivery. These will have to be fought for as part of a wider struggle for equity and
social justice.
The high maternal mortality rales in most of the developing countries, despite
advances in health care, have prompted several studies analyzing the main causes of
maternal death and groups at risk, so that medical care can be appropriately directed.
However, the role of the health services system itself, both in preventing a woman with
a complication in pregnancy or delivery from seeking medical help and in providing a
woman who reaches a medical facility with appropriate care, has rarely been looked
into. Of the several links in the chain of events that culminate in a maternal death, the
role of an inadequate health care system characterized by misplaced priorities seems to
be vital. This article attempts to put together evidence to this effect, using data from
maternal mortality studies in several developing countries.
It is common practice for hospital-based studies on maternal mortality to look into
“avoidable factors”: factors that, if avoided, could have prevented the maternal death. In
a number of cases, the researchers state explicitly that the avoidability of deaths was
evaluated by standards realistic under the circumstances prevailing in that country at
that lime. The discussions in this article arc based on such accounts.
international Journal of Health Services, Volume 22, Number 3, Pages 513-528. 1992
© 1992, Bay wood Publishing Co., Inc.
513
zed
me
rth
sal
ng
he
ho
an
a
-')•
gjs
,s*
th
as
te
et
ar
id
:n
)r
g
1
n
it
e
y
Health Care Systems and Maternal Deaths / 515
514 / Sundari
Delayed Arrival or Nonarrival at a Health Facility
“PATIENT FACTORS,” OR INACCESSIBLE
HEALTH SERVICES?
One of (he standard categories into which avoidable factors arc classified is what
are known as “patient factors." Patient factors, as the name suggests, arc deemed
faulty action on the part of the patient, for which the health care system is not respon
sible and about which it is helpless to do anything. Table 1 gives an overview of
the proportion of maternal deaths attributed to various patient factors in different
studies (1-8).
Tabic 1
Maternal deaths with “patient factor" as an avoidable factor
in selected developing countries
Country: hospital/rcgion
(reference no.)
Factor
____________
No. of all
maternal
deaths (%)
Years
19781981
Malaysia: all
government health
facilities
in Krian district (1)
Refusal to go to hospital
Handled by traditional birth attendant
and relatives; delayed medical aid
Handled by traditional birth attendant
alone; no medical aid
95 (10%)
182 (20%)
Vietnam:
22 institutions (2)
Patient not presented
Patient noncompliancc
22(17%)
13(10%).
19841985
Pakistan: Civil
Hospital, Karachi (3)
Patient’s or relations’ attitude
Deficient management by traditional
birth attendants
85 (67%)
11(9%)
19791983
Malawi: Kamuzu
Central Hospital,
Lilongwe (4)
Patient delay
29 (48%)
1985
Tanzania: Muhimbili
Medical Center,
Dar-es-Salaam (5)
Delay in arrival
Interference with pregnancy
11(7%)
2(1%)
1983
India: 41 teaching
institutions (6)
Delay by patient or relatives
2.109 (45%)
19781981
India: Anantapur
district (7)
Lack of early and adequate antenatal
care
Termination of pregnancy by
unqualified personnel
18 (8%)
19841985
Zimbabwe: Harare
Maternity Hospital,
Harare (8)
Late presentation
Refusal of treatment
Unbooked
8 (16%)
2 (4%)
5 (10%)
________ _
164(18%)
18(8%)
1983
Of the various patient factors identified in studies, patients' nonarrival and delayed
arrival at a medical facility feature prominently. It is also mentioned in some
cases that the patient’s and her relatives’ attitudes were incorrect, leading to a
preference to deliver at home with the help of relatives and/or traditional birth
attendants, rather than go to a hospital or health center. Instances of the patient’s refusal
of treatment arc also mentioned. (Delays due to distance and transportation problems
arc discussed later.)
There may be a number of reasons why women do not seek medical care during
pregnancy and delivery. The first of these is probably a lack of awareness of ftc
seriousness of the problem. <t Anantapur, India, when family members of women who
died were asked if they were aware of the seriousness of the problem, more than
one-fifth indicated that they did not comprehend the seriousness of the patient’s condi
tion. Of those who knew about the seriousness, the great majority took steps to call a
health worker/doclor or to move the patient to a hospital (7). Studies of maternal deaths
in the Tangail and Jamalpur districts of Bangladesh indicate that women who developed
complications during pregnancy more often received medical help prior to death than
women who developed complications during labor and delivery or post partum (9,10).
These studies indicate that the seriousness of complications encountered during preg
nancy, and of specific complications such as toxemia that lead to convulsions, is
probably more apparent than the seriousness of prolonged labor or postpartum sepsis.
This illustrates the failure of the health care system to reach out to the population with
important health messages. If women knew how to identify danger signals that calFfotf
immediate medical attention, a large majority of them would certainly attempt to rcactf
a health facility, f
Poorer and higher parity women remain uncovered by medical services, whereas
relatively well-off and lower parity women who arc not at any special risk benefit the
most (11). Poorer women and women with large families may find it difficult to get
away from work at home and on the farms, often at the cost of their lives. In Zaire, for
example, 13 of 20 maternal deaths occurred during the first five months of planting and
harvest, seasons when the need for women’s work in the field can make women
reluctant to go to the hospital (12). Lack of available money is. of course, a majol
deterrent!®!! seeking medical help. That economic factors arc an important intervening
variable in access to health care is evident from a study in Oran, Algeria, between 1971
and 1980 (13). The maternal mortality rate plunged from 157/100,000 live births in
1971-1975 to 91/100,000 in 1976-1980. One of the reasons for this decline was that
after 1974-1975, when fees for medical services were waived in public hospitals, the
number of unassisted home deliveries was greatly reduced.
There may be a number of other reasons why women prefer home deHwry^^t^d_by
a traditional birth allendant or relatives. These include the unfamiliar setting al the '
health facilit^whcrc the woman would be attended to by strangers, in the absence of her
family and friends and the physical and moral support they offer; Impossibility of being
attended to by male doctors, unacceptable in sonic cultures; the nonlolcrance by hospital
staff of cultural practices related to childbirth, sucIPas consump'tion’of special foods and
practice of certain rituals-;'the total lack of sympathy and understanding on the part of
Health Care Systems and Maternal Deaths / 517
516 / Sundari
health personneljf and not least, the belief that childbirth docs not need medical inter
ference. All of these reasons arc valid and cannot be ignored or disclaimed.
Failure to Seek Legal Abortion, or Interference with Pregnancy
Another patient factor often mentioned is the failure to seek a legal abortion, or
interference with pregnancy. A detailed discussion of the complex issues surrounding
why women do not seek legal abortions, or why they interfere with their pregnancies
instead of preventing a pregnancy, is beyond the scope of this article. Some of the
underlying reasons may be similar to those that explain why women do not seek medical
help during childbirth: not knowing that abortions can be legally obtained, lack of
information about where such services arc available, and lack of resources._Thcrc are,
however, many essential differences arising from laws that severely restrict abortions in
several countries, and the social, cultural, and religious pressures against seeking an
abortion where it may be available. In addition, the degree of privacy afforded by a
traditional abortionist may be a factor. The least that can be said is that “failure to seek
a legal abortion" cannot be classified neatly as a patient factor for which the woman
alone is responsible.
Whatever the reasons for a woman’s not going to a medical facility for pregnancyrelated problems, the consequences arc serious enough to warrant corrective action. To
give an example from Kenya, several women who died of maternal causes in the
Kenyatta National Hospital between 1972 and 1978 arrived in a poor condition after
futile management had been attempted at home for many days (14). This was especially
true of women who had illegal abortions. Most of those who died of puerperal sepsis had
delivered at home. One patient who had delivered at home with the assistance of a
midwife had been treated for nearly a week before she was admitted to the hospital. In
Togo, again, women referred to the Centre Hopitalicrc Universitaire de Lome during
1977 included many with uterine rupture that had occurred several days earlier at home
and had not been detected (15).
Nonuse ofAntenatal Care
The next most important patient factor mentioned in studies is the nonuse of antenatal
care by pregnant women. This is disturbing given the overwhelming evidence that the
lack of antenatal care increases the risk of maternal death.
make several antenatal visits spread over the gestation period, so that complications that
arise at different stages may be identified and followed up. In Zaire (1981-1983) the
maternal mortality rale was 250/1 (X),000 live births for those who had made four or
more antenatal visits, 270/100,000 for those who had made between one and three visits,
and a very high 3,770/100,000 for those who had no antenatal care at ail (12). Similarly,
in a study of three hospitals in Senegal, 20 percent of the women who died had no
antenatal care, compared with only 2 percent in the control group; and only 40 percent
of them had made three or more visits, compared with 75 percent in the control group (19).
The ease for early and adequate antenatal care is clear. The obstacles to use of
antenatal care need Io be investigated. There arc some clues to the possible reasons for
nonuse in these same studies. A community study from Ethiopia found that just as in the
ease of institutional delivery, it is the better-off and lower parity women who use
antenatal care adequately (11). Use of antenatal care decreased with increasing parity,
both in hospitals and in the Maternal and Child Health clinics. The extent of nonattendancc among the high-risk women who were currently para 5 to para 8 was 35 percent,
and that for women who were now para 8+ was 44 percent. Sixty percent of those who
did not receive antenatal care had unwanted pregnancies. Women with unwanted
pregnancies who did receive antenatal care tended to visit Maternal and Child Health
clinics, which were free of cost.
The failure of higher parity women to seek antenatal care may not only result from
lack of time and money. They may feel it is unnecessary to seek antenatal care,
especially if their earlier pregnancies were problem-free. In the case of unwanted
pregnancies out-of-wedlock, hesitation to seek antenatal care is understandable. As for
high parity women with unwanted pregnancies, the very reasons for which the preg
nancy was unwanted may also impose constraints in seeking antenatal care. The women
may also not feel motivated for self-care.
The deficient quality of antenatal care may be another major deterrent. A study of
Primary Health Centers in India found that women attending antenatal screening were
not screened either for anemia or for high blood pressure or proteinuria to detect the
risk of eclampsia (20). This can be a cosily shortcoming, as judged from a study in
Mozambique: more than 80 percent of the women who died had attended antenatal
clinics, and yet there were deaths from preventable causes such as anemia and eclampsia
(21, 22). Poor quality of antenatal screening and the indifferent attitude of health
personnel in health facilities can destroy women’s faith in the usefulness of antenatal
care. Darc we blame the women if they decide that it is not worth expending their scarce
According to the famous Zaria maternity survey that monitored 22,725 deliveries
in Ahmado Bello University Hospital in Nigeria, antenatal care was associated with
resources on what may be a futile exercise?
a reduction in maternal mortality in all age-parity groups (16). In American University
of Beirut Medical Centre, Lebanon, the maternal mortality rale for those who had
antenatal care was 19/100.000, whereas the rate for those without antenatal care was
197/100,000 (17). In Vietnam, only 34 percent of women who died had attended
Transportation Problems
antenatal clinics, compared with 74 percent in the control group, a statistically signifi
cant difference (2).
ambulances or other means of transportation to health facilities, and inadequate means
of transporting emergency cases from peripheral to referral hospitals make the essential
difference between life and death in most developing countries. In a heart-rending and
extreme cxampl^rpm a Tanzanian study, a rural woman had to walk 70 kilometers after
the onset of lab^^ reach a hospital, only to collapse on arrival (23).
Early antenatal care is important. In Thailand, mothers who started antenatal care in
their first and second trimesters of pregnancy had lower maternaljnortalily rates than
those who did not start antenatal care until the third trimester (18).^® also necessary to
In many instances, the late arrival of a patient at a hospital, usually classified as a
patient factor, is the result of lack of transportation methods. Poor roads, lack of
Health Care Systems and Maternal Deaths / 51
518 / Sundari
Late arrivals and referrals account for a disproportionately large number of maternal
deaths in hospitals. The following examples illustrate the magnitude of the problem:
• In Centre HGpitalicre Univcrsitairc de Cocody, Abidjan, Ivory Coast, in 1986, the
maternal mortality rate was 2,000/100,000 deliveries for those who had been transferred
from within the urban zone, 3,000/100,000 for those who had been transferred from the
suburban area, and 6,000/100,000 for those who had been transferred from rural
areas (24).
• In the Maternity Hospital, Katmandu, Nepal, 40 percent of the women who died
arrived in a very poor condition; 17 percent were unconscious. Forty-five of the 81
deaths (56 percent) occurred within the first day, 38 of them within the first eight
hours (25).
• In an Aden Hospital, 73 percent of deaths were of women from rural areas who had
to travel a long way. Ten percent of the women who died were dead on arrival, and
another 15 percent died within an hour of arrival (26).
• In Zaire, all but two (90 percent) of the women who died were admitted in a critical
condition. The most common complication was prolonged labor (greater than 18 hours)
due to fclo-pelvic disproportion or malprcscntation. Sixteen of the 20 women who died
had been in labor for more than 18 hours, and nine of these had been in labor for 48
hours. The risk of death was more than 400 times greater for those who had been in labor
for more than 48 hours than for those who had labored 12 hours or less. Prolonged labor
resulted in a ruptured uterus in 14 eases, which increased the risk of death more than
100-fold (12).
• In Togo, women referred to Centre Hopitalicrc Univcrsitairc de Lome during 1977
included cases of uterine rupture that had occurred several days earlier (15).
• In a study of 48 hospitals throughout Tanzania in 1986, 63 percent of the 247
women who died had to travel more than 10 kilometers to the hospital where they
eventually died. Of these, 37 percent lived more than 30 kilometers away (27).
• In Krian district, Malaysia, 73 deaths (8 percent) were due to poor transportation
methods, and a further seven deaths occurred cn route from one hospital to another (1).
When the hospital is far away, not only the distance but also the mode of transport
becomes an important determinant of how soon medical help becomes available and,
consequently, of survival chances. In Anantapur, India (1984-1985), 41 percent of all
maternal deaths occurred at home, and 9 percent en route to a hospital. Of 140 women
who were taken to hospital in a serious condition, 96 (69 percent) were transported by
' public bus. 27 (19 percent) by bullock carts, five (3 percent) by manually drawn
rickshaws, and only 12 (9 percent) by motor-driven vehicle or by ambulance. Twentyfour women died on the way to hospital, and another 54 died immediately on arrival (7).
These problems arc accentuated when the cause of death is a difficult-to-anticipatc
complication such as postpartum hemorrhage. In Gambia, where an extremely high
maternal mortality rate has been recorded (2,360/100,000 live births), 11 of a total of 15
deaths occurred within four hours after deliver and were associated with hemorrhage or
sudden collapse; there were no resuscitation facilities at the nearest dispensary, and the
government hospital al Banjul was several hours’ journey away, including a ferry
crossing of the river Gambia (28).
Weather conditions may also affect the possibility for rapid transportation to hospita
A study covering three hospitals in Senegal found that maternal deaths from hemorrhaj
and uterine rupture occurred 1.7 times and 3.5 times more frequently in the four w<
months between July and October, and suggested that this is probably because of tl
way rain paralyzes transportation on mud roads and foot paths through which paticn
have to be transported (19).
All of the patient factors discussed above are a consequence not only of geograph:
inaccessibility but of the social, cultural, and economic inaccessibility of health service
to pregnant women. Could we not consider attributing responsibility for these factors t
the patient a ease of “victim blaming”?
FAILURES IN THE HEALTH SERVICES DELIVERY SYSTEM
When other obstacles arc overcome and women with a complication in pregnancy c
childbirth finally reach a health facility, there may be yet other problems that jeopardiz
their chances of survival. Personnel and equipment arc scarce, and health facilities ar
often unable to cope even with the small proportion of affected women who arrive. Th
quality of care is far from satisfactory, and may be summed up as “doing too little, fo
late.” Table 2 shows the proportion of maternal deaths attributed to various “hcalt
service factors” in different studies (2, 6, 8, 29, 30).
Shortage of Trained Personnel
Many countries have a shortage of trained personnel not only at the specialist level
but all down the ladder to the midwife. An extreme example is that of Gabon, whetthere is a shortage of trained obstctricians-gynecologists: six of the nine provinces c
Gabon do not have the services of a specialist obstetrician. In addition, health center
and even provincial hospitals do not have 24-hour services (31).
Even where the situation is not quite so bad, understaffing of health facilities is ;
common problem. In Malawi, at Kamuzu Central Hospital, Lilongwe, medical staf
were at times required to be at the Central Hospital and the Old Wind Maternity three
kilometers away at the same time, and this alone had contributed to maternal death it
some cases (4).
Another problem is that staff have inadequate or inappropriate training and canno
cope with obstetrical emergencies. Cameroon is a unique ease in point. A hospital studv
in Yaounde found that the incidence of deaths from ruptured uterus was high not only
because of the poor standards of midwives in rural hospitals, but because specialists in
referral hospitals were trained abroad and could not handle eases of uterine rupture (32)
Health personnel interviewed in a 48-hospital study in Tanzania stated that, in theii
opinion, the following were among factors contributing to high maternal mortality (27)
• Scarcity of medical and paramedical personnel, especially in rural areas;
• Poor on-the-job training of health staff at all levels;
• Low salaries, poor working conditions, etc., for health workers, leading to lack ot
motivation.
Health Care Systems and Maternal Deaths / 521
520 / Sundari
Maternal deaths with “poor patient management in hospital" as an avoidable factor,
selected developing countries
Country: hospilal/rcgion
(reference no.)
Factors
No. of all
maternal
deaths (%)
Years
Vietnam: 22 institutions
(2)
Delay in diagnosis
Wrong diagnosis
Delay in treatment
Wrong treatment
Delay in referral
Inappropriate referral
68 (53%)
28 (22%)
80 (63%)
47 (37%)
77 (60%)
1 (8%)
19841985
Malawi: Health centers
and referral hospitals
in Central Region (29)
Medical staff factors
Nursing staff factors (includes
failure to diagnose, failure to
initiate appropriate treatment,
delay in referral)
30 (28%)
26 (24%)
1977
Zimbabwe: Harare
Maternity I lospital,
Harare (8)
Failure to diagnose/delay in
diagnosis
Failure to operate/ delay in
operation
Failure to give appropriate
treatment
Poor operative technique
Overtransfusion
Anesthetic problem
4(8%)
1983
South Africa: 267
hospitals throughout
the country (30)
Delay in diagnosis
Delay in consultation or transfer
Judgment errors in diagnosis
Treatment given “loo little,
too late”
Surgical and anesthetic problems
11(1%)
25 (3%)
11 (1%)
87 (11%)
India: 41 teaching
institutions (6)
Defective obstetric care
5 (10%)
2 (4%)
2(4%)
2(4%)
1 (2%)
19801982
24 (3%)
1,525(32%)
19781981
The unsatisfactory working conditions of lower-level health workers often lend to be
overlooked, but may be a key cause of the scarcity of health personnel so vital to the
improvement of coverage of maternal health services.
Lack of Equipment and Facilities
The absence of a blood bank or of facilities for transfusion can be one of the most
catastrophic inadequacies in a health facility, and^xl is one of the most frequently
encountered. A paticnl with hemorrhage may not s^^/e to reach the referral hospital.
In Gabon, a study from Centre HSpilalicrc de Libreville mentions that patients suffering
from hemorrhage often were kept waiting until a donor with a matching blood group
was found, before operative intervention (31). In some studies showing a high incidence
of deaths from hemorrhage, absence of a blood bank was often a contributing factor.
For example in Vietnam, where 48 percent of maternal deaths in selected hospitals
during 1984-1985 were from hemorrhage, lack of blood led to deaths in 46 eases
(36 percent) (2). In Kenyatta National Hospital, Kenya, no blood was available for a
patient admitted in a highly anemic condition due to postpartum hemorrhage, until she
died a day later (33).
Lack of other facilities and equipment is mentioned in many other studies. For
example, the study of L’hflpital Arstridc le Dantcc, L’hopilal Principal, and Centre
Abbas Ndao in Senegal (1986-1987) found that 70 percent of the 152 maternal deaths
were attributable to lack of equipment and facilities (19).
In the hospital at Libreville, Gabon, mentioned above (31), there was overcrowding,
with a bed occupancy rate of 130 percent. Supplies of drugs were inadequate, and
treatment was delayed until the patient’s family bought the drugs from a pharmacy.
There were even inordinate delays in transferring the patient to the operative block. In
Vietnam, lack of drugs was responsible for 26 deaths (20 percent), and lack of other
equipment for 14 deaths (11 percent) (2).
The study of maternal deaths in Kenyatta National Hospital also mentions over
crowding; patients often had to share beds and mattresses, leaving them vulnerable
to cross-infection within the hospital. There was not enough clean linen, and
even basic equipment such as gloves and antiseptic solution fell short of require
ment (33). The lack of basic equipment in conjunction with overcrowding and
the scarcity of trained personnel has led to an increase in in-hospital sepsis
rates. Sepsis deaths increased from 8 percent of maternal deaths in 1953-1960 to
17 percent in 1961-1971, and stood at 12 percent in 1975-1982 in a hospital
study from Durban, South Africa; during this period the maternal mortality rales
also rose (34, 35). The reasons for this increase were overcrowding and nonadherence
to aseptic and antiseptic principles when doing vaginal examinations, among other
things. In Sudan, deaths from puerperal sepsis in the Khartoum Teaching Hospital,
Khartoum, increased from 10 percent of all maternal deaths in 1968-1972 to as high
as 32 percent in 1978-1982 (36). And in Venezuela, a study in Concepcion Palacios
maternity hospital, Caracas, covering the period 1939-1974, found that while (he
maternal mortality rate declined from 196/100,000 live births in 1939-1963 to
125/100,000 in 1964-1972, it subsequently rose to 144/100,000, owing to an alarming
increase in post-cesarian section and puerperal sepsis deaths during the last ten years of
the study (37).
Lack of equipment is a more acute problem in most peripheral hospitals; the
Kenyan study found that of 92 women referred to Kenyatta National Hospital from
peripheral hospitals, in 43 eases the anesthetist or the medical officcr-in-charge was
not available. In 19 of these eases the hospital had no facility for operative delivery,
in 21 no blood was available, and in nine eases the hospital had no water or electricity.
An added problem was that the hospital admitted high-risk patients when it had
no facilities Io tackle the problem, or had diagnosed the problem loo late, delaying
522 / Sundan
Poor Patient Management
Inappropriate action by health staff in treating patients has been identified in several
studies as a factor contributing to maternal deaths.
Delay in diagnosis and treatment and inadequate treatment arc often responsible for
maternal deaths. There seem to be inordinate delays in initiating treatment even when
the patient’s condition is critical, for reasons quite apart from lack of equipment and
facilities. Crucial decisions arc delayed, and not infrequently, wrong decisions arc made.
Standard procedures for patient management arc often absent, which makes it difficult
for nursing staff and junior doctors to take appropriate action in emergency eases. Also,
decision-making and initiation of sophisticated procedures in hospital settings arc fre
quently concentrated in a small number of senior doctors and specialists, while other
members of staff arc restricted to carrying out instructions.
A study of Kenyatta National Hospital illustrates some eases of poor patient
management. Lack of proper investigations of the etiological causes of infection led
to an inappropriate choice of drugs and nonresponse of the microorganism to
therapy. Decisions for operative interventions were at times taken loo late, and the
operations were entrusted to junior doctors. In one instance, a woman admitted
for sepsis following abortion had to undergo one colpotomy and two laparotomies
within a space of 10 days because the pelvic abscess was not properly drained
in the first two procedures. Another instance of patient mismanagement in the
same hospital was of two women with ruptured ectopic pregnancies who virtually
lost their entire blood volume before they received laparotomy because cross-matching
of blood, for transfusion was inordinately delayed. Both women died following
laparotomy (33).
In another study from the maternity and children’s hospital in Saudi Arabia (19781980), mismatched blood transfusions were a factor in two of 29 deaths, one from
hemorrhage and one from septic abortion (38). Delays in decision-making by the health
personnel occurred in two instances: in a ease of uncontrollable hemorrhage during
cesarean section and in a patient with antepartum hemorrhage, in which ease there was
delay in deciding about definitive surgery. In another instance the avoidable factor was
clinical, namely, combining major surgery with cesarean section in a peripheral hospital
with limited facilities. Delay in decision-making and failure to initiate prompt intensive
care were responsible for several first-hour deaths in R.M.C. Hospital, Imphal, India
(39). In five eases, immediate surgical interventions by experienced obstetricians could
have prevented death.
A confidential inquiry into all maternal deaths in Jamaica between 1981 and
1983 gives a very useful analysis of avoidable patient management factors with respect
to three major causes of maternal death: hemorrhage, sepsis, and eclampsia (40).
According to this inquiry, some of the factors contributing to deaths from hemor
rhage were:
• Delays in midwives’ appreciating the extent of blood loss and contacting a doctor;
• Delays in starting and inadequate resuscitative procedures for blood loss, partly due to
unavailability of blood or plasma in many of the smaller hospitals:
Health Care Systems and Maternal Deaths / 523
* Delays in manual removal of the placenta in patients with retained placenta, or
attempting this procedure without the necessary preliminary establishment of a
reliable intravenous infusion;
• Inadequate use of ergometrine.
In the ease of deaths from sepsis the avoidable factors were:
• Inadequate surveillance of body temperature in women with a prolonged first stage of
labor, and post delivery;
• Not giving antibiotics to women with prolonged rupture of the membranes;
• Inadequate bacteriological investigations in women with puerperal pyrexia;
• Reluctance to use aggressive treatment with broad-spectrum antibiotics for women
with puerperal pyrexia.
Avoidable in-hospital factors that were responsible for deaths from eclampsia
included:
• Absence of relevant information on antenatal surveillance symptoms and signs
(c.g., weight gain, blood pressure readings) at the time of admission to hospital;
• Inadequate monitoring of patient's blood pressure and urine, particularly on admission
and immediately following delivery;
• Delay by hospital staff in initiating appropriate treatment when signs of preeclamptic
toxemia were found or the patient had convulsions, the delay being due to lack of
coordination among various levels of staff;
• Lack of a clear-cut clinical-therapeutic strategy for dealing with patients with
eclampsia.
Problems related to operative techniques and administration of anesthesia also claim
a large number of maternal lives, and routinely appear as a cause of death in most
hospital studies of maternal mortality. One of the highest rates for maternal deaths from
complications of anesthesia has been reported from Ivory Coast (110 deaths/100,000
live births) (41), and high rates of death associated with cesarean sections have been
reported from Egypt (222/100,000 live births) (42) and Malawi (142/100,000 live
births) (4).
A good proportion of deaths related to complications of cesarean section and anes
thesia may in fact be related to the poor condition of the patient prior to the operation.
Surgical procedures arc often undertaken on emergency admissions as a last recourse,
with the knowledge that survival chances arc limited. However, the sharp increase in
post-cesarean section sepsis in instances such as in Caracas, mentioned above (38),
point to faulty in-hospital procedures. In Cuba, again, cesarean delivery was identified
as a risk factor associated with maternal death in a study covering the period 1980-1984
(43). Forty-one of the 54 eases of death from sepsis during that period followed a
cesarian section, and 13 deaths from complications of anesthesia were also simul
taneously associated with cesarean section. In another example from Sudan, a study of
all cesarean sections carried out in the Khartoum hospital between 1978 and 1982 found
Health Care Systems and Maternal Deaths / 5
524 / Sundari
that of 24 maternal deaths following cesarean section (of a total of 140 maternal deaths),
only six could be attributed to underlying causes (36).
Clearly, the performance of medical systems in saving maternal lives entrusted to
them is far from satisfactory. This is unfortunate, considering the difficulties that women
must overcome in order to reach a referral facility. They have to leave their families
behind, expend a great deal of money in finding a quick means of transportation, and
find a suitable person to accompany them. The person accompanying has to find the
means and money to stay in a strange town or city during the period of the patient’s
treatment. And if the patient should die, quite apart from the fact that it would greatly
distress her to be away from family and friends in her last hours, transporting the body
back home would prove both difficult and expensive.
We hope that the existence of a number of studies looking into avoidable in-hospital
factors in maternal deaths demonstrates a commitment to effecting the required changes
wherever possible.
CONCLUSIONS
The prevention of maternal deaths requires far-reaching social and economic changes
beyond the confines of the health care system. The factors that make the natural
processes of pregnancy and childbirth highly risky and even fatal for poorer women arc
structural; so arc the factors that influence the value women place on their personal
well-being, and those that influence their ability to seek health care for themselves. The
last depends crucially on resources such as time, money, and information that women
have at their disposal, and whether they have the authority for decision-making.
However, this does not absolve the health care system of its responsibility to make
fundamental changes in both the structure and the delivery of health services. From the
discussions in this article, certain areas stand out as priorities for action. These arc
presented not as policy recommendations to the medical status quo—whose priorities
are, more often than not, determined by the interests of those in power and by their own
professional interests—but rather as a proposal for action by health activists.
CThc starting point of an agenda for action would be to call for a drastic reallocation of
national resources with a larger share for the health sector, and a substantial allocation
within the health budget for the health care of women, of which maternal health care is
one component. The health expenditure of a vast majority of countries falls short of 5
percent of gross national product. Less than half of this is allocated to “primary health
care” (a term that has come to be used to define all health care below the secondary and
referral levels, as opposed to the principle enunciated in the Alma-Ata Declaration). A
minuscule amount of this allocation is spent on maternal and child health care, in which
child health and family planning get the lion’s share of the resources compared with
f. maternal health. And although it is well known that maternal health cannot be improved
without improvement of women’s health in general, as far as the health care system is
concerned women count only as mothers and have no existence prior to or after a
pregnancy and delivery. Also, the disproportionately large share of resources allocated
to family planning programs (often a cuphcmisn^or population control programs), at
the cost of other aspects of maternal health carc.^J in no way be justified.
Appropriate reallocation of resources for women’s health care would have to beg
with strengthening health services at the community level. Women who arc in greate
need of health care, and who run the greatest risk of maternal death, have the lea
resources to seek medical help. They can only be reached if services are available do
to home, and ideally at their very doorsteps. What is needed is the deployment ■
thousands of community health workers who arc also equipped for maternal health car
Training traditional birth attendants and local women to provide domiciliary care
perhaps one of the best ways to invest resources. However, action in this direction h.
been disappointing. Far from being one of the cornerstones of the strategy for preventio
of maternal mortality and morbidity, it remains a low-priority activity, carried out in
sporadic and haphazard manner.
The next step in appropriate resource allocation would be to equip the first referr.
levels with the necessary supplies, equipment, and personnel. The World Healt
Organization guidelines on essential obstetric functions at the first referral level identif
eight groups of functions that should be available at a health facility catering to
population of 100,000. Among these arc surgical functions such as performing ccsarca
sections, surgical treatment of severe sepsis, and laparotomy for treatment of utcrin
rupture; anesthetic functions; and blood-replacement functions. This would bring abou
an estimated 5 percent reduction in the number of maternal deaths (44).
Shortage of (rained personnel is often cited as a major barrier to upgrading firs
referral facilities. This is usually the result of the strict hierarchy in the division of labo
among health personnel, and inflexible notions held by doctors regarding the cthica
propriety of entrusting complicated interventions to lower level staff. The Centrt
Medical Evangelique’s Nyakunde, Aba, and Aru hospitals in the Upper Zaire regior
have successfully overcome such barriers. Here, nurse practitioner surgeons deliver al
types of labor, normal or complicated. A study of their performance has shown that thi
outcome of complicated labor in the hands of the nurse practitioner surgeons is com
parable to the outcome of such-cases in the hands of physicians (45). Training nursing
and midwifery staff to deal with complicated deliveries is clearly a viable option
but may not be welcome to the medical establishment, which would resent such ar
encroachment on its territory.
There have been a number of such creative interventions aimed at better utilization ol
scarce resources for maternal health care. In Ekedwani hospital, Malawi, for example.
an antenatal waiting shelter was opened for “high-risk” women, to deal with the problem
of distances and transport. This greatly reduced the maternal mortality rate, obstetric
emergencies having become a thing of the past (46).
The second major area for action is improving the quality of care in health facilities.
This involves more than ensuring the availability of equipment and supplies and trained
personnel; it also entails making the health services more socially accountable. There
should be careful record-keeping, and records should be accessible Io the public. Even-
maternal death and every complicated delivery should be carefully scrutinized. Prevent
ing the recurrence of an “avoidable factor" should be a medical priority. Inappropriate
organizational and managerial procedures that cause inordinate delays in instituting care
must be challenged: it is not unusual for a patient to be kept wailing while paperwork is
being^^nplctcd or because the person authorized for decision-making is not present.
Morc^portantly, seeking health care should cease to be the dehumanizing experience
Health Care Systems and Maternal Deaths / 527
526 / Sundari
it now is, devoid of respect and consideration or even compassion on the part of health
personnel.
The third and perhaps most urgent area for action is to assist and equip those most
affected by the problem of high maternal mortality—women (and men) from the
most deprived sections of society—to actively participate in demanding the changes
outlined above.
The existing state of affairs in the health care system that contributes to high maternal
mortality is not the consequence of mere inept planning or poor organizational and
managerial capabilities. It is a reflection of the priorities set by an elitist system in which
the poor and powerless do not count. We do not expect the demands made in these pages
to be handed down from above. They have to be fought for, as part of a much wider
struggle for equity and social justice.
REFERENCES1
Karim. R. Overview of Maternal Mortality in Malaysia and the Application of the Risk
Approach Strategy in Maternal Health. Paper presented al the Seminar on Maternal Health,
Kemcnlcrian Kesthatan, Malaysia, 1982.
2.
Vietnam, Institute for the Protection of Mother and Newborn. Maternal Mortality in
Selected Areas of Vietnam. Paper presented at the Interregional Meeting on the Prevention
of Maternal Mortality, Geneva, November 11-15, 1985. Unpublished WHO document no.
FHE/PMM/85.9.8.
3.
Ahmad, Z. Maternal mortality in an obstetric unit. J. Pakistan Med. Assoc. 35: 243-248,
1.
4.
1985.
Keller, M. E. Maternal mortality at Kamuzu Central Hospital for 1985. Med. Q. (Malawi) 4:
13-16. 1987.
Justensen, A. An analysis of maternal mortality in Muhimbili Medical Centre, Dar cs Salaam,
July 1983 to June 1984. J. Obstet. Gynaecol. East Central Afr. 4: 5-8, 1985.
6.
Bhasker Rao, K. Report on the Maternal Mortality Committee of the FOGSl, 1978-1981.
Federation of Obstetricians ’ and Gynecologists ’ Societies of India, New Delhi, 1984.
7.
Bhatia, J. C. A Study of Maternal Mortality in Anantapur District, Andhra Pradesh, India.
Indian Institute of Management, Bangalore, 1986.
8.
Crowther, C. A. Maternal deaths at the Harare Maternity Hospital during 1983. South Afr.
5.
9.
Med. J. 69: 180-182, 1986.
Alauddin, M. Maternal mortality in rural Bangladesh: The Tangail District. Stud. Fam. Plann.
10.
17: 13-21, 1986.
Khan, A. R., et al. Maternal mortality in rural Bangladesh: The Jamalpur district. Stud. Fam.
Plann. 17: 7-12, 1986.
11.
Kwast, B. E., cl al. Report on Maternal Health in Addis Ababa. Swedish Save the Children
,
Federation, Addis Ababa, 1984.
12.
Smith, J. B., et al. Hospital Deaths in a High Risk Obstetric Population: Karawa, Zaire.
Unpublished document. Family Health International, Durham, 1985.
13.
Gana, B., and Louadi, T. La mortalite maternelle en milieu hopitalier: le cas d’Oran.
Universite d’Oran, Institute de Sciences Sociales, Departement de Demographic, Oran,
14.
Algeria, 1982.
Makokha. A. E. Maternal mortality—Kenyatta National Hospital, 1972-1977. EastAfr. Med.
J. 57: 451-460. 1980.
The unpublished documents in this reference list were referred to from the data base and documentation
on maternal mortality maintained by the Division of Family Health. World Health Organization, Geneva,
Switzerland.
Vovor, M., and Hodonou. Togo. Paper presented at the WHO Regional Multidisciplinary
Consultative Meeting on Human Reproduction, Yaounde, December 4-7. 1978.
16.
Harrison, K. A. A Review of Maternal Mortality in Nigeria with Particular Reference to the
Situation in Zaria. Northern Nigeria 1976-79. Paper presented at the WHO Interregional
Meeting on Prevention of Maternal Mortality, Geneva, November 11-15, 1985. Unpublished
WHO document no. FHE/PMM/85.9.12.
17.
Mashini, I., el al. Maternal mortality in the American University of Beirut Medical Centre
(AUBMC). bit. J. Gynaecol. Obstet. 22: 275-279. 1984.
18.
Ratlanporn, P. 'Ihc Internal Factors Affecting Maternal Mortality. Thesis submitted to the
Mahidol University, Bangkok, 1980.
19.
Correa, P., et al. Rapport final de 1’ctudc sur la mortalite maternelle a Dakar, Senegal. Causes
et mcsurcs a prendre pour I’amcliorcr. Unpublished report. Dakar. Senegal, 1987.
20.
Indian Council for Medical Research. Evaluation of Quality of Family Welfare Services at
PHC Level—Report of34 PHCs. New Delhi, 1987.
21.
Songadc, F. Analisc dos casos de mortes matemas ocorridas nosprimeiros 7 mcscs de 1984.
Boletin Informative do Servico de Ginecologia Obstetrica. Hospital Central, Maputo.
February 1985.
22.
Songadc, F. Maternal Mortality al Maputo Central Hospital, Mozambique. Paper presented al
the FIGO Congress, Berlin, September 1985.
23.
Price, T. G. Preliminary reports on maternal deaths in the Southern I lighlands of Tanzania in
1984. J. Obstet. Gynaecol. East. CentralAfr. 3: 103-110, 1984.
24.
Berardi, J. C., et al. Evaluation du benefice de 1’installation d’unc structure obstetrico-chiurgicalc dcccntralisce en terme de reduction de la mortalite maternelle et des transferts en Cote
d’Ivoire. Unpublished paper, CHU de Cocody, Abidjan, Ivory Coast, 1987.
25.
Malta, D. S. Study of Causes of Maternal Mortality in Selected Hospitals in Nepal. Paper
presented at the Interregional Meeting on the Prevention of Maternal Mortality, Geneva.
November 11-15, 1985. Unpublished WHO document no. FHE/PMM/85.9.9.
26.
Ahmed Ali, A. A Review of Maternal Mortality at Abood Maternity Hospital. Aden from
1962-1986. Unpublished paper. Abood Maternity Hospital, Aden, Democratic Yemen. 1987.
27.
Murru, M. Hospital Maternal Mortality in Tanzania. Master’s Dissertation, Royal Tropical
Institute, Amsterdam, 1987.
28.
Greenwood, A., et al. A prospective study of pregnancy in a rural area of the Gambia, West
Africa. Bull.WHO 65: 635-644, 1987.
29.
Bullough, C. Analysis of maternal deaths in the Central Region of Malawi. East Afr. Med. J.
58: 25-36,1981.
30.
Boes, E. G. M. Maternal mortality in Southern Africa, 1980-82. South Afr. Med. J. 71:
158-161,1987.
31.
Nlomc-Nzc, R., et al. La mortalite maternelle au Centre Hopitalicre de Libreville, Gabon.
Unpublished paper. Libreville, Gabon, 1987.
32.
Lekc, R. J. Outcome of pregnancy and delivery al the Central Maternity, Central Hospital
Yaounde. Ann. Univ. Sei. Sante 4: 322-330, 1987.
33.
Aggarwal, V. P. Obstetric emergency referrals to the Kenvatta National Hospital. East Afr.
Med. J. ST. 144-149, 1980.
34.
Crichton, D., and Knobel, J. The principles of prevention of avoidable maternal death. South
Afr. Med. J. 47: 2205-2210, 1973.
35.
Melrose, S. B. Maternal deaths at King Edward VIII Hospital, Durban. South Afr. Med. J. 65:
161-165, 1984.
36.
Abbo, A. H. Preventable factors in maternal mortality in Khartoum Teachine Hospital. Arab
Med. J. 4( 11.12): 23-28. 1982.
37.
Aguero, O., cl al. Mortalidad matema en la matemidad Concepcion Palacios, 1939-1974.
Rev. Obstet. Ginecol. Venezuela 37: 361-366, 1977.
38.
Chatlopadhyay, S. K., cl al. Maternal mortality in Riyadh, Saudi Arabia. Br. J. Obstet.
Gynaecol. 90: 809-814, 1983.
39.
Devi, Y. L., and Singh, J. Maternal morbidity: A ten year study in R.M.C. Hospital. Imphal.
J. Obstet. Gynaecol. India, 37: 90-94, 1987.
15.
528 / Sundari
40.
Walker, G. J., cl al. Maternal Mortality m Jamaica. Paper presented at the Interregional
Meeting on the Prevention of Maternal Mortality, Geneva, November 11-15, 1985. Unpub
41.
42.
lished WHO document no. FHE/PMM/85.9.10.
Bohoussou, K. M., et al. La mortalite matcmcllc au cours de la parturition ct la post-partum
immediat. Etude hopitalicrc. Afr. Med. 25(239): 125-130, 1986.
Abdullah, S. A., et al. Maternal Mortality in Upper Egypt. Paper presented at the Interregional
Meeting on the Prevention of Maternal Morbidity, Geneva, November 11-15,1985. Unpub
WHO document no. FHE/PMM/85.9.18.
43. lished
Famot,
U. C. Maternal Mortality in Cuba. Paper presented at the Interregional Meeting on the
Prevention of Maternal Mortality, Geneva, November 11—15, 1985. Unpublished WHO
FHE/PMM/85.9.13.
44. document
Worldno.
Health
Organization. Essential Obstetric Functions at the First Referral Level. Report
of a Technical Working Group, Geneva, June 23-27, 1986. FHE/86.4. Geneva, 1986.
45.
Maroja, L. T. The Role of Medical Auxiliaries in Operative Obstetrics in Rural Zaire.
Master’s Dissertation, Institute of Child Health, University of London, London, 1984.
46.
Knowles, J. K. The Antenatal Waiting Shelter as an Important Factor in Reducing Maternal
Mortality. Unpublished paper. Ekedwani, Malawi, 1986.
Direct reprint requests to:
Dr. T. K. Sundari
Centre for Development Studies
SOWING THE SEEDS OF NEO-IMPERIALISM:
THE ROCKEFELLER FOUNDATION’S
YELLOW FEVER CAMPAIGN IN MEXICO
Armando Sol6rzano
The Rockefeller Foundation’s campaign against yellow fever in Mexico sought to
advance the economic and political interests of U.S. capitalism. The campaign was
implemented at a time of strong anti-American sentiments on the part of the Mexican
people. With no diplomatic relationships between Mexico and the United States, the
Rockefeller Foundation presented its campaign as an international commitment.
Thus, Foundation doctors became the most salient U.S. diplomats. At the same time
they made sure that the Mexican yellow fever would not spread to the United States
through the southern border. The by-products of the campaign went beyond the
political arena. Special techniques to combat the vectors allowed the Rockefeller
Foundation’s brigades to change the anti-American sentiments of the people. When
the campaign ended, the Foundation had already set in place the foundation for the
modern Mexican health care system. Benefits from the campaign also accrued to
President Obregon, who used the campaign to strengthen his position of power.
Mexican doctors adopting a pro-American attitude also allied with the Rockefeller
Foundation to gain reputation and power within the emerging Mexican State.
Prasanth Nagar Road, Ulloor
Trivandrum 695 011
Kerala
India
The Mexican health care system is clearly an extension of the U.S. model of mcdicint
(1-3). Was this the result of a benevolent flow of medical and technological assistance
from the United States, as some authors might claim (4, 5)? Or should the historica
process of the formation of the medical system in Mexico alert us to examine the broadci
influences of foreign medical programs in the social, political, and medical institutions';
The overwhelming ideology of philanthropic institutions and the rhetoric of inter
national medical cooperation compel the social analyst to question what is bchinc
altruistic intentions (6). The critical approach represented by the Political Economy ol
Health maintains that the introduction of medicine in less-developed societies sets in
motion very complex interactions affecting the productivity of (he local labor force
(7-9). Other transformations brought by medicine arc perceived in the political balance
of a country (10,11), in the institutions of medical education (12). and in the production
of a class-based delivery of health care services (13). The extensive involvement ot
medical philanthropy in Central and Latin America makes it necessary to analyze the
consequences of their public health and medical programs. It is not an exaggeration to
The Rockefeller Foundation funded the archival research for this article.
International Journal of Health Services, Volume 22, Number 3, Pages 529-554, 1992
© 1992, Baywood Publishing Co., Inc.
529
Soc. Sei. Med. Vol. 38. No. 8. pp. 1091—1110. I°°4 ,
Copyright
1994 Elsevier Science Lie [ZU
Printed in Great Britain. All nghls reserved " I
0277-95:
TOO FAR TO WALK: MATERNAL MORTALITY IN
CONTEXT
Sereen Thaddeus1 and Deborah Maine2
'The Center for Communication Programs, Johns Hopkins University, 111 Market Place. Suite 310,
Baltimore, MD 21202-4024, U.S.A, and 2Center for Population and Family Health, Columbia University.
60 Haven Avenue, New York, NY 10032, U.S.A.
Abstract—The Prevention of Maternal Mortality Program is a collaborative effort of Columbia
University's Center for Population and Family Health and multidisciplinary teams of researchers from
Ghana, Nigeria and Sierra Leone. Program goals include dissemination of information to those concerned
with preventing maternal deaths. This review, which presents findings from a broad body of research, is
part of that activity.
While there are numerous factors that contribute to maternal mortality, we focus on those that affect
the interval between the onset of obstetric complication and its outcome. If prompt, adequate treatment
is provided, the outcome will usually be satisfactory; therefore, the outcome is most adversely affected
by delayed treatment. We examine research on the factors that: (1) delay the decision to seek care; (2)
delay arrival al a health facility; and (3) delay the provision of adequate care.
The literature clearly indicates that while distance and cost are major obstacles in the decision to seek
care, the relationships are not simple. There is evidence that people often consider the quality of care more
important than cost. These three factors—distance, cost and quality—alone do not give a full understand
ing of decision-making process. Their salience as obstacles is ultimately defined by illness-related factors,
such as severity. Differential use of health services is also shaped by such variables as gender and
socioeconomic status.
Patients who make a timely decision to seek care can still experience delay, because the accessibility
of health services is an acute problem in the developing world. In rural areas, a woman with an obstetric
emergency may find the closest facility equipped only for basic treatments and education, and she may
have no way to reach a regional center where resources exist.
Finally, arriving at the facility may not lead to the immediate commencement of treatment. Shortages
of qualified staff, essential drugs and supplies, coupled with administrative delays and clinical mismanage
ment. become documentable contributors to maternal deaths.
Findings from the literature review are discussed in light of their implications for programs. Options
for health programs are offered and examples of efforts to reduce maternal deaths are presented, with an
emphasis on strategies to mobilize and adapt existing resources.
Key words—maternal mortality, obstetric complication, developing countries, health services utilization
INTRODUCTION
Every year about 500.000 women worldwide die
due to complications associated with pregnancy and
childbirth [1, p. 1], Unfortunately, maternal aspects
of Maternal Child Health have all too often been
relegated to secondary priority within the child sur
vival revolution [2], However, emerging information
and concern with this high rate of maternal mortality
precipitated the foundation of the Safe Motherhood
Initiative (SMI) and the Prevention of Maternal
Mortality Program (PMM) in 1987.
The Safe Motherhood Initiative (SMI) was for
mally launched at a conference held in Nairobi,
Kenya. It calls for concerted action at the local,
national and international levels to reduce the high
rates of maternal mortality and improve women's
health in the developing world [3]. SMI differs from
other health initiatives in that it focuses on the
well-being of women as an end in itself. The preven
tion of death of pregnant women is considered to be
the key objective, not because death adversely affects
children and other family members, but because the
women are intrinsically valuable.
Within SMI, there are proposals for a variety of
interventions. These include programs aimed at im
proving the health status of women who become
pregnant, at improving women’s access to health
services during pregnancy and at improving the qual
ity of medical care available to women who experi
ence complications during pregnancy and delivery.
There are several similarities between the problems
experienced by health planners and promoters within
SMI and those experienced by other health initiat
ives, including issues of distribution, utilization and
quality of services. PMM thought it worthwhile to see
what findings from research in related fields might be
applicable to the challenges faced by SMI. The PMM
Program is a collaborative effort of Columbia Uni
versity's Center for Population and Family Health
(CPFH) and multidisciplinary teams of African
researchers in Nigeria, Ghana and Sierra Leone.
1091
1092
Sereen Thaddeus and Deborah Mainz
Sponsored by the Carnegie Corporation of New
York and the John D. and Catherine T. MacArthur
Foundation, this partnership seeks to strengthen the
capabilities of African institutions in developing,
implementing and evaluating preventive programs.
Furthermore, an essential component of our program
is to disseminate information useful to researchers,
program planners and policy makers concerned with
preventing maternal deaths. This review is part of
that activity.
We conducted a multidisciplinary literature review
to gather information that can guide programmatic
effort in the prevention of maternal mortality.* In
reviewing a broader body of literature than that
dealing strictly with maternal mortality, we are view
ing maternal mortality as an instance of a generic
problem. Our aim in doing so is to derive insights
from a broader body of research and experience,
notably in the social sciences, that can be applied in
SMI. The articles we selected cover the developing
world, with an emphasis on Africa.
We are not claiming to consider all possible factors
that may contribute to maternal deaths. For example,
we are not dealing here with background factors such
as nutrition.! The focus of our review is the interval
between the onset of an obstetric complication and its
outcome. The reason is that even among well-nour
ished, well-educated women who receive prenatal
care, a sizable proportion develop serious compli
cations during delivery. While there is still a lively
debate within SMI about the relative importance of
various kinds of interventions, there can be no doubt
that the interval we have chosen to concentrate on is
crucial to reducing maternal deaths [4],
This paper first presents a conceptual framework—
the three phases of delay—which identifies obstacles
to the provision and utilization of high quality, timely
obstetric care. We then present the findings of our
literature review as they relate to these three phases
of delay. Potential applications of the findings and
•We produced short abstracts of the studies reviewed.
entering them in a computerized database. This database
is available to anyone interested in using it. modifying it,
or adding to it. Interested persons will need to have
PROCITE. the bibliographic software used to enter,
edit, and retrieve abstracts. For more information, con
tact Ana Pagan at the following address: Center for
Population and Family Health. Columbia University
School of Public Health. 60 Haven Avenue. New York.
NY 10032. U.S.A.
tReaders interested in the literature on these background
factors are referred to the excellent review by J. Leslie
and G. Rao Gupta. Utilization of Formal Services for
Maternal Nutrition and Health Care in the Third World.
International Center for Research on Women. Washing
ton. DC. 1989.
^Except where otherwise noted, our discussion of the de
cision to seek care and the utilization of health care
services focuses exclusively on modern medical care.
since the major complications we are concerned with are
not treatable at the traditional health care level. There
fore. when we talk about seeking care, we mean modern
medical care.
directions the PMM program has taken are then
discussed. The review points to an approach which
prioritizes practical, measurable interventions de
signed to improve the availability and accessibility of
services, which should in turn mitigate factors which
impede the decision to seek these services.
THE CONCEPTUAL FRAMEWORK: THE THREE PHASES
OF DELAY
We know from the clinical literature that about
75% of maternal deaths result from direct obstetric
causes, such as hemorrhage, obstructed labor, infec
tion, toxemia and unsafe abortion [5]. We also know
from this same literature that a majority of these
deaths could have been prevented with timely medical
treatment. Delay, therefore, emerges as the pertinent
factor contributing to maternal deaths. Hospital
based investigators of maternal mortality have long
bemoaned patients’ delay in coming for care. How
ever, to blame the patient for the delay would be
simplistic. We view delay as having three phases:
Phase I delay
Delay in deciding to seek care on the part of the
individual, the family, or both. Examples of factors
that shape the decision to seek care include the actors
involved in decision-making (individual, spouse, rela
tive, family); the status of women; illness character
istics; distance from the health facility; financial and
opportunity costs; previous experience with the
health care system; and perceived quality of care.j
Phase II delay
Delay in reaching an adequate health care facility.
Examples include physical accessibility factors, such
as distribution of facilities, travel time from home to
facility, availability and cost of transportation and
condition of roads.
Phase III delay
Delay in receiving adequate care at the facility.
Relevant factors include adequacy of the referral
system; shortages of supplies, equipment, and trained
personnel; and competence of available personnel.
Although some proportion of maternal mortality is
a result of all three phases of delay, any one phase can
prove fatal. Phase' here connotes placement in a
temporal order, from the onset of complications to
treatment. While there does exist complex interplay
between phases, one type of delay is not linked
inextricably with another. Anticipating concerns that
a universal model such as this loses sieht of the
specific pathways exhibited in different places, we will
simply note that maternal death in areas where
aistances to health facilities are large and services
poor are comparable to maternal deaths in New York
City, where a woman may live next door to a hieh
tecnnology hospital but still die because of pover’tv
and its attendant impact on the decision to seek care.
Maternal mortality in context
The model as presented is universal insofar as both
of these cases fit the framework.
FINDINGS
Our findings are presented chronologically:
prospective patients begin their health-care-seeking
process with the decision to seek care, then they try
to reach a health facility where they can receive care.
Figure 1 is a schematic representation of how the
various factors discussed affect the interval between
onset of illness (specifically, an obstetric compli
cation) and its outcome.
1093
Phase I Delay: Decision to Seek Care
The factors that affect the decision to seek care are
often those discussed as ‘barriers’ or ‘constraints' to
the utilization of services in the literature on health
care seeking behavior. Numerous researchers have
observed that increasing the availability of services
(for instance, by building more facilities or expanding
health programs) does not always increase the use of
services. This finding has stimulated research into
factors that might account for the underutilization of
services.
Our review indicates that the barriers most
Fig. 1. Tne three delays model.
109-
Serees Thaddeus and Deborah Maine
commonly studied and discussed are distance, cost,
quality of care and sociocultural factors. In what
follows, we present findings concerning the influence
of each of these factors on the decision to seek care.
We also present our assessment of the relationships
among these factors and the hierarchy of their influ
ence on the decision to seek care.
Distance
The distance separating potential patients from the
nearest health facility has been shown to be an
important barrier to seeking health care, particularly
in rural areas [6-10], Distance exerts a dual influence:
long distances can be an actual obstacle to reaching
a health facility, and they can be a disincentive to
even trying to seek care. In addition, the effect of
distance becomes stronger when combined with lack
of transportation and poor roads. Potential patients
who have to walk or ride a mule over rugged terrain
will take longer to reach a facility. Distance will
therefore be a greater obstacle for them, and act
as a greater disincentive to efforts to seek care, than
for those who can travel by motorized vehicles on
relatively good roads.
Distance as a disincentive to seeking care plays an
important role in Phase I delay. However, the two
influences—disincentive and actual obstacle—are re
lated and often difficult to disentangle. Thus, some of
the findings presented below are conjectural.
The impact of distance as a consideration in the
utilization of health services has been assessed in a
variety of ways, including community-based inter
views and analysis of facility records [11]. In one
series of interviews in Oyo State. Nigeria, respondents
explained that they had not sought care because the
facility was too far or. alternatively, that their choice
of facility was made as a function of distance [12].
In studies using records from health facilities,
findings often indicate that the highest proportion of
users are located close to the facility—e.g. within a
radius of five miles or kilometers—and that the
proportion of users declines as the radius increases
[6. 13, 14],
A third way in which the role of distance has been
assessed is by looking at the severity of the condition
in which patients arrive at the facility and relating it
to how far they had to travel. The hypothesis is that
those patients who arrive at the facility in an ad
vanced stage of illness probably had to travel further
than those who reached the facility in a less advanced
stage of illness. This scenario highlights the role of
distance as actual obstacle. However, some re
searchers extrapolate further, and propose that those
patients who had to travel further probably also
waited until the illness became serious before deciding
to seek care. Presumably they waited longer because
distance was acting as a disincentive to seek care
earlier, thus delaying their decision [14], For example.
a case-control stud} of bacterial meningitis among
Navajo children in New Mexico revealed that the
total distances travelled by cases and controls were
similar. However, the mean distance travelled on
unpaved roads was 10 miles for cases, compared to
1-4 miles for controls. The author suggests that the
distance travelled on unpaved roads acted as a disin
centive and delayed the caretakers’ decisions to seek
care until complications of the initial disease devel
oped [15]. In a Nigerian study, the percentage of
individuals seeking treatment within one week of
illness onset declined as distance from the treatment
facility increased [10].
Some studies indicated that contrary to investi
gators' expectations, physical proximity does not
necessarily increase utilization [16], As one study in
Kenya’s Meru District illustrates, road improvements
significantly reduced travel distance and time to
health centers in the district. However, admission
rates and patterns at the two mission hospitals most
affected by these changes did not show substantial
improvement. According to the author, road im
provements alone do not guarantee increased utiliz
ation, as institutional barriers, such as the financial
cost of treatment at the fee-charging mission hospi
tals, may limit the advantages of shorter distances
[17]The magnitude of the impact of distance on the
decision to seek care appears to be shaped by other
factors as well, such as the severity of the condition
and the reputation of the provider. Stock’s data from
Nigeria show an effect of distance on utilization, yet
he stresses that there are differences in the size of the
effect according to illness and the perceived effective
ness of the health care provider. Tuberculosis, for
instance, is an illness for which respondents con
sidered medical care essential. In such cases, the
nature of the illness and quality of care appeared to
be more important than distance, and people did
travel far to obtain care [10].
These and other studies suggest that the impact of
distance is shaped by other factors and that reasons
for nonuse often lie in institutional accessibility fac
tors, such as the cost and quality of care, to which we
now turn.
Cost
Another variable that receives considerable atten
tion in the literature is the financial cost of receiving
care, which includes transportation costs, physician
and facility fees (when they exist), the cost of medi
cations and other supplies, and opportunity costs.
Cost and distance often go hand in hand as consider
ations in the decision-making process, as longer
distances entail higher transportation costs [18].
The effect of cost of services on utilization is
commonly assessed through interviews and surveys of
users and nonusers in which respondents are asked to
give reasons for their choice of actions when they are
ill. If a large proportion of respondents give financial
constraints as a major reason for not seeking care, or
for seeking one lorrn of care rather than another, this
Maternal mortality in context
f)
1095
indicates that cost of services was an important factor medication are only some of the cost considerations
affecting utilization. Much to our surprise, the litera facing individuals in their decision to seek care.
The other important component is the opportunity
ture indicates that compared to other factors, the
financial cost of receiving care is often not a major cost of the time used to seek health services. Time
determinant of the decision to seek care [12]. A survey spent getting to. waiting for and receiving health
conducted among a sample of 680 Ibo, Yoruba and services is time lost from other, more productive
Hausa people in Nigeria revealed five factors that activities, such as farming, fetching water and wood
influenced people’s decision to seek traditional or for fuel, herding, trading, cooking and so on. As
western medical care: Respondents ranked cost and women carry out a large majority of these tasks, the
distance fourth and fifth, respectively [19], Kloos value of their time and the competing demands made
et al. reported that in Ethiopia, cost of services was on it are important to consider.
In many parts of the developing world, prospective
often a less important consideration in utilization
than were the quality of services and perceived patients, especially women, do not travel alone to a
health facility: They are accompanied by other adults
efficacy of the treatment [20].
We found only a few studies that assessed the effect and by children who cannot be left at home alone
of changes in the fee structure on utilization levels because caretakers are not available. All these ad
[21]. Recent data from Nigeria show a drastic decline ditional people swell the cost of transport [27], Often.
in hospital births, apparently as a result of the family members accompanying patients must incur
country’s deepening economic crisis. Researchers at the costs of staying in a town where the health
the Ahmadu Bello University Teaching Hospital services are offered. Furthermore, the availability of
(ABUTH) in Zaria found that obstetric admissions others to help with household chores, to look after
declined sharply between 1983 and 1985, the year that children or to accompany patients to the facility can
the government instituted fees for prenatal care and be a factor in the decision to seek care [13].
delivery. Obstetric admissions to ABUTH decreased
It should be stressed that the cost/benefit ratio of
further in 1988, when patients were required to pay using medical services may be viewed very differently
for some of the essential supplies. The researchers in emergency cases [24], However, we did not find
note, however, that admissions for complicated ob information on factors influencing decision-making
stetric cases increased during the 1983-1988 period, under emergency conditions.
suggesting that the increased price did not deter
utilization by women with obstetric complications. Quality of care
Further examination of hospital records indicated
Quality of care is an important consideration in the
that the incidence of maternal deaths in the hospital decision to seek care. Our review found that where
increased by 56% between 1985 and 1988, whereas it potential patients have access to more than one
had remained stable between 1983 and 1985. Hospital facility, their perception of the quality of care offered
staff believe that this rise in maternal deaths may at these facilities often takes precedence over con
be associated with increasing costs that act to delay cerns about distance [28]. Annis found that in the
the decision to use the hospital until the woman's Guatemalan highlands, government health posts
condition is critical [22].
seemed to be conveniently located, yet that proximity
Unfortunately, we did not find any studies that did not guarantee utilization, probably because the
compared actual fees charged by various providers facilities were understaffed and underequipped and
and then related the fees to income levels and to thus unable to provide quality care. Detailed on-site
utilization. In fact, a few studies suggest that govern inspection of 83% of the operating health posts
ment facilities may be underutilized precisely because showed that more than half were understaffed, under
they are free [23, 24],
equipped. or both. Annis thus stressed that “the
More generally, the literature simply does not current low utilization of Ministry facilities reflects
provide systematic evidence that cost of services is a poor quality of services—and certainly not physical
major barrier to seeking care in the developing world. access nor mysterious ‘cultural barriers' ” [16, p. 522].
These findings seem to contradict anecdotal reports
The role that quality of care plays in the decision
from developing countries such as those mentioned to seek care is related to people's own assessment of
above. Perhaps other study designs are needed to service delivery, which largely depends on their own
fully explore the circumstances in which the cost of experiences with the health system and those of
services poses a major and a definitive barrier to care. people they know.
In addition to fees for services, there is evidence in
The two mechanisms through which quality of care
the literature that the cost of medications is often very affects the decision to seek care are satisfaction or
high [24. 25]. The cost of medicines is most likely to dissatisfaction with the outcome (e.g. effectiveness of
affect compliance with prescribed treatment. How the treatment and remedies prescribed), and satisfac
ever. to the extent that the cost of drugs figures in the tion or dissatisfaction with the service received (e.g.
decision to seek care, it can be expected to delay or staff attitudes, hospital procedures, availability of
discourage that decision. The financial cost of health supplies, efficiency) [10.19.29], When patients are
services in the form of provider fees and the price of dissatisfied with services, the reason more often than
SSM 11,1—c
1096
Serees Thaddeus and Deborah Maine
not lies in institutional factors, such as the procedures
performed, staff attitudes and long waiting times.
These factors will act as inhibitors of future utiliz
ation, thus affecting the decision to seek care [30].
Furthermore, modem medical facilities have a
culture of their own. which often clashes with the
culture of potential users [30]. The lack of emotional
support and privacy in the hospital setting, compared
with the home, and disruption of household respon
sibilities as a result of hospital confinement are some
of the complaints which contribute to women’s
dissatisfaction with maternity services [23,31].
Although a focus on cultural barriers to seeking
modem obstetrical care may inappropriately de
emphasize institutional inadequacies and economic
considerations, several studies have shown that
beliefs associated with traditional birth practices
act as disincentives to seeking such care. For example,
Sargent’s ethnographic studies of the Bariba in
Benin suggest that where infanticide is still practised,
modem medical culture comes into conflict with
beliefs, creating barriers. Traditional Bariba belief
holds that witches may be identified at birth, and an
entire cosmology provides a rationale for infanticide.
Although the values and beliefs of that society
are in flux, and witches are increasingly ‘managed’
through less drastic procedures, infanticide
persists.
In Pehunko (Benin), extrinsic factors such as distance, time,
and lack of support services rendered cosmopolitan support
services unavailable to most women. But even where cosmo
politan practitioners were available to attend home deliver
ies, this alternative was viewed with suspicion for fear that
witch detection and management might be obstructed.
Moreover, the rural ideal was solitary delivery in which a
woman demonstrated her courage and stoicism, enhanced
her prestige, and had the fiexibilitv to keep or reject the child
[32. p. 206],
While Sargent’s most recent and far-reaching ma
terial acknowledges the saliency of time, distance,
cost and government policy factors, and that “modifi
cations in medical and religious beliefs and practices
occur in conjunction with hospital use.” [32, p. 23].
she maintains that belief is central to the decision
making process [fbfrf.]. Our review suggests that be
liefs, as they relate to the etiology of illness and
maternal complications, also play some part in the
decision whether to seek modem obstetrical care.
However, these beliefs play less and less of a role as
societies change through urbanization and increasing
recognition of the efficacy of modern medical treat
ment.
In addition to the above examples of what may be
seen as general hospital policy, there are those pro
cedures specific to childbirth that women dislike or
fear [33], Women may fee] uncomfortable having to
expose their genitals in the hospital ward [23], or they
may intensely, dislike the positions favored by hospi
tals for delivery [34], Other specific hospital pro
cedures that inhibit utilization because women may
fear them include surgical operations such as
cesarean sections [35] and episiotomies [36].
Finally, how the prospective patient expects to be
treated by providers and staff at the health care
facility is an important dimension of the patient’s
assessment of the quality of care. If the facility has a
reputation for unfriendly staff, rude service providers
and humiliating treatment, the prospective patient
may delay the decision to seek care until the serious
ness of her condition necessitates overcoming all
barriers [24, 30. 31,37, 38].
Leslie and Rao Gupta identify corruption as
another important dimension of staff attitudes [39].
Where ‘little presents’ help to get medicines and
supplies, corruption may indeed delay the decision to
seek care by increasing patient dissatisfaction and, of
course, by swelling the costs of seeking care [24].
We have sketched some of the interactions between
distance, cost and quality of services as they appear
from our review of the literature on utilization of
services. A fuller understanding of the decision to
seek care needs to take into account other factors
related to the illness itself.
Illness factors
The literature clearly shows that health-care-seeking behavior is strongly influenced by the character
istics of the illness as perceived by individuals. To
begin with, prospective health care users must recog
nize that an abnormal condition exists. The perceived
severity and the perceived etiology of the disorder
then shape the decision to seek care. The studies we
reviewed describe one or more of these illness factors
without necessarily drawing conclusions about their
role in the health-care-seeking process.
Recognition. Before deciding to seek treatment.
people need to recognize that they have a condition
requiring specialized attention [40],
A recent survey conducted in six of Senegal’s 10 regions
indicated that women in these regions lack basic infor
mation on signs and symptoms of obstetric complications.
One-quarter of the women interviewed could not name a
single complication. Only 13 percent recognized fever, and
10 percent prepartum hemorrhage, as important danger
signals. Some women even said that fever, dizziness and
pallor were signs of a normal pregnancy [41],
Although pregnancy is considered a normal life event
among respondents [to a qualitative survey in Jamaica], a
childbirth was perceived as potentially dangerous to the
majority of the women interviewed. However, most women
were familiar with only the common symptomatic com
plaints of pregnancy, and less than 10% of women could
Recognition of illness is denned by the patient’s
view of reality, not by the health professional's
medical criteria, with which it may or mav not
coincide [42.43], .Moreover, individuals' assessment
of a health condition can be influenced by the preva
lence of the condition. In a classic study in medical
sociology. Zola emphasized that in populations
Maternal mortality in context
where a particular condition is widespread, it is
perceived as normal, natural, inevitable "and thus to
be ignored as being of no consequence" [44. p. 615].
In addition, the perception of a condition as in
evitable is often accompanied by the perception that
it is not amenable to treatment, that nothing can be
done to manage it [20].
Pregnancy and childbirth are ubiquitous events.
Although acknowledged as potentially risky, preg
nancy and delivery are commonly considered natural.
normal work for women. In other words, they are
often not seen as illnesses for which medical expenses
are justified and a hospital room booked [23. 36,45].
Furthermore, just as pregnancy is considered a nor
mal event, death during labor and delivery may
sometimes be considered ‘normal' or inevitable. Such
fatalistic views can lead to the perception that the
condition is not amenable to treatment, and can thus
act as effective barriers to a timely decision to seek
care. The recognition of a health condition can also
be shaped by sociocultural prescriptions and in
terpretations. Among the Bariba of Benin, for
example, labor that lasts up to a day is considered
normal and thus is not recognized as dangerous
[33, 46],
In parts of Africa, prolonged obstructed labor is
taken to be a sign of the woman’s infidelity
[45.47-49]. Obstructed labor is thus interpreted as
punishment for adultery and not recognized as a
medical problem. It is believed that the woman must
‘confess her sins’ so that the delivery will progress
smoothly, thus precluding the decision to seek medi
cal care for the complication.
Finally, mention should be made of situations in
which a health problem is recognized, but care is not
sought because of the fear of social or legal sanctions.
Those suffering from a condition they view as shame
ful or stigmatizing may recognize its seriousness, yet
the fear of punishment and ostracism can prevent
them from seeking appropriate care. For example.
venereal diseases are often denied, unreported and
untreated [20]. Vesicovaginal fistulae and compli
cations resulting from unsafe induced abortion often
remain unreported, therefore untreated, because of
ostracism and shame in the former and the fear of
sociolegal sanctions in the latter [34 .50-53]. Certainly
in the case of an unwanted pregnancy, the condition
and the need for care are both recognized. However,
fear, shame and desperation can act as powerful
barriers and lead to disastrous consequences as
women seek illicit and unsafe abortion, attempt to
self-abort and. in extreme cases, commit suicide
[54-57],
Severity. In addition to recognition of a health
condition, the perceived severity of an illness is a very
important factor in the decision to seek care. Utiliz
ation of services appears to be influenced by the
recognition of symptoms and the assessment that the
svmptoms are serious enough to justify medical care
[is. 42. 58].
1097
The perception of a condition as normal or minor
interacts with cost and distance in the decision to seek
care. Just as certain conditions (such as pregnancy)
are perceived as ‘natural’ and therefore not requiring
medical care, conditions that are perceived as minor
also do not justify the expenses of money, time and
travel effort often involved in medical care [10.20].
Cosminsky and Scrimshaw report that residents on
the Guatemalan plantation that they studied tended
to use low-cost remedies to treat minor conditions
and then move to more expensive resources if the
illness progressed [59].
It is important to note that we did not find any
studies showing that illness severity was not an
important factor or that it played a lesser role than
other variables as a consideration in the decision to
seek care. This is in contrast with the findings of
studies examining the role of distance, cost and beliefs
about illness causation, all of which reveal much
variation in the importance of these factors.
The aforementioned studies indicate that the per
ceived severity of the condition may well be an
overriding factor in the decision to seek appropriate
care. Furthermore, there is an interaction between
severity of illness and other factors involved in the
decision. Specifically, there is a reluctance to incur
costs when the disorder is perceived as non-threaten
ing or self-limiting. However, the perception of these
expenses as a barrier seems to decrease dramatically
when the disorder is perceived as serious, debilitating
or life-threatening, and the perceived benefits of
seeking care seem to outweigh the constraints. As
perceived severity increases, utilization of services
increases and the impact of distance and cost in
decision-making decreases.
It should be noted that most of the studies we
reviewed assume that the decision to seek care is
a process that occurs in stages. While this may
be the case for conditions with a slow’ onset, it is
unclear what happens in medical emergencies (e.g.
postpartum hemorrhage).
Etiology. Once the decision to seek care is justified
by the perceived severity of the illness, a key factor
in determining the type of care (self, traditional.
modem or a combination of the three) that will be
sought is the cause to which the illness is attributed
by patients and their families.
Our review indicates that while beliefs about illness
causation do sometimes play a role in the decision to
seek medical care, this role is not as important as it
might have been a few decades ago, when the efficacy
of medical care was less well accepted in the develop
ing world [27], Furthermore, while traditional medi
cine is still relatively more available than modern
medical care in rural areas, there is ample evidence
from most parts of the developing world that the
trend is toward utilization of both systems for treat
ment of most conditions.
Medical anthropologists and sociologists, such as
Cosminsky and Scrimshaw [59], Foster [27], Lasker
1098
Seres’ Thaddeus and Deborah M.
[24] and Young [IS] reject the view that beliefs about
illness causation generally lead to decisions not to
seek medical care. They argue that people are empir
ical and pragmatic, as opposed to ‘unscientific,’ or
‘irrational.’ that they base their health care decisions
on an assessment of available and accessible re
sources.
The important lesson from anthropological studies
of health beliefs is that a narrow focus on ‘cultural
barriers’ obscures the role that institutional inade
quacies and economic considerations play in the
decision to seek care. Nonetheless, variation across
cultural groups and across health conditions remains
great, and beliefs about illness causation do some
times affect the decision to seek medical care. As we
noted earlier, the belief that obstructed labor is
caused by a woman's infidelity is widely held—for
example, in Sierra Leone, Liberia, Ghana and
Zimbabwe. It should serve as an important reminder
of the types of factors that need to be identified by
research and addressed by programs. It also illus
trates that at the heart of many factors that limit
access to care is the status of the women in the
society.
Women's status
Women's status is composed of the educational,
cultural, economic, legal and political position of
women in a given society. While women's status
generally underlies and shapes women’s access to
health services, there are specific ways in which it
directly affects and delays the decision to seek care.
In this section, we focus on how women's access to
health services is limited by constraints on their
autonomy.
In countries as diverse as Nigeria, Ethiopia.
Tunisia. India and Korea, studies show that women
do not decide on their own to seek care: the decision
belongs to a spouse or to senior members of the
family [10, 20. 23. 41. 60-■62]. Furthermore, women’s
mobility is limited in certain areas because they need
permission to travel. Often this permission must be
granted by the spouse or the mother-in-law '[10],
Where women’s mobility is severely restricted be
cause of such cultural prescriptions, efforts to seek
timely care may be thwarted. According to Harrison,
in Zaria, Nigeria, “no matter how obvious the need
for hospital management becomes for the girl who
develops obstructed labor, permission to leave home
for hospital can usually be given only by the husband;
if he happens to be away from home, those present
are often unwilling to accept such responsibility” [34,
p. 385]. In Ethiopia, women tend to use those primary
care facilities within walking distance from their
homes, because of “cultural restrictions placed on
[their] travel outside the community" [20. p. 1013],
For a woman with obstetric complications, access
limited to the nearby primary care centers is not of
much help. These facilities are usually not equipped
to deal with obstetric complications, and further
delay can occur through staff errors and misdiagno
sis.
.
In addition to identifying the major factors gener
ally shaping the decision to seek care, our review
indicates that these constraints often apply unequally
to women. Consider the example of distance. We
have discussed how overcoming this barrier largely
depends on mobility: Individuals with access to mo
torized vehicles are more mobile than those with
access only to bicycles or donkeys, who are in turn
more mobile than those who can rely only on their
feet. Yet among the strict Muslim communities of
northeastern Nigeria, women are not allowed to ride
bicycles or donkeys. Although these means may be
physically present in the community, they are effec
tively unavailable to women [10],
Women’s status also interacts with the cost of
treatment in the decision to seek care. The literature
on the preference for male children provides evidence
that the consideration of cost in the decision to seek
care is applied unequally to males and females [26],
Witness for example the impact of son preference on V
access to health services, a phenomenon best docu
mented for Asia, specifically India and Bangladesh.
and to a lesser extent, for the Middle East [63] and
Africa [38, 64].
In Bangladesh, as elsewhere, private physicians' fees are
much higher than those of other providers. Parents con
sulted private physicians three times as often for their sons
as for their daughters. Moreover, the purchase of drugs
prescribed by physicians was about three times as frequent
when the prescnption was for a bov as when it was for a girl
[65].
Especially where resources are scarce, parents’
health care seeking behavior and expenditures often
reveal a preferred investment in their sons’ health.
Even where health care services and transportation
were both free of charge, such as in Matlab,
Bangladesh, parents still used the services far more
frequently for injured or ill boys than for girls [66]. *■
It is evident that the low value placed on females
adversely affects their utilization of health services.
However, this link has been generally overlooked. As
Royston and Armstrong have recently pointed out.
“sex discrimination as a contributory factor to ma
ternal mortality has been largely ignored, [and] has
been hidden within the general issue of poverty and
underdevelopment which is assumed to put every
one... at an equal disadvantage in health terms” [67.
pp. 45—46]. Stemming from the low status of women.
reluctance to allocate resources or assign importance
to female health inhibits the decision to seek modem
medical care when complications associated with
pregnancy and childbirth arise.
In many parts of the developing world, women
consider childbearing as their only means of gaining
status. Thus, women often find themselves in a
paradoxical situation: high fertility is their main
channel to improving their status, but it increases
their risk of maternal death. Even in some societies
.Maternal mortality m context
where women are financially independent, they derive
pride and prestige chiefly from their roles as mothers
[68]. Sargent s study of the Bariba of Benin illustrates
yet another way in which pregnancy and childbirth
confer status on women.
1099
away were of higher economic status and more
commonly owned cars or motorcycles than did those
living closer to the clinic [7],
Educational status
Education is measured by the number of years of
formal schooling. In developing countries, men gen
erally have higher educational levels than women.
Our review reveals two major findings with respect to
the role of formal education in the decision to utilize
health services: (1) that its role is not clear-cut; and
In such situations, a woman’s efforts to gain esteem (2) that the mechanisms through which education
and enhance her status have direct implications for may play a role are not well understood.
the recognition of complications and delays in the
Most of the studies reviewed show that utilization
decision to seek care if they do develop.
of medical services increases with increasing levels of
None of the studies reviewed examines utilization education. The positive association repeatedly docu
of services by women who are financially indepen mented is that between mother’s education and use of
dent, who are autonomous in their decision-making child health services and child survival technologies
and who derive status and prestige from roles other [76-78]. The presence of a positive association be
than motherhood alone. Furthermore, the role of tween educational level and use of adult health
women’s informal power is rarely addressed. Re services is not as consistent [75], However, survey
search in such contexts is much needed. It might results from Ethiopia, Jordan and the Philippines
mitigate some of the gloominess described above. indicate a significant positive association between
The potential contribution of such research can be use of prenatal care services and level of womens’
gleaned from preliminary' results of focus-group re education [56. 58, 78],
search conducted in Enugu, Nigeria. Women partici
The mechanisms through which education might
pating in the focus groups argued that although their affect the decision to use health services are not well
husbands are the overall decision-makers, the women understood. It has been hypothesized that education
are financially independent. Access to cash, they affects individuals by introducing them to a new
slated, was the most important factor in the decision ‘modem’ culture [77]; that increasing levels of edu
to seek care. This means that in case of a medical cation increase knowledge and awareness by shaping
problem, the women do not need to wait for their thought patterns—for example, by acting as “medi
husbands, as they have ready access to cash and are cation against fatalism” [76]; and that education
able to pay for the expenses incurred [69].
increases access to information. A related hypothesis
is that education increases self-confidence and
Economic status
imparts respect and influence [76].
The literature describes statistical associations be
There is evidence in the literature that higher levels
tween economic status and the utilization of services. of education may not guarantee higher levels of
However, the mechanisms through which this associ health services utilization [11,24,42, 43]. Some stud
ation operates are not specified. Possibilities include: ies suggest that with increasing education, individuals
(1) income constraints; and (2) characteristics of the depend more on self-care and self-prescribed medi
health care facilities serving the poor that may dis cation and postpone the visit to a facility until after
courage use [20,70,71], What is clear, however, is these methods fail to produce a cure. However, it may
that morbidity and mortality rates are higher among also be that the better educated are generally health
ier, thus requiring less care than the less educated.
groups of low economic status [20, 52, 56. 72—74],
Although there are not many studies that show a
Most of the studies reviewed indicate that econ
omic status affects the use of health services. In negative relationship between education and utiliz
general, these studies find that utilization increases as ation of health services, they are important, because
economic status increases [9,12,75]. In studies by they illustrate that the explanation of differential
Kwast et al. in Addis Ababa, Ethiopia, economic utilization cannot be reduced to one variable. In
status was measured by income, house ownership and addition to their education, literate and illiterate
occupation. The lowest rates of prenatal clinic attend individuals alike rely on their past experience of
ance and the highest rates of home delivery were health services as a source of information. Further
found among women from the lowest economic more. focusing on education as a main factor in poor
status groups [56,73]. Data from Iraq show that utilization levels in effect lets the health system ’off
consultation rates for all health facilities rose from 67 the hook.’ It obscures the fact that there are often
per 100 illness episodes for low-income households to institutional factors that deter utilization and it
103 for those in the high income bracket [13], In ignores the potential effect of outreach activities.
The experience of declining infant mortality inde
Calabar. Nieeria. distance did not deter patients from
using the familv health clinic: Patients living further pendent of education in countries such as Cuba.
To the Bariba.-birth represents a rare opportunity for a
woman to demonstrate courage and bring honor to both her
family and that of her husband by stoic demeanor during
labor and delivery. The woman who manages to deliver
without calling for assistance until the child is bom is
especially esteemed [33, p. 291],
1100
Semen Thaddecs and Deborah Maine
China. Costa Rica and Sri Lanka illustrates what
Cleland and van Ginneken call the “equalizing influ
ence of health services" [78]. Declines in infant mor
tality were sharp among offspring born to illiterate
mothers in China and to those with less than four
vears of schooling in Costa Rica. Over time, accessi
bility and availability of medical services in these
countries reportedly decreased differentials in infant
and child mortality that had been associated with
levels of parental education.
By contrast, there are instances where neither
strong national investments in education nor achieve
ment of a high literacy rate appeared to have any
effect on that country’s high mortality rate. Bullough
has pointed out that countries with high under-five
mortality rates spend about three to five times as
much on education as on health. He further notes
that Paraguay and Tanzania are examples of
countries that "manage to combine high literacy rates
with high maternal mortality rates: adult female
literacy 85 percent and 80 percent, maternal mortality
rate 469 and 370/100 000 live births” [80. p. 1119].
In its purest form, the decision to seek medical care
is a behavioral response to a perceived need created
by an illness. The complexity of the real world,
however, introduces variability and constraints into
this process. It is therefore simplistic to relate people’s
underutilization of services to their ignorance, illiter
acy, poverty, laziness or superstition. Rather, under
utilization is often related to people’s knowledge,
based on previous experience, that facilities are far
away and often difficult to reach, that they may be
closed, that needed drugs may be out of stock, and
that staff are often less than helpful and polite. In
other words, the actual accessibility of services is
often at the heart of the matter (Fig. 2).
Phase II Delay: Reaching a Medical Facility
The accessibility of services plays a dual role in the
health-care-seeking process. On the one hand, it
influences people's decision-making, as outlined
under the rubric of Phase I Delays. On the other
hand, it determines the time spent in reaching a
facility after the decision to seek care has been made.
This latter effect we term Phase II Delay.
Interviews with pregnant women in rural Kenya indicated
that 47 percent of the women intended to deliver in a
hospital, 40 percent intended to deliver at home and 13
percent had not yet decided at the time of the interview. Of
those who had decided to deliver in a hospital, only 36
percent actually did so. The rest had not changed their
minds—they were simply not able to reach the hospital [81],
The data further indicate that 84 percent of the women in
the sample had received prenatal care; that the majority of
the women and their relatives could recognize risk factors;
and that women who experienced difficulties with previous
deliveries were significantly more inclined to plan for a
hospital delivery than were those who had a history of
uncomplicated deliveries. Yet a sizable proportion of
women could not act on their informed decision because
they lived far from the hospital, which they could reach only
by walking or by waiting for a passing lorry [81],
Here, distance and the unavailability of public
transportation were not considerations that delayed
the decision to seek care. They were actual obstacles
that prevented women from reaching the hospital.
Factors that create Phase II Delays include the
location of health facilities, the travel distances that
result from this distribution and the transportation
means necessary to cover the distances. In other
words. Phase II Delays result from the actual
accessibility of health services.
Phase II delays are very common, particularly in
rural areas, yet they are not systematically docu
mented in the literature. Rather, researchers have
typically focused on the individual and institutional
characteristics that inhibit the timely use of services.
The perspective that users and providers are the only
actors in the health-care-seeking process prevails
throughout the literature. By focusing exclusively on
the two poles of the health-care-seeking process, this
perspective fails to take into account all that happens
on the way to the health care facility.
Phase II delays have important programmatic im
plications. For instance, it is of little use to identify
high-risk pregnant women who should deliver in the
hospital and to raise the community’s awareness of
risk factors if the women are unable to reach the
hospital, as in the Kenyan example cited above.
Gathering data on delays that face patients who are
trying to reach a facility is thus an important research
effort that can serve to guide programmatic interven
tions.
Distribution offacilities
There is a general shortage of medical care insti
tutions in the developing world. In addition, existing
facilities are more often than not concentrated in and
around urban areas. Governments plan to have rural
areas served by a network of regional and district
hospitals in large towns, primary health centers,
health posts and dispensaries. In many cases, how
ever. this network does not function as planned. All
studies reviewed indicate that inhabitants of urban
areas have better access to health facilities than do
rural inhabitants [20.24], In the Syrian Arab Repub
lic, 30% of all government and 19% of all private
hospital beds are concentrated in Damascus, the
capital city. Also, 65% of the nation’s health centers
are located in urban capitals of governorates. Health
care providers are also in short supply and unevenly
distributed. Of the country's 221 obstetricians. 78
(35%) practice in the capital city. In contrast, only
nine obstetricians practice in the rural areas, and four
of them are located in Damascus governorate. This
means that there are only five obstetricians in the
country's remaining 13 governorates [82],
A concern for equitable distribution seems to
have guided the allocation of health resources in a
few countries. According to Cardoso, the Cuban
Ministry of Health has paid particular attention to
the rural areas in establishing a network of hospital
Maternal mortality in context
1101
Fig. 2. Phase I delay, detail.
facilities that would be accessible to the entire
population. Existing hospitals were enlarged
and new hospitals were built in the rural areas [83].
Unfortunately, the Cuban model does not appear
to be widespread. Of course, Cuba is a relatively small
country, a factor which probably facilitates the im
plementation of such policies. Still, there are many
small countries where distribution of resources is
much less equitable.
Travel distances
The uneven distribution of facilities has impli
cations for travel distances between women and even
the closest facility, let alone a specialist referral
hospital. The issue of access is therefore an acute
problem for rural inhabitants in most developing
countries. Examples of actual travel distances cited in
the literature gives an idea of the magnitude of the
no:
Serees Thaddeus and Deborah Maise
problem [11.23.52]: People from a rural fanning
community in Mexico had to travel 30 km to reach the
nearest medical facility [84]; in Ethiopia, rural
patients had to walk between 15 and 18 km to the
nearest town where Land Rover service was available
to transport them-to the nearest medical facility [20],
Travel distance can be measured as a straight line
between two points—e.g. the house and the hospital.
But people often cannot follow a straight line to reach
a facility. The nature of the terrain and the condition of
the roads often dictate that distances will be longer
[69, 85],
Transportation
In addition to travel distance, the scarcity of trans
portation in developing countries is also a harsh reality
[24.88]. In Tanzania, a woman with placenta previa
“died only 20 miles from the Consultant Referral
Hospital because the Land Rover assigned to her
medical center was being used by an unauthorized
person at the time, and she bled to death at the
roadside waiting for a taxi" [89, p. 104],
As a result, inhabitants of rural areas commonly
have to walk or improvize means of transportation to
reach a health care facility [72, 90]. For example, “In a
remote area of Bangladesh, seriously ill patients were
often carried to the clinic on a chair because there were
no vehicles available to transport them" [14],
The patient’s condition can, of course, deteriorate
with increasing delays in reaching a treatment facility,
making the condition more difficult to treat once the
facility is reached—that is, if the patient is still alive
upon arrival.
Deaths on the way to the hospital
Not all individuals who decide to seek care at a
medical facility arrive there in time to be treated; some
die while trying to get there. Deaths on the way to
seeking care may result from the joint effect of Phase 1
and Phase II delays: There might have been a delay in
the decision to seek care, which was further aggravated
by the long distances and/or the unavailability of
transportation. But it is entirely possible that the
decision to seek care was timely, yet the poor distri
bution of facilities and the resulting distances separ
ating people from services accounted for the delay and
therefore caused the death.
In addition, it must be specified that reaching a
health facility does not necessarily mean the end of the
health-care-seeking journey. If the nearest facility is a
peripheral health center not equipped to treat the
condition or even to administer essential first aid.
seriously ill patients will have to go on to another,
better equipped institution. By the time the patient
reaches an adequate health facility, the delays will have
further increased the risk of a death en route.
Data on such deaths are scarce. Hospital-based
studies are not helpful, since they include only deaths
that occur in the institution. Community-based re
search is more relevant, but deaths on the way to
seeking care are sometimes counted as deaths at home.
Of all studies reviewed, the literature on maternal
mortality proved to be the richest source of data on
deaths occurring on the way to seeking care [76.91.92]
(Fig. 3).
A 1984 investigation of maternal mortality in 287 Chinese
cities, districts and counties revealed that 15 percent of all
recorded maternal deaths occurred on the way to the
hospital. They were all in rural areas [93].
In Addis Ababa. 13 percent of maternal deaths recorded
over a two-vear period occurred on the wav to the hospital
[94].
Phase III Delay: Receiving Adequate Treatment
Today. Mary, the lady who helps us in the house, came late
to work. I told her off for being late and asked why. She said
that one of her townswomen ... had died in the hospital
while giving birth to a baby. This was her fifth delivery. She
was not from a far off village but from Sokoto city itself. She
had not gone too late to hospital but rather gone on
time.... By the time they found a vehicle to go to hospital.
by the time they struggled to get her an admission card, by
the time she was admitted, by the time her file was made up.
by the time the midwife was called, by the time the midwife
finished eating, by the time the midwife came, by the time
the husband went and bought some gloves, by the time the
gloves were brought to the hospital, by the time the midwife
was called, by the time the midwife came, by the time the
midwife examined the woman, by the ume the bleeding
started, ... by the time the doctor was called, by the lime
the doctor could be found, by the time the ambulance went
to find the doctor, by the time the doctor came, by the time
the husband went out to buy drugs. IV set, drip and bottle
of ether, by the time the husband went round to look for
blood bags all round town, by the time the husband found
one and by the time the husband begged the pharmacist to
reduce the prices since he had already spent all his money
on the swabs, dressings, drugs and fluids, by the time the
haematologist was called, by the time the haematologist
came and took blood from the poor tired husband. ... by
the time the day and night nurses changed duty, by the time
the day and night doctors changed duty, by the time the
midwife came again, by the time the doctor was called, by
the time the doctor could be found, by the time the doctor
came, by the time the t’s had been properly crossed and all
the i’s dotted and the husband signed the consent form, the
woman died. Today the husband wanted to sell the drugs
and other things they never used to be able to carry the body
of his wife back to their village but he could never trace [the
body] again in the hospital [95],
This excerpt from a letter sent to us by a colleague
provides a vivid illustration of Phase III delays—those
that occur at treatment facilities. Delays in the delivery
of care are symptomatic of the inadequate care that
results from shortages of staff, essential equipment,
supplies, drugs and blood as well as inadequate man
agement. Late or wrong diagnosis and incorrect action
by the staff are other factors that contribute to delays
in the timely provision of needed care. All these
deficiencies in the quality of the care provided at health
facilities are frequently mentioned in the literature.
In addition to identifying the diagnoses in cases of
maternal death, some hospital-based studies deter
mine whether or not the deaths were avoidable. They
generally find that while a small number of maternal
deaths are unavoidable, the large majority are either
Maternal mortality in context
entirely or probably preventable. For example, 98%
of institutional deaths studied in Tanzania [87]; 94%
of maternal deaths studied in Cali, Colombia [96];
88% of those studied in Vietnam [97]; and 80% of
those studied in Jamaica [98] and in Lusaka, Zambia
[88], were judged preventable by the respective inves
tigators.
Insufficient and unqualified staff, clinical misman
agement of patients, unavailability of blood, short
ages of essential drugs and missing supplies and
equipment limit individuals' access to lifesaving pro
1103
cedures. According to a technical working group
formed by the World Health Organization in 1986.
these deficiencies "represent a failure on the part of
the health services to seize the last chance to save a
woman" [99, p. 2]. This technical working group also
identified seven obstetric functions that are essential
at the first referral level to save the life of emergency
obstetric patients. Accordingly, district and subdis
trict hospitals should be able to perform cesarean
sections, administer anesthetics and blood transfu
sions, perform vacuum extraction, carry out suction
Factors Affecting /
: Utilization and Outcome
Fig. 3. Phase II delay, detail.
Sereen Thaddeus and Deborah Maine
curettage for incomplete abortion, insert intrauterine
devices'and perform tubal ligation or vasectomy. The
capacity to perform these essential obstetric functions
provides a guideline against which to evaluate the
quality of care described in the following findings.
Ill-staffed facilities
Insufficient numbers of medical and nursing per
sonnel at a facility necessarily lead to delays in
patients’ receiving the care they need. This shortage
is often not only a matter of staff numbers, it is
also a matter of competence. In other words, there
is a shortage of trained, qualified personnel
[57. 87, 98,100]. In a study of maternal mortality at
the University Teaching Hospital (UTH) in Lusaka,
Zambia, “the most worrying finding [was] that an
avoidable hospital factor was present in 52 percent of
cases” [88, p. 77]. Hospital factors identified included
poor intrapartum assessment, failure to correct ane
mia, missed diagnosis of ruptured ectopic pregnancy
and unavailability of the anesthetist. The investi
gators argue that all these factors could be "reduced
or eliminated” [ibid.]. Numerous other studies report
similar cases of clinical mismanagement from Colom
bia [96]. Kenya [101], Malawi [102], Vietnam [97], and
Zambia [88. p. 77],
Ill-equipped facilities
A lack of equipment and supplies plagues health
facilities in most regions of the developing world.
There is little question that this situation is due in
part to the very real issue of limited resources. But it
is often perpetuated by poor management and organ
ization of the available resources. Difficulty obtaining
blood for transfusion assumes paramount import
ance in the management of several major obstetric
complications and is often identified as an avoidable
factor delaying the provision of adequate care
[56. 103, 104], For example, blood shortages were
implicated in 35% of hospital maternal deaths in
rural Tanzania [89], 39% in Malawi [102], and 36%
in Vietnam [97]. At Korle-Bu Teaching Hospital in
Ghana, prepartum hemorrhage was an indication for
9% of the cesarean sections performed in 1971. The
investigators argue, however, that patients who might
be treated conservatively if blood were available are
sectioned as the quickest way of stopping the bleed
ing. They maintain that the situation would improve
considerably if the maternity unit had its own blood
bank [105],
Inadequate supplies of essential drugs, such as
antibiotics and ergometrine, are other avoidable
factors that contribute to phase 3 delays. Such short
ages occur at all levels of the health system
[16.26.56.87.97], In Ilorin University’s Teaching
Hospital in Nigeria, some patients were without any
antibiotics until the third day after a cesarean section.
because their relatives were not abie to buy the drugs
immediately and they were not in stock at the hospi
tal pharmacy. Sepsis caused 82% of the deaths in this
hospital study. Most of these would have been pre
vented with a course of antibiotics [106].
In brief, the vast body of literature documenting
medical and nursing staff shortages, failures in the
clinical management of complications and shortages
in essential supplies indicates that the quality of care
in many institutions is inadequate. These studies
show that blaming the patient for seeking care late
obscures the fact that the health care system often
fails the patient (Fig. 4).
DISCUSSION
In the preceding sections of this paper, we have
presented findings from a great variety of studies to
help us elaborate some of the factors that may
contribute to delay in preventing deaths among
women with obstetric complications. We now piece
together these various factors to examine the larger
picture.
Obtaining medical care for women with obstetric
complications begins with the recognition of danger
signs. Access to such information and understanding
of the gravity of symptoms, such as bleeding or
prolonged labor, help a woman and her family to
seek timely treatment. Even when women and their
families recognize danger signals and understand the
need for medical care, they are also aware that there
is not much the medical facility can do for her when
there is no trained doctor or nurse-midwife, when
blood shortages are regular and when equipment is
frequently broken. People do not bother to seek care
when they know that they probably will not be cured,
that they are even likely to die in the hospital.
Unfortunately, and despite the efforts of many dedi
cated and hardworking health providers, this is the
state of affairs in many facilities in the developing
world. Under such circumstances, people’s decisions
not to use the health facilities available to them make
sense.
The process of obtaining medical care unfolds
within the confines of the health care system. In
defining the components of this system, it is import
ant to speak not only of the providers, but also of the
users as part of that system. As with any system,
changes introduced into one component can effect
changes in other components. Thus, the objective
obstacles encountered in Phases II and III feed back
into the subjective decision-making of Phase I, link
ing the user of health services and the provider of
these services into the same system.
To apply what has been learned in this literature
review, one can begin with a brief discussion of
program strategies. The factors identified as con
tributing to delay were the following: distance, cost.
quality of care, illness characteristics.'women’s status^
economic status and educational status. As Fia 1
showed, these factors all influence a woman and'her
family in their home as they decide whether to seek
medical care lor her. Interventions designed to affect
Maternal mortality in context
Factors Affecting
Utilization and Outcome
1105
1
Phases of Delay
i
Phase 1:
Socioeconomic/'
- Cultural
Factors
• Deciding to Seek-
Care
Phase II;
Accessibility of’
Facilities
Identifying and
Reaching Medical
Facility
' -| Actual .QuaHtyJot Car® j
-'<^Fiy ^efifeatEaciiit^s'kX
Jus(aff:numixts
:LyJ^
- competence of personnel .
?^oriy.:EqujP^-jEaciuifes^
z-.unavmtabrt^ii.Wood-CJ
unavailability, of.drugs?.~:r
rv-Lunavwlabiltty.-.ofl«the.r.:.y?':?
■equipment. .
Kherd^unency^problemsz^
;qnadequBf«{Mariagemert^T^SilS
•Zrjhcorie<rt:diagn6sj» enri/Bofion?
Fig. 4. Phase III delay, detail.
these factors, however, must operate at quite different
levels.
Consider, for example, distance and cost. Both
these factors affect people’s decisions to seek care;
there is, however, relatively little that individuals or
families can do to influence these factors. Rather, in
order to make systematic and widespread changes in
these factors, the government must take steps to
improve the distribution and financing of medical
care. Even so. there are some actions that can be
started on a smaller scale and may help reduce the toll
of maternal deaths. Some of these are discussed
below.
Distance
The physical distance between people and medical
care in developing countries is a problem that will
take a substantial amount of time, money and politi
cal will to solve. However, there are several compara
tively inexpensive measures that could reduce
maternal deaths by reducing travel distance to health
services. Simply expressed, either pregnant women
1106
Sereen Thaddeus and Deborah Maine
have to move closer to the services, or the services
have to move closer to the women.
The first option has been implemented in the form
of maternity waiting homes, which provide modest
accommodation close to the hospital for pregnant
women who live far-away. These women can live in
the home during the last few weeks of their preg
nancy. then be transferred at the onset of labor or any
complication to the nearby local hospital for delivery.
A number of countries—such as Cuba [107], Colom
bia. Uganda and Zaire—are experimenting with ma
ternity waiting homes. Unfortunately, there are no
studies to date that evaluate the impact of maternity
waiting homes on deaths among women from compli
cations. Such programmatic research is much needed.
While maternity waiting homes will be practical
and useful in some situations, they are not the
solution to the uneven distribution of obstetric care
in developing countries. To deal with this problem, a
number of programs are being planned in which
community members will be helped to prepare for the
eventuality of obstetric emergencies either by setting
aside funds to pay for public transport or by arrang
ing with owners to make their vehicles available in
emergencies.*
The second option—that of moving the services—
was endorsed by a WHO Working Group on the
Organization of Maternal Health Care, which
stressed that "programmes should be guided by the
axiom that al] services should be provided at the most
peripheral level of the health system at w'hich this can
be done effectively” [99. p. 9].
It is not reasonable to propose that definitive
treatment of obstetric complications (such as ce
sarean section) be made available at all health facili
ties. Even so. many women's lives would probably be
saved if health centers in rural areas were at least able
to provide first aid to women with complications. In
three isolated Gambian villages, the single most
important factor contributing to mortality declines
“has apparently been the on-the-spot. 24-hr avail
ability of a physician or qualified midwife" at the
clinic [108 p. 912]. In addition, free transportation to
and from the clinic was provided, and the clinic
physician or midwife assisted at home deliveries.
According to the authors, transfer to a hospital in
cases of major difficulties could be achieved within
3 hr. No pregnancy-related deaths have been
recorded in the project area since 1975. This is in
contrast to statistics from a nearby non-project vil
lage where, in 1981-83. there were 24.2 maternal
deaths per 1000 women of childbearing age.
One of the common suggestions for extending the
coverage of maternity care services is to train tra
ditional birth attendants (TBAs). since there are
many societies where they still conduct a large pro’These programs have beer, planned in the contexi of the
PM.M collaboration with teams of African researchers.
Implementation began in 1991.
portion of the deliveries. While there may be other
benefits to such training (e.g. reducing the incidence
of tetanus among newborn imams), it does not
address the problem of major obstetric compli
cations. many of which cannot be predicted. For
most major complications, there is little that a TBA
can do in the way of treatment, although existing
trainins prosrams would do well to include more on
first aid measures.
Quality of care
Some of the program options for improving quality
of care have already been mentioned, for instance.
upgrading peripheral facilities to provide obstetric
first aid and even treatment. But there are also actions
that can be taken to improve the services in large
hospitals. For example, in a major teaching hospital
in Nigeria, the obstetric operating theatre has been
closed for more than a year because the anesthesia
equipment needs repair. Consequently, women who
need emergency obstetric surgery have to wait until
they can be operated on in the hospital’s all-purpose
theatre. Reducing Phase III Delay in this case does
not require equipping a whole operating room, it just
requires repairing the available equipment.
As noted in our review, lack of essential supplies is
a common problem in developing countries. Usually,
this is part of much wider economic problems, involv
ing devalued currencies, reduced purchasing power,
poor balance of trade and stringent structural adjust
ment policies. Such issues are. for the most part.
beyond the scope of health programs. Even within
these difficult conditions, however, there is often
something that can be done to reduce their impact. In
an African country. PMM staff have observed a
■people’s store' set up in the courtyard of a large
clinic. This store operates on a revolving fund started
with clinic money. It sells items that are out of stock
in the clinic pharmacy (which depends on the govern
ment’s central store for supplies). The people's store
buys its supplies from merchants in the town at
wholesale prices. Thus, the people’s store saves
patients and their families both time and money.
There are many other options for improving qual
ity of care in health facilities, including training
programs and expanding roles for nurses and mid
wives. The few mentioned above are intended only to
illustrate that relatively simple innovations are poss
ible even under very difficult economic conditions.
Cost
This is one of the most difficult factors for which
to propose program options at any level. In the past
decade, household incomes and purchasing power
have been declining in many countries along with
government spending in general and for health care
in particular. In addition, importing drugs and
supplies requires hard currency, which ~ many
countries must allocate instead to servicing their
debts with foreign banks.
Maternal mortality in context
At the same time, grass roots development contin
ues in the face of these constraints. Farmer-run coop
eratives already allow individuals to pool limited
resources and negotiate a better deal in the market
place. Similarly, a community group, such as a
women’s organization, could use the profits of an
income-generating activity toward the bulk purchase
of generic drugs to stock a local clinic. Such a group
could cooperate with an area hospital toward the same
end. making the drugs available to patients at cost. The
need for creative experimentation and the involvement
of interested nongovernmental organizations is great
and may be the most fruitful direction at present.
Economic educational and women's status
Here again, extensive changes will require policy
changes at a very high level. Policies and measures to
improve women's status, for instance, are being
adopted at the global, national, and local level [109].
The United Nations Convention on the Elimination of All
Forms of Discrimination Against Women is. in effect, an
international bill of rights for women. The convention was
adopted by the United Nations General Assembly in 1979
and by early 1988. it had been ratified by 94 nations [110],
Lasting change lies in the structure of a society and
change must occur at the top as well as at the grass
roots. Thus, people in health programs must put
government proclamations into action, and even an
ticipate them, if necessary, to ensure that women's
status becomes more than a topic at cabinet meetings.
‘Your wife's health is important; look after her' was the
theme for a community education program in northern
Nigeria. Men in the communities targeted were reminded of
the importance of women's health and the need for maternal
care through posters and radio broadcasts. In addition.
separate discussion groups were held with men and women
(most of whom are in purdah). Participants were told about
activities to promote the role of women in development
locally, nationally and globally. Women's health needs were
also discussed and experiences and perceptions of home and
hospital delivery were exchanged [111).
Illness characteristics
The literature reviewed indicated that people's rec
ognition of illness and their perception of its severity
are important influences on the decision to seek care.
From a program point of view, this is an encouraging
finding, because the recognition of danger signs during
pregnancy, labor and delivery can be addressed
through community-level programs. A Senegalese sur
vey revealed that women lacked information about
obstetric complications. In response, the government
of Senegal plans to provide community education on
pregnancy care and obstetric complications through
women's groups [41]. In other countries, lack of infor
mation may not be a problem. Women and their
families could have enough knowledge to seek care in
a timeiy fashion. They may face other obstacles, such
as distance, the cost of services and their inadequate
quality.
HO"
The PMM experience
Many of the practical applications of our con
clusions from the literature review become apparent in
the above discussion. Indeed, several asoects of the
PMM program take their cues from the conclusions we
suggest here. As mentioned earlier, the PMM program
works through a network of teams of researchers and
practitioners in Ghana. Nigeria and Sierra Leone. In
each country, solutions to problems associated with
maternal mortality are different. As a part of their
operations research projects, teams first conducted
situational analyses of health facilities and focus group
research to determine barriers to utilization of services
and areas where the quality of these services may be
improved. The PMM Network's activities to date have
focused attention on hospitals (improving the avail
ability of drugs and supplies, improving hospital man
agement and quality of care), on secondary health
■facilities (expanding and decentralizing provision of
emergency obstetric care, improving staffing and
skills), and finally on communities (improving emer
gency transportation, improving the availability of
blood, providing first aid. and encouraging the early
treatment of complications). The PMM project has
adopted a strategy of meeting the community half
way. feeling that it is counter-intuitive to educate and
motivate the community about seeking emergency
obstetric care until services and accessibility are
adequate.
Although women experience delays beginning with
the decision to seek care, the PMM approach starts at
the other end—with receiving care at the emergency
obstetric care facility. The schematic diagram in Fig. 1
is helpful in pointing out our rationale: all the factors
affecting utilization and outcome of Phase II and III
Delays—distance, transport, roads, cost and quality of
care—are crucial variables in the Phase I decision
making process.
Programs must recognize that even ‘low risk'
women develop obstetric complications, and that
provision of prenatal care, food and vitamin sup
plementation programs, and training of traditional
birth attendants in safe, hygienic birthing practices
may be of limited efficacy. Additional locally relevant
research should be conducted when designing more
community-based interventions, such as involving tra
ditional birth attendants in the reduction of maternal
mortality. Prenatal screening programs, whether these
involve traditional birth attendants or not. may not
bring the benefits they intend to bring, since their
epidemiologic sensitivity has traditionally been
disappointingly low. Also, it is widely assumed that
traditional birth attendants are influential in encour
aging or discouraging patients and their families
from seeking necessary obstetric care: dearly.
more research is needed in this regard. Certainly
research and education efforts should be directed at
decision-makers as thex are identified—e.g. mothersin-law. husbands, religious leaders, etc. The PMM
Sereen Thaddeus and Deborah Maine
I IOS
Network works with community leaders to encourage
their participation as educators, advisors and mobilizers.
CONCLUSIONS
In conclusion, we believe that given large gaps in
the literature regarding factors affecting the utiliz
ation of health services, high priority should be given
to field-based research that can elaborate the factors
leading to delay in different settings by focusing
simultaneously on circumstances facing women in the
community and in the health facility. We believe that
programs to reduce maternal deaths are more likely
to succeed if they are based on gathering data on
these various components and then devising interven
tions that will address them.
The next step is thus for people involved in the Safe
Motherhood Initiative to assess the situation in their
respective regions and implement program options
based on their findings. We also urge people to
evaluate their interventions: only if programs are
systematically evaluated will we be able to say
whether they were effective in reducing delay.
We hope that this article encourages a fresh per
spective on the prevention of deaths among women
with obstetric complications.
Acknowledgements—This monograph is the result of a team
effort, and the contribution of several individuals must be
acknowledged. Sharon Stash was the driving force behind
the literature review in its early stages. As graduate research
assistants with the program. Sheryl McCurdy. Voahangi
Ravao, Jack Kjlcullen. Pamela Skripak, Laura Sanders and
Schuyler Frautschi contributed their valuable skills at
various stages.
We greatly appreciate comments on various drafts of this
paper from Angela Kamara. Joe Wray. James Allman.
Norman Weatherby and Allan Rosenfield of Columbia
University and Annette Ramirez of Hunter College.
We especially thank James McCarthy, director of CPFH.
for the time he took to comment on and discuss several
drafts.
We would also like to thank Ana Pagan for production
assistance and Mary button O’Connor for copy editing.
Finally, we must express our immense gratitude to fhe
Carnegie Corporation of New York for their financial
support and for the inspiration provided by Drs
Adetokunbo Lucas and Patricia Rosenfield.
REFERENCES
Abou Zahr C. and Royston E. Maternal Mortality: A
Global Factbook. World Health Organization. Geneva.
1991.
2.
Rosenfield A. and Maine D. Maternal Mortality—A
Neglected Tragedy: Where is the ’M' in ’MCH’? The
Lancet. 2. 83-85. 1985.
3.
Starrs A. Preventing the Tragedy of Maternal Deaths:
A Report of the International Safe Motherhood Confer
ence. Nairobi. Kenya. Feb. 1987.
4.
Maine D. Safe Motherhood Programs: Options and
issues. Center for Population and Family Health.
Columbia University. Neu York. 1991.
5.
World Health Organization. Prevention of Maternal
Mortality: Report of a World Health Organization
1.
Interregional
6.
Meeting.
11-15
November.
1985.
Geneva. 1986.
Frederiksen H. S. et al. Epidemographic Surveillance:
A Symposium. Monograph No. 13. Carolina Popu
lation Center. University of North Carolina. Chapel
Hill. 1970.
Freeman D. H. Jr et al. A categorical analysis of
contacts with the family health clinic. Calabar, Nige
ria. Soc. Set. Med. 17, 571, 1983.
8.
Lennox C. E. Assessment of obstetric high risk factors
in a developing country. Tropical Doctor. July. 125.
1984.
9.
Roghmann K. J. and Zastowny T. R. Proximity as a
factor in the selection of health care providers: emer
gency room visits compared to obstetric admissions
and abortions. Soc. Sci. Med. 13, 61, 1979.
10.
Stock R. Distance and the utilization of health facili
ties in rural Nigeria. Soc. Sci. Med. 17, 563, 1983.
11.
Orubuloye I. 6. and Caldwell J. C. The impact of
7.
public health services on mortality: a study of mor
tality differentials in a rural area of Nigeria. Popul.
Stud. 29. 259. 1975.
12.
Egunjobi L. Factors influencing choice of hospitals: a
case studv of the northern part of Oyo State, Nigeria.
Soc. Sci.'Med. 17, 585, 1983.
Habib O. S. and Vaughan J. P. The determinants of
health services utilization in southern Iraq: a house
hold interview survey. Ini. J. Epidemiol. 15, 395, 1986.
14.
Rahaman M. et al. A diarrhea clinic in rural
Bangladesh: Influence of distance, age, and sex on
attendance and diarrheal mortalitv. Am. J. Publ. Hlth
72, 1124, 1982.
15.
Williams R. Meningitis and unpaved roads. Soc. Sci.
Med. 24, 109, 1987?
13.
Annis S. Physical access and utilization of health
services in rural Guatemala. Soc. Sci. Med. 15, 515.
1981.
17.
Airey T. The impact of road construction on hospital
in-patient catchments in the Meru District of Kenva.
Soc. Sci. Med. 29, 95. 1989.
18.
Young J. C. Non-use of physicians: Methodological
approaches, policy implications, and the utility of
decision models. Soc. Sci. Med. 15, 499, 1981.
19.
Nnadi E. E. and Kabat H. F. Choosing health care
services in Nigeria: A developing nation. J. Trop. Med.
Hyg. 87. 47. 1984.
20.
Kloos H. et al. Illness and health behavior in Addis
Ababa and rural central Ethiopia. Soc. Sci. Med. 25,
1003. 1987.
21.
Yoder R. Are people willing and able to pay for health
services? Soc. Sci. Med. 29, 35. 1989.
22.
Ekwemou C. C. et al. Structural adjustment and health
in Africa. The Lancet 336, 56-57, 1990.
23.
Auerbach L. S. Childbirth in Tunisia: Implication of a
decision-making model. Soc. Sci. Med. 16. 1499. 1982.
24.
Lasker J. N. Choosing among therapies: Illness behav
ior in the Ivory Coast. Soc. Sci. Med. 15, 157. 1981.
25.
Abu-Zeid H. A. H. and Dann W. M. Health services
utilization and cost in Ismailia. Egypt. Soc. Sci. Med.
21. 451. 1985.
26.
Dor A. and Van der Gaag J. The Demandfor Medical
Care in Developing Countries: Quantity Rationing in
Rural Cote d'Ivoire. Living Standards Measurement
Study Working Paper No. 35, The World Bank.
Washington. D.C. 1988.
27.
Foster G. Medical anthropology and international
health planning. Soc. Sci. Med. 11. 527. 1977.
28.
Ivun F. Hosnnal service areas in Ibadan Citv. Sor. Sci.
Med. 17. 601. 1983.
29.
Mwabu G M. Health care decisions at the household
level: Results of a rural health survev in Kenva. Soc.
Sci. Med. 2. 315. 1986.
30.
Finerman R. D. Experience and expectation: conflict
16.
Maternal mortality in context
and change in traditional family health care among the
Quichua of Saraguro. Soc. Set. Med. 17, 1291, 1983.
31.
Wedderbum M. and Moore M. Qualitative Assessment
of Attitudes Affecting Childbirth Choices of Jamaican
Women. MotherCare Project Working Paper: 5, Nov.,
1109
fistula in northern Nigeria. J. Biosoc. Sci. 13. 139.
1981.
Tahzib F. Epidemiological determinants of vesicovagi
nal fistulas. Br. J. Obstetrics Gynaec. 90, 387. 1983.
54.
Alauddin M. Maternal mortality in rural Bangladesh:
the Tangail district. Stud. Fam. Planning 17, 13. 1986.
1990.
Khan A. R. et al. Maternal mortality in rural
32.
Sargent C. F. Maternity. Medicine and Power: Repro 55.
Bangladesh: The Jamalpur District. Stud. Fam. Plan
ductive Decisions in Urban Benin. University of Califor
ning 17, 7, 1986.
nia Press, Berkeley, 1989.
Kwast B. et al. Report on maternal health in Addis
33.
Sargent C. Obstetrical choice among urban women in 56.
Ababa September 1981-Septcmber 1983. Sponsored by
Benin. Soc. Set. Med. 20, 287, 1985.
the Swedish Save the Children Federation. Addis
34.
Harrison K. A. Obstetric fistula: One social calamity
Ababa. Ethiopia. 1984.
too many (commentary). Br. J. Obstetrics Gynaecol.
57.
Mhango C., Rochat R. and Arkutu A. Reproductive
90.
385, 1983.
mortalitv in Lusaka, Zambia, 1982-1983. Stud. Fant.
35.
Chavez L. R., Cornelius W. A. and Jones O. W.
Planning 17, 243. 1986.
Utilization of health services by Mexican immigrant
58.
Abbas A. A. and Walker G. J. A. Determinants of the
women in San Diego. Women Hhh 11, 3. 1986.
utilization of maternal and child health services in
36.
Ityavyar D. A. A traditional midwife practice, Sokoto
Jordan. Int. J. Epidemiol. 15, 404, 1986.
State, Nigeria. Soc. Sci. Med. 18, 497, 1984.
Cosminsky S. and Scrimshaw M. Medical pluralism
37.
Feierman E. K. Alternative medical services in rural 59.
on a Guatemalan plantation. Soc. Sci. Med. 14, 267.
Tanzania: a physician’s view. Soc. Sci. Med. 15, 399,
1981.
1981.
Abasiekong E. M. Familism and hospital admission in
38.
Bamisaiye A. Selected factors influencing the coverage 60.
rural Nigeria: a case study. Soc. Sci. Med. 15. 45. 1981.
of an MCH clinic in Lagos, Nigeria. J. Trop. Pediat.
61.
Murthv N. Reluctant patients-the women of India.
30, 256, 1984.
• Leslie J. and Rao Gupta G. Utilisation of Formal
Wld Hlth Forum 3. 315. 1982.
62.
Sich D. Traditional concepts and customs in preg
Services for Maternal Jiutrition and Health Care in the
nancy. birth and postpartum period in rural Korea. In
Third World. International Center for Research on
Traditional Birth Practices: An Annotated Bibliography
Women, Washington, D.C., 1989.
40.
Stein C. M. and Muir J. The causes of delayed
(Edited by Edouard L. and Foo-Gregory L. H.).
diagnosis of cancer of the cervix in Zimbabwe. Cent.
World Health Organization, Geneva, 1985.
63.
Cook R. Current knowledge and future trends in
Afr. J. Med. 32, 29, 1986.
41.
Dia A. et al. Maternal mortality in Senegal: contribut
maternal and child health in the Middle East. J. trop.
ing factors in the health system and the community.
Pediat. 33. 3 1987.
64.
Glik D. C., Parker K. and Hetegikamana G. M. B.
Draft report. 1989.
42.
Sharp K.., Ross C. E. and Cockerham W. C. Symp
Integrating qualitative and quantitative survey tech
toms, beliefs, and the use of physician services among
niques. Int. Q. Community Hlth Educ. 7, 181. 1986—87.
the disadvantaged. J. Hhh Soc. Behavior 24, 255, 1983.
65.
Hossain M. M. and Glass R. Parental son preference
43.
Tanner J. L.. Cockerham. W. C. and Spaeth J. L.
in seeking medical care for children less than five years
Predicting phvsician utilization. Med. Care 21, 360,
in a rural community in Bangladesh. Am. J. publ. Hlth
1983.
78,
1349, 1988.
44.
Zola I. K. Culture and symptoms: an analysis of 66.
Chen L.. Huq E. and D'Souza S. Sex bias in the family
patients’ presenting complaints. Am. Social. Rev. 31-,
allocation of food and health care in rural Bangladesh.
615. 1966.
Pop. Dev. Rev. 7, 55. 1981.
45.
Peterson K. J. Brong midwives and women in 67.
Royston E. and Armstrong S. Preventing Maternal
childbirth: Management of uncertainty in a division
Deaths. World Health Organization. Geneva. 1989
A of labor. In Traditional Birth Practices: An Annotated
68.
van de Walle F. and Ouaidou N. Status and fertility
■ Bibliography (Edited by Edouard L. and Foo-Gregory
among urban women in Burkina Faso. Int. Fam.
L. H.). World Health Organization. Geneva, 1985.
Planning Perspectives 11, 60. 1985.
46.
Sargent C. Utilization of national health maternity 69.
The prevention of maternal mortality network, bar
services in a northern district of People’s Republic of
riers to treatment of obstetric emergencies in rural
Benin. Rural Africana Fall-Winter, p. 77. 1980-81.
communities of West Africa. Stud. Fam. Planning 23,
47.
Kargbo T. K. Certain practices related to delivery. In
279-291, 1992.
Traditional Birth Practices: An Annotated Bibliography
70.
Favin M., Bradford B. and Cebula D. Improving
(Edited by Edouard L. and Foo-Gregory L. H.j.
Maternal Health in Developing Countries. World Fed
World Health Organization. Geneva, 1985.
eration of Public Health Associations. Washington.
48.
Marshall R. et al. Traditional practices affecting the
D.C., 1984.
health of women and children in Liberia. In Traditional
71.
Rundall T. G. and Wheeler J. R. C. The effect of
Birth Practices: An Annotated Bibliography (Edited by
income on use of preventive care: An evaluation of
Edouard L. and Foo-Gregory L. H.). World Health
alternative explanations. J. Hlth Soc. Behavior 20, 397.
Organization. Geneva. 1985.
1979.
49.
Mutambirwa J. Pregnancy and childbirth among the 72.
Bhatia J. C. A study of maternal mortality in AnanthaShona of Zimbabwe. In Traditional Birth Practices: An
pur District. Andhra Pradesh. India. Unpublished
Annotated Bibliography (Edited by Edouard L. and
paper. 1986.
Foo-Gregory L. H.). World Health Organization.
73. Kwast B. E. Epidemiology of maternal mortality in
Geneva. 1985.
Addis Ababa: a community-based study. Paper pre
50.
Bleek W. Induced abortion in a Ghanaian family.
sented at the World Health Organization Interregional
African Studies Rev. 11. 103. 1978.
Meeting on the Prevention of Maternal Mortality.
51.
Figa-Taiamanca I et al. Illegal abortion: an attempt
Geneva. 11-15 Nov.. 1985.
to assess its cost to the health services and ns
'4. Kwast B. E. and Liff J. M. Factors associated with
incidence in the communitt. Int. J. Hhh Sen. 16. 375.
maternal mortality in Addis Ababa. Ethiopia. Int. J.
1986.
Epidemiol. 17, 115. 1988.
-2. Murphy M. Social consequences of vesico-vaginal
75.
Okafor S. 1. Factors affecting the frequency of hospital
53.
1110
Sereen' Thaddeus and Deborah Mai.<e
trips amonz a predominantly rural population. Soc.
Sci. Med. 17. 591. 1983.
76.
Caldwell J. C. Education as a factor in mortality
decline: An examination of Nigerian data. Popul. Slud.
33, 395, 1979.
77.
Caldwell J. C. and Caldwell P. Education and literacy
as factors in health. In Good Health and Low Cost
(Edited by Halstead S. B., Warren J. A. and Walsh
K. S.). The Rockefeller Foundation, New York. 1985.
78.
Cleland J. G. and van Ginneken J. K. The search for
pathways of influence. Soc. Sci. Med. 27, 1357, 1988.
79.
Wong E. L. et al. Accessibility, quality of care and
prenatal care use in the Philippines. Soc. Sci. Med. 24,
927, 1987.
80.
Bullough C. H. W, Letter to the editor. Br. J. Ob
stetrics Gynecol. 96, 1119, 1989.
81.
Voorhoeve A. M., Kars C. and van Ginneken J. K.
Modem and traditional antenatal and delivery care. In
Maternal and Child Health in Rural Kenya (Edited by
van Ginneken J. K. and. Muller A. S.), p. 309. Croom
Helm, London, 1984.
82.
Fathalla M. F. Assignment Report Maternal Health in
Syria, December 19-29. 1982. World Health Organiz
ation, Geneva. 1983.
83.
Cardoso U. F. Maternal mortality in Cuba. Paper
presented at the World Health Organization Inter
regional Meeting on the Prevention of Maternal Mor
tality, Geneva, 11-15 Nov., 1985.
84.
Young J. C. and Garro L. Y. Variation in the choice
of treatment in two Mexican communities. Soc. Sci.
Med. 16, 1453, 1982.
85.
World Health Organization. Safe Motherhood Confer
ence. Nairobi, Kenya, 10-13 Feb., 1987.
86.
Fortney J. A.. Susant I.. Gadalla S. er al. Reproductive
mortality in two developing countries. Am. J. Publ.
Hlth 76, 131, 1986.
87.
Mtimavalye L. A., Justesen A. and Ngwalle E. Survey
on institutional maternal deaths in four regions of
Tanzania, July 1983-December 1984. Preliminary re
port, unpublished. 1984.
88.
Hickey M. U. and Kasonde J. M. Maternal mortality
at University Teaching Hospital, Lusaka. Med. J.
Zambia 11, 74, 1977.
89.
Price T. G. Preliminary report on maternal deaths in
the South Highlands of Tanzania in 1983. J. Obstetrics
Gvnecol. East Central Africa 3, 103, 1984.
90.
Schulpen T. W. J. and Swinkels W. J. A. M. The
utilization of health services in a rural area of Kenva.
Trap. Geogr. Med. 32, 340, 1980.
91.
Chen R.-J. Maternal mortality in Shanghai, China.
Paper presented at the World Health Organization
Interregional Meeting on the Prevention of Maternal
Mortality, Geneva, 11-15 Nov., 1985.
92.
Dervisoglu A. Maternal mortality in Turkey. Paper
presented at the World Health Organization Interre
gional Meeting on the Prevention of Maternal Mor
tality, Geneva, 11-15 Nov., 1985.
93.
Lingmei Z. and Ding H. Analysis of the causes of
maternal death in China. Bull. Wld Hlth Org. 66, 387,
1988.
94.
95.
Kwast B. E.. Rochat R. W. and Kidane-Mariam W.
Maternal mortality in Addis Ababa, Ethiopia. Stud.
Fam. Planning 17, 288. 1986.
Tahzib F. College of Health Sciences, University of
Sokoto, Nigeria, personal communication. 21 Mar..
1989.
Rodriguez J. et al. Avoidable mortality and maternal
mortality in Cali, Columbia. Paper presented at the
World Health Organization Interregional Meeting on
the Prevention of Maternal Mortality, Geneva. 11-15
Nov., 1985.
97.
Institute for the Protection of Mother and Newborn.
Maternal mortality in selected areas of Vietnam. Paper
presented at the World Health Organization Interre
gional Meeting on the Prevention of Maternal Mor
tality, Geneva, 11-15 Nov., 1985.
98.
Walker G. J. A. et al. Maternal mortality in Jamaica:
A confidential inquiry into all maternal deaths in
Jamaica 1981-1983. Paper presented at the World
Health Organization Interregional Meeting on the Pre
vention of Maternal Mortality, Geneva, 11-15 Nov.,
1985.
99.
World Health Organization. Essential obstetric func
tions at first referral level to reduce maternal mortality.
Report of a Technical Working Group. Geneva, 23-27
June, 1986.
100.
Stein C. M., Gelfand M. and MacDougall C. N.
Cancer of the colon and rectum in Zimbabweans. Cent.
Afr. J. Med. 31, 88, 1985.
101.
Aggarwal V. P. Obstetric emergency referrals to
Kenyatta National Hospital. E. Afr. J. Med. SI, 144,
1980.
102.
Bullough C. H. W. Analysis of maternal deaths in the
central region of Malawi. E. Afr. Med. J. 58, 25, 1981.
103.
Okafor L. A.. Orhue A. and Sahu B. B. Blood
transfusion in obstetrics and gynaecology: pattern,
problems and prospects. E. Afr. Med. J. 63, 63,
1986.
104.
Megafu U. Factors influencing maternal survival in
ruptured uterus. Int. J. Gynaecol. Obstetrics 23, 475,
1985.
105.
Klufio C. A., Ardayfio S. A. W„ Nartey I. N. and Kissi
S. A. Y. A retrospective survey of caesarean sections
at Korle Bu Teaching Hospital, Accra. 1971: A review
of 1077 cases. Ghana Med. J. 12, 142. 1973.
106.
Qjo V. A.. Adetoro O. O. and Okwerekwu F. E. O.
Characteristics of maternal deaths following cesarean
section in a developing country. Int. J. Gynaecol.
Obstetrics 27, 171, 1988.
107.
Cardoso U. F. Giving birth is safer now. Wld Hlth
Forum 7, 348, 1986.
108.
Lamb W. H. et al. Changes in maternal and child
mortality rates in three isolated Gambian villages over
ten years. Lancet 20 Oct., p. 912, 1984.
109.
Communique in the New Nigerian, 13 Nov., 1989.
110.
Byrnes A. Convention on the Elimination of All Forms
of Discrimination Against Women. 7th CEDAW/
WRAW Report, 1988.
111.
Activity report submitted to the International
Women’s Health Coalition.
96.
Page 1 of 9
ADVANCE UNEDITED VERSION
Committee on the Elimination of Discrimination
against Women
Twenty-second session
17 January-4 February 2000
Consideration of reports of States parties
India
Initial report
1. The Committee considered the initial report of India (CEDAW/C/IND/1)
at its 452nd, 453rd and 462nd meetings, on 24 and 31 January 2000
(CEDAW/C/SR.452, 453 and 462).
(a) Introduction by the State party
2. The representative informed the Committee that India had ratified the
Convention in July 1993 with two declarations and one reservation. She
indicated that the preparation of the report had been preceded by wideranging consultations with a number of women’s organizations. She noted
that India had ratified a number of international human rights instruments
and that the Indian Constitution prohibited discrimination on the basis of
sex, as well as providing for affirmative action for women. India had
initiated a consultative process in preparation for the Fourth World
Conference on Women and was among the first countries to unreservedly
accept the Beijing Platform for Action.
3. The representative indicated that among recent achievements in the
implementation of the Convention had been the establishment in March
1997 of a parliamentary committee on empowerment of women, and the
passage of constitutional amendments to reserve for women 33.33 per cent
of the seats in the Panchayati Raj institutions at the local self-government
level in rural areas and municipalities in urban areas. She also stated that a
bill had been introduced in late 1999 which would reserve not less than one
third of the total numbers of seats filled by direct elections in the LokSabha
(House of the People) and State Legislative Assemblies for women.
4. The representative described the national machinery for women’s
advancement coordinated by the Department of Women and Child
Development, which is headed by a cabinet minister assisted by a minister
of state. The National Commission for Women, established in 1992, served
Page 2 of 9
as a statutory ombudsperson for women, while the Central Social Welfare
Board networked with nearly 12,000 women’s NGOs. Institutional
mechanisms for women’s advancement also existed at state level. The
representative highlighted the ninth five-year plan (1997-2002), which had
identified the empowerment of women as a strategy for development and
mandated early finalization of a national policy on empowerment of
women. She indicated that pending the adoption of the national policy,
many mechanisms identified therein had already been put in place.
Recently, the Prime Minister’s Office had directed that a review be made of
the impact of gender mainstreaming in ministries and departments.
5. The representative indicated that progressive legislation to promote the
interests of women existed at both state and central levels, and that the
Government had tasked the National Council of Women to oversee the
implementation of constitutional and legal safeguards for women. The
review of 39 laws was under way; recommendations for amendments,
including those with regard to the Immoral Traffic (Prevention) Act, had
been submitted; and a draft bill on violence against women had been
prepared. Lok adalats (people’s courts) and parivarik mahila lok adalats
(family women’s courts) had been established to provide less formal
systems of justice delivery. India had a tradition of public interest litigation
and the Supreme Court had issued landmark judgements, including on
sexual harassment at the work place and child prostitution. Several training
institutes had also introduced gender sensitization training for judicial
officials.
6. The representative described steps which had been taken to revise
curricula and textbooks from a gender perspective, and the efforts of the
Ministry of Information and Broadcasting to ensure projection of positive
images of women in the media. Measures to address prostitution and
trafficking in women had included a proposal to amend the Immoral Traffic
(Prevention) Act to widen its scope and increase penalties; the appointment
of special police officers; and the establishment of protective homes and
child development and child-care centres for the children of sex workers. A
plan of action to combat trafficking and commercial sexual exploitation of
women and children and to integrate victims into society had been
developed, and India had actively participated in the drafting of the South
Asian Association for Regional Cooperation (SAARC) Convention on
Preventing and Combating Trafficking in Women and Children for
Prostitution.
7. The representative indicated that at the Fourth World Conference on
Women, India had committed itself to increasing investment in education to
6 per cent of gross domestic product (GDP), but that target had not been
achieved to date although the overall growth in literacy among women had
been higher than that of men in recent years. Intensive efforts to address
gender differentials in literacy and education were continuing, and included
the establishment of girls’ learning centres in order to meet the needs of
girls who were unable to access formal education.
8. The representative informed the Committee that International Labour
Organization (ILO) standards were reflected in Indian labour laws and the
Page 3 of 9
Government had been seeking to extend maternity benefits to all women,
and to provide child care for working women. Guidelines for employers
with respect to sexual harassment had been established in a Supreme Court
judgement, and legislation reflecting those guidelines was being prepared.
Efforts to recognize women’s work in the informal sector and reflect it in
the national census and to provide workers in the sector with labour
protection had been initiated.
9. Significant improvements in women’s health had been achieved in the
last decade, although the high maternal mortality ratio remained a concern.
The recently launched reproductive and child health programme sought to
address women’s health in a holistic manner. Measures to address
HIV/AIDS had been introduced and legislative and other strategies to
confront female infanticide and sex-selective abortion had also been
adopted.
10. The representative indicated that rural women constituted almost 80 per
cent of the female population, and the Government had introduced quotas
and women specific schemes to ensure that they received an equal share in
rural development and agricultural programmes.
11. The major religious communities’ personal laws had traditionally
governed marital and family relations, with the Government maintaining a
policy of non-interference in such laws in the absence of a demand for
change from individual religious communities. However, the Family Courts
Act, providing that family matters, such as marriage and maintenance, came
within the jurisdiction of the family courts, which incorporated informal
procedures and counselling services, had been adopted. The representative
drew attention to legislation concerning dowry-related violence and the
provision of the Penal Code and Evidence Act regarding cruelty to a wife
by her husband or his relatives.
12. In conclusion, the representative emphasized India’s determined,
concrete and sustained efforts to eliminate poverty and social disability and
empower the poor and vulnerable.
(b) Concluding comments of the Committee
Introduction
13. The Committee welcomes the submission of the initial report of India.
While noting that the report conforms to the Committee’s guidelines, it
does not provide adequate information relating to implementation of some
articles and the general issue of violence against women. The Committee
further notes that the report was submitted with some delay. The report also
does not contain information on measures taken to implement the Beijing
Platform for Action. The Committee appreciates the detailed written and
oral responses of the delegation during the consideration of the report,
which provided important additional information.
Page 4 of 9
14. The Committee notes that the report and the oral and written responses
do not provide adequate statistical data, disaggregated by sex and the States
of the Union, and information on the implementation of affirmative action
measures for scheduled castes.
15. The Committee notes with concern that the Government does not intend
to review the declarations entered to article 16(1) and 16(2) of the
Convention.
Positive aspects
16. The Committee recognizes that India has guaranteed in its Constitution
fundamental human rights that can be enforced by an application to the
Supreme Court. The Committee commends in particular the recognition of
a fundamental right to gender equality and non-discrimination, and a
specific enabling provision on affirmative action in the Constitution.
17. The Committee appreciates the contribution made by the Supreme
Court of India in developing the concept of social action litigation and a
jurisprudence integrating the Convention into domestic law by interpreting
Constitutional provisions on gender equality and non-discrimination.
18. The Committee commends the introduction of a range of policies and
programmes by the Government of India over the last years to improve the
situation of women. It notes with appreciation that those programmes have
contributed to some extent to improving the quality of social indicators for
women in various states of the union. The Committee welcomes the
proposal to formulate a new gender empowerment policy and the directives
sent from the Prime Minister’s office to mainstream gender issues and a
rights approach to development at the national level.
19. The Committee commends the Government of India for establishing the
National Commission for Women and state commissions for women with
responsibility for developing action plans on gender and proposals for law
reform.
20. The Committee commends the Government for introducing affirmative
action measures that have enabled 33 per cent of seats in local government
bodies to be reserved for women. It welcomes the proposed bill to reserve
33 per cent seats in state and national assemblies for women, and the
assurance in the oral presentations that 30-40 per cent coverage will be
provided for women in programmes that give access to credit.
21. The Committee commends the Government for introducing legislation
that has banned sex-selective abortions. It welcomes the amendments to the
law on nationality, which confer equal rights on men and women.
Page 5 of 9
Factors and difficulties affecting the implementation of the
Convention
22. The Committee notes that India has a very large and mainly rural
population living in absolute poverty and that feminization of poverty and
growing income disparities prevent the advantages of economic
development being transferred to women.
23. The Committee considers that widespread poverty, such social practices
as the caste system and son preference, as reflected in a high incidence of
violence against women, significant gender disparities and an adverse sex
ratio, present major obstacles to the implementation of the Convention.
24. The Committee notes that the existence of regional disparities is an
impediment to the effective implementation of the Convention.
Principal areas of concern and recommendations
25. The Committee notes that the Convention and the Beijing Platform for
Action have not been integrated into policy planning and programmes.
While there have been several national plans in the pre and post-Beijing
period, the Committee notes that these adopt a welfare approach toward
women.
26. The Committee recommends that the proposed gender empowerment
policy integrate the Convention and the Beijing Platform of Action and a
rights-based approach.
27. The Committee considers that inadequate allocation of resources for
women’s development in the social sector and inadequate implementation
of laws are serious impediments to the realization of women’s human rights
in India.
28. The Committee urges the allocation of sufficient and targeted resources
for women’s development in the social sector, as well as full
implementation of relevant laws.
29. The Committee notes that there are many gaps in the legislative
framework. The Committee considers that there is an urgent need to
introduce comprehensive legislative reform to promote equality and the
human rights of women.
30. The Committee recommends that proposals of the National Commission
of Women on law reform be used in preparing new legislation, and that the
Commission be entrusted with the task of developing working papers on
legal reform in critical areas, within a time-frame.
31. The Committee notes that steps have not been taken to reform the
personal laws of different religious and ethnic groups in consultation with
Page 6 of 9
them so as to conform with the Convention. The Committee is concerned
that the Government’s policy of non-intervention perpetuates sexual
stereotypes, son preference and discrimination against women.
32. The Committee urges the Government to withdraw its declaration to
article 16 (1) of the Convention and to work with and support women’s
groups as members of the community in reviewing and reforming these
personal laws. The Committee also calls upon the Government to follow the
directives principles in the Constitution and Supreme Court decisions and
enact a uniform civil code which different ethnic and religious groups may
adopt.
33. The Committee is concerned that India has not yet established a
comprehensive and compulsory system of registration of births and
marriages. The Committee notes that inability to prove those important
events by documentation prevents effective implementation of laws that
protect women and girls from sexual exploitation and trafficking, child
labour and forced or early marriage. The Committee is also concerned that
failure to register marriages may also prejudice the inheritance rights of
women.
34. The Committee calls _.upon the Government to provide adequate
resources and establish a system of compulsory registration of births and
monitor implementation in cooperation with women’s groups and local
bodies. It urges the Government to withdraw the reservation to article 16(2)
of the Convention.
35. The Committee is concerned that the fundamental right to education
under the Constitution recognized by the Supreme Court has not been
realized by providing girls with equal access to primary and secondary
education. It notes that budgetary allocation for education is still far below
India’s commitments with regard to the Beijing Platform for Action.
36. The Committee urges the Government to take affirmative action, set a
time-frame and provide adequate resources for primary and secondary
education so as to give girls equal access to education and eradicate adult
illiteracy among women. It calls upon the Government to make primary and
secondary education compulsory by introducing and enforcing relevant
regulations.
37. The Committee is concerned that the fundamental rights recognized in
the Constitution can be enforced only against state actors and in the event
of inaction on the part of the state. It also notes that the private sector,
where a great number of women are employed and which is expanding in a
period of transition to market economic policies, is not covered by
Constitutional standards.
38. The Committee recommends that a sex discrimination act be introduced
to make the standards of the Convention and the Constitution applicable to
non-state action and inaction.
39.
The Committee is concerned that there is a high incidence of gender
Page 7 of 9
based violence against women, which takes even more extreme forms
because of customary practices, such as dowry, sati and the devadasi
system. Discrimination against women who belong to particular castes or
ethnic or religious groups is also manifest in extreme forms of physical and
sexual violence and harassment.
40. The Committee urges the Government to implement existing legislation
prohibiting such practices as dowry, devadasi and caste-based
discrimination. It calls upon the Government to strengthen law enforcement
and introduce reforms proposed by the National Commission on Women
and women activists in regard to the law on rape, sexual harassment and
domestic violence.
41. The Committee recommends that a national plan of action be developed
to address in a holistic manner the issue of gender-based violence, in line
with the Committee’s general recommendations 19 and 24. It calls upon the
Government to provide statistics and information on violence against
women in its next report.
42. The Committee is concerned that women are exposed to the risk of high
levels of violence, rape, sexual harassment, humiliation and torture in areas
where there are armed insurrections.
43. The Committee recommends a review of prevention of terrorism
legislation and the Armed Forces Special Provisions Act, in consultation
with the Human Rights Commission, the National Commission of Women
and civil society, so that special powers given to the security forces do not
prevent the investigation and prosecution of acts of violence against women
in conflict areas, and during detention and arrest. The Committee
recommends that women be given an opportunity to make their
contribution to peaceful conflict resolutions.
44. The Committee recommends the introduction of gender sensitization
and human rights programmes for the police, the security forces and
medical professionals, in addition to programmes already undertaken.
45. The Committee is concerned with the continuing discrimination,
including violence, suffered by women of the Dalit community, despite the
passage of the Scheduled Castes and Scheduled Tribes (Prevention of
Atrocities) Act of 1989.
46. The Committee urges the Government to enforce laws preventing
discrimination against Dalit women and prohibiting the devadasi system. It
urges the Government to introduce affirmative action programmes in such
areas as education, employment and health so as to provide life chances to
Dalit women and girls and create an environment conducive to their
progress. The Committee calls upon the Government to set a time-frame for
those interventions and provide information on the progress made in the
next report.
47. The Committee is concerned that women and girls are exploited in
prostitution and inter-state and cross-border trafficking. It is also concerned
Page 8 of 9
that those women are exposed to human immunodeficiency virus/acquired
immunodeficiency syndrome (HIV/AIDS) and health risks and that existing
legislation encourages mandatory testing and isolation.
48. The Committee calls upon the Government to review existing
legislation on trafficking and forced prostitution and to strengthen law
enforcement. It recommends the development of bilateral and inter-state
controls and reintegration and advocacy programmes to prevent the
exploitation of women and girls in forced prostitution and trafficking.
49. The Committee notes with concern that maternal mortality rates and
infant mortality rates are among the highest in the world. It also notes the
adverse sex ratio and the incidence of sex-selective abortions due to son
preference despite the law banning that practice. It notes that family
planning is only targeted for women.
50. The Committee recommends the adoption of a holistic approach to
women’s health throughout the life cycle in the country’s health
programme. It urges the Government to allocate resources from a "women’s
right to health" perspective, following the guidelines of the Committee’s
general recommendation 24. The Committee calls upon the Government to
elicit the support of medical associations in enforcing professional ethics
and preventing sex-selective abortions. The Committee also recommends
that the Government obtain the support of the medical profession in
creating awareness on the urgent need to eliminate practices associated with
son preference.
51. The Committee is concerned with the low participation of qualified
women in the administration and the judiciary, including family courts and
lok adalats or conciliation tribunals.
52. The Committee urges the Government to take affirmative action to
increase women’s participation in the judiciary and lok adalats, and provide
gender-disaggregated data in its next report.
53. The Committee is concerned with significant disparities in economic
activity rates for men and women. It is concerned that the practice of debt
bondage and the denial of inheritance rights in land result in gross
exploitation of women’s labour and their impoverishment.
54. The Committee requests the Government to enforce laws on bonded
labour and provide women with self-employment opportunities and
minimum wages in home-based production and the non-formal sector. It
calls upon the Government to review laws on inheritance urgently and to
ensure that rural women obtain access to land and credit.
55. The Committee is concerned that the National Commission on Women
has no power to enforce its proposals for law reform or intervene to prevent
discrimination in the private or public sector. It notes that the National
Commission and state commissions are not supported by adequate financial
and other resources. It also notes that the National Commission on Women
is not as well resourced or as empowered as the Human Rights Commission
Page 9 of 9
of India, and that it has no formal link with the state women’s commissions.
56. The Committee recommends that NGOs be represented on the National
Commission of Women. The Commission’s powers should be as wide as
those of the Human Rights Commission and include a complaints
procedure. The Committee recommends that state commissions be placed
on a legal basis, be established in all States, and strengthened and linked
with the National Commission.
.
57. The Committee is concerned that despite the willingness of the
Government to work with NGOs and women’s groups women activists and
human rights defenders are exposed to violence and harassment in the
communities in which they work.
58. The Committee urges the Government to strictly enforce the law and
protect women activists and human rights defenders from, acts of violence
and harassment.
The Committee encourages India to deposit its acceptance of the
amendment to article 20, paragraph 1, of the Convention concerning
the Committee’s meeting time.
60. The Committee urges the Government to sign and ratify the Optional
Protocol to the Convention as soon as possible.
59.
61. The Committee requests that the Government responds in its next
periodic report to the specific issues raised in its concluding comments.
62. The Committee encourages the wide dissemination in India of the
present concluding comments in order to make the people, civil society and
Government sectors aware of the steps that have been taken to ensure de
jure and de facto equality of women, as well as further steps that are
required in that regard. It also requests the Government to disseminate
widely in all local languages the Convention, its Optional Protocol, the
Committee’s general recommendations and the Beijing Declaration and
Platform for Action.
Concepts on Comprehensive Health Care of
The Community specialy women and Children.
1.
The Health Care system should be tpwards positive and
correctional rather than on the curative approach.
2
The
system
looks
at
the
root
of
the
problem,seen, observed,or even discussed rathan at the
problem per -se.
3.
Realisation of the fact that the system should be
location specific and the programme to be reliable and
acceptable to the community.
4
Helath care is not to be considered as a temporary
measure but should be treated as_ a-continued effort
towards the Human development.
5
This calls for the effor to involve the community at
the time of planning itself,promote organisations of
the peopleto take charge of their Health and gradually
reduce the dependency on the Government alone.
6.
To have a "sustained health" it necessarily should
have lonkages horizontally which also effect or affect
the health status in a community,food production
hygiene safe drinking water environmental situation
are such linkages.
7
In order to have an action plan for the activities the
health educational level of the community is vital
8
The groups which take the responsibility need to plan
a system to maintan as an integral part of system
9
Within the overall efforts thespecial needs of the
section of the community need to be attended to in
endemic areas like malaria,goitre fluorosis and others
7.
The growth of children in the community should be the
indicator on the health status within the community.'
NUTRITION:
1.
Children in the age of 7 months and 2 requires
nutritional supplements as the foundation of Health.
2.
I rrespective of the fact whether a group requires are
not all the children in the community need to be
involved in the programme
3.
Designining a diet with local foods have more chances
of the chil receiving the food and accepting it.
-24
One hot meal need to be provided for the infants and
pre-schoolers .in order to ensure availability of the
nourishment,
5
Special foods need to be given separately to the
children needing these nutrients like iodine but by
and large normal food should be the pattern (to give
more of what they have)
6.
Mothers who need nutrtional care should also be given
the food (cooked food foe some time) in order to
protect the child to be born
7.
Ensuring the aviaslbility of’these foods in the PDS
should be treated as a requirement and part of the
approach.
8.
Nutrition education as support communication need to
be planned at the begining and the messages to be
location specific.
9
Gramsabhas need to be involved in selecting the needymother s of the community.
10.
Economic.capability of the mothers should be part of
the nutritional planning,
11.
Status of the girl child need to be focussed in the
whole approach.
Some Random
Thoughts
Independant body to monitor provide feedback under CEO.
District committee to make the policy assessment of the
implementation of the programme.This body to realise the
interfacing of the actvities as well, specifically the
food production socio-economic action plan
(Feedback to the State).
Nutrition programme to be under the women and childwelfare
with the support of coordinating committee.
PHE to be responsible for the drinking water
Establishment of training unit for two or three districts
Promotion of women Health cooperatives
villages
Special cell in
TB.Malaria Aids
the
district
for
for a cluster of
the
diseases
like
Development of norms of indicators for the positive health
Promotion of gram panchyats to fixup priority
Strengthening the existing the Institutions as per
details of TASK FORCE,including man-power improvement
the
Involvement of local district colleges for study on going
assessment, and research.
Central body to be given resposibility for the Research and
coordination
Sustained effort on Health Nutrition Education and FAMILY
POPULATION
Information support for the people who are involved.
uCH 2-
High mortality despite good care-seeking
behaviour: a community study of childhood
deaths in Guinea-Bissau
M. Sodemann,1 M.S. Jakobsen,’ K. Molbak,2I.C. Alvarenga Jr.,3 & P. Aaby4
The care-seeking behaviour of mothers of 125 children deceased aged 1-30 months was investigated by
verbal autopsy in an urban area of Guinea-Bissau. A total of 93% of the children were seen at a health centre
or hospital during the 2 weeks before death. In a previous survey covering the period 1987-90 we found that
tr% of the children who died had presented for consultation (8); despite this increase in care seeking, infant
^g>r,ality had not decreased. Comparison of elapsed time from disease onset to first consultation between
^ildren who died and matched surviving controls indicated that the interval was shorter for children who died
than for those who survived (odds ratio (OR) = 0.7; 95% confidence interval (Cl): 0.5-0.99). Of the 125
terminally ill children, 56 were hospitalized. A total of 20 children died on the way to hospital or while waiting
in the outpatient clinic. Lack of hospital beds resulted in 15 mothers being refused hospitalization for their
child Of hospitalized children, 42% were discharged as improved or recovered during the 30 days preceding
death. These results reveal a need for improved hospital admission criteria, improved recognition of the
symptoms of serious illness, better discharge criteria, and the implementation of quality assurance systems
for health services.
Introduction
Mam studies have reported a significant decrease in
child mortality following general improvements in
primary health care (PHC) (J. 2). Such decreases are
mainly the result of improvements in antenatal care
and vaccination coverage; the effect of diarrhoeal
disease programmes is less unequivocal. However, as
vaccines and antenatal care cannot entirely eradicate
the problem of excess childhood mortality in devel
oping countries, better case management of severely
ill children is clearly needed.
improvements in the management of severely ill
children are often based on audits of case histories
with fatal outcomes (3). However, few studies in
developing countries have investigated care-seeking
wiaviour prior to death in serious childhood illness
border to improve case management (4-6). Mortal-
Department of Epidemiology and Social Medicine, University of
Aamus. Hoegh-Guldbergsgade 10. DK-8000 Aarhus C, Denmark;
and Danish Epidemiology Science Cenfre, Statens Seruminstilul.
Copenhagen. Denmark. Reauests for reprints should be sent to Dr
: Danish Epidemiology Science Centre. Statens Seruminstilul.
Copenhagen; Denmark.
: Ministry of Health. Bandim. Bissau. Guinea-Bissau.
' Danish Epidemiology Science Centre. Statens Seruminstitut,
Copenhagen. Denmark: and Projecto de Saude, Bandim. Bissau.
Guinea-Bissau.
Reprint No. 5771
ity surveys have found large variations in the propor
tion of children seen at a health facility before dying
(7-10). It is important to explain why mortality re
mains high among under-5-year-olds in settings with
easy access to health care facilities. For example, in a
rural area of the Gambia, where 80% of children
were fully immunized and PHC programmes had
been active for 10 years, infant mortality was still
120 per 1000 live births in 1990 (11). In the Bandim
suburb of Bissau, Guinea-Bissau, we previously re
ported that the infant mortality was 94 per 1000 and
under-5-year-old mortality 215 per 1000, despite the
presence of two health centres, a mother-and-child
health clinic and an outpatient clinic (8).
We conducted the present study on patterns of
care-seeking behaviour prior to a child’s death to
investigate child mortality on the basis of the moth
er’s experience. The aim was to obtain individual
case histories that could be used to improve patient
management in primary health care programmes
and thereby lower childhood mortality in developing
countries.
Subjects and methods
Study area
The study was carried out in the suburbs Bandim 1
and Bandim 2 of the capital Bissau. Guinea-Bissau.
The population of approximately 25000 persons
5 World Health Organization 1997
M. Sodemann et al.
is served by two local health centres (with senior
nurses consulting), one mother-and-child health
clinic (with physicians consulting) as well as an out
patient clinic at the paediatric ward of the national
hospital (with hospital paediatricians consulting).
All inhabitants live within 1km of a health centre
and within 3 km of the mother-and-child health clinic
and outpatient clinic. Apart from a small one-time
charge levied for a child’s vaccination chart, no fees
were charged at health facilities in Bissau during the
study period. Since 1979. the area has had a demo
graphic and health surveillance system that covers
the following: registration of all pregnancies and
births: and for children less than 3 years of age. rou
tine collection, by means of 3-monthly visits to all
houses, of information on vaccinations, infections.
nutritional status, migrations, and deaths. Morbidity
and care seeking are monitored by weekly house
hold interviews. Traditional remedies for severe dis
eases are not generally the first treatment choice.
Study population
The cohort followed in the present study consisted of
all 1347 children born in Bandim 1 or 2 between 1
May 1992. and 30 April 1993. Deaths were ascer
tained by means of the routine surveillance system.
Two additional rounds of data collection were car
ried out in 1993 and 1994: furthermore, a census of
the entire population was performed in 1994. Verbal
autopsies were conducted by two of the authors
(MS & ICA) and a specially trained Guinean mid
wife. Interviews were carried out from July 1992 to
November 1994. by which time the youngest children
in the study cohort were 18 months of age and the
oldest children 30 months of age. Median time from
death to interview was 7 months (25-75th percentile:
6-9 months) The immediate cause of death was
determined by combining information from the
verbal autopsy, the morbidity survey, and a register
of hospital diagnoses. Morbidity information was
considered valid if the child had been followed up
until death, and hospital diagnoses were considered
valid when the child had been hospitalized for more
than 24 hours. Hospital records were available for 43
of 56 hospitalized children (76.8%). A probable
cause was determined for 93% of all deaths. In this
study, “hospitalization" was defined as hospitaliza
tion at any time during the 30 days preceding death.
regardless of subsequent discharge from hospital.
Households with deaths were divided into two
socioeconomic status groups: group 1 (50 mothers)
consisted of households with two or more of the
following: corrugated iron roof, television, inside
toilet, and electricity, group 2 (75 mothers) consisted
of households with less than two of these charac
teristics. Socioeconomic information was obtained
from the health surveillance system.
Statistical methods
Sample means were compared with the Student's ttest for normally distributed data, but the KruskallWallis test was used when sample variances were
significantly different. In bivariate analyses, back
ground factors were controlled for by means of a
Mantel-Haentzel stratified analysis of two-by-two
tables. A nested case-control study was carried out
by matching a control to each fatal case. The cor^j>'
was chosen from among children in the study poJPt'
lation participating in a weekly morbidity survey.
age-matched (=1 month), had experienced an epi
sode of disease within the same month as the fatal
case, was seen at a health centre or a hospital, but
survived at least 3 months following the episode.
Time to consultation was measured as the number
of days between the onset of illness and the first
consultation. The odds ratio was calculated as the
ratio of discordant pairs, and 95% confidence inter
vals (CI) were calculated with Miettinen's tesl^jased
approach (12).
Results
Childhood mortality in the study group
All deaths of live-born children (248/1347) were in
vestigated by verbal autopsies with the mother, or
the nearest relative if the mother was absent. The
circumstances, timing, and location of each contact
with health care personnel during the fatal illness
were recorded during the interviews. The proportion
of stillbirths was 55 per 1000 births, perinatal mortal
ity was 81 per 1000 births, and infant mortality 91 per
1000 live births. However, only post-neonatal dea^^
(125/1347) were included in this analysis.
Of the 125 such cases. 114 had verifiable in
formation on care seeking. Of these. 106 children
(93%) were seen by a health professional during
the 14 days preceding death. Of the eight others.
two died on the way to consultation, three died
suddenly and unexpectedly, and three from dis
eases ascribed to traditional ceremonial causes.
Compared with our previous mortality survey m
the same city, the behaviour reported here re
presents a significant reduction in the risk of not
beine broucht to a health facility (risk ratio =
0.3: 95% Ch 0.2-0.7) (6). Moreover. 33 (26.4%) of
the deaths occurred in hospital, whereas in the
previous survey 45% of deaths occurred in hospital.
A total of 23 children (18.4% of deaths) died
WHO Bulletin OMS. Vol 75 199’
M. Sodemann et al.
at home after being discharged from hospital. No
information on the location of death was available
for seven children.
Time to consultation
To determine whether mothers delayed consultation
in fatal cases, we performed a nested case-control
study. It was possible to match a surviving control for
93 cases. Equal delay occurred in 9 of the matched
pairs. In 35 matched pairs, the case exhibited the
longest delay and in 49, the control. Cases were more
likely to have a shorter delav than controls, with an
odds ratio of 0.70 (95% CI: 0.50-0.99).
First consultation and hospitalization
The place of first consultation according to cause of
death is shown in Table 1. The median lime from
onset of symptoms to first consultation was inde
pendent of child's age. ethnic group, mother’s educa
tion. socioeconomic status, and cause of death.
Of the 47 children first seeking care at a health
centre, only 23 (49%) were admitted to hospital and.
of these. 20 only after the mother sought consulta
tion more than once. Of the 38 children first seeking
care at the outpatient clinic at the paediatric ward. 22
(58%) were admitted to hospital. Immediate hospi
talization was more likely among children presenting
at the outpatient clinic first than for children present
ing at the health centre (risk ratio = 5.0. 95% CI:
2.0-12.5). Children taken to a health centre survived
longer (median. 8 days: 25-75lh percentile; 2-24
days) following first consultation than children ini
tially taken to the paediatric ward (median. 2 days:
25-75rh percentile: 0-8 days: P = 0.01). No differ
ence in survival time after first consultation was
found between children hospitalized immediately
(n = 18) and others (n = 20: P = 0.8). After control
ling for mother's education, socioeconomic status.
and child’s age. there were no differences in place of
first contact with the health system. However, chil
dren with diarrhoea were more likely to contact a
health centre first. Of those children surviving al
least 2 days from first consultation without hospitali
zation, 39* (84.8%) later reattended a health facility.
Hospitalization: reasons for refusal
or discharge
Of the 114 deaths for which we have information.
103 children (90.3%) presented al hospital one or
more times during lheir terminal illness. Of these.
10 children died on the way to hospital and 10 while
waiting for treatment in the outpatient clinic (Table
2). Of the remaining S3 children. 56 (67.4%) were
206
admitted either at the first visit (n = 22) or at a
subsequent visit; of those admitted. 18 children died
the day of admission. For the 61 children not admit
ted at first consultation. 15 of the mothers stated they
were turned away from the outpatient clinic having
been informed that their child should be hospital
ized. but that there were insufficient beds. Refusal of
admission did not depend on mother’s education.
socioeconomic status, or child’s age (P = 0.9).
Elapsed time since disease onset (>14 days) in
creased the risk of refusal (risk ratio, 2.4: 95% Cl:
0.9-6.6).
Of the 56 children admitted to hospital,
(41.7%) were discharged before death, with the
of discharge being independent of socioeconomic
status (P = 0.44) and child's age (P = 0.35). Of these.
9 children were discharged as "cured”. 10 as “im
proved” or “recuperating”. 1 was discharged by
the mother, and 2 had no status information at
discharge.
Case histories
Six representative case histories depicting the man
agement problems of severe childhood illness in the
study area are shown in Table 3.
Discussion
Despite a high percentage of children with fatal ill
ness obtaining treatment from a health professional.
infant mortality' in the study suburban area of
Guinea-Bissau has continued to be high: (1987-90.
94 per 1000:1992-93.91 per 1000). The proportion of
children who later die after presenting for consulta
tion both at health centres and hospitals has in
creased significantly since our previous mortality
survey (5)7
Among physicians and other health care workv
ers m developing countries, a common explanati^
for high childhood mortality is that, as mothers ai^
believed to be incapable of caring for a severely ill
child, children are brought to care too late. More
over. they do not recognize severe symptoms and
may seek traditional care first. However, the present
study indicates that mothers sought care sooner in
cases of fatal illness than in other cases.
Conceivably, seriously ill children would have a
better chance of survival if they were treated at the
outpatient paediatric ward than at a health centre.
The ratio of mothers choosing a health centre as site
of first consultation to mothers choosing the paediat
ric ward was the same, regardless of mother’s educa
tion. socioeconomic status, child’s age. and ethnic
group. Moreover, the chance of being admitted imWHO Bulletin OMS Vol 75 199“
I
Table 2: Place of first consultation and subsequent care seeking
Not hospitalized:
Hospitalized:
1 leallh centre
Outpatient clinic
Mothor-andchild
hoallh clinic
Hospital or hoallh
clinic In the interior
No information
on place
No consultation
No information
on consultations
Total
Directly
3
18
0
1
—
_
22
Aller ono or
more reconsullatlons
20
2
4
Total
hospitalized*
home*
Died on (ho way
to outpatient
clinic
23 (11)
22 (6)
2(1)
19(11)
7(6)
2(1)
2
3
0
Died white wailing
lor consultation at
outpatient clinic
3
5
1
3(2)
—
Total not
hospitalized
on place of
24
16
3
_
6
—
47
38
5
j1
3
0
—
4(3)
—
—
—
—
_
6
4
2
—
_
g
A
_
7
g
30
56 (23)
41 (20)
10
10
62
7
125
5(2)
* Figures in parentheses are number of children subsequently discharged who died outside hospital.
e
M. Sodemann et al.
Table 3: Typical case histories
Girt, 9 months of age. presents at health centre with diarrnoea
and vomiting after 2 days of illness; given oral rehydralion salts
ana sent home: next day mother seeks care for child at another
health centre; after 2 more days, mother presents child at
outpatient paediatnc clinic, where the child is given oral
rehydration salts and sent home: 20 days later child dies without
receiving additional care.
Boy. 4 months of age, presents at outpatient paediatric clinic
with diarrhoea and vomiting after 2 days of illness; given oral
rehydration salts and sent home; 3 days later mother seeks
care for child at outpatient paediatnc clinic: child grven oral
rehyoration salts and sent home, 10 days later, child collapses
at home and mother ta*es child to outpatient paediatric clinic;
child is sent home without treatment and dies same day.
Boy. montns of age. presents at outpatient paediatric clime
with hign fever after 1 day of illness; given medication and sent
home (mother told no: enough hospital beds): child suffers
generalized seizures at home, and next day mother returns to
outpatient paediatric clinic with child comatose, after waiting 2
hours, child sent to laboratory for tests and dies witnout
receiving additional care.
Boy. 9 months of age. hosoitalized twice within 2 months for
high fever and multiple ooiis: eacn time discharged as ’cured';
2 weeks after last discharge child dies at nome with fever and
convulsions.
Girt, 7 montns of age. presents a: motner-and-chilc health
clime wiin hign fever and chills after 2 days of illness: giver.
chloroouine and paracetamol and sen: home; same day child
worsens, and mother seeks care at outpatient paediatnc clinic:
child dies before receiving aoditionai care.
vomiting, and constipation after i wee* o< illness, chile given
lemcn juice ano sent home: after no improvement, mother seeks
care same day at outpatient paediatric clinic: child aomittea:
after waiting more than 1 hour for a biooe samoie. and then
wailing for tne fatner to buy tne necessary drugs (which were
not in stock at hospital), child oies witnout receiving additional
mediately to the paediatric ward of the hospital was
remarkably lower for children presenting initially at
a health centre than for children presenting initially
at the outpatient paediatric ward. It is therefore pos
sible that health centres retard needed hospitaliza
tion. As health centers were visited more frequently
than in our previous mortality survey, this could
have serious implications.
Apart from five children dying suddenly at
home or on the way to their first consultation, only
five children were not presented for consultation
at hospital, which is a marked decrease from our
previous survey. However, it is significant that so
few fatally ill children were admitted to hospital.
even from among those who first presented at the
outpatient paediatric ward. In many cases, the reason
was a shortage of beds. There were nine terminally
ill children attended by a paediatrician at the out
patient clinic 48 hours prior to death without being
admitted. The risk of refusal of admission after
consultation at the outpatient paediatric ward was
higher if symptoms had a duration of more than 14
days, indicating that chronic illness was less likely to
be’seen as requiring hospitalization. This is signifi
cant. as the two most common chronic illnesses, per
sistent diarrhoea and malnutrition, both have a very
high mortality (5). Since children not returning for a
second consultation died rapidly (median survival.
1 day) mothers* lack of knowledge does not explain
why children were not hospitalized. Children not
hospitalized after a first visit to the outpatient paedi
atric clinic died as rapidly as those who were; it is
therefore unlikely that refusal of admission was
based exclusively on clinical criteria. Hospitalizatij
was not influenced by socioeconomic status, mon-.er’s education, child’s age. or ethnic group. How
ever. verbal autopsies suggested that hospitalization
was obtained more easily if a mother knew a staff
member in rhe outpatient clinic.
A considerable proportion of children died
waiting for consultation at the outpatient clinic or
laboratory. Some of these deaths could probably
have been avoided by means of a revision of clinic
procedures and by training health personnel to
recognize children requiring immediate care.
A major problem is the high proportion of chil
dren dying at home after discharge from hospital. In
light of discharge status, this could not have been
caused by mothers fleeing the hospital with dying
children. No sociocultural factors were related to
risk of discharge, suggesting that inadequate recog
nition by medical staff of the potential consequences
of illness or nosocomial infections may have been
responsible. If so. this problem has been aggravated
since our previous mortality survey, since a larger
proportion of hospitalized children later die at home.
The number of beds in the paediatric ward remained
constant between the two surveys. Hence, demand
for limited bed space may have contributed to some
premature discharges. Hospital beds can be occu
pied for long periods of time by chronically
children suffering from malnutrition, persistent di^
rhoea. complications resulting from cerebral ma
laria. or tetanus. A clearer distinction between acute
and long-term illness in terms of management and
the need for care, as well as a more strict set of rules
for admission and discharge could potentially lower
demand for bed space.
The present mortality survey consists of case
histories with a fatal outcome. Since medical con
sultations for terminally ill children represent only a
small fraction of all consultations for sick children.
this survey may be biased as an evaluation of the
adequacy of health system procedures. However.
the present study does point to a number of specific
problems in case management. Previous studies anaWH0 Buiicim QMS. Vol 75 1997
High mortality despite good care-seeking behaviour in Guinea-Bissau
lysing care-seeking behaviour have focused particu
larly on traditional beliefs and practices that prevent
mothers from seeking proper medical care (5. 6. 9).
However, our experience suggests that it may be
equally important to examine the quality of the
medical care provided. This is supported by a Mexi
can study using verbal autopsies in a similar way. In
an area where no household was farther than 30
minutes from a health facility. 60% of the deaths in
children occurred at home and 80% of these children
had received qualified medical care within 3 days of
death (4).
j^For dealing with problems associated with
st.Jrely ill children WHO/UNICEF recommends
"integrated management of the sick child", which
combines the principles learnt over the past 15 years
in disease-specific health programmes into a unified
approach to managing childhood illness (73). This
initiative focuses on improvements in health-worker
performance and changing family behaviour in rela
tion to sick children. Training courses for the inpa
tient case management of sick children have also
been developed.
The present analysis clearly supports the need
for such initiatives. Surveys analysing fatal cases can
be a valuable tool, and can serve as a cost-effective
means for health care workers to identify areas for
improvements in the case management of severely ill
children. Improving the management of such chil
dren may be as important for decreasing childhood
mortality as vaccination and antenatal care pro
grammes have been, especially in countries with
poorly educated and badly paid health care workers.
Inadequate supplies, physical facilities, and equip
ment may also contribute to the persistence of high
childhood mortality in Bissau. Such constraints em
phasize improved health system management as a
means of better using available resources.
A key step in improving case management
r^uld be the establishment of an effective triage
* Jem that singles out seriously ill children as soon
as they come to a health facility and ensures that
appropriate action is taken. More formal criteria for
admission, referral, and discharge are also needed.
accompanied by clinical and system-management
training of staff. Finally, measures should be taken to
assure the quality of services provided by health care
workers, e.g. by medical audit or the use of epide
miological methods such as those used here. These
findings could be extended to the health services of
other developing countries: however, important dif
ferences may exist depending on available resources.
personnel, and payment systems. Hence, additional
studies investigating the case management of severe
illness at the primary health care and hospital levels
>n other countries are warranted.
WHO Buteon OMS. Vol 75 1997
Acknowledgements
We are indebted to Angelina Da Silva and Queba Djana
for assistance during interviews and identification of
mothers. This study was supported by the Science and
Technology for Development Programme of the European
Community (contract No. TS3-CT92-0060) and by the
Danish Council lor Development Research (grant No.
104.DAN8/535).
Resume
Une mortalite elevee malgre la
recherche de solns appropries: resultats
d’une enquete communautaire sur les
deces d'enfants en Guinee-Bissau
Bien que de nombreuses etudes aient fait etat d'un
declin significatif de la mortalite infantile a la suite
d'ameliorations generales des soins de same primaires, la vaccination et les soins prenatals ne
peuvent supprimer a eux seuls la surmortalite infan
tile dans les pays en developpement. Une prise
en charge plus efficace des enfants gravement
malades est done necessaire. Rares sont les
etudes qui ont die faites dans les pays en devel
oppement sur la recherche de soins appropries
comme moyen d'ameliorer la prise en charge des
entants gravement malades. La presente enquete
sur la demande de soins avant le deces a ete
conduite pour analyser le probleme de la monalite
infantile en fonction de lattitude de la mere. II
sagissait de recueillir des antecedents medicaux
individuals en vue d'ameliorer la prise en charge
des cas dans le cadre de programmes de soins de
same primaires et ainsi. de reduire la mortalite in
fantile dans les pays en developpement.
La demande de soins par les meres de 125
enfants decedes entre 1 et 30 mofs a ete etudiee au
moyen d'autopsies verbales dans une zone urbaine
de Guinde-Bissau. Tous les habitants sont a moins
de 3 km d'un centre de same. Au total. 93% des
enfants avaient ete retjus dans un centre de same
ou un hopital dans les deux semaines ayant pre
cede leur ddees. Notre precedents enquete, sur
la periode 1987-1990, avait montre que 78% des
meres des enfants decedes les avaient montres en
consultation; toutefois, malgre cette augmentation
de la demande de soins, la mortalite infantile n'a
pas baisse. Si I'on compare le temps ecoule entre
I'apparition de la maladie et la premiere consultation
pour les enfants decedes et des temoins survivams
appanes. il apparail que cet mtervalle avait ete plus
court pour les enfants qui sont decedes que pour
ceux qui ont survecu (odds ratio = 0.7: intervals de
M. Sodemann et al.
confiance a 95% = 0,5-0,99). Sur les 125 enfants
qui etaient en phase terminale, 56 ont ete hospital
ises. Vingt sont decedes lors du transport a I'hopital
ou en attendant d’etre vus en consultation dans
un dispensaire. Faute de lits disponibles, 15 meres
se sont vu refuser I'hospitalisation de leur enfant.
Sur les enfants hospitalises, 42% ont ete declares
en meilleure sante ou gueris et renvoyes chez eux
dans les 30 jours ayant pr6c6de leur deces. Ces
resultats montrent qu’il est necessaire d'ameliorer
les criteres d'hospitalisation, la reconnaissance
des symptomes des maladies graves et les cri
teres de sortie et de mettre en oeuvre des systemes d’assurance de la qualite des services de
sante.
La solution prdconisee par I’OMS et I’UNICEF
pour le traitement des enfants gravement malades
est la “prise en charge integree de I’enfant malade"
qui associe les principes acquis depuis 15 ans
dans le cadre de programmes de lutte centre des
maladies determinees en une approche uniforme et
coherente de la prise en charge des maladies de
I’enfance. La presente etude montre tres clairement
que de telles initiatives sont necessaires. Les
enquetes sur les cas monels peuvent etre un instru
ment precieux et fournir aux agents de sante un
moyen d’un bon rapport cout/efficacite de deter
miner les domaines dans lesquels des ameliora
tions doivent etre apponees a la prise en charge
des enfants gravement malades.
Pison G et al. Rapid decline in child mortality in a rural
area of Senegal. Internationaljournal of epidemiology,
1993, 22: 72^80.
Another audit. Lancet, 1988,1: 450-451.
Gutierrez G et al. Study of the disease-health
seeking-death process: another use of the verbal
autopsy. International journal of epidemiology, 1994,
23: 427-428.
5.
Sutrlsna B et al. Care-seeking for fatal illness in
young children in Indramayu. West Java. Indonesia.
Lancet. 1993, 342: 787-789.
6.
Snow RW et al. Factors influencing admission to
hospital during terminal childhood illnesses in Ke^^
Internationaljournal of epidemiology, 1994,23:1 (■ }
1019.
7.
De Francisco A et ai, Comparison of modality be
tween villages with and without Primary Health Care
workers in Upper River Division. The Gambia. Journal
of tropical medicine and hygiene. 1994, 97: 69-74.
8.
Molbak K et al. Persistent and acute diarrhoea as the
leading causes of child modality in urban GuineaBissau. Transactions of the Royal Society of Tropical
Medicine and Hygiene. 1992. 86: 216-220.
9.
Shamebo D et al. The Butajira rural health project in
Ethiopia, modality pattern of the under fives Journal
of tropical pediatrics. 1991. 37: 254-261
10.
Mirza NM et al. Modality patterns in a rural Kenyan
community. East African medical journal. 1990. 67:
823-829.
11.
Alonso PL et al. A malaria control trial using
insecticide-treated bed nets and targeted chemopro
phylaxis in a rural area of The Gambia. West Africa. 2.
Modality and morbidity from malaria in the study area.
Transactions of the Royal Society of Tropical Medi
cine and Hygiene, 1993, 87(suppl 2): 13-17.
12.
Kirkwood BR. Essentials of medical statistics.
Oxford, Blackwell Scientific Publications, 1988: 179-
2.
3.
4.
References
1.
Greenwood BM et al. Evaluation of a primary health 13. World Health Organization, Division of Diarrhoeal
care programme in the Gambia. II. Its impact on mor
and Acute Respiratory Disease Control. Integrated
tality and morbidity in young children, journal of tropi
management of the sick child. Bulletin of the World
cal medicine and hygiene. 1990, 93: 87-97
Health Organization. 1995, 73: 735-740.
How we have the ‘movement’
’ but the fascists haw the women!
is a time to listen to the different resonances of
JLwomen in song, in folk tales, in grandmother’s
stories, in symbols; a time to create new spaces, to
seek new knowledge, to find new possibilities for our
times. ”
So said the invitation to the Fourth National
Conference on Women’s Movements in India, to
hundreds of women activists across the length and
breadth of this country. But even more loud and clear
from audio and video cassettes around the country
can be heard the shrill and hysterical shriek of a
woman :
“Declare without hesitation that this is a Hindu
Rashtra, a nation of Hindus.
We have come out to
strengthen the immense Hindu Shakti into a fist. Do
not display any love. This is the order of Ram
The
Koran exhorts them to lie in wait for idol worshippers,
to skin them alive, to stuff them in animal skins and
torture them until they ask for forgiveness
Let there
be a conflagaration than this slow torturous
simmering.
We could not teach them with words,
now let us teach them with kicks
Let there be a
bloodshed once and for all.
Now we will not only
shed our own blood, but the blood of others, too.
That Mahatma Gandhi led you to ruin.
Tie up your
religiosity and kindness into a bundle and throw it in the
Jamuna maiya
Any non-Hindu who lives here does
so at our mercy..... ”
Ominous and blood-thirsty words these; and that
too from the mouth of a woman — Uma Bharati,
elected to the highest body of the land — Parliament.
And she is not the only woman spewing communal,
nay fascist hate and poison amongst the people today.
There’s Sadhvi Ritambhara who has come out of her
ashram and vowed not to rest content till a Hindu
Rashtra is established. Listen to what she has to say:
“We want to teach the Muslims a lesson — either
they come to heel and surrender to our will in Ayodhya,
or we shall take it by force.
We don’t believe in this
kind of secularism
”
Which are the times in which we women activists
from all over India are meeting today? Those of the
invitation or those of Uma Bharati, Vijayaraje Scindia
and Sadhvi Ritambhara? Will these fascist women
permit the crores of women of our country to quietly
listen “to the different resonances of women in
song”? Or is it increasingly going to be the ‘fate’ of
our women to hear only the wails of bitter anguish as
their homes are looted or burnt down, or the screams
of outrage as a husband or infant is stabbed to death?
And folk tales—will it be tales from the
Panchatantra or the Jatakas, or will it only be sinister
and gory tales of “how Babar destroyed a mandir to
build a masjid, how the Muslims demanded partition
and Pakistan and got it, how the Sikhs and Kashmiris
are terrorists and butchers, etc., etc.”
And as for grandmothers’ stories, will they be like
those of yesteryear, full of the milk of human
kindness, about repentance even if an ant is killed
underfoot, about the teachings of our great Indian
sages, sants and saints who down the years taught the
people of their times as well as future generations to
show care and concern for the wretched of the earth?
Or will grandmothers and mothers now teach their
sons and grandsons only about revenge and how they
must avenge the murder and slaying of their near and
dear ones, the cruel destruction of their hearts and
hearths and the crushing underfoot of their lives and
livelihoods?
And symbols — will they continue to be of
women’s life-giving and life-sustaining shakti, of her
destructive powers over evil and wrongdoing
symbolised in Kali, of her deep knowledge of life and
society symbolised in Saraswati? Or are today’s
symbols increasingly going to be bricks and jyots,
trishuls and swords, acid bulbs and AK 47s.
“A time to create new spaces. " Where, one might
well ask? Where will the women victims of Gonda
and Baroda, Ahmedabad and Hyderabad, Agra and
Aligarh, Chandigarh and Srinagar and of innumerable
other towns and cities too shameful to enumerate,
create new spaces? In burnt-out bastis and strife-torn
mohallas'! In makeshift refugee camps or
disease-filled migrant colonies?
"We must find new possibilities for our times ....... ”
What new possibilities are there for women caught in
the throes of a fundamentalist mania that has
engulfed entire towns and cities, talukas and districts,
making them simmering cauldrons that can be ignited
and set aflame at the slightest rumour or whisper!
We have been asked “to express our ideas and
experiences, feelings and problems through a cultural
medium of our choice”. To express ourselves through
“songs, skits, plays, paintings, tableaus” etc Honestly
can we really sing and dance with gay abandon and
joy while a ghastly death dance is enacted all arm.nd
us? Do we wish to enter the footnotes of history .«
women who fiddled while India burnt?
Not merely fundamentalism, but FASCISM!
Of what use?
We are aware that some of the feminists gathered
here will dismiss our views as alarmist. Perhaps to
them all talk of fascism is an unnecessary phobia.
So simple to dismiss the present communal
conflagration as just another bout of riots which
have regularly erupted in our country since 1947. So
easy to make believe that sooner or later the riots
will be quelled and the women’s movement left in
peace to discuss patriarchy in the home, sexual
stereotypes in the mass media and how women
should regain control over their bodies. So simple
to satisfy our feminist consciences by just
ritualistically having a sub-theme in the National
Conference
on
the
“topic”
of religious
fundamentalism, in which we plod through the same
old groove of personal laws and Shah Bano, Roop
Kanwar and sati, when the country is threatened
Of what use are workshops on “women studies and
the national planning policy” to the millions of
Kashmiri women who are being kept within the
Indian nation only at the point of a gun? Can the r
most stringent tightening of rape laws help when
women are gang-raped during a communal
holocaust or while under military occupation? Do
the much-trumpeted family courts set up to
‘sympathetically deal’ with marital disputes, have
any chance in front of the Khalsa courts of the
Khalistanis? What property rights can we talk of for
women whose families have lost whatever property
they possessed in communal riots or terrorist
violence? Is it not a joke to exhort women “to unite
and reclaim the night” when fascist lumpen
elements control the towns after sundown? Can our
preoccupation with how daughters and mothers eat
last and least, have any meaning when entire
families are being pushed into semi-starvation and
destitution due to weeks-long curfews; when traders
make use of the breakdown of all civil life to hoard,
blackmarket and sell onions for Rs. 40 a kg, never
mind other foodstuffs and foodgrains? Can our talk
of women having rights in the matrimonial home or
in the ancestral property, have any meaning when
they have lost hearth and home and are rotting in
refugee camps? Some feminists have taken
patriarchy to such absurd levels by claiming “Men
kill. Women give birth”! What meaning and
direction can such anti-male chauvinism give us in
such troubled times, when fanatic sadhavis are
exhorting people to kill their non-Hindu
neighbours! When the majority who have fallen
victims to the bullets of the fundamentalists happen
to be men struggling against fascism! For 40 years,
our feminist sisters have boldly proclaimed,
“Sisterhood is powerful”! Can we talk of any
sisterhood with the likes of Uma Bharati and
Ritambhara and thousands of other fanatic women
who teach hatred, revenge and aggression!
with not merely fundamentalism but fascism.
Let’s wake up. Fascism is a million times more
rapacious and bestial than fundamentalism.
Fundamentalism mobilised the people of its
community “to defend religion” from the interference
of our half-hearted secular state. Fascism is a
ferocious mass movement which aims to make
fundamentalism
the
state
power
itself.
Fundamentalism primarily stifled working and toiling
women. Fascism will not spare even ‘liberated’ and
‘emancipated’ women from the bourgeois and petty
bourgeois class.
Kashmir is already in the control of Muslim
fascists who are not merely fundamentalists. These
fascists are beyond caring whether section 125 of the
Cr.P.C. goes against the Shariat or not. They are
fighting for . secession and an Islamic state joined to
Pakistan. The Khalistanis in Punjab are already a
state within a state, while the Hindu fascists have
made it clear that their aim is a Hindu Rashtra. This
cataclysmic transformation from our present
half-hearted ‘secular and democratic’ state to
theocracy and fascism has already unleashed the most
rabid criminalisation and militarisation of social life.
Senas of armed thugs control every city and
town.Their fascist attacks have been defended by sane,
educated sections of society as “teaching those
anti-national Muslims a lesson”. Huge parts of the
country are under military rule, with its
house-to-house raids, its inevitable rounding up of
innocents, imprisonment without trial, and torture.
This brutalisation of our people has in a flash
exposed how the so-called gains of the women’s
movement have indeed been built on sandy
foundations. It has brought to the fore as never
before, the inherent impotence of the women’s
movement as we know it today, to deal with the
monster of fascism.
2
In fact, the most uncomfortable question forced by
life on the women’s movement today is: How come
the fascists with all their backward views about
women’s inequality, with all their support for
reactionary personal laws, have succeeded in winning
over millions of women to their cause? On the other
hand, how come the women’s movement with all its
opposition to reactionary personal laws, with all its
progressive views about women’s equality is impotent
to break the stranglehold of the fascists on women? It
is time to ask ourselves: How come the feminists have
the ‘movement’, but the fascists have the women?
This question demands soul-searching from all of us,
who believe that an awakened womanhood can stand
between democracy and fascism, between social peace
and communal anarchy, between sanity and collective
madness.
Can there be herstory without her concerns?
The first point to realise is that the women’s
movement has by and large refused to make the
primary concerns of the majority of women its
special concern. The majority of the women of our
country arc working and toiling women, homeless,
landless and overworked •— bordering between
survival and death. Their primary concern has been
that under 40 years of ‘secular rule’, their self-worth
has been raped, their collective identity has been
shattered, their self-respect has been destroyed,their
dignity has been insulted, their will has been broken
and their dreams and future torn to shreds.
again
declared
that
adulteration
and
blackmarketeering of rations denial of drinking
water and toilets, extortion of donations for school
admission etc, etc, are not women’s problems but
“general problems”.
When the women’s movement has by and large
bypassed the overwhelming majority of women all
these years, is it surprising that these women are
bypassing the women’s movement today? And can
there be any real struggle against fascism, unless these
women are organised and mobilised?
In fact by overlooking these women, the women’s
movement has left the field open for the fascists to
play on the emotions and hopes of our women. Is it
surprising then that they are attracted to the fascists
who constantly talk of restoring the pride of their
respective communities, who boast of reclaiming back
their lost dignity and identity, who magnetically draw
the degraded unemployed youth and their mothers
with visions of a new future? Is it surprising then that
the fascists appear as saviours of women when they
forcibly close down liquor shops and cinema halls
showing obscene films, when they promise jobs and
small business to their sons by driving out the
“outsiders” or getting rid of “the other community”?
When our so-called secular state has robbed women
not only of their meagre possessions but insulted and
humiliated them adding insult to injury, is there any
reason for women to defend this state from the
clutches of the fascists?
When women lose their homes over and over again
due to brutal evictions, what self-worth can she cling
to ? When she and her family are hunted like animals
from one forest to another by corrupt forest officials,
what is left of her pride? When she is forced to
defecate on railway tracks and has to fight for even a
bucket of water, what is left of her dignity? When she
is constantly forced to fall at the feet of one labour
contractor or another, when unscrupulous middlemen
rob her of her hard-earned labour, when she is
reduced to begging and pleading with vicious
moneylenders, is there anything left of her will?
When she has to bear up with the sexual assaults of
the landlords, just in order to get work the next day,
what is left of her self-respect? When landlessness
and debt forces her family to migrate to the city
pavements, what is left of her collective identity?
When she sees her tiny children working from dawn
to dusk just in order to survive, when she sees her
married daughters reduced to skin and bones due to
hard work and drudgery, is there any future to live
for? When she sees her husband forced into
unemployment and reduced to an alcoholic, what
rainbow-like dreams are there for her?
The second point to realise is that the primary
obsession of the women’s movement has been the
discrimination between the sexes — a burning and
immediate question for women of the bourgeois and
climbing middle class, but of marginal importance
Let’s do some soul-searching
to the overwhelming mass of working and toiling
women. The women’s movement has been
Has not' the women’s movement by and large
insulated itself from this collective degradation
suffered by the overwhelming majority of women?
Have not most women’s organisations (exceptions
granted) regarded mass evictions of slum dwellers
and tribals from their homes as not “women’s
issues”, and hence of no direct concern to the
women’s movement? Have not many in the women’s
movement (exceptions granted) consciously closed
their eyes to the millions of families reduced to
landlessness due to landlordism and moneylending,
claiming these are not specifically “women’s
problems”? Has not the women’s movement by and
large failed to protest against the pernicious
contract system which has strangulated millions of
women at work, including those involved in
household industry — all under the plea that this is
a trade union problem and does not concern the
women’s movement! Have not feminists time and
When obsession leads to regression
over-concerned with how daughters are given less
food than sons in the homes of the poor, while the
major concern of the woman of the house, has not
been this discrimination but how to feed her
half-starving, family. The women’s movement has
fought for property rights for women, but what
appeal can this have for the millions of women who
belong to the propertyless class? The women’s
movement has spoken of land pattas and house
pattas for women, but to women who are landless
and homeless, the patta is all-important, rather than
whether she or her husband will be the owner. The
women’s movement has demanded that the
matrimonial home should be in the name of the
woman, while women living in the slums are less
afraid of being thrown out by their husbands than
by the government’s demolition squads which make
her whole family homeless. For the women’s
movement, the giving and taking of dowry is an
insult to womanhood and a reflection of her
3
Majlis-e-Itehadul-Mussalmeen (MIM), responsible
for the present riots in Hyderabad, runs among
other things an ITI, a polytechnic, an engineering
follege, a medical college, an Institute for Islamic
and Arabic studies etc.,all of which not only receive
money from the Islamic fundamentalist regimes of
Saudi Arabia and Pakistan but also from the
Secular Democratic Republic of India. Even more
widespread and pernicious has been the stranglehold
of the RSS (indicted in several riots by government
commissions) over education. The RSS runs more
than 10,500 institutions and institutes all over the
country, with again lavish grants from the Secular
Democratic Republic of India.
While this state was in the few and far between
times giving women activists of the ‘autonomous
women’s movement’ access to the government mass
media like Doordarshan and AIR, it was hourly
opening up this mass media to the fundamentalists of
all religions. Also note, how while the
Jamaat-e-lslami, the Shiv Sena, the Khalistanis, the
VHP, etc., have used the mass media in print and
celluloid, audio and video, to spew their communal
poison, the state has pretended to see no evil and
hear no evil.
Our tragedy
The tragedy is that the women’s movement has by
and large gratefully accepted these crumbs, believing
that with a little bit of more petitioning and
pressure, the crumbs will become morsels. Today
leave aside getting more, the growing fascist forces
are snatching even the crumbs from our mouths.
E.g. in Chandigarh, Khalistani fascists are forcibly
preventing college girls from even wearing clothes
of their choice, while our ‘secular and democratic’
state watches helplessly.
The worst sufferers are those who belong to the
so-called ‘autonomous women’s movement’. We say
so-called, because this movement has in fact been tied
to the patronage and apron strings of this very
‘democratic and secular’ state. Instead of being
autonomous of all political parties who swore by the
merits of this ‘secular and democratic’ state, it was
miserably tied to their outlooks. Is it surprising that.
in a period of rising fascism when these ‘secular and
democratic’ parties become irrelevant, like in Punjab
and Kashmir, the ‘autonomous women’s movement’
has become impotent and paralysed?
Let’s be honest. All this talk of autonomy was
meant primarily to segregate the women’s movement
While our ‘democratic and secular’ state was
from any emerging revolutionary and democratic
attempting to set up a few family courts as token
movement. In short, to isolate the women’s movement
gestures of its ‘concern for women, in distress’, it was
from the very forces capable of taking on the fascists.
giving full and free rein to the fundamentalists forces..
to set up their own Personal Law Boards, with legal
sanction to decide in vital matters of family life such Why the exploiters need fascism
as marriage, divorce, maintenance, custody and
guardianship of children, inheritance, etc. Further, Today the most reactionary sections of the exploiter
these “protectors of religion” were being allowed to classes do not have much use for even the facade of
a ‘secular and democratic’ state which has served
maintain a tight grip over their communities as well
as to brutally excommunicate, boycott and ostracise their purpose for 40 years. Today their interests can
only be protected by a fascist party presiding over a
all those who even questioned, let alone opposed
repressive state machinery, purged of secular and
their slavish fatwas and edicts.
democratic elements, and supported by fascist senas
from the outside. Today, since the exploiter classes
We ask all women activists to look around them. cannot even promise, let along give, the basic
Who runs more trusts meant for the welfare of necessities of life to the masses, they need fascist
women? Progressive women organisations or organisations which will constantly whip up
fundamentalist organisations? Who runs more fundamentalist frenzy and keep the masses divided
orphanages, ashrams, destitutes homes, boardings for and in a state of fanaticism. If this requires that
deprived children? Progressive women groups or entire regions of the country be under military rule,
fundamentalist organisations? Who runs more clinics, so be it.
dispensaries, ambulance services, hospitals (all of
Only through such a fascist ‘stability’ can the
urgent importance to mothers)? Progressive women
or fundamentalist organisations? Who runs more imperialists get their huge foreign debt serviced every
hostels or homes for women? Progressive women’s year on the sweat and blood of the people. Only
trusts or fundamentalists’ trusts? Just find out how through such a ‘stability’ can the masters of the
many crores of rupees in government grants, tax fascists get further loans to buy more guns and extort
exemptions, exemptions from Urban Land Ceiling more commissions. Only through such fascist control
Acts, have been provided by our ‘secular and can India compete internationally as the land of sants,
democratic’
state
to
these
fundamentalist mahatmas, and spiritualism as well as the source of
organisations. Only then will we understand how the the cheapest of cheap labour. Only through this
women’s movement has received crumbs while the brutalization can our exports be made ‘competitive’ in
international markets.
fundamentalists have gobbled up the cake.
5
This drive for cheap labour will demand the
dismantling of whatever meagre protective legislation
exists for women, eg., restrictions on night duty,
working in underground mines, etc. However, the
fascists need not take the ignominy of this crime on
their heads. Some feminists have already demanded
the withdrawal of all protective legislation under the
plea that this protection violates “gender equality”
and affects women’s employment.
Breakdown of sisterhood
Through all this it is becoming increasingly clear
that the growth of fascism will break asunder the
“oneness and unity of sisterhood” which has been
an article of faith for many feminists. Leave aside
the Uma Bharatis, many women especially from the
growing middle class who have acquired the goodies
of life can only be afraid of losing them due to the
growing insecurity and the anarchy of social and
political life. It is not difficult to sell them the need
for a strong repressive state. Many women have
been ‘liberated’ enough to own shares and play the
stock market. Such women may even sneer at
Advani’s Toyota Yatra, during parties and social
gatherings. But will they be able to resist the appeal
of the BJP which will more and more appear to
them as the only party which can prevent a stock
market crash?
to come, this anti-fascist women’s movement will
attract the best daughters of our land who refuse to
seek their liberation outside the emancipation of the
millions of exploited and oppressed women of ot>:
country. Today such activists are struggling alongside
contract workers, dalits, tribals, landless, homeless
and other oppressed sections of the population. The
growing forces of fascism will make it necessary for
them to be autonomous of state patronage and the
outlook of the so-called secular and democratic
parties like the Congress. It will make it necessary for
them to be more linked to the anti-fascist
revolutionary movement. It is these women activists
who will radically redefine the women’s movement as
India enters the turbulent 90s.
This anti-fascist women’s movement can only grow
from strength to strength — despite repression,
despite fascist attacks, despite momentary 'osses and
defeats. As the ugly face of fascism bares its fangs,
this women’s movement will receive the support and
protection of millions of working and toiling women
— simple women whom bourgeois feminists have
hitherto sneered or dismissed as “backward, illiterate,
superstitious and religious”.
The anti-fascist women’s movement will give rise
to its own irony. It’s ranks may be depleted of many
‘liberated, secular, rational’ feminists who will desert
There is no need to mourn the breakdown of this the movement, while women who religiously fast for
sisterhood. The anti-fascist women's movement can > their husbands or go to pilgrimages for a son will surn
only be strengthened by such polarisation. In the days out to be its strongest allies.
22 December 1990
Presented at the Fourth.National Conference on Women’s Movements in India,
at Calicut, Kerala, December 28-31, 1990.
AN APPEAL
TODAY our country is on the brink.
Fundamentalists of all religions arc increasingly
using fascist methods to achieve their ultimate
goal — of a fascist theocratic state. What this will
mean for the men and especially the women of our
country, can well be imagined.
We believe that the power and strength of the
AWAKENED women of our country can combat
and stem the forces of fascism. But for this the
women’s movement will have to re-direct itself and
grow into a strong anti-fascist women’s movement.
It is for this reason that we have put down our
views sharply and critically, in order to initiate a
healthy debate on the present weaknesses, and
more importantly, on the crucial and historic tasks
that face the women’s movement today. We hope
that our criticism will be taken in the spirit in
which it has been made.
We call upon all those interested to add to,
correct and criticise what we have put forward, so
that together we can fulfil the responsibility that is
ours TODAY.
Stree Jagruti Samiti
254, Ambedkar Nagar,
M.l.D.C. Road No. 8,
Andheri (East),
Bombay 400 093.
9, New Gurupanpalya Slum,
Behind Drive-in Theatre,
Off Bannerghata Road,
Bangalore 560 081.
Position: 708 (10 views)