RF_NUT_13_SUDHA.pdf
Media
- extracted text
-
RF_NUT_13_SUDHA
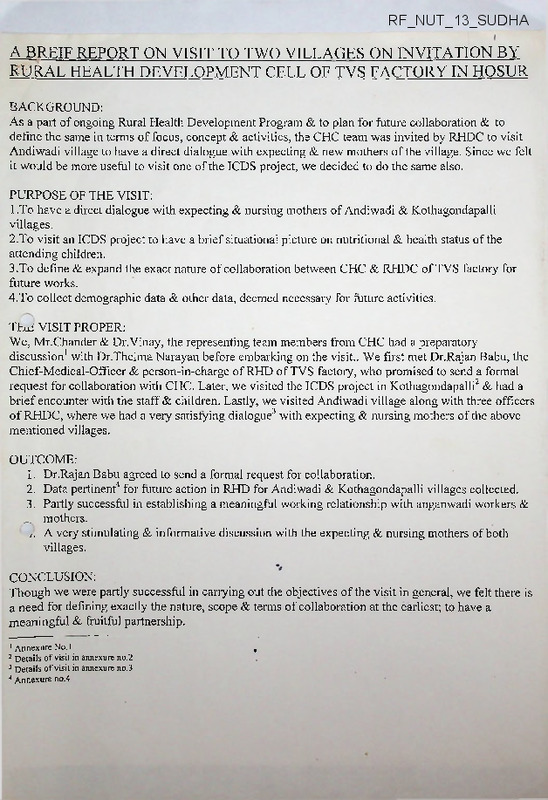
A BREIF REPORT ON VISIT TO TWO VILLAGES ON INVITATION BY
RURAL HEALTH DEVELOPMENT CELL OF TVS FACTORY IN HOSUR
BACKGROUND:
As a part of ongoing Rural Health Development Program & to plan for future collaboration & to
define the same in terms of focus, concept & activities, the CHC team was invited by RHDC to visit
Andiwadi village to have a direct dialogue with expecting & new mothers of the village. Since we felt
it would be more useful to visit one of the ICDS project, we decided to do the same also.
PURPOSE OF THE VISIT:
To have a direct dialogue with expecting & nursing mothers of Andiwadi & Kothagondapalli
l.
villages.
To visit an ICDS project to have a brief situational picture on nutritional & health status of the
2.
attending children.
To define & expand the exact nature of collaboration between CHC & RHDC of TVS factory for
3,
future works.
To collect demographic data & other data, deemed necessary for future activities.
4.
THE VISIT PROPER:
We, Mr.Chander & Dr.Vinay, the representing team members from CHC had a preparatory
discussion1 with Dr.Thelma Narayan before embarking on the visit.. We first met Dr.Rajan Babu, the
Chief-Medical-Officer & person-in-charge of RHD of TVS factory, who promised to send a formal
request for collaboration with CHC. Later, we visited the ICDS project in Kothagondapalli2 & had a
brief encounter with the staff & children. Lastly, we visited Andiwadi village along with three officers
of RHDC, where we had a very satisfying dialogue3 with expecting & nursing mothers of the above
mentioned villages.
OUTCOME:
1. Dr.Rajan Babu agreed to send a formal request for collaboration.
2. Data pertinent4 for future action in RHD for Andiwadi & Kothagondapalli villages collected.
3. Partly successful in establishing a meaningful working relationship with anganwadi workers &
mothers.
Z A very stimulating & informative discussion with the expecting & nursing mothers of both
villages.
CONCLUSION:
Though we were partly successful in carrying out the objectives of the visit in general, we felt there is
a need for defining exactly the nature, scope & terms of collaboration at the earliest; to have a
meaningful & fruitful partnership.
1 Annexure No. 1
2 Details of visit in annexure no.2
3 Details of visit in annexure no.3
4 Annexure no.4
,
ANNEXURE NO 1
PREPARATORY DISCUSSION WITH Dr.THELMA NAP-AYAN
A very iusiguuiil discussion with Dr.Thelma Narayan, ior whicuDr, vmay arrived laic, during which she
eave us anoverview of what should be our focus during the visit & oriented us towards the exact job at
kcn/i tka avow
u-*** v<*rious data to be collected stressed on the need for forma!
agreement & imponance of establishing a good rappon with concerned people. She also cautioned us
about carefully selecting the method of pedagogy, appropriate to the group The discussion gave ns that
IICDS PROJECT
Kothagondapalli, a village, is a 10 min drive from TVS Factory, where RHDC of TVS has been working
iu various capacities since 1954.
OBSERVATIONS:
1 The anganawadi is housed within the campus of Government school with a separate room &
kitchen to itself.
9 The hnildino as a whole was constructed hv the Government The ‘nnliftino’ in terms of naintinv
maintenance, toilet provision, gardening, enclosure construction <5c maintenance of play Helu is
undertaken by RHDC.
4. The anganawadi was spacious, cieaniy maintained with a separate, ciean kitchen with a gobar gas
fuelled stnve for cookino
j.
lucre was enougn space ror cmiuren to p>ay witmn tne room, aioert witnout enougn toys.
6. There is afiess to drinkma water & clean toilet.
*7
Tknro tvoc o Irvxvr o4*A*»z4«>r*AA rxT
r>-P "2 -C r\r»1xr 0/1 tvnrc
fQOCOri rrirrf^n
was me famess of me anganawadi from Their houses.Chiidren present at me time of visit were
reasonably healthy & most of them were well nourished However there were a few malnourished
vmjLuicil{ iuCiv iS a iict-u jlvi a uGiaiiou Stuuy vi uuc Same Wuivu WaS pvSipvucu due tv lavK vi
time).
C
TKa
kointy
woo
vAtv
All At»UrlrAv» WArA mor^A +q xirock 4iA,'r T»o*»i4c
& say meir prayer before being served food, with each chiid gening a separate piate for eating.
The children seemed more than ready to cooperate with a stranger & happily submitted themselves
ior vAdiiufiduun oy Dr. vinay.
10. The staff members were cooperative & friendly with us. They' seemed very well informed about
their duties & seemed to be doing the same reas onab ly well. They also seemed to be genuinely
interested in meir work. They aiso reported enough support from Government in terms of supply
of food # medicines
Various lunctioiis pcrlormcu by the stall as told by thein are as lollowsi
> Nutritional supplementation to all children in the age group of 0-6 years & all expecting &
lactating mothem r^,he'*z also followed differential Quantity as prescribed by the authorities
ANC for expecting mothers including tetanus immunization every 2nd Monday of the
month with help of visiting ANM.
0
r Imnmmzaiioii of all cliildieu. as prescribed by authorities, on every 2nd Wednesday of the
month with heln of visiting ANM.
> Distribution of IFA tablets’ to expecting mothers & all girls between 11-19 years,
administration of Vitamin-A to ail children at 6 months of age & then 2mi every 6 months
til! 5 years of age,distribution of paracetamol, albendazole A clotrimazole to people in
need.
>
j»
>
>
z-
Referral services for sick people.
Health education to all women between 15-45 ’’ears
Non-formai education to all children between 2-6 years of age.
Periodic meetings with women, adolescent girls & with village lemslative council.
ivlaiuiciiuiive 01 icCOfuS luCiiiuiiig gi'OWiu iiluiiituiuig, geiicial health 01 children &
performing ^nsex duty.
1iX.
1 livovrvi, CUV LjllXim^ UVAVVV -iron
>>UU iUo
CUV UlUVlllV; V»X VXXK/ OVUll
o^nrfc VI MUIrUvvr.
111U111U1111 U.1VXWA VUU1W
yUJUUl ^JUL, "V
dmy so imponam, due to acute shortage in the suppiy of growth chans by ihegovemmenti
1? The efaff WAS enthusiastic in fiirther imnrnvemente of the ancanawadi in general A readv to nive.
ilcip ui wnaievci way uiey Can.
IMPRESSION:
before any improvements are suggested.
ANNEXURE N0.3
THE D1AL0UGE PROCESS AT ^NDIWADI WITH EXPECTING & NURSING MOTHERS OF
BOTH VTT.T AGP.S
expecting & nursing mothers of above mentioned two villages. The meeting was arranged by RHDC &
piace in the beaurifui cl secure anganawadi of Andiwadi viiiage.
The dialogue was held in a very informal manner, with the participants and resource persons mingling
a planting planted m wilderness & not cared! It helped to break the ice & also gave the woman an ideal
platform to start the dialogue. Then on the dialogue continued with good participation & some of the
observations as made by Dr.Vinay are as follows:
1 The participating group was a good mixture, of woman from different economic levels, though it
Caiiuvt v© Said SO vf uldi SOCial vlaSS.
2. Only 2-3 participants were very active & others answered only when questioned. 1'here was not
3. me coordinator was articulate, expressive & tactful, stimulating the women to think & participate.
4. The knowledge of most of the participants regarding child health &. rearing was commendable.
the effectiveness of dialogue):
> Mr.SJC: Why should you feed children?
Women: “To fill stomach; io help in growih;io maintain health of the children".
> Mr.SJC: When should breast feeding started? Weaning-When & how?
W omen. BF just after the birth; no prclactcal feeds to be given; Weening to start in 3-6 months
Withragi porridge & other soft foods; confusion among the group regarding marketed baby foods
& on informing^ by US, that they era not necec<;ary, one even questioned US bv askinn how crane
then that the doctor prescribes it?; most said they have never bottle fed their babies!
> Mr.SJC.' Tmmnnization-When. T-Tow many?
Women: Most of them knew of Ol’V, BCG, DPT, but not many knew of Measles vaccine. Also
they were ignorant of number of doses of each & tlie disease agamst which different vaccines were
health.
Mr.SJC: What are their ‘unmet needs’?
women:!. v>my rice not cnongu, varictj
2. Need more playthings.
4. Make ‘baiawadi’ attractive to children, so that they ‘love’ to come there.
> Mr.SJC: Why do they think some children are not attending anganawadi?
make their children dirty'1; some fear that there will be sharing of plates; distance problem;
Mr.SJC: Any other significant problem they wanted to discuss?
Women: Most of them strongly felt something is needed to he done to children of coolies, as the
anganawadi closes till then parents return home from their work.
Women: rood; preschool- so that their children become smart; to see that ‘headache" is transferred
to someone else for atlcast sometime!
Women: (Alter some minutes of silence) “You give the suggestions
then we will see how we
IMPRE S SIGN:
most important being the dangerous misconception of Govt, supplied ‘supplementary nutrition1 as a
‘replacement’ to
nutrition^ which TTiakes the basic objective of IGOS ^h^mp nf Snmnwinv child
nutrition", a distant dream. Also there is need io further the health knowledge or mothers regarding doses
of immunization & other aspects of child care. It seems necessary to consider how best can we make
conveniently overlooked is ‘the street children1 problem, it is an emergency problem which needs to be
addressed on a war fooling. Also it is pertinent for us to now evolve a strategy for effective 6comm»miiy
participation’ if we aic to make Rural Health Development a reality.
( (SX5J- -
.
4
f
L,
!&>'
?O^q\dS1^Y|
W^OkRFWG
CSLUCWD
Tokd
Va^UtK
"WUDfcEN
f4ki<3
0-(>w ’|~ram
Co-t'i]
^Q^faxc^YY<S^(JoUi
MAW<kdi
V°>G3>
3<50.' IO\3
\<Al
IW '153
|J-gArn
35-36™
<?3h
A US
® BoVVi
\fiJdxx.^y>
Wxie pBtc'DS-E.
W
•2:Q
lx>
W <w4> \hkta(^
\y)
Ph^ecfc
xmAc.ts
•
SEX
R fillO IN WTLWEn
6-6-4
O~(jCD
7-I6<y>
fj-36w
.jf-Sfcrn Su-t-j
.Arte
*Qrt
<iNG
11
13
6
3
liv-iao
’
2Q
AGOtfT WE iOS
®?^ese^)u^
JFWOW £ mHAGO^-DAVALUl
PW\
Mndkhkwe/n
1 ecn^^di
>
T7-
S'-5
j:5
131
- 36'.IQ
a&'33
PROTECTS
^MehwoerJi
VnVU U
93-’5t
a
o^T-N.
^n^acG
^vOpo^oA
nejQjA ^ufa^e.
® sta^ ■-
Kofaa^oYicRfolU
}>A^6voawacLi
AnrbvJadA
SoGmm >
C?e»xm&i
$ Hhi.Ual^na
fc. t1«5 )'
. 3a^ftwwa
^•Ah0|-
S- 6.9.051 M
(ji Oy\YA$nfop
A V\hK . Io^Iqm rr>i
Mli3G| ~
P..1U36/-
b) tta • fk>\Vx
o) Y\wi.\)o.'ft<w)W
p,- LUof'
t-bA • Se.4Va
ftAUO|~
$)M to
OBStRvAW >
The^e
tW'^'fauX,
is a
c^cLime
Vn
g-^tWd
o-W^l^ W>khv>C^ M(WiO
M cKU^.f.TV,^ u a
CAHSe
>
fogin
fcfK w
d^dHve
fa)
Co^tfc/-
^XvoIjqy),
9sn,
SRINIVASAN SERVICES TRUST
Jayalakshmi Estate, No.8, Haddows Road, Nungambakkam, Chennai -6
30.11.2004
To
Dr. Thelma Narayanan,
Community Health Cell - CHC
No. 367, Srinivasa Nilaya,
Jakkasandra I Main, I Block,
Koramangala,
Bangalore - 560 034.
Ph : 25531518(080)
Sub : Nutrition Programme for 5 Villages.
Dear Dr,
In continuation of discussing we had with Mr. Chandar & Dr. Vinay on the above subject
we would request you to assess under 5 children and conduct Nutritional Programmes
for the following 5 Villages. We would also request you to send the outline of the program
and the cost involved.
a.
b.
c.
d.
e.
Kothakondapalli
Bommandapalli
Bathalapalli
Andivadi
Belagondapalli
Expecting an early reply.
Ref: CHC/2004/
10nd December 2004
Dr. A. Rajan Babu,
Chief Medical Officer,
Srinivasan Services Trust,
Jayalakshmi Estate, No.7,
Haddows Road,
Nungambakkam,
Chennai 6
Dear Dr. Rajan Babu,
Thank you for your letter. I have been on leave due to the serious illness of my
father and hence the delay in replying.
We are also currently busy with a training programme and with preparations
for a National Public Hearing on the right to health care being jointly organized
by the NHRC and the Jan Swasthya Abhiyan during mid- December in Delhi.
We would be able to assist you in January 2005. Dr.Vinay is presently in
Gadchiroli in Maharashtra and will be back in the last week of December 2004.
From a community health perspective it is better for your team with the local
health workers to conduct the nutritional programmes yourselves. We could
conduct the survey along with your team so that local skill development takes
place. We could assist in the process of participatory planning, implementation
and review of the nutrition intervention. Baseline and later measurements
would help the community to know if there is any impact following introduction
of the intervention.
We will keep in touch with you in this regard.
With best wishes,
Yours Sincerely,
For Community Health Cell
Thelma Narayan
Co-ordinator
k
P.S : Enclosed is a copy of the Peoples Charter on HIV/AIDS launched by
the Peoples Health Movement at the International AIDS Conference in
Bangkok in July 2004. Enclosed also is a Arogya Kalajatha Book of
songs on health issues. It also has a kannada translation of the AIDS
charter.
DFA
Report on field visit to Kothakondapalli. proaarmme bv TVS
Dr. Rajan Babu the chief medical officer and Mr.Kamalakanna the social welfare
officer of TVS company in Hosur visited Community Health Cell on 13th July 2004.
They requested for the support of CHC in addressing the problems pertaining to
nutrition and environmental and personal hygiene among the people in the villages
where the company is working.
The Community Health Cell team consisting of;
1.
Ms. Pamasini Asuri,
2.
S.J.Chander.
3.
Prasanna Saligram
Visited Kothakondapalli villages near TVS Company in for assessing the nutrition
programme on 22nd July 2004. We are given to understand that TVS Company is
working in six villages around the TVS Company where government is implementing
the ICDS Progarmme.
TVS Company is organizing self-help groups in all these
villages. These self-help groups make chapathis and supply them to TVS Company's
canteen.
According the filed worker Mr. Gangadharaiah, he collects information
regarding the children's nutritional status from the anganawadi centers and given to
the company.
The team was accompanied by Mr.Ganngadhariah to Kothakondapalli as he could
not give satisfactory answers to CHC team members, Dr. Rajan Babu was requested
to come to the field to provide information regarding the prevailing situation. Before
Dr. Rajan Babu could arrive the village the team had interacted with the anganawadi
worker and also reviewed the records used for growth monitoring. According to Mr.
Gangadharaiah; "there are no malnourished children. However, all the children were
within I & II Degree"
During our visit, 30 out of 35 children were present at the anganawadi center. The
scale against, which the children weighed used, by the ICDS Programme in Tamil
Nadu does not contain source and basis. According the CHC team there Is errors In
the scale for example a child born with 2.5 kgs of birth weight should gain 9kgs of
weight at three months, according to the scale 7.5 kgs as acceptable. The
1
supplementary feeding powder packet supplied by the government does not reveal
what it contains for example wheat/corn, it is difficult to infer if it contains wheat or
com.
According to our observation all children seemed undernourished and running low
temperatures. It was suooested to have a health check up and monitor the children
for general health problems. The anganawadi worker and the filed staff of TVS are
unable to interpret the data that they have documented regarding children's growth
monitoring.
It was suggested to check for helminthes infection and assess types of food children
get at home and its quantity in order to overcome calorie gap in diet intake both at
home and ICDS center. This is important for preventing brain damage, which could
occur during the first 11/2 years of the child's life, as it is difficult to repair later. It
appears that the children are not weighed regularly on monthly basis. The food
supply during the week to children, during the week the menu seems to be
satisfactory and its effect is not documented therefore it is difficult to asses.
It was suggested that not to depend on weight for age indicator alone for measuring
the weight for children as a child suffering from mild kwashiorkor could also show an
increase in weight.
It was suggested to make a follow up plan for children in two categories separately;
one for children below two years and children above two years. This is important to
understand the foilwing matters; food habits at home; the quantity of food given its
quality and how much is consumed; who normally feeds child and how the family
assesses the growth of a child for planning. There might exist misconception
regarding diet given to children, which must be identified and addressed.
It would be helpful if medical examination and weighing is done once in two months
for all children under two years for assessing their general decease pattern and
monitoring the growth. Finally it was suggested to involve mothers among the group
by training them and involve them for creating awareness and support the
programme on day-to-day basis.
2
&
-
nxv *1
••J
*
VI x^MvaiVivX* diIU
Environment hygiene. (Villages covered by TVS, Haritas at Hosur)
Dr .Rajan Babu and Mr. Kamalakannan of TVS came to Community Health Cell on
22ndly July and 27th August 2004 to request to help them in addressing the problem of
Nutrition and environmental hygiene. During the discussion it was discussed and agreed
that a collective process would be evolved with the community than implementing a
project to address the problem. Therefore the following visits were proposed to have
dialogues with the various groups were necessary.
CHC team members have made three visits so far to Asses the situation. The first visit
was made by a team of three people consisting of Ms. Padmasini Asuri Nutrition expert,
Mr. SJ.Chander Community Health and Sociology background and Mr.Prasanna
Communication background. Following were the observation made during the visit. The
first visit was made to Kothakondapalli anganwadi centre. The team had a dialogue with
the Anganwadi worker, Dr. Rajan Babu and Mr. Gangadharappa of TVS. The children
appeared sickly, running low-grade temperature. It was observed that the chart used for
recording the weight of the children is misleading in categorizing the grades of
malnutrition as the chart was shows less weight for the age.
During the second visit, the CHC team members had in interaction with the anganwadi
workers. All the anganwaid workers for the six centers were present for the meeting.
Couples of ayahs were also present. All of them expressed their willingness to work
together in addressing the nutrition problems of children. They are demotivated by lack
of supportive supervision and cooperation from their superiors. They expressed their
dissatisfaction over their salaries. They said they are made to work more for less salary.
Their knowledge on nutrition seems satisfactory; however an assessment would be
helpful before conducting the training programme for fine-tuning their knowledge and
skills. Without motivating the anganwadi workers, improving the infrastructure facilities
would not make much impact on the health and nutrition status of children.
The third was made to interact with the mothers. Eight mothers were present for the
discussion from three villages
In'1? • ‘
’ ’’
’••••"> >- --
nutritional needs of their ehildren adequately, later when probed they expressed that there
is a problem with the poor families where both the parents are working as coolies.
Childcare is a problem after anganwadi center as the children are left on the street or left
to care of the elderly until their parents return from work. It was reported that many of the
poor families arc unable to provide adequate food for their children.
The mothers
nuBundorBland that the food given al the anganwadi center is adequate, they do not know
it is only a supplementation. The angawadi teachers expressed absenteeism as a problem.
They said the following are the reasons; children want to be free, do not want to be
confined within four wall, no toys and distance. They said malting available more toys
and improve the quality food could attract more children. It was observed that there were
more boys than girls in (he register, we wonder if there is a problem of sex ratio.
Physical structure of anganwadi centers is excellent TVS has helped in providing toilet
and water facilities, they are also providing biogas facilities for cooking. The surrounding
of the villages appeared untidy. There is a need to work with the village leaders and if
there are any village level committees.
It is not clear, what is the extent of the problem of nutrition. Therefore it is suggested that
a sample survey may be necessary. It would also be helpful to assess the knowledge
attitude and skills of andganwadi workers and mothers.
Anganwadi workers told us that they regularly monitor the growth of children. However
it would be helpful do an assessment of a small sample to know how well growth
monitoring is done.
PROTECT PROPOSAL FOR NUTRITINAL STATUS OF CHILDREN (0-6YEARS) IN
6 VILLAGES IN HOSUR TALUKA
AIM: Assessment of nutritional status of children between 0-6 years of age in 6 villages
of Hosur taluka of Krishnagiri district of Tamilnadu state & to plan & enable measures
to mitigate malnutrition in children & to promote the development of children & ensure
them a healthy childhood.
OBJECTIVES:
■
■
■
To assess the nutritional status of children aged 0-6 years in 6 villages of Hosur
taluka where health division of Community Development department of TVS
Motors (TVSM) is working.
To identify the various factors; social, economical, political, educational &
cultural; that affect the nutritional status of the children in that area.
To plan & enable the local community & Community Development department
of TVSM to take collective action to adapt & maintain rational & appropriate
nutritional practices of the children to restore their nutritional status to normalcy
& maintain the same.
THE PROCESS:
The whole project will be taken in two phases:
1.
Assessment phase including collection & analysis of child nutrition data &
2.
Post assessment action phase includes evolving a plan to enable the local
community & health division of Community Development department of TVSE
to take collective action to adapt & maintain rational & appropriate nutritional
practices of the children.
ASSESSMENT PHASE:
It includes the following processes:
* An action based & participatory community approach will be the guiding
principle for the whole process. Meeting the local people & building working
relationship with them will be the first step of the project. Local people includes
the staff at health division of Community Development department of TVS
Motors, the community leaders of all 6 villages, representatives from parents,
women, men, children & elderly groups of the community, the anganwadi
workers & ANMs of the area. The meeting would serve as a place to:
o Know the willingness of the community to participate in the project
o Inform & discuss, with all parties involved, the objectives & methodology
of the project
o To understand & build rapport with the community
o To involve every stake holder in decision making process
o To finalize the logistics of the assessment phase of the project
To collect past records, whatever is available, regarding the health status
of the children in the community
o To build a causal model of malnutrition
Methodology used for the assessment of nutritional status of the children would
be a 'cross sectional study' of all the children through house to house visits &
recording their weight using Salter scale & height (for children >2 years)/length
(for children <2 years) using fibre glass scale/infantometer. The data will be
collected with the involvement of the local people. The data collected will be
collated with the past records of the children to assess the nutritional status. The
NCHS values for weight & height of children, as recommended by WHO, will be
used as the reference values to draw inferences.
In addition, based on the causal model of malnutrition, a questionnaire designed
to study the various factors; social, economical, political & cultural; that affect the
nutritional status of the children in that area will be administered to a
representative sample of the different groups in the community.
The process will be designed & implemented with full participation of the local
people. The community will be asked on how best can we involve them in the
process (& also will be asked to provide 2 volunteers in each village for the entire
process to move forward. Then, the volunteers will be involved in a discussion
where the whole process of the project will be discussed with them & their needs
identified. In addition, their inputs will be incorporated in the design of the
questionnaire. A training program to build capacity of the volunteers to
undertake the project themselves will be planned.)
o
■
■
■
COMPONENTS OF THE ASSESSMENT PHASE:
1.
Meeting with the local people: Meetings will be held with local communities &
staff members of RHDC of TVSE with the objectives mentioned earlier. Also,
these meetings will be made participatory & will be used to serve the following
requirements:
■ Build a team within these villages to assist us in the project. In addition,
capacity building of the same to be undertaken during the process of
project execution to enable them to continue the work in future
■ Construct a simple & functional
hypothetical causal model of
malnutrition
2.
Collection of vital statistics: It is important to have a general picture of the
community in which a health program is being planned. Apart from helping us
in providing on the demographic profile of the region & an approximate number
in the target group (children of 0-6 years), it also helps in giving a broader
picture of the overall health status of the children in the region. RHDC can obtain
the same from the local governmental authorities. The data deemed pertinent for
the project are number of children in 0-6 year age group, sex ratio in the same
age group, IMR, 1-4 mortality rate, vaccination coverage, life expectancy of the
area, spacing of the child birth, details of families with 0-6 year old children &
any other deemed necessary during actual process.
3.
Collection of previous records of the children: Such as growth charts, birth
certificates, under 5 health records, records from pre primary child care centres &c.
any other records pertaining to the health of the children under study.
4.
Clinical examination: Clinical examination of all the children to search for
specific signs of malnutrition to be carried out. The specific signs of malnutrition
that will be looked in each child will be as follows:
• Hairs: Sparse, thin, easy pluck ability, hypo pigmentation, without sheen,
flag sign
• Eyes: Dry eyes, Bitot's spots, keratomalacia, xeropthalmia, pallor
• Tongue & mouth: Sore, red & glazed tongue; cheilosis; pallor
• Skin: Erythema, Hyper pigmentation, raw hypo pigmentation; easy
bruisability; dry, inelastic & mosaic skin; phrynoderma
• General appearance: Wasted muscles & bony prominences; no fat under
the skin; protuberant abdomen; generally apathetic or highly irritable
child; child which has stopped feeding; oedema;
5.
Anthropometric measurements: The height & weight of each child is to be
measured & then weight for age (under weight), weight for height/ weight for
length (acute malnutrition) & height for age/ length for age will be calculated for
a sample of children. The age of the child in question will be assessed according
to the data in birth record or if no such data is available using the local calendar
or an approximate age is calculated using the clinical examination. All
measurements are to be obtained under standard conditions using standard
equipment & standard techniques. The NCHS values of height & weight for age
in children will be used as reference values to draw conclusions. The same will
be recorded on a growth chart & the importance of maintaining the same in
future will be stressed. If previous records of weight & height are available, the
same will be collated with the current measurements to know the trend of
nutritional status & to identify the 'at risk age', if any, in the community.
Community survey: Once a simple & functional causal model of malnutrition is
built & major determinants for the cause of malnutrition identified, analysis of
the data will be taken up & priority areas for intervention will be identified.
A period of one month is envisaged to be the time period to carry out all the above
activities. Once, the above process is over, the project moves into the post- assessment
action phase.
6.
PROJECT PROPOSAL FOR NUTRITIONAL ASSESSMENT OF CHILDREN IN 6
VILLAGES IN COLLOBORATION WITH RHDC OF TVSE FACTORY IN HOSUR
AIM: Assessment of nutritional status of children between 0-6 years of age in 6 villages of
Hosur taluka & to plan & enable measures to mitigate malnutrition in children, if it is
prevalent, & to promote the adequate development of children & ensure them a healthy
childhood.
OBJECTIVES:
■
■
■
To map out the magnitude of the burden of malnutrition as a health ptoblem in
children between 0-6 years of age in 6 villages of Hosur taluka.
To identify the various factors; social, economical, political & cultural; that affect the
nutritional status of the children in that area.
To plan & enable the local community & RHDC of TVSE to take collective action to
adapt & maintain rational & appropriate feeding practices of the children to restore
their nutritional status to normalcy & maintain the same.
THE PROCESS:
For the sake of convenience, the whole project will be taken in two phases:
1. Assessment phase
2. Post assessment action phase includes analysis of the data collected during the
assessment phase & evolving a plan to enable the local community & RHDC of
TVSE to take collective action to adapt & maintain rational & appropriate feeding
practices of the children.
ASSESSMENT PHASE:
It includes the following processes:
■ Meeting the local people & building working relationship with them. Local people
includes the staff at RHDC of TVSE, the community leaders of all 6 villages,
representatives from parents, women, men, children & elderly groups of the
community, the anganwadi workers & ANMs of the area. The meeting would serve
as a place to:
o Know the willingness of the community to participate in the project
o Inform & discuss, with all parties involved, the objectives & methodology of
the project
o To understand & build rapport with the community
o To involve every stake holder in decision making process
o To finalize the logistics of the assessment phase of the project
o To collect past records, whatever is available, regarding the health status of
the children in the community
o To build a hypothetical causal model of malnutrition
■ Methodology used for the assessment of nutritional status of the children would be
a 'cross sectional study' of all the children through house to house visits & recording
their weight using
height (for children >2 years)/length (for children <2
years) using
. The data will be collected with the involvement of the local
people. The data collected will be collated with the past records of the children to
■
■
assess the nutritional status. The WHO/ICMR values of height & weight for age in
children will be used as reference values to draw conclusions.
In addition, based on the hypothetical model of malnutrition, a questionnaire
designed to study the various factors; social, economical, political & cultural; that
affect the nutritional status of the children in that area will be administered to a
representative sample of the different groups in the community.
The process will be designed & implemented with full participation of the local
people. The community will be asked on how best can we involve them in the
process (& also will be asked to provide 2 volunteers in each village for the entire
process to move forward. Then, the volunteers will be involved in a discussion
where the whole process of the project will be discussed with them & their needs
identified. In addition, their inputs will be incorporated in the design of the
questionnaire. A training program to build capacity of the volunteers to undertake
the project themselves will be planned.)
COMPONENTS OF THE ASSESSMENT PHASE:
1. Meeting with the local people: Meetings will be held with local communities &
staff members of RHDC of TVSE with the objectives mentioned earlier. Also, these
meetings will be made participatory & will be used to serve the following
requirements:
■ Build a team within these villages to assist us in the project. In addition,
capacity building of the same to be undertaken during the process of project
execution to enable them to continue the work in future
■ Construct a simple & functional hypothetical causal model of malnutrition
2. Collection of vital statistics: It is important to have a general picture of the
community in which a health program is being planned. Apart from helping us in
providing on the demographic profile of the region & an approximate number in the
target group (children of 0-6 years), it also helps in giving a broader picture of the
overall health status of the children in the region. RHDC can obtain the same from
the local governmental authorities. The data deemed pertinent for the project are
number of children in 0-6 year age group, sex ratio in the same age group, IMR, 1-4
mortality rate, vaccination coverage, life expectancy of the area, spacing of the child
birth & any other deemed necessary during actual process.
3.
Collection of previous records of the children: Such as growth charts, birth
certificates, under 5 health records & any other records pertaining to the health of
the children under study.
4.
Clinical examination: Clinical examination of all the children to search for specific
signs of malnutrition to be carried out. The specific signs of malnutrition that will be
looked in each child will be as follows:
•
•
•
•
•
Hairs: Sparse, thin, easy pluck ability, hypo pigmentation, without sheen, flag
sign
Eyes: Dry eyes, Bitot's spots, keratomalacia, xeropthalmia, pallor
Tongue & mouth: Sore, red & glazed tongue; cheilosis; pallor
Skin: Erythema, Hyper pigmentation, raw hypo pigmentation; easy
bruisability; dry, inelastic & mosaic skin; phrynoderma
General appearance: Wasted muscles & bony prominences; no fat under the
skin; protuberant abdomen; generally apathetic or highly irritable child; child
which has stopped feeding; oedema;
5.
Anthropometric measurements: The height & weight of each child is to be
measured & then weight for age (under weight), weight for height/ weight for
length (acute malnutrition) & height for age/ length for age (chronic malnutrition) ?
should this also be used to children>2 years? will be calculated for each child. The
age of the child in question will be assessed according to the data in birth record or if
no such data is available using the local calendar or an approximate age is calculated
using the clinical examination. All measurements are to be obtained under standard
conditions using standard equipment & standard techniques. The WHO/ICMR
values of height & weight for age in children will be used as reference values to
draw conclusions. The same will be recorded on a growth chart & the importance of
maintaining the same in future will be stressed. If previous records of weight &
height Eire available, the same will be collated with the current measurements to
know the trend of nutritional status & to identify the 'at risk age', if any, in the
community.
6.
Community survey: Once a simple & functional hypothetical causal model of
malnutrition is built & major determinants for the cause of malnutrition identified,
a questionnaire will be designed to study the identified factors; social, economical,
political & cultural; & will be administered to a representative sample of the
different groups in the community with the help of local people.
A period of one month is envisaged to be the time period to carry out all the above
activities. Once, the above process is over, the project moves into the post- assessment
action phase.
Report of visit to TVS community development project in Hosur
On 7lh March 2005 a meeting was held with the anganwadi workers working in the
following five villages; Andhivadi, Kothakondapalli, Romandapalli, Relakondapalli and
Bathalapalli to finalize the nutritional assessment of under five children. The anganwadi
workers clearly indicated that they are de motivated to work as they are paid a very
meager salary (honorarium) they said they are not doing their work as per the conceptual
framework given by the Integrated Child Development Services project. They said if
TVS considers providing them some support it would motivate them to collaborate with
the initiative of TVS in improving the health and nutritional status of children. They did
not say this as a condition.
Regarding areas of concern for improving the anganwadi centers they said many children
are going to private nursery schools and others not motivated to come to the center. For
this they said, if TVS could help in providing additional supplementary food like the
government gives an egg on Thursdays and the attendance goes high on Thursdays. They
also said if they children could be provided with uniform it will motivate the parents
sending their children to private nursery schools to send them to the anganwadi centers.
On 19,h March 2005 it was decided to start the assessment at Kothakondapalli and it was
communicated to Dr.Rajanbabu of the Chief Medical Officer of TVS. When we went to
Kothakondapalli on 18U1 at 9 am. there were only four children in the center. We waited
there for the teacher and the ayah to come, at about 10 am the ayah came with a basin full
of cow dung for the Gobargass plant installed for the cooking. The ayah said the teacher
had gone for a meeting and she would not be coming. She was busy cutting the
vegetables for the food that she was planning to cook and the children were playing on
their own in the center. Few mothers and relatives of the children came there to drop the
children.
We started the assessment at about 10 am and could not continue after assessing about 10
children, as wc could not elicit the information about the name of children and their
mothers and also their date of births. Since we had to leave these columns incomplete we
decided to stop the assessment and planned to continue when the anganwadi teachers was
there and their parents were informed. We met the self-help group members of TVS and
explained to them about the proposed nutritional interventional plans. They said they
would support the initiative. Some of them said that their children are also in the
anganwadi and they were not happy with the way the anganwadi center is functioning as
their children not taught well and taken care. After meeting the self-help group members
we went to Bomnadapalli, there were about 15 children in the aganwadi and the ayah was
busy cooking the food. Here too the anganwadi teachers had gone for the meeting. We
went to meet the panchayt president’s house to seek his support. Mr. Srinivas Reddy was
not there but his family members said they would convey the message to him and gave us
his phone number to talk to him. We met the self-help group leader Ms. Prema and two
other women, they said they would support the initiative planned by TVS. During the
afternoon we had meeting with Dr. Dhakshinamoorthy, he said we had to assess all the
children under five years of age, which was contrary to the plans that we had. We had
decided to assess all the children who are coming to aganwasdi and assess about 20% of
the children who are not coining to the center. We told him if we have to consider
assessing all the under five children, we need to revise our budget. We also told him that
we will only assess the nutritional status and build the capacity of mothers, self help
group members, anganwadi workers and TVS staff we will not do the intervention alone
for TVS. We also discussed the concern of the aganwadi workers and appointing a
female health staff by TVS. Dr. Dhakshinamoorthy said that TVS will not consider
appointing such a person and regarding the grievance of the anganwadi workers, he said
TVS would not consider offering any support to them too. He suggested that we could
have planned their support as part of their budget. Later he took us to Kothakonda palli
and Belagondapalli to meet the key informant in the village and to identify the places
where we could establish the assessment centers in the village. After this he dropped at
the Hosur bus station at 5 pm.
Ref: CHC/2005^
June 13, 2005
Ms. Padmasini Asuri
Nutrition, consultant
Jayanagar,
Bangalore
Dear Madam,
Greetings from Community Health Cell!
You have been supporting our nutrition intervention for the Community Development
Programme of TVS Motor Company in Hosur during the past few months. Your support
is highly appreciated both by CHC and TVS Motor Company. I would like to request
you to continue to support in planning and implementing appropriate intervention based
on the finding of the recent assessment carried out in five villages. The next meeting with
all the anganwadi workers, CDPO and TVS staff is planned for 20th June,2005 at. 2.00
pm, at Community Health Cell. Kindly facilitate the discussion and planning process. We
shall make arrangement for you conveyance.
With warm regards
Yours sincerely
^STChander
For Community Health Cell
Field Training Coordinator
Ref; CHCpoy05
8th August,2005
Dr. Rajan Babu
Srinivasan Services Trust
Jayalakshmi Estate
No.8, Haddows Road
Nungambakkam
Chennai - 600 006
Dear Sir
Greeting from Community Health Cell
Subject: Partial payment for our services towards nutrition intervention project.
Please find furnished below the details of our service charges towards the nutrition
intervention project of TVS Company in five villages in Hosur taluk.
Sl.No
1.
2.
3.
4.
5.
Description of cost
Resource fee for the preliminary visits for 7 days
for two people @ Rs. 1000 for one person and Rs.
500 for another person.
Equipment for measuring height and weight
Travel during the assessment phase
For 20 days @ Rs. 400 per visit for two people
Resource fee during assessment phase
@ Rs. 500 for one person and Rs. 300 for another
person
cko-W
Total
<
(Rupees thirty nine thousand five hundred only)
With regards
Yours sincerely
ftfChander
For Communty Health Cell.
Total
Rs. 10,500.00
Rs. 5,000.00
Rs. 8.000.00
Rs. 16.000.00
Rs. 39,500.00
Budget for Nutritional assessment and intervention in five villages'TJ^ZE^it
SI. No
1.
2.
3.
4.
Description of cost
Preliminary visits
7 visits by two resource person
@Rs. 1000 per one person and Rs.500.00 per another
person 7X1500.00= Rs. 10, 500.00
Resource charges during intervention phase
For 24 days two visits in month by two people @Rs.I500
per visit 24X1500= Rs.36.000.00
Printing and stationery
Equipment for measuring height and weight of children
Travel
During assessment Phase
For 20 days @ Rs. 400.00 per visit for 2 people
400X20
During intervention phase
@Rs.4OO per visit for two people for 24 days
Rs.400X24 = Rs.
Total
Rs. 10, 500.00 /
Rs. 36,000.00
Rs.
Rs.
5,000.00
5,000.00 J
Rs.
8,000.00
Rs.
9,600.00
Rs.
4,000.00
5.
Training programme
Two one day training programmes
@ Rs. 2000.00 per day
Rs.2x2000= 4,000.00
Total
(Rupees seventy eight thousand one hundred only)
Rs. 78,100.00
.
lrb&!
-*
Technical Comments on the activities of ICDS
programme support from TVS Medical Unit Hosur.
This comment has been written after a single visit to the Anganwadi
center of Government of TN that has the support of TVS unit at Hosur.
Hence it is limited to what had been observed at the time of visit.
The Situation:
The village Kothaguntapalli is about few kms from Hosur Factory. The
Anganwadi is one the centres of ICDS. There was a teacher and an ayah
manning the children, A typical Anganwadi center with lackluster in
various aspects, this is attached to the primary school of the village.
There was a ‘Salter Scale ‘ hanging in the middle of the room, (perhaps
to indicate that the center was an Anganwadi) There were about 25
children, out of enrolment 35. It was about a month since the centre had
been opened for the current year.
The strength of Anganwadi Positive points ;The Govt of TN had
provided the teacher with the chart which is almost a ready- reckoner for
the teacher to classify the children according to the nutritional status.
Naturally the teacher lacked in depth understanding of the purpose of the
chart, She merely records the wt and had mentioned that most of the
children were normal or in grade 1 Similarly the chart had been given for
the weight for the expectant mothers, who are also the beneficiary of the
centre. Both the charts did not show the reference standards. I could not
check the weight recorded as the register was not in the class. The fact
that an effort to help the teacher to record the weight, utilising the
figures provided in the chart shows the concern of the authorities.
The Ration given to the children as per the Governmental instruction is
as under
WEANING FOOD (as found on the label) Composition per 100 g.
Cereal (wheat/Maize/ Bajra------52 g
Ragi
----- 05 g
Bengal gram — 12 g
Jaggery
----- 30 g
Nutritional facts
per 100g Calories 350
Protein
8.5 g
The ration permitted of the ready mix to the children . The processed
powder is mixed with boiled and cooled water to make into laddoos
50 g ball for the under two yrs and 100 g balls for the above 2 yrs upto
5yrs. As soon as the children arrive the balls are sserved The under twos
have the laddos and return with the mothers while the anganwadi
children get the midday meal as well. The ration per child /day are
as Rice
80 g , dhall 10 g- oil 2 g In addition on Mondays
potatoes are given, Tuesdays Greengram Thursdays
1 egg while on
Wednesdays and Fridays no additional item is provided .
Through this meal as per the calculation the children get 290 calories
and 6.5 g Protein thus during the day with laddo and meal the
anganwadi children get in total 640 calories (RDA 1230 )
15 g Protein (RDA 25 g)
The food provided during the day gives about 50% of RDA and is quite
good. According to the ‘consultant’ of the team the normal status
children in the class is to the extent of 70-80% (!) But the Team had also
taken the wt of children who do not attend the anganwas\di class and the
wt recorded shows children with normal wt also to the extent of 75 %
What is the impact of the meal provided ?
My observations: The support given by the Government of TN in
providing a ready reckoner is a good start. But beyond this there were no
information whether the the children me given any vitamin /mineral
supplements. Whether the medical checkup was done or notwas not
known. The children looked rather weak and stunted in growth.Though it
is difficult to weigh the children of that age certain care need to be taken
during weight recording. Since we did not see any data of individual
child’s growth rate one does not know whether the normal child is on the
borderline or well above. There was no individual weight card. When the
children are getting the calorie gap filled in with the meal and laddoos,
there should be some difference between the anganwadi and nonanganwadi attending children. Weight alone is inadequate to rate the
child’s nutrtional status. Some of the standards, recommended
maintained in India and elsewhere are stated below.
Standards available to assess the nutritional status of the children :
On the recommendations of the WHO the standards of National Centre
for Health Statistics (NCHS)is the reference point recommended in
India. The median value of NCHS is taken as Indian reference standard
(copies enclosed) Normally the classification of nutritional status are
Ht for age wt for age as well as wt for ht.
1. According to Gomez standard the classification details are :
Normal
above 90% of Indian standard
I st degree mal-nutrition
75-90 %
II nd degree
60-75
III rd degree
<60 %
Reference is 50th centile
2 The Indian Academy of Pediatrics (LAP)
Normal
I st degree
II nd
III rd
Iv th
above 80%
70-80 %
60-70
50-60
< 50%
To confirm the nutritional status weight alone is inadequzte. Height for
age is also essential and weight for ht as well as wt for agegrefer to the
table) A proper medial checkup need to be done at the beginnng to check
for possible infection or infestation ,other factors that would inhibit the
absorption of the nutrients by the body,
With the average availability of 650 calories even the mal nourished
should be able to show some improvement and move up in the scale.
Since the teacher appears to be not so trained in the technical details
including the weighing of the child in the balance ,A-close observation
whether the children are eating what is served would give more
information about the children and the instruction received from their
mothers.
It is said that every child has the same growth potential if properly
nourished. It us thus necessary as not to accept lower standards as
“Indian “
4
With my handicap of limited information received on the spot, I make
the following suggestion for the TVS team who are graciously
supporting the Government’s effort in the area of child development
The suggestions are:
1. Check the scale used by the Anganwadi as the spring needs to be
strengthened.
2. Weigh the children individually as to wt for age ,measure the ht for
age with reference to the NCHS 50th centile (as per the chart) of
the Anganwadi group and record their status. Measurement of
arm-girth would be also useful if the doctors have the time. This
data of individual child , the team could keep in their office and
not share with the teacher till certain facts could be deduce
3
The teacher can continue her exercise. This can be corrected once
the doctors ares sure of the data. For this reason a close supervision
of the anganwadi school children need to be done’
As to their eating habits alertness and interest. A close observation of
children’s eating habit is required to find out whether they do get
their share and consume the food served. This one of the team
members can do continuously for a week or two during the meal
time The same person should make enquiries about the food that is
given by the mothers at home to compute the food availability for the
growing child
4.
Provide the medical check up for possible corrections if required
The children should be weighed periodically (once in three
months) to observe the growth during the period and also see the
difference between Anganwadi and outside.
6. To weigh the other children bathroom scale (platform type)
should be avoided..
7. Conduct under two advisory centers as this age is very crucial to
promote the potential growth factor in the child
8. To conduct this it should be considered as Health-nutrtion
education programme.
8.1
Select intelligent mothers and train them on few facts
of nourishment and health care of the under two yrs,
and make them as para- teachers/mother-teachers to
teach minimum of five mothers in their peer group,
5.
5
8.2
8.3
8.4
Conduct nutrition and health education classes to
give a holistic information on water,hygiene and food
requirements
The clinical classes should be a positive under two
Programme and not just cater to the sick children
alone. This would enable the mothers to a understand
and help in maintaining the weight chart as well as
provide possible adequate nourishment at home
Encourage the mother- teachers to participate and help
the anganwadi specially during meal time. This can
be done by the selected mother-teachers in turn
A comparative findings of local situation with that
of anganwadi will be useful for other areas
alsowhere anganwadi programme is executed. In TN
With time bound project the TVS team can show the way to
organize Under Twos in Anganwadi centres
The above activities are only a suggestion to improve the condition
of the children and the approach to anganwadi with TVS support.
0
D. HANUMANTHA RAO AND K. VIJAYARAGHAVAN
154
.155
TEXTBOOK OF HUMAN NUTRITION
Table 2: Median Values (50th percentile) Weight for Height for Boys and Girls
Table 1: Median Values (50th centUes) of Heights and Weights of
Boys and Giris (0-60 months) — NCHS
Height
(ems)
Ref: WHO. Measuring change in nutritional status. Guidelines for assessing the nutritional impel of
supplementary feeding programmes for vulnerable groups. WHO. Geneva. 198.1.
Expected Weight (kg)
Boys
Giris
Heighl
Expected Weight (kg)
<UnV
Boys
Girls
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
14.2
14.5
14.7
15.0
15.2
' 15.5
15.7
16.0
16.3
16.6
16.9
17.1
17.4
17.7
180
18.3
13.9
14.1
14.3
14 6
14.9
15.1 .
154
15.6
15.9
16.2
. 16.5
16.7
17.0
17.3
17.6
17.9
112
113.
114
115
116
117
1 18
119
120
121
122
19.3
19.6
20.0
' 20.3
20.7
21.1
21.4
21.8
22.2
22.6
23.0
J8.9
19.2
19.5
20.3
20.6
21 0
21.4
21.8
21 8
22.7
126
127
128
129
24.8
25.2
25.7
26.2
24 6
25.1
25.7
26.2
132
133
134
135
136
137
27.8
28.4
29.0
29 6
" 30.2
30.9
28 0
28-7
29.4
30.1
30.8
31.5
19.9
Kef: WHO Measuring change In nutritional status. Guidelines for assessing the nutritional impact of
tupplementary feeding programmes for vulnerable groups. WHO. Geneva, 1983.
GROWTH CHART - BOYS
156
TEXTBOOK OF HUMAN NUTRITION
(IAP-Clast®atlon - NCHS standards)
CLASSIFICATION OF NUTRITIONAL STATUS
Relatively speaking, weight, height and arm circumference have come to be considered
the most sensitive parameters for assessing nutritional status of under fives. Several
methods have been suggested for the classification of nutritional status ,based on these
measurements.
The anthropometric data can be expressed in a number of ways in relation to. refer- ■
ence data: (a) by the use of mean and standard deviation values, (b) by calculating per
centages of the median value of reference population which is assigned as 100 per cent,
and (c) by comparing with percentiles of the reference data, where median value is the
50th centile.
Weight for Age
Various methods have been suggested to classify children into various nutritional grades
using the body weights. The most widely used classification is the Gomez classification
(Gomez et al., 1956), in which the children are classified as having first, second or third
degree malnutrition if their weight for age is in the range of 75—90%, 60-75% or less
than 60% respectively of the reference median. All children whose weight is 90% and
above are categorised as normal. The selection of cut-off levels was based on the clini'cal/hospital experience in Mexico. Gomez et al. (1956) observed a marked difference in
mortality during first 48 hours between children with second degree malnutrition (6075% of median) and those with third degree malnutrition (< 60% of median). The Indian
Academy of Paediatrics (IAP) recommends the following classification : 80%, 70-80%,
60-70%, 50-60% and < 50% as normal, first, second, third and fourth grtde of mal
nutrition respectively (LAP, 1972). This classification is currently used by the Integrated
Child Development Scheme (ICDS) for selecting beneficiaries and growth monitoring
(Chart 1). As such, most of the classifications, based on weight for age use arbitrary cut
off points. Normal growth is considered to encompass values within two standard devia
tions of the mean. Since body weight does not follow Gaussian distribution, use of mean
and standard deviations for classifying children into differenet grades of nutritional
status may not be appropriate. To overcome these problems. Ramnath, et al. (1993),
recommend use of 5th percentile of reference values as the cut-off point to classify
children as normal and malnourished. They suggest that the weight below the 10th per
centile values of the community (ICMR data) may be considered as indicative of severe
degree of malnutrition. When these criteria were used, their analysis indicated that 80%
of NCHS median appeared appropriate to decide whether children were normal or mal
nourished. The current criterion of 60% of reference median for grading the children as
suffering from severe degree of malnutrition and 80% of reference median as cut-off be
tween 'normals' and malnourished, appears to be the most reasonable. A summary of
these classifications is given in Table-3.
GROWTH CHART - GIRLS
(IAP classification - NCHS standards)
SI.
No
Name of the
Village
1. Andhivadi
2. Kothakondapalli
I
3. Kothakondapalli
II
4. Bathalapalli
5. Bomandapalli
6. Belagondapalii
Number of
houses
Population
Male
Female
356
289
1551
1345
838
665
713
680
Male
134__
54
Female
86
70
167
640
312
328
52
56
108
370
182
433
1829
992
2132
937
514
1033
892
478
1099
110
44
103
115
40
89
225
84
192
0-5 population
Non SC
Total
220
124
Male
97
Female
63
Scheduled
Caste
Male Female
37
23______
Preliminary discussion on the finding of the nutritional assessment carried out in five
Miinties of the meeting
1. The following people from TVS company were present
2. Dr. Rajan Babu Chief Medical Officer
6. Mr. Ami tab . Community Development officer
llie following people from C11C were present
1.
Ms. Padmansim Asuri. Nutrition Consultant
2.
Mr. SJ.Chandcr, Field Training Coordinator
3.
Dr. Vinny. C?omrnunity Health Fellow
Before starling the presentation on the findings of the study. Ms. Padmasini clarified with the
TVS team to what extent, the concept of ICDS is being understood by the project staff of the
ICDS. The TVS team gave the feed back that it is not well understood by them. She said
ICDS is not merely a nursing teaching the number and rhymes to the children, it was started
to i’ldu in the over a.u development oi tnc child. it is not training centre out correctional
centre, helping addressing the child’s health and development needs. ICDS should focus on
personal hygiene, food hygiene and socialization. ICDS should take two years children too,
and asked if they take them; the answer was no.
Ms. Padmasini wanted to know if the ICDS project of the Krishnagiri district has a medical
officer to look into (he health needs of the children. She said if the government docs not have
one they should accept the role oi 1 VS medical officers.
Later she explained the standard used for assessing the nutritional status by the National
Centre for Health Statistics.. She explained what is percentile, particularly the 50th percentile
Later Mr.S J.Chander of CIIC made a presentation on ihe rinding of the study. The total
number of children covered by the study was 640 which include 313 girls and 327 boys
between 0-60 months of use.
■ Boys
. Girts
Total
i 7,7%
25,3%
___ ; 9.7%____ j 21.1%
■ 17.3%
i 46.4%
! 15.5%
:| 16.7%
! 32.2%
I 2.7%
; 1.4%
4.1%
|
j
i
It was noted that only 17% are normal and 78.6% were mild and moderate and 4.1 percent
were severe. Data on each village was also presented with comparison between boys and
girls. It was found that Bathala paili was the lowest and Andhiwadi was the highest. The TVS
team explained that residents of Andliiwadi are economically better off and the'residents of
Balhlapaiii arc poor. Il was observed that over all the girls seems io bee belter that the boys. Il
was observed that the malnutrition was present more in the 12-24 months age frequency. This
was explained as that this could uiie the increasing need of dietrary intake as the olav activity
of the child increase but the child may not be getting sufficient food. The TVS team
members asked why some cluldrcn cat mud. It was explained that the children that the
children could be suffering from calcium deficiency.
Ms. Padmasini said regarding the causes of mild malnutrition, it could he that the children are
not getting adequate food; as they children are growing the mother’s milk may not be
sufficient for the children and parents may not be aware of the required dietary intake for
children. Mother’s health status is important for delivering a normal child is important.
Children, who have experienced many episodes ot diarrhoea, should be ted double the
amount of food. It is important to know if the mothers know this and can they afford.
Education of diarrhoea and food hygiene is important in preventing. Worm infestation also
could be one of the causes A sick child my drop in growth but should regain in the next few
months. Others causes such as the economic status of the family particularly Hie-mother’s is
important for the nutritional status of a child.
Regarding the moderate state, it is likely to remain the same unless something drastic is done.
Regarding growth monitoring, she said it is not necessary that the children be weighed every'
month: it is OK if they' are weighed once in two or three months but weighing is important.
She said weighing is important; it is like the child’s horoscope.
Action plan
It was suggested that the mothers and community development staff of TVS should focus on
normal and mild children in preventing further mal nutrition. Moderately malnourished
cluldrcn should be attended by the anganwadi workers and the severely malnourished
children should be attended by a doctor. It was suggested to send a report with the findings of
the study io Tamil Nadu government. The meeting concluded with the decision that on 20"
TVS team with the anganwadi workers and CDPO’s will come to CHC for discussion and
drawing up a joint action plan.
By : S.J.Chandor
9*° June 2005
4
fxjvT- 1 3>»
Risks & Benefits
Justice
Informed consent
Public Health Research
Ethics in Nutrition Intervention Research
Common infections precipitate malnutrition, which in turn reduces resistance. This facilitates
further infections, which again lead to increased nutrition deficit. The 1960s was a period of
developing awareness of interactions between infections and malnutrition. Up to then the
research on and organisation of programmes for these two issues were separate enterprises.
So a national medical research institute, with multi-disciplinary participation of
scholars/researchers, decided to undertake a nutrition intervention study in a Primary Health
Centre area somewhere in North India with financial support from the International - UN and
state agencies and Indian government. The main objective/purpose of the study was to
determine if there was a synergism in. the programmes to control malnutrition and infections
similar to the known synergism between these problems. The child nutrition programmes at
that time (1960s) placed emphasis on nutritional rehabilitation, which treated children with
severe conditions like marasmus and kwashiorkor. This study was a step forward to
examining the synergism between malnutrition and infections to practical policy and
programmes.
The researchers felt that the only way that the synergy between malnutrition and infection in
the young infants and children could be examined was to find groups with high prevalence of
malnutrition and common infections and then study them to see what happens when efforts
were made to selectively reduce each type of condition. The nutrition project was conducted
in four clusters of 10 villages. Care was taken to ensure comparability between different
groups of villages and also sufficient separation in order to minimise communication among
villagers who received different service packages. To avoid random events particular to a
specific village from affecting the research process, at least two villages were selected from
each experimental or control group.
The total population covered in the two nutrition and population studies was 35,000 people in
26 villages distributed in clusters as experimental groups within 3 community development
blocks. On an average in the 10 nutrition study villages there were 1000 children below 3
years of age with each experimental group having an average of 200-300 children. In the
neighbourhood PHC, in 1955-60, the death rate for infants below age 1 was 156 per 1000 live
births. For the children 0-4 years of age, the mortality rate was 27 per 1000 population.
The researchers sought the cooperation of the villages and negotiated with them until the
combination of service interventions assigned to the village was accepted. There was no
compulsion for families to cooperate, but all village leaders agreed to help persuade all the
families to participate in the survey.
The following interventions were undertaken - the three nutrition villages received nutrition
care; the 2 health care villages received health care mainly for infection control and the third
received services for both. There were two control villages. The nutritional input consisted of
twice daily food supplements consisting o calorie fortified milk in the mid morning and
porridge made from crushed wheat, milk powder, raw sugar and oil in the mid after noon,
with a combined nutrient value of400 calories and 11 grams of protein.
Findings: The study found that nutrition care alone or in combination with health care
significantly improved both weight and height of study children beyond 17 months of age. At
36 months, children from the Nutrition intervention villages or the Nutrition and Health Care
intervention villages weighed on an average 560 gms. more and were 1.3 cm taller than those
in control villages. A male higher caste child from a nutritional input village or a nutrition
and health care input village averaged about 2 kilogrammes more in weight and 6 cm more in
height at 36 months than a female, lower caste child from the control village. Perinatal
mortality was significantly reduced in the nutrition and nutrition and health care input
villages compared with only health care villages (31 vs 45 perinatal deaths per 1000 live and
still births) and it was higher in the control villages ((57 per 1000 live and still births). This
was due to the supplementation of all mothers with iron and folic acid and additional feeding
for mothers at nutritional risk. Neonatal mortality and post-neonatal mortality significantly
reduced by one third to half in villages where health care or nutritional inputs were provided
vis-il-vis control villages.
Many years after the study was conducted, some Indian researchers expressed reservations
about the idea of undertaking a study in such settings and the ethical justification for
continuing to study a control group even though the implications of nutritional deprivation on
child survival were clearly established. The study researchers contended that even in control
villages, if the health workers found that a child was dying, going blind or suffering from
other illnesses that would leave permanent damages, the worker was instructed to call the
doctor to start intensive care. Others have justified the study saying that, (a) in the late 60s
and early 70s this was the understanding of scientific and ethical research. The scientists had
done their best to ensure scientific validity by conducting and documenting the study
carefully and drawing appropriate and cautious conclusions, (b) The study did not cause any
additional harm and all that researchers did was to make use of an existing
condition/situation.
Questions for discussion
1.
Who are the participants in this study and how would the researchers should-obtain their
informed consent for participation?
2.
What are the risks and benefits of participation in each arm of this study?
3.
What standard of care in each arm should be mandatory in order to conduct this study?
4.
Do the participants in each arm have a right to receive additional benefits after the
conclusion of the study, and if so, what and for how long?
5.
What kind of community engagement would be required for a study of this kind?
6.
In order to do this study, who all must consent? In order to obtain their consent, what
information each one needs to be provided? Would the researchers require different kinds of
consent for form for each?
(By Mala Ramanthan and Amar Jesani)
2
Risks and benefits - Informed consent -Methodology to study natural history of disease
An Indian study of the natural history of cervical cancer
Cancer of uterine cervix is the most frequent neoplasm among women in India. The epidemiological
evidence available in mid-1970s supported a spectrum of heterogeneous epithelial lesions antedating
invasive cervical cancer. The biological behaviour of these pre-cancerous lesions was not clearly
understood. It was felt that identification of relevant risk factors and the detection and management
of the pre-cancerous lesions were important in the prevention and control of invasive cancer of the
uterine cervix, more so in a resource poor setting of India. Such knowledge will help the health
services to selectively intervene early only in those women having high-risk cervical lesions. This
would enable the country to use its scarce health resources more efficiently.
Study design and methods: With such a goal, scientists.of a national institute in India designed amulti-disciplinary study. The study was carried out from 1976 to 1990. From 1976 to 1986, 120,471
women attending the gynaecologic outpatient departments of six major hospitals in a metropolitan
city were screened, and cervical smears of 117,411 collected along with clinical history and other
parameters. All women were called to the hospital clinics after 15 days to take reports of their
cervical smears. Of 117,411 cervical smears collected, 30,399 (25.9%) were negative, 84,889
(72.3%) showed inflammation, 1,910 (1.6%) had dysplastic lesions and 213 (0.2%) were malignant.
As women reported back to clinics of hospitals after 15 days to collect their reports, those women
who were having dysplasia were approached for recruitment in a study to observe or follow them up
for long time in order to understand the causative factors and biological behaviour of the dysplasia.
Some of those without any dysplasia and malignancy were recruited as matching control. On
recruitment the researchers collected detailed epidemiological information as well as biological
material for cytological (study of cells), histo-pathological (study of tissues to study manifestations
of disease), serological (study of body fluids) and immunological studies from all participants.
The recruitment of these participants started a fortnight after the first batch of women was screened
in 1976, and the last batch ofrwomen was recruited following the last screening in 1986. Of the
1,910 women who showed cervical dysplastic lesions in the screening, 1,163 (61%) were
“registered”/recruited for long term “follow up’Vobservation of their cervical lesions. Moderate and
severe dysplasia cases were followed every three months, mild dysplasia every six months and
controls annually. At each of the follow up, biologic material for cytopathologic and serologic
investigations was collected. Biopsy was not mandatory during the course of follow up. However,
50% of the dysplasia cases, included in the long-term follow up category, were randomly subjected
to biopsy. Any woman in non-biopsy group showing a higher grade of cytologic abnormality and/or
clinical suggestion of higher grade of lesion underwent biopsy.
No follow up of women was done after the study ended in 1990.
A paper of the researchers published in an international journal in 1987 stated that, “A formal
informed consent in writing from subjects included in the study is not standard practice in India.
However, all women registered for long-term follow up were informed about the objective and the
purpose of the study and also the cooperation that would be required from them. The individual
registered as a dysplasia case was informed that she had a lesion that could either regress to
normalcy or progress to higher grades of atypicality and was then given the option of either being
followed or of being discharged from the study. Patients choosing the latter alternative (15%) were
appropriately managed”. It also stated that, “For obvious ethical reasons, the end point of the study
in any case was carcinoma in situ (CIS) at which time appropriate treatment was offered”.
Findings: Analysis of the data up to the end of March 1986 by researchers showed that progression
rates (from dysplasia cases to malignancy) per 100 women-years of follow up was 0.65 for mild,
17.7 for severe and 2.7 for all dysplasia. The corresponding figure in the control group was 0.21. The
cumulative risk for developing malignancy during any time of follow-up over a period of 72 months
was 5.11% for the mild and 27.91% for moderate dysplasia and 13.76% for all dysplasia. In
moderate dysplasia group, one out of 3 would develop malignancy in 72 months and in severe
dysplasia group 41.86% or almost one out of two in 30 months (few women with severe dysplasia
were followed up beyond 30 months as majority were moved out of the cohort due to undergoing of
hysterectomy or cone-biopsy). The diagnosis at detection of malignancy (total 71 cases) was:
“Carcinoma In Situ''’ (CIS - a localised cancer not yet invading surrounding tissues) in 35 (49.3%),
CIS with spread in lymph glands in 20 (29.2%), CIS with micro-invasion in 7 (9.8%) and CIS with
invasive cancer in the remaining 9 (12.6%).
Contribution to the policy making: Reportedly, by 1986 the findings of this study on cervical
cancer with special reference to its natural history had been extensively used in the planning of
National Cancer Control Programme for India for control of cervical cancer. Several socio
demographic and biological parameters studied in this project indicated pointers for identifying
“high risk” group of pre-cancerous lesions from those of relatively “low risk”. This is of
considerable relevance for control of cervical cancer and for optimisation of limited specialised
health services in India.
Controversy: In 1997, a national daily front-paged a report saying that the national institute that
conducted this study had not obtained proper informed consent of the women participants as per the
ICMR’s guidelines of 1980 which provided an elaborate procedure and written documentation of the
consent. Besides, they had allowed so many women to develop cancer without offering best
treatment for the dysplasia available at that time. The health and women activists and some leading
professionals criticised the study. The researchers defended by saying that at that time written
informed consent was not considered mandatory for doing the._study-.and..the women were -mostly
illiterate so it was difficult to take written consent. They claimed that though many women
developed malignancies, during the study period none of them died, and so there was no harm
caused to them. And over and above everything, the research provided very valuable information
that eventually went into the making of a national programme and thus in long run saving lives of
scores of women.
Questions:
1.
Please identify potential risks all participants would be exposed to during and after the completion
of the study.
2.
What were the measures taken by the researchers to minimise potential risks? What more could
have been done?
3.
What are the benefits to the participants from the study? What are the benefits to the society and
science from the study? What could be done to increase these benefits?
4.
How far the autonomy of women participants respected in the study? What difference the written
informed consent could have made on the conduct and outcome of the study?
5.
If you were asked to do research on natural history of a disease using the design and methods of
this study, would you do it? Why?
(By Amar Jesani)
2
Sadhavis, Sexuality and Societal morality
In a medium sized city in India with two medical colleges, a religious sect was having a
group of sadhvis undertaking religious as well as social work. This sect has a very sizeable
following in the city. Some of these sadhavis were working in collaboration with an NGO
doing work among children for last two decades. One of the works of the NGO was to
educate and rehabilitate street children in few Children’s Homes established by it. sadhvis of
this sect were managing one of these homes for last five years. They had left their homes in
their early age and fully dedicated themselves to religious and social work. One of them was
45 years and another 38 years old. They were very popular in the community for their
dedication, caring nature and simple life-style. The children’s home run by them had two
rooms - one big room was serving as dormitory to sleep at night and in the day-time place
for educational classes 21 children (all boys) housed in the Home. The second small room
had two coats and tables and chairs where these two sadhavis used to live. A door connected
both the rooms, and both rooms had a door each opening to the outside courtyard
independently. At night the children slept in the dormitory, the room connecting two rooms
used to remain locked from the side of the sadhvis room and if any child needed assistance
of theirs, he had to knock. The young inmates of the were provided basic education and
taught skills - most of them started doing some work in the city or elsewhere using such
skills by the age of 14 or 15 years and used to leave this Home. The sadhavis and the NGO
used to maintain contact with them as these rehabilitated children looked at the Home as
their own home and sadhavis like their mother.
One day, at around 5 in the morning a small child needed assistance of the sadhavi, he
knocked at the door of sadhavis' room several times, but did not get any response. Hearing
noise other children got up and they all knocked. The children went to the courtyard and
knocked another door of the sadhvis’ room, found it not-locked, went inside, and found both
sadhavis in a pool of blood and dead. The children were panicky they shouted for help, the
neighbours came rushing. The news spread like wildfire in the town, the priest and other
sadhavis of the sect gathered in no time. They all and children were crying around the dead
bodies when police.reached the scene. The police had hard time to get all of them out,
cordon off the area and look for the clues. Both sadhavis were stabbed but no weapon was
found. A team of forensic experts also visited the scene ofcrime.
Next day morning, there was a bandh in the city to pay respect to the deceased, and the
newspaper ran the front-page story of the murder, and wrote with superlative language
articles on the dedication and popularity of the sadhavis, and above all, blasted the police for
deterioration of the law and order. Speculations were rife about the involvement of a
powerfill underworld gang having political connections and the cause talked about was its
attempt to get the Children’s Home which had, with small building, courtyard and garden;
large amount of land. The police said that they were on the trail of murderers but they would
be able to say more after the post-mortem were conducted on the bodies. The Chief Minister
of the State gave a statement expressing sympathy with the head of the sect to which these
sadhavis belonged to, and severely pulled up the police chief for inefficiency and negligence.
The post-mortem of both bodies was conducted by early afternoon.
On the second day after the murder, three of the four newspapers published in the city front
paged different story on the murders and the sadhavis. Citing a reliable source, they said that
the autopsy had revealed they were not raped but at the same time it showed that they were
used to sexual intercourse and one of them was also suffering from a sexually transmitted
disease. They also stated that perhaps police was investigating sadhavis ’ relationship with
ex-inmates of the Home - the boys who grew up there and subsequently moved to some
other towns; and also with some sadhus or priests of the sect who were frequent visitors of
the Home and with the head of the NGO. In these stories there were indirect references to the
licentious behaviour of the men and women who were supposed to remain pure. With the
publication of these stories, the public outcry on he murder suddenly died down, even the
priests of the sect stopped giving statements, and in the next few days the furore was gone,
the media shifted the story to inside pages and mainly reported statements of police about the
progress of investigation.
After about three months of the murder a meeting of the sadhavis took place where all of
them revealed that since the murder, their image in the community had gone down, people
were regarding them as of loose moral character and they were finding it difficult to continue
with their work. At that time, a lawyer, journalist and a doctor along with few other publicspirited individuals constituted an investigation team. These sadhavis provided them with a
copy of the autopsy report and they went around for two weeks interviewing doctors, who
were involved in doing autopsy, police officers, newspaper reporters and many others. It was
discovered that apart from findings of injuries that killed them there were only two other
positive findings. In both the hymen was found absent or torn, and vaginas were patulous;
and there was a small inaugural wart near vagina of the younger woman. The autopsy report
was dated seven days after the murder and the doctor, who did the autopsy refused to take
responsibility of the kind of interpretation given by the media. He also said that at the time of
autopsy his senior professor was present and he actually had taught five students from
medical college on these bodies. The said professor had actually said some uncharitable
things about women in general and the morality of sadhavis and sadhus in religious sects.
The professor refused to talk to the team saying that he had not done autopsies. The team
also discovered that few years back both sadhavis had undergone D&C at the public hospital
due to some severe menstrual problems. The reporters of the newspapers claimed that they
had written truthfully whatever was reported to them but they refused to divulge their source.
Whenthe investigation team - released its report-there was furore in public. While
acrimonious debates continued in the media, the followers of the sect that had kept quite for
so long, suddenly felt that the sadhavis of their religion were deliberately maligned, and they
protested. However, the murderers of sadhavis were never found and the police closed the
files.
QUESTIONS:
1.
Did doctors and reporters do anything wrong? What? Why did they do it? Were they
correct in refusing to apologise?
2.
Was it correct for a citizens’ team to do its own investigation in this episode? Why? What
are the rights and ethical responsibilities of the team?
3.
What are the ethical obligations of forensic doctors?
(By Amar Jesani)
2
Community & Culture
Privacy and confidentiality
Publication & dissemination
Qualitative research
Research, community and culture
An NGO working with lower caste and class people in 40 villages in an economically
underdeveloped North Indian hilly state (province) obtained funding for commencing public
health work on HIV/AIDS. One of the objectives of the project was to design intervention
strategies for prevention of the spread of HIV by training members of large number of NGOs in
the state. In order to design its training programme, it decided to undertake a study in its villages
to understand the socio-economic and behavioural factors responsible for the spread. A
qualitative study using Focus Group Discussion (FGDs) and In-depth Interview techniques was
designed. The study was completed in six villages covered by the NGO, a quick data analysis
done, and using this data, a small booklet in Hindi was prepared, and 500 copies printed in Sept
1999 for use as background material for the training. No paper was written for publication in the
journal. Some copies were sent out to other NGOs and individuals. The short-course training
programme commenced, in few months after the publication of the booklet.
Seven months after the publication, a copy of the booklet reached one of the Hindi newspapers
published from the state. The newspaper accused the NGO of publishing pornographic and
obscene material, and maligning and polluting Indian culture. Soon other newspapers in the
region picked up the story. A left-wing political group was first in criticising them in order to
show the kind of work foreign funding agencies were encouraging on low-priority-issue of the
HIV/AIDS in the region. But it was soon sidelined and replaced by extreme-right wing political
parties and Hindu religious fundamentalist organisations. A week after the newspaper reports,
mobs comprising the latter groups simultaneously attacked the head office of the NGO in the city
and one of its community centres at a village where training-sessions were on. During the attack,
the Police arrested 11 persons, including the heads of the NGO and even visitors to the NGO.
Ostensibly, this was done to protect them from being lynched by the crowd. At the police station,
however, they were booked under provisions dealing with obscenity (a bailable offence), making
of statements provoking public mischief (a non-bailable offence), etc. The Bar Council of the
city resolved that no lawyer would appear on behalf of those arrested. The NGO was ordered to
stop all activities (whether or not these were related to the booklet in question) and bank
accounts, including personal accounts of the workers and their family members were frozen. The
bail application for six arrested members of the NGO was rejected, they were handcuffed and
paraded through the streets of the city on their way from the prison to the Court. The litigation to
get them released lasted 40 days, and when it became clear that they could not be kept in the
prison, the state government made unsuccessful attempt to invoke National Security Act to keep
them in the prison. On their release, the work in those villages continued with the community
support, but the NGO was forced to shift its office to a neighbouring state.
The study finding contained in the booklet explained that being an economically underdeveloped
region, majority of people were very poor and many men had left their families and migrated to
prosperous region to find work. These men, while visiting home were bringing STD and HIV.
Absence of men and the insufficient money received by families were forcing some women to
promiscuous activities and also forcing them to sell their bodies, particularly, to the high-risk
groups of men like the truck drivers passing on the highways. It also found that protection during
sex was virtually absent because most women did not know about it or they had no control over
it. Besides, while the high prevalence of STD was known, the community did not have much
understanding about the HIV. The booklet did not give names of the participants and the villages
where the study was conducted. However, the study covered only six villages and there were
certain indirect references to individuals in those as well as other villages. There was no report of
any participant of the study protesting or joining the protests by political and religious groups.
The obscenity charge related to three passages in the booklet (total of 2-300 words in booklet of
20,000 words), all of them direct quotes from the qualitative data collected. These passages
explicitly described the sexual behaviour using colloquial language without any refinement.
At the time of this episode the state government, was controlled by the right-wing Hindu
fundamentalist party. The new elections were approaching and there were reports that this party
was losing support. Besides, one of the powerfill central (federal) government ministers of this
party hailed from this region, and his authority in the state party was under pressure. He took
deep interest in this episode. Interestingly, around the time of this episode about half a dozen
qualitative studies on sexual behaviour were published as reports or journal papers. All of them
used more sexually explicit quotes and were more lax in preserving anonymity of the
respondents than the booklet of the NGO. However, all of them were published in English, and
none of them faced any protest.
Questions:
1.
Did researchers violate rights of the participants and the community while undertaking and
reporting the research? What is the specific nature of each violation?
2.
Unlike therapeutic research, the academic behavioural research is often not accompanied or
followed by action-for behavioural change. What are the dilemmas 'and pitfalls involved when
the community based action group undertakes research on sensitive issue with an intention to
affect changes in the community?
3.
At the community level, there is a big overlap of cultural, social and political dimensions.
What kind of competencies required for undertaking research on sensitive issues in the
community?
4.
Should the researchers share major findings of their study with the community in the language
they understand? If so, what precautions need to be taken in disseminating findings of tire study
to participants and the community?
5.
Ethics attempt to protect human rights of the participants. The researchers are also vulnerable
to human rights violation. What are the ways to protect human rights of the researchers?
(By Amar Jesani)
2
NUTRITION PAPER OF THE MONTH
April 1995
New global perspectives on overcoming malnutrition1'
V. Ramalingaswami
American Journal of Clinical Nutrition, 1995; 61:259-63
Copyright 1995 American Society for Clinical Nutrition
' UNICEF New York
Nutrition Section
April 1995
PRESENTED BY
Dr. M.N. KULKARNI
Special Article
New global perspectives on overcoming malnutrition1-3
V Ramalingaswami
The ICN process
I am honored to be asked to make this presentation in the
aftermath of the International Conference on Nutrition (ICN),
held in December 1992 and reflect on the perspectives gained
in the process before this august gathering. The ICN is a critical
step in the continuing process of strengthening commitment
and action to prevent and alleviate nutritional problems wher
ever they occur. The preparatory committee meeting held in
August of 1992, which was technical in nature, reviewed the
main background document of the conference: Nutrition and
Development—A Global Challenge and the draft of the “World
Declaration” and “Plan of Action for Nutrition.” These and
numerous other documents were the result of a synthesis of
information, experience, and ideas gleaned from a variety of
sources through an unprecedented historic process spread over
two years, representing the coalescence of two main streams of
activity (Figure 1). One stream, the Ground Reality Stream,
started in countries with the preparation of 116 country papers
constituting a unique repertoire of country scenarios, both
developed and developing, followed by regional meetings of
technical representatives of the countries of each region, finally
ending in the preparatory committee meeting. Country partic
ipation was a signal feature of the ICN preparatory process.
Countries have been primed and poised for real action at the
ground level.
The other stream was the Stream ofSaepce. Its output was
a critical analysis of eight priority areas for policy and action so
as to enable planners and policymakers in different sectors to
have a shared perception and common understanding of the
spectrum of causality for a coherent approach to interventions
at the national level. Experts from around the world, a specially
designated Advisory Group of Experts (AGE), the Sub-Com
mittee on Nutrition of the Administrative Coordination Com
mittee of the United Nations (UN; ACC/SCN), the UN agen
cies, Bilateral and International Development Agencies, the
International Union of Nutrition Societies (IUNS), and Non
governmental Organizations (NGOs) provided valuable inputs
throughout the preparatory phase. The ICN itself, which met in
December 1992, was attended by more than 1000 country
representatives from 159 member states and the European
Community, as well as by representatives of 15 organizations
and bodies of the UN system and more than 150 other inter
governmental and nongovernmental organizations. Indeed, the
active participation of nongovernmental organizations in such
large numbers was an outstanding feature of ICN. “The World
Declaration” and “Plan of Action for Nutrition" were reviewed
in depth and adopted by this high-level ministerial mini-sum
mit, providing the political driving force needed to move from
rhetoric to action (1). The ICN thus represents an upward
synthesis of knowledge and experience in nutrition in a bot
toms-up approach, starting with countries, followed now by
downward support and action ending in countries.
After the ICN, action has shifted almost immediately to
countries and regions. The goal is to develop in each country a
national action plan, sharpen, correct, and fine-tune the plans
already made by countries at the beginning of the ICN process,
with priorities, goals, targets, time scales, monitoring, identi
fication of resource needs, and their mobilization, and above
all, national capacity building.
The World Declaration and Plan of Action
The World Declaration is about what needs to be done and
the “Plan~of Action"'~is"al>out how it~is to Te'done, The
Declaration identifies the root causes of malnutrition as pov
erty, deprivation, social inequality, lack of education, and
growth of population out of proportion to the natural resource
endowment. It recognizes that nutritional well-being is an
essential prerequisite to effective learning and a key objective
of human development Despite appreciable worldwide im
provements in nutritional status, life expectancy, and adult
literacy, the ICN viewed with deep concern the fact that 780
million people in developing countries—20% of their com
bined populations—still do not have access to enough food to
meet their basic daily needs. There is a high prevalence and an
increasing number of malnourished children under 5 y of age in
parts of Africa, Asia, Latin America, and the Caribbean, 192
million. More than 2 billion people still suffer from or are at
risk of micronutrient deficiencies producing an array of dis
abilities and developmental disorders on an unprecedented
scale. The prevalence of low birth weight, the single most
powerful predictor of death in the first few months of life, still
stands at 19% for developing countries as a whole with figures
reaching 30% and beyond among the teaming millions of South
Asia, whereas for developed countries this figure stands at 6%.
At the same time, there is a changing global picture of chronic
noncommunicable diseases related to excessive or imbalanced
dietary intakes often leading to premature death (Figure 2).
1
From the All India Institute Of Medical Sciences, New Delhi, India.
2
Presented to the XV International Congress of Nutrition, Adelaide,
Australia, on September 27, 1993.
3
Address reprint requests to V Ramalingaswami, All India Institute of
Medical Sciences, Department of Pathology, Ansari Nagar, New Delhi,
110029, India.
Am J Clin Nutr 1995;61:259-63. Printed in USA. © 1995 American Society for Clinical Nutrition
259
RAMALINGASWAMI
260
TABLE 1
Factors influencing nutrition—the troika
FIGURE 1. Tbe International Conference on Nutrition process. Tbe
Ground Reality Stream on tbe left, tbe Stream of Science on the right
AGE, Advisory Group of Experts.
In reality, the “World Declaration on Nutrition” is about
human development—about human vulnerability, care and car
ing, natural and manmade disasters, historical negligences, and
ecological handicaps of women resulting in excessive time
losses and energy drain, lifestyles and behavior, debt and
adjustment, General Agreement on Tariffs and Trade (GATT)
and the Uruguay Round, household food security and produc
tive assets of the poor, and about food aid not only for human
survival during emergencies but also as a stepping stone to
development and self reliance.
The Declaration calls on member states to make all-out
efforts to eliminate the following before the end of the decade:
7) famine and famine related deaths, 2) starvation and
nutritional deficiency diseases in communities affected by
natural and manmade disasters, and 3) iodine and vitamin A
deficiencies.
Causes of Death
1985
2015
Factor
Elements
Food
Availability
Access
Quality
Safety
Health
Health services
Lifestyles
Care
Mothers
Households
Communities
The member states also pledged to reduce substantially
within this decade widespread chronic hunger and undemutrition especially among women, children, and elderly people;
other micronutrient deficiencies including that of iron; dietrelated communicable and noncommunicable diseases; social
and other impediments to optimal breast-feeding; and inade
quate sanitation and poor hygiene, including unsafe drinking
water. The approach was broad, resting on the tripod of food,
health, and care (Table 1).
Health and care
The Plan of Action for Nutrition provides a technical frame
work for the preparation of national plans of action and, iden
tifies nine strategies. The key is competent local action follow
ing a strategy that is flexible and sensitive to local factors. The
emphasis is on location specificity; building on existing struc
tures; on ongoing activities; on what people already know; on
identification of technically sound, implementable activities;
and on choices of areas that are amenable to immediate inten
sification. Much enthusiasm was generated by the ICN, which
should not be allowed to dissipate by too much time being
spent on elaborate planning exercises in a “planning dream.”
The science and experience gathered at this historic XV Inter
nationa! Congress of Nutrition could serve as a most valuable
catalyst to the implementation of post-ICN follow-up activities.
Global perspectives
Permit me now to step aside from the content of the Decla
ration and Plan of Action for Nutrition to reflect on some
global perspectives for overcoming malnutrition arising out of
the ICN experience.
The concept of care
CIRCULATORY
■I
OTHERS
CANCER
■■
PREGNANCY
INFECTIONS
□Tj
injury
M
PERINATAL
FIGURE 2. Estimated and projected distribution of the major causes of
death in developing and industrialized countries, 1985 and 2015. Adapted
with permission from Bulutao, Lopez, and Stevens. 1989.
Of the three comerstones of nutritional well-being, food,
health, and care, which were expanded into nine strategies in
the ICN Plan of Action, special mention may be made of the
care and caring concept. The vulnerable include not only
infants^ young growing children, and mothers, but also oftenneglected adolescent girls, elderly people, and disabled and
displaced people. One may ask: What is left of the human life
cycle? The entire life cycle seems to have vulnerabilities all
along, from womb to tomb. Perhaps a case can be made for
paying special attention to young school-age children as well,
for malnutrition and poor health in this group are linked to low
rates of enrollment, high absenteeism, early dropping out, and
GLOBAL PERSPECTIVES ON MALNUTRITION
261
low achievement (2-4). Enhanced child survival and the postTABLE 2
Monitoring and evaluation of iodine-deficiency diseases
Jomtien Conference activities spurring enrollment for primary
education are enlarging the pool of primary school learners.
Monitoring
There is evidence relating a child’s attention deficits, learning
Urine iodine
disabilities, and sensory impairments to general and micronu
Blood spot thyroid-stimulating hormone
trient malnutrition and intestinal helminth infestation. There
Evaluation
are safe, effective, and logistically feasible approaches avail
Control of cretinism
able at low cost and it is hoped that the post-ICN activities will
Control of goiter
give due emphasis to the collective health and educational
Intelligence tests of children
benefits of improved nutrition and,health of school-age_chilSocial indications
dren. Such an approach will be synergistic to the other ongoing
improvements in the quality of teachers and educational infra
structure. When" health and nutrition interventions in school
Micronutrient malnutrition
children are coupled with the incorporation of the correspond
Micronutrient malnutrition is represented by the vicious
ing knowledge base into the school curriculum, a sustainable
troika of deficiencies of iodine, iron, and vitamin A (7). Their
behavioral change can be effected in children and when chil
dren, teachers, and parents are involved together, great change ‘ wntinued persistence (Table 2) leads one to ask why society is
failing to utilize optimally some of the commonplace contrican occur (2-4).
.butions of science and technology. The answer is clear, techTo go back for a moment to the care concept, it is rather
daring and extends beyond children across the whole spectrum Lnology yiejds-its full benefits only when used within a framer work of social development and community organization. The
of vulnerability in the human life cycle. It is an enabling ['ultimate barrier toTmowIedgeapplication todeveloping"countransition _from dependency to independency, autonomy, and
- tries is management, with its complement of information, in
maturity. Of particular importance is breast-feeding and adeformed judgement, continuous tuning of policy, surveillance,
quateweaning practices, the success of which depends on good
and a participatory approach. In dealing with the problem of
nurturing and emotional support given by mothers, caretakers,
micronutrient malnutrition, diversification of diets to provide
family members, and the society in general. Early psychosenthe micronutrients in requisite quantities on a continuing daily
sorial and affective stimulation in conjunction with nutritional
basis as a long-term measure, indeed, as an all-time measure, is
inputs can accelerate recovery from severe marasmus (5). The
advocated strongly, whereas short-term measures such as sup
International Code of Marketing of Breastmilk Substitutes, the
plementation for immediate alleviation are to be regarded not
breast-feeding data banks, the baby-friendly hospitals, the lac
as ends in themselves but as preludes to sustainable solutions.
tation training centers, and the training materials are instru
The International Council for the Control of lodine-defiments for enlarging and strengthening care. Improvement of
ciency Diseases (ICCIDD), WHO, and UNICEF have updated
complementary feeding of infants and young children by using
projections of numbers of people living in areas considered to
locally available foods that are safe and fulfill nutritional needs
be at risk of iodine deficiency from 1 billion persons estimated
in major ecological zones in different socioeconomic groups is
last year at the time of The World Health Assembly to 1.6
paramount to overcome the hazards of the weaning process.
billion persons at the present time. Iodine deficiency is a
The first and most dangerous year of life still remains a
community disease that affects virtually all of a community’s
challenge and is being addressed by the World Health Orga
members to some degree and is regarded as the greatest single
nization (WHO) and the United Nations Children’s Fund
cause'of preventable brain damage and mental retardation (8).
(UNICEF).
The good news is that there is acceleration of efforts in every
region of the world in the control of iodine-deficiency diseases,
so much so that thought is now being given to verifiable criteria
Monitoring and surveillance
that indicate the elimination of iodine-deficiency diseases by
The ICN makes a strong plea for regular assessment and
the year 2000. This is a track reminiscent of that followed for
nutrition monitoring by each country, within its resource lim
smallpox eradication in the past and now being followed in the
itations, especially of its vulnerable groups, and leading to
Americas for polio eradication. Actions against iodine-defi
positive policy and project responses. It advocates innovative
ciency diseases are afoot in many African countries. The WHO
efforts such as_risk mapping, sentinel sites, and rapid appraisal
has just launched a Micronutrient Deficiency Information Sys
techniques, in addition_to_using traditional indicators such as
tem and the first working paper on iodine-deficiency diseases
anthropometry, birth weights, breast-feeding prevalence, di
jointly produced by WHO, ICCIDD, and UNICEF has just
etary intakes, and biochemical markers of nutrients and clinical
come out. At this point I would like to pay a tribute to that
signs. As an example, some of the indicators used in monitor
distinguished Australian, Dr Basil Hetzel, for the crucial role
ing and evaluation of control of iodine-deficiency disorders are
he is playing in iodine-deficiency disease control. It looks as if
given in Table 2. The study of socioeconomic status and
the total elimination of this ancient scourge of humankind is
distress factors is of value in disaster prediction and prepared
likely to be achieved by the end of this decade, this century,
ness against ecological calastrophies such as lack of or excess
and this millennium. May Adelaide and this Congress signify
rainfall, seasons of wasting and increased disease transmission,
the final ascent!
and abundance of disease vectors. Emergency preparedness
We are not so happily situated with regard to iron deficiency,
requires solid technical support in countries to build national
although here too there are signs of significant movement. The
capabilities for coping with nutritional emergencies (6).
numbers of anemic or iron-deficient subjects continue to be in
262
RAMALINGASWAMI
the high range of over 2 billion, with devastating effects on the
physical, social, and economic fabric of society. There is an
extraordinary opportunity for a determined attack on iron de
ficiency. The elimination of this single micronutrient defi
ciency can do more than any other program to achieve the goals
of human development because all age groups and both sexes
are affected. Greater attention paid to the logistics of uninter
rupted supply and flow of iron supplements, and to counseling
and confidence-building in the recipients of tablets, are hopeful
signs of possible progress in this area. The recent study in
China that showed that the discomfort from iron tablets can be
drastically reduced when they are given on a weekly schedule
adds to the optimism on this front. The weekly dosage schedule
is not only a convenient unit of time, it also exceeds the time
it ^akesTorintestinJmucosal ^eUs_ta-turn_over_in_humans.
Administenng”a'supplementarydose every 7 d will enable the
intestinal mucosal cells loaded with iron from a previous dose
to be shed. WHO, United Nations University, and UNICEF are
proposing to do a major study to determine the practicality and
likely effectiveness of adopting country-wide weeklyjlpsage
schedules based on primary health ruire systems, as is used in
China (9)~
' ~~
I have little to add with respect to vitamin A deficiency,
perhaps the most dramatic of the micronutrient deficiencies. A
lasting solution to the problem of vitamin A deficiency lies in
the context of overall development and in fostering the in
creased cultivation and consumption of carotene-rich foods.
School gardens and kitchen gardens are essential for increasing
the intake of dark-green leafy vegetables_and-orange-colojed.
vegetables and fruits. Red pumpkins, carrots, yellow sweet
' potatoesTiomatoes, papayas, mangos, and bananas with yellow
cores in addition to dark-green leafy vegetables provide an
answer and exclusive breast-feeding is essential. It is clear that
small children can meet their vitamin A requirements by eating
green leafy vegetables (10).(Leaves_can save^children’s eyes
and liyes. Each country will have to determine the place of
short-term solutions and immediately available means such as
massive dosing with vitamin A for improving vitamin A status
of groups that continue to be at greatest risk. A surveillance
system to monitor the micronutrient status of the vulnerable
population and their diets is an essential prerequisite for an
effective policy for the control of micronutrient deficiencies
and for the interaction and phasing out between short- and
long-term approaches (11).
Nutrition and noncommunicable diseases—
a question of behavior and lifestyle
The social affirmation of preventive and promotive practices
will be needed to tackle chronic noncommunicable diseases.
Human lifestyles and behavior hold the key to the future health
of humans. The fact that declines in mortality from noncom
municable disease had occurred to a considerable extent
through preventive actions including diet changes in several
industrialized countries is an argument for initiating similar
programs in an anticipatory way in developing countries in
demographic and epidemiological transition or in the posttran
sitional phasefCpmplete understanding bf all factors cannot be
a precondition to intervention, or else heaith>ievelopirient
wouldno?have?dvanced to the extent that it has (12). We have
the scientific knowledge to create a world in which some of the
chronic diet-related afflictions such as coronary heart disease
and stroke can be made to decline through policies related to
smoking and physical activity, dietary energy intake, the intake
of total and saturated fats, salt and free sugars, complex car
bohydrates, dietary fiber, and stress reduction. I exclude phar
macological means from the pursuit of behavior and lifestyle
interventions.
Economic growth is essential for development, but while
pursuing it, it is possible through preventive and promotive
action to avoid the ascent of “diseases of affluence.” Free
enterprise, market economics, and Thatcherism are the eco
nomic orthodoxies today, but the desire is for economic growth
with environmental sustainability and equity as was addressed
in the Rio Conference.. Does equity ogam. by gravity, by a
trickle-down phenomenon, or by active social development”
policy? AfanyrateTwe are backtothe basics, namely promo
tion of balanced, wholesome, safe, culturally acceptable, and
aesthetically attractive diets. J
Nutrition and public health in transition—
what lessons have we learned from history?
A journey through nutritional history
The growing frequency of diet-related noncommunicable
diseases in developing countries and the coexistence of preand posttransitional disease spectra in population groups in
several developing countries, the so-called “double burden,” is
all too familiar. For instance, obesity is already prevalent in
some developing countries, among the poor in middle income
countries, and among the well-to-do in low income countries.
There is a rerun of patterns of nutritional diseases of affluence,
if I may use that term, in those developing countries entering
the posttransitional phase at an accelerated rate over the past
30-40 y. The McCarrison Society in the United Kingdom
discussed this subject in OxSrd. Sir Robert McCarrison, who
wqsjhe founder of India’s National Institute of Nutrition, ancT
whomTIiad’tli^priviiege to knowuTfiis postretirement years at
Oxford in the late 1940s and early 1950s, influenced me in
developing an interest in iodine deficiency diseases in the
Himalayas. He served as a young Indian Medical Service a
officer in Gilgit in the western Himalayas in the early years of "
this century. He was struck by the fine physique, powers of
endurance, and relative freedom from disease of the local
people and conceived the idea that those characteristics might
be related to their diet. He spent a good part of his professional
life pursuing this idea and his experiments with Sikh, Bengali,
and Madrasi diets are well known. He wrote in 1932 that a diet
most likely to maintain physical efficiency and health is “a diet
composed of any whole cereal grain or mixture of cereal
grains, milk and milk products, legumes, green leafy vegeta
bles, root vegetables, fruit and water, with meat occasionally
added” on festive occasions (13). McCarrison advocated the
-Oslo breakfast, reputed to be good for'Norwegian children.
which was similar to his own prescription. The breakfast
served free to Norwegian children in those days consisted of
500 mL milk, whole-meal bread with butter, whole-meal rusks
(or raw carrot, an apple or orange, and whey cheese.
The return of outbreaks of the ancient scourges’of pellagra,
beriberi, and scurvy in refugees today is a negation of the
GLOBAL PERSPECTIVES ON MALNUTRITION
history of human progress. Food for refugees, their health,
nutrition, and survival, are issues troubling human conscience
today. The numbers of these refugees have risen despite the
end of the Cold War.
In nutrition, one sees_a repetition of history in time and
_spac?, It would seem a wise policy to go back to some of the
nutritionally sound and wholesome principles and practices in
indigenous and traditional systems befgrejhey^areJost in the
avalanche of modernity. Mahatma Gandhi once said, “I have
notifingTbTeacETEeworld; truth and non-violence are as old as
the hills.” Some part of poor peoples’ traditional diets may be
worth emulating, for example, less meat and more vegetables.
(R Longhurst, personal communication, 1993).
The UN system
The UN agencies have a special responsibility for the fol
low-up of ICN. They need to strengthen greatly their collabo
rative and cooperative mechanisms at all levels, from global to
local, especially at national and local levels (14). The ACC/
SCN is assigned an important role in promoting interagency
linkages. The new ethic is decentralization to provinces, dis
tricts, and local areas with communities taking more leadership
and responsibility. An overalTintersectoral framework is es
sential for nutritional improvement, fully recognizing the es
sential role that individual sectors have to play. Decentraliza
tion means taking action closer to people with the involvement
of local government and local community leaders, accountabil
ity, and community empowerment through the effective use of
communication and education. Someone told me the other day
to “Take health away from the hands of the accountants and put
it in the hands of the people.” It is not that we need accountants
lessbutthat we need accountaBilitymore! There should be
greaterreronciliation andliarmonizationof_Agencyjnandates.
Rapid response to country needs is one ofthesecrets oFsuccess
and dependency on local or regional expertise wherever feasi
ble is conducive to progress.
Conclusion
As I come to the end of this presentation, a kaleidoscope of
images impinges on my mind. The post-ICN follow-up ap
proach is to view the problem of nutrition in a holistic, inter
disciplinary, and intersectoral manner. It conceives nutrition as
a means, a measure, a fruit of development, and as part of an
ethic in which people and communities hold the master key. A
dominant image is a shift from central to provincial and district
levels. Increased access to and control of resources by women
is another dominant image as is also the biological and psy
chosocial needs of adolescents. Yet another image is that
chronic endemic food insecurity, uncontrolled population
growth, degradation of the environment, rapid unplanned ur
banization, and inequities are critical determinants of malnu
trition to be addressed. The nutritional status of a population is
263
an exquisite indicator of overall development, and nutrition
monitoring and surveillance and a systematic flow of informa
tion are essential prerequisites for disaster preparedness, for
targeting vulnerable groups, and for longer-term policy and
program development Our policies must reflect the growing
ethic of lifestyle change and personal responsibility for health.
More effective use must be made of research guiding policy
and action and for finding solutions to unresolved problems.
The link between scientific evidence,-popular concern,_and.
potitKaTresponse is sought to be strengthened by the ICN
process. Despite^the prevailing conflicts, much destruction, and
death, there is a conducive new international environment.
There is renewed faith in the UN system. The search for hope
is urgent and promising in a world less divided.
I am grateful to the authorities of the XV International Congress on
Nutrition in Adelaide for permission to publish this presentation.
References
International Conference on Nutrition. Final report of the conference.
Rome: FAO and WHO, 1992.
Levinger B. Nutrition, health and learning. Current issues and trends.
School nutrition and health, no. 1. Educational Development Corpo
ration, 1992.
3.
Musgrove P. Feeding Latin American children. An analytical survey of
food programmes. World Bank Report no. 9526 - LAC, 1991.
4.
HRO Dissemination Notes: Human Resources Development and Op
erations Policy. Enhancing investments in education through better
nutrition and health, no. 7. Washington, DC: World Bank, 1993.
5.
Monckeberg F. Discussion of malnutrition and its emotional aspects in
Latin America. Child Health 1991;2:1-5.
6.
WHO Executive Board. International Conference on Nutrition. Report
by the Director-General, EB 91/3. Geneva, Switzerland: WHO, 1993.
7.
Ramalingaswami V. Challenges and opportunities—one vitamin and
two minerals. World Health Forum 1992;13:222-30.
8.
Hetzel B. A global perspective of iodine deficiency. IDD Newsletter
1991 ;7.
9.
WHO, UNU, UNICEF. Master protocol: population studies on the
relative effectiveness of weekly and daily iron supplementation in
pregnant women, adolescent girls and preschool age children. Geneva,
Switzerland: WHO, 1993.
10.
Rahman MM, et al. Can infants and young children eat enough green
leafy vegetables from a single traditional meal to meet their daily
vitamin A requirements? Eur J Clin Nutr 47:68-72.
11.
Greiner T. Combining short and long term vitamin A deficiency
control programs. News on Health Care in Developing Countries
1992;Vitamin A:27-9.
12.
Ramalingaswami V. To foresee is to govern. Address presented at
plenary session on politics, economics, and ethics of cardiovascular
disease intervention at the International Heart Health Conference.
Victoria, British Columbia, Canada, 27th May 1992.
13.
McCarrison R. Problems of nutrition in India. Nutr Abstr Rev 1932;
2:1-8.
14.
Heyward EJR. The United Nations system and nutrition: the need for
change in a more democratic world. Fifth Annual Martin J Forman .
Lecture. Helen Keller International, June 15, 1972.
1.
2.
Nut - 12-A Tragedy Unfolding: Tribal Children Dying in Attappady
Vol - XI.IX No. 2, January 11,2014 | Manikatidan A.D
The continuing deaths of infants and children due to malnutrition in Attappady, the only tribal
block in Kerala, reflects the state government’s apathy towards addressing issues germane to the
tribals residing in the region.
Manikandan A.D (alungal09@gmail.com) is a PhD candidate at School of International
Relations and Politics. Mahatma Gandhi University, Kottayam, Kerala, and ICSSR Institutional
Doctoral Fellow al the Centre for Economic and Social Studies (CESS), Nizamiah Observatory
Campus, Begumpet. Hyderabad.
Introduction
Malnutrition deaths of infants/children are highly prevalent in India. The country accounts for 29
% (3.09 lakh) of all first-day deaths globally (Singh: 2013). The extent and severity of
malnutrition deaths of infants/children, however, differs among various social groups and states.
For instance, malnutrition deaths are highly prevalent among socially marginalised groups such
as tribals, fisherfolk and dalits, and rampant in socio-economically backward states such as
Bihar, Jharkhand, Madhya Pradesh, Rajasthan and Uttar Pradesh (Khera: 2008). But it is
shocking to see in Kerala —a state with superb achievements in human development, people’s
planning, governance, and women’s literacy- an alarming rate of malnutrition deaths of tribal
infants/children. The UNICEF Report (2013) observed that a total of 39 deaths had been reported
from Attappady tribal block in Palakkad district between April 2012 and May 2013. Major
causes included asphyxia, acute respiratory distress syndrome, aspiration, apnoea, preterm and
low birth weight, development growth delay, and intrauterine growth retardation (IUGR). C D
Rozario (2013) noted that 36 children had died in the past 16 months (from January 2012 to
April 2013) as compared to 25 and 32 starvation deaths in 1996 and 1999 respectively. [1] The
Times ofIndia (2013) came up with the more shocking estimate of “58 malnutrition deaths in the
past 20 months” in Attappady tribal block. The Ekbal Committee Report (2013) said that in
2013 about 30 children died within a few hours/days of their birth. A team of experts from the
National Institute of Nutrition (2013) visited Attappady tribal block for studying infants or
children deaths and reported that the infant mortality rate (IMR) there was 66 as compared to
14.1 deaths per 1000 live births in the rest of the state. [2]
In light of these facts some pertinent questions need to be addressed. Why is the infant/ children
mortality rate very high among the tribal groups in Kerala? Why is the government unable to
stop this phenomenon even after implementing so many social security/welfare schemes and
laws, including the Forest Right Act, Restriction of Transfer of Land and Restoration of
Alienated Land Act?
Incidence and Intensity of Health and Nutritional Problems in Attappady
Attappady tribal block, established in 1962, is located in Palakkad district of Kerala, east of the
Silent Valley in the Western Ghats, one of the world’s most famous biodiversity hotspots. In
1901, this region was mostly forested and inhabited exclusively by hills tribes. Forest coverage
which was 82% in 1959, came down to 19.7 % in 1996. The share of tribal population came
down to 40.9% in 2001 from 90% in 1951. The share of scheduled caste (SC) population among
the total population was 4% while that of general category was 55%. According to 2001 figures,
a total of 66,171 persons reside in Attappady, of which 27,121 persons are tribals (40.9). Out of
27,121 tribals, 20,883 persons (77%) belong to the Irula group (non-primitive), 3,487 persons
(13%) belong to Muduga group (non-primitive) and 2,755 persons (10%) belong to Kurumba
group (primitive). There are 189 tribal hamlets with a total of 8,585 tribal households. As per a
study, 83% of the tribal population was poor in 1997 (Institute for Societal Advancement 2006).
According to the Kerala Institute of Local Administration (KILA) (2008), there are 8,589 tribal
households in Attappady block, of which 6,180 tribal households have ration cards; out of these
25.34% of households hold APL (Above Poverty Line) ration cards, and rest of them hold BPL
(Below Poverty Line) ration cards. What is more shocking is that around 2,400 tribal households
do not even have ration cards. The literacy rates of tribal males and females is 64% and 56%
respectively (KILA 2008) while male and female literacy rates in the rest of Kerala stand at 96%
and 92% respectively (Census 2011).
Kerala, a state with a robust performance in the health sector, received a jolt from a report of
the Comptroller and Auditor General (CAG) of India, which stated that as per the World Health
Organisation (WHO) growth standard the percentage of malnourished and severely malnourished
children in Kerala as on March 2011 stood at 36.9% and 0.8% respectively (The Hindu: 2013).
This is not surprising because the situation of malnutrition and related health problems is
abmysal among socially vulnerable groups in the state of Kerala. For instance, the incidence and
intensity of malnourishment and health problems are high among tribal groups, fisherfolk and the
like in Kerala. C D Rozario (2013) has observed that among adivasi children of 12 months or
less, 9.1% are severely underweight, 32.2% suffer from severe stunting and 7% suffer from
severe wasting. At the same time, it was found that 54% of children from the fisherfolk
community below the age of 6 were malnourished.[3]
The status of nutrition of tribal children is appalling in Attappady tribal block in the Palakkad
district of Kerala. One of the first tribal blocks to be established in India, Attappady is one of
the most backward blocks in Kerala. Tribal groups are suffering from extreme starvation and
malnourishment even after 50 years of its formation. A study by Kerala Institute of Local
Administration (KILA) (2008) reveals that 48% of the total tribal households are poor. Kerala
has received another pertinent jolt from the CAG after a report prepared by the National Institute
of Nutrition showed that the overall prevalence of underweight, stunting and wasting among the
children attending a health camp at Tribal Specialty Hospital at Kottathara in Attappady tribal
block was very high -78.6%, 77.8%, and 53% respectively. The overall prevalence of anaemia
was 85% among women, with 56% having mild anaemia, 28% moderate anaemia and 1% severe
anaemia.
A recent survey conducted by Thampu, a non-governmental organisation (NGO) dealing with
tribal rights, found that out of the 300 tribals affected by malnutrition 200 were children.
K.Venugopal, the district medical officer, said that 412 cases of anaemia and 67 cases of
malnutrition had been noticed by the health department (The Hindu: 2013). The Integrated Tribal
Development Programme conducted a survey between 11 April 2013 and 19 April 2013 in
Attappady, covering 7,565 households and a population of 23,599, and found that the number of
tribal people with anaemia/malnutrition was 463/69, the number of children aged below five with
anaemia/ malnutrition was 68/57 and lactating mothers with anaemia and malnutrition was 62/ 0
(The Hindu: 2013). The UNICEF Report (2013) observed that weight of the mothers at delivery
ranged between 39 and 45 kgs. The Ekbal Committee (2013) said that most women had
undergone abortion more than once and almost all children examined suffered from anaemia and
malnutrition. Difference between the nutritional status of Kerala’s general rural populace and
that of Attappady could be as high as 50% (Suchitra: 2013). Considering these dismal statistics,
Attappady can be called Kerala’s “sub-Saharan Africa”.[4]
Causes of Malnutrition Deaths
The death toll of infants due to malnutrition and related health problems has risen between
January and December 2013 (The Hindu: 2013). The newspapers have come up with shocking
estimates of infant deaths in Attappady. According to The Hindu, 52 infant deaths were reported
from Attappady in the past 17 months (3 July 2013). The Times of India said that as many as 58
malnutrition deaths were reported in the tribal hamlets in the past 20 months (27 September
2013).
A survey of literature on malnutrition and related health problems in Attappady points towards
several reasons for extreme poverty and malnutrition deaths in the region. The most pertinent
among them are as follows[5]: land alienation of the tribals; loss of traditional shifting
cultivation; loss of traditional food items such as ragi, chama, cholam, veraku, thina, thuvara,
honey, tubes, roots, medicinal vegetables, etc.; neglect of the tribal people and inaction by the
departments of Tribal and Social Welfare and Health; failure of public distribution system; poor
performance of Mahatma Gandhi National Rural Employment Guarantee Scheme (MGNREGS);
contrary to the practices in other places, the anganwadis do not distribute eggs, milk, and
bananas among tribal children; lack of essential drug supplies such as Mesoprestol and Magsulf
for delivery and childbirth related medical emergencies;
disempowerment of the adivasi
communities; failure of Attappady Hill Area Development Society (AHADS), a Japanese
funded project, which works towards ensuring a sustainable livelihood and ecology; and
institutional delays and inefficiency in implementing the laws, schemes and projects meant for
tribal groups in Attappady.
Conclusions
It is well understood that malnutrition and related health problems are some of the most
important issues facing the country. Socially marginalised groups, women and children in
particular, in many states are the worst victims of this problem. It is shocking to note that Kerala
- a state with the remarkable achievements in human, and social (health) indicators - has
excluded the tribal groups from its so-called achievements[6]. It shows that development in
human and social (health) sectors is as not inclusive as claimed by the state. For instance, more
than 60 tribal infant/children died due to the combined impacts of loss of indigenous food items,
poor public distribution system, unavailability of alternate nutritious food and the loss of
employment opportunities, which led to widespread starvation along with high malnutrition and
related health problems (Ekbal Committee: 2013) in the past 24 months in Attappady, the only
tribal block in the state of Kerala.
In order to increase livelihood opportunities and ensure health of tribal groups in Attappady, the
following suggestions may be useful. Right to common property resources or right to commons
needs to be implemented keeping in mind that many indigenous/traditional communities have
depended upon the common property resources for centuries or even millennia. This right should
meet long-term livelihood and health security of the tribal groups in India. Right to health needs
to be enacted. A Special Land Distribution Act for Attappady needs to be implemented since the
tribal groups have lost more than 10,000 acres of land (The Hindu 2013, Ekbal Committee: 2013,
Rozario: 2013). Deployment of a Central Development Force (CDF), a special police wing to
capture or arrest those who are not the implementing schemes/programmes meant for socially
weaker sections should be considered seriously. A culturally sensitive approach to the
implementation of MGNREGS should be looked into. This essentially means that the chief
onnooppan of each tribal hamlet should be granted powers to plan, execute, monitor and
evaluate the rural employment guarantee scheme in tribal areas/ belts. Formation of tribal sabhas
or hamlet sabhas and tribal self-help groups should be encouraged. Engineering, medical and
higher education institutions with special provisions for tribal students should be opened in the
area. Investment in the transportation sector should be enhanced to improve the accessibility and
connectivity of tribal groups. The quality and quantity of health services provided by both public
and private sector in Attappady should be upgraded. [7]
Notes
[1]
Attappady had experienced starvation deaths among tribal groups in the past, but its intensity was relatively low
(Rozario 2013: 16).
[2]
Recent estimate shows that Kerala’s infant mortality rate is 12/ 1000 live births (The Hindu, 28 Dec. 2013: 9);
Bakshi (2010).
[3]
RIGHTS, in their submission, have referred to the above survey conducted by National Nutrition Monitoring
Bureau (NNMB on children from Adivasi communities up to the age of 12 months. Theeradesha Samrakshna
Samithi has made a submission referring to its survey in Alappad Panchayat, a marine fisher Grama panchayath in
Alappuzha district, which has 8 fishing villages and found that more than 50% of the children there are
malnourished.
[4]
See Manikandan (2013a).
[5]
See for more details The UNICEF Report (2013), National Institute of Nutrition Report (2013), Dr. B. Ekbal
Committee Report (2013), Rozario (2013), the newspapers such as The Hindu, The Times of India, Deepika and
Deshabhimani.
[6]
See for more details Soman and Rajasree (1994), Kerala Calling (2005), Kerala Human Development Report
(2005), Shivakumar (2010), Bakshi (2010) Raman (2010), Vasanth (2013), Ittyipe (2013), and Ekbal (2013a,b).
[7]
See for more details the UNICEF Report (2013) and Suchitra (2013)
Position: 1290 (6 views)