RF_NUT_6_SUDHA.pdf
Media
- extracted text
-
RF_NUT_6_SUDHANUT 6.1
INSTRUCTIONS
FOR
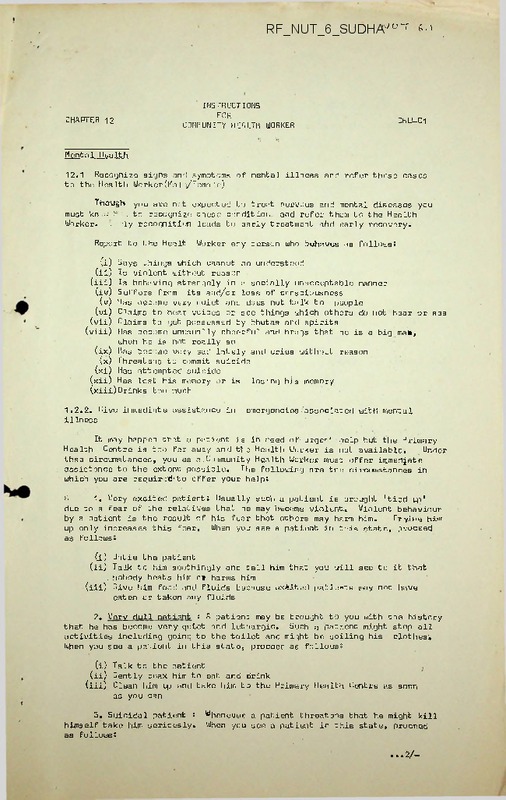
COMMUNITY HEALTH WORKER*(i)
CHAPTER 12
CHW-C1
Mental Health
12.1 Recognize signs and symptoms of mental illness and refer these cases
to the Health Worker(Male/Temale)
you are not expected to treat nervous and mental diseases you
h .. to recognize these conditioi.: and refer them to the Health
'ly recognition leads to early treatment ahd early recovery.
Though
must kn
Worker.
-
Report to the Healt
Worker any person who behaves as follows
*
(i) Says things which cannot be understood
(ii) Is violent without reason
(iii) Is behaving strangely in a socially unacceptable manner
(iv) Suff ors from fits and/or loss of consciousness
(v) Has become very quiet and does not talk to people
(vi) Claims to hoar voices or see things which others do not hear or see
(vii) Claims to get possessed by bhutas and spirits
(viii) Has become unusually cheerful and brags that he is a big ma»,
when he is not really so
(ix) Has become very sad lately and cries without reason
(x) Threatens to commit suicide
(xi) Has attempted suicide
(xii) Has lost his memory or is losing his memory
Drinks
(xiii)
too much
1.2.2. Give immediate assistance in
illness
emergencies-'associated with mental
It may happen that a patient is in need of1 urge1-' help but the Primary
Health Centre is too far away and the Health Worker is not available
*
Under
thse circumstances, you as a.Community Health Worker must offer immedjate
assistance to the extent possible. The following are the circumstances in
which you are required-to offer your helps
>1
1. Very excited patient; Usually such a patient is brought 'tied up
*
due to a fear of the relatives that he may become violent.. Violent behaviour
by a patient is the result of his fear that others may harm him.
Trying tvim
up only increases this fear. When you see a patient in this state, proceed
as follows.
(i) Untie the patient
(ii) Talk to him soothingly and tell him that you will see to it that
. nobody beats him o» harms him
(iii) .Give him food and fluids because ex-iited pat.i.eats may not have
eaten or taken any fluids
2. Very dull patient s A patient may be brought to you with the history
that he has become very quiet and lethargic. Such a patient might stop all
activities including going to the toilet and might be soiling his clothes'.
When you see a patient in this state, proceed as follows!
(i) Talk to the patient
(ii) Gently coax him to eat ar.d drink
(iii) Clean him up and take him to the Primary Health Centre as soon
as you can
3. Suicidal patient *
himself take him seriously.
as follows;
Whenever a patient threatens that he might kill
When you see a patient in this state, proceed
...2/-
: 2 :
'
See that c-’mocne is axwoyg with ths patient until he is taken
to a doctor
(ii)
Remove all sharp instruments and poisons from within his reach
(i)
4.
Person who has had too mu»h alcohol: People may get irritable and even
violent after drinking. ' The best way to deal with a drunken person is to let
the patient sleep.
5.
Fits:
When you see'a
patient with fits, proceed as follows:
(i) Take the patient to a safe place and see that he does not get hurt
by hitting himself against ’a hard object
(ii) Put. a rolled-up piece of cloth in the mouth so that the patient does
not’bite his tongue
(liii) Do not give him anything to drink during or soon after the fit.
It
might choke him.
■
6.
Without wasting any time take the patient to the doctor if mental
symptoms have appeared .immediately or soon after:
(i) Child birth(ii) High fever
(iii)
Head
injury
(iv)
Fits
(v)
Dog bite ,
12.3
.
Educate the community .about mental illness
You must make the people under your care aware of.the following facts:
1.
2.
3.
4.
5.
6.
7.
Mental illness is like any other illness and is not due to bhutas,
spirits or witchcraft
There is no shame in having a case of mental illness in tho family,
just 'as there is no shame in having a person with fever
Mental illness can be cured. The recovery is quick and may-be complete
if the patient is seen in the early stages
The treatment of mental illness is prolonged and must be continued
according to the advice of the doctor even after the patient becomes
apparently normal
Marriage is not a cure for mental illness.
The stress of married life
will only increase the problem
A mentally disturbed patient bn treatment must be kept occuoied in
whatever job ho can do. Keeping the patien unoccupied makes
him more disturbed.
One must not make fun of patients with mental illness.
It makes them
worse and induces them to excitement.
,
////////
programme
TOPIC:
"Organising Nutrition Rehabilitation in a village
set up".
9.30 - 10.00
Introduction of the participants
10.00 - 11.00
'Concept of Nutrition Rehabilitation
in a village set up1.
11.00
11.15
Break
11.15
12.15
Group Discussion
15
1.00
Presentation of the groups
1.00
2.00
Lunch
2.30
4.00 p. m,
Field trip to the Bangalore Baptist
Hospital
Slides; use of health education material
Use of simple anthropometric equipments.
G R 0 U P-.'S
1.
What are the different Nutritional problems seen in the
community what are its causes, effects and the cure sought?
2.
What are the problems inter-related to Malnutrition?
Social? economic? Cultural?
3.
What are the factors to be considered in teaching nutrition
to members? What are the 'methods to be adopted?
The media for rural education. Evaluation techniques, in
education
4.
How will- you integrate the other services with Nutrition
Rehabilitation or surveillance in the community?
2
= 2 =
Concept of Nutritional Rehabilitation and. Nutritional
Surveillance:
Vanaja Ramprasad,
Bangalore Baptist Hospital.
The economic liability of malnutrition in the growing popu
lation is the concern of many nations all over the world.
It is a modest estimate that in India about 30% of the
vulnerable group of population is malnourished or under
nourished.
long
The most desirable and lasting solution depends upon/term
measures aimed at social and economic development. This calls
for motivation of so many people and large capital invest
ments and sustained efforts for long periods, before any
change can be noticed.
•
•
Meanwhile, the situation calls for immediate and specific
attention. The idea that the malnourished child requires
hospitalization is still very widespread. While it. is
obvious that extremely severe cases should be hospitalized,
it is now realised that a large proportion of advanced
cases require simply a proper diet. Hospitalized children when
treated successfully hav-c- a relapse because treatment a cone
fails to correct the underlying cause of illness which is in
his home. Effective education based on their understanding,
their educational background and their food and financial
resources is'a must for a lasting impact on the mothers.
It is here that the Nutrition Rehabilitation has its genesis.
The concept of Nutrition Rehabilitation centres was initiated
way back in the year 1955, by Dr. Jose M» Bengoa, Since,
then a number of countries including Algeria, Brazil, Haiti,
Nigeria, Philippines and now India have set up Nutritional
Rehabilitation Centres.
It is an established factor that the rehabilitation centres
should be a part of a more comprehensive child health programme.
Objectives of N.R.C.
1.
2.
The primary aim of an NRC is education.
Rehabilitation of the malnourished child with well balanced
diet1 of local goods.
To include in the education not only practical nutrition but
the elements of personal hygiene and good sanitary practices.
4.
To have the centre, house and operate it in a way that is
as close as possible to the conditions prevailing in the
community.
3.
To study the knowledge, attitude, and practice of the
people prior to exposing them to health education.
6.
To study pertinent information about people, their problems
regarding health, their understanding and misconceptions
about certain aspects of life situations, their customs
and beliefs.
5.
3
= 3 =
7.
To identify ’those who will perform health services in the
operational phase of the programme.
NUTRITIONAL EDUCATION:
Since the mother determines completely the food the child
eats, her nutritional knowledge needs to improve.
Past
efforts at educating peasant mothers have been largely
frustrating. Effective education of peasant women requires
that several basic facts of the problem be given serious
attention. The process of learning should be very non-formal
since for most part these mothers are illiterates. What these
women need to learn in terms of nutrition and general child care
is simple. Everything that is taught must be usuable within
the framework of an extremely limited family income.' Knowledge
of the art of combining locally available food in a way that
will meet the food needs of the young child should be imparted
to them.
Education process starts with an active desire for-such a '
centre, from the village. Usually this requires a series of
meeting with community leaders, convincing them of their local
needs and determining the extent to which the community is
able and willing to support the centre.
A thorough knowledge of the people to be educated is very
essential, apart from the. thorough investigation that is needed
to study the nutritional problems of children under five. With
this basic information the message- should be-directed at the
problems. The lessons Conducted should be relevant and appro
priate, apart from being clear and easily understood.
Use- of demonstrations is an effective method of teaching.
bedause seeing is believing . Use of flash cards, flip
charts or flannel graphs should be relevant to the local
situations. Use of the weight card’ in educating the mother
is extremely Valuable. The long term results of a rehabi
litation centre can be explained with due credit to the■
education programme.
NUTRIT TONAL RECUPFRATION:
Although Kwashiorkor has been known and treated for more than
three decades there- arc- many variations in its therapy through
the world. Various aspects of Protein Calorie ’Malnutrition;
have to be understood before treatment can be undertaken,
especially in their own homes. Literature suggests two
clinical types of Protein Calorie Malnutrition; i.e.
Kwashiorkor and Marasums sometimes seen in the same community
children exposed to the same dietary environment. This is the
result of adaptation or non-adaptation to■dietary habits or
other stress in which the functional status of the adrental
cortex and adrental hypophyseal axis plays an active role.
As a result of continuous protein-calorie deficiency, loss
of subcutaneous tissue occurs and muscle protein may break
down resulting in severe wasting as seen in clinical cases
of marasums.
It is possible that some children may be
biochemically adapted if on the other hand, the child fails
to adapt to the dietary restriction and is not protected by
muscle wasting, it may develop signs of Kwashiorkor in wich
the biochemical integrity is not maintained. Several 'studies
show that the biochemical integrity is better.maintained in
marasums then in Kwashiorkor. Plasma proteins and aleumin
serum enzyme? like lipase, amylase and esterase and blood
urea are found to be normal in marasmic children while
these values were markedly lowered in children suffering from
Kwashiorkor.
Livers of children suffering from Kwashiorkor
have invariably been found to be heavily infiltrated with
fat while livers of marasmic children are free from fatty
infiltration. With this background let us discuss about the
appropriate treatment at different stages.
TREATMENT :
As long as severe diarrhoea persists, the child needs hospita
lization and under medical care is kept on NPO. The traditional^
and safe method of introducing food to the child is half strength
milk with sugar. As the. child is able to accept the milk, the
dilution is decreased gradually to full strength milk. The next
stage is when solid foods are given to provide 4 gms of protein
and 150-200 calories per kg'of body weight.
The treatment of Kwashiorkor consists of providing protein food
of biological value in an easily assimilable form Considering
the severe shortage of milk, it cannot be the practical answer.
Whild we resort to the use of protein rich foods of vegetables
origin, there are certain disadvantages. 1. They contain
indigestible carbohydrate which may swell and interfere in the
digestion and absorption of proteins. 2. Many of them contain
odiferous and bitter principles which effect their palatibility.
The criteria of selection of the vegetable food recommended are:
1.
It should be rich in protein. 2. Locally available and
reasonably cheap. 3. Commonly acceptable and 4. Suitable
j
for use in the daily diet in various forms. Literature .provides "
evidence of ample experiments conducted with peanut, proteins
and roasted Bengalgram dhal powder, The following alternate
suggestions could be introduced: 1. Defatted peanut protein
powder and milk in the ration of 3:1, reconstituted to provide
4 gms of protein and 150 to two hundred calories per kg. body
weight arrived at, from the average of actual and expected
body weight. The second alternative is with dehusked roasted
behgal gram powder in the form of a toffee.
The third alternative is plain yoghurt.
So much for tackling cases of Kwashiorkor with severe oedma.
But whenever there is a child over 2 years falling the third
degree malnutrition or as per the arm circumference in the
'Red' area, neither severe marasmus nor Kwashiorkor, the
following recommendation is made based on the finding from
the children fed at the NRC.
5
The blend made of the locally available material consists of
ragi, gg dhal, D.G.N., flour and jaggery
*
The following
details give- the nutritive value of the blend.
Cal
Prot
Calcium JFe
Vit A'' Cost
43.00
60.4
(j ,u)
Ragi
'
gg dhal
D.G.N. flour
Jaggery
Total
30 oms 98.4
2.19
20 gms • 66.8" 4.40
10 gms 38,0
4.0
25 gms 95.5
0.1
85 gms 302.75 11.19
103.2
15.0
20.0
20.0
138.2
/
n
/) 9.8
.17
--20 gms
*
312.55 11.26
79.00 3.3 461.0
217.2 9.7 589.8
-
Add mc-thi’
Requirement of-child
1-3 years 1200 17/18/20
4-6 years 1500 22
Pregnant women
Lact-ating women
" 3300 55 gms
' 3700 65 gms
4 to 5
4 to 5
1.92 12.6
1.7 . 4.8
2.8
6.4
15 - 20' 'mg 1000
15 - 20 mg 1200
1 gm 40 mg •
1 gm 30 mg
-3000
4600
(Education for Preparation in their homes)
Considering the requirement , 85 gms' of the blend gives the above
quantities of the requirement. When used as a supplement it
fills up the existing, gap of calories', proteins and. vitamin
A especially in children and iron in pregnant and lactating
women, who are anaemic..
Whenever advise needs.to be given regarding preparation of the
.mix .at home the following approximate measures have been
arrived at ■
•Ragi
30 x'100 3 kg
• gg dhal
20 x’100 2 kg
• g.n. flour 10 x 100 1 kg
•Jaggery
25 x'100 2-£ kg
/3
/3
/3
/3
= 1 kg
= 3/4kg (little less)
=
kg
= 3/4kg (little less)
Alternate, ingredients should be suggested.
= 6 =
Composition, Nutritive Value- and Cost of the Ready to
Consume formulatipns .
Cost
Ingredients
Rs. ps.
Jowar-Fcngal Gram Formulation
131
92
71
96
3.9
5.6
3.3
0.1
0.04
0.06
0.05
0.04
12.9
0.19
3.9
6il
3.3
0.1
0.04
0.05
0.05
0.04
13.4
0.18
4.1 .
5.6
5.6
0.1
0.04
0.06
0.05
0.04
13.1
0.19
128
87 '
71
96 ■
4.1
6il
3i3
Oil
0.04
0.05
0.05
0.04
382
13.6
0.18
2.7
5.6
3.3'
0.1
0.04
0.06
- 0.05
0.04
11.7
0.19
2.7
6.1
3.3
0.1
0.04
0.05
0.05
0.04
12.0
0.18
37.5
Roasted Jowar flour .
Roasted be ng al gram dhal flour 25.0
Roasted groundnuts
12.5
Jaggery
25.0
. 390
100.0
Jowar green gram foi mulation
Roasted jowar flour
37.5
131
Roasted green gram dhal flour 25.0
87
■ Roasted groundnuts
12.5
71
Jaggery
96
25.0
385
100.0
■JVid.ze-bencaJL gram formulation
Roasted maize flour
37.5
128
Roasted bengal gram dhal flour-25.0
92
Roasted ground nuts
12.5
71 ’
Jaggery
25.0
96
387
100.0
Maize-green qram forinulation
Roasted maize flour
Roasted green gram dhal flour
Roasted ground, nuts
Jaggery
37.5
25.0
12.5
25.0
100.0
■
Raqi-benqal qiram formijlation
Roasted rggi flour
37.5
123
Roasted bengal gram dhal flour 25.0
92
Roasted groundnuts
12.5
71
Jaggery
96
' 25.0
100.0
382
Ragi-grecn qr am formuliation
Roasted ragi flour
37.5
123
Roasted green gram dhal flour 25.0
87
Roasted’ groundnuts
71
12.5
Jaggery
25.0
96
100.0
377
7
7
NUTRITIONAL., SURVFILIANCF:
Malnutrition amongs.t the agricultural population is hidden
beneath the surface in apparently normal children and is not
obvious to the naked eye. The majority of the children with
mild to moderate malnutrition and even some suffering from
severe malnutrition remain undetected. Between extreme
manifestations of malnutrition and full health there is a
wide "grey area" in which the body mechanisms arc not working
fully effiencitly. Hence it is crucial to detect malnutrition
in its early stages. (Refer the training manual chapter 8)
here in the early signs and symptoms of malnutrition arc
described, and where the 'at risk factors are discussed.
Some of the points to be- noted while- advising simple changes
in food habits are also mentioned.
Meaningful education must start with recongition of the
situation in which the people find themselves, their atti
tudes and the resources actually or potentially available to
them.
Family welfare through education of in family planning which
is of direct relevance to improving nutrition, since mal
nutrition is frequently more- common in large families and
especially in those- families where children arc- closely
spaced, must also be promoted by the health workers.
For sustained benefit to be derived, the active cooperation
of the community has to be enlisted.
Local people can be
trained to maintain hand pumps or to administer simple drugs
in conduction with supplementary feeding and nutrition
therapy.
@ @ @ @ @
ms/17578/*
pAJT 6-3
ASSESMENT OF NUTRITIONAL STATUS OF A COMMUNITY
The Nutritional status of a community is the sum of the nutritional status
of tha individuals who Form ,t het community.
(l) Longitudinal
(2)
Cross Sectional
Clinical Examination
Anthropometiic Examin ition
Biochemical Exaninat ■. n
Laboratory Examir.atio >
V
VI
VII
Dietary Examination
Study if Vital Statistics
Asses ’itit <.f Ecological Factors
Types of Survey :
I
II
III
IV
I
Clinical Examination
(1)
(2)
General
appearance
Hair 8
(3)
(4)
Face 2
Eyes :
(5)
(6)
(7)
(8)
(9)
(1U)
(12^
Lips ?
Tongues
Teeth 2
Gums 2
Glands ?
Skin 2
Nails 2
*nma 2
Ra chit xu.
changes s
Internal
(13)
5 Zv+.
.
Normal built/Thin built/sickly-
Normal/ddtl and dry/dyspigmented/thin and sparse/easily
pluckablc'flag sign
Diffuse dtoigmentation/naso-labial dyssobacea/mcon face
Conjunctiva-normal/dry on exposure for
*
min/dry and
wrinkled/bitct’ s spots/brown pigmentation/angular
conjunctlvitis/pale conjunctiva Cornea-normal/dryness/
hazy or noa^ue
Normal/anguiar/stomatitis/chcilosis
Normal/pale end flabby/red and raw/fissured/geographic
Norma 1/bleedir.e
Thyroid enlargcnent/parditid enlargement
Norml/dry and scaly/follicular hyperkeratosis
Koi lony chia
in dependent parts
Knock-knees- or bor legs/cpiphysoal enlargcmont/beading
Motor weakness/HacpatomeQaly/p-’' chomotor changc/mental
nonfusion/sensory “loss/loss of position scnsc/loss of
fibration sense/loss of ankle -.nd-knee jerks/calf
cndcrness/cardinc enlargement/tachycardia.
Anthropometric ExairatAi- i
(1)
(2)
(3)
Weight (kg)
Height (cm)
Mid-upper-arm circumfeaOncQ (cm)
(4)
(5)
(6)
Ho- d circumference (cm)
Ch..st circumference (cm)
Sk\n fold- Tricopes, subscapular,
(7) Cai f circumference
Composite
(1)
wt „
(Ht)2
100
x
(2) :crm_Cjj?q1BB_perenco
Head circ'Knfo>->nC0
(3)
Calf circumference
Height
III
(1)
(2)
(3)
(4)
Protein 2-
Total scrum-protein
(5)
Serum albumin
Urinary urea
(6)
Vitamin A s— Serum Vitamin A
.(7)
Serum carotene
V -tamin C 2- Serdm ascorbic acid
(8)
Urinary ascorbic acid
Vitamin D
Serum alkaline phospha- (9)
taso in young children
Thiamine 2— Urinary thiamine
Blood pyruvate
Riboflavins •- Urinary riboflavine
Niacin
Urinary N-mothyl nico
tinamide
Iron *S- H.aornQgicein
Serum iron
Iodine :- Urinary iodine
Tests for thyroid function
IV
Laboratory Examinejions *
(l)
(2)
(3)
V
Dietary Examinations (1)
(2)
(3)
(4)
VI
v:so nit-ached Diet Surve .-.chedule)
bieighment of raw f-.-.-’s
Weighmcnt of ceokc
■ ’cods
Oral questionnire n chod
Checking bf stock inventor1/ -
Study of Vital Statistics
(1)
(2)
(3)
VII
Haemoglobin ■ (specify method)
Stool » nsgntive/asei rias ia/ahcylns tonins is/nir.rdiasia/apocbi--sis/
strongyloif ■s/'jthsrs (state) ’
Slood sm-~.r - nega--: jc/W.T./8.T./Filaria'
Infant mortality rate
(4) Perinatal
Neonatal mortality rate
(5) mortalit-.for (1-4) years grsiypStill Birth rate
(6) Life expo;
ctancy
(7) Hospital statistics
flssesment of Ecological F- ctors
(l) Conditioning influences
(4) Socio-economic factors
(2) Cultural influences
(s) Health and educational services
(3)
Food productiot
6-m
II. BALANCED DIETS IM TERMS OF STANDARD CUPS AND SPOONS
The balanced diets For different categories of
people are given in terms of standard cups and spoons in
the following table':
Table-1:- Balanced Diet for Adult Man('Moderate worker)
Food Stuff
Qty
(g)
Approximate
volume in std.
cup and std.
spoon.
Number
I. CEREALS
1. Rice
2. Wheat flour
335
140
1-3/5
1
50
30
1/5
6 std. sp.
125
1-4/5
100
3/5
2 medium sized ones
75
1/2
12-15 or a
handful
II. PULSES
1. Redgram dhal
2. Blackgram dhal
III. GREEN LEAFY VEGETABLE
1. Amaranthus
3 bundles
IV. Roots and Tubers
Photato
V. OTHER VEGETABLES
Beans
VI. fruit
Orange
30
-'
3 segments.
VII. Milk
200
4/5
-
VIII. Fats and oils
40
2/5
40
1/5
IX. Sugar & Jaggery
-
2
Table-II: Balanced Diet for an Adult Women (Moderate Worker)
(1)
(2)
(4)
(3)
I, CERFAL
1. Rice
2. Wheat.
230
120
1
-4/5
II. PULSES
1. Redgram dhai
2. Blacl'.gram dial
45
25
-1/5
5 std. sp.
125
1-4/5
75
1/2
1
1/2
12-155or a
handful.
- ■
III. GREEN LEAFY VEGETABLE
Amaranth
3 bundles,
TV, ROOTS AND TUBERS
Potato
V. OTHER VEGETABLES - Beans
75
VI. FRUITS- - Orange
30
VII. AU Ik
200
4/5
VIII. Fats and Oils
35
1/5
30
6 Std. sp. -
IX. Sugar and Jaggery
3 segments
or a quarter
fruit.
-
Table-Ill: Addition. ■ A’ . jwance for Pregnancy and Lactation
Lactation
Pregnancy
Food Stuff
Appx. Vol.
in std.cup
Appx.Vol.
in std.cup. No.
N0,
I. CEREALS:
Rice
Wheat
50
1/5
-
40
60
1/5
2/5
20
2 std.sp.
II. PULSES:
Redgram dhal
III. GREEN LEAFY
VEGETABLE
VI. Milk
V. Fats & Oils
25
2/5
3 /4 bun-25
dies
125
i
-
125
15
■2/5
3/4bundles
1/2
4 std.sp.
= 3 =
Table - IV: Balanced Diet for a Child between the Age
3-6 years ('Ref. - 6 years old child)
Food Stuff
Qty
(g)
Appr.Vol.in
std. cup
(1)
(2)
(3 J)
140
60
3/5
2/5
30
15
15
6 std. sp.
3 "
3 "
;
75
1-1/5 std.cup
No.
I. CEREALS
1. Rice
2. Wheat flour
—
-
II. PULSES
1.. Redgram dhal
2. Blackgram dhal
3. Other grams
III. GREEN LFAFY VEGETABLE:
Amaranth
1-4 bundles
IV. BOOTS AID TUBERS
Potato
50
2/5
50
2/5 std.sp.
8-10 in no.
5 segments.
"
1 medium size
V. OTHER VEGETABLES
Beans
VI. FRUITS
Orange
VII. Milk
•,
VIII. Fa’ts and Oils
IX.
Sugar and Jaggery
50
2/5 std.cup.
250
1 ’
"
25
7
std.sp.
40
8 std. sp..
4
Table - w : Balanced Diet for a Child Between the. Age 1-3 years
_____ '_________________ (Ref 3 .xeax- old .child 1----------- ---------------(2)
(1)
(3)
(4)
—-
I. CEREALS
'
' '
1. Rice
2. Wheat
90
60
2/5
2/5
-
25
10
15
5 std.sp
*
2 std.sp.
3 std.sp.
-
50
4/5 cup
1 bundle
30
2/5 cup
1 small
30
2/5 cup
5--7 in no.
II. PULSES
1. Redgram dhal
2. Blackgram dhal
3. Greengram dhal
III. GREEN LEAFY VEGETABLES:
Amaranth
IV. ROOTS AND TUBERS ,
Potato
V. OTHER VEGFTAPLFS
Beans VI. FRUITS - Orange
50
VII. Milk
300
VIII. Fats and Oils
20
6 std.sp.
30
6 std. sp.
EX'. Sugar and Jaggery
ms/18578/'
5 segments
1-1/5
-
II. BALANCED DIETS IN TERMS OF STANDARD CUPS AND SPOONS
The balanced diets for different categories of
people are given in terms of standard cups and spoons in
the following table:
Table-1: Balanced Diet for Adult Man(Moderate worker)
Approximate .
volume in std •
cup and std:
spoon.
Food Stuff
Number
I. CEREALS
1. Rice
2. Wheat flour
335
140
1-3/5
1
50
30
1/5
6 std. •Sp.
125
•1-4/5
100
3/5
2 medium
sized one;
75
1/2
12-15 or a
handful
II. PULSES
1. Redgram dhal
2, Blackgram dhal
III. GREEN LEAFY VEGETABLE
J. Amara.nthus
3 bundles
IV. Roots and Tubers
Photato
V. OTHER VEGETABLES
Beans
VI. FRUIT
Orange
30
-
3 segments.
VII. Milk
200
4/5
-
VIII. Fats and oils ■■
. 40
2/5
-
IX. Sugar & Jaggery
40
1/5
_-_
__ —__ - —
__ —__ —__ —
2
1
Table-II: Balanced Diet for an Adult Women (Moderate Worker)
I, CEREAL
1. Rice
2. Wheat
230
120
1
-4/5
II. PULSES
1. Redgram dhal
2. Blackgram dhal
45 •
25
-1/5
5 std. sp.
125
1-4/5
75
1/2
1
1/2
12-15Jor a
handful.
•
.
-
III. GRFEM LEAFY VEGETABLE
Amaranth
3 bundles.
a
IV. ROOTS AND TUBERS
Potato
V. OTHER VEGETABLES - Beans
75
VI. FRUITS - Orange
30
VII. Milk
200
4/5
VIII. Fats and Oils
35
1/5
30
6 Std. sp. -
IX. Sugar and Jaggery
3 segments
or a quarter
fruit.
Table-III: Additional Allowance for Pregnancy and Lactation
Pregnancy
Food Stuff
Qty
(g)
— ———--------—-------- =——= ——:
Lactation
Appx.Vol.
Qty Appx.Vpl.
..
in std.cup. ’ ‘
(g) in std.cup
--- = ——=--- = — * —•—-——. ——— —----— ——— — —tz — — — —-— »■ —— —~ —
I. CEREALS:
Rice
Wheat
50
1/5
40
60
1/5
2/5
20
2 std.sp.
II. PULSES:
Redgram dhal
III. GREEN LEAFY
VEGETABLE
VI. Milk
V. Fats & Oils
VI. Sugar £ .’3-
25
2/5
3/4 bun-25
dles
125
i
-
125
15
2/5
-
3/4bundles
1/2
4 std.sp.
= 3 =
Table - IV: Balanced Di«-t for a Chil' between the Age
3-6 years (Ref. -•6 years old child)
Food Stuff
Qty
(g)
Appx.Vol.in
std. cup
, (1)
(?•)
' (3)
140
60
3/5
2/5
30
15
15
6 std. sp.
3 ”
3 "
75
1-1/5 std.cup
No.
-
-
I. CEREALS
1. Rice
2. Wheat flour
-
II. PULSES
1. Redgram dhal
2. Blackgram dhal
3. Other grams
•
HI. GREEN LFAFY VEGETABLE:
Amaranth
1-4 bundles
IV. BOOTS A:!D TUBERS
Potato
50
2/5
50
2/5 std.sp.
8-10 in no.
5 segments.
”
1 medium size
V. OTHER VEGETABLES
Beans
VI. FRUITS
Orange
50
2/5 std.cup.
VII. Mik '
250
1
"
VIII. Fats and Oils
25
7
std.sp.
40
3 std. sp.
IX. Sugar and Jaggery
•
4
Table - v
: Balanced Diet for 'a Child Between the Age 1-3 years
-=_==_==_==_==_=t:_==XH^L^L=^-^_Q^_-^l.y=sX= ==_=■= ==_=_-=
(1)
(2)
“ "
(3j
"
"(4) "
I. CEREALS
1. Rice
*
2. Wheat
90
60
2/5
2/5
-
25
10
15
5 std.sp.
2 std.sp.
3 std.sp.
-
50
4/5 cup
1 bundle
30
2/5 cup
1 small
30
2/57rup
5-7 in no.
II. PULSES
1. Redgra.m dhal
2. Bladkgram dhal
3. Greengram dhal
III. GREEN LEAFY VEGETABLES:
Amaranth
IV. ROOTS AND TUBERS
Potato
V. OTHER VEGETABLES
Beans -
VI. FRUITS
Orange
50
5 segments
VII. Milk .
300
VIII. Fats and Oils
20
6 std.sp.
30
6 std. sp;
IX. Sugar and Jaggery
ms/13578/*
1-1/5
-
II. BALANCED DIETS IN TERMS OF STANDARD CUPS AND SPOONS
The balanced diets for different categories of.
people are given in terms of standard cups and spoons in
the following table:
Table-1: Balanced Diet for Adult Man(Moderate worker)
Food-Stuff
Qty
(g)
Approximate
volume in std.
cup and std.
spoon.
Number
I. CEREALS
1. Rice
2. Wheat flour
335
140
1-3/5
1
50
30
1/5
6 std. sp.
125
'1-4/5
100
3/5
2 medium s
sized ones
1/2 .
12-15 or a
handful
II. .PULSES
1. -Redgram-dhal
2. Blackgram dhal
III. GREEN LEAFY VEGETABLE
1. Amaranthus
3 bundles
IV. Roots and Tubers
Photato
V. OTHER VEGETABLES
Beans
75
■
VI. FRUIT
Orange
3 segments.
30
VII. Milk
200
4/5
-
VIII. Fats and oils
40
2/5
-
40
1/5
-
IX. Sugar & Jaggery
2
2
Table-II: Balanced Diet for an Aduit Women (Moderate Worker)
1
II
II
ii
_ (3)__
_
1
II
II
II
i
1
i
'l-'l
_
St-
_(2)
_
I
ii
(1)
I, CEREAL
230
120
1. Rice
2. Wheat
1
-4/5
II. PULSES
1. Redgram dhal
2. Blac.kgram dhal
' -45'
25
-1/5 .
5 std. sp.
125
1-4/5
75 J
1/2
III. GRFEM LEAFY VEGETABLE
Amaranth
3 bundles.
IV. ROOTS ALP TUBERS
Potato
V. OTHER.VEGETABLES - Beans
75
1
’ 1/2
VI. FRUITS -.'Orange
30
VII. Milk
200
4/5
VIII. Fats and Oils
35
1/5
12-15Jor a
handful.
3 segments ’
or a quarter
fruit.
-
IX. Sugar and Jaggery
30
6 Std
*
sp. =—=--==.—=—-=—=—=—=—=—=—=—=—=—=—=--=—=- —=—=—=--- =—
Table-III: Additional Allowance for Pregnancy and Lactation
Pregnancy
Food Stuff
Qtv
(g)
Lactation
Appx.Vol.
in std.cup. 1J0’
Qty
(g)
Appx.Vol.
in std.cup
40
60
1/5
2/5
I. CEREALS:
Rice
Wheat
50
1/5
II. PULSES:
Redgram dhal
III. GREEN LEAFY
VEGETABLE
VI. Milk
-• & Oils
20
25
125
2/5
'
2 std.sp.
3/4 bun-25
dies
2/5
-
1/2
125
1r
3/4bundles
= 3 = '
Table - IV: Balanced Diet for a Child between the Age
3-6 years (Ref. - 6’years old child)
Appx.Vol.in
std. cup
N».
(2)
(3)
_ (4) _
140
60
3/5
2/5
*
30
15
15
6 std. sp.
3' n
3 "
75
1-1/5 std.cup
Food Stuff
(i).
.
I. CEREALS
1. Rice
2. Wheat flour
•
.11. PULSES
1. Redgram dhal
2. Blackgram dhal
3. Other grams
III. GREEN LEAFY VEGETABLE:
Amaranth
L-i
bundles
IV.' ROOTS AND TUBERS
Potato
-
50
S/5
50
2/5 std.sp.
8-10 in no.
5 segments.
1 medium size
V. OTHER VEGETABLES
Beans
VI. FRUITS
50
2/5 std.cup.
VII. Milk
250
1
"
vui; Fats' and Oils
25
7
std.sp.
40
8 std. sp.
Orange -
IX. Sugar and Jaggery
4 =
Table - n : Balanced Diet for a Child Between the Age 1-3 years
____________________ __4Ref i--3 v£i
old xhildj_______ —
•
(1)
■
(2)
__(4)
(3)
I. CEREALS
1. Rice
2.’ Wheat
90
60
2/5
2/5
-
25
10
15
5 std.sp.
2 std.sp.
'3 std.sp.
-
50
4/5 fujp
30
2/5 cup
1 small
30
2/5 cup
5-7 in no.
“ Hi, PULSES
1. Redgram dhal
2. Blackgram dhal
3. Greengram dhal
III. GREEN LEAFY VEGETABLES:
Amaranth
IV. ROOTS AND TUBERS
Potato
1 bundle
*
V. OTHER VEGETABLES
Beans VI. FRUITS - Orange
5 segments
50
' VII. Milk
300
VIII. Fats and Oils
20
6 std.sp.
30
6 std. sp
IX. Sugar and Jaggery
******
*
ms/18578/
1-1/5
-•
i^/{JT 6-q
11.
3ALAFCSP
DIETS IF,.T--irr.3 o.? 3TA?DA"D CUPS.-AKD SPOOKS
The balanced diets for different categories of people
are giver in terms'of standard cups and spoons in the following
table:
Table-1: Balanced Diet for Adult Mar(Moderate worker)
~j?d stuff
Qty
(g)
Approximate
volume in the
std.cup and
std.spo-.'r.
335
140
1-3/5
1
50
30
1/5
6 std.sp.
Number
Ie CKRB/tLS
1. Rice
2. '■.heat flour
II. PULSES
1. Redgram dhal
2. Blackgram dhal
III. SL’rar
T7I.. ’3LE
1. Amaranthus
3 bundles
125
1-4/5
100
3/5
2 medium sised ones
75
1/2
12-15 or a hard ful
■ X£. R’ ^TS ’AFP TLW-3
Potato
V. STH ;■> VEGETABLES
Bears
VI. BRUIT
Orange
VII. Milk
VIII. Fats ard oils
IX. Sugar & Jaggery
30
-
3 segments.
200
4/5
-
40
2/5
-
40
1/5
-
Table - Ils Balanced Diet for an Adult Woman
(Mo derate Worker)
I. cerJlL
1. Rice
2. Wheat
230
120
1
-4/5
II. PULSES
1. Red gram dhal
2. Blackgramdhal
-1/5
std.sp.
-
125
1-4/5
3 bundles.
75
1/2
45
25
5
TABLE
III.
Amaranth
J-D TUIDJtS
1
V. OTHER VEGETABLES - Beans
75
1/2
12-15 or a hand
ful.
VI. FRUITS - Orange
30
-
VII. Milk
200
4/5
3 segments: or a
quarter fruit.
-•
35
1/5
-
30
6 std. sp.
VIII. Fats and Oils
IX. Sugar and Jaggery
-
.
„
Table - III? Additional Allowance for Pregnancy. Hnd-Lactatipn.
Lactation
Pregrarcy
Foodstuff
Qty
<g)
Appx.Vol.
in" std. cup
No.
50
1/5
-
Appx. vol.
ir std.cup
Nb.
I. GER' .AIS ?
Rice
Wheat
II.
40
60
1/5
2/5
20
2 std.sp.
PULSES;
Redgram dhal
HI.
IV.
GREe I' leafy
vegetable
25
2/5
3/4 hurdles
25
2/5
Milk
125
A
-
125
1/2
V.
Fats <3: oils
VI.
Sugar & Jaggery
10
2 std.sp.
-
3/4 burdl
15
4 std.sp.
20
4 std.sp.
Table - IV? Balanced Diet for a Child between the Age 3-6 Years
(Ref. - 6 years old child)
No.
Foodstuff
Qty
(g)
Appx.vol.ir
std.cup
1
2
3
140
60
3/5
2/5
30
15
15
6 std.sn.
3 "
3 “
75
1-1/5 std. cup
1-Jr bundles
50
2/5
1 medium size
4
I. CEREALS
l.Rice
2. Wheat flour
-
II. PULSES
l.Redgramdhal
2.Blackgr&m dhal
3.Other grams
in. green leafy vegetable?
Amaranth
IV. Boots nrd Tubers
potato
«
i
7.
4
3
2
JTHER vegetables
Bears
50
2/5 std.sp. 3-10 ir no.
2/5 std.cup 5 segments.
VI. FRUITS'
Orange
50.
•711. Milk
250
1
VIII. Fats and Oils
25
7 std.sp.
40
8 std.sp.
IX. Sugar and Jaggery
"
Balanced Diet for a Child Between the Age 1-3 Years
(Ref: 3 year old child)
Table-V:
1
3
2
4
I. cereals
1. Bice
2. .’-.'heat
So
2/5
2/5
-
25
10
15
5 std.sp.
2 std.sp.
3 std.sp.
—
-
50
4/5 cup
1. bundle
90
II. PULSES
1. Redgram dhal
2. Blackgram dhal
3. Greengram dhal
III.
green LEAFY VEGETABLES:
Amaranth
17.
HOOTS AMO TUBERS
P«^ato
30
2/6 cup
V.
OTHER VEGETABLES - Beans
30
2/6 cup
Sx5?xxr:xns.
1 small
5-7 in no.
5 segments.
71.
FRUITS - Orange
50
Ssl/S ±h3j£Sx
VII.
mMXarcIXMXM Milk
20 300
$X5TfefcXS£<. 1-1/5
VIII.
Fats and Oils
20
6 std.sp.
Sugar and Jaggery
30
6 std.sp.
IX.
- - - -
_
VITAMIE AND MINERALS
Daily Requirement for an adult
6 -6
Vitamin A
3000 I.U.
1. Xeropthalmia. Bli i-inc-ss
2. Decrease Resistanc; to URTI
3. Inner Ear DGafness
4. -^Cne^
Vitamin D
400 I.U.
1. Rickets in children
2. Osteomalacia in adults
Thiamine
1.5 mgms
1. ’Beri Beri
-2. Neuritis
Riboflavine
1.5 mgms
• Nicotinic Acid
15 mgms
Cyanocobalamine
1 mcg.
Pathothemic Acid
3 mgms .
Choline Parent substance
acetylcholine
and a constituent
of Lecithin
2 gms
Deposition of fat in liver and
Haemorrhagic degeneration, of
liver and kidney
Ascorbic acid
50 gms
1. Scurvy
2. Decrease resistance to infection
,
. Angular Stomatitis
. PhotopfroL-Ls
Glossitis
Pellegara
Anaemia
1. Chick Pellagara
2. Hair growth
Folic acid
1.5 mgms.
Vitamin E & K
Not known
1. Vitamin E - sterility in male
2. Vitamin K - Bypopiotbrnmbinaemia
Ca.
1 gm.
1. Bo/ne defects
2. Hair
3- Blood disease
Iron
15 mgms.
Anaemia
Fluoride, Ion
in water
1-2 ppm
Dental caries
■
Anaemia
. .
■ :
Essential Fatty acids nutritionally important and necessary for growth.
They are Linoleic, Linolenic and Arachidonic acids. They ■’innot be synthosiaed
in the body and have to be supplied in the diet. Linol'eir- and Linoenic acid
are of vegitable origin and present in cotton seed, groundnut and linsee oils
while Arachidonic acid is of fish and animal origin. E.F.A. regulate
cholesterol metabolism.
DAILY BALANCED DIET FOR AN ADULT
flveeflG-E
XNblMO
Bier •
Cereals (rice chiefly milled)
Dhal (red gram)
Green vegetable (cabbage)
Potatoes Cauliflower - cSExv
Banana - Inij-JOi
Oils & fats
Sugar (in tea, coffee & sweets)
Milk (cow)
Mutton
Egg
Agathi
ss- 1 IS' "
* ?>s
..
«7 ■'
Gms
■300
100
100
100
100
150
50
100
100
200
50
50
Cals
(340x3) 1020
355
2"
9”
3C
15C
45C
40C
6'
(194x1) 38S
S5
45'
3? U _
' DEB. RTMB NT OF PREVENTIVE ft SOCIAL MEDICINE
ST. JOHN'S MEDICAL COLLEGE, BANGALORE 560034-
EXERCISES IN NUTRITION AND DIETETICS
Q - I,
A family consists of the following .members:
a) Old lady of 60 years (40 kg.)
An adult male going to office (55 kg.)
An adult female (45 kg)
Two sons and two daughters of 15, 15, 11 and 7 years of-age.
Give a schedule of balanced
}
diet for this family in terms of Rice, Pulses,
Greenleafy vegetables,
L__, P„.k
Root vegetables, other vegetables, milk, sugar, fish,
meat, egg and oil.
Coefficient value of the family:
ANSWER:
a)1 Old lady
b ) Adult male
c ) Adult female
dj) Son, 15 years
e ) Son, 15 years
f<) Daughter, 11 years
g.) Daughter, 7 years
0.9
1.0
0.9
1.0'
1.0
0.8
0.7
6.5
Total
Requirement of Balanced Diet for the family
gms
Oz.
1.
Rice
400 x 6.5
=
2520
gms
14
^8.2 Oz.
2.
Pulses
85 x 6.5
=
535.5
gms
3
,18.9 oz.
3.
G.L. Vegetables 114 x 6.5
=
718.2
gms
4
25.2 oz.
85 x 6_5
=
535.5
gms
Other vegetables 85 x 6.5
=
535.5
gms
_ .. 3
X
18;,9 oz.
~IsAoz.
18.91 oz.
4.- Root vegetables
5.
6.
Fruits
• 85 x 6.5
--
55b. 5
gms
3
7.
Milk
2b4 x 6.5
=
1789.2
gffle
10
63.0(02.
8.
Sugar
57 x 6.5
=
359.1
gms
2
,12.6 oz.
9.
Fish & meat
85 x 6.3
=
535.5
gms
10. Eggs
7 eggs
11. Oil
57 x 6.3
=
359.1
/ / .: 18.9 oz.
3
gms
1
7 eggs
2
12.6 bz.
We require for the above family 2400 x 6.3 = 15,120 calories. The above
diet yields approximately 3000 x 6.5 calories. Hence, it is sufficient for the
- - ---------- . family.
Q - II.
ixU-c Clew
A family consists of an adult male (55 kg.), and adult female (45 kg.)
and a child of 5 years weighing 15 kgs. On a diet survey of this
family, it was observed that the consumption per day in terns of the
proximate principles and nutrients was aS follows:-
- <f X Proteins
OHO
Fats
..
..
...
ft
cue.,
150 gms.
2000 gms.
100 gms.'
v£t. A.
Vit. B.
V£t. C.
eo-AA.prMHX-'j
Comment on the quantity! and quality of the diet.
1000 I.U.
10 mgm.
150 mgm.
1
b) Suggest improvements confining your attention to the above
nutrients only.
, , •_ ft
"
ANSWER: —
l^i‘
•
Requirements
1. Proteins
‘Male
2< CH0
450. gm.
60 'gm.
Female
+
+
+
+
55 gm.
l$-42$ %eX 3. Fats
3500 IU
4. Vit. 'A'
Child
45 gms.
450 gms.
40 gms.
3500 IU
+
+
+
+
52.5 gms.
=
152.5 gms.
180.0 gms.
=
1080.0 gras.
40.0 gms.
=
160.0 gms.
3500.0 IU
=
10,500.00 IU
In terms of Retinol and daily requirement will be 750 micrograms for the
adult and for the child of 5 years 300 micrograms. It comes to 750 + 750 +
300 = 1800 micrograms. One'I.U. of Vit. 'A1 = 0.3 mg. So, 10,500 I.U. will
be 3,150 micrograms.
'
?
1
=
5 gms.
..50+50+40
+
+
=
140 Egm
5. Vit. *
B'
(Thiamine)
6. Vit. 'C'
..
i. COMMENTS:
Quantity: . Calories requirement 1 + 0.9 + 0.5 = 2.4 coefficient
■ = 5,760 calories.
■
..
2
The above diet will provide Proteins 150 x 4
CHO
,2000 x 4
Fats
100 x 9
= 600 calories
= 8000
-do= 900
-do-
= 9400 calories
Total
' It is more than ample.
QUALITY
:-
Proteins
Fats
Vit. B
:
:
:
Just short:
Short\
Sufficient:
CHO - more than ample
Vit^. A - very much short
Vit. O— sufficient.
■IMPROVEMENT: Cut out CHO (Cereals) an<k increase the pulses, milk or includ
egg. Fat requirement can be met by increasing oil or ghee (60 gms). Vit.A
or Betinol is very much short of requirements and leafy vegetables like
araaranath, drum stick leaves and other vegetables like carrot; fruits like
papaya should be included in the diet. Vit.'B & C are sufficient.
Q - III., A mother with an,, infant of 6 months old wants to start her child
with artificial feeding with buffalo’s milk. What is the quantity
of the buffalo's milk and the number of feeds per day that'you
would advise? What other advise you would like to give to the
mother about the feeding with the buffalo's milk? Considering the
deficiencies in the milk, what supplements would you advise?
ANSWER:
Buffalo milk yields 118 calories/100 gms. A child of 6 months
(normal), weighing 6.7 kg. will require 600 calories. The child
therefore, requires 600/118 = 5 or 500 gms. of milk or 16 to 17 oz.
of milk. This milk must be diluted with water to reduce the fact
concent, and sugar must be added to increase the CHO content.
Composition: Buffalo milk
Human milk
= Fat
= Fat
8.8
3.4
sugar 5.1
sugar 7.4
i.e. the milk must be humanised.
Thus, 16 to 17 ozs. of diluted milk must be given in 4 feeds (8 hrs, once)
during day and one feed before going to bed. Milk is deficient in Iron
and Vit. C. Hence, fruit juices and green leafy vegetables mashed should
be given as supplements.
’
f' 'r'" '<2.C C'
6-8
ROP LT.'S ON NUTRITION
NUTRITION;
1. A family consists of an adult male (55 kq) and an adult female
(45 kg) and a child of 5 years weighting 15 kg. On a diet survey
of this family it was observed that the consumption per day in
terms of the proximate principles and nutrients arc as follows:
Protein
Carbohydrates
Fats
Vit A
Vit
150 gms.
OOOc'Caloris
100 gms.
1000 I.U.
10 mgm
150 mem
Suggest improvements confim ing your attention to the above
nutrients only.
2.
On analysis, it was found that diet of an adult male doing
moderate work contained following nutrients:
a) CHO
b) Fat
c ) Protein
d) Vit A -
250 g
e) Thiamine
30 gs
f | Vit C
4000 I.U. hj Calcium
Iron
0.5 mg
25 mg
0.5 mgm
10 mg
a) Comment, on the quantity and quality of the diet?
3.
A mother with an infant of 6 months old, wants to start her child
with artificial feeding with bufallo's milk. Calculate the
quantity of the buffalo's milk and its strength and the number of
feeds per day that you would advise? Considering r.the defici
encies in the milk, enumerate the supplments to be advised for
this child from your knowledge of commonly available food stuffs.
4.
As a medical officer of a PNC what would you do if you come
across Vit A deficiency conditions among many members of a family?
5.
Put up a balanced diet for a family consisting of a father, a
lactating mother and a boy aged 12 years.
6.
In your practice as a family physician you encounter nutritional
deficiency cases in a family. What investigations would you
conduct to determine that it is due to lack of proper diet?
Give the composition with quantity, of a balanced diet in a
family consisting of father 40 years, mother 35 years, one son
15 years, two daughters of 10 years and 6 years respectively.
7.
Describe how you would conduct a diet and nutrition survey in a
boarding hostel having 100 students in the Primary school age
group and suggest measures to improve the nutritional status of
these students.
8.
A family consists of the following members:
a) Old lady of 60 years (40 kg);
b) An adult male going to office (55 kg);
c ) An adult female (45 kg);
d) Two sons and two daughters of 15, 13, 11 and 17 years of age.
Give a schedule of balanced diet for this family in terms of Rice,
Pulses, Grecnlcafy vegetables. Root Vegetables, other vegetables,
milk, sugar, fish meat, eggs, and oil.
.2
2
9.
10.
Prescribe a diet for a family of A whose monthly income is Rs.400/>
of father, mother, sons and daughter.
Comment on the following daily diets
i) Raw rice polished
ii) Pulses
iii) Grcnleafy vegetables
iv) Erinjals
v) Putter milk
vi) Sugar
- 16 oz.
- 1 oz.
- 4 oz.
- i- pz.
- 4 bz.
oz.
480 gms.
30 gms.
15
15 gms.
120 gms.
15 gms.
11. Suggest improvements without increasing the cost of the diet
very much?
12.
Comment on the following
a) Pasteuriser’ milk is positive for phosphotase test.
b) Infant should be started on solid diet after 6 months of age.
c ) Mixed cereals is desirable than a single cereal in our diet.
Dale :
Syr>el
£ . Z^zo p e cxa 0^7 <-*> - F^CJZ-
n/o.E' ^/c^UzT-ez^/^evo?/^
^1 ■
cJt'fW'- jj'io-'^j*'’
Dale: IGIIWI
h-
3.
zTrsa-c.
i/.
A^L<-O <&r~>eJ
- P e#.
<zf j
Crr->
- ></^
-ncto
*
S. 3fcrcJ^-e^iX< oJ
Pc.J^
^=>,
P>e-^e^-)l^cr>^
PE’^
7.
P^S'-'--^
>iolE C^P-e^
PEnJZ C..ho^yr I /-3o-zL^i b-dr
WEIGHT II! KIL0G7.
/\) UT;
Fig. 11.3: .Weight curve chart
2. ^ensuring Itid-arn Circumference:. The identification of children who
are nalnourislied can .also be done by measuring the distance around the
uid-am. This should be done by having the art1, hang loese at the side
of the body and placing the aw circumference scale at tho r.dd—point
as shown in fig. 11.4a & b. Any child between the ages of one and five
years is considered to bo malnourished if this neasurc: ’.ent is less tZian
12.8 cm.
*
.Ccntd/65-
: 65 :
GUIDE TO lUTPITIOri
IMMUNIZATION SCHEDULE
SLLLFGX
?r."'or;-: at birth or as seen
Mfcr as possible
Szjaination of Scar
REAGCIJkTION ,at ono year '
an every three years,
threafter
?SRCULOSIS (D.G.G)
Date”'
six nonth;;.
Date
Date
Date
: -ent. .Continue breast feeding as long -as
possible’ and introduce the following solids
gradually.
FCUF.T-J. MDHH
ji
Binary: at birth, er as;,soon
ater as possible
fenination of Scar
I x .C ,H ♦ CARD II
BIRTH TO ONE; YEAR: Breast Feed •
Breast nilk' is noteipugh for the baby after
Date
(Triple. Vaccination)
rioarytfren 4th month
Date
r.wo injections at interval
Date
c: 8-12 •weeks
;
Date
•BISTER; 1-1/2 - 2 years
Date
____________
5 years
__________
ILIGhKELITIS (Oral trivalent vcseine)
Binary: fron /th month
Date
tree doses by mouth
■S Jj-6 weeks interval ■____________ Date
YRHOID-FARATYIHQID
• binary: at 1-1/2 years or latter Date
'wo doses at 7-10 days
'nicrval
Date
)C£STER: Two dooes at 7-10 days
interval every year_____________ Date
1?^ HEP.LA. - TETANUS
Binary: when triple vaccine
?.c given durinr.infancy
Date
"V- injections at 8-12 weeks
ve-iks interval
.
. _
Date
ELoTEftiOne injection at 5 years Date
doctor/nurse will, record the date of
firing the injection and tell you when to
or.-r the child for inc next one._________
Child’ Card
(To be kept with the nother)
He needs additional nourish-
•”
• /'
Introduce fresh cow, buffalo, goat or tinned
powder , milk if breast milk is insufficient.
Rice, Buji, Ragi (Dhalia) etc-, well cooked
to a soft consistency and sweetened.
Vegetables like potato, carrot, cooked and
nashod.fi'
f.
f
•
Mashed ripe banana-sweetened, orange/
sweet liue/tonatu juice.-
SIXTH MONTH
In addition to solid foods..already given
introduce the following:
Tread,' biscuits, dlials like Bengal gran,
lentil.,. red. gran - well - cooked, Fishboiled, '':'eat--■ well- cooked and tender,
Bggs-half boiled, ■ Curd, butter-milkCIsanna (Casein), vegetables like cauli
flower, Cabbage, cucumber, etc,. All
fruits.
QIC YEAR
Child can share the ..family food, except hot
and spiced foods.
Do not wait for the baby to cut his teeth
to give solid foods. He will digest well
cooked vegetables, rice;, puji,' etc.., even if
he has no teeth to- chew then. .
•,
Wash your h ands oefore preparing food, cooking
or feeding.
All foed for the baby should be freshly prepared,
no left-over be. given.
All utensils like cups, spoons, bottles etc.
should be washed in boiled water and kept covered.
. EHC/S .0/1 .C .D. Centre
Registration No.
Vil2
Name:.
h/F
Date first seen:
Date of birth :
Or ■
Nb.. of brothers:
birt
Religion:
Sisi.
Diet:
Vegetarian/Noi'.
Hothe r1 s nano:
Occupation:
Fahtor’s name:
Occupi.tic>n
:
Address
:
Medical notes:
Blood Group :
Allergies:
Other infomation:________
Family Planning status of pt
Have your child weighed regv'
Weight will be marked on thi
Bring your cliild to the cent?
nonth till his second birthd ;
every three months’ till his 1
birthday and any tine he doc
appear well. Protect your c'
fron diseases by giving him 5.
actions shown on this card.
services aro given without -;
Ministry of Health and Fanil;.
planning, llirnan Bhavan, Now
LJ___1
1
7cu
■Yellow |
1?i->cli
Groon
13.5cr.
,
|
17«5cr
(adapted from
hal-nour-- Possible lornal
Adnan Shakir
ishcd: ■
I-al-HGtri .
& David I 'orloy-1
"bj.Cll
'
The levcot.P 758■759, .April 20,
1974
'
■
•
Colour Code
Fed'.
--'o-r 12‘.5C'-: 'Salnouxi
cd
“i : '■ 12.5-13~5c Possible
nalnutii'
tion
’>'■
over 13'5cm Kornal
Fig: 1'1 >Zb: Arr- eircurfcronco tape
3 m .©uft^cdristics of Cnildron who are likely to Develop ■ iiJiiutri'bicn:
The systematic search for •; alnourishcd children 'in .the comunity can be very
fruitful when your effort s arc ■ concentrated .among those who have certain
social claaractcristics which are as foliotv’s: ■i.
i. The ‘child is. one of twins.
di.-'The child has no living parents or has a stepmother.
iii. The child is eared for during .'the day by a n older sister or brother
while the mother, works.
'
iv. The .child hop a younger sistdr or brother and the difference in age
is leas tha1? one year.
v. There are four oi- more children in the fondly.
vi. The child belongs to a migrant-family.
vii. jhe child
obviously thinner and' s.rllor than i','1'crc of his ago.
: 68 :
c. AriEemia _(scq section 11.8.4)
d ."'Vitamin 'deficiencies
Vitamin A: Dryness of ’ the eyes-oeeurs due 'to ^he lack of
vitamin A in the didt-’of young .children (see s'ection 11 .8.5).
Vitamin : Signs of symptoms of vitmain B deficiency include:
A sere mouth and tongue, cracks-and sores at the angles of
tlic mouth, rain, numbness and reduced sensation in 'the limbs.
lii. Vit'njain 0: .Persons who do not consume sufficient amounts of fresh
fruits and vegetables containing vitamin 0 develop spongy,
"bleeding gums,"'"loosening of the teeth, and ha,emorrhages under
the skin.
iy. Vitamin D: Rickets is a disease, .caused by a deficiency of
-------vitamin D in the diet, or '.lack of exposure of the skin to
sunlight. It can result in permanent deformities in the bones
5,
(see fig.11.7). Signs and symptoms include soreness and tender?.
ness of the-body,-delayed eruption of teeth, bulging of the bones of
of the head in young children, bow legs,, beading of the ribs
and deformities of the pelvic bones and spine.
i.
ii.
c • Tineral deficiencies:
i.
Calcipm: A deficiency.of calcium in the diet can result in '
rickets, interference with the clotting of blood, deformities
of bones such as knock-faicos and poor teeth.
ii.
Icdine: .Goitre is a disease characterized by swelling in the
front of the neck (see fig.11.8) . It occurs most' frequently
in areas where the food and water arc doficine in iodine.
The increasing use of iodized salt by-persons living in such
areas has decreased the number of people affected by goitre.
ANY -PERSON WHO HAS SIGI'S CR SYMPTOMS OF MALNUTRITION SHOULD BE
FURTHER SCREENED SINCE HE HELL OFTEN HAVE -MCRE THAN ONE NUTRITIONAL
DEFICIENCY.
: 69 :
3
*
11.8
KWASHIORKOR AND I BRASI US
,
■ If an infant or prc-school child (under five years) is found to have
any of the following signs and symptoms, proceed as follows:
j
■ Kwashiorkor
Iferasnus
I 1-fi.sorable arid apathetic.
Generr-l appearance
. Oedema of feet- and leg^
Yes
' No
'
Appearance of fade
Fat or "noon" face
Thin or "old nan’s"
face
Hair colour und texture
.-Lighter than in others
or reddish and brittle
Normal colour and
Springy
Below normal
Very much below
nonrial
Thin and flabby
Very thin, bones
showing
Stretched- and taut,
also ha.s flaking of
skin -
Shrivelled and
wrinkled
•4
Weight
Muscles
,
Skin --
Appetite
...
'
. .................
Accepts fo’cd offered '
Refuses food
:
Arrange' for
transport- to •
the FHC "
''
Alert to people anc
surroundings
Instruct '.nether to
■increase 'quantity ■ ■
of feeds
.
Refer
t
Inform tlic Health Worker (Female.)
-
To-check for oedema," see section 21.4
Roth of the above children have severe nalnutrition and must be referred
to the Primary Health Centro for furtlier treatment. -Unless prompt re
ferral is made, such children nay die *
11.8.4
ANAEMIA
Anaemia is a condition -which is commonly found in pregnant and nursing
wonen and in children
*
(For causes, signs and symptoms of anaemia see section 21.5).
: 70 :
ONE CF YOUR IMPORTANT TASKS AS A HEALTH WORKER IS TO IDENTIFY
ANAEMIC WOMEN AID CHILDREN IN THE COMMUNITY ASEARLY AS POSSIBLE
SO THAT THEY CAN BE TREATED PROMPTLY AND BE TAUGHT HOW TO PREVENT
THE RECURRENCE OF THIS CONDITION.
1. Facts tliat you should know about anaemia and. health
'
i.
Children who arc anaemic suffer from minor illnesses more often
than those who are healthy,, and the illness is' often more severe
. ' than in normal children.
ii- The incidence of anaemia and its effect on health is highest among.pregnant and nursing women and pre-school children.
ili’. Pregnant women who arc anaemic often have serious complications,
e.g., haemorrhage during childbir :h, and produce babies who are
also anaemic at birth.
.....
iv. Anaemic invididuals generally take a longer tine to recover from
infections.
■' .. F£g. 11.9: Examining the ye fer anaemia
2.
Method for identifying those are are anaemic: There are several ways
that canto used to find those who arc anaemic as you make your houseto-house visits. Look for mothers and children whoso skin is pale and
those who tire easily and have little energy since these are the signs
that are commonly associated wifti anaemia. Such persons should further
be examined aS follows:
i.
Pull down the lower eyelid to look a;t the colour of the conjunctiva
(see fig.11.9).
■ •
'
REMEMBER TO WASH YOUR HANDS BEFORE DOING THIS A'D S3 CAREFUL. HOT TO
TCV^i
CONJUNCT-IVA SVY® CTOS ON
MAY ~ 'r ■'1_'rI]FE'n’T0”r
: 7t :
If the conjunctiva is pale pink or colourless, the person is
anaemic.;- A bright pink conjunctiva usually means that there
is no ahaeria.
ii.
Bill down the lown the lower lip to look at the colour of the
mucosa lining tbe mouth.' If it is very pale pink or colourless
the person is ahaoijic. A ’ right pink mucosa usually neans that
there is no. anaemia.
iii . Find out the.percentage of haemoglobin using a Tallquist colour
scale.
~
Procedure f>r determining anaemia using the Tallquist method.
Remember that before doing any procedure, especially one that is
connected with Ibsing blocd, you must get the cooperation of the individual
by explaining;
'
-why it'is needed;
i.
ii.
how it will:be.donp;
iii.
whether there trill be any pain or discomfort associated with it.
Proceed as follows:
’
'
1. Collect and assemble the equipment, viz.
i.
Sterile Hagedorn needle embedded in a cork and kept in a
container of spirit so that the tip remains covered by the dis-infoctant- (sec fig. 11.10a & b).
ii.
Spirit or Sp.vlon.'
-Cotton
iii.
wool.
iv.
Tallquist papers and colour.scale.
_________
2.
Fig.11.10:-Hagedorn needle
■
Carry out the technique: Any procedure that breaks the skin may
load to infection so it is important to take certain precautions on
pricking the skin.
: 72 :
i.
wash your hands and allow then to dry by shaking in'the air.
ii.
Hold, the individual’s finger, usually tho left ring finger,
.’or loft big toe tightly for about 10 seconds to collect a
• good supply of blood.
iii.
Wipe tho aroa to be pricked, i.c. the side of the finger tip
or big toe with cottonwool moistened with spirit or Savlon
and allow to dry.
iv.
Remove the needle from its container, shake off any excess
spirit, and prick the finger or toe with a quick jabbing notion.
v.
Squeeze tho finger until a large drop of blood appears and blot
it into a piece of the Tallquist paper (sec fig.11.10b).
vi.
Take a piece of cottcn wool moistened with spirit on the finger
and ask the person to press it lith his thumb until bleeding
steps.
;
vii.
Compare the colour of the bleed on the paper with the colour
on tho Tallquist scale to determine- the haemoglobin. level.
viii.
Record the haemoglobin level on the individual’s health card.
ix.
Explain the test result to the individual.
3.
Administration of iron and folic acid as prophylaxis against nutri
tional anaemia in mothers and children
Eligibility for iron and folic acid: Tho following criteria arc to
be used tc determine who arc eligible to be given ■ iron and folic
acid and who should be referred to tip Primary Health Centre:
i. All pregnant and nursing women who have 10 gms (70 per cent)
haemoglobin or less according to the Tallquist scale should be
referred to the Primary Health Centre for treatment. If the
haemoglobin level is between 10 to 12 gms (70 to 80 per cent)
■ given iron and folic acid tablets.
ii.
AH family planning acceptors who have 10 gms haemoglobin or
loss, according to the Tallquist scale diould be referred to
the Primary Health Centre for treatment. If tho haemoglobin
level is 10 to 12 grarn^, give iron and folic acid tablets.
iii.
All infants-and pe-school children..(under five years) who have
8 grams haemoglobin or.less according to tho Tallquist scale,
should be referred to the Primary.Health Centre for treatment.
If tho haemoglobin level is 8 to 12 grans give iron anf folic
acid.
■.
r
■
Dosage of iron and folic acid:
Form of
drug
Dosage of
folic acid
Pregnant and
Tablets
nursing women
and family planning
accepters
0.5 mg daily
Children under 5
years
'’
0.1 ng daily
Category
Tablets 'or
liquid
...
' Dosage of
ferrous sulphate
180 ng daily
........
Give the treatment for three months.
week supply of the drugs.
60 ng daily
Dispense a two to four
Health teaching related to treatment: Individuals who arc anaemic
and arc being given iron and folic acid tablets need to have tho follow
ing information:
. : 73 :
i. Iren and folic acid aro special drugs that arc needed by the
body for raising the haemoglobin content in the blood.
Tc be effective, both drugs' must be taken daily in the proscribed .
dosage together with feeds rich in iron.
iii.
Foods rich in iron such as leafy vegetables that arc available
locally should bo included.in the daily diet.
iv.
Tedause the drugs can irritate the stomach they should always be
taken with seme food or at ncaltino•
v.
The tablets will, make the fao'ccs black, but this is an expected
action or iron and should not cause alarm or worry.
vi.
If the person has symptoms such as diarrhoea or"indigestion, she
should inform you about this since the dosage or frequency of the
drugs may have to bo charged.
vii.
After three months of treatment tht blocd test will be repeated to
find out the haemoglobin level.
viii.
To avoid accidental ingestion of .the drugs by small children, the
medicines should bo kept cut of their roach.
ix.
A fresh supply of drugs can bo obtained either at the subcentre or
from the health worker.;
ii.
I'feking follow-up contacts: Follow-up activities can be carried out when
the individual comes to the subcontre, or during bene visits. Points to
remember include the following:
i. If the individual docs not cone to the subcentre Within two to
four weeks after the drugs arc dispensed, make a■heme visit to
assess -tolcranfc to the drugs, side-effects if any, regularity in
talcing the tablets, and whether foods rich in iron have been
added to the diet.
ii. Listen to complaints related to taking drugs and reassure the indivi
dual.
iii.
Dispense a two to four week supply of the drugs if needed by the
individual, but urge her to ob ain then fren the subcentre on a
regular basis.
iv.
Han tc repeat the Tallquist test after the individual has been
taking the drugs for three months.
Records and reports: You are required tc maintain the following records and
reports pertaining to the iron and folic acid tablets that you have dispensed
to eligible persons in the community (see Annoxurc 1116 Forms A, B and 0
in the Supplement tc the Manual).
a.
Individual recipient’s health record: The individual card of the
pregnant or nursing woman, dild, or family planning. acceptor
should include:
i. the date cf the blo< d test and the haemoglobin level;
ii. the date of commencing-the prophylactic treatment, dosage
of the drug, and the number of tablets dispensed;
iii.
the date cf the repeat ;blood tost.-.and the haemoglobin'level;
iv.
the date whpn- .thc drug was stopped'and the reasons for
.stopping it.
Register of beneficiaries: Enter the card number, date of enrolment,
nano, age-and- category of each beneficiarynnd date of stopping the
treatment (see.Ferm A) .
c.
Steck register: The number cf tablets received, issued and in
balance on each date are recorded in the sbeck register (see Form B).
d.
Monthly report to the Primary health Centre: This is a consolida
tion of -the information in Nos. 2 and 3 above (sec Form C).
b.
11.8.5 VTTAJUn A DEFICIENCY
Indra.
Vitamin A deficiency in the diet is a very serious health problem in
largo number of j ro-schcol children have eye symptoms as a result
’
• 't arc deflate t in vitr.’.dn
J
: 75 :
specific dates for coverage of eligible children.
Select the nest easily accessible location in the village
to facilitate attendance and -.rake arra.ngcucnts for its use.
iv.
Deci I . on the content and ; etlicds to be used for pr c-progra-.no
publicity and health education of village leaders and parents.
v.
Bsti -..-t' - amount of drug needed and procure the supply and
er librat^. -. s; ..ns or droppers from th. Tri ar - Hee 1th Centre.
Store th. drug in a cool, dry place.
vi.
Select sirplc tas’-s to be dene by volunteers and train the
c'.T.runit;• r.ci.icl'crs to assist with the pregra'.r, io‘.
iii.
Coordinate ig activities with the Health Worker (Female): Your
task is tr r.dr.iinist-„r vitamin A to as r.'-any children aged one to five years
as possible in each village. In order to achieve a high coverage cf such
children and to avoid duplicati.- n of administration, y u will need to work
closely with the Health Worker (Female) since y u will he th be raking visits
to the same f*ar riHat different intervals for delivery cf specific health
services.
Procedure for adri. istering vita; in A solution;
Use a 2 i li spoon (supplied with the vitamin L solution)
nodicine dropper which is calibrated to -jeasuro the 2 la!
unit dose (2 rd.) which is prescribed (seo ftgj11.1l).
2. Instruct the aether to'hold the baby in her ley. with the
head, raised, so that thc; solution can bo placed in the side of
the nouth or on the tongue.
3 • Administer the drug slowly to avoid the risk of choking.
4.
If •■the-’child spits cut the initial dose, repeat the procedure.
1.
Fig:1l .'11: Elastic..spoori for dispensing vitamin A solution
Health teaching related to vitamin A: loach the p-oople, especially '
parents, elders in he family and leaders, about the value of adding foods
rich in vitamin A to the d aily diet.
records and reports: (soc Annoxure 11. 7, Ferns A, B and C in the
Suppler, ent’ to the rianual).
: 76 i
1 • Individual recipient's health record: Record the details of
vitamin A administration in the individual child's health
record t'lat is kept at the subccntro.
2.
Register uf beneficiaries: Note the date of enrolment, nans,
address and age of each beneficiary and date of administration
of vitamin A solution (sec Form A).
3.
Stock Register: Enter the receipt, issue and balance of vitamin
A solution on ea.chob.to (sde Form B).
4.
Honthly report to the Primary Health Centre: This is a consoli
dation of the information in lies.2 and 3 above (see Form C).
PROTEIN FO® SOURCES
PROTEIN FOODS
RATING
Vegetable sources
Bengal gran dal
Black gran dal
Cow pea
Green gran dal
• Horse gran
Lentils
Pbas (dry)
Red gran dal
Soya bean
Groundnut
XX
XX
XX
XX ••
XX
XX
XX
XX
XXXX
XXX
Bajra
Cholan (Jowar)
Ragi
Rico
Wheat
X
X
X
X
X
Animal sources
Choose
Phnir (Cottage cheese)
I ilk
Eggs
Ourds
Fish (fresh)
Fish (dried powder)
Moat (goat or mutton)
xx
XX
X
vy
VV
XXX5F
XX
Legend:
X = 5 to 15 grr.is protein per 100 grams edible portion.
XX = 15 to 25 grans protein per 100 grans edible portion.
XXX = 25 to 35 grans protein -per 100 grans edible portion.
XXXX = 35 to 45 grans protein per 100 grans edible portion.
* powdered fish contains more than 45 grans of protein per 100 grans
edible portion.
NOTE: Food values in annexuros 11.1, 11.2, 11 .3 and 11.4 are based on
tables included in 'Nutritive Value of Indian Foods' by 0. Gopalan,
• B.V. Rana Sastri and S.C, Balnsubrananian, MEN Publication, 1976.
: 77 i
VITAMIN A FOOD SOURCES
rec?i cgitaiicjg vivd-in a
RATING
Vegetable sources
i’-aranth loaves (chaulai)
Acaranth Stcns
£_.thua loaves
I?c t greens (tops)
. otcl leaves
Carrot (loaves)
Cclocasie (arvi)
Fenugreek loaves (nothi)
lango (ripe)
i ant leaves
Mustard (loaves)
Faraya (ripe)
Itippkin- • •
■ - ■ ’ Radish (tops)
Spinach
Turnip (teps)
Ian
Aa.
XX
Zxj'-Jl.
X
XX
xxxx
■ ■
'
•■■ ‘ '
X
A
-V
A
-•y
XjQ
XXXX
*
J
Aninal sources
■
butter
Cheese
Fish liver oils
Ghee
ialk (frosh)
Sheep, liver
Vanaspati
Whole powdered uilk
X
JZXXS
**
X
JS
XXX3?;-*
A
Legend:
X
XX
XXX
XXXX
= 1,000 to 5,COO units vitanin A per 100 grans edible portion.
= 5,000 tc 10,000 units vitanin A per 100 grans edible portion.
= 10,000 to 15,000 units vita.-.'in A per 100 grans edible portion.
= 15,000 to 20,000 units vitanin A per 100 grans edible portion.
Less than 1,000 units of vitanin A pox ^OO gns... edible portion.
More than 20,000 units of vitanin A per 100 gris. edible portion.
: 73 :
IRON FOOD SOURCES
FOODS COlSUIKD® TROil
FiTIIIG
Vegetable sources
Bajra
Barley
Cholan
Ragi
Rice (flakes)
(hand pounded)
(rdllod)
Wheat (whole)
Bengal gran
Black gran
Ccw pea
Green gran (1-foong)
Lentils
Rod gran dal
Soya bean
Lnaranth (tender)
Boot greens
Carrot leaves'
Cauliflower greens
Colocasia (black leaves)
(green leaves)
Coriander leaves
Dm.-stick loaves
Knol-khol greens
lustard loaves
Noon loaves (tender)
Radish leaves
Turnip greens
Vella kccrai
lutton or goat neat
Eggs (hen)
Fish noal (dry powder)
liver (shoe)
Khqa. (Buffalo rille whole)
X = 5 to 10 ng. iron per 100 grans edible portion.
XX = 10 to 15 ng. iron er 100 gms edible portion.
XXX =15 to 20 ng. iron per 100 grans edible portion.
XXXX = 20 to 25 ng. iron per 100. grans edible portion.
* Less than 5 rig. fron per 100 grans edible portion.
** Iforc than 25 ng. fren per 100 grans edible portion.
1 79 :
CALCIUM FOOD SOURCES
FOODS' CONTAIUING CALCIUM
' WING ' '
-
Vegetable sources
" Ragi
Bengal gran dal
_____ Balck gran„dal_________ ..
Cow' pea
Green gr^n (Moong) dal
Lentils
Red' gran
Soya bean
...
.
X
•
' X.' '
■’X' ■
xxxx
Aninal sources
. Cheese
Curds
Fish (dried)
Khnor
Khoa (Buffalo) ..........
(Cow)
Milk (Buffalo)
................... (Cow)
**
xxxx
XX" ■
*XXXXF
*
XaCF
■
*»
xxxx
xxxx9*
xxxx
7
•
Xa
Legend:
X = 50 to 100 ng. calciun per 100 grans edible portion.
XX =100 to 150 ng. calciun per 100 grans edible portion.
XXX = 150 to 200 ng. calciun per 100 grans edible portion.
XXXX = 200 to 250 ng. calciun per 100 grana edible portion.
**Moro than 250 ng. calciun per 100 grans edible portion.
KUTEITIGUS RECIPES FOR VULIERABIE GROUPS (REGIOilJlSl)
FORTH
1.
Wheat Bcsan ledco
Ingredients
Wheat flour
Bengal gran flour (bcsan)
Groundnut
Jaggery (gur)
Quantity
6 teaspeens
6 teaspoons
10 kernels
4 teaspoons
Method
1 • Roast wheat flour and bongal gran flour.
2.
Roast groundnut, renovo the skin and crush coarsely.
3.
Make jaggery syrup and add the flour nixturc and groundnut to it.
4.
Mix well and Dake into balls.
........................... ..................... Contd/SO-
: 80 :
Uutritivc value:
339 calories
12.5 gm protein
Suitable for: Infants, pro-schcrl children and school children.
NOTE: Wheat flour can be substituted by any other cereal flour.
Bengal gran flour can be substituted by any other pulse
flour.
2.
Bajara Khichiri
Ingredients
Quantity
Bajara (millet)
Green gran dal
Rico
Leafy vegetables
Salt to taste
Water
6 teaspoons
6 teaspoons
2 teaspoons
4 tcaspocns
Method
1.
Bick bajara and grind ib coarsely, sxrinkliiig- a little water on it.
2.
Renovo the husk of the bajara by washing it.
3- Soak it overnight in a little water.
4. Soak dal and rick for an hour after washing it.
5.
Tut dal and rice, bajara, and leafy vegetables chopped coarsely in
a dogchi.
6.
Add salt and water.
7• Cook for 20 minutes or so.
Nutritive value:
250 calories
11.4 gm protein
Suitable for: Bro-school children, school children, pregnant and
nursing women..
3« Faushiik Roti
Ingredients
Quantity
Wheat flour
Bengal gram flour
Green leafy vegetable, e.g., palak
7 teaspoons
5 teaspoons
2 teaspoons
1 teaspoon = 5 gms.
Vanaspati (margarine)
salt to taste
Water as required
2 tcaspocns
Method
1. Sifb together bosun and wheat flour.
2. Wash green leafy vegetables, chop finely and mix with the flour3.
Add salt and water aid knead to a stiff dough.
4» Roll cut chapati a.nd place on heated tawa.
5.
Turn when slightly done.
6.
Pour a teaspoon of fat into the tawa and fry the chapati on
both sides•
Nutritive value:
307 calories
9.8 gm pretoin
suitable for: school children and pregnant and nursing women.
: 81 :
Sprouted Horse Gran/Green Gran Savoury
4.
Ingredients
Quantity
Horse grar/Greon gran
Onion
potatoes
Ifengo powder (anchor)
Salt and spices to taste
Fat
6 teaspoons
2 teaspoons
10 teaspoons
1 teaspoon
1 teaspoon
Method
1. Soak gran in warn water overnight.
2. Drain water and put gran in wot cloth and hang in a warn place.
keep sprinkling water. Sprouts will appear 2 days.
3.
Wash sprouted gran.
4.
Chop onion and potato finely.
5.
Fry onion and potato in fat and cook until .potato is done.
6.
Add sprouted gran and cok for 5 ninutes.
7« Add salt, spices and nango powder.
Nutritive value:
217 calories
7«3 gn protein
Suitable for: school children and pregnant and nursing wonen.
SCOTH
5.
Wheat Umana
Ingredients
Quantity .
Broken wheat
Onion
Oil
Black gran dal (udath)
Drunstick leaves '
Dried chillies
rhstard seeds
Curry loaves
Salt to taste
Water as required
6 teaspoons
2 teaspoons
2 teaspoons
2 teaspoons
1 bunch
a few
a few
a few
Method
1. Fry nustard seeds, chill ies, curry leaves and dal in oil until
brown.
2. Add broken wheat and fry until brown.
3.
Ad’ chopped onions and chopped drunstick leaves.
4.
Add watorand salt and cook over low fire until done.
Nutritive value:
237 calories
5.9 gn protein
Suitalbe for: Infants, pre-school and school children, and pregnant
and nursipg wonen.
6.
Tapioca Frriidge
Ingredients
Quantity
Tapioca (naravalli)
MUk
Jaggery
Grated coconut
Water as required
6 teaspoons
half cup
2 teaspoons
2 teaspoons
ejot
HARVARD
WIGHT
AGES
50th
!
PERCENTILE
BOYS
3 MONTHS'1
5.72
1
5.62
5.67
|
7.58
j
7.26
7.42
6
"
i
MEAN
GIRLS -| WEIGHT
1
60^
of
3.40
•4.45
1
9
"
1 YEAR
|
II
9.07
|
10.07
2
|
1
8.71 j
|
9.75
9.91
11.11
' 11.27
|
6.76
12.43
j
1
7.46
11.43
li
"
I
12.57
!
5.33
8.89
I
1
12.29
!
2i
"
|
13.61
i
13.43
3
"
|' 14.61
I
14.42 J‘ 14.51
5.95
• 8.11
13.52
8.71
1
4
5
"
n
16.51
! 18.37
i
16.42 ,| 16.46
!
18.37
| 18.37
50 th
PERCENTILE
9.88
1
11.02
balanced diets for children
•
Veget
arian
(gm)
Cereals
Pulses
Green leafy vegetables
Other vegetables J
Roots and tubers $
Fruits
Milk
Fats rand oils
Herat and fish
J
Eggs
|
Sugar -nd. jaggery
School children
Pre-school Children
3
*
1
7-9 years
4-6 years
yo&rs
Hon-vege Veget
arian
tarian
(gm)
Nor.-vege- ! Vsgot—
tarian
• arian
: u)
(gm)
Non-vogetarinn
(^)
arian
(S* 9
Non-vege
tarian
(gm)
150
50
aj
i un
40
50
200
GO
75
200
50
250
70
75
250
60
75
320
70
100
320
60
100
30
30
50
50
50
50
75
75
50
300
20
50
200
20
50
250
25
50
200
25
50
250
30
50
200
30
50
250
35
50
200
35
30
-
30 .
-
-■ 30
|
30
30
1
40-
40
50
. 1—__ ___ —___
KG1661976
| _10-12 ;years
J
' 50
2 50
•--- — ,___ _
B/iANCED DISTS FOR ADOLESCENT BOYS AND GIRLS
GIRL s
B 0 Y S
15-15 years
Vegetarian
)
*
(g
Non-vegetarian
(gm)
j
1
450
70
100
75-
■
|
75
30
430
50
ICO.
75
75
30
150
40
30
□U
30
— — — - •- — -...........
Cereals
Pulses
Green 3 tafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Meat and fish
Eggs
Sugar and. jaggery
Groundnut';
'
■250
35
1
30
13-18 years
1
16-18 y■ears
...!
:Veget-.rian Nonvegetarian I Vegetarian ■ Nonvegetarian
(gm)
(gm)
M
I
(-^)
—
- ............... - - - --------------------- 1
'■
• 450
70 ■ .
i
ioo
|
75 .
100
30
250
,45
~
,
;
i
i
40
*
50
;
[
■
j
1
1
j
■ :
i
350
50
100
75
100
30
150
50
30
30
40
*
50
. I
1
1
I
. *An additional 30 gm of fats and oils can ho included in the diet in place of groundnuts.
KGj661976
350
70
150
75
75
30
250
35
—
30
!
350
50
150
75
75
30
150
40
30
30
50
?
_ __________
;•
j
i
I
1
balanced diets for adolescent boys and girls
BOYS
'
13-15 years
Vegetarian
(gm)
| Non-vegetarian
i
(gm)
GIRLS
16-18 years
13-18 years
i Vegetarian : Nonvegetarian ; Vegetarian j Nonvegetarian
(gm)
:
(gm)
'
(gm)
(gm)
1
Cereals
Pulses
•
Green leafy vegetables •
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Meat and fish
Eggs
Sugar and jaggery
Groundnuts
!
430
70
100
75
75
30
250
35
1
1
—
-
i
30
I
1
430
50
100
75
75
30
150
40
30
30
30
i
i
450
70
100
75
100
30 .
250
45
~
40
*
50
350
:
•
i
50
100
75
100
30
150
50
30
!
w
:
40
*
50
i
i
!
i
i
|
i
!
350
70
150
75
I
'
l
i
75
30
250
35
i
!
—
30
■
;
!
,
!
'
i
I
350
50
150
75
75
30
150
40
30
30
30
KG-^61976
) l '9 J-O /v
*An additional 30 gm of fats and oils can be included in tho diet in place of groundnuts.
BALANCED DIETS FOR CHILDREN
School children
Pre-school Children
Veget-
arian
(gm)
Cereals
Pulses
Green leafy vegetables
Other vegetables J
Roots and tubers jj
Fruits
Milk
Fats and oils
Meat and fish
5
Eggs
J
Sugar and jaggery
_—_ —_ —_ —_ —_ —_ —_ —_ —_ —_ —_ —_ —_ —_ —_ —
KG1661976
150
50
50
i
4-6 years
1
1-3 years
Non-vege Veget
arian
tarian
(gm)
! (gm)
150
40
50
1
'
200
’(30
75
10-12 years
7-9 years
Non-vegetarian
(gm)
200
50
75
Veget- 1
arian
(gm)
250
70
75
Non-vege
tarian
(gm)
Vegetarian
(gm)
Non-vege
tarian
(gm)
320
70
100
320
60
100
250
60.
75
30
30
50
50
50
50
75
75
50
.300
20'
50
200
20
50
250
25
50
200
25
50
250
30
50
200
30
50
250
• 35
-
30
-
30
50
200
35
i
30
30
30
_—____ _ ___
40
40
30
| 50
L
50
_—_—_ —_ —. 1 — ——_—— — —_ — _
-
_
|
50
____ —_ —_ —_ —
BALANCED DISTS FOR ADULT WOMEN
Sedendary work '
Heavy work
Moderate work !
Veget- j'Non-vege- Veget Ilon-vegc- i Veget Non-veg
arian •tarian
.arian :tarian
| arian ![tarian
■ (gm) i (gm)
(gm)
| (gm) ; (gm)
j (gm)
, .... wa
— —— ... . .. _ r-.~ ——’ «- _
_- — — —
• ~ .. —
Cereals
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Sugar and jaggery
M^at and fish
Eggs
Ground nuts
: 500
. 60
■ 125
. 75
50
50
• 200
; 50
: 50
—
—
■ —
500
: 45
i 125
' 75
! 50
i 50
j 100
55
; 50
• 50
i 50
• -
■ 550
i 70
, 125
• 75
75
' 50
, 200
' 55
• 50
—
. —
-
■
i
,
■
550
55
125
75
75
50
100
40
50
50
50
—
!:
i
.
'
i
I
i
■
:
475
70
125
130
100
50
200
40
40
: *
40
!1
!
j
I
!
I
1
:
i
i
Additional allowances
during
1 Pregnancy
1 Lactation
1
(gm)
:
(gm)
1
1
50
~
25
j
-
—
100
10
i
25
—
1
125
;
125
10
—
!
!
!
15
20
—
-
475
55
125
100
100
.50
■
100
45
40
50
50
*
40
i
i
*An additional 25 gin. of fats and oils can be included in the diet in place of groundnuts
KG1661976
zG
-4
BALANCED DIETS FOR ADULT MAN
I
Moderate work
Sedendary work
Cereals
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Meat and fish
Egg
Sugar and jaggery
Groundnuts
*An additional
KG1661976
1
Vegetarian
Nonvegetarian
(era)
(gm)
(gm)
400
>J
100
75
75
30
100
40
30
30
30
-
475
80
125
75
100
30
200
40
400
70
100
75
75
30
200.
35
!
:
|
!
1
1
I
;
i
!
1
■
30
i
;
!
i———■±—=—
Heavy work
Vegetarian jNonvegetariani Vegetarian j Nonvegetarian
40
(gm)
475
65
125
75
100
30
100
40
30
30
40
-
:
:
1
;
■
:
,
I
~~m
i Z“Z ~ ~~ ■ i ***
»«~w
■■
•
(gm)
|
'
i
1
j
|
650
80
125
IOC
100
50
200
50
!
;
!
:
i
i
;
—
i
55
!
*
50
in5— ■■ ~~~ h
(gm)
i~n i
30 gm. of fats and oils can be included in the diet in place of groundnuts.
650
65
125
100
100
30
100
50
30
30
55
*
50
BALANCED DIETS FOR ADULT NOMEN
Additional allowances
Moderate work |
Heavy work
'
________ during
Veget- ;jion-vegc- iVeget- ;IIon-vegG- iVeget-1 Non-vege- i Pregnancy
1 Lactation
’arian ■tarian
(gm)
j
(gm)
: arian • tarian
i
.arian tarian
> (gm) j (gm).______
: (gm)
(gm)
(gm)
; (gm)
Sedendary work !
Cerc.-ls
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Kilk
Fats and oils
Sugar and jaggery
Meat and fish
Egg's
Ground nuts
: 300
60
: 125
75
50
■ 30
• 200
■ 30
•
. —
—
• -
i 300
: 45
i 125
: 75
' ‘ 50
i 30
i 100
35
• 30
■ 30
* 30
-
i'35O
. 70
: 125
' 75
75
• 30
: 200
‘ 35
30
. —
—
-
:
!
•
i
■
’350
-53
125
75
75
30
100
40
30
30
30
-
I
,
.
;
;
i
i
!
!
'
475
70.
125
IX100.
A'
200
4<?
40
—
—
*
40
I
|j
I
1
i
j
!
475
50
—
*125
100
100
30 ■
100
45
40
30
30
1 25
! ~
| _
i .40
*
i
j
:
1
—
125
10
100
1.1
Ii
—
125
15
20'
—
—
-
*An additional 25 gm. of fate and oils can bo included in the diet in place of groundnuts
KG1661976
BAIuWCED DIETS FOR ADULT MAN
I
Moderate work
Sedendary work
------— . — — —
(gm)
(sn)
!
(gm)
' !
(gm)
— — ... — — — — - |----------- --- .. i-------------------------- — —----- — —. ■ ~ -- "" — — — — • 1 — — — — — —1 — — —----- -------
Cereals
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Meat and fish
Egg
Sugar and jaggery
Groundnuts
*An additional
KG1661976
Heavy work
Vegetarian j Norivegetarian' Vegetarian iNonvegetarian
Vegetarian iNonvegetnrian
(gm)
I
(g’n)
400
70
103
75
75
30
200
35
j
1
i
-
30
i
!
400
55
:
:
i
;
!
100
75
75
30
100
40
30
30
i
30
'
475
80
125
75
100
30
200
40
—
—
i
40
!
:
i
:
475
65
125
75
100
30
100
40
30
30
:LU
■
1
i
1
1
I
'
I
■
i
!
650
80
125
100
100
1
!
|
1
I
650
65
125
100
100
30
200
50
-
1
!
1
30
100
50
30
55
*
50
i
30
55
*
50
30 gm. of fats and oils can be included in the diet in place of groundnuts.
PROTEIN-ENERGY MALNUTRITION
PEM can be defined as a range of pathological conditions arising
from a deficiency of protein and energy, and is commonly associated with
infections. It occurs more frequently in infants and young children but
is also observed in adolescents and adults, mostly lactating women, espe
cially during periods of famine or other emergencies.
PEM covers a wide spectrum of pathological conditions, the extremes
being nutritional marasmus and kwashiorkor (4, 5). In practice, a large
proportion of PEM cases occupy an intermediate position and are referred
to as "marasmic kwashiorkor". The definitions of nutritional marasmus and
kwashiorkor are as follows!
Nutritional tnarasmus! a condition characterized by very low body weight
for age, loss of subcutaneous fat, gross muscle wasting, and absence of
oedema. . It is observed more frequently in.infants and very young children.
Kwashiorkor? a condition characterized by oedema and low body weight
for age. The following signs may be also present but are by no means uni
versal or very marked » muscle wasting, dermatosis, hepatomegaly, hair
changes, diarrhoea, anc mental changes. The serum albumin level is low.
The syndrome is most frequently observed .in children aged 1-3 years and is
precipitated by an infection or more commonly by a series of infections
occurring successively or concurrently.
The manifestations o~ severe PEM vary widely according to the nature
of t'no causative factors, the time for which they operate, and tho age Of
the patient. Moreover, a cnild with nutritional marasmus may develop
marasmic kwashiorkor and a child with marasmic kwashiorkor may present a
picture of-nutritional marasmus after the oedema subsides, from the pub
lic health point of view, it is often more convenient not to emphasize the
distinctions but to use tho more general term "protein-energy malhutrition".
Thera has been a tendency in the past to understimatc marasmus and to focus
attention on kwashiorkor.
It is now recognized that the proportion of
marasmic children in the world is increasing steadily, especially in urban
and periu.-ban areas.
Besides the children suffering from the most severe forms of protoin
energy malrutrition-namely, kwashiorkor, marasmic kwashiorkor, and marasmus
a much greater number display a moderate or mild form of this type of mal
nutrition. The main characteristics of these children is that their weight
for-age’ anc weight-for height ratios are low in comparison with those of
well-nourished children.
finally, some children may-have a low weight—for—age ratio while their
weight-for height is normal. Although these children are small for their
age, there is no apparent sign of actual malnutrition because of the more
or less proportionate decrease in body dimensions. The term "nutritional
uw.jx.p-orn" has been .isod to describe this condition.
Protein-malnutrition results from the interaction of several
factors, among whisk, two are more or less directly responsible for the
disease and act synergistically. They are (l) a quantitatively insuffi
cient and qualitatively i,nriGquatc dietary intake, and (2) infectious pro
cesses such as gast mint estii si nnd respiratory infections and infectious
diseases of childhood (11, 12).
2
PRINCIPAL FEATURES OF PROTEIN-ENERGY MALNUTRITION
Marasmus
Features
Essential features
(1) Oedema
(2) Wasting
(3) Muscle wasting
(4) Growth retardation
in terms of body
weight
(5) Mental changes
Variable features
(1) Appetite
(2) Diarrhoea
(3) Skin changes
Kwashiorkor
Lower legs, sometimes
face, or generalized
Gross loss of subcutaneous Less obvious;sometimes
fat, "all skin .and bone"
fat, blubbery
Severe
Sometimes
Severe
Less than in marasmus
None
Usually none
Usually present
Usually good
Often (past or present)
Usually none
Usually poor
Often (past or present)
Oft on, diffuse depig
mentation; occasional,"flaky-paint" or
"enamel" dermatosis
(4) Hair changes
Often sparse-straight
Texture may be modified
but usually no dyspigmenta- and silky;dyspigmentation-greyish or reddish
tion
(5) Moon face
Often
None
(6) Hepatic enlargement None
Freqyeht,although it is
not observed in-some
areas
Biochemistry/pathology
Normal or slightly decrea-.Low
sed
Urinary urea per
Normal or decreased
Low
g of creatinino
f3) Urinary hydroxyLow
Low
■■’'oline index
(4) Ser^.frjg amino
Elevated
Normal
acid rav-q
(5) Anaemia
Common;iron or folate
May be observed
deficiency may be
associated
(6) Liver biopsy
Fatty infiltration
mal or atrophic
(l)
(2)
Serum albumin
rJ^JT 6'"a
VITAMINS
Oh fine and fat was Ralph the Rat,
And his eye was cold, clear grey
How mournful that he ate less fat
As day succeeded day.
Tin he found each cornea daily hornier,
Lacking its Vitamin A.
’I missed my Vitamin A my dear, ’
The Rat was heard to say.
.
’And you’ll find your eyes will keratinize
If you miss your Vitamin A.’
B
Now polished rice is extremely nice
At a high suburban tea
But Arbuthnot Lane remarked with pain,
That it lacks all Vitamin B.
’Ard Beri-Beri is very very
Hard on the nerves' says he,
'Oh take your Vitamin B my dears,'
I heard that surgeon say.
'If I hadn't been fed on standard bread
I wouldn't be here today.'
0
The scurvy flew through the schooner's screw,
As they sailed the Arctic Sen.
They were far from land and their food was canned
So they got no Vitamin C
For 'Eevils the use of orgnge juice'
The skipper had said, said he.
They were victualled with pickled pork,
my dears,
Those mariners bold and free.
Yet life's but brief on the best corned beef
If you don't get Vitamin C.
D
The epiphyses of Jemima's kneed
Were a truly appalling sight
For the Rickets strikes where it jolly well likes,
If the Vitamin D's not right
Though its plots we foil with cod-liver oil
Or some Ultra-Violet light
So swallow your cod-liver oil, my dears,
And bonny big babes you'll be
Though it makes you sick, its a cure for rickets,
And teeming with Vitamin D.
' E
Now Vitamin D, A, B, and C,
Will ensure that you'ie happy and strong.
But that's no use you must reproduce
Or the race won't last for long.
So Vitamin E is the stuff for me
rind its praises end my son
We 'll double the birth-rate yet my dear
If we ell eat Vitamin E
We can blast thd hopes of Marie Stopes
By taking it with our tea.
lyjur G'l S'
MALNUTRIT ION
Malnutrition has been defined as "a Pathological state resulting from
a relative or absolute deficiency or excess of one or more essential
nutrients, this state being clinically manifested or detected only by bio
chemical, anthropometric or physiological tests111.
Four forms of malnutrition have been distinguished,
(l) Under
nutrition s This is the condition which results when insufficient food
is eaten over an extended period of time.
In extreme cases, it is called
starvation.
(2) Overnutrition s This is the pathological state resulting
from the consumption of excessive quantity of food over an extended period
of time. The high incidence of obesity, atheroma and diabetes in western
societies is attributed to overnutrition.
(3) Imbalance S It is the
pathological state resulting from a disproportion among essential nutrientswith or without the absolute deficiency of any nutrient. (4) Specific
deficiency s It is the pathological state resulting from a relative or
absolute lack of an individual nutrient.
Classification of Nutritional Diseases ?
The WHO Expert Committees on Nutrition (1962, 1971) proposed the follow
ing classification of nutritional diseases .
Nutritional Diseases 2
HYPOALIMENTATION ;'
1.
Protein-calorie Malnutrition (PCM)
(a) Kwashiorkor
(b) Nutritional marasmus
(c) Severe PCM, unqualified
(d) Moderate PCM, unspecified
(e) Other PCM
(f) Malnutrition, unspecified
(g) Nutritional dwarfism
3.
Vitamin deficiency
(a)
(b)
(c)
(d)
(e)
(f)
(g)
(h)
(i)
(j)
Vitamin A deficiency
Thiamine deficiency
Niacin deficiency
Ariboflavinosis
Deficiency of other 0 complex
vitamins
Ascorbic acid deficiency
Vitamin D deficiency
Sprue
Vitamin K deficiency
Vitamin E deficiency
2. Mineral deficiency
Iodine
(b) Fluorine
(c) Selenium
(d) Calcium
Others
4. Other Nutritional deficiencies
Essential fatty acid deficiency
Individual amino acid
deficiency
(c)
Other states and unspecified
(a)
(b)
HYPERALIMENTATION s
FOOD TOXICANTS s
(a)
(b)
(c)
(d)
(e)
(f)
(a)
(b)
(c)
Obesity
Hypervitaminosis A
Carotenaemia
Hypervitaminosis D
Fluorosis
Other
Lathyrism
Epidemic dropsy
Aflatuxicosis
p. t. o.
Diseases of the Blood and Blood Organs ?
PERNICIOUS ANAEMIA s
(a)
Subacute combined degeneration
NUTRITIONAL DEFICIENCY ANAEMIA s
(a)
(b)
Iron deficiency anaemias
Other deficiency anaemias (folic acid, vitamin B^, vitamin Bf
protein)
INDICATORS OF MALNUTRITION l
It will be useful, to bear in mind the'.following, "-indicators of malNutrition" while assessing the nutritional status as well as evaluation
of nutrit.ional programmes in a community.
(l) Statistical?
(-2) Anthropometric ?
(a) the mortality in the age-group
under one year (especially 6-12
months).
(b) the mortality in the age group
1-4 years.
(c) the ratio of deaths of children
less than 5 years of age to
total deaths.
(3) Clinical?
(a) the weight of the newborn.
(b) the percentage of newborn.
weighing less than 2,500 grams
(c) the height and weight of
children aged up to 5 years
(d) the. average weight of 7-year
old children' entering school.
(e) The index weight/height is
regarded as a simple and
reliable indicator of the
nutritional status of preschool
children in a community. An
index of 0.15 has been used as
a dividing line between wellnourished' and mal-nourished
children.
(4) Dietary Examination?
(a) the number of cases of mal(a)
nutrition admitted annually
in hospitals and health centres, (b)
(b) diagnosis of individual nutrition
al deficiency diseases.
(c)
the proportion of pregnant women
with less than 10 g of haemoglobin
per 100 ml of blood in the last
trimester of pregnancy.
Intake of calories, proteins
and other nutrients ?
Studies of dietary habits.
Degrees of Malnutrition?
While studying malnutrition ininfancy and childhood with special
reference to kwashiorkor, Gomez(l955) was able to draw up the fallowing
classification by assessing the percentage of underweight in relation to
average
(l) First Degree Malnutrition:
Weight between 85 and 75 per-cent of
the theoretical average for the age
(2) Second Degree Malnutrition?
Weight between 75 and 60 per cent of
the theoretical average for the age
(3) Third Degree' Malnutrition?
Weight below 60 per cent of
the theoretical average for the
age.
NJT G'lfa
NUTRITION
Xi Ik: It is an ideal food for infants and children and a good supplementary
food for adults. It is nearly a complete food existing in nature. It contains
all the nutrients.
Composition:
Gms, per 100 gms
Cow's milk
Buffalo's mill
Human -ilk
3:2
4.1
4.4-'
67
4.3
8.8
5.0
117
1.1
5.4
7.4
65
Protein
Fat
- Lactose
Calories
Rich:
in calcium
Deficient:
I+ is deficient in iron and vitamin C
Daily req ui rem - nt:
Adults
.
Children
Expectant mothers
10 oz Or 284 gfflo 1,1.on--vegetarian
requirement - 20 oz or 568
20 oz
40 oz
Milk borne infections: from the animal - Bovine tuberculosis, (Brucellosis)
anthrax, achin^mycosis, Q. Fever
from the human - typhoid, paratyphoid, dysenteries,
handler &
cholera, dip.”. /‘er-ia, infective
environment
hepatitis.
Prevention:
Pasteurization - if effectively.done - phosphatase test will be
Boiling
negative
Nice: Main cereal consumed in south India, cheapest source of energy a;Z
contributes 70-80?? of calories. Main source of thiamine and nicotinic acid.
By virtue of its quantity it provides nearly 50% of protein requirements.
Proteins of rice is of better quality than wheat although th? protein content
of wheat is more-.
. —Composition:
Gms, per 100 gms
mgm
Protein
CHO
Fat
Th'a-line
Nicotinic
Raw rice(mld)6.8
78.2
0.5
0.06
1.9
-'6.4
79.0
O.A
0.21
3.8
Parboiled rice is superior in nutritive value to raw rice .is regards the
thiamine and nicotinic acid are concerned.
Daily requirements:' 14 «zs or 400 gms. If milled raw rice ’6 being consumed,
it can oe partially substituted by wheat, jowar or rag'.. This improves the
nutritive value of the diet (N.B. 100 gms or rice cont-.ins more proteins th°n
in 100 gms of milk).
Wheat: Next to rice, wheat is the most important cereal
Daily requirements:
14 oz or 400 gms
Composition:' (whole wheat)
Per .100. gms
rX
11 r o ’ 4,-ma
Fat
CHO
Thiamine
Niacin
1.5 as
71.2 fins
O.45mgms
5.60ingms
Though it has protein to the extent of 11.8% itlacks in lysine. It is a good
source of thiamine and niacin.
Millets: Jowar and Ragi : - Jowar is deficient in lysine and has an excess
of leucine. The consumption of jowar is occasionally found to be associated
with pellagra.
Ragi is a popular millet in South India. It is very rich in calcium, and is
a ‘'air source of iron, phosphorous and thiamine.
-2requircments:
In combination with cereals daily
or 400 gms.
Composition:
a
14 oz
•Gms, per 100 gms
Jowar
Ragi
Prdein
gm
CHO
Calcium
gm
1C.4
7.3
72.6
72.0
25.0
344.0
Pair-ess Pulses are next in importance to cereals as an er icle of diet in
India. The common pulses ased are red gram, green gram, black gram dnal, Ben ;
gram, dry beans, and dried peas.
Pulses are rich in protein containing about 20-25 g of protein per 100 gms. In
vegetarian diets, pulse- are the main source of protein. Pulse ■ are good sources
cf B g'->up vitamins, especially thiamine and riboflavine. Sprouted pulses are
good sources of vitamin C.
.daily requirements;
5 oz or 85 gms
Proteins %
Bengal gram
Black gram
Reg gram
Green gram
17.1
24.0
22.3
24.0
I4g-ji per 1C>0 gms
mgm
nigra
ro.^m
Thiamine
Nia;Cin
Riboflavine
—————
0.3
0.42
0.45
.0.47
2. 9
2. 0
2. 9
2. 1
0.15
0.37
0.19
0.39
mgm
Iron
——
10.2
9.1
5.8
7.3
Groundnuts: Groundnuts or Peanuts are e xtensively grown in India. It is
rich in fat, protein is equal to pulses. It is also rich in nicotinic acid,
thiamine and riboflavine.
Composition:
Per 100 vms
Protein
Fat
CHO
Thiamine
Riboflavine
Nicotinic acid
■ -• lv requirements:
25.3%
40.1%
26.1%
0.9 mg®
Ou 13 mgm
19.9 ®gm
!
j!
ji
j!
j
j
Groundnuts after
extraction of fat is a cheap
and rich source of proteins
ln combination with pulses 3 oz
Green leafy vegetables: Eg. spinach, amnrsnth. fenu greek, cabbage are cheapest
protective foods. These are excellent source of carotene and vitamin C.
They are also good sources of calcium,, iron, riboflavine and folic acid. They
provide cellulose which acts as roughage. It plays an important role in persons
who go on diet to cut down calories.
vai-.ly requirements:
4 oz or 114 gms.
<:?1: Eg. groundnut oil, gingelly oil etc. vegetable fat..It is 100% fat,
yields 900 calories per 100 gms. Contains no vitamin, contains more of
polyunsaturated fatty acid's. Lowers the serum cholestrol.
~v-ily requirements:
2 oz or 57 gms
Ghee:
Animal. Except for little moisture it nearly cent per cent fat. Yields
cetween 820 to 895 calories. Good sou’-ce of vitamin A (200 i.u./lOO gms)
contains more of saturated fatty acid and hence tries to raise serum cholestrol.
Iajly requirements:
In coinbination with other fat like oil 2 or. (l-T.B.
vegetable fats.usually do not cont-'i u vitamin A)
’’’’anaspathi: Popular cooking media in our country. It is manufactured by
’■yurogeaation of vegetable oils. On hydrogenation saturated fatty acid content
Gives
*
increases.
about 700-i.u. of A and 150 i.u. of 'D' per 100 gms. It is
?00% fat and yields 900 calories.
•:i?.v requirement: In combination with other fats 2 oz.
1 v-so • re added by manufacturers according to governr.-t r^.gulatiors.
NUTRITION
Milk: It is an ideal food for infants and children and a good supplementaryrood for adults. It isi nearly a-complete food existing in nature. It contains
all the nutrients.
Composition:
Gms. per 100 gms
Protein
Fat
Lactose
Calories
Rich:
Cow's milk
Buffalo's milk
Human milk
3.2
4.1
4.4
67
4.3
8.8
5.0
117
1.1
3.4
7.4
65
-
in ealeixim
Deficient: I+ is deficient in iron ard vitamin C
Daily requirement:
Adults
10 oz or 284 gms (fnon- zegetarian 3
Children
Expectant mothers
\jers
20 oz'
40 oz
requirement - 20 oz or 568 gms)
Milk borne infections: from the animal - Bovine tuberculosis, (Brucellosis)
»
anthrax, achinomycosis, Q, Fever
from the human - typhoid, paratyphoid, dysentries,
handler &
• cholera, diphtheria, infective
environment
hepatitis.
Prevention:
Pasteurization - if effectively done - phosphatase test will be
Boiling
negative
Ric_2.: Main cereal consumed in south India, cheapest source of energy and
contributes 70-80% of calories. Main source of thiamine and nicotinic acid.
By virtue of its quantity it provides nearly 50% of protein requirements.
Proteins of rice is of better quality than wheat although the protein content
o ? wheat is more.
.
Composition:
Gms, per 100 gms
m.-m
mgm
CHO
Fat
Thiamine
Nicotinii
Raw rice(mld)6.8
78.2
0.5
0.06
1.9
6.4
79.0
0.4
0.21
3.8
Protein
Parboiled rice is superior in nutritive value to raw rice -n. regards th j
thiamine and nicotinic acid are concerned.
Daily requirements: 14 ozs or 400 gms. If milled raw ric? <s being consumed,
it can be partially substituted by wheat,.jowar or ragi. This improves tne
nutritive value of the diet (N.B. 100 gms or rice contains mere proteins than
in 100 gms of milk).
Wheat: Next to rice, wheat is the most important cereal
Daily requirements:
14 oz or 400 gms
Composition: (whole wheat)
Protein
Fat
CHO
Thiamine
Niacin
Per 100 gms
11.8 gms
1.5 gms
71.2 gms
0.45mgms
5«50mgE&
Though it has protein to the extent of 11.8% it lacks in lysine. It is a good
source of thiamine and niacin.
Millets: Jowar and Ragi : - Jowar is deficient in lysine and has an
of leucine. The consumption of jowar is occasionally found to be assoc^g^B
with pellagra.
•_>’
Raai is a popular millet in South India. Tt is vo"v
Doily requirements:
Ip combination, wit’-, cereals daily requirement is 14 02
or 400 gms.
Gms, per 100 gms
Composi-tion:
Jowar
Ragi
Prdvin
gm
OHO
gm
Calcium
gm
10.4
7.3
72.6
72.0
25.0
344.0
Pulses: Pulses are next in imports. nee to cereals as an article of diet in
India. The common pulses used are red grain, green gram, black gram dhal, Bengal
gram, dry beans, and dried peas.
Pulse: are rxch in protein containing about 20-25 g of protein per 100 gms. In
veget: r?an diets, pulse" are the main source of protein, lulse- are good source
cf B grjv.p vitamins, especially thiamine and riboflavine. Sprouted pulses are
good sources of vitamin C.
Daily requirements;
5 oz or 85 gms
Proteins %
Bengal gram
Black gram
Reg gram
Green gram
17.1
24.0
22.3
24.0
Mg.a per 100 gms
mgm
mgm
mgm
Thiamine
Niacin
RibofJ avine
0.3
0.42
0.45
0.47
0.15
0.37
0.19
0.39
2. 9
2.0
2. 9
2.1
mgm
Iron
10.2
9.1
5.8
7.3
Groundnuts: Groundnuts or Peanuts are extensively grown in India. It is
rich in fat, protein is equal to pulses. It is also rich in nicotinic acid,
thiamine and riboflavirie.
Composition:
Per 100 .-ms
Protein
■ Fat
CHO
Thiamine
Riboflavine
Nicotinic acid
Daily requirements:
25.3%
40.1%
•
26.1%
0,9 mg®
0113 ■mgm
19.9 mgm
Groundnuts after
extraction of fat is a cheap
and rich source of proteins
1^ combination with pulses 3 oz
Green leafy vegetables: Eg. spinach, amaranth, fenu greek, cabbage are cheapest
protective foods. These are excellent source of carotene and vitamin C.
They are also good sources of calcium, iron, riboflavine and folic acid. They
provide cellulose which acts as roughage. It plays an important role in persons
who go on diet to cut down calories.
Daily requirements:
4 oz or 114 gms.
Oil: Eg. groundnut oil, gingelly oil etc. vegetable fat. It is 100% fat,
yields 900 calories per 100 gms. Contains no vitamins contains more of
polyunsaturated fatty acids. Lowers the serum cholestrol.
Daily requirements:
2 oz or 57 gms
Ghee: Animal. Except for little moisture it nearly cent per cent fat. Yields
between 820 to 895 calories. Good source of vitamin A (200 i.u./lOO gms)
contains more of saturated fatty acid and hence tries to raise serum cholestrol.
Pai
.requirements:
In combination with other fat like oil 2 oz (n.B.
vegetable fats usually do not contain vitamin A)
Vanaspathi: Popular cooking media.in our country. It is manufactured by
hydrogenation of vegetable oils. On hydrogenation saturated fatty acid content
Givas
*
increases.
about 700 i.u. of A and 150 i.u. of *D' per 100 gms. 1^ is
100% fat and yields 900 calories.
: requirementi In combination with other fats 2 oz.
id by manufacturers according to s-ovo-nnm ■■>■><-
-3Sugar & Jaggery: These are cax+o>iy'1rate foods. Sugar is
p.-r; carbohydrate
foot and contains no proteins, fats or minerals. 490 cal./lOO gm.
Jaggery: Is used in place of sugar, 383 cal./lOO gms. I’: is also rich
source of iron 11.4 mgm/100 g.
Daily requirement:
Sugar/and/or Raggery - 2 oz or 57 gms.
Eggs: It js an important source of animal protein. It contains also the
nutrients except CHO. It contains protein, fat, calcium, all the vitamins
except C. Ifc is a complete protein containing all essential amino acids.
Composition:
Protein
?at
Minerals
K Cals
Es.j]y requirement:
■loot and tubers:
13.3$
];.3<
1$
1+3
1 egg (1-g- oz)
Generally used as vegetables.
Potatoes, tapioca, carrot, onion, raddish. Those especially potatoes are
rich in CHO. Poor source of fat and protein. Good source- of calcium and
phosphorous.
Carrot rich in carotene
Potatoes rich in vitamin C
Daily requirement:
3 ozs or 85 gms.
ARAYAN
9. LANGFORD ROAD. BANGALORE-25, INDIA.
=
/o^,
=
Sz =
3
/Viiaeiz, -
> 7 r>^>^j-
v;rc -
~<o ^7
L< rr’>
■
/_<dAy
te>^
KU.y^£'
—
1^^
Oxjj
V.1'
C?JclxJLa
T1IX- £J 'O-X. 6>( ,
^Xsx^SA^^ijsX?-
f=>£ ^.r^l'.
V^U2j-^„/„Colfe^'iCcJ.
‘221!!?-. .j.
,•
__ rr~»gcaJ^ r >°-A-o 0JL4 , ftulxe^ _____
@ fxXvU-^ptuPU, ■_ -
. ^1G ~Js3o.
__
w
I^Cd^^Q
Z^L^/pa^=7i^
JLcI'''-.
,
_ : buJlc) -,
M-uSSl '
.cAaJWa£<O_.._ .
~.,/PP
-p^r • ’aa^r
J Jt-^cb -cfc-hL,
Qjk^d^Jd ." c?».rZr^- ^cJkot
Gi^-^ .$ , L^bZkC'" _ xjoJLlM.
. d^2^Jk^L^ko.ct
JeS.^utO.
/\A.uj z g> JLi-ttJicjLP _
VkJA-\j2 f
,Q?,
\z)
a-d-d
ho Petb^ -
^“r
-
/Dz'e-A'
A^2x-?/^/
Afek //X „
^csTj'cjj^p^y-t^cJ
/-tealfl~\
l^ll^
NUT
6'tT-
: 51 :
NUTRITION
Nutrition- is the study of foods and their actions or effects on the
body. Good nutirtion means that the body is getting the required food
and is-able to make use of it. Nutrients are substances with special
functions which are found in feed and which are necessary £>r growth and
development of the body, repair of the body tissues, and protection of
the body against disease. They are of six types, viz., proteins,
carbohydrates, fats vitamins, minerals and water..
People general ly eat or drink when they are hungry or thirsty and,
on auspicious occasions, they may eat or drink special foods, the foods
that people cat every day are usually not selected on the ba. sis of their
nutritive value, but because of family habit, religion, or social custom.
It has been found that many such dietary practices, especially those
that are related to feeding infante, young children and pregnant women
are not based on body requirements.
SOME TRADITIONAL FOOD HABITS AND CUSTOMS ARE HARFUL TO HEALTH. ' ~
Because of e ating an unbalanced diet, many young children in India
are frequently ill due to infections, are retarded in their physical
growth, and their mental development is negatively affected. 'Unless
good nutritional guidance is' given, accepted and practised by their
parents, such children will become adults who have chronic ill, health
and are unable to make their full contributicn as productive members'
of the community.
In addition, infants may be born weak and malnourished because their
mothers had poor diets during pregnancy. Because many women do noteat the
amount and -kind of f oed that their bodies require during pregnancy and
afterwards, they become weak, have little energy to care for their babies
and are unable to produce breast milk in the amounts needed by growing
infants.
NOT EATING CERTAIN FOODS EVERY DAY CAN CAUSE:
i.
WEAK INFANTS CF LOW BIRTH WEIGHT/
it. INSUFFICIENT HD DUCTION OF EEEAST MTTK.
. iii. RETARDED PHYSICAL AND MENTAL GROWTH .
iv. ILLNESS At© ■DEAlTTES’HSUlMTY AMONG INFATS AND iBE-ECWOt CHILDREN.'
•11 .1
ERINCIPLES OF NUTRITION
In order to be able to assist individuals and families to learn
about and be 'able to practise good nutrition, you must know the principles
of nutrition.
1.
Food is necessary for keeping the cells and tissues of the body
alive and for maintaining normal body functions.
2. An adequate daily fluid intake is necessary for maintaining
the.fluid balanced diet includes.
J. A balanced diet includes:
i.
a'sufficient number of calories;
ii.
adequate amounts of proteins, fats and carbohydrates;
.iii. adequate amounts of vitamins;
iv.
adequate amounts of minerals.
.................................. Contd/52_
: 50 :
10.12 .3
INFORMING COUPLES ABOUT WHAT CAN BE DONE
Points for emphasis should include the following facts:
Infertility can be overcome in rany cases by treatmen or
advice.
Treatment will require more than one visit to the doc'fetr.
There is a need for both the husband and the wife to undergo
physical examination and special tests to determine the cause
to infertility.
iv.
Learning new sex techniques may be part of the treatment.
v.
Advice and treatment for infertility are available from the
male and female doctors and may given at She subcentre at
the time pf their weekly visits, or at the PHO, or at the
District hospital if■specialized treatment or investigations
are required.
i.
ii.
iii.
REFERRING COUPLES FOR SERVICES
10.12.4
‘In malcing referrals, make sure that the couple:
know where and when to go for advice;
know what to expect at the clinic;
know that both of them vri.11 have to undergo investigation
and treatment;.
iv.
have a referral chit, which gives their name, address, and
the nature of their problem, and which is signed by yourself
and gives the name of your subcentre. In this way, should
specific follow-up be needed, such instructions can be noted
by the doctor and returned to you by the couple.
i.
ii.
iii.
10.12.5
FOLLOW-UP VISITS
You should schedule a visit to the home within two weeks after
the initial referral is made to find out if the couple had been to the
clinic and whether they are in need of any a ssistance in following the
prescribed treatment. . You may often find that it tikes more than one
visit and dissuasion in the home to convince infertile couples that
something can be done for them. Another problem that may be encountered
in that although the man may be willing for his wife to submit to an
examination tests, he may refuse to do the same himself. In such a
situation, he may be willing to listen to some other man in the vi 11 age
who has benefited from such procedures.
10.12 .6
RECORDS AND REPORTS
You are expected to record the usual details of referrals made
in the health card of the couples and to submit the required reports.
REMEMBER
i.
ii.
iii.
iv.
PREGNANCY CZ_N BE PLANNED TO PROTECT' THE HEATH OF THE MOTHER
AND CHUD .
PREGNANCY CAN BE PREVENTED TO CONTROL FAMILY SIZE.
PREGNANCY CAN BE TERMINATED IF IT IS UNWANTED.
INFERTILE’ COUPLES’ CAN BE HEALPED TO HAVE’ A CHILD .’
.Contd/51-
PROTEINS
Approx.
Vegetable Sources
cost
Horse grari
Rs .3 per
Kg.
March to October
xxx
Bengal gram
Rs .2/2 5 per
Kg.
Throughout year
XX
Moong dal
Rs .2/25 per
Kg.
Throughout year
XX.
Wheat
Rs.1.29 per
Kg--------
Throughout year
Buffalo Milk
Rs .2/- per
Kg.
Throughout year
Eggs
Rs.4/- to 5/“ .Throughout year
psr dozen
Fish
Rs .8/— to
Rs .12/- per
Kg.
-
-
Rating
Seasonal availability
X
...-----
.
Animal Sources
XX
■
. .X.
January to April
September to December
XX
Annexure 11.1 contains a list of protein-food sources available
in India. Refer to this list of prepare your own list of protein sources
available in your area.
• ■
Similar kinds of food source lists, can also be made for other
nutrients such as vitamin A, iron, or calcium which are also often
deficient in the diets of infants and young children (see annexures
11.2, 11.3 and 11.4).
11.3.1
JRCTEIN Or BODY-BUILDING FOODS
Foods that contain proteins are needs by the.body daily for
repairing and' replacing cells. Adequate amounts of this nutrient are
especially important in the diets of pregnant and nursing women, infants
and young children because they have extra needs in addition, to normal
requirements, Pregnant women need extra protein foe ds to take care of the
needs of the growing foetus. A;nursing mother needs more body-building
foods to replace what she gives to her bcby through breast feeding.
Infants and young children are growing at a very rapid rate and require
proteins fqr healthy growth. and development.
11.3.2
CARBOHCT^JES OK EMERGY-GIVING FOODS
In order to run, play or work, we need foods that give us energy
Carbohydrates in certain .foods provide the body with energy. The
amount required by a person depends on the kind of activity he carries
out and the time for which it io done. A man who is breaking stones all
day will need more energy-giving foods than a man who sits in his shop.
Children, especially pre-school children, are often not fed .frequently
enough during the day so that they do not receive an adequate amount
of carbohydrates. When this happens, children become less active and
tire easily.
.C-outa/52-
Foods rich in carbohydrates include the following:
i.
ii.
iii.
iv.
Sugar, jaggery and honey.
Cereals such as wheat, rice, fillet, suji, maize.
Vegetalbes such as potato, sweet potato, tapioca, yams.
Fruit suchaas bananas, jackfruit,chikku, mango.
11.3 .3. FATS CE CO NCENTR/JED-ENELGY FOODS
Foods that contain fats are needed by the body because they
supply concentrated energy, prevent dry, scaly, skin, help in the absorption
of vitamin D, and improve the flavour of food
*
Because they are a concen
trated source of energy, fats supply twice as much energy as . the same, amount
of proteins or carbohydrates. This means that smaller amounts of fats are
needed in the daily diet to meet the body requirements.
Foods rich in fits include the following.:
-Vegetable sources:
■
-i. Cooking oils such as cocoanut, mustard; sesame (til) of
groundnut oil
Animal sources:
i.
ii.
iii.
11.3 4
Butter and ghee- - ...
Milk, curds and cheese
Fish and fatty meat
VITAMINS CT. EROTECTIVE FOODS
-
Vitamins are substances which are found in small quantities in
several kinds of food. They are needed by tte body for normal growth and-maintenance of cells.
The body" requires vitamins in small amounts. Since
the body cannot produce these substances, food sources are very important.
There are several kinds of.-vitamins. Some'are needed foi good
vision and healthy eyes (Vitamin A), others for blood formation (Vitamin B),
others are needed in the. diet for strong teeth and bones '(Vitamin D), and
others for increasing resistance to infections and early healing of wounds
(Vitamin C).
■ ’
■ -
■
1. Vitamin Ai In order to prevent nutritional blindness in ycungg
children due to vitamin A deficiency in the diet, people must be informed
about the kinds of feeds that contain this important substance and must be
encouraged to include it in their daily diet. In order to prevent night
blindness and dryness of the eyes all 'children ffom one to five years
are being given vitamin A solutiin twice e. year. Foos, rich in vitamin A
include tire following:
Vegetable sources:
i.
Green leafy vegetables and yellow fruit like' mango and papaya
and. .vegetables like yellow pumpkins a.nd carrots.
Animal Sources :
. Eggs and liver
i.
ii.
Milk and curds
TEACHING FAMILIES- -HOW -TO -HiEVENT- -NIGHT- BLINDNESS IN YOUNG CHELSREN -IS
A VERY IMPORTANT HEALTH EDUCATION ACTIVITY FOR AIL HEALTH WORKERS,
2.
Vitamin B; Vitamin B is a complex vitamin consisting of
several components which have various special functions.
: 52 ••
4« Different types of fo’d provide different kinds end
quantities of nutrients.
5. The age, activity, state of health and rate of growth
decide the amount and kinds of nutrients that are required
by the body for healthy growth and for the maintenariB of
good health.
FUNCTIONS AMD VAHJE-S OF NUTRIENT'S IN FOOD
11.2
All foods contain nutrients in varying amounts. Some foods
are made up of only one type of nutrient whereas others may include more
than one nutrient, e.g., cooking ail consists entirely of fat, while rice
consists mostly of carbohydrates but also contains some protein. Because
of this characteristic, foods can be classified according to the amount
of the various nutrients that they contain. It is very useful to know
which foods contain a large amount of a given nutrient so that these can be
-selected to meet the requirements of the body.
REMEMBER THAT -A GOOD- DIET IS A USED DIET COI'S-ISTIMG OF- DIFFERENT KINDS
OF FOIDS WHICH COICTAIN THE NUTRIENTS NECESSARY FOR GOCD HEARTH.
Each of the six nutrients that are found in food has its own
special functions to perform in the body. These functions 'are as follows:
i. Proteins are necessary- for growth. They help in repairing
worn-out body cells and in the formation of blood and
antibodies which arej';ncedcd for building up resistance to
infection.
ii. Fats and carbohydrates provide the body with energy or fuel
• to carry out its various daily activities•' ’
Hi. Vitamins and riinerale arc necessary for the development
• - of the blood colls, help to maintain good vision and strong
teeth and bones, and help to promote normal growth . iv. Water comprises more than half the weight of the body and
is essential for the proper functioning of body cells and
for maintaining the fluid- balance of the body.
11.3
.
FOOD-SOURCES GE NUTRIENTS
When, a food, contains a,.( very high amount, of a given nutrient#
it is called a feed source,, e.g., pulses and. dais.and very good, food .
sources for protein, .while potatoes and bananas are good food sources
for carbohydrates, but ore a poor.source of protein.
Protein is the- nutrient that is the'most important for infant
and child nutrition, hut it is the one that is most often missing in their
diet. It is, therefore',’ necessary ’to have infbrSation about**
pfbtein
sources so that;this can b e conveyed at every opportunity to parents
arid'others’who’care for children.' Because the different geographical'
qreas in the country produce varied kinds of vegetables which contain these
nutrients and the dishes that are prepared differ according to locality,
it is not possible to list all of them here. More accurate and realistic
information Which is based on local conditions Cante complied by you with
the assistance of the Health Worker (Female1) by de ^loping a list of
protein food sources for the villages within the subcontre. A sample
form is given below
.....
,*
.Contd/53-
: 53 :
These include the following:
They assist in the breakdown and absorption of food.
They are necessary for keeping the skin and mucous members
healthy.
iii.
They are necessary for the proper development and function
ing of the nervous system.
iv.
They arc necessary for the formation of the blood cells.
i.
ii.
Foods rich in vitamin B complex include the following:
Vegetable sources:
i.
ii.
iii.
iv.
v.
■
‘
Jhrboiled rice and unpolished rice
Cereals and mill p+.
Groundnuts
Riises
Legumes.
Animal sources:
i.
ii.
iii.
Milk and milk products
Eggs
Meat, liver and fish.
3.
Vitamin C: This vitamin is necessary to keep the body tissues
intact and to help in repair of the tissues. It also helps to protect the
body against infection.
Vitamin C is very easily destroyed and hence foods containing
this vitamin should not be exposed to a ir and heat.
Foods rich in vitamin C include the following:
i. Citrus fruits such as oranges and lemons.
ii.
Quava, tomato and amla.
4.
Vitamin D: Vitamin D is necessary for the absorption and
utilization of calcium a.nd phosphorus and hence lack of this vitamin causes
unhealthy teeth and skeletal deformities such as are seen in rickets.
Sources of vitamin D are as fellows;
i.
ii.
iii.
Exposure to sunlight is the cheapest way to obtain this
vitamin.
Fish liver oils have a very high content of vitamin D.
Butter, ghee, groundnut oil and eggs alsocontain vitamin D.
LEI-EMBER THAT EXFOSUKE TO SUNLIGHT ALONE IS JOT ENOUGHT IF THE
DIET IS DEFICIENT IN FAT . '
• -
11.3.5 MINERALS Oh HIOTECTIVE FOODS
Minerals are needed by the body for the formation of blood. The
development of strong teeth and benos, and for regulating certain body
processes such as blood clotting. There are a number of minerals that
are required in minute quantities by the body. However, calcium and
iron are two of the important minerals which are needed by everyone,
especially by pregnant and nursing women and children who are growing.
Feeds rich in calcium include the following:
Vegetable sources:
i. Lagi ■ •
ii. Green leafy vegetables.
: 55 :
Animal Sources:
i. THTk, cheese
*
Focds rich in iron include the following:
Vegetable sources:
i. Bajra and ragi
ii.
Green leafy vegetables.'
Animal' sources:
i. Fed neat, lever and eggs.
Iodine is another mineral which is essential for noraal grox/th
and development including the rate atxhich food is used by tie body.
The deficiency of this mineral in the daily diet is the cause of goitre. '
Foods rich in iodine include the following: ,
i. Fish of all types
ii. Vegetables w ich are grown in areas close to- the .sea•
Salt which is fortified with iodine is used in areas where goitre
is prevalent.
11.3.6
WATER di. FLUIDS
An adequate daily fluid intake ia important for healthy functioning
of the body. Abnormal losses from vomiting, diarrhoea and high fevers can
cause dehydration (drying up of body fluids), which is a serious condition,
especially among infants and young children. Fluids in the fern of itrilk
juices, other beverages and fruits and vegetables which are pulpy can be
used to supply the daily needs cf the body.
TO PREVENT DEATH FROM DEHYDRATION CAUSED BY EXCESSIVE FLUID LOSSr
•HiOMJT FLUID REPLACES .ENT IS NECESSARY ES EECIA11Y IN INFANTS A®
YOUNG CHUDEEN. :
11.4
■ A BALANCED DIET
Nutrition experts have been able'to find out what combination
cf feeds is needed in the daily diet for healthy growth and development.
However, this information has nc.t yet reached many who live in the
villages so that they continue to eat only those focds that have been
eaten by their families for generations and as a result often suffer
from various kinds of malnutrition. Often they are unaware that pregnant
women, nethers who are nursing their babies, and rapidly growing jraung
children need noro of- certain feeds to prevent .their becoming ill-nourished.
A BALANCED DIET IS ONE WHICH IS MADE UP OF FOODS THAT CONTAIN ALL THE~
-NECESSARY- -NUTRIENTS IN THE REQUIRED AMOUNTS- Al© PROPORTIONS TO MIOTA-I-N
HEALTH (SEE FIG.
.1) ._________________ •
A balanced diet is necessary for gb<d health. It is especially
important that pregnant and nursing woncn,’ infants and young children have
a oalancod diet, because these groups are most likely to develop malnutri
tion.
..................................... Contd/56-
; 56 :
People need to know how a balanced diet will improve their health,
what fo< ds should bo included, how much it will cost, where to obtain
the required feeds and even hew to prepare feed properly so that nutrients
are not discarded or lost due tc improper cooking.
Since you will be the only health worker making regular house-tohouse visits in the twilight ,area,..ycu should know about balanced diets
for pregnant a-nd nursing women, and children, and proper feeding methods
frf infants.
11.4.1
DAILY BALANCED DIET FOR A HiEGNANT OK NURSING WOMAN
i. Iiilk, curds or lassi
-
2 tumblers
Select one or more fo- ds from each of these five groups:
-"t”
Oarbohyir--.-1-; f ■ is .—ch ;.-s lioed, Rice. Wheat, Fbtato, Sugar,
: 57 :
Group B: Protein focds such as Meat, Fish, Eggs, Milk, Groundnut, Dal,
Beans
Group 0: Fruits such as Orange, Banana, Ninbu(Line), Papaya, Mango
Group D: Vegetables such as Feas, Capsicun, Carrots, Bhindi (ladies’
Ungers), Brinjal, Tomato, Korela (bitter gourd), Cawliflower,
Palak (spinach), and Methi (fenugreek)
Group E: Fatty focds such as Ghee, Oil, Butter
Fig: 11.1: A balanced diet
ii. Pulses, e.g., beans or dal
iii.
Cereals e.g., rice or wheat
iv.
Green leafy vegetables
v.
Eggs
vi.
Fruit (seasonal) •
-
twice
3 tines
at least once
'
One every day or every
other day
1 portion daily
Nursing mothers need more fluids including an extra, glass of rrilk
each day.and extra servings of yellow arid green leafy, vegetables and
cereals *
If-.the pregnant or nursing woman is vegetarian’and does not-eat eggs,
or cannot afford to get milk, she should be.encouraged:
i.
to eat a handful of groundnuts each day;
ii. to increase the pulses to 3 tines a day.
■ Anaemia is commonly found in pregnancy and causes the woman to feel
weak and become easily tired. . This can usually be prevented by including
a serving of a green leafy vegetable in the daily diet, and by talcing tire
iron and folic acid,tablets which are distributed at the subcentre or on
the hone visits by the health worker.
In sone connunities women eat leris during pregnancy becuase they
believe that they will then ■ have a smaller baby and an easier delivery.
People need to knew that this is a harmful practice which can lead to mal
nutrition in the mother and low birth weight <bf the infant who is also
malnourished.
REMEMBER THAT a SMALL BABY AT BIRTH HAS LESS CHANCE OF SURVIVAL AND IS
ICTE LIKELY TO GET SICK BECAUSE GF LOW RESISTANCE TO INFECTION.
BALANCED DIET FOP INFANTS (ZERO TO 12 MONTHS)
11.4.2
The major points to remember about the diet for and feeding of
infants are as fallows:
1.
Breast milk is the best food for infants up to the age of six’
months because:
i.
it is clean and-safe;
ii. it contains all the necessary nutrients;.
iii.
no cost is involved.
2.
*
3
.
*•,
.
..
After four months, all infants need to be given'solid food
since breast nilk does not supply all the nutri'erits that a rapidly
growing baby requires.
- ?■
During weaning the ’first’ focds should be semisolid in consistency
e.g., mashed rice, millet,, banana or potatoes. Gradually solid
foods from vegetable and animal sources containing protein must
be added so that the infant receives'a balanced diet.
: 58 :
Remove the infant’s portion of food before spices are added
for the rest of the family otherwise the baby will develop «' ’ - -'
diarrhoea
*
5.
Give the baby a spoonful of food at first and gradually inc: ease
the amount given over a period of weeks.
4.
The addition of foods other than milk to the infant’s diet
should be done gradually over a period of tine rather than
all at once.
7 • Glean hands and utensils and fresh foed are necessary for
preventing infections. Food must be kept covered so that flies
do not sit on it. Water sho Id be obtained from a safe source
of supply or boiled if possible. Never feed an infant with left
over foods because they are very’likely to be spoiled and will
cause illness.
8. If the mother does jot produce enough breast milk, do not
suggest the use of a bottle and nipple; use of a cup and
spoon is safer since they arc easier to keep clean.
9. Breast feeding should be continued throughout-the-first year
so that the infant continues to receive valuable protein from
■ this source.
_________________________
___:___________ 66_______________________________
REMEMBER THAT THE 1AJ0L CAUSES OF MNUTHTION IN INFANTS AND YOUNG
CHHDREII ARE:
i.
DELAY IN ADDING SOLID FOODS TO THEIR DIET .
ii. NOT FEEDING THEM FREQUENTLY ENOUGH.
iii.
THE LACK OF ECDY-EUILDING PROTEIN FOODS .
iv.
INSUFFICIENT FOODS CONTAINING VITAMIN A .
11.4.3
BALANCED DIET FOR THE PRE-SCHOOL CHILD (ONE TO FIVE YEARS)
Children between the ages of eno and five years are often neglected
and underfed by their mothers. This happens because mothers do not know
that these children need proportionately more food for their size than is
needed by adults. Becuae they arc growing at a fast rate and the growth
is continuous, they need extra amounts of body-building protein food and
energy-giving foods.
In nariy poor families, young children are breast-fed until they
are two or three years old and are not given any other foods eaten by the
rest of the family. This practice results in a high incidence of kwashi
orkor and marasmus; the former of which is caused by a deficiency of protein
and calories in the diet, while the latter is dte to deficiency of calories.
AFTER FOUR MONTHS- CF- AGE, A DIET CONSISTING CF ONLY BREAST MIK IS
INADEQUATE ■
A daily diet for children one ta five years should include the
following:
Milk
Cooked cereal - pulse
mixture (khichiri, clalia,
idli or groundnuts)
3.
Green leafy vegetables
(Palak, chawli) and yellow
vegetable or fruit (carrot
pumpkin, papaya, mango)
4« Cooked cereal or millet
(rice, wheat, ragi)
1.
2.
-
-
1 tumbler
8 to 12 level spoons
-
4 ’to 8 level spoons
4 to 16 level spoons or
1 to 2 chappatis
~~
: 59. :
5- Egg
or dal
or fish/noat
6. Fresh fruit
(banana, guava or
Tomato)
Ono
4 to 8 level spoons
4 to 8 level sppons
one portion
The feeds for the child under two years should be small in amount
and should be given at shorter intervals tlian for the rest of the family.
The following foods should be avoided in the diet of young children:
i.
Highly spiced dishes and.' curries.
ii. Foods made with large amounts of sugar.
iii.
"Very greasy foods.
iv.
Poorly cleaned, insufficiently cooked, or improperly mashed foods.
Dietary instructions are easier to follow for most individuals when
they understand the amounts to be eaten in terms of commonly used measures
(see fig. 11.2). When utensils are not available in the home, you will
liavo to give instruct] ons regarding the quantity to be consumed in terms
of a ’a handful of dal’, or ’one banana’, etc.
Fig. 11.2: Common household measures
The amount of food which a child can eat at one meal depends on
his health, body size and physical activity.
CHAPTER 8
•
INSTRUCTIONS
FOR
COMMUNITY HEALTH WORKERS
CHW-C I
Nutrition
Good nutrition means that - the body is getting the required food
and is able to make use of it.
Malnutrition occurs when.a person does not
get the proper kinds of food in the amounts that arc needed for keeping
healthy.
8.1
Identify css,<swith signs and symptoms of malnutrition among pre-school
childrcn(one to five years) and refer them to the Health Worker(Male/Female)
It is important for you to identify malnourished children under five
years of age as early as possible because they develop serious ill effects
when they are improperly fed. Within this age group the children between
six months and three years are most liable to develop malnutrition and,
therefore, you should concentrate on looking for malnutrition in this age
group.
Whenever you find a malnourished child in the community, you should
refer the child to the Health' Worker(MaIc/Fomale)
The early signs and symptoms of malnutrition which you should look for
are the following?
1. The child is ; ft on sick because of low resistance to infection
2.
It has a dry, scaly or rough skin
3.
Ifr has dry eyes and tends to stumble after dark
4.
It fails to gain weight regularly or loses weight
5.
It has cracks at the corners of the mouth(see slide Nut-1)
6.
.It has a sore mouth and tongue
7.
It has bleeding from the gums
8.
It has soreness and tenderness of the body
9.
It tires easily and has little energy
10.
It has a pale pink-or colourless lower eyelid or lower lip
The later signs and symptoms of malnutrition which you
are the following:
should look for
1. The child is smaller in size and considerably thinner than other
children of the same age
It may become easily breathless when playing
It may look miserable and show no interest in people or surroundings
It has hair which is lighter coloured than in others or which is
reddish and brittle
5.
It has swelling of the feet and logs and peeling of the skin
(see slide Nut-2)
6.
It is very thin with bones showing and wrinkled skin (see slide Nut-3)
7.
It has eyes which no longer shino and the surface of which is
rough and dull
8.
It has sores on the surface of the eyes
9.
It has bumps tin the front portion of the hend(see slide Nwt-4)
10.
It has bowing of tho legs(sec slide Nut-4)
11.
It has bead-shaped lumps along the ribs on either side of the
breastbone(see slide Nut-4)
2.
3.
4.
You should also be especially alert to the possibility of finding a
malnourished child when tho conditions in his family are as follows?
1. The child is one of twins
2.
The child was much smaller than usual at birth
3.
Breast feeding was stopped before the child was three months old
4.
The child has no living parents
5.
The child belongs to a migrant family
; 2 :
6.
7.
8.
9.
10.
Ths mother has low intelligence
There are four or more children in the family
The family belongs to the poorest group in tho community
The child's brother or sister is less than one year younger
The child is cared f ' during the day by an older brother or
sister without paren -al supervision
8,2
Identify cases with signs and symptoms of anaemia in pregnant and nursing
women and childrenfand refer them to the Health Worker(Male/Female) for
t
treatment
Anaemia is a' condition of the blood resulting from aninsufficient amount
of iron in the body
*
In India the most common causes of anaemia are malnutrition
malaria and hookworm infestation. However, in women additional causes of
anaemia are frequent pregnancies, repeated abortion and severe bleeding before,
during nr after delivery. You can identify thosowho are anaemic in the
community in the following ways •
1. Look for mothers and children who have a pale skin and nails and
who tire easily
Pull down the lower eyelid and note whether the lining is pale
(see slide Nut-5)
3.
Pull down the lower lip and note whether the lining is pale
(see slide Nut-6)
2.
Whenever you find pregnant or nursing women or young children who have
any combination of these signs and symptoms, you should refer them to the
Health Worker (Flale/Female) for treatment. If iron and folic acid are prescribed,
assist the Health Worker in distributing the drug.
8.3
Assist the Health Worker(^ale/Female) in administering vitamin A
solution as prescribed to children from one to five years of age
You should assist the Health Worker^ale/Female) in the following ways? .
1. Find out from the leaders of the village suitable dates six months
apart for administering vitamin A solution, and inform the
Health Worker
2.
Suggest to the Health Worker a central, shady place for holding
the clinic so that it is easily accessible to all
3.
Get the community to provide the followings
(a)
(b)
(c)
(d)
A table for equipment ,
Flats or charpoys for seating
Adequate supply of drinking water
Facilities for washing hands and spoons
'
'
Prepare a list of children between the ages of one and five for your
village according to the instructions given by the Health Worker
5.
Visit the homes on the day before the date scheduled for the'
administration -of vitamin A solution to remind families where and
when to assemble
6.
Greet those who come for vitamin A solution and see that they are
administered the drug according to their turn
7.
Ask the adult accompanying a child who is to be given the vitamin A
solution to hold the child in her/his lap with the head raised so
that the solution can be placed in the side of the mouth or on the
tongue(see slide Nut-7)
8.
Assist the Health Worker as required during administration of
vitamin A solution
9.
Inform adults accompanying children to the clinic approximately when
the next dose of the drug will be administered in tho village and tell
them that regular six monthly doses are necessary for preventing
vitamin A deficiency in children until they are 5 years of age.
4.
.
s 3 s
8.4
Teach families about the importance of breast feeding and the introduction
of supplementary weaning foods
The major factors which arc responsible for malnutrition in infants and
young children are poverty,- incorrect family food habits and parental ignorance
regarding proper feeding and diet for this ago group. You should talk about
the following whenever you teach a family about how they can improve the
diet for infants and young childrens
1. Breast milk is the best food for infants up to the age of six months
because it is clean and safe, it contains all the necessary nutrients
and there is no cost
2.
Breast feeding should continue throughout the first year
3,
It is: dangor.pus to use a bottle and nipple for feeding babies when
the family do not have the necessary facilities for boiling the
articles and keeping them clean. Whenever breast feeding is not
possible a cup and spopn should be used
4.
After a baby is four months'" old, he needs to be give supplementary
weaning food since breast milk does not supply all the nutrients that
a rapidly growing baby requires
5.
The- first solid foods which are given to the baby should be soft,
without roughage or spices and semi-solid in consistency, e.g., ripe
banana, well-cooked mashed rice, millet or potatoes.
Remove the
infant's portion of the family food before spices are added as otherwise
the baby will develop diarrhoea
6.
Give the baby a spoonful of new food at first and gradually increase
the amount given over a poriod of weeks
7.
Supolcmentary weaning foods' should be added gradually over a period
of time rather than all at once
8.
Clean hands and utensils and freshly prepared food aro necessary for
preventing infections
9.
By six .months of age the baby should be given dal, green leafy
vegetables, egg yolk, chapati, roti or bread and fish or meat
10.
By the time the child is one year old, it should be eating all the
foods(without spices) eaten by the family daily
8.5
Educate the community about nutritious diets for mothers and children
It is important to educate the community about proper diets for mothers
and children.
The major points which you should stress about improving diets
for mothers and children are the following!
1. If a pregnant woman does not eat' sufficient amounts of the right
kinds of food every day. She is likely to have a weak, low-birth
weight infant and insufficient breast milk.
2. Contrary to some common beliefs, pregnant women need more rather
than less food throughout pregnancy
Pregnant and nursing women should eat larger quantities of the
regular family meals especially dal, leafy green vegetables and
cereals, i.e. rice, chapati -and roti, and milk whenever available
4.
If the pregnant or nursing woman does not eat eggs or cannot afford
to have milk, she should eat ahandful of groundnuts each day, and
have two servings of dal or have a serving of ragi daily
5.
If children under five years do not receive the right amount and
type of food every day, physcial and mental growth are retarded and
illness and even death may result
6.
Children over one year of age should be given all well-cooked foods
in the family diet instead of diluted foods such as gruel or cor.jee.
Hot spices for young children should be avoided
7.
The child under three years foust be fed two or more snacks or sma.l
meals between the family meals so that he will get the amount of ^ood
his rapidly growing body requires.
8.
A nutritious diet is one that consists of a variety of foods
selected from each of the five groups needed to meat the requirements
of the body(see slide Nut-8)
3.
: 4 ;
9.
A family meal can be improved and made more nutritious by making simple
changes as follows?
Add a handful of groundnuts or any dal to rice or wheat to. be
prepared for the meal’. Whenever possible add egg, fish or
meat to the meal
(b)
Include green leafy vegetables in the meal daily
(c)
Use a combination of .cereal and millet or■cereal-millet-pulse
preparation instead of a single caroal
(d)
Serve well-washed vegetables such as carrot, cabbage or tomato
raw instead of cooked
(e)
Servo unpolished, hand-pounded or parboiled rice instead of
milled rice
(f)1 Use the water in which rice or vegetables are cooked for making
soups or adding to the curry
(g)
Serve sprouted channa or moong either raw or lightly cooked
as often as possible
(a)
10.
Cheap and locally available nutritious foods should be used for
family meals.
///////////
/xj'J'T
1st August 1972.
G-'2-0
Nutrition S-oinar
Indian diet - Nutrition education.
-•fHeats
i) Average Indian Diet.
ii) Suggestions for improving the diet.
a) Health eduction, pamphlets.
References:
b) Economics of die^s by Lt. Col. Amircband.
Anoraal balanced diet designed to meet "ur energy
Introduction - Normal diet:
requirements, to build and rebuild, tissues and furnish vitamins and minerals
Salts to maintain gO'd health, is one which contains the barie of foodstuffs
There are a) cereals, b) pulses c) milk and milk
in sufficient quantities.
products d) Fresh fo ds e) fruits f) leafiy vegetables and g) Roots an', tubers.
Mainly there are two tvpes - a) uri.a- ‘.md h) Rural.
Indian diet:
In the rural
area, the main foodstuffs’- consumed are cereals like ragi, jowar and rice and
pulies such as redgram, hors’gram, field beans etc.
the staple diet being
ragi among the poorer class and wheat and rice among the middle class.
Many
families do not use vegetables daily and fruits are onl'- occasionally used.
The menu pattern as fonn
Break fast
Lunch and
Dinner
b-
our work in Sampangiram nag: r is as dllows:
2 iddly or dosai or uppama.
5
S
Ragi balls or chapathi
Tur dhal rasam
milk 1 glass
Vegetables leafy
150 gras.
50 gms.
100 gms.
100 gms.
Butte
CHO - 50$
fat - 30;prot -20$
Food value
Amount
Ragi flour
Dhal
But1 er milk
G.L.Veget■ les
CHO
gms.
Prot
gms.
105
30
5
6
11
11
5
4
~31~~
150 gms.
50 gms.
100 gms.
100 gms.
156
Fat
g'S.
2
1
Calories
Kcals .
1
' 500
180
120
40
13
840
Q
Then taking brsjakfast as equal to half a meal,, and. adult has 2-J- meals a
and his consumption per day is - CHO - 390 gras.
Prot - 50 gras.
fats - 30 gras.
Caloridie value - 2100 K cals.
Thio diet lacks in proteins and
in fat.
The energ- requirement for a.moderate
worker per day is about 3000 k als and we see that about 30$ of the total energy
requirement is not met in this diet.
So there is a great difference between the diet most satisfactory and the diet
now available to the greater part of our population.
The leasf we can do is
to reduce this diference between the actual and optimimum sandards by using
what is available nos- economically and wisely.
This is economic-' of diets.
A factor of great importance in relation to this is the prevention of good
wastage.
Poverty is one of the causes but not the greatest cause of malnutrition.
The beet food is a-fte-roften the cheapest.
The biggest single cause is ignorance.
J
\
contd....2/-
-2In man'. cases the most nutricious part of the food being prepared is either boiled
or thrown away.
The following are some of the examples.
In the case of wheat and ricewhich are the commonest Cereals consumed,
1. Cereals:
the outer skin is discarded in the processes of milking.
This part conta ns
proteins, mineral salts and vitamin B in higher proportions.
Whole wheat - 7r> gluten, finer grain flover.
white flour - finest 6$ gluten.
(maida)
Similarly hand pounded rice is more nutricious than mill polished rice.
Some people
are in the habi'. of wabhing - ■>» rice several times befiore cooking and throwing it
away after each washing.
in this manner.
The water soluble mineral salts and vitamins are discarded
The rice should be cooked, so that there is no surplus water left
after corking.
II Pulses
-
in proteins and the outer skin contains vitamins
There are extremely rich
B in greater abundance than cereals.
There should be consumed in this whole state
instead of soaking them in water and discarding the outer skin.
Ill
Vegetables
are extremely rich sources of mineral salts and vitamins.
in this ca e occurs in several ways.
Wastage
A point of importance is the sslection of
the proper edible portion of the vegetables.
a) The outer green leaves of cabbage are about 10 times as rich in vitamins as the
pale inner ones, and should not be removed
and discarded in preparation.
About
15 grms of the green top of turnips and radish, can meet the daily requirement of
vitamins A and C and
the daily need of calcium and 1/3 rd that of iron.
b) Sometimes the water in which the
egetable is boiled is thrownaway.
This water
contains the soluble mineral salts and vitamins C and A to a considerable degree.
d) Some of the vegetables can be eaten without being cooked for eg. carrots, beetroot,
tomatoes, bettuce etc. and this preserves the heat cemifive vitamins.
Conking
- To reduce loss in cooking, the vegetables should be eu cut into as large
a piece as possible, and should not be cut or pieced long before cooking.
should be cooked in a minimum
The vegetables should
They
uantity of water and the vessel should be covered.
be added after the water begins to boil, as this prev-nts
oxidation of vitamins first by destruction ofthe oxidising rnoymes and secondly
jky removing the dissolved carbon-di~oxide.
^-heating should be avoided.
The food should be served .while hot and
Roots ad tubers should
be steamed and not boiled
their skin.
Sona „„
nation." for improving the diet:
With locally available foods and within
economic means of the people.
♦
contd....2/-
a) Encourage a mixed cereal diet - instead of eating rice, ragi or wheat
exclusively so tha' the nutriants lacking in one is made rup in the other.
b) Comparatively in expensive pulses, dhals and meets co bined and properly
used would provide almost the sane nutrients as milk and meat,
of ground nut contains
for eg. 100 grins
27 grins of protein, 40 grins of fat, 20 grms of CHO and provides
about 550 cals of energy.
c) Increased use of sprented pulses, leafy tops of vegetables like cauliflower,
Knol-khal and Radish, and n-nce- methods of cooking to prevent loss of nutrients
and vastage ran significantly e
increasing the cost.
the nutrifice value of the diet witbut
°fRl Tlorsl
?.<~5r^> YC-6^>
‘"7/eS v ^/"Leo
— C^e-r-L.^-csjkoYC^Ci^S .
/"ci/? <= ,.o z
y?/<7 ^ 7^
UJ' ft
6CX)/-<p
- Mj5±±^^i^tc-haJS
_
v—
5q-<£U2-.
^SXa_XkJ y
I
_ )-to>^-£. '-^-p
"■• e.2t^J ,^;
(t
.be-o
daLa_A_^(
Ujye?<l-J2-AA-^-Up
<JLQ ‘c^'
XaJ>M
k
£
'
f'^°2s/- -sv-LLu^ <7^'.
,—
X-’V O-gxP-CU^ojJ,
,?U co.
__ A.
■P-qLo.
<^3r>
W'Srvg
'
k/ • ‘~ ^c-
J $n rl
k
i. . _ a . > ?
12
(-j>x_Q>c-JlXLi'
T^~
<>rr\.Q_LCU_p
ci-ax-Lo^r-^-!
Z&C£1K-U^M
ver
La
c?ts2_>iL
I^LClo-C UU3 '
pcN
jS-(
—
-
p^-xP'e-^x
“
IC^OaxXaS^Jm^
Q^-Lqaa-Q.--
eAe^-p^
AJXCokJ-xj
rricaJlcx^J-A^X'-O
■'
—® 2^?ci
p^Y, qLqA'OUIj^c^^ —3
',) Uua-gLm-'
a)
tnj©A-vv<-<XU-txcxA
5
CiAcn'oc.
it>
/a<^
b)
P)
fp=sz=a^.
/ M>?oU
bcs^,
/
'
p-r^C^
L^> /ncrtc^Kcm.
7
/
is>
^LieP pcJi-e^
10 l'k-Q
•xjj rtc~"'
^2©e^-Oee-E>r>t5rvUc_
,
-2-t eJ-l~Lg
S"CSt> WvQ
'.
IGATION
£
FACTS
ABOUT
OUR
DIET
An important factor contributing to malnu
trition in India is lack of awareness about
the importance of balanced diet and
want of knowledge about locally available
and
relatively
inexpensive
foodstuffs
which can be consumed to prevent or
overcome malnutrition.
One of the most significant findings of mo
dern nutritional research is that calorie protein
malnutrition in growing infants can lead to
serious ill-effects, resulting
in mental
retardation and even irreversible brain
damages.
It has been reported by nutri
tionists that many pre-school children in
several regions in our country suffer from
mental dwarfism.
During the months of
breast feeding, children normally grow at
a rate comparable to well-nourished children,
but after six months of age, if weaning food
Nutrition is accomplished by the con
sumption of the right food in proper
amounts and correct proportions. The
primary step towards elimination of malnu
trition is, therefore, to make available to
people different kinds of foodstuffs in
amounts and quality required to achieve a
balanced diet.
of cases is progressively retarded. It is there
fore necessary that proper care is taken
Balanced diet is essential to sustain good
health. We take food not just to make life
possible but to lead a healthy and active
life. Food contains many nutrients required
to make the body grow, keep it health. |
of infants at this stage.
and provide energy for work.
is not given, growth of children in a majority
Essential nutrients present in food are
carbohydrates, proteins, fats and oils,
vitamins and minerals and, of course, water,
which helps in vital processes of the body.
A complete and balanced food should
contain elements which are essential to
good nutrition—proteins to build muscles
and tissues; carbohydrates and fats to
supply energy; mineral salts to develop
healthy bones and blood and vitamins for
healthy life and growth of the body.
age, sex, physical work and other physio
logical conditions.
A manual labourer
engaged on heavy work requires more of
energy-giving food than a person doing
office work. A growing child requires more
protein and minerals per kg. of his body
weight than an adult. Pregnant women
and nursing mothers require more protein
and minerals because of physiological
changes taking place during this period of
their lives.
The requirements for the body of the
^various nutrients—carbohydrates, proteins,
fats, vitamins and minerals—depend on
A diet containing all the required nutrients
in proper quantities and proportions has,
therefore, to be taken by an individual
depending upon such factors as age, sex,
working conditions etc., to meet the
requirements of the body. A diet which
satisfies these needs is known as a balanced
diet. It can be prepared by a judicious
combination of foodstuffs from the following
food groups:
(a)
Energy-yielding Foods
Foods rich in carbohydrates and
fats are called 'energy-giving foods'.
Cereals, roots and tubers, dry fruits,
sugar, oils and fats are included in
this group.
(b)
Body-building Foods
Foods rich in proteins are known
as 'body-building foods'. Milk, meat,
fish, eggs, pulses, oilseeds, nuts and
low-fat oilseed flours are good ex
amples of such foods.
(c)
Protective Foods
Foods rich in proteins, vitamins
and minerals are termed 'protective
foods'. Milk and milk products, eggs,
liver, green leafy vegetables and
fruits form part of this group.
The diet of a vast majority of people in
India is predominant in cereals and defi
cient in other essential nutrients. Improve
ment in the diet can be brought about
generally, by diversifying it in such a way
that the consumption of cereals, wherever
high, is reduced and that of other items of
food which provide the needed proteins,
vitamins and minerals, increased. The use
of such foods, wherever available, as also
of those saved from loss through preserva
tion and the application of science and
technology, can help in an overall improve
ment in nutrition. There is also considerable
scope for utilising the available foods more
effectively by reducing nutritional losses
through improved techniques of cookery.
Prolonged boiling or frying of food results
in considerable loss of nutrients. Adequate
care has, therefore, to be taken to see that
food is properly cooked.
Nutritional requirements and balanced diets
for individuals of different age groups as
well as functions of nutrients and their
sources are given in the succeeding tables.
The data presented in these tables are based
on compositions given in the book “Nutritive
Value of Indian Foods" published by the
National Institute of Nutrition, Indian
Council of Medical Research, Hyderabad.
NUTRIENTS
FUNCTIONS
TABLE 1
1
FUNCTIONS OF
NUTRIENTS
__________________ AND
THEIR SOURCES
PROTEIN
To build and repair body tissues, muscles
and vital fluids like blood; to help form
enzymes and antibodies to fight infection.
2. FAT
To serve as a concentrated source of energy
and supply fat solvable vitamins.
3. CARBO
HYDRATES
To supply energy to the body.
4. VITAMIN A
To help keep the skin and mucous mem
branes healthy and to protect against night
blindness.
w
RICH SOURCES
Fresh or dried milk, cheese, curd, oilseeds and nuts, soyabean,
yeast, pulses, meat, liver, fish, egg and cereals.
Butter, ghee, vegetable oils and fat, oilseeds and nuts, fish liver oils
and egg yolk.
Cereals, millets, roots and tubers, such as potatoes, sweet potatoes,
yam, tapioca etc., and sugar and jaggery.
Fish liver oils, liver, milk and milk products (curd, butter, ghee)
carrots, fruits and green leafy and yellow vegetables.
TABLE I
FUNCTIONS
NUTRIENTS
--
5. VITAMIN B 1
(Thiamine)
For normal appetite and digestion, healthy
nervous system, and to help change good
carbohydrates into energy for work.
6. VITAMIN B 2
(Riboflavin)
To help the cells use oxygen, to keep vision
clear and smooth, skin without scaling I
around mouth and nose or cracking at the
corner of the mouth
7. NIACIN
To preserve health of the skin, functioning
of the stomach and intestines and nervous
system.
8. VITAMIN C
To help cement body cells together, strenc£v\
then the walls of blood vessels, provia/'’/
resistance to infection and help in healing.
%
(Continued.)
FUNCTIONS OF
NUTRIENTS
AND
THEIR SOURCES
RICH SOURCES
Liver, eggs, pork, legumes, pulses, nuts, oilseeds, fruits, yeast, whole
grain cereals and parboiled rice.
Milk, skim milk, curd, cheese, eggs, liver and leafy vegetables.
Cereals, whole-grains, meat, liver, yeast, oilseeds, nuts, legumes
and pulses.
Tfynla, guava, citrus fruits, fresh vegetables, salad, and green
Jrouted pulses.
TABLE I
NUTRIENTS
FUNCTIONS
9. VITAMIN D
To help the body absorb calcium and to help
build strong teeth and bones.
10. CALCIUM
AND
PHOS
PHORUS
To help build bones and teeth as also the
blood to clot and assist muscles and nerves
to react normally.
11. IRON
To combine with protein to make haeomoglobin—the red substance in the blood
which carries oxygen to the cells.
(Continued.)
FUNCTIONS OF
NUTRIENTS
AND
THEIR SOURCES
Id SOURCES
Sunlight butter, cheese, fish liver oil, ghee, egg yolk and milk.
Milk and milk products, leafy vegetables, small fish, cereals,
whole-grains, and gingelly seeds.
Liver, yeast eggs, vegetables, oilseed nuts, legumes
brown sugar (jaggery), dried fruits and leafy vegetables.
pulses
Sedentary work
Moderate work
Heavy work
Vege
tarian
a,,
(gm)
Non
vege
tarian
(gm)
(gm)
Non
vege
tarian
(gm)
(gm)
*vege
tarian
(gm)
Cereals
400
400
475
475
650
650
Pulses
70
55
80
65
80
65
Green leafy vegetables
100
100
125
125
125
125
Vege
tarian
Vege
tarian
TABLE II
BALANCED
___________ DIETS
_____________ FOR
ADULT MAN
Other vegetables
75
75
75
75
100
100
Roots & Tubers
75
75
100
100
100
100
Fruits
30
30
30
30
30
30
Milk
200
100
200
100
200
100
Fats and oils
35
40
40
40
50
50
Meat and fish
—
30
—
30
—
30
Eggs
—
30’
—
*
30
—
30’
Sugar & Jaggery
30
30
40
40
55
55
Groundnuts
__
__
__
50”
5
__
•
)
• One egg.
** An additional 30 gm. of fats and oils can be included in the diet in place of ground
nuts.
1
Sedentary
work
3
TABLE III
Cereals
300
300
350
350
475
475
50
Pulses
60
45
70
55
70
55
-
10
125
125
125
125
125
125
25
25
75
75
75
75
100
100
50
50
75
75
100
100
—
—
Fruits
30
30
30
30
30
30
_
Milk
200
100
200
100
200
100
125
125
Fts&o,s
30
35
35
40
40
45
—
15
30
30
30
30
40
40
10
20
30
—
30
—
30
—
—
*
30
—
30’
—
*
30
—
—
—
—
—
* *
40
* *
40
—
—
BALANCED Other vegetables
|
Roots & Tubers
FOR
ADULT
WOMAN
----------------------------------------------------
Sugar & Jaggery
Meat & Fish
Eggs
3
Additional
allowances
during
Heavy
work
Vege- Non- Vege Non Vege Non Preg Lacta
tarian vege- tarian vege tarian vege nancy
tion
tarian
tarian
(gm) (gm) (gm) (gm) (gm) (gm) (gm) (gm)
________________
----------------------------------------------------
Moderate
work
Groundnuts
—
100
__
• One egg.
” An additional 25 gm. of fats and oils can be included in the diet in place of
groundnuts.
Girls
Boys
13-15 years
13-18 years
Non
vege
tarian
(gm)
Vege
tarian
(am)
Non
vege
tarian
(gm)
Vege
tarian
(gm)
(gm)
veg'tarian
(gm)
Cereals
430
430
450
450
350
350
Pulses
70
50
70
50
70
50
Green leafy vegetables
100
100
100
100
150
150
Other vegetables
75
75
75
75
75
75
Roots & tubers
75
75
100
100
75
75
Vege
tarian
TABLE IV
BALANCED
DIETS FOR
ADOLESCENT
BOYS &
- -------------------------------------------------- ___________ GIRLS
16-18 years
Fruits
30
30
30
30
30
30
Milk
250
150
250
150
250
150 ,
Fats & oils
35
40
45
50
35
40
Meat & fish
—.
30
_
30
__
*
30
Eggs
*
30
30
*
30
Sugar & jaggery
30
30
40
40
30
Groundnuts
—
—
50"
50”
—
30
JX
’ One egg.
" An additional 30 gm. of fats and oils can be included in the diet in place of
groundnuts.
Pre-school children
1-3 years
TABLE~V
BALANCED
DIETS
_____________ FOR
CHILDREN
School children
4-6 years
7-9 years
10-12 years
Vege-
Non Vege Non Vege Non Vege Non
vege tarian vege tarian vege tarian vege
tarian
tarian
tarian
tarian
(gm) (gm) (am) (gm) (gm) (gm) (gm) (gm)
Cereals
150
150
200
200
250
250
320
Pulses
50
40
60
50
70
60
70
60
Green leafy vegetables
50
50
75
75
75
75
100
100
75
320
Other vegetables "|
30
30
50
50
50
50
75
Fruits
50
50
50
50
50
50
50
50
Milk
300
200
250
200
250
200
250
200
Fats & oils
20
20
25
25
30
30
35
Roots & tubers
J
35
Meat & fish ■]
*
30
e
Eggs
*
30
*
30
J
Sugar & jaggery
* One egg.
*
30
30
30
40
40
50
50
50
50
C
TABLE VI
DAILY
ALLOWANCES
OF NUTRIENTS
FOR INDIANS
Group
MAN
WOMAN
(RECOMMENDED
BY THE NUTRITION EXPERT
GROUP IN 1968)
Particulars
Calories
Proteins
(gm)
Sedentary work
Moderate work
Heavy work
2400 ■)
2800 k
3900 J
Sedentary work
Moderate work
Heavy work
Pregnancy
(second half of pregnancy)
Lactation (up to 1 year)
19001
2200 U
3000 J
4-300
45_ |
i7) 1
+1GT
4-700
+20 J
55
I
Calcium
(gm)
Iron
(mg)
Vitamin A
Retinol or ^-carotene
(Mg)
(Mg)
3000 j-
0-4 to 0-5
J&4 to 0-5
A
▼
20
750
Thiamins
(mg)
1-2
2-0
11-0
Riboflavin
(mg)
Nicotinic
acid (mg)
1619 1r
1-3
1-5
2-2
26 J
30
750
40
750
30001
y3000 J
1-5
+0-2
1-0
1-2
i ■/
4-0-2
131
15 [
20 J
+2
30
1150
4600
4-0-4
4-0-4
+5
1-0
Ascorbic
acid(mg)
Folic
acid
(Mg)
Vitamin
100
1
50
100
1
50
150-300]
b
150 J
50
80
(Mg)
1-5
Vitamin
D
(I.U.)
TABLE Vj
(Continued.)
Calories
Particulars
Group
Proteins
(gm)
INFANTS
___________ DAILY
ALLOWANCES
OF NUTRIENTS
FOR INDIANS
0-6 months
120/kg.
2-31-8/kg
7-12 months
100/kg.
1-81-5/kg
CHILDREN
1 year
"1
2 years
L
3 years J
4-6 years
7-9 years
10-12 years
1500
1800
2100
17
18
20
22
33.
41
1200
ADOLESCENTS
13-15 years
Boys
Girls
2500
2200
55s
50j
16-18 years
Boys
Girls
3000
2200
60)
50 J
Position: 1368 (5 views)