RF_NUT_5_SUDHA.pdf
Media
- extracted text
-
RF_NUT_5_SUDHA
A mother’s grief
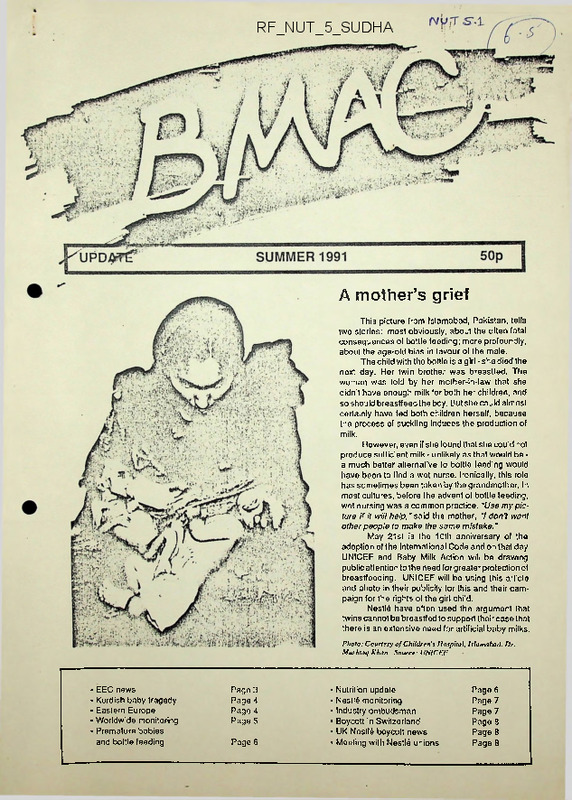
This picture from Islamabad, Pakistan, tells
two stories: most obviously, about the often fatal
consequences of bottle feeding; more profoundly,
about the age-old bias in favour of the male.
The child with the bottle is a girl - she died the
next day. Her twin brother was breastfed. The
woman was told by her mother-in-law that she
didn't have enough milk for both her children, and
so should breastfeed the boy. But she could almost
certainly have fed both children herself, because
the process of suckling induces the production of
milk.
However, even if she found that she could not
produce sufficient milk - unlikely as that would be a much better alternative to bottle feeding would
have been to find a wet nurse. Ironically, this role
has sometimes been taken by the grandmother. In
most cultures, before the advent of bottle feeding,
wet nursing was a common practice. "Use my pic
ture it it will help,"said the mother, "I don't want
other people to make the same mistake.'
May 21st is the 10th anniversary of the
adoption of the International Code and on that day
UNICEF and Baby Milk Action will be drawing
public attention to the need for greater protection of
breastfeeding. UNICEF will be using this article
and photo in their publicity for this and their cam
paign for the rights of the girl child.
Nestld have often used the argument that
twins cannot be breastfed to support their case that
there is an extensive need for artificial baby milks.
Photo: Courtesy of Children's Hospital, Islamabad. Dr.
Mushtnq Khan. Source: UNICF.F
• EEC news
• Kurdish baby tragedy
• Eastern Europe
• Worldwide monitoring
• Premature babies
and botlle feeding
Page 3
Page 4
Page 4
Page 5
Page 6
• Nutrition update
• Nestl6 monitoring
• Industry ombudsman
• Boycott in Switzerland
• UK Nostl6 boycott news
• Meeting with Nestld unions
Page 6
Page 7
Page 7
Page 8
Page 8
Page 8
Baby Milk Action
This newsletter (2nd edition) Is produced by Baby Milk Action, the coordinators of the UK Noslld boycott. It is
written and edited by Gay Palmer, Andrew Radford, Patti Rundall, Stuart Reid and Lisa Woodburn. Baby Milk Action is
a member of the International Baby Food Action Network (IBFAN), a network of over 100 groups working for the pro
tection of infant health in over 60 countries. Baby Milk Action aims to halt the commercial promotion of bottle feeding and
to protect and promote good and appropriate infant nutrition.
We aim to produce a newsletter every 6 months. However, campaigning, lobbying and monitoring commitments
may make this impossible. Contributions and letters are welcomed but we cannot guarantee to use them as space is
limited. Please write if you have any information which may bo useful to us.
Baby Milk Action's development education work is funded mainly by the EEC, Save the Children, Oxfam, Christian
Aid, CAFOD, UNICEF and UK churches. For our campaigning work we rely on donations, membership subscriptions
and income from the sale of materials. If you find this newsletter interesting and would like to help us, please consider
joining or sending a donation. Baby Milk Action is a small organisation, Nestle is the largest food multinational in the world.
Baby Milk Action, 23 St. Andrew's Street, Cambridge CB2 3AX. Tel: Q223 464420. Tel/Fax: 464417
Area Contacts
Our network of area contacts has expanded to 47 activists
following a training day in April. Baby Milk Action intends to hold a
health workers training day in September and an area contacts
training day in Scotland in the Autumn. Anyone interested in becom
ing more active is welcome to attend. A list of area contacts is included
with this newsletter • and we are always looking for additions to it...
New materials
Wake up to the facts: a 6th display poster has been added to
the original series of five mentioned in the last Update. Colour photos
of breastfeeding mothers and babies can also be hired at a nominal
charge.
Baby Milk Action leaflets: A4 folded leaflets with information
on Baby Milk Action and our campaigns.
Breastfeeding a Global Priority, UNICEF (VHS video). 25
minutes. Available for hire: £5 from Baby Milk Action.
Competition
results
This is the
winning caption from
the competition in the
last BMAC Update.
The winner Is Mrs E.
Tent of Saffron
Walden. Runners up
prizes have been
sent to Rhoda Ui
Chonaire of Ireland
and Hermit Singh
Randhawa of New
castle.
Hmm, this one’s not tlcud yet.. better f>ive it another bottle.
BMAC UPDATE Sumnwr INI Pig« 2
Hospital booklet
withdrawn
Bradford Health Authority has been forced to
withdraw a booklet entitled A Guide to Maternity Services
after complaints about full-page adsfor Cow& Gate and
Farley's baby milks which appear on the inside covers.
The message conveyed doubly undermines the Gov
ernment's stated support for breastfeeding by a smaller
advertisement inside which urges readers to support
advertisers “by using their products and services.'
Oldham, North Tyneside, West Norfolk and Cam
bridge HAs have allowed ads to appear in similar book
lets - some of which contain no other information about
infant feeding. We understand that a firm in the Mid
lands arranges for these guides to be paid for by
advertising.
Why we need a law not a
voluntary Code
A health worker reports that companies continue
to dump free baby milk at The Queen Elizabeth II
Hospital in Welwyn Garden City .
Companies feel that as the UK Code is voluntary
they are free to ignore some of its provisions. They are
placing a wide interpretation on ‘professional evalu
ation and research' and are asking for cooperation from
paediatricians for 'research.' Since all the babies for
whom statistics of any kind are being collected are the
subject of research, the manufacturers are dumping
free supplies and at the same time asking health
workers to take part in joint research.
Baby Milk Action Area Contact for Hertfordshire,
Louise Lotz has volunteered to help with the monitoring
and reporting of Code violations in the UK. Louise has
been shocked at the volume of promotional literature
that she has found in hospitals, clinics and supermar
kets and says that it is clear that companies are delib
erately trying to sabotage breastfeeding.
Monitoring...
Tragedy of Kurdish babies
News reports of Kurdish babies dying during their desper
ate flight from Iraq imply that mothers are too malnourished to
breastfeed. For the refugees, who were mainly middle class and
well fed, the long walks into Iran and Turkey must have caused
great shock and stress. Nevertheless, breastfeeding rates in Iraq
are low (in some areas only 30% at 3 months) so the majority of
the babies were already bottle feeding before they left Iraq.
Lactation performance is unlikely to be affected in such a
short time and so those mothers who were breastfeeding and
whose milk diminished from the stress of the journey could
probably, with the right help and encouragement, have rees
tablished their supply. Baby Milk Action Director, Dr Tony Cos
tello, of the Institute of Child Health, London, visited Iraq for Save
the Children and confirmed this. “In my view a very significant
toumber of children, especially babies, died because they were
Ibottle fed. This is a wealthy, population who had been largely con
vinced that bottle feeding is better than breastfeeding. In the
response to the crisis, it was tragic that insufficient attention was
given to the promotion of oral rehydration and the possibility of
relactation.’ Janey Hampton, also with Save The Children,
visited hospitals in Iran where many of the Kurdish mothers were
giving birth. She was not surprised that so many mothers were
bottle feeding since they were given no encouragement to
breastfeed when they gave birth. It was standard practice for
babies to be separated from their mothers at birth for 6 hours.
Indeed if the babies were anything but "100% normal", ie, forceps
delivery, twins, low-birth weight, they went straight to special care
units (often for weeks) where mothers were forbidden to enter. All
babies in incubators were bottle fed. Of course, everything should
be done to ensure that milk reaches babies who genuinely need
it (indeed, the Code specifically allows companies to give in those
circumstances) but this tragic episode illustrates the dangers of
relying on imported products and inappropriate methods of feed
ing.
While the reports talked repeatedly about baby milk short
ages, Nestld claimed to have lost sales of about 60,000 tonnes
' of powdered milk to Iraq and Kuwait during the embargo and used
this as one of the reasons for their decline in profits for 1990.
Nestld claims that 17 kg of milk powder are neodod Io lood a baby
for 6 months. But if all babies in Iraq and Kuwait were exclusively
bottle fed for 6 months, only 13,804 tonnes would be needed.
Eastern Europe: baby
milk companies muscle in
Most baby milk distribution in Eastern Europe is con
trolled by governments, but the situation is changing with
the introduction of the 'free market'. Already, excellent
Eastern European milk banks are closing due to lack of
funding and an assumption that commercial baby milk will
replace donated breastmilk. Nestld, Milupa and others are
invading the new markets, with aggressive promotion that
undermines breastfeeding. Fortunately IBFAN groups are
being formed; although not yet properly funded, they have
the enthusiasm essential for any consumer campaign.
Nestle have bought the East German infant formula
Manasan and the price has doubled; they are also planning
a production unit in eastern Germany. Baby milk is pro
moted aggressively in Germany and mothers in the east
are already receiving quantities of gifts and samples.
In Hungary, Milupa are handing out information
booklets containing promotional messages and have or
ganised a paediatric conference. Nestle plan to set up pro
duction sites there.
Phillip Lunts, a Baby Milk Action Director, visited
Poland and found tins of Nestld’s Guigoz with baby pictures
on the label. The text was mainly in English with only the
preparation instructions in Polish.
In Czechoslovakia, where national baby milks are on
prescription only, Milupa products are marketed near the
German border. A Prague shop window had a promotional
display of Chicco bottles and teats. IBFAN also discovered
that South Africa had suggested donating breastmilk sub
stitutes here as aid. A Czech paediatrician told the aid
negotiators, "There’s no need, if we have a shortage of our
own, there is Milupa.”
In October 1990, The first WHO Conference on
Nutrition for Europe took place in Budapest and Baby Milk
Action's Gay Palmer and Dr. Clarke of the UK Department
of Health presented their views in the Infant Feeding
workshop. In April 1991, Gay Palmer ran the infant feeding
section at the Nutrition Policy Workshop in Prague, organ
ised by the London School of Hygiene and the Prague
Institute of Hygiene and Epidemiology.
Ten years of the International Code - any progress?
Company promotion continues to lure mothers and health workers
away from breastfeeding, concludes a worldwide survey of baby
food marketing published by the International Baby Food Action
Network (IBFAN). Andrew Radford of Baby Milk Action analysed
monitoring information sent by researchers working in over 80
countries, comparing it with the requirements of the International
Code of Marketing of Breast-milk Substitutes.
Chart 1: The State of the Code by Company shows lip service to
the Code alongside aggressive marketing. The 10 years since the
Code’s adoption shows improved labelling and reduced direct
advertising. However, 10 companies fail to use local language
labels and 11 still use baby pictures. Five companies are
highlighted as the worst: Nestld, Wyeth, Milupa, Meiji, and Hipp.
Company marketing practices have evolved since 1981 and large
BMAC UPDATE Summw IWl P>0« <
budgets are spent on developing new promotion methods
which get round the Code's restrictions and undermine
breastfeeding. Follow-on milks, unheard of 10 years ago,
are now promoted by almost every company. Pre-term,
soya and hypo-allergenic formulas and baby milks which
purport to cure diarrhoea are promoted and marginalise
breastmilk.
Chart 2: Slate of the Code by Country, documents the
measures taken to implement the International Code by the
governments of 169 countries. Only 9 countries have
adopted the Code as law although 12 have a good voluntary
code. Twenty eight have parts of the Code as law but 66
have so far failed to take any action. The charts are available
from Baby Milk Action: £1.50 each or £2.50 for 2.
Changes in European laws
EC allows high
sugar levels
A loophole in the compositional
standards of the new EC Directive will
allow infant formulas and follow-up milks
Faced with mounting consumer pressure and publicity, the EC Commission
agreed on 15 March, the final day of consultation, to important changes to the Directive
on baby milks. Although the final version contains loopholes and omissions, it does
not contradict the WHO Code and will improve breastfeeding protection in Europe.
The final Directive will permit free supplies only to babies who have to be led on
infant formula. The previous wording would have allowed free milk to be given to all
babies who are bottle led. The UK can now keep retain its ban on free supplies to
maternities. Now wording permits countries to ban advertising if they wish. This
means that the UK, (who wanted a ban on advertising) havo no excuse not to ban the
baby milk ads currently flooding hospitals. Baby pictures on labels and froo samples
will be banned. The Commission refused to change the age range of follow-up milks
(they will be allowed from 4 months) despite the fact that most EC member states had
supported the 6 month age limit in 1987. The Directive does not cover other bottle fed
foods (sweetened drinks, special milks etc), exports or bottles and teats.
The Commission came under pressure from all sides: from governments - the
UK and Dutch Governments were strong in thbir support for the WHO Code; from
MEPs • who threatened to overturn the Directive if it did not satisfy their demands; from
over 1,000 health, consumer and development agencies; from the public - the Com
mission allegedly received over 1500 letters; and from Wl IO and UNICEF - UNICEF's
Executive Director, James Grant wrote to Jacques Delors, the President of the
Commission describing the unmodified Directive as a serious setback in our efforts
to promote exclusive breastfeeding for the first 4-6 months.
Patti Rundall of Baby Milk Action and Bas van der Heide, of the Dutch IBFAN
group, WEMOS, who organised the lobbying met with the Commission in February.
The Chair of the Standing Committee discussed possible changes so that at least
countries could honour their commitment to the Code.
Press attention mounted until the last day with three BBC programmes, French
radio, Danish TV, Reuters and numerous journalists pressuring the Commission to
explain why they were insisting on such a bad Directive. The Commission admitted
to Reuters that free supplies were necessary mainly for the survival of the market.
The Commission's advisory committee, the Scientific Committee on Food, is
not required disclose its industry interests. IBFAN has asked the Commission to
address this issue. Please write to your MP or MEP or to Minister for Health, the Rt
Hon Virginia Bottomley, at the Department of Health, 79 Whitehall, London, SW1A
2NS, to ask for the whole of the Code to be adopted as law in the UK
Weaning Directive
Following the baby milk Directive comes a draft Commission Directive on
weaning foods. This draft covers only labelling and composition and does not address
promotion. It allows weaning foods to be labelled as suitable from 3 months, WHO
states; ‘The provision of foods other than breastmilk before about four months of age
is unnecessary and may also be harmful. "Please send comments to: Alison Maydom,
Consumer Protection Division, Ministry of Agriculture, Fisheries and Food, Ergon
House, 17 Smith Square, London SW1P 3JR. The first meeting is in June.
to contain 40-50% sugars - and 75% of
these sugars can be tooth-damaging
sucrose or glucose syrup. Product la
bels will not have to reveal sugar con
tent and can even claim - if glucose
syrup is used - that they are 'sucrose
free'. For more information on sugar,
contact Jack Winkler, Action and Infor
mation on Sugars, 28 St Paul St, Lon
don N1 7AB. 071 226 1672.
Milupa condemned on
sugar levels
Milupa have been found guilty by
a Frankfur( court of marketing a dan
gerous product with insufficient instruc
tions for use. The case was brought by
the parents of two children who suffer
from painful tooth decay alter being
bottle fed with Milupa infant teas. The
Federal Health Department had previ
ously issued warnings about this baby
bottle syndrome but Milupa only in
cluded a warning in small print on an
accompanying loallut. Infant teas and
drinks are high in sugar and, when they
are bottle fed, lead to serious tooth
decay. The Department of Health's
1989 COMA report on tooth decay
states that “for infants and young chil
dren simple sugars (eg sucrose, glu
cose or fructose) should not be added
to bottle feeds."
Another 27 similar cases are
awaiting judgment In Germany, each
claiming over US$27,000 in damages
from Milupa. Lawyers say that in Ger
many alone there are around 100,000
children sufferlngfrom baby bottle syn
drome. In German hospitals newborns
are routinely fed these sweetened teas
and baby milk promotion is widespread.
Small wonder that the breastfeeding
rate is as low as 3% at 3 months in
some areas. These drinks are now
aggressively marketed in the UK •
Boots, Robinsons and Cow & Gate pro
mote varieties in bottles designed to
carry a teat. A study in Camden shows
that 11% of bottle fed children suffer
from dental caries.
0MAC UPDATE Summer 1W1 P«9«
Boycott news ,
General Synod to debate
the boycott
/ Nestle overreact as boycott
is launched in Switzerland
The General Synod of the Church of England is to debate
a motion proposed by the Bishop of Leicester calling for
support for the Boycott - possibly in July.
Baby Milk Action meets Nescafe shop
stewards
On 3 May, Andrew Radford and Patti Rundall of Baby
Milk Action met senior shop stewards from the Nescafe factory
in Burton on Trent and representatives of the Transport and
General Workers Union (TGWU). The Nescafe workers had
been worried that the increasing success ol the boycott was a
threat to jobs. The meeting provided an opportunity for all to
express their concerns.
NestIG make no secret of the fact that "because of
rationalisation and rostructuring measures... it is feared that
jobs will be eliminated." According to the International Union
of Food Workers 1,597 jobs are to be lost due to restructuring
in France alone. If the boycott is successful, Nestld will bo
forced to change their practices before profits are reduced to
a level where job losses become necessary.
On behalf of those present. Bob Harrison, TGWU
National Secretary, expressed concern (or our campaign to
protect mothers and children from exploitation. Ho said ho
would report back to his members who would decide on further
action;
Midwives endorse boycott
In December 1990, the Royal College of Midwives called
upon its 36,000 mombnrs to boycott Noscalo and other Ner.tlrt
products and condemned "Nestld's dangerous marketingprac
tice of providing free baby milk formula to maternity wards in
developing countries". (See Boycott endorsers list.)
Stars pull out
Richard Briers has contacted a Baby Milk Action sup
porter to say that he will no longer advertise Nescafe. Felicity
Kendall is already an endorser. Nothing has been heard from
Paul Eddington. Sarah Greene has also stopped advertising
Nescafe.
Nestle have filed a complaint against the three national
Swiss TV stations for biased reporting in screening Yorkshire
TV's Vicious Circles and Australian TV's Formula Fix in Feb
ruary. The programmes, which were screened the day before
the Swiss boycott was launched, document the consequences
of marketing of baby milk by Nestld and other companies in
Pakistan and the Philippines. The films wore shown after
Neslld had made repeated attempts to intimidate the stations
into withdrawing them. Swiss broadcasting legislation requires
all programmes to be balanced and, in their complaint to the In
dependent Media Licensing Commission ol Switzerland, Neslld
claim that thn 1V companies have violated this rule.
Annolies Allain of the International Organisation of
Consumer Unions made the point, "Here was the largest and
holiest of Swiss companies being challenged on home turf."
For a country with a unique 'protection of personality' law
which prohibits criticism of a Swiss company the films amounted
to heresy. Two days before the Swiss programmes were due
to be screened, Neslld hold a press briefing with selected
'friondly'journalists. Thoy showed clips from both films without
permission, in breach of copyright, and refused to allow
anyone from Swiss TV's documentary department to attend.
The documentaries, which have been shown without com
plaint in several other countries, wore followed by a debate
between Neslld spokesperson Franrjois Porroud and Dr. Juan
Perez from the Philippines. Nestle's defence was superficial.
They maintained that not only did their formula save babies'
lives but that breastfeeding has no relationship to infant mor
tality rates.
Nestld's reaction backfired and stimulated the interest
ol the Swiss procs which reacted sceptically to the company's
protestations. Dr Jim Tulloch of tho World Health Organisation
wrote to Swiss Television to challenge Nestle's claims on the
quality ol the programme saying, “To infer....that breastfeed
ing is not important in reducing the risk of mortality in infancy
is absolutely incorrect from the scientific point of view. "The
Christian Medical Commission of the World Councilol Churches
wrote in support of tho programmes.
Nestle shareholders wrote to Nestld President, Helmut
Maucher, expressing concern at the company's response to
the programmes: "Wo thought this typo of reaction, ofplaying
down the facts and ofprofessing a perfectly clean conscience
had been relegated to the museum of tho sevonties, at the
famous Born court case..." In 1974, a Bern Third World group
Actionsgruppe Dritte Welt translated
War on Want's report The Baby
Killers asNestle Kills Babies.
Nestld sued (or libel.
This case also
backfired and
resulted
in wide
spread
publicity
for the
issue.
A carloon from a Swiss newspaper making novel
use of Nesiltf’s birds and nest logo.
rvuT
THE DANGER OF UNDER FEEDING
Kwashiorkor and marasmus are two diseases caused by
insufficient intake of food. This leads to deficiency of
calories (energy) and protein (body building material).
VICTIMS
Kwashiorkor and marasmus occur most commonly in children
between 1—5 years of age. Breast milk is sufficient for
children only upto the age of 4 months. Supplementation
with cereals, pulses, milk and eggs after the age of 4 months
is essential. If this is delayed or not done,-children do
not grow properly and kwashiorkor and marasmus develop.
SIGNS AND SYMPTOMSs
■
OEDEMA: Children with kwashiorkor first show swelling of
the legs. Later, the face and the whole body may
also, become swollen.
C
o'
<$■
£
SkIN CHANGES:
The skin becomes rough and sore.
HAIR CHANGES:
-------------- •------- ’—
"
The hair may become scanty and also change colour
from black to various shades of brown. The child
also becomes irritable and disinterested in his
surroundings.
v
Children with marasmus become very thin and feeble due
to wasting of muscles. However, there is no oedema.
TREATMENT: ’
o
The child should be made to eat more food at frequent
intervals. Severe cases with loss of appetite should Le
treated at the hospital. Milder cases can be treated at home.
The diet must contain protein and energy rich foods. A
Combination of cereals, millets, pulses and oilseeds will
provide the necessary nutrients. If possible, milk, eggs
or flesh foods should also be given.
It is important to treat infections and diarrhoea
promptly.
The National Institute of Nutrition, Hyderabad has
formulated an energy-protein rich mixture to treat protein
calorie malnutrition at the home level. It consists of
wheat, roasted Bengal gram dhal, groundnuts and jaggery.
hese ingredients can be suitably changed depending upon
local availability. The comoosition of the mixture is
given belows
•?’
- 2 -
Whole wheat (roasted)
s
40 grams
Bengal gram (roasted)
8
16 grams
Groundnut
*
10 grams
s
20 grams
(roasted)
Oaggery
86
TOTAL
Calories
. : • 330
Protein
:
11.3 grams.
Many children with protein calorie malnutrition have been
treated with this food, mixture.A-picture of one - of these
children is shown below, 'he child showed improvement after
a few weeks and was completely cured within 3 months.
rvuT b-
-,tH CELL
-loor)St- Marks Road
*...
,,,
INFANT
'■. |
.560 001
FEEDINGS
Breast milk is a nutritious food and meets, the baby's
requirements fully till the 4th month of life.. Later'; breast
milk alone is net enough to meet the nutritional needs of the
growing child. This, calls for additional food supplements.
If additional foods are not given, the baby does not grow
properly and can show stunted growth.
DEINING
v
The gradual switching over of the child from breast milk
one to other foods is called 'weaning'.
'Fast rural .Indian mother do not give supplementary foods
because of the fear that infants will not be able to digest
solid or even semi—solid foods. This is Unfortunately a wrong
belief. The right type of foods- cooked in the right way and
introduced gradually are easily digested and will greatly benefit
the child.
The first foods added to the child's diet, after 4 months can
be in the liquid form. Buffaloe's or cow's .milk, mashed
vegetables like potatoes, tender beans, carrots and green leafy
vegetables can be safely given. Many mother add too much water
to milk.thus making it less nutritious. This practice should
be discouraged.
Introducing new foods to infants is not always very easy as
some infants may not accept them readily, but the mother should
continue to coax the child till he accepts it.
At the age of 5-6 months cereals and millets can be
introduced in the form of porridges. Small amounts of pulses
should be added to the preparation to make it more nutritious.
The belief that pulses are gas producing and cause distension
on the stomach should not exclude the use of pulses in infant
feeding. Infants tolerate a fairly good amount of pulses. Green
leafy vegetables should also be added, since they provide many
nutrients like vitamins. A and C, Iron and Calcium.
These nutrients are essential for good vision, blood
formation and healthy bones. A preparation using cereal,
pulses and greens is given below?
KICHEDI
Rice
- 3^- table spoons (50 Grams)
Greengram dhal (roasted) - 2
table spoons
(25 grams)
Leafy vegetables
(Palak or Amaranth)
bundle
(15 grams)
Salt
— 1
As required
Cort
2 -
METHOD
Rice and dhal are cleaned, washed and cooked together.
Palak is cooked and strained through a clean cloth. The
vegetable juice is adr'ed to the cooked rice-dhal mixture.
Salt
is added and mixed.
Soft ripe fruits should be mashed and given to the baby.
A ripe bababa is relished by all babies. Orange and sweet lime
juices are good sources of vitamin C. These, however, are more
expensive than are green leafy vegetables.
It should be remembered that clean vessels and boiled
and cooked water should be used while preparing any food supplement
Hands should be cleaned well before preparing the food.
Eggs and flesh foods can be fed to the infant aound the
first year of life whenever they are available and can be afforded
by the parents. Initially the egg should be given in a soft
boiled form.
If the mother is busy with other work and cannot prepare
fresh supplements every day, she can prepare ready mixed by roasting
cereals and millets (like wheat, ragi and bajra) and pulses (like
Bengalgram and .greengram) and powdering them separately. These
powders can be mixed and stored in clean tins for a few months.
Small amounts of'these powders can be prepared as porridges and
fed to babies.
An example is given below..
R A G I N A
Ragi
-4 tablespoons (60 gms)
Bengalgram dhal(roasted)- 4 teaspoons (
Sugar
20 gms)
- 3-Jr tablespoons (50 gms)
flETHOD
Powder all the ingredients and cook in sufficient water.
Addition of milk makes the porridge more nutritious.
The amounts indicated for each recipe are meant to be
given per day per child. They should be distributed in the child's
diet in equal amounts during the. whole day. Instead of ragi or
bajra, wheat can be used. Similarly, any type of pulse can be used
insted of Bengalgram dhal.
Such.supplements started at the proper time will go a
long way in keeping the infant healthy and assuring proper growth.
3 -
RECIPES THAT NEED TO BE COOKED
GRAM
WHEAT
PORRIDGE
oqj
INGREDIENTS?
Roasted wheat flour
; 40 grams ( 2% tablespoons)
Powdered, roasted Bengal . 25 gramg (
gram
Powdered, roasted
groundnut
Spinach ( or any other
leafy vegetable)
tablespoons)
10 grams ( 12 tea spoons )
. 3Q gj?amg (
bundlg
METHOD;
Roast groundnut, wheat and Bengalgram and powder them.
Mix the wheat, Bengalgram and groundnut powders and prepare a Watt er
by addition of jaggery dissolved in a suitable amount of water and
made into a thin syrup.
Boil spinach in water till soft.
Mash and strain through a
clean cloth.
Add the vegetable juice to the batter and cook for a few
minutes with continuous stirring still semi-solid.
COMMERCIAL RECIPES
GROUNDNUT
BISCUITS
INGREDIENTS;
Groundnut (roasted)
s 25 grams (
Wheat flour(roasted)
S 25 grams ( 1% tablespoons)
Sugar
s 20 grams ( 4 tea spoons
Baking powder
; a pinch
Salt
; to taste
tablespoons)
)
METHOD
Powder the main ingredients and mix them. Add baking powder and
salt and mix thoroughly. Make a stiff dough by kneading the mixture.
Role like chapatis.
Cut out any shape desired with tin-lids or any sharp instruments.
Place the biscuits.on metal trays and bake them well on heated sand in a
dekchi. (The dekchi should be kept covered with a lid and pieces of live
charcoal kept on the lid to ensure uniform all-round heating).
Remove the,biscuits when they are goldenbrown
this usually takes about 20 minutes.
The quantities indicated are for use as a sup
plement per child per day. Similar biscuits can be prepared
using Bengalgram, gingelly seeds, cowgram and horsegram.
: 51 ■
NUTRITION
Nutrition is the study of foods and their actions or effects on the
body. Good nutirtion neans that the body is getting the required food
and is able to make use of it. Nutrients are substances with special
functions which are found in food and which are necessary for growth and
development of the body, repair of the body tissues, and protection of
the body against disease. They are of six types, viz., proteins,
carbohydrates, fats vitamins, minerals and water.
People generally eat or drink when they arb hungry or thirsty end,
on auspicious occasions, , they may eat or drink special foods, the foods
that people cat every day are usually not selected on the basis of their
nutritive value, but because of fe.mily habit, religion, or social custom.
It has been found that many such dietary practices, especially those
that are related to feeding infante, young children and pregnant women
arc not based on body requirements.
SOME TRADITIONAL F PCD HABITS AND' CUSTOIS ARE HARFUL TO HEALTH.
Because of e ating an unbalanced diet, many young children in India
are frequently ill due to infections, are retarded in their physical
growth, and their mental development is nega.tively affected. Unless
good nutritional guidance is given, accepted and practised by their
parents, such children will become adults who have, chronic ill health
and are unable to make their full contributicn as productive members
of the cor-TEiunity.
In addition, infants may be born weak and malnourished because their
mothers had poor diets during pregnancy. Because many women do not eat the
amount and kind of food that their bodies require during pregnancy and
afterwards, they become weak, have little- energy to care for their babies
and are unable to produce breast milk in the amounts needed by growing
infants.
NOT EATING CERTAIN FOODS EVERY DAY CAN CAUSE:
i. WEAK INFANTS CF LOW BIRTH WEIGHT.
ii. INSUFFICIENT PRODUCTION OF BREAST MILK.
iii.
RETARDED PHYSICAL AND MENTAL GROWTH .
iv. 'ILLNESS AND’ D’EMJFES'mTlXLlY^MO'NG INFATS AND WiS’CHO’PL’ CHILDREN. ’
11.1
PRINCIPLES OF NUTRITION
In order to be a.ble to assist individuals and families to learn
about and be able to practise good nutrition, you must know the principles
of nutrition.
Food is necessary for keeping the cells and tissues of the body
alive and for maintaining normal body functions.
2.
An adequate daily fluid intake is necessary for maintaining
the fluid balanced diet includes.
3.
A balanced diet includes:
1.
i. a sufficient number of calories;
ii.
adequate amounts of proteins, fats and carbohydrates;
•iid. adequate amounts of vitamins}
iv.
adequate amounts of minerals.
.................. .’Contd/52-
FROTEI1S _
Approx.
Vegetable Sources
cost
Horse gram
Rs .3 per
Kg.
March to October
XXX
Bengal gram
Rs .2/2 5 per
Kg.
Throughout year
■XX
Moong dal
Rs .2/25 per
Kg.
Throughout year
XX
Rs.1.29 per
-Kg.................
Throughout year
X ■
Buffalo Milk
Rs .2/- per
Kg.
Throughout year
XX
Eggs
Rs. 4/- to 5/“
per dozen
Throughout year
X
Fish
Rs.&/- to
Rs .12/- per
Kg.
-
January to April
September to December
XX
Wheat
Seasonal availability
Rating
Animal Sources
Annexure 11.1 contains a list of protein food sources available
in India. Refer to this list of prepare your own list of protein sources
available in your area.
Similar kinds of feed source lists can also be made for other
nutrients such as vitamin A, iron, or calcium which are also often
deficient in the diets of infants and young children (see annexures
11.2, 11.3 and 11.4).
11.3.1
JROTEIN EF BODY-BUILDING FOODS
Foods that contain proteins are needs by the body Hni ly for
repairing and replacing cells. Adequate amounts of this nutrient are
especially.important in the diets of pregnant and nursing women, infants
and young children because they have extra needs in addition to ncrmal
requirements, Pregnant women need extra protein foe ds to tafte care of the
_needs of the g-owing foetus. A nursing mother needs more body-building
foods to replace what she gives to her beby through breast feeding.
Infants and young children are growing at a very rapid rate and require
proteins for healthy growth and developnent.
11.3.2
CARBOWB/JES OR ENERGY-GIVING FOODS
In order to run, play or work, we need foods that give us energy
Carbohydrates in certain foods provide the body with energy. The
amount required by a person depends on the kind of activity he carries
out and the- time for which it is done. A man who is breaking stones all
day will need more energy-giving foods than a man who sits in his shop.
Children, especially pre-schocl children, are often not fed frequently
enough during the day so that they do not receive an adequate amount
of carbohydrates. When this happens, children become less active and
tire easily.
...................Contd/52-
: 52 :
Foods rich in carbohydrates include the following:
i.
Sugar, jaggery and honey
*
ii.
Cereals such as wheat, rice, millet, suji, maize.
iii-.-¥eg®taLbos such as potato, sweet potato, tapioca, yams
*
iv.
Fruit suchaas bananas, jackfruit, chikku, mango.
11.3.3. FATS CT. CONGENrRATED-ENETcGY FOODS
Foods that contain fats are needed'by>the body because they
supply concentrated energy, prevent dry, scaly- skin, help in the absorption
of vitamin D, and improve the flavour of ford
*
Because they, are a. concen
trated -source of energy, fats 'Supply twice as much energy as the same amount
of proteins or carbohydrates
*
This means that smaller amounts of fats are
needed in the daily diet to meet the body requirements •
- •
Foods rich in&ts include the following:
Vegetable sources:
.Cooking oils such as cocoanut, mustard, sesame (til) or
i.
groundnut oil
Animal sources:
i.
ii.
iii.
11.3.4
Butter and ghee
Milk, curds and cheese
Fish and fatty meat
VTTAI-ilNS CT. EROTECTIVE FOODS
Vitamins are substances which are found in small quantities in
several kinds of food. They are needed by the body for normal growth and :
maintenance of cells.
The body requires vitamins in small amounts. Since
the body cannot produce these substances, food sources are very important.
There are several kinds of vitamins. Seme are needed for good
vision and healthy eyes (Vitamin A)., others for blood formation (Vitamin B),
others are needed in the diet for strong teeth and bones (Vitamin- D), and
others for increasing resistance to infections and early healing of wounds
(Vitamin C).
1.
Vitamin A: In order to prevent nutritional blindness in youngg
children due to vitamin A deficiency in the diet) people must be informed
about the. kinds of foods that contain this important substance'and must be
encouraged to include it in their daily diet. In order to prevent night
blindness and dryness- of the eyes all children from one to five years
are being given vitamin A solutiin twice a, year. Foos rich in vitamin A
include the following:
Vegetable sources:
i.
Green leafy vegetables and yellow fruit like mango and papaya
and vegetables like yellow pumpkins and carrots.5
Animal Sources :
i.
Eggs and liver
-ii. Milk and curds
•
TEAMING FAMILIES- HOW TO -HlEVENT- -NIGHT BLUENESS IN YOUNG CHTTJlHENqs
A VERY IMPORTANT HEALTH EWCjaiOjO^
FOR AIL HEALTH WORKERS.
.
2.- Vitamin B: Vitamin B is a complex vitamin consisting of
several components which have various social functions.
: 52 :
4- Different types of fo-'d provide different kinds and
quantities of nutrients.
5.
The ago, activity, state of health and rate of growth
decide the amount and kinds of nutrients that are required
by the body for healthy growth and for the maintenane of
good health.
11.2
FUNCTIONS AND VAHJE-S OF NUTRIENTS IN FOOD
A~I~1 foods contain nutrients in varying amounts. Some foods
are made up of only one type of nutrient whereas others may include more
than one nutrient, e.g., cooking ail consists entirely of fat, while rice
consists mostly of carbohydrates but also contains some protein. Because
of this characteristic, foods can be classified according to the amount
of the various nutrients that they contain. It is very useful to know
which foods contain a large amount of a given nutrient so that these can be
•selected to meet the requirements of the body.
RE1EMBER THAT -A GOOD DIET IS A IDfflD DIET CONSISTING OF- DIFFERENT KINDS
OF FO(DS WHICH COl-iTAIN THE NUTRT EICTS NECESSARY FOR GOOD HEALTH.________
Each of the six nutrients that are found in food has its own
special functions to perform in the body. Those functions ’are as follows:
Proteins are necessary for growth. They help in repairing
worn-out body colls and in the formation of blood and
antibodies which are needed for building up resistance to
infection.
ii. Fats and carbohydrates provide the body with energy or' fuel
to carry out its various daily activities..
iii. Vitamins and minerals are necessary for the development
of tire blocd cells, help to maintain good vision and strong
teeth and bones, and help to promote normal growth.
iv.
Water comprises more than half the weight of the body and
is essenti: 1 for the proper functioning of body cells and
for maintaining the fluid balance of the body.
i.
11.3
FOOD SOURCES OF NUTRIENTS
When a food contains a very high amount' of a given nutrient^
it is called a feed source, e.g., pulses and dais and very good food
sources for protein, while potatoes and bananas are good food sources
for carbohydrates, but are a poor source of protein.
Protein is the nutrient that is the most important for infant
and child nutrition, hut it is the one that is most often missing in their
diet. It is, therefore, necessary to have information about protein
sources so that this can be conveyed at every opportunity to parents
and others who care for children. Because the different geographical
areas in the country produce varied kinds of vegetables which contain these
nutrients and the dishes that are prepared differ according to locality,
it is not possible to list all of them here. More accurate and realistic
information which is based on local conditions can he ■ compel'.ed by you with
the assistance of the Health Worker (Female) by de ^loping a list of
protein food sources for the villages within the subcentre. A sample
fora is given below
, „ k.. .
Contd/53-
: 53 :
These include the following:
They assist in the breakdown-and absorption of food.
They are necessary for keeping the skin and mucous members
healthy.
iii.
They are necessary for the proper development and function
ing of the nervous system.
iv.
They arc necessary for the formation of the blood cells.
i.
ii.
Foods rich in vitamin B complex include the following:
Vegetable sources:
• 'i. Parboiled rice and unpolished rice
ii.
Cereals and millet
iii.
Groundnuts
iv.
Ibises
v.
Legumes
Animal sources:
i.
Mik and milk products
ii- Eggs
iii.
Meat, liver and fish.
3. Vitamin C; This vitamin is necessary to keep the body tissues
intact arid to help in repair of the tissues. It also helps to protect the
body against infection.
Vitamin 0 is very easily destroyed and hence foods containing
this vitamin should not be exposed to air and heat.
Foods rich in vitamin C include the following:
i.
ii.
Citrus fruits such as oranges and lemons.
Guava, tomato and'amla.
4«- Vitamin D: Vitamin D is necessary for the absorption and
■utilization of calcium and phosphorus and hence lack of this vitamin causes
unhealthy teeth and skeletal deformities such as are seen in rickets.
Sources of vitamin D are as follows:
i.
ii.
iii.
Exposure to sunlight is the cheapest way to obtain this
vitamin.
Fish liver oils have a very high content of vitamin D.
Butter, ghee, groundnut oil §.nd eggs also_ contain vitamin D.
DE1®FBER THAT EXPOSURE TO SUNLIGHT ALONE IS PICT ENOUGHT IF TIE
DIET IS DEFICIENT IN FAT ♦
11.3.5
■ ■
MINERALS CTl HIOTECTIVE FOODS
Minerals are needed by the body for the formation of blood. The
development of strong .teeth and bones, and for regulating certain bedy
processes such as bleed clotting. .There are a number of minerals that
are required in minute quantities by the body. However, calcium and
iren are two of the important minerals which are needed by everyone,
especially by pregnant and nursing-women and children who are growing.
Feeds rich in calcium include the following:
Vegetable ‘sources:
i.
ii.
Lagi
. .
Green leafy vegetables.
: 55 :
Animal Sources:
i.
1 Hlk, cheese •
Focds rich in iron include the following:
Vegetable sources:
ii Bajra and ragi
ii.
Green leafy vegetables.
Animal sources:
i.
hod neat, lever and eggs.
Iodine • is another mineral, which is essential fcr normal growth
and development including the rate at which food is used by tie body.
The deficiency cf this mineral in the d aily diet is the cause of goitre •
Focds rich in iodine include the ■ fallowing:
i.
ii.
Fish of all types
Vegetables w ich are grown in areas close to the sea.
Salt which is fortified with iodine is used in are.as whore goitre
is prevalent.
11.3.6
WATER 01 FEU IDS
An adequate daily fluid intake in important for healthy functioning
of the body. Abnormal losses from vomiting, diarrhoea and high fevers can
cause dehydration (drying up of body fluids), which is a serious condition,
especially among infants and young children. Fluids in the fem of tri Ik
juices, other beverages and fruits and vegetables which are pulpy can be
used to supply the daily needs of the body.
TO PREVENT DEATH FROM DEHYDRATION CAUSED BY EXCESSIVE FLUID LOSS?-PROMPT FLUID REPLACES ENT IS NECESSARY ESTECIA11Y IN INFANTS /.ND
YOUNG CHUDEEN.
11 .4
■ A BALANCED DIET
Nutrition experts: have been able-to find out what combination
cf feeds is needed in the daily diet for healthy growth arid development.
However, this information has not yet reached many who 'live in the
villages so that they continue to eat only these feeds that have been
eaten'by their families for generations and as a result often suffer
■from various kinds of malnutrition. Often they are unaware that pregnant
women, mothers who are nursing, their babies j-. and rapidly growing young
children need more cf- certain foods to prevent their becoming ill -iv»ri .ghed.
A BALANCED DIET IS ONE WHICH IS MADE UP OF FOODS THAT CONTAIN ALL THE~
NECESSARY- -NUTEIENrS IN THE REQUIRED AMOUNTS AND PROPORTIONS TO MATNTA-T-N
HEALTH (SEE FIG. 1* .1).________________________________________
*
A balanced diet is necessary for good health. It is especially
important that proghant and nursing women,, infants and young children have
a balanced diet because these groups are most likely to develop malnutri
tion.
• ................................ Contd/56-
; 56 :
People need to know how a balanced diet will improve their health,
what fo> ds should be included, how much it will cost, where to obtain
the required foods and even how to prepare feed properly so that nutrients
are not discarded or lost due to improper cooking.
Since you will be the only health worker making regular house-tohouse visits in the twilight area, you should know about balanced diets
for pregnant and nursing women, and children, and proper feeding methods
frf infants.
DAILY BALANCED DIET FOP A PREGNANT OR NURSING WOiO
11.4.1
Select one or more fo- ds from each of these five groups:
a
.
....
f:-'ch
road, Rice. Vfcc-.t. Ebtat- , Sugar,
: 5? :
Group B: Protein foods such as Meat, Fish, Eggs, Milk, Groundnut, Dal,
Beans •
Group C: Fruits such as Orange, Banana, Ninbu(Line), Papaya, Mango
Group D: Vegetables- such as Feas, Capsicum, C: rrots, Bhindi (ladies’
fingers), Drinial, Tomato, Korela (bitter gourd), Cauliflower,
Palak (spinach), and Methi (fenugreek)
Group E: Fatty fo< ds such as Ghee, Oil, Butter
Fig: 11.1: A balanced diet
ii. Pulses, e.g., beans or dal
iii. Cereals e.g., rice or wheat
iv. Green leafy vegetables
v. Eggs
.
,
vi.
Fruit (seasonal)
twice
3 times
at least once
One every day or every
other day .
1 portion daily
Nursing mothers need more fluids including an extra' glass of milk
each day and extra servings of yellow and green leafy vegetables and;
cereals.
If the pregnant or nursing woman is vegetarian and does not eat eggs,
or cannot afford to get milk, she should be encouraged.:
to eat a handful of groundnuts each day;
to increase the pulses to 3 tines a day.
i.
ii.
Anaemia is commonly found in pregnancy and causes the woman to feel
weak and become easily tired..This can usually be prevented by including
a serving of a green leafy vegetable in the daily diet, and by taking the
iron and folic acid tablets which are distributed at the subcentre or on
the home visits by the health worker,.
In sone communities women eat less during pregnancy becuase they
believe that they will then • have a smiler baby and an easier delivery.
People need to knew that this is a harmful practice which can lead to mal
nutrition in the mother and low birth weight <bf the infant who is al an
malnourished.
REMEMBER THAT A SPALL BABY AT SUITE HAS LESS CHANCE OF SURVIVAL AMD IS
ME T.TKTCT.V TO CRT SICK BECAUSE CF LOW RESISTANCE TO INFECTION.
11
2
*
4
BALANCED DIET FOR. INFANTS (ZERO TO 12 MONTHS)
The major points to remember about the diet for and feeding of
infants are as follows:
1.
Breast milk is the best food for infants up to the age of .six
months because:
.
;
< ..
i.
ii.
iii.
it is-clean arid safe;
....
it contains all the necessary nutrients
no cost is involved.
•> ■
’’
..
After four months, all infants need to be given solid, food
since breast mi,1k does not supply all the nutrients that a rapidly
growing baby requires.
3- During weaning the ’first’ foods should be semisolid in consistency
e.g., mashed rice, millet, banana or potatoes. Gradually solid
foods from vegetable and animal sources containing protein must
be added so that the infant receives a balanced diet.
2.
: 58 :
4« Remove the infant’s portion of food before spices.are added
for the rest of the family otherwise the baby will develop «'
diarrhoea.
.
5 • Give the baby a spoonful of food at first and gradually inc: ease
the amount given over a period of weeks.
$*• Tho addition of foods other than milk to the infant’s diet
should be done gradually over a period of tine rather than
■ all at once.
7.
Glean hands and utensils and fresh foed are necessary for
preventing infections. Fbcd must be kept covered so that flies
do not sit on it. Water she Id be obtained from a safe source
of supply or boiled if possible. Never feed an infant with left
over foods because they are very likely to be spoiled and will
cause illness.
. '
.
8.
If the mother does jot produce enough breast milk, do not
suggest the use of a bottle and nipple; use of a. cyp and
spoon is safer since they are easier to keep clean.
9.
Breast feeding should be continued throughout the first year
so that the infant continues to receive valuable protein from
•
■
this source._____
'________
_
_____ ■ ____66
REMEMBER THAT THE MAJOR CAUSES OF BKNUTlfi liON IN INFANTS AND YOUNG
CHILDREN ARE:
i.
DELAY IN ADDING SOLID FOODS TO THEIR DIET .
ii . NOT FEEDING THEM FREQUENTLY ENOUGH .
iii.
THE LACK OF .CQDY-BUILDING EROTEIN FOODS .
iv.
INSUFFICIENT FOODS' CONTAINING THAI-UN A .
11.4.3
BALANCED DIET FOR THE JREASCHOOL CHILD (ONE TO FITE YEARS)
Children between the ages of one and five yoarp are often neglected
and underfed by their mothers. This happens because mothers do not know
that these children need proportionately more food for -uheir size than is
needed by adults. Becuae they are growing at a fast rate and the growth
is continuous, they need extra amounts of body-building protein food and:
energy-giving foods.
In many poor families, young children are breast-fed until they
are two or three years old and are not given any other foods eaten by the
rest of the family. This practice results in a high incidence of kwashi
orkor and marasmus, the former of which is caused by a deficiency of protein
and calories in the diet, while the latter is due to deficiency of calories.
AFTER FOUR MONTH
*
GF AG?, A DIET CONSISTING CF ONLY BREAST MILK IS
INADEQUATE ..
■ ~
A daily diet for children one -fo five years should include the
following:
1. Milk
2. Cooked cereal - pulse
mixture (khichiri, dalia,
idli or groundnuts)
3. Green leafy vegetables
(Ralak, chawli) and yellow
vegetable or fruit (carrot
pumpkin, papaya, mango)
4. Cooked cereal or millet
(rice, wheat, ragi)
-
1 tumbler
8 to 12 level spoons
-
4 to 8 level spoons
4 to 16 level spoons or
1 to 2 chappatis
: 59.:
5« Egg
or dal
or fish/noat
6.
Fresh fruit
• (banana, guava or
Tomato)
-
-
One
4 to 8 level spoons
4 to 8 level spoons.. , «
one portion
The feeds for the child, under two- years should be snail in amount
and should be given at shorter intervals than for the rest of the family.
The following foods should bo avoided in the diet of young children:
i.
Highly spiced dishes and curries.
ii.
Foods made with largo amounts of sugar.
iii.
Very greasy foods.
iv.
Poorly cleaned, insufficiently cooked, or improperly mashed foods.
Dietary instructions are easier to follow for most individuals when
they understand the amounts to be eaten in terms of commonly used measures
(see fig. 11.2). When utensils are not available in -the home, you will
have to give instructions regarding the quantity to be consumed in terms
of a 'a handful of dal’, or' 'one banana1, etc.
Fig. 11.2: Common household measures
Mc|
°£
Child can eat at one meal depends on
has health, body size and physical activity.
: 60 :
In the preparation and serving of food for children, it is
necessary to follow certain procedures in order to:
i.
ensure that the food is safe and clean;
' ii. preservo the nutrients in food;
iii.
nake the food more easily digestible.
These-procedu’ es are as follows:
1. Before preparing food or feeding the child, wash the hands
and utensils with C^-ean water.
Use unpolished hand-pounded or parboiled rice instead of
pplished rice.
3.
Whenever possible use only fresh fruits and vegetables.
. 4- Do not expose picked vegetables to sunlight.
5.
Clean and wash vegetables before cutting or slicing then.
6.
Avoid soaking cut vegetables in water before cooking.
7.
To reduce the incidence of diarrhoea caused by indiegestible
fords, nake then soft and digestible by:
2.
a.
b.
c.
d.
8.
- ■
soaking dried foods before cooking;
removing husks from grains;
cooking until soft;
mashing feeds.
Do. not throw away the water used for cooking vegetables but
use it for preparing soups or other dishes.
Avoid prolonged cooking, reheating already cooked foods, or keeping then warn over a period of tine..
MANY FAMILY DILTS CAN ffi IMIKOVED’ BY THE AbDUION OF:
i.
MORE HJLSES CR DAIS
x ii • GREEN LEAFY VEGETABLES
iii.
YELLOW FRUIT OR VEGETABLES
THESE/CHANGES GAN BENEFTjC All' IN THE' HOUSEHOID'.
Additional methods for increasing the nutritional values, of-foods
are as follows:
1. Sprouting pulses, i.e. Bengal gran, black gran or green gran,
increases the vitamin 0 and' ribonilavin (vitamin B) content.
Such processing also increases the digestibility of pulses
so that they are especially good foods for young children.
Sprouted pulses should be prepared and served either raw
or lightly cooked-in order to preserve the nutrients. .
2.
Fermenting cereal and dal increases the vitamin B content
■ of both foods. This is commonly done in South India, e.g.,
in preparing idli and dosa.'
3« Mixing a pulse with a cereal as in Khichadi increases the
quality of the protein eaten.. Less of each is required for
meeting-the daily requirements.
In annexure 11.5 a few nutritious recipes-are included. These
are selected according to the foods available: in the noritem, southern,
eastern and western regions of India.
11 .5
KITCHEN GARDENS
Encouraging families to plant kitchen gardens and to eat the produce
should, also bo considered a part of your work in the delivery of nutrition •
services tc tile’people who live in the area.
: 61.:
They need to be helped to understand how growing fruits and
vegetables for the family will help then to cat better and improve their health
health. Other benefits of kitchens gardens arc as follows:
i.
Less money is needed to buy food.
' ii. Fresh produce usually tastes better.
aii. Fresh fruits and vegetables contain more nutrients than those
that have been picked earlier, handled and transported.
iv.
Sullage water can be utilized, and is, at the same time, disposed
of in. a hygienic way.
You can help families who want to "plant a kitchen garden by giving
then advice so that they cs.n decide where to locate' it, uhe size of the
plot needed, and the amount and kinds of vegetables or fruit to be grown.
' If they require more information than you are able to provide, you can refer
them to the local agricultural, worker who is attached to the Block Development
Office.
Kitchen gardens should be located:
i.
ii.
iii.
iv.
v.
near to the house for easy care;
near to the source of water;
sc that there is exposure to the sun;
in rich soil;
on land with a gentle slope and with good drainage.
In deciding the size of the plot, the family should- consider:
i. the time available. to cultivate it;
ii.
the number of members in the family.
In deciding the amounts and kinds of vegetables and fruit to grow,
the following factors should be considered.:
i.VJhat arc their food preferences?
Do
ii.
they need sone to eat fresh and others to store?
_iii .Which vegetables are needed to improve the family diet?
Is
iv.
fresh water or sullage water used for watering the garden?
(see also section 6.2.1)
EACH FAMILY SHOULD BE ENCOURAGED TO PL/.i-T AND E/J? THE VEGETABLES
Al® FRUIT THAT THEY- GROW IN THE KB? CHEN GARDEN SO THAT THEIR DIET
IS IMJROVED .‘
11.6
MAKING EFFECTIVE VISITS FOR IMPROVING FAMILY NUTRITION
In order to "alee your nutrition education activities effective, you
will liavc te collect or find out specific information related to the diet
ary habits and practices of. the community in order to decide how best to
assist them to improve their food habits. The information that you should
collect includes the following:
1 • The Banes of locally available foods, especially those that are
rich sources of proteins, minerals, and vitamins.
The typos of fo<d which arc being eaten or not being eaten bv
the family.
3.
Whether or not the pregnant and nursing women in the family are
being provided with extra amounts of food cr special foods.
4« The kinds of fo ds which- are toeing fed. to children above four
months of ago.
5.
The duration of breast feeding.
6.
Whether supplementary snacks are being given to young children
betr cn ••.oals until, thrnr rrc, nh"'n +.-> t
n fll-’n fn.T'il-'- -'cal.
2.
:62 :
7.
8.
11.7
Fbople * s knowledge about the nutritional value of fbods
and methods for preserving the nutrients of food.
Whether the family can afford to implement the suggested
changes in dietary practices.
HEALTH EDUCATION
Sone of the topics which you should talk about in relation to
inproving the diet are as follows:
1. Pregnant and Nursing Women
i. The need to include more proteins, vitamins and minerals
as well as additional calories in the daily diet.
2.“Pre-school Children.
i. Tlie continuation of breast feeding for the first year as
breast milk can supply protein to supplement the diet.
The importanace of nixing pulses and dais with the staple
cereal to increase the quality of protein.
iii.
The methods of preparing, food so as to make it softer
and more digestible.
iv.
The.importance of avoiding spices in the child's diet.
v.
The need for including body-building foods, protective
foods and energy-giving foods in tho 'cliild’s daily diet.
vi.
The importance of cleanliness in the preparation and
solving of food.
■ vii.’The need to ensure that the child gets a sufficient daily
diet-.
ii.
NUTRITION TEACHING FOR CHANGING BEHAVIOUR BECOMES MORE EFFECTIVE
WHEN FAMILY JRIOR-ITIES Ad© FEASIBILITY ARE OONSIDEIED AJ© THE • •
INFORMATION OR MESSAGE IS CLEARLY RELATED TO THE -IDENTIFIED PROBLEM.
11 .8
I-iALl-UTRITIOH
Malnutrition is a condition which occurs when the. body does not
get the proper kind of food an tho amounts that are needed for maintaining
health.
MALMJTRETION IS A COMMON HEALTH HIOBLEM -AMONG YOUNG CHILDREN IN
Iim. • EIGHT OUT OF EVERY TEN IRE-SCHOOL CHILDREN SUFFER FROM SO IE
DEGREE OF MALNUTRITION.________________________________________________
11.8.1
WHAT YOU SHOULD KNOW ABOUT 1 A.LLUTRIT ION
1. Poverty and parental ignorance regarding proper feeding
and diet for infants .and young children in addition to
incorrect family f ood habits and customs are nnj or factors
responsible, for malnutrition.’
2.
A failure to gain weight, or loss of weight in young children
.. are signs of early malnutrition.
■'3. Serial or repeated weighing is the best method for identifying
malnourished children.
4.
Early identification and correction of malnutrition are
important because severe malnutrition permanently affects the
physical and mental devel op.ientof chil dren and may load to
death.
: 63 :
’
5« Children who develop infections with-fever or who have worms
or repeated bouts of diarrhoea can develop rialnutrition if care
is not taken to meet the extra food requirements of the body.
6. Tlie larger the size of the family, the more likely is it that
one or more children will be malnourished.
7.
iJlien a child is ill, food and fluids should not be withheld but
should be given in order to prevent malnutrition.
8.
The largest number of malnourished children are between six months
and three years of age. Look for malnutrition in this age group
in the community.
9» The most common conditions caused by poor diet and incorrect
eating habits are:
i. Kwashiorkor, from lack of protein, e.g., dais, grams, milk
and eggs, as well as lack of calories.
Nutritional marasmus, from insufficient calories because of
not eating enough focd. ■
i ii. Anaemia, from lack of foods containing iron and vitamins,
g.,
e.
green leafy vegetables, eggs and foods from animal
sources,
iv.
Night blindness from lack of foods containing vitamin A,
e.g., yellow fruits and vegetables.
- Rickets from lack of foods containing vitamin D, and fats
v.
such as butter, groundnut oil, and eggs.
ii.
■ '
11.8.2
IDEIffIFICASION OF- MILHUTRITION IN IRE-SCHOOL CHILDREN
Young children have low nutritional reserves and, therefore,
require a relatively higher amount of calories and. proteins in order that !.
they may grow and develop normally, Insufficient foods of the right kind
in the diet of a young child will result in malnutrition.
There are several methods commonly used for identifying children
who are malnourished in a community. This can be done by:
1. Weighing and measuring children regularly.
2.Measuring the circumference of the upper arm.
3
.Systematically looking for children who are more likely thah
others to develop malnutrition.
4« Systematically looking for children who show signs and
symptoms of nutritional deficiency.
Your major responsibility is to identify children who are rialnourished as early as possible so that curative measures can be started prompt
ly.
1. Regular Weighing and Measuring: The best way to identify" young
children who are malnourished is to weigh and. measure then regu
larly (monthly for infants and at three to six month intervals
for those who are older). Those children who do not show consis
tent, growth and weight, gains over tine are either sick or mal
nourished (see Weight" Curve Chart, Fig. 11.3)..
Children arc usually weighed and measured in the clinics held at
the subcentres or by the health workers who nake regular domicil ia-ry visits.
Follow the directions on the Weight Curve Chart in deciding what action to
take when the weight of the.children is below line I (see fig. 11.3).
.Contd/64-
WEIGHT
in KILOff'I
PAFSiTS SHOULD D3 LiCCi t-AGSD 10 TAICE TULIP GHUDL3E KEGUURLY TO THE
OLZIO AT l.n. S\.TQT-'.TBU F" k 1IZTL1.'’ 2Wl;&’I0iJ, ’JEIGiilSG AI0 ?EASUR-
Weights of average well-fed healthy children should
be above'the uppernost line I.'
Children whose weight’ fails between lines I’and in.
arc tinder-nourished and require supflenontrry. feed
ing at litae»
Children whose weight falls below lino III
several;
rialncurishcd. Consult the doctor an.! follow hi s 'at Ivie:
Children whose weight falls below line IV will have tp
be hospitalized for- troatuent.
Fig. 11.3: ’’eight curve chart
2.
^ensuring Idd-ara Oircunfcren.ee: The identification of children who
are nalnourished can also bo done by rseasurihg tJ .c distance around, the
rdd-am. This should bo done by bavin;' the anti lianr-; lor.se at the side
•of the body and. jfLacing t?'.c ari.i circuuforcncp. sc.-Io s.t
? r.id-pcint
us showp in fig. 11.A:; h b. Any cliild between the ages -:f one and five
5=-oars is considered to be nalncurishe'." if this neastu'evsent is less than
12-8 cn.
*
'
.Ccntd/65-
: 65 :
IMMUNIZATION SCHEDULE
GUIDE TO BUTRITIOi!
S.'EjLFOX
hnirry: at birth or as soon
lifer as possible
feination of Scar
REACCIiLATION at one year
an- overj three years,
threafter
Date?
pate
Date
Date
D ,te
V.SERCU LOSIS (D.C.G)
Hnary: at birth er as soon
£ter as possible
Saoination of- Scar
Date
Date
^IHEHERIA-WHOOPING OOUGH3TAAUS)
(Triple Vaccination)
.-inarysfren /th month
Two injections at interval
?: 8-12 weeks
SISTER: 1-1/2 - 3 years
BIRTH TO 01® YEAR: Breast Feed’
Breast nilk is not enough for the baby after
six riontte. He needs additional nouritsh'• -ent• Continue breast feeding 'as long ab
possible and introduce the .following solids
gradually.
FOURTH liOBTII
Introduce frosh cow, buffalo, goat or tinned
powder nilk if breast i.-.ilk is insufficient.
Bice, Suji, Ragi (Dhajia) etc., well cooked
to a soft consistency and sweetened.
Vegetables like potato, carrot, cooked and
nashod.ft
' -+
hashed ripe banana-sweetened, orange/
sweet line/tonato juice.
Date
SIXTH liOnTH
Date
In addition to solid foods already given
Date
introduce the following:
•
Date
Bread,; biscuits,.dials’like; Bangal gran,
5 years
_________ _lentilj. red. gran' - well - cooked, FishILIOlu'ELITIS (Oral trivalent v;accine)
boiled, Boat - well- cocked and' tender,
Date
binary: fron /th -month
Eggs-half boiled, Curd, buttor-mlk-Clianna (Casein),, vegetables like cauli
iree doses by mouth
Z-6 weeks interval
Date
flower, cabbage, cucunbor, etc. All
HTPHOTD-FARATYRHOID
fruits.
Ol.G YEAR
rirary: at 1-1/2 years or l?ttier Date
'wo doses at 7-10 days
Child can share the. fa’lily food, except hot
■ interval
Date
and spiced foods. BOOSTER: Two doses at 7-10 days
Do not wait for the baby to cut his teeth
interval every year
Date
to give solid foods. He will digest well
cooked vegetables, rice, suji, etc., even if
TZPHTHEFXA - TETANUS
he has no teeth to chew then. .
rbinary: when triple vaccine
Wash your h a.nds oefore preparing food, cooking
given durin!" infancy
Date
or feeding.
•V- injections at 8-12 weeks
All foed for the baby should bo freshly prepared,
vo?ks interval
Date
no left-over be given.
£C-STER:One injection at 5 years Date
All utensils like cups, spoons, bottles etc.
doctor/nufse will record tine date of
should, be washed in boiled, water and kept covered.
gring the injection and toll you when to
srpg the child for the next one.________
i-I .C .H . CARD II
Child’ Card
(To be kept with the riother)
FHC/S .0/1 .C .D. Centre
.Registration No.
Vil"
••Katie:
. L/T .
. Date first seen:
Date of birth :
Orlc.
No. of brothers:
birt
Religion:
Sistr.
Diet:
Vegetarian/NcnHbther’n nano:
Occupation:
Fatter's name:
Occura.ti.on
:
Address a
:
Medical notes:
Blood Group :
Allergies:
Other infornation: ■_______ ,
Fatiily Hanning status of pt
Have your child weighed regt:.
Weight will be narked on thi
Bring your child to the cent:
month till his second birthd .
every three months till his’ f.
birthday and any tine he dot..,
appear well. Protect your cln
from diseases by giving hit; j.
zations shown on this card.
services are given without ■■■:'.
Ministry of Health and Fanil’,
planning, Birman Bhavan, New .
: 66 :
;.l
j|
5
j
0
7cci
I
|
“
Rod
u _
“
/ Acllovz I
12»5cli
I
Green
13 -5on
j
ARi; ar.?a.; j-epeece scale
---------------------------------------Colour Code
17.5cn
(adapted from
Ifel-nour- Possible Norml
iidnan Shakir
ished
Ifel-nntri
Sc David. Mbrloy-1
tion
The Lancet.P 758759, April 20,
1974
under 12.5cm Malnaurished
Yellow 12.5-I3~5cm Possible
mlnutritionGreen, over 13.5cm Normal
Red
Fig: 11.4b: Arm circumfcronco tape
3.
Characteristics' of Chaldron who' arc likely to Develop ihlnutrition:
The system tic search for :alnourished children in the cbpmnity can bo very
fruitful when your effort s are concentrated among those who have certain
social characteristics which are as follows:
i. The child is one of twins.,
ii.
The child has no living parents or. has a stepmother.
iii.
The child is cared for during the day by an .oldor sister or brother
while the mother works.
iv.
The child hah a younger sister or brother and the difference in ago
is loss than onc year,.
v.
There are four or more children in the, family. «
. vi. The child belongs to a migrant family4"'’('4,1
■<
'
vii.
Tho child .is obviously thinner and svrUef’ than others of his ago.
and which can cause sxgnxiacaau
.
. . .
occur in infants anl y'ung children, whereon others arc seen in persons
ox all aces. A feu er. ?, bo fatal or canto the underlying cause of death,
while others way lead to serious disability. Those diseases arc. as
follows:
Kwashierker (Protein Deficiency) is a serious disease which develops
in young children, usually between one and t> re.; years, who arc fed
diets which lack sufficient amounts of protein
calories to meet
body requirements (see fig.-11.5) • It can also .-l_’.olcp in previous
ly malnourished children following diseases such as measles, whoop
ing cough and .lalaria. If adequate treatment is not provided,
clnldrc.n with kwashiorkor can die (see section 11 .8.3) .
Fig : 11.5: Kwashiorkor
b.
i-ferasnus (see fig. 11.6) i.s the technic?! tor for the severely
wasted, undernourished- child or adult. It is a sorioud disease
which, can occur at any age when a person docs net oat or got enough
food which is require-’ by his body. In young children the condition c
often dcvolcps during the second year when breast feeding stops and
provision is not rads for giving Ilion sufficient amounts of nilk and
other feeds to meet the daily requirements, e.-;., small supplementary
feedings until the child is able to consume sufficient feeds during
tlic regular family meals (see section 11.8.3).
BeSHICRKOF. At© hARASiUS ARE DlSEASrS lu'.-’H SERIOUS COSWllwCE-S SCfbSE
’ll- I'?'CAUSE TUySSo
D li'TIi. ’E’iTD H-IHSTOZi. 'lTT ■ ‘
yg':
: 68 :
c.
d.
Anaemia (soo section.11.8.4)
Vitanin .deficiencies'
..
---•
i. Vitanin A: Drynefes of the eyes occurs due to the lack of
vitanin A in the diet of young-children (sec section 11.8.5).
Vitamin 3: Signs' of symptoms of vitrain 'B'deficiency include:
A sore mouth and tongue, cracks and sores at tho angles of
the "icruth, jain; numbness and reduced sensation in tho limbs.
iii.
Vitamin 0: Persons who do not consume sufficient anejunts of fresh
fruits and vegetables containing vitanin C develop spongy,
bleeding guns, loosening of tho teeth,--and- haemorrhages under
. ' the skin.
- iv. Vitamin D: Rickets is a disease caused by a deficiency of
. vitamin D in the diet, or lack of exposure of thc-skin to
sunlight. It can result in permanent deformities in the bones
.. - (see-fig ."1T;7) • Signs and symptoms include soreness pnd tender
ness of tho body, delayed cruption of teeth, bulging |of the bones of
of the head in young children, bow legs, beading of the ribs
-and; deformities of the pelvic bones.and-spine.
ii.
c. Mineral deficiencies: <
i. Calcium: A deficiency of calcium in the diet can result in
rickets, interference with the clotting of blood, deformities
. of bones such as knock-knees and poor tooth.
ii.
Iodine: .Goitre is a disease characterized by swelling in the
front of the neck (see fig.11.8) . It occurs most frequently
in areas whore the food and water arc doficine in iodine.
The increasing use of iodized salt by persons living in such
- areas has decreased the number of people affected by goitre.
ANY PERSON WHO HAS SIGIS Gt SYMPTOMS OF MALNUTRITION SHOULD BE
FURTHER SCREENED SINCE HE WILL OFTEN HAVE .HO1E THAN ONE NUTRITIONAL
DEFICIENCY.
: 69 :
3
*
11.8
KWASHIORKOR AID KEASIDS
If an infant or pre-school ' chi 1 d (under five years) is found to have
any of the following signs and symptoms, proceed' as follows:
|
7
Kwashiorkor
I Miserable and apathetic
General appearance
Oedema of feet and' leg^"
i’ferasnus
Mr
Alert to people anc
■ surroundings
‘ No
Yes
Appearance of face
Fat or "noon" face
Thin or "old.nan’s"
face
Hair colour and texture
Lighter than in others
or reddish.and brittle
Normal colour and
Springy
Weight
Below normal1
Muscles
Thin and flabby
Very thin, bones
showing .
Skin
Stretched and taut,
also has flaking of
skin
Shrivelled' and
wrinkled
Refuses'afood
Accepts feed offered '
/
Appetite
I
•
’
•
Very much below
normal
y
Arrange for
transport to ■ the PHO
Instruct mother to
-increase quantity •
of feeds '
Refer
Inform the Health Worker (Fenale)
*To check for oedema, see section 21«4
Roth of the above children have severe malnutrition and must bo referred
to the Primary Health Centre for further treatment. Unless prompt re
ferral is made, such children may die•
11.8.4
ANAEMIA
Anaemia is a. condition which is commonly found in pregnant and nursing
women'and in children.
(For causes, signs and symptoms of anaemia see section-21.5)•
: 70 :
ONE (F YOW IMF0P.TA1T TASKS AS A HEALTH WORKER IS TO IDENTIFY
ANAEMIC WOMEN ill-D CKIIDREH IN THE COMDNTTY ASEARLY AS POSSIBLE
SO THAT THEY CAN BE TREATED EROMITLY AID HE TAUGHT HOW TO PREVENT
THE RECURRENCE CF THIS CONDITION. '
1. Facts that you should know about anaemia and health
i. Children who are anaemic suffer from minor illnesses more often
than those who aro healthy, and. the illness is often nore severe
than in normal children.
ii.
The incidence-of ana.enia and. its effect on health is highest amongl
pregnant and nursing women and ’pre-school children.
iii.
Pregnant women who aro anaemic often have seripus complications,
c.g., haemorrhage during childbir h, and produce babies who are
also anaemic at birth.
iv.
Anaemic invididuals generally take a longer time to recover from
infections.
Fig. 11.9: Examining the ye for anaemia
2.
Method for identifying those are are anaemic: There are several ways
that cante used to find those who are anaemic as you make your houseto-house visits. Look for mothers and children whose skin is pale and
those who tire easily and have little energy since these are the signs
that are commonly associated wife anaemia. Such persons should further
be examined as follows:
i. Pull down the lower eyelid to look at the colour of the coniu, ^tiv(sec fig.1-1.9).
BEIEiPER TO WJSHJOUK HANDS BEFORE DOING THIS AD BE CAREFUL. NOT TO
2r'.C0HJUNCT7V --""GE CWJG i>H
_0 ,.'SE INFECTION .
: 71 :
If the conjunctiva is pale pink or colourless, the person is
anaemic. A bright pink conjunctiva usually moans that there
is no anaemia.
%ii. Full down tho lown the lower lip to look at the colour of the
mucosa lining the mouth. If it is very pale pink or colourless
the person is anaemic. A 1 right pink mucosa usually means that
there is no anaemia.
iii . Find out the percentage of haemoglobin using a Tallquist colour
scale •
1
Procedure f>r determining anaemia using the Tallquist method.
Eembmbcr that befqrc doing any procedure, especially- one that is
connected with losing blood, you must get the cooperation of the individual
by explaining;
- i • why it is needed;ii. how it will bo done; <
\
iii.
whether there will be any pain or discomfort associated with it.
Proceed as follows:
.
■>
1. Collect and assemble the equipment, viz •
i. Sterile Hagedorn needle embedded in a cork and kept in a
container of spirit so that the tip.remains covered by the dis
infectant (see fig.11.10a & b).
ii. Spirit or Sp.vlon.
iii.
Cotton wool•
iv.
Tallquist papers and colour scale.
Fig.11.10: Hagedorn needle
2.
Carry out tho technique: Any procedure that breaks tho skin nay
load to infection so it is important- to take certain precautions on
pricking the skin.
: 72 :
■'
3.
i. wash ycur hands and allow then to dry by shaking in the air.
,,ii. Hold the individual's finger, usually the loft ring finger, •
, ;; ot; loft! big
*
too tightly for about 10 seconds to collect a
goed supply? o f.blood•
iii.
Wipe the area, to be pricked, i.c. the side of the finger tip
er big toe with cotton w ool noistoned .with spirit or Savlon
and allow to dry.
‘
'
iv.
Renovo the needle from its container, shake off any excess .
spirit, and prick the finger or toe with a quick jabbing notion.
v.
Squeeze the finger until a large drop of bleed appears and blot
it into a piece of the Tallquist paper (sec’ fig.11.10b).
vi.
Talco a piece of cotton wool noistoned with spirit on the finger
and ask the person to press it with his thunb until bleeding
steps.
vii.
Compare the colour of the bleed on the paper with the colour
on -the Tallquist scale tc dctcraino the hacnoglobin level.
viii.
Record the hacnoglobin level on the individual's health card.
ix.
Explain the test result to the individual.
Mninistration of iron and folic acid as prophylaxis against nutri
tional anaemia in mothers and children
Eligibility for iron and folic acid: The following criteria.arc to
be used tc determine who arc eligible to be given iron and folic
acid and who should be referred to the Primary Health Centre:
i* All pregnant and nursing women who have 10 gms (70 per cent)
hacnoglobin or less according to the Tallquist scale should be
referred to the Primary Health Centre for treatment. If the
haemoglobin level is between 10 to 12 gns (70 to 80 . per cent)
given iron' and folic acid tablets.
ii. All family planning acceptors who have 10 gms haemoglobin or
less, according to the Tallquist scale should be referred to
the Primary Health Centre for treatment. If the haemoglobin
level is 10 to 12 gran?, give iron and folic acid tablets..
iii.
All infants aud .pc-school children (under five years) who have '
8 grans haemoglobin or less according to the, Tallquist scale,
should bo referred to the Primary Health Centre for'treatment.'
If the hacnoglobin level is .8 to 12 grans give iron anf folic
acid.
Dosage of iron and folic- acid:
Form of
drug
Dosage of
folic acid
Pregnant and
Tablets
nursing women
and family planning
accepters
0.5 mg daily
180 ng daily
Children under 5
Tablets or
years.................... ‘" liquid
0.1 mg daily
60 mg daily
Category
Give the treatment for three months.
week supply of the drugs.
Dosage of
ferrous sulphate
Dispense a two to four
Health teaching related to treatment: Individuals who are anaemic
and are being given iron and folic acid tablets need to have the follow
ing informaticn:
: 73 i
ii Iren and folic acid arc special drugs -that arc needed by the
body for raising the haemoglobin content in the blood.
ii. Tc be effective, both drugs must be taken daily in the prescribed
dosage, together with feeds rich in iron;
iii.
Foods rich in iron such as leafy vegetables that-arc available
locally should be included in the daily diet .
iv.
defense the drugs can irritate the stomach they should always be
taken with seme food or at mealtime.
v.
The tablets will make the faeces black, but this is an expected
action or iron and should not cause alarm or worry.
vi.
If the person has symptoms such a s diarrhoea or indigestion, she
should inform ycu about this since the dosage or frequency of the
drugs may have to be charged. ,
vii.
After three months of treatment tht blood test will be repeated to
find out the haemoglobin level.
viii.
To avoid accidental ingestion of the drugs by small children, the
medicines should bp kept cut of their roach.,
ix.
A fresh supply of drugs can be obtained either at the subcentre or
from the health worker.
feking follow-up contacts: Follow-up activities can be carried out when
1the individual comes to the subcentre, or during borne visits. Points to
remember include the following:
i. If the individual does not cone to the subcentre within two to
four weeks after the drugs arc dispensed, make a hone visit to
assess tolcranfc to the'drugs, side-effects if any, regularity in
talcing the tablets, and whether foods rich in iron have been
added to the diet.
■ ii. Listen to complaints related to taking drugs and reassure the indivi
dual.
iii.
Dispense a two to four week supply of the drugs if needed by the
individual, but urge her to ob ain them from the suboentre on a
regular basis.
iv.
Plan to repeat the Tallquist test after the individual has been
taking the drugs for three months.
Records and reports: You are required to maintain the following, records and
reports pertaining to the iron and folic acid tablets that ycu have dispensed
to eligible persons in the community (soo Annexure 1116 Forms A, B and 0
in the Supplement to the Manual).
. a. Individual recipient’s, health record: The individual card of the
pregnant or nursing woman, dild, or family planning acceptor
should include:
i. the date of the blocd test and the haemoglobin level;
ii. the date of commencing the prophylactic treatment, dosage
of the drug, and the number of tablets dispensed;
■ iii. the date of the repeat blocd test and the haemoglobin level;
iv.
the date when the drug ®s stopped and the reasons for
stopping it.
'
b. Register of beneficiaries: Enter the card number, date of enrolment,
name, ago and category of each beneficiary a nd date, of stopping the
treatment (see.Ferm A).
c. Steck register: The number of tablets received, issued and in
balance on each date are recorded' in the stock register (see Form B).
d. Monthly report to the Primary Health Centre: This is a consolida
tion of the information in’ Mos. 2 and 3 above (sec Form C).
11.8.5
VTTAMHT A DEFICIENCY
Vitamin A deficiency in the diet is a very serious health problem in
Indi?.. A large number cf rro-schccl cliildron have eve symptoms as a result
" •” i??t arc doficic-t in vitamin/..
: 75 :
specific dates for coverage of eligible cliildron.
Select the nest easily accessible location in the village
to facilitate attendance and rake arrangements for its use.
iv.
Decide on the content and methods to be used for irc-programno
publicic; -.-.nd health education of village leaders -.nd parents.
iii.
v. Estimate the amount of drug needed and procure the supply and
calibrator s; . ns or drop, ere from th., Pr.jr.r7- Health dentro.
vi.
Store the drug in a cool, dry place.
Select simple tas’ s to be done by volunteers and train the
community monebers to assist with the programme.
Coordinating activities with the Health Worker (Female): Your
task is to administer vitamin a to as many children aged one to five years
as possible in each village. In order to achieve a high coverage of such
children and to avoid duplication of adi.iinistra.tion, y u will need to work
closely with the Health Worker (Female) since y u will ho th be making visits
to the same families at different intervals for ckSSvoi'y of specific health
services.
Procedure for administering vitamin A solution;
1. Use a 2 ml. spoon (supplied with the vitamin A solution) ®r.
medicine dropper which is calibrated to measure the 2 lakh dr
unit dose (2 ml) which is prescribed (see fig.11.11).
2.
Instruct the mother to hold the baby in her lap with the
head raised sc- that the solution can be placed in the side of
the mouth or on the tongue.
3.
Administer the drug slowly to a.void the risk of choking.
4.
If the child spits out the initial dose, repeat the procedure.
Fig:11.11: Elastic spoon for dispensing vitamin A solution
Health teaching related to vitamin A: ToaCh the people, especially
parents, elders in he family and leaders, about the value of ad'ling foods
rich in vitamin A to the d aily diet.
Eocords and reports: (see Annoxure 11. 7, Ferms A, B and C in the
Supplement to the Manual).
■■
i
: 76 :
?7 'I’i-lividyc.l..r.QciriQpt!s.,.h^lttL,rccord: Record the details of
vitanin i. a':inisti’aticn-iii th&
■i?JMSdds;d«caltli
record thaPis'fccw at the subcentre.
2.
Register of beneficiaries: Note the date'' of;■'enrolcent, nano,
address and age of oa.ch beneficiary and'-datc ofl'adbinistration
-.of yitaqin L solution (see Torn A).
-.3.'Steel’.' : c:ylstc.r:--Enterj{iic receipt;'.issjic jxnrl/balance of vitanin
. 1. .sdlutihvdn.
j- j rd/?- =. 1 ’.p;
4«:-'cr.tl;lyLrdpert to thc-’Rri.’.-'ory ''Hd^.lih. i)cnt,tc;:/T-his/gia a consoli;
' datioh of 'tho‘infoiX.£tiibh:'iri Fids i2": and'-3j?i$BycL‘(ggg;.JForn C).
.HiCTELH.FPCD SOffiCES
•I .- of.'HiDTEin FOOpS.-- .
. IATING;.iwb
Tv-Jiv
Vegetable sources
XX
- 'XX
Bengal gran dal
. ..
Black gran dal
Cow 'pea
Grcpi^-gran dal
~.Horse.gray.............. ';\' ;
-- _ .... dentals
Feas vGtey)
----- Red .,pran dal
Soya’bean
. .............. .................
Groundnut
Bajra
Cholan (Jowar)
Ragi
Rico ■
’Wheat .
’ .
XX\
. ..XX’
■ixx ■'■■■
■---- ..jZiA
■■■■
XX
’ '
.xccx
. v . XXX .
-;:p
X
. X
x .
. X "
X
-r
’
Anir nl ” s curco s
Cheese
■
Pa.nir (Cottage cheese)
iaik
- ; Eggs
.
1
Curds
Fish (frosh)
■ Fish (dried powder)
p
ifcat.(goat or rutton)
r
-'
■■
x^' '
■. - ■•.>’ SC--. ’-U- 1CX
X-. .
•. '
. : XX ■
’’
r
' .iex .
Legend:
X = 5 to 15 gras protein per 100 grans edible portion.
XX 4.15 to 25 grans protein per 100 grans edible portion..
2XX-. ="25 to 35 grans protein per 100 grans edible portion.,
XJQQL f. 35. t,o, 45. gypns, protein., per. 100- grans edible portion. .
.
* powdered fish contains nbro'than-45 grans- of. protein .per .100 grans
edible portion.
- .
NOTE: Food values in annexuros 11.1, 11.2,?11>3.and 11.4 arc. based on
tables included in 'Nutritive Value of Indian Foods' by C. Gopalan,
V.
B.
Lana Sastri and S.0. Balasubrananian; JO Publication, 1976•
VHAtgK L FOOD SCTir.CES .
FOODS COKPAI.'TTIG VITA111: A
Vegetallc sources
Amaranth leaves (chaulai) ’
Amaranth Stems
Bathua leaves
Beet greens (tops)
Betel leaves
. Carrot ('leaves):
Cclecasia (arvi)
Fenugreek leaves (ncthi) •
Tango (ripe)
J tint loaves
Mustard' (loaves.).
Papaya (ripe)
Rimpkiri'"- • ............'
Budish (tops)
Spinach
Turnip (tops)Ian
Animal sources Butter
Cheese
Fish liver oils
.
Ghee
- rilk (frosh) ■ ■ Shoepi-liver
— -Vanaspati
■ ,Whole powdered milk
-
2X2
*
X
**
XXXI
Legend:
X
XX
-2X
DD1XX
= T,000 to 5, COO units vitamin A per 100 grans edible portion.
= 5,000 tc 10,000 units vitamin A per 100 grans edible portion.
= '10,000 to 15,000 units vitamin A per 100 gratis alible portion^
= 15,000 tc 20,000 units vitamin A ; or 100 gratis edible portion.
Loss than 1,000 units of vitamin A per 100 gras, edible’ portion.
■ More than 20,000 units of vitamin A per 100 gms. edible portion.;
.'.Contd/78-
: 78 :
mon food samcES
FOODS COIiilTUNG UlOil
whig
Vegetable scurccs
bajra
Earley
Chelan
Bagi
Bice (flakes)
(hand pounded)
(nilled)
tiheat (whole)
Bengal gran
Elack gran
Ccw pea
Green gran (Moong)
Lentils
Ecd gran dal
Soya bean
Amaranth (tender)
Beet greens
Carrot leaves
Cauliflower greens
Cqlocasia (black leaves)
(green leaves)
... Coriander.leaves .. ....
Drumstick leaves
_ Knolrkhol. greens
Mustard loaves
Keen leaves (tender)
Eadish leaves
Turnip greens
Vella kocrai
Animal .sources
XXX
**
XXXX
xxx
**
XXXX
. .
Mutton or goat .peat
Eggs (hen) .
Fish.peal (dry powder)
Liver (shoe)
Khqa (Buffalo milk whole)
Legend:
X = 5 to 10 mg..iron per 1 00-grans edible portion.
XX = 10 to 15 ng. iron er 100 grns edible portion.
XXX = 15 to 20 ng. iron per 100 grans edible portion.
XXXX = 20 to .25 ng. iron per 100 grans edible portion.
* Less than 5 ng. from per 100 grans ediblo portion.
*
«
More than .25 ng. fireri per 100 gratis edible portion.
: 79 :
CALCIUM FOOD SOURCES
FOODS
"
'-'r
\
Vcgctablg.. sources
. J.)-.’. 'n -L'
;
- " r ■"
■Eagi.
Bengal., gran dal
BaJ.cE' gran-dal- . ............ ..
Cow 'pea
Green.gran (Mbong) dal
LenW s
Red .gran
S oyay’be'an
-
Animal sources
(.',£
Cheese
... Curds-------- - ---------------------- '■—————
Fish (dried)
Khp.er
•
Khoa (Buffalo)
' (Cow)
Milk (Buffalo) ■
■ '(■Cow) I. ,i 'h .
or
'
•■■XXXI 1
O.-m.X.L'
.-i'M
'- 7
'
XXXX;*
' '
- '■ ;cC^■
Legend:
= 50 to 100 rig. calcium. per 100 -grana edible £®rtioii.: .
XX-.= 100 to 150 ng. calcium per 100 'grans ■edible pciticn.
XXX = 150 to 2C0 rg. calcium yor 100 grams .edible portion.•
XQS = 200 to 250 ng. calcium per 100 grans edible-portion.
**M6rd than 250 ng. calcium per .100 grans edible. pertipn.-.'
KUSETTICUS EEGIEES FCR-VULNERABLE GROUTS ,(REGIOIlflSE)~ '
■: ’
NORTH
'
1. Whcat'Bcsan Lr.dco
- ■ Ingredients • • —
Wheat flour
Bengal gram flour'(besan)
Groundnut
•Jaggery (gur),
,
Method
’'
'
-
—
p
. ..
Quantity''
6 teaspoons
6 teaspoons
10 kernels ...
• 4-toaspo.ojis...
"
■
j ■=.
1. Eoast wheat' flour and -bengal gran -flour. -. 1
. '■
2.
Roast groundnut, remove the skin and crush coarsply..3.
Make-jaggery syrup and add-the flour.mixture ■ and groundnut to it.
A.
Mx well end make into balls.
.C
: 80 ;
liutritivo value:
339 calories
12.5
gn protein
Suitable for: Infants, pro-school children and school children.
NOTE; Wheat flour can be substituted by a ny other cereal flour,
Bengal gran flour can bo substituted by any other pulse
flour.
2. Bajara Khichiri
Ingredients
Quantity
Bajara (nillct)
Green gran dal
Rice
Leafy vegetables
Salt to taste
Water
6 teaspoons
6 teaspoons
2 teaspoons
4 teaspoons
Method
1. Fick bajara and grind it coarsely, sprinkling a little water on it.
2.
Renovo the husk of the bajara by washing it.
3.
Soak it overnight in a little water.
4.
Soak dal and rick for an hour after washing it.
5• Put dal and rice, bajara, and leafy vegetables chopped- coarsely in
a dcgchi.
6.
Md salt and water.
7« Cock for 20 ninutes or so.
Nutritive value:
250 calories
11.4 gn protein
Suitable for: Fro-school children, school children, pregnant and
nursing wonen.
3. Faushtik Roti
Ingredients
Quantity
Wheat flour
Bengal gran flour
Green leafy vegetable, e.g., palak
7 teaspoons
5 teaspoons
2 teaspoons
1 teaspoon = 5 gas.
Vanaspati (nargarino)
salt to taste
Water as required
2 teaspoons
Method
1. Sift together bosan and wheat flour.
2.
Wash green leafy vegetables, chop finely and nix with the flour.
* Add salt and water and knead to a stiff dough.
3
4« Roll cut chapati and place on heated tawa.
5- Turn when slightly done.
6. Four a teaspoon cf fat into the tawa and fry the chapati on
both sides.
Nutritive value:
.
307 calories
8
*
9
gn protein
suitable for: school children and pregnant and nursing wonen.
4. Sprouted Horse Gran/Green Grau Savoury
•Ingredients
Quantity
Horse gran/Green grail
6 tca.spoons
2 teaspoons
10 teaspoons
1 teaspoon
potatoes
Mango powder (anchor)
Salt and slices to taste
Fat
1 teaspoon
fethod
1. Sca£ gran in warn water overnight.
2. Drain water and put gran in wet cloth and hang in a warn place.
keep sprinkling water. Sprouts will appear 2 days.
3. Wash sprouted gran.
4. Chop onion and potato finely.
5. Fry onion and potato in fat and cook until potato is done.
6. Add sprouted gran and cock for 5 ninutes.
7. Add salt, spices and naiigo powder.
Nutritive value:
217 calories
3
*
7
gn protein
Suitable for: school children and pregnant and nursing wonen.
SCTJTH
5. Wheat Uwana
ingredients
Quantity
Broken wheat
Cnion
Oil
Black,gran dal (udath)
Drunstick loaves
Dried chillies
iiistard seeds
Curry leaves
Salt tc taste
Water as required
6 teaspoons
2 teaspoons
2 teaspoons
2 teaspoons
1 bunch
a few
a few
a few
Method
1. Fry mustard seeds, chiPies, curry loaves and dal in oil until
brown.
2. Add broken wheat and fry until brown.
3. Ad chopped onions and chopped drunstick leaves.
4. Add watcrand salt and cook over low fire until done.
Nutritive value:
237 calories
5.9 gn protein
Suitalbe for: Infants, pre-school and school children, and pregnant
and nursing wonen.
6. Tarioca Ftrridge
Ingredients
Quantity
Tapioca (uaravalli)
Milk
Jaggery
Grated coconut
Water as required ,
6 teaspoons
half cup
2 teaspoons
2 teaspoons
: 82 :
Method
'■
1. Pool and cut tapioca into snail pieces, and took in water until
soft.
2.
Ad1. hi~lk and cocl until seni-solid.
3.
Add jag;.cry and coconut and cock for a few □inute's.
Nutritive value:
2^8 calorics
4.1
gn protein
Suitable for : infants and pre-school children.
Ingredients
Quantity
Kagi Hour
Roasted Bengal gran Hour
Jaggery
Grated coconut
Oil (groundnut)
Water as required
6 teaspoons
1/2
2teaspoons’
31/2
teaspoons
1 teaspoons
1-1/2 teaspoons
Method
1. Dissolve jiggcry in water.
2.
Mix ragi flour and roasted Bengal gran flour. Add to dissolved
jaggery.
3 • Add coconut and prepare a thick dough.
.
4.
Prepare adai and fry c.n a greased tawa.
Nutritive Value:
299 calorics
6.1
gn protein
Suitable for: scho 1 children and pregnant and nursing wenen.
8.
Cholan Httu
Ingredients
Quantity
Cholan flour (nillet)
Roasted Bengal gran flour
Grated coconut
Jaggery
Salt
Water as required
6 teaspoons.
5
teaspoons .■
1 teaspoon
4
teaspoons
a pinch
Method
1. Sieve raw cholan flour.
2.
Mix cholan flour, Bengal gran flour and salt.
3« Add grated coconut.
4.
Ad". two teaspoons of wator and nix well.
5.
Add jaggery powder and stoan for 15 ninutes.
Nutritive value:
305 calories
9.1
gn protein
Suitable for: infants, .-re-school and school fin. Aren.
'EAST
PpUshtik Khichiri
Ingrddicntq
Quantity
Rico
D.-J. (lentil)
Potatoes
Green papaya
5 teaspoons
10 teaspoons
6 teaspoons
6 teaspeonr
: 83 :
Ono
Small 'piece
Onion (small)
Ginger
Salt and spices to taste
Water ag required
Ifethod
1 . Clean rice and dal and wash separately.
2.
Boil water in a degchi.
3.
Add rico, chopped onion and ginger and s pices.
4» Cook until rice is half done.
5
. Add dal and vegetables •
6.
Cook until soft.
7.. Add oil and salt to taste.
Nutritive value:
309 calories
6.7
gn protein '
Suitable for: infants, pre-school and school children
and pregnant and nursing wonoh.
10.
Bengal Grau Burfi
Ingredients
Quantity
Boasted Bengal gran flour
'
Jaggery
.. .
Cardspon
■
...
Water - sufficient to make a syrup.
10 tor.spoons
10 teaspoons
a pinch
Ifethod
1. Make a .syrup with jaggery and water.'
2.
Adi Bengal granfLcur and nix thoroughly.
3.
Add a pinch of cardauou.
4.
Transfer mixture into a greased plate and spread.
5.
Out when cool.
Nutritive value:
375 calories
11.0 gn protein
Suitable for: prc-schocl and' school children, pregnant
and nursing women.
WEST
11.
Sprouted Grau Salad (Usal)
Ingredients
Quantity
Sprouted green gran
Green.chillies, cumin, mustard
seeds and salt to taste
Lino
'
Coriander leaves
Oil (groundnut)
10 teaspoons
' •
One small bunch
half toaspon
Method
1 . Wash the sprouted gran and retain the husks.
2.
Adi" salt, chopped chillies and. coriander to the gran.
3.
Heat oil, and fry cumin and nustard seeds until
spluttering stops.
4.
Mix all the ingredients, garnish with line and servo cold
Nutritive value:
180 calories
11 gn p-rotein
Suitable for: school chaldron, pregnant and nursing w<?Qon
84 :
12. Khandvi
Ingredients
Quantity
Bengal gran flour
Curds
Water
Salt
Turmeric
Oil (groundnut)
Mustard seeds
Green chilly (chopped)
Coriander leaves
half cup
half cup
one cup
half teaspoon
1 teaspoon
1 teasp •-n
1/4 taspc.cn
one
snail bunch
frfethcd
1. liix curds, water and gran flour. seeing that there are no lunps.
2. Add salt, turmeric, 'chilly and half tea spoon, oil.
3.
Cock,- stirring all the while so that there arc nc lunps.
4« When thick, test by placing a little on the back of a greased.
thali and seeing if it can be rolled off.
5• Spread on the back of the thali and let it set.
6.
Out into long strips and make strips into rolls.
7’Hcat oil and fry mustard seeds until they stop spluttering.
8. Four over the rolls, Garnish with coriander loaves.
Nutritive value:
242 calories
13.2
gn protein
Suitable for: pre-schcbl and schorl children, pregnant and nursing
women.
*
13
Groundnut Milk
Ingredients ‘
Groundnut kernels
Water (lukewarm)
Quantity
.
half cup
2-1/2 cups
Method
1 • Fick the kernels And discard shrunken aid spoilt kernels.
2. F-oast kernels on a tawa for "5 to 10 minutes.
3.
Renovo pink skin of kernels;
4.
Soak kernels in water overnight.
5 • Drain off water and grind the kernels to a fine paste • Add a little
water if necessary.
6. Add two and half cups of lukewarm water and stir vigorously for
5 minutes .7.
Filter through a clean mull cloth (loose weave) and collect the
milky fluid'. .
8.
Boil the milk, stirring continuously to get rid of the nutty flavour.
9.
Serve hot or cold with sugar to taste.
(This rrilk can also bo used for preparing curds as followas:
To a cup of cold groundnut milk add one teaspoon of cow's or
buffalo's rrillc curd, and set overnight).
Nutritive value:
550 calories
25 gn protein
Suitalbe for: infants, pre-echocl and school children, pregnant
and nursing women.
COMM'JNIIY HEALTH CELL
/1,(First FloorJSt. Marks Roari
BANGALORE • 560 001
The art of selling 'baby killers'
By Shahnaz Anklesaria
least mention
somewhere that the
suffer malnutrition, disease or death
bottle should be sterilised each time
because they are bottle fed
instead before use? “Every mother
knows
of being breast fed.
this should be done, but she does not
If a mother bottle feeds her child do it. Why ? She may be too lazy or
when she can just as easily
breast
too busy or feels it is clean...” he
feed it, she is signing its death warr
replies. It is not his job to caution
ant, say doctors. If the bottle and the
her of the danger to her child.
nipple are not thoroughly
sterilised
I persist. Cigarette manufacturers
before each use, children have been
add the blurb about cigarette “smok
known to die of diarrhoea. If the milk
ing being injurious to the health” in
in the bottle is not thoroughly boiled,
their advertisements. Can he not
it can be lethal for the child. If while
work out something similar ? “Unless
using baby food the mother mixes
it with unboiled or partially
boiled
water, cholera or typhoid can
kill
the baby. Overdiluted baby food has
led
to malnourishment.
Mother’s
milk, besides having none of these
nr HE International Baby Food
defects, in fact provides the infant
A Action Network (IBFAN) has
with antibodies necessary to combat
documented 200 violations by 19
infections like gastroenteritis.
companies in 33 countries of the
A WHO/UNICEF organised con
WHO/UNICEF 1979 recommen
ference in October
1979 issued a
dations. This evidence, the report
statement saying, “It is the respon
says, showed only the tip of the
sibility of society to promote breast
iceberg of the promotion of in
feeding and to protect pregnant mo
fant feeding products by the in
thers from any influence that could
fant food industry.
disrupt it.” To thwart media mani
What
the
document , clearly
pulation, it was
agreed that there
shows is the unwillingness of the
should be no
sales
promotion or
infant food industry to modify its
advertising to the public of products'
practices voluntarily. As long as its
which can be breast milk substitutes.
means of promoting infant feeding
The confidence of mothers is thorou
products are considered “legal”,
ghly shaken by such sale promotion
the immoral and unethical nature
tactics.
of that promotion is ignored.
In India, advertisements of some
a directive comes from the Govern
ment we won’t do it.”
Why not ? Then the real reason for
the resistance slips out. “If the glass
(of the bottle) and the nipple is not
of a good quality, it will spoil with
constant sterilisation.”
Does he have an opinion on the
subject of breast feeding as opposed
to the bottle? “We do not deny that
mother’s milk is the best.” And again
later, “We know that breast feeding
is the best. Bottle feeding cannot be
Unethical promotion
brands of baby food concede that
breast feeding is the best. “Remem
ber mother’s milk is far the best for
baby. It is extremely difficult to sub
TJ E looks trapped. For just one
stitute for breast milk.” says
one.
“ fleeting instant, a genuinely
But such soft-pedalling by baby food
horrified look flashes into eyes. He
manufacturers is offset by the aggre
is a manager of an advertising
ssive advertisements of bottle and and
agency, one of the several all over
nipple manufacturers.
Nowhere do
the country to have released adver
their advertisements warn buyers
tisements proclaiming the worth of
of how fatal it is to use their products
artificial baby milk, feeding
bottles ,
without sterilisation.
and nipples. All this at a time when
“It could all be the doctor’s ima
people the world over are becom
gination.
Diarrhoea
and sickness
ing increasingly militant against their
could have occured for other rea
use.
sons,” is one advertising manager’s
Both baby food and the feeding
reply.
bottle are now called baby
killers.
BABY FOOD AD :
immoral and unethical
It has been estimated that over
10
But does he not owe it to the con
million Third World infants annually sumer and to advertising ethics to at
Below are some of the WHO/
UNICEF recommendations (prin
ted in bold letters) and evidence
of how the companies have flouted
them.
* “There should be no sales pro
motion, including promotional ad
vertising, to the public of products
to be used as breast milk substi
tutes or bottle fed supplements and
feeding bottles.”
In
practice,
companies
like
Abbot, Cow and Gate, Dumex,
Glaxo, Lijempf, Mead Johnson,
Morinaga, Nestle (whose vice-pre
sident claimed in May 1979, “We
do not advertise our brands of in
fant formula to consumers in deve
you.” Such examples of statements
You will have living evidence before
you.” Such examples of statements
Some
advertisements, says
Mrs’
Basrur, are a direct appeal to the
mother’s selfishness. For instance, one
advertisement promoting a feeding
bottle claims that breast feeding your
child is just not “convenient”. You
CONTINUED ON NEXT PAGE
baby foods
loping countries”), Wyeth, have all
advertised their products through
posters, radio, newspaper and free
sampling.
* “Facilities of the health care
system should never be used for
the promotion of artificial feed
ing.”
In public, health centres, in ma
ternity homes and hospitals of the
developing countries several baby
food companies have been advertis
ing their products. Milk nurses
talk to mothers and distribute sam
ples and literature at clinics and
hospitals in Turkey, Barbados and
South America. Mothercraft nur
ses give lectures to
mothers in
Kenyan clinics
providing posters
and booklets promoting Glaxo
products. Nestle provides
free
bottles to
government clinics in
Martinique advertising a product
“Guigoz”. These bottles are dis
tributed directly to poor mothers.
* “Promotional
distribution of
samples of breast milk substitutes
through health service channels
should not be allowed.”
Cow and Gate, Abbot, Borden
Dumex, Glaxo, Mead Johnson,
Morinaga, Lijempf, Nestle, Wyeth
were among the larger companies
found distributing promotional su
pplies. In Puerto Rico, Abbot pro
vides Similac discharge kits with a
tin of ready-to-feed concentrate,
Htmmat July 11, 1980
compared to that.” Then why in the
actual advertisement is the very op
posite said ? For instance an advertise
ment claims “You feel everything he
has should be the best ... we agree.”
Another Hindi advertisement for a
feeding bottle reads,
“Give
your
child milk through (the brand name
of the feeding bottle) and be without
fear. Your beloved child will grow
contrary to medical evidence are too
numerous to cite.
Irate members of the
Consumer
Guidance Society of India
(CGSI)
complain that such advertisements in
fact draw perfectly healthy mothers
away from breast feeding their infants
and to the bottle. “It is very difficult
to fight the constant indoctrination of
these advertisements,” says Mrs Kri
shna Basrur of the CGSI.
vitamins and a nursette to breast
feeding mothers at community
hospitals. A nurse in one hospital
in Barbados said “We don’t have
to buy anything from Cow and
Gate -— they give us all kinds of
free samples. We have a cupboard
full.”
they gets a bonus if they meet the
monthly sales target and a commis
sion if the monthly target is ex
ceeded.
* “No personnel paid by compa
nies producing or selling breast
milk substitutes should be allow
ed to work in the health care sys
tem.”
Abbot, Dumex, Dutch Baby,
Glaxo, Mead Johnson had no pic
torial instructions, some had no
preparation instructions, others had
had labels in English in countries
where Creole and French are the
local languages and Nestle did not
advise using sterilised utensils.
In Peru a doctor reported that
the director of the Neonatology
Department in the hospital Maternidad is employed by Nestle and
also works in the Nestle pediatric
clinic. Nestle has exclusive rights in
providing milk to that hospital. It
is the largest in Lima. Mothercraft
nurses are still employed by Nestle
to work in rural community health
clinics. After a hospital official in
Lesotho refused to allow Nestle
mothercraft nurses to lecture to
mothers, three Nestle executives
visited the official and oflered him
an all-expenses paid trip through
out South Africa, funding for the
Southern Africa pediatrics confe
rence in Lesotho and a possible job
offer when the official’s
current
contract expired.
Glaxo employs nurses in Trini
dad as sales representatives and
* “Foods for infants and young
children ... should be labelled
to indicate proper and safe home
preparation.”
* “Products that are not suitable
alone as weaning foods, such as
sweetened condensed milk ...
should ... not be packed, labelled,
advertised or otherwise promot
ed ... as a complement or substi
tute for breast milk.”
Four
international companies
were reported promoting sweetened
condensed milk products for in
fants. None of them carried an
explicit message about the superio
rity of breast milk. In fact in its
advice on breastfeeding, a Nestle'
booklet circulated in Sierra Leone
said about breastfeeding, "Do not
feed him at night, you and baby
must rest,” and “Do not give the
breast too often”.
------
S, A.
BABY FOODS — from page 13
do not have babies because it is a
matter of convenience,’’ storms Mrs
Basrur. If mothers were
educated
about the dangers that arise from
neglecting to breast feed, they would
put in a for more effort to do so, she
says.
“It is the manufacturer’s responsi
bility to check if what we are claiming
is justified or not,” is the ad man’s flat
rejoinder to any accusations. In other
words, he is helpless. It is either the
mother’s fault, the doctor's ignorance
the art of
good
management..
moulding
our varied resources—
human, natural,
technological—for the
common good.
Shriram seminars and courses are part of
this moulding process... which involves
executives in a ceaseless interchange of
ideas, discussion of modern techniques,
evaluation and reconsideration of policies.
So that the Shriram organisation is const. antly infused with fresh dynamism... and
our resources are utilised to the optimum.'
SHRIRAM FERTILISERS AND CHEMICALS
or the manufacturer’s responsibility.
His job is just to sell — any product.
1 march across to a manufacturer
of feeding bottles and nipples. Does
he know of the bottle-feeding contro
versy ? Yes. He is' politely disintere
sted. Is he aware that bottle-feeding
kills? “All this advice should be given
by the doctor.”
Could he at least mention on the
packaging that the bottle and nipple
must be sterilised before each use? “It
is mentioned — look”. What I see is
the word “sterilizable” among three
-other words proclaiming the bottle’s
uniqueness. But that is not the same
as a direct warning.
“Mothers do
not care. The consumers who
buy
our product are the upper class and
upper middle class. Their doctors
should educate the mothers about
the importance of sterilisation,” he
insists. Even when hospitals tell
mothers to shield the nipple,
they
still do not bother to do so.
tificate.
ISI uses British standards?
And I export my bottles to Britain.”
Besides, what can he do if the ma
ternity homes themselves specify that
every expectant mother must
bring
a feeding bottle
along with
other
necessities ?
Now the Central Indian Ministry of
Social Welfare has organised a work
ing group to set up a code of conduct
for the manufacture and promotion
of baby food along the lines of the
code formulated by WHO/UNICEF
in October 1979. One hopes that
the code, which is being formulated,
will be strong and effectively, imple
mented.
He says he sells 200,000 to 300,000
bottles a month. Then it cannot be
only the higher income groups who
buy his bottles. “OK also the lower
middle class”. Forget class, I tell
him, lakhs of children are vulnerable
because he chooses not to warn their
mothers.
Finally he
concedes, “I
never realised it from this angle.”
The nipples that he produces have
a wider range of consumers.
“In
villages you can buy them for 25 paise
each.” His Bombay unit alone sells
12 lakhs each month, and his Ban
galore unit, three and a half lakhs.
I tell him that the rural children are
the easiest victims of death by diarr
hoea and cholera because they
are
fed powdered milk diluted with un
clean water or the cow’s milk is un
boiled. All this the children suck in
from the nipples he produces. Besides
there is danger of the nipples being
uncovered and
contaminated.
So
would he consider ceasing production
of these nipples? “Never.” I am infor
med that nipple manufacturing is a
big cottage industry with at least 60
to 70 known manufacturers. “At least
we can guarantee the quality of what
we produce.”
.
Can his products withstand regular
sterilisation ? Yes, of course. Perhaps
it has passed the Indian Standard In
stitute tests? “I not need an ISI cer
aMMAT July 11.1U80
COMMUNITY HEALTH .CELL
47/1. (First Floor)St; Marks Road
drinking to whose heaith?w“l0'1E'5S<‘°°1
There are many products which claim to pro
with malnutritioned children can get the same
mote health. Generally, these products are costly
amount of calories and protein from other food
and only the upper class can afford them. But they
sources much cheaper. Recently, the Government
are precisely the people who do not need them.
of India forced the Beecham subsidiary, Hindus
Their normal food is more nutritious if properly
tan Milkfoods, to remove the untrue claim “twice
eaten.
ent
The damage however is on the less afflu
and
the
poor
who
try
to
imitate
such
as good as milk” from the Horlicks label.
manufacturers of Horlicks are also
The
known to
consumerism but cannot afford. This is similar to
falsely claim: “the only one that doctors all over
trying to smoke king-size
the world recommend”. This is simply unethical.
the poor rural youth
costly cigarettes in a delusion that he is living
Horlicks is dinned into doctors over and over
The economic
by repeated visits by sales representatives, spon
and social damage of these ads on a poor society
sored seminars of the health professionals and
various other kinds of direct and indirect gifts.
"life king-size” as the ads claim.
are terrible.
The Horlicks and Bournvita stories are classic
examples of advertisements dictating habits. In
Britain,
both
Horlicks
a'nd
mainly as mild soporifics.
Bournvita are sold
In England, Bourn
vita is the "good night drink” which "helps sleep
come naturally”.
In India, it is the ideal “health
Such are the attempts to “persuade” the health
profession in the country. Because of such per
suasions Horlicks corners about 53 per cent of the
Rs. 43 crores a year health drinks market.
Both
Cadbury and Hindustan Milkfood Manufacturers
makers of Bournvita and Horlicks (and
Boost)
taste” which
respectively, are reported tojbe spending about
means
it can be presumably taken in waking
hours.
Strange for an “Olympic drink” indeed!
Rs 1 crore of the nearly Rs 1.75 crores spent by
all food drink manufacturers in high pressure
drink
for
strength, vigour
and
Horlicks has similar claims. It is true that both
advertising.
Horlicks and Bournvita are relatively good foods.
Cost breakups of some of these health drinks
But on the other hand, as the Social Audit Re
can be shocking. Liberal cost estimates for Pfi
zer’s Protinex would give one rupee for the con
port points out',their calorific value and protein
content can be compared with that of any good
cereal
or pulse and there is certainly nothing
tents and two rupees for the package material
while it is sold in the market for over Rs 15
unique about them as nutrients, as some of the
claims may suggest." The well fed 10 per cent of
India can do without these drinks.
And the poor
HEALTH FOR THE MILLIONS/APRIL-JUNE 1981
The damage caused by baby foods (infant for
mula) is only too well known.
is
However, what
not well known is a more blatant intrusion by
In the villages of the Goan taluk Sattari, there
known there—nache is the cheapest of the millets.
Now
Nestle
(which has a poor reputation
are women with adequate breasts
but still can
among people working in rural health care) have
This is because they have poor
decided to enter this ragi baby food business
and that is certainly likely to boost up the costs,
commercial companies into a poor child's diet.
not breast-feed.
diets due to low incomes. Yet their children are
as healthy and even stronger than those city
children brought up on expensive cereal mixtures
by upsetting ragi prices and wrecking the poor
child’s diet.
and formula foods. The Sattari women feed their
new born children on ragi or nache
as
Who is becoming healthy at whose expense?
it is
ao embarrass mg vitamin
Many thousands are on these dosages either
“Vitamin E is one of those embarrassing vita
mins,” write Sir Stanley Davidson and Reginald
with or without the advice of doctors. The indus
Passmore
try happily supplies. Such wasteful medication
in their standard text book Human
Nutrition and Dietetics (4th edition, 1970) "that
and overdose of Vitamin E leads to false security
have been identified, isolated and synthesized by
and
physiologists and
care.
Luckily,
human
body.
biochemists and then handed
to the medical profession with a suggestion that
a
use should be found for them—without any
satisfactory evidence to show that human beings
postpones or ignores real proper medical
the drug
is not harmful to the
The same cannot be said of other
vitamins and “multivitamin" tablets.
Fat, soluble Vitamins A and D, if taken in large
are ever deficient of it or even that it is a neces
doses too long produce serious or even fatal
sary nutrient for man.”
intoxication or chronic illness. It is not yet known
This makes Vitamin E an ever easier target for
than
whether large amounts of the single element of
vitamins.
B complex produces any imbalance. But never
Vitamin E occurs in large stores in human fatty
theless they are sold at high costs and in more
tissue and even though special diets have exclud
than the required amounts. For instance, Surbex-
ed Vitamin Efor months on end there is enough
T contains 15, 10, 5, 5 and 2 times the neeeded
in the human storage deports to sustain adequate
daily amount of vitamins Bj, B2, B, Bo and Bi2
respectively (based on ICMR recommendations).
commercial
exploitation
other
levels. Vitamin E has no toxicity, no matter what
quantities are consumed. Thus, with some imagi
nation and repression of information, Vitamin E
can be sold for almost anything. And indeed, at
one time or the other it has been sold in ever
increasing quantities for one or more
of
the
following conditions or uses, with no supporting
scientific evidence: ageing, acne vulgaris, after
shaving tenderness, allergies, amyotrophic lateral
sclerosis,
angine
pectoris,
atherosclerosis,
cancer, chronic cystic fibrosis, chronic
mastitis; coronary heart disease, cosmetic skin •
hemolytic
anaemia,
People have been made to believe that they
need vitamins. Both physicians and patients have
fallen for the glossy ads and sales
promotion.
The busy executives, at whom these vitamin ads
are normally directed, do not require any vitamins
for their psychosomatic illnesses
like headache,
bodyache etc.
cystic
conditions, diabetes mellitus; frigidity, habitual
abortion,
Becosules exceed the recommended daily require
ments by 50, 12, 5 and 5 respectively.
hypercholestero-
They believe B-complex may solve their prob
lems, little realising most of the costly B-complex
is flushed out of their body as its physiologically
iaemia, infertility, lupus erythematosis, macrocytic
required amount is small, and excessive amounts
anaemia, muscular dystrophy, myasthenia gravis,
cannot be stored in the body.
peptic ulcer, rheumatic fever, scleroderma under
arm deodorant, venous thrombosis.
their US counterparts) had decided to permit sale
22
Some time ago, drug authorities in India (like
HEALTH FOR THE M1LLIONS/APRIL-JUNE 1981
of only two categories of vitamin formulations:
therapeutic (for example, 50 mg of vitamin
B!
authorities seem to have quietly shelved the idea,
presumably due to pressure from the drug lobby.
Times study revealed that such a
to treat beriberi) and prophylatic (containing just
An Economic
enough vitamins to overcome deficiencies, for
legislation would affect atleast 571
instance, about 1 mg of vitamin Bj as per ICMR).
at a cost of atleast Rs 1.5 crores to its manu
facturers. One understands the enthusiasm of
the drug industry to thwart any such legislation^
In tee US, such a regulation has helped reduce a
great deal of
abuse.
However,
in
India,
the
formulations
tonics
Waterbury's Yellow label Tonic is one of the
brand leaders in the tonics market.
They claim
the usual benefits for tonics like it stimulates
appetites and build bodies.
Each teaspoonful of
Waterbury's contains just 3 mg of iron and only
one-tenth of which may be absorbed in the body.
The ICMR recomends atleast 10 mg of iron daily
for men, and 20-30 mg for women. Obviously
Waterbury’s will be insufficient for most.
Actually, on analysis it is found that the tonic
has 10 per cent alcohol content (like most other
tonics) and it is this which stimulates the appe
tite. So much for tonics as appetite-stimulants!
Similarly,
Incremin
C,
the
tonic
with
the
Giraffe drawing, claims to increase growth be
cause it contains a vital amino acid called lysine,
which the human body cannot synthesise itself.
But even a handful of peas can provide six times
the 300 mg
of lysine that is present in each
teaspoon of Incremin. The manufacturer’s claim
that
Incremin
turns
“extra
eating
growth” is at best a half-truth and
into
extra
medically
unsubstantiated. The other constituents of Incre
min are just an economic waste—10 times more
vitamin Bn 25 times more vitamin Bi._. and twice
that of vitamin Ba than needed daily.
The tonic Femibon belongs to that school of
tonic manufacturers who play up the iron defi
ciency theme. The tonic is meant exclusively for
menstruating women and the ad-copy goes
like'
“.. .you need twice as much iron as a man.. .your
As usual, the target women groups of Femibon
tonic consumers
do get enough
iron and the
daily diet does not normally provide you this
poorer women who do need cannot afford it, and
in any case there are less costly formulations
extra iron you need."
and ways to get iron. Also, subclinical doses of
HEALTH FOR THE MILLIONS/APRIL-JUNE 1981
23
haematinics (drugs such as iron and vitamins)
used in such mixtures have been known to cause
serious consequences
of suppression of early
signs of anaemia.
Another group
of
irrational tonics
phosphates—Neurophosphates.
is the
Hemiphos,
BG
Phos are some members of this group. Nervous
tissue consists mainly of combinations of phos
phates and fatly substances called phospholipids,
Stretching this fact a bit too Imuch, Waterbury’s
ads till the other day used to claim that it con
tained “phosphates to tone up your system."
This
is
a
typical example of drug marketing
cleverness.
The patient pays for the attractive bottle, the
alcohol percentage, the synthetic
flavour (e.g.
Dex-Orange and some vitamins added in some
irrational doses.
More than that he pays for the
Doctor I've taken the tonic. But I starved for days to,buy it
advertisements.
common coid war
There is as yet no proved cure for the com
mon cold. Indeed no one has isolated a common
cold virus, if any. There is a not so well-substan
tiated belief (sparked by Linus Pauling) that
vitamin C cures cold.
Manufactures have cashed
with
patients who have allergic rhinitis, it may
prove effective. This deludes the patient into
believing he was cured of what to him was a cold.
A dangerous side-effect of such
drugs is that
they dry secretions in the respiratory passage
on this controversy. Coldarin tablets, for in
stance, claim, with 50 mg of Vitamin C per tablet,
ways, causing them to go into spasms.
you can build your body resistance and fight
the market usually contain expensive brands of
colds.
All that 50 mg of Vitamin C is effectively
The many cold tablets and capsules sold in
aspirin with
harmful drugs like phenacetin, use
down the drain—most of it will be washed out
less drugs like Vitamin C and antihistamines, or
with urine the very next day.
ineffective ones like phenylephrine or ephedrine.
Coldarin and other brands
like
Vicks
500
Similarly, the many cough drops (like Vicks,
claim decongestant properties to clear “running
Halls, Strepsils) contain subclinical
nose and sinus”. Most of these drugs contain, a
dextromethorphan (a cough depressant), ephed
class of drugs called sympathomimetic amines
(like ephedrine) which given by nonoral routes
can cause blood vessel constriction. Orally, these
rine (which helps widen the bronchial passage
tingling sensation when applied locally, some
drugs are not well-absorbed, and in the form of
what
drops cause local decongestion. However, as a
coughs).
reputed pharmacological guide puts it, “No con
vincing evidence of benefit from oral use of such
equally effective.
active ingredients like antibiotics, antiseptics and
drugs to relieve nasal congestion in colds has
yet been presented.". Also many of these nasal
impressive to an uninitiated consumer. Indeed so
ways)
and menthol
like
doses
of
(which causes a pleasant
eucalyptus
oil,
but
does
not cure
Good old grandma's concoctions are
Sometimes they contain other
local anaesthetics.
The'combination can be very
decongestants are known to be harmful for people
impressive, that Strepsils alone has a sales turn
being treated for high blood presure.
over of more than one crore rupees per year!
Similarly, antihistamines
like Viko-y
useless in the common cold war.
24
1,
are
But sometimes
*
*
*
HEATLH FOR THEMILLIONS/APRIL-JUNE 1981
n\jT
COMMUNITY HEALTH CCU.
57/J,(First Floor)Sc. Marks <ioad
BAMGALOHE- 560 003
All Field Directors
All Field Secretaries
TO:
FROM:
DATE:
S'-a
23rd June, 1981
John Clark, Campaigns Unit
Baby Milk Code
You may already have heard that this year's World Health Assembly agreed on an
International Code of Marketing of Breastmilk Substitutes by 118 votes to one
against (the US) and three abstentions.
Hie key points of the code are:1)
There should be no advertising or other forms of promotion to the general
public of products within the scope of the code (breastmilk substitutes,
feeding bottles and teats).
2)
Manufacturers and distributors should not provide, directly or indirectly,
to pregnant women, mothers or members of their families, samples of products
within the scope of the code.
3)
Only objective and consistent information on infant and young child feeding
should be provided to the public. This should not encourage the abandonment
of breastfeeding or carry brand advertising of products within the scope
of the code.
4)
No facility of a health care system should be used for the purpose of
promoting products covered by the code.
5)
The use of "professional service representatives", "mothercraft nurses" or
similar personnel provided or paid for by manufacturers or distributors is
forbidden.
6)
Feeding with infant formula (home prepared or manufactured) should be
demonstrated only by health workers or other community workers if necessary;
and only to mothers or family members who need to use it. The information
given should include a clear explanation of the hazards of improper use.
7)
Only factual and ethical information should be provided to health workers.
Manufacturers and distributors should not give gifts of any kind and
donations to health care institutions should not seek in any way to promote
products covered by the code.
8)
Labelling should stress the superiority of breastfeeding, should not idealise
bottle feeding by using images of well babies or other images to imply
medical endorsement of the product but should instead give full instructions
for safe home preparation’.
9)
Company employees should not receive a commission on sales as this encourages
inappropriate marketing methods.
,-jvtY
■ •• ■°‘t' continued............
- 2 -
You could help ensure compliance with this code in three ways:-
a)
Notify the Campaigns Unit of any violations of the above points with full
details (including names, place names, date, etc) and evidence (or
photographs). We will then share the information with the WHO (who have
been mandated to monitor compliance with the code) with industry (which
have promised to take corrective action) and with other baby food
campaigning groups.
b)
Either share this invitation with project holders and any other contacts
in the field of health or who are likely to be interested in this issue or
let us know names and addresses of those who we should approach directly.
c)
Let us know any trustworthy and accurate researcher or journalist who would
be prepared for a modest fee to undertake a short monitoring of compliance
with the code in the locality (this would include scanning literature etc.
for advertisements, collecting infant feeding literature available at
hospitals and clinics etc., assessing the use of free samples and the
activities of marketing personnel, investigating any inducements offered
to health care workers, analysing the labels of products etc).
Undoubtedly the code (at present an international recommendation) would be
more effective if translated into law by national governments. If you,
project holders or other contacts have any influence within the health
ministry please encourage the consideration of legislation. The WHO are
only too happy to provide legal, nutritional and marketing advice on
appropriate legislation. The Campaigns Unit can supply English copies of
a WHO paper on "Relevant National Legislation" and provide names within the
WHO Secretariat of people who would assist. In any event, please keep us
informed of any moves towards legislation that you hear of.
Oxfam's involvement in the UK in the campaign in support of the code has
been very effective (you may like to read the enclosed account or at least
the summary of lobbying activities at the World Health Assembly). The
issue provides a rare chance for staff and volunteers at home to join with
field staff in a campaign with truly international ramifications.
Thank you for any contribution you can make to this campaign.
COMMUNITY HEALTH CELL
S7/-J,(First FloorlSt. MarksRoad
C/066
BANGALORE-560 001
CIRCULAR
TO:’
FROM:
All Regional Organisers
Area Directors
Education and Youth Officers
Div Heads
Departments in Oxfam House
John Clark
Not for Publication
DATE:
10th June, 1981
STOP PRESS ll/6/81~ Cow and Gate - the UK company
with which Oxfam has developed a very constructive
dialogue told me that it and it's Dutch sister company
Nutricia are pulling out of the industry federation
ICIFC in disgust at the way ICIFI members tried to
subvert the World Health Assembly.
HOW THE BREAST WAS WON
Summary
Over 90 people from 40 countries took part in the lobbying at last month's World Health
Assembly to encourage support for the proposed International Code of Marketing of
Breastmilk Substitutes. The exercise was highly successful and was praised by many
delegates including the president of the Assembly in her dosing address. Several of
the lobbyists worked on or had close connection with Oxfam supported health projects.
Intensive anti-code lobbying also ' took place amidst political intrigue. This involved j
several top company executives, a spurious new organisation called Voice of the World's r
Children (which alleged completely falsely that the prestigious International Paediatric
Association was opposed to the code), and a company lawyer who represented himself as the
Guatemalan delegate until he was exposed as an imposter.
Documents leaked from Washington to lobbyists showed that the US government.was more
concerned about the political implications of the code (particularly the precedent of
restrictions on multinational corporations) than the health considerations. It was
anxious that the code had been revitalised after its efforts to water it down and now
presented problems to the-US and "particularly to US industry".
A second leaked cable revealed the influence on US government thinking by industry and
Nestle in particular. The cable described a plan by industry hard-liners to "thoroughly
discredit" the WHO and "provoke a North-South split" by generating "a confrontation at
the upcoming World Health Assembly".
In the World Health Assembly debate delegates criticised the anti-code lobbying as well as
persuasive baby milk promotional tactics in developing countries. On the other hand, they
stressed the important role Non Government Organisations had to play in monitoring the
code and promoting breastfeeding.
A.
very controversial early closure of the debate angered and confused several delegates
leading to the rather unsatisfactory vote of 93 countries for the code, 3 against and
9 abstentions. A re-vote the next day, however, yielded the resounding 118 votes for,
1 against (the US) and 3 abstentions. The UK delegation played a very positive role in
the debate and in the build up towards it.
It is now quite clear that attempts will be made to extend the successful WHO - NGO
cooperation in the developing of a code governing the marketing of pharmaceuticals.
The baby milk code has resulted in the first major political defeat for Reagan (himself
involved in the decision to vote No). Two top USAID officials resigned in protest and
the US spokesman on human rights, Ernest Lefever, has been forced to resign after it
came to light that his successful lobbying for the US "No" vote stemmed from his financial
connection with Nestle.
Lefever's private organisation, the Ethics and Public Policy Center, received some 025,000
for sending an article smearing the baby food campaign to hundreds of thousands of people
on a Nestle-provided mailing list. A leaked Nestle memorandum describes the use of this
article as a successful example of "third party rebuttals" but warned that "Nestle should
not be seen to be the dominant subscriber to the Ethics and Public Policy Center".
Finally I outline the possible future involvement of Oxfam in this issue.
I apologise for the length of this circular but can assure you that it makes interesting
reading.
- 2 -
The Lobbying for the Code
At the start of the main lobbying operation (a week or so before the code was debated)
there were about 20 to 25 people from Non Government Organisations (NGOs) in about a
dozen countries. This rose to some 90 people from 40 countries in the YMCA hotel in
Geneva which was also used as a meeting place. The lobbying was conducted under the
common name of the International Baby Foods Action Network (IBFAN). Amongst the
lobbyists were people working with Oxfam supported health projects in Kenya, Zimbabwe,
Bangladesh and Yemen and several others who had close connection with Oxfam.
Besides running a general office (mostly for taking phone messages) we had the use of an
office in the UN Geneva Head Quarters (the Palais des Nations) where the assembly was
taking place, and of the NGO Lounge there, where we held daily briefing meetings for
lobbyists.
We produced 3 briefing kits for delegates, press and lobbyists. Functions we divided
amongst ourselves were:- Steering Committee (to decide on strategy and work for the
next day), Press work, Regional Coordinators (to coordinate lobbying of the six WHO
geographic regions of the world), WHO liaison and overall lobbying coordination. Also
on a daily basis we took it in turns to:- staff the two offices, chair the meetings,
observe and report on the meetings of the Assembly, orient newcomers to the lobbying
process, photocopy and prepare documents.
—
The lobbying itself (talking to the delegates) was mostly conducted in the coffee bar and
cafeteria. It ranged from brief chats to inquire casually what the delegate's attitude
was towards the code, to very involved series of meetings and sharing of information.
The delegations we had closest contact with were Norway, Algeria, Sweden, Samoa and
Jamaica. We also had very good contact with delegations of Denmark, India, Kuwait,
Turkey, Canada and Yemen. The UK delegation was also surprisingly positive and friendly
considering the attitude it had taken at last year's World Health Assembly (very close
to the US position).
Most delegations were very ready to talk with us though some obviously felt "over-lobbied"
at times - something we had to be very sensitive to. Many delegates (including the
President of the Assembly in her closing speech) thanked the NGOs for the positive role
they had played and still had to play. Undoubtedly very many delegates found our
material useful.
Anti Code lobbying
We were not by any means the only lobbying force at the Assembly. Several very senior
baby milk company executives were also taking every opportunity to talk with delegates.
The manufacturers federation - the International Council of Infant Food Industries (ICIFI)
- ran a "Hospitality Suite" at Geneva's poshest hotel - open at all times to delegates and
press. ICIFI also circulated to delegates a letter (criticising the code) and the ICIFI
Charter which bore on its cover a quotation from the UK's chief medical officer. This
brought a sharp reply from Dr Harris the Head of the UK delegation in the form of an
opai letter to the assembly rebuking the possible false impression given of association
between ICIFI and the UK, and pledging instead full UK support for the code.
Industry supporters circulated a letter purporting to come from the "All India Medical
Students Association" with the letterhead falsely claiming affiliation to the
International Federation of Medical Students' Associations". The letter implied that
Indira Gandhi (who gave India's opening address at the assembly) did not fully support
the code. In response the chief Indian delegate Dr I. D. Bajaj circulated a letter
refuting the claims made by the Assocation saying "for a variety of reasons, including
the date of the letter and the apparently motivated manner in which excerpts have been
quoted therein have created grave doubts about the bona fides of the communication".
Perhaps the most intriguing lobbying was conducted under the name of the specially formed
"Voice of the World's Children (VWC).
- 3 One of its fierce attacks on the code was a letter it circulated to delegates claiming
that .the International Paediatric Association (IPA) was opposed to the code. (This
letter was handed out by the same person who was distributing ICIFI material though
ICIFI denied any knowledge of the organisation). It happened that Turkey's Chief
Delegate, Dr Dogramaci, is also head of the IPA. He repudiated the VWC claim during the
Assembly's debate on the code saying that it was "absolutely unfounded".
Even more incredible is the story of the Guatermalan Stooge. Two Mexican IBFAN lobbyists
overheard a Guatermalan - Antonio Carerra - describing by phone a strategy to confuse the
code debate by introducing a long series of ammendments. Investigations showed that he
was not an official delegate, though he had been sitting in Guatemala's chief delegate's
seat. He left the Assembly just before his credentials were challenged. A reliable
source told us that "the Guatemala delegation has confirmed that the "imposter" is a
lawyer employed by Nestle".
Leaks from Washington
The issue of the code was seen by the US government as being an all important political
battle. Unlike Britain where the government line was decided by the Department of Health,
in Washington the views of the State Department and the White House overruled those of their
health department. President Reagan himself was involved in the final decision to vote
against the code.
Several leaked documents from Washington tell a fascinating story of the influence
powerful companies can have on governments. These were extremely useful documents in the
lobbying process. The first leaked cable was from the US government to governments of
other countries via their US embassies. It said that the code presented problems for the
US government and "particularly US industry". There was the fear that "adoption of this
code could stimulate WHO interest in further codes" - mentioning pharmaceuticals as a
possibility and there was a complaint that the strong wording particularly of the
resolution accompanying the code "envisions a code in the form of a binding regulation
and reasserts a number of controversial factors that the US government and others have
been able to remove from the text of the code in the course of the negotiations". The
cable asked for the views of other governments - besides putting forward the US objections.
It contained no mention of the health of infants.
The second leaked cable was from the US Ambassador in Geneva (Helman) to the US State
Department. It described a plan by members of ICIFI to "thoroughly discredit" the WHO.
The cable reported on a conversation between Nestle official Geoffrey Fookes and
Ambassador Helman:
"Industry's goal is to provoke a North-South split. He (Fookes) said there were the
"hawks" in the international group (ICIFI) who truly desired to see a confrontation at
the upcoming World Health Assembly".
"Fookes reported that ... the "hawks" in ICIFI want to persuade their governments to
oppose the code, thus precipitating a decision by the World Health Assembly to issue a
mandatory code which will be challenged in the International Court of Justice on
procedural irregularities in the development of a 'regulation'". Fookes stated that the
governments of Canada, Australia and WGermany had indicated that they would make this
challenge. Later the Canadian chief delegate, Dr Maureen Law, made it clear that her
government did not have and never had such a plan.
The cable also revealed that industry was more concerned about voluntary groups' insistence
that they keep to the code than the pressure on them from governments.
The decision by the US government to oppose the code showed that it was more influenced by
industry pressure such as described in this cable, than they were by the health arguments
in favour of the code.
- 4 The WHA debate on the code
The code and the accompanying resolution were introduced to the Assembly on the afternoon
of 20th May by Dr Mark, the Norwegian Director General of Health. He stressed that this
was a subject of Health not Trade and called for a concensus. 51 countries then indicated
that they wanted to speak, an impressive confirmation of the importance of this issue.
First the Swedish delegate took the floor speaking for the five Nordic countries and
voicing strong support. He stressed the important role played and to be played by NGOs.
Next the Dutch delegate voiced support on behalf of the 10 EEG countries (the UK had
played an important role in encouraging the 10 to speak with one voice). Switzerland,
Brazil and Canada all gave their support as did the Turkish delegate in an impassioned
speech in which he said "if a mother is showered with clever publicity and sometimes free
samples of breastmilk substitutes she cannot be expected to make the best choice for her
baby". The Indian delegate referred to the anti code lobbying as "the only contamination
in the otherwise clinical atmosphere of Geneva" and explained that his government had
already "drafted a legislative framework which I think will fit our national situation".
Tunisia referred to company marketing practices as "questionable to say the least" and
Central African Republic said that he wouldn't want to see the present draft code
weakened "by maneuvers in the corridor".
Unfortunately, at this point the Belgian delegate butted in with a motion of closure of
the debate. Such a motion can be put at anytime and has to be voted on straight away.
j
Normally, however, delegates are sensitive enough to allow a good number of contributions
on a controversial issue before moving a closure. In this case with so many countries
anxious to speak it was an untimely move especially as very few Third World delegations
had spoken and several important blocks of countries had not had a chance to air their
views. The motion of closure was carried but several delegates were extremely angry.
When the vote on the code came immediately afterwards, Bangladesh and Chad joined the US
in voting against the code - purely as a form of protest. Several other delegations were
angry or confused and abstained from the vote and many more delegates - expecting that the
debate would go on for several more hours yet - had slipped out of the assembly. The
result, then, was a rather disappointing 93 votes for, 3 against and 9 abstentions.
Luckily, at the plenary of the Assembly on the next day the Samoan delegate called for a
re-vote which yielded the resounding 118 countries for, 1 against (the US) and 3
abstentions (Japan, Argentina and S. Korea).
In brief
a) Two visitors from the European Parliament (an Italian M.E.P. and the researcher for
the Development Group) observed the code debate and met with some of the European
lobbyists to discuss what contribution the European Parliament could make to ensure the
code's success.
b) After the debate officials of WHO outlined a plan they had developed for monitoring
compliance with the code in countries which were willing to participate.
c) IBFAN held its first international congress after the Assembly finished with over 90
participants from 40 countries. The major thrust was ensuring a closer link between the
First World and Third World groups and so making the monitoring operation much more
effective.
d) It is very likely, following the successful formulation of the baby food code, that
a pharmaceutical code will be attempted. This will be discussed at WHO's Executive Board
in January and again at next year's World Health Assembly. An attempt to pre-empt this
was made by the International Federation of Pharmaceuticals Manufacturers Association
when during the assembly they announced the formation of their own marketing code. Oxfam
has obtained copies of this. It clearly has such gaping loopholes that it is unlikely
that this will contribute towards more appropriate marketing. It was widely felt in
Geneva that NSOs had an important role in encouraging the drafting and implementation of
a more effective code.
.
’
- 5 -
US Resignations
Before the code debate news came from Washington that two senior government aid officials
had pledged their resignation if their government did not reverse its decision to vote
against the code. They were Dr Stephen Joseph (USAID's top health official) and Eugene
Babb (USAID's top agriculturalist). In describing the decision to oppose the code as
"unconscionable" they triggered off what was described as the first major internal split
in the Reagan administration.
The split widened last Friday when for opposite reasons Ernest Lefever was forced to
resign his very senior government post - a move described by Harry Jackson of the
Guardian as the first important political defeat for Reagan. The Senate Foreign Relations
Committee had voted against Lefever's appointment as the White House spokesman on Human
Rights.
The key incident in the Committee's 5-J- hour session was described by the Guardian:- "Mr
Helms, who was the nominee's strongest advocate and his staunchest supporter on the
committee, asked once more about the Nestle corporation's donations to Mr Lefever's Ethics
and Public Policy Center and whether the money had influenced a favourable report on
powdered milk sales to the Third World. Since Mr Lefever had persistantly and firmly
denied any connection, Senator Helms was presumably seeking another formal denial for the
record. To his, and every other member's astonishment, Mr Lefever reversed himself and
said the money and the report had been linked and that he had solicited a contribution
from Nestle before commissioning the report".
An internal memorandum between top Nestle officials which was leaked some months ago had
revealed Nestle's close links with Lefever. Nestle had paid some #25,000 to Lefever's
Ethics and Public Policy Center which in return circulated hundreds of thousands of copies
of a Fortune magazine article which was a fierce criticism of the international baby food
campaign. Nestle provided Lefever with the address list of people to send the article to.
The memo showed that Nestle" were very satisfied with the use of the Fortune article ("The
credibility of third party rebuttals of the activists' case was also unanimously endorsed
and the Fortune article, together with the interests of the Ethics and Public Policy Center
is the best opportunity we have had yet to put the record straight,and must be fully
exploited") but it was stressed "Nestle" should not be seen to be the dominant subscriber to
the Ethics and Public Policy Center".
The entire memorandum provides a rare and interesting insight into mechanisms by which
large companies counter criticism and seek to buy "positive image development". Copies of
this memorandum are availbe from me.
Oxfam's role
The major role for NGOs now (besides the general promotion of breastfeeding) is two foldr
monitoring compliance with the code and encouraging governments to translate the code into
national laws. Oxfam with its wide network of field staff and project holders could play
an important role in this. Already our investigation of the problem in the Yemen has
been well praised by the Yemeni delegate and others in the Yemen government. Examples
of violations of the code received by Oxfam would be shared with WHO and industry as
well as the IBFAN clearing house and interest in formulating legislation would be directed
to appropriate advisors.
And finally
Very soon I intend producing the final issue (for the time being) of Baby Milk Action
which will mostly be a digest of the above.
April, 1974
Weighing for nutrition surveys
Z3ATE.
5
3
to
//
/Z- &
W \ TH \p I 5?
^j-NEW MOON ©A?
MAN MARV
Fig. II.
O
^ushya itiasanL m
Uhogi
1973 English Months and Equivalent Telugu Months and Festivals.
groups in all. An average size village can be
completely surveyed in 2 working days, for we
would expect 180 pre-school children in a
village of 1000.
In our mobile under five clinics one trained
dai last year weighed and graded 20,000 child
ren at the rate of 20-60 per hour, using the
hanging scale,
indigenous calendar, and
Morley type weight chart. Of course part of
the reasons for this efficiency is that one per
son, not too highly trained, concentrates on
weighing as her main work. As she weighs
however, she has time to give nutrition and
family planning advice. With any other type
of weight for age chart, this efficiency would
not be possible.
The mother keeps
the
record—is this
wise ?
Can the mother be trusted with the child’s
record ? We trust her to look after the child,
so why not the record too ? After 20 months
in very poor city colonies, 88 % were recover
able at the door. This was despite shelling
HI YEAR
Fig. Ill
Volume XI Number
B.M.. Laugesen
of the city for 2 weeks of. war resulting in
panic evacuation of the mothers and their
children to the countryside, where they had
to live in grass huts for 4 weeks. They took
their records with them, and some got lost.
In non-border areas: 94% have been recovered
compared with 4% of outpatient records lost
in the same hospital2.
The advantages of this method are firstly
a speed up of service to the patient in the child
clinic, and a freeing up of staff for more use
ful patient care. Secondly, the record is an
important tool for educating parents and other
health workers and indigenous doctors to take
more intelligent interest in child health3.
The disadvantages mainly relate to fear that
patients may lose the record. However, many
hospitals succeed in losing a sizeable percent
age of records, as any doctor knows who has
tried to pull records more than a year old for
study. For special research projects these
records or a duplicate may be kept at the clinic,
but for service purposes, we have found it
faster and easier, to trust the mother to keep
the child’s record. This statement is based
on some 10,000 record cards entrusted to
patients every year in Ferozepur, Punjab, and
on the experience of many other hospitals in
India, and in many other countries.
2.
For local events and indigenous calen
dars a check should be made as to which
indigenous calendar is used by the local
village women, Saka, Lunar or Bikrami
Samvat. In a village, local events might
include wars, floods, drought, electrifi
cation and roading of the village.
3.
Child Health Records in 12 regional
languages for very low cost are avail
able. As the child will attend 3 times
in the first year and again in following
years the cost per visit is thus only a
few paise. An explanatory brochure on
use of these parent retained records is
available also.
4.
For scales, child health record and
brochure enquire from—
Coordinating Agency for Health Plann
ing,
C 45 South Extension Part 2
New Delhi 110049.
REFERENCES
Proceedings of the workshop on “Protein Calorie
Malnutrition”; ecology and management, organi
sed on 24-25 July at Bombay by malnutrition
Staff equipment and costs
Sub-Committee, Indian Academy of Pediatrics
1.
In busy urban clinics the best results
edited by P.M. Shah of J .J. Hospitals, Bombay.
are obtained if one person can specia
2.
Cutting WAM (1970) Annual Report of Nutri
lise in weighing of children. The staff
tion Rehabilitation Unit, weight card study.
costs in Ferozepur mobile and static
C.S.I. Hospital, Jammalamadugu, Andhra
under fives clinics worked out at 10
Pradesh.
paise per child visit (2 workers took care
of 30,coo patient visits in 1972). And
this price includes the diet advice, feed
ing demonstrations given to those with
malnutrition, and
family
planning
advice given and supplies issued.
288
1.
3.
Shah PM: (1972) report given to the “Care of
Under-fives” workshop at Hyderabad, October,
1972, sponsored by Indian Academy of Pedia
trics and Coordinating Agency for Health
Planning.
©I?
INDIAN PEDIATRICS
Volume XI Number 4
jA Weight Chart and Weighing Scale for Nutrition
Surveys and Grading of Malnutrition in Clinics
*
M.
B.
Laugesen
Abstract
For accurate diagnosis of protein calorie malnutrition we need accurate weight,
accurate age, and a convenient weight for age graph. Such things are available locally
at reasonable cost. The weight chart described allows grading of children into 5 standard
grades of nutrition, with speed and accuracy.
Accurate weight can be obtained by por
table light weight scales
weighing only
2 kilograms. This is an Indian version of the
famous English Salter scales, and a scale
accurate upto 20 kg is available, and thus all
pre-school children can be weighed with the
some scale (Fig. I).
The child is suspended in a canvas or
strong cloth holder, while small newborns may
be suspended by the four corners of a cloth
wrapper. We notice that children are less
upset by the suspension method of weighing
than by the usual platform or cradle type of
scale, which gives a feeling of insecurity.
In clinics the scale is suspended by wire from
anj' convenient hook or peg or from the leg
of an upturned string bed.
In door to door surveys, the scale is held
up by hadd till the child is weighed. If two
cloth holders are used, and the next child is'
put into it by his mother, children can be
weighed much faster by this scale than by
beam balance scales. Also mistakes are less
likely with reading of a dial scale. And com
pared with use of a floortype bathroom scale
it is much more accurate, and subtraction
errors from this are eliminated.
The scale is marked in tenths of a kilo.
Although it is a spring scale, it should be noted
that techological improvements in metals for
springs have made more accurate scales
possible.
Accurate age
Calendars using the indigenous months,
full moon dates, local festivals and other local
events, with conversion to English months and
dates, can be compiled by each hospital, and
even for each village, and mounted behind
clear X-Ray paper, and given to the registra
tion clerk for the child clinic, or to the person
doing a nutrition survey (Fig. II).
In a survey of 1,000 children coming to
mobile clinics for the first time, there was no
increase in the number of children at 12, 24,
36 or 48 months of age as would be expected
if parents could not remember accurately. (The
literacy rate in this area was less than 40% in
1971). This is because of the use of indigenous
months—local events calendar—where appro
priate. In the case of illiterate hospital clean
ing staff, the month of birth given several
years later when checked against hospital
birth records was not more than one month
wrong.
Convenient weight for age graph
*From the Community Health Department,
Frances Newton Hospital, Ferozepur, Punjab, now
at Coordinating Agency for Health Planning, Delhi.
Paper read at Symposium on Protein Calorie
Malnutrition, Postgraduate Institute of Medical
Education & Research, Chandigarh, February, 1972.
Traditional weight for age graphs require
calculation of the child’s age every time the
child is seen. But Morley, working in Nigeria,
designed a health record that uses calendar
months along the bottom of the weight for age
285
Volume X1 Number 4
13.M. Laugesen
graph. Thus age is automatically calculated,
without further work, every time the child is
seen.
care, but they are not as they look, in that a
definite minimum standard of good care is
assumed, which many hospitals are still not
equipped to provide.
These health records have been used widely ,
in many mission hospitals, in village model
health care programmes, and are now being
printed by several State Governments.
This weight chart can be used by matri
culation-pass clerks and trained dais, and
probably by those of lesser education, for
clerks and auxiliary midwives have learnt to
use these records efficiently in a day or two.
Grading of malnutrition is made auto
matic with this weight for age graph
The Nutrition subcommittee of the Indian
Academy of Pediatrics1 has defined protein
calorie malnutrition in terms of low weight-for
age thus :
81-100% of Harvard
Standard (this is shown
as the ‘road to health’
on the weight chart,
shaded in red.;
71-80% of Harvard
Standard
nutrition good
malnutrition grade 1
61-70% of Harvard
Standard
malnutrition grade 2
60% br less of Harvard
Standard
malnutrition grade 3
(The Harvard standard or median or 50th per
centile is given for each in Nelson’s textbook
of Pediatrics)
Fig. I Hanging Scale for an accurate weight
This card has been modified for India by
adding suitable food pictures, including space
for family planning, and adding local languages.
To make it useful up to school entry age, the
weight graph extends up to six years of age.
These child health records have greatly
simplified the delivery of high quality health
286
This standard allows international com
parisons and sidesteps the difficulty of obtain
ing large groups of healthy children for local Z
weight-for-age standards, which vary enor
mously in India with social class.
Two lines to separate the 3 grades of
malnutrition are dotted on the weight graph,
below the road to health (Fig. HI).
The speed and efficiency of this method
Using these weight charts and hanging
scale, tn 1 day, 2 workers were able to weight
graph and grade 85 children’s nutrition into
five grades and into six years of life, 30 sub-
April, ip74
Weighing for nutrition surveys
I
a?##©
2.
3
w
T
5
&
7
8
8
/o
77/|z= | ^ | 5 I at 1 r 1
^WEW MOON W
sIANUARV
Fig. II.
Z2
TH
• Pa&hua ifoasauz —
__ 1__ Lr±J__ 1
!
Z3
S
Bhogi
1
1973 English Months and Equivalent Telugu Months and Festivals.
groups in all. An average size village can be
completely surveyed in 2 working days, for we
would expect 180 pre-school children in a
village of 1000.
In our mobile under five clinics one trained
dai last year weighed and graded 20,000 child
ren at the rate of 20-60 per hour, using the
hanging scale,
indigenous calendar, and
Morley type weight chart. Of course part of
the reasons for this efficiency is that one per
son, not too highly trained, concentrates on
weighing as her main work. As she weighs
however, she has time to give nutrition and
family planning advice. With any other type
of weight for age chart, this efficiency would
not be possible.
The mother keeps
the
record—is this
wise ?
Can the mother be trusted with the child’s
record ? We trust her to look after the child,
so why not the record too ? After 20 months
in very poor city colonies, 88% were recover
able at .the door. This was despite shelling
III YEAR
Fig. HI
Volume XI Number
B.M. Laugesen
of the city for 2 weeks of war resulting in
panic evacuation of the mothers and their
children to the countryside, where they had
to live in grass huts for 4 weeks. They took
their records with them, and some got lost.
In non-border areas: 94% have been recovered
compared with 4% of outpatient records lost
in the same hospital2.
The advantages of this method are firstly
a speed up of service to the patient in the child
clinic, and a freeing up of staff for more use
ful patient care. Secondly, the record is an
important tool for educating parents and other
health workers and indigenous doctors to take
more intelligent interest in child health3.
The disadvantages mainly relate to fear that
patients may lose the record. However, many
hospitals succeed in losing a sizeable percent
age of records, as any doctor knows who has
tried to pull records more than a year old for
study. For special research projects these
records or a duplicate may be kept at the clinic,
but for service purposes, we have found it
faster and easier, to trust the mother to keep
the child’s record. This statement is based
on some 10,000 record cards entrusted to
patients every year in Ferozepur, Punjab, and
on the experience of many other hospitals in
India, and in many other countries.
2.
For local events and indigenous calen
dars a check should be made as to which
indigenous calendar is used by the local
village women, Saka, Lunar or Bikrami
Samvat. In a village, local events might
include wars, floods, drought, electrifi
cation and reading of the village.
3.
Child Health Records in 12 regional
languages for very low cost are avail
able. As the child will attend 3 times
in the first year and again in following
years the cost per visit is thus only a
few paise. An explanatory brochure on
use of these parent retained records is
available also.
4.
For scales, child health record and
brochure enquire from—
Coordinating Agency for Health Plann
ing,
C 45 South Extension Part 2
New Delhi 110049.
REFERENCES
Proceedings of the workshop on “Protein Calorie
Malnutrition”; ecology and management, organi
sed on 24-25 July at Bombay by malnutrition
Staff equipment and costs
Sub- Committee, Indian Academy of Pediatrics
1.
In busy urban clinics the best results
edited by P.M. Shah of J.J. Hospitals, Bombay.
are obtained if one person can specia
2.
Cutting WAM (1970) Annual Report of Nutri
lise in weighing of children. The staff
tion Rehabilitation Unit, weight card study.
costs in Ferozepur mobile and static
S.I.
C.
Hospital, Jammalamadugu, Andhra
under fives clinics worked out at 10
Pradesh.
paise per child visit (2 workers took care
of 30,000 patient visits in 1972). And
this price includes the diet advice, feed
ing demonstrations given to those with
malnutrition, and
family
planning
advice given and supplies issued.
288
1.
3.
Shah PM: (1972) report given to the “Care of
Under-fives” workshop at Hyderabad, October,
1972, sponsored by Indian Academy of Pedia
trics and Coordinating Agency for He'alth,
Planning.
Iga ST IPH 3FR
an 5’1 nt qjl irl
?a nta n ai«r gz ngtt arfiqi
Use this strip to measure the left arm of
young
children every month between first and fifth birthdays.
t
xa
nt nfg aran 'H nfa nr mar fair gt tn n arnn
anal i ng n^m
11 sa n^t nt mat mar faa
?gr | i nm at ^anr gt mar faaiar nrfgn i ant ng
arpia ainr i srsr mr nfari gt an nt art mar feafa
rgar irfga i
i>. G\'
Healthy child
If the black end of the strip comes opposite the green, the child
is getting enough food. Keep feeding him enough food. If he
becomes sick, give him soft food till he is better.
5a n^n a fatr ata ar atm fair qfa in a arna mar t I
5W n^ ar anra mar srait g I 5a at gi ita mrar ma
at a^ia g i 5?t Sift aim nr am art at sraia 11 art
5a epffa nt mat mar agt fair anr at ng hi nt aaar | i
Child Needs Care
If the black end of the strip comes opposite the yellow, the child
needs more food every day. Begin feeding some soft food.
,__
-
\
—-
jJlav
quit arrar nfa a nswr anrcia aaar | i
snrsr nfa a aaat at? atat gt mat ft i
srtfa nt snn araf a | i 5H a^r
facj 'fitft nr mar
fair ma ifa n anfa arar 11
nt afan arar mt
nt aga asaa | I wr nrnt arnr a faar at
ai at
anar | i
fan a afa nr
nri mar tar nrf^n i ani
?a nnr arnr nr *
nft airn ant agt faaat | at ara gt
ntfarr atr a^ nt ngfa a snrar aim ntfaq ,i
Child in danger
If the black end of the strip comes opposite the red, the child
needs more food. If he does not get enough food he may die.
Feed him more of what he usually eats. Feed him five or six
times a day. If he has not started to eat soft food, START NOW.
Feed him more food than before.
With more food the child grows healthier.
With more food his arm grows thicker.
fsrfT'Tr ainr nf greft
t,
^H’HT
3JTEIT
441
Hm %
T'T urnr
nrfgn i
nil ?aar
tarnr fan *f <itn ar ®:
nra'i Jf atz
feimr
aifgif i
srua <n 4^ 3r f<=rq
nrar sarar a(V gfar i
a^ aft at zat sh at
5i~m jftat | an
aftarz % aat ata
sr?t 11
snq-
URjft 'Fta
crar um % a^W art a *
faa a saar tnrnr rart
at aaw | : arzt<Y
araa, = atFzat, ?
arztzt am, j® at ar
aa, qar Fma aa,
'ter 55, ah artf trar
ara ar aasft fan
ahan srata aarrr g i
By the time a child is one year old, he should eat half
as much food as his mother.
The child may be much
smaller than his mother, but he needs lots of food to
grow properly. Mother gives this food in 5 or 6 meals.
Then the child does not have too much food to eat at
one time.
A one year bld child needs this every day : 2 cups rice, 2
small rotis, 1 cup dal, A cup green leafy vegetables, some
oil, some gur, some milk and any fruit or vegetable
which the family can afford.
nterf zr tm g i nn atn
arn
44 vftfarr I RFT
afk ^'4 %
4 vftFsflT I 3T4 ^fatr
44 4rmr fazr fw Tn % nnm arrar | l
Use for children between 1st & 5th birthday
Acknowledgements :
Three colour strip — Morley & Shakir April 74, Lancet, p 758
N-12
ARM CIRCUMFERENCE STRIP & FOLDER
(C) VOLUNTARY HEALTH ASSOCIATION OF INDIA
C-14, COMMUNITY CENTRE
Safdarjung Development Area,
New Delhi 110016
You can measure the fatness of a child's arm. Place
the plastic strip around the middle part of the child's
LEFT upper arm. Put the black end beside the
coloured part of the strip. See which colour the
black end comes opposite to.
CHILD’S BANGLE FOR THE DIAGNOSIS OF
UNDERNUTRITION
Dr. Murray Laugesen
It is rarely that we learn from the obvious, we are
so immersed in our technical expertise. Thousands of
Punjabi Children waved their arms covered in bangles
at us from 1969-73 but not till recently was it realized
that a thing as simple as a child’s bangle could sift
malnourished from the well nourished.
The Principle of the Bangle Test
The bangle measures arm circumference.
With
good nutrition, arm circumference does not vary much
from one to five years of age and varies little between
boys and girls. But it varies according to the state of
nutrition of the child from 10 eras to 16 eras arm
circumference. As the dividing line between the fat
and the thin, we chose a bangle of 4.0 ems diameter.
Due to its flexibility, this was found in practice to
pass up arms of up to 13.2 ems circumference.
Uses of the Bangle Test :
(i) In clinic practice. The bangle will select out
those children whose mothers need special advice on
feeding more solid food. It is also useful as a pre
operative check of nutritional status. Every toddler
child can and should be screened. It takes no longer
than feeling the pulse in an adult. It is so cheap,
every worker in the child clinic can use one.
(ff) Selection of villages for feeding programmes :
When the 4.0 ems bangle was tested in April-May 1975
on 300 children age 1 to 4 years we found that—
In a scarcity village
in Orissa
27 out of 100 children
were bangle positive.
In a Delhi slum
23 out of 100 children
were bangle positive.
In a Delhi low-income
colony
12 out of 100 children
were bangle positive.
The bangle gave the same ranking for nutritional
status to the three communities as other methods such
as weight for age and arm circumference. The bangle
can be used for simple surveys, measuring the children
in every fifth house and including all castes and
groups. In this way, during the time of scarcity, we
can decide quickly which villages are most in need of
feeding programmes.
The bangle is also useful in monitoring the nutri
tional status of sample villages in Districts and States
where food scarcity is likely to occur due to recent
crop failure. A rising percentage of bangle positives
in sample villages scattered over several Districts can
be helpful in getting needed food to the affected areas
in good time.
(Hi) Selecting children for feeding in each village :
The bangle positive children will include all those
with marasmus or third degree protein calorie malnu
trition (that is, all with weight for age 60% or less of
the Harvard standard, or below the lower dotted line
on the growth charts published by Voluntary Health
Association of India).
If the bangle goes above the elbow, the child needs
extra food. Based on tests on 300 children, we can
however be more precise, if we know the age of the
child at last birthday.
Age 1 : If the bangle goes above the elbow, the
weight of age is under 75% of Harvard standard. The
bangle will select all cases of second and third degree
malnutrition.
Age 2 : If the bangle goes above the elbow, tfc/e
weight for age is under 70% (below the second to
bottom dotted line of the growth charts published by
Voluntary Health Association of India). The bangle
will select most of such second degree malnutrition
case and all of the third degree.
Age 3 : The bangle will select out all children
below 65% of Harvard standard weight for age (all the
third degree cases and all the worst of the second
degree).
The author is Community Health Consul
tant with the Voluntary Health Association of
India, C-45, South Extension, Part II,
New Delhi-49. In this article Dr. Laugesen
brings out his findings about measuring malnu
trition amongst children in the age group of
one to four years by a simple device. A
child’s bangle 4.0 ems. in internal diameter
can diagnose undernutrition and marasmus in
individuals and communities. The bangle
test is based on the principle that arms circum
ference in the toddler varies little with age
but varies greatly with nutritional status, (zl
sample bangle of the correct size will be mail
ed out free on request to TNAl office.)
Ed.
An illustration of
Child's Bangle :
The bangle is passed
up the arm in one
straight push. If it
goes above the
elbow the child is
malnourished. No
attempt Is made to
twist it or force it.
Age 4 : The bangle will select out the very few
children with marasmus or third degree malnutrition
in this age group. The bangle will not select out
second degree malnutrition at this age.
The bangle favours children under the age of 3,
female children who have been under weight for a
long time. These are the groups in which most of the
malnutrition deaths will occur. With the bangle test
we can identify these children and take preventive
action.
(tv) Monitoring offeeding programmes
A youth on a cycle can monitor one feeding centre
daily. He measures the children with the bangle, dur
ing the hour of feeding. He can use the feeding re
gister. From this the number who are bangle positive
can be kept note of, each week or fortnight. As the
body weight can fall by 10% per week in total famine,
at least fortnightly checks are needed in famine areas.
A rising percentage of bangle positives means that the
ration is not sufficient or that it is not reaching the
children.
Action plan when the Bangle Test is positive :
In times of food scarcity, extra food needs to be
fed to the affected children in the affected villages. The
village people can be recruited to use the bangle in
selecting out only those village children who need such
special care. In ‘normal’ times, the custom has been
to give only breast milk for the first year of life. The
mother is repeatedly encouraged to feed solid food, as
often as possible, in as much quantity as possible,
from the fourth month of age. If this is done, very
few children need die of malnutrition.
• Reference
Laugesen, Child’s bangle for nutrition screening, submitted
for Indian Paediatrics of August 1975.
Acknowledgement
Thanks are due to Mr. Jamal Masih for assistance in
measuring 200 children in Delhi; to Miss M. Mills and the staff
of Christian Hospital, Diptipur for assistance in measuring 100
children in Orissa, to Gopal Dutia and UNICEF for the use of
photographs, and OXFAM for travelling expenses.
Reprinted from The Nursing Journal of India, August, 1975 issue
Specification
Strong metal case painted blue,
zinc plated steel hooks.
White dial, black figures.
Graduations
25 kg. x ’/, kg.
Approx. Weight
with Hook
2%lb./1.2 kg.
The taring screw allows
for approximately 5%
adjustment either side of
zero.
Approx. Overall
Length________
16"/406mm
IVBodel 225 FEW
Portable Baby
Weigher
152mm/6" Dial
The divisions on the scale match those on the Road-To-Health chart.
This scale has. been developed in conjunction with the
INTERMEDIATE TECHNOLOGY Development Group
to fulfil a need in developing countries where the control
of child health is largely accomplished by medical auxiliaries
visiting villages with no other transport than bicycles.
Prototypes of these scales have already been tested in
Zambia and the specification has been worked out in
conjunction with the medical authorities in both Zambia
and Kenya.
THE UNIT is supplied in a pack, consisting of one scale,
five pairs of weighing trousers manufactured from terylene,
P.V.C. coated and a shoulder bag of similar material.
The shoulder bag is made to accommodate the scale and
weighing trousers and afford some degree of protection to
the scale during transit.
The pack of 5 weighing trousers enables mothers to prepare
their babies and save weighing time.
1-10 Packs
...... ...... £8.50 each
11-25
£8.15
26-50
£7.95
51-75
£7.80
76-100
£7.65
Above 100 subject to special quotation
Prices
Quantities up to 100
available ox stock from
C.M.S. Weighing Equipment Ltd.,
18, Camden High Street,
London NW1 0JH
Phone: 01-387 2060
2.2
CdMMuNii v
health cell
47/1, (First FlsorJSt, Marks Hoad
VKAi
W. 23
Re 1-00
BAWGALOaE-580 001
CHILD'S BANGLE FOR THE DIAGNOSIS OF
UNDERNUTRITION
Dr. Murray Laugesen
It is rarely that we learn from the obvious, we are
so immersed in our technical expertise. Thousands
of^Punjabi Children waved their arms covered in
bangles at us from 1969-73 but not till recently was it
realized that a thing as simple as a child’s bangle
could sift malnourished from the well nourished.
The Principle of the Bangle Test
The bangle measures arm circumference. With
good nutrition, arm circumference does not vary
much from one to five years of age and varies little
between boys and girls. But it varies according to the
state of nutrition of the child from 10 ems arm
circumference. As the dividing line between the fat
and the thin, we chose a bangle of 4.0 ems diameter.
Due to its flexibility, this was found in practice to
pass up. arms of up to 13.2 ems circumference.
Uses of the Bangle Test :
(i) In clinic practice. The bangle will select out
those children whose mothers need special advice on
feeding more solid food. It is also useful as a pre
operative check of nutritional status. Every toddler
child can and should be screened. It takes no longer
than feeling the pulse in an adult. It is so cheap,
every worker in the child clinic can use one.
(ii) Selection of villages for feeding programmes :
When the 4.0 ems bangle was tested in April-May 1975
on 300 children age 1 to 4 ; irs we found that—
In a scarcity village
in Orissa
In a Delhi slum
In a Delhi low-income
colony
27 out of 100 children
were bangle positive.
23 out of 100 children
were bangle positive.
12 out of 100 children
were bangle positive.
crop failure. A rising percentage of bangle possitives
in sarnble villages scattered over several Districts can
be helpful in getting needed food to the affected areas
in good time.
(Hi) Selecting children for feeding in each village :
The bangle positive children will include all those
with marasmus or third degree protein calorie malnu
trition (that is, all with weight for age 60% or less of
the Harvard standard, or below the lower dotted line
on the growth charts published by Voluntary Health
Association of India).
If the bangle goes above the elbow, the child
needs extra food. Based on tests on 300 children, we
can however be more precise, if we know rite age of
the child at last birthday.
Age 1 : If the bangle goes above the elbow, the
weight of age is under 75% of Harvard standard. The
bangle will select all cases of second and third degree
malnutrition.
Age 2 : 1 f the bangle goes above the elbow, the
weight for age is under 70% (below the second to
bottom dotted line of the growth charts published by
Voluntary Health Association of India). The bangle
will select most of such second degree malnutrition
case and all of the third degree.
Age 3The bangle will select out all children
below 65% of Harvard standard weight for age (all
the third degree cases and all the worst of the second
degree).
The author was Community Heulth Consultant
with
the
Voluntary
Health
Association
of
India,
C-14, Community Centre SDA, New Delhi-110016.
The bangle gave the same ranking for nutritional
status to the three communities as other methods such
as weight for age and arm circumference. The bangle
can be used for simple surveys, measuring the children
in every fifth house and including all castes and
groups. In this way, during the time of scarcity, we
can decide quickly which villages are most in need of
feeding programmes.
In
this article Dr. Laugesen brings out his findings about
measuring malnutrition amongst children in the age
group of one to four years by
a
simple device-
A
child’s bangle 4.0 ems. in internal diameter can diag
nose undernutrition and marasmus in individuals and
communities.
The bangle test is based on the principle
that arms circumference in the toddler varies little
The bangle is also useful in monitoring the nutri
tional status of sample villages in Districts and States
where food scarcity is likely to occur due to recent
with age but varies greatly with nutritional status.
—Ed
An illustration of Child's
Bangle : Trie bangle is
passed up the arm in one
straight push-
if it goes
above the elbow the ch Id is
m&lrtoutishcd. No attempt is
made to twist it or force it.
The bangle favours children under the .age of 3,
famale children who have been under weight for a
longtime. These arc the groups in Which most of the
malnutrition deaths will occur. With the bangle test
we can identify these children and take preventive
action.
Action plan when the Bangle Test positive :
In times of food scarcity, extra food needs to be
fed to the affected children in the affected villages.
The village people can be recruited to use the bangle
in selecting out only those village children who need
such special care. In‘normal’times, the custom has
been to give only breast milk for the first year of life.
The mother is repeatedly encouraged to feed Solid
food, as often as possible, in as much quantity as
possible, from the fourth month of age.
If this is
done, very few children need die of malnutrition.
(iv) Monitoring offeeding programmes
Reference
Age 4 : The bangle will select out the very few
children with marasmus or'third degree malnutrition
in this age group. The bangle will not select out
second degree malnutrition at this age.
■ A youth on a cycle can monitor one feeding
centre daily. He measures the children with the bangle
during the hour of feed,ing. He can use the feeding
register. From this the number who are bangle
positive can be kept note of, each week or fortnight.
As the body weight can fall by 10% per week in total
famine, at least fortnightly checks arc needed in
famine areas. A rising percentage oft bangle positives
means that the ration is not sufficient or that it is not
reaching the children.
Reprintedfrom The Nursing Journal of India,
August, 1975 issue
Laugescn, Child’s bangle for nutrition screening, submitted
for Indian Paediatrics of August 1975.
Acknowledgement
Thanks are due to Mr. Jamal Masih for assistance in
measuring 200 children in Delhi: to Miss M- Mills and the staff
of Christian Hospital, Diptipur for assistance in measuring 100
children in Orissa, to Gopal Dutia and L NjCEF for the use of
photographs, and OXFAM for travelling expenses.
For. more copies write to :
Voluntary Health Association of India,
C-14, Community Centre,
Safdarjung Development Area,
New Delhi-110 016
CHILD’S BANGLE FOR THE DIAGNOSIS OF
UNDERNUTRITION
Dr. Murray Laugesen
It is rarely that we learn from the obvious, we are
so immersed in our technical expertise. Thousands of
Punjabi Children waved their arms covered in bangles
at us rrom 1969-73 but not till recently was it realized
that a thing as simple as a child’s bangle could sift
malnourished from the well nourished.
The Principle of the Bangle Test
The bangle measures arm circumference.
With
good nutrition, arm circumference does not vary much
from one to five years of age and varies little between
boys and girls. But it varies according to the state of
nutrition of the child from 10 cms to 16 cms arm
circumference. As the dividing line between the fat
and the thin, we chose a bangle of 4.0 cms diameter.
Due to its flexibility, this was found in practice to
pass up arms of up to 13.2 cms circumference.
fe,
Uses of the Bangle Test :
(i) In clinic practice. The bangle will select out
those children whose mothers need special advice on
feeding more solid food. It is also useful as a pre
operative check of nutritional status. Every toddler
child can and should be screened. It takes no longer
than feeling the pulse in an adult. It is so cheap,
every worker in the child clinic can use one.
(if) Selection of villages for feeding programmes :
When the 4.0 cms bangle was tested in April-May J975
on 300 children age 1 to 4 years we found that—
In a scarcity village
in Orissa
27 out of 100 children
were bangle positive.
In a Delhi slum
23 out of 100 children
were bangle positive.
In a Delhi low-income
colony
12 out of 100 children
were bangle positive.
The bangle gave the same ranking for nutritional
status to the three communities as other methods such
as weight for age and arm circumference. The bangle
can be used for simple surveys, measuring the children
in every fifth house and including all castes and
groups. In this way, during the time of scarcity, we
can decide quickly which villages are most in need of
feeding programmes.
The bangle is also useful in monitoring the nutri
tional status of sample villages in Districts and States
where food scarcity is likely to occur due to recent
crop failure. A rising percentage of bangle positives
in sample villages scattered over several Districts can
be helpful in getting needed food to the affected areas
in good time.
(Hi) Selecting children for feeding in each village :
The bangle positive children will include all those
with marasmus or third degree protein calorie malnu
trition (that is, all with weight for age 60% or less of
the Harvard standard, or below the lower dotted line
on the growth charts published by Voluntary Health
Association of India).
If the bangle goes above the elbow, the child needs
extra food. Based on tests on 300 children, we can
however be more precise, if we know the age of the
child at last birthday.
Age 1 : If the bangle goes above the elbow, the
weight of age is under 75% of Harvard standard. The
bangle will select all cases of second and third degree
malnutrition.
Age 2 : If the bangle goes above the elbow, the
weight for age is under 70% (below the second to
bottom dotted line of the growth charts published by
Voluntary Health Association of India). The bangle
will select most of such second degree malnutrition
case and all of the third degree.
Age 3 : The bangle will select out all children
below 65% of Harvard standard weight for age (all the
third degree cases and all the worst of the second
degree).
The author is Community Health Consul
tant with the Voluntary Health Association of
India, C-45, South Extension, Part II,
New Delhi-49. In this article Dr. Laugesen
brings out his findings about measuring malnu
trition amongst children in the age group of
one to four years by a simple device. A
child’s bangle 4.0 cms. in internal diameter
can diagnose undernutrition and marasmus in
individuals and communities. The bangle
test is based on the principle that arms circum
ference in the toddler varies little with age
but varies greatly with nutritional status. (A
sample bangle of the correct size will be mail
ed out free on request to TNAl office.)
Ed.
An illustration of
Child’s Bangle :
The bangle is passed
up the arm in one
straight push. If it
goes above the
elbow the child is
malnourished. No
attempt is made to
twist it or force it.
Age 4 : The bangle will select out the very few
children with marasmus or third degree malnutrition
in this age group. The bangle will not select out
second degree malnutrition at this age.
The bangle favours children under the age of 3,
female children who have been under weight for a
long time. These are the groups in which most of the
malnutrition deaths will occur. With the bangle test
we can identify these children and take preventive
action.
'
(tv) Monitoring offeeding programmes
A youth on a cycle can monitor one feeding centre
daily. He measures the children with the bangle, dur
ing the hour of feeding. He can use the feeding re
gister. From this the number who are bangle positive
can be kept note of, each week or fortnight. As the
body weight can fall by 10% per week in total famine,
at least fortnightly checks are needed in famine areas.
A rising percentage of bangle positives means that the
ration is not sufficient or that it is not reaching the
children.
Action plan when the Bangle Test is positive :
In times of food scarcity, extra food needs to be
fed to the affected children in the affected villages. The
village people can be recruited to use the bangle in
selecting out only those village children who need such
special care. In ‘normal’ times, the custom has been
to give only breast milk for the first year of life. The
mother is repeatedly encouraged to feed solid food, as
often as possible, in as much quantity as possible,
from the fourth month of age. If this is done, very
few children need die of malnutrition.
Reference
Laugesen, Child’s bangle for nutrition screening, submitted
for Indian Paediatrics of August 1975.
Acknowledgement
Thanks are due to Mr. Jamal Masih for assistance in
measuring 200 children in Delhi; to Miss M. Mills and the staff
of Christian Hospital, Diptipur for assistance in measuring 100
children in Orissa, to Gopal Dutia and UNICEF for the use of
photographs, and OXFAM for travelling expenses.
Reprinted from The Nursing Journal of India, August, 1975 issue
VOLUNTARY
C-14,
HEALTH
Community Centre,
Safdarjung
Phone : 652007, 652008
ASSOCIATION
Development Area,
OF INDIA
New
Delhi-110016
Telegrams : VOLHEALTH New Delhi-110016
VHAI-249
EXERCISE ON GROWTH CHARTS FOR UNDER: FIVES
And Indigenous Calendar
These records are central to all activities in the Under Fives
Clinic, and are now coming into use in many countries. .'
To understand how they are used let us take for our example
Bobbi who was 2 years old when seen in summer of 1976 and
we will complete a chart for her. Her mother-says Bobbi was born
in May.
'
’
Turn the chart sheet until the boxes in which we fill in the months
are down the left hand side . (Fig.l)
Fill-in the month of birth, which in; this
case is May, in the first space of each
year. You will notice that this first
space is more heavily outlined. Write
'MAY' in each of these.
Then fill in the other months, as shown,'
for 2 years.
Once this calendar is completed, we
never need calculate the age again
How old was Bobbi in July, 1976?
months
Turn the chart so that the kilogram weights are down the left hand side.
Now, when the child is weighed each month put a large dot in the month
space. (Fig.2)
Bobbi, Bom May 197^
197^ Weight in kilograms 197^7
May
6.5
May chO •
4.0
June
7.5
June
8.0
4.5
July
July
Aug
8.5
5.5
Aug
9.0.
Sept
Sept. 6.0
9.0
Oct.
6.5
Oct.
9.5
Nov
Nov. Did not attend
Dec. ’ 2.5
Dec. 7.0
Had whooping cough jan.7> 10.0
197$ Jan
Feb r 9,5
Did not attend
March 10.0
Feb. Still away
April 10.5
March 6.0 Measles
April 5.5 To Nutrition Feeding
Centre with marasmtw
1.
What-are-iha-advantages in. the
2.
what are the advantages of this record ------------------------ ’——■—n
over six pages of clinical notes?--——-—-—------------ -—■—
mother keeping this record?
3,
List some of the reasons for Bobbi g---- --—*-■
----- —-
loss of weight following whoopingcough and measles >■
4.
The child illustrates one of the
problems in timing DPT
irnmimi-za^irm
What is this?
EXERCISE IN USE OF INDIGENOUS CALENDAR
- -------- —'
When was the child born?
Mother says Bobbi was bom at amavasya. This was in the month
of Baisakh after Baisakhi. We look, at the indigenous calendar (VHAlr^l5)
1974
1975
Baisakh
mid April to mid May
Amavasya in
Baisakh
22 April
11 May
Baisakhi
13 April
13 April
Which month was Bobbi really bom in ?
1.
Rural mothers often do not know the English calendar. —-----------------How many health workers would know the village calendar?----------------
2.
Would it be easier to record on the growth chart all months —-;-------as indigenous or "desi" months from the beginning, without--------------translation?
-------------------------------------------------------------------------------
'3.
How would we make up an indigenous calendar?------------- ------- .-----------Which of these events would be important in your area?---------------------- :
Phases of moon
_________________________________
Desi months
______________ __________
Local village festivals and markets _______________________
Events such as floods, famind, new road
Seasons for planting and harvest.
4.
Which languages would be needed and which staff would find
it useful?
--------------------------------
FIGHTING
MAL-NUTPJT.I'O:N
WITH
'HYDERABAD
M 8 X '
INDO-DUTCH PROJECT FOR CHILD WELFARE
(STICHTING NEDERLANDS KINDERHULP PLAN)
Chevella Block, Hyderabad District, A. P,
Protein packets made out of1 local seasonal crops, such as jowar
or ragi, gram-dhal, ground-nut and jaggery have helped in
eradicating diseases of mal-nutrition in nearly 7,000 children in
the selected villages of Chevella Block of Hyderabad District.
Each packet of 70 grams contains:
Wheat or Jowar
Bengal Gram
Ground-nut
Jaggery
Defatted Soya Flour
.. 35.0 gms.
.. 1 1.0 gms.
.. 6.0 gms.
.. 11.5 gms.
.. 6.0 gms.
Protein content of
Calories
Vitamin-A'
... 10 gms.
250
... 50 IU
Cleaning, roasting and grinding
Mabila
is done by local members of
mandals who earn a marginal profit of about 3 to 4
paise per packet, the monthly consumption being 3,000 packets
The results of using these packets in the past three years are:
Reduction of oedema fluid in first week,
Increase of weight from second week.
Disappearance of oedema, improvement in mental changes,
subsidence of diarrhoea and puffness of face in second week.
Increase of weight at the end of 4 weeks (0.66 kg. average.)
Manner of Feeding:
As plain powder, or
with milk as. porridge, or
as jaggery balls (laddoos), or
in bread cakes (ch'apathies). ’
To convince the villagers that protein packets can be made by
them with local ingredients, a nutrition demonstration unit has
been
established at Kanakamamidi, where seasonal crops are
being grown by a local farmer on one hectare land, donated to
the Indo-Dutch Pioject. -Mahila mandals will use the produce
for preparation of protein'packets
(Balwadis) and creches.
for the Nursery Schools
This provides a chain of demonstra
tions - growing of local high yielding crops, method of prepa
ring protein packets at the village level, utilising the packets in
different ways for mothers and childern, controlling mal-nutrition and encouraging local mothers to use this ‘mix’ at home
Nutrition Demonstration Unit
Information regarding project acitvities can be had from
Dr.H.W.Butt, Director, Indo-Duch Project for Child'Welfare
$-3-885, Somajiguda, Hyderabad - 500 004.
Tel. 3 5 9 3 8.
Res. Tel. 3 3 40 8,
Link with maDnutrition
his issue of Health Dialogue looks at the link between
acute respiratory infections and nutrition.. Children who are
severely malnourished have a much greater risk of dying from
pneumonia than other children, yet it is more difficult to
recognise pneumonia in severely malnourished children. A
recent study showed that children with severe malnutrition
often have pneumonia without the usual clinical signs — fast
breathing or chest indrawing.
This means that all severely malnourished children with
cough or difficult breathing should be admitted to hospital and
treated for severe pneumonia.
Much still needs to be learnt about pneumonia in these
children, but research suggests giving either a combination of
benzypencillin plus gentamicin, or chloroamphenicol
intramuscularly should be the first choice of action.
The link between ARI and nutrition is two-way.
Malnutrition means a child is more likely to develop
pneumonia. Unless particular attention is given to feeding sick
children, respiratory infections can cause a well nourished
child to lose weight and become malnourished.
High fever, a block nose and fast breathing can interfere
with normal feeding. Articles inside discuss how to overcome
these problems and provide guidelines on how to make sure
children receive the nutrients they need.
Finally, this issue contains a success story from
Pakistan. It is difficult to carry out research as part of the
day-to-day work of a busy hospital. However, Pakistan's
Children Hospital introduced a simple ARI register to collect
data on the success of introducing standard case
management, which has produced extremely encouraging
results. (See page 8)
We would strongly advise other hospitals and health
centres to collect data in a similar way so that feedback can
be obtained on the impact of ARI programme activities.
Gathering such evidence of a reduction in deaths, or costs,
can be an important way to convince health workers and
families that this approach really works.
Harry Campbell
(ARI News Issue No. 30)
In this issue :
□
H
H
■
Nutrition
Micronutrients
Case Study
Communication
CMAI
AHRTAG
Christian Medical
Association
of India
Appropriate Health
Resources & Techmnologies
Action Group
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
NUTRITION
Feeding sick children
Children with respiratory
infections need nourishing food
to help them to recover. Kenneth
Brown provides
recommendations on appropriate
diets for children of different age
groups and how to overcome
feeding problems.
Little research has been done into
appropriate diets for young children
with acute respiratory infections, so
there are few specific guidelines on
how to feed children during and
after respiratory infections.
However, a lot of research has
been done into feeding children who
have diarrhoea, which shows that
most children with diarrhoea should
be fed the same diets as healthy,
well nourished children. It is likely
that this is also true (with only a
few exceptions) for children with
ARIs.
Therefore this article describes
general recommendations for
feeding healthy children of different
ages, and then discusses some
• changes that might be necessary for
children with ARIs.
Exclusive breastfeeding
It is well established that
exclusive breast-feeding (giving
breastmilk only, with no other foods
or fluids, including water) is the best
way to feed young infants. It
ensures that infants grow well and
protects them from diarrhoeal and
respiratory infections.
However, there is some debate
about when to introduce
complementary (weaning) foods. If
these foods are introduced too
early, an infants's breastmilk intake
is reduced and replaced with less
suitable sources of nutrients, and
the infant is exposed to infection.
But on the other hand, if
complementary foods are introduced
too late, an infant's growth and
development may be delayed due to
inadequate nutrient intake. Current
recommendations are that
Q
complementary foods should be
introduced between four and six
months of age.
Research recently completed in
Honduras provides new information
on when to introduce complementary
foods. In the study, exclusively
breastfed four-month-old infants
were randomly assigned to two
groups; one group continued to be
breastfed exclusively until six
months of age while the other group
was fed high quality, industrially
processed complementary foods,
such as rice cereal with egg yolk,
and mashed fruits and vegetables,
in addition to breastmilk. High
quality complementary foods were
chosen in order to identify possible
benefits of introducing
complementary foods early.
However, there was no
difference in infant's growth from
four to six months of age between
the two groups. Total energy intake
was similar in both groups. Infants
who received complementary foods
consumed less breastmilk, despite
mothers continuing to breastfeed
them as frequently as when they
were exclusively Breastfed. The
infant's feeding and growth
continued to be studied in their
second six months of life with both
groups receiving home-prepared
complementary foods. Infant's
acceptance of food and patterns of
growth were not affected by whether
they had been exclusively breastfed
or received complementary foods at
4-6 months of age.
The results suggest there was
no advantage in introducing
complementary foods before six
months of age. However, most of
the infants studied had normal
birthweights (weighing 2,500 grams
or more) which may have affected
the results. More research needs to
be done to find out whether these
recommendations are relevant to low
birthweight infants whose mothers
may be more likely to be
undernourished.
Complementary feeding
Once complementary foods are
introduced, breast-feeding should be
continued for as long as possible,
as breastmilk is a high quality
source of easily absorbed energy,
protein, vitamins and minerals.
Complementary foods given in
addition to breastmilk should be
carefully chosen to provide the
nutrients required by growing ■
children. A good diet is one where
meals combine foods with different
nutrients (sometimes called multimixes) including:
1
•
local staples (such as cereals
or starchy vegetable tubers)
•
protein sources (such as beans,
groundnuts, meat, eggs, milk or
fish)
• foods rich in vitamins and
minerals (vegetables, fruits or
animal products) and, if
necessary:
e
extra sources of energy (oils
and sugars).
Foods given to children should
be: readily available locally,
acceptable to families, and able to
be prepared in a form that a young
child can easily eat (e.g. mashed).
It is important that the mixed
diet is rich enough in energy so that
children can get the energy they
require before their stomachs are
full. This is called energy
concentration: the energy a food
contains per volume of the food.
For example, a watery gruel has a
low energy concentration. Children
are likely to feel full and not
manage to eat enough of it to
provide adequate energy.
Energy concentration is
measured in kilocalories per 100
grams of food. If children are fed
four times a day they need at least
80 kilocalories/100g serving of food;
if they receive three meals a day
they need 120 kilocalories/100g.
Watery cereal gruel commonly fed to
infants being weaned in West Africa
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
NUTRITION
is well below the recommended
energy concentration (at 25-30 kcal/
100g). Full fat animal milks are
also low in energy concentration
(60-70 kcal/100g). Mashed root
vegetables (100 kcal/100g) and
cooked rice (100 kcal/100g) are
about the required energy
concentration, while bread (300-400
kcal/100g) has high energy
concentration.
If common complementary
foods have a low energy
concentration, this can be increased
by adding fats or oils (such as
butter or oil) which have a very high
^jergy content. However, only
▼.nail amounts of fat or oil should
be added, otherwise children may
satisfy their energy needs and stop
eating before they have taken in
enough other nutrients such as
protein or micronutrients (small
amounts of vitamins and minerals
which the body needs to function
well). Ideally, health workers
providing advice to families on
increasing a food's energy
concentration should consult a
trained nutritionist first.
A major challenge to health
workers, nutritionists and programme
planners is to ensure that local
mixed diets provide the full range of
micronutrients. Sometimes local
diets are deficient in a particular
^cronutrient. In some cases it may
be necessary to provide
micronutrient supplements or add
the missing micronutrient to
industrially produced foods ( such as
adding iodine to salt). However, the
main focus should be to ensure that
local communities have access to
good mixed diets which provide the
full range of nutrients required.
Dr. Kenneth Brown, Programme
in International Nutrition,
Department of Nutrition, 3150
Meyer Hall, University of
California, Davis, CA, 956168669, USA.
For more information about
nutrition for children write to
AHRTAG for a list of further
reading.
1. Cohen R J et al. Effects of
age of introduction of complemen
tary foods on infant breast milk
intake, total energy intake, and
growth: a randomised intervention
study in Honduras, Lancet
1994;343:288-93
ARI News issue No.30)
Advice specific
to ARIs
• Children with ARI may have
feeding problems for several
reasons
• Any infection, especially if fever
is present, may reduce a child's
appetite.
• An infant with a blocked nose
may find feeding difficult
because he or she is having to
breathe through the mouth.
o Fast breathing or respiratory
distress makes feeding difficult
and can lead to the child
choking or inhaling food into the
lungs.
For these reasons, special
nursing or home care may be
needed and feeding practices may
have to be adapted as described
below.
Fever There is little scientific
information on how to stimulate
the appetite of febrile children
with infections. Some health
workers believe that reducing
fever by giving paracetamol may
help overcome lack of appetite,
but there is no good evidence to
support this.
The most important thing is to
advise families and care givers to
continue to offer sick children a
nutritious diet and encourage them
to eat, so that as soon as their
appetites return they can easily get
the nutrients they need. In the
recovery period, children should be
offered small amounts of food
more frequently than usual to give
them the chance to correct any
nutritional loss which may have
occurred during the illness.
Blocked nose If a child's ■
nose is blocked by thick mucus,.
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
someone in the family should be
shown how to clean the child's
nose, using a soft, clean cloth,
dipped in lightly salted water. The
cloth should be rolled until it is
pointed, then inserted gently into
the child's nostril and turned
around.
Fast breathing or respiratory
distress If the child is breathing
very rapidly (more than 80 breaths a
minute) it may be advisable to stop
normal feeding until the child's
breathing settles down in order to
reduce the risk of inhaling food into
the lungs. In a hospital setting,
with access to the right equipment
and good nursing care, nasogastric
feeding can replace normal feeding
(although there is a risk of inhaling
food with this procedure also).
If a child is normally breastfed,
but is unable to suckle for a short
time, show the mother how to
express her milk. Expressed
breastmilk could be fed to the baby
through a nasogastric tube. Even if
it is decided not to use a
nasogastric tube, expressing
breastmilk will help ensure that the
mother's breasts do not become
uncomfortable and will help
maintain her breastmilk supply so
that the child can easily start
breast-feeding again when he or
she is better.
Dr. Kenneth Brown
MICRONUTRIENTS
Vitamin A dteftetency
prevention is best
Does giving Vitamin A
supplements to children
hospitalised with pneumonia
improve their recovery? Chris
Kjolhede, Anne Gadomski and
Fracisco Chew report on new
research.
\/itamin A deficiency is a serious
public health problem in many
developing countries, causing
damage to people's eyesight and
weakening children's resistance to,
and recovery from, infections.
Several large studies have
shown that giving high dose vitamin
A supplements (also known as
retinol) 2-4 times a year to children
in places where vitamin A
deficiency is widespread can reduce
overall childhood mortality.
However, it is not clear
whether vitamin a supplementation
can prevent acute respiratory
infections such as pneumonia or
reduce the number of deaths
associated with ARI.
A link between vitamin A
deficiency and acute respiratory
infections has been reported in
some studies, but it is not known
which is the cause and which is
the effect. However, it is clear
that ARI can cause a temporary
lowering of vitamin A levels. One
explanation for this is that vitamin
A or retinol is lost in the urine of
people with acute infections.
Studies of vitamins
supplementation during measles
have shown a beneficial effect,
with a reduction in both the
incidence of post-measles
pneumonia and deaths from
pneumonia. However, most deaths
D
from pneumonia (more than 80
percent) are not linked to measles.
Vitamin A supplementation has
■ not shown a clear benefit in infants
under one year old. This age
group is particularly important
because that is when most cases
of, and deaths from, ARI occur.
Does Vitamin A speed recovery?
Our study investigated whether
high dose vitamin A supplements
given to children hospitalised with
pneumonia could enable them to
recover faster. Children aged 3-4
months admitted with pneumonia to
a Guatemalan hospital were divided
randomly into two groups and given
eithe.r a vitamin A capsule or
placebo (a capsule without any
medical benefit) in addition to' the
usual antibiotic and supportive
treatment for pneumonia. Neither
researchers nor parents knew which
children had received which
capsules.
However, the main lesson is
clear. Efforts should focus on
preventing malnutrition, including
vitamin A deficiency, before a child
becomes ill, rather than trying to
treat it during an acute illness.
Dr Chris Kjolhede and Dr Anne
Gadomski, The Mary Imogene
Bassett Research Institute,
f)
1, Atwell Road, Coopperstown,
New York 13326-1394, USA.
Dr. Francisco Chew, INCAP,
carretera Roosewelt,
Guatemala City, Guatemala.
1.
Stephensen CB et al. Vitamin
A is excreted in the urine
during acute infection. Am j
Cloin Nutr, 1994; 60: 388-92.
We then assessed children's
recovery, including breathing rate,
oxygen absorption and fever.
There were no significant clinical
differences between those who had
received vitamin A and those who
had received the placebo.
Our conclusion is that treating
non-measles related pneumonia
with vitamin A in addition to normal
pneumonia treatment does not
improve infants' and children's
recovery. Two possible reasons for
this in the hospital setting studied
might be that only severe
pneumonia cases were treated or
that children were brought to
hospital late in the course of
pneumonia.'
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
NUTRITION
Foedong pracioces
l V [ alnutrition Is common in
young children in India even though
the incidence of Marasmus has
come down considerably and one
hardly sees any child with
Kwashiorkor. The most vulnerable
period is 6 months to 2 years.
According to the National Family
Health Survey, 1992-93, around 5060% of children were malnourished
by two years and the prevalence
plateaus after that. Stunting was a
jpajor problem and was present in
Almost half the children. According
to the National Nutrition Monitoring
Bureau Survey 1988-92, stunting
was present in 60% of children
between 1-5 years. This sad state
of affairs is due to a high infection
rate at this age and a lack of
understanding regarding the child's
food requirements. Furthermore,
when a child is ill with fever, acute
respiratory infection, diarrhoea etc.,
he/she loses appetite and is not
inclined to eat. Many families have
a mistaken belief that a sick child
needs less food and that he/she
can only digest porridge, diluted
milk, fruit juice etc. Most energy
rich foods are considered bad for a
sick child.
Exclusive breast-feeding
It has now been well.
established that exclusive breast
feeding protects the child from
infections such as diarrhoea and
respiratory infections.
Unfortunately even though almost
all women do breastfeed the baby,
the iniciation is delayed in the
belief that colostrum (perceived as
blocked milk and looks like pus) is
not good for a baby. Various
fluids and herbal mixtures some
with laxative effect including castor
oil, are given for the first day or
two, and sometimes even longer.
There is also a misconception that
there is no milk secretion, as on
squeezing the areola, only a few
drops ooze out. Giving water is
also quite common even after
breast-feeding has been
established. Many mothers go
back to their work fairly soon, and
they start giving some diluted
animal milk in addition to
breastmilk to get the child "used
to it". The health professionals
too are guilty of advising prelacteal feeds. A few studies have
shown that exclusive breast
feeding indeed is not common
even though almost every mother
breastfeeds naturally and doesn't
have to be persuaded to do so.
It is obvious therefore that
benefits of exclusive breast-feeding
need to be emphasised and the
mother, the family and the
community made aware of it. For
a working mother, there is a
dilemma and difficult choices have
to be made. It is necessary
therefore, that government,
employers, family and the
community helps to create
conditions in which the mother can
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
exclusively brestfeed her baby for
at least four months. Recently
the role of stress, migration of the
husband to urban areas in search
of work, alcoholism etc. has also
been highlighted.
In addition to breast milk,
some semisolids need to be
introduced around 4-6 months.
Most family foods can be modified
and made suitable for. the child.
These should be energy rich, and
the quantity has to be increased
gradually. Watery supplements
such as juices, dal water, khichri
water etc. should be strongly
discouraged. Energy density of
semisolids can be increased by
adding oil butter, ghee or sugar.
The child's energy requirement is
high but the stomach is small and
so he/she needs to be fed 5-6
times a day. It has to be
emphasised that illness is not a
contraindication for giving the
normal family food, which the child
was having earlier. Most illnesses
depress appetite, and so the child
needs to be coaxed to eat. Poor
energy density foods from hawkers
should be discouraged. These
NUTRITION
increase the risk of diarrhoea also.
Breast-feeding should be continued
for as long as possible as
breastmilk is an excellent source
of energy, proteins, vitamins and
minerals.
The cultural beliefs in "cold"
and "hot” foods should not be
condemned outright. With proper
explanation, this obstacle can be
overcome, or an alternative
suggested.
Fruits such as mosumbi, apple,
grapes and pomegranates are
traditionally considered to be
beneficial during illness and families
spend a great deal of money to
buy these rather than the energy
rich, banana, mango, papaya,
chickoo etc.
The Indian diet is usually a
mix of cereals and legumes and
hence rich in proteins.
Fermented foods too are
popular in most parts of India.
They are. rich in vitamihs.
Malting is practised in some
parts of India and amylase
produced as a result of malting
helps to reduce the viscosity
and the child can eat a larger
quantity. The grain is
dampened to allow it to
germinate, then it is dried,
dehusked and ground. The
malting process increases the
content of riboflavin, niacin and
iron. Porridge made from
malted flour is less thick
because of the presence of
amylase and more flour can be
used to make porridge as
compared to ordinary flour.
This increases the energy
density of food. Food is less
viscous and hence easier to
eat. Ragi malt is used
extensively for feeding young
children in South India.
It is imperative that all the
health workers, ICDS functionaries
and others who are in contact with
the community help to take the
right messages regarding young
child feeding in health or during an
illness not only to the mother but
to the whole family. Their training
has to be tailored to meet this AV
requirement.
Dr. Shanti Ghosh
Scientific Editor
Health Dialogue
The Child Survival and Safe
Motherhood Programme (CSSM)
The Child Survival and Safe
Motherhood Programme (CSSM)
was launched by the Ministry of
Health and Family Welfare in
August 1992 with the objective of
improving the health status of
women and children and reducing
maternal, infant and child mortality
rates. The access to women and
children established under the
immunisation programme is now
being utilised to intensify other
services related to maternal and
child health. All the districts will
be covered by 1997. The
programme will cost Rs. 11255.8
million over a seven year period
and is supported by the World
Bank and UNICEF. CSSM
programme underlines the high
priority by the central and state
□
governments to improving the
health status of women and
children and reducing maternal,
infant and child morbidity and
mortality. The programme is geared
to fulfil the goals set for the year
2000.
Goals for the year 2000
Infant mortality rate
50
Under 5 mortality rate
70
Maternal mortality rate 200/100,000
Births
Crude birth rate
21
Crude death rate
9
Life expectancy
Male
Female
63 years
65 years
Elimination of polio and
neonatal tetanus
Service coverage
Antenatal coverage
100%
Information to couples
about child spacing
100%
Effective couple protection
rate
Immunisation coverage
Deliveries by trained
attendant
65%
100%
100%
The package of services
For the children:
•
Essential new born care
including exclusive breast
feeding
»
Immunisation
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
NUTRITION
•
Appropriate management of
diarrhoea and acute respiratory
infections
o
Vitamin A prophylaxis
•
Early registration of pregnancy
Antenatal care and early
identification of maternal
complications
•
Immunisation
•
Prevention and treatment of
anaemia by universal coverage
with Iron Folic Acid (IFA)
tablets
f
•
Promotion of clean deliveries
and deliveries by trained
personnel
•
Promotion of institutional
deliveries
•
Management of obstetric
emergencies
c
Birth spacing
Essential new born care
Delivery practices
25% or more deliveries in each
state to be institutionalised and
100% to be conducted by trained
personnel by 2000.
•
Create awareness about
essential new born care among
health care providers
•
Improve maternal care and
promote birth spacing.
Upgrading PHCs with labour
rooms and other basic essentials.
The programme addresses
the major cause of morbidly and
mortality in women and children
which are preventable by readily
available and cost effective
interventions. Retraining of the
medical and paramedical
personnel is an important activity
to ensure high quality of
services. Vaccines, drugs and
equipment kits are being
provided to ensure availability of
essential supplies in adequate
quantities.
Train health care providers
including TBAs and ICDS
functionaries to identify women with
maternal complications, bad
obstetric history or any high risk
factor.
For the mother
•
•
Train clinicians in the First
Referral Units and district
hospitals for the care of the
sick new born
The existing health facilities in
the rural areas are being upgraded
to equip them to handle emergency
obstetric cases.
e
• Resuscitation of new borns
with asphyxia
•
Prevention of hypothermia
a
Interventions for the reduction of
Maternal Mortality
f'
Prevention of infections
Exclusive breast-feeding
o
o
Referral of the sick new born
Strategies
At least one dai will be
trained in each village.
Training on diarrhoea has
been integrated with the training on
ARI and new born care. For
management of ARI, contrimoxazole
tablets are included in drug kit
supplied to the sub-centres.
The existing health facilities in
the rural areas will be upgraded to
equip them to handle emergency
obstetric cases.
Relevant equipment for
newborn care is being provided at
the PHCs and district and sub
district hospitals.
e
e
0
Strategies
0
Institutional delivery for women
at high risk
0
Immediate referral and
appropriate care of
emergency obstetrics
complications.
In the districts under the
CSSM, retraining of the medical
and paramedical personnel is an
important activity to ensure high
quality of services and an
integrated implementation of field
activities. Drugs and equipment
kits are being provided to all
districts under CSSM to ensure
availability of essential supplies in
adequate quantities. Reporting
forms for surveillance of all the
childhood diseases and monitoring
of performance of the interventions
under the CSSM programme have
been integrated.
o
Safe and clean delivery
practices.
Dr. Shanti Ghosh
•
Train health personnel in new
born care
•
Provide basic facilities for
essential new born care for
low birth weight and sick new
borns in the first referral units
and district hospitals
Advice to women with
medical problems to avoid
pregnancy till health
improves.
Birth spacing
TT 2 doses and I FA tablets
Early treatment of maternal
complications
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
CASESTUDY
Case management works
Mushtaq Khan and Gul Rehman
describe how training in ARI case
management reduced mortality
from pneumonia and led
decreased antibiotic use and cost
savings.
Acute respiratory infections are the
leading cause of childhood illness
and deaths in Pakistan. They cause
more than a quarter of deaths in the
community of children under five
years old and a third of hospital
deaths in the same age group. ARIs
are also the major cause of childhood
illness in Pakistan.
Management of ARI may be
complicated by: delay in seeking
medical help; wrong or late diagnosis
by a health worker; inappropriate
drugs being prescribed; or antibiotic
instructions not being followed.
Pakistan launched a national
ARI control programme in 1989 with
dual aims of reducing deaths from
pneumonia of children under five,
and rationalising the use of
antibiotics and other drugs in treating
children with ARIs. The programme
promotes standard case
management--the use of simple signs
such as fast breathing and chest
indrawing to diagnose pneumonia.
Antibiotics are only recommended for
pneumonia, acute tonsillitis, acute
otitis media and mastoditis, not for
simple coughs and colds. The use of
commercial cough mixtures, many of
which contain multiple ingredients, is
also discouraged.
Training begins
Training in ARI case
management began in 1990. Twenty
ARI training units have been
established for this purpose. One of
these units is based at the Children
Hospital in Pakistan's capital,
Islamabad. Both staff of the
Children Hospital and health workers
Q
from other hospitals and clinics are
trained at the unit.
The Children Hospital has 230
beds for medical, surgical and
neonatal patients. It has an out
patient department where 350-400
children are seen from 8 am - 2 pm.
At other times children are referred to
the hospital's emergency department.
From January 1990 to December
1991, all doctors regularly employed
at the hospital were trained in ARI
case management at four-day
training courses. Standard ARI case
management was introduced in the
out-patient and emergency
departments.
Children with severe or very
severe pneumonia seen in the
outpatient or emergency departments
are admitted to hospital. Other
children with ARIs are sent home.
Their care givers are advised on
home care, and antibiotics are given
to children with (non-severe)
pneumonia, acute otitis media or
streptococcal sore throat.
Since January 1990 details of
children with ARIs have been
recorded in special ARI registers.
Standard terms-no-pneumonia,
pneumonia, severe pneumonia, and
very severe pneumonia-are used in
this register. To assess the
impact of case management, in
patient records of children with
ARIs between 1989-1992 were
analysed, and antibiotic prescription
in the out-patient department was
studied.
Assessing improvement
During this period the ARI
case fatality rate (percentage of
children admitted to hospital with
ARIs who died) was more than
halved (11.6% to 4.3%). This
decrease was significantly greater
than the reduction in overall
mortality (percentage of children
admitted to hospital with‘any illness
who died) Which fell from 8.7% to
7.3%. Antibiotic use in the out
patient department was reduced by
two-thirds (54.5% to 18.7%).
Our results indicate that
standard ARI case management
using simple clinical signs reduces
ARI mortality and reduces antibiotic
use even in a teaching hospital.
Reduction in antibiotic use and
the use of low-cost standard
antibiotics also leads to cost savings.
In the Children Hospital we saved to
equivalent of over pounds 2,000 in
one year alone, reducing the total
antibiotics budget for the out-patient
department by a third.
Professor Mushtaq A Khan,
National Co-ordinator and
Programme Manager, and
Dr. Gul Rehman, National ARI
Control Programme, Children
Hospital, Pakistan Institute of
Medical Sciences, Islamabad,
Pakistan.
(ARI News Issue No. 30)
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
COMMUNICATION
Advising mothers
Cathy wolfheim describes a
new WHO training initiative aimed
at improving the way health
workers advise mothers on how
to manage diarrhoea at home.
Some health interventions depend
mainly upon adequate supplies of
drugs and equipment and health
workers' skills to deliver the right
treatment. However, good
management of diarrhoea also relies
^1 mothers being able to treat their
children's diarrhoea at home.
How well mothers care for
children with diarrhoea depends
largely on how messages have been
communicated by health workers.
There are three main guidelines
for home management of diarrhoea:
•
give the child more to drink than
usual
•
continue usual feeding,
including breast-feeding if the
child is being breastfed
•
take the child to a health facility
if danger signs appear
Mothers and other care givers
need to know these rules so that
they can apply them when their
children are ill. People who have
heard the rules before may need to
be reminded.
One of the most effective
means of communication is two
individualstalking. Sometimes called
"face-to-face, or one-to-one”
communication. It allows an
immediate exchange of information
and ideas.
Health care workers often do
face-to-face communication. They
are usually respected as good
sources of information, and they are
in regular contact with many parents
through their day-to-day work.
However they may need help in
improving their communication skills.
Integration with clinical training
WHO has recently developed a
training guide called 'Advising
mothers' which aims to teach health
workers to communicate more
Summary of steps taught in training activities
ASK What was done for the child before coming to the health centre
and listen carefully. Were drinks given? What sort? How much? .Was the
child given food? What food? How much? Any other treatment?
PRAISE the mother's helpful actions. Every mother bringing a child
for care has done something right, even if it is only the fact that she has
sought medical help.
ADVISE the mother about other things she can do to help her child.
Even if a mother has taken most of the correct steps, she is likely to
welcome further advice such as danger signs to watch out for if the child
gets worse, or advice on preventing further episodes' of diarrhoea. Make
sure you do not overload her with information, choose the most important
points.
CHECK that the mother has understood. AS her to describe what she
will do when she returns home. This is better than asking: 'Do you
understand?' She would probably answer 'yes', because she may be too
embarrassed to say no. If possible, ask her to demonstrate what she will
do, e.g. preparing an oral rehydration solution.
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
effectively using the simple process,
ask, praise, advise, check (see
bottom left). The training activities
in the guide are designed to be
included in courses on clinical
management of diarrhoea so that
communication skills are given the
same importance as clinical skills
such as diagnosis or treatment.
Alternatively, the training activities
can be run as a separate 1/2 day
course for health workers who have
already been trained in clinical
management of diarrhoea. Rather
than attempting to produce
communication 'experts', the training
aims to teach a few essential
communication skills to health
workers.
The training guide emphasises
the value of practising new skills.
Practice helps participants to become
familiar with listening and giving
advice, and convinces them that the
process works. In the same way that
practice is important when learning to
do new things such as driving a car
or diagnosing illness. It is also
important when learning how to talk
to mothers more effectively, and how
to use visual aids. In the training
activities some skills are first
practised as exercises, then
participants are given the opportunity
to practise the skills in a real life
situation with mothers whose children
have diarrhoea.
Cathy Woifheim, ODD, WHO,
CH-1211 Geneva 27, Switzerland.
Editors'note: In this issue of
DD we refer to advising mothers
since mothers usually bring children
to clinics.
However, other people often
look after sick children,
grandmothers, fathers, olderchildren
and other family members. The
same skills should also be used to
communicate with them.
COMMUNICATION
A good question
The way health workers ask
questions is very important. Good
questioning will allow a real
exchange of information between you
and a mother. Questions can be
used for several purposes; finding
out basic information, getting more
information about something a
mother has said, finding out what a
mother already knows, and checking
whether she understands and
remembers what you have told her.
There are two basic types of
questions:
Closed questions
These are questions that need
only yes or no as an answer. For
example, 'Did you prepare ORS
solution? ' Have you continued
feeding your child?' Closed questions
What is communication?
Communication is the
exchange of information. In
health programmes, the aims of
this exchange are to reach a
common understanding and to
change or reinforce certain
behaviours that promote health.
The word 'exchange' is vital.
Think about how two people hold
a conversation. First, one person
talks and the other listens. Then,
based on what the first person
has said, the second person
responds. Information and ideas
are exchanged between the two.
The course on advising
mothers is also based on
exchanging ideas. It starts with
a health worker asking a mother
key questions; then praising the
mother, so the mother knows she
is being listened to; then health
worker giving the mother advice
based on what the mother
already knows and does.
often begin with the words; have,
has, did, do, are or will. These sorts
of questions are useful when you
need to find out simple information,
such as whether a mother prepared
ORS solution or continued feeding a
child.
However, closed questions are
very limited. If a health worker only
asks closed questions, a mother will
have little opportunity to say anything
apart from yes or no. The chance to
find out other important information
will have been missed.
Closed questions can also lead
a mother to answer what she thinks
the questioner wants to hear. For
example, if you ask:' Did you give
your child ORS solution?' Then she
might say yes because she thinks
that is the correct answer. If you ask
instead 'What did you do for your
child with diarrhoea?' It is more likely
that she will describe what she
actually did, since she has not been
prompted to remember ORS.
Open questions
These are questions that
require a mother to say much more
than just yes or no. Such questions
encourage her to describe what she
did, explain why she did it, or outline
what she understands about
managing childhood diarrhoea.
Open questions often begin with:
What? When? Why? How?
Examples:
What did you do when you
realised your child had diarrhoea?
How much has your child had to
drink?
How do you prepare ORS
solution?
When finding out what home
care the child has received, it is
useful to use a combination of closed
and open questions as the following
example shows.
HEALTH WORKER: Has your
child been drinking lots of liquids?
MOTHER:No.
HEALTH WORKER:What seems
to be the problem?
MOTHER: She was vomiting as
well as having diarrhoea, so I
thought if I gave her something to
drink it would increase her vomiting.
Source : CDD, WHO, 1993
Advising Mothers. CDD/93.2
fT)
Copies of the 'Advising
mothers' training guide are available
to trainers and managers of health
care providers. Write to CDD,
WHO, CH-12311 Geneva 27,
Switzerland.
Practical exercise for training
courses.
This exercise aims to help you
think about different ways of asking
questions. Please change each
closed question into an open
question.
Example
CLOSED: Do you know about the
importance of giving more fluids to
a child with diarrhoea?
OPEN: How much will you give
your child to drink?
Exercise
1 .CLOSED: Do you understand
what you should do at home now?
OPEN:..............................................
2.CLOSED: Do you have a one litre
container at home to measure
water for mixing ORS?
OPEN:..............................................
3. CLOSED: Do you know when to
bring your child back to the health
centre? "
OPEN:...............................................
Suggested answers on page no.11
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
COMMUNICATION
A
Examples of training activities
story-telling
/vsk participants to form small
groups. Give each group a copy of
the following story for one group
member to read aloud while the
others listen carefully.
Ana comes to the clinic with her
very young baby. She has lost her
health card and feels very frightened
to tell the health worker. The health
worker shouts at Ana: 'Where is your
alth card?'Ana whispers a
response. The health worker shouts:
'If you cared more about this little
baby you wouldn't forget to bring that
card!'
Ana looks down and hand over
the child who is crying. The health
worker weighs the child, shakes her
head sadly, and writes information in
her book without telling Ana what
she is writing.
Ana is frightened and worried.
She thinks: 'is there something wrong
with my daughter?' The health worker
then speaks very quickly to Ana.
"Your daughter is under-weight. Give
her more food more often, especially
fruits and vegetables. Breastfeed
her frequently. That's all! Next time,
bring your health card!'
Ask participants to discuss and
write down on a chart:
(a) what did the health worker do
that showed poor
communication?
(b) what will Ana do as a result?
(c) suggest specific things the
health worker could have done
to ensure better communication.
In the same way as before, ask
a spokesperson from each group to
report on the group's discussion.
In the end, it may be worth
suggesting some of these points if
groups have not already mentioned
them.
(a) The health worker spoke
quickly, wrote information
without telling Ana, gave orders
- instead of information.
(b) Ana may worry, get
discouraged, lose hope, forget
the message, feel bad that she
cannot buy enough fruit and
vegetables, decide not to return
the next time, tell her family and
friends about the harsh person.
(c) The health worker could ask,
listen to Ana, praise, advise,
check.
Source: Learning to listen to
mothers, Nutrition Communication
project, Academy for Educational
Development.
(Dialogue on Diarrhoea,
Issue No. 58)
Suggested answers to practical
exercises on page 11
Open questions
1 What will you do for your child
when you return home?
2 What containers do you have
at home for mixing ORS?
3 What signs would show that
you need to bring your child
back to the health care?
Simple language
1. Mix the contents of this ORS
packet with three soft-drink
bottles of water. Then give
your child a cupful every time
she has diarrhoea.
2 After the diarrhoea is over,
your child needs to eat more
than usual. It is a good idea
to give her snacks between
meals or an extra meal each
day.
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
m
COMMUNICATION
Active listening
^3 ood communication is atwo-way
process with both health workers and
mothers listening to one another,
respecting each other's viewpoints
and learning from one another.
Unfortunately, we have probably
all seen examples of one-way
communication where health workers
talk'down' to mothers, lecture them,
or criticise them. These mothers are
likely to go away feeling
misunderstood and humiliated. As a
result, many of them will be unwilling
to visit a health centre again.
Listening is a particularly
important skill. Many of us might
think we do this every day and do not
need training in it. But do we listen
with our full attention and really try
to understand, rather than just
hearing the words and reaching our
own conclusions?
Very few of us could claim to be
perfect listeners. But with training,
many of us can improve our listening
skills.
Active listening involves:
•
•
•
•
giving our full attention to the
person speaking.
concentrating on what the
persons is saying
respecting the speaker's
viewpoint
checking that we have
understood what the speaker is
saying.
It does not involve:
•
Carrying out another task at the
same time switching off and
thinking about other things
interrupting the speaker telling
the person that they are wrong.
Active listening builds
relationships by showing the other
person that we take what they say
seriously and accept them. It helps to
avoid misunderstanding. It
encourages people to speak fully and
frankly because they know their ideas
will be listened to.
Much of active listening is
common sense. The following points
may help you to focus on how to
listen more actively.
•
Give the speaker your attention
and make time for them.
Different cultures have different
ways of showing this. For
example, in some cultures it
may involve looking at the
person, making eye contact and
nodding.
o
Be ready to summarise what the
person has said. This helps to
check yourunderstanding and
to demonstrate it to the other
person. You may like to use
expressions like:' Are you
saying....?
o
If you do not understand, as, it
is better ask: Tm not sure I
understand the point
about.... Can you explain it
again,1 than to ignore what the
person is saying.
•
Encourage the speaker if he or
she seems uncertain. This may
take the form of asking open
ended questions such as:' And
what happened next?', or
making supportive comments or
gestures. Sometimes silence
can be a way of encouraging,
you do not have to say
something.
o
Try not to respond until it is
clear that the speaker has
finished.
Two-way communication takes
more time and effort than giving
instructions, but it is time well spent
when it results in improved care of
children.
Source: The Open University,
1991. Managing Yourself, Block-1,
Book 2. Managing Voluntary and
Non-Profit Enterprises.
‘‘DcaZaytceHealth Dialogue is published
quarterly by the Christian Medical
Association of India and is
available in English. It has a
circulation of over 22,000 in India.
Scientific editor : Dr. Shanti Ghosh.
Executive editor : Ms. Latika Singha.
Editorial advisory group :
Dr. Cherian Thomas, Dr Shanti Ghosh,
Ms. Razia Ismail, Dr. M.K.Bhan
Dr. Narender Gupta, Dr. Beverley
Booth, Dr. Kalindi Thomas,
Dr. Alfred Edwards.
DTP input : Ms. Susamma Mathew,
Ms. Sandra Mark.
Distribution & mailing list :
Ms. R. Kamakshi.
Co-director and head of programmes
and publishing
services (AHRTAG):
Mr. Richard Manning.
Executive editor child health
programme (AHRTAG):
Ms. Kate O’Malley.
Dialogue on Diarrhoea
Scientific editor : Dr. William Cutting.
ARI News
Editor-in-chief : Dr. Harry Campbell.
Technical editors : Prof. Peter
Burney (UK); Dr. Anthony Costello (UK);
Prof. Michael Levin (UK); Prof. David
Miller (UK).
Ahrtag address :
AHRTAG
Farringdon Point
29-35 Farringdon Road
London ECIM 3JB, UK
£
Tel. : +44 171 242 0606 (International)
Fax : +44 171 242 0041 (International)
E mail : (Geonet) GEO2:AHRTAG or
(Internet) ahrtag @ geo2.geonet. de
The views expressed in Health
Dialogue are not necesssaily those of
the editorial advisory group.
Christian Medical
Association of India
Plot No. 2, A-3,
Local Shopping Centre,
Janakpuri, New Delhi - 110058
Phones : 5521502, 5599991
5599992, 5599993.
Telex ; 31-76288 CMAI IN,
Fax : 011-5598150
©
Laser Typeset & Printed by :
New Life Printers (P) Ltd.
Mukherjee Nagar, Delhi - 110 009
Tel.: 7244855, 7243396
Health Dialogue, Issue no. 3, August 1995, Published quarterly by CMAI.
3ftf
WT
^TJTTT ife, nf fefoft-1 10001 gTTT WfSRf 5T4T R^ST
'-TRa uteo-t
M)<Y<MI<4 gTO nfsa I
fJ U T
3W
toft Firecr furerr ’To,
hih.H a
£1 /OU
*
*
/OM
ai £j /OU"
iMjJf
HO
n Ki
- 3> 3
Hi
IfhH ]'O
4 -m
Ih b lk fr life
± X h ll M b
h MB,H
h
h Jjaut JbJJzh h ilk u MH1 feHJjihj h hjh 11 JihJJ2hJ
3,1
EFE 5TT gTET
pERT RTE 5 fEE 5> 55E 5 ERF 5 f[E5-
fEdl RFE EF EE. EFgt .EF EEXET "TEfFEf”. ETE5F TTE gF EFEF
Sf? ET eekTi g I
g I 5E EFE E EFFgF E TpFE sftg EE gFE EEEF
XE f=ieI[h*1 EE EFET 5 -HlHdR TT ttIHW '-bHdTTt,
fu 5 g?RTT ET IPRWgd, RfE-EfvPT F H EFERT, W EE EFET,
^rr^r
EE EE «IS«(ST ET
EFT E?T Pti'tilqa gt RETT g I
Tjr»T
idr
EES EE
i
■■n^Rd -d^r, ^^r<d nrr. ^fr^, dpjir, ^^d <t,
EE EFET, dEFEK ER 5TET gtt TEER Ef^EET, EtEET E
Eg PEdTpEH TER, 'EIRE, Eg 5TpR EF EHH' E EETF
etet srrar g1 ?et ePePfef Rtef etRft
Eg (qcifttl EFEF EFET E girt I g I
ttrr, ettt sfk
fEp<ET, fd MER HJI'-t'E I 5 Eg fqei(nd STET EFET E gTET g I
faeifEE ‘sft’2 :—■_ Eg ferfER srfatex gTE
■qiqvi ET pRETHI P*1 ^1 % ^1 dr-pl E gTET g I ttldd ERFT, <l«ll,
ETEE EFT TFfcFEF ETTE EtT SFRF FEFEf TT gET E ‘3El
EEE E Eg ferfEE ER gt TT5T | I SET: EETET ETt EF^TF
FjfFzft ETTE EI«Y EfeTET EFp TEEE T ^TT ET5 gt F3T EEF
G(»in+< ■EJpRE ETT, frrfTET, Pw~|-+< EEEFEF, FERTT,
ElfgM, I gE fqelpH'l TT meM EF Pee EferEt EFE E EFE EFET
EFE, fTEX Ek SER ETTpR 5E ferfEE T RR® XftE g I
E EtT ST gF qad E M + HT EllgH I
terfirE ‘ET Efsivre' TT EFEFE TEF, pETiETX pRRTpER
faETfa^ ‘3t’
•<t’2 EE TEp T EFFTE EF'E Td STIST g ftFEE EtgT gTET g
EET ETR % TTET EFtE ET EE ET5 g I
PrETPEE ‘Ht’
pRdl’pER ‘Ep’ TXPg EF 3FEEFF EFT EEfeff FEET | Eh
fgCTfEE ‘St’ gPgsET E|t EFET EE ETgE EET^ ql?l EE
EFT T5IE E EgTEEF gtET t I E^f EE EFTEE gPgSEF TF EFE
EE ETT fk^EE TTE EF EESeP EkFIET T Tfg EFT gEET TT
Pete ere efe fm eft t'fef’tte ere e Eg eweP g i
5FER EFF 5E EF TTE'F E E35 E EEE TSET g I
U5 EEFEF, EE fECTfEE EFT MI Rd EE EEE ETET E1TJE g I
gE fEEFfEE EFt EFEt gFE E TTg-EfEET E 5tEF gFF E
$7 EEEt g I EEgf E EFT TEE ETE5F t, Eg EgEftEF gE 5T5
EE E%rl g fc ETgTT E fECTfEE ‘EV E?t EFEF g I
(EFET. EEE pTEE EETT, EF0! EE ERp, c^E SftT 58F EF
EETTEf E Ep Eg fgdFpEE EFET 3FTET g I
fazrfaa
aft Ms
ga aqi
--- ag 3TFRT dqr SI’ST UH | I
fTR
gr <dMi qar 4=ni<< qg '41'1'ir ar ?rfaqr dnaHr g i
gprr WH d/g H qq>HT arfga gqnq HJFT Hat A1TO d?a
Cm^tM'T
* < fdeifad ■TOT a gH TltT |
qgfga 5® ‘qnq aW ah ‘q qrqq apq’ ara’
(vi<aa g i M4>id qqq vraa him asa a (qeifa at qrr aara
gt arar g I
—tt[eMdi faar ®t?r gr 4+ii> i
—afcrar ah tttt qq hrt mar feaaq a aar? i
—ti fo»iq'i ifl< 4>mi qq ■'■'■" ■■ qiat a uh ah qqqq qr
qqqf urq gr qqq q qr afta a i
—qrqqr qq
qr fqq gaar gr qiat qq faaa a a Mai
aag qqr qrc ah aaa qq aar qqqr< hr i araar M4>it
q> qn qfq
mht tsrqq qq mn ut qq 'pq? q^r i
tht q ttw <qq ^ra 11 ?q qnr qr qn ufcrqr
qr qqqq q qqtq fqrqr qr qqqn | i
—qqq^ h qqr qHT qrrft qr q qS i qrr qrq qrfq qqn
q qq'rq qr? i
—qfsqqr qqqq q ran qrqr rrnr strhet q qr?, qqrftr
rrrrr ju fqqrfqq qn §t rsnq (' i
H^qqar UTH
q§ qrq u?r qrq
fq; niF-q % fqq atetq, qqi
aftr qqr\r qq sqq
% hw fddlCqq xt 3R<t
5 i qrfrT arqqr fqrqrqqqnf % fqrq fqfrfqq arfqqrq
qiq nq § i q-jfq q ^q g-r qi? fqerfrrq fqq f at at
qrisj-qqrqf qrt stqr a q rsteq, qqq sn a ataq qqrx
qrqq qr snai' ararqar % qnqa 5a qqqq qfcr qrar q
qqqta q§i qrr <q^ 1
q^ a<t 5 fq: ^q fqqfaa aa a fasifaa qrt ntfa<ri
qi faarfaq-qraa q^f rarcl? aqqr ar qqqq aiar a au,
qfa qi a»st qq aaq q^t qrT qqqt, faraj ^q fqfraa
aa a qr©
aarra aferaf afta giaf qrt naw at
qtT §t aqr^ | 1
srfaqrta fasrfaat art snanqrar aga atfr arar arafa
aR^tara ar faaiara a gtat g, fqrra a arfaara g ata
gar? abra a gqqq gtar qnat g 1
IN CHILDREN UNDER
TWO IN RURAL INDIA
Dr. Tara Gopaldas
Dr. Sunder Gujral
November 20,1998
CARE INDIA
B 28 Greater Kailash 1
P O Box 4220
New Delhi 110048
Phones 6221728 6418421 6418422 6441948
6470254 6470258 6470299 6471527
TCN1362 CARE INDIA
Fax 91 11 648 3007 91 11 647 3098
E Mail cbox@careindia.org
FOREWORD
INDIA
Both the Government of India and CARE-lndia have prioritized a response to the problem
of malnutrition among young children in India. Increasing the precentage and number of
children 6 to 24 months who receive and consume a supplementary meal is a key
intervention to addressing the problem of malnutrition, as this age group is particularly at
risk of growth faltering.
Dr. Tara Gopaldas and Sunder Gujral review the scenario of malnutrition among children
in this age group in India; the role of supplementary nutrition in filling nutritional gaps; and
specifically CARE-lndia’s efforts in promoting the receipt and consumption of a
supplemental meal among children 6 to 24 months of age. The report provides a summary
of efforts to improve access, availability, acceptability and utilization of foods at the
community level. It also highlights Health Days where Take Home Rations are provided
as an effective means for achieving improved coverage rates of receipt and consumption
of supplemental food among children in this age group. The report benefits from the
inputs of a number of field staff-, guidance provided by Dr. Sanjay Sinho, and final formatting
and editing done by Dr. Ranjani Saxena, Rina Dey and Suresh Babu.
CARE invites your comments and collaboration in implementing some of the key
recommendations made in this report.
Sincerely,
CARE INTERNATIONAL
CARE’Australia
CARE Canada
CARE Danmark
CARE Deutschland
CARE France
CARE Italia
CARE Japan
CARE Norge
CARE Osterreich
CARE UK
CARE USA
Gita Pillai
Director, Nutrition and Health
The views expressed in this Working Paper are those of the authors alone and may not be reflective of the opinions of CARE India.
ADDRESSING NUTRITIONAL GAPS IN CHILDREN UNDER TWO IN RURAL INDIA
A REVIEW OF CARE-INDIA'S APPROACH
Tara Gopaldas and Sunder Gujral
1.1
NUTRITIONAL STATUS OF CHILDREN UNDER
TWO IN INDIA
1.2
NUTRITIONAL REQUIREMENTS FOR INDIAN
CHILDREN 6 TO 24 MONTHS OF AGE
It is now well recognized that most of the children under
two years of age, especially children 6 to 18 months,
are extremely undernourished, underweight and
stunted. More than half of the world's underweight
children live in just three countries, namely, India,
Bangladesh and Pakistan. The National Family Health
Survey (1992-93) has found the prevalence of under
nutrition to be very high in India. The survey found more
than half (53%) of all children under age four to be
underweight and a similar proportion (52%) to be
stunted. 21-29% of children were severely
undernourished according to weight for age and height
for age measures. One in every six children was found
to be excessively thin (wasted). It further documented
that undernutrition varied substantially by the age of
the child, being highest after first six months.
Undemutrition was particularly high in Bihar and Uttar
Pradesh, while the problem of wasting was most evident
in Bihar and Orissa; which also have among the highest
infant mortality rates in the country.1
The nutrient requirements for early infants (6-12 months)
and children 1-3 years as recommended by the
Indian Council of Medical Research, 1992 is set out
in Table 12.
Table 1
Recommended Daily Allowances for Infants
(6 -12 months) and Children (1-3 yrs)
There are several factors operating synergistically to
hasten the rapid decline to undernutrition, especially
from the sixth month of life. These are: the child may
have been bom low birth weight; lack of and/or total
unsuitability of complementary foods; repeated
episodes of diarrhoeal and respiratory infections;
unhygienic personal, and environmental conditions;
unsafe drinking water and poor'
sanitation; limited, distant, slow
and non-affordable access to
preventive and curative health
services; poor income levels,
illiterate and working parents;
ignorance of simple and doable
caring practices and large
families (especially in North
India) with narrow or no birth
spacing.
Group
Particulars
Infants
6-12 months
Children
1-3 years
Body wt (Kg)
Net Energy (kcal/d)
Protein (g/d)
Fat (g/d)
Calcium (mg/d)
Iron (mg/d)
8.6
843
14
25
500
12
350
1200
0.6
0.7
8.0
0.4
25
25
0.2
. 12.2
1240
22
25
400
12
400
1600
0.6
0.7
8.0
0.9
40
30
0.2-1.0
Vitamin A (pg/d)
P - Carotene (pg/d)
Thiamin (mg/d)
Riboflavin (mg/d)
Nicotinic acid (mg/d)
Pyridoxine (mg/d)
Ascorbic acid (mg/d)
Folic acid (pg/d)
Vitamin B-12 (pg/d)
The Indian Council of Medical Research. New Delhi. 1992
The dietary guidelines for the infant (6-12 month) and
the 1-3 year age group as per the National Institute of
Nutrition (NIN), 1998 are
reproduced in Table 23. It is
evident from the table that,
our rural, tribal and urban
children aged 6 to 24 months
are in no way fortunate enough
to receive the balanced diet
recommended by NIN. In North
and West India, the children
under two receive minuscule
amou'nts of dal-roti, while in
South and East India they receive rice and sambhar/
dal. The child, fortunately, is on breast-milk right into
his third year. The NFHS found breast-feeding to be
universal in India, with 95% of all children born in the
four years preceding the survey having been breast
fed. However, among children aged 6-9 months, less
than one third were receiving solid or mushy food
(amount unspecified) in addition to breast-milk'.
status of the vulnerable age group. Data from one such
projects, CARE-lndia’s Project Poshak, 1975 is
produced in Figs. 1 to 3. These data represent the
average daily intake of the experimental group that
received the supplementary nutrition of vitamin-mineral
fortified and sweetened Instant-Corn-Soya-Milk (ICSM),
breast milk and some home diet and a matched control
group that did not receive the supplementary nutrition4 5.
Table 2
Balanced Diet for Infants and Children.
Food Groups
One can see glaring deficits in the control group relating
to calories, vitamin C, calcium and iron, in the infant
(6-11 months). The deficit gets accumulated with respect
to calories, vitamin A, vitamin C, calcium and iron in the
12-23 months old child. This is because the volume of
breast milk drops and the amount of complementary
home diet are very meager. Data show that the 2-3 years
old child is able to fend for himself/herself better than the
younger age groups as he/she is practically on the home
diet. Great deficiencies in vitamin A and vitamin C persist.
Infants
Children
(6-12months) (1-3 years)
Amount/
Amount/
day(g)
day(g)
.
Cereals and Millets
45
15
Pulses
Milk (ml)
500
Roots and Tubers
| 50
Green Leafy Vegetables 25
Other Vegetables
25
Fruits
100
Sugar
25
Fats/Oils (visible)
10
120
30
500
50
50
50
100
25
20
Most of the ICDS rural infants have to depend on fortified
supplementary food to obtain their RDA of vitamins and
minerals, at least partially. Every attempt should be
made therefore to see that the complementary or
supplementary food is fortified with 80% to 100% of the
child’s RDA, especially that of vitamin A, B-complex, C,
Source: Dietary Guidelines for tndans-A Manual. The National Institute of Nutrition, 1998.
Note: Top milk of 200 mi has to be given even in case of breast-fed infants
Items listed in the NIN balanced diet for infants and
young children such as top milk, roots and tubers, green
leafy vegetables, fruits, fats and oils and sugar are
luxuries beyond the means or comprehension of any
typical rural (CDS household. These expensive items
of fruits, vegetables, milk and pluses are the dietary
avenue to supply vitamins and minerals to the young
child, which most ICDS-rural households cannot afford.
iron, and zinc; is low-bulk (soupy), yet ‘high in nutrient
density’, so that, the child can consume all or at least
almost all of his/her ration in one or two sittings; and
gets to-the home‘of most children under two, through
delivery channels such as Take Home Rations(THR).
1.3
ROLE OF SUPPLEMENTARY NUTRITION IN
FILLING NUTRIENT GAPS
=
_■
Supplementary nutrition is a nutritional | ~ J ■
intervention, which aims to make up
for the deficit in the child s diet. The
J
supplement provides the child with
energy, proteins and micronutrients. Various nutritional programs have >^4..-.
demonstrated the importance of
supplementary nutrition and the
difference it has made to the nutritional -------• r
2
These three important conditions need to converge, if the
rural ICDS children are to benefit from supplementary food.
It is of utmost importance that policy makers, implementers
and the public health and nutrition community recognise
these facts. It is unfortunate that not even nutritionists and
:
dieticians have sufficiently realised that
:
T .. the consistency, nutrient-density and
■■
amount an infant can consume at a sitting
T'.
vary enormously for a 6-9 months old; a
~ 9
months old; a 12 -15 months old,
< and so on till the child reaches his/her
second birthday. More operational
research and field-testing need to be
7 •• done in this area
Data reproduced from Project Poshak
Fig. 2: AVERAGE DAILY NUTRIENT INTAKE OF EXPERIMENTAL AND CONTROL GROUPS
OF PRESCIIOOL CHILDREN 12 TO 23 MONTHS OLD (EXPLORATORY PHASE)
'
* '/j Retinol + Carotene
3
TABLE 3
Nutrition and Health Days (with or without THR)
Geographic
coverage
State
Andhra Pradesh
|
AWCs/Villages initiated
Blocks initiated
FY '98
Plan
Total
achieved
HI
CB
BN
FM
2083
16
1428
16
103
1325
15
Nil
Nil
Bihar
AWCs/Villages initiated
Blocks initiated
165
9
165
9
110
3
55
6
Nil
Nil
Madhya Pradesh
AWCs/Villages initiated '
Blocks initiated ■
2000
35
2267
40
295
3
1208
15
764
22
Nil
Orissa
AWCs/Villages initiated
Blocks initiated
775
16
775
16
100
675
15
Nil
Nil
Rajasthan
800
18
324
11
38
1
286
10
Nil
Nil
:
AWCs/Villages initiated
Blocks initiated
Uttar Pradesh
,
’
AWCs/Villages initiated
Blocks initiated
11684
99
9341
99
283
3
1913
19
7145
77
Nil
West Bengal
■
1
AWCs/Villages initiated
Blocks initiated
712
21
2
14
1
7
Nil
Nil
Total
‘
AWCs/Villages initiated
18219
197
14321
943
13
5469
81
7909
99
Nil
Blocks initiated
193
empowering mothers to improve the health and
nutritional status of themselves and that of their infants;
and forging collaboration and partnerships with the GOs,
NGOs, and CBOs (Community Based Organizations).
2 CARE-INDIA.S UNIQUE NUTRITION AND HEALTH
DAY STRATEGY FOR REACHING THE MAXIMUM
NUMBER OF CHILDREN UNDER TWO IN THE ICDS
CARE-lndia assists the ICDS in seven states of India,
namely Andhra Pradesh (AP), Bihar, Madhya Pradesh
(MP), Rajasthan, Orissa, Uttar Pradesh (UP), and West
Bengal'3--4. CARE has taken a bold step in formally
reinstating THR as its food delivery system for pregnant,
lactating, and children under two years of age. This was
the delivery system it pioneered and piloted in MP,
through Project Poshakm the seventies, which is often
quoted4 5
Table 4'
Total CARE-lndia Assisted ICDS Areas
I States
AP
I Blocks 108
$
WB | Total:
War MP
Orissa Rajasthan
UP
157
134
104 177 | 915
CARE
146
89
. .r--
Cjir.'?,
'y-
The overriding and immense advantage of THR is
accessibility and coverage. THR enabled the vital
contact between mother and children under two and
the Anganwadi center (AWC) to be made. Once this
was achieved, a tremendous improvement in selected
indicators, such as receipt of THR in the past two days;
breast feeding started within 6/8 hours of birth;
complementary food started from 6 to 10 months was
notedTaKe5.
It has recently gone operational with its innovative
Integrated Nutrition and Health Program (INHP) from
October 1996. Extremely practical synergies between
nutrition and health have been planned and
implemented along with ration distribution, for the
pregnant, lactating women and children under two in
the ICDS. INHP places emphasis on improving women’s
health and nutrition to achieve reductions in neonatal
mortality; preventing and managing infections;
preventing and rehabilitating from malnutrition since
malnutrition is the underlying cause of 67% of all deaths
due to infection and a significant factor in low birth weight
and intra-uterine growth retardation.
Table5
Improvement in Selected Nutrition Performance Indicators
in the Children Under Two in High Impact Blocks
The Nutrition and Health Sector of CARE-lndia has
shown the way by organizing nutrition and health-days,
where both the functionaries of the ICDS (Anganwadi
Worker and Supervisors) and health (Auxiliary Nurse
Midwife) are present. During these nutrition and health
days, children under two are weighed and the THR is
distributed. Mothers willingly help and participate. This
is an excellent mechanism and strategy that needs to
be taken-up by the entire national ICDS. The magnitude
of Nutrition and Health Days being held in CARE areas
is detailed in table 3.
Perfonnance
Indicator .
(Results for
Q4LHI)
Its overall strategies,
therefore,
rightly
concentrate
on
increasing coverage of
the hitherto ’invisible
categories'
of
pregnant, lactating
women and children
under two years of age;
All States
AP
UP
MP
FY
'97
BLS
FY BLS
97—
FY
97
BLS
FY
97
BLS
Supple
mentary
Nutrition %
6-24 months
(past 2 days)
68
41
87
57
NA
11
72
22
Breast
Feeding %
giving within
6/8 hours
65
35
33
29
NA
66
43
8
Comple
mentary
Feeding %
6-10 months
giving mushy
food
75
46
62
56
NA
49
NA
52
Source: Ref. 9. John N.: CARE-lndias INHP Results Reports. Achievements versus Plans
(FY 1997 Vs FY1996). 1998; and Ref 10. Pfei G: CARE-lnda’s Integrated Nulnbon and Health .
Program (1995-2000)
5
3.1
repeated demonstrations of cooking and feeding THR
to meet the special needs of infants 6-9 months;
9-12 months; 12-15 months and so on. The nutrition and
health staff as well as the mothers will realize how much a
cooked portion of a single ration will be and how much of
this an infant of a specific age group can consume over a
reasonable period of time (say 20 minutes). This kind of
practical and visual education will immediately
communicate to both ICDS staff and mothers.
IMPROVING OUTREACH AND ACCESS TO FOOD
As of March 1996,5,614 ICDS-projecis covering 21.3
million beneficiaries have been sanctioned by the
GOI. The seven states where CARE-lndia is assisting
the ICDS have particularly large numbers of projects.
Interrupted delivery of supplementary nutrition has been
a perennial problem in the ICDS. Delivering the food
component from the block to the
AWCs especially the far-flung ones
has also been a perennial logistical
and monitoring problem. Even
within the village, the generally
‘invisible’
categories
of
beneficiaries at the AWC have
been the pregnant/lactating
women and children under three.
The problem of outreach and
contact becomes aggravated
during the harvesting seasons.
2. It would be useful if-the
nutrition and health days are
held every 15 days rather than
every month, with one of the
days reserved only for children under two years of age and one
exclusively for the mothers
(pregnant and lactating). The
village elders and members of
the village panchayat should be
encouraged to participate and
get actively involved.
3.
The strategy of using
comrriunity change agents to
ensure that the services of ICDS
are understood by all; and to
roundup all children under two
years of age, and their mothers
is an excellent strategy for
outreach.
It could be
universalized in the ICDS.
The Planning Evaluation
Organization (PEO) Evaluation,
19766 and the ICDS National
Evaluation in 19927 pointed out
that children under three could not
make it on their-own to the
/4/^a/»iwf'center(AWC). Project
Poshak in MP 19754 5, also
showed that children below three
could not be transported every day to a feeding center for
spot feeding. This problem is even more accentuated for
children under two, especially in scattered tribal hamlets,
hilly areas or even within a village. CARE- India’s baseline
survey, 1997 reports that 40% children under two years of
age were brought to the AWC in the past one week for spot
feeding, a figure often grossly over-reported by the
Anganwadi worker (AWW)!6
4.
Setting up of 'seasonal creches’ will enhance the
THR and should be considered for both mothers and
child beneficiaries. Since, mothers will have to stay back
on nutritional and health days, some monetary
compensation for doing so may be considered by the
village panchayat.
5.
Opening sub-centers for facilitating outreach in
scattered hamlets
Possible solutions
6.
An alternative delivery system is dry ration
distribution on a predecided frequency, which increases
the receipt of food to the home of the child under two.
The CARE-lndia 1998 Results Report, indicates That
1. Take home rations have been successful in reaching
children under two. However, the THR has to be made
attractive and meaningful to the mothers in order that they
come regularly to collect the THR especially designated
for children under two. Possible areas that can be
strengthened are counseling on the child's weight and
THR had succeeded in reaching over 68% of children
under two in all states (High Impact Blocks); and as
high as 87% ih AP9.
6
Table 6
Nutrient value of CSB and Oil
Nutrient Value
Percentage
RDA
26
319 Kcal
53
11.7g
1105IU
69
47
0.33 mg
13.00 mcg
43
26,00 mg
65
520.00 mg
130
11.70 mg
98
1.95 mg
39
108
32.50 ppm
3.2
IMPACT ON AVAILABILITY AND ACCESSIBILITY
OF FOOD TO CHILDREN UNDER TWO
65g Ration of CSB
+8gofOil
Food Energy
Protein
Vitamin - A
Riboflavin
Folic Acid
Vitamin C
Calcium
Iron
Zinc
Iodine
1. It was very clear from the
field visits to the three
states, that the THR had
helped to reach food to
almost all the registered
beneficiaries.
2z In-hard-to-reach
hamlets and villages as in
MP, there is no other
substitute for THR.
Source: Nutrient Requirements and Recommended Dietary Allowances for Indians. The Indian
Council of Medical Research. New Delhi. 1992
3. The nutritional and
health days (once a week,
fortnight or month) were immensely successful in getting
the ICDS and Health functionaries at a fixed place and
at a fixed time. Since, it was mandatory for the mother
to bring her baby, all the target beneficiaries were
available for health .services like immunization and for
regular monthly weighing. It is an ideal situation where
need-based demonstrations of how to prepare the THR
and feed the baby can also be done. The mothers
cheerfully volunteered to help in the distribution of THR.
A sense of ownership and responsibility was instilled in
each mother when she paid her rupee on the nutrition
health day for the comprehensive set of services.
Assuming the child 6 to 24 months consumes his/her
entire ration, this would satisfy the GOI requirements of
delivering 300 Kcal and 12 g protein per child per
feeding day and address the nutrient gap of calories in
their usual diet. However, the nutritional gap in vitamins
and mineral remains.
1. CSB and Salad oil are excellent complementary foods.
The only problem with the CSB is that it is gritty or grainy in
texture. When cooked it becomes pasty and nonhomogenous to touch and taste. It is not appropriate for
the early infant or even the late infant. The bulk and
pastiness does not facilitate the consumption of the full
ration. Children upto one year of age and even upto two,
have a poor swallowing reflex and are slow feeders. Hence,
feeds that are nutrient dense but liquid/ go down faster,
without spillage or waste. There are many options to
enhance its acceptability.
• Fine-grind it. This could be done in USA itself.
• Extrude CSB rather than roast it. Extrusion will
powder the product and will thoroughly cook it. This
could be done in USA too.
• Blend in Salad oil, extra vitamins, minerals and 5%
ARF (Amylase-Rich-Food). This should be done
at the final stage.
e All these processing actions can be done at the
manufacturing end, and the specially processed
food can be separately bagged and demarcated
for children under two.
4.
Cross infections among 60 children under three
being huddled in a small AWC were avoided.
5.
There was much more accountability by the ICDS
staff for supplementary food distributed.
6.
The responsibility for caring for vulnerable children
under two was transferred to the mother and the family.
7.
Repeated cooking and feeding demonstrations done
on the nutrition and health days can prove to be a
powerful nutrition-education instrument.
3.3
ACCEPTABILITY OF THE FOOD BY CHILDREN
UNDER TWO
CARE-lndia supplies Corn-Soya-Blend (CSB) and
Salad oil (SO) to the ICDS program. Table 6 depicts
the percentage contribution of a single ration of 65 g
CSB + 8 g salad oil to the RDA of child under two years
of age.
2. If this is not possible, Modem Foods Ltd. Delhi can
process it in this way for at least UP. Further, since the
RTE for UP is swe.etened with sugar (25%),
we would strongly urge CARE-lndia to consider
7
replacing 5 to 10% of the sugar with an
equivalent amount of commercial
Barley-Malt Powder (cheaper than
sugar). We would also urge CARE-lndia
to consider bringing up the levels of
the vitamins and minerals to 80% of an
one-year-old Indian child's RDA2-Table5.
3.
Both Project Poshak15 and M/s
IESSCO Pvt. Ltd.12 have noted that
most Indians like a fried/roasted/
caramelized smell and flavor. If within
manufacturing and/or processing costs,
the addition of a synthetic smell/flavor
could be considered.
4. M/s IESSCO Pvt. Ltd., have also reported that
about half the UP mothers in focus group discussions,
felt that the CSB-RTE was not suitable for children
under two years of age12. They felt it was too dry, caused
diarrhea, and children under two could not consume
their ration. The RTE had to be made semi-solid with
milk or water. They felt the dry RTE choked the young,
child. However, the CSB-RTE in gruel, haiwaw daiia
form was suitable.
5. The concept of ‘hot’ and ‘cold1 foods are firmly
entrenched in most rural and tribal populations. For
instance, especially in MP and UP home-diets made
out of wheat, ghee, milk, jaggery and pulses, all
considered ‘hot’ would be appropriate for the cold and
rainy seasons; whereas rice, curd, lassi, groundnuts
and sugar (cold foods) are fed to the child in summer5*.
Likewise, CSB/oil recipes and ingredients should be
adapted to the season.
3.4 IMPROVING UTILIZATION
Although there is clear evidence that the strategy of dry
ration distribution on a predecided frequency increases the
delivery of food to the homes of children under two, it is still
a question as to how much of the THR gets into the
stomachs of the children under two. There is a lack of
sufficient appreciation among all concerned, namely, the
ICDS health and non-health staff, INHP-CARE-lndia
staff, community and mothers, that unless a major portion
of this food is fed to the intended children, he/she will
not improve in weight or health. It is possible that children
under two will consume only a fourth
to third of the ration, while the rest is
consumed by other siblings and the family.
Possible solutions
1. CARE-lndia is actively promoting
the concept of feeding the total amount
of dry ration to children under two. This
has to be done by the ICDS-staff, health
staff, panchayat, village health
practitioners, village school teachers,
change agents and adolescent girls.
2. Change agents, and adolescent
girls can advice and ensure that the
food is given to the children under two'in the house,
while the children above two are fed at the Anganwadi.
This will minimize sharing.
3.
On the nutrition and health days, repeated cooking
demonstration of recipes might be done. A single
demonstration 'child’ of 6, 9,12 months can be fed in
front of the mothers group. They will then learn two
important facts: a) the amount that can be consumed
by the infant; b) that the amount consumed per sitting
will increase with age. Even a few months difference in
age would make a big difference in consumption. By
18 months, the child would probably consume the entire
ration at a sitting.
4. Mothers can be requested to bring their home
tumblers or katoris. These can be calibrated for CSB
and oil single rations.
5.
The mother should be encouraged and counseled
to give the full ration in small amounts over 2-4 feeds.
She must be told to feed children under two when the
children above two are at the Anganwadi Center.
Minimization in ‘sharing’ can be achieved in this way. The
above concept was not found to be strong at any level
(ICDS, NGO, Health Staff or even the CARE-lndia-INHP
Staff). It needs to be built into the capacity building strategy.
6. All concerned should become familiar with the
number of pieces a particular single ration would yield
e.g. how many iaddoos, 'dosaisot the amount of halwa,
sheera, payasamdtc. This concept also does not exist
presently.
3.5
INCREASING PALATABILITY OF THE FOOD FOR
CHILDREN UNDER TWO
enterprising about varying the CSB-oil recipes for children
1. The Regional Profile for ‘Malnutrition in South Asia',
UNICEF, 1997 strongly recommends the use of the ARF
technology as a manageable, practical and traditional
technology to increase energy intake of traditional low
energy-gruels13. We would go a step further and strongly
endorse the adoption of the ‘ARF Technology’ for the
immediate improvement of the CSB-THR ration’4,9. Any
germinated cereal grain powder is an Amylase-Rich-Food.
Due to germination, the amount of an enzyme called pamylase increases enormously. It is this enzyme that is
responsible for rapidly liquefying even bulky or pasty CSBoil rations. Hence, the THR becomes smooth and semi
liquid while retaining all its good
nutrition. Adding amylase rich food
to the CSB enables children under (v
two to drink the cooked ration in
one or two feeds1"’34
.
3.6
APPROPRIATENESS OF THR FOR
REHABILITATION
2. For children under two,
especially children under one, it is
the consistency and texture of the
complementary food that are of
paramount importance. However,
in a mother-child dyad, it is she
who decides. Most Indian mothers
under two years.
Children in grade III and IVare usually very anorexic. Hence.
it is very necessary that they be given frequent small feeds
ofthe CSB-oil-THR (double ration). The amount of vitamins
minerals consumed will be in direct proportion to the amount
of THR consumed. Even if 50% of the THR or one single
ration is consumed, it will certainly bring up the depleted
macro and micro nutrient status of the child. The feeds
could be made nutrient-dense but liquidy with Commercial
Barley Malt Powder-ARF, or with Ragi-Malt powder, which
tribal groups of AP make as local
weaning food. The mother or
caregiver should make the feeds
as palatable as possible by
cooking it in milk, where sugar or
jaggery should be added. Mashed
banana and soft mashed rice with
some oil (to increase the calorie
value of the food) could also be
given. The mother should be
counseled to devote some time
and patience in feeding the child.
The family should be made to
realize that some money for milk,
banana, jaggery has to be spent by them for nutritional
rehabilitation. Double ration of CSB-oil cannot rehabilitate
by itself. Preliminary project monitoring data indicate that
diarrhea and ARI case management at the home level is
excellent since the inception of INHP9. Perhaps the change
agents, the AWWs and the adolescent girls can help the
mothers of sick children, by being available to make small
CSB-oil-ARF-feeds.
.
4j'7
:
" VI
1
'
like a caramelized or roasted taste
and flavoring. Both the mothers.
and the babies like it sweet. Intake by children is definitely
better with a sweet tasting preparation5*.
3. Sweet tasting or ‘liquidy’ da/ia, rabadi or kheer type of
recipes would be most suitable for the early infant in MP
and UP. It would be the payasam counterpart in AP
4. The older child (1-2 years) may like laddu, which the
mother can make by roasting the grainy CSB in the Salad
oil, add some jaggery and fashion into laddus, haiwa, sattu
or prashad. Salty preparations would be chapati, paratha,
dosai or uppumav. Our interactions with the mothers in
UP, MP and AP (particularly in UP) showed that most of
the mothers generally wanted to cook only tw'o times
(morning and evening), perhaps due to fuel and time
constraints. They usually chose to make the dish that was
most convenient for them. For instance, roti in UP, MP,
and uppumam AP. Sweetening the CSB with jaggery or
sugar was a special treat. In short, the mothers were not
3.7
VIEWS OF THE IMPLEMENTERS AND
BENEFICIARIES ON THE THR
A. The ICDS and health staff
The entire gamut of implementers, namely, the ICDS
staff of CDPOs, supervisors and AWWs were fully in
favor of the THR strategy. Apart from the high coverage
and receipt of the supplementary food as compared to
center-based feeding, the THR and nutrition and health
days had made the administration and logistics much
9
D.
simpler. For the first time both ICDS and Health Staff
came together at the AWC on.a fixed date and a fixed
time. Hence, both Nutrition and Health Services were
delivered to mother and child. Since
mothers had to come with their
under- two children only once a
month, compliance was very high.
Empowerment of the community
and beneficiaries was a new and
welcome feature. The catalytic role
of the CARE-lndia-INHP staff was
highly appreciated in all three States.
B.
The CARE-lndia-INHP staff
CARE-lndia-INHP staff voiced
all the advantages and the one
disadvantage of the sharing of THR. Much of the credit
for the success of nutrition and health days, in all the
three States, goes to the CARE-lndia-INHP staff. CARElndia-INHP staff have a particularly good relationship
with the community, village revenue officer, panchayat,
beneficiary households, change agents, CBOs, NGOs
and AnganwadNloft.&ts. They were confident that the
battle of ‘full portion size' and the reduction in ‘sharing’
could surely be won, as the CSB and oil had traveled
all the way from USA to practically every rural/tribal
household of registered beneficiaries in the 7 states.
They said that they were not aware that the children in
the age group of 6-36 months were actually three
different population segments as far as the dietary
habits and problems were concerned. They now
realized why the early infant could not consume much
of the CSB and salad oil THR.
C.
The Mothers/Pregnant and Lactating Women
The women beneficiaries were unanimously appreciative
of the strategy. The most advant
ageous reasons according to
them was time saved, having food
at home, independence as to when
to cook and how much to cook,
ability to feed both children under
three and above three two times a
day,
and
sharing
the
food with other needy members
of the family (they were quite
open about this). Some said they
did not like the oil being mixedup with the CSB. Mothers in AP
took a lively interest in the 'single-ration' cooking
demonstration and its subsequent feeding to a healthy
7-month-old child.
4.
GLOBAL AND NATIONAL EXPERIENCE OF FOOD
DELIVERY MECHANISMS
Beaton and Ghassemi in their excellent review of
> Supplementary Feeding Programs for Young Children
in Developing Countries, 1982 concluded that ‘Take
Home’ food delivery systems were effective in achieving
greater coverage of children under two at much lower
cost20. In the seventies, there was a spurt in testing ■
various types of supplementary feeding programs,
namely, On-site, take-home and nutritional rehabilitation
programs. Anthropometric gains attributable to ‘Take
Home.' feeding programs ranged from 21% to 75%21.
Moffat, in Uganda (1973) and Aiderman etal in Jamaica
(1977); The Asia Research Organization in the Philippines,
(1976); Khare etal in Maharashtra (1976); and Gopaldas
etal in MP (1975), were able to show extremely impres
sive reduction in grade II and III degree malnutrition
ranging from 27% to 75%. The major Indian studies on'
THR are: CARE-lndia's Project Poshakm MP (1970-75)45;
The Sidney Cantor/ATAC Study on ‘take-home’ dry food
as a distribution system in Tamil Nadu (1973)22; The
Evaluation of the India Population Project, Karnataka
(1981 )a; and the Maharashtra study by Khare et al, (1976)
*.
The findings of all the international and national studies
went heavily in favor of the THR for the children under
three, except for the one fact that there was some
‘sharing’ or dilution of the THR at home.
Community leaders and change agent strategy
All groups were very positive about the THR. The
Sarpanchs felt that the'mothers and the community were
full participants and that the health of the mothers and the
community had improved. The change agents who had
been chosen for their leadership qualities stood out as far
as confidence went. They were knowledgeable about the
THR (except importance of portion size), and the nutrition
and health services offered to the mother and the child in
the INHP. None of the change agents in AP had more than
2 children. Hence, they were good role models for other
mothers.
10
a month. One of the nutrition and health/take
home ration days could be exclusively for individual
counseling and/or attention to the registered
beneficiaries.
Advantages of the THR
• Very high geographic outreach
• Covers majority of under two population
• Convenient for the mothers
• Less expensive than fed-on-site
• Minimizes cross infections
• More realistic child care education and caring
practices for the mother
• Mother can feed what the child likes in
frequent feeds J
• The THR rations have definitely reached the
household level. The current problem is to closely
monitor and test out strategies that will ensure
that children under two years of age consume more
of the THR.
• The Village Panchayat, the local CBOs, the Change
Agents and the adolescent girls could all be used
for household level monitoring, counseling and
actual demonstrations of how it is to be used for the
beneficiary child only. This is bound to reduce
'sharing' of the food with other siblings or other adult
family members.
• Treats malnutrition in its milieu
e Child is more emotionally secure at home
• Ensures weight gain inspite of ‘sharing’.of the
THR/_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
5.
CONCLUSIONS
• THR is the most appropriate food delivery system
for children under two years of age.
e
• There are many ways to enhance the concept of a
. full THR ration for children-under two. They are as
under:
If combined with nutrition and health days and the
use of village level change agents, it becomes an
extremely strong and practical way to make the
supplementary food available and accessible to
children under two.
— On nutrition and health days, repeated cooking
and feeding demonstrations of a single ration
must be done with infants of specific ages,
namely, 6,9,12 months and so on. The mothers
and ICDS staff will learn two important facts: 1)
the amount that has to be and is actually
consumed by the infant, and 2) that the amount
of THR consumed per sitting increases with age.
• The present CSB-SO can be made more
acceptable/palatable for children under two by
incorporating the ARF-technology; by making it
ready to eat; and by making it sweet.
— Storage canisters for the ration and calibrated
tumblers/katoris to cook the correct amount at
home.
• Some sharing or dilution of the THR is inevitable.
However, all attempts must be made to ensure that
the beneficiary child consumes a major portion of
THR.
6.
— The mother should be encouraged/counseled
to give the full ration divided over 2-4 feeds to
children under two when the older siblings are
away at the AWC. The problem again and again
is that minuscule amounts are fed to children
under two years of age.
RECOMMENDATIONS
6.1 RECOMMENDATIONS ON THE FOOD
DELIVERY SYSTEM
• THR has been shown to be the best food delivery
system for children under two years of age. It should,
therefore be used universally in the ICDS.
— All concerned should become familiar with the
number of pieces a particular Single Ration would
yield, e.g. how many laddus, dosais or the
amount of ha/wa, sheera, payasam etc. This
concept does not exist presently.
• THR can be immensely strengthened by seeing that
the strategies of the ration distribution, nutrition and
health days and village level change agents,
converge.
— The training and capacity building programs
for all should be greatly strengthened by
incorporating the above concepts.
• THR distribution should be done at least two times
12
child’s Recommended Daily Allowance. Now there
is quite a wide variation in thisTat>e6. Since vitamins
and bio-available iron come from expensive dietary
sources which is beyond the economic capability
of an average ICDS household to supply to its
children under two, the CSB ration may be the child's
major avenue to satisfy his/her micronutrienthunger.
— Appropriate strategies should be worked out
for the agriculturally peak months. Rural
communities work in the fields for about six
months in a year. Institution of'Seasonal Creches',
distribution of increased levels of RTE-THRs,
and compensating mothers monetarily, forcollecting the rations may be some of the strategies to
be considered.
o The present roasted RTE
for UP should be periodically
checked for its micronutrient
content.
6.2
RECOMMENDATIONS
TO IMPROVE ACCEPTABILITY
A. Make changes in the
physical characteristics
of the CSB.
• CSB is grainy and gritty.
I The grits are very hard. At
the simplest level the CSB
can be find ground at the
manufacturer's end, for
children under two. A gritty
product could cause gastrointestinal problems in
these children.
Offer nutrient dense but
low-bulk rations.
The CSB-oil ration on
cooking becomes thick, pasty
and voluminous. This is not
appropriate for children under
two (especially children under
one year of age). Incorporate
5% Commercial Barley Malt (CBM) Powder. This
can be most easily done at the manufacturing end.
CBM is very cheap in the USA (20 cents per Kg.),
and can be adjusted towards 5 gm of corn. CBM
being the richest source of p -Amylase, will instantly
'liquefy' the cooked up ration. Children under two
find it easy to drink but not swallow a solid or pasty
THR ration. This will go a long way to solve the major
problem of ‘portion size'. Acceptability and intake
by the child will go up markedly.
C.
• If possible, extrusion technology can be employed
on raw corn and raw defatted Soya. This will result
in a completely cooked and homogeneous
powdered CSB. This again is most easily done at
the manufacturer’s end. Such a product will have
very suitable physical characteristics for feeding the
children under two.
e
If this is difficult to operationalize, the mother/ care
giver of the children under two may be counseled
to fine grind the CSB in her household chakki.
Alternatively, the AWC-helper/Change Agents/
adolescent girls/CBOs can do this on the day before
the nutrition and health day and THR distribution
day.
® If this is not possible, a distribution of 150 gm
CBM powder can be considered for 30 days at a time. The mother can bring a small container or
dabba for this. Alternatively, a one time screw-top
container may be considered.
o
• Sieving of the CSB by mothers at home must be
discouraged. It divides the ration and renders it
nutritionally imbalanced.
Make changes in the micronutrient composition
of CSB
• The USA manufacturer may be supplied with the
micro nutrient requirements of a one-year-oldlndian-childTsbB'. He may be able to add 80% of the
B.
In some areas, communities traditionally germinate
/■^/(Tribal AP) or have been taught to germinate
wheat (Rajasthan). Such germinated cereal
powders are rich sources of ARF that the community
or its households can acquire and use.
• The vital importance of nutrient dense but low bulk
foods needs to be introduced into Training and
Capacity Building right from the national to the
household level.
13
6.5
RECOMMENDATIONS TO IMPROVE NON-FOOD
FACTORS THAT INFLUENCE THE NUTRITIONAL
6.3
RECOMMENDATIONS TO IMPROVE
PALATABILITY
STATUS
A. For the Supplementary food
• Safe drinking water, personal hygiene of the mother
and the child under two and a reasonably clean
house environment.
• Infants definitely like a sweet food. If economically
feasible, the ration can be sweetened (10 to 15%)
at the manufacturer's end. The RTE for UP is
25% sweetened.
•
• Most children living in rural, tribal and urban settings
are infected with worms. Biannual deworming with
single dose Albendazole or Mebendazole would
go a long way to improve the child’s nutritional
status.
If not possible, mothers could be encouraged to'
offer a sweet gruel to the extent possible.
• If some top milk or seasonal fruit can be offered,
this will add to palatability and nutrition.
• A small family norm. AP leads the way in this
respect. A child under two years of age automatically
gets more attention from his/her mother if he/she •
• Use of chillies and strong spices should be
discouraged for this age group.
a single child or has only one other sibling. In this
respect, it may be a good strategy to put the mothers
of small norm families in MP and UP on a pedestal.
B. For the Home Food
Mothers/care-givers can be encouraged to add some
thick unspiced dal to soft-boiled rice and add even half
a teaspoon of oil to the dish. The same can be done
with potato, yam etc. In case of dal-roti, the /o//must be
made mushy in the unspiced dal. This may be done in
boiling water or even hot tea, if cte/cannot be afforded.
The amount should be at least half-a-cup. Usually a
teaspoon or two is offered, offering of such minuscule
amounts continues to be a problem. ■
6.6
RECOMMENDATIONS FOR MULTI-STATE
OPERATIONAL RESEARCH STUDIES
• Depending on the recommendations accepted,
simple Seven-State-Operational Research Studies
could be designed and conducted.
• To the extent, possible CARE-lndia-INHP staff could
be trained to collect the data required; or
alternatively the State-Level-Research -Institutions
used by Foundation for Research in Health Services
(FRHS) could be considered.
6.4
RECOMMENDATIONS TO REHABILITATE
SEVERELY MALNOURISHED CHILDREN
• Product tests of THR with and without ARF need to^
be designed and field tested.
w
• The severely malnourished children under two years
of age are 5% in AP, 16% in MP and 14% in U.P8.
These children more than any other category need
low-bulk’ yet “high nutrient density foods”.
• Product tests of UP sweetened RTE-THR with
and without ARF similarly needs to be designed
and field tested.
6.7
RECOMMENDATIONS TO PRODUCE AND
CIRCULATE PUBLICATIONS ON TAKE HOME FOOD
DELIVERY MECHANISMS
• Nutritional Rehabilitation with amylase liquefied
feeds has been successfully done in Bombay,
Chandigarh and Saudi Arabia. The CSB-Oil THR
needs to be given more often, namely, 6-8 times
over the day.
• Project Poshak, may be reproduced and widely
circulated. It is considered the most definitive work
on take home food delivery mechanisms.
• Parents have to be prepared to spend a little more
on foods such as milk, banana, sugar, oil and green
coconut water etc.
• Summary of the above Project may be translated
into regional languages and circulated
14
7.
REFERENCES
15.
John C. and Gopaldas T: Reduction in Dietary
Bulk of Soya Fortified Bulgar Wheat Gruels with
Wheat Amylase-Rich Food. UNU Food and
Nutrition Bulletin, 1988; 10 (4); 50-53.
16.
Tara Gopaldas, Suneeta Deshpande, Urvi
Vaishnav, Neha Shah, Pallavi Mehta, Sashi
Tuteha, Shubhada Kanani and Kashmira Lalaani:
The Transfer of a Simple Dietary Bulk Reduction
Technology of Weaning Gruels by AmylaseRich Foods (ARFs) from Laboratory to Urban
Slum. UNU Food and Nutrition Bulletin, 1991; 13
(4): 318-321.
17.
Tajjuddin K.M.: Studies on Nutritional
Rehabilitation with ARF. Unpublished Ph.D.
results, 1990.
18.
Mujoo R.: Studies on Commercial Barley Malt.
Unpublished Ph.D. results, 1993.
19.
Gopaldas T and Deshpande S: The Miracle of
Germinated Cereal Grain Powders. Daya
Publishing House, Delhi, 1992.
20.
Beaton G.H. and Ghassemi H.: Supplementary
Feeding Programs for young children in
Developing Countries. Am. J. Clin. Nutr, 23,
707-15., 1982.
21.
Austin J.E. and Zeitlin M.F.: Nutrition Inter
ventions in Developing Countries—An Overview.
Published by Oelgeschlager, Gunn and Hain,
Publishers Inc., Cambridge Mass, USA, 1981.
22.
Devadas R. P.: Take Home System Vs On-thespot feeding Proc. Nutr. Soc. India. 15, 68,1973
(As a part of the Sidney Cantor Study, T.N.).
23.
India Population Project, Karnataka: Nutrition
Component. National Institute of Nutrition,
Hyderabad, 1981.
24.
Khare R.D., Shah P.M., and Junnarkar A. R.:
Management of Kwashiorkor in its milieu; a
follow-up for fifteen months. Ind. J. Med. Res.
64 (8),1119,1976.
1. International Institute for Population Sciences
(UPS) 1995. NationalFamily Health Survey (MCH
&
Family Planning), India 1992-93. Bombay. IIPS
2. Nutrient Requirements and Recommended Dietary
Allowances for Indians, The Indian Council of
Medical Research, New Delhi, 1992.
3.
Dietary Guidelines for Indians-A Manual. The
National Institute of Nutrition, 1998.
4.
Gopaldas T etal: Project Poshak, Vol. .One, and
1975, printed by CARE-lndia, New Delhi.
i 5. Gopaldas T etal: Project Poshak, Vol. Two 1975,
printed by CARE- India, New Delhi.
6.
Planning Commission Evaluation Report on the
ICDS (1976-78). New Delhi, India, Planning
Evaluation Organization, New Delhi, 1982.
7.
National Evaluation of the ICDS. National Institute
of Public Co-operation and child development,
New Delhi, 1992.
8.
Nirmala Murthy: CARE-lndia's Integrated Nutrition
and Health Program. The Baseline Survey Report
(Consolidated for 7 states), Part II, 1997.
9.
Johri N.: CARE-lndia’s INHP Results Reports.
Achievements versus Plans (FY 1997 Vs FY
1996), 1998.
10.
Pillai G: CARE-lndia's Integrated Nutrition and
Health Program (1995-2000).
11.
Johri N.: CARE-lndia's Nutrition and Health SectorProgram update, 1998.
12.
Consultancy Report by IESSCO Pvt. Ltd. On UP’s
RTE. Cited as an Appendix in Ref. (10).
13.
Malnutrition in South Asia: A regional Profile.
Edited by Stuart Gillespie. UNICEF, S. Asia, 1977.
14.
Gopaldas T: Fighting infant malnutrition with
amylase complementary foods. Nutriview, 2,
1998/2.
HEALTH BASICS:
WEAW8MG
Breastmilk is the best and safest food
for young babies. Older babies need
extra foods as well as breastmilk. It is
important that babies are given extra
foods as well .as breastmilk at the right
age. and in sufficient amounts, to
enable them to grow and stay healthy.
Too little food, given too late, or
inadequate food with too few nutrients
may lead to poor growth and malnutri
tion. The malnourished child will get
sick more often and will be less able to
fight off illnesses such as diarrhoea.
Weaning foods can. however, be very
dangerous for babies. If they are not
hygienically prepared they can be a
major source of infection. This Health
Basics insert describes good weaning
practices to help families prevent diar
rhoea in their children.
What is weaning?
Weaning means giving family foods in
addition to breastmilk. Weaning is a
gradual process by which the infant
becomes accustomed to the adult diet.
It is not good for babies to stop giving
breastmilk when new foods are first
being given — weaning foods do not
replace breastmilk, they complement
it. As the baby gets older it needs more
food to grow and stay healthy. The
number of breastfeeds can be reduced
slowly as the baby starts to eat more
and more family foods. However, it is
important to remember that until the
age of about two years babies can still
receive an important amount of
nourishment .from breastmilk.
start to need extra food'in addition.to
breastmilk because they are growing
fast and. breastmilk is no longer
enough.
When to start giving extra foods?
Start by giving one or two teaspoons a
day of carefully mashed food in addi
tion to regular breastfeeds. Do not use
a feeding bottle. Slowly increase, the
number of meals and the amount of
food given. By the age of eight months
most babies need four ‘meals' a day
including a variety of foods, in addition
to regular breastfeeding. At one year
old a child should be able to be given all
types of family foods, although the
food may still need to Be softened or
mashed. At this age a child needs to eat
about half the daily amount of food its
mother eats.
Feed babies using a clean cup and
spoon. Do not add water to the wean
ing food. Watered down weaning food
does not have enough nutritional
.value, and if the water is dirty or con
taminated the baby will probably get
diarrhoea. Patience is needed when
babies are first starting to eat family
foods — while they are learning to eat
this way they may often spit out the
food — this does not mean that they are
Weaning foods should be given to the
baby at about the age of four to six
months. At four months most babies
How should weaning foods be
given, and how often?
Produced by Dialogue on Diarrhoea, AHRTAG, 1 London Bridge Street, London SE1 9S.G, U.K.
WEANING
not hungry. Let the baby get used to
one food for a few days before intro
ducing another.
Weaning foods should ideally be:
• high in energy:
• easy to digest;
• low in bulk and viscosity (not too
thick):
• fresh and clean:
• inexpensive and easy to prepare;
• not too highly seasoned.
What are good weaning foods?
A thick creamy porridge made from the
basic food of the community is a good
weaning food for babies. The basic
food or staple is cheaper than most
other foods and is usually eaten by the
family at most meals. Examples of
basic foods'includc:
• cereals — maize
— wheat
— sorghum
— oats
— barley
— bread (soaked in gravy,
milk, or tea)
— rice
• ' roots
— cassava
— yam
— cocoyam
— potato
— sweetpotato
• starchy
fruits
— plantain
— breadfruit
— banana
On their own. especially when cooked
in water, most cereals, grains and roots
are too low in energy. Some oil or fat
(or sugar) should be added to the por
ridge to make it richer and easier to
swallow and digest.
Adding oil
increases the energy value of the wean
ing porridge.
Give, this porridge in addition to
breastmilk for about two weeks — after
this time babies need other foods as
well as breastmilk and porridge to pro
vide enough energy and a balanced
diet. It is important that weaning foods
contain oils, fats or sugars; fruits; dark
green vegetables or orange or yellow
fruits; and food from animals or fish or
from legumes (for example lentils).
These different types of food provide
energy; vitamins; and proteins. The
best type of weaning meals should con
tain something from all of these groups.
Continue to give breastfeeds regularly
between meals.
Examples of types of foods from these
groups are:
• peas and beans
These are as good as food from animals
for providing protein but are cheaper.
They need to be cooked thoroughly and
mashed to make them easily digestible
for
babies.
Examples
include
chickpeas, cowpeas, groundnuts, soya
beans, split peas, lentils, blackeye
beans, peanuts, red beans, navy beans.
• oils, fats or sugars
These add extra energy to the weaning
porridge or cereal dishes. Sugars are
not as good as oils or fats and will also
damage teeth. Examples include: corn,
palm,
groundnut,
coconut
and
sunflower oils, ghee, butter, mar
garine, lard, any animal fat.
•Peis and beans
•Pood from. zva
animals • UJ
•Dark green vege
tables and orange
and yellow fruits
and vegetables ■
• food from animals and fish
These are good for babies but are usu
ally more expensive than peas and
beans. Examples include meat, fish.
offal, eggs, milk, and food made from
milk such as cheese and yoghurt, curd.
cottage cheese.
• dark green leafy vegetables, and
orange and yellow vegetables and fruits
Babies need these foods to prevent eye
damage and possibly blindness from
shortage, of Vitamin A. Examples
include: spinach, kale, tomatoes, car
•fruits ■
rots,
amaranth,
sweet
cassava,
pumpkin leaves, calalu, pumpkin and
pawpaw.
• fruits
Before giving these to babies they
should be'peeled carefully or washed in
clean water, then mashed or the juice
squeezed out. If water is added to the
juice it must be clean; otherwise babies
may get diarrhoea. Examples include:
oranges, pumpkin, tomato, banana.
Pupaya. mango, pineapple.
Produced by Dialogue on Diarrhoea, AHRTAG, 1 London Bridge Street, London SE1 9SG, U.K.
WEANING
Food from the family pot
Family foods, that is foods that the rest
of the family normally eat can give
babies all the nourishment they need
without any additional cost. There is no
need to buy expensive commercially
manufactured weaning^ foods. Talk to
mothers about what the family usually
eats and help them to decide which
foods would be suitable to give a young
baby. Family pot feeding — giving the
family food in a mashed form, without
or before adding hot spices or extra
salt, and adding something extra like
oil. an egg, and extra dark leafy vegeta
bles — is best. Put the child’s food in a
separate dish or bowl so that it is possi
ble to see how much he or she cats.
Also make sure that the bowl or plate
and utensils used by the child are clean.
This also encourages the child, as it gets
older to learn to feed itself. Make sure
that the child's hands are clean.
Cooking weaning foods
Cooking
equipment,
particularly
stoves, plays a vital role in the health
of the family or community. Safe,
economical stoves are essential to pro
vide heat and light and to cook safe and
nutritious meals.
A good cooking stove helps to ensure
that weaning foods are well cooked and
properly reheated. A stove should be:
Careful preparation of weaning foods helps
to prevent diarrhoea.
• safe (so that children do not burn or
scald themselves);
• easy to use and suitable for frequent
use;
• fuel efficient, i.e. should not waste
or use too much fuel, or produce too
much smoke;
• be capable of cooking and reheating
food thoroughly and boiling water
using minimal fuel and time.
Food that has not been cooked or
reheated thoroughly may contain diar
rhoea-causing
germs
(pathogens).
Cooking food thoroughly so that it
boils can make it safe" by destroying
these pathogens (e.g. bacteria and
parasitic eggs). Cooking food can also
improve its flavour, making it more
palatable for children, and the addition
of other ingredients can increase the
nutritional value of the food. (Badly or
over-cooked food on the other hand
can cause loss of nutrients and contri
bute to malnutrition). Cooking food
also makes it easier to chew and digest
and helps the body to absorb nutrients
from it.
Preparing weaning foods
Contaminated weaning foods give
babies diarrhoea. Careful preparation
and storage of weaning foods keeps
them safe. Follow these rules for safe
preparation of weaning foods:
• wash hands before preparing food;
• if possible prepare weaning foods
immediately before they will be
eaten;
• wash all utensils before preparing
food, and scrub chopping boards
and tables;
• cook or boil food well;
• reheat food thoroughly if it has been
kept for more than two hours, until it
boils. Boiling food will kill any
germs that may have contaminated
the food while it has been stored. Let
it cool before giving it to the baby;
• mash foods up with a clean pestle,
fork or spoon. Never use a sieve as
these are difficult to keep clean;
• use the cleanest water available for
making weaning foods and for wash
ing uncooked foods. If possible boil
Produced by Dialogue on Diarrhoea, AHRTAG, 1 London Bridge Street, London SE1 9SG, U.K.
WEANING
the water if it has not come from a
clean source such as a tap or water
pump. Boiling water will kill the
germs that cause diarrhoea.
Storing weaning foods
• Do not store weaning foods for more
than two hours if possible. Keep
them stored in clean covered con
tainers that keep out flies and other
insects.
• Keep in a cool shady place out of
direct sunlight if possible.
• If food has been kept for more than
two hours reheat it thoroughly so
that it boils.
Why do weaning age babies get
malnourished?
This is usually because:
• they are not given the right sort of
weaning foods or enough food;
® they grow very fast and need plenty
of energy rich foods — more for
their size than older children or
adults;
• they may be taken off the breast too
early, or suddenly, i.e. as soon as
extra foods arc given;
• they have small stomachs and do not
get food often enough. Two or three
meals a day like the rest of the family
is not enough for the weaning age
baby;
• they do not have enough teeth to
chew, and need food that is soft and
easy to swallow.
The weanling with diarrhoea
As at any other age. the weanling with
diarrhoea must be given plenty of
appropriate fluids and continue to cat
plenty of nourishing food to help
recovery and ensure that there is no.
growth retardation.
Weaning education
Before talking to mothers about which
weaning foods to give, you will need to
be aware of the family’s socio-economic
status, and availability of different
types of foods, particularly those which
are seasonal. Some existing beliefs
about foods and feeding are beneficial.
others may be more harmful, but make
suggestions tactfully and explain how a
weaning diet can be made more
nutritious using local foods. In many
places you may also need to win over
the support of the grandmother if you
Why do weaning age babies often
get diarrhoea?
• After four to six months of age
babies have lost some of the
protection against disease given to
them by their mothers at birth
, (maternal
antibody)
and
from
breastmilk.
Personal hygiene and weaning
foods
Hands should be washed before prepar
ing weaning foods and before feeding
them to the baby, particularly after
using the latrine. Unwashed hands can
pass on diarrhoea germs via food to the
baby. Mothers should be especially
careful to wash lheir hands, with soap if
available, after cleaning their baby’s
bottom.
Remember: cool, covered, clean cooked
food is safe food but
faeces, flies, filth, fingers
can mean dirty unsafefood.
• They may also get diarrhoea from
the new foods that they are being
given if these are prepared or given
to the baby with dirty hands and
utensils. Food that is not stored
safely, but which is left uncovered
and open to dirt and flies, or kept in
dirty containers, will quickly go bad,
become contaminated and may give
babies diarrhoea.
• Also at this age babies start to move
around more, put things in their
mouths, and are more likely to come
into contact with germs and dirt.
However, they are too young to have
built up much immunity themselves
to protect them against diseases sue.h
as diarrhoea.
Hands should he washed before preparing
weaning foods.
Produced by Dialogue on Diarrhoea, AHRTAG, 1 London Bridge Street, London SE1 9SG, U.K.
WEANING
Home and community weaning food
production
This can be done:
• at home using a cereal staple plus
legume/sced/nut mixture. The mixture
should be easily reconstituted and
should have a shelf life of at least one
week (simple grinding devices to reduce
the time and work involved are recom
mended); or
• at community level through community
groups. Women's groups can initiate and
operate communal production/incomc
generating activities which may or may
not be subsidised. The use of oils, pine
apple juice, papaya juice and fermenta
tion methods as well as germination can
decrease the viscosity of weaning foods.
Community level activities should have
an educational and health component
and should be integrated into, for exam
ple, children’s supplementary feeding
programmes.
There arc several approaches to
decreasing the viscosity and bulk of
weaning food. Fermenting sorghum pro
duces enzymes which decrease viscosity,
as used in Tanzania. In South India, fer
mentation of rice and legumes is used to
decrease viscosity. With bulky staple
foods common in Asia and Africa, a
small child would have to consume about
1 kilogramme of cooked rice or cooked
banana to obtain only 1.000 calories.
Small children cannot cope with such
enormous quantities of staple foods to
meet their energy needs. More energy
dense,'less bulky, low viscosity foods for
young children should be promoted.
•
are to change what mothers feed to
their young children.
For example, there are, in India,
beliefs about the digestibility of certain
foods and their consistency. Far too
often watery gruels or lentil water or
thin vegetable soups are given in the
belief that the baby will not be able to
digest anything else. But these have no
or very little energy value. Beliefs in
■hot" and ‘cold’ foods or, for example,
that cereals are bad for the liver, should
not be condemned, but can be over
come with patience and alternatives
suggested. Many mothers believe that
their baby needs expensive or special
foods, which they cannot afford. They
may also ask how the child can eat
proper food before it has any teeth.
Emphasise that this is not a problem if
the food is properly mashed and soft.
Feeding the weaning child
Points to remember
• Feeding is a matter of using good
sense. Like adults, babies may like a
particular food more than another,
and may be more hungry on some
days than others. No two babies are
the same in which foods they like
more than others. Some babies
prefer sweet things while others
prefer salty things. Make allowances
for this.
• Mealtimes should be pleasant and
‘force’ must not be-used in feeding.
Remember that learning to swallow
semi-solid food may be difficult for a
baby who only knows how to suck
the breast.
o If a particular food is refused, do not
offer it again for a few days. Try
something different.
Acknowledgements
This DD insert is based on an article
by Dr Shanti Ghosh and material ■
from:
• Learn More About Breastfeeding
and Weaning. League of Red Cross
and Red Crescent Societies 1987.
• Primary Health Care Technologies
at Family and Community Levels.
Aga Khan Foundation, UNICEF.
WHO, 1986.
• Feeding Mother and Child. The
Caribbean Food and Nutrition Insti
tute.
• Prevention of Diarrhoea. Supervis
ory Skills WHO, 1987.
Produced by Dialogue on Diarrhoea, AHRTAG, 1 London Bridge Street, London SE1 9SG, U.K.
RESOURCE LIST
Addresses for organisations supplying books/manuals, audiovisuals, and newsletters, are listed under sources of information and materials
• Voluntary Health Association of India World Federation of Public Health Associa
(VHAI), 40 Institutional Area, South of tions. Programmes Activities for Improving
Weaning Practices. Information for Action
IIT, New Delhi — 110 016, India.
• World Health Organisation (WHO), Nut Issue Paper. 1984.
• American Public Health Association,
rition Unit, 1211 Geneva 27, Switzerland. WHO. Guidelines for Training Community
International Health Programmes, 1015
• World Federation of Public Health Associ Health Workers in Nutrition. WHO Offset
Fifteenth Street, N.W., Washington,
ations (c/o American Public Health Publication. 2nd Edition-. 1986.
C. 20005, USA.
D.
Nutrition Educational Materials Listing.
Association, USA)
• Caribbean Food & Nutrition Institute.
• World Neighbors, 5116 North Portland WHO. 1984.
PO Box 140. Kingston 7, Jamaica.
Show and Tell. Nutritional Educational
Ave. Oklahoma City, OK 73112, USA.
• Child-to-child Programme, Rm 833,
Programme. UNESCO. 1985.
Institute of Education, 20 Bedford Way,
BOOKS/MANUALS
London WC10AL.UK.
• Clearinghouse on Infant Feeding & Mat Cameron M & Hofvander Y. Manual on
ernal Nutrition, American Public Health
Feeding Infants and Young Children. AUDIOVISUALS
Association. 1015 Fifteenth Street. N.W.
Oxford University Press. 1983
Washington, DC20005, USA.
Child-to-child Programme. Child-to-child Videos
How to Wean Your Baby. A 20 minute video
• Find Your Feet, 13-15 Frognal, London
Reader: Good Food.
NW3. UK.
Caribbean Food & Nutrition Institute cassette & slidc/audio cassette. 1986. CFNI.
• Intermediate Technology Publications
(CFNI). A Guide to Feeding the Weaning Lucky Gary. A 10 minute video on weaning
Ltd., 103-105 Southampton Row. Lon Age Group in the Caribbean. 1982 and aimed at eastern Caribbean audiences.
don WC1B 4HH. UK.
Improving Weaning Practices in the Carib CFNI.
• International Nutrition Communication
bean. Self Learning Modules for Commun Slides
Service (INCS), Education Development
Weaning Foods & Energy. TALC, UK.
ity Workers. 1986.
Centre, 55 Chapel Street, Newton, MA.
Ebrahim GJ. Nutrition in Mother and Filmstrips
02160. USA.
Filmstrips available on feeding babies suita
Child Health. Macmillan. 1983.
• Institute of Nutrition & Food Sciences,
Ghosh S. The Feeding and Care of Infants ble for audiences in Guatemala. Nepal,
University of Dhaka, Dhaka 2, and Young Children. Voluntary Health Philippines. World Neighbors, USA.
Bangladesh.
Flipchart
Association of India (VHAI). 1985.
• International Children's Centre, Chateau
Hollis C. Using Communications To Solve Infant Care & Feeding. World Neighbors.
de Longchamp, Bois de Boulogne.
Nutrition Problems. International Nutrition USA.
F75016. Paris, France.
Communication Service. (INCS) 1986.
Flaimelgraph
• League of . Red Cross & Red Crescent
Israel R.. & Lamptcy P. Nutrition Training Scries includes: Feed Your Children Often,
Societies, 17 Chemin d& Crcts, P.O. Box
Manual Catalogue for Health Professionals, Give Your Child Plenty of Soup. TALC.
372, 1211 Geneva 19, Switzerland.
Trainers and Field Workers in Developing UK.
• London School of Hygiene & Tropical Countries. (INCS).
Medicine, Department of Human Nutri Joint WHO/UNICEF Nutrition Support
tion. Keppel Street. London WCi 7HT.
Programme. JNSP Nutrition Learning Pac NEWSLETTERS
UK.
kages, Package 4: Young Child Feeding.
• Macmillan Press Ltd., Houndmills,
League of Red Cross & Red Crescent Bulletin of the Nutrition Foundation of the
Basingstoke, Hampshire RG2I 2XS.
Societies. Learn More About Breast Feed Philippines. Nutrition Foundation of the
UK.
ing & Weaning. 1987.
Philippines.
Bi-monthly,
English
&
• National Food & Nutrition Committee,
Nutrition Handbook for Community Work Tagalog, Subscription.
PO Box 2223, Government Buildings. ers in the Tropics. Macmillan/CFN I. TALC. Cajanus Magazine, Caribbean Food & Nut
Suva, Fiji.
UK. 1986.
rition Institute. Quarterly, English. Sub• Nutrition Foundation of India, B 37 GulPacey A. Gardening for Better Nutrition. scription.
moher Park. New Delhi, India.
Intermediate Technology Publications. The Fiji Food & Nutrition Newsletter, The
• Nutrition Foundation of the Philippines.
1978.
National Food & Nutrition Committee.
Inc., 107 E. Rodriguez Sr., Boulevard,
Proceedings First Asian Household Nutri Fiji, English, Subscription.
Quezon City, PO Box 3, Philippines.
tion Appropriate Technology Conference. Nutrition, Division of Nutritional Sciences,
• National Institute of Nutrition, Indian
Colombo. Sri Lanka. UNICEF 1981.
Cornell University. USA. English, Free.
Council
of
Medical
Research.
Ritchie J.A.S. Nutrition & Families. Mac Nutrition & Development. Ministry of
Hyderabad 500007, India.
millan. 1983.
Health, Papua New Guinea. Quarterly,
• Ministry of Health, Nutrition Section,
Royal Tropical Institute. Mauritskade 63. English, Subscription.
Box 2084, Konedobu, Papua New
1092 AD Amsterdam. The Netherlands. Nutrition News. National Institute of Nutri
Guinea.
Ready-made Weaning Food Mixtures in tion, India. English, Free.
• Oxford University Press, Walton Street,
Developing Countries. 1983.
Nutrition News, Institute of Nutrition and
Oxford OX2 6DP.
De Swccmer C., el al Manual for Child Nut food sciences, Bangladesh. Quarterly,
• Teaching Aids at Low Cost (TALC), PO
rition in Rural India. VHAI.
English, Subscription.
Box49, St. Albans. Herts. AL1 4AX.
Trcgoning M.A.. & Bova G.S. Better Child Mothers & Children. American Public
• Tanzania Food & Nutrition Centre, Box
Care. TALC. UK.
Health Association. English. French.
977, Dar cs Salaam, Tanzania.
UNESCO, Nutrition Education Series. Spanish, Free.
• UNESCO, Nutrition Education Prog
Issue 10. Easy to Make Teaching Aids for Tanzanian Food & Nutrition Journal. Tan
ramme,- 7 Place de Fontenoy, 75700.
Nutrition Teaching Learning. 1984.
zanian Food & Nutrition Centre. Tanzania.
Paris, France.
UNICEF. The UNICEF Home Gardens English, Subscription.
• UNICEF, UN Plaza, 4/1234C, New York
Handbook — For People Promoting Mixed Vitamin A + Sieve. Rodalc Press Informa
10017, USA.
Gardening in the Hurnid TYopics.
tion Services, 33E, Minor Street. Emmaus,
• Urban Resource Systems, 783 Beuna
Wade 1. City Food Crop Selection in Third PA 18098, U.S.A. English, Free.
Vista West, San Francisco, CA 94117,
World Cities. Urban Resource Systems. Xerophthalmia Club Bulletin. 31 Observat
USA.
198.6.
ory Street, Oxford, U.K. English, Free.
Produced by Dialogue on Diarrhoea, AHRTAG, 1 London Bridge Street, London SE1 9SG, U.K,
Published in India by L ^) d . S. M ukarji General Secretary,
C M A l.^ n behalf o f Ahrtag, London.
SOURCES OF INFORMATION
AND MATERIALS
DIET FOR CHILDREN
First 4 months - Only mother’s milk. No Water.
From 5th month.onwards /with
Breast feeding to continue. Add following foods as advised.
Stari^boiled and cooled water with a small glass. No need
for use of bottle at any age.
1.
Cereals ; Home made dalia (Porridge) or suji kheer or thin
seera with ghee or soaked bread or mashed boiled rice or phir. _ni made from rice powder and mi'lk may be started after
completion of 4 months.
One or two teaspoons are given
twice a day in between two feeds around 8 AM and 7 J?M..Keep
increasing every 3rd or 4th day to the amount accepted.
Later on, may also add cereals around 2 P.M.
2.
Mashed banana can be added a week after starting the cereal.
It may be mashed with malai or milk - a quarter banana to
begin with.
Increase by quarter every succeeding week
to the limit accepted. This can be given with cereal or
at another feeding time. You can interchange banana with
apple sauce (Cut peeled apple into small bits; boil it
with some sugar; mash in a mixer or with fork).
Once
prepared, it may be kept in a covered jar in a cool place
or in a refrigerator for 3 to 4 days.
Other seasonal
fruits like pears ( boiled), papaya, mango, chikoo etc.
can also be given.
3.
Soft-boiled egg; Add a week later.
Boil the egg in water
forSminutes arid then cool in running water. Commence with
one tea spoon of the yellow with a pinch of salt and/.br
sugar to taste. Gradually increase by tea spoon increments
adding the white of the egg so that baby may use the
whole egg in about 4 weeks from the commencement.
4.
Mashed and well-cooked vegetable : Add a week later, with
ghee or butter or cooking oil and salt and sugar.
Begin
with 2 to 4 tea spoons just preceding any other feeding
and increase progressively. (Dark green leafy vegetables,
carrots, peas and pumpkin are preferable items).
5.
Dahi ; Add a week later, sweetened and/or salted, two
or four tea spoons to begin with;' increase progressively.
6.
Mashed and well cooked khichri or rice and dal ;
Add 1-2
weeks later, with salt and/or sug^r and ghee or coking
oil or butter.
Begin with 2 to 4 tea spoori and increase
to the quantity accepted by the baby.
As items 2 to 6 are added, do not stop or reduce previous
ones. The object is to foster more tastes and increase
quantity to the amount accepted. Patience and perseverence
are key words.
In case you have started feeding solids
with a bigger baby, you can always begin with a larger
amount and increase rapidly.
N.B. In families with history of allergy ( Asthma, Eczema),
avoid addition of egg, cocoa preparations (like Chocolate),
juices and wheat preparations until the completion of 6
months. With a strong family history of allergy, it may
even be better to avoid all foods other than breast milk
in the first 6 months of like.
Around 9 months ; Add undiluted cow’s or buffalo’s milk
with a glass.
If the milk contains too much fat, remove
cream. Continue mother's milk.
2
After one year ; Mother's milk can be continued upto 2 years.
Give cow's'or buffalo's milk from a djlass (2—3 times).
Gradually let the child get used to food made at home.
Children who do not eat enough at a time should be offered
food every 2-3 hours.
But do not force. Make sure that
enough protein containing foods are given ( like pulses,
gram, peanuts, peas, beans, egg, fish mutton, liver).
Sprouted gram or moong is very nutritious.
Green,
orange, red and yellow vegetables are essential;.cheapest
seasonal fruits should be preferred.
If child doesn't
like milk , give milk preparations like curds, Encourage
the child to eat with spoon or with own fingers.
Washing
hands before and after meals should be encouraged. Chapati
should be made from whole wheat flour.
Polished rice is
not as healthy as par^boiled rice. Scrape vegetables like
Potatoes instead of peeling them. Water in which rice or
vegetables have been boiled should be utilised.
Do not
overcook the vegetable. Avoid too much spices. Avoid
chocolates, sweets, biscuits, cold drinks, sharbats, flavou
ring agents etc. as far as possible .
SIMPLE REMEDIES FOR COMMON ALIMENTS
1.
Watery motions
Do not starve. Let the patient eat or drink what he/she
likes. May prefer rice preparations, curds, banana, pota
toes, stewed apple. If breast-fed, continue breast-feeding.
Water - 1 litre =(Capacity of 2 ) Mix; Taste. The sol-:
dairy milk
)ution should not teste
bottles)
)more salty than tears.
Salt - 1 teaspoon
) For younger children
) use 3/4 teaspoon of
Sugar - 8 teaspoons
) salt.
Add lime juice (sour/sweet) or orange juice to taste
(Some children prefer without juice. They may prefer juice
separately.). Keep this solution in a refrigerator or a
cold place. Consume as much as possible. For teenagers,
aim at 2 glasses ( 8 Oz glass) after each loose motion.
For younger children, one glass after each loose motion
(if child doesn't take much at a time, give few sips
every 5-10 mts. day and night). The idea is to ensure
ensure enough urine output.
(Make fresh solution after
24 hours) Where possible, boil the water and cool it
before adding salt and sugar.
Once the solution is ready,
do not boil it.
2.
Fever
Do mot be scared of fever.
It is our friend.
it helps
us fight infection. Avoid drugs for lowering
temper
ature. Prefer physical methods like keeping the skin
cool,light clothing, fan or AC, sponging of whole body with
tap or stored water, cold packs on forehead or limbs and
free flow of air into the room.
If an infant is prone to
convulsions with sudden rise of fever, use paracetamol
(like Crocin, Pyrigasic, Calpole or Metacin) tablets/
syrup.
Infants - 1/2 to 1 teaspoon. Children - 1 to 2
teaspoons. Teenager 1 tablet. Can repeat after 4 hours
if required.
3
3.
Cough :
Mix 2 parts of honey to 1 part of lime juice.
1/2 teaspoon (say for a baby around 3 months) to 1
tablespoon (say for an adolescent)every 3-4 hours.
4.
Blocked nose
Water - 4 ounces (120 ml) Mix, boil, cool
Salt - 1/4 teaspoon
) 2-3 drops into each nostril.
5.
Burn
Pour cold water, colder the better. Do not apply any
ointment.
6.
Minor injury s
(in an immunised person) - Just wash with soap and
water, nothing else need be done.
7.
If symptoms persist or the looks of the child cause
anxiety, consult your Doctor.
NUTRITIONAL REQUIREMENTS OF CHILDREN
Years '
‘4-'6”
Calories
Protein (g./kg)
....
Calcium (mg.).
Iron (mg)
•Retinal, .(ug.) -
'■
1 -9
10-12“
1,500
1,600
2,100
2,500 (boys)
2,200 (girls)
1.66
1.59
43
1.44 (boys)
1,40 (girls-)
. .400.-500.
400-500
600-700
600-700
15-20
25 (boys)
35 .(girls)
15-20
..
15-20
300--------
400
.
Thiamine-. . . - .
-.
Vitamin C (mg)
30-50
Vitamin D (i,u.) — ..
400 .
Vitamin B^—(ug)- -
-1.5........... ..
Folic acid, (ug)
50-100 .
' 13-75 " ’
.
603..
• --
.
,7.50
0.5 mg., per 1,000 calories consumed
.
.
"
"0t5Q
130
... 5^5
50—100
■
' 30-50 ~ '
“ 30-50 ’
■ •
- - ..100
.
2,0
...
50-100
•
100
2.0......................
50-400 . ..
RECOMMENDED NUTRIENT ALLOWANCES DURING
PREGNANCY AND LACTATION
■
Indian
Reference Woman
-......... (sedentary work)
Calories
Protein (c)
Calcium (mg)
Iron (mg)
Vitamin A (ug)
Vitamin D (iu.)
Thiamine (mg/1,000 calories)
Riboflavine
"
Niacin
"
Ascorbic acid
Folic acid (ug)
Vitamin 012 (ug) . - • ■
-
1,900
45
400-500
20
750
100
0.5
0.55
6. 6
30
100
2.0
Pregnancy
(second half)
+ 300
1,000
40
750
400
0.5
0,55
6.6
50
150-300
. . 3.0 ■
Lactation
+ 700
65
1.000
30
+ 400
400
0.5
0.55
6.6
50
150
-.2.5
HEALTH, NUTRITION AND EDUCATION
INDIA : AN INTEGRATED APPROACH
OE
GIRLS
IN
Jon E. Rohde
"’Hie health and nutrition of the girl today will affect
the health and survival of the future generation, because
d'? is the mother of tomorrow and no future cmi be built.
■>r an edifice that Is not strong and healthy and which Is
corioded with discrimination and Injustice al every level."
Shmitl Ghosh (Jndian Pediatrics, January, 1 98G)
"'Die most crucial segment-of our population from the
no i't. of view of the "quality" of our future generation are
today’s young girls who are < Just - on the threshold of
marriage and motherhood. Their attainments and competence
w).!l be the major determinants of the health and nutrition
of children of the next generation. It Is precisely alsu this
soi|i<i?nt of our population that has been sadly neglected
in all our development, and educational programmes."
C.
Gopalan - NFI liullotiiu January, 1984)
DacAf{round
More
than
two-thirds
of
India's
children
are
Id nl nourished, growing slower, smaller and with more
>illness and loss stamina than their more fortunate
peers. Remarkably more than one-third of Indian btililes are
born malnourished or low birth weight (LBW), less than 2.5
kilograms, LBW babies are more likely, to be Infected and
far more likely to din than babies of normal weight.
Mortality Is 3-5 times higher In LBW babies, accounting for
hall’ to 2/3 of all Infant deaths. Evan amongst the well to
do LBW babies are born : upto seven per cent In Western
countries, a similar percentage among the well to do In
Journnl of education and Social Change
India. But other developing countries have far lower rates
of LBW, globally estimated to be 15%. Even In Africa the
estimate is only 20% LBW birth and In Latin America
12-15%. It Is the hit'll rate of LBW that determines Initially
high Infant mortality, high malnutrition. Low birth weight
Is the first major problem facing India's next generation.
I low can this problem be addressed ? Feed the mother
well while she Is pregnant, belter ante-natal care, fewer
Infections In the mother, are frequent answers and they are
all right to a degree but the hard fact Is that the small
size of Indian mothers is Itself a major cause of low birth
weight. Small body size Is the best predictor of the LBW
baby : mother less than 145 cins tall, less than 40 kgs
In weight. In much of the country up to 30% of the
mothers full into these categories and have LBW rates of
two, three or four times more ^han other women In the.
same socio-economic setting, ihe other group Cuui.rlutitliig
mosl LBW Is adolescent girls having their first pregnancy.
Upto 50% of these births arc LBW. What cun be done ?
Maternal size. Is fixed, This piijMrr describes a strategy
ilia1, can address In a short term a major part of this
problem at the root cause, maternal size and nutrition.
Girl children in India
With important exceptions,, such as the state of
Kerala, girl children experience higher mortality, , and
particularly, higher rules of malnutrition than-boy children,
in their earliest years of life. Efforts to Include them In
food supplement programmes, such as ICDS, are partly
successful, but the majority of rural and poor urban girls
rencli the age of adolescence some twelve to fifteen
centimetres shorter than their well-to-do peers In the same
society. Repeated efforts to reach them at the youngest
pgej hpve been relatively unsuccessful.
However, a second unexploited opportunity presents
Itself, as every girl on' reaching adolescence will undergo
puberty and this period of two to three years of hormone
stimulation changing the body of a girl to that of a
woman, Is accompanied by a growth spurt. Careful studies
have shown that even children who are stuhted and
niiihiourlshed throughout childhood, If fed adequately during
the adolescent growth spurt under the Influence of the
normal body hormones, will experience c.utch-up growth and
74
Health, Nutrition And Education Of Girls In India :
achieve an adult size, almost as great or Indeed as great
as children who were better nourished throughout their
young childhood.
One African sutdy (AJCN
36,
527,
1082)
demonstrated complete cutch-up during adolescence of a
cohort of girls who at age 10 years were’ fully 20 cm
stunted In comparison to a normally nourished cohort. Only
a normal diet In adolescence led to this remarkable catch
up growth. Thus adolescent growth spurt in girls offers an
opportunity, provided there is-an adequate diet, to make
up for deprivation of the past.
Interestingly, in each girl this happens at a slightly
different age, but the age Is not what is Important. At the
firs: sign of puberty, (the Initial development of the breasts
Is the earliest sign that the endocrine system has started
to secrete the hormones that mediate the transition from
a young girl .to an adult woman), If fed extra food, catch
up growth could occur. The maximal rate, of growth occurs
at the Initiation of puberty - to wait for menarche is
clearly too late. Not only a taller and heavier adult woman
but also one with larger organ systems and a greater
capacity
to
bear
children
successfully
will
result.
Particularly the growth of the pelvis In this period will
reduce the dangers of. child birth and make that process
easier and safer, reducing maternal mortality as well ns
perinatal deaths. Of particular Interest Is the predictable
decline in LBW incidence associated with taller, heavier
mothers. In a study of 341 prlm.lparous women (first baby)
maternal weight and height explained 38
of birth weight
variation (Bhatia - Indian Pediatrics, 1984, 2 1:365), Adole
scent growth spurt Is the great opportunity for society to
give |:o Its daughters what they did. not receive .as young
children, full healthy growth.
Literacy and Mothering Skills
.
It Is well known' that the most Important factor for
determining the survival of a child is the literacy of the
mother. Literate women make far better use of health
services, feed their children better, have better nourished
and healthier children who die at far lower rates, even half
those of illiterate mothers. But Is It literacy the ability to
read and write that accpunts for this difference? There Is
evidence that In fact It Is mothering skills and the social
status of the mother that accounts for this Important
difference. The literate mother ’ tends to know her rights
and Social Cliamjn
and opportunities and will make better use of ante-natal
care services, health care and institutional delivery or at
least assistance from u trained mid-wife. She knows more
about feeding children, getting them immunised, and she
is more likely to accept family planning methods and space
her ' children. Perhaps even more Important, she views
herself, and Is viewed by her family, as a poison whose
opinion matters and she participates more fully In the
decision making process of the family. Literacy grunts
power and status, both In the eyes of the woman herself
as well as the people she lives with.
For the little girl who has not had the opportunity for
school or has had to drop out, adolescence offers ti new
opportunity to attain some of the. skills, self-respect and
community esteem accorded to her literate sisters. II,
during this period, she Is involved In a programme to pro
vide her with knowledge and skills of’ motherhood and she
is
recognized
for
these,
say
with
a
"certificate of home
ccomics", even If she Is not fully literate, she may
tu.lilcive the level of acceptance, a level of self confidence
and n level of knowledge, and ability to assure the survival
of her child. A proposal to this effect was made some two
year:; ago by Dr. C. Gopalatt, President,Nutrition Foundution
of Judin, hut litis not apparently been given serious
consideration (NF1 Bulletin 5,1,1984),
li
imrluis,
may be by working in an Auganwadl assisting and
for
children
or
in. some
similar
village
based
programme. There she herself could receive supplementary
fpod and would he trained In certain essential mothering
skill ; child feeding, child Immunisation, importance of moni
toring of growth of the child and practical ways of Impro
ving a child'snutrition using oral rehydrallon for diarrhea,
importance of periodic vitamin A, basic hygiene, and
■impiovement of the environment, all aimed at preventing
illness and Improving the child's health and growth. She can
learn about her own health and, partlculaily, as adolescence
comes upon her, about the changes taking place In her own
body. She can learn about the physiology of reproduction
ant! of contrucupti® mid wiii be better prepared to enter
Into marriage both as a wife and mother with a fuller
understanding of her own body and physiology and of the
benefits to her and her family of planned fertility. She may
learn specific skills of caring for children, of washing them,
7G
Health Nutrition And Education Of Girls In Jndl.*
feeding them, preparing foods; the most, modern concepts
of health and nutrition can be taught to Iler during tills
time. Perhaps in addition, she could learn useful household
skills in cooking or sewing, agricultural skills to help her
contribute to the Income of her family or to her own
financial Independence when she Is married.
After completion of the programme, during which she
has received supplemental education, supplemental feeding
and improved her own health and growth, having passed
through adolescence, the young woman is provided with a
certificate simiiui to a scliool leaver which will perl'.aps
enhance her status In her family's eyes and those of her
in-laws when she Is married.,
For Tomorrow'a Generation Today r
fa programme to assist adolescent girls in growth,
health, education will have rapid pay-offs. These girls, who
would enter a programme today at an average age of I I
or 1'2 years, can be expected to be having their first child
within the next seven to ten years, a child who under the
present circumstances have a 5j0% or greater chance of
beiiLBW. Improved diet during adolescence might add
5-10 cm to adult height and several kilograms body mass
thereby reducing maternal risk during first pregnancy and
substantially reducing the problem of LBW. Programme
graduates would rapidly show benefits to their families mnd
Io society of the Investment made In them during the years
of their adolescent growtli spurt when their minds and
bodies would be adequately nurtured to better serve them
in their adulthood as a woman, as a mother, as a.wife, as
a 'member of the society. This Is In a very real sense our
last opportunity to make up to these girls for what they
did not receive during their young childhood years. It is an
opportunity to dramatically affect the nutrition and survival
of Clio next generation of children in India. It is a chance
for a better tomorrow, today.
ooo
77
C6MNIUNVTV ^"'^arksftoa<i
NUTRITION
47/'l,(.‘:'rstF’°^rF.£.5G0 00l
BftNGAtORi-
\
/-ilk: It is an ideal food for infants and children and a good sipplementary
food fcr adults. It is nearly a complete food existing in nature. It contains
all the nutrients.
Compoeition:
Gms, per 100 gms
Cow's milk
Buffalo1 s mil c
Human milk
3.2
4.1
4.4
67
4.3
8.8
5.0
117
1.1
3.4
7.4
65
Protein
Fat
Lactose
Calories
Rich:
in calcium
Deficient:
I+ is deficient in iron and vitamin C
Daily requirement:
Adults
"Children 7
''
Expectant mothers
10 oz or 284 gms i.on-vegetarian
requirement.- 20 oz or 568 gms)
20 oz
40 oz
bilk borne infections: from the animal - Bovine tuberculosis, (Brucellosis)
anthrax, achinomycosis, Q. Fever
from the human - typhoid, paratyphoid, dysentries,
handler &
cholera, diphtheria, infective
environment
hepatitis.-
Prevention:
Pasteurization - if effectively done - phosphatase test will be
Boiling
negative
Rice: Main cereal consumed in south India, cheapest source of energy and
contributes 70-80$ of calories. Main-source of thiamine and nicotinic acid.
By virtue of its quantity it provides nearly 50$ of protein requirements.
Prote?rs’of rice is of better quality than wheat although rhe protein content
of wheat is more
*.
■ ■ - . ... —-
Composition:
Gms, per 100 gms
mgm
Protein
CHO
Fat
Raw rice(mld)6.8
78.2
-'6.4
79.0
mgm
Thiamine
Nicotin-i
0.5
0.06
1.9
0.4
0.21
3.3
Parboiled rice is superior in nutritive value to raw rj.ce as r ;gards the
thiamine and nicotinic acid are concerned.
Daily requirements: .14 .zs or 400 gms. If milled raw rice is being consumed,
it can be partially substituted by wheat, jowar .or ragi. This improves, the
nutritive value of the diet (j t.Bi 100 gms or rice contains more proteins than
in 100 gms ef milk).
Wheat: Next to rice, wheat is the most important cereal
Daily requirements:
14 oz or 400 gms
Composition: (whole wheat)
rritoin
Fat
CHO
Thiamine
Niacin
Per 100 gms
11,9 gins
1.5 gms
71.2 gms
O.45mgms
Though it has protein to the extent of 11.8$ it lacks in lysine. I-t is a good
source of thiamine and niacin.
Millets: Jowar and Ragi : - Jowar is deficient in lysine and has an excess
of leucine. The consumption of .jowar is occasionally found to bo associatea
with pellagra.
Ragi is a popular millet in South India. It is very rich in calcium, and is
a fair source of iron, phosphorous and thiamine.
Daily requirements:
Ip combination with cereals daily requirement is 14 oz
or; 400 gms.
Composition:
Gms, per 100 gms
Jowar
Ragi
Prctein
gm
OHO
gm.
Calcium
gm
10.4
7.3
72.6
72.0
25.0
344.0
Pulses: Pulses are next in importance to cereals as an article of diet in
India. The common pulses used are red gram, green gram, black gram dhal, Bengal
gram, dry beans, and dried peas.
Pulses- are rich in protein containing about 20-25 g of protein per 100 gms. In
vegete .1 an diets, pulse" are the main source of protein. Pulse" are good sources
of B group vitamins, especially-thiamine and riboflavine. Sprouted pulses are
good sources of vitamin C.
Daily rsquinaments:
3 oz or 85 gms
Proteins %
Bengal gram
Black gram
Reg gram
Green gram
Mgm per 100 gms
mgra
mgm
mgm
Thiamine
Riboflavine
Niacin
mgm
Iron
10.2
9.1
5.8
7.3
Groundnuts; Groundnuts or Peanuts are extensively grown in India. I-t is
rich in fat, protein is equal to pulses. It is also rich in nicotinic acid,
thiamine and riboflavine.
17.1
24.0
22.3
24.0
Composition:
0.3
0.42
0.45
0.47
0.15
0.37
0.19
0.39
2.9
2.0
2.9
2.1
Per 100 gms
Protein
Fat
CHO
Thiamine
Riboflavine
Nicotinic acid .
Daily requirements:
25.3%
40.1%
26.1%
0,9 mg®
Q.'IS -mg®
19.9 -mgm
!!
!
!
j!
1i
j
Groundnuts after
extraction of fat is a cheap
and rich source of proteins
In combination with pulses 3 oz
1
Green leafy vegetables: Eg. spinach, amaranth, fenu greek,. cabbage are cheapest
protective foods. These are excellent source of carotene and vitamin C.
Thoy are also good sources of ’calcium, iron, riboflavine art folic -acid. Tbey
provide cellulose which acts as roughage. It plays an important role in persons
who gc on diet to cut down calories.
Daily requirements:
4 oz or 114 gms.
Oil: Eg, groundnut oil, gingelly oil etc. vegetable fat. It is 100% fat,
yields 900 calories per 100 gms. Contains no ^i’amin, conta-.’rs more of
polyunsaturated fatty acids. Lcwer.: the serum cholestrol.
Daily requirements:
2 oz or 57 gms■
Ghee: Animal. Except for little- moisture it nearly cert per cent fat. Yields
between 820 to 895 calories. Good sourcb of vitamin A ;2C0 i.u./lOO gms)
contains more of saturated "fatty acid and hence tries to ra.se serum cholestrol.
Daily requirements:
In combination with other fat like oil 2 oz (n.B.
vegetable fats usually de not contain vitamin A)
^anaspathi: Popular cooking media in our country. It is manufactured by
hydrogenation of vegetable oils. On hydrogenation saturated fatty acid content
increases.*
Gives about 7)0 i.u. of A and 150 i.u. of 'D1 per 100 gms. If is
10C% fat and yields 900 calorics.
Dj.jCv requirement: In combination with other fats 2 oz.
-5-
Sugar & Jaggery: Those are carbohyc!ra<.e foods. Suga” is
pur. cerbchyr?
food ard contains no proteins, fats or minerals. 400 cal./j.OO gm-.
Jaggery: Is used in place of sugar. 383 cal./I00 gms. It is also rich
source of iron 11.4 mgm/100 g.
Dail;- requirement:
Sugar/and/or •',ag-.-ory - 2 os or 57
Bags: It is an important source of animal protein. It contains also she
natrients except CHO. It contains protein, fat, calcium, all the vitamin
except C. It is a complete protein containing all essential amino acids.
Couyositiou:
Protein
Pat
Minerals
K Cals
Daily requirement:
fleet and tubers:
13-37’
13-3^
1^
1+3
1 egg (1-y os)
Generally used as vegetables.
Potatoes, tapiooa, carrot, onion, raddish. These especially potatoes are
rich in CHO. Poor source of fat and protein. Good source of calcium and
phosphorous.
Carrot rich in carotene
Potatoes rich in vitamin C
Daily "equirement:
3
ozs or 85 gms.
//^XlW//
Me* //A
17
Scjex’exi
£
Apl vlX^
c^j
Lx^o<y Cc^
I. jduKzK^
do
^i^ryycr>^)l<^aKc-^
b? A/s Adu^-u.'
^LxyCyO C^nxu2-z^)/^x
P~o)la>-l^J oyO
3
/SolZo
A>y
d4l>~>
goo
—
— Affv
/t^gK^x,
ptyrra^a^
Ko
P^zcl-av Al/C
/ C^L^K Tn-<ce
/-o CCt£ Z&o.'j
-p^V LXXa^s
' '
"
iv- \ _
frxTMSS
MureinoN of rue scuoot -aoep cuw
an unfortified biscuit and cold drink. The biscuits and cold
drinks were distributed daily during the school week,
during the first two hours of the school day, for a period of
12 months. No intervention took place during school
holidays or on public holidays. Distribution and
consumption took place under close supervision and
compliance was recorded daily. To exclude parasitic
infestations as a confounding factor, the children of both
groups were dewormed.
The 12-month intervention resulted in a significant
improvement in blood levels of vitamin A, ferritin, iron,
haemoglobin, haematocrit and in urinary iodine levels in
the group who received the fortified biscuits compared to
the unfortified group. The greatest improvement in vitamin
A and ferritin status was seen in children with low values
at the start of the study, while the intervention had little
effect on those with adequate status: i.e., those that
needed it most benefited the most from the intervention.
The prevalence of low serum vitamin A levels (<20 pg/dl)
dropped from 39% to 12%, of low serum ferritin levels
(<20 pg/I) from 28% to 14%, and of anaemia (<120 g/l)
from 30% to 16%. There were no significant reductions in
the group receiving the unfortified biscuit. The prevalence
of low urinary iodine levels (<1 Opg/dl) in the fortified group
decreased from 98% to 30% after 6 months, and to 5%
after 12 months. In the unfortified group the prevalence
decreased from 96% to 90% and 34% after 6 months and
12 months, respectively. The iodisation of salt became
compulsory in South Africa during the second half of our
study, thus contributing to the improvement in iodine
status in both the fortified and unfortified groups. There
was no reduction in the prevalence of goitre, which was
21% at the baseline assessment; a 12-month period may,
however, have been too short to reverse an already
enlarged thyroid. The biscuit was well accepted and 74%
of the children indicated that they would prefer more than
the three biscuits they were receiving. The price of three
biscuits is US$0.05 per child per day and provides
191 kcal. The cost of fortification itself is US$0.86 per child
per year.
no preparation, is easy to distribute and has
a long shelf life. It is also easy to monitor and therefore
less open to misuse or corruption.
Dealing with the hidden hunger of micronutrient
deficiencies through food fortification is regarded as a
short- to medium-term solution to address an immediate
need. Longer-term solutions will include nutrition
education in schools and communities with regard to the
need for diverse diets. Should a fortified biscuit be
implemented in school feeding, it is recommended that it
be accompanied by a relevant nutritional message which
would put the fortified biscuit in the diet into perspective.
Using a micronutrient fortified biscuit and cold drink in
school feeding is feasible, effective and practical, and can
seriously be considered for addressing micronutrient
deficiencies in school children. The role of nutrition
education as a long-term solution should, however, not
be overlooked.
The biscuit is now commercially available and is actively
marketed at the primary school level by the food industry,
using the scientific results to promote its use in school
feeding programmes throughout South Africa. Once in
place, an effectiveness study will be carried out.
Lize van Stuijvenberg, Senior Scientist, P.O. Box 19070, Tygerberg,
7505, South Africa. Tel: 27 21 9380911 x 264 Fax: 27 21 9380321
Email: lvanstui@eagle.mrc.ac.za AJS Benade is Programme leader of
the Nutritional Intervention Programme, Medical Research Council,
Cape Town, South Africa. Mailing address: Medical Research Council,
PO Box 19070, Tygerberg 7505, South Africa. Tel: 021 938 0283 Fax:
021 938 0321 Email: sbenade@eagle.mrc.ac.za The information
contained in this article is also'available as a technical report and a
policy brief issued by the MRC. Both are available free of charge on
request from Dr Benade.
A danger of school feeding is that parents may reduce the
food provided for children at home. Using a biscuit as a
vehicle for fortification eliminates this problem, because it
is seen as a snack rather than a meal and therefore
unlikely to replace meals given to the child at home. In this
study the biscuit intervention had no effect on the number
of children who ate breakfast before coming to school, nor
on the number of children bringing food to school.
Additional advantages of using a biscuit are that it needs
7?
N'TV'g'
UNITED NATIONS |||
j
I
§
is
I
iJ
§
£
through the Life cycle...26
News and Views...29
Nutrition in Emergencies. ..36
Letters to the Editor... 40
Courses, Meetings and Announcements. ..44
Information Resources...49
Programme News...52
Publications...65
J'-'iTE" NAT C‘»S ADMtNISTRAT. ,'E CO'/M.TTEE ON COORDINATION
'
<’
'SUi
SUB-COMMITTEE ON NUTRITION
(ACC/SCN)
The ACC/SCN is the focal point for harmonising the policies and activities in nutrition of the United Nations system. The role of the SCN
I is to serve as a coordinating mechanism, for exchange of information and technical guidance, and to act dynamically to help the UN
i respond to nutritional problems. The SCN is responsible for overseeing the direction, scale, coherence and impact of the UN response
to the nutritional problems of the world.
■ The Administrative Committee on Coordination (ACC), which is comprised of the heads of the UN Agencies, recommended the
1 establishment of the Sub-Committee on Nutrition in 1977, following the World Food Conference (with particular reference to Resolution
j V on food and nutrition). This was approved by the Economic and Social Council of the UN (ECOSOC). The SCN held its first Session
| in 1977 in Rome.
The UN members of the SCN are FAO, IAEA, IFAD. ILO, UN, UNDP, UNEP, UNESCO, UNFPA, UNHCHR, UNHCR, UNICEF, '
|- UNRISD, UNU, WFP, WHO and the World Bank. From the outset, representatives of bilateral donor agencies have participated i
j actively in SCN activities. Non-governmental organisations are also involved. The SCN is assisted by the Advisory Group on Nutrition ■
i (AGN), comprised of six nutritional scientists and practitioners of world repute from different regions. The Secretariat is hosted by WHO :
; in Geneva.
: The SCN undertakes a range of activities to meet its mandate. Annual meetings have representation from the concerned UN Agencies, :
i from 10 to 20 donor agencies, the AGN, as well as invitees on specific topics; these meetings begin with a symposium on subjects of j
i current importance for policy. The SCN brings certain such matters to the attention of the ACC. The SCN sponsors up to nine working I
; groups on specialised areas of nutrition.
I The SCN compiles and disseminates information on nutrition, reflecting the shared views of the agencies concerned. Regular reports I
on the world nutrition situation are issued. Nutrition Policy papers are produced to summarize current knowledge on selected topics. ;
I SCN News is normally published twice yearly and reports on the nutritional status of refugees and displaced persons (RNIS) four times .
! per year. As decided by the Sub-Committee, initiatives are taken to promote coordinated activities • inter-agency programmes,
! meetings, publications -- aimed at reducing malnutrition, primarily in developing countries.
^V/l/£tX'No'.16 was edited by Catky Needkant
Tke nutrition in emergencies section was compiled, by Jane Wallace
We are most grateful for contributions as skown in Sources after articles
Illustrations by Lindsay Barrett
A/fa'fTis issued in July and December each year by the Secretariat of the UN ACC Sub-Committee on Nutrition.
Your contributions to future issues would be most welcome.
fJcaims to help the sharing of experience in nutrition.
If you wish to receive additional copies of Sk'V /JEi-jQ or would like to suggest other names to be added to our distribution list,
please write to us:
I Chairman: Dr Richard Jolly
; Special Advisor to the Administrator
i United Nations Development Programme
. One United Nations Plaza, New York, NY 10017. USA
i Telephone: 1 212 906 5764, Fax: 1 212 906 6661
I EMail: Richard.Jolly@undp.org
Technical Secretary: Dr Sonya Rabeneck
ACC/SCN c/o World Health Organization
20, Avenue Appia
CH-1211 Geneva 27, Switzerland
elephone: 1 41-22 791 04 56. Fax: 1 41-22 798 88 91
EMail: accscn@who.ch
> A’A.-' .< •A.T -.S'aims to provide information for those concerned with international nutrition.
Publication of items in
.
E'.. /does not imply endorsement of views given, nor necessarily the
official positions taken, by the ACC/SCN and its member agencies.
The status of quotes and other material is generally indicated in the text and/or sources.
Items in Ec'/J /JEhJEmay be reproduced without prior permission, but please attribute to the ACC/SCN
(/Je. gratefully acknowledge funding assistance from.
tke Government of tke Netkerlands and USQID
for tke preparation. and printing of tkis issue of
'MESEEEE FT2.OM EEE EUAi/ZMEW
SCN’s 21rt If ear and- 25^ Session:
a wottky celebration, in. Oslo-, Norway
The 21s1 anniversary of SCN's founding and its 25111
Session was an important occasion. UN Agencies,
Bilaterals and the Advisory Group on Nutrition (AGN) were
present in force, with a new participant - the Asian Devel
opment Bank. With more NGO participants than ever
before, the turnout for the opening of the Symposium Challenges for the 21s1 Century: A Gender Perspective on
Nutrition Through the Life Cycle - was probably a record,
and the opening addresses by the Norwegian Minister of
International Development and Human Rights Dr Hilde
Frafjord Johnson, and Dr Gro Harlem Brundtland,
Norway's former Prime Minister and Director-General of
WHO, made the event very special. It was most fitting
that this 25” Session of the SON was hosted by a national
records), my opening remarks underlined some of the
SCN's pioneering achievements:
o
its very creation by ECOSOC in 1977 as a
'triumvirate' (Dick Heyward’s terminology) - the UN
Agencies, Bilaterals and the AGN. It is probably the
first interagency committee of the ACC to include civil
society as an integral part of its structure;
o
SCN’s leadership in proposing and mobilising action
in key areas of nutrition: iodine deficiency, vitamin A
and iron;
o
the establishment of interagency mechanisms for
reporting on key areas of nutrition, the Reports on the
World Nutrition Situation, the Nutrition Policy Papers,
the regular reports of the Refugee Nutrition
government - Norway - a first in SCN history.
Information System;
The Session itself was full and substantive. The various
working groups spent the weekend discussing scientific,
policy and programmatic developments and developed
priorities and recommendations for action (for a summary
of discussions see page 24). Highlights of the Session
included:
o
the presentation by Philip James on the preliminary
findings of the Commission on Nutrition in the 21s1
Century, which provoked lively discussion and
debate (see SCN 25“’ Session report, available from
the SCN Secretariat in Geneva or on the SCN web
site - http://www.unsystem.org/accscn/ );
o
the 1998 Abraham Horwitz Lecture - a most lively and
unforgettable presentation on breastfeeding by Isatou
Semega-Janneh;
o
the presentation of the Third Report on the World
Nutrition Situation, with its encouraging news of the
significant progress over the last two decades in
reducing stunting in all regions of the world (except
Sub-Saharan Africa);
o
the splendid presentation by Mercedes de Onis and
Cutberto Garza on the WHO research project to
develop a new reference for child growth.
The 25” Session gave us an opportunity to look back at
c
SCN's basic work in providing a forum for strengthen
ing coordination - by sharing information on past and
future activities, and by reviewing implementation of
major international commitments made at the World
Summit for Children, the International Conference on
Nutrition and the World Food Summit.
I hope all of us left Oslo with a new sense of opportunity
and challenge. For all the progress, high levels of under
nutrition are still an outrage and violation of the human
right to food and nutrition in a world where global
consumption totals $24 trillion and where we now have
knowledge and practical examples of how undemutrition
can be rapidly reduced.
Soon we will have a draft report setting out the elements
of a strategic plan for enhanced interagency collaboration
to accelerate action to achieve nutrition goals. Sonya
Rabeneck, Lilian Marovatsanga and I have visited UN
Agencies for discussions in the preparation of this report.
Already one clear lesson has emerged - that there is as
much need to strengthen nutrition priorities and .coordina
tion within agencies as there is to strengthen coordination
between agencies. As SCN Chairman, I wish all SCN
participants and SCN's wide group of supporters every
success as we respond to the' nutrition challenges ahead.
the vision and creativity of the SCN's founders. With the
help of George Beaton (who had reviewed the SCN
------------ —
AAA PAAA
Tke CLGN cuuL Current Members
The Advisory Group on Nutrition (AGN) provides
assistance and advice on policy and the science of
nutrition to the SCN. It is comprised of nutritional
scientists and practitioners of world repute from
different regions (see SCN News No. 15 p2
. for details of current members).
After six years of service, Jak Jervell retired
from the AGN in March 1998. Jak contributed
enormously to the work of the AGN and we thank him
greatly for his work. He can be contacted by email on
.'.jak.jervell@klinmed.uib.no
Update on Q.GN CotivitLes and.Discussions
some promise for greater coordination and interaction at
the country level. Furthermore, future visits by AGN
members will focus on countries with successful
experiences in country level coordination, and it is
intended that during such visits, AGN members will help
with strengthening interagency work and catalysing
coordination.
Other activities and discussions;
0 The AGN recently addressed the question of using
food balance sheets (FBS) to determine the
micronutrient content of food supplies. They
concluded that this is potentially very useful and
should be explored further, however at present, using
the FBS to calculate figures for micronutrient
availability is premature.
0
In considering what actions are necessary to reduce
malnutrition globally, the AGN is examining the
current activities of the UN lead agencies, and
reviewing key agency documents to identify
successful approaches.
0
The AGN will provide advice to the SCN Secretariat
in a project aimed at comparing different methods of
anthropometric data analysis being used to estimate
malnutrition in young children, with the purpose of
defining the best approach to use in future analyses.
0
In recent discussions of the role of multiple vitamin
and mineral supplementation in maternal nutrition,
the AGN concluded that early trials of
supplementation in pregnancy should be closely
monitored to evaluate any adverse effects. In
addition, more research is needed on the
effectiveness of generalised medicinal supplement
ation before this practice can be recommended for
adoption at the community level. The need for
controlled randomised clinical trials with large
numbers of subjects is considered necessary before
multinutrient supplementation is considered at the
policy level.
The AGN met at the SCN’s 25th Session, held in Oslo,
Norway in March 1998. During the latter half of 1997, the
AGN undertook assessment missions to two countries
(Zimbabwe, Bangladesh) to look at coordination at country
level. This work was highlighted as being important to the
SCN in fulfilling its mission to harmonise and enhance the
effectiveness of food and nutrition programmes.
The AGN members found that while there was good
cooperation and information sharing between UN
agencies, coordinated action tended to occur on an ad hoc
basis and usually as a result of strong leadership by
certain individuals, rather than because of a formal
institutional policy. Coordinated actions between UN
agencies were found to be most effective in response to
acute emergency situations such as famine or civil strife.
The lack of intersectoral coordination of action, follow-up to
plans of action, and programme implementation at the
country level was reflected in the words of one national
planner;
‘Nutrition is everybody's business
and nobody's responsibility"
A copy of the full. AGN report, ‘Report of the Meeting of the
Advisory Group on Nutrition at the Twenty-Fifth Session of the
Sub-Committee on Nutrition, Oslo, Norway, 26 March 1998’, is
On a positive note, the process of thematic planning, led
by UNDP (see SCN News No. 15 p43) was seen to offer
available on request from the ACC/SCN Secretariat, c/o WHO,
20 Avenue Appia, CH-1211 Geneva 27, Switzerland. Fax: 41
22 798 8891 Email: accscn@who.ch
aJUFF.iFiONJ OF
rue
FOFOOL-FFbO dF'LP
There are more children of school age, and more children going to school than ever before. Around 90% of the world’s
children now survive beyond their 7>h birthday’. These successes raise new concerns. Ill health and nutrition
compromise both the quality of life of school-age children and the potential to benefit fully from what might be the only
education they receive.
In many developing countries there are more teachers than health workers and more schools than clinics. The
infrastructure of the school system therefore provides an opportunity for health services to reach children in a
cost-efficient way.
This feature brings together a variety of articles, and reports of two new publications on the health and nutrition of J
school-age children. The papers range in content from the assessment of nutritional status in school-age children, to ;
examples of school-based nutrition and feeding prdgramriies in different countries. The nutritional concerns of school 1
children in industrialised countries-concernsthat arealsoemerging in some areas of thedeveloping worid-arealso
presented..
..
_ _
_■ _____ ;__' - '' ■ _■
..
OVERVIEW TO THE FEATURE
The first article in this feature presents new data from the
Partnership for Child Development, showing that nutrition
problems of school children may be greater and more
widespread than previously thought (see page 4).
Furthermore, anaemia data from the database on iron
deficiency being developed by WHO indicate a higher
prevalence of anaemia in school-age children than in
pre-school children, although data are limited (see page 7
of this feature). It is likely, therefore, that the scale of
nutritional problems in school-age children may have pre
viously been underestimated. Indeed, one of the main
conclusions from the meeting of the SCN Working Group
on Nutrition of School-age Children*
2 in Oslo this year is
that more data on the health and nutrition of school-age
children are needed to assess the scale of their problems.
A survey of donor and agency support for school health
and nutrition programmes is presented on page 8 of this
feature. This review reveals a surprisingly broad-based
support for school nutrition and health programmes and
calls for stronger collaboration between UN agencies,
bilateral agencies, NGOs and the implementing countries.
• ' ' •
The article on nutrition of school-aged children in Mongo
lia provides information about food and nutrient intakes of
school children, and describes how the very low intake of
fruit in school-age children is responsible for the intake of
some essential vitamins and minerals falling below
Mongolian normative values (see page 10). This descrip
tion draws on information from an extensive dietary
survey report, which is one of the few nutrition studies in
Mongolia that has been translated into English.
There is concern that school-based systems fail to benefit
children who are not enrolled in school, but who may be
the most in need. Although this remains a problem,
school feeding programmes can motivate children to
attend school and can motivate parents to enroll their
children. Food-for-school programmes, such as the
national programme in India described on page 13, for
example, provide 'take home’ food to children with high
attendance records, and are often implemented to
increase enrolment and attendance, particularly for girls.
Furthermore, 'school health days' could bring in non
enrolled children to receive treatments, and thus provide
effective outreach to the community at large.
' UNICEF. The State of the World's Children, 1995.
2 A copy of the report from the Working Group on Nutrition of School-age Children (summarised dn page 25), is available on request from the SCN
Secretariat, c/o WHO, 20 Avenue Appia, CH-1211 Geneva 27, Switzerland. Tel: 41 22791 0456 Fax:41 227988891 Email:accscn@who.ch
7
/JEUS' fJO. 16, JUL V igg?
Practical experience gained by the Partnership for Child
Development indicates that school-based health and
nutrition programmes are feasible and effective, with clear
potential to improve the nutrition and growth of school-age
children (see below). Examples of school feeding pro
grammes presented in this feature show varied success.
In India, the government-funded Nutritional Support to
Primary Education Programme (NSPE) is working well in
rural areas. By the end of 1998, it is expected that the
whole country will be covered by this programme (see
page 13). The new school feeding programme being
implemented in designated ‘poor’ villages in Indonesia, is
still in its early days. Funded entirely by the government,
the recognition of its importance for the long-term future of
Indonesia is signified by the fact that funding support has
been maintained in spite of the recent economic crisis (see
page 15). In South Africa, a case study has shown that
vitamin and mineral fortification of biscuits results in a
significant improvement of micronutrient status when given
as a snack to school children. The biscuit is now commer
cially available and is actively marketed at the primary
school level by the food industry (see page 16). School
feeding programmes in Kenya however, have suffered
from lack of funds. The Kenyan case highlights the need
to monitor programme impact in order to develop more
cost-effective approaches. Some other lessons that have
emerged from Kenya include the key role of parents in
sustaining school feeding programmes, the concerns of
safety and quality of food from vendors and hawkers, and
the problems of money given to children for food being
spent on drugs (see page 18).
The rising prevalence of obesity among school children,
and the need for health education to focus on healthy
eating is also presented in this feature. The article on
page 22 provides an example of this focus on healthy
eating, with the development of guidelines that promote
healthy eating for school children in the USA . Nutrition
concerns facing industrialised countries, and, increas
ingly, by some groups in developing countries include the
problems of dietary excess and obesity, eating disorders
and the future risk of chronic disease. The article on
page 19 discusses these nutrition concerns. It also
discusses the changing lifestyles and dietary patterns in
industrialised countries, which are resulting in personal
preferences driving the nutritional patterns of school
children, rather than the availability of food itself. Finally,
a study in Nepal has shown that in more affluent schools
where convenience snacks are available, school chil
dren’s food habits are changing towards a preference for
modem convenience foods of poor nutritional quality
(see page 21).
We would like to thank Andrew Halt (PCD, Oxford University)
for helpful comments during the preparation
and editing of this feature.
/
THE PARTNERSHIP FOR CHILD DEVELOPMENT: PROMOTING THE HEALTH,
NUTRITION AND EDUCATION OF SCHOOL-AGE CHILDREN
by Andrew Hall and Don Bundy
he Partnership for Child Development (PCD) was
established in 1992 to conduct and promote
operations research on school health and nutri
tion programmes, and to undertake research on the health
and health education of school-age children (1). The
establishment of the PCD was a response to the growing
number of children who were surviving to school-age - a
group which typically comprises between 20% and 30% of
the population.
r
The 1993 World Bank Development Report, 'Investing in
Health' identified school health and nutrition programmes
as one of 5 priorities for public health initiatives. This,
however, was based largely on theoretical analyses and
there was little prior experience of large-scale
4
,— programmes. The first aim of the
pcd therefore, was to gain practi|
d
cal experience of the processes,
/\ \
costs and issues involved in
Joi Id Development establishing school health pro
grammes in a variety of settings.
The PCD was set up as a consortium of donors,
countries and technical institutions to develop the inter
sectoral collaborations necessary to establish or
strengthen school health programmes. The Scientific
Coordinating Centre for the PCD is based at Oxford
University in the U.K. This international initiative helps to
provide technical assistance and support in order that
low-income countries can monitor and evaluate the
PFATUXES
MummoM of rue oeuoo(.-a&eD cuw
costs, processes and impact of programmes. The pro
grammes established so far have emphasised the devel
opment of national collaborations as a part of locally
managed programmes, the core of which is the essential
partnership between the health and education sectors.
There are now PCD research programmes or activities in
more than 14 countries around the world, supported by a
broad range of international agencies (UNDP, WHO,
UNICEF, World Bank), bilateral agencies (USAID, UK
DFID), and charities (Rockefeller Foundation, Edna Mc
Connell Clark Foundation, James S. McDonnell Founda
tion, Wellcome Trust and Save the Children Federation).
The practicality of the school-based approach
A core activity of the PCD is to evaluate large-scale
demonstration school health and nutrition programmes.
These are typically implemented by governments through
the existing school system rather than through the
traditional health infrastructure. The support for national
programmes provides an opportunity for the typical unit of
decentralised administration - usually the district - to
develop methods and skills on a scale that is operationally
informative and representative. In practice, the school
based health services evaluated so far have ranged in
size from to 45,000 children in Viet Nam to over 3 million
children in India. In Tanzania, for example, the PCD
programme, called Ushirikiano wa Kumwendeleza Mtoto
Tanzania, is being implemented by a collaboration be
tween four ministries working in three districts of Tanga
Region, and currently involves about 350 schools and
120,000 pupils.
The experiences of implementing these programmes have
confirmed the practical benefits of the school-based ap
proach and have led to some important conclusions (see
Box below).
The effectiveness of the school-based
approach
Although the impact of school health services on growth,
nutritional status, parasitic infections and, in some
countries, on cognitive functions, is being evaluated as a
part of PCD programmes, this article will focus on
nutrition. Evaluations are typically in the form of annual
surveys of children both in districts where the programme
is being implemented and in adjacent, comparison
districts where programme implementation has not yet
started.
The percentage of school children in five
countries of the PCD showing evidence of
undernutrition
□ Stunting (height-for-age <-2 SD below the NCHS reference)
□ Underweight (weight-for-age <-2 SD below the NCHS reference)
B Wasting (weight-for-height <-2SD below the NCHSreference)
The baseline surveys have shed new light on the extent
of undemutrition and ill-health experienced by school-age
children. A recent analysis of anthropometric measure
ments of about 14,000 schoolchildren in Ghana, Tanza
nia, Indonesia, Viet Nam and India (see graph above)
found that a large proportion of children have stunted
height and low weight when compared with NCHS refer
ence values. Wasting is less common, although over
Box: The practicality of the school-based approach - conclusions
0
Simple, safe and effective health services such as deworming and micronutrient provision (required periodically ;
but infrequently) can be provided through the school system.
0
With minimal training, teachers can feel positive about providing health care to children, as long as the task :
doesn’t take up too much of their time. In addition, children and parents are willing to accept teachers in this role
and may perceive schools in a more favourable light as a result of such programmes.
0
A school-based system is not expensive, mainly because an existing infrastructure is used. For example, in the
African programmes of the PCD it costs 3-4 US cents per child to deliver an annual standard-dose tablet to treat
intestinal worms. While a more complicated treatment, such as. praziquantel to treat the disease urinary i
schistosomiasis, is more expensive to deliver at between 21-67 US cents per child, it is still relatively
inexpensive compared with many other health, nutritional or educational interventions. The experiences of the I
PCD in both Africa and Asia have illustrated that the education and health sectors can implement a school- ■
based programme at very low cost (2).
e
SdUJULV iggt
20% of school children studied in Viet Nam and India have
low weight-for-height (3). Data on the haemoglobin con
centrations of 3,000 children in four of these same coun
tries, reveal that anaemia is very common in Tanzania and
Ghana (4), and is least common in school children studied
in the Red River Delta of Viet Nam (see adjacent graph).
This may be largely related to the occurrence of hookworm
infection, urinary schistosomiasis and malaria in the
African programmes. Urinary iodine and serum vitamin A
data from Ghana, Tanzania and Indonesia have indicated
that deficiencies of these micronutrients are more localised
in nature.
Surveys conducted after the programmes have been im
plemented are showing that school health services can
have an impacton a broad range of health and educational
outcomes. In Tanzania, for example, the children who had
participated in the programme showed an average addi
tional gain in height attributed to treatments with albenda
zole and praziquantel, of 1.5cms over 16 months, and an
average increase in haemoglobin concentration of 4.8 g/l.
There is, however, a large margin for further improvement.
In Ghana, where evidence of better growth and improve
ments in educational achievements were also observed,
the PCD programme is now investigating whether teachers
can administer iron tablets to children once a week for a
school term, and assessing what impact it would have on
haemoglobin concentrations.
,fB as eLine, surveys kave skecL
new kg kt on tke extent
of undernuirition and- ill-kealtk
experienced. by sekool-age ekikken”
Action-oriented research
The PCD also provides a focus for a broad range of
research activities in the field of school health with the aim
of improving interventions and health education, and to
develop better measures of outcome. For example,
o a large study of the impact of treating parasitic
infections on children's cognitive functions and educa
tional performance is being undertaken in Tanzania;
o studies are being done in Ghana and Tanzania to see
how children perceive the pictorial messages used in
health education materials with the aim of making
them more easily understood;
o studies have been done in Ghana of children to
investigate the health and social factors that are asso
ciated with not being enrolled in school because such
children will miss out on both education and school
6
The percentage of school children
who were anaemic (haemoglobin <120g/l)
in four PCD countries
o
health services; and
a randomised trial is being done in Viet Nam to see
if health educalon prevents reinfection with
intestinal worms.
The future
Efforts are now being made to scale up school health and
nutrition programme activities and to help countries to
develop and implement their own programmes by means
of programme toolkits and guides. To this end,.the PCD
is working with WHO, UNICEF, the World Bank and with
other international agencies working in the field of school
health (see page 8).
The PCD is also beginning new research studies. To
strengthen the body of scientific evidence on the impact
of school-based nutritional interventions, large-scale ran
domised trials are planned for Ghana and Tanzania to
look at the outcome of programmes providing iron with
and without anthelmintics in terms of growth,
haemoglobin concentrations and educational achieve
ments, and in Viet Nam of anthelmintics alone. Research
studies are also underway in Uganda and India to look at
the benefits of nutritional interventions such as vitamin A
and anthelmintics as a part of early childhood develop
ment programmes, with the aim of improving the readi
ness of pre-school children for education.
Although experience of school health programmes and
knowledge of the health and nutritional problems of
school-age children is growing, there is still a lot to be
done and much to be learned. The authors would be
delighted to learn from others about their experiences
and research and can place summaries of programmes
and activities on a forthcoming School Health and Nutri
tion site on the Internet and look forward to hearing from
you.
References
1.
Partnership for Child Development (1997).
Better health,
nutrition and education for the school-aged child. Transactions
of the Royal Society of Tropical Medicine and Hygiene 91,1-2.
2.
Partnership for Child Development (1998a). Cost of school
based drug delivery in Tanzania. Health Policy and Planning, in
press.
3.
Partnership for Child Development (1998b). The anthropo
metric status of school children in five countries in the Partner
ship for Child Development. Proceedings of the Nutrition Society
57,149-158.
4.
Disease, Oxford University, South Parks Road, Oxford
0X1 3PS, UK. Tel: 44 1865 281231 Fax: 44 1865 281245 Email:
child.development@zoo.ox.ac.uk Web: http://www.ceid.ox.ac.uk/child/
Partnership for Child Development (1998c). The health and
nutritional status of school children in Africa: evidence from
school-based health programmes in Ghana and Tanzania.
Transactions of the Royal Society of Tropical Medicine and
Hygiene, in press.
Don Bundy (Head of Centre) and Andrew Hall (Field Programmes
Coordinator) are at the Scientific Coordinating Centre for the Partner
ship for Child Development at Oxford University. Partnership country
programmes are coordinated by: Dr. Sam Adjei (GPCD, Health Re
search Unit, P.O. Box 184, Accra, Ghana); Prof. Charles Kihamia
(UKUMTA, P.O. Box 9383, Dar es Salaam, Tanzania); Prof. Satoto
(Mitra, Research Institute, Diponegoro University, Semarang, Central
Java, Indonesia), Prof. Tara Gopaldas (124/B, Varthur Road, Nagavarapalayam, Bangalore 560016, India); Prof. Ha Huy Khoi (VPCD,
National Institute of Nutrition, 48 Tang Bat Ho, Hanoi, Viet Nam).
For further information, please contact Andrew Hall at the Scientific
Coordinating Centre, Partnership for Child Development, Wellcome
ANAEMIA IN SCHOOL-AGED CHILDREN
by Bruno de Benoist and Yun Ling
ron deficiency is the most widespread micronutrient
deficiency in the world today. The anaemia it causes is
a major problem among women and young children,
but there is growing evidence that it is also a problem
among school-aged children. Its importance as a public
health problem in school-aged children deserves greater
attention not only because of its deleterious effects,
which include lower school achievement due to impaired
cognitive development, fatigue §gd poor attention span,
and increased morbidity because of reduced resistance
to infection, but also because of the large numbers of
school-age children affected. Indeed, recent estimates
based on the WHO global database suggest that 7.8% of
school-aged children in industrialised countries and 53%
in developing countries are anaemic. Prevalences are
highest in Asia (58.4%) and Africa (49.8%) where around
half of school-aged children suffer from anaemia. More
over, in developing countries, the proportion of schoolaged children with anaemia is much higher than that of
pre-school children (see graph).
Prevalence of anaemia in pre-school and
school-age children
I
These estimates should be interpreted cautiously since
they are based mainly on subnational surveys from a
limited number of countries for the regions mentioned.
They nevertheless serve to draw attention to anaemia as
a problem of public health importance in this age group
and highlight the need for more information on its
magnitude and causes so that appropriate control mea
sures can be adopted. Countries in general, and devel
oping countries in particular, can ill afford to allow their
youth be damaged by so devastating a public health
problem as anaemia.
i
Pre-school children (0-4y) ■ School-age children (5-14y)
Data come mostly from subnational surveys. For pre-school
children, data are from 118 countries equally distributed
between regions; for school-aged children, data are from 30
countries mainly from Africa (9 countries), Asia (10 countries)
and America (9 countries).
Anaemia is defined from
haemoglobin concentration using 110g/l as cut-off for the 0-4y
age group, and 120g/l as cut off for the 5-14y age group.
The WHO Micronutrient Deficiency Information System (MDIS) in
cludes three databases on iodine, vitamin A and iron (see page 59).
The database on iron deficiency (from which information has been
taken for this article) is currently being developed, and WHO welcomes
new contributions to this database. For further information about how
to contribute to the database, please contact Bruno de Benoist, Pro
gramme of Nutrition, WHO, 20 Avenue Appia, CH-1211 Geneva 27,
Switzerland. Tel: 41 22 791 3412 Fax: 41 22 791 4156 Email:
debenoistb@who.ch
TJcUJ tJGujg>JO. 16, JUL V Tee?
SCHOOL-BASED HEALTH AND NUTRITION PROGRAMMES:
A SURVEY OF DONOR AND AGENCY SUPPORT
by Don Bundy, Judy McGuire, Andrew Hall and Carmel Dolan
/
here are more children of school age and more
children attending school than at any time in
human history. These children are one of the
most accessible population groups from a public health
perspective because they are gathered together on an
almost daily basis and because they are supervised by a
trained workforce of teachers. They are also a group which
can benefit considerably from nutrition and health
interventions: good health and adequate nutrition promote
both physical growth and learning, while good health and
nutrition education at school age can lay the foundation for
life-long good health.
Given the apparent opportunities for school-based health
and nutrition programmes, the SCN Working Group on
Nutrition of School-age Children commissioned a survey of
what donors and agencies are actually doing for school
children. The survey method was to conduct key
informant interviews over a two-month period in early
1998, and to present the results for further discussion at
the Working Group meeting in Oslo, April 1998 (see page
25). A major conclusion of this review process was that
there was much more happening in school nutrition and
health than was commonly perceived, and also that the
activity involved UN, financial, bilateral and NGOs in part
nership with implementing countries.
Many UN agencies have strategies or policies on school
based health and nutrition. UNICEF has articulated a
school health and nutrition strategy that encompasses
sound school policies and the rights of school children,
skills-based health education, a healthy school environ
ment, and improved access to health services for school
children. UNDP was a founding co-sponsor of the Partner
ship for Child Development in 1992 and has continued to
support operations research into the contribution to
sustainable human development of health and nutrition at
school age. WHO launched a Global School Health
Initiative in 1996 with a focus on health promoting schools
and regional networks’. The Health Education and
Promotion Division is the focal point for the 8 Divisions
which contribute to the steering group for school health
and nutrition, but some 22 divisions at WHO are reported
to be active in this area. UNFPA supports reproductive
health programmes for adolescents in 98 countries, and
school-based HIV/AIDS prevention activities in 95
countries. UNESCO supports the integration of HIV/AIDS
education into the school curriculum and is a co-sponsor
of UNAIDS, which has a specific working group on school
based interventions. UNESCO also provides technical
support for the WFP's school feeding activities which are
underway in some 60 countries. FAO is currently field
testing school-based nutrition education materials to pro
mote dietary diversification and food security (see page
53).
Perhaps because school health and nutrition pro
grammes are necessarily intersectoral, many of these
activities are being implemented in partnership. This has
been achieved formally, for example, by UNAIDS efforts
to promote HIV/AIDS education in schools, co-sponsored
by UNICEF, UNESCO, UNFPA, WHO and the World
Bank. A looser partnership was created by the UNICEF
School Based Initiative in 1994 which, through a series of
technical support group meetings in Asia, Africa and the
Americas, brought together WHO, UNFPA, UNESCO,
the World Bank and NGOs to create a ‘Situation Analysis
Tool for School Health and Nutrition Programming’
(available on request from the PCD, see contact informa
tion on page 10). This partnership continues to grow: the
tool has been evaluated by WHO in 5 African countries,
with support from the Edna McConnell Clark Foundation,
and is currently being evaluated for use in Spanish
speaking and Francophone countries by PAHO and US
AID.
It appears that few bilateral agencies have specific
policies which promote the health and nutrition of school
children, but nevertheless most contribute significantly.
Since 1992, CIDA has provided Can$87 million for nutri-
'Editor’s note: A new WHO fact sheet (No.92; June 1998) on ‘WHO’s Global School Health Initiative: helping schools to become
‘Health-Promoting Schools" is available on the web at http://www.who.ch/. The goal of the WHO Global School Health Initiative is to
increase the number of schools that can be called 'Health-Promoting Schools'. Such schools are characterised by their constant
strengthening of capacity to provide a healthy setting for living, learning and working. Further information can be obtained from the recent
WHO publication ‘Promoting Health through Schools', 1997, WHO Technical Report Series 870. pp.94 CHF 17 (CHF 11.90 in developing
countries). Available from WHO distribution and sales, CH-1211 Geneva 27, Switzerland. Tel: 41 22 791 2477 Fax: 41 22 791 4857
Email: publications@who.ch
FEATUKtS
^umiriOM of r/Jo gcuooL-agep ouw
tion projects. These actions specifically help school chil
dren: e.g., the elimination of iodine deficiency disorders
(IDD) and vitamin A deficiency in school girts in the Indian
Sub Continent, and school-based IDD monitoring in South
America. The CIDAA/VFP Women's Health and Nutrition
Facility targets 0.9 million women and 2.2 million children,
including school children, in 15 low-income countries with
food, micronutrients and deworming. DFID, UK, supports
the integration of health and nutrition education into school
curricula, funds the School Health Action and Training
Project for teachers in 700 schools in Delhi and Bombay,
provides USS7 million worth of school-based health ser
vices in Andra Pradesh, and has provided water and
sanitation for 800 schools in Kenya; yet DFID has no
specific policy for the health of the school-age child.
DANIDA, NORAD and SIDA also have no specific policy
for the health of the school child, but provide major sup
port for information-education-communication (IEC) and
life skills to promote health - particularly reproductive
health - to be integrated into school curricula. For exam
ple, the Regional Adolescent Social and Reproductive
Health Project implemented by AMREF in Kenya, Tanza
nia, Uganda and Ethiopia is co-funded by NORAD and
SIDA. In 1997, GTZ identified adolescents as a neglected
group, and recommended increased programming in life
skills training for youth health, HIV/AIDS and nutrition particularly in Africa. USAID has both a policy for promot
ing the health of school children - in Africa and the
Americas - and active programmes providing school
based health services, including interventions (such as
micronutrient provision and deworming) and skills-based
health education.
Much of the practical implementation of school health and
nutrition activities is undertaken by international or local
NGOs, even if funded by bilateral and other agencies. A
survey of 10 major INGOs revealed that all were active in
IEC and skills-based health education in schools, and a
majority were promoting a healthy school environment and
the provision of school-based health and nutrition
services. These programmes are often very substantial.
World Vision (Canada), for example, has a CIDAsponsored Can$25 million programme in Ethiopia, Ghana,
Malawi, Senegal and Tanzania that will, as one compo
nent, provide IEC, vitamin A and iron to school children
and sanitation to schools. Catholic Relief Services is
providing school-based IEC, feeding, specific micronutri
ents and first aid kits, in various combinations, in 10
countries, while Save the Children Federation (USA) is
providing school-based IEC with or without micronutrient
supplements and deworming in 15 countries. The cover
age of IEC may be very extensive, for example, the
Children's Health and Environment maga
zine supported by CARE in Thailand is read by more than
one million students in 31,000 schools.
The multilateral financial organisations also play an in
creasingly important role. The Inter American Develop
ment Bank and the Asian Development Bank both pro
vide loans in support of school nutrition and health pro
grammes. The Worid Bank was amongst the first to
identify school-based health and nutrition programmes as
remarkably equitable and cost-effective interventions that
contribute to human capital and social capital develop
ment. The World Bank, mainly through the International
(Courtesy of UNHCR)
Development Association, currently supports pro
grammes that seek to deliver a simple package of locally
relevant health and nutrition interventions through
schools, delivered on a scale that is a benefit rather than
a burden on the education services. Such activities are
typically small components (2% to 9%) of universal basic
education projects (with total budgets in the range of
US$35 to 60 million), but are also components of health
and nutrition projects (with total budgets in a similar
range), community funds for health, nutrition or education
(with total budgets in the range of US$50 to 110 million),
and Sector Investment Projects (with total budgets in the
US$100s of millions). To enhance responsiveness to the
needs of client countries, the Worid Bank has entered into
productive partnerships with UN agencies (e.g., PAHO/
WHO in Latin America and the Caribbean), INGOs (e.g.
SCF (USA) in Africa) and technical groups (e.g. the PCD)
as part of an International School Health Initiative (for
further details of Worid Bank activity see page 22 ‘Class
Action' by Joy del Rosso and Tania Marek).
Overall, this survey reveals surprisingly strong and broad
based support for school nutrition and health pro
grammes. There may be a need to explore ways to build
beyond the current levels of collaboration, and perhaps the
SCN Working Group on Nutrition of School-age Children
can contribute to this. Almost all UN agencies, funds and
organisations with a mandate in health, nutrition or educa
tion have a specific policy to promote the health and
nutrition of the school-age child, and most have active
programmes in this area. The bilateral donors are active in
the area, but curiously few have articulated specific health
and nutrition policies for school children. This may reflect
the ambiguities of the intersectoral status of some school
“health” activities; school feeding, for example, is often
seen as promoting school attendance and learning, and
thus as contributing to educational rather than health
outcomes. Or it may reflect a lack of recognition that
programmes to promote adolescent health - a major area
of current emphasis for prevention of HIV/AIDS, substance
abuse, and violence - are frequently school-based in low
income countries. The INGOs have clearly grasped this
concept, and are expanding tljpir definition of school
health and nutrition to include school-based services, such
as snacks, micronutrient provision and deworming. It
seems to be this minimum package - health education and
simple, well-tried health and nutrition services, both deliv
ered through schools - that is emerging as a practical
definition of a school-based health and nutrition pro
gramme.
This survey is a work in progress. If you would like a copy of the latest
draft of the report, or if you would like to contribute to the survey,
please contact Andrew Hall at the Scientific Coordinating Centre of the
Partnership for Child Development, The Wellcome Trust Centre for the
Epidemiology of Infectious Disease, University of Oxford, South Parks
Road, Oxford 0X1 3PS, UK. Tel: 44 1865 281231 Fax: 44 1865
281246 Email: child.development@zoology.ox.ac.uk
The survey was supported by a World Bank Special Grant and was
conducted by Carmel Dolan with the Partnership for Child Develop
ment. The Partnership for Child Development programmes and activi
ties are supported by the UNDP, the WHO, the British Department for
International Development, UNICEF, the World Bank, the Edna Mc
Connell Clark Foundation, The Rockefeller Foundation, the James S.
McDonnell Foundation, and the Wellcome Trust.
Don Bundy is at the Human Development Network Education Depart
ment at the World Bank, Washington D C. and at the Wellcome Trust
Centre for the Epidemiology of Infectious Disease, University of Ox
ford; Judith McGuire is at the Latin American and Caribbean Human
Development Network at the World Bank, Washington D.C.; Andrew
Hall is in the Scientific Coordinating Centre of the Partnership for Child
Development, University of Oxford; Carmel Dolan is a Freelance
Consultant.
NUTRITION OF SCHOOL-AGED CHILDREN IN MONGOLIA
by Ruth English
he population of Mongolia (2.3 million people) is
relatively young, with 38% under the age of 15
years (1). Fifty-two percent of the Mongolian
population live in urban areas and 48% live in rural areas,
with approximately 20% of the population being nomadic.
Since the break-up of the Soviet Union at the beginning of
the decade, the economy of Mongolia has been in
transition, changing from a communist-based to a
capitalist-based economy. This has meant much hardship
for the Mongolian people. As the support base for the
agriculture system and the social welfare programme
services has eroded, agricultural production has fallen
drastically and unemployment and poverty are increasing.
The cities have large numbers of people concentrated in
ger (tent) settlements with 60,000 families in the capital
city of Ulaanbaatar. There are associated problems relat
ing to safe drinking water, adequate sanitation and waste
disposal, and increased levels of soil pollution. These
living conditions contribute to ill-health and an unsatisfac
tory quality of life.
T
Education situation
Educational achievement has been high with a 95%
literacy rate, 98% primary school coverage, 88% cover
age for 8 years of schooling and 15% in higher levels.
However this may be falling with increasing poverty and
unemployment.
Nutrition situation of school children nutrient intake
From 1993 to 1996, the National Nutrition Research
Centre conducted dietary surveys on some 21,000 per
sons, including school children. The data collection
comprised a 24-hour recall of food eaten the previous
day, using a questionnaire form for response. The report
of the Nutritional status of the Mongolian population (2)
details the nutrient intakes of pre-school and school-age
children in four age groups: 4-7y, 6-10y, 11-14y, and
15-17y. For the two older age groups, the nutrient
intakes of boys and girts were estimated separately.
MUreiTiONJ OF FUE qeuool-aeed omld
Nutrient intakes of school children in Mongolia
Nutrients
Age Groups
4-7y
8-10y ,
Boys
Girls
Boys
Protein (g)
75.6
69.0
64.7
56.2 i
73.0
Fat (g)-Plant
8.7
14.4 .
29.9 ___
9.3 .
Fat (g) - Animal
22.4
" ~ 31.1 ___
25.4
39.8 ~
-a: a - 7c:ai
11-14y
____ 40.6 ___23 9
70.5
38.2
144
34.0 ,
Carcohydrate (g)__
284.8
286.4 ____2_565____ 202.2
48.4
274.2 |
Energy (kcal)
1711
1780
1920
1378
1824 |
|' 'uamin
(mg)
[ >-ramm S1 (mg)
i • :=~.n 52 (mg)
' '•L2:-n (2191_______
: i m9)
’ a: ........ g
... r ,
0.70
0.50
1.28
0.57
0.67
0.88
___ 0.90
0.94
0.75
0.98
____ 0.91
0 94
0.89 .
0.85
1.10
8.54
8.87
20.3
7.70
10.5;
8.1
14.7
10.9
10.8
180
202 :
720
186
217 |
16.7
___ 11.0 ;
15.0
12.1
16.0 |
18:16 66
16:20:64
14:23:53 . 16:25:56
16:24:60 I
p: energy from
The energy intakes of the younger age groups are high in
comparison with those in the 11-14y Snd 15-17y age
groups - particularly in girls (see table above).
With regard to micronutrients, intakes of some essential
vitamins and minerals in all age and sex groups are below
the recommended levels developed for the Mongolian
population (3). In particular, intakes of vitamin C, vitamin
B-2, and calcium are low, although the calcium intakes of
boys aged 11-14 years appear to be adequate. Iron
intake could be considered low for girls of puberty age
(11-14y and 15-17y). However, this level of intake may
actually be adequate as a major source of the iron would
be in the form of the more absorbable haem iron from
meat products.
Food intake among school children
The average daily intakes of foods for school children
(aged 4-17y) are as follows:
Meat and meat products
158.6g
Milk and milk products
282.4g
Flour and flour products
205.3g
Butter
6.0g
Fat
0.4g
Rice
211.6g
Fruit
4.6g
The
figures
for
vegetable
consumption were not included in
the report. The very low intake of
Girls
fruit and possibly also vegetables
_£7A
was responsible for the low intake
11.2
of
some vitamins (e.g., vitamin C)
29 0
and minerals, which fell well below
40 2
the normative values for nutrient
211.0
1435
intakes developed for Mongolia in
1981 (3). It was noted that eggs
0.60
and rice were not consumed at all.
0.82
The low intake of milk and milk
0.88
products explains the overall low
8.00
intake of calcium and vitamin B-2,
16.8
while the low consumption of veg
227
etable oil, butter, milk and milk
12.4
products result in the generally low
intake of fat.
16:25:59
15-17y
Nutrition situation of school children - malnutrition
There is evidence of nutrient deficiency diseases among
school children in Mongolia. Meat and dairy products
have traditionally formed the main part of the adult diet
with flour and flour products. Dietary patterns have been
changing over the period of economic transition, particu
larly in relation to the consumption of milk and milk
products. Especially in the cities and towns, the availabil
ity of milk has been decreasing, partly due to a break
down in the milk marketing systems from rural to urban
areas.
Underweight
The National Nutrition Research Centre has conducted a
series of anthropometric surveys in children under 5
years of age to determine the prevalence of
undemutrition in young children in this country. While
the overall prevalence of underweight (low weight-for
age) has decreased from 1992 to 1996, there has been
an increase from 29.4 to 42% amongst children aged
25-48 months and from 0 to 13% amongst children aged
49-60 months. These results are indicative of an increas
ing problem of malnutrition and growth failure in children
as they enter the school system.
Micronutrient deficiencies
There are three priority micronutrition deficiency diseases
in Mongolia that primarily affect women and children:
fJO.i 6. JULY
0
0
0
Vitamin D deficiency. There is a major problem of
vitamin D deficiency in Mongolia. Surveys have iden
tified prevalence rates of rickets varying from 6% to
68% in different populations, with an average preva
lence rate at 3 years of 26.5%. In the 1992 child
survey, 44.7% of children under five had one or more
signs of rickets with bowing of the tibia being the most
common sign. The cause of vitamin D rickets in
Mongolia is as yet ill-defined, but the data indicate that
many children cany the handicap of bone malforma
tion from rickets through their school years into adult
hood.
Iron deficiency anaemia: The prevalence of iron defi
ciency is now reported to be as high as 28.8% in
pregnant women and 43.6% in children below five
years of age. No data are available on the prevalence
of iron deficiency anaemia in children of school-age.
Iodine deficiency diseases: In 1992, 1490 children
aged 7-12 years from eight schools, were examined to
determine the prevalence of iodine deficiency disor
ders (IDD). Two of the eight schools were on remote
state farms. The survey showed an overall preva
lence of 41% (range 24-83%), with children in the
Bulgan area or Aimag, most at risk. Clinical signs of
dysfunction of the thyroid were identified in 1.5% of
the children. Overall, it is estimated that 28% of the
population has goitre. Iodine fortification of salt is the
major strategy being pursued to reduce and control
IDD. Six plants produce salt in Mongolia. In 1996, it
was estimated that 40% of households were using
iodised salt. The small additional cost of fortified vs.
unfortified is reported to be a deterrent to purchase
of the iodised salt by poor families.
Other micronutrient deficiencies: In some country
reports, reference is also made to the risk of vitamin A
and vitamin C deficiencies in Mongolia. One survey
indicated a prevalence of night blindness in 4.5% of a
group of children, as reported by mothers. No evidence is
available indicating that vitamin C deficiency has been
clinically identified in school children or adults in
Mongolia.
References
1.
State Statistical Office of Mongolia. Mongolian economy and
society in 1996. Uaanbaatar, 1997.
2.
National Nutrition Research Center.
Nutritional status of
Mongolian population. Ulaanbaatar, 1997.
3.
Ministry of Agriculture and Industry. Physiological norms for
nutrient intakes for the Mongolian population. Ulaanbaatar,
1981.
Ruth English is a Nutrition Consultant and Honorary Research Consul
tant at the Department of Social and Preventive Medicine, University of
Queensland, Australia. Postal address: P.O. Box 1491 Noosa Heads,
Qld, Australia. Tel/Fax: 61 7 5449 2015 Email: renglish@ozemail.
com.au This article is based on information obtained during a consul
tancy in Mongolia in May/June 1997.
SCHOOL FEEDING PROGRAMMES
^
*
y^
chool feeding programmes are one of several
V,.
interventions that can address some of the
csO nutrition and health problems of school-age
children. If properly designed and effectively implemented,
school feeding programmes can achieve a number of
goals:
0
0
0
0
0
12
alleviate short-term hunger, thus increasing attention
and concentration span;
encourage (or be used specifically to encourage)
enrolment by girls and improve retention;
motivate children to attend school and motivate
parents to enroll their children in school;
contribute to better nutrition and address specific
micronutrient deficiencies in school-age children
(especially iron and iodine deficiencies which directly
affect cognitive development);
increase community involvement in schools.
A series of three documents entitled “School Feeding
Programmes: Food for Education' have been prepared
by Joy del Rosso under the auspices of the Partnership
for Child Development (see page 4) to provide
governments, agencies and organisations with up-todate information:
Part I: Summary of Major Issues and Recommendations
Part II: A Review and Annotated Bibliography
Part III: Guidelines for School Feeding Programmes to
Contribute to Improving the Effectiveness and Efficiency of
Education
Copies are available on request from the Partnership for Child
Development, Wellcome Trust Centre for the Epidemiology of
Infectious Disease, Oxford University, South Parks Road, Ox
ford 0X1 3PS, UK. Tel: 441865 281231 Fax: 44 1865 281245
Email: child.development@zoo.ox.ac.uk Web: http://www.ceid.
ox.ac.uk/child/
FEATURES
_____________________ MumiTiOM OF FldE SCHOOL -a<$EP CHILO
INDIA’S NATIONAL PROGRAMME OF NUTRITIONAL SUPPORT
TO PRIMARY EDUCATION PROGRAMME (NSPE)
by Tara Gopaldas
n August 15"1 1995 (India’s 48th Independence
Day), the Government of India launched the
National Programme of Nutritional Support to
Primary Education (NSPE). A number of converging and
positive factors contributed towards the launch of NSPE.
These were:
0
0
0
0
0
0
0
0
a strong political commitment at both central and state
levels to universalise primary education;
the decision by the Government of India to redeem the
national pledge of allocating 6% of the national income
for primary education;
successive bumper harvests, the success of the ‘Green
Revolution' and the development of a large-scale public
distribution system;
the excellent report of the Committee on Mid-Day-Meals
(1) which is the Plan of Action instrument for the NSPE’;
numerous research studies and publications in the
1980s and 1990s stressing the link between nutritional
status and educational performance;
a number of national and international surveys and
studies to highlight the extremely poor nutritional and
health status of the school child;
some success stories of the cost-effectiveness of
improving the micronutrient (iron, iodine, vitamin A) and
health (intestinal parasites, impaired sight and hearing)
status of the school child in the classroom itself;
the strong recommendation of the Government of India
that the NSPE should forge links with school health on
the one hand, and with India's Integrated Child Develop
ment Services (ICDS - see SCN News No. 15 p27) on
the other.
Aims, coverage and budget of the NSPE
The main aim of the NSPE is to give a boost to the
universalisation of primary education in India by
increasing enrolment and attendance at schools, and
simultaneously improving the nutrition education of the
school child (aged 6-15y). It is much more a food for
education scheme than a food for nutrition and health
scheme as it is based on supplying those students with a
good school attendance record with grain (wheat or rice)
over a period of time. A school child with 80% attendance
is supplied with 3kg grain per month for 10 academic
months per year. The child or parent is expected to collect
1 The NSPE is the current Mid-Day-Meal Programme (see SCN
the grain from the designated ration (or public distribu
tion) shop in the village.
The quantity of grain ration was guided by the findings of
a 1990-1992 Eight-States Diet and Nutrition Survey
conducted by the National Nutrition Monitoring Bureau
(2). The survey found that the nutritional status of the
rural school child was very poor, with only 6% classified
as ‘normal’ when compared to the NCHS growth refer
ence. The survey reported an average deficit of 620kcal
and about 7g protein per day when compared to the
Indian Recommended Daily Intake for this age group.
School boys eating a hot cooked meal in the classroom.
(T. Gopaldas)
The NSPE has been operational for around three years.
In 1995-6, 225,000 schools and 33.5 million school chil
dren were covered by the NSPE. This number rose to
some 370,000 schools and 55.4 million school children in
1996-7. Attendance also increased from 21 million
children in 1994 to 55 million in 1997. The NSPE has also
helped to boost enrolment in primary schools.
All 32 states and union territories (UTs) of India are
implementing the NSPE. Seven of these 32 states and
UTs, namely, Gujarat, Haryana, Jammu & Kashmir,
Kerala, Madhya Pradesh, Orissa, Tamil Nadu and the UT
of Pondicherry, are providing school children with a hot
cooked mid-day meal. This is usually a cereal-pulse
preparation with some condiments and seasonal vegeta
bles. The remaining states and UTs either prefer not to
give meals, or are not ready at present to make the
necessary arrangements for provision of a hot cooked
meal and have opted to provide school children with 3kg
of grain per month for an 80% attendance record.
News No. 14 p23).
77
g&J
/JO-16. JULV ',???
Once the ‘hot cooked meal’ becomes the norm in India,
with the majority of states and UTs providing hot meals,
5kg per month of grain per school child for 10 academic
months will be supplied within those states and UTs that
are not able to run a 'hot cooked meal’ programme. This
is based on the argument that other members of the family
in addition to the school child will consume the 'take-home'
grain ration.
The NSPE is a 100% Central Government sponsored
scheme. The cost of the food grains and transportation
are borne by the Central Government. In the case of hot
cooked meals, the States or UTs have to bear all other
costs (kitchens, cooks, fuel etc.) Rs.8000 million was
spent in 1996-7 (equivalent to approx. 190 million US$),
and Rs.9600 million has been allocated in 1997-8
(equivalent to approx. 225 million US$).
cooked meal variant have to be assessed. Above all, if
the NSPE has an important nutritional status improve
ment objective, then its impact in this crucial area has to
be evaluated.
How can the present NSPE be made to have a more
nutritional and health slant?
0
0
0
0
Preliminary reports indicate that the NSPE is working well
in the rural sector but not so well in the urban sector where
the ration shops may be located far away.
0
0
School girls receiving iron, vitamin A and anthelmintics in
the classroom. (T. Gopaldas)
Monitoring and evaluation
The Government of India is developing a computerised
Management Information System with the assistance of
the National Informatics Centre in New Delhi in order to
record data on enrolment, eligible beneficiaries for NSPE,
and quantity of food grains allocated, collected and
utilised. The system is not, as yet, fully operational as
training at the state and UT level is required.
An ail-lndia process and impact evaluation of the NSPE is
urgently required. The reactions of the main actors,
namely the school child, the teacher, and the local ration
shop keeper are yet to be evaluated. Similarly, whether or
not linkages have been formed with the primary health
centres, the village Panchyats and the ICDS has to be
ascertained. Furthermore, the advantages and disadvan
tages of the ‘take home’ grain ration versus the hot
76
The NSPE must put nutrition and health objectives
ahead of enrolment, retention and drop-out objectives.
The NSPE must set a time-frame, say by the year
2000, where every primary and middle school child will
receive a hot cooked meal.
The NSPE must insist that a good brand of iodised salt
be used in the hot cooked meal variant. India has the
capability to produce the required quantity of iodised
salt.
In Indian communities, school-aged children are the
age group most heavily infected with intestinal para
sites. Hence, periodic deworming is a must. India has
the capability to produce the required quantity of an
thelmintics and dosing can and should be given by the
teacher in the classroom.
Weekly iron supplementation can and should be given
by the teacher in the classroom. India also has the
capability to produce the required quantity of iron
supplements.
India is one of the most vitamin-A deficient countries in
the world. Legislation should make it mandatory that
red palm oil, which is abundantly rich in p-carotene, be
used in the hot cooked meals.
At present, India has a school-age population of
approximately 200 million children. Policy-makers and
implementers of the NSPE must realise that it would
benefit the school child more to give him/her a health
package of deworming, iron, vitamin A and iodine, rather
than just grain. At Rs.10 (approx. 0.2 USS) per child per
year, such a health package, delivered in the classroom
throughout India, would cost Rs.2000 million a year
versus a yearly expenditure of some Rs.10 000 million
for the grain. The best proposition would be to give the
school child both the hot meal and the health package in
the classroom.
References
1. Nutrition Support to Education: report of the Committee on
Mid-Day-Meals, New Delhi, May 1995.
2. Diet and Nutrition Surveys in Eight States of India on Rural
Children (6-11y).
National Nutrition Monitoring (Rural) Sur
veys. National Institute of Nutrition, Hyderabad, 1990-2.
Tara Gopaldas is Director of Tara Consultancy Services, 124-B,
Varthur Road, Nagavarapalya, Bangalore-93, India. Tel: 91 80
5242999 Fax: 91 805288098
_________________________________________ MUTlZiriOM OF TUS €CUOOL-a6£P C/-HLP
SCHOOL FEEDING IN INDONESIA: A COMMUNITY BASED PROGRAMME
FOR CHILD, SCHOOL AND COMMUNITY DEVELOPMENT
by Lisa Studdert and Soekirman
In July 1996, Indonesia initiated a national school
feeding programme. Initially implemented in all officially
♦designated 'poor' villages except those on the islands of
Java and Bali, the programme expanded in year-2 of
implementation to include all 'poor1 villages throughout
Indonesia. The programme now provides a nutritious
snack three times a week to 7.2 million primary school
children. In developing this programme, the Government
of Indonesia has adopted a unique approach to school
feeding with community-based implementation involving
several community groups, utilisation of local foods, and
education and health components. This design is aimed
at an overall programme goal of human resource develop
ment while addressing several objectives that target
human, economic and social development at the
community level. The sustainability of the programme will
depend on the empowerment of all involved people especially women. The objectives and the programme
design recognise that improvement in children's health,
nutritional status and educational achievements requires
interventions that extend beyond the school child in the
schoolyard or classroom.
Human resource development in Indonesia
The Government of Indonesia has recognised human
resource development as a key objective of its second
(current) 25-year Development Plan. In the 1970s, the
government launched a primary school development pro
gramme ensuring that every village in the country has a
primary school. Building on this, the current 5-year Devel
opment Plan (1994/95-1998/99) has directed that all chil
dren should receive a minimum of nine years of schooling.
There was concern, however, that these efforts have
focused more on the infrastructure and policy than on the
child and the child's capacity and ability to be in school
and leam and progress effectively. Surveys in the early
1990s showed that up to 70% of children in 'poor' villages
were consuming less than 70% of the their daily energy
requirements; up to 40% of children are anaemic and
between 50-80% of children have worm infections. More
over, it is estimated that each year around 1.2 million
children - or 4.2% of the eligible population - drop out of
school.
Thus, the Programme Makan Tambahan Anak Sekolah
(supplemental food for the school child - PMT-AS) was
pilot tested in several provinces in the early 1990s and
introduced as a national policy, with presidential endorse
ment, in 1996. Expenditure in 1997/98 was over US$ 100
million.
PMT-AS: the why and how
The objectives of the PMT-AS programme are divided
into those for the school child, those for the school and
those for the parents and community.
PMT-AS Objectives
For the child:
-reducing absenteeism;
-alleviating short-term hunger;
-increasing total energy intake:
-educating children on topics of
health and nutrition;
-reducing worm infection rates
through the provision of deworming
medication twice yearly.
For the school:
-improving teachers knowledge on
teaching health and nutrition topics.
For the parents
and community:
-knowledge and involvement of
parents in children's health, nutrition
and education;
-increased demand and appreciation
for local agricultural produce.
Implementation of the programme revolves around the
provision of a mid-morning 'snack' to primary school
children three days per week through the school year (9
months). The term 'snack' is deliberately used so that
there is no impression that the food is a meal that
replaces food children would receive at home thus ensur
ing, as much as possible, that the snack received is
additional and not substitutional. Children are also given
deworming medication twice per year.
Funds, based on a per-snack, per-child, per-day amount
are sent from the national level directly to the local level.
Only the school principal may withdraw funds from the
bank, and only with a snack menu plan co-signed by the
heads of the local women's and parent's associations.
The menu plans are prepared at the community level with
technical advice from Ministry of Health personnel. It is
stipulated that menus must use locally produced foods
and that the snack must contain a minimum of 300
calories and 5g of protein. The compulsory use of locally
produced foods is key to ensuring PMT-AS funding is
that work on a rotating basis. Support and guidance are
expected from the village leader, local Ministry of Health
and Education officials and school officials.
A programme for the future and in a crisis
It is intended that the PMT-AS school feeding pro
gramme will be a long-term government initiative in
Indonesia. Funded entirely by government resources,
the recognition of its importance for the long-term future
of Indonesia is signified by the fact that funding support
has been maintained in spite of the economic crisis that
has recently affected Indonesia.
Hypothetical relation between PMT-AS and village
economy
directed into, and kept within, the local economy. Hence,
PMT-AS provides incentives for intensified local produc
tion as well as for home garden produce and school
gardens. Through this mechanism, PMT-AS is expected
to contribute to national poverty eradication programmes
(see diagram above).
The process for food purchase and preparation is not
strictly defined, but training and guidelines have been
provided suggesting that the local women's association
(PKK) and the school parents association (BP3) develop a
system acceptable and appropriate to that community.
Observations in the field have shown a wide range of
practices involving between 1-15 women - some villages
with a core group that does all the work, others with teams
In the life of such a programme it is still early days. The
government plans to start comprehensive monitoring and
evaluation activities in the coming year - year 3 - of
implementation. The results of these activities will be
used to modify and enhance implementation processes
and related training activities and guidelines. Moreover,
these results should start to assess programme impacts
so that the value of this programme can be analysed,
appreciated and shared with other nutrition, health and
education policy makers and programme planners
around the world.
Lisa Studded is a doctoral student at Cornell University, Ithaca, New
York, USA, carrying out research in Indonesia in 1998 on the PMT-AS
programme. Tel (c/o UNICEF, Jakarta): 62 21 570 5816 Fax: 62 21
571 1326 Email: lisa@cim.com.au or Ijs10@cornell.edu Dr Soekirman is Professor of Nutrition at the Agriculture University, Bogor,
Indonesia. Tel: 62 21 7987 993 Fax: 62 21 7987 130 Email:
skirman@rad.net.id
ADDRESSING MICRONUTRIENT DEFICIENCIES IN PRIMARY SCHOOL CHILDREN
WITH FORTIFIED BISCUITS
by Lize van Stuijvenberg and Spinnie Benade
ady in 1995, after having been approached by the
community leaders of a rural village in KwaZuluNatal, South Africa, the South African Medical
Research Council undertook a cross-sectional nutritional
survey in that community. The results showed deficiencies
of iron, iodine and vitamin A; the prevalence of vitamin A
and iodine deficiencies exceeded the level regarded by the
WHO as a public health problem. These deficiencies were
also present among the children attending the local pri
mary school, despite the fact that a school feeding
scheme, whereby the children received a cooked meal five
days each week, had been in operation for a period of two
years prior to the survey. 16% of the children were stunted
and 2% were underweight.
E
An intervention study, in collaboration with the local
community leaders and the food industry, was then
undertaken to determine whether the micronutrient defi
ciencies present in the school children could be allevi
ated through food fortification. A shortbread type of bis
cuit was identified as a suitable vehicle for fortification. A
similar biscuit is sold by the shops in the area and is very
popular amongst the school children. The biscuit was
fortified with [3-carotene, iodine and iron (50% of the
RDA), while a cold drink served as a carrier for vitamin C
which was necessary to enhance the absorption of the
iron. Two hundred and fifty-two 6-11-year-old children
were randomly allocated to a group that received a
fortified biscuit and cold drink, or to a group that received
FFATUKES
MumrriokJ of rue school -a&eo cuw
an unfortified biscuit and cold drink. The biscuits and cold
drinks were distributed daily during the school week,
during the first two hours of the school day, for a period of
12 months. No intervention took place during school
holidays or on public holidays. Distribution and
consumption took place under close supervision and
compliance was recorded daily. To exclude parasitic
infestations as a confounding factor, the children of both
groups were dewormed.
The 12-month intervention resulted in a significant
improvement in blood levels of vitamin A, ferritin, iron,
haemoglobin, haematocrit and in urinary iodine levels in
the group who received the fortified biscuits compared to
the unfortified group. The greatest improvement in vitamin
A and ferritin status was seen in children with low values
at the start of the study, while the intervention had little
effect on those with adequate status: i.e., those that
needed it most benefited the most from the intervention.
The prevalence of low serum vitamin A levels (<20 pg/dl)
dropped from 39% to 12%, of low serum ferritin levels
(<20 pg/l) from 28% to 14%, and of anaemia (<120 g/l)
from 30% to 16%. There were no significant reductions in
the group receiving the unfortified biscuit. The prevalence
of low urinary iodine levels (< 1Optg/dl) in the fortified group
decreased from 98% to 30% after 6 months, and to 5%
after 12 months. In the unfortified group the prevalence
decreased from 96% to 90% and 34% after 6 months and
12 months, respectively. The iodisation of salt became
compulsory in South Africa during the second half of our
study, thus contributing to the improvement in iodine
status in both the fortified and unfortified groups. There
was no reduction in the prevalence of goitre, which was
21% at the baseline assessment; a 12-month period may,
however, have been too short to reverse an already
enlarged thyroid. The biscuit was well accepted and 74%
of the children indicated that they would prefer more than
the three biscuits they were receiving. The price of three
biscuits is US$0.05 per child per day and provides
191 kcal. The cost of fortification itself is US$0.86 per child
per year.
no preparation, is easy to distribute and has
a long shelf life. It is also easy to monitor and therefore
less open to misuse or corruption.
Dealing with the hidden hunger of micronutrient
deficiencies through food fortification is regarded as a
short- to medium-term solution to address an immediate
need. Longer-term solutions will include nutrition
education in schools and communities with regard to the
need for diverse diets. Should a fortified biscuit be
implemented in school feeding, it is recommended that it
be accompanied by a relevant nutritional message which
would put the fortified biscuit in the diet into perspective.
Using a micronutrient fortified biscuit and cold drink in
school feeding is feasible, effective and practical, and can
seriously be considered for addressing micronutrient
deficiencies in school children. The role of nutrition
education as a long-term solution should, however, not
be overlooked.
The biscuit is now commercially available and is actively
marketed at the primary school level by the food industry,
using the scientific results to promote its use in school
feeding programmes throughout South Africa. Once in
place, an effectiveness study will be earned out.
Lize van Stuijvenberg, Senior Scientist, P.O. Box 19070, Tygerberg,
7505, South Africa. Tel: 27 21 9380911 x 264 Fax: 27 21 9380321
Email: lvanstui@eagle.mrc.ac.za AJS Benade is Programme leader of
the Nutritional Intervention Programme, Medical Research Council,
Cape Town, South Africa. Mailing address: Medical Research Council,
PO Box 19070, Tygerberg 7505, South Africa. Tel: 021 938 0283 Fax:
021 938 0321 Email: sbenade@eagle.mrc.ac.za The information
contained in this article is also’available as a technical report and a
policy brief issued by the MRC. Both are available free of charge on
request from Dr Benade.
A danger of school feeding is that parents may reduce the
food provided for children at home. Using a biscuit as a
vehicle for fortification eliminates this problem, because it
is seen as a snack rather than a meal and therefore
unlikely to replace meals given to the child at home. In this
study the biscuit intervention had no effect on the number
of children who ate breakfast before coming to school, nor
on the number of children bringing food to school.
Additional advantages of using a biscuit are that it needs
7?
)
UO.-.C-, JULY
SCHOOL FEEDING PROGRAMMES: LESSONS FROM KENYA
by Ruth Oniang’o and Agnes Kimokoti
’he National School Milk Programme launched by
■
Presidential Decree in 1978, was a move to
V
contribute to better health and nutritional status of
school children. The costs of running this programme,
however, have become unaffordable by the government,
and as such, the operational targets of the programme can
no longer be met. A second school feeding programme
aimed at improving both nutritional and educational out
comes began in WFP-assisted areas where schools not
only fed children, but also promoted nutrition education.
This is now a nation-wide programme, although the phas
ing out of support by WFP means that its future is
uncertain, in both of these cases, financial support seems
to be the major constraint. There is a need to look into
alternative mechanisms and more cost-effective strategies
of supporting child nutrition.
cates the carrying of packed lunch to school by
every child and discourages parents as much as
possible from giving their children money. This ap
plies especially to children who commute daily to
school. The Nutrition and Health Unit is also
encouraging schools to establish their own school
gardens. This would go a long way towards
minimisation of expenses of buying food, for both
schools and parents.
0
Apart from giving the actual food, the Unit is also
concerned with providing nutrition education and
sensitising the public to proper nutrition and feeding
habits, diet diversification and food quality and
safety. This is done deliberately through the school
curriculum, posters and during parent-teacher meet
ings. According to the head of the Unit,
considerable success has been achieved in this
area.
0
In urban and peri-urban slum areas, NGOs are
involved with provision of food for school children.
However, there is a need for the government to
coordinate all school feeding activities. Continuous
monitoring is also necessary in order to formulate a
programme that is beneficial to children, manage
able by the schools and affordable by the parents.
Issues for consideration
Some issues to be borne in mind when considering school
feeding programme design and implementation in Kenya
include the following:
0
Kenya has had a tradition of providing school lunches,
either through government or community mecha
nisms. Parents play a key role in school feeding.
Where they can, parents support a scheme that pro
vides a hot meal for their children. In such cases,
vendors and hawkers are discouraged because of
food safety and quality concerns. In arid and semi-arid
areas, where families have few resources, parents
make only a modest contribution. Government- and
WFP-supported schemes have targeted such areas
with the aim of encouraging school enrolment and
attendance. It is these areas where the majority of the
population is illiterate and the enrolment is fragile so
that incentives are required to motivate school enrol
ment and retention.
0
Some parents are able to afford to give their children
a packed lunch or money to buy food. However, it has
been observed that when children are given money,
they buy snack foods of low nutritional quality, or
spend their money on something else entirely. With a
growing drug problem among Kenyan youth, parents
are hesitant to give food money to their children for
fear that this will be spent on drugs.
0
The Nutrition and Health Unit has developed recom
mendations relating to school feeding. The Unit advo
Ruth Oniang’o is an AGN Member and Professor of Food Science and
Nutrition at the Jomo Kenyatta University, College of Agriculture and
Technology, P.O. Box 62000, Nairobi, Kenya. Tel: 254 151 22646/9
Fax: 254 2 583294 Email: oniango@iconnect.co.ke Agnes Kimokoti
is a Senior Lecturer at the University of Nairobi, Faculty of Education,
P.O. Box 30197, Nairobi, Kenya.
FFATUftES
A/C/re/77<2A/ OF n-IF CCUOOL-A66D CUW
MALNUTRITION AMONG SCHOOL CHILDREN IN INDUSTRIALISED COUNTRIES
by Andrew Tomkins
I
oor nutrition in school children seriously
compromises their health and learning capacity
and sets up a disastrous trend towards damaging
dietary patterns which affect the prevalence of disease in
adults. There is disturbing evidence that the nutritional
status among school children is deteriorating. In previous
generations, anaemia, rickets and poor growth were
associated with low socio-economic status. However,
current radical changes in lifestyle among both poorer and
better-off strata in industrialised countries, mean that
personal preference about foods, fashion, physical activity
levels and the media are now driving the nutritional
patterns of school children more than the availability of
food itself.
Traditional nutritional programmes focus on the provision
of an adequate diet so that children can maintain a good
level of health and benefit from the opportunities to leam
at school. However, health and nutrition of school children
are also of critical importance for determining the
prevalence of adult diseases such as ischaemic heart
disease, hypertension, certain types of cancer and
diabetes. Failure to address the nutrition of school children
probably explains why so many programmes aimed at
preventing adult disease have had very limited impact.
This article concentrates on the nutritional problems facing
industrialised countries, such as those in Europe and
North America, but there are many communities in other
continents where the nutritional status of children in betteroff families is more akin to the industrialised nations, than
to malnutrition syndromes of anaemia, hunger and
stunting. Current epidemics of premature mortality among
adults in less developed countries also have important
origins in schoolchild nutrition.
Nutritional problems of school children
Obesity. There is a steadily increasing epidemic of
obesity among school-age children. Age-adjusted body
mass index (BMI: weight divided by height squared) cen
tres are now available on the basis of which around 15%
of UK children have a BMI of over 25. This figure has
increased steadily over the last 2 decades. Using linked
longitudinal data, up to 60% of obese children remain
obese when they are restudied in their early 30s. Obesity
in children is associated with a decreased willingness to
become involved in physical activities and sports, leading
to a much lower level of fitness. Obesity in children is also
a major risk factor for adult disease.
Hypertension. Several longitudinal studies show an in
crease in levels of blood pressure among older children
leading to hypertension in adulthood. While there are few
immediately visible problems as a result of increasing
blood pressure in adolescents, it is of concern that as
such trends continue into adult life, they will increase the
risk of heart attacks and strokes.
Eating disorders. While overweight is a major problem
among school children, there is an increasing prevalence
of anorexia nervosa and bulimia, especially among girls.
The widespread, current social vogue, driven by the
media and advertising agencies, which dictates that it is
more beautiful to be thin, is a key factor driving the eating
patterns of school children. This has devastating impacts
on mental and physical health, school performance and
family relationships.
Dental disease. Despite the enormous publicity and
health promotion about the effect of confectionery on
dental caries, dentists still find poor levels of dental health
among many school-age children.
Anaemia is still a problem, especially in countries such as
the UK where certain ethnic groups, such as Asians, may
be disadvantaged and have dietary patterns which
increase the risk of iron deficiency.
Antioxidant deficiency.
Many adult diseases such as
coronary heart disease and some forms of cancer are the
result of the interaction between toxic agents, which
generate free radical release, and lack of antioxidants
which prevent disease by scavenging the free radicals.
Toxic agents include excessive fat intake and cigarettes.
There is a disturbing deficiency of certain antioxidants
such as vitamin C because of rather low levels of fruit
intake by many school children. Soft drinks and
confectionery make up an increasing proportion of
children's diets.
Hunger. Children who do not eat before coming to school
do not perform so well at school. Increasingly, children
‘fend for themselves’ and many leave home without
breakfast.
Changing lifestyles and dietary patterns
Major societal change has occurred such that 'family
meals’, when parents and children sit down together to
eat and talk, are much less common than in previous
decades. Children are often given money to buy food
7j7
G&J fJgujgfJO.iS, JULY
during the day and even when they do eat at home, there
are increasing trends towards use of convenience pre
prepared foods rather than traditional meals. The ‘eat and
go' culture and decreasing levels of social interaction
between parents and children mean that children 'choose'
rather than 'are told' what to eat.
Schools have a great potential. Nutrition and health
Convenience foods frequently have high levels of dietary
fat; many surveys show that school children eat over one
third of their energy as fat. Children tend to have high
sodium intakes as a result of the spices and sauces which
are an integral part of many fast foods and snacks.
issues should be incorporated into the curriculum from
an early stage, with boys learning just as much about
food, its values and preparation, as girls. Self-learning
activities, such as 'Child-to-Child' approaches are
effective at stimulating 'learning by doing’. In disadvan
taged areas, where many children come to school with
out breakfast, concerned school authorities can start
‘breakfast clubs' where children can begin the day with a
better nutritional state. Suitable foods include nutrientdense porridges, suitably enriched or fortified biscuits or
locally prepared nutrient rich-snacks.
Physical exercise and fitness among children is decreas
School governors or councils have responsibility for mon
ing. As a result of increasing community violence, danger
and parental fear, children are more frequently taken to
school by car or bus rather than walking or cycling. Many
schools have sold playing fields in recent years in order to
provide income to pay teachers and have reduced staff
salaries for supervision of physical activities such as team
games and individual exercise. Provision for physical
activity in inner cities is a special problem. Recent studies
show that children take very little exercise which is
vigorous enough to increase heart rate significantly.
Increased consumption of toxic agents such as cigarettes,
alcohol and drugs all put a stress on the antioxidant
capacity on the body to overcome their degenerative
effect. Advertising aimed at school children is now a major
focus of the food industry. While most governments
prohibit cigarette advertising aimed at the young, no
government has any policy aimed at reducing the
consumption of certain foods by school children.
Action for nutritional improvement
There are several ways of improving
nutrition of school children. Children them
selves should be the focus. Few people,
other than the marketing units of the major
confectionery and snack food industry, have really
addressed their needs or wishes. Health promotion which
starts with children's own perceptions and enables them to
look at their wishes for health and feeling “good" both now
and in the future are essential. Participatory approaches
are likely to be more acceptable and effective rather than
lectures which are considered “boring".
Parents need guidance. With the decreasing tendency of
many parents/carers to provide cooked meals for children,
and in certain circumstances, a low level of knowledge of
how to prepare even a basic meal, there is a need to
improve parenting as a focal point for improving the family
dietary intake.
20
itoring academic standards in schools. They can also
ensure adequate quality of nutrition within the curriculum
and catering services. Only food of appropriate nutritional
standards should be provided by school catering agen
cies. School governors also have the ability to limit the
promotion and advertising of less nutritionally valuable
foods obtainable by automatic vending machines which
provide snacks for cash.
Community councils have statutory powers to licence
fast food vendors who target their sales towards school
children. They also have opportunities to provide local
events which promote healthy diets and physical activity.
The media and food industry have enormous
responsibility. The fashion industry has a responsibility
for promoting beauty as something other than thinness.
The food industry has a responsibility for promoting foods
which can contribute to a better dietary intake.
Social services identify children from poor families who
need particular income support and subsidise school
meals for certain children. Despite their efforts, recent
studies in the UK show that poor families still find it
difficult to buy enough of certain foods such as fruit, even
though energy intakes may be so great that their children
are overweight.
Transport policies are crucial. Both city and rural councils
need to develop a physical activity policy, especially
within an overall transport policy such that children are
able to cycle and walk to school safely and find safe
places to take vigorous exercise.
Government policies. Improving nutrition of school chil
dren cannot be achieved by a government policy from
one ministry alone. It needs concerted, focused work
between ministries of health, agriculture, education,
sports and social welfare. Governments need to liase
with local community voluntary groups such as in the
FEATURES
K/unZiTiOKj of rue £cuool-a£6p cwcp
Health Cities Project of WHO and in the Health Action
Zones now starting in the UK. If Governments recognised
that such policies do not just address issues of childhood,
but are crucial for longer term issues of adult health and
national development they would take school child nutri
tion much more seriously.
Nutrition Professionals. It is the task and challenge for
nutrition professionals to inform and stimulate action by
government and community alike. With increasing
independence, it is increasingly children,
rather than their parents, who decide what to eat. The
challenge for any policy maker or programme manager is
to understand their needs and wishes and promote di
etary intakes that will provide better health for them
selves, both now and in their adult years.
Andrew Tomkins is Director of the Centre for International Child Health,
Institute of Child Health, University College London, 30 Guilford Street,
London WC1N 1EH, UK. Tel: 44 171 242 9789 Fax: 44 171 404 2062
Email: a.tomkins@ich.ucl.ac.uk
TRENDS IN THE INTAKE OF READY-TO-EAT FOOD1 AMONG
URBAN SCHOOL CHILDREN IN NEPAL
by Indira Sharma
In 1996, a cross-sectional study was conducted in an
I urban Nepalese school to assess the food behaviour of
S school-aged children in relation to ready-to-eat food
(REF) intake, its impact on nutritional status and nutri
tional composition of meals eaten. 610 school children
aged between 9-11 years from middle income families
were included in the study. Consumption of seven widely
available REFs - namely biscuits, bread, noodles, snack
packets, potato chips, low cost doughnuts and dalmoth (a
snack prepared from beans) - was assessed. Demo
graphic and socio-economic data were collected and a
questionnaire was developed to gather information on
food choices and preferences.
The frequency and amount of REF intake was recorded
for each child over a period of one week. Results showed
that children consumed at least one or two items of REF
every day. The average frequency of REF intake was 1.9
times per day, and the amount consumed was 125g per
day. This provided 439 (+/-127 SD) calories on average
per day - approximately 20% of the total energy require
ment of children in Nepal. When classified according to
the level of REF consumption, the majority of children
(59.6%) had moderate consumption (300-500 calories),
27.7% had high consumption (>500 calories) and 12.7%
had low consumption (<300 calories).
Compared with traditional foods, REFs were preferred by
the majority of school children (687%). Taste preference,
convenience and affordability were the foremost criteria in
choosing REFs. In the majority of cases, parents were
responsible for introducing REFs into their children's diets.
The role of advertising in influencing children's choices
was also considered relevant by 80% of children. Among
the many socio-economic factors, per capita income and
mother's education level was found to be positively asso
ciated with REF consumption.
A subsequent, in-depth study conducted on a representa
tive sub-sample of school children drawn from the low-,
moderate- and high-consuming groups compared the
nutritional status of the children in the three groups.
There were no significant inter-group differences in
height, weight, or in the energy and protein density of
meals eaten by the children. The intake of pulses, green
leafy vegetables, fruits and milk was, however, found to
significantly decrease with increasing REF consumption.
Taste preferences for new food products are slowly
changing children's food habits from eating conventional
foods to preferring modern convenience foods.
Presently, this change in eating behaviour is seen mainly
in snacking patterns, however this may further extend to
main meals. Thus, the results obtained from this study
indicate changing food habits with an increase in REF
intake by (middle-income) school children in Nepal. Is it
expected that this trend will further accelerate in the
future because of ongoing technological developments in
the food industry - encouraged by government policies leading to an increased rate of REF production. Further
more, per capita income and women’s education level are
also expected to increase.
Considering these points, it is advisable to take timely
precautions for the prevention of the deleterious effects
stemming from the intake of industrially processed ready-
' Ready-to-eat foods are defined in this article as 'industrially produced processed food characterised by food additives, low fibre, high salt and sugar
containing foods that are expensive compared with home-made traditional foods'.
21
rJO.r 6. JULY Tee?
to-eat foods which are deficient in micronutrients such as
calcium, iron, and vitamins A, B and C. The loss of various
nutrients during processing suggests a possibility of their
fortification with different nutrients. Caution must be taken
however regarding the addition of harmful food additives,
especially artificial colours and flavours. Labelling in all
manufactured foods should be made mandatory. Nutrition
education for mothers should include the adverse effects
of food containing high levels of sodium, fat, sugar, food
additives and low levels of fibre, and the improvement of
children's diets by compensating the deficient components
with other rich sources. Finally, the importance of
balanced diet with special emphasis on the formation of
good food habits should form an integral part of nutrition
education for school children in Nepal.
Indira Shanna, Tribhuvan University, Padma Kanya Campus, Bag
bazar, Kathmandu, Nepal. Tel: 977 1 414482 Fax: 977 1 418907
Email: sushil@mos.com.np The full research article describing these
studies was published in the journal of ‘Asian Regional Association for
Home economics- 1996. Vol. 3 pp 22-27 (Editor Dr. Soojae Moon.
Dept of Food and Nutrition, Yonsel University, Seoul, Korea).
CDC'S GUIDELINES FOR SCHOOL HEALTH PROGRAMS TO PROMOTE
LIFELONG HEALTHY EATING
/
he key to promoting health in children of schoolage is education, and the best opportunities for
V
positively influencing the health of this age group
are found in the school (World Health Report, 1998, p85).
Most young people in the United States make poor eating
choices that put them at risk for health problems. For
example, over 84% of young people in the US eat too
much fat; 51 % eat less than one serving of fruit a day; and
8% of high school girts take laxatives or vomit to lose
weight or prevent weight gain. The consequences of
unhealthy eating include an increased risk of obesity (the
percentage of young people who are overweight in the US
has more than doubled in the past 30 years), lower
intellectual performance, ill health and premature death in
adulthood. On the other hand, the benefits of healthy
eating patterns in childhood include promotion of optimal
health, growth and intellectual development, the preven
tion of iron deficiency anaemia, obesity, eating disorders
and dental carries, and the prevention of long-term prob
lems such as coronary heart disease. Establishing
healthy eating habits at a young age is therefore critical,
and schools can help young people improve their eating
habits by implementing effective policies and educational
programmes.
Agir a I’ecole. Pour de meilleurs resultats
scolaires par I’amelioration de la sante et de la
nutrition dans les pays non industrialises
(Banque Mondiale, 1998)
par Joy Miller del Rosso et Tonia Marek
A partir d'exemples concrets, cette publication montre
qu'une sante et une nutrition deficientes limitent
I'acquisition du savoir par les eleves et reduisent les taux
22
The Division of Adolescent and School Health of the US
Centers for Disease Control and Prevention, has
developed a series of guidelines, one of which is the
Guidelines for School Health Programs to Promote Life
long Healthy Eating. These guidelines identify the most
effective policies and programmes that schools can im
plement in order to promote healthy eating choices.
Seven recommendations are included in the guidelines.
These include the development of a school policy on
nutrition, the implementation of nutrition education, the
integration of school food services and nutrition
education, suitable staff training, family and community
involvement and programme evaluation.
These guidelines are available on the Internet at http://www.cdc.gov/
nccdphp/dash. The document 'CDC's Guidelines for School Health
Programs to promote lifelong healthy eating - at-a-glance' is available
from CDC, National Center for Chronic Disease Prevention and Health
Promotion, Division of Adolescent and School Health, ATTN, Re
source room, 4770 Buford Highway, Mailstop K-32, Atlanta, GA
30341-3724. Tel: 1 770 488 3168.
Source: CDC. Guidelines for School Health Programs to promote
lifelong healthy eating. MMWR 1996; 45 (No.RR-9), and brochure
'CDC's Guidelines for School Health Programs to promote lifelong
healthy eating - at-a-glance’.
d’inscription et de frequentation scolaires.
Plusieurs interventions d'un cout modique et d'une haute
efficacite, deja realisees ou a entreprendre par les Etats
afin d'ameliorer la sante et la nutrition des populations
scolaires, y sont exposees.
L'ouvrage recapitule comment ces ameliorations peuvent
se traduire par un renforcement des capacites individuelles grace a une incidence benefique sur les taux de
reATuxes
Mure.iric>kJOFruE GcMot-ageD cuw
secularisation, I'assiduite, les performances scolaires, la
productivite economique et sur la sante des futures
generations.
who has developed to
the peak of his or her potential will be
happier and learn better, and will
ultimately grow up to become a more
fully engaged, productive citizen.
On distingue cinq chapitres: “Les enfants d'age scolaire:
une population a risque"', “Situation couteuse, remedes
peu couteuiC; “Accroissement de la productivite et amelio
ration de la sante communautaire"; “Agif', “Logons a
retenii".
Deux annexes competent I'ouvrage:
‘Informations necessaires pour une analyse de la situation
des enfants d’age scolaire en nutrition et sante", et une
liste par pays de projets finances par la Banque Mondiale
et lies a la nutrition et a la sante de la population d'age
scolaire.
Class Action. Improving School Performance
in the Developing World through Better
Health and Nutrition (World Bank, 1996)
by Joy Miller del Rosso and Tonia Marek
This publication shows concrete
evidence that with poor nutrition and
ill health, the learning capacity of
children, and school enrolment and
attendance rates are reduced.
A discussion on a variety of low-cost
and highly efficient actions that gov
ernments have taken and can take to
improve the health and nutrition of
school age children is provided. The book summarises
how improvements in these areas will lead to gains in
human capital development through its beneficial effects
on school enrolment, attendance, and performance, eco
nomic productivity, and the health of future generations.
60pp. US $10. English and French versions are available from The
World Bank, P.O. Box 960, Herndon, VA 20172-0960, U.S.A. Tel: 703
661 1580 Fax: 703 661 1501 Email: books@woridbank.org World
Bank publications can also be ordered via the World Bank website at
http://www.woridbank.org/html/extpb/ordfornVordform2.htm
Nutrition, Health and Child
Development (1998)
In the countries of Latin America and the Caribbean infant
mortality rates have been steadily decreasing over the
past few decades, with more children surviving past
infancy than ever before. As more and more children live
to school age, the quality of life and concerns for achiev
ing optimal physical and psychological potential and to
benefit fully from education become paramount. A child
This publication, arising from a work
shop jointly organised by the Tropi
cal Metabolism Research Unit
(TMRU) of the University of the West Indies, and PAHO in
1995 in Jamaica, examines how and to what extent
nutrition, health, and stimulation can affect children's
cognitive and social development and their ability to learn
in schools. By examining recent research, the authors
explore such topics as undernutrition, iron and iodine
deficiencies, neonatal feeding, short-term food depriva
tion, parasitic infections, and psychosocial deprivation.
They also review results from early childhood interven
tions, including nutritional supplementation and psycho
logical stimulation, as well as interventions in later child
hood, including school feeding and deworming pro
grammes.
Although no formal consensus statement of the workshop
was issued, the technical editor, Sally GranthamMcGregor, summarises the main findings of the workshop
in an appendix. With respect to school-age children,
these include the following:
0
0
0
0
0
There is now reasonably strong evidence to support a
detrimental effect of undernutrition on school-age chil
dren's development.
The effects of iodine deficiency on the cognitive
development of school-aged children is equivocal and
more data is needed.
High risk school-aged children benefit from iron
supplementation and school feeding programmes.
New data are emerging on the interactions between
different nutritional and health conditions, such as
undernutrition and missing breakfast, or undernutrition
and parasitic infections.
Improving children’s health and nutrition while they
attend highly inadequate schools is unlikely to improve
their achievement levels, thus, health and nutrition
interventions for school-aged children should be
integrated into educational improvement programmes.
268 pp. US $36 (US$26 in developing countries). A joint publication by
the Pan American Health Organization, the Tropical Metabolism Re
search Unit of the University of the West Indies and the World Bank.
Scientific Publication No.566. Copies of this book can be ordered from
PAHO Sales and Distribution Center, P.O. Box 27, Annapolis Junction,
MD 20701-0027, USA. Tel: 1 301 617 7806 Fax: 1 301 206 9789
Email: paho@pmds.com or via the PAHO website at http://
www.paho.org
23
Zcd/J Vfur>JO.
duC V itf?
A ^dHHA^AF^AdlAA/^C/AdA’A’/^AFrP
2>/^k'^^S7<)A7^ dQ-d
On the occasion of the SCN’s 2$h Session in Oslo, Norway (26 March - 2 April, 1998), eight working groups met to discuss
scientific, policy and programmatic developments, and to develop priorities and recommendations for action. Presented
here are summaries of the discussions and decisions taken during these meetings. Full reports of each of the working
group meetings are available on request from the SCN Secretariat, c/o World Health Organization, 20 Avenue Appia,
t CH-1211 Geneva 27, Switzerland, Tel: 41 22 791 0456 Fax: 41 22 798 8891 Email: accscn@who.ch
Nutrition, Stkits ancL44umanTiigkts
Household Food. Security
There is a growing interest in a human rights approach to
food and nutrition among SCN members, attributed in part
to the UN reform process to incorporate human rights
approaches in all programme activities. This move away
from a basic needs approach means that people can not
only express their needs for, but also claim their rights to
adequate food and nutrition.
The working group heard a number of presentations on
different agencies’ approaches to household food
security as an integrated part of a larger livelihood secu
rity approach. These included a presentation of CARE's
Household Livelihood Security approach to assessment,
action and monitoring, and a presentation by FAO of the
document ‘Household Food Security and Nutrition:
The working group discussions were guided by a
document prepared by WANAHR1 entitled 'The Promotion
and Protection of the Human Right to Food and Nutrition
by ACC/SCN Members', which identifies challenges and
opportunities for the SCN in defining, adopting and
monitoring a human rights approach to food and nutrition.
Prominent among these is the need to develop an IEC
(information-education-communication) strategy on the
right to food and nutrition in close collaboration with the UN
High Commissioner for Human Rights (UNHCHR).
One of the main recommendations of this working group
was that the Symposium at the 26th Session of the ACC/
SCN in 19992 have the theme ‘The Substance and Politics
of a Human Rights Approach to Food and Nutrition Poli
cies and Programming'. This recommendation was ap
proved by the SCN.
Iodine. Deficiency Disorders (IDD)
The remarkable success by countries and the international
community in eliminating IDD has been greatly helped by
commitment and prioritisation at all levels. However, in
some countries, interest is declining and sustainability is
emerging as a major concern. In response, the working
group drew up 10 key requirements for sustainability of
programmes and urges the ACC to maintain its commit
ment to the elimination of IDD.
The working group also discussed the need to improve
coordination of databases, the relative merits of different
kits to measure iodine in salt and urine, and the issue of
IDD elimination as a human right.
Approaches and Experiences of FAO'.
The working group proposed that a workshop on
promoting household food security in Africa be organised
during 1998, and that agencies prepare brief summaries
of highlights in the household food security area, focus
ing on one or two countries with successful programmes
as examples. The working group is currently addressing
the problems of targeting household food security inter
ventions, and the operational methods required to target
such interventions.
Breastfeeding and Complementary Feeding
Seven issues were discussed by the working group:
maternity legislation, the care approach, complementary
feeding, Code implementation, the Baby-Friendly
Hospital Initiative, the economic value of breastfeeding,
and HIV and infant feeding in the context of vertical
transmission. For the latter, the urgent need for detailed
practical guidance to manage the distribution of breast
milk substitutes for use by infants of HIV-positive mothers
was stressed. This was subsequently addressed at a
WHO-UNAIDS-UNICEF technical consultation on HIV
and infant feeding (Geneva, 20-22 April 1998 - page 63).
The 1942 ILO Maternity Protection Convention No.103,
which includes the right to maternity leave, cash benefits
and medical benefits, is currently being revised and will
be presented by the ILO in the year 2000 for considera
tion. The working group reaffirmed that UNICEF and
WHO will work with ILO to ensure the protection of
breastfeeding rights of working women. Further informa
tion is available through the new WABA webpage on
'World Alliance for Nutrition and Human Rights ’The 26” Session of the SCN will be held at the office of the UNHCHR in Geneva, Switzerland, April 1999.
F6ATUK6S
Chairs and Rapporteurs for SCN Working Groups, 1998
Rapporteur(s)
Nutrition, Ethics and Human
hjgnts
Chair(s)
Urban Jonsson
(UNICEF)
Wenche Barth Eide
& Uwe Kracht
leoine Deficiency Disorders
Graeme Clugston
Frangois Celange
Household Food Security
Bia Clay (FAO)
Lawrence Haddad
(IFPRI)
Breastfeeding and
Complementary Feeding
Lida Lhotska
f UNICEF)
Felicity Savage
(WHO)
Nutrition of School Age
Children
Judith McGuire
(Wdrld Bank)
Andrew Hall (PCD)
Rita Bhatia
(UNHCR) & Anne
Ca.lanan(WFP)
Judith Appleton
(OXFAM-GB)
Nevin Scrimshaw
(UNU)
Gary Gleason
(INF) Rainer Gross
(GTZ), Fernando
Viteri (UNU) & Ray
YiptUNICEF)
Joanne Csete
Martin Bloem (HKI)
Working Group
.•r-i’-r-n nf PsfftrasQ anri
displaced People
Vitamin A Deficiency
breastfeeding rights of women at http://www.elogica.com.
br/waba/working.htm
Nutrition of Sekool-Clge CklMren (see page 3)
Recent data suggest that nutritional problems in school
age children may be greater and more widespread than
previously thought. There are a number of activities aimed
at improving the nutritional status of school-aged children,
including school feeding programmes, school health and
nutrition programmes (micronutrient provision, deworm
ing, nutrition eduction and first aid), HIV prevention pro
grammes, and water and sanitation projects.
The working group made three main recommendations.
Firstly, more data on the nutritional status of schoolchil
dren are needed; secondly, the reference values on
growth and anaemia need to be reviewed; and thirdly,
there is a need to identify examples of good practices and
success stories.
Nutrition of "Refugees and D is placed "People
Thu Oxfam report ‘Acceptability and Use of Cereal-Based
Foods in Refugee Camps' (see page 39) was presented.
It was agreed that as a follow-up, plans to hold a meeting
to discuss levels of micronutrient fortification in blended
foods will be explored.
Panel discussions on 'How Food Aid Works' reflected
perspectives and constraints for providing food aid by
ICRC, WFP, USAID and CIDA. The working group agreed
to continue discussions on appropriate indicators for
assessment of needs and impacts, and to better under
stand the processes of emergency food aid provision.
Iron Deficiency Control
Iron deficiency and iron deficiency anaemia has conse
quences for cognition, resistance to infection, physical
performance, metabolic impairments, morbidity and mor
tality. The working group recommended that govern
ments, agencies and NGOs use an integrated strategy to
reduce iron deficiency in combination with other micronutient deficiencies (e.g., vitamin A deficiency), based on a
life cycle approach and focusing mainly on preventive
measures. An integrated strategy should include a com
bination of dietary approaches, fortification of appropriate
foods and supplementation of the most vulnerable
groups. It was stressed that the focus of supplementation
during pregnancy should be expanded to include young
children (because of its impact on cognitive development)
and non-pregnant women (so that women enter preg
nancy with sufficient iron stores).
It was also recommended that iron deficiency prevention
programmes be linked with related health programmes
such as breastfeeding promotion, prevention of other
nutritional deficiencies, reproductive health and mea
sures to control infectious diseases - especially malaria
and intestinal helminth infections.
Vitamin Cl Deficiency
The number of young children with sub-clinical vitamin A
deficiency has been estimated by WHO/UNICEF and
reported in the WHO/UNICEF MDIS report (1995). How
ever, the working group expressed caution in citing the
figure because of methodological difficulties, and recom
mended that WHO and UNICEF use a new method to
update the prevalence and numbers.
The discussions of the working group covered a number
of issues, including a presentation of the Bangladesh
national vitamin A deficiency survey (in which access to
home gardens was shown to play a role in addition to
supplementation in reducing vitamin A deficiency), a
presentation of the Nepal study on supplementation dur
ing pregnancy and maternal mortality (see SCN News
No.15 p27) and a discussion of the near-crisis in
Guatemala whereby the government considered revoking
a law to fortify sugar with vitamin A.
A new initiative (the Global Vitamin A Initiative, supported
by UNICEF, USAID, Ml and CIDA) to accelerate progress
towards the elimination of vitamin A deficiency as a public
health problem was also presented to the working group.
g&j fJ£U€ kjo. i6, juc y mt
AH^T^AATA FfZdFl THE QfrlPdQAFl
CHALLENGES FOR THE 21st CENTURY:
A GENDER PERSPECTIVE ON
NUTRITION THROUGH THE LIFE CYCLE
The Symposium on Challenges for the 21st Century: 'A Gender Perspective on Nutrition through the Life Cycle’ took
place on 30-31 March 1998 during the SCN’s 25th Session in Oslo, Norway. Following the opening address by Richard
Jolly, SON Chairman, the Minister of International Development and Human Rights in Norway, Hilde Johnson, welcomed
participants to Norway. IVe were delighted that Dr Gro Harlem Brundtland presented the keynote address on ’Food,
Nutrition and Health in a Global Perspective’.
■
■
The Symposium was chaired by Kaare Norum, Director and Professor at the Institute for Nutrition Research, Oslo,
Norway. Presented here are the abstracted the presentations, including the abstract of the 1998 Abraham Horwitz
Lecture, 'Breastfeeding: From Biology to. Policy’ by Isatou Semega-Janneh.
The report of the proceedings of the Symposium are expected to be published in October and will be available from the
SON Secretariat, c/o World Health Organization, 20 Avenue Appia, CH-1211 Geneva 27, Switzerland. Tel: 41 22 791
0456 Fax: 4122 798 8891 Email: accscn@who.ch Details of all SCN publications are regularly updated on pur website:
i http://www.unsystem.org/accscn/
i
■
i
THE GLOBAL NUTRITION CHALLENGE IN THE MILLENNIUM:
PRESENTATION OF THE MAIN REPORT
by Philip James
(Commission Chair and Panel of Commission Members)
Rowett Research Institute. Scotland
Following the ACC/SCN meeting in Kathmandu in 1997, a
Commission was established to consider the need for new
initiatives, particularly in relation to the persistent burden of
childhood protein-energy malnutrition. The contributions
of UN and other international agencies to this endeavour
were seen as the crucial components of any new plan. A
reassessment of global trends in health has revealed that
a range of issues needs to be tackled in a new coordi
nated way if the plea for the human right to health is to be
converted into action. A preliminary perspective will be
presented.
NUTRITION CHALLENGES AND GENDER IN ASIA
by Suttilak Smitasiri
Institute of Nutrition, Mahidol University, Thailand
Though science has increased knowledge leading to the
improvement of nutrition in the past fifty years, recent
reports indicate that malnutrition is still a contributory factor
to half of the deaths of our children today. In Asia, during
this same period, there have been many successful nutri
tion interventions which have demonstrably changed nutri
tion situations. Prevalence and numbers of malnutrition in
the populations in general, are going down but progress
26
among countries and different areas within countries are
often uneven. South Asia, for example, still has the
world's highest prevalence of childhood malnutrition and
some countries in South East Asia still have widespread
problems. Moreover, the recent Asian economic crisis
will undoubtedly challenge all nutrition workers as to how
to improve or maintain nutrition situations in the region.
FEATURES
Thailand is an Asian country which has made good
progress nutritionally in the past twenty years. In this
paper, the author attributes Thailand's success to good
strategic thinking of leaders in the field of nutrition and
development, a determined commitment of several sec
tors, good participatory action plans, systematic monitor
ing and most importantly, an effective social mobilisation
process at all levels. Essential elements in the Thai
holistic nutritional development process which led to rapid
progress are discussed. The issue of gen
der in the development process is critical to the success
of empowering women, men, families and communities in
taking positive actions towards nutritional change. A
gender issue in the Thai context is discussed and synthe
sised. Lastly, some remedial suggestions are made
which might be helpful to other countries, particularly
those in South Asia.
ACHIEVING THE 2020 VISION, WITH SPECIAL REFERENCE TO
GENDER ISSUES
by Per Pinstrup-Andersen
International Food Policy Research Institute
Achieving good nutrition for all is within reach. However,
while business as usual is likely to reduce the number of
malnourished people, a different approach is required to
achieve universal food security and good nutrition. The
2020 Vision for Food, Agriculture, and the Environment is
a world where every person has access to sufficient food
to sustain a healthy and productive life, where malnutrition
is absent, and where food originates from efficient, effec
tive, and low-cost food systems that are compatible with
sustainable use of natural resources.
require new or strengthened partnerships between indi
viduals, households, farmers, local communities, the pri
vate sector, NGOs, national governments, and the inter
national community. It will require a change in behaviour,
priorities and policies. And it will require strengthened
cooperation between industrial and developing countries,
as well as among developing countries. Failure to take
action will lead to persisting hunger and poverty, continu
ing degradation of natural resources, increasing conflicts
over scarce resources, and widening gaps between the
rich and poor.
The action needed to achieve the 2020 Vision falls into six
priority areas discussed in the paper. Such action will
GENDER AND NUTRITION IN THE GLOBAL BURDEN OF DISEASE, 1990 - 2020
by Alan Lopez
World Health Organization, Geneva, Switzerland
Reliable information on the causes of disease and injury in
populations, and how these patterns of ill-health are
changing, is a critical input into the formulation and evalu
ation of health policies and programmes, and for the
determination of priorities for health research and action.
Such assessments must take into account not only
causes of death, but also the impact of non-fatal outcomes
and the comparative, importance of major health hazards
or risk factors.
The Global Burden of Disease Study, which commenced
in 1992, is perhaps the first comprehensive assessment of
global health conditions, providing quantitative estimates
of premature death and disability from over 100 diseases
and injuries, and 10 major risk factors, for 8 geographical
regions of the world, by age and sex. Contributions from
death, disability and risk factors have been assessed
using a time-based metric of future potential years of life
lost or lived with a disability, namely Disability-Adjusted
Life Years, or DALYs.
In 1990, about 1.3 billion DALYs were lost as a result of
new cases of disease and injury in that year, almost 90%
of which occurred in developing regions. Of the global
total, about 52% of DALYs lost in 1990 arose from male
mortality and morbidity, compared with 48% among fe
males. The pattern of DALYs lost varied quite markedly
between the sexes. For example, at ages 15-44 years,
the leading causes of DALYs lost for women (worldwide)
2?
EcJA UEuJE AO. :c:, JULY ree>
were depression, tuberculosis, anaemia, suicide, bipolar
disorder and obstructed labour whereas for men the lead
ing causes were road traffic accidents, depression, alcohol
use, homicide, tuberculosis and war.
Of the 10 major risk'factors evaluated, malnutrition was by
far the leading contributor to DALYs worldwide, causing an
estimated 16% of the global burden of disease in 1990
(18% in developing regions), with the contributions to
disease burden being particularly evident in Sub-Saharan
Africa (33%) and India (22%).
Projections of the burden of disease were made based
on scenarios according to the degree of optimism or
pessimism about changes in the variables used to project
health status. The baseline assumptions suggest that by
2020, ischaemic heart disease will be the leading cause
of DALYs worldwide (rising from 5th place in 1990),
followed by depression (4th), road traffic accidents (9th),
stroke (6th), chronic obstructive pulmonary disease
(12th) and lower respiratory infections (1st). On current
trends, tobacco is expected to be the leading underlying
cause of death and disability worldwide in 2020, causing
more deaths (8-9 million) than AIDS, tuberculosis and
complications of childbirth combined.
AAAAF/AFl EAfZuiTS LEdTAfZE
BREASTFEEDING: FROM BIOLOGY TO POLICY
bylsatou Semega-Janneh
Department of State for Health, Social Welfare & Women's Affairs, The Gambia
The biological benefits of breastmilk and breastfeeding for
mothers and infants in both developing and industrialised
countries are well documented. Recent research findings
have demonstrated physiological, immunological, psycho
logical and economic factors in favour of exclusive breast
feeding for up to 6 months. Global trends, however, show
that exclusive breastfeeding is practiced by a minority of
mothers only. This may be attributed to a combination of
cultural, social, economic and political factors.
This paper discusses the importance of providing local
communities with adequate information about the advan
tages of breastmilk and exclusive breastfeeding and the
equally important need for public support through govern
ment commitment and encouragement. The example
given is that of the Baby Friendly Community Initiative
(BFCI), implemented by the Ministry of Health in 12 com
munities in The Gambia. It shows how communities
equipped with enough information can be motivated into
action to promote breastfeeding. It also shows the critical
role of government encouragement and support and how
positive results from field trials can be subsequently trans
lated into national policy.
In the BFCI, community members, both men and women,
were trained and certified as Village Support Groups on
Infant Feeding. Innovative ways of disseminating informa
tion were used by them to educate mothers and fathers on
maternal and infant nutrition, environmental sanitation and
personal hygiene. Evaluation of the intervention has
demonstrated that while exclusive breastfeeding was
initially practiced by none, all mothers now do so and the
term as translated into the local Mandinka language Susudiri Timaringo - is a password in all the communi
ties. The Ministry of Health has now launched exclusive
breastfeeding as a policy objective and will gradually
enable the project to go from pilot to national scale.
International commitment to breastfeeding is well
recognised in the form of declarations, strategies and
global initiatives. The paper, however, calls for more
aggressive ways for SON member agencies, through
their specialised areas of work, to further stimulate
national and local governments to view breastmilk as a
critical natural food resource that must be optimally
utilised in the best interest of the child, family and
society.
Policy options would include public and community
support to pregnant and lactating mothers and also
adequate nutrition, care and advice. Legal protection in
the form of regulated maternity leave for women in the
formal sector should be strengthened while solutions
must be sought for the majority of women working in the
informal sectors.
Finally, the potential impact of HIV/AIDS on the safety of
breastmilk and breastfeeding must be reviewed including
solutions that do not jeopardise breastfeeding of infants
everywhere.
U6IA/5 AMP
Urban Malnutrition: a Rising Policy Problem
access to poverty and malnutrition data, disaggregated into
Over the period 2000-2025, the rural population of the develop
two points in time. The data show that for 9 out of 14 countries,
the absolute number of underweight1 children in urban areas is
rural and urban areas, for a number of countries over at least
ing world is projected to increase from 2.95 billion to 3.03 billion.
Over the same period, the urban population of the developing
world is projected to double - from 2.02 billion to 4.03 billion
(United Nations Centre for Human Settlements, UNHCS, 1996).
increasing. These 9 countries constitute a large percentage of
the developing world given that they include China, Nigeria,
Egypt, and the Philippines.
While we can be sure that the number of people living in urban
For the majority of the countries studied:
areas in the developing world will increase rapidly in the next 25
0
the number of urban poor is increasing;
0
the share of the urban poor in overall poverty is increasing;
years, we do not know how many of them will be poor and
undernourished. Furthermore, we do not know whether the
0
the share of urban preschoolers in overall numbers of
0
the number of underweight preschoolers in urban areas is
underweight preschoolers is increasing; and
absolute number of urban poor and undernourished will increase
more quickly than the rural number. In other words,
O
will there be a shift of poverty and undernutrition from rural
increasing (see graph below).
to urban areas?
O
are the opportunities for (and constraints to) income gener
ation, food security and improved nutrition different for
those living in urban areas compared with those living in
rural areas?
0
Tka Locus of poverty and undernutrituyn.
appears to be changing from
rural to urban areas
what do the answers to these questions imply for policy
research and for policymaking in urban areas?
Why is more research needed on urban poverty and under
nutrition?
Research at the Food Consumption and Nutrition Division of the
Despite this upward trend in the numbers, there is surprisingly
International Food Policy Research Institute (IFPRI) has begun
little research on urban poverty, food insecurity and malnutri
to provide some answers to these questions. Newly assembled
tion. The available research is often fragmented by issue or by
data suggest that the absolute number of poor and undernour
discipline.
ished in urban areas is increasing and is accounting for a
utilise and generate rich case-study data, these studies are
growing share of overall poverty and malnutrition.
frequently limited in terms of the general conclusions that they
Moreover, while many of the studies within cities
can draw about other areas of the city or the city as a whole.
Data to analyse trends in rural/urban comparisons of poverty
The dynamics of urban poverty and the links to rural poverty
and child malnutrition, are extremely scarce. IFPRI sought assis
also have been under-researched. Finally, community, NGO,
tance from colleagues at the World Bank and WHO and gained
and municipal and national government responses to urban
Percent of all Underweight Children that
Reside in Urban Areas
'Underweight is defined as weight-for-age <-2SD below the NCHS reference median value
2<3
>JO. 16. JUL ¥ i‘‘t
poverty and malnutrition have not been systematically docu
mented and evaluated with a resulting set of best practices.
The authors argue that this closing of the rural-urban gap is a
In. 1997 approximately 30 million, acres
worldwide were planted- with
genetically modified, crops
sufficient basis to call for more research on urban poverty, food
and nutrition issues. The demand for urban food and nutrition
Environmental and safety concerns
policy research is rapidly outstripping the existing stock. Further
There are major concerns about the environmental impact and
research in this area is likely to have large payoffs in terms of
safety of genetically modified crops. One of the main environ
assessment, analysis and action.
mental concerns is the effect that the introduced genes will
Based on a forthcoming IFPRI Discussion Paper (1998), 'Growing Urban
Poverty and Undemutrition and the Urban Facts of Life: Implications for
genetically modified crops and wild-species.
have once they are released into the environment. No one
Research and Policy' by Lawrence Haddad, Marie Ruel and James
Garrett. Copies of discussion papers can be obtained from FCND,
IFPRI, 2033 K Street, N W„ Washington, D.C. 20006, USA. Tel: 1 202
862 5600 Fax: 1 202 467 4439 Email: ifpri@cgnet.com This note was
prepared by Bonnie McClafferty at the FCND, IFPRI. See also page 54
for further details about IFPRI’s recent activities in nutrition.
Data Sources: WHO Global Database on Child Growth and Malnutrition;
(WHO 1997, see page 68); UN Population Divisions Urban and Rural
Areas by sex and age: The 1992 Revision, UN 1993, and World
Urbanization Prospects: The 1994 Revision (1995).
knows the long-term consequences of interbreeding between
Nutritionally, there are questions as to whether the introduction
of a new gene could disturb metabolic pathways within the
plant such that the proportions of fats, carbohydrates and other
constituents are altered. Specifically, there is concern that the
introduction of a new gene may increase the production of
toxins in the plant, or indeed, be itself toxic.
There is also debate over the possible transfer of antibiotic
resistance genes to the gut of livestock fed with genetically
modified maize, and the possibility of eventual transfer to
humans.
Genetically-Modified Crops:
Finally, there is the issue of consumer choice.
the Social and Ethical Issues
have a right to know what they are eating and drinking. As US
Consumers
growers do not segregate genetically modified soya from
The Nuffield Council on Bioethics (UK) - an independent body
traditionally-bred soya, countries importing US soya are unable
established to consider major ethical issues arising from devel
to track which products are derived from genetically modified
opments in medicine and biology - has recently started an inquiry
crops. Within the UK, a general aim of regulations has been
into the ethical issues raised by genetically modified crops.
A
that people should have a choice about whether to consume
Working Party has been established to discuss this issue and a
genetically modified foods. Given the difficulties of separating
report will be published early in 1999.
genetically modified foods, however, labelling has become a
major issue in Europe.
Implications for developing countries
Genetically modified crops may potentially offer substantial
benefits to developing countries, such as increasing yields and
What are genetically modified crops?
in contrast to traditionally bred varieties, genetically-modified
plants have foreign or synthetic DNA inserted directly into their
cells to confer desirable characteristics such as disease resis
tance or improvement of storage or processing characteristics.
This method of genetic improvement has obvious benefits for
agriculture.
The private sector has invested heavily in this
technology, and most scientists, who have spent years develop
ing and perfecting the techniques involved, believe that such
crops are safe to grow and eat.
improving food consumption. However, it is likely that technol
ogy will continue to be directed towards the needs of rich
countries, and it is unclear whether developing countries will
have access to these new technologies.
There is also the
danger that new genetically modified products will undermine
the market for commodities from developing countries. The
United Nations Environmental Protection agency (UNEP) has
adopted non-binding guidelines for the management of the
release of genetically modified organisms'.
However, many
developing countries cannot afford to implement what some
see as essential safeguards when genetically modified crops
Genetically modified soya, maize and cotton are increasingly
enter the environment or food chain. Some have argued that
grown in the United States, and genetically modified crops are
lower safety standards are justified.
already entering the human food supply in parts of Europe. In
some areas of the world, however, these crops are being grown
in the absence of a free press and with little public awareness of
' Tzotzos, G.T. Genetically Modified Organisms.
science.
Biosafety. Wallingford, UNIDO, UNEP. CAB International, 1995.
Copies will soon be available to order from the UNEP website at
http://www.unep.org
30
A Guide to
As part of the inquiry, the Nuffield Council on Bioethics is inviting
The momentum for a new global drive for nutrition has perhaps
comments on the development of genetically modified crops and
never been greater, underpinned as it is by the message from
the implications for consumers, the environment and the current
the UN Secretary-General Mr. Kofi Annan in his proposal for UN
regulatory framework. The Council would also like to hear views
reform launched in 1997, that human rights shall resume a
on the way in which ethical issues are being approached, now
central place throughout the work of all United Nations agen
and in the future.
cies, programmes and funds. Also, the celebration of the 50th
anniversary of the Universal Declaration on Human Rights this
Please send your comments to: Dr Sandy Thomas, Secretary to the
Working Party on the Genetic Modification of Crops, Nuffield Council on
Bioethics. 28 Bedford Square, London WC1B 3EG, UK. Tel: 44 171
631 0566 Fax: 44 171 323 4877 Email: ncob@cableinetco.uk by
August 31st 1998. As the Council may publish some of the views
expressed, please make it clear if you wish your response to be treated
in confidence. Further information can be found in the consultation
document 'Genetically Modified Crops: the Social and Ethical Issues',
available on the web at http://www.shef.ac.uk/~doe/ or from the Nuffield
Council on Bioethics
year has put into focus the human rights movement and its
linkages to peace and economic and social development as the
two other fundamentals of the UN Charter.
Specifically, the offer by the UN High Commissioner for Human
Rights to host the 26tn ACC-SCN Session in Geneva on April
12-151999, is a sign that nutrition may in the future figure much
more centrally on the UN agenda at large. It is now up to the
SCN and its participants to become better informed about the
human rights system and the challenges it offers to the UN, to
Source: The Nuffield Council on Bioethics consultation document
‘Genetically Modified Crops: the Social and Ethical Issues', April 1998.
member countries, and to civil society in partnership for a move
that may make a difference. The 26“'SCN Session in 1999 wili
provide an opportunity for advancing understanding through its
symposium ‘The substance and politics of a human rights
Human Rights and Nutrition in the SCN
The 25“’ Session of the ACC-SCN saw a breakthrough in the
recognition of linkages between nutrition as a development goal
and nutrition as a human right. Over the last two SCN sessions Ghana (1996) and Kathmandu (1997) - there has been increas
ing recognition of the international human rights system as a
hitherto unexplored opportunity for strengthening nutrition analy
sis and advocacy, and for strengthening action towards sustain
able access for all to adequate food and nutritional well-being.
A human rights approach can embrace broad nutrition policy
issues and give added support to ongoing and future nutrition
relevant programmes. The advantages of using the human
approach to food and nutrition policies and programming ".
which will take place on April 12,1999.
By Wenche Barth Eide (Institute for Nutrition Research / School of
Nutrition, University of Oslo, P.O. Box 1046 Blindern, 0316 Oslo,
Norway. Tel: 47 22 85 1375 Fax: 47 22 85 1376 Email:
w.b.eide@basalmed.uio.no ) and Uwe Kracht (World Alliance for Nutri
tion and Human Rights (WANAHR), Viale delle Medaglie d'Oro 415,
00136, Rome, Italy
Tel/Fax: 39 06 35 40 9595
Email:
kracht@flashnet it), rapporteurs for the SCN Working Group on Nutri
tion, Ethics and Human Rights. See also page 24. The background
document provided by this Working Group ‘The Promotion and Protec
tion of the Human Right to Food and Nutrition by ACC-SCN Member
Agencies: Obligations and Opportunities', is available by email from
Wenche Barth Eide (address above).
rights system of internationally agreed legally-based norms,
institutions and procedures to strengthen the cause of ending
hunger and malnutrition, is becoming better understood by the
nutrition community.
There is also a growing recognition that the nutrition community
itself can, through the SCN mechanism, play an important role in
strengthening the work of the United Nations in promoting eco
nomic, social and cultural rights and in particular, the right to
food and nutrition. The contributions by SCN participants include
the provision of data, the documentation of experiences from
efforts that do or do not work, and the dissemination of a
comprehensive understanding of the linkages between nutrition
goals and other development.goals. This would improve the
content of the obligatory periodic reports by member states (that
have ratified the human rights conventions relevant to food and
nutrition), and enhance the analysis by expert treaty bodies,
notably the Committee on Economic, Social and Cultural Rights
(CESCR) which has a Secretariat at the UNHCHR office in
Geneva.
A Multinutrient Package for
Tea Plantation Workers for Better Health,
Productivity and Profitability
Results from a study to evaluate the effects of micronutrient
supplementation on tea plantation workers and their families in
India have demonstrated a significant, positive impact on the
workers' health and productivity.
Initiated in 1996, the study
was conducted in the plantation district of Chikmagalur, Kar
nataka State, South India - a district with endemic iodine
deficiency disorders (IDD), and high prevalences of iron defi
ciency anaemia and vitamin A deficiency (VAD). The overall
objective of the project was to intervene for nine months with a
multinutrient package of supplemental iron (240mg ferrous
sulphate twice a week), vitamin A (1600 IU once a week) and
iodised salt (30ppm for daily cooking in the household), and to
evaluate the effects of this intervention on the health, productiv
ity and profitability of the workforce and their families.
77
QjkJ
>JO. 16, JUL Y
Breastfeeding Promotion:
A Cost Effective Intervention
Investing in breastfeeding promotion is among the most costeffective interventions for child survival, equal to conventional
practices such as immunisations and vitamin A supplementa
tion, and surpassing oral rehydration therapy. This is the main
conclusion from the Breastfeeding Cost-Effectiveness Study,
conducted in Brazil, Honduras, and Mexico, initiated in 1992.
The aim of the study was to provide comparative data on the
A tea plantation, India. (T. Gopaldas)
cost-effectiveness of breastfeeding promotion. To determine
the impact of the breastfeeding promotion programmes, preva
The workers were responsible for dosing themselves and their
family members.
A simple IEC (information - education -
lences and rates of exclusive breastfeeding were compared for
two groups of women:
communication) sheet on the dosing regimen and benefits was
developed in the local Kannada language and was distributed to
the workforce at frequent intervals throughout the intervention
period.
1. those who delivered at a hospital with a breastfeeding
promotion programme;
2. those who delivered at a nearby hospital without such a
programme.
Significant improvements in the health of the workforce and their
dependents were observed: haemoglobin levels increased (from
The programme involved 17 specific breastfeeding promotion
108g/l to 121g/l in females and from 116g/l to 140g/l in males);
activities during hospitalisation for childbirth. Results showed a
clinical signs of iron deficiency, VAD and IDD were significantly
significant impact on breastfeeding (see graph below and refer
reduced (49%->11%, 19%->14% and 17% ->7%, respectively);
ences 1 and 2).
and common health problems and hospital referrals decreased.
Above all, the intervention created a feeling of being cared for,
and the majority of the workforce reported that they 'felt better’,
Breastfeeding status in programme and control
hospitals
‘ate more’ and felt less tired’. Marked improvements in worker
productivity were also observed with an increase in the average
amount of tea plucked (and hence increased income) over the
intervention period.
The total number of pluckers employed
decreased over the intervention period. The analysis of prof
itability showed that the total cost of the micronutrient package
(Rs 43,050, or Rs 61.5 (about US$1.5) per worker + family per
annum) was recovered in the cost of labour saved (Rs 111,800).
India is the largest producer of tea in the world, accounting for
nearly 30% of the global production of tea. The tea industry in
India is unique in that it employs 40-50% women workers. The
workforce live on the plantations and their health and welfare are
the general responsibility of the estate’s management.
This
project, funded by OMNI-ILSI, was jointly planned and imple
mented by Tara Consultancy Services and the management of
To determine costs, each hospital programme was described in
terms of activities undertaken for breastfeeding promotion. The
nature and level of resources (personnel, facilities and materi
als) associated with each activity were then determined and the
direct institutional costs and savings of breastfeeding promotion
the tea estate, and used the plantation's own infrastructure and
for one year were determined. Programme maintenance costs
This approach,
of recurrent activities were itemised. All resources were identi
on-going management information systems.
together with a simple intervention and the empowerment of the
fied and valued in terms of their economic or opportunity costs.
workers to take care of themselves and their families, has
A discount rate of 3% was used to calculate the annual value for
ensured the continuation (and funding) of the intervention by the
capital goods. From the profile of costs developed, the differ
management after the project ended in early 1998.
ence in incremental costs between breastfeeding promotion at
Based on the report 'A Multinutrient Package lor Tea Plantation Work
ers for Better Health, Productivity and Profitability, by Tara Gopaldas
and Sunder Gujral. Tara Consultancy Services, Bangalore, India, 1998.
For further information and a copy of the report, please contact Profes
sor Tara Gopaldas, Director, Tara Consultancy Services, ‘Saraswati’,
124/B, Varthur road, Nagavarapalya, Bangalore - 560 093, India. Tel:
91 80 5242999 Fax: 91 80 5288098.
72’
the programme and control hospitals, incremental savings per
birth, and net incremental costs per birth was obtained.
Cost-effectiveness was calculated by determining the reduction
in risk of diarrhoea and acute respiratory infection (ARI) from
hospital differences in the prevalence of exclusive and partial
breastfeeding. Mortality effects of differences in these breast-
comprehensive support and educa
tional activities for mothers is to miss
out on an extremely cost-effective
health investment. As the results from
this
study
show,
hospital-based
breastfeeding promotion results In
dramatic improvements in the dura
tion of exclusive breastfeeding and is
also one of the most cost-effective
interventions available to improve in
fant and child health.
References:
1.
Perez-Escamilla R, Letter CK, Segall,
AM, Rivera A, Trevino-Siller S, Sanghvi T.
(1995) Exclusive breastfeeding duration is
associated with attitudinal, socioeconomic
and biocultural determinants in three Latin
American countries. J Nutr, 125 2972-2984.
feeding practices were derived by using relative risks for mortal
ity for diarrhoea and ARI previously reported (3). Demographic
and Health Survey data were used to make assumptions about
baseline prevalences of diarrhoea and ARI in infants less than
six months of age, and hence the number of diarrhoeal and ARI
deaths averted.
Although the Mexico programme appears to be the most costeffective (graph above), its cost-effectiveness stems largely
from capitalising on the savings from less use of infant formula,
2.
Lutter CK, Perez-Escamilla R, Segall A, Sanghvi T, Teruya K,
Wickham C. (1997) The effectiveness of a hospital-based breastfeed
ing promotion programme to promote exclusive breastfeeding among
low-income women in Brazil. Am J Public Health, 87(4) 659-663.
3.
Victora CG, Vaughan JP, Lombardi C, Fuchs SMC, Gigante LP,
Smith PG, Nobre LC, Teixeira AMB, Moreira LB, Barros FC. (1987)
Evidence for protection by breast-feeding against infant deaths from
infectious diseases in Brazil. The Lancet ii 319-321.
4.
Horton S, Sanghvi T, Phillips M, Fiedler J, Perez-Escamilla R, Lutter
C. Rivera A and Segall-Correa A. (1996) Breastfeeding and priority
setting in health. Health Policy and Planning 11(2) 156-168.
which was not the case in Brazil and Honduras. Given the low
rate of coverage and the extremely short duration of exclusive
breastfeeding, Mexico is an example of a programme in which
objectives of coverage and effects are not being met and for
which additional investments are needed.
The range of cost-effectiveness estimates obtained in this
analysis provides an indication of expected values in different
programme and policy contexts (graph above).
When com
By Chessa Lutter, Regional Advisor, Food and Nutrition Program, Pan
American Health Organization, 525 Twenty-third Street, N.W., Wash
ington, D.C. 20037-2895, USA. Tel: 1 202 974 3871 Fax: 1 202 974
3682 Email: lutterch@paho.org This study was supported by the US
Agency for International Development under the Latin American and
Caribbean/Health and Nutrition Sustainability Project contract to Uni
versity Research Corporation (LAC-0657-C-00-0051) and subcontract
to International Science and Technology Institute (90/01/3700). The
study director was Dr. Tina Sanghvi.
pared to the interventions to control diarrhoea, breastfeeding
promotion in all three countries compared favorably with ro
tavirus and measles immunisation. When breastfeeding pro
Breastfeeding Promotion:
motion includes a shift from formula to almost no formula
The Haitian Experience
feeding, as in the case of Mexico, its cost-effectiveness is
comparable to other health interventions, including iodisation of
salt ($5 per DALY gained), vitamin A supplementation ($9), or
short course chemotherapy for tuberculosis ($3).
However,
even after savings that result from the elimination of formula
have been fully exploited and no longer can be used to offset
As the 1991-94 political crisis wore on in Haiti, women were
forced to spend more time away from home in an effort to
provide for their family’s survival. As a result, exclusive breast
feeding for three months plummeted from 13% in 1987 to 3% in
1995(1,2).
other costs, as in the case of Brazil and Honduras, breastfeed
ing promotion still remains a highly attractive intervention, simi
In response, the breastfeeding promotion programme started in
lar to the Expanded Programme on Immunisation Plus and
1994 with the introduction of the Baby Friendly Hospital Initia
vitamin A supplementation.
tive. This was followed by a one-year national breastfeeding
promotion campaign, launched in 1995 by the Minister of
Eliminating formula feeding and instituting ‘rooming-in’ have
been appealing options for policy makers eager to realise their
savings potential.
However, limiting breastfeeding promotion
activities to these changes without the next step of establishing
Health. A coordination committee oversaw the activities which
included:
0 wide partnership with churches, NGOs, the Haitian Medical
Association, local cooperatives, and youth organisations;
77
rJEvJSUO.iC-, JULY iggg
promotion by traditional birth attendants, priests, voodoo
0
Box 2: Lessons learned
priests, youth, community workers, and health workers;
testimonies on the values of breastfeeding by mothers
0
0
' who had successfully breastfed exclusively for six months;
The political crisis in Haiti pro
voked large-scale migration within the country, disrup
mass media support in the form of promotional materials,
0
Breastfeeding promotion can play an important role in
crisis management.
tion of many social mechanisms, breakdown of public
radio broadcasting, audiotapes with the programme jingle
health services, and a sharp deterioration of the health
and breastfeeding messages played in local taxis, and
situation.
promotional activities in local markets.
Promotion of and support for exclusive
breastfeeding for six months provided parents with
better skills to avert the threat of disease and ensure
The campaign became a national event that drew the attention
survival of their young infants.
of the press and national authorities. Momentum peaked in
1996 when both the President and the Prime Minister partici
0
The importance of community empowerment ensured
0
A chain reaction can be generated by mobilising suc
that communication efforts led to sustainable behaviour
pated in several events to celebrate the World Breastfeeding
change, which goes beyond the life of the programme.
Week.
The breastfeeding promotion programme was one of the most
successful and visible social development programmes imple
cessful mothers to share their experiences with others.
0
Involving fathers and male leaders in the process of
mented in Haiti during these difficult times. Key messages on
building a breastfeeding movement is important. Their
breastfeeding had reached nearly every village.
Moreover,
proven enthusiasm and involvement in providing sup
various intervention areas throughout the country reported
port for breastfeeding gave the impression that their
dramatic increases in the rate of exclusive breastfeeding for six
indifference to child care is as much born out of igno
months from 0% to more than 50%, while cases of severe
rance and lack of capacity as it is a ‘macho’ behaviour.
diarrhoea and malnutrition declined. Factors responsible for
the success of the programme are summarised in Box 1 below.
There were problems however, and a number of lessons were
breastfeeding programme as virtually all sectors in the country
learned (Box 2, above right).
suffer from lack of national interest.
Box 1: Success factors
0
Adoption of a community-based strategy which
0
Testimonies of healthy babies as a result of exclusive
fostered wide mobilisation and participation.
breastfeeding.
0
Ease with which breastfeeding promotion integrates
into cultural ceremonies because of its association with
References
1. Cayemittes M, Chahnazarian A. Survie et sante de I'enfant en Haiti
(EMMUS-I). Port-au-Prince, Institut Haitien de I'Enfance, 1989.
2. Cayemittes M, Rival A, Barrere B, Lerebours G, Amedee Gedeon M.
Enquete mortalite, morbkiite et utilisation des services (EMMUS-II)
Haiti 1994/95. Port-au-Prince, Institut Haitien de I'Enfance; Calverton,
Macro International, Inc., 1995.
By Menno Mulder-Sibanda and Flora S. Sibanda-Mulder, do UNICEF/
WCARO, B.P. 443, Abidjan 04, Cote d'Ivoire. Tel: 225 42 32 27 Fax:
225 21 05 79 Email: mmsfssm@globeaccess.net
new life, health, happiness and love.
0
Economic hardships, which facilitated the communica
tion of messages on the economic value of breast
feeding.
The programme was engineered by a small number of highly
motivated organisers (despite efforts to engage as many peo
ple in the process as possible), and most key players have now
moved on. It has now lost momentum, although behavioural
changes have been sustainable. In addition, many institutions
and NGOs have integrated breastfeeding promotion into their
regular activities. However, the goodwill among policy-makers
and decision-makers is fading in the absence of a constant
reminder. This is of particular concern because legislation on
the marketing of breastmilk substitutes has not been adopted in
Haiti, and the protection of breastfeeding in the work place
(including markets) needs to be emphasised and promoted.
The biggest weakness in the programme is that it has not
secured national support for promotion, protection and support
of breastfeeding.
74
Unfortunately, this is not unique to the
The national breastfeeding promotion campaign year ended with a mural
painting competition in the Port-au-Prince metropolitan area. The winning
murals were compiled in a 1997 calendar that was developed to sensitise
and inform the public on the Code on the Marketing of Breast Milk
Substitutes. This picture shows one of the winning murals.
News from the World Alliance for
Breastfeeding Action
The World Alliance for Breastfeeding Action (WABA) arose out
of the 1990 Innocenti Declaration. It is a conglomerate network,
consisting of large and small networks, interested individual
organizations and interested individuals. WABA has a very flat
structure, but as a democratic entity, still has to organise respon
sibilities. WABA therefore has a Steering Committee; a small,
hard-working Secretariat in Penang led by its most able Director;
an International Advisory Council; Regional Focal Points; and
eight Task Forces.
World Breastfeeding Week, 1-7 August 1998, will have the
The Alliance makes maximum use of electronic media. Much of
theme 'Breastfeeding: the Best Investment'.
WABA's global interaction goes via cyberspace, although being
electronically literate is no prerequisite for joining the Alliance.
True to its grassroots responsibilities, WABA will always find a
way of getting messages across, be it by hand or foot, mouth,
pigeon or snail mail!
agenda in June, 1999.
There is a looming threat that the
WTO’s rules will override national legislation on worker's rights
issues. This might be counteracted if maternity protection at
work is recognised as 'core labour standards' of special impor
tance, and which will continue to be under the protection and
Breastfeeding: the best investment
jurisdiction of ILO in the future.
This year, WABA has chosen ‘Breastfeeding: the Best Invest
ment as the theme for the World Breastfeeding Week (August
The workshop finally adopted a "Quezon City Declaration"
1-7,1998). A number of economic studies reviewed in WABA's
which summarises the concerns of the WABA partners and
action folder for the 1998 World Breastfeeding Week, provide
asks for continued vigilance as well as sharing of positive
powerful arguments for advocacy efforts with governments,
experience.
health care institutions, employers, funding agencies and others.
For example, in Iran an increase in exclusive breastfeeding from
HIV and breastfeeding
10% in 1991 to 53% in 1996, saved US$50 million on the cost of
At the June meeting in the Philippines, the WABA Steering
importing of breastmilk substitutes.
Committee issued a position statement on HIV and breastfeed
ing. In brief, the WABA SC is concerned that the full economic
This year's World Breastfeeding Week materials from WABA
and health consequences of the recent WHO/UNAIDS/UNICEF
provide all the information needed to calculate some of the
policy on HIV and infant feeding have not been adequately
economic losses that artificial feeding implies. The information
analysed (see page 63). Alternatives to infant formula such as
also emphasises that breastfeeding is worth more than its cost
expressed and heat-treated human milk are listed in the policy
savings. Advocacy should begin on the basis that breastfeeding
guides, but their use has not been adequately studied and is not
is a woman's right; advocacy messages can then go on to show
explained in the same detail as is infant formula use.
that efforts to protect, support and promote breastfeeding will
yield significantly reduced costs for health care and for infant
WABA emphasises that the single most important condition that
These savings may help to reduce foreign exchange
must apply if infant formula is used systematically in high
foods.
HIV-prevalence areas is that only generic labelling of tins of
spending.
formulae be permitted. Finally, WABA recommends that the
Breastfeeding, women and work: from human rights to
creative solutions
WABA has just concluded its annual Steering Committee (SC)
meeting, which was held in Quezon City, the Philippines. Prior
to the meeting, a workshop entitled 'Breastfeeding, women and
work: from human rights to creative solutions' was held
(sponsored by SIDA).
Numerous ideas were presented and
discussed for creative solutions to the difficult situation breast
feeding mothers find themselves in when they have to combine
'mother work and other work'.
ILO is updating its Conventions concerning maternity protection
provisions - a subject that will be on their annual meeting
health workers who live with the counselling problems on a
day-to-day basis be heard and that they be given resources to
study their own situation and propose appropriate remedies.
By Elisabet Helsing, co-chair, Steering Committee, WABA. The World
Breastfeeding Week action folder, and other WABA information is
available from the WABA Secretariat, P.O. Box 1200,10850 Penang,
Malaysia. Fax: 60 4 657 26 55 Email: secr@waba.po.my Further
information about the 1998 World Breastfeeding Week, other WABA
activities and more action ideas are available on the WABA website at
http://www.elogica.com.br/waba/ The coordinator of the World Breast
feeding Week, Denise Arcoverde from Brazil, is also responsible for
bringing the Alliance into the electronic age, and can answer questions
on this (origem@elogica.com.br).
36
iJO.rC-, JULY
In Praise of Nevin
A message from Richard Jolly, on behalf of the SCN
A symposium, followed by a gala banquet, was held on June 26th 1998 at MIT Laboratory of Human Nutrition, in honour of the enduring
and broad ranging contributions made by Nevin Scrimshaw during his distinguished career. The event was held during Nevin's 80"’ year.
Richard Jolly, Chairman of the SCN, relayed the following message to Nevin during this important event.
We thank you Nevin, for your leadership and inspiration from the very beginnings of the ACC/SCN, throughout its life and to the
SCN's latest meeting a few months ago in Oslo. Way back in 1955 you helped bring to birth the Protein Advisory Group, to provide
the advice UNICEF needed for its child-focused programmes. Seven or eight years before that you had inspired Hans Singer to
write the first UN publication on economic development and children, drawing on your early research on nutrition and cognitive
development in infants and young children.
All this stretches to 50 years - yet you remain ever young in your vitality, enthusiasm and freshness of mind. So many of the good
things of the SCN have grown from your own leadership and commitment: you organised in the UNU the first SCN meeting on
nutrition and economic adjustment policy, you have been the force behind the working group on iron deficiency, endlessly pressing
for practical actions to tackle the most widespread of all micronutrient deficiencies. You have been by far the most dedicated
supporter of all the SCN's work and activities - at once forthright and practical, upright and professional and always wonderfully
generous and creative. You have made these contributions both in your own name but always carrying with you the strong
support of the UNU.
“Human progress is neither automatic nor inevitable. Even a superficial look at history reveals that no social advance rolls on the
wheels of inevitability.
Every step towards the goals of justice requires sacrifice, suffering and the tireless exertions and
passionate concern of dedicated individuals." So said Martin Luther King, of the giants who give leadership and of the ordinary
citizens who together become the force of social movements and human progress.
We thank you, Nevin, for being one of these individuals - one of the giants of nutrition as well as a committed citizen of humanity
- who has helped and succeeded to bring real and widespread advance in nutrition in so many countries over the last half century.
We thank you for your wisdom and vision - and for your boundless energy and impact in carrying vision into practical action. We
look forward to many further occasions of working with you and being inspired by your words, research, writings and ideas.
AjumiriOAj
‘KJ
£t-J£££££(£d££>
Health Intelligence Network for Advanced
WHO intends to provide such vital health data proactively for
Contingency Planning (HINAP)
decision making and planning purposes through development
of the Health Intelligence Network for Advanced Contingency
’....The Goma refugee problem pointed out that epidemiological,
nutritional, environmental, economic, and social information re
quired to effectively mobilise resources was net available in a
timely fashion...' (Professor Nancy Mock, Tulane University In:
‘Public health crisis prevention, mitigation and recovery: Linking
relief and development', March, 1996).
Planning or HINAP. An abundance of valuable information
already exists but implementing agencies such as IOM, ICRC,
UNHCR and NGOs such as MSF are obliged to contact various
sources (e.g„ different programmes and offices of WHO) for
advance planning purposes. This is not only inconvenient, but
may be impossible under emergency circumstances.
The Rwanda crisis of 1994, resulting in an estimated 50,000
deaths from cholera amongst refugees in Goma, and the subse
A core team at WHO in Geneva is working to develop an
quent repatriation of over one million refugees back to Rwanda in
information management system for those involved in complex
1997, clearly demonstrated the need for advance health informa
humanitarian emergencies with sudden population displace
tion and risk mapping for effective contingency planning. Deaths
ments. The project's major objective will be to consolidate,
from preventable diseases would be avoided if vital health data
filter, organise and redistribute background information and
were available in advance.
existing data to the right people at the right time in an easy-to-
36
UNITED NATIONS
ADMINISTRA T/VE COMMITTEE ON COORDINA TtON
SUB-COMMITTEE ON NUTRITION
Secretariat: ACC/SCN, c/o World Health Organization
20, Avenue Appia, CH-1211 Geneva 27, Switzerland
Tel: 41-22 7910456 Fax: 41-22 798 88 91 Email: accscn@who.ch
Web: http://www.unsystem.org/accscn/
(zeroers om r^e world mutRaTiOM
Third Report on the World Nutrition Situation, December 1997
Update on the Nutrition Situation 1996, November 1996
Update on the Nutrition Situation, November 1994
Second Report on the World Nutrition Situation, Volume II, Country Data, March 1993
Second Report on the World Nutrition Situation, Volume I, Global and Regional Results,
October 1992
Supplement on Methods and Statistics to the First Report on the World Nutrition Situation,
December 1988
First Report on the World Nutrition Situation, November 1987
AdLL/Zd/F ^TAr6-OF-rU6-AS.r C£/2i£5 (G&A)
policybiZcusSiOM pafsff
Nutrition and Poverty, by S. Gillespie, N. Hasan, S. Osmani, U. Jonsson, R. Islam, D. Chirmulay,
V.Vyas & R. Gross. November 1997 (SOA No.16)
How Nutrition Improves Report based on ACC/SCN Workshop held on 25-27 September 1993 at the
15th ILINS International Congress on Nutrition, Adelaide, Australia by S. Gillespie, J. Mason, R.
Martorell. (SOA No. 15)
Controlling Vitamin A Deficiency Report based on ACC/SCN Consultative Group Meeting held in
Ottawa July 1993. Prepared by Gillespie and Mason, January 1994. (SOA No.14)
Effectiveness of Vitamin A Supplementation in the Control of Young Child Morbidity and
Mortality in Developing Countries, by G.H. Beaton, R. Martorell, KJ. Aronson, B. Edmonston, G.
McCabe, A.C. Ross, B. Harvey. December 1993. (SOANo.13)
Nutritional Issues in Food Aid Report of symposium on "Nutritional Issues in Food Aid” held at the
19th Session of the ACC/SCN in Rome, February 1992. Includes papers on the support of public works
by food aid as a nutrition intervention, which age groups should be targeted for supplementary feeding,
effects of supplementary feeding in the growth of children with infection, experiences of feeding
programmes, and protecting refugees' nutrition with food aid. August 1993. (SOA No.12)
Nutrition and Population Links ■ Breastfeeding, Family Planning and Child Health. Papers from
the ACC/SCN 18th Session Symposium, held at UNFPA, New York, February 1991. Papers include
"Nutrition and Family Planning Linkages: What More Can be Done?" by Sandra Huffman,
"Reproductive Stress and Women's Nutrition by Reynaldo Martorell and Kathleen Merchant,
"Breastfeeding, Fertility and Population Growth" by Roger Short, "Nutrition and its Influence on the
Mother-Child Dyad" by Prema Ramachandran, and with final comments by Miriam Labbok, Barry
Edmonston, and Beverly Winikoff. (SOA No. 11)
Nutrition-Relevant Actions - Some Experiences from the Eighties and Lessons for the Nineties Book developed from the
original background paper for the ACC/SCN ad hoc group meeting held in London in November 1990. Proposes a
framework for the analysis of policies and programmes affecting nutrition, before reviewing experiences during the 1980s in
several countries, and moving on to consider options for improving nutrition in the 1990s. Complements and expands on
Supplement to SCN News No.7. Prepared by Stuart Gillespie and John Mason, October 1991. (SOA No. 10)
Controlling Iron Deficiency Report of ACC/SCN workshop held in Trinity College, Dublin, June 1990. Focuses on iron
supplementation and practical means of improving large-scale programmes. Also introduces fortification and diet change.
Gives information from six large-scale programmes. Prepared and edited by Gillespie, John Kevany, and John Mason,
February 1991. (SOA No. 9)
Managing Successful Nutrition Programmes Report of ACC/SCN workshop held at IUNS meeting in Korea, August 1989.
Includes reports on 16 large-scale nutrition programmes, and summary of discussions on targeting, staff issues, community
participation, management information systems, sustainability and replicability. Edited by Joan Jennings, Stuart Gillespie,
John Mason, Mahshid Lotfi and Tom Scialfa, October 1990. (SOA No. 8)
Appropriate Uses of Child Anthropometry Report based on workshop held by ACC/SCN, June 1989. Basic concepts,
uses for screening, growth monitoring, population assessment, and surveillance. Prepared and edited by G. Beaton, A.
Kelly, J. Kevany, R. Martorell, and J. Mason, December 1990. (SOA No. 7)
Women and Nutrition Background, and papers presented at SCN Symposium, held at UNICEF, New York, February
1989. Papers include "Beating the Zero Sum Game" by McGuire and Popkin, "Reflections from India and Pakistan" by
Chatterjee and Lambert, "Grameen Bank Experience" by Quanine, "Improving the Nutrition of Women in Tanzania" by
Kisanga, "Nutrition Security System at Household Level" by Bajaj, "Issues in Need of a Global Focus" by Ghassemi, October
1990. (SOA No. 6)
Malnutrition and Infection - A Review, by A. Tomkins and F. Watson, October 1989, reprinted June 1993 (SOA No. 5)
Women's Role in Food Chain Activities and their Implications for Nutrition, by Gerd Holmboe-Ottesen, Ophelia
Mascarenhas and Margareta Wandel, May 1989. (SOA No. 4)
The Prevention and Control of Iodine Deficiency Disorders, by Basil S. Hetzel, March 1988, reprinted June 1993. (SOA
No. 3)
Delivery of Oral Doses of Vitamin A to Prevent Vitamin A Deficiency and Nutritional Blindness, by Keith P. West Jr
and Alfred Sommer, June 1987, reprinted June 1993. (SOA No. 2)
- Ct periodic. review of developments in. international
nutrition, compiled from information, available to- the Q.CC/SCN,
publiskedtwiee yearly. Contains features, news and views,
programme news, and reviews of publications (Free of charge],
No.16, July 1998 - features: Nutrition of the School-aged Child; A summary of Working Group
discussions, Oslo 1998; Abstracts from the Symposium on Challenges for Challenges for the 21st Century: a Gender Per
spective on Nutrition through the Life Cycle
No.15, December 1997 - features: Effective Programmes in Africa for Improving Nutrition; the 10th Annual Matin J. Forman
Lecture: How are we doing in International Nutrition?
No. 14, July 1997 - features: The Nutrition Challenge in the 21st Century: What Role for the United Nations? Meeting the
Nutrition Challenge: A Call to Arms; Update on the Nutrition Situation, 1996; Poor Nutrition and Chronic Disease Part II;
Effective Programmes in Africa for Improving Nutrition.
No. 13, late 1995 - features: Interview with Dr A. Horwitz, SCN Chair, 1986-1995; Behavioural Change and Nutrition Pro
grammes; and Poor Nutrition and Chronic Disease Part I.
No. 12, early 1995 - features: The Role of Care in Nutrition - A Neglected Essential Ingredient; Summary of findings from
the recently published ACC/SCN "Update on the Nutrition Situation, 1994"; Specific Deficiencies Versus Growth Failure:
Type I and Type II Nutrients; and Enrichment of Food Staples Through Plant Breeding. A New Strategy for Fighting
Micronutrient Malnutrition.
No.11, mid 1994 -- features focussing on Maternal and Child Nutrition: Adolescent Growth; Prepregnancy Nutritional Status
and its Impact on Birthweight; Maternal Nutrition During Pregnancy as it Affects Infant Growth, Development and Health; The
Consequences of Iron Deficiency and Anaemia in Pregnancy on Maternal Health, the Foetus and the Infant; Impact of
Maternal Infection on Foetal Growth and Nutrition; Maternal Micronutrient Malnutrition: Effects on Breast Milk and Infant
Nutrition, and Priorities for Intervention; Vitamin A Deficiency in the Mother-Infant Dyad; Maternal Protein-Energy Malnutri
tion and Breastfeeding; and Maternal Nutritional Depletion.
No. 10, late 1993 - features: Nutrition and Food Aid, Nutrition and Human Rights, The Nutrition Transition.
No.9, mid 1993 -- Focus on Micronutrients. Features: Addressing Micronutrient Malnutrition, Micronutrient Deficiency - The
Global Situation, Effectiveness of Vitamin A Supplementation in the Control of Young Child Morbidity and Mortality in
Developing Countries, Zinc Deficiency - Is It Widespread but Under-Recognized?
No.8, late 1992 - features: Highlights of the World Nutrition Situation, Food Prices and Nutrition, Food Security and Nutrition
1971-91 - Lessons Learned and Future Priorities, Long-Term Effects of Improved Childhood Nutrition.
No.7, mid 1991 -- features: Refugees' Nutrition Crisis, Breastfeeding, Birth Spacing and Nutrition, Community-Based
Development - From a Programme Towards a Movement, Micronutrient Intakes, Incomes and Prices. Supplement: Some
Options for Improving Nutrition in the 1990s -- Reviews experience of policies and programmes, and grouping nutrition
issues, leads to identifying options as building blocks for future action.
No.6, late 1990 - features: Preventing Anaemia, Policies to Improve Nutrition - What Was Done in the 80s, Weaning Foods
-- New Uses of Traditional Methods, (out of print).
No.5, early 1990 - features: Nutrition and School Performance, Uses of Anthropometry, Malnutrition and Infection (Part II),
Flows of External Resources for Nutrition.
No.4, late 1989 - features: Update on the Nutrition Situation, Women and Nutrition, Malnutrition and Infection (Part I),
Targeted Food Subsidies, (out of print).
No.3, early 1989 - features: Does Cash Cropping Affect Nutrition?, Nutrition in Times of Disaster.
Nos. 1 and 2, March 1988 -- features: Vitamin A Deficiency, Urbanization, World Nutrition Situation, Economic adjustment
(limited number of copies remain available).
^OUNFlZV
^FUPieS
Brazil: The improvement in Child Nutritional Status in Brazil: How Did it Occur? by R. F. lunes & C. A. Monteiro.
September 1993.
Egypt Review of Trends, Policies and Programmes Affecting Nutrition and Health in Egypt (1970-1990), by H. Nassar, W.
Moussa, A. Kamel & A. Miniawi. January 1992.
India: Nutrition in India, by V. Reddy, M. Shekar, P. Rao & S. Gillespie. December 1992.
Indonesia: Economic Growth, Equity and Nutritional Improvement in Indonesia, by I. T. Soekirman, G. S. Idrus Jus'at & F.
Jalal. December 1992.
Tanzania: Nutrition-Relevant Actions in Tanzania, by F. P. Kavishe. April 1993.
Thailand: Nutrition and Health in Thailand: Trends and Actions, by Y. Kachondham, P. Winichagoon & K. Tontisirin.
December 1992.
Zimbabwe: Nutrition-Relevant Actions in Zimbabwe, by J. Tagwireyi, T. Jayne & N. Lenneiye. December 1992.
(Z6FU66E UUrgjrtoKJ iMFOfZF/FFiOM Qz'^FFM
•Report on tke nutrition situation of refugee and displaced populations.
Puhllsked every tkree montks wttk an interim, electronic, mail update.
PUBLICATIONS ORDER FORM IS OVERLEAF
UNITED NATIONS
ADM/N/STRA T/VE COMMITTEE ON COORDINA T/ON
SUB-COMMITTEE ON NUTRITION
PUBLICATIONS ORDER FORM
My full postal address is:
Name:
PLEASE PRINT CLEARLY
Address:
Please send me the following ACC/SCN reports and nutrition policy discussion papers:
[_]
[_]
[ ]
First Report on the World Nutrition Situation (1987)
Supplement on Methods and Statistics to the First Report on the World Nutrition Situation (1987)
Second Report on the World Nutrition Situation, Volume I, Global and Regional Results (October 1992)
[ 1
□
Second Report on the World Nutrition Situation, Volume II, Country Data (March 1993)
Update on the Nutrition Situation (November 1994)’
U
Update on the Nutrition Situation, 1996: Summary of Results for the Third Report on the World Nutrition Situation (Late 1996)
[J
[J
[_]
[J
[_]
[J
[_]
[_]
[_]
Third Report on the World Nutrition Situation (December 1997)
SOA No.2 Vitamin A (1987) (Reprinted 1993)’
SOA No.3 Iodine (1988) (Reprinted 1993)’
SOA No.4 Women's Role in the Food Chain (1990)’
SOA No.5 Malnutrition and Infection (1990)"
SOA No.6 Women and Nutrition (1990)’’
SOA No.7 Appropriate Uses of Child Anthropometry (1990)'
SOA No.8 Managing Successful Nutrition Programmes (1991 )"
SOA No.9 Controlling Iron Deficiency (1991)’’
[_]
[J
SOA No.10 Nutrition-Relevant Actions - Some Experiences from the Eighties and Lessons for the Nineties (1991)
SOA No.11 Nutrition and Population Links - Breastfeeding, Family Planning and Child Health (1992)’
□
[J
SOA No.12 Nutritional Issues in Food Aid (1993)
SOA No.13 Effectiveness of Vitamin A Supplementation in the Control of Young Child Morbidity and Mortality in Developing
Countries (1993)"
[_]
L]
[_j
SOA No.14 Controlling Vitamin A Deficiency (1994)’’
SOA No. 15 How Nutrition Improves (1996)’’
SOA No. 16 Nutrition and Poverty (1997)"
Please send me the following Country Case Studies
LJ
[J
Brazil, September 1993
Egypt, January 1992
LI
U
India, December 1992
Indonesia, December 1992
L]
[J
Tanzania, April 1993
Thailand, December 1992
[J Zimbabwe,
December 1992
Please send me the following Back numbers of CctiJ k)E1NS[Unfortunately, No. 4, 6 and 12 are out of print]
[J
LI
U
[J
No. land 2, March 1988
No. 3, early 1989
No. 5, early 1990
No. 7, mid 1991
L]
U
Please check this box if you would like to be placed on the mailing list for CdU kJElA/S
Please check this box if you would like to be placed on the mailing list for Refugee Nutrition Information System
LI
LI
LI
No. 8, late 1992
No. 9, mid 1993
No. 10, late 1993
[J
[J
[J
No. 11, mid 1994
No. 13, late 1995
No. 14, July 1997
Checking a box [J means you will automatically receive IhisAhese document(s) when available if you are requesting from outside Aus
tralia, Europe, Japan, New Zealand, North America. However, if requesting from within Australia, Europe, Japan, New Zealand, North
America, checking this box means you undertake to remit US$16/15~ to the ACC/SCN upon receipt of each publication.
PLEASE SEND THIS ORDER FORM TO:
ACC/SCN, do World Health Organization, 20, Avenue Appia, 1211 Geneva 27, Switzerland
Tel: 41 22 7910456 Fax: 41 22 796 8891 EMail: accscn@who.ch
Or use the order form on our website at http://www.unsystem.org/accscn/
use format (e.g., World Wide Web, regular hard copy bulletins,
CD-ROM, email, faxback, etc.).
Some of the objectives of the WFP/UNICEF collaboration are to
prevent famine-related deaths and malnutrition - including mi
cronutrient malnutrition - and to restore or provide access to
HINAP will focus on country situations where latent or low-level
health services, water supplies, sanitation and other basic
tensions have not yet attracted significant attention but could
services for families, with particular attention to unaccompanied
escalate. It could assist decision-making in order to spur preven
children. This collaboration is also intended to improve the
tative measures where possible, and contingency planning
condition of women, on the premise that strengthening opportu
where necessary. Examples of information that could be col
nities for women is a major factor in overcoming hunger and
lected for countries of origin and countries of asylum include:
poverty.
0
0
health data such as epidemic risks, incidence and preva
lence of communicable diseases and vaccination coverage,
Specifically, WFP is responsible for assessing overall food
nutritional status and country health profiles;
needs and logistics and will mobilise and provide non-food
basic ethnographic data on populations at risk of displace
items necessary for the transport, storage and distribution of
ment;
food commodities. UNICEF will be responsible for mobilising
0
capabilities of in-country NGOs and UN Agencies;
and providing non-food items (e.g., food cooking equipment,
0
description of the country’s disaster plan, if any;
emergency shelter material, soap). Food commodities will be
0
level of health professional training in the country of origin
appropriately fortified, and UNICEF will be responsible for
which may help in recruiting and training of refugee health
covering any unmet micronutrient needs through supplement
workers;
distribution or the provision of vitamin and mineral mixes.
0
logistics information such as warehouse capacity, price and
availability of fuel, air and road access and telecommunica
UNICEF, in consultation with WFP will also identify require
tions capacity;
ments for strengthening caring capacity, access to safe water,
0
local and regional laboratory capabilities;
sanitation, health services, and education. Both organisations
0
in-country production capacity for and/or availability of
will promote, protect and support breastfeeding practices in
drugs, jerry cans, cooking kits and other needed items.
emergencies.
Some initial HINAP data is expected to become available on the
Web in late 1998. The address will be http://www.who.ch/eha/
This project is supported by the US Stale Department's Bureau for
Population, Refugees and Migration (BPRM), the British Department for
International Development (DFID) and the US Centers for Disease
Control and Prevention (CDC). For further information, please contact:
Eric K. Noji, M.D., M.P.H., Senior Medical Officer and HINAP Coordina
tor, Division of Emergency & Humanitarian Action, WHO, 20 Avenue
Appia, CH-1211 Geneva 27, Switzerland. Tel: 41 22 791 2705/2754
Fax: 41 22 791 4844 Email: nojie@who.ch
For copies of the WFP/UNICEF MOU please contact Diana Populin at
WFP.Tel: 396 6513-2214 Fax: 396 6513-2817 Email: populin@wfp.org
IDPs and the Human Rights Commission
At the Sri"1 Session of the Commission on Human Rights
(Geneva, 16 March - 24 April 1998), the report ‘Further Promo
tion and Encouragement of Human Rights and Fundamental
Freedoms, Including the Programme and Methods of Work of
the Commission: Human Rights, Mass Exoduses and Displaced
Persons’was presented. The addendum to this report, 'Guiding
New UNICEF/ WFP MOU
Principles on internal Displacement', addresses the specific
needs of internally displaced people (IDPs)' worldwide by iden
A new memorandum of understanding (MOU) between UNICEF
tifying rights and guarantees relevant to their protection. The
and WFP was signed in February 1998. The MOU details the
Principles reflect and are consistent with human rights law, and
working arrangements between the two organisations with re
are intended to be a persuasive statement that should provide
spect to joint activities in emergency and rehabilitation opera
not only practical guidance, but also an instrument for public
tions. The MOU applies where WFP and UNICEF have agreed
policy education and consciousness-raising.
to work as partners in situations caused by natural or man-made
disasters where people remain in their country of origin, and
includes internally displaced people.
Specific reference to food and nutrition is made in principles 7,
10 and 18. Principle 7 sets out one of the guarantees to be met
when authorities undertake displacement after having ensured
In these situations, WFP and UNICEF provide a comprehensive
range of services to safeguard the health and nutrition of the
affected population, with an emphasis on the most vulnerable
groups. This joint approach is designed to make optimal use of
each agency's strengths. The cooperation will maximise the
efficiency of the agencies while avoiding duplication of efforts.
Internally displaced people are defined, for the purposes of these
Guiding Principles as 'persons or groups of persons who have been
forced or obliged to flee or to leave their homes or places of habitual
residence, in particular as a result of or in order to avoid the effects of
armed conflict, situations of generalised violence, violations of human
rights or natural disasters, and who have not crossed an internationally
recognised State border.' (para 2, Guiding Principles E/CN. 2/1998/53/
Add.2).
37
UGUJS MO.16, JULY uri
that no alternative courses of action exist. This is to ensure "that
ties as general free food distribution or targeted feeding of the
such displacements are effected in satisfactory conditions of
most vulnerable groups, supplementary and therapeutic feed
safety, nutrition, health and hygiene, and that members of the
ing, food-for-work/agriculture, rehabilitation and monitoring. It is
same family are not separated." (E/CN.4/1998/53/Add.2). Princi
estimated that emergency food aid reached more than 11.5
ple 10 discusses the elimination of starvation as a method of
million beneficiaries during the reporting period (data was not
Efforts are underway to
combat Principle 18 specifies that all IDPs have the right to an
available from four programmes).
adequate standard of living which, at a minimum, means safe
coordinate more closely with the ACC/SCN on monitoring
access to:
nutritional status of beneficiaries through the Refugee Nutrition
b
essential food and potable water;
0
basic shelter and housing;
0
appropriate clothing;
0
essential medical services and sanitation.
Information System.
The assessment found that significant progress was made
through new programme approaches in 1997. FFP/ER intro
duced innovative measures to meet the challenge of timely
Regarding humanitarian assistance, Principles 24-26 stipulate
food aid delivery within the context of an established system
that all humanitarian assistance be carried out in accordance
which normally take 120-150 days. These include the use of
with the principles of impartiality and without discrimination. The
USDA procurements to ensure the arrival of food grains within
primary responsibility for providing assistance rests with the
two months of the start of the procurement process, and the
national authorities - international organisations and others can
prepositioning of $5 million worth of commodities at US ports
offer their services in support of IDPs. Assistance will not be
for immediate loading in case of a sudden-onset emergency.
diverted, in particular for military or political reasons, and persons
This has been used successfully to meet El-Nirio emergency
engaged in humanitarian assistance shall be respected and
food aid needs in Sudan, Somalia and Central America. Other
protected from attack or other acts of violence.
Source: ‘Further Promotion and Encouragement of Human Rights and
Fundamental Freedoms, Including the Programme and Methods of Work
of the Commission: Human Rights, Mass Exoduses and Displaced
Persons', Report of the Representative of the Secretary-General, Mr
Francis Deng, submitted pursuant to Commission on Human Rights
resolution 1997/39, and Addendum, 'Guiding Principles on Internal
Displacmenf. (E/CN:4/1998/53, E/CN.2/1998/53/Add.2, Resolution
1998/50). Both documents are available on the UNHCHR website at
http://www.unhchr.ch/html/menu4/chrrep/98chr53.htm and http://
www.unhchr.ch/html/menu4/chrrep/98chr53a2.htm, respectively, or from
High Commissioner for Human Rights/Centre for Human Rights, Palais
des Nations 8-14, Avenue de la Paix 1211, Geneva 10, Switzerland. Or,
High Commissioner for Human Rights/Centre for Human Rights, United
Nations New York, NY 10017, USA.
measures are a two-year planning for long-term or complex
emergencies with funding requirements reviewed annually
against needs. This will enable implementing partners to better
address ‘transition’ and longer-term issues like rehabilitation,
improving the programme planning and approval process by
introducing a proposal guideline and checklist, and a new
standardised grant document.
Accomplishments and lessons learned are illustrated by coun
try case studies and data on various performance indicators,
Expected “results” of the R4 process include:
0
populations;
delivery of food aid target groups on schedule;
0
improved planning and implementation from relief activi
ties to development, including specific attention to avoid
USAID’s Results Review and
Resource Request (R4) process
As part of USAID's' management-for-results efforts, the Food
For Peace/Emergency Division (FFP/ER) is monitoring progress
in achieving its objective of meeting the critical food needs of
targeted groups in emergencies. This is done through its Results
Review and Resource Request (R4) process which assesses
factors affecting programme performance and summarises
progress made during the fiscal year. Thirty-five programmes
improved targeting of food aid to the most vulnerable
o
the negative impacts of food aid in programme design and
implementation (‘do no harm’);
0
strengthened capabilities of cooperating sponsors and
host country entities to manage emergency food aid.
For further information on USAID's Food for Peace Emergency Pro
grams, please contact: David Garms, Emergency Division, Office of
Food for Peace, USAID, 1300 Pennsylvania Avenue, Washington DC
20523, USA. Tel: 1 202-712-5834 Fax: 1 202-216-3039 Email:
dgarms@usaid.gov
implemented by the WFP, private voluntary organisations and
government agencies in 24 countries, primarily in Africa, were
included in the review process in 1997.
Most programmes assessed (76%) in the 1997 review were
responding to complex emergencies, and undertook such activi'USAID's Office of Food for Peace, Emergency Division (FFP/ER),
administers the U.S.Govemment's P.L 480 Title II emergency food aid.
Title II development activities related to food security with a primary
focus on household nutrition and agricultural productivity are under
taken by the Development Division.
Vitamin C Fortification of Food Aid
Commodities: Final Report (1997)
institute of Medicine
Over the last five years, there has been considerable interest in
micronutrient fortification of rations provided in international
food relief programmes.
In 1995, a pilot programme was
initiated by USAID to increase the vitamin C content of corn-soy
blend (CSB) and wheat-soy blend (WSB) from 40mg/100g to
ability of fortified blended foods, and the feasibility of cereal
90-100mg/100g (see also SCN News No. 15 p36-7).
fortification at the local level in three refugee situations (Nepal,
Ethiopia and Tanzania).
This new report reviews and evaluates the pilot programme,
determines the cost-effectiveness of scaling up vitamin C fortifi
The report was presented and discussed at the meeting of the
cation, makes recommendations concerning the advisability of
SCN Working Group on the Nutrition of Refugees and Dis
placed People during the ACC/SCN’s 25lh Session in Oslo,
increasing vitamin C fortification and discusses alternative mech
anisms for providing vitamin C to refugee populations at risk for
1998. The following is taken from the Working Group report1.
vitamin C deficiency.
The nutritional situation and nutritional content of the rations for
Scurvy outbreaks have been reported among refugee popula
each of the three sites are included in the report to give
tions who are wholly dependent on emergency relief rations.
background and context. Summaries of preferences at each
With the exception of a mild recurring scurvy outbreak among
site between items provided in the ration are described.
In
Bhutanese refugees in Nepal, all other outbreaks in the past two
addition, preferences among ration and non-ration food items
decades have been among refugee camps in the Greater Horn
are included.
Differences in preferences were found to be
of Africa (Ethiopia, Kenya, Somalia and Sudan). As only about
related to differences in age of the consumer, potential for sale,
7% of all US-supplied fortified blended foods is designated for
familiarity of food type, cooking time required, cooking methods
use in these countries, the Committee concluded that the costs
and type of meal.
The study also conducted a preliminary
of increasing vitamin C levels in all (100%) US-supplied fortified
assessment of the opportunities for fortification of cereals at
blended foods could not be justified, and suggested alternative
different levels (household, camp, regional, national).
approaches for the prevention of scurvy. These include provid
ing vitamin C-containing foods (such as locally available fruits or
The main findings of the report are as follows.
vegetables, or tomato paste) as part of the emergency ration
0
to long-term commitment to this by donors, and consider
tion of commodities in the country or region where the emer
able technical and management expertise.
gency is occurring. Specifically, the report recommends that:
0
0
0
ate where the distributed staple grain is acceptable and
food aid commodities should not be increased;
consumed in milled form rather than as whole grain.
health surveillance systems in refugee camps should be
0
the uniformity of the vitamin and mineral fortificant through
Household-level fortification of cereals during pounding or
grinding did not appear to be feasible. However, a fortifica
populations at risk should be targeted with appropriate
tion powder (premix) could be added to family meals
vitamin C interventions;
0
Camp-level fortification of cereals would be most appropri
the level of vitamin C fortification of US-supplied blended
strengthened to monitor populations at risk of scurvy;
0
Regional-level fortification of cereals would require ade
quate milling capacity close to the population, a medium-
package, increasing access to local markets, and local fortifica
during cooking.
0
out the blended foods should be improved.
The evidence suggested that selecting a food vehicle for
fortification should be context-specific.
Factors that need
to be assessed include: familiarity and food, resale and
100pp. US $15 (in the US); US $18 (international). Copies are available
from the National Academy Press, 2101 Constitution Avenue, N.W., Box
285, Washington, DC 20055, USA. There is a 20% discount when
placing orders through the National Academy Press Web online book
store (http://www.nap.edu). The report is also available to download
free of charge from the same website.
cultural value.
0
No evidence emerged of rejection on cultural grounds of
any of the blended foods investigated. In general, where
blended foods were familiar, they were accepted, however
unfamiliarity did not indicate low acceptability. The report
highlights some technical and operational issues of quality
control and timely supply of local products.
Acceptability and use of Cereal-based Foods
in Refugee Camps (1998)
An Oxfam Working Paper by Catherine Mears
with Helen Young
135pp. UK12.95; US $18.95 Available from Oxfam, c/o BEBC, PO
Box 1496, Parkstone, Dorset BH12 3YD, UK or in the USA, from
Oxfam, c/o Humanities Press, 165 First Avenue, Atlantic Highlands, NJ
07716-1289.
Episodes of scurvy, pellagra, and beriberi among refugees
during the 1980s were a startling reminder of the inadequacies
and failures of the international humanitarian response. Fortifi
cation of the cereal staple and the provision of a fortified blended
food are key strategies identified for prevention of micronutrient
1 A full report of the Working Group meeting (see also page 25) is
malnutrition in refugee settings. This report publishes the find
available from the SCN Secretariat, c/o WHO, 20 Avenue Appia,
CH-1211 Geneva 27, Switzerland. Tel: 41 22 791 0456 Fax: 41 22
798 8891 Email: accscn@who.ch
ings of a study, conducted by OXFAM-GB and funded by Ml
through CIDA, and UNHCR, to investigate the use and accept
July mt
LeTretze
Wru.e
SPtTOZ
This section aims to encourage positive discussion and debate about current issues in the field of
international nutrition, including reponses to articles published in SCN News.
Your letters and comments would be most welcome.
Dear Editor,
We have read with interest the edited version published in SCN
sources, improved access to good quality and safe food, and
News No. 15 of the Forman Memorial Lecture on 'How are we
better overall development and improved incomes and employ
doing in international nutrition' which was delivered by F. James
ment. This FAO work is essential to the programmes of all
Levinson at the recent IVACG Meeting in Cairo.
countries in attacking the basic causes of hunger and malnutri
Mr. Levinson
based his lecture on a questionnaire sent to persons he selected.
tion.,
None of these questionnaires were apparently sent to anyone at
FAO or WHO, despite our work to provide member countries
Mr. Levinson's paper includes a ranking of a list of entities
worldwide with authoritative normative information and policy
working in nutrition on the basis of his questionnaire.
The list
guidance needed for better nutrition, food, agriculture and health
in itself is curious since it omits several ACC/SCN members
programmes and our daily work with involved government agen
with broad or specific interests in nutrition, such as UNESCO,
cies, the international community, academia, NGOs and others
IFAD, IAEA, UNHCR, the World Food Programme, UNFPA and
involved in nutrition improvement activities.
UNDP. Although FAO has been working on international nutri
tion and nutrition improvement for more than 50 years, we note
Although his lecture is concerned with international nutrition, Mr.
that we have finished last in the questionnaire results which
Levinson does not mention the FAO/WHO sponsored December
indicates somewhat of a bias among those polled and a definite
1992 International Conference on Nutrition (ICN). The ICN was
failure to appreciate the critical nature of access to adequate
attended by over 2,000 persons interested in nutrition with
supplies of good quality and safe food as the first and foremost
delegations from 159 countries and was the first and only inter
requisite for good nutrition.
national and inter-governmental conference on nutrition.
The
ICN took a broad approach to nutritional improvement and its
Certainly the ICN brought the topic of improved nutrition and
recommendations call for action in a coordinated and coopera
reduction of malnutrition to centre stage and prepared a very
tive manner by all concerned. In addition, the ICN recommenda
clear plan of action showing all the things that need to be done.
tions were fully endorsed and incorporated into the 1996 World
The heads of state and government and high level ministers
Food Summit Declaration and Plan of Action.
from 180 countries who attended the World Food Summit
renewed the commitment of all countries to ICN goals and
FAO and WHO have worked closely together, and with other
emphasised the need for access by all to adequate supplies of
interested international organisations at the global, regional and
good quality and safe foods as essential to assuring food
national level to prepare and implement ICN mandated national
security and eliminating hunger and malnutrition.
plans of action for nutrition. These ICN follow-up activities have
in international nutrition should do their best to implement all of
elevated nutrition to a much higher priority in many countries.
its recommendations and work together on the basis of our
This has attracted significant levels of government and other
different mandates to cooperatively address all of the ICN
resources for preparing and implementing effective policies,
concerns. While there was little appreciation of FAO work over
programmes and activities devoted to better food supplies,
the years by those polled, we at FAO will continue our efforts to
household food security, improved health care and education,
implement the ICN recommendations to improve the nutritional
All involved
poverty alleviation and improved overall development. In fact, in
status of all, and to continue to do our best to actively cooper
FAO Governing Body meetings, the member governments of
ate with all.
FAO have regularly given strong support to our nutrition-related
activities, particularly in regard to our ICN follow-up work.
In
By John R. Lupien, Director, Food and Nutrition Division, FAO.
addition, FAO has over many years played a major role in
Via dalle Terme di Caracalla, 00100 Rome, Italy. Tel: 396 5705
promoting better agriculture, food supplies, gender equality in
3330 Fax: 396 5705 4593 Email: john.lupien@fao.org
agriculture, environmental protection and rational use of re
60
'
A Reaction to James Levinson’s 10th Annual Martin
Forman Memonal Lecture (SCN News No. 15), pre
sented in the form of a letter to the student 'Erica'
I propose that we - once and for all - have the courage to
separate PEM from micronutrients interventions as two com
pletely different entities, two different universes and two totally
different challenges. Only then will we avoid nutritionists run
Dear Erica,
ning away from the more difficult choices and challenges in the
You probably did not expect that a concerned question of yours
battle against (the real) malnutrition.
to Professor Jim Levinson would propel you to some notoriety,
Your question allowed Dr Levinson to go into some depth on
I am sorry, Erica, to disagree not only with the respondents, but
something that has worried us for many years, namely how we
also with Dr Levinson on the centrality of the issue of intera
are doing in international nutrition. Reading his response to you,
gency infighting. It exists, and it is a disappointment, granted.
I found much that I could identify with. But I also found things for
But it is not the main obstacle to a faster progress. The issue of
which I have a slightly different view and that would help you
a lack of commitment by governments to meaningful nutrition
even better judge what you are-planning to get involved in your
interventions was chosen as another major obstacle. But this
future career. That is why I am writing you this sequel letter.
argument has been made too often, always keeping it as a
blanket statement, almost as a slogan.
It is time we must
Judging the most important advances in nutrition in the last 10
analyse this in more depth; only then will we learn how to tackle
years, the survey respondents chose advances in reverting
it better. The frequent absence of project evaluation, also cited
micronutrient deficiencies.
Most
as a constraint, I am convinced is on purpose; this allows
nutritionists still like ‘silver bullet’ fixes, primarily because they
agencies to continue pouring money into actions that do not
But, at its roots, PEM is more
much alter the balance of power at the base of the disempower
of a political problem; it is the biological translation of a social
ment that breeds malnutrition. Further, I do agree that bureau
This came as no surprise.
move within the technical realm.
disease.
cratic problems in getting things done are a great burden.
Of the four next choices for important advances that were
Jim Levinson concludes from these responses above some
chosen, I can agree with two: greater community involvement in
thing that I cannot agree with. He says that this shows that ’the
programmes (not so much projects), and increased attention to
major negative factors faced in international nutrition are not
care practices addressing women and children. But for the other
...structural... constraints, but rather problems that the nutrition
two, I have slightly different interpretations: it is not that we now
community.... can...control’. I could not disagree more.
have a ’better understanding of the causes of malnutrition; we
major negative factors I think are indeed structural and related
have rather reached a point in which we have convinced more
to the basic causes of malnutrition. Most is ultimately a matter
people about the ’correct’ conceptual framework of the causality
of empowerment.
of malnutrition, one that considers the latter an outcome of those
sustained (and sustainable) bottom-up activism to revert mal
different levels of causality.
Further, I take exception to the
The
In the years to come, it will take a more
nutrition on the scale that is needed.
suggestion that having achieved better designs and manage
ment of nutrition interventions in the last 10 years, this has led us
to significantly better resolve the problems of PEM - design and
management are not the main constraints our nutrition interven
tions have had in the last 10 years.
The main top-to-bottom,
often palliative thrust of them has been (and still is) the main
constraint. We have not started addressing all underlying and
basic causes of malnutrition yet I was definitely surprised, Erica,
to read the next major advance chosen by respondents: 'greater
sensitivity to the importance of nutrition counselling'-, this just
shows the ethnocentric bias of the respondents.... as if
’counselling’ would solve the problems of poverty and inequity...
The respondents were also asked to rank international agen
cies in terms of how they had served the field of international
nutrition. Low rankings received by agencies we thought major
nutrition actors do not necessarily reflect them having lost their
funding or commitment to international nutrition; it rather re
flects that they probably embraced the wrong approaches to
solve malnutrition in the last 10 years (perhaps those that were
too sectoral?). Lower current funding, in my view, reflects
nothing more than one more swing of the pendulum that has
affected international nutrition funding following the fashion
swings in the thinking of the international community. (Or is it
that we have little to show for the increased funding we enjoyed
The same bias can be found when respondents chose reduced
funding as the major problem or constraint to achieving better
results in the battle against PEM. If additional funding is used for
the wrong priorities and interventions, we might as well not have
it! As pertains to available funding going more for field opera
tions than for research, this is a shift that may be pointing to the
fact that we do know what to do, we just have to apply it
in the last few years...?).
The politics of it all is at the very centre of international nutrition.
With this fait accompli, it should be clear that you cannot
escape the responsibility of taking a political stand on nutrition
yourself.
This will help you to question your own current
education, as well as all that you see out there in the job market
that is waiting for you shortly.
rationally and courageously, even against the opposition of the
powers that be.
Dr Levinson is right, Erica, when he tells you that the current
state of affairs in international nutrition ‘will pose increasing
47
Q?>J >JElj€/JO.16, JULY ifrf
frustrations' and challenges for you and your generation.
My
doubts though come from looking at how politically uninterested
country plans as one of their choices in the ’most important
advances' category.
your generation of students in America and Western Europe has
become. If you are one of them, don’t worry, you will not face
But, let me be clear. The data I presented in the lecture was a
increasing frustrations and malnutrition will continue to plague
summation of responses from a large number of individuals
this worid in the years to come.
around the world. A 50% response rate is remarkably high for
an internationally mailed questionnaire of this sort. I was able
In closing, Erica, Jim Levinson conveys to you his confidence
and optimism that our work has the ability to make a difference.
The question is which difference.
It is not a matter of an
to assure that the information was accurately analysed and
tabulated.
To say that the material is ’inaccurate’ is only to
question the judgements of the respondents.
increasing number of activities in international nutrition taking
place in developing countries; it is a matter of what kind or type
John Lupien may be correct in chiding me for excluding from
of activities. Issues of inequity are at the base of the problems at
the organisation/agency rankings a number of other UN organi
hand, and if nutrition is used as a port of entry to revert such
sations which do have some nutrition involvement. The desire
inequity I would share his optimism. But we need your upcoming
here was only to make the questionnaire manageable - as it
generation, Erica, to get the job done.
was, there were 16 organisations or groups or organisations to
rank. I took my cues on which to include from several interna
By Claudio Schuftan, MD, IPO Box 369, Hanoi, Vietnam.
Tel/
Fax: 84 4 8260780 Email: aviva@netnam.org.vn
tional colleagues and two major international figures, one each
from Africa and Asia.
I won’t try to respond to all of Claudio Schuftan’s interesting
A response by Jim Levinson...
remarks, but will comment briefly on a few. First, I think Claudio
is correct about underlying structural and political problems
which deserve more attention from the development commu
Dear Editor,
nity as a whole.
Second, I’m in complete agreement with
Claudio's contention with respect to the micronutrients/PEM
I am delighted that my Forman Lecture has generated so much
discussion. In my invitation to deliver the Lecture I was asked by
imbalance. In fact, his letter to the SCN News, which he copied
to me earlier, generated considerable correspondence and an
Dr. Horwitz to be ‘original, stimulating and even provocative’.
eventual letter from the two of us and V. Ramalingaswami
One measure of success on the last of these was the comment
which will be published in The Lancet this summer.
made by one listener who came up to me after the Lecture and
said jocularly, “I hope you have tenure!"
Claudio and I may agree to disagree on the importance of the
‘infighting’ issue which was identified by respondents as such a
As mentioned in the Lecture, I grew up with the greatest respect
major negative factor in international nutrition.
for both FAO and WHO, and continue to believe that both
mention that, since presenting the Lecture, I've been absolutely
provide important services. I utilise many of them myself on a
swamped with messages from individuals around the world
regular basis. As indicated, I am genuinely saddened to see that
confirming the insidious effect that such infighting has had on
these UN technical agencies do not elicit the same level of
our community. Several individuals even have asked that the
confidence, at least within the nutrition community that they once
issue be placed formally on the agenda of the SCN.
But I should
did. Rather than responding defensively, I would hope that these
organisations would view the Lecture as an invitation to recap
What pleases me most is that the Lecture and SCN's publica
ture that confidence.
tion of it, have served the purpose of presenting these impor
I should correct a few factual errors in the letters. First, re John
consideration.
tant issues to the nutrition community at large for our common
Lupien’s comment about the questionnaire, it was, in fact, sent to
a considerable number of FAO and WHO officials, John included.
By Jim Levinson, Director, International Food and Nutrition
Many of these persons have acknowledged to me personally
Center, School of Nutrition Science and Policy. Tufts Univer
both that they received it. and that they completed and returned
sity, Medford MA. 02155, USA.
it. Additionally, rather than ignoring the FAO/WHO sponsored
Fax: 1 617 627 3887 Email: jlevinson@emerald.tufts.edu
International Conference on Nutrition (ICN), I specifically in
cluded it together with the development of country plans of action
on a list from which respondents were invited to select the four
most important advances in international nutrition over the past
10 years. Nineteen percent of respondents included the ICN and
62
Tel: 1 617 627 3223 x2284
I feel that Werner and Sander's arguments would have been
better supported with more focus on issues such as abuse of
Claudio Schuftan's review of Werner and Sanders' new book
'Questioning the Solution' (SCN News No.15 p58) cannot go
medical treatment of diarrhoea (antidiarrhoeals or antibiotics),
poor motivation and supervision of health workers, etc., but
unchallenged. David Sanders kindly gave me a copy of the book
applied to ORS, I found it unconvincing because ORS has been
on his recent visit to Darwin, so I certainly bear him no malice,
one of the great successes of diarrhoeal management upon
but this book is too far from evidence-based medicine for my
which we need to build.
approval. Indeed, the science is used too selectively to justify a
political perspective. Many important claims are made with no
References:
data to support them. In the end, it is political rhetoric instead of
1.
Morales E. Craig LD, MacLean WC, Jr. (1991) Dietary management
of malnourished children with a new enteral feeding. J. Am, Diet.
Assoc. 91(10) 1233-8.
2.
Nichols BL, Dudley MA, Nichols VN, Putman M, Avery SE, Fraley
JK, Quaroni A, Shiner M, Carrazza FR. (1997) Effects of malnutrition
on expression and activity of lactase in children. Gastroenterology
112(3)742-51.
3.
Wright EM, Hirsch JR, Loo DD, Zampighi GA. (1997) Regulation of
Na+/glucose cotransporters, J, Exp. Biol. 200(Pt 2) 287-93.
4.
Pappenheimer JR, Karnovsky ML, Maggio JE Absorption and
excretion of undegradable peptides: role of lipid solubility and net
charge (1997). J. Pharmacol Exp. Ther. 280(1) 292-300.
5.
Mazumder RN, Kabir I, Rahman MM, Khatun M, Mahalanabis D.
(1996) Absorption of macronutrients from a calorie-dense diet in mal
nourished children during acute shigellosis. J Pediatr. Gastroenterol.
Nutr. 23(1) 24-8.
6.
Northrop Clewes CA, Lunn PG, Downes RM. (1997) Lactose
maldigestion in breast-feeding Gambian infants. J Pediatr Gastroen
terol Nutr 24(3) 257-63.
7.
Brewster DR. Manary MJ, Graham SM. (1997) Case management of
kwashiorkor: an intervention project at 7 Nutritional Rehabilitation
Centres in Malawi. Eur J Clin Nutr 51 139-47.
good medicine. This is especially disappointing as a sequel to
' Where there is no doctor’, which deserved its good reputation.
The basic argument is for salt-sugar solution (SSS) which can be
made up at home instead of ORS in packets, which has been a
recurring theme of public health debate, and I am not unsympa
thetic to that argument. But there have been so few sustainable
SSS projects in which families have been shown to remember
the formula of the safe solution when children have diarrhoea
that this book’s argument is unsustainable. ORS has been an
important advance for health facilities, so it is a pity this book
appears to discredit it without making a convincing case from an
evidence perspective. However, it is true that the emphasis on
oral rehydration ignored (until recently) the importance of persis
tent diarrhoea and malnutrition. I would favour home-based
programmes under circumstances where health facilities were
inadequate, but not as a universal programme for diarrhoea, and
certainly not always instead of ORS in packets.
As a paediatrician treating children with diarrhoea, I am too
aware of the need for potassium in rehydration solutions and the
dangers of incorrect sodium concentrations in home-based solu
By David Brewster, Head of Paediatrics & Clinical Dean, North
ern Territory Clinical School, PO Box 41326, Casuarina, Dar
tions. Of course mistakes can be made with packets going into
win, Australia. Tel: 61 8 89228765 Fax: 61 8 89228286 Email:
a glass of water instead of a litre, but health facilities need to use
david.brewster@health.nt.gov.au
the best solution and that means with potassium. Of course,
empowering people to manage their children's diarrhoea without
the need for health workers is fine, but not in order to deny them
optimal treatment which is still accessible to most populations
even in very poor countries like Malawi and Zimbabwe (where I
have worked). This book does not provide any evidence that
home-based solutions are more accessible as a sustainable and
effective intervention than ORS made widely available through
all levels of health facilities. Successful home-based SSS pro
jects have needed enormous educational and promotional activi
ties, which are excellent but expensive and difficult to sustain.
Cereal-based ORS does seem to have marginal benefits in
some of the studies, but not in all. However, the nutritional
benefits do not seem to be greater than with early refeeding of
malnourished children. The work of Nichols, Lunn, Pappen-
heimer, Wright and others (see references) on the intestinal
mucosa now allow us for the first time to design appropriate diets
for malnourished children during early rehabilitation which will be
tolerated and lead to faster transition to a high energy rehabilita
tion diet and recovery. So it is improved diets rather than just
cereal-based ORS which are needed.
Corrigendum. Guiding principles for feeding infants and young chil
dren during emergencies (SCN News No.15 p. 37). Copies of the final
version of the Guiding Principles will be available for general distribu
tion only later in 1998. In addition, our footnote at the bottom of the 2”
column should have read: Editor's note: World Health Assembly resolu
tion WHA45.34 reaffirmed 'that during the first four to six months of life
no food or liquid other than breastmilk, not even water, is required to
meet the normal infant's nutritional requirements, and that from the age
of about six months infants should begin to receive a vanety of locally
available and safely prepared foods rich in energy, in addition to
breastmilk, to meet their changing nutritional requirements'. The
complementary feeding portion of this resolution was reiterated in
resolution WHA 47.5, which urged 'fostering appropriate complemen
tary feeding practices from the age of about six months, emphasising
continued breastfeeding and frequent feeding with safe and adequate
amounts of local foods'. The scientific basis for these recommenda
tions is the 1995 report of the WHO Expert Committee on 'Physical
Status: the use and interpretation of anthropometry'.
63
>JO. 76 JULY
orrery)
Troffi)
Hu
|gh
dOU(2.f?£f5, H6ZTZ7/U^5 AMD AMMC>UMC£M£MT£> jW
Dr Gro Harlem Brundtland Elected
Director General of WHO
DR GRO HARLEM BRUNDTLAND was bom in Oslo,
Norway. She studied medicine at the University of Oslo,
from which she obtained her M.D. degree in 1963.
received a Masters degree in Pubic Health from Harvard
years as medical officer at the Norwegian Directorate of
of the World Health Assembly
Health, and for 6 years as Assistant Medical Director at the
(WHA), Geneva, 11-16 May 1998.
Oslo Board of Health, Department of School Services. In
This five-year term will start on July
21a 1998. In her speech to the
Environment, a position she held for 5 years. Appointed
WHA, Dr Brundtland immediately
Prime Minister for the first time in 1981, she held this
affirmed her conviction that soci
position three times, and in total, was Head of Government
eties can be changed and that
poverty can be fought. "The chal
lenge goes to all of us. WHO can
Source: WHO website
http://ww.who.ch/
She
Dr Gro Harlem Brundtland was
elected to the post of DirectorGeneral of WHO at the 51s' Session
and must change. It must become
more effective, more accountable,
more transparent and more recep
tive to a changing world.”
University in 1965, following which she served for two
1974, Dr Gro Hariem Brundtland was appointed Minister of
for more than 10 years.
Among her numerous international positions, Dr Gro
Harlem Brundtland chaired the World Commission on Envi
ronment and Development (starting in 1983), which coined
the concept of 'sustainable development' and made recom
mendations leading to the Earth Summit in Rio de Janeiro
in 1992.
Describing the priorities and reorganisation which she intends to
start implementing "from the very first day", Dr Brundtland said
that programmes and activities will be organised around key
functions focusing on four areas of concern: communicable
Roger Shrimpton - New Chief of Nutrition,
UNICEF
diseases, non-communicable diseases, building sustainable
health systems and advocating health. Some activities will be
organised into projects.
Among the first priorities for such
projects, she proposed to “Roll Back Malaria, by developing a
new health sector-wide approach to combat the disease at
global, regional and country levels." A second priority is tobacco:
"We need to address a major cause of premature death which is
Roger Shrimpton was appointed Chief of Nutrition, Programme
Division, UNICEF, New York on 29 December 1997, following
the move of David Alnwick from Chief of Nutrition to Chief of
Health (see SCN News No. 15 p38). Prior to his appointment,
Roger served as Senior Programme Officer in Jakarta,
Indonesia.
dramatically increasing... Tobacco is a killer."
Roger joined UNICEF in 1984 as Nutrition Officer in Sao Luis,
Dr Gro Harlem Bruntland concluded her speech by saying, "I
Maranho in the North-East of Brazil.
He also served in the
envisage a world where solidarity binds the fortunate with those
Brasilia office for two years, coordinating health and nutrition
less favoured. Where our collective efforts will help roll back all
support to the North-East of Brazil.
the diseases of the poor. Where our collective efforts assure
assignment as a Research Associate with Cornell University's
universal access to compassionate and competent health care.
Food and Nutritional Policy Programme, he returned to the
Following a two-year
Bringing the world one step closer to that goal is our call for
Brasilia office in 1989 as Senior Project Officer. In 1991, Roger
action."
joined the Jakarta Indonesia office where he remained until his
transfer to New York.
In mid-June, a list of provisional organisational clusters (ten
clusters in total) placed Food Safety and the Programme for
Nutrition in the 'Health, Environmental and Sustainable Develop
ment' cluster, with Food Aid Programmes and the Division of
Child Health and Development in the 'Health Care Delivery'
cluster.
Sources: Transcript of Dr Brundtland's speech to the 51“ WHA, 1998.
WHO press release WHA/3.
44
Milla McLachlan - Nutrition Advisor
for the Human Development Network
at the World Bank
Milla McLachlan was appointed nutrition advisor for the Human
Development Network at the World Bank on June 81" 1998.
Prior to her appointment, Milla worked at the Development Bank
of Southern Africa and was chairperson of the Nutrition Society
of Southern Africa.
ship between growth retardation in rural Mexican children and
impaired intersensory integration, while an investigator in the
Children's Hospital of Mexico, provided the first convincing
evidence that malnutrition influenced learning and behaviour.
Milla has taught food and nutrition in Botswana, has lectured in
food science and adult education at the University of Stellen
bosch and was head of department at the University of Zulu land.
She has written many publications on nutrition, the most recent
of which is 'Bold Choices: Making the South African Nutrition
Strategy Work’, written with Pauline Kuzwayo
The findings, graphically presented in his famous lecture
'Children of the White Dust,' stimulated the research that has
now confirmed the relationship in dozens of studies from all
parts of the world. Variations in growth among children in
middle and upper income families bore no relationship to differ
ences in intersensory integration.
Cravioto also described the relationship between marasmickwashiorkor and reduced cognitive performance. This work
complemented the significant concurrent work of Fernando
Monckeberg in Chile showing a similar and lasting effect of
marasmus in infancy. Cravioto was a charismatic teacher who
inspired generations of paediatricians and nutritionists to under
stand and take into account the impact of malnutrition on the
physical and mental growth of children.
Rafael Flores Ayala - New Research Fellow
From 1961 to 1966 he left Mexico to serve as Associate
for the Fourth Report
Director of the Institute of Nutrition of Central America and
Panama (INCAP). While there he replicated his famous land
The SCN and 1FPRI are collaborating on the production of 'The
mark study of undernutntion in children and demonstrated his
World Nutrition Situation: Fourth Report'
To this end, Rafael
outstanding influence on students as a leader of the summer
Flores Ayala has been appointed to conduct research, analyse
course in Public Health Nutrition. He also had responsibility for
and interpret global, regional and country trends in nutrition
INCAP's relationship with its member countries to assist them in
indicators, leading to the publication of the Fourth Report in
the application it its research findings and formulation and
December 1999. Rafael will work closely with the SCN Secre
implementation of national nutrition policies.
tariat in Geneva and the Division of Food Consumption and
Upon returning to Mexico, he became the Director for the next
Nutrition at IFPRI in Washington, USA.
16 years of the National Programme for Integrated Family
Of Guatemalan origin, Rafael has worked at the Institute de
Development of the National Institute of Science and Technol
Nutrition de Centro America y Panama (INCAP) for most of his
ogy and continued active field research. At the time of his death
career. At INCAP he initially worked as a statistician, becoming
he was on the faculty of the National Institute of Human
head of the Statistical Unit in 1982. In 1993 he was appointed
Communication of the Autonomous University of Mexico still
head of the Transfer of Science and Technology Program, and
conducting research on nutrition, growth, and development.
two years later he became head of the Nutrition and Health
Program. In 1989, Rafael obtained a doctorate in public health
From 1966 to 1971, he was Director of Training in the Chil
from the Department of Biostatistics, University of California at
dren's Hospital of Mexico. He also served for several years as
Los Angeles, USA.
Assistant Director of the Applied Nutrition Division of FAO in
Rome. He was a visiting professor at Cornell University, Mas
Rafael has experience in technical cooperation activities
sachusetts Institute of Technology, and the University of Wash
throughout Central and South America.
His main interests
ington in the United States and universities in the United
include the generational effects of malnutrition and the causal
Kingdom and Sweden. He received honors and awards from
mechanism between malnutrition, infection and diet. Rafael will
many countries and was a member of 25 national and foreign
start work on the Fourth Report in August 1998.
scientific societies.
In addition to his wife Maria Cristina he is survived by a son,
Joaquin Cravioto - In Memoriam
Alejandro, and daughter, Patricia, both of whom worked with
him in his research, as well as three grandchildren. With his
Joaquin Cravioto, one of the hemisphere's pioneer paediatric
death the world has lost one of the last of the remarkable
nutritionists, died in Mexico City on April 9,1998. Born in Mexico
founders and leaders of modern paediatric nutrition.
on September 12,1933, his seminal observations of the relation
By Nevin Scrimshaw, UNU.
Oik) UEcjS iJO.iS, JULY nrt
The 8lh European Nutrition Conference
Lillehammer, Norway, 17-19 June 1999
national human rights, especially economic, social and
cultural rights;
0.
(NNS), the Federation of European Nutrition Soci
0
8
(preliminary):
0
nutrition and genetics;
0
antioxidants and nonnutrients from fruits and
and action.
Topics addressed in the course will include:
0
0
obesity in Europe;
0
the nutrition of the foetus and the young child;
0
dietary lipids and health;
0
classical micronutrients;
0
bone development and osteoporosis;
0
0
an overview of the international human rights normative
system;
the content and implementation of economic, social and
cultural rights;
vegetables;
0
enable participants to recognise the possible advantages
of a human rights approach to nutrition analysis, advocacy
eties (FENS) and the European Academy of Nutri
tional Sciences (EANS), the S"1 European Nutrition
Conference will cover the following main topics
address human rights issues as they relate to food and
nutrition;
Organised by the Norwegian Nutrition Society
0
human rights institutions, mechanisms and procedures for
promoting and monitoring food and nutrition policies and
programmes;
0
human rights standards and recommendations by major
food and nutrition policy;
0
human rights data bases and information gathering;
food safety and security.
0
communication about the right to food and nutrition as
UN development conferences;
human rights.
The conference aims to provide a inspiring forum for interactive
exchange by any group interested in food and nutrition: scien
tists, clinical nutritionalists, food technologists and producers,
policy-makers, students, health workers, dietitians, home
economists, public health nutritionalists and administrators and
journalists.
In addition to the course coordinators (Wenche Barth Eide and
Siri Damman), guest lecturers from various institutions will lead
the sessions, which may include a few intensive weekend
seminars. The course will be participatory and interactive and
a substantial amount of time will be required for individual
reading.
For further scientific information, please contact Sigrid Berge, Norwegian
Nutrition Society. Schweigaards gate 33B, N-0191 Oslo, Norway. Tel:
47 22 17 35 40 Fax: 47 22 17 35 38 Email: sigrid berge@nilf.nlh.no
The conference organiser is Trude Arnesen, P.O. Box 14, N-2601
Lillehammer, Norway. Tel: 47 61 25 17 05 Fax: 47 61 25 65 15 Email:
lillarra@sn.no Further information and requests for a second announce
ment leaflet are available on the Web at http://www.nutrition.uio.no/Nse/
8thFENS_EANS/
To be admitted to the course, the student must have a first degree in
human nutrition or equivalent documented knowledge, and a good oral
and written working knowledge of English. Participation is limited. For
further information and application forms, please contact Marius
Bergh, Study Administrator, Institute for Nutrition Research I School of
Nutrition, P.O. Box 1046, Blindern, 0316 Oslo, Norway. Tel: 47 22 85
1342 Fax: 47 22 85 13 41 Email: marius.bergh@basalmed.uio.no or
Siri Damman, course coordinator, Tel: 47 22 85 13 79 Email:
siri.damman@basalmed.iuo.no
Nutrition and Human Rights the Rights Way to Approaching Nutrition
Challenges in the Future?
A graduate/postgraduate course
Institute for Nutrition Research/School of Nutrition,
University of Oslo, Norway. 5 Oct-3 Dec 1998
International Conference on Infant and Pre
School Child Nutrition
Celebrating 50 years of the University of Ibadan
16-21 Nov 1988, Department of Human Nutrition,
University of Ibadan, Nigeria
'Everyone has the right to a standard of living adequate for the
The overall purpose of this conference is to bring together
health and well-being of himself and his family, including food,
internationally renowned scientists and practitioners to discuss
clothing, housing and medical care...” Article 25 of the Universal
current issues and future directions on infant and pre-school
Declaration of Human Rights, adopted 50 years ago by the UN
child nutrition.
General Assembly.
scientists will be encouraged to participate more actively in the
On the 50” anniversary of the Universal Declaration of Human
Rights, the Institute for Nutrition Research and School of Nutri
tion at the University of Oslo, Norway is for the second time
With an emphasis on Africa, young African
debate on appropriate strategies for reducing under five malnu
trition and mortality. The conference will also review progress
made by the State Parties in Africa to achieve the commitments
made at the 1990 World Summit for Children and the 1992ICN.
offering a two month graduate/postgraduate credit course on
Nutrition and Human Rights. The aims of the course are to:
0
4^
introduce participants to the evolution and practice of inter
Topics covered will include:
0
nutrition of the pre-term and term infant;
0
exclusive breastfeeding and maternal care;
0
indicators and the choice of indicators;
0
nutritional requirements of infants in health and disease;
0
from data to information;
0
nutritional implications of culture in infant feeding practices;
0
presentation and communication of information;
0
complementary feeding, quality and safety;
0
evaluation.
0
feeding the pre-school child.
Active participation will be emphasised through individual and
The conference will consist of a series of plenary lectures,
debates, symposia, workshops, oral and poster presentations in
simultaneous english-french translation.
To obtain a copy of the conference booklet, giving full details of the
programme, including application forms, registration forms and informa
tion about registration fees, travel and accommodation, please contact
Professor Isaac 0. Akinyele, Coordinator, International Conference on
Infant Nutrition, Department of Human Nutrition, University of Ibadan,
Ibadan, Nigeria. Tel: 234 2 810 5859 Fax: 234 2 810 5272 Email:
laolu.akinyele@skannet.com.ng or for countries other than Nigeria, Dr
Serge Treche, Directeur de Recherche, ORSTOM, Lab de Nutrition
Tropicale. Centre ORSTOM, 911 Avenue Agropolis, BP 5045, F34 032,
Montpellier, Cedex, France. Tel' 33 4 6741 6295 Fax: 33 4 6754 7800
Email: treche@mpl.orstom.fr
group work, including case studies, computer practicals and
computer-assisted learning.
This course is is jointly organised by ORSTOM (the French Research
Institute for Development through Cooperation, Nutrition Unit, WHO
collaborating center for nutrition, Montpellier, France), IMT (Institute of
Tropical Medicine, Nutrition Unit, Antwerp, Belgium) and the Interna
tional Course in Food Science and Nutrition, University of Ghent,
Belgium For more information please contact Pierre Traissac, CISN,
Montpellier 98, Laboratoire de Nutrition, Centre ORSTOM BP 5045,
34032 MONTPELLIER Cedex 01, France. Tel: 33 4 67 41 61 70 Fax:
33 4 67 54 78 00 Email: traissac@mpl.orstom.fr
IBFAN International Meeting on the Issue of
Infant Feeding in Emergency
and Relief Situations
Split, Croatia, 22-24 October 1998
2nd International Course on Nutrition
Surveillance / 2eme Cours International:
This three day international meeting, facili-
Surveillance Nutritionnelle
October 19 to November 6,1998
19 octobre ■ 6 novembre 1998, Montpellier, France
tated bylhe International Baby Food Action
Network (IBFAN), is targeted at NGOs
working in humanitarian relief, funding
agencies (governments, churches and others), UN agencies,
La surveillance nutritionnelle est un volet important des Plans
recipient communities and other interested parties.
d'action mis en oeuvre par plus de 108 pays, a ce jour, a la suite
de la Conference Internationale sur la Nutrition (Rome, 1992).
The major objective of the meeting is to ensure a consistent
Au Sommet Mondial de [Alimentation, en novembre 1996, les
approach to infant feeding in emergencies globally.
Etats participants se sont egalement donne pour objectif d'etablir
cally, the meeting aims to:
des systemes d'information sur I'insecurite et la vulnerability
0
alimentaire. L’objectif du cours est de repondre a la demande
d'information/formation pour apprehender au mieux les implica
Renseignements: ORSTOM - LNT, B.P. 5045, F-34032 - Montpellier
Cedex 01, France. P. Traissac, tel: 33 4 67 41 61 70 Telecopie: 33 4
67 54 78 00 Courrier electronique: traissac@mpl.orstom.fr
devise strategies to ensure that policies are transformed
into action;
0
form a working group to prepare a framework for future
national meetings and for international consultation.
A number of issues will be addressed at the meeting, including:
0
The purpose of nutrition surveillance is to provide regular, rele
vant and timely information for early warning of impending
raise awareness of key issues among international NGOs,
humanitarian relief agencies and donor agencies;
b
nels de la nutrition, de la sante publique, de [agriculture, im-
pliques dans des pays en developpement.
raise the issues of infant feeding in emergencies higher up
the agenda of all concerned organisations;
0
tions et les moyens de mise en oeuvre d'activites de surveillance
nutritionnelle. Ce cours est destine en priorite a des profession-
Specifi
inappropriate donations of infant formula and baby food as
aid;
0
nutrition emergencies, for on-going programme management
lack of awareness and implementation of existing guide
lines;
and for the development, implementation, monitoring and evalu
0
the impact of inappropriate infant feeding practices;
ation of policies and programmes.
This three week course,
0
lack of training of health and aid workers on infant feeding;
taught in French, is aimed at people dealing with nutrition
0
training of trainers in the field;
surveillance in developing countries. Specific topics include:
0
gaps in information and knowledge among NGOs and UN •
0
the causal approach to nutrition problems;
0
concepts and methods in nutrition surveillance;
0
lessons from the past;
0
identification of users;
For further information, please contact Margreet Houndijk, Wemos
Foundation, P.O.Box 1693, 1000BR Amsterdam, The Netherlands.
Tel. 31 20 420 22 22 Fax: 31 20 620 50 94 Email, wemos@tip.nl
0
set up of nutrition surveillance activities;
Web: http://www.wemos.nl/ or http://www.gn.apc.org/ibfan/
agencies working in emergencies.
4?
16, JULY zggf
S&4ME0 - TROPMED Short Courses
The programme will be of particular interest to physicians and
other health professionals such as dietitians, government
The SEAMEO-TROPMED Regional Center for
Community Nutrition is a training and research
policy-makers, and all those who confront the health implica
tions of obesity in society.
centre for all South East Asian countries, located at
the University of Indonesia.
The SEAMEO-
TROPMED Community Nutrition Training Programme consists of
an MSc in nutrition (2 years), a Doctor of nutrition (3 years), a
diploma programme in management of community nutrition (3
months) and a field research programme (6-8 months).
The residential, fully inclusive fee is UK £1,490. For further informa
tion and a full prospectus, please contact the Information Manager,
International Seminars, The British Council, 1 Beaumont Place, Oxford
OX1 2PJ, UK. Tel: 44 1865 316636 Fax: 44 1865 557368 / 516590
Email: international.seminars@britcoun.org Further information, in
cluding an application form, can also be found on the Web at http://
www.britcoun.org/seminars/
In addition, the SEAMEO-TROPMED Nutrition Training Pro
gramme offers several short courses on specific community
nutrition topics aimed at improving the professional's knowledge
and skills. For 1998-99, the following short courses are offered:
0
The 16th Leeds Course in Clinical Nutrition
15-18 September 1998
Nutrition, aging and non communicable diseases (Aug/Sept
1998)
This course is intended to provide a thorough grounding in all
0
Nutritional epidemiology (31 Aug -18 Sept 1998)
aspects of clinical nutrition and will appeal to clinicians, dieti
0
0
Micronutrients programme (1 Sept -11 Sept 1998)
ZOPP1 and nutritional planning and management (21 Sept
others with interests in patient nutrition.
-9 Oct 1998)
0
Public health system and nutrition (12 Oct - 23 Oct 1998)
0
Nutritional anthropology and communication planning for
community nutrition programmes (23 Nov -18 Dec 1998)
0
Food safety and food control (4 Jan-15 Jan 1999)
For further information and to obtain application forms, please contact
the Training Programme Coordinator, The SEAMEO-TROPMED Re
gional Center for Community Nutrition, University of Indonesia, 6,
Saiemba Raya, Jakarta 10430, Indonesia. Mailing address; P.O. Box
3852, Jakarta 10038, Indonesia. Tel: 62 21 330205 / 3913932-3 Fax:
62 21 3907695 / 3913933 Email: gtzseame@indo.net.id or
stropmed@rad. net.id
Obesity: a Global Challenge
A British Council international Seminar
11-17 October 1998, Aberdeen
Directed by Professor P. Trayhurn and Professor W.P.T. James,
tians, hospital pharmacists, nursing staff, nutritionalists and
Lectures will include 'The effects of dietary changes in colonic
diseases in Africa’ by Dr A.R.P. Walker, Johannesburg; ‘The
psycho-biology of appetite’ by Prof. J.E. Blundell, Leeds;
'Managing nutritional problems of patients with stroke’ by Prof.
K.W. Woodhouse, Cardiff; and 'Medical management of obe
sity' by Dr P. Kopelman, London. This year's mini-symposium
is entitled ‘Geographic trends in clinical nutrition’.
This course is approved for a total of 16 hours C.M.E. by the Royal
Colleges of Physicians of London and Surgeons of England, and also
has PGEA approval (17h A/B). Application forms and further informa
tion are available from Samantha Armitage, Course Secretary, Clinical
Nutrition, School of Continuing Education, Continuing Education Build
ing, Springfield Mount, Leeds LS2 9NG, UK. Tel: 44 113 233 3241
Fax: 44 113 233 3240 Email: s.armitage@leeds.ac.uk Web: http://
www.leeds.ac.uk/aed/cehome/shortc/clinut.htm
The Doris Howes Calloway
Endowed Fund in Human Nutrition
this seminar is intended to provide an overview of our current
understanding of obesity - its prevalence, causes, conse
quences - and examine strategies for treatment.
In recognition of Professor Doris Howes Calloway's scholar
ship, research, teaching, and contributions to the field of human
nutrition throughout the world, the College of Natural Re
The main topics will include:
0
public health (international perspective, health conse
0
quences);
body fat (distribution, body composition, endocrinology);
0
energy balance (food intake, dietary surveys, energy expen
o
0
sources at UC Berkleley, California, USA, has recently estab
lished the Doris Howes Calloway Endowed Fund in Human
Nutrition. Perhaps best known for her research on protein and
energy requirements in a career spanning 50 years, her re
search agenda has included topics ranging from protein
diture);
metabolic pathways and space research to the composition of
causes (genetics, neuroendocrinology of feeding and ther
indigenous diets and food and nutrition policy.
mogenesis);
The Fund will be used to support continued research and teaching in
human nutrition. For further information, including details of how to
contribute to the Fund, please contact Rosemary Lucier, Director of
College Relations, College of Natural Resources, University of Califor
nia, Berkeley, USA. Tel: 1 510 643 8861 Email: lucier@nature.
berkeley.edu
treatment (dietary, exercise, behavioural, pharmacological
etc.).
1 Objective Oriented Program Planning (ZOPP - Ziel Orientierte Projekt
Planning)
ituFOiZM/AriOkJ fffouffff
©
New Vitamin A and Iron Email
Visit the ACC/SCN website at
Discussion Groups
Illi R#
http://www. unsystem, org/accscn/
ZJ
The International Vitamin A Consultative Group (IVACG)
United Nations
AOirOSTFH WE CCMUTTEE ON ODCFCfW TKN
and the International Nutritional Anemia Consultative
Group (INACG) have launched two new email discussion
SUBCOMMITTEE ON NUTRITION
groups to promote networking and sharing of information
and expertise related to vitamin A deficiency and nutritional
anaemia, respectively. By subscribing to the lists, email
WELCOME TO THE SCN HOME PAGE
messages can be sent to a group of participating sub
Sj\
*A !
■1
/
j
Discussion Group
—5 SX
*
IS
by
LatestNews-
scribers who receive the message simultaneously within
’ ThoACCTSCN
Is the focal point for
>
harmonizing th© policies and ’
activities on nutrition of the j
United Nations system. The
role of the SCN is to serve as
a coordinating mechanism,
for exchange of Information
and technical guidance, and
t0 act dynamlcal|yto h8,p,he
UN respond to nutritional
problems.
minutes. Postings to the two groups should reflect either
vitamin A deficiency, or iron deficiency and iron deficiency
anaemia, as well as strategies to control these public health
problems.
The discussion group is a 'closed' list, i.e., the IVACG or
INACG Secretariats monitor subscriptions to the list. To
subscribe to one or both of the groups, send an email
message to majordomo@lists.ilsi.org
in the body of the
message type either SUBSCRIBE VITAMINALIST then
RNIS No.23 di»ponibl« <n funcits »t «n
RNIS No.23 J»JilJbl« in french ind ;npl!<h
fl
w'
leave one space and type your email address (to subscribe
j I
to the vitamin A discussion group), or SUBSCRIBE IRON-
SCN News No.18 du« out thi
* Juty. 'Nutrition of th« SohooFApcd Child mH b« th«
LIST then leave one space and type your email address (to
subscribe to the iron discussion group). It is not necessary
to write in the subject line of the message.
Launched in March 1998, the SCN website provides general
information about the SCN, details of SCN publications including
an online order form, RNIS and SCN News online, and useful
links to other nutrition-related websites. The website is updated
regularly. New items include:
Discussion group: Enter the discussions from the homepage.
Participate via the website or by emailing accscn@who.ch
The Third Report on the World Nutrition Situation: Now
3se listserves are a service provided by the IVACG and INACG
retariats. The ILSI Research Foundation's Human Nutrition Insti
tute serves as the IVACG and INACG Secretariats through Opportuni
ties for Micronutrient Interventions (OMNI), a project of the global
Bureau for Programs, Field Support and Research, USAID. For
specific questions about the discussion groups, please contact Laurie
Aomari or Maribel Flewitt, IVACG/INACG Secretariat, ILSI Human
Nutrition Institute, 1126 Sixteenth St., N.W. Washington, D.C. 200364810. Tel: 1 2026599024 Fax: 1 202 659 3617 Email: omni@ilsi.org
Web: http://www.ilsi.org/ivacg.html or http://www.ilsi.org/inacg.html
available to view and download in portable document format.
The Reproductive Health Library (RHL) - a
Clinical Nutrition Update Service
New Electronic Journal by WHO
The email-based Arbor Clinical Nutrition Updates are available
free to nutritionalists, physicians and other health professionals.
In March 1998, a new peer reviewed electronic journal; the
Some 4800 nutrition and health professionals in 90 countries
Reproductive Health Library (RHL), was launched by WHO in
worldwide receive the updates each week. As a subsidiary
service to the Arbor Nutrition Guide on the Web (http://arbor-
England, China, Mexico, South Africa, Thailand, India and
Uruguay. RHL contains:
com.com/), the nutrition updates contain abstracts of current
clinical nutrition research, comments on the research, and infor
•0
systematic reviews of clinical trials on priority reproductive
0
expert commentaries on the relevance of the review find
health topics;
mation on the best nutrition resources available on the Internet.
The editor-in-chief, Dr Tony Helman, is keen to reach a wider audience
with the Clinical Nutrition Updates. If you would like to receive the
updates on a regular basis, either fill in the form on the Arbor Nutrition
Guide website or send an email to helmant@ozemail.com.au
ings for developing countries;
0
practical advice on the management of reproductive health
problems.
...
,,
...continued on page 51
16, JULY
Low-Cosf Newsletters and Journals for Nutritionists
The following list, compiled by the Nutrition Society UK, provides information on low-cost publications that give up-to-date information
on human nutrition.
Breastfeeding Briefs from the International Baby Food Action Network / Geneva Infant Feeding Association, CP 157,1211 Geneva 19,
Switzerland, (breastfeeding)
Carotenoid News from Human Nutrition and Dietetics, M/C 517, University of Illinois at Chicago, 1919 W Taylor St. Chicago, IL60612,
USA. (carotenoids)
Child Health Dialogue from Healthlink (formerly AHRTAG), 29-35 Farringdon Rd, London EC1M 3JB, UK. Email: info@healthlink.org.uk
(control of child diseases particularly malnutrition, diarrhoea, malaria, measles and respiratory infections)
Community Eye Health from the International Centre for Eye Health, Institute of Ophthalmology, 27-29 Cayton St., London EC1V 9EJ,
UK. (eye health, vitamin A deficiency)
Field Exchange from Emergency Nutrition Network, Dept Community Health & General Practice, 199 Pearse St, Trinity College, Dublin
2, Ireland. Email: foreilly@tcd.ie (nutrition in emergencies)
,
|
Food, Nutrition and Agriculture from Food Policy and Nutrition Division, Food and Agricultural Organization, 00100 Rome, Italy, (food,
nutrition, food policy, food regulations)
;
I
IDD Newsletter from Dr J.T. Dunn, International Council for Control of Iodine Deficiency Disorders, Box 511, University of Virginia Medical
Centre, Charlottesville. VA 22908, USA. Email: jtd@virginia.edu (iodine deficiency research, policies, country reports)
1
I
UDIEJCIG Annual Report from Executive Secretary International Dietary Energy Consultancy Group, do Nestle Foundation, Box 581,
1001 Lausanne, Switzerland, (activities, publications and research on dietary energy)
!
IFPRI Report from International Food Policy Research Institute, 1776 Massachusetts Ave NW, Washington DC 20036, USA. ifpri@cgnet.
I
com (food security, food policy, research)
Mothercare Matters from Mothercare Matters, John Snow Inc., 1616 N. Fort Myer Drive, 11th floor, Arlington, VA 22209, USA. (maternal
i
and neonatal health/nutrition)
1
NFI Bulletin from Nutrition Foundation of India, 13-37 Gulmohar Park, New Delhi 110049, India, (nutrition research, programmes, India)
i
NU News on Health Care in Developing Countries from International Child Health Unit, University Hospital, S-751 85 Uppsala,
i
Sweden (health care, nutrition)
I
Nutrient News from National Institute of Nutrition, Tamaka, Hyderabad 500 007, India, (nutrition, India)
OMNI Update from OMNI Project, John Snow Inc., 1616 N Fort Myer Drive, Arlington, VA 22209, USA . Email: omni_project@jsi.com
j
■
(micronutrients, USAID projects)
PAMM Newsletter from Program against Micronutrient Malnutrition, Dept. International Health, Rollins School of Public Health, Emory
University, 1518 Clifton Rd, Atlanta, Georgia 30322, USA. Email: vanderha@sph.emory.edu (micronutrients, training)
,
RNIS (Refugee Nutrition Information System) from from ACC/Sub-Committee on Nutation, do WHO, 1211 Geneva 27, Switzerland.
!
Email: accscn@who.ch (nutrition of refugees and displaced people)
Safe Motherhood from Division of Family Health, World Health Organization, 1211 Geneva 27, Switzerland. Email: abouzah@who.ch
(maternal health)
SCN News from ACC/SCN, do WHO, 1211 Geneva 27, Switzerland. Email: accscn@who.ch (nutrition, UN and other agencies)
Sight & Life Newsletter from Task Force SIGHT & LIFE, PO Box 2116, 4002 Basel, Switzerland. Email: martin.frigg@roche.com
■
(xerophthalmia)
I
WHO Collaborating Centres for Nutrition Newsletter from Lifestyles & Health Unit, WHO/EURO. Scherfigsvej 8, 2100 Copenhagen,
|
Denmark. Email:sal@who.dk (European nutrition)
I
Xerophthalmia Bulletin from Dr D.S. McLaren, International Centre for Eye Health, 27 Cayton St, London EC1V 9EJ, UK. (vitamin A,
i
j
vitamin A deficiency)
This list of English-language publications was compiled by Ann Burgess at the Nutrition Society, 10 Cambridge Court, 210 Shepherds Bush, London W6
7NJ, UK. Most of the publications are free of charge to people working in low income countries, but it is advisable to check before ordering. If you know
of other useful, low-cost nutrition publications, the Nutrition Society will be very happy to hear from you. Please write to the Publications Committee on
the Nutrition Society at the address above, or email Ann Burgess at annburgess@sol.co.uk The Nutrition Society thanks everyone who has supplied
information. Further information about the Nutrition Society can be found on their website at http.7Avww.nutsoc.org.uk/
50
...continued from page 49
Included in the topics (27 reviews and 22 commentaries) cov
In conjunction with this, an email newsletter is also available
ered in the first issue, are nutritional supplementation during
called ID21NEWS which provides regular updates and sum
pregnancy, and breastfeeding.
maries of the latest research finding that have been added to
Primarily intended for use in developing countries, RHL aims to
make available the most reliable and up-to-date medical infor
mation to health workers in order to promote evidence-based
care in the area of reproductive health. Prior to the RHL, such
information was typically scattered in numerous papers and
journals, making it difficult for health practitioners to get a good
overview of all the data available on a given subject
The
systematic reviews included in the RHL are taken from the
Cochrane Library' and are based on data from controlled clinical
the ID21 collection.
A system whereby each digest can be
automatically requested via email is currently being developed.
To subscribe to ID21NEWS, send a blank email message to:
id21news@ids.ac.uk and in the subject field, write: subscribe
id21news
The ID21 team would welcome any practical suggestions for making
this online service more useful or accessible in the future. Please
email Alistair Scott at id21@sussex.ac.uk
trials published in major medical journals worldwide.
RHL is provided on a 3.5 inch diskette and requires no special knowl
edge of computers to access and read. Subscription to RHL is free of
charge for health workers in developing countries. Availability in
developed countries will be restricted to scientists and institutions
working closely with WHO or in developing countries. It is produced
jointly by HRP (the UNDP/UNFPA/WHO/World Bank Special Pro
gramme of Research, Development and Research Training in Human
Reproduction) and RHT (WHO's Division on Reproductive Health), in
association with the Cochrane Collaboration.
For further information, and to obtain a copy of RHL, please contact
Jitendra Khanna, Special Programme of Research, Development and
Research Training in Human Reproduction, WHO, 20 Avenue Appia,
CH-1211 Geneva 27, Switzerland. Tel: 41 22 791 3345 Fax: 41 22 791
4171 Email: khannaj@who.ch
Source: WHO Press Release, 4 March 1998.
ID21: a New Development Research
Reporting Service
Nutrition Materials Available from TALC
The new Teaching-Aids at Low Cost (TALC) 1998 catalogue
includes the following nutrition related materials.
Books
State of the World's Children (1998) UNICEF £2.50
Community Nutrition for Eastern Africa (1994) Burgess & others £7.00
Nutrition Handbook for Community Workers (1993) CFNI £5.20
Helping Mothers to Breastfeed (1992) Savage King (also in Spanish)
£3.00
Nutrition for Developing Countries (1992) Savage King & Burgess
£9.50
Protein Energy Malnutrition (1992) Wateriow£5.00
Slide sets
Each set contains 24 slides and a script. Prices are £5.50 for self
mounting sets, £7 for mounted sets and £11 for sets in a folder:
Malnutrition in an Urban Environment - revised 1997
Undernutrition in Young Children: signs and causes - revised 1997
Complementary Foods and Energy - revised 1997
Breastfeeding (also in French) -1990
Breastfeeding Problems (also in French) - revised 1993
The ID21 (Information for Development in the 21st Century)
development research reporting service provides access to the
latest and best UK-based development research from aca
demics, NGOs and consultants. This new online service con
tains hundreds of policy-relevant findings on critical global devel
opment issues. These include agriculture and rural livelihood
issues, and food, water and environmental security issues.
Backed by the UK Department for International Development,
this Internet-based system links development research and re
searchers directly to policy makers and development practition
ers around the world through a new website at http://
Accessories
TALC Direct Recording Scale (plastic scale, wall chart and plasticised
Child Health charts - also available in Arabic, French, Nepali, Por
tugese, Spanish and Zulu) £16.50
See How They Grow wall chart £0.60
Child Health charts (also available in above languages) £0.25
Weight for Height chart £5.25
Language stickers available in French, Portugese and Spanish £1.75
Insertion tape for measuring arm circumference (39cm) £0.25
Insertion tape for measuring head, chest and abdomen circumferences
(100cm) £1.00
www.id21.org/ Hosted by the Institute of Development Studies,
the key feature of ID21 is a searchable online collection of short,
one-page (500-word) digests of the latest social and economic
research studies across 30 key topic fields.
' The Cochrane U’brary is a regularly updated electronic library de
signed to provide a scientific basis for informed healthcare decision
making. It is available on disk and CD-ROM (email info@update.co.uk
for more information). Details can be found on the web at http://
For further details, or to order any of the above items, please contact
TALC, PO Box 49, St Albans, AL15TX, UK, Tel: 44 1727 853869 Fax:
44 1727 846852 Email: talcuk@btintemet.com All prices are in
pounds sterling. Post and packing for books and accessories is 30%
of total order surface (minimum £2.75) or 60% airmail (minimum
£3.75). The price of slide sets includes surface postage. Payment by
sterling cheque, Visa or MasterCard or International Money Order.
Contact TALC for other methods of payment. All materials are avail
able in English. Submitted by Ann Burgess Email: annburgess@
sol.co.uk
hiru.mcmaster.ca/cochrane/
51
kJEuSiJO.i6, JULY
____________
PLZOgeAMMb LJElA/f?
A6£AJCi£5tZ£POlZr £W £££i^ A££i\5i£i££> iM KJUTTZtTiOAJ
FAO
Preventing Micronutrient Deficiencies
elaborated guiding principles for effective risk communication
within the risk analysis framework.
The workshop on the ‘Prevention and Control of Micronutrient
Malnutrition through Food-based Approaches in SAARC Coun
tries' was held in Dhaka, Bangladesh, from 17-20 November
1997.
It was sponsored by FAO in collaboration with the
Thrasher Research Fund (USA) and the Micronutrient Initiative
and was organised by the Agricultural Research Council of
Bangladesh. All SAARC countries - India, Pakistan, Bangladesh,
The Consultation focused on two primary goals - the creation
of more openness and transparency in the entire risk analysis
process through the use of risk communication and the in
creased involvement of all interested parties (i.e., the govern
ment, industry, consumer organisations, etc.) in risk communi
cation during the risk management process. The report of the
consultation will be available later this year.
Nepal, Sri Lanka, Bhutan and the Maldives - participated in the
workshop. Renowned experts working in the SAARC and other
Asian countries were invited to present papers and discuss
Comparative Analysis of Nutrition
various facets of food-based approaches for the control and
Interventions Workshop in Thailand
prevention of micronutrient malnutrition.
FAO, in collaboration with the Institute of Nutrition at Mahidol
The workshop reviewed the current status of the problems of
University, organised a workshop on Comparative Analysis of
micronutrient deficiencies in SAARC countries and discussed
Nutrition Interventions, held in Bangkok, Thailand, 2-4 June
food-based approaches for their control including the role of fruit
1998. The preparatory work and proceedings of the workshop
and vegetable gardening, small animal rearing and the aquacul
has provided a major contribution towards the development of
ture at household level, processing and preservation to improve
a manual on this subject. The manual will be based on lessons
food security and nutritional value, nutrition education for improv
learned and wisdom accrued from comparative analyses of
ing consumption and selection of micronutrient-rich foods, and
interventions, to identify what works and what does not. It is
food fortification for improving food quality and nutritional value.
intended as a source of advice and inspiration for current and
The workshop participants agreed that food-based approaches
are the preferred, most practical and sustainable strategy for the
prevention of micronutrient malnutrition and for the control of mild
micronutrient malnutrition in SAARC countries. They recom
mended that food-based actions should be an integral part of all
action programmes, both short- and long-term. They advised that
planned nutrition interventions by providing information on
strategies, approaches and procedures that are known to have
resulted in successful outcomes in past and ongoing interven
tions. The manual is intended to create an understanding of the
need for ongoing monitoring to improve the cost-effectivenes
and outcomes of nutrition interventions.
SAARC countries look at their farms and not at their pharmacies
for the solution of these problems.
A report containing the
Development of a National Nutrition Training
recommendations, conclusions and technical papers is available
Programme for South Africa.
from the FAO Food and Nutrition Division (contact details below).
A Technical Cooperation Project
Expert Meeting on Risk Communication1
with the Government of South Africa
The Reconstruction and Development Programme of the Gov
A Joint FAO/WHO Expert Consultation on the Application of Risk
Communication to Food Standards and Safety Matters'was held
in Rome on 2-6 February 1998. The meeting was attended by 18
experts who identified strategies for crisis situations such as
ernment of South Africa has developed an integrated nutrition
strategy aimed at reducing hunger and malnutrition.
To this
end, FAO is working with the Government of South Africa to
strengthen staff training programmes.
food-borne disease or illness outbreaks and for use in on-going
risk communication activities. The experts recommended ways
Specifically, FAO has helped the Government of South Africa to
to overcome the barriers to effective risk communication and
sensitise top policy-makers, mid-level administrators and pro
gramme managers to nutrition problems, their causes and
' The Codex Alimentarius Commission has defined risk communication
as: 'the interactive exchange of information and opinions concerning
risk among risk assessors, risk managers, consumers and other inter
ested parties.'
52
potential solutions, and to increase national capacity to under
take community programmes through the training of resource
persons and trainers of community nutrition workers.
It is
currently undertaking a needs assessment for the development
information and greatly increase the amount of material to be
of future university training/teaching programmes in human nutri
incorporated into FIVIMS.
tion. The project is expected to be completed in August 1998.
FlVIMS will rely on a set of indicators to provide a comprehen
Nutrition Education for School Children
sive picture of the food and nutrition situation in a country. This
will include food trade and production, market conditions, liveli
hood systems, social institutions, cultural attitudes, natural re
A major component of FAO’s normative work on nutrition in
sources, health and sanitary conditions and feeding practices.
volves nutrition education for the public. FAO encourages the
Thus, FIVIMS can enable users to describe the food and
development of practical and effective programmes of nutrition
nutrition situation, discern trends in the prevalence of undernu
education in primary schools in developing countries. In co
trition and provide an analysis of the major causal factors.
operation with the School Nutrition Education Section of The
Netherlands Nutrition Centre, The Hague, FAO is developing a
planning guide for nutrition education in primary schools. The
Within this framework, the Food and Nutrition Division is creat
ing NUTRIDAT, a system to assemble and disseminate infor
materials to be developed are partially based on the expressed
mation about people who are underfed, undernourished or
needs of government school staff who have responded to a
at-risk of becoming so. The database is currently located and
questionnaire inquiring on the current state and shortcomings of
maintained at the central level with copies of relevant country
nutrition education in schools in English-speaking countries.
data being made available at the regional and sub-regional
levels for trend analysis and policy work. FAO is collaborating
Currently, a planning guide for school inspectors and school
supervisors is being prepared to allow them to initiate, support
and guide nutrition education for schoolchildren in all schools in
developing countries. A draft version of this planning guide will
with WHO and other agencies in sharing data for NUTRIDAT
with a view to linking data from different agencies.
Direct
access to NUTRIDAT Central will be possible through the
Internet and available on CD-ROM in 1999.
be reviewed and field tested in the beginning of 1999. Comple
mentary documents, such as a teacher’s guide and examples of
good practice in nutrition education in primary schools in devel
NUTRIDAT contains anthropometric information, and where
available, consumption data at household level and food supply
oping countries, will also be prepared. These documents will be
at national and sub-national level, as well as statistics on health
particularly useful in schools which have adopted the WHO
and demography. The FAO database emphasises information
approach of Health-Promoting Schools (see page 8) but do not
on adults and school-age children.
require that a school is member of the WHO programme. With a
view to further enhance the benefits of the two programmes for
In addition to NUTRIDAT, FAO’s Nutrition Country Profiles
the assisted countries, special efforts are being made to actively
provide concise analytical summaries of the food and nutrition
collaborate in the world-wide School Health Initiative, promoted
situation in individual countries. This information is presented in
by the WHO and its respective regional networks for Health-
the context of information and background statistics on food-
Promoting Schools. This collaboration will strengthen ongoing
related factors such as agricultural production, and other se
nutrition education through emphasising the food-based ap
lected economic and demographic indicators. The information
proach. This is hoped to have lasting positive effects on the food
is presented in a disaggregated fashion; trends and sub
and nutrition situation of schoolchildren, their dietary attitudes,
national differences are highlighed when available. The profiles
practices and choices.
include consistent and comparable statistical data that are
presented in a combination of colourful graphical displays,
World Food Summit follow-up:
tables and maps, each supported by a short explanatory text.
Nutrition Information Systems
Nutrition mapping is an innovative component of the profiles
To assess progress made in reaching the 1996 World Food
The maps combine information such as anthropometric status,
Summit goals for reducing undemutrition, FAO is developing the
micronutrient deficiencies, and energy and nutrient consump
that presents the data in a visible and eye-catching manner.
Food Insecurity and Vulnerability Information and Mapping Sys
tion where available, with information about safe water supplies
tem (FlVIMS). This is part of the international effort to assess the
and education, to provide an immediate comprehensive picture
nature, extent, magnitude and severity of malnutrition and to
of the geographical distribution of vulnerable groups at sub
monitor trends over time.
national level. With this visual aid, the locations of populations
FAO is requesting each country to provide the results of their
most recent food and nutritional status surveys so that the
database can be updated frequently.
Many data collection
activities have been undertaken in developing countries that
need to be documented and catalogued at the international
level. Identifying sources of such data with the help of govern
ments and NGOs would prevent the neglect or even loss of this
with major nutritional problems are clear.
The maps also
highlight gaps in information alerting policy makers that addi
tional data collection is necessary. Nutrition country profilescan
be requested from Food and Nutrition Division.
Source: FAO Food and Nutrition Division, Via delle Terme de Cara
calla, 00100 Rome, Italy. Fax: 396 5225 4593 Email: FoodQuality@FAO.org or Nutrition@FAO.org Web: http://www.fao.org/waicent/faoinfo/economic/esn/nutri.htm
53
G&J fJEujg >JO.i 6, JULY
----------
IAEA
----------
Among the most important events of 1997 for nutrition activities
at the International Atomic Energy Agency (IAEA) were two
major reviews. The first review focused mainly on the resources
growth faltering in infants. Other possibilities for joint projects
are currently being explored with WFP, UNHCR and FAO.
For further information oh any of these projects, please contact Robert
Parr, Head, Section of Nutritional and Health-Related Environmental
Studies, IAEA, P.O. Box 100, A-1400 Vienna, Austria. Tel: 43 1 2060
21657 Fax: 43 1 20607 Email: R.Parr@iaea.org
needed to ensure the sustainability of the health programme and
on the identification of appropriate topics for coordinated re
search. The second review was concerned with thematic plan
---------- \FPR\ -----------
ning for future technical cooperation projects. Both reviews had
very positive outcomes; consequently there is a significant ex
pansion in IAEA's nutrition activities expected in the near future.
Urban Malnutrition
There are nine current and planned coordinated research pro
jects (CRPs: see SCN News No. 15 p50) involving applications of
isotopes for which funding is available:
Preliminary results from work by Lawrence Haddad, Marie Ruel
and James Garrett at IFPRI indicate that urban undemutrition is
growing both in absolute terms and in terms of the share of
0
o
0
0
1995-9. Development and application of isotopic techniques
overall undernutrition. Rural areas still contain the majority of
in studies of vitamin A nutrition.
undernourished children (except for Brazil), but the gap is
1995-9. Reference Asian Man (dietary intake and body
closing rapidly. The authors conclude that there is a need for
composition for selected trace elements of relevance to
more research on identifying the main constraints to urban food
radiological protection).
security and good nutrition and on understanding the basis of
1996-2000. Isotopic evaluations of maternal and child nutri
effective community, programme and policy responses (see
tion to help prevent stunting.
page 29).
1998-2001. Isotope-aided studies of nutrient interactions in
Links between Women’s Status and
Child Nutrition
developing country populations exposed to multiple nutri
0
tional deficiencies.
1998-2001. isotopic evaluations in infant growth monitoring
(in collaboration with WHO's Multicentre Growth Reference
Study).
O
1998-2001. Application of nuclear techniques in the preven
tion of denerative diseases (obesity and non-insulin depen
dent diabetes) in ageing.
o
1999-2002.
Development and validation of isotopic and
complementary tools for nutritional assessment of iron sta
tus in developing country populations.
0
1999-2002.
Development and validation of isotopic and
complementary tools for nutritional assessment of zinc sta
tus in developing country populations.
0
2000-2003.
Development and validation of isotopic and
complementary tools for nutritional assessment of house
hold food security in developing country populations.
Ongoing and planned technical cooperation projects have a
Preliminary results from work by Lisa Smith and Lawrence
Haddad at Emory University and IFPRI indicate that women's
status has a large positive and significant impact on child
nutrition in the developing world.
Utilising data from a wide
range of carefully documented sources, a cross-section time
series data set was constructed with some 180 data points
covering approximately 64 developing countries from 1970-
1996. Country fixed-effects methods were employed to esti
mate the impact of per capita dietary energy supplies, female
secondary school enrolments, access to clean water and the
ratio of male to female life expectancy (the proxy measure of
women's status relative to men) on low weight-for-age preva
lence for children under five.
Of the four factors, women's
relative status has the largest elasticity with respect to child
underweight prevalence'. The variable has a particularly
common theme in trying to make practical use of nuclear and
strong effect for South Asia, a result in line with work suggest
isotopic techniques to assess the impact of national nutrition
ing that women's status is key to reducing child malnutrition
programmes. Typical examples include studies of micronutrients
there.
(iron, zinc, vitamin A), breastmilk volume, energy expenditure
and body composition. Individual technical cooperation projects
New Partnership with CARE International
have recently been carried out in Cameroon, Chile, Ethiopia,
Peru, Sierra Leone and Sri Lanka, and new ones are currently
IFPRI’s multi-country programme on 'Urban Challenges to
being started in Chile, Ethiopia, Senegal and Venezuela. Larger-
Food Security and Nutrition1 led by Marie Ruel and James
scale regional projects are in the planning stage in Latin America
Garrett has established a new partnership with CARE Interna
and East Asia. A new project is also expected to start soon in
tional in an effort to be more effective in linking research to
Indonesia, in collaboration with UNICEF, which will use isotope
programming in urban areas. Over the last six months, IFPRI
techniques in support of UNCEF’s multi-country field trials of the
efficacy of iron and zinc supplementation to reduce anaemia and
' Elasticity: the percentage change in one variable resulting from a
one percent change in another variable.
sa
and CARE have collaborated in carrying out urban livelihood
assessments in Bangladesh, Tanzania, Togo and Ghana as part
of the initial diagnostic phase in CARE's urban programme
development. Honduras is next on the list. Additional collabora
For further information, please contact Bonnie McClafferty, Outreach,
FCND, IFPRI, 1200 Seventeenth Street, NW, Washington D.C. 20036,
USA. Fax: 202 467 4439 Email: b.mcclafferty@cgnet.com or ifpri@cgnet.com
tive work is planned to work jointly on follow-on phases such as
project design, implementation, monitoring and evaluation.
--------------------
UNICEF Meeting in Tanzania
Develops Proposal for Community-based
UNICEF --------------------
All countries represented at the meeting formulated plans for
further development of the household and community compo
nent of IMCI and other community-based programmes.
Programmes to Support IMCI
Some of the main conclusions and findings from the meeting
UNICEF and WHO are collaborating in the development and
implementation of the Integrated Management of Childhood
Illness (IMCI) programme (see SCN News No.15 p56). Collabo
ration to date has largely focused on the integration of manage
ment at the level of the health facility, for which WHO has taken
the lead. In the last year, a community and household compo
nent of IMCI has been developed, including strategies for
community-based nutrition activities. Many of the deaths associ
ated with the five IMCI diseases (malnutrition, acute respiratory
infections, diarrhoea, measles and malaria) need improved pre
ventive measures at the community and household levels.
UNICEF is leading the development of the IMCI components at
these levels.
are as follows:
1.
of information on what works, yet systematic documentation of
these community-based experiences and utilisation of this
information to inform better programme design is lacking. A
need was expressed for countries to undertake a more system
atic review of community-based programmes. A more critical
examination is required of the community processes to ascer
tain that repeated Triple A cycles are indeed taking place and
that projects/programmes are not ‘locked’ into actions based on
only the first round of assessment and analysis.
2.
In late April, the UNICEF Eastern and Southern Africa Region
Nutrition Network held a meeting in Morogoro, Tanzania that
Better attention to documenting lessons learned
The various case studies showed that there is already a wealth
Scale of community-based programmes
The UNICEF Nutrition Strategy promotes community-based
nutrition-oriented programmes as the best way to accelerate
included planning for IMCI at the community level based in large
reduction of child malnutrition.
part on existing experiences with community-based nutrition
effort over the last decade to promote community-based pro
programmes. The meeting drew a total of 78 participants from
grammes, there are still too few examples of programmes
Despite a lot of training and
19 African countries. Participants included government repre
operating at a scale commensurate with a potential for a
sentatives from health, nutrition and IMCI coordinating units;
significant nutrition impact. UNICEF staff and other partners
UNICEF staff in health, nutrition, water and sanitation, communi
involved in these efforts need new kinds of training for this
cation and evaluation; representatives of WHO, USAID, BA
SICS, AMREF1, and a number of research institutions.
purpose.
Among the community-based programmes described in detail at
The meeting discussed at length the concept of IMCI and the
the meeting were the Madagascar Project NAC, the Kisarawe
opportunities it brings to promote improvement in nutrition and
District (Tanzania) Child Survival, Protection and Development
better management of childhood diseases through promotive,
3.
(CSPD) programme, the Zambia community breastfeeding pro
Household and community component of IMCI
preventive and curative interventions.
Renewed attempts to
motion, community child heath projects coordinated by AMREF,
promote community-based nutrition programmes are neces
and various community malaria and hygiene interventions. The
sary. Both through IMCI and independent of it, the pursuit of
meeting also provided an overview of IMCI, including the con
community-based nutrition programmes should be accelerated
cept, components and strategies for the household and commu
across the region. An agreement was reached on the need for
nity component. There were sessions on communication and
individual countries to review what was already on the ground
social mobilisation, monitoring and evaluation and a field visit to
and develop further what may need to be done in order to
several sites of the Morogoro District CSPD programme.
strengthen or operationalise household and community-based
programmes. The draft country proposals were a reflection of
this, with several countries having proposed core nutrition-type
1 The African Medical Research Foundation - an NGO based in Nairobi
with activities all over East Africa.
community-based interventions including growth promotion,
55
fJO.16, JULY iggt
breastfeeding, adequate complementary feeding and others
9.
proposing to build upon mother support groups, community
All participating countries developed draft plans for strengthen
malaria interventions, and water and sanitation groups.
ing community-based programmes. These plans need to be
Next steps
further discussed at country level. The UNICEF offices in the
4. Advocacy
There was optimism on strengthening community-based inter
ventions but concern for how to get governments to give
community-based interventions more importance.
phase one IMCI countries - Madagascar, Tanzania, Uganda,
South Africa, and Malawi - will receive funds from USAID to
help implement their plans.
Renewed
advocacy, making the case for the importance of nutrition to
national development, is needed. The 1998 State of the World's
Children Report on nutrition has put the case forward that
nutrition is a lever that can accelerate and potentiate economic
development. Good nutrition is also a right that governments
have committed themselves to achieving by signing the Conven
tion on the Rights of the Child.
A meeting report is available on request from Roger Shrimpton,
UNICEF, Mail code TA-24A, 3 United Nations Plaza, New York, NY
10017, USA. Tel: 1 212 824 6368 Fax: 1 212 824 6465 Email:
rshrimpton@unicef.org For further information, please contact Vincent
Orinda at UNICEF Health Section (email: vorinda@unicef.org) or Jim
Tulloch, CHD, WHO, 20 Avenue Appia, CH-1211 Geneva 27, Switzer
land. Tai: 41 22 791 2632 Fax: 41 22 791 4853 Email: tullochj@who.ch
5.
Community level‘workers’
Action at community level relies on a cadre of community level
’mobilisers”. The necessary support to mobilisers from the next
level in service delivery, especially from extension workers, was
Evaluation of UNICEF Support for Universal
Salt Iodisation in South Asia
not always forthcoming. The question of appropriate ratios of
mobilisers to facilitators requires further discussion. The issue of
payment of community-based workers was an area of concern
that needs to be analysed carefully in each country. In various
countries, the decision to pay community workers had already
been made and some had included such considerations in their
local government and decentralisation initiatives. The issues
around cost-effectiveness and sustainability need to be thought
through for each country. Ways of sustaining the motivation of
the community workers though non-monetary and in-kind sup
universal salt iodisation (USI) effort in South Asia. Over the last
progress towards USI in South Asia, resulting from concerted
government intervention and support from agencies and
donors. Progress has been so great that the type of assistance
that can be usefully provided by agencies and donors is
changing. This evaluation aims to take, stock of the UNICEF
contribution country-by-country over the last five years and to
guide the process of planning for UNICEF’s future support.
port also need to be developed.
6.
UNICEF is undertaking an evaluation of its support to the
few years, there has been a tremendous acceleration in
The evaluation will include:
Gender issues in community-based programmes
Health and nutrition programmes have not yet adequately facili
0
for improved care at household level.
It was proposed that
0
careful attention be given to this in further development of
household and community IMCI and community nutrition pro
comparison of UNICEF USI inputs with those of other
development agencies and government resources;
0
Communication and social mobilisation
The focus of communication pro
grammes seems to be on behaviour modification and not on
informed choices. Implementation of communication strategies
has to be well founded in the understanding of what motivates
people to change and which behaviours are the most important
measurement of the extent to which UNICEF’s efforts
have tried to stimulate demand and the extent to which
Many nutrition and health outcomes are determined by be
haviours at houshold level.
measurement of the inputs and outputs of the UNICEF
support programme;
0
grammes.
7.
assessment of the current situation with regard to avail
ability of iodised salt at the household level;
tated the process of drawing in men and fathers in programming
they have been aimed at stimulating supply;
0
assessment of the degree to which the private sector has
supported the iodisation of salt; and
0
examination of the quality of supply and legislation en
forcement.
The
The evaluation is being coordinated by a steering committee
UNICEF programme communication group at UNICEF head
chaired by the UNICEF Regional Monitoring and Evaluation
quarters is developing tools that will be made available to guide
Officer for South Asia. A questionnaire was sent to all UNICEF
country offices in their communication strategies.
country offices in South Asia in late 1997 to collect data
for achieving improved health and nutrition outcomes.
8.
specifically for the evaluation. Findings will be analysed by an
Technical support areas
Countries identified areas for which additional support is required
to further action on community-based programmes.
These
include planning for communication and social mobilisation; pro
posal development; orientation and training for household and
community IMCI; assessing care-seeking behaviours; and com
munity monitoring and information systems.
56
independent evaluator, discussed with the wider Nutrition Initia
tive in South Asia group (NISA) and reviewed by an external
panel. The main output of the evaluation will be a 30-40 page
report - stage one of which is expected to be finalised by
September 1998.
Both WHO and ICCIDD will be asked to act as external review
attending schools in rural areas.
ers of a draft report version of the evaluation. If they agree, their
education, a tiny fraction of female children in Herat and Kanda
views will be annexed in the final version of the report.
har regions did attend school at the time of the survey. These
The steering committee is actively seeking offers of persons wishing
formally to review the evaluation. For further information, please
contact Roger Pearson, Regional Monitoring and Evaluation Officer,
UNICEF South Asia, P.O. Box 5815, Lekhnath Marg. Kathmandu,
Nepal. Tel: 977 1 417 082 Fax: 977 1 419 479 Email: rpearson@
uncrosa.mos.com.np
Despite the ban on female
informal schools were maintained underground by mothers who
defied the law against female education.
The survey showed that nationally, 25% of children aged 6-35
months were wasted and 52% were stunted.
Stunting rates
were higher among boys than among girls throughout the
country. Highest stunting rates were seen in Kandahar region,
The 1997 Afghanistan Multiple Indicator
where 63% of boys and 59% of girls were stunted. These data
indicate considerably higher levels of malnutrition than have
Baseline Survey
previously been documented, making Afghanistan one of the
worst affected countries in the world.
Afghanistan has been in a state of conflict for almost 20 years,
leading to large-scale displacement and almost total collapse of
the country’s infrastructure. With an annual per capita income of
Vitamin A deficiency (assessed by self-reporting of night blind
ness), was reported in about 3% of the children (aged 12-23
approximately US S220 (in 1994), Afghanistan is consistently
months) surveyed in Jalalabad and Kandahar. Nationally, 12%
ranked among the poorest countries in the world. Access to
of children had received a vitamin A capsule, with higher
populations within the country over the last two decades has
coverage of vitamin A distribution in Jalalabad and Kandahar.
been sporadic at best, and consequently the national situation in
National goitre rates (assessed by self-reporting of visible goi
terms of health and sanitation has been unclear.
ter) were 7.5 cases per 1000 people.
In 1997,
UNICEF undertook a multiple indicator survey in Afghanistan.
Technical support was commissioned from CIETIntemational’.
Assessment of breastfeeding practices showed striking differ
This is the first national-level survey carried out in the country for
ences in reporting from (and opinions of) women and men.
25 years, and gives baseline indicators for development and
Women reported that only 25% of infants were exclusively
relief programmes including health, nutrition, education, food
breastfed to 4 months, whereas men tended to overestimate
security, water and sanitation.
this figure.
The survey included over 60,000 people from 96 sentinel com
For food security, 42% of households reported that they had
munities representing the five operational regions of the country.
sufficient food in the week prior to the survey, implying that 58%
Mortality rates were very high: maternal mortality rates were
did not.
around 400 per 100 000, and infant mortality rates were 140-150
per 1000. Female literacy was extremely low: less than 5% of
rural women, and around 10% of urban women aged 15-49
years old knew how to read and write.
School attendance
For further information, please contact Roger Pearson, Regional Moni
toring and Evaluation Officer, UNICEF South Asia, P.O Box 5815,
Lekhnath Marg, Kathmandu, Nepal. Tel: 977 1 417 082 Fax: 977 1
419 479 Email: rpearson@uncrosa.mos.com.np
figures reflected this dismal situation, with only 7% of girls
WHO
The Innocenti Declaration:
Continuing towards its Targets
---------------------
centi Declaration, and to identify areas where more effort is
needed, the Programme of Nutrition recently gathered informa
tion in this connection in four WHO Regions. Information has
The Innocenti Declaration on the Protection, Promotion and
thus far been received from 57% (108) of WHO's 191 member
Support of Breastfeeding, adopted in 1990, includes a number of
states, many of which have made considerable progress to
operational targets. It calls upon international organisations to
wards achieving the operational targets of the Innocenti Decla
draw up action strategies for protecting, promoting and support
ration.
ing breastfeeding, including global monitoring and evaluation of
0
their strategies.
To assist countries in their efforts to monitor and assess
progress towards achieving the operational targets of the Inno’ An NGO registered in the USA dedicated to building the community
voice into planning and better governance.
Breastfeeding committees: Several countries have breast
feeding committees (58 % in the Africa Region (AFR),
22% in the Region of Americas (AMR), 65% in the Eastern
Mediterranean Region (EMR), and 63% in the European
Region (EUR)) and Baby-Friendly Hospital Initiative com
mittees (74% in AFR, 80% in AMR, 53% in EMR, and 71%
in EUR). These committees are composed of representa
tives from relevant government departments, NGOs, edu-
5?
Ql/J iJEbJg/JO. ie, JUL ¥ 759?
0
cational institutions, health professional associations and
Diego, California, USA), and UNICEF. The monitoring tools will
infant-food manufacturers.
National breastfeeding policy. Sixty-eight percent (AFR),
be published at the end of 1998.
72% (AMR), 82% (EMR), and 60% (EUR) of countries have
For further information, please contact Randa Saadeh, WHO Pro
gramme of Nutrition. Tel: 41 22 791 3315 Fax: 41 22 791 4156 Email:
formulated national breastfeeding policies, and 57% of
saadehr@who.ch
countries have plans of action for implementing the BFHL
0
Baby-Friendly Hospitals: The 4 WHO Regions have 13,526
‘Promoting Breastfeeding in Health
hospitals with maternity services. There were 2,430 hospi
tals designated as being baby-friendly at the end of 1997,
Facilities: a Short Course
compared with 943 hospitals at the end of 1995. 4,578
for Administrators and Policy-makers’
hospitals are targeted to become baby-friendly (1,554 hos
by WHO I Wellstart International
pitals in AFR, 1,294 in AMR, 950 in EMR, and 780 in EUR).
0
International Code of Marketing of Breast-milk Substitutes:
Many governments have taken responsibility for adopting,
implementing and monitoring the Code (61% in AFR, 80% in
AMR, 53% in EMR, and 49% in EUR). Some countries are
in the preliminary stages of drafting national measures for
this purpose, while still others have hardly begun.
0
Free and low-cost supplies of breastmilk substitutes'. The
distribution of free and low-cost breastmilk substitutes has
ended in 5,949 hospitals (1,967 in AFR, 995 in EMR, 1,468
in EUR and 1,519 in the AMR).
0
Maternity legislation: Governments of WHO member states
are using different means to protect, promote and support
breastfeeding by enacting imaginative maternity protection
legislation (87% in AFR, 100% in AMR, 94% in EMR and
89% in EUR) and by providing information on breastfeeding
This short course (WHO/NUT/96.3) which provides practical
guidance on policy and administrative changes needed to
promote breastfeeding in health facilities, is available in Arabic,
English, French, Russian and Spanish, and will soon be avail
able in Italian and Portuguese. It has thus far been given in
Egypt, Ghana, Kenya, Lithuania, Malaysia, Saudi Arabia,
Spain, Swaziland, the UK, Ukraine and the USA. The course
has had a major impact on BFHI status and progress.
For
example, in Ukraine alone, the course has been given twenty
times and has prompted the establishment of a national breast
feeding committee and development of a breastfeeding policy.
In Brazil, it is planned to integrate the course into the overall
national training plan for breastfeeding, and it is seen as a tool
to sensitise decision-makers and obtain their commitment to
becoming baby-friendly.
through the mass media, i.e., television and radio pro
grammes, newspaper articles and breastfeeding weeks.
The course is currently being used as the main advocacy tool
to target private and university hospitals.
The WHO Programme of Nutrition has consolidated the survey
results in 'The Innocenti Declaration: Progress and Achieve
ments', Parts I, II and III, published in the Weekly Epidemiologi
cal Record (73(5): 25-30,1998; 73(13): 91-94,1998 and 73(19):
For further information, please contact Randa Saadeh, WHO Pro
gramme of Nutrition. Tel: 41 22 791 3315 Fax. 41 22 791 4156 Email:
saadehr@who.ch
139-144,1998).
Joint WHO/Tufts Consultation on
Nutrition Guidelines for Healthy Ageing
This exercise will be repeated every 3 years, and the information
collected will be included in the reports by the WHO Director-
General to the World Health Assembly. To facilitate this process,
In view of the growing number and proportion of older members
the Programme of Nutrition has added a module on Innocenti
in populations of both developed and developing countries and
targets to the WHO Global Breastfeeding Data Bank, and these
the increase in diet- and lifestyles-related chronic noncommuni
will be seen as part of the Nutrition Surveillance system.
cable debilitating diseases affecting the ageing population,
For further information, please contact Randa Saadeh, WHO Pro
gramme of Nutrition. Tel: 41 22 791 3315 Fax: 41 22 791 4156 Email:
WHO and the USDA Human Nutrition Research Center on
saadehr@who.ch
Aging at Tufts University, Boston, USA, organised a joint
Consultation on Nutrition Guidelines for Healthy Ageing from 26
to 29 May 1998. The specific objectives of the Consultation
The Baby-Friendly Hospital Initiative (BFHI)
were:
0
to review scientific and epidemiological evidence regard
In assisting countries to maintain the credibility and sustainability
ing the role of diet and other lifestyle factors, including
of the BFHI, the Programme of Nutrition is continuing to develop
physical activity, in health protection and promotion and
re-assessment and monitoring tools based on the WHO/UNICEF
noncommunicable diseases prevention in ageing popula
BFHI Global Criteria. The monitoring tools are intended to aid
data collection on key indicators related to BFHI and infant
tions; and
0
to develop a report of a practical nature that will constitute
feeding practices. They have been field-tested in Poland and
an authoritative source of information for member country
Bolivia, (Oman and Malaysia to follow) in close collaboration with
governments, nutritionists, medical practitioners, nurses,
Wellstart International (a WHO collaborating centre based in San
elderly care-providers, social workers and others.
The agenda of the Consultation included a wide spectrum of
Currently, this database incorporates survey data from 91
subjects related to nutrition and the functional and health status
countries. Population rates of BMI, or mean BMIs are classified
of ageing populations.
according to the standard BMI cut-off points—i.e. 18.5, 17.0,
These included assessment of nutri
tional status, nutrition and chronic diseases, water metabolism
and 16.0 for Grades 1, 2 and 3 undernutrition (thinness) in
and dehydration, alterations in sensory systems, nutrition and
adults, and 25.0, 30.0, and 40.0 for overweight, obesity and
immune function, nutrition behaviour and cognitive function,
severe obesity in adults. Some 61 countries (covering 70.4% of
nutritional requirements and dietary guidelines. The Consultation
the adult population worldwide) have national mean BMI data,
also reviewed the demographic, epidemiological and social as
whilst 30 other countries have complete data sets including
pects of ageing with particular emphasis on a developing coun
mean BMI and prevalences below and above the standard BMI
tries perspective and discussed the community support for im
cut-off points.
provement of nutrition, physical activity and behaviour (life
styles) of ageing populations.
The report of the consultation will be published by the end of 1998. For
further information, please contact R. Buzina, WHO Programme of
Nutrition. Tel: 41 22 791 3316 Fax: 41 22 791 4156 Email: buzinar@
who.ch
WHO welcomes new contributions to this database. For further
information about how to contribute to the database, please contact
Yun Ling at the WHO Programme of Nutrition. Tel: 41 22 791 3322
Fax: 41 22 791 4156 Email: lingy@who.ch
WHO Consultation on Behavioural Aspects
of Preventing Obesity
Joint Consultations between WHO and FAO
The FAO/WHO consultation process seeks to periodically bring
together world experts on specific questions where areas of
responsibility overlap. The consultations are expected to draw
conclusions and make recommendations that provide the best
and most scientifically sound advice and information possible for
Member States.
and its Associated Problems
A WHO Consultation to address behavioural aspects of obesity
prevention and its associated problems is planned for 1-3
October 1998 in Tokyo, as part of WHO's efforts to develop
global, regional and national strategies for preventing and
managing the increasing global public health problem of obesity
(see also page 71).
Joint FAO/WHO Expert Consultation on Carbohydrates in Hu
The Consultation aims to:
man Nutrition: The purpose of this Consultation was to review
0
review and analyse emerging trends of nutrition transition
the full scope of carbohydrates in foods, including their role in
and behavioural factors contributing to the development of
human diet, the effects of processing on their digestibility, their
overweight and obesity;
use in manufactured foods, and their role in disease conditions
0
review various country experiences in promoting healthy
0
develop guidelines for effective behaviour-related strate
(see SON News No. 14 p34). The report of the Joint FAO/WHO
Consultation on Carbohydrates in Human Nutrition has just been
diets and lifestyles with respect to obesity;
published in the FAO Food and Nutrition Series (No. 66,1998)
gies to prevent and manage obesity as a public health
and is available from FAO (Sales and Marketing Group, Food
and Agriculture Organization, Viale delle Terme de Caracalla,
00100 Rome, Italy. Tel: 39 6 5705 5727 Fax: 39 6 5705 3152
problem;
0
identify methodologies for implementing and monitoring
behavioural strategies for controlling and reducing obesity.
Email: Publications-sales@fao.org).
Multisectoral strategies aimed at reducing obesity and its envi
Joint FAO/WHO Consultation on Vitamin and Mineral Require
ronmental determinants, and to improve knowledge about obe
ments in Human Nutrition: This Consultation will take place from
sity, its prevention and management, will be developed.
21-30 September 1998 in Bangkok, Thailand (see SCN News
Methodologies will be identified for designing effective
No.15p48)
community-based nutrition programmes to promote the choice
of appropriate diets and healthy lifestyles by individuals and
WHO Global Database on Obesity and
Body Mass Index (BMI) in Adults
This database was established in 1996 by the Programme of
families.
For further information please contact Chizuru Nishida, WHO Pro
gramme of Nutrition. Tel: 41 22791 3317 Fax: 41 22791 4156 Email:
nishidac@who.ch
Nutrition, and is being steadily built up. The aim is to provide an
up-to-date instrument—the only one of its kind—for establishing
IDD, Vitamin A Deficiency and Anaemia
the magnitude and distribution of obesity and underweight in
Data show that many countries
In the last fifteen years, WHO, UNICEF and ICCIDD have
have problems of obesity and undernutrition, occurring side-by-
worked with governments to combat IDD by ensuring adequate
adult populations worldwide.
side.
iodine intake through consumption of iodised salt. As a result,
the elimination of IDD as a public health problem by year 2000
is no longer an utopian view for a large number of countries. A
UZuZ UO. 16, JULY
report on the progress achieved by countries to control IDD will
Specific nutritional deficiency outbreaks still occur in refugee
be submitted to the next World Health Assembly in 1999. How
populations, and in other severely deprived or famine-affected
ever, programme sustainability is still a critical concern (see also
population groups.
The Programme of Nutrition is currently
SON working group discussions, page 24). In addressing this
writing guidelines on how to manage and prevent these defi
issue, WHO is currently assessing the quality of IDD monitoring,
ciencies.
and the WHO/UNICEF/ICCIDD document on ‘Indicators for as
lished shortly:
sessing Iodine Deficiency Disorders and their Control through
0 Scurvy and its prevention and control in major emergencies.
Salt Iodization' (WHO/NUT/94.6, WHO Geneva, 1994) is being
0 Thiamine deficiency and its prevention and control in major
revised.
The following three technical reviews will be pub
emergencies.
WHO, UNICEF and other organisations launched a 4-year pro
ject starting initially in Africa in 1998, to provide vitamin A
supplements to pre-school children during immunisation contacts
and to women at delivery.
0 Pellagra
and its prevention
and
control
in
major
emergencies.
Joint WHO/UNHCR Initiative to Develop
Guiding Principles for Caring for the
In order to assist public health staff to design and implement
programmes for control of iron deficiency and its consequences
Nutritionally Vulnerable during Emergencies
- especially anaemia - WHO, with UNICEF and UNU is about to
publish 'Iron deficiency: Assessment prevention and controf
In an effort to implement the World Declaration and Plan of
Action for Nutrition of the ICN, the WHO Programme of Nutri
(WHO/NUT/98.6 WHO Geneva).
tion has been examining aspects of care-related nutritional
To assess the magnitude of micronutrient malnutrition, monitor
vulnerability and household food and nutrition insecurity to
the impact of programmes on populations, and assess the
develop strategies for caring for the nutritionally vulnerable
soundness of proposed strategies, WHO maintains the Micronu
during emergencies.
trient Deficiency Information System (MDIS) which includes three
databases on iodine, vitamin A and iron. The iodine and vitamin
A deficiency databases have already been published, and are
currently being revised. The database on iron deficiency is still
In order to develop consolidated strategies for caring for the
nutritionally vulnerable during emergencies, a joint WHO/UN
HCR Technical Consultation on Caring for the Nutritionally
Vulnerable during Emergencies was held in Rome, 24-27
being developed.
February 1998, hosted by the National Institute of Nutrition.
WHO welcomes new contributions to all MDIS databases. For further
information about how to contnbute, please contact Bruno de Benoist,
Programme of Nutrition, WHO, 20 Avenue Appia, CH-1211 Geneva 27,
Switzerland Tel: 41 22 791 3412 Fax: 41 22 791 4156 Email:
debenoistb@who.ch
Two
background
documents
were
prepared
for
the
Consultation:
o Caring for the Nutritionally Vulnerable dunng Emergencies:
a Review and Implications for Policy.
0 Caring for the Nutritionally Vulnerable during Emergencies
Nutrition in Emergencies
(an annotated bibliography).
The Programme of Nutrition is very frequently called upon by
other UN organisations, humanitarian/relief NGOs, and member
states to provide technical advice on management of nutritional
emergencies, famine, or other disaster situations.
The Pro
gramme of Nutrition provides technical inputs for strengthening
capacities at national, subnational, and also international levels
for the management of nutrition in emergencies. This is done
through the production of guidelines, norms, criteria, methodolo
gies and information on the monitoring/surveillance and manage
ment of nutrition in emergency settings, and through information
dissemination and training.
Guiding principles for feeding infants and young children during
emergencies, 1997 (see SCN News No.15p37).
A three-part practical manual pack: This pack, due be published
by the end of this year, is for field staff working at the operational
level in emergencies and for programme managers. It includes
methods to calculate group nutrition requirements, assess and
monitor nutrition status, and also includes information on food
distribution and selective feeding.
Specific aims of the Consultation were to:
0 examine care-related and behavioural aspects of nutritional
vulnerability and household food insecurity during emergen
cies, and to possibly develop approaches for assessing and
monitoring these aspects of nutritional vulnerability;
0 develop strategies and guiding principles for promoting
household food and nutrition security and caring for the
nutritionally vulnerable during emergencies, to be used as
the basis for developing policies and programmes as well as
training modules to assist health personnel and others
working in emergencies;
0 identify research needed in the area of care, household food
and nutrition security and emergencies.
The Consultation provided a forum for exchanging information
and experiences of experts, country representatives, NGOs,
bilateral and international agencies. It compiled information on
nutritional vulnerability, determining factors and possible ap
proaches for assessing care-related nutritional vulnerability
during emergencies. The Consultation also developed generic
6o
guiding principles for each vulnerable group, to be applied and
lished its estimates of per capita consumption of raw agricul
incorporated into policies and programmes, and to serve as a
basis for training modules to assist health personnel and others
five regional diets (WHO/FSF/FOS/98.3). Finally, a full report is
working in emergencies.
now available on the joint FAO/WHO Consultation on Food
tural commodities and certain semi-processed commodities for
Consumption and Exposure Assessment of Chemicals in Food,
The generic guiding principles are being finalised by WHO in
collaboration with UNHCR, UNICEF and various NGOs.
The
including food additives, contaminants, residues of pesticides
and veterinary drugs and certain nutrients which was held
final document will also include simple tools for applying and
10-14 February 1997 in Geneva (WHO/FSF/FOS/97.5 - see
implementing the guiding principles. A draft document will be
SCN NewsNo.15p55}.
ready to be circulated for expert peer review in late 1998.
For further information, and to request copies of the documents listed
above, please contact Chizuru Nishida, WHO Programme of Nutrition.
Tel: 41 22 791 3317 Fax: 41 22 791 4156 Email: nishidac@who.ch
Disinfection of Fruits and Vegetables
WHO, jointly with FAO and in collaboration with the National
Sanitation Foundation International, USA, has prepared a docu
For further information about any of activities of the Programme of
Nutrition and requests for documents, please contact the WHO Pro
gramme on Nutrition, WHO, 20 Avenue Apcza, CH-1211 Geneva 27,
Switzerland. Tel: 41 22 791 3326/3321 Faz: 41 22 791 4156 Email:
ment on current practices with regard to disinfection of fruits
and vegetables. The document provides a review of the haz
ards associated with fruits and vegetables, and the efficacy of
different disinfection methods on the hazards. The report will
clugstong@who.ch
be available from the WHO Food Safety Unit (contact details on
next page) in September 1998.
Food Safety for Nutritionists
Food Safety: GEMS/Food
A WHO/lndustry Council for Development (ICD) Course on
The Global Environment Monitoring System / Feed Contamina
tion Monitoring and Assessment Programme /GEMS/Food),
which now includes participating institute1" s from over 70 coun
tries worldwide, collects and evaluates information on evels and
trends of contaminants in food, their contrixitfon to total human
exposure and significance with regard to pcofic health and trade.
GEMS/Food continues to provide informatzfl from its database,
held at the WHO Food Safety Unit, Geneva x /arcus users,
including the Codex Alimentarius Commisscn and its subsidiary
bodies. The Programme is described in a 'ew ororxere (WHO/
FSF/FOS/97.9) available from the WHG Fxc Safety Unit
Food Safety for Nutritionists is organised annually in Indonesia
as part of the MSc Programme carried out by the South Asian
Ministers of Education Organization (SEAMEO) in collaboration
with the German Technical Cooperation Agency (GTZ). The
objectives of the training course are to promote understanding
of food safety and to enable participants to effectively reduce or
prevent foodborne diseases. The training course is open to all
candidates desiring to be trained in food safety.
A training
package entitled 'Food Safety for Nutritionists' is made avail
able to the participants of the course, which consists of nine
modules, lecture notes, set of overheads and student handouts.
The course lasts for two to three weeks (see page 48 for more
(contact details on next page).
details).
During 1997, GEMS/Food conducted two Anai-/xai Cuality As
surance (AQA) studies. The first - on pesxxe mizxres - was
coordinated by the WHO Collaborating Oerre for Pesticide
Databank on Foodborne Disease Outbreaks
Analysis and Training located at the G7Z =esoGde Service
The Food Safety Unit, WHO is maintaining a global databank
Project in Eschborn, Germany. A repcr of Its stucy is now
available from the WHO Food Safety Unt foo-ac: oatails on
on food borne disease outbreaks published in the literature. The
next page). The second - on heavy "ea aoayss - was
conducted in cooperation with the WHO Cotexraor.G Centre for
causative agents, number of people affected, signs and symp
Food Contamination Monitoring at the Eg // 'Sxoesnstitut fur
was prepared and consumed, and factors contributing to the
gesundheitlichen Verbraucherschutz urc
outbreak.
/ersrrai tedizin),
databank collects epidemiological data, including data on
toms, food vehicle involved, place where the implicated vehicle
Berlin, Germany and the report should ie szaiaoe from the
The databank has been developed to meet the increased
Food Safety Unit shortly.
demand for epidemiological information on foodborne disease.
GEMS/Food has also recently issued e 'ez'sec <ersion of
The objective is to compile epidemiological information neces
'Guidelines for Predicting Dietary Intake or
Fssidues’
sary for a variety of purposes, for example, the application of
(WHO/FSF/FOS/97.7), which offers simcie
xacxe methods
Hazard Analysis and Critical Control Point (HACCP), risk as
for assessing possible exposure to pesficcas casae 'S Tie best
sessment, health education in food safety, and understanding
use of available information. In addition.
"as pub
the role of food in the transmission of diseases.
61
JULY iegg
For further information and to obtain copies of any of the documents
mentioned above, please contact the Food Safety Unit, Programme of
Food Safety and Food Aid, WHO, 20 Avenue Appia, CH-1211 Geneva
27, Switzerland. Tel: 41 22 791 2555 Fax: 41 22 791 4807 Email:
foodsafety@who.ch WHO Food Safety documents are also increasingly
available on the web at http7Avww.who.ch/fsf/
Box;: Global-Health. Targets to 2020
1
Increase equity in health and use the health equity index
■
of childhood stunting.
2
Improve survival and quality of life, indicated primarily by
reductions in maternal and child mortality rates and'
increased life expectancy.
3
Health for All in the 21st Century-
Reverse global trends for tuberculosis, HIV/AIDS,
malaria, tobacco-related diseases and violence/trauma.
4
the Nutrition Elements
Eradicate and eliminate certain diseases (measles, lym
phatic filariasis, Chagas disease, leprosy, trachoma and
vitamin A and iodine deficiencies).
Since 1978, when the policy on Health for
5
Conference, political, economic, environ
6
7
8
9
Establish and strengthen operational global and national
10
health information and surveillance systems.
Develop and enhance health research programmes at
WHO, aimed at formulating a new global
health policy.
A briefing document is
available, together with the policy which
Improve access everywhere to comprehensive high
quality essential health care.
cations for health has resulted in an inten
sive worldwide consultation process led by
Develop, implement and monitor national policies con
sistent with HFA.
a renewed vision and model of health to
suit these new trends and their huge impli
Promote healthy life styles and discourage health dam
aging ones in all countries.
mental and social changes have occurred
on an unprecedented scale. The need for
Improve access in all countries to safe drinking water,
sanitation, food and shelter.
All (HFA) was adopted at the Alma-Ata
global, regional and country levels.
has been endorsed by the World Health
Assembly during its Session in May 1998.
In building on the strengths of the original policy, Health for All in
the 21st Century sets out, for the first two decades of the 21s'
century, global priorities and targets which will create the condi
tions whereby people everywhere will have the opportunity to
reach and maintain the highest attainable level of health through
out their lives. It gives added emphasis to 'health as a human
right'; to gender sensitivity; and the paramount importance of
addressing poverty and inequality as both root causes and
results of ill health.
define priorities for resource allocation (see Box). Achieving
these targets will ensure that the overall goals of HFA are met.
How do nutrition concerns fit into the new HFA vision?
Nutrition is central to the first health target, where stunting rates
will be used to assess equity within and between countries as a
basis for promoting and monitoring equity in health. Stunting
(defined as height-for-age more than two standard deviations
below the reference value) has been recommended by WHO1 as
an ideal indicator for determining priorities for allocation of re
It measures the
cumulative deficient growth associated with long term factors
such as chronic insufficient daily food intake, frequent infection,
poor feeding practices and possibly the low socioeconomic status
of households. The initial quantitative target utilised for equity is
' WHO Technical Report Series, No. 854,1995.
62
are stunted should be less than 20% in all countries and in all
Nutrition is also specifically addressed elsewhere in the new
HFA vision. In the second health target, a child mortality rate of
less than 45 per 1000 live births has been set for the year 2020.
In setting this target, the health community has undertaken to
give priority to providing resources to the IMCI (integrated
management of childhood illnesses), which aims to reduce the
impact of the five major causes of death in children - one of
Ten new global targets have been set out to spur action and to
sources to improve equity in health care.
that by the year 2020, the percentage of children under 5y who
specific subgroups within countries.
which is malnutrition (see SCN News No.15, p56).
More
directly, the fourth health target specifies that by the year 2020,
vitamin A and iodine deficiencies have been eliminated. By the
same year, target 5 states that through intersectoral action,
major progress will have been made in making safe food
available to all.
Fulfilling the HFA vision
To achieve these targets, the document emphasises that com
mitted action is needed. At the national level, governments will
be responsible for creating an enabling environment for action
in support of HFA. And it is the role of WHO, as the world’s
health advocate, to stimulate global action, provide global
leadership for HFA and build strategic alliances with other UN
agencies, the World Bank, NGOs, the private sector and other
relevant partners in pursuit of HFA goals at all levels.
’
For general information about Health in the 21s Century, please contact
Dr Roberta Ritson, WHO, Division of Policy Programme and Evaluation,
Policy Action Coordination Team, 20, Avenue Appia, CH-1211 Geneva
27, Switzerland. Tel: 41 22 791 2557 Email: Ritsonr@who.ch', or Mr
Chris Powell, WHO, Division of Health Promotion, Education and Com
munication, Health Communications and Public Relations, 20, Avenue
Appia. CH-1211 Geneva 27, Switzerland. Tel: 41 22 791 2888 Email:
powellc@who.ch. For specific information on nutritional aspects
please contact the Programme of Nutrition, WHO (Tel: 41 22 791 3326
Fax: 41 22 791 4156 Email: clugstong@who.ch). Based on the WHO
document A51/5 and briering summary ‘Health for all in the twenty-first
century'. Further information about Health for All in the 21“ Century
can be found on the WHO website at http://www.who.ch/hfa/index.htm
WHO / UNAIDS / UNICEF
Technical Consultation on HIV and Infant Feeding
Geneva, April 20-22 1998
Three million children worldwide have been infected with HIV.
cies. The meeting was also attended by representatives of
Most have been infected through transmission of the virus from
breastfeeding specialised NGOs and the infant formula
their HIV-positive mother. About two thirds of mother-to-child
industry.
transmission occurs during pregnancy and delivery, and about
one-third through breastfeeding.
The number of children in
fected with HIV is rising, reflecting the increase in numbers of
Recommendations and outcome of the meeting
In addition to the key recommendation of increasing access to
women of childbearing age who are infected. In 1997 alone,
replacement feeding for HIV-positive women, the need to im
more than half a million children were infected worldwide, and in
prove access to voluntary and confidential HIV counselling and
a growing number of countries, HIV is now the single most
testing, particularly for pregnant women, and counselling on
important cause of child death.
infant feeding, was emphasised.
Following the adoption of the Joint Policy Statement on HIV and
Participants also endorsed the need to implement measures to
Infant Feeding in 1997, WHO, UNAIDS Secretariat and UNICEF
prevent breastfeeding from being undermined among HIV
developed a set of three comprehensive guidelines to assist
negative women and among those who do not know their HIV
decision-makers and health care managers to implement the
status.
policy:
distributing and making available breastmilk substitutes should
0
HIV and Infant Feeding: Guidelines for Decision-makers.
0
HIV and Infant Feeding- A Guide for health care managers
0
There was consensus that methods for procuring,
comply with the International Code of Marketing of Breast-milk
WHO/FRH/NUT/CHD 98.1, UNAIDS/98.3, UNICEF/PD/
Substitutes (see page 67) and subsequent resolutions of the
NUT (J) 98-1.
World Health Assembly.
and supervisors, WHO/FRH/NUT/CHD/98.2, UNAIDS/98.4,
Strengthening health care services was also a priority, particu
UNICEF/PD/NUT (J) 98-2.
larly reproductive health services in developing countries, to
HIV and Infant Feeding: A review of HIV transmission
implement interventions that would reduce HIV infection in
through breastfeeding, WHO/FRH/NUT/CHD/98.3, UN-
women and reduce mother-to-child transmission of HIV and
AIDS/98.5, UNICEF/PD/NUT (J) 98-3.
ensure care and social support for HIV-positive mothers.
The documents recognise that HIV can be transmitted through
A full report of the meeting 'Technical Consultation on HIV and Infant
breastfeeding. The documents also cover all alternative feeding
Feeding: Implementation of Guidelines WHO/CHD/98.15, WHO/FRH/
NUT/98.4, UNAIDS/)(,6, UNICEF/PD/NUT(J)98-4' is in preparation,
and will be available on request from the Division of Child Health and
Development or the Nutrition Programme at WHO, Geneva, or from the
UNAIDS Documentation Centre, Geneva, or the Nutrition Section,
UNICEF New York, TA -24A, 3 UN Plaza, New York, NY 10017, USA.
The three documents listed above are available upon request from
Randa Saadeh, WHO Programme of Nutrition. Tel: 41 22 791 3315
Fax: 41 22 791 4156 Email: saadehr@who.ch (CHF16, CHF11.20 in
developing countries).
options which are: commercial formula, home-prepared formula,
heat treated mother’s milk, milk from an established milk bank,
wetnursing by a relative and earlier cessation of breastfeeding.
The documents express the need to support the use of safe
alternatives to breastfeeding when an HIV-positive mother
makes a fully informed choice not to breastfeed and selects one
of the above options. They also strongly emphasise that breast
milk remains the optimal source of nutrition for the majority of
infants, including all infants of mothers not tested for HIV.
Implementation of the guidelines was discussed during a meet
Sources: Felicity Savage (WHO/CHD), Ludmila Lhotska (UNICEF) and
Randa Saadeh (WHO/NUT).
ing convened by WHO in Geneva (April 20-22, 1998) that
brought together representatives of governments from countries
most affected by HIV/AIDS, scientists, and United Nations agen
63
Gc/J K)Eu€)JO.ie, JULY
The World Bank
Nutrition Lending Update
is the first new World Bank supported project in The Gambia
The graph shows the latest figures for regional nutrition lending
since 1994. The Participatory Health, Population and Nutrition
by the World Bank. South Asia and Latin America regions have
Project will have far-reaching beneficial impacts on the health
the highest estimated lending for nutrition, although the Africa
of The Gambia’s most vulnerable populations - particularly
region has the highest number of projects that allocate funds to
infants, children, and women of reproductive age - by improving
health services and promoting the active participation of individ
nutrition.
uals and communities in ensuring their own health.
Yearly average of nutrition lending by
region in millions of USS
Prepared through an extensive consultation process involving
NGOs, community members, other donors, and the govern
ment, the project takes an integrated approach to improving
family health. World Bank financing will support preventive
■ AFR
BLAC
qSAS
□ ECA
□ MENA
health care activities, as well as support policy and programme
development. A grassroots education programme will encour
age community awareness, community involvement in health
services, promote safe sex behavior, and strengthen basic
health and nutrition. Training for health care workers, the
FY91-95
,
FY96-2000
Fiscal year
The graph shows an overview of the average lending figures per year
over the fiscal periods 1991-95 and 1996-2000. All numbers are based
on projections; i.e. not actual disbursement.
expansion of family planning services and HIV/AIDS prevention
programmes, and upgrading and maintenance of existing
health infrastructure are also included.
The Philippines
The World Bank has approved a US$19 million loan to the
Philippines for an Early Childhood Development (ECD) Project
Recently Approved Projects
that will provide services to reduce childhood mortality and
promote the physical and mental development of Filipino chil
Madagascar
dren, particularly those who are most vulnerable and disadvan
The World Bank recently approved a US$27.6 million equivalent
credit for a project to improve the nutrition for children and
pregnant and breastfeeding women in Madagascar. The project
will focus on reducing the number of underweight children,
combatting vitamin A and iron deficiency, and reducing helminth
taged. The project also aims to establish an effective partner
ship between national and local governments in the provision of
ECD services. It is designed to assist in compensating for past
government under-spending in human resource development
and poverty alleviation.
infections. An educational component will increase awareness of
malnutrition and its causes. This Community Nutrition II project,
The project is part of a 10-year ECD Programme which seeks
which will be national in scope, builds on the successful World
to expand and upgrade existing ECD programmes in the
Bank-supported community nutrition project Projet de Securite
Philippines. One component of the project will involve supplying
Alimentaire et de Nutrition currently operating in two provinces.
crucial inputs to maintain and upgrade five region-wide ECD
The project will have several components. A Community Nutri
tion Programme will support community-based growth monitoring
and growth promotion campaigns involving the weighing of chil
dren less than 3 years old.
Pood supplementation will be
available for malnourished children as well as pregnant women,
and vitamin A supplements will be given to young children and
breastfeeding mothers. A School-Based Nutrition Programme
will promote good nutrition and hygiene, provide iron and de
worming tablets, and treat children aged 3-14 years for worms
both in and out of school. The project will also assist in financing
nutrition-related activities in the health and agriculture sectors.
The Gambia
The World Bank recently approved a US$18 million equivalent
credit for a project to improve family health in The Gambia. This
programmes covering immunisation, improved management of
sick children, prevention and control of micronutrient deficien
cies (iron, iodine, vitamin A) through food fortification, educa
tion of parents on how to stimulate and promote young child
development and improved curricula and health services for
children in Grade 1.
For more information,
please contact Claudia Rokx
(crokx@woridbank.org), or Claire Hervey (Tel: 1 202 473 8294 Fax: 1
202 473 7917 Email: chervey@worldbank.org) at the World Bank,
1818H Street NW, Washington DC 20433. To obtain project docu
ments please contact the World Bank's Public Information Center
(PIC), 1776 G Street, NW, Room GC1-300, Washington DC 20433.
Tel: 202 458 5454 Fax: 202 522 1500 Email: pic@wortdbank.org
Further information about the World Bank's recently approved projects
can be found on the Web at http://www.woridbank.org/
Sources: C. Rokx, C. Hervey and World Bank 1998 press releases.
RECIPES FOR INFANTS AND TODDLERS
POTATO PUDDING
Dried potato chips powder 60 g.
Horse gram dhal powder
25 g.
Groundnut cake powder
30 g.
Baking soda
a pinch(half tea-spoonful)
Method : The flours are mixed and a semisolid batter is
prepared. Oil or dalda is smeared on an luminimum pan and the
batter is poured into the oiled pan. The vessel is covered with
a greased paper and tied up and steamed.
RAGI PUDDING
Ragi flour
50 g.
Bengal gram dhal flour
Groundnut cake powder
Jaggery
Baking soda
12.5 g.
12.5 g.
20 g.
a pinch
Method: Same as for preparation of Potato pudding.
CHOLAM PUDDING
White cholam flour
Groundnut cake powder
Food Yeast
Jaggery
Cumin seeds
30 g.
15 g.
5 g.
12.5 g.
One-fourth teaspoonful
Method: Same as for preparation of Potato pudding.
THENAI ADAI
Thenai flour (roasted)
Groundnut cake powder
(roasted)
Jaggery
Dalda
25 g.
25 g.
20 g.
One-eighth teaspoonful
Method: The dough is prepared with jaggery syrup and small
balls are made and spread in rounds or squares on the palm.
The rounds are placed on a greased hot iron plate. They are kept
turning over and over till cooked.
THENAI IDDLY
Thenai
Bengal gram dhal
Salt
100 g.
50g.
to taste (enough for 8 iddlies)
Method: The Thenai grains and Bengal gram dhal are ground and
mixed to a thick batter and kept overnight. In the morning
iddly moulds are filled up and steamed till they are well codied.
2
2
CHOLAM IDDLY
White cholam grains
Cow gram dhal
Salt
100 g.
50 g.
(for 8 iddlies)
Method: The grains and dhal are soaked for a few hours. They
are ground together into a fine paste in a stone mortar. The
paste is kept overnight. The thick batter is poured in iddly
moulds and steamed till it is well cooked.
SAMAI BALLS
Samai flour
Black gram dhal flour
Salt
60 g.
30 g.
to taste
Method: The dhal is cooked till soft and salt is added. The
samai flour is mixed in water to a thick paste and added to the
m.ashed dhal. It is cooked with just enough water, poured into
a plate and while still warm, balls are made.
CHOLAM SCRU WITH DHAL
White Cholam
Red gram dhal flour (raw)
Tomato
Salt
100 g.
30 g.
30 g.
(Blanched and the juice extracted
and sieved)
to taste
Method: The cholam grains are cooked and when it is well done,
the dhal powder is added and cooked well for 20 minutes. It is
removed from the fire and tomato juice is sprinkled. It is
served warm to the child.
READY-TO-USE INFANT FOODS
GROUNDNUT CAKE PORRIDGE
Groundnut cake powder roasted
Green gram dhal flour roasted
Palm jaggery
50 g.
15 g.
25 g.
Method: The two flours are mixed in hot water and a semi-solid
batter is prepared. Jaggery is prepared in the form of a syrup.
The semi-solid batter is added to the boiling syrup and kept
stirred. It is boiled for 10-15 minutes in an open vessel over
low fire. It is served to the infants before it gets cold.
.. .3
3
GP.CUM?NUT CAKE POWER/JACK FRUIT SEED POWER/PORRIDGE;
Jack fruit seed flour (roasted)
Groundnut cake flour
Palm jaggery
25 g.
50 g.
25 g.
Method : Same as for preparation of Groundnut cake powder.
PREPARATION OF JACK FRUIT SEED FLOUR;
Jack fruit seeds are peeled of theskins and sliced
thin and washed repeatedly in cold water It is boiled for 15
minutes and dried in sun. The dried seeds are ground to flour.
The flour can be kept for days if kept free from dampness.
SOURCE: Swasth Hind - June 1980.
Position: 21 (125 views)