RF_L_7_A_SUDHA.pdf
Media
- extracted text
-
RF_L_7_A_SUDHA.
L~
Programme
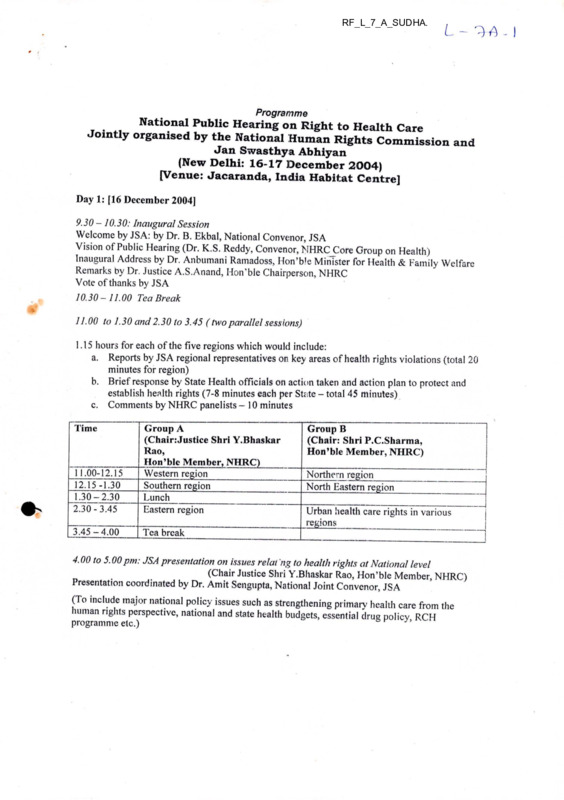
National Public Hearing on Right to Health Care
Jointly organised by the National Human Rights Commission and
Jan Swasthya Abhiyan
(New Delhi: 16-17 December 2004)
[Venue: Jacaranda, India Habitat Centre]
Day 1: [16 December 2004]
9.30-10.30: Inaugural Session
Welcome by JSA: by Dr. B. Ekbal, National Convenor, JSA
Vision of Public Hearing (Dr. K.S. Reddy, Convenor, NHRCCore Group on Health)
Inaugural Address by Dr. Anbumani Ramadoss, Hon’ble Minister for Health & Family Welfare
Remarks by Dr. Justice A.S.Anand, Hon’ble Chairperson, NHRC
Vote of thanks by JSA
10.30 - 11.00 Tea Break
11.00 to 1.30 and 2.30 to 3.45 (two parallel sessions)
1.15 hours for each of the five regions which would include:
a. Reports by JSA regional representatives on key areas of health rights violations (total 20
minutes for region)
b. Brief response by State Llealth officials on action taken and action plan to protect and
establish health rights (7-8 minutes each per State - total 45 minutes)
c. Comments by NHRC panelists - 10 minutes
12.15-1.30
1.30- 2.30
2.30- 3.45
Group A
(Chair: Justice Shri Y.Bhaskar
Rao,
Hon’ble Member, NHRC)
Western region__________
Southern region____________
Lunch___________
Eastern region
3.45-4.00
Tea break
Time
Tl.00-12 J 5
Group B
(Chair: Shri P.C.Sharma,
Hon’ble Member, NHRC)
Northern region
North Eastern region
Urban health care rights in various
regions
4.00 to 5.00 pm: JSA presentation on issues relat 'ng to health rights at National level
(Cllair Justice Shri Y.Bhaskar Rao, Hon’ble Member, NHRC)
Presentation coordinated by Dr. Am it Sengupta, National Joint Convenor, JSA
(To include major national policy issues such as strengthening primarv health care from the
human rights perspective, national and state health budgets, essential drug policy RCH
programme etc.)
- I
Day 2: |17 December 2004]
9.30 to 12.30: Parallel sessions on key health rights issues, 45 minutes each
(JSA presentation 20 minutes, discussion 15 minutes, panelist comments 10 minutes)
Group A: 9.30 to 11.00\ Session 1
(Smt. Reva Nayyar, Secretary, Women & Child Development to chair
Shri S.S.Brar, Joint Secretary (RCH), Deptt. of Family Welfare.
Women’s right to health care
Children’s right to health care
Session 2: 11.00 to 12.30: Shri Chaman Lal, Special Rapporteur, NHRC to Chair
Dr.P.K.Dave, NHRC Expert Group on Emergency Medical Care:Co-chair
(subject to confirmation)
Mental Health Rights
Health Rights in situations of conflict and displacement
Group B: Session 1 9.30 to 11.00: Shri V.K. Arora, Addl. DG, Health Services to chair
Dr. D. Banerjee, Vice-Chairperson, JSA-co-chair
Right to essential drugs
Health rights in the context of the Private medical sector
Session 2: 11.00 to 12.30 : (Dr S.Y.Quraishi, Additional Secretary
& Project Director, NACO to chair)
Dr. N.H.Antia, Chairperson, NHRC Core Group on Health: co-chair)
Health rights in the context of the HIV-AIDS
Occupational and environmental health rights
12.30-1.30
Lunch
1.30 to 2.15: Plenary presentation by ISA Rapporteurs [Dr. Vandana Prasad and Mr. Amitava
Guha] on the key health rights issues emerging from two parallel sessions
[Chair: Shri S.S.Brar, Joint Secretary' (RCH), Deptt. of Family Welfare to chair]
2.30 to 4.15: Towards a National action plan to establish, fulfil and monitor the Right to HealthCare
1. Statement by Mr. Paul Hunt, United Nations Special Rapporteur on Right to Health [Ms.
N.B. Sarojini to read oufthe Statement]
2. People’s actions to establish the Right to Health Care (Dr. Abhay Shukla, National Joint
Convenor, JSA)
3. JSA-NHRC joint presentation on a National action plan to establish, fulfil and monitor
the Right to Health Care (Shri Y.S.R. Murthy, Deputy Secretary (Research), NHRC and
Dr. T. Sundararaman, National Joint Convenor, JSA)
4. Responses from Union Health Ministry (Shri P. Hota, Secretary, Health & Family
Welfare)
5. Concluding remarks by Dr. Justice A.S. Anand, Hon’ble Chairperson, NHRC
6. Vote of thanks by Shri Y.S.R. Murthy, Deputy Secretary (Research), NHRC
National Public Hearing on the right to health care
Jointly organized by the National Human Rights Commission and Jan Swasthya Abhiyan
The programme on started on time with the welcome address delivered by Dr. Ikbal convener of
JSA. He welcomed the dignitaries and the delegates. Dr. Ikbal in his address mentioned this event
is an historical one as this is the first time a Human Rights Commission was collaborating with
civil society agencies in addressing a issue.
Followed by the welcome address Dr. Ikbal shared the vision of public hearing/. Dr. Srinath Reddy
in his address mentioned that right to health is a human right and denial of access to health care is
violation of human right. He mentioned the need for comprehensive primary health care approach
in meeting the health needs of citizens of this country. He also mentioned that the present
understanding that the public private partnership for the benefit of the poor needs a critical analysis.
Finally he said community participation is crucial in the success of any programme. He concluded
his speech by saying that the goal of Jan Swasthya Abhiyan’s Right to Health Care campaign is to
strengthen accessibility of public health services.
Followed by Dr. Reddy the Honrable Minister for health and family welfare Dr. Anbumani
Ramdoss delivered the inaugural address. Dr. Ramdass in his address said right to health care is*
un amental right. He referred to the constitution of WHO which says; that every one has the right
to enjoy health at the highest attainable standard. He also referred to the Universal Declaration of
Human Rights by the General Assembly of the United Nations, which says that all human beings
are born free and equal in dignity and rights.
\(
He referred to the WHO's definition of health and said health care is complex issue. He mentioned
the need to balance between the various aspects in health care, which include curative preventive
promitive. He also mentioned the determinants of health such as water, sanitation and nutrition He
said the rural population put together to with the urban poor constitute 90% of the population to
whom the health care is important, he pointed the need for changes in the health care delivery
system, he said he was particularly concerned about the quality. He mentioned about the doctor
patient ratio in India he said, even if we put together the practitioners of all system of medicine the
doctor patient ratio in India comes one doctor per 800 population. He said the hospital beds
available at present in the country, which is about one million barely sufficient. He justified the
need for public private partnership by mentioning that the public sector contribution in health care
is only 17/o, he emphasized the need for streamlining. Here he mentioned about the need for
accreditation of health care facilities that area available in the county and the need for health
regulatory authority. He also mentioned about need for essential drugs guidelines and said he is
concerned about particularly about the list not being available regarding the life saving drugs
While referring to private sector he mentioned about the need for checking quackery.
^delineatinfthTneeds 3''
reCOmmendations Put forth b> JSA't is commendable for the efforts
creation. He said he is also concerned about safe mother hood by which the MMR could be brought
down he said he particularly concerned that MMR is stagnant for the past three decades He said
that the prime minister is concerned about two key issues the health and education which are alike
Alcohol: No Ordinary Commodity. A summary of the book -Alcohol & Public Policy GroupPage 1 of 10
I
THE GLOBE
,
X ' G1 b a I A i c o ii o t P o H c y A M i.
■■■
Alcohol: No Ordinary Commodity. A summary of the bo
Alcohol & Public policy Group
Alcohol Policy and The Public Good, published in 1994, was a modern landmark in ah
policy. Here, with the kind permission of the editor of the journal Addiction, we repr<
summary of its successor. Alcohol: No Ordinary Commodity — Research and public pi
(Babor et al. 2003). The first part of the book describes why alcohol is no ordinary
commodity, and presents epidemiological data on the global burden of alcohol-relate
problems. The second part of the book reviews the scientific evidence for strategies
interventions designed to prevent or minimise alcohol-related harm: pricing and taxi
regulating the physical availability of alcohol, modifying the drinking context, drinkii
counter measures, regulating alcohol promotion, education and persuasion strategic
treatment services. The final Section considers the policy making process on the loca
national and international levels, and provides a synthesis of evidence-based strateg
interventions from a policy perspective.
Setting the policy agenda
The purpose of this volume is to describe recent advances in alcohol research that have direct
to alcohol policy on the local, national and international levels. Alcohol policies serve the inter
public health through their impact on drinking patterns, the drinking environment and the hee
services available to treat problem drinkers. Public health concepts provide an important vehh
manage the health of populations n relation to the use and misuse of beverage alcohol by hel
communities and nation states to design better preventative and curative services. Alcohol po
been implemented throughout histpry to minimise the effects of alcohol on the health and saf<
population but only recently have ese strategies and interventions been evaluated scientific.
No ordinary commodity
In many countries, the production and sale of alcoholic beverages generates profits for farmer
manufacturers, advertisers and investors. Alcohol provides employment for people in bars anc
restaurants, brings in foreign curre icy for exported beverages and generates tax revenues for
government. Alcoholic beverages a-e, by any reckoning, an important, economically embedde
commodity.
However, the benefits connected w th the production, sale and use of this commodity come at
enormous cost to society. Three imbortant mechanisms explain alcohol's ability to cause medi
psychological and social harm:
• (1) physical toxicity
• (2) intoxication and
• (3) dependence.
Alcohol is a toxic substance in terms of its direct and indirect effects on a wide range of body •
http://www.ias.org.uk/publications/theglobe/0 5issue3/globe0303_p3.html
12/22/2004
He also mentioned about the need to work towards checking the trend regarding HIV/AIDS in
India. He said there is need for legislative measures in checking discrimination against people
affected by HIV/AIDS.
He said his government is concerned about health that is the reason why the new programme is
being planned ie the rural health mission in 17 states, which are backwards. About the health
budget he said that the governement would increase from the present .9% to 2%.
Finally he said that the judiciary has created havoc in medical education and he would be interested
to discus the same with the chairperson of NHRC.
Justice Anand in his remark said that India is welfare state therefore it is the duty of the government
to provide health care for all its citizens. He referred to article 21, which talks about right to life and
argued right to health leads to right to life. He said without addressing the following three areas it is
difficult to achieve development; he referred to poverty, health care and education. He illustrated a
case where a patient in West Bengal was denied health care in many places. He also expressed his
concerned about the health indictors, though life expectancy has gone up but indicators such as
IMR and MMR being stagnated. Regarding access to essential drugs he said only 35%of the
population are accessible. Regarding health budget he said it should go upto 3-5%. The inagural
session came to an end by vote of thanks by Dr.Sarojini of Sama.
Living dangerously: The World Health Report, 2002
Page 3 of 3
"Legislation enables risks to health to be reduced in the workplace and on the roads, whether
the wearing of a safety helmet in a factory or a seat belt in a car. Sometimes laws, education
persuasion combine to dimiroish risks, as with health warnings on cigarette packets, bans on t
advertising, and restrictions on the sale of alcohol."
The report is particularly concerned with the increase in alcohol consumption in poorer, devek
countries: "All of these risk factors -- blood pressure, cholesterol, tobacco, alcohol and obesity
the diseases linked to them ard well known to wealthy societies. The real drama is that they r
increasingly dominate in low mortality developing countries where they create a double burde
of the infectious diseases that always have afflicted poorer countries. They are even becominc
prevalent in high mortality developing countries." |
The Globe (links to previous issues)
This issue of The Globe (link to index)
\
(Global Alcohol Policy Alliance|Alliance House
12 Caxton Streetj London | SW1H 0QS| Tel: 0207 222 40011 Contact Gapa
Copyright 2003
http://www.ias.org.uk/publications/theglobe/02issue4/globe0204_p3.html
Home
12/22/2004
L- ^^3
WESTERN REGION PUBLIC HEARING
ON
RIGHT TO HEALTH CARE
29 JULY 2004
BHOPAL, MADHYA PRADESH
Recommendations from the Public Hearing
Legal Measures
Enactment of a State Public Health Act in each state, which would outline the
mandatory health care sen ices which must be made available to the people as a right at
various levels of the public health system. This act would specify which services and
standards of care must be made available at the community, sub-centre, PHC, CHC,
Sub-district and District hospital levels, as well as the preventive and promotive
measures that the government would undertake.
> Enactment of a Clinical Establishments Regulation Act in each state to ensure
minimum standards, adherence to standard treatment guidelines and ceilings for costs of
essential medical services in the private sector. For example, the Bombay Nursing
Home Regulation Act 1949 - Maharashtra, may be substantially modified and
improved to effectively regulate the quality of private medical services in the state.
> Private practice presently allowed to Government health care providers should be legally
banned, and those doing it should be promptly punished.
Independent Social Monitoring and Redressal System
> Preparing lists ofspecific services and supplies that would be guaranteed at all levels of
the public health system; wide dissemination and public display of these lists in all
relevant facilities.
> A system of regular independent monitoring of the functioning of the health care
system at all levels - encompassing state, district, city / town, block and community
levels. Representatives of state level health sector coalitions, social organizations
involved in health-work along with representations from the beneficiary population, in
conjunction with relevant health officials, should be entrusted with this independent
monitoring.
> An effective redressal mechanism at block, district and state levels for persons with
complaints regarding quality of health care, or those who have suffered denial in any
form. This mechanism should be transparent, should involve health sector coalitions and
social organizations, and should be independently reviewed on a periodic basis. A
department or position of Swasthya Lok Ayukta may be created especially to address
complaints and to ensure that rational guidelines are followed.
>
Budgetary Measures
Immediate doubling of public health-care expenditure by State governments and
further increase to at least 3% of the State Domestic Product in next five years in
keeping with provisions in the Common Minimum Programme.
1
Per capita allocation for public health care for rural areas should be increased and
made equal to that for urban areas.
> Immediate doubling of drug budget for rural health facilities.
>
Measures to improve functioning of the health system and attention to special groups
Standard Treatment Protocols should be implemented regarding care to be provided at
various levels of Health Care Facilities, so that the necessary quality is maintained.
> The full range of comprehensive health services should be guaranteed at all levels of
the public health system, these health services must be ensured as a right. In exceptional
cases of failure by the public system to provide any such health service to a patient, there
should be a mechanism wherein care may sought from designated private facilities
following standard treatment protocols. Such registered and regulated facilities could
give relevant care to the patient, and the state could reimburse them at standard rates,
ensuring that the patient is not deprived of any essential care at time of need.
> Guaranteed availability of essential drugs relevant to the level of service, in all public
health facilities. A mechanism to ensure that if any health care facility is unable to
provide any of the essential drugs that are supposed to be available at that level of health
care, the expenses incurred by the patient on this ‘outside prescription’ should be
promptly reimbursed. All health care providers in both public and private sector should
prescribe according to the essential drug list, and prescribe drugs by their generic
names.
> A comprehensive statewide policy to provide Primary Health Services to urban areas.
Adequate health services need to be provided in all cities and small towns. Expansion of
Urban health care infrastructure, especially of health posts and of outreach health
services keeping in mind the needs of the growing slum population.
> Filling of all the vacant posts and construction of buildings for Sub-centres and other
facilities.
> A new scheme to provide a Community Health Worker in every village or habitation of
the state should be launched. As part of such a scheme, in tribal areas the Community
Health Worker should be operative at hamlet level. For example, in Maharashtra under
the Pada Swayam Sevak scheme, the full potential of the Pada Swayam Sevaks (PSSs),
in tribal districts now needs to be realised by upgrading their role as has been done in
innovative projects. This may be done by ensuring substantially upgraded training,
integration of curative and preventive roles and preference being given to women in the
selection process.
> Regarding womenfs access to health care, availability of all services in a woman
friendly and sensitive manner at public health facilities must be ensured. This should
include assured round the clock maternity services at Sub-centre and PHC level; assured
emergency obstetric and neonatal care at CHC level; facility of diagnosis and treatment
of Reproductive Tract Infections and of infertility, and woman friendly, quality abortion
services. Simultaneously, quality health care for women beyond reproductive health
such as availability of services by women doctors; supply of iron tablets to all anaemic
women irrespective of being pregnant or not; care for victims of domestic violence, and
other services relevant to women’s health must be ensured.
> Training of staff to increase its sensitivity to groups with special health care needs like
women, children, old people, the mentally and physically challenged.
> Greater sensitivity towards mentally unwell, institutionalised patients, provisions for
proper counseling. Provisions for consent procedures, facilities for legal aid and
measures for rehabilitation and family contact.
>
2
>
All coercive measures, including incentives and disincentives for limiting family size,
which result in violations of human rights, must be stopped immediately.
The norms for maintaining quality of service during tubectomy operations must be
strictly followed. For any violation, of these norms responsible persons must be suitably
held accountable and punished. The ‘camp approach', which often results in poor
quality operative care and violation of various aspects of women’s rights, needs to be
seriously reviewed immediately.
>
The other recommendations are:
1.
Public Health facilities should guarantee a Health Centre within walkable
distance with qualified doctors and infrastructure.
2.
Facility to refer patients with serious ailments to specialized hospitals including
transport (Ambulance or Vehicles) with minimum facilities to give life sustaining
treatment during transit.
3. Drugs availability at reasonable rate within reach of common man
a) Supply of quality drugs
b) Ban of spurious drugs envisaging violation as grave crime entailing severe
punishment.
c) There should be a Drug Price control Policy,
Violators should be held
accountable, including penal action.
4.
Social responsibility of providing 10% of free service or service on nominal
charges fixed by the State should be made mandatory for all Corporate Hospitals
and Private Nursing Homes with regular accountability entrusted to a body
created by the State to monitor the system.
>
Visit of Mobile Hospitals with adequate infrastructure and doctors, at least twice a
month, to a village to treat the ailing people where there is no hospital facility and
refer serious patients to Health Centres or District hospitals.
>
To examine the children in all primary and middle schools regularly twice a year
and send report to DMs and/or Collectors, along with names and attestation of Head
Master and Sarpanchs of the village.
>
The diet specialist doctors should prepare a list of food articles available in local
area and prepare a chart showing the proportions of food articles to be taken by
3
children, young boys and girls, pregnant women, old citizens and women from
weaker sections, etc. for strengthening the nutrition of body and to end malnutrition.
This exercise should be made every year and published in local language, put up on
Notice Board of Panchayat offices, Schools and Hospitals of every village.
>
It should alsQ: publish that the parents should examine their children regarding their
hearing problems, vision, speech, etc. immediately they notice any one symptom so
that at young age itself the same could be treated.
>
The Gram Panchayats (full body) and recognized Non-Governmental Organisations
at village, taluq, and district levels should send quarterly reports about the
functioning of hospitals in their village stating presence or absence of doctors, the
period for which one is absent or no doctor is posted at all, including women
doctors, nurses, other medical staff of hospital and availability of drugs to the
District Medical Officer, Collector or Commissioner, Director of Medical Services
of the State and one to the Health Secretary.
>
A Monitoring body should be formed with Chief Secretary as Chairperson, Health
Secretary, Director of Medical Services and Secretary in-charge of Vigilance as
Members to scrutinize the reports and suggest action to be taken immediately as
time-bound programmes. The reports of Monitoring Committees should be placed
before the Assembly every six months for consideration of elected representatives.
4
NATIONAL HUMAN RIGHTS COMMISSION AND JAN SWASTHYA
ABHIYAN
SOUTHERN REGION PUBLIC HEARING ON THE RIGHT TO HEALTH CARE
HELD ON 29™ AUGUST, 2004 AT CHENNAI
KEY FINDINGS AND RECOMMENDATIONS IN RESPONSE TO ORAL AND
WRITTEN TESTIMONIES
for the States of Kerala, Tamil Nadu, Andhra Pradesh, Karnataka and Pondicherry
1. Access to Primary Health Care through the public sector health system
Primary health care is understood in a more limited way as services made available
through Sub-Centre (SCs), Primary Health Centres (PHCs) and Community Health
Centres (CHCs).
•
Pondichery received positive community response regarding the availability and
quality of primary health care services.
•
There were no complaints from Kerala though issues regarding essential drugs,
environmental health and trauma care were raised which come within a broader
understanding of primary health care(covered in item 5,6,7).
•
In Karnataka and AP the irrational siting of PHCs (possibly under political
pressure) made access to health care very difficult and sometimes impossible.
Some of the farthest villages were 40 - 50 kms away, and in other cases there
was no easy bus access to PHCs / SCs. In AP subcentres that were supposed to be
there were non-existent on non-functional. In Tamilnadu, Karnataka and AP
there were problems with regard to quality of care, referrals and staff attitudes.
Recommendation 1.
•
The siting / distribution and physical accessibility of PHCs and subcentes must be
ensured. They should provide good quality services during the prescribed
timings. Indicators and mechanisms for monitoring quality of care need to be
developed and used. No money should be taken for services that are to be
provided free. The citizens charter for services at PHCs should be prominently
displayed and implemented. Staff vacancies need to be filled up and staff needs
such as quarters, toilets, water supply and electricity need to be ensured.
Adequate provision of medicines, laboratory equipment and consumables,
registers etc is a basic requirement. Maintaining staff motivation through good
management practices will help improve the quality of services and to foster a
relationship of mutual respect and trust between providers and people.
1
•
State and Central health budgets would need to be increased as per the National
Health Policy 2002 and the Common Minimum Programme commitments.
Distribution of the health budget between the primary, secondary and tertiary
levels of care would also need to follow norms, such as 65%, 20% and 15%
respectively.
2. Urban health care
There were several instances where the urban poor suffered adversely due to lack of
access to health care and to basic determinants such as lack of access to safe potable
water and sanitation.
Recommendation 2.
•
The urban poor should have access not just to family welfare services but to
comprehensive primary health care through health centres which cater to 50,000
people.
•
Provision of safe potable water and sanitation is necessary to prevent morbidity
and mortality due to water-borne diseases.
•
User fees in institutions like NIMHANS need to be reconsidered as they have
resulted in lack of access to care. Urban poor families including migrants often
do not have ration cards and BPL cards. Rural and urban poor patients coming
from other places do not carry all these cards (if they have them) when they come
to hospital in times of illness.
•
Corruption and rude behaviour in institutions like Kidwai Institute of Oncology
as well as in IPP VIII Centres need to be checked.
•
Pourakarmikas from Hyderabad Metro Water Works and those in other cities and
towns need to have access to basic preventive, promotive and curative care,
including safety gear and equipment.
3. Private sector health care
The case of death of a teenaged girl following treatment of gastroenteritis by a
private practitioner (with an unusual medical qualification) raised the need for:
Recommendation 3.
•
Regulation of the private medical/health sector by government and professional
bodies. Liability of practitioners and payment of compensation where death or
disability results from improper treatment or negligence.
2
•
Unnecessary surgeries such as hysterectomies
be curbed.
as was reported from AP should
4. Women’s access to health care and gender concerns
It was painful to hear testimonies from women about the poor treatment they received
even for ANC/PNC and family planning services and the lack of respect and privacy.
Recommendation 4
•
The camp approach should not be used for tubectomices / sterilizations. Good
quality , safe contraceptives need to be available in health centres at different
levels, with adequate facilities for screening follow-up and discussion about
possible side-effects. Patient feedback on quality of care should be regularly
taken and acted upon.
•
Medical and health care should be made available to women and children as close
to their residence as possible.
•
Privacy and respect should be ensured for women and girls during medical
examination and treatment.
•
The large number of hysterectomies at young ages taking place in AP without
adequate medical justification needs to be urgently looked into and curbed. The
commercialization of medical practice does not benefit persons or families and
requires social control.
•
There should be 24 hour PHCs functioning in every taluk for emergency obstetric
care and CHCs should have gynecologists and anesthetists. Due to the shortage
of anaesthetists medical officers with a 3 - 6 month training in aneasthesia could
be authorized to give anaesthesia.
5. Environment and Health
Strong testimonies were presented from Kerala, Tamilnadu and AP on the adverse
impact on human health resulting from exposure to toxins from industries / factories,
and pesticides. This problem exists throughout the country.
Recommendation 5.
•
The Department of Health at state and central level needs to have structural
mechanisms through which it can function along with other agencies likes the
pollution control board, ministry of environment and forests etc. to implement
regulatory and preventive measures, and to provide for occupational health and
safety, as well as access to medical care where environmental injury has
occurred. In short there is need for a public health response to environmental
health problems.
3
6. Access to Essential Medicines and rational therapeutics
The use of irrational and sometimes harmful, banned and bannable medicinal drugs
and preparations was raised as an issue of concern in Kerala. This problem exists in
all states.
Recommendation 6.
•
Rational drug' policies, essential drug lists standard treatment guidelines and
formularies need to be adopted in the public and private sector, and more
importantly they should be used and regularly updated.
Existing and new mechanisms for continuing education of medical practioners
and allied health professionals need to be actively used for this purpose.
•
Measures to increase consumer awareness and good pharmacy practice need to be
widely instituted.
7. Trauma Care
This came up strongly from Kerala, but is applicable in all states.
Recommendation 7.
•
With the rising number of traffic and other accidents early trauma care using
standard protocols need to be ensured through provision of infrastructure and
training. Preventive measures such as use of helmets and seat-belts should be
mandatory.
8. Mental Health
The following problems were experienced by groups working in the different states lack ol access to mental health care by rural poor due to centralized mental health
care available mainly in city and town based institutions; stigma, discrimination and
abuse; lack of medical and health personnel with adequate training in mental health;
non-availability of drugs; lack of public awareness about mental health
Recommendation 8.
•
Medical and psychosocial care ;and support for persons with mental illness should
be available in a decentralized manner. This will require adequate training and
continuing education,
Public awareness and sensitivity also needs to be
increased.
9. Public Health issues
Other public health issues raised included prevalence of Vit. A deficiency (AP);
discrimination faced by patients with AIDS who required surgery (AP); death of TB
patients due to lack of access to treatment (Karnataka).
4
Recommendation 9.
National guidelines regarding these public health issues need to be followed.
Increasing community involvement and feeling of community ownership of health
institutions and programmes would help in better outreach and quality. Training and
involvement of community health workers / social health activists would provide a
valuable link.
10. Follow-up and monitoring of implementation of recommendations arising from
the Public Hearings on the Right to Health Care.
Recommendation 9.
•
A mechanism needs to be established at state level for joint monitoring by the Jan
Swasthya Abhiyan and officials from the state department of health regarding the
follow-up of recommendations. They will report to the NHRC. NHRC officials
may also visit to observe and monitor the follow-up whenever necessary.
Accountability and communication with the local communities is of greatest
importance.
afc * * j|c * $ 9(c
5
NORTHERN REGION PUBLIC HEARING
ON
RIGHT TO HEALTH CARE
26th SEPTEMBER, 2004
LUCKNOW, UTTAR PRADESH
Recommendations at a Glance
Recommendations by The Northern Region Public Hearing, NHRC-Jan Swasthya
Abhiyan:
Regulation and Monitoring
• Enactment of State Public Health Acts, which would outline the mandatory health
care services that would be guaranteed at all levels of public health system as a
right.
• Regulatory mechanism at state level to ensure the quality of private medical
services by implementing minimum standards standard treatment guidelines and
ceiling for costs of essential medical services.
• A system of regular independent review of the functioning of the public health
system at state, district and community levels. This review ,every 3 to 6 months
should involve JSA and other social representatives.
• An effective redressal mechanism for persons or communities who have suffered
denial of health care in any form .This mechanism should involve JSA and other
social representatives.
Strengthening public health system
• Tripling the public health budget in next five years, to increase it to at least 3% of
SDP as per the Common minimum programme.
• Allocation of adequate budget for drugs, which would involve at least doubling of
state drug budgets. Guarantee of essential drug at all levels.
• Provision of adequate infrastructure including buildings, equipments ,vehicles and
maintenance for all public health facilities. Filling of all vacant posts at various
levels.
• Women are often denied access to health care because of insensitive attitude of
health staff and inadequate facilities. Keeping this in mind .availability of ad
health services for both reproductive and non reproductive health needs to be
guaranteed women friendly manner at all public health facilities.
• Universalisation of ICDS, including strengthening of child health related
services. Guarantee of immunization, nutritional supplementation and other
essential preventive child health services. Ensuring school health services and
mid-day meals.
•
•
•
•
A comprehensive statewide policy to provide primary health services to urban
areas. Expansion of Urban Health care infrastructure, especially of health posts
and of outreach health services.
A new scheme to provide a community health worker in every village of the state
should be launched. This should effectively involve communities,Panchayats and
local organizations.
Regarding mental health, much greater sensitivity towards mentally unwell,
institutionalized patients , provisions for proper counseling and measures for
rehabilitation and family contact.
All coercive measures for limiting family size must be stopped immediately. The
tubectomy camp approach, which often results in poor quality operative care and
violation of various aspects of women’s rights, needs to be reviewed.
State level recommendations:
Recommendations for Health Sendees in Delhi
Uhere are three over-arching issues applicable to all public health institutions:
a. With Delhi being a city-state and the national capital with a historical
development of multiple local bodies there is a multiplicity of providers. The
respective roles of Govt, of India, Govt, of Delhi and the local bodies need to be
clearly spelt out and well coordinated.
b. There is a need to rationalize and integrate the functioning of the public health
agencies. The Dr. Pattanayak Committee had given its recommendations for
restructuring the health services of the Municipal Corporation o Delhi in 2001-02
but it has largely been ignored. There is a need to consider its implementation.
c. Health personnel (including doctors) need to be in position through regular
appointments and their performance should be ensured through administrative and
community regulatory mechanisms.
2. Strengthening of Primary Level Institutions
a. Peripheral areas lack institutional coverage; these areas require special attention
and should be expanded
b. Equipment and infrastructure backup should be available in dispensaries and
PHCs including laboratory support and emergency backup sen ices
c . Vacant posts of personnel should be filled up, their allocation rationalized and
regular attendance and performance ensured
d. The Maternal & Child Welfare Centres and Family Welfare Centres should
provide full range of primary gynaecologic and paediatric sen ices.
e. The sub-centre network should e expanded in rural areas that should be linked to
the respective PHCs.
f. Public health programmes and personnel need to be reorganized/restructured and
these institutions need to integrate with the local curative institutions.
g. Involvement of local communities (through Local Health Committees, for
example) in local level planning and implementation of services; the departments
of health, water, sanitation and social welfare should be involved and accountable
to these local committees.
3. Secondary Level Hospitals
a. 100 bedded hospitals and 30/40 bedded colony hospitals should have full range of
secondary level services operational from its inception; hospitals like Sanjay
Gandhi Hospital, Mangolpuri took more than 10 years to develop all services the present new hospitals are in a similar state.
b. The secondary level institutions should be linked with the local primary level
institutions with a proper referral mechanism.
c . Secondary level specialty services and requisite equipment and supplies should be
available.
d. Rational prescribing practices should be implemented.
e. Special emphasis needs to be given on environmental and occupational health
problems
4.1 ertiary Level Hospitals (all agencies)
a. The above measures will decrease unnecessary overload at this level.
b. Adequate supply of drugs and supplies, based on rational drug formularies,‘should
be available.
c. Internal medical audit mechanisms should be instituted.
5. With strengthening of these three levels we should
«
be able to ensure that social security
services like CGHS, Railways and ESIC should not be sending their patients to private
corporate institutions.
6. a. Reporting of notifiable diseases and medical certification of deaths should be strictly
implemented by all institutions (government and private) and private practitioners.
b. Public should have access to information about availability of services at each level,
availability of beds at a point of time; other linkages like networking of blood banks are
also necessary.
7. a. Independent monitoring of health services through social audit
b. Grievance redressal mechanisms within each agency providing public health services.
8. There are 4 state level medical colleges and one national apex institute (ARMS) There
should not be any more increase in medical colleges. The content of medical education
needs to be appropriate for operationlising the public health services as detailed above including raining for managerial roles, a public health perspective and rational
therapeutics. Training of field workers need to be strengthened.
Recommendations for Health Services in Himachal Pradesh
•
•
•
Rationalization of staff
Filing up of all vacant posts
Contract system be abolished
•
•
•
•
•
•
•
Free diagnostic tests and no user charges
Each PHC should have a lady doctor
Per Diem system for different trainings be removed.
Incentive for trained birth attendant for promoting safe deliveries
Basic facilities at sub centre level be ensured
Separate and independent IEC Bureau be established with trained staff in health
education.
Work load of Anganwari workers should be decreased.
Recommendations for Health Services in Uttar Pradesh
•
Establish, adopt, recognize health as a fundamental right of all citizens including
vulnerable, displaces, slum dwellers and poor.
• The Primary Health care system should be made accountable to Panchayats in
rural and urban areas including JSA.
• Privatization or commercialization of health should be totally banned and
regulated by the state.
• Poor, marginalized, deprived, migrant and other vulnerable groups should be
accorded identity, accessibility and availability of health care system free of cost.
• Indian system of Medicines should be treated at par with modern medicines and
should be mainstreamed.
• Social security to senior citizens, children, disabled and women should be
specially provided.
• All the policies related to health, child development and women empowerment
should be seen in totality and not in isolation.
• All forms of user charges should be removed and health care should be provided
free of cost.
• The denial of health care and negligent care should be made accountable to
people and arrangement of redressed should be in place.
• The essential drug list should be made public and state should ensure the
reasonably quality and adequate essential drugs to all health facilities.
• The incentive and disincentive in family planning programme should be removed.
• Two child norm and coercive population policies should be removed.
• Government should honour the “Health for all goals and adopt the PHA charter
EASTERN REGION PUBLIC HEARING
ON RIGHT TO HEALTH CARE
RANCHI
11 OCTOBER , 2004
Recommendations:
The public hearing on the denial of right to health care that was held in Ranchi on the 11th
of October, heard a number of cases of denial from the five states of Bihar, Jharkhand,
Chhattisgarh, Orissa and West Bengal.
Of the over 70 cases presented orally and about 150 cases submitted in writing, there
were a few recurrent themes.These included
a. High degrees of illegal fees and denial of treatment if these are not paid - in
public health facilities.
b. Poor quality of service in many public health facilities.
c. Absence of any services in remote tribal areas.
d. Denial of right to safe drinking water.
e. Lack of food security and malnutrition related illness.
f. Expensive, irrational drug prescription along with lack of availability of essential
drugs in public health facilities.
g- Lack of emergency obstetric care services and safe abortion services
h. Lack of emergency services for a wide variety of emergencies - notably
accidents, burns, snakebites.
i.
Lack of referral transport system to access emergency services.
J- Poor access to sterilisation services and poor quality of sterilisation services.
k. Weak public health response to epidemics and sudden increase in infectious
deaths in certain areas.
After listening to the testimonies the panel has decided to take cognisance of only a
small part of them as individual human rights cases . Though the other individual cases
are also heart-rending the panel thought it more useful to pursue the systemic causes
behind these failures. For these systemic issues that underlie the denial of the right to
health care the panel makes the following 15 recommendations which are forwarded to
the state governments for implementation.
A Vigilance Mechanism must be build up in each state health department with
assistance and in coordination with the police department. This vigilance should
be proactive and not only responding to complaints. Its focus should be to prevent
Hegal charges in public health facilities, and private practice inside public health
facilities or in public hours.
2. All public health facilities should have display boards that state what are the legal
user fees if any , declare that payments other than these are illegal and inform
where to register a complaint in this regard.
1.
1
3. Vigilance also needs to be exercised against unnecessary referrals to nursing
homes, clinics, diagnostic services. To be effective on this the state governments
have to issue orders disallowing public health staff from referring to nursing
homes, clinics or diagnostic services where they have a monetary advantage or
commission..
4. Monitoring structures for health programmes should be established/strengthened
at the district and block levels with the inclusion of panchayat representatives and
civil society partners who are active in advocacy work.
5. Monitoring structures for CHCs, civil hospitals and district hospitals should be
established by either strengthening existing patient welfare societies or creating
them. These would also have vigilance functions.
6. Independent of the above two there should be a grievance redressal mechanism
where those who have been denied quality care- in the private or public sector
can go to for registering their grievance and seeking relief.
7. All areas which have had no doctor for over an year and all those areas which
have had no nurse/midwife for over an year should be publicly notified as
medically and paramedically underserved and a special package of measures must
be undertaken to provide some temporary relief and access to care for these areas.
( eg visiting doctor- pvt or public, mobile clinic. NGO, etc). This special package
adopted may be made in consultation with all interested parties especially the
States^should have a transparent non-discriminatory transfer policy such that
8.
doctors and other paramedical staff serve by rotation in difficult areas. During
such service in difficult areas a special package of measures including financial
incentives to support such doctors should be adopted. These two steps are critical
to address the problem of lack of doctors in difficult rural areas.
States should have a state drug policy and /or adopt a state drug action p
9. which ensures that the states formulate an essential drug list and all the drugs o
this list are available at all public health facilities without interruption, and that
the prescription and use of irrational, expensive drugs and the use of hazardous
and banned drugs is curbed in both the private and public sector. This would also
need to specify better drug information to both the patient and the prescribers.
10 The state should adopt a time bound action plan/road map by which e: cn ica
gaps in the provision of good quality emergency obstetric services,sterilisation
services, safe abortion services, and basic surgical emergency servicesf burns ,
accidents) can be provided in a network of referral centers such that there: is at
least one such center per eveiy 100000 population. This action plan should be a
detailed publicly stated commitment and should have an year by year milestone,
so that even if the entire plan would take ten years to implement, the monitoring
committees and the public would know whether each year, that year s goals are
being achieved.
11. The most immediate measure for closing specialist gaps in the referral center
would be transferring of surgeons and gynaecologists and anaesthetists so that this
norm for the provision of emergency and referral level care is met in as many
facilities as possible. In the absence of a transfer policy well-qualified specialists
2
languish in peripheral centers losing their skills while key facilities, which needs
their services, go without them.
12. The governments may publicly notify what are the services it would be providing
at the level of the habitation, at the level of subcenters,at the level of PHCs, CHCs
and district hospitals along with quality indicators. This should be accompanied
by similarly graded standard treatment protocols. This is essential for public
knowledge and for monitoring. This will also help prevent unreasonable
expectations from the public - for certain services may be available only at the
district or block level and not at every PHC as may be expected. But this needs to
be publicly notified.
13. The governments should set up a medical services regulatory authority- analogous
to the telecom regulatory authority- which sanctions what constitutes ethical
practice and sets and monitors quality standards and prices of services - both in
the public and even more importantly in the private sector.
14. A Public Health and Health Services Act that defines the rights of food security,
safe drinking water, and other determinants of health and the citizens’ rights to
enjoy them along with the rights to medical services that are accessible, safe,
affordable needs to worked out. This act would make mandatory many of the
recommendations laid down above and would make more justiciable the denial of
health care arising from systemic failures as had been witnessed during the public
hearing.
15. Implementation of the Supreme Court order regarding food security and the need
to universalise ICDS programmes and mid day school meal programmes remains
a priority that this panel also endorses.
3
RECOMMENDATIONS OF
NORTH EAST REGIONAL PUBLIC HEARING ON
RIGHT HEALTH CARE
GUWAHATI
DATE: 28th NOV 2004
Budgetary Measures:
1. The state Health budget on Health budget on health care to be doubled with
immediate effect.
2. The drug budget for PHC and CHC in the state should be doubled.
3. In the pre monsoon season, extra stocks and inventory of all essential medicines
to be made available in government hospitals in rural areas to deal with possible
disruption in supply.
4. Contingency plan to deal with healthcare arising during and post flood situation
in the state with special staff assigned for such work.
Legal Measures:
1. Enactment of a State Public Health Act in each state, which would outline the
mandatory health care services which might be made available to the people as a
right at various levels of the public health system. This act would specify which
services and standards of care must be made available at the community, sub
centre. PHC, CHC, Sub-district and District hospital levels, as well as the
preventive and promotive measures that the government would undertake.
2. Enactment of a Clinical Establishment Regulation Act in each state to ensure
minimum standards, adherence to standard treatment guidelines and ceilings for
costs of essential medical services in the private sector.
3.
Private practice presently allowed to Government health care providers should be
legally banned, and those doing it should be promptly punished.
4. Policy for primary health care in the state should be adopted and implemented.
1
5. Standard Treatment Protocol for treating of all common ailments should be
prepared and enforced.
6. The clear and distinct regulatory act for private nursing homes should be made.
7. Public hearing should be organized on a regular basis in all the North Eastern
State in every district of Assam.
8. Private practitioners should have a uniform and affordable rate to make medical
treatment accessible to all.
Measures to improve functioning of the health system and attention to
special groups:
1. Standard Treatment Protocols should be implemented regarding care to be
provided at various levels of Health Care Facilities, so that the necessary quality
is maintained.
2. The full range of comprehensive health services should be guaranteed at all
levels of the public health system, these health services must be ensured as a
right. In exceptional cases of failure by the public system to provide any such
health service to a patient, there should be a mechanism wherein care may be
sought from designated private facilities following standard treatment protocols.
Such registered and regulated facilities could give relevant care to the patient,
and the state could reimburse them at standard rates, ensuring that the patient is
not deprived of any essential care at time of need.
3. Guaranteed availability of essential drugs relevant to the level of service, in all
public health facilities. A mechanism to ensure that if any health care facility is
unable to provide any of the essential drugs that are supposed to be available at
that level of health care; the expenses incurred by a patient on this “outside
prescription” should be promptly reimbursed. All health care providers in both
public and private sector should prescribe according to the essential drug list,
and prescribe drugs by their generic names.
4. A comprehensive statewide policy to provide Primary Health Services to urban
areas. Adequate health services need to be provided in al cities and small towns.
2
Expansion of urban health care infrastructure especially of health posts and of
outreach health services keeping in mind the needs of the growing slum
population.
5.
Filling up of vacant posts and construction of buildings for Sub centres and
other facilities. A new scheme to provide a community Health Worker in every
village of the state should be launched.
6. Regarding women’s access to health care, availability of all services in a women
friendly and sensitive manner at public health facilities must be ensured. This
should include maternity services, pre natal and neonatal care etc.
7. A scheme for community Health Worker in every village should be launched.
8. Urban Health care infrastructure should be expanded and PHC services should
be made available in all towns and cities. Emphasis should be given to slum
dwellers.
9. Malaria is a major problem in the state. Special action plan to deal with malaria
in the north east states with emphasis on vector control and ecological measure
along with universal availability of anti malarial drugs.
Independent Social Monitoring and Redressal System
1. Apart from the above steps, a system of regular independent monitoring of the
functioning of the heath care system at all levels should be taken up.
2. An effective redressal mechanism at block, district and state levels for persons
with complaints regarding quality of health care and for those who have suffered
denial of health care in any form.
3
> Enactment of a State Public Health Act in each state, which would outline the
mandatory health care services which must be made available to the people as a
right at various levels of the public health system. This act would specify which
services and standards of care must be made available at the community, sub
centre, PHC, CHC, Sub- district and District hospital levels.
> Enactment of d Clinical Establishments Regulation Act in each state to ensure
minimum standards, adherence to standard treatment guidelines and ceilings for
costs of essential medical services in the private sector. For example, the Bombay
Nursing Home Regulation Act 1949-Maharastra, may be substantially modified
and improved to effectively regulate the quality of private medical services in the
state.
>
The clear and distinct regulatory act for private nursing homes should be made.
> Public hearing should be organized on a regular basis in all the North Eastern
States and in every district of Assam.
> Private practitioners should have a uniform and affordable rate to make medical
treatment accessible to all.
4
The Urban Health Services in India: Towards Prevention of Human Rights
Violations
[Submission at the National Human Rights Commission Hearing,
National Level, New Delhi, 16th December, 2004]
An Overview
The focus of public health services planning and development in post
Independence India has been,
rightly, the rural populations. The urban
population even today constitutes less than 30% of India’s people and the urban
health indices show a better profile than the rural. Yet several large and small
studies have demonstrated the inadequacy of our State and society in providing
basic and comprehensive health services, so essential for the Right to Life, to
this relatively privileged population. All regional hearings organised by the JSA
and NHRC on the Right to Health Care have provided evidence of violation of the
right in urban people. While each state and region has its own special features, a
national overview and some common issues are being highlighted.
•
Urban areas constitute a wide diversity by size of population and land
area, condition of amenities and health care services. (Tables in
annexure).
Water,
sanitation,
housing
and
other
environmental
dimensions become greater problems as concentration of people on land
increases.
•
Disparity of economic and social status is more marked in the urban areas
as compared to the rural. 40-60% of all urban citizens live in the slums or
unauthorised colonies with poor socio-economic status, poor housing and
low standards of amenities. The health status indices of the different
sections demonstrate a direct correlation between socio-economic status,
the health of the poor even showing worse figures than the rural in some
instances.
•
On the other hand, the urban areas have the highest concentration of
health services, both public and private.
•
Public services in urban areas are relatively low at the primary level,
especially in' terms of community outreach. The secondary and tertiary
services are more highly developed; all secondary and tertiary institutions
are situated in urban areas. Private services are high at all three levels.
The secondary and tertiary hospitals serve both the urban and the rural
people.
•
The lack of focus on the planned development of a ‘comprehensive health
service system’ in urban areas has been officially recognised atleast since
the 1980s, with the Krishnan Committee report of the central government.
•
Major lacunae that clearly exist today are the following:-
•)
Lack of access to services by the poor.
")
Physical mal-distribution of services and mal-distribution of resources
within the health services. The lack of peripheral services, multiple
authorities providing services and overlapping responsibility of the
institutions and agencies, as exemplified by Delhi’s health services,
leads to overcrowded hospital OPDs and wards. While rationalising of
existing infrastructure has been repeatedly recommended, no action
has been taken in this direction.
iii)
Major weaknesses in functional quality of the public services exist
because of the load on them, with a user profile that has lower
resources to supplement the services provided than the private sector
users. Nevertheless these cannot be reasons to excuse the kind of
violation of rights of the citizens and of the patients coming to the
institutions. Evidence of gross misinformation, negligence, poor social
interaction by doctors abounds. The rude, aggressive behaviour of
paramedics and other staff of health institutions with those who come
to these institutions in times of crisis for some solace can only be
called criminal.
iv)
While our focus is the provision of services by the public sector, impact
of the private sector on the pubic services needs to be recognised. The
private sector issues largely pertain to services in urban areas where T
they too tend to concentrate. The issue of free land to private
corporates without their fulfilling the obligations in the contract are
issues of urban governance. Public funds being siphoned to support
the private sector through the social insurance (CGHS, ESI etc.),
instead of going to strengthening of public services, are issues of
concern. The private services also set up models of engage in greater
practice of over-medication and prescribing of unnecessary medical
interventions which, besides adding to costs also bring in iatrogenic
diseases due to the side-effects etc., which adds to the burden on the
public health services
The Presentations in the Session
1. Mr S.J.Chancier, Community Health Cell, Bangalore, presents conditions
from the Southern region, focusing on the issues of barriers to access to
services of the urban poor.
2. Dr. C. Sathyamala, Epidemiologist, presents data from a recent study that
highlights the impact of economic conditions, and that the poor still rely upon the
public services despite the problems they face.
3. Dr. Kamla Ganesh, Retd Professor of Obs. & Gynae, and ex-MCH adviser to
the Delhi govt., presenting findings of her excellent investigation into the
reasons for maternal deaths of women coming to the IPP-VIII MCH centres for
ANC/delivery. Basically highlights the institutional flaws and the need for support
to health care personnel in performing their duties.
4. Dr. Sanjay Nagral’s presentation on the Mumbai and Maharashtra situation
and the impact of public private linkages in terms of access and the quality of
services.
5. Dr. Rajib Dasgupta, Centre of Social Medicine & Community Health, JNU,
presents the recommendations.
Recommendations for Preventing Human Rights Violations by the Urban
Health Services in India
1. Rationalising the struc ture of health services
•
Almost all large urban centres suffer from the problem of multiplicity of health
service delivery agencies. The respective roles of state government and local
bodies as health service oroviders in urban areas need to be clearly defined.
Should local bodies be confined to primary health care services only? The
general trend is that local bodies are resource-constrained and therefore the
‘burden’ of secondary and tertiary health care institutions are borne by the
state governments. Secondary and tertiary care institutions are/will almost as
a rule be located in urban centres and also act as referral units for the
general/district health services. That argument will de facto imply that urban
local bodies confine themselves to the primary level only. Though the
Bombay Municipal Corporation operates services at all level including medical
colleges that is an exception than a rule as the financial health of the
organisation supports such endeavours.
•
Recommendations of Committees appointed so far - Krishnan Committee,
Pattanayak Committee- to rationalise and integrate existing public health
agencies need to be adopted
and
implemented. The Pattanayak
Committee was appointed in the aftermath of the Dengue Epidemic in
Delhi to restructure the services of Municipal Corporation of Delhi. It
essentially recommended reorganisation of the services on the basis of
municipal wards and suggested changes for personnel and services to
that effect. It also recommended strengthening of certain key
public
health institutions like Infectious Diseases Hospitals. Epidemiology Units
and Public Health Laboratories for epidemic forecasting and better
management of outbreaks, particularly of infectious diseases.
•
Public health programmes operate vertically in most urban areas. Though
Ward Health Units exist in some cities/towns, rarely do they deliver
integrated comprehensive services. What is delivered is (as is common in
the rural system also) selective primary health care or programmes in
campaign/mission mode like Pulse Polio. There is a need to integrate and
rationalise the manpower and services.
Prevention programmes need to address all sections rather than target only
•
the poor. Urban local bodies, and their personnel, are oriented largely
towards slum populations. However, public health cannot be bought ‘off the
shelf and urban local bodies will have to address all sections of the
population more comprehensively rather than adopting a sectoral approach. It
means that non-slum areas get ignored this is reflected in various house-tohouse campaigns. Vector breeding is actually often higher in better-off
households that have more containers.
•
Support services like blood banks, ambulance services and hearse van
services should be networked with all level of institutions for efficient
functioning and reduction of response time.
2. Strengthening of Primary Level Institutions :
•
Peripheral areas of towns and cities (generally populated by poorest
segments) often lack institutional coverage; these areas require special
attention and institutional coverage should be expanded.
•
All health posts should provide outreach services to slum and slum like
areas through ANM and MPW.
•
Monitoring primary health services should be included as a responsibility
of the Ward committees.
•
New guidelines on the role and functioning of the health post system in
view of an integrated and decentralised primary health care programme
need to be developed and implemented uniformly across all the Municipal
bodies in the state.
•
Equipment and infrastructure backup should be available in dispensaries.
•
Vacant posts of personnel should be filled up, their allocation rationalised and
regular attendance and performance monitored and support provided against
the inherent medical and legal hazards of the occupation.
•
Maternal and Child Health Centres / Family Welfare Centres should provide
full range of primary gynaecologic, obstetric and paediatric services; special
emphasis needs to be given to emergency services and institutional deliveries
whenever indicated.
•
There is a need to train and integrate dais who operate in lower income
groups of urban areas with the formal primary health care system.
•
Public health programmes and personnel need to be reorganised/restructured
and these institutions need to integrate with the local curative institutions.
•
Communities (through Local Health Committees, for example) should be
involved in local level planning and implementation of services; the
departments of health, water, sanitation, education and social welfare should
be involved and accountable to these local committees.
•
The experience of contracting of service delivery to private agencies and
NGOs, e g. School Health Services, immunisation services, IEC field
campaigns
and
cremation
ground
services
should
be
reviewed;
comprehensiveness of services, coverage, follow-up, cost-effectiveness and
sustainability should be some of the criteria on which the ‘new’ services are to
be evaluated.
•
Birth and death registration procedures should be made transparent and
citizen friendly.
3. Strengthening of Secondary and Tertiary Level Institutions
•
Primary and secondary level services need to be available and accessible to
prevent overload of tertiary hospitals, that is almost a rule across urban
centres of India. These institutions should be linked with the local primary
level institutions with a proper referral mechanism.
•
Secondary level speciality services and requisite equipment and supplies
should be available.
•
Rational prescribing practices should be implemented. Experience of Delhi
and other cities where efforts have been made in this direction should be
reviewed and lessons drawn.
•
Adequate supply of drugs and other consumables, particularly, live saving
drugs and equipment must be ensured. The purchase procedures should be
transparent. The model of Tamil Nadu Medical Supplies Corporation can be
adopted.
•
Special emphasis needs to be given on environmental and occupational
health problems.
•
Social security services like Central Government Health Services (CGHS)
and Employees’ State Insurance Corporation (ESIC) and other employee
medical benefits in public institutions should not refer patients to the private
corporate hospitals and instead should integrate and network with secondary
and tertiary level public institutions. This will allow public funds to be used for
strengthening of public services rather than be siphoned off to private
services. It will also build pressure for the strengthening of public institutions.
4. Institutional Structures and Procedures for Constant Monitoring and
Strengthening
•
Clinical auditing of deaths of patients can go a long way in making the
services sensitive to their own weaknesses in patient management
practices. This should be made mandatory and brought back as a live
practice so as to improve medical care and prevent negligence.
Grievance redressal mechanisms must be available within each institution
and for public health services as a whole. Measures for informing users of
the services about the mechanisms must be a responsibility of the
institution and the health services.
Social audit mechanisms must be instituted to make the services
responsive to community needs.
Co-ordinator. Dr. Ritu Priya, Centre of Social Medicine & Community Health,
JNU.
Health of the urban poor in Karnataka
Areas of concerns
By S.J.Chander
Community Heath Cell
Introduction
AT least 22 per cent of Karnataka's urban population lives in insecure and unhygienic urban
slums. In September 1999, the Karnataka Slum Clearance Board (KSCB) identified 2,322
slums in the State with a population of around 23.79 lakhs, which is 17 per cent of the total
urban population. Bangalore alone accounted for 362 slums with a population of 5.9 lakhs.
This appears to be an underestimate of the actual figures.
In 1993 itself the National Sample Survey, 49th round estimated the slum population was at
32.2 lakhs, making it around 23 per cent of the total urban population in the State. The same
study estimated the population of Bangalore's slums at 10 lakhs1. Bangalore
experienced an exponential growth of slums in the 1990s, from 444 slums in 1991 with a
population of 1.12 million, to 763 slums with 2.2 million in 1998-99 with a population of,
about 20 per cent of the city's population. The most recent data, from the 2001 Census, lists
733 slums in Bangalore. (The Hindu, June 3, 2003)
The present health care services made available for the urban poor are family welfare and
family planning oriented. The word Primary Health Care has been used inappropriately by
many agencies including the government and voluntary organization. Their understanding is
no way close to the definition for Primary Health Care that the World Health Organization
(WHO) gave during the Alma Ata declaration in 1978.
It is presumed that urban poor do not lack health care facilities, as most of the health care
facilities are concentrated in the urban areas. This may be true but the question for which one
must find an answer is to what extent these facilities are really accessible, available and
affordable to urban poor. The present model excludes the important elements such as water
and sanitation, Health education in the Primary Health Care Approach that the WHO
advocates. Treatment of minor ailment is also inadequate and unsatisfactory which is one of
the eight elements of Primary Health Care specified by WHO. Recent interaction with some
of the community members revealed that some of the urban health centers do not have anti
rabies vaccines and treatment for tuberculosis. The health problems faced by the urban poor
are largely due substandard living conditions and lack of health awareness. Alcoholism and
Tobacco are another major problems, which takes away limited economic resources available
for the families. The problem of alcoholism not only takes away the resources, it constantly
causes psychosocial problems in the families. Unless these issues are addressed satisfactorily
improvement in the health status of the poor cannot be achieved.
1 Karnataka Housing Revolution, Parvathi Menon in Frontline Magazine. Vol 19, Issue 13 June - July 5,2003
1
Substance abuse, exploitation by unqualified providers (quacks), and use of hazardous
biomass fuels for cooking have direct health consequences that are often overlooked.
Alcoholism
Alcoholism is another major problem that puts pressure on the limited income of
the urban poor. The survival of the alcohol industry to a large extent depends on the poor.
The major portion of the income that the man earns goes in for alcohol, depriving the families
the money for nutritious food and educational needs. One of the serious consequences of
alcoholisms is violence, particularly against women. Do we need more studies to confirm to
get into action?
Water and sanitation
The urban poor not only suffer from inadequate water supply and sanitation, they also suffer
from poor quality of services that area available to them. One fifth of all urban households
lack access to water supply and 60 percent of urban households live without access to
sanitation. In slums, 40 percent of households are without access to safe drinking water, and
90 percent without access to sanitation. Per capita daily consumption of water in Class I cities
is less than 142 litres, reaching a low of 50 litres in some cities.3
Recently, Jansahyog a (Bangalore based voluntary organization) collected water samples
from 12 slums. The results revealed that all the 12 samples were contaminated. A report
published by UNDP titled ‘Urban Poverty and Deprivation’ gives the following statistics
regarding the health status of the urban poor; diarrhoeal deaths account for 28 percent of all
mortality, while acute respiratory infections account for 22 percent. Nearly 50 percent of
urban child mortalitv is the result of poor sanitation and lack of access to clean drinking water
in the urban slums.4 One of the testimonies presented for the public hearing in Bangalore, a
14-year-old girl died of gastro enteritis. She was treated by a private practitioner who was a
quack. She could have been saved had she been to qualified health personnel. However the
primary cause of the problem is due to water and sanitation.
Housing
By the year 1997, the total housing shortages in India was estimated at 13.66 million units,
out of which 7.57 million units would be in the urban areas. More than 90% of this shortage
is for the poor and the low-income category. In 1999, the Karnataka Slum Clearance Board
(KSCB) identified 2,322 slums in the State with a population of around 23.79 lakhs It is
estimated that there are about 2,60,000 households in the slums of Bangalore city. Only 10%
of the slum household in the Bangalore city has RCC roofing, which is built by government,
NGO/CBO and the communities’ themselves.5
Land
The living conditions where the urban poor are living in most places are far below the
standard for human habitation, lacking potable drinking water, facility for disposal of solid
and liquid waste and housing. The majority of the slums are located on the land owned by the
Government/Municipality or private landlords. People who are residing on non-declared slum
are constantly under the threat of demolition and eviction. Many of the services of
3,4 www.UNDP India-reports-urban poverty
5. PROOF Network, Bangalore
2
government programmes are not extended to non-declared slums. They are deprived of both
the health services and basic amenities. The Karnataka Slum Clearance Board (KSCB) has
the authority to declare a slum under section 17 of the Karnataka Slum Areas Act 1973
Health care delivery services for the urban poor
The process of urbanization further adds pressure on the limited resources available to the
urban poor. The existing health care facilities provided by the Bangalore Mahanagara Palike
(BMP) which has; 38 maternity homes, 6 referral hospital, 55 health centers developed under
the IPP VIII Programme and 19 family welfare clinics are barely sufficient for the 12 percent
of the five million residents of Bangalore city (The Hindu daily 4th January 2003) the same
report comments that bulk of the budget goes for solid waste management and salaries of the
staff at the dispensaries and hospitals. The report also said that essential drugs are not
available for poor free of cost and the poor cannot afford to purchase them from private
chemist shops. These services may be geographically accessible but does it cater to the needs
of the people living in the slums. Regarding availability, it is the private practitioners who are
available at the time of need and convenient to the urban poor.
Health services provided by the BMP are largely family welfare and family planning, which
is only one of the eight elements of the primary health care approach, suggested by WHO.
These services have many problems such as:
Inadequate staff
Of the 36 vacancies, 9 of them are on study leave ranging from 2-5 years. BMP has recently
recruited 6 doctors. Remaining 21 posts are vacant and it is likely to be vacant until the
government changes its policy on recruitment. At a group discussion held among the self
help group members around an urban health centers Bangalore, the participants said “
Doctors are not available in the health center, they are very irregular. The doctor comes late
and leaves early. If doctor is there, the nurses won’t be there. Even if they are available do
not provide good care. ”
Corruption
Though services at the all the urban health center are supposed to be given free but none of
the services are available free of cost to the urban poor, whether it is during out patient or in
patient care. The participants during the group discussion said, “ If they give an injection and
tablet they demand Rs.I5” the practice of demanding money for showing the babies to the
mother and her relatives after delivery still continues. The staffs at the health center demand
Rs. 400 for the male child and Rs.200 for the female child. The women delivered said unless
one pays the staff would not attend. A woman stays closer to a health center said they
demand money Rs.500 to Rs.600 for conducting medical termination of pregnancies. Many
women who are unable to pay carry on with the pregnancy though they don not want another
child within a short space.
Ill-treatment
Women who have undergone the experience of deliveries said they the words the health staff
use are humiliating. They said the verbal abuse takes place when they were not able to push
the baby during labor. Some of them have experienced physical attack such as pinching badly
on their legs and thighs. Another women who went to government hospital for treatment of
cancer of the esophagus received the worst from the staff. While disclosing her the diagnosis
3
she was told, “ the disease that you got will kill you. When she went for chemotherapy the
health staff scolded her when she had to remove her magalsuthra “ you are going to die, why
do you need this, this has only cultural significance. She said by hearing this she wept
bitterly.
People’s perception of their needs
A study conducted by Commonwealth Association for Mental Handicap and Development
Disabilities (CAMHADD) recently elicited the following as the priority of needs of the urban
poor; safe drinking water, toilet, underground drainage, trauma care, education and
prevention of alcoholism and empowerment of women to resist alcoholism. The report also
emphasized the need for creating better job opportunities and motivation of better living
conditions.6
A group discussion held recently among the self-help group members in a slum reveled the
following: “They give same medicine for all problems, the medicine they give does not help
us get cured. ’’ They gave these suggestion for improving; Doctor should be available till 4.00
pm and treat them well. The place should be kept clean
Conclusion
There is a need for improving the quality of existing services particularly with regard to staff
attitude; keeping the health centers corruption free and keeping them clean. The present
health care delivery system should move beyond family welfare, family planning to
comprehensive primary health care focusing on determinants of health. It should give greater
emphasis on preventive and promotive aspects.
6 Indian Express, 28th February 2003
4
G\
Policies Affecting Health Care and
Violation of Health Rights
Presentation by the Jan Swasthya Abhiyan
National Public Hearing on Right to Health Care
Jointly organised by the National Human Rights Commission and
Jan Swasthya Abhian
(New Delhi: 16-17 December 2004)
Section I: The Policy Framework
Health services in India at the time of Independence were a function of the socio-economic and
political interests of the colonial rulers. The post - independence era witnessed a real effort at
providing comprehensive health care, and in extending the infrastructure of health services.
However the improvements in our health delivery system did not match the needs of the vast
majority of our people. After initial efforts in the first two decades after independence, the
country’s commitment to providing affordable and easily accessible comprehensive health care
services suffered due to lack of adequate resources being pledged for the same. So much so that
the Govt.’s “Statement on National Health Policy”(1982) was forced to state In spite of such
impressive progress, the demographic and health picture of the country still constitutes a cause
for serious and urgent concern.”
Thus, neither the stated commitment of the Government, nor its implementation, was able to
make a significant dent in the status of health or in health care delivery systems. In addition, the
impact of an urban elitist bias in medical education as well as in medical services detracted from
the ability of the Indian State in providing Health care to the poor as well as those in rural India.
Continued emigration of doctors, rush for super specialities, development of corporate hospitals
and polyclinics, and an incredibly large and near universal trend to irrational use of drugs and
technology are all trends that are a consequence of this bias. As a result, the major disease-load of
the population has continued to be unacceptably high and, in recent years, health indicators like
Infant and Child Mortality Rates have started stagnating after the downward trends seen earlier.
As noted earlier, the Indian State’s allocation for health care has been extremely low by global
standards, resulting in a large majority of people having to access the private sector. Even the
meagre allocation for health has not been optimally utilised, resulting in extremely pool quality of
services provided by the public sector. Thus, to a very large extent, health services and health
care in India tends to respond to the existing ‘market demand’. The vast health needs of the
majority of the people do not figure as part of this “demand” for there is neither the awareness nor
the organization nor their participation in the making of these decisions. This trend has
accelerated since the initiation of neoliberal economic reforms in the country from the late 80s
Neoliberal “Reforms” — Impact on Health Care
This situation was compounded with the initiation of neoliberal economic reforms in the country
in 1991. These reforms marked a major shift in the government's policy towards social sectors
like health. These policies sought - by way of fiscal austerity measures - to cut Govt, spending
and subsidies in social sectors, reduce direct taxes, increase administered prices, liberalise trade
by reducing tariff rates and providing other incentives for foreign investments, privatise public
<
enterprises, deregulate the labour market, etc. The policies were designed to clear the path for
withdrawal of the State from the social sectors like health, education, food security, etc. The
ideological barrage associated with the reforms package served to confer legitimacy to the virtues
of the private sector and the market. In the process, the supposed inability of the state to sustain
funding of education, medical care and public health, programmes for provision of drinking
water, etc., seems to have gained acceptance.
The immediate fallout of the new policies was a cut in budgetary support to the Health sector.
The cuts were severe in the first two years of the reform process, followed by some restoration
subsequently. Thus, outlay on Health fell from 1.9% of plan investment in 5th Plan to 1.6% in first
two years of 90’s, and then increased marginally to 1.8%in 8th Plan outlay.This squeeze on the
resources of states was distributed in a fairly secular fashion over expenditures incurred under all
developmental heads. Health care was a major casualty as the share of states constitutes a major
portion of expenditure. A similar kind of squeeze in resource allocation was felt in all
programmes, largely financed by the states, including water supply and sanitation. As a result of
the rollback on expenditure on health care, the expenditure by the Govt, on health care has fallen
from 1.4% of the GDP in 1991 to 0.9% in 2002.
Compression of funds available with states has had a number of far reaching effects. Generally,
expenditures on infrastructure (buildings, rentals, salaries, etc.) tend to take up an inordinately
large part of total expenditure. They constitute 70-80% (or more) of expenditure for most major
programmes, and the trend is most distorted in the case of rural programmes, viz. rural hospitals
and primary health centres. Faced with limited funds, the burden of cutbacks are increasingly
placed on supplies and materials. Ultimately a skeletal structure survives, incapable of
contributing in any meaningful manner to amelioration of ill-health.
Expenditure patterns on health care are grossly skewed in favour of urban areas. Expenditure cuts
further distort this picture with the axe on investment falling first on rural health services. As a
result of this rolling back of state support to health care the first major casualty in infrastructure
development has been the rural health sector. There has been a perceptible slowing down in
infrastructure creation in rural areas.
The extent of cuts in health sector funding by the state and the consequent impact, as part of the
refonn process are, in a sense, peripheral issues. The central issue that needs attention is the
theoretical underpinning of the reform process vis a vis state involvement in social sectors like
Health. It is important to note that structural adjustment policies are geared to restructure the
economy in a certain manner and not to improve welfare measures. Reforms initiated in this
country and elsewhere start from the premise that present levels of subsidies to the social sectors
are unsustainable. So prescriptions for restructuring of the health sector are designed, not to
provide the best possible health care but to maximise outputs from greatly reduced state support.
India's situation in terms of spending of Health Care is different from most developing countries
on tw o counts. At 6% of GDP spent on health care, India spends more on health care in percent
terms than most developing countries. At the same time, at 16%, government spending of the
total expenditure on Health Care, India is one of the lowest in the world, both in actual terms as
well as in percentage terms. It may be contrasted with 70-80 per cent share of expenditure on
health care by governments in most of N.Europe, and even the 44 per cent expenditure by the
government in the U.S. While successive Five-Year Plans have shown a fall, in percentage terms,
in allocation for health care, the present mantra of liberalisation is being used to legitimise further
privatisation in the health sector. Health expenditure in India is thus already heavily distorted in
favour of the private sector. It should be understood that the extremely low level of public
funding in India is not a new phenomenon. In fact successive Five Year Plans have shown a fall
in percentage terms, in budget allocation for health care.
There has been little effort towards sustained investments to build up health care infrastructure in
the country. To be fair, periods of stagnation have been punctuated by sporadic efforts to enhance
public health funding. Mention may be made in this context of the National T.B. and Malaria
programmes of the fifties and sixties and the Primary Health Care Programme in the late
seventies and early eighties. In the case of all these programmes, much of the earlier gains were
frittered away as the initial infrastructure created was not supported in later years by matching
investment. In fact between 1985-86 to 1990-91 there was already a major slow down or decline
in State expenditures on Medical and Public Health. This was more glaring in the case of capital
expenditures for setting up of new infrastructure.
Misplaced Emphasis on Vertical Programmes
This is not to suggest that optimal use has been made of public health expenditure in the country
before the reforms process. In fact, quite to the contrary. Much of the blame for what is today
being termed the “resurgence of communicable diseases” lies in strategies adopted well before
the reforms programme in the country. These strategies relied on various centrally administered
programmes (vertical programmes) for disease control and prevention. Such programmes
included the National programmes on Tuberculosis, Malaria, Leprosy. Immunisation, Diarrhoeal
diseases, Blindness and Family Planning. With no integration at the level of delivery, these
programmes were insensitive to local conditions, unresponsive to local needs, highly
bureacratised and inefficient. These programmes were accountable to officials situated in the
national and state capitals, and had little or no scope for flexibility’ based on local conditions.
Local populations were indifferent and in some cases hostile to such programmes, resulting in fair
measure to the very poor utilisation of Government health facilities in many areas.
Oblivious to these trends the government has geared itself towards the show-casing of the
"market orientation" of health care policies. Investment in the private hospital sector was very
low in the 1970s, but since then it has grown at an exponential rate. This was fuelled by a slowing
down of investment by the State and simultaneous incentives given to the private sector in the
form of soft loans, subsidies and tax exemptions. In recent years new medical technologies have
further added to the impetus, with increasing participation from the Corporate sector. This
coupled with the impending entry of insurance multinationals, has cleared the path for the Indian
health care sector being taken over by forces that control the global "market" for health care. In
the process, the health needs of an overwhelming majority of Indians are being increasing!)
ignored.
Penetration of the Private Medical Sector
The abandonment of the government's basic duty in providing health care facilities has greatlx
enhanced the ability of the private sector to penetrate into the health sector. The distinction
between health care and medical care is important and needs to be noted. Health care involves a
lot more than just medical care, i.e. diagnosis and treatment of illnesses. Health care involves
nutrition, drinking water and sanitation facilities, good housing, and a lot more. These aspects of
health, for obvious reasons are not provided by the private medical sector.
6)3
But what of the medical care that is provided by the private sector? There is a fundamental
contradiction that exists in the concept of private medical care. By definition private medical care
can survive only if it is profitable. What logically follows is that a private medical care provider
stands to profit from ill-health—the more people fall ill and the longer they remain ill, the larger
the profit for the care provider! Additionally, as the poor have less money, much of the so called
^quahty’pnvate sector tends to be concentrated more among the better off citizens while the
quacks’ serve the poor.
We have commented earlier about the fact that developed economies continue to pledge resources
- on public funded health care—to the tune of 70-80% of total health care costs. They do so, not
out of any altruistic motives, but because conventional wisdom dictates that health care in the
private sector is expensive and inefficient. And yet, our government wishes to argue that
privatisation of health care leads to more efficient utilisation of resources!
In spite of all the virtues of the "free-market" that are being sought to be foregrounded, the private
sector is thriving because of a host of direct and indirect subsidies it receives from the
government It is ironical that a government which declares that it makes poor economic sense to
subsidise health care for the poor, provides such subsidies to the private and corporate medical
sector, which caters exclusively to the needs of the rich. Thus, after providing medical education
at a very nominal cost the government provides concessions and subsidies to private medical
professionals and hospitals to set up private practice and hospitals.
The government also provides incentives, tax holidays, and subsidies to private pharmaceutical
and medical equipment industry. It allows exemptions in taxes and duties in importing medical
equipment and drugs, especially for expensive new medical technologies. The government has
allowed the highly profitable private hospitaTsector to function as trusts which are exempt from
taxes, thereby exempting them from contributing to the state exchequer even while being allowed
to make huge profits. Moreover, medical and pharmaceutical research and development is largelx
carried out in public funded institutions but the major beneficiary' is the private sector. Manx
private practitioners are given honorary positions in public hospitals, which they use openly to
promote their personal interests.
The decade of the nineties has seen another transition taking place in the private health sector.
Prior to this, the private sector consisted of a large number of individual practitioners and private
tospitals and nursing homes run by medical professionals. For the first time, today, we see the
entry of the organised corporate sector in medical care. As the practice of medicine becomes
more technology intensive, the role of the medical professional is becoming narrower. The
control of technology has thus become the key factor in determining who or which entity controls
private medical care. Corporate entities, given their ability to invest in ’’state of the art” medical
technologies, are fast wresting control of the medical care ’’industry'”. Henceforth, the return on
investment made by such corporations, and not any esoteric concept of professional ethics, will
determine the kind of care |provided.
‘
‘ corporates try to maximise profits they will attempt to
As
further push up cost of medicalI costs by introducing high cost technologies, and expensive
iagnostic aids and medicines. This is not merely an imaginary futuristic scenario. In the United
States, such an approach to medical care has lead to health care costs being the highest in the
world. Alongside the move towards reduced support to health care facilities, the government^
new-found fascination with health insurance is designed to facilitate privatisation of the health
sector.
National Health Policy 2002
The National Health Policy announced by the Government in 2002 is a continuation of the trends
indicated earlier. An examination of the new policy shows that is most eloquent where it is silent.
It completely omits the very concept of comprehensive and universal health care and in fact
primary health care itself is reduced to primary level care!. In contrast, the National Health Policy
of 1983 (NHP 1983) had said: “India is committed to attaining the goal of “Health for All by the
Year 2000 A.D.” through the universal provision of comprehensive primary health care services’’^
The new policy, thus, departs from the fundamental concept of the NHP 1983 and the Alma Ata
declaration of 1978, for “Health for all by 2000” to which India was a signatory. Though it does
mention the importance of investing in infrastructure, the new policy is conspicuously silent on
the concept of the village health worker -- the first contact in the primary health care system or on
the need to have good public referral services. By its silence, the policy pro\ ides a framework for
the dismantling of the whole concept of primary health care. Significantly, the section on policy
prescriptions is entirely silent on the content of the primary health care system.
Similarly while there is talk of the need for standardised regimens of treatment and the need for
essential drugs, it does not take on the issue of the need of price control for drugs. Also the policy
is practically silent about pharmaceuticals and their impact on health care — thereby virtually
accepting that the Ministry of Health has no role in formulation of the drug policy. This is even
more surprising given the fact that a new Drug Policy was announced by the Ministry of Industry
in 2002 just a short while after the announcement of the Health Policy. The new drug policy has
recommended further relaxation of price and production controls on drugs.
Other important concerns are either ignored or referred to only in passing in the new policy. The
importance of an intersectoral approach in health planning is mentioned only to be ignored . In
the same way the policy has a four-line section on women’s health, without any specific
proposals being spelt out. Child health is not even afforded a separate section, and is dealt with
through passing references. It is silent on child nutrition in spite of the shameful fact that a half of
children below 5 are malnourished in India - a dubious distinction that India shares with only one
other country (Bangladesh) in the world.
The policy betrays a total lack of understanding regarding the need to create a medical education
system oriented to the needs of primary care, and instead is steeped in the bias of urban specialist
based health care. On the other hand it is entirely silent about the bane of private medical colleges
and the need to stop the setting up of new private medical colleges and regulate these institutions.
The section on Research in the policy harps on “frontier areas” and medical research. There is no
understanding of the necessity to initiate and sustain research on public health. There is no
mention of the necessity to regulate medical research and to develop ethical criteria in this regard.
A perusal of the new policy throws up many fundamental concerns. The policy admits that public
health investment has been “■comparatively low”. The policy recommends welcome increase in
public health expenditure from the present 0.9% of GDP to 2.0% in 2010. However the quantum
suggested is too little and comes very late. It falls far short of the 5% of GDP that has been a
long-standing demand of the health movement and recommended by WHO long back. Moreo\ er
the Draft projects that public expenditure in 2010 will be 33% of total health expenditure - up
from the present 17%. But even 33? o is lower than that of the average of any region in the globe
today - India would continue to be one of the most privatised health systems in the world even in
2010! W hile even the small increase in health financing can make some difference this can only
happen if distribution is equitable and if the allocation of resources is to improve services in
backward areas and not for increasing use of technology or subsidy to the private sector. While
the document does mention that part of the allocation would be used for strengthening
infrastructure it does not say where and other issues of allocation are however apparently not
important enough to merit discussion in the policy document. The policy also is eloquent on the
inability of states to increase expenditure on health care and laments that the allocation by states
has in fact decreased in the past decade. There is a veiled attempt to castigate the states for their
inability to increase expenditure. Such insinuations are uncalled for without a detailed analysis of
the manner in which the liberalisation process has shattered the financial stability of states.
Top-Down Prescriptions
The new' policy, for all the rhetoric on community participation, is replete with “top down”
prescriptions. While admitting the wastage involved in running Centrally sponsored and
controlled vertical disease control programmes and envisaging their integration in the
decentralised primary health care system, it goes on to recommend that we would need to retain
many of them! On the other hand the policy is delightfully vague about actual devolution of
responsibility and financial powers to Panchayat Raj Institutions (PRIs) and relocation of
accountability to appropriate levels of local self-governments. In the absence of such clarity there
is the danger of the primary health care system becoming a Collector driven exercise, which is
controlled by the Centre — thereby defeating the entire effort at decentralisation. In fact the
policy suggests that local self-governments be ‘assisted’ by social activists, private health
professionals, MLAs/MPs and Govt officials.
The policy also has a rather naive understanding of the reasons for lack of utilization of OPD
services by the public. They seem to feel that providing drugs (though an important part) is all
that is needed - the poor quality of, or lack of other equipment, the absence of staff as well as the
emphasis on Family planning are all not even realised! Again, the vision of further training of and
extending the duties of paramedicals totally overlooks the fact that these personnel are already
overworked
Prescriptions for Further Privatisation
Numerous formulations in the policy, in various forms, clear the way for even greater
privatisation of the health care system. The policy says, ^the NHP will
suggest policy
instruments for implementation ofpublic health programmes through individuals and institutions
of civil society^. This constitutes a veiled attempt to clear the way for sub contracting public
health to NGOs. The policy proposes to employ user fees in public hospital, couched in the usual
sugar coating of it being introduced for those who can pay. Global experience of user fees at any
level shows that they serve only one purpose — to drive out the poor and the indigent. Proposal
of user fees in a Health Policy is objectionable. The policy suggests targeting of primary health
care for resource allocation but this should not constitute an argument for the legitimisation of the
government's retreat from providing comprehensive and quality secondary and tertiary care. The
policy hints at this possibility in different sections and also hints at “encouraging” the private
sector to occupy the space that would be left vacant. It conveniently forgets that part time doctors
will lack commitment even more that present doctors. It also ignores the implications of
privatization for the National Health Programs. The policy document also discounts the data that
shows that for critical inpatient care 45% of the poorest continue to depend upon the public sector
hospitals.
The policy talks about using Indian health facilities to attract patients from other countries. It also
suggests that such incomes can be termed as “deemed export” and should be exempt from taxes.
This formulation draws from recommendations that the industry has been making and specifically
from the “Policy Framework for Reforms in Health Care”, drafted by the prime Minister s
Advisory7 Council on Trade and Industry, headed by Mukesh Ambani and Kumaramangalam
Birla. Such a proposal, termed by many as “health tourism”, will divert our best resources to
serve the interests of the global health market and create islands of brain and resource drain
within the country. The use of domestic facilities for treating patients from outside the country
may be encouraged only if such use is restricted to less than 10% of the facilities of any
institution. The policy also, talks of encouraging '"the setting up ofprivate insurance instruments
for increasing the scope of the coverage of the secondary and tertiary sector under private health
insurance packages”. Further, there are repeated references in the policy about “valuable’
contributions made by the private sector and the need to “encourage” more such contributions.
While the policy is repeatedly critical of the public health system (justifiably so) there is no
criticism of the ills of the unregulated private medical care system, though reference is made to
the need to develop regulatory norms.
In brief, the new policy identifies many of the gross deficiencies of the existing health care
scenario, proposes a substantial rise in central government expenditure on health care and has
some other positive features like the proposed regulation of the Private sector. However, it
constitutes an abandonment of the Alma Ata declaration, and legitimises, further privatisation of
the health sector.
Policy on Population Control - Targeting Women
Population control policies in India have changed in nomenclature in the last 4 decades. But what
has remained constant is that they have been a major obsession for planners in this country.
However, evidence indicates that the programme can hardly be held responsible for the few
success stories in population planning in the country - Kerala and Tamil Nadu. Kerala’s success
in achieving results comparable to the developed world - vis-a-vis both demographic and health
indicators - have been widely attributed to factors such as high minimum wages, land reforms,
high literacy rates and access to universal health care. Much of Tamil Nadu’s success in pegging
down birth rates in recent years is being attributed to improved child survival due to the massive
statewide feeding programme for undernourished children and improved communication
facilities. Both experiences strengthen the maxim that “development is the best contraceptive”.
Population control strategies have tended to be paternalistic, prescriptive and coercive. It is a
strategy which starts from the belief that the poor breed prodigiously and it is the nation’s duty to
cap their unbridled fertility. Such programmes are inappropriate not only because they victimise
women, but also because they do not work. Such a strategy has undermined the effectivity of the
general health care infrastructure as well as the faith that women have in this infrastructure to
address their real concerns. Most programmes, have tended to view women as assembly line
appendages required to produce babies. Thus a woman’s health becomes important only when she
is pregnant or lactating. But in India 65% of deaths in women are due to infection related causes
and only 2.5% of deaths are related to childbirth. Even among women in the reproductive age
group only 12.5% of deaths are due to childbirth associated causes. Gender discrimination starts
very early. Girls are more likely to die than boys, between the ages ot 1 and 5 years. The risk of
dying at that age is 43% higher for girls -- one of the largest sex-based mortality differences in
the world.
Nomenclature notwithstanding, the new policy carries withm it the basic core of ember pohci
which made them unacceptable to large sections of women m this country. Women need'access
family planning services because of their own health needs^ Eut ^^.^^hdce
o de
women have a choice, that women are in a position to make decisions about their choice.Jr1 orde
for a policy to centre-stage women’s concerns and needs, it should revolve aroun
p
g
addresses women’s health in all its dimensions and not just their wombs.
The National Population Policy (2000) was an advance because it clearly stated that '^nt.ves
and disincentives would not be part of the National Policy. It affirmed the
of
government towards voluntary and informed choice and consent of citizens M avadtng J
reproductive health care services, and continuation of the target free approach
[ f
family planning services". Unfortunately this has translated poorly into actual actio and^coercmn
remains a cornerstone of the State’s attempts at population stab.hsation In fact man) State
Governments, have legislated to promote the so called “Two Child Norm and continu tci use
coercive methods like laws that disbar people with more than two children from contesting
elections.
The promotion of the two-child norm in « gender insensitive society has led to s
distortions The most glaring is the rapid proliferation of the heinous practice of sex-selcc
XZs The recent tnsns dam shelving a rapid fall in child-sex ratios across the country ,s a
matter of extreme concern.
Pharmaceutical Policy
The first comorehensive National Policy on pharmaceuticals was announced by the Government
"m
h.s been'revised in 1936,1995 .nd 2002.
continues to be formulated by the Ministry of Chemicals and Fertilisers and not by the Ministry
of Health. As a result the Policy has always been deficient m addressing issues related
and access.
The Policy announced in 2002 brought in new changes aimed at allowing a rise mJP^es. In
X^meVdmento^
of^MBut off-Patent Drugs
^Yndia
fact prices of some top selling drugs are higher in India than those in Canada and the UK.
In the New Policy, in one sweep, the volume of pharmaceuticals under price= control has-been
reduced from an estimated 40 per cent to just 25 per cent of tie tota lug^nu
'
have clearly shown that prices of drugs start rising as soon “ contiols
r"'"ov . Control
evident in 1995-96, after the last round of price decontrol effected th.ough th?
8P
Order (DPCO) 1995 Further, in almost all segments, the brand leader for a particular drug t
U,e tend
'1’e Mghes. tume.ert is —y
of the most expensive (n> son,, e.ses«... .s
6xi>
expensive!). This flies in the face of the argument that market forces and competition stabilises
drug prices.
The new policy has attempted to justify the price decontrol with the plea that this shall boost
R&D expenditure in the pharmaceutical sector. When concerns (legitimate in our view) were
raised that amendment of the Indian Patents Act would result in rise in Drug Prices, the ministry
of chemicals and fertilisers had consistently claimed that any rise in prices would be kept in check
through mechanisms in the DPCO. It is extremely surprising that now that we are moving
towards a Product Patent regime (the amendment to the Patents Act is presently pending in
parliament), there should be talk of diluting Price Controls. Price Controls have already been
diluted in the past decade and only 40 per cent of the turnover of the industry was under price
control prior to the new policy. Any further dilution would mean virtual abandonment of price
controls. It must also be noted in this context that most country, including virtually all developed
countries have mechanisms in place that control prices of drugs.
Pharmaceuticals have an unique characteristic - those who need drugs most are the least likely to
be able to pay for them. Thus even a small increase in prices results in the "costing out" from the
market of a large number of people. In a country where half a million people die of Tuberculosis a disease that can be treated by over a dozen drugs - because drugs are unaffordable, such a
license to profiteer is inhuman. The imminent rise in drug prices comes at a particularly
unfortunate juncture. The public health delivery system is in shambles and large parts of it are
being dismantled or privatised. Drug supplies at public health facilities are at an all time low. This
has already forced poor consumers to pay for medicines even if they are being treated in public
facilities. Any further price rise can only push such patients to the brink of penury.
Any Drug Policy has to start with the premise .that drugs are not like any other industrial products
or consumer goods. Unlike say, washing machines or cars, availability of affordable drugs may
make the difference between life and death for millions of people. A Drug Policy, thus, has to
address the issues of quality, indigenous manufacture, availability of essential drugs, review of
existing irrational and hazardous drugs, and affordability of drugs that are available. The new
policy does not address any of these.
New Directions in Policy
Since the National Health Policy 2002 was announced, there has been a change of Government in
the country. Hopes of a change in direction were stoked by some positive declarations of intent in
the Common Minimum programme of the newly installed UPA Government. It stated, for
example, that: “The UFA government will raise public spending on health to at least 2-3% of
GDP over the next five years with focus on primary health care”. The CMP also underlined its
commitment to focus on Primary Health Care. It also stated that: “The UFA government will take
all steps to ensure availability of life-savings drugs at reasonable prices” However the hopes
raised by such positive commitments have been belied in the ensuing months.
The first budget by the UP A Govt, provided no additional budgetary support for health care,
thereby rendering meaningless its commitment to increase public spending on health. There have
been no concrete moves to impose price controls in order to bring down the spiralling rise in drug
prices.
The Government’s commitment to Primary Health Care is now being sought to be implemented
through the proposed Rural Health Mission. However a reading of the initial drafts of the
proposed Mission raise many disturbing concerns. The scheme proposes to hand over large parts
o tie public health system to private providers and NGOs. It lays emphasis on the need to lev\
user fees inorder to maintain the infrastructure. It is not committed to strengthening the public
lealth infrastructure, but instead proposes to fill the gaps in the infrastructure through private
sector participation. An impression is being created that the non-functioning of the public health
system is a legitimate reason for resorting to privatisation of the structure. The move towards
casualisation and privatisation is evident from the fact that the central Govt, has recently
advertised for district level posts of district managers and other personnel in six states of India to
manage activities of SCOVA (autonomous organisations registered by the state Govts.under the
direction of the central Govt.). These personnel are to ensure increasing participation of NGOs
and other private institutions in health care. In some states (like Rajasthan) posts of Medical
Officers in PHCs are being abolished. In essence, thus, there appears to be a trend towards
moving further away from any commitment in providing comprehensive health services by the
government.
It is also a matter of deep concern that the Common Minimum programme refers to “sharplv
tengeted population control programmes in 150 Districts''* This amounts to providing tacit
clearance to coercive measures to control population. Not only are such measures violative of
basic human rights, they have also been shown to be almost entirely useless in stabilising
population. The CMP’s position on this stands in clear variance with the National Population
Policy 2000, which had been formulated on the basis of a wide national consensus.
Section II: Wide Ranging ImpactDenial of Health Care at All Levels
The consequences of the policies related to health care are being widely felt. Some glaring
instances include the following:
•
•
•
•
•
•
•
•
•
•
•
Infant and Child mortality snuffs out the life of 22 lakh children every year, and there
has been very little improvement in this situation in recent years. We are yet to achieve the
National Health Policy 1983 target to reduce Infant Mortality Rate to less than 60 per 1000
live births.2 More serious is the fact that the rate of decline in Infant Mortality, which was
significant in the 1970s and 80s, has slowed down in the 1990s.
130,000 mothers die during childbirth every year. The NHP 1983 target for 2000 was to
reduce Maternal Mortality Rate to less than 200 per 100,000 live births. However. 407
mothers die due to pregnancy related causes, for every 100,000 live births even today. In fact,
as per the NFHS surveys in the last decade Maternal Mortality Rate has increased from 424
maternal deaths per 100,000 live births to 540 maternal deaths per 100,000 live births.
Three completely avoidable child deaths occur every minute. The four major killers
(lower respiratory tract infection, diarrheal diseases, perinatal causes and vaccine preventable
diseases) accounting for over 60% of deaths under five years of age are entirely preventable
through better child health care and supplemental feeding programs. The most recent estimate
of complete immunization coverage indicates that only 54% of all children under age three
were fully protected.
About 5 lakh people die from tuberculosis every year, and this number is almost unchanged
since Independence! 20 lakh new cases are added each year, to the burgeoning number of TB
patients presently estimated at around 1.40 crore Indians!
India is experiencing a resurgence of various communicable diseases including Malaria,
Encephalitis, Kala azar, Dengue and Leptospirosis. The number of cases of Malaria has
remained at a high level of around 2 million cases annually since the mid eighties. B\ the
year 2001, the worrying fact has emerged that nearly half of the cases are of Falciparum
malaria, which can cause the deadly cerebral malaria.
A growing proportion of Indians cannot afford health care when they fall ill. National
surveys show that the number ofpeople who could not seek medical care because of lack of
money increased significantly between 1986 and 1995. The proportion of such persons
unable to afford health care almost doubled, increasing from 10 to 21 % in urban area>. and
growing from 15 to 24% in rural areas in this decade.
Forty percent of hospitalised people are forced to borrow money or sell assets to cover
expenses.
Over 2 crores of Indians are pushed below the poverty line every year because ot the
catastrophic effect of out of pocket spending on health care.
Irrational medical procedures are on the rise. According to just one study in a community in
Chennai, 45% of all deliveries were performed by Cesarean operations, whereas the WHO
has recommended that not more than 10-15% ot deliveries would lequiie Cesarean
operations.
Due to irrational prescribing, an average of 63 per cent of the money spent on prescriptions
is a waste. This means that nearly two-thirds of the money that we spend on diugs max be for
unnecessary or irrational drugs.
The pharmaceutical industry is rapidly growing -- yet only 20? o of the population can access
all essential drugs that they require. Many drugs are being sold at 200 to 500 percent profit
margin, and essential drugs have become unaffordable for the majority of the Indian
population.
The above facts, startling as they are in their own right hide severe disparities between the well
off and the poor, the urban residents and rural people, the adivasis and dalits and others, and
between men and women. They include:
The Infant Mortality Rate in the poorest 20% of the population is 2.5 times higher than that
in the richest 20%) of the population.
A child in the 'Low standard of living' economic group is almost four times more likely to
die in childhood than a child in the better off'High standard of living’ group. An Adivasi
child is one and half times more likely to die before the fifth birthday than children of other
groups^.
A girl is 1.5 times more likely to die before reaching her fifth birthday, compared to a boy!
The female to male ratios for children are rapidly declining, from 945 girls per 1000 boys
in 1991, to just 927 girls per 1000 boys in 2001. This decline highlights an alarming trend
of discrimination against girl children, which starts well before birth (in the form of sex
selective abortions), and continues into childhood and adolescence (in the form of worse
treatment to girls).
health problems, is six
A person from the poorest quintile of the population, despite: more
i
times less likely to access hospitalization than a |person from the richest quintile. This means
that the poor are unable to afford and access hospitalization in a very large proportion of
illness episodes, even when it is required.
The delivery of a mother, from the poorest quintile of the population is over six times less
likely to be attended by a medically trained person than the delivery of a well off mother,
from the richest quintile of the population. An adivasi mother is half as likely to be
delivered by a medically trained person.
The ratio of hospital beds to population in rural areas is fifteen times lower than that for
urban areas.
The ratio of doctors to population in rural areas is almost six times lower than the
availability of doctors for the urban population.
Per person, Government spending on public health is seven times lower in rural areas.
compared to Government health spending for urban areas.
•
•
•
•
•
•
•
•
The above are a direct consequence of the virtual dismantling of the public health infrastructure,
as shown by the following state of Primary Health Centres:
•
•
•
•
•
Only 38% of all PHCs have all the critical staff.
Only 31% have all the critical supplies (defined as 60% of critical inputs), with only 3%
of PHCs having 80% of all critical inputs.
In spite of the high maternal mortality ratio, 8 out of every 10 PHCs have no Essential
Obstetric Care drug kit!
Onl} 34% PHCs offer delivery services, while only 3% offer Medical Termination of
Pregnancy.
A person accessing a community health centre would find no obstetrician in 7 out of 10
centres, and no paediatrician in 8 out of 10.
Women’s Right to Health Care: Reiterating State Obligation
Background document of the presentation
(based on international and national documents related to the title)
to the
National Human Rights Commission
and the
Ministry of Health and Family Welfare, Government of India
at the
National Public Hearing on Right to Health Care (Jan Sunwai)
(jointly organized by the NHRC and the Jan Swasthya Abhiyan)
Manisha Gupte
Research Assistance: Namrata Kavde
Mahila Sarvangeen Utkarsh Mandai (MASUM)
Pune, Maharashtra
December 2004
1
State obligation with respect to the right to health care has been understood in
international treaties^ broadly under the following categories:
Respect: The obligation to respect requires States to refrain from interfering directly or
indirectly with the enjoyment of the right to health.
Protect: The obligation to protect requires States to take measures that prevent third
parties from interfering with what article 12 guarantees.
Fulfill and promote: the obligation to fulfil requires States to adopt appropriate
legislative, administrative, budgetary, judicial, promotional and other measures towards
the full realization of the right to health.
The General Recommendation No. 24 of the Convention on the
Elimination of All Forms of Discrimination Against Women (1979)
spells out the above state obligations succinctly in the following way:
13. The duty of States parties to ensure, on a basis of equality of men and women, access
to health-care services, information and education implies an obligation to respect,
protect and fulfil women's rights to health care. States parties have the responsibility to
ensure that legislation and executive action and policy comply with these three
obligations. They must also put in place a system that ensures effective judicial action.
Failure to do so will constitute a violation of article 12.
14. The obligation to respect rights requires States parties to refrain from obstructing
action taken by women in pursuit of their health goals. States parties should report on
how public and private health-care providers meet their duties to respect women's rights
to have access to health care. For example. States parties should not restrict women's
access to health services or to the clinics that provide those services on the ground that
women do not have the authorization of husbands, partners, parents or health authorities,
because they are unmarried or because they are women. Other barriers to women's access
to appropriate health care include laws that criminalize medical procedures only needed
by women punish women who undergo those procedures.
15. The obligation to protect rights relating to women's health requires States parties,
their agents and officials to take action to prevent and impose sanctions for violations of
rights by private persons and organizations. Since gender-based violence is a critical
health issue for women. States parties should ensure:
(a) The enactment and effective enforcement of laws and the formulation of policies,
including health-care protocols and hospital procedures to address violence against
women and sexual abuse of girl children and the provision of appropriate health services;
(b) Gender-sensitive training to enable health-care workers to detect and manage the
health consequences of gender-based violence;
(c) Fair and protective procedures for hearing complaints and imposing appropriate
sanctions on health-care professionals guilty of sexual abuse of women patients;
1
(d) The enactment and effective enforcement of laws that prohibit female genital
mutilation and marriage of girl children.
16 States parties should ensure that adequate protection and health services, including
trauma treatment and counselling, are provided for women in especially difficult
circumstances, such as those trapped in situations of armed conflict and women
refugees.
17. The duty to fulfil rights places an obligation on States parties to take appropriate
legislative, judicial, administrative, budgetary, economic and other measures to the
maximum extent of their available resources to ensure that women realize their rights to
health care. Studies such as those that emphasize the high maternal mortality and
morbidity rates worldwide and the large numbers of couples who would like to limit their
family size but lack access to or do not use any form of contraception provide an
important indication for States parties of Possible breaches of their duties to ensure
women's access to health care. The Committee asks States parties to report on what they
have done to address the magnitude of women's ill-health, in particular when it arises
from preventable conditions, such as tuberculosis and HIV/AIDS. The Committee is
concerned about the evidence that States are relinquishing these obligations as they
transfer State health functions to private agencies. States and parties cannot absolve
themselves of responsibility in these areas by delegating or transferring these
powers to private sector agencies. States parties should therefore report on what
they have done to organize governmental processes and all structures through
which public power is exercised to promote and protect women's health. They should
include information on positive measures taken to curb violations of women’s rights by
third parties and to protect their health and the measures they have taken to ensure the
provision of such services.
Women of the World - Women^s Health in India
By Victoria A. Velkoff and Arjun Adlakha
International Programs Center, Issued December 1998.
1. Over 100,000 Indian Women Die Each Year From Pregnancy-Related Causes
India has a high maternal mortality ratio—approximately 453 deaths per 100,000 births
in 1993. The level of maternal mortality varies greatly by state, with Kerala having the
lowest ratio (87) and two states Madhya Pradesh and Orissa having ratios over 700
(UNICEF, 1995). This differential maternal mortality is most likely related to differences
in the socioeconomic status of women and access to health care services among the
states. The high levels of maternal mortality are especially distressing because the
majority of these deaths could be prevented if women had adequate health services
(either proper prenatal care or referral to appropriate health care facilities) (Jejeebhoy and
Rao, 1995). In fact, the leading contributor to high maternal mortality ratios in India is
lack of access to health care (The World Bank, 1996).
2
2. Few Pregnant Women Receive Prenatal Care
The National Family Health Survey (NFHS) of 1992-93 found in the 4 years preceding
the survey that 37 percent of all pregnant women in India received no prenatal care
during their pregnancies (UPS, 1995). The proportion receiving care varied greatly by
educational level and place of residence. Nearly half of illiterate women received no care
compared to just 13 percent of literate women. Women in rural areas were much less
likely to receive prenatal care than women in urban areas (42 percent and 18 percent,
respectively). Most women who did not receive health care during pregnancy said they
did not because they thought it was not necessary (UPS, 1995). Thus, there is a definite
need to educate women about the importance of health care for ensuring healthy
pregnancies and safe childbirths. Another reason for the low levels of prenatal care is
lack of adequate health care centers.
3. One in Five Maternal Deaths Related to Easily Treated Problem
Anemia, which can be treated relatively simply and inexpensively with iron tablets, is
another factor related to maternal health and mortality. Studies have found that between
50 and 90 percent of all pregnant women in India suffer from anemia. Severe anemia
accounts for 20 percent of all maternal deaths in India (The World Bank, 1996). Severe
anemia also increases the chance of dying from a hemorrhage during labor.
4. Excess Female Deaths
Several studies have found that one of the reasons for the poor health of Indian women is
the discriminatory treatment girls and women receive compared to boys and men (Das
Gupta, 1994; Desai, 1994). The most chilling evidence of this the large number of
“missing women” (i.e., girls and women who have apparently died as a result of (past and
present discrimination). Recent estimates place this number at approximately 35 million
(The World Bank, 1996). In other words, there is a deficit of 35 million girls/women who
should be part of the population but are not. Differential treatment of girls and boys in
terms of feeding practices and access to health care is among the factors responsible for
higher female mortality. Causes of death for children aged 1 to 4 show girls dying at a
higher rate than boys from accidents and injuries, fever, and digestive disorders—all
causes that are related to living conditions and negligence (Government of India, 1995).
1. Respect
Refraining from denying or limiting equal access for all persons;
Abstaining from enforcing discriminatory practices as a State policy;
Abstaining from imposing discriminatory practices relating to women's health status and
needs;
3
Refraining from prohibiting or impeding traditional preventive care, healing practices and
medicines, from marketing unsafe drugs and from applying coercive medical treatments;
Refraining from limiting access to contraceptives and other means of maintaining sexual
and reproductive health;
Refraining from censoring, withholding or intentionally misrepresenting health-related
information;
»!
Refraining from preventing people's participation in health-related matters;
Refraining from unlawfully polluting air, water and soil, from using or testing nuclear,
biological or chemical weapons;
Refraining from limiting access to health services as a punitive measure;
Fundamental Rights guaranteed by the Indian Constitution
Article 14 Equality before law
Article 15 Prohibition of discrimination on grounds of religion, race, caste, sex or place
of birth.
Article 21 Protection of life and personal liberty
Article 1 of the Convention on the Elimination of All Forms of
Discrimination Against Women (1979) defines ‘discrimination” against women :
The term "discrimination against women" shall mean any distinction, exclusion or
restriction made on the basis of sex which has the effect or purpose of impairing or
nullifying the recognition, enjoyment or exercise by women, irrespective of their marital
status, on a basis of equality of men and women, of human rights and fundamental
freedoms in the political, economic, social, cultural, civil or any other field.
Article 16 (and article 5) of the General Recommendation 19 to the CEDAW
22. Compulsory sterilization or abortion adversely affects women’s physical and
mental health, and infringes the right of women to decide on the number and
spacing of their children.
Universal Declaration of Human Rights (1948)
4
Article 1 All human beings are bom free and equal in dignity and rights.
Article 2 Everyone is entitled to all the rights and freedoms set forth in this Declaration,
without distinction of any kind.
Article 3 Everyone has the right to life, liberty and the security of person.
The International Covenant on Civil and Political Rights (1976)
Article 1
1. All peoples have the right of self-determination (to freely pursue their economic,
social and cultural development).
Article 2
1. State Parties to abstain from distinction of any kind, such as race, colour, sex,
language, religion, political or other opinion, national or social origin, property,
birth or other status.
Article 6
1. Every human being has the inherent right to life. This right shall be protected by
law. No one shall be arbitrarily deprived of his life.
The International Convenant on Economic, Social and Cultural Rights
(1976)
Article 1 All peoples have the right of self-determination (to freely pursue their
economic, social and cultural development).
Article 2 The States Parties to present Covenant undertake to guarantee that the rights
enunciated in the present Covenant will be exercised without discrimination of any kind
Article 3 The States Parties to the present Covenant undertake to ensure the equal right
of men and women to the enjoyment of all economic, social and cultural rights set forth
in the present Covenant.
2. Protect
To adopt legislation or to take other measures ensuring equal access to health care and
health-related services provided by third parties;
5
To ensure that privatization of the health sector does not constitute a threat to the
availability, accessibility, acceptability and quality of health facilities, goods and
services;
To control the marketing of medical equipment and medicines by third parties;
To ensure that medical practitioners and other health professionals meet appropriate
standards of education; skill and ethical codes of conduct.
To ensure that harmful social or traditional practices do not interfere with access to preand post-natal care and family-planning;
To prevent third parties from coercing women to undergo traditional practices, e.g.
female genital mutilation;
To take measures to protect all vulnerable or marginalized groups of society, in particular
women, children, adolescents and older persons, in the light of gender-based expressions
of violence.
To ensure that third parties do not limit people’s access to health-related information and
services.
3. Fulfill
To give sufficient recognition to the right to health in the national political and legal
systems, preferably by way of legislative implementation;
To adopt a national health policy with a detailed plan for realizing the right to health.
To ensure provision of health care, including immunization programmes against the
major infectious diseases;
To ensure equal access for all to the underlying determinants of health;
To ensure that public health infrastructures provide for sexual and reproductive health
services, including safe motherhood, particularly in rural areas.
To ensure the appropriate training of doctors and other medical personnel:
To ensure the provision of a sufficient number of hospitals, clinics and other healthrelated facilities.
To promote and support the establishment of institutions providing counselling and
mental health services, with due regard to equitable distribution throughout the country.
To include the provision of a public, private or mixed health insurance system which is
affordable for all.
6
To promote medical research and health education;
To adopt measures against environmental and occupational health hazards and against
any other threat as demonstrated by epidemiological data;
To take positive measures that enable and assist individuals and communities to enjoy the
right to health;
To fulfil (provide) a specific right contained in the Covenant when individuals or a group
are unable, for reasons beyond their control, to realize that right themselves by the means
at their disposal;
Article 25 of the UDHR
1. Everyone has the right to a standard of living adequate for the health and well
being of himself and of his family, including food, clothing, housing and medical
care and necessary social services, and the right to security in the event of
unemployment, sickness, disability, widowhood, old age or other lack of
livelihood in circumstances beyond his control.
2. Motherhood and childhood are entitled to special care and assistance. All
children, whether born in or out of wedlock, shall enjoy the same social
protection.
Article 12 (of the ICESCR)
The States Parties to the present Covenant recognize the right of everyone to the
enjoyment of the highest attainable standard of physical and mental health.
Article 11 (of the CEDAW)
1. States Parties shall take all appropriate measures to eliminate discrimination
against women in the field of employment in order to ensure, on a basis of
equality of men and women, the same rights, in particular:
(f) The right to protection of health and to safety in working conditions, including the
safeguarding of the function of reproduction.
Article 12 (of the CEDAW)
1. States Parties shall take all appropriate measures to eliminate discrimination against
women in the field of health care in order to ensure, on a basis of equality of men and
women, access to health care services, including those related to family planning.
2. Notwithstanding the provisions of paragraph 1 of this article, States Parties shall
ensure to women appropriate services in connection with pregnancy, confinement and the
post-natal period, granting free services where necessary, as well as adequate nutrition
during pregnancy and lactation.
7
4. Promote
To undertake actions that create, maintain and restore the health of the population;
Such obligations include:
(i)
fostering recognition of factors favouring positive health results, e.g. research
and provision of information;
(ii)
ensuring that health services are culturally appropriate and that health care
staff are trained to recognize and respond to the specific needs of vulnerable
or marginalized groups;
(iii)
ensuring that the State meets its obligations in the dissemination of
appropriate information relating to healthy lifestyles and nutrition, harmful
traditional practices and the availability of services;
(iv)
supporting people in making informed choices about their health.
Directive Principles in the Indian Constitution
Article 38 and 38{(i)}| State to secure a social order for the promotion of welfare of the
people (in which justice, social, economic and political, shall inform all the institutions of
the national life).
Article 47 Duty of the State to raise the level of nutrition and the standard of living
and to improve public health Article 41 Right to work, to education and to public assistance in certain case
Article 42 Provision for just and humane conditions of work and maternity relief
Article 43 Living wage, etc., for workers
Special attention needs to be drawn to Article 39, which eloquently spells out the ways in
which the above may be achieved:
(a) that the citizens, men and women equally, have the right to an adequate means of
livelihood;
(b) that the ownership and control of the material resources of the community are so
distributed as best to subserve the common good;
(c) that the operation of the economic system does not result in the concentration of
8
wealth and means of production to the common detriment;
(d) that there is equal pay for equal work for both men and women;
(e) that the health and strength of workers, men and women, and the tender age of
children are not abused and that citizens are not forced by economic necessity to enter
avocations unsuited to their age or strength;
(f) that children are given opportunities and facilities to develop in a healthy manner
and in conditions of freedom and dignity and that childhood and youth are protected
against exploitation and against moral and material abandonment.
The National Population Policy (India) of 2000 re-introduces incentives and
disincentives for the adoption of a small family norm. These are violative of women’s
right to a life with dignity. Unless promotive measures are adopted by the government,
women will never have the power of negotiation within and outside their homes to decide
upon the number of children they wish to have.
Some of the promotional and motivational measures for adoption of the small family
norm as suggested by the National Population Policy (India) of 2000:
o
o
o
o
o
Panchayats and Zila Parishads will be rewarded and honoured for exemplary
performance in universalising the small family norm, achieving reductions in
infant mortality and birth rates, and promoting literacy with completion of
primary schooling.
The Balika Samridhi Yojana run by the Department of Women and Child
Development, to promote survival and care of the girl child, will continue. A cash
incentive of Rs. 500 is awarded at the birth of the girl child of birth order 1 or 2.
Maternity Benefit Scheme run by the Department of Rural Development will
continue. A cash incentive of Rs. 500 is awarded to mothers who have their first
child after 19 years of age, for birth of the first or second child only.
Disbursement of the cash award will in future be linked to compliance with ante
natal check up, institutional delivery by trained birth attendant, registration of
birth and BCG immunisation.
A Family Welfare-linked Health Insurance Plan will be established. Couples
below the poverty line, who undergo sterilisation with not more than two
living children, would become eligible (along with children) for health insurance
(for hospitalisation) not exceeding Rs. 5000, and a personal accident insurance
cover for the spouse undergoing sterilisation.
Couples below the poverty line, who marry after the legal age of marriage,
register the marriage, have their first child after the mother reaches the age of
21, accept the small family norm, and adopt a terminal method after the
birth of the second child, will be rewarded.
9
Recommendations for government action (General Recommendation 24
of the CEDAW)
29 States parties should implement a comprehensive national strategy to promote
women’s health throughout their lifespan. This will include interventions aimed at
both the prevention and treatment of diseases and conditions affecting women, as well as
responding to violence .against women, and will ensure universal access for all women
to a full range of high-quality and affordable health care, including sexual and
reproductive health services.
30 States parties should allocate adequate budgetary, human and administrative
resources to ensure that women's health receives a share of the overall health budget
comparable with that for men's health, taking into account their different health needs.
General Recommendation 19 of the CEDAW
Violence and Women
Background
7. Gender-based violence, which impairs or nullifies the enjoyment by women of
human rights and fundamental freedoms under general international law or under
human rights conventions, is discrimination within the meaning of article 1 of the
Convention. These rights and freedoms include.
g) The right to the highest standard attainable of physical and mental health;
Article 12 of GR 19 of CEDAW
19. States parties are required by article 12 to take measures to ensure equal access to
health care. Violence against women puts their health and lives at risk.
20. In some States there are traditional practices perpetuated by culture and tradition that
are harmful to the health of women and children. These practices include dietary
restrictions for pregnant women, preference for male children and female circumcision or
genital mutilation.
Beijing Declaration and Platform for Action, Fourth World Conference
on Women, 1995.
The BDPFA details out the following strategic objectives that the State need to fulfill
with reference to women and health:
io
o
Increase women's access throughout the life cycle to appropriate, affordable
and quality health care, information and related services:
o
Strengthen preventive programmes that promote women's health
o
Undertake gender-sensitive initiatives that address sexually transmitted
diseases, HIV/AIDS, and sexual and reproductive health issues
o
Promote research and disseminate information on women's health
o
Increase resources and monitor follow-up for women's health.
The International Conference on Population and Development (ICPD),
1994
o
Endorses a new strategy, which emphasizes the numerous linkages between
population and development.
o
Focuses on meeting the needs of individual women and men rather than on
achieving demographic targets.
o
Key to this new approach is empowering women and providing them with more
choices through expanded access to education and health services and promoting
skill development and employment.
o
Advocates making family planning universally available by 2015, or sooner, as
part of a broadened approach to reproductive health and rights, and calls on
Governments to make these resources available.
o
Includes goals in regard to education, especially for girls, and for the further
reduction of infant, child and maternal mortality levels.
o
Addresses issues relating to population, the environment and consumption
patterns; the family; internal and international migration; prevention and control
of the HIV/AIDS pandemic; information, education and communication; and
technology, research and development.
Vienna Declaration and Programme of Action, World Conference on
Human Rights, 1993.
o
Reaffirms the solemn commitment of all States to fulfill their obligations to
promote universal respect for, and observance and protection of all human rights
and fundamental freedoms for all.
o
Recognises the right of self-determination of all peoples.
o
Reiterates that the human rights of women and of the girl-child are an inalienable,
integral and indivisible part of universal human rights.
11
o
Urges for the full and equal participation of women in political, civil, economic,
social and cultural life, at the national, regional and international levels.
o
Considers eradication of all forms of discrimination on grounds of sex as primary
objectives of the international community.
o
o
o
Endorses that gender-based violence and all forms of sexual harassment and
exploitation, including those resulting from cultural prejudice and international
trafficking, are incompatible with the dignity and worth of the human person, and
must be eliminated.
Considers that the human rights of women should form an integral part of the
United Nations human rights activities, including the promotion of all human
rights instruments relating to women.
Urges Governments, institutions, intergovernmental and non-governmental
organizations to intensify their efforts for the protection and promotion of human
rights of women and the girl-child.
o
Emphasises the full and equal enjoyment by women of all human rights.
o
Stresses the importance of working towards the elimination of violence against
women in public and private life.
Urges the eradication of all forms of discrimination against women, both hidden
and overt.
of the highest standard of
o Recognizes the importance of the enjoyment by women
physical and mental health throughout their life span.
o Reaffirms, on the basis of equality between women and men, a woman's right to
accessible and adequate health care and the widest range of family planning
services, as well as equal access to education at all levels.
o
12
Recommendations to the NHRC
and to the Ministry of Health and Family Welfare, GOI
1. stop violation of women’s rights in the family planning programme
2. dismantle the “camp approach” in family planning
3. remove disincentives in family planning, especially those related to maternity
benefits, ration cards and political participation
4. remove incentives (gun licenses, for example)
5. user-fees, privatisation of health services and exorbitant fees for medical
education need to be done away with
6. regulation of the private sector (pharmaceuticals, medical profession, health
service providers etc) is essential for people’s rights to be protected
7. budgetary allocations to health cannot be reduced. This policy amounts to
violation of people’s right to health care
8. women should not be seen merely as mothers or potential mothers. Their health
needs must be addressed in a holistic manner - mental health, occupational health,
problems of ageing, cancers, STDs, RTIs and HIV-AIDS need to be addressed
from a gender framework
9. universal access to comprehensive and quality health services, irrespective of
capacity to pay is the only way to achieve the right to health care for all Indian
people, including women
10. health, being an indicator of the quality of life, cannot be achieved unless
measures to improve the social determinants of health are adopted
11. promotive measures, such as access to schooling (and to higher education),
gainful employment, job security, equal wages, workers’ benefits, access to
resources (family, community and national) and the right to inheritance of
property (home, land, assets etc) need to be put into place for health and well
being to become a reality for Indian people, especially women
*******
13
mF
At'A
CONVENTION ON THE ELIMINATION OF ALL FORMS OF DISCRIMINATION
AGAINST WOMEN (1979)
Article 1
•i
For the purposes of the present Convention, the fetm "discrimination against
women" shall mean any distinction, exclusion or restriction made on the basis of
sex which has the effect or purpose of impairing or nullifying the recognition,
enjoyment or exercise by women, irrespective of their marital status, on a basis
of equality of men and women, of human rights and fundamental freedoms in the
political, economic, social, cultural, civil or any other field.
Article 2
r>
States Parties condemn discrimination against women in all its forms, agree to
pursue by all appropriate means and without delay 'a policy of eliminating
discrimination against women and, to this end, undertake:
(a) To embody the principle of the equality of men and women in their national
constitutions or other appropriate legislation if not yet incorporated therein and to
ensure, through law and other appropriate means, the practical realisation of this
principle;
(b) To adopt appropriate legislative and other measures, including sanctions
where appropriate, prohibiting all discrimination against women;
(c) To establish legal protection of the rights of women on an equal basis with
men and to ensure through competent national tribunals and other public
institutions the effective protection of women against any act of discrimination;
(d) To refrain from engaging in any act or practice of discrimination against
women and to ensure that public authorities and institutions shall act in
conformity with this obligation;
(e) To take all appropriate measures to eliminate discrimination against women
by any person, organisation or enterprise;
(f) To take all appropriate measures, including legislation, to modify or abolish
existing laws, regulations, customs and practices which constitute discrimination
against women;
(g) To repeal all national penal provisions which constitute discrimination aqainst
women.
Article 3
States Parties shall take in all fields, in particular in the political, social, economic
and cultural fields, all appropriate measures, including legislation, to ensure the
full development and advancement of women, for the purpose of guaranteeing
them the exercise and enjoyment of human rights and fundamental freedoms on
a basis of equality with men.
1
Article 4
1. Adoption by States Parties of temporary special measures aimed at
accelerating de facto equality between men and women shall not be considered
discrimination as defined in the present Convention, but shall in no way entail as
a consequence the maintenance of unequal or separate standards; these
measures shall be discontinued when the objectives of equality of opportunity
and treatment have been achieved.
2. Adoption by States Parties of special measures, including those measures
contained in the present Convention, aimed at protecting maternity shall not be
considered discriminatory.
Article 11
1. States Parties shall take all appropriate measures to eliminate
discrimination against women in the field of employment in order to
ensure, on a basis of equality of men and women, the same rights, in
particular:
(f) The right to protection of health and to safety in working conditions, including
the safeguarding of the function of reproduction.
Article 12
1. States Parties shall take all appropriate measures to eliminate discrimination
against women in {he field of health care in order to ensure, on a basis of equality
of men and women, access to health care services, including those related to
family planning.
2. Notwithstanding the provisions of paragraph 1 of this article, States Parties
shall ensure to women appropriate services in connection with pregnancy,
confinement and the post-natal period, granting free services where necessary,
as well as adequate nutrition during pregnancy and lactation.
2
GENERAL RECOMMENDATION NO. 24 of the CEDAW
Women and Health (Article 12)
(Twentieth session, 1999)1
1. The Committee pn the Elimination of Discrimination against Women, affirming
that access to health care, including reproductive health, is a basic right under
the Convention on the Elimination of All Forms of Discrimination against Women,
decided at its twentieth session, pursuant to article 21, to elaborate a general
recommendation on article 12 of the Convention.
Background
2. States parties’ compliance with article 12 of the Convention is central to the
health and well-being of women. It requires States to eliminate discrimination
against women in their access to health-care services throughout the life cycle,
particularly in the areas of family planning, pregnancy and confinement and
during the post-natal period. The examination of reports submitted by States
parties pursuant to article 18 of the Convention demonstrates that women's
health is an issue that is recognized as a central concern in promoting the health
and well-being of women. For the benefit of States parties and those who have a
particular interest in and concern with the issues surrounding women's health,
the present general recommendation seeks to elaborate the Committee's
understanding of article 12 and to address measures to eliminate discrimination
in order to realize the right of women to the highest attainable standard of health.
3. Recent United Nations world conferences have also considered these
objectives. In preparing this general recommendation, the Committee has taken
into account relevant programmes of action adopted at United Nations world
conferences and, in particular, those of the 1993 World Conference on Human
Rights, the 1994 International Conference on Population and Development and
the 1995 Fourth World Conference on Women. The Committee has also noted
the work of the yyorid Health Organization (WHO), the United Nations Population
Fund (UNFPA) and other United Nations bodies. It has collaborated with a large
number of non-govemmental organizations with a special expertise in women's
health in preparing this general recommendation.
4. The Committee notes the emphasis that other United Nations instruments
place on the right to health and to the conditions that enable good health to be
achieved. Among such instruments are the Universal Declaration of Human
Rights, the International Covenant on Economic, Social and Cultural Rights, the
International Covenant on Civil and Political Rights, the Convention on the Rights
of the Child and the Convention on the Elimination of All Forms of Racial
Discrimination.
' Contained in document A/54/38/Rev.1, chapter I.
3
5. The Committee refers also to its earlier general recommendations on female
circumcision, human immunodeficiency virus/acquired immunodeficiency
syndrome (HIV/AIDS), disabled women, violence against women and equality in
family relations, all of which refer to issues that are integral to full compliance
with article 12 of the Convention.
6. While biological differences between women and men may lead to differences
in health status, there are societal factors that are determinative of the health
status of women and men and can vary among women themselves. For that
reason, special attention should be given to the health needs and rights of
women belonging to vulnerable and disadvantaged groups, such as migrant
women, refugee and internally displaced women, the girl child and older women,
women in prostitution, indigenous women and women with physical or mental
disabilities.
7. The Committee notes that the full realization of women's right to health can be
achieved only when States parties fulfil their obligation to respect, protect and
promote women's fundamental human right to nutritional well-being throughout
their lifespan by means of a food supply that is safe, nutritious and adapted to
local conditions. To this end, States parties should take steps to facilitate
physical and economic access to productive resources, especially for rural
women, and to otherwise ensure that the special nutritional needs of all women
within their jurisdiction are met.
Article 12
8. Article 12 reads as follows:
"1. States parties shall take all appropriate measures to eliminate discrimination
against women in the field of health care in order to ensure, on a basis of equality
of men and women, access to health-care services, including those related to
family planning.
"2. Notwithstanding the provisions of paragraph 1 of this article, States parties
shall ensure to women appropriate services in connection with pregnancy,
confinement and the post-natal period, granting free services where necessary,
as well as adequate nutrition during pregnancy and lactation."
States parties are encouraged to address the issue of women's health throughout
the woman's lifespan. For the purposes of the present general recommendation,
therefore, "women" includes giris and adolescents. The general recommendation
will set out the Committee's analysis of the key elements of article 12.
Key elements
Article 12 (1)
9. States parties are in the best position to report on the most critical health
issues affecting women in that country. Therefore, in order to enable the
4
Committee to evaluate whether measures to eliminate discrimination against
women in the field of health care are appropriate, States parties must report on
their health legislation, plans and policies for women with reliable data
disaggregated by sex on the incidence and severity of diseases and conditions
hazardous to women's health and nutrition and on the availability and cost
effectiveness of preventive and curative measures. Reports to the Committee
must demonstrate that health legislation, plans and policies are based on
scientific and ethical research and assessment of the health status and needs of
women in that country and take into account any ethnic, regional or community
variations or practices based on religion, tradition or culture.
10. States parties are encouraged to include in their reports information on
diseases, health conditions and conditions hazardous to health that affect women
or certain groups of women differently from men, as well as information on
possible intervention in this regard.
11. Measures to eliminate discrimination against women are considered to be
inappropriate if a health-care system lacks services to prevent, detect and treat
illnesses specific: to women. It is discriminatory for a State party to refuse to
provide legally for the performance of certain reproductive health services for
women. For instance, if health service providers refuse to perform such services
based on conscientious objection, measures should be introduced to ensure that
women are referred to alternative health providers.
i. ■
I
12. States parties should report on their understanding of how policies and
measures on health care address the health rights of women from the
perspective of women's needs and interests and how it addresses distinctive
features and factors that differ for women in comparison to men, such as:
(a) Biological factors that differ for women in comparison with men, such as their
menstrual cycle, their reproductive function and menopause. Another example is
the higher risk of exposure to sexually transmitted diseases that women face;
(b) Socio-economic factors that vary for women in general and some groups of
women in particular. For example, unequal power relationships between women
and men in the home and workplace may negatively affect women’s nutrition and
health. They may also be exposed to different forms of violence which can affect
their health. Girl children and adolescent girls are often vulnerable to sexual
abuse by older men and family members, placing them at risk of physical and
psychological harni and unwanted and early pregnancy. Some cultural or
traditional practices such as female genital mutilation also carry a high risk of
death and disability;
(c) Psychosocial factors that vary between women and men include depression
in general and post-partum depression in particular as well as other
psychological conditions, such as those that lead to eating disorders such as
anorexia and bulimia;
(d) While lack of respect for the confidentiality of patients will affect both men and
women, it may deter women from seeking advice and treatment and thereby
5
adversely affect their health and well-being. Women will be less willing, for that
reason, to seek medical care for diseases of the genital tract, for contraception or
for incomplete abortion and in cases where they have suffered sexual or physical
violence.
13. The duty of States parties to ensure, on a basis of equality of men and
women, access to health-care services, information and education implies an
obligation to respect, protect and fulfil women’s rights to health care. States
parties have the responsibility to ensure that legislation and executive action and
policy comply with these three obligations. They must also put in place a system
that ensures effective judicial action. Failure to do so will constitute a violation of
article 12.
14. The obligation to respect rights requires States parties to refrain from
obstructing action taken by women in pursuit of their health goals. States parties
should report on how public and private health-care providers meet their duties to
respect women's rights to have access to health care. For example, States
parties should not restrict women's access to health services or to the clinics that
provide those services on the ground that women do not have the authorization
of husbands, partners, parents or health authorities, because they are unmarried
- or because they are women. Other barriers to women's access to appropriate
health care include laws that criminalize medical procedures only needed by
women punish women who undergo those procedures.
15. The obligation to protect rights relating to women's health requires States
parties, their agents and officials to take action to prevent and impose sanctions
for violations of rights by private persons and organizations. Since gender-based
violence is a critical health issue for women, States parties should ensure.
(a) The enactment and effective enforcement of laws and the formulation of
policies, including health-care protocols and hospital procedures to address
violence against women and sexual abuse of girt children and the provision of
appropriate health services;
(b) Gender-sensitive training to enable health-care workers to detect and
manage the health consequences of gender-based violence;
(c) Fair and protective procedures for hearing complaints and imposing
appropriate sanctions on healtn-care professionals guilty of sexual abuse of
women patients; ».
(d) The enactment and effective enforcement of laws that prohibit female genital
mutilation and marriage of girt children.
16. States parties should ensure that adequate protection and hearth services,
including trauma treatment and counselling, are provided for women in especially
difficult circumstances, such as those trapped in situations of armed conflict and
women refugees.
6
17. The duty to fulfil rights' places an obligation on States parties to take
appropriate legislative, judicial, administrative, budgetary, economic and other
measures to the maximum extent of their available resources to ensure that
women realize their rights to health care. Studies such as those that emphasize
the high maternal mortality and morbidity rates worldwide and the large numbers
of couples who would like to limit their family size but lack access to or do not
use any fonm of contraception provide an important indication for States parties
of possible breaches of their duties to ensure women's access to health care.
The Committee asks States parties to report on what they have done to address
the magnitude of women's ill-health, in particular when it arises from preventable
conditions, such as tuberculosis and HIV/AIDS. The Committee is concerned
about the evidence that States are relinquishing these obligations as they
transfer State health functions to private agencies. States and parties cannot
absolve themselves of responsibility in these areas by delegating or transferring
these powers to private sector agencies. States parties should therefore report
on what they have done to organize governmental processes and all structures
through which public power is exercised to promote and protect women s health.
They should include information on positive measures taken to curb violations of
women's rights by third parties and to protect their health and the measures they
have taken to ensure the provision of such services.
V
18. The issues of HIV/AIDS and other sexually transmitted diseases are central
to the rights of women and adolescent girls to sexual health. Adolescent girls an
women in many countries lack adequate access to information and services
necessary to ensure sexual health. As a consequence of unequal power relations
based on gender, women and adolescent girls are often unable to refuse sex or
insist on safe and responsible sex practices. Harmful traditional practices, such
as female genital mutilation, polygamy, as well as mantal rape, may also expose
girls and women to the risk of contracting HIV/AIDS and other sexually
transmitted diseases. Women in prostitution are also particularly vulnerable to
these diseases. States parties should ensure, without prejudice or discrimination,
the right to sexual health information, education and services for all women and
girts, including those who have been trafficked, even if they are not legally
resident in the country. In particular, States parties should ensure the rights of
female and male adolescents to sexual and reproductive health education by
property trained personnel in specially designed programmes that respect their
right to privacy and confidentiality.
19. In their reports, States parties should identify the test by which they assess
whether women have access to health care on a basis of equality of men and
women in order to demonstrate compliance with article 12. In applying these
tests, States parties should bear in mind the provisions of article 1 of the
Convention. Reports should therefore include comments on the impact that
health policies, procedures, laws and protocols have on women when compared
with men.
7
20. Women have the right to be fully informed, by properly trained personnel, of
their options in agreeing to treatment or research, including likely benefits and
potential adverse effects of proposed procedures and available alternatives.
21. States parties should report on measures taken to eliminate barriers that
women face in access to health-care services and what measures they’ have
taken to ensure women timely and affordable access to such services. Barriers
include requirements or conditions that prejudice women's access, such as high
fees for health-care services, the requirement for preliminary authorization by
spouse, parent or hospital authorities, distance from health facilities and the
absence of convenient and affordable public transport.
22. States parties should also report on measures taken to ensure access to
quality health-care services, for example, by making them acceptable to women.
Acceptable services are those that are delivered in a way that ensures that a
woman gives her fully informed consent, respects her dignity, guarantees her
confidentiality and is sensitive to her needs and perspectives. States parties
should not permit forms of coercion, such as non-consensual sterilization,
mandatory testing for sexually transmitted diseases or mandatory pregnancy
testing as a condition of employment that violate women's rights to informed
consent and dignity.
23. In their reports, States parties should state what measures they have taken to
ensure timely access to the range of services that are related to family planning,
in particular, and to sexual and reproductive health in general. Particular attention
should be paid to the health education of adolescents, including information and
counselling on all methods of family planning.
24. The Committee is concerned about the conditions of health-care services for
older women, not only because women cften live longer than men and are more
likely than men to suffer from disabling and degenerative chronic diseases, such
as osteoporosis and dementia, but because they often have the responsibility for
their ageing spouses. Therefore, States parties should take appropriate
measures to ensure the access of older women to health services that address
the handicaps and disabilities associated with ageing.
25. Women with disabilities, of all ages, often have difficulty with physical access
to health services. Women with mental disabilities are particularly vulnerable,
while there is limited understanding, in general, of the broad range of risks to
mental health to which women are disproportionately susceptible as a result of
gender discrimination, violence, poverty, armed conflict, dislocation and other
forms of social deprivation. States parties should take appropriate measures to
ensure that health services are sensitive to the needs of women with disabilities
and are respectful of their human rights and dignity.
8
Article 12 (2)
26. Reports should also include what measures States parties have taken to
ensure women appropriate services in connection with pregnancy, confinement
and the post-natal period. Information on the rates at which these measures have
reduced maternal mortality and morbidity in their countries, in general, and in
vulnerable groups, regions and communities, in particular, should also be
included.
27. States parties should include in their reports how they supply free services
where necessary to ensure safe pregnancies, childbirth and post-partum periods
for women. Many women are at risk of death or disability from pregnancy-related
causes because they lack the funds to obtain or access the necessary services,
which include antenatal, maternity and post-natal services. The Committee notes
that it is the duty of States parties to ensure women's right to safe motherhood
and emergency obstetric services and they should allocate to these services the
maximum extent of available resources.
Other relevant articles in the Convention
28. When reporting on measures taken to comply with article 12, States parties
are urged to recognize its interconnection with other articles in the Convention
that have a bearing on women's health. Those articles include article 5 (b), which
requires States parties to ensure that family education includes a proper
understanding of maternity as a social function; article 10, which requires States
parties to ensure equal access to education, thus enabling women to access
health care more readily and reducing female student drop-out rates, which are
often a result of premature pregnancy; article 10 (h), which requires that States
parties provide to women and girts access to specific educational information to
help ensure the health and well-being of families, including information and
advice on family planning; article 11, which is concerned, in part, with the
protection of women's health and safety in working conditions, including the
safeguarding of the reproductive function, special protection from harmful types
of work during pregnancy and with the provision of paid maternity leave; article
14, paragraph 2 (b), which requires States parties to ensure access for rural
women to adequate health-care facilities, including information, counselling and
services in family planning, and (h), which obliges States parties to take all
appropriate measures to ensure adequate living conditions, particularly housing,
sanitation, electricity and water supply, transport and communications, all of
which are critical for the prevention of disease and the promotion of good health
care; and article 16, paragraph 1 (e), which requires States parties to ensure that
women have the same rights as men to decide freely and responsibly on the
number and spacing of their children and to have access to the information,
education and means to enable them to exercise those rights. Article 16,
paragraph 2 proscribes the betrothal and marriage of children, an important
factor in preventing the physical and emotional harm which arise from early
childbirth.
9
Recommendations for government action
29. States parties should implement a comprehensive national strategy to
promote women's health throughout their lifespan. This will include interventions
aimed at both the prevention and treatment of diseases and conditions affecting
women, as well as responding to violence against women, and will ensure
universal access for all women to a full range of high-quality and affordable
health care, including sexual and reproductive health services.
30. States parties should allocate adequate budgetary, human and administrative
resources to ensure that women's health receives a share of the overall health
budget comparable with that for men's health, taking into account their different
health needs.
31. States parties should also, in particular:
(a) Place a gender perspective at the centre of all policies and programmes
affecting women's health and should involve women in the planning,
implementation and monitoring of such policies and programmes and in the
provision of health services to women;
(b) Ensure the removal of all barriers to women's access to health services,
education and information, including in the area of sexual and reproductive
health, and, in particular, allocate resources for programmes directed at
adolescents for the prevention and treatment of sexually transmitted diseases,
including HIV/AIDS;
(c) Prioritize the prevention of unwanted pregnancy through family planning and
sex education and reduce maternal mortality rates through safe motherhood
services and prenatal assistance. When possible, legislation criminalizing
abortion should be amended, in order to withdraw punitive measures imposed on
women who undergo abortion;
(d) Monitor the provision of health services to women by public, non- ’
governmental and private organizations, to ensure equal access and quality of
care;
(e) Require all health services to be consistent with the human rights of women,
including the rights to autonomy, privacy, confidentiality, informed consent and
choice;
(f) Ensure that the training curricula of health workers include comprehensive,
mandatory, gender-sensitive courses on women's health and human rights, in
particular gender-based violence.
10
GENERAL RECOMMENDATION NO. 19 of the CEDAW
Violence against women
(Eleventh session, 1992)2
Background
violence is a f°m of discrimination that seriously inhibits
? T 1QP b" y 0 enjOy n9hts and freedoms on a basis of equality with men.
rnJT198? the Committee recommended that States should include in their
reports information on violence and on measures introduced to deal with it
(General recommendation 12, eighth session).
spcti™ !enth !,ession in 1991’ 'f was decided to allocate part of the eleventh
session to a discussion and study on article 6 and other articles of the
exototet on r
Cnnfora
t0 S'6006 t0WardS W°men and the sexual harassment and
Of woryien- That subject was chosen in anticipation of the 1993 World
* i,S
mit!ee concluded that not ali th® reports of States parties adequately
based vinT C°Se corinect|on between discrimination agqinst women, gender
full imolemlrn6; and eolations of human rights and fundamental freedoms. The
to eliSS X^ZZ^s,a,es 10 ,ake posi,“measures
pol^VnT:^6/"996516" t0 States parties that in reviewing their laws and
fniSn;
reporting under the Convention, they should have regard to the
g comments of the Committee concerning gender-based violence.
General comments
suEnn S Y
'nC/
aCtS that infliCt physical- mental or sexual harm
baspri
S °f SuCh acts’ coercion and Other deprivations of liberty. GenderX
may breach Specific provisions of ,he Convention, regardless of
whether those provisions expressly mention violence
human nnhtatedH y,ol®nce' which imPairs or nullifies the enjoyment by women of
human riohtq E fundamental freedoms under general international law or under
ConvAntin J
nVen l0nS' IS dlscrim|nation within the meaning of article 1 of the
convention. These rights and freedoms include:
(a) The right to life; ’•
(b) The right not to be subject to torture or to cruel, inhuman or deqrading
treatment or punishment;
Contained in document A/47/38.
11
,0 hU“"
°f
(d) The right to liberty and security of person;
Jhe r'9ht to equal protection under the law;
() I he right to equality in the family;
h The rinh!!° th® h'9hest standard attainable of physical and mental health;'
r Th
r9h °Jus and favourable conditions of work.
acts oef violenrl1100 apPlies to violence perpetrated by public authorities. Such
human rights la J’anZZ
State'S obli9ations under general international
Convention
U
Conventions. in addition to breaching this
restriZ toPZlZh'h°WeVlr’hhat discnmination under the Convention is not
5) For PYAmnJ
Or Ori behalf Of Governments (see articles 2 (e), 2 (f) and
all aporoonZ
2
Convent,on calls on States parties to take
oersoPn omfn ™eastjres to eliminate discrimination against women by any
human riohTc
°f T^56' Under 9eneral international law and specific
faZ a^w h du!ZtS’ Sta‘eS may alS° be responsible for private acts? they
Comments on specific articles of the Convention
Articles 2 and 3
10. Articles 2 and 3 establish a
a comprehensive obligation to eliminate
discrimination in all its forms in addition
..’-j to the specific obligations under articles
5-16.
Articles 2 (f), Sand 10(c)
SdS
such V oleZ
rCVS a fOrm of Protection or control of women. The effect of
th 'TeaZeXvm T P yS'Ca' and mental inte9rity of women is to dePrive
of
freedoms ZL ?’ exercise and knowledge of human rights and fundamental
he underivZ r
C°mment addresses mainl/ ^tual or threatened violence
maintain wnmZ
T6'!065 °f these forms of Sender-based violence help to
particioation and tn ,!iUbc’rdinate roles and contribute to their low level of political
12 These ah Jud
7
°f education' skills and work opportunities.
depicZ ani ntSr
to
propagation of pornography and the
Article 6
13. States parties are required by article 6 to take
forms of traffic in women aUd exploLro';fo^rh^StuZofTomen50^^5 a"
12
14. Poverty and unemployment increase opportunities for trafficking in women. In
addition to established forms of trafficking there are new forms of sexual
exploitation, such as sex tourism, the recruitment of domestic labour from
developing countries to work in developed countries, and organized marriages
between women from developing countries and foreign nationals. These
practices are incompatible with the equal enjoyment of rights by women and with
respect for their rights and dignity. They put women at special risk of violence
and abuse.
15. Poverty and unemployment force many women, including young girls, into
prostitution. Prostitutes are especially vulnerable to violence because their
status, which may be unlawful, tends to marginalize them. They need the equal
protection of laws against rape and other forms of violence.
16. Wars, armed conflicts and the occupation of territories often lead to increased
prostitution, trafficking in women and sexual assault of women, which require
specific protective and punitive measures.
Article 11
17. Equality in employment can be seriously impaired when women are
subjected to gender-specific violence, such as sexual harassment in the
workplace.
18. Sexual harassment includes such unwelcome sexually determined behaviour
as physical contact and advances, sexually coloured remarks, showing
pornography and sexual demands, whether by words or actions. Such conduct
can be humiliating and may constitute a health and safety problem; it is
discriminatory when the woman has reasonable ground to believe that her
objection would disadvantage her in connection with her employment, including
recruitment or promotion, or when it creates a hostile working environment.
Article 12
19. States parties are required by article 12 to take measures to ensure equal
access to health care. Violence against women puts their health and lives at risk.
20. In some States there are traditional practices perpetuated by culture and
tradition that are harmful to the health of women and children. These practices
include dietary restrictions for pregnant women, preference for male children and
female circumcision or genital mutilation.
Article 14
21. Rural women are at risk of gender-based violence because traditional
attitudes regarding the subordinate role of v.omeri that persist in many rural
communities. Giris from rural communities are at special risk of violence and
sexual exploitation when they leave the rural community to seek employment in
towns.
13
22. Compulsory sterilization or abortion adversely affects women's
Physical and mental health, and infringes the right of women to decide on
tne number and spacing of their children.
V'0'ence 's.one
ths most insidious forms of violence against
men. t is prevalent in all societies. Within family relationships women of all
ages are subjected 4o violence of all kinds, including battering, rape, other forms
troHTXUa assau't’ mental and other forms of violence, which are perpetuated by
aaitional attitudes. Lack of economic independence forces many women to stay
n violent relationships. The abrogation of their family responsibilities by men can
a orm o violence, and coercion. These forms of violence put women's health
of equality 'mpa'r their abil'ty to ParticiPate in family life and public life on a basis
Specific recommendations
24. In light of these comments, the Committee on
the Elimination of
Discrimination against Women recommends:
(a) States parties should take appropriate and effective measures to overcome
ail forms of gender-based violence, whether by public or private act;
(b) States parties should ensure that laws against family violence and abuse,
rape sexual assault and other gender-based violence give adequate protection
o a women, and respect their integrity and dignity. Appropriate protective and
support services should be provided for victims. Gender-sensitive training of
juaiciai and law enforcement officers and other public officials is essential for the
effective implementation of the Convention;
(c) States parties should encourage the compilation of statistics and research on
he extent, causes and effects of violence, and on the effectiveness of measures
to prevent and deal with violence;
(d) Effective measures should be taken to ensure that the media respect and
promote respect for women:
(e) States parties in their report should identify the nature and extent of attitudes
customs and practices that perpetuate violence against women, and the kinds of
yio ence that result. They should report the measures that they have undertaken
to overcome violence, and the effect of those measures;
(f) Effective measures should be taken to overcome these attitudes and
practices. States should introduce education and public information programmes
No S igs?)'0316 prejudices' which hinder women's equality (recommendation
opecific preventive and punitive measures are necessary to overcome
trafficking and sexual exploitation;
(hLStates parties in their reports should describe the extent of all these problems
an the measures, including penal provisions, preventive and rehabilitation
measures, that have been taken to protect women engaged in prostitution or
suoject to trafficking and other forms of sexual exploitation. The effectiveness of
tnese measures should also be described;
14
sLuKperoS.teWS Pro0'!<:'UreS and remSdieS’ in°luain9 “-"Pensaton,
harassmentP^eS' Sh°l"d l"ClUde 'n lheir rePorts «0™atlon on sexual
ha“' a"a
other fonnsot
violence6 ranA^c
eStabhSh °r SUpport Services for
of family
refuoee 'sSlif ? aSS^ 3nd °ther fOrms of 9ender-based violence including
(I) S?ates
7 Ha'n?d hea'th WOrkers’ rehabilitation and counselling-'
9
late TcXI «S hdUldc“em?„ea8lJreS ,0 °Ver“™
Ptaettes and should
t^oo^thtendatiDn No. 14) in reporting m'htPa^Mssues' °" ,ema'e C'rCUmCiS'On
aPP™P"a'e 00^^
at’Odldn beCaUSe °f laCk O'
shouid Mieatethe'most rep°«s,®h°uld stale the extent of ihese problems
(o) States narfiAc h
access^ tn
,
S ha have been taken and their effect
enSUre that services for victims of violence
and
are
SPeCia' SerViC6S are
provided to isolated commTnitS
emolovmZn^n t0 pr°tect them fram violence should include
domestic wife
thS monitor,n9 °f the employment training and
conditions of
'naturalvtolence'aXTusem'’
,0 'Ura' '™nen' ,he extenl a"a
to support and orner semS
a
Z ara Subiect’their oeed ,or aM «“ess
violence;
services and the effectiveness of measures to overcome
W cSpenaltE
viblenoe
P
S
,O 0Ver0°me ,amil' ™tence stioutd Mude:
"ooossaty and civil remedies in case of domestic
SatSX^memoT defenCe °' hOn°Ur in ra!|M ,0 lha
B'SE£Fe, "ne9?nd'?eS
,am"y v'0,ence'
abuse, and9"™ the^S'venS’eT'’-.1”6 "T* 0' d°meS,iC vl0tence and sa*dal
taken;
P ventlve’ Pun|t've and remedial measures that have been
a" 16931 and °ther measur« that are
nL^U^f^pro'vid^eSpf19
violence, including, inter alia-
pr° ectlon of women against gender-based
compensatory^provisbnT^o' DratAct"19 96031 sanctions’ civil remedies and
including, inter alia violencA and
harassmer^TTt^wXiace
h
women against all kinds of violence,
family' 56X631 aSSault and sexual
15
torhTnnl1^^038^68’indUClin9 public informatio" and education programmes
fiii\ p9e attltudes concerning the roles and status of men and womenLnrt
Ve measures, including refuges, counselling, rehabilitation and
violence
f°r W°men Wh° are thG V'Ct'mS °f Vi°lenCe Or wh0 are at risk of
thIt\hNrhSSteSHPa ues should report on a"forms of gender-based violence, and
of viniPnrJ PCT ShpU d inciude al1 available data on the incidence of each form
M tS th and °n thS effeCtS Of Such violence °n the women who are victimsorevenHvl !nden°? ? S‘ateS partieS Sh0Uld include information on the legal,
aZ Xnm
prolectlve measures that have been taken to overcome violence
against women, and on the effectiveness of such measures.
16
OIILD HEALTH; KEY STRATEGIES AND INTERVENTIONS
. Rational Public Hearing On Denial Of Health Care Services
_.rganisedI By Jan Swasthya Abhivan and National Human Rights Commission
The India Habitat Centre, New Delhi le*1'-!?11' December, 2004
The Situation
parameters oS ovZlstlte "LaTaXa^
independence have slowed down or even plateaued. Residual problems seem to be more
intractable and demand greater systemic changes in the overall socio economico political
context as well specifically in the systems of health care themselves. Factors of class
caste geography and gender complicate the situational analysis of the smallest health
problem and confound any planning that does not adequately take them into account.
imultaneous y, solutions that are technocentric rather than oriented towards public
health, overall trends of cutting back on public health expenditure and promoting
privatised systems of health care and consequent escalations in costs of health care are
putting health out of reach of a vast proportion of our children.
This paper does not intend to go into a description of status of child health since the data
hat exists is largely uncontested, or if at all, errs on the side of showing a picture better
han what exists in our expenence. Nevertheless, some facts are presented below to set
me stage ror our recommendations;
Infant and Child mortality snuffs out the life of 22 lakh children everj- year, and
there has been very little improvement in this situation in recent years. We are yet to
achieve the National Health Policy 1983 target to reduce Infant Mortality Rate to less
than 60 per 1000 live births. More serious is the fact tliat the rate of decline in Infant
Mortality, which was significant in the 1970s and 80s. has slowed down in the 1990s
(.See diagram below)
IMR Trends in India 1960-2000
w
r 180
^2 150
£ 120
- 90
o 60
5
o
CL
30
0
1960
1970
1980
1990
1995
2000
Years
India —A1
India Urban —«S—India Rural
The current annual reduction rate deaths is estimated to be 2.3 % each year and if India
intends to achieve MDGs by 2015, it should be three times the reduction rate.
•
•
Three completely avoidable child deaths occur every minute. If the entire country
were to achieve a better level of child health, for example the child mortality levels of
Kerala, then 18 lakh deaths of under-five children could be avoided every year. The
four major killers (lower respiratory tract infection, diarrheal diseases, perinatal
causes and vaccine preventable diseases) accounting for over 60% of deaths under
five years of age are entirely preventable through interventions aiming at prevention
of child malnutrition through education of families like prenatal care, newborn care,
optimal infant and young child feeding, (exclusive breastfeeding during first six
months, continued breastfeeding along with appropriate and adequate complementary
feeding beginning after six months to two years or beyond) , hygiene etc., and for
older children supplemental feeding programs. The most recent estimate of complete
immunization coverage indicates that only 54% of all children under age three were
fully protected. Only about 40% babies are exclusively breastfed and 33% are given
timely complementary feeds.
Diarrhea, dysentery, acute respiratory infections and asthma continue to take their toll
because we are unable to improve environmental health conditions. Around 6 lakh
children die each year from an ordinary illness like diarrhea. While diarrhea itself
could be largely prevented by universal provision of safe drinking water and sanitary
conditions and ensuring optimal infant and young child feeding. These deaths can be
prevented by timely administration of oral rehydration solution, which is presently
administered in only 27% of cases.
Survivors are underweight and underdeveloped as we see from the existing data half
of our under three children are underweight and their development is potentially
compromised.
Poverty and gender
• The Infant Mortality’ Rate in the poorest 20% of the population is 2.5 times higher
than that in the richest 20°/o of the population. In other words, an infant born in a poor
family is two and half times more likely to die in infancy, than an infant in a better off
family.
• A child in the 'Low standard of living' economic group is almost four times more
likely to die in childhood than a child in the better off 'High standard of living group.
An Adivasi child is one and half times more likely to die before the fifth birthday than
children of other groups.
• A girl is 1.5 times more likely to die before reaching her fifth birthday, compared to
a boy! The female to male ratios for children are rapidly declining, from 945 girls
per 1000 boys in 1991. to just 927 girls per 1000 boys in 2001. This decline
highlights an alarming trend of discrimination against girl children, which starts
well before birth (in the form of sex selective abortions), and continues into
childhood and adolescence (in the form of worse treatment to girls).
• Children below 3 years of age in scheduled tribes and scheduled castes are twice as
likely to be malnourished than children in other groups.
7
1million children are wage labourers. Many more participate in a major way
m household work and sibling care activities. Many thousand of these live on the
streets in grave danger to their health and welfare.
•
•
3-10 /o of all children suffer from disability. The sendees that exist for children with
special needs are highly inadequate.
According to NACO estimates on fthe basis of prevalence, 55,000 children would be
already infected with HIV /AIDS iin the year 2003. Of course, many more would
have a parent or parents who are affected or who have been orphaned.
Key Strategies
Of course, overall strategies for combating poverty and discrimination on grounds of
gender and caste are an absolute requirement for any health care intervention. More
specifically, as malnutrition sets in during first three years, focus must be on under threes
starting from pregnancy. Food security of the under three, safe water and sanitation play a
uge preventive role. Following this, interventions need to be made in the specific
programmes, schemes and delivery mechanisms relating to child health and development.
Adequately trained and skilled Anganwadi workers, nurses ,village health workers and
ANMs, Functional PHCs and subcentres, availability of medical doctors/paediatricians at
appropriate levels of primary care, availability of neonatal units with trained staff,
availability of free essential drugs including those required for PPTCT are other major
requirements.
At the outset, it needs to be acknowledged that rectifying the situation requires a
multisectoral and comprehensive approach to child health ^involving all sections of
society but necessarily families, the health care system, education, labour and welfare
systems of the country and governance at all levels. Convergence cannot be left to the
will or competence of implementing individuals but needs to be set into systems that are
workable.
Based on our experience, the key strategies that would make the maximum dent on the
existing situation of child health are as follows:
1. Ensuring that good quality antenatal care is accessible to all women.
9
Ensuring that all home deliveries are carried out by trained birth attendants and
promoting institutional delivery by providing access and good quality maternity
sei vices, (prevention of neonatal mortality due to asphyxia and prematurity)
3. Adopting Preventing child malnutrition early' approach rather than a treatment
approach
4. Preventing the proportion of deaths due to sepsis in the neonatal period.
5. Promoting early and exclusive breastfeeding for the first six months, and adequate
complementary feeding after six months by good communication of correct
/ 3
information, skilled assistance and help and supporting breastfeeding women by
maternity entitlements and creches on work sites.
6. Ensuring the food security of children by strengthening the PDS and making
appropriate food available for children through it, by promoting correct child
feeding practices, offering supplementary nutrition to all children through
universalising the ICDS and the mid day meal scheme.
7. Ensuring meaningful growth monitoring through tracking the individual child,
care of childhood illnesses, deworming, iron supplementation, health checks and
vaccination through a systematic and functional convergence between the AWC
and PHC systems.
8. Ensuring systematic school health checks in all schools, public and private with
capacity building of personnel on adolescent health issues including ‘life skill
training’.
9. Making elementary education, including ECCD, free and universally available.
10. Ensuring that this is inclusive for children with special needs.
Recommendations
W’e understand that many of these concerns are being addressed through fresh planning
vis a vis RCH II, ICDS, the Rural Health Mission and other policies and programmes
being considered by the Ministry of Health and Family Welfare.
Jan Swasthya Abhiyan members have also been making recommendations to some of
these through the National Advisory Council as well as by participating in planning
sessions organised by the Ministry.
In order to translate the strategies enumerated above to realities on the ground, some firnl
steps will have to be taken. Our recommendations for immediate action are as follows;
1. The national health policy barely takes cognizance of child health issues. This
should be reworked immediately giving due space and priority to child health and
preventing malnutrition in children.
2. All positive changes will require enhanced budgetary allocations for health and
child health and development in particular. We recommend an overall increase in
the health budget by a minimum of 0.5% of the GDP each year over and above
the current 0.9%. Programme-specific increases are mentioned in points that
follow.
3. AN Ms and AWW can be made responsible for registration for maternity
entitlements and maternity benefit schemes for better coverage.
4. A large cadre of dais need to be identified and trained to cover the needs ol
women giving birth at home while centres are being set up to allow larger
numbers to choose institutional delivery.
5. Identify and ensure optimal infant and young child feeding as a major preventive
intervention for growth and development.
6. Inclusion of infant and young child feeding indicators in the ICDS, MPR and
Nation/State/Division/District/Block/Circle/Village/ urban slum level monitoring
and review systems.
7. Introduce village child health and development report cards compiled by the
PRI/and frontline workers into block/district and so on.
8. Setting up of a National Resource Centre on Infant and Young Child Feeding,
linked to State Resource Centres and District Resource Units/training teams.
9. Mechanisms to implement the Infant Milk Substitutes, Feeding Bottles and Infant
Foods (Regulation of Production, Supply and Distribution) Act 1992 as amended
in 2003 should be in place at district level with Annual review plans.
10. The Creches for Working and Ailing Mother’s Children Scheme with revised
norms and enlarged outlay needs to be revived and made available to the full
range of women’s groups. Currently, approximately 15000 Creches are provided
under the Scheme where as the need is for 8 lakhs. The Scheme has been
evaluated and the norms need urgent revision. Funds need to be allocated for
expansion of the Scheme to meet the need. Cost of Day care/ creche arrangements
is estimated at Rs 15 per day per child ( Care/ nutritional supplements/ learning
activities/ health care) .It is estimated that 60. million children 0-6 years require
this service. Anganwadi come creche scheme needs to be made operational
wherever necessary.
11 Creches at working places provided under Labour Legislation require to be
enforced. Funds from the industry via Cess Acts can made available and
manpower requirements can be co-ordinated with training strategies to develop a
range of trained creche workers. (It may be noted that the collection of cess in
Delhi has not yet been started despite the fact that the Act was passed in 1996)
12. Universalisation of the ICDS with priority to dalit, tribal and urban areas should
happen in accordance with the Supreme Court judgement by design. This requires
a credible plan to extend the reach of ICDS to all 14 lakh habitations in the
country in a time-bound manner, say within two years. Adequate funds need to be
made available for his to happen as well as to support the state budgets for
nutrition through the ICDS.
13. All sanctioned projects that are not “operational” should be operationalised
immediately, as per Supreme Court orders.
14. The allocation for nutrition per child should be increased to Rs 3 per child per
day.
15. Iron supplementation should be made available to all children along with periodic
deworming.
16. Staffing gaps pertaining to the ICDS should be met with urgency.
17. Basic infrastructural requirements such as running water, toilets, separate space
tor cooking, weighing machines and toys should be ensured on a priority basis.
18. Anganwadi workers to get adequate remuneration and suitable skills training to
perform their role as health communication agents and nutrition counsellors
especially for infant and young child feeding.
19. She should not be asked to perform several other roles she is asked to do
/ S
presently.
20. There should be a systematic convergence between the AWW, ANM and any
proposed or existing village health worker/ASHA/ Mitanin through processes
such as pre fixed mother and child health days ( CARE model).
21. All village health workers/ASHA etc should have a clear mandate to give
priority to child health interventions specially for infant and young child feeding
and should be trained appropriately (Mitanin model, Gadchiroli model, CARE
model)
22. This convergence (between ‘health, family welfare, women and child
development and education) should systematically extend to district and block
level (UP GVS model, CARE model). Representatives of groups working on
relevant health issues (JSA, BPNI, Right to Food Campaign etc) should be
included at all levels, from State to district, wherever possible.
23. Vitamin A supplies need to be ensured and maintained.
24. Immunisation drives such as pulse polio must be organised carefully to ensure
that routine immunisation is not being neglected.
25. Measles coverage must be achieved to 100% on a priority basis.
26. Nutritious cooked mid-day meals should be provided to all children up to class 8
throughout the year.The minimum norm of Rs 2 per child per day for 'conversion
costs', proposed by the Commissioners of the Supreme Court, should be extended
throughout the country. Full quality safeguards must be in place.
27. All states should extend mid-day meals to Class 8 from 1 July 2005 at the latest.
28. Strict instructions should be issued to the effect that central assistance for mid-day
meals is intended as a supplement to the resources already provided by state
governments, and not as a substitute for them.
29. The proceeds of the Education Cess should be clearly ear-marked for elementary
education including ECCE and nothing else. The Cess should be paid into a
dedicated non-lapsable account. The additional financial allocations associated
with the Cess in 2004-5 (i.e. the net addition to financial allocations already made
in the interim budget) should be clearly spelt out by the Central Government.
Also, these allocations should be made available immediately and not at the end
of the financial year.
30. The school health scheme needs to be made mandatory for all private and public
schools and should include annual general health checks, vision and dental
checks, immunisation and deworming, iron supplementation and adolescent
health counselling.
Prepared for Jan Swasthya Abhiyan by Dr Vandana Prasad (Consultant Paediatrician),
Dr Arun Gupta (Regional Coordinator, International Baby Food Action Network(IBFAN)
Asia Pacific, Dr Jean Dreze (Delhi School of Economics) and Ms Devika Singh
(Consultant, Mobile Creches).
C6
..L'3^-10
'
CADocuments and Settings\Admimstrator\Desktop\Presentation on Mental Health Rights.doc
Presentation on Mental Health Rights during
National Public Hearing organised by NHRC and JSA
I. Background
This presentation is a <compilation
" ’ of issues related to people with mental illness in India
and is based on them
their experiences. The compilation is
i a result of collective effort of a
gi°uP o People comprising of those who have had personal encounters with mental
illness,
mness, field staff of organizations involved iin mental health and other stakeholders,
n ormation has also been gathered from secondary sources to substantiate the claims
made m this document.
Health Economics
a. Assessment of burden in mental illness
thei Global burden of disease with disability adjusted life vears
(DALYs) shows that Mental and neurological conditions are among the most
important contributors; for instance in 1999 they accounted for 11% of the DALYs
ost due to all disease and injuries. Among all the mental and neurological disorders
c epression accounts for the largest proportion of the burden. Almost everywhere'
the prevalence of depression is twice as high among women as among men Four
other mental disorders figure in the top 10 causes of disabilitv in the world, namely
alcohol abuse, bipolar disorder, schizophrenia and obsessive-compulsive disorder.
b. Social Impact
Negative social attitudes towards the mentally ill are the barriers to reintegration
and acceptability. These adversely affect social and family relationships'
employment, housing, community inclusion and self-esteem. Equally they create
arners to equality of treatment options and limit accessibility to best treatment
practices and alternatives. Unfortunately, often medical and hospital personnel also
shaie negative attitudes towards people with mental illness.
c. Economic Impact
The economic impact of mental disorder is wide ranging, long lasting and large,
easurable causes of economic burden are health and social service needs, impact
on families and caregivers (indirect costs) lost employment and lost productivitv
Crime and public safety.
Studies from countries with established economies have shown that mental
disorders consume more than 20% of all health service costs.
In the case of poor people with mental illness in Rural areas, families are unable to
go or treatment because in addition to the cost of transport, the accompanvina
icimily member loses a days wages.
d. Legal Impact
llu laws i elated to mental health in India - such as the Mental Health Act 1987 and
nnMn^Lr^'1? to contracts (including marriage and property), contribute to
aiginahzation of people with mental illness.
»„ Menlal
'D°CUn’'"'S “nd
RighK doc .
them is found to be^entonv'niPprTc15 16831 SeParat'on of life partners if one of
concerned doctors CS nX”ll'a
iss“
XXD"OrS
false certificates to those desiring to
Asra
of fX,
sign any proper'^rented documente otXXXmXh
“T*
Provides for guardians to manage the affaX
lth Act 1987Sibiings also take advantage of this clause to d° P“SOnS W‘th mm,al illnessand ln fact ensure that the illness persists" ) that bp
11
person
demand his/her right.
P
th f h s not weI1 enough to
n«X be hosXXXX815' ‘nfTS "here the pa'ient is vioIenl and
II. Determinants ofMental Health
L
Socio economic factors
canteexpXdXo“ aXhichlXpre''ale“e rates of Psychiatric disorders
are exposed to greater levels foualiti
mUtU.a y exclusive. First, poor people
psycholoo-ical advpr >
k- 7
ty 3nd quantity) of environmental and
distress. They hive X^fficulf0^"5
1S °f
and P^ological
services. In India these service
3jCesSmg formation and mental health
poor: informatton ri XXX «
and costly, and responsibilities of t-h i
factors contribute to cZntitv
/
X" °U‘ °f
i d lterate P°PuIations, transport is difficult
. SerViC6S *
Not OnIy do th<^
psychotic forms of mental ilhiss^sTeTlf
als° triS°er non-
Considerable evidence points m H P
T depression and anxiety disorders,
depression in women b^h of wl 1
of Psychological distress and
families of people widX„ / a X'*'0"8
^Proportionately,
livelihood. cXg fa h X „ a"'^ '0 'T '/ f
Aa
family
S
P 1S°n 3S Wel1 as meetinS the high costs of illness in die
ii.
fSocial attitudes and Belief si stem
Social attitudes
<
.;.a and
belief systems are attitudinal hurdles in accessing treatment
This coupled with stigma and
discrimination manifests itself in subjecting the
person with mental illness and
his/her family to social boycott and other human
rights abuses.
Social boycott social June? 111 Preventin8 Pe°PIe with mental illness from
participating in
chons, marriages, ceremonies and going to religious
places.
village in Jharkhand.
ness and started spending time in the village temple even durine
odd hoin-s of the night. The viUages^uspeeted that she was pSg
^umcnts and Settn^AdministratodDeskto^Presentation
on Mental Health Rights.doc
C. Gender issues - ’ '
- Women who are mentally
mentally ill
U1 are
are often
often subjected to
physical and sexual
--J abuse. Destitution of women with mental illness is
an, where there are women
Xis vXwtxw’t™"6 giri wi,h
hangedthe' rTeldslXX
‘“’a f" d'scussion-al1 •>« men i
unkind and miles away Tm cmS
*“ -
is <™1- i
and dementi,
or where she came from a™8 dlSlrict'N° °”e knetv who she
sh. was
„
•ahen to a short 3U, home^Xr^'^SS" ----- > and
ESr^&oX^-
child
came frnn^ R
re8ained her memory and remembered where she
The discrepa
becomes the
woman
care.
f°r WOmen’ where she in long term
remarries.
the man
Violence agatnsr
50 % of women h<
20 % to
W% to 15 % of women report
£ e°C°UntrieS reveaI
partner. The high prevalence of t J t
haVe S6X with their intimate
, with the consequent high rate of post fraumTtO ^hlCh WOmen of a11 aSes are exposed
are most affected by this disorder
’
UmatlC Stress dlsorder ^plains why women
s™'± ® eIm h” :‘ratoi”terpre8”"a>'
arp^ctaXd'sc^
reimed bemth
n a„d
XS.
d- Family Support system
poor ftmilie,. ««on“„ ow“f"hee°r‘dXmtion o”h'1 l"1”0" S-'S"'’’S
XT
among
'"e
cases. Where blacksmiths were asked °'gan'“t“’ns har-e come across several such
dlness.
WUL "■sked to
shackles foe the person with mental
J3
Documents and Settings\Administrator\Desktop\Presentation
on Mental Health Rights.doc
Hl. Current scenario
i- Denial of services
'Z° PrT‘ atIas 2002- ,he ,ndia
psychologists. Most of them work in citiprM™ S°Cial workers and 1000 clinical
With problems live in rural areas THp D ! Tax
whereas the 70%
people
available in a mere 100 districts across the h 1
HeaIth Program makes treatment
“a,lhrgram * X
how^lha dH'
district hospitals and some hosnitals in caniud f
‘j:
th'
w
aUth°nties hardly indent medicines. In
- A recent study (Reddy 2001)
because they have been abandoned ly
but
pa,imts a“ ab“
care of hospitals
a. Almost 2/3 of long stay patients have
been in hospital for over 5 years and one
fourth have stayed for more than 15 years.
SrinX°/90%° Punt 'tyTT
P“™Iia '
g
w /o, 1 une - 73 /o, Baroda - 72%, Calcutta - 70% and Indore - 68%
stey
- >»
e.' hr 'thT t
PatiTtS Were diaSnosed with schizophrenia
patients are voluntary boardT^R17 Oriented instltutions a vast majority of long stay
R-chi - 75%,TXXuT"dr%.
8
" 98%' Hyderabad - 83%' RinPaS - 78°' CIP
are largely Instit^tilnl/iTnahTe °f JreSently available psychiatric services is that they
iii Absence of <TX
Urban baSed’ Moreover they are inadequate
’
audit of services foi people Zth
? preSently there is no mechanism for user
service providers. This puts then, at ris’k rfZ “anttolZct'1161’'"
,lK
Facilities0 for 'after care'and transf
SerViTS
PreS6nt
CHniCaI in natUre'
based.
‘
transfer of care to the community are very few and urban
IV. Recommendations/Issues for action
C:'D0C“m“'S j”4
on Mental Health Rights.doc
A. Mental Health law reforms
government needs to spf
n
Participation from all stakeholders especS wt
Ref°rm Think T^k with
■service and significant individuals in H ^t
P™317 Stake holder- the users of the
Premise that the users of thl servLinartheir lives.
tT' We
tO m°Ve
—1 sect
unable to comment
want. The voluntary sector and private
,C°mment on determine what they
private sector need to have
P'ann.„g slage. lt wil,
a
X'.
’ r°,e in lhe
people w™''XaTXl'MtaXo 11/'
fol legislative change eventually.
Parhamentarians to be able to lobby
°
A • Legal Measures
The Mental Health Act flQATA
psychiatric and private nuisinJhn
U^akstic minimum standards for the
........ -......
•
•
the means for getting rid of •^tUhOnallzatlon / medical certificates often become
MHA Sec 81 caSn be
J
nCOnvenient wife (Sections 19 & 20)
and „rfit to Be at
X.
‘
hospital, so that they are centers fo T ™
There is need of putting ob X
t
7 between the family and the
h°USeS °f Custody•
authorities, psychiatric institutions and marisT6
mental heaIth
to persons with mental illness in least restr8. 3Cy m °rder to Provide treatment
welfare agencies within civil society to assXbe e"V"Tn’ent and in,eract wieh
Persons win, menlal illness. Sec SI neei to ,
t T''™ a"d 1"te8ra“on °f
B B^X-nXS'-“’—' ~
of altadoX^Xilhe p?"entage SToX”' X'05
cK. '’Ot leSS
5% °f 'Be totaf budX
a,tent“>" in
reSO”“S Sh°U,d
improve functioning of heflth services
are interesting in spile of
h—
“ t0
based
CdOocumettts ami Seuit^AdministratonOe^p^,,,,.,,, on MenlaI Hea|1|, Rights d I
md—q >h=
s«vltpTovt:XTiders and have
issuesMdlS into'
Can.lake ,s to
mental hcplfh
need is to institutionalized p1™118 cu™cula o{ a11 hoping professionals. The
teachers nurses do tor '
linkages w.fh existing providers of training for
work and facilitate incluston of 1 ’
existing curricula The mod, ?'
postSraduates in Psychology and social
"’T”
* ‘SSU“ a"d skills in ,heir
Technica, resourceb''
Quality assurance and standards of care
hXtio^
consensus for servtoe provX 2
development (suXtSXX
O" e'’lda'“
S“PPOrt
D. Provision of Services for mental health
a. Supervise domiciliary after care
from the institution to the program which facilitates the transfer of care
community. This should include financial
compensation for caregivers
b. Promotive mental health
services such as barefoot counselors earlk*
identification and referral
c. .Access to all poverty alleviation and welfare programs
ii. Proactive di
in cases of hum!
e.
fh°r«ed\llit„T'i2<!d rrViCeS 10 a“ Vul"™bl' groups
women, children
such as violencetet^m 3™
??a,"ra'
““ "’ade disaste«
, terronsm and riots, victims of dowry, child sexual abuse etc.
VI Social Monitoring system
a User Audit - There is also
a need for consumer and civil societv led ongoing qualitv
audit of services so as to
ensum a decreased risk of violation of rights of people with
mental illness. This quality assurance is only possible through a public-private
partnership.
Uk Adaalate
communities should also be pan of the audit mechanisms.
VII. Information Education and Communication
J6
C:\Documents and Settings\Administrator\Desktop\Presentation on Mental Health Rights.doc
based cadres of service providers and have included caregivers and users of the
service in provision of care.
The second step that the government can take is to mainstream mental health
issues and skills into existing training curricula of all helping professionals. The
need is to institutionalize linkages with existing providers of training for
teachers, nurses, doctors, graduates and postgraduates in psychology and social
work and facilitate inclusion of basic mental health issues and skills in their
existing curricula. The modules for such integration can be made by the
Technical resource Group proposed earlier.
Quality assurance and standards of care
Mental health services need to have mechanisms for assuring quality. In. the
present scenario, quality assurance is not being provided by any of the sectors.
Institutional care still has some statutory parameters to follow, but the other
components of care are largely unmonitored and there is a lack of accountability.
There is a need for standardized protocols of care based on evidence and
consensus for service provision.
Facilities at the district level for diagnosis, treatment and care by qualified and
trained mental health personnel. Paramedical support for mental health and
development (standard treatment protocol)
Study and research on alternative good health care systems such as AYUSH
(Ayurveda, Unani, Sidda and Homeopathy)
D. Provision of Services for mental health
a. Supervise domiciliary after care program which facilitates the transfer of care
from the institution to the community. This should include financial
compensation for caregivers.
b. Promotive mental health services such as barefoot counselors - early
identification and referral
c. Access to all poverty alleviation and welfare programs
d. Proactive district legal aid committees who can be approached in cases of human
rights violations, exploitation and abuse.
women, children,
e. Provision of specialized services to all Vulnerable groups
the aged, destitute, sexual minorities, victims of natural and man made disasters
such as violence, terrorism and riots, victims of dowry, child sexual abuse etc.
VI Social Monitoring system
a. User Audit - There is also a need for consumer and civil society led ongoing quality
audit of services so as to ensure a decreased risk of violation of rights of people with
mental illness. This quality assurance is only possible through a public- private
partnership.
Lok Adaalats and communities should also be part of the audit mechanisms.
VII. Information Education and Communication
I
C:\Documcnts and Settings\Administrator\Desktop\Presentation on Mental Health Rights.doc
a. Cultural and locally appropriate educational material needs to be developed in
collaboration with NGOs
b. Mental health website
c. Need for training medical professionals and strengthening undergraduate
medical curriculum
d. Development of a National mental health resources center
e. Mental health should become part of school curriculum and teachers training
IX Ethical guidelines
There is a need for periodic review and effective implementation of ethical guidelines in
issues such as Use of ECT, drug related research etc.
J
3-4^) 0
C:\WlNDOWSl\Temporary Internet Files\Content.IE5\01 AR8XQR\Right to Essential drugs final.DOCC:\WINDOWSl\Temporan- Internet
Files\Content.IE5\Ol AR8XQR\Right to Essential drugs fmal.DOC
Kight to Essential Drugs
Modern Medicines form an essential component of modern Health Care. But it needs to be
understood that while a very large number of drugs are present in the market today, only a small
fraction of these provide significant benefit. Further, out of these, i.e. about 2000 drugs which have
been proved through research to be effective and safe, only about 300 are considered ‘essential’.
Essential Drugs (EDs) are those which can cater to the majority of the needs of a population in a
country and hence according to the World Health Organization they must be available at all times
in adequate quantities in the relevant health care centres. Countries should be self-reliant in the
production of the EDs, and the EDs should be accessible and affordable to all.
Unavailability of EDs can cause death or serious complications, which may lead to long-term
impairment of health. Hence availability of EDs is a human right. In India however, this right is
being violated in both public and private sector.
Access to essential Drugs in India is compromised at various levels. Estimates say that only
about 20% of the population has access to all essential drugs they need. Whi le the country is largely
self-reliant in production of essential drugs, and in fact exports in excess of 40% of the total volume
of drugs produced, our own people are denied access. This denial takes place today because drug
prices continue to be high and thus unaffordable, the public health system spend too little on
procuring drugs, and there is widespread production and prescription of irrational and hazardous
drugs.
Our suggestions about key policy measures to ensure availability of EDs to all the people are
as follows:
Availlability of EDs in the Public Health Care Facilities
In the public health services, a graded ED list should be prepared which would list which
drugs should be available for Primary Health Care with Community Health Workers, (CHWs), in
Sub-centres and Primary Health Centres (PHCs); for secondary health care in Community Health
Centres (CHCs), Rural Hospitals (RHs) and for tertiary care in District Hospitals and Medical
College hospitals. The National Essential Drug List (NEDL) needs to be graded accordingly. The
lists of EDs which must be available at different health care centres must be widely, readily
available and the list for the relevant centre should be available at the centre. The authorities have
to ensure that the patient does not have to buy any medicine included in this list. If in exceptional
cases the patient has to purchase any of the medicines from this list, this expense should be
reimbursed to him/her. Unless this provision is made, there would not be any effective mechanism
for people to ensure that they get EDs without paying from their pocket. Unavailability of EDs in
sufficient quantities is a violation of human rights as it can jeopardise life and health of the people.
Annual requirements of these health care centres need to be estimated and accordingly
supplies, inventories need to be maintained. This is not being done and there are gross, frequent
shortages of EDs at all levels, as has been complained by health-activists and borne out by available
studies. To give an example, only about 20% of the patients go to the Primary Health Centres and
even half of their requirement is not met. A large proportion of patients are given prescriptions to
purchase medicines or have to pay the doctor for these medicines, which the doctor keeps with him
as private stocks.
One study indicates that the drug-supply to the PHCs needs to be doubled to cater to the
current drugs needs. In Maharashtra, this would require only Rs. 100 million, compared to the
overall health budget of the Maharashtra govt, of Rs. 20000 million. It is thus possible to ensure the
availability of EDs at all times, and this availability should be part of the basic health services as a
matter of human right.
The drug companies in the public sector have been marginalized during the last 20 years. This
process needs to be halted and public sector drug companies need to have an important role to play
C:\WINDOWSl\Ternporary Internet Files\Content.IE5\Ol AR8XQR\Right to Essential drugs final.DOCC:\WINDOWSl\Temporary Internet
[•'iles\Contont.IE5\01AR8XQR\Right to Essential drugs final.DOC
in the supply of life saving, essential drugs, as this availability can not be left entirely to the market
forces.
For the procurement of drugs for the Public H ealth facilities, a transparent procurement
mechanism similar to that adopted by the Tamil Nadu Medical Service Corporation should be
adopted.
Access to EDs in the private sector
An estimated 90% of the annual drug consumption of about Rs. 20,000 crores in India is
through private purchases made by households. A large proportion of this sale consists of sale of
unscientific fixed dose combinations and of non-essential drugs. Though EDs too are available and
sold in significant proportion, they are not accessible to every body because of lack of adequate
purchasing power. The primary barrier in the effective accessibility of EDs in the private sector is
their high prices due to profiteering by the drug companies. This profiteering of the is seen from
various indicators like • The higher share prices and bonuses of drug-companies.
• Huge price-differences between the branded formulations iin the retail market and
corresponding formulations in the generic drug market.
• The procurement prices of some drugs by the Tamil Nadu Medical Services
of the retail
Corporation (a public sector procurement agency) are as low as 2 to 10% of
market prices of these drugs.
. t
Drugs are not only a life saving essential commodity but also the one in which consumer pays
but doctor decides’. Moreover, patients are in need of urgent relief and hence have very htt e
choice but to buy the prescribed medicines urgently at whatever price the medicines are available in
the retail market. Unlike in the West, in India most of the patients are out of any institutional
coverage, and hence are further vulnerable to face the powerful drug industry as individual buyers
°f “Sese to together make a strong ease for ineluding all EDs in the Drug Price Control
Order (DPCO). In 1994 the government announced its new policy on Drugs and Phaimaceuticals.
While continuing the trend set in 1986, the Govt, reversed all positive features of the 1978 drug
policy which had helped to built a self reliant industry, the best of its kind in the third woild, and
comparable to those in many developed countries. In the new policy the Govt, granted major
concessions to the industry in terms of reduced price and production controls. They included the
slashing down of the number of drugs under price control and increase in returns allowed tor bu k
drug manufacture. Further the DPCO of 1995 (based on the 1994 Drug Policy) has used purely
market based criteria for selection of drugs in DPCO and has totally neglected Essential Drugs as a
criterion. Thus, over the years the number of drugs under price control has been slashed from 343
in 1978, to 166 in 1987, and to 74 in 1994. The 2002 Policy and the new DPCO seeks to further
slash the span of price control (to about 25-30 drugs only) but the new DPCO has been stayed by
the Courts because of a Public Interest Litigation challenging the new order. Hence many of the
even life saving drugs are currently not in the DPCO. This policy has to change and all EDs have to
be included in the DPCO.
Price controls need also to be matched with production controls to ensure that companies do
not shift production from essential drugs that are under price control to drugs that are not essential
but are outside controls. Otherwise there will be shortages of EDs and proliferation of non-essential
drugs.
Weeding out of Irrational and Hazardous Drugs
Irrational and hazardous drugs, which exist in the market, are an unnecessary burden on
consumers, and take away resources from what should be spent on essential drugs. While the Drug
Technical Advisory Board (DTAB) is supposed to monitor the presence of such drugs, its
functioning has been far from satisfactory. There is urgent need to revamp the DTAB, broaden its
powers and have the DTAB play a proactive role in weeding out such drugs from the market.
C:\WINDOWSl\Temporary Internet Files\Content.IE5\Ol AR8XQR\Right to Essential drugs final.DOCC:\WINDOWSl\Temporary Internet
Files\Content.IE5\OlAR8XQR\Right toEssentialdrugsfmal.DOC
Adverse Drug Reaction Monitoring
These efforts need to be matched with the setting up of Adverse Drug Reaction Monitoring
centers across the country, so that there is an ongoing mechanism to monitor the incidence of
adverse drug reactions. All developed countries have such mechanisms, and it is indeed a shame
that India, with arguably the second largest scientific manpower in the world and the most
developed pharmaceutical industry in the developing world, is yet to set up an effective mechanism
to monitor hazards related to drug consumption.
Quality Control
It is estimated that 40% of drugs consumed in the country are substandard or spurious. Over
much larger number of Drug Inspectors, and changes in the Drugs and Cosmetics Act t0 Provl
more powers to Drug Inspectors. A transparent mechanism by which consumers and
professionals can file complaints about drug quality should also be instituted.
of unethical methods - ranging from providing wrong
promotional activities of drug companies.
Amendment to the Indian P^ent
under the WT0, India is required to amend its
As per the provisions c
comnliant regime There has been extensive debate within the
Patent Laws to provide for a TRIPS compliant regime, mere
country about what the contours of India’s Patent Laws should be. 1 he 1970 Act sei
;
well and was instrumental in development of the indigenous industry - to a point ^liei e tlu. 1' d <
pharmaceutical Industry is the leader in the developing world. It is thus imperative that any
fundamental changes in the 1970 Patents Act need to be carefully examined so as not to
compromise the interests of the country, both in terms of our ability to safegaurd the health of ou
people and our interest in promoting a self-reliant indegenous Pharmaceutical Industry.
There is a wide consensus that domestic laws, while being 1 RIPS compliant, need to make lull
use of “flexibilities” available in the TRIPS agreement. This was reiterated in unequivocal terms by
the WTO Doha Declaration on TRIPS Agreement and Public Health (2001), which, inter aha.
commented that countries have the sovereign right to enact laws that safeguard domestic interests.
It recognised the gravity of public health problems in developing countries and clearly provided
that member countries had the right to protect public health to promote access to medicines for all.
In pursuance of the necessity to make India’s Patent Laws TRIPS compliant, the Indian
Parliament has enacted two legislations through the Patents (Amendment) Acts of 1999 and 2002.
In order to fulfil the conditions in the TRIPS agreement, a Third Amendment is now to be tabled in
Parliament. The Patents (Amendment) Bill of 2002 did not make full use of the flexibilities
available in the TRIPS agreement, which were further emphasised in the Doha Declaration
The draft Bill is entirely inadequate in addressing domestic concerns relating both to health
care and development of the indigenous industry. The least that that the Indian government needs to
do is to pro-actively use the space created by the Doha declaration in order to ensure that all newer
EDs which have Public Health importance are kept out of the new patent regime. Otherwise in
coming years, Indian people will be increasingly denied their right to essential drugs.
Concept Note on the Private sector in Health Services for NHRC Hearings
Any attempt to locate the role of the private sector in health
services within a rights framework has to take into account the
extent of poverty and the type of services provided by this sector.
Since the private sector caters to those who have the ability to pay
for services, there is serious concern regarding accessibility,
especially for a large percentage of the population that lives below
the poverty line. Another important concern is that the private
sector focuses only on curative services and therefore fragments a
comprehensive approach that includes the preventive, promotive
and rehabilitative inputs in the health services. The private sector
has grown over the last three decades due to a weak public health
service infrastructure and recent policies that have offered a variety
of subsidies, has furthered this process. The abdication of the state
to provide health services has ‘pushed’ people to the private sector
as a result of which only those who are able to pay for services can
access these services.
The private sector occupies a significant presence in the
delivery of health services at the primary, secondary and tertiary
levels of care.
Over the last two decades there has been a
significant growth in the number of institutions providing health
services across states and rural/urban areas. The increase in the
number of institutions is reflected in the utilization patterns as well.
Studies show that a significant proportion of the population utilizes
the services of private practitioners, trained and untrained, for minor
ailments requiring out patient care.
fnl
For in patient care requiring hospitalization one finds that
there has been a shift from the public to the private sector
especially among the upper and middle classes.
While those
belonging to the lower income groups rely much more on the public
sector they are also accessing the secondary and tertiary level
private hospitals.
It is well established that the private sector is characterized
by plurality and heterogeneity. At the primary level it consists of
individual practitioners, at the secondary level there is enormous
variation in the size of operations, bed strength, and types of
services and cost of services.
The tertiary level consists of
specialist hospitals with varying patterns of ownership (trust,
corporates, private limited concerns), type of services and also cost
of services. Given this heterogeneity with little or no regulations as
a result serious concerns have been raised by health researchers
and activists regarding access, price, quality, type and equity for
people who utilize these services.
Another important concern is
that the private sector provides curative services for the treatment
of a
number of communicable diseases.
These curative
interventions constitute an important input into the strategy for
prevention
of communicable disease, therefore,
it must be
mandatory for private institutions to report cases treated to the
public health service system. Suitable systems for reporting by the
private sector to the public health services need to be worked out.
In the treatment of communicable diseases the private sector
needs to follow the
standardized treatment
procedures as
prescribed by the National Disease Control Programmes.
It is often assumed that the private sector provides better
quality of services as compared to the public sector. Studies have
shown that there is variability in standards in terms of training of
personnel and infrastructure across levels of care that influences
the quality of the services given.
Similar variability is seen for
pricing of services with no transparency in the pricing of services.
Often a patient accessing a private facility cannot anticipate the
cost that he or she is likely to incur at the end of the treatment
process. Given the profit motive of the private sector unnecessary
testing, procedures and irrational use of drugs have been reported
in various studies. The high cost incurred is a burden, especially
for those who belong to the lower income groups. Studies have
shown that high costs of medical care are a major cause of rural
indebtedness for lower income groups. The world over, especially
in countries where organized healthcare systems exist, insurance is
an important mechanism of financing healthcare, whether provided
by private providers or public facilities.
Insurance is an important financing mechanism to sustain a
private health economy at one level and at another level insurance
is also a mechanism to regulate and control medical practice. In
Canada, Europe, Australia, Japan and some Asian and Latin
American
countries
insurance
operates
with
a
publicly
controlled/regulated healthcare system and hence it is sustainable
but in the USA, as also in India, insurance deals largely with private
markets
and
hence
insurance
in such
countries
is
grossly
inequitable and unsustainable. India has to learn from the non-USA
experience in developing its health insurance markets.
In the absence of professional or governmental regulations,
the private sector cannot be held accountable.
There is lack of
transparency and information for the person seeking care and there
(v\3
to few mechanisms tor redressa, of grievances arising out of
~ practices and. medica. neg.igence in the private sector
e inclusion of medica, services in the private sector under the
f°r dealing »ith
of ZZ T0" AC' WaS S
Of med,cal negligence. There were a tew cases that were filed with
consumer courts in different parts ot the country and there have
been some landmark judgements. However these are few when
compared to the extent of the problem since majority of cases
mvolvmg medical negligence go unreported.
within thn
At,'hiS 'UnCtUre " iS ™POrta"'t0 address ,he prablems
aspects
6 SeCt°r and eV0'Ve mechanisn1s ^ring various
•
Review, amend and imptement the existing tegisiations
concerning various aspects of the private sector.
Evolve effective review,
monitoring
and
regulation of
s andards ot private medical and paramedical institutions
and tor different leveis ot service providers. At the Central
and State levels there is a need to enact an Act for clinical
establishments
tor
hospitals,
nursing
homes,
clinics.
Pathological labs, diagnostic centres addressing issues of
standards and quality of care.
•
Evolve mechanisms tor periodic audit ot clinical Interventions
m private nursing homes and hospitals with reference to
gynaecological and obstetrics, cardiology, orthopaedics
•
Create a mechanism tor social audit tor reviewing quality in
private
hospitals,
medical
medical
meoicai
anH
and
paramedical
colleges/institutes.
•
Registration
of
imaging
Reproductive Technologies
technologies
and
Assisted
be made mandatory.
pA
Review and evolve operative criteria for assessing ‘profit’
•
and ‘non profit’ status of hospitals.
Private hospitals undertaking research have to be registered
.
with the appropriate government institution.
For all human clinical research trials must have clearance
•
under the
appropriate
clause
under the
Drugs
and
Cosmetics Act. Mechanisms for getting clearance, reasons
for giving the clearance by the appropriate authority,
providing information regarding the research undertaken and
its results should be made public.
Direct government subsidies should not be given to
•
corporate
hospitals.
For
any
past
violations
of
conditionalities, appropriate compensation should be paid by
these corporate hospitals to the government before any new
business deals are made. The compensations must include
penalty for the occupation of the land and non-provision
free/concessional services over the period of violations.
•
Build systems for reporting and monitoring of cases treated
in the private sector to the public sector.
.
Transparency with regard to pricing of services.
.
Proper maintenance of medical records and access to
•
patients to these records.
Abide by the conditionalities when receiving government
subsidies.
Rama V. Baru and Imrana Qadeer
Centre of Social Medicine and Community Health
JNU, New Delhi
Ravi Duggal, CEHAT, Mumbai
Annexure
Summary of Qureshi Committee report
The terms of reference, laid down by the government of Delhi to the constituted
high level committee of enquiry for hospitals in Delhi (Chaired by Justice A. S.
Quereshi), in 2001 were
a)
To review the existing free treatment facilities extended by the
charitable and other hospitals who have been allotted land on concessional
terms/ rates by the government.
b)
To suggest suitable policy guidelines for free treatment facilities for
needy and deserving patients uniformly in beneficiary institutions in particular to
specific the diagnostic, treatment, lodging, surgery, medicines and other facilities
that will be given free or partially free.
c)
To suggest a proper referral system for the optimum utilization of the
free treatment by deserving and needy patients.
d)
To suggest a suitable enforcement and monitoring mechanism for the
above including a legal framework.
Findings and recommendations.
The inquiry that lasted for eleven months tabled the following findings and
recommendations.
The existing free treatment facilities extended by charitable and other hospitals
who have been allotted land on concessional terms/rates are inadequate, erratic
and far from what was desired. The reasons that were mostly attributed by the
hospitals were on various fronts.
1) Few hospitals questioned the financial prudence and viability of ventures on
offering free services. They feel it to be an unwarranted and huge financial
burden.
2) Other hospitals present their case in a different way, they claim to be the
purchasers of the land and feel in no way obliged for free services.
3) But some hospitals, who agree that they had been either allotted or leased
land from the government, claim that free service is not mentioned in any of the
agreements.
4) A few hospitals who claim that they are not charitable hospitals and therefore
not liable for free services.
5) In the government’s conditionality there is no precise definition of the ‘poor’,
who can be considered eligible for free treatment. And there has not been an
agreement over what constitutes free services.
The policy guidelines and recommendations of the inquiry are
* The government needs to intervene and to take action against all cases who
have contravened the terms and conditions of allotment. The allotments and
leases could be cancelled and necessary fresh agreements specifying fresh
and uniform terms and conditions. The committee also suggests that the
tariff subsidised has been too low and could be charged on nominal market
rates. And the new agreement should look into the reconstitution of the
managements with at least three nominees of the Delhi government on
board of all managements. And all defaulters should be made to pay
compensation which could be constituted as a welfare fund to benefit the
poor.
•
Regarding the policy for treatment the committee recommends certain
guidelines. They would include on the issue of free treatment the committee
defines free treatment to be completely free
and not partly free. The
patient virtually will not have to pay anything in both O.P.D. and I.P.D.
including medicines and medical consumables. The extent of offering free
services would be 10% of the total beds in I.P.D. and 25% of the total
number of patients in O.P.D. uniformly.
•
Every hospital should have committee to
screen and if necessary investigate
to ascertain the patients who are really poor and deserve free services. And
all such services rendered should be directed to
a newly constituted
monitoring cell under D.G.H.S. on periodic basis. And there should be strict
penal provisions for any non- compliances.
•
All patients referred should be through hospitals
with referral letters to the
monitoring cell stating and justifying the reasons for referral to a super
speciality hospital. Individual or institutions or other bodies of government or
non-government are not eligible for any references.
•
The committee recommends a drastic overhauling of the existing legislation
and suggests bringing in a new legislation that would be comprehensive and
properly monitoring all private medical institutions irrespective of just free
services but also on other larger and pressing issues.
Indraprastha Apollo Hospital
The Indraprastha Apollo Hospital is
a collaborative venture with the government
of the Delhi. The Delhi government has purchased the land of 15 acres for Rs 4
crores and has leased out to the hospital for a period of 30 years. The
government collects a token rent of just one rupee from the hospital as subsidy
with an agreement that stipulates to treat poor patients free of service and that
would be one thirds of the total number of beds, the hospital was planned to be
a 600 beds hospital and hence it is believed that 200 beds will be for poor
Al S
patients. However on inquiry it was found that there had not been any free
services for 200 beds but only 140 beds out of a total of 650 beds is being
earmarked for free services. And the services that are offered are also not totally
free.
The paradox is that the Delhi government owns 26% of the equity shares valuing
Rs.23 crores of the hospital, it has further invested Rs. 15 crores in the
construction of the hospital, has its appointees on the board of management and
still, the result is far from the desired. An overall investment of Rs.40 crores and
further subsidies in terms of land import of equipments have all meant nothing
for the Delhi’s poor. And the reasons cited are huge economic burden if such
services are rendered, which is indeed far from true. It is indeed a blatant
violation of an agreement and a fraud on public funds invested in the whole
project.
PH
13
Summary of presentation on Environmental and
Occupational health rights at National Public hearing on
Right to Health Care, 16-17th December 2004
Presentation by Occupational Health and Service Committee and the Corporate
Accountability Desk of The Other Media
In India, child mortality rates due to environmental hazards and toxins are on the rise,
with about 55% originating in perinatal period. Apart from traditional environmental
risks, modern hazards like air pollution, exposure to agro-industrial chemicals and toxic
wastes are increasingly influencing people’s health and wellbeing in India. It is
estimated that India spends about Rs. 4,660 crore every year to make up for
health damages caused solely by ambient air pollution alone (Aggarwal et al, 1999).
A World Bank study found that one person in Delhi dies every hour due to air pollutionrelated respiratory diseases.
Death and injury caused by environmental pollution are preventable. However, because
it is the poor and people from socially oppressed castes that are predominantly and
disproportionately affected by pollution and environmental disturbance, preventive
measures are slow to come. This is a form of environmental racism that is prevalent in
our health and environment policies. In fact, the National Health Policy is very shallow in
terms of its discussion of environmental/occupational health, and does not analyse
environmental health as a class or caste issue.
The National Health Policy 2002 (NHP 2002) has only now reached the stage where it
has acknowledged Environmental and Occupational Health as an issue: "The ambient
environmental conditions are a significant determinant of the health risks to which a
community is exposed. ” It goes on to state that “This Policy envisages that the
independently-stated policies and programmes of the environment-related sectors be
smoothly interfaced with the policies and the programmes of the health sector, in order
to reduce the health risk to the citizens and the consequential disease burden". The
policy also recognized “sub-standard” working conditions and vulnerability of workers,
specially children in such kind of workplaces. Therefore, the policy explicitly stated:
"NHP-2002 envisages the periodic screening of the health conditions of the workers,
particularly for high- risk health disorders associated with their occupation."
This understanding of the effects of environment on community and worker health is not
new. The Factories Act and the Workman’s Compensation Act recognise the impact of
the workplace environment on workers, and mandates preventive, diagnostic and
rehabilitative measures to protect worker health. However, the law is not implemented,
at least in part because resources and incentives are not provided to implement the law.
Similarly, it is not known, or likely, that th© NHP's lofty vision is matched by
commensurate budgetary allocations. Indeed, research on environmental health finds
no mention in the health research section of the NHP 2002. The Policy states that it
“envisages an increase in Government-funded health research to a level of 1 percent of
the total health spending by 2005; and thereafter, up to 2 percent by 2010. Domestic
medical research would be focused on new therapeutic drugs and vaccines for tropical
diseases, such as TB and Malaria, as also on the sub-types of HIV/AIDS prevalent in
the country."
oi-
Despite the obvious link between health, and the living and working environments,
coordination between the Ministries of Environment, Health and Labour is pathetic.
This is evident from the fact that the public health care system does not work to detect,
treat or prevent environmental or occupational diseases. Neither does the health
department seem to see a role for itself in environmental and occupational health
issues.
Issues relating to occupational health:
•
It is estimated that between 100,000 and 150,000 workers are killed in workplace
accidents and that there are two million new cases of occupational diseases per
annum. (Stirling Smith)
• The official estimates for deaths at work are incomplete partly due to poor
reporting mechanisms, but greatly due to non-applicabiiity of legislations on a
large section of work places that constitute the bulk of workforce, that is in the
informal sector.
• Informalization of work has added more uncontrolled workplaces and more
insecure workforce - women and children.
• Deaths from occupational diseases will be greater than those from accidents.
The majority of these deaths are preventable, without expensive imported
technology.
Occupational safety and Health is neglected as a development issue and as a
human rights issue.
The Factories’ Act does not give rights to workers and trade unions to approach
courts in cases of violation of occupational safety at workplaces.
Because pollution-impacted people, including workers and contract workers, are
predominantly and disproportionately from poor and politically disadvantaged
communities, they do not have the political or economic strength to sustain longdrawn legal cases, or to fight for the implementation of favourable court orders
subsequently.
Doctors (Factory doctors, government or private doctors) are not trained to
detect Environmental and Occupational Health problems either in individuals or
in communities and to report them as an important preventive tool.
Pollution control measures, environmental standards or pollution norms are
made with an attention to the financial health of the industries that are regulated
than to the health of workers, the community or the environment.
The amounts given as compensation to workers for lifetime injuries due to
occupational hazards are meager.
Some of the key issues relating to Environmental health:
While the kinds of industries and the number of people living within the impact range of
pollution may differ from place to place, the problems faced by and the demands of
workers and communities living along or near the fenceline of polluting factories is
identical throughout the country.
issues with regard to health in pollution-impacted communities:
01
•
•
•
•
•
•
•
•
High rates of morbidity among exposed people, especially women and children.
Because women, children stay at home and, hence, in a polluted atmosphere all
day long, they (along with and factory workers living v/ithin the pollution-impacted
community) are worse affected than men or others who may have relief from
pollution for at least the time that they leave the polluted environment to work
elsewhere.
Children are routinely identified as one of the most affected groups.
Pollution-related diseases are treated symptomatically and without any real
understanding of toxic injuries.
For most pollution-impacted communities, medical expense takes a
disproportionate share of income. Added to that, health problems - particularly
for the daily wage earners who constitute the bulk of the pollution-impacted —
also mean a loss of income due to lost work days.
Regulatory authorities regularly stand the Precautionary Principle on its Head.
Anecdotal evidence, testimonies of pollution-impacted people, complaints and
even simple studies seem to be inadequate to move district authorities, the
health department and the Pollution Control Board into action. Rather than act on
this evidence, they demand conclusive proof of harm from complainants or
belittle their claims as exaggerated, or motivated by greed.
Flawed values and belief system: Many officials at regulatory authorites believe
that pollution is inevitable, and that communities - particularly the poor and
workers — cannot be choosy about the kinds of jobs or “development* they get.
They also recommend "reason” and "patience" to complainants, saying that the
pollution has to be reduced gradually keeping in mind the need to balance the
interests of the industry and the community. This attitude condones pollution and
authorizes the ongoing exposure of communities to pollution.
Alarmingly, the Health Department is noticeably absent from the discussion
around the issue of health in pollution-impacted communities. In the absence of
any steps to stop exposure to pollution, there is little that can be done to improve
the health status of pollution-impacted communities.
The local Government and medical and emergency infrastructure (hospitals,
police, fire department) lack the training, understanding, infrastructure and
resources to deal with an industrial accident or emergency. None of the
communities hosting a hazardous plant is any better equipped today to deal with
a Bhopal style disaster than it was 20 years ago.
Recommendations to address issues of Environmental and Occupational
health within the health and environment policy framework:
1. Recognizing and addressing Environment and Occupational Health issues as
integral part of community health issues by facilitating greater interaction
between Health, Labour and Environment ministries.
2. Seeking out and engaging with labour organisations and community gioups in
developing an understanding of the health issues and the solutions.
3. Update the list of scheduled occupational diseases under Workman s
Compensation Act based on the Precautionary Principle, and initiate a process to
prepare a similar schedule and compensation mechanism for communities
resident near polluting industries.
03
4. Improvement in the existing infrastructure and institutions like Employees’ State
Insurance Corporation, Public Health Care centres to detect, diagnose, treat and
report Environmental and occupational health problems.
5. Expansion of the ESIS to include the informal sector. ESI Corporation may
already have the financial strength to do so and may not require additional
finances.
6. Notify areas around polluting industries as "Zones of Environmental Health
Concern."
7. In the health administration infrastructure (ESI, PHC, GH etc) covering "Zones of
Environmental Health Concern," deploy specialised environmental health cells or
retrain existing health department staff to deal with a) long-term monitoring health
among pollution-impacted communities; b) providing long-term specialised health
care to people living, working within such Zones; c) cases of acute poisoning by
industrial chemicals.
8. In such zones, set up Local Area Committees, involving elected panchayat
leaders, representatives from women's self-help groups and public interest
organisations with a demonstrated commitment to working on issues of pollution
and/or health. Such committees should be vested with authority and provided
training to monitor health and the functioning of health care infrastructure, report
on pollution incidents, and supervise efforts to reduce pollution.
9. Stop Ongoing Exposure, Stop Pollution: Working with the Ministry of
Environment and the Central Pollution Control Board, the Ministry of Health
should deploy a plan for toxics use and release inventories in factories, and for
reducing the use of toxics in a timebound manner.
10. Deploy an emergency plan to contain the damage already done to children’s
health, and initiate measures for the rehabilitation of children’s health.
11 Operationalise the Polluter Pays Principle: Polluting industries maximize their
profits by externalizing the costs of pollution to the community in the form of
transferred health care costs to repair pollution-related health damage. These
industries should be made to pay for the health care of pollution-impacted
communities and for the specialized health care infrastructure required in such
communities.
12.Operationalise the Precautionary Principle, and use the Precautionary Principle
rather than a cost-benefit analysis to guide decision-making on the matter of
environmental health. Pollution standards and pollution-control mechanisms
should be based on health criteria rather than on issues of economic viability of
industries.
13. The Health Department should play a proactive role in ensuring that practices to
prevent harm are followed within industries. They should do this by coordinating
with the Factories Inspectorate.
14. The Health Department should facilitate the routine monitoring of workers health
data that is required to be, but is not, collected under the Factories Rules to
identify problems (if any) of occupational diseases among them.
15. The Factories Inspector should be directed to diligently perform his/her functions,
particularly in regard to maintaining industrial safety and ensuring emergency
response by industry. The Inspector should also ensure that only trained workers
are deployed on hazardous jobs and contract workers are not used for such
activities.
16. Hospital infrastructure in the areas near polluting industries should have trained
personnel and equipment to deal with cases of industrial injury and poisoning.
0^
17. Th© Diotrict Adminiotration should be inetructed to asoietthe victim or hio/her
survivors in accessing compensation and/or pension. An interim compensation
fund should be created with advance contributions from polluters.
18. NHRC should direct the Pollution Control Board to show zero tolerance to
polluters.
19. A National Commission on Pollution Impacted Communities (including workers
and communities) should be constituted to understand the special needs of
pollution-impacted communities, and recommend specialised infrastructure to
deal with the same.
0^
Health Rights in the context of HIV infection and AIDS
Presentation by the Jana Swasthya Abhiyan
National Public Hearing on Right to Health Care
Jointly organised by the National Human Rights Commission and
Jan Swasthya Abhian
(New Delhi: 16-17 December 2004)
HIV/AIDS is a developmental issue that calls for social and political action. It is also a public health
issue that requires people-oriented health and medical interventions. Such responses require
democracy, pro-people inter-sector policies, good governance, people's participation and effective
communication. They should be rooted in internationally accepted human rights and humanitarian
norms [‘People’s Charter on HIV/AIDS’ by People’s Health Movement].
The widespread abuse of human rights and fundamental freedom associated with Indian
constitution has emerged as a serious issue in the last two decades after the origin of epidemic in
India. Protection of human rights is essential to safeguard the human dignity in the context of HIV
infection and AIDS. This paper draws upon five important areas where violation of human rights in
the context of HIV infection and AIDS in health sector has been reported in India.
1. Universal Access To Treatment For PLHAs Through Public Health System
Providing equitable access to comprehensive treatment for HIV infected people is crucial to the
overall HIV infection and AIDS scenario in India. Comprehensive healthcare for those who have
infected with HIV/AIDS include opportunity for them to lead healthy lifestyle which include costeffective nutritional input, psycho-social support eel, access to treatment for the opportunistic
infections and access to anti-retroviral therapy. The inability of people living with HIV/AIDS to
access treatment is violating the ‘Right to Life' under the India’s constitution. The ‘Right to Life”
guaranteed by the constitution has been interpreted by the Supreme Court to include the “Right to
Health' [Eg. Vincent Panikulangara Vs Union of India, 1987]. Many international commitments for
which we are a signatory also mandate the state to provide access to treatment for those who are
affected by HIV/AIDS [Eg. UNGASS Declaration of Commitment].
The Alma Ata Declaration of 1978 promised health for all by 2000 through primary health care
approach. Verticalisation of public health systems, changing economic priorities, invasion of private
interests into political decision-making and lack of political determination lead to undermining of our
public health system. This breakdown of public health and primary health care systems over the
last two decades has proved to be highly detrimental to the capacity of our health system to cope
with the treatment and care of HIV/AIDS.
One of the important components of treatment for the HIV/AIDS infected people is Anti-retroviral
Therapy. Effective therapy inhibit the viral replication and reduces the viral load. This results in
lower frequency of opportunistic infection and helps the infected people to lead more productive
lives. The decision taken by the Government of India to provide treatment to one hundred thousand
people starting from 1st of April 2004 in six high prevalence states was an important step. However
the majority the people who require anti-retroviral therapy are outside this commitment. It has also
been noted that the pace at which the programme is rolling out even in the identified states is not at
a desirable level and also some of these states are facing logistic problems. One major reason for
this is the collapse of our public health system which make it handicapped to handle and monitor
Anti Retroviral Therapy. Though the programme has been announced as free of cost, it is totally
objectionable that certain elements of cost recovery from users have nevertheless been brought
into the public provision of Anti-Retroviral Therapy through the back door. The present programme
vulnerabl
307 SeC°nd ''H6 theraPy
Pe°Ple Wh° fail 'n the
,ine therapy highly
Informed consent and proper counseling of patients is essential and should be mandatory before
starting the treatment. The counseling should include detailing the nature of life long treatment,
possibility of resistance, toxicity of anti retroviral drugs. Provision of anti retroviral should ensure
maintaining and respecting the right to confidentiality of the PLHAs, proper monitoring of the
patient clinically and also providing necessary psycho-social support. Another important point of
caution is the likelihood of abuse of Anti-retrovirals by the unregulated private health sector in India
[as in the case of tuberculosis treatment where hundreds of different treat regimes, most of which
are irrational are being practiced by the doctors]. This should be avoided as such a practice can
result in drug resistance as well as exploitation of the patients.
Increased cost of anti-retroviral drugs decreases government’s ability to procure medicines. The
impact of TRIPS on cost of drugs will be one aspect that will make treatment out of reach for most
of Indian PLHAs. Government of India should make maximum use of the provisions available
within TRIPS and also pursue other options like overhauling and expanding system of price control
of medicines. Revamping of public sector drug manufacturing units is another crucial step in
making sure the availability of medicines at critical times.
Recommendations
1. Governments should develop and strengthen health system based on comprehensive Primary
Health Care principles and include the treatment and care interventions for peoples livinq with
HIVand AIDS under it.
2. Government should ensure free and universal access to treatment for opportunistic infections,
provision of anto-retrovirals whenever necessary and required monitoring tests to all people
living with HIV and AIDS. Make nutritional inputs and psychosocial support part of HIV and
AIDS care. Special attention should be paid to gender issues and treatment access of women
living with HIV infection. There is increasing number of children living with HIV/AIDS and their
need for treatment should be also be attended to.
3. Cost recovery elements in the present programme to provide anti-retroviral therapy in select
high prevalence states should be stopped..
4. Treatment protocol required for the administration of anti retrovirai drugs and drugs for
opportunistic infection should include guidelines for counseling and informed consent. Take
necessary steps to ensure that the same protocols are followed by the private sector.
5. Ensure the availability and affordability of all essential medicines including those required for
the treatment of people living with HIV and AIDS, by expanding the DPCO and making the
process of price control transparent.
6. Make use of the flexibility available with in TRIPS agreement and include supporting provisions
in to the amendment to the patent Act. Accessibility and availability of medicines should be
ensured by limiting patents to new chemical molecules and revamping the existing compulsory
license mechanisms.
7. Revitalise the public sector pharmaceutical manufacturing units so as to cater to the needs
arising out of situation under TRIPS.
2. Prevention of Parent To Child Transmission
Perinatal transmission of HIV infection accounts for about 2.74% of all HIV infection in India. In the
absence of any preventive steps, the risk of vertical transmission from an infected mother to child is
about 30 to 35%. Historically the prevention of parents to child transmission was looked only as a
technical/clinical issues of treating the mother and child to prevent vertical transmission. However it
needs to be viewed from a rights perspective of all the people in child’s life whose well being will
enable fulfillment of child’s life.
Unfortunately our weak health system provides limited access for anti-natal care leaving many who
require preventive measure against vertical transmission out of reach. Unless the health systems
are equipped to provide ante-natal care services to most of pregnant women, the chances of most
of the infected pregnant women accessing Voluntary Counseling Testing [VCT] and Prevention of
Parent To Child Transmission [PPTCT] are rare. The availability of VCT and PPTCT should be
universal by making it part of health systems based on primary health care strategy.
Right to autonomy and bodily integrity is recognised in all law including the fundamental rights in
the constitution - article 21 - right to life and personal liberty. However despite the recognition of
the right to autonomy and bodily integrity in the law, large number of women visiting the ante natal
clinics in India are routinely prescribed HIV test as part of a battery of tests. In India a number of
cases have already been reported where pregnant women are subjected to HIV screening without
proper pre test counseling and on diagnosis of HIV infection, they are denied post test counseling.
It should also be ensured that HIV infected pregnant women are not coerced into abortion by
health system staffer relatives and the choice should be given to the pregnant women. Availability
of voluntary testing facilities with compulsory provisions for pre and post test counseling is a must
for safeguarding the mothers right to take an informed decision regarding testing, continuation of
her pregnancy and also for receiving treatment for PPTCT.
PPTCT programme which look only at the right of the child and ignoring the rights to life of people
connected with the child is unacceptable. Treatment and care should also be made available to
HIV positive mothers and other infected members of the family. Adequate support systems need to
be built within the community for the affected and infected children.
The risk of transmission of infection to child through breast milk is about 15 percent. But given
India’s high infant mortality rate, the protection benefits of breast feeding against Diarrhoea and
other life threatening infections far outweigh the risk of transmission through breast feeding. Every
HIV positive women has the right to an individual evaluation of the best feeding option for her child.
If she decides so, all required support should be made available to enable this.
V3
Recommendations
1. Ensure that women visiting antenatal centres are not targeted and taking informed consent and
pre and post test counseling should be part of any screening for HIV infection in pregnancy.
2. Accepting or refusing testing should not have detrimental consequences to the quality of
prenatal care offered.
3. Access to PPTCT should be universal. It should not be viewed in isolation as a procedure to
prevent vertical transmission and all people related to the life of the child especially the mother
should get anti-retroviral drug therapy, if required
4. Women s reproductive heaith rights should be respected in aspects of the programme to
reduce the risk of parents to child HIV infection. Woman’s decision based on proper informed
consent should be mandatory for all important decisions including continuation of pregnancy,
PMTCT intervention, breast feeding of the child etc.
3. Consent and counseling issues related to testing/screening for HIV
The principle of consent is based on the fundamental principle of autonomy of an individual, which
has been recognised within the meaning of the right to life and personal liberty under Article 21 of
the Constitution of India. Based on this principle, the most important reason for taking consent from
a person before testing and treatment is to respect human dignity and bodily integrity. Another
reason for taking consent is clinical; as the efficacy of any treatment improves substantially through
a patient's co-operation, faith and confidence. For those delivering treatment, obtaining consent
also provides a defense to a criminal charge of assault or battery or a civil claim for damages or
trespass to a person. Therefore, it is necessary for a health care worker (including counsellor) to
take consent and explain the implications and risks involved as part of the duty to care. Mandatory
testing, which is not based on informed consent, is a violation of the right to autonomy and has had
have negative public health consequences and has proven to be detrimental to HIV prevention
efforts.
The concept of consent has three discrete but equally important aspects: first, consent is valid only
if the person giving it is competent to do so; second, consent must be properly informed, third,
consent must be given voluntarily. The patient/client has a right to all the information relevant to the
decision of whether or not to consent to a particular diagnostic test, a test to determine the line of
treatment or the line of treatment itself. Informed consent implies informing the patient/client of the
implications of the tests and treatment and risks involved in the treatment prior to taking consent
from the patient. Therefore, consent for necessitates (a) a duty on the health care worker to take
informed consent from the patient, as a part of the duty to care; (b) a right of the patient to have
knowledge and information of the options available and the risks involved in testing and treatment,
so as to enable the patient to make an informed choice.
The question that arises is how much should be disclosed to the patient to ensure that consent is
informed. In England, the standard of care which a doctor is required to exercise in discharging
her/his duty to inform the patient of risks inherent in the treatment is the same as that required by a
doctor in his diagnosis and treatment, namely to act in accordance with a practice accepted by a
body of skilled and experienced medical professionals. In the U.S., the doctor must disclose all
"material risks"; what are material risks is based on the "prudent patient" test i.e. a risk is material
"when a reasonable person would attach significance to the risk." In Canada, the doctor must
/V^
disclose known, probable, special or unusual risks. The law requires that objective and subjective
factors be taken into consideration. The objective factors are what a reasonable patient would
complain of, the subjective factors are the "particular concerns" and "special consideration affecting
a particular patient" to determine whether the patient would have refused treatment if informed of
possible risks. In Australia, the doctor has a duty to warn the patient of a material risk inherent in a
proposed treatment. It would be a material risk if a reasonable person would attach significance to
it. This duty is subject to therapeutic privilege. In India the concept of consent is not fully developed
in tort law and references may be made to the principles laid down in the Indian Contract Act and
the Indian Penal Code.
There are situations where consent cannot be taken from the patient and is taken from the next of
kin or guardian of the patient. This is also referred to as proxy consent and is particularly relevant
in the case of children. Consent for diagnosis and treatment of children is generally taken from the
parents or an adult next of kin of the child. However, in certain circumstances law recognises that a
child may consent depending on the age of the child and the ability of the child to understand the
nature of the diagnosis or treatment. In England, a young person of 16 years of age may be treated
as an adult and is presumed to have the capacity to decide. In most states in the U.S., minors who
are at least 12 years of age can consent for an HIV test or treatment. The paramount consideration
remains the best interest and welfare of the child when evaluating which actions are permissible,
even if consent is taken from the minor. However, under the NACO Policy consent for testing has
to be taken from the minor’s guardian. Studies and experiences have indicated that a large
percentage of minors are sexually active and take drugs and need services related to sexual health
and HIV etc. Experiences have also shown that minors are unwilling to access services with a
guardian. Many minors such as those living on the streets have no guardians and want to access
services independently.
Law provides for exceptions in certain circumstances. Thus, if a person is unable to give consent
because s/he cannot understand the nature and consequence of the diagnosis or treatment due to
mental incapacity, medical practitioners are under a duty to act in the best interest of the person. In
England, no person can give or withhold consent to treatment on behalf of a mentally incapacitated
patient. The medical practitioner has a duty to assess the capacity of the patient and make an
informed decision about the treatment. If the patient lacks capacity, then the medical practitioner is
to act in the best interest of the patient. Similarly, during an emergency where, for instance,
obtaining consent from an unconscious patient would not be possible, the medical practitioner can
lawfully treat the patient and is required to act in the best interest of the patient so as to preserve
life.
In light of the above, it is indicative that health programme that does not maintain the dignity of
patients or deprives them of their basic rights is violative of their fundamental and human rights. No
individual should be made to undergo a mandatory test for HIV. A person, who has the mental and
physical capacity to make a decision, has an absolute right to choose whether to consent to testing
and/or medical treatment, to refuse it or to choose an alternative. It is also important that informed
consent is taken in writing after explaining to the patient, in a language that s/he understands, the
risks and implications of a particular test or treatment. The patient has a right to refuse and/or
withdraw consent prior to the test being conducted. Principles relating to consent also mandate pre
and post-test counselling as fundamental to any process of obtaining informed consent.
Recommendations
/v^>
1) Ensure that consent to testing for HIV has to be accompanied by pre and post test
counselling.
2) Ensure that consent for HIV testing, treatment and research is taken in a language and
manner that is best understood by the person.
3) Ensure that the counselling is of a high quality and that it is done in a non-judgmental and
sensitive manner. The protocols for pre-test and post test counselling and training of
counsellors should be reviewed through a consultative process.
4) Ensure that every institution involved in HIV related testing, treatment and research should
develop counselling protocols for women and children to ensure that decision-making is
independent and informed.
5) Ensure that persons between the ages of 12 and 16 years be allowed to consent for a HIV
test and only in cases where the health care provider evaluates in writing that the person
lacks the capacity to consent should consent be taken from the parent/guardian. A clear
policy needs to be developed for the same.
6) Ensure that that protocols for taking consent for treatment is developed that includes giving
information in a language and manner best understood by the person, on risk and benefits
of the proposed treatment the alternatives that may be available, including the nature of
the HIV disease, the treatments available for it (including the possible failures, toxicity etc),
the stages when they can be administered, their duration, the likely expenses, the when
they can be administered, their duration, the adherence requirements.
7) Formal training of counsellors should be made mandatory and training facility should be
made available at various regions of the country.
8) Norms for testing and counselling should be part of 'code of medical ethics’ prepared by
the Medical Council of India [MCI} and MCI and state medical councils should take action
against those registered medical practitioners who are violating the norms.
9) Ensure that any proposed research on HIV/AIDS is thoroughly examined for ethical
standards and that consent protocols are developed to inform the potential research
subject in a language and manner best understood by him/her of the aims, methods,
sources of funding, any possible conflicts of interest, institutional affiliations of the
researcher, the anticipated benefits and potential risks of the study, the discomfort it may
entail and the right to abstain from participation in the research or to withdraw consent to
participate in the research at any time.
4. Stigma and Discrimination in health care settings
Discrimination lies at the root of all legal and human rights issues in the HIV/AIDS context. It is
because of the fear, ignorance and stigma associated with HIV/AIDS that PLHAs are treated
prejudicially and unequally.
a/6
However the reality is quite different and discrimination is rampant vis-a-vis PLHAs in the
healthcare setting. This is further accentuated for certain marginalized populations. For instance
women, sex workers, drug users and prisoners find themselves discriminated in healthcare
irrespective of their HIV status. The positive status of such individuals/groups, however, further
marginalizes them and decreases access to health services even more. Those who do not fall
within these populations but are HIV+ also suffer immense discrimination in healthcare. Not only
would increase in access to healthcare benefit PLHAs, it would have a positive public health impact
on society at large in preventing the spread of the epidemic.
The Right to Healthcare
The right to be treated equally and the right to health are fundamental rights guaranteed under the
Indian Constitution and basic human rights found in all international human rights documents. In
the Indian constitutional context it is the State’s obligation to provide healthcare for all. However,
the right of equality and healthcare is available only against the State and not against private
bodies. Therefore, it is the widely felt experience of many PLHAs that they are discriminated
against and refused treatment by private healthcare institutions due to their positive status. Even
state-run healthcare institutions discriminate against PLHAs in many ways. These include an
outright refusal to treat, physical isolation in wards, early and inappropriate discharges, delays in
treatment, on condition of higher charges being levied and prejudicial comments and behaviour.
It has been held by the Indian Supreme Court, however, that both public and private healthcare
institutions have a duty to treat all those in emergency situations although the latter is not obliged
to treat persons in other circumstances. Yet, both public and private healthcare institutions
continue to discriminate based on HIV/AIDS status.
Anti-discrimination Legislation
In certain jurisdictions medical standards prescribe that a healthcare worker must treat every
patient as HIV positive and carry out medical procedures and take precautions based on this
assumption. These jurisdictions also prescribe anti-discrimination legislation that makes treatment
of PLHAs obligatory even on private healthcare.
In India however, there is an absence of anti-discrimination legislation. Therefore, private
healthcare is free to refuse treatment to PLHAs, as it almost always does.
Manifestations of Discriminatory Practices
As mentioned above, many PLHAs are denied their basic fundamental right to health due to the
discriminatory practices carried on by healthcare institutions. Discrimination manifests itself in
. many ways in a healthcare setting. For instance, PLHAs have their case papers often hung on their
beds with bold and conspicuous notations on them indicating their positive status. This is done in
order to 'warn' others and leads to prejudicial comments and mistreatment by healthcare staff.
Bodies of people deceased due to HIV/AIDS-related causes are treated in an undignified manner.
Often healthcare staff refuses to handle such bodies. If they do, then the bodies are often dumped
in plastic bags with ‘HIV’ written across the bags, which is unnecessary. Even after this the
unclaimed bodies are not disposed off with dignity but are left to decay. Sometimes relatives are
charged extortionate amounts for handling of such bodies.
Hospitals have been seen to refuse treatment to PLHAs stating that PLHAs can be treated from
home and that admission in the institution is unnecessary. PLHAs are also discharged early by
hospitals, prior to completion of treatment; on the pretext that the PLHA’s health is improving and
does not require supervision. Healthcare institutions sometimes grant a bed to the PLHA but
discharge him/her in a few days without having analysed his/her condition or prescribed any
treatment.
Sometimes PLHAs are treated by healthcare institutions and in the middle of treatment are asked
to do an HIV test. Once the test results are seen as positive the PLHA is removed from the
institution in the middle of treatment.
Pregnant women in private nursing homes are tested for HIV by a single, non-confirmatory ELISA
test. If they are found positive, they are refused treatment at the nursing home, and are directed for
delivery to public hospitals.
User charges are being imposed by public hospitals even though treatment in such institutions is
meant to be free. Accessibility to treatment, therefore, is further reduced. Inaccessibility or denial of
treatment causes PLHAs to access quacks instead, and to rely on spurious medications. The long
term consequence of this will be their worsened health condition and the increase of society’s
overall vulnerability to HIV infection.
Public hospitals too deny treatment to PLHAs. They often try to avoid surgical procedures on some
pretext. This includes suggesting a non-invasive but inappropriate course of treatment. This
method of treatment, and sometimes-outright refusal, is often meted out to PLHAs from certain
marginalized communities such as injecting drug users and sex workers on the basis of their
appearance. The only study done on patient-to-healthcare worker transmission by the Centre for
Disease Control, United States Government indicates that the chances of such transmission are
remote and the paramedical staffs is more at risk than the physician or surgeon. (CDC data shows
that of the 52 cases 48 were of paramedical staff.) There are no similar studies in the Indian
context but anecdotal data show similar trends. It may be pointed out that the results may be
different considering the difference in the manner and context in which the health care sector
functions.
It was reported that doctors, well informed about the manner in which HIV may be transmitted,
refuse to touch HIV+ patients, thereby increasing the stigma among less trained personnel and
attending family members. Healthcare workers sometimes disclose the status of PLHAs to
colleagues although the same is totally unnecessary. This sharing of information leads to
discrimination by the entire healthcare staff due to the stigma surrounding the infection and already
marginalized populations; separate wards, which can be in most shabby conditions, are maintained
for PLHAs and also labelled as such.
Concerns of Healthcare Workers
There is a right in lav; of a health care worker to a safe working environment. Due to the fear,
ignorance and stigma around HIV/AIDS, many healthcare workers are afraid to treat PLHAs. Such
fear can be mitigated if healthcare workers are provided a safe working environment. This in turn
may reduce the discrimination suffered by PLHAs.
It has been argued, even by public healthcare institutions, that providing basic universal
precautions to healthcare workers is not a matter of priority. As such, it has been seen that these
universal precautions, (including gloves and sheet, and in the HIV context, post-exposure
prophylaxis (PEP1)), which ought to be considered an essential part of the functioning of healthcare
institutions, whether dealing with HIV or any other condition, are not provided to healthcare
workers. In these circumstances, it is contended that they are free to deny treatment to PLHAs.
NACO is supposed to reimburse expenses incurred on PEP and Universal Precautions to public
healthcare institutions. Even though NACO policy envisages provision of PEP and Universal
Precautions, in reality, the same is not available. Where available, red tapism prevents
reimbursement of costs as assured. Also there is no proper government policy on universal
precautions and this is not treated as a priority issue.
The healthcare workers argue that the institution owes them a standard of care, which necessitates
provision of universal precautions. In the absence of these precautions would a healthcare worker
be justified in refusing treatment, especially with public hospitals and their emergency wards being
burdened as they are?
Certain other issues that require discussion arise in the healthcare context. For instance, whether
the healthcare worker have a right to refuse treatment to a person who shows symptoms of
HIV/AIDS but is unwilling to be tested. This is of special significance especially in the public
healthcare setting where the duty of the state to provide health care is of paramount importance.
What are the rights of the healthcare worker -in the event of being infected in the course of
employment? In such an event the institution is bound to take care of the worker’s medical needs,
especially in light of the fact that the healthcare workers have a right to a safe working environment
including universal precautions.
It is the experience of many persons that because of their positive status, healthcare institutions
charge them large amounts of money, which are otherwise not charged to those with other
illnesses. This is often done on the pretext that the healthcare worker needs to spend an extra
amount for protective gear. Thus the burden of providing universal precautions falls on the PLHAs,
making access to care even more remote.
Recommendations
1) The government should make efforts to ensure that discrimination of PLHAs and those
associated with HIV/AIDS in both the private and public health sector is prohibited. This
can be achieved through legislation and sensitization programmes with healthcare
workers.
2) Ensure that health care workers including paramedical staff have the right to a safe
working environment where they are provided with universal precautions, PEP etc for
which protocols should be developed.
PEP is a combination drug regimen, which if administered within a certain time, can prevent the
healthcare worker infected b\' needle stick injury from becoming H1V+.)
3) oZutfons'
Staff iS Pr°Vided With trainin9 on the effective use of universal
precautions, reporting in case of exposure and PEP administration.
5. Confidentiality issues in healthcare settings related to positive status
01 P*'acy an<1 PlayS an
in 'he HIV/AIDS
of the nd* dual
J’'! a'e rampant As
later, this is not only an issue
of confidpntiaiih th?
b also °ne that actual|y serves the general public interest. In the context
riaht tn rnnfi/ f |.ma,n ,ssue that squires to be addressed is whether a positive person has the
D„7le“
Approaches to the Issues around Confidentiality
emerged3-6 the baht's oUhe id'
Wherein
aPParent|y Polarised views have
nrni ♦ iu ne . S f he ind,VKjual versus the
At by
hv
the rights
rights of
of the
the community
community. ItIt is
is araued
argued th
that
prevalenceof th
COmmunityis not made aware of the
remedipH h f n PfndemicI and 15 therefore at greater risk of getting infected. This should be
remedied by full disclosure of the positive status of all persons.
arXnfposte SiSS"’1 R
(he c“ZXitself. This
wZ,K,in8 “es ,tas
HIV/AIDT^deed^fAmN
ma'ntainin9 confidentiality does not contribute to the spread of
wavs rnnfdAnt dn emp'oyed In the aPPr0Priate context and in creative and culturally sensitive
Z ? 2X2 t02crease the spread of HIV/AIDS-For instance’in >he ind-
function under ZtX
entiahty may require to be adaPted where voluntary testing centres
area /rooms% sZ
HsPacek constraints and do not have the luxury of separate counselling
ci«
X eV°'Ved t0 enSUrS that confidentiality is respected even in
presence of others, as is oZ^heS
'S
t0
3 P"’8 StatUS " the
Also, it is sometimes seen that a woman’s test result is not collected by her, but by a male member
of the family. Sometimes a patient is too ill to go to collect the test result him/herself and a friend or
relative does so instead. In these circumstances the question whether the healthcare worker
should give the results to the relative or whether s/he should insist on the patient collecting the
results. Either choice raises different issues. For example, the situation at the patient’s home may
not be amenable to maintaining confidentiality. If the policy is that the relative may be given the
result, a method of monitoring whether she/he has the informed consent of the patient to collect the
result will have to be evolved.
Whether it is appropriate for the counsellor to make home visits despite the likelihood that family
members may become aware of the patient’s condition is a question that will have to be addressed
in a culturally sensitive manner. This dilemma is compounded in cases where ART (Anti Retroviral
Treatment) is being provided and follow up treatment is necessary, but where the person does not
return for treatment.
Young people including adolescents are unable to access health care services including HIV
testing and sexual health information because many health care providers do not view them as
having rights equivalent to adults and therefore would often violate the principle of medical
confidentiality. One of the key issues in testing and reporting of results is whether or not to involve
a youth’s parents/guardians in the process. Many young people may not wish to involve anyone in
decisions relating to sexual or reproductive health services or HIV testing and treatment. In other
countries the age at which a minor can access confidential testing varies between 12 to 16 years.
Breach of Confidentiality
Breach of confidentiality manifests itself in many ways. Due to the stigma and fear surrounding
HIV/AIDS, it is the experience of many positive persons that once their status is disclosed they are
denied many services especially in the healthcare and employment setting. Often test results are
shared, without the HIV positive patient’s consent, with other healthcare personnel, family
members, relatives, neighbours, friends, colleagues and employers. Instead, maintaining
confidentiality is seen to benefit and integrate positive people into mainstream society.
In the healthcare setting, it is seen that some hospitals have a practice of writing HIV in block
letters on patient case papers. These papers go from department to department for tests etc. Also,
it is common that these case papers are attached to the patient’s bed. These practices are
ostensibly to warn healthcare workers to be more wary of occupational exposure when providing
services to PLHAs, but often result in discriminatory practices. Strategies need to be evolved so
that the health services may be provided to PLHAs without compromising on either the right of
health care workers to a safe working environment or the duty of confidentiality. Such strategies, it
is suggested, would include mechanisms of ensuring availability of universal precautions (gloves
etc) to health care workers and clear and enforceable rules regarding confidentiality.
Often hospitals assign separate wards to HIV/AIDS patients. This exposes positive persons to
breach of confidentiality and discriminatory practices.
In the employment setting confidentiality is breached at various stages. During recruitment
employers often insist on knowing the status of the prospective employee and doctors, working for
the employer, divulge the same. This occurs even at stages of routine medical examinations during
employment. The question that arises in such circumstances is whether a doctor is obliged to
inform the employer and how this is balanced with the duty of confidentiality towards the patient.
Some employers argue that the employee’s immediate superior should be informed of her/his HIV
status, to facilitate informed action in emergency situations. It has also been argued that the duty to
maintain confidentiality would vary in circumstances where the employee remains regularly absent
from work. Policy and rules with respect to these issues need to be clearly identified.
Breach of confidentiality is also seen in other situations such as at the time of an insurance claim.
The question that arises often in this context is whether a healthcare worker is under an obligation
to disclose the HIV status of a person to an insurance company enquiring into the cause of death
or whether an alternative answer would suffice.
Exceptions to Confidentiality
The case for maintaining confidentiality limits non-disclosure. Although confidentiality is maintained
between the healthcare worker and patient it is the duty of the positive person to notify his/her
spouse/sexual partner/needle-sharing partner of his/her positive status. This is where counselling
plays a vital role. However the argument in favour of disclosure sometimes goes to the extent of
contending that the duty to notify the partner is not just the positive person’s obligation but also
extends to the healthcare worker.
It is important to note that the law does recognise exceptions to the rule of confidentiality. Such
exceptions arise in a situation when the public interest to disclose outweighs the public interest to
maintain confidentiality. It has also been held that disclosure is permissible (to another doctor) if it
is for the treatment/interest of the patient. Confidentiality can also be breached when a person is
compelled by law to breach it. Although there is no clear policy, some courts have held that where
a special relationship exists (such as between counsellor and client) and there is a foreseeable
danger to an identifiable third party, confidentiality can be breached by a healthcare worker. This
reasoning could be applicable in a situation where, despite extensive counselling, a person
continues to engage in high-risk activity for example refuses to practice safer sex with his/her
sexual partner. In a situation where a person refuses to disclose HIV status to partner and is
unable to have protected sex, the healthcare provider would need to assess if the client would face
any dire consequence as a result of the disclosure and only then decide to disclose or not. For
example women who test positive first might fear abandonment and violence on disclosure.
Beneficial Disclosure
Closely linked to the principle of confidentiality is the notion of beneficial disclosure. This implies
disclosure that is made for the benefit of the affected individuals including the PLHA, his/her sexual
and drug-injecting partners and family. Beneficial disclosure is voluntary, respects the autonomy
and dignity of the affected individuals and maintains confidentiality as appropriate. Apart from
beneficial results for the people affected, it is intended to lead to greater openness about HIV/AIDS
in the community and meets the ethical imperatives of the situation where there is need to prevent
onward transmission of HIV. Such beneficial disclosure maintains individuals’ human rights,
prevents discrimination, and improves public health in the form of prevention and care efforts.
Promoting beneficial disclosure with its elements of voluntariness and confidentiality serves a direct
public health function, because it encourages people to access HIV prevention and care services.
Beneficial disclosure also serves the purpose of opening up the HIV/AIDS epidemic. As more
people feel able and willing to disclose their status, there grows a critical mass of individuals and
families within a community, and indeed within a nation, who are openly involved in dealing with
the pandemic in positive and supportive ways. The challenge is to create an environment in which
people will come forward for testing, counselling, prevention and care.
Recommendations
1. Information that is taken, disclosed, recorded in connection with HIV counselling, testing,
treatment or research should be kept confidential.
2. Ensure that disclosure of information imparted in confidence cannot be divulged unless
with written informed consent.
Make sure that Health Care Institutions institute data protection measures to protect
confidentiality of PLHAs.
4. Ensure that protocols are developed for disclosure to partner based on existing laws and
policies. The protocols would need to address the issue of violence and abandonment that
women might experience on disclosure. A health care worker notifying a partner should
follow the protocols.
5. Confidentiality of minors accessing HIV and related services should be ensured to improve
their accessibility to such services. A clear policy should be developed for the same.
/V/5
L-^IS-
Health Rights In the Context of Conflict and Fundamentalism
(Renu Khanna SAHAJ, PUCL-Vadodara Shanti Abhiyan )
Introduction
The last thirty years have seen protracted conflict in several parts of India. And it appeals
as though we have to live with (or rather live in) situations of chronic conflict. I beheve
that it is imperative to draw attention to the gendered health consequences of conflict and
*e xJolaZ ol women’s reproductive and sexual rights and make these an important part
the violation o.worn
v
presentation thus explores consequences of
the General Recommendation 24 of Article 12 of CEDAW.
My own interest in
X
“s“e
™supported
•*>*from’10 hiEhl'8l’, ,1“heal*'’ ”"SK1““e! °f
violence and the issues that need to be addressed.
Nature of Conflict
Conflict and wars have always existed through history and rape and other kinds of sexual
globalization driven economic policies, revolutionary class struggles, separais
autonomy struggles and the general failure of the democratic agenda, have all contributed
to radicalized politics. Smaller groups are asserting their right to cultural surxiva1 ai
political power and seriously challenging the state as the sole souice of legitimate
political power and the concept of the state as a neutral umpire.
Technology and the strategy of annihilation have resulted in wars not simply being
fought on the ‘front’. Sites of confrontation, with the ‘other are the market place, the
school the community well or the water tap. Institutions of the State (like the police and
to some extent even the lower judiciary in India), are subverted to further the divisive
agenda of the State. The objective is to destroy the social fabric of society, and the
strategy is to create institutional terror, to permeate social relations, and psychologically
demoralize the community by creating suspicion and hatred.
Analysis reveals that conflict and violence in several parts of the region are initiated and
sustained by a nexus of, usually, right wing fundamentalist forces and their agents at
various levels (APDC 2000, Manchanda 2000). Here by fundamentalist, I do not mean
fundamentalism as defined in just the leligious sense. I define fundamentalism to denote
dogmatic rigid worldviews, intolerance of the ‘other’, and construction of an entire frame
work, not often amenable to reason, and a certain system of (il-)logic to legitimize a
worldview.
Violence in Gujarat
The violence in Gujarat began after a carriage of a train carrying Hindu activists, was set
on fire, in Godhra, on February 27, 2002 There are several theories around who set the
train on fire. The dominant version is that following an altercation between the Hindu
activists and a Muslim tea seller, and possibly an attempted molestation of the tea
seller's young daughter, on the Godlira railway piattonn, a Mualini mob sot th© train on
fire. In the Godhra train burning, fifty-eight people were killed many of them women and
children. The activists were returning from Ayodhya, a north Indian town, where they
supported a campaign led by the Vishwa Hindu Parishad and allied organsiations, to
construct a temple of the Hindu God Ram on the site of a sixteenth century mosque
destroyed by Hindu militants in 1992. The VHP claims that the mosque was built on a
site that was the birthplace of Ram.
Between February 28 and March 2, 2002 a three day retaliatory killing spree by Hindus
left hundreds dead and thousands homeless and dispossessed. The looting and burning ot
Muslim homes, shops, restaurants, and places of worship was also widespread.
The Gujarat government chose to characterize the violence as a '‘spontaneous reaction to
the incidents in Godhra. Findings of several independent human rights groups, and.civil
liberty organizations, indicate that the attacks on Muslims throughout the state were
planned, well in advance of the Godhra incident, and organized with extensive police
participation and in close cooperation with officials ot the Bharatiya Janata Party (Indian
People’s Party. BJP) state government.
The attacks on Muslims are part of a campaign of Hindu nationalist organizations to
promote communal tensions to further the BJP’s political rule-a movement that is
supported at the local level by militant groups that operate with impunity and under the
patronage of the state. The Hindu nationalist organisations, collectively referred to as the
sangh parivar (or ‘‘family” of Hindu nationalist groups) promote the argument that
because Hindus constitute the majority of Indians, India should be a Hindu state, contrary
to the spirit of the founders of the Constitution of the Indian State which was, and is,
avowedly secular.
The state of Gujarat and the central government of India initially blamed Pakistan for the
train massacre. The heightened fears of terrorism since September 11 were exploited by
local Flindu nationalist groups and the local press which printed reports of a "deadly
conspiracy” against Hindus by Muslims in the state.
In the weeks that followed an estimated 2000 Muslims were killed and around 200,000
displaced.
Sexual Violence
The sexual violence perpetrated on Muslim women and young girls was unimaginable.
Many women were killed after being raped and mutilated. Those who survived report
that sexual violence consisted of forced nudity, mass rapes, gang rapes, mutilation,
insertion of objects into bodies, cutting of breasts, slitting the stomach and reproductive
organs, carving Hindu religious symbols on the body parts of women.
Majority of the survivors did not register rape complaints with the police. This is hardly
surprising. Given the hostility of the police and the wrong recording of even the simpler
FIRs (those related with the sequence of events and damage to property), the police were
hardly going to encourage the registering of sexual crimes. Additionally, deeply
internalized notions of shame and honour prevented women from registering their
complaints. So while there are no official figures of the number of women subjected to
sexual crimes, women’s groups estimate that a minimum of 350 women must have been
assaulted and raped.
Health Consequences of the Violence in Gujarat
A report of the Medico Friend Circle, a group of individuals concerned about social
issues in medicine, documented the varied and multidimensional consequences of the
violence in Gujarat. In addition to the obvious physical injuries inflicted by burns, arms
and weapons, there was considerable mental trauma and stress, there was hunger due to
curfews, isolation and hiding, and infections and epidemics due to living in inhumanly
unsanitary conditions of refugee camps.
Sexual health consequences of rape among women who survived - unwanted
pregnancies, STIs - must have subsequently been there, they were not picked up at that
time by the fact finding teams possibly because the trauma of the rape over shadowed all
else. Pregnancy outcomes were affected by sexual and other kinds of violence. Women
reported premature deliveries, miscarriages and abortions. Deliveries took place in relief
camps in overcrowded, unsanitary conditions because Muslim women could not access
health services due to insecurity.
Apart from these direct health consequences of violence, there were the indirect and long
term health consequences. The continuing economic boycott of the Muslims, and deaths
and injuries of the males, led to increasing impoverishment and therefore chronic hunger
among the poorer Muslims. Because of fear of their safety, girls are being married off
early, they become mothers earlier with all the consequences of adverse maternal and
child health.
Community health projects in Ahmedabad among the urban poor Muslims report that
even eighteen months after the onset of violence, women are reporting menstrual
irregularities and lactation failure (SANCHETNA, personal communication).
Response of the Health Care System
What was the response of the health care system in Gujarat? Did it provide first aid and
humanitarian services to all injured without considering which group they belong to? Or
did conscious and sub-conscious prejudices result in discrimination during service
provision? Did the health care system recognize injuries and other consequences of
sexual offences? Was the health care system geared to creating an enabling environment
in which women could safely seek treatment for injuries due to sexual violations?
Experience of the Gujarat violence indicates that there were several lacunae in the
response of the health care services. (However, while mentioning the lacunae we would
also like to place on record that we also came across individuals who put themselves at
risk to provide services to the injured and suffering regardless of which community they
belonged to.) The following lacunae were observed:
Medical records failed to document medical evidence of violence — death
certificates and postmortem reports failed to mention injuries due to police firing
or stabbing.
.
• Health services failed to acknowledge the seriousness of psychological trauma
and did not adequately address PTSD
. There was a lack of acknowledgement of sexual violence. Medical records of
dead or injured women failed to mention sexual abuse. Despite women coming
to hospitals in conditions that indicated sexual assault, doctors failed to recognize
this. Because of women’s negative experiences at the hands of the health care
providers, even in ‘normal’ times, and for ‘normal’ events (like childbirth),
wUnpraMe sexually
sexnallv assaulted women did not approach health care providers for
vulnerable
medical examinations and recording of evidence.
• While most doctors performed their duties neutrally and did not actively
discriminate against any community, very few were proactive in defending the
rights of their patients.
• Hospitals preferred to prematurely discharge Muslim patients rather than provide
them protection and ensure their safety.
•
These lacunae need to be examined in the light of the obligations of the State as defined
in the General Comment No. 14 of the Committee of Social, Economic and Cultural
Rights and the General Recommendation 24 of Article 12 of CEDAW. The State failed
to uphold its obligation to respect the right to health and the obligation to protect the
rights of minority women to access health care services in the situation of engineered
violence against the Muslims. Muslim women did not feel safe to reach health care
facilities. The State also failed in its obligation to fulfil - it did not take positive
measures ‘to enable and assist individuals and communities to enjoy the right to health;
fulfil or provide a specific right contained in the Covenant when individuals or a group
are unable, for reasons beyond their control, to realize that right themselves by the
means available at their disposal. ’ Committee on Economic, Social and Cultural Rights.
General Comment 14, E/C. 12/2000/4.
CEDAW ‘s General Comment No.24 says that State’s obligation to respect rights
requires state parties to refrain from obstructing action taken by women in pursuit of
health goals. For example, State parties should not restrict women’s access to health
services. The obligation to protect rights relating to women’s health requires state
parties, their agents and officials to take action to prevent and impose sanctions for
violations of rights by private persons and organizations. Since gender-based violence is
a critical health issue for women, State parties have to
• ensure the effective enforcement of protocols and procedures to address violence
against women and girls
• protective procedures for hearing complaints
• ensure adequate protection and health services including trauma treatment and
counseling.
The duty to fulfill rights include positive measures taken to curb violations of women’s
rights by third parties. Budgetary, economic and other measures were required to provide
sanitation and health facilities in the health camps.
Failure to uphold these obligations construes violation of article 12.
Issues that need to be addressed
The State has to specify what measures it will take in situations of violence and conflict
to uphold its obligations to respect, protect and fulfil sexual and reproductive rights of
women as well as their right to health care in situations of conflict. Some of our
recommendations are:
1. Health care system has to be reorganized so as to become more accessible and
conducive for all categories of vulnerable groups to access services in situations
of conflict.
2. Health care system, forensic departments and law enforcement institutions have to
interact in facilitative and gender sensitive ways.
3. There is need to rethink on the rape law, definition of rape, identity of perpetrator,
medical examination and evidence to establish rape in the context of conflict
situations where mass and gang rapes occur.
4. Health care delivery systems need to' recognize that sexual violence is meant to
not just inflict injuries but also to scar the psyche - humiliation and shame. In
addition to the physical mjuries, psychological trauma has to be recognized and
addressed by the health care system.
5. Health care providers need to recognize and acknowledge sexual offences and
sexual injuries.
6. Health services need to be organized in refugee camps.
References
(i)
(ii)
(iii)
(iv)
Griffen, Vanessa (Ed.), Marginalised Women: Documentation on Refugee
Women and Women in situations of Armed Conflict, Asian and Pacific
Development Centre, GA 3 Programme, Kuala Lumpur, (2000).
Citizen’s Initiative, Hard ^acts, Centre for Social Justice, Ahmedabad, (2002).
Citizen’s Committee for Extraordinary Report on Gujarat, Submissions to the
CEDA W Committee for Seeking Intervention on Gender Based Crimes and
the Gendered Impact or the Gujarat Carnage (2002).
Medico Friends Circle, Carnage in Gujarat: A Public Health Crisis, (2002).
Renn Khanna email: sahajbrc@.icenet.co.in
NATIONAL PUBLIC HEARING ON RIGHT TO HEALTH CARE
ORGANISED BY NHRC & JSA ON 16-17 DECEMBER 2004, NEW DELHI
NHRC Recommendations for a
National Action Plan to Operationalise the Right to Health Care
Within the broader framework of the Right to Health
Objectives of the National action plan
• Explicit recognition of the Right to Health Care, to be enjoyed by all citizens
of India, by various concerned parties: Union and State Governments, NHRC,
SHRCs and civil society and other health sector civil society platforms.
• Delineation of essential health services and supplies whose timely delivery
would be assured as a right at various levels of the Public Health System.
• Delineation of citizen’s health rights related to the Private medical sector
including a Charter of Patients Rights.
• Legal enshrinement of the Right to Health Care by enacting a Public health
services Act, Public health services Rules and a Clinical Establishment
Regulation Act to regulate the Private medical sector.
• Operationalisation of the Right to Health Care by formulation of a broad
timetable of activities by Union and State Governments, consisting of the
essential steps required to ensure availability and accessibility of quality health
services to all citizens, which would be necessary to operationalise the Right to
Health care. This may include a basic set of Health Sector reform measures
essential for universal and equitable access to quality health care, and guidelines
regarding the budgetary provisions to be made available for effective
operationalisation.
• Initiation of mechanisms for joint monitoring at District, State and National
levels involving Health departments and civil society representatives, with
specified regularity of monitoring meetings and powers to monitoring
committees. In parallel with this, an institutionalised space needs to be created for
regular civil society inputs towards a more consultative planning process. These
should be combined with vigilance mechanisms to take prompt action regarding
illegal charging of patients, unauthorized private practice, corruption relating to
drugs and supplies etc.
• Functional redressal mechanisms to be put in place at District, State and
National levels to address all complaints of denial of health care.
Recommendations under the action plan
Recommendations to Government of India / Union Health Ministry
• Enactment of a National Public Health Services Act, recognizing and
delineating the Health rights of citizens, duties of the Public health system,
public health obligations of private health care providers and specifying broad
legal and organisational mechanisms to operationalise these rights. This act
would make mandatory many of the recommendations laid down, and would
make more justiciable the denial of health care arising from systemic failures,
as have been witnessed during the recent public hearings.
1
I
This act would also include special sections to recognise and legally protect
the health rights of various sections of the population, which have special
health needs: Women, children, persons affected by HIV-AIDS, persons with
mental health problems, persons with disability, persons in conflict situations,
persons facing displacement, workers in various hazardous occupations
including unorganised and migrant workers etc.
• Delineation of model lists of essential health services at various levels:
village / corrimunity, sub-centre, PHC, CHC, Sub-divisional and District
hospital to be made available as a right to all citizens.
• Substantial increase in Central Budgetary provisions for Public health, to
be increased to 2-3% of the GDP by 2009 as per the Common Minimum
Programme.
• Convening one or more meetings of the Central Council on Health to
evolve a consensus among various state governments towards operationalising
the Right to Health Care across the country.
• Enacting a National Clinical Establishments Regulation Act to ensure
citizen’s health rights concerning the Private medical sector including
right to emergency services, ensuring minimum standards, adherence to
Standard treatment protocols and ceilings on prices of essential health
services. Issuing a Health Services Price Control Order parallel to the Drug
Price Control Order. Formulation of a Charter of Patients Rights.
• Setting up a Health Services Regulatory Authority - analogous to the
Telecom regulatory authority- which broadly defines and sanctions what
constitutes rational and ethical practice, and sets and monitors quality
standards and prices of services. This is distinct and superior compared to the
Indian Medical Council in that it is not representative of professional doctors
alone - but includes representatives of legal health care providers, public
health expertise, legal expertise, representatives of consumer, health and
human rights groups and elected public representatives. Also this could
independently monitor and intervene in an effective manner.
• Issuing National Operational Guidelines on Essential Drugs specifying the
right of all citizens to be able to access good quality essential drugs at all
levels in the public health system; promotion of generic drugs in preference to
brand names; inclusion of all essential drugs under Drug Price Control Order;
elimination of irrational formulations and combinations. Government of India
should take steps to publish a National Drug Formulary based on the
morbidity pattern of the Indian people and also on the essential drug list.
• Measures to integrate National health programmes with the Primary
Health Care system with decentralized planning, decision-making and
implementation. Focus to be shifted from bio-medical and individual based
measures to social, ecological and community based measures. Such measures
would include compulsory health impact assessment for all development
projects; decentralized and effective surveillance and compulsory notification
of prevalent diseases by all health care providers, including private
practitioners.
2
•
Reversal of all coercive population control measures, that are violative of
basic human rights, have been shown to be less effective in stabilising
population, and draw away significant resources and energies of the health
system from public health priorities. In keeping with the spirit of the NPP
2000, steps need to be taken to eliminate and prevent all forms of coercive
population control measures and the two-child norm, which targets the most
vulnerable sections of society.
• Active participation by Union Health Ministry in a National mechanism for
health services monitoring, consisting of a Central Health Services
Monitoring and Consultative Committee to periodically review the
implementation of health rights related to actions by the Union Government.
This would also include deliberations on the underlying structural and policy
issues, responsible for health rights violations. Half of the members of this
Committee would be drawn from National level health sector civil society
platforms. NHRC would facilitate this committee. Similarly, operationalising
Sectoral Health Services Monitoring Committees dealing with specific health
rights issues (Women’s health, Children’s health, Mental health, Right to
essential drugs, Health rights related to HIV-AIDS etc.)
• The structure and functioning of the Medical Council of India should be
immediately reviewed to make its functioning more democratic and
transparent. Members from Civil Society Organisations concerned with health
issues should also be included in the Medical Council.
• People’s access to emergency medical care is an important facet of right to
health. Based on the Report of the Expert Group constituted by NHRC (Dr.
P.K.Dave Committee), short-term and long-term recommendations were sent
to the Centre and to all States in May 2004. In particular, the Commission
recommended:
(i)
Enunciation of a National Accident Policy;
(ii)
Establishment of a central coordinating, facilitating, monitoring
and controlling committee for Emergency Medical Services (EMS)
under the aegis of Ministry of Health and Family Welfare as
advocated in the National Accident Policy.
(iii)
Establishment of Centralized Accident and Trauma Services in all
districts of all States and various Union Territories along with
strengthening infrastructure, pre-hospital care at all government
and private hospitals.
•
Spurious drugs and sub-standard medical devices have grave implications for
the enjoyment of human rights by the people. Keeping this in view all
authorities are urged to take concrete steps to eliminate them.
•
Access to Mental health care has emerged as a serious concern. The NHRC
reiterates its earlier recommendations based on a Study “Quality Assurance in
3
Mental Health” which were sent to concerned authorities in the Centre and in
States and underlines the need to take further action in this regard.
Recommendations to State Governments / State Health Ministries
• Enactment of State Public Health Services Rules, detailing and
operationalising the National Public Health Services Act, recognizing and
delineating the Health rights of citizens, duties of the Public health system and
private health care providers and specifying broad legal and organisational
mechanisms to operationalise these rights. This would include delineation of
lists of essential health services at all levels: village / community, sub
centre, PHC, CHC, Sub-divisional and District hospital to be made available
as a right to all citizens. This would take as a base minimum the National Lists
of essential services mentioned above, but would be modified in keeping with
the specific health situation in each state.
These rules would also include special sections to recognise and protect the
health rights of various sections of the population, which have special
health needs: Women, children, persons affected by HIV-AIDS, persons with
mental health problems, persons in conflict situations, persons facing
displacement, workers in various hazardous occupations including
unorganised and migrant workers etc.
. Enacting State Clinical Establishments Rules regarding health rights
concerning the Private medical sector, detailing the provisions made in the
National Act.
• Enactment of State Public Health Protection Acts that define the norms tor
nutritional security, drinking water quality, sanitary facilities and other key
determinants of health. Such acts would complement the existing acts
regarding environmental protection, working conditions etc. to ensure that
citizens enjoy the full range of conditions necessary for health, along with the
right to accessible, good quality health services.
• Substantial increase in State budgetary provisions for Public health to
parallel the budgetary increase at Central level, this would entail at least
doubling of state health budgets in real terms by 2009.
• Operationalising a State level health services monitoring mechanism,
consisting of a State Health Services Monitoring and Consultative
Committee to periodically review the implementation of health rights, and
underlying policy and structural issues in the State. Half of the members of
this Committee would be drawn from State level health sector civil society
platforms. Conesponding Monitoring and Consultative Committees with
civil society involvement would be formed in all districts, and to monitor
urban health services in all Class A and Class B cities.
• Instituting a Health Rights Redressal Mechanism at State and District
levels, to enquire and take action relating to all cases of denial of health care
in a time bound manner.
• A set of public health sector reform measures to ensure health rights
through strengthening public health systems, and by making private care more
accountable and equitable. The minimum aspects of a health sector reform
4
framework that would strengthen public health systems must be laid down as
an essential precondition to securing health rights. An illustrative list of such
measures is as follows:
1. State Governments should take steps to decentralize the health services
by giving control to the respective Panchayati Raj Institutions(PRIs)
concerning the government hospitals up to the district level. Enough funds
from the plan and non plan amount should be devolved to the PRIs at
various levels. The local bodies should be given the responsibility to
formulate and implement health projects within the overall framework of
the health policy of the state. The elected representatives of the PRIs and
the officers should be given adequate training in local level health
planning. Integration between the health department and local bodies
should be ensured in formulating and implementing the health projects at
local levels.
2. The adoption of a State essential drug policy that ensures full availability
of essential drugs in the public health system. This would be through
adoption of a graded essential drug list, transparent drug procurement and
efficient drug distribution mechanisms and adequate budgetary outlay.
The drug policy should also promote rational drug use in the private
sector.
3. The health department should prepare a State Drug Formulary based on
the health status of the people of the state. The drug formulary should be
supplied at free of cost to all government hospitals and at subsidized rate
to the private hospitals. Regular updating of the formulary should be
ensured. Treatment protocols for common disease states should be
prepared and made available to the members of the medical profession.
4. The adoption of a Universal community health worker programme
with adequate provisioning and support, so as to reach out to the weakest
rural and urban sections, providing basic primary care and strengthening
community level mechanisms for preventive, promotive and curative care.
5. The adoption of a detailed plan with milestones, demonstrating how
essential secondary care services, including emergency care services,
which constitute a basic right but are not available today, would be made
universally available.
6. The public notification of medically underserved areas combined with
special packages administered by the local elected bodies to close these
gaps in a time bound manner.
7. The adoption of an integrated human resource development plan to
ensure adequate availability of health humanpower at all levels.
8. The adoption of transparent non-discriminatory workforce management
policies, especially on transfers and postings, so that medical personnel
are available for working in rural areas and so that specialists are
prioritised for serving in secondary care facilities according to public
interest.
5
I
9. The adoption of improved vigilance mechanisms to respond to and limit
corruption, negligence and different forms of harassment within both the
public and private health system.
•
•
Ensuring the implementation of the Supreme court order regarding food security,
universalising ICDS programmes and mid day school meal programmes, to
address food insecurity and malnutrition, which are a major cause of ill-health.
People’s access to emergency medical care is an important facet of right to health.
Based on the Report of the Expert Group constituted by NHRC (Dr. P.K.Dave
Committee), short-term and long-term recommendations were sent to the Centre and
to all States in May 2004. In particular, the Commission recommended:
(i)
Enunciation of a National Accident Policy;
(ii)
Establishment of a central coordinating, facilitating, monitoring
and controlling committee for Emergency Medical Services (EMS)
under the aegis of Ministry of Health and Family Welfare as
advocated in the National Accident Policy.
(iii)
Establishment of Centralized Accident and Trauma Services in all
districts of all States and various Union Territories along with
strengthening infrastructure, pre-hospital care at all government
and private hospitals.
• Spurious drugs and sub-standard medical devices have grave implications for the
enjoyment of human rights by the people. Keeping this in view all authorities are
urged to take concrete steps to eliminate them.
•
Access to Mental health care has emerged as a serious concern. The NHRC
reiterates its earlier recommendations based on a Study “Quality Assurance in
Mental Health” which were sent to concerned authorities in the Centre and in States
and underlines the need to take further action in this regard.
Recommendations to NHRC
• NHRC would oversee the monitoring of health rights at the National level by
initiating and facilitating the Central Health Services Monitoring Committee,
and at regional level by appointing Special Rapporteurs on Health Rights for
all regions of the country.
• Review of all laws/statutes relating to public health from a human rights
perspective and to make appropriate recommendations to the Government for
bringing out suitable amendments.
Recommendations to SHRCs
• SHRCs in each state would facilitate the State Health Rights Monitoring
Committees and oversee the functioning of the State level health rights
redressal mechanisms.
6
Recommendations to Jan Swasthya Abhiyan and civil society organisations
•
JSA and various civil society organisations would work for the widest
possible raising of awareness on health rights - ‘Health Rights Literacy’
among all sections of citizens of the country.
7
NARMADA BACHAO ANDOLAN
Maitri Nhvas,.Dhadgaon P.O, Nandurbar, Maharashtra
Ph: 02595-220620
62 M.O Marg, Badwani, Madhya Pradesh - 45155 J
Telefax: 07290-222464
C/o B-13 Shivam-Flats, Ellora Park Baroda 390007,
Gujarat. Telefax: 0265-2282232
Health Rights in Situations of Conflict and Displacement
A Brief Note Jointly prepared by
Ms. Yoghd Khanolkar, Dr.Revathy Joshi and Dr. Suhas Kothekar
The National Public Hearing on Right to Health Care, as we understand, is part of a
process to understand, assess and analyze issues related to health towards creating better
awareness of health rights among the people. This initiative by NHRC clearly indicates that the
demand for total health is not merely a secondary' issue but an important component of human
rights.
/
WHO defines that ‘"Health is physical mental and social wellbeing and not merely
absence of diseases”. So while curative aspects are normally given more importance, any attempt
at attaining lull health rights should have preventive measures as the priority. Hence a deeper
understanding and analysis of the causes of illness and disease is necessary.
We understand Displacement as a Physical, Emotional and Social crisis because it
severely destroys the traditional health patterns and systems which have evolved out of
generations of living in specific community oriented atmosphere. Due to human made
displacement like Big Dams. High Ways. Mining, Military' Firing Range, Privaiizaiion of coastal
sea resources. Tourism, Sanctuaries, Industrial disasters like Bhopal Gas Tragedy, Communal
riots or War, the affected peoples - most of them being the so called weaker sections like
adivasis, daliu, women, children and minorities - finds their Right to Health Care brutally
violated.
One significant example of this violation can be seen in the Narmada Valley’ where the
health of the dam affected adivasis are deteriorating day by day. whether in the flood affected
areas in the valley or in the resettlement sites. While tlie State policies and laws and even the
Supreme Court (in its October 2000 verdict) endorses the argument that displacement improves
health and livelihood means of the affected, this is not based on any detailed study per fie. This
new of the educated urbanized policy makers need to be challenged. The reality fa that, since
health or well being fa directly connected to livelihood and community relationships, forced
displacement which does not provide £de<iuate alternative resources, will had to violation
of health rights. Providing physical resources is not enough. It is necessary to ensure that the
affected groups arc enabled to maintain their social and cultural life. In most situations this is not
possible.
The Existing policies and laws are not sufficiently addressing the complex issue of the
violation oi health rights due to displacement. This may not be primarily due to a lack of effort
but a problem with the perspective and the methodologies used so far. A more participatory
process, with definite involvement of the displaced peoples will initiate a fresh path in the search
for ensuring bener health care rights to the affected populations.
VIOLATION OF RIGHT TO HEALH AND HEALTH CARE AS A CONSEQUENCE OF
DISHzACEMENT IN THE NARMADA VALLEY
Many of us may remember the news clippings from Harsud (M.P.) this monsoon wherein
the residents of this city, displaced by the large dam Indira Sagar were made to demolish their
homes with their own hands and said to be rehabilitated in Chanera, the rehabilitation site. Few
days later we also learnt that in this rehabilitation site women had no place to go to toilet
Imagine the plight of a pregnant woman. Along with the tanker supplying drinking water, there
used to be an official announcement telling “Do not use this water for drinking without boiling'
and of course availability of fiiel was a problem too. Things have been worse in many more
villages but often there is no access to let the world know about it.
z
We have been working for several years with die people displaced by Sardar Saroyar
project. one of the two mega dams on the Narmada and would like to present some data and
share our experiences with you all who respect the basic human rights. Even though the
Governments on their computers/website shows number of project affected people (PAFs) at the
dam height of 110 meters in each of the three states, namely Maharashtra. Madhya Pradesh and
Gujarat as ‘ZERO’, there are at least 11000 PAFs still stay ing in the original villages, some of
them haring dissatisfied with and returned from the rehabilitation sites. They have been facing
numerous problems but here we summarize just the few that affect their HEALTH directly.
(SLIDE NO 1 and 2).
Given bdow are some of the Factors that affect the Health ofthe displaced people.
a) The loss ot fertile land leading to scarcity of food, severe anemic condition of people
in general and of women in particular. The children borne to such anemic mothers, if
surviving are also severely anemic.
b) Malnutrition in children leading to deaths (but under-reported by the governments as
the health personnel do not reach the villages facing submergence and thus not
haring easy access.) causes severe traumatic condition in parents, at times leading to
mental sickness.
c) Fatal contamination of water because of submergence, leading to complaints of
frequent stomach upset and fever and even incidences of death in children showing
symptoms of gastroenteritis.
d) Stagnant bock waters of the dam causing increase in mosquito home diseases, such as
Malaria.
e) Difficulties in reaching out to free flowing river leading to unhygienic conditions and
increase in skin infections such as scabies.
f) Decrease in the availability of fish, the only protein source for these tribals resulting
from the stagnation of the river leads to decrease in general resistance and increase in
g) Complaints of not feeling well.
h) Decrease in the availability of fruits and edible roots (rhizomes) because of
destruction of the forests.
i) Submergence of forests and decomposition of trees may be adding tome toxic
compounds and possibly leading to complaints of stomach upset
j) Unnatural deaths because of
• Drowning as a result of getting trapped in the sludge (silt)
plai upon the
• Being eaten up by
oy crocodiles (As the crocodiles have lost, their breathing places
big rocks in the river as a result of increased back water level, they have to come to the
banks for breathing).
• Poisonous snake biting e\^n while sleeping on cot. (Poisonous snakes from the
submerged forests, having been displaced from their natural habitat get more aggressive
and attack people in the areas surrounded by water)
Status of Health Care services in these villages
Most of these villages do not have any easy access to the primary health centre.
There is no health care worker paying regular visits.
There is no information about many health related programs announced bv the
Government such as Antyoday Yojana, Mid-day meals or even allowance available to the
pregnant and lactating women.
If at all a patient reaches a rural hospital, s.'he is not given proper attention .There is an
inclination to send the patient to the Civil hospital which is further away and the patients’ family,
even though below’ the poverty line, is asked to make their own arrangements for transporting the
patient The hospital’s vehicle or driver is not available or there is no fund for diesel.
Thus, the displaced always experience very callus and humiliating treatment from most
of tte staff members. All this adds to their stress. Having lost their traditional rights to Natural
resources, like land, river, fish, forest minor produce and traditional medicines, they are forced to
move out to city slums in very unhygienic conditions and work as labor on a day to day basis.
Thus they are economically and socially in a very vulnerable situation. This may force them to
get trapped into various illegal activities, addictions and sexual harassments, thus increasing the
risk of being exposed to various new diseases like AIDS.
16 December 2004
Narmada Bachao Andolan
Section III: Violation of Health Rights in India
ire and their impact on access to health
Const^tional provisions
provisions in
in the
the country
country and
and International
International covenants
signed by India.
.TlLi„^rs^S'X3°.T t’TiT’i r”““in8
protection of life and personal libertv f11011 2
.0 live With h„™„
health facilitil
' 1» "S
‘o S“ aS,:' Th
8
Declaration.51316
Wishes,
of the Constitution guarantees
Sf"Pr‘m: Cf“ h“ h'M ,h“ ,h' ■*
to I,fe and the go.emtnent has a constitutional obligation to provide
»('XiSiZ°f±
ot Which
"8ht “
C“,i“” - "»
°r
e.« p™„ is a
let us also examine some the key covenants which India has ratified
aCC6SS aS deSCribed earlier are evide-e of violation of the
^°theVn a'ttSZMhe Inte™ational Covenant on Economic, Social and Cultural Rights (ICESCR)
and the Umted Nanons Convention on the Rights of the Child fCRC^
International Covenant on Economic, Social and Cultural Rights
=S== —■~ SSi-.-s
■a==:::::=~z~' —“
This right has been elaborated upon and clarified by the General Comment
14 of the UN
onunittee on Economic, Social and Cultural Rights, adopted in the year 2000*
ics‘sarr:Ti
k
iinplemeoioiion". Recognition of the riolu to h^'hl
India, hence this oblign.L ™,.i!ts Ji.MM.
" e8"i'“,e
of legislative
I"
413
“..and to adopt a national health policy with a detailed plan for realizing the right to health “.
No such plan exists in the National health policy 2002.
“States must ensure provision of health care, ”
Gross deficiencies in provision of health care by the Government have been described in the
previous section..
“...including immunization programmes against the major infectious diseases, and ensure equal
access for all to the underlying determinants of health, such as nutritiously safe food and potable
drinking water, basic sanitation and adequate housing and living conditions. ”
“Public health infrastructures should provide for sexual and reproductive health services,
including safe motherhood, particularly in rural areasT
India’s high maternal mortality rate at 408 per lakh live births, poor coverage of antenatal and
delivery' services indicate large scale violation of this right.
“States have to ensure the appropriate training of doctors and other medical personnel, the
provision of a sufficient number of hospitals, clinics and other health-related facilities, and the
promotion and support of the establishment of institutions providing counselling and mental
health services, with due regard to equitable distribution throughout the country. ’’
There are large scale inequities in availability of doctors and hospital beds between urban and
rural areas as shown below
The General Comment 14 also clearly specifies certain Core obligations of states related to the
right to health:
“43 ... States parties have a core obligation to ensure the satisfaction of, at the very least,
minimum essential levels of each of the rights enunciated in the Covenant, including essential
primary health care. ”
“(a) To ensure the right ofaccess to health facilities, goods and services on a non-discriminatory
basis, especiallyfor vulnerable or marginalized groups; ”
Vulnerable groups such as rural and tribal populations suffer from denial of physical access to
quality health services; one fact which exemplifies the consequence of such denial is that the
tribal population, which constitutes only 8% of the total population, contributes 50% of the
malarial deaths in the country. The large sections of the population living in poverty sufier from
lack of financial access concerning private medical services. For example, a person from the
poorest quintile of the population, despite more health problems, is six times less likely to access
hospitalization than a person from the richest quintile.
“(d) To provide essential drugs, as from time to time defined under the WHO Action Programme
on Essential Drugs; ”
All Essential drugs remain inaccessible for an estimated 80% of the population.
“(e) To ensure equitable distribution of all health facilities, goods and services:
There is grossly inequitable distribution between urban and rural areas as described earlier.
“(ft To adopt and implement a national public health strategy and plan of action, on the basis of
epidemiological evidence, addressing the health concerns of the whole population; the strategy’
and plan of action shall be devised, and periodically reviewed on the basis ofa nartim ,
,
transparent process; they shall include methods, such as right to £1^^ ^ “ >
There is neither such a national public health strategy, nor are we aware of anv
r
“d 1""p,lr"" review; n°r l“ve
Motors .nd beni.rks “e°„
The General comment 14 has clearly specified ‘Violations of the obligation to fulfil’ as followsJ- Violations of the obligation to fullfil occur through the failure of States parties to take all
ado^-T t0~e,he^lizaIi0n °f‘he ^t to health. Examples incLTthe^
P
plement a national health policy designed to ensure the right to health for evervone ■
°fpubliC reS°UrCeS which resuIts in the ^n-enjoyment
Er lure .
I , by
or
particularly the vulnerable or marginalized- the
fadu e to monitor the realization of the right to health at the national level, for exampie by
dentifying right to health indicators and benchmarks; the failure to take measures to reduce the
lequitable distribution of health facilities, goods and services; the failure to adopt a gender
PracficallZl oft
thefai'Ure t0 reduCe infant and ma^nal mortality rates
}
of these violations exist on a consistent and continued basis as described earlier.
FinaHy the GC 14 has specified the desirability of a national legislation on Right to healthshould consider adopting a framework law to operationalise their right to health
mole
S^teSy The Rework law should establish national mechanisms for monitoring the
implementation ofnational health strategies and plans of action "
omtormg Hie
Needless to add, no such legislation or framework exists in India.
United Nations Convention on the Rights of the Child
The United Nations
Convention 011 ^ie Rights of the Child entered into force in 1990 and was
.
ratified by India in
in 1992. Article 24 of CRC clearly mandates the right to health and health care
for children:
Article 24
•7. States Parties recognize the right of the child to the enjoyment of the highest attainable
farfefshal^f af,O-facilidesfor the ^^nt of illness and rehabilitation of health. States
cZ^
°
"°
iS depriVBd O^his Or her r^> of access ito such health
With 18 lakh avoidable child deaths taking place in
India every year, it is obvious that this right
remains largely unrealized
d.. States Parties shall pursue full implementation of this right and, in particular,
shall take
■appropriate measures:"
"(a) To diminish infant and child mortality: "
The expected decline in both IMR and CMR has not taken place during the 1990s. The current
acZe MDGXiofrtSVtS
*
“ ,O
IS
"(b) To ensure the provision of necessary medical assistance and health care to all children with
emphasis on the development ofprimary health care; ”
Gross inequities exist in access to health care for children in rural areas compared to urban areas,
and for children from poor families compared to those from well off families. For example,
children from the bottom income quintile suffer a 2.5 times higher infant mortality compared to
children from the top income quintile; children from lower standard of living households suffer
3.9 times higher child mortality, compared to children from the higher standard of living
households.
"(c) To combat disease and malnutrition, including within the framework ofprimary health care,
through, inter alia, the application of readily available technology and through the provision of
adequate nutritious foods and clean drinking-water, taking into consideration the dangers and
risks of environmental pollution; ’’
According to National Institute of Nutrition data, 92% children in rural areas suffer from
malnutrition. Only 54% of all children under age three are fully protected with immunisation.
Around 6 lakh children die each year from an ordinary illness like diarrhea, almost all these
deaths would have been prevented if safe drinking water and sanitary conditions were available.
"(d) To ensure appropriate pre-natal and post-natal health care for mothers; "
Only 20 percent of mothers receive all of the recommended types of antenatal care, Nearly twothirds of births are delivered at home and 83 percent of women who give birth at home receive no
postpartum care.
"(e) To ensure that all segments ofsociety, in particular parents and children, are informed, have
access to education and are supported in the use of basic knowledge of child health and nutrition,
the advantages of breastfeeding, hygiene and environmental sanitation and the prevention of
accidents;"
Only about 40% babies are exclusively breastfed and only 33% are given timely complementary
feeds. The life saving Oral Rehydration Solution is presently administered in only 27% of cases
of diarrhea in India.
"(f) To develop preventive health care, guidance for parents and family planning education and
services. "
The above mentioned sample facts illustrate the large scale deficiencies in preventive health care
for children. As far as guidance for parents is concerned, according to the CAG report on ICDS
centres, in QI per cent of the ICDS projects, no health awareness activities were carried out. This
was due to non availability of media, defective projectors and other equipment, lack of training
for use of equipment and of course, general lack of time and motivation.
This overview demonstrates that violation of health rights, which have been mandated in certain
international covenants ratified by the Govt, of India, is not occasional or accidental, but is
universal, large scale and related to systemic issues.
6.1^
Section IV: Initiatives to Remedy the Situation
It is but obvious that a large number of initiatives are required to remedy the present situation
Some immediate steps related to the health care system that need to be taken include:
National Public Health Act mandating assured provision of basic health services: The
Union health ministry max initiate the process by having a discussion in the Centra]
Council on Health (including all state health ministers) and developing a consensus on
the issue. Passing a ‘National Public Health Act’ (stipulated long back by Bhore
committee-1946 and Mudaliar Committee-1961), which would specify a set of basic
health services to be available to all as a right, including legal obligations of public and
private health care providers, health rights of citizens, standards of care and certain
proportion of public funds to be earmarked for public health. State governments to pass
corresponding ‘State public health services rules’ within specified time.
• Making health care a fundamental right by suitable constitutional amendment. The
formulation of a National legislation mandating the Right to Health care, with a clearly
defined comprehensive package of health care, along with authorization of the requisite
budget, being made available universally within one year.
• The Government should undertake a review of the National Health Policy (2002) to
foreground the Primary Health Care approach and the goal of Universal access to
comprehensive health care: along with elimination of measures to promote the private
medical sector and ‘medical tourism’.
• Significant strengthening of the existing public health system with commitment to
quality coverage and equity, especially in rural areas, by assuring that all the required
infrastructure, staff, equipment, medicines and other critical inputs are available, and
result in delivery of all required sendees at the primary secondary and tertiary levels.
These would be ensured based on clearly defined, publicly displayed and monitored
norms. Health services need to be integrated and vertical programs must be phased out
• The declining trend of budgetary allocations for public health needs to be reversed, and
budgets appropriately upscaled to make optimal provision of health care in the public
domain possible. At one level adopting a fiscal policy of block funding or a system of per
capita allocation of resources to different levels of health care, with an emphasis on
Primary Health Care will have an immediate impact in reducing rural-urban inequities by
making larger resources available to rural health facilities like Primary health centres and
Rural hospitals. Simultaneously, the budgetary allocation to the health sector must be
increased substantially, targeting the 5% of GDP as public expenditure on health care as
recommended by the WHO.
e
If the public health system fails to deliver it should be treated as a legal offence, remedy
for which can be sought in the courts of law. The public system must ensure all elements
of care like drug prescriptions, diagnostic tests, child birth services, hospitalization care
etc.
Universalisation of the ICDS scheme should be undertaken in a time bound framework,
along \\ ith the convergence of the scheme with state health sen ices.
• There is a need for a range of policy measures to eliminate discrimination, and to provide
special quality and sensitive services for women, children, elderly persons, unorganised
sector workers, 111V-AIDS affected persons, disabled persons, persons with mental health
problems and other vulnerable groups. Similarly, situations of conflict, displacement and
migration need to be addressed with a comprehensive approach to ensure that the health
rights of affected people are protected.
•
61)^
•
•
•
•
•
•
Putting in place a National legislation to regulate the private health sector, to adopt
minimum standards, accreditation, standard treatment protocols, standardised pricing of
services etc. Also a mechanism to be put in place to regulate private medical colleges.
The government operationalise a system and set up a central fund for procurement of
essential drugs. Such a central fund could be utilised for procurement of a set of essential
drugs in all states, to be made available through Sub-centres, PHCs and CHCs. This fund
could be matched by a state essential drugs fund and transparent, rationalised procurement
and distribution system at state level. The model being pursued in Tamil Nadu could
possibly be examined for this purpose.
Effective drug price control and promotion of rational drugs'. Steps be taken to impose
price control on all drugs of the National Essential Drug List in a phased mannei. This
would require amendment of the DPCO (2002) and a thorough review of the 2002 Drug
Policy.
The state should introduce a new community-anchored health worker scheme, and
implement it in a phased manner with involvement of people s organizations and
panchayati raj institutions, in both rural and urban areas, through which first contact
primary care and health education can be ensured.
All state level coercive population control policies, disincentives and ordeis should be
removed and disproportionate financial allocation for population control activity should
not be allowed to skew funding from other important public health priorities.
Sreamlining of medical education to create a basic doctor ensuring a wider outreach and
improvement of access to health care services in all areas. Regulation of the growth of
capitation based medical colleges
GIS
PEOPLE'S HEALTH CHARTER
We the people of India, stand united in our condemnation of an iniquitous global system that, under the garb ot
“globalisation" seeks to heap unprecedented miser, and destitution on the overwhelming majority of the people on this
globe. This system has systematically ravaged the economics of poor nations in order to extract profits that nurture a
handful of powerful nations and corporations. The poor, across the globe, arc being further marginalised as they arc
displaced from home and hearth and alienated from their sources of livelihood as a result of the forces unleashed by this
svstem. Standing in firm opposition to such a system we reaffirm our inalienable right to comprehensive health care that
includes food security; sustainable livelihood options; access to housing, drinking water and sanitation; and appropriate
medical care for all; in sum — the right to HEALTH FOR ALL, NOW!
The promises made to us by the international community in the Alma Ata declaration have been systematically repudiated
by the World Bank, the IMF. the WTO and its predecessors, the World Health Organization, and by a government that
functions under the dictates of international Finance Capital. The forces of “globalization" through measures such as the
structural adjustment programme arc targeting our resources — built up with our labour, sweat and lives over the last fifty
vears — and placing them in the service of the global “market" for extraction of super-profits. The benefits of the public
sector health care institutions, the public distribution system and other infrastructure - such as they were - have been
taken away from us. It is the ultimate irony that we arc now blamed for our plight, with the argument that it is our
numbers and our propensity to multiply that is responsible for our poverty and deprivation
We declare health as a justiciable right and demand the provision of basic health care as a fundamental constitutional right
c ;ery one of us. We assert our right to take control of our health in our own hands and for this the right to:
• A truly decentralised system of local governance vested with adequate power and responsibilities and provided with
adequate finances;
• A sustainable system of agriculture based on the principle of “land to the tiller", linked to a decentralized public
distribution system that ensures that no one goes hungry;
• Universal access to education, adequate and safe drinking water, and housing and sanitation facilities;
• A dignified and sustainable livelihood;
• A clean and sustainable environment;
• A drug industry geared to producing cpidcmiologically essential drugs at affordable cost;
• A health care system which is responsive to the people's needs and whose control is vested in peoples hands;
Further, we declare our firm opposition to:
• Agricultural policies attuned to the needs of the “market" that ignore disaggregated and equitable access to food
• Destruction of our means to livelihood and appropriation, for private profit, of our natural resource bases;
• The conversion of Health to the mere provision of medical facilities and care that arc technology intensive, expensive,
and accessible to a select few;
< 'he retreat, by the government, from the principle of providing free medical care, through reduction of public sector
expenditure on medical care and introduction of user fees in public sector medical institutions, that place an
unacceptable burden on the poor;
• The corporatization of medical care, state subsidies to the corporate sector in medical care, and corporate sector health
insurance;
> Coercive population control and promotion of hazardous contraceptive technology.
• The use of patent regimes to steal our traditional knowledge and to put medical technology and drugs beyond our
reach;
® Institutionalization of divisive and oppressive forces in socictv ^ueb as fundamentalism, caste 'u.:: c-iv. and the
attendant violence, which have destroyed our peace and fragmented oi.r solidarity
In the light of the above we demand that.
1. The concept of comprehensive primary health care, as envisioned in the Alma /\ta Declaration should form the
fundamental basis for formulation of all policies related to health care. The trend towards fragmentation of health
delivery programmes through conduct of a number T ■
pr -:;!J. be reversed National health
programmes be integrated within the Primary Health Care system with decentralized planning, decision-making and
implementation Focus be shifted from bio-medical and individual based measures to social, ecological and community
based measures.
2. The primary' medical care institutions including trained village health workers, sub-centres, and the PHCs staffed by
doctors and the entire range of community health functionaries be placed under the direct administrative and financial
control of the relevant level panchayat raj institutions. The overall infrastructure of the primary health care institutions
be under the control of panchayati raj and gram sabhas and provision of free and accessible secondary and tertiary
level care be under the control of Zilla Parishads, to be accessed primarily through referrals from PHCs. The essential
components of primary’ care should be:
• Village level health care based on Village Health Workers selected by the community and supported by the Gram
Sabha / Panchayat and the Government health services;
• Primary Health Centers and subcentres w ith adequate staff and supplies which provides quality curative services at
the primary health center level itself with good support from linkages;
• A comprehensive structure tor Primary Health Care in urban areas based on urban PHCs, health posts and
Community Health Workers;
• Enhanced content of Primary Health Care to include all measures which can be provided at the PHC level even for
less common or non-communicable diseases (c.g. epilepsy, hypertension, arthritis, prc-cclampsia, skin diseases)
and integrated relevant epidemiological and preventive measures.
• Surveillance centres at block lc\cl to nieiii:. r the
^luaUuii and tertiary care with all speciality
services, availaiblc in every district.
A comprehensive medical care programme financed by the government to the extent of at least 5% of our GNP, of
which at least half be disbursed to panchayati raj institutions to finance primary level care. This be accompanied by
transfer of responsibilities to PRIs to run major parts of such a programme, along with measures to enhance capacities
of PRIs to undertake the tasks involved.
4. The policy of gradual privatisation of government medical institutions, through mechanisms such as introduction of
user fees even for the poor, allowing private practice by Government Doctors, giving out PHCs on contract, etc. be
abandoned forthwith. Failure to provide appropriate medical care to a citizen by public health care institutions be made
punishable by law.
5. A comprehensive need-based humanpowcr plan for the health sector be formulated that addresses the requirement for
creation of a much larger pool of paramedical functionaries and basic doctors, in place of the present trend towards
over-production of personnel trained in super-specialities. Major portions of undergraduate medical education, nursing
as well as other paramedical training be imparted in district level medical care institutions, as a necessary complement
to training provided in mcdical/nursing colleges and other training institutions. No more new medical colleges to be
opened in the private sector. Steps be taken forthwith to close down private medical colleges charging fees higher than
state colleges or taking any form of donations, and to eliminate illegal private tuition by teachers in medical colleges.
At least an year of compulsory rural posting for undergraduate (medical, nursing and paramedical) education be made
mandatory, without which license to practice not be issued. Similarly, three years of rural posting after post graduation
be made compulsory.
6. The unbridled and unchecked growth of the commercial.private sector be brought to a halt. Strict observance of
standard guidelines for medical and surgical intervention and use of diagnostics, standard fee structure, and periodic
prescription audit to be made obligatory. Legal and social mechanisms be set up to ensure observance of minimum
standards by all private hospitals, nursing/matcrnitv homes and medical laboratories Prevalent
of offering
commissions for referral to be made punishable by law. For this purpose a body with statutory po-y.-rs be constituted,
wiuch has due representation from peoples organisations and professional organisations.
7. A rational drug policy be formulated that ensures development and growth of a suit reliant industry for production of all
essential drugs at affordable prices and ot proper quality. The policv should, on a priority basis:
• ban all irrational and hazardous drugs;
• introduce production quotas and price ceiling for essential drugs;
• promote compulsory use of generic names.
• regulate advertisements, promotion and marketing of all medications based on ethical criteria.
• formulate guidelines for use of old and new vaccines;
• control the activities of the multinational sector and restrict their presence only to areas where they are willing to
bring in new technology:
• recommend repeal of the new patent act and bring back mechanisms that prevent creation of monopolies and
promote introduction of new drugs at affordable prices;
• promotion of the public sector in production of drugs and medical supplies, moving towards complete self-reliance
in these areas.
X. Medical Reseach priorities be based on morbidity and mortality profile of the country , and details regarding the
direction, intent and focus of all research programmes be made entirely transparent. Adequate government funding be
provided for such programmes. Ethical guidelines for research involving human subjects be drawn up and
implemented after an open public debate. No further experimentation, involving human subjects, be allowed without a
proper and legally tenable informed consent and appropriate legal protection. Failure to do so to be punishable by law .
All unctical research, especially in the area of contraceptive reseach. be stopped forthwith. Women (and men) who.
without their consent and knowledge, have been subjected to experimentation, especially with hazardous contraceptive
technologies to be traced forthwith and appropriately compensated. Exemplary damages to be awarded against the
institutions (public and private sector) involved in such anti-people, unethical and illegal practices in the past
9. All coercive measures including incentives and disincentives for limiting family size be abolished. The right of
families and women within families in determining the number of children they want should be recognised.
Concurrently, access to safe and affordable contraceptive measures be ensured which provides people, especially
women, the ability to make an informed choice. All long-term, invasive, systemic hazardous contraceptive
technologies such as the injectables (NET-EN. Depo-Provcra. etc ), sub-dermal implants (Norplant) and anti fertility
vaccines should be banned from both the public and private sector. Urgent measure be initiated to shift to onus of
contraception away from women and ensure at least equal emphasis on men's responsibility for contraception
10.Support be provided to traditional healing systems, including local and home-based healing traditions, for systematic
research and community based evaluation with a view to developing the knowledge base and use of these systems
along with modern medicine as part of a holistic healing perspective^
1 1 Promotion of transparency and decentralisation in the decision making process, related to health care, at all levels as
well as adherence to the principle of right to information. Changes in health policies to be made only after mandatory
wider scientific public debate.
□ Introduction of ecological and social measures to check resurgence of communicable diseases. Such measures should
include:
• integration of health impact assessment into all development projects;
• decentralized and effective surveillance and compulsory notification of prevalent diseases like malaria. TB by all
health care providers, including private practitioners;
• reorientation of measures to check STDs/AIDS through universal sex education, checking social disruption and
displacement and commercialisation of sex, generating public awareness to remove stigma and universal
availability of preventive and curative services, and special attention to empowering women and availability of
gender sensitive services in this regard.
13 Facilities for early detection and treatment of non-communicable diseaseslike diabetes,
be available to ail att appropriate levels of medical care.
cancers, heart diseases, etc. to
14 Women-centered health initiatives that include:
• awareness generation for social change on issues of gender and health, triple work burden, gender discrimination in
nutrition and health-care:
• preventive and curative measures to deal with health consequences of womens' work and domestic violence:
• complete maternity benefits and child care facilities to be provided in all occupations employing women, be they in
thq,organizcd or unorganized sector;
• special support structures that focus on single, deserted, widowed women and commercial sex workers; gender
sensitive services to deal with reproductive health including reproductive system illnesses, maternal health,
abortion, and infertility;
• vigorous public campaign accompanied by legal and administrative action against female feticide, infanticide and
sex pre-selection.
15.Child centered health initiatives which include:
• a comprehensive child rights code, adequate budgetary allocation for universalisation of child care services, a
expanded and revitalized ICDS programme and ensuring adequate support to working women to facilitate child
care, especially breast feeding;
• comprehensive measures to prevent child abuse and sexual abuse;
• educational, economic and legal measures to eradicate child labour, accompanied by measures to ensure free and
compulsory elementary education for all children.
16.Special measures relating to occupational and environmental health which focus on:
• banning of hazardous technologies in industry and agriculture;
• worker centered monitoring of working conditions w ith the onus of ensuring a safe workplace on the management.
• reorientation of medical services for early detection of occupational disease;
• special measures to reduce the likelihood of accidents and injuries in different settings, such as traffic accidents.
industrial accidents, agricultural injuries, etc.
I 7. Measures towards mental health that promote a shift away from a bio-medical model towards a holistic model of
mental health. Community support and community based management of mental health problems be promoted.
Services for early detection and integrated management of mental health problems be integrated with Primary Health
Care.
IS.Measures to promote the health of the elderly by ensuring economic security, opportunities for appropriate
employment, sensitive health care-facilities and. when necessary, shelter for the elderly.
19. Measures to promote the health of physically and mentally disadvantaged by focussing on the abilities rather than
deficiencies. Promotion of measures to integrate them in the community with special support rather than segregating
them; ensuring equitable opportunities for education, employment and special health care including rehabilitative
measures.
20.Effective restriction on industries that promote addictions and an unhealthy lifestyle, like tobacco, alcohol, pan masala
etc., starting w ith an immediate ban on advertising and sale of their products to the young, and provision of services for
de-addiction.
Jan Swasthya Abhiyan contact addresses
B. Ekbal,
National Convenor, JSA
Vice Chancellor
University of Kerala
Trivandrum
Ph: 0471-306634(0)
0471- 444362(R)
e-mail.
Abhay Shukla
Amit Sen Gupta
JSA National Secretariat
Jt. Convenor, JSA
C/o CEHAT
Delhi Science Forum;D-158,
Flat No. 3 & 4, Plot No. 126
Lower Ground Floor,] Block,
Aman Tcrracc-E, Dahanukar Sakct, New Delhi-110017
Colony, Kothrud,
Ph: 011-26862716/26524324
Pune -411029
Ph: 020-2545141 / 25452325
e-mail:
Amitava Guha
Jt. Convenor, JSA
FMRAI,
372/21 Russa Road East
Kolkata- 700 033
Ph. 033-24242862(0)
e-mail:
Thelma Narayan
Jt. Convenor, JSA
Community Health Cell
No. 367. Srinivasa Nilaya.
Jakkasandra 1st Main,
Koramangala 1st Block,
Bangalore-560034
Ph:
080-5531518
5525372
e-mail :
Sarojini
Member, National Secretariat
Sama, 1st Floor
J-59, Sakct
New Delhi- 17
Ph: 011-26968972 / 26850074
e-mail:
T. Sundararaman
Jt. Convenor, JSA
Director,
State
Health
Resource Center
Kahbadi. Raipur - 492001
Phone:
0771-2236104,
2236175
I e-mail:
Vandana Prasad
Member, National Secretariat
L- 91, Sector 25
Noida, UP, 201301
Phone: 0120-2536578
e-mail:
For getting in touch with the international Peoples Health Movement contact:
Ravi Narayan
PHM Global secretariat
C/o Community Heath Cell
No. 367, Srinivasa Nilaya,
Jakkasandra 1st Main,
Koramangala 1st Block,
Bangalore-560034, Karnataka
Phone: 080 -51280009
Mira Shiva:
Voluntary Health Association of India
40, Insitutional Area, South of Delhi, New
Delhi,
110016
phone: 011-2330634(0); 6855010(R ).
Email: mirashiva@yahoo.com
Yet another way of getting in touch with the PHM network is to visi* its website - which
has a compendium of information about PHM and the contact addresses.
The website for PHM is
a'
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Pagel
Monday, November 29,2004
| O N L JJM E Y
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
I
I
COMPENSATION
— Arts. 21 and 32 — Compensation — Lunatic undertrial
prisoner languishing in jail for over 30 years — No action taken by
ACMM and jail authorities — Medical treatment provided only after High
Court intervened — Thus there has been complete violation of Art. 21
as also provisions of Prisons Act, CrPC and Lunacy Act — Accountability
not fixed so far — Under directions of the Court the undertrial has been
accommodated in the home maintained by Missionaries of Charity
(Brothers) at Kancharapara (W.B.) for the time being — Considering
the undertrial's present mental and physical health, direction for
payment of some interim compensation to him would not be of any
avail — He has no known relatives either — Therefore, as an interim
measure, the Court directed that a sum of Rs two lakhs shall be paid by
the State of West Bengal to the Missionaries of Charity (Brothers),
Howrah, by way of donation
(Para 6)D3181^ R.D. Upadhyay v. State ofA.P.,
(2001) 1 SCC
437 : AIR 2000 SC 1756 : 2000 Cri LJ 2277.
Bench Strength 3. Coram : DrA.S. Anand, C.J. and M. Jagannadha
Rao, V.N. Khare, JJ. [Date of decision : 29-11-2000]
[Search Text : MENTAL HEALTH ACT]
O V-v->
i I d
I
I
O'/
O C« Q I
ce.
Supreme Court Case Finder 2004, CopyrigiiL © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Monday, November 29, 2004
PON LINE T
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
SERVICE LAW
MEDICAL BENEFITS
Reimbursement of medical expenses — Room rent paid to
hospital includible — In absence of availability of specialised
treatment of a particular heart disease in the State Hospitals of Punjab,
permission given by the Director with the approval of the Medical Board
to get the treatment in an approved hospital outside the State and the
State Government servant concerned referred to one of such hospitals
(AIIMS at New Delhi, in this case) — In such circumstances, rent room
paid to the hospital by the government servant, held, reimbursable to
him by the State and could not be denioo on the ground of being
contrary to para (vii) of Government Resolution dated 25-1 -1991 as
right to health is integral to the right to life and the Government is
under a constitutional obligation to provide health facilities — Punjab
Government Letter No. 7/7/85/5 HBV/2498 dated 25-1-1991 —
Constitution of India — Article 21 — Health care — Right to health —
Govt, under a constitutional obligation to provide health facilities
The respondent, an employee of the State Government of Punjab,
had a heart ailment. Since, specialised treatment for that ailment was
not available in the hospitals maintained by the State Government, he
was given permission by the Director and approval by the Medical Board
to have treatment outside the State. His case was referred to AIIMS at
New Delhi. The question was whether while reimbursing his medical
expenses the room rent paid to the hospital by him was to be included
therein.
The State Government pleaded against the inclusion on the
ground of being contrary to para (vii) of its Resolution contained in letter
dated 25-1-1991. Rejecting that plea and allowing the employee's
appeal,
Held :
It is now settled law that right to health is integral to the right to
life. Government has a constitutional obligation to provide health
facilities. If the government servant has suffered an ailment which
requires treatment at a specialised approved hospital and on reference
whereat the government servant had undergone such treatment therein,
it is but the duty of the State to bear the expenditure incurred by the
government servant. Expenditure, thus, incurred requires to be
reimbursed by the State to the employee.State of Punjab v.
Mohinder Singh Chawla,
(1997) 2 SCC 83 : 1997 SCC (L&S) 294 :
AIR 1997 SC 1225 : (1997) 1 SLR 745.
-vx-Bench Strength 2. Coram : K. Ramaswamy and G.B. Pattanaik, JJ.
[Date of decision : 17-12-1996]
[Search Text
" RIGHT TO HEALTH"]
I
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Tuesday, November 30, 2004
This product is licenced to JANVIKAS (CSJ).. Vastrapur, Ahmedabad
|O N L I N E
SERVICE LAW
MEDICAL BENEFITS
— Reimbursement of medical expenses — Room rent paid to
hospital includible — In absence of ayailability of specialised
treatment of a particular heart disease in the State Hospitals of Punjab,
permission given by the Director with the approval of the Medical Board
to get the treatment in an approved hospital outside the State and the
State Government servant concerned referred to one of such hospitals
(AIIMS at New Delhi, in this case) — In such circumstances, rent room
paid to the hospital by the government servant, held, reimbursable to
him by the State and could not be denied on the ground of being
contrary to para (vii) of Government Resolution dated 25-1-1991 as
right to health is integral to the right to life and the Government is
under a constitutional obligation to provide health facilities — Punjab
Government Letter No. 7/7/85/5 HBV/2498 dated 25-1-1991 —
Constitution of India — Article 21 — Health care — Right to health —
Govt, under a constitutional obligation to provide health facilities
The respondent, an employee of the State Government of Punjab,
had a heart ailment. Since, specialised treatment for that ailment was
not available in the hospitals maintained by the State Government, he
was given permission by the Director and approval by the Medical Board
to have treatment outside the State. His case was referred to AIIMS at
New Delhi. The question was whether while reimbursing his medical
expenses the room rent paid to the hospital by him was to be included
therein.
The State Government pleaded against the inclusion on the
ground of being contrary to para (v/7) of its Resolution contained in letter
dated 25-1-1991. Rejecting that plea and allowing the employee's
appeal,
Held :
It is now settled law that right to health is integral to the right to
life. Government has a constitutional obligation to provide health
facilities. If the government servant has suffered an ailment which
requires treatment at a specialised approved hospital and on reference
whereat the government servant had undergone such treatment therein,
it is but the duty of the State to bear the expenditure incurred by the
government servant. Expenditure, thus, incurred requires to be
reimbursed by the State to the emoloyee.^s1
State of Punjab v.
Mohinder Singh Chawla,
(1997) 2 SCC 83 : 1997 SCC (L&S) 294 :
AIR 1997 SC 1225 : (1997) 1 SLR 745.
-v-Bench Strength 2. Coram : K. Ramaswamy and G.B. Pattanaik, JJ.
[Date of decision : 17-12-1996]
[Search Text
:
"(1997)
2 SCC 83")
I
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Tuesday, November 30, 2004
|ON LINE X
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
HEALTH CARE
— Arts. 21 and 32 — Medical aid — Denial of emergency medical
aid by govt, hospitals — Compensation for — Remedial
measures directed — Govt, duty-bound to provide timely medical
assistance to persons in serious/moribund condition — Medical facility
cannot be denied by govt, hospitals to such patients on ground of
non-availability of bed — Petitioner 2 (a member of Petitioner 1 Samiti)
sustaining serious head injuries and brain haemorrhage not admitted in
various State-run hospitals m city (Calcutta) oecause of non-availability
of bed and ultimately given treatment as indoor patient in a private
hospital as a result of which he incurring expenditure of Rs 17,000 —
Writ petition filed by petidoner being aggrieved by the indifferent and
callous attitude on the part of medical authorities of the State hospitals
— Held, denial of medical assistance to the petitioner by the State
hospitals amounted to violation of right to life under Art. 21 — State
directed to pay Rs 25,000 to petitioner as compensation — Enquiry
Committee headed by a retired Judge of High Court appointed by State
Govt, to conduct enquiry and recommend remedial measures —
Recommendations made by the Committee (para 10) accepted by the
State Govt, and directions issued by the Govt, on that basis for dealing
with the patients approaching health centres/OPDs/Emergency
Departments of govt, hospitals (paras 11 to 13) — Apart from those
recommendations, directions also issued by Supreme Court in order to
ensure availability of proper medical facilities for dealing with emergency
cases (para 15) — Other States should also take necessary steps in the
light of the recommendations of the Committee, directions of the State
of W.B. and further directions given by Supreme Court — State cannot
avoid its constitutional obligation on ground of financial constraints
The Constitution envisages the establishment of a welfare State at
the federal level as well as at the State level. In a welfare State the
primary duty of the Government is to secure the welfare of the people.
Providing adequate medical facilities for the people is an essential part
of the obligations undertaken by the Government in a welfare State. The
Government discharges this obligation by running hospitals and health
centres which provide medical care to the person seeking to avail of
those facilities. Article 21 imposes an obligation on the State to
safeguard the right to life of every person. Preservation of human iife is
thus of paramount importance. The government nospitais run by the
State and the medical officers employed therein are duty-bound to
extend medical assistance for preserving human life. Failure on the part
of a government hospital to provide timely medical treatment to a
person in need of such treatment results in violation of his right to life
guaranteed under Article 21. In the present case there was breach of
the said right of Petitioner 2 guaranteed under Article 21 when he was
denied treatment at the various government hospitals which were
approached even though his condition was very serious at that time and
d h
Supreme Court Case Finder 2004, Copyright © 1969-2004, FBC Publishing Pvt. Ltd.
Paoe 2
Tuesday, November 30, 2004
FonT’ine "f
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
he was in need of immediate medical attention. Since the said denial of
the right of the petitioner was by officers of the State, in hospitals run
by the State, the State cannot avoid its responsibility for such denial of
the constitutional right of the petitioner. In respect of deprivation of the
constitutional rights guaranteed under Part III of the Constitution the
position is well settled that adequate compensation can be awarded by
the court for such violation by way of redress in proceedings under
Articles 32 and 226 of the Constitution. The petitioner should, therefore,
be suitably compensated for the breach of his right guaranteed under
Article 21 of the Constitution. Having regard to the facts and
circumstances of the case, the amount of compensation is fixea at Rs
25,000.
It is the constitutional obligation of the State to provide adequate
medical services to the people co preserve human life. Whatever is
necessary for this purpose has to be done. The State cannot avoid its
constitutional obligation in that regard on account of financial
constraints. In the matter of allocation of funds for medical services the
said constitutional obligation of the State has to be kept in view. It is
necessary that a time-bound plan for providing these services should be
chalked out keeping in view the recommendations of the Committee as
well as the requirements for ensuring availability of proper medical
services in this regard as indicated by the Court and steps should be
taken to implement the same. The State of West Bengal alone is a party
to these proceedings. Other States, though not parties, should also take
necessary steps in the light of the recommendations made by the
Committee, the directions contained in the memorandum of the
Government of West Bengal dated 22-8-1995 and the further directions
given herein by us.
The Union of India is a party to these proceedings. Since it is the
joint obligation of the Centre as well as the States to provide medical
services it is expected that the Union of India would render the
necessary assistance in the improvement of the medical services in the
country on these lines.
As regards the Medical Officers who have been found to be
responsible for the lapse resulting in denial of immediate medical aid to
Petitioner 2 it is expected that the State Government will take
appropriate administrative action against those officers.^1
Paschim
Banga Khet Mazdoor Samity v. State of W.B.,
(1996) 4 SCC 37.
-v* Bench Strength 2. Coram : S.C. Agtawal and G.T. Nanavati, JJ.
[Date of decision : 6-5-1996]
[Search Text
:
"(1996)
4
SCC 37"]
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Monday, November 29, 2004
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
|ONLINE
CONSTITUTION OF INDIA
ARTICLE 32
/ Ih
Tn Ch<7U>-t See.
PUBLIC INTEREST LITIGATION (PIL)
PARTICULAR INSTANCES
— Arts. 32 and 21 — PIL — Ranchi Mental Hospital —
Mismanagement of — Report submitted by Chief Judicial Magistrate,
Ranchi revealing shocking and inhuman conditions in the hospital in
which large number of patients kept — Proper running of hospitals and
providing medical attention to every citizen is the obligation of the State
and it is difficult for Supreme Court to monitor management of a
hospital located far off — But State Government taking an indifferent
attitude and in spite of several interim orders of the Supreme Court and
assurances held out by the State, defects still not remedied — In the
circumstances change in administration necessary so as to give a totally
new 'service to patient' orientation to the institution — In the
circumstances a Committee of Management appointed by the Supreme
Court with a sitting High Court Judge as its Chairman — Directions
given to the Committee for proper functioning, management, funds etc.
— Parties, including the Committee, at liberty to move the Court from
time to time - Mental Health Act, 1987, Ss. 5, 13, 37, 39 and 77 D3181^
Rakesh Chandra Narayan v. State of Bihar,
1989 Supp (1) SCC 644
: AIR 1989 SC 348 : 1989 BUR 13.
Bench Strength 2. Coram : Ranganath Misra and M.N.
Venkatachaliah, JJ. [Date of decision : 27-9-1988]
Rakesh Chand Narain v. State of Bihar, 1986 Supp SCC 576, referred to
[Search Text
:
"MENTAL HEALTH ACT"]
Supreme Court Case Finder 2004, Copyright © 1969-2004,
EBC Publishing Pvt. Ltd.
Pa9e 1
Monday, November 29, 2004
| ON L I N E
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
MENTAL HEALTH ACT, 1987
— Ss. 3 to 8 — Suo motu action by Supreme Court — Detailed
directions issued to Central and State Govts, as well as UTs
regarding implementation of Act and undertaking awareness
campaign with special rural focus - Only licensed mental health
care institutions to be allowed to function — Compliance report to be
submitted within three months of date of Supreme Court's order Report to state specifically that no mental patient is chained in any part
of the State or UT — State/UTs having no govt.-run mental health
hospital to take steps to establish the same and file affidavit informing
Supreme Court within one montn of steps being taken — Constitution of
India - Art. 21 - Health care, Art. 21 - Mental Health
D31814
r^th
Chained Inmates in Asylum Fire in T.N., In re v. Union of
India,
(2002) 3 SCC 31 : AIP. 2002 SC 979.
«-**• Bencli Strength 3. Coram : M.B. Shah, B.N. Agrawai and Ariiit
Pasayat, JJ. [Date of decision : 5-2-2002]
[Search Text : "MENTAL HEALTH ACT"]~
’
--------------
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Tuesday, November JO, 2004
I O N L IJM E
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
HEALTH CARE
— Arts. 21, 41 and 47 — Right to healthy life — Held, is the
obligation of the State but Government is justified in limiting the
facilities to the extent permitted by its financial resources — Hence, the
decision of the appellant-State to restrict financial assistance to its
employees for medical treatment, within the resources of the State,
held, not violative of Art. 21 — Therefore deletion of list designated
private hospitals and payment at private hospitals at specified rates
fixed by Govt, not violative of Art. 21 — Service Law — Allowances —
Medical Allowance — Reimbursement of medical expenses
The respondents in this case were aggrieved by the change in
policy affected by the appellant-Government in regard to reimbursement
of medical expenses to its serving and retired employees. According to
previous policy promulgated in 1991, reimbursement of medical
expenses charged by certain designated hospitals like, Escorts, Apollo,
etc., were admissible. However, according to new policy promulgated on
13-2-1995, treatment could be had from any hospital but
reimbursement of medical expenses was to be restricted ''... to the
level of expenditure as per the rate fixed by the Director, Health and
Family Welfare, Punjab for a similar treatment package or actual
expenditure which ever is less". The new policy further laid down as
follows : ' 'The rate for a particular treatment would be included in the
advice issued by the District/State Medical Board. A Committee of
technical experts shall be constituted by the Director, Health and Family
Welfare, Punjab to finalise the roles of various treatment packages."
There were further instructions that reimbursement of medical expenses
will be according to the rates as prevalent in the All India Institute of
Medical Sciences (AIIMS).
The contention of the respondent was that in Surjit Singh case ,
the Supreme Court had already upheld reimbursement for treatment at
Escorts, and therefore now it would not be permissible for the
appellant-State to change its policy.
Declaring the new policy as constitutionally valid,
Held :
Right of one person correlates to a duty upon another, individual,
employer, Government or authority. The right of one is an obligation of
another. Hence the right of a citizen to live under Article 21 casts
obligation on the State. This obligation is further reinforced under Article
47, it is for the State to secure health to its citizens as its primary duty.
No doubt Government is rendering this obligation by opening
Government hospitals and health centres, but in order to make it
meaningful, it has to be within the reach of its people, as far as possible,
to reduce the queue of waiting lists, and it has to provide all facilities for
which an employee looks for at another hospital. Its upkeep,
maintenance and cleanliness has to be beyond aspersion. To employ the
best of talents and tone up its administration to give effective
Supreme Court Case Finder 2004, Copyright © 1969-2G04, EBC Publishing Pvt. Ltd.
Page 2
Tuesday, November 30, 2004
I O NI L I N E
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
contribution. Also bring in awareness in welfare of hospital staff for their
dedicated service, give them periodical medico-ethical and
service-oriented training, not only at the entry point but also during the
whole tenure of their service/Since it is one of the most sacrosanct and
valuable rights of a citizen and equally sacrosanct sacred obligation of
the State, every citizen of this welfare State looks towards the State for
it to perform this obligation with top priority including by way of
allocation of sufficient funds. This in turn will not only secure the right of
its citizen to the best of their satisfaction but in turn will benefit the
State in achieving its social, political and economical goal. For every
return, there has to be investment. Investment needs resources and
finances. So even to protect this sacrosanct right, finances are an
inherent requirement. Harnessing such resources needs top prioritv.
The State can neither urge nor say that it has no obligation to
provide medical facility. If that were so, it would be ex facie violative of
Article 21. Under the new policy, medical facility continues to be given
and now an employee is given free choice to get treatment in any
private hospital in India but the amount of payment towards
reimbursement is regulated. Without fixing any specific rate, the new
policy refers to the obligation of paying at the rate fixed by the Director.
The new policy does not leave this fixation to the sweet will of the
Director but it is to be done by a committee of technical experts.
No State or country can have unlimited resources to spend on any
of its projects. That is why it only approves its projects to the extent it is
feasible. The same holds good for providing medical facilities to its
citizens including its employees. Provision of facilities cannot be
unlimited. It has to be to the extent finances permit. If no scale or rate
is fixed then in case private clinics or hospitals increase their rate to
exorbitant scales, the State would be bound to reimburse the same. The
principle of fixation of rate and scale under the new policy is justified
and cannot be held to be violative of Article 21 or Article 47 of the
Constitution.
Answer to the question whether the modification of the policy by
the appellant-State by deleting its earlier decision of permitting
reimbursement at the rates charged by the Escorts and other
designated hospitals, is justified or not, will depend upon the facts and
circumstances. The Court would not interfere with any opinion formed
by the Government if it is based on relevant facts and circumstances or
based on expert advice.
Any State endeavour for giving best possible health facility has
direct co-relation with finances. Every State for discharging its obligation
to provide some projects to its subject requires finances. Article 41 of
the Constitution gives recognition to this aspect.
The appellants have explained that earlier under the 1991 policy,
bulk of the budget was being taken away by a few elites for such
treatment like heart ailment etc. to the detriment of a large number of
other employees who suffered. Hence the facility of reimbursement of
full charges at designated hospitals was withdrawn even under the old
1
i
|
i
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 3
Tuesday, November*30, 2004
ONLINE^
This product is licenced to JANV^KAS (CSj), Vastrapur, Ahmedabad
policy. It has to be held that the appellant's decision to exclude the
designated hospitals is not violative of Article 21 of the Constitution.
For the aforesaid reasons and findings, the new policy dated
13-2-1995 of the appellant-Government is upheld. It is further held that
the new policy is not violative of Article 21 of the Constitution.
State of Punjab v. Ram l.ubhaya Bagga,
(1998) 4 SCC 117 : 1998
SCC (L&S) 1021 : AIR 1998 SC 1703 : 1998 Lab IC 1555 : (1998) 2 LLN
973.
Bench Strength 3. Coram : S.B. Majmudar, M. Jagannadha Rao and
A.P. Misra, JJ. [Date of decision : 26-2-1998]
[Search Text :
(1998)
4 SCC 117]
1
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd
Pa9e 1
Tuesday, November 30, 2004
ONLI N E
!
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
ENVIRONMENT PROTECTION
— Art. 21 — Use of pesticides and chemicals causing health
hazard affects Art. 21 — PIL for banning import, production,
distribution, sale and use of 40 named insecticides and/or additives
which are alleged to be causing health hazard and which are said to
have already been banned in USA and other advanced countries —
Steps a heady taken by Central Govt, in totally prohibiting some of the
insecticides/additives and in permitting restrictive use of some ofher
insecticides/additives — In the circumstances, a Committee of four
senior officers from four different Ministries involved directed to be
constituted with a view to make coordinated efforts — Use of Internet
to gather the latest information suggested 'as* 4 Ashok (Dr) v. Union of
India,
(1997) 5 SCC 10 : AIR 1997 SC 2298.
Bench Strength 2. Coram : S.C. Agrawal and G.B. Pattanaik JJ
[Date of decision : 2-5-1997]
[Search Text
:
"(1997)
5 SCC 10"]
- ------------
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Monday, November 29, 2004
I’o N L I N E
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahrnedabad
CONSTITUTION OF INDIA
ARTICLE 21
HEALTH CARE
— Arts. 21, 39(e) and Preamble — Right to health of a worker
falls under Art. 21 — Health does not mean mere absence of sickness
but complete physical, mental and social well being — Universal
Declaration of Human Rights, Arts. 22 to 25 — International Convention
on Economic, Social and Cultural Rights — Labour Law — Committee on
Labour Welfare, 1969, Paragraph 5.77 of Chapter 5
Per K. Ramaswamy, J.
Right to livelihood springs from the right to life guaranteed under
Art. 21. The health and strength of a worker is an integral facet of right
to life. The aim of fundamental rights is to create an egalitarian society
to free all citizens from coercion or restrictions by society and to make
liberty available for all. Right to human dignity, development of
personality, social protection, right to rest and leisure as fundamental
human rights to common man mean nothing more than the status
without means. To the tillers of the soil, wage earners, labourers, wood
cutters, rickshaw pullers, scavengers and hut dwellers, the civil and
political rights are ' mere cosmetic' rights. Socio-economic and cultural
rights are their means and relevant to them to realise the basic
aspirations of meaningful right to life. The Universal Declaration of
Human Rights, International Convention on Economic, Social and
Cultural Rights recognise their needs which include right to food,
clothing, housing, education, right to work, leisure, fair wages, decent
working conditions, social security, right to physical or mental health,
protection of their families as integral part of the right to life. Our
Constitution in the Preamble and Part IV reinforces them compendiously
as socio-economic justice, a bedrock to an egalitarian social order. The
right to social and economic justice is thus a fundamental right.
The term health implies more than an absence of sickness.
Medical care and health facilities not only protect against sickness but
also ensures stable manpower for economic development. Facilities of
health and medical care generate devotion and dedication to give the
workers' best, physically as well as mentally, in productivity. It enables
the worker to enjoy the fruit of his labour, to keep him physically fit and
mentally alert for leading a successful, economic, social and cultural life.
The medical facilities are, therefore, part of social security and like
gilt-edged security, it would yield immediate return in the increased
production or at any rate reduce absenteeism on grounds of sickness,
etc. Health is thus a state of complete physical, mental and social well
being and not merely the absence of disease or infirmity. D381^ C.E.S.C.
Ltd. v. Subhash Chandra Bose,
(1992) 1 SCC 441 : 1992 SCC
(L&S) 313 : AIR 1992 SC 573 : 1992 Lab IC 332 : (1992) 1 LU 475 :
(1992) 1 LLN 353.
Bench Strength 3. Coram : Ranganath Misra, C.J. 1 and M.M.
Punchhi 2 and K. Ramaswamy 3, II. [Date of decision : 15-11-1991]
Supreme Court Case Finder 2004, Copyright © 1969-2C04, EBC Publishing Pvt. Ltd.
Pa9e 2
Monday, November 29, 2004
|ONLINE
[Search Text
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
:
•' RIGHT TO HEALTH"]
*
*
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Monday, November 29, 2004
(ONLINE
This product is licenced to JANVIKAS (CS?), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
n
io
HEALTH CARE
— Arts. 21, 38, 39(e), 41, 43, 48-A, 300 and 32 & 142 Occupational health hazards — Right to health and medical aid
of workers during service and thereafter, is a fundamental right
— Court can give directions in appropriate cases to State or its
undertakings/ instrumentalities, company or private employer
to make the right meaningful and to pay compensation to
affected workmen — Workmen employed in asbestos industries
affected by asbestosis and becoming prone to lung cancer and
related ailments — PIL filed to enforce their fundamental right
— Held, employer obliged to provide protective measures to workmen
— Asbestos industries bound by directions in ' 'All Safety in the Use of
Asbestos" issued by ILO — Asbestos industries further directed to
maintain health record of workmen during service and after retirement,
conduct their Membrane Filter Test and compulsorily insure their health
coverage; Union and State Govts, directed to review the standards of
permissible exposure limit and to consider monitoring of small-scale
factories as well; and Inspectors of Factories directed to send the
workers examined by ESI hospital for re-examination by National
Institute of Occupational Health — Workers found to be suffering from
occupational health hazards, entitled to compensation of Rs 1 lakh
payable by the factory concerned — Labour Law — Factories
Act, 1948, Ss. 89 and 112
Right to health and medical care to protect his health and vigour
while in service or post-retirement is a fundamental right of a worker
under Article 21, read with Articles 39(e), 41, 43, 48-A and all related
articles and fundamental human rights to make the life of the workman
meaningful and purposeful with dignity of person. The right to health of
a worker is an integral facet of meaningful right to life, to have not only
a meaningful existence but also robust health and vigour without which
the worker would lead a life of misery. Lack of health denudes him of his
livelihood. Compelling economic necessity to work in an industry
exposed to health hazards due to indigence to bread-winning for himself
and his dependants, should not be at the cost of the health and vigour
of the workman. (Paras 25 and 24)
Facilities and opportunities, as enjoined in Article 38, should be
provided to protect the health of the workman. Provision for medical
test and treatment invigorates the health of the worker for higher
production or efficient service. Continued treatment, while in service or
after retirement is a moral, legal and constitutional concomitant duty of
the employer and the State. The State, be it Union or State Government
or an industry, public or private, is enjoined to take all such action which
will promote health, strength and vigour of the workman during the
period of employment and leisure and health even after retirement as
basic essentials to live life with health and happiness. The health and
strength of the worker is an integral facet of the right to life. Denial
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Pa9e 2
Monday, November 29, 2004
Ionline y
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
thereof denudes the workman of the finer facets of life violating Article
21. The right to human dignity, development of personality, social
protection, right to rest and leisure are fundamental human rights of a
workman assured by the Charter of Human Rights, in the Preamble and
Articles 38 and 39 of the Constitution. Facilities for medical care and
health to prevent sickness ensures stable manpower for economic
development and would generate devotion to duty and dedication to
give the workers' best physically as well as mentally in the production of
goods or services. Health of the worker enables him to enjoy the fruits
of his labour, keeping him physically fit and mentally alert for leading a
successful life, economically, socially and culturally. Medical facilities to
protect the health of the workers are, therefore, the fundamental and
human rights of the workmen. (Para 24)
Disease occurs wherever the exposure to the toxic or carcinogenic
agent occurs regardless of the country, the type of industry, job title,
job assignment or location of exposure. The disease will follow the trail
of the exposure and extend the chain of carcinogenic risk beyond the
workplace. It is the exposure and the nature of that exposure to
asbestos that determines the risk and the diseases which subsequently
result. The development of the carcinogenic risk due to asbestos or any
other carcinogenic agent does not require a continuous exposure. The
cancer risk does not cease when the exposure to the carcinogenic agent
ceases, but rather the individual carries the increased risk for the
remaining years of life. The exposure to asbestos and the resultant long
tragic chain of adverse medical, legal and societal consequences, remind
the employer or the producer of their legal and social responsibility not
to endanger the workmen or the community or the society. They not
absolved of the inherent responsibility to the exposed workmen or the
society at large. They have the responsibility — legal, moral and social
to provide protective measures to the workmen and to the public or all
those who are exposed to the harmful consequences of their products.
Mere adoption of regulations for the enforcement has no real meaning
and efficacy without professional, industrial and governmental resources
and legal and moral determination to implement'such regulations. (Para
In an appropriate case, the court would give appropriate directions
to the employer, be it the State or its undertaking or private employer
to make the right to life meaningful; to prevent pollution of workplace;
protection of the environment; protection of the health of the workman
or to preserve free and unpolluted water for the safety and heaith of the
people. The authorities or even private persons or industry are bound by
the directions issued by the Supreme Court under Article 32 and Article
142 of the Constitution. (Para 28)
In public law claim for compensation is a remedy available under
Article 32 or Article 226 for the enforcement and protection of
fundamental and human rights. The defence of sovereign immunity is
inapplicable and alien to the concept of guarantee of fundamental rights.
There is no question of defence being available for constitutional
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 3
Monday, November 29, 2004
lONLINE
o
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
remedy. It is a practical and inexpensive mode of redress available for
the contravention made by the State, its servants, its instrumentalities,
a company or a person in the purported exercise of their powers and
enforcement of the rights claimed either under the statutes or licence
issued under the statute or for the enforcement of any right or duty
under the Constitution or the law. (Para 29)
The Government of India issued model Rule 123-A under the
Factories Act for adoption. Under the directions issued by the Supreme
Court from time to time, all the State Governments have by now
amended their respective rules and adopted the same as part of it but
still there are yearning gaps in their effective implementation in that
behalf. It is, therefore, necessary to issue appropriate directions. In the
light of the rules ' 'All Safety in the Use of Asbestos" issued by the ILO,
the same shall be binding on all the industries. Therefore, it is not
necessary to issue any direction to the Union or State Governments to
constitute a committee to convert the dry process of manufacturing into
wet process but they are bound by the rules not only specifically
referred to in the judgment but all the rules in that behalf in the above
ILO rules. The Employees' State Insurance Act and the Workmen's
Compensation Act provide for payment of mandatory compensation for
the injury or death caused to the workman while in employment. Since
the Act does not provide for payment of compensation after cessation of
employment, it becomes necessary to protect such persons from the
respective dates of cessation of their employment till date. Liquidated
damages by way of compensation are accepted principles of
compensation. In the light of the law above laid down and also on the
doctrine of tortious liability, the respective factories or companies shall
be bound to compensate the workmen for the health hazards which are
the cause for the disease with which the workmen are suffering from or
had suffered pending the writ petitions. Therefore, the factory or
establishment shall be responsible to pay liquidated damages to the
workmen concerned. (Para 30)
Accordingly, all the industries are directed (1) to maintain and
keep maintaining the health record of every worker up to a minimum
period of 40 years from the beginning of the employment or 15 years
after retirement or cessation of the employment, whichever is later; (2)
the Membrane Filter Test to detect asbestos fibre should be adopted by
all the factories or establishments on a par with the Metalliferrous Mines
Regulations, 1961 and Vienna Convention and rules issued thereunder;
(3) all the factories whether covered by the Employees' State Insurance
Act or Workmen's Compensation Act or otherwise are directed to
compulsorily insure health coverage to every worker; (4) the Union and
the State Governments are directed to review the standards of
permissible exposure limit value of fibre/cc in tune with the international
standards, reducing the permissible content as prayed in the writ
petition referred to at the beginning. The review shall be continued after
every 10 years and also as and when the ILO gives directions in this
behalf, consistent with its recommendations or any convention; (5) the
Cl'
r-v
bOJ
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 4
Monday, November 29, 2004
[o N L I N E'—'r
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
Union and all the State Governments are directed to consider inclusion
of such of those small-scale factory or factories or industries to protect
health hazards of the workers engaged in the manufacture of asbestos
or its ancillary products; (6) the appropriate Inspector of Factories, in
particular of the State of Gujarat, is directed to send all the workers,
examined by the ESI hospital concerned, for re-examination by the
National Institute of Occupational Health to detect whether all or any of
them are suffering from asbestosis. In case of the positive finding that
all or any of them are suffering from the occupational health hazards,
each such worker shall be entitled to compensation in a sum of rupees
one lakh payable by the factory or industry or establishment concerned
within a period of three months from the date of certification by the
National Institute of Occupational Health. (Para
Consumer
Education & Research Centre v. Union of India,
(1995) 3 SCC 42 :
1995 SCC (L&S> 604 : AIR 1995 sc 922 : (1995) 2 LU 768.
Bench Strength 3. Coram : A.M. Ahmadi, C.J. and M.M. Punchhi and
K. Ramaswamy, JJ. [Date of decision ; 27-1-1995]_________________
[Search Text :
" RIGHT TO HEALTH"]
(
)
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Monday, November 29, 2004
I’o N L I N E
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
RIGHT TO HEALTH
— Right to health and medical care during service and post
retirement is a fundamental right of a worker under Art. 21 r/w
Arts. 39(e), 41, 43 and 48-A — Court can give directions to State, its
instrumentalities, Company or private employer to make the right
meaningful and pay compensation to affected workmen — Workers of
asbestos industries found to be suffering from occupational health
hazards were entitled to compensation of Rs 1 lakh payable by the
factory concerned t3181’^ Consumer Education & Research Centre v.
Union of India,
(1995) 3 SCC 42 : 1995 SCC (L&S) 604 : AIR 1995
SC 922 : (1995) 2 LU 768.
Bench Strength 3. Coram : A.M. Ahmadi, C.J. and M.M. Punchhi and
K. Ramaswamy, JJ. [Date of decision ; 27-1-1995]
[Search Text :
" RIGHT TO HEALTH’']
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
• Monday, November 20, 2004
ION LINE
This product is licenced to JANVIKAS (CSS), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
f
1) Ct
WtUf
—------ -----------------------
ECOLOGY
— Arts. 21 and 32 — Vehicular pollution in Delhi — Directions
given in M.C. Mehta case (1998) 6 SCC 63 - Overriding effect of,
over statutes — Having been issued to safeguard the people's right to
health under Art. 21, held, the said directions override the provisions of
every statute including MV Act — Moreover, emission norms fixed by
MV Act for diesel vehicles, held, are in addition to and not in derogation
the requirements of Environment (Protection) Act — Hence, bus
operators complying with the norms fixed by MV Act, held, 'could not
merely for that reason, bypass the directions given in M.C. Mehta case
— Motor Vehicles — Motor Vehicles Act, 1988, S. 110(l)(g) — Motor
Vehicles — Central Motor Vehicles Rules, 1989, Rr. 115 and 116 —
Environment Protection and Pollution Control — Environment
(Protection) Act, 1986, Ss. 3, 6 and 7
^ParaJ?D3181^ M-c- Mehta v- Uni'on of India (Delhi vehicular air
pollution),
(2001) 3 SCC 756 : AIR 2001 SC 1948.
Bench Strength 3. Coram : Dr AS. Anand, C.J. and B.N. Kirpal V.N.
Khare, JJ. [Date of decision : 26-3-2001]
[Search Text :
" RIGHT TO HEALTH"]
*
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Tuesday, November 30, 2004
Po N L I N E f
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
MEDICAL PROFESSION
MEDICAL ETHICS
— Duty to maintain secrecy — Exception — Disclosure for
protecting an identifiable person against- health risk — Decision in Mr
' X' v. Hospital ' Z', (1998) 8 SCC 296 — What it decided and what it did
not — Held, that decision decided only that the revealing of the
appellant's HIV-positive status to the relatives of his fiancee did not
violate his right in any manner — Other observations made by the
Supreme Court in that case, such as those relating to the appellant's
suspended right to marry, held, were uncalled for — Practice and
Procedure — Obiter dicta — Observations not necessary for resolving
the issue made — Status of — Constitution of India — Art. 141 —
Obiter dicta. Art. 141 — Status of observations not necessary for
resolving the issue — Family Law — Marriage — Suspended right to
marriage — Pena! Code, 1860, Ss. 269 and 270
In Mr 'X' v. Hospital 'Z', (1998) 8 SCC 296, the Supreme Court
had rested its decision on the facts of that case that it was open to the
hospital or the doctor concerned to reveal such information to persons
related to the girl whom he intended to marry and she had a right to
know about the HIV-positive status of the appellant. Therefore, there
was no need for the Supreme Court to go further and declare in general
as to what rights and obligations arise in such context as to right to
privacy or confidentiality or whether such persons are entitled to be
married or not or in the event such persons marry they would commit
an offence under law or whether such right is suspended during the
period of illness. Therefore, all those observations made by the Supreme
Court in the said matter were unnecessary, particularly when there was
no consideration of the matter after notice to all the parties concerned.
(Para 6)
Therefore, it is held that the observations made by the Supreme
Court in that case except to the extent of holding that the appellant's
right was not affected in any manner in revealing his HIV-positive status
to the relatives of his fiancee, were not called for. (Para
Mr
‘ 'X" v. Hospital ' 'Z",
(2003) 1 SCC 500.
Bench Strength 3. Coram : S. Rajendra Babu, P. Venkatarama
Reddi and Arun Kumar, JJ. [Date of decision : 10-12-2002]
Mr 'X' v. Hospital ' Z', (1998) 8 SCC 296, limited
[Search Text
:
"(2003)
1
SCC 500"]
Supreme Court Case Finder 2004, Copyright © 1969-2004, EBC Publishing Pvt. Ltd.
Page 1
Tuesday, November 30, 2004
|ONLINE
This product is licenced to JANVIKAS (CSJ), Vastrapur, Ahmedabad
CONSTITUTION OF INDIA
ARTICLE 21
GENERALLY
— Art. 21 — Conflict between fundamental rights of two parties
— Right to privacy of one and right to healthy life of the other —
Which one to prevail — In such a case, only that right which would
advance public morality or public interest, held, would be enforceable —
Judges' duty towards morality, stated — Jurisprudence — Morality and
the law — Judicial process — Moral aspects — Regard to by Judges
Where there is a clash of two Fundamental Rights as in this case
right to privacy of one party as part of right to life and right to lead a
healthy life of another party which is also a fundamental right under Art.
21, the right which would advance the public morality or public interest,
would alone be enforced through the process of court, for the reason
that moral considerations cannot be kept at bay and the Judges are not
expected to sit as mute structures of clay in the hall known as the
courtroom, but have to be sensitive, '' in the sense that they must keep
their fingers firmly upon the pulse of the accepted morality of the day".
38 * Mr X' v- Hospital 'Z',
(1998) 8 SCC 296.
Bench Strength 2. Coram : S. Saghir Ahmad and B.N. Kirpal, U
[Date of decision : 21-9-1998]
But See Mr ' ' X" v. Hospital ’ 'Z", (2003) 1 SCC 500
[Search Text
:
(1998)
8
SCC 296]
►
Position: 708 (10 views)