15711.pdf
Media
- extracted text
-
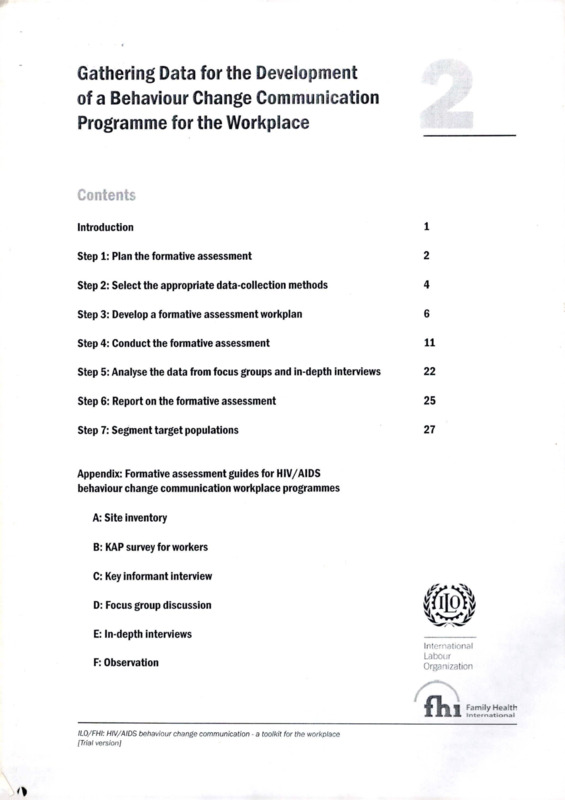
Gathering Data for the Development
of a Behaviour Change Communication
Programme for the Workplace
Contents
Introduction
i
Step 1: Plan the formative assessment
2
Step 2: Select the appropriate data-collection methods
4
Step 3: Develop a formative assessment workplan
6
Step 4: Conduct the formative assessment
11
Step 5: Analyse the data from focus groups and in-depth interviews
22
Step 6: Report on the formative assessment
25
Step 7: Segment target populations
27
Appendix: Formative assessment guides for HIV/AIDS
behaviour change communication workplace programmes
A: Site inventory
B: KAP survey for workers
C: Key informant interview
D: Focus group discussion
E: In-depth interviews
F: Observation
International
Labour
Organization
JL
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
fl Family Health
International
Introduction
This booklet offers users a framework for collecting data to form the basis of an HIV/AIDS
behaviour change communication (BCC) programme for the workplace. Gathering data
for BCC is generally called a ‘formative assessment’ and is defined as the gathering of
in-depth information about the programme’s target groups to design effective behaviour
change communication activities. 'Formative’ means the formation or development of
a body of information through which to assess or determine the nature of a population.
Formative assessments will be conducted during the planning stage of the BCC
programme’s development. A formative assessment provides a thorough understanding of
current conditions, practices and attitudes among target populations. This understanding
is essential for designing appropriate BCC interventions, as well as workplace HIV/AIDS
programmes and policies.
This booklet describes the research methods available for gathering information, along
with guidelines on how to select and use these methods. The appendix contains guides for
designing a BCC formative assessment for the workplace.
Reading and using this booklet will enable a team or facilitator to:
■
■
■
■
■
■
■
plan the formative assessment;
select the appropriate data-collection methods;
develop a formative assessment workplan;
collect the data;
analyse the data;
develop a formative assessment report; and
segment the target populations in preparation for BCC programming.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
2
Step 1: Plan the formative assessment
A. Defining your goals
The goals of rhe BCC formative assessment in the workplace are:
■
■
■
■
■
■
■
to identify opportunities, resources and potential barriers to BCC activities;
to understand different target populations’ behaviours, attitudes, likes and dislikes,
hopes and fears for the future;
to specify the target populations’ current knowledge, attitudes and behaviours
regarding HIV/AIDS;
to identify the target populations’ specific interests and concerns regarding HIV/AIDS
and the type of programming and support they need;
to define their social networks and their high-risk settings (i.e., environments that can
lead to high-risk behaviours—for example, bars, brothels and truck stops, where sex
workers operate);
to involve them in the behaviour change process; and
to identify ways to increase HIV/AIDS-related health-seeking behaviour.
B. Gathering data
Achieving these main purposes means reviewing the information already available about a
particular workplace, and identifying what additional information is necessary.
The following categories may help when collecting information for the formative
assessment.
The broader environment
■
■
■
Data on the epidemic in the country/region (including the main modes of HIV
transmission)
Role of national, regional or local government in addressing HIV/AIDS in the
workplace (e.g., workplace strategy as part of national HIV/AIDS plan)
Information and services available from community-based or AIDS service
organizations.
The work environment
■
■
■
■
■
■
■
■
■
■
■
■
Existing programmes, policies and practices at the workplace for HIV/AIDS
prevention, care and support
Condom distribution
Basic health care
Sexually transmitted infection diagnosis and treatment
Access to voluntary HIV testing and counselling
HIV/AIDS/tuberculosis treatment, care and support (including antiretroviral therapy)
Workplace policy
Workplace committees (e.g., health and safety)
Basic and in-service training programmes
Normally planned events
Worker organization(s); what kind of support workers receive from their union
Categories of workers by job function, education, gender, income and ethnicity.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
3
Worker knowledge, attitudes, values and beliefs
■
■
■
■
■
■
■
■
■
■
Current knowledge, attitudes and behaviour regarding HIV/AIDS
Level of interest in developing HIV/AIDS programmes
Specific interests and concerns related to HIV/AIDS (e.g., housekeeping staff in a
hospital in Kenya were afraid to clean the rooms of AIDS patients)
HIV-positive workers who are open about their status with employers and co-workers
Treatment of workers living with HIV/AIDS
Attitudes towards people living with HIV/AIDS at the workplace
Behaviours, attitudes, hopes and fears for the future, likes and dislikes
Social networks
Potential high-risk settings
Current health-seeking behaviour
Communication mechanisms
■
■
■
How people get information ar the workplace (e.g., newsletter, bulletin board, staff
meetings, training sessions, new employee orientation)
Trusted sources of information
Media habits
Identifying information that is currently available
To identify relevant information that is already available, you will need to conduct a review
of work already carried out by previous programmes. Potential sources of information may
include:
■
■
■
■
■
■
■
■
ILO country profile or status reports regarding HIV/AIDS and the world of work;
UNAIDS country fact sheets;
past studies and reports on HIV/AIDS;
surveys of HIV/AIDS knowledge, attitudes, practices and beliefs among the target
population;
government epidemiological data and health surveys pertaining to HIV/AIDS;
local university dissertation research;
other organizations’ studies; and
studies conducted in the selected workplace.
There may be no need to have focus group discussions and in-depth interviews with the
target populations if the relevant data already exist. Instead, information gaps may be
identified and a questionnaire developed on the basis of the missing information. In this
way, valuable and scare resources may be preserved for use in other areas of the programme.
Identifying necessary additional information
Once existing studies and data have been reviewed, there may still be gaps in information
about the key target populations. It is important to systematically categorize these gaps in
preparation for gathering additional data for rhe formative assessment.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
4
Step 2: Select the appropriate data-collection methods
Once you have reviewed the existing data, you will need to collect rhe additional
information needed for the BCC formative assessment. The following methods may be
used to do this.
Site inventories help assess how target populations are structured in geographic and social
space and how they network with other populations. Sire inventories usually focus on
informants who are knowledgeable about the geography and social structure of the area and
experienced with BCC interventions. Inventories can also provide an overview of existing
resources useful to the programme, such as HIV/AIDS-related services available both at
the workplace and in the surrounding community, media opportunities and local partners.
This exercise is easy to carry out at the workplace.
KAP surveys for workers consist of a list of questions with a range of pre-determined
responses. Surveyors generally use these questionnaires to learn more about workers’
knowledge, attitudes and practices with regard to HIV/AIDS. HIV/AIDS knowledge can
include misconceptions, prevention strategies and modes of transmission. Becoming more
aware of workers’ attitudes, such as how they feel about condoms, will help you determine
which topics your BCC programme should focus on. In addition, the practices that
workers engage in will help you ascertain which activities would be most beneficial at your
workplace. Knowledge, attitude and practice surveys are relatively simple to conduct and
. can provide baseline data for programme development.
Key informant interviews are conducted with people who are highly knowledgeable about
the topic under investigation and who are linked to target populations. Key informants
may include opinion leaders, local health providers and experts from the target population.
Key informant interviews provide an insider’s view of the structural, organizational, social
and cultural context of the workplace or community. They also give insights into the target
populations behaviour. This activity serves as the basis for the methods that follow.
Focus group discussions are conducted with eight to ten representatives of the target
population, and require a skilled moderator. These discussions reveal major issues and
patterns, including both shared and conflicting ideas about target population behaviour.
They also allow interviewers to assess potential reasons for a target population adopting a
particular behaviour.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
I
5
In-depth interviews can take place with workers from different departments at the
workplace and from different levels of management. They can also include representatives
from human resources and medical departments, as well as union and health and safety
representatives (if relevant). In the community, interviewees may include labour leaders,
health-care providers and representatives from local non-governmental organizations
that provide HIV/AIDS services. These individual assessments are necessary for an indepth look at rhe intimate individual perspectives, beliefs, motivations and logic behind
behaviour. They may also show how such behaviour fits into the broader social context.
Observation can help to confirm or refute results found through the methods outlined
above. Observation involves choosing a setting of interest, such as a truck stop, to see how
the workers engage in social and work activities. It helps in describing social networks,
high-risk settings and the steps or influences that lead to high-risk behaviours.
BCC assessment monitoring involves the results of one method informing the content
and structure of another. This feedback and revision will lead to more refined assessment
protocols. For example, data obtained from the inventory exercise may reveal additional
questions that will need to be put to management. Information from in-depth Interviews
with management may lead to questions for staff group discussions.
Each method can inform the development of other methods or help in determining if
another method is needed. Developing a good BCC programme is an investigative process.
Factors to consider when choosing methods:
■
■
■
■
Level of existing information
Human and financial resources at your disposal
Diversity of target populations
Time available
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
6
Step 3: Develop a formative assessment workplan
Once the data-gachering activities have been selected, a review of the suggested
methodology and of the kinds of questions to be included in each guide should be carried
out. ThixS will help define the scope of the assessment and determine which human and
financial resources are necessary. Some activities may be curtailed if human and financial
resources are limited. The Family Health International publication Qualitative Methods: A
Field Guide for Applied Research in Sexual and Reproductive Health is a valuable resource
that covers topics such as planning research, methods, sampling and ethics.
To develop a workplan, you will need to:
A. set up the needs assessment team;
B. select the sample;
C. select key informants and information collection approaches;
D. create assessment tools based on the toolkit guides; and
E. train interviewers.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
7
A. Set up the needs assessment team
What are the roles of the different assessment team members?
The assessment team can be as simple or as extensive as is necessary to com plere your needs
assessment. For example, if your needs assessment is small, then hiring one consultant
could be enough. However, a larger assessment team will be necessary if you want to
include multiple workplaces, review secondary resources, map each workplace, and use
several of the qualitative formative assessment methods described below.
The assessment team may include programme staff, a consultant or a team of consultants,
and representatives from the workplace. The roles outlined below are examples of how you
might want to organize your assessment team if the needs assessment is on a larger scale.
You can also combine tasks so that one person fills two roles.
Assessment leader:
The person who provides technical leadership and oversight; the
BCC programme coordinator might fill this role.
Assessment coordinator: The person in charge of logistics. He/she works in close
collaboration with the partnership interviewers, setting up
meetings, communicating with the rest of the team and
carrying out other organizational duties.
Partnership interviewers: Members of the community who help recruit participants and
identify respondents and interview sites. These people might
help record responses and observations such as facial expressions
and body language during focus group discussions, or they
might keep a log of the discussion if a tape recorder is not
available.
Interviewers:
People who perform field tasks such as interviews, observations
and moderating.
The programme coordinator may choose to maintain a formal role in the team or to act in
an advisory capacity. The BCC assessment team should make decisions about how to set up
a workable system to conduct the assessment. How the team is constituted will depend on
the situation.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
8
How to establish a timeline
It is advisable to develop a timeline for assessment activities prior to assigning specific tasks
to ream members. The assessment leader should work with team members to develop a
timeline based on the overall BCC programme calendar. Together, this team can determine
the pace of work.
The workplan will need to specify the roles and responsibilities of each ream member
and an appropriate timeline for assessment activities. For example, if the team decides to
conduct four focus group discussions with long-distance truck drivers from 6 to 8 July, it
will be necessary to organize logistics and conduct the interviews.
It is important to make several field visits to the selected sites to gain the support of
the community and of those at the workplace for the formative assessment before
implementing it. Site visits help you understand when, where and how to conduct the
formative assessment, and encourage collaboration with stakeholders.
Table I: Example of timelines for interviews
Method
1 week
Inventory
In-depth interviews
Focus group
discussion
How long
How many
How often
When
1-5 July
3 key informant
interviews
(plus review of
documents)
90 minutes
15 interviews
2 per day
7-12 July
1 hour
3 groups
1 per day
6-8 July
Table 2: Assignment example
Who
What
Assessment coordinator
Organize focus group
discussions for truckers
When
15-17 June
■ Meet with trucker
union
■ Meet with truckers
■ Coordinate venue
Organize focus group
discussions for
secretaries
17-19 June
■ Meet with secretaries
■ Coordinate venue
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
9
B. Select the sample
Tlie first task is to select the workplace to be assessed. In many cases, this will already be
apparent. But you may also have to identify specific areas within the site.
Next, the respondents must be selected. Here are some suggestions for doing this:
■
■
■
■
■
Always keep in mind rhe populations you are targeting.
Go to sites or observe events that are easier to get to (or arrange).
Go to the sites when people are most cooperative: for example, when members are on
break or at the beginning or end of the day. Times for research may be different than
times for setting up interviews: for example, you might contact secretaries during a
coffee break but schedule the interview for the following day, when they are not busy.
Always take advantage of opportunities that occur.
Always follow up on leads about where you can find the people you are seeking.
C. Select key informants and information-collection approaches
(See Step 2, page 4.)
D. Create assessment tools based on toolkit guides
(See Step 2, page 4, and the appendix of Booklet 2)
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
10
E. Train interviewers
Once you have developed the assessment tool and are ready to implement it, you will need
to schedule a training session for the interviewers on your team. The training will provide
them with information and skills on how to conduct an interview and/or group discussion
using the tool.
The activities listed below are examples of what to include in the training.
Day 1: Getting to know the tool
The main goal of the first day is to provide interviewers with background knowledge on the
tool. Begin by walking interviewers through the tool, explaining the reason for including
the questions or topics and what you hope to learn from the interviewees. The trainer
should provide enough background information so that interviewers feel confident. The
main concepts to cover include:
■
■
■
■
modes of transmission and prevention strategies for HIV and other sexually
transmitted infections;
HIV/AIDS activities at the workplace;
stigma and discrimination; and
knowledge of HIV/AIDS workplace policies.
Interviewers should learn about general questionnaire/interview administration issues,
such as obtaining consent, establishing rapport with a respondent, and the need for
standardization of questions.
Day 2: Role play
The main activity of the second day is role plays. In role plays, one interviewer pretends
to be an interviewee while another administers the questionnaire or interview. Others
watch and, at designated times defined by the training facilitator, may offer suggestions
for improvement and/or may point out good qualities. After all interviewers have assumed
both roles, they should repeat the exercise with interviewers playing rhe part of a ‘difficult’
interviewee. After each session, the group should discuss the strengths and weaknesses of
the interviewer, as well as possible ways of probing the interviewee. During the role plays,
interviewers should gain good knowledge of questionnaire/interview administration. They
should learn to handle clients who answer vaguely or not at all. They should also be able to
filter out superfluous information and to note multiple answers.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
11
Step 4: Conduct the formative assessment
The same behaviour may mean different things to different people. Talking with the target
population can yield insights about the rationale behind their actions that help in designing
effective communication products and activities aimed at altering behaviours.
The BCC assessment team will work with respondents to produce answers about topics of
interest. The success of the assessment depends on the quality of the relationship between
the respondent and researcher as well as on rhe level of interaction.
For formative assessment methods 2 to 7, described below, there are associated guides in
the appendix, which provide examples of how to modify or adapt a programme, if needed.
Method 1: Review of existing information
Method 2: Site inventory
Method 3: Knowledge, attitude and practice (KAP) survey for workers
Method 4: Key informant interview
Method 5: Focus group discussion
Method 6: In-depth interview
Method 7: Observation
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
12
Method 1: Review of existing resources
Reviewing existing resources includes consulting existing studies and reports on HIV/
AIDS, on the selected target population, and on the selected workplaces. Resources that
cover HIV/AIDS-related issues can be useful in the design of successful BCC workplace
interventions. Reviewing existing resources can yield much of the required information,
saving time and money. Any gaps in the available information can be covered by a
questionnaire or interview that focuses on the missing information.
Method 2: Site inventory
You can conduct the initial site visit and the site inventory at the same time. Both require
meeting with managers, supervisors and line workers to outline the systems, structures and
opportunities at the workplace. It is also a good opportunity to build partnerships between
programme and workplace staff. Through the site inventory, you can:
■
■
■
chart the organizational and physical structure of the workplace;
identify the main target populations, worker organizations, and workplace activities
and services; and
identify opportunities for integration of HIV/AlE)S-related activities into existing
services or for easy creation of new services.
The site interview can be conducted by reviewing available documents that describe the
organizational structure of the workplace, and by interviewing key staff to gain more up-todate information about services, programmes, activities, associations and newsletters. The
results of the site inventory will help in identifying opportunities and gaps for integration
and/or addition of HIV/AIDS behaviour change communication activities. (See the
appendix, page A-l, for a site inventory guide.)
Method 3: Knowledge, attitude and practice (KAP) survey for workers
The KAP method is a quantitative method used in HIV/AIDS studies and programmes.
A statistician will need to be on your team so you can accurately analyse the results. KAP
surveys are often used in a pre/post-test design to rapidly assess the population’s knowledge,
attitudes and practices regarding a certain disease or area. In a pre/post-test design, the
programmers and/or researchers can determine whether there have been any changes that
could possibly be attributed to the interventions.
KAP surveys often give the programmers/researchers new insights about the target
population. However, there are disadvantages to this approach. For example, in any survey,
the respondents may give you answers that they think you want to hear. The respondents
may also answer untruthfully in areas that are very personal, such as their sex lives or their
feelings towards people with HIV. In addition, the many “yes/no” answers to many of the
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
13
questions do not allow the researcher to explore the question in depth. Often, qualitative
methods need to be conducted as well to get a fuller picture of the lives of the target
population. The in-depth information from the target population is especially important
when designing behavior change communication programmes.
Method 4: Key informant interview
Key informants are experienced people with direct, expert knowledge of the subject under
study. Key informants may include:
■
■
■
■
worker representatives;
focal points from trade unions and employer organizations;
representatives from the health facility that serves the target population; and
staff from organizations that provide HIV/AIDS services to the target population.
It could also be relevant to interview:
■
■
■
■
representatives of the ministries of labour and health;
representatives of the national HIV/AIDS programme;
private sector leaders who understand HIV/AIDS issues; and
relevant non-governmental organizations.
It is important to include representatives from all levels of workplace personnel—from top
management to line workers—and from different departments. Staff from medical services
and human resource departments, as well as health, safety and union representatives (where
they exist), should be high on the list of interviewees.
Talking to people from these groups will help in determining who the experts are. For
example, when talking to garage owners, it is useful to ask who the lead mechanic is or who
most people look up to in the garage. Similarly, when speaking with apprentices and other
mechanics, you can ask which of their colleagues is most knowledgeable about the garage
and possible HIV/AIDS-related activities. People identified repeatedly as experts may be
promising key informants.
Try to probe potential key informants to make sure that they really are experts before
accepting them as key informants and investing time in interviewing them. Look for a
long record of involvement; direct, personal experience; and comments rich in situational
and contextual detail and examples. Be wary of informants whose comments are limited to
generalities. If your informant's reply is satisfactory, you can proceed. If not, thank them
politely and tactfully discontinue the conversation.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
14
How to gain information from key informants
There are numerous ways of acquiring information from key informants. This can be done:
■
informally;
■
■
■
■
through formal introductions;
via in-person interviews;
through telephone interviews; and
with formal techniques, such as written questionnaires.
Try to apply the following principles when conducting key informant interviews:
■
■
■
■
■
■
Begin with truly exploratory, flexible, open-ended questions and pursue all
unanticipated, but important, issues that arise.
Never tell people they are wrong, give non-verbal clues, or offer value judgements.
Share your own experiences (without disclosing strong views), if doing so relaxes
informants.
Never move to a new topic until you have completely explored the topic under
discussion.
Make detailed notes on each informant's comments.
Interpret and summarize the key informant interviews, perhaps using the following
steps:
■ First, make a list of all areas, categories of places, addresses, days and times when/
where risky activity occurs.
■
Second, produce a summary (in point form) of the key points made by each key
informant.
■
Third, make a summary (in point form) of the separate key informant summaries.
■
Divide the summary into areas of major and limited agreement and consider
possible explanations for inconsistencies.
The following strategies can help in determining whether the information received is
reliable:
■
■
■
■
■
■
Be attentive to internal inconsistencies in the comments of key informants and explore
these inconsistencies in a reassuring way.
If some conclusions seem questionable, try to determine whether an informant has
drawn them from a single, memorable incident.
Ask whether key informants’ experience qualifies them to make a statement whose
reliability seems uncertain.
Consider carefully whether rhe attitude the informant holds towards the workplace
may have influenced particular answers.
Compare answers of different key informants, looking for contradictions and points of
consistency.
Compare the information gathered from key informants with that yielded by other
methods.
Key informant interviews will help yield the following information:
■ An overview and in-depth information on rhe workplace and its social context
■ Perceptions and insights into target population behaviour
■ Information about human resources for the forthcoming BCC programme.
ILO/FHI: HIV/AlDS behaviour change communication - a toolkit for the workplace
[Trial version]
15
You can also ask key informants to suggest questions for possible use during in-depth
interviews and focus group discussions, should you choose to use these methods. (See the
appendix, page C-l, for a key informant interview guide.)
Method 5: Focus group discussion
Focus group discussions involve gathering a group of people from the workplace to
thoroughly discuss important issues such as HIV/AIDS and related interventions. A
group leader guides the discussion, using a series of carefully chosen questions. Individual
in-depth interviews are often preferable to focus groups for examining personal, sensitive
or complex issues, while focus groups are useful for producing ideas, examining group
interaction and its effects, developing and testing educational materials, and refining health
services.
Workplace focus groups can generate important information by:
■
■
■
■
identifying worker perspectives on employers, unions, medical services and other
benefits that help determine what type of BCC HIV/AIDS programme to develop;
identifying high-risk behaviours and helping to determine the areas of prevention
training that are most critical to the workplace;
identifying which HIV/AIDS-related issues are of most concern to workers; and
assessing the workplace environment regarding discrimination and stigma towards
HIV-positive workers, or employee needs with regard to care and support, including
testing and treatment issues.
A focus group discussion is not meant to be a problem-solving session, nor is it a decision
making group. At best, it is a discussion among participants rather than a series of two-way
communications between the moderator and individual participants. Ideally, the moderator
will ensure that participants feel free to express their thoughts and opinions openly, that all
topics of the focus group discussion guide are presented, and that the discussion is broad
and deep. One of the goals should be to foster an in-depth discussion among participants
about their knowledge, attitudes and behaviours with regard to HIV/AIDS. The skill and
experience of the moderator will determine the quality of the information gathered.
If possible, a skilled moderator should be hired. If not, informal group discussions are still
a good way to learn about workers’ knowledge, attitudes and practices, as well as what they
would like to see in a workplace HIV/AIDS programme. Be aware, however, that informal
group discussions do not constitute a genuine qualitative research method.
In focus group discussions, the interaction of participants should stimulate richer responses
and allow for new and valuable thoughts to emerge. It is not necessary for the group to
reach a consensus, or for people to disagree, although this may occur. The objective is to get
high-quality information in a setting where people can consider their own views in light of
the views of others.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
16
Focus group composition
The composition of the discussion group should include workers from different
departments or a particular target audience (e.g., janitors). Focus group discussions are
usually easier to conduct and generate better results if participants are of similar age, sex,
education, socio-economic background, occupation and fluency in the language used.
However, you may waive some of these criteria if the goal is to hold a discussion among
a broad cross-section of the workplace. It is usually important to be careful when mixing
people of different status. For example, in workplace settings, workers may have difficulty
speaking freely among supervisors and managers.
Size
The ideal group size is eight to ten people. This gives everyone a chance to talk and permits
a sufficient range of contributions. The number should seldom be below six or above 12.
Number of sessions needed
There are no firm guidelines about the ideal number of group discussions, although, as
a rule, three sessions are held for each variable (males vs. females, in-school vs. out-of
school youth) and sessions are continued until no new information comes up. Participants
usually begin to repeat information over the course of three group discussions. At least one
focus group discussion should take place in each geographical region where a difference in
information might appear.
Session length
Each session should last from one-and-a-half to two hours.
Setting and seating arrangement
Choose a site where it is easy to hear people speak. It should be accessible, private, quiet,
comfortable, and in a non-threatening environment. Select a site where the presence of
an observer will not disturb the group. It should also be large enough to seat eight to 12
people in a circle, as this makes it harder for anyone to dominate the discussion.
The seating arrangement should avoid showing status. Ser up seating so that the moderator
has good eye contact with everyone and every participant is equidistant from the moderator
and in view of the other participants. The group leader should sir in the circle with
everyone else and avoid standing in front of the group or doing anything else that suggests
higher status. A circular seating plan usually fulfills these requirements.
Moderator technique
The moderator should not be (or seem) judgemental or try to dominate. He/she should
convey warmth, enthusiasm and interest, encourage everyone to participate, and quietly try
to control dominant participants.
When the group discussion is over, the leader should invite concluding comments, thank
the group as a whole (noting how helpful they have been and citing specific insights they
have provided), and thank them individually.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
17
Topic guide
Before holding a focus group discussion, it is important to agree on the objective. For
example, a focus group in the early stage of an intervention may be concerned primarily
with the social and sexual context of HIV risk. A focus group held when an intervention
is well established may examine participants’ responses to intervention services and
programme adjustments needed. However, some themes are likely to be consistently
important throughout a programme. These include how to remove barriers to condom
use and how to improve the accessibility, acceptability and uptake of sexually transmitted
infection management and other services.
Once the objective is clear, you will need to prepare a question guide. This guide must not
be too long or the focus group will be rushed and superficial. In general, about ten to 12
questions are sufficient.
Topic guides will have this general structure:
1) Warm-up and explanation
A) Introduction
B) Purpose
C) Procedure
D) Self-introductions
2) Topics (four to eight major ones with a total of ten to 12 questions)
3) Closure
Develop your own topic guide, using one or more of the following guides as a model. (See
the appendix, page D-l, for a focus group discussion guide.)
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
18
Method 6: In-depth interview
What is an in-depth interview?
An in-depth interview is an extended and formalized conversation. This type of interview
focuses on a good informant from the target population. In-depth interviews are openended and use many of the same principles discussed above for key informant interviews.
As noted earlier, key informants have expert knowledge of other peoples’ lives, while
in-depth informants are experts about their own lives. It is customary to interview key
informants several rimes and in-depth informants once.
In-depth interviews focus on obtaining in-depth information about why the target
population engages in certain behaviours. This includes aspects of high-risk behaviour,
beliefs, motivations and the logic behind their behaviour.
While the main goal of the in-depth interview is to gather information, it also makes key
target populations feel that they are being consulted and helps bring them on board as
allies or partners.
Preparation
Define the purpose of the interview. Prior to interviewing, the person developing the
assessment instrument must define the information required.
Script the interview. In-depth interviews require a format and process that entail the
preparation of a script or protocol. You will need to prepare, pilot and review detailed
questions with the interviewer and with representatives from the target population before
conducting the interview.
Prepare the interviewee. Confirm the time and place of the interview before it takes
place. Before beginning, summarize the main topic areas. Explain to the interviewee
the contribution of the interview to the assessment and to the programme. Assure the
interviewee that you will respect confidentiality and tell her/him how much time the
interview will take.
Interview
Try to make the interview feel more like a conversation than a survey. Let the respondent
do most of the talking.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
19
Recording the interview
■
■
■
■
■
You may want to tape rhe interview. This may help to convey your intention to ger it
right’, and it encourages considered responses, while ensuring a back-up if the original
notes are lost. Ask permission to tape and offer to stop taping on request. However,
raping is optional, as no recorder may be available and it might inhibit the respondents
from speaking freely.
While conducting the interview, pause to allow the respondent to gather her/his
thoughts, but not long enough to raise uncomfortable feelings.
Take notes even if you are taping, so that you have a back-up copy of the interview in
case your tape does not work. Return to key questions that have incomplete responses,
using oblique questions to reveal additional facets.
Tell the interviewee that you may follow up if you still have questions.
Tell the interviewee that a summary of the interview will be available and that he/she
will be welcome to look ar it. This will raise the level of credibility of your programme.
After the interview
■ Immediately after each interview, fill in the blanks in your notes while the interview is
still fresh in your mind.
■ Contact the interviewee for follow-up information, if necessary.
■ Provide a summary of the interview notes to the respondent for approval, if requested.
(See the appendix, page E-l, for an in-depth interview guide.)
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
20
Method 7: Observation
Why observation?
The goal of observation is to obtain evidence about the social networks and the settings
for risk and influences that lead a target population to engage in risky sexual behaviour.
Observation allows you to see things that interviews do not reveal and to use this
information to amplify data or to ask additional questions of rhe target population.
Observation also reaffirms or contradicts information obtained as a result of other
activities.
What to observe
In a workplace setting, you might observe who talks to whom, who the natural leaders are,
where people spend their time (which may be good venues tor future BCC activities), how
they access information, and to what extent they use facilities or resources (e.g., do workers
take advantage of the health services? Are educational events well-attended? Who attends?).
You may also have an opportunity to observe situations that lead to high-risk behaviours
(e.g., do workers typically go out drinking after work?).
When and how to use observation
Information about your target population should help you to determine when to observe,
what to look for, and where to go to see who is in the social networks and what the highrisk settings are. (See Table 3 below for an example.)
Table 3: Observation locations
Locations for:
Secretaries
Bank tellers
Truckers
Front desk
Bank lobby
Truck park
Outside boss’s office
Break room
Bars/clubs
Lunch room
Neighbouring bar
Garages
The observer can be a non-participant or participant (an observer who joins the activities
as if he/she is a member of the population under observation). A non-participant observer
can be more objective, but sometimes activities arc too private or the people being observed
are too defensive to allow an outsider to observe. It is important that the person making the
observations be able to objectively record what he/she sees so that the data collected truly
reflect what is occurring.
Once on location, the observer should let events unfold as freely as possible in order to
observe the target population, networks and the culture, and to identify behaviour patterns.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
21
How to make observations
■
■
■
■
You may start by writing down everything that goes on in a blank notebook (field
notes). Describe who you see, what they are doing and the setting they are in. There
cannot be too many details when you are observing. These notes will help you
form hypotheses about what is going on and to compare what you discover during
observation with what you discover during interviews. You should take notes to help
ensure validity of the data-collection and -interpretation processes. You should also try
to confirm your data with members of the target population.
You may use audio- and/or videotape. Recording the essential elements of your
observations requires knowing what you are looking for.
In addition to your own observations, you can use the observations of others, journal
notes, or anything else that reveals the culture of the target population.
As you proceed with your observations, try to develop a synthesis of what you are
seeing, and then compare new information with information already synthesized. If
necessary, revise your synthesis and continue until you believe you have an accurate
picture of what is occurring.
The framework shown below might help you to better organize your observations.
Note that you can revise these categories to reflect the local situation. (See the appendix,
page F-l, for an observation guide.)
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
22
Step 5: Analyse the data from focus groups and in-ciepth
interviews
Purpose of data analysis
Dara analysis of focus group discussions and in-depth interviews involves reviewing the
statements made by participants on each topic to determine:
■
■
■
■
what the audience members already know and what misinformation they have;
why they behave the way they do;
how comfortable they feel discussing a topic, what they want to know, and what they
need to know; and
how they want to receive information, what they believe, and why.
Analysis should bring to the surface some of the underlying factors or reasons for
participants’ behaviour or beliefs, as well as some ideas for arguments that you may use to
motivate them to alter their behaviour or to allay their fears or doubts. Well-conducted
in-depth interviews and group discussions will provide data that can serve to improve
or modify counselling and service delivery, develop behaviour change communication
materials, and design training programmes.
After each in-depth interview or group discussion (or as soon as possible on that same day),
the facilitator and note-taker should review the notes together and, if possible, listen to
the audiotape(s) of the interview or group discussion to fill in any gaps in the notes. They
should jot down initial overall impressions and findings while the conversations are still
fresh in their minds. These initial notes often capture key findings as well as the atmosphere
of rhe interview or group. Certain emotional and interactive events are easily forgotten as
the team prepares for the next interview or group discussion. The quality of the notes will
directly influence the outcome of the data analysis.
Organizing notes
Organizing notes, after filling in any gaps, helps the project team understand the data
collected. Here is one method for doing this:
■
■
■
■
■
Photocopy notes. If photocopying is not possible, use coloured pencils for coding rhe
margin of the note-taker’s original notes, with a different colour assigned to each main
topic.
Place asterisks next to particularly ‘quotable’ passages (e.g., comments that might
actually be used as messages or as text under a pictorial message).
Write out key questions or topics from the discussion guide on the top of separate
sheers of paper.
Cur up the photocopy of rhe notes and glue all rhe information relevant to each
discussion question on the appropriate sheer of paper. Create new sheets labelled with
appropriate question headings for data that do not fit under any existing discussion
questions. Try to group the new data by question or issue.
Once you have cut and pasted all the notes onto sheets with headings, review the
information for each question. (Note: If you have used the margin colour-coding
method, take one topic at a time and read the coded items in rhe notes to see what
informants said and felt about each topic.)
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
23
■
■
Write a summary of the major findings for that question and, if possible, include some
participant quotes supporting the finding(s).
Review all the organized notes to see if programme staff can identify any emerging
patterns that confirm or refute assumptions about the research question. Those
organizing the discussion notes should be able to fill in these blanks:
Most of the participants said
Some of the participants said
A few of the participants said
■
Decide if it is necessary to add, change or delete any of the discussion questions
or probing questions to get the information you are seeking. Remember not to
automatically discount responses given by only a few people or that you had not
expected to hear. If you suspect that there may be an important underlying reason for
the comment, or that it may be an issue that is important to others, include questions
in subsequent focus groups to check out rhe finding.
Use of computer programmes
Several computer programmes are now available to help in organizing the information
gathered. Two popular programmes, NUD*IST and Ethnograph, are available from
SCOLARI Sage Publications Software (www.SColari.CQ.uk/). Other programmes such
as Ez-Text are available free of charge from the US Centers for Disease Control website
(www.cdc.gov/hiv/softwarc/ez-text.htm).
When deciding whether to use manual tabulation or computer-assisted analysis, consider
the following:
■
■
■
■
The programmes timeframe and resources. A computer programme will not code the
data or do the analysis for you. However, once you have coded the data, you can use a
programme to print out all coded text by topic area and do searches by several codes.
The computer will count everything. If one person makes similar statements several
times, the remarks may be inaccurately attributed to several group members,
concluding more consensus than is warranted.
Programme support staff may require the appropriate training to use the computer
programs.
Programme managers may decide that computer analysis is more suitable for analysing
qualitative data gathered for a large research project (where use of tapes followed by
transcription is part of the process) than for analysing a small series of focus group
discussions to identify relevant messages for designing pictorial materials.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
24
Comparing data across interviews or groups
After conducting all the in-depth interviews and group discussions, compare responses
from the various interviews and groups. Gather the responses for a specific question from
all of the interviews and groups, and, using either of the systems described above, write a
summary of the major findings for each question, including participant quotes. Identify
any patterns that may be useful.
If you do not have a software package to help you analyse the results, you will have to do it
manually.
Do not quantify results
Remember that this is qualitative research, which has the objective of describing a situation
or target population. Quantitative research, by contrast, is meant to report numbers
and quantify findings. While you are looking for trends in qualitative research, it is not
appropriate to quantify the results by counting or creating percentages for the number of
participants in the interviews or groups who give similar responses. Participants represent
only a small proportion of the population; thus, the findings from group discussions and
in-depth interviews cannot be generalized to the entire population.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
25
Step 6: Report on the formative assessment
The information collected will contribute to rhe development of an HIV/AIDS BCC
strategy for the workplace and can also help justify broader programming at the workplace
and in the surrounding community for HIV/AIDS prevention, care and support. You
should also disseminate rhe results of the formative assessment to the target groups at the
workplace. Interacting with target groups could provide rhe assessment team with more indepth data for the final analysis, conclusions and intervention recommendations.
Purpose of a formative assessment report
Once data analysis is complete, a formative assessment report should be produced. 1116
report should include opportunities, resources and potential barriers for BCC interventions
and broader HIV prevention at the workplace. It should also summarize information on
the target population’s knowledge, attitudes, behaviours, fears, goals, motivations and
interests with regard to HIV/AIDS prevention, care and support. Your programme can
disseminate information to target groups during BCC sessions, summarize the information
in a newsletter, or post it on a bulletin board, depending on information channels at the
workplace.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
26
Suggestions for report-writing
While the information is fresh, the programme manager should designate someone to
summarize the research findings in a report. This need not be a lengthy, official document;
the objective of this qualitative research is to gain useful information about the workplace
and rhe target groups at that workplace so that meaningful HIV/AIDS programmes can be
developed and implemented.
Be sure to include the following elements in the report:
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
Number of in-depth interviews and focus group discussions conducted for each
category of participant
Location of each in-depth interview and focus group discussion (city, clinic, home,
etc.)
Length of time spent in each interview and discussion
Major findings, including:
Existing HIV/AIDS prevention, care and support activities at the workplace and/or
community
Organization of the workplace and staff
What the target population knows about HIV/AIDS and the existing activities and
services at the workplace
What members of the target population think they know about HIV/AIDS
What the target population would like to know about HIV/AIDS
How members of the target population feel about important issues such as HIV/AIDS
stigma and discrimination at the workplace
What they do and why they do it
Wtys they believe they can be motivated to change certain behaviours
Barriers to change
Patterns (trends) in the data
Suggestions for communication strategies, messages, and improved and relevant new
materials.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
27
Step 7: Segment target populations
It is important to differentiate between rhe various groups in particular target populations.
The formative assessment will shed more light on these groups and will provide
information on gatekeepers, and primary and secondary populations. Although target
populations m ay be segmented during the formative assessment, additional groups may
also be identified.
You can further segment rhe target population following analysis of the formative
assessment data. The results will supply programme staff with a basis from which to
further segment the primary target population. A number of factors will help determine
subdivision of the population, including the following:
High-risk behaviours
Gender
Age
Location
Position at the workplace
Ethnicity
Language
See Table 4 below for an example of how to organize the information collected about the
different segments of the target population.
Table 4: Characteristics of primary and secondary populations
Characteristics
Primary
populations
Unmarried secretaries
♦
♦
♦
♦
♦
Married secretaries
♦
♦
♦
Low wages
Their bosses
Feel vulnerable
Lack of control
Do not want to loss their
position
Feel pride in job
Have more children than
unmarried
Do not feel as vulnerable as
unmarried
Often feel lack of control
over working environment
Characteristics
Secondary
populations
♦
♦
♦
Husbands/boyfriends
♦
♦
Most respect secretaries
Some take advantage of their
position
Some feel like secretaries “owe”
them
Happy that wives and/or
girlfriends can work
Worry about men flirting with
them
Workplace stakeholders may reach a consensus about whether or not further
segmentation is necessary. Further assessments should be undertaken if there are gaps
in the initial results and stakeholders express the need for a more conclusive analysis.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
Gathering Data for the Development
of a Behaviour Change Communication
Programme for the Workplace
Appendix
Contents
This appendix includes guides for the data-collection methods outlined in
Booklet 2, namely:
A: Site inventory
B: KAP survey for workers
C: Key informant interview
D: Focus group discussion
E: In-depth interviews
F: Observation
K
Here are a few ideas to keep in mind when reading and adapting rhe guides:
- Many of the guides include sample questionnaires to apply to prospective respondents.
Each questionnaire contains a wide array of potential questions. When developing a
questionnaire that is appropriate for the workplaces or sectors involved, choose those
questions that are most important and relevant for the target populations.
- As a rule, try to limit the number of interview questions to 12-15. Respondents probably
have limited time and may suffer from 'interview fatigue' if asked too many questions.
- You will find many of the same questions in the guides to site inventories, key informant
interviews, focus group discussions, and in-depth interviews. The same questions may yield
different information in the context of each method.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-l
Appendix A: Site inventory guide
Why conduct a site inventory?
Site inventories can help:
■
■
■
■
identify existing workplace services into which BCC activities can be integrated;
put information needs in perspective, allowing you to understand what information
you really need;
obtain useful background information; and
avoid the duplication of research when adequate information already exists.
As a research method, conducting site inventories can also help determine:
■
■
■
■
■
■
■
■
■
■
■
■
■
■
the approximate size and categories of staff within an organization;
staff hierarchies;
organizational structures;
major target groups—for example, in a flower farm, these might include field workers,
packers, drivers, support staff and health staff;
major target areas, such as headquarters, departments, satellite offices;
major stable and mobile target groups and the relative size of each;
existing health and education services at the workplace;
health, education, social and non-governmental organization services in an area;
the social and sexual culture of the workplace;
potential interventions;
a general idea of resources required for interventions;
the broader environment, including:
■ data on the HIV epidemic
■
roles of national, regional or local government in addressing HIV/AIDS
programme development at the workplace (e.g., BCC programmes, materials and
messages)
■
information and services available from community-based or AIDS-service
organizations
existing workplace initiatives that will support your BCC programme, including:
existing programmes, policies and practices at the workplace for HIV/AIDS prevention
and care
■ HIV/AIDS education programmes
■
condom distribution
■
diagnosis and treatment of sexually transmitted infections
■
access to voluntary HIV testing and counselling
■
available HIV/AIDS and tuberculosis treatment services, including antiretroviral
therapy
■
access to other health-care services
■
monitoring of quality and assessment of impact and effectiveness
■
workplace policy
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-2
■
■
■
worker organizations: what kind of support do workers receive from their union?
employee knowledge, attitudes, values and beliefs, including:
■ current knowledge, attitudes and behaviour regarding HIV/AIDS
■
level of interest in developing HIV/AIDS programmes
■
specific interests and concerns related to HIV/AIDS (e.g., housekeeping staff in a
hospital in Kenya were afraid to clean rhe rooms of AIDS patients)
■
whether there are people at the workplace or in the community who are HIV
positive and open about their status to their employers and co-workers
■
how employees living with HIV/AIDS feel about the treatment they receive at
work
communication mechanisms, including:
■ how people get information at rhe workplace (e.g., newsletter, bulletin board, via
staff meetings, training sessions, new employee orientations, through word-ofmouth)
■
who the trusted sources of information are
■
what peoples favourite media are and how often they access them
Steps for conducting an inventory
■
■
■
■
■
■
Review documents carefully, noting major departments and offices.
Consult with people who are familiar with each department, asking them to provide
further detail.
Visit the workplace and familiarize yourself with the site. During this visit, develop a
plan to conduct a more detailed inventory of the site, by subdividing it into smaller,
more manageable units and identifying focal points for further inventory.
Develop a detailed key and organizational chart stating staff and structures for each of
the features.
During the inventory, also note the following:
■ The latest estimate of the workplace population
■
Geographical distribution of the target population (for exam pie, if yo:u are working
with Bank X, note how many branches it has).
■
The general infrastructure, and which health and educational facilities are available
at the worksite.
On the basis of this information, assess whether it is feasible to initiate interventions in
the entire site or whether to limit interventions to subsites. In making this assessment,
consider these factors:
■ If the workplace population is too large, it may be advisable to limit activities to
subgroups, at least initially.
■
In widely dispersed workplaces, it may be better to choose particular sites for
initial activities.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-3
Sample questionnaire for site inventory on the national
perspective on HIV/AIDS at the workplace
To map out a broader picture of HIV/AIDS at the workplace, you may want to interview
staff from key ministries operating HIV/AIDS-related activities at the workplace, such as
the Ministry of Health and/or the Ministry of Labour. You might also want to interview
representatives from business organizations and labour leaders. Remember to choose a
maximum of 12—15 questions, based on your needs and objectives.
Epidemiology
■
Are there existing studies that provide insights into workplace target populations?
What are the incidence and prevalence of HIV?
What are the incidence and prevalence of sexually transmitted infections?
Role of government
■
■
■
■
■
■
What role has the national, regional and/or local government been playing in
addressing HIV/AIDS programme and policy development at the workplace?
Are there existing laws, guidelines or other regulations that address HIV/AIDS as it
relates to workplaces? What are they? Are any under development? (Get copies of these
documents, if possible.)
Do any of these laws or guidelines address discrimination against HIV-positive
employees?
Which government ministries or other bodies have been most active in issues relating
to HIV/AIDS and the workplace?
What role is the Ministry of Labour playing in this regard?
How could the Ministry’s capacity to promote and support the development of
workplace programmes and policies be enhanced?
Role of community
■
■
■
■
Do you know of other assistance programmes (whether run by government, labour
unions, non-governmental organizations or private firms) that have been helping
businesses with workplace-based HIV/AIDS programmes and policy development? If
so, please name and describe them.
Would you say they have been successful? Why or why not?
What do you think could be done differently to help make these workplace HIV/AIDS
policies and programmes (even) more successful?
Are there particular areas of need in workplace HIV/AIDS programme planning that
have nor been addressed and that you think should be?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-4
Role of business sector and labour unions
■
■
■
■
What are businesses and/or labour unions doing to respond to HIV/AIDS?
Are there enterprises that provide workplace-based HIV/AIDS education and
prevention services? How typical is that?
Are there employer organizations, or an existing business coalition on HIV/AIDS, that
do or could focus on HIV/AIDS and the workplace?
Are labour unions active in HIV/AIDS prevention, care and support?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-5
»
Sample questionnaire for site inventory on HIV/AIDS
at the workplace
People you might interview to map out a picture of HIV/AIDS at the workplace include
human resource managers, health and safety representatives, medical officers, trade union
leaders, and other enterprise spokespersons.
Remember to choose a maximum of 12—15 questions, based on your needs and objectives.
i
Workplace profile, unions and socio-cultural influences
Workplace profile
■
■
■
■
■
■
■
■
■
■
How many people are currently employed within each category of employee? (Break
down by gender, age and locale such as headquarters, province, district, factory, etc.)
What are the levels of education of the different categories of personnel (technical,
managerial, office support, etc.)?
What level of training and experience is required for each category?
What is the strategic importance of each category for the effective functioning of the
workplace?
Does the targeted workplace provide education/prevention programmes?
What services are being provided at the workplace (e.g., education sessions,
management of sexually transmitted infections, tuberculosis diagnosis and treatment,
condom distribution)?
What efforts exist to provide workers with access to voluntary HIV testing and
counselling?
What services exist for the care, treatment and support of HIV-positive employees and
their partners (e.g., treating opportunistic infections, proving antiretroviral therapy)?
Describe any health-related benefits offered to employees. For example:
■ Retirement benefits
■
Disability payments
■
Funeral expenses/burial fees
■
One-time payment of death benefits/life insurance
■
On-going family support
■
Other benefits
If a worker is known to have HIV/AIDS, do the benefits continue, remain rhe same, or
end?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
CPHE ‘ SOCHARA^
Koramangala
^<41 {CLIC) *
A-6
Workplace unions
■
■
Are one or more unions represented at the workplace?
If so, which unions are represented and how many staff at the workplace belong to
each union?
Number of employees
Number of employees
Number of employees
Union name
Union name
Union name
How interested are unions in HIV-related issues?
X
Socio-cultural influence
■
■
■
■
■
■
What laws, government policies, agencies and pressure groups influence and limit
various organizations and activities?
What are the prevalent religious practices?
What religious obstacles might there be to HIV programming?
What is the situation concerning stigma and discrimination (e.g., fear of revealing
status, reluctance to undergo HIV counselling and testing, lack of faith in
confidentiality of services, fear of stigmatization by fellow workers and community,
etc.)?
What factors affect peoples purchasing power and spending patterns (e.g., alcohol
consumption, sex work, affordability of condoms and health care)?
Is there peer pressure to drink alcohol and have sex with sex workers?
Vulnerable groups at the workplace
a. Understanding vulnerability
■
■
■
■
What features make it more or less likely that the workers at a specific workplace will
contract HIV infection?
Do certain male employees spend long periods away from home and family?
Do young, unmarried female workers seek to supplement their incomes through sex
for money?
Is there sexual coercion within the workplace—for example, do older men in power
pressure younger women working for them to exchange sex for better working
conditions?
b. Identifying susceptible groups
■
■
■
■
Which categories of employees (if any) are most likely to be susceptible to HIV
infection?
Are certain groups among employees particularly exposed to infection? (Examples
include health workers exposed to blood products, and employees who are away from
home for extended periods of time.)
Why are they exposed?
What are the gender and age characteristics of the most susceptible groups?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-7
HIV/AIDS programming at the workplace
a. Management support for HIV interventions
■
■
■
■
What is managements perception of its role in HIV/AIDS prevention, care and
support?
Is HIV/AIDS programming perceived as a benefit to the workplace?
What is managements perception of the enterprise’s potential for loss of skilled
workers and the cost of replacement?
Given the known and predicted rates of HIV prevalence, how many people does
management expect to become ill or die each year over the next ten to 15 years in each
category of employment?
b. Workplace HIV/AIDS interventions
■
Do employees have access to health services at the workplace related to prevention or
care of HIV/AIDS? If so, please specify. Are any of the Following offered?
■ HIV/AIDS focal point
■
Special HIV/AIDS budget
■
Full-time nurse
■
Information dissemination, including:
— Open poster display
— Peer education
— H1V/AIDS discussion committees
— Guest speakers
■
■
■
■
■
■
■
Condom distribution
■
Testing and diagnosis of sexually transmitted infections
■
Voluntary and confidential HIV testing
■
Counselling services
■
Tuberculosis treatment
■
Antiretroviral therapy
■
Antiretroviral treatment for women during pregnancy
■
Referral systems (to HIV/AIDS services in the community)
Do HIV/AIDS services reach all employees?
Do employees use the services?
Do employees trust the confidentiality of the services?
Which HIV/AIDS prevention, care and support services do employees most use and
accept?
Which of these services do they least use and accept?
What are some of the reasons employees give for accepting or not accepting HIV/
AIDS services and activities?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-8
€
c. Prevention strategies
■
■
■
■
What prevention strategies has your organization set up?
Do these strategies target specific populations?
What is the cost of these activities?
Are the efforts punctual (e.g., an isolated education session) or regular (an on-going
programme)?
d. Entry points for HIV/AIDS behaviour change communication at the workplace
■
■
■
■
■
What health-related activities does the organization offer (e.g., health and safety
training, first aid, counselling services, free medications, etc.)?
What work-related training does the organization offer?
How are announcements made (e.g., noticeboards, employee newsletters, pay package
notes, flyers, posters, etc.)?
Does the organization make use of washrooms to convey messages (hygiene messages.
advertisements, etc.)?
What social and recreation activities exist?
HIV/AIDS policy at the w<rorkplace
a. Workplace policies
■
Does the organization have a written policy statement dealing with HIV/AIDS at the
workplace? If so, what does it contain?
■ Statement on HIV/AIDS as a workplace and labour issue
■
How HIV/AIDS affects company growth
■
Prevention of discrimination on the basis of HIV status
■
Requirement to explain policy to employees
■
Assurance that the working environment is healthy
■
Protection of confidentiality
■
Prohibition of screening or testing for employment and other decisions such as
training and promotions
■
Assurance that HIV/AIDS is not a cause for termination of employment
■
Entitlement of all employees to company benefits
■
Assurance of equal treatment of employees, including gender equality
■
Provision of care and support for people living with HIV/AIDS in the home
■
Company HIV/AIDS budget
Conclusion
The site inventory is a framework for all ensuing work. After completing the site inventory
exercise, subsequent assessments and interventions can be planned around it. During
interventions, mapping can be repeated at regular intervals (usually annually), to ensure
that information is up to date.
ILO/FHI: HIV/AlDS behaviour change communication - a toolkit for the workplace
[Trial version]
A-9
Once the inventory has been carried out, the information can be summarized on the
following chart, indicating those characteristics of the workplace that support the
behaviour change communication objectives (assets) and those that may present barriers to
the initiative (gaps) and should be modified or changed.
Workplace assets
Workplace gaps
!
ILO/FHI: HIV/AlDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-l
Appendix B: KAP survey guide
Sample questionnaire for workers
I
ILO WORKPLACE EDUCATION PROJECT1
I
WORKER SURVEY
DATE:
/
J
DAY MTH YEAR
S'
Questionnaire number:
Interviewer:
Workplace:
Interviewer Instructions (READ OUT LOUD): “My name is ... I am assisting the ILO
HIV/AIDS Workplace Education Project in interviewing people at your workplace to see
what they understand about HIV and AIDS. The information from this interview will help
rhe ILO to develop and monitor a programme designed to assist you in protecting yourself
against HIV, with help from your employer and the people who work here. You have
been selected randomly from a list of all the workers at this [ministry, enterprise, informal
sector association]. There are XX other workers who were also selected randomly from this
[ministry, enterprise, informal sector association].
Confidentiality and consent: “I’m going to ask you some personal questions about
what you think about HIV and AIDS and about your sexual behaviour. Your answers are
completely confidential. We will not ask your name and will not record it anywhere. We
will not tell anyone else your answers to the questions. You do not have to answer any
questions that you do not want to answer. However, your honest answers to these questions
will help us to better develop a programme for this workplace. We would greatly appreciate
your taking part in this interview. Tie interview will take about 30 minutes. Would you be
willing to participate?”
(Signature of interviewer certifying that informed consent has been given verbally by
respondent)
1 This workers’ survey was developed by Management System International (MSI) as part of the project performance
monitoring tools for the ILO/USDOL International HIV/AIDS Workplace Education Programme. For National
Project Coordinators: The questions in yellow have been added to the generic workers’ survey developed in accordance
with the project performance monitoring plan to specifically address BCC issues.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
f'
!
s
i
I
B-2
Section 1: Socio-demographic Information
- NOT LINKED TO INDICATORS
Number
Questions and filters
Q101
Sex of respondent
Q102
How old were you on your last birthday?
Skip to
Coding categories
Male
1
Female
2
Age in completed years
[__ ]
Q103
Q104
Q105
Have you ever attended school?
What is the highest level of school you
completed?
Don’t know
88
No response
99
Yes
1
_____ No
Primary
£
Secondary
2
Higher
3
No response 99
Worker 1
What is your position at work?
Management
Other (specify:.
Q106
How long have you been working here?
1
2
.)
Don't know
88
No response
99
0 to 6 months
1
6 to 12 months 2
1 to 2 years
Q107
3
More than 2 years
4
No response
99
Married
What is your current marital status?
Single
Divorced
Separated
No response 99
Q108
Spouse
Who do you currently live with?
Relatives or friends
Alone
Other
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-3
Section 2
HIV/AIDS-related knowledge and attitudes
Number
Questions and filters
Q201
Have you ever heard of HIV or the disease called
AIDS?
Skip to
Coding categories
NOTE: QUESTIONS 201-207 ARE NOT LINKED
TO INDICATORS; THEY ARE FOR GENERAL
INFORMATION
Yes
1
No
2
->202
END
Don’t know 88
No response 99
The next set of questions asks you about how you heard about HIV/AIDS.
Q202
From what sources have you heard about HIV/
AIDS?
Mass media
Health provider outside
workplace
Interviewer: check appropriate boxes
Workplace clinic
Labour union representative
NGO
Family or friends
Co-worker
Other source
Q203
Which was the best source of information for
you about HIV/AIDS?
Mass media
Health provider outside
workplace
Interviewer: check one box
Workplace clinic
Labour union representative
NGO
Family or friends
Co-worker
Other source
Q204
What sources of information on sexual health do
you find most credible?
Interviewer: check appropriate boxes
Mass media
Health provider outside
workplace
Workplace clinic
Labour union representative
NGO
Family or friends
Co-worker
Other source
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-4
Q205
What sources of information on sexual health do
you find most credible at the workplace?
Interviewer, check appropriate boxes
Printed materials
Health provider at workplace
Workplace clinic
Labour union representative
Co-worker
Other source
Q206
How are announcements made at the
workplace?
Noticeboards
Interviewer: check appropriate boxes
Employee newsletters
Emails
Pay package notes
Flyers
Posters
Word of mouth
Other
Q207
What occasion(s) bring(s) most of the employees
together?
Meetings
Lunch
Breaks
After-work events
Encounters in hallways
Other
The next questions ask you about how you can become infected with
HIV, the virus that causes AIDS. The first question uses the term “sex”.
By this we mean vaginal, oral or anal sex. When we use the word “sex”
in other questions, it will always mean vaginal, oral or anal sex.
Q208
Can you become infected by having unprotected
Yes
1
sex with a person who is infected with HIV?
No
2
Don’t know 88
No response 99
Q209
Can you become infected from a transfusion of
blood or blood products?
Yes
1
No
2
Don’t know 88
No response 99
Q210
Can you become infected by sharing needles
Yes
1
with a person infected with HIV?
No
2
Don’t know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-5
Q211
Can a HIV+ mother infect her unborn child?
Yes
1
No
2
Don't know 88
No response 99
The next questions ask you about how you can keep from becoming
infected with HIV, the virus that causes AIDS.
Q212
Can you keep yourself from becoming infected
by having faithful sexual partners who are not
infected with HIV?
Yes
1
No
2
Don’t know 88
No response 99
Q213
Can you reduce the chance of becoming infected
by using condoms during sex?
Yes
1
No
2
Don’t know 88
No response 99
Q 214
Can you keep yourself from becoming infected
by having no sex?
Yes
1
No
2
Don’t know 88
No response 99
Q215
I
Can you become infected by having unprotected
sex with a person who looks healthy?
I
Yes
1
No
2
Don’t know 88
No response 99
Q216
Is excessive use of alcohol or drugs a
contributing risk factor to becoming infected
with HIV?
Yes
1
No
2
Don’t know 88
No response 99
Q217
Is there a difference between HIV and AIDS?
Yes
1
No
2
Don’t know 88
No response 99
Q218
Can you always tell if someone has HIV by
looking at them?
Yes
1
No
2
Don’t know 88
No response 99
The next questions ask you how you feel about using condoms if you
have sex with a person other than your spouse(s)
Q219
Do you believe a condom should be used if
you have sex with a person other than your
spouse(s)?
Yes
1
No
2
Don't know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-6
Q220
Do you believe you know how to use a condom
correctly?
Yes
1
No
2
Don’t know 88
No response 99
Q221
Do you believe that it is acceptable for married
men to use condoms at home?
Yes
1
No
2
Don’t know 88
No response 99
Q222
Do you believe that it is acceptable for single
men to use condoms?
Yes
1
No
2
Don’t know 88
No response 99
Q223
Do you believe that it is acceptable for married
women to use condoms at home?
Yes
1
No
2
Don’t know 88
No response 99
Q224
Do you believe that it is acceptable for single
women to use condoms?
Yes
1
No
2
Don’t know 88
No response 99
The next set of questions asks you how you feel about people who have
HIV or AIDS.
Q225
Would you be willing to work alongside a co
worker who is HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q226
Would you be willing to use the same toilet as a
co-worker who is HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q227
Would you be willing to eat food at a company
canteen prepared by a co-worker who is HIV
positive?
Yes
1
No
2
Don't know 88
No response 99
Q228
Would you be willing to share utensils with a co
worker who is HIV-positive?
Yes
1
No
2
Don't know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-7
Q229
[ Would you be willing to buy food prepared by a
’ vendor who is HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q230
Would you be willing to hold hands with
someone who is HIV-positive?
Yes
1
No
2
Don't know 88
No response 99
Q231
Would you be willing to share a room with
someone living with HIV/AIDS?
Yes
1
No
2
Don’t know 88
No response 99
Q232
Would you be willing to receive medical
treatment from a health-care worker who is HIV
positive?
Yes
1
No
2
Don’t know 88
No response 99
Q233
Would you be willing to utilize the services of a
barber or a hairdresser who is HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q234
Do you feel that a teacher who is HIV-positive
should be allowed to continue teaching?
Yes
1
No
2
Don’t know 88
No response 99
Q235
Do you feel that HIV-positive children should
be allowed to stay in school with uninfected
children?
Yes
1
No
2
Don’t know 88
No response 99
Q236
In the last 3 months, have you known of
someone at your workplace gossiping about a
co-worker suspected of being HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q237
In the last 3 months, have you known of
someone at your workplace refusing to work
with a co-worker suspected of being HIV
positive?
Yes
1
No
2
Don’t know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
- SOCHARAX^
Koramangala
rTcuci"*
B-8
Q238
In the last 3 months, have you known of
someone at your workplace refusing to eat with
a co-worker suspected of being HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q239
In the last 3 months, have you been aware
of a situation in which employees received
negative treatment because they were known or
perceived to have HV or AIDS?
Yes
1
^240
No
2
->241
Don’t know 88
No response 99
Q240
If so, who treated the employee known or
perceived to have HIV or AIDS negatively?
Interviewer: check appropriate boxes
Co-workers
Supervisors
Managers
Labour representatives
Other
Q241
In the last 3 months, have you been aware
of a situation in which employees received
positive treatment because they were known or
perceived to have HV or AIDS?
Yes
1
->242
No
2
243
Don’t Know 88
No response 99
Q242
If so, who treated the employee known or
perceived to have HIV or AIDS positively?
Interviewer: check appropriate boxes
Co-workers
Supervisors
Managers
Labour representatives
Other
The next set of questions asks how your employer treats people who
might have HIV/AIDS.
Q243
Do you believe a physically fit worker at your
workplace would be fired if he or she was known
to be or was suspected of being HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
Q244
Do you believe a physically fit worker at your
workplace would be denied promotion, salary
increases, training or other career development
opportunities if he or she was known to be or
was suspected of being HIV-positive?
Yes
1
No
2
Don’t know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-9
Section 3
HIV/AIDS-related services
Number
Questions and filters
Skip to
Coding categories
The next questions asks you about HIV/AIDS services that you may
have received at the workplace
Q301
Are you aware of any HIV/AIDS services
available at your workplace?
Yes
1
-^302-316
No
2
■401
Don’t know 88
No response 99
Q302
If so, which HIV/AIDS-related services at your
workplace are you aware of?
Interviewer: please check boxes
Education
Condom availability
STI treatment/information
VCT/information
Care and support/information
Other
Q303
Brochures
What kinds of HIV-prevention materials exist at
your workplace?
Posters
Interviewer: check appropriate boxes
Books
Information sheets
Other.
Q304
Brochures
What kinds of HIV-prevention materials do you
prefer?
Posters
Interviewer: check appropriate boxes
Books
Information sheets
Other
Q305
What kind of HIV-prevention education exists at
your workplace?
Interviewer: check appropriate boxes
Presentations
Facilitated discussions
Informal discussions
Peer education
Support programmes for those
living with HIV/AIDS
Other
Q306
What kind of HIV-prevention education do you
prefer?
Interviewer: check appropriate boxes
Presentations
Facilitated discussions
Informal discussions
Peer education
Support programmes for those
living with HIV/AIDS
Other
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
->303-306
8-10
Q307
In the past 6 months, have you received any
HIV/AIDS education, such as a training course,
that was led by an expert or peer counsellor at
your worksite?
Yes
1
No
2
Don't know 88
No response 99
Q308
In the past 6 months, have you requested and
received condoms at the workplace?
Yes
1
No
2
Don’t know 88
No response 99
Q309
If so, were the condoms consistently available
WHEN REQUESTED?
Yes
1
No
2
Don’t know 88
No response 99
Q310
In the past 6 months, have you requested
and received information at the workplace
on resources in the community that provide
treatment of sexually transmitted infections?
Yes
1
No
2
Don’t know 88
No response 99
Q311
In the past 6 months, have you requested
and received information at the workplace
on resources in the community that provide
voluntary HIV counselling and testing?
Yes
1
No
2
Don’t know 88
No response 99
Q312
In the past 6 months, have you requested
and received information at the workplace on
resources in the community that provide care
and support services and AIDS treatment?
Yes
1
No
2
Don't know 88
No response 99
Q313
Does your workplace’s HIV/AIDS education
reach all of the employees?
Yes
1
No
2
Don’t know 88
No response 99
Q314
Do employees use the HIV/AIDS-related services
available to them at the workplace?
Yes
1
-^Q315
No
2
—+Q316
Don’t know 88
No response 99
Q315
Education
If so, which services do they use?
Condoms
STI treatment
VCT
Antiretroviral therapy
Other
Q316
Do employees trust the confidentiality of the
HIV/AIDS services at the workplace?
Yes
1
No
2
Don’t know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-ll
Section 4
HIV/AIDS policy
»T^
1
The next set of questions asks you about your knowledge of HIV/AIDS
policy or guidelines at your workplace.
Q401
Q402
Yes
1
—»Q402
No
2
—>Q501
Don’t know 88
-♦Q501
No response 99
^Q501
Does your employer have an HIV/AIDS policy (or
HIV/AIDS guidelines) that protects employees
who have HIV/AIDS?
What are the components of that workplace HIV/
AIDS policy (or guidelines)?
Interviewer: please check boxes of components
mentioned by respondent
Dialogue between
management/workers
Non-discrimination
No mandatory HIV test
No denial of employment
Healthy work environment
Medical confidentiality
No job termination if fit to work
Same opportunities as others
Gender equality
HIV-prevention education
.)
Other (.
Q4O3
According to workplace policy (or guidelines),
do management and workers engage in regular
dialogue to ensure the successful implementation
of HIV/AIDS policy and programmes?
Note: Questions 403-408 are not directly linked to
an indicator - they evaluate level of knowledge for
104. THESE QUESTIONS MAY BE DISREGARDED
FOR INFORMAL SECTOR_______________________
Q404
According to workplace policy, do all employees
have the right to the same treatment regardless
of their HIV status?
Yes
1
No
2
Don’t know 88
No response 99
Yes
1
No
2
Don’t know 88
No response 99
Q405
According to workplace policy, are job applicants
or workers protected from mandatory HIV testing
for employment or promotion?
Yes
1
No
2
Don’t know 88
No response 99
Q406
According to workplace policy, are employees’
medical records confidential?
Yes
1
No
2
Don’t know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-12
Q407
According to workplace policy, are employees
informed of first aid procedures that would protect
them against HIV infection?
Yes
1
No
2
Don't know 88
Q408
According to workplace policy, is basic first aid
equipment available to employees to protect
them against HIV infection (gloves, for example)?
No response 99
Yes 1
No
2
Don't know 88
Q409
According to workplace policy, do workers have
the right to education at the workplace on HIV
prevention, transmission and treatment?
No response 99
Yes 1
No
2
Don’t know 88
No response 99
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-13
Section 5
HIV/AIDS-related practices
Number
Questions and filters
Coding categories
Skip to
The next set of questions asks about your sexual behaviour. We
recognize that this part is sensitive and we appreciate your honest
answers to the questions. This will help us better design an HIV/AIDS
programme for your workplace.
Q 501
Yes 1
—»Q501
No
2
—►end of
Don’t know 88
questions
Are you sexually active?
Note: Question not related to an indicator
No response 99
Q502
Yes 1
^Q503
2
—►end of
Don’t know 88
questions
If so, do you have a sexual partner other than your
spouse(s)?
Note: Question not related to an indicator
No
No response 99
Q503
In the past 3 months, have you had sex with a
person other than your spouse(s)?
4
Yes
1
—►Q504
No
2
Q505
Don’t know 88
I
No response 99
Q504
Yes
1
No
2
Don’t know
88
If so, did you use a condom the last two times you
had sex with person(s) other than your spouse(s)?
No response 99
Q505
If you have had multiple sexual partners in the
past, have you intentionally reduced the number
of those partners in the past 6 months in order to
reduce the risk of HIV?
Yes
1
No
2
Don’t know
88
No response 99
Q506
Yes
1
No
2
Don’t know
88
Do you feel you are at risk of becoming infected
with HIV or another sexually transmitted infection?
No response 99
Q507
Yes
1
—508-512
No
2
—510
Don’t know
88
Are certain employees at the workplace more
vulnerable to HIV infection than others?
No response 99
Q508
Females
If so, who?
Males
Those who travel
Other
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
B-14
Q509
If so, why?
Multiple sexual partners
Not using condoms
Sharing needles
Not being faithful to spouse
Partner is not being faithful
Other
Q510
Do you think you can change your behaviours to
reduce your risk of becoming infected with HIV?
Yes
1
No
2
Don’t know
88
No response 99
Q511
Do you think men at your workplace can change
their behaviours to reduce their risk of becoming
infected with HIV?
Yes
1
No
2
Don’t know
88
No response 99
Q512
Do you think women at your workplace can
change their behaviours to reduce their risk of
becoming infected with HIV?
Yes
1
No
2
Don’t know
88
No response 99
THANK YOU VERY MUCH FOR TAKING PART IN THIS INTERVIEW.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
*
C-l
Appendix C: Key informant interview guide
Sample introduction to key informant
Good morning/ahernoon/evening! Thank you for raking rhe rime to speak with me today.
My name is. 1 work for
and come from
. (Note-taker/
observer introduces her/himseif.)
I would like to discuss some health issues that affect your workplace, including HIV/AIDS.
I’m interested in all your ideas, insights, comments and suggestions. I’d like you to know
that there are no right or wrong answers to any of the questions I will ask you. Your point
of view is of the greatest importance during this interview. All comments—both positive
and negative—are welcome.
To avoid missing any points that you make during our conversation, I would like to use
a tape recorder. I want you to know that all your comments are confidential and will be
used for research purposes only. To protect your confidentiality, your hill name will not
be recorded. I will be happy to answer any questions that you may have at the end of our
conversation.
Sample questionnaire for key informants
People to interview in order to get a better picture of the target population and their
specific vulnerabilities to HIV might include those who have been at the workplace for a
long time, those who are perceptive about their workplace environment and colleagues,
and those who are willing to share their insights with you.
The objective of key informant interviews focused on the target population differs from
that of key informant interviews for site inventory. The goal of the site inventories is to gain
a better understanding of the national and local HIV/AIDS environment related to the
workplace. The goal of key informant interviews of the target population is to gain a better
understanding of the population, which, in turn, will contribute to the design of effective
behaviour change communication programmes. Therefore, these key informant interviews
should focus on the ‘Behaviour change communication questions’, which begin on page C-7
of this guide. You should choose only a few of the questions listed under other headings
below (if any), to complete key informant interviews.
Remember to choose a maximum of 12—15 questions, based on your needs and objectives.
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
C-2
Socio-demographic information, workplace profile, unions, and
socio-cultural influences
Key informant profile
Name of organization:
Location:
Job title/grade:
Salary:
Age:
Sex:
Education level:
Religious affiliation:
Marital status:
Number of children:
Ethnic group:
Workplace profile
■
■
■
■
■
Briefly describe the structure of the enterprise.
What are the different categories of personnel (technical, managerial, office support,
etc.)?
What is the total number of personnel at your workplace?
How many people are currently employed within each category of employee? (Break
down by gender, age and locale such as headquarters, ministries, district, or other
locations.)
Are you familiar with any other programmes (whether run by government, labour
unions, non-governmental organizations or private firms) that have been helping
businesses with workplace-based HIV/AIDS programmes and policy development? If
so, please describe.
■ Would you say they have been successful? Why or why not?
■
What, if anything, do you think could be done differently to make workplace
HIV/AIDS policies and programmes (even) more successful?
■
Are there particular areas of need in workplace HIV/AIDS programme planning
that you think should be addressed and have not been thus far?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
5
C-3
Socio-cultural influence
■
■
■
■
■
■
What laws, government policies, workplace policies, agencies, churches or pressure
groups influence this organization’s ability to implement HIV/AIDS-reiated activities?
(Ask each question individually—first about laws, then about government policies,
then about workplace policies, etc.)
What religious practices are prevalent at this workplace? Do they help or hinder HIV/
AIDS-related activities?
Are there any religious obstacles to HIV/AIDS programming (e.g., church’s view on
HIV prevention)?
What is the situation concerning stigma and discrimination in relation to HIV/AIDS
(e.g., fear of revealing HIV-positive status, lack of faith in confidentiality of services,
fear of stigmatization by fellow workers and community, etc.)?
Do you think your workforce would be willing to undergo voluntary counselling and
testing for HIV? What about you? What do you think the benefits of HIV counselling
and testing might be?
Is there peer pressure at rhe workplace to do things such as drink alcohol, dress a
certain way and/or have sex with other workers? Please explain.
Knowledge, attitudes and beliefs about HIV/AIDS
Understanding vulnerability
■
■
■
Are certain employees at the workplace more vulnerable to HIV infection than others?
(Probe on females vs. males, those who travel vs. those who do not, etc.) Please explain.
Is there sexual coercion within the workplace (e.g., do older men pressure younger
women who work for them to exchange sex for better working conditions)?
Do you think you are at risk of contracting HIV?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
C-4
Knowledge, awareness and perceptions of HIV/AIDS
■
■
■
■
■
■
■
■
■
What can you tell me about how [insert name of the target population here, e.g., rhe
employees of X Company] think HIV and other sexually transmitted infections are
transmitted and prevented?
Do [name of target population] know the difference between HIV and AIDS?
Do they know about the length of time an HIV-positive person can live with no
symptoms before developing opportunistic infections (i.e., AIDS) and, finally, dying?
Are they aware of the possibility of mother-to-child transmission of HIV? Please
explain.
Do they think it is possible to get HIV by having casual contact with HIV-positive
people? Please explain.
Where are they in the process of behaviour change (e.g., unaware, informed/aware,
concerned, knowledgeable and skilled, motivated to change, ready to change, have
tried or tested the new behaviour, or have adopted and maintained safer behaviour)?
What is their estimation of their personal risk of becoming infected with HIV and
other sexually transmitted infections?
If they do not feel that they are at risk, what is their reason for this?
Which peer groups and significant others are most important to them?
HIV/AIDS programming at the workplace
Management support for HIV/AIDS-related activities
■
■
■
■
■
Is the HIV epidemic taken seriously at your workplace?
What is management’s perception of its role in HIV prevention, care and support
when an employee is living with HIV/AIDS, and in the elimination of HIV/AIDSrelated stigma and discrimination?
Is HIV programming perceived as a benefit to employees?
What is management’s perception of the potential for loss of skilled workers and of the
cost of replacement?
Given the known and predicted rates of HIV prevalence, how many people does
management expect to become ill or die each year over the next ten to 15 years in each
category of employment?
Union support for HIV/AIDS
■
If unions exist, how interested are they in HIV-related issues?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
C5
♦
HIV/AIDS at the workplace
■
■
■
■
5
■
■
■
■
■
■
■
What are businesses and/or labour unions in the country doing to respond to HIV/
AIDS?
What do you believe yoi>ur employer and/or union should do to assist workers in
preventing HIV?
What do you think your employer and/or union would do if they knew an employee
had AIDS?
Do employees have access to health services at the workplace related to HIV
prevention or care? If so, please list those services. Could include:
■ HIV/AIDS focal point
■
Special HIV/AIDS budget
■
Full-time nurse
■
Information dissemination, such as:
■
Open poster display
■
Peer education
■
HIV/AIDS discussion committees
■
Guest speakers
■
Condom distribution
■
Testing and diagnosis of sexually transmitted infections
■
Voluntary and confidential HIV testing
■
Counselling services
■
Tuberculosis treatment
■
Antiretroviral therapy
■
Antiretroviral treatment for women during pregnancy
■
Referral systems (to HIV/AIDS services in the community)
If a preventive education programme on HIV/AIDS at the workplace exists, how
would you describe it?
■ Basic facts in brochures, posters, etc.
■
A short presentation (30—60 minutes) of factual information about HIV/AIDS
■
A longer programme or discussion about HIV/AIDS such as attitudes towards
AIDS, experiences with HIV, or support and care issues
■
A formal peer education programme for HIV/AIDS (if one exists, please describe
the programme and how it began)
■
Education or support programmes for workers living with HIV/AIDS
■
Education or programmes for workers on sensitivity to HIV-positive co-workers
Do HIV/AIDS services reach all employees?
Do employees use the services?
Do employees trust the confidentiality of the services?
Which HIV prevention and care services do employees most use and accept?
Which of these services do they least use and accept?
What are some of the reasons employees give for accepting or not accepting HIV/
AIDS services and activities?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
C-6
■
■
■
■
What do you think this organization should do in terms of HIV/AIDS programming
that it is not currently doing?
What was the cost of HIV/AIDS-related activities at the workplace last year? What is
the cost of such activities this year? Who or what organization/ agency is funding these
activities?
Are these activities temporary (isolated events) or regular (ongoing programmes)?
Are any collaborative groups involved in these activities?
Entry points for workplace behaviour change communication
■
■
■
■
■
■
What health-related activities does the organization offer (e.g., health and safety
training, first aid, counselling services, free medications, etc.)?
What work-related training does the organization offer?
How are announcements made (e.g., noticeboards, employee newsletters, pay package
notes, flyers, posters, etc.)?
What occasion(s) bring most of the employees together? How often do these gatherings
occur and how long do they last?
Does the organization make use of washrooms to convey messages (hygiene messages,
advertisements, etc.)?
What social and recreational activities exist?
HIV/AIDS policy at the workplace
■
■
Is there a workplace HIV/AIDS policy in this organization? If so, could you please
explain it to me and could I have a copy of it?
What is the policy of management regarding em ployees who are HIV-positive and
those living with AIDS?
HIV/AIDS-related practices
■
■
■
■
■
■
■
Based on your observation and personal contacts, what do you think are the behaviours
that put employees most at risk of contracting HIV and other sexually transmitted
infections?
How do they currently understand and practise preventive behaviours?
What do they see as rhe benefits of changing their high-risk behaviours?
What do they see as the disadvantages of changing their high-risk behaviours?
What pressures make it difficult for them to change their high-risk behaviours?
What power do they believe they have to change their behaviours? If it is limited,
please explain why and by whom or what.
What would it take for them to change to a safer behaviour or to continue practising a
safer behaviour?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
C-7
Behaviour change communication questions
Media preferences and habits
■
■
■
■
■
■
Which radio and television programmes do [insert name of target population here]
prefer?
What is the language of the broadcast?
When do they listen to or watch these programmes?
What print media do they prefer (e.g., newspapers, magazines, pamphlets, booklets,
comic books, picture books, etc.)?
What kind of music do they listen to?
What kind of traditional theatre do they attend?
Sources of information
■
■
■
■
■
■
■
When and where do [insert name of target population here] usually get information
about topics related to sexual health?
How do they communicate with their friends (email, telephone, in person, etc.)?
Where do they meet? When? Who is in their immediate social network?
What are the sources of information on sexual health that they find most credible?
Who is their trusted source of information at the workplace?
If they had a question about HIV/AIDS, whom would they consult in the community?
At the workplace?
When and where would it be best to talk to them about HIV prevention, to distribute
condoms and to offer treatment services for sexually transmitted infections, and who
could do this most effectively?
Which teaching aids would help you learn the most in group information
sessions (e.g., videos, slide shows, overhead projectors, flipcharts, picture codes,
demonstrations, role plays, etc.)?
Fears and hopes
■
■
■
■
■
■
■
■
How do [insert name of target population here] see themselves in ten years’ rime?
What are their hopes and dreams for the future?
What would be the best thing that could happen to them in the future?
What do they need to help them realize their hopes and dreams?
What can they do specifically to realize their hopes and dreams?
What is the biggest obstacle to them achieving their long-term goals?
What fears do they have about the future?
What is the biggest threat that they face today that could affect their future?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
C-8
1
Stigma and discrimination
■
■
■
■
■
What is being done to ensure that employees are not discriminated against and that
they receive prevention and education services at rhe workplace regarding HIV/AIDS?
Are you familiar with any support organization for people who are HIV-positive?
Are there employees who are HIV-positive who are open about their status to their
employers and co-workers?
Are you aware of a situation in which employees/workers received different treatment
because they were known or perceived to have HIV/AIDS? If so, please describe.
Who treated the employee known or perceived to have HIV/AIDS differently?
■ Co-workers
■
Supervisors
■
Managers
■
Labour representatives
■
Others (specify)
Conclusion
■
Do you have any other ideas or recommendations about what kind of HlV-preventionand-education programmes should be implemented for the benefit of workers?
■ At the workplace?
■
■
In the community?
Is there anything else you would like to tell me?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
D-l
D: Focus group discussion guide
Sample introduction for focus group discussions
Good morning/afternoon/evening! Welcome to our group discussion. My name is.
I work for
her/himself).
and come from. (Note-taker/observer introduces
We’re here today to talk about certain health issues that affect your workplace, including
HIV/AIDS. We are interested in all your ideas, insights, comments and suggestions. There
are no right or wrong answers. All comments—both positive and negative—are welcome.
Please feel free to disagree with one another. We welcome all points of view. We want this
to be a group discussion, so you need nor wait for me to call on you to speak.
To avoid missing any points that you make during our discussion, I would like to use a
tape recorder. I want you to know that all your comments are confidential and will be used
for research purposes only. To protect your confidentiality, your names will not be recorded.
We will be happy to answer any questions you may have at the end of the discussion.
You can leave at any time during the discussion and you do not have to talk about anything
that makes you uncomfortable. Do I have your permission to start the group discussion?
Socio-demographic information and discussion
Introduction
■
■
■
What are the main problems you face?
How do you solve them?
What do you do when on leave and at weekends?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
D-2
Knowledge, attitudes and perceptions about HIV/AIDS
Levels of knowledge about HIV/AIDS
■
■
■
■
■
■
■
■
■
■
■
■
■
What do HIV and AIDS stand for?
What is a sexually transmitted infection?
Name three common sexually transmitted infections.
How are HIV and other sexually transmitted infections transmitted?
Do you know colleagues/friends who have ever had a sexually transmitted infection?
How did they treat it?
How can HIV be prevented?
What are the signs and symptoms of AIDS?
What are opportunistic infections?
What is the length of time between infection with HIV and the progression to AIDS?
How can HIV infection pass from a mother to her child?
What forms of social/sexual contact and activity do not involve a risk of HIV
transmission?
What is voluntary HIV counselling and testing?
Perception of HIV
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
■
What are your thoughts about HIV?
What are your thoughts about other sexually transmitted infections?
What do your co-workers and friends think about HIV and other sexually transmitted
infections?
Do you think you are at risk of becoming infected with HIV or other sexually
transmitted infections? Please explain.
Which behaviours do you think put you at risk of contracting HIV and other sexually
transmitted infections?
Which behaviours do you think put your friends at risk of contracting HIV and other
sexually transmitted infections?
Do you think your partner is faithful to you?
How do men react when their female partners ask them to use a condom?
How would you react if your casual partner refused to use condom?
Why do some colleagues and friends agree to sex without a condom?
How do you feel about undergoing HIV counselling and testing?
What do you think are the benefits of HIV counselling and testing?
[For women] Would you consider undergoing HIV counselling and testing before
getting married and before becoming pregnant in the future?
What would you do if you found out that your co-worker was HIV-positive?
What would you do if you found out that you were HIV-positive?
Is there peer pressure to drink alcohol, dress fashionably and/or have sex with sex
workers?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
D-3
Understanding vulnerability
■
■
■
■
■
■
What features of your workpl ace make it more or less likely for workers to contract
HIV infection?
Which categories of employees (if any) are likely to be exposed to HIV infection?
Do some employees spend long periods away from home and family?
Do you know of colleagues who have been approached on the job for sexual favours in
exchange for better working conditions and other benefits?
If they don’t agree, what happens?
If they agree, what happens?
HIV/AIDS programming at the workplace
■
■
■
What HIV/AIDS prevention, care, support and treatment services are available to you
at your workplace?
What is your opinion about your employers/union’s response to HIV/AIDS?
What kinds of HIV/AIDS programmes/services would you like to see at the
workplace?
HIV/AIDS policy at the workplace
■
■
Does your organization have a policy about HIV/AIDS at the workplace? If so, could
you please explain it to me?
What is the policy of management regarding employees who are HIV-positive and
those living with AIDS?
HIV/AIDS-related practices
■
■
■
■
■
■
■
■
What behaviours put you most at risk of becoming infected with HIV and other
sexually transmitted infections?
How do protect yourself from HIV infection?
Do you want to change any of your behaviours that may put you at risk of contracting
HIV? Please explain.
What do you see as the benefits of changing your high-risk behaviour?
What do you see as rhe disadvantages of changing your high-risk behaviour?
What pressures make it difficult for you to change your behaviour?
What power do you believe you have to change your behaviour? If it is limited, why is
that, and by whom or what?
What would it take for you to change to a safer behaviour or to continue practising a
safer behaviour?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
D-4
Behaviour change communication questions
Media habits
■
■
■
■
Which are your favorite radio and TV programmes and when do you watch or listen to
them?
What is the language of the broadcast?
Which newspapers do you read? Magazines? Pamphlets? Booklets? Comic books?
Picture books?
What kind of music do you like?
Which kind of traditional theatre do you attend (local drama, concert party, story
telling, etc.)?
Sources of information on HIV/AIDS
■
■
■
■
■
■
■
■
When and where do you usually get information about topics related to sexual health?
Who or what is your trusted source for health information at the workplace?
How do you communicate with friends (in person, by email, on the telephone)? Where
do you meet your friends? When? Who is in your immediate social network?
What peer groups and significant others are most important to you?
What are your preferred sources of information on health-related topics?
What are the sources of information on sexual health that you find most credible?
When and where would be the best times to talk to you about HIV prevention, to
sell or distribute condoms and to provide treatment services for sexually transmitted
infections? Who could do this most effectively?
Which teaching aids would help you learn the most in group information
sessions (e.g., videos, slide shows, overhead projectors, flipcharts, picture codes,
demonstrations, role plays, etc.)?
Fears and hopes
■
■
■
■
■
■
■
How do you see yourself in ten years’ time?
What would be the best thing that could happen to you in the future?
What do you need to help you realize your hopes and dreams?
What could prevent your hopes and dreams from being realized?
What are the biggest obstacles to you not achieving your long-term goals?
What fears do you have about the future?
What are the major barriers/hindrances you currently face that could affect your
future?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
"-Wi’
Stigma and discrimination
■
■
■
■
■
/
What is the organization doing to ensure that employees are not discriminated against
and that they receive prevention and education services at the workplace regarding
HIV/AIDS?
Are you familiar with any support organization for people who are HIV-positive?
Are there employees who are HIV-positive who are open about their status to their
employers and co-workers?
Are you aware of a situation in which employees/workers received different treatment
because they were known or perceived to have HIV? If so, please describe.
Who treated the employee known or perceived to have HIV/AIDS differently?
■ Co-workers
■
Supervisors
■
Managers
■
Labour representatives
■
Others (specify)
a
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
D-5
E-l
Appendix E: In-depth interview guide
Sample introduction to in-depth interviewee
Good morning/afternoon/evening! Thank you for taking rhe time to speak with me today.
(Note-taker/
My name is. I work for
and come from
observer introduces her/himself.)
I would like to discuss some health issues that affect your workplace, including HIV/AIDS.
I’m interested in all your ideas, insights, comments and suggestions. Id like you to know
that there are no right or wrong answers to any of the questions I will ask you. Your point
of view is of the greatest importance during this interview. All comments—both positive
and negative—are welcome.
To avoid missing any points that you make during our conversation, I would like to use
a tape recorder. I want you to know that all your comments are confidential and will be
used for research purposes only. To protect your confidentiality, your full name will not
be recorded. I will be happy to answer any questions that you may have at the end of our
conversation.
Socio-demographic information and introduction
Key informant profile
Name ol organization:
Location:
Job title/grade:
Salary:
Age:
Sex:
Education level:
Religious affiliation:
Marital status:
Number of children:
Ethnic group:
Number of years at current position:
Area in which you live:
Hobbies:
Introductory questions
■
■
■
■
■
■
What are the main problems you face?
How do you solve them?
What are your expenditures for the month?
What are your sources of income?
How much do you earn per month?
What do you do when on leave and at weekends?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
E-2
Knowledge, attitudes and perceptions about HIV/AIDS
Knowledge levels
■
■
■
■
■
■
■
■
■
■
■
What do HIV and AIDS stand for?
How are HIV and other sexually transmitted infections transmitted?
Name three common sexually transmitted infections.
Do you know a colleague or friend who has ever had a sexually transmitted infection?
How can HIV be prevented?
What are the signs and symptoms of AIDS?
What are opportunistic infections?
What is the length of time between infection with HIV and the development of AIDS?
How can HIV infection pass from a mother to her child?
What forms of social/sexual activity or contact do not involve a risk of HIV
transmission?
What is voluntary HIV counselling and testing?
Perception of HIV
■
■
■
■
■
■
■
■
■
■
■
■
What are your thoughts about sexually transmitted infections? What are your thoughts
about HIV and AIDS?
Do you think you are at risk of getting a sexually transmitted infection? Do you think
you are at risk of becoming infected with HIV? Please explain.
What peer groups and significant others are most important to you? Do you think
your partner is having sex only with you?
How do men react if their female partners ask them to use condoms?
How would your partner react if you asked him/her to use a condom?
What would be your reaction if your partner refused to use a condom?
Are your co-workers concerned about sexually transmitted infections? Are they
concerned about HIV?
What do you see as the benefits of adopting safer sexual behaviour (e.g., practising
abstinence, being faithful to one partner, using condoms)?
[If interviewing a female] Would you undergo HIV counselling and testing before
becoming pregnant?
[If interviewing a male] Have you ever undergone HIV counselling and testing? Would
you like to? Why or why not?
What would you do if you found out that one of your co-workers was HIV-positive?
What would you do if you found out that you were HIV-positive?
HIV/AIDS programming at the workplace
■
■
■
Which HIV/AIDS prevention, care, support and treatment services are available to you
at your workplace?
What is your opinion about your employer/union response to HIV/AIDS?
What kinds of workplace programmes/services related to HIV/AIDS would you like to
see?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
E-3
3
HIV/AIDS policy at the workplace
■
■
Does this organization have a policy on HIV/AlDSat the workplace? If so, could you
please explain it to me?
What is the management’s policy regarding HIV-positive employees and those living
with AIDS?
HIV/AIDS-related practices
■
■
■
■
■
■
■
■
■
What behaviours put you most at risk of becoming infected with HIV and other
sexually transmitted infections?
How do protect yourself from HIV infection?
Do you want to change any of your behaviours that may put you at risk of contracting
HIV? Please explain.
What do you see as the benefits of changing your high-risk behaviour?
What do you see as the disadvantages of changing your high-risk behaviour?
What pressures make it difficult for you to change your behaviour?
What power do you believe you have to change your behaviour? If it is limited, please
explain why, and by whom or what.
What would it take for you to change to a safer behaviour or to continue practising a
safer behaviour?
Do you know of a colleague who has been approached on the job for sexual favours in
exchange for certain benefits? Have you ever had an experience like this?
Behaviour change communication questions
Media habits
■
■
■
■
■
a
What are your favorite TV and radio programmes? When do you watch or listen to
them?
What is the language of the broadcast?
What print media do you prefer (e.g., newspapers, magazines, pamphlets, booklets,
comic books, picture books, etc.)?
What kind of music do you prefer?
What kind of traditional theatre are you exposed to in your community (local drama,
concert party, story-telling, etc.)?
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
,^/>CPHE - SOCHA
(
Koramangala
}®}]
E-4
c
Sources of information
■
■
■
■
■
■
■
When and where do you usually get information about topics related to sexual health?
Who or what is your trusted source for health information at rhe workplace?
How do you communicate with your friends (telephone, email, in person)? Where do
you meet your friends? When? Which friends do you see every few weeks?
What are your preferred sources of information on health-related topics?
What are the sources of information on sexual health that you find most credible?
When and where would be the best times to talk to you about HIV prevention,
distribution of condoms and treatment services for sexually transmitted infections, and
who could do this most effectively?
Which teaching aids would help you learn the most in group information
sessions (e.g., videos, slide shows, overhead projectors, flipcharts, picture codes,
demonstrations, role plays, etc.)?
Fears and hopes
■
■
■
■
■
■
■
How do you see yourself in ten years’ time?
What would be the best thing that could happen to you in the future?
What do they need to help you realize your hopes and dreams?
What could prevent your hopes and dreams from being realized?
What are rhe biggest obstacles to you achieving your long-term goals?
What fears do you have about the future?
What are rhe major barriers/hindrances that you currently face that could affect
whether or not you achieve your goals?
A
>
Stigma and discrimination
■
■
■
■
■
What is being done to ensure that employees are not discriminated against and that
they receive prevention and education services at the workplace regarding HIV/AIDS?
Are you familiar with any support organization for people who are HIV-positive?
Are there employees who are HIV-positive who are open about their status to their
employers and co-workers?
Are you aware of a situation in which employees/workers received different treatment
because they were known or perceived to have with HIV/AIDS? If so, please describe.
Who treated the employee known or perceived to have HIV/AIDS differently?
■ Co-workers
■
Supervisors
■
Managers
■
Labour representatives
■
Others (specify)
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
c
Appendix F: Observation guide*
Location:
Observer(s):
Approximate number of target population:
Date:
Date/time
observation began:
Date/time observation
ended:
Date/time recording
began:
Describe the situation/context.
Describe the activities of the target population.
Describe who is present.
Describe social networks/membership.
Which language(s) are used?
What are the high-risk behaviours?
Which other behaviours are associated with these high-risk behaviours?
*
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
Date/time recording
ended:
'J
F-2
Which factors trigger high-risk behaviours?
Which factors maintain high-risk behaviours?
4
Who are the potential members of the target population that are not engaging in high-risk
behaviours)? Explain.
Which other people interact with the target population? What influence do they have?
What other observations should be made?
*Some of the questions listed above were obtained from the following source:
Developing Workplace HIV/AIDS Policies and Programmes: Needs Assessment Guide.
AED/Smart Work, October 2002. lit tp: //w vvvv. smartwork. o rg/reso u rces/pd I7n eedsassessment.pdf
ILO/FHI: HIV/AIDS behaviour change communication - a toolkit for the workplace
[Trial version]
*
*
Position: 1368 (5 views)