MEASUREMENT AND EVIDENCE KNOWLEDGE NETWORK.pdf
Media
- extracted text
-
1
/FvjfiEnJcer
^SORbNE^r
KrJDbOt-^^fr^
Aj£T^>C>^y<
£
1
c O^ae
(9rJ
D£-TERH/M>6a//S
ibCQlr^ e>AA\i~jV_.
CS-bH
I
2x>q^
y
9
/
‘
*
>
■
Page 1 of 1
Community Health Cell
From:
To:
Cc:
Sent:
Attach:
Subject:
"Josiane Bonnefoy" <josiane.bonnefoy@gmail.com >
"Thelma Narayan" <chc@sochara.org>
"Liliana Jadue" <ljadue@udd.cl>; "Francisca Florenzano" <fflorenz@gmail com>- "Mike Kelly"
<Mike.Kelly@nice.org.uk>; "Antony Morgan" <Antony.Morgan@nice orq uk>
Friday, March 31, 2006 5:44 AM
Arrangements for M&E KN Meeting at Santiago.doc; Measurement and Evidence Knowledge
Network.xls; Agenda Draft 31thMarch.pdf; Paper 1 - Methodology Paper 040206.pdf; Paper 2
CSDH - Conceptual framework.pdf; Paper 3 - Consultation on Measurement - Report of
Proceedings.pdf
M&E KN First Meeting Santiago 2006 - Dr. Narayan
Dear Thelma,
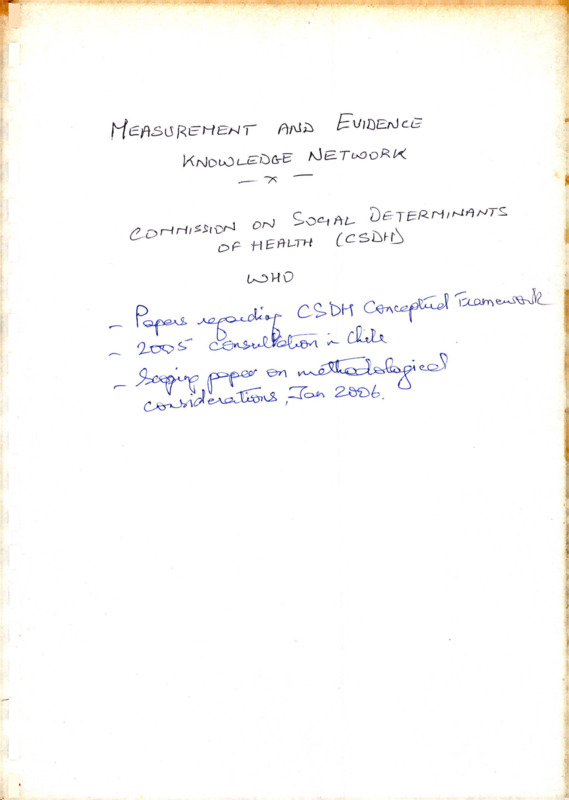
Please find enclosed information for our First Meeting of the Measurement and Evidence Knowledge Network.
We are attaching the following documents for your information:
1. Arrangements for M&E KN Meeting at Santiago
2. Measurement and Evidence Knowledge Network:
3. Agenda Draft 31thMarch
We are enclosing the following essential reading for the meeting:
Paper 1 - Methodology Paper 040206
Paper 2 - CSDH - Conceptual framework
Paper 3 - Consultation on Measurement - Report of Proceedings
I would appreciate if you could confirm the reception of this mail.
If you would like any further information, please do not hesitate to contact me,
Looking forward to meeting you, I wish a nice and safe trip.
Best regards,
Josiane Bonnefoy
3/31/2006
MEASUREMENT AND EVIDENCE KNOWLEDGE NETWORK
FIRST MEETING
1 • Flight arrangements
Following consultation with all you, itineraries have been agreed and tickets have
been forwarded to you. Please note that once you receive your tickets, the cost of any
changes made to these flights will be at your own expense.
Visa, travel insurance and other travel-related costs
You are responsible for obtaining your own visas for Chile and countries in transit,
wherever required. On arrival in Chile, we will reimburse you for the cost of visas and
any airport taxes on receipt of invoices only. Please bring these invoices with you.
Please note that weecannot •be •held
- - responsible for any costs associated with travelrelated problems, including health problems, experienced during the; course of the
meeting.
3. Meals and accomodation
The Measurement and Evidence Knowledge Network will cover the costs of each
participant’s accommodation, meals and transport from and to the airport.
Accommodation is booked until the date of the agreed return flight and meals will be
provided for the same period.
4. Airport pick-ups
On the basis of the agreed flight times, we will make arrangements for you to be
picked up at the airport on arrival. Please look for a representative of Transvip
standing outside the gates immediately after you clear Customs, in the arrival hall. If
you do not see the person who will be waiting for you, please approach the Transvip
counter. You may have to wait a short while for other participants to arrive on
different flights.
Please do not use other means of transport since it is already booked for you. This
means that you do not have to pay for the service because we have already taken care
of it. We will also arrange transport for you back to the airport after the meeting.
5. Accommodation arrangements
The meeting will be held at the InterContinental Santiago Hotel, with contact details
as below:
Hotel InterContinental Santiago
Av. Vitacura #2885 Las Condes
Santiago CHILE
Tel: (562) 394 2000 | Fax (562) 394 2075
http://www.intercontisantiago.com/
1
Upon arrival please inform at the reception desk that you are part of the group booked
by the Universidad del Desarrollo for the Measurement and Evidence Knowledge
Network Meeting.
6. Climate
At present we are in autumn, with decreasing temperatures, at the moment ranging
during the day between 8° and 24° Celcius.
7. Health precautions
No specific health precautions are necessary for Santiago.
8. Currency
At the moment, 1 US Dollar is equivalent approximately to $ 520 (Chilean pesos) and
1 Euro to $ 625 (Chilean pesos).
If you are bringing dollar notes, please take into account that USD 100 notes
beginning the series with AB and CB (years 1996 and 2001) are not accepted.
Nearly all credit cards are accepted. The most commonly used are: Visa, MasterCard,
Dinners and American Express. ATM machines accept Plus and Cirrus. You will find
them at the airport if you need to have some cash immediately.
We very much look forward to seeing you.
(iosiane.bonnefoY@gmail.com)
or
my
colleague
(fflorenz@gmail.com ) with any queries.
Please contact myself
Francisca
Florenzano
Our phone numbers at the University are:
Josiane Bonnefoy
+56 (2) 299 9423
Francisca Florenzano
+ 56 (2) 299 9305
Liliana Jadue
+56 (2) 299 9423
Fancy Fredes (Secretary) : +56 (2) 299 9423.
Only in case of emergency:
Josiane Bonnefoy :
Francisca Florenzano:
Home: +56 (2) 273 5626
Mobil: 09-2247800
Upon arrival to the hotel you will receive information on who will be at the venue to
contact you.
We wish you a nice and safe trip to Santiago.
Best regards,
Josiane Bonnefoy
2
World Health Organization
Commission of Social Determinants of Health
Measurement and Evidence Knowledge Network Members
i/
______ • Name
Dr Francisco Espejo
Country
Chile
________ E-mail address
Francisco.Espeio@wfp.org
%• Dr Mark Exworthy
United Kingdom M.Exworthy@rhul.ac.uk
3,. Dr Gao Jun
China
gaoiun@moh.gov.cn
Institution and Postal address
Chief School Feeding Service
Strategy Policy and Programs Division
Policy and External Affairs Department
UN World Food Program
Via CG Viola 68
Parco dei Medici
00148 Rome
Italy
______ TelePhone:
Phone:+39 06 6513 2064
Fax:+39 06 65132854
School of Management
Royal Holloway
University of London
Egham
Surrey TW20 OEX
United Kingdom_________________
Deputy Director,
Center for Health Statistics Information,
Ministry of Health,
1 Nalu Xizhimenwai
Xicheng District,
Beijing, 100044,
China
Phone:+ 44
Fax: + 44
Phone: + 86
Fax:+ 86
_________ Name
4. Dr Ichiro Kawachi
Country
Japan
S' . Prof. Johan Mackenbach
The Netherlands l.mackenbachffierasmusmc.nl
. Dr Landon Myer
South Africa
lmyer@cormack.uct.ac.za
India
chc@sochara.org
Dr Thelma Narayan
■z. Prof. Jennie Popay
_________ E-mail address
Ckawach@aol.com
United Kingdom i.popay@lancaster.ac.uk
______ Institution and Postal address
Department of Society, Human
Development and Health
Harvard University
Kresge Building
7th Floor
677 Huntington Avenue
Boston, MA 02115
USA_________________________
Department of Public Health
University Medical Center Rotterdam
Erasmus University
P.O. Box 1738
3000 DR Rotterdam
The Netherlands
School of Public Health and Family
Medicine,
University of Cape Town,
Anzio Road,
Observatory 7925,
Cape Town
South Africa______________________
Coordinator
Community Health Cell
# 367, Srinivasa Nilaya,
1 st Main, Jakkasandra,
1st Block Koramangala,
Bangalore - 560 034
India
Professor of Sociology & Public Health
Institute for Health Research
Lancaster University
Lancaster LA 1 4YT
UK
_______ TelePhone:
Phone:+1 (617)432 0235
Fax+1 (617)432 3123
Phone: + 31
Fax: + 31
Phone:+ 27 (21)406 6661
Fax:+27 (21)406 6764
Phone: + 91 (80) 255 31518
Telefax: + 91 (80) 255 25372
Phone: + 44 (0) 1524 592493
Fax:+ 44 (0) 7734058761
________ Name
Dr Peter Tugwell
Country
Canada
_ ______ E-mail address
elacasseffiuottawa.ca
Institution and Postal address
Canada Research Chair in Health Equity
Director,
Centre for Global Health
University of Ottawa
Institute of Population Health
1 Stewart St.
Room 202
Ottawa, Ontario KIN 6N5
Canada
[C>.
a
UK-
____ TelePhone:
Phone:+1 (613) 562 5800 ext
1945
Fax:+1 (613)562 5659
World Health Organization
Universidad del Desarrollo
National Institute for Health
and Clinical Excellence
Commission on Social Determinants of Health
Measurement and Evidence Knowledge Network First Meeting
Santiago, Chile: April 6th - 8th, 2006
Hotel InterContinental Santiago
Avda. Vitacura 2885, Las Condes
Santiago, Chile
Agenda
Draft
Objectives of the Meeting:
I. To launch the Measurement and Evidence Knowledge Network, and provide a
face to face discussion, reflection and proposal on the Network’s subject, tasks
and key deliverables.
2. To agree -the key principles that will steer M&E KN’s work, so as to
provide guidance to the work carried out by the Commission’s main streams:
civil society, country work and knowledge networks.
3. To present and discuss applied experiences of evaluation at different levels:
civil society, country and international cooperation agenciesTofboth upstream
and downstream interventions.
4. To agree M&E KN’s working organisation and methodology, distribution of
responsibilities, links with different CSDH’s components, use of SharePoint,
and timeframe of KN’s activities.
5. To agree on a framework for the collection, appraisal and synthesis of
evidence across knowledge networks.
6. To identify the necessary pieces of work and the main themes for position
papers and how these will be commissioned by the M&E KN.
7. To suggest date and topics to be dealt with in the Second M&E KN Meeting.
Expected outcomes of the meeting:
1. Shared understanding of M&E KN’s role, responsibilities, tasks and key
deliverables.
2. Definition of M&E KN’s working methodology and timeframe.
3. Clarity on individual members’ responsibilities.
4. Preliminary inventory of experiences of evaluation of interventions on social
determinants of health equity known by members.
5. Agreement on necessary pieces of work and on main themes for position
papers and how these will be commissioned.
6.
Proposal of date for Second M&E KN Meeting and highlights of subjects.
Thursday 6th April
19:30
Dinner
Welcome address from representatives of:
Ministry of Health
HDD, Dr Pablo Vial and Dr Liliana Jadue
NICE, Professor Mike Kelly
WHO/CSDH, Ms Sarah Simpson
Introduction of Knowledge Network members and invited observers.
Friday 7th April
9:00 - 13:00 First session: The Measurement and Evidence Knowledge Network
Chair: Jeanette Vega
Rapporteur: Francisca Florenzano
Objectives:
1. To introduce the Commission on Social Determinants of Health, and the
organisational context in which the M&E KN will work.
2. To present the Measurement and Evidence Knowledge Network: its
background, purpose, special characteristics (cross-cut), tasks and key
deliverables.
3.
fo examine members representation in the network and to agree on how to
deal with potential gaps in representation.
4. To agree on the meeting’s working methodology and expected outcomes.
5. To introduce the preparatory work and the key principles guiding the KN’s
work.
2
9:00 - 9:30 Introduction
Dr Josiane Bonnefoy & Professor Mike Kelly
•
Objectives of Meeting
•
Expected outcomes of Meeting
•
Structure of agenda.
9:30-10:30
Commission on Social Determinants of Health
Ms Sarah Simpson, Secretariat, WHO Geneva & Ms Tanja Houweling
Secretariat, UCL London.
•
•
Social Determinants of Health and WHO’s position on the subject.
Conceptual framework of the Commission on Social Determinants
of Health.
•
CSDH Components: Commissioners, Knowledge Networks,
Country Work, Civil Society, Secretariat and linkages.
Knowledge Networks: Themes.
•
(20’ presentation and 40’ discussion)
10:30-11:00 Break
11:00-12:00 Measurement and Evidence Knowledge Network Update on work to date
Dr Josiane Bonnefoy
•
M&E KN Hub History:
(a) Measurement Consultation meeting, Santiago, March
2005 - main themes and conclusions
First meeting of Knowledge Network hubs, Ahemedabad,
India, September 2005Fourth meeting of Commissioners,
Teheran, Islamic Republic of Iran, January 2006.
(b) Work with other knowledge networks to date.
4
•
M&E KN Members:
(a) Preliminary composition of network - criteria, potential
gaps, etc.
(b) Terms of reference: hub, network members and virtual
members.
(c) Expected outcomes.
(20’ presentation and 40’ discussion)
12:00-13:00 M&E KN Scoping Paper
Professor Mike Kelly
3
•
•
Presentation (30 mins)
Discussion (30 mins) - (key issues arising, noted for later
discussion of key issues)
13:00-14:00 Lunch
14:00-18:30 Second session: Measurement and Evidence: developing a shared
perspective and approach
Chair: Sarah Simpson
Rapporteur: Antony Morgan
Objectives:
1. To present the conclusions arrived at the Santiago Consultation,
March 2005, in order to state from where are we taking a step
forward.
2. To identify the key issues for the..Network to consider in gathering
and synthesizing evidence on:
(a) methods for evaluating action on the social determinants
of health (given absence often of RCTs).
(b) equity/inequality measurement tools for setting targets
and monitoring and evaluating - these could be
integrated into health information systems e.g.
household surveys etc.
1. Presentations:
• Introduction and outline of session (5-10 mins)
• Brief presentation of main conclusions of the Santiago
Consultation, March 2005 on evaluation methodologies.
Ms Francisca Florenzano (20 mins).
• Example of a concrete evaluation of intervention carried out by
NICE, to identify the challenges. Mr Antony Morgan (20 mins).
2. Discussion and identification of key issues.
Saturday 8th April
8:30-13:00:
Third session: Developing a framework for the collection,
appraisal and synthesis of evidence: working with knowledge
networks and developing our future guidance
Chair: Josiane Bonnefoy
Rapporteurs: Sharon Friel and Tanya Houweling
4
» 'vO
c-
Objectives:
1. To agree on how are we going to collect, collate and synthesise the
network’s own evidence on evaluation methodologies and
experiences.
2. To agree on the recommendations to Knowledge Networks on how
to collect, collate and synthesise their networks’ evidence.
8.30-9.15
Summary key points from day 1 discussions
Professor Mike Kelly
9.15-10.30
Two working groups focussing on
•
•
•
•
•
What type of evidence is needed to support sound recommendations
and what are the methodological implications?
How to incorporate evidence coming from different sources, i.e.,
civil society, country and international levels.
What criteria to discern whether small-scale interventions or
experiences can be scaled up to the macro level?
How to develop attributable fractions analysis of interventions.
What approaches and methods will be used to gather evidence?
NB there may be other questions to consider in addition to these
10.45-11.15 Working group report back.
11.15- 13.00 Discussion, summary and next steps
Group 1: Rapporteur: Sharon Friel:
Group 2: Rapporteur: Tanya Houwling
13:00- 14:00 Lunch
14:00-18:30 Fourth session: Key foci and activities for MEKN
Chair: Mike Kelly
Rapporteur: Josiane Bonnefoy
Objectives:
To finalise key issues to be considered by Network
To determine priority activities for network
To identify main pieces of work to be commissioned by network
To identify links with other CSDH streams of work (country work
and civil society process)
5. To agree on roles of network members in relation to work
prioritised
6. To agree on network members’ terms of reference.
7. To clarify process, mechanisms and timing of future
communication among network members
1.
2.
3.
4.
5
T
J cJLa.J
v.0
8. To identify other people or experiences that could be drawn on in
undertaking work
9. To identify date and activities for second network meeting (subject
to discussion with missing members)
10. To finalise overall timeplan for network activities
Discussion:
•
•
•
•
20:00
Agreed outcomes from meeting and key issues
(a) Scope of the work and priority activities
(b) Potential gaps, challenges and ways forward with MEKN
approach
Linking to other streams of CSDH work
Other KN planning
(a) Roles of network members
(b) Share Point and communication among network
(c) Second meeting date and purpose
(d) Overall timeplan
Summary and conclusion.
Dinner.
6
WORLD HEALTH ORGANISATION
COMMISSION ON THE SOCIAL DETERMINANTS OF
HEALTH
MEASUREMENT AND EVIDENCE KNOWLEDGE
NETWORK
METHODOLOGICAL CONSIDERATIONS RELATING TO THE
DEVELOPMENT OF THE EVIDENCE BASE ON THE SOCIAL
DETERMINANTS OF HEALTH: SCOPING PAPER ORIGINALLY
PREPARED FOR THE WHO COMMISSIONERS’ MEETING TEHRAN, IRAN
JANUARY 2006
Michael P Kelly, Josiane Bonnefoy, Antony Morgan, Francisca
Florenzano
The National Institute for Health and Clinical Excellence (NICE) (UK) and
the Universidad del Desarrollo (UDD) (CHILE)
Draft 2 February 4th 2006
METHODOLOGICAL CONSIDERATIONS RELATING TO THE
DEVELOPMENT OF THE EVIDENCE BASE ON THE SOCIAL
DETERMINANTS OF HEALTH
Draft 2 February 4th 2006
2
1. Introduction
1.1. Commission on the Social Determinants of Health
A
{
In 2005, the Director General of the WHO set up a global Commission on the Social '
Determinants of Health (CSDH). The Commission’s mission consisted of four
elements:
1. learning: the consolidation, dissemination and promotion of knowledge that
demonstrated the imperative and necessity for action on the social
(J
A
determinants of health and informed policy and effective, equitable
interventions on the social determinants;
u
2. advocacy: the identification and promotion of opportunities for action on the
key social determinants for policy makers, implementing agencies and the
wider society;
3. action: the speeding up and supporting of processes that initiated, informed
(j
and strengthened actions to integrate knowledge about social determinants
within public health policy and practice; and
i
6
4. leadership: the support, enhancement and development of the public,
political, technical and institutional leaders to help them inform, advocate and
deliver the desired change in understanding and action.
The overarching objective of the Commission was to lever policy change by learning
from existing knowledge about the social determinants of health (SDH) and turning
j
that learning into actionable global and national agendas. As part of the learning
element, a number of Knowledge Networks (KNs) were established to synthesize
knowledge. This knowledge would inform the Commission about opportunities for '
improved action on SDH by fostering the leadership, policy, action and advocacy
needed to create change.
The purpose of the Knowledge Networks was to organize knowledge:
•
on priority associations between the social determinants of health and
health inequities across different country contexts with attention to
widespread cross-cutting determinants such as gender inequality;
•
on the extent to which prioritized social determinants of health in relation
to globalization can be acted upon, exemplified through successful
national and global policies, programmes and institutional arrangements;
r O’
4
*
j
•
to stimulate societal debate on the opportunities for acting on the social
determinants of health; and
•
to inform the application and evaluation of policy proposals and
programmes in relation to the social determinants of health nationally,
across regions and globally, assessing implications for both women and
men.
The themes for the KNs included: C?
•
Early Child Development
•
Health Systems
•
Urban Settings
Social Exclusion
•
Employment Conditions
Globalization
•
Women and Gender Equity
•
Measurement and Evidence •
The themes of the last two KNs were cross-cutting,^
The Measurement and Evidence Knowledge Network (MEKN) will work with the
other KNs on the measurement, appraisal, evaluation and synthesis of evidence
relating to the social determinants of health. This paper outlines the principles that
will inform the approach of the MEKN.
As part of the launch of the Commission on the Social Determinants of Health which
took place in Santiago in Chile in March 2005, an expert consultation for the
Measurement and Evidence KN was held. The purpose of the meeting was to begin
a consensus building process towards the development of guidelines on assessing
and evaluating programmes and policies on the social determinants of health.
Following the consultation the National Institute for Health and Clinical Excellence
(NICE) in London, England and the Universidad del Desarrollo (UDD) from Santiago,
Chile were selected as the organizational co-hubs for the Measurement and
Evidence Knowledge Network (MEKN).
5
1.2 The social determinants of health and health inequalities
Globally there have been impressive improvements in overall indicators of health
over the last several decades. None the less, health inequalities within and between
countries persist and in many cases have widened and have continued to widen in
the recent past (WHO, 2004). This is in spite of the fact that the pursuit of equity and
the reduction in health inequalities has been a goal of some national (Graham,
2004a; 2004b) and some international policies (World Health Organization, 1981;
1985; 1998a; Ritsatakis, 2000; Braveman, et al, 1996; Braveman, 1998, United
Nations, 2000).
The first premise for the development of a methodology for working on the social
determinants of health is a statement of a value position. The explicit values
underpinning the development of the methodology is that the health inequalities that
exist within and between societies are unfair and unjust. This is not a scientifically or
rationally derived principle; it is a value position which asserts the rights to good
health of the population at large. It stands in contrast to the value position that
argues that differences in health are a consequence (albeit an unfortunate
consequence) of the beneficial effects of the maximisation of individual utility in the
market. It is important to state this at the outset that individual and collective utilities
may be at odds with the rights to health. The debate about social determinants takes
place within a sometimes explicit but usually implicit tension between the competing
claims of rights and utilities. Arguably these claims and counter claims are
irresolvable through rational discourse. In short, to uphold one person’s or group’s
rights is to interfere with some other individual or group’s utilities - and vice versa
(Macintyre, 1984). This applies in health as it does within in other spheres of human
conflict.
It is important therefore to be very clear about questions of inequality and inequity and the
values that inform the discussion. Whitehead describes health inequality as ‘measurable
differences in health experience and health outcomes between different population groups
- according to socioeconomic status, geographical area, age, disability, gender or ethnic
group’. Inequality is about objective differences between groups and individuals
measurable by mortality and morbidity. Whitehead describes ‘health inequity’ as
‘differences in opportunity for different population groups which result in for example,
6
unequal life chances, access to health services, nutritious food, adequate housing etc.
These differences may be measurable; they are also judged to be unfair and unjust
(Whitehead, 1992). Leon et al (2001) point out that health inequalities and health
inequities within countries do not mean the same thing and the related values may be
different As a consequence solutions to tackling health inequalities cannot be universally
applied to all situations and the importance of applying these solutions in context must be
noted. However, regardless of context, cultural differences and differing systems, the
position taken by the MEKN is that systematically differential patterns of health outcomes
which have their origins in social factors are unfair and unjust. The explicit value position is
that this is morally indefensible and that there is an imperative to find solutions to this state
of affairs. Moreover, because the origin is social they are the product of human agency.
Because they are the product of human agency they are potentially changeable through
human agency.
Although such human agency will operate through political, economic and biomedical
systems, they must be underpinned by an evidence based approach. And this is the
second premise - commitment to an evidence based approach. However, there are
a number of difficulties; the present paper offers some solutions to those difficulties.
The difficulties may be briefly stated. There are conceptual problems of attribution.
So it may be argued that pursuing equity in health means eliminating the social
determinants of health inequalities. These determinants are in turn systematically
associated with social disadvantage and marginalization (Braveman, 2003). The
major factors may be relatively easily delimited. The unequal distribution of the
social and economic determinants of health such as income, employment, education,
housing, and environment produce inequalities in health (Graham, 2000). However
while the general relationship between social factors and health is well established
(e.g. Marmot & Wilkinson, 1999; see also Solar & Irwin, 2005 for a review), the
relationship is not as well understood in causal terms, as it is readily observed (Shaw
et al 1999). The causal pathways of inequalities in health are empirically and
theoretically underdeveloped. Consequently the policy imperatives necessary to
reduce inequalities in health are not easily deduced from the known data.
There have been many attempts to develop policy on the basis of what is known, and
on basis of the observed relationships. The results have not been particularly
impressive, partly because the evidence base is weak - there is a very rich literature
describing health inequalities, especially in developed countries, but a dearth of good
studies explaining what can be done about it (Millward et al 2003) - and partly
7
, 0
I
, /Xj: >>( £
1
because policies which damage health and increase health inequalities have
prevailed. The evidence base is further hampered by a lack of systematic studies of
the effects of policy. The contours of inequality are not well described. The degree to
which changes in inequalities can be measured is ill defined (Killoran & Kelly, 2004).
The difference between the determinants of health and the determinants of
inequalities in health is often confused (Graham & Kelly, 2004; Graham, 2004a,
2004b, 2004c). The health of populations and the health of individuals is frequently
elided (Heller, 2005). And, finally, the link between the proximal and distal
determinants of health are poorly conceptualized and integrated into research (WHO,
2004).
In the face of these difficulties a thoroughgoing evidence based approach means
finding the best possible evidence about the social determinants (NHMRC, 1999).
The most sophisticated and technologically advanced search strategies and
systematic review procedures should be used (Glasziou et al 2004, Jackson &
Waters 2005a, 2005b) along with traditional forms of scholarship. The definition of
best evidence should be made on the basis of its fitness for purpose and on the basis
of its connectedness to research questions (Glasziou et al 2004). Those research
questions are the ones which deal with the effectiveness of interventions to-change
the social determinants. While there will be gaps in this evidence and some of it will
be more powerful than other parts. Therefore the strength of evidence alone should
no£driye the strength of policy recommendation (Harbour & Miller, 2001). Never the
less it is taken that is axiomatic that an evidence based approach offers the best
hope of tackling the inequalities that arise as a consequence of the operation of the
social determinants. The evidence will provide the basis for understanding and the
basis for action (Greenhalgh, 2001). Linking evidence based to health policy will
require the identification of appropriate and culturally sensitive mechanisms (Rawlins,
2005; Briss, 2005).
There are of course some important caveats about the evidence based approach.
There will have to be a recognition that strength of evidence alone is not sufficient as
a basis for making policy (NHMRC 1999) and that it is possible to have very good
evidence about unimportant problems and limited or poor evidence about very
important ones. Therefore a distinction must be drawn between absence of evidence,
of poor evidence and evidence of ineffectiveness. The two former are not the same
as the latter. It will need to be recognised that the links between scientific knowledge
and policy and practice are not linear and that the scientific evidence base is
8
generally imperfect in its own methodological, theoretical and empirical terms.
Consequently the connection between evidence and policy and practice inevitably
involves matters of judgements (Kelly et al 2004). This leads to a commitment to the
principle that the application of research findings to non research settings requires an
understanding of the local context and the tacit knowledge and the life worlds of
practitioners and end users. It also means that evidence hierarchies must be used
flexibly.
2 Principles
2.1 Initial Conceptual Ideas
Solar and Irwin (2005) developed a discussion paper for the CSDH ‘Towards a
conceptual framework for analysis and action on the social determinants of health’ to
set out the conceptual foundations for the work of the commission. It put forward a
framework (drawn from existing models and frameworks,) for the social determinants
of health which aimed to:
•
clarify the mechanisms by which social determinants generate health
inequities
•
show how the major determinants relate to each other
•
provide a framework for evaluating which social determinants of health are
the most important to address
•
map specific levels of intervention and policy entry points for action.
The framework also highlights 3 key issues that need to be addressed if effective
action is to be taken on the social determinants of health:
1. to distinguish between the structural (e.g. income and education) and
intermediate (e.g. living and working conditions, population behaviour, food
availability) determinants of health
2. to understand and make explicit what is meant by the socio-political context
(encompasses a broad set of structural, cultural and functional aspects of a
social system whose impact on individuals).
3. to take account of the actions that need to be taken at different levels (macro,
meso, micro) in order that inequalities in health can be tackled (i.e. to alter the
configuration of underlying social stratification, and those policies and
interventions that target intermediate health determinants).
9
The MEKN drew on these ideas to develop a set of principles for thinking about
measurement evaluation and evidence issues relating to the social determinants of
health.
2.2 Defined Principles for MEKN
■
Principle 1 Methods and epistemology
r
iSi-KSP
The data and evidence which relate to social determinants of health come from a
variety of disciplinary backgrounds and methodological traditions. The evidence
about the social determinants comprises a range of ways of knowing about the
biological, psychological, social, economic and material worlds. The disciplinary
differences arise because social history, economics, social policy, anthropology,
politics, development studies, psychology, sociology, environmental science and
epidemiology, as well as biology and medicine may all make contributions. However,
each of these has its own disciplinary paradigms, arenas of debate, agreed canons,
and particular epistemological positions. Some of the contributions of these
disciplines are highly political in tone and intent. And in spite of a great deal of
research endeavour and comment as well as practical attempts at problem solution,
there is also a great deal which is not known about the causes of inequalities in
health.
In short, although the empirical subject matter of the social determinants of health is
diverse, that diversity is given an added layer of complexity by the disciplines
involved and that those disciplines do not reach an easy consensus on the nature of
knowing the material nor its interpretation. When the ways of knowing and
understanding within the worlds of policy makers, politicians, NGOs, as well as of the
people whose lives are directly affected by the social determinants, the degree of
complexity could be potentially debilitating. As an evidence base therefore it has a
number of problems: it is drawn from a diversity of disciplines using different
methods, it is incomplete, and it is it is biased in various ways, including political and
ideological bias. This does not mean it is unusable; it means we must devise ways of
sorting out the disciplinary differences, of filling the gaps and of reducing the bias
while valuing the diversity.
It is therefore inappropriate to rule out evidence and data a priori on the basis of its
disciplinary and methodological provenance. The immediate task is to find the best
1
tv-
evidence, from whatever source it comes, defined by the extent to which it has used
an appropriate method to answer the research question. It is axiomatic that to assert
the superiority of one type of knowing over another will be unhelpful. A range of types
of knowledge and knowing will be important (Kelly, 2004; Berwick, 2005). A
pluralistic approach will therefore be necessary. The question which must be asked is
what we know, suitable for what we need to do?
The principles involved are very straightforward and have been the premise of
philosophical thought for millennia (Plato, 1974). Humans use different forms of
knowing and different forms of knowledge for different purposes. There is no
necessary hierarchy involved until we need to discriminate on the basis of fitness for
purpose. It is necessary to describe the criteria for acceptability and fitness for
purpose and this the MEKN will do. The task will involve doing this across a range of
different knowledge types. This does not mean that all knowledge and knowing in
general, or of the social determinants of health in particular, is of equal value. It
means we have to develop multiple criteria to determine fitness for purpose, to judge
thresholds of acceptability and critically appraise the knowledge on this basis.
Principle 1 therefore promotes the use of a wide range of methodologies to assess
the success of interventions and policies which aim to address the social
determinants of health. This is familiar territory. Indeed, much has been written over
the last 30 years about the most appropriate means of evaluating the work of social
and community programmes aimed at reducing health inequalities. During the 1980s,
increasing expectations within public services towards evidence-based decision
making led to a desire from those working in the field of health promotion to establish
a credible scientific basis for their work. Early attempts to summarize the evidence of
‘what works’ borrowed methodologies employed by biomedicine to systematically
review evaluations of the effectiveness of health promotion interventions.
Traditionally, a systematic review process was used to assess evaluations in terms of
their methodological merit and measures of effectiveness. To allow long-term follow
up over time, this type of evaluation requires dedicated and substantial research
resources and those with specialist evaluation expertise who can advise on
appropriate research designs and methods, implement these and conduct the
appropriate analysis. One of the biggest problems with this form of evaluation is
providing evidence of a causal link between the project being evaluated and the
outcome measures. Experimental and quasi-experimental research designs go some
11
way towards addressing this problem, although these designs are regarded by many
as a research design that is neither feasible nor desirable for community-based
interventions.
The findings from reviews of scientific studies highlight the tensions inherent in
searching for the limited amount of health promotion that has been evaluated or will
fit into the biomedical model of evidence. Some of the key questions include:
•
What counts as evidence?
•
How do certain perspectives on evidence limit the focus of our endeavours in
evaluating the impact of health promotion?
•
What kinds of explanatory models might help us to ask better questions?
•
What does this mean for indicators of outcome in evaluation studies?
These questions have been considered by a WHO Working Group (1998b), who has
put forward a set of core features for the evaluation of health promotion.
They are:
•
Participation. Each stage of evaluation should involve, in appropriate ways,
those who have a legitimate interest in the initiative. Those with an interest
can include: policy makers, community members and organizations, health
and other professionals, and local and national health agencies. It is
especially important that members of the community whose health is being
addressed be involved in evaluation.
•
Multiple methods. Evaluation should draw on a variety of disciplines and
methods.
•
Capacity building. Evaluations should enhance the capacity of individuals,
communities, organizations and governments to address important health
promotion concerns.
•
Appropriateness. Evaluations should be designed to accommodate the
complex nature of health promotion interventions and their long-term impact.
The MEKN aims to identify what types of instruments exist or need to be developed
to measure the impact of a social determinants approach to improving health, as it is
mediated through the health system. In doing so, it will promote the use of combining
methodologies and to building a strength of evidence and will avoid disciplinary wars
aiming to promote the use of the right method of evaluation to answer specific
questions.
12
1
Participants involved in the expert meeting held in Chile in 2005 to accompany the
launch of the Commission also called for the need to ensure:
•
a balance in the type of evidence drawn upon: consult systematic reviews
(such as the Cochrane and Campbell databases of relevant interventions),
but also aim to develop an 'evidence jigsaw’, including for example,
descriptions of policy-making processes (e.g. detailed case studies of
successful as well as failed policy initiatives in the area of social
determinants).
•
Different kinds of evidence are used for policymaking depending on the
question being asked. Policymakers have recommended that researchers
should help them with the task of piecing together the ‘evidence jigsaw’
(Whitehead et al. 2004). The ‘jigsaw’ would encompass different types of
evidence - for example, evidence about the potential effectiveness of policies
(from experimental, quasi-experimental, and observational studies); evidence
on the diagnosis and/or causes of problems that could contribute to the
development of appropriate interventions/programmes; evidence on costs
and cost-effectiveness.
•
The purpose for which the evidence is used should be made explicit. It is also
important to recognize that evidence is produced for different kinds of
purposes, including: mobilizing political will, purchasing "buy-in” from the
public, demonstrating success, predicting outcomes, and monitoring
progress.
The MEKN will pay particular attention to the role of qualitative research in assessing
the effectiveness of approaches to address the social determinants of health.
Professor Jennie Popay has proposed two different models to describe the ways in
which qualitative evidence contributes to the evidence base for policymaking
(Presented at the March 2005 Chile CSDH Meeting).
1) The enhancement model assumes that qualitative research adds something
“extra” to the findings of quantitative research - by generating hypotheses to
be tested, by helping to construct more sophisticated measures of social
13
phenomena, and by explaining unexpected findings generated by quantitative
research.
2) The epistemological model views qualitative evidence as making an equal
and parallel contribution to the evidence base through: (a) focusing on
questions that other approaches cannot reach; (b) increasing understanding
by adding conceptual and theoretical depth to knowledge; and (c) shifting the
balance of power between researchers and the researched (Popay
unpublished). Importantly, the epistemological model views qualitative
evidence as not necessarily complementing quantitative evidence, but / '
sometimes conflicting with it.
Qualitative research can play two key roles as part of the evidence base for the
social determinants of health: (a) providing insights into the subjectively perceived
needs of the people who are to be the targets of the interventions and programmes
aimed at addressing the social determinants of health and health inequalities (giving
people a ‘voice’); and (b) helping to unpick the ‘black box' of interventions and
programmes to deepen understanding about factors shaping implementation, and
hence, impact (Roen et al; Arai et al 2005). One major difference between the
qualitative and quantitative traditions concerns the notion of replicability and
generalizability. Obviously generalizability within the qualitative tradition is of a
different kind to that which is possible in an experiment or a survey (Popay
unpublished). With regard to judging the external validity of qualitative evidence,
Popay notes: ‘The aim [in the qualitative tradition] is to identify findings which are
logically generalizable rather than probabilistically so’ (Popay et al. 1998). It should
also be noted that there is a rapidly growing literature on methods for the synthesis of
qualitative research and of mixed methods research (see for example, Dixon Woods
et al 2004; Popay & Roen, 2003).
There must therefore be a commitment to methodological pluralism and
epistemological variability and a commitment to the view that epistemological
positions should not be viewed as mutually incompatible. The argument that there is
an inherent incompatibility between objectivist and subjectivist approaches is to be
explicitly rejected in favour of the view that there are different ways of knowing, and
that different ways of knowing can and do play different roles in the ways that human
actors use knowledge and information. However, in certain circumstances and for
certain purposes some forms of knowing are more practically useful. The polarization
of knowledge into objectivist and subjectivist approaches is unhelpful and misleading
14
(See Gomm & Davies, 2000; and Gomm et al 2000 for a review of helpful ways to
describe different methodological approaches). The view that all knowledge is
relative and of equal value is to be rejected in favour of a view which defines the
relevance and the salience of knowledge according to its practical value in given
circumstances.
Principle 2: Gradients not gaps
There are conventionally three different ways in which the inequalities are described:
health disadvantage, health gaps and health gradients (for a full discussion of this
see Graham, 2004a, 2004b, 2005. and Graham & Kelly, 2004). Health disadvantage
simply focuses on differences, acknowledging that there are differences between
distinct segments of the population, or between societies. The health gaps approach
focuses on the differences between the best and worst off. The health gradient
approach relates to the health differences across the whole spectrum of the
population acknowledging a systematically patterned gradient in health inequalities.
Conceptually, narrowing health gaps means raising the health of the poorest, fastest.
It requires both improving the health of the poorest and doing so at a rate which
outstrips that of the wider population. It is an important policy goal. It focuses
attention on the fact that overall gains in health have been at the cost of persisting
and widening inequalities between socioeconomic groups and areas. It facilitates
target setting. It provides clear criteria for monitoring and evaluation. An effective
policy is one which achieves both an absolute and a relative improvement in the
health of the poorest groups (or in their social conditions and in the prevalence of risk
factors).
However, focusing on health gaps can limit the policy vision. This is why the
approach advocated here is one of normally aiming to reduce health gradients. The
penalties of inequalities in health affect the whole social hierarchy and usually
increase from the bottom to the top. Thus, if policies only address those at the bottom
of the social hierarchy, inequalities in health will still exist and it will also mean that
the social determinants still exert their malign influence. The approach to be adopted
by the MEKN will involve tackling the whole gradient in health inequalities rather than
only focusing on the health of the most disadvantaged. The different meanings
associated with health inequalities and health inequity is sometimes conflated. The
principle here is to make the conceptual distinction clearly and to argue for a very
15
clear approach based on the whole population gradient. The only significant caveat
is that where the health gap is both very large and the population numbers in the
extreme circumstances is high, a process of prioritising action by beginning with the
most disadvantaged would be prioritised.
This approach is in line with international health policy. The founding principle of the
WHO is that the enjoyment of the highest attainable standard of health is a
fundamental human right, and should be within reach of all ‘without distinction for
race, religion, political belief, economic or social condition’ (WHO, 1948). As this
1/
implies, the standards of health enjoyed by the best-off should be attainable by all.
The principle is that the effects of policies to tackle health inequalities must therefore
(
extend beyond those in the poorest circumstances and the poorest health. Assuming
■(
that health and living standards for those at the top of the socioeconomic hierarchy
continue to improve, an effective policy is one that meets two criteria. It is associated
with (i) improvements in health (or a positive change in its underlying determinants)
for all socioeconomic groups up to the highest socioeconomic group and (ii) a rate of
improvement which increases at each step down the socioeconomic ladder. In other
words, a differential rate of improvement is required: greatest for the poorest groups,
with the rate of gain progressively decreasing for higher socioeconomic groups. It
'
locates the causes of health inequality, not in the disadvantaged circumstances and
r-x
health-damaging
behaviours of the poorest groups, but in the systematic differences
....................................................
in life chances, living standards and lifestyles associated with people’s unequal
positions in the socioeconomic hierarchy (Graham & Kelly, 2004).
Principle 3: Causes: determinants and outcomes
o
Principle 4 is that MEKN will use as a basis for developing the evidence a causal
model which crosses from the social to the biological.
What is generally missing in the analysis of social factors and health is the kind of
underlying certainty about effectiveness and cause which we have come to expect
with respect to clinical medicine. Clinical medicine has its own uncertainties of
course. Aetiology is sometimes unknown or tenuous. The effects of treatments are
r
also uncertain (Chalmers, 2004). The disease categories used by medicine to
describe pathology, are not essentialist but are nominalist and therefore change and
evolve over time. Data and evidence are surrounded by uncertainty (Griffiths et al
0
2005), and the skill of the doctor is in the end about working through and with these
uncertainties, not resolving them.
J)
16
f
But not with standing the uncertain and contingent nature of the understanding of bio
medical processes, medicine operates very successfully with an underlying
epistemological principle which is that health outcomes have preceding causes and
that the isolation of cause is the basis of effective intervention. In the case of
inequalities in health real pathological changes in the human body occur, but in
highly patterned ways in whole populations. The key assumption made here is that
both the pathologies and their patterning have causes. There will be social and
biological causes working in tandem. The task is to map that process as a way of
developing an explanation. In classic scientific terms there must be covering scientific
social and biological laws (Hempel, 1965). What needs to be explained is why the
biological systems in the human body change in ways that are determined by social
circumstances. At the heart of the problem of the social determination of health and
the corresponding inequalities in health is this. The molecules in the human body
behave differently according to the social position someone occupies, according to
their job, according to their experience of class and ethnic relations, according to
their education, and according to a whole range of social factors which impact on
them over their life course. Their immunity, their nutritional status, their resilience,
their ability to cope, all act as mediating factors, but ultimately there is a biologically
plausible pathway from a number of social factors or social determinants to biological
structures in the individual human body.
In the biological clinical realm the randomized controlled trial provides the best way of
determining what the mechanisms of cause are and what precisely it is, that is
effective (Chalmers, 1998). The randomized controlled trial provides the most secure
basis for valid causal inferences about the effects of treatments (Chalmers, 1998).
Inter alia, to what extent can similar methods be applied in the social realm?
It has been argued that before 1948 clinical medicine was dominated by what today
we would call theoretical and political positions and largely untested paradigms
(Cochrane, 1972; Doll, 1998). It is suggested that these practices were tested
empirically by individual clinicians, but were never subject to the kind of deep
rigorous scrutiny which the clinical trial permits (Greenhalgh, 2001). Effectiveness
was in much more tenuous territory than it is today. Doll has argued (Doll, 1998) that
1948 was a watershed because it was the year that the streptomycin trial for treating
pulmonary tuberculosis reported. The methodological breakthrough was that
effectiveness could be plainly demonstrated. Although of course in 1948, the clinical
17
trial still had many years to go before it found general acceptance (Cochrane, 1972),
the fundamental principle was established and the causal premise was in grasp.
The question is to what extent is the study of the social determinants of public health
governed by untested paradigms? To what extent is the study of the social
determinants led by theory rather than by evidence of effectiveness? If it is to be led
by evidence of effectiveness the question of cause has to be confronted head on.
Moreover, even if the goal of seeking causes is aspirational, given the current state
of knowledge, that there are causal mechanisms at work, and that these may
eventually be discerned, is a guiding principle.
The approach to be adopted is that of separating necessary and sufficient conditions.
The necessary condition is/are the preceding phenomenon which needs to be
identified and be described without which the succeeding phenomena will not occur.
The sufficient conditions will describe the degree or volume which is required to
produce an effect. A true causal model would permit the statement, ‘if a then always
b’. By identifying the necessary and sufficient conditions it is possible to develop such
statements (Davidson, 1967). A true causal model would also account for the nature
of the relationship between a and b. This is what Hempel (1965) called the covering
law. Of course, because the subject matter is going to be surrounded by varying
degrees of uncertainty, the initial models or model will be weaker than a true causal
model. However, it is the degree of precision of the true causal model that should be
the goal, and unravelling necessary and sufficient conditions is the starting point
With respect to the social determinants of health, we are able to identify some of
what are the necessary and the sufficient conditions but the nature of which are
which, is very unclear. The core candidates can be listed relatively easily because
—--------- --------...
- ———"——
the literature has explored them at length: occupational exposure to hazards,
occupational experience of relations at work (degree of self direction), the biological
aging process , the experience of gender relations, the experience of ethnic relations
including direct experience of racism, home circumstances, degree and ability to
exert self efficacy especially through disposable income, dietary intake, habitual
behaviours relating to food, alcohol, tobacco and exercise, position now and in the
past in the life course, schooling, marital status and socio economic status. These
are the media through which the direct effects of the social world impacts directly on
the life experiences and exert direct effects on the human body. They in turn are
linked to macro variables like the class system, the housing stock, the education
18
system, the operation of markets in goods and labour and so on (see Solar & Irwin,
2005).
However, just listing the factors, neither tells you what the linkages actually are, nor
what the covering law is, nor what the biologically plausible relations actually consists
of. As Smith (2004) has argued, if we combine all the dimensions of social
differences into one construct, like socio economic group, this precludes discussion
of the policy relevant options (Smith, 2004), but it also precludes proper explanation.
There is clearly an urgent need for these processes to be modelled.
The problem of multi faceted causation will need to be considered in the modelling
process. It is clear that there are likely to be a range of factors involved in the
explanatory framework, and the component parts of the model will need to be
delineated. However, this must not degenerate into simply arguing that it is very
complex, because this is no explanation at all (Cohen, 1951). Modelling in a multi
factorial way allows the delineation of the necessary and sufficient conditions.
The evil causes evil fallacy (Cohen, 1951) also needs to be avoided in this modelling
process. Antonovsky (1985; 1987) called this the pathogenic approach. By this he
meant, a search for system dysfunction, or the identification of the breakdown of
idealized social systems. He argued that the social and medical sciences were
dominated by a pathogenic orientation. Applied to health inequalities, a pathogenic
argument is that health inequalities are a pathological deviation from an idealized
better state caused by some kind of pathological mechanism. The pathological
mechanisms are usually said to be things like global capitalism, political decisions,
failing health care systems and poverty. This is unhelpful on two counts. First,
idealised perfect non pathological social systems do not exist, and the pathology
which is identified as the cause is not an explanation, it is a political statement about
values. The value system is used as the explanation. Now that it is not to say that the
tackling of health inequalities and the associated suffering and premature mortality
are not worthwhile things to do, nor that is a value position of which to be diffident
(see above). Quite the contrary, it is a prime value which should drive forward
research and action. But a value, which determines that something is bad (or good),
is not the same thing as an explanation.
To understand health inequalities we must turn to a concept of cause which has its
origins in positivistic and rationalist thought and which in effect mirrors the kinds of
19
precision about cause which clinical medicine is capable of delivering. This, it will be
argued, requires a classical scientific explanation: neither an historical nor a
sociological explanation will do (Danto, 1968). This is because the phenomena being
explained are not historical or social: they are physical. An explanation which stops at
the social level is insufficient for these purposes. We need a model of cause which
traverses a number of levels of analysis which academic disciplines traditionally keep
separate. Some of the observed patterns which are manifested in mortality and
morbidity data are no doubt accounted for genetically or other purely biological
mechanisms, but it seems inconceivable that the health variations which follow so
closely sets of social arrangements could all be accounted for in this way. Other
processes are at work and they are amenable to causal analysis which asserts the
primacy of a pathway from the social to the biological. This does not undermine any
other form of analysis like a sociological one which operates at the level of the social,
nor does it preclude bringing aspects of the sociological explanations into play. But
the principles of cause should be applied to the issue in question across the social
and biological. In this sense the concern is not really inequalities in health, but much
more specifically the social determinants of inequalities in illness. The research
question is to find out what the social determinants of mortality and morbidity are.
This will lead further to use the distinction between the determinants of health and
the determinants of inequalities in health. The commitment to addressing the social
determinants of health is often summed up in the phrase ‘tackling the determinants of
health and health inequalities’. Such phrases can create the impression that policies
aimed at tackling the determinants of health are also and automatically tackling the
determinants of health inequalities. What is obscured is that tackling the
determinants of health inequalities is about tackling the unequal distribution of health
determinants.
Focusing on the unequal distribution of determinants is important for thinking about
policy. This is because policies that have achieved overall improvements in key
determinants such as living standards and smoking have not reduced inequalities in
these major influences on health. Positive trends in health determinants can go handin-hand with widening inequalities in their social distribution. As these examples
suggest, distinguishing between the overall level and the social distribution of health
determinants is essential for policy development. When health equity is the goal, the
priority of a determinants-oriented strategy is to reduce inequalities in the major
influences on people’s health. Tackling inequalities in social position is likely to be at
20
the heart of such a strategy. It is the pivotal point in the causal chain linking broad
(‘wider’) determinants to the risk factors that directly damage people’s health.
Therefore the model of cause needs to be articulated. The evidence should be
interrogated to determine what phenomena are attributed to other phenomena. Are
necessary and sufficient conditions specified, is the causal chain concerned with
proximal, intermediate or distal causes, and what are the plausibility levels of the
proposed mechanisms? In brief are we able to find patterns which point to strong
causal or associational relationships? To what degree are we able to discern a
consistent direction in the evidence, and to what degree are the patterns of the
results or the conclusions of studies broadly similar? Is there a relationship which
suggests that more of the exposure or the intervention produces more of an effect? If
there is then we have a much clearer sense of potential cause and are able to map
out what the proposed mechanisms are.
The level, or levels of analysis, needs to be identified (Kelly, Charlton and Hanlon,
1993). This means examining the evidence, and regardless of its disciplinary
provenance, assessing whether the dynamics of what is described could plausibly
work at a physical, societal, organisational, community or individual level. In other
words, to what degree is the policy or intervention based on biological, social,
technical plausibility? To what extent is it possible to ascertain time periods and the
chronology in the evidence? Are the purported relationships logically possible in
chronological terms? Do certain events precede others? What dynamic processes in
terms of the component parts of social systems are described? This is particularly
important in multi factoral explanations, where the sequencing of events may be
hidden, or at least difficult to discern and where, as we noted above, multi factoral
explanations are often no explanations at all.
Principle 4: Social Structure
Principle 4 aims to make more explicit the range of dimensions of inequalities that
need to be considered when building an evidence base on how best to address the
social determinants of health, including ethnicity, gender, sexuality, age, area,
community and religion (Anthias, 1990; 1992). These represent linked but separate
dimensions of inequality. Whilst these discrete dimensions of social difference are
seldom denied as important, they are under developed empirically and theoretically
in the literature on social determinants. Consequently, the relationships between the
different dimensions of inequality and the ways they interact with each other to
21
produce health effects, are hardly to be found in the extant evidence at all (Graham &
Kelly, 2004). This is a point of very considerable importance because, it is clear from
the evidence that does exist, that different segments of the population respond very
differently to identical public health interventions. This means that we need to
anticipate a wide range of responses to policies across and within societies, by virtue
of the nature of the variation in populations.
What these different and variable axes of differentiation have in common is that they
result in differences in life chances. These differences in life chances are literal: there
are marked social differences in the chances of living a healthy life. This has been most
systematically captured in occupation-based measures of socioeconomic position - but
differences in people’s health experiences and their patterns of mortality are observed
across other axes of social differentiation. It is an important challenge to develop
measures of inequality that embraces these axes. If, as the evidence suggests,
dimensions of disadvantage interlock and take a cumulative toll on health, these
dimensions need to be summed in order both to map and to understand the health
penalty of social inequality.
One of the key principles therefore for the MEKN is that there are different axes of
social difference (Graham & Kelly, 2004) and that these dimensions overlap (Davey
Smith et al 2000). Within different axes of differentiation, like gender, different
aspects interplay as well, like income access to power and prestige (Bartley et al
2000). The specific health impacts will be mediated by proximal factors like social
position, specific exposures, the nature of specific illnesses and injuries and their
social significance in different cultural contexts (Whitehead et al 2000). The model
which will be developed will also need to account for the fact that these different
aspects of social difference vary independently of each other. But they also coalesce
together in varying ways to produce overall patterns of advantage and disadvantage.
Material and environmental disadvantage accumulate through the life course and in
particular childhood disadvantage is associated with disadvantage in later life
(Benzeval et al 2000). The two building blocks which will be used to develop these
ideas are those of the life course and the life world. Life course epidemiology shows
how socially patterned exposures during childhood, adolescence and early adult life
may operate via chains of social, biological or psychological risk (Kuh et al 2003;
Graham & Power, 2004). The purpose of life course epidemiology is to build and test
theoretical models that postulate pathways linking exposures across the life course to
22
later life health outcomes (Kuh et al 2003). The life world is a social space, part
physical, but predominantly cognitive and subjective. The life word is where we
experience the social structure first hand in the form of opportunities, barriers,
difficulties and disadvantage. Schutz (1964, 1967; 1970) conceptualized the totality
of the experience of the life world as a series of concentric circles. The innermost
circle is the one where the everyday contacts and routines are highly predictable and
are therefore taken for granted, which are salient and immediate and which tend
most of the time to be the most important. There are more distant parts of the life
world. It is important to note that the innermost circle of the life world may not be, and
Schutz never suggested it would be, a place that was benign and cosy. It may be
violent and bullying. It may be cold and unforgiving. It may be unpleasant and
chronically difficult. It will be the place where discrimination and disadvantage are
experienced. However, it constitutes the centre of the existence of the person. This is
because life worlds are the building blocks of social life. It is the point where social
structure impacts on the individual. The life world is where the causal mechanisms of
health inequalities operate, and the pathways to ill heath can be described. It is the
bridge between the social and the biological.
The importance of this idea for patterning of health is that health is an outcome of the
accumulated effects of a variety of social and biological factors which impact on
people at distinct periods in the life course in the life world. These factors act both
positively and negatively as well as cumulatively. MEKN will therefore proceed on
this conceptual basis.
So what is the model of social structure, if any, in the evidence? This means
considering the extent to which the evidence is sensitive to the relations between
groups and individuals and in particular the social variations and differences in the
population. The important differences along the dimensions of age, gender, religion,
caste, occupation, mobility, place, residence, status grouping, and class
membership.
Principle 5: Social Dynamics
Principle 5 highlights that the social systems and sub systems which make up
societies are not static objects, they are constantly changing and therefore the
relationships which give rise to the outcome of health inequalities and differences are
themselves also changing in terms of their force and in terms of their salience at any
given moment.
23
In compiling evidence across knowledge networks it is important therefore to reflect
on the historical dimension with respect to the social determination of health. Whilst
inequalities in health seem to be a characteristic of all modern contemporary
societies, the shape they currently have is not a given, is not set in stone. It is instead
something which changes. The question is whether there is any discernible historical
patterning which would help us to understand what is going on, and what the
processes involved actually are.
The starting point for such analysis is the path breaking work of Antonovsky (1967).
In what was one of the very earliest attempts to review historical and contemporary
evidence about inequalities in health in a systematic way, Antonovsky showed that
inequalities were a common feature of all advanced social systems. Examining data
from more than thirty international studies he argued that the inescapable conclusion
was that social class influenced a person’s chance of staying alive. Historically he
noted a variation of about 2:1 between the extremities of the social classes, although
he saw this differential narrowing in the mid nineteen sixties. This class differential
held even though overall death rates were declining. He noted that whatever the
index used, or however the class system was represented, almost invariably the
lowest social classes had the highest mortality rates (Antonovsky, 1967).
He went on to demonstrate that there was an important characteristic in the historical
differences between the most and the least advantaged across different societies. He
observed that where the overall rates of mortality were high, the differences in
mortality between the best and the worse off tended to be relatively small. This, he
claimed, characterised societies in the early period of industrialization. As rates of
economic growth increased, and particularly as industrialization evolved, the patterns
of mortality began to improve for both the most and the least advantaged, but at
differential rates. The middle and upper classes seemed to derive the health
dividends of industrialization earlier. The mortality rate of the most advantaged
improved at a faster rate than the rate of mortality of the least advantaged. The result
was that the differences between the most and least advantaged got bigger.
However, as time went on, the rate of improvement for the middle and upper classes
began to slow, while the rate of improvement for the least advantaged began to
increase, resulting in a narrowing of the difference.
This led Antonovsky to suggest that where death rates are relatively high or low, the
24
difference between the most and the least advantaged will tend to be relatively small,
but where the rates of mortality are mid range the difference between the most and
the least advantaged will be relatively high. Since the publication of these data in the
mid 1960s this pattern seems to have evolved still further. For example the gradient
in countries like Britain seems to have begun to steepen again over the last forty
years or so, and in some countries of the former Soviet block the increase in health
inequalities in recent time has been dramatic. One conclusion to be drawn from
Antonovsky’s earlier work, combined with the more recent data, is that health
inequalities are part of long term social, political and economic trends and are linked
to the playing out of policies and historical events and underlying changes in the
social structure and the division of labour in society in ways that require an
explanation in their own right.
The interesting thing about this is the shape of the curves Antonovsky described.
Both extremes are close together and the middle much further apart. One conclusion
to draw from this is that it describes a pattern that is linked to some underlying
process of modernization/ industrialization, and there are some compelling biological
(the prevalence of infectious disease, the nature of infant mortality) as well as social
(the nature of the housing stock, the appearance of decent sanitation and safe
drinking water in particular), set of factors at work. Certainly the chronology of events
would lead one in that direction. The other important conclusion is that these data
demonstrate namely that inequalities in health are not fixed, but rather are variable at
different historical time periods.
One of the more interesting ways of trying to make sense of global type data is to try
to evaluate it in the context of data from different spheres. One of the most striking
examples of this is in relation to work by Victora and colleagues (2000). They
propose the idea of the inverse equity hypothesis. Drawing on data relating to the
implementation of child health programmes in Brazil, they note a very similar, almost
identical set of curves to that described by Antonovsky, although over very much
shorter time horizons. They note that whenever there is a new programme
introduced, the children of the better off benefit sooner and to a greater extent than
the children of the poorer sections of society. The improvements do impact on the
less advantaged but later, and there is an inevitable catching up process. Critically
Victora and colleagues argue for the inevitability of this process ceteris paribus. It
operates at a much shorter time frame than the kinds of historical epochs which
Antonovsky was interested in, but the same pattern emerges. Victora et al also note
25
that these effects compound one another in the sense that they children of the more
well to do are inevitably always in front since the benefits of the next new
intervention(s) will have already kicked in, before the poorer cohorts have caught up
with last one. So. although the overall effect is of health improvement, the constantly
repeated cycles tend to reinforce the inequalities giving them the impression of being
constant, when in fact they are each the product of successive waves of differential
responses to successive interventions.
Several important ideas follow from this. If health inequalities as measured by the
differences between different groups are not fixed, but rather constantly reinforced
and reproduced, then the search for the distal causes should be in the cycle, or
rather in the reasons why inequities reproduce themselves in each cycle in this way.
The intermediate determinants are to be located in factors in the delivery of
intervention, rather than in some abstract entity called society, the economy or the
political process. These would in turn be mediated by the proximal factors in the life
course and the life world.
The key idea here then is the nature of dynamic change, not as interesting historical
data but as central to the explanatory process itself.
Principle 6 Explicating bias
The last test to be applied relates to ideological or political bias. The problem of
values and politics and their particular role in generating knowledge has been a
longstanding theme in the social and the political sciences (Weber, 1948). The
solution though is relatively straightforward. All knowledge is potentially and actually
ideologically or politically biased. The solution is to acknowledge this fact and to seek
to make the biases explicit, even if the writer has sought to conceal their own
prejudices. This is an imperfect science, but is workable in two stages. First being
able to describe any political bias that is inherent in the argument, and then second,
to seek to determine whether the political biases have influenced the interpretation of
and the selection of the evidence.
It must be acknowledged that values determine the way knowledge is constructed
and generated in the first place and in the ways that it is interpreted and used. This
explicitly recognises that knowledge and knowing can never be value free. However,
the way to move through the problem of values is not to try to produce value neutral
science but to aim to make values explicit, to the reader, the author and the user.
26
Recognition must be made that although knowledge and knowing are socially
constructed, it is still possible to develop knowledgeable understandings of physical
and social phenomena and that the search for better understanding is a worthwhile
and important goal of science.
Because knowledge is socially constructed bias will be an inherent part of any
knowledge based activity. The overarching goal in reaching understanding of
phenomenon is the reduction of and the demonstration the reduction of bias. In
whatever field of knowledge we are working our aim should be to uncover bias and
manage it. This is equally true in detecting possible sources of bias in trial data or
meta analysis as it will be in interpreting the results of qualitative investigations or the
evaluations of policy programmes. That knowledge is a social construct is not
denied, but that knowledge is the most valuable tool for tackling health inequalities
and understanding their social determinants is axiomatic. Knowledge is better than
prejudice and is critical to making progress. It is imperative to expose political and
ideological biases in the selection of and interpretation of evidence.
3. Into action
3.1 Translating evidence for policy and practice
It must be recognised that in public health and related interventions context, culture
and human behaviour and social differences in the population play a greater
mediating role than in clinical interventions and that therefore different forms of data
and evidence will be called into play, external validity will be inherently problematic
and the time from intervention to outcome will generally be long term (Briss 2005).
Evidence is an essential but not sufficient basis for policy action. Several other
ingredients besides evidence are involved in the policy-making process, including
political will, transferability of evidence into appropriate social strategies, and
scalability into different contexts and settings. The policy-making process is often
poorly understood by researchers (Petticrew et al 2004; Whitehead et al 2004;
Lomas et al 2005).
It may be argued that focusing on the evidence base and the individualised
interventions which typically populate it has the effect of ignoring the more important
macro level determinants of health and the degrees to which inequity is tolerated and
sustained through policies at national and local levels. Inequalities in health reflect
wider inequalities (and therefore decision-making across a wide policy spectrum). At
27
a micro level, too, reliance on the evidence base works against a recognition or
assessment of the effects of synergy and also underestimates context-specific
aspects. In order to obviate these problems there are a number of further questions
which need to be asked of the evidence (Kelly et al 2004).
An explicit attempt should be made to assess the transferability of interventions from
one setting to another. For example, are the interventions feasible, culturally
acceptable and appropriate, and possible to scale-up in developing countries? What
are the financing, budgetary and institutional implications of national interventions
and of scaling up local interventions? What factors or processes affect change in
countries and systems? Under what conditions are policy/programme changes
associated with improvements in population-level health and greater equity in health?
Such factors and their relative contribution to change should be analyzed.
The MEKN will work towards proposing approaches for using the evidence on
integrating the SDH and health equity goals into national and global policy and
planning. One particular approach that may be helpful in articulating the processes
involved in effective approaches is ‘Programme Evaluation’ put forward at the expert
meeting on measurement held in March 2005. Programme evaluation (PE) in this
respect is defined as a systematic set of practices to improve and account for public
health actions, and to forecast a range of “plausible futures” stemming from policies.
Evaluation is a driving force for planning effective public health strategies, improving
existing programmes and demonstrating the results of resource investments (Milstein
& Wetterhall 1999). The foundation of PE consists of a well-described sequences of
steps (engaging stakeholders, describing the programme - including the use of logic
models, focusing the evaluation design, gathering credible evidence, justifying the
conclusions, and ensuring the use and sharing of lessons learned) that has been set
forth by the CDC’s Programme Evaluation Framework (Milstein & Wetterhall 1999),
the Community Toolbox (http://ctb.lsi.ukans.edu/ctb/c30/ProgEval.html ) and
elsewhere. Beyond formal evaluation systems, PE also encompasses a wider
spectrum of methods and approaches (such as system dynamics simulation models)
to observe and interpret programmes, and to stimulate further observations.
Within its sequences of steps, PE subsumes virtually all of the methods and tools
considered during the meeting and described above. Thus, planning for action within
a PE framework incorporates systematic reviews of previous research, Health Impact
28
Assessment, as well as additional steps such as power mapping and eliciting public
opinion. The real utility of PE may lie at the country engine level.
4.Proposed programme of work for MEKN and key deliverables
This paper has set out a range of issues which are key to advancing our
understanding of the social determinants of health. It has puts forward a set of
principles which will guide the approach taken by all the thematic knowledge
networks in their task to organise and synthesis evidence and knowledge that
promotes a social determinants approach to health development.
In particular, these principles emphasise the need to focus on knowledge that:
•
Supports reductions in health gradients to ensure that standards of health
achieved by the best off can be attained by the whole population.
•
Demonstrates the added value of using diverse methods to build certainty
about the right approach to be taken to address the social determinants of
health (e.g. Whitehead’s ‘evidence jigsaw’).
•
Attempts to incorporate a multi-faceted causation model of health and health
inequalities.
•
Takes account of all the dimensions of social difference including ethnicity,
gender, sexuality, age, area, community and religion to ensure that
recommendations for action are sensitive to a range of contexts.
•
Incorporates a historical perspective to finding out what works best to address
the social determinants of health and recognises the dynamic nature of the
social systems that influence people’s lives.
These principles will also be used to frame the forthcoming activities of the MEKN.
The activities will also be guided by the ongoing work being carried out by the WHO
secretariat to developing the overarching conceptual framework for the Commission’s
work.
The National Institute for Health and Clinical Excellence and the Universidad del
Desarrollo will collaborate with a small group of experts in the field of measurement
and evidence specifically to fulfil the aims and objectives of the MEKN particularly
focusing on:
29
1. Definitions of Evidence-. What constitutes evidence when measuring the effects of
policy and interventions aimed at tackling social determinants and health
inequalities? In the absence of a control group, what constitutes evidence? What
are the standards for levels of evidence for both quantitative and qualitative
techniques used to illustrate the relationship between a social determinants
approach and improved health outcomes and greater health equity? The
following key areas will form the basis of the approach to the evidence - causes
of inequalities, dimensions of variation in population, the relationship between
individual behaviour and social systems and a typology of evidence and methods.
2. Measurement - Selection of indicators: What types of indicators accurately reflect
the effect of a social determinants approach on health and health systems?
(Referring to health systems conceptualized as complex social systems with
flexible boundaries that shift with the emergence of new social realities). Should
indicators be predominantly outcome or process oriented? In the case of the
former: should they reflect a change in absolute numbers, relative numbers, or a
change in trends?
3. Measurement - Evaluation methodologies: What types of instruments exist or
need to be developed to measure the impact of a social determinants approach
to improving health, as it is mediated through the health system?
4. International perspectives on links between social determinants and health:
Analyse evidence on the robustness of the associations between SDH and
health/ health equity across different country contexts.
5. Action on the social determinants: upstream interventions: Collate and
summarise evidence and suggest national and global policies, programs and
institutional arrangements that modify the association between SDH and health
equity and enhance opportunities for greater health equity, taking into
consideration women's as well as men's concerns and experiences.
6. Action on the social determinants: mainstreaming downstream interventions:
Document and assess the processes and mechanisms required to mainstream
and scale-up successful examples of incorporating social determinants (SD) into
health programs and policies.
7. Developing Frameworks for Action: Propose approaches for using the evidence
on integrating the SDH and health equity goals into national and global policy and
planning.
30
8. Using effective dissemination strategies: Identify and engage institutions and
actors to contribute to the production, dissemination and use of knowledge for the
proposed policies and programs across different regions.
9.
Working in partnership with the Commission: Engage with the Commission
components (country work, civil society organizations and global initiatives,
themed knowledge Hubs, WHO technical liaison) to exchange knowledge and
learning. In particular to provide technical support to the themed KN’s through the
shared workspace by providing regular current awareness bulletins on the
measurement, evaluation and synthesis of evidence relating to the social
determinants of health (e.g. advice on identifying literature, quality and quantity of
evidence required for evaluation approaches, methods and tools for assessing
the strength of the evidence and evidence-based prioritization of
recommendations).
31
As a result of these activities the MEKN will:
•
Establish a global network of researchers, policy makers and agencies on the
theme of measurement and that connect the developing and developed
worlds.
•
Organise and host two MEKN meetings.
•
Develop a series of position papers relating to issues arising out of this
scoping paper to improve knowledge and action on issues of definition,
measurement, synthesis, evaluation and implementation of actions to address
the social determinants of health.
•
Moderate online discussions through SharePoint about key measurement and
evidence issues to assist other Knowledge Networks and Commission
streams of work.
Other activities and products may arise out of the first meeting of the Knowledge
Network which will take place on the 7th and 8th of April 2006 in Santiago, Chile.
32
References
Anthias, F. (1990). Race and class revisited- conceptualising race and racisms. Sociological
Review 38:19-42.
Anthias, F. (1992). Connecting race and ethnic phenomena. Sociology 26: 421-38.
Antonovsky, A. (1967). Social class, life expectancy and overall mortality. Millbank Memorial
Fund Quarterly 45: 31-73.
Antonovsky, A. (1985). Health Stress and Coping. San Francisco: Jossey Bass.
Antonovsky, A. (1987). Unravelling the Mystery of Health: How People Manage Stress and
Stay Well. San Francisco: Jossey Bass.
Arai, L., Roberts, H., Roen, K., Popay, J. (2005). It might work in Oklahoma but will it work in
Oakhampton? What does the effectiveness literature on domestic smoke detectors tell us
about context and implementation? Injury Prevention 11 148-151.
Bartley, M., Sacher, A., Firth, D., Fitzpatrick, R. (2000). Dimensions of inequality and the
health of women, in Graham, H. (ed) Understanding Health Inequalities. Buckingham: Open
University Press.
Benzeval, M., Dilnot, A., Judge, K., Taylor, J. (2000). Income and health over the lifecourse:
evidence and policy implications, in Graham, H. (ed) Understanding Health Inequalities.
Buckingham: Open University Press.
Berwick, D.M. (2005). Broadening the view of evidence based medicine. Qual Saf Health
Care 14: 315-16.
Braveman, P. (1998). Monitoring Equity in Health: A Policy Oriented Approach in Low- and
Middle Income Countries. Geneva: World Health Organization Department of Health Systems
(WHO/ CHS/ HSSZ 98.1).
Braveman, P. (2003). Monitoring equity in health and health care: A conceptual framework.
Journal of Health Population Nutrition 21(3): 181-92.
Braveman, P., Tarimo, E., Creese, A. et al (1996). Equity in Health and Health Care: A WHO
Initiative. Geneva: World Health Organization, October 1996 WHO/ARA 96.1.
Briss, P. (2005). Evidence-based: US road and public health side of the street. Lancet 365:
828-830.
Chalmers, I. (1998). Unbiased, relevant and reliable assessments in health care. British
Medical Journal 317: 1167-68,
Chalmers, I. (2004). Well informed uncertainties about the effects of treatments: How should
patients and physicians respond? British Medical Journal 328: 475-76.
Cochrane, A.L. (1972). Effectiveness and Efficiency: Random Reflections on Health Services.
London: British Medical Journal/Nuffield Provincial Hospitals Trust.
Cohen, A.K. (1951). Juvenile Delinquency and the Social Structure, PhD Thesis, University of
Harvard.
Danto, A.C. (1968). Analytic Philosophy of History. Cambridge: Cambridge University Press.
33
Davey-Smith, G., Chaulsley, K., Lambert, H., Paul, S., Fealon, S., Ahmad, W. (2000).
Ethnicity, health and the meaning of socio economic position, in Graham, H. (ed)
Understanding Health Inequalities. Buckingham: Open University Press.
Davidson, C. (1967). Causal relations. Journal of Philosophy 64: 691-703.
Dixon-Woods, M., Agarwal, S., Young, B., Jones, D. and Sutton, A. (2004). Integrative
Approaches to Qualitative and Quantitative Evidence. London: Health Development Agency.
Doll, R. (1998). Controlled trials: the 1948 watershed. British Medical Journal 317: 1217.
Glasziou, P., Vandenbroucke, J., Chalmers, I. (2004). Assessing the quality of research.
British Medical Journal 328: 39-41.
Gomm, R. & Davies, C. (eds) (2000). Using Evidence in Health and Social Care. London:
Open University Press.
Gomm, R., Needham, G., Bullman, A. (eds) (2000). Evaluating Research in Health and Social
Care. London: Sage.
Graham, H. (ed) (2000). Understanding Health Inequalities. Buckingham: Open University
Press.
Graham, H. (2004a). Social determinants and their unequal distribution: clarifying policy
understandings. Milbank Quarterly 82: 101-24.
Graham, H. (2004b). Tackling health inequalities in England: remedying health
disadvantages, narrowing gaps or reducing health gradients. Journal of Social Policy 33:115-
Graham, H. (2005). Intellectual disabilities and socioeconomic inequalities in health: an
overview of research patterns, determinants and challenges. Journal of Applied Research in
Intellectual Disabilities 18 101-111.
Graham, H. & Kelly, M.P. (2004). Health Inequalities: Concepts, Frameworks and Policy.
London: Health Development Agency.
Graham, H., & Power, C. (2004). Childhood Disadvantage and Adult Health. London: Health
Development Agency.
Greenhalgh, T (2001). How to Read a Paper: The Basics of Evidence Based Medicine.
London: BMJ Books.
Griffiths, F., Green, E., Tsouroufli, M. (2005). The nature of medical evidence and its inherent
uncertainty for the clinical consultation: qualitative study. British Medical Journal 330:511.
Harbour, R. & Miller, J. (2001). A new system for grading recommendations in evidence
based guidelines. British Medical Journal 323:334-6.
Heller, R. (2005). Evidence for Population Health. Oxford: Oxford University Press.
Hempel, C.G. (1965). Aspects of scientific explanation, in Hempel, C.G., Aspects of Scientific
Explanation and other Essays in the Philosophy of Science. New York: Free Press.
Jackson, N. & Waters, E. (2005a). For the Guidelines for Systematic Reviews in Health
promotion and Public Health Task Force, Criteria for the systematic review of health
promotion and public health interventions. Health Promotion International 20: 367- 74.
34
Jackson, N., Waters, E. (eds) (2005b). Systematic Reviews of Health Promotion and Public
Health Interventions. The Cochrane Collaboration. The Cochrane Public Health Field.
www.vichealth.vic.qov.au/cochrane.
Kelly, M.P., Speller, V., Meyrick, J. (2004). Getting Evidence into Practice in Public Health.
London: Health Development Agency.
Kelly, M.P., Charlton, B.G., Hanlon, P. (1993). The four levels of health promotion: An integrated
approach. Public Health 107: 319-326.
Kelly, M.P. (2004). Foreword in Dixon-Woods, M., Agarwal, S., Young, B., Jones, D. Sutton,
A. Integrative Approaches to Qualitative and Quantitative Evidence. London: Health
Development Agency.
Killoran, A. & Kelly, M.P. (2004). Towards an evidence-based approach to tackling health
inequalities: the English experience. Health Education Journal 63: 7-14.
Kuh, D., Ben-Shlomo, Y., Lynch, J., Hallqvist, power, C. (2003) Life course epidemiology. Journal
of Epidemiology and Community Health 57: 778-83.
Leon, D., Walt, G., Gilson, L. (2001). International perspectives on health inequalities and policy.
British Medical Journal 322: 591-94.
Lomas, J., Culyer, T., McCutcheon, C., McCauley, L., Law, S. (2005). Conceptualizing and
Combining Evidence for Health System Guidance. Ottawa: Canadian health Services Research
Foundation.
Macintyre, A. (1984) After Virtue, Notre Dame: University of Notre Dame Press.
Marmot, M. & Wilkinson, R. (eds) (1999). Social Determinants of Health. Oxford: Oxford
University Press.
Milstein, R.L. & Wetterhall S.F. (1999). Framework for programme evaluation in public health
MMWR48:No. RR-11.
Millward, L, Kelly, M.P., Nutbeam, D. (2003). Public Health Interventions Research: The
Evidence. London: Health Development Agency.
NHMRC (National Health and Medical Research Council) (1999). A Guide to the Development,
Implementation and Evaluation of Clinical Practice Guidelines. Canberra: National Health and
Medical Research Council.
Petticrew, M., Whitehead, M., Macintyre, S.J., Graham, H., Egan, M. (2004). Evidence for
public health policy on inequalities: 1: The reality according to policymakers. Journal of
Epidemiology and Public Health 58:811-16.
Plato (1974). The Republic, translation and introduction D. Lee. Hamondsworth: Penquin.
(Second Ed).
Popay, J., Rogers, A. and Williams, G. (1998). Rationale and standards for the systematic
review of qualitative literature in health services research. Qualitative Health Research 8-34151.
Popay, J. (2005). Qualitative research and the epidemiological imagination - a vital
relationship. Unpublished manuscript circulated at meeting. Chile Measurement Consultation
meeting Commission on Social Determinants of Health, Santiago, Chile.
Popay, J. and Roen, K. (2003). Using Evidence from Diverse Research Designs: A
Preliminary Review of Methodological Work. SCIE Report No. 3, November 2003. ISBN 190481-2-05-8. UK: Social Care Institute for Excellence.
35
Rawlins, M. (2005). 5 NICE years. Lancet 365: 904-8.
Ritsatakis, A. (2000). Experience in Setting Targets for Health in Europe. European Journal of
Public Health 10:4 (supplement): 7-10.
Roen, K., Arai, L., Popay, J. and Roberts H. (2005). Preventing children’s injuries: Exploring
methodological issues in the systematic review of qualitative evidence. Social Science and
Medicine (in press).
Schutz, A. (1964). Collected Papers: II Studies in Social Theory. The Hague: Martinus Nijhoff.
Schutz, A. (1967). The Phenomenology of the Social World, trans G. Walsh & F Lehnert
Evanston III: North Western University Press.
Schutz, A. (1970). On Phenomenology and Social relations: Selected Writings. Chicago:
Chicago University Press.
Shaw, M., Dorling, D., Gordon, D. and Davey Smith, G. (1999). The Widening Gap-Health
Inequities and Policy in Britain. Bristol: Policy Press.
Solar, O. and Irwin, A. (2005). Towards a conceptual framework for analysis and action on the
social determinants of health. Discussion paper for the Commission on the Social
Determinants of Health. Internal Paper
Smith, J.P. (2004). The Impact of SES on Health over the Lifecourse. Unpublished.
United Nations (2000). United Nations, The General Assembly, United Nations Millennium
Declaration, A/RES/55/2.
Victora, C.G., Vaughan, J.P., Barros, F.C., Silva, A.C. and Tomasi, E. (2000). Explaining
trends in inequalities: evidence from Brazilian child health studies. Lancet 356 1093-1098.
Weber, M. (1948). Science as a vocation, in Gerth, H.H. & Mills, C.W., From Max Weber:
Essays in Sociology. London: Routledge & Kegan Paul.
Whitehead, M. (1992). Perspectives in health inequity. International Journal of Health
Services 22: 429-45.
Whitehead, M., Diederichsen, F., Burston, B. (2000). Researching the impact of public health
policies on inequalities in health, in Graham, H. (ed) Understanding Health Inequalities.
Buckingham: Open University Press.
Whitehead, M., Petticrew, M., Graham, H., Macintyre, S., Bambra, C. and Egan, M. (2004).
Evidence for public health policy on inequalities: 2: Assembling the evidence jigsaw Journal
of epidemiology and Community Health. 58:817-21.
WHO (1948). Constitution of the World Health Organisation. London: WHO.
WHO (1981). Global Strategy for Health for All by the Year 2000. Geneva: World Health
Organization.
WHO (1985). Targets for Health for All. Copenhagen: World Health Organization Regional
Office for Europe.
WHO (1998a). Health 21 - Health for All in the 21st Century. Copenhagen: World Health
Organization Regional Office for Europe.
WHO (1998b). Health Promotion Evaluation: recommendations to policy makers. Report of
the WHO European Working Group on Health Promotion Evaluation. Copenhagen: WHO.
36
WHO (2004). Priorities to Take Forward the Health Equity Agenda: Report from the Task
Force on Health System Research Prionties for Equity in Health. Copenhagen: WHO.
37
COMMISSION ON
SOCIAL DETERMINANTS OF
HEALTH
(0)
Towards a Conceptual Framework for Analysis and Action
on the Social Determinants of Health
Discussion paper for the Commission on Social Determinants of Health
DRAFT
5 May 2005
CSDH Conceptual Framework
DRAFT
This draft paper was prepared for the second meeting of the Commission on Social
Determinants of Health by the Commission secretariat, based in the WHO Health Equity
Team, Office of the Assistant Director-General, Evidence and Information for Policy Cluster,
WHO Geneva. The principal writers were Orielle Solar and Alec Irwin. Valuable input was
provided by the other members of the Commission secretariat, in particular Jeanette Vega.
Any errors are solely the responsibility of the principal writers.
2
CSDH Conceptual Framework
DRAFT
TABLE OF CONTENTS
1. INTRODUCTION
4
2. SOCIAL DETERMINANTS: DEFINITIONS; DIFFERENCE FROM INDIVIDUAL RISK FACTORS.
.......................................................................................................................................................................... 4
3. DEFINING CORE VALUES: SDH AND HEALTH EQUITY
.5
4. PURSUING EQUITY THROUGH HEALTH POLICY: HEALTH DISADVANTAGE, GAPS AND
GRADIENTS
.
9
5. MODELING HEALTH DETERMINANTS AND THE PATHWAYS TO INEQUITY ...
11
5.1 Dahlgren and Whitehead: layered influences......................................................
5.2 Diderichsen et al. : social stratification and disease production......................
12
5.3 Ma ckenba ch etal.: selection AND CA USA TION.................................................................
13
5.4 Brunner, Marmot and Wilkinson: multiple influences across the life-course
5.5 Synthesis........................... .......................................................
13
14
6. PROPOSED CONCEPTUAL FRAMEWORK FOR THE CSDH
6.1 Structural and intermediate social determinants
6.2 Socio-political context..............................................
6.3 Levels for policy action on SDH...............................
6.4. Selection of specific themes for the CSDH..........
11
16
,17
18
19
20
7. INTERVENTION AND POLICY DEVELOPMENT MODELS FOR ACTION ON SDH
,26
7.1K. Stronks framework...................................................................................................
7.2 M. Whitehead and G. Dahlgren framework..............................................................
7.3 Diderichsen etal. framework.....................................................................................
7.4. Synthesis: key policy principles.................................................................................
,26
,27
28
30
8. CONCLUSION
31
REFERENCES
,33
3
CSDH Conceptual Framework
DRAFT
1. Introduction
The Commission on Social Determinants of Health (CSDH) has affirmed its desire to be
judged not only on the scientific rigor of its analyses, but on the policy and institutional
changes catalysed in countries through Commission advocacy and partnership. To set
feasible objectives for its political work and send consistent messages to partners and the
public, the CSDH requires clarity on basic conceptual issues. These include:
• The concept of social determinants of health (SDH)
• The values that ground the Commission's analysis and policy recommendations
• The pathways by which SDH affect health status and outcomes
• How SDH relate to health inequities
• The most important SDH for the Commission to address, and why
• Appropriate intervention levels and entry points for policy action on SDH
• The ultimate goal of SDH policies (improving average health status or reducing
health inequities)
This paper outlines a conceptual framework we hope can serve as a basis for discussion and
clarification of these issues within the CSDH. The paper in its current form is an early draft,
which aims to open debate rather than furnish definitive answers. It summarizes the results of
an initial phase of research and analysis by the CSDH secretariat. The paper will pass
through subsequent iterations to incorporate input from Commissioners and yield a final
document succinctly laying out the conceptual foundations of the Commission’s work.
The paper begins by recalling the CSDH definition of social determinants and some
methodological implications. It then takes up the question of values. We propose the concept
of health equity as a cornerstone for the Commission's normative framework. Applying
equity criteria, we consider the implications of policy approaches focused respectively on: (1)
tackling health disadvantages in targeted population groups; (2) reducing health gaps; and (3)
addressing the health gradient across the full spectrum of socioeconomic positions. The next
section of the paper reviews several models that have sought to explain relationships among
SDH and their causal role in generating health inequities. Drawing lessons from these
approaches, we propose a comprehensive SDH framework that situates the major
determinants and clarifies levels for policy action. Using this model, we then show how and
why a set of key thematic foci for the Commission's work have been proposed. Finally, we
review several evaluative frameworks the CSDH could use in developing policy
recommendations and suggest some principles to ground those policy choices.
2. Social determinants: definitions; difference from individual risk factors
The social determinants of health (SDH) can be understood as the social conditions in which
people live and work, or in Tarlov’s phrase "the social characteristics within which living
takes place". SDH point to both specific features of the social context that affect health and
to the pathways by which social conditions translate into health impacts. The SDH that merit
attention are those that can potentially be altered by informed action2.
4
CSDH Conceptual Framework
DRAFT
The concept of SDH originated in a series of influential critiques published in the 1970s and
early 1980s, which highlighted the limitations of health interventions oriented to the disease
risks of individuals. Critics argued that understanding and enhancing health required a
population focus, with research and policy action directed at the societies to which
individuals belonged 3. A case was made for "refocusing upstream" from individual risk
factors to the social patterns and structures that shape people's chances to be healthy. Integral
to these critiques is the argument that medical care is not the main driver of people's health.
Instead, the concept of social determinants is directed to the "factors which help people stay
healthy, rather than the service that help people when they are ill". 4
In some contexts, health determinants have continued to be conceptualized primarily as
characteristics of the individual, such as a person's social support network, income or
employment status. Population are not merely collections of individuals, however; the causes
of ill health are clustered in systematic patterns, and in addition effects on one individual may
depend on the exposure and outcomes experienced by other individuals.5 This flows from the
fact that the determinants of individual differences regarding some characteristic within a
population may be different from the determinants of differences between populations.6 In
this light, it is useful distinguish two kinds of etiological questions: the first seeks the causes
of cases, the second the causes of incidence. When we talk about social determinants, we
wish to understand how the causes of individual cases relate to the causes of population
incidence . Why do we observe a graded relationship between social position and health
status that affects people at all levels of the social hierarchy? How is this gradient shifting
over time? Are the factors determining health changing for the better? Is it the same for
everyone? Where and for whom are they changing for the worse?8
3. Defining core values: SDH and health equity
A reflection on values will necessarily be part of Commissioners' shaping of a conceptual
framework. We propose the concept of health equity as a foundation for this reflection.
Health equity can be defined as the absence of unfair and avoidable or remediable differences
in health amon^ populations or groups defined socially, economically, demographically or
geographically.
geographically. 9 Health inequity involves more than mere inequality, since some health
inequalities (e.g., the gap in average life expectancy between women and men) cannot
reasonably be described as unfair, and some are neither preventable nor remediable. Inequity
implies a failure to avoid or overcome inequalities in health that infringes human rights
norms or is otherwise unfair. Health inequities have their roots in social stratification.10
Health inequity thus defined is a moral category deeply embedded in political reality and the
negotiation of social power relations.
The social determinants of health are not necessarily the same as the social determinants of
health inequities.11 Among the many social factors and processes that influence health, some
but not all will be found to be significant contributors to health gaps among different social
groups. It would be possible to promote SDH policies that might improve average health
indicators in a country without altering the extent of health disparities between privileged and
disadvantaged groups. A key question for the CSDH then becomes the following: is
improving average health indicators a sufficient objective for the policies the Commission
5
CSDH Conceptual Framework
DRAFT
will recommend, or should probable positive effects on health equity be a central criterion for
the CSDH in selecting policy options?
We argue that the Commission should concentrate its attention on SDH that are major causes
of health inequities, and that the policies recommended by the Commission should be
policies that can be expected to have a substantial positive health equity impact. However,
neither the philosophical value of the concept of health equity nor the desirability of a pro
equity approach to health policymaking can simply be assumed. It is necessary both to justify
health equity conceptually and to "give arguments for the government's responsibility to
reduce socioeconomic health differences".12 13 A number of valuable philosophical accounts
of health equity and arguments for the political application of the concept have been put
forward recently. Many of these contributions emanate from Amartya Sen or adopt his
categories. It will be useful to recall the broad outlines of several of these arguments, giving
particular attention to those that emphasize the political translation of health equity.
Stronks and Gunning-Schepers (1993) have drawn on the work of Sen, Berlin and others to
construct an argument for government action on health inequities rooted in a theory of social
justice. They argue that a just society is characterized by providing equally to all its members
a high degree of freedom, specifically the "positive freedom" to choose from among a range
of desirable options the life plan that most fully agrees with the particular individual's
conception of the good life. A just government does not promote one particular conception of
the good life. It leaves the choice of life plans open to individuals. However, a just
government is obligated to provide the enabling conditions that make it possible for each
individual to freely choose her life-plan. "The capability to be as healthy as possible is such a
condition," since the presence or absence of this basic capability "determines the life plans
from which an individual can choose". To the extent that social conditions can be shown to
constrain the health capability of some people within a society, creating inequalities in
people's opportunity to exercise positive freedom, a government is under obligation to take
action on these social determinants in order to guarantee equality in the chances for health.
Importantly, the factor to be equalized is not health status but health opportunity, since
individuals may employ their positive freedom to choose a way of life that compromises
health in the pursuit of other goods. This underscores that health inequalities per se are not
inherently problematic, since such "inequalities that are the result of free choices made by an
individual are acceptable". The principle of justice applied here "does not require everyone to
have the same level of health, but it demands such a distribution of determinants of health, to
the extent they can be controlled, that every individual has the same possibilities to lead a
long and healthy life".14
In recent work, Anand (2004) has further clarified the grounds for regarding health equity,
and not just average levels of health achievement, as a public policy concern. In convergence
with Sen, Anand stresses that health is a "special good" whose fair distribution merits the
particular concern of political authorities. There are two principal reasons for regarding
health as a special good: (1) health is directly constitutive of a person's well-being; and (2)
health enables a person to function as an agent.15 Inequalities in health are thus recognized as
"inequalities in people's capability to function". When such inequalities arise as a
6
CSDH Conceptual Framework
DRAFT
consequence of individuals' different social positions, a grave breach of the political principle
of equality of opportunity has occurred. Assuring the fair distribution of health among
members of the society should thus be regarded as a primary responsibility of just
governance.
Ruger (2005) has developed similar arguments, linking Sen’s capability approach with
Aristotle's political philosophy. "While recognizing the interrelatedness of health and other
valuable social ends, such as education," Ruger "emphasizes the importance of health for
individual agency the ability to live a life one values". Health is seen as sustaining all other
aspects of human flourishing or capability. Thus, promoting an equitable distribution of real
opportunities for health emerges as a fundamental task of public policy. "Public policy
should focus on individuals’ capability to function, and health policy should aim to maintain
and improve this capability by meeting health needs".16
A values framework based on health equity provides strong support for an SDH agenda.17,18
Meanwhile, policy action on social determinants can also be justified using a variety of other
normative approaches, in particular human rights. The 2000 General Comment on the right to
health by the UN Committee on Economic, Social and Cultural Rights characterized the right
to health is an "inclusive right" extending "not only to timely and appropriate health care but
also to the underlying determinants of health".19 Authoritative interpretations of international
human rights accords thus acknowledge the responsibility for governments to act on SDH
and may facilitate the translation of this responsibility into policy. Further reflection will be
required to clarify complementarities and possible tensions between equity and human rights
approaches to SDH, in light of recent analyses of the plurality of moral frameworks used to
legitimate health actions.20,21
To summarize, the concept of health equity provides a robust ethical foundation for the work
of the CSDH. A close relationship exists between health equity and social determinants, both
conceptually and in political terms. Substantial progress cannot be made on health equity
without action on the social determinants of health. On the other hand, at a time when health
inequalities between and within countries are the focus of increasing concern22, the potential
contributions of SDH measures to health equity constitute an important scientific, ethical and
political argument for action on SDH.
The preceding discussion represents only a first step in defining a values framework for the
CSDH. It is proposed that a working group of Commissioners with special interest in this
area take forward, with support from the secretariat, the project of developing this analysis.
The results will be submitted to the full Commission for review and input. The discussion
above points to several issues for this deeper exploration. These include the following
questions, roughly ranked from broader to more circumscribed:
•
A rigorous analysis of social determinants may lead to the conclusion that
significantly reducing health gradients would require profound structural changes in
many contemporary societies, e.g., in the functioning of markets and the
redistributive role of the state. Is the CSDH prepared to "own" such ideas, and what
forms of political philosophy will guide its deliberations and recommendations in this
7
CSDH Conceptual Framework
DRAFT
respect? Much recent discussion of health equity has been subtended by models of
social justice derived from liberal thinkers, in particular John Rawls, for whom liberal
market democracy remains the paradigm of appropriate social organization among
well-ordered peoples". Rawls' ideas (and liberal democracy itself, where it may exist)
clearly still have much to offer. Yet an analysis of contemporary societies in terms of
health equity should be prepared to test and challenge the liberal democratic paradigm
itself — both at the level of Rawls' idealized abstractions and, more importantly, at the
level of "really existing market democracies".
•
A number of important and insufficiently clarified issues cluster around the notions of
individual freedom, personal agency and choice. An equity-based SDH model
appears to stand in a complex relationship to prevalent ideas of freedom and
responsibility. On the one hand, an equity approach seeks to equalize opportunities,
not outcomes, and maintains that health differences arising through individual free
choice are acceptable; on the other, an analysis of structural determinants implies that
certain forms of "free choice" (e.g., low-paid workers' "choice" to smoke more
heavily than members of higher socioeconomic groups) are in fact shaped by social
forces largely beyond the individual's control. A robust analysis of equity and SDH
will need to develop a clear account of the scope and limits of personal freedom, as
constructed and/or negated in different social contexts and through diverse forms of
social constraint and conditioning. Of use in developing such an analysis will be Paul
Farmer's notion of "structural violence",23’24 as well as accounts of the distortion of
personal agency through systemic social oppression proposed by social scientists like
Philippe Bourgois.25 In reflecting on SDH, equity and individual agency, it should not
be neglected that, in societies where health is regarded primarily as a private matter,
the motif of "personal responsibility" has been deployed politically precisely to
absolve government of responsibility for addressing health inequities and responding
more actively to the health needs of poor and excluded groups.
This topic and the preceding point could perhaps best be summarized by stressing that
a credible health equity framework must equip itself with a robust theory ofpower.
This is in keeping with the observation that health inequities derive most
fundamentally from the differential allocation of power and wealth to social
positions. Sen's work on capabilities, rationality and freedom will again open
valuable lines of enquiry in this respect, especially if crossed with a concrete analysis
of the mechanisms and practices of manipulation, exclusion, disinformation and
disempowerment deployed in contemporary societies, both authoritarian and
nominally democratic. Philosophy should do more than simply describe an ideal of
human freedom (or equitably distributed human health). It must also show how we
might begin to advance towards that ideal in concrete political terms.
•
Human rights analysis emphasizes not only substantive rights, but also people's right
to informed participation in the decision-making processes that affect their lives and
the exercise of their liberties. Sen's work on the process aspect of freedom explores
related concerns.27 It will be important to clarify to what extent the concept of health
equity implies a process aspect and how the relevant procedures might be specified.
8
CSDH Conceptual Framework
DRAFT
Will health equity, in its concrete social and political operationalization, stipulate the
participation of communities and other stakeholders in decision-making relative to
health and health equity agendas (including action on SDH)? How might such
participation be structured? What would be its precise objectives? At what level(s)
would it take place, and who would be included? Ranaan Gillon has suggested what
might be at stake in such choices by asking, in the framework of a discussion of value
judgments about health equity, if it would not be appropriate for the taxpayers whose
contributions fund national health programmes to be invited to vote on the broad
composition of health sector budgets (e.g., proportion of spending devoted to
prevention vs. curative care, special benefits for vulnerable groups, etc.).28 Such a
debate is of course just one entry point to a broader discussion about the modes of
participation and community ownership required for a robust operationalization of
health equity.
More work is clearly needed on the translation of philosophical principles of health
equity into the practice of planning and resource allocation at the various levels of
government. A broad commitment to equity does not pre-determine priority among
the different moral criteria that may legitimately be used at national and local levels
in allocating scarce health resources. These criteria include, for example, allocation
based on: need; maximization of individual benefit; and maximization of benefit at
the population level. These criteria are all "morally respectable" but can, and in many
cases will, lead to conflicting judgments on how resources available to promote
health and social welfare should be invested (Gillon). It will be important to continue
work currently underway to see if a health equity model of the type presented above
can shed light on these operational issues, which are clearly of relevance to planners
and programme implementers in countries: constituencies among whom the CSDH
needs to be taken seriously.
4. Pursuing equity through health policy: health disadvantage, gaps and gradients
Today, health equity is increasingly embraced as a policy goal by international health
agencies and national policy makers.29 As Hilary Graham has shown, however, political
leaders’ commitment to ’’tackle health inequities» " can be interpreted in different ways and
authorize a variety of distinct policy strategies.
Three broad policy approaches to reducing health inequities can be identified: (1) improving
the health of disadvantaged population groups through targeted programmes; (2) closing the
health gaps between those in the poorest social circumstances and better off groups; (3)
addressing the entire health gradient, that is, the association between socioeconomic position
and health across the whole population.
To be successful, all three of these options would require action on SDH. All three constitute
potentially effective ways to alleviate the unfair burden of illness borne by the socially
disadvantaged. Yet the approaches differ significantly in their underlying values and
implications for programming. Each offers specific advantages and raises distinctive
problems.
9
CSDH Conceptual Framework
DRAFT
Programmes to improve health among disadvantaged populations have the advantage of
targeting a clearly defined, fairly small segment of the population and of allowing for relative
ease in monitoring and assessing results. Targeted programmes to tackle health disadvantage
may align well with other targeted interventions in a governmental anti-poverty agenda, for
example social welfare programmes focused on particular disadvantaged neighborhoods. On
the other hand, such an approach may be weakened politically precisely by the fact that it is
not a population-wide strategy but instead benefits sub-groups that make up only a relatively
small percentage of the population. Furthermore, this approach does not commit itself to
bringing levels of health in the poorest groups closer to national averages. Even if a targeted
programme is successful in generating absolute health gains among the disadvantaged,
stronger progress among better-off groups may mean that health inequalities widen.
An approach targeting health gaps directly confronts the problem of relative outcomes. The
UK's current health inequality targets on infant mortality and life expectancy are examples of
such a gaps-focused approach. However, this model, too, brings problems. For one thing, its
objectives will be technically more challenging than those associated with strategies
conceived only to improve health status among the disadvantaged. "Movement towards the
[gap reduction] targets requires both absolute improvements in the levels of health in lower
socioeconomic groups, and a rate of improvement which outstrips that in higher
socioeconomic groups". Meanwhile, Graham argues that gaps-oriented approaches share
some of the underlying moral ambiguities of the focus on health disadvantage. Health-gaps
models continue to direct efforts to minority groups within the population (they are
concerned with the worst-off, measured against the best-off). By adopting this stance, "a
health-gaps approach can underestimate the pervasive effect which socioeconomic inequality
has on health, not only at the bottom but also across the socioeconomic hierarchy". By
focusing too narrowly on the worst-off, gaps models can obscure what is happening to
intermediate groups, including "next to the worst-off groups that may also be facing major
health difficulties.
Tackling the socioeconomic gradient in health right across the spectrum of social positions
constitutes a much more comprehensive model for action on health inequities. With a health
gradient approach, "tackling health inequalities becomes a population-wide goal: like the
goal of improving health, it includes everyone". On the other hand, this model must clearly
contend with major technical and political challenges. Health gradients have subsisted
stubbornly across epidemiological periods and are evident for virtually all major causes of
mortality, raising doubts about the feasibility of significantly reducing them, even if political
leaders have the will to do so. Public policy action to address gradients may prove complex
and costly and, in addition, yield satisfactory results only in a long timeframe. Yet it is clear
that an equity-based approach to social determinants, carried through consistently, must lead
to a gradients focus.
Importantly, as Graham argues, strategies based on tackling health disadvantage, health gaps
and gradients are not mutually exclusive and need not be cast as rivals. The approaches are
complementary and can build on each other. "Remedying health disadvantages is integral to
narrowing health gaps, and both objectives form part of a comprehensive strategy to reduce
10
CSDH Conceptual Framework
DRAFT
health gradients". Thus a sequential pattern emerges, with "each goal add[ing] a further layer
to policy impact". Of course the relevance of these approaches and their sequencing will vary
with countries' levels of economic development and other contextual factors. A targeted
approach may have little relevance in a country where 80% of the population is living in
extreme poverty. Here the CSDH can contribute by linking a deepened reflection on the
values underpinning an SDH agenda with country-level contextual analysis and a pragmatic
mapping of policy options and sequencing.
5. Modeling health determinants and the pathways to inequity
Over the past 15 years, several models have been developed to show the mechanisms by
which SDH affect health outcomes, to make explicit the linkages among different types of
health determinants; and to locate strategic entry points for policy action. Influential models
include those proposed by: Dahlgren and Whitehead (1991); Diderichsen and Hallqvist (1998,
subsequently adapted in Diderichsen, Evans and Whitehead 2001); Mackenbach (1994);
Marmot and Wilkinson (1999). These models are particularly important in making visible the
ways SDH contribute to health inequities among groups in society.
5.1 Dahlgren and Whitehead: layered influences
Dahlgren's and Whitehead's frequently cited model explains how social inequalities in health
are the results of interactions between different levels of causal conditions, from the
individual to communities to the level of national health policies (see figure on next page).30
Individuals are at the centre of the picture, endowed with age, sex and genetic factors that
undoubtedly influence their final health potential. Moving outward from the centre, the next
layer represents personal behaviors and lifestyles. People in disadvantage circumstances tend
to exhibit a higher prevalence of behavioral factors such as smoking and poor diet, and will
also face greater financial barriers to choosing a healthier lifestyle.
Social and community influences are represented in the next layer. These social interactions
and peer pressures influence personal behaviors in the layer below, for better or worse.
Indicators of community organization register fewer networks and support systems available
to people towards the lower end of the social scale, compounded by the conditions prevalent
in area of high deprivation, which have a fewer social services and amenities for community
activity and weaker security arrangements. At the next level up, we find factors related to
living and working conditions, food supplies and access to essential facilities and services. In
this layer, poorer housing conditions, exposure to more dangerous or stressful working
conditions and poorer access to services create differential risks for the socially
disadvantaged.
Overarching all other levels are the economic, cultural and environmental conditions
prevalent in society as a whole. These conditions, such as the country's economic state and
labor market conditions, have a bearing on every other layer. The standard of living achieved
in a society, for example, can influence an individual's choice of housing, work and social
interactions, as well as eating and drinking habits. Similarly, cultural beliefs about the place
11
CSDH Conceptual Framework
DRAFT
of women in society or pervasive attitudes to minority ethnic communities can influence their
standard of living and socioeconomic position.31
Living and working
conditions
/ Work
wnvifonfrwnt
c/'
<&/
Education
e/
7^
UrxwnployTnentX
Water and
sanitation
Vx/
00/
Agriculture
and food
production
Health
care
services
ft
Housing
Age, sex and
hereditary
factors
5.2 Diderichsen et al.: social stratification and disease production
Diderichsen's and Hallqvist’s 1998 model was adapted by Diderichsen, Evans and Whitehead
(2001). This model emphasizes how social contexts create social stratification and assign
individuals to different social positions. People’s social position determines their health
opportunities. In the diagram below, the process of assigning individuals to social positions is
shown as (1). The mechanisms involved are "those central engines of society that generate
and distribute power, wealth and risk", for example the educational system, labour policies,
gender norms and political institutions. Social stratification in turn engenders differential
exposure to health-damaging conditions (II) and differential vulnerability (III), as well as
differential consequences of ill health for more and less advantaged groups, shown as
mechanism (IV). "Social consequences" refers to the impact a certain health event may have
on an individual’s or a family's socioeconomic circumstances. This model includes a
discussion of entry points for policy action, an aspect we will take up in a later section.
Social
Context
I
>
Social Position
I
II
II
Specific exposure
I- Disease or injury
Policy
Context
I
IV
Social Consequences of illhealth
12
CSDH Conceptual Framework
DRAFT
5.3 Mackenbach et al.: selection and causation
Mackenbach’s model emphasizes the mechanisms by which inequities in health are generated:
selection vs. causation. The number "1" marks the selection processes represented by an
effect of health problems at adult ages on adult socioeconomic position, and by an effect of
health in childhood on both adult socioeconomic position and health problems at adult ages.
The number "2" is the causation mechanism is represented by the three groups of risk factors
which are intermediary between socioeconomic position and health problems (Lifestyle
factors, structural/environmental factors, psychosocial stress-related factors). Childhood
environment, cultural factors and psychological factors are included in the model, which
acknowledge their contribution to inequalities in health through both selection and
causation.3
Adult
socioeconomic
position
Incidence of health problems at adult ages
t
1
1
2
2
>
1
d. - childhood environment
e. - cultural factors
f - psychological factors
a. - Lifestyle factors
b. - structural/environmental
factors.
c. - psychosocial stress-related
factors.
2
2
1
g.- health in childhood
5.4 Brunner, Marmot and Wilkinson: multiple influences across the life-course
This model was originally developed to connect clinical (curative) and public health
(preventive) perspectives on health. It was subsequently applied to the social process
underlying health inequalities as a model of the social factors that both cause ill health and
contribute to health inequalities. The model is included in the United Kingdom’s Acheson
report, introduced explicitly to illustrate how socioeconomic inequalities in health result from
differential exposure to risk- environmental, psychological and behavioral- across the life
course
This model links social structure to health and disease via material, psychosocial
and behavioral pathways. Genetic, early life and culture factors are further important
influences on population health.
13
CSDH Conceptual Framework
DRAFT
Social structure
MATERIAL FACTORS
PSYCHOLOGICAL
Social
environment
i
HEALTH
BEHAVIOURS
4
>
BRAIN
Neuro-endocrine
and immune
response
Pathophysical changes
Organ impairment
Early life
Genes
Culture
Well - being
Mortality
Morbidity
5.5 Synthesis
The various models we have examined (along with others not reviewed in detail here) seek to
explain the mechanisms that generate health inequities via SDH. From these proposals,
several themes emerge as deserving special attention, including ’’selection vs. causation”, the
"specific determinants” perspective and the ’’life course” approach. Life course analysts argue
that policies that prevent an accumulation of risk in the critical biological and social periods such as prenatal development, the transfer from primary to secondary school, entry to the
labor market and^exit from the labor market - should be especially important in protecting the
most vulnerable . Ongoing debates reveal differences with respect to the incorporation of a
life course perspective, however. Certain models are restrictive in this area, while others give
strong priority to childhood events and conditions.
Other revealing differences can be noted among the models surveyed in our research. Some
models ignore the reverse effect of health on socioeconomic position, while others
incorporate it explicitly. Some make biological pathways explicit, while others leave this
aspect unaddressed. (One could argue that biological pathways are more relevant for clinical
intervention and less so for policymaking.) Health care service and systems are rarely
accorded a place in the models, reflecting the fact that the concept of social determinants was
originally introduced into debates about public health to underscore the importance of
nonclinical factors in shaping the health of individuals and populations.36
14
CSDH Conceptual Framework
DRAFT
A comprehensive SDH model should achieve the following: (a) clarify the mechanisms by
which social determinants generate health inequities; (b) show how major determinants relate
to each other; (c) provide a framework for evaluating which SDH are the most important to
address; and (d) map specific levels of intervention and policy entry points for action on
SDH. Each of the models we have examined makes an important contribution, yet none on
its own fully meets these requirements. However, by combining elements of various models,
we can arrive at a synthetic construct that may advance the debate. The schema below is the
first stage of such a synthetic model. A more developed version is presented and discussed in
the next section, in which we will take up the question of specific thematic foci for the
Commission. As a preliminary step, the model sketched below attempts to draw together the
more significant insights of the approaches reviewed in the preceding pages.
I
X
w
Socioeconomic
position
H
Z
Specific
determinants
or individual's
social position
<D
Differential
Health Status
wCD
O
u
J
Q
H
3
o
Q
J
<
u
o
GO
CZ)
Structural or social
determinants of
inequities in
health. E.g. : social
stratification via
education, labour
market, income,
social cohesion.
Social
inequities
3
Pathway or
intermediary
determinants or social
determinants of health.
E.g. living and
working condition,
health behaviours, life
course, health and
social care.
Differential
exposure and
vulnerability
Differential
Health and
Wellbeing
Differential
access to
Health
System
>
Reading from left to right, we see the social and political context (including political
institutions and economic processes) giving rise to a set of unequal socioeconomic positions.
Groups are stratified according to income levels, education, professional status, gender,
race/ethnicity and other factors. This column of the diagram ("Socioeconomic position")
locates the underlying mechanisms of social stratification and the creation of social inequities.
These socioeconomic stratification mechanisms can be described as structural determinants
of health or as the social determinants of health inequities. These mechanisms configure the
health opportunities of social groups based on their placement within hierarchies of power,
prestige and access to resources.
15
CSDH Conceptual Framework
DRAFT
Moving to the right, we observe how these socioeconomic positions then translate into
specific determinants of individual health status reflecting the individual's social location
within the stratified system. Based on their respective social status, individuals experience
differential exposure and vulnerability to health-compromising factors. The model shows that
a person's socioeconomic position affects his/her health, but that this effect is not direct.
Socioeconomic position influences health through more specific, intermediary determinants.
Those intermediary factors include material conditions, such as working and housing
conditions; psychosocial circumstances, such as psychosocial stressors; and also behavioral
factors, such as smoking. The model assumes that members of lower socioeconomic groups
live in less favorable material circumstances than higher socioeconomic groups, and that
people closer to the bottom of the social scale more frequently engage in health-damaging
behaviors and less frequently in heath promoting behaviors than do the more privileged.
A distinctive element of this model is its explicit incorporation of the health system.
Socioeconomic inequalities in health can in fact be partly explained by the "feedback" effect
of health on socioeconomic position, e.g., when someone experiences a drop in income
because of a work-induced disability. Persons who are in poor health less frequently move up
and more frequently move down the social ladder than healthy persons. This implies that the
health system itself can be viewed as a social determinant of health. This is in addition to the
health sector's key role in promoting and coordinating SDH policy. On this point the UK
Department of Health has argued that the health system should play a more active role in
reducing health inequalities, not only by providing equitable access to health care services
but also by putting in place public health programmes and by involving other policy bodies
to improve the health of disadvantaged communities37.
6. Proposed conceptual framework for the CSDH
The diagram below adds further elements to the schema just discussed. The expanded model
seeks to summarize visually the key lessons of the preceding analysis and to organize in a
single comprehensive framework the major categories of SDH; a specific set of
recommended thematic foci for the Commission; and a mapping of potential levels of policy
action. The graphic is necessarily somewhat complex, since it seeks to represent in schematic
form an intricate social and political reality. We will "walk through" the diagram, spelling
out the links among its components. This framework makes visible the concepts and
categories discussed in this paper. It also locates the specific social determinants on which
we propose that the Commission focus its work and provides a context for understanding
why these particular determinants might be given priority. Before taking up the question of
proposed thematic foci, it is helpful to become familiar with this expanded version of the
framework. Key issues are: (a) structural vs. intermediate determinants; (b) what is meant by
socio-political context; and (c) levels at which inequities in health can be tackled.
16
CSDH Conceptual Framework
DRAFT
WHO Equity Team social determinants framework38
DIFFERENTIALS CONSEQUENCES
§
E
Z E
H E
Program Social assistance :
return and/ or maintenance
Social status
2
O « «
o-g
•j
<
«
u O ~
s-H
ft. c u
J H ©
<0.0
K .«
5 «
SOCIAL
STRATIFICATION
Income
Education'
Sexuality
Gender
Ethnicity
(racism)
Cohesion social
( Social exclusion)
h
HEALTH
SYSTEM
Sickness
and
Disability
_ _____ I
DIFFERENTIAL EXPOSURE ■
DIFFERENTIAL VULNERABILITY
TJ
>
O
- Living conditions
- Working conditions
- Food availability
- Barriers to adopting
health-related
behaviour.
Type of
Intervention :
-Life course
eg Early child
Selective
o
I
|
'
m
>
rj
Zone e g
Human
Delivery
service
personal
and no
personal
e.g. Priorities
Diseases
5
Social position
SOCIAL DETERMINANTS
"STRUCTURE"
Globalization
1
Specific exposure
SOCIAL DETERMINANTS
"INTERMEDIARY "
. in
if
6.1 Structural and intermediate social determinants
Fleshing out the previous schema, this framework likewise identifies two major groups of
determinants, structural and intermediate, providing specific examples of each. Structural
determinants are those that generate social stratification. These include the traditional factors
of income and education. Today it is also vital to recognize gender, ethnicity and sexuality as
social stratifiers. A central point for us is the aspect of social cohesion related to social
capital. Intermediate determinants flow from the configuration of underlying social
stratification and, in turn, determine differences in exposure and vulnerability to health
compromising conditions. Here the literature reflects ongoing discussions regarding the
accumulation of exposures and about selection. We include in the category of intermediate
determinants: living conditions, working conditions, the availability of food, population
behaviours and barriers to adopting healthy lifestyles. Relevant population groupings for
analysis and action on intermediate determinants can be defined in various ways. We
introduce two examples of groups selected (1) by greater vulnerability (children) and (2) by
geography (slum dwellers).
The health system itself should also be understood as an intermediate determinant. The role
of the health system becomes particularly relevant through the issue of access, which
incorporates differences in exposure and vulnerability. This is closely related to models for
17
CSDH Conceptual Framework
DRAFT
the organization of personal and non-personal health service delivery. The health system can
directly address differences in exposure and vulnerability not only by improving equitable
access to care, but also in the promotion of intersectoral action to improve health status.
Examples would include food supplementation through the health system. A further aspect of
great importance is the role the health system plays in mediating the differential
consequences of illness in people's lives. The health system is capable of ensuring that health
problems do not lead to a further deterioration of people's social status and of facilitating sick
people's social reintegration. Examples include programmes for the chronically ill to support
their reinsertion in the workforce, as well as appropriate models of health financing that can
prevent people from being forced into (deeper) poverty by the costs of medical care.
6.2 Socio-political context
This framework differs from some others in the importance attributed to the socio-political
context. This is a deliberately broad term that refers to the spectrum of factors in society that
cannot be directly measured at the individual level. 'Context' therefore encompasses a broad
set of structural, cultural and functional aspects of a social system whose impact on
individuals tends to elude quantification but which exert a powerful formative influence on
patterns of social stratification and thus on people's health opportunities. Within the context
in this sense will be found those social and political mechanisms that generate, configure and
maintain social hierarchies, such as the labour market, the educational system and political
institutions.
The most relevant contextual factors, i.e., those that play the greatest role in generating social
inequalities, may differ considerably from one country to another.39 For example, in some
countries religion will be a decisive factor, in others less so. Contextual differences militate
against one-size-fits-all policy approaches to address SDH. Since the mechanisms
producing social stratification will be different in different settings, certain interventions or
policies are likely to be effective for a given socio-political context but not for others.
Meanwhile, the timing of interventions with respect to local processes must be considered, as
well as for example partnerships, availability of resources, and how the intervention and/or
policy under discussion is conceptualized and understood by the participants at national and
local levels.40
The specificities required for an appropriate understanding of context may vary with the
specific health determinants on which one wishes to act. For example, the most relevant
contextual elements for action on early child development will differ from those most
relevant to globalization or health systems. In general, the construction/mapping of context
should include at least four points: (1) political systems and processes, including definition of
needs, existing public policies on determinants, patterns of discrimination, civil society
participation, and accountability/transparence in public administration; (2) macroeconomic
policy, including fiscal, monetary, balance of payments and trade policies; (3) policies
affecting factors such as labor, land and housing distribution; (4) public policy in areas such
as education, social welfare, medical care, water and sanitation.41
18
CSDH Conceptual Framework
DRAFT
To set feasible policy goals, these general considerations should be supplemented with
another, more health-specific element of contextual analysis, namely an assessment of the
social value placed on health. The value placed on health and the degree to which health is
seen as a collective social concern differ greatly across regional and national contexts. We
have argued elsewhere, following Roemer and Kleczkowski, that the social value attributed
to health in a country constitutes an important and often neglected aspect of the context in
which health policies must be designed and implemented.
__ 4^In
In constructing
constructing a typology of
health systems, Roemer and Kleczkowski have proposed three domains of analysis to
indicate how health is valued in a given society:
• The extent to which health is a priority in the governmental /societal agenda, as reflected
in the level of national resources allocated to health.
• The extent to which the society assumes collective responsibility for financing and
organizing the provision of health services. In maximum collectivism (also referred to as
a state-based model), the system is almost entirely concerned with providing collective
benefits, leaving little or no choice to the individual. In maximum individualism, ill
health and its care are viewed as private concerns.
• The extent of societal distributional responsibility. This is a measure of the degree to
which society assumes responsibility for the distribution of its health resources.
Distributional responsibility is at its maximum when the society guarantees equal access
to services for all.43
These criteria are important for health systems policy and evaluating systems performance.
They are also relevant to assessing opportunities for action on SDH.
Increasingly, global institutions and processes influence the socio-political contexts of all
countries, in many cases constraining the autonomy of national actors, including states.
Global trade agreements, the deployment of new communications technologies, the activities
of transnational corporations and other phenomena associated with globalization also directly
impact health determinants at various levels. Hence the inclusion in the framework of
globalization as a crosscutting factor with implications for all components of the model.
6.3 Levels for policy action on SDH
It will be crucial for the CSDH to identify the level(s) at which it will seek to promote change
in tackling SDH through policy. The framework helps to situate these levels, clarify their
relationships and suggest the scope and limits of policy action in each area. The crucial basic
distinction is between policies that seek to address structural determinants, i.e., to alter the
configuration of underlying social stratification, and those policies and interventions that
target intermediate health determinants.
Drawing on Diderichsen et al., a typology or mapping of entry points for policy action on
SDH identifies the following major options, marked by darkly shaded boxes within the
framework: social stratification; differential exposure/differential vulnerability; and
differential consequences. First is the option of altering social stratification itself, by
reducing "inequalities in power, prestige, income and wealth linked to different
socioeconomic positions". For example, policies aimed at diminishing gender disparities
19
fl
CSDH Conceptual Framework
DRAFT
will influence the position of women relative to men. In this domain, one could envisage an
impact assessment of social and economic policies to mitigate their effects on social
stratification. Further to the right side of the framework, we see other levels where policies
could engage: by decreasing people's differential exposure to health-damaging factors; by
lessening the vulnerability of disadvantaged people to the health-damaging conditions they
face; and by intervening through health system to reduce the differential consequences of
ill-health. Policy options should marshal evidence for the range of interventions (both
disease-specific and related to the broader social environment) that will reduce the
likelihood of unequal consequences of ill health. For instance, additional resources for
rehabilitation might be allocated to reduce the social consequences of illness. Equitable
health care financing is a critical component at this level. It involves protection from the
impoverishment arising from catastrophic illness as well as an understanding of the
implications of various public and private financing mechanisms and their use by
disadvantaged populations.
These issues will be explored in greater depth in a later section of the paper, on
intervention and policy development models for action on SDH.
6.4. Selection of specific themes for the CSDH
Clearly, the CSDH cannot hope to address the full range of social determinants illustrated in
the above framework. Reasoned choices must be made regarding specific topics on which the
Commission will focus its knowledge-building activities, policy recommendations and
advocacy. While the selection of themes is by no means rigidly fixed at this date, a set of
proposals have been developed over the past months through research by the secretariat and
the Chair, consultations with experts inside and outside WHO, and the initial discussions
among Commissioners during their first meeting in Santiago. The following section outlines
the thinking that has led to a specific set of recommendations regarding priority themes for
the CSDH. Commissioners are invited to consider this rationale on their way to finalizing a
list of themes for the Commission's Knowledge Networks, commissioned papers and other
products/activities.
Some preliminary points merit attention. First, it is clear that for most if not all key SDH,
precise data on the burden of morbidity and mortality directly attributable to these factors are
not available. This means that a simple quantitative ranking of SDH by associated burden of
disease is not yet (and may never be) feasible. (Whether such a ranking, if feasible, would be
desirable is a separate question into which we will not enter here.) Inevitably, then,
assessments of the relative importance of particular SDH must be developed in the absence
of exhaustive quantitative data; all such assessments will involve a more or less openly
"political" aspect.
The selection of recommended areas of work for the Commission has been strongly shaped
by a concern with addressing "orphan" areas, i.e., important areas relatively neglected by
previous research and heretofore insufficiently addressed by interventions. The evidence base
concerning interventions on health determinants is not large.45 However, an important
finding from the available literature is that not all major determinants have been targeted for
20
CSDH Conceptual Framework
DRAFT
interventions. In particular, social factors rarely appear to have been the object of
interventions aimed at reducing inequity. In contrast, interventions are more frequently aimed
at the accessibility of health care and at behavioral risk factors. Regarding the accessibility of
health care, a majority of policies are concerned with financing. A notably high proportion of
interventions are aimed at those determinants that fall within the domain of regular
preventive care, including behavioral factors (individual health promotion and education).
Fewer interventions have been found targeted at determinants that do not come under the
direct responsibility of the health service or of public health organizations, e.g., factors in the
social environment. In general, the smaller the number of determinants addressed by a
particular type of intervention, the more frequently that sort of intervention is used.46 In other
words, people have an understandable appetite for simplicity. But simple models do not
always lead to satisfactory results.
Interventions and policies on structural determinants of health constitute key orphan areas in
the determinants field. More work has been done on intermediary determinants (decreasing
vulnerability and exposure), but interventions at this level frequently target only one
determinant, without relation to other intermediary factors or to the deeper structural factors.
Interventions from the health system have generally been limited to issues of access,
moreover focused largely on the financing component and on education activities to promote
healthy behavior change. Interventions have not often had the scope to grapple seriously with
the social barriers to healthy behavior. The CSDH can ensure that it brings genuine valueadded to the determinants field by targeting research and advocacy on such neglected areas.
The following aspects informed the development of a proposed list of foci for the
Commission:
J Themes that impact on the gradient of health inequity, that is, those areas that are closely
related to the construction and maintenance of social stratification.
S Themes that incorporate a life course perspective, given the powerful impact of such
factors on health inequities, linked to the possibility to address, through a life-course
approach, groups facing unusually high health vulnerability.
Themes particularly closely related to the health system and thus to the special
responsibilities and opportunities of the health sector in tackling inequities in health. All
themes selected should reflect policy areas in which the health sector can realistically
expect to exert influence, favoring the implementation of SDH interventions and scaling
up towards more comprehensive equity-oriented policies.
Themes reflecting fast-growing health problems predominant in developing countries.
Themes reflecting a strong concern in all countries, implying consequences both for
developing and developed countries.
Themes that would engage groups experiencing high exposure and vulnerability to the
social determinants of health inequities.
Themes that are already widely recognized as important SDH, such that from the start the
Commission s work could focus, not on trying to convince partners of the theme’s
relevance, but instead on seeking and promoting effective interventions and policies to
respond to the problem.
21
CSDH Conceptual Framework
DRAFT
In what follows, we explore in some detail the basis for selection of each of the
recommended themes, in keeping with the general criteria just outlined.
6.4.1 Focus on areas that directly impact the health gradient: gender and social exclusion.
Part of the CSDH value-added will be supporting countries not only in tackling intermediary
determinants, but in implementing more ambitious policy options that can get at the deeper
structural sources of health disparities. Gender and social exclusion have been identified as
key structural determinants. They point to social forces that directly shape health inequities.
As such, they are of central relevance for the Commission. At the same time, gender and
social exclusion constitute structural determinants upon which the health system can actually
intervene (directly or indirectly) and which can be incorporated into health sector
programming, including but not limited to the delivery of clinical health services.
From a gender perspective, two central social determinants of health are: (1) the multiple
impacts of the sexual division of labor; and (2) gender-based differential access to the
resources that enable direct payment for medical services or participation in public or private
insurance schemes. Both aspects are important for the analysis of gender and health equity.
Social exclusion is a major factor in shaping health inequities and is closely linked to a wide
range of other SDH, as well as to social capital. The concept of social capital has increasingly
been viewed as relevant to explaining patterns of health inequalities in communities. It is also
informing policy and intervention options aimed at reducing health inequalities, particularly
through effort and investment in building social capital in ways that can generate health
benefits in socially disadvantaged communities. More broadly, policymakers increasingly
view the potential of social capital for generating economic, social and health outcomes as a
reason why working with communities and building social cohesion is a prerequisite to
tackling deprivation and inequities.47 Social cohesion and community engagement therefore
become central for turning policy into practice. A growing body of empirical work tests the
relationship between health and measures of social capital. Meanwhile, although positive
effects of social capital on health have been identified, many questions remain to be
addressed. Specific intervention studies may provide a way forward that allows for more
precise testing of how health benefits might flow from specific elements of social capital.48
6.4.2 Including a life-course perspective: early child development. Some studies shows that
a principal explanation for the persistence and worsening of inequalities is the way in which
health (both good and bad) is transmitted from generation to generation through economic,
social and developmental processes, and that the advantages and disadvantages are reinforced
in adult life. A life-course approach focuses on the different elements of the experience of
health, from the moment of conception through childhood and adolescence to adulthood and
old age. The life-course model describes the causal pathways of health inequalities and links
these to broad social and economic factors as well as to studies of child development. It
reveals critical points in the transitions from infancy through childhood into adult life, where
an individual may move in the direction of advantages or disadvantages in health. This
approach shows that mainstream policies in health, education and social welfare do not
always provide enough protection for people at these crucial turning points. The patterns are
not uniform, varying by social class but also by ethnicity. Social circumstances influence
22
CSDH Conceptual Framework
DRAFT
health at all ages, but have particularly strong effects in utero, in infancy and in childhood.
For many people, physical, emotional and cognitive development patterns are effectively
fixed in childhood, with beneficial or harmful effects on subsequent health.
Such findings suggest that, to develop robust strategies for promoting health equity through
social determinants policy, the CSDH requires a specific focus on early child development.
Researchers have identified three main routes for the transmission of advantage and
disadvantage through early childhood conditions and experiences: (1) poor childhood social
circumstances predict poor adult circumstances; (2) poor childhood circumstances cause poor
childhood health; and (3) poor adult circumstances determine poor adult health. Focusing for
present purposes just on the first of these paths of transmission, we can observe that poor
childhood social circumstances relate to poor adult circumstances in several ways. For
example, education is still the major route out of disadvantage, but poorer children perform
educationally less well than better-off children. Children not staying on in education, or not
entering employment or training at 18, are a particularly high-risk group. Children from
poorer backgrounds are much more likely to get into trouble with the police, to be excluded
from school, or to become a teenage parent, all of which make moving up the social
hierarchy more difficult. Meanwhile, analysts question whether some current policies on
education, social welfare, employment, crime and health are helping solve these problems or
are themselves part of the causes.49 50 The Commission can make an important contribution
at this key intersection of health sciences, policymaking and social values.
6.4.3 Focus on areas closely connected with health systems. As previously discussed, the
various models that have tried to explain the functioning and impact of SDH have not made
sufficiently explicit the role of the health system as a social determinant. In some instances,
the relevance of the health system has been seen as limited to its role in giving (or denying)
access to preventive and curative services to vulnerable and exposed groups, particularly
with regard to financial barriers. On the other hand, intersectoral action for health has at
times been promoted as a major axis of health policy, with greater or less emphasis and
varying degrees of success.51
Overall, the orientation of health systems policy has rarely included intervention on SDH.
There is ample evidence that SDH dramatically impact health and substantially constrain the
health opportunities of vulnerable groups; yet the direct, independent actions that the health
system can undertake with respect to SDH are limited. What, then, should health systems do
- particularly with regard to SDH and health inequities? Little guidance is currently available
on these questions. This gap in knowledge and leadership represents a space in which the
Commission to make a significant contribution.
Even if the health system is not itself considered as a direct determinant of health inequities,
it influences how people move among the social strata. Benzeval, Judge and Whitehead
argue that the health system has three obligations in confronting inequity: (1) to ensure that
resources are distributed between areas in proportion to their relative needs; (2) to respond
appropriately to the health care needs of different social groups; and (3) to take the lead in
encouraging a wider and more strategic approach to developing healthy public policies at
both the national and local level, to promote equity in health and social justice.52 In opting to
23
CSDH Conceptual Framework
DRAFT
engage centrally with health systems, the CSDH will moreover underscore that health
systems play a fundamental role, together with other social sectors, in preventing negative
social consequences of ill health. It will highlight and reinforce the capacity of the health
sector to place health equity goals, implying SDH actions, on the agendas of other
governmental sectors.
From this perspective, two strategic themes are defined. The first, on priority public health
conditions, primarily concerns the integration of SDH policies and actions into traditionally
defined health programmes, such as those targeted at specific diseases. This will include
aspects such as equitable access to service delivery (promotional, preventive and curative)
for different health problems. In addition, a focus is recommended on health systems
properly speaking, whose work will embrace intersectoral action; promoting equitable access
at the systems level (including financing and the organization of services); and indirect health
actions that affect SDH.
6.4.4 Focus on vulnerability and high exposure: employment conditions. Human
production is the basis for both welfare and health. There is a clear correlation between gross
national product (GNP) , income level, living standards and average life expectancy when
nations are compared, but also notable differences in health and life expectancy between
socioeconomic strata and occupational groups within nations.
Differences in working conditions and work-related health status have been reported for
centuries. The spur for improvement has been the often appalling working conditions,
especially for manual workers, who are likely to be poorly educated and have low incomes.
Even when the health of manual workers improves, health inequalities do not necessarily
diminish, as occupational groups with a better education also benefit from welfare
improvements and increased economic resources. The main foci for improvements in workrelated health are awareness of the health aspect in the planning of work and production; the
eradication or control of known hazards; and improvements in the work environment. But
even when theses '’classic" occupational hazards have been corrected, inequalities in health
remain between higher and lower positions in the workforce, indicating the potential for
further improvement.
Occupation is the most important criterion of social stratification in advanced societies and is
the basis of the categorization of socioeconomic groups. Social approval depends largely on
ones type of job, professional training and level of occupational achievement. Furthermore ,
type and quality of occupation, and especially the degree of self-direction at work, strongly
influence personal attitudes and behavioral patterns in areas not directly related to work, such
a leisure, family life, lifestyle, education and political activity . Research from the past two
decades has demonstrated the importance of the place and content of work and their effects
on coronary heart disease, mental health and musculoskeletal disorders, but many
workplaces still have unacceptable safety risks and exposures.53 54 On the other hand ,
unemployment or changes in employment status have been shown to be linked to changes in
health.
24
CSDH Conceptual Framework
DRAFT
For the CSDH employment conditions should include both internal factors (workplace) and
external factors (social, economic, governance structure and legal context) related to
employment. Evidence will be provided on the health effects of internal factors including:
psychological stress; physical and ergonomic risks; toxic chemical exposure; and
employment conditions like income, job security, flexibility in working hours, job and task
control, and employment-related migration. Evidence from a variety of different country
contexts and vulnerable population subgroups such as migrants and child workers will be
examined. Low self-esteem due to job insecurity and lifestyle choices associated with type of
employment will also be considered. The effectiveness of engineering and administrative
control measures, employment and industrial relations policy and worker safety legal
frameworks—which are external factors that seek to mitigate the effects of the internal
factors—will be mapped and analyzed. A concerted effort will be made to examine
programmes that include workers' and labour associations in the development of
interventions and policy.
6.4.5 Focus on fast-growing problems: urban settlements. Part of the Commission's
opportunity to add value will involve engaging themes whose impact on global health is
destined to expand rapidly in the coming years, and which have not yet registered sufficiently
with the health community. The theme of urban settlements and in particular the health
challenges of slum dwellers constitute a vast and growing challenge for developing countries.
Interventions in this area imply the integration of actions simultaneously addressing a range
of health determinants.
Urban slums are characterized as unplanned informal settlements where access to services is
minimal-to-nonexistent and where overcrowding is the norm. The last ten years have seen a
dramatic increase in the number of slum dwellers worldwide. Urban development has
historically been seen as both a cause and solution for social inequalities in health. However,
environmental and individual gradients within urban areas occur everywhere and are resistant
change. Urban environments are influenced by the degree and type of industrialization,
quality of housing, accessibility of green spaces and by transport, an increasing concern.35
Slum upgrading includes: physical upgrading of housing, water and sanitation, infrastructure,
and the environment; social upgrading through improved education; violence reduction
programmes; better access to and improved health services; governance upgrading through
participatory processes; community leadership and empowering civil society through
knowledge and information.
6.4.6 Globalization. Globalization can be regarded as a social macro-determinant. As shown
in the framework, global processes exert a powerful impact at all levels of the social
production of health: on the evolution of sociopolitical contexts in countries; on social
stratification; and on the configuration of numerous specific determinants (e.g., working
conditions, food availability). Among the most relevant aspects of globalization for the work
of the CSDH are: market access, trade barriers and liberalization, integration of production of
goods, commercialization and privatization of public services, and consumption and lifestyle
patterns.
25
CSDH Conceptual Framework
DRAFT
While recent years have seen a rapid expansion of interest in globalization and health,
numerous important questions remain inadequately explored.56 By framing global processes
as macro-determinants of health and health equity and marshalling the appropriate evidence
to clarify these links, the CSDH can shed fresh light and open new perspectives. Above all,
there is a need to identify and evaluate policy options through which national policymakers
can respond to the challenges posed by globalization and capitalize on its opportunities. It is
necessary to identify and characterize the degree of negative or positive health impact of
globalization in specific cases: not only to clarify relevant causal processes, but as a
contribution to evaluating the impact of interventions and policies on other social
determinants of health. We are interested both in how global processes have shaped
countries' sociopolitical contexts and in how the various modalities and tendencies associated
with globalization have impacted countries' capacity to intervene successfully on other SDH.
Meanwhile, the need for a new moral framework for globalization has been underscored by
current actors and analysts, including the ILO-sponsored World Commission on the Social
Dimension of Globalization: "The governance of globalization must be based on universally
shared values and respect for human rights. Globalization has developed in an ethical
vacuum, where market success and failure have tended to become the ultimate standard of
behaviour, and where the attitude of'the winner takes all' weakens the fabric of communities
and societies". 7 Using its health equity framework, the CSDH will identify policies that can
foster a more equitable distribution of globalization's benefits and a fairer portioning-out of
opportunities for human flourishing.
7. Intervention and policy development models for action on SDH
The CSDH will consolidate evidence around its thematic foci not just to strengthen the
scientific knowledge base, but above all to catalyze action. Action in this context primarily
means public policies and interventions to tackle health inequities via SDH. To guide policy
development, the type of schema presented above - which shows the levels of SDH and their
pathways of causal influence — must be combined with a mapping of political structures,
opportunities and processes. In other words, a scientific "imaging" of the way social
determinants differentially impact health must be overlayed with a political grid. The result
would be a comprehensive framework that could both locate the real sources of health
problems at the social level (accurate diagnosis) and help identify politically workable
solutions (effective prescription).
Our review of the literature has identified three particularly suggestive models for
intervention and policy development on SDH. We will analyse these three proposals in turn.
Throughout, it will be useful to recall the distinction between specific interventions (e.g., an
innovative health education programme or a change in the organization of a screening
programme) and broader policies (e.g., changes in income distribution or in the government
mechanism for allocating health care resources).
7.1 K. Stronks framework
This model was proposed in the context of the Dutch national research programme on
inequalities in health.58 The programme report highlights three phases of analysis for the
implementation of interventions and policies on SDH:
26
CSDH Conceptual Framework
DRAFT
J Phase one involves filling in the social background on health inequalities in the specific
country or socioeconomic context. The impact of each social determinant on health varies
within a given country according to different socioeconomic contexts. Four intervention
areas are identified:
• The first and the most fundamental option is to reduce inequalities in the
distribution of socioeconomic factors or structural determinants, like income and
education. An example would be reducing the prevalence of poverty in the lowest
socioeconomic groups.
• The second option relates to the specific or intermediary determinants that
mediate the effect of socioeconomic position on health, such as smoking or
working conditions. Interventions at this level will aim to change the distribution
of such specific or intermediary determinants across socioeconomic groups, e.g.
by reducing the number of smokers in lower socioeconomic groups, or improving
the working conditions of people in lower status jobs.
• A third option addresses the reverse effect of health status on socioeconomic
position. If bad health status leads to a worsening of people's socioeconomic
position, inequalities in health might partly be diminished by preventing ill people
from experiencing a fall in income, e.g., as a consequence of job loss. An example
would be strategies to maintain people with chronic illness within the workforce.
• The fourth policy option concerns the delivery of curative healthcare. It becomes
relevant only after people have fallen ill. One might offer people from lower
socioeconomic positions extra healthcare or another type of healthcare, in other to
achieve the same effects as among people in higher socioeconomic positions.
S Phase two of the analysis concerns effectiveness. Having identified the possible
strategies to tackle health inequalities, one must form an idea of the effectiveness of those
strategies. There is clearly a lack of evidence on the effectiveness of interventions to
reduce inequities in health. Reviews have shown that many interventions have been
undertaken, including health promotion and measures within the healthcare sector.
However, only a few them have been evaluated with respect to their effect on the size of
socioeconomic inequities in health.59
Phase three looks at political feasibility. The question is: can one actually implement a
given intervention in daily practice? Could it be scaled up to constitute a realistic policy?
Enabling factors, opportunities and potential barriers to a specific policy or intervention
must be clearly identified: examples would include legal constraints, norms and values,
financial barriers, etc. A certain intervention judged successful in one country might not
fit with the cultural norms of other countries, such that its implementation there might not
yield the predicted positive effects.
7,2 M, Whitehead and G. Dahlgren framework
The framework proposed by Whitehead and Dahlgren indicates four interrelated levels to
which policies can be addressed: strengthening individuals; strengthening communities;
improving access to essential facilities and services; encouraging macroeconomic and culture
change.60
T1
CSDH Conceptual Framework
DRAFT
The first level is strengthening individuals. Here, policy responses are aimed at
supporting individuals in disadvantaged circumstances, using person-based strategies.
These policies adopt the premise that building up a person's knowledge, motivation,
competence or skills will enable them to alter their behavior in relation to personal risk
factor, or to cope better with the stresses and strains imposed by external health hazard
from other layers of influence. Examples would include stress management education for
people working in monotonous conditions; counseling service for people who become
unemployed to help prevent the associated decline in mental health; and supportive
smoking cessation clinics for women with low incomes. The potential effect of this
policies would be more indirect - counseling services for people who are unemployed are
not going to reduce the unemployment rate, but may ameliorate the worst health effects
of unemployment and prevent further damage.
J The second level is concerned with strengthening communities. This is focused on how
people in disadvantaged communities can join together for mutual support and in so
doing strengthen the whole community's defense against health hazards. The community
development strategies at this level recognize the intrinsic strength that families, friends,
voluntary organizations and communities can have , over and above the capabilities of
individuals working in isolation. These policies recognize the importance to society of
social cohesion, as well as the need to create conditions in deprived neighborhoods for
communities dynamics to work.
J The third policy level focuses on improving access to essential facilities and services.
These policies tackle the physical and psychosocial conditions in which people live and
work, ensuring better access clean water, sanitation, adequate housing, safe and fulfilling
employment, safe and nutritious , food supplies, essential health care, educational
services and welfare in times of need. Such policies are normally the responsibility of
separate sectors, often operating independently of each other but with the potential for co
operation. In this point is necessary program or action integrated.
J The fourth policy level is aimed at encouraging macroeconomic or cultural changes to
reduce poverty and the wider adverse effects of inequality on society. These include
macroeconomic and labors market policies, the encouragement of cultural values
promoting equal opportunities and environmental hazard control on a national and
international scale.
7.3 Diderichsen et al. framework
As mentioned above (section 5.2), the Diderichsen model identifies four entry points or
levels of action for interventions and policies: influencing social stratification; decreasing
differential exposure to health-damaging factors; decreasing vulnerability; and preventing
unequal consequences of ill health that can deepen social inequities.
Decreasing social stratification itself. While social stratification is often seen as the
responsibility of other policy sectors and not central to health policy per se, Diderichsen
and colleagues argue that addressing stratification is in fact "the most critical area in
terms of diminishing disparities in health". They propose two general types of policies in
this entry point: first the promotion of policies that diminish social inequalities, e.g., labor
28
CSDH Conceptual Framework
DRAFT
market, education, and family welfare policies; second a systematic impact assessment of
social and economic policies to mitigate their effects on social stratification. In the figure
below, this approach is represented by line A.
S Decreasing the specific exposure to health-damaging factors suffered by people in
disadvantaged positions. The authors indicate that, in general, most health policies do not
differentiate exposure or risk reduction strategies according to social position. Earlier
anti-tobacco efforts constitute one illustration. Today there is increasing experience,
however, with health policies aiming to combat inequities in health that target the specific
exposures of people in disadvantaged positions, including aspects such as unhealthy
housing, dangerous working conditions and nutritional deficiencies. In the figure, this
approach is represented by line B.
S Lessening the vulnerability of disadvantaged people to the health-damaging conditions
they face. An alternative way of thinking about modifying the effect of exposures is
through the concept of differential vulnerability. Intervention in a single exposure may
have no effect on the underlying vulnerability of the disadvantaged population. Reduced
vulnerability may only be achieved when interacting exposures are diminished or relative
social conditions improve significantly. An example would be the benefits of female
education as one of the most effective means of mediating women’s differential
vulnerability. This entry point is shown below by line C.
S Intervening through the health system to reduce the unequal consequences of ill-health
and prevent further socioeconomic degradation among disadvantaged people who
become ill. Examples would include additional care and support to disadvantaged
patients; additional resources for rehabilitation programmes to reduce the effects of
illness on people’s earning potential; and equitable health care financing. This entry point
appears in the figure as line D.
Social
Context
>
Social Position
1 A
B
Specific exposure
C
Policy
Context
......> I —
Disease / injury
D
<
<■
Social Consequences of ill
health
29
CSDH Conceptual Framework
DRAFT
7.4. Synthesis: key policy principles
The intervention frameworks just reviewed should be seen in the light of our earlier
discussion on health disadvantage, gaps and gradients (section 4). Following Graham, we
argued that improving the heath of poor groups and narrowing health gaps are necessary but
not sufficient objectives. A commitment to health equity ultimately requires a health
gradients approach. A gradients model locates the cause of health inequalities not only in the
disadvantaged circumstances and health-damaging behaviors of the poorest groups, but in the
systematic differences in life chances, living standards and lifestyles associated with people's
unequal positions in the socioeconomic hierarchy.61 While interventions targeted at the most
disadvantaged may appeal to policymakers on cost grounds or for other reasons, an
unintended effect of targeted interventions may be to legitimize poverty, making it both more
tolerable for individuals and less burdensome for society.62 ’63'64 Health programmes
(including SDH programmes) targeted at the poor have a constructive role in responding to
acute human suffering. Yet the appeal to such strategies must not obscure the need to address
the structured social inequalities that create health inequities in the first place.65
Health equity is not only about good or bad health outcomes. It fundamentally concerns
health opportunities. These opportunities must be considered in the elaboration of
interventions and policies addressing SDH. This means asking what interventions and
policies most effectively promote health opportunities. Are health opportunities best
enhanced by focusing action on the groups that are currently most severely affected in terms
of health outcomes? Where does such an approach leave those groups that, without being
among the most severely affected, experience vulnerability in terms of health opportunities?
In the medium term, such vulnerable groups will begin to reproduce the health results now
seen in the groups with the worst outcomes. Among groups suffering vulnerability in terms
of health opportunities, will we find only people with very low incomes, women or people
with certain ethnic or religious backgrounds? The social patterning of health opportunities is
highly complex. This is why inequity gradients in SDH cannot be excluded when
governments set objectives and build programmes. Including these gradients as an explicit
area of policy action can assure that interventions and policies have an impact on health
opportunities.
Specific interventions are selected and shaped according to more overarching policy
frameworks. Thus, in addition to identifying potential intervention levels on SDH, principally
following Diderichsen et al., we believe it is necessary to specify the policy principles within
which interventions are implemented. The principles or modalities highlighted involve:
intervening upon and shaping the socio-political context; developing policies from the
standpoint of the community, with community participation in decision-making; developing
intersectoral action, including the incorporation of SDH actions emanating from non-health
sectors; and the prioritization of actions proven genuinely effective in tackling health
inequities.
The figure below summarizes these ideas. The horizontal arrows mark the levels of
intervention on SDH. Here, these levels are placed in relation to the policy modalities that
can or should be implemented. The vertical arrows identify four policy principles we believe
30
CSDH Conceptual Framework
DRAFT
are essential from the perspective of the CSDH. The first underscores the need for
responsiveness to the socio-political context of each country and region. This is a central
element for the development of policies adapted to the real capabilities of developing
countries and not shaped according to pre-determined recipes. The second vertical arrow
represents the principle of community participation in decision-making, underscoring as a
central aspect of the CSDH the inclusion and participation of civil society. The third arrow
represents intersectoral action, implying not only policies and actions managed from within
the health sector, but also the integration of interventions and actions by other sectors that
have included contributing to health within their goals. Partner sectors will likely include
education, transport and housing, among others. The fourth vertical arrow recalls the need to
focus on effective interventions: action based on evidence, evidence for action.
Diagram: new action on pathways and policies 66
Principles for policies on SDH
Socio-political
Context
0
>
a>
Community
participation in
decisions
Intersectoral
action
Targeted
effective
intervention
Decrease differential exposure
Decrease differential vulnerability
c
Improving access include differential exposure and vulnerability
£
Decrease differential consequences
I
■S
Decrease stratification social
8. Conclusion
This draft paper has sketched a framework on social determinants of health intended to
catalyze discussion within the CSDH. The paper in its present form is of course not a
finished product, but a tool to stimulate shared thinking and advance debate. It is a step in a
process whereby Commissioners, supported by the CSDH secretariat, will reach shared
understandings on a set of fundamental conceptual issues important for the coherence and
efficacy of the Commission's work. The paper has sought to clarify the concept of social
determinants; to suggest a coherent values basis for action on SDH rooted in health equity;
and to sketch a model locating intervention levels and entry points for policy action on SDH.
31
CSDH Conceptual Framework
DRAFT
The key element of the framework presented here is the distinction drawn between structural
and intermediate social determinants of health, also thought of as social determinants of
health equity and more specific determinants of health. As we have noted, the feasibility of
directly impacting health inequities requires intervention on structural determinants.
However, such action will demand profound and possibly quite slow processes of social
change and will only yield results in the long term. When will these processes begin? Are
they even possible? Skepticism regarding the current feasibility of fundamental change is
understandable. This being the case, if it is not possible to act directly upon the structural
determinants, might one be able to identify pathways to influence them indirectly? The
actions that can be undertaken by the health system have major relevance in this regard. It
may be possible to influence and model the system in such a way as to bring us closer to the
capacity to directly address the social determinants of health inequities.
The sustainability of health sector-led interventions on SDH and the underlying policy
structure are inseparably related. It is not possible to maintain continuity in SDH
interventions (e.g., incorporation of SDH into health programmes, intersectoral actions and
programmes) if such interventions are not supported by broader, enabling government
policies in the health sector and the whole range of other sectors. At the same time, a broad
policy approach incorporating social determinants will not have any real impact if is not
translated into specific, concrete interventions that apply these ideas at national and local
levels. For the health sector, this final point implies a new perspective on the elaboration of
goals and plans and on the deployment of health actions.
32
CSDH Conceptual Framework
DRAFT
References
1 Tarlov A. 1996. Social determinants of health: the sociobiological translation. In Blane D, Brunner E,
Wilkinson R (eds). Health and social organization. London: Routledge. 71-93.
2 Krieger N. A glossary for social epidemiology J. Epidemiology Community Health 2001; 55;693-700
3 Graham H. [complete]
4 London Health Observatory 2002 review of the London Helath Strategy High- level Indicators.
5 Evans T, Whitehead M, Diderischsen F., Bhuiya A., Wirth M. Challenging inequities in health from ethics to
action Oxford University Press 2001.
6 Marmot M. Economic and social determinants of disease Bulletin of the World Health Organization, 2001,79
(10) pag 988 -989.
7 Rose G. Sick Individuals and Sick Populations International Journal of Epidemiology Vol 14 n° 1 1985.
8 Performance measurement and performance management in OECD health systems J. Hurts , M Jee-Hughes
2001 .
9 WHO Equity Team working definition.
l0Socioeconomic position includes both material and social resources as well as rank or status in a social
hierarchy or hierarchies. Social positions derive from, and are generated by, a particular social context, meaning
that classifications of social position will vary across societies and historically. In some countries gender, race
or religion plays a major part in what position a person occupies. Because there is a range of structures of
inequality everyone occupies multiple social positions: for example a white, gay man in a manual occupation or
a heterosexual, Indian woman in a managerial occupation. Graham H, Kelly MP. Health inequalities: concepts,
frameworks and policy. 2004. NHS Briefing Paper.
11 Hilary Graham Social determinants and their unequal distribution : Clarifying policy understandings The
Milbank Quarterly, Vol 82, n° 1,2004 ( pp.101-124)
12 Stronks K, Gunning-Schepers L. 1993. Should equity in health be target number 1? European Journal of
Public Health 1993;3: 104-111.
13 Sen, "Why health equity?"
14 Stronks K, Gunning-Schepers L. 1993. Should equity in health be target number 1? European Journal of
Public Health 1993;3: 104-111
15 Anand S. 2004. The concern for equity in health. In Ananad S, Peter F, Sen A (eds). Public health, ethics and
equity. Oxford: Oxford UP.
16 Ruger 2005
17 Sen, "Why health equity?"
18 Ruger 2004.
19 General Comment and Questions and Answers p 10.
20 Alkire S, Chen L. Global health and moral values. Lancet 2004; 364:1069-74.
21 London L. 2003. Can human rights serve as a tool for equity? EQUINET policy series 14.
22 Numerous refs
23 Farmer P. 2003. Pathologies of Power.
24 Farmer P. Infections and inequalities.
25 Bourgois P. 2003. In search of respect: selling crack in el barrio. New York: Cambridge UP.
26 Diderichsen, Evans and Whitehead. 2001. The social basis of disparities in health. In Evans et al. (eds). 2001.
Challenging inequities in health: from ethics to action. New York: Oxford UP.
27 Sen, Rationality and Freedom.
28 Gillon R. Value judgements about health equity.
29 Graham H. Tackling inequalities in health in England.
30 LJ Gunning-Schepers Models: instruments for evidence based policy . J Epidemiology Community Health
1999;53:263.
31 Tackling Inequalities in health : an agenda for action : a review of policy initiatives M. Benzeval, K.Judge.
M.Whitehead.
32 Mackenbach , Van de Mheen, Stronks A Prospective cohort study investigating the explanation of
socioeconomic inequalities in health in the Netherlands Social Science Medicine 1994: 38:299-308.
33 Acheson Report
34 Hilary Graham
33
CSDH Conceptual Framework
DRAFT
35 Bartley blane british journal
36 Hilary Graham
37 J, Mackenbach, L.J. Gunning-Schepers How should interventions to reduce inequalities in helath be
evaluated ? Journal of Epidemiology and communities Health 1997;51:359-364
38 Based in : Reducing inequalities in health a European Perspective J. Mackenbach, M Bakker 2002;
Generating evidence on interventions to reduce inequalities in Health : the Duch case K. Stronks Scand J
Public Helath 30 Suppl 59 ; Evans T, Whitehead M, Diderischsen F., Bhuiya A., Wirth M. Challenging
inequities in health from ethics to action Oxford University express 2001.
39 Socieconomic inequalities in health , Part 1 , Mackenbach , Bakker, Kunst and Diderichsen . reducing
Inequalities in health : European Perspective. 2002.
40 National evaluation of Health Action Zone ,The final report of the tackling inequalities in health module
Michaela Benzeval Queen Mary 2003.
41 Rockefeller Health Equity programme , from Concept and trends in research on Social determinants of Health
in Latin America and the Caribbean J.A. Casas WHO.
42 Orielle HSR and repro health paper.
43 Solar O, Irwin A, Vega J. 2004. Equity in Health Sector Reform and Reproductive Health: Measurement
Issues and the Health Systems Context. WHO Health Equity Team working paper, [i] Kleczkowki BM, Roemer
M, Van Der Werff A. 1984. National health systems and their reorientation toward health for all: guidance for
policymaking. Geneva: WHO.
44 Diderichsen et al
45 Mark Petticrew , Sally Macintyre. What do we Know about effectiveness and cost - effectiveness of
measure to reduce inequalities in Health ? University of Glasgow 2001.
46 Gepkens A, Gunning - Schepers LJ Interventions to reduce socio-economic health differences: a review of the
international literature European Journal public Health 1996; 6:218-226.
47 Cabinet office 2002 Social capital: a discussion paper Performance and innovation Unit. London
48 Tackling Health inequalities: turning policies into practice? Hunter D. Killoran A. NHS Health
Development Agency.
Childhood disadvantage and adult health: a lifecourse framework . Hilary Graham,Institute for Health
Research, Lancaster University; Chris Power, Centre for Paediatric Epidemiology & Biostatistics, Institute of
Child Health, London Health Development Agency. NHS.
50 Clyde Hertzman , Making Early Childhood development a priority : Lesson from Vancouver May 2004
Canadian Centre for Policy Alternative .
51 Background paper and sources cited.
52 Ref
53 Work related policies and interventions, Chapter 6: Hogstedt C., Lundberg I. Edited Mackenbach , Bakker,
Reducing Inequalities in Health : European Perspective. 2002.
54 Regeneration &neighbourhood change Curtis S.,Cave B, Courts A. Quenn Mary University of London Paper
prepared for HAD seminar . Appendix Employment. 2002
55 Mark McCarthy Urban Development and health inequalities . Scand J Public Health 2002: 30 :Suppl 59 :
59-62.
56 Kawachi and Wamala; numerous other refs
57 Ref
58 K. Stronks Generating evidence on interventions to reduce inequalities in health : The Dutch case.
Scandinavia Journal public Health 30 ( suppl 59) pp 21-25.
59 Gepkens A, Gunning - Schepers LJ Interventions to reduce socio-economic health differences: a review of the
international literature European Journal public Health 1996; 6:218-226.
60 M Whitehead ,Tacling inequalities in helath : a review of policy iniciatives
61 H. Graham , M P. Kelly Health inequalities : concepts, frameworks and policy. Briefing paper NHS Health
development Agency 2004
Petticrew M, Macintyre S. 2001. What do we know about effectiveness and cost - effectiveness of measures
to reduce inequalities in health ?
63 Macintyre S, Petticrew M. 2000. Good intentions and received wisdom are not enough. Journal of
epidemiology and Community Health 54 :802-803.
34
CSDH Conceptual Framework
DRAFT
64 H. Graham , M P. Kelly Health inequalities : concepts, frameworks and policy. Briefing paper NHS Health
development Agency 2004.
M . Petticrew , S. Macintyre. What do we Know about effectiveness and cost - effectiveness of measure to
reduce inequalities in Health ? 2001 Oliver A. Cookson R. McDaid D Issues Panel for Equity in Health Niffield
Foundation , London .
66 Elaborated equity team Adapted model Diderichsen and Mackenbach
35
Commission on Social Determinants of Health (CSDH)
Report of Expert Consultation for Measurement Knowledge Network
Santiago, Chile
March 21 -24, 2005
REPORT OF PROCEEDINGS
and RECOMMENDATIONS
July 2005
1
EXECUTIVE SUMMARY
Preliminary Guidelines for CSDH Knowledge Networks Review and Analysis Activities
Introduction
The following is an executive summary and notes from a WHO-sponsored consultation on the
measurement of social programs that was held in March 2005. The purpose of the document is
to provide broad terms of guidance to the Knowledge Network review and analysis work and to
provide suggestions to the Commission on how to document change processes.
This document should be read in conjunction with other CSDH background documents
such as the overall Commission strategy outlined in ‘Imperatives and Opportunities for Change’
and the conceptual framework titled ‘Towards a Conceptual Framework for Analysis and Action
on the Social Determinants of Health.’
A three step process
In order to meet the goal of the Knowledge Networks (KN) to synthesize knowledge to inform
the Commission of opportunities for improved action on SDH by fostering the leadership, policy,
action and advocacy needed to create change, each KN is recommended to consider the
following steps:
Step 1 - Rapid mapping of evidence and policy.
•
Canvass a broad and inclusive spectrum of evidence on social determinants of health and
health inequalities, including:
-
knowledge from formal research (both qualitative and quantitative)
-
knowledge from practice (including case studies), and
-
experiential knowledge (from policy makers, program managers, international
donors and program beneficiaries).
•
Identify priority areas and gaps in knowledge, taking into account variations in contexts
across regions of the world, interactions between social determinants, and relevant
stakeholders.
Ensure a balance in the type of evidence drawn upon: consult systematic reviews (such
as the Cochrane and Campbell databases of relevant interventions), but also aim to
develop an “evidence jigsaw”, including for example, descriptions of policy-making
2
processes (e.g. detailed case studies of successful as well as failed policy initiatives in the
area of social determinants).
•
The composition of expertise within each KN should include, at a minimum,
representation of qualitative research and policy expertise, as well as ideally, historical
expertise.
Step 2 - Reviewing the prioritized policy options
•
In the second step, evidence gathered during the mapping stage should be systematically
appraised, using explicit criteria appropriate for each study design (e.g. quantitative and
qualitative evidence). Criteria for appraising different study designs are available in the
literature and should be consulted (for example: Jackson N & Waters E. Systematic
reviews of health promotion and public health interventions.
The Cochrane
Collaboration 2005; and Spencer L, Ritchie J, Lewis J, Dillon L, Quality in qualitative
evaluation: A framework for assessing research evidence. London; Government Chief
Social Researcher’s Office, 2003, etc).
•
How strong and consistent (geographically, across different contexts, across time) are the
measured relationships between interventions on specific SDH and improvements in
health and health equity? Are the interventions focused on changing gradients of overall
inequalities in health or on reaching the groups with lowest health indicators (eg targeting
lowest quintile, closing gaps or reducing overall gradients of inequalities)?
•
An explicit attempt should be made during this stage to assess the transferability of
interventions from one setting to another. For example, are the interventions feasible,
culturally acceptable and appropriate, and possible to scale-up in developing countries?
•
What are the financing, budgetary and institutional implications of national interventions
and of scaling up local interventions?
•
Change processes: what factors or processes affect change in countries and systems?
Under what conditions are policy/program changes associated with improvements in
population-level health and greater equity in health? Such factors and their relative
contribution to change should be analyzed.
3
Step 3 - Formulation of recommendations
•
Steps 2 and 3 should be independently conducted. Sometimes strong recommendations
are justified even on weak evidence, and vice versa. The criteria or basis for specific
recommendations can for example be drawn on the basis of social justice; economics;
public health burden; etc.
•
Each KN should as a minimum run a screening checklist (through the application of
Health Impact Assessment) to each of their recommendations, in order to give some
indication of the nature, scale, severity, probability, and distribution of potential health
impacts.
4
A.
OVERVIEW OF EXPERT CONSULTATION
1.
Purpose of the meeting:
The purpose of the meeting was to develop guidance on assessing and evaluating interventions,
programs, and policies that are aimed at affecting the social determinants (SD) of population
health and health inequalities.
2.
Goals:
The three overarching goals of the expert consultation were to:
1. Begin discussions towards developing expert consensus on the sources of evidence for
social determinants of health and health inequalities.
2. Provide guidance to the CSDH’s Knowledge Networks in assessing evidence on social
determinants of health, including identification of appropriate methods, tools, and best
practices.
3. Develop a programme of work for the CSDH’s Measurement Knowledge Network.
3.
Meeting participants
Participants at the meeting represented a broad range of constituencies involved in the evaluation
of knowledge and the application of diverse sources and types of evidence to policies. They
included representatives of the Cochrane and Campbell collaborations with experience in
systematic reviews of public health, social, educational and health service interventions,
qualitative researchers, practitioners from the Health Impact Assessment community, and
program evaluation/planning experts (see Annex I for list of participants).
B.
TOWARDS DEVELOPING ASSESSMENT AND EVALUATION GUIDELINES
FOR SOCIAL DETERMINANTS
1.
The Nature of Evidence
1.1
“Evidence” refers to any type of observation, whether gathered through qualitative or
quantitative methods, or whether arising from randomized controlled experiments or
uncontrolled case studies. Although the term “evidence-based” (as in “Evidence-Based
5
Medicine”) has become associated, at least in some quarters, with findings generated by
randomized controlled trials (RCTs), there is increasing acknowledgment of alternative
ways of “learning” and gaining valuable knowledge about the determinants of health,
such as through qualitative research.
For example, the Cochrane Collaboration has
moved away from its earlier focus on ranking the quality of evidence based exclusively
on study design; instead turning to address issues such as “What is the appropriate
evidence given the question being asked?’
Qualitative ways of knowing are being
increasing incorporated into systematic reviews of policy evidence (Jackson & Waters
2005).
1.2
Evidence is an essential but not sufficient basis for policy action.
Several other
ingredients besides evidence are involved in the policy-making process, including
political will, transferability of evidence into appropriate social strategies, and scalability
into different contexts and settings.
The policy-making process is often poorly
understood by researchers (Petticrew et al. 2004; Whitehead et al. 2004). For instance,
the strength of the evidence on any particular topic is not necessarily proportional to the
strength of recommendations that should follow.
The latter depends upon values,
contexts, and judgments about net benefits and harms.
Sometimes, strong
recommendations for policy are justified on weak evidence, and vice versa. Overall,
there is a need to devote further resources to understand: what are the determinants of
global public health policymaking.
1.3
Different kinds of evidence are useful for policymaking.
Policymakers have
recommended that researchers should help them with the task of piecing together an
“evidence jigsaw” (Whitehead et al. 2004). Such a “jigsaw” would encompass different
types of evidence - for example, evidence about the potential effectiveness of policies
(from experimental, quasi-experimental, and observational studies); evidence on the
diagnosis and/or causes of problems that could contribute to the development of
appropriate interventions/programmes; evidence on costs and cost-effectiveness.
In
addition to considering a diverse “jigsaw” of study designs addressing different kinds of
questions, it is also important to recognize that evidence is produced for different kinds of
6
purposes, including: mobilizing political will, purchasing “buy-in” from the public,
demonstrating success, predicting outcomes, and monitoring progress.
1.4
Expanding the scope of “admissible” evidence in the field of social determinants does not
mean sacrificing rigor or doing away with the need for systematic reviews. Qualitative
and quantitative researchers alike agree that their respective approaches are amenable to
systematic review. Systematic reviews -- regardless of whether they are conducted in the
quantitative (GRADE Working Group 2004; Jackson & Waters 2005) or qualitative
fields (Popay et al 1998; Spencer et al. 2003), or involving both qualitative and
quantitative evidence as in the EPPI reviews (at the Institute of Education in London) involve established conventions forjudging the “trustworthiness” or robustness of the
research, for assuring the transparency of methods employed, for the assessment of the
technical quality of the research in the context of qualitative research, and the
transferability of findings to other settings. The strength of systematic reviews is that
they provide a rigorous process to evaluate what has been conducted before; a focus on
what works; and perhaps more importantly, what doesn’t work.
2.
The Role of Randomized Controlled Trials
2.1
Randomized trials have been viewed as the “gold standard” in medical interventions
(such as the effect of taking a pill X to prevent disease Y).
By experimentally
manipulating the treatment, randomized trials have the ability to weed out problems such
as selection and endogeneity that often plague observational studies, as well as to uncover
any unintended consequences of treatment.
2.2
Although RCTs have been carried out in many clinical settings (e.g. hormone
replacement therapy, drugs to treat high cholesterol), as well as in a number of social
policy issues (e.g. the negative income tax, early childhood education, welfare-to-work
programmes), they have not been attempted as often in the field of the social
7
determinants of health.1 In some instances where RCTs have been done, the findings
have been at odds with the observational findings (although this phenomenon is by no
means confined to the field of social determinants). For example, two recent randomized
trials of social support provision following major illness -- the ENRICHD Trial (2003)
and FIRST Trial (Glass et al. 2004) -- failed to confirm findings from earlier
observational studies of a health-protective effect of social support. Experts have argued
I
that these RCT findings do not necessarily disprove the observational evidence. Thus,
according to Cohen et al. (2000): “social support is not a variable; it is a process that
arises through interaction between people. Nor is social support a commodity that can be
“delivered” or abstracted from its relational context” (Cohen et al. 2000, p. 17). In other
words, translating observational evidence into testable interventions continues to pose
challenges in the field of social determinants.
3.
The Role of Qualitative Evidence
3.1
Two different models have been described for the ways in which qualitative evidence
contributes to the evidence base for policymaking (Popay unpublished).
The
enhancement model assumes that qualitative research adds something “extra” to the
findings of quantitative research - by generating hypotheses to be tested, by helping to
construct more sophisticated measures of social phenomena, and by explaining
unexpected findings generated by quantitative research. By contrast, the epistemological
model views qualitative evidence as making an equal and parallel contribution to the
evidence base through: (a) focusing on questions that other approaches cannot reach; (b)
increasing understanding by adding conceptual and theoretical depth to knowledge; and
(c) shifting the balance of power between researchers and the researched (Popay
unpublished). Importantly, the epistemological model views qualitative evidence as not
necessarily complementing quantitative evidence, but sometimes conflicting with it.
3.2
Qualitative research can play two key roles as part of the evidence base for the social
determinants of health: (a) providing insights into the subjectively perceived needs of the
1 For recent examples in the area of housing, see , the Moving to Opportunity housing voucher experiment
conducted by the US Department of Housing and Urban Development (Kling et al. unpublished), or the He Kainga
Orazigfl/Housing and Health Research Programmeme conducted in New Zealand (Howden Chapman in press).
8
people who are to be the targets of the interventions and programmes aimed at addressing
the social determinants of health and health inequalities (giving people a “voice”); and (b)
helping to unpick the “black box” of interventions and programmes to deepen
understanding about factors shaping implementation, and hence, impact (Roen et al. in
press; Arai et al. in press).
3.3
One major difference between the qualitative and quantitative traditions concerns the
notion of replicability and generalizability.
Obviously generalizability within the
qualitative tradition is of a different kind to that which is possible in an experiment or a
survey (Popay unpublished). With regard to judging the external validity of qualitative
evidence, Popay notes: “The aim [in the qualitative tradition] is to identify findings which
are logically generalizable rather than probabilistically so” (Popay et al. 1998). It should
also be noted that there is a rapidly growing literature on methods for the synthesis of
qualitative research and of mixed methods research (see for example, Popay & Roen,
2003)..
4.
The Role of Health Impact Assessment
4.1
Health Impact Assessment (HIA) is a tool for prospectively forecasting the impacts of
interventions on health and the distribution of health.
HIA differs from systematic
reviews in that its primary purpose is to predict the outcomes of a proposed policy (as
compared to retrospectively rating the quality of existing evidence). It is important to
emphasize that HIA is not a planning tool. Rather, its utility is as a prospective tool for
forecasting the positive and negative impacts of policies that have already been proposed.
4.2
Although the application and diffusion of HIA to public health decision making is still in
its early stages, the methodology is already sufficiently robust so that structured
guidelines exist for their implementation (see for example, the 1999 Gothenburg
Consensus Statement, as well as the European Policy Health Impact Assessment Guide
2004). No policy is immune from HIA scrutiny. There was consensus among meeting
participants that HIA need not be prescribed for the individual CSDH Knowledge
Networks; however, they ought to be mainstreamed within health systems and
9
government decision making processes, even in developing countries.
Much work
remains to be done to make this a reality, including the need for local training and
capacity building to undertake HIA, possibly with financing from WHO. To date, there
has been only limited application of HIA to macro-economic policy decisions.
In
addition, the use of HIA itself needs further systematic study, i.e. what is the evidence of
their impact on policy decisions?
4.3
Among practitioners of HI A, tension exists between its different uses. Some view it as a
technical decision support tool, while others view it as a mechanism for engaging the
community affected by the proposed policy (i.e. it is a part of the democratic decision
making process). This tension is reflected in who actually ends up conducting the HI A professional experts or members of civil society representing the affected communities?
HIAs vary with respect to the extent of community consultation and participation versus
capture’ by professionals. In addition, HIAs are often unclear about the degree of
uncertainty surrounding forecast impacts. HIAs are frequently conducted under severe
time and resource constraints. There is a role for WHO to create a library of HIAs in
developing countries (for example, Thailand has conducted about fifty HIAs so far), and
to make these accessible to other settings.
4.4
Equity-focused HI A (EFHIA) is a special subset of HIAs intended to forecast the impacts
of policies on health equity outcomes (Mahoney et al. 2004). Here, clarity is required in
specifying the exact equity outcomes that are being considered -
for example, (a)
improving the health of the worst off; (b) reducing the gaps between the best and worst
off; or (c) reducing the overall gradient across the socioeconomic hierarchy.
These
outcomes - referred to respectively as minimizing health disadvantage, narrowing the
health gaps, and reducing health gradients (Graham & Kelly 2004) - may not be
simultaneously achievable within the context of a given policy intervention, and EFHIA
needs to specify which target is being evaluated.
10
5.
The Role of Programme Evaluation
5.1
Programme evaluation (PE) is a systematic set of practices to improve and account for
public health actions, and to forecast a range of “plausible futures” stemming from
policies. Evaluation is a driving force for planning effective public health strategies,
improving existing programmes and demonstrating the results of resource investments
(Milstein & Wetterhall 1999).
The foundation of PE consists of a well-described
sequences of steps (engaging stakeholders, describing the programme - including the use
of logic models, focusing the evaluation design, gathering credible evidence, justifying
the conclusions, and ensuring the use and sharing of lessons learned) that has been set
forth by the CDC’s Programme Evaluation Framework (Milstein & Wetterhall 1999), the
Community Toolbox (http://ctb.lsi.ukans.edu/ctb/c30/ProgEvaI.html ) and elsewhere.
Beyond formal evaluation systems, PE also encompasses a wider spectrum of methods
and approaches (such as system dynamics simulation models) to observe and interpret
programmes, and to stimulate further observations.
5.2
Within its sequences of steps, PE subsumes virtually all of the methods and tools
considered during the meeting and described above. Thus, planning for action within a
PE framework incorporates systematic reviews of previous research, Health Impact
Assessment, as well as additional steps such as power mapping and eliciting public
opinion. There was no firm consensus at the meeting, however, about where the PE
approach should be positioned within the scope of work to be undertaken by the CSDH.
For example, should PE be embedded within individual Knowledge Networks, or should
it be adopted as an integrative function of the Measurement Knowledge Network? The
real utility of PE may lie at the country engine level. In order for PE to be valued by
stakeholders, it is recommended that a specific portion of the budget be set aside for this
activity (e.g. 10% as recommended by the 6th Global Health Promotion Conference and
the 2000 Mexico Declaration) during the 3rd phase of the CSDH.
6.
Remaining Gaps
6.1
There is currently lack of information about how much evidence on social determinants
exists for developing countries. Nor do we know the extent to which evidence on SD
11
from developed countries is transferable or scalable to developing country contexts.
Robust criteria exist for assessing the quality of evidence (both qualitative and
quantitative), as well as for applying the existing evidence to plan, forecast and monitor
the impacts of policies in the SD field. However, the infrastructural capacity has been
hitherto lacking to apply these approaches in the developing world. Each Knowledge
Network should include strong representation from a diversity of regions to ensure
capacity building as well as knowledge transfer (including lessons that could be applied
from developing regions to the rest of the world).
62
In addition to the methods and tools considered at the meeting, there is a need to expand
coverage to alternative systematized approaches to evaluating evidence - for example,
participatory approaches to research and evaluation, exemplified by community-based
participatory research (CBPR) and community asset-mapping.
C.
TOWARDS
A
STANDARD
REVIEW
PROCESS
FOR
KNOWLEDGE
NETWORKS - PRELIMINARY RECOMMENDATIONS
Background
The KN work is essential to the success of the entire CSDH. The focus of the KN work over the
next 18 months is to:
1. Analyse evidence on the robustness of the associations between SDH and health/
health equity across different country contexts.
2. Evaluate evidence and suggest national and global policies, programmes and
institutional arrangements that modify the association between SDH and health equity
and enhance opportunities for greater health equity.
3. Document and assess the processes and mechanisms to mainstream and scale-up
successful examples of incorporating SD into health programmes and policies.
4. Propose approaches for using the evidence on integrating the SDH and health equity
goals into national and global policy and planning.
12
5. Identify and engage institutions and actors to contribute to the production,
dissemination and use of knowledge for the proposed policies and programmes across
different regions.
6. Engage and dialogue with wider country, regional and global processes of the
Commission to exchange knowledge and learning.
1.1
Each Knowledge Network should establish a three step process in conducting
standardized reviews of evidence on SD: (i) an analytic and strategic review paper; (ii)
systematic reviews of selected policies and interventions; and (iii) formulation of
recommendations.
1.2
The first step for each Knowledge Network should be a rapid mapping exercise to
identify potential policies for review and to prioritize them.
This should not be a
comprehensive review, but should be transparent and reasonably broad. Knowledge
Networks should not - indeed they cannot afford to -- confine themselves to considering
only randomized trial evidence on social determinants. Each KN should adopt a broad
and inclusive spectrum of approaches to gathering and synthesizing evidence, including:
•
Knowledge from formal research (both qualitative and quantitative)
•
Knowledge from practice (including case studies)
•
Experiential knowledge of professionals, policy makers, and people who are to be the
targets of interventions.
1.3
During the mapping stage, each KN should identify priority areas as well as gaps in
knowledge, and should take into account:
•
Variations in context across regions of the world
•
Variations by socially stratifying factors
•
Interactions between social determinants
•
Relevant stakeholders for the social determinant, including the public sector,
private sector, and civil society.
13
1.4
During the mapping stage, case studies might be considered for identifying best practices,
hypotheses, useful frameworks, and issues that should be considered in systematic
reviews (the 2nd step) of selected policy options.
The review step should be also
informed by overviews of available systematic reviews (such as the Cochrane and
Campbell databases of relevant interventions, or the York University database of public
health interventions), theoretical frameworks, and consultation.
The process should
largely rely on structured reflection informed by the foregoing sources (as well as
additional sources), but it should not be a systematic review and caution should be taken
to not just focus on policies where there is the best evidence.
1.5
Each Knowledge Network should pay careful attention to the use of language:
•
Take care that the use of the term “systematic review: does not become equated
with only (randomized) controlled studies
•
Take care that the language used is inclusive and engages sectors outside of health,
i.e. avoid being “healthiest”.
1.6
1.7
The composition of each Knowledge Network should:
•
Include representation of qualitative research expertise
•
Ideally include policy expertise (policy analysis as well as policy practitioners)
•
Ideally include historical expertise.
The second step should consist of reviewing the prioritized policy options, and should be
systematic in nature.
The evidence considered during this step should include
unpublished studies in the grey literature, and canvas a wide range of study designs
including case studies where appropriate. Explicit criteria applicable for all KNs should
be used for selecting studies that are included (although this has yet to be developed), and
the selected studies should be critically appraised using criteria that are appropriate for
each study design (e.g. qualitative and quantitative).
Steps should be undertaken to
evaluate the transferability of interventions from one setting to another.
A broad
spectrum of approaches should be considered for synthesizing knowledge, e.g. systematic
reviews, meta ethnography as well as realist synthesis.
14
1.8
There is a need for coordination and management moving from the 1st to the 2nd step to
avoid duplication across Knowledge Networks, to identify potential gaps, and to ensure
that the questions (the policy options) that are prioritized are appropriately broad. It is
our understanding that the CSDH Secretariat is planning this for their meeting in India in
September, 2005.
1.9
It is important that the 2nd and 3rd steps (formulation of recommendations) are separated,
particularly concerning judgments about the quality of evidence and how compelling it is.
Sometimes, strong recommendations are justified on weak evidence and vice versa. The
Commission needs to consider how to manage this process, including identifying who is
responsible for making the policy recommendations. The Commission also needs to
consider how the recommendations should be formulated in such a way that they take
into account the need to apply them in vastly different settings, and to take account of
different contexts, cultures and values.
1.10
The Knowledge Networks should not use the limited time and resources they have to
undertake comprehensive reviews of the association between social determinants and
health. This would take time, resources, and would be difficult to accomplish given the
complexity of the relationships. It would be better to focus directly on the question of
what we can do.2
1.11
Consideration should be given to asking the Knowledge Networks to undertake case
studies given that the evidence for many upstream interventions will be limited, including
the quality of available case studies.
1.12
Perspectives and values need to be local. Knowledge Networks can provide guidance
regarding how to take these into account, and should incorporate these into reviews of the
evidence (for example, identifying potentially important moderating factors). Networks
2 Of course, in some instances there may be no evidence about “what to do”, in which case the KN might usefully
spend time reviewing evidence on causality in order to assist in the formulation of interventions & programmemes
which can then be evaluated.
15
should not undertake systematic reviews of this evidence outside of the context of
reviewing the effects of policies.
1.13
The Measurement Knowledge Network should be tasked with developing a set of
guidelines on how each of the Knowledge Networks should conduct and report their
standardized reviews. A number of resources already exist that could be easily adapted
and modified.
1.14
The Networks and the Commission should not hide uncertainty. Given that there is likely
to be uncertainty about most recommendations, one of the mandates given to the
Networks should be to provide explicit suggestions on how policies should be evaluated
so as to reduce some of the most important areas of uncertainty.
1.15
There is a need to devote further resources to understanding: what are the determinants of
global public policymaking, i.e. towards understanding “how change happened”, as well
as detailed case studies offailed policy initiatives.
D.
TOWARDS
INCORPORATING
HEALTH
IMPACT
ASSESSMENT
IN
KNOWLEDGE NETWORKS - PRELIMINARY RECOMMENDATIONS
1.1
Each Knowledge Network should as a minimum apply a screening checklist to each of
their recommendations, in order to give some indication of the nature, scale, severity,
probability, and distribution of potential health impacts.
1.2
The CSDH should financially support the building of capacity to carry out HIA in
countries working with the CSDH (e.g. through organizing regional training workshops).
1.3
The results of HIA should be used to prioritize policy options in the work of the
Commission.
16
1.4
The Commission should adopt the principles of HIA as adumbrated in the Gothenburg
Consensus Statement with its broad socio-environmental view of health, and HI As should
be:
•
Equity-focused based on the distributional impacts of social determinants of
health
1.5
•
Adapted to the institutional, social and cultural context of each region
•
Applied to all policies, including global policy initiatives.
In order to be able to undertake HIA, it will be necessary to devote further resources for
gathering baseline health data at the country level, and ensure that these data are broken
down on the basis of core indicators to analyze distributional impacts.
17
Annex I
KNOWLEDGE NETWORK FOR MEASUREMENT:
Santiago, Chile: 21-24 March 2005
-List of ParticipantsCommission Chair and His Office
Prof Sir Michael Marmot
Head of Department
Department of Epidemiology and Public Health,
University College London
Ruth Bell PhD
Department of Epidemiology and Public Health University College London
.
■■■
-
Commissioners
•____
Dr. Monique Begin
Dean Faculty of Health Services
University of Ottawa School of Management
Measurement Experts
IB
Dr Aluisio Barros
Associate Professor
Programa de Pos-gradua^ao em Epidemiologia
Universidade Federal de Pelotas,
Dr Tony Blakely
Associate Professor
Department of Public Health,
Wellington School of Medicine and Health Sciences,
University of Otago
Dr Maria Teresa Cerqueira
Chief of the Unit of Healthy Settings
Pan American Health organization
Dr Adam Coutts
Postdoctoral Research Fellow
Magdalene College, University of Cambridge, CB3 OAG, UK
Dr Ligia de Salazar
Professor and Director of the Public Health Technology Evaluation Center
18
Dr. Francisco Espejo
Chief School Feeding Service
Strategy Policy and Programs Division
Policy and External Affairs Department
UN World Food Program
Dr Mark Exworthy
Senior Lecturer
School of Management, Royal Holloway - University of London,
Dr Paul Gertler
Professor of Economics & of Health Services Finance
University of California, Berkeley
Dr Elizabeth Harris
Director
Centre for Health Equity Training Research and Evaluation
School of Public Health and Community Medicine, UNSW &
Division of Population Health, South Western Sydney Area Health Service,
Dr Philippa Howden Chapman
Director, Housing and Health Research Programme
University of Otago,
Dr Liliana Jadue
Director
Institute of Epidemiology and Public Health Policies,
Faculty of Medicine, Clinica Alemana - Universidad de Desarrollo
Dr Ichiro Kawachi
Director
Harvard Center for Society and Health
Department of Society, Human Development and Health,
Harvard School of Public Health,
Professor Mike Kelly
Director of Evidence & Guidance
The Health Development Agency
Dr Meri Koivusalo
Senior Researcher
STAKES (National Research and Development Centre for Welfare and Health)
Mr Bobby Milstein
Evaluation Coordinator
Centers for Disease Control and Prevention
Dr Andy Oxman
Researcher
Informed Choice Research Department,
Norwegian Health Services Research Centre,
Professor Jennie Popay
Professor, Sociology & Public Health
Institute for health research, Lancaster University
19
Dr Alex Scott-Samuel
Senior Lecturer in Public Health and
Director, International Health Impact Assessment Consortium (IMPACT)
Division of Public Health, University of Liverpool,
Dr Venkatasubramanian Sankaranarayanan
Assistant Profesor
Department of Society, Human Development and Health,
Harvard School of Public Health,
Dr Haluk Soydan
Research Professor
University of Southern California
School of Social Work
Mr Decharut Sukkumnoed
Researcher and Research Co-ordinator
HPP-HIA Program, Health Systems Research Institute,
Elizabeth Waters
Chair of Public Health
School of Health and Social Development, Deakin University
Chile Delegation
BB
Dr Hernan Sandoval
Chilean Ambassador in France
Dr Patricia Frenz
Coordinadora Reunidn Subsecretaria de Salud Publica
Ministerio de Salud
Dr. Ximena Aguilera
Jefa Division de Planificacidn Sanitaria
Ministerio de Salud
Mr. Camilo Cid
Departamento Economia de Salud
Division de Planificacion Sanitaria
Ministerio de Salud
Dr. Jorge Jimenez
Profesor del Departamento Salud Publica
Departamento de Salud Publica
Facultad de Medicina Pontificia Universidad Catblica
Dr. Rodrigo Salinas
Jefe Depto. Bioetica y Salud Basada en Evidencia
Ministerio de Salud
Dr. Tito Pizarro
Jefe de Nutricion
Ministerio de Salud
20
Oscar Arteaga
Jefe Divisibn Academica de Politicas y Gestion
Escuela de Salud Publica, Universidad de Chile
REFERENCES
Arai L, Roberts H, Roen K, Popay J. It might work in Oklahoma but will it work in Oakhampton?
What does the effectiveness literature on domestic smoke detectors tell us about context and
implementation? Injury Prevention 2005 (in press).
Cohen S, Underwood LG, Gottlieb BH. Social Support Measurement and Intervention. A Guide
for Health and Social Scientists. New York: Oxford University Press, 2000.
European Policy Health Impact Assessment. A Guide. 2004.
Glass TA, Berkman LF, Hiltunen EF et al. The Families in Recovery from Stroke Trial (FIRST):
Primary study results. Psychosom Med 2004;66:889-97.
GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ
2004;328.
Graham H & Kelly MP. Health inequalities: concepts, frameworks and policy. NHS Health
Development Agency Briefing Paper. 2004, 12 pp.
21
Howden-Chapman P, Crane J, Matheson A, et al. Retrofitting houses with insulation to reduce
health inequalities: Aims and methods of a clustered, randomised community-based trial. Soc
Sci Med 2005 (in press).
Jackson N & Waters E. Systematic reviews of health promotion and public health interventions.
The Cochrane Collaboration 2005.
Kling J, Liebman J, Katz L, Sonbonmatsu L. Moving to Opportunity and tranquility:
Neighborhood effects on adult economic self-sufficiency and health from a randomized housing
voucher
experiment.
(unpublished
manuscript
accessed
at:
http://www.ksg.harvard.edu/ieffreyliebman/papers.htm)
Mahoney M, Simpson S, Harris E, Aldrich R, Stewart Williams J. Equity-focused Health Impact
Assessment Framework.
University of Newcastle, Sydney: Australasian Collaboration for
Health Equity Impact Assessment (ACHEIA), 2004.
Milstein RL & Wetterhall SF. Framework for programme evaluation in public health. MMWR
1999;48:No. RR-11.
Petticrew M, Whitehead M, Macintyre SJ, Graham H, Egan M. Evidence for public health policy
on inequalities: 1: The reality according to policymakers. JECH 2004;58:811-16.
Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative
literature in health services research. Qualitative Health Research 1998;8:341-51.
Popay J. Qualitative research and the epidemiological imagination
a vital relationship.
Unpublished manuscript circulated at meeting.
Popay J & Roen K. Using Evidence from Diverse Research Designs: A Preliminary Review of
Methodological Work. SCIE Report No. 3, November 2003. ISBN 1-90481-2-05-8. UK: Social
Care Institute for Excellence.
22
Roen K, Arai L, Popay J, Roberts H. Preventing children’s injuries: Exploring methodological
issues in the systematic review of qualitative evidence. Soc Sci Med 2005 (in press).
Spencer L, Ritchie J, Lewis J, Dillon L. Quality in qualitative evaluation: A framework for
assessing research evidence. London; Government Chief Social Researcher’s Office, 2003.
Whitehead M, Petticrew M, Graham H, Macintyre, Bambra C, Egan M. Evidence for public
health policy on inequalities: 2: Assembling the evidence jigsaw. JECH 2004;58:817-21.
Writing Committee for the ENRICHD Investigators. Effects of treating depression and low
perceived social support on clinical events after myocardial infarction. The Enhancing Recovery
in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA 2003;289:3106-16.
23
Position: 1776 (4 views)