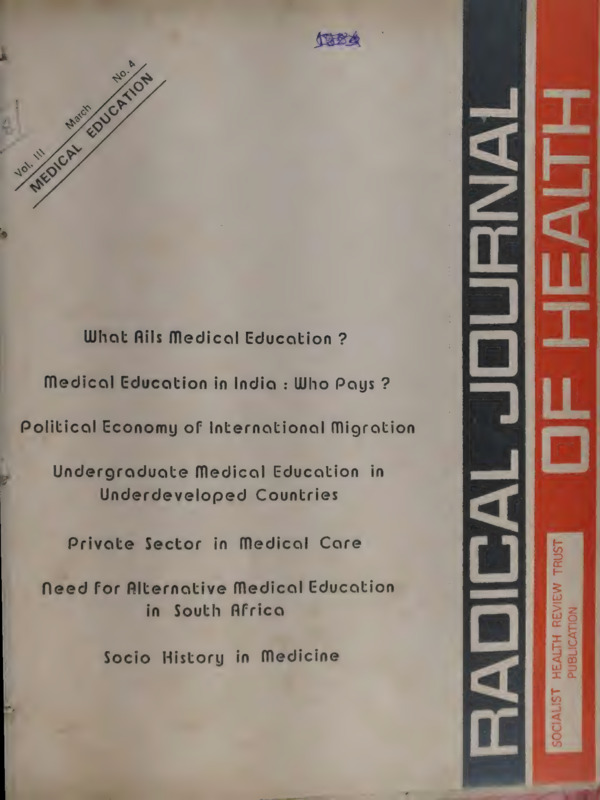
Radical Journal of Health 1989 Vol. 3, No. 4, March - Medical Education.pdf
Media
- extracted text
-
own 18
What Ails Medical Education ?
Medical Education in India : Who Pays ?
Political Economy of International Migration
Undergraduate Medical Education
Underdeveloped Countries
Private
Need
Sector
in Medical
in
Care
for Alternative Medical Education
in South Africa
Socio
i
History
in Medicine
0 igOw
|
= =
Z <q
or
es aT |
O LL
J
-_
ef
2
O
cf
or
CJ
PUBLIC
SOCIALIST
REVIEW
HEALTH
TRUST
Voinne 10) la
29
No.4
:
ION
MEDICAL EDUCAT
1
Editorial Perspective
WHAT AILS MEDICAL
Ajoy Mitra
Sujit K.Das
Amar Jesani, Manisha Gupte,
Padma Prakash, Ravi Duggal
Collective
Ramana
Imrana
Dhara, Vimal
Balasubrahmanyan
Quadecr, Sathyamala C (Delhi),
EDUCATION
?
MEDICAL EDUCATION IN INDIA: WHO PAYS
of
health
journalRavi Duggal
radical
Working Editors :
Editorial
By
?
13
:
(AP),
Dhruv
POLITICAL ECONOMY
MIGRATION
OF INTERNATIONAL
T.K: Ishi
Mankad (Karnatak), Binayak Sen, Mira Sadgopal (M
-P), Anant Padke, Anjum Rajabali, Bharat Patankar,
Jean D'Cunha, Srilatha Batliwala (Maharashtra) Amar
Singh Azad (Punjab), Smarjit Jana and Sujit Das
(West Bengal)
Editorial Correspondence :
Radical Journal of Health
C/o 19 June Blossom Society,
UNDERGRADUATE MEDICAL EDUCATION IN ~
UNDERDEVELOPED COUNTRIES : THE CASE OF
PAKISTAN
S. Akbar Zaidi
36
60A, Pali Road, Bandra (West)
Bombay - 400 050 India
Update
DEFINING QUACKS
RURAL DOCTORS IN THAILAND
Printed and Published by :
38
Dr. Amar Jesani for
Socialist Health Review Trust from C-6 Balaka
Swastik Park, Chembur Bombay 400 071
Printed at:
Omega Printers, 316, Dr. S.P. Mukherjee Road,
Belgaum 590 001, Karnataka
Annual Subscription Rates :
Rs. 30/- for individuals
Rs. 45/- for institutions
Rs. 500/- life subscription individual
US dollars 20 for the US, Europe and Japan
US dollars 15 for other countries
We have special raics for developing countries.
SINGLE COPY: Rs. 8/-
(All remittances to be made out in favour of Radical
Journal of Health.
Add Ry. 5/- on outstation
cheques)
A Brief Survey
PRIVATE SECTOR
Rama V. Baru
IN MEDICAL
CARE
40
NEED FOR ALTERNATIVE MEDICAL
EDUCATION IN SOUTH AFRICA
R.H. Philpott
42
SOCIO HISTORY IN MEDICINE
Padma_Prakash
46
Book Review
era tPA ee e e
5a.
a
Ne ert
Pd ye
‘
‘
=
«
=r
at Perspective
a
=
¢
E ANCES
wae
x
‘ay
if
A
3
ive Pe
?
?
What Ails Medical Education?
are being voiced from various platforms
ns medical education in India for quite some time. Its
ucts, the doctors, are alleged to be found wanting
€serving in the rural milicu. The medical curriculum
ing blamed for such deficiencies in medical graduates
“€rudite schemes are being prescribed from time to
- But curiously, the role of medical teachers has
fed the attention of the commentators. That teachers
with their teachers which is often life-long— the implication being that the teacher-student relationship js extended
beyond the boundaries of Alma Mater.
In the earlier days, doctors were inéucted
into the
teaching job in various ways. In government institutions,
doctors were appointed as teachers in medicat colleges at a
a 1987, medical teachers were kept, by an apparent
ensus, Outside the purview of the exercise on the as-
ripe age after they had served their due period in nonteaching hospitals spread all over the state. A good number of doctors who acquired post-graduate qualifications,.
were also offered teaching posts on an honorary basis. In
the non-government medical colleges, almost all teachers
were on honorary terms or managed to secure a token
salary. This honorary system, though advantageous to the
employer, had not been resented by the employees. Appointment to a teaching job in a medical college is a very
prestigeous position in the mcdical profession. It brings
renown, uplifts status and quickly establishes the teacher
in the field of private practice. People look upon medical
ption that they are something special. Political author-
teachers as the most learned, accomplished and_ skilful
and officials look upon medical teachers not primarily
eachers, but as doctors first—taking the job of teaching
among the doctors; such an attitude works as a one-way
ticket to success in private practice. There are, of course,
ch might clarify the role of teachers in medical cduca-
ing to clinical disciplines, are daily engaged in the treatment of patientsin indoor and outdoor services. They are
ga profound role on the nature and quality of educagoes without saying. This role has been discussed and
lysed from various aspects in different forums. The
4 of medical teachers in medical education, however,
escaped such analysis, presumably because it is taken
> grante
d that there is nothing special to discuss. On the
sthand, in the gencral dcbate on pay and service conms of teachers, even during the Alt India Teachers’
a secondary one and medical graduates as by products
ncalth care system. Here we will explore the elements
The prevailing picture in West Bengal has served as
|.
jodel which may differ in many respects from state to
e but shares their essential characteristics.
certain. grounds for such belief. Mcdical teachers belongin a position to experiment with different curative technologies on the hospital patients, perfect them in hospital
practice and then apply those technologics profitably in
trains the
fhe world of medical education is small. Teachers and ‘their private practice. Hospital job not only
but also keeps him abreast of
ents soon become known to each other. An intimate doctor to be a skilful one
.
tionship develops between the teacher and the taught in continuing developments in the curative technology
ny instances. Thus teachers influence the students not
State of Medical Education
life
of
sphere
s
other
in
also
but
life
academ
ic
their
y in
Western medicine was imported in India and initially
their personality and behaviour.
the curriculum and contents of education were necessarily
a
of
compo
is
sed
educat
ion
medica
of
l
subject
The
borrowed. Over the years the curriculum underwent many —
aber of disciplines each of which being a speciality by changes and the teaching methods steadily adopted themHf has its own conclave of functioning.. Teachers of
at this Indian reality
a
i
‘by
journals
ch discpline have their separate associations,
selves to the Indian reality. A look
will reveal that production of doctors was stepped up rapthe
idly, after. independence with a vicw lo expanding
medici
ne
into
level
the
underof
s
graduate
¢ integrated at the
facilities of curative medicine to the largest section
to
have
doctors, state
ABBS) where teachers of different disciplines
people. To employ the increasing number of
method
integra
any
ted
state
Howeve
r,
eract with each other.
services underwent rapid expansion; employees
health
been
not
launched, and pri‘teaching at the under-graduate level . has
insurance (medical benefit) scheme was
discicach
faciliti es for the
olved as yet. In the post-graduate education,
vate industrial sector opened up medicare
ee
rate of expansion stabiine functions separately.
employces. In the seventies, the
special
ist
It was found
act as
a paradoxical situation emerged.
In the clinical discipline, teachers also
and
lised
tors and consultants, ie they are erigaged in treating
for doctors was aquoorcd,
thatthe employment markct
all disciplines
d/or academic forums. At the same time,
i
q
. This has been
Baticnts in hospitals attached to the colleges
|
a
-
opportunities
abroad
were
reduced,
the es ni
he
a sustaincd Laacantyaeetd
live, doctors ¥° :
e turned tremendously compeu
Mrumental in the development of
i | practic
pine se
The young doctors
con the teachers and students,
enter 95 ea
wate and post-graduate qualifications,
their link and relationsniy
of medical practice and retain
farch 1989
started swelling and
the employment exchange
employment. Paripassu,
tors resorted to agitation fur
the
/
. largest section of the people, particularly the rural poor
remained deprived of the minimum facilities of life-saving
curative medicine. Pandits traced the source of this paradox in the quality of medical education. It was propounded that medical education was lopsided; the curativebiased western model failed to properly equip the doctor
to tackle the health problems of the Indian people. It was
because of this western model, doctors settle in urban areas, itch to migrate to western countries, and practice individual medicine. It was, therefore, proposed that community medicine should be taught and emphasised more and
more in the curriculum. New syllabi were introduced accordingly. The department of preventive and social medicine was created and upgraded; the internship period was
extended from six months to one year, the R.O.M.E. programme was introduced to give field training to medical
students, But the broad community of teachers, who were
expected to turn this new revised programme into reality,
were not taken into confidence during this entire exercise.
_ In fact, community medicine eventully came to be another
subject to be taught by the department of PSM and was
required to be learned by the students for examination
purposes. Thus community medicine remained a paper
exercise; it was not even practised anywhere to serve as a
demonstrative model for the students. Neither educational
administrators nor teachers had any field knowledge or
experience about what community medicine aimed at.
_ Teaching method underwent little change except adopting themselves to the changing content of the syllabus and
changing structure of examination. An integrated teaching
approach, by which the student could have a holistic view
of the world of medicine as well as the aim of community
medicine and which would have enabled him to appreciate
the importance of studying different subjects in the preclinical and clinical courses to prepare him to be a doctor,
was not taken into consideration. Even the modest WHO
sponsored programme of integrated teaching in Maternit
lum within the framework authorised by MCI, pr
examination and confers degrees and diplomas. Government, who runs the colleges, admits students, appoints .
teachers and provides the material infrastructure for teach-;
ing, including the hospital.
Over the years, control by the MCI and the University
has been reduced to a notional character and the Governmental control, which is exercised largely by bureaucrats
who are neither doctors nor teachers, has steadily tight- —
ened its grip. This control is exercised through financial |
allocation and through appointment-transfer-promotion of
teachers. The teacher actually enjoys a large amount of
freedom of manoeuvre in his/her own area of activity ie
actual teaching and examination where external supervi-
sion and control is minimal, often non-existent. But the
teacher has to bow to the bureaucratic fiat whenever called
upon to do so.
|
|
A sinister trend is being noticed in the medical fiel
in West Bengal since 1983. The ruling party, in its zeal to
enlarge its sphere of influence, is (mis)using administra-
tive machinery in order to exercise its control over every
level of medical education. The Left Front government
has constituted different committees for selection of teachers, for elevation of their academic rank at every level and
|
their transfer. These committees are being manned by ~
pliant people who owe allegiance to the ruling party.
Those who are not ready to be used as plectrum are being
deprived of their dues. Further, the ruling party, by virtue —
of its control over the university administration, has
played havoc in admission to under-graduate and post-
gfaduate courses, through manipulation over examination
results—evén prior disclosure of questions has been alleged on several Occasions in the mass media. The most
scandalous practice which has made headlines is the system of admitting in the MBBS course, wards of ministers,
MLA, police officers, businessmen etc, who have been’
unsuccessful in the admission test, through special power
& Child Health where jeachers from the.discipline of of the chief minister. This indirect political control is —
Paediatrics, Obst. & Gynaec. and P.S.M. join together in undermining academic independence as a whole and bodes
a limited way, to explain to the students the disease process in thesqcial context and the methodsof tackling it,
remained limited to only three centres in India. There also
it is being followed perfunctorily. The object of teaching
had been and still remains to be an exercise
to prepare the
Student for the examination. .
|
Control of Medical Education
There are three agencies for control. Med
ica
l Council
of India (MCT) determines the over
all standard. MCI pre-
Scribes minimum qualification of
eligibility
of siudents
_ and teachers, necessary material
requirements of a niedicn’
college eg space, laboratory,
teaching aids etc, sets
teacher-student ratio, student-b
ed ratio etc and auth ee
curriculum. Affiliating Univer
sity sets up detailed YR
2
ill for the future.
)
Status of Medical
Teachers
The status of medical teachers in the world of medical
education is determined by a number of factors, eg (a)
The speciality or subject; (b) The status of the teacher’in
medical practice; (c) The status of the teacher in profession/service.
The subject taught has a lot to do with the status of a
teacher. Clinical subjects eg medicine, surgery, obstetrics
and gynaecology, eye, ENT etc where diagnosis and
management of diseases are dealt with, are accorded extraordiiary importance for the reason that these subject’
deal with the living beings—patients who need succour, »
The non-clinical subjects eg anatomy, physiology, pharma-
Radical Journal ofHealth
i ta
ae
:
cology, biochemistry etc, do not deal with patie
nts and
hence are treated as unavoidable nuisances. Para-clinica
l
subjects eg pathology and radiology, though do not
make
direct interventions in treatment, have nevertheless
to
age of
eligibility for
lecturership.
come in contact with patients and hence, are given
some
importance. PSM comes nowhere amongst these divisions
and hence, ignored like the non-clinical ones. In the prac-
tice of medical care also, doctors (and teachers) belonging
to clinical disciplines are looked upon by the entire society.
as the real persons of importance. Policy-makers, planners
and administrators are concerned with clinical subjects
only. Progressive commentators on health leave out nonClinical and para-clinical subjects from their deliberations,
people at large do not even recognise the teachers dealing
with these disciplines as doctors. Students search for ideals
among the clinical teachers.'In West Bengal, only teachers
of clinical discipline and radiology are allowed the privilege of private. practice so that these all-important persons
do not suffer from financial deprivation. These privileged
teachers thus can live as members of the upper economic
class of the society and pose as role models for the students.
A look at the remuneration enjoyed by the medical
teachers is relevant here. On the salary scale, medical
teachers are situated below the level enjoyed by general
college and university teachers. General teachers have been
enjoying UGC pay scale since 1973, whereas medical
teachers in West Bengal were given the benefit of UGC
scale only in 1981. General teachers now enjoy a much
higher pay-scale as recommended by the Mehrotra commission while medical teachers are still lagging behind in
the old UGC scale. In the report of the second Pay Commission (1977-80) of the government of West Bengal, the
_- member-secretary observed
It is doubtful whether conditions of service
of the teaching posts on the UGC pay-scale are
exactly the same as those teaching posts in
West Bengal Health Service. The teachers in
the other academic institutions who are in receipt of UGC pay-scale have a limited number
of instructional periods in a week. They enjoy
vacation and holidays which are not similarly
available to the teaching posts in the medical
line. This difference apart, the holders of
teaching posts in West Bengal Health Service
have to do hospital duties which are onerous in
nature. The tremendous pressure of population
on hospital services has made their duties all
the more onerous. There exists a good case for
distinguishing the tcachers in the medical insti-
tutions from their counterpart in the other academic institutions.
The points for distinction. are as in the table:
given
In West Bengal, the clinical teachers have been
College
Teache
Medical
Teachers,
period) requirement.
1973 | 18 hrs/
Years
week.
1981
Years
the option of private practice in lieu of a 30 percent cut in
their salary; in addition—they are debarred from the highest pay-scale (ie their pay-scale is limited to Rs. 700—
1900). Consequently, the amount of gratuity and pension
also is small. The clinical teacher, therefore, is asked to
perform the whole-time job of teaching, whole-time job
of a clinician in the hospital and thena whole-time engagement in private practice— a task obviously impossible
for a human being. The teacher, in reality, is confronted
with a choice to prefer one whole-time job among these
three and he, like the average citizen, opts for the profitable one ie private practice. It is a somewhat universal
picture that the clinical teachers are accustomed to look
upon their salary as a sort of fringe benefit and concen-
trate on private practice with a fierce dedication to earn as
much as they can while the opportunity exists. No wonder, when the state governments in Bihar, Orissa, Andhra
Pradesh, Assam etc, withdrew the privilege of private
practice, clinical teachers fought at every stage to retain it.
In West Bengal, private practice for medical teachers was
prohibited in 1982. A case was instituted at the high court
and the order was stayed. Soon after, the health portfolio
which was under RSP—a constituent of the Left Front,
was taken away by the major partner of the Front—
CPI(M). The new health minister showed reluctance in
implementing the order and the merry atmosphere of private practice continues. Needless to mention, private practhan
tice not only offers a return of several times more
engaging
the salary figure but also demands a sincere and
for a
possible
attention from the clinician. It is simply not
do justice to the
clinician successful in private practice to
job of teaching
and hospital
tasks.
He has to make
a
choice, set up a priority.
Then again, among
the medical teachers, non-clinical
respect and envious Onteachers, deprived of status and
fortunes are a frustrated
looker of their clinical colleagues,
lot who
in their
have lost interest both in teaching and
subject. A good number of them
find solace in unauthor-
;
March 1989
oe
es
OT ee te ee
ised clandestine private practice while others lament. West
Bengal has two post-graduate medical colleges where all
teachers are forbidden private practice. Their conduct follows the line of the under-graduate non-clinical teachers,
ie either clandestine private practice or disinterest in job.
This system of private practice to compensate the clinical teachers has given rise to the following problems:
i) Practising teachers are inclined to settle in Calcutta
where the market for private practice is lucrative and are’
reluctant to accept transfer to another medical college,
particularly a distant rural one as it would disrupt the
practising network which they have diligently built up
with years of effort. The rural medical colleges (there are
three in West Bengal) therefore, suffer from a perpetual
shortage of teachers.
ii) There is always a long waiting list of doctors possessing eligibility for a teaching post in clinical disciplines
and under the unavoidable influence of the law of demand
and supply, this situation has resulted in rampant corrup-
_
tion in the matter of teaching appointments. The competi-
tion for a teaching post in clinical disciplines has further
intensified due to preference for a Calcutta posting. Con- sequently, clinical teachers try their utmost to retain their
Calcutta-posts and resort to questionable means including
inciting students to launch agitation demanding the. retenit tion of their favourite teachers.
tii) Non-clinical
disciplines perpetually
suffer from
dearth of teachers, not to speak of competent teachers.
_ Aspiring teachers vie for a teaching post in the clinical
discipline and barring a few, opt for the non-clinical diseipline only when they fail in their endeavour. They accept
such postings reluctantly and then try somehow to live
with it.
\
iv) Appointments in the post-graduate colleges are like_ wise resisted as these are “compulsorily non-practising.
Teachers in these institutions being non-practising not only
suffer financially but also are placed on a lower level of
social recognition than the practising ones. Thus they become frustrated and reluctant. Standard of post-graduate
medical education has; therefore, deteriorated considerably. In the absence of any incentive, rescarch work, required to be conducted by students, have been turned into
paper exercises only. Practical training for students is lopsided. Even among the post-graduate students there is keen
competition for the clinical disciplines resulting in corrupt
practices in admission and examination; while non-clinical
disciplines suffer from dearth of applicants.
What is To Be Done?
The standard of teaching has steadily deteriorated over
the years. Zealous attempts to politicise health service has
undermined the morale of the doctors including teachers.
Non-clinical teachers have little interest. in teaching.
4
Teachers of clinical disciplines look upon such appoint-—
ments as a means of personal aggrandisement and of earning money. Students are merely after the degrees which
they would use as capital for their business in medical
practice. They have learned the bitter truth that connections in places of influence will fetch them their desired
objective—an under-graduate or post-graduate degree/diploma. In such a context, attempts to devise a meaningful
methodology of teaching or to revise the curriculum have
little relevance. Whatever might be the objective of such
an exercise it should not be forgotten that it is the teachers, after all, who are expected to implement the programmes. If objective conditions are not set up so that the
tcachers participate actively, no programme will succeed.
Another aspect of this messy situation is worth pointing
out. The degradation of standards of education makes its
own impact on standards of medical practice. Commercialisation apart, scientific excellence in medical care is
conspicuous by its absence. Bereft of a rational approach,
medicine is being practised as a shot in the dark. Unscientific drugs are being used at random. Modern safer and
more effective investigative and operative technologies
have not reached even the upper strata of medical practitioners. The less said about clinical research the better. In
fact, in the absence of a continuous updating of knowledge, a sort of quackery is rampant even among practitioners holding post-graduate qualifications, not to speak of
general practitioners.
Frankly speaking, in the practice of modern medical
science, science is the real victim in India. Low levels of
scientific knowledge among the medical profession, particularly teachers, have rendered them easy prey to the
profiteering campaign of drug and equipment industry.
Medical literature, produced mostly by teachers, has not
made any positive significant contribution to the development of medical science in the country. An unsavoury
example may be cited to give an idea about the hollowness of the medical establishment. Two years ago at the
national conference of the orthopaedic surgeons, a paper
was presented as a critique of a number of original.
research articles published during last several years in the
orthopaedic journal. Analysing the crucial contents of the
articles and citing evidence, this paper revealed that all
articles were the products of plagiarism without acknoledgement from the articles published in foreign journals.
Scrutiny may show that the picture is no different in other
specialities.
Independence or autonomy of teachers, updating of
Standards and ‘check and balance’ in career prospect are
the areas needing consideration afd overhauling. Independence starts with the removal of financial dependence
on private practice. The last two Central Pay Commissions
(Continued on Pg. No. 48)
‘
Radical Journal of Health
_
Medical Education in India: Who Pays?
ravi duggal
It is with the aid
i of publicj resources that medical
'
education and the subsequent production of medical hwmanower has consolidated
it.
é
P
ted itself. Most of this humanpower finds its way into the private sector. Even worse there
has been @ sustained migration of doctors mostly to developed countries. This
we feel is a serious concern.
Public resources must be used for public benefit.
MEDICAL education in India is almost entirely the re- tion, the other is the concentration of the outturns from
sponsibility of the state. Ironically between 2/3rds and medical colleges in the urban areas (see table 3), even in
3/4ths of those qualifying from public financed medical
the state health sector which can be seen. Between 1952
schools participate in the private sector. This means for and 1983 the number of hospital beds had increased 3 1/2
every three allopathic doctors the government trains at the times but as a ratio to the population it had increased 4
cost to the public exchequer for its own health services, it barely twice. Thus in the fitst plan period there was one
hospital bed for 2717 population but in 1983 the availabilalso trains seven doctors for the private sector at public
cost. Besides this a more or less similar pattern exists for ity of beds had increased to one bed for 1362 population,
But, this aggregate picture -is misleading because of the —
education (Ayurveda, , Unani,
non-allopathic medical
gre?
Siddha and Homoeopathy) which together accounts for concentration of available facilities in urban areas.
the first and sixth plan periods the ~
Thus between
twice the number of allopathic doctors. As though this
beds changed from one per 706 —
of
hospital
availability
drain on the public exchequer is not enough, out of every
:oo
population to one per 395 in the urban areas in compari- ig
100 allopathic doctors going to the private sector between
eee
M
Ps
popufrom
Lie
9438
was
rural
change
areas
to
where
son
the
34 and 57 have been migrating out of the country each
year, mostly to developed capitalist ones, and recently also lation per bed to 5937 population. Since the distribution {
to the Gulf countries. This is indeed gross injustice to the of medical humanpower data is not available in a <7
be —
poor Indian masses who have contributed their mite in gregated form the distribution of hospital beds may
i
plan
first
the
in
Thus
assumed as an indirect indicator.
training these doctors in the hope that they will in turn
period only 39 percent of hospitals and 23 percent of beds na
care for them. However, the focus here is not the dynamwere in rural areas when 80 percent of the population ‘ b
ics of this injustice, which is so openly and unashamedly
*
practised, but to view in a historical perspective the
growth and financing of medical education in India.
Prior to the First Five Year Plan there were 28 medical
colleges (unless otherwise specified we mean allopathic),
all except one being publicly owned, from which about
2500 doctors graduated every year. By the end of the
Second Five Year Plan the nutnber of medical colleges
had doubled and the doctor outturn increased 2 '/, times,
and at the start of the Fourth Five Year Plan the number
of medical colleges had quadrupled and doctor outturn
increased six times (see table 1 and 2). Most of this
growth was in the state sector and with the aid of public
e in
resources. After the Fourth Five Year Plan the increas
but exmedical education facilities have been very small
penditure has increased at a galloping pace.
ges in
As of present (1987) there are 123 medical colle
the governthe country with 102 being owned and run by
corporament or other public bodies like the municipal
ges). The
tions (four colleges) and universities (three colle
private bodremaining 21 colleges are owned and run by
assistance or
ies, with most of them getting some financial
the colsubsidies or support from the state in conducting
public resources
leges. Thus, it is largely with the aid of
production of
that medical education and the subsequent
|
,
medical human-power has consolidated itself
ly of doctors is
This drain of public resources, especial
n of medical educaonly one dimension of the expropriatio
March
1989
lived there. In contrast in 1983 when about 76 percent of
the population was in rural areas the availability of medi- ne
cal care facilities in comparison to urban areas had de- Aa
clined to 26 percent of hospitals and 17 percent of beds in "
rural areas. In 1987 the number of hospital beds in rural
areas declined further (from 1894 in 1983 to 1633in —
1987) accounting for only 21 percent of all hospitals, the
proportion of beds stayed at around 17 percent. In the —
case of government hospitals the situation is equally bad—
ruin 1983 of all government hospitals a quarter were in
only —
ral areas and of all hospital beds in the state sector
While
10 percent were in rural areas (CBHI/GOI, 1985).
available,
there is no direct data of medical humanpower
census
1981
the
to
except 1981 census data — according
only 28
of all working (main earners) allopathic doctors
all nurses and midpercent worked if rural areas and of
(Census/GOI,
wives 38 percent were in rural areas
1987).
there .are
Besides allopathic services and humanpower
— ayurveda,
non-allopathic institutions and humanpower
In terms of health care unani, siddha and homocopathy.
in these systems of
facilities (hospital and dispensaries)
facilities is fairly small
medicine, the ratio to allopathic
1s far larger
of medicine
but humanpower of these systems
3 and 4). Also, in
Tables
than that of the allopathic (see
a much larger proportion
comparison to allopathic doctors,
56
found in rural areas —
of non-allopathic doctors are
census. Thus in the year
percent according to the 1981
.
ee
1986-87 there were totally 830, 400 doctors of all systems
of medicine, besides 210,000 nurses and over 10,000 dentists (see Table 4). In addition to this in the same year
there were 372,140 paramedics (ANMs, MPWs, Midwives
and LHVs) (CBHI/GOI, 1988). If we take doctors of all
the systems and calculate the ratio of doctors to population
we find that in India one doctor exists for every 935 persons, and assuming the rural/urban distribution of the
1981 census we estimate that in 1986-87 for rural arcas
there is one doctor per 1574 persons (for allopathic one
A ONE
te
let el
1
ee
‘medical education’ under the medical account section. The
data on state expenditure on medical education being
lysed here is for the period 1951-52 to 1982-83, a total
32 years, from the First Five Year Plan to the middle
the Sixth Five Year Plan. The expenditure reported here i
‘revenue expendituyse’'— that is, expenditure incurred
of revenues collected by the state and covers the uni
government and all state and union territory governments,
This expenditure includes only the component spent
medical,
dental
and
nursing colleges.
hospital
The
per 6116 persons) and for urban areas there is one doctor
per 421 persons (for allopathic one per 793 persons).
Thus it is amply clear that humanpower resources in
the health sector as regards the number of doctors is quite
adequate, establishing the fact that medical education in
terms of supply of doctors has kept pace with the growth
of population and is today at a level (or supply) that is
sufficient to meet the needs of the country's population.
However, the hitch is that it does not meet the needs of
the people because a large majority of ,doctors take up
private practice, concentrate in urban areas or migrate
abroad — in fact, more allopathic doctors migrate abroad
other supportive services needed for medical and nursing
education are not included in this amount—this component
of expenditure is not available separately. Capital expendi-
than go to rural areas of India.
possible to calculate how much is spent on training of
each medical person because detailed breakups of expenditure on each category of personnel are not available and
the supportive, administrative and hospital costs incurred
for training are also not known. Performance budgets of
states may provide this information but for macro analysis
this information is too voluminous to put together because
it is available for each college separately. Even here,
:
As stated earlier, medical education in India has been
almost wholly financed by the public exchequer. This
money comes mostly from tax revenue collected by the
government from the people. Direct payment by students
in the form of fees etc is presently very small.
Before we look at the data on medical education expenditure it will be in order to explain in some detail the
structure of the state health sector financing.
State health expenditure is divided into three major
heads called ‘medical’, ‘public health’ and ‘family welfare’.
‘Medical’ is further divided into ‘allopathy' and ‘other systems of medicine’ (non-allopathic). The main sub-heads
under allopathy are (a) direction and administration (b)
medical relief (c) education, training and research (d)
ESIS and CGHS (e) and other sub-heads, and under ‘other
Systems’ there are separate sub-hcads for ayurveda, unani,
siddha and homoeopathy. ‘Public Health’ is divided into
‘Public health and sanitation’ and ‘sewerage and water supply'— the former being mainly expenditure on communicable diseases prevention programmes and_ the latter
mainly rural and urban water supply schemes. The 'Family Welfare' account includes expenditure on rural and
urban family planning services and maternity and child
health services.
All the three accounts have a ‘capital outlay’ section
which is mostly construction activity. Thus, under 'medical’ the main sub-heads are construction, expansion and
improvement of (a) hospitals, dispensaries and health
centres and (b) medical colleges. Under ‘public health’ it
includes almost entirely water supply schemes and under
‘family welfare’ construction of family planning centres.
In this article we are concerned with the sub-head
ture is excluded from 'medical education expenditure’. We
will deal with this separately.
Between 1951-52 and 1982-83 the state's expenditure
on medical education has been substantial. It has seen a
healthy growth of 2.8 percent per year in sharp contrast to
1.4 percent growth rate of total state health expenditure
and only 1.24 percent growth of total government expenditure (CAG/GOI, various years).
~ At this stage we would like to emphasise that it is not
Table 1
Medical Education Infrastructure
1951-52 to 1986-87 (figures at end of period)
Reference
years
Plan I 1952-56
Plan II 1957-61
Plan III 1962-66
Medical
Colleges
Nursing
institutions
Dental
colleges
Number
Percent
Private
41
60
87
7.3
5.0
9.2
241
208
254
7
12
14
94
105
106
111
123
9.6
8.6
8.5
10.8
17.0
259
270
283
324
374
ae)
15
17
25
26
Plan holiday
1967-69
Plan IV 1970-74
Plan V 1975-79
Plan VI 1980-83 @
1986-87
EEE
@ 4 year period including 1979-80 annual plan and
first three years of Sixth Plan.
Source : Health Information of India (earlier called
Health Statistics of India and Pocket Book
of Health Statistics ), CBHI, GOI, various years.
Radical Journal of Health
lOWwever, the Supportive costs cannot
be know
same figure). Whether this approach is correct is debatable
but the fact that a supportive structure of a teaching hospitalisneeded for medical education cannot be discounted.
Whether the present type of teaching hospital is the right
type is a different question altogether but the inclusion of
the entire cost of teaching hospitals as part of medical
(see Table 6). If we assume this proportion for Indi
a for education, we feel, is perfectly justified — and this cost
the year 1983 then the cost per doctor to the state for only
today (1988) in Maharashtra is Rs. 80 million per teaching
_ the medical college component works out to Rs. 8495
1.78,
hospital (for JJ Hospital and Grant Medical College, Bom: In the same year, given the average cost of Rs. 50 million bay the cost
is Rs. 150 million). Besides, administrative
” pet medical college and teaching hospital (on the basis of
and capital costs have not been included.
data for Maharashtra) the annual cost per qualifying stuIn the First Plan period the state spent Rs. 66.4 million
dent for the teaching hospital (excluding medical college on medical education. (See Table 5) During this period
. expenditure indicated above) works out to Rs. 372,312.35.
12,520 MBBS doctors, 657 postgraduates, 142 dentists and
Let us also assume that this entire cost is necessary for 9345 nurses and general nurses qualified from the 41
training of medical humanpower. Taking the same propormedical colleges, 7 dental colleges and 241 nursing
zfpon of 84 percent as expenditure for MBBS doctor train- schools/centres. (Table 1 and 2). This expenditure working
Wang Rs. 312,742.37 becomes the teaching hospital cost per out to Rs. 13.28 million per year, was 5.3 percent of all
doctor and the total cost per doctor totalling to Rs. expenditure on medical services by the state and 3.5 per-
Id studies at the teaching hospital level
will ay.
ng down these costs. For instance,
in Maharashtra
S0f the total expenditure on medical educatio
n for the years
1981 to 1989 on an average 84 percent was
spent on
training of MBBS doctors and the rest on othe
r personnel
397,694.15
(Please note that we are taking one year's
_ expenditure on medical education and teaching hospitals to
_ be the cost of the 4", years. This method is perfectly okay
| because in any one year there are 5 batches of medical
| students. Thus if we divide the above figure by five we
| will get per medical student cost per year and if we again
|
multiply by 4 '/, -we prefer 5 — we come back to the
‘
cent of the expenditure on total health care (including FP,
public health and water supply) spent by the state. (Table
5). More than one - half of this expenditure was by the
union government and the three provinces of Bombay,
(Gujarat and Maharashtra) West Bengal and Madras
(Tamil Nadu). This concentration of expenditure in these
provinces continues even today. (See Table 7).
Table 2 : Outturn of Medical Personnel 1951-52 to 1982-83
Reference years
MBBS Doctors
Desitists
|
:
Post-graduates
Nurses
General
(Medical & Dentist)
(BSc)
Nurses
Nurse/
Doctor
Outturn
Ratio
12520
(2504)
I
145
(29)
657
(131)
132
(26)
1:1.34
:
1708
(342)
141
(28)
9213
(1843)
12196
(2439)
1:1.30
Plan II
|
16047
(3209)
579
(116)
Plan III
4
24631
(4926)
1210
(242)
4002
(800)
286
(57)
20355
(4011)
719
saan
HE
1 an IV
(8831)
55818
(350)
2338
(1289)
8198
(97)
570
(5428)
28981
oS
1:1,
Plan Holiday
q:
an V
Z
VI@
26494
1015
16284
290
3866
1.
(11164)
(468)
(1640)
(114)
(5796)
oer
63350
2410
15860
976
29891
:2.
(12670)
(482)
(3172)
(195)
(5978)
age
2133
17296
1032
ae
46870
30501
(11718)
(533)
(7625)
(258)
—, (4324)
plan and st three years of Sixth Plan period
@ 4 year period including 1979-80 annual
are annual average.
Figures are total for period, and parentheses figures
e
,®
Source :
Health Information of India
(carlier called Health Statistics of India
and
GOI, various years.
Pocket Book of Health Statistics ). CBHI,
March 1989
s
DPR
RTE
_—_
SAB WE,
In the Second Plan period, expenditure on medical education almost tripled in contrast to less than doubling of
health expenditure. The average annual expenditure on
medical education during this period had increased to Rs.
38.04 million which was 8.3 percent of state health expenditure. (Table 5) This is reflected in the 46 percent increase in the number of medical colleges, a 28 percent
increase in outturn of MBBS doctors and over 2 '/, times
increase in post-graduates,
;
Between the Second and Third Plan periods state medical expenditure leaped again by 2 '/, times averaging Rs.
93.3 million per year during the Third Plan period. The
number of medical colleges had more .than doubled now
in comparison to the First Plan Period, and the outturn
too had leaped to 24631 from 16047 in the Second Plan
— a 53 percent increase. The post-graduate outturn again
increased at a much faster rate of 134 percent betwcen the
Second and Third Plans. Medical educatibn expenditure in
the Sth and 6th Plan annual expenditure to Rs. 680.1
million and Rs. 1467.07 million, respectively. (Table 5
This is a phenomenal expenditure when we consider
fact that!between 80 percent to 85 percent of this goes
production of medical graduates and that 75 percent o
these graduates go to the private sector. By any standar
this is a phenomenal drain on the resources of the publi
exchequer.
As if this is not enough there is another aspect of thi
drain of resources. Since the First Plan period the migra
tion of doctors to other countries, especially developer
ones, has been very high. In the First Plan period 81
doctors were migrating every year. In 1986-87 this figun
had reached 5304. (Table 8). At this figure in comp
son the outturn' of medical graduates than in the Fi
Plan, 32.35 percent of doctors migrated abroad and ;
1986-87 40.8 percent did so. This high rate of migra’
is very closely linked to imperialism. Our entire medic
the Third Plan period, increased to 12 percent of medical
services expenditure and 7 percent of health care expenditure. (Table 5).
;
The pattern of growth continued through the Plan Holiday and Fourth Plan period when state expenditure on
medical education was 14.3 percent and 16 percent respectively, of state medical services expenditure (Table 5). By
the end of the Fourth Plan there were 105 medical col-
Table 3:
Medical Care Facilities (Public and
Private) 1951-52 to 1986-87
Reference __ Hospiyears
tals
Dispensaries
_PHCs_ Hospital Popu-—
(only
Beds
lation
rural) (exclu- (millding
leges in India (96 owned by public bodies) and the out-
turn of medical graduates in the Fourth Plan period was
55,818 medical graduates and 8198 post graduates. By this
time the production of dentists had picked up and every
year about 468 dentists were qualifying. However, the
growth in the production of nurses remained slack, as
even in the Fourth Plan period only one nurse was being
produced for every two MBBS doctors. (Table 2).
The situation in the Fifth and Sixth Plans did not
_ change very drastically. Between the Fourth and Fifth
period the production of post graduates almost doubled.
The
-fatio of production of nurses to doctors worsened
in the
Fifth Plan, though improving slightly in the
Sixth Plan
(Table 2). The expenditure on medical education
in these
two Plans stabilized at about 13 percent of medic
al serv-
ices expenditure and 7 percent of health Care
expenditure.
The average annual expenditure on medical educa
tion in
the Fifth and Sixth Plan was Rs. 60.8.94
million and Rs.
1187.43 million, respectively (Table 5). Today
(1988) this
expenditure is about Rs. 3000 million (estimated by
author) and against this about 13,000 medic
al graduates,
4500 postgraduates, 700 dentists and
10,00 nurses are
being produced. Besides this there is capita
l expenditure
incurred every year. This data in the national accounts
is
available only from 1974. Thus in the 5th
and 6th Plan
periods
if capital
expenditure
on
medical
education
is
added to the medical education expenditure,
we see. that
capital expenditure accounts for 10.5 percent
and 19 percent of this combined expenditure, respec
tively, increasing
ions)»
PHC)
Plan I
i!
3307
7194
725.
(39.3)
Plan II
3054
(32.8)
Plan III
mage be a|
(32.5)
Plan Holiday 4023
(30.7)
Plan IV
4014
.
(25.2)
Plan V
6168
(29.1)
PlanVI@
7181
(26.4)
1986-87
7764
(21.0)
(84.0)
9406
(53.3)
(10231
(78.9)
10440
(79.1):
10200
(71.6)
15968
(69.8)
21780
(59.4)
25871
(53.2)
(23.0)
2695
(15.8)
4631
(18.0)
4919
3{ZE-0)
5283
(21.0)
5423
(17.4)
7210
(17.4)
14145
145297
229634
306518
328323
355361
476942
53637
594747
(17.6)
@ 4 year period including 1979-80 annual plan and
Ist three years of Sixth Plan Period. Figures at end
period,
Figures in brackets are percent rural.
Source : Health Information of India (earl
ier
of
called
Health Statistics of India and
Pocket Book of Health Statistics ).
CBHI, GOI, various years.
Statistical Abstract of India —1984,
CSD, GOT, 1985.
~
y
8
Radical Journal ofHea
education curriculum is western oriented. Doctors are
trained in a system which best suits the system of developed capitalist countries. This encourages migration. Not
and of imperialism (through migration). To conclude we
feel that the outturn of medical education needs to be
regulated. Public resources must be used for public benefit
:only this but international funding and via it policy too only— this should be the principle in regulation. The mix
plays its role in causing the continuation of the existing of expenditure also needs to be changed. More resources
system. For instance all the schools of medical excellence
have to be committed to the production of nursing profes(AIIMS, PGIMR etc.) have been set up with assistance of sionals whose numbers are only one-fourth of what should
imperialist agencies. As an example, between 1950 and exist in India today. Thus a drastic change is needed in
1974, nearly 99 percent of all health sector assistance by the investment and expenditure policy for medical education in India to change radically the growth patterns of
the Rockefeller Foundation to India went to medical education and research, including attractive fellowships for medical education and expenditure on it. This change is
even more urgent presently, given the wave of privatisastudy abroad (Rockefeller Foundation, ‘various years).
Thus, not only do doctors go to the private sector but a tion. In 1988, for instance, 13 new medical colleges have
significantly large number migrate to other countries as been sanctioned, bringing the total to 146 medical colleges; and the striking feature of this is that 12 of these
well.
colleges were in the private sector. The danger here is that
This, we, feel is a serious concern. We are not against
‘Jthe investment of medical education; in fact, if necessary, . even private colleges are funded through public finances.
Like education in general, this is also true of medical edu- investment must be increased. What is wrong is the drain
cation.
:
of public resources for the benefit of the private sector
Table 4 : Medical Humanpower 1951-52 to 1986-87
Number Registered at End of Period
ant
t
irri
Reference years
Dentist
Allopathic
Nurses
‘Homeopaths
AT
Ayurveds
Unani
Siddha
Doctors
PAPAS aN RE SE
RPO
AP
1 ELLE
OO
|
Plan I
76904
3003
24724
NA
NA
NA
NA
:
Plan Il
85784
4181
39350
27468
73382
NA
NA
Plan Ill
111580
4731
59914
NA
NA
NA
NA
Plan Holiday
138744
5485
77824
110514
155828
24530
15413
Plan IV
200003
6559
106751
145434
223109
30400
18128
Plan V
255138
8487
154230
112638
233824
28737
18357
Plan VI @
297228
8725
170888
123852
251071 °
28382
11532
1986-87 *
340000
10000
210000
150000
300000
28800
11600
|
Ist three years of Sixth Plan, period
-— @ 4 year period including 1979-80 annual plan and
* estimated by author.
NA = Not available
of dentists, is not vey reliable.
Note : The registered data, with the exception
Source : Same as Table 1.
Q
March
1989
‘tm,
se?
*
a
-a
Ae |
1951-52 to 1982-83
Table 5: Medical Education Expenditure
Years
¢
;
—
i
on a/c
Receipts
of medical
education
(fees etc)
ucatiion
esee
5
otninARS
ARIPA
ts
Ca
dd
ay
SE
aN
“ie
ehae
<i
=e
5.33
3.47
12.6
8.25
5.20
9.6
11.99
7.01
40.92
(13.64)
8.4
14.28
7.14
76.60
5.8
16.06
7.25
23.9
es
.
(4.78)
;
(38.04)
Plan III
466.5
Hs
Plan holiday
486.06
(162.02)
Hoes
Plan IV
1319.95
44.85
(8.97)
(93.3)
(263.99)
re
(15.32)
Plan V
3044.70
(608.94)
356.15
(71.23)
16.95
(15.39)
2.5
12.79
7.21
;
Plan VI
4749.72
1118.56
76.28
C7
13.33
6.95
(1187.43)
(279.64)
NR
SE
ert
Son
iTAME
ae
tcse
28.7
(3.81)
,
190.2
Ay
ale
a
Peo
1.3
Expenditure
19.05
oe
(13.28)
Plan II
Service
Expenditure
yp
66.4
Plan I
Total Health
Medical
i
Bees
:
Medical Education
Expenditure as
percent of
Percent } of
expenditure
received as
fees etc.
re a
(19.07)
ar
sh
Figures are total for period in Rupees million. Figures in brackets are annual average. @ 4 year period including 1979-80
annual plan and Ist three years of Sixth Plan period.
Source: Combined Finance and Revenue Accounts 1951-52 to 1982-83, Comptroller and Auditor General of India, GOI,
nS
oe
rr
.7‘.
>
‘
;
various years.
Table 6 : Medical Education and Teaching Hospital Expenditure in Maharashtra : 1981-1989
Rupees in Millions
Reference
Year
1981-82
1982-83
1983-84
1984-85
1985-86
1986-87
1987-88*
1988-89@
10
Medical
|
Education
Expenditure
Medical
Colleges
Expenditure
Teaching
Hospitals
Expenditure
Total Medical
Education
Expenditure
(1)
(2)
(3)
(1+3)
112.49
12-21
143.70
150.24
162.11
186.68
203.48
244.87
97.71
104.63
121.54
124.96
138.82
158.11
172.39
192.32
239.03
241.87
272.46
299.83
334.69
399.41
447.78
393.67
351.52
364.08
416.16
450.07
496.80
586.09
651.26
638.54
Column 2
as percent of
column 1
86.9
85.6
84.6
83.2
85.6
84.7
84.7
78.5
Radical Journal of Heals
_
*
@
CCU
Note:
Revised estimate
Budget estimate
Expenditure only for eight government owned medical colleges, excludes 3 municipal owned colleges of
Bombay and 1 private college.
Source : Performance Budget of Department of Medical Education and Drugs, Ministry of Health and Family
Welfare, Government of Maharashtra, 1983-84 to 1988-89.
Table 7 : Medical Education Expenditure in Selected Major States 1951-51 to 1982-83
State
i
Plan I
Plan II
|
R
1952-56
Union Government
Maharashtra
_ Gujarat
Tamil Nadu
West Bengal
0.94
27
7.08
2.24
(included in Maharashtra)
2.18
ot to
A
1.65
1.31
Percent share of
_ above govts.
a
_ Andhra Pradesh
_ Karnataka
_ Kerala
~
1957-61
;
31.9
bs aE!
aera
0.58
0.02
0.30
Plan Il
Plan
Plan IV
Plan
1962-66
Holiday
1967-69
1970-74
1975-79
1980-83
5.24
9.22
—6411
6.44
2.91
12.71
11.92
8.35
ISS
8.36
16.62
23.08
13.80
25.91
13.24
149.00
48.92
22.62
46.30
37.73
295.33
112.41
47.43
77.00
68.17
50.0
vrs
50.1
34.0
35.1
Tn mn
10.36
4.91
5.18
14.56
6.56
9.76
20.63
1 ee
13.69
38.97
29.20
26.34
75.04
60.15
52.94
4.59
5.82
8.47
8.74
1520
11.87
43.44
25.73
59.43
40.99
UO
i
0a,
5.36
1.09
1.98
1.25
se
V_— Plan VI@
4.10
8.03
4.40
6.32
/ Goa, Daman & Diu
a
Uttar Pradesh
Madhya Pradesh
0.69
|Wigyh4
0.81
2.89
Bihar
ajasthan
0.32
0.21
0.35
0.78
2.38
1.44
3.17
1.59
3.58
4.49
8.18
6.12
Sai
10.59
14.00
12.80
9.27
16.30
24.07
19.34
15.96
25.97
16.54
12.87
42.53
46.11
26.2220.28
0.98
2.39
9.55
Tadd
8.98
. 19.62
36.40
Ske
3.89
20.78
12.84
38.47
58.38
issa
Assam
Punjab
—
nee
(included in Punjab)
—-
1.16
1.67
2.23
Union territory
0.33
2.76
0.09
1.08
3.52
11.71
23.83
INDIAN TOTAL
13.28
38.04
93.30
162.02
263.99
608.94
1187.43
Haryana
Jammu and Kashmir
Other States &
ns.
Figures are Annual Average of Period in Rupees Millio
three years of 6th plan.
first
and
@ 4 year period including 1979-80 annual plan
Source: Same as Table 5.
thageh. 1080
/
Table 8: Migration of Doctors to Other Countries: 1951-52 to 1986-87
|
He
a
:
a
Reference Years
No. of Doctors Migrating
Plan I
Plan II
Plan II
4050
5175
5950
Plan Holiday
7200
Plan IV
Plan V
15450
21300
Plan VI @
18548
1986-87
Annual
Avcrage
st
810
1035
1190
.
:
2400
3090
4260
4637
5304
5304
@ 4 year period including 1979-80 annual plans and first three years of Sixth Plan.
Source : Health Information of India, CBHI, various years
=
f
The Brain Drain Study: Phase I — Analysis of ordinary passport issued during 1960-67, IANR, 1970.
*
_ [This article has been prepared from data that was col-
:
lected by the author and other colleagues at the Foundation
for Research in Community Health on a research project
study on State Financing in India sponsored by the India
Council for Medical Research]
—
References :
CAG/GOI
CBHI/GOI
1985
CBHI/GOI
id
: Health Information of India, 1987
CBHI, GOI.
3
a3;
: Combined Finance and Revenue Accounts
Comptroller and Auditor General of India.
GOI, various years.
: Directory of Hospitals in India 1985
- Central Bureau of Health Intelligence,
GOI, 1986.
|
Rockefeller : Annual Report, various years.
|
Foundation
REPRODUCTIVE
AND GENETIC
ENGINEERING.
A
"i
pie
‘
2 [Journal of International Feminist Analysis] (published three times in
a year) RGE is designed to
facilitate the development of feminist multi-disciplinary and international
analysis on the new reproductive technologies and genetic engineering and their impact on women
worldwide. The policy of
the journal Is to recognise the use and abuse of women as central
to the development of reproductive
technologies and genetic engineering and to highlight the relevan
ce of the application to these technologies to the past, present and emerging social and political
conditions of women.
)
RGE is edited by International Editorial Collective and
Editorial Advisory Board.
Subscription :
One year (institution) $75
Two year (institution) $ 142.5
One year (individual) $ 25
Send International Demand Draft or
Money Order to :
Reproductive and Genetic Engincering Perg
amon Journals Limited,
Headington Hill Hall, Oxford Ox3 OBW
England
Radical Journal of Health
Fsmn
Political Economy
Cem
cont i ee:
Of SO
Fs
Pea
Sb
ee
Tk hay
ae
pee
Be
<'5
of International Migration
ie
Indian Physicians to United States
t k ishi
(Saran and Eames 1980, Fisher 1980). There is,
however,
tive is needed to fully understand this recent movem
ent
The purposes of this paper are 1 ) to present a theoretical frame
work to explain this phenomenon within the context of the international political economy, and 2 ) to apply this framew
ork to the migration of Indian physicians to
the United States for the period between the mid-60s to the mid-70s.
This study is part of a larger project by the
researcher
on a comparative study on the international migration of physicians
and nurses from Asia, mainly from
India, Korea (republic) and the Philippines.! (This article has been reprinte
d from South Asia Bulletin, Vol I, No
eI; £982.)
_
BEFORE
presenting the theoretical framework, previ-
Ous theories on international migration should be bricfly
mentioned.’ The first major theory deals with ‘push’ and
‘pull’ factors operating separately at the countries of origin
and destination of migration. The weakness of this theory
lies in its failure to see the complex relationship between
_the two sides of migration. Morcover, the theory tends to
:focus on individual motivations to migrate. The second
theory is the ‘equilibrium’ theory from a neoclassical eco“nomic model. This explains international migration as a
“natural process of the movement of people to reduce exist-.
ing inequalities in the supply and demand of lajyour, as
well as in the incomes between the countries of origin and
destination.
However,
this
approach
cannot
explain
non-economic variables such as immigration laws. Furthermore, this ignores the fact that international migration,
many occasions, resulted in unequal development, as in
he case of migration to western Europe (Paine 1974).
Literature is increasingly available on international migration from a new perspective (Bach 1978, Bonacich and
Hirata 1980; Castells 1975; Petras 1981; Burawoy 1976;
Portes 1978). This perspective tries to sce the international
migration of labour within the context of 'core-periphcral’
relationship. In other words, immigration serves as a deliberate tool to further the economic development of developed countries (DCs), while emigration
the distorted
development
is caused by
of less developed
countries
(LDCs), influenced by the dominance of DCs over LDCs.
The following study is based on the above approach
and tries to examine the validity of the approach by ap-
plying it to a case study on the migration of physicians
from India to the United States.
The basic variables for the proposed theoretical framework are as follows:
Py The labour need for the economic development of DCs;
2) The role of the labour sector in DCs;
3) The role of the governments of DCs;
March- 1989
4) The labour surplus caused by the failure of LDCs in
economic development;
5) The role of the governments of LDCs;
\
6) The role of the labour sector in LDCs;
7) The cultural, economic and technological hegemony of
DCs over LDCs.
DCs with successful economic growth up until the early
70s required a larger labour force in construction, services
and professional ficlds. Also, a
‘dual labour market’
(Piore 1979), which produced a division in the primary
and secondary sectors of industries, as well as in occupations, existed, Foreign labour filled the absolute shortage
of labour, and the shortage created by the dual labour
market as well.
The labour sector in DCs was very sensitive to immigration, particularly when domestic economies were declining. Fears of competition with foreign labour and lowering effects on salaries by foreign labour were aroused.
This pressure from the labour sector in relation to the labour needs for economic growth was the concern of DC |
governments.
As a result, from time to time, DC govern-
ments accommodated the above counter pressures, and manipulated the import of foreign labour with various legislations and regulations.
In response to the labour needs of DCs, LDCs filled
these needs with their labour surpluses. In fact, the emiphasis on gross national products for development plans in
LDCs, by and large, neglected unemployment problems.
Second, the neglect on the economic development of rural
areas caused severe problems in urbanisation. Furthermore,
the emphasis on the expansion of capital-intensive induslogy
trics with the assistance of foreign capital and techno
In
nous
indige
resulted in'a retreat in the development of
dustrics. As such, emigration pressure from various Segments of the dislocated population
rosc
The governments of LD¢ "s ¢ ither
the emigration
of
their own
peopl
ignored
Of encouraged
Indeed,
“migration
emigrati
MUCT
Sta
served as a safety-valve for the acute unemployment situ- ~ labour is crucial for
tion in the context of the political economy
ation in LDCs. Furthermore, remittances sent by emigrants
LDCs.
from abroad became indispensable for LDCs to acquire
The following is a case study of the migration of I
the foreign exchange needed for their development strate-
gies and debts in foreign loans. Generally speaking, however, the labour sector as a collective in LDCs was weak
in influencing government policies. Therefore, the labour
sector had nearly no influence on emigration itself. Nevertheless, in the administrative and professional sectors (including the medical profession) entrenched personnel suc-
cessfully maintained their positions by excluding new en-
aeehs
oa
or)
ae
seme”
\al
trants. In the general context of slow development, these
frustrations faced’ by recent graduates forced many of
—
them to emigrate.
Aside from the above framework, an understanding of
the cultural, economic and technological hegemonics of
DCs over LDCs which had a tremendous impact on
migration from LDCs to DCs should be incorporated.
Through these hegemonies, the flow of capital, technology, information and goods from DCs to LDCs apparently
contributed to the emigration of people from LDCs to
DCs.
|
The following piece of information is significant in
order to grasp the above concept. The US Government
dian physicians to the United States from the mid-60s
the mid-70s. This case could be considered as part of the
‘brain drain’. Although the theoretical framework discus
earlier does not specify the migration of high level manpower, such migration can be similarly regarded as a phenomenon of international labour migration duc to the role
it has played [Portes 1978]. Thus, the framework discussed will be used to analyse the following case study.
The reason why physicians are of particular interest is that
more data and literature is available for this group than
for other occupational groups, and second, that the number of physicians who came to the United States is remarkable.
The period from the mid-60s to the mid-70s was particularly chosen for study because it was during this ume
that, in a historical context, the international migration of
physicians was most prominent. This means that beginning
in the early 60s this migration phenomenon became acute
and declined after the mid-70s. This case study, thus, focuses around this period; however, on certain occasions, as
recently began to concern itself with international migraneeded, the period prior to and after the mid-60s to midtion in terms of its foreign policy, because most countries
70s will be touched upon.
;
with high emigrant populations were major recipients of
US foreign assistance, major partners of US trade and
Magnitude of Immigration From India
targetted areas of US direct investment [US Agency for|
In viewing the immigration of Indian physicians to the
International Development 1980; Morrison 1980]. MoreUnited States, it should be understood that this phenomeOver, most countries of emigration were of the more developed countries among LDCs. This fact may suggest
non is only part of the general trend of the emigration of
that the process of economic development in those counAsian Indians to other parts of the world during the 60s
tries was much telated to the emigration of their own
and 70s. One major trend was. the immigration to DCs,
people despite, or because of, their intimate relationship
mainly the United States, the United Kingdom and CanBid
AME
Ce
megs
ee
EMEA
«|
SEY
1yes
Mae
Nee
eNO
Oyen
Se
Men
NMR
aR
S=ee
7)PORES)
. with the United States.
ada.* Another trend which became important recently was
Before concluding this section, two points should be the immigration to the oil-producing Middle East [Mcmentioned. First, freedom to leave countries: was granted,
Carthy 1979]. With this in mind, the magnitude of the
freedom to enter other countries was not. In this respect,
migration of Asian Indians, particularly of physicians, will
the economic advantage of DCs over that of LDCs greatly
eh
api
th
tale
be described later.
influenced the direction of international migration.
As Table 1 shows, the number of Indian immigrants to
Second, the relationship between DCs and LDCs was the United States has been considerable since the passage
mutually interdependent, although not under equal terms.
of the Immigration Act of 1965. Prior to 1965, the immiDCs had an overwhelming amount of power over LDCs
gration of Asians in general was severely restricted under
through the movement
of various factors such as Capital,
technology, military and information. Through this, the
world economy became more and more Systematically integrated into a global unit. In this respect, international
migration cannot be comprehended if considered in isolation from the above perspective.
International migration was sought after in DCs as a
cheap and substitutable labour source to alleviate the labour shortage. At the same time, multinational corpora-
tions left DCs in search of a cheaper labour force in the
LDCs. Thus, the concept of an international division of
the McCarran-Walter Act of 1952. Among various occu-
pational categories, professionals and technical workers
were the largest. This was, of course, due to the preference for professional immigrants in the immigration law.
As a matter of fact, Table 1 shows that a significant
number of Indian immigrants was admitted under the third
preference of the immigration law, which includes professionals, scientists and artists, although, since the mid-70s,
more non-professionals are tending to immigrate.
(See
Table 1)
In addition to the immigration statistics, the number
of
14
Radical Journal of Health
~.
er
‘tudents was significant.
The reas on
“this was that Physicians who
were exchange visitors
re, first, potential immigrants, and
second, performing
ties and work in similar areas as were
immigrant physi-
uans.
As for Students, they were importan
t because many
Stayed in the United States to seek employme
nt opportunies after completing their studies.4 Table 2
indeed, indithe magnitude of the numbers of Indian exch
ange
visitors and students, as well as those who adjus
ted their
peatuses to immigrants while remaining in the
United
States. (See Table 2)
c However, as both Tables 1 and 2 clearly show, a deClining trend. existed in the immigration of professionals
a
of those adjusting from non-immigrant statuses to perManent residents. This was mainly due to the further in-
flux of relativesof US citizens and immigrants, and partly
sue to a restriction on the admittance of professional
famigrants, particularly physicians, as will be discussed
ater.
_Regarding the Foreign Medical Graduates (FMGs) receiving US licenses for the first time, their proportions to
he total number of those receiving licenses rose from 5.1.
percent
in
1950
to 22.4
percent
in
1968
[Kabra
976:600].
In terms of Indian physicians, unfortunately, no
shronological data, except for some fragmented data, is
vailable. For example, a survey of Indians in the New
‘ork Metropolitan Area in 1978-79 showed that 16 per-
sent were doctors [Leonhard-Spark and Saran 1980: 154].
New York State was the state which the largest number of
new Indian immigrant, 24.1 percent between 1970-76,
declared as their destination upon arrival [US Immigration
d Naturalitation Service: 1970-76]. This fact implies the
‘istence of a significant number of Indians immigrant
#hysicians in the United States. Also, Table 3, although
“Hh of a recent period, shows the magnitude of these
imbers. This data, particularly in 1972, illustrates the
existence of a significant proportion of Indian physicians
to the total number of immigrant and exchange visitor
physicians in the United States. (See Table 3).
| In short, although accurate data on the number of In-
dian physicians in the United States is not available, the
magnitude of immigrants, as well as exchange visitors
apparently increased greatly after 1965. A study in India
f the Council of Scientific and Industrial Research also
fevealed in 1973 the significance of the outflow of Indian
Nc tors, along with scientists and engineers [Kabra
1976:75).
US Need For Foreign Medical Graduates
onals in the
In 1970, the percent distribution of professi
Jnited States was
rH
14.6, while those in 1950 and 1930
8.6 and 6.8 respectively [Chen
1980 : 144]. This
was partly a conscYA ge in occupational distribution capit
al by modern tniwence of the demands for human
Ch 1989
—
tures for health care in the United States? Sorkin
[1977:2], in answering this, states that the growing expenditures were mostly attributed to the utilisation of health
Care services and to inflation, but little to population
growth because it was proportionately low. [See Table 4].
The most significant reason for the greater utilisation of
health care services was the introduction of the centralisation of the health care system in the United States since
the second world war. In the public sector, the basic
change occured in 1966 with the Social Security Amendments to implement Medicare and Medicaid. Thus, the
public expenditures for health care and the rate of total
expenditures drastically increased since then, as seen in
Table 4 [Sorkin 1977: 2].
In the private sector, total expenditure rose sharply due
to a big expansion in health insurance plans, which were:
sucessfully resisted by the American Medical Association
(AMA) before the second world war (Kim 1981: 150)
Another aspect of the demand for physicians was due to a maldistribution of physicians in the health service system
in the United States. This meant, for example, that native
physicians tended to choose suburban areas as sites for
their more profitable private practices. Therefore, it left
4,000 to 6,000 unfilled positions per year in the inner-city
hospitals [Mick 1975:
15, 18 and 19].
However, despite the fact that a drastic increase in the
demand for physicians existed in the United States, the
AMA failed to respond positively. It maintained a restrictive attitude towards the expansion of medical schools, as
well as towards the expansion of national health services
[Hock 1970: 27].:The physician/population ratio actually
declined from 1950 to 1960 as seen in Table 4. In fact,
such a ‘cartel-like guild’ attitude was intended to keep the
income of the physicians high [Adams and Dirlam 1968:
260]. As already evident, although the AMA is not a labour group, it played a similar role as the labour sector
described in the theoretical framework of this study. In
short, the AMA pressured for the maintainance of the
prestige and high incomes of US physicians by attempting
to retain a monopoly on the labour supply.
import
Thus, facing a severe shortage of physicians, the
pard,
of FMGs (Foreign Medical Graduates) was neede
als. As
ticularly for intern and residency positions in hospit
one third of all the
a matter of fact, during the mid-70s,
FMGs, which
medical graduates in the United States were
included many Indians. The result was to divide the physician population
two classes:
of this country,
natives and
FMGs
ie the United
[Mick
1975:
States, into
14 and
17}.
tla
cae
la
ean
EN
ls
all
A
hh
Ah
tk
ae
Sayaa
aI
iTit
re
=
TCOS
Moreover, it was natural that the import of FMGs was
desired because it was quicker and cheaper than producing
native medical graduates [Reddy 1974: 376]. It should be
added that FMGs were faced with problems in state licensure and underemployment. This meant that many FMGs
failed the state licensure examinations which allowed them
to practice their professions, and that many worked in
lower-skilled jobs such as technicians and assistants.°
Considering the shortage of physicians caused by the
expansion of health care services and the reluctance of the
AMA to produce physicians according to the proportionate
need in the United States, the US government passed various provisions so that foreign professionals, mainly Asians
_ remaining in the United States, could become immigrants,
Te
ee
American medical profession not to rely on
cians. English language ability and the quality of
ance in the delivery of health care “were reasons given.
—
States were se-
;
Thus, the influx of FMGs
to the United
verely interrupted. Of course, this new legislation greatly
affected various hospitals in need of FMGs [Stevens et al
1978: 273-275]. It should be added that due to several
health legislations after 1963, the rate of increase in the
number of US medical graduates switched from 0.8 percent for the 1956-66 period to 4.8 for the 1966-73 period
[Sorkin 1977: 87-103]. Therefore, by the late 70s, it was
expected that US medical graduates would absorb the
shortage. Thus, it can be said that the role of FMGs was
temporarily to fill the shortage created by the delay in a
sufficient production of US medical graduates.
As already clear, in addition to the US need for FMGs,
even before 1965.° Otherwise, Asian professionals were
unable to become immigrants under the McCarran-Walter
Act of 1952, which barred the admission of large numbers
of Asian immigrants. Consequently, in 1965, despite the
reluctance on the part of public opinion to admit non_white immigrants, other pressures from thé government
and business communities succeeded in changing the McCarran-Walter Act in order to receive more professional
immigrants. Interestingly, this change was paralleled with
as well. The-ne.t question to be asked, then, is, "Why did
the expansion
many
of higher
educational
systems
in many
Third World countries. According to the new immigration
law which became fully effective in 1968, professionals
were, categorized under the third preference [Public Law
89-236]. It is needless to say that the influx of FMGs,
including Indians, into the United States partially relieved
the shortage of physicians, particularly in hospitals in this
country.
In addition to the major change in immigration laws,
other legislation in regard to the migration of physicians
should be mentioned. First, the screening test for FMGs in
1958 by the Educational Council for Foreign Medical
Graduates (ECFMG) was established. The test was admini-
stered in various countries outside of the United States,
and FMGs had to pass the tests in order to be employed in
the United States. Second, the Mutual Educational and
Cultural Exchange Act of 1961, which provided the exchange Visitor Program, was modified in 1970 in a manner so that the two year foreign resident requirement for
exchange visitors before they were eligible to become
immigrants, was eased. This amendment [Public Law 91-
225] offered incentives to exchange visitors to adjust their
Statuses. In fact, the number of ad justed FMGs became the
major group of new immicrant entries, as Table 1 sug-
gests [Stevens, ei ai 1975: 440].
However,
the trend surely changed after the United
States tightened the entry of FMGs
with the Health Pro-
fessionals Educational Assistance Act of 1976, under the
Congressional assumption that there was no longer a short-
age of phyicians in the United States. This act applied
to
both FMG immigrants and exchange visitors. Behind this
legislation, pressute existed from the various bodies of
the
various legislation and regulations similar to a ‘tariff policy’ [Thomas 1968: 40] played a significant role in the
supply and demand of physicians in the US market. The *
international migration of FMGs to the United States was
manipulated by different interest groups such as hospitals
and the AMA (:: quasi-labour group), and the government,
FMGs
in the United States come
from particular
countrics such as India?”
Indian Reply To US Need
In India as in the educational expansion of most LDCs,
higher education, in particular, was considered very essen-
tial for economic development in the face of an increasing
importance of human capital. In fact, the annual growth —
rate in college enrollments and the total expenditures in
higher education were 10 to 13 percent in the 50s and 60s
(IIchman 1974: 121]. Any attempts to restrict admissions
in higher education was avoided because they were unpopular and politically unwise [Tobias 1968: 39]. More-
7
over, in addition to the inability of the Indian government
to control the output of graduates due to its decentralised
System in higher education [Domrese 1970 : 226], several
—
five-year development plans failed to absorb the graduates
into the Indian domestic labour market, leaving severe™
unemployment [Puttaswamaiah 1977: 79-106]. In short,
the lack of coordination between education and human
power planning caused educated unemployment, which led
to the emigration of many cducated people from India.
With regard to physicians in India, the situation was the
same, although not as severe as for scientists and engineers
[Ghosh 1979: 281]. The expansion of medical education
in India after the nation's independence was great, particularly during the Third Five-Year Plan between 1961 and
1966. According to Mathur [1971: 76, 77 and 93],
the
actual annual intake of medical students rose from
2,675
in 1951 to 11,106 in 1968, along with a-tripling
in the
number of medical colleges. And, the estimated
surplus of
16
Radical Journal of Health
’
, Stag
tors IT the future supply and demand of doctors in
~~ India, utilising various methods to estim
ate projected
snumbers, were 13,000 in 1971, and 32,000 in 19768
onetheless, as long as a shortage of physi
cians in terms
ofa physician/population ratio existed, the
production rate
_ of medical graduates was expected to be larger
than the
_ growth rate of the population in India according to
Indian
_ Planners [Tobias 1968: 140]. How could this contr
adictory
_ phenomenon be explained?
_
a
One explanation lies in the maldistribution of physi: cians in India. This meant that most physicians refused to
_ work
in rural areas or public services because of lower
_ Temunerations and the lack of facilities available in those
_ areas. Physicians were concentrated in big cities and de-
_ veloped
areas
where
higher
income
was_
expected.
{Marthur 1971: 61]. In the economic sense, the purchasing
‘powerof medical services in rural areas could not mect
the expectations of medical graduates in terms of the ex-
pected high incomes and the cost for training these physi-
_ cians. In addition, the lack of logistical -facilities in rural
"areas and public services created a reluctance among phy-
[Dandekar
1968:
217-219}.
Thus,
the conflict
between
seniors, or established gencrations, and juniors, was serious, and many young professionals could not better their
opportunities in India. In effect, ‘elite feudalism’ {[Khadria
1978: 103] maintained the status quo of established professionals and prevented the incorporation of increasing
professionals. Such negative factors, of course, facilitated
the emigration of professionals, including physicians.
Upon considering the factors influencing the emigration
of professionals, what were the responses of the Indian
government? The situation of a brain drain was repeatedly
discussed by LDCs. Yet, there was no definite assessment
in regard to whether the migration of high-level manpower was a loss to the countries which produced emigrants, and how the LDC governments could prevent their
people from leaving their countries.
Wie
_ _ India was not an exceptional case. Although India tried
to discourage the ‘brain drain,’ it was actually not among
the most urgent issues needing to be resolved, as will be
described later. There were more acute problems caused
by underdevelopment. The government, overall, could not |
_ Sicians with specialized training to work there. Therefore, _ effectively control the exodus of its high-level manpower.
es
a mere consideration of the physician/population ratio in’
It was only in 1958 that the Indian government took
“India, as a whole, could not be a sufficient indicator in
concrete action in establishing the Scientists Pool for
planning the output of physicians. As Gish [1975: 5-7]
qualified Indians abroad. The objective of the pool was to
_ describes, the maltraining and malutilisation of physicians
_ should also be regarded as being importantin understand:ing this unequal distribution between city and countryside.
provide temporary placement for persons returning from
abroad with high qualifications, mainly in science, technology and medicine, until they could find permanent
In short, a lack of coordination between the desire to
expand the production of medical graduates and an inabil-
posts in India [Abraham 1968: 88-90]. However, the pool
system proved to be ineffective in encouraging qualified
ity on-the part of the country to utilise these graduates,
persons abroad to return home because it did not coordi-
along with the maldistribution of physicians caused unemployment problems for physicians, mainly in the major
cities of India. Nonetheless, the employment concern of
nate its efforts with existing employment opportunities and
conditions in India [Domrese 1970: 250; Abraham 1968:
105-6; Tobias 1968: 190]. Moreover, although the govern-
,ndian economic
ment
development was treated as a minor
’ problem. The emigration of Indian physicians, therefore,
could be seen at least, as an alternative to resolve the
unemployment problem by individual physicians sccking
_ prospective jobs in other countrics,
In terms of the employment structure of professionals
_ in India, particularly that of physicians, it is not clear how
the government viewed the emigration of their professionals. However, it should be mentioned that, as Banerjea
1975: 192] notes, favouritism, nepotism and seniority in
appointments and promotion affected the younger professionals.
Through
of favouritism
the use
nepotism,
and
only those having political and personal ties with the hiring sclection commitices
and promotion
personnel tended
to be selected. Thus. the qualifications of those secking
of secondary
concern.
| Of course, this type of practice was also common
in other
appointments
or promotions
were
IDCs.
The professional structure inherited from a British
model also limited the opportunity for juniors, or younger
generations,
in terms
of positions,
as
well
as
income
tried to bring
back
high-level
manpower
from
abroad, it did not intend to prevent them from leaving
India.
ye
Concerning the medical fields, the government did take
some actions against the emigration of physicians, One
such action was the government banning of tests given by
the Educational Council for Foreign Medical Graduates
(ECMFG), which screened FMGs for work in US hospitals as interns and residents. Indian physicians, however,
were still able to take the tests in neighbouring countries.
Another action required medical graduates from state
medical colleges in India to serve the public health system
in medical fields for a limited period [Abraham 1968:
abso110]. These measures were apparently based on the
lute shortage of physicians in India as earlier mentioned,
and the
resulting from the low physician/population ratio,
maldistribution of physicians in the country.
cians, the
Although not particular to the case of physi
ation of high
role of the Indian government in the emigr
, is discussed
level manpower, including medical manpower
below.
As previously stated, the government
did not ser
19
March 1989
ously concern itself with the emigration situation. For
example, in a report by the Education Commission for
1964-66, a statement indicated that the 'brain drain’ issue
was over-exaggerated.? What were the underlying reasons
behind the neglect on the part of the government concern-
ment did not want to be scrutinised over the human righ
of people to leave the country freely by heavily taxing
people [Bhagwati 1976: 13]. To the contrary, as in
case of the emigration to the Middle East, the governmen
even encouraged the emigration of its own people whethe:
they were labourers or professionals due to acute uneming this very issue?
It appears that there were two major reasons for the. ployment and the lack of foreign exchange in India.
neglect. One was that the government was unable to tackle
the problem of unemployment, in gencral, and of its educated people in particular. This implied that the issue was
‘overflow’ not ‘brain drain’ [Baldwin 1970: 358]. Whether
_ Or not it is appropriate to use the term ‘overflow,’ it is
definite that the’ emigration of high-level manpower, including physicians, served as a 'safety-valve’ against the
acute unemployment situation [Blaug 1969; 161]. It was
also true that educated unemployment was a_ political
threat to the state because the educated were influcntial
enough to address their own concerns.
US. Indian. Linkage
It has, thus far, been argued that the emigration o
Indian physicians to the United States was caused mainly
by US demand, and partly by a surplus of physicians in
India resulting from the underdevelopment of the country.'
Also mentioned was that population movement as such
was directly promoted by immigration legislation in the
United States. However, in the final section of this paper,
the linkage between the two perspectives, the United
_ Another reason was related to the foreign exchange — States and India, will be discussed. In fact, the US-Indian
reserve. India, as one of the developing countries, reccived political economyis a basis for understanding the migra.
:
\
a large amount of foreign capital through forcign assis- tion.
_ tance and direct, foreign investment in order to develop its _. Beginning in 1956 through the Second and Third FiveYear Plans, the Indian government emphasised the expan- economy. Nevertheless, in doing so, India became largely
: 2 reliant on foreign capital historically from the United “sion-of the public sector by introducing heavy industries.'?
of industiresin the
Kingdom and contemporarily from the United States. It is As a matter of fact, the development
production
of
goods,
particularly
steel,
machinery and
_ needless to say that foreign exchange was also required to
_ pay off debts accumulated through foreign loans, and the chemicals, was accelerated during this period. On the
import of oil, machinery and technology. ©
other hand, this tendency to place an intensive emphasis
In relation to the emigration issue, the governments
on the heavy industries of the public sector caused reac‘Tefusal to grant foreign exchange for the operation of the
Association for Service to Indian Scholars and Technicians.
(ASSIST)
in the United States and the United kingdom,
tions in the Indian economy, as a whole. For example, by
ignoring other sectors of the economy, eg agriculture and
“small enterprises, such problem as stagnant agricultural
which was to coordinate Indian high-level manpower from ©production and the existence of widespread manual indusabroad and provide placement in India, implied a priority | trices were perpetuated. This situation led to an imbalance
set on foreign exchange by the government [Tobias 1968:
in trade because India had to import agricultural goods as
192]. Such concerns were reflected in the control of for- well as machinery and equipment, and to maintain its ineign exchange acquired through the Reserve Bank of In- vestments throughout.
the Five-Year Plans. In addition, by
dia. And in the case of medical graduates, they were able _heglecting light industries, where its strength was, India's
to receive foreign exchange conditionally [Domrose 1970: exporting powers were weakened. Therefore, Table 6 il246 and 247]. In short, as Blaug [1969: 159] states, the lustrates the trade deficit expanded from the late 50s to
‘brain drain’ was unfavourable, but the foreign exchange
- problem was worse.
Along with the decline in foreign exchange reserve, the
importance of remittances sent by Indians abroad began to
play a significant role in acquiring foreign exchange,
as
Table 5 iflustrates.!° Various measures taken by the govemment to encourage the emigration of Indians into the
Middle East were such an example [Nadkarni 1978].
In
respect to the emigration to the United States, the situati
on
was not clear, but a large amount of remittances to
India
was, naturally, expected.'' (See Table Ss):
In sum, the overall policy of the government regar
ding
the emigration of professionals consisted in posing
few or
no obstacles to their leaving the country. There
is no
doubt that, unlike the Soviet Union, the Indian
govern-
the late 60s. However,
the domestic market which was to
absorb the output of newly built heavy industries remained
weak. This was due to the continuing existence of the
widespread poor segments of the Indian economy, which
was perpetuated by the industrialisation policy. As a result
of this gap between the primary and secondary sectors of
the economy, India, lacking the capital to import goods
and to maintain its industrialisation policy, began to rely
on foreign capital, either in the form of aid or direct investments. (Sce Table 6).
In looking at Table 6, it is obvious that the proportion
of Indian import from the United States increased from
13.1 per cent in 1955-56 to 38.0 per cent in 1965-66, and
also that the United Kingdom underwent a decline in its
influence,
18
Radical Journal of Heatth
Sucha shift in i
:
eaten aoe influence from the United Kingdom to
aE
,
was
a clear manifestati ion of the US
:
ony over India during this perod, a
|
amer Asian countries. - Table
Fable 77 illustrates eee
the magnitude of
§B foreign
aid
throughout
the
world
the 1
oe
rid. To be sure, India
as
the largest recipient of US foreign aid throughout
th
mid-50s to the late 60s. s. O Of course, , this was due
piweas
to the2
:
:
economic potential and strategic importance of India as
noted by the US agency for International Devel
966: 106]. : The US shareare in
i foreign aid to IndiaMaes
Res
1966:
was the
largest, at 51 per cent, not mentioning the share from the
Vorld Bank, which was primarily US controlled [Ito
1972: 126]. (See Table 7).
,
the development of the indigenous technology of India.
Therefore, Indian telent became isolated and was not able
to contribute to the country's own technological development [Ray 1971: 2061]. As long as India depends on
multinationals for capital and technoiogy. India will continue to rely on the imported technology of the United
States.
Of course, in addition to the monopolisation of technology by the United States, the gap in the absolute amount
of expenditures and the percentages to the gross national
product (GNP) in Research and Development between the
United States and India, 34 billion dollars,or Rs 26,000
crore (3.4 percent of the GNP), and Rs 150 crore (0.43
While Indo-US economic relations were deepened percent) respectively in 1971-72, perpetuated the existing
a rough trade and aid, direct foreign investment in India US hegemony in technology [Banerjea 1975: 190-191].
of the United States, which
As _such, the technology
SO was outstanding beginning in this period. The US
are increased 9 per cent in 1955 to 27 per cent in 1968,
: “hile that of the United Kingdom declined from 83 perent to 41 percent in 1955 and 1968 respectively [Ito
1972: 131). This meant that India ceased to be a monopo-
was notavailable in India, became attractive to Indian professionals, including physicians, who wanted to pursue ~
further research and training. Several surveys do indicate
convincingly that professionals who leave their countries
and live in the United States permanently do so largely for
the research facilities and logistical supports available only
ed market for the United Kingdom, while the United
ates became more influential. In fact, as Table 8 shows,
3} investment in India, through US affiliations and rupee in the United States
mpanics controlled by US capital, as well as technologi-
t
[Oh 1977; Cortes 1974].
However, it was not only individuals who sought US
| collaborations, increased tremendously beginning in the
s (See. Table 8).
India did not take a policy of export expansion until
technology but institutions in India as well. This point
needs clarification since India, from its colonial period,
the output of Indian industrialisation. A huge deficitin
tute of Technology, Kanpur,
modelled itsclf after the United Kingdom. Yet, as the
United States came to lead the world in technology, US
carly 60s. Capital flowed mainly from the United
on Indian educational and research institutions
aics in the form of aid and private investment, which ‘influence
nt. A typical example was the Indian Instiindispensable for the increase and/or maintenance became appare
Became
established through the assis-
-
;
to pay
“the balance of payments in India made it difficult
by
‘soar previously received. The situation was aggravated
tance of the United States [Sreenivasan 1978}.
7jpPrace of US aid. With this crisis in India, India
from the US
received 6 million dollars for its construction
rned with
government. Among private foundations conce
temporary
Tuye Indo-Pakistan War of 1965, along with the
anged its development policy after 1965 by devaluating
b e rupee, relicving economic control by moving towards
en revolution’ and
iberalisation, implementing the ‘gre
private sector. Necden phasising the development of the
ng
modification was to accommodate a stro
! less to pa
ld Bank, belonging to
itside pressure, primarily the Wor
by the United States. In
ne Aid-India Consortium, led
on foreign collaboration
is respect, having already relied
ar, the Indian economy
From the United States in particul
within the US hemisphere.
ce became deeply involved
understanding the migration
‘Important, particularly for
the hegemony of US techF physicians, is the factor of
ains,
As Kabra [1976: 53] expl
wlogy over that of India.
in
became a common feature
| technological ‘colonialism’
e
Sinc
nt of multinationals.
Iidia through the instrume
own technology which was
iultinationals utilized their
for
was brought from abroad
and
ge
chan
l
inua
cont
Mer
keep up
impossible for India to
J (aie use, it was
, largetechnology. As a result
‘digest the imported
wed down
n collaboration, slo
eig
for
h
wit
n
le industry,
th 1989
AllIn relation to the medical field, the case of the
se it
India Institute of Medical Sciences was notable becau
public health and medical research, the Rockfeller
Founda-
Indian Association was most active with its grant to the
Education [Sodeman
tion for the Advancement of Medical
for teaching and
1971: 168-170], and provision of funds
colleges and institutes
rescarch equipment to many medical
clearly a very important
in India. Family Planning was
1978: 170-71).
project of the Foundation [Mukherji
gy and equipment for
The introduction of US methodolo
led individual students and
teaching and research no doubt
cation in ‘the United States.
graduates to seck higher edu
ad programmes encouraged
Also, needless to say, studyabro
ically
were another factor. Iron
by the Indian government
technoland importing westem
the purpose of absorbing
not well
abroad programme was
ogy through the studydid not
number of students who
achieved due to the large
Ay
return home.
HT
h as
of elite institutions, suc
The fact that graduates
Post
us
gio
sti
and returned with pre
Kanpur, wenl abroad
.
+9
‘re
ono
Wen vit
tions, suggests that, although these graduates
19
oO
|
TABLE 1
1960-1978.
Indian Immigrants, Professionals, Exchange Visitors and Students to the United States,
:
=
SUAr
th
|
a
‘ae
dai."
Immigrants
|Exchange
Visitors
Students
Professionals,
Technical and
Percentage of
total immigrants
1960
1961
391
421
1,337
01,579
1,591
1,947
'
118
139
30.2
33.0
1962
LSA,
1,567
2,029
min
PS
197
197)
1972
0
0
|
1977
as
ee
1978
LO Ea
2,242
5,392,
AIO
16,926 —
12,779
1974
19757
(2/244
4.048
th eee
1978
TOTGRA
5,963
2,507
4,682.
+
1969
5
2:535uahun
4,158 4g ae
1,782
2,527
2,458
4,642
“966
1967
2,402
1,969)
8
1,427
See
L126
Mii
MROD
29,753 .
1,009
1,000
ey
Goa
5,683:
Oy
ATA
ve: AGRE
nal
2640
2 OG
\ 3,202
|
Aer
50.7
34.7
34.0
|
1,424
2,474
1
57.9
53.3
|
2 Bo
46.8
HAT)
pee |
54,941
37.6
48.4
BRO
52.7.
48.3
17,543
PEE RTT
0.
4,266),
30.6
aie
595
220
198
eerie
4 GTR)
ey ee 540.2)
TSI
4
Sse
2,104
2.025.)
2,558
1,879
2,029
5, 12,073
1,173
634.
RRP
1963
1964
96S
1968
5
Beth
YEAR
WUE
Ss CB AOR
|
he om
a
3
Bats
2
.
e
°)"
39/0.
36.6
4,731
}
~
37.7
e
a eG TSG
0 re ata
4
22.8
*The numbers do not include those admitted hanes July 1 to September 30, 1976 since the:physical |
year of the
Immigration and Naturalization Service changed from July through June to October through Sere in 1977.
Sources: a. U.S. Immigration and Naturalization Service (1960-1977)
EE)
Oe
ed. _.b,
U.S. Immigration and Naturalization Service (LOTS)
Adjusted Indian Immigrants.
ae
YEAR
4 Ee
r
Re
Total adjusted if
i
ic
ie
* >, 3)Students
ie
.
vie
Ae
ane:
|
‘Status of entry |
Spouses and children
of Students
Brak
|
ey,
cp
|
1P06
1,789
1967
1968
1969
1,015
2,822
2,276
2,719
Lee
1,703
1,383
15967
345
410
525
ae
6,144
2,925
955
1870
3,886
P
7,810
hey
4,823
oe
3,962
anee
=
ni
tes
2,249
2,940
dep
Mis
Exchange
Visitors
:
Spouses and
Children of
|
os
Re
AY
11
83
73
bit
52
40
73
a4
836
.
63
554
Body
1,332
1,636
260
1,047
1,264
1,703
814
4,188
374
1,901
406
497
299
4,463
4,146
266
2,009
1,576
181
540
417
333
492
219
364
4,430
* See the footnote in Table 1.
1,996
440
<-9s
:
Exchange Visitors
ae
is
‘
|
y
at
ae
ae
heart
277
218
Sources: Same as Table 1.
20
Radical Journal of Heal
TABLE 3.
1960 ce 965 a
2 ar a 25,856
| as) Dd
12,909 “19,461
AMOR
38,892 69 201 “gat
59
Le ne a
29,357. 43,810. 71,361.
AMEE 16,395."
9,535 25,391 “501870.
, pri AE 8 Da EG aay a 41.6
oa ae ESE 275. (805, 348 408
i)
ag
diag’
Oa,
Yi
151,326 “165,069 179,979
153
466
88
(193,526 208,
hagit
i “213,032,
Bik s.
|
esoftheCensus (1977 : it,94.100
gee,
U.S.Bureau of the Census (1965: 11).
+ aih ¢
“i fe .)
@
Se)
“
eens i ie
;
ih
5,
ee)
eee
mM
eas
Hale)Ne
PARLES$?)
tees
Indian Private Transfer Payments*
Vy
1960/61
;
.
*
—
.
408 million Rupees.
826 million Rupees.
949 million Rupees.
1,364 million Rupees.
1964 receipts of pensions, retirement
benefits on private account.
urce : India (Republic). Central Statistical Organization (1974: 233-238)
Yarch- 1989
|
;
yh
;
;
i
j
;
j
iSsi
ie
j
5 of savings,
avings,
remittances
of missionaries,
reccipts
remittances,
maintenance
transfer payments include
Private
fers, and since
:
:
1965/66
1970/71
|
AMOUNT
YEAR
1955/56
.
0 4 tab
ae
neg
migrants,
mig
trans-
"Fe Ta T
TABLE 6
Rupees).
India, by Principal Countri es (million
Value of Imports into Exports from
Imports of Merchandise
1965/66 (%)
1970/71 (%)
11,216
14,085
16,342
199(1.8)
110(1.4)
1,225(10.9)
651(8.4)
296 (2.6)
245(3.2)
608(5.4)
383(5.0)
2(19:4)
2,17
1,998(25,8) .:,
3,276(29.2)
1,016(13.1)
159(1.4)
72(0.9)
305(2.2)
1,371(9.7)
341(2.4)
793(5.6)
1,501(10.7)
5,348(38.0)
83265.)
1,172(7.2)
1,075(6.6)
916(5.6)
834(5.1)
- 1,268(7.8)
4,530(27.7)
1,06 1(6.5)
1970/71 (%)
1960/61 (%)
1955/56 (%)
HOROR!
Sa Ge OS
eel eIS
PPRRIS
7,144
Total
“Canada
Germany (Fed.)
Iran
Japan
UK.
U.S.A.
US.S.R.
Exportsof Merchandise
;
1955/56 (%)
1960/61 (%)
1965/66 (%)
eee
6,324
8,016
301(5.0)
1,644(27.2)
853(14.1)
33(0.5)
349(5.5)
1,707(27.0)
— 998(15.8)
288(4.6)
5717(7.1)
1,448(18.1)
_——:1,470(18.3)
929(11.6)
2,021(13.3)
1,700(11.2)
2,068(13.6)
2,098(13.8)
-1,710
-4,892
-6,069
-1,098
oe
_
Total
|
3
:
e.
Japan
UK.
USA.
US.S.R.
s’
Trade Deficits
us
Source: India (Republic), Central Statistical Organization (1974: 206-211)
Be
i
a
:
\
Major Recipient Countries of U.S. Government Foreign Aid, 1955-1975 (in millions of dollars).
1955a
e
(1965a
1960a
sh MMO denen ASIN S Ses DLN Cita ie Me ee eee
4,909
Total, net
2
!
Brazil
-
China (Taiwan)
s
4,590
42
a7
109
109
523
118
India
a
5,052
153
49
1970a
eee
1975b
es
5,695
93
14
8.681
193°
191
854
434
243
167
314
Pakistan
349
198
229
Turkey
97
101
140
88
73
301
418
eae
Vietnam (South)
186
203
Source: a. U.S. Bureau of Census (1970: 872-875)
.
342
134
b. U.S. Bereau of the Census (1977:859).
TABLE 8
U.S. Investment in India (in millions of Rupees).
Mace
470
Source: Mukerji (1978: 126).
ne
726
Complied from the data of the
,
1968
1972
1976
22
Gea OL. eam
67
261
279
Korea (Rep.)
|
—
|
TABLE7
:
15,244 |
1,660
4,223
Reserve Bank of India.
4.850
*5,100
*estimated
Radical Journal of Hea
&
Ser
im,
«
Sets aa
¥
it
si
igrating, they played a role in perpetuating the trend
_ of modelling the educational system in India
along the
This hegemony of the US over India began to incorporate
- ignored or downgraded the culture of India. Thus it could
be understood why the foreign-educated were considered
close doors to immigrants, and the LDCs and individual
immigrants must rely on DC policies, even though indi- ~
India within the US sphere. This linkage is the very factor
lines of educational institutions in the US. Natura
lly, in for understanding the exodus of Indian physicians to the
the case of FMGs, there was an expressed conce
rn in ‘the United States."
_ United States regarding the purchase of pharmaceut
In this.respect, international migration can be considicals
and equipment by other countries (including India) ered as an analogy
to internal migration because after the
through FMGs. This meant, when FMGs returned to their influx of urban capital and system
of production into rural
home countries, it was expected that they purchase and areas, people were pushed
out. Today, a similar relation| introduce products from the US into their countries [US
ship is exercised at an international dimension. Indeed, the
_ Select Commission on Immigration and Refugee Policy movement of people from LDCs to DCs plays a role in
1980 : 216-217].
establishing an international division of labour, while still
:
In regard to the cultural aspect of migration, the ‘coloother factors of movement, capital and technology, occur
nial’ mentality which was formally created through British - in an Opposite direction, as earlier mentioned.
_ Tule in India should be considered. That is, in India, the
It should be stressed also that DCs are very much reBritish educational model was considered superior to that sponsible for inducing migration from LDCs for the sake
Of the Indian [Munjee 1975 : 17]. A similar attitude was
of their economic development, and whenever the situreflected towards US culture after the decline of British ation changes, they are able to limit the entrance of immi,
7 influence in India. This indealisation of western culture grants. It is the DCs which have the option to open or
superior in their fields in India even though they might
viduals may profit from the migration. Thus, the issue of — the contribution made to the development of DCs by the
__ not have had efficient skills [Munjee 1975: 17]. In lookinternational migration of high-level. manpower from
ing at the ‘neo-colonial’ relationship with the United
_ States, the attitude, although difficult to measure, is sig- LDCs has also been discusssed, a phenomenon referred to
nificant.It is well-known that the ‘demonstration effect’ as the reverse transfer of technology [Kabra 1976; Mainwhich came forth with the influx of western goods stimu- strean 1974]. Indeed, generally speaking, freedom of
_ lated Indian minds. On the other hand, those who went to _mobility is widely acknowledged; however only the free-
affluent societies such as the United States became accus_ _ tomed to the small conveniences of the United States, and
dom to leave countries
countries is not.
is granted, the freedom
thus, did not return [Daendekar 1968: 215]. _
ea
a
In addition, ‘neo-colonial’ ties with the United States
contributed to the emigration of Indian phyicians through
the network of Asian Indian communties in the United
_
|
_ [This study. was partially funded by the institute of American Culture, UCLA, to whom I am grateful. I am particularly
flow between India and the
indebted to Don T Nakanishi, professor at UCLA, for his help-
United States. For instance, the Directory of Approved
Internships and Residencies by the AMA played a signifi-
many of my friends at the Asian American Studies Center pro-
States,
-
Notes
to enter
and the information
ful comments on parts of this paper. It is needless to'say that
me with stimuli for this study. Also, I need to mention
vided
cant role in informing FMGs of the opportunities in the ‘that the research assistantship at the Center under the auspices
United States [Stevens et al. 1978 : 95].
of Lucie C Hirata and Edna Bonacich, professors at UCLA and
In sum, the United States, backed. by an overwhelming
flow of capital goods, technology, and information, intervened in India’s own economic development and incorpo-
rated India within its sphere. With an understanding of
this relationship, which was not equal in nature, reasons
behind the migration of Indian physicians to the United54
States can be seen.
under unequal
terms . between
DCs
and
ing
LDCs. In the case of India, the United States, replac
50s, exercised an over» the United Kingdom after the late
movement of
? whelming influence on India through the
into India.
capital, goods, technology and information
March 1989
and Vasant Kaiwar for their comments and encouragement. ]
on Pilipino.
1. As part of my project, I have done another case study
.
See Ishi [1982].
migrational
interna
on
re
literatu
2. For a Critical review of previous
tion theories, see Bach [1978] in details.
te of the non-retum
4. According to Oh [1977: 33], the estima
In conclusion, it should be emphasised first that the
phenomenon of migration is not a separate issue from interdependence
to two editors of the South Asia Bulletin, Sucheta Mazumdar
[1977].
3. For an overview on Indians abroad, see Tinker
Conclusion
Ww
UC Riverside respectively, provided me with various opportunities to further my interest in this field. Finally, I am thankful
rate of
Indian students was 59.5 per cent.
th profesionals in the
5. Regarding the problems faced by Asian heal
ittees
York State Advisory Comm
United States, both California and New
vei
efforts to address the needs
made
to the US Commission on Civil Rights
Rights, —
Civil
on
ssion
Commi
US
See
of Asian health professionals.
Com
fornia Advisory
mittee
6.
Committee
[1975] and New
[1980]
For
manpower
a
historical
concems,
see
of
immigration
[1967]
in details
development
Awasthi
York
State Advisory
laws
in
r
is
relation
i
7. Chen
[1980]
describes
of the Immigration
the background
and
Nationality Act of 1965 in respect to who pressured its passage.
8. The various methods used by Mathur [1971: 80-81] to estimate the .
supply and demand of doctors are as follows: 1) Supply was estimated
from the assumption that no new medical college would be added, and
the annual intake capacity of 15,000 would be fully met. 2) Demand was
estimated a) from doctor/population ratio norms, b) the relationship between stock of doctors and the growth of national income, c) the relationship between demand for doctors and the stage of economic development-the fitting of the regression curve of doctors on national income to
the data of different countries, -and d) the component approach.
9. Cited in Pandit [1968: 109]. Also, in Reddy [1974: 375] cited that
the Financer Minister of India in 1968 said the brain drain was not a loss
i
to India.
10. The trend of increasing remittances countinued after 1975 when
the incentives for non-resident Indians to invest in India were taken by
Workers and Class Stn
Castells, Manuel 1975 ‘Inunigrant|\
in Advanced
Capitalism: The Western European
Experience,’ Politics and Society, 5 (1), 33-66.
Chen, Helen 1980 ‘Chinese Immigration into the United States
: An Analysis of Changes in Immigration Policies, Unpublished Ph D dissertation, Brandeis University.
Cortes, Josefina R 1974 ‘Factors Associated with the Outflow.
of High-Level Philippine Manpower to the U.S. A,’ East-West,
Population Institute. Proceedings of Conference on
International Migration i i the don icenes June 10-14,
Honolulu.
4
V M 1968 India, Walter Adams edited, The Brain|
Dandekar,
;
Drain, New York :The Macmillan Co., 203-232.
Domrese, Robert J 1970 'The Migration of Talent from India’,
‘the government [Rele 1976: 270}.
in the: Committee on International Migration of Talent, Insert,
11. According to a survey, approximately 60 percent of the Indians .
in
metropolitan New York area send remittances to relatives in India of
national Migration of Talent, New York: Praeger, 215-257.
—
Rirw
100 US dollars or more per month [Thottathil and Saran 1980 : 245].
Dublin, Thomas D 1974 ‘Foreign Physicians: Their Impact
on —
Ere
4
12. The following argument is based on a study by Ito [1972] in
respect to Indian economic development after the second world war.
13. The study on the migration of Indian physicians from India to the
United kingdom and the United States, and of British physicians from the
|
US Health Care, Science, 185, August 2, 407-414.
Fisher, Maxine P. 1980 The Indians of New York City: A Study
|
of Immigrants from India, New Delhi: Heritage Publishers. _
ou
__.
United Kingdom to the United States, should be fascinating. Along with
_ the US hegemony on research and development, and the establishment of
a national health service system in the. United Kingdom, many UK phy~~“sicians went to the United States while many Indian physicians filled the
_ shortage in the United Kingdom partly caused by the exodus of UK physicians. However, Indian qualifications were only recognised up until
at im 1975. Afterwards, it became difficult for Indian physicians to emigrate to
the United Kingdom [Smith 1980: 1-12]. In 1976, the United States also
Mae
a mopored stricter requirements as mentioned in this paper.
References _
:
S Aiieatignn, PM
from Abroad;
fie
of Policies,
Programmes
and
Problems, Manpower Journal, 3 (4), 83- 117. (India)
wae
Adams, Walter and Dirlam, Joel B 1968 ‘An Agenda for Ac-
a
Journal, 11 (3), 7-18. (India)
Ghosh, B N 1979 'Some Economic Aspects of Indian Brain |
Drain into the USA,' International aeitig ti2 4, ape789
(Switzerland).
Iichman, Warren F 1974 ‘People inPlenty’ :Fe dualied Reeatd
ployment in India’, in Amrik Singh and Philip G Altbach, —
eds, The Higher Learning in India, Delhi :Vikas Publishing
- House Pvt Ltd., 119-136.
|
India (Republic) 1974 Central Statistica Organisation, Statis-
eee
1968 ‘Regaining High Level Indian Manpower
A Review
Gish, Oscar 1975 ‘Medical Brain Drain Rewisted’, Manpower —
tical Abstract. —
’
Ishi, T K 1982 ‘International Division of Stor’ The migration
of Pilipino physicians to the United States’, paper presented —
at National Conference ofthe Association for Asian Pacific
tion,’ in Walter Adams edited The Brain Drain, New York:
American Studies, held on February ssf University of
The Macmillan Co., 247- 263.
California, Berkeley.
;
Ito, Shoji 1972 'Dokuritsugono Dikusenasigens Hattento |
Keizaiteki-Juzoku, (The Development of Monopolistic Capi.tion Laws, Manpower Journal, 3 (3), 58-74. (India)
tal and Economic Dependence after Independence), in Heiji
Bach, Robert L 1978 "Mexican Workers in the United States: A
Nakamura
Edited, Indo Gendaishino Tembo, (The Prospect
a
Study of Migration and Social Change,’ Unpublished Ph D |
of Indian Contemporary History), Tokyo : Aoki Shoten, 99Dissertation, Duke University.
Awasthi, S P 1967 Manpower Aspects of Ee
Immigra-
:
a
n
=—
Baldwin, George B 1970 ‘Brain Drain or Outflow? Foreign Affairs, 48 (2), 358-372.
___
#
a;
fe
ape
Banerjea D. 1975 ‘Brain Drain, Its Causes and Remedies,’ Science and Culture, 41 (5), 190-194. (India)
Bhagwati, Jagdish N and Partington Martin, eds. 1976 Taxing
the Brain Drain I: A Proposal, Amsterdam:
Publishing Co.
North-Holland
Blaug, R Layard M and Woodhall, M 1969 Causes of Gradu-
ate Unemployment indndia, London; Allen, Lane, The Penguin Press.
Bonacich, Edna and Hirata, Lucie Cheng 1980 ‘International
Labour Mirgation. A theoretical Orientation’, Unpublished
manuscript; 1980.
Burawoy, Michael 1976 The Functions and the Reproduction
of Migrant Labor Comparative Material from Southern Africa and the United States,’ American Journal of Sociology,
81 (5); 1050-87.
151.
Kobe, Kamal Nayan, 1976 Political Epa
of Brain Drain:
Reverse Transfer of Technology, New Delhi: Arnold Heinemann.
Khadria, Binod Kumar 1978 ‘Brain Drain-The wi atae Péxipec:
tive : A Comment’, Journal of Higher Education, 4 (1), 101105 (India).
Kim, Illsoo 1981 New Urban Immigrants: The Korean Community in New York, Princeton, New Jersey: Princeton University Press.
Leonhard-Spark, Philip J and Saran Parmatma 1980 ‘The
Indian
Immigrant in America : A Demographic Profile’, in Parma
tma
Saran and Edwin Eames editors, The New Epunics: New
York,
Praeger.
Mainstream
Stream,
Mathur,
1974 Set
Tranter of Technology’,
13 (11-12), 43-50. (India)
Main-
P N 1971 ‘Demand and Supply of Doctors in india,
|
1951-86,’ Manpower Journal, 7(1-2), 58-96
. (India)
24
Radical Journal of Health
y, John W Jr 1979 ‘Asian Labor Emigrat
Veta
jn! et
es
am
as
is
n toike
b OPEC States’, lmegula: Paper 8, December. US Agency
for International Development Office of Development plan
‘ning Asia Bureau.
Merriam, Marshal F 1969 Brain Drain Study at I.1.T.
Kanpur:
Opinions and Background of Faculty and Senior Staff,
Kanpur, India+ Indian Institute of Technology Kanpur.
Mick, Stephen S 1975 'The Foreign Medical Graduates’, Scientific American, 232 (2), 14-21.
Morrison, Thomas K 1980 'The Relationship of U. S. Aid,
Trade and Investment to Migration in Major Sending Countries,, US Agency for International Development, September.
Mukherji, Sadhan 1978 India’s Economic Relations with USA
and USSR: A Comparative Study, New Delhi: Sterling Publishers PVT Lid.
Munjee, Aslam 1975 ‘Why Do Our Experts Leave?', Illustrated
Weekly of India, 96 (29), 17-19. (India)
Nadkarni, Vithal C 1978 ‘Racket at the Airport?’, Illustrated
Weekly of India, 99 (25), June 18, 30-31. (India)
_ Oh, Tai K 1977 The Asian Brain Drain: A Factual and Causal
Analysis, San Francisco: R and E Research Associates.
Paine, Suzanne 1974 Exporting Workers: The Turkish Case,
- London: Cambridge University Press, Department, of Ap-
Medical Moar New York, The Josiah Macy, ‘iFounda.
tion, 163-172.
Sorkin, Alan L 1977 Health Manpower; An Economic Perspective, Lexington, Mass: Lexington Books.
Sreenivasan, Sheilu 1978 'Foreign-Aided ITT Education’, Journal of Higher Education, 4 (2), 187-200. (India)
Stevens, Rosemary, Goodman, Louis Wolf and Mick, Stephen
+ yt
S 1978 The Alien Doctors: Fore'gn Medical Graduates in
American Hospitals, New York: Wiley.
-------- et al. 1975 ‘Physician Migration Reexamined', Science,
—
190 (4213) October 31, 439-442.
2,
Thomas, Brinley 1968 "Modern Migration’, in Walter Adams,
editers, The Brain Drain, New York: The MacMillan Co., 29-
_
49.
Thottathil, Pelis A and’ Saran, Parmatma 1980.'An Economic
Profile of Asian
Indians’, in Parmatma
Saran
and
.
Edwin ca
Eames, editers., The New Ethnics, New York: Praeger, 233-
246.
Tinker, Hugh 1977. The Banyan Trees: Overseas Emigrants. é
from India, Pakistan, and Bangladesh, Oxford: Oxford Uni-. )
versity Press.
ibe
Te
plied Economics, Occasional Paper 41. _
Pandit, Harshida 1968 ‘Brain Drain: A Problem’,Unitedeg
12 (2), 109-114. (India)
Tobias, George 1968 India’s Manpower Sieiees ‘Revised, ‘
1947-1967, Bombay: N M Tripathi Private Lid. United_
States, Agency for International Development 1980 ‘Interna- A
tional Migration and Development: Implications for AID
Programs and Policies, AID/PPC, March 7.
an
a
the Modern World Economy’, in Mary M Kritz et al, editors.,
_ Global Trends iinpen New York: von forie Aa
nomic Assistance Programs FY 1967, Summary Presentation
. ;
“to the Congress, March.
dre
Petras, Elizabeth McLean 1981 ‘The Global Labor Meike ‘i —Agency for International Development 1966 Proposed Eco-bay
- Studies, 44-63.
Piore, Michael 1979 Birds of Powmase Misrott haber and
Industrial Societies, New York :Cambridge University Press.
(uc
Mey
the United States. a :
*i
Portes, ‘Alejandro 1978’ Migration and nian
Politics and Society, 8 (1), 1-48. .
—Commission
Ray, Kamalesh 1971 ‘Unemployment and Brain Drain’, Economic and Political Weekly, 6 (39), Sep 25, 2059-
‘—Commission on Civil Rights 1980 New York State Advianeyh :
Committee, Asian Americans: An arg for Action, A CNR
2063. (India)
Reddy, Amulya Remar N 1974 ‘The Brain Drainin Amrik
—Immigration and Naturalization Service 1960-1977 Annual‘
Puttaswamaiah, K 1977 Unemployment in India: ‘Policy for
Manpower, New Delhi: Oxford and IBH Publishing Co.
Singh and Philip S$ Altbach Editers., The Higher Learning in
India, Delhi: Vikas Publishing House Pvt Ltd., 373-394.
Rele, S J 1976 ‘Incentive for Non-resident Indians’, Eastern
.
‘Economics, 67 (6), August 6, 270-271. (India)
New
Saran, Parmatma and Eames, Edwin, Editers 1980 The
Ethnics: Asian Indians in the United States, New York:
Praeger.
Smith, David J 1980 Oversease Doctors in the National Health
Service London: George Berridge and Co. Ltd.
Sodeman,
William
A
1971
‘United
States
Programs
to
Strengthen Medical Education in Developing Countries’, in
John Z Bowers and Lord Rosenhcim, editers, Migration of
March-1989
on Civil Righa: 1975 California ie Ns
Committee, A Dream Unfulfilled: Korean
Health Professionals in California, May.
and
Pilipino ee
i
i
ference Summary, February.
Reports.
—-Immigration and
Yearbook.
National Science
“p
Naturalization
Foundation
Servic 1978
1972
Scientists,
Statistical bs
Me
Engingarsi
and Physicians from Abroad ; Trends Through F iscal Year iy
1970. NSF 72-312.
Policy ;
— Select Commission on Immigration and Refugee
ss.
1980 Second Semi-annual Report to Congre
Manpower
Van Hock, F J 1970 The Migration of High Level
: Moulfrom Developing to Developed Countrics, The Hague
ton.
\
Undergraduate Medical Education in
Underdeveloped Countries: The Case of Pakistan
s akbar zaidi
The type of medical education of a country is closely linked with its system of health care. Any health care system,
t.
with its own peculiarities, requires a certain type of doctor who can function effectively in the given environmen
The same is the case with underdeveloped capitalist countries, such as Pakistan, where a skewed, elitist, curative
model of health care exists. In Pakistan, where the literacy levels in the native tongue are very low, medicine is
taught in English, and nearly all prescribed textbooks are written in and for the West. Conditions specific to
Pakistan, such as the degree of cheating in exams, the time lost due to closure, and the level of debate concerning
the medical system may find their parallel in other UDCs. Since it is the social and economic forces, which in the
of health care and medical education, one cannot expect any significant
final analysis, determine the system
improvement within the existing class structure. (Reprinted from Social Sci. Med. Vol. 25, No.8) —
\
economic formation, the new socio-economic formation
may not be able to bring in a new radical programme for
which is, to a great extent, modelled on that found in de- ’ medical education overnight. Clearly, the superstructure
~ veloped countries (DCs). A salient feature of this type of and its parts will take much longer to change than will
the base. Nevertheless, a revolution in society will have
health care is that it is essentially curative in nature. However, as the degree of social and economic development in its affects on the health system, which, as experience
. THE historical evolution of most underdeveloped countries
(UDCs) has resulted in a pattern of medical and health care
UDCs still lags behind that in the DCs, the resulting model
of health care is of a peculiar and distorted kind, and is in
most cases, not as successful as that found in DCs [1-8].
Pg”
es.
=
Fil
yet
from
the world
in the last 40 years shows,
will be
greatly improved and expanded. For example, almost all
socialist countries have made impressive gains in the
health status of their people, thanks to the programmes
of basic nutrition, housing, sanitation, water and educa-
The main feature that has evolved’ from this (curative
care) type of health structure is the dominant role of the
ee
er
age
oe
tion which now reach a majority of the population. Thus,
doctor in administering medical care. The preferable pyramidal structure for health personnel, where there should physicians in thcse socictics will be aided by the ex_ be more auxiliary health workers assisting each doctor, is panded health infrastructure in their attempts to eradicate
disease. This advantage is clearly lacking in capitalist
in most UDCs, inverted [S, p 18]. These doctors have thus
UDCs.
.
4
become the ‘frontline’ health workers, whether they function at urban hospital or district level. The role a doctor
Furthermore, there is a difference in the position of
;;
performs in any socicty is determined by the system of
health and medical care in the country, which in turn is
largely determined by the socio-economic formation preva-
_
Jent there. Furthermore, the model of medical education,
the process through which doctors are produced, is tied in
very Closely with the model of health care in that country
and with the demands and perceived needs of the people or |
their ruler. If the model of health care in a capitalist UDC
1s one which is urban-based, hospital and curative care oriented and determined by the workings of the market
_ mechanism resulting in a small minority of the population
having any feasible access to the system, the doctor will go
through a number of years of medical school so as to be
able to work effectively in such an environment.
In socialist oriented countries, attempts will be made to
make the doctor's role radically different and to involve
him in social and community oriented health projects. This,
however, is easier said than done, and a mere desire is not
a sufficient condition to fulfill such political tasks. Given
the fact that the medical education system before social
change in these UDCs was one governed by the old socio-
doctors in the health system's matrix in capitalist and socialist UDCs. In capitalist UDCs, the doctor (and thus
medical education) plays a more dominant role since
supporting health infrastructure are lacking. In socialist
oriented UDCs, other factors in the health matrix begin
to play an increasing role. That is not to belittle the role
of doctors and the importance of medical education in
socialist oriented UDCs. Experience from these countries
shows that by realising the importance of the role of
doctors, concerted efforts are made to change the medical
Curriculum and to produce doctors oriented to the needs —
of the local environment. However, as has been argued
above, the results may take time to bear fruit, as
remnants of the old system may cause hindrances.
This paper will examine the issues relating to medical
education in UDCs. After a bricf overview of UDCs in
general, we will turn to the particular case of Pakistan,
a
post-colonial state, and critically evaluate the syste
m of
medicine and medical education in this country.
The final section will deal with the possibility of refor
m in
medical education.
26
Radical Journal of Health
iF
ica
en ae
,
it
_ Heal
th Caree and Medica
l Educat
ion aein UDC's!
A great deal of litcrature exists which deals
with the
model of health care in UDCs [1-22]. Most of
these authors have limited their analysis directly to the model
of
health care, and have only indirectly approached the question of medical education.
However, as we have argued,
the two are very closely related.
Most of the present UDCs were, at one time colonies of
the western nations. Their economic and social system
s
have been greatly influenced by the colonialists and despite their ‘independence’ they still follow Closely norms
and regulations left behind by their masters.
When the colonialists first took over, the overall socicty
and economy of these countries were transformed, and the
medical and health facilitics were brought in line with the
changing ‘super-structure’. The colonial administrators re~ quired a model of health care which would cure the ills of
their own people, their military and their burcaucrats.
5
SEES
Say Zoe
more equitably distributed, health services are free etc. [2
27]. Mozambique too, is following a similar path and ir
dications show that the health status of her population i
also improving [28]. What is important to point out her
is that these countries have not only had a change of gov
ernment, but there has been a substantial transformatio
in their economic structure. They have gone from a no
socialist mode of production (form of the economy) to
socialist one, where the distribution of power and re
sources rests with the people and their true representatives
The people have collectively been able to decide what i
best for them and have taken action for their own better
ment and welfare without having to confront a hostile rul
ing class. This importance of the change in the mode o
production has been emphasised by Navarro as he argues
"abundant empirical evidence cxists to show that the mos
country and actively built up this ‘western’ type
of health
care, usually at the expense of the indigenous system
important changes in the health of the underdevelope
countries’ populations during the last 20 years have oc
cured in revolutionary Socialist underdeveloped countrie
via changes in their economic, political and social struc
tures, independently of and outside the health care sector
which had existed earlicr. As a select few of the locals
were incorporated into the closed circles of the colonial-
[11, p. 169].
In underdeveloped capitalist countries, for the function
ists, a new elite was formed. Members of this small clique
ing of the inequitable and elitist model of health care, th
the westerners, one of which was the access to western
doctor who can function within the norms as definedb:
medical care. When the colonisers left the foreign lands,
the local elite had been so 'westernised' that they emulated
in with the larger movements of the international econ
They thus set about ‘importing’ medicine from their home
mie
were also able to afford some of the luxuries brought by medical college has provided just the right graduate:.
their masters in practically all fields
[1, 7].
The pattern of health care that has evolved in most of
the capitalist UDCs is one based on curative care, and the
workings of the socio-economic and political systems are
such that health care has come to cater essentially for the
rich and the elite [2, 8]. This model of health care has a
predominantly urban bias in the distribution of facilitics,
and thus the majority of the population, usually rural, are
denied the right to have access to health care [15]. And, it
is not all the urbanites who have access to health care.
Since medical and health care is sold like any other commodity in the market, most of the urban poor cannot afford the escalating costs of mcdical care either, In underdeveloped capitalist countries, we have argued that the
socio-economic system, with its resulting class structure is
largely responsible for this type of urban bascd clitist
model of health care [8]. This model, along with a general low priority given to health care and discase elimination is responsible for the very high communicable disease
pattern in these countrics. However, there are a few UDCs
which have at least made sincere attempts to solve the
problems of their people.
The cases of China, Cuba, and Nicaragua are worth
citing. In all these countries, there has been an improvement in the health status of the population. The infant and
child mortality rate have fallen, facilities have come to be
that society. Just as the economy of a UDC is closely tic
omy, and is dependent on the developed countries, so to
is its system of health care. Similarly, the medical colleg
is linked closcly with the pattern of medical education it
the dominant (often ex-colonial) country. This is despit
the fact that the real needs of the UDCs, as defined b
their discase patterns and limited resources, are differen
from the DCs.
oh
Even in Tanzania after the Arusha Declaration, the cur
riculum in the medical schools ‘mimicked’ that of th
West with a content which is clearly unsuitable to th
needs of the local environment.
A major factor whicl
determines the need to achieve an ‘international’ standart
is the faculty. This desire for acceptance by universit
authorities in the West, forces them to adopt western con
cepts of ‘academic standards’. The result is that "much 0
the curriculum is thus objectively being determined fron
outside the country" [16, p 47; also see 6,8]
Gish [14], Gish and Godfrey [19] and Horn [18] hav
shown how this type of western-oriented medical educa
tion results in a ‘brain drain’ of professionals to the devel
to in
oped countries, Gish and Godfrey argue that due
care |
equities in the functioning of the market, medical
also skewed
in a manner
which
suits the rich, The. pro
stan
spective doctor goes through an institution "Whose
ar
and
n
dards’ are generated by New York and Londo
possibilities 0
mostly unrelated to the problems and
the bourgeol
UDCs" [19, p 6]. The reason for this is that
57
d/
March-1989
ae
——_—~S
Aa Bd ae
oie
ic, who controls most of the resources in a country, reuires the latest and best in medical care and thus try to
roduce
‘comparable’
doctors
at home
[2]. This interna-
onalisation of doctors only helps the developed countries.
‘he migrating doctors subsidise these countries as they do
ot have to go through the expensive process of producing
heir own doctors, while the social cost of producing them
; borne.by the poorer UDCs.
Not only does this internationalisation assist migration,
ut by maintaining foreign standards, severe internal disortions also arise. Since medical students are taught their
raft in hospital settings, as is done in the West, they of-
tion ha s been
iS
UDCs, Thus
uncritically adopted by most JD
ough specific to Pakithe case study presented below, alth
stan, will clearly echo
the situtation prevalent in other
UDCs.
Case of Pakistan
Up to 1947, what are now India and Pakistan, were one
country ruled by the British. Any history that they had
until that time, was broadly the same, albeit, regionally
specific in character. In the field of health services too,
this is largely true with the exception that what is now
and
Pakistan, had a greater influence of Muslim and Arab culture than did present-day India.
ural and thus remain ignorant of the social causes of dis-
Debabar Banerjiis a leading authority in the field o
en fail to interact with
‘communities’,
both
urban
ase. Since the disease patterns in UDCs are quite differnt from
those
in DCs, the way to deal with them must
Iso be different. Medicine taught in the hospital setting is
ften not sufficient to deal with the complexities of disase in UDCs. The unfortunate outcome of this type of
nedical education is a hospital-oriented doctor who has
een taught to function in urban settings with the help of
nodern and sophisticated technology. With such technolo-
social aspects of medicine in the sub-continent. He has
written extensively on. the historical evolution of medical
and health facilities in India and has shown how British
imperialism imposed its values on Indian society and
trampled on the indigenous health system that had existed
until then. The colonialists developed their own system of
health care (the ‘western’ system) and recruited a select
few of the local elite to take over the entire political and
ies and facilities lacking in rural areas, a large number of administrative system after they left in 1947 [1, 6-8].
loctors would choose not to go there, thereby denying the, :
The resulting medical and health services system inher-
ightof the rural population to have access to doctors. ited by Pakistan is one which is modelled on the West (in
With the concentration of doctors and facilities in urban
particular Britain), being primarily hospital-oriented and
ireas, the limited finances of the health budget are spent based in cities. More than 90% of health facilitics
are in
ere, where only a minority of the population lives [8,20- _ urban areas and the disparity shows no sign of improving —
ee
ae
ayn factor closely linked to the functioning of urban
ased doctors having a primarily curative approach, is the
wescribing of drugs in great abundance. Since medical
are, as it is practised,is linked with the doling out of
nedicine, this type of doctor and health care model also
-ontributes in supporting the drug industry. The drug in-
[8]. The medical colleges in the country centre around this
hospital-based approach to health care and look towards
New York and London for guidance and inspiration.
There are at present 17 medical colleges in the country? —
with an annual intake exceeding 4300 students (there are
at present more than 22,000 students enrolled). Two of
these are exclusively for women while all the others are
co-educational. There has been a great increase in the
her link in the exploitation of the UDCs by the West [29.
number of medical collegesin the last decade mainly due
30).
to the populist rhetoric of the Bhutto Government— in
_ Another important aspect of medical education has been 1971 there were
only seven medical colleges in the counucidly examined by Banerji [1, 6, 7]. He says that in the
try. Some of these colleges were set up purely on political
sourse of their medical education, the students "who
expediency, in cities which lacked even supporting inframostly belong to the upper classes, get furt
Structure (eg Nawabshah, and Larkana—Bhutto's home
alienate
from the masses of the people" [7, p. 33]. her
The coloniald . town). Due to excess
production, the present government
sharacter of the health services, affecting medical educahas not only put a stop to the increase in the number of
ion, also played its role in "shaping the value system and medical
colleges,
he social outlook of the Indian physicians" [1, p. 1334). _ admission capaci but has also decided not to increase the
ty of the existing colleges. Ad-hoc and
This class based alienation makes them further dysfuncanarchic policies, usually short-term, appear quite reguional in the UDC, especially in the rural areas and urban
larly, and despite weighty five-year and annual
plans
slums, where due to their class position, they are often not
there is seldom, if any, planning at all.
ible to relate to the poor. The doctor thus produced cater
The curriculae of all the medical colleges in
the counimarily to the elite of their country, or then, go off to
try are identical and the colleges come under the
he West or the oil-rich countries where they feel more at
acgis of
the Pakistan Medical and Dental Council (PMD
C). This
lome professionally (and often even socially)?[21].
body, apart from regulating and streamlining
medic
al eduThis ‘western’ model of health care and medical educacation, also looks at the ethical aspects of medic
al practice
justry in most UDCs is foreign owned and acts as a fur-
Radical Journal of Health
;
; ae rag
+
Serial
Number
woe
ee
oe.
\5
’
if Ags
fe
at
we
t
st ig
~ fy Tiger
a?
tie
;
7 ee
eV
r
q
Total number
Subject and year
of hours
Percent
| 800
200
600
24.5
6.2
18.5
When. examined
Years I and II:
1.
Zi
3.
Anatomy with histology
Bio-chemistry Physiology
4
Human relations, sociology,
community orientation, medical ethics
5.
Pakistan studies and islamic ideology
Year Ill:
6. _Pharmacology
including
therapeutics
7.
General pathology (microbiology parasitology)
8.
Forensic medicine and geouges <3t
Years IV and V :
oF
Community medicine (IV year)
10.
Medicine including applied: physiology
11. Surgery including applied iri
ee 7 ae 53 Orthopaedic surgery
13. Obstetrics and gynaecology
14. Paediatrics
“ES, Opthalmology _
16.
ENT.
—
17.
VD and skin
|
ws
Pe
EP
OAR
100
—
Bick
100
3.1
ist professional
300.
9.2
300
2nd professional
—
60
1.8
3rd_ professional
100
145.7
145°
20
eagle
Eek
Be hel
7
Ist professional
lst professional
1st professional
B, y
6.2!
4.8?
a
2nd_ professional
3rd!professional
_ Final’|
Final
sa
Mats
:
7
Fa _
80
25
50
13),
30} §
15
0.9
0.9
—
Final |
Final —
100
80
12.34
2.5
3rd_ professional
aregae
Lert
3250,
100.00
Final
ee
Pathology (general and | eoiat se me
microbiology and parasitology (IV year)
19. ee:
conference, orientation, etc.
me
Cat
;
e
ig
®
re be
aly?
es
,
+
%
3
Os
h
, laclides no. 4.7 Includes no. 17. Includes no. 12, * Includes no. 7. 5 Includes no. 14 and no. 17. A
Source :GT). ph
+f
_
iB
‘and actsas a control on Fen uta BeTheE hesy consists of
senior professionals in bureaucratic positions and the principals of all the colleges. For all practical purposes, the
PMDC docs. little work that is of any profound signifi_ canceto the system of medical education. However, it
does exercise some control over the curriculum of the
_ medical colleges and determines the courses to be studied.
The last major change occurred in 1975, when the PMDC
laid down the present curriculum for the MBBS degree.
Since then some insignificant changes have been made,
notably in the shifting of the subject of community medicine from one year to another. Another recent change is
the introduction of Pakistan Studics and Islamiat (Religious Studies) in the first year of medical school [31].
Education in a Medical College
A student enters
medical
college after
12 years of
schooling, the last four of which have already determined
the choice of the student (or in most cases, his parents’)
towards
medicine.
However,
a miniscule
proportion
of
those who in their ninth year of school opted for medicine
eventually get to medical college. Further, admission to
March-1989
ja
Py
A
{
wa
Wied
:
i
é
ey
etian| school is not limited to merit, me‘a quota system. is
exists which permits some second class students to enter.*ae
Thus competition from an early age is fierce, and only Ry,
those who excel, or have the right connections, or ne
regional or social backgrounds, are admitted.
rit’
The medical degree, MBBS, is spread over five years
e
h
er
with four professional exams. Years One and two consti<
tute the course work for the first professional exam, with — |
a professional exam cach year for the remaining three f
years (see Table 1). Clinical teaching starts from the third
year, where students are supposed to spend 2 or 3 hours a
day for a period of nine months with one month per
ward, The third ycar group is taught how to examine patients but is not given Iectures on diseases and is largely
it is
selftaught. Attendance to the wards is compulsory, as
bigger
to classes, but as the group gets larger because of
by the
intake, it gets more unmanageable and as learning
stay
bedside gets more difficult, more and more students
and cager
away. Eventually only the core group of bright
competence w ho
ones remain, while the ones with lesser
|
need more attention stay away.
importance
Community medicine is rarely given much
Table1). Prein UDCs, and Pakistan is no exception (see
ct which
subje
the
viously, there used to be ‘ficld trips’ in
h centers,
took students to see sewerage plants, rural healt
y mediand other such institutions. Even then, communit
stucine had a ‘curative’ institution bias. Rarely did the
or rural,
dents interact with a ‘community’, whether urban
and often these trips were considered ‘fun trips’ and ‘outings’. Now this procedure has been replaced by discussions
and seminar groups for a period of one month each year.
Thus, the discussions by the alicnated students relates
to ‘communities’ of which they have no first-hand
knowledge. Due to a lack of training in the social sciences, they are also unable to see the social mechanisms at
work in the environment. Even the patients that come to
the wards are usually from urban backgrounds, so exposure to rural disease patterns is totally lacking [20, 21].
oe
must be honorary.
cism of the
criti
our
The basic issue with which we start
The memodel of medical education is that of language.
tan, is
dium of instruction in all medical colleges in Pakis
English; Pakistan, like India, is a country
with different
Cornationalities and cultures, each region having its Own
are
s
responding language. Although the official language
English and Urdu, the entire population cannot speak
Urdu, leave alone English. The regional languages have
preference over the official ones, especially in the interior
of all the four provinces. Further, only 26 percent of the
population is literate (in any language). Thus, of those 26
percent one can presume that very few would be able to
read and write English. Even fewer would have English as
a mother tongue. Moreover, although medical education is
in English, schooling can be in any regional or national
Further, the students are not taught in detail about
common diseases such as typhoid and malnutrition, but
instead, surgery, pathology, etc are emphasised. The stu-
language. A student may speak his mother tongue at
home, he may use another language for primary and secondary education, and yet a third for. professional educa-
crative returns. A post-graduate in community medicine
may be more qualified to deal with discases in a poor
years of school life in a language other than English, he.
or she will be confronted with a ‘foreign’ language once
he enters medical college. This foreign medium of education means that very few students from per-medical
‘dents are advised to specialise in subjects which offer lu-
rural community, but he would indced have a hand-to-
‘mouth existence. There is no social value attached to
community medicine in this socicty and little or no demonstration effect exists. Thus, for students to reject com-
‘munity medicine and specialise in neurosurgery is sad, but
nevertheless, understandable.
|
a Lending facilities in the college libraries are poor and
tion. That means
that although a student has spent 12
schools will actually be able to learn much in medical
colleges. This preference for English shows a bias towards
the elite and westernised urban based minority who are
accustomed to English in their homes and educational institutions. Members of this elite, apart from being able to
so students have to buy most of thcir books. Nearly all
learn more, and with much more case, claim the best
expensive, although now most of them are printed in
Pakistan, or published in the Far East. In the first year a
Thus, discrimination on a class basis is reinforced through
“student is required to buy the greatest number of books
which are also the most expensive. 'Gray's Anatomy’ alone
medicine were taught in either the regional or national
language, the international mobility of doctors would fall
books are written by western authors and thus are fairly ‘house jobs, followed by the most lucrative job offers.
the medium of instruction in medical colleges. Further, if
costs close to Rs. 700 and the bare minimum cost for dramatically. This is a situation which the elite, whether
books in the first year comes close to Rs. 1700. If a stu- doctors or laymen, will not readily accept [21].
ae wishes to purchase medical ‘atlascs', he must spend a The problem of language is not restricted to the lecture
great
deal
more.
Further,
the desire
for ‘latest’
books | halls alone. Students have to take histories from patients,
_means that since editions change very fast and the matcrial
changes as well, students cannot usually work
with scec-
ond-hand books from their senior colleagues. By the end
of the final year, the students have spent between five to
|seven
Si
thousand rupees for their very basic books and if
they want a few more necessary texts, they must spend
further Rs. 3000-4000. The costs in many individual cases
can be substantial.°
fo, Al the end of the five years in medical college (which
in Pakistan due to ‘disruptions’ usually extends to seven),°
the students are supposed to do a ‘House Job’ (internship)
for a period of one year. Six months are spent as a junior,
while the other six are spent as senior house officer in the
“same or another speciality. Again, the opportunity to work
‘in a certain ward is based on merit, with about 30-40 doc-
‘tors per ward. Of these only a few are paid, while the rest
30
if not in the mother tongue of the patient, then in the
local or regional language. A student who does not even
know the names of the most basic diseases in the national
language,
will have
substantial
difficulty
in finding out
what is bothering the patient. There will be very little
communication between the two, if at all. Langauge, however, is only a minor barrier compared to the cultural
barrier that exists between the patient and doctor. In most
post-colonial socictics, a separate ‘culture’ exists for the
clite, and even a mastery of the language will not necessarily close the cultural gap between the two (21).
The books that are used in medical colleges in Pakistan
are in most cases written by foreign authors—mostly
American
and British.? These books cater, primarily, to a
western audicnce in medical schools in developed countrics. They are written in, and for, a specific socio-ecoRadical Journal of Health
4-*
no
ic culture and environment dealing with a particular
health and disease pattern. The fact that they are used in
4
‘Ss without any changes, causes a few problems. Since
the authors have the DC student in mind, quite naturally
they talk more of diseases found in the West than in Pakistan or other UDCs. The main diseases in Pakistan which
are caused by infections
and are communicable have more
or less been wiped out in the West. Further, a great number of diseases in UDCs have their roois in social and economic conditions which are far removed from the hygienic western hospitals in the countries of the authors.
Thus, some diseases which are very common in Pakistan,
such as typhoid and diptheria would
be treated as 'interesting and rare’ cases in the West, and would not be given
the importance they deservein the texts.
___._ The average size of a class in medical colleges exceeds
’ 250 students— in some colleges it is more than: 400.
- With such an unfavourable student-teacher ratio, it be-
comes very difficult to learn anything in class. Further,
_ the audio-visual facilities that exist in all medical colleges
are very poor, and thus most ofthe students arein effect,
_
_
not participating in the learning process.
One important factor which upholds the existing system
of education is the role of the teachers. With very few
exceptions,
all are foreign qualificd. In fact, it is very
helpful for teachers to be foreign qualified if they intend
to rise to the post of professor.’ These tutors lead their
-
students through the course they went through— first cdu-
cation in Pakistan, followed by essential forcign training
to learn the latest teachniques. These students if they come
back, either end up in large hospitals in the city or else
attempt to go and settle abroad where lucrative jobs await
them.'°
as
bias
The irony of the medical education system is that with
is quite significant. One observer quoting medical students, wrote in a local newspaper: "there was a question
on typhoid ... we ignore small items. We prepare diseases
which have complex, lengthy treatment so we could fill
up pages. Typhoid has a simple treatment. Nobody bothered to study it. We strongly protested (to the invigilator)
and cheated, of course" [32]. (This happens where every
third day, six or seven cases of typhoid turn up in the
wards). It is estimated that as many as 90 per cent of the
Students cheat. Cheating is not only limited to written
exams,
the oral
exams,
which
should be a safeguard
against cheating, are also subject to unfair means. There is
a case where a student got.a distinction in a subject by
giving his tutor a diamond. Other students have been
known to arrange for forcign trips for their teachers,
while still others have paid for the petrol of their teacher's
car for the whole year. Cheating in educational institutions
of all types, at all stages is epidemic, yet few active measures are taken to deal with the problem.”
|
There is an anomaly which is probably unique to Pakistan. Some medical colleges in the country, although
functioning under the PMDC regulations are not recog-
nised.
The degrees of the Chandka Medical College, set
up in 1972, are as yet not acceptable to the post-graduate
medical centres of the country. Two other colleges which ~
have been functioning for a number of years have only
recently been recognised. This essentially means that a
student may complete five years of medical school and yet
be legally unable to practice medicine.”
The present government of Pakistan has repeatedly.
played the nationalism and religion ‘cards’ as a means to —
extend its rule in the country. It has thus introduced the
subjects.
Pakistan Studies and Islamiat, in the curriculum —
of medical colleges. In fact, of all subjects taught in the
4000 new graduates a year, not all can be absorbed in the first year they are probably the most important. If a stuexisting health system. This leaves many unemployed, and dent fails in cither of the two he or she will not be allowed to reappear in the subject and will be declared
the numbers keep on increasing at a very fast rate indeed.
failed in all subjects. Apart from the argument that reliThis expanding cumulative unemployment ariscs despite
the fact that very few people in rural areas have access to gious studies have nothing to do with medicine, the level
of instruction in these two subjects is similar to that of
doctors who tend to converge in the more lucrative urban
intermediate (class XI and XII), and is thus a repetition of
areas. The medical education system has taught the doctor
to deal with sophisticated equipment
and modern technol- the previous years. However, in this case, they not only
nce
ogy. In a rural areca he is completely lost without his ‘add to the burden of work, but with so much importa
tools. Further, the disease pattern is also different, and he granted to them, cause unnecessary anxicly.
may findythat unless he is aware of rural sociology, politics and economics, or is a native of the rural arcas, he
will not be able to function
effectively
[8, 13, p. 217,
20).
|
The examination system.in medical colleges acts as a
major contributor to the poor quality of doctors produced.
With the emphasis on essay-type exams held at the end of
the year, with journal work and orals (viva-voce) playing
a small part, irregularities are quite widespread.
It is not possible to assess exactly the amount of chcat-
ing. but one can, on casual observation, clearly sce that it
March- 1989
Although the problems mentioned
above may be spe-
ities,
cific to Pakistan, many UDCs can find some similar
s in the
However, the level of debate concerning reform
poor standard
medical system in this country, 1s of a very
|
compared to other UDCs, such as India.
ed an important
Since health care itself is not consider
h sector gets only
priority of the government —the healt
issues related to | epee
0.6 percent of GNP—any
attention,
within the health system receive even less
Very
h deals with prob
little research is done in Pakistan whic
Nevertheless, a few
lems related to medical education
f
government publications do exist which indicate the altitude of the doctors and concerned bureaucrats. However,
since they echo the elitiest bias in medical thought, the
q
i
“
wt
ites
ri
‘3
the helnt i am
ae at
the mass level. Further, with a Pe
government, any semblance of debate and dialogue if it
gets underway, is heavily biased in favour of the existing
status-quo. The media is totally controlled by the governrecommendations if followed, can prove quite disastrous
ment, where inhabitants of the country are given their
to the welfare of the masses of the country.
daily dose of 'newspeak’. With such an atmosphere existA commission set up in 1960 (33), to study the medical
the country (lacking
and health sector came up with some recommendations ing within the social conditions of
place
‘dealing with medical education. Some salient points of any significant opposition), any reforms that take
be
will
They
above.
will be similar to those mentioned
the report are worth noting.
The report recommended that "since children of medi- totally cut off from social réality and will at best be only
‘cal practitioners will have seen at first hand what will be ‘cosmetic’. Thus, to await reforms from the ruling class
‘expected of them by the community, therefore a bias to- to suit the masses, is both native, and unrealistic. As long
wards the children of medically qualified parents (in the as ‘things are in control’. and the status-quo remains —
stable, the government have no need to cater to rag
Zcase of admission to medical college) should be exercised"
but to those whose interest it serves.
|
(33, p. 46). Such an attitude is reflective of the medical
lobby which wishes to perpetuate its own hold on the
Possibility of Reforms >
_profession. The prominent professors and physicians who
Asthe title of this section suggests, we will deal with
control the health system wish their offspring to enjoy
the fruits which they have tasted.
The class nature of
"medical professionals is thus further re-inforced. (21).
_ This is evidenced by another recommendations which
iccepts the fact that many students’ "knowledge of English
_ isinsufficient for them to profit from their course of stud“ies!
(33, p. 56).
recommendations for reform in the medical education sysWe will essentially deal with the sugges-_
tions put forward by Gish and Godfrey (19). We feel that
their recommendations are indeed ideal and if followed —
tem in UDCs.
through would result in an excellent system of medical
Rather than suggest a conversion to the | education and health care which would fit the require-
mother tongue of the students, the writers of the report
ments of UDCs almost perfectly. As we proceed to show,
eee the teachers in medical schools to give their students
"practice in speaking, reading and writing English" (33,
P:56). The elite, who are fluent in English and need no
however, their recommendations are good only on paper
and as they have ignored the social and political forces
active in UDCs, cannot be implemented in capitalist un- —
‘practice’, would HSVen nee have an ae
derdeveloped countries very easily.2
hand in the
'ssystem.
_ The elitist bias is feahel pee by thefact that the
‘Teport gives only four lines out of 20 pages to community
“medicine. This is so because the elite amongst the doctors
are the last who will need to see a rural community or an
“urban slum, since most of their clients will be well-to-do.
“urbanites. Thus even if they. were taught community
medicine, they would have little opportunity to put it to
“practice.
_ The western- orientation of medical education in this
“country is further reinforced by the recommendations of
the report. It suggests that the more ‘enterprising’ men
“and women who can make the ‘necessary arrangements’
4should complete their training in the United States or Brit-
ain.
In fact, another report goes even further.
_ Ahmed (34), argues, that not only should the physician
‘training programme maintain international standards of
quality, but since the cost of producing medical personnel
As low, the world price is high, "the setting is ideal for
developing an export market" (34, p 12). The object of
medical education, according to the author is to "produce
a graduate within our resources who is accepted internationally" (34, p. 13). (The report was funded and published by the Public Health Association of Pakistan!)
There exists little consciousness about social issues in
this country, either at the political/oureaucratic level, or at
Gish and Godfrey start their paper with a critique of |
neo-classical reforms rejecting ‘the framework on which
they are based. Their alternative framework accepts an
international
market
'e 4
for professional
skills into which
UDCs are well-integrated. Their suggestion is a withdrawal from the market, essentially arising from. a
changed focus in educational policy which should deal
with internal needs rather than external markets.
They
have presented some specific recommendations to which
we now tum.
(Their paper deals primarily with UDC
commonwealth governments.) °
The authors have given 11 different recommendations
for UDCs which are summarised as follows: (i) an end to
use of British qualifications; (ii) no more foreign professional examinations in UDCs and an end to advertisement
and recruitment by developed countries; (iii) disaffiliation
from western-dominated international professional associations; (iv) permission for students to go abroad only on
‘relevant’ courses. (v) the development of local courses
and qualifications which are more suitable to local needs
and thus less acceptable to the western employers— a
‘deinternationalisation' of doctors and medical education;
(vi)
regional cooperation for higher education; (vii)
the use of
the national languages as the medium of instructi
on. (viii)
improved rewards and job content; (ix) .various
controls
to dissuade overseas study; (x) rejection of
various, other
32
Radical Journal of Health
|
f
"
ne ”
as eee
ed Sak
tee
Sao
‘
Sl
es
;
"¥
eee
he
ae
Benn er’,
BRN
ee
ae
pet a Ra te RN
eth
Waatside thehealthsector) interests; and (xi) the restriction” in the control of the people of their own
of the output of doctors in UDCs to the number that can
be absorbed at home (19, pp 8-10).
Let us now proceed to examine each of their recommendations. Firstly, an end to British qualifications must
take place not only at medical college level, but also at
school level. At present the vast chain of 'O' and 'A' level
schools all over the commonwealth offers the elite the opportunity to acquire British education while sitting at
home. They have a great deal to lose by denying themselves this privilege and one sees no reason why they
should give this up. Again, the author's second point:
ee eet ar wy
destinies, these
reforms are possible. Mosambique is an example of a
country in which such change has occurred and it has carried Out some of the reforms recommended by Gish and
Godfrey. They have 'de-internationalised' their doctors,
teaching them more about their own country than about
the colonial nations. This has resulted in a more socially
conscious, ‘new' doctor, required by and suitable to the
needs of Mozambique (28, 35).
Wehave analysed the issues involved in the model of
medical education in UDCs, and have treated Pakistan as a
sional exams in the country, those with money can easily
fly to London or San Fransisco and take the relevant ex-
case study. The factors that come out most clearly are that
medical education is a reflection, in the final analysis, of _e
e
eeeeh
the socio-political structure in the country.
»
The present form of medical education in capitalist Re’
ams there.
UDCs is elitist in nature and is a major impediment to an
although Pakistan has ended the sitting of foreign profes-
;
Recommendation (v) requires substantial changes in the
equitable distribution of health care. This type of medical —
model of health care. Of course, UDCs should have locally specific courses so that they can function in the local
education, often in a ‘foreign’ language, favours the domi- _
nant classes and produces a doctor who works best in an
environment, but again, as has been argued above in the
way the class system exists, the rich want a certain type of
doctor who is well acquainted with the latest and best
techniques in major hospitals in the East, and not in the
poor areas at home. It is quite clear that the doctor produced in UDCs favours and belongs to certain class, and
urban-hospital setting either in the home country or in the
West. Such a doctor is heavily incapacitated in rural set-
this class, in all essence, determines the type of doctor to
be produced and supports the ‘international’ curriculum
(1,2,8,21).
Instruction in the national language, as we have shown
above, also chips away the advantage of the elite for
whom English has become a mother tongue. By introducing the national language (which is itself controversial, say
in India), members of the lower classes will have access to
the domain of the elite, again a hard-won privilege which
they will not give up easily. Further, UDC governments
can if they wish, discourage overseas study, but if a
monetary mechanism
is used, the rich can over-ride it. It
seems doubtful that any other means will be used, especially since the children of the elite are the ones who are
most likely to go abroad. Even local production cannot
really be restricted, as the burgeoning middle classes will
clamour for their rights as well.
Essentially, the above discussion looks at the relation-
ship of the elite (the dominant class/classes) with the government. We argue that the dominant class has substantial
control on the government and on the distribution of
health resources in a country (2). Further, in the absence
of any significant challenge or opposition, we sce no reason why the ruling class should carry out policies to hurt
its own interests, This is mainly what Gish and Godfrey
have recommended—the government working for the
‘masses’ at the expense of the elite. This is clearly a probHowever, in
lem in underdeveloped capitalist countrics.
countries
where
there has been
significant social change
and mass participation and genuine democracy has resulted
March-1989
tings, as he has not been trained in line with the needs of _
the country.
ae
The case of Pakistan is peculiar in some cases, but in ~
most of the broader issues concerning medical education,
she is like other dependent UDCs. A lack of clear plan-—
ning and the interests of those in power have often deter-
mined the path of medical care and the growth of medical ee
educational institutions. The system of medical education —
requires a restructuring to suit the true needs of the Re
people. Clearly, mere rhetoric on the part of the govern-
ment will fail to achieve this aim.
needed
What is essentially
is a change at the political and economic
—
level —
which will in turn affect the health care system and the~
system of medical education, and will thus determine new |
priorities. In a new society, a people-oriented package is
to be devised, in which a newly designed medical educa- —
tion programme should play an important role alongside
other ingredients of the health matrix.
[I am greatly indebted to Mchreen for her invaluable comments and suggestions. The editors of this Journal also deserve ee
e
eS
gratitude for some excellent comments on the first draft.]
References
(1)
servBanerji D. Social and cultural foundations of health
1974.
1333,
ices systems. Econ. Polit. Wkly IX,
(2)
Navarro
(3)
The
underdevelopment
health of underdevelopment:
of health
or the
an analysis of the distribu-
Latin America. Int. J.
tion of human health resources in
Tn
Hith Serv. 4,5, 1974.
lism in
socia
h care and
Modell H. and Waitzkin H. Healt
"Chile.
(4)
V.
Monthly Rev. 29-40: May, 1975.
B. Health care in developBenyoussef A. and Christian
399 408, 1977.
ing countries. Soc. Sci Med. 11,
Prise al:
ha
ei.
,
Health: Sector Policy Paper. ‘World Bank, Washington
D.C. 1980.
Banerji--D.
(6)
Sie
|
medicine
Western
in developing
countries
Tavistock,
London,
Whyence me
i
S.A.: evid
id
~ (20) Za
rural areas
students:
(21) Zaidi S.A. The,class composition of medicalPolit.
Wkly
some indictions from Sind, Pakistan. Econ.
21, 1756-1759, 1986.
1984.
Banerji D. Health and family planning services in inde-
(7)
(22)
India: policies, programmes and prospects.
pendent
(Draft of a chapter in a book: India 1947-72: A Social
Report), mimeo, Centre for Social Medicine and Community Health, Jawaharlal Nehru University, New Delhi,
not dated (n/d).
Zaidi S.A. The urban bias in health facilities in Pakistan.
Soc. Sci. Med. 20, 473-482.
Ugalde A. The role of the medical profession in public
health policy making the case of Colombia. Soc. Sct.
Med. 13C, 109 120, 1979.
(23)
stan Devl. Rev. In press.
Roemer M.I-Political ideology and health care: hospital
patterns in the Phillipines and Cuba Int. J. Hlth Serv. 3,
,
487, 1973.
(24)
Britain Cuba Resouree Centre. Health in Cuba. Newslet-
(25)
— 14A, 435-444, 1980.
of the ideological and political
Navarro V.A critique
position of the Brandt Report and the Alma Ata Declaration. Int J.. Hlth Serv. 14, 159 1984.
) King M. Medical Care in Underdeveloped Countries.
Walt G. and Vaughan P. and introduction to the primary
hea!th care approach in developing countries. Ross Institute of Tropical Hygiene Publication No 13, London,
17 March, 1985.
(26)
The Guardian. Manchester,
(27)
Bossert T.J. Health policy making in a revolutionary
context: Nicaragua 1979-81, Soc. Sci. Med. 15C, 225231, 1981.
(28) Walt G. and Melamed A. (Eds) Mozambique : Towards a
Peoples Health Service. Zed, London,
1984.
9)
Banerji D. Community health needs and Indias drug
industry, mimeo, Centre of Social Medicine and Community Health, Jawaharlala Nehru University, New
Dethi, 1983.
Bell,
(30)
Patel S.J. (Ed.) Pharmaceuticals and health in the Third
World. J. Wid Devi. Special Issue, 11, 1983.
Sharpston M.J. Uneven geographic distribution of medi-
(31)
Pakistan Medical
Oxford University Press, Nairobi, 1966.
Bryant J. Health and the Developing World.
Cornell
‘University Press, Ithaca, N.Y., 1969.
Gish
O. Doctor
London,
Migration
and World
Health.
1971.
al care: a Ghanian case study. J. Devi. Stud. 8, 205-222,
1972.
a
Segall M. The politics of health in Tanzania.
_ Bader M.B.
and Dental Council.
Regulations for
the Degree of Bachelor of Medicine
and Bachelor of
Surgery, ammended
Dev.
International
upto April 1981, to be effective
from the Academic Session of 1981. Ministry of Health,
: = Change 4, 39, 1972-73
~
1981.
1981.
_ fessional values and economic interests. Soc. Sci. Med.
16)
PakiZaidi S.A. Issues in the health sector in Pakistan.
ter. London,
A. Physicians control of the health sector: pro-
| Ugalde
rs
527-534, 1986.
“the case of India.In Health and Illness in Developing
Countries (Edited by Blizard P.).
a survey.
Islamabad,
1981.
transfer of medical
technol-
(32)
DAWN, Karachi, 13 May, 1984.
0gy— ‘An analysis and a proposal for
monitoring. /nt. J. Hlth Serv. 7, 443, 1977.
effective.
(33)
Government of Pakistan. Report of the Medical Reforms
Commission. Karachi, 1960.
Hom J. Brain drain and health priorities
AmericaZJnt. J. Hlth Serv. 7, 434,1977.
in Latin
(34)
Ahmed
A. A critical study of health manpower
programme
Gish O. and Godfrey B.A. reappraisal of the brain drain—
- with special reference to the medical profession. Soc.
Sci. Med. 13C, 1, 1979.
in Pakistan.
Pakistan, Lahore,
(35)
Mozambique,
Public Health Association of
1976.
Angola
and
Guinea Information
Revolutionary practice in health.
London,
training
Centre,
People Power No 13,
1979.
Notes
_ Our
discussion
is stricted
to underdeveloped
capitalist
_ countries and we have purposely ignored developed counoid
a
.
__ tries. It is true that in advanced capitalist countries health’
.
*
.
.
.
care is fairly well distributed and accesssible to all, but this
is a different issue, and we believe that comparisons be-
tween DCs and UDCs (whether capitalist or not) are quite
:
a irrelevant and out of context.
2
It must be emphasised that it is not doctors who are at fault,
but the cldss system by which they are produced and in
which
3
they function.
Of the 17 colleges, all but one are government owned. The
Aga Khan University: is the only private University in the
country and is linked closely with McMasters, McGill and
Harvard Universities. It however also follows PMDC regulations, but has the ‘advantage, of not only foreign trained
personnel, but expatriates on their faculty,
Each college has its own ‘quota system’, A certain percen
tage of seats are given on merit, while the others
are reRadical Journal of Health
|
apeineinenie
dine
s at hethe Arm
A J
-ex-service —
a
:
“4 dents
oe Phin
-
ke
5
;
Ussi=Rs.
:
ee
PO)
and fo
ae
ae?
well . extra-curricular activities and
in the relatively less important subject of forensic medi-
aes ake erprivileged areas Gages are usually
:
17/- annual per capita income
e
.
e colleges,
due to
: cine, biochemistry and physiology.
10
in Pakistan is
:
=
for many weeks
as SO
ay
percent of doct
3
oduced i
i
eae
dent sitting in the corridors diligently working away. On }
each’ year
adding up to a minimum of two years in a medical students
college life.
ee
o
About four of the 20 essential’ books are written by Paki-
no previous visit had the author seen students so busy. On
~
enquiry it was revealed that each and every one was mak-
fs
ing notes to pass on to students in the examination hall.
12 The PMDC reiterates its claim that the level of teaching at
stani authors. There is an unfortunate twist to this, in that
the few books written by Pakistan authors are unfortunately of extremely poor quality, but are nevertheless,
made compulsory if the author happens to be teaching the
course.
As many
Speaad:
11 The author on a visitor to medical college found every stu-
local (college) or national politics
and disturbances, are closed
7
three were not foreign "qualified.
=a
fedical Co lege, only ee
these colleges is not up to ‘standard’ and thus their doctors ea
are not ‘properly’ qualified.
s
13 Although Gish and Godfrey's recommendations are meant
to reduce the exodus of physicians from UDCs, we feel
_
that since it is the education system which causes the
_
8 The Army Medical Collge m Rawalpindi run on very disci-
migration in the first place, their recommendations need
plinary (military) lines, admits only 100 students a year.
to be discussed as they are extremely cogent and worth- eo
Liaquat Medical College in Hyderabad admits 447.
while.
|
g
Economic and Political Weekly
i.
A journal of current affairs, economics and other sociai sciences
;
Every week it brings you incisive and independent comments and reports on current problems plus a
re
number of well-researched, scholarly articles on all aspects of social science including health and medicine,
“i-
environment, science and technology, etc.
‘ie
Some recent articles:
es:
Mortality Toll of Cities— Emerging Pattern of Disease in Bombay : Radhika Ramsubban and Nigel Crook
Famine, Epidermics and Mortality in India—A Reappraisal of the Demographic Crisis of 1976-78: Ronald
va
Lardinois
Malnutrition of Rural Children and Sex Bias:
Geography of Secular Change in Sex Ratio in 1981:
Illina Sen
Occupational Health Hazards at Indian are Earths Plant:
;
925
Institutions/Companies one year Rs 325, Two years Rs 625, Three years Rs
One year Rs 250, Two years Rs 475, Three years Rs 700
hers Rs 200
Concessional Rates (One year): Students Rs 150; Teachers and Researc
(Please enclose certificate from relevant academic institution)
Hitkari House, Shahid Bhagatsingh Road, Bom[All remittances to Economic and Political Weekly, 284,
ed, please add Rs 14 to outstation cheques for
bay 400038. Payment by bank draft or money order preferr
collection charges]
on health and related subjects
A cyclostyled list of selected articles in EPW
is available on request
—————
ll
ae
oe
Be
T V Padmanabhan
Inland Subscription Rates
Individuals Only:
a
os
Amartya Sen and Sunil Sengupta
Family Planning and the Emergency—An Unanticipated Consequence : Alaka M Basu
Ecological Crisis and Ecological Movements : A Bourgeois Deviation?: Ramachandra Guha
Environment Conflict and Public Interest Science : Vandana Shiva and J Bandhyopadhyay
March-1989
:
; ;
fe |
“i 4g
4
ae
UPDATE
News and Notes
Defining Quacks
CONSUMER Week this year was celebrated by meetings
organised by several organisations such as the Consumer
Guidance Society of India, Grahak Panchayat etc on
health and health related issues like medical care and
quackery, responsible medical practice etc. While these
to take action against the doctors which the Lentin Commission had named as being responsible, by their negligence, for the tragedy at the J.J.Hospital. One may legiti-
mately ask: Is this a body to enforce medical ethics or a
body to Iegalise quackery?
the
Of course, the MC does take prompt action on certain
_| process can never take off unless certain uncasy questions
| are confronted.
issues such as promptly de-registering a non-practising
filmstar doctor for advertising. Or more recently, the
Maharashtra Medical Council issued a statement ‘threatening’ the doctors who supported Dr Bal in his fight
against victimisation with ‘dire consequences’. His supporters, it will be recalled are agitating against the sinister role played by Dr Sudhakar Sane in his personal
capacity as Vice President of the Managing Committee of
Dhanvantri Hospital from where Dr Bal was dismissed.
Dr Sane happens to be the current president of the Maharashtra Medical Council and so the MMC sought to
provide protection for him for his personal ill-deeds.
Why, was Dr Bal victimised by Dr Sane and his
friends in the managing committee of Dhanvantri Hospital? Because he is the secretary of ACASH, a consumer
organisation which along with others sought to get the
HDEP drugs banned, started a campaign against the unscientific claims made to sell analgin by the industry and
so on. Thus so-called qualified doctors and their premier
body have chosen to victimise those who are fighting
against the quackery of medical professionals.
It is really ironic and tragic that in the consumer week
the president of the Maharashtra Medical Council was invited by the CGSI to speak on Consumer Education in
Medical Practice. Not only that, the CGSI which supported Dr Bal and the drug consumer movement till recently has decided to dump both Dr Bal and the campaign for rational use of drugs in favour of such medically-organised quackery. We cannot help wondering at
the kind of education that this protector of the high
priest of medical quackery will give to lay people
. In
are
commendable
efforts
at consumer
education,
|
Is it enough to define quacks as those who do not
| have appropriate degrees and qualifications? Such practitioners are, of course, quacks. But there are also those
| who practise ‘quackery’ even though they possess requi| Site qualifications and degrees. These are the properly
| registered doctors who pursue irrational practices and
| therapy. We illustrate this with just two instances :
|
(a) Several surveys and our own experience shows
4 that a majority of patients who approach doctors receive
|injections regardless
of their ailment.
Is this rational
| practice? Medically, injections are given only in three
| situations—life threatening conditions; when the paticnt
| has severe vomiting and cannot retain oral medication
| and; when the drug is not available in oral form, such as
| insulin. Aren't these doctors who prescribe injections in| discriminately also ‘quacks’ of a sort?
} — (b) Such quackery became even more visible during
;the recent controversy regarding high dose estrogen pro|gesterone (HDEP) drugs. No standard text book of media cine or pharmacology recommends such HDEP drugs.
a Moreover, they aré known to cause serious harm to the
| foetus when taken by pregnant women.
And yet, this
| drug with a multicrore-rupee market was freely pre| scribed and used by doctors not only for pregnancy test: ‘ing but even to induce abortions. Further, when the Su-
| Preme
By
Court ordered a public enquiry: to decide
whether the irrational and potentially
harmful
on
drug be
| banned, some of these doctors chose to give glowing tcs-
is timonials in support of the drug. Is this responsible
:
2 medical practice or is this ‘quckery' to help the
drug
| industry?
jie
The Medical Council of India is charged with the re_ | sponsibility of regulating medical practice which
includes
curbing quackery. What has it becn doing? It has never
come out against irrational practices such as the propoga| tion of the ‘injection culture’ by doctors; it has kept
a
dubious silence on the issue of the doctors’ role in push-
ing hazardous drugs; and even worse, it has not bothered
any case, do people who either indulge in this
sort of
‘quackery’ or give them protection by refusing
to confront the issues have any moral right to be
part of consumer mectings? They are really the ‘accus
ed’ and not the
‘educators’,
Isn't it time to take the bull by the
horns and confront
the medical establishment with thes
e issues?
(Press release from Medico Fri
end Circle, Bombay
Group on March 18, 1989.)
36
Radical Journal of Health
Rural Doctors in Thailand
IN accord with a world-wide change in attitude about
health services the government in Thailand has adopted
a health policy centred on community services and a
better balance between prevention and cure. However
there are problems with the implementation of the policy. These problems were raised at a seminar held recently in Bangkok about the role of community hospitals in public health development. Jointly organised by
the Rural Doctors’ Association (RDA) and the Ministry
of Public Health (MOPH),
tended the seminar.
some 400 rural doctors at-
The government policy, as laid out in the previous
Fifth (1982-1986) and current Sixth (1987-1991) National Health Development Plans, talks of participation
in development, basic minimum needs, primary health
care, decentralization and intersectoral collaboration.
Nobody disputes the soundness of the policy. And few
into the practice of medicine. Contemporary medical
education is often centred on accomplishing skills at utilizing medical technology, ignoring the inter-dependence
of body, mind and spirit. Thus, training of all health
personnel is inadequate in instruction on both the principles of primary health care and the dependence of
physical health on social and spiritual well-being.
While*it is true that considerable gains have been
made towards achieving equity in health expenditure,
further redistribution is essential if the health status of | |
the poorest Thai people is to improve.
A former chairperson of RDA and now a member of |— '
the Health Planning Division, MOPH, Dr. Suwit Wibul-
phonprasert explained this further. "If the proportion of | 3
the health budget spent in rural areas, now a relatively
fair 63 per cent of the total, is dissected further it can be
seen that half of it goes to provincial hospitals and more
would dispute the progress made to date. The number of
than two-thirds of the remainder goes to district hospi- | _
doctors in the rural areas has more than doubled over
the past six years. This year 63 per cent of the health
budget will be spent on rural services, compared to 43
per cent in 1981. All villages have local village health
personnel, and almost all districts have hospitals. In
general, the government's policy is well approved of and
is having some positive results.
The RDA though is critical of the actual implementation and argues that the potential positive effects have
been hampered by a budget that does not adequately reflect the policy, and poor education for all health personnel about the principles of primary health care.
As already mentioned, over the past six years the
number of doctors working in the rural areas has more
than doubled. However as the chairperson of RDA, Dr.
tals." Thus the vast bulk of the budget is used for hospi- | —
Supatra Sriwanichakorn
pointed out, "This still repre-
tal services.
Now is the time to concentrate on health services at |©
sub-district and village level. The projected 9 percent in-
crease
in the ‘district/sub-district’ item of the health
budget will almost all go to the sub-district level. There
are plans to employ nurses in all the Health Centres as
well as to increase the availability of Mobile Health |
Teams for weekly visits to the Health Centres. However, |—
should this become merely an outreach extension of the |
hospital it cannot be considered a true diversion of funds |
.
towards primary health care.
disof
The RDA is also advocating more autonomy
trict hospitals so that decisions about implementation of ie
policy can be made locally with local conditions in a
mind. Decentralisation is the key-word. "But you have
to differentiate between delegation and decentralization"
Dr. Suwit cautioned. Delegation is handing down the responsibility for some decisions from one officer to anfull
other. Decentralisation should go hand-in-hand with
decommunity participation. That is, power should be
volved to the recipients of health services.
not disputThe Rural Doctors’ Association is certainly
sents less than 10 per cent of the more than 14,000 doctors nationwide while more than 80 per cent of the
population are rural residents.” Thus in the north-east of
Thailand, the poorest region, the ratio of doctors per
head of population in 1984 was 1:15,554 while Bangkok
could boast a ratio of 1:1,321.
In addition to this only 45 per cent of these rural
nt's public
ing the general direction of the governme
doctors have worked there for more than two or three
that much more
health strategy. They do believe though
years. The government currently requires medical graduof
to accelerate the health development
done
be
could
»
after
years
three
for
hospital
rural
ates to work in a
Thailand— for all of its people.
graduation. Thus the majority are relatively inexperienced and rush back to the city after their compulsory
rural service.
A further concern of several speakers at the seminar
was the dehumanising effect of the modern medical sys-
tem. Several speakers reiterated the necd to inject ‘spirit’
March- 1989
:
For further information, contact
Dr. Supatra Sriwanichakorn,
Chairperson,
Rural
Doctors’
Association,
Bua Yai Community Hospital
Nakorn Ratchasima 30120
THAILAND
a
Tbe
ff OME EL oe Te
oe ae
e
~
Private Sectur in Medical Care
(A Brief Survey)
rama
Vv baru
le venture and has proThe increasing penetration of high technology equipment is making medical care a profitab
hospinursing a
vided a fillip to the expansion of the private sector, which in health care comprise clinics,
development? What are
tals, pathological labs and diagnostic centres. What are the factors which have led to this
the implications for health care?
WHILE only a few years back there were hardly any
hospitals which offered super specialist services outside
major metropolitan centres, now a large number of private
hospitals and diagnostic centres have come up in all major
cities. Some of these organisations are corporate enter-
prises
which are run like regular business concerns by
floating shares in the market. Big business groups like
- Tata, Hinduja, Modi and Escorts and regional groups like
_ Standard Organics Lid in Hyderabad and Apollo Hospitals
Ltd. in Madras have diversified into Medical care
_
Whether in larger hospitals, nursing homes, diagnostic
- centres or pathological labs, high technology medical
: equipment like scanners
nuclear gamma
camera, _ lithot-
_ fipers, auto-analysers and the like have come
to play a
crucial
purposes.
role
for diagnostic
and
therapeutic
= Nearly 80% of al] medical equipment is imported through
- companies like Siemens of Germany, General Electric of
_ USA, Dornier and Hitachi.! Although equipment costs are
__ high, imports are rising quickly. While in 1980 alone Rs.
20 crore worth of equipment was imported, by 1986-87 it
_ ports are expected to rise at the rate of twenty percent
_ annually for the next three years. The trend of increase in
Modinagar with emphasis on specialities like paediatric,
cardiology and cancer treatment. The project is valued
around Rs.200 million and is nearing completion. Apart
from this several smaller projects have been initiated in
major cities of North India. In New Delhi the cancer
treatment facility for the 1000 bed All India Institute of
Medical Sciences is being developed in cooperation with
the Rotary Club of New Delhi. The estimated cost of this
project is to reach over Rs. 100 million. In addition a
number of large hospitals and diagnostic centres have also
been set up with NRI collaboration in New Delhi.
A sizeable number of large private hospitals
have
mushroomed in States like Maharashtra, Kerala and
Andhra Pradesh over the last few years. In Maharashtra,
Bombay has threé or four large projects in the offing. The
Hinduja business family from London is funding the expansion and renovation of their 100-bedded National Hospital to a 300-bedded modern general hospital with the
latest diagnostic equipment. The hospital proposes to offer
specialised services in opthalmic and orthopaedic surgery.
The Indian Cancer Society in Bombay has initiated the
construction of a new cancer hospital which is valued at
Rs. 200 million. Yet another 200-bedded hospital is being
built by the Mahavir Health Foundation which is a chari-
table trust. The estimated cost of this project is Rs. 100.50
Vee
_ medical equipment
the government has reduced import
_ duties from 107 per cent to a mere 40 per cent. In addi_ tion, total duty exemption has been granted to hospitals
2 -and diagnostic centres willing to treat at least 40 per cent
S of their patients free of cost. In the case of non-resident
»
a
Indian (NRI) investors exemption from import duties is
granted if at least 25 per cent of the patients are offered
__ free treatment.
:
The liberalisation of import duties coupled with increase in the income of middle and upper middle classes
has resulted in the demand for consumer durables and
luxuries. This, naturally, has had an effect on health care
as well. A number of large projects have been initiated
and several existing hospitals are being expanded and up-
graded by business groups and private trusts across several
States in the country.
According to a market survey report by a leading pharmaceutical company, in Uttar Pradesh, the Modi group of
industries
38
is establishing
a super
specialist
hospital
in
million and will specialise in cardiac and kidney diseases.
The Bhatia General Hospital which is run by a private
trust in Bombay has been expanded at a cost of Rs. 20
million with super specialist service like cardio-therapy,
ultra sonic imaging and clinical analyses equipment. The
mushrooming of private hospitals in Maharashtra is by no
means confined to Bombay. Karad town in Satara district
of Maharashtra has a 200-bed private hospital started with
an investment of Rs. 30 million to provide for construction and initial costs. Since the project is located in a
small town it is expecting to provide services to surrounding villages as well.
In Kerala there has been a state-wide boom in private
hospitals. According to a Survey conducted by the Burea
u
of Economics and Statistics in 1986, there were
1,953
government institutions with a bed strength of 38,133 as
against 3,585 private hospitals with 50,766 beds? While
ati like Trivandrum and Cochin have their share
of high
“Sapte medical centres, it is by no means restricted to
the larger cities. In fact high technology
medical care has
Radical Journal of Health
—
4
rated
e'
‘into uate towns a ee
in some
en partsof. Kerala. According «: a report it is not uncommon
to find private hospitals in villages having scanning and
diagnostic cum therapeutic equipment being used for treatment of patients.
Apart from big business groups and private trusts establishing hospitals with sophisticated equipment, regional
business groups have also entered this arena. Apollo Hospitals Lid, a Madras-based corporate concern was one of
the first to establish a super specialist hospital in South In-
result of fe:a “number of large and repional Gignes :
groups and doctor enuepreneurs are diversifying into this —
areca. Institutions which use high-tech equipment are nolonger confined to the metropolises but are penetrating a
semi-urban and even rural areas.
oak
There are several reasons for the burgeoning of the pri-a
vate sector. Firstly, although the public sector has ex-
panded considerably since independence, the meagre investments made by the state have been inadequate in meet- _
ing rising
demand. This ‘pent-up’ demand is increasingly
dia. Recently, the same concern has initiated another proj-
being met by the private sector. Secondly, the increase in
ect in Hyderabad with an initial investment of Rs. 12 mil-
incomes of the middle and upper middle classes, in recent _
years, has resulted in the demand for durables and luxuries —
which is reflected in medical care as well. Thirdly, advancement in medical technology has pushed up the cost
of medical care making it a profitable business venture.
oe coupied with liberalisation of import duties on higt
echnology equipment has led to mushrooming of ne
lion tO cover construction and equipment costs.? Several
such projects are being initiated in Andhra Pradesh by
business groups and private trusts in collaboration with
Non-Resident
Indians.
Standard
Organics Ltd, a Hydera-
bad-based corporate concern has also made inroads into
health care. The Standard Organics Ltd which is essentially a pharmaceutical concern has diversified into leasing
of medical equipment and have set up diagnostic centres in
several major cities in the country.*
In a recent announcement a group of Andhra non-resident Indian doctors based in California are initiating superspeciality hospitals project in Hyderabad, Vijayawada and
Visakhapatnam. The cost of each of these projects is estimated at Rs. 30 crores and will consist of over 300-bed
hospital, 200 nursing quarters, 100 physician quarters, a
hundred room three star hotel, a thousand seater auditorium and four lecture halls. In addition to providing super
specialist services the foundation seeks to "bring about
medical and health awareness in rural and semi-urban
populace through continuing medical education programmes with accent on rural health.* Apart from these
large projects a number of smaller ventures have already
been initiated in the several major towns. In Hyderabad a
local business group has initiated a super speciality hospital
valued at Rs. 7.60 crores is nearing completion.*
Calcutta is yet another metropolis where somie leading
business groups from Madras have applied for permission
to the government for land to build super specialist hospi-
tals. In addition in a recent announcement the State is
planning to hand over some ‘sick’ government hospitals to
industrialists and NRIs in order to improve the functioning
of these insititutions.’
Although this brief survey is by no means exhaustive, it
is certainly indicative of the emerging scenario in the private sector. While it is well known that both the statc-
supported medical service and private medical care have
been co-existing since independence, in more recent years
the latter has been growing and diversifying. The private
sector in health care comprises, clinics, small, medium and
large nursing homes, hospitals, pathological labs and diagnostic centres.
care institutions across the country.
be 2
Quite clearly, the increase in imports of medical equi reat
ment has hiked the cost of medical care. Since most of the
high technology equipment is employed for diagnosti ic
purposes, testing has assumed an important role in treat- —
ment. As a leading specialist remarked "these days doctors
depend excessively on sophisticated testing procedut
which have often led to unnecessary testing". Althou
import of medical equipment is on the rise there has be
no effort to either regulate the growth or prescribe mi i
mum standards for the running oF these enterprises. He
to a secondary position. With the increasing commodi i
cation of medical care and the demand to treat it as
industry, it is mandatory that the government prescrit i
References
:
1. (Market Survey on Medical equipment), Confidential report
prepared by a oe pharmaceutical concern, Hyderabad,
.
1987.
2. Cited in Pillai. S, ‘A Flourishing Business’ in /ndia Today
January 31, 1988, p. 149.
3. India: Market Survey... Op. cit.
h Services:
4. Baru, R. Factors Influencing Variations in Healt
Pradesh, UnpubA Study of Selected Districts of Andhra
arlal Nehru Unilished M. Phil thesis submitted to Jawah
versity, New Delhi, 1987.
in The Hindu, January 20,
5. Advertisement of Indus Hospitals
1988.
6. Indian Express,
April
1987.
7. Times of India, January 24, 1988.
Increasing penetration of high technology
equipment is making medical care a profitable venture and
has provided a fillip to the expansion of this sector. As a
39
March- 1989
ee
a
a
SAD
oo wae ee eu wecor,
Need for Alternative Medical Education in South
F.
Alrica
r h philpott
many eminent doctors. But
Medical education was introduced in South Africa in 1922 and has since produced
needs or more disturbtoday the universities are not producing doctors appropriately trained either for current
There is an urgent need to radically transform the medical course and
ingly, for a post-apartheid future.
curriculum. (Reprinted from Critical Health, 1988)
DOCTORS first completed their medical education in the
University of Cape Town in 1922. The early medical
teachers brought their curriculum with them, mainly from
the United Kingdom. They produced many first rate doc-
tors and in the decades since, many graduates have attained international acclaim. There have been a number of
intra-university curriculum reviews but these have tended
- to add more and more
to an already overfull course.
In
1985, the South African Association for Medical Education (SAAME) held a national review of medical education in South Africa, but very few of the recommendations have had any effect on our medical schools. Our
universities are neither producing graduates appropriate to
the needs of our country at present nor, more disturbingly, for the post-apartheid future. This paper sets out
Eine of the reasons why we urgently need alternative
_ie medical education to help solve the scrious health care
pe blems in this country, remembering that it will be six
_ years after the new curriculum is established before the
¥ first graduates appear.
Maldistribution of Health Services
Doctors tend to practice in the kind of environment
5
a
ie
oy
Ri hcre they are taught and so it is understandable that they
. find their security in city practice, cither in this country or
Overseas. It is true that it will take more than a changed
eo. to entice doctors to practice holistic medicine in
__ the neglected parts of our country, but if we don't change
__ the education we provide, no amount of structural change
:
in
the health service will bring about improved health care
_for the people of South Africa. Doctors need to be trained
in the context of where their services are needed most.
i
Not only does maldistribution operate geographically
: but also in the emphasis on specialities. For example,
s Many specialist obstetricians with a minimum of twelve
_ years of training spend the bulk of their time doing nor_ mal deliveries for extra-ordinarily high fees while primary
_ health care for the poor is seriously neglected.
_
The major portion of clinical teaching is provided in
_ teferral, high-technology teaching hospitals, where the
_ bulk of the country's health budget is spent. This gives
_ Students a view of health care that suggests that doctors
_ only deal with rarities and that sophisticated monitoring
systems and laboratory investigations are not only indis_pensable, but immediately available.
The teaching: hospital glorifies high-technology curative
medicine and surgery and gives limited consideration to
preventive and promotive health. Role models have a ma-
jor influence on the development of a medical student's
approach to medical practice, and with the emphasis given
to curative medicine and the down-playing of preventive
and promotive care, it is little wonder that the same pattern persists in succeeding generations.
There is a need for a medical faculty to develop expertise in the various specialities but this does not promote
the most appropriate basis for medical education. It has
engendered unhealthy competitiveness for curriculum time,
space and status. Each department advances its own course
for survival sake and as a result produces a curriculum
more suited fo specialists in the discipline. Such structures
are not suited for the undergraduate education of a ‘core’
doctors. Instead, there is a need for strong central depart- ments of medical education that co-ordinate cross-discipline, integrated programmes of problem-based learning.
Medical students who graduate from our medical
schools have every right to presume that health care is
dependent primarily, or even exclusively, on doctors.
Their doctor teachers in the hospital are on top of the pile
and project other health workers as auxiliaries. Medical
students are scldom introduced to other health workers, let
alone train with them. Again it is understandable that our
graduates have little experience of working in teams and
that our country's health service is, in the words of David
Werner (author of the book Where There is No Doctor)
community oppressive rather than community supportive.
Doctors are expected to have all the knowledge and wisdom and are not shown how to consult the communities
they are meant to serve. They have been trained to be
consultants before they learn to consult and to direct before they have learnt to serve.
The tencts of western medical practice are taught as if
no other belief and practices have any place in a country
with such a multiplicity of cultures. Our very failures
Should alert us to the need to examine others’ successes
and to incorporate them into new learning opportunities
for our students. A salutary research study conducted in
Zimbabwe needs to be heeded by our medical educators.
Groups of 100 rural and 100 urban women (many of
whom were university graduates) were asked where they
would wish to be delivered of their next baby and who
they would like as their attendant. The majority in
both
groups wanted the safety of hospital or maternity clinic
but 100 percent of the rural and 90 percent of the
urban
woman preferred to have a traditional birth
attendant
(TBA) with them during their labour. Few
doctors even
40
Radical Joxrnal of Health
.‘
f
1
ee
We Pee,
ac
Tr Ae oar
Ue rege eras 5a
+
iF
eth
LS SES ES
ae?
eR
ee
ee
a
_ Fecognise that the overwhelming majority of women on ~ demands of
the new century. We subscribe to Health for
this continent are delivered by TBAs. Instead they write
Ail
by
the
year
2000" but are not equipping graduateto.
s
____ Off such patients as 'unbooked’ or 'defaulters'.
We interpret meet that challenge. Rather than multiplying
3
scribe, in spite of the fact that we never explain
ed what
they were for. We also forget that our patients have an
entirely different world view that iaforms their under-
i)
nity or the individual patient level, Problem-solving will
ensure a multi-disciplinary approach to medical education —
and will equip students to absorb and apply new knowledge as it becomes available. It will also ensure that each :
Subject discipline is dealt with accordin$ to its merits, the
merit of the solution to common life-saving problems in
the first instance, and later, any other problem that may
standing of the aetiology and therefore treatment of ill-
faculties in the university. How can we expect students to
accept other disciplines such as agriculture, economics,
sociology and education as being important, if not more
present itself. Students progress when they know how to
important, than medicine in providing health and whole-
explore knowledge rather than just memorise it.
rams
We manage to drain every atom of motivation and en-—
University, which is not only a contradiction in terms, but
ricula, which in the first three years can only suggest t
health care is all about. The consequences are a country
that can boast the first heart transplant while within walk-
specimens in bottles. How much more exciting it is to
ness of care? We even call one of our schools a Medical
__
Wa |
is that they will be called on to do whether at the commu-—
ness.
.
Not only do we compartmentalise within our medical
faculties, but we isolate the medical schools from all other
»
adhe
content we
need to provide students with problem-solving skills, for it
_ compliance as meaning taking the host of tablets we pre-
;
t
thusiasm that students bring with them by our layered
cu
more evidence of our failure to understand what holistic | Students that life is filled with laboratories, cadaversan
a small group of first year students deciding on the a
ing distance of the particular hospital involved, there are.
omy, physiology, pathology etc that they need to expk |
townships with no piped water. The need for a multi-dis-
and learn to enable them to solve a particular clin
ciplinary approach to teaching extends beyond the com-—
i
fe
problem. By the end of a course of suitably chosen: pr
partmentalised medical school to cross the academic barri- _ _lem-solving studies they will have not only learnt:
ers in the university. It is only when engineers and agri- principles and content of each subject in the curricul e
culturists link with sociologists and physicians in formulat- but they will see how it all fits together in helping them
ing new curricula that the ill-health caused by factors re- solve the problems. Experience with such curricula has
lated to each of these disciplines will be addressed. It all shown that students have to be restrained from over-studyseems so obvious, but until we are brave enough to create
ing rather than driven through the early years of bored
new educational structures, our students will retreat into
.
their academic enclaves instead of becoming the new pio| neers of health care in Southern Africa.
This is not the language of our medical teachers. We
interpret the effects of state systems on community and
individual health, and therefore demand
that politics and
health care be kept in separate compartments.
In spite of the fact that many of our students come
from the oppressed communities, their awareness and understanding is not encouraged by the majority of their
teachers, and the only oasis in the midst of a year of non-
contextualised teaching is the annual Students Conference,
at which academic staff are conspicuous by their absence.
The Medical Course
This statement hardly needs elaborating, yet we are all
guilty of adding every new discovery to the curriculum,
without taking anything out. Each new discovery should
remind us that much of the content in today's curriculum
will be out of date by the time our students are in practice
and our volumes of content
will not prepare them for the
Ned
‘
RRS
sets in at junior schools. Children, left to themselves,
are
experiential, self-directed learners until the schools get”
hold of them, From then on the teacher takes control, at d
presumes that all children learn at the same pace. Consequently they are regimented into large classrooms, told
keep quict and listen to the teacher. The only difference
medical school is that the classes are many times larg
protects our academic safety. Few of us have experienced
the oppressive effects of apartheid, the major cause of
poverty and ill-health in the midst of this land
of great
wealth. Without this experience, our teachers are unable to
.
ing the natural spirit of adventure and exploration. The Tot
are the privileged ones and we are comfortable with our
___
élitist positions and the status quo and bureaucracy that
;
Medical schools are not entirely to blame for suppres-_
~
and the teachers do not even hold an education diploma,
My only surprise has been the rapidity with which fourth —
year university rote learners respond to the liberating ex te
perience of changing from an emphasis on whole-class iY
lectures to the fun of problem-solving in small groups. —
We have shown that it works at that late stage of the cur-
riculum, so why not start that way from the first year of
the medical course?
Of all countries in the world today, South Africa in
1s .
particular needs a liberated educational system. Not only
this the most appropriate way to learn but it equips people
to seck after truth and justice in every sphere of theif |
|
lives.
educaThis outline of the need for alternative medical
'
of
ion
direct
the
tion. in South Africa must point us In
community-based,
community
lem-solving education
oriented,
as the solution
integrated,
to our
prob+
needs,
4]
March-1989
y=
|
Socio History in Medicine
padma
prakash
the class in charge. Even the content
Medical curricula is in the long run determined by the socio -political needs of
m content of one under graduof these disciplines reflects these needs. This article examines the history and curriculu
ate discipline in medicine—preventive and social medicine.
THE practice of medicine has undergone tremendous expansion and diversification. Several factors have contributed to
the transformation of medical practice, Some internal and
others external not the least significant of which have been
social, political and economic. From time to time medical
education has reflected these changes in the practice of
‘medicine. This amalgamation of current practice with train-
|
appear to follow any particular sequential logic. A first
chapter on what is presumably meant to be a history of
medicine is followed with a series genetics and health, sociology and health, environment and health. In a sense of
course, the chapterisation is indicative of the entire approach to the subject— that the understanding of the preventive and social aspects of medicine can be so compart-
ing has not taken place in either a smooth progression or as
a matter of course. For example while improved methods of
mentalised. There appears to be no continuity between the
chapters. This criticism will perhaps become clearer when
we deal with these chapters in greater detail.
Our main criticism is that the book projects a certain
‘of knowledge in epidemiology
picture of medicine, medical practice, and of the role of the
doctor. This creates and reinforces an ideology which is
biased against certain sections of society. Moreover it delineates for the medical graduate a methodology for understanding social phenomena which views society as a Static,
rigidly divided structure. According to this viewpoint the
diagnosis and treatment have become part of the training of
‘medical graduates with relative rapidity, the growing body
and in the sociology of
health and illness have been all but ignored in the under-
‘graduate medical curriculum. This marginalisation of the
OXiological perspective
has had consequences for the de-
velopment of medical education and inevitably for the na‘ture of health care.
;
can each be studied separately, can even be
It is the character of the dominant group/section/class in
components
ociety which determines
the trends and content of medical
modified, improved, changed. For instance, that health be-
sducation. This dominance
however, is not because of
haviour can be changed without altering the social location
umerical strength but is a consequence of the historical
evelopment of society. Again, what constitutes the require-
of the individual or family concerned. This affords the right
health characteristics of the class/group. For the require-
grounding for the view that medical solutions can not only
be independent of social factors, but in fact they over ride
the latter and can even affect social change. While undoubt-
“ments are rooted in the socio-political needs of the class in
edly medicine in history has contributed to socio-cultural
nents of this dominant class is not just derived from the
charge. In fact not only is the curricula determined largely
ythese factors, but even the content of these disciplines is
ailored to match and sustain the ideological requirements of
he dominant Class. To illustrate, we examine in the follow_ing the history and curriculum content of one undergraduate
department, viz preventive and social medicine (PSM). This
isa relatively new field, having been introduced as a distinct discipline only in the second quarter of this century. In
F india separate departments of PSM were established only in
the late fifties. What were the factors leading to the intro“duction of PSM into the undergraduate curriculum? What
“has been its orientation and what is its current content?
4” _ For the purpose of examining in detail the undergradu~ate curriculum content of PSM we have taken The Textbook
of Preventive and Social Medicine by J. E. Park and E.
Park as a typical illustration. The content preventive and
social medicine can only be understood against this back-
“ground, Specifically, we have looked at Parks’ Textbook of
eee
Medicine assuming it to illustrate the typical
curriculum
followed in the department in any undergraduate
;
.
3
course.
t
‘42
The textbook is divided into 18 chapters which don't
changes, that it has itself been a product of society is some-
thing which is entirely missing in this world view projected
by textbooks such as Parks’.
Simultaneously, the book also projects society as a
homogeneous entity where everyone has equal access to the
conditions which make for health. There is no recognition
of the fact that health status, especially in third world conditions is an indicator of the class location (20). This may
be best illustrated by the manner in which the authors discuss the problem of malnutrition. Socio-economic factors
are listed only as one among the many aspects of the ecology of malnutrition.
The text manages to de-emphasise the fact that malnutrition especially under-nutrition which is the major problem in India, is largely rooted in the lack of purchasing
power of certain sections of the population which in tur
is
again both a cause and consequence of the lack of politica
l
power to demand and obtain the wherewithal to
lead comfortable lives, live in healthy surroundings and work
at nonhazardous occupations. Leave alone the issue of
class in
society, the book does not even admit sex discrimination
in
society. Surely a book published in 1985 cannot
claim to be
Radical Journal of Health
ee
ea
Noe
bye,
Monaware of
data on this matter. Any number of studies have
: ‘aps me women suffer to a greater extent from the probsenor raga “98 do men. Again, in dealing with tu-
iribution
ofdes
the tideide; eS
Pts
(resi
ough
the rural-urban
veh and
Sh
ida
the >age
sex trends,
differences
are remarked
upon.
¢
In general the book tends to medicalise all prablems
conceming
health.
Such
as
for
instance
malnutrition.
Clearly, a social problem it is regarded as a 'medical' problem with social causes and repercussions. Even worse is the
way the authors treat mental illness where although social
pathological are listed— only third to organic and hered-
_ Ity— the solutions offered stress mainly early diagnosis and
_ Tehabilitation just as in any medical problem. The point is
_ except for a small proportion of cases which have organic
| and hereditary roots, the majority are symptoms of social
» distress which become manifest in individual aberrations.
/ They can hardly be resolved by ‘early diagnosis’ of individual cases. The solution lies in the early diagnosis
of social
distress, which clearly according to Parks is beyond the
purview of the doctor.
Not surprisingly, the solutions offered by the authors to
any of the range of health problems are either individualist
mnie
=
=
rm
Modem medicine has its roots in this body of knowledge
even though today it may bear little resemblance to it. In
consequence the contributions of early medical practitioners
and thinkers such as Hippocrates, Galen, are regarded as
distinct and separate from that beginning with say, Parcelsus
(who “publicity burnt the works of Galen and attacked
superstition and dogma in medicine"), Vasalius ("who
demonstrated some of Galen's errors") and Ambroise Pare
(who "revived surgery and became the father of modern
surgery"). While it is true that developments in
medicine after the sixteenth century represent a break with
the past, the continuity of empirical traditions which is so
characteristic of the field does not feature in the narration.
The middle ages (‘dismissed by the authors of the book
as the dark ages'') saw the development of two distinct tra-
ditions of medicine, which were to become competitive in a
later period. The inflexibility of the codes of the Catholic
church, the widening gap between Church medicine and the
people, the famines and plagues, the growing impoverish-
ment provided an impetus for the growth of a more acces-_ iy
sible cheaper medical care. Folk medicine which had con- —
tinued to exist outside the Church, largely in the hands of
women, began to encroach upon Church medicine ? Many
historians have seen the witch hunts which were rampant in
or abstract. That is, what the individual can and must do to
Europe in the tenth to fourth centuries as the manifestation
avoid falling ill or how the government or more often the
health services can offer appropriate measures. That preven-
of the attempts by the Church to usurp the folk knowledge
lised by the rich feudal lords, the richest of them being the
through social action of a group or community. Thus it
_ completely misses out the crucial role the doctor can play in
such action by providing the group or community with information etc. In fact right through the book the doctor is
regarded as a person being apart and slightly above the rest
of society.
Church, and the other practised by and accessible to the lay
Letus now look more closely at some of the chapters
? in the book. The first, purported to be a history of medicine runs to nine pages. It is pertinent here to note that this
is the only department in the undergraduate medical course
where the history of medicine figures at all. It was in 1955
recommended the introduction of history as part of the
PSM curriculum. In Parks’ textbook we have a travelogue
through time, enumerating the ‘advance’ of medical knowlinteredge rather than an account of the dynamic
medicine and society. The authors’
relationship between
approach is a historical dealing with the developments not
in time periods taking into account the social and economic
structures of the time, but rather as geographical categories.
We
have for instance, paragraphs dealing with primitive
medicine, Indian medicine, Chinese, Egyptian, Greek and so
on. This gives a false notion that the growth of knowledge
of ‘Nain medicine has been circumscribed by boundaries
tions and states. In fact, although there were characteristic
developments in different countries in numerous: periods of
history, there has also been a process of dissemination and
——
assimilation
March
1989
between
the various
centres
of civilisation.
5a
and quell the competing tradition of medicine, one monopo-
be brought about
tion of illness can fost effectively
a
poor’.
é‘
|
Park reviews the beginnings of modern medicine, that —
is in the 16/17th centuries without ever referring to the tremendous changes that were occuring in the social fabric of
the time. So great was the intellectual impact of these discoveries in the field of medicine, that they in turn influenced other sciences and social ideas as well. For instance
William Harvey was the first to consciously use scientific
methodology in the biomedical sphere. He also used concepts of quantification to arrive at a hypothesis. And used
the concept of the human body as a mechanical system with
the heart as pump. These are concepts which are integral to
clinical medicine today.
Parks' history fails to recognise and trace the ideological trends which are current to this day in medical practice.
This would have been possible only if the dynamic interacFor extion between medicine and society is admitted,
, cultural
ample, the predominant social structure of society
enth
ninete
the
practices and prejudices of the seventeenth to
or the other into
centuries, were assimilated in some form
and medicine
the concepts and content of modern science
ingly, medicine's
which were then evolving.’ Not surpris
a white, adult male.
model of a ‘normal’ human being was
and non whites were ‘abBy definition, therefore, women
the development of
normal’. These ideas have influenced
understanding of particular
medicine and set limits on the
43
.
pathologies and illness syndromes. Similarly, the mechanistic concept of the body as a machine, as distinct from the
mind was to limit the growth of medical knowledge for
generations.
At the same time because medicine adapted the domi-
nant ideas of the period, and because it continued to retain
its long-standing status in society, it was used to reinforce
and substantiate these social myths. Thus for example, because
women
were
by definition all physiological,
condi-
tions experienced by them, menstruation, childbirth etc,
were regarded as being abnormal and treated as illnesses.’
Society in tum promoted and perpetuated these ideas by
taking resort to medical opinion. This fact that throughout
history medicine and its practitioners have largely been oriented towards supporting and sustaining dominant ideas,
often to the detriment of the socially oppressed classes is an
important aspect of history unfortunately given a miss by
_Parks' textbook. In short, the first chapter of the book is a
- disoriented, disjointed account of history which really ought
not to have been there at all. If at all the history of medi_ cine is to be taught to medical students, it ought to receive
a more coherent, sociological treatment than the one pre-
§ had
tas, as Parks would call it) is not reco
that
others
than
that some groups are more empowered
these power relationships cannot be altered without shakin
the very roots of society.
Society has been defined in a number of ways by di
ferent sociologists. In the evolutionary model all societies
pass through definite stages of development. For some so-_
cial thinkers like Durkhiem the most important dimension
of society is the degree of specialisation within it which is—
progressively complex as societies pass through the different —
. stages. In the structural functionalist model it is the interrelationship of social institutions rather than the individual or
group which is to be emphasised.*° Talcott Parsons modelled
his conception of society on the theory of homeostasis and ||
saw society as constantly attempting to balance its citer s
when upset by imternal a 3
rium by automatic ao.
external forces.
Parks’ textbook appears to have no use at all for with
variety of ways in which thinkers have understood society.
This is even more true of the other ‘concepts’. Certainly it
is utterly ridiculous to try to define socialism in 14 eenyg
lines.
What little there is of sociology in the textbook. is &
a? sented here.
Sociology of Medicine
almost entirely Parsonian. Talcott Parsons developed ‘the
eu “We now look at two chapters which give us an idea of concept of the sick role in his writings have greatly influenced medical sociology. According to this understanding 2,
e the sociological concepts presented by the authors. The
- book deals with sociology more as a set of terms to be there are four essential aspects of the sick role— the sick
» defined rather than as a body of knowledge with a long . person is exempted from his normal social role responsibili-_
history. Like other disciplines sociology. too, a plethora of ties; the sick person cannot help being ill; the sick person is
- theories, orientations and schools of thought have richly expected to get well as soon as possible and finally he is
_ contributed to dts development. Park however, is either
expected to seek help in getting well. Parscns therefore _
:unaware of these developments |or regards but one school of emphasised the need to control sickness. Consequently, so~ thought as being important. This approach will undoubtedly
cial control is clearly a function of the medical each)
-leave the medical student with a slightly jaundiced view of ment.’
|
- the discipline. More importantly, the book ‘does not deal
Not surprisingly of course, the textbook deals with so- -f
with methods of sociological analysis which are so necescial institutions such as the family as being “the most pow- i¢
sary for the delivery of health care.
erful example of social cohesion" which have existed in all
The chapter on ‘sociology and health’ deals with the
societies. "The family is a primary unit in all societies." It
- following '‘concepts in sociology": society, social structure,
is well-accepted today that the family, defined as the au_ social institutions, role, socialism, socialisation, social
thors do viz, "a group of biologically related individuals
_ control mechanisms, customs, culture, acculturation,
living together and eating from a common kitchen.” was
_ Standard of living, social problems, social pathology, social
not in fact a primary unit in all societies. Quite clearly, the
surveys, case study, field study, communications and social
Parks notion of the family is patriarchal: "The family is .
defence in that order. Need we say anything at all about
bridge between generations and between fathers and sons.”
_ this? One is hard put to understand the logic and the purAnd again, "The family provides social care by .. - giving .
pose of such a list of 'concepis'. Admittedly these are terms
Status in a society to its members ie use of family names..."
which need to be explained, but they are not concepts. Even
At one point the book talks of how the "freedom of wives”
the terms cannot be understood by mechanical definitions.
has enlarged and of how "the young wife in India.. brings
Each has to be understood historically, its meaning often
to a marriage not only a dowry but a professional or semihaving changed with time and the context. Moreover, even
professional education and she seeks a professional career."
the choice of ‘concepts’ so defined appears biased. Such imThere are several points to be made here. First, the changed isis)
}
net
portant concepts as social movements, or social change
and
what they constitute, do not figure here.
It is also significant that in defining social structure
the
inherently conflicting relationship between classes (or
stra-
44
ing family structure is a consequence of a number
of factors, economic, cultural and social and second,
the status
women in the family and their role, as well as
the functions
of the family are not universally the same. Even
within one
Radical Journal of Health
—_—
=
ARC
ae
i re
y vary with ‘class, region and culture
He third,
it is true that dowry is a widespread phenomena, to
ne as an inevitable and accepted feature of socjety is
quite correct.
discussions on the family in the textbook are par-
ticularly important because ‘social and community medicine’
confers a significant role on the family in disseminating its
message. Thus for instance, the family's traditional role or
rather the role of the women in the family, ‘in child bearing, health and nursing care, are the via media through
which ideas can be propogated from generation to generation, thus ensuring the perpetuation of the social structure as
it exists currently.
live together in peace and health. (5) The human body is a
mechanical system and organs are component parts which
may be repaired or replaced. In the same fashion all health
problems may be reduced to the malfunctioning of a particular part of the subsystem. Biological man rather than the
social human being is the ideal. (6) Health is defined and
understood in terms of an individual's productive capacity
and not the quality of life. By this definition, a worker is —
termed healthy as long as he can achieve a certain level of
productivity. The individual must therefore be helped to
maintain this level of productivity irrespective of whether
he feels healthy.In short, PSM justifies existing socio-eco- _
nomic and political formation by arguing that the aberra- " i
Another chapter which is a hotch potch is the one on tions seen in the system are not intrinsic to
it but area
community} health, After attempting to define health in a result of individual behaviour and may be smoothed over | any
crudely
chanistic way and outlining the relationship be- by persuading individuals in ‘communities’ to accept their—ee
‘tween h th‘and development, the chapter moves on to a fault. and remedy the situation. An approach to medicine. ae=
leninition of disease— the interaction of the agent, host and which has the potential to show up the inhcrent contradic- ."
nvironmet itetc, and then on to a description of health situ- tions in patriarchal class society which in reality determine ix
_3
ation and thehealth services. While such an explanation for the health status of a society, has effectively been defused. eeBe
-unders nding disease may be useful, it can also tend too
mechanical. Evidently the result of the interaction of the.
three is” often much greater than the sum of the three.
Morcover, i
it is not possible to change the nature of one
without inevitably altering the other two. Altering, say the
disease agent may not be possible without simultaneously
changing the characteristics of the other two.
“Nowhere in all this do we find a definition of commu-
The exercise underiaken here is only illustrative, but ee<a
does indicate that the orientation of preventive and social
medicine
reinforces
the socio-political
‘
framework. which
papers over major contradictions in socicty. It helps to jus- :Ay
tify existing socio-economic and political formation by ar a
guing that the aberrations seen in the system, in this case in ‘
the health status of the population, are not intrinsic to it butia :
are a result of individual behaviour or minor faults which .
nity. This iis a concept which has created much discussion may be smoothed over or repaired. If the practice of mediamong sociologists.
If by community
is meant a group | cine is to become more relevant, it is here in the wa
7
which shares common socio-political features, then a village
ment of PSM that the restructuring must start.
comprises several communities and it is absurd to talk of a
village community as if it is homogeneous. Community
[This article is an abridged version of a paper appearing infige!
an anthology on Medical Education published by the Medico hee
Friend Circle. a the Press)] |
;
a Cb):
medicine is a meaningless Za
defined.
To
if ‘community’ is not
sum up, in this book preventive and Social siedicine
Notes
changes so as to balance the changes in nature. (2) The activities of the individual are the major reasons for ill health
—— viz, use of unclean water sources causes typhoid, cholera etc, smoking causes cancer, inadequate iron intake
causes anaemia, babies die because mothers don't breastfeed,
workers die because their work environment is unhealthy
and so on. The object of PSM is to teach medical students
to help individuals, alter their lifestyles without damaging
social institutions and norms. (3) The social and political
forces in society do not significantly affect the development
of medicine or health policy, and the history of thought
(including medicine) may be viewed as a set of isolable,
distinct phases with little spillover. (4) society is generally
uniformly cohesive. Although there are groups and stratas,
they do not have inherently conflicting interests and may
March
1989
biasa ;
1. J D Bemal in fact delineates the significant cdhinibuliane of | a
medieval Christiandom to science while at the same time, a
has the following characteristics : (1) Ill health is viewed as
‘a consequence of the interaction of man and nature where
the changes in the latter are beyond our control. The essence of medicine is to help 'man' make the necessary
a
2.
cautioning against the trend to glorify the period. Modern
science grew out of the superceding of the medieval worldfey
a
. picture (Science in History Vol II, Penguin)
See The Political Economy of Health by Doyal and Peinel)i
4.
Pluto Press London.
Leo Huberman Man's Worldly Goods, 1968 and Hughes
}
Pennethorne, Witchcraft, 1965, Penguin.
for
1981
on,
Oppressi
Sexual
and
Sce Brian Easlea, Science
5
1976.
Midwives
Barbara Ehrenreich and Deidre English, Witches,
3,
critical reading of nineteenth century biology and Hilda
Smith, 'Gynaecology and Ideology in 17th century England’ in Liberating Women's History by Bemice Caroll
and Nurses,. Glass Mountain Pamphlet, 1980.
sociology which
6. A brief but comprehensive introduction to
defines the canvas of the discipline is Alex Inkeles, What
the Foundais Sociology? published by |®entice Hall in
tions of Modern
7
Talcott
Parsons,
The
Sociology
Social
Serics,
System
19
Book
Review
An Uneasy Relationship
‘sucheta
amin
(Second Edition), pp 344,
Law and Medical Ethics by J K Mason and Smith McCall R A, Butterworth 1987
but every legal duty is
$ 12.95. It should not be correct to say that every moral obligation involves a legal duty,
453.
founded on a moral obligation — Lord Chief Justice Coleridge in R.V. Instan (1893) 1QBat
THIS second edition of the book takes account of recent
legislation and much of the text, including chapters on reproductive techniques, consent and euthanasia has been rewritten. There is also a new chapter on the treatment of the
elderly and the Mental Health Act 1983 is also considered.
‘With the introduction it covers five major topics viz: reproductive medicine, medical practice, death, research and ex-
perimentation) and psychiatry and the law. The list of cases
and table of statistics along with appendices is also given.
The first section on evolution of medical ethics briefly
follows the progress through the earlier periods to the organisation of modern medicine. This section also introduces
medical ethics and legal intervention in medicine. The crucial question raised is that of determining the extent to
which medical decisions should be the object of legal scrutiny and control. Two extreme views exist, one that holds
that the medical profession should be left to regulate itself
and that it alone should decide what-is acceptable conduct.
The contrary view expressed, denies doctors the right to
regulate their relationship
with their patients ie reserving for
- the medical profession the right to decide on issues of life
and death is an improper derogation from an area of legiti_ mate public concern andan encrochment by clinicians into
what is, properly, social policy. Broadly speaking these conflicting views are those of two groups representing the
medical profession holding the first viewpoint and the pa_ tients who are treated by these medical professionals holding the latter view-point. The legal system then is faced
with the classic problem of doing justice to both parties.
The fear of the medical profession must be taken into account while the legitimate claims of the patient cannot be
ignored.
The second section dealing with reproductive medical
covers (a) A Reform of Sex Law? (b) Modern Reproductive
Technology (c) Control of Fertility (d) Abortion (e) Prenatal and Wrongful Life (f) Neonaticide and selective treat-
_ment of the newborn.
Under the topic a reform of sex law, this book deals
briefly with application of law with regard to sexual intercourse, rape, homosexuality, incest, transexualism etc. "Full
expression of ones sexuality is now advocated in some
countries by responsible educational authorities. Medical
knowledge and expertise are moving to serve the changing
needs of people. It is doubtful on the other hand if our
present sex laws to accurately reflect current public
46
mores". The topic of rape ie sexual intercourse without
consent briefly but concisely brings out various issues related to the subject. They almost take a stand when they
state "our feeling is that ‘rape’ is essentially an act of vio_
lence in which sexuality plays only a secondary part. It also
brings out the outdated existing laws in the United King- —
dom where rape, to be raped requires intercourse per wy
vam.' There is a brief mention of approach to rape in a
=
ferent countries. There is a humane though condescen ing
|
and
ls
homosexua
attitude taken by the authors towards
transexuals. As for incest when it is sexual abuse on children by a trusted elder then there can be no place for law '
‘that protect such abusers.
Modern reproductive technology has been extensively —
covered in this book. Being
a very sensitive issue needing —
intense consideration of both legal and ethical issues. The —
authors seem to be taking a very practical view when they ~
state ‘methods are now available for by-passing the natural — :
process. Almost inevitably, these sometimes conflict with—
laws which were mainly fashioned before such techniques —
were considered.
ag
If we look at the different reproductive techniques of- —
od
fered at their exorbitant rates, it is a highly commercialised
process. So let us not be under the impression that it is
concern for childless couples that such techniques have %
emerged. Why are absurd techniques like amniocentesis in
vogue today? Is it to help facilitate female foeticide under
=
‘the garb of helping correct genetic defects? Why should fascist ideas of eliminating imperfect foetus be encouraged? In
almost all cases the woman who has to go through all the
painful procedure has someone else making decisions for
her. The major being the ‘stigma’ attached to being infertile.
Surrogate motherhood is a mockery of motherhood the way
it stands today. The word someone had coined ‘technological adultery' would more apt here. There is so much about
abortion and laws relating to it. Why is not the woman left
to decide whether she wants to abort or not? It is her body,
her right to decide. If the socio-economic pressures are the
main reason a woman goes in for abortion, why aren't laws
passed to deal with exploitation that is going on. Instead of
whether the heart was beating at the time the foetus was
aborted?
”
The chapter on medical practice looks into issues relat
ing
to medical confidentiality, consent to treatment,
treatment
of the aged. The above mentioned issues are point
s of conRadical Journal of Health
=
-
‘
fl
wee law aad edical ilies. The Bhi have prey sented the issues illustrated with actual cases. Laws relating
- to medical ethics emerged as a safeguard againsi expivitation by of the medical profession. Being a reflection of the
to look within, to question our motives.
The extent to which psychiatry can operate as a political
or social weapon constitutes
its importance in the current
‘debate. A broad sympathetic view may prevent the unjust
: capitalist social structure, compensations (torts) will be depunishment of those who are truly not responsible for their
_ manded for medical malpractices. ‘It is inevitable because
action but it may also prove to be socially damaging if
the patient has his/her right since ‘they are paying for the criminals are left free under the garb of insanity. The inesservices. Counsel regarding treatment of the aged is a clear
capable task then becomes one of charting a course between
indication of the economic climate and is unlikely to be fol- Scyulla and Charybdis. To achieve this the criminal law
lowed in the foreseeable future.
should adhere to a broad definition of insanity (such as in —
The topic on ‘Death’ deals with diagnosis of death, dona- Scottish or French formulae : refer page 307) which allows
_ tions of organs and transplantation, euthanasia Biomedical
maximum leeway for a court to take into account expert |
human experimentation, Research on children and foetal evidence while at the same time avoiding necessarily being
bound to an acceptance of psychiatric notions of reponsibil_ experimentation. Issues over which medical profession could
ity.
.
_ exert their power. Euthanasia whether active or passive,
voluntary or involuntary is reflective of a person's right to
This book is a good reference volume with its pragmatic. :
_ life. The question I would like to raise is whose life is it? approach to different issues illustrated by actual cases. It —
covers topics relating to law and medical ethics in United
Donation of organs and transplantation is once again based
Kingdom., These issues can hardly be considered applicable —
= on financial gains except a few philanthrophists who would
_ donate organs from the goodness of heart. Though research in Indian context where law itself if negligent, let alone ‘
is necessary for its benefits to humanity, the way it is used medical ethics.
- for commercial purposes leaves one aghast. Then we need
oh
SUBSCRIPTION
RENEWALS
Is this your last subscribed issue? A prompt renewal from you will ensure that your
copy is mailed directly from the Press. Many of our issues have sold out fast! So book”
your copies by renewing your subscription now!
Our new subscription rates:
For individuals—Rs. 30/- (four issues)
For institutions—Rs. 45/- (four issues)
for all other countries
Foreign institutions: US $ 20 for US, Europe and Japan US $ 15
(special rates for developing countries)
Life subscription:
Rs. 500/-
Health , B'bay. Please write
D.D.s, cheques, IPOs to be made out to Radical Journal of
e don't forget to add Rs. 5/- on
your full name and correct address legibly. And pleas
outstation cheques.
March
1989
a ol
‘ontd from: Pg. No.4)
peatedly stressed that scientists and technologists ought to
-accorded-higher status and emoluments. The Shrivastava
ymmittee, MCI and other highly placed authorities un-
vivocally recommended non-practising terms for the
edical teachers. The administration has not taken their
commendations in the right spirit. There has developed a
xus of mutual interest between the political-bureaucratic
thority and the teaching community,
Politicians of all
ades and bureaucrats enjoy the free services of teacher-
rh:
ph
Sroneuniad than in ‘the field ‘of medical | education.
-
The o
attitude towards both science and society ‘is involved. The
student is influenced not only by the teachings and preach-
ings of the teacher but is influenced most by the teacher's
practice. The teacher's admonition against indiscriminate
use of antibiotics or random use of steroids cuts little ice
with the student when the latter discovers the very teacher's:
indiscriminate and random prescriptions in private practice.
The student thus learns the difference between theory and
practice and this influence is intensive and sustained, shap-
ecialists who also make the costly medicare facilities of
ing the professional career and attitude of the student. The
2 state hospitals available to the former out-of-turn. It is
deed difficult to find a political leader or a high governent official who is not personally obliged to a medical
acher. In fact, one of the topmost physicians of Calcutta
enly maintained unauthorised private practice throughout
4 entire length of his service career occupying nonactising posts, which included the topmost posis in the
st-graduate medical coliege and the health service in West
ngal: _this enterprising doctor professionally served the
teacher's conduct, in its turn, is detemined by his/her posi- —
tion in the society and the profession. Social and economic
—
f ministers and ministers during both Congress and Left
itregimes. ‘Unless: this pernicious system of private
actice is removed, other measures will be infructuous.
| discriminations in the matter of pay, promotion and re-
ement benefits should be resolved.
More and more uni-
compulsions dictate terms.
In the conflict between pursuit —
of science and commercial gain, the latter generally prevails. _Medical education cannot wait for the development —a
of the intrinsic goodwill of the teachers.
ements and procedure for assessment could be devised and
given: a trial. If this is done, then the present system of
aminations based on subjective assessment could be
rown away and be replaced by periodic objective assessent. of students at‘every: crucial level of curriculum and
ining.
hs
The task of updating of knowledge should not be left to
dividual initiative. Updating includes revision and is
pendent on research.
It may be emphasised that the
aching community is the most effective force in research
id the poor siate of medical research in India is actually a
flection of the teaching community.
The Bhore Committee observed in 1946.
"No special facilities are available for the training
teachers in the different subjects of the medical currilum... Broadly speaking medical research receives little
no attention in the medical colleges of India.
The
thorities responsible for staffing and financing the medi| colleges are usually ignorant of the importance of
search in relation to the achievement of a correct attitude
mind in the students... " The role of teachers in shapy the make-up students is crucial ahd nowhere is it more
<7]
are taken to ensure job satisfaction, medical colleges will if
always remain short of dedicated teachers. Unless the stan-—jb 3
dard of teachers is improved, teaching can never
improve and consequently medical care cannot improve, however, grandiose or rational might be the curriculum orks,
methodology of teaching. Unfortunately this profound role ee
of teachers in medical education is yet to be popes micein
8
India.
ae
rsily.control should be introduced replacing government
ntrol, There should be a declared. policy of transfer in
insferable services. Lastly and most importantly, there
ght to be a system of assessment of performance accom-
nied by incentives and disincentives. This is perhaps the
Ostcontroversial area and difficult to operate. Because,
edibility of assessment ‘depends upon the credibility and
mpetence of assessors. Still, a structural framework for.
Unless measures
" Njoy Mitra’.
Sujit K.Das ss
Appeal to Subscribers/Readers
We. regret that the last few issues of the|
Radical Journal
This has been
of Health
have been delayed.|
because of printing and other]
—
difficulties, none of which fortunately are insur-|
mountable.
We hope to bring the publication |—
up-to-date in the next couple of months. Please}
_
bear with us!
=
The RJH is for you and is sustained mainly by| _
the support of regular readers like you. So far
the journal is being subsidised by donations from
concerned individuals. We would not like to pass
on the burden of the extra cost to our readers by
increasing the subscription rates.
The Socialist
Health Review Trust, the publisher of RJH has
Started a campaign for creating a corpus fund
which can continue to racists the extra cost as far
as possible.
We appeal to you and your friends to gene
rOusly contribute to this fund. All dona
tions may
be made payable to the Socialist Health
Review
Trust and are exempted from Income
Tax under
Section 80G of the Income Tax
Act.
:
Radical Journal of Health
-~”
~
ih
ol
Why don't you write for us?
This rcstial:is a collective effort of many individuals active or interest
ed in the ficld of healt): Or interested in
calth issues. The chief aim of the journal is to provide a forum of exchange
of ideas and for gencrating a debate on
Kenton
and theoretical issues in health for a radical or Marxist perspective. We believe
that only through such
teraction can a coherent radical and marxist Pte of health and health care be evolved
.
Hack issue. ofthe journal highlights one theme, but it also publishes (i) Pics
artic i
issues Gi) Commentaries, reports, shorter contributions outside the main theme.
on articles published in
213 you wae eewrite on any of these issues do let us know immediatcly. We have to work three months
ahead of
e dateof publication which means that the issue on Medical Technology is already being worked on. A full length
rticle should not excecd 6,000 words and the number of references in the article should not exceed 50. Unless a
therwise stated, authors’ names in the case of joint authorship will be printed in alphabetical order. You will
ppreciate that,wehave a broad editorial policy on the basis of which articles will be accepted.
We have an alithor’s style-sheet and will send it to you on request.
te
eprint articles are as in the original and are NOT as per our style.
a]
a>-
Please note that the spellings and referencing 6 a
We would Ne like to reccive shorter articles, commentaries, views or reports. This nced not be on the themes i
easementioned. These articles should not exceed 2,000 words. Please do Wri and tell us what you think of this es ‘Allmickee shguldbe sent in duplicate. They should be neatly typed in double spacing on one side of the sheet.
his is
i necessary because we do not have office facilities here and the press requires all materials to be typed. But if —
_is impossible for you to get the material typed, do not let it stop you from sending us your contributions in a neat
andwriting on one side of the paper. Send us two copies of the article written in a legible handwriting with words
Lee
tas: Spaced.
Y
| The best way to Srpsiallise and clarify ideas is to put them down in writing. Here's your opportunity to interact
‘ough your ihr and forge links with others who arc, working on issues of interest to you.
WORKING
ee
eae
a
EDITORS
I
:
j
Please send me Radical Journal of Health for one year (four issues). I am sending
as subscription and/or donation by Demand Draf Y
Rs.
Cheque. (DD and cheque in favour of Radical Journal of Health and for cheque add Rs.5, if
{
outside Bombay).
i
j
|
ee
Name
SO SI
EES
:
i
:
f
Ee
ee
ay
assalient!) PIN
agli
: : : : : : : : : ! : : : : : : i : i | : j : :
Sgbes
:
4
Ms
:
}
,
;
,
:
*
On Eliminating Quackery
-
:
to secure
efforts
their curative
privileges;
types
only
the
guardian-
consolidating belief in authority,in the best of
of the
patronising
cases, producing
state
which
as education,
under
put
were
patients
the
the government,
ship of
police state. The
modern
is to
of knowledge
and
of certain
of
doctrines
a sterile scholarship; as long
from primary
school, to univer-
- establish the equal rights of free citizenship
sity is not throughout based on perception by
“must therefore,
Our
maintenance
automatically
be against
the
of the law of quackery.
senses,
We
an and
must (now) ask how the state...
shall
prevent
quackery.
Forit can-
not be denied that it lies in the public interest
to restrain as far as possible the treatSeat
eee
‘i
:
mentof patients
- The
main
= tion. If we
by ignorant
persons.
of
standing
side
in natural
will
correspondingly
_ frequent.
The
more
of
become
perfect
the
state,
more
practical medical
the
laymen,
ia
educational
scientific
which
would
judgement
cated
but
common
remain
cal
authority
the
constitute
tions, the more realiable will be the physi-
medical
cians,
pass
— and that
‘‘accredited
by the
government’’
and
officially recommended
to the lamyen and the
‘ “greater will be the confidence they will meet
and acquire. . . . But just as important, or peruate
Ae
.
ov haps even more so, is
the educatioH n of the
ft
a
a large fund of
a
turn
logical
will
educated
a
ee
be lacking |
to form his
physicians
only
and
the
and
unedu-
laymen
the
as the outstanding people,*
anda
court,
exa nina-
the
servilely
privy
medical
ard
thought,
layman
his
Not
as well
will.
the
on
also
a
careful
with
the basis
enable
education, the stricter
ri and the more
to
faculty
independent
history,
pseudophysicians.
that
aim
positive knowledge in the natural sciences
level
as
not
.
educational
of
it does
by critical
by side
the
well
as
<=
sound, genuine and unadultered human under-
Own
quackery
and
power
is educa-
as
of the
ge
the
democracy
physicians
institutions
long
of
tool
raise
as
maintain and increase
by
a
.
the transmission
their
main
.
.
.
.«
.
;
to
devote
schools
As long as our
layman.
in their special
tended to protect physicians
interests,
in-
were
quackery
against
laws
The
subordinate
resounding
to
medi-
title such as
or
sanitary
counsellor
a
most
lucrative
shingle
quack.
.
..
Let
which
postulate,
a few
now
as
Out to be an actual
a
for the
generations
appears
pious
necessity,
will
as
just
wish
will
a cultural
achievement.
—
Rudolf
Virchow
:
a
EEE
Ss
ee
» tog
eyerre
7.
~
-
a
a
’
F
, A
‘
*
.
m
,
>
2
ae
7
*
Ta!
ee
a
*
-
a
eptaieaeit
‘
P
>
* a
7
;
a Serine
a Se: =
Mn?
;
_
7
‘
rer
ean:
.
a
.
z
nee
eneOPN
eine
el
gy
.
petals:
4
cs
gi
re
ete
Ls
ee
SSS
ita
——
=
SE
Position: 3092 (2 views)