RF_DIS_6_A_SUDHA.pdf
Media
- extracted text
-
RF_DIS_6_A_SUDHA
Polio News
.
.
.
'
■
-.
-
-
'
■
WHO
.
.
w
-/W
- v
■■./
■
unkef
-
Post-certification
era
TCG reviews 3 hightransmission" countries
Aventis Pasteur
donates more OPV
Page 2
Page 5
Page 6
A Newsletter for the Global Polio Eradication Initiative
Department of Vaccines & Biologicals
World Health Organization
in association with Rotary International,
Centers for Disease Control and Prevention
and the United Nations Children's Fund
!
2002: Lowest number of polio infected
countries ever - but more cases
T most seven countries will
still be endemic for polio at
the close of 2002 compared
to 10 countries last year.1
S'
Furthermore,
the
vast
majority of cases - more than 85% - are
A
® W
Polio eradication highlights2002:
■ EURO certified polio-free. Combined with the
'
WHO's Region of the Americas (1994) and Western
Pacific Region (2000), more than three billion
people in 134 countries now live in certified-zones
■ No polio detected in Sudan or Ethiopia
■ Improved access in countries affected by complex
emergencies - Afghanistan, Angola and Somalia
■ Type IIpoliovirus has not been detected for the
past threeyears
TCG Findini
I I 11j I I 1. 11J I I I
confined to just nine states/provinces of
76 within India, Nigeria and Pakistan.
Despite this geographical restriction in
transmission, a five-fold increase in cases
in northern India and Nigeria will result
in more cases for 2002 (1461 to date)
than for 2001 (483 total). The northern
India state of Uttar Pradesh alone
accounts for more than 60% of the global
total {see pages 3 and 5 for more details).
Four endemic countries - Afghanistan,
Egypt, Niger and Somalia- have lowintensity transmission with fewer than
25 cases combined. ♦
THE GLOBAL TECHNICAL
CONSULTATIVE GROUP (TCG) FOR
POLIOMYELITIS ERADICATION
Due to the approach of the end
2002 target date for stopping
transmission, and the evolution
of research on post-certification
immunization policy, the
Global TCG held a special
interim meeting
13-14 November 2002 in
Geneva. Much of this issue of
Polio News highlights
the TCG's findings.
, —•
’ All data in this issue of Polio News is as of 3 December 2002.
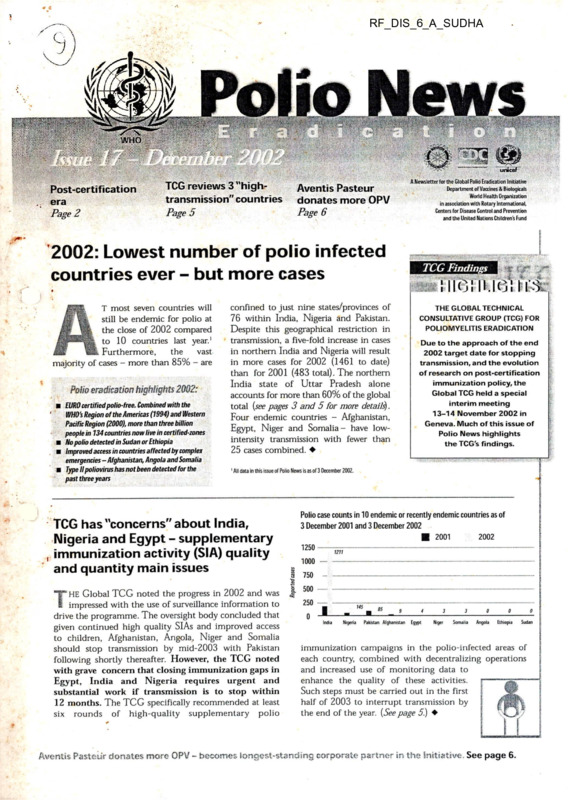
Polio case counts in 10 endemic or recently endemic countries as of
TCG has "concerns" about India,
Nigeria and Egypt - supplementary
, immunization activity (SIA) quality
and quantity main issues
*STK HE Global TCG noted the progress in 2002 and was
I impressed with the use of surveillance information to
drive the programme. The oversight body concluded that
given continued high quality SIAs and improved access
to children, Afghanistan, Angola, Niger and Somalia
should stop transmission by mid-2003 with Pakistan
following shortly thereafter. However, the TCG noted
with grave concern that closing immunization gaps in
Egypt, India and Nigeria requires urgent and
substantial work if transmission is to stop within
12 months. The TCG specifically recommended at least
six rounds of high-quality supplementary polio
3 December 2001 and 3 December 2002
■ 2001
1250
2002
1211
1000
| 750
t 500
£
250
0
145
JL
India
Nigeria
85
9
Pakistan Afghanistan
4
3
3
0
0
0
Egypt
Niger
Somalia
Angola
Ethiopia
Sudan
immunization campaigns in the polio-infected areas of
each country, combined with decentralizing operations
and increased use of monitoring data to
enhance the quality of these activities.
Such steps must be carried out in the first
half of 2003 to interrupt transmission by
the end of the year. {See page 5.) ♦
Mentis Pasteur donates more OPV - becomes longest-standing corporate partner in the Initiative. See page 6.
Technical tips
Risks of polio paralysis in the post-certification era'
Part One
’Risk
category’'
POST C-^l li-ICAllON
IMMUNIZAl lOi'l POLICY
■
\
Risks of polio paralysis
from continued use of
oral polio vaccine
Risk
fregueriRy
Esiifftertffd global
anniii}} buraen "
VAPP
1 in 2.4 million doses
of OPV administered
250-500 cases per year
cVDPV
One episode per year
in 1999-2001
(Haiti, Madagascar,
the Philippines,)
Approx. 10 cases per
year (total of 29 cases
in three years)
iVDPV
19 cases since 1963,
with 4 continuing to
excrete; no secondary
cases
<1 case per year
Inadvertent release
from an IPV
manufacturing site
One known event in
early 1990s
No cases
Inadvertent release
from a laboratory
None to date
Intentional release
None to date
FRAMEWORK FOR THE ASSESSMENT & MANAGEMENT
OF PARALYTIC POLIO IN THE POST-CERTIFICATION ERA
The November interim meeting of the TCG endorsed the
framework which has been developed to summarize the
risks of paralytic poliomyelitis in the post-certification
era. This framework will be particularly important for
discussing post-certification immunization policy with
OPV-using countries and for developing policy decision
models. The framework divides the risks into two
major categories: (a) those due to vaccine-derived
polioviruses and (b) those due to the handling of wild
poliovirus stocks.
Risks of paralysis from
mishandling of wild
poliovirus
This page summarizes the research to date on the nature and
magnitude of the risks of vaccine-derived polioviruses as
presented to the November TCG. The next issue ofPolio News will
include an update on the risks of polio paralysis due to the
handling of wild poliovirus stocks, with a special focus on the
progress in containment.
‘ Study and data collection is ongoing lor a
' ’ Under current polio immuniza
s
(see table on the right)
Risks from the continued use of
oral polio vaccine (OPV):
VAPP, cVDPV and iVDPV
key factor in the risk assessment for OPV-using
countries is the small but continuing risks of
paralytic polio due to OPV. These include vaccine
associated paralytic polio (VAPP), the emergence of
circulating vaccine derived polioviruses (cVDPVs) and
excretion of VDPVs from immunodeficient people
(iVDPV). Preliminary estimates presented to the TCG on
the total global burden of disease due to VAPP, measured in
terms of the number of cases per birth cohort, is 250-500
cases per year. Although the risk of emergence of a cVDPV
appears to be even lower than VAPP, it is conditional on
factors such as the level of population immunity and
immunity gaps. Screening of >5000 Sabin polio isolates and
enhanced global surveillance for cVDPVs over the past
three years has documented cVDPV on just three occasions
at a frequency of one episode per year. These three recent
cVDPV outbreaks resulted in a total of 29 cases, but
experience from the pre-eradication era in Egypt suggests
that cVDPVs may establish endemicity under certain
conditions. The iVDPV burden from 40 years of use of
OPV stands at 19 cases globally with just four patients
continuing to excrete poliovirus today. There have been no
secondary cases. New research is underway on further ways
of expressing the risks from cVDPVs and iVDPVs, and will
be presented to the Global TCG meeting on an ongoing
basis. ♦
□
1
Vaccine derived poliovirus
(VDPV) investigation and
response guidelines
J SING the data and experience available at the end of
B 2002, the TCG endorsed interim guidelines for
responding to the isolation of VDPVs. These
guidelines emphasize the need for a mop-up response to (a) any
AFP cases from which a VDPV is isolated which has greater
than 1% genetic drift and recombination with a group C non
polio enterovirus and (b) any cluster of AFP cases from which
a common VDPV is isolated (see below). The guidelines state
that in all other instances the first response should be an
appropriate epidemiological, clinical, immunologic and
virologic investigation. If there is an identified immunization
coverage gap, whether geographic or demographic, this(
’d
be addressed while the investigation is ongoing, xuese
guidelines will be updated as additional information becomes
available. The WHO guidelines on response to wild poliovirus
are also being updated to include the VDPV investigation and
response guidelines. ♦
B
g
Decision-tree for responding to the isolation of a vaccine-derived poliovirus (VDPV)
2 AFP cases’
mop-up
Immediate mop-up if VDPV has >1% drift
and recombination with a non-polio Group C
enterovirus
Otherwise evaluate for gap in population immunity
0 AFP.cases = investigate
Ifyes immunize and
investigate
' duster in time and space with same VDPV
If no investigate
AFP and polio roportincjf year-to-date (data received at WHO Geneva as of 03 December 2002)
2001 (as of 04 December 2001)
Non-polio
AFP rate
Adequate stool
specimens
Polio
confirmed cases
Wild polio
virus cases
Non-polio
AFP rate
Adequate stool
specimens
Polio
confirmed cases
African Region
2.9
39
10*
0
110
European Region
1.32
157
3**
2.9
0.98
2.25
83%
1.24
83%
1.53
1.19
2
178
1.17
South-East Asia Region
Western Pacific Region
1.63
84%
88%
1.46
0
329
1.2
Global total
72%
76%
84%
90%
84%
87%
82%
70
Region of the Americas
Eastern Mediterranean Region
1.79
85%
164*
0
99
0
1211
0
1474
1.81
178
0
418
93%
88%
Wild polio
virus cases
151
0
99
0
1211
0
1461
■ Vacdne derivedpolio virus. In 2001, in the American Region, in Dominican Republic 3 cases and in Haiti 2 cases.
In 2002, in the Alnun regton, in Madagascar, 4 cases
■' Importation ol wildpoliovirus into the region
Wild poliovirus map
I imolinC” total wild poliovirus and date of most recent wild
poliovirus by country as of 03 December 2002
03 December 2001 - 02 December 2002
.'..OSes
'
-v.. ■
■'■■V"-
........
..
------- '' 4,”
.i-r;'
3 _I
r
India
Pakistan
Nigeria
Egypt
Afghanistan
Somalia
Niger
1238
89
...................
145
4
9
4
4
,,
Seine: Data at WHOGeneva as ol 03 Deamber 2002
Importations
Zambia
*3
Most ream importation usesAms
* 2
• *-*i<**r.*TS4*i
Burkina Faso
1
as at date ol going tnprint
NIDs calendar for selected countries
Region
Country
AFRO
Cameroon__________
Central African Republic
Chad______________
Equatorial Guinea
Gabon_____________
EMRO
Nigeria_____________
Afghanistan_________
February 2003
Type of activity
Intervention
January 2003
Type of activity
Intervention
March 2003
Type of activity
Intervention
21-Jan/SNIDs ZOPV R°und2
21-JanZ NIDs ZOPV Round?
21-JanZ NIDs ZOPV R°und2
21-Jan Z NIDs ZOPV Round 2
21-JanZ NIDs ZOPV Round 2
25-JanZ NIDs ZOPV Round i
00-MarZ SNIDsZOPVRound?
00-MarZ SNIDs Z OPV «°und i
00-MarZ NIDsZOPVR^i
00-MarZ SNIDsZOPVRoundi
Egypt______________
Iraq_______________
Somalia____________
Pakistan____________
Yemen_____________
SEARO
OO-Feb/ MBs/OPV
i
28-JanZ SNIDsZOPVRoundi
OO-JanZ NIDsZOPVRound?
00-MarZ NIDsZOPVR°u"d2
03-MarZ NIDsZOPVRoundi
29-Mar/ NIDs/ OPV
Bangladesh_________
India______________
Maldives___________
05-JanZ NIDsZOPVR°undi
OO-JanZ SNIPsZOPV«°und2
Myanmar___________
Nepal______________
Thailand
12-JanZ NIDsZOPVRound?
Vit A
09-Feb/NIDs/OPV Round?
08-Feb/ NIDs/OPVRound 2
04-JanZ NIDsZOPVRqu^1
21-JanZ SNIDsZOPVRound?ZVitA
This calendar reflects information known to WHO/HQ at the time ofprint. Some NIDs dates are preliminary and may change; please contact WHO/HQ for up-to-date information.
□
f
News and announcements
Polio News [
Decern*. MB Q ggj (g) |
Dozens of US.Rotary club members help immunize
millions of children against polio in Africa
I
a
!
Ll
i
'1 !
Nigerian Rotarian immunizes a child in northern Nigeria. Ihis part of the country continues to
have the highest levels of transmission of wild poliovirus in Africa.
| N support of Rotary’s goal of a polio-free world
I by 2005, more than 150 Rotary members from
the United States flew across the Atlantic to
participate in national immunization days (NIDs)
in Ethiopia, Ghana and Nigeria in October and
November 2002. American Rotarians teamed up
'*Trick-or-Treat for UNICEF"
raises funds for polio
THE United States Fund for UNICEF is
i donating all the proceeds from its 52nd annual
“Trick-or-Treat for UNICEF” campaign to the
global effort to eradicate polio. Every 31 October
in the United States, kids dress up in celebration
of Halloween and go door-to-door to “Trick-orTreat” for sweets and funds for UNICEF. The US
Fund’s “Trick-or-Treat” for UNICEF anticipates
raising more than US$ 4 million, from the 2002
campaign, including US$ 850 000 from the
United Nations Foundation, and it was one of the
Fund’s most extensive efforts involving a record
number of corporate partners and distribution of
20 million donation boxes - more than four times
the number distributed in 2001.
GAVI breakout session on polio
“TTHE polio eradication programme has enhanced
i vaccine delivery systems and capacity in dozens
of countries with equipment, institutional
arrangements such as the laboratoiy network and
more than 2500 skilled people. Participants at the
November 2002 Partners’ meeting of the Global
Alliance for Vaccines and Immunization (GAVI) in
Dakar, Senegal joined a breakout session to discuss
the potential future roles of this polio infrastructure.
EPI managers from several countries including
Nigeria and Bangladesh noted the importance and
value of maintaining capacity to further strengthen
immunization services. The group recommended
that countries have a strong voice in determining
the best ways to ensure the polio infrastructure is
used to forward the GAVI objective of 80% routine
immunization coverage in 80% of districts in every
country. ♦
with their local counterparts to help with vaccine
delivery, volunteer recruitment and trans
portation, and community mobilization and
education. Seattle-based Rotary Club member
Ezra Teshome led 85 Rotary members to his home
country of Ethiopia. “It was moving to see the
families’ hope at the NIDs,” said Teshome. “Some
had walked for miles and miles to get their
children vaccinated.” Brad Howard of the
Oakland California Sunrise Rotary Club brought
34 Rotarians to Ghana. “Something like this
gives people the chance to make a difference one
person at a time,” he said. As the top private sector
contributor to polio eradication, Rotary has
given USS 182 million to eradicate polio on
the African continent and committed more than
USS 500 million worldwide. ♦
The Fund’s regional offices worked to educate
children and adults about polio and its ongoing
effects in the remaining endemic countries.
US mayors officially declared 31 October as
“Trick-or-Treat for UNICEF” day in 144
American cities. The campaign gave children in
schools, youth groups and clubs the chance to
help raise money for the Global Polio Eradication
Initiative, knowing that every dollar they collected
would help immunize children against polio. ♦
Photographer
.IjM Salgado- urges
support for Horn
of Africa polio
activities
O HOTOGRAPHER Sebastiao Salgado, who has
i worked tirelessly with polio partners to
document eradication efforts around the world,
made the case for support to polio activities in the
Horn of Africa at a Polio Partners’ meeting in
Nairobi in September. Salgado was the keynote
speaker at the gathering of partner agencies, donor
and country representatives, convened to address
the challenges in Ethiopia, Somalia and Sudan.
Along with ensuring access in conflict-affected
areas and maintaining local political commitment,
securing the US$ 50 million required for polio
activities between 2003 and 2005 in the region
was considered the key challenge.
Ambassadors from Belgium, Ethiopia and the
United States, representatives from various
countries, international organizations, non
governmental organizations (NGOs), the US
Centers for Disease Control and Prevention
(CDC) and Rotary International participated in
this successful event. ♦
□
TCG Review
I Country focus I
SS
Pakistan ~ The model for
quality work
The November 2002 interim meeting of the
TCG reviewed eradication activities in the
remaining polio-endemic countries. The TCG
recognized progress in all countries and
singled Pakistan out for praise in particular.
However it had "grave concerns" about the
possibility of stopping transmission within
12 months in Egypt and India, Nigeria.
INCE 2000, Pakistan’s polio eradication
W programme has steadily improved. With
continued strong work it may be the first of the
remaining ’ high transmission” countries to stop
transmission. In contrast to Nigeria and India
where cases have increased five-fold in 2002, new
cases in Pakistan have declined by 10% and
transmission has been reduced significantly in the
traditional reservoir areas. The TCG emphasized
that Pakistan’s programme is strong overall, and
that success is due mainly to continued multiple
rounds of high-quality SIAs particularly in the
face of decreasing caseloads and virus lineages.
Other strong areas of the programme include the
careful analysis and use of surveillance data to
inform programme decisions and diligent follow
up of independent monitoring data prior to and
following SIAs. Government commitment is high
at national, provincial and, increasingly, district
levels. To stop transmission, the TCG endorsed
Pakistan’s SIA plans for four rounds of NIDs
and four rounds of subnational immunization
days (SNIDs) in 2003 along with the strategy to
concentrate on identified reservoir and high-risk
areas. ♦
TCG comparison of eradication activities in the three "high-transmission"
countries in 2002
Key activities
Pakistan
Nigeria
India
Number of rounds of
large-scale SIAs in 2002
4NIDs,4SNIDS
2NIDs, 4SNIDS
2NIDS, 1SNID
Management of
operations
Joint national/
international teams at
national, state and
substate levels
Joint national/
international teams at
national and state
levels
Joint national/
international
teams at national
level
Monitoring of SIA
quality
Independent 3" party
monitoring began in
early 2002
Independent
monitoring began in
late 2002
Independent
monitoring
began in late
2002
India - Wanted: higher
quality, quantity SIAs
| IISTORICALLY, India’s progress in polio
t i eradication has been unprecedented in the
world, with the virus circulation drastically reduced
from almost every district in the country to two
states in just a few years. The most progress
occurred in 1999-2000, when India undertook 10
national or subnational immunization campaigns
in a 24-month period. In contrast, only three largescale SIAs took place in 2001. The result? A five
fold increase in cases in 2002 (1211 at 4 December
2002) over 2001 (just 268 for the year). These cases
are primarily (75%) centred in Uttar Pradesh (UP)
- the major reservoir for polio in India and the
world. At year’s end, the area with the highest
transmission in western UP had reseeded many
other districts, including Gujarat and West Bengal
which had been free of endemic polio in 2001.
Data shows this major outbreak is the result of gaps
in the quality of immunization activities, and that
minority populations in western Uttar Pradesh are
the most severely affected by these gaps. The
Global TCG considers that India - the state of
Uttar Pradesh in particular - constitutes the
greatest risk to the achievement of global polio
eradication.
Moving forward, the TCG is recommending
an increased number of better quality SIA
rounds, including four rounds in the areas of highintensity transmission in the first half of 2003.
These must reach every child under five years of
age, particularly children in minority populations.
The TCG also recommends sufficient high-quality
staff to manage polio eradication at national, state
and substate levels, and the formation of substate
operational groups to manage polio eradication
activities across a number of districts, with the
support of partner agencies. ♦
Nigeria ~ political ownership
key
IB J HILE an increase in reported cases in 2002
wV (145 to date) over 2001 (56 total) is partly
due to improvements in surveillance quality,
transmission in several states of northern Nigeria
remains intense. Despite the increase, however,
cases have been geographically restricted, with just
seven states, all in northern Nigeria, reporting over
90% of cases, and two states, Kano and Kaduna,
with half of the total for the country. Virological
evidence demonstrates that many of the strains
causing disease in prior years are no longer
circulating, and there are a limited number of
strains remaining in circulation in 2002.
The TCG noted data showing that until very
recently most children under five years of age had
received insufficient (<3) doses of OPV in several of
the remaining endemic states. Although data from
the September SIAs indicate improvement, the
states of Kano and Kaduna in particular need to
ensure high-quality SIAs, as the current coverage
rates, while at 75-80%, are still too low to
interrupt transmission of wild poliovirus. The
TCG concurred with the national plan for three
rounds of high-quality SNIDs in the highest risk
states in the first half of 2003. The TCG also
emphasized that the high level of government
commitment at national level needed to be matched
at state and local government Area levels. ♦
CONC:-
□
Resource mobilization
Recent donations:1
.7-
Polio firmly on the agenda
for Africa-Europe discussions
USS 32 million for 2003-2005 polio eradication
activities in Africa
| N the final communique of the Second Africa-Europe
I Ministerial meeting held in Ouagadougou, Burkina
Faso in November, African Foreign Affairs ministers
noted the significant progress made toward polio eradi
cation in Africa and called on European Union Member
States to mobilize adequate funds to finish the job.
The inclusion of polio eradication in the
Ouagadougou communique sets the stage for polio erad
ication to be discussed at the European Union-African
Union Summit in April and for Polio Advocacy Group
follow up with European governments for additional
funding for polio eradication in Africa. ♦
Aventis
Pasteor
donates
30 million
doses of
polio
vaccine
° _9
1¥
i
i
David Williams, CEO of Aventis Pasteur, signed on for
the final push to eradicate polio during a ceremony
with WHO Director-General Gro Harlem Brundtland
and UNICEF's Executive Director Carol Bellamy at the
UN Seaetariat in New York in November 2002.
A
S West African countries launched a massive co
ordinated effort to immunize 60 million children
against polio, the world’s largest vaccine manufacturer,
Aventis Pasteur, donated 30 million doses of oral polio
vaccine to the Global Polio Eradication Initiative. The
donation - the third by Aventis Pasteur - is valued at
USS 3 million, and makes Aventis Pasteur the longeststanding corporate partner of the Initiative.
Materials available:
The report of the November 2002 interim meeting of the Global Technical
Consultative Group for poliomyelitis eradication is available electronically in English.
US$ 3 million worth of oral polio vaccine for
2002-2005 in Africa
USS 9.6 million for oral polio vaccine in Pakistan
USS 14.5 million for 2002-2003 polio activities in
key countries and regions, including India, Nigeria
and Pakistan
USS 100 000 for polio activities in EMR0 countries
USS 8.2 million for oral polio vaccine and
surveillance activities in Bangladesh in 2003-2004
USS 27.4 million in global funding, with a focus on
Africa, and for activities in Nepal
"’J - -u?,'-
'
’
The Aventis Pasteur donation is already making a
difference, with almost 3 of the 30 million doses
earmarked for November’s polio immunization
campaign in Liberia.
At a recent signing ceremony attended by
David J. Williams, President and Chief Executive
Officer of Aventis Pasteur, Gro Harlem Brundtland,
Director-General of WHO and Carol Bellamy,
Executive Director of UNICEF, Mr Williams signed a
banner pledging Aventis’s commitment to end polio.
“The Initiative has already made tremendous
progress and we admire the remarkable work done by
WHO, Rotary International, CDC, UNICEF and
millions of volunteers around the world,” Williams
said. “This donation is just one example of Aventis
Pasteur’s commitment. We are very proud of our
involvement with the Global Polio Eradication
Initiative.” ♦
Forthcoming events 2003
Date
Event
Venue
20-28 January
4-6 February
WHO Executive Board
Geneva, Switzerland
25-27 March
Rotary IPPC meeting
AFRO Regional Certification Committee
24-25 April
Global TCG
Evanston, USA
Yaounde, Cameroon
Geneva, Switzerland
The Progress2001 (WHO/POLIO/02.08) report is now available in French.
To register to receive Polio News, either in print or by email, or to receive any of the items above, email:
poliocpi&who.int or call +4122 7912657.
mm
< U Polio News
Manypolio documents are available on the web site at:
www.polioeradication.org
i---------------------------------------------------------------------------------------------------------------------------------------------------------------------- 1
| Please fill out tltit respoasf' coupon anti return it to Polit> News, £Pl, Deftartment ot
i Vaccines and tiialogicais, Docuntent Centre, iNnrld Health Organiiation. CH-1211
i Geneva 21, if you wt>ulii Hht) to cartlinuv receivirttj this publication.
*
i
j 7 would like to receive this publication regularly.
[ Name:
I
] Institution:
; EWorld Health Organization 2002.
; All rights reserved. The designations emptayed and the presentation of the material in
: this publication do not imply the expression of any opinion whatsoever on the part of the
j World Health Organization concerning the legal status of any country, territory, city or area or
of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on
maps represent approximate border lines for which there may not yet be full agreement
I
i Address:
The World Health Organization does not warrant that the information contained in this
publication is complete and correct and shall not be liable for any damages incurred as a result
of its use. Polio News is published quarterly by EPI, WHO Headquarters, Geneva, Swntzerland,
and part funded by USAID. Published data reflects information available at time of print
! Please also send this publication to:
i
| Name:
All comments and feedback on Polio News should be sent to:
Department of Vaccines and Biologicals, WHO, Geneva.
i
| Institution:
.
Tel.:
[ Address:
i=-
J
Fax:
Email:
Web site:
+41227913219
+41 227914193
polioepi@>who.int
http://www.polioeradication.org
I
i
WHO
Rotary and CDC special edition (see pages
.
Supplementary immunization
in polio-free areas
Greatly missed:
DrTaky Gaafar
Page 2
Page 6
European Region certified polio-free
P OR some 870 million people living in the 51 Member
i States of the European Region of the World Health ’
Organization (WHO), June 2002 heralded the most
important public health milestone of the new millennium.
The historic decision to certify the Region polio-free was
announced at a meeting of the European Regional
Commission for the Certification of Poliomyelitis
Eradication (RCC) in Copenhagen on 21 June. Certification
of the Region, which stretches from Iceland to Tajikistan and
includes the Russian Federation, confirms the potency and
transferability of polio eradication strategies.
The European Region has been free of indigenous
poliomyelitis for over three years, in the presence of
certification-standard surveillance. The region’s last case
caused by an indigenous wild poliovirus occurred in eastern
Turkey in November 1998, when a two-year-old
unvaccinated boy was paralysed.
Poliovirus imported from polio-endemic countries
remains a threat to the region. In 2001 alone, there were
three polio cases among Roma children in Bulgaria and one
non-paralytic case in Georgia, all caused by poliovirus
originating in south Asia. At the certification meeting,
Sir Joseph Smith, Chairman of the RCC cautioned that,
“ Throughout the European Region, ongoing vaccination and
surveillance is vital. The risk ofpoliovirus being imported into
Europe will continue until we eradicate polio globally.”
m
f'KI
I
iJ
■
1
i
!
Coordinated national immunization campaigns, known as Operation MECACAR, were instrumental in achieving
a polio-free European Region. MECACAR involved 18 polio-endemic countries and areas in the European and
Eastern Mediterranean Regions of WHO.The synchronization of immunization among neighbouring countries
has become a model for eradicating the disease globally.
—- r’
unierf
A Newsletterfor the Global Polio Eradication Initiative
Department of Vaccines & Biologicak
World Health Organization
in association with Rotary International,
Centers for Disease Control and Prevention
and the United Nations Children's Fund
Historic milestone \
<
’ '
‘
R
V
&
■e
0'
e>
SWi’ f-
•
u /T7
WW
® Certified polio-free
/
Not yet certified polio-free
Certification of the European Region means over half the
countries of the world -115 countries and areas - are now
certified polio-free. The European Region is the third of the
six WHO regions to be certified - the Americas and the
Western Pacific were certified in 1994 and 2000 respectively.
"To get where we are today required
the full commitment and
cooperation of each of our
51 Member States, the hard work of
public health workers in the field and
the firm support of international
partners in coordination with WHO."
DrMarcDanzon
WHO Regional Director for Europe
21 June 2002
In addition to maintaining high
immunization coverage, surveillance and
the ability to respond to imported cases,
European countries are now cataloguing
all laboratory stocks of poliovirus as part of the global plan
to ensure effective containment in a polio-free world. ♦
G8 leaders commit to raising
funds to eradicate polio by 2005
ft. FRICA was a centrepiece of this year's G8 Summit,
Jb held on 26-27 June in Kananaskis, Canada. With the
Africa Action Plan, G8 leaders responded to the
New Partnership for Africa’s Development (NEPAD)
launched by African leaders last year. Health is one of
the components of the plan, and polio was prominently
featured. Jean Chretien, Prime Minister of Canada and
G8 Summit Chairperson, summarized the
outcomes of G8 discussions: “In addition to
our ongoing commitments to combat (other
diseases), we committed to provide sufficient
resources to eradicate polio by 2005”. ♦
See back page for further details on the G8 pledges.
i
! Technical tips j
Supplementary immunization
in polio-free areas
EVEN the risk of spread of imported wild
B w polioviruses (importations occurred into
Bulgaria, Georgia and Zambia in 2001 alone),
the Global Technical Consultative Group (TCG) on
Polio Eradication has re-evaluated the role of
supplementary immunization activities (SIAs) in poliofree areas. The TCG decided that it is important
polio-free areas continue to use periodic national
immunization days (NIDs) or extensive sub-national
immunization days (SNIDs) to maintain population
immunity. The occurrence of the recent vaccinederived poliovirus outbreaks in the presence of low
population immunity (Hispaniola, Madagascar,
Philippines — see box) provides further argument for
achieving and sustaining high immunization coverage,
ideally through routine immunization services.
Consequently, the seventh meeting of the Global
TCG recommended:
■ Polio-free countries which border endemic areas, or have
very low immunization coverage, should continue
to conduct NIDs or SNIDs, as appropriate, on an
annual basis.
Polio compatible cases
Surveillance for acute flaccidparalysis (AFP) in Madagascar has detected a cluster
of four cases of paralytic poliomyelitis from which type-2 vaccine-derived
polioviruses have been isolated. Preliminary data indicate that these patients,
residing in the Tolagnaro district of Toliara province in southeastern Madagascar,
had onset ofparalysis between 20 March and 12 April 2002. None ofthe children
affected was fully vaccinated. Vaccination coverage data suggest that during
1999,37% ofchildren aged under one year had received three doses of OPV. The
genetic sequencing studies on these viruses are compatible with an outbreak of
paralyticpolio due to a circulating vaccine-derived poliovirus (cVDPV).
In July, a joint mission by the Ministry of Health, the Pasteur Institute of
Madagascar, WHO and UNICEF in Madagascar recommended that countrywide
NIDs be undertaken in September and October 2002, using a door-to-door
strategy. Further NIDs are planned in spring 2003, after the rainy season, in
Toliara and other districts at risk ofpoliovirus transmission.
To read the WER/MMWR report, visit
www.cdc.gov/mmwr/preview/mmwrhtml/mm5128a5.htm
■ Countries which have been polio-free for at least three
years, but have not achieved or maintained a level of
'2l90% routine immunization of infants with OPV
(OPV3 coverage), should continue to conduct NIDs
at least every three years, to prevent the
accumulation of susceptibles and protect against the
importation of wild polioviruses. In larger countries,
where appropriate, SNIDs should be conducted to
cover those states or provinces with lower than 90%
coverage. ♦
Reported polio compatible cases in 2002*
ECOGNIZING the high number of
polio compatible cases reported
II W in 2001, ar its seventh meeting
the Global TCG reaffirmed its
recommen-dations that all countries
a
D
should maximize efforts to obtain two
adequate specimens from every acute
flaccid paralysis (AFP) case,
J
prioritize investigation and follow
up of cases with inadequate jgp
specimens, and ensure all
potentially compatible cases are ® BMffl
referred to an appropriately
trained expert group for classification within 90 days of onset.
At this stage of the Global Polio
Eradication Initiative, the careful analysis of
|
data on polio-compatible cases is critical. Polio|
compatible cases should be monitored and B
mapped at least monthly, with field
1
investigations of all compatible cases, including
’
active case search, with particular attention to
clusters of cases. Data on polio compatible cases
should be used to identify areas for improving
surveillance quality and areas at risk of wild
poliovirus circulation. ♦
J £>
o
a
® Polio compatible case
BB Endemic region
* Data from 1 January 2002-5 September 2002
See Polio News Issue 12, July 2001 and Issue
Febnuiry 2002, respectively, [or further information on classifying AFP cases
and the role of expert groups for case classification; see the TCG’s full recommendations on polio-compatible cases in the seventh
meeting report. For electronic copies please contact polioepi@iuho.int or Tel: +41 22 791 3219-
□
AFP and polio reporting year-to-date comparison of 2001-2002
2002(as of 10$
2001 (as of 10 September 2001)
Non-polio Adequate stool
AFP rate
specimens
Confirmed
polio cases
Wild polio
virus cases
Pending
cases
Non-polio Adequate stool
specimens
AFP rate
r2002)_____________]
Confirmed
polio cases
Wild polio
virus cases
Pending
cases
African Region
2.80
71%
159
17
780
106
1.11
77%
9*
0
456
2.80
0.93
83%
Region of the Americas
90%
0
92
0
395
Eastern Mediterranean Region 1.90
83%
80
49
511
2.14
88%
41
41
413
European Region
1.12
82%
2**
2
252
1.32
83%
0
0
384
South-East Asia Region
1.41
84%
76
1443
1.43
85%
407
407
1626
Western Pacific Region
1.19
87%
0
1 030
1.19
87%
Global total
138
81%
144
4472
1.70
85%
76
0
327
554
N/A
__2
349
540
3167
• Vaccine derived poliovirus
** Importation of wild poliovirus
Wild poliovirus map
total wild poliovirus and date of most recent
wild poliovirus by country from 10 Sep 2001
to 09 Sep 2002
10-Sept-2001 to 10-Sept-2002
2OO1
Dec Jan Feb Mar Apr May Jun Jut
India
X
'.
|
Pakistan^
.... - ‘ . 540
'.
93
Afghanistan Fl .
•
6
'W '
I.:-.
l\J
' >' •■■■
Nigeria
119
.'k <.
Somalia >
Egypt
importation
(
•
Wild virus type 1
r
•
Wild virus type 3
•
....................
•
...... -
- ----
‘ ' 5
2
Source: Dalo al WHO Gtnm as o< 10 September 2002
Date of/mooned cases/virus
Importations
Zambia
, y
Algeria
Wild virus type 1 and 3
Endemic countries
NIDs calendar for selected countries
Region
Country
AFRO
Central African Republic
Oct 2002
Type of activity
Intervention
Nov 2002
Type of activity
Intervention
17-Dec/NIDs/0PV“VVitA
Chad
9-Nov/ SHIDs/OPV
17-Dec/ NIDs/OPV“ Wit A
2-Nov/ NIDs/OPV“VVitA
21-Dec/NIDs/OPV “z
17-Dec/ NIDs/OPV“WitA
Equatorial Guinea
Eritrea
EMRO
SEARO
Dec 2002
Type of activity
Intervention
6-Dec/ NIDs/OPV“WitA
Ethiopia
25-Oct/NIDs/OPV
Madagascar
30-0ct/HiDs/OPV“2
West African Block* & Nigeria
5-Oct/ NIDs/OPV“WitA
Afghanistan
22-0ct/ NIDs/OPV“4
Egypt________
1-Oct/ NIDs/OPV^111
Somalia
1-Oct/SNIDs/0PV“3
Sudan
29-Oct/NIDs/OPVRound’
Southern Sudan
**7-0ct/ SNIDs/OPV“s
Pakistan
23-Oct/ NIQs/OPVRounri4
9-Nov/ NIDs/OPV
17-Dec/SNIDs/OPVRound}
l-Nov/NIDs/OPVfi’^i
16-Dec/MDs/0PV“2
4-Nov/ SNBs/OPV Round 6
17-Nov/ SNIDs/OPV “2
India
*The West African Block is Benin, Burkina Faso, Cameroon, Cape Verde, Cdte d'Ivoire, Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Mali, Mauritania, Niger, Senegal, Sierra Leone and Togo.
This calendar reflects information known to WH0/HQ at the time ofprint. Some NIDs dates are preliminary and may change; please contact WH0/HQ for up-to-date information.
**At time ofprint, the Southern Sudan SNIDs were suspended due to flight restrictions.
o
Spearheading partners:
Rotary International
Gates Foundation
how much can be accomplished when a group selflessly
uses every ounce of the political capital at its disposal to
recognizes Rotary for its
improve the health of the worlds poorest children.”
As the world’s first and one of the largest
critical advocacy role
humanitarian service organizations with 1.2 million
U OTARY’S efforts to
kU eradicate polio were
recently honoured with the
US$ 1 million 2002 Gates
Award for Global Health
| from the Bill & Melinda
I Gates Foundation.
During the award
| ceremony on 30 May, Bill
I Gates Sr, President of
the
Foundation
said,
“What has been achieved
since Rotary International
Luis Vicente Giay, Chairman of the Rotary
Foundation of Rotary International, receives the
courageously committed
Gates award from Bill Gates Senior, President of
the Bill & Melinda Gates Foundation.
to eradicate polio defies
description. Every time we see a world leader
administering polio vaccine to a child, or hear about a
war being stopped somewhere so children can
---- be
__
vaccinated, we can thank Rotary for demonstrating
I
nF
I
members, Rotary is the lead private sector contributor
and volunteer arm of the global partnership dedicated
to eradicating polio.
In 1985, Rotary created PolioPlus — a programme
to immunize all children against polio by Rotary’s
100th anniversary in 2005. To date, Rotary has
committed more than US$ 493 million to the
protection of two billion children in 122 countries.
In addition, Rotary’s Polio Eradication Advocacy
Task Force has played a major role in decisions by
donor governments to contribute over US$ 1.5 billion
to the effort. This year, in an effort to help close the
funding gap, Rotary is embarking on its second
membership fundraising drive, entitled Fulfilling Our
Promise: Eradicate Polio,, with the goal of raising an
additional US$ 80 million for polio eradication. Rotary
and the United Nations Foundation are also
collaborating in a joint appeal for funding from private
corporations, foundations and philanthropists to help
secure urgently needed funds by the end of 2002. ♦
. .. ________________ ^.1
Rotary recognizes polio An international profile
eradicatfQ^gfepions'
ft S part of its ongolng^-advocacy efforts, Rotary
>> publicly recognizes world leaders who have
made outstanding contributions to global polio
4 eradication. Eveline Herfkens, the former
Minister for Development Cooperation of the
Netherlands, was presented with the Polio
Eradication Champion Award on 7 May 2002, by
Luis Vicente Giay, Chairman of the Rotary
Foundation of Rotary International, for her
leadership in securing US$ 110 million in
contributions from the Netherlands Government
to support polio eradication.
Rotary also presented key members of
Congress in the United States with the Polio
Eradication Champion Award on 15 May 2002,
acknowledging their ongoing support of the polio
eradication initiative. In the 2002 fiscal year,
Congress appropriated US$ 129-9 million to the
global polio eradication effort. First time
recipients of the award include: Senator Richard J.
Durbin, (D-IL), Rep. Maurice D. Hinchey
(D-NY), Rep. Benjamin Gilman (R-NY), Rep.
Mark Steven Kirk (R-IL), Rep. John Peterson (RPA), and Rep. Michael McNulty (D-NY). Past
recipients were also honoured for their continued
support. Other leaders who have been honoured
with this award include the former United States
President William Jefferson Clinton, former
Prime Minister of the United Kingdom Rt. Hon.
John Major, First Lady of Egypt Mrs Suzanne
Mubarak and UN Secretary-General Kofi Annan.
At Rotary's Convention, Wane
Annan, the lawyer and artist
married to UN Secretary-General
Kofi Annan, spoke on "The
Importance of Volunteers in
Today's World." Following her
address, Rotary International
President Richard King and
Chairman of the Rotary
Foundation Luis Vicente Giay
presented her with the Rotary
Award for Humanitarian Service.
Photo: Rotary International
ORE than 18 000 Rotary club members from
I w I 125 countries gathered in Barcelona for Rotary’s annual
convention this June. Despite their different political, cultural,
and historical backgrounds, a common mission united
Rotarians: promoting peace and building better communities.
The convention included a focus on worldwide health and
polio eradication, where Rotary club members shared best
practices of working with governments and other
nongovernmental organizations. The convention included the
election ofthefollowing new Rotary leaders:
■ Bhichai Rattakul of Thailand took office as the new
President of Rotary International on 1 July 2002. A
Member of Parliament for nine terms since 1969 and
Leader of the Democrat Party, he has served his country
as Foreign Minister, Deputy Prime Minister, Speaker of
the House of Representatives and President,-xof the
Parliament.
\
■ Glen W. Kinross of Australia is the new Chairman of The
Rotary Foundation of Rotary International. As .a member
of the International PolioPlus Committee, Mr. Kinross is
■■
dedicated to the global effort to eradicate polio.
El
1
W-.
Spearheading partners:
Centers for Disease Control and Prevention
CDC technical partner in polio eradication
f'J
£
Deborah Moore microbiologist examines cultures for the presence of poliovirus at the CDC polio laboratory
in Atlanta, United States.
■f" HE Atlanta-based US Centers for Disease Control
I and Prevention (CDC) has been a spearheading
partner in the global polio eradication initiative since
1988. CDC’s niche in the initiative lies in its technical
support and funding for large supplies of oral polio
vaccine (OPV) and operational costs for mass
immunization campaigns.
CDC is perhaps best known for its wide-ranging
technical support. For example, the poliovirus
laboratory at CDC functions as one of the global
specialized laboratories in the polio laboratory
network. Among the four spearheading partners, CDC
____
■
/
'
works as the “virus detective,” using its state-of-the-art
virological surveillance expertise,
or genetic
fingerprinting, to identify the strain of poliovirus
involved in an outbreak and pinpoint its exact
geographical location and origin. Each year CDC
scientists at the polio laboratory test more than
6000 specimens and isolates from around the world.
CDC also assigns short- and long-term technical
experts to WHO and UNICEF offices worldwide to
provide epidemiologic, programmatic, and managerial
assistance to support surveillance and polio immu
nization campaigns in developing countries. These
include members of the Stop Transmission of Polio
(STOP) teams since 1999 (see below) and public
health scientists who analyse surveillance data and
investigate outbreaks of polio, especially in areas within
or bordering polio-free zones. Most recently, CDC staff
members have conducted polio outbreak investigations
in Bulgaria and the Philippines.
In addition, CDC is one of the major funders for the
purchase of OPV used in supplementary immunization
campaigns such as NIDs. In the fiscal years of
2001 and 2002, CDC contributed approximately
US$ 115 million through UNICEF for this purpose.
CDC also provides technical resources to assure that the
purchased vaccine is targeted to achieve polio eradication
objectives. ♦
__________________
- HEALTWfEft « PSOPLE "
STOP programme: providing field support where it's
needed most
a
UR job is to help strengthen surveillance
networks for polio ... we have to know where
the disease is and where it isn’t, and we have to move
fast. Its the most exciting job I’ve ever done,” wrote a
member of the first Stop team sent from CDC in 1999.
This captures the essence of what the STOP
programme is all about: rapidly deploying human
resources to the field to support national polio
eradication programmes.
Based on the model used by smallpox eradication
teams in the 1960s and 1970s, STOP team members
collaborate with local and national counterparts from
the Ministry of Health, WHO, and UNICEF. Their
duties include:
■ supporting, conducting, and evaluating active
surveillance for acute flaccid paralysis (AFP);
■ assisting with polio case investigations and follow
up, and
■ assisting with planning, implementing, and
evaluating supplemental immunization activities,
including house-to-house mop-up operations.
Each day is different. Team members may work
with local religious leaders to overcome community
rumours about the safety of OPV; train traditional
healers about AFP surveillance; hire a boat to a remote
island to investigate a suspected polio case; or give a
presentation to health officials on immunization
campaign coverage.
In partnership with WHO and Rotaiy, CDC
launched the programme in 1999, ind since then has
deployed 11 teams, comprising 386 members, to
34 countries. Prior to leaving for their three-month
assignments, participants; receive one week of training
conducted by CDC and WHO staff in Atlanta. The
partnership that supports STOP has expanded from
WHO, Rotary, UNICEF and CDC to also include the
Canadian Public Health Association.
Perhaps one of the best tributes to the programme
is the fact that after completing their field assignments,
one in four team members have continued to work in
polio eradication with CDC, WHO or UNICEF.
To learn more about the STOP programme, the qualifications
sought, and hou> to apply, visit
httptHwww. cdc.gov/nip/global/default. htrn
s
News and announcements
Canada supports NIDs in Nigeria
As part of the social mobilization effort in preparation of the forthcoming NIDs, Mme Chretien, the
First Lady of Canada, and Mrs Danjuma (representing Mrs Stella Obasanjo, who was attending the
Cote d’Ivoire meeting of First Ladies) arrive at the Bamishi village in the area council of Kuje near
Abuja on 5 April to attend a polio immunization session.This advocacy event coincided with the visit
of the Prime Minister of Canada, Jean Chretien, to Nigeria.
phDfo: © UNICEF/Noble Tholari
De Beers
flying for polio eradication
Obituaries
Dr Taky Gaafar, Regional Adviser, Vaccine Preventable Diseases and
Immunization (VPI), and Coordinator, Disease Surveillance Eradication and
Elimination in the WHO Eastern Mediterranean (EMR) Office, passed away
on 4 July in Cairo. Dr Gaafar was first associated with WHO as short-term
consultant in smallpox eradication in Bangladesh in 1975 and in Somalia
(1979-1981). Dr Gaafar had a long association with Alexandria University,
latterly as a Professor in the Department of Public Health, Faculty of
Medicine from 1985 —1994. He actively tookpart in a number of WHO EMR
activities during this time, including national/interregional training courses,
intercountry workshops and indepth programme reviews. Dr Gaafar became
Regional Adviser, VPI at WHO EMR office in January 1995. He will be sorely
missed by all those who had the privilege and pleasure of working with him.
Abdi Risak Mahmed Farah, laboratory technician working for WHO
in Somalia as Regional Polio Eradication Officer for Mudug Region, was
tragically killed in a car accident on 5 May on his way back to his wife and
children from a monthly meeting. His organizing skills and openness,
transcending clan dimensions, had been the single most important factor in
bringing NIDs to as many children as possible in this otherwise hard-toreach area. His relentless effort in detecting AFP cases made a difference
within his first few months with the programme. Working in Mudug Region
is particularly challenging, as its regional town ofGalkayo is the geographic
centre of war-torn Somalia. Abdi Risak is greatly missed by his family, his
colleagues, his community and the programme.
Dr Sekou Victor Sangare, former Expanded Programme on
Immunization (EPI) Manager ofCote d'Ivoire, passed away on 14 June in
Abidjan. Having left EPI management around two years ago,
Dr Sangare undertook several assignments for the Vaccine Preventable
Diseases department at the WHO Africa office as a consultant; his last
assignment was a mission to the Gambia and Guinea in February2002.
He will be much missed.
Suzanne Spencer, Head of Information and Communication at De Beers, doing a wing walk for her
Day of Hope challenge, through which she raised over £1000 (around US$ 1500) for the Global
Polio Eradication Initiative. Seen here on the top wing of a 1940 Boeing Stearman Bi-plane,
Suzanne was wearing £100 000 (around US$ 150 000) of diamonds to gain publicity and raise
awareness for the global bid to eradicate polio.
photo @ BeefS
Bruno Cor be, recent consultant to WHO in Goma, the Democratic
Republic of the Congo, and long-time member ofstaff with Medecins Sans
Frontieres (MSF), died on 11 March in Martillac, France. Mr Corbe joined MSF
in 1986, going to Sudan and Mozambique as a logistical expert, then to Iraq,
Somalia, Afghanistan and Angola. Later at MSF headquarters, hejoined
missions to Bosnia, Chechnya, Rwanda and Kivu. In 1987 he launched the
MSF-Logistics central purchasing offices in Lezignan. In 1993, he was
appointed Logistics Director at MSF's Brussels headquarters and later, a
member of the MSF-France Board of Directors and the MSF-Belgium Board.
"The influence of his work and personality are indelibly stamped on the
history of MSF"
Worid Press Photo award winner:
polio eradication in Eritrea
"Polio in the press"
i.'..
1
;
Hews media
• Europe declared polio-free but cash shortage hampers rest ofthe world Agence France Presse (21.06.02)
• Silent polio carrier highlights risk - Georgina Kenyon, BBC Online (22.07.02) *
• Polio casein Burkina Faso - BBC Online (30.07.02)
Scientific articles
• Chemical Synthesis ofPoliovirus cDNA: Generation ofInfectious Virus in the
Absence of Natural Template - Jeronimo Cello, Aniko V. Paul, and Eckard
Wimmer, Science (11.07.02) *
• Public Health Dispatch: Poliomyelitis - Madagascar, 2002 - Morbidity and
Mortality Weekly Report (MMWR) (19.07.02)
For copies ofthese and other recent articles, please contactpoljoepi@who.int or
Tel: + 41 22 7913219
• *The implications ofthese aspects ofthe risk assessment for post-certification immunization
policyforpolio will be covered in the December edition ofPolio News.
Photographer Stefan Boness won an award in the 'science and technology' category of the World
Press Photo awards for his portrayal of a young girl receiving polio vaccine at a health station in
the village of Dresa in Western Eritrea, taken in December 2001.
Photo© Stefan Boness/lpon
British Airways 'Change for Good'
donation funds Zambia NIDs
RITISH AIRWAYS (BA) staff travelled to Zambia at the end of July
to observe the country’s recent SNIDs and mop-up campaigns.
A US$ 700 000 donation from BA’s Change for Good/UNICEF
fundraising partnership provided all of the OPV and social mobilization
requirements for the July round.
High quality supplementary immunization activities were essential to ensure
that virus from the five polio cases found in Zambia in 2001-2002, all importations
from eastern Angola, did not reestablish poliovirus transmission in the country.
Zambia’s SNIDs aimed to reach at least 1 million children under the age of five.
§
The BA team observed the campaign at close quarters from the country’s
Ndola (Copperbelt) region. Gaining hands-on experience administering OPV to I
©
children, the team also joined vaccinators in the region’s door-to-door campaign. s
£
Later, the imponance of cross-border campaigns was underlined when the team
In Chililabombwe, a town in Zambia’s Copperbelt region on the
travelled to the Zambia/Democratic Republic of the Congo border to observe
country's border with the DRC,the tiny fingernail of a newborn baby i
joint immunization activity between the two countries.
covered with harmless gentian-violet paint to indicate that she has
been vaccinated against polio.Zambia's July SNIDS, funded by BA's
Since 1994 BA’s ‘Change for Good’ campaign has raised more than
Change for Good programme, reached over a million children.
US$ 16 million in support of UNICEF programmes around the world. ♦
1
I
Cease-fires pave the way for direct access to children
5',-
EASE-FIRES in two of the ten countries considered
polio-endemic at the outset of 2002 have resulted in
OPV reaching many children who had likely never
been vaccinated before.
SUDAN: Some parts of the remote Nuba mountains,
located in the central part of war-ravaged Sudan, have been
inaccessible by direct UN humanitarian relief operations in
the region for decades. As a result of a cease-fire signed on
19 May 2002, Initiative partners have been able to gain
direct access to some areas for the first time, successfully
completing three rounds of
polio SNIDs in the Nuba
region. Almost immediately
following the cease-fire, WHO,
in partnership with UNICEF,
seized the opportunity to
launch
the
immunization
campaign, despite difficult
logistics. Landmines severely
hampered the movement of
vaccination teams, and the
mountainous terrain and lack
Photos: WH0/P. Blanc
of roads meant that teams frequently had to walk for over
ten hours a day and climb steep mountain slopes in severe
heat to access remote villages. In the villages themselves,
where there is a dearth of education and health
infrastructure, social mobilization efforts had to be
intensified in order to explain the threat of polio and the
reasons for the campaigns. Despite the difficulties, an
average of 45 000 children were reached in each round.
ANGOLA: The April cease-fire in Angola has led to similar
success for polio eradication, providing the opportunity to
vaccinate hundreds of thousands of children who had been
unreachable for years due to the conflict. The discovery of
Angolan children with polio paralysis just across the border in
Zambia in late 2001 demonstrated the reality of wild virus
transmission in eastern Angola. At that time, the possibility of
conducting successful immunization activities in the east was
not assured. However, the 4 April ceasefire opened the
formerly inaccessible areas, allowing SNIDs and mop-up
campaigns in April and May. For the June and July NIDs,
logistical support from the army, nongovernmental
organizations and about 30 000 volunteers meant children in
150 newly-accessible municipalities, 37 “quartering and
family areas” and children in internally displaced persons
camps were vaccinated against polio. In total, close to
4.5 million children were reached in Angola during the
June round, and the final round of NIDs took place in
late August - all synchronized with neighbouring countries.
The knowledge provided by this ‘direct access’ to
inaccessible populations in both Sudan and Angola has a
major impact on the confidence of the polio status of each
country. To date, Sudan has not isolated a wild poliovirus
since April 2001. Angola’s last recorded virus was in
September 2001, though the recent importations to Zambia
suggest that transmission is ongoing in eastern Angola. With
continued access and strong AFP surveillance, these countries
can reach the goal of being polio-free by the end of 2002. ♦
Recent donations.-* ■
Resource mobilization
DeBeers staff members:
European certification and
G8 commitment provide
backdrop for enhanced
resource mobilization efforts
US$ 5000 of undesignated funds, allocated to Guinea Bissau for
operational costs
LL levels of the polio partnership are actively
working to address the Initiative's most critical
issue: filling the US$ 275 million funding gap.
On 21 June, as the European region of WHO
was certified polio-free, WHO's Director-General,
Dr Gro Harlem Brundtland, wrote an exceptional
appeal to all European development ministers, citing
the necessity of an extraordinary show of support for
polio eradication in order to reach the goal of a poliofree world — therefore protecting the collective
investment already made by the European region.
At the June 2002 G8 Summit in Kananaskis,
Canada, G8 leaders pledged to fill the Global Polio
Eradication Initiative's US$ 275 million funding gap
as part of the Africa Action Plan. The partnership is
now working with G8 member states to help to
operationalize this pledge. At the Summit, Canada
pledged US$ 32 million in new funding over three
years. Canada and the UK, which has since committed
an additional US$ 25 million, are now preparing to
advocate with the other G8 countries. A meeting of the
Africa Personal Representatives of the G8 leaders
towards the end of this year will be the crucial forum
for translating the G8 pledges into actual resources. ♦
This autumn, the document'Estimated external financial resource
requirements for 2003-2005' will be published. It will summarize the
global resource requirements and highlight the budget needs for all
endemic countries and countries at high risk of wild poliovirus
transmission - providing the basis for resource mobilization efforts.
Materials available:
A
The polio eradication Progress Report 2001 is available
in English in print and electronic format.
The first edition of the polio eradication endgame
I
briefing pack is available in English and French - it is |
also available electronically on
/
USS 32 000 raised throug
US$ 10.5 million to purchase OPV for Bangladesh, Ethiopia,
Ghana, India, Nigeria and Sudan
7
I
I .
GZ.
www.polioeradication.org
Hew Zealand:
US$ 43 000 contributed to the Rotary Foundation to support
activities in Indonesia
Norway:
US$ 6.8 million in undesignated funding to the global
programme
SSI''.
Private Sector Appeal:
us$ 1.7 million for polio activities in Angola and the Democratic
Republic of the Congo as well as support for CDCs STOP team
programme
US$ 3.75 million in private sector campaign donations from
Wyeth, Baxter, Tellabs and Pew Charitable Trust for polio
activities in Ethiopia, India, West Africa and for the African Polio
Laboratory Network
' '
Trickor Treat:
US$ 3.4 million for polio activities in Pakistan and Afghanistan,
which attracted a US$ 850 000 match from the UN Foundation
United Kingdom:
US$ 7.8 million in undesignated funding
'll
the Global Polio piod^tia^TsUoihe expresses irsgiatmude to alldonots.
^Donations annauntjedsince Mine's JSMay2^2,
Wyeth donates US$ 1 million
to Global Polio Laboratory
Network
\
n
is
Photo: WHO
Dr Gro
right) joined Jack Blane, director of the Rotary's Polio
Eradication Private Sector Campaign (middle right), in
Geneva this June at a ceremony where US-based
pharmaceutical company Wyeth pledged
US$ 1 million to polio eradication.
Tommy Thompson, United States Secretary of Health and
Human
Services
(far
Human Services (far left)
left) looked
looked on'as
on as Kevin
Kevin Reilly,
Reilly,
President ofWyeth Vaccines and Nutrition (middle left)
presented the contribution to the Polio Eradication
Private Sector Campaign (jointly sponsored by The Rotary
Fmindatinn
Foundation nf
of Dntarv
Rotary IntamaftAnal
International nnJ
and fka
the IbG+aJ
United
Nations Foundation).The gift will support the African
Region of the Global Polio Laboratory Network in their
efforts to identify the last reservoirs of wild poliovirus.
As part of Wyeth's commitment to the Initiative, now
spanning six years, this is the company's second
US$ 1 million contribution to support the Global Polio
Laboratory Network.
Forthcoming events 2002
Date
Event
21-22 September Rotary International Meeting of National Advocacy Advisors
25 September
Horn of Africa Polio Partners'meeting
7-11 October
Meeting of Interested Parties
22-24 October
Rotary IPPC Meeting
11 & 15 November Global Polio Management Team Meeting
12 November
WHO/UNICEF MoH Consultation for Priority Countries
13-14 November Meeting of the Global TCG
25-29 November Pan American Health Organization
Special Centennial Meeting on Vaccines
2-5 December
Task Force on Immunization
Venue
Zurich, Switzerland
Nairobi, Kenya
Geneva, Switzerland
Evanston, US'
Geneva, Swi
j
Geneva, Switzerland
Geneva, Switzerland
Washington DC, USA
Abuja, Nigeria
Many polio documents are available on the web site at:
www.polioeradication. org
• Please fill out this response coupon and return it to Polio News, EPI, Department of
i Vaccines and Bialogkals, Document Centre, World Health Organization, CH-1211
| Geneva 22, if you would like to continue receiving this publication or
■ send an e-mail to polioepi^who.int
i / would like to receive this publication regularly.
I Name:
I Institution:
| Address:
i
1
'
World Health Organization 2002.
All rights reserved.The designations employed and the presentation of the material in
this publication do not imply the expression of any opinion whatsoever on the part of the
World Health Organlxation concerning the legal status of any country, territory, dty or area or
of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on
maps represent approximate border lines for which there may not yet be full agreement.
The World Health Organization does not warrant that the information contained in this
publication is complete and correct and shall not be liable for any damages incurred as a result
of its use. Polio News is published quarterly by EPI, WHO Headquarters, Geneva, Switzerland,
and part funded by USAID. Published data reflects information available at time of print.
i Please aha send this puhlicutiou to:
i Name:
I Institution:
i Address:
;
All comments and feedback on Polio News should be sent to:
Department of Vaccines and Biologicals, WHO, Geneva.
§
Tel.:
4-4122791 3219
I
Fax:
4-4122791 4193
Email:
polioepi@who.int
3
Web site:
http://www.polioeradication.org
_____________
ill
I
o
BMC Public Health
BioMed Central
Open Access
Research article
Polio eradication initiative in Africa: influence on other infectious
disease surveillance development
Peter Nsubuga*1, Sharon McDonnell1, Bradley Perkins2, Roland Sutter3,
Linda Quick3, Mark White1, Stephen Cochi3 and Mac Otten3'4
Address:1 Division of International Health, Epidemiology Program Office, Centers for Disease Control and Prevention, Atlanta, Georgia, USA,
2Division of Bacterial and Mycotic Diseases, National Center of Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia,
USA, 3Vaccine Preventable Disease Eradication Division, National Immunization Program, Centers for Disease Control and Prevention, Atlanta,
Georgia, USA and 4Regional Office for Africa, World Health Organization, Harare, Zimbabwe
Email: Peter Nsubuga* - pnsubuga@cdc.gov; Sharon McDonnell - semO@cdc.gov; Bradley Perkins - bap4@cdc.gov;
Roland Sutter - rsutter@cdc.gov; Linda Quick - maq2@cdc.gov; Mark White - mhwl@cdc.gov; Stephen Cochi - scochi@cdc.gov;
Mac Otten - ottenm@whoafr.org
* Corresponding author
Received: 17 September 2002
Accepted: 27 December 2002
Published: 27 December 2002
B/VIC Public Health 2002, 2:27
This article is available from: http://www.biomedcentral.eom/l47l-2458/2/27
© 2002 Nsubuga et al; licensee BioMed Central Ltd. This is an Open Access article: verbatim copying and redistribution of this article are permitted in all
media for any purpose, provided this notice is preserved along with the article's original URL
Abstract
Background: The World Health Organization (WHO) and partners are collaborating to
eradicate poliomyelitis. To monitor progress, countries perform surveillance for acute flaccid
paralysis (AFP)- The WHO African Regional Office (WHO-AFRO) and the U.S Centers for Disease
Control and Prevention are also involved in strengthening infectious disease surveillance and
response in Africa. We assessed whether polio-eradication initiative resources are used in the
s.uryeillance for and response to other infectious diseases in Africa,
Methods:
During October
I999-March
——
2000, we developed and
—
administered a survey
questionnaire to at least one key informant from the 38 countries that regularly report on polio
activities to WHO. The key informants included WHO-AFRO staff assigned to the countries and
Ministry of Health personnel.
Results: We obtained responses from 32 (84%) of the 38 countries. Thirty-one (97%) of the 32
countries had designated surveillance officers for AFP surveillance, and 25 (78%) used the AFP
Resources for the surveillance and response to other infection^
In 28 (87%) countries, AFP
program staff combined detection for AFP and other infectious diseases. Fourteen countries (44%)
had used the AFP laboratory specimen transportation system to transport specimens to confirm
other infectious disease outbreaks. The- majority pf thv-^evntnor thnr poQormpd AFP surveillance
adequately (i.e., non polio AFP rate = 1/100,000 children aged <15 years) in 1999 had added 1—5,
diseases to their AFP surveillance prograrn.
Conclusions: Despite concerns regarding the targeted nature of AFP surveillance, it is partially
integrated into existing surveillance and respnn^ ^rpips in multiple African countries. Resources
provided for polio eradication should be used to improve surveillance for and response to other
priority infectious diseases in Africa.
Page 1 of 6
(page number not for citation purposes)
BMC Public Health 2002, 2
Background
The polio-eradication initiative has led to the largest in
flux of public health resources into Africa since the small
pox-eradication campaign, comprising both human
resources and infrastructure investment [1,2]. Public
health professionals have debated the merits and demerits
of the polio-eradication initiative, regarding the priorities
of developing countries. Supporters of the initiative have
reported on the high benefit-cost ratio of eradication
[1,2]. Among the demerits cited is that polio has a lower
public health importance as compared to other infectious
diseases - many of them epidemic prone - in poor coun
tries [1-3]. An investigation of the impact of the polio
eradication initiative on the status of funding for routine
immunization revealed that the amount of funding for
routine immunization activities has not increased over
the years and that whether eradication funding will be
available for other public health interventions when polio
is eradicated is unclear [4). Anecdotally reported merits
and benefits of the polio-eradication initiative have in
cluded increased national enthusiasm and funding for Ex
panded Programs
on
Immunization,
enhanced
surveillance capacity for other diseases, strengthened pub
lic health laboratory capacity, and improved epidemio
logic skills [2]. We report the results of a survey regarding
the impact of the polio-eradication initiative on the sur
veillance for other infectious diseases in Africa.
In 1989, the African Regional Office of the World Health
Organization (WHO-AFRO) adopted the global goal of
eradicating».poliomyelitis by the year 2000, and in 1995,
member countries initiated specific polio-eradication
strategies including acute flaccid paralysis (AFP) surveil
lance. Resources are deployed primarily through surveil
lance officers, development of a functional regional
laboratory network, logistics, cold-chains, communica
tions, and transportation [5-7]. To ensure that the polio
eradication strategies were efficiently and effectively im
plemented, countries were divided into five epidemiolog
ical blocks on the basis of geographic proximity, similarity
in infrastmeture, and program needs. These country
groupings included central, eastern, southern, and west
ern epidemiological blocks and Countries in Special Cir
cumstances (i.e., Angola, Democratic Republic of the
Congo, Ethiopia and Nigeria) [5]. By 1999, 38 countries
regularly reported polio/AFP surveillance data to WHOAFRO.
In September 1998, to share resources, and improve effi
ciency, WHO-AFRO adopted the Integrated Disease Sur
veillance and Response (IDSR) strategy, which aims to
improve surveillance and response by integrating infec
tious disease surveillance programs [8,9]. The IDSR strat
egy is based on core activities and support functions that
are required to perform infectious disease surveillance, ep-
http://www.biomedcentral.eom/1471-2458/2/27
idemic preparedness, and response |l,10,11]. Core activi
ties include case-patient detection, registration, and
confirmation; reporting, analysis, use, and feedback of da
ta; and epidemic preparedness and response (e.g., out
break investigations, contact tracing, and public health
interventions). Support functions include coordination,
supervision or performance evaluation, training, and re
source-provision for infrastructure, including communi
cation. The Centers for Disease Control and Prevention
(U. S. Department of Health and Human Services) (CDC)
provides technical and financial support to WHO-AFRO
for both IDSR and the polio-eradication initiative, along
with the U. S. Agency for International Development and
other partners.
Methods
We performed a survey to determine the impact of AFP
surveillance on the surveillance for and response to other
infectious diseases. The objectives of the survey included
describing the characteristics of AFP surveillance pro
grams in WHO-AFRO, how surveillance activities for AFP
and other infectious diseases have been combined, the
contribution of AFP surveillance to the surveillance of
other infectious diseases, and the effect of adding surveil
lance and response to other infectious diseases on the per
formance of AFP surveillance. We also used the experience
of AFP surveillance programs to obtain a description of
the constraints to strengthening infectious disease surveil
lance in Africa. We targeted the 38 countries that regularly
report AFP surveillance and polio eradication activities to
World Health Organization (WHO).
We developed, pilot-tested, and translated into French a
survey questionnaire. The questionnaire was adminis
tered to at least one key informant per country by tele
phone, electronic mail, and in person during December
1999-April 2000. The key informants included Ministry of
Health officials and WHO country assignees. Non-polio
AFP rates are used as an indicator of the sensitivity of AFP
surveillance programs. A sensitive AFP surveillance pro
gram should be able to detect a background rate of >1 case
of non-polio AFP per 100,000 children aged <15 years in
any geographic area (province, country,' region etc.) per
year. Non-polio AFP rates are reported monthly to WHO
and compiled annually. We abstracted data regarding
non-polio AFP rates from the WHO website [12]. Data ac
cruing from this survey were entered and analyzed using
Epi Info version 6.04 [13].
Results
We obtained data from 32 (84%) of the 38 countries that
regularly report on polio/AFP surveillance activities in Af
rica to WHO (Figure 1). The highest response rates were
from the southern epidemiological blocks (all nine coun
tries) and the Countries in Special Circumstances (all four
Page 2 of 6
(page number not for citation purposes)
http://www. biomedcentral .com/1471 -2458/2/27
BMC Public Health 2002, 2
often uneasy regarding entrusting others with gathering
surveillance data that are crucial to targeting and evaluat
ing their programs. Therefore, ongoing training monitor
ing and periodic external evaluations should provide the
quality assurance and credibility that integrated surveil
lance and response programs will need to reassure manag
ers that they are basing decisions on reliable information.
This survey had a few limitations and we were unable to
obtain responses from all the targeted countries. In certain
countries, we could not contact possible respondents be
cause of difficulties in communication, which could have
led to introduction of bias in the survey because the non
respondents might have had substantially different an
swers to our questions than the respondents. Another pos
sible limitation was that respondents were reporting on
themselves and could have lacked objectivity additional
ly, the future employment and/or career development of
the respondents may likely depend on their capacity to
support other control programs and this may have intro
duced a bias in answering the questionnaire, although
there is no way to determine this for certain. Further, the
tool that we used did not have questions on the accepta
bility of AFP surveillance and the feasibility of IDSR and
we also did not evaluate the cost of IDSR or the cost to
maintain and sustain the infrastructure of the polio erad
ication initiative after polio is eradicated. We determined
the performance of the AFP surveillance programs solely
by non polio AFP rates because of the lack of widely used
surveillance and response indicators at the time of the sur
vey, however WHO-AFRO and CDC have recently begun
work on a list of core indicators that will help monitor
and evaluate the implementation of the IDSR process.
The findings of this survey have important implications
for WHO-AFRO's initiative to improve surveillance, epi
demic preparedness, and response in the African region.
First pnlin-eradication initiative staff, financial resources.
and infrastructure can be used as one strategy to build
IDSR in Africa, Because additional funds are needed for
surveillance now and will be needed after polio is eradi
cated, other disease-specific programs, especially those fo
cusing on epidemic prone diseases like malaria, might
consider investing in general infectious disease surveil
lance following the polio example. Second, as surveillance
and response capacity are developed in Africa, adding new
diseases to existing or new surveillance systems should be
on the basis of indicators of the surveillance system's ca
pacity not to overload the surveillance system. Finally, the
cadre of new people trained in surveillance by the polio
eradication initiative should be used for IDSR, and career
paths should be provided for them as one lasting legacy of
the poliomyelitis-eradication campaign in Africa.
Competing Interests
None declared
Author Contribution
PN conceived and carried out the study and drafted the
manuscript. SM conceived and carried out the study. BP,
RS, LQ, MW, SC and MO participated in the design and
coordination of the study. All authors read and approved
the final manuscript.
References
I.
2.
3.
4.
5.
6.
7.
8.
9.
IO.
il
12.
13.
14.
ls.
16.
Taylor CE, Cutts T and Taylor ME Ethical dilemmas in current
planning for polio eradication. Am j Public Health 1997, 87:922-5
Sutter RW and Cochi SL Ethical dilemmas in worldwide polio
eradication programs [Comments]. Am J Public Health 1997,
87:913-6
Lee JW, Melgaard B, Hull HF, Barakamfitiye D and Okwo-Bele JM
Ethical dilemmas in polio eradication. Am J Public Health 1998,
88:130-2
Levin A, Jorissen J, Linkins J and McArthur C Impact of polio erad
ication initiative on donor contributions to routine immuni
zation. Special Initiative Report No. 36. Bethesda, AID: Partnerships for
Health Reform Project, Abt Associates Inc 2001,
Okwo-Bele JM, Lobanov A, Biellik RJ, Birmingham ME, Pierre L and
Tomori O Overview of poliomyelitis in the African Region
and current regional plan of action. J Infect Dis 1997, 175(Suppl
l):SI0-5
Centers for Disease Control and Prevention Progress toward po
lio eradication Africa, 1996. A4MWR 1997, 46:321-4
World Health Organization, Regional Committee for Africa Ex
panded program on immunization: Disease control goals;
the countdown has started. Brazzaville: World Health Organization,
Regional Office for Africa, resolution AFRJRC45IR5 1995,
World Health Organization, Regional Office for Africa Integrated
disease surveillance strategy, a regional strategy for commu
nicable diseases 1999-2003. Harare: World Health Organization Re
gional Office for Africa 1999,
World Health Organization: Regional Office for Africa Regional Com
mittee resolution AFR/RC48/R2 1998,
World Health Organization An integrated approach to commu
nicable disease surveillance. Weekly Epidemiological Record 2000,
75:1-8
Centers for Disease Control and Prevention Assessment of infec
tious disease surveillance, Uganda 2000. A4A4WR 2000, 49:6879
Online AFP Surveillance Data, World Health Organization 2000,
Dean AG, Dean JA, Coulombier D and Brendel KA Epi Info, Ver
sion 6: a word processing, database, statistics program for
epidemiology on microcomputers. Centers for Disease Control
1994,
Kleinau E Management of health information systems In: Design
and implementation of health information systems (Edited by: Lippeveld T,
Suaerborn R, Bodart C) Geneva, Switzerland, World Health Organization
2000, 176-197
_ .
Centers for Disease Control and Prevention Updated guidelines
for evaluating public health surveillance systems: recom
mendations from the guidelines working group. A1A1WR ^001,
50(No. RR-13):
World Health Organization, Regional Office for Africa Protocol for
the assessment of national communicable disease surveil
lance and epidemic preparedness and response systems. AFR/
IDS/OI.I 2000,
Pre-publication history
The pre-publication history for this paper can be.accessed
here:
http://www.biomedcentral.eom/1471-2458/2/27/prepub
Page 6 of 6
(page number not for citation purposes)
http://www.biomedcentral.eom/1471 -2458/2/27
BMC Public Health 2002, 2
Table 2: Major contribution of acute flaccid paralysis surveillance to surveillance for other diseases and constraints to disease
surveillance in 32 African countries - 2000
(%)
Contribution of AFP Surveillance
n
Improvement of disease surveillance
12
(38)
Improved infrastructure or resources
7
Increase awareness about surveillance or capacity building
7
Increased personnel for surveillance
3
(22)
(22)
(9)
Constraints to Disease Surveillance
Lack of staff
9
Lack of funds
7
Lack of vehicles or fuel
3
(28)
(22)
(9)
Lack of training
2
(6)
Lack of political commitment
I
(3)
Total
32
countries that had prudently added other diseases to their
AFP surveillance programs were also able to perform AFP
surveillance adequately. However, the survey also indicat
ed that additional staff firndfr-nnd -politiraLcommitment
might be required if in fact-inn* disease surveillance and re
sponse is to improve in Africa.
Substantial fixed costs are involved in building and main
taining national surveillance and response systems and a
limited number of countries can afford the cost of dupli
cative systems [14]. Other targeted and substantially fund
ed disease control programs (e.g., HIV/AIDS, malaria,
tuberculosis) need to consider following the pya.mpfa nf
AFP surveillance and make investments in thp.ciirypilhnrp
and response infrastructure at the country level. Many of
these categorical programs desire improved timeliness
and completeness of district reporting and evidence-based
decision making, which can be addressed by implement
ing IDSR activities.
AFP surveillance programs have instituted laboratory sys
tems in countries and have formed networks between and
within countries and with WHO-AFRO by providing port
able computers with modems, telephone/facsimile lines,
and electronic mail connections. Our survey results indi
cated that detection and confirmation of outbreaks of oth
er infectious diseases has been conducted by using the
To support surveillance activities as a necessary compo
resources and infrastmeture of the AFP surveillance labo
nent of disease prevention and control activities, an ur
gent need exists to develop a consensus core set of
ratory network, including the specimen transportation
system. This can be further strengthened into a network of
surveillance and response indicators that are field-tested
laboratories that can support the IDSR strategy. Joint in
and that can be monitored routinely in a similar manner
formation-sessions for clinicians regarding polio-AFP sur
to the polio indicators, in addition to the existing surveil
lance evaluation frameworks [15,16]. These indicators can
veillance and other diseases of public health importance
within countries are already occurring and can be
then guide the strengthening of surveillance systems and
strengthened into a collaborative training effort for IDSR.
the integration of other diseases into targeted disease-speStronger links among epidemiologists and laboratorians * cific programs,
are necessary to improve outbreak detection and control.
Contributions that were identified and attributable to the
Our study determined that the majority of diseases that
presence of AFP surveillance programs indicate that polio
are integrated into AFP programs are vaccine-preventable ■ eradication programs have gone beyond a purely vertical
diseases, (e.g., measles and neonatal tetanus), indicating
approach (i.e., disease-specific) toward one that is more
an ongoing linkage with other vaccination programs and
horizontal (i ° , ryFtPm<? development)- Improvements of
disease-prevention activities. Other diseases included in
infrastructure, capacity building, and provision of person
AFP surveillance programs were epidemic-prone diseases
nel can be used to develop the overall surveillance system
(e.g., cholera and meningitis), reflecting the importance
for infectious diseases as long as the categorical program
of epidemic response in general. Among the countries that
policies clearly support this approach. A lack of resources
achieved the surveillance target for AFP in 1999, the ma
(e.g., staff, funds, vehicles, or fuel) were the main con
jority included 1-5 other infectious diseases in the AFP
straints to infectious disease surveillance that were identi
surveillance program, indicating that the judicious addi
fied in the survey - interestingly, training was not
tion of a few diseases to a program such as AFP surveil
identified as a top constraint, possibly indicating that
lance is feasible without adversely affecting the primary
trained personnel already exist, at least within the AFP sur
veillance program. Managers of categorical programs are
program.
Page 5 of 6
(page number not for citation purposes)
http://www.biomedcentral.eom/1471-2458/2/27
BMC Public Health 2002, 2
-
-
Eastern Mediterranean WHO Region
_,r i
AFRO
Responded
AFRO
Did not respond
Figure I
African Region WHO (AFRO) Countries Surveyed — 2000
countries). The lowest response rate was from the central
epidemiological block where only two of the four coun
tries responded.
Thirty-one (97%) of the 32 countries had designated sur
veillance officers working on AFP surveillance, with a me
dian number of 10 per country. Twenty-seven (84%) of
the 32 countries had an annual AFP surveillance budget
ranging from $10,000 to $1.8 million (median:
$125,000). The majority AFP surveillance programs (26
[81%]) had >1 dedicated vehicles. In the majority of
countries (27 [84%]), the AFP surveillance program was
started after the general infectious disease surveillance
program.
Detection for other infectious diseases was combined
with AFP detection in 28 (90%) countries (Table 1). In 28
(90%) countries, staff from the AFP program took respon
sibility for informing clinicians and other health practi
tioners regarding other infectious diseases while
conducting training in AFP surveillance. Fourteen coun
tries (44%) had used the AFP laboratory specimen trans
portation system to transport specimens to laboratories
for confirmation other infectious disease outbreaks.
Fifteen (47%) of the 32 countries performed AFP surveil
lance adequately (i.e., non polio AFP rate = 1/100,000
children aged <15 years) at the end of 1999 (Figure 2).
Eleven (73%) of the 15 countries that performed AFP sur
veillance adequately had also added 2-5 diseases onto
their AFP surveillance program. Both countries that added
>5 diseases onto their AFP surveillance program per
formed AFP surveillance inadequately.
A total of 25 (78%) of the 32 countries had combined AFP
surveillance with surveillance for other infectious diseas
es. The most common diseases added to surveillance for
AFP were other childhood vaccine-preventable diseases:
measles in 24 (96%) and neonatal tetanus in 22 (88%).
The other diseases added to the AFP surveillance programs
tended to be epidemic-prone diseases (e.g., cholera in 17
[68%], meningitis in 16 [64%], or yellow fever in 11
[44%]), and depended on the epidemiological patterns in
the responding countries.
When the respondents were asked to illustrate major con
tributions attributable to the AFP surveillance programs,
12 (38%) described an improvement of national disease
surveillance (Table 2). Other contributions cited were im
proved infrastmeture or resources, increased awareness re
garding surveillance or capacity building, and increased
Page 3 of 6
(page number not for citation purposes)
BMC Public Health 2002, 2
http://www.biomedcentral.eom/1471-2458/2/27
6
w
5
E
2
D)
O 4
CL
>»
4-^
□ 3
o
O
o
E
□
z
w
2
i -B
0
■
_f
0
_ _ ___
2
3
4
5
6
Number of Diseases Added to AFP Surveillance
□ Adequate H Inadequate
Adequate performance = Non polio AFP rate > 1 per 100,000 children less than 15 years old
Inadequate performance = Non polio AFP rate < 1 per 100,000 children less than 15 years old
Figure 2
Effect of integration of other diseases on the performance of acute flaccid paralysis (AFP) surveillance using 1999 non polio AFP
rates in 32 African countries
Table I: Integration of surveillance and response for other diseases with the acute flaccid paralysis surveillance program in 32 African
countries - 2000
Attribute
n
(%)
Use AFP resources for surveillance for other diseases
Combine detection for other diseases with AFP
Inform clinicians about other diseases when informing them about AFP
Use AFP laboratory transportation system for other diseases
26
28
27
14
(81)
(90)
(87)
(44)
Total
32
personnel for surveillance. Major constraints to general
disease surveillance that were identified included a lack of
staff to perform surveillance, a shortage or lack of funds,
lack of vehicles or fuel, lack of training, and a lack of po
litical commitment.
Discussion
Our survey revealed that, among the African countries that
conducted AFP surveillance and reported to WHO in
1999, the majority had designated surveillance officers,
vehicles, and annual budgets. .Moreover, most of the na
tional polio eradication programs combined the surveil
lance for and response to AFP with other infectious
diseases^ (Jur investigation also revealed that certain
Page 4 of 6
(page number not for citation purposes)
7
Policy and Practice
The impact of the Global Polio Eradication Initiative on the
financing of routine immunization: case studies in Bangladesh,
Cote d'Ivoire, and Morocco
Ann Levin,1 Sujata Ram,2 & Miloud Kaddar2
Abstract To determine if the Global Polio Eradication Initiative (PEI) affected financing of routine immunization programmes, we
compared sources and uses of funds for routine immunization programmes and PEI activities in Bangladesh, Cote d'Ivoire, and Morocco for
the years 1993-98. We also examined funding trends for these years in these countries and assessed the effect of the initiative on the
availability of specific resources in national immunization programmes, such as cold-chain equipment and personnel time spent on
activities related to national immunization days and surveillance of poliomyelitis and acute flaccid paralysis. We found that all three
governments and the majority of donors and international organizations continued to fund routine immunization programmes at levels
similar to those before the PEI, Trend analysis also indicated that financinglor routine immunization in each of the countries continued to
increase after the PEI was introduced. The results show that the PEI did not reduce funding for routine immunizations in these countries.
Keywords Poliomyelitis/prevention and control; Immunization programs/economics; Financing, Government/trends; Financing,
Organized/trends; Health expenditures/trends; Comparative study; Case report; Bangladesh; Morocco; Cote d'Ivoire (source: MeSH, NLM}.
Mots des Poliomyelite anterieure aigue/prevention et controle; Programmes de vaccination/economie; Financement par
gouvernement/orientations; Organisation financement/orientations; Depenses de sante/orientations; Etude comparative; Cas clinique;
Bangladesh; Maroc; Cote d'Ivoire (source: MeSH, IN5ERM).
Palabras clave Poliomielitis/prevencidn y control; Programas de inmunizacion/economia; Financiamiento gubernamental/
tendencias; Organizacion del financiamiento/tendencias; Gastos en salud/tendencias; Estudio comparative; Informe de caso;
Bangladesh; Marruecos; Cote d'Ivoire (fuente: DeCS, B/REME).
Bulletin of the World Health Organization 2002;80:822-828.
Voir page 828 !e resume en francais. En !a pagina 828 figura un resumen en espano/.
Introduction
Considerable progress has been made in eradicating polio
myelitis, thanks to the Polio Eradication Initiative (PEI), led by
WHO, the United Nations Children’s Fund (UNICEF), and a
number of bilateral donors. However, the initiative has
required considerable financial and other resources from
ministries of health and other local and external sources, which
raised the question as to whether resources for routine
immunizations were adversely affected by the focus on the
PEI. In the 1990s, global funding for routine immunization
programmes in developing countries declined sharply for
several reasons, including funding reductions from the United
States Agency for International Development (USAID) after
the cold wax- ended; competition from health services, such as
those for human immunodeficiency virus (HIV)/acquired
immunodeficiency syndrome (AIDS) and other health
priorities; and a reduction in UNICEF funding after Universal
Child Immunization ended in 1990. During the 1990s,
initiatives to control and eliminate diseases also became more
frequent.
The PEI began in 1988 and has since reduced the global
incidence of poliomyelitis. The WHO Region of the Americas
was the first region to certify eradication in 1994, although one
outbreak of vaccine-derived poliomyelitis has since occurred.
The WHO Western Pacific region was certified poliomyelitis
free in October 2000, and the WHO European Region was
declared poliomyelitis free in June 2002. The two regions with
the highest incidence of poliomyelitis are the WHO African
Region and the WHO South-East Asia Region, although the
frequency of cases is much lower than a decade ago.
Critics of eradication initiatives have argued that thev
divert resources and undermine efforts to maintain and
strengthen routine health services. In the least-developed
countries poliomyelitis eradication has had both positive and
negative impacts on the development of health systems (7, 2).
The positive impacts on routine health services resulted from
the emphasis on social mobilization and improving manage
ment as part of the targeted initiatives. In poorer countries,
however, targeted immunization programmes diverted re
sources away from routine services, especially during mass
immunization campaigns.
Other studies also found that poliomyelitis eradication
efforts had both positive and negative impacts. The develop
ment and strengthening of acute flaccid paralysis surveillance
in the Philippines, for example, improved surveillance for other
diseases (5), whereas poliomyelitis eradication initiatives in the
1 Senior Research Associate, Family Health International, 4301 Connecticut Avenue, Northwest, # 280, Washington, DC 20008, USA (email: alevin@pcdc.org).
Correspondence should be addressed to this author.
2 Consultant, Partners for Health Reform Project, Abt Associates Inc., Bethesda, MD, USA.
Ref. No. 01-1341
822
Bulletin of the World Health Organization 2002, 80 (10)
013139 1 VVNOIXVNM3XNI
NVA
ONIliaiSlSOO M V V H N V V
1861 SONIS TV SOW3AA ONtXHOIXS X >19 3 AA 3XHOVO3D 3Z3O XIHNVA
N3a3O1ANI38 13H
MOOQ N 3 O N V 3 S O N 11 3 >1 >11 AA X N O N1
N 3 AA H O 9 A N3
N3NNVW NVA OI3HONOZ39 30 NVA N393X3893A X3H
XHD39N3SN3W 133S93AINn N33 SI ai3HONOZ3D 3 T V HI X d O
Polio eradication and the financing of routine immunization
Lao People’s Democratic Republic, Nepal, and United
Republic of Tanzania had both positive and negative impacts
on the health system, depending on the level of development
of the health system, the management capacity of personnel,
and the level of integration of the health infrastructure (4).
Positive impacts were more likely when sufficient planning was
in place. It should be noted, however, that these three countries
may not have been representative of other countries in their
respective regions.
In the present study, we examined whether trade-offs
occurred for routine immunization programmes, when
governments, donors, and international organizations pro
vided funding for the PEI.
Data collection
We collected data in Bangladesh, Cote d’Ivoire, and Morocco —
chosen as pan of a larger study on the financing of immunization
programmes — since the countries had a mix of financing
sources and were located in different geographical regions.
However, the countries all had diphtheria, pertussis, and tetanus
coverage rates greater than 60% and are not representative of
countries with programmes that function less well.
We collected information on sources and uses of funds
for routine immunization programmes and poliomyelitis
eradication activities by the governments, donors, and other
contributors (5—7). Although poliomyelitis eradication activ
ities only began in 1995—96, funding for surveillance and
planning activities began in 1993-94. The sources of financing
included national governments, local (regional) governments,
donors, international organizations, and the private sector.
Morocco differs from the other two countries since it
was already conducting national immunization days before the
PEI was started as a means of supplementing routine
immunization activities. National immunization days were
used to improve immunization coverage, since disparities in
coverage rates existed, particularly in rural areas. When the
initiative began, poliomyelitis immunization for children aged
1—5 years old was included in national immunization days.
Expenditure was divided into recurrent and capital
expenses. Recurrent expenditures occurred within one year or
less, such as personnel salaries and supplies. Capital expendi
tures were for items that lasted longer than a year, such as
equipment and land. Interviews were conducted with key
informants to obtain in-depth information on the immuniza
tion programmes and long-term prospects for financing.
Better estimates of the role of governments in financing these
activities were obtained by including the value of personnel
time in the analysis, although the analysis did not attempt to
separate out the contributions from different levels of staff.
Funding data for trend analyses were converted to United
States dollars so that data from different sources could be
compared. Nominal dollars — which give the value at current
prices — were used because inflation of the United States
dollariwa|s0 low htbcffing-1993aj2’000.
"iO" of the initiative on financing
roupiftesimraw®za>ti/3a6 we^Ci cammed by trend analysis when
information8^^8 aya!lla'bfe.
determine whether the rate of
funding for routine immunizations had decreased, routine
immunization HtidlrigAv^ dbrnpared with that for poliomve.
Hvauaisw? atM00\
• j i i
i
' r
litis eradication acf^yiltig^.a\^^Jso examined whether the rate of
funding iracreasa i slowed i rance poliomyelitis eradication
activities were 1 introduced.'Z/In addition, specific funding
SOW3M 5NI1H3IJ.S
Bulletin of the World Health Organization 2002, 80 (10)
r
°
sources were investigated to determine whether individual
flows increased or decreased over the same period.
The contributions of the governments of Bangladesh,
Cote d’Ivoire, and Morocco for routine immunization
programmes and national immunization days were examined
separately to assess how governments allocated national
immunization programme resources to immunizatiort and
poliomyelitis eradication activities. The study also examined
whether the governments contributed to the PEI, and
examined whether this had long-term effects on financing
for their routine immunization programmes.
The possibilities for long-term financing for routine
immunization, poliomyelitis eradication, and other health
activities were determined from discussions with contributors
and key informants, such as ministry officials and donor
representatives.
Spending trends for routine immunization
and the PEI
The trends in expenditures on routine immunization and
poliomyelitis eradication in Bangladesh and Cote d’Ivoire were
examined to assess whether expenditures for routine im
munization changed as poliomyelitis eradication activities were
introduced. Morocco was not included, as there was
insufficient information on past expendimres. In Bangladesh,
expenditures between 1993 and 1997 on routine immunization
comprised an approximately constant 6-7% of total health
sector expenditures (Table 1). Funding for poliomyelitis
eradication was also fairly constant at 2% of total health
expenditures. However, the annual increase in expenditure was o
only 1.6% for poliomyelitis eradication, while those for routine 0
immunization and the health and population programme „
increased by 11—12% (Table 1).
* <
In Cote d’Ivoire, expenditures on the PEI, routin'^ °
immunization, and the health sector increased between 199& =»
and 1998 (Table 2). In this country, PEI expenditures were equivalent to NID spending because no information was i
available on spending on surveillance. Expenditures on routing l!
immunization as a percentage of health sector expenditures
remained the same during this period.The expenditures on th£
PEI increased more rapidly during this period (22-27%), z
although the value in United States dollars of the expenditure;^
was relatively low and ranged from only 1.1% to 1.8% of tot^l ™
health sector expenditures. The funding for the entire national immunization programme increased at a slower rate (9.1°/(g °
than the health budget as a whole (11.3%).
> ®
z
Funding trends for routine immunization
and polio eradication
;
°
o
For all three countries, we examined funding trends for the PEjJ and for routine immunization by source, to determine whetheT a
some sources reduced their funding for routine immunization after the PEI was introduced. In Bangladesh, funding for routine z
immunization either stayed the same or increased for mo&
funding sources (Table 3), and the government of Bangladesh ’
increased its funding for routine immunization, despite some
fluctuations. The level of funding of other agencies, such as >
USAID and WHO, did not significantly change during the*
period. The three-year moving average^ ,pf funding gonttibutionsl
were USS 315 099, USS B4'9C3@,hiacMUS$ ^OChO^^fe^USAIDW j
soiais/w
Policy and Practice
Table 1. Annual expenditure for polio eradication, routine immunization, and the health and population programme,3
Bangladesh, 1993-97, all sources of funding
Annual expenditure13
Health activity
Average annual
change (%)
1993
1994
1995
1996
1997
Polio eradication
Annual expenditure (US$ in thousands)
Annual change (%)
0
NAC
7 104
NA
7 601
7.0
7 306
-3.9
7 430
1.7
1.6
Routine immunization
Annual expenditure (US$ in thousands)
Annual change (%)
19 833
NA
24 869
25.4
19 292
-22.4
25 379
31.6
27 826
9.6
11.1
Total: polio eradication and routine immunization
Annual expenditure (US$ in thousands)
Annual change (%)
19 833
NA
31 974
61.2
26 893
-15.9
32 685
21.5
35 257
7.9
18.7
Health and population programme
Annual expenditure (US$ in thousands)
Annual change (%)
% of expenditures on PEI to total health programme
% of expenditures on routine immunization
to total health programme
268 100
NA
NA
7.4
343 400
28.1
2.1
7.2
357 31 1
4.1
2.1
5.4
399 591
11.8
1.8
6.4
412 574
3.2
1.8
6.7
11.8
2.0
6.6
3 Includes all expenditures on health, including routine immunization and the Global Polio Eradication Initiative.
b Expenditures have been converted to USS (thousands) to account for inflation during the study period.
c NA = data not available.
Table 2. Annual expenditure for polio eradication, routine immunization, and the health sector, Cote d'Ivoire, 1995-98, all
sources of funding
Average annual
change (%)
Annual expenditure3
Health activity
1995
1996
1997
1998
Polio eradication
Annual expenditure (US$ in thousands)
Annual change (%)
NAb
NA
2 009c
NA
2 442d
21.5
3 099
26.9
24.2
Routine immunization
Annual expenditure (US$ in thousands)
Annual change (%)
NA
NA
7 224
NA
7 409
2.6
7 876
6.3
4.4
Total: polio eradication and routine immunization
Annual expenditure (US$ in thousands)
Annual change (%)
NA
NA
9 234
NA
9 852
6.7
10 976
11.4
9.1
132 572
NA
182 566
37.7
173 542
-4.9
175 559
1.2
11.3
Health sector
Annual expenditure (US$ in thousands)
Annual change (%)
3 Expenditures have been converted to US$ (thousands) to account for inflation during the study period.
b NA = data not available.
c It was assumed that the government contribution towards operational expenses was the same as that in 1998.
d It was assumed that the German Development Bank contributed USS 278840 (amount contributed the previous year).
and USS 143 749,US$ 158 151, and USS 184 890 for WHO (the k quantified, since the Agency was still making contributions to the
amounts refer to averages of data from three years, beginning u routine immunization programme indirectly. Since UNICEF no
longer had funds to purchase vaccines, the government of
with the base year, base year + 1, and base year + 2. Although
Bangladesh used its World Bank loan instead to purchase
UNICEF funding for the routine immunization programme did
vaccines. Funding for the PEI stayed at about the same level for
i decrease in 1997—98, this could be attributed to the introduction
most sources (Table 3), with the exception of the government of
of the sector-wide approach in the health sector, rather than to a
Bangladesh, which gradually decreased its contributions.
reallocation of funds to the PEI. The Swedish International
In Cote d’Ivoire, the government, the European Union
Development Agency and other donors that previously
Development Fund, and the German Development Bank all
funnelled contributions to routine immunization (for cold-chain
increased funding for routine immunization between 1996 and
equipment and vaccines) through UNICEF, instead provided
1999 (Table 4). The contribution from WHO remained the
their aid as sector-wide pooled funding. The exact contributions
same, while that for UNICEF declined slighdy, for unknown
for the Swedish International Development Agency could not be
824
Bulletin of the World Health Organization 2002, 80 (10)
ai3T39 1VVNOIIVNHUNI
NVA N3a3O3ANI38 13H 8000 N 3 O N V 3 S D N IT 3 >1 8 I AA X N O Nl N3MnO«A N3
-DNmBXSTSOa HVVH NW
1861 SONIS TV S O W 3 AA DNIXHOtXS X X 8 3 AA 3XH3VO3O 3Z3O XIONVA
N3NNVW
NVA
OIBHONOZaD 30 NVA
N3H3X3083A X3H
XH338N3SN3W T33S83AINn N33 SI ai3HONOZ30 3TVHIX8C
Polio eradication and the financing of routine immunization
Table 3. Funding sources for routine immunization and polio eradication activities, Bangladesh, 1993-97
Source
Funding3 for routine immunization
1993
1994
1995
1996
1997
Government of Bangladesh
World Bank
UNICEFb
USAIDC
WHO
Government of Japan
9 329
2 876
11 461
265
134
0
16 657
4 872
6 246
300
200
0
15 260
2 989
6 382
379
96
0
16 387
2414
10419
278
357
475
17 676
9 342
179
242
100
494
Total funding for routine immunization
24 067
28 275
25 108
30 333
28 034
1993
1994
1995
1996
1997
Government of Bangladesh
UNICEF
CDCd
USAID
WHO
Rotary International
Government of Japan
0
0
0
0
0
0
0
3130
1193
315
121
603
1637
0
1113
349
315
165
603
1601
3281
1003
312
315
198
572
1497
3213
723
343
735
125
4
1608
4437
Total funding for polio eradication
0
7001
7429
7113
7976
Source
Funding3 for polio eradication
a Funding data have been converted to US$ (thousands) to account for inflation during the study period. The figures in this table do not include all expenditures and
are therefore lower than the total expenditure figures in Table 1.
b UNICEF = United Nations Children's Fund.
c USAID = United States Agency for International Development.
d CDC = United States Centers for Disease Control and Prevention. CDC contributed funds for national immunization days through UNICEF and consequently it is not known
whether double counting occurred for this funding.
reasons. The contributions of the government of Cote d’Ivoire
for poliomyelitis eradication also increased (Table 4). While the
contributions of a few donors, such as USAID (through
WHO), were lower for 1999 than those for 1998, Japan and
UNICEF have filled the gap when required. The contributions
of the7_ government of Cote d’Ivoire to both routine
immunization and national immunization days increased.
The government of Japan pledged to support the PEI and
designated its contribution for the cold chain, while the
German Development Bank, which has a history of supporting
routine immunization but not poliomyelitis eradication,
designated its contribution for routine immunization.
In Morocco, the government was the main financier of
both the routine immunization programme and the PEI, in
contrast to the situation in Bangladesh and Cote d’Ivoire. In
1995 Morocco began to finance all of its vaccines using its
World Bank loan (a non-International Development Associa
tion loan). The contribution of international agencies to the
immunization programme comprised only about 4% of total
costs (6). The contributions of the government of Morocco
increased for both routine immunization and PEI activities
(Table 5, Table 6). For the routine immunization programme,
the increases occurred because population growth required
additi<bti^lzWshi3ftSS-1-5i^ pt^ramme improvements required
PEI> an acceleration in the
impkmcntatioaoafafitivitias- increased contributions.
8 00 9 8 9 fr-Ot- I £+ XVd
,
8 8 1 889 t-
OZ - I £ +
T3X f
Long-term$ gwprospects
for financing routine
VI Hawi 3 N 3H1
immunizations*««ooo.
£691 snsisod
In Bangladesh Jong*tetm iprospects for financing routine
immunizatibfisJah'd health tyftems have changed little since the
SOW3AA DNIXHOI'XS
Bulletin of the World Health Organization 2002, 80 (10)
PEI was introduced. Two donors, the government of Japano
and Rotary International, used not to fund routine immuniza-0'
tion activities, and even though they currendy provide funds*
for poliomyelitis eradication activities, this situation vgll<
probably change. Rotary International has a particular interest®;
in funding poliomyelitis eradication activities and other speciBoprogrammes, such as AIDS Education, and is unlikely tofinance other immunization activities. Also, even though tSeJ
government of Japan has provided funding for routifie^
immunization vaccines since 1995-96, interviews of staff pf2
the Japan International Cooperation Agency in Dhal&,
Bangladesh, in February 1999 indicated that this contributipnz
would end in a few years (Y. Ando, personal communication^
1999).
° ™
The effect of the PEI on the long-term financing™
prospects for Cote d’Ivoire is unclear. If a donor uniqudy^
funded the PEI, loss of this funding would not impact*
funding for other programmes. Also, the government of Cdted’Ivoire has gradually increased its contribution for polig-<
myelitis eradication activities and this additional funding could^
be available for other health sector activities after the PEIm
finishes.
-•
o 2
In Morocco, the most favourable long-term prospects^
are for the additional resources generated by the government,
for poliomyelitis eradication vaccines. When the PEI ends, itls2
possible that the additional contributions of the government^
could be transferred to the routine immunization programme,”
since the funds may have been “institutionalized.” The°
government could have directed the additional poliomyelitis1’
eradication funds for the national immunization programme tci
purchase other vaccines and supplier .insj:q:acJ, h as, hepautia ,
B vaccines and disposablaisvninge^A However^ it> 12 Jess likejl I
SOIAIBAM
Policy and Practice
Table 4. Funding sources for routine immunization and polio eradication in Cote d'Ivoire, 1996-99
Source
Funding3 for routine immunization
1996
1997
1998
1999
Government of Cote d'Ivoire
European Union Development Fund
German Development Bank
WHO
UNICEF6
5 170
1 720
299
NAd
34
5 303
1 764
306
NA
34
5617
1 869
325
27
37
5 870
1 953b
7 280c
29
11
Total funding for routine immunization
7 224
7 409
7 876
15 144
Funding3 for polio eradication
Source
1996
1997
1998
1999
Government of Cote d'Ivoire
Operational costs
Personnel
Rotary International
Donations through WHO
Local donations
Government of Japan
USAID1 through WHO
WHO-C6te d'Ivoire
UNICEF
NA
610
NA
626
294
752
711
691
1 161
0
0
NA
NA
50
375
26
1 166f
NA
NA
50
279
12
1 1209
624
9
50
509
8
298
8
218
Total funding for polio eradication
1 821
2 243
3 140
2 443
h
a Funding data are given in USS (thousands).
b Financing was blocked due to fraud.
f
c The increase in financing was due to the purchase of cold-chain equipment.
d NA = data not available.
e UNICEF = United Nations Children's Fund.
f Contribution for cold chain.
9 National Immunization vaccine and operating costs.
h According to WHO, 1998 funds from the government of Japan were used in 1999 to buy vaccines and for operational costs.
1 USAID = United States Agency for International Development.
that these resources could have been generated without highlevel support, such as that of the PEI and the royal family’s
strong support and advocacy of the national immunization
days.
Discussion
Government financing
Our findings indicate that since poliomyelitis eradication
activities were introduced in Bangladesh, Cote d’Ivoire, and
Morocco, government financing for routine imrnumzation
^ctiyitie^jncrejsgd. 1° Cote d’Ivoire and Morocco, the
governments also increased their contributions to the PEL
The results suggest that no trade-offs were made in Cote
d’Ivoire and Morocco, and that instead the governments
\ increased their overall financing of both routine immunization
[and poliomyelitis eradication. In Bangladesh, the government
concentrated its limited resources on routine immunization
rather than on poliomyelitis eradication activities. This was an
appropriate choice for the government, since the routine
coverage did not increase during 1993-97.
External financing
Financing of routine immunization programmes by most
external sources of funding stayed the same (Bangladesh) or
increased (Cote d’Ivoire) over the five-year study period. The
only organization that decreased its contributions to routine
immunization during this period was UNICEF, but the
826
decreases were probably associated with factors other than the
reallocation of funding to the PEI. Some donors (e.g. Rotary
International) concentrated their funding on either routine
immunization or on poliomyelitis eradication activities and did
not need to make any funding trade-offs.
Three important funding sources for the PEI in the
countries studied, the United States Centers for Disease
Control and Prevention (CDC)? the government of Japan, and
Rotary International, focused most of their resources on this
initiative. It should be noted that CDC and the government of
Japan did not finance the PEI programme in Morocco. In only
one case was funding also provided for routine immunization
— Japan financed the purchase of measles vaccine in
Bangladesh — but this contribution was relatively small.
Other donors provided funding only for routine
immunization activities (e.g. the German Development Bank
in Cote d’Ivoire and the Swedish Internationa] Development
Agency in Bangladesh). Only a few organiza.tiQps (USAID,
WHO, and UNICEF) funded both activities in at least two of
the three countries. None appeared to be reducing their
funding significantly for routine immunization activities, with
the exception of UNICEF in Bangladesh and Cote d’Ivoire.
In Bangladesh and Cote d’Ivoire, funding for routine
immunization activities from most sources generally stayed the
same or increased. Where funding decreased, the decline was
attributed to reasons other than the reallocation of funds to the
PEI. In Morocco, where most of the funding was from the
Bulletin of the World Health Organization 2002,80 (10)
Y
N VA N 3 O 3 O 1 A N I 3 8
SNmaisiJoo awn
1861 SONIS IV SOW3M DNIXHOIXS XM83M 3XHDVO3O 3Z3O XIONVA '1HD38N3SN3H 133S83AINn N33 SI ai3HaNOZ3O STVWIXdO
nvv
13H UOOQ NSQNVTSDNnSXXIAAXNO N I
N 3M D O 8 A N 3 N 3 N N V W
"013139 1VVNOI1VNM3XNI
N V A N3B313^83A X 3-i-J
N V A ai3HQNOZ3D 3a
Polio eradication and the financing of routine immunizatk
Table 6. Government expenditure3 for routine immunization,
Morocco, 1994-97
Table 5. Funding sources for polio eradication, Morocco,
1993-983
Funding for polio eradication6
Funding source
1993
Government
of Morocco
Vaccines
Personnel
Total
1994
1995
1996
1998
336 742 930 1131
1855d 1910 1968 2027
2191 2653 2898 3158
NAC
NA
NA
NA
NA
NA
115
331
NA
115
15
NA
121
NA
USAID9
115
603
NA
Total
718
446
130
Donor
UNICEF6
Rotary International1
1997
64
NA
24
93
NA
NA
57
185
117
57
a WHO provided funding for National Immunizations days (6), but the exact
amount contributed during the study period is not known.
b Expenditures have been converted to USS (thousands) to account for inflation
during the study period.
c NA = data not available.
d The figure is based on the 1997 value, adjusted for a 3% annual inflation rate.
e UNICEF = United Nations Children's Fund. UNICEF funding supported
surveillance and social mobilization activities.
f Rotary International funding supported the purchase of vaccines (in 1993
and 1994), social mobilization activities (1995), and cold-chain equipment
purchases (1997).
9 USAID = United States Agency for International Development. USAID funding
supported information, education, and communication activities, including
meetings.
government, any decrease in funding by donors would have
been due to reasons other than financing the PEI.
Prospects for long-term financing of routine
immunizations
In Cote d’Ivoire and Morocco, government funding for
poliomyelitis eradication activities increased during the study
period. To try to keep these funds after the PEI ends and have
Pthem allocated to the health sector, policy-makers and
I programme managers should make plans for the funds and
[begin lobbying to keep them within the health sector. However,
much of the additional funding for the PEI is from donors that
| provide financing specifically for this activity and not for routine
immunization; consequenriy, the prospects for maintaining
funding from them after the initiative ends are jigLclga;, The
government of Japan may choose to shift its funding from
poliomyelitis eradication to routine immunization, since it funds
the latter activity in some countries, but it is not clear that it will
do so. It is also possible that donors, such as Rotary International
and other international organizations, will shift their funding to
another disease eradication initiative, if one is initiated. Despite
these concerns, some funds for the PEI were for capital
expenditures on equipment and vehicles, which could be used
by the
Wp^^pp/pgramme after the PEI ends.
Expenditure
1994
1995
1996
1997
Personnel
Vaccines
Maintenance/overheads
4347
719
165
4477
893
4750
170
4612
1001
175
Totals
5232
5541
5789
6218
Increase (%)
NAb
5.9
4.5
7.4
1287
181
3 Expenditure is given in USS (thousands).
b NA = data not available.
It is likely that there were costs in choosing to support
poliomyelitis eradication activities in each country, rather than
improving the routine immunization programmes. For
example, the funds could have been used to introduce
“new” vaccines such, as that for hepatitis B, or to provide
more social mobilization activities for routine immunization.
On the other hand, without high-level advocacy, it is possible
that these other activities could not have attracted the
additional funding that the high-profile PEI did and they
would not have had sufficient finance.
Limitations of the study
One limitation of the study was that the three study
countries were not representative of countries with lower
immunization coverage rates. It is possible that the impact of <
the PEI on financing for routine immunizations would be
more adverse in countries with weaker immunization
□
programmes and low coverage. Also, we did not determine
o
whether the policy and financing decisions of international
2
°
agencies were made at headquarter or regional levels, since we investitigated funding
_ only at the country level. Finally, this - <
study examined the impact of the PEI on funding for routine
immunization
we cannot
regarding
its 3^
theand
financing
of draw
otherconclusions
health services
in the
impact: on
countries studied.
C I
n -3
Acknowledgements
o 0
by the PEI funds of the Child z
This study was su[ipported
x
Survival Division of USAID, Office of Health and Nutrition, z
and coordinated by the Partnerships for Health Reform. z CD
m
Implementation of the study in each country would not have > "
been possible without the support of the ministries of health, 2
national immunization programme coordinators, and colla- o °
borating agencies. We also thank Marty Makinen of the > ®
Partnerships for Health Reform, and Bruce Aylward and Jean- z
Marc Olive of WHO for their comments. Finally, we express
for the continued support and encourage- z 0
our a[appreciation
x
ment of Ellyn Ogden, USAID Child Survival Division.
X
°z
Conflicts of interest: none declared.
ttZS9Zt' OHIDXSOd
1NSOW3MMMM :13NH31NI
TN SOH3M®SOW3M :HVW-3
900989t’-0Z-|£+ X V J
88f 8 8 9 ►-0Z- I £+ 131
SQNV1H3H13N 3HJ
wvauaiswv us oooi
£691 snsisod
SI IVVMISN VWH3113
NDllva 1'1 no i SQH 3M
SOW3M 9NI1H3I1S
Bulletin of the World Health Organization 2002, 80 (10)
11 V
aO3
H 11 V 3 H
a(lMai3M3M ai3HaNOZ3D
S0IAI3
Policy and Practice
Resume
- ----- —-------
5^ h! 1ST*sur le finan«ment de la vaccination de routine:
etudes de cas au Bangladesh, en Cote d'Ivoire etau Maroc
Pour determiner si I'initiative pour ('eradication de la poliomyelite a
le personnel a des activites en relation avec la surveillance de la
eu un impact sur le financement des programmes de vaccination de
poliomyelite et de la paralysie flasque aigue. Nous avons trouve que
routine, nous avons compare les sources et ('utilisation des fonds
les trois gouvernements et la plupart des donateurs et des
destines aux programmes de vaccination de routine et les activites
organismes internationaux ont continue a financer les programmes
de cette initiative au Bangladesh, en Cote d'Ivoire et au Maroc
de vaccination de routine au meme niveau qu'avant I'initiative.
pendant les annees 1993 a 1998. Nous avons egalement examine
L'analyse des tendances a egalement montre que le financement
les tendances du financement pour cette meme periode dans ces
de la vaccination de routine dans chaque pays a continue a
pays et evalue I'effet de I'initiative sur la disponibilite de certaines
augmenter apres le lancement de I'initiative. Les resultats montrent
ressources au sein des programmes nationaux de vaccination,
que I'initiative pour I eradication de la poliomyelite n'a pas reduit le
comme I'equipement de la chaine du froid et le temps consacre par
financement des vaccinations de routine dans ces pays.
Resumen
-------------------
de Er^di”ci°n de la Poliomielitis en la financiacion de la inmunizacion
sistematica. estudios de casos en Bangladesh, Cote d'Ivoire y Marruecos
A fin de determinar si la Iniciativa de Erradicacion de la
a actividades relacionadas con la vigilancia de la poliomielitis y la
Poliomielitis (IEP) afectaba a la financiacion de los programas de
paralisis flaccida aguda. Observamos que los tres gobiernos y la
inmunizacion sistematica, comparamos la procedencia y el uso de
mayon'a de los donantes y las organizaciones internacionales
los fondos destinados a dichos programas y a las actividades de la
siguieron financiando los programas de inmunizacion sistematica
IEP en Bangladesh, Cote d'Ivoire y Marruecos durante los ahos
en medida parecida a como Io habian hecho antes de la IEP. El
1993-1998. Tambien examinamos las tendencias de la financia
analisis de tendencias mostrb ademas que la financiacion de la
cion a Io largo del citado periodo en esos paises y evaluamos el
inmunizacion sistematica en cada uno de los paises siguio
efecto de la iniciativa en cuanto a la disponibilidad de recursos
aumentando tras la introduccion de la IEP. Los resultados
especificos en los programas nacionales de inmunizacion, como el
muestran que esta no mermo los fondos dedicados a la
equipo de las cadenas de frio y el tiempo dedicado por el personal
inmunizacion sistematica en esos paises.
References
1. The impact of the Expanded Programme on Immunization and the Polio
Eradication Initiative on health systems in the Americas. Final report of the
Taylor Commission. Washington (DC): Pan American Health Organization;
2. Taylor C, Curts F, Taylor ME. Ethical dilemmas in current planning for
poliomyelitis eradication. American Journal of Public Health 1997;87:922-5.
3. TangermannR, Costales M, FlavierJ. Poliomyelitis eradication and its impacton
primary health care in the Philippines. Journal ofInfectious Disease 1997-175
Suppl 1:5272-6.
4. Mogedal 5, Stenson B. Disease eradication: friend or foe to the health system?
Synthesis report from field studies on the polio eradication initiative in
Tanzania, Nepal, and Lao PDR. Geneva: World Health Organization; 1999
(unpublished document of November 1999, available on request from the
Department of Vaccines and Biologicals, 1211 Geneva 27, Switzerland).
828
5. Levin A, Siddiqi M, Howlader S, Routh S, Rasul I, Ram S. Case study on the costs
and financing ofimmunization services in Bangladesh. Bethesda (MD):
Partnerships for Health Reform, Abt Associates Inc.; 1999 Special Initiative
Report No. 21.
6. Kaddar, M, Mookherji S, DeRoeck D, Antona D. Case study on the costs and
financing ofimmunization services in Morocco. Bethesda (MD): Partnerships
for Health Reform, Abt Associates Inc.; 1999. Special Initiative Report No. 18.
7. Kaddar M, Tanzi V, Dougherty L. Case study on the costs and financing of
immunization services in the Cdte d'Ivoire. Bethesda (MD): Partnerships for
Health Reform, Abt Associates Inc.; 2000 Special Initiative Report No. 24).
Bulletin of the World Health Organization 2002, 80 (10)
013138 1VVNOI1VNH31NI NVA N 3 a 3 O 1 A N .1 3 8 13H 8000 N 3 a N V 1 S D N 11 3 H X I AA X N O Nl N 3 AA H O 8 A N 3 NBNNVH
DNiiiBisiaoa awn nvv
1861
SONIS IV SOW3AA DNIIHDIIS X X 8 3 AA 3XH3VO3D 3230 XIANVA
aiBHaNOZBD 30 NVA
NVA OI3HONOZ3D
N383X3883A X3H
XHO38N3SN3H 133S83AINn N33 SI ai3HONOZ3D 3 3 V W IX d C
CB
o
o
3 O
z <
on 0
o
O
-n ”
o n
z
O
z
o
z m
> Z
z o
o m
O m
O
□
in
m
Z
o <
Z r
o
m
7>
O
O z
a
t>t>9IOCIt’
WVa«31SHV XAX
Z z
ZZZS9ZI> OMIOlSOd
1N SOM3M MMM :13NB31NI
O
1N SOW3M@SOH3M niVW-3
c
800 989t’-0Z-|E + XVd
o
88£ 889 t’-OZ-l E+ 131
SaN VTd3H13N 3 Hl
wvaaaiswv as 0001
£69 1 snsxsod
si ivvaisNvwaana
HOHVaiinOd S0H3W'
SOW3M DNI1HDI1S
a o j
ariMai3H3M
ai3HaNOZ3D
soiAia
: ..
| Qoc. u me ryja-hon
BH
Public Healm Policy Forum
Public Hcullh Policy Forum
rhea, measles, and malnutrition.1" Hou
much oi the global savings from polio
eradication uill help poor countries ad
dress their priorities, especially consider
ing that eradication is possible onl\ uith
the cooperation of such countries .'
I
H
I
B ■
ii
?
Ethical Dilemmas in Current Planning
for Polio Eradication
abstract
Intensification of polio eradica
tion efforts worldwide raises con
cerns about costs and benefits for
poor countries. A major argument for
global funding is the high benefit
cost ratio of eradication; however,
financial benefits are greatest for rich
countries. By contrast, the greatest
costs are borne by poor countries: the
| Pan American Health Organization
I has estimated that host countries bore
* 80% of costs for polio eradication in
the Americas. The 1988 World Health
Assembly resolution setting up the
Polio Eradication Initiative canied
the proviso that programs should
strengthen health infrastructures.
Drastic cuts in donor funding for
health make this commitment even
more important. Two international
evaluations have reponed both posi
tive and negative effects of polio and
Expanded Programme on Immuniza
tion programs on the functioning and
sustainability of primary health care.
Negative effects were greatest in
poor countries with many other
diseases of public health importance,
b If poor countries are expected to
I divert hinds from their own urgent
| priorities, donors should make solid
commitments to long-term support
for sustainable health development.
(Am J Public Health. 1997;87:922925)
•
• \ hat Are the Costs, and Who
Pays?
DPH' 'V,D' MPH- FRCPlC}- Feli^ Curts. MRCP. MD.
MBCHP ,\4Sc. FFPHM. and Mary E. Taylor. MHS
Introduction
In 1988. the World Health Assembly
unanimously approved the goal of polio
eradication by the year 2000 with the
proviso that a global partnership should
strengthen health care systems.' As pro
grams for a polio-free world intensify to
meet the end of the century deadline, there
are growing concerns about the global
commitment to suppon sustainable health
services.
A basic policy question is. How will
global goals and local priorities be bal
anced. and what are the ethical implica
tions of current choices? The specific
underlying questions are as follows:
Should poor countries, with many health
problems that could be controlled, diven
their limited resources for a global goal
that has low priority for their own
children? When wild virus remains only
in a few sites, will rich countries, and the
global organizations they infiuence. pro
mote eradication as a single-focus activ
ity? Should poor countries expect donors
to improve upon past expenence and use
the opportunity and financial benefits
from polio eradication to build sustainable
health systems for the world's neediest
children?
Who Will Benefit Most from
Polio Eradication?
Progress in eradication is most evi
dent in countries that already have wellestablished health infrastructures.--5 Now
those countries face the dilemma of how
long they will have to sustain immuniza
tion and surveillance costs. National polio
control costs the United States S23O
million annually, which is equivalent to
about 76% of USAID contributions to
child survival worldwide.” Also, while the
■!
922 American Journal of Public Health
United States has had no cases of
wild-type poliomyelitis since 1979, an
average of nine cases each year have been
linked to oral polio vaccine.7 Thus, there
would be two immediate benefits for
countries such as the United States.
Globally, benefit-cost analyses
project that polio eradication benefits will
exceed costs by 2007. with cumulative
savings of S13.6 billion by 2040? Savings
are .primarily in the cost of acute care and
rehabilitation from paralysis. Such sav- ings accrue almost entirely in industrial
ized countries, because paralyzed children
in poor countries have little access to care.
Changing the "base case" assumption for
developing countries from 33% access to
0% access has virtually no effect on the ?>'■
global benefit-cost analysis, while changes wj?.
in assumptions for industrialized countries have large effects.
Elimination of paralytic poliomy- 'SA3
elitis will obviously benefit every country.
However, benefits for children in poor
countries must be balanced against many ;>
more common threats to health and lifeEven in Southeast Asia and sub-Saharan
Africa, where polio incidence remains
?
highest, polio is responsible for less than
2% of years lived with disability.9 Poorf^ i
countries naturally give priority to prob-?
lems such as pneumonia, malaria, diar-j^^^ Carl E. Taylor and Mary E. Taylor are with the^*
Department of International Health. Johns Hop-’'
kins School of Hygiene and Public Health.
Baltimore. Md. Felicity Cutts is with the;
Depanment of Epidemiology and Population
Sciences. London School of Hvgiene and TropP
cal Medicine. London. England.
Requests for reprints should be sent to Carfj
E. Taylor. DPH. MD. Depanment of Interna
tional Health. Johns Hopkins School of Hygiene
and Public Health. 615 N Wolfe St. Baltimore,
MD’noS.
Editor’s Note. See related comment by ■
Sutter and Cochi (p 913) in this issue.
ftI£
Bl-
fe
..... .
1
'
Donor support for global immuniza
tion peaked with the Universal Child
Immunization Initiative in the early 1990s
and has declined since then." External
lunding for polio eradication is targeted
for polio vaccine procurement (especially
•r National Immunization Days), intemaonal technical advisers, cold chain equip
ment. and laboratories for surveillance.
U^Yglopine country' governments are ex
pected to fund the remaining costs, and all
but (he poorest countries are also expected
to finance an increasing proportion of
other Expanded Programme on Immuniza
tion vaccine costs.12 In the Americas, host
: wemments and communities have con"uted about 80% of polio eradication
•.■•as.-’ Major cuts in donor funding for all
health programs are being justified by
growing use of terms such as self-reliance
in financing services, decentralization,
and community participation.1-'-14 When
liK-al communities finance their own
health care, preventive services such as
immunization will have to compete with
other concerns. People reasonably com. •'* benefits of polio eradication wiih
’^merits of alternative services for their
children.
International contributions are in
creasingly earmarked for polio vaccines
and their delivery systems.8 The global
polio eradication strategy includes three
methods for vaccine delivery: routine
immunization services; National Immuni•-uion Days, conducted twice a year for 5
vears with a goal of 90% coverage in
polio-endemic countries: and mop-up
vaccination in high-risk areas identified
by surveillance.-’-3 It has been postulated
that high coverage with National Immuni
zation Davs^ repeated for several years.
may be sufficient to eradicate polio.13 This
v-ould be a sharF break from accepted
policy, which stresses increasing vaccinahon coverage for ail Expanded Pro
gramme on Immunization antigens and
effective surveillance to respond rapidly
to suspected polio outbreaks.16 In the
African region, the average coverage rate
■or infants for three doses of oral poliovjvaccine was only 58% in 1995.
tpenence with National Immunization
Days has been mixed. Despite high
coverage of campaigns in eastern and
southern Africa, eylx repons suggest ih.it
alternative commimiix-bused siratceiex
would provide more long-term benefit* in
West African countries w itli ueak health
inlrastmcture (R. Knippenberg. written
communication. March 1997). Little is
known about the effort and resources
needed for alternative strategies in the
poorest countries.
Estimates of vaccine delivery costs
through routine services, derived mainly
from studies conducted a decade ago.
range from S6 to more than S20 per child
for the original six Expanded Programme
on Immunization vaccines, with an aver
age of SI5.1017 Community contributions
are typically much larger, especially for
activities, such as National Immunization
Days, that depend on volunteer and
intersectoral efforts. Xhe opportunity costs
to communities and health services are
great, diverting’ lime and effort from oihi-r
aptivjiips—Ln (he past 15 years, structural
adjustment policies for economic reform
promoted by international banks have
caused governments to cut health care
budgets by a third In ,'! hnlf in mi-wt
sub-Saharan African rnimtpp^ is public
sector salaries are becoming increasingly
meaningless in some countries where
health workers live largely on per diems
from vertical programs. Any consider
ation of cost must include incentives
given to health personnel to compensate
for current public sector working condi
tions.19 Estimates are needed of the true
health investments required for hard-toreach groups in which wild virus strains
will presumably remain longest.
^Eradication is. by.definition. sustain
able. since the virus would no loncer
exist. However, this does not equate.
automatically with developing the sustain
able health systems implied in the World
Qealth Assembly resolution Prinririe* m
low-income countries include safe mother
hood. common childhood infections, tuber
culosis. sexually transmitted diseases, and
family planning/reproductive health.10
These programs differ from polio eradica
tion in their target groups, control strate
gies. and need for sustained contact with
beneficiaries. Rebates about how global
target-driven programs affect sustainable
primary health care have polarized policy
discussions since the 1978 Alma Ata
World Conference on Primary Health
Care. Both positive and negative lessons
were learned from eradication programs
such as the smallpox initiative.20 From the
malaria eradication efforts of the 1960s.
ue.should luxe learned not tn extrapolate
>ucccs\es from Hie re^t of the uorld
automatically to the poorest countries m
Africa and .Via,/’^
What Is the Past Experience?
Of particular value is the experiences*.^'
of the I'JXHs. We summarize nou the
results of two recent evaluations of the
impact of the Expanded Programme on
Immunization and polio eradication on
primary health care systems and the
sustainability of immunization pro
grams.11--' (Carl E. Taylor chaired the
Commission on the Impact of the Ex
panded Program on Immunization and the
Polio Eradication Initiative on Health
Systems in the Americas.-'2 Mary E.
Taylor was the principal researcher who
gathered and analyzed field data and
wrote the report of the steering committee
for the United Nations Children's Fund
study." Felicity Cults was a member of
both evaluation learns.)
A 1995 repon by a Pan American
Health Organization commission" used
in-depth rapid assessment procedure meth
ods in six Latin American countries repre
sentative of those with wild poliovirus
transmission in 1984. Positive and nega
tive findings were carefully analyzed by
interviewing sizable samples of four
groups: polio eradication health workers,
health workers in other services, knowl
edgeable public officials, and community
representatives. Excellent support for this
2-year effort to gather objective informa
tion was provided by the Pan American
Health Organization's Polio/Expanded
Programme on Immunization group. TJie
overall,conclusion was that nolio eradica
tion contributed positively to health sys
tems and helped generate a "culture.of
prevention" in these middle-income epuntnes with well-established health infra
structures. Most positive was the promo
tion of social mobilization and intersectoral
cooperation, two of the Alma Ata primary'
health care goals that have been the most
difficult to implement. The Expanded
Programme on Immunization strength
ened managerial, epidemiological, and
laboratory capacity and was an important
catalyst for donor coordination. The man
agement. laboratory, and surveillance sys
tems helped in measles elimination activi
ties.-'
However, a common negative effect
in the poorer countries was that targeting
of immunization programs i-:nK,»ri diver
sion of resources and effon at "the
expense of other health activities " Neea-
June .1994, Vol. 87. No. 6
Vol. 87. No. 6
American Journal of Public Health 92?
■
F!I
K
JI I
I
.k
'S’
H
I<
II
S'
li
I
i, *
Public Heallh Pnlicj Knrum
Public Health Policj Forum
live observations were made when social
mobilization protluced excessive topdown pressure and ■negative feelings
about repeated visits for onlv one pur
pose." A strone conclusion was that tiie
benefits ol polio eradicaiion in the Ameri
cus can be directly applied io nolii vinuktng onlv in countries with established
and sustainable health systems, strong
leadership al central :nnl district levels, a
well-oreamzed infrastructure, and local
ownership and decision m;ikin»
A 1995 United Nations Children’s
Fund study" focused on the sustainability
of universal child immunization in achiev
ing 80% coverage with all Expanded
Programme on Immunization vaccines bv
1990. Case studies in six countries in
Africa and Asia, along with a desktop
review of global activities, were con
ducted. The greatest achievement was
reported to be raising the immunization
coverage of infants worldwide to 80% in a
short time period, although only some
what more than hall ol developing coun
tries reached 80%. Universal chikfimmunization helped focus global attention on
pjXYeiuian and demonstrated that services
could effectively reach the periphery.
However, the increase in g I o ba I
coverage obscured problems^in many
■poor cnuntnas. In the African region. 25%
of countries reported 80% or higher
coverage for three doses of oral poliovirus
vaccine in 1990. but only 17% achieved
this rate in I994/95.24 In the case study
countries, health service personnel said
that, because universal child immuniza
tion goals were set globally and negoti
ated politically, there was Ijttle local
involvement in setting targets, which were
imposed on national health systems and
communities. Vjien health systems were
weak, universal child immunization tended
to overtide local delivery strategies and
create parallel and unsustainable systems
ol hliiincm1,’ vaccine supply, iransoorr
and supervision. Top-down social mobili
zation increased apparent local participa
tion. but communities were simply told
what to do. Conflict resulted between
local demand lor integrated services,
especially essential drugs, and national
immunization targets.
When donor support for recurrent
costs waned after 1990. little capacity or
commitment to maintain coverage re
mained in poor countries. In an indepen
dent study in Ghana.- a district medical
officer said. "The approach used was:
here is the money, go out! We want 80
percent by December." A 1992 review
reported that a rapid rise in coverage was
followed by a fall; the rate leveled off at
approximate!} 32%.
What Have We Learned?
Have the inteniational agencies plan
ning polio eradicaiion heeded these les
sons? Projections of high benefit-cost
ratios are based on time limits for different
regions? If implementation is delayed,
costs will rise substantially, as rich coun
tries continue intensive surveillance and
mop-up activities. Gradually developing
programs will seem more costly than
originally anticipated. Benefit-cost ratios
are very different when seen from the
perspective of poor countries. Direct costs
from paralytic polio are low. and relative
risk judgments emphasize other priorities.
In any case, the costs of routine immuniza
tion must be met for a growing number of
vaccines.
Donors exert great influence on1
health systems in poor countries; for
example, they contribute, on average.
19.5% of health expenditures in subSaharan Africa (40% or more in 13
countries), as compared with an averaae
ot less than 2% in the rest of the world.26
We consider it shortsighted for donors to
use their considerable influence to pro
mote polio eradication if this delays or
diverts long-term investment by poor
countries in sustainable health systems. It
would still be a good bargain for rich
countries to use projected benefits from
polio eradication to help build sustainable
health systems in poor countries. A solid
commitment by donors to long-term aid
(with clear process indicators) that builds
sustainable services could ensure continu
ing benefits in poor countries and reduce
the potential for the spread of other
diseases. Health systems development
should include community representation t
in decision making, the shared setting of j
References
1. World Health Assembly. Global Eruduution ot Poliomveliris h\ die Year T'hH).
Geneva. Switzerland: World Health Organi
zation; 1988. Resolution WHA4I.2S.'
2. De Quadros C.A. Strategies lor disease
contrul/eradicaiion in the Americus. In:
Cults IT. Smith PG. eds. l<nemotion and
World Health. Chichester. Englund: John
Wiley & Sons Inc: 1994:17-34?
3. Hull HF. Ward NA. Hull BP. Milstien JB.
de Quadros C. Paralytic poliomyelitis;
seasoned strategies, disappearing disease
Lancet. 1994:343:1331-1337.
4. Pmgress tow ard global poliomyelitis eradi
cation. MMW’R Morl) Monai W'ldv Ren
IW5:44:273-28I.
5. Report of die 1st Meetim- of die Global
Commission for die Certification of die
Eradication of Poliomyelitis. Geneva. Swit
zerland: World Health Organization: 1995
WHO/EPI/GEN795.6.
6. PubL 104-107. 11()Stat 706(1996).
7. Sutter RW. Onorato IM. Patriarca PA.
Current poliomyelitis immunization policy
in the United States. PediatrAnn. 1995T9702-706.
8. Ban KJ. Foulds J. Patriarca P. Global
eradication ol poliomyelitis: benefit-cost
analysis.-Bn// World Health Organ. 1996:
resistance in the final Mages of the South
Asian smallpox eradication campaign.
1973-|y-’5. s»c Sei Med. |W5:4l:6U_
M5.
21. SiJdiqi J. World Health mid Wi.rld Polities.
Part III Ctise Study: 7 he Mulariti Eradica
tion Pmeruimite. Columbia. SC: L’niver'ilx of South Carolina Press: 1995:12'192.
_2. The Impact ol the Expanded Pniyram on
linnuinizatidii and the Polio Eradication
Initiative on Health Systenix in the . \nierieu.s. Report of the Taslor Commission.
Washington. DC: Pan American Health
Organization: 1995.
23. De Quadrns C.A. Olixe J-M. Hersh BS. et
al. Measles elimination in the Americas.
Exolving strategies. JAMA. 1996:275:224229.
24. EPI Information System—Global Summars. Geneva. Switzerland: World Health
Organization: 1996, WHO/EPI/CEISAJb.l)?.
25. Lafond A. Siotatnmv Primary Htuidt
Can-. London. England: Earth-can Publica
tions Ltd: 1995:140.
26. Michaud C. Murrav CJL. External .i-.mstance to the health 'cctor in deveiopine
countries: a detailed analysis. Im-2-''I). In"
Murrav CJL. Lopez AD. eds. Global
Comparative Assessinenis in the Health
Sector Disease Burden. Expenditures and
Inicrventum Packages. Geneva. Switzer
land: World Health Organization: 1994157-170.
9. Murray CJL. Lopez AD. Quantifying
disability: data, methods and results’ In:
Murray CJL. Lopez AD. eds. Global
Comparative Assessments in die Health
Sector. Disease Burden. Expenditures and
Intervention Packages. Geneva. Switzerkind: World Health Organization: 1994:55-
10. World Bank. World Development Report
1993: Investing in Health. Oxford. En
gland: Oxford University Press Inc: 1993.
11. Taylor ME. LaForce FM. Basu RN. Cutts
F. Ndumbe P. Steinglass R. Sustainability
of Achievements: Lessons Learned from
Universal Child Imnumization—Report of
a Steering Committee. New York. NY:
United Nations Children’s Fund: 1996.
12. Expanded Programme on Immunization.
Vaccine Supply. The First Line of Defense.
Geneva. Switzerland: World Health Organi
zation: 1993.
13. Health Strategy for UNICEF. New York.
NY: United Nations Children’s Fund:
1995.
14. Bridging the Gaps. Geneva. Switzerland:
World Health Organization: 1995.
15. Cruz RR. Cuba: muss polio vaccination
goals and priorities, and local ownership /
program. 1962-1982. Rev Infect Dis 19846.S408-S412.
and control of resources and services.
16. Jamison DT. Torres AM. Chen LC. Mel
Building of infrastructure was what
nick JL. Poliomyelitis: what are the pros
was promised in the unanimous World
pects for eradication and rehabilitation?
Health Assembly resolution. The consor
Health Policy Plann. 1991:6:107-118.
17.
Brenzel L. The Cost of EPI: Lessons
tium of donors who have the most to gain
Learned from Cost and Cost-Effectiveness
from rapid eradication should not only
Studies of Immunization Programs. 7
bear most of the costs of eradication
REACH project paper 1990 (unpublished
document. Basics Project. Suite 300. 1600
activities but also fulfill that promise.
Wilson
Blvd. Alexandria. V.A 22209).....
Polio eradication will be a gift to the 21st
18. Evans I. SAPping maternal health. Lancet.
century only if donors and governments
1995:346:1046.
act in partnership to ensure long-term
19. Abel .Smith B. The world economic crisis,
part I: repercussions on health. Health
benefits for the least developed countries
Policy Plaint. 1986:1:202-213.
and poorest communities.
-0. Greenough P. Intimidation, coercion and
. ............. -
|
Erratum
1997-87-543Sr5^Sen
AdamS B- Annotation: eiSarette smoki"g- nutrition, and binhweieht.
The name of the second author. Barbara Abrams.
Am J Public Health.
was incorrectly printed as Barbara Adams.
924 American Journal of Public Health
June 1997. Vol. 87. No. 6
£
IW. Vol. 87. No. 6
American Journal of Public Health 925
•
Page 1 of 1
Main identity
inriyiHmumrffT* rn HHamfe.
From:
To:
Sent:
Attach:
Subject:
”amol" <amol__p@vsnl.com>
<drugactionindia@heaithyskepticism.org>
Wednesday, January 07, 2004 8:24 AM
Polio Rupa Chinai.rtf: Polio-Kale.rtf
[drugactionindia] polio eradication
Dear all.
Dr Ashok Kale and Dr N. S Deodhar two public health experts in Pune have also fundamentally questioned the
objective of eradicating polio virus. Attached herewith is a news report prepared by Rupa Chinai on this debate
and Dr. Kale's note. The power point presentation by Dr. Deodhar is a big file. I would send it those who ask for it.
With Regards,
Sincerely Yours,
Anant Phadke
WISH YOU A MEANINGFUL, PEACEFUL NEW YEAR I
Anant & Sandhya Phadke,
8, Amey Ashish Co-op. housing society,
Near Kokan Express hotel, off Karve Road,
Kothrud, Pune 411029.
phone no. - 020 5460038
Drug Action India is hosted by Healthy Skepticism. If there arc problems contact
peter(5)healThy skepticism, org
ft \
1/7/04
1/7/04
e
I
{ Deleted: ....
Ipri^hidiK
i.think..thatjhe:..^&Linent aboiit polio accounting.^
s^pnd^..tael
isthat
UAe.polio.yiiusJroiii ilie ^itli..and.heiice.to stop...diepolio
small pox. Hence I suggest that the argument about gross over-estimation of polio
induced lameness be shifted to the end.
be a^pad.id<^to start.by..quoting.Pr...N:..S-Dcodhar. fo
health e?®.^.in.Pun&..Ifeye.p.^^..^
academic programme on polio eradication in School of Health Sciences, Pune
5Juiyersity..I>r:...Kale;.was the main pr^ntCT
commentator.
..Ihope,..you wpuldfind these; changes suggested.betowm the track<h^g« modex
useful.
WR
SY
Anant Phadke
By Rupa China!
Mumbai:
Speaking at a recent academic programme on polio eradication in School of Health
•
...Dr.-;
^.4..fi.!4...^Py.!s.e‘Pplip^Strategy is.aHe
expl^n^--‘‘yvernation .has.no .jBli^t whai-^-ever on eiwironnw^
the virus. Secondly, even with more than 3 doses of OPV many children are not folly
protected and may either get paralytic polio or get infected & discharge the virus in the
faec^enyironment. A small pCTcentage of “Jmmuni^d
infection of’polio .and.are thus.able to spread.the\dni.s.
Thus, there arc enough number of such susccptiblcs to get infected, allowing polio virus
to multiply and disseminate in the environment under unsanitary conditions
; itself'and by ch^cc exme.^
I
!
jrwfr\s*y that the aim of
polio-eradication (meaning eradication of the vHid
polio virus from the earth and not merely elimination
of polio-disease) is unattainable and the current
'pulse polio' programme is diverting attention and
resources from more urgent, pressing health problems.
Unlike smallpox, the polio virus is not a suitable
microbe for eradication, they said.<PI>
Ashok Kale, Pune based community medicine expert and
chief of the medical wing of the Akhil Bharatiya
■
Deleted: The polio virus only
contributes to zo per cent of
limb ptavlysi> aue». Dai* fruiu Zudia, die
Americas «
aral Vi«*banu publiHliwl ni rvptiLMl
scientific journals, .•
clearly establishes that a substantial
pruporikm 01 •>
pafiente of Acute Flaccid Paralj'sis arc
not due to the »
polio virus but due to seme c&er
enteroviral
iufwi>uu.<PI> *
Experts say these findings have majcr
imphcaticns on
India's pursuit of the Rs.500 crore a year,
pulse polio' jxutpauiuv, which i» pari 01 au
international .■
effort aimed at erradjeatiug the wild polio
virus from the lace at the earth. <PI> Fur mauy years there has botsi au
ussuniptiociy even to :•
the medical fraternity, frat limb-lameness
or paralysis implied polio. Extrapolation of
polio «
prevalence m the country’ was calculated
on fee basis
of detection of such cases in sample
surveys, leading io exaggefaiioa of the polio figures. <PI> ■
Recent studie? hxve now shown that
physical symptoms
of polio are mimicked by a number of
other viral mfectioiih like ECHO, Coxackie and
Jspsnere
Encephalitis. New international
guidelines now require that confinnahon of polio cases require
labot aiory testing of stool samples for detection of
&e wild polio virus <PT> «
With the implementation of surveillance
activities and ■>
isolation of the wild polio vims from the
Stool y
vimples of Acute Flaccid Paralysis
(AbPjcases, it was w
found that ibe number of polio cases
never exceeded 20
per cent In India, this was evident in
papers^
published by the Indian Academy of
Ptidudrics and Ibe »
Indian Journal of Pediatrics. For instance
intiie vear 2002 out of 9 711 msRS of AFP tfw* polio
virus was fuuud iu 1,600 ubei (16 per ceul). TLe
rwtfhwd y
______
Deleteci: n medical experts
f ... [1] I
Grahak Panchayat said, "It is clearly impossible to
j eradicate polio aiid hence to stop the^polio y^ination4 like. m
small pox.:¥.
India
is chasing an unattainable mirage. The resources and
effort mobilised for the polio programme are not
cost-effective. It also adversely affects other
health-care programmes. The sensible approach is to
have a control programme with routine oral polio
vaccination, as part of the national child
immunisation programme Eradication meanwhile, should 7
be left to elimination of poverty, malncurishmcnt and
‘
sdriiiation’’.<PI>
Placing too much emphasis on vaccination as a strategy
for controlling polio is meanwhile, fraught with
problems, said Anant Phadke, a public health expert
with the Centre for Enquiry Into Health and Allied
Tliemes. The oral polio vaccine involves use of die
live but weakened polio virus, which can mutate and I
I rivert back to its vdld form. ^Persons
J
with immune deficiency are known to shed the polioT
’.nrus for several years after receiving the vaccine, ,
and this poses a threat to the cominunily that sulfei s
from poor access to clean water and sanitation.
WHO-declared 'polio free zones', such as Haiti, saw a
polio epidemic a decade after it was assumed that the
country had freedom from the disease. Investigations
by the Centre for Disease Control in the US found that
the weakened virus used in the OPV had mutated back to
its wild state, causing paralytic disease in a group
of children who had either not been vaccinated or had
not received a complete course of the vaccine. <PI>
While advaiiced .countries, .like the US discarded the use of OPV, because.OPV is .known 7
tq.hayethe
;
potential to cause vaccine developed polio’, and took to the
injectable Inactivated Polio Vaccine (IPV), which uses
the killed polio virus, India since the past eight
years, has continued to pump its children with
excessive doses of OPV, through repeated rounds of the /'
'pulse polio* campaign launched since 1995.<PI>
I
The IPV does not however provideFa feasible option
either. Apart from being expensive -- a 100 times
costlier than the OPV ~ it cannot assure safety
either. It cannot act against the multiplication of
the wild polio virus found in the human gut. <PI>
A conference of pediatricians in Mumba i early this
year, warned that the current emphasis on polio is
...
( Deleted: and to stop poiio vaccimmon J
• Deleted: OPV is known to have toe .
potential to cause vaccine developed
polio'.
backfiring in states like UP, where public resistance
to such vaccination campaigns is being reported.
Pursuing thKT1elnsTveTm^t^1^61io^radication
activities is overlooking the enormous costs, and r )
forced health authorities to turn a blind eye to
I
damage dene by ether diseases Icng thcu^it tc be
waning over tlie years. In some areas ofUP,
poiio-eradication is the only public health activity
being done by the slender public health staff experts
said<PT>
^.^c..fertbcr..^gy.cs...“®cppUoyimsqniy..ccntife
hnib p^ysis cas«>..Data.from.^
^.4...Y.i®3^..P.uhiished in.reputed;..sdenufic journals,.
clwly..e^Ushes.titet a^b^antji proportion.of
PMfentsAarte
poho virus but due to some
A
infection. <PI>
iS^imdingshave.m^or.iin£iicafrgn.s.on
India's..pursuit of te..Ife.-5W.g:orea..Yew,.lpulse ft
PQlig\pro^rammex which is p^ of
effort.
the face of the earth. <PI>
| For. m^y .y.ws thCTe^
! the medical fraternity, that limb-lameness or
/
paralysis implied P.olio...^
prwdence.in.frie country .wM.c^.OTlat^.pn.theb^.is
of ddectjon.of.such, .^es m...^
/
IO
of Ae pouo
Recent studies have now shown that physied ^mptpms
< .QhpliQ..ar.e.mimicked..W
infedions.i&e.ECHO,.Coxacldean^
I
Enc^halitis. .Newu^
that:.confrrmadqno£.ppho c^sr^
testing of stool samples for detection of the wild
polio.virus. <PI>
.With.the implemOTtation of su^
l^l§gonp£tiiewnd polio virus from fteshwl
sampies of Acute Flaccid
found that the number of polio cases never exceeded 20
per cent...Tn India, this was
published.by.the.In$M
Iiidi^i.Jpuni^..ofP^atriw ;.rpr
2.QQ?. out. of 9,71 i. cases .of AiJ. .the.poijp.y^
found in 1,600 cases (16 per cent). The rest had
/
P^vsisfrom other cwi^s. Such
a
me pouo virus only conlriDUTes to zu per cent oi
limb paralysis cases. Data from India, the Americas
and Vietnam, published in reputed scientific journals,
clearly establishes that a substantial proportion of
patients of Acute Flaccid Paralysis are not due to the
polio virus but due to some other enteroviral
infection.<Pl>
Experts say these findings have major implications on
India’s pursuit of the Rs.500 orore a year, pulse
polio’ programme, which is part of an international
effort aimed at crradicaiing the wild polio virus from
the face of the earth. <P1>
For many years there has been an assumption, even in
the medical fraternity, that limb-lameness or
paralysis implied polio. Extrapolation of polio
prevalence in the country was calculated on the basis
of detection of such cases in sample surveys, leading
to exaggeration of the polio figures. <PI>
Recent studies have now shown that physical symptoms
of polio are mimicked by a number of other viral
infections like ECHO, Coxackic and Japanese
Encephalitis. New international guidelines now require
that confirmation of polio cases require laboratory
testing of stool samples for detection of the wild
polio virus. <PI>
With the implementation of surveillance activities and
isolation of the wild polio virus from the stool
samples of Acute Flaccid Paralysis (AFP)cases, it was
found that the number of polio cases never exceeded 20
per cent. In India, this was evident in papers
published by the Indian Academy of Pediatrics and the
Indian Journal of Pediatrics. For instance in the year
2002 out of 9,711 cases of AFP, the polio virus was
found in 1,600 cases (16 per cent). The rest had
paralysis from other causes. Such evidence is also
demonstrated in studies from the Americas and
Vietnam. <PI>
The costly Mirage of Polio Eradication
Dr. Ashok Kale
Almost everybody seems to be convinced that in the very near future. India would eradicate polio;
in near future, the whole world will have eradicated polio and like small-pox, after a few years polio
vaccination would be stopped.
AUached below, is Qie article of Alan Dove, which convincingly argues (hat it will not be possible to
stop poiio-vaccinauon in the developed countries. At the end, I have drawn my conclusion from his article,
have commented upon it and have added a couple of points.
The Polio EradWtlgfi Effort: Should Vaccine Era^cttfon Be Next?
Alan W.
Vincent R. Racaniello
http;//w ww. sciencemag. org/help/
* i'he authors are at the Department of Microbiology, Columbia *
University College of Physicians and Surgeons, New York, NY
100.32, USA.
♦
To whom correspondence should be addressed. E-mail: vrri@columbia.edu
of smallpox ranks as one of medical science's greatest contributions to public health, saving
millions from disease and eliminating the need for vaccination. The World Health Organization (WHO),
in cooperation with the Centers for Disease Control and Prevention (CDC), Rotary International, and
governments around the world, is in the process of completing another such accomplishment, but in a
considerably different social climate and with a different pathogen. The worldwide effort to eradicate
is likely to reach its goal by 2003, if current levels of funding and cooperation continue. Vv^ile we applaud
tills goal and tire piogi ess that lias been made, we feel that the crucial final steps in the campaign need to
be reconsidered.
The WHO has implemented a plan that takes advantage of the seasonal nature of poliovirus spread.
National Immunization Days (NIDs) arc held during the winter, or ’’polio-low season.M They involve
massive publicity campaigns, followed by door-to-door visits to unvaccinated households. Additional doses
of the vaccine arc distributed as needed during the "high season,” wdicn outbreaks occur. This approach
maximizes the effect of vaccination and bypasses many of the logistical difficulties of a year-round effort
I he ISSn campaign uses live Sabin oral pplip vaccine (OPV) exclusively, because it is cheaper
than inactivated pjHto vaccine (IPV) and does not require trained personnel and sterile needles
(1 Resources which many lesser developed countries lack. The WHO also rigorously tracks cases of
infantile paralysis and screens sewage and river water for poliovirus in targeted areas. Whenever an
outbreak is detected, a local immunization campaign is carried out to prevent the virus’ spread (2 ). The
results of the
effort have been impressive. Poliomyelitis caused by wild-type poliovirus (wild
peiio) is rapidly vanishing from even the most remote regions worldwide. The CDC projects that the world
will be jwlie-tree by 2003 (3), leaving behind a medical infrastructure for vaccination that can then be used
in a campaign against measles. Under this plan, polio vaccination will be stopped by 2005, which will save
about 5200 million a year in vaccine-associated expenses in the U.S. alone (3).
After this date, iaboratoiy stocks of poliovirus would veiiher be destroyed or restricted to high -level
containment facilities (3). While this plan is promising, it is not complete. Because the WHO is relying on
OPV. certification of an area as “polio-free’ is accurate only by a narrow definition: no wild polio
detectable in the population, sewage, or the drinking water over a. period of yean? Because Sabin strains
mutate readily back to
virulentforms (4), potentially pathogenic viruses are still being released into the aquifers. Vaccineassociated poliomyelitis will still occur in these ’’fwiftHfree’’ areas, at rates of 1 in 300,000 (5) to 1 in
500,000 (6) recipients of OPV. Because recycling of waste water is ncccssaiy in many parts of the world,
virus excreted by vaccinees may persist indefinitely (7). A broader, more intuitive definition of^W^i^HiW
would be elimination of both vaccine and wild strains-a goal that cannot occur if only OPV is used.
Difficulties in distribution and lack of medical resources are cited as reasons for using OPV, but
terminating the effort without making a transition to IPV contradicts theWHO goal of establishing an
infrastructure for future
campaigns. One way to accomplish both goals would be to continue
wiib
vaccination
until
IPV
can
be
distributed
worldwide.
Then
htfp.//216.2.39.41.100/search?q=cache:K1c5dnb2fiBT X)J:aimicro2cpmc.cohii,nbia,edu/Polio1ab/_________
3http://216.239.41.100,/search?q~cachc:Kk5dnb2sBLQJ:cumicro2.cpmc. columbia.cdu/Pcliclab/________
3Http./721u.239.41.100/search?q-cache:Kk5dnb2sBLQJicumicro2.cpnic. coluiubia.edu/Poliolab/3(he
campaign would not be an isolated effort, but part of a broader public health initiative (8). Before
vaccination can be stopped safely, it will be necessaiy to destroy most existing viral stocks and restrict
access to the remainder to prevent accidental and deliberate release. For smallpox, virus stocks were
located in only a few institutions before
which meant that inventory control was relatively
straightforward. There is no central record of poliovirus stocks, which arc distributed among hundreds, or
possibly thousands, of silos. Without an accurate inventory, it is unlikely tiiat all virus stocks can be found
and destroyed. For example, during structural
studies of coxsackievirus Bl, an enterovirus, it was discovered that the virus stock was contaminated with
pbiib (9). This incident emphasizes the difficulty in identifying poliovirus repositories in research
laboratories. Experience with influenza virus suggests that accidental release of an infectious agent from
laboratory stocks may occur (10). As with smallpox, there is the possibility that some wild xdrus will
survive for long periods in the environment (11,12). Even if total virus destruction could be accomplished,
the small size of the poliovirus genome (7.5 kb), whose sequence is known (13, 14) and whose
complementaiy DN A is infectious (15), would make it possible tor a. terrorist to synthesize a. new stock.
In the post-vaccine world, the susceptible population would increase each year and the large number of
potential sources of reintroduction would soon constitute a major threat Vaccination of laboratory would
either be destroyed or restricted to high-level containment facilities (3). While this plan is promising, it is
not complete. Because the WHO is relying on OPV, certification of an area as " j^Sa-free" is accurate only
by a narrow definition: no wild ppKe detectable in the population the sewage, or the drinking water over a
period of years. Because Sabin strains mutate readily back to personnel who are studying the virus or
maintaining emergency vaccine stocks then creates a dilemma. If workers are vaccinated with OPV, they
will shed live poliovirus into the environment Use of IPV would allow these workers to act as carriers
(because infection of the gut is still possible), increasing the probability of an outbreak. For smallpox, the
fact tiial vaccine and virulent strains differ substantially made it possible to avoid this difficulty.
To evaluate die potential impact of a single reintroduction of poliovirus into the post-vaccine world, we
can use the 1992-93 Dutch epidemic as a model, in this incident 67 cases of paralytic poliomyelitis were
reported, but the virus spread to many more individuals. High levels of vaccination with IPV meant that the
paralytic cases were restricted almost entirely to members of a religious group that
refused the vaccine (16). Within this subpopulation and its immediate contacts, the virus spread very
efficiently; ~7% of the children in this group were actively secreting wild palin in a. single sampling
taken during the epidemic (17). This epidemic occurred in a nation with high standards of health care,
where paralytic cases w’ere reported promptly and additional doses of TPV and OPV were distributed tn
the affected area immediately. Such high standards ofpreparedness are unlikely to continue after
cessation ofvaccination, hi a city of 10 million unvaccinated individuals, a rough estimate vrould be
dial a single release of virus could resull in 7000 paralytic cases. IL would lake more Qian 700 years of
vaccination to produce that number of cases of vaccine-associated paralysis m the U.S.
The control of poliomyelitis has substantially improved the quality of life worldwide, and the
completion of this task will allow lesser developed countries to focus on other public health issues To
succeed, however, the polio WOte’Ooii effort should take a balanced approach as part of a larger
campaign to improve health and sanitation.
REFERENCES
1. "Global poliomyelitis eradicaitoii by the year 2000. Plan of action" (WHO, Geneva, 1996).
2 S. E. Robertson, et al , Bull WHO 72, 907 (1994) [Medline]
3 . O. Kcw, in a lecture at the American Society for Virology’ Annual Meeting, London, Ontario, 1996.
4. P. D. Minor, e/ cz/., Biologiccih 21, 357 (1993) [Medline].
5. J. L. Melnick, Clm. Immvnother. 6,1 (1996).
6. A. J. Beale, Pediab. Ir^cL DiaAQ, 970 (1991) .
7. H. Knoiie, Gesundheitswesen51, 351 (1995) [Medline].
8. T. A. Swartz, Public Health Rev.21,157 (1994).
9. E. Arnold, personal communication.
10 K. Nakajima, etal.} Nature 274. 334 (1978) [Medline].
11. C. J. Hurst, ct al.. Can. J. Microbiol.35,474 (1989) [Medline].
12. M. V. Yates ei al., Appl. Envir. Micro. 49, 778 (1985).
13. V. R. Racanielioand D. Baltimore, Proc. Natl. Acad. Set. U.S.A.'Jb, 4887 (1981) [Medline].
14. N. Kitamura, et al., Nature291, 547 (1981) [Medline].
15. V. R. Racanielloand D. Baltimore. Science 214
Points not covered in Dove’s article The limitation of Dove's article is that though the article creates enough basis to question the aim of
eradication of polio, it docs not do so. This is perhaps because, based in the US, he has no concrete idea
about how in (lie third world countries, the polio-eradication programme is diverting attention and
resources from more important, pressing health problems.
I would argue that it’s clear from impossible io eradicate polio and to stop polio vaccination. Hence
in India the special efforts taken and money being spent under the illusion that polio eradication is possible
is all uncalled for. As in the case of smallpox, if by polio-eradication, is meant elimination of the wild
poliovirus from the earth's environment; so that polio-vaccination becomes unnecessary forever; this aim is
unattainable. But if we take a more limited view dial by polio-eradication we mean absence of clinical
cases of Acute Flaccid Paralysis (AFP) due to the polio-virus, the extra-efforts being taken for the 'mop up
operations' on detection of polio-cases and for National Immunization Days for Polio-vaccination, are not
cost-effective, they also adversely affect other heaith-care programmes in India. Hence these special
efforts be abandoned. Instead a more cost-effective, realistic policy of systematic efforts to increase the
coverage of routine OPV be carried out. Secondly such medical technical measures must be backed up with
healthy developmental measures like eradication of mass-poverty and hence malnourishmenl as well as
universal improvements in water and sanitation. Its only then can we bring down to almost zero, even with
routine immunization, die incidence of AFP due to the polio-virus. To tty to achieve elimination of the wild
poliovirus from the earth's environment, without radical improvement on ihe front of nutrition, water,
sanitation, poverty-eradication is a medico-technical mirage. The sensible approach would be to have a
control programme with OPV and leave eradication to elimination of poverty, malnourishmcnt and
sanitation.
There arc three more problems with the polio eradication strategy which have not been address by
Dove.
1) Data from the Americas, from Vietnam and how even from India (Mumbai, U.P) clearly establishes
that a substantial proportion of patients of Acute Flaccid Paralysis are not due to the polio torus but due to
some other enteroviral infections.1’2,3’4 In the Americas, over the period 1989-91. 838 (67) isolates were
NPFV (non polio entero viruses) out of 6000 ^Tn Vietnam (1995), out of 22 AFP cases only one case had
wild polio virus in stool sample, while three had NPEV and twelve had Japanese Encephalitis Virus in
their fauces ?. hi one of the Sentinel Centres of Mumbai, in Ihe year 98-2000, out of 98 cases of AFP,
only 13 were due to polioviruses and 18 due to NPEV. ’. Even in Uttar Pradesh, in 1998, in a stuay,out of
563 AFP cases, 163 (29 %) showed Polio viruses in their faeces as compared to 191 (34 %) of NPEV4
However, this fact was not known earlier in India when the incidence of polio-induced lameness was
estimated in die eighties. All limb-lameness was assumed to be due to die polio vinises and hence there
has been gross overestimation of polio-induced lameness and consequently a gross underestimation of the
uoai-efucacy of polio-vaccination.
2) Carl Taylor has any way pointed out that the cost-efficacy has been calculated in the context of
western countries, with the focus on savings on expenses on paralysed children admitted for treatment
and recovery,. These calculations are not valid for India.
3) Dove has not touched upon the political economy of polio-vaccination
To pursue the mirage of eradication of the polio-virus, the logical step is to shift to
Injectable Polio Vaccine (IPV), despite the fact that it is exorbitantly costlier than the
OPV. Yet the Indian Academy of Pediatrics has recommended this measure! Such a
measure would serve the interests of the IPV manufacturers. Unlike the Sabin vaccine,
the IPV has no action at the gut level, and hence it will not decrease the circulation of the
wild-virus. This strategy it will therefore, not eliminate the wild polio virus from the
environment. The only advantage would be, unlike the Sabin vaccine, it will not cause
vaccine induced polio. That is why it is being used in the rich countries.
The rich countries are interested in eradication of polio in developing countries because they can not
stop the costly IPV programme in their own countries till polio is eradicated in the poor countries also.
They are pulling pressure on lhe poor countries to lake up Uris polio eradication programme; (hough, for the
poor countnes, it means diverting resources from more pressing issues. India is spending Rs. 500 crores a
year for the polio-eradication programme, only 20% of which is grant from the international agencies. In
some areas in UP, polio-eradication programme is the only public health activity being done by the slender
public health staff
The rich countries want to stop their expenditure on IPV and hence the poor countries have been
brainwaslied into taking up Hie unattainable aim of polio-eradication. The ultimate result would be the
failure to achieve poiio-eradication in both the rich and the poor countries. But in the meanwhile, vested
interests would have earned a lot of money!
References :
1. Dietz, J. Andrus, S.Cochi,et al. Epidemiology and clinical characteristics of Acute
Flaccid Paralysis associated with Non-Polio Enteroviruses : the experience in the
Amencas„Bulletm WHO, 1995,73 (5), 597-603.
2. Solomon, Racheel Kneen et al, Poliomyelitis-like illness due to Japanese Encephalitis
vims,The Lancet,vol 351, April 11,1998,1094-1097.
3. Kantharia, Bawadekar, AFP surveillance Experience From a Sentinel Centre, IAP
Maharashtra State Conference Souvenir, December 2001, page 113.
4. Amit Kapoor, A. Ayyagari and T.N Dhole, Non-polio Enteroviruses in Acute Flaccid
Paralysis, Indian Journal of Pediatrics, volume 68—October, 2001, pages 927-929.
5. Carl E. Taylor, Ethical Dilemmas in Current Planning for Polio Eradication,
American Journal of Public Health. June 1997. vol 87. No. 6. ng 922-925.
*********
vs
IPPPH - Profile
pagina 1 van 2
Close Print
Initiative on Public-Private
Partnerships For Health
Profile
Global Polio Eradication Initiative (GPEI)
Contact Person(s)
Address
Mr. Olivier Rosenbauer, Communication Officer
Global Polio Eradication Initiative (GPEI)
World Health Organization
20 Avenue Appia
Geneva 27, 1211, Switzerland
Tel: +41 22 791 3832
Fax: +41 22 791 4193
Email: rosenbauero@who.int
http://www.polioeradication.org
Mission / Objective
- To interrupt transmission of the wild poliovirus globally and certify all WHO
regions polio-free by the end of 2005.
- To conduct effective and high quality supplementary immunization
activities, including national immunisation days and mop-up campaigns to
interrupt wild poliovirus transmission.
- To develop and sustain certification standard surveillance and laboratory
systems that can rapidly identify polio-infected areas.
- To ensure laboratory containment of wild poliovirus stocks.
- To develop a consensus strategy to stop polio immunisation after
certification of eradication.
- To use polio eradication to strengthen and expand routine immunisation
services.
Disease / Condition
Polio
Product / Service
Technical and financial support for all polio eradication activities, including
supplementary immunization activities (ie. National Immunization Days),
and acute flaccid paralysis surveillance including a global laboratory
network. Support for routine immunization services, along with Vitamin A
supplementation during polio National Immunization Days.
Legal status
No separate legal status. WHO programme.
Established
1988
Major Participants
Public sector
World Health Organization (WHO), World Bank, UNICEF, Danish Agency for
Development Assistance (DANIDA), Belgium, Government of, Italy,
Government of, Japan, Government of, US Agency for International
Development (USAID), UK Department for International Development
(DFID), US Centers for Disease Control & Prevention (CDC), Canadian
International Development Agency (CIDA), Netherlands Ministry for
Development Cooperation. Ministries of Health of all recently or currently
polio endemic countries, including India, Pakistan, Afghanistan, Nigeria,
Niger and Egypt.
Non-profit sector
Bill & Melinda Gates Foundation, Australian International Health Institute.
Rotary International, De Beers, governments of Finland and Germany,
Rotary Foundation and the United Nations Foundation.
Commercial sector
Aventis SA. Wyeth and De Beers.
Major funders
Governance
US Agency for International Development (USAID), Japan, Government of,
Bill & Melinda Gates Foundation, Canadian International Development
Agency (CIDA), US, Government of, Netherlands, Government of, UK
Department for International Development (DFID). Rotary International, the
United Nations Foundation.
A programme spearheaded by WHO, Rotary International, the US Centers
for Disease Control and Prevention and UNICEF. WHO provides the overall
technical direction and strategic planning for the management and
coordination of the initiative.
x
http: //www. ippph. org/data/summary_sheet.cfin?id=77
29-5-2003
d^Cjf
IPPPH - Profile
Disclaimer Statement
Source: Partnerships for Health
pagina 2 van 2
Email: info@iDPph.org
http://www.ippph.org/data/summary_sheet.cfin?id=77
Global Polio Eradication Initiative (GPEI)
Last Updated: 2003 January 29.
29-5-2003
issue
World's press watches polio
Contents
x « j ITH the lowest number of polio\/\ f endemic countries ever, the world’s
V V press is focused on the Global Polio
Eradication Initiative (GPEI). In the first few
months of 2003, a number of major media
outlets ran feature length stories on the
Initiative. The New York Times ran a front
page story on the rise in polio cases witnessed
in India last year, the Los Angeles Times
published a five-page spread on Rotary
International’s role as the catalyst of the
campaign, while USA Today ran a feature on
world-renowned photographer Sebastiao
Salgado and his work in publicizing polio.
These pieces were followed by items in the Wall
Street Journal and both BBC World television
and radio, focusing on the February
immunization campaign in India.
Many media stories highlighted the fact that
never before in the Initiative s history have so
few' countries remained endemic with wild
Immunization
after polio
Page 4:
Madagascar heroes
honoured
Page 5:
Emir of Kano & Rotary
fight polio
Page 6:
Polio in cash crunch
poliovirus.
The features went
on to focus on the
importance of reaching and vaccinating every
child under the age of five, if polio is to be
eradicated from those remaining countries, i
UNICEF plays crucial
role in mobilizing
communities
R Iqbal Baig has been treating families in
India's Meerut City for decades. Over
time he has seen the city s population
grow to 1.2 million and, more recently, a change
in his job. In India - the country with the
world’s largest number of cases - Dr Baig is
now 1 of 2500 Community Mobilization
-T. 'r.
:
F
I'm
oW?
5
’I
i
1
K Sr
Iqbal Baig (left), Subaida Khatoon (second from left) and Mohammed Farhat (center)
receiving a briefing from UNICEF Field Coordinator, Kshitij Joshi (right)
Page 2:
Coordinators employed by UNICEF in Uttar
Pradesh. The state of 170 million people
accounts for 65% of the world’s polio cases.
Dr Baig works with a team to reach households
and ensure all children under five years of age
are immunized against polio.
This is one view into the people and efforts
behind social mobilization activities in India
during the largest polio immunization
campaigns in the w'orld, targeting 165 million
children. Social mobilization is an important
component of eradicating polio to raise
awareness about immunizing all children;
influence attitudes to generate support for
eradication; and promote behaviour that
ensures no child is missed. In India, ten days
before this year’s national immunization days
(NIDs), television and radio advertisements,
many featuring India s best known celebrity,
Amitabh Bacchan, aired countrywide.
Meanwhile, social mobilization efforts in Uttar
Pradesh focus on 3000 high-risk villages.
Today, Dr Baig and his team are
intensifying efforts so parents have their
children vaccinated before the upcoming
monsoon season when torrential rains create an
environment that exacerbates poliovirus
transmission. "We must motivate every
resisting family, newcomer, and parent
of newborns, before the rain sets in,” Dr Baig
sighed. “We have to try harder.
For the first time since the
launch of the GPEI in 1988,
the programme faces an
unprecedentedfunding crisis
in the first quarter of2003,
resulting in planned
immunization activities
being scaled back in some
recently endemic countries.
A global
race...
’ I
/
Photo: ® Rotary Intemolional/JM dibaui
for a global
victory
•
WHO
ISSN 1727-3730
A Newsletter for
the Global Polio Eradication Initiative
Department of Vaccines & Biological?
World Health Organization
in association with Rotary International,
United Nations Children's Fund and the
Centers for Disease Control and Prevention
unicefM
USAID recognizes Ellyn Ogden's contribution to polio eradication. See page 4.
Technical tips
- -J
Part Two
The importance of containment
Framework for the Assessment and Management ofParalytic Polio
in the Post-Certification Era
The November 2002 interim meeting of the Technical Consultative Group (TCG)
endorsed the framework (see below), which has been developed to summarize
the risks of paralytic poliomyelitis in the post-certification era. This framework
will be particularly important for countries using Oral Polio Vaccine (OPV) and
for developing policy decision models.The framework divides the risks into two
major categories: (a) those due to vaccine-derived polioviruses (VDPVs) and
(b) those due to the handling of wild poliovirus stocks.
In continuation from Polio News issue 17, which focused on risks associated
with the use of OPV, this issue summarizes the nature and magnitude of the
risks related to handling wild poliovirus stocks.
Risks of polio paralysis in the post-certification era**
!
Hisk
category
Risk
Estimated global
annual burden*
Frequency
Risks of polio paralysis VAPP
1 in 2.4 million doses of
from continued use of (n«ine-<u«uitedparaMi<i»i>oi OPV administered
oral polio vaccine
.........................................................................
cVDPV
One episode per year in
(circulating iKtmuknvtd polio)
1999-2001
(Haiti, Madagascar,
the Philippines,)
iVDPV
(immuno-defkienl rraMon of
wcorw-derrwif polio)
19 cases since 1963
with 2 continuing to
excrete; no secondary
cases
Risks of para lysis from Inadvertent release from None to date
mishandling of wild
a laboratory
poliovirus
Inadvertent release from One known event in
an IPV manufacturing
early 1990s
site
Intentional release
250-500 cases per year
Approx.10 cases per
year (total of 29 cases
in three years)
<1 case per year
No cases
None to date
• Study and data collection is ongoing lor all categories
" Under current polio immunization policies
"p HE Global Certification Commission for the Eradication
I of Poliomyelitis (GCC) will declare the world free of
wild poliovirus transmission only when no wild poliovirus
has been found for at least three years and appropriate
measures have been implemented. Laboratories and
inactivated polio vaccine (IPV) manufacturers will be the
only remaining sources of wild poliovirus. “Experts agree
that the current risks and consequences associated with
inadvertent release of wild poliovirus arc small, but we have
to ensure a defined global containment strategy is in place
to reduce those risks to the lowest possible level for now and
in the future,” says Dr Walt Dowdle, External Consultant
to the Global Polio Eradication Initiative (GPEI) and head
of the US containment effort. The 1978 laboratory
associated smallpox outbreak in the United Kingdom
emphasizes the need to address laboratory containment
issues for infectious agents that no longer exist in nature.
According to Dowdle, though, the challenges of polio
containment are quite different from smallpox. Most
obvious is the fact that many more laboratories around the
world have wild poliovirus containing materials, as polio is
a popular research tool and can cause clinically unapparent
infections. This may potentially leave some laboratories
unaware of the presence of wild polio in stored clinical
materials. Additionally, large quantities of the wild virus
are necessary for production of poliovirus vaccine. For these
reasons, the global survey for laboratories with wild
poliovirus will involve nearly 100 times the number
surveyed for smallpox. “With a containment strategy in
place, the risks of accidental release can be further
minimized,” concluded Dowdle. ♦
Poliovirus release - possible occurrence and consequences deemed 'low'
\ki HILE the risk of release due to mishandling of the wild
V V poliovirus is low-; the GPEI is actively addressing all
three potential scenarios in which this might occur.
Scenario 1: accidental release from a laboratory
Between 1941 and 1976, 14 cases of paralytic polio
occurred among laboratory workers. Since then, the
population has been immunized and safety of laboratory
technology has improved to a degree that makes
inadvertent release of infectious virus much less likely.
However, since laboratories will be the only remaining
source of the virus once natural circulation is interrupted,
it is important to take stock of all wild poliovirus now to
ensure that laboratories with wild poliovirus are operating
under appropriate biosafety conditions. Nearly 170
countries and territories worldwide have initiated
national surveys of all biomedical laboratories to identify
poliovirus materials, encourage destruction of unneeded
materials, and implement appropriate biosafety
conditions.
Scenario 2: accidental
manufacturing site
release
from
an
IPV
Large quantities of live poliovirus are used in the
production of IPV. One case of inadvertent release was
recorded in the early 1990s, occurring during a period of
universal immunization when no containment strategies
existed. To prevent a repeat of this situation, such risks are
being adequately managed. Manufacturers have worked
closely over the past 18 months with biosafety experts and
WHO to implement more stringent containment
practices at manufacturing facilities. In February 2003,
the
WHO
Expert
Committee
on
Biological
Standardization (ECBS) convened to finalize the
guidelines for an increased containment process for all
manufacturers. As IPV manufacturing sites are located in
industrialized countries, consequences of a potential
release would be limited as these countries are planning to
maintain high population immunity with IPV for the
foreseeable future, and sanitation infrastructure is high.
Scenario 3: intentional release
This scenario is the least likely to occur, due to ongoing
use of polio vaccines globally and the inherent limitations
of poliovirus as biological weapons or bioterrorist tools.
However, full evaluation of this risk depends on the polio
immunization policies that arc adopted worldwide in the
post certification era. Most countries which have been
suggested as potential targets for an intentional release
plan to maintain population immunity with IPV for the
foreseeable future, markedly reducing the probability of
an intentional release and the implications in the unlikely
event of such an occurrence. <
Surveillance and immunization
AFP and polio reporting, year-to-date (data received at WHO Geneva as of25 February 2003)
2002 (as of 25 February 2003)
2001 (as of25 February 2002)
i Non-polio
AFP rate
Region
African1
Americas
Eastern Mediterranean
European
South-East Asia
Western Pacific______
2-20
1.13
Adequate
specimen rate
1.78
83%
1.39
1.61
88%
81%
.
Pending
cases
Non-polio
AFP rate
476_ j
326 ~ i
3.00 4 82%
1.20
92%
63
0
89%____ J0n__
83%
139....
.. 81%
i
Wild polio
virus cases
ZZHEZZZiiE;
F 1.89
L 1-23
Global total
Confirmed
polio cases
236 .
560__ [
610
2461
268
0
472
268
0
533
214-
Wild polio
virus cases
Pending
cases
201
942
328
82
236
582
438
2608
0
0
.......OL'..2'SEZZ.119.
139
r.
Adequate
Confirmed
specimen rote polio cases
82%
0
0
82%
1595
1595
88%_________ 0_________ 0_
84%
1928
1915
1.19
1.92
1.33
1.90
1 for African Region, pending cases refers to pending laboratory results.
Importation.
f"5 Vaccine derived polio virus. In 2001, in the American region, in Dominican Republic 3 cases and in Haiti 7 cases. In 2002, in the African region, in Madagascar, 4 cases.
Wild poliovirus map
TiffiShOBJ
total wild poliovirus and date of most recent wild
poliovirus by country' from 25 February 2002 to
24 February 2003
25 February 2002 --24 February 2003
Ci
|
-
f pl %
2003
Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb
*•
■MS?
India
Pakistan
Nigeria
■■
jiAfghanistan
Egypt
Somalia
Niger
93
M
'4
I
iiiiportsttioiis:
Burkina Faso
Zambia «1
5 Z
Importation
<» WiB virus type 1
• Wild virus type 3
df
u
;
Some:Dao a WHO 6enero a ofiS FebruaryMl
n» DVXSM MD«neS
*41*
MMtmipY e*rRr<*»«i
wuarart*
WWtl
OMffffM 9t MQ4 48 M
17
totawy.
w ao < t fcamrwx • •wemwj trr «tn to Un
♦ Wild vrus type 1 and 3
F] tndewiK reannies
ar«t urs wr w»a Mtaw «<>«» U
*&4v«4*ari4<tffUN mn «Mnw«iu
WWtMW Mfl VX4M 4<r<*4 (>*
CtaM>»»DiC • O* r»f* mi
1 ;
Snapshots from NIDS...
. I'
B 2J
I
W 1 y
NIDs calendar for selected countries
Region
Country
AF^O
Angola
Niger
Nigeria
EMRO
Afghanistan
April 2003
Type of activity
Intervention
Intervention
June 2003
aciiviiy
Intervention
27-June/NI0/0PVRo‘"’d1
26-April/:.-4,/0PV«-^
....... 29-May/:/^/0PV^
01,05,26-April / SNIbs / OPV
15-April/ J /OPV^i
20-MayA
/OPV^VVit A
02-May/
Egypt
SEARS
May 2003
Pakistan
15-April/4: / OPV fioun«i2
Somalia
April/ ■
Sudan
01,13,17-April/i
03-June/S J; /OPV«0“nti1
/OPV'«
/ppyRoundZ
Bangladesh
April/;;' /OPVR”und..'./yitA
..947May/M4/OPyBo“nd2
India
06-April/SNL /OPVRounii1
18-May/ >‘4- /OPV2
This calendar reflects information known to WHO/HQ at the time ofprint. Some NIDs dates are preliminary and may change; please contact WHO/HQ for up-to-date information.
News and announcements
Rotary raising urgently needed funds
to eradicate polio
p OTARY members are more committed than ever to
lA achieving a polio-free world. To that end. Rotary' has
embarked on a new drive to raise USS 80 million by June
2003. In addition, Rotary is reaching out to the public by
way of a global advertising campaign. The ads, which are
prominently appearing on television and in magazines in
Australia and Canada during February and March, target
receptive business and professional people. These ads are
also being distributed as public service announcements
worldwide.
In addition, a special add is airing on United Airlines’
in-flight television network from February to April on all
national and international flights. Passengers will be
directed to a corresponding advertisement in United
Airlines’ “Hemispheres” magazine. The ad will give
instructions on how to make a contribution to polio
eradication.
Anyone wishing to contribute can send donations to:
The Rotary Foundation - Polio, P.O. Box 75133, Chicago,
IL 60675-5133, USA. Or Visit: www.rotary.info 4
Madagascar heroes recognized as
tragedy overshadows NID
SIX people participating in an NID in Madagascar
tragically died in October 2002, when their helicopter
crashed while returning from successfully delivering
polio vaccine to difficult-to-reach areas of the country.
The helicopter was on its way back after finalizing the
delivery of vaccines for the second phase of the NID
when the accident occurred. The names of the six vic
tims, Lt Colonel Davisa Ratsimandah: Lt Colonel Michel
Nernet Miharivelo: Lt Colonel Emmanuel Rakotoniaina:
Lt Flavien Yamicole; Andre Jaonera; and Major Solo
Ratsimbazafy, have been nominated as ‘Polio Eradication
Heroes of the CDC Foundation. The ‘Heroes Fund’ was
established to assist families financially who have lost
loved ones during polio eradication activities.
The activity will be remembered for the tragic death
of the six Polio Eradication Heroes. 4
I
F
A Red Crescent volunteer in Pakistan
administers the oral polio vaccine to a child.
Over 490 volunteers worked tirelessly to raise
awareness about immunization activities,
and personally immunized over360 000
children in 2002.
Pakistani Red
Crescent
volunteers
instrumental
in reaching
hard-to-reach
areas
□ AKISTANI
Red
I Crescent volunteers
are turning out by the hundreds to help stop the
virus. In 2002, the Pakistan Red Crescent Society
actively recruited 491 men and women volunteers
to systematically mobilize target communities for
supplementary immunization activities (SIAs).
Driving through the streets with megaphones,
going door-to-door, the volunteers distributed
100 000 polio fact sheets (in English, Urdu and
other languages), polio information stickers,
brochures, badges, pens and banners, while
posting over 90 000 posters announcing
upcoming immunization campaigns. The Red
Crescent’s unique community-based advantage
proved essential in visiting specific population
groups in many otherwise hard-to-reach areas. By
the end of the year, the Red Crescent volunteers
alone had immunized well over 360 000 children.
“Our volunteers did a fantastic job.” commented
Dr Fazil Moin, Secretary-General of the Pakistan
Red Crescent Society. “Each and every one of
them personally immunized over 900 children.
Because they belong to target communities, the
service they offer is uniquely valuable in reaching
areas
which
otherwise
would
remain
unvaccinated. It was a tremendous achievement
and one we hope to build on in 2003." In 20012002, Red Cross and Red Crescent volunteers have
helped promote polio immunization days in
Afghanistan. Bangladesh, Chad, Congo, the
Democratic Republic of the Congo. Egypt. Ethiopia,
Iraq. Liberia, Niger, Nigeria. Pakistan, Sierra Leone.
Somalia and Sudan. 4
USAID Global Health Bureau recognizes Ellyn Ogden's contribution
to polio eradication
£
§
&
1
Eiiyn Ogden highlights the
importance of polio eradication at a
recent donor meeting.
r llyn Ogden, USAID Polio
C Eradication Coordinator, has
been granted the prestigious
Sustained Outstanding Achieve
ment Award by the Global
Health Bureau, USAID, in
Washington DC. The award
recognizes Ogden’s tireless commitment to polio eradication
across the globe. “This official
°
recognition is more than
deserved, commented Richard Greene. Director,
Office of Health, Infectious Diseases and Nutrition
of the USAID Bureau for Global Health. “Ellyn’s
energy and commitment are second to none, having
fought polio not just centrally, but first-hand in the
field in countries such as the Democratic Republic of
the Congo, Egypt and Ethiopia.” Greene cited Ms
Ogden’s leadership in championing social
mobilization activities, gaining increased support by
local NGOs at national levels, and working to
improve routine immunization services as examples
of her many distinguishing characteristics.
Ms Ogden has been involved in polio eradication
since 1997, when she took on the global challenge as
USAID Polio Eradication Coordinator. USAID has
allocated more than USS 200 million to the Polio
Eradication Initative since 1996. 4
Country focus
Rotary steps up global
volunteerism
a USTRALIAN and Canadian Rotary members rang
/v in the New Year while volunteering during the
January 2003 NID in Cameroon. Another Rotary
group of 85 from the United States joined members
from Ethiopia to help immunize children against
polio in that country. And, another group of Rotary
members travelled to Nigeria in November, where
their efforts were honored with a visit from the Emir
of Kano, who also took part in the NID by
immunizing local children.
Earlier, in October 2002, Rotary continued its
high level of support to India by approving a grant
of almost US$ 5 million for eradication activities in
that country, bringing Rotary’s total contributions
there to more than USS 46 million. Among other
things, the grant helped pay for hiring local
vaccinators, to go house-to-house. In November
2002, Rotary International President Bhichai
Rattakul called on Rotary leaders in India to
“redouble your efforts’ to achieve polio eradication
in Uttar Pradesh.
As an answer to this call. Rotary placed an
information advertisement of a pro-immunization
speech given at Moradabad by Dr. Naseem Ahmed,
Vice-Chancellor of Aligarh Muslim University, in a
number of newspapers for wider outreach.
In addition, 65 Rotary members from Canada
and the United States joined Indian Rotarians,
health workers, and other volunteers in the six day
effort to vaccinate 165 million children under the
age of five years. ♦
I
“i
Rotary International volunteers from around the world are joined by the Emir of Kano in Nigeria to
raise awareness of immunization campaigns.
Democratic Republic of the Congo: maximizing the polio experience
Polio infrastructure makes measles
campaign possible
A model polio-free country
AN 13 December 2002, a measles campaign was
kJ launched in the North Kivu and East Kasai
provinces of the Democratic Republic of the Congo
(DRC) to immunize all children between 6 months
and 15 years of age. To maximize immunization
coverage for the event, the government organizers,
with the assistance of UNICEF and WHO, drew on
the experience and infrastructure of the GPEI to both
plan and implement the campaign. Organizers
adapted past polio successes to produce maps, organize
cold chains for the vaccines, target social mobilization
activities at schools, parents, and political
administrators, and encourage parents and children to
take advantage of the services offered. Nearly
3.2 million children were immunized (an estimated
96% coverage). “The polio eradication experience
made the success of this activity possible,"
commented Dr Brad Hersh, EPI Medical Officer at
WHO, Geneva. “The polio programme provided a
perfect framework to reach almost all children and
prevent many measles deaths.”
i a IITH an increasing number of countries attaining
VV polio-free status, it is important to maintain
vigilance and political commitment to ensure wild
poliovirus is not reintroduced into a polio-free
country. The DRC is a model example of a country
doing exactly that.
Since confirming its last case of polio on 29
December 2000, the DRC has taken a number of
steps to maintain its polio-free status, including
continuing
SIAs,
consistently
improving
surveillance, and increasing the level of routine
immunization.
The success of the DRC’s post-polio programme
is all the more extraordinary considering the
country’s infrastructure remains disjointed after
more than a decade of civil war. Most roads are still
impassable, making logistical organization of SIAs
difficult. Volunteers, health workers and equipment
often have to be transported by sea or air, putting a
tremendous strain on human and financial resources.
Despite this, the DRC continually maintains its
political commitment to polio eradication - and it is
paying off, as the country just celebrated its second
polio-free year. 4
H
A*
fi. flu
;
"A:
1
I
.^1
A child is protected against measles, during one of many mass immunization campaigns across Africa
Recent donations:’
Resource mobilization
Funding shortfall prompts cutbacks
p XTREMELY encouraging interL_ national support to and endorse
ment of the Initiative in 2002 was
overshadowed by an acute funding
shortfall at the start of 2003, leading
to an abrupt curtailing of some
activities in the first half of the year.
Due in part to the global economic
downturn of the past two years, a
number of key partners informed
WHO late in 2002 that it would not
be possible to provide expected yearend resources. While the resultant
scaling back of activities presents new
risks to the rapid achievement of a
polio-free world, the risks are
manageable if sufficient funding is in
place by June 2003 for activities
planned in the second half of the year.
In response to this acute funding
gap. the Initiative has re-prioritized
and subsequently scaled back
activities, particularly in the WHO
Regions for Africa and the Eastern
Mediterranean. By the end of
January 2003, plans had been made
to cancel national or subnational
polio immunization campaigns in
more than 10 recently endemic
countries, cut national surveillance
budgets by an average of 30 percent
and reduce the length of contracts of
most polio-funded international and
national staff. ♦
Japan: a solid global polio partner
| N 1980, Japan made
I history when it
eradicated polio, but
the. country s mission
to eliminate polio lias
transcended Japanese borders.
Long before the launch of the
GPEI in 1988, Japan had worked
with governments of nearby
countries to eliminate polio. In the
late 1960s and early 1970s, Japan
helped provide the Philippines and
Thailand with vaccines, equipment
and human resources to vaccinate
children against polio. In 1980.
Japan began helping Brazil produce
quality polio vaccine and provided
equipment and technical experts.
With the 1988 launch of the
GPEI, Japan strengthened its com
mitment to end polio and provided
aid to Bangladesh, China and Laos,
Indonesia, Kenya, Niger and
Pakistan. Over the past decade,
Japan's generosity has spanned
the globe. It has provided US$ 230
Materials available:
e Weekly Epidemiological Record:
Progress towards poliomyelitis eradication in
Egypt, 2002 (issue no. 1 ?, 28 March 2003)
Progress towards poliomyelitis eradication in
India, 2002 (issue no. 10,7 March 2003)
| |
million to help countries obtain
vaccines and construct cold chain
facilities. That commitment has made
Japan the fourth largest donor to
the GPEI while helping to immunize
600 million children around the
world.
Even today, as Japan faces
economic dilemmas at home, it
remains a steadfast partner in the
endeavour to end polio. At a Decem
ber ceremony in Islamabad, the
Government of Japan announced its
USS 9.6 million pledge to Pakistan for
2003 activities to eliminate polio from
the country. The contribution raised
Japan's total donation to Pakistan's
polio eradication efforts since 1996
to USS 38.5 million. “We are com
mitted to fighting infectious diseases
worldwide, as it is viewed by
Japan as a global issue requiring
approaches based on global partner
ships." said Mr Minoru Shibuya,
Japan’s Ambassador to Pakistan, at
the ceremony. ♦
Forthcoming events 2003:
Technical Consultative Group - 24-25 April
ss World Health Assembly -19-28 May
® Rotary International PolioPlus Committee
Meeting - 27-29 May
® Rotary International Convention 1-4June
©World Health Organization 2003. Ail rights reserved. The designations employed and the
rUII UKWS presentation of the material in this publication do not imply die expression of any opinion
whatsoever on tile part of the World Health Organization concerning the legal status of any
country, territory', city or area or of Its audionties, or concerning the delimitation of its frontiers or boundaries. Dotted
lines on maps represent approximate border lines for which there may not yer be full agreement. The World Health
Organization does nor warrant that the information contained in this publication is complete and correct and shall not
be liable for any damages incurred as a result of its use. Folio News is published quarterly by EPl. WHO Headquarters.
Geneva. Switzerland, and parr funded by USAID. Published data reflects information available at. time of print.
Finland
USS 90 000 for Polio Reference Laboratory in
Finland
Italy
USS 80 OOO for Polio Reference Labonitury in
Rome
USS 100 000 for polio inununizaion activities in
Somalia and Sudan
Rotary International
USS 2.6 million as rapid response grants for 2003
polio activities in Angola, the Democratic
Republic of the Congo. Ethiopia. India, Nigeria,
and a grant to AFRO for surveillance activities.
United Kingdom
USS 4.75 million in global funding for polio
activities
USS 340 000 for AFP surveillance in Myanmar
United States of America
USS 133 million for 2003 global polio eradication
activities distributed through the US Centers for
Disease Control and Prevention and USAID.
Tne Global Polio imiication Initiative expresses its gratitude to all
donors.
*Donations announced since Polio News 17 December 2002.
PAG pursues funding
opportunities
-T" HE Polio Advocacy Group (PAG)
I is involved in a number of
activities to help fill the funding gap.
Established to coordinate the
resource mobilization efforts of the
partners and exploit their relative
strengths, the PAG is an informal
partnership between Rotary Inter
national, the UN Foundation,
UNICEF and WHO.
The PAG made an urgent appeal
to the donor community and partners
in late 2002 to help fill the critical
2003 funding gap of USS 75 million
for polio eradication activities. It
appealed to donors to have funds
available before mid-2003, to ensure
scheduled activities continue in the
second half of the year.
The G8, during its last Summit in
June 2002, vowed to provide the
funding required for polio eradication
activities in Africa. Following
commitments by Canada and the UK,
appeals have been made to the other
G8 countries to fulfill their commit
ment before tire upcoming G8 Summit
in Evian, France in June 2003.
Discussions with the European
Commission were reconvened in an
attempt to reprogramme unspent EC
Health Sector funds for polio
eradication in priority countries.
Support was approved in the amount
of US$ 25 million for India and
USS 12.9 million for Nigeria. This
funding builds on the EC’s
contribution for polio eradication
activities in Nigeria that amounted
to over USS 18 million. A
All comments and feedback on Polio News
should be sent to:
Department of Vaccines and Biologicals,
WHO, Geneva.
Tel.:
+41 22 791 3219
Fax:
+41 22 791 4193
Email:
polioepi@who.int
Web site:http://www.poiioeradication.org
I
f
I
I
•A
■
West Africa launches final assault on polio - 60 million African children to be vac...
pagina 1 van 3
- fe-A-1
English | Espahol i F
World Health Organization
Media Centre
Home
Countries
Search
r
Location: WHO > WHO Sites > Media Centre > Press Releases
Health Topics
Cl.printabie version
Publications
Research Tools
WHO Sites
Media Centre
West Africa launches final assault on polio - 60 n
African children to be vaccinated
Press Releases
Events
Fact Sheets
Notes for the
Press
12 November 20021new york/geneva - With West African countries
in the midst of vaccinating millions of children against polio, the
world’s largest vaccine manufacturer,^l^tis.^asteur,.h^
donated 30 million doses of oral polio vaccine to the Global Polich
Eradication Initiative/
Statements
Multimedia files
This week, 16 West African countries are uniting to vaccinate all
children under five within their borders.* Immunization campaigns
over the past two years have driven the number of polio-endemic countries in
all-time low. In 1999, 20 African countries were polio-endemic, but to date tl
three are considered endemic.**
This success is due to the Global Polio Eradication Initiative, a broad partners
deliver polio vaccine to every child under five. The Aventis Pasteur donation
making a difference, with almost 3 million of the 30 million doses bound for
immunization campaign in Liberia.
“We are further strengthening the solidarity which has brought us to the cusp
free world, and will indeed push us to full success/ said Dr Gro Harlem Brur
Director-General of the World Health Organization, at a recent signing cerem
United Nations in New York.
The Global Polio Eradication Initiative is spearheaded by the World Health C
Rotary International, the US Centers for Disease Control and Prevention and
Aventis Pasteur - the longest standing corporate partner in the Global Polio E
Initiative - has donated 120 million vaccine doses since 1997 and targeted its
African countries affected by conflict, including Sierra Leone and the Sudan,
appear to be polio-free.
ii
“We are so close to beating this crippling disease in Africa and worldwide,” s
Bellamy, Executive Director of UNICEF, “but we are not there yet. We have
focused and committed and encourage support from all comers - from endem
donor countries and the health industry - so all children can be immunized. TJ
will help these countries finish the job and ensure no more African children a
by this easily preventable disease.”
David J. Williams, President and Chief Executive Officer of Aventis Pasteur,
company in the world devoted entirely to vaccines, signed a banner pledging
commitment to end polio. “The Initiative has already made tremendous progr
http://www.who.int/mediacentre/releases/pr86/en/
13-12-2002
West Africa launches final assault on polio - 60 million African children to be vac...
pagina 2 van 3
admire the remarkable work done by WHO, Rotary International, CDC, UNI<
millions of volunteers around the world,” Williams said. “This donation is j w
example of Aventis Pasteur’s commitment. We are very proud of our involve
Global Polio Eradication Initiative.”
About the Global Polio Eradication Initiative
Since its launch in 1988, the Global Polio Eradication Initiative has reduced j
transmission from 125 countries and an estimated 350 000 cases, to just ten c
beginning of 2002. Of these just three - India, Nigeria and Pakistan - have hat
high-intensity transmission, while the remaining seven - Afghanistan, Angola
Ethiopia, Niger, Somalia and Sudan - each have fewer than eight cases to date
The final challenge to stopping transmission of wild poliovirus in Africa is to
children are reached with polio vaccine - particularly those in the conflict are;
city of Mogadishu in Somalia; those in eastern Angola, and all children undei
Nigeria. With the support of governments and millions of volunteers, the Initi
requires USS 275 million to fund polio eradication activities through 2005 an
is required for African countries.
To help meet the current funding challenge, Rotary members worldwide have
a major campaign to raise US$ 80 million by the year 2003. To date, Rotary 1
contributed USS 182 million to eradicate polio throughout the African contin<
committed USS 510 million worldwide. In addition to raising funds, Rotary n
donate their time and personal resources during National Immunization Days
this year, Rotary members from countries around the world have joined Rotai
polio endemic countries to help immunize children against polio.
Other partners in the Global Polio Eradication Initiative coalition include: the
of countries affected by poliomyelitis; private foundations (e.g. United Natioi
Foundation, Bill & Melinda Gates Foundation); development banks (e.g. Woi
donor governments (e.g. Australia, Austria, Belgium, Canada, Denmark, Finl
Germany, Ireland, Italy, Japan, Luxembourg, Netherlands, Norway, United K
United States of America); the European Commission; humanitarian organize
International Red Cross and Red Crescent movement) and corporate partners
Pasteur, De Beers and Wyeth). Volunteers in developing countries also play e
million have participated in mass immunization campaigns.
* The participating West African countries are Benin, Burkina Faso, Cape Ve
Ghana, Guinea, Guinea-Bissau, Ivory Coast, Liberia, Mali, Mauritania, Niger
Senegal, Sierra Leone and Togo.
** The three African countries with laboratory-confirmed transmission are N:
all cases on African continent to date in 2002); Niger and Somalia. In additioi
cases among Angolan refugees in western Zambia (February 2002) and positi
environmental samples from Egypt demonstrate ongoing transmission in Ang
Egypt. See www.polioeradication.org for details on incidence of polio in eacl
For more information contact:
information Officer
WiH©*
Telephone: +41 22 791 4688
Mobile phone: +41 79 254 6815
Email: mcnabc^whp.int
http: //www. who. int/medi ac entre/rel eases/pr86/en/
13-12-2002
West Africa launches final assault on polio - 60 million African children to be vac...
pagina 3 van 3
New York
Telephone: +1 212 326 7566
Email: ekramer@unicef.org
Averfti?"
Lyon, France
Telephone: +33 4 37 37 7273
Email: Koren.Wolman-Tardv@aventis.com
I .EmpJ.Qy.rn©nt I Qtb.e£...UN..S.ite!S I Search | Site. Mgp I Suggestions
© CPPXriah.^
http://www.who.int/mediacentre/releases/pr86/en/
13-12-2002
t
WORLD HEALTH ORGANIZATION
EB111/32
21 November 2002
EXECUTIVE BOARD
111th Session
Provisional agenda item 10.5
Eradication of poliomyelitis
Report by the Secretariat
1.
In 1988, the Forty-first World Health Assembly (resolution WHA41.28) established the goal of
the global eradication of poliomyelitis by the end of the year 2000. At the time the resolution was
adopted, an estimated 350 000 poliomyelitis cases were occurring each year, and at least 125 countries
were endemic for poliovirus. In 1999, the Fifty-second World Health Assembly, in resolution
WHA52.22, called on Member States to accelerate eradication activities to interrupt the chains of
transmission of wild-type poliovirus and to introduce laboratory containment of wild-type poliovirus.
As a result of this acceleration, only 10 countries1 were still endemic for wild-type poliovirus at
2.
the end of 2001, and just 483 laboratory-confirmed cases of poliomyelitis were reported in those
countries. The absence of cases during that year from countries historically considered as major
reservoirs of wild-type poliovirus, particularly Bangladesh and the Democratic Republic of the Congo,
also demonstrates that the eradication strategies are sound. On 21 June 2002, the independent Regional
Certification Commission certified the WHO European Region poliomyelitis-free, bringing the total
number of such certified regions to three, with a total population of more than 3000 million people in
134 countries, areas and territories. By 12 November 2002 the number of countries affected by
poliomyelitis was the lowest ever, with only seven known to be endemic.
3.
In 2001-2002, a framework for assessing and managing the risks of poliomyelitis in the post
certification era was created, drawing on extensive research results, in order to facilitate national and
international deliberations on future poliomyelitis immunization policy. Planning is under way for
extensive consultations with Member States to determine how these risks may influence national
policy on the use of poliomyelitis vaccines after global certification.
4.
Increasing attention is being given to optimizing and documenting the role of the infrastructure
of the Global Polio Eradication Initiative in contributing to the attainment of other health goals. In
2001, for example, a survey of 1015 WHO staff funded by the Global Polio Eradication Initiative
found that 91% of international staff and 100% of national staff are devoting an average of 44% and
22%, respectively, of their time to strengthening routine immunization and surveillance systems.
Specific milestones have been established and indicators developed to monitor progress in this area.
1 Afghanistan, Angola, Egypt, Ethiopia, India, Niger, Nigeria, Pakistan, Somalia, and the Sudan.
EB111/32
ISSUES
5.
Over the next 12 months an intensive global effort will be required to eradicate poliomyelitis
from the remaining endemic areas. Of particular importance will be to close the gaps in the quality of
supplementary immunization activities to ensure that all children receive oral poliomyelitis vaccine in
India, Nigeria and Pakistan, which, as of 12 November, accounted for 98% of cases in 2002 (90% of
these cases are found in nine of the 76 states or provinces of those three countries) (see Annex,
Figure 1). Concerted action will be needed to stop the low-level but geographically extensive
transmission of poliovirus in Egypt and Niger.
6.
In Afghanistan, the Mogadishu area of Somalia, and eastern Angola, continued improvements in
access to immunization of all children are crucial to interrupting the final chains of poliovirus
transmission in these “low transmission” areas.
7.
For all the WHO regions to be in the process of poliomyelitis-free certification by 2005, the
quality of surveillance of acute flaccid paralysis must be raised to certification standard, especially in
33 countries in the WHO regions of Africa (23 countries), the Eastern Mediterranean (7) and SouthEast Asia (3) (see Annex, Figure 2).
8.
In terms of progress toward laboratory containment of poliovirus, by August 2002, 122 Member
States had initiated a national survey, and, of those, 76 had completed and submitted an inventory of
laboratories holding wild-type polioviruses and potentially infectious materials. Global certification
will require that all countries complete these activities to ensure that any retained materials are handled
in appropriate biosafety conditions.
9.
Implementing the necessary eradication, surveillance, certification and containment activities
largely depends on whether the shortfall in funding of US$ 275 million for the period 2003-2005 is
met.
ACTION BY THE EXECUTIVE BOARD
10.
2
The Executive Board is invited to note the report.
EB111/32
ANNEX
Figure 1. Reported cases of poliomyelitis due to
transmission of indigenous wild-type poliovirus, by country,
in 2002*
(data as of 12 November 2002)
1000
900
800
700
600
500
400
300
200
100
0
896
14470-
India
Nigeria
8
3
2
Niger
Somalia
3
Pakistan Afghanistan Egypt
* In addition to the countries referred to in this Figure, the isolation of wild-type poliovirus from Angolan
refugees in Zambia suggests ongoing transmission in Angola during 2002.
who 02.198
Figure 2. Performance of acute flaccid paralysis surveillance
for the eradication of poliomyelitis in 2002 in the three
WHO regions yet to be certified as free of poliomyelitis
(data as of 12 November 2002)
Certification standard
F
I Achieved
E2 Not achieved
3
- 6 A-3
*
WORLD HEALTH ORGANIZATION
FIFTY-FIFTH WORLD HEALTH ASSEMBLY
Provisional agenda item 13.7
A55/11
27 March 2002
Eradication of poliomyelitis
Report by the Secretariat
BACKGROUND
1.
The Forty-first World Health Assembly (resolution WHA41.28) established the goal of
eradication of poliomyelitis by the year 2000. Recognizing that, despite substantial progress and sound
strategies, transmission of wild poliovirus would continue in some Member States beyond the target
date, the Fifty-second World Health Assembly, in resolution WHA52.22, called for acceleration of
eradication activities, additional funding and the introduction of laboratory-containment activities.
2.
Acceleration of eradication activities between 1999 and 2001 has resulted in a 28%
improvement in poliomyelitis surveillance, a two-thirds reduction in the number of endemic countries
and a 92% decline in reported poliomyelitis cases since resolution WHA52.22 was adopted in May
1999. Poliomyelitis is now at its lowest point ever, with 473 cases due to indigenous wild poliovirus
reported in 10 countries in 2001 (as of 12 March 2002) compared with an estimated 350 000 cases in
more than 125 countries in 1988 (see Annex). On 29 October 2000, the Western Pacific became the
second WHO Region to be certified poliomyelitis-free.
3.
All Member States endemic for poliomyelitis have conducted “intensified” national
immunization days and have improved surveillance in response to the call for acceleration. To
maximize the impact, 16 West African countries synchronized national immunization days in OctoberNovember 2000 and 2001. Angola, Congo, Democratic Republic of the Congo and Gabon
synchronized three rounds of intensified national immunization days in July-September 2001.
Afghanistan, Islamic Republic of Iran and Pakistan continued to synchronize activities. Under the
leadership of the United Nations Secretary-General, many United Nations organizations, in
partnership with humanitarian and nongovernmental organizations, supported Member States in
carrying out these activities.
4.
Critical to achieving this acceleration have been large unearmarked contributions for
poliomyelitis eradication to WHO totalling US$ 308 million during 1999-2001, from the governments
of the Netherlands and the United Kingdom of Great Britain and Northern Ireland, the Bill & Melinda
Gates Foundation and the United Nations Foundation. During the same period, additional
contributions to the eradication initiative, through either multilateral or bilateral channels were made
by Rotary International and by the European Commission; the governments of Australia, Austria,
Belgium, Canada, Denmark, Finland, Germany, Ireland, Italy, Japan, Luxembourg, Norway, Oman,
United Arab Emirates, United Kingdom of Great Britain and Northern Ireland and United States of
America; Aventis and De Beers.
A55/11
5.
The Global Action Plan for Laboratory Containment of Wild Polioviruses1 is now being
implemented. National task forces have been appointed in 114 countries and areas: 36 in the Western
Pacific Region; 50 in the European Region; 19 in the Eastern Mediterranean Region; seven in the
South-East Asia Region; and two in the Region of the Americas. Over 90 countries have already
begun compiling exhaustive lists of biomedical facilities to be surveyed, with more than 70 000
laboratories listed as of January 2002. Twenty-nine countries have completed the pre-eradication
phase activities and submitted national inventories of laboratories.
ISSUES
6.
Five of the 10 remaining endemic countries constitute the “high transmission” areas of northern
India, Pakistan and Afghanistan, and Nigeria and Niger. Stopping poliomyelitis worldwide by the end
of 2002 requires reaching all children in these areas with multiple rounds of supplementary
poliomyelitis immunization in 2002. In the five “low transmission” countries of Angola, Egypt, and
the Hom of Africa (Ethiopia, Somalia and Sudan), the risks that poliomyelitis will not be rapidly
stopped include deterioration in security and/or suboptimal strategy selection and implementation.
7.
In contrast to the maximum biosafety and containment of regulations in place for smallpox
virus, the goal for laboratory containment of wild polioviruses is the implementation of appropriate
biosafety procedures depending on the level of risk. The WHO Global Action Plan for Laboratory
Containment of Wild Polioviruses was revised in 2002 to reflect this emphasis and outline the action
needed in Member States.
8.
The importance of defining poliomyelitis immunization policy for the post-eradication era has
been highlighted by outbreaks caused by circulating vaccine-derived polioviruses in the Philippines
(2001) and the Dominican Republic and Haiti (2000-2001). To facilitate this policy development, a
full programme of work is being implemented, which includes evaluation of the future risk of such
outbreaks and the feasibility and implications of each of the post-eradication immunization policy
options.
9.
A “Meeting on the impact of targeted programmes on health systems: a case study of the Polio
Eradication Initiative” was held in Geneva from 16 to 17 December 1999.2 To build on the finding that
opportunities for strengthening health systems could be better exploited, WHO is working to ensure
that the lessons from poliomyelitis eradication and the infrastructure are used to improve the delivery
of other immunization services and surveillance for other diseases of public health importance. This
may require substantial human resources, as more than 2000 immunization personnel, funded by the
Global Polio Eradication Initiative, have been critical for national capacity-building for this
undertaking.
FUTURE ACTION
10. The funding gap of US$ 275 million to the end of 2005 is now the single greatest threat to the
goal of poliomyelitis eradication. To ensure that the funding requirements are met in a timely manner,
commitments are needed from partner agencies and Member States, whether endemic or non-endemic.
1 Document WHO/V&B/99.32.
2 See document WHO/V&B/00.29.
2
A55/11
11. In Member States that are endemic for poliomyelitis and undergoing humanitarian crises,
particularly Afghanistan, Angola, Democratic Republic of Congo, Somalia and the Sudan,
poliomyelitis eradication activities need to be emphasized as a crucial part of the humanitarian agenda
in order to facilitate the prompt interruption of transmission.
12. Global certification of poliomyelitis eradication, targeted for 2005, requires that all Member
States will have first completed the pre-eradication phase activities set out in the global action plan for
the laboratory containment of wild polioviruses, including establishing a national inventory of all
facilities holding potentially infectious materials.
13. The Director-General will continue to submit an annual report to the Executive Board on
progress towards the eradication of poliomyelitis and the development of post-eradication policy.
ACTION BY THE HEALTH ASSEMBLY
14.
The Health Assembly is invited to note the report.
3
A55/11
ANNEX
ERADICATION OF POLIOMYELITIS: PROGRESS
Endemic countries: 1988 and 2001
J
/
'V V
5^
/
X___ J
'K >
V
F
° ^Jr
SIB
-6
J)
pl
1
o
o
o
o
o
o
o
©
■B
a
g
o
a
/7q’
1988
350 000 cases
LB. yB
IlbiL,
\
■tf
v z "‘‘01
. W/
aTTF
W-
o
o
o
o
a
o
ga
§
a
2001
473 cases*
laboratory confirmed as of 12 March 2002
4
f H WORLD HEALTH ORGANIZATION
EXECUTIVE BOARD
103rd Session
Provisional agenda item 3
EB103/7
27 November 1998
Poliomyelitis eradication
Report by the Director-General
BACKGROUND
1.
In 1988 the Health Assembly established a goal to eradicate poliomyelitis globally by the year 2000.1
Recognizing that a focused eradication goal could facilitate the development of health care systems, the
Health Assembly specified that poliomyelitis eradication should be conducted within the Expanded
Programme on Immunization (EPI) and the context of primary health care.
2.
Routine immunization systems are now delivering poliomyelitis vaccine and other EPI antigens to
80% of the world’s infants. National immunization days for poliomyelitis eradication have been conducted
in all endemic countries with the exception of the Democratic Republic of the Congo and Liberia. Eightynine countries will conduct national immunization days in 1998, targeting an estimated 470 million
children, approximately three-quarters of the world’s population aged less than five years. Many
immunization days are being internationally coordinated either within or between WHO regions, including
the “Kick Polio Out of Africa” campaign. Operation MECACAR (Eastern Mediterranean and European
regions), and the simultaneous immunization days among countries of the South Asian Association for
Regional Cooperation. Surveillance of acute flaccid paralysis has been established in all poliomyelitis
endemic countries, fully integrated in a global network of 133 poliomyelitis laboratories. Truces have been
declared for immunization campaigns in Afghanistan, El Salvador, Peru, Philippines, Sri Lanka, Sudan,
and Tajikistan.
3.
If the current rate of progress is maintained, poliomyelitis can be eradicated globally by the year
2000 or shortly thereafter. Since 1988 the number of cases reported by WHO Member States has fallen
by 85%. Poliomyelitis eradication was certified in the Region of the Americas in 1994, three years after
the last case occurred in Peru. In the Western Pacific Region the last case occurred in Cambodia in March
1997. As of mid-1998, only 50 countries were still considered to be polio-endemic, mainly in South Asia
and sub-Saharan Africa (Annex).
4.
Eradication of poliomyelitis will benefit the world by preventing hundreds of thousands of cases of
paralysis each year, and producing direct savings of US$ 1.5 thousand million each year after
immunization is stopped. The eradication initiative has already revitalized immunization programmes in
many countries, helping to re-establish the cold chain and improve routine coverage. Improved integrated
1 Resolution WHA41.28.
EB103/7
surveillance systems, trained health staff and the global virology laboratory network are additional legacies.
In 43 countries, the distribution of vitamin A during national immunization days has prevented blindness
and reduced deaths from measles and other infectious diseases. Because of the “slack” in many health
systems, combined with the availability of new funding, there has not been a major disruption in other
health services or diversion of funds. The eradication of poliomyelitis in the Western Hemisphere has led
the Region of the Americas to adopt a measles elimination target.
ISSUES
5.
The poliomyelitis eradication initiative is now in a crucial phase, with some of the most difficult
countries still remaining endemic. Six countries (Bangladesh, Ethiopia, India, Nepal, Nigeria and Pakistan)
are major reservoirs of poliomyelitis, where large populations, high birth rates, crowded areas with poor
sanitation and insufficient routine immunization facilitate poliovirus transmission. Implementing
eradication activities is especially challenging in seven countries affected by conflict (Afghanistan, Angola,
Liberia, Sierra Leone, Somalia, Sudan and Tajikistan). The Democratic Republic of the Congo is a unique
challenge, a major reservoir affected by conflict.
6.
During the initial phases of poliomyelitis eradication, countries paid 80% to 90% of the total cost.
However, the lower levels of infrastructure and health resources available in the remaining poliomyelitis
endemic countries mean that a high percentage of the eradication cost has to be paid from external sources.
Political will and financial resources are urgently needed to accelerate the eradication initiative and to avoid
delays that would both threaten the success to date and substantially increase the overall cost. Such support
also needs to continue in those countries that are now poliomyelitis-free, as the quality of surveillance and
immunization has already started to decline in some areas.
7.
As more countries become free of the disease, the risk posed by laboratory stocks of wild poliovirus
increases substantially. If wild poliovirus were inadvertently released after immunization is stopped,
circulation could be re-established. WHO has drawn up a global action plan and timetable for safe
handling and maximum laboratory containment of wild polioviruses and potentially infectious materials.
This plan calls for countries to inventory laboratory stocks of wild polioviruses, destroy stocks of no
scientific value and move the remaining stocks to interim repositories starting in 1999.
FUTURE ACTION
8.
Eradication activities must be accelerated in the 14 most difficult countries, with additional rounds
during national immunization days in many areas. Data deriving from surveillance of acute flaccid
paralysis must be improved in order to identify accurately areas where wild polioviruses continue and to
target large scale house-to-house “mopping-up” immunization to halt transmission. Truces for
immunization need to be secured in countries affected by conflict. All countries must ensure that highquality immunization days reach all children aged less than five years.
9.
WHO’s advocacy is needed to secure the political support and funds necessary to conduct these
activities. WHO estimates that a total US$ 700 million is needed from external sources over the next three
years, the current shortfall being US$ 350 million. An emergency fund is needed to permit a rapid and
effective response when windows of opportunity open in countries that are affected by conflict or are
politically isolated.
2
EB103/7
10. Implementation of WHO’s plan of action for containment of wild polioviruses should start in 1999.
A coordinating group needs to be set up, with the authority to oversee the process, provide guidance to
WHO, and report formally to the Global Commission for the Certification of the Eradication of
Poliomyelitis.
ACTION BY THE EXECUTIVE BOARD
11.
The Executive Board is invited to consider the following draft resolution:
The Executive Board,
Noting the report of the Director-General on the global eradication of poliomyelitis.
RECOMMENDS to the Fifty-second World Health Assembly the adoption of the following
resolution:
The Fifty-second World Health Assembly,
Reaffirming WHO’s commitment to the global eradication of poliomyelitis by the end
of the year 2000;
Recognizing that substantial progress has been made towards eradication of
poliomyelitis, with large geographic areas of the world now free of poliomyelitis, and a fall
of 85% in annually reported cases since global eradication began in 1988;
Noting, however, that as of May 1999 a number of countries of south Asia and subSaharan Africa remain poliomyelitis-endemic, some of which are either affected by conflict
or constitute densely populated wild poliovirus “reservoirs”.
1.
URGES poliomyelitis-endemic Member States to accelerate eradication activities by
conducting additional immunization rounds each year, on either a national or subnational
basis; to improve the quality of national immunization days by ensuring that every child is
reached; to implement house-to-house “mopping-up” campaigns; and to enhance
surveillance by ensuring that all cases of acute flaccid paralysis are detected and promptly
investigated;
2.
URGES poliomyelitis-free Member States to sustain high levels of immunization
coverage and poliovirus surveillance until eradication is certified globally;
3.
URGES all Members States:
(1) to mobilize the human and financial resources necessary to accelerate
eradication in poliomyelitis-endemic countries;
(2) to begin in collaboration with WHO, the process leading to the laboratory
containment of wild poliovirus;
4.
REQUESTS the Director-General:
3
EB103/7
(1) to urge all partners to facilitate acceleration of the initiative to eradicate
poliomyelitis during the critical period 1999 to 2001;
(2) to collaborate with other organizations of the United Nations system and other
international bodies in arranging truces in countries affected by conflict for eradication
and facilitating activities;
(3) to help mobihze the necessary financing to implement eradication activities,
including establishment of an emergency fund to meet the needs of countries affected
by conflict, countries classified as major wild poliovirus reservoirs, and other countries
in particularly difficult circumstances;
(4) to collaborate with Member States in the establishment of a mechanism for
overseeing the process of laboratory containment of wild poliovirus.
4
EB103/7
ANNEX
COMPARISON OF “KNOWN OR PROBABLE” WILD POLIOVIRUS
TRANSMISSION IN 1988 AND BY JANUARY 1998
Wild poliovirus 1988
Sir
Known or probable wild
poliovirus transmission
Wild poliovirus 1998
W
*
■sin
(f <
J
111 v?
f
s'i'
k. -afiSB
■
17 u
t_
7’
■
Known or probable wild
poliovirus transmission
5
WHA41.28 Global eradication of poliomyelitis by the year 2000
The Forty-first World Health Assembly.
Appreciating the rapid progress being achieved by the Expanded Programme on
Immunization as evidenced by coverage for a third dose of poliomyelitis or
diphtheria/pertussis/tetanus vaccines of over 5090 of children under the age of one year in
developing countries, as well as by the prevention of the death of more than one million
children from measles neonatal tetanus or pertussis, and the prevention of the crippling of
nearly 200 000 children through poliomyelitis annually in these countries;
Confident that these coverage rates will continue to rise rapidly and be sustained, in pursuit
of the goal endorsed by the Thirtieth World Health Assembly” in 1977 (resolution
WHA30.53) - the provision of immunization for all children of the world by 1990 - and will
lead to further marked reductions in the incidence of most of the target diseases;
Aware that poliomyelitis is the target disease most amenable to global eradication, and that
regional eradication goals by or before the year 2000 have already been set in the Regions
of the Americas Europe and the Western Pacific;
Recognizing that the global eradication of poliomyelitis by' the year 2000 a goal cited in the
Declaration of Talloires, represents both a fitting challenge to be undertaken now, on the
Organization's fortieth anniversary, and an appropriate gift, together with the eradication of
smallpox, from the twentieth to the twenty-first century;
Noting:
(1) that achievement of the goal will depend on the political will of countries and on the
investment of adequate human and financial resources;
(2) that this achievement will be facilitated by the continued strengthening of the Expanded
Programme on Immunization within the context of primary health care and by improving
current poliomyelitis vaccines and clinical and laboratory surveillance;
(3 ) that efforts to eradicate poliomyelitis serve to strengthen other immunization and
health services, especially those for women and children;
1. DECLARES the commitment of WHO to the global eradiction of poliomyelitis by the year
2000;
2. EMPHASIZES that eradication efforts should be pursued in ways which strengthen the
development of the Expanded Programme on Immunization as a whole fostering its
contribution, in turn, to the development of the health infrastructure and of primary health
care;
3. INVITES Member States which have covered at least 70% of their target populations
with a protective course of poliomyelitis vaccine, and which continue to have cases of
poliomyelitis, to formulate plans for the elimination of the indigenous transmission of wild
poliomyelitis viruses in ways which strengthen and sustain their national immunization
programmes;
4. ENCOURAGES Member States which have not yet attained a 70% coverage rate to
accelerate their efforts so as to surpass this level as quickly as possible through means
which also improve and sustain the coverage for the other vaccines included within the
national immunization programmes;
5. REQUESTS Member States which have confirmed the absence of the indigenous
transmission of wild poliomyelitis viruses to sustain their success and to offer their
technical expertise, their resources and support to countries still working to achieve this
goal;
6. URGES all Member States:
(1 ) to intensify surveillance to ensure prompt identification and investigation of cases of
poliomyelitis and control of outbreaks and accurate and timely reporting of cases at national
and international levels;
(2 ) to make all possible efforts to permit the rehabilitation of as many as possible of the
children who still become disabled by poliomyelitis;
7. THANKS the many partners already collaborating in the Expanded Programme on
Immunization (including the United Nations agencies, multilateral and bilateral development
agencies, private and voluntary groups and concerned individuals), especially UNICEF for its
overall efforts and Rotary International for its "Polio Plus" initiative, and requests them to
continue to work together in support of national immunization programmes, including
activities aimed at the eradication of poliomyelitis, and to ensure that adequate resources
are available to accelerate and sustain these programmes;
8. REQUESTS the Director-General:
( 1 ) to strengthen the technical capacities of WHO in order to be able to respond better to
requests from governments for collaboration in:
(a) strengthening planning, training and supervision within national immunization
programmes and undertaking country-specific evaluation to facilitate corrective action
towards achieving the goal of eradication in countries with coverage of less than 70%;
(b) improving programme monitoring and evaluation at national, regional and global levels;
(c) improving national disease surveillance systems to permit the rapid control of outbreaks
and the investigation and confirmation of clinical diagnoses of poliomyelitis through
serological and virus isolation techniques;
(d) strengthening clinical laboratory services;
I
(e) improving the quality control and production of vaccines;
(2) to pursue efforts to promote the development and application of new vaccines, other
new technologies and knowledge that will help to achieve the eradiction goal;
(3) to seek from extrabudegtary contributions the additional resources required to support
these activities;
(4) to submit regular plans and reports of progress concerning the poliomyelitis eradication
effort through the Executive Board to the Health Assembly, in the context of the progress
being achieved by the Expanded Programme on Immunization.
Hbk Res., Vol. Ill (1st edj, 1.16.1 (Fifteenth plenary meeting, 13 May 1988 -Committee B,
fourth report)
OFFICE OF THE UNITED NATIONS HIGH COMMISSIONER
FOR HUMAN RIGHTS
ft,
STATUS OF RATIFICATIONS OF THE PRINCIPAL
INTERNATIONAL HUMAN RIGHTS TREATIES
As of 02 May 2003
The international human rights treaties of the United Nations that establish committees of experts (often referred to as "treaty bodies") to monitor their implementation are the following:
(1) the International Covenant on Economic, Social and Cultural Rights (CESCR), which is monitored by the Committee on Economic, Social and Cultural Rights;
(2) the International Covenant on Civil and Political Rights (CCPR), which is monitored by the Human Rights Committee;
(3) the Optional Protocol to the International Covenant on Civil and Political Rights (CCPR-OP1), which is administered by the Human Rights Committee; and
(4) the Second Optional Protocol to the International Covenant on Civil and Political Rights, aimed at the abolition of the death penalty (CCPR-OP2-DP).
(5) the International Convention on the Elimination of All Forms of Racial Discrimination (CERD), which is monitored by the Committee on the Elimination of Racial Discrimination;
(6) the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), which is monitored by the Committee on the Elimination of Discrimination against Women;
(7) the Optional Protocol to the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW-OP);
(8) the Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment (CAT), which is monitored by the Committee against Torture;
(9) the Convention on the Rights of the Child (CRC), which is monitored by the Committee on the Rights of the Child;
(10) the Optional Protocol to the Convention on the Rights of the Child (CRC-OP-AC) on the involvement of children in armed conflict;
(11) the Optional Protocol to the Convention on the Rights of the Child (CRC-OP-SC) on the sale of children, child prostitution and child pornography.
(12) the International Convention on the Protection of the Rights of All Migrant Workers and Members of Their Families (MWC), which was adopted by the General Assembly in 1990 and will enter into force when
20 States have accepted it;
The following chart of States shows which are a party (indicated by the date of adherence: ratification, accession or succession) or signatory (indicated by an "s" and the date of signature) to the United Nations
human rights treaties listed above. Self-governing territories that have ratified any of the treaties are also included in the chart. As at 02 May 2003, all 189 Member States of the United Nations and 4
non-Member States were a party to one or more of these treaties.
(7>
-> (
’ C
02 May 2003
CESCR
Afghanistan
24 Jan 83a
24 Jan 83
Albania
04 Oct 91“
04 Oct 91
Algeria
12 Sep 89
12 Sep 89
Angola
10 Jan 92“
10 Jan 92
a
;a~
CRC
CEDAW
06 Jul 83a
06 Mar 03
01 Apr 87 28 Mar 94
11 May 94“
11 May 94
11 May 94“ 27 Feb 92
19 Sen RQa
14 Feb 72*
22 May 96“
12 Sep 89* 16 Apr 93
.fOS Aua 02
s:05 Aug 02
15 Jan 97“
CCPR0P2
a
s:05 Aug 02
Andorra
CEDAWOP
CERD
CCPR0P1
CCPR
s:05 Aug 02 02 Jan 96
17 Sep 86“
06 Dec 90
25 Oct 88d
01 Aug 89“
19 Jul 93“ 06 Oct 93
10.Ian 92“
Antigua and Barbuda
15 Oct 02
s:28 Feb 0G
24 Sep 86* 05 Dec 90
CRCOPAC
CRCQPSC
MWC
20 Sep 02a
30 Apr 01
30 Apr 01
30 Apr 02
10 Sep 02
Argentina
08 Aug 86
08 Aug 86
OR Ana R6“
02 Oct 68
15 Jul 85
Armenia
13 Sep 93!
23 Jun 93
23 .Inn 93
23 Jun 93“
13 Sep 93“
13 Sep 93 23 Jun 93
Australia
10 Dec 75
13 Aug 80
25 Sen 91 “
02 Oct 90“
30 Sep 75*
28 Jul 83
08 Aug 89' 17 Dec 90
s:21 Oct 02
s:18DecO1
Austria
10 Sep 78
10 Sep 78
10 Den R7
02 Mar 93
09 May 72’
31 Mar 82
07 Sep 00
29 Jul 87* 06 Aug 92
01 Feb 02
s:06 Sep 00
Azerbaijan
13 Aug 92“
13 Aug 92
27 Nov 01 “
22 Jan 99“
16 Aug 96“
10 Jul 95“
01 Jun 01
16 Aug 96“ 13 Aug 92 “
03 Jul 02
03 Jul 02
11 Jan 99“
Bahamas
05 Aug 75d
06 Oct 93“
Bahrain
27 Mar 90“
18 Jun 02“
11 Jun 79“
06 Nov 84“
07 Sep 00
07 Sep 00
s:07 Oct 98
a
20 Feb 91
06 Mar 98“ 13 Feb 92 a
07 Sep 00
05 Oct 98“ 03 Aug 90
Bangladesh
05 Oct 98“
07 Sep 00
Barbados
05 Jan 73“
05 Jan 73
05 .Ian 73“
08 Nov 72“
16 Oct 80
09 Oct 90
Belarus
12 Nov 73
12 Nov 73
30 Snn 92“
08 Apr 69
04 Feb 81
13 Mar 87 02 Oct 90
Belgium
21 Apr 83
21 Apr 83
17 Mav 94“
07 Aug 75*
10 Jul 85
s:10 Dec 99
25 Jun 99* 16 Dec 91
06 May 02
s:06 Sep 00
Belize
s:06 Sep 00
10 Jun 96
14 Nov 01
16 May 90
09 Dec 02 “
17 Mar 86“ 02 May 90
s:06 Sep 00
s:06 Sep 00
Benin
12 Mar 92“
12 Mar 92
30 Nov 01
12 Mar 92
s:25 May 00
12 Mar 92“ 03 Aug 90
s:22 Feb 01
s. 22 Feb 01
s:26 Mar 73
31 Aug 81
22 Sep 70
08 Jun 90
27 Sep 00
12 Apr 99 26 Jun 90
16 Jul 93d
01 Sep 93d
04 Sep 02
01 Sep 93“ 01 Sep 93 d
20 Feb 74“
13 Aug 96“
27 Mar 68*
01 Feb 84
08 Dec 98
12 Mar 92“
Bhutan
Bolivia
12 Aug 82“
12 Aug 82
Bosnia and Herzegovina
03 Mar 92d
01 Sep 93
Brunei Darussalam
d
08 Sep 00
Botswana
Brazil
12 Ana R2“
24 Jan 92“
24 Jan 92
a
01 Mar 95
16 Mar 01
24 Jan 02“
14 Nov 01“
01 Aug 90
s:10 Nov 01
12 Oct 00“
s:07 Sep 00
04 Sep 02
13 Dec 96“
s:06 Sep 00
s:06 Sep 00
08 Sep 00 14 Mar 95 a
28 Jun 02
28 Sep 89 25 Sep 90
27 Dec 95 a
2
02 May 2003
CESCR
Bulgaria
Burkina Faso
Burundi
21 Sep 70
04 Jan gg3
09 May 90*
ICPI
CCPROP1
26 MarQ?’
21 Sep 70
04 Jan 99
a
09 May 90
a
CCPROP2
10 Aug 99
04 Jan 99 a
a
CAI
CRCOPAC
CRCOPSC
08 Aug 66*
08 Feb 82
16 Dec 86* 03 Jun 91
12 Feb 02
12 Feb 02
18 Jul 74a
14 0ct87a
s:16 Nov 01
04 Jan 99* 31 Aug 90
s:16 Nov 01
s:16 Nov 01
27 Oct 77
08 Jan 92
s:13 Nov 01
18Feb93a 19 Oct 90
s:11 Nov 01
IRC
30 May 02
19Dec86a 11 Jan 93
s:05 Oct 01
s:05 Oct 01
24 Jun 87* 13 Dec 91
07 Jul 00
s:10 Nov 01
04 Jun 92a 04 Jun 92 a
10 May 02a
10 May 02a
09 Jun 95a 02 Oct 90
s:03 May 02
s:03 May 02
30 Sep 88 13 Aug 90
s:15 Nov 01
07 Feb 03
04 Oct 88 03 Mar 92
s:15 Mar 01
03 Dec 02
08 Dec 87 28 Jan 91
s:06 Sep 00
s:06 Sep 00
27 Jun R4a
24 Jun 71
23 Aug 94
a
19 Mav 76a
14 Oct 70
10 Dec 81
06 Aug 93
a
19 Mav 00a
03 Oct 79a
05 Dec 80*
OR Mav R1 a
16 Mar 71
21 Jun 91a
23 Apr 92
09 Jun 95a
17 Aug 77a
09 Jun 95a
2R Mav 9?a
20 Oct 71*
08 Dec 89
29 Dec 81a
04 Nov 80
02 Sep 81
19 Jan 82
s:22 Sep 00
31 Oct 94a
s:22 Sep 00 23 Jun 93
11 Jul 88a
26 Jul 82
14 Oct 93
26 May 92
Cameroon
27 Jun 84a
27 Jun 84
Canada
19 May 76a
19 May 76
Cape Verde
06 Aug 93“
Central African Republic
08 May81!
08 May 81
a
Chad
09 Jun 95a
09 Jun 95
a
Chile
10 Feb 72
10 Feb 72
China
27 Mar 01
Colombia
29 Oct 69
19 May 00a
s:05 Oct 98
29 Oct 69
29 Oct 69
05 Aug 97a
Comoros
05 Oct 83
a
05 Oct R3a
18 Oct 02a
s: 10 Dec 99
s:10 Dec 99
IWC
s:16Nov01
s:13Nov01
a
s. 27 Jun 00
15 00192* 15 Oct 92
15 Oct 92a
26 May 92a
05 Oct 83a
CEDAWOP
s:06 Jun 00
28 Nov 83
Cambodia
Congo
CEDAW
lERD
16 Sep 97a
s:24 Sep 93
24 May 95
s:22 Sep 00
a
06 Jun 97 a
Cook Islands
Costa Rica
29 Nov 68
29 Nov 68
Croatia
08 Oct 91d
12 Oct 92
d
24 Jan 03
29 Nov 6R
05 Jun 98
16 Jan 67*
04 Apr 86
20 Sep 01
11 Nov 93’ 21 Aug 90
12 Oct 95a
12 Oct 95a
12 Oct 92d
09 Sep 92d
07 Mar 01
12 0ct92d 12 Oct 92
15 Feb 72
17 Jul 80
s: 17 Mar OC
17 May 95 21 Aug 91
21 Apr 67’
23 Jul 85a
26 Apr 02
18 Jul 91* 07 Feb 91
27 Feb 01
01 Jan 93d 22 Feb 93 d
Cuba
15 Anr 92
10 Sep 99*
d
10 Apr 02
13 May 02
s:13Nov00
25 Sep 01
s:08 Feb 01
Cyprus
02 Apr 69
02 Apr 69
Czech Republic
01 Jan 93d
22 Feb 93
d
22 Fah 93 d
22 Feb 93d
22 Feb 93d
Cote d'Ivoire
26 Mar 92a
26 Mar 92
a
05 Mar 97 a
04 Jan 73a
18 Dec 95
18 Dec 95a 04 Feb 91
Democratic People's
14 Sep 81a
14 Sep 81
a
27 Feb 01a
21 Sep 90
01 Nov 76a
01 Nov 76
a
21 Apr 76a
17 Oct 86
18 Mar 96 28 Sep 90
12 Nov 01
12Nov01a
Denmark
06 Jan 72
06 Jan 72
09 Dec 71*
21 Apr 83
27 May 87* 19 Jul 91
28 Aug 02
s:07 Sep 00
Djibouti
05 Nov 02a
05 Nov 02
a
17 Jun 93
a
20 Sep 02 a
20 Sep 02a
30 Nov 01
Republic of Korea
Democratic Republic of
01 Nov 76 a
the Congo
Dominica
17 Jun 93a
06 Jan 72
24 Feb 94
05 Nnv 02 a
05 Nov 02a
31 May 00
02 Dec 98a
05 Nov 02* 06 Dec 90
15 Sep 80
13 Mar 91
3
02 May 2003
CESCR
CCPR0P1
CCPR
CCPR0P2
CAT
CRC
CRCOPAC
CERD
CEDAW
CEDAWOP
25 May 83a
02 Sep 82
10 Aug 01
s:04Feb85 11 Jun 91
s:09 May 02
22 Sep 66a
09 Nov 81
05 Feb 02
30 Mar 88' 23 Mar 90
s:06 Sep 00
01 May 67
18 Sep 81
CRCOPSC
MWC
s:06 Sep 00
05 Feb 02a
12 Jul 02“
19 Feb 93“
Dominican Republic
04 Jan 78a
04 Jan 78
04 Jan 7Ra
Ecuador
06 Mar 69
06 Mar 69
OR Mar 89
Egypt
14 Jan 82
14 Jan 82
El Salvador
30 Nov 79
30 NOV 79
06 Jun 95
30 Nov 79“
19 Aug 81
Equatorial Guinea
25 Sep 87“
25 Sep 87
25 San 87“
08 Oct 02“
23 Oct 84“
Eritrea
17 Apr 01“
23 Jan 02
01 Aug 01“
05 Sep 95“
03 Aug 94
Estonia
21 Oct 91“
21 Oct 91
21 Oct 91“
21 Oct 91“
21 Oct 91“ 21 Oct 91
Ethiopia
11 Jun 93“
11 Jun 93
23 Jun 76“
10 Sep 81
13 Mar 94“ 14 May 91
11 Jan 73d
28 Aug 95
13 Aug 93
14 Jul 70’
04 Sep 86
29 Dec 00
30 Aug 89’ 21 Jun 91
11 Apr 02
s:07 Sep 00
28 Jul 71“
14 Dec 83
09 Jun 00
18 Feb 86’ 08 Aug 90
05 Feb 03
06 Feb 03
29 Feb 80
21 Jan 83
08 Sep 00 09 Feb 94
s:08 Sep 00
s:08 Sep 00
29 Dec 78“
16 Apr 93
s:23 Oct 85 08 Aug 90
s:21 Dec 00
s:21 Dec 00
s:06 Sep 00
s:06 Sep 00
a
23 Feb 93“
21 Oct 91 “
Fiji
04 Apr 91
25 Jun 86“ 06 Jul 90
s:04 Apr 01
08 Oct 02“ 15 Jun 92 a
19 Aug 75
19 Aug 75
19 Ann 75
France
04 Nov 80“
04 Nov 80
17 Feb R4“
Gabon
21 Jan 83“
21 Jan 83
Gambia
29 Dec 78“
22 Mar 79
09 Jun 88“
Georgia
03 May 94“
03 May 94
03 Mav 94 “
22 Mar 99“
02 Jun 99“
26 Oct 94“
01 Aug 02“
26 Oct 94“ 02 Jun 94 a
Germany
17 Dec 73
17 Dec 73
25 Ann 93“
18 Aug 92
16 May 69’
10 Jul 85
15 Jan 02
01 Oct 90’ 06 Mar 92
Ghana
08 Sep 00
08 Sep 00
08 Sen 00
08 Sep 66
02 Jan 86
s:24 Feb 00
08 Sep 00 05 Feb 90
Greece
16 May 85“
05 May 97
05 Mav 97 “
18 Jun 70
07 Jun 83
24 Jan 02
06 Oct 88’ 11 May 93
Grenada
06 Sep 9T
06 Sep 91
s:17 Dec 81
31 Aug 90
Guatemala
19 May 88“
06 May 92
2R Nov 00“
18 Jan 83
12 Aug 82
Guinea
24 Jan 78
24 Jan 78
17 Jun 93
14 Mar 77
09 Aug 82
Guinea-Bissau
02 Jul 92“
s:12 Sep 00
ff12 Sftn 00
s:12 Sep 00
23 Aug 85
Guyana
15 Feb 77
15 Feb 77
10 Mav 93 “
15 Feb 77
17 Jul 80
19 May 88 14 Jan 91
19 Dec 72
20 Jul 81
06 Feb 91
Haiti
Honduras
17 Feb 81
25 Aug 97
ft-19 Dftc 65
Hungary
17 Jan 74
17 Jan 74
07 Snn RR“
Iceland
22 Nov 79
22 Aug 79
22 Ann 79“
08 Sep 00
s:07 Sep 00
s:07 Sep 00
10 May 02
10 May 02
05 Nov 90
10 May 02
05 Jan 90“ 06 Jun 90
10 Oct 89 13 Jul 90
s:12 Sep 00
01 May 69
Holy See
07 Feb 03“
a
Finland
05 May 97“
14 Mar 03
18 Apr 02
17 Jun 96“ 10 Jul 90
a
08 Sep 00“
s:08 Sep 00
s:08 Sep 00
09 Jun 95
s: 15 Aug 02
s:15Aug 02
26 Jun 02“ 20 Apr 90
24 Oct 01
24 Oct 01
05 Dec 96“ 10 Aug 90
14 Aug 02a
09 May 02“
02 Oct 01
09 Jul 01
s:12 Sep 00 21 Aug 90
10 Oct 02“
03 Mar 83
24 Feb 94“
01 May 67’
22 Dec 80
22 Dec 00“
15 Apr 87’ 08 Oct 91
02 Apr 91“
13 Mar 67’
18 Jun 85
07 Mar 01
23 Oct 96’ 28 Oct 92
14 Mar 03
s:12 Sep 00
4
02 May 2003
CESCR
India
10 Apr 79"
CCPR
CCPROP1
CCPROP2
10 Apr 79
Indonesia
:erd
CEDAW
03 Dec 68
09 Jul 93
25 Jun 99"
13 Sep 84
;ai
crc
s:14 0ct97 11 Dec 92
s:28 Feb 0C
CRCOPAC
CRCOPSC
s:24 Sep 01
s:24 Sep 01
18 Nov 02
s:07 Sep 00
MWC
a
28 Oct 98 05 Sep 90
13 Jul 94
24 Jun 75
24 Jun 75
29 Aug 68
Iraq
25 Jan 71
25 Jan 71
14 Jan 70
13 Aug 86"
Ireland
08 Dec 89
08 Dec 89
29 Dec 00*
23 Dec 85"
Israel
03 Oct 91
03 Oct 91
03 Jan 79
03 Oct 91
Italy
15 Sep 78
15 Sep 78
05 Jan 76’
10 Jun 85
Jamaica
03 Oct 75
03 Oct 75
04 Jun 71
Japan
21 Jun 79
21 Jun 79
Jordan
28 May 75
28 May 75
Iran (Islamic Republic
CEDAWOP
of)
OR Dac RO
15 Sen 7R
18 Jun 93’
14 Feb 95
Kazakhstan
Kenya
01 May 72"
01 May 72
a
15 Jun 94 a
08 Sep 00
11 Apr 02* 28 Sep 92
03 Oct 91 03 Oct 91
s:14 Nov 01
12 Jan 89* 05 Sep 91
10 May 02
10 May 02
19 Oct 84
14 May 91
10 May 02
s:08 Sep 00
15 Dec 95"
25 Jun 85
29 Jun 99" 22 Apr 94
s:10 May 02
s: 10 May 02
30 May 74’
01 Jul 92
13 Nov 91 24 May 91
s:06 Sep 0G
s:06 Sep 00
26 Aug 98’
26 Aug 98"
26 Aug 98" 12 Aug 94
10 Apr 03
24 Aug 01
13 Sep 01’
09 Mar 84"
21 Feb 97" 31 Jul 90
28 Jan 02
s:08 Sep 00
22 Sep 00
24 Aug 01
11 Dec 95 a
Kiribati
Kuwait
21 May 96’
21 May 96
a
Kyrgyzstan
07 Oct 94"
07 Oct 94
a
Lao People's
s:07 Dec 00
07 Ont 05 ’
s:07 Dec 00
15 Oct 68’
02 Sep 94’
05 Sep 97"
10 Feb 97"
22 Feb 74’
14 Aug 81
14 Apr 92"
15 Apr 92’
14 Apr 92" 15 Apr 92
12 Nov 71"
21 Apr 97’
05 Oct 00" 14 May 91
04 Nov 71"
22 Aug 95’
05 Nov 76’
17 Jul 84
04 Jun 93
03 Jul 68’
16 May 89"
16 May 89" 16 Apr 93
08 Mar 96" 21 Oct 91
22 Jul 02’
05 Sep 97" 07 Oct 94
a
12 Feb 03"
08 May 91 ’
Democratic Republic
Latvia
14 Apr 92"
14 Apr 92
a
Lebanon
03 Nov 72’
03 Nov 72
a
Lesotho
09 Sep 92’
09 Sep 92
a
Liberia
s:18Apr67
22 Jun 94’
07 Sen 00’
s:18Apr67
s:06 Sep 00
a
s:01 Feb 02
s:01 Feb 02
s:10 Oct 01
13 Nov 01" 10 Mar 92
s:06 Sep 00
s:06 Sep 00
s:08 Sep 00
Libyan Arab Jamahiriya
15 May 70"
15 May 70
a
Liechtenstein
10 Dec 98’
10 Dec 98
a
10 Drc 9Ra
10 Dec 98’
01 Mar 00’
22 Dec 95"
24 Oct 01
02 Nov 90* 22 Dec 95
s:08 Sep 00
Lithuania
20 Nov 91"
20 Nov 91
a
20 Nov 91 ’
28 Mar 02
10 Dec 98
18 Jan 94"
s:08 Sep 00
01 Feb 96 31 Jan 92 a
20 Feb 03
Luxembourg
18 Aug 83
18 Aug 83
1R Aim R3’
12 Feb 92
01 May 78*
02 Feb 89
s:10 Dec 99
29 Sep 87* 07 Mar 94
s:08 Sep 00
s:08 Sep 00
Madagascar
22 Sep 71
21 Jun 71
07 Feb 69
17 Mar 89
s:07 Sep 00
s:010ct01 19 Mar 91
s:07 Sep 00
s:07 Sep 00
s:07 Sep 00
s:07 Sep 00
Malawi
22 Dec 93’
22 Dec 93
16 Mav R9’
21 Jim 71
a
11 Ji in 96
11 Jun 96"
12 Mar 87’
s:07 Sep 00
11 Jun 96’ 03 Jan 91
a
a
5
02 May 2003
CESCR
CCPR0P1
CCPR
CCPROP2
CERD
Mali
16 Jul 74“
16 Jul 74
Malta
13 Sep 90
13 Sep 90
24 Or.t 01 “
a
13 Sen 90 “
29 Dec 94“
CEDAWOP
:ai
CRC
CRCOPAQ
CRCOPSC
05 Jul 95
17 Feb 95 a
24 Apr 84a
01 Jul 93a
11 Feb 91
s:10May02
10 May 02
16 Jul 74“
10 Sep 85
26 Feb 99“ 21 Sep 90
16 May 02
16 May 02a
27 May 71*
08Mar91a
13 Sep 9(> 30 Sep 90
10 May 02
s:07 Sep 00
s:11 Nov 01
s:11 Nov 01
15 Mar 02
15 Mar 02
06 Dec 91“ 21 Jun 93
14 Nov 01
s:26 Jun 00
24 Jan 02“ 06 Jul 90
s:12 Nov 01
s:12Nov01
22 May 02
02 Oct 01
Malaysia
Maldives
CEDAW
05 Dec 00“
MWC
05 Oct 93
Marshall Islands
Mauritius
12 Dec 73“
12 Dec 73
Mexico
23 Mar 81“
23 Mar 81
a
16 May 91
13 Dec 88
10 May 01“
12 Drc 73“
30 May 72“
09 Jul 84“
s:11 Nov 01
09 Dec 92“ 26 Jul 90
15 Mar 02
20 Feb 75
23 Mar 81
15 Mar 02
23 Jan 86* 21 Sep 90
Mauritania
a
08 Mar 99
05 May 93 “
Micronesia (Federated
States of)
Monaco
28 Aug 97
28 Aug 97
Mongolia
18 Nov 74
18 Nov 74
Morocco
03 May 79
03 May 79
28 Mar 00“
16 AnrQ1“
21 Jul 93“
21 Jul 93
Mozambique
27 Sep 95“
20 Jul 81
18 Dec 70
22 Jun 93“
21 Jun 93 21 Jun 93
18 Apr 83“
16 Apr 97“
14 Sep 99“ 26 Apr 94
22 Jul 97“
15 Jul 91
Myanmar
Namibia
28 Nov 94“
28 Nov 94
s:12 Nov 01
Nauru
2ft Nov 94 “
28 Nov 94“
28 Mar 02
06 Aug 69
11 Nov 82“
23 Nov 92“
26 May 00
06 Mar 03“
a
28 Nov 94“ 01 Oct 90
s:12Nov01 27 Jul 94
s:12 Nov 01
.<5-12 A/nu 01
a
16 Apr 02
16 Apr 02
s:08 Sep 00
s:08 Sep 00
Nepal
14 May 91“
14 May 91
14 Mav ft1 a
04 Mar 98“
30 Jan 71“
22 Apr 91
s:18 Dec 01
14 May 91“ 14 Sep 90
s:08 Sep 00
s:08 Sep 00
Netherlands
11 Dec 78
11 Dec 78
11 Rpc 7ft
26 Mar 91
10 Dec 71’
23 Jul 91
22 May 02
21 Dec 88' 06 Feb 95
s:07 Sep 00
s:07 Sep 00
New Zealand
28 Dec 78
28 Dec 78
2fi Mav R9 a
22 Feb 90
22 Nov 72
10 Jan 85
08 Sep 00
10 Dec 89' 06 Apr 93
12 Nov 01
s:07 Sep 00
Nicaragua
12 Mar 80“
12 Mar 80
12 Mar ft0“
15 Feb 78“
27 Oct 81
s: 15 Apr 85 05 Oct 90
Niger
07 Mar SO1
07 Mar 86
07 MarR6“
27 Apr 67
08 Oct 99“
05 Oct 98“ 30 Sep 90
Nigeria
29 Jul 93“
29 Jul 93
16 Oct 67“
13 Jun 85
s:08 Sep 00
s:08 Sep 00
s:13 Jun 00
02 Oct 01
s:26 Sep 01
s:26 Sep 01
s:08 Sep 00
13 Sep 72
13 Sep 72
13 Sen 72
05 Sep 91
06 Aug 70'
21 May 81
05 Mar 02
09 Jul 86' 08 Jan 91
09 Dec 96 “
Oman
Pakistan
19 Apr 91
20 Dec 95 “
Niue
Norway
28 Jun 01
21 Jun 93
21 Sep 66
12 Mar 96“
12 Nov 90
6
02 May 2003
CCPR
CCPROP1
CCPROP2
:erd
CEDAW
CEDAWOP
CR(
04 Aug 95
Palau
Panama
JAI
08 Mar 77a
08 Mar 77
OR Mar 77
21 Jan 93®
Papua New Guinea
16 Aug 67
29 Oct 81
27 Jan 82a
12 Jan 95a
10 May 01
CRCOPAC
CRCOPSC
08 Aug 01
09 Feb 01
24 Aug 87 12 Dec 90
02 Mar 93
Paraguay
10 Jun 92®
10 Jun 92
10 Jan 95 a
s:13 Sep 00
06 Apr 87a
14 May 01
12 Mar 90' 25 Sep 90
27 Sep 02
s:13 Sep 00
Peru
28 Apr 78
28 Apr 78
03 Ort R0a
29 Sep 71’
13 Sep 82
09 Apr 01
07 Jul 88’ 05 Sep 90
09 May 02
09 May 02
Philippines
07 Jun 74
23 Oct 86
?? Ann R9a
15 Sep 67
05 Aug 81
s:21 Mar 00
18 Jun 86® 21 Aug 90
s:08 Sep 06
s:08 Sep 00
Poland
18 Mar 77
18 Mar 77
07 Nov 91 ®
05 Dec 68*
30 Jul 80
26 Jul 89' 07 Jun 91
s: 13 Feb 02
s:13Feb 02
Portugal
31 Jul 78
15 Jun 78
03 Mav 83
24 Aug 82a
30 Jul 80
09 Feb 89* 21 Sep 90
s:06 Sep 00
s:06 Sep 00
11 Jan 00® 04 Apr 95
25 Jul 02a
14 Dec 01®
s:06 Sep 00
s:06 Sep 00
s:08 Feb 02
s:08 Feb 02
18 Oct 01
17 Oct 90
Republic of Korea
10 Apr 90®
10 Apr 90
a
a
05 Dec 78'
10 Anr 90®
Republic of Moldova
26 Jan 93®
26 Jan 93
Romania
09 Dec 74
09 Dec 74
20 Jul 93a
Russian Federation
16 Oct 73
16 Oct 73
01 Ort 91 ®
Rwanda
16 Apr 75®
16 Apr 75
27 Feb 91
a
Saint Lucia
09 Nov 81®
09 Nov 81
a
09 Nov R1 ®
27 Dec 84
09 Jan 95® 20 Nov 91
a
26 Jan 93®
01 Jul 94®
15 Sep 7(?
07 Jan 82
s:06 Sep 00
18 Dec 90® 28 Sep 90
11 Nov 01
04 Feb 69'
23 Jan 81
s:08 May 01
03 Mar 87' 17 Aug 90
s:15FebO1
16 Apr 75®
02 Mar 81
24 Jan 91
23 Apr 02 a
15 Mar 02®
25 Apr 85®
24 Jul 90
14 Feb 90d
08 Oct 82®
16 Jun 93
09 Nov 81®
05 Aug 81®
01 Aug 01® 26 Oct 93
25 Sep 92®
29 Nov 94
s:05 Jun 00
s:05 Jun 00
Saint Kitts and Nevis
Saint Vincent and the
26 Apr 02
22 Jul 76a
Qatar
MWC
a
28 Nov 95 26 Jan 93
s:13 Sep 00
05 Jul 95
Grenadines
Samoa
San Marino
Sao Tome and Principe
18 Oct 85®
s:31 Oct 95
18 Oct 85
a
1R Or.t R5 a
K'Ofi Sftn 00
s:31 Oct 95
Saudi Arabia
13 FaH 78
Senegal
13 Feb 78
13 Feb 78
Seychelles
05 May 92®
05 May 92
a
05 Mav 92 ®
Sierra Leone
23 Aug 96®
23 Aug 96
a
23 Ann 96®
15 Dec 94®
12 Mar 02
s:18SepO2 25 Nov 91 a
s:06 Sep 00
s:31 Oct 95
a
23 Sep 97®
08 Sep 00
19 Apr 72'
05 Feb 85
07 Mar 78®
06 May 92®
02 Aug 67
11 Nov 88
28 May 93d
28 May 93
d
2R Mav 93
22 Jun 99
28 May 93d
28 May 93d
s:06 Sep 00 14 May 91
s:06 Sep 00
23 Sep 97® 26 Jan 96 a
26 May 00
s:08 Sep 00
05 Oct 95®
Singapore
Slovakia
s:06 Sep 00
21 Aug 86' 01 Aug 90
s:08 Sep 00
s:08 Sep 00
09 Jun 99®
05 May 92® 07 Sep 90 a
s:23 Jan 01
s:23 Jan 01
15 Dec 94®
25 Apr 01 18 Jun 90
16 May 02
17 Sep 01
s:15 Sep 00
05 Oct 95
17 Nov 00
a
28 May 93d 28 May 93 d
s:07 Sep 00
s:30 Nov 01
7
02 May 2003
CESCR
CCPR
06 Jul 92
a
CCPR0P1
CCPR0P2
CERD
CEDAW
CEDAWOP
CAT
16 Jul 93“
10 Mar 94
06 Jul 92d
06 Jul 92d
s:10 Dec 99
16 Jul 93u 06 Jul 92 d
17 Mar 82d
06 May 02a
06 May 02
10 Apr 95 a
Slovenia
06 Jul 92d
Solomon Islands
17Mar82d
Somalia
24 Jan 90“
24 Jan 90
South Africa
s:03 Oct 94
10 Dec 98
2ft Ann 02“
28 Aug 02“
10 Dec 98’
15 Dec 95
Spain
27 Apr 77
27 Apr 77
25 Jan 85
11 Apr 91
13 Sep 68“
05 Jan 84
Sri Lanka
11 Jun 80“
11 Jun 80
03 Oct 97 “
18 Feb 82“
05 Oct 81
Sudan
18 Mar 86“
18 Mar 76
Suriname
28 Dec 76“
28 Dec 76
a
15 Mar 84d
06 Dec 71
Sweden
06 Dec 71
06 Dec 71
Switzerland
18 Jun 92“
18 Jun 92
a
Syrian Arab Republic
21 Apr 69“
21 Apr 69
a
Tajikistan
04 Jan 99“
04 Jan 99
a
Thailand
05 Sep 99“
29 Oct 96
The Former Yugoslav
18 Jan 94d
18 Jan 94
d
1? Dec. 94“
21 Oct 87’ 06 Dec 90
08 Mar 02
15 Oct 02“
03 Jan 94“ 12 Jul 91
08 Sep 00
24 May 84“
24 May 84
a
30 Mar ftft “
MWC
18 Dec 01
11 Mar 96“
s:04 Jun 86 03 Aug 90
s:10 May 02
s:10May02
08 Jan 86’ 29 Jun 90
20 Feb 03
s:08 Jun 00
26 Jun 02
s:07 Sep 00
05 Aug 02 a
05 Aug 02“
s:17Ju!01
s:17 Jul 01
02 Mar 93
02 Mar 93“
08 Sep 95
24 Apr 03
06 Dec 71’
02 Jul 80
16 Jun 94“
29 Nov 94“
27 Mar 97
02 Dec 86’ 24 Feb 97
21 Apr 69“
28 Mar 03“
15 Jul 93
11 Jan 95“
26 Oct 93“
s:07 Sep 00
28 Jan 03“
09 Aug 85“
14 Jun 00
18 Jan 94d
18 Jan 94d
s:03 Apr 00
01 Sep 72“
26 Sep 83“
26 Jan 95
s:08 Sep 00
06 Jul 01
11 May 90
04 Jan 99“
s:08 Sep OG
s:08 Feb 02
07 Apr 69“
Swaziland
CRCOPSC
10 Dec 98* 16 Jun 95
21 Mar 77“
2ft Dar. 76“
CRCOPAC
24 Jan 90“ s:09 May 0
26 Aug 75
24 Jan 90“
CRC
11 Jan 95“ 26 Oct 93
a
08 Jan 02
27 Mar 92 a
12 Dec 94d 02 Dec 93
Republic of Macedonia
Togo
s:15 Nov 01
s:15 Nov 01
06 Nov 95 “
16 Feb 72“
Tonga
04 Oct 73
12 Jan 90
06 Dec 91
18 Mar 69
13 Jan 67
20 Sep 85
23 Sep 88’ 31 Jan 92
02 Jan 03
13 Sep 02
s: 15 Aug 00
s: 15 Aug 00
16 Sep 02
20 Dec 85“
02 Aug 88’ 04 Apr 95
s:08 Sep 00
19 Aug 02
s:13 Jan 99
01 May 97“
01 May 97
29 Sep 94“
01 May 97“
25 Jun 99“ 20 Sep 93 a
06 Oct 99“
22 Sep 95 a
03 Nov 86“ 17 Aug 90
06 May 02 a
30 Nov 01“
14 Nov 95“
24 Feb 87 28 Aug 91
s:07 Sep 00
s:07 Sep 00
Trinidad and Tobago
08 Dec 78“
21 Dec 78
Tunisia
18 Mar 69
Turkey
Turkmenistan
a
01 Mav 97 “
11 Jan 00“
Tuvalu
Uganda
21 Jan 87“
21 Jun 95
Ukraine
12 Nov 73
12 Nov 73
United Arab Emirates
18 Nov 87’ 01 Aug 90
a
14 Nnv 95
21 Nov 80“
23 Jul 85
25 Jul 91 “
07 Mar 69’
12 Mar 81
20 Jun 74“
29 Oct 02
s:07 Sep 00
03 Jan 97
8
02 May 2003
CCPR
CESCR
20 May 76
20 May 76
11 Jun 76a
11 Jun 76
s:05 Oct 71
08 Jun 92
Uruguay
01 Apr 70
01 Apr 70
Uzbekistan
28 Sep 95a
28 Sep 95
United Kingdom of Great
CCPR0P2
CCPR0P1
10 Dec 99
:a'
:erd
CEDAW
07 Mar 69
07 Apr 86
08 Dec 88’ 16 Dec 91
27 Oct 72a
20 Aug 85
11 Jun 91
21 Oct 94
s:17 Jul 80
21 Oct 94* s:16 Feb 9
23 Dec 02
23 Dec 02
30 Aug 68’
09 Oct 81
24 Oct 86* 20 Nov 90
s:07 Sep 0G
s:07 Sep 00
28 Sep 95a
19 Jul 95a
28 Sep 95a 29 Jun 94
08 Sep 95
07 Jul 93
29 Jul 91' 14 Sep 90
s:07 Sep 0G
09 May 02
20 Dec 01
20 Dec 01
31 Jan 03
10 Oct 02
CEDAWOP
CRC
CRCOPAC
CRCOPSC
s:07 Sep 0G
s:07 Sep 00
MW(
Britain and Northern
Ireland
United Republic of
a
24 Apr 03a
Tanzania
United States of America
21 Jan 93
01 Anr 70
a
28 Sfin 95 a
Vanuatu
10 May 78
Venezuela
10 May 78
Viet Nam
24 Sep 82a
24 Sep 82
Yemen
09 Feb 87a
09 Feb 87
a
Yugoslavia
12Mar01d
12 Mar 01
<1
06 Sad 01
Zambia
10 Apr 84a
10 Apr 84
a
10 Anr 84 a
Zimbabwe
13May91a
13 May 91
a
REMAINING SIGNATORIES
22 Feb 93
10 Mav 78
a
06 Sep 01a
26 Jul 01
10 Oct 67
02 May 83
09 Jun 82a
17 Feb 82
28 Feb 90
18 0ct72a
30 May 84a
05 Nov 91a 01 May 91
12 Mar01d
26 Feb 82
12 Mar 01^ 03 Jan 91
04 Feb 72
21 Jun 85
07 Oct 98a 06 Dec 91
13 May 91a
14 May 91a
11 Sep 90
13 May 02
15 Feb 01a
■i
d
CESCR
CCPR
CCPR-OP1
CCPR-OP2-DP
GERD
CEDAW
CEDAW-OP
CAT
CRC
CRC-OP-AC
CRC-OP-SC
MWC
7
8
5
7
8
2
33
12
2
63
68
10
146
149
104
49
166
172
50
132
191
51
50
21
(&)
TOTAL STATE PARTIES
Notes:
The dates listed refer to the date of ratification, unless followed by:
an "a" which signifies accession,
"d", which signifies succession, or
"s", which signifies signature only.
(&) Among non-State parties.
* indicates that the state party has recognized the competence to receive and process individual communications of the Committee on the Elimination of Racial Discrimination under article 14 of the
CERD (total 40 state parties) or of the Committee against Torture under article 22 of CAT(total 52 state parties).
9
/
■
WHO/V&B/00.29
ORIGINAL: ENGLISH
DISTR.: GENERAL
Meeting on the impact of
targeted programmes on
health systems:
a case study of the Polio
Eradication Initiative
WHO, Geneva, 16-17 December 1999
DEPARTMENT OF VACCINES
AND BIOLOGICALS
World Health Organization
Geneva
2000
The Department of Vaccines and Biologicals
thanks the donors whose unspecified financial support
has made the production of this document possible.
This document was produced by the
Expanded Programme on Immunization
of the Department of Vaccines and Biologicals
Edited by Health and Development Networks (www.hdnet.org)
Ordering code: WHO/V&.B/00.29
Printed: September2000
This document is available on the Internet at:
www.who.int/vaccines-documents/
Copies may be requested from:
World Health Organization
Department of Vaccines and Biologicals
CH-1211 Geneva 27, Switzerland
• Fax: + 41 22 791 4192 • E-mail: vaccines©who.int •
© World Health Organization 2000
This document is not a formal publication of the World Health Organization (WHO), and all rights are
reserved by the Organization. The document may, however, be freely reviewed, abstracted, reproduced
and translated, in part or in whole, but not for sale nor for use in conjunction with commercial purposes.
The views expressed in documents by named authors are solely the responsibility of those authors.
ii
Contents
Abbreviations
v
A cknowledgemen ts
vii
Executive summary
ix
1.
Introduction
1
2.
Background
3
3.
Summary of the meeting...............................................
5
3.1 Study methodologies and broad findings..............
3.2 Major areas of PE impact on health systems and
services delivery.........................................................
3.3 Remaining information gaps...................................
3.4 Recommendations......................................................
3.5 Next steps: optimizing opportunities of targeted
health programmes....................................................
5
. 8
11
11
4.
Conclusions
15
5.
References
17
Annex 1: Agenda
19
Annex 2: List of participants
21
Annex 3: Summary table of new studies on PE
27
Annex 4: Summary of presentations, discussion and comments
28
Annex 5: Using polio eradication (PE) activities to strengthen
routine immunization: the 10-step programme........
46
12
iii
Abbreviations
AFP
acute flaccid paralysis
AIIMS
All India Institute of Medical Sciences
BASICS
Basic Support for Institutionalizing Child Survival
CDC
Centers for Disease Control and Prevention (USA)
CIDA
Canadian International Development Agency
CORE
The Core Group - Child Survival Collaborations and Resources
Group
DANIDA
Danish International Development Agency
DFID
Department for International Development (UK)
DTPS
Three doses of diphtheria-tetanus-pertusis vaccine
EC
European Commission
EPI
Expanded Programme on Immunization
GAVI
Global Alliance for Vaccines and Immunization
GCC
Global Certification Committee
GLP
good laboratory practices
ICC
Interagency Coordinating Committee
IndiaCLEN
India Clinical Epidemiology Network
KFW
German Development Bank
LABNET
Global Polio Laboratory Network
MCH
maternal and child health
NGO
nongovernmental organization
NID
national immunization day
NORAD
Norwegian Agency for Development Cooperation
OPV
oral polio vaccine
PAHO
Pan American Health Organization
PE
polio eradication
PHC
primary health care
PHR
Partnerships for Health Reform
PPI
Pulse Polio Immunization
V
QA
quality assurance
QAP
quality assurance project
QM
quality management
SNID
subnational immunization day
TB
tuberculosis
TCG
Technical Consultative Group
UCI
Universal Childhood Immunization
UN
United Nations
UNICEF
United Nations Children’s Fund
USAID
United States Agency for International Development
VVM
vaccine vial monitors
WHA
World Health Assembly
vi
Acknowledgements
The time and efforts of the many people that helped produce this report are gratefully
acknowledged. In particular, Ms Andrea Gay (UN Foundation, Washington) who
served as rapporteur at the meeting, and Ms Ellyn Ogden (USAID, Washington).
vii
Executive summary
On 16-17 December 1999, WHO convened a meeting on the impact of targeted
programmes on health systems: a case study of the Polio Eradication (PE) Initiative.
Much progress has been achieved in PE, but tension exists within polarized camps
of opinion about whether eradication activities have been implemented in a way that
maximizes their potential positive impacts on immunization and health systems,
and minimizes any negative effects. This debate has prompted a series of studies to
try and understand the dynamics between PE and other health systems issues more
thoroughly.
The meeting reviewed six recent studies assessing the effects of the PE on
immunization and broader health systems development. The primary areas of impact
of PE were summarized in the following categories: management: relations with the
community and social mobilization: strengthening immunization and health systems;
opportunity costs; effect on routine EPI and other health services; promotion of
vitamin A; promotion of intersectoral collaboration; improvement in laboratory
services; disease surveillance; and financial effects on routine immunization and health
care budgets.
There is no debate that PE holds the potential for positive synergies and impact on
health systems. Determining the extent to which this has been achieved has proven
to be a difficult task, as most findings have been country-specific and cannot therefore
be generalized. The studies presented at this meeting found no overwhelming
evidence of either great positive or serious negative impact on national health systems.
However, it is widely accepted that there are “missed opportunities” associated with
PE.
The main operational conclusions are that:
Polio eradication does not automatically have a positive health systems impact,
nor grave disruption or diversion. Commonly the studies found mixed positive
and negative effects, with no firm conclusion in either direction.
More positive impacts can only be achieved by having specific health systems
objectives and targets, and an explicit process for monitoring progress.
Most negative impacts can be averted through better planning.
ix
The recommendations from the meeting summarize the next steps required to optimize
the opportunities of PE to strengthen health systems while minimizing threats.
First, there are actions that can be taken immediately to ensure greater synergy
between PE and health system strengthening, including a renewed focus on routine
immunization, linking acute flaccid paralysis (AFP) to surveillance for other diseases,
and using PE training and supervision activities to benefit other health services as
well.
Second, there is broad agreement that the health systems strengthening potential
of PE has been hindered by the lack of an explicit monitoring framework
(including specific objectives and targets) for this part of the PE goal. Prompt action
needs to be taken to redress this situation, including (i) the development and
dissemination of a simple and useable matrix of indicators for planning and monitoring
the health systems strengthening and routine immunization services impact of PE;
and (ii) selection of an oversight committee to monitor country-level and global
progress towards the health systems strengthening part of the PE goal.
Third, there remain some important gaps in our understanding of PE that need yet to
be documented.
Fourth, health systems strengthening cannot be achieved by, nor is it the responsibility
of, PE alone. Stronger linkages need be forged with groups and specialists working
on health systems development in order to fully maximize the impact of PE, maintain
political and financial commitment to immunization, and to help guide health sector
reform decisions that may affect immunization services.
Finally, the World Health Assembly (WHA) goal of eradicating polio while
strengthening health systems is more than an empty promise. A sincere commitment
and environment of goodwill does exist among the PE partners to realize the full
vision of the WHA goal. This is perhaps best captured in the words of one of the
researchers present at the meeting who stated that although it was our duty to
“first do no harm” - for the legacy of polio eradication, however, this would be
setting our ambitions far too low.
X
1. Introduction
The meeting on the impact of targeted programmes on health systems: a case
study of the Polio Eradication (PE) Initiative was held in Geneva, Switzerland
from 16 to 17 December 1999. Dr Daniel Tarantola, Special Adviser to the
WHO Director-General, opened the meeting and welcomed the participants
(see Annex 1: Agenda).
The World Health Organization (WHO) was represented by staff from WHO
headquarters, the Regional Offices for Africa, the Americas, Europe and the Eastern
Mediterranean. The United Nations Children’s Fund (UNICEF) was represented
by headquarters’ staff. Also present were representatives and key polio eradication
stakeholders from the UN Foundation, Canadian International Development Agency
(CIDA), United States Agency for International Development (USAID),
Centers for Disease Control and Prevention (CDC), European Commission (EC),
Global Alliance for Vaccines and Immunization (GAVI), Department for International
Development, UK (DFID), Norwegian Agency for Development Cooperation
(NORAD), World Bank, The Core Group - Child Survival Collaborations and
Resources Group (CORE), Basics Support for Institutionalizing Child Survival
(BASICS), and country managers from Lao People’s Democratic Republic (PDR),
Nepal and Tanzania, etc. (see Annex 2: List of participants).
In 1988 the Forty-first World Health Assembly (WHA) committed WHO to the
goal of “global eradication of poliomyelitis by the year 2000” emphasizing that this
should be “pursued in ways which strengthen the development of immunization
programmes as a whole, fostering its contribution, in turn, to the development of the
health infrastructure and of primary health care
In December 1999, with the goal of polio eradication fast approaching, WHO felt it
appropriate and timely to gather partners together to share, discuss and review new
information and data assessing the impact of polio eradication on health systems.
The objectives and expected outcomes of the meeting were as follows:
Objectives:
•
To review and discuss the findings of the WHO study of the impact of polio
eradication activities on health systems functioning and development.
•
To share other complementary assessment efforts.
•
To identify any missing information or additional studies that are needed.
•
To agree on a methodology for assessing the health systems impact of polio
eradication.
WHO/V&B/00.29
1
Expected outcomes:
•
Identify strategies for strengthening health systems through PE activities.
•
Develop a dissemination strategy for findings to influence future planning and
implementation of PE activities and achieve maximum health system benefits.
•
Reach a consensus on a revised methodology for the assessment of PE impact
on health systems and recommendations on next steps.
This report provides a summary of the discussions, main findings/conclusions,
and recommendations resulting from the meeting.
Impact of targeted programmes on health systems: a case study of PE
2
iiiipui uuiL iur une wnoie nn programme in Lao FDK. Surveillance was found
to be weak in Nepal and Tanzania. Linkages and partnerships were forged but
WHO/V&B/00.29
5
commonly not exploited for other health purposes. The external inputs were
generally found to be additional with new donors mobilized. No diversions of
national funds were registered. The national contribution to PE was mainly in
the form of substantial human resources.
Overall, the positive impacts were strongest in Lao PDR where PE has
established a basis for services that did not exist before. In Nepal and Tanzania
there were striking examples of missed opportunities and some negative impacts.
Important methodologically, it was noted that the potential positive impacts
tend to be “softer” and more long-term and thus harder to establish. Whereas
the potential negative impacts tend to be disruptive in nature and thus more
apparent and easily measurable. It was also noted that it was difficult to compare
countries due to differing capacity and contextual factors (i.e. health reform,
decentralization). In summary, the study found neither any outstanding
“automatic” positive impact of PE on health systems, nor grave disruption or
diversion. Recognizing the great potential that PE has, the main operational
conclusions were that: (i) most negative impacts can be averted through better
planning; and (ii) positive impacts can only be systematically ensured by having
clear objectives and instituting effective planning procedures to reach these
objectives.
In India, the All India Institute of Medical Sciences (AIIMS) and the India
Clinical Epidemiology Network (IndiaCLEN), with financial support from
USAID, carried out in-depth interviews and focus group discussions with
2163 stakeholders ranging from the Prime Minister and key decision-makers
to mothers in the community. The study was implemented over two years
(1997-98) and covered 24 diverse districts in 15 major states (and is still
ongoing). The AIIMS/IndiaCLEN study concluded that the effects of PE on
the health system had mostly been positive but that there were “threats” that
had to be recognized explicitly and dealt with pre-emptively. The study indicated
that PE had strengthened management capacity, improved social mobilization,
and increased confidence in the health care system. None the less, better planning
was required to minimize the disruptions caused by the national immunization
days (NIDs).
In 1999 with funding from USAID, the Partnerships for Health Reform (PHR)
project conducted a study in Bangladesh, Cote d'Ivoire and Morocco,
to determine the impact of PE on the financing of national immunization
programmes and to the extent possible, the health system as a whole.
Using trend analysis and a review of budget and financial expenditure records,
the study found that funding (including government) for routine EPI activities
has been increasing since the introduction of PE in each of the three countries.
Typically donors have concentrated on funding either routine EPI or PE and
have not made trade-offs in their support. Only a few organizations have been
funding both activities. None appear to be reducing their funding for routine
EPI activities, with the exception of UNICEF in Bangladesh. Informal reports
however, suggested that USAID had made some reductions in routine EPI
funding in other countries in West Africa as a result of financing PE activities.
Overall it was noted that the funding for national immunization programmes
(routine EPI and polio eradication activities) has been increasing at a higher
rate than for the health budget as a whole. The study could not draw conclusions
as to whether there were trade-offs in the provision of funding for immunization
activities versus other health activities.
UdEALnTX
6
Impact of targeted programmes on health systems: a case study
A
Throughout the summer of 1999, the Quality Assurance Project (QAP),
with funding from USAID, conducted a study to determine if the Global Polio
Laboratory Network (LABNET) could be cited as a “best practice model”
given that many other public health programmes rely on laboratory results to
guide programme decisions (e.g. malaria, TB, or HIV). Using site visits and
interviews, the key purpose was to identify the quality principles subscribed
to by the LABNET that have contributed to its success and to determine
whether these principles can be applied to other health programmes and or
health systems to improve their outcomes. The study found that the LABNET
effectively uses quality assurance (QA) activities in the clinical laboratory
setting to achieve, according to internationally recognized scientific, standards,
the stature of good laboratory practices (GLP). In addition, QA activities are
used to monitor compliance with GLP in clinical laboratories. The laboratories
visited displayed a sincere commitment and sense of pride at being involved
within the network. The findings reveal that the network demonstrates
six quality principles: leadership; systematic and regular quality assurance
activities (such as performance standards, monitoring); ongoing training and
capacity building; effective communication; recognition and accreditation; and
accurate documentation and data management that is used to inform programme
implementation. The achievement of these principles was found to be especially
noteworthy given the context of minimum equipment/supplies and resource
constraints. The study concluded that the substantive and numerous quality
principles found in the LABNET may serve as benchmarks for closing
performance gaps in other laboratories or health programmes.
In 1999, UNICEF carried out a rapid assessment of the impact of PE on routine
EPI and other health activities in two countries: Benin and Niger. The countries
were selected based on their performance (Niger as a low performer, Benin as
a high performer). The assessment process included a qualitative review of
available documentation, interviews with key actors, and field visits to two
districts. The main issues considered were EPI coverage, time/workloads,
social mobilization/information, education and communication (IEC),
cold chain, integration of other health interventions, reaching the unreached,
budget allocations, and surveillance. The UNICEF assessment also concluded
that there was little evidence of either a positive or negative impact of PE on
routine immunization and other aspects of primary health care. Key obstacles
to better interaction between EPI and PE were identified: late start of NIDs
planning process due to factors beyond national control; lack of consolidated
and integrated social mobilization/IEC strategies; and generally poor
distribution of operational resources and budgets for routine EPI and other
health activities at the district level (this was less of an obstacle in Benin where
the Bamako Initiative makes funds available). The integration of vitamin A
with NIDs was noted as a positive impact but there were missed opportunities
to develop more systematic inventory monitoring for the cold chain,
and to integrate (AFP) surveillance with other disease surveillance efforts
(it was noted the relative importance of this would increase as the countries
began to embark on more human resource intensive active AFP surveillance).
WHO/V&B/00.29
7
3.2
Major areas of PE impact on health systems and services delivery
Presentation and discussion of the study findings highlighted a number of specific
areas of impact of PE. These included:
Management: all of the studies that addressed this issue (WHO, AIIMS/
IndiaCLEN, and UNICEF) concluded that PE had had some positive impact
on health systems management. For example, in Nepal the NIDs were the
first activities where funds had been released directly to regions and districts.
In Lao PDR, PE helped promote a new district strategy that stressed health
care delivery closer to the community There was also recognition that much
more could have been done to institutionalize the good management practices
engendered by PE.
Relations with the community and social mobilization: consistent with the
Taylor Commission findings, there was also consensus from the two in-depth
studies that PE helped improve the community’s perceptions of the health
services, including the political support given to the health care system.
For example, in India the NIDs improved the confidence of mothers in health
workers and helped change their perception that health workers were only
interested in family planning. Generally, PE social mobilization efforts have
been widespread and successful.
Strengthening immunization and health systems: the studies concluded that
PE eradication has not had a very strong positive or negative impact on
immunization and health systems, although the long-term implications may
not be realized for many years. This time horizon is of significance given that
the observed negative impacts of PE tend to more easily measurable in the
short-term, while the potential positive benefits are more long-term in nature
and consequently more difficult to quantify. Meeting participants agreed that
polio eradication did have indirect opportunity costs in that attention given to
other aspects of strengthening immunization programmes was not as great as
it could have been (e.g. health sector reform, safe injections, or introduction of
new vaccines). In order to avoid this indirect consequence and to increase the
likelihood that PE has positive spin-offs there should be specific goals for system
strengthening agreed to at the outset with established indicators for regular
monitoring and reporting.
Opportunity costs: some observers have expressed concern that there are
significant opportunity costs associated with PE, when health staff are taken
away from other important activities to focus on NIDs. The WHO study
addressed this issue explicitly, assessing the amount of time health workers
devoted to PE in Lao PDR, Nepal and Tanzania. The investigators calculated
that the demands of PE on work time increased towards the peripheral level
of the health system where staff spent as much as 12 days per year on this
activity (about 5% of their working time). The effect of this on the delivery of
other health services, however, depended very much on staff productivity.
In the three countries examined in the WHO study, PE activities were not felt
to have compromised other activities, due to substantial “slack” in the system.
The UNICEF assessment also examined staff time allocation and in West Africa
documented a more highly concentrated effort at the central/regional level
8
Impact of targeted programmes on health systems: a case study of PE
(between 66-100% of time over the 3-4 month NIDs planning
and implementation period) and less at the district and health facility level
(35% and 25% respectively over a 3-month time period concerning
NIDs - or approximately 18-20 days per year). The review of activity records
found no clear positive or negative impact on the delivery of services as a
consequence of staff time spent on NIDs, and the report similarly observed
that districts with low baseline health services activity were unlikely to be
negatively affected by NIDs.
Delivery of routine EPI services: one of the most debated aspects of PE is
whether it interferes with routine immunization activities. Only the WHO
and UNICEF studies examined this issue quantitatively and their analysis was
hampered by the lack of survey data on coverage rates and coincidental health
reforms such as decentralization. The WHO study concluded that the
relationship between PE and routine immunization coverage was hard to assess.
Both Lao PDR and Nepal experienced an increase in routine coverage after
NIDs began but this coincided with an expansion in the number of peripheral
health facilities. In Tanzania, health sector reforms, including decentralization,
“overshadowed any possible impact” of PE on routine services. The UNICEF
study found no effect of PE on routine immunization coverage in Benin and
that the poor performance in Niger did not improve. It concluded that there
was little evidence of either positive or negative PE impacts on routine
immunization but identified a number of “missed opportunities” and a need to
be more proactive. Negative impacts could have been avoided with better
planning thereby lessening last minute pressures on the health system. All studies
included qualitative findings and anecdotes, both positive and negative, on the
effect of PE on other aspects of routine immunization services.
Delivery of other health services: there has also been considerable debate
about whether PE has disrupted other ongoing health services and the
three studies examining this issue concluded that disruptions had occurred and
in some cases may have been serious. For example, in Nepal family planning
activities were “somewhat” hampered by NIDs. However, the WHO study
examined routinely reported monthly data on maternal child health (MCH)
services and found that they showed the same seasonal variation as before PE
began. The AIIMS/IndiaCLEN study found that half of all stakeholders
interviewed believed that PE had actually improved primary health care (PHC)
services, although concern was expressed that villagers might come to expect
other health services to similarly be delivered house-to-house. The two major
studies and the UNICEF appraisal concluded that many of the negative effects
of PE could have been prevented with better planning.
Promotion of vitamin A: NIDs associated with PE have been used as a vehicle
for distributing vitamin A capsules to children from 6 months to five years of
age. This is now being carried out in over 50 countries worldwide and has met
with widespread acceptance and appreciation of parents. Given the large
expected impact of vitamin A supplementation (23% reduction in overall
mortality among children 6 to 59 months of age according to a meta-analyis of
8 randomized trials), there is broad consensus that this is a significant positive
contribution of PE to child survival.
WHO/V&B/00.29
9
Promotion of intersectoral collaboration: the two in-depth studies indicated
that PE was a good example of effective intersectoral collaboration.
For example, in a number of countries it was found that collaboration
mechanisms established for PE provided useful models for other programmes.
However, it was noted that Interagency Coordinating Committees (ICCs)
that had been established to assist PE were not always used to help strengthen
the immunization programme as a whole.
Improvement in laboratory services: As a result of PE there has been
considerable cooperation among the 150 laboratories involved in identifying
the poliovirus. It appears that this unique cooperation, through a process of
strict quality control, accreditation, and regular communication, has led to a
substantial improvement in the accuracy and quality of these laboratories.
Disease surveillance: the three studies addressing this issue found that
AFP surveillance had been introduced in all countries, but the WHO-study
noted insufficient quality of implementation in Nepal and Tanzania.
Overall, there had been relatively little spin-off in terms of strengthening
surveillance capacity for other priority diseases. It was agreed that there was
potential for wider positive effect in this regard.
Financial effects of PE on routine immunization and health care budgets:
the detailed analysis of immunization financing in Bangladesh, Cote d’Ivoire,
and Morocco, funded by USAID, concluded that: (i) funding for routine
immunization has increased since PE began; (ii) government funding of routine
immunization has increased since PE was initiated; and (iii) in Cote d’Ivoire
and Morocco, but not Bangladesh, the government has increased its annual
expenditure on PE. These results suggest there was little financial trade-off
between PE and routine immunization. Although the impact on the financing
of other components in the health budget was beyond the scope of the study,
it was noted that the funding for national immunization programmes
(routine EPI and PE) has been increasing at a higher rate than for the health
budget as a whole. The WHO study attempted to examine the impact of PE on
financing of other health services in Lao PDR, Nepal and Tanzania, but found
no evidence that it has reduced the financial resources available for other
programmes. Investigation of this issue in the UNICEF assessment was
inconclusive. Supplementary information presented by WHO during the
meeting demonstrated that of the estimated US$ 319 million in external donor
funding for PE in 1999, over 80% was funding that was not previously targeted
for developing country immunization services (Ms J. Linkins/WHO,
17 December 1999). As much as 50% of the external PE financing was from
funding sources such as Rotary International that have not previously
contributed to official development assistance for health.
10
Impact of targeted programmes on health systems: a case study of PE
3.3
Remaining information gaps
The participants of the meeting raised important concerns about programmatic gaps
that have not been included in the studies described above, but which should be
considered to complete the assessment of the legacy of PE. The gaps identified by
participants included:
The impact of PE on equity in access to health services.
The impact of PE on community ownership of their health agenda.
The long-term impact and lessons learned from the global partnership and
agency coalition that PE has mobilized to achieve a worldwide objective
(e.g. the translation of political will into resources for action, public/private
partnership; development of policy and regulatory agreements; interagency
collaboration; global lessons/impact).
The geopolitical impact of cross-border and regional collaboration necessary
for PE.
The peace-building impact of “Days of Tranquillity”, “Corridors of Peace”,
and negotiated humanitarian cease-fires to achieve PE in war-torn countries.
The childhood morbidity and mortality impact of integrating vitamin A
supplements with PE activities.
Further documentation of the impact of PE on laboratory capacity (differences
before and after PE).
The opportunity costs and effect on PE on routine immunization.
3.4
Recommendations
There was consensus that conducting further country studies to seek more evidence
to prove or disprove the hypotheses that eradication efforts are good or bad for
health systems would not add much to our current knowledge. The urgency is to
implement what is already known about how to optimize the benefits and minimize
the threats of PE. Towards this end, the participants identified a series of specific
action-oriented next steps for immediate implementation by PE staff, for health
systems staff, and for future eradication initiatives. These are outlined in Section 3.5.
There was strong agreement among the participants of the meeting that the
immunization and health systems strengthening potential of PE has been hindered
by the lack of an explicit monitoring framework (including specific objectives and
targets) for this part of the WHA goal declared in 1988. As a consequence,
there have been many “missed opportunities” to manage PE with a more balanced
and effective approach. Nevertheless, it is not too late. A sincere commitment and
environment of goodwill among the PE partners to realize the full vision of the
WHA goal does exist.
WHO/V&B/00.29
11
To meet this challenge, the participants of the meeting proposed the following
recommendations:
1)
Develop and disseminate a simple checklist with key indicators for monitoring
the impact of PE on (i) delivery of immunization services; and (ii) health systems
at the country level (the matrix presented in the WHO study could serve as a
starting point). Ideally this monitoring tool should be used to raise awareness
of the potential positive and negative effects of PE, facilitate more systematic
and broader documentation of country experiences, and ensure that polio
strategy implementation is modified to fully exploit opportunities for systems
strengthening (see Annex 5 for draft checklist and indicators).
2)
Compile all the existing documentation and studies on the impact of PE into
an overview “state-of-the-art” paper or collection. Much is already known
and this should be made easily accessible and shared widely.
3)
Initiate efforts to document remaining information gaps in knowledge of the
impact of polio eradication. These include: the global partnership story;
the impact of adding vitamin A to polio NIDs; Days of Tranquillity;
cross-border and interregional initiatives; social mobilization and community
ownership; PEI and equity in health; the polio laboratory network;
and intersectoral collaboration.
4)
Establish an oversight committee as part of the accountability framework for
the immunization and health systems strengthening aspect of the PE goal.
For example, one participant suggested that the terms of reference for the
Global Certification Committee (GCC) or other existing body could be
expanded to include this responsibility. This issue should be discussed and
decided at the next Technical Consultative Group (TCG) meeting
(Geneva, May 2000).
5)
Engage broader participation of those with influence and expertise in the area
of health systems to ensure that the opportunities of targeted programmes are
fully exploited and the threats to health systems minimized (see Section 3.5).
3.5
Next steps: optimizing opportunities of targeted health programmes
Clearly, targeted health programmes provide opportunities and synergies for
strengthening health systems if appropriate action is taken. The meeting participants
recognized that there were certain activities that the PE staff and partners could
implement directly and that are considered to be within their direct line of
responsibility. Other activities that would help to fully realize the potential positive
benefits of PE require the participation and buy-in of a wider range of people with
different spheres of influence. This second group of activities would take longer to
implement, but the participants noted that without their active participation,
little would move forward.
12
Impact of targeted programmes on health systems: a case study of PE
I.
Proposed immediate actions for PE staff
a)
Development, field testing, dissemination and follow-up of a checklist
(see Annex 5 for draft checklist and indicators), based on the findings of the
studies presented to date, that would help guide PE activities in order to
maximize the positive impacts under their direct sphere of influence.
b)
Document both positive and negative anecdotes about the impact of PE.
c)
Polio plans should be nested within broader and more comprehensive
EPI plans. There is a need for a renewed focus on routine immunization.
d)
Expand district level micro-planning to include EPI and disease surveillance
in addition to polio. Use the information from PE to improve planning for
other programmes.
e)
Make NIDs training schedules available in order to avoid disrupting activities
planned for other programmes. Use PE training and supervision activities to
benefit other health services.
f)
Assure vulnerable programmes protected during NIDs, e.g. TB, routine
immunization, emergency care.
g)
Expand Interagency Coordinating Committees (ICCs) to include action
planning for EPI and disease surveillance; enhance membership by inviting
key opinion leaders and stakeholders to participate.
h)
Budgets should include polio and non-polio needs; the ICCs with support from
WHO should track non-polio funding with the same level of detail as the polio
funding.
i)
Integrate other diseases into AFP surveillance systems as locally appropriate.
IL
Proposed actions for health systems staff
a)
Develop plans and implementation strategies to transfer health systems
strengthening skills and lessons learned to other programmes.
b)
Develop, track and monitor indicators to measure the impact of PE on broader
health systems. Include indicators to monitor interaction of sector reform on
routine immunization services.
c)
Develop a strategy and plan of action for documenting financial and political
commitment over time.
d)
Report back at polio/immunization and health sector meetings.
e)
Recognize and highlight for health systems experts the implications of PE for
other targeted programmes.
HI.
Proposed actions for future eradication activities
Meeting participants reviewed the conclusions and recommendations of the
Report of the Workshop on Disease Elimination/Eradication and Sustainable Health
Development (Salsibury D, 1998). There is much which is already known about the
“best practices” for disease eradication initiatives; the challenge is to implement this
knowledge. Participants endorsed the workshop recommendations and enhanced
them with additional suggestions (in italics);
WHO/V&B/00.29
13
a)
Eradication initiatives should be implemented with the support of broad
coalitions of partners. Great efforts should be made to build consensus and a
shared sense of mission among United Nations agencies, the donor community
(both public and private sector) and participating communities. Planning must
involve partnerships among all stakeholders.
b)
Managers of eradication initiatives should respect the importance of other,
ongoing public health programmes being promoted and implemented by the
ministry of health and by other staff, internationally, nationally and locally.
c)
To the extent possible, peripheral level decision-makers should be allowed to
reach centrally established targets in a flexible and locally appropriate way.
Similarly, when centrally driven priorities are set, those with responsibility at
the peripheral level, who may have considerable autonomy for resource
allocation, should understand their role within the wider objective.
d)
Successful eradication programmes are good examples of effective
management. The programme activities should further the development of
leadership and managerial skills among health personnel, building programme
management capacities which the staff involved can carry to other health
programmes, especially at the district level. Identify opportunities for capacity
building and ways to measure change.
e)
Surveillance of programmatic processes and outcomes (reduced morbidity and
mortality) is important for successful eradication. The initiatives must
demonstrate the principles of effective surveillance and actively develop and
implement integrated surveillance systems which can readily be adapted to
meet the needs of other national priority programmes after eradication is
achieved.
In addition, the participants suggested the following:
f)
There must be a genuine willingness to learn from and document any negative
effects in order to address them.
g)
Any future disease control initiatives similar to PE should set specific goals for
assisting health system development and collect baseline data against which to
measure progress.
h)
Strengthening health systems contributes to eradication and vice versa. Specific
objectives should be identified and indicators for successful strengthening of
the health care system should be used to monitor and report on progress.
i)
Risk factors should be identified for future eradication programmes, particularly
to guide and alert specific groups of countries that may be more vulnerable.
J)
Eradication activities must be planned with an accurate assessment of resource
needs to ensure success. In addition, there is a need to look beyond the traditional
funding sources for new partners.
k)
To develop a culture of prevention and health promotion, more attention should
be paid to social mobilization and message development at all levels.
14
Impact of targeted programmes on health systems: a case study of PE
4. Conclusions
There is no debate that PE holds the potential for positive synergies and impact on
health systems. Determining the extent to which this has been achieved has proven
to be a difficult task, as most findings have been country-specific and cannot therefore
be generalized. The studies presented at this meeting found no overwhelming
evidence of either great positive or serious negative impact on national health systems.
However, it is widely accepted that there are “missed opportunities” associated with
PE.
The main operational conclusions are that:
Polio eradication does not automatically have a positive health systems impact,
nor grave disruption or diversion. Commonly, the studies found mixed positive
and negative effects, with no firm conclusion in either direction.
More positive impacts can only be achieved by having specific health systems
objectives and targets, and an explicit process for monitoring progress.
Most negative impacts can be averted through better planning.
The recommendations from the meeting summarize the next steps required to optimize
the opportunities of PE to strengthen health systems while minimizing threats.
First, there are actions that can be taken immediately to ensure greater synergy
between PE and health system strengthening, including a renewed focus on routine
immunization, linking AFP to surveillance for other diseases, and using PE training
and supervision activities to benefit other health services as well.
Second, there is broad agreement that the health systems strengthening potential
of PE has been hindered by the lack of an explicit monitoring framework
(including specific objectives and targets) for this part of the PE goal. Prompt action
needs to be taken to redress this situation, including (i) the development and
dissemination of a simple and useable matrix of indicators for planning and monitoring
the health systems strengthening and routine immunization services impact of PE;
and (ii) selection of an oversight committee to monitor country-level and global
progress towards the health systems strengthening part of the PE goal.
Third, there remain some important gaps in our understanding of PE that need yet to
be documented.
WHO/V&B/00.29
15
Fourth, health systems strengthening cannot be achieved by, nor is it the responsibility
of, PE alone. Stronger linkages need to be forged with groups and specialists working
on health systems development in order to fully maximize the impact of PE, maintain
political and financial commitment to immunization, and to help guide health sector
reform decisions that may affect immunization services.
Finally, the WHA goal of eradicating polio while strengthening health systems is
more than an empty promise. A sincere commitment and environment of goodwill
does exist among the PE partners to realize the full vision of the WHA goal. This is
perhaps best captured in the words of one of the researchers present at the meeting
who stated that although it was our duty to “first do no harm” - for the legacy of
polio eradication, however, this would be setting our ambitions far too low.
16
Impact of targeted programmes on health systems: a case study of PE
5. References
Arora NK, et al. Pulse Polio Immunization Program Evaluation 1997-98.
New Delhi: All India Institute of Medical Sciences', 1999: 271.
Aylward RB, Bilous J, Tangermann, RH, et al. Strengthening immunization services
in the Western Pacific through the eradication of poliomyelitis. Journal of Infectious
Diseases 1997; 175 (suppl. 1): 268
Aylward RB, Hull HF, Cochi SL, Sutter RW, Olive JM, Melgaard B.
Disease eradication as a public health strategy: a case study of poliomyelitis
eradication. Bulletin of the World Health Organization, 2000; 78(3):285-297.
Goodman T, Dalmiya N, de Benoist B, Schultink W. Polio as a platform:
using national immunization days to deliver vitamin A supplements. Bulletin of the
World Health Organization, 2000; 78 (3): 305-314.
Hull HF, Tangermann RH, Aylward RB, Andrus JK. (letter). Eradication of
poliomyelitis. Lancet. 1999; 354: 1910.
Lee JW, Melgaard B, Hull H, Barakamfitiye D, Okwo-Bele JM. Ethical dilemmas
in polio eradication (letter). American Journal of Public Health. 1998; 88:130-131.
Levin A, Ram S. The Impact the Polio Eradication Campaign on the Financing of
Routine EPI: Findings of Three Case Studies. Bethesda: Partnership for Health
Reform, University Research Co.; 1999.
MacAulay C, Verma M. Global Polio Laboratory Network: A Model for Good
Laboratory Practice - A Study of the Quality Principles within the Global Polio
Laboratory Network. Bethesda: Quality Assurance Project, University Research
Co.; 1999.
Melgaard B, Creese A, Aylward RB, Olive J-M, et al. Disease eradication and
health systems development. Bulletin of the World Health Organization, 1998;
76 (suppl. 2): 26-31.
Mogedal S, Stenson B. Disease eradication: friend or foe to the health system?
Synthesis report from field studies in Tanzania, Nepal and Lao PDR.
(WHO/V&B/00.28).
WHO/V&B/00.29
17
PAHO/WHO. The Impact of the Expanded Programme on Immunization and the
Polio Eradication Initiative on Health Systems in the Americas: Final Report of the
“Taylor Commission”. March 1995. Pan American Health Organization,
Washington.
Roisin A. Assessment of the Impact of the Polio Eradication Initiative and
National Immunization Days (NIDs) on Routine EPI and Other Ministry of Health
Activities. UNICEF 1991 (unpublished draft report).
Salisbury D. Report of the Workgroup on Disease Elimination/Eradication
and Sustainable Health Development. Bulletin of the World Health Organization,
1998; 76 (Suppl. 2): 72-79.
Sutter, R, Cochi, S. Comment: Ethical dilemmas in worldwide polio eradication
programs. American Journal of Public Health, 1997; 87:913-916.
Tangermann RH, Costales M, Flavier J, et al. Poliomyelitis eradication and
its impact on primary health care in the Philippines. Journal of Infectious Diseases,
1997; 175 (suppl.): 272-76.
Taylor Commission. The Impact of the Expanded Programme on Immunization and
the Polio Eradication Initiative on Health Systems in the Americas.
Washington, DC: Pan American Health Organization; 1995.
Taylor C, Cutts F, Taylor ME. Ethical dilemmas in current planning for polio
eradication. American Journal of Public Health, 1997;87:922-925.
Taylor C, Taylor ME, Cutts F, Ethical dilemmas in polio eradication, (letter).
American Journal of Public Health', 1998; 88: 1125.
World Health Organization. Challenges and strategies for health systems
development. (WHO document HDP/97.3 1997)
18
Impact of targeted programmes on health systems: a case study of PE
Annex 1:
Agenda
Thursday, 16 December 1999
13:30-14:00
Registration
14:00-14:15
Welcome/opening remarks
Session 1
Targeted programmes and health
systems development
14:15-14:30
WHO’s health systems perspective
Polio eradication/EPI perspective meeting objectives
Mr O. Adams
Dr B. Melgaard
14:30-14:45
Disease eradication and health systems
development: A summary of the debate
Dr D. Salisbury
14:45-15:00
Discussion
Session 2
Evaluating the impact of polio
eradication on Health Systems
15:00-15:30
Multicountry assessment of the impact
of polio eradication activities on health
systems functioning and development:
summary of case study methodology
15:30-16:00
Coffee
16:00-16:30
Multicountry assessment of the impact
of polio eradication activities on health
systems functioning and development:
summary of case study results
16:30-17:30
Discussion
18:00
Cocktails
WHO/V&B/00.29
Dr D. Tarantola
Dr S. Mogedal
Mr B. Stenson
19
Friday, 17 November 1999
9:00-9:45
Dr N.K. Arora
All India Institute of Medical Sciences
Evaluation of the Pulse Polio Immunization
programme: summary of methodology and
results
9:45-10:30
Discussion
10:30-11:00
Coffee
11:00-11:30
Summary of ongoing polio eradication
impact studies
- financing of Polio Eradication
Campaigns in Bangladesh,
Cote d’Ivoire and Morocco
(Partnerships for Health Reform)
-
Lessons learned in the development
of the Global Polio Laboratory
Network (Quality Assurance Project)
Dr C. McCaulay
-
Experience in West Africa - Benin,
Niger (UNICEF)
Dr J. Zucker
11:30-12:30
Discussion
12:30-14:00
Lunch
Session 3
Next steps: optimizing opportunities of
targeted health programmes
14:00-14:15
Summary of methodology issues and
information gaps
14:15-15:00
Discussion
15:00-15:30
Coffee
15:30-15:45
Next steps: identifying strategies for
strengthening health systems through PE,
and dissemination of lessons learned
15:45-16:30
Discussion
16:30-17:30
Conclusions and recommendations
20
Dr A. Levin
Dr P. Ndumbe
Ms E. Ogden
Dr D. Salisbury
Impact of targeted programmes on health systems: a case study of PE
Annex 2:
List of participants
Dr C. Akim. EPI Programme Manager, Ministry of Health, P.O. Box 9083,
Dar es Salaam, Tanzania
Tel: +255 51 450404; Fax: +255 51 450089
Dr Narendra K. Arora, Department of Pediatrics, All India Institute of Medical
Sciences, Ansari Nagar, New Delhi 110029, India
Tel: +91 11 6853125, +91 11 6526096: Fax: +91 11 686 2663
E-mail: nkmanan@hotmail.com
Dr Chanpen Choprapawon, Thailand Health Research Institute (THRI),
National Health Foundation, 1168 Soi Phaholyothin 22, Phaholyothin Rd,
Ladyao, Jatujak, Bangkok 10900, Thailand
Tel: +66 2 939 2239: Fax: +66 2 9 939 2122
E-mail: chanpen@health.moph.go.th
Dr Stephen L. Cochi, Director, Vaccine Preventable Disease Eradication
Division, National Immunization Program, Centers for Disease Control and
Prevention (CDC), 1600 Clifton Road, Mailstop E-05, Atlanta, GA 30333, USA
Tel: +1 404 639 8252; Fax: +1 404 639 8573
E-mail: slcl@ccic.gov
Dr M. Dawar, Canadian International Development Agency (CIDA),
200 Promenade du Portage, Hull, Quebec, KIA 0G4, Canada & Department of
Health Care & Epidemiology, Faculty of Medicine, James Mather Building,
5804 Fairview Avenue, Vancouver, B.C., Canada V6T123
Tel: +1 819 994 7091; Fax: +1 819 997 9049
E-mail: mdawar@interchange. ubc.ca
Mrs Marleen Dijkman, National Institute of Public Health and the Environment
Vaccine Division, Antonie van Leeuwen hoeklaan g, Bilthoven, The Netherlands
Dr Somthana Douangmala, Director, National Center for Paediatric Infectious
Diseases, National EPI Manager, National Institute of Hygiene and Epidemiology,
Ministry of Health, Vientiane, Lao People’s Democratic Republic
Tel: +856 21 350027; Fax: +856 21 350067
WHO/V&B/00.29
21
Dr Fidel Font, International Federation of Red Cross and Red Crescent Societies
(IFRC), Case postale 372, 1211 Geneva 19, Switzerland
Tel: +41 22 791 730 42 22; Fax: +41 22 733 03 95
Ms Andrea Gay, United Nations Foundation, 1301 Connecticut Avenue NW,
Suite 700, Washington, D.C. 20036, USA
Tel: +1 202 887 9040 Fax: +1 202 887 9021
E-mail: agay@unfoundation.org
Dr Tore Godal, Executive Secretary, Global Alliance for Vaccines and
Immunization, UNICEF, Palais des Nations, 1211 Geneva 10, Switzerland
Tel: +41 22 909 5020: Fax: +41 22 909 5931
E-mail: tgodal@unicef.ch
Mr Richard Greene, Chief, Child Survival Division, US Agency for International
Development, Washington, D.C. 20523-3700, USA
Tel: +1 202 712 128; Fax: +1 202 216 3702
E-mail: rgreene@usaid.gov
*Mr Klaus Hornetz, Senior Health & Population Adviser, Kreditanstalt fur
Wiederaufbau, D-60045 Frankfurt am Main, Germany
Tel: +49 69 74 31 36 00; Fax: +49 69 74 31 29 44
E-mail: bettina. tewinkel@kfw. de
Dr Inaam U1 Haq, Health and Population Programme Officer, Department for
International Development (DFID), British High Commission, Development
Section, Diplomatic Enclave, Ramna 5, P.O. Box 1122, Islamabad, Pakistan
Tel: +92 51 206071/75; Fax: +92 51 823017/823439
*Dr Jacques Laruelle, Senior Programme Officer, Belgian Administration for
Development Cooperation, Belgium
Tel: +32 2 519 0752; Fax: +32 2 519 0570
E-mail: m4.vnu@badc.fgov.be
Dr M. Lakshman, Department of Pediatrics, All India Institute of Medical
Sciences, Ansari Nagar, New Delhi 110029, India
Tel: +91 11 6853125/6593692; Fax: +91 11 6853125
E-mail: mlvel@hotmail.com
Dr Ann Levin, Abt Associates, Partnership for Health Reform (PHR), Hampden
Square, 4800 Montgomery Lane, Suite 600, Bethesda, MD 20814-5341, USA
Tel: +1 301 913 0500: Fax: +1 301 652 3618
E-mail: ann_levin@abtassoc.com
*
22
Unable to attend
Impact of targeted programmes on health systems: a case study of PE
Dr Benjamin Loevinsohn, World Bank, 1818 H. Street N.W., Washington,
D.C. 200443, USA
Tel: +1 202 473 7948; Fax: +1 202 522 2955
E-mail: bloevinsohn@worldbank.org
Dr Catherine MacAulay, Senior Quality Assurance Advisor,
The Quality Assurance Project (QAP), University Research Corporation,
7200 Wisconsin Avenue, Suite 600, Bethesda, MD 20814, USA
Tel: +1 301 941 8414: Fax: +1 301 941 8427
E-mail: cmacaulay@urc-chs.com
Dr Sigrun Mogedal, Chief Technical Adviser for Social Sector Development,
Norwegian Agency for Development Cooperation (NORAD), P.O. Box 8034
Dep. N-0032 Oslo, Norway
Tel: +47 22 240202; Fax: +47 22 242031
E-mail: sigrun. m ogedal@n ora d.no
Dr Peter Ndumbe, Centre for the Study and Control of Communicable Diseases,
Faculty of Medicine and Biomedical Sciences, B.P. 8445, Yaounde, Cameroon
Tel: +237 31 51 04; Fax: +237 31 51 78
E-mail: camdiagnostix@camnet. cm
Mr David Newberry, Children’s Health Senior Advisor, CARE, 151 Ellis Street
NE, Atlanta, GA 30303 2439, USA
Tel: +1 404 681 2552; Fax: +1 404 577 1205
E-mail: newberry@care.org
Ms Ellyn Ogden, Polio Eradication Coordinator, US Agency for International
Development (USID), G/PHN/HN/Child Survival, 1300 Pennsylvania Avenue,
Room 3-07-070, 3rd Floor, Washington, D.C. 20523-3700, USA
Tel: +1 202 712 5891; Fax: +1 202 216 3702
E-mail: eogden@usaid.gov
*Mr FL Pigman, Vice-Chairman, IPPC, Rotary International, 5303 W 850 N,
Ambia, Indiana 47917, USA
Tel: +1 765 869 5821; Fax: +1 765 869 4821 (home),
Tel: +1 847 864 4527 (Evanston)
Dr Peter Poore, Save the Children Fund, 17 Grove Lane, London SE5 8RD, UK
Tel: +44 171 703 5400; Fax: +44 171 703 2278
Dr P. Procacci, Health Adviser, Eastern and Central Europe, Asia,
Directorate for Development Cooperation, Ministry of Foreign Affairs,
Unita Tecnica Centrale, Via S. Contarini 26, 1-00142, Italy
Tel: +39 06 3691 6266: Fax: +39 06 324 0585
E-mail: procacci@esteri.it
*
Unable to attend
WHO/V&B/00.29
23
*Dr Pia Rockhold, Technical Adviser, Royal Danish Ministry of Foreign Affairs,
2 Asiatisk Plads, DK-1448 Copenhagen K, Denmark
Tel: +45 33 92 02 31: Fax: +45 32 54 05 33
E-mail: piaroc@um.dk
Dr E. M. Saether, Doctoral Student, Ragnar Frisch Centre for Economic
Research, Health Economics Research Programme, University of Oslo,
Gaustadalleen 21, N-0349 Oslo, Norway
Tel: +47 22 95 88 19: Fax: +47 22 95 88 25
E-mail: e.m.sather@frisch. uio.no
Dr David Salisbury, Principal Medical Officer, Department of Health,
707 Wellington House, 133-155 Waterloo Road, London SEI 8UG, UK
Tel: +44 171 972 4488; Fax: +44 171 972 4468
E-mail dsalisbu@doh.gov.uk
Dr Shreebatsa P. Shrestha, Research Group for Health Economics and
Development, Senepa., Lalitpur 2, Nepal
Tel: +977 1 529371, 977 1 524699
E-mail: reghed@htp.com.np
Mr Richard L. Skolnik, The World Bank, 1818 H. Street, N.W, Washington,
D.C. 20433, USA
Tel: +1 202 458 0298; Fax: +1 202 477 0397
E-mail: rskolnik@worldbank.org
Mr Robert Steinglass, Immunization Coordinator, BASICS,
1600 Wilson Boulevard, Suite 300, Arlington, VA 22209, USA
Tel: +1 703 312 6800; Fax: +1 703 312 6900
E-mail: rsteingl@basics.org
Mr Bo Stenson, 2182 Route de Pitegny, F-01170 Gex, France
Tel: +33 450 41 69 24; Fax: +33 4 50 28 3249
E-mail: bo.stenson@wanadoo.fr
*Dr Carl Taylor, Johns Hopkins University, Baltimore, MD 21205-2179, USA
E-mail: ctaylor@jhsph.edu
Dr John Tomaro, Director of Health Programmes, Aga Khan Foundation,
13 avenue de la Paix, CH-1202 Geneva, Switzerland
Tel: +41 22 909 7200; Fax: +41 22 909 7291
*Dr Fran^oise Varet, Chef de division du developpement sanitaire et social,
Ministere delegue a la coopeeration et a la Francophonie, 20 rue Monsieur,
F-75700 Paris 07 SP, France
Tel: +33 1 53 69 31 47; Fax: +33 1 53 69 37 19
*
24
Unable to attend
Impact of targeted programmes on health systems: a case study of PE
Ms Linda Vogel, United States Mission to the United Nations Office and other
International Organizations, Case postale, 1292 Chambesy, Switzerland
Tel: +41 22 749 4111: Fax: +41 22 749 4880
Mr J. Waslander, Permanent Mission of the Kingdom of the Netherlands to the
United Nations Office and International Organizations at Geneva,
Chemin des Anemones 11, Case postale 276, 1219 Chatelaine, Switzerland
Tel: +41 22 795 15IT, Fax: +41 22 795 1515
E-mail: waslander@gev.minbuza.nl
Dr Jane R. Zucker, Health Adviser, UNICEF, 3 United Nations Plaza, TA-ZYA,
New York, NY 10017, USA
Tel: +1 212 824 6312: Fax: +1 212 824 6460
E-mail: jzucker@unicef.org
WHO Secretariat
Regional offices
Dr O. Babaniyi, WHO Regional Office for Africa (AFRO), Parirenyatwa
Hospital, P.O. Box 773, Harare, Zimbabwe
Dr M. Landaverde, HPV/HVI, WHO Regional Office of the Americas/Pan
American Sanitary Bureau (AMRO/PAHO), 525 23rd Street, N.W, Washington,
D.C. 20037-2895, USA
Dr M. H. Wahdan, Assistant Regional Director, WHO Regional Office for the
Eastern Mediterranean (EMRO), P.O. Box 1517, Alexandria - 21511, Egypt
Dr G. Oblapenko, Medical Officer, WHO Regional Office for Europe (EURO),
8 Scherfigsvej, DK-2100 Copenhagen 0, Denmark
WHO headquarters staff
Director-General’s Office (DGO)
Dr D. Tarantola, Senior Policy Adviser, DGO
Health Technology and Pharmaceuticals Cluster (HTP)
Dr M. Scholtz, Executive Director, HTP
Department of Vaccines and Biologicals (VAB), Health Technology and
Pharmaceuticals Cluster (HTP)
Dr B. Melgaard, Director, VAB/HTP
Dr Maureen Birmingham, Coordinator, Vaccine Assessment and Monitoring
(VAM), VAB/HPT
Dr J.-M. Olive, Acting Coordinator, Expanded Programme on Immunization
(EPI), VAB/HTP
Dr B. Aylward, EPI/VAB/HTP
Ms Tracey Goodman, EPI/VAB/HTP
WHO/V&B/00.29
25
Communicable Diseases Cluster (CDS)
Dr D. Heymann, Executive Director, CDS
Dr N. Zagaria, Strategy Development and Monitoring for Eradication and
Elimination (CEE), Department of Communicable Diseases Control,
Prevention and Eradication (CPE), CDS
Dr D. Klaucke, Department of Communicable Disease Surveillance and
Response (CSR), CDS
Dr Petra Heitkamp, Stop TB, CDS
Department of Organization of Health Services Delivery (OSD), Evidence and
Information for Policy Cluster (EIP)
Mr Orvill Adams, Director OSD/EIP
Dr J. Heldrup, OSD/EIP
Ms B. Stilwell, OSD/EIP
Dr Prabhat Jha, Department of Research Policy and Cooperation (RPC), EIP
26
Impact of targeted programmes on health systems: a case study of PE
Annex 3:
o
g
Summary table of new studies on PE
Ko
co
Title of study/date
Authors/lnstitution
Location
Methods
Study Objective
Disease eradication:
friend or foe to health
system (1999)
S. Mogedal (DiS, Centre for Partnership in
Development, Oslo) and B. Stenson
(Division of International Health Care
Research (IHCAR) Karolinska Institutet,
Stockholm)
Lao PDR, Nepal and
Tanzania
Systematic country review, interviews,
statistical and document review using health
systems capacity assessment framework of
indicators
Impact of PE on
health systems
Pulse Polio
Immunization
Programme
Evaluation 1997-98
and 1998-99
N.K. Arora and M. Lakshman
(All India Institute of Medical Research,
AIIMS-lndiaCLEN, Delhi)
India
Interviews and focus group discussions with
key informants/stakeholders at all levels e g. decisions-makers, planners, NGOs
community
Impact of PE on
health services
delivery
The impact of PE
Campaign on the
Financing of Routine
EPI: Findings of
Three Case Studies
(1999)
A. Levin, and S. Ram (Partnership for
Health Reform, University Research
Co., Bethesda)
Bangladesh,
Morocco,
Cote d’Ivoire
Trend analysis of source and use of funds,
survey
Immunization
financing
Global Polio
Laboratory Network:
a model for good
laboratory practice
C. MacAulay and M. Verma
(Quality Assurance Project, University
Research Co., Bethesda)
USA (CDC),
South Africa,
Uganda, India
Observation of laboratory practices and
interviews with laboratory staff
Polio laboratory
network
Benin, Niger
Consultant field visit, interviews, document
and coverage review
Routine
immunization
services
(1999)
ro
Assessment of the
A. Roisin (UNICEF consultant, New York)
effect of PE and NIDs
on routine EPI (1999)
Annex 4:
Summary of presentations,
discussion and comments
1.
Targeted programmes and health systems development
Presentation by Mr Orvil Adams, Director ORD/EIP, WHO, Geneva
Introduction
The key elements of WHO’s approach to health systems development include:
a)
An overall set of goals:
•
•
•
•
To improve the health of populations.
To enhance the responsiveness of the health system to meet the
expectations of populations.
To improve on the non-health dimensions of interaction with the health
system.
To promote fair financing and reduce financial risk.
b)
An overall objective to have a positive impact on health systems concerned
with services to the poor in such key functional areas as service delivery, human
resource development, financing, and stewardship.
c)
A monitoring function: to track when and what reforms are introduced in
countries; to document changes in performance; and to explain key factors
involved in the changes to inform decisions of policy-makers.
d)
The design and development of a set of indicators to measure changes in
performance and health and build capacity to measure the achievement of the
stated goals and objectives. (Note: It is important to remember that EPI has
one good indicator - coverage - but other indicators of the immunization system
are weak.)
The challenge is to link polio eradication efforts with health system performance and
essential health systems functions (outlined in b. above).
Commen ts/discussion
What is less clear is how far polio eradication activities can go to help meet the aims
of this framework and the extent to which polio eradication can influence the broader
health systems. Polio eradication cannot rebuild the health system nor is it meant to.
In addition, there is no guarantee that a greater emphasis on these issues through
PE and/or through EPI will have a major impact on health systems strengthening
more broadly. We need to be realistic about what can be done - broader development
efforts are necessary.
28
Impact of targeted programmes on health systems: a case study of PE
While eradication programmes, in general, should not be held responsible for curing
ills of existing health systems they can help promote the following:
Consensus and coordination among a broad coalition of partners essential for
eradication initiatives.
Respect for other ongoing public health programmes by managers of
eradication initiatives.
Flexibility of peripheral level decision-makers in reaching centrally established
targets.
Effective management and leadership transferable to other health programmes.
Successful eradication programmes are powerful examples of effective
management and leadership.
Adaptation of improved and effective surveillance to meet needs of other public
health system programmes after eradication is achieved.
Programme planning by defining the roles of training, human resource
development, community mobilization, health policy, finance and resource
mobilization.
The positive impact of eradication programmes can be improved by avoiding the
following pitfalls:
Capacity building without appropriate attention to health information systems
and evaluation.
Building parallel structures where human resources are siphoned away thus
jeopardizing existing programmes.
Concentrating on central level over community levels.
Missing opportunities to link with other programmes.
Underestimating the financial and human resources required to complete the
job.
Promoting strategies that may not be the most cost effective.
Lack of transparency with policy- and decision-makers about all aspects of
the programme: technical, financial and political.
2.
Disease eradication: friend or foe to the health system?
Presentation by Dr Sigrun Mogedal, Chief Technical Adviser for Social
Sector Development, NORAD and Mr Bo Stenson, Consultant, Gex,
France
Introduction
This study was commissioned in 1998 by WHO to develop a methodology for
assessing the impact of polio eradication on health systems. The methodology was
field tested in three countries: Lao PDR, Nepal and Tanzania. A summary synthesis
report outlines the methodology, the findings from the country studies, discusses the
major issues involved, and provides recommendations for action. Individual reports
of the country case studies are also available.
WHO/V&B/00.29
29
Methods and data collection
The first part of the methodology development involved establishing a framework
of indicators for describing the structure and capacity of key health systems functions:
policy context, national capacity, service delivery, training and supervision and social
mobilization. In addition, the main immunization systems areas of infrastructure,
financial and human resource inputs were explored. A summary table of generally
perceived PE potential for both positive and negative effects was compiled.
This framework and indictors were applied and pursued through reviews of
documents, statistics and interviews with concerned individuals at the central (national)
as well as the provincial and district levels in one or a few selected districts of each
country studied. The findings in relation to this set of indicators were finally assessed
in relation to health system context and functions, to identify vulnerable and strong
system elements and discuss the conditions for positive and negative PE impact.
A summary of the indicator framework and overview of the findings (including missed
opportunities or potential positive impact that was not realized or could not be traced)
is provided in Annex 4 of the study’s final report.
Despite efforts to use a common framework for describing health system
capacity and assessing impact, comparing countries has obvious methodological
limitations. Tanzania is a country with a comparative wealth of data in relevant
areas. This was especially so in the province/district chosen for the peripheral study,
Morogoro. Lao PDR is characterized by a paucity of data especially with regards to
health financing. In Nepal the availability of data at the central level was similar to
Tanzania, while the data availability at the district level was not so complete.
Summary and conclusions
In the area of policy context mainly positive impacts were registered. Organizational
capacity findings pointed in both directions, mostly positive in Laos PDR and Nepal
with negative examples from Tanzania. Service delivery showed no major impact in
either direction. In training and supervision, delays and disruptions were registered
as well as increased capacity.
Improvements of the cold chain through polio eradication were especially important
for the whole EPI programme in Lao PDR. Surveillance was found to be weak in
Nepal and Tanzania. Linkages and partnerships were forged but generally not
exploited for other health purposes. The focus on national immunization days (NIDs)
was found to be stronger than on strengthening routine immunization.
The external inputs were generally found to be additional and new donors had been
mobilized. No diversion of national funds was registered. The national contribution
to polio eradication was mainly in the form of substantial human resources, especially
at the lower levels.
The positive impacts stand out in Lao PDR where polio eradication has established
a basis for services that did not exist before. In Nepal and Tanzania there were
striking examples of missed opportunities and some negative impacts.
30
Impact of targeted programmes on health systems: a case study of PE
Contextual factors, especially the capacity of the health system, are essential in
mediating the effects of polio eradication. Health reforms may overshadow the impact
of polio eradication.
A potential for synergies at several levels was found, requiring coordinated planning.
Thus leadership at the central and operational levels with responsibilities beyond the
specific intervention becomes crucial.
The main operational conclusions are that:
Most negative impacts of PE can be averted through better planning.
Positive impacts can only be achieved by having clear objectives and instituting
effective planning procedures to reach these objectives.
Recommendations for medium-term action:
Eradication partners
•
To give due attention to how planning and implementation of eradication can
give benefits to health systems.
WHO
To develop guidelines for the strengthening of health systems and support
countries in their implementation.
To establish a monitoring system that makes it possible for the global community
to benefit from country experiences with eradication programmes.
Countries
To take specific action to create better synergies through a renewed emphasis
on routine immunization and identification of opportunities provided by health
reforms.
To make the scheduling of the final phase of PE predictable and coordinate it
with other training, supervision and service activities.
To integrate surveillance of other diseases with acute flaccid paralysis (AFP)
surveillance.
To set objectives and establish long-term monitoring systems (including specific
indicators of PE impact) to be followed and acted upon as appropriate.
Recommendations for immediate action for:
All involved
To renew emphasis on routine immunization.
To integrate other diseases surveillance into AFP.
To plan training and supervision in order that it can be strengthened rather
than disrupted by PE.
To exploit PE partnerships for other health purposes.
To collect data and report on routine immunization as part of PE programme.
WHO/V&B/00.29
31
Commen ts/discussion
Meeting participants felt that this study provided good information and would help
to depolarize the intensity of the debate of the past years. There was general agreement
that within the context of each country studied, it was possible to find positive and
negative impacts, meaning both are possible.
Participants were in further agreement that more needs to be done to promote the
positive impacts of eradication and minimize the negative consequences. The polio
eradication effort cannot afford to waste opportunities/resources or cause indirect
harm through benign neglect.
Some participants felt that the findings are very useful for looking at individual
countries, but they are limited in their usefulness for characterizing the impacts at
global level.
Participants agreed that some of the impacts of PE might not be evident for several
years. It will be important for WHO to continue to monitor the impact, both on
routine immunization and broader health systems. It was recommended that
WHO monitor this situation closely, take a pro-active approach to intervening should
there be a need, and to revisit these findings periodically, by reporting back at regional
and global meetings.
Other examples of the impact of polio eradication were noted by meeting participants.
These include:
WHO staff, representing countries in EMRO cited, anecdotally,
additional positive impacts of polio eradication including: improved image of
health ministries because of polio success stories (Egypt, Sudan, Yemen);
social mobilization efforts that have been used for EPI as well as PE;
ceasefires extended beyond polio NIDs to deliver other health services;
cold chain improvements important for EPI; surveillance systems improved
and beginning to be used for other diseases; management systems for NIDs
being used for other efforts; and, increased coordination among activities.
WHO staff, representing countries in EURO cited, anecdotally,
additional positive impacts including: improved interregional coordination;
improved managerial skills, EPI is now part of national budgets in most
countries; strengthened cooperation between health sectors/professionals;
increased social mobilization: greater access to previously unreached
sub-populations; improved morale of health professionals; strengthened
diphtheria control efforts; an increase in DTPS coverage for at least three
countries.
32
Impact of targeted programmes on health systems: a case study of PE
Summary and conclusions
1)
Intersectoral coordination was recognized as a compelling factor for successful
implementation at the district level and lower. NGOs were not very active in
the tribal and hilly areas.
2)
Logistics issues, particularly transportation, drew the attention of over half of
the district and block officers. In rural and urban areas, NGOs often provided
a significant proportion of vehicles. This problem was magnified in the absence
of NGOs. Enumeration of children in remote areas was also a difficulty.
3)
Simplicity of the programme was mentioned as an important reason for success.
The service utilizers notably appreciated that the immunization posts were
near their homes and the programme was conducted on holidays - further
reiterating the need for services that are easily available, accessible, affordable
and acceptable.
4)
Cooperation and participation by the community, especially by the local leaders
and influential person was important.
5)
There was a uniform opinion among the providers that the image and credibility
of health systems had been enhanced since the onset of PPI. People were now
more familiar with the activities of the health department. Relationships between
the health workers and community had improved due to increased frequency
of their interaction. A majority of community stakeholders confirmed these
perceptions.
6)
Existing health services, as measured by indicators for immunization coverage,
maternal and child health activities, and antenatal care services were either
not influenced or had shown some improvement.
7)
There was a temporary relocation of resources (personnel and materials) from
all participating departments for carrying out PPI activities. Vehicles were
requisitioned from a large number of departments and private sources for up
to four weeks in connection with the last two PPIs.
8)
Most of the health workers said that their routine and specific activities were
adversely affected due to their participation in the PPI programme but the
magnitude of this impact was not defined.
9)
There has been a 10% decline in routine immunization coverage since 1994,
more in some states. It is difficult to ascribe this deterioration in programme
performance to any particular factor. While there appears to be some dislocation
of services with PPI for 4-6 weeks around the NIDs, the coverage rates reflect
achievements for the whole year. All categories of stakeholders including
utilizers, did not perceive any adverse effect of PPI on routine services.
Nevertheless, it is noteworthy that almost half of the mothers and pregnant
women were not aware of the services provided by the health department and
appeared dissatisfied with their overall performance.
34
Impact of targeted programmes on health systems: a case study of PE
Using eight indicators to assess the impact of PPI programme on the health system,
the main conclusions of the evaluation were as follows:
Relationships between health workers and community improved across country.
Image of and confidence in health institutions improved.
Morale of health workers improved.
Mixed view of effect on other health programmes although mostly positive.
Availability of drugs and other services increased.
Overall there is benefit with better behaviour of health workers cited.
Awareness of other health programmes increased and demand for services
increased.
Some social barriers were broken down.
EPI rates declining before PPI cycles started; some service disruption but
unclear cause.
Recommends tions
1)
Allocation of resources (both material and manpower) for the PPIs should be
built into the yearly calendar of activities of all participating departments to
minimize the negative impact.
2)
Although most of the health functionaries maintained that there was either no
adverse impact or there was some beneficial effect of PPI on the delivery of
other ongoing health programmes, one-half of the utilizers were unaware of
the existing health programme and hence would not have been using those
services.
3)
There was unanimity among stakeholders that the relationship between
health workers and the community had improved with the onset of PPI and
this in turn also improved the image and credibility of the health department.
There is now a need for an awareness campaign about the other ongoing
programmes and services to improve service utilization. Apparently,
expectations of the health department could also be heightened. If the health
system does not respond to the community expectations, health programmes
including PPI can face adverse effects in subsequent cycles.
Comments/discussion
Meeting participants commended AIIMS-IndiaCLEN for the thorough and detailed
attention to rigorous qualitative research methods. The amount of data and the
programmatic implications were very impressive. The government was pleased with
the study and has asked AIIMS-IndiaCLEN to conduct a similar study for their
HIV/AIDS programme. This was noted as a good spill-over effect from polio,
both for AIIMS-IndiaCLEN in their ability to apply their methodology to other
programmes, and for the Government of India and their desire to monitor the process
and progress of another large health programme.
WHO/V&B/00.29
35
When asked about politicians’ views of polio eradication, the researchers responded
that interviews with ministers found no conflict with party lines. In fact, they wanted
polio eradicated during their tenure to gain prestige from success.
Some meeting participants expressed strong concern about several potential,
unintended consequences of polio eradication:
That house-to-house immunization raises expectations that health services will
be brought to their door.
That polio is having a more significant impact on routine immunization,
in India, than is currently documented.
The researchers commented that while some respondents stated that they expected
the health system to now deliver NIDs’ vaccine to their door, it was not known that
these same people expected all immunizations or all health services to now be
delivered to their door. Findings from other countries (e.g. Afghanistan) also suggest
that people’s expectations of house-to-house delivery of immunizations and potentially,
other health services, is growing as a result of the NIDs. There is sufficient concern
to suggest that AIIMS-IndiaCLEN try and get more information to better determine
the real expectations of people. The researchers said they would address these issues
in the next evaluation.
A number of participants knowledgeable about the variation in capacity in Indian
states, raised questions about generalizing the findings. It was recommended that
the researchers disaggregate and compare their data by state, and district if possible.
It would be very informative to learn more about how to increase political
commitment where capacity is weak; how to build on the management capacity
existing at district/local levels to be more successful in strengthening system in future.
The researchers assured the group that they will look at the data by state and district
more closely.
4.
Financing of polio eradication campaigns in Bangladesh,
Cote d’Ivoire and Morocco (Partnerships for Health Reform)
Presentation by Dr Ann Levin, University Research Co., Bethesda,
Maryland, USA
Introduction
Numerous researchers have found it difficult to obtain substantive data about the
impact of the polio eradication campaign on the financing of health systems.
The USAID-funded Partnerships for Health Reform (PHR) project, via its
immunization financing initiative, is undertaking a study on the financing of the
polio eradication (PE) initiative. The purpose of the study is to determine the impact
of the eradication campaign on the financing of national immunization programmes
and to the extent possible, the health system as a whole.
The study examines whether trade-offs occur when governments, donors and
international organizations provide funding for polio eradication (PE). Do they reduce
their funding for other activities such as routine immunization programmes in order
to shift funding to PE? Or are they able to provide funding for both activities?
36
Impact of targeted programmes on health systems: a case study of PE
Are governments providing funding for PE or do they assume there are sufficient
resources and concentrate on providing resources for other activities such as routine
EPI? It is also important to ascertain whether the increased knowledge about the
benefits of immunizations from the PE is attracting new funding for the national
immunization programme and other health sector activities and that their long-term
funding prospects may be improving. This study seeks to determine the impact of
the polio eradication campaign on the financing of long-term programmes of the
health sector such as the routine EPI programme.
WHO estimates that the global campaign towards PE will reach its peak of activity
in 1999 to 2001. During this critical period, the biggest challenge will result from
the shift in focus from logistical strategies to financial strategies. WHO is estimating
that US$ 700 million will be necessary during this time for eradication efforts.
Although external support from donors is substantial, additional resources will be
required to cover projected shortfalls in funding.
What impact do resource allocation decisions for eradication campaigns have on the
provision of routine services? Critics of eradication campaigns have argued that
eradication activities divert resources and undermine the efforts to maintain and
strengthen routine health services.
Methods and data collection
The effect of the PE on the financing of routine immunization activities and health
systems is analysed in terms of two dimensions: 1) short-term effects on funding;
and 2) long-term effects on financing of the national immunization programme and
health systems.
The short-term effects of PE on financing of routine EPI are examined using trend
analysis when this information is available. First, the funding of routine EPI and
health sector activities is examined and compared with funding for NIDs to determine
whether a decrease or the decline in the rate of increase has occurred for these
activities during the time when polio eradication activities were introduced.
In addition, the changes over time of funding from specific sources is investigated to
determine whether these individual flows have increased or decreased during this
time period.
The contributions of the governments (including personnel) in each of these countries
for routine immunization programmes and NIDs is examined separately to assess
how governments have divided available resources for their national immunization
programme among routine EPI and polio eradication activities. It is also important
to examine whether governments are making substantial contributions to PE and
possible long-term effects on financing for their immunization programme.
Long-term financing possibilities are discussed in terms of findings from information
on types of contributors as well as discussions with key informants in the case study
countries.
WHO/V&B/00.29
37
The data collection took place in three countries: Bangladesh, Cote d’Ivoire and
Morocco. These countries were chosen because data had already been collected from
them for PHR’s immunization financing studies. Specifically, they all have a mix of
financing strategies, are in different geographical regions, and two out of the three
are using a financing mechanism (UNICEF’s Vaccine Independence Initiative) to
purchase vaccines.
Information has been collected on source and use of funds for routine immunization
programmes and polio eradication activities by the governments, donors and other
contributors. The funds are disaggregated by type of expenditure such as personnel,
supplies, transport, and equipment. The sources of financing include the following:
government, donors, international organizations, local (regional) governments, and
the private sector.
Expenditure information is divided into recurrent and capital expenses. Recurrent
includes any expenditure that last for a time period of less than one year such as
personnel salaries and supplies. Capital includes longer-term expenditures that last
longer than a year such as equipment and land.
The data on contributions of the central government, donors, and international donors
were collected from ministries of health, donor databases (e.g. SIDA), and projects
that support NG Os. In addition, separate surveys were initiated when the data on
contributions were not available. For example, a survey of municipalities was
conducted to obtain data on contributions of local governments towards the national
immunization programme in Bangladesh.
The calculation of personnel time was undertaken through multiplying the number
of days and percentage of total work time spent on the activity by salary of the type
and number of workers. For example, in Bangladesh, health assistants were estimated
to spend 40% of their time on routine expanded programme on immunization (EPI)
and 8% of their time on national immunization days (22 days for 2 NIDs) and their
salaries were multiplied by 0.40 to get the cost of their time spent on this activity.
Interviews were conducted with a large number of key informants to obtain in-depth
information on the immunization programmes and long-term prospects for financing.
Summary and conclusions
A summary of some of the main findings from this assessment of financing of polio
eradication activities, routine EPI, and health budgets are the following:
Three of the main funders of the polio eradication campaign in these
countries - Rotary International, the Government of Japan, and GDC are
focusing most of their resources on this campaign. In only one case was funding
also provided for routine EPI - Japan’s financing of measles vaccine in
Bangladesh.
Other sources of finance (donors) provide funding only for routine EPI
activities, e.g. KFW in Cote d’Ivoire, SIDA in Bangladesh.
The governments in each of the three countries as well as UNICEF and WHO
are funding both activities.
38
Impact of targeted programmes on health systems: a case study of PE
The ministries of health in each country have taken different approaches to
funding of routine EPI and polio eradication activities :
-
-
-
in Bangladesh from 1993/4-1997/8, the Ministry of Health has been
increasing its contributions to the routine EPI programme, but decreased
their funding for polio eradication activities;
in Cote d’Ivoire, the contribution of the Ministry of Health has increased
gradually both for routine EPI activities and the polio eradication
campaign;
in Morocco, the Ministry of Health, with assistance from a World Bank
loan, has increased its funding for both activities so that it is now financing
most of the costs of routine EPI and the polio eradication campaign.
The funding for routine EPI activities has been increasing in each of the three countries.
Funding by the governments have been increasing for routine EPI activities during
the period since the polio eradication activities were introduced. In Cote d’Ivoire
and Morocco, the governments have also been increasing their contributions to the
polio eradication campaign. The results suggest that no trade-offs were made in
Cote d’Ivoire and Morocco. Instead, the governments have increased their overall
financing of routine EPI and polio eradication. In the case of Bangladesh,
the Government chose to concentrate its limited resources on routine EPI rather
than polio eradication activities. This is an appropriate choice for the Government
since the routine coverage appears to be declining.
Most donors1 (e.g. Rotary International) have concentrated on funding for either
routine EPI or polio eradication activities, and did not need to make any trade-offs
regarding their funding. Only a few organizations - one donor, USAID, and two
international organizations, WHO and UNICEF - are funding both activities.
None appear to be reducing their funding for routine EPI activities,2 with the
exception of UNICEF in Bangladesh.
It is likely, however, that there were opportunity costs in choosing to support polio
eradication activities in each country rather than making improvements to the routine
EPI programme. The funds could have been used to support the introduction of
“new” vaccines such as hepatitis B, to provide more social mobilization activities
for routine EPI, etc. On the other hand, it is possible that these other activities could
not have attracted the additional funding that the high-profile polio eradication
campaign did, and they would not have had sufficient financing.
1
2
Although the Government of Japan is providing funding for both routine EPI and polio
eradication in some countries, it is funding primarily polio eradication activities in the three
countries in this study.
It should be noted that informal reports suggest, though, that some reductions in USAID funding
for routine EPI activities have occurred in other countries in West Africa as a result of introducing
financing for polio eradication activities.
WHO/V&B/00.29
39
This study has concentrated on funding for routine EPI and cannot draw conclusions
regarding the impact of polio eradication on the financing of other health services in
these three countries. It should be noted, however, that the funding for national
immunization programmes (routine EPI and polio eradication activities) has been
increasing at a higher rate than the health budget as a whole. It is possible that some
trade-offs in the provision of funding for immunization activities versus other health
activities are being made. However, without more information, no conclusions can
be drawn.
The long-term financing prospects can be divided into two types: 1) government
funding for polio eradication activities, and 2) funding of donors and international
organizations. In two of the three countries in the study, Cote d’Ivoire and Morocco,
the funding for polio eradication activities has increased during the time period
investigated, particularly in the latter case. One possibility is that, after the polio
eradication campaign is finished, the additional funding can be kept for the national
immunization programme and be used to strengthen it.
Since much of the additional funding for polio eradication activities is from donors
that provide financing for this activity and not routine EPI, the long-term prospects
of obtaining funding from them is not clear. For example, the Government of Japan
may choose to shift its funding from polio eradication to routine EPI (since it is
funding the latter in some countries), however, it is not clear that they will do so.
It is also possible, however, that, funders such as Rotary International and international
organizations will shift their funding to another disease eradication campaign such
as measles.
In addition, it should be noted that some of the funding for the polio eradication
campaign has been for the capital costs of financing equipment and vehicles,
they have provided additional resources that can be used by the routine EPI
programme that will last for several years.
In summary, the study found that:
a)
Most donors concentrate on funding either EPI or polio eradication.
b)
The governments, UN programmes, USAID fund both.
c)
The role of a government as a funding source is different in each country.
d)
Funding for EPI increased.
e)
Government funding for polio eradication activities increased in two countries
so may be reprogrammed.
f)
Funding of capital goods by donors has long term use for other programmes.
g)
The need for a long-term plan of how to shift from polio activities to new
activity is recommended.
h)
There is a role for donors and international organizations to assist countries to
plan for improvements to national immunization programmes.
40
Impact of targeted programmes on health systems: a case study of PE
Comments/discussion
Participants noted the important gap that this study addresses, that of the
financial impact of polio on country programmes. While good data was presented on
country-level budgets, when asked about trends in donor funding, PHR showed a
graph of USAID’s funding trends for polio and routine immunization. As polio funding
increased, resources for routine immunization decreased. USAID representatives at
the meeting stated that the two were indeed interrelated and a result of the earmarks
required by Congress (USA) for polio eradication (the earmark was not additional
funds, but had to be taken from within the existing programme.). Trends for other
donors were not available, however, WHO presented supplementary information
on funding sources for PE in 1999. That data demonstrated that of the estimated
US$ 319 million in external donor funding for PE in 1999, over 80% was funding
that was not previously targeted for developing country immunization services.
As much as 50% of the external PE financing was from funding sources such as
Rotary International that have not previously contributed to official development
assistance for health.
Temporally, the decline in routine immunization in many countries in the early 1990s
coincided with a contraction in donor funding for immunization. Many participants
identified this as one of several contributing factors that influenced the decline in
routine immunization during this time. Others pointed out that the WHO country
case studies indicated that decentralization might have played an even greater role
in reducing coverage. PHR could not generalize whether country budgets had
compensated for the reductions in donor funding, thus making government support
for immunization more sustainable.
The participants recommended that WHO undertake further analysis of trends in
donor funding for polio and routine immunization.
5.
Lessons learned in the development of the Global Polio Laboratory
Network (quality assurance project)
Presentation by Catherine MacAulay, University Research Co., Bethesda,
Maryland, USA
Introduction
This study, funded by USAID, was conducted by the Quality Assurance
Project (QAP) to determine if the Global Polio Laboratory Network (LABNET)
can be cited as a “best practice model” given that many other public health
programmes rely on laboratory results to guide programme decisions (e.g. malaria,
TB, or HIV/AIDS). With increased attention on integrated surveillance and the use
of data to drive decision-making for public health, USAID and other donors are
interested in cost-effective strategies for collecting relevant disease information.
A key purpose was to identify the quality principles subscribed to by the LABNET
that have contributed to its success and to determine whether these principles can be
applied to other health programmes and or health systems to improve their outcomes.
WHO/V&B/00.29
41
QAP cast its analysis of LABNET’s success in providing laboratory support to the
Global Polio Eradication Initiative in terms of quality management (QM) quality
assurance (QA) techniques that the network uses to ensure high quality performance
in detecting and tracking the wild poliovirus. Quality assurance is a systematic process
for closing the gap between actual performance and the desired outcome. Accurate
and timely detection, identification and reporting of the virus’ geographic origin are
crucial to the polio eradication effort.
Offering QAP’s view of the LABNET in QM and QA terms will provide other
laboratories and health programmes with an analytical framework that may serve as
a benchmark for assessing their own program’s performance.
LABNET consists of 150 laboratories, distributed throughout the world, at the
international, regional and national levels. These laboratories conduct scientific testing
to isolate and identify the wild poliovirus in stool specimens collected from patients
with acute flaccid paralysis (AFP). This scientific testing is critical to the eradication
strategy. The deployment of a sophisticated science to track the virus’ geographical
origins provides the catalyst, i.e. scientific confirmation of a polio case, to trigger the
appropriate mop-up vaccination operations that concentrate on the populations at
risk for viral contamination.
The design and implementation of strategies for the network were modelled after
the Pan American Health Organization’s (PAHO) Latin America Polio Network.
PAHO/WHO decided to be highly selective in incorporating laboratories into the
network and deliberately restricted the number of laboratories to optimize
proficiency, logistics and communication. This also allowed for better oversight and
support (mentoring and coaching) by PAHO/WHO for the laboratories in the
network. Laboratories were selected based on their level of overall high performance
(reputation), and strategic location, ensuring that health care facilities had reasonable
access and timely response from a functioning polio laboratory. From the outset
criteria were established for laboratory performance. It has been a conscious decision
to keep the network small and focus on quality, defined as accurate and timely
reporting.
Accreditation is conducted annually. The accreditation process is an on-site visit
designed to assess an individual lab’s compliance with WHO’s standards for
proficiency, management, and reporting.
By incorporating strict performance standards and quality control elements into the
accreditation process the laboratory network can consistently produce reliable results
regardless of whether the specimen was analysed in Atlanta or Lucknow. The
successful development of the laboratory network and the experience to date of
using performance-based standards is a noteworthy contribution of the Polio
Eradication Initiative.
42
Impact of targeted programmes on health systems: a case study of PE
Methods and data collection
The evaluation took place over a period of several months in the summer of 1999.
It was conducted by researchers with experience in QA and Good Laboratory
Practice. Five laboratories in Africa (2), India (2) and the USA (1) were visited and
the researchers attended laboratory network directors’ meetings. QAP observed
first hand the laboratories functions and practices and reviewed the Global Polio
Laboratory Network on the merits of their quality management principles that have
contributed to the global network becoming a best practice model for good laboratory
practice. The researchers observed the laboratory practices and interactions with
staff including laboratory directors, laboratory managers, laboratory supervisors,
virologists, laboratory technicians, and data managers.
The establishment and maintenance of QM/QA activities is clearly a management
responsibility and unless management is committed to QA it will not happen.
The laboratories conduct many QM/QA activities on a regular basis through
supervision visits, data tracking and accreditation processes.
Summary and conclusions
The study found that LABNET’s structure and operational approaches do implement
key QM/QA principles and practices, providing a model that can be applied to other
health programmes. LABNET effectively uses QA activities in the clinical laboratory
setting to achieve, according to internationally recognized scientific, standards,
the stature of good laboratory practices (GLP). In addition, QA activities are used
to monitor compliance with GLP in a clinical lab.
The laboratories visited displayed a sincere commitment and sense of pride at being
involved within the network. As one laboratory worker said in India; “The community
respects us more knowing we are accredited and I go home at night knowing that
my work might save (prevent) one family the pain of a paralysed child.”
The findings reveal that the network demonstrates six quality principles that have
helped achieve their high quality of success and which are factors that contribute to
the network’s success in supporting the PEI efforts. These six quality principles
exemplify QM/QA in practice throughout the network:
1)
Leadership (strong management and global accreditation process).
2)
Quality assurance activities become institutionalized (standards developed,
quality monitoring and improvement, teamwork).
3)
Accrediation (recognition of compliance).
4)
Capacity building (education, data management training, feedback).
5)
Communications (professional, between laboratories, with programme
implementers/EPI managers regular and frequent e-mails).
6)
Documentation (network-wide, information used for improvement of
programme management).
WHO/V&B/00.29
43
Management science supports that an organization’s leaders set the tone.
“In a learning organization leaders are designers, stewards, and teachers. They are
responsible for building organizations where people continually expand their
capabilities to understand complexity, clarify visions, and improve shared mental
models - that is they are responsible for learning.” (The Fifth Discipline, P. Senge,
1990).
In this regard the study concluded that WHO leadership has been exemplary and is
replicated in style and substance at every level within the network. WHO has created
a vision for the laboratory network and has effectively communicated this to all
participants. Management is professional, approachable, collaborative,
anti-bureaucratic and friendly. This approach keeps everyone in LABNET motivated,
on-track and dedicated. Communication is vertical and horizontal. Training and
education are targeted and tailored to individual settings and aimed at improving
shortcomings highlighted during the annual accreditation review. Seen more as peer
review, accreditation visits serve as problem-solving opportunities involving all
laboratory staff, and thus becomes an interactive learning experience for all
participants. Data management is given as much attention as specimen analysis.
While the study was not able to collect information on the costs of operating the
laboratory network, donors provide resources, time and expertise. LABNET is not
fully funded and efforts are under way to secure additional resources. QAP did not
investigate the reasons why some laboratories left the network prior to this study;
this remains an area to be explored.
Comments/discussion
Most participants agreed that the development of the laboratory network is a
remarkable achievement. Several people noted that the study could be strengthened
further by providing more details on the status of the laboratory’s performance prior
to inclusion in the network. It is important to answer the questions: How did polio
eradication activities bring added value to the laboratories? What changes resulted?
What proportion of the polio eradication resources go to support the laboratory
network? Is it possible to estimate how much staff time was invested in developing
the laboratory from its baseline to its current level of functioning? How will these
laboratories be sustained after polio is eradicated? There was also agreement that
the reasons why a few laboratories left the network should be explored.
This information could provide important guidance for the development of other
laboratory networks.
44
Impact of targeted programmes on health systems: a case study of PE
6.
UNICEF experience in West Africa - Benin, Niger
Presentation by Dr Jane Zucker, Health Adviser, UNICEF, New York
Introduction
In 1999 UNICEF carried out a rapid assessment of the impact of PE on routine
EPI and other health activities in two countries: Benin and Niger.
Methods and data collection
The countries were selected based on their performance (Niger as a low performer,
Benin as a high performer). The assessment process included a qualitative review of
available documentation, interviews with key actors, and field visits to two districts.
The main issues considered were EPI coverage, time/workloads, social mobilization/
IEC, cold chain, integration of other health interventions, reaching the unreached,
budget allocations, and surveillance.
Summary and conclusions
Like the WHO study, the UNICEF assessment also concluded that there was little
evidence of either a positive or negative impact of PE on routine immunization and
other aspects of primary health care.
Key obstacles to better interaction between EPI and PE were identified:
Late start of NIDs planning process due to factors beyond national control.
Lack of consolidated and integrated social mobilization/IEC strategies.
Generally poor distribution of operational resources and budgets for routine
EPI and other health activities at the district level (this was less of an obstacle
in Benin where the Bamako Initiative makes funds available).
The integration of vitamin A with NIDs was noted as a positive impact but there
were missed opportunities to develop more systematic inventory monitoring for the
cold chain, and to integrate AFP surveillance with other disease surveillance efforts
(it was noted the relative importance of this would increase as the countries began to
embark on more human resource intensive active AFP surveillance).
Comments/discussion
Participants noted that there were other factors in Niger, such as the coup, that may
have contributed to the decline in EPI and for the diversion of funds. Participants
urged UNICEF to quickly finalize and disseminate the report of the assessment
(no document was available at the meeting), so that the findings could be available to
all for review.
WHO/V&B/00.29
45
Annex 5 :
Using polio eradication (PE) activities
to strengthen routine immunization:
the 10-step programme
Draft Checklist
PE activity
1. ADVOCACY:
To achieve PE, sustained
political and financial
commitment is necessary
at all levels.
Actions to strengthen
routine immunization
Are you doing this (yes/no)?
How to improve?
Combine efforts: explain to
decision-makers that PE
depends on strong routine
immunization services; state
the importance and needs of
routine immunization in all
PE advocacy opportunities.
Highlight the context: when
reporting NIDs coverage
compare with routine
coverage for DPT3 and
measles (e.g. publish tables
comparing district coverage)
Troubleshoot: use highvisibility of NI Ds to solve
administrative and technical
bottlenecks that affect routine
immunization and impede
PE (i.e. slow release of funds,
staffing).
2. PARTNER COORDINATION:
PE relies on coordinated
partners to ensure that all
resource requirements are
addressed.
Think bigger: ensure that
Interagency Coordinating
Committee (ICC) meets
throughout the year; expand
mandate of ICC to include
routine immunization.
3. INFORMATION,
EDUCATION,
COMMUNICATION (IEC):
Nationwide multisectoral
awareness is critical for PE.
Generate demand: include
messages in NIDs training,
materials, or media events
about other EPI vaccines and
the need for children to be
fully immunized (e.g. where
and when to receive other
immunizations).
4. SOCIAL MOBILIZATION:
Active participation of
community leaders,
volunteers, parents, and
private sector is needed to
achieve PE.
Maintain involvement: use
the organizations, media and
people mobilized for PE to
support the delivery of routine
immunization services in all
areas (e.g. develop social
mobilization plan for routine
immunization).
46
Impact of targeted programmes on health systems: a case study of PE
PE activity
5. PLANNING:
Comprehensive strategic
and annual micro-planning
is necessary for PE to reach
every child with oral polio
vaccine (OPV).
Actions to strengthen
routine immunization
Are you doing this (yes/no)?
How to improve?
Share plans early: to avoid
disruptions to other health
services, share planned NIDs
dates widely with all health
programmes.
Double up: use PE micro
planning and training
opportunities to improve
planning of routine
immunization services
(e.g. frequency, sites, etc).
Use data: encourage use of
NIDs target population data
for routine immunization, if
these are more accurate than
official data.
6. COLDCHAIN/LOGISTICS:
PE requires effective
logistics and cold chain to
ensure safe and potent
administration of OPV
with minimum wastage.
Protect the investment: ask
NIDs partners to invest in cold
chain that meets EPI
standards, and to support the
preventive maintenance,
spare parts and training to
keep it functioning for routine
immunization.
Waste not, want not: use
good vaccine management
practice in NIDs to reinforce/
teach stock management for
routine vaccines (e.g. to
adjust OPV requirements and
redistribute stock after NIDs).
Exploit technology: provide
training on the use of vaccine
vials monitors (WMs) as a
management tool for routine
immunization services.
7. SERVICE DELIVERY &
SUPERVISION:
PE needs to provide high
quality services (OPV) at
point of delivery in NIDs and
routine immunization.
WHO/V&B/00.29
Build capacity: use PE
training opportunities to
refresh routine immunization
skills and knowledge.
Work together: combine
surveillance and routine
supervisory visits; ask PE
surveillance officers to check
fridge temperatures, stock
levels, knowledge of WMs, etc.
47
Actions to strengthen
routine immunization
PE activity
8. SURVEILLANCE:
High-performing, timely AFP
surveillance system is
essential to achieve PE.
Get integrated: gradually
include other priority diseases
with AFP surveillance and
reporting. Train AFP
surveillance officers; develop/
adapt case investigation and
reporting forms.
9. INJECTION SAFETY:
PE offers opportunities to
promote safe injection
practices.
Play it safe: ensure that any
NIDs activity that includes
injectable vaccines has a
detailed plan of action to
ensure safe injection and
waste disposal at all levels.
Establish safe practices/
systems for routine
immunization.
10. MONITORING:
Achievement of the PE goal
requires careful monitoring.
Track impact on system:
make a commitment to
“achieve PE in ways that
strengthen routine
immunization systems”.
Use nine key indicators to
monitor and document the
impact of PE on strengthening
routine immunization (see
attached List of Impact
Indicators). Analyse and use
collected information to take
corrective action, and report
progress periodically.
Are you doing this (yes/no)?
Howto improve?
Nine key indicators (draft)
Monitoring the impact of polio eradication (PE)
on routine immunization programmes
i)
Trends in routine immunization coverage:
Monitor and analyse annual DTPS and measles coverage by district over
time.
2)
Trends in financial resources:
Trend analysis of annual financing (external and national) of PE compared
to financing (external and national) of routine immunization services (if
possible also compare to overall health sector budget/expenditures).
48
Impact of targeted programmes on health systems: a case study of PE
3)
Surveillance:
•
4)
Cold chain improvement:
•
5)
Inclusion of vaccine vial monitor (VVM) training for PE campaign
activities.
Partner coordination:
•
9)
Existence of PE communication and social mobilization plan that includes
routine immunization (and if appropriate, surveillance).
Vaccine logistics:
•
8)
In countries with vitamin A deficiency problems, delivery of vitamin A
is integrated with routine immunization services.
Information, education, and communication:
•
7)
Percentage of district cold stores with full complement of functioning
equipment and system for maintenance.
Integration of other services:
•
6)
Number of other diseases integrated with “active” AFP surveillance
activities.
Interagency Coordinating Committee (ICC) is used for broader health
sector coordination (mandate and membership are not PE-specific).
Human resource development:
•
WHO/V&B/00.29
Systematic use of PE micro-planning to improve the delivery of routine
health services.
49
"pl5 - G
WHO/V&B/02.12
ORIGINAL: ENGLISH
4
Vaccines ana io ogica s
Report of the seventh meeting of the
Technical Consultative Group (TCG) on the
Global Eradication of Poliomyelitis
IS
t
Geneva, 9-11 April 2002
World Health Organization
■
1
if
||||^
aliiife
1 M *
8
WHO/V&B/02.12
ORIGINAL: ENGLISH
Vaccines and Biol ogical 5
Report of the seventh meeting of the
Technical Consultative Group (TCG) on the
Global Eradication of Poliomye) ItlS
Geneva
II
WHO
World Health Organization
’ r 11 April 2002
The Department of Vaccines and Biologicals
thanks the donors whose unspecified financial support
has made the production of this document possible.
This document was produced by the
Expanded Programme on Immunization
of the Department of Vaccines and Biologicals
Ordering code: WHO/V&B/02.12
Printed: October 2002
This document is available on the Internet at:
www.who.int/vaccines-documents/
Copies may be requested from:
World Health Organization
Department of Vaccines and Biologicals
CH-1211 Geneva 27, Switzerland
• Fax:+ 41 22 791 4227 • Email: vaccines@who.int •
© World Health Organization 2002
All rights reserved. Publications of the World Health Organization can be obtained from Marketing
and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland
(tel.: +41 22 791 2476; fax: +41 22 791 4857; email: bookorders@who.int). Requests for permission to
reproduce or translate WHO publications - whether for sale or for noncommercial distribution - should
be addressed to Publications, at the above address (fax: +41 22 791 4806; email: permissions@who.int).
The designations employed and the presentation of the material in this publication do not imply the
expression of any opinion whatsoever on the part of the World Health Organization concerning the legal
status of any country, territory, city or area or of its authorities, or concerning the delimitation of its
frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may
not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are
endorsed or recommended by the World Health Organization in preference to others of a similar nature
that are not mentioned. Errors and omissions excepted, the names ofproprietary products are distinguished
by initial capital letters.
The World Health Organization does not warrant that the information contained in this publication is
complete and correct and shall not be liable for any damages incurred as a result of its use.
ii
Contents
Abbreviations........
.. v
Executive summary
vii
1.
Summary of conclusions and recommendations
1
2.
Stopping wild poliovirus transmission................................................
4
2.1 Resource requirements and resource mobilization.......................
2.2 Endemic countries and strategic priorities for 2002 ......................
4
5
Priorities in the pre-certification era.................................................
10
3.1 Certification-standard surveillance................................................
3.2 Containment of laboratory stocks of wild poliovirus....................
3.3 Supplementary immunization in polio-free areas...........................
3.4 Post-certification immunization policy development....................
3.5 Programme oversight, administration and human resources........
3.6 Milestones for the Global Polio Eradication Initiative 2002-2003
10
14
15
16
19
21
3.
Annex 1: Agenda
23
Annex 2: List of participants
26
iii
Abbreviations
AFP
acute flaccid paralysis
AFR
African Region
AMR
Region of the Americas
cVDPV
circulating vaccine-derived poliovirus
DR Congo
Democratic Republic of the Congo
EAG
expert advisory group
EMR
Eastern Mediterranean Region
EPI
Expanded Programme on Immunization
EUR
European Region
GAVI
Global Alliance for Vaccines and Immunization
ICC
Interagency Coordinating Committee
IPV
inactivated polio vaccine
NID
national immunization day
OPV
oral polio vaccine
SAGE
Scientific Advisory Group of Experts
SEAR
South-East Asia Region
SIA
supplementary immunization activity
SNID
subnational immunization day
TAG
Technical Advisory Group
TCG
Technical Consultative Group
TFI
Task Force for Immunization
VDPV
vaccine-derived poliovirus
WPR
Western Pacific Region
V
Executive summary
The seventh meeting of the Global Technical Consultative Group for Poliomyelitis
Eradication (TCG) in April 2002 noted that progress towards the eradication
goal has been considerable. All of the major 2001 programme milestones had been
achieved either in full or in part (see table 3). Most importantly, reported polio cases
had fallen from 2971 to 480 between 2000 and 2001, with only 10 countries remaining
polio-endemic at the start of 2002 (figure 1).
The TCG recognized, however, that substantial risks to achieving the eradication
target remain. Of these, the funding gap of US$ 275 million constitutes the greatest
threat (figure 2), especially as it could increase by US$ 150 million, should polio
transmission continue into 2003. Closing the funding gap should be the highest
priority of the partnership.
Among the 10 endemic countries that now constitute three “high transmission” zones
(north India, Pakistan/Afghanistan, Nigeria/Niger) and three “low transmission”
zones (Horn of Africa, Angola, Egypt (figure 3)) the TCG was particularly concerned
with India, which reported 56% of global cases in 2001, and Egypt, where the extent
of transmission has been severely underestimated. The TCG was also alarmed that
an inappropriate response to wild poliovirus, such as happened in Mauritania
in 2001, could still occur at this late stage. Priorities were defined for each
endemic country, with the establishment of a national technical oversight body
(Technical Advisory Group - TAG) recommended for each.
In reviewing the priorities for non-endemic countries, the TCG questioned the
adequacy of acute flaccid paralysis (AFP) surveillance in some areas due to weak
AFP quality indicators and/or the high number of polio-compatible cases, especially
in Africa (table 1). Southern Africa, the Horn of Africa and Indonesia were identified
as priorities for improving surveillance. Although impressed with the progress in
containing wild poliovirus laboratory stocks (table 2), the TCG emphasized the need
for national coordinators and action plans in all polio-free countries by
end-2002. Based on an analysis of population immunity in polio-free areas (figure 7),
the TCG decided that all polio-free countries bordering a polio-endemic area should
conduct national immunization days (NIDs) or subnational immunization days
(SNIDs) annually; all other countries which lack 90% routine infant immunization
should continue NIDs at least every three years.
The TCG evaluated the work on development of post-certification immunization
policy, and identified key data gaps in several areas: the transmissibility
of vaccine-derived polioviruses (VDPVs), prevalence of long-term excretors
(i.e. in middle-income countries), quality of laboratory containment, vaccine
vii
stockpiles, inactivated polio vaccine (IPV) efficacy in developing countries and oral
polio vaccine (OPV) production in the post-immunization era. Policy decision models,
reflecting how the range of possible research outcomes could affect post-certification
policy, would also need to be developed and tested through 2003.
Having deliberated on all of the major polio eradication issues, the TCG reviewed
and updated the 2002-2003 milestones for each of the objectives detailed in the
Global Polio Eradication Strategic Plan 2001-2005 (table 3).
viii
1. Summary of conclusions
and recommendations
Rapid progress continues towards the global interruption of wild poliovirus
transmission. Between 2000 and 2001 the number of countries considered
endemic for polio has decreased from 20 to 10 (figure 1). High-quality surveillance
data is increasingly guiding the implementation of national programmes.
The number of reported polio cases has declined from 2971 in 2000 to 480 in 2001
(as of April 2002, figure 3). Within the remaining endemic zones, progress is indicated
by decreasing geographic extent of virus transmission and a reduced number
of circulating virus lineages. Wild poliovirus type 2 has not been isolated since
October 1999.
Figure 1: Polio-endemic countries, 2000-2001
Polio-endemic in 2000
Polio-endemic in 2000 and 2001
The considerable progress towards global polio eradication was only possible through
intense efforts in endemic countries and because of continued generous support from
the international polio eradication partnership. During the past year, an additional
US$ 425 million was raised to cover polio eradication activities through 2005.
Nevertheless, a funding gap of US$ 275 million remains (figure 2), which must be
urgently closed.
WHO/V&B/02.12
1
Global polio eradication efforts have brought considerable benefits. Since 1988,
polio eradication has prevented an estimated four million children from being crippled
for life, and averted at least one million childhood deaths, both through polio
vaccination and the provision of vitamin A during NIDs. Further improvements in
targeted social mobilization and information efforts have been an important element
of success. Countries increasingly utilize polio eradication activities to further
improve routine immunization services and disease surveillance.
However, the TCG is very concerned that only eight months remain to reach
the goal of interrupting virus transmission globally by end-2002. Intense,
greatly accelerated efforts during the remainder of 2002 and continued strong political
support will be needed both to improve surveillance everywhere to reliably find and
characterize all remaining foci of transmission, and to intensify supplementary
immunization activities (SIAs), especially in high-risk areas, to reach all remaining
unimmunized children.
Despite the considerable progress made, the TCG considers that the three zones
of high-intensity transmission represent the major risks to the global eradication
goal: northern India, Pakistan/Afghanistan and Nigeria/Niger (figure 3).
Of particular concern is northern India, which accounted for approximately half of
all virus-confirmed polio cases reported globally in 2001, and from where wild virus
was imported into polio-free areas elsewhere in India and into other countries
(Bulgaria and Georgia). In addition to these high transmission areas, low intensity
transmission continues in the Horn of Africa (Ethiopia, Somalia, Sudan),
Angola and Egypt. The TCG is concerned that the extent of virus transmission in
Egypt had been severely underestimated until recently (figure 4), requiring urgent
improvements in the quality of surveillance and supplementary immunization.
The recent isolation of wild poliovirus in West Africa, genetically related to a virus
found in Mauritania in 2001, probably indicates a continuing focus of transmission
in West Africa that had not been previously detected due to suboptimal surveillance.
Response activities targeted at this focus to date have not been adequate.
Continuing transmission of wild poliovirus is the result of suboptimal implementation
of polio eradication strategies in the remaining endemic countries. High-quality AFP
surveillance is essential to identify problems and high-risk areas, and to guide
supplementary immunization efforts (figures 5 and 6). The TCG is impressed
with the overall improvements in surveillance, especially in Africa. However,
serious technical and programmatic concerns about surveillance quality remain.
Failure to collect sufficient clinical information and adequate stool specimens,
lack of 60-day follow-up examination, and absence of expert review has resulted in
the classification of large numbers of AFP cases as polio-compatible (table 1),
particularly in African countries. This raises the possibility of missing ongoing virus
transmission. The infrastructure of surveillance systems in many African countries
remains fragile, requiring considerable continuing technical and administrative
support and timely provision of adequate resources.
2
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
The TCG notes that, in addition to the rapid progress made toward stopping wild
poliovirus transmission, there has also been considerable progress in the programme
of work on the post-certification phase of polio eradication. The objectives of this
programme of work are to address (1) the risks of re-introduction of virus into the
population from laboratory stocks or long-term carriers, (2) the risks of emergence
of VDPVs, and (3) the management of response activities, should these be needed in
the post-eradication era. Considerable work remains to be done, particularly in
establishing consensus on post-certification immunization policy.
The TCG had noted during its sixth meeting (May 2001) that substantial efforts and
resources will be required through 2010 and beyond, to sustain high-quality
AFP surveillance, to maintain high population immunity until consensus on
post-certification immunization policy is reached, and to manage the risks of reintroduction of poliovirus post-certification. The programme has begun to prepare
estimates of resource requirements for the post-certification era; however, further
work will be needed in this area.
WHO/V&B/02.12
3
2. Stopping wild poliovirus
transmission
2.1
Resource requirements and resource mobilization
At its 2001 meeting, the TCG regarded the funding gap as the major risk to the
initiative. While substantial progress has been made, there remains a serious gap of
US$ 275 million for the period 2002-2005 (figure 2, the gap for 2002 is $80m).
If virus transmission is not interrupted globally by end-2002, the funding gap will be
even larger, over US$ 150 million above current projections for 2003-2005 in a
worst-case scenario (i.e. if all endemic areas were to fail to stop poliovirus transmission
in 2002).
Figure 2. Required and pledged/projected financial resources
as well as funding gap for polio eradication, 2002-2005
Rotary International
United Kingdom
Other
Japan
Funding gap =
US$ 275 million
USAID
Canada
US CDC
World Bank IDA
Credit to Govt, of India
Germany
Netherlands
External resources required = US$ 1000 million
Pledged/projected = US$ 725 million
Conclusion
The availability of sufficient financial resources remains critical to the success of the
global polio eradication initiative. The TCG urged all partners to maintain the highest
possible levels of support through certification.
4
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Recommendations:
•
WHO and UNICEF should publish, by September 2002, revised estimates
of the financial resource requirements for polio activities for the period
2003-2005. In addition to detailing the external financial resources required,
this document should reflect, as much as possible, the contributions of the
endemic countries themselves, as well as the financial implications of continued
wild poliovirus transmission into 2003.
•
The estimates of requirements for the post-certification period do not yet provide
adequate information to the partnership. Based on various post-eradication
scenarios outlined during the seventh TCG meeting, the estimates should be
further refined by September 2003.
2.2
Endemic countries and strategic priorities for 2002
The TCG reviewed the current epidemiology in “high transmission” areas,
noting the geographic and/or molecular evidence of ongoing progress in each of
these areas. In summary, there has been a 50% reduction in the number of endemic
districts in India, a 50% reduction in virus-confirmed cases in Pakistan/Afghanistan
and recent localization of transmission in Nigeria to the north/north-west of the
country (figure 3). In all “high transmission” countries, detailed programme guidance
and strategic priorities for 2002-2003 have been defined by joint national-international
technical advisory bodies (i.e. the Polio Expert Advisory Group in India and the
Technical Advisory Group on Polio Eradication for Pakistan and Afghanistan) or an
expert review (i.e. February 2002 National and International Review of Polio
Eradication in Nigeria).
Figure 3: Polio-endemic countries and wild poliovirus, 2001
Wild vims importations
(from South Asia)
Wild vims of
uncertain origin
Wild vims importation
(from Mauritania)
Wild vims importation
(from Angola)
WHO/V&B/02.12
□ Polio-endemic country
# 1 wild virus case
A Wild virus importation
Of the five “low transmission” countries, only Somalia, Angola and Egypt have had
wild poliovirus confirmed polio cases since 1 May 2001. However, surveillance is
suboptimal in Ethiopia, and surveillance gaps remain in Angola and the Sudan.
Of note, the recent wild poliovirus importation into western Zambia confirmed
ongoing virus transmission in eastern Angola. In Egypt, environmental sampling
confirmed that circulation of multiple lineages of wild poliovirus type 1 is widespread
in Upper (possibly also in Lower) Egypt, indicating that problems in implementing
AFP surveillance limit its sensitivity (figure 4). Joint national-international technical
advisoiy groups (TAGs) have now been established for Egypt, the Sudan and Somalia.
Figure 4: Environmental surveillance for wild poliovirus, Egypt, 2000-2001
Oct 00 Jan 01 Apr 01
Jul 01
Oct 01
Governorate
5
JK
0
Tanta
Beni Sueif
___ nJ..,.. iiblI iB■ M
Minya
______________
E
Abu Qurkas
s EZl
- narOi-_.____ ■o o.
•g
JUL
—(
^2
E .
I : !■
D
z
Mallawy
i
it
, al. L
Asiut
£1
El
n
■ H Mt m Mt W M
—
H Positive sample
Negative sample
Dairut
Sohag
Qena
.■UL
Aswan
Oct 00 Jan 01 Apr 01
Jul 01
Oct 01
Despite clear progress in African countries west of Nigeria, a further focus of ongoing
wild poliovirus transmission may exist in West Africa. Following the isolation of
wild poliovirus type 1 during the first half of 2001 in Mauritania (of uncertain origin,
possibly imported), wild poliovirus was recently found again in an area north of
Mauritania. Comprehensive investigation, as well as complete surveillance and
immunization response, are urgent.
Conclusions
Continued progress towards interruption of wild poliovirus transmission reaffirms
that polio eradication is technically and operationally feasible. Insufficient financial
resources continue to pose the greatest threat to the eradication initiative. At the
country level, heightened attention needs to be paid to the high transmission areas,
particularly India. Additionally, special attention is needed for Egypt, and Mauritania
and its neighbouring countries.
6
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Following a review of the recommendations made recently by country-level TAGs,
the TCG endorsed the surveillance and immunization strategies outlined for each of
the remaining endemic countries during this critical year for the global initiative.
The TCG notes the significant efforts to improve social mobilization and information
activities in most endemic countries. These efforts will have a positive impact on
SIA quality and should be continued and further expanded.
The TCG agreed with the following proposal of the global polio eradication
partnership as the priority order for resource allocation for country level activities;
a)
sustaining the surveillance infrastructure worldwide;
b)
ensuring sufficient supplies of oral polio vaccine;
c)
ensuring high quality SIAs in endemic countries; and
d)
promoting the quality of SIAs in recently endemic countries.
Given the progress in eradication in 2001 in the remaining endemic countries,
areas affected by conflict are of increasing importance to global eradication.
While governments and polio partner agencies have made further progress to access
children in conflict-affected areas, additional well-organized efforts to identify and
access critical areas will be needed in 2002.
Because of the rapidly evolving nature of poliovirus transmission worldwide, it would
be premature to revise the target date for the cessation of transmission. The Global
TCG does recognize, however, that the intensity of virus transmission in the “high
transmission” areas, the security concerns in other endemic areas, and the necessary
infrastructure work in Egypt, will make it necessary for the initiative to plan for a
full programme of work through 2003.
Recommendations:
•
The programme should continue to review and update specific contingency
plans on a six-monthly basis to deal with potential resource gaps.
•
Highest priority should be given to intensify and improve the quality of SIAs
in known endemic areas, guided by reliable surveillance data. Results of
systematic efforts to monitor and evaluate SIA quality should be used for
immediate action to correct problems, and should be documented and provided
to the respective countiy-level TAGs.
•
Country-level TAGs or expert advisory groups (i.e. EAG in India) are
performing an essential function in endemic countries. All countries endemic
for polio in 2001 that do not have an advisoiy group should establish and
convene such a group by September 2002. The terms of reference of country
level TAGs/EAGs should include;
-
-
WHO/V&B/02.12
critical review of the evolving epidemiology of polio in the country;
identification of the risks to achieving eradication, with respect to plans,
strategies, and implementation of surveillance and supplementary
immunization activities;
recommendations as to the appropriate strategies and activities to achieve
eradication targets, particularly in the areas of supplementary
immunization and surveillance.
7
Country-level TAGs/EAGs should be convened by and report to the
Minister of Health and meet at least annually. Meetings may need to be
convened eveiy six months in rapidly evolving programmes. Whenever possible,
TAGs/EAGs should be joint national-international bodies with an appropriate
mix of expertise in disease control and eradication. To facilitate collaboration
with the Global TCG, country-level TAGs/EAGs should include a
representative of the Global TCG, wherever possible. The outcome of country
level TAG/EAG meetings should be documented in brief reports, which should
include a summary of key data upon which the strategic recommendations are
based.
During the course of the meetings of country-level TAGs or EAGs,
or immediately thereafter, country programmes (i.e. the Ministry of Health
(MOH), WHO, UNICEF and other relevant implementing agencies)
should translate the recommendations into an operational programme of work.
These work plans should define roles, responsibilities and timelines to guide
the work of the partnership for the subsequent 6-12 months.
Social mobilization activities have only recently been accelerated in many
countries. All major endemic countries should have completed an evaluation
of progress in addressing social mobilization needs by September 2002.
Polio teams in endemic countries with conflict-affected areas should provide a
detailed analysis by end-July 2002 to identify those areas where serious access
problems persist and to indicate which potential mechanisms may exist to obtain
access for immunization and surveillance activities.
The TCG should convene again in late 2002 to review all available data,
and to further comment on the probable timeline towards stopping wild
poliovirus transmission in each of the remaining endemic countries.
The partnership will be made aware of TCGs conclusions.
Country specific recommendations:
•
India: SNIDs should be brought forward to the earliest possible time in
the period recommended by the recent EAG (e.g. July and August 2002).
Maximum use must be made of both surveillance and SIA quality data to assure
the highest possible coverage of very young children, especially in minority
groups. It is urgent to systematically evaluate the impact of efforts to improve
SIA quality over the last six months and to utilize this valuable information to
optimize coverage during the upcoming SIAs.
•
Mauritania/West Africa: the possibility of a focus of previously undetected
transmission in western Africa is of great concern. The WHO Secretariat should
urgently clarify the situation by end-May 2002, so that all affected countries
can plan and implement response activities as soon as possible.
•
Egypt: the TCG is impressed by the frank assessment by the Egypt TAG of
problems affecting the national polio eradication programme (see figure 4).
The TCG urges the MOH Egypt to review the oversight of the programme at
national level and requests partner agencies to provide the appropriate technical
and financial support.
8
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Angola: an unprecedented opportunity currently exists to access children in
all parts of Angola. All partners, especially the government of Angola,
are urged to move quickly to achieve safe and effective access to all Angolan
children during the planned mid-year NIDs.
Pakistan: the TCG concurs with the strategy of targeting high-risk areas within
the country, in addition to focusing on joint virus reservoir areas shared with
Afghanistan.
Afghanistan: the re-establishment of an effective programme in Afghanistan
should be a global priority. All partners, including the Special Representative
of the UN Secretary-General to Afghanistan, all UN agencies, and the
provisional Government, are urged to give polio eradication efforts high priority
and visibility, in order not to delay the interruption of transmission in
Afghanistan, and not to threaten regional and global progress
Nigeria: at this critical juncture of the programme, efforts to improve the
quality of SIAs must be intensified, and results reported back to the regional
Task Force for Immunization (TFI) and the global TCG. Specific efforts are
needed to coordinate activities with Niger. Plans for the formation of an EAG
for Nigeria should be carried through and the first meeting held no later than
July 2002.
Niger: coordination of surveillance and supplementaiy immunization efforts
with Nigeria should be a priority until both countries are polio-free.
DR Congo: continued efforts should be made to reduce the number of
polio-compatible cases through timely and accurate case classification.
A progress report on this work should be made to the next meeting of the
regional TFI and global TCG.
Hom of Africa: countries in the Hom of Africa (Ethiopia, Somalia, Sudan,
and surrounding countries) should ensure appropriate coordination of
surveillance and immunization activities, to ensure that no high-risk groups
are missed.
Ethiopia: improving the quality of surveillance should remain the focus of
efforts over the next 12 months. An expert advisory group for Ethiopia should
be formed by September 2002. Particular attention should be given to
coordination of surveillance and supplementary immunization efforts between
the Ethiopian region V and Somalia.
Somalia: access to the remaining area of transmission in Mogadishu and
Lower Shabelle is critical if polio is to be eradicated; all partners,
especially UN agencies, are urged to advocate for access and to provide support
in accessing these areas for polio eradication work.
Sudan: continued attention should be paid to the quality of the national
laboratory, with double-testing of specimens until quality indicators improve.
All partners are urged to maintain the coordination between programmes
covering northern and southern Sudan and to assure that access to all children
is sustained.
WHO/V&B/02.12
9
3. Priorities in the
pre-certification era
3.1
Certification-standard surveillance
The sensitivity of surveillance for wild poliovirus was evaluated by the TCG,
beginning with a review of the key indicators (non-polio AFP rates, adequate
specimen collection rates, laboratory accreditation) focusing on the Eastern
Mediterranean Region (EMR), South-East Asia Region (SEAR) and African Region
(AFR) (figures 5 and 6). There has been improvement in AFP surveillance in the
priority countries of Nigeria, Angola and DR Congo. Considerable gaps remain
however, particularly in Indonesia, southern Africa and the Horn of Africa.
Figure 5: Non-polio acute flaccid paralysis (AFP) rate, WHO African Region,
Eastern Mediterranean Region and South-East Asia Region, 2001
10
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Figure 6: Percent of AFP cases with adequate stool specimens, WHO African,
Eastern Mediterranean and South-East Asia regions, 2001
I
I
Adequate stool specimen rate <60%
-I Adequate stool specimen rate 60% - <80%
I Adequate stool specimen rate >80%
y
At its last meeting, the TCG made extensive recommendations on the use of AFP
cases classified as “polio-compatible” to identify surveillance gaps and areas of
potential risk of wild virus circulation. Supplementary information on surveillance
sensitivity is now available from genetic sequencing data, environmental sampling
and surveillance reviews.
Conclusions
While there have been recent improvements in the timeliness and accuracy of AFP
case classification, there remain a large number of polio-compatible cases in many
countries following adoption of the virological classification scheme during 2001,
particularly in the African Region (table 1). This clearly indicates that the mechanisms
for reviewing potential polio-compatible cases are not yet well enough developed.
Large numbers of polio-compatible cases represent a failure of the surveillance system.
WHO/V&B/02.12
11
Table 1: Acute flaccid paralysis, stool specimen collection, confirmed-polio
cases and polio-compatible cases, by WHO region, 2001
*
Compatibles
(% of total AFP)
AFP
Adequate Stool
specimens
Confirmed
polio
AFR
8 541
72%
68
946
(11.1%)
AMR
2189
90%
10
9
(0.4%)
EMR
3858
83%
140
77
(2.0%)
EUR
1752
81%
3
5
(0.3%)
SEAR
10646
83%
268
221
(2.1%)
WPR
6527
88%
3
12
(0.2%)
Global
33 513
81%
492*
1270
(3.8%)
Region
Global total includes all wild-virus confirmed cases and 12 cases associated
with vaccine-derived poliovirus, data as of 8 April 2002
The sequencing data presented to the TCG demonstrate high AFP surveillance
sensitivity in India and Pakistan but reaffirm concerns as to the sensitivity in Egypt.
Sequencing data on viruses detected in 2001 also confirms the need to further enhance
sensitivity in Somalia, West Africa, the Sudan and Angola.
The TCG notes that AFP surveillance can be developed to certification-standard
levels in countries affected by conflict. Despite concerns as to AFP sensitivity in
conflict-affected areas, performance indicators and international surveillance reviews
(e.g. DR Congo) demonstrate that AFP surveillance quality in these areas, supported
where necessary by special surveillance activities such as “active search”, can reliably
identify wild poliovirus transmission.
The TCG recognizes the increased difficulty of international transport of laboratory
reagents, supplies and samples in the period following 11 September 2001, and the
increased demands that this is making on the laboratory network. Wherever possible,
specific constraints to rapid transport should be identified so that they can be
appropriately addressed.
12
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Recommendations:
•
The TCG notes the value of AFP surveillance reviews and recommends that:
all endemic countries that have not conducted a surveillance review within
the last 12 months, or a review of polio activities that incorporated
surveillance, should complete such a review by end-2002;
any polio-free country that has been unable to achieve or maintain
certification-standard AFP surveillance and has not conducted a
surveillance review within the last 12 months should complete such a
review by end-2002, with particular priority given to the relevant
countries of southern and eastern Africa;
the methodology of surveillance reviews should be comparable across
countries. Standard tools should be developed drawing on the experience
of previous reviews.
Given the inter-regional nature of some geographic blocks (e.g. the Hom of
Africa) WHO HQ should be coordinating the mapping of key surveillance
indicators across regional boundaries, with the distribution of these maps and
appropriate surveillance data to the concerned teams on a quarterly basis.
-
•
•
Recognizing the high number of polio-compatible cases, the TCG reaffirms
the importance of recommendations of previous meetings stating that all
countries should:
maximize efforts to obtain two adequate specimens from every AFP
case;
prioritize investigation and follow-up of cases with inadequate specimens;
ensure all potentially compatible cases are referred to an appropriately
trained expert group for classification within 90 days of onset;
monitor and map polio-compatible cases at least monthly, and conduct
field investigations of all compatible cases, including active case search,
with particular attention to clusters of cases;
use data on polio-compatible cases to identify areas for improving
surveillance quality and areas at risk of wild poliovirus circulation.
At this stage of the Global Eradication Initiative, the careful analysis of data
on polio- compatible cases is critical. The use of data on polio-compatible cases
to identify surveillance gaps and high-risk areas should be strengthened by:
-
•
the augmentation, by June 2002, of guidelines for expert groups to include
a standard format for the analysis of potential compatible cases;
re-briefing of expert groups in all countries with high proportions of
polio-compatible cases;
close scrutiny of the classification and use of compatible cases
during surveillance reviews, including the reasons for classification as
polio-compatible.
An interim report on surveillance quality in the African Region should be
presented to the next meeting of the Regional TFI. The report should emphasize
the mechanism for the assessment of potential polio-compatible cases,
and contain an analysis of cases classified as polio compatible, and of the
proportion of cases with inadequate specimens that have 60-day follow-up.
-
•
WHO/V&B/02.12
13
Data on polio-compatible cases, and the trends in classification of these cases,
is lacking at global level. The TCG requests a summary report to be included
at the next TCG meeting, providing data on the trends in compatible cases
over time, comparison of characteristics of polio-compatible cases with other
non-polio AFP cases and polio-confirmed cases (e.g. age, vaccination status),
and outcomes of the investigation of clusters of compatible cases.
The TCG notes and supports the mechanism proposed by the Global Laboratory
Network meeting (March 2002) for the distribution and updating of genetic
sequencing data on polioviruses. The system should be brought into operation
as soon as possible. The TCG should receive an update on the status of the
system by end-2002 with full details by mid-2003.
The TCG notes and supports the proposal of the Global Laboratory Network
meeting (March 2002) to develop global guidelines for environmental
surveillance by July 2002. These guidelines should incorporate previous WHO
guidelines on the programme response (both immunization and surveillance)
to wild poliovirus isolations from the environment.
The TCG noted with concern the low percentage of stool specimens arriving
at the laboratory within three days of collection, in almost all regions.
Priority should be given to improving this indicator in all regions, with a report
to the TCG in 2003 on the status of the indicator, the constraints to achieving
it, and the potential implications, if any, for wild poliovirus isolation.
3.2
Containment of laboratory stocks of wild poliovirus
An overview of the progress with global laboratory containment was presented,
and the TCG noted the progress in all WHO regions, especially in the European
Region (EUR) Member States (table 2). The TCG was also updated on the major
revisions to the global action plan for laboratory containment, resulting from WHO
consultations in October 2001 and March 2002.
Table 2: Progress with global laboratory containment, status March 2002
Coordinator
Plan
Lab list
Survey
Inventory
Non- endemic AMRO (48)
2
2
1
1
0
EURO (51)
48
27
28
22
0
WPRQ (36)
36
36
36
36
9
EMRO (23)
17
17
1
1
1
SEARO (10)
3
3
0
0
0
AFRO (48)
0
0
0
0
0
Global (216)
106 (49%)
85 (40%)
66 (31%)
60 (28%)
10 (5%)
WHO region
Endemic
14
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Recommendations:
•
The second edition of the global action plan for laboratory containment should
be completed by end-July 2002, and widely circulated.
•
WHO should urge all non-endemic countries to appoint a national containment
coordinator or task force and establish a national plan of action by end-2002,
with particular emphasis on countries of the Americas, as well as appropriate
polio-free countries of SEAR and EMR.
•
Potential tools for the validation of the containment process at the national
level should be developed, pilot tested and reported to the TCG by mid-2003.
•
Further studies should be conducted, in at least two additional countries,
to assess the risk of wild poliovirus in those materials identified as
“potentially infectious” in the course of establishing national inventories in
large industrialized countries. This experience should be reported to the TCG
by mid-2003.
3.3
Supplementaiy immunization in polio-free areas
Given the risk of spread of imported wild polioviruses (Bulgaria, Georgia, Zambia)
WHO has re-evaluated the role of supplementary immunization in polio-free areas.
The analysis presented to the TOG (figure 7) demonstrates the importance of poliofree areas continuing to use periodic NIDs or extensive SNIDs to maintain population
immunity. The occurrence of the recent vaccine-derived poliovirus outbreaks
(Hispaniola, Philippines) in the presence of low population immunity provides further
argument for achieving and sustaining high immunization coverage, ideally through
routine immunization services.
Figure 7: Population immunity by age, assuming 50% OPV3
immunization coverage and 15% secondary exposure
1
0)
c
E
E
c
o
ti
o
CL
o
Q.
TJ
O
ro
E
(/)
LU
0.9
0.8
0.7
0.6
0.5
i_______ Z_____________
I
i\
1
—
I—
0.4
Routine vaccination
0.3
0.2
:mal antibodies
0.1
0
Secondary exposure
, ,^7-,. ....................................
1
4
. . .l
7 10 13 1 6 19 22 25 28 31 34 37 40 4 3 46 49 52 55 58 61
Age (months)
WHO/V&B/02.12
15
Recommendations:
•
In all countries, plans for SIAs should be integrated with broader multi-year
national immunization plans, including those developed in conjunction with
proposals for Global Alliance for Vaccines and Immunization (GAVI) support,
where applicable.
•
Polio-free countries that border endemic areas, or have very low immunization
coverage, should continue to conduct national or subnational immunization
days, as appropriate, on an annual basis.
•
Countries that have been polio-free for at least three years, but have not
achieved or maintained a level of 90% routine immunization of infants with
three doses of OPV (OPV3 coverage), should continue to conduct NIDs at
least every three years, to prevent the accumulation of susceptibles and protect
against the importation of wild polioviruses. In larger countries,
where appropriate, SNIDs should be conducted to cover those states or
provinces with lower than 90% coverage.
•
Where provision of resources for SIAs in polio-free countries is an issue, priority
should be given to countries in high-risk situations and with the lowest routine
coverage.
•
The ongoing research on the frequency and risk factors for circulating
vaccine-derived polioviruses (cVDPVs) should be used to evaluate the potential
role of supplementary immunization activities following regional certification.
3.4
Post-certification immunization policy development
The TCG reviewed progress with the two-part agenda to enable an evidence-based
decision on the most appropriate immunization option (s) in the post-certification
era.
The first area of work, the research agenda, is proceeding well. Despite screening
over 2100 Sabin-like isolates, no new episodes of cVDPV have been identified.
Follow-up of the 12 long-term excretors identified during 40 years of OPV use has
found that only two are known to continue to excrete, while data from the UK and
USA suggest that persistent excretion occurs in at most 0.01-1% of persons with
severe immunoglobulin-deficiency diseases. In the area of “new” vaccines, a review
of the regulatory issues for monovalent OPV will be available by mid-2002 as well
as initial estimates on the size of the stockpile required. The field component of the
IPV study in Cuba to address immunogenicity and mucosal immunity in such settings
has been completed. A study of the circulation of OPV-derived viruses before,
during and after a switch to IPV in New Zealand has been designed to measure the
effect of IPV on VDPV circulation.
Draft scenarios for IPV demand were discussed with manufacturers in March 2002,
and UNICEF is preparing an exploratory request for proposals to determine the
potential supply and public sector price. A proposal to prepare a clinical trial lot of
Sabin-IPV is under consideration such that clinical trials could be implemented in
2003 with immunogenicity data available by 2004. To better understand the potential
impact of OPV campaigns on the dynamics of VDPVs, systematic analyses of data
on Sabin-like isolates after supplementary immunization activities will be completed
by mid-2002.
16
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
The second area of work involves international consensus-building on policy for the
post-eradication era, including evaluation of the economic, political, operational and
financial implications of each option. Through advice from policy-makers,
primarily from developing countries, the April 2002 meeting of the Global Health
Forum on post-certification immunization policy development held in Annecy,
France, just before the TCG, has generated critical information required to develop
national policy for the post-certification era. This forum has also led to suggestions
on appropriate mechanisms for discussing and generating policy consensus.
The TCG was presented with a detailed communications and public information
plan to keep countries and interested parties abreast of the issues, and to work towards
consensus on important issues related to post-certification immunization policy.
The TCG also was briefed on the potential role of the International Health
Regulations in the post-eradication era.
Conclusions
While acknowledging progress in implementing the programme of work related to
the development of post-certification policy development, the TCG notes the
following remaining gaps: (1) type of vaccines, size and operating procedures
necessary for managing the vaccine stockpile needed for the post-immunization era;
(2) the incidence and relevance of chronic excretion of polio vaccine virus;
(3) the determinants of increased transmissibility of circulating vaccine-derived
polioviruses; (4) operational and epidemiological issues surrounding the routine use
of IPV; (5) assembling information in ways (i.e. decision models) that make it easier
to arrive at actual policy decisions; and (6) the working relationship between the
programme and vaccine manufacturers is not yet as close as is desirable.
Recommendations:
•
The TCG makes the following recommendations to address the remaining
major gaps in research and programmatic information needed for the
development of post-certification immunization policy:
-
-
Vaccine stockpile for the post-imm uniza tion era’, preliminary information
on the potential size, type of vaccines and operating procedures for this
stockpile should be available in 2003. The size of this stockpile should
be guided by an understanding of how population susceptibility could
evolve after immunization stops, the potential spread of poliovirus in
various populations, and various sensitivities of surveillance to detect
virus. A working group should be formed to accelerate work in this
area.
Long-term excretors of polio vaccine virus: the work to evaluate the
incidence and potential risk posed by severe immunodeficiency syndromes
should be expanded in middle-income countries. Further work should
be done to evaluate the potential transmissibility of viruses from such
patients and the potential role of antiviral therapies in clearing the
excretion.
-
WHO/V&B/02.12
OPVproduction in the post-immunization era: the programmatic work
should be expanded to include an evaluation of the time, costs and other
factors involved in restarting OPV production after immunization with
OPV has been discontinued.
17
Transmissibility of VDPVs: further work should be done to understand
the markers of transmissibility of VDPVs, particularly the utility of
recombination with non-polio enteroviruses as an indicator of the risk
of VDPV circulation.
IPV in developing countries: given the complexities (and uncertainties)
with routine IPV use in developing countries, a multi-year pilot/
demonstration project of IPV routine use (combined with related
operational research) should be explored in a tropical island setting.
Recognizing the progress in the programmatic and scientific research
agenda for development of post-certification immunization policy for polio,
WHO should develop policy decision models over the next 12 months
that reflect how the range of possible research outcomes would affect
post-certification policy development. To better understand how differing risk
perceptions might influence national or regional policy development,
these decision models should be tested with a range of experts familiar with
policy development in representative geopolitical areas. The outcomes of this
work and its implications should be presented to the TCG in 2003.
-
Experience gained from implementation of the communications plan should
be used to review and revise that plan by June 2003. This should include further
delineation of the goals, objectives and target audiences, the provision of
communication tools for national programmes and how the communication
plan will be evaluated. The results of this review should be presented to the
TCG in 2003.
The work being undertaken by different institutions, on the economic and
financial implications of the possible post-certification immunization scenarios,
should be consolidated by mid-2003 to provide a comprehensive view of the
potential resource requirements.
Recognizing the value of the March 2002 meeting with manufacturers on polio
vaccine demand post-2005, WHO and UNICEF should plan regular meetings
(at least annually, but more frequently if requested by manufacturers) to
exchange information and provide a forum for discussion of the vaccine supply
implications of policy options.
WHO should, by September 2002, refine and make widely available the
framework it is using for assessing and managing the risk of polio
re-introduction or re-emergence once immunization against polio has been
stopped.
WHO should present to the TCG in 2003 an outline of the cross-cluster
programme of work for the post-certification era, including biosafety,
surveillance and response, and health systems strengthening.
18
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
3.5
Programme oversight, administration and human resources
The TCG reviewed the findings of the two major evaluations of the polio initiative
that had been conducted in 2001, with particular attention to the thematic evaluation
commissioned by the WHO Director-General. The TCG examined the
recommendations that the composition and operations of the global oversight body
be revised to ensure it can fully and efficiently address all post-certification issues.
In considering the optimum expertise and mechanisms for its future work, the TCG
noted that its role had been changing with the advent of country-level oversight
groups and the increasing attention already being given to laboratory containment
and post-certification policy. The TCG also recognized that there are an increasing
number of international and national fora for partners to review progress and stay
abreast of evolving issues and challenges (e.g. Scientific Advisory Group of Experts
(SAGE), regional TCGs and the TFI).
Since 1999 the TCG has commented on the need to enhance the WHO administrative
support to polio eradication activities. The administrative challenges posed by the
rapid increases in human and financial resources (see figure 8) have been compounded
by the fact that most of this growth has been in countries with the weakest banking
and security infrastructures. The TCG was impressed with how responsive WHO
administration at all levels had been to prior TCG recommendations.
The administrative mechanisms developed to support polio eradication at global,
regional and country level have enhanced the capacity of the programme to deal
with rapidly evolving situations. The TCG is concerned, however, that this level of
support must be maintained and where possible expanded in the period leading up to
certification, particularly in the endemic regions and countries. In this critical stage
it is vital to maintain the mechanisms developed to improve the speed and efficiency
of administrative support. The TCG endorsed the plans to better monitor the
performance of this support.
Further to the 2001 TCG recommendation to document the impact of the polio
infrastructure on other health services, the results of an extensive survey on the
work of WHO polio-funded personnel was presented. Initial analyses found that
91% of polio-funded personnel are regularly engaged in routine immunization
activities, 65% had participated in measles or tetanus campaigns in 2001 and 68%
conducted surveillance for other diseases. The TCG was impressed by the information
documenting that polio eradication teams, consisting of well-trained cadres of
motivated professionals, have played a major role in supporting broader immunization
programmes and overall health systems. Polio eradication teams represent a veiy
valuable national resource, which countries should plan to continue to take advantage
of, even beyond certification of polio eradication.
WHO/V&B/02.12
19
Figure 8: Increase in the number of polio-funded staff working at global,
regional and country level from 1988 to 2002
2500
[—I Country level
2qqq___|
£
5
(0
o
■5
a
1950
| Regional office level
H Global (HQ) level
1400
1500
Mb*
-Q
1000
E
3
z
500
224
14
53
1988
1995
0
1999
2000
2002
Year
Recommendations:
•
As future meetings of the Global TCG will increasingly focus on specific
technical or policy issues for the post-certification era, WHO should ensure
that the size of these meetings promotes and facilitates appropriate scientific
presentation and discussion of the issues.
•
Given the need to limit the size of future Global TCG meetings, WHO and
the polio partnership should consider convening occasional public meetings,
with invitation to all interested parties, to share information on the status of
global polio eradication.
•
Given the evolving role of the Global TCG, WHO should identify additional
TCG members to strengthen expertise in the areas of international policy
development, virology and biosafety. In expanding the TCG, efforts should be
made to achieve a better gender balance.
•
Recognizing that the move of the African Regional Office to Brazzaville will
result in a transition period for support services, the TCG would like to be
kept informed about progress in maintaining a high level of administrative
support for poliomyelitis eradication activities in the Region.
•
The analysis of the survey of WHO polio-funded personnel on their work in
other immunization and surveillance activities should be completed and
disseminated widely to all partners.
•
The TCG reaffirms the need for human resources planning to ensure that all
vital functions for achieving and maintaining polio-free status through global
certification and beyond are maintained. This plan should be submitted to the
next meeting of the TCG.
20
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
3.6
Milestones for the Global Polio Eradication Initiative 2002-2003
The TCG reviewed progress against the milestones outlined in each of the five
major areas of the Global Polio Eradication Strategic Plan 2001-2005 (table 3).
While the five major areas of work outlined in the Plan continue to be appropriate
for the polio eradication partnership, however, on the basis of experience gained
over the past 24 months there is a need to review and revise the scope of three of the
areas (i.e. supplementary immunization, post-certification immunization policy,
and impact of polio eradication on health systems), as well as the milestones for
2002-2003.
Recommendation:
The TCG concurs with the revised scope of work and milestones of the
Global Polio Eradication Initiative Strategic Plan 2001-2005, as detailed in
table 1 below.
WHO/V&B/02.12
21
Table 3: Objectives and milestones for the
Global Polio Eradication Initiative, 2002 and 2003
Objective
Milestones 2002
Milestones 2003
Interruption of
poliovirus
transmission
• Transmission of wild poliovirus will be
stopped in all countries.
• EUR will be certified polio-free.
• Maintenance of global pofio-free status.
Supplementary
immunization
activities (SIAs)
Endemic countries
• 34 NIDs/year and mop-up campaigns
will continue in all countries that were
endemic in 2000-2001, using a house-tohouse strategy.
Polio-free countries
• Continued annual SIAs in all high-risk
polio-free countries and long-term SIA
plans established for all countries with
OPV3 <90%.
Endemic countries
• 3-4 NIDs/year and mop-up campaigns will
continue in all countries that were endemic in
2001-2002, using a house-to-house strategy.
Certification
standard
surveillance
AFP surveillance
• Certification-standard surveillance will be
achieved and maintained in all regions and
in >90% of countries.
Certification
• National Certification Committees will be
established in all countries including all
endemic and recently endemic areas.
AFP surveillance
• Certification-standard surveillance will be
achieved in all countries of AFR, EMR and
SEAR.
Certification
• Regional Certification Committees receive
preliminary reports from National Certification
Committees of all countries which have been
polio-free for greater than 3 years.
Containment of
wild poliovirus
stocks
Process
• National Task Force / Coordinator and
National Plans of Action for laboratory
containment are established in all
non-endemic countries.
Outcomes
• National laboratory surveys are initiated in
all non-endemic countries of AMR, EMR,
EUR, SEAR with complete inventories
in WPR.
Process
• Regional plans of action are established lor
the “post wild poliovirus interruption’ phase
in AMR, EUR and WPR.
Polio-free countries
• Continued annual SIAs in all high-risk
countries, and other polio-free countries with
<90% OPV3 conducting SIAs at least
every 3 years.
Outcomes
• National laboratory survey initiated in all
countries with inventories complete in AMR,
EUR and the non-endemic countries of
EMR and SEAR.
Development of
post-certification
immunization
policy
Data generation
• All programmatic data required for policy
development has been identified or collected.
Policy development
• A framework is developed for assessing
and managing post-certification risks of
polk) re-introduction or re-emergence.
Data generation
• All scientific research data required for policy
development is being collected.
Policy development
• At least one forum is held with key policy
makers in each geopolitical block to receive
comments on the risk framework and post
certification immunization policy options.
Strengthening
health systems
through routine
immunization and
surveillance
Routine immunization
• Five of the countries with a large polio
infrastructure will have explicit phased plans
linking that infrastructure with the routine
EPI goals.
Surveillance
• All countries using AFP surveillance will
have established a timeframe for expansion
to indude the notification of at least tetanus
and measles cases with laboratory capacity
to diagnose measles.
Partnership
• Lessons learned from the Interagency
Coordinating Committees (ICCs) are
documented, with best practices defined.
Routine immunization
• Ten countries with a large polk) infrastructure
will have explicit phased plans for linking that
infrastructure with the routine EPI goals.
22
Surveillance
• All countries using AFP surveillance will
have induded at least tetanus and measles in
the system and established laboratory
capacity to diagnose measles.
Partnership
• ICC best practices are disseminated and
introduced, at least in the 74 countries
receiving GAVI assistance.
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Annex 1:
Agenda
Tuesday, 9 April 2002
08:00-08:30
08:30-08:50
08:50-09:00
Registration
Opening statements
Introductions, election of officers and adoption of agenda
Day 1:
Stopping polio transmission
Session 1:
Programme objectives and overview
09:00-10:00
2001 eradication activities, milestones and
TCG recommendations
Special report: resource mobilization activities and outcomes
Discussion
Session 2:
Endemic countries - status, risks and priorities
10:00-10:30
High intensity transmission areas
- Northern India
10:30-11:00
Coffee break
11:00-13:00
- Pakistan and Afghanistan
- Nigeria and Niger
Low intensity transmission areas
- Hom of Africa: Ethiopia/Somalia/Sudan
- Egypt
13:00-14:00
Lunch
14:00-15:00
15:00-15:30
- Central Africa: Angola/Democratic Republic of the Congo
Stopping polio transmission: summary of 2002-2003
supplementary immunization activities and OPV supply
15:30-16:00
Coffee break
16:00-18:00
Closed session of the Global TCG: recommendations on
sessions 1 and 2
WHO/V&B/02.12
23
Wednesday, 10 April 2002
Day 2:
The polio endgame
Session 3:
Priorities in the pre-certification era
09:00-12:30
Gaps in global AFP surveillance:
- AFP performance indicators including compatible cases
- Global Laboratory Network performance and
sequencing data
- Environmental sampling data
- Conflict-affected countries and areas
Laboratory containment: progress and proposed revisions
to the global plan of action
10:30-11:00
Coffee break
Role of supplementary immunization after interrupting polio
transmission
12:30-14:00
Lunch
Session 4:
Development of post-eradication polio immunization policy
14:00-15:30
Status of programmatic and scientific research:
- Frequency of VDPV circulation and chronic excretors
- Monovalent OPV and Sabin-IPV
- IPV efficacy in the developing country setting
- Impact of pulse OPV on VDPV circulation
Potential vaccine requirements for the post-eradication
policy options
15:30-16:00
Coffee break
16:00-18:00
Closed session of the Global TCG: recommendations on
session 3 and 4
24
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Thursday, 11 April 2002
Day 3:
The polio endgame (continued)
Session 4:
Development of post-eradication polio immunization
policy (cont.)
09:00-10:30
Factors influencing post-eradication policy - Report of
the IGH Forum
International Health Regulations and the post-eradication era
Programme of work in endgame communications
10:30-11:00
Coffee break
Session 5:
Programme administration and milestones
11:00-12:30
Administration: management and capacity for the polio
eradication initiative
Human resources - current status, activities and future plans
Polio eradication initiative milestones for 2002-2003
12:30-14:00
Lunch
Session 6:
Closing
14:00-15:30
TCG conclusions and recommendations
15:30-16:00
Coffee
Session 7:
Closed session of the Global TCG
16:00-17:00
Report finalization and other business
WHO/V&B/02.12
25
Annex 2:
List of participants
Technical Consultative Group
* Dr I. Arita, Agency for Cooperation in International Health, 4-11-1
Higashi-machi, Kumamoto City 862, Japan
Dr R.N. Basu, A73 Yojna-Vihar, New Delhi 110092, India
Dr P. Figueroa, Department of Epidemiology, Ministry of Health, Kingston,
Jamaica (Rapporteur)
Dr Mohammed Suleiman Ali Jaffer, Ministry of Health, PO Box 393,
Muscat, Sultanate of Oman
(also serves as member of the Global Certification Commission (GCC) and Chair,
Steering Committee on Research for the Development of Post Eradication
Immunization Policy)
Professor F.K. Nkrumah, Noguchi Memorial Institute for Medical Research
(NMIMR), University of Ghana, PO Box LG 581, Legon, Ghana
(also serves as member of the Global Certification Commission (GCC))
Dr W Orenstein, Centers for Disease Control and Prevention,
National Immunization Program, 1600 Clifton Road, Atlanta, GA 30333, USA
(Chair)
Global Commission for the Certification of the Eradication of Poliomyelitis
Professor A. Adams, National Centre for Epidemiology and Population Health,
Australian National University, Canberra ACT 0200, Australia
Dr A. Deria, 28 Claudia Place, Augustus Road, GB-London SW19 6ES,
United Kingdom
Professor S.G. Drozdov, Institute of Poliomyelitis and Viral Encephalitis of
the Academy of Medical Science of the Russian Federation, Moscow 142782,
Russian Federation
’Professor Jan Kostrzewski, Department of Epidemiology, National Institute of
Hygiene, 24 Chocimska Street, PL-00-791 Warsaw, Poland
Dr R. Leke, Department of Immunology and Microbiology, Faculty of Medicine,
University of Yaounde, Yaounde, Cameroon
Dr C. de Macedo, SMDB Conjunto 01 Casa 05, Lago Sul, Brasilia,
DF 71680-010, Brazil
Unable to attend.
26
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Professor Nath Bhamarapravati, Center for Vaccine Development,
Institute of Sciences and Technology for Development, Mahidol University
at Salaya, Nakhonchaisri, Nakhonpathom 73170, Thailand
* Dr EC. Robbins, Department of Epidemiology and Biostatistics,
School of Medicine, Case Western University, 10900 Euclid Avenue,
Cleveland, OH 44106-4945, USA
Sir J. Smith, 95 Lofting Road, Islington, GB-London, N1 1JF, United Kingdom
Dr Wang Ke-An, Chinese Academy of Preventive Medicine (CAPM),
27 Nanwei Road, Beijing 100050, People’s Republic of China
Technical advisers
Dr J.K. Andrus, Institute for Global Health, University of California,
74 New Montgomery Street, Suite 508, San Francisco, CA, USA
Dr E. Feinglass, Institute for Global Health, University of California,
74 New Montgomery Street, Suite 508, San Francisco, CA, USA
*Mrs Maureen Best, Office of Laboratoiy Security, Health Canada,
HPB Building #7, Post Locator 0700A1, Tunney’s Pasture, Ottawa,
ON KIA OL2, Canada
’Dr N.K. Blackburn, National Institute for Virology, Private Bag X4,
Sandringham 2132, Johannesburg, South Africa
Dr S. Cochi, Centers for Disease Control and Prevention,
National Immunization Program, 1600 Clifton Road, Atlanta,
Georgia 30333, USA
*Dr J. Deshpande, The Enterovirus Research Centre, Indian Council of Medical
Research (ICMR), Haffkine Institute Compound, Acharya Donde Marg, Parel,
Mumbai 400 012, India
Dr W. Dowdle, The Task Force for Child Survival and Development,
750 Commerce Drive, Suite 400, Decatur, Georgia GA 30030, USA
Dr T. Hovi, Head, Department of Microbiology, National Public Health Institute
(KTL), Mannerheimintie 166, FIN-Helsinki 00300, Finland
Dr O. Kew, Centers for Disease Control and Prevention, 1600 Clifton Road,
Atlanta, GA 30333, USA
Dr D. Salisbury, Department of Health, Room 607A, The Communicable Disease
and Immunisation Team, Skipton House, 80 London Road, GB-London SEI 6LH,
United Kingdom
Dr H. van der Avoort, Laboratory of Virology, RIVM, Antionie Van
Leewenhoeklaan 9, Box 1, NL-3720 Bilthoven, The Netherlands
Dr W. Lim, Head Virus Unit, 9/F Public Health Laboratory Centre,
382 Nam Cheong Street, Kowloon, Hong Kong, People’s Republic of China
Unable to attend.
WHO/V&B/02.12
27
Steering Committee on Research for the Development of Post Eradication
Immunization Policy
Dr J. Clemens, International Vaccine Institute, Kwanak PO Box 14,
Kwanak-Ku, Seoul 151-600, Republic of Korea
Dr P. Fine, London School of Hygiene and Tropical Medicine, Keppel Street,
GB-London, WC1E 7HT, United Kingdom
Professor Y. Ghendon, Frunzenskaya nab. 36, Flat 26, Moscow, 119146,
Russian Federation
Dr P. Minor, Division of Virology, National Institute for Biological Standards
and Control (NIBSC), Blanche Lane, South Mimms, GB-Potters Bar,
EN6 3QG, United Kingdom
Dr N. Takeda, National Institute of Health (NIH), 4-7-1 Gakuen,
Musashimurayama, Tokyo 208, Japan
Dr P. Wright, Department of Pediatrics, Division of Infectious Disease,
Vanderbilt University Medical Center, 1161 21st Avenue South, Nashville,
TN 37232 2581, USA
Countiy representatives
Dr A. Akhgar, Director of Primary Health Care, Afghanistan
Dr W.P. Kandolo, EPI Programme Manager, Democratic Republic of the Congo
Dr Tesfanesh Belay, Head of Family Health and Dr Yigzaw Asnakew, EPI
Programme Manager, Ethiopia
Mr J.P. Sharma, Secretary of Family Welfare, Uttar Pradesh, India
Mr A. Amanullah, Secretary of Family Welfare, Bihar, India
Dr S. Sarkar, Assistant Commissioner Secretary of Family Welfare,
New Delhi, India
Dr A. Barkire, EPI Programme Manager, Niger
Dr A. Awosika, Coordinator, National Programme on Immunization, Nigeria
Dr R. Hafiz, National EPI Manager, Pakistan
Dr A. El Sayed, EPI Director, Sudan
28
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Polio Eradication Core Partner Organizations
Rotary International
Mr W. Sergeant
Mr P. Carpenter
Dr R. Scott
United Nations Children's Fund (UNICEF)
Mr C. Tinstman
Dr J.M. Okwo-Bele
Dr S. Mahendra
Dr A. Golaz
Dr V. Lara
Mr B. Isselnou
Dr K. Vanormelingen
Dr P. Salama
Dr M. Costales
Mr T. Sorensen
Dr R. Davis
Dr M. Babille
Dr R. Aziz
Dr Q. Al-Nahi
Mr M. Pecho
Ms T. De Bodt
Dr T.O. Kyaw-Myint
Ms J. Bailey
Ms S. Hall
Dr C. Dricot d’Ans
Ms L. Desomer
Dr M. Sheth
Centers for Disease Control and Prevention (CDC)
Dr R. Keegan (Unable to attend)
Ms D. Johnson
Dr V. Caceres
Dr M. Pallansch
Mr P. Zuber
Implementing Partners
Francois Bompart, Aventis Pasteur Limited, Connaught Laboratories Ltd,
1755 Steeles Avenue West, Toronto, Ontario M2R 3T4, Canada
Global Alliance for Vaccines and Immunization (GAVI)
Dr V. Pellegrini, International Federation of Pharmaceutical Manufacturers
Associations (IFPMA)
’Developing Countries and Vaccine Manufacturers Network (DCVNM)
Dr B. Moriniere, International Federation of Red Cross and Red Crescent
Societies (IFRC), 17 Chemin des Crets, 1211 Geneva 19, Switzerland
’International Committee of the Red Cross, Geneva, Switzerland
Unable to attend.
WHO/V&B/02.12
29
Donors’ and Partners’ governments
Ms S. Barrow, Canadian International Development Association (CIDA)
’Gates Foundation
’Ireland
Dr Y. Chiba, Department of International Cooperation, National Medical Centre,
Japan
Ms M. Middelhoff, Permanent Mission of the Kingdom of the Netherlands to the
United Nations Office and International Organizations at Geneva, the
Netherlands
Dr I. Orstavik, National Institute of Public Health, Norway
’Rockefeller Foundation
United Kingdom of Great Britain and Northern Ireland
Ms Andrea Gay, United Nations Foundation, 1301 Connecticut Avenue, NW,
Suite 700, Washington, DC 20036, USA
Ms Ellyn Ogden, United States Agency for International Development (USAID)
’Wellcome Trust
World Bank, 1818 H Street, MSN 3-301, Washington, DC 20433, USA
WHO Secretariat - regional and country offices
Regional Office for Africa (AFRO), Harare, Zimbabwe
Dr O. Babaniyi
Ms Y. Kerr
Dr S. Okiror
Dr M. Otten
Dr O. Tomori
Dr K. Kapitaine
Dr A. Gasasira
EPI subregional offices, African Region
Dr R. Eggers, ICP Eastern Block, Kenya
Dr D. Nshimirimana, ICP Western Block, Cote d’Ivoire
Dr J. Rasoarimalala, ICP Central Block, Cameroon
AFRO country offices
Dr R. Gama-Vaz, Angola
Dr M. Kamwa, Democratic Republic of the Congo
Dr A.B. Gaye, Democratic Republic of the Congo
Dr F. Oyewole, Ethiopia
Dr A. Jack, Nigeria
Unable to attend.
30
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
Regional Office for the Americas (AMRO), Washington, DC, USA
Mr P. Carrasco
Dr M. Landaverde
Regional Office for the Eastern Mediterranean (EMRO), Cairo, Egypt
Dr H. Wahdan
Dr T. Gaafar
Dr F. Kamel
Dr H. Ashgar, Laboratory Coordinator
EMRO country offices
Dr A. Mounts, Pakistan
Dr N. Sadozai, Afghanistan
Dr S. Haithami, Sudan
EPI subregional offices (EMRO)
Dr H. Jafari, PAK/AFG/IRN
Dr E. Durry, SOM/SUD
Regional Office for Europe (EURO), Copenhagen, Denmark
Dr S. Wassilak
Dr G. Oblapenko
Dr G. Lipskaya
Dr N. Emiroglu
Regional Office for South-East Asia (SEARO), New Delhi, India
Dr B. Burkholder
Mr J.-G. Tezier
Dr A. Thapa
SEARO countiy offices
Dr G Hlady, India
Regional Office for the Western Pacific (WPRO), Manila, Philippines
Dr Y. Baoping
Dr S. Roesel
Dr W. Antowiak
WHO headquarters, Geneva, Switzerland
Other clusters
Dr D. Nabarro, Executive Director, DGO
Dr A. Asamoa-Baah, EXD/EGB
Mr Maryan Baquerot, EXD/GMG
Dr D. Heymann, EXD/CDS
Dr Johanna Larusdottir, Director EHA
Ms H. Wild, Director, FNS
WHO/V&B/02.12
31
HTP cluster
Dr Y. Suzuki, EXD/HTP
Dr D. Tarantola, Director, V&B
Dr B. Aylward, V&B/Polio
Dr J. Bilous, Coordinator, EPI
Dr M. Birmingham, Coordinator, VAM
Mr F. Caillette
Dr E. de Courville, VAM
Mr H. Everts, EPI
Dr D. Featherstone, VAM
Dr J. Fournier, ATT
Dr S. Lambert, QSB
Mr C. Maher, V&B/Polio
Ms M. Mailhot
Dr J. Milstien, Coordinator, ATT
Ms L. Muller, V&B/Polio
Dr B. Nkowane, EPI
DrJ.-M. Olive, EPI
Dr R. Sutter, VAM
Dr R. Tangermann, EPI
Mr C. Wolff, VAM
Dr D. Wood, QSB
32
Seventh meeting of the Global Technical Consultative Group (TCG), April 2002
The Department of Vaccines and Biologicals was
established by the World Health Organization
in 1998 to operate within the Cluster of
Health Technologies and Pharmaceuticals. The
Department's major goal is the achievement of a
world in which all people at risk are protected
against vaccine-preventable diseases.
Five groups implement its strategy, which starts
with the establishment and maintenance of norms
and standards, focusing on major vaccine and tech
nology issues, and ends with implementation and
guidance for immunization services. The work of
the groups is outlined below.
The Quality Assurance and Safety ofBiologicals team
team ensures the quality and safety of vaccines
and other biological medicines through the devel
opment and establishment of global norms and
standards.
The Initiative for Vaccine Research and its three
teams involved in viral bacterial and parasitic
diseases coordinate and facilitate research and
development of new vaccines and immunizationrelated technologies.
The Vaccine Assessment and Monitoring team
assesses strategies and activities for reducing
morbidity and mortality caused by vaccinepreventable diseases.
The Access to Technologies team endeavours to
reduce financial and technical barriers to the intro
duction of new and established vaccines and
immunization-related technologies.
The ExpandedProgramme on Immunization develops
policies and strategies for maximizing the use of
vaccines of public health importance and their
delivery. It supports the WHO regions and countries
in acquiring the skills, competence and infrastructure
needed for implementing these policies and strate
gies and for achieving disease control and/or
elimination and eradication objectives.
Department of Vaccines anid Biologicals
Health Technology and Pharmaceuticals
World Health Organization
CH-1211 Geneva 27
§
WHO
Switzerland
Fax:+41 22 791 4227
Email: vaccines@who.int
or visit our web site at: http://www.who.int/vaccines-documents
.I
Global
I
I I t
Eradication
Initiative
Certification of global polio eradication
I he purpose
"Certification" is the independent verification of wild poliovirus eradication. The Global Polio Eradication Initiative aims to
certify the world polio-free by the end of 2005. Certification of global polio eradication will be possible only when all
regions have been certified polio-free and all pre- and post-eradication wild poliovirus containment tasks have been
completed (see fact sheet on Containment of wild poliovirus stocks). Global certification will be an important milestone in
the development of post-eradication immunization policy for polio.
The process
The process for cerHffcation of global polio eradication
The Global Certification Commission (GCC),
established by the Director-General of WHO in
1995, is responsible for setting the process and
criteria for certification and ultimately deciding
whether to certify global polio eradication.This
requires at least three years of zero polio cases
due to wild poliovirus in the presence of
certification-standard surveillance in all six
regions.The GCC also requires all six regions to
provide data demonstrating full implementation
of the pre- and post-eradication containment
activities outlined in the WHO global action plan
for the containment of wild polioviruses1 prior to
global certification.
Global Certification Commission
Regional
Certification
Committees
->
PAHO
AFR
EMR
EUR
SEAR
WPR
Certification Committees
National
Surveillance and laboratory personnel
In contrast to individual countries being certified free of smallpox, an entire WHO region must be certified polio-free. For
this to happen, every country and area in a region must provide evidence consistent with there being no indigenous wild
poliovirus cases for at least three years, under conditions of certification-standard surveillance for the virus. Surveillance for
acute flaccid paralysis (AFP) is the gold standard for certification, though other surveillance strategies have been accepted
for some countries that have long been polio-free and have high levels of sanitation and strong health systems. The
capacity of a country to detect and investigate sufficient AFP cases in the absence of polio demonstrates that the poliovirus
would be found if it were present.
This certification documentation is collected and verified by national certification committees (NCCs) and provided to a
regional certification commission (RCC), which then decides on the basis of the data whether the region can be certified.
The RCCs are independent panels of 8 - 10 internationally recognized experts in public health, epidemiology, virology
and/or clinical medicine. The finalization of documentation is a multi-year, iterative process involving dialogue between the
NCCs and the RCC. The documentation must also illustrate the capacity to detect, report and respond to "imported" polio
cases.
Once a region is certified polio-free, and before global certification can be considered, all countries within the region must
maintain certification-standard surveillance and implement post-eradication containment measures.
1 WHO global action plan for laboratory containment of wild polioviruses, WH 0/V&^^3
World Health Organization
ks(
►
Poliovirus importations do not affect certification status if they
are dealt with promptly and do not establish prolonged or
extensive circulation of poliovirus (e.g. less than one year with
limited geographic spread).
After global certification, stopping polio immunization will
additionally require that vaccine-derived polioviruses do not
continue to circulate and that a global stockpile of vaccine is
available if needed (see fact sheet on Post-eradication
immunization policy for poliomyelitis).
The GCC has highlighted the importance of three acute
flaccid paralysis (AFP) performance indicators in particular
for demonstrating the interruption of wild poliovirus
circulation2. Even in the absence of wild poliovirus
circulation, surveillance systems should:
H detect at least one case of non-polio AFP per
100 000 population aged less than 15 years annually;
E collect adequate stool specimens from at least 80% of
AFP cases; and
fi test all specimens at a WHO-accredited laboratory.
2 For certification-standard criteria, see Report of the second meeting of the Global Commission for the
Certification of the Eradication of Poliomyelitis, Geneva, 1 May 1997, WH0/EPI/GEN/98.03.
The progress
Meeting annually since 1995, the GCC has established the process and criteria for certification as outlined above. Polio-free
status has been certified by RCCs in the WHO Region of the Americas in September 1994 and the WHO Western Pacific
Region in October 2000. No indigenous wild poliovirus has been found in either region subsequently, validating the process
and criteria for certification. As no indigenous wild poliovirus has been isolated under conditions of certification-standard
surveillance in any Member State of the WHO European Region since November 1998, that Region is on track for
certification in 2002.
The WHO African Region, Eastern Mediterranean Region and South-East Asia Region have made excellent progress toward
the target of stopping wild poliovirus circulation by the end of 2002, with only four countries, five countries, and one
country reporting confirmed indigenous wild poliovirus circulation, respectively, as of 20 January 2002.
All regions have established RCCs, which report and raise issues to the GCC annually.
The challenges
National certification committees - NCCs must be established in all countries, with UN-supported data collection and
verification mechanisms for areas without recognized national governments.
Timely completion of the pre- and post-eradication phases of the WHO global action plan for laboratory
containment of wild polioviruses - the laboratory containment programme must be accelerated, especially in
industrialized countries, if global certification is to be achieved on time (see fact sheet on Containment of wild poliovirus
stocks).
Surveillance in conflict-affected areas - achieving certification-standard surveillance in areas affected by conflict,
particularly parts of Angola, remains a challenge. Certification cannot be achieved until there is confidence that circulation
of wild poliovirus in these areas has been stopped.
Sustaining the surveillance infrastructure - this infrastructure will need to be sustained in all countries through
global certification and beyond. Thus sufficient financial, human and technical resources will be needed for the foreseeable
future to reap the full benefits of polio eradication.
Circulation of vaccine-derived poliovirus (VDPV) - prolonged or extensive VDPV circulation may postpone regional
certification (in regions not yet certified) or require re-evaluation of regional certification status (in certified regions).
Recognizing that VDPVs can rarely cause polio outbreaks, a process is being developed for verifying the absence of VDPV
circulation in the post-eradication era.
Maintaining high polio immunization coverage - it is vital that all countries maintain childhood immunization
coverage of more than 80% through routine immunization services, supplementary immunization activities ora
combination of both. o
cle2<e <docu rreotem Uct?/
xZcoLcin?
/For more information on certification, please contact Dr Rudi Tangermann (WHO/Geneva),
/
Tel: +41 22 791 4358, email tangermannr@who.int
f
..— ■
.....
'
ke,
-niinnr
f
Further reading
Report of the second meeting of the Global Commission for the Certification of the Eradication of Poliomyelitis, Geneva, 1 May 1997, WHO/EPI/GEN/98.03.
;Report of the sixth meeting of the Global Commission for the Certification of the Eradication of Poliomyelitis, Washington DC, 28-29 March 2001, WHO/V&B/01.15.
Report of the sixth meeting of the Global Technical Consultative Group for Poliomyelitis Eradication, Geneva, 7-10 May 2001, WHO/V&B/01.32.
WHO global action plan for laboratory containment of wild polioviruses, ^HOAy&B/99.31
For more information on polio eradication, visit: www.polioeraication.org
I
WHO/V&B/02.13
ORIGINAL ENGLISH
Vaccines an J Biological s
Certification of tke Global Eradication of Poliomyelitis
Report of tke seventh meeting of tke Global Commission
for tke Certification of tke Eradication of Poliomyelitis
neva, 12 April 2002
World Health Organization
ill
v < *
W'-
*
WHO/V&B/02.13
ORIGINAL: ENGLISH
Vaccines and Biol ogical s
Certification of tke Global Eradication of Poliomyeli IS
1
Report of tke seventk meeting of tke Glokal Commission
for tke Certification of tke Eradication of Poliomye ins
Geneva7 12 April 2002
e
> World Health Organization
WHO
The Department of Vaccines and Biologicals
thanks the donors whose unspecified financial support
has made the production of this document possible.
This document was produced by the
Expanded Programme on Immunization
of the Department of Vaccines and Biologicals
Ordering code: WHO/V&B/02.13
Printed: October 2002
This document is available on the Internet at:
www.who.int/vaccines-documents/
Copies may be requested from:
World Health Organization
Department of Vaccines and Biologicals
CH-1211 Geneva 27, Switzerland
• Fax:+41 22791 4227 • Email:vaccines@who.int •
© World Health Organization 2002
All rights reserved. Publications of the World Health Organization can be obtained from Marketing
and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland
(tel.: +41 22 791 2476; fax: +41 22 791 4857; email: bookorders@who.int). Requests for permission to
reproduce or translate WHO publications - whether for sale or for noncommercial distribution - should
be addressed to Publications, at the above address (fax: +41 22 791 4806; email: permissions@who.int).
The designations employed and the presentation of the material in this publication do not imply the
expression of any opinion whatsoever on the part of the World Health Organization concerning the legal
status of any country, territory, city or area or of its authorities, or concerning the delimitation of its
frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may
not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are
endorsed or recommended by the World Health Organization in preference to others of a similar nature
that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished
by initial capital letters.
The World Health Organization does not warrant that the information contained in this publication is
complete and correct and shall not be liable for any damages incurred as a result of its use.
ii
Contents
Abbreviations
iv
1. Introduction
1
2. Region of the Americas
3
3. European and Western Pacific Regions
5
4. Eastern Mediterranean and South-East Asia Regions
7
5. African Region
9
6. Laboratory containment
11
7. The GCC mandate and circulating vaccine-derived
poliovirus (cVPDV)................................................
13
8. GCC membership and operating procedures
15
Annex 1: Agenda
17
Annex 2: List of participants
18
iii
Abbreviations
AFP
acute flaccid paralysis
AFR
African Region
AMR
Region of the Americas
AMRO
WHO Regional Office of the Americas
ARCC
African Regional Certification Commission
EPI
Expanded Programme on Immunization
EMR
Eastern Mediterranean Region
EMRCC
Eastern Mediterranean Regional Certification Commission
EUR
European Region
EURCC
European Regional Certification Commission
GCC
Global Commission for the Certification of the Eradication of
Poliomyelitis
ICCPE
International Commission for the Certification of Poliomyelitis
Eradication from the Americas
ICCPES
International Commission for the Certification of Poliomyelitis
Eradication in the South-East Asia Region
IPV
inactivated polio vaccine
NCC
National Certification Committee
PAHO
Pan America Health Organization
RCC
Regional Certification Commission
SEAR
South-East Asia Region
TCG
Technical Consultative Group on global polio eradication
cVDPV
circulating vaccine-derived poliovirus
WHO
World Health Organization
WPR
Western Pacific Region
WPRCC
Western Pacific Regional Certification Commission
iv
1. Introduction
Sir Joseph Smith, the chairman of the Global Commission for the Certification of
the Eradication of Poliomyelitis (GCC, the “Commission”), convened the seventh
meeting of the GCC on 12 April 2002, in Geneva, Switzerland.
Welcoming members of the GCC on behalf of Dr Gro Harlem Brundtland,
Director-General of the World Health Organization (WHO), Dr Daniel Tarantola,
Director, Department of Vaccines and Biologicals, expressed his confidence that
the GCC would again provide help and guidance to facilitate the successful
continuation of the global and regional process towards eventual certification of the
interruption of wild poliovirus transmission.
GCC members attending were:
•
African Region: Dr Rose Leke, Chair, African Regional Certification
Commission (ARCC), Professor F. Nkrumah, Member, African Regional
Certification Commission (ARCC);
•
Region of the Americas: Dr Carlyle de Macedo, Member, Western Pacific
Regional Certification Commission (WPRCC);
•
Eastern Mediterranean Region: Dr Mohammed Suleiman Ali Jaffer,
Chair, Eastern Mediterranean Regional Certification Commission (EMRCC),
Dr A. Deria, Member, Eastern Mediterranean Regional Certification
Commission (EMRCC);
•
European Region: Sir J. Smith, Chair, European Regional Certification
Commission (EURCC) and Chair, Global Certification Commission (GCC);
Dr. S. G. Drozdov, Member, European Regional Certification Commission
(EURCC);
•
South-East Asia Region: Professor Natth, Chair, International Certification
Commission for Poliomyelitis Eradication, South-East Asia Region (ICCPES);
•
Western Pacific Region: Dr A. Adams, Chair, Western Pacific Regional
Certification, Commission (WPRCC), Dr Wang Ke An.
WHO/V&B/02.13
1
All GCC members had attended the preceding seventh meeting of the
Technical Consultative Group (TCG) on global polio eradication from 9 to
11 April 2002. Presentations and discussions at the TCG meeting had provided GCC
members with a comprehensive global and regional overview of the current status
of the eradication initiative, including detailed country-specific information about
programme components relevant for certification, such as the quality of acute flaccid
paralysis (AFP) surveillance, accuracy of AFP case classification, progress in
laboratory containment of wild poliovirus and status of the programme of work
towards the development of a post-certification immunization policy. The GCC
concurs with all TCG recommendations related to the improvement of surveillance.
Based on the detailed technical briefing at the TCG meeting, the Commission focused
its agenda on the following certification-specific objectives:
•
receive and discuss updates on certification activities in each WHO region, with
special emphasis on the European and African regions;
•
discuss the increasing importance of laboratory containment activities, especially
the emerging need for validating containment, and to align certification and
containment efforts more closely;
•
consider the possible implications of new information on circulating vaccinederived polioviruses for the certification process; and
•
discuss issues related to GCC membership.
2
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
2. Region of the Americas
The GCC notes that progress is being made with respect to several March 2001
GCC decisions related to the Region of the Americas (AMR). Surveillance quality
overall seems to have been maintained during 2001 compared to 2000;
however, both AFP rates and stool collection completeness still show considerable
variation by country, and within large countries (e.g. Brazil). Haiti - where the last
known cVDPV case had onset of paralysis in July 2001 - did not to reach certification
standard AFP surveillance quality in 2001.
During its 2001 meeting, the GCC had urged all WHO regions to assure that,
prior to global certification, updated country level data be examined and verified by
an independent regional mechanism, preferably regional commissions for the
certification of polio eradication (RCCs). The GCC had recommended that regions
should consider maintaining regional and national certification bodies beyond regional
certification; both the Western Pacific and European Region are following this
recommendation. Neither the Regional Certification Commission nor country-level
national certification committees (NCCs) were maintained in the Americas following
regional certification in 1994. While the WHO Regional Office for the Americas
(AMRO) Secretariat reported on plans to identify and appoint an independent group
for verifying regional certification status, such a body has not yet been identified and
designated.
Laboratory containment of wild poliovirus had not yet been introduced as a
requirement for regional certification of the Americas in 1994. The GCC had
requested (March 2001) that a regional plan of action for laboratory containment,
based on the global containment plan, be prepared for the Americas, and notes that
efforts to implement containment have begun in the Region. The AMRO Secretariat
plans to form country-level containment committees and to appoint national
containment coordinators in AMR countries; these activities are in an early phase.
Establishment of national containment groups provides an opportunity to have a
body at the national level that could also perform duties similar to a
National Certification Committee, which were disbanded in AMRO after
certification. Therefore, the AMRO Secretariat considers to use these national groups
working on laboratory containment, to assess and verify national polio-free status,
and relay this information to the regional level, though consideration needs to be
given to potential conflict of interest and whether or not these groups will have the
relevant expertise to fulfil the certification role. National containment groups are
implementing bodies typically composed of members from the laboratory/biosafety
community and may not have relevant epidemiological and clinical expertise to
re-evaluate the country’s polio free status.
WHO/V&B/02.13
3
GCC decisions:
1.
The quality of AFP surveillance in several countries of the Americas
(i.e. Haiti, Brazil) is of concern and efforts are needed to assist countries to
reach and maintain satisfactory AFP surveillance performance.
2.
The GCC continues to be concerned about the limited progress in re-establishing
independent regional capacity to verify the maintenance of polio-free status
before global certification and reiterates the need to establish such a body.
3.
The GCC concurs with the AMRO plan to establish national committees
for laboratory containment and to expand the committee’s terms of reference,
and if necessary membership, to also perform a function similar to national
certification committees. However, the exact terms of reference of these groups,
in particular their capacity to deal with certification issues and mode of interaction
with the regional level, need to be clarified once an independent regional body
to verify polio-free status has been formed.
4.
The GCC requests the AMRO Secretariat to provide a detailed progress report
on the above issues at the next GCC meeting planned for early 2003.
4
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
3. European and
Western Pacific Regions
European Region (EUR). The European Region is likely to become the third
WHO region to be certified as free of indigenous wild poliovirus transmission during
the second half of 2002. The 51 EUR Member States had submitted final update
documentation on their polio-free status to the RCC/EUR. At its most recent meeting
in March 2002 in Copenhagen, the RCC reviewed all available evidence on
polio-free status, including the final written country reports, presentations from
16 countries, and a comprehensive data analysis of each of the European Region’s
six epidemiological zones. The RCC focused on several main issues:
•
the evidence for the absence of transmission of indigenous wild poliovirus,
including the interval since wild poliovirus was last identified in the country;
•
the capacity of the country to identify re-established transmission of wild virus
following an importation, and to effectively respond to importations to prevent
indigenous transmission;
•
progress in laboratory containment, and
•
the capacity of countries to sustain polio-free status after certification.
In addition to AFP and virological surveillance data, polio immunization coverage
rates, and reported polio cases by year, the RCC also took account of a range of
supplementary evidence, including national morbidity and mortality data, and also
the status of the national health care system. The RCC requested NCCs to endorse
a statement of their rationale for concluding that no transmission of indigenous wild
poliovirus had occurred in their countries for the past three years. Following their
March 2002 review, the RCC concluded that:
indigenous wild poliovirus transmission had not been detected in the European
Region for more than three years,
satisfactory progress had been made in laboratory containment,
spread of wild poliovirus following an importation into polio-free areas of the
Region would quickly be detected and responded to, and that
EUR countries were likely to be able to sustain polio-free status following regional
certification.
WHO/V&B/02.13
5
The RCC/EUR specifically noted that the results of surveillance and immunization
response activities conducted in Georgia following the wild poliovirus importation
identified during the fourth quarter of 2001 had not yet been fully documented.
The RCC expects, however, that Georgia will submit satisfactory evidence to prove
that the imported virus had not re-established transmission, and that this evidence
will be available in time to allow regional certification to occur in the third quarter of
2002.
The RCC/EUR proposes to follow the practice adopted in the Western Pacific Region
of meeting annually after regional certification in order to monitor NCC’s reports
on their evidence for continued freedom from wild virus transmission, and their
further progress in laboratory containment.
Western Pacific Region (WPR). Following certification of the absence of indigenous
wild poliovirus in October 2000, the RCC/WPR conducted (in October 2001) the
first meeting of an RCC following regional polio-free certification. The RCC/WPR
noted the high quality of continued cooperation of countries and NCCs,
which continue to function and work effectively in all WPR countries to assure that
polio-free status post-regional certification is sustained. Most countries were able to
report on continued high-quality surveillance, immunization and laboratory
containment activities. The RCC/WPR endorsed several specific recommendations
made by the regional technical advisory group on immunization and polio eradication
(TAG) towards maintaining high-quality surveillance, following polio-free
certification, and specifically on stool specimen transport.
In view of the emergence of a circulating vaccine-derived poliovirus (cVDPV) in the
Philippines in 2001, the WPR RCC requested that the potential implications of VDPV
circulation for polio-free certification be addressed at the global level.
The GCC notes that, while further progress towards containment occurred in the
Western Pacific Region, Australia, China, Japan, Malaysia and the Philippines have
not yet completed phase 1 containment activities (national inventory of laboratories
holding infectious or potentially infectious material).
GCC decisions:
1.
The GCC recognized that activities at country and regional level towards
regional certification of the absence of indigenous wild poliovirus transmission
in the European Region have been of sufficiently high quality to allow regional
certification to occur later this year. The GCC requests, however, that the RCC
closely scrutinize final country data from Georgia in their June meeting to assure
that the documented importation did not result in re-established indigenous
transmission.
2.
The GCC commends countries of the Western Pacific Region for their successful
efforts to sustain and document polio-free status following regional polio-free
certification, and urges all WPR countries that have not yet completed phase 1
laboratory containment activities to reach this important milestone by the end
of 2002.
6
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
4. Eastern Mediterranean and
South-East Asia Regions
Both the Eastern Mediterranean and South-East Asia regions (EMR and SEAR
respectively) are still engaged in interrupting transmission in two of the three global
“high intensity transmission areas” - the Pakistan/Afghanistan epidemiological block
and northern India, as well as in three countries with low intensity transmission,
most notably Egypt. The GCC appreciates that international technical advisory
groups at global (TCG) and country level (country TAGs) are now regularly reviewing
progress and making specific recommendations to accelerate progress towards
interrupting transmission, including the strengthening of surveillance.
Certification activities have progressed as planned in both EMR and SEAR,
where AFP surveillance quality in 2001 had reached levels commensurate with
certification. In most countries this was achieved at both the national and first
subnational levels. Designated and functioning National Certification Committees
and expert groups for case classification in all countries provide the necessary structure
on which formal certification activities can be conducted.
Eastern Mediterranean Region (EMR). Five of the remaining 10 endemic countries
are in EMR; however, there is good overall progress towards interrupting
transmission in the Region. Increasingly reliable surveillance documents that only
few foci of “low intensity transmission” remain in Sudan (South Sudan) and
Somalia (Mogadishu area), despite ongoing conflict and complex emergency situations
in both countries. Continued improvements of strategy implementation in
the Afghanistan/Pakistan epidemiological block further reduced the extent of
transmission in these countries during 2001. Events in Afghanistan following the
11 September terrorist attack did not have a significant negative impact on eradication
activities in Afghanistan, though it has compromised surveillance quality in some
key areas. The situation in Egypt, where the extent of virus transmission was severely
underestimated until recently, will require urgent improvements in the quality of
surveillance and supplementary immunization.
To date, the RCC/EMR has received and favourably reviewed preliminary
national reports from 15 of 23 countries, with preliminary reports pending from 8
countries (including Pakistan). The RCC/EMR has prepared a special abbreviated
format for annual update reports from NCCs to the RCC; this format was used
for annual update reports submitted from eight countries of which three
(Oman, Saudi Arabia and Tunisia) included a preliminary report on laboratory
containment. In March 2002, a meeting was conducted to update and brief chairs of
EMR national certification committees and national expert review groups on the
current status of polio eradication, focusing on issues relevant for certification,
surveillance and accuracy of AFP case classification.
WHO/V&B/02.13
7
South-East Asia Region (SEAR). India is the only remaining endemic countiy in
the Region. With certification-quality AFP surveillance during 2001 in all other SEAR
countries, transmission is likely to be interrupted in these areas, most notably in
Bangladesh (last wild virus in mid-2000).
Even though the total number of cases reported from India did not decrease between
2000 and 2001, there was a marked reduction in both the geographic extent of
transmission (50% reduction in the number of endemic districts) and the biodiversity
of circulating virus lineages (from 8 to 3). Only parts of the northern Indian states of
Uttar Pradesh and Bihar were endemic in 2001.
Of particular relevance for certification, the timeliness and accuracy of AFP case
classification through the Indian national expert review committee has met
international standards. Through appropriate application of the virological case
classification and specifically the polio-compatible concept, the India programme
identifies and collects additional information on polio-compatible cases within three
months of paralysis onset. High-quality clinical follow-up data is collected for virtually
all cases with inadequate specimens. As India moves toward a wild-virus free status,
the practice of thorough follow-up and scrutiny of polio-compatible cases will lead
to more accurate final case classification and allow increased confidence in having
interrupted wild virus transmission in all parts of the countiy.
The RCC/SEAR has met most recently in March 2002 and reviewed
preliminary national reports from eight countries and update reports from two
(Sri Lanka and Thailand) of 10 countries in the Region. NCCs in all SEAR countries
have now collected basic data on polio activities, largely based on the draft format
proposed by WHO. However, there is still more work needed to ensure the
completeness of the required data and to further develop the database of essential
national documentation. The SEAR/RCC noted that the highest priority must
currently be afforded to achieving the objective of eradicating all foci of wild poliovirus
transmission in India. This priority far outweighed all other activities related to polio
eradication and its certification in SEAR. The SEAR/RCC will meet again in
September 2003.
GCC decisions:
1.
The GCC concurs with recent recommendations made by the global TCG and
countiy TAGs that accelerated efforts towards interrupting wild poliovirus
transmission in the remaining endemic countries of EMR and in India should
receive the highest priority.
2.
The GCC encourages both RCCs and the WHO Secretariat to increasingly
coordinate certification activities between EMR and SEAR, through cross
attendance at meetings and the ongoing informal exchange of information.
8
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
5. African Region
Compared to other WHO regions, eradication and certification activities
commenced most recently in the African Region (APR). However, significant progress
towards interrupting wild virus transmission and establishing reliable surveillance is
being made in the remaining endemic countries of the Region, notably in the
Democratic Republic of Congo, Ethiopia, Nigeria, and in large parts of West Africa.
The GCC specifically commends the continued high level of political support for
polio eradication in a number of African countries.
However, the implementation of eradication strategies, particularly high-quality
AFP surveillance and accurate AFP case classification, and the certification process,
face a number of specific challenges in AFR.
The GCC noted the AFR/RCCs substantial concern about:
•
the challenges to interrupting transmission in Nigeria;
•
continued low performance of routine immunization systems;
•
weak cross-border coordination, especially of supplementary immunization
activities;
•
the need to urgently improve surveillance in several countries of the southern
block (i.e. Madagascar, Mozambique, South Africa); and
•
recent evidence suggesting that an important focus of ongoing virus transmission
may have been missed in Western Africa (Mauritania and surrounding countries)
through suboptimal surveillance and response.
Since the March 2001 meeting of the GCC, national certification committees
and national expert committees (NECs) for case classification have been appointed
in 41 of 46 APR countries. At three intercountry meetings attended by members of
the AFR/RCC, NCC and NEC chairs of 37 of 41 countries were oriented to polio
eradication and the process of RCC review of country documentation. The meeting
was held with assistance from WHO/HQ, WHO/EUR and WHO/WPR.
Progress in certification in the African Region has been more difficult than anticipated.
Challenges include:
•
several countries (Algeria, Equatorial Guinea, Mauritania and Sierra Leone)
have not yet nominated NCCs and a NEC;
•
in more than half of the 37 countries where the NCC chairs had participated in
regional orientation meetings, other NCC members have not yet been briefed
in turn;
WHO/V&B/02.13
9
•
other difficulties to make designated committees fully functional, such as
insufficient support for NCCs locally (inadequate administrative support,
problems in making meeting per diems available);
•
limited administrative and technical staff support at AFRO to conduct the
required multicountiy meetings.
The RCC/AFR is concerned that the importance of certification is not yet fully
acknowledged by a number of countries, negatively affecting implementation of the
certification process.
GCC decisions:
1.
The GCC requests WHO to urgently strengthen the managerial and
administrative support necessary for efficient implementation of the certification
process in member states of the African Region.
2.
Recognizing the large number of recently endemic countries in the
Region, certification activities in Africa should continue to be the first priority
for receiving technical support from WHO staff with certification experience
(e.g. PAHO, WPRO, WHO/HQ).
3.
The RCC/AFR should request AFRO to assure that, by the end of 2002,
NCCs are designated and made functional in all countries, with completion of
the orientation of all NCC chairs and members.
4.
The GCC is concerned about the lack of progress towards revitalizing
AFP surveillance in Madagascar and other countries of southern Africa,
and fully endorses the global TCG’s recommendations in this regard.
10
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
6. Laboratory containment
The GCC notes that progress is being made in all regions towards laboratory
containment, particularly in the European and Western Pacific regions. As part of
the pre-certification phase of containment, more than 80 000 laboratories worldwide
(in all regions except APR) are now listed in national registers of bio-medical
laboratories to be surveyed, and more than 50% of these laboratories have already
responded to the survey. To date, 450 laboratories worldwide have been identified
as having wild poliovirus infectious material. Guidelines for containment in inactived
polio vaccine (IPV) production facilities have been drafted, and will be published
during the first half of 2002.
RCCs reported progress in many countries towards closer aligning and coordinating
certification and containment activities at the national level. However, progress in
several regions (AMR) was not as fast as had been expected (see regional sections
above). The GCC is concerned that, although regional and national certification
groups are now expected to coordinate certification and containment efforts more
closely, the actual reporting requirements on containment are not clear.
The GCC appreciates that the second edition of the global action plan for laboratory
containment will better define several key issues relevant for effective laboratory
containment, and therefore for certification, most notably:
•
the biosafety requirements for wild poliovirus infectious and potentially infectious
materials, depending on risk assessments,
•
the need for containment of vaccine-derived polioviruses, and
•
better definition of storage conditions.
The second draft of the global plan also highlights the fact that specific
recommendations on containment for the post-certification era can only be made
following decisions on post-certification policy.
The GCC encourages the ongoing efforts to develop methods to confirm and validate
laboratory containment achievements and notes that consideration is given to form
technical groups to facilitate national validation efforts.
WHO/V&B/02.13
11
GCC decisions:
1.
The updated version of the global plan for laboratory containment of wild
polioviruses should be finalized, published and made available to the GCC and
RCCs as soon as possible.
2.
The GCC urges the Secretariat to review containment documentation needs at
national and regional level, and to continue efforts to develop methods for national
authorities to validate reported containment achievements. The GCC requests
the Secretariat to report on the proposed validation methods, including the
development of relevant guidelines, during the next GCC meeting.
3.
Regional certification commissions, in consultation with WHO regional
secretariats, should consider the potential value of RCC subcommittees on
laboratory containment to work more closely with biosafety oversight groups
active in large countries and at the regional level.
12
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
7. The GCC mandate and
circulating vaccine-derived
poliovirus (cVPDV)
Noting the additional information and data on cVDPV presented during the
April 2002 meeting of the global TCG, the GCC acknowledges that further progress
was made in understanding cVDPV and the possible implications of cVDPV for the
global eradication effort. The global polio laboratory network has agreed on standard
nomenclature to categorize VDPVs and has established special screening methods
to improve the sensitivity of existing laboratory surveillance to assure the timely
detection and characterization of VDPV. Of note, all cVDPVs found to date showed
recombinations with non-polio enteroviruses in the non-structural region of the virus,
a possible marker to facilitate the detection of cVDPV.
The GCC further notes progress in other research to better define the epidemiology
and duration of shedding of Sabin viruses following immunization campaigns.
In addition to ongoing research studies in Cuba, the programme has begun to analyse
data derived from AFP surveillance to study patterns of Sabin virus isolation in
relation to supplemental immunization activities (SIAs). Preliminary results using
data from India suggest that Sabin virus is not shed for more than four weeks following
campaigns. Final results of this work will become available within a year.
Prospective screening and retrospective analysis of more than 3400 SABIN isolates
from AFP cases reported since 1999 from all WHO regions is consistent with the
assumption that the circulation of neurovirulent VDPV is a very rare event.
Despite the considerable increase in surveillance sensitivity, cVPDV has not been
found again since the detection of cVDPV in 3 children in the Philippines between
March and September 2001. Sensitive AFP surveillance in Haiti, the Dominican
Republic and the Philippines indicates that cVPDV transmission in all three countries
was interrupted through well-implemented supplementary immunization campaigns
with oral polio vaccine (OPV).
The GCC, during its 2001 meeting, reaffirmed that the objective of its activities,
as outlined in the report of the first meeting of the GCC in May 1995, is to certify
the global interruption of the transmission of wild polioviruses. An additional
prerequisite for global certification - the need to complete the laboratory containment
process - was added in 1997. The GCC had noted in 2001 that the full benefits of
eradication will only be realized in the absence of cVDPV, and that the potential
implications of cVDPV for the certification process must remain under review.
The GCC had urged WHO to continue its research on cVDPV, taking account of
the need for methods to verify the absence of VDPV.
WHO/V&B/02.13
J
io ’
GCC decisions:
1.
The GCC reaffirms its 2001 decision to encourage WHO to continue its work
to understand cVDPV, to improve surveillance sensitivity for cVDPV, and to
create a mechanism to verify cVDPV absence after the certification of wild
poliovirus eradication.
2.
While acknowledging the need to verify the absence of cVDPV once the
eradication of wild poliovirus has been certified globally, the GCC re-emphasizes
that the main objective of its work remains the certification, when and if
appropriate, of the interruption of wild poliovirus transmission globally.
3.
In view of currently available data on cVDPV and the probable rarity of
cVDPV emergence, the GCC considers it premature to discuss an expansion of
its own mandate to also include verification of the absence of cVDPV following
certification of wild poliovirus eradication. This verification task may well be
accomplished through another mechanism and by another group.
14
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
8. GCC membership and
operating procedures
The GCC noted the importance of the independence of all experts serving on
WHO technical advisory groups and oversight bodies. The GCC has previously
discussed the issue of potential conflicts of interest among its members and in one of
its 2001 decisions, stressed the need for independence of certification bodies at global
and regional level. Specifically, GCC and RCC members should remain separate
from the implementation of polio eradication activities, but can participate in activities
such as country visits to review the status of polio eradication and to promote
certification activities.
The GCC noted that the overlap of membership between regional and global
commissions (all RCC chairmen are also GCC members) had proved very useful for
its work. The only potential conflict of interest that may arise from this
cross-membership would be in relation to the certification of a region. However,
several GCC members also serve on other polio eradication-related technical advisory
groups at global, regional and national level, with direct influence on programmatic
activities. These groups include the global TCG, WHO’s global steering committee
on polio research, as well as regional and national TAGs, with differing terms of
reference.
Cross-membership of GCC (or RCC) members on technical consultative
Groups (global or regional level) or technical advisory groups (TAGs) may be
perceived as incompatible with the strict assessment function of a certification group.
Although TCGs and TAGs are not actually implementing the programme, both exert
a direct influence on programme implementation as their advice and guidance is
directly translated into programmatic action.
The GCC also noted that the Commission has not been able to work with the
full number of members (13) originally designated by the Director-General of WHO,
as two members had been unable to attend meetings for several years. At the same
time, the GCC believes it could benefit from enhanced expertise for some technical
areas of the GCC’s work (i.e. laboratory containment, emergence of cVDPV).
The group discussed the value of appointing additional members with expertise in
enterovirology, molecular biology and biosafety in particular.
In discussing the issue of reporting needs from RCCs to the GCC, the Commission
noted that such reporting requirements had not yet been standardized, for either
certified regions or those yet to be certified. RCCs are also requesting more detailed
guidelines on the reporting of progress in laboratory containment, in particular from
country level (NCCs or containment task forces).
WHO/V&B/02.13
15
GCC decisions:
1.
The WHO Secretariat should review for the GCC the cross-appointments of
GCC members in polio eradication technical oversight bodies to identify
potential conflicts of interest. The Secretariat should develop a matrix listing
names, structure, roles and objectives of all relevant polio eradication committees
and groups to facilitate future GCC deliberations on this issue. Any new GCC
members should not be members of technical oversight groups.
2.
Dual membership in a regional and the global certification commission does not
constitute a conflict of interest, provided that GCC members from a particular
region abstain from voting on issues related to polio-free certification of their
own region.
3.
Recognizing that only 10 of the original GCC members are currently fully active
in the work of the Commission, the GCC reiterated the importance of ensuring
a full complement of at least 13 active members representing all WHO regions.
The GCC concurred that the Commission should continue to have two
representatives from each WHO region (ideally including the RCC chairperson),
with the origin of the 13th member at the discretion of the Director-General of
WHO. Given that some members may not be able to fully cany out their duties,
the GCC Chair should use a set of “attendance rules” to discuss future
participation with any member who should miss three consecutive meetings.
4.
In appointing new members, the GCC requests that the Director-General of
WHO give consideration to the geographic knowledge and/or specific technical
expertise of a candidate for GCC membership. Areas of expertise to consider
are virology (especially enterovirology), molecular biology and biosafety.
Also, as much as possible, the gender balance of the Commission should be
addressed. GCC members are able to provide names of potential candidate GCC
members for the consideration of DG/WHO.
5.
The GCC further recognizes the need to summarize, in a single document,
the GCC Terms of Reference, membership issues, role of the WHO Secretariat,
and operating principles (including relationship to RCCs), with a special focus
on standardizing annual reporting requirements from RCCs to the GCC before
and after regional certification. It is suggested that this document be compiled
by the Secretariat, then reviewed and updated by the Commission as a standing
agenda item at future meetings. The updated document could then serve as an
Annex to all future reports of the Commission, superseding any previous
documents.
6.
Annual GCC meetings should be convened as dedicated 2-day meetings,
potentially at WHO regional offices, to provide appropriate support to regional
and national certification efforts. The next meeting of the GCC should be
conducted in early 2003 in the African Region. GCC members should also
continue to have the opportunity to follow the deliberations of the global TCG
on polio eradication.
16
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
Annex 1:
Agenda
08:45-09:00
Opening
Administrative remarks
09:00-10:30
Status of 2001 GCC decisions and
issues arising from the WHO meeting
of certification focal points (Dec 2001)
WHO/HQ
Discussion points:
• GCC mandate with respect to VDPVs
• GCC cross-membership in technical
oversight bodies
• Selection of new GCC members
10:30-11:00
Coffee break
11:00-12:30
RCC reports - EUR, SEAR, EMR,
WPR and AMR
12:30-14:00
Lunch
14:00-14:30
RCC report: APR, with special focus
on the certification process in the
WHO Region for Africa
RCC Chairperson
14:30-15:30
Issues arising from the seventh
TCG meeting
GCC Members
RCC Chairpersons
Discussion points:
• GCC capacity to validate laboratory
containment
• Proposed GCC and RCC activities
through mid-2003
15:30-16:00
Coffee break
16:00-17:00
Finalization of decisions of the
GCC Chairperson
seventh GCC meeting
17:00
WHO/V&B/02.13
Closing
17
Annex 2:
List of participants
Global Commission for the Certification of the Eradication ofPoliomyelitis
Professor A Adams, National Centre for Epidemiology and Population Health,
Australian National University, Canberra, ACT 0200, Australia
Dr A Deria, 28 Claudia Place, Augustus Road, London, GB-SW19 6ES, UK
Professor SG Drozdov, Institute of Poliomyelitis and Viral Encephalitis of the
Academy of Medical Science of the Russian Federation, Moscow 142782,
Russian Federation
* Professor Jan Kostrzewski, Department of Epidemiology, National Institute of
Hygiene, 24 Chocimska Street, PL-00-791 Warsaw, Poland
Dr R Leke, Department of Immunology and Microbiology, Faculty of Medicine,
University of Yaounde, Yaounde, Cameroon
Dr C de Macedo, SMDB Conjunto 01 Casa 05, Lago Sul, Brasilia,
DF 71680-010, Brazil
Professor Nath Bhamarapravati, Center for Vaccine Development, Institute of
Sciences & Technology for Development, Mahidol University at Salaya,
Nakhonchaisri, Nakhonpathom 73170, Thailand
Professor FK Nkrumah, Noguchi Memorial Institute for Medical Research
(NMIMR), University of Ghana, PO Box LG 581, Legon, Ghana
* Dr FC Robbins, Department of Epidemiology and Biostatistics,
School of Medicine, Case Western University, 10900 Euclid Avenue, Cleveland,
OH 44106-4945, USA
Sir J Smith, 95 Lofting Road, Islington, London, GB-N1 1JF, UK
Dr Wang Ke-An, Chinese Academy of Preventive Medicine (CAPM),
27 Nanwei Road, Beijing 100050, People’s Republic of China
Dr Mohammed Suleiman Ali Jaffer, Ministry of Health, PO Box 393, Muscat,
Sultanate of Oman
Unable to attend.
18
Report of the seventh meeting of the Global Commission for the Certification of Poliomyelitis
WHO Secretariat
Regional offices
Regional Office for Africa (AFRO)
Dr S Okiror
Regional Office for the Americas (AMRO)
Dr M Landaverde
Regional Office for the Eastern Mediterranean (EMRO)
Dr MH Wahdan
Regional Office for Europe (EURO)
Dr G Oblapenko
Regional Office for South East Asia (SEARO)
Dr Arun Thapa
Regional Office for the Western Pacific (WPRO)
Dr S Roesel
WHO headquarters
Geneva, Switzerland
Dr D Tarantola, Director, Department of Vaccines and Biologicals (V&B)
Dr B Aylward, Polio Eradication Group (PEG), V&B
Dr Esther de Gourville, Vaccine Assessment and Monitoring (VAM), V&B
Dr R Tangermann, PEG/V&B
Dr C Wolff, VAM/V&B
WHO/V&B/02.13
19
t
The Department of Vaccines and Biologicals was
established by the World Health Organization
in 1998 to operate within the Cluster of
Health Technologies and Pharmaceuticals. The
Department's major goal is the achievement of a
world in which all people at risk are protected
against vaccine-preventable diseases.
Five groups implement its strategy, which starts
with the establishment and maintenance of norms
and standards,focusing on major vaccine and tech
nology issues, and ends with implementation and
guidance for immunization services. The work of
the groups is outlined below.
The Quality Assurance and Safety ofBiologicals team
team ensures the quality and safety of vaccines
and other biological medicines through the devel
opment and establishment of global norms and
standards.
The Initiative for Vaccine Research and its three
teams involved in viral, bacterial and parasitic
diseases coordinate and facilitate research and
development of new vaccines and immunizationrelated technologies.
The Vaccine Assessment and Monitoring team
assesses strategies and activities for reducing
morbidity and mortality caused by vaccinepreventable diseases.
The Access to Technologies team endeavours to
reduce financial and technical barriers to the intro
duction of new and established vaccines and
immunization-related technologies.
The Expanded Programme on Immunization develops
policies and strategies for maximizing the use of
vaccines of public health importance and their
delivery. It supports the WHO regions and countries
in acquiring the skills, competence and infrastructure
needed for implementing these policies and strate
gies and for achieving disease control and/or
elimination and eradication objectives.
Department of Vaccines aniid Biologicals
Health Technology and Pharmaceuticals
World Health Organization
CH-1211 Geneva 27
Switzerland
WHO
o
u
Fax:+41 22 791 4227
Email: vaccines@who.int
or visit our web site at: httpy/www.who.int/vaccines-documents
WHO/Polio/00.05
Distr.: General
G^-Cl
Global
I
isi
-1
E r a d i c a t I
I
i t i a t i v e
Strategic Plan
2001 - 2005
Department of
Vaccines & Biologicals
f
Health Organization
2000
THE GLOBAL POLIO ERADICATION INITIATIVE
Table of contents
Glossary of key terms and abbreviations
iv
Executive summary
vii
1. Background
1.1 Progress and current status of the Global Polio Eradication Initiative
1.2 Polio Eradication strategies and quality of implementation
1
1
2
2. The Strategic Plan 2001-2005: goal, objectives, timelines, and key milestones
3
3. Components of the Strategic Plan 2001-2005
3.1 Intensify NIDs and mop-up campaigns
3.2 Achieve certification-standard surveillance
3.3 Contain laboratory stocks of wild poliovirus
3.4 Develop a consensus strategy for stopping polio immunization
3.5 Strengthen national immunization programmes (EPI)
4
4
4
5
5
6
4. Implementation of the Strategic Plan: challenges and solutions
4.1 Major challenges
4.2 Other challenges
7
7
8
5. The role of partners
10
6. Financial resource requirements, 2001-2005
12
7. Beyond 2005: activities during the post-certification era
14
Annex 1: Priority actions by countries according to status of polio eradication
15
Annex 2: Rounds of supplementary immunization activities in polio-endemic and
recently endemic/high-risk countries
16
Annex 3: Annual objectives for years 2000-2005
18
iii
THE GLOBAL POLIO ERADICATION INITIATIVE
3. Acute flaccid paralysis (AFP) surveillance and laboratory investigation: AFP surveillance is
established in all polio-endemic or recently endemic countries to ensure that all cases of poliomyelitis
are detected. The goal of AFP surveillance is to report and investigate “any case of acute flaccid
(floppy) paralysis, including Guillain-Barre Syndrome, in a child aged less than 15 years and any case
of suspected polio in persons of any age”. A number of indicators have been established to monitor the
performance of AFP surveillance systems. Most importantly, even in the absence of wild poliovirus cir
culation, surveillance systems should be capable of (1) detecting at least one case of AFP per 100 000
population aged less than 15 years’, (2) collecting adequate stool specimens from at least 80% of AFP
cases, and (3) testing all specimens at a WHO-accredited laboratory.
An international laboratory network has now been established under the auspices of WHO, consist
ing of national laboratories which undertake virus isolation and identification, regional reference
laboratories which differentiate wild and vaccine viruses, and specialized reference laboratories which
support the network and conduct genetic sequencing studies on wild viruses to assist the identification
of routes of transmission. All network laboratories must successfully complete an accreditation process
and use established indicators to monitor their performance.
4. Mop-up campaigns: AFP surveillance data are used to identify the final chains of wild poliovirus
transmission in each geographical area. In these areas, two doses of OPV are administered to all
children aged less than five years, regardless of their prior immunization status, by immunization teams
that go house-to-house. These intensive immunization campaigns improve coverage and ensure that
the most difficult-to-reach children are immunized, thereby interrupting the last chains of wild
poliovirus transmission. In addition to delivering supplemental OPV doses, mop-up activities often
include an active search for AFP cases.
V
THE GLOBAL POLIO ERADICATION INITIATIVE
4. Implementation of the Strategic Plan:
challenges and solutions
Eradication Initiative has been mainly dependent
on multilateral funding mechanisms and Rotary
International, and, more recently, on foundation
funding. From 2001 to 2005, stronger efforts will
be undertaken to increase public and private sector
support for the eradication activities of polio
endemic countries. In particular, bilateral support
for the eradication activities of the ten global prior
ity countries (Afghanistan, Angola, Bangladesh,
Democratic Republic of the Congo, Ethiopia,
India, Nigeria, Pakistan, Somalia and Sudan) will
be critical to success.
ul] implementation of the five main components outlined in the Strategic Plan
jL.
2001-2005 will be a challenge. Key chal
lenges to implementation and possible solutions
that partners in the eradication initiative can bring
to bear are summarized below. In particular, advo
cacy for polio eradication is required at the global
and country level to surmount challenges, ensure
sufficient resources are available to all countries,
maintain political support, and secure societal sup
port.
4.1 Major challenges
Maintaining political commitment in all countries
Sustaining political commitment from the highest
levels of government is particularly challenging in
the face of a disappearing disease, but remains
key to ensuring high-quality activities in both
polio-endemic and polio-free countries. Some
polio-endemic countries plan to stop NIDs despite
having surveillance below certification standard.
Experience has conclusively demonstrated that such
actions jeopardize progress because low-level
poliovirus transmission can continue undetected for
years in areas with suboptimal surveillance. Political
commitment, particularly monitoring by the head
of state of the progress towards eradication, is key
to:
Securing access to all children, especially those in
conflict-affected countries
The success of the UN Secretary-General and other
global and national-level authorities in establishing
access, cease-fires, and “Days of Tranquillity” for
NIDs in Afghanistan, Democratic Republic of the
Congo, Peru and elsewhere has demonstrated the
feasibility of working successfully in conflict-affect
ed areas. These efforts must be expanded, drawing
upon the strengths of the UN Secretary-General’s
office, many UN agencies, the International Red
Cross and Red Crescent movement, and other new
and existing partners who can operate in countries
affected by conflict.
Improve the quality of NIDs and other SIAs
so that house-to-house immunization activi
ties reach all children by, for example,
enlisting multisectoral support.
Ig: Implement early and aggressive use of
extensive mop-up campaigns.
B Improve or maintain the quality of AFP
surveillance.
E Improve or maintain routine immunization
coverage.
Ensuring adequate financial resources from the
public and private sectors
Necessary financial resources must be secured to
purchase OPV, plan and implement NIDs, SNIDs
and mop-up campaigns (e.g. hiring and deploying
all necessary national and international staff, trans
portation, social mobilization, communications),
and cover surveillance and laboratory costs. To
ensure sufficient resources, advocacy for the Global
Polio Eradication Initiative is required at the global
and country levels. Thus far, the Global Polio
7
THE GLOBAL POLIO ERADICATION INITIATIVE
Communicating the progress of the Global Polio
Eradication Initiative
Effective communication is an essential element for
all of the components of this Strategic Plan.
Communication issues include meetings to ensure
exchange of experience and information (e.g.
between EPI programme managers and laboratory
directors); technical policy meetings held annually
to review progress and further develop policies
within the global initiative; media coverage for
public awareness and advocacy, and newsletters for
feedback to all health staff. O
Improving social mobilization
Markedly enhanced social mobilization efforts will
be essential to improving NIDs/SNIDs/mop-up
quality. Social mobilization efforts will enlist key
community networks and leaders - such as religious
organizations and womens groups - to ensure that
appropriate messages are developed and delivered to
the target population. Multifaceted mechanisms
will be enlisted to transmit messages, including use
of the media (print, radio and television), banners,
posters, and megaphones. Additional staff will be
enlisted to support these activities.
9
THE GLOBAL POLIO ERADICATION INITIATIVE
Eradication Initiative at the global level. Financial
donors at the global level of the initiative include:
dren in hard-to-reach areas, such as in conflictaffected countries.
K Foundations:
• Rotary Foundation
• Bill & Melinda Gates Foundation
• United Nations Foundation
• Organization of the Petroleum Exporting
Countries (OPEC) Foundation
Additional partner organizations play critical roles
at the regional and country levels to support polio
eradication. Of particular note is the Micronutrient
Initiative of Canada whose support includes ensuring
administration of vitamin A capsules during NIDs
and development of training materials. UN funds,
agencies, and programmes such as the World Food
Programme, United Nations High Commissioner
for Refugees, United Nations Office for the
Coordination of Humanitarian Affairs and
Operation Lifeline Sudan, have been key to imple
menting SIAs. Specific activities of these partner
organizations include:
K Corporations:
• Aventis Pasteur
• De Beers
• International Federation of Pharmaceutical
Manufacturers Association (IFPMA),
representing Pasteur Merieux Connaught
(now Aventis Pasteur), Chiron, Smith-Kline
Beecham, and Wyeth-Lederle.
® Participation in ICCs at country, regional, and
global levels.
Provision of financial and human resources.
E Technical support.
E Strategy implementation at country level
through, for example, volunteers for social
mobilization and NIDs, transportation, and
communications.
® Multilateral agencies:
• European Union
• World Bank
Nongovernmental organizations (NGOs), and
humanitarian
organizations such as the
International Red Cross and Red Crescent move
ment, Medecins San Frontieres (MSF), Save the
Children Fund, World Vision, CARE, and the
umbrella-organization CORE, are also key part
ners, particularly through assisting with micro
planning, training, transport, surveillance and
administration of supplementary immunization.
Many NGOs play a unique role in accessing chilFigure 4:
Past contributions received, 1985-2000
Belgium
Australia
European Union
.Other'
Netherlands___ __
Germany----------United Nations Foundation
Denmark—
Bill & Melinda Gates
Foundation
Japan
z
Rotary International
Civil society advocates and special ambas
sadors: leading celebrities from the arts, sciences,
entertainment, and sports fields provide their per
sonal talents to increase the profile of the eradica
tion initiative. Key advocates for the polio eradica
tion initiative include UNICEF Special
Representatives Ms Mia Farrow, Ms Claudia
Schiffer,
WHO
Goodwill
Ambassador Ms Martina Hingis,
basketball star Mr Dikembe
Mutombo, renowned photogra
US CDC
pher Lord Snowdon and the
Federation Internationale de
Football Association (FIFA).
Total received
US$1 450 million
Financial resources provided have
supported all aspects of the initia
USAID
tive, including planning of
national polio eradication activi
ties, social mobilization and train
ing; strengthening of laboratory
World Bank
IDA loan to Government of India capacity; and review meetings and
evaluations. O
UK
* Other includes past contributions from the Agency for Cooperation in International Health (Japan); American Association for World
Health (USA); Aventis Pasteur; Custom Monoclonals International (USA); De Beers; Finland; Institut Merieux; Ms Martina Hingis;
Italy; Japanese Committee for "Vaccines for the World’s Children"; Malaysia; Millennium Fund; Norway; Portugal; Republic of Korea;
11
THE GLOBAL POLIO ERADICATION INITIATIVE
Figure 6:
Status of financial resource requirements by year
400t
US$340m
350 -
[
i
: 11
150-t--------
100-
0-
El Shortfall
□ Funds projected
□ Funds pledged
US$300m
’ .
US$180m
-w.
US$95m
USS 85m
2004
2005
JIB
ii
2001
2002
2003
Year
13
THE GLOBAL POLIO ERADICATION INITIATIVE
Annex 1: Priority actions by countries
according to status of polio eradication
Status of polio eradication
Endemic countries (30 countries at
end of year 1999)
Definition: countries with virological
and/or epidemiological evidence of
endemic poliovirus circulation during
the past 12 months.
J
Priorities:
E. Intensify NIDs and conduct mop-up
campaigns every year until poliovirus
transmission is interrupted.
E Improve surveillance to accurately
target NIDs and mop-up cam
paigns.
E Strengthen routine immunization
activities.
J
'
■
Endemic (virologic or epidemiologic evidence of virus in 1999)
High-risk for poliovirus transmission
Low-risk for poliovirus transmission
Data as of August 2000
Certified polio-free
Recently endemic/nigh-nsk countries
(25 countries at end of year 1999)
detected for > 1 year, but at high risk of ongoing low-level indigenous virus
Definition: countries with no polio
a
or sustained transmission of imported virus due to: (1) geographic proximity to an endemic country, (2) low
routine immunization coverage, and/or (3) inadequate surveillance.
Priorities:
Maintain NIDs (or SNIDs if low routine coverage is limited to specific areas).
B Establish certification-standard surveillance.
B Conduct inventory of laboratory stocks for containment purposes.
E Strengthen routine immunization services.
Low-risk countries (101 countries at end of year 1999)
Definition: countries with no polio detected for > 1 year and at low risk of indigenous virus or sustained trans
mission of imported virus due to (1) high routine immunization coverage; (2) lack of proximity to endemic
countries; and/or (3) maintenance of high-quality surveillance.
Priorities:
K Achieve/maintain certification-standard surveillance.
Inventory laboratory stocks for containment purposes.
E Strengthen routine immunization services.
E Conduct polio supplementary immunization activities in areas of low coverage.
Countries certified polio-free (36 countries at end of year 1999)
Definition: countries certified polio-free by a regional certification commission (only AMR as of 15 August
2000).
Priorities:
£ Contain laboratory stocks of polioviruses.
B Maintain certification-standard surveillance.
E Strengthen routine immunization services.
E Consider polio supplementary immunization activities in areas of low coverage.
15
THE GLOBAL POLIO ERADICATION INITIATIVE
Section 2: Recently endemic/high-risk countries:* number of NI Ds rounds (unless SN IDs specified)
AFR
Burundi
Eq. Guinea
Gabon
Gambia
Kenya
Madagascar
Malawi
Mauritania
Mozambique
Namibia
Rwanda
Senegal
Tanzania
Uganda
Zambia
Zimbabwe
EMR
Djibouti
Iran
Yemen
2000
2001
2002
2003
2004
2005
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
SNIDs
2
2
SNIDs
SNIDs
SNIDs
SNIDs
SNIDs
2
2
SNIDs
SNIDs
SNIDs
SNIDs
SNIDs
SNIDs
SNIDs
SNIDs
2
2
2
2
SNIDs
2
2
SNIDs
2
2
SNIDs
SNIDs
2
2
2
2
2
SNIDs
2
2
2
SNIDs
2+SNIDs
2
2
2
SNIDs
SNIDs
SNIDs
2
2
2
2
2
SNIDs
SNIDs
SNIDs
2
SNIDs
SNIDs
SNIDs
SNIDs
SNIDs
EUR
Tajikistan
Turkey
Turkmenistan
Uzbekistan
SEAR
Myanmar
Sri Lanka
2
SNIDs-
2
2
SNIDs
SNIDs
Section 3: Low-risk and certified countries*
Many low-risk and certified countries must continue to guard against polio importations by conducting SIAs,
either full NIDs or SNIDs. For example, virtually all certified countries of AMR are planning to continue full
NIDs through 2005, the target date for global certification. Similarly, the Global TCG stated that NIDs must
be continued in all countries recently endemic for polio. Discontinuation of NIDs should only be considered
in countries with OPV coverage > 80%, no documented wild poliovirus for the last three years, and certifica
tion-standard surveillance for at least one year. Global vaccine forecasts take these recommendations into
account.
*as of end 1999
17
THE GLOBAL POLIO ERADICATION INITIATIVE
Table 2: Milestones to be achieved by end of year 2001
▼ Objectives
▼ Milestones 2001
Interrupt transmission of
wild poliovirus
4 Wild poliovirus transmission will be stopped in all countries except five to ten
countries in Asia and Africa.
Intensification of NIDs
and mop-up campaigns
All endemic countries will conduct either at least four rounds of intensified NIDs or
three consecutive NIDs (with SNIDs in high risk areas) as well as mop-up campaigns
(except India that will conduct two rounds of NIDs and two SNIDs.)
Certification-standard
surveillance
4- All countries in AFR will achieve certification-standard surveillance.
The South-East Asia and Eastern Mediterranean regional certification commissions
will have established national certification committees in all countries.
Containment of wild
poliovirus stocks
< National inventories will be completed and all wild polivirus infectious and
potentially infectious materialswill be contained under BioSafetylevel(BSl)-2/polio
conditions in AMR, EUR, WPR and 14 countries of EMR.
< Regional guidelines for implementation will be created in AFR and SEAR.
0 National plans of action, task force, and inventory process will start in remaining EMR
countries where polio transmission has been stopped.
❖ Interim wild poliovirus repositories will be examined and validated in AMR, EUR and WPR.
Consensus strategy for
stopping immunization
4* All research studies to determine the strategy for stopping vaccination will be at least
at the data collection phase.
Strengthening routine
immunization services
4 The lessons learned from polio eradication will be applied for use in strengthening
routine immunization programmes, including use of the checklist to optimize the
impact of polio eradication on immunization systems.
< Immunization management training modules will begin to be updated to incorporate
lessons learned from polio eradication.
Table 3: Milestones to be achieved by end of year 2002
▼ Objectives
▼ Milestones 2002
Interrupt transmission of
wild poliovirus
4- Wild poliovirus transmission will be stopped in all countries.
Intensification of NIDs
and mop-up campaigns
Intensified NIDs will continue in Angola, DR Congo and Nigeria.
NIDs or SNIDs, and mop-up campaigns will continue in all countries that were
endemic or high-risk in 2000 or 2001.
Certification-standard
surveillance
4* EUR will be certified as polio-free.
Certification-standard surveillance will be maintained.
National certification committees will be established in all AFR countries.
> The role of environmental surveillance will be defined.
Containment of wild
poliovirus stocks
< Global certification containment requirements will be implemented in AMR and
EUR (upgrade to BSL-3/polio).
Global certification containment conditions will be completed in WPR (completion
of upgrade to BSL-3/polio)
4“ Interim wild poliovirus repositories will be examined and validated in AFR and SEAR.
Consensus strategy for
stopping immunization
< Multiagency meeting will be held to assess the status and findings of research studies.
Strengthening routine
immunization services
# ICCs will monitor routine immunization services in all recently endemic countries.
Updated immunization management guidelines will be completed.
19
THE GLOBAL POLIO ERADICATION INITIATIVE
Table 6: Milestones to be achieved by end of year 2005
▼ Milestones 2005
▼ Objectives
Intensification of Ml Ds
and mop-up campaigns
Conduct NIDs and/or SNIDs in any remaining high-risk countries at least until
Certification-standard
surveillance
< All regions will be certified polio-free and global certification will be achieved.
< Supplemental surveillance will be completed as recommended by the Global
global certification is achieved.
Certification Commission.
♦ Containment requirements for certification will be attained globally.
Final global wild poliovirus repository(ies) will be operational.
The draft global plan of action for post-OPV era containment procedures will be
Containment of wild
poliovirus stocks
developed.
.
..
■
.
.
-
.
.
■
■
•
.
-
;
'■
Consensus strategy for
stopping immunization
< Specific recommendations for stopping polio immunization will be presented to the
World Health Assembly for endorsement.
Strengthening routine
immunization services
National polio-funded staff will be assimilated into routine immunization
programmes, and will continue to work toward the GAVI goal of reaching routine
- -
EPI coverage of 80% in 80% of districts globally.
< All countries that included vitamin A in NIDs have integrated vitamin A into routine
immunization programmes, as appropriate.
21
Jose Utrera
Mi
Home
Help
Intended for Health Professionals
Search/Archive
Feedback
Table of Contents
PDF of this article
Email this article to a friend
Respond to this article
Read responses to this article
PubMed citation
Related articles in PubMed
Download to Citation Manager
See Correction for this article
This article has been cited by other articles
Search Medline for articles by:
Yamey, G.
Alert me when:
New articles cite this article
r Collections under which this article appears:
International health
BMJ 2002;325:1236-1240 ( 23 November)
Education and debate
WHO in 2002
Faltering steps towards partnerships
Gavin Yamey, deputy physician editor, Best Treatments.
BMJ Unified, London WC1H 9JR
qyamey@bmj.com
Public-private partnerships for health have been a defining feature of Gro Brundtland's term as director
general of WHO. How-is WHO performing in its role as a partner?
WHO must "reach out to others," said Gro Brundtland in her first speech after her election as director
general of the organisationAThis statement heralded a new era of partnerships between WHO-and
other health agencies, the private sector, and civil society-(box I).2 In this article, I examine how WHO
is performing-in these alliances, with a particular focus on Roll. Back Malaria.- X__________________
Summary points
Gro Brundtland's election as director general heralded a new era of partnerships between WHO and other heal
agencies, the private sector, and civil society
WHO has found it hard to let go of its traditional role as being "in charge" of global health activities
The Roll Back Malaria partnership has been plagued by a lack of clear governance and ineffectiveness at cour
WHO could play an important role in helping countries coordinate new global health initiatives with health syste
strengthening
The organisation needs to articulate a clear policy on working in partnerships, including proper safeguards in it*
interactions with the private sector
—
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 1 of 9
Malaria causes about 3000 deaths a day, over 90% of which are in sub-Saharan Africa.5 It is both a
disease of poverty and-a cause of poverty (fig 1), slowing economic growth by 1.3% per-year in
endemic areas.5 Roll Back Malaria (RBM) was launched-in 1998 as Brundtland's "pathfinder" project,^
bringing together-the biggest players in health with the aim of halving the malaria-death rate by 2010.
Fig 1. Global burden of malaria
w
w
u
(Credit: WHO)
View larger version (47K):
[in this window]
[in a new window]
______________ ®_________________________
!t has had two major successes. Firstly, it brought together more than 90 multilateral, bilateral, nongovernmental, and private-organisations. Secondly it has raised the profile of malaria,-particularly
through its April 2000 summit in Nigeria.5
rZ]
Box 1: Public-private partnerships involving WHO^
European Partnership Project on Tobacco Dependence
Global Alliance for TB Drug Development
Global Alliance to Eliminate Lymphatic Filariasis
Global Alliance to Eliminate Leprosy
Global Alliance for Vaccines and Immunization
Global Elimination of Blinding Trachoma
Global Fire Fighting Partnership
Global Partnerships for Healthy Aging
Global Polio Eradication Initiative
Global School Health Initiative
Multilateral Initiative on Malaria
Medicines for Malaria Venture
Partnership for Parasite Control
Roll Back Malaria
Stop TB
UNAIDS/lndustry Drug Access Initiative
David Alnwick, Roll Back Malaria's project manager, said that "when RBM was formed, a very
deliberate, very considered position-was taken to try to avoid a burdensome, cumbersome, formal
governance-structure." But Roll Back Malaria recently commissioned Richard-Feachem, executive
director of the Global Fund, to lead a team-in evaluating the alliance, and the team found that the
projecfs-loose governance structure made the very concept of partnership-unclear. The roles of each
partner were undefined, and this "looseness-and uncertainty is confusing to the partners themselves; it
allows-the partners to avoid responsibility and to put blame on others;-and it is also confusing to clients
at the country level."5
One damaging aspect of this looseness is that it encouraged WHO to "go it alone" and make
decisions without adequate consultation-with partners. Rather than being a true alliance, Roll Back
Malaria-was "a WHO programme with friends."5 A recurring theme in my-interviews with WHO's
partners was their fear that WHO was using-its new alliances to get back in the driver's seat in
international-health policy making. "WHO speaks a language of partnership,"-said one senior member
of a global health agency, "but the reality-is of insecurity and control-freakery."
Brundtland rejected this accusation. WHO cannot be criticised in this way, she said, "because we are
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 2 of 9
hentaZp^n f Practlce’ -'t says. "partners yield most of the responsibility for RBM to-WHO, and
then blame WHO for what goes-wrong.
A new rote- for WHO
“■
As global health cooperation fragments into many different partnerships, WHO is being asked to olav
rou^hp",?
r°le7!te—W Str°ng leadershiP buL^°^Ye greater voice to its padnars -The role
could be described as leading from the middle, rather-than the-front.
11 ■Srri?K|jUSt Wlth'n Ro11 Back Malaria that WH0 must give more room to its partners but also in the
joint UN programme on-HIV and AIDS (UNAIDS), an alliance of UN agencies and the World-Bank
aimed at alleviating the global impact of the epidemic (table)
View this table:
[in this window]
[in a new window]
Number of adults and children (age <15 years) living with HIV infection or AIDS, end of 2
From igse, WHO took the lead on HIV control activities through its Global Programme on AIDS
used®? to form UNd°"orsJ But in the mid-90s donors cut their funding and-
used it to form UNAIDS. This was partly a protest against the-leadership of the former director general
WHO ThSnf
T h°rUNA'DS W0U'd take 3 more multlsectoral approach-than
'
Th w \ u
? c°nfldence frorn donors had a profound-effect on WHO. Instead of asking itself
what it could still contnbute-on HIV and AIDS, it battled with its partners to regain its primacy'n this
area. Peter Plot executive director of UNAIDS, says that-the spilt was "like a really bad divorce There
was a fantasy of bringing UNAIDS back into-WHO."
uivoice. mere
S3'd'n°7 needs t0 redefine itself given that the architecture of global health has
w
amount-°f ener9y was spent fighting each other, particularly WHO Unicef-the
World Bank, and UNDP [the United Nations Development Programme].-[The fighting] was on territory
and policies, with WHO claimmg-it was the controller, that they were in charge. The world is-changecHn
e meantime. That s why I'm saying that WHO still-has to look for its place in the-world "
uZnlld35 reinvi9°rated WHO'S AIDS Programme, which is providing technical expertise to
?9^ 9 9U'dance to-ooontnes on drug treatment of HIV, including prices? Piot-believes
nwTff° rfh?U d C?n<;eu,tx7te °n thlS klnd Of 9uldance.-and not try to become the leader of the world's
need a global pllnS ail partTe^"n9e'
°f
lnternatiOnal A>DS-Society, agreed: "We
►
Governance
estabhsh'q]rtX* "“‘I’’ “ Yate u“«re'tV. saM tha> "»HO has not been willing or able to
“SXXTXm.P9'™® and ,his be9S ,he ‘"'esto to*WH0
•»
Buse believes that the best model for achieving shared governance is the one used by legally
independent partnerships, such-as the Medicines for Malaria Venture and the Global Alliance for-TB
Drug Development "I hese have established boards," he said,"with explicit fiduciary and oversight
Sliced JrivatlsecS.^
“ management is resP°nsible, with representation-from both
soisfteHS^v96"^ “d'? ad°Pt thiS kind °f modeL One Partnership that has done
ronfr^tn mb tA d
Vab,CClneS and lmmunization (GAVI).s It is housed within-Unicef but—in
contrast to most partnerships housed within WHO—it-has a governing board that represents oublic
X^s PartnerS-The b°ard haS 11 members'thr- whom are Representatives9Seveio^ng
Box 2: A framework for good governance of partnerships involving WHO^
fl Partnerships should:
f
—t
*
-
Establish clear goals, roles, responsibilities, and decision making structures
?onsider the means of monitoring and enforcing decisions
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 3 of 9
'
“—““’er*" ab““ d“'”°" '"abi"9 structures, funding, resourc
Document and publicise details of the process and outcomes of the partnership
Governing bodies should:
• Be widely representative
‘
^“eXSion™” '™1”9 ""“b '’"“b”9 iB p0s“0n 88te’«b -W Par'1C"’a,i” 0' ™8“to“88
’
*t:
oft™, lack me materia,
Country support
Willem van de Put is director of HealthNet International, a non-governmental organisation that
co aborates with WHO in post-conflict-zones, where malaria is often rife. He had high expectations ofmnrh a?t T
But We're dlsaPPointed." he said, "that something-so widely advfrtised with so
TV,
Mone^
|
l0n’ ‘urn® °ut t0 be’no more than the sum °f its Parts. If we want to do malaria work -we're
RB"
isan
»"•
is »
A£country level, Roll Back Malaria’s presence and activities are often criticised as ephemeral There
has been no push, -said Fred Bmka, who used to work with Roll Back Malaria and who-is now at the
University of Ghana, to try to get something done-on the ground.” WHO's regional offices are
important to Roll Back-Malaria's success. "Some regions have done well" said Binka -"but the African
2“
Mver- The reg»n gets blamed far underpeXing ’. said
yet headquarters-gave no support, no capacity strengthening" (box 3),
Box 3: Malaria in the African region
----------- ------------------
Roll Back Malaria faces its greatest challenge in sub-Saharan Africa. Malaria is Africa's leading cause of
mortality in children under 5. It accounts for 40% of public health expenditure, and up to half ofall moatient
admissions and outpatient visits in areas where transmission of malaria is high 2 The cheapest antimalarlal
drug, chloroquine, is rapidly losing its effectiveness in almost all countries where malaria i/endemic.
re9IOnal offlc® f°r Africa (AFRO) has an important role to play in Roll Back Malaria's malaria control
Hklh r
c.urrently located ln Harare, but at least part of the office is moving to Brazzaville a move that i<
afro” T«kte ' m°He 's°lated' Unfortunately, a "politicized and inflexible bureaucracy impedes the ability of ’
S,S"'are S,re“ed ,0 Capa* antl "**,he
.-1"88 ,he ne“S“V b"™" and "nanc”1
donSe
Most countries are helpless-ltej
Malaria is endemic in 42 African countries, said Binka, yet the partnership created only three malaria costs in
« balan.
“^~al at l-
Roll Back Malaria partners have agreed that an important immediate step will be to create "inter aoencv infer
provide coordinated and continuous support to a small group o °c"ies
rmnVrfnn^r31^110,"
that R°" BaCk Ma,aria's 3lobal and re9ional processes have made little
£"'7or"rvhSeiT''=
be in douCbtU
V
’
BaCk Ma,ana CannOt Sh°W results soon’its credibility-and future will surely
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 4 of 9
,°9eth'r “
Drug production in Addis Abada, Ethiopia
r
ir
(Credit: P VIROT/WHO)
if
View larger version (103K):
[in this window]
[in a new window]
term> hig
e go.-
One of the obstacles facing the new public-private initiatives is that they are being rolled out in
countries with weak health-systems. For example, an assessment oTGAVI's impact on four Africancountries raised concerns about whether these countries were sufficiently-prepared and resourced to
roll out the new vaccine initiativeAThere is a.tensjonbetween a donor-driven global partnership aimingfor short term, high profile goals and the need for countries-to broadly develop their health systems.
< Partnerships tend to-"pick the low hanging fruit"—they concentrate their efforts on-getting quick results
I rather than building up the wider systems-needed to address the broader burden of-disease.
V(
P
Another related problem is that partnerships rarely synchronise their activities with emerging
processes within countries-aimed at developing their health systems. The evaluation of Roll-Back
Malaria found that the initiative was not linked up to sector-wide-approaches, where donors contribute
to a single pot of fundslhatsupport a country's whole health sector ratherThan individual-disease
programmes.^! Nor was it linked .tojhe World Bank's-poverty reduction strategies1^ or its programme
of debt relief-for heavily indebted poor countries.13
►
Are partnerships undermining WHO’s core activities?
Poor countries do not have the resources to coordinate the bewildering array of new public-private
partnerships with programmes-aimed at health systems support. WHO arguably has the mandate,though not the budget, to help governments with this coordination.-Public-private partnerships could
inadvertently mid ermine WHO's-core activities, including country support, by diverting resources-away
from such activities. If the donor community concentrates-its spending on these partnerships, which
are mostly single disease-programmes, and if WHO also diverts its resources towards them,-there will
be fewer resources at WHO's disposal for its core activities.Children talk about malaria during Gro Brundtland's visit to Nigeria, 2001
1
- w f
4^’
a
•r
(Credit: P VIROT/WHO)
View larger version (92K):
[in this window]
[in a new window]
Brundtland denies that this will happen. The increase in voluntary donations to WHO during her term,
she said, shows that-more funds are flowing to the organisation. But donors are still-earmarking these
for specific vertical programmes, and so a question-remains over how WHO's less glamorous but
increasingly important-country support work will be-funded.
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 5 of 9
■"'
t t IV
f 01 !wl
Some academics worry about the private sector's involvement in partnerships for health.
Could
the private sector,-they wonder, distort the public health goals of the UN agencies?-Carol Bellamy,
chair of the board of the Global Alliance for Vaccines-and Immunization and executive director of
Unicef, has warned-that "it is dangerous to assume that the goals of the private-sector are somehow
synonymous with those of the United Nations,-because they most emphatically are not."—
But the private sector has a vital role to play in improving global health, and WHO must engage with it.
The difficult question-is how close this engagement should be. Roll Back Malaria's recent-partnership
with the company Novartis, for example, has caused-alarm among some malaria experts (box 4).
Box 4: WHO’s partnership with Novartis: cause for concern?
Roll Back Malaria is seeking alternatives to chloroquine for treating malaria in resistant areas. There is partici
interest in combinations of drugs that include derivatives of artemisinin. Paul Garner, professor at the Liverpo
School of Tropical Medicine, said that "there are good strategic and scientific reasons to use artemisinin drug
combination with other drugs, as these slow the development of resistance, but there should be good evident
that the particular combinations are at least as effective as other regimens to cure patients."
In areas where multidrug resistant malaria is emerging, Roll Back Malaria is advising governments to use
artemisinin based combination drugs to treat the disease. The only combination drug ready for use is one tha
produced solely by Novartis: artemether-lumefantrine (Coartem). It is expensive, and the company has agree
provide it for use in malaria endemic countries at what it states is the cost of production. Recently a systemat
review of the drug found that it was more effective than chloroquine in chloroquine resistant areas, but less
effective than some cheaper alternatives.^ The authors, of whom Garner is one, found insufficient research
evidence to compare it adequately with sulfadoxine-pyrimethamine, one of the main drugs in use in Africa.
Given this lack of proved effectiveness, said Garner, why did Roll Back Malaria not insist that the company
conduct proper studies comparing its effectiveness against existing antimalarial regimens? Why is the projec
particularly promoting Novartis' drug as first line treatment for malaria?
When I interviewed David Alnwick, Roll Back Malaria's project manager, boxes of Coartem were on display ir
office. "Should I take the boxes of Coartem down," he asked, "when the press or TV come? No. Why have I c
them up there? Because at the moment this is the best single drug around for treating malaria in countries th
have got multidrug resistant malaria. Should I be ashamed of the fact that we've worked with Novartis to impr
access to developing countries to the drug? Absolutely not. Why not? Because I think we're entirely open, an<
have been open, in saying that it is a real pity that Novartis is the only group in town making this drug. While t
may own the intellectual property on this particular drug, there are four or five similar drugs out there waiting t
developed."
Hans Hogerzeil, a member of WHO's essential drugs and medicines policy group, said that "there are
different ways for WHO-to be in contact with commercial companies" and each requires-different rules
of engagement. WHO's tropical diseases programme,-for example, must work closely with industry to
develop new drugs.-But WHO's essential drugs department should be "totally fire-walled-off, because
we, through the expert committee, have to finally-decide, independently, is this a good drug or not—is
it recommendable,-is it-safe?"
WHO knows it must tread carefully in its interactions with industry and has formulated guidelines for its
* staff to govern-these.12 It is Jindear,,however, how closely the guidelines-are being followed across the
organisation, and they are vague-about important issues such as screening potential corporate
i partners.-Until WHO addresses this vagueness, it will continue to stumble-into situations in which it
1 seems to be too close to the private-sector. Many WHO staff, for example, were amazed that the
official-lobbyist of the pharmaceutical industry was asked to write a policy-paper on generic drugs for
WHO's Commission on Macroeconomics-and Health.One senior WHO insider said that the episode
showed-a "fatal error of judgment" on Brundtland's-part.
►
TaWno
-..afc
Daniel Tarantola, one of Brundtland's senior policy advisers, said: "We are now in a phase of taking
stock—looking at the-good and the bad in these alliances, and recreating and refocusing-what we do."
He believes that the lessons from partnerships to-date point to a few important questions. What sort of
composition-should they have? What should their relationships to governments-be? When should they
and should they not involve the UN-system?
This kind of appraisal is desperately needed. WHO has not articulated a clear and consistent policy on
working in partnerships,-and yet it is increasingly entering into them. Not all staff embrace-the new
direction that WHO is taking, and yet this diversity of-opinion is rarely heard. The organisation needs a
sound policy-that has come from a process of open discussion and-debate.
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 6 of 9
.
W3
.
, &w <
J
W ,«sc3 ;•
WHO has yet to find its feet as a partner in a global health landscape that is becoming dominated by
partnerships. An analysis-of Roll Back Malaria shows that WHO could fulfil an important-new role,
helping to define the governance of partnerships and-the responsibilities of each partner. It is well
placed to support-countries in the local implementation of new global health initiatives,-and in
coordinating these initiatives with strengthening of health-systems, but it is unclear how it will get the
funds to do so.-Proper safeguards in its interactions with the private sector-will go a long way towards
inspiring confidence that these initiatives-are truly serving public-health.
i
- vw gme ■ i h
aci
Competing interests: The BMJ receives submissions and commissions papers from many WHO
authors, but GY is no longer involved in this process. GY now works for BMJ Unified, a joint venture
between the BMJ Publishing Group and United Healthcare Services Inc (www.besttreatments.org ).
h
F c o tn d ■ ■' s
This is the third of five articles
Kt
1.
2.
3.
4.
5.
6.
7.
8.
9.
a
r-
World Health Organization. Dr Gro Harlem Brundtland, director-general elect, The World Health Organizatio
to the fifty-first World Health Assembly, Geneva, 13 May, 1998. Geneva: WHO, 1998. www.who.int/directorgeneral/speeches/1998/index.html (accessed 5 Nov 2002).
Reich MR. Public-private partnerships for public health. In: Public-private partnerships for public health. Carr
Harvard University Press, 2002:1-18. www.hsph.harvard.edu/hcpds/partnerbook/chap1.PDF (accessed 15 b
World Health Organization. Fact sheet No 203. Roll Back Malaria. Geneva: WHO, 2002. www.who.int/inffs/en/fact203.html (accessed 15 Nov 2002).
World Health Organization. Launch of Roll Back Malaria. Geneva: WHO, 1998. www.who.int/directorgeneral/speeches/1998/english/1 9981030 un.html (accessed 15 Nov 2002).
Yamey G. African heads of state promise action against malaria. BMJ 2000; 320: 228.
Feachem R, Medlin C, Daniels D, Dunlop D, Mshinda H, Petko J, et al. Achieving impact: Roll Back Malaria
phase. Final report of the external evaluation of Roll Back Malaria. August
29 2002. http://mosquito.who.int/cmc upload/0/000/015/905/ee.pdf (accessed 15 Nov 2002).
Godlee F. The World Health Organisation: WHO's special programmes: undermining from above. BMJ 199f
182[Free Full Text],
World Health Organization. Sources and prices of selected drugs and diagnostics for people living with HIV/
Geneva: WHO, 2002. www.who.int/medicines/library/par/hivrelateddocs/prices-eng.pdf (accessed 15 Nov 2(
Brugha R, Starling M, Walt G. GAVI, the first steps: lessons for the Global Fund. Lancet 2002; 359: 435-
438nSlirMedlinel.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
Buse K, Waxman A. Public-private health partnerships: a strategy for WHO. Bull World Health Organ 2001;
754[ISI1[Medlinel.
Garner P, Flores W, Tang S. Sector-wide approaches in developing countries. BMJ 2000; 21: 129-130.
Verheul E, Rowson M. Poverty reduction strategy papers. BMJ 2001; 323: 120-121[Free Full Text],
World Bank. The HIPC Initiative, www.worldbank.orq/hipc/about/hipcbr/hipcbr.htm (accessed 15 Nov 2002).
Yamey G. Global vaccine initiative creates inequity, analysis concludes. BMJ 2001; 322: 754[Free Full Text],
Richter R. 'Partnerships' between UN agencies and transnational companies: a critical perspective. In: Heat
International. Public-private 'partnerships'. Amsterdam: Health Action International,
2000. www.haiweb.org/campaign/PPI/seminar200011 .html#item3 (accessed 15 Nov 2002).
Bellamy C. Public, private and civil society. Statement of Unicef executive director to Harvard international d(
conference on "sharing responsibilities: public, private and civil society," Harvard University, Cambridge, MA
1999. www.un.org/partners/business/unicef14.htm (accessed 15 Nov 2002).
World Health Organization. Guidelines on working with the private sector to achieve health outcomes. Gene’
2000. www.who.int/gb/EB WHA/PDF/EB107/ee20.pdf (accessed 5 Nov 2002).
Bale EH. Consumption and trade in off-patented medicines. Commission on Macroeconomics and Health W(
paper series, Paper No WG 4:3. www.cmhealth.org/docs/wg4 paper3.pdf (accessed 15 Nov 2002).
Omari AA, Preston C, Garner P. Artemether-lumefantrine for treating uncomplicated falciparum malaria. Co(
Database Syst Rev 2002;(3):CD003125.
UNAIDS. UNAIDS at Barcelona. Global estimates of HIV/AIDS epidemic as of end
2001. www.unaids.org/barcelona/presskit/barcelona%20report/Global estimate.pdf (accessed 13 Nov 2002)
© BMJ 2002
This article has been cited by other articles:
► HOME
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 7 of 9
D. Aitken
WHO responds
BMJ, January 25, 2003; 326(7382): 217 - 218.
[Full Text] [PDF]
Rapid responses:
Read all Rapid responses
Co-artemether versus sulphadoxine-pyrimethamine: is a comparative study necessary?
Stephen Toovey, et al.
bmj.com, 28 Nov 2002 [Full text]
WHO's policies on public-private partnership: the need for reform
Kent Buse
bmj.com, 29 Nov 2002 [Full text]
Public/Private Partnership Between Novartis and Co-artemether r
Phil M Rush, et al.
bmj.com, 6 Dec 2002 [Full text]
PDF of this article
Email this article to a friend
Respond to this article
Read responses to this article
PubMed citation
Related articles in PubMed
Download to Citation Manager
See Correction for this article
Search Medline for articles by:
Yamey, G.
Alert me when:
New articles cite this article
? Collections under which this article appears:
International health
Home
Help
Search/Archive
Feedback
Table of Contents
»mi c
British Journal of Opthalmoloqy
© 2003 BMJ Publishing Group Ltd
Printed for Jose Utrera, 17 Feb 2003, 12:28
Page 8 of 9
A-.
&
2002, 77, 97-108
No. 13
Weekly epidemiological record
Releve epidemiologique hebdomadaire
29 MARCH 2002, 77th YEAR / 29 MARS 2002, 77* ANNEE
No. 13, 2002, 77, 97-108
http://www.who.int/wer
Contents
97
Outbreak news
98
Progress towards the global
eradication of poliomyelitis,
2001
107 Influenza
108 Criteria used in compiling the
infected area list
108 International Health
Regulations
Sommaire
97
Le point sur les epidemies
98
Progres vers I'eradication
mondiale de la poliomyelite,
2001
107 Grippe
108 Criteres appliques pour la
compilation de la liste des
zones infectees
108 Reglement sanitaire
international
WORLD HEALTH
ORGANIZATION
Geneva
ORGANISATION MONDIALE
DE LA SANTE
Geneve
Annual subscription / Abonnement annuel
Sw. fr. / Fr. s. 230-
6.5001.2002
ISSN 0049-8114
Printed in Switzerland
OUTBREAK NEWS
LE POINT SUR LES EPIDEMIES
Dengue/dengue
haemorrhagic
fever,
Brazil. As of 19 March, the health authorities
had reported 104 469 cases of dengue and
40 deaths in Rio de Janeiro state. In the city of
Rio de Janeiro, the municipal health author
ity reported a total of 49 149 cases and
435 cases of dengue haemorrhagic fever, with
a total of 29 deaths.
Dengue/dengue hemorragique, Bresil. Au
19 mars, les autorites sanitaires avaient signale
104 469 cas de dengue et 40 deces dans 1’etat de
Rio de Janeiro. Dans la ville de Rio de Janeiro, les
autorites sanitaires municipales ont signale au
total 49 149 cas et 435 cas de dengue hemorragi
que, avec au total 29 deces.
The dengue outbreak is the largest in the
state’s history, and the authorities have im
plemented an intensive ongoing campaign
to control the epidemic. Included are social
mobilization activities to involve the com
munity in eliminating breeding sites of mos
quitoes and in taking measures to avoid be
ing bitten by mosquitoes, as well as state and
municipal vector control programmes.
La flambee de dengue est la plus serieuse dans
1’histoire de cet etat, et les autorites effectuent
une campagne intensive pour lutter contre 1’epidemie. Cette derniere comprend des activites de
mobilisation sociale pour impliquer la communaute dans 1’elimination des sites de reproduc
tion des moustiques et dans la prise de mesures
pour eviter de se faire piquer par les moustiques,
ainsi que des programmes de lutte contre les
vecteurs au niveau de 1’etat et de la municipalite.
Ebola, Gabon (update).’ On 20 March, the
Ministry of Health reported 60 confirmed
cases, including 50 deaths. Suspect cases
continue to be investigated.
Ebola, Gabon (mise a jour).1 Le 20 mars, le Mi
nistere de la sante a signale 60 cas confirmes,
dont 50 deces. Les enquetes se poursuivent quant
aux cas presumes.
Ebola, Congo (update).2 As of 22 March,
32 confirmed cases, including 19 deaths, had
been reported in villages in Cuvette region;
18 contacts are being followed. Ebola haem
orrhagic fever has now been laboratoryconfirmed in the Kelle area.
Ebola, Congo (mise a jour).2 Au 22 mars, on
avait signale 32 cas confirmes, dont 19 deces,
dans des villages de la region de Cuvette; 18 con
tacts sont suivis. La presence de la fievre hemorragique Ebola dans la zone de Kelle a ete confir
mee en laboratoire.
Meningococcal disease, Burkina Faso
(update).1 As of 20 March, 3 579 cases had
been reported, including 544 deaths (case
fatalityrate, 15%), from all parts of the coun
try. The epidemic threshold has been
reached in 12 out of 15 districts, and 13 dis
tricts are on alert for reaching the threshold.
Vaccination campaigns were carried out in
2001 and recently in 2002 .
Meningococcie, Burkina Faso (mise a jour).1
Au 20 mars, 3 579 cas avaient ete signales, dont
544 deces (taux de letalite, 15%), dans tout le
pays. Le seuil epidemique a ete atteint dans 12
des 15 districts, et 13 districts restent en alerte au
cas oil le seuil serait franchi. Des campagnes de
vaccination ont ete effectuees en 2001 et recemment en 2002.
' SeeNo.11,2002,p.81.
2 See No. 7,2002, p. 49.
1 VoirN°11,2002,p.81.
2 Voir N° 7,2002, p. 49.
70gr0Up W135 has been lab°«-
ory confirmed m cases from 5 districts by the WHO Col
Kur OMS de ,eftrence el de redmX’E’J
coilabora-
Oslo, Norvege. Une cellule de crise a ete etahP
r"eni,1S0C0‘lues.
la same. Une equipe de 1’OMS coll h
b 16 Par 6 Mlnistcrc de
afin dedefinirlameflleu™
“ de Cette ceUule
presence de la sonchl wi£
t
“ntre la flambee, vu la
veillance epidemiologique, la lofleciTel^all'^dXlTamV"'
13 ra0b‘I1Sat-on sociale, la formation et la coofomaXlt
'
Progress towards the global
eradication of poliomyelitis, 2001
thfS WortdOHrafhat4iOn initiatiVe’launched folIowi"g
Progres vers I'eradication mondiale de la
pohomyelite, 2001
the 1988 World Health Assembly resolution to eradicate
poliomyelitis worldwide, has made remarkable nm
From 1988 through the end of 2001, foTnX of cC
nes where polio was endemic decreased from > 125 to 10
2002U Derrent
2°01 (aS °f 10 March
2002) a percentage decrease of > 99%. Wild-type 2 polio
despHe^01 “ deteCted W°rldwide
OrtoberS
despite improving surveillance. Two WHO regions - the
Americas and the Western Pacific - have been certified free
indigenous wild poliovirus. The European Region has
lilX ri lndlgen°US
POliOV‘™s ^ce 1998 and L
likely to be certified polio-free in 2002.
However, considerable remaining challenges to f
' '
the global
s.i
de cas de poliomyelite estime a 350 000 en fl
•
< 1 000 cas en 2001 (an 10 mars 2t)n^ c t
, 88 e 1 passe a
poliovirus sauvage de tvoeTn’
’ .
de > 99%- Le
puis octobre 1999
/P
pas ete detecte dans le monde de-
DeuxrX de roMS^r/
t0U>rS pl- ^“ce.
ont ete certifi” exempts
°CCldental ~
Region europeenne esttemntf d^T SaUVage autochtone- La
»... d^, tet miei, i., “x’STCependant, les problemes considerables r------que rencontre encore 1’ef-
"S
into nnP
d C°ntlnUed lmP°rtations of wild poliovirus
mo polio-free areas, and the detection of circulating vac
cine-derived poliovirus in the Philippines.
g
ainsi qu>en L^h et en
poliovirus sauvage dans des rZionf'e
Soudan ~
continu« de
sent egalement des problemes, ainsi qm7aPdXcfio^dTXeiIlte-P0’
circulant derives de la souche vaccinle aux Ph^pines"
*
This article reviews global progress achieved during 2001
and summarizes the current status of the initiative
Implementation of polio eradication strategies
XX XXXX Z“ ”b““ *• -
«
The global polio eradication initiative relies on high-qualty implementation of 4 main strategies: routine infant imacfivifiesdurin1111
■ SUppIementary immunization
activities during national immunization days (NIDs) sur
veillance for wild poliovirus through reporting and X
ogical testing of all cases of acute flaccid para!ysis (AFP)
mong children aged < 15 years, and targeted mop-up im
cTnfe foe™ CamPaignS On“ VirUS “dssion haf be-
Routine immunization coverage with 3 doses of oral polio
aged<Tmonfo PV3)’ reTed gl°bally am°ng Children
1 foo
f
*S’ remain«i relatively unchanged between
differences in
81%
82%’ respectively- Substantial
the If
n
eaSt between WH0 regions, with
the African Region reporting the lowest OPV3 coverage
rates (51/om 1999 and 55% in 2000). Routine immunizl
98
’
--------------------------------------------------------------------------------
SUSSEX” “• monde chez les enfants ages de <n mo- \ " S1gnalee dans le
meme entre 1999 et 2f)nn I «io/ on
CSt reStee relatlvement la
tion coverage continues to be low in the 10 countries (ex
cept Egypt) endemic in 2001 (Map I), including the re
maining endemic states of Bihar and Uttar Pradesh in
India. In the absence of good routine OPV coverage, the
only means for countries to reach the immunity levels nec
essary to interrupt wild poliovirus transmission is to in
crease the frequency and quality of supplementary immu
nization campaigns.
de la vaccination systematique reste faible dans les 10 pays d’endemie (a 1’exception de 1’Egypte) recenses en 2001 (carte I), et notamment en Inde, dans les etats du Bihar et de 1’Uttar Pradesh. En 1’absence d’une bonne couverture systematique par le VPO, le seul
moyen pour ces pays d’atteindre le degre d’immunite necessaire
pour interrompre la transmission du poliovirus sauvage consiste a
accroitre la frequence et la qualite des campagnes de vaccination
supplementaire.
All endemic and most recently endemic countries con
tinued to conduct supplementary immunization activities
during 2001. An estimated 575 million children in 94 coun
tries received nearly 2 billion doses of OPV during
300 rounds of NIDs, sub-NIDs or mopping-up activities. All
countries used well-supervised house-to-house immuni
zation in part or all of the target area for supplementary
immunization activities as the primary means to further
increase their quality in order to reach the highest possible
coverage of children aged < 5 years.
En 2001, tous les pays d’endemie et d’endemie tres recente ont
poursuivi leurs activites de vaccination supplementaire. On estime
a 575 millions le nombre d’enfants qui, dans 94 pays, ont re$u pres
de 2 milliards de doses de VPO a 1’occasion de 300 JNV, sous-JNV,
ou operations de ratissage. Dans tous ces pays, la vaccination portea-porte, dument supervisee dans certaines parties ou dans 1’ensemble des zones cibles des activites de vaccination supplementaire, a
ete le principal moyen utilise pour accroitre la qualite des services
et parvenir a la couverture la plus elevee possible chez les enfants de
< 5 ans.
The quality of AFP surveillance to indicate reliably the
presence or absence of wild poliovirus has further im
proved in all WHO regions and endemic countries
(Table 1). In 2001, all regions and endemic countries
reached levels of AFP reporting sufficiently sensitive for
polio-free certification and often far exceeding the re
quired annual non-polio AFP rate of at least 1 AFP case per
100 000 population aged <15. Progress in AFP reporting
between 2000 and 2001 was particularly notable in the Afri
can Region, especially in Angola, Ethiopia and Nigeria.
Similar progress is seen in improving the rehability of virological surveillance through the collection of adequate
stool specimens. In 2001, all WHO regions, except for the
African Region, reached and surpassed the certification re
quirement of collecting 2 adequate stool specimens from
at least 80% of AFP cases. This indicator also came close to
certification quality in the African Region, where it in
creased from 50% in 2000 to 71% in 2001.
La qualite de la surveillance de la PFA s’est encore amelioree dans
toutes les regions de 1’OMS et dans tous les pays d’endemie, indiquant de maniere liable la presence ou 1’absence de poliovirus
sauvage (Tableau T). En 2001, toutes les regions et tous les pays
d’endemie ont atteint des niveaux de notification des cas de PFA
suffisamment sensibles pour pouvoir certifier 1’absence de la poliomyelite, niveaux depassant souvent de loin le taux annuel de PFA
non poliomyelitique exige, qui est d’au moins 1 cas de PFA pour
100 000 habitants de < 15 ans. Entre 2000 et 2001, les progres de la
notification des cas de PFA ont ete particulierement visibles dans la
Region africaine, surtout en Angola, en Ethiopie et au Nigeria. Des
progres similaires sont observes dans 1’amelioration de la fiabilite
de la surveillance virologique, grace a la collecte adequate d’echantillons coprologiques. En 2001, toutes les regions QMS sauf la Re
gion africaine ont atteint ou depasse la norme exigee pour la certi
fication, qui est de recueillir 2 echantillons coprologiques conformes pour au moins 80% des cas de PFA. Get indicateur s’est egalement rapproche de la qualite exigee pour la certification dans la
Region africaine, oil il est passe de 50% en 2000 a 71% en 2001.
The 147 laboratories collaborating in the WHO-accredited
global polio laboratory network continued to provide con
sistent quality support to the programme. Improvements
in AFP reporting and specimen collection considerably
increased the workload for most laboratories, especially in
the African laboratory network, where the number of stool
specimens increased by 56%, from 11 891 in 2000 to 18 515
in 2001. Globally, 64 443 stool samples were tested from
32 041 AFP cases in 2001, with results for 92% of cases re
ported within 28 days after receiving specimens in the na
tional laboratory. Improvements in the efficiency and lo
gistics of stool specimen handling and transport between
collaborating laboratories in many countries allowed fur
ther reductions of the unavoidable reporting delay be
tween the onset of paralysis and the reception of final labo
ratory results. For example, in the Indian laboratory net
work, this interval has been reduced to 40 days or less on
average.
Les 147 laboratoires collaborant au reseau mondial des laboratoires de la poliomyelite agrees par 1’OMS ont continue a fournir un
soutien regulier et de qualite au programme. Les ameliorations
apportees a la notification des cas de PFA et a la collecte des echan
tillons ont considerablement accru la charge de travail de la plupart des laboratoires, surtout dans le reseau des laboratoires africains, oil le nombre d’echantillons coprologiques a progresse de
56%, passant de 11 891 en 2000 a 18 515 en 2001. Dans le monde,
64 443 echantillons coprologiques ont ete testes pour 32 041 cas de
PFA declares en 2001, les resultats de 92% d’entre eux ayant ete
rapportes dans les 28 jours suivant la reception des echantillons au
laboratoire national. Les ameliorations apportees sur le plan de
1’efficacite et de la logistique du traitement et du transport des
echantillons coprologiques entre les laboratoires collaborateurs
dans de nombreux pays ont permis de reduire encore les inevita
bles retards de notification dus au temps ecoule entre I’apparition
de la paralysie et la reception des resultats de laboratoire finaux.
Par exemple, dans le reseau des laboratoires indiens, ce delai a ete
reduit en moyenne a 40 jours au plus.
Impact on wild poliovirus transmission
The initiative’s progress towards global interruption of
wild poliovirus transmission from 2000 to 2001 is charac
terized by the following main achievements:
Effets sur la transmission du poliovirus sauvage
Dans le cadre de cette initiative, les progres realises en vue de 1’interruption mondiale de la transmission du poliovirus sauvage entre 2000 et 2001 se caracterisent par le bilan suivant:
RELEVEEPIDEMIOLOGIQUEHEBDOMADAIRE, N° 13, 28 MARS 2002
99
the decrease in the number of countries with endemic
transmission from 20 to 10, reducing the number of
wild-virus confirmed polio cases reported globally
from 719 (2000) to 473 (2001 provisional total as of
10 March 2002);
transmission est
e po lomyelite confirmes dus au virus sauvage notifies dans le
monde, nombre qui est passe de 719 (2000) a 473 (2001, total
provisoire au 10 mars 2002);
the decreasing geographical spread of virus transmis
sion within each country, often within affected provinces
or states (e.g. Afghanistan, India, Nigeria, Pakistan);
le retreassement geographique de la transmission du virus
dans cheque pays, souvent au sein des provinces ou des Etats
touches (par ex., Afghanistan, Inde, Nigeria, Pakistan);
- the reduced biodiversity of circulating virus, indicated
by fewer numbers of virus substrains circulating sepa
rately in endemic countries;
- la biodiversite reduite des virus circulants, revelee par le nom
bre p us reduit de sous-souches virales circulant separement
dans les pays d’endemie;
F
- the decrease in the number of circulating virus types: of
the 3 wild poliovirus types, type 2 has not been isolated
since October 1999, and type 3 was isolated only in Af
ghanistan, India, Nigeria, Pakistan and Somalia in 2001.
Table 1 AFP surveillance quality and confirmed polio
Tableau 1 Qualite de la surveillance de la PFA et cas
la diminution des types de virus circulant:
...
---- ----- —***a>ts: sur les 3 types de
hrP ^USriaUVageS’
tyPe2 n’a PaS
iSOk dePuls °«°bre 1999, et le type 3 n’a ete isole qu’en Afghanistan, en Inde, au
Nigeria, au Pakistan et en Somalie en 2001.
cases by WHO region, 2000 and 2001 and in countries endemic during 2001-
de poliomyelite confirmes par Region QMS. 2000 et 2001 et par pays d’endemie
en 2001a
AFP cases reported
Cas declares de PFA
Annualized non-polio
AFP rateb
TauxdePFAnon
poliomyelitique annualiseb
AFP cases with
adequate specimensc
_____
Cas
de. PFA avec
echantillons conformed
Total confirmed
(clinical + virological)
Total des cas confirmes
(diniques + virologiques)
Virus-confirmed
cases
Cas confirmes
virologiquement
(%)
Region/Country* - Region/payse 2000
Africa - Afrique
Angola
Ethiopia - Ethiopie
Niger
Nigeria
Americas - Ameriques
Eastern Mediterranean Mediterranee orientale
Afghanistan
Egypt - Egypte
Pakistan
Somalia - Somalie
Sudan - Soudan
Europe
South-East Asia Asie du Sud-Est
India - Inde
Western Pacific Pacifique occidental
5 936
8 444
213
345
93
979
149
552
2 076
Global - Monde
2001
229
1 931
2 186
2000
2001
2000
2001
2000
2001
2000
2001
1.50
1.60
0.70
1.20
0.70
1.21
2.96
2.40
50%
55%
45%
37%
71%
66%
47%
80%
67%
1 863d
115
152
33
638
12
113
1
1
6
51
10'
160
55
3
2
63
1
1
28
0
51
0
505
120
4
199
96
79
0
140
11
5
116
7
1
3
287
27
4
199
46
4
0
140
11
5
116
80%
83%
74%
91%
84%
59%
74%
81%
1.90
4.40
3.80
1.13
36%
80%
89%
3 253
252
275
1 152
161
213
257
1 562
129
269
303
1 645
1 818
1.41
1.08
1.28
1.53
2.16
1.35
1.12
10 758
8103
10 658
7510
1.82
2.03
1.79
1.86
78%
82%
83%
83%
591
265
268
268
272
265
268
268
6 894
6 552
1.49
1.40
90%
88%
0
3'
0
0
30 562
33 510
1.57
1.61
75%
84%
2 971
537
719
473
3 852
1.89
1.69
1.19
2.32
4.09
2.15
1.23
70%
50%
90%
71%
50%
49%
An’mS1 °f|- °20°2’"D°nn4eS P°Ur2001 endatedu 10mars2002.
; Two stool specimens cEedXirtAdays
24-48^
Vaccine-derived poliovirus. - Poliovirus derive de la souche vaccinlle
During 2001, only 10 countries documented indigenous
transmission of wild poliovirus, decreasing from 20 en
demic countries by the end of 2000. A number of central
and western African countries were endemic in 2000, but
found no virus m 2001 despite sensitive AFP surveillance
approaching certification quality: Bangladesh, Benin, Cen
tral Afncan Republic, Chad, Congo, Cote d’Ivoire, Demo
cratic Republic of Congo, Ghana, Iraq and Nepal also iso
lated virus in 2000 but were no longer endemic in 2001.
ioo
6
7
1
2
P°i' ’ °0 00° PerS°nneS de <15 ans-
ParPayS,°n'apparatel^^
En 2001, seuls 10 pays ont documente une transmission autochtone
de poliovirus sauvage, alors qu’ils etaient 20 a la fin de 1’annee 2000
Un certain nombre de pays d’Afrique centrale et occidentale
etaient des pays d’endemie en 2000, mais n’ont isole aucun virus en
00 malgre une surveillance sensible de la PFA, proche de la
qualite necessaire a la certification; ce sont: le Bangladesh, le
Benin, le Congo, la Cote d’Ivoire, le Ghana, 1’Iraq, le Nepal, la Repu“ had Centrafricaine’la R«Publique democratique du Congo et le
'
WEEKLY EPIDEMIOLOGICAL RECORD. NO. 13, 28 MARCH 2002
P2
S
Map 1 Wild poliovirus cases, 2001 (10 endemic countries)
Carte 1 Cas de poliovirus sauvage, 2001 (10 pays endemiques)
8
L_J.
£>3 0^
5
§
o
g
5
Wild virus importation: Bulgaria and Georgia/
Importation de virus sauvage: Bulgarie et
George
c?
1g
01
//
UJ
NJ
CO
I
o
s
Q
6o
£
Probable wild
virus importation:
Mauritania/
Importation probable
de virus sauvage:
Mauritanie
O
O
o
O
o
o
Wild virus importation:
Zambia/
Importation de virus
sauvage: Zambie
6
Q,
i 2| Polio endemic countries / Pays d'endemie poliomyelitique
\\
v
Vyl
o
U Wild virus importation I Importation de virus sauvage
'I
The designations employed and the presentation of material on this map
do not imply the expression of any opinion whatsoever on the part of the
World Health Organization concerning the legal status of any country, territory,
city or area or of its authorities, or concerning the delimitation of its frontiers
or ooundaries.
[S] 1 wild virus case /1 cas de virus sauvage
Les designations utilises sur cette carte et la presentation des donnees
qui y figurent n'impliquent, de la part de I’Organisation mondiale de la Sante,
aucune prise de position quant au statut juridique de tel ou tel pays, territoire,
ville ou zone, ou de ses autorites, ni quant au trace de ses frontieres.
WHO, 2002
tooftrt^fl
<Juall,>' improved from 2000 to
2001 ln all WHo regions and endemic countries, the
number of reported polio cases decreased further, with
10 M537,tOtal conflrmed polio cases reported in 2001 (as of
10 March 2002), of which 473 are wild-virus confirmed
719ewe7ewld971 10131 C°nfirmed cases in 2000- °f which
19 were wild-virus confirmed. Since there are still AFP
catfon'in
2°01 PendinS flnal classififor 200, ’ reglOnS’ theJotal number of confirmed cases
fo^ooi will mcrease, but is expected to remain below
B==£==S~=
dus a des virus sauvages. Cornme il y a encore dans routes les rl
ladassmcation dX?Xe"rnoX^wtaYd'eTa
2001 va augmenter, mais devrait rester inferieur a I OOT.
hkh m?6 10 remaining endemic countries constitute the
high-transmission areas of Afghanistan, northern India
Niger, Nigeria and Pakistan. Due to their large, dense popu ’
ktions, India, Nigeria and Pakistan have traditionally been
major poliovirus reservoirs. Virus transmission in endemc areas of these countries, as weU as bordering areas of
Afghanistan and Niger, is still intense, although le extent
of transmission is rapidly decreasing. Following a rapid
^crease m the extent of wild virus transmission in India
between 1997 and 2000,' wild poliovirus types 1 and 3 con
tmued to be transmitted during 2001, mainly in the north-
“u 65 °f Blhar and Uttar Pradesh' The total
numb
didlo df
7^confirmed cases reported from India
r rn 1
ease from 2000 (265 c^es) to 2001 (268 cases as
Of 10 March 2002). However, closer epidemiological ana’lyXd1”^65 11,31 °nly 3 poliovirus type 1 lineages circub
reolned" 17
’
fr°m 8 “ 200°- FeWer districts
reported wild-virus confirmed polio cases during 2001 as
compared to 2000 (63 vs. 87 of 530 total districts in India)
Most of the virus found during 2001 in Indian districts out
side the states of Bihar and Uttar Pradesh was not found to
fewmm6"0115
but originated ” one of the
gaming northern Indian foci which remained en-
iTnf
,Ug, 0Ut
Wh°le year' ThuS>Virus found “ 42 of
infected districts during 2001 was considered indige
nous to these districts, while virus found in the remaining
the V
ln 2001 could be traced to an importation from
the known endemic areas of Bihar and Uttar Pradesh.
smn ^n'th1^ geographical sPread of Virus transmis
sion m the Afghanistan-Pakistan epidemiological block
has further decreased from 2000 to 2001, particularly in the
Cinq des 10 pays d’endemie restants representent des zones de forte
sion 6Cr01t rapidement- APres une diminution rapide de 1’exten
on geographique de la transmission du virus sauvage en Inde
ob ervee entre 1997 et 2000,' les poliovirus sauvages de twes 1 ef t
ont continue a etre transmis en 2001, principalenfent danTles etats
confcme1111'6 "T B’har ''
PradeSh-Le nombre total de cas
2000
3 P°110VlruS sauvage notifi“ en Inde n’a pas baisse entre
2000 (265 cas) et 2001 (268 cas au 10 mars annal r
S
analyse epidemiologique plus fine indique que seuksTligTeVde
m
? tyPe 1 °nt C,rCUie en Inde “ 2001, contre 8 en looo
Moms de districts ont notifie des cas confirmes de poliomyelite a
2001
districts7nd-
nS ’
P
2000
deS
‘outre 87 sm Us
tr0UVas en 2001 dans les
istricts mdiens autres que ceux du Bihar et de 1’Uttar Pradesh
n etaient pas autochtones, mais provenaient de 1’nn Hac
i
foyers qui subsistent dans le nofd
des eTZ6 T1710ng de 1’ann“'AlnSi’les virus trouv& dans 42
des 63 districts mfectes en 2001 ont ete considers comme autoch
“aTtre
“ PU daterminer ciue ceux trouves dans ks
de l-Uttar Pmd“
r6Si°nS
du Bihar
noliomSrt61 r®ensi°n S^graphique de la transmission du virus
tan ont enZdiXIen^eXoS^p^eXX'
2 virus reservoirs shared between these countries (NorthWest Frontier province with adjoining provinces of Eastern
Afghanistan; and Northern Balochistan with South-West
Patsatantanhar°?nd Kandahar)' Progress * evident in
Pakistan, where large population centres in Punjab and
Snrer°TeS
al°ng
molecular
vidence indicating decreasing virus biodiversity. However
multiple virus foci did remain in 2001 in all provinces of
Pakistan, with particularly intense transmission in NorthWest Frontier province, a localized outbreak of type 3 virus
during the second half of 2001 in south-western Punjab
pcovince, and remaining foci in northern and southern
Sindh. Progress from 2000 to 2001 was remarkable in Af
ghanistan, where wild poliovirus transmission appears to
-ceased outside the 2 joint reservoirs, including in
northern and north-western Afghanistan, which both had
endemic transmission in 2000.
grandes agglomerations se sont retrouvees exemptes de virus dans
les provinces du Pendjab et du Sind, et ou des donnees moleculatre
’"diquent une diminution de la biodiversite virale. Toutefois en
001, de nombreux foyers viraux sont restes actifs dans 1’ensemble
des provinces pakistanaises, avec une transmission particulierement m ense dans la province frontaliere du nord-ouest, une flamdan 7
V‘7S
ty?e 3 aU C°UrS du deu”eme semestre 2001
dans la province du Pendjab et des foyers toujours actifs dans le
remt61 6 M U
Pr°Sr“
entre 2000 et 2001
ete
remarquables en Afghanistan, ou la transmission du poliovirus
sauvage semble avoir cesse en dehors de ces 2 reservoirs «
ment dans lenord et le nord-ouest de 1’Afghanistan, ou la transmis
sion etait endemique en 2000.
transmis
' See No. 34,2001, pp. 258-262.
102
’ Voir N° 34, 2001, pp. 258-262.
WEEKLYEPIDEMIOLOGICAL~RECORO, NO. 13,
While endemic transmission was found throughout
Nigeria in 2000, transmission during 2001 seems to have
become more focal to the northern states of Nigeria, and
adjoining parts of Niger.
Tandis que la transmission etait endemique dans 1’ensemble du
Nigeria en 2000, en 2001 elle semble s’etre cantonnee aux etats du
nord et aux regions voisines du Niger.
Ethiopia, Somalia and Sudan in the Horn of Africa, as well
as Angola and Egypt, are considered to be low-transmis
sion countries. The intensity and geographical spread of
virus transmission decreased in Angola between 2000 and
2001, despite marked surveillance improvements; however,
transmission may still be missed in areas with conflictrelated access problems, as shown by the importation of
poliovirus to Zambia from eastern Angola in 2001. Docu
mented through both AFP and environmental surveillance,
several lineages of wild poliovirus continue to circulate in
Egypt despite many years of implementing eradication
strategies. Virus transmission in Sudan is clearly focal, with
only 1 virus-confirmed case reported during 2001 in the
presence of close to certification-quality AFP surveillance.
Improvements in AFP surveillance quality, as well as highquality supplementary rounds, increasingly suggest that
virus transmission in Ethiopia is also limited. Few virusconfirmed cases (all wild-virus type 3) were found in
Somalia in 2001, despite improved surveillance following a
wild poliovirus type 1 outbreak in 2000 in the area around
Mogadishu.
L’Ethiopie, la Somalie et le Soudan dans la Corne de 1’Afrique, ainsi
que 1’Angola et 1’Egypte sont consideres comme des pays de faible
transmission. L’intensite et 1’extension geographique de la trans
mission virale ont diminue en Angola entre 2000 et 2001, malgre
une amelioration marquee de la surveillance; toutefois, cette trans
mission peut encore passer inaper<;ue dans des regions oil il y a des
problemes d’acces lies a des conflits, comme l’a montre 1’importation en Zambie d’un poliovirus venu de I’est de 1’Angola en 2001.
Plusieurs lignees de poliovirus sauvages, documentees par le biais
tant de la surveillance de la PFA que de la surveillance de 1’environnement, continuent de circuler en Egypte malgre la mise en oeuvre
de strategies d’eradication depuis de nombreuses annees. La trans
mission du virus au Soudan est nettement limitee a des foyers, avec
settlement 1 cas confirme rapporte en 2001 en presence d’une sur
veillance de la PFA ayant la qualite requise pour une presque certi
fication. Les ameliorations apportees a la qualite de la surveillance
de la PFA, ainsi que des tournees de vaccination supplementaire de
qualite, laissent de plus en plus a penser que la transmission du
virus est egalement limitee en Ethiopie. On a trouve peu de cas
confirmes en Somalie en 2001 (tous dus au pohovirus sauvage de
type 3), malgre une surveillance amelioree a la suite d’une flambee
de poliovirus sauvage de type 1 survenue en 2000 dans la region de
Mogadiscio.
During 2001, 3 polio-free countries detected importations
of wild poliovirus: Bulgaria and Georgia in the European
Region, and Zambia in the African Region. It is not clear
whether wild virus detected in Mauritania in 2001 repre
sents indigenous transmission or an importation. Virus
importations were rapidly reported and triggered largescale surveillance and immunization response activities,
thereby containing further spread.
En 2001, 3 pays exempts de poliomyelite ont detecte des importa
tions de poliovirus sauvage: la Bulgarie et la Georgie dans la Region
europeenne et la Zambie dans la Region africaine. On ne sait pas si
le virus sauvage detecte en Mauritanie en 2001 represente une
transmission autochtone ou une importation. Ces virus importes
ont ete rapidement signales et ont declenche une surveillance a
grande echelle ainsi que des activites de vaccination, qui ont per
mis d’endiguer leur propagation.
Circulating vaccine-derived poliovirus (cVDPV),
2000-2001
After immunization with OPV, vaccinees excrete Sabin-|
strain virus for a limited time. However, very rarely, vaccine|
derived polioviruses (VDPV) may acquire the neuroviru^
lence and transmission characteristics of wild-type polio-i
virus. Polio cases due to circulating type 1 VDPV (cVDPV)|
were found in Haiti and the Dominican Republic (Hispa-|
niola island) during 2000 and 2001 (21 virus-confirmedl
cases), and in the Philippines during 2001 (3 virus-1
confirmed cases). Type 1 cVDPVs in both the Hispaniola^
and Philippines episodes showed more than 2% differenc^
from Sabin virus (VP1 region of genome), and may hava)
circulated for 2 years before paralytic cases were detected^
Low immunization coverage may be a risk factor fo^
VDPVs to assume wild-type characteristics.
Poliovirus circulants derives de la souche vaccinate
(2000-2001)
Apres une vaccination par le VPO, les sujets vaccines excretent du
virus de la souche Sabin pendant une duree limitee. Toutefois, et ce
tres rarement, il arrive que des poliovirus derives de la souche vaccinale acquierent la neurovirulence et les caracteristiques de
transmission du poliovirus sauvage. Des cas de poliomyelite dus a
un tel virus vaccinal circulant de type 1 ont ete trouves en Haiti et en
Republique dominicaine (ile d’Hispaniola) en 2000 et en 2001
(21 cas confirmes), ainsi qu’aux Philippines en 2001 (3 cas confirmes). Les virus vaccinaux de type 1 incrimines lors des episodes
survenus a Hispaniola et aux Philippines ont montre une difference
par rapport au virus Sabin superieure a 2% (region VP1 du genome)
et ont peut-etre circule pendant 2 ans avant qu’on ne detecte des cas
de paralysie. La faible couverture vaccinale peut constituer un facteur de risque pour que le virus derive de la souche vaccinale prenne les caracteristiques du type sauvage.
The programme’s response to cVDPV included mass cam
paigns with OPV, which interrupted cVDPV circulation on
Hispaniola island. Campaigns have been conducted with
the same objective in the Philippines in early 2002. The
global polio laboratory network has established addition
al procedures to identify suspect Sabin isolates, i.e. isolates
showing more than 1% difference to original Sabin virus in
the VP1 region of the genome. Suspect isolates are immedi-
La reponse du programme devant 1’apparition de ces poliovirus
derives de la souche vaccinale a ete d’organiser des campagnes de
vaccination de masse par le VPO, qui ont permis d’interrompre la
circulation du virus vaccinal virulent dans Pile d’Hispaniola. Des
campagnes ont ete menees aux Philippines dans la meme inten
tion. Le reseau mondial des laboratoires de la poliomyelite a mis
en place des procedures supplementaires permettant d’identifier
les isolements de virus Sabin suspects, c’est-a-dire les isolements
RELEVEEPIDEMI0L06IQUE HEBDOMADAIRE. N° 13, 28 MARS 2002
103
2 inn ft
°r genet'C S^uenang studies. More than
2 100 Sabin strain isolates from AFP cases, primarily
from 2000 and 2001 cases, have now been screened and
no additional cVDPVs were detected, except for the
Philippines.
Polio endgame considerations
Progress in 3 key activities will constitute the global polio
endgame: certification of the absence of indigenous wild
poliovirus; containment of wild poliovirus laboratory
stocks, and the development of a post-eradication immunization policy for polio.
montrant une difference superieure a 1% par rapport au virus Sabin
sonUmmeTt 'e8’0"
g“°me' CeS isolement® ™spects
sont immediatement sounds a des etudes de sequence genetique. A ce pur, plus de 2 100 isolements de souche Sabin provenant
e cas de PFA, survenus prmcipalement en 2000 et en 2001, ont ete
analyses et aucun poliovirus derive de la souche vaccinal n’a ete
detecte, sauf aux Philippines.
Aspects relatifs a la derriere phase de la lutte centre la
poliomyelite
rent hTS
^7 3 tyPeS d’aCtivitf5S
constitueront la dermere phase de la lutte centre la poliomyelite: la certifiment”/6 t fT d> P°110virus sauva8e autochtone; le confine
ment des stocks de poliovirus sauvages de laboratoire; et I’elabora
pohomS
Certification of the absence of indigenous wild poliovirus
occurs on a regional basis, requiring that, with high-quality
surveillance in place in all countries in a WHO region a
wild-virus free period of at least 3 years has passed. Ex
perience in 2 WHO regions (Americas and the Western
Pacific, certified polio-free in 1994 and 2000, respectively)
has shown that the process and criteria for certifying the
WHn-'F0"
lndl8enous ^d poliovirus are sound.
WHOs European Region is likely to be certified in mid
Certification is closely linked to containment. Once trans
mission of wild poliovirus is interrupted globally, diagnos
tic and research laboratories and vaccine production facil
ities will represent the only remaining reservoirs of wild
poliovirus. The goal of containment is to minimize the risk
o inadvertent or intentional reintroduction of wild polio
virus from a laboratory or vaccine production site into human circulation. Countries need to identify all laboratories
storing wild poliovirus or potentially wild-virus infectious
material to ensure proper handling or disposal of such
materials under appropriate biosafety conditions. In keep
ing with the Global Plan of Action for Laboratory Contain
ment of Wild Polioviruses, 120 of 216 non endemic coun
tries (56%) have already started implementing these preera ication phase activities. Ninety-eight countries (45%)
are currently conducting a national survey of biomedical
laboratories and 34 (16%) of these have finalized a national
inventory of laboratories confirmed to be storing wild
poliovirus materials. Most of these countries are in the
Western Pacific or European regions, although in every
WHO region there are now some countries that are begin
ning activities. In contrast to regional certification, certifi
cation of global polio eradication will be possible only
when all WHO regions have been certified polio-free and
all pre- and post-eradication phase tasks have been completed.
Given the rapid progress made towards interrupting wild
poliovirus transmission, the programme of work to devel
op post-eradication immunization policy has been
accelerated WHO and its partners are coordinating
an agenda of research to broaden the knowledge base to
wards building a global consensus on the safest and most
effective polio immunization strategy for the post-eradica104
,<P°SMradiCatiOn» de
centre la
La certification de 1’absence de poliovirus
poliovirus sauvage autochtone
opere au niveau regional et exige que, disposant d’une surveillanexemn^dr ]anS.t°US leS payS d'Une ragion OMS, une penode
exempte de poliovirus sauvage d’au moins 3 ans se soil ecoulee
L experience que 1 on a des 2 regions OMS certifiees exemptes de
en lXye™raeriqUeS *
°CCidenta1’ resPecti~t
mL et.2000) a montre que le processus et les criteres de certifidesTa Re^ 1Catl°n
P°UovirUS sauvage autochtone sont solides. La Region europeenne de 1’OMS devrait etre certifiee exempte
au miheu de 1’annee 2002.
exempte
La certification est etroitement associee au confinement. Une fois
a transmission du poliovirus sauvage interrompue dans le monde
les laboratoire;> de diagnostic et de recherche et les etablissements
de production de vaeem representeront les seuls reservoirs restants
de poliovirus sauvage. L’objectif du confinement est de reduire au
maximum le risque de remtroduction accidentelle ou intentiondn danTr^ 1“ lab°ratOires ou d’un site de production de vacin dans la population humaine. Les pays doivent recenser tous les
laboratoires qui conservent du poliovirus sauvage ou des materiels
potentiellement infectieux, afin de faire en sorte que ces derXs
soient mampules ou elimmes dans des conditions de securite bioogique appropnees. Conformement au Plan d’action mondial
pourle confinement des poliovirus sauvages en laboratoire, 120 des
216 pays de non-endemie (56%) ont deja commence a mettre en
muvre ces aetvites de la phase «pre-eradication». Qua“«
dix-huit pays (45%) menent actueUement une enquete nationlie
sur les laboratoires biomedicaux et 34 (16%) d’entre eux ont finali
se un inventaire national des laboratoires dont il est confirme qu’il
“fervent du poliovirus sauvage. La plupart de ces pays sont situes
dans les regions du Pacifique occidental ou de 1’Europe, bien que
dans chacune des regions de I’OMS il y ait desormais des pays qui
demarrent ce type d’activites. Contrairement a la certification r"
gionale, la certification de 1’eradication mondiale de la poliomyehte ne sera possible que lorsque toutes les regions de I’OMS auront
certifiees exemptes de poliomyelite et que les taches des phases
pre et post-eradication auront ete menees a bien.
Etant donne les progres rapides realises pour interrompre la trans
mission du poliovirus sauvage, le programme de travail visant a
ler?L’OMSnetP
qUe
VaCCinatlOn P°«-eradication a ete accevmmrn T
r partenalres ““donnent actueUement un pro
gramme de recherche visant a elargir le corpus des connaissances
afin de parvemr a un consensus mondial sur la strategic de vaccina
ion antipohomyelitique la plus sure et la plus efficace pour la
penode qui suivra 1’eradication.
WEEKLY EPIDEMIOLOGICAL RECORD. NO. 13, 28 MARCH 2002
Editorial note. Strongly supported by the global polio
eradication partnership,2 the world moved closer than ever
before to interrupting wild poliovirus transmission global
ly during 2001, through continued intense polio eradica
tion activities in the remaining endemic countries, accel
erated in countries affected by conflict. Main achievements
for 2001 include the reduction to 10 endemic countries
globally, and further reductions of both the extent of trans
mission and the diversity of virus lineages within these
countries.
Note de la redaction. Grace au soutien sans faille du partenariat
pour I’eradication mondiale de la poliomyelite,2 en 2001 le monde
a ete plus proche que jamais auparavant de 1’interruption totale de
la transmission du poliovirus sauvage, du fait de la poursuite d’activites intenses d’eradication de la poliomyelite dans les pays d’en
demie restants, activites qui ont ete accelerees dans les pays en
proie a des conflits. Les principales realisations de 2001 sont la
reduction a 10 du nombre de pays d’endemie dans le monde, accompagnee de la reduction de 1’extension geographique de la
transmission et de la diversite des lignees virales dans ces pays.
Eradication activities continued in conflict-affected coun
tries. Thirty-five million children received vaccine in
Afghanistan and Pakistan at the height of the crisis in late
2001. Both Angola and the Democratic Republic of the
Congo successfully participated in the synchronization of
central African NIDs. 2001 saw unprecedented political
commitment supporting national polio eradication ef
forts, with heads of state launching NIDs in central and
western Africa and India. Two traditional large poflovirus
reservoir countries, Bangladesh and the Democratic
Republic of the Congo, did not isolate wild poliovirus, de
spite high-quality surveillance. The European Region is
likely to become the third WHO region to be certified po
lio-free, in 2002.
Les activites d’eradication se sont poursuivies dans les pays en
proie a des conflits. Trente-cinq millions d’enfants ont re^u le vaccin en Afghanistan et au Pakistan au plus fort de la crise, fin 2001.
L’Angola et la Republique democratique du Congo ont participe
avec succes a la synchronisation des JNV en Afrique centrale. L’annee 2001 a vu un engagement politique sans precedent en faveur des
efforts nationaux d’eradication de la poliomyelite, des chefs d’Etat
ayant lance les JNV dans le centre et 1’ouest de 1’Afrique et en Inde.
Deux grands reservoirs de poliovirus traditionnels, a savoir le Ban
gladesh et la Republique democratique du Congo, n’ont pas isole
de poliovirus sauvage, malgre une surveillance de qualite. La Re
gion europeenne devrait devenir la troisieme Region QMS a etre
certifiee exempte de poliomyelite, en 2002.
However, a number of serious challenges remain to reach
ing the global polio eradication goal. The combination of
large, dense populations, poor sanitation and low routine
immunization coverage in Niger/Nigeria, Afghanistan/
Pakistan and northern India may cause transmission in
these countries to continue into 2003, unless eradication
activities during 2002 are even more targeted and of higher
quality. Delays in interrupting transmission could also oc
cur in conflict-affected endemic countries if conflicts
should intensify, security deteriorate, or access to children
not be sustained. National polio eradication efforts cannot
be successfully implemented by the health sector alone
and will fail unless supported by strong political commit
ment and multisectoral mobilization at all administrative
levels. The current global funding gap of US$ 400 million
for activities from 2002 to 2005 needs to be closed urgently.
Toutefois, un certain nombre de problemes serieux doivent etre
resolus avant de pouvoir atteindre 1’objectif d’eradication mondia
le de la poliomyelite. L’association entre des populations importantes et denses, des services d’assainissement mediocres et une
faible couverture vaccinate systematique en Afghanistan/Pakistan,
au Niger/Nigeria et dans le nord de 1’Inde, pourraient faire que la
transmission se poursuive dans ces pays en 2003, a moins qu’en 2002
les activites d’eradication soient encore plus ciblees et de meilleure qualite. Des retards concemant 1’interruption de la transmission
pourraient egalement se produire dans les pays d’endemie en proie
a des conflits si ces derniers devaient s’intensifier, et la securite se
deteriorer ou Faeces aux enfants ne pas etre maintenu. Les efforts
nationaux d’eradication de la poliomyelite ne peuvent etre mis en
oeuvre avec succes par le seul secteur de la sante et echoueront s’ils
ne sont pas appuyes par un engagement politique fort et une mobi
lisation multisectorielle a tous les echelons administratifs. Il convient de combler d’urgence 1’actuel deficit de US$ 400 millions qui
existe pour le financement des activites dans le monde entre 2002 et
2005.
The programme has identified and defined the key risks to
eradication in each country and is implementing country
specific response plans. Following a successful example in
India, technical advisory groups of experts have been
formed for most remaining endemic countries, with sup
port from the global polio eradication partnership. These
groups regularly review a country’s programme status and
advise on optimal strategy implementation. Genetic se-
Le programme a recense et precise les obstacles importants a 1’eradication dans chaque pays et est en train de mettre en oeuvre des
plans permettant de les surmonter. Suivant un exemple qui a reussi
en Inde, pour la plupart des pays d’endemie restants, et avec 1’aide
du partenariat pour 1’eradication mondiale de la poliomyelite, des
groupes consultatifs techniques d’experts ont ete constitues. Ces
groupes examinent regulierement 1’etat du programme d’un pays
et le conseillent sur la meilleure fa^on de mettre en oeuvre la stra-
2 The Global Poliomyelitis Eradication Initiative is spearheaded by WHO, Rotary Interna
tional, the Centers for Disease Control and Prevention (United States) and UNICEF.The
poliomyelitis eradication coalition also includes: the governments of countries affected
by poliomyelitis; private foundations (e.g. United Nations Foundation, Bill & Melinda
Gates Foundation); development banks (e.g. World Bank); donor governments (e.g.
Australia, Austria, Belgium, Canada, Denmark, Finland, Germany, Ireland, Italy, Japan,
Luxembourg, Netherlands, Norway, United Kingdom and United States); the European
Commission; humanitarian organizations (e.g. the International Federation of Red Cross
and Red Crescent Societies) and corporate partners (e.g. Aventis Pasteur and De
Beers). Volunteers in developing countries also play a key role: 10 million have par
ticipated in mass immunization campaigns.
1 L'lnitiative mondiale d'eradication de la poliomyelite est menee par TOMS, le Rotary International,
les Centers for Disease Control and Prevention (Etats-Unis d'Amerique) et I'UNICEF. La coalition en
vue de I'eradication de la poliomyelite comprend egalement: les autorites des pays touches par la
poliomyelite; des fondations privees (par ex. Fondation des Nations Unies, Fondation Bill & Melinda
Gates); des banques de developpement (par ex. la Banque mondiale); des pays donateurs (par ex.
I'Allemagne, I'Australie, I'Autriche, la Belgique, le Canada, le Danemark, les Etats-Unis d'Amerique,
la Finlande, I'lrlande, I'ltalie, le Japon, le Luxembourg, la Norvege, les Pays-Bas et le Royaume-Uni);
la Commission europeenne; des organisations humanitaires (par ex. la Federation intemationale des
Societes de la Croix-Rouge et du Croissant-Rouge) et des partenaires des entreprises (par ex.
Aventis Pasteuret De Beers). Les benevoles despays en developpement ont egalement joue un role
important: 10 millions d'entre eux ont participe aux campagnes de vaccination de masse.
RELEVEEPIDEMIOLOGIQUEHEBDOMADAIRE, Np 13, 28 MARS 2002
105
quencmg data are now being used more systematically to
identify and target the main poliovirus reservoir areas. The
quality of supplementary immunization activities to reach
every child has further improved through better supervised
house-to-house immunization. Better social mobilization
and information activities are addressing campaign fatigue
and the decreasing motivation and even non-compliance
ot both parents and vaccinators in some areas.
Through placement of international and national polio
eradication staff at country (often also province) level, AFP
surveillance systems everywhere have dramatically im
proved, even m countries severely affected by conflict such
as Angola. Surveillance quality in most countries is ap
proaching or has reached certification quality, allowing the
programme to confidently confirm or rule out the pres
ence of wild poliovirus in most areas. Expert groups for
case classification now exist in most countries to improve
the accuracy of final AFP case classification. The consider
able decrease globally in the total number of confirmed
cases between 2000 and 2001 should be noted, particularly
in the African Region, mainly due to the acceleration of
supplementary immunization, but partly reflecting the fact
that most countries have now switched from clinical to
virological case classification criteria. Using virological
criteria, AFP cases are no longer confirmed on clinical
grounds, but only if wild poliovirus is isolated. As expert
groups for case classification begin to work in African
countries, it will be a leading priority to reduce the large
number of AFP cases currently classified as polio-compat
ible m the African Region.
Interagency coordination committees at regional, national
and often subnational level coordinate partner and multi
sectoral support for the polio eradication programme and
focus on fund-raising at the regional level. These commit
tees, created for polio eradication, are increasingly also
being used to coordinate partner input to strengthen rou
tine immunization and activities of the Global Alliance for
Vaccines and Immunization (GAVI). Polio eradication
continued to have other positive impacts on routine im
munization services and disease surveillance. In 2000 and
2001 alone, polio funds were used to purchase over
700 vehicles for immunization and surveillance. It is esti
mated that 30% of the cold chain in sub-Saharan Africa has
been refurbished through polio eradication funds. About
80% of the 2 000 health staff recruited with polio funds are
also regularly involved in planning and implementing rou
tine immunization services.
Continued political commitment to polio eradication, ac
cess to children in conflict-affected countries and adequate
funding are all preconditions for interrupting poliovirus
transmission by the end of 2002. Given continued improve
ments in surveillance to pinpoint areas of virus circulation,
further progress in improving the quality of immunization
campaigns, and the availability of appropriate funding, the
polio eradication goal is within reach. Concurrently, the
106
tegie. Les donnees du sequence genetique sont desormais em
ployees plus systematiquement afin d’identifier et de cibler les
pnncipales zones servant de reservoir au poliovirus. La qualite des
activites de vaccination supplementaire visant a atteindre chaque
enfant s est amehoree grace a une vaccination porte-a-porte mieux
supervisee. De meilleures activites de mobilisation sociale et d’information doivent faire face a la lassitude engendree par les campa
gnes et a la baisse de motivation, voire au non-respect des regies
dont font preuve les parents et les vaccinateurs dans certaines
regions.
Par le truchement du detachement de membres du personnel na
tional et international d’eradication de la poliomyelite dans les
pays (et souyent aussi dans les provinces), les systemes de sur
veillance de la PFA se sont spectaculairement ameliores partout,
meme dans les pays en proie a des conflits graves comme 1’Angola.’
a quahte de la surveillance dans la plupart des pays est voisine ou
a atteint la quahte exigee pour la certification, permettant au pro
gramme de confirmer ou d’infirmer avec assurance la presence du
poliovirus sauvage dans la plupart des regions. Des groupes d’ex
perts de la classification des cas existent desormais dans la plupart
Pays afin d’ameliorerTexactitude de la classification des cas de
. La diminution considerable enregistree partout dans le mon
de dans le nombre total de cas confirmes entre 2000 et 2001 est a
noter, en particulier dans la Region africaine, et est principalement
due a 1 acceleration des activites de vaccination supplementaire
mais reflete en partie le fait que la plupart des pays sont desormais
passes des cnteres de classification cliniques a des criteres virologiques. A 1’aide de ces criteres virologiques, les cas de PFA ne sont
plus confirmes a partir de resultats cliniques, mais seulement si le
poliovirus sauvage est isole. Parce que des groupes d’experts de la
classification des cas commencent a travaiher dans les pays africains, 1 une des premieres priorites consistera a reduire le nombre
important de cas de PFA actuellement classes comme etant com
patibles avec la poliomyelite dans la Region africaine.
Des comites de coordination interorganisations a I’echelon regio
nal, national et souvent sous-national coordonnent I’appui partenanal et multisectoriel au programme d’eradication de la poliomyehte et sont axes sur la coUecte de fonds au niveau regional. Ces
comites, crees pour 1’eradication de la poliomyelite, sont egalement de plus en plus employes pour coordonner la participation
des partenaires aux efforts visant a renforcer la vaccination systematique et les activites de 1’Alliance mondiale pour les vaccins et la
vaccination (GAVI). L’eradication de la poliomyelite a continue a
avoir d autres effets positifs sur les services de vaccination systema161 surveiUance de la maladie. Pour les seules annees 2000 et
2001, les fonds ont ete utihses pour I’achat de plus de 700 vehicules
destines a la vaccination et a la surveillance. En Afrique subsahanenne on estime que 30% de la chaine du froid a ete remise a neuf
deS f°ndS destin^s a Eradication de la poliomyelite. Pres de
80/o des 2000 membres du personnel de sante recrutes avec ces
fonds participent regulierement a la planification et la mise en
oeuvre des services de vaccination systematique.
Un engagement politique continu, le libre acces aux enfants dans
les pays en proie a des conflits et un fmancement suffisant consti
tuent 1’ensemble des conditions preambles necessaires a 1’interruption de la transmission du poliovirus d’ici la fin 2002. Pour
autant qu’on continue a apporter des ameliorations a la surveillan
ce afin de reperer les regions oil le virus circule, qu’on progresse
encore pour ameliorer la qualite des campagnes de vaccination et
qu on dispose d’un fmancement approprie, 1’objectif d’eradication
—
WEEKLY EPIDEMIOLOGICAL RECORD. NO. 13, 28 MARCH 2002
agendas for certification, containment and policy develop
ment for the post-eradication era need to be aggressively
implemented. The experiences from Hispaniola and the
Phihppines with cVDPV demonstrate that, following the
interruption of wild poliovirus transmission, continued
high-quahty surveillance and high routine immunization
coverage are needed to screen for and prevent the emer
gence of cVDPV.
The global community must ensure that the enormous in
vestment already made for polio eradication is protected
and that endemic countries are fully supported in the final
phase of their massive programme. B
Influenza
Australia (22 March 2002).1 An outbreak of influenza was
detected in a nursing home of elderly residents in Mel
bourne. Over 40 polymerase chain reaction tests were car
ried out, further to which 5 patients tested positive for influ
enza A(H3N2). This is the second outbreak reported since
January 2002.
Chile (19 March 2002)? In March, morbidity due to acute
respiratory infections remained at baseUne level both in
adults and children. One influenza B virus was isolated
from a 9-year-old girl in Santiago, which is a B/Sichuan/
379/99-like strain.
Greece (1 March 2002)? The rate of influenza-like illness
has remained very low. No influenza virus has been identi
fied by antigen detection nor isolated.
Latvia (19 March 2002)? Influenza activity remained at
widespread level, although the intensity of outbreaks has
started to decrease. A local outbreak of influenza A(H3N2)
was detected in a trauma centre. To date, 30 influenza
A(H3N2) viruses were A/Moscow/10/99-like strain and
36 influenza B viruses were B/Sichuan/379/99-like.
New Caledonia (23 March 2002).5 Following the first influ
enza A case reported in February, 3 new influenza A cases
were detected during the third week of March.
Norway (16 March 2002).4 The number of influenza-like
illness cases is stiU increasing in the northern part of the
country, with a rate remaining above the 2% outbreak
threshold. Most viruses detected were influenza A. In the
rest of the country, the consultation rate for influenza-like
illness has declined. With the exception of 1 influenza B
virus belonging to this winter’s new Victoria-like strain, all
viruses characterized to date are similar to the current vac
cine strains.^
1 See No. 5,2002, p. 38.
2 See No. 43,2001, p. 336.
3 See No. 7,2002, p. 56.
4 See No. 12,2002, p. 95.
5 See No 50,2001, p. 400.
RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE. N° 13, 28 MARS 2002
de la poliomyelite est atteignable. Simultanement, les programmes
de certification, de confinement et d’elaboration des politiques
pour la periode qui suivra 1’eradication doivent etre mis en oeuvre
energiquement. Les experiences d’Hispaniola et des Philippines
avec les virus derives de souches vaccinales demontrent que, suite a
1’interruption de la transmission du poliovirus sauvage, il faut assu
rer une surveillance continue, de qualite, et une couverture elevee
par la vaccination systematique pour prevenir 1’emergence de
virus-vaccinaux virulents, ou les depister.
La communaute mondiale doit faire en sorte que 1 investissement
considerable deja realise pour 1’eradication de poliomyelite soit
protege et que les pays d’endemie soient entierement soutenus
dans la demiere phase de leur programme de masse. 1
Grippe
Australie (22 mars 2002).’ Une flambee de grippe a ete detectee
dans une maison de retraite a Melbourne. Plus de 40 tests par PCR
{polymerase chain reaction) ont ete effectues, a la suite desquels
5 patients se sont averes positifs au virus grippal A(H3N2). Il s agit
de la deuxieme flambee signalee depuis Janvier 2002.
Chili (19 mars 2002)? En mars, la morbidite causee par les infec
tions respiratoires aigues s’est maintenue a un niveau de base tant
chez les adultes que chez les enfants. Un virus grippal de type B, tres
proche de la souche du vaccin B/Sichuan/379/99, a ete detecte chez
une fillette de 9 ans, a Santiago.
Grece (1 mars 2002)? Le taux de syndromes grippaux est reste tres
faible. Aucun virus grippal n’a ete isole ou identifie par detection
antigenique.
Lettonie (19 mars 2002)? L’activite grippale etait toujours a un
niveau general bien que 1’intensite des flambees ait commence a
diminuer. Une flambee locale de grippe A(H3N2) a ete detectee
dans un centre de traumatologic. Jusqu’a present, 30 virus grip
paux de type A(H3N2) etaient de souche analogue a A/Moscow/
10/99 et 36 virus grippaux de type B, de souche analogue a
B/Sichuan/379/99.
Nouvelle-Caledonie (23 mars 2002)? Suite au premier cas de grip
pe A signale en fevrier, 3 nouveaux cas de grippe A ont ete depistes
au cours de la troisieme semaine de mars.
Norvege (16 mars 2002)?Le nombre de cas de syndromes grippaux
continue d’augmenter dans le nord du pays, avec un taux se maintenant au-dessus des 2% du seuil epidemique. La plupart des virus
grippaux detectes etaient de type A. Dans le reste du pays, le taux de
consultations pour syndromes grippaux a diminue. A 1 exception
d’un virus grippal B de souche analogue au nouveau virus Victoria
detecte cet hiver, tous les virus caracterises sont similaires aux sou
ches du vaccin actuel. S
' Voir N° 5,2002, p. 38.
2 Voir N°43,2001, p. 336.
3 Voir N° 7,2002, p. 56.
4 Voir N° 12,2002, p. 95.
‘ Voir N° 50,2001, p. 400.
107
Where to obtain the WER through Internet
(1)
connect to the WER pages at the following address:
http://www.who.int/wer/
(2)
Comment acceder au REH sur Internet?
WHO WWW server: Use WWW navigation software to
Par le serveur Web de I'OMS: A I'aide de votre loqiciel
D
duREHbl'X" WWW'
* la Pa9e d'accue
du REH a I adresse suivante: http://www.who.int/wer/
E-MAIL list: An automatic service is available for re
ceiving notification of the contents of the WER and
short epidemiological bulletins. To subscribe, send
an e-mail message to majordomo@who.ch The
subject field may be left blank and the body
of the message should contain only the line subscribe
wer-reh. Subscribers will be sent a copy of the table of
contents of the WER automatically each week, together with
other items of interest.
Criteria used in compiling the infected
area list
governmental information is used):
y
L Anarea ? !ntered in the list on rece'Pt of information of:
(i) a declaration of infection under Article 3;
(n) the first case of plague, cholera or yellow fever that is
..... n.either an imported case nor a transferred case;
(m) plague infection among domestic or wild rodents;
(iv) activity of yellow-fever virus in
vertebrates other than man
using one of the following criteria:
2)
Par courrier electronique: Un service automatique de distribution
du sommaire du REH et de brefs bulletins epidemiologiques est
disponible par courrier electronique. Pour s'abonner a ce service
il suffit d envoyer un message a I'adresse suivante'majordomo@who.ch. Le champ «Objet» peut etre laisse vide
et, dans le corps du message, il suffit de taper subscribe wer-reh
Les. abonnes recevront chaque semaine une copie du sommaire du
KtH, amsi que d autres informations susceptibles de les interesser.
Cnteres appliques pour la compilation de la
liste des zones infectees
Conformement au Reglement sanitaire international les criteres suivants
sont appliST!* *i0"
a jour de la liste des zone?in“(seules
»nt
utilisees les informations officielles emanant des
-------------- gouvemements).
I. Une zone est portee sur la liste lorsque ^Organisation a recu:
(i)
‘
____________
une declaration
d'infection, au terme de ('article 3;
(ii) nil
notification
. , . . du .premier
-r cas de peste, de cholera ou de fievre jaune
( ' n 'est ni un
____
qui
cas importe ni un cas transfere(iii) notification de la presence de la
et chez les rongeurs'sauvages? ''
(iv) notification de I'activite
------------- du v*rus amaril chez les vertebres autrpq
rants:hOrnme' determin*e par '-application de I'un des criteres sui-
(a) the discovery of the specific lesions of yellow fever in
the liver of vertebrates indigenous to the area; or
a)
d^Prt-h6-^
cripdon ou65
(b) the isolation of yellow fever virus from
any indigenous
vertebrates.
II. An area is deleted from the list on receipt of information as followsth WaS dezClared infected (Artide
jt is deleted from
the list on receipt of a declaration under Article 7 that the area is
tree from infection. If information is available which indicates that
free fr°m infection durin9 the time intervals
stated in Article 7, the Article 7 declaration is not published the
area remains on the list and the health administration concerned is
queried as to the true situation;
(") lf ?e ^aie?7ed the ,ist for reasons other than a declaration
under Article 3 (see I, (n) to (iv) above), it is deleted from the list on
rAertei|Pt7°fIne?atlVu Weekly reports of the time intervals stated in
Article ?. In the absence of such reports, the area is deleted from
the list on receipt of notification of freedom from infection (Article
thettnnaXd case me
7
elap5ed SinCe
b)
sp™fi<'ues de la fievre jaune dans le foie
’ k"™ 'nd'9dnG d" territ0're ou de la circons-
',irUSJde la Kvre iaune chaz n'importe quel vertebre de la faune indigene.
M
II. Les zones sont radiees de la liste dans les conditions suivantes' I'r^n"6 r ete d^C,ar'e infeCt*e (artide 3)' elle est radiee de la liste lorsque
‘S'iatlon r^0,t une notification faite en application de I'artide^
suivant aquelle la zone est mdemne d'infection. Si I'on dispose de renseiHn!n6ntH,ndiqUant T 3 ZOne n a pas
indemne d'infection pendant
e periode correspondant a la duree indiquee dans ('article 7, la notification
prevue par Article 7 n'est pas publiee, la zone reste sur la liste et
.. quant""ion"'^
h0""" ““
II) Si la zone a ete portee sur la liste pour des raisons autres que la reception de
de7a iSp 7 preVUe P3r l'artide 3 (voir'' W a
ci-dessus), elle es^ radit
de la liste lorsque des rapports hebdomadaires negatifs ont ete recus
pendant une periode dont la duree est indiquee a ('article 7. A defaut de tels
indin? S' •a|'Z°tne|eS7t r?dl^e de 13 liste ,ors9ue- au terme de la periode
d infectio'^SV' ' °r9aniSatiOn
"’exemption
■^ERNATIONAL HEALTH REGULATIONS / REGLEMENT SANiTAIRE INTERNATIOMAL----------- -------------------------
Notifications of diseases received from 22 to 28 March 2002 / Notrfh
---------------- lotions de maladies refues du 22 au 28 mars 2002
Cholera / Cholera
Africa / Afrique
Mali
Cases / Deaths
Cas / Deeds
20.11
...1
Uganda / Ouganda
...n.ii-3.ni
Zanzibar
».56
ll.III
,..16
0
8
0
Cases / Deaths
Cas / Deeds
Europe
Czech Republic / Republique 15.11
tcheque .....................
------- 1(0
Germany/ Allemagne
15.III
------1(0
0
0
i = imported.
WWW access • http://www.who.int/wer
E-mail • send message subscribe wer-reh io majordomo@who.int
Acces WWW • http://www.who.rnt/wer
Fax: (+41-22) 791 48 21/79142 85
Courrier electronique • envoyer message subscribe wer-reh a majordomo@who int
Editor: vallanjonm@who.int
Fax: (+41-22) 791 48 21/791 42 85
Redactrice: vallanjonm@who.int
108
WEEKLY EPIDEMIOLOGICAL RECORD. NO 13, 28 MARCH 2002
Global
WHO/POLIO/02.04; updated January 2002
S- 6^^' X.
Post-eradication immunization policy for poliomyelitis
The purpose
The ultimate goal of disease eradication is to interrupt circulation of the target organism on a global scale such that control
measures can be discontinued.1 As with smallpox eradication, there will be benefits and challenges to stopping polio
immunization. Stopping immunization would eliminate side effects such as vaccine-associated paralytic polio (VAPP). From
an economic perspective, cessation of polio immunization could save hundreds of millions of dollars every year.
Many of the challenges to stopping polio immunization are similar to those faced by smallpox, including effective
laboratory containment of the virus. Unlike smallpox, post-eradication immunization policy for polio is further complicated
by the fact that oral polio vaccine (OPV) has caused paralytic polio outbreaks and there has been long-term excretion of
vaccine-derived poliovirus from immunodeficient persons.Thus the challenge to stopping OPV would be: 1. protecting
susceptible populations from possible outbreaks due to circulating vaccine-derived poliovirus (cVDPV) and 2. minimizing
the risk of a poliovirus reintroduction from immunodeficient persons, laboratories or vaccine production sites in the future.
The process
The process for developing post-eradication immunization policy for polio
Given the need for international consensus on a post
eradication immunization policy for polio, the final
decision will rest with WHO Member States represented at
their annual meeting, the World Health Assembly (WHA).
Through broad consultation and an extensive programme
of work, the Global Technical Consultative Group for
Poliomyelitis Eradication (TCG) is developing potential
policy options for consideration by WHO's Strategic
Advisory Group of Experts (SAGE), prior to eventual
presentation to the World Health Assembly.
Policy option
development
Recommendation to
Director-General/WHO
Resolution to
Member States
Air®.! TCG on
IMdkation
____ x
Oversight of research
proposals and studies
Ifealth
■>
ibly
■
The agenda of work developed by the TCG includes programmatic work, new scientific research, and policy development, to
be completed by 2002,2003 and 2004 respectively. All relevant programmatic data will be collected by WHO and UNICEF on
issues such as inactivated poliovirus vaccine (IPV) price, production capacity, potential introduction costs, the frequency of
VDPV circulation and VDPV surveillance. Overseen by the TCG's Steering Committee on Research, new scientific data will be
generated on key issues such as the efficacy of IPV in developing country settings and the frequency, significance and
potential impact of long-term vaccine virus excretors.To support policy development, the political, economic and
operational implications of each of the potential policy options will be evaluated.
Surveillance confirms that polio outbreaks due to circulating vaccinederived polioviruses (cVDPV) are rare, but possible. An estimated 10
billion doses of oral polio vaccine (OPV) were administered
worldwide between 1997 and 2001; only two episodes of polio
outbreaks due to cVDPV have been confirmed in that period: in
Hispaniola (2000-1) and the Philippines (2001).
11
World Health Organization
Recognizing that it will take time to collect these data, and to
establish an international consensus on post-eradication
immunization policy for polio, plans have been made to
continue using OPV in most countries for the foreseeable
future.
1 Global disease elimination and eradication as public health strategies, Supplement No. 2 to Volume 76,1998, of the VJor
The progress
Since 1997 theTCG and its technical advisers have studied
the evolving issue of post-eradication immunization
policy for polio, supplemented by several meetings of
experts to address specific issues.
After certification of polio eradication, individual decisions by countries
to stop or continue oral polio vaccine (OPV) use could place populations
that no longer use the vaccine at risk of exposure to circulating vaccinederived polioviruses (cVDPV). For this reason, any cessation of OPV use
would require an internationally coordinated approach.
In March 1998, WHO convened the first meeting of experts on stopping polio immunization, which concluded that
"Vaccination with OPV should stop and vaccination with IPV can stop when there is (a) sufficient assurance of the global
eradication of wild type polioviruses, (b) suitable laboratory containment of remaining stocks of wild polioviruses, and (c)
evidence that VDPV will circulate for only a limited period in the post-vaccination era." The sixth meeting of the TCG
identified a further criteria: that a global stockpile of vaccine is available if needed, with a clear strategy for its use.
In January 2000, WHO convened a second meeting of experts on "New polio vaccines for the post-eradication era'; which
concluded that the development of a new vaccine would pose formidable regulatory and manufacturing challenges.
Consequently, a meeting in September 2000 on regulatory challenges to licensing vaccines for the post-eradication era
focused on monovalent OPVs (for controlling type-specific outbreaks) and IPV based on Sabin strains (to replace the wild
poliovirus strains currently used in IPV).
The detection of two polio outbreaks caused by circulating VDPV - in Hispaniola in 2000-2001 and the Philippines in 2001
gave new urgency to post-eradication immunization policy development and highlighted the challenges to maintaining
polio surveillance and immunization in countries/regions that are polio-free.
In May 2001, WHO convened a steering committee to guide, monitor and evaluate the ongoing research agenda for post
eradication policy development, under the direction of theTCG. New research was already commissioned by November 2001.
In the January 2002 edition of Clinical Infectious Diseases,2 the TCG summarized the current status of the polio "endgame"
and noted that, though challenging, there are compelling reasons for discontinuing OPV as soon as possible following
eradication.Three scenarios for stopping OPV were outlined:
1. coordinated discontinuation of OPV (with or without IPV, depending on national decision);
2. replacement of OPV with IPV in all countries;
3. development of new live vaccines that would not cause VAPP and would not be transmissible.
The TCG stated that WHO's three-part agenda of work must be completed before a final decision can be made as to the
feasibility of the most appropriate strategy.
The challenges
Coordinating post-eradication immunization policy - many countries may want to stop immunization against
polio as soon as circulation is interrupted globally. However, individual country decisions to stop or continue OPV use could
place populations at risk from cVDPVs.
Vaccine security in the pre- and post eradication eras — as global certification approaches, an increasing number
of countries may wish to use IPV, though production capacity is currently limited. At the same time, sufficient OPV must be
available for routine immunization for the foreseeable future and for stockpiling against outbreaks in the post-eradication
era. The appropriate range and quantity of vaccines must be ensured.
Funding for timely completion of the research agenda - the research agenda involves an ambitious programme
of work requiring more than US$ 1 million per year. The timely completion of necessary research is essential to define
options and make policy decisions on stopping polio immunization.
Sustaining the surveillance infrastructure and immunization coverage - see fact sheet on Certification of
global polio eradication.
For more information on the development of post-eradication immunization policy,
please contact Dr David Wood (WHO/Geneva), Tel.: +41 22 791 4050, email woodd@who.int or
Dr Roland Sutter (WHO/Geneva), Tel.: +41 22 791 4682, email sutterr@who.int
Further reading
Report of the meeting on the scientific basis for stopping polio immunization, Geneva, 23-25 March 1998, WHO/EPI/GEN/98.12.
New polio vaccines for the post-eradication era, Geneva, 19-20 January 2000, WHO/V&B/00.20
"Polio vaccines for the post-eradication era: regulatory and biosafety issues';20-21 September 2000 (in print).
Report of the sixth meeting of the Global Technical Consultative Group for Poliomyelitis Eradication, Geneva, 7-10 May 2001, WH0/V&B/01.32.
2 “Endgame’Issues for the Global Polio Eradication Initiative, CID 2002:34 (1 January 2002)
For more information on polio eradication, visit: www.polioeradication.org
Global
■
i b
. to
I
Z',:
t
I 1
i w
Eradication
initiative
WHO/POLIO/02.02; updated January 2002
• 13
Containment of wild poliovirus stocks
I he purpose
Certifying the world polio-free requires not only stopping the circulation of wild poliovirus in human populations, the only natural
reservoir, but also minimizing the risk of an accidental or intentional reintroduction of wild poliovirus into the community from a
laboratory or vaccine production site. The WHO global action plan for laboratory containment of wild polioviruses1 aims to locate
laboratories worldwide that store wild poliovirus and potentially infectious materials, and ensure that those materials are handled
under appropriate biosafety conditions in the post-eradication era.
Completion
of all pre- and post-eradication containment measures is a
| The recent intentional spread of anthrax and increased media atten
prerequisite of global certification of polio eradication.
tion to smallpox have raised questions about poliovirus as a potential
bioterrorist agent. Poliovirus however is currently a low-level risk
relative to agents such as smallpox and anthrax: polio's public health
impact and dissemination potential are low while preparedness to
detect and control polio is high. Containment, vaccine stockpiling
measures, sustained surveillance and polio immunization policy for
the post-eradication era will deter the use and limit the impact of
poliovirus as a bioterrorist agent in the future.
That the last case of smallpox actually occurred as a result of a
laboratory containment failure in Birmingham, England in 1978, one
year after global eradication of smallpox, serves as an important
reminder of the need for effective containment.
The process
The process of laboratory containment of wild poliovirus was developed through international consultation. Beginning in 1997, a draft
action plan was widely distributed for comment, resulting in publication of the WHO global action plan for laboratory containment of
wild polioviruses in 1998. In 1999, the World Health Assembly unanimously passed resolution WHA52.22, urging all Member States" to
begin the process leading to the laboratory containment of wild poliovirus.."
The containment action plan consists of three phases: pre-eradication, post-eradication, and post-global certification. The pre
eradication phase requires that:
1. National authorities in all countries survey laboratories to identify those with wild poliovirus infectious or potentially infectious
materials and encourage destruction of all unneeded materials.
2. Laboratories retaining such materials institute enhanced biosafety level-2 (BSL-2/polio) procedures.
3. National authorities develop a national inventory of all laboratories with wild poliovirus materials.
4. Member States begin planning for implementation of biosafety requirements for the post-eradication phase.
Laboratories should be requested to conduct a search for all wild poliovirus infectious and potentially infectious materials which include
not only viral isolates and clinical specimens from poliomyelitis cases but also faecal samples, throat swabs, or environmental samples
that were collected for any reason at a time and place of wild poliovirus circulation and stored in a manner known to preserve
poliovirus.
The post-eradication phase begins one year after detection of the last wild poliovirus anywhere in the world. It requires all laboratories
possessing wild poliovirus infectious or potentially infectious materials to implement recommended containment procedures (currently
enhanced biosafety level-3 or BSL 3/polio) OR transfer such materials to WHO-designated repositories OR render such materials noninfectious, or destroy them, under appropriate conditions.
s n
&
World Health Organiration
1 WHO global action plan for laboratory containment of wild polioviruses, WHQ)V^79^3^^
y
It*.
- f
ft
B'V*'
The progress
Although a tremendous logistical challenge, effective laboratory containment is operationally feasible, as progress in the
European and Western Pacific regions demonstrates. Worldwide, as of mid-October 2001, authorities in 110 countries had
appointed a national task force and started the containment planning process: 2 of 47 Member States in the Americas;
17 of 24 in the Eastern Mediterranean; 48 of 51 in the European Region; 7 of 10 in Southeast Asia; 36 of 36 in the Western
Pacific. Seventy countries had already begun compiling exhaustive lists of biomedical facilities to be surveyed, with more
than 60 000 laboratories listed. Eleven countries had completed all pre-eradication phase activities and submitted a
national inventory of laboratories.
Although it is not possible to guarantee that all laboratories with wild poliovirus infectious materials will be identified,
implementation of the global action plan substantially reduces the chance of an accidental reintroduction of wild type
poliovirus from a laboratory.
Inactivated poliovirus vaccine (IPV) is produced using large volumes of high concentration, non-attenuated wild poliovirus
strains. WHO is working with IPV manufacturers and regulatory authorities to appropriately contain poliovirus strains used
in IPV production. Containment guidelines for IPV manufacturers will be published in 2002.
A second, updated edition of the WHO global action plan for laboratory containment of wild polioviruses, incorporating lessons
learned from two years of experience with implementation of laboratory containment, will be presented to the Global
Technical Consultative Group for Poliomyelitis Eradication in April 2002.
The challenges
Implementation of the global action plan - the scale of laboratory containment presents a significant operational
challenge requiring commitment from political leaders, diligence from national authorities implementing the action plan
and goodwill from laboratories worldwide.
IPV manufacturing sites - IPV production facilities handle large volumes of high concentration, non-attenuated wild
poliovirus strains, making appropriate containment especially important and challenging.
For more information on containment, please contact Mr Chris Wolff (WHO/Geneva),
Tel.: +41 22 791 4524, email labnet@who.int
Further reading
WHO global action plan for laboratory containment of wild polioviruses, WH0/V&B/9932.
Guidelines for implementing the pre-eradication phase of the global action plan for laboratory containment of wild
polioviruses, WHO/V&B/00.21.
Summary sheet: Poliovirus and bioterrorism.
For more information on polio eradication, visit: www.polioeradication.org
The History of Polio Eradication
1999
The second anniversary of the last case in the Western Pacific falls in March.
A large polio outbreak occurs in Angola with more than 800 cases and 50 deaths.
The UN Secretary-General agrees to negotiate truces for immunization in the Democratic
Republic of Congo.
Dr Gro Harlem Brundtland, Director-General of WHO vaccinates children during a
National Immunization Day in Cote d'Ivoire and urges the country to set a standard for the
region.
Dr Brundtland appeals to governments and donors to accelerate polio eradication.
6.5 million children are vaccinated during house to house immunization in Pakistan.
National Immunization Days are conducted in war-torn Liberia.
1998
An estimated 470 million children aged under five years are immunized during National
Immunization Days.
The National Immunization Days are conducted for the first time in Somalia and South
Sudan.
Nigeria and India improve their surveillance in a matter of months.
The Rotary International Network of Polio Eradication Advocacy Advisors expands to
Europe and Asia.
1997
•
•
•
•
An estimated 450 million children aged under five years are immunized during National
Immunization Days in 97 polio-endemic countries.
250 million children are vaccinated during National Immunization Days held
simultaneously in China, India, Bhutan, Pakistan, Bangladesh, Thailand, Vietnam and
Myanmar.
134 million children are immunized on a single day in India.
The last case of polio in the Western Pacific region is found on 19 March. She is a 15month-old girl called Mum Chanty living near Phnom Penh in the Mekong River area of
Cambodia.
1996
•
•
•
•
•
Nelson Mandela officially launches the Kick Polio Out of Africa campaign.
The Organization of African Unity (OAU) adopts the Yaounde Declaration of Support for
the Expanded Programme on Immunization, including polio eradication.
420 million children are immunized during National Immunization Days.
A large polio outbreak in Albania, which had been free of wild poliovirus for 18 years,
spreads to neighbouring countries.
The last case of polio is identified in China.
1995
•
Operation MECACAR (Mediterranean, Caucasus, Central Asian Republics and Russia) is
launched: National Immunization Days are coordinated in 19 adjacent countries of the
European and Eastern Mediterranean Regions of WHO. More than 56 million children are
immunized.
consecutive year) to allow children
to be immunizedS^NationlH^
•
India crgXsTSSa' SSSTd“° —™g
1994
of Polio EradicationCertlfled POl'°’free by the lnternational Commission for the Certification
’ S £Si4 Sin
1992-1993
rel£us°Xoanlinproves^hhftriTmportJd°poliovirusUPf^h°
immunity levels are low.
•
P
P
t0 be immunized for
ov rus stlH constitutes a threat wherever
The virus spreads to Canada.
The Global Polio Laboratory Network
is formally established to facilitate high quality
virologic investigation in all countries.
1991
The last case of polio occurs in the Americas in September
called Luis Fermin Tenorio living in Junin, Northern Peru.
He is a three-year old boy
1990
. EsESEEF"
““s»'reaffim
? eoZge »X"'Za,“ '"“”e
Moppmg-up activities are conducted in the Americas.
1989-1990
••
^XSal ”°
reported both years.
1988
has raised US $247 million
fundraising campaign to raise US $120 million
1987
Rotary International launches a campaian to raise li^ $100 rv»;ir
<•
provides the necessary impetus to begin the polio eradication inTtSe
9
P°li0 “
1985
The Pan American Health Organization (PAHO) launches an initiative to eradicate polio in
the Americas by 1990.
The Universal Childhood Immunization Initiative is launched jointly by UNICEF and WHO,
with the aim of reducing child mortality through effective immunization.
1970-1980
Lameness surveys demonstrate that polio is widespread in many developing countries,
leading to the introduction of routine immunization with OPV in almost all national
immunization programmes.
1979
The last case of smallpox in the world occurs in Somalia.
1978
A polio outbreak occurs in the Netherlands and spreads to Canada and the US the
following year.
1974
The World Health Assembly passes a resolution to create the Expanded Programme on
Immunization (EPI) to bring basic vaccines to the world's children.
EPI aims to build on the success of smallpox eradication and make immunization for
children’s diseases available worldwide.
1961
Dr. Albert Sabin develops a "live" oral vaccine against polio (OPV). OPV rapidly becomes
the vaccine of choice for most national immunization programmes in the world.
Immunization campaigns in Cuba and in Eastern Europe demonstrate that wild poliovirus
can be eliminated in large geographic areas, providing the basis for eradication.
1959-60
Mass OPV campaigns are conducted in Czechoslovakia and Hungary.
1955
Dr. Jonas Salk develops the first vaccine against polio, an inactivated (killed), injectable
polio vaccine (IPV).
1948
Thomas Weller and Frederick Robbins succeed in growing poliovirus in live cells, which
lays the foundation for the development of any vaccines against polio. Six years later they
receive the Nobel Prize for their work.
The World Health Organization is established.
1938
later becomes the March^f Dimes6aPfundrXinqTr36''^^ * thS
States' ™s
support the fight against polio.
’
fUndraisln9 organization focusing on research to
1931
Sir Macfarlane Burnet and
Dame Jean MacIMamara identify several types of poliovirus,
known as Types 1, 2, and 3.
1916
b°th Sides of the
and^ceteratesPrese^chTnVhow^
Ocean
1908
•
Austrian physicians Karl ILandsteiner and Erwin Popper make the first hypothesis that
polio may be caused by a virus.
1907
Dr Ivar Wickman, a Swedish paediatrician, categorizes the different clinical types of polio.
1894
The first significant outbreak of infantile
paralysis, subsequently identified
is documented in the United States.
as poliomyelitis,
1840
time develop",ng^he ZrylhaF the^difeiT’may beTo°f P°liomyelitis' for the ^st
are used well into the 20th century.
Y b conta9lous- Von Heine’s treatments
1789
polio, entHledDeWy of
thS
knOWn Cl'n'Cal descrlPtlon of
1580-1350 BC
polio has been endemicfo?^hous^nds ofhyea^shered le9’ 1630103 00 3 Staff’ su99ests that
I
\l.
•J
jJ J
'
lu-------
npi6/^^s
Lessoq of
Global Polio Eradication Initiative (GPEI) in India
This draft paper is being circulated to seek comments, views and collaborations
for further refining this paper
Prepared for
Society for Action In Community Health (SACK)
D-1 Gulmohar Park,
Delhi 110049
By Dr. Qnkar Mittal
Contact E-mail: O Mittal@r6diffmail.com
Phone- (91)-98 181-10784
I
i
CONTENTS:
Page No
Abstract
3
Executive Summary
3-5
1. INTRODUCTION
6-11
2. The story of the polio eradication program in India
• The strategy and its implementation
• The financial resources
• The actors
• The achievements and limitations
-12
3. Where to go from here on pulse polio and polio eradication
32
Annex-1 Some Views on the polio eradication program in India -
37
Annex-2- Measurement, prioritization and benefits of polio eradication in
India
44
Annex-3. Lessons for health policy and international cooperation for health
in India
58
Annex-4- a proposal for a paper on vaccination policy in India
Lessons from Global Polio Eradication Initialise in India- draft paper-04/23/03
68
9
[Abstract: The paper suggests that the inability of the pulse-polio program to
achieve polio eradication in India should surprise no one. This should not be
misconstrued as a failure of a gigantic effort by lakhs of health workers and
million of volunteers and participants in the program in the last seven years. The
limitations of the efficacy of the oral polio vaccine and low routine immunization
coverage in several parts of the state were well known to WHO and all the other
important decision-makers in the country. Despite this the case for early
eradication of polio was over-pushed and the risks of the failure were
underplayed. At the end, the bluff has failed to achieve the success in the
gamble. However the global leaders of this initiative have no accountability for
this failure and it has happened in the past with other eradication programs like
Malaria. Nevertheless, there are important lessons for health policy making in the
country and the role of international cooperation in health].
Executive Summary
Key Issues:
1.
The paper is an initial overview of the GPEI in India. It attempts to
address the three key issues arising from failure to meet the target of polio
eradication in India: (i) was it fair to impose the ambitious target of polio
eradication on India and other developing countries and the world which implies
that a single case of polio anywhere would be tantamount to the failure of the
entire global initiative? Could we have not managed better with less
ambitious and more feasible target of polio reduction and control; (ii) did we
have a sound technical basis and operational strategy to embark on this superambitious polio eradication program? ; (ii) If yes, what went wrong with the
implementation of this strategy and (iii) if not, then what were the interests and
influences that played key role in pushing this superambitious objective
and strategy in India and globally? The inferences made in this paper are based
on the available information on the issue. It is perhaps not possible to avoid
hasty conclusions and ideological biases while stimulating discussion and
debate, especially while all the data and information has not been placed on the
table. We invite the readers and the experts in the field to place other facts
and information on the table, challenge the inferences made in this paper
and provide alternative interpretations and explanations.
Failure of the Seven Years effort in India to achieve polio eradication
2.
It is argued here that while the magic bullet of pulse polio and intensive
pulse polio immunization (IPPI) might have contributed to the reduction of the
transmission of poliovirus in India and other developing countries, it has
singularly failed to achieve the eradication of polio The deadline of the year
2000 for achieving polio eradication has already passed. It is a naked truth now
for everyone that this goal is not going to be achieved in the near future.
Therefore the intensive pulse polio immunization (IPPI) strategy has lost its
meaning altogether and should be abandoned immediately. The foremost
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
3
reguirement now is to drop the sword of urgency to achieve polio
eradication.
3.
The paper makes a plea for an independent review of the future strategy
April 2003 onwards to decide the future of the IPPI and other SIAs in India. There
is an urgent need to learn lessons from the failure of the program if we have to
avoid repealing the same mistakes in the new phase of the program beginning
from April 2003. This would also reguire a review of the lead role played by the
international agencies like WHO, UNICEF and World Bank in this program in
order to avoid being misled by them in future.
Real Magnitude of the Problem: Is polio eradication an overarching priority?
4.
It is also argued that WHO estimates of polio cases in India (and globally)
were perhaps gross overestimates when it launched the global polio eradication
program in 1988. Considering that in India, the confirmed polio cases amongst
the reported AFP cases are just 10-20 % of the total, the previous estimation
of the paralyses attributed to polio virus requires a review.
5.
It further describes, how everyone including WHO, UNICEF and World
Bank have admitted that polio eradication is not a priority for the
doveloping countries. Yet tho program has boon justifiod on tho most flimsy
argument that it may result In small savings to the western countries on tho
expendrture on the polio vaccination once the polio eradication is achieved
globally. This is a most phony justification for flogging the already weak health
systeni5 of the developing countries to this exhausting marathon run. The billions
of dollars spent on this program could have been more efficiently utilized to solve
more pressing problems and the rehabilitation of the decaying health systems of
the developing countries. It calls for making realistic exercise of estimation of
the opportunity cost of implementing this program and opportunities lost in
not implementing the more appropriate programs.
The Politics of WHO-Why Did it over-push the case for eradication?
6.
It is further argued that WHO over-pushed the case for eradication of
poliovirus in India by using the example of Latin American countnes that was not
really applicable in the Indian situation. It also underplayed the risks of the
failures to achieve the polio eradication in India and other developing countries
due to well known limitations in India and other developing countries. These
imitations were (i) very low routine immunization coverage in certain states in
India and (ii) the low efficacy of the OPV in providing sufficient immunity in India
and other developing countries. WHO also overemphasized the possible
enefits from the global eradication of poliovirus and it underplayed the
negative 'mpacts on the general health services and the risks and costs of
the failure of the program. It did all this against its own wisdom It narrates
how, after the failure of Malaria Eradication Programs globally, eradication
became a bad word’ in WHO, notwithstanding the success achieved in small
Lessons from Global Polio Eradication Initiative in India- draft paper-(M/23/03
4
pox eradication earlier. It asserts, therefore that WHO, in its organizational
wisdom could not have, on its own, embarked on a global eradication program
for polio. Based on the information available, it is difficult to figure out what
influences have played a role in WHO for pushing the polio eradication as an
utmost urgency for the developing countries. We admit our failure in solving
this riddle and invite others to help us in this endeavor.
7.
The paper suggests that: the Global Polio Eradication Initiative (GPEI) is
yet another negative exercise in mismanaging the health priorities and programs
in the developing countries. The UN institutions, their corporate philanthropic
partners and the gullible health bureaucracies, technocracies and political
leaderships of the developing countries, all are equal partners in this futile and
absurd exercise. We also question the right of the G-8 nations and
international philanthropies like Gates Foundation to provide earmarked
resources for particular disease control programs and thereby distorting the
health policies, priorities and programs of the developing countries. This is
the biggest blemish on the international cooperation in health. Considering that
global commitments are involved, it is necessary for India to play a more
proactive role with the governments of the other SAARC countries and the
African countries where WHO is pushing the program for the last several years.
The paper also calls for learning lessons from the entire GPEI for the functioning
of WHO and the GPPP within WHO.
The way forward for India
8.
There is a greater urgency to make critical decisions for strengthening
the health systems in India. Only this can enable us to strengthen the routine
immunization program and achieve the polio eradication in due course. There
is no shortcut to this process.
9.
The positive lessons should be drawn from the gigantic efforts made by
lakhs of health workers and millions of volunteers and participants in the program
throughout the country. The program should be publicized as a success in
reducing the transmission of poliovirus in the country and not a failure, just
because some cases are still occurring. The live contact made with millions of
poor and disadvantaged people for the first time by the country’s health systems
should be strengthened for health improvements in other areas and with
involvement of the newly activated civil society.
10.
It also draws attention to the right of compensation for those who have
suffered from Vaccine Induced Paralytic Poliomyelitis (VIPP). It also calls for
comprehensive rehabilitation of those suffering from residual paralyses (due to
poliovirus and other causes) and not to ignore the issue in our quest for defeating
the virus.
Lessons from Global Polio Eradication Initiative in India- draft papcr-(U/23/03
5
1. INTRODUCTION
Polio is an infectious disease caused by poliovirus. The disease can strike at any
age but affects mainly children under three (50-70% of all cases) and causes
paralysis. In follows infection with any one of the three related enteroviruses:
polioviruses type 1, type-2, or type 3. The virus usually enters through mouth and
then multiplies inside the throat and intestines. The incubation period is 4-35
days and the initial symptoms include fever, fatigue, headache, vomiting,
constipation ( or less commonly diarrhea), stiffness in neck, and pain in the limbs.
Once established, poliovirus can enter the bloodstream and invade the central
nervous system spreading along nerve fibers. As it multiplies, the virus destroys
the motor neurons, which activate the muscles. These virus cells cannot be
regenerated and muscles no loner function. Muscle pain, spasms and fever are
associated with rapid onset of acute flaccid (floppy) paralyses. Polio paralyses is
almost always irreversible. The muscles of leg are affected more often than arm
muscles. More extensive paralysis, involving the trunk and muscles of thorax and
abdomen, can result in quadriplegia. In most severe, often fatal, cases, poliovirus
attacks the motor neurons of the brain stem reducing breathing capacity and
causing difficulty in swallowing and speaking (bulbar polio). Without adequate
respiratory support, bulbar polio can result in death by asphyxiation.
Although polio paralysis is the most visible sign of polio infection, less than 1% of
polio infections ever result in paralysis. Most cases, as many as 90%-produce no
or very mild symptoms and usually go unrecognized. The remaining cases(“abortive polio”) involve mild flue like symptoms common to other viral
infections-mild fever sore throat, abdominal pain, vomiting-but do not result in
paralysis. About 5%-10% of all polio infections result in aseptic meningitis.
Global Context:
Since 1980s, some experts had been making a strong advocacy for mobilizing
the global opinion in favor of polio eradication. Based on the ‘scientifically rational
evidence’, they developed a strong case for desirability and feasibility of global
polio eradication. They pleaded that “ if the world unites in a global effort to
eradicate polio, we can look forward to the day when parents need no fear that
polio will cripple their children and when that money that today is allocated to
polio vaccination and rehabilitation can be diverted to other health priorities. This
seemingly “fool-proof case" was backed by WHO from the 1988.
However there were already debates amongst the experts nationally and
internationally about the efficacy of OPV in the developing countries and the
dangers of outbreaks of epidemics due to loss of natural immunity and
Ia ssoiis I t om Global Polio l<t adication Initiative in India- dr aft paper-0 1/23/03
()
incomplete coverage with OPV vaccination. Different solutions were being
suggested to meet this challenge. However these debates were ignored
complotoly when tho pulso polio was launched in 1994-95 due to vigorous efforts
by a combination of forces. These issues bounced back with vengeance in
subsequent years.
In the year 1988 the World Health Assembly made the declaration for the global
polio eradication to be achieved by the year 2000. In the year 1999, a special
session of the global assembly met again to press for achieving this objective by
the year 2000. In between the pulse polio program as the chosen strategy to
achieve this objective got the backing from the G-8 nations, World Bank, the
vaccine industry and global philanthropies. This also suited the gullible third
world bureaucracies as easy short-cut solutions and opportunities for mass
mobilization for health has always been a great narcissistic enterprise for them.
The GPEI or Global Polio Eradication Initiative is being portrayed as the “war
between polio virus and polio vaccine” . The monitoring screens of the
www.npsindia.org project the figures for the cases of Acute Flaccid Paralyses
(AFP) and the confirmed poliovirus cases month by month and year by year for
the last five years. The real battle has more story in it than you can watch on the
screen. UN institutions playing the mixed roles of advisers, implementers,
monitors and purchasers of vaccines; the magnanimity of the bilateral donors’
world bank and Gates Foundation and Rotary International for liberally financing
this very expensive program; the hidden and invisible hand of the vaccine
industry in influencing and pushing the program; the other minor players in the
form of thousands of health workers, lakhs of volunteers and millions of mothers
and children all anxious and confused at this ordeal, in the states, districts,
cities and urban slums and villages and their incentives motivations and faults;
and the future battles that will be fought globally, nationally and locally on the
soil of victory or defeat of this campaign.
This is a feeble attempt to narrate a fragmented story. Only those who are sitting
on the highest policy making bodies and who are the esteemed v/eavers of this
story can collectively help to complete this fragmented story. Individually they
may not be aware of its various facets or may be they have not even given it a
thought. To complete the jigsaw puzzle- you need the genius of Agatha Christie
or Sir Arthur Coyle
The Indian Context:
It is a mind-boggling exercise to find out the actual incidence of AFP cases due
to poliomyelitis infection in India in early nineties (see annex-2 for details). There
appears to be reasonable ground to believe that Polio was already on the decline
in India when the pulse polio program had been started in the year 1994-95.
Several states in India were already polio free. This may have been due to better
availability of sanitation and potable water to the population as well as the child
Lessons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
7
vaccination program launched in the country since the early eighties. With
continued effort in promoting the general vaccination program in the country the
polio cases would have further declined in number.
Eight Years ago, in the year 1994, some of the leading pediatricians in the city of
Delhi had approached the then Health Minister of the Government of National
Capital Territory of Delhi to undertake the Pulse Polio Program for eradication of
polio in the city of Delhi. In the same year the States of Tamilnadu and Kerala
also took up the pulse polio campaign. GOI subsequently took it up as a
National Program in the year 1995, in the hope that it will be possible to eradicate
the polio from the country, just as small pox and guinea worm had been
eradicated earlier. This resolve was further helped by the promise of liberal
support for financial grant by the international agencies to meet the costs of the
entire exercise. The purpose of this paper is to inform those who are seeking
answers to the impasse we seem to have reached on the Polio Eradication
Initiative in India after 26 rounds of National and Sub-National
immunization days for pulse polio at the expense of nearly a few billions of
rupees. Despite the promise to meet the cost by grants from the bilateral aid,
India has been forced to take a loan of $21 Omillion from World Bank-IDA in the
year 2000 and more loans would be required in the near future for the same
purpose for this very expensive strategy. The cost calculations for the program
do not include the administrative costs and the negative effects on the general
health services by devoting utmost priority time for the planning and
implementation of these exercises at increasingly frequent intervals. We would
like to use it as a case study to sensitize on the various facets of health policy
making in India under the varied global influences.
More immediately, the following issues are highlighted in this paper (Under
Preparation):
Goal: - What is the problem that we are trying to solve? Are we addressing the all
the paralytic illnesses of the childhood or just those attributed to the poliovirus
infection; the magnitude of the problem compared to other childhood and adult
morbidity and mortality; Change in the case definition from clinical to virological
and contribution of this to decline in the reported cases of poliomyelitis.
Desirability: - Why do we want to give priority to solve this problem urgently^
Control vs. Eradication
'
Strategy of eradication and feasibility: - how do we want to solve this problem?
Shift in India from the earlier strategy of 2 NIDs to the fast track approach of
Intensive Pulse Polio Immunization (IPPI) in 1999-2000 and its results. The
experience of Americas and Europe and other countries in Polio Eradication.
Lessons from Global Polio Eradication Initiative in India- draft papcr-0-1/23/03
8
Resources: How much resource we are putting into this. Expenditure incurred on
the program till date; mobilization of resources from international grants and
loans; future needs for resource mobilization if we continue to use the current
exorbitantly expensive strategies.
Responsibility and Accountability: Who are the players involved; the technical
leadership provided by the WHO and its alliance partners to the GPEI in India;
the interest of G-8 nations and role of WHO advocacy for the GPEI; the hidden
hand of the vaccine industry.
Recommendations: Where Do we go from here, what should be the appropriate
way forward keeping in view the successes achieved and not achieved till date.
What lessons should we learn for health policy and international cooperation?
The main events of this story are captured in very brief below.
1950s - Discovery of SALK and SABINE Vaccines
1960s Polio Elimination from USA
1978-Global Eradication of small pox
1984- Rotary International Initiative on Global Eradication of Poliomyelitis
1985-lndia starts EPI; The Pan American Health Organization (PAHO) launched
an initiative to eradicate polio in Americas by 1990.
Year 1988
In May the World Health Assembly resolved Global Polio Eradication by the year
2000, About 35,000 polio cases reported world-wide ( the estimated number of
cases by WHG-3,50,000)
Year 1990
i
World Summit fo^Children in New York endorsed the polio eradication goal
Year 1991
•
Number of reported cases brought down to 13,500.
•
Emerging polio free zones identified, including the Pacific Rim, southern and
eastern Africa, North America, the Middle East, and Western Europe
Ixssons f n>m Global Polio Eradication Initiative in India- draf t paper-04/23/03
9
•
Last case of polio in Americas, involving a three-year-old child in Peru.
•
Western Hemisphere declared Polio Free
•
Vigorous advocacy by WHO and other experts for the Global eradication of
Polio
•
Debates around the efficacy of OPV in the developing countries
1992
WHO revised plan of action for polio eradication urged greater political
commitment, increased funding and improved surveillance systems
1993- WDR report on health
1994 - Delhi, Kerala, Tamilnadu launch Pulse Polio Program
1995- GQI launches Pulse Polio Campaign for polio eradication
1997 - In India AFP surveillance and laboratory network operationalised through
WHO support
Western Pacific declared polio free
1998- Europe Declared Polio Free
1999- Shift in strategy; Intensive Pulse Polio Immunization launched in India
2001 - Indian strategy turns full circle - renewed stress on routine immunization
strengthening. India takes World Bank loan. New vaccines introduced in the
selected districts by GOI in the routine immunization program.
2002-03- 1400 confirmed case despite total number of 26 rounds
Of the NIDs and SNIDs (in high-risk states); other routine immunization for
polio and not counting the large number of mop-up rounds.
FACT SHEET OF POLIO ERADICATION PROGRAMME IN INDIA 1995-2003
Year
Number
of Budget
Cases
rounds
Ix-ssons from Global Polio Eradication Initiative in India- draft papcr-(M/23/()3
10
1995-2000
95-2NID
96-2NID
2001-2005
nearly
$
for
million
years
200
five
95
96
97-2NID
97-524
98-2NID
98-1931
99-00-see next
99-1126
October
1999- $ 450 million plus
2001Twelve other items could
rounds in total be
nearly
600
NIDs and SNIDs. million plus 30
In addition Mop up percents
costs
rounds
and calculated for GOI
outbreak
contribution
in
immunizations.
kind
Some
children
were subjected to PLUS
excess
18 doses in 18 expenditure
months.
incurred in 19992000
265 cases in 2000
and 27 cases till
September 2001.
No
Cases
expected
next
year,
Battle
against
polio
nearly won.
2001-02-
Final case tally in
2001- 268
2 NIP and 1 SNIP
2002-03
1400 in 2002
2 NIDs plus ?
2003-04
i
proposed 4 NIDs
and 4 SNIDs till
February 2004
Lessons from Global Polio Eradication Initiative in India- draft |)a|)er-(M/23/03
II
2. The STORY OF POLIO ERADICATION IN INDIA:
(FOR SOME OF THE ISSUES IN DETAIL SEE ANNEX-2)
2.1 HOW TO ACHIEVE ERADICATION-THE STRATEGY
Before the launch of Pulse Polio
Routine Immunization program in India
°VeSal' l.l?d'a. hfs made fair|y 9°od progress on immunization. The country
reported that it had met the 90%coverage with EPI vaccines. Later it became
clear that reported coverage had been substantially over-reported False
optimism based on over-reported coverage contributed to a plateauing in
program performance in the first half of 1990s. The best recent estimates
suggest overall coverage is now about 55-60%. Nevertheless the number of
cases of vaccine preventable diseases has continued to go down Polio
cases declined from 24,000 in 1988 to 3854 in 1998 notwithstanding greatly
improved reporting of disease. The number of reported measles cases declined
ram 2,48,000 in 1987 to 34,000 in 1998, but actual number of cases is much
higher at both points of time. India accounts for at least one quarter of all
measles cases globally”.
The debate on the efficacy of polio vaccine
From the inception of the WHO Expanded program of immunization (EPI) the
author and the WHO experts were in complete disagreement as to what
adequate immunization is. While the WHO EPI experts insisted that 3 doses of
OPV for 85% of infants were sufficient to control poliomyelitis, the author insisted
that they were not. The results of very carefully conducted studies in Vellore in
1970 s had shown that the protective vaccine efficacy was in the region of 75%.
,.... Immunization against poliomyelitis is adequate only when poliomyelitis has
been completely prevented- both at individual level and at the community level
We knew that poliomyelitis continued to occur in individual children even after
receiving 3 doses of OPV. Had this phenomenon- vaccine failure-been quantified
and investigated, we would not have been in this sorry state of affairs as we find
ourselves today in which half the children with poliomyelitis are indeed
immunized with 3 doses of OPV. The high frequency of vaccine failure in itself
was an indictment against the 3 dose schedule."- T. Jacob John
Pulse Polio launched
The strategy evolved in two phases- the first phase was from the year 1995-99
when two roqnds of pulse polio were done each year in the form of National
Immunization Days (NIDS). In the second phase beginning from end of 1999
Intensive Pulse Polio Immunization Activities were launched that included NIDS^
lessons from Global Polio Eradication Initiative in India- draft papcr-(M/23/()J
12
SNIDS, Mop-UP Rounds and house to house visits for giving the OPV dose to
the children who were not reaching to the booths. This is described in some
details in the following pages:
The First Phase- Year 1995-98
In the year 1995 the overall strategy had four main components:
•
Maintaining high routine immunization coverage
•
Providing supplementary immunization campaigns nationwide
•
To boost levels of polio immunity - National Immunization Days-NIDs
•
Developing effective surveillance systems capable of detecting and
investigating every case that could be poliomyelitis
•
Localized immunization campaigns once the incidence of polio is
reduced to a few pockets
The PPI program consists of the second and fourth components of the
strategy outlined above. It was expected to last five years over which time the
focus of attention would shift from nationwide supplementary immunization
campaigns to ‘mopping up” operations.
WHO recommendation was that NIDs target all children under five years of
age. In India it had been decided to restrict the target group to the under
threes for both pragmatic and logistical reasons. MOHFW believed that the
scale of operations required to immunize 75 million children in one day twice
within six weeks stretches their capacity to the limit, and to add a further 50
million children to the target group would constrain the system. The additional
cost was not believed to be justified and thought to be difficult to meet. As the
great majority of polio victims were in less than three years old, the technical
implication of restricting the immunization coverage to this group would be to
extend the time taken to eradicate polio by one or two years.
The major activity in the first year was to be to provide extra doses of oral
polio vaccine (OPV) to all children under 3 years of age in India on a single
day regardless of previous immunization. An estimated 75 million children
were to be immunized twice in two rounds six weeks apart. Children in their
first year of life were to continue to receive three doses of OPV (and a fourth
doses in the second year) under the routine polio eradication strategy.
Risks
The main risks to project success in the first year were assessed as:
Lessons from Global Polio Eradication Initiative in India- draft paper-(M/23/03
13
•
•
•
Weak institutional capacity in some states reduces immunization
coverage.
Strategies to reach high risk pockets are not appropriate
Lack of transport prevents timely delivery of vaccines.
Despite the risks identified above, the PPI was expected to have a successful
outcome in its first year, defined as achieving immunization coverage of not
less than 70 percent nationwide. Countries that have undertaken PPI program
and were successful in eradicating polio after four or five years achieved
coverage rates in the first year of their program of 70 percent or higher e.g.
China and Brazil. Both countries saw a very large drop in the number of
reported polio cases in the second year of the PPI directly attributable to good
immunization coverage achieved in the first round of NIDs.
It was expected that the coverage would be much higher in some states than
others. Based on expert advice, the average coverage per state was
expected to range from 90 percent plus in the southern and western states
down to 55 percent in the problem states of Uttar Pradesh and Bihar, and
some parts of Madhya Pradesh and Orissa. Coverage in rest of India was
expected to be 75 percent.
The risk of project failure was therefore very low in the first year. The main
risks over the life of the project was assessed, as the performance of
the weaker states will negate the gains earned elsewhere and that
incomplete surveillance would weaken follow-up monitoring capacity.
GOI was stated to be aware of these risks and planning to tackle them in the
second year of the PPI.
i
Justification- see annex-2
Indicators of success
The main indicator used to iudqe the initial outcome of the NIDs was the
number of polio doses administered divided by the target population. The PPI
project aimed for 100 percent coverage, while knowing that this is never
achieved in practice. Coverage of more than seventy percent in the first year
was considered satisfactory and coverage of more than 8o percent was
considered good.
Ihe standard indicator used to measure the short term impact of NIDs was
the fall in number of reported polio cases in the following year. This was
expected to be steep typically very steep where coverage was either
satisfactory or good. It was reported that following a mass polio immunization
Lessons from Global Polio Eradication Initiatec in India- draft papcr-()4/23/03
14
campaign in Delhi in late 1994, which achieved good coverage, the number of
reported polio cases fell from 963 in 1994 to 66 cases in the first eight months
of 1995.
The indicator of project impact over 4-5 years implementation period included
• continuing drops in the number of recorded polio cases each year,
• a fall in the number of areas classified as high/risk;
• the disappearance of the number of types of polio virus ( there are
three types and type 2 normally disappears first)
• and finally no cases of polio reported.
The second phase -1999-2003
Assessment of last three years
It was clear that all but last of the indicator of project success had been
achieved.
NIDs in India had consistently reached 90% or more of the targeted
children. This was backed up by high quality surveillance which has
increased the non-polio AFP rate to more than 1 per 100,000, managed
an appropriate stool collection rate of 72% and provided laboratory results
on time in more than 80% of cases. Virologicaly confirmed cases of polio
had dropped from 1932 in 1998 to 173 in 1999. P2 cases had reduced to
just six and are now confined to one state. P3 spread was between Delhi
Uttarpradesh and Westbengal and PI whilst more generalized' is
predominantly found in UP. P1 lineage was decreasing and there was an
overall decline in biodiversity. Progress in India had a substantial impact
on the global eradication initiative, and the Indian model was now being
replicated worldwide.
However, even 10% of children missed by PPIs means that an estimated
13 million children were not captured.
A number of issues led the GOI and WHO to consider revisions to the
existing strategy:
•
Lack of a consistently high cushion of immunity through
good routine immunization coverage
•
Additional rounds of NIDs or sub-NIDs (SNIDs) are
appropriate in areas where poliovirus transmission had
previously persisted. - or in areas where the routine
immunization prograrT does not attain high coverage. In
north eastern Brazil,' NIDs of three rounds were required to
achieve polio eradication. In large parts of China, four
lessons from Globa! I’olio Eradication Initiative in India- draft papcr-04/23/03
I5
rounds of NIDs/sub-NIDs per year allowed the country to
reach polio zero in only two years.
•
The efficiency of immunization - i.e. probability that the
vaccine fully protects an individual against infection and
paralytic disease depends on how well individuals respond
to the vaccine.
•
Considerations to increase the number of rounds centers on
the need to interrupt transmission by the agreed target date
as well as the relative number size and conditions of the high
risk areas in the country
•
Birth rates are so high that the absolute number of children
in the annual birth cohort is large.
A meeting of the Indian and international experts on polio eradication was
convened in early May 1999 to review the Government of India’s polio
eradication strategies. Drawing on the lessons above the group of experts
recommended modifying the eradication strategies and these were
accepted by the government.
>
The New Approach in 1999- Intensive Pulse Polio Immunization
i
India will conduct four nationwide OPV immunization rounds of PPI
.• between October 1999 and January 2000. In addition, eight priority states
will conduct two statewide supplementary PPI rounds between February
to April 2000. Unlike during previous rounds, both fixed-post and intense
house to house immunization will be used during each planned round
1999 to 2000 to assure that all eligible children are identified and
immunized.
Each round would last three to four days
Table: A comparison of the strategies in the two phases:
1995
2000
Estimated expenditure -Rs 200 crores
per year
Estimated expenditure- Rs 600 crore
per year
25 percent resources were to be spent
by the state government. The rest from
All Expenditure is mobilized from
external aid. In addition to grants, loan
Lessons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
16
the grants. No loan was envisaged.
was taken from the world Bank
Strategy
■ NID as SIA for 2-3 years- 2
campaigns per year
Strategy
■
After that localized campaigns in
selected pockets for a few years
■
The routine polio immunization
will take place regularly
■
Even after going on for five
years it will go on for three more
years. Strategy after that was
still to be decided
-
More NIDS,
Only children upto the age of three
years were given the polio drops
SNIDS introduced in eight states
where polio cases are still
occurring,
■ mop up rounds
Polio drops given to children upto five
tears of age
A great stress was laid on completing
the entire pulse process in a single day
as a technical necessity
The process was now being allowed to
be completed over a period of one
week.
■
No house to house visits
Though a target of one hundred
percent coverage was kept, it was
expected and envisaged that 70 to 80
percent coverage can be achieved and
this will be sufficient to bring down the
number of cases significantly
House to house visit are part of the
entire process
Routine immunization was almost
negligible in UP, Bihar and Jharkhand
Stress was now to achieve hundred
percent coverage which is impossible
to achieve
Role of WHO- Technical adviser
Role of UNICEF- technical advice
Pendulum continued to shift on the
intensification pulse polio immunization
and strengthening routine immunization
Role of WHO extended to monitor,
surveillance, implementation support
and supervision of the program
Role of UNICEF- contractor
purchasing all external vaccines
for
Contractor for trie expensive social
mobilization programs
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
17
There was greater overt emphasis on
epidemiological justification for the
entire program- the control and
eradication of the disease
The emphasis has shifted now on the
economic justification of the eradication
and need to save on the cost of the
polio vaccine in future. It is now agreed
that this is not an epidemiological
priority for the developing countries
and they should make this effort in the
global interest (i.e. of the developed
nations saving on the cost of the
vaccine)
Risk and benefits of NIDs in the period
The process of PPI thus far has been characterized by a centralized technocratic
ally driven and non consultative approach, captured in one stakeholder
perception that “there is compulsion from authorities to give polio drops.”
Strategic decision on intensifying the program through increasing the number of
NIDs and adopting house Io houso strategies wore taken centrally with no
consultation with those likely to be most affected, i.e. frontline health staff or
vaccine acceptors. Similarly there was no consideration to identify user and
provider concerns and priorities within formulation of national media strategies.
Under PPI, all districts in the country were Itasked
‘ ‘ to immunize everyj child under
5 years old eight times in the next 18 months. In high-risk districts this could be
up to 12-18 times, including the SNIDs and the mop-up rounds. The degree of
intensification, in particular opportunity cost to mothers bringing children to booth,
confusion on the part of acceptors as to the need for this intensification and the
demand on volunteers had not been explored with stakeholders in ways that
could inform the program.
Table: Total NIDs and SNIDs in India till date:
1994
1995-96-97-98
1999-2000-
NIP_______
SNIP
2 in Delhi, Kerala and Nil
Tamilnadu
2 per year-total 8 all over Nil
country
24Ih Ocfober 1999~
27th February 2000
21s* November-1999
26th March 2000
19th December-1999
Lcssons from Global Polio Eradication Initiative in India- draft paper-(M/23/(l3
IS
2000-01
2001-02
2002-03
2003-4
Total NIDs and SNIDs
All over the country
excluding Mop-Up rounds
23rd January-2000
IO111 December 2000
21s1 January 2001
2nd December-2001
20111 January-2002
5ld January-2003 ~
9"1 February-2003 ~
April-03
19_______________ '
26
27lh February 2000
5,FrNovember-20d6
"i?'1 October-2001
29^ September 2002
17lh November 2002
7
It is clear from the above that a child born in a high risk state in April 1998 would
be expected to get 18 doses of pulse polio, three doses of routine immunization
and other doses in the mop-up rounds in course of first five year of his or her life.
2.2 FINANCIAL RESOURCES MADE AVAILABLE
During our interaction we were surprised to hear from some of the
top decision-makers that that resource constraint was never an issue for
the health sector and it was always possible to find financial resources for
a good cause. It was difficult to pull these people into a debate on whether
these resources could be put to better use elsewhere?
The projected resource requirements for Pulse Polio Immunization have
continued to increase in the different phases of the program. The
allocation in the tenth plan for Pulse Polio for the year 2002-03 is rupees
400 crore- 240 crore for purchase of vaccine and 160 crore for operating
cost. [400 crore is almost one-fifth of total family welfare program recurring
expenditure in India in 1997-98.] The total allocation for pulse polio is 1450
crores - (870 crore for purchase of vaccine and 580 crores for the
operating cost).This is much lower than actual projections made for
the donor agencies. The estimated resource requirement for the year
2001-05 has been placed at Rs 3000 crores. -See belowIt would be important to bear in mind that the cost of Govt, of India on EPI
vaccine purchase in 1998/99 was rupees 75 crore and in 199/2000 98
crores-(the expenditure on polio vaccine was nearly Rupees- 40 crores
per year? ). The tenth plan document has earmarked a total of 1410
crores rupees for the immunization program.
The resources have been made available in the last seven years by the
donor agencies for the purchase of vaccines, publicity of the program
(IEC), and strengthening the surveillance. In important chunk of resources
Lessons from Global Polio Eradication Initiative in India- draft pa|>er-04/23/()3
19
have been provided directly to UNICEF and WHO for managing different
aspects of the program. The gaps in the available resources have been
made from the loan of the World Bank.
Financial Commitment for external donors:
S
S
J
J
J
1995-96- $ 5 million;
1996/97-$ 34 million;
,
1997/98-$37.8 Million
1998/99-$ 51.87 million.
2001435- projected partner contribution- $ 226 million projected cost
$563 million
No cost calculations have been done for the staff time and other local
resources invested in the program as well as the opportunity cost of the
volunteers’ time and mothers time for participating in this program. World
Bank has estimated domestic inputs into Polio campaign at US$30 million
for expenditure related to booth management, transportation, anganwadi
workers, school teachers and other NGO activities. An additional US$26
million is estimated for indirect GOI inputs including staff and
management.
Sustainability- According to World Bank, given the nature of nature of polio
elimination approach, financial sustainability is not an issue since
campaign will end with elimination. In fact total earmark of polio may not
be used. At the time of the loan (year 2000), it was expected that need for
more campaigns in year 2 and 3 of the project will depend on the findings
of the surveillance system. If, as expected, the pockets of remaining wild
poliovirus are localized, campaigns will be scaled back producing
budgetary savings that can be applied to strengthening routine
immunization. It also suggested that there is always a risk that complete
elimination will not take place requiring additional funds in the future. The
strong surveillance system, however, and the targeted mop up strategy
should minimize that risk.
Some details on donor funding
The cost projection for at the beginning of the IPPI phase in 1999 are
given below:
In the year 1999- cost projections (in $ million)
1999- 20002000- 2001
1 /9.04 (including GOI cont.)
179.04
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
20
2001- 2002
2002- 2003
2003- 2004
8.40
8.40
8.40
The costs projections for the program during 2001-2005
These were further revised later on. The DoFW prepared in the year 2000
an alternative estimated Resource Requirement -ERR to seek funds from
the donor agencies. This totaled $ 563.48 million or nearly Rs. 3000
crores.
Table: Estimated Resource Requirement for Polio Eradication-year
2001-05
NID/SNID
Vaccine___________
211.55
T raining-Micro-planning
20.10
Transport____________
25.15
Mobilisation
of 55.02
vaccinators/supervisors
IEC and social mobilisation
56.64
Supplies and logistics
3.14
371.60
Mqp Up Immunization
35.54_______________
1.83________________
9,61________________
9.40
9.82
69.26
Subtotal-
•
•
•
•
Supplementary Immunization- $ 440.87 million
AFP Surveillance- $ 51.25 million for WHO
Containment of wild polio virus- 0.25
Strengthening routine immunization- 71.12
•
Total - $ 563.48 million
•
GOI Contribution in Kind estimated to be 30% of the above cost
estimates
Projected partner contribution- $226.64 million
Shortfall- 337.75
In response to this, the donors made Year by year commitments and no
long-term commitments
Box: Donor commitment for polio eradication in India in year 2000
Lessons from Global Polio Eradication Initiative in India- draft papcr-(M/23/03
21
Partner
GDC
DANIDA
Italy
Japan
KFW
Netherlands
Rotary Inti
Rotary Corporate
Campaign
UN Foundation
USAID
World Bank
UNICEF
Contribution in $ million (year 2001)
50
5.80
6.0
38.0
10.0
6.70
1.45
5.0
2.0
14.52
86.42 (RCH Project?)
?
In order to met the resource gap, India mobilized an interest free loan
from IDA World Bank for the polio eradication. The loan from World
Bank was taken under the India The Immunization Strengthening
Project ( a hidden name for polio eradication program)
Project ID- INPE-7330
Loan - Government of India
Date - April 2000
Total finances
Amount - US $142.6 Million
Project implementation period- 3.5 years- (2001-04)
Project components
Polio Eradication: US $100 million
J Strengthening Routine Immunization: US $38.0 million
s Strategic Framework development for vaccine preventable diseasesUS $4.4.million
UNICEF will be the procurement agent for the vaccines. For other items
like cold chain equipment, stoves, sterilizers, cards, registers printing and
some medicines, contractors acceptable to Bank will be engaged.- How
much commission for UNICEF- to be explored further
Box- various Cost of vaccine - to be explored further
>
>
>
>
According to International Public Health 2001- $ 0.02/dose
One of the 1999 document - $ 0.07 per dose
Estimates for global savings- $ 0.48 per dose
Total cost of vaccine in 1999-2000 $ 77.30 million or 350 crores
lessons from Global Polio Eradication Initiative in India- draft |)apcr-(N/23/()3
22
At the request of Government of India, the donors have made the
following financial resource available for WHO-lndia
Table: Budget for WHO strategy Framework
•
•
•
•
•
Policy and Strategy development
Supplementary Immunization
AFP Surveillance
Program and resource management
Strengthening Immunization Services
Total
1,50,000
13,726,250
40,278,684
5,875,000
3,700,500
$ 63,730,434
Or nearly 300 croers -
WHO also charges 10% administrative charges over and above the cost
estimates
It will be interesting to note in this context, the commitment of donors’
resources globally for the GPEI
Table: Global Contributions for pulse polio in $ million
SOURCE- www.unicef.orq/newsline/poliopkinvestn~ient.htm
US (CDC-USAID)_________________
Rotary International
_____________
United Kingdom__________________
Japan______________________
Netherlands
Germany
Bill and Milinda Gates Foundation
Denmark
UN Foundation
598
462
341
200
110
65
50
35
31
Total $1892 million or nearly Rs
10,000 crores
Total contribution of DFID till 2000 to polio eradication was 130 million
sterling pounds including 60 million in Indian subcontinent. Total financial
requirements to ensure polio eradication by 2005 were estimated to be $
1bn of which $550 million were already pledged in the year.
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
23
2.3 WHO ARE INVOLVED IN THE SOLUTION OF THE PROBLEM
Policy process - Governance and institutional issues
India began its universal immunization program in 1985 which included
giving three doses of OPV to children in their first year of life and a fourth
dose in the child’s second year. As a result the number of polio cases in
India began to fall steadily. In 1988 India adopted the WHA resolution on
polio eradication. The first strategy adopted was to take a staged
approach under which eleven states were targeted in an effort to eradicate
polio in part of the country. The intention was to repeat the exercise in
other states once the first stage was completed. This strategy which relied
on routine immunization program did not achieve its goal.
In 1994 India undertook mass immunization (PPI) campaign in Tamilnadu
Kerala and New Delhi, on top of the routine immunization program, which
were successful in greatly reducing the number of reported polio cases in
the first eight months of 1995.
M°lJFW oblamod the final approval for the 1995/96 PPI campaign from
tho Stalo Ministers and Socrotarios in the middle of July 1995. Thoy hold a
meeting al the end of July to which officials aid donors and NGOs were
invited to explain what would be involved and to request support for the
•
•
•
•
•
•
Ministry/ Cabinet
Planning commission Parliamentary standing committee
Administrators -vs technocratsICMR, NICD
Centre state district officers CMOs panchayats- demand driven or
supply driven
• Professional groups-civil society
• CAG
• Vaccine Industry• Role of dissenting voices what are the appropriate forums for
debate
• WHO/UN
The strategic Plan 2001-2005 was launched at Global Polio Partners
summit in September 2000 in New York
Box. Partners in Global Polio Eradication Initiative (GPEI)
International Partnership of
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
24
Rotary International
UNICEF
CDC -USA
UN Foundation
Bill and Melinda Gates Foundation
Governments of Denmark; Italy; Japan; Germany; USA; UK
World Bank
Rotary Corporate Campaign
Private Companies-De Beers; Vaccine Manufacturers
World Bank and DFID have provided majorities of resources
Woddhea^Ith Assembly(WHAJ^affinne^ar^endorse^Tc^
of activities in 1999.
|
BMBB1
Global Technical Consultative Group —
•
7 International experts on immunization, surveillance and disease
eradication
2.4 WHAT HAS BEEN THE ACHIEVEMENTS AND FAILURES
It is time to take stock of the situation and see what has been achieved so
far and how far do we need to go down this route before the desired
success is achieved. We also need to assess the costs that are involved
in the future.
Eight years later the goal is far from achieved. The WHO-lndia has
developed a very elaborate surveillance system for detecting polio cases
in the country. In the year 1998, 1932 cases were reported and this came
down to 268 in the year 1999. However this number has increased to
nearly one thousand four hundred (1400) in the year 2002 (excluding the
vaccine induced cases). This has disappointed everyone and the hope of
achieving the polio eradication by the end of 2001 in India and globally,
has become dismal now.
Table: No of polio case after Pulse Polio Campaign in India
Year
No of AFP cases
No
of
cases
poliomyelitis
of
confirmed :
___________________
Lessons from Global Polio Eradication Initiative in India- draft paper-0-4/23/03
25
1990
10408
1997
8098 or 3047
524
1998
9466
1931
1999
9587
1126
2000
?
265
2001
7470
268
2002
6153
1400
Non-polio AFP rate increased from 0.22 in 1997 to above 1.9 in May 2000
due to better surveillance.
Expected non-polio AFP Rate- 1 case per 1,00,000 population of children
below
15 years of age.
TABLE-1 SECULAR DECLINE OF POLIO CASES AND FIVE YEARLY
UPSWINGS
1981
1982
1987
1988
1992
1993
93-98
98-2002
20,000__________
38,Q00UPSWING
20,000___________
28,000-UP SWING
6,000
8000
UPSWING IN 1998
UPSWING IN 2002
(The polio has not been a notifiable disease till 1997 (?). Earlier estimates
of polio cases have been made from the national lameness surveys. The
reported cases are those largely picked up from the formal system and
reaching the polio specialized centers.
Total affected districts- 86
Bihar-22; Chatisgarh- 1; Delhi-7; Gujrat-6; Haryana-3; Jharkhand 7.
Madhya Pradesh -1; Maharashtra-3; UttarPradesh 405; Uttranchal- 7;
West Bengal -16
Lessons from Global Polio Eradication Initiative in India- draft papcr-()4/23/03
26
Wild Polio Virus- 2002-1556 cases in 16 States
Uttar Pradesh
Bihar
West Bengal
_Ha_ryana
Rajastahn
Gujrat
Delhi________
Madhya Pradesh
Jharkhand______
Uttranchal
.M.?_h^_rashtra
Orissa
Punjab______
Chandigarh_____
Chattisgarh
J&K
P-1
P-3
1121
119
44
100
1
2
32_
30
24
20
20
12
11
6_
4 ~
2
5
3
J__
1_
1 '
Intra-typic differentiation and vaccine Induced cases:
While the confirmed cases are being reported more openly the
compatible cases are not. There are no open reports on the vaccineinduced cases. There are no open reports on the vaccination profile
of the polio-affected cases.
Table: Intratypic differentiation of polio isolates from AFP cases
ERC India
2001
Wild
Poliol
Polio2
Polio3
'Vaccine
209
113
0
70
56____________ 126 ’
Vaccine Mix 101
Wild Mix -3
2002________
Wild
Vaccine
435
58
0
36
45,__________' 72
Vaccine Mix 44
Wild Mix 0
Lessons from Global Polio Eradication Initiative in India- draft pa|)er-04/23/03
27
1
-
AFP Cases postive for polioAl! Wild
All VI
a
678
261
310
813
480
190
non
The failures in the implementation of the program:
The meeting of the expert advisory group -polio-that met in Lucknow
on the 25 and 26lh of November 2002 — in its final conclusions and
recommendations sums up the situation as follows
Why has a resurgence of polio occurred in India ? A lack of accountability
and supervision in the health system in UP has allowed a large proportion
of children to remain under immunized despite multiple rounds of
immunization and the expenditure of hundreds of millions of rupees.
Routine immunization coverage has remained unacceptably low in
UP and Bihar, contributing to the pool of susceptibility. Detailed
evaluation of surveillance, immunization coverage and sequencing data
shows several factors contributed to this situation:
First children in Western UP, particularly in the Muslim community, have
constantly been missed both during SIAs and for routine immunization.
Data from AFP surveillance shows that in the past several years at least
10% of children with non-polio AFP in UP had received 3 or fewer doses
of OPV ( 16% in 2002), allowing continued circulation of multiple lineage
of P1 virus, and P-3 in addition. Among Muslim children in U.P. , 20% of
children are under immunized. UP has remained the major source of virus
in India throughout this time period.
Major political, managerial and operational barriers remain to be overcome
to achieve eradication in India. Unless these barriers are urgently
addressed by the national and state governments (especially in UP) in
close cooperation with polio eradication partner organizations, polio
transmission could continue beyond 2003. Polio- Free States in India, as
well as other countries, continues to face a major risk from reintroduction
of polio-virus from endemic areas of northern India.
According to Planning Commission 10th Plan document
lessons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
28
"However it is a matter of concern that over the last five years coverage
under routine immunization has not improved. There are sections of
population who escape both routine immunization and pulse polio
immunization. As a result, though there has been a substantial decline in
the number of polio cases, this was not sufficient to enable the country to
achieve zero polio incidences by 2000. .
Quality of surveillance
Issues have already been raised about the quality of surveillance and the
criteria of 1.5cases per 1 lakh population under the age of fifteen - see
papers from Dr SKMittal. The implications are that we may still be
missing the cases and the presumption that surveillance has improved
may not be correct. In fact some of the Medical officers have alleged that
cases are being detected now more while they were still occurring in 2000
and 2001.( see below for global surveillance)
The impact of the eradication program on tlic routine immunization
program
There are anecdotal reports on the decline of the routine immunization
program everywhere in the country due to exclusive attention dedicated to
pulse polio, though no surveys have been carried out by any responsible
agency to authenticate this information. Pediatricians are reporting
reemergence of some of the vaccine preventable diseases like
tuberculous meningitis and diphtheria that had almost disappeared in the
last one decade. “
The administration is engaged throughout the year on pulse polio -All
other activities are neglected - some say that it is self evident and
requires no proof - other says that where is the proof - three district study
conducted by UNICEF and WHO in UP- Within India there is not sufficient
aff^TT t0 SU"eSt th3t routine immunization program is being adversely
A study by Sekhar Bonu, Manju Rani and T Baker (John Hopkin
University) comparison of NFHS-I and NFHS-II data
Four major findings emerge from the study that have program and policy
implications! (a) significant increase in coverage of first polio due to the
PPI campaign; (b) a significant drop out between first and third dose of
Ia-smhis from Global Polio Eradication Initiath
c in India- draft papcrdM/23/0J
29
•
polio despite the campaign (c) moderate reduction in gender; caste; and
wealth based inequities, but no reduction in religion -or residence based
inequities in polio immunization coverage as a result of PPI; and (d)
negligible effect of the PPI campaign on levels and inequities in coverage
of other non-polio EPI vaccinations. This is certainly not in line with
expectations of the 41st World health Assembly, and other advocates of
PPI who expected strengthening of national immunization programs and
health infrastructure as a consequence of mass immunization campaigns
(de Quadros&Handerson,1993; Goodman et al., 2000’ Hull and
Aylward,2001)
Contrary to above study - International findings from a study conducted by
John Hopkins using social science methodology including interviews with
health staff in a number of countries where polio has been eradicated
showed positive and negative benefits but concluded that there were net
benefits from NIDs. The largest benefit came from increased coordination
among sectors such as health education and commerce leading to greater
coordination on other health programs and also greater awareness in
general public about the befits of disease prevention program in general.
Other studies (AllMS 2000; Gounder, 1998; Hull, Ward, Hull, Milstien &de
Quadros, 1994). However, almost all these studies are qualitative and
anecdotal in nature, mostly based on interviews with community leaders or
health staff. In addition, some of the studies reported some disruption of
^OoT)1163^ aCtiVitieS 3S an outcome of PPI (AIIMS-2000; Rajum et al.,
WHO- 1997- Taylor Commission Report
Taylor Commission has reported positively/ on the impact of polio
eradication program in Americas. Commission’s report published in 1995,
pointed out that most countries in the Americas were already had a wellorganized health system and infrastructure when polio-eradication started.
And it cautioned against applying the findings of the report too closely to
countries where health services had not yet reached the majority of the
population. Not all the response obtained in the interviews by Taylor
Commission were positive. Some of the complains were: "both funds and
personnel were being directed to polio eradication while other programs
competed for scarce resources; failure to integrate polio eradication with
other health programs; concern that door to door immunization might
establish a paternalistic attitude to health ^services and reduce attendance
in health centres; in some of the poorest and least developed countries in
Colombia, Mexico, and Brazil there were reports of resistance to
immunization due to repeated home visits to immunize children.”
According to Planning Commission 10th plan document- “ data from
NFHS indicates that there has not been any decline in the immunization
Ia-ssohs from Global Polio Eradication Initiative in India- draft papcr-04/23/03
30
coverage in the 1990s. However none of these states have achieved
coverage level of over 80 percent; coverage level in states like Bihar, Uttar
Pradesh and Rajasthan was very low. The drop out rates between the
first, second and third doses of oral polio vaccine and DPT have been very
high in most states. Lower coverage of around 20 % is reported for
measles as compared to other vaccines. One of the main reasons for
not achieving 100 percent routine immunization, is the focus in
campaign mode programs in health and family welfare.
The
Department of family welfare has now taken up a scheme for
strengthening routine immunization. Tenth plan will concentrate on
...discouraging campaign mode operations which interfere with
routine services.
Routine Immunization In States
Coverage Evaluation Survey UNICEFState
%ge coverage
Bihar
21
50
53
69
73
75
77
80
88
91
93
95
96
97
JJP_____
Rajasthan______
West Bengal
Madhya Pradesh
Haryana_______
Andhra Pradesh
Orissa_________
Karnataka______
Gujrat_________
Punjab________
Maharashtra
Kerala______ _
Tamilnadu
Lessons from Global Polio Eradication Initiative in India- draft |>a[>cr-()-l/2J/0J
31
3. WHERE DO WE GO FROM HERE
It was hoped that just as Latin America had become 'polio-free' in the early
nineties so elsewhere the same approach would have the same success. The
sense of frustration in India is further compounded by the fact that, in last few
years -WHO has declared some of the poorest countries in the Western Pacific
'polio-free' and even countries like Bangladesh have reported no polio cases in
the last few years. Only India, Pakistan, Nigeria and some other African countries
are reporting polio cases. This frustration is also leading to the communalization
of the whole issue in India and a particular community is being blamed for the
failure of the entire global expensive campaign.
When pulse polio was launched, it was demanded that at least 95 percent
coverage of the under-five children should be achieved if the desired goal is to be
achieved. It was no body’s case to demand 100 percent coverage. However an
impossible case is now being made that each and every child should get the
polio dose if the goal of eradication is to be achieved and even if one child is
missed, this is sufficient to break the control chain. Moreover we are now being
told that even if one case is reported from a country of one billion,
anywhere, entire campaign would be treated as failure and WHO would not
be able to label India and World polio-free. The country has been trapped in
the success criteria imposed by WHO and we are finding difficult to wriggle out of
this situation in an honorable manner.
In this context it would be useful to note that between 2000-03, 23 countries are
still reporting confirmed cases of poliomyelitis. Outs of these eight countries were
still reporting cases in the year 2002.
Box: 23 Polio Virus Endemic Countries 2000-02
Year-2002
Pakistan;lndia;Egypt;Nigeria;Somalia;Afganistan;Burkino-Faso;Niger; Zambia
Year 2001
Above and ...Algeria; Angola; Georgia; Bulgaria; Sudan; Mauritiana
/
Year 2000
Above and ...DRC; Iran; Cape Verde; Congo; Nepal; Ghana; Bangladesh; CAR?;
Cote d’lvore; Chad; Benin; Myanmar; Iraq; West Bank; Gaza Strip
It would also be useful to note that polio compatible cases have been reported
from all the regions of the world in the year 2002 . This is also true for American
and Western pacific as well as European regions that have been certified as
polio free by WHO. This puts a very fundamental question mark on any success
in achieving polio eradication anywhere in the world.
Lessons Innn Clolnil Polio Enulimlion Initialivc in India drall paper-O 1/2.1/11.1
I
African
American
East
Mediterran
ean_______
European__
South East
Asian_____
Western
Pacific
2002-Total
2001
AFP cases
Confirmed
Polio
835'9
2023
4501
206
0
117
0“
1737
12855
Wild Virus
117
Polio
Compatibl
c
111 __
4
47
Pending
classificati
on
1129
496 “
214
0_
1556
0_
1556
4
27'1
336
969
6143
0
0
9
412
35708
31515
1879
501
1866
443
446
2147
3556
W3
3527
WHO Global Surveillance- 1997- WHO in collaboration with national
governments, has established a network of over 80 laboratories to provide
virological surveillance. There are three tiers, each providing specialized
services; over 60 national laboratories, 16 regional reference laboratories, and
six global specialized laboratories. The laboratory network provides the only
means of identifying where poliovirus persists and where eradication activities
should be targeted. When no cases of polio are occurring, the laboratory network
will play a crucial role in certifying the eradication of polio- by certifying the
absence of wild poliovirus. At this stage surveillance may also entail analysis of
stool specimen from healthy children in high-risk areas and possibly of sewage
and wastewater as well.
Today there is an urgent need to step up the quality of surveillance in many
countries. Of the 116 countries where polio is- or was until recently —endemic,
less than 10 percent are meeting the essential criteria of reporting at least one
case of acute flaccid paralysis for every 1,00,000 children under 15. Even worse
at the end of 1996, 25 polio endemic countries
,
Box
i
WHO - Vaccine Preventable Diseases: Monitoring System 2002 Global
Summary
By the end of year 2001, reported polio cases had declined by 99% compared
with 1988, and only ten countries remained endemic. From 2000-2001 the
decline has continued, especially in AFR. Nevertheless a change in case
definition (from clinical to virological classification) explains partially this
decrease.
Ia'S-soiin from Global
Eradication Initiative in India- draft pa|)cr-(N/23/l)J
33
The tenth plan document states that medical goal of polio eradication is to
prevent paralytic illness due to polioviruses by the elimination of wild poliovirus
so that children need not be immunized perpetually. India will probably achieve
zero incidence of polio by 2004. If there are no more cases over the next three
years, the country will be declared polio free. When this is achieved, steps will be
taken to ensure 100% coverage under routine immunization for another
decade.
It also states that due to danger of vaccine mutant virus, several countries that
have eradicated polio have shifted to injectable killed polio vaccine after
elimination of the disease. India along with other South Asian countries may have
to consider all these options and prepare appropriate strategies during tenth
plan.
There are various shades of marketplace and expert opinions on this issue
•
•
•
•
•
•
•
We cannot wait for water and sanitation to be corrected for eradication of
polio
We cannot wait for health systems to be corrected for delivery of the polio
vaccination through the routine immunization
Wo must pursue this strategy and achieve the desired results
Money is not the issue- we must eradicate this evil-which paralyses
millions of the children in the third world
We cannot go back from our commitment after spending so much time
and energy
The negative consequences of not doing the complete job i.e. not
achieving the polio eradication- it could cause worse epidemics now that
we do not have the protection of natural immunity anymore
We have made enough efforts, there is already fatigue set in and nothing
more will be achieved in pursuing it any further
( see annex-1 for more details on this)
There are also natural concerns on the impact of the failure in certain states in
India on polio free states and on adult population in an environment where there
is loss of natural immunity.
Way Forward:
It is clear that the target of achieving the polio eradication by 2000 is postponed
substantially. Even if it is achieved in India after some years, other Asian and
African countries may not be able to achieve it or there may be resurgence in the
countries that have already received it due to vaccine mutant virus. The demands
of certification are even more stringent and even after achieving zero case status
and certification, the decision to discontinue with polio vaccination and make the
cost saving on the vaccine remains a far dream. It is therefore suggested that
Lessons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
34
the we should no longer be pushed to meet the target date of the Global polio
Eradication. The push given in the form of IPPI is not justified again? However,
the WHO and the expert group may try to justify it on flimsy grounds
The ultimate justification given by WHO to push this strategy on India and few
other countries is that a polio free world will lead to saving on cost of one billion
dollar per year for polio vaccination by the countries of the developed world and
1.5 billion by the entire world. This, in our humble opinion, is not a sufficient
reason to hold the entire health establishment of India to ransom for the pursuit
of this objective, if it is not feasible to achieve it for a variety of reasons in near
future and we have no reasons to feel frustrated or ashamed by it.
We would like us to shift to the original strategy and not go in for IPPI (
intensive Pulse Polio Immunization) any more. That is our sum total of
recommendation for the policy makers at this stage.
Suggested Course of Action
> With draw Supplementary Immunization Activities- like NIDs and SNIDs,
review the role of MOP rounds and outbreak immunization, while routine
immunization coverage is still low
> Use experience and lessons of the seven years efforts to take serious
action on strengthening the health systems including the routine
immunization
>. Continue surveillance but use the network to extend it to other diseases
too. Link it to the general surveillance project.
> An independent review of the technical and operational strategy should be
done. The lead partners of the GPE1 should not guide this. The national
government with other donors and World Bank should develop a common
viewpoint on( this issue. Some of the issues for this review should be
following:
The flimsy argument on the saving of 1.5 billion on the cost of polio
vaccine- should this be the beacon light of the polio eradication
program and its ultimate justification?
J Could we have done the same with less money? Impact of
oversupply of resources on one program within the health system/
What does the CAG report say?
Independent study of the impact on the general health services and
the indirect cost of the polio program
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
35
z Role of UNICEF and WHO in provision of technical advise- Is there
a conflict of interest involved- how many experts are paid by the
vaccine industry
z Two new elements introduced- Vaccine mutated wild polio virus in
areas where WHO has certified polio free- and the advocacy of
IPV- who will bear the cost of this costly vaccine
Donor Responsibility
> Resource projections in the new circumstances, how many resources
donors are ready to commit- prior warning to the national government
Some experts have pushed the target date to 2015. Planning
?orTn JS'°n haS a!SO made Similar Pr°jections- Do we have resources
for an expensive strategy?
More basic issues
ev^uati0n of the Pegram should be undertaken to learn
Srh05
stren9thenin9 the health systems in the country and
reaching the poorest and marginalsed populations.
'h'6' Ca"S f°r national governments to be in lead in
reform of WHO- why should then donors provide funds for the WHO in
direct imPlementation role. Do we want to make WHO
?E 35 private contractors ,for provision of global public
g ods- the new mantra of the international aid? GPPP and the
influences on WHO
uie
I
Priorities- How much of priorities should be given to vaccine
preventable diseases, Are these the priorities of the developing
countnes? Review of BOD and DALY etc MECH has called for
and the Snt h CHil S0C'ety t0 deCidS the health priorities of ‘he poor
and these should not be determined merely on the basis of the
epidemiological data.
< Make a case to make available donor resources into the general pool
and not targeted to specific disease control programs
a-
Review GAVI/ Vaccine industry
Lessons In>m Global Polio Eradication Initiative in India- draft paper-04/23/03
36
Anncx-1
The current views
It is amazing to find so sense of helplessness amongst those who know that things have
been wrong from the beginning. They also feel helpless that now we have no other choice
but to continue with this folly. On the other hand there are views that either show
ignorance or cynical. There is no view tliat reflects the urge to find the truth and correct
where things have gone wrong. Therefore, the program continues, as before and the
nation suffers. Here is a collection of views, opinions and reactions of a cross section of
people who had some role in the program-
1.
WRONG OR RIGHT -WE HAVE COME THUS FAR. WE CANNOT GO
BACK NOW. WE MUST ERADICATE POLIO. WHO WILL BE RESPONSIBLE FOR
THE NEGATIVE RISKS OF ABANDONING THE PROGRAM MIDWAY? - A
MOST COMON REACTION.
2. I he polio eradication program was a great opportunity for us to spend the resources
that were committed to the health sector in India but these were lying un-spent- the tap
was always kept open for pulse polio because it was fthe real potential to spend the
money- views from task managers of the bilateral donors and multilateral
------------------ 1 agencies.
3. Our Chief from the headquarters was blaming
for messing
messing up
up the
the entire
entire
blaming WHO
WHO for
program. It was a waste of opportunity costs and story of opportunity lost. This amount
of money could have done wonders for the health of the poorest. However when he
joined the formal meeting, his stance; was changed completely- inside views from several
bilateral and multilateral agencies.
I
agencyJorjhcj3PEI
^OjI-CJnJonnaljacwfron^
Box:
I he GPU is based on political decision- not on a rational or technical decision.
Who sets policy - GOI or WHO? It is certainly GOI and not WHO
Il is wrong to say that WHO is playing a role in implementation. Il is GOI that is
implementing.
1 he 1 PPI tliat began in 1991 did not deliver the goods because GOI did not agree with it
completely, as advised by WHO. It did not keep with the suggested approach. The
dilleiences emerged on more Mop-Up rounds suggested by GOI instead of more SNIPS
and NIL>s recommended by W110.
There is a politico-economic” side to the whole argument- India cannot unilaterally
withdraw from the program.
Lessons from Global Polio Eradication Initiative in Indi
draft papcr-04/23/03
37
WHO has been emphasizing for long that Muslim Population as a group is refusing to
accept immunization. However, Indian government has not agreed to raise it as one of the
issues in the poor implementation of the program.
Health systems strengthening cannot be the approach now. We need the ‘Juggernaut’ or
the ‘Sledge hammer’ to complete the task.
Donors will be ready to put more money for polio eradication under RCH-2. This has to
be pursued and cannot be given up.
Need to clarify whether the cases polio in non-high-risk states are occurring amongst the
migrants or the virus originating from one place is attacking the still vulnerable
population in the non-high risk states.
The World Health Assembly gave the mandate to WHO to take up polio eradication.
WHO as an organization had never advocated for this. In fact Eradication is a bad word
in WHO.
Other related issues on vaccination
Polio Surveillance
Program (NPSP)and the World Bank Served kmc" Project and Xht L'e^nV^
surveillance should incorporate all vaccine preventable diseases.
Under the Immunization Strengthening Project funded by World Bank for India, no
strategic framework for immunization has been developed as yet by GOI. This project is
not providing funds fof hepatitis B vaccination project, 'fliesc arc being funded by GAVI
Conspiratorial nexus, as reported in EPW paper, between Hepatitis B and GAVI is not a
fair statement. China is using GAVI funds at provincial level without including hepatitis
B vaccination.
The GAVI project has increased the equity gap in India. It is being implemented in those
districts that already have high immunization coverage for other vaccine preventable
diseases. GOI is coming to donors for asking for more funds for hepatitis B. There is
need to review the approval of funds process for GAVI. It does not get usual clearance
from Finance and DEA as in the case of other externally funded projects.
Need to understand the murky influences on WHO - the private foundations and
transnational corporations.
5. One View from an International
i
adviser who worked in the WHO SHARP region
office for GPEI in the initial years:
Lessons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
■i
The most important person in the program in the WHO SEARO office was.........Who is
credited with the polio eradication in the Latin American region. For him the most
important activity was to establish the network of high-class laboratories for the viral
testing in India and in the region for the surveillance purpose. The issue of very low
coverage of routine immunization in certain population groups came in as an important
issue early in the program. Il was suggested that it was very important (o give priority to
establish mechanisms for routine polio-immunization in these populations groups to
overcome their resistance. However, this advice was ignored.
6..
“ We were participating in the program to do some good work. We were never
aware of these complex dimensions of the entire issue. We are hearing this for the first
time - common reaction of large number of the Medical officers who were nlayino
a lead lole in the implementation of the program.
/
“ We must not forget the most important fact- it is not GO! that is running the
program^ It is the WHO. WHO is the master of this program. The opinion of Indian
maTr a8ainSt the opinion of the white-skinned experts. I had opposed
c m bPaid any attentlon t0 my advice. It is only now when the program is
tailing that they are calling me to seek my views. Ultimate decisions still rest with them.
, V”60,?8 15 Ca"ed excluslvcly of Indian experts, I am ready to reveal the complete
liulh.
One senior most iiKernational authority on the global eradication of polio
8
“All those who were sincerely implementing the program were sidelined because
they were opposed to mishandling of funds.” One medical officer
9.
We had oppdsed the IPP1 from the beginning. But we were sidelined. We had to
sacrifice the coveted positions in WHO. Those who were ready to speak the party line got
the prize postings.” - One medical officer
10..
“Can anyone answer this question as to 1how many doses of polio vaccination
should a child get before he can be guaranteed protection from polio?'In my district all
poho cases have already received four or five doses of vaccine. And why does not
somebody focus into the poverty angle because all children getting polio arc from poorest
socio-economic strata. It is obvious to us that it is the conspiracy of the transnational
vaccine manufacturers to impose this program on us. There is no other logic for this
program. But we arc helpless.” One CMO in one of the districts in U.P.
''' ipl|>>Cri'/dian Aca,dJc,ny of Pediatrics in its resolution in the year 2000 had opposed the
11 11. We were told by the government that it was an administrative decision and not a
techmeal decision and it has to be carried out. One of the senior most secretaries said
that if do not follow WHO recommendation, the blame will come on us. So we have
no choice. — One senior pediatrician in (lie city
12 Ihi!"dl.an
.°f. pediatrics> the Indian Medical Association and other
important professional bodies iare supporting this
' program. How can health ministry
or planning commission have a different view
on this, against the views of these
Lessons from Global Polio Eradication Initiative in India- draft papcr-(U/23/03
39
professional bodies, 'fhey have even gone to Human Right Commission to claim
hepatitis B vaccination as the human right of the children. Only if these bodies are
convinced, can it be possible for us to take a different view on polio eradication. Till
then we have to continue with this policy. If somebody has to approach us on this
issue- it should be through these bodies.” -one senior official and adviser.
13.
“lam on record to have opposed this program as not being a priority when 1 was
with Planing commission. But my note was not even forwarded to the health ministry” One retired senior most functionary of the Government
14.
“Who is going to listen to you. There is plenty of free floating money in this
progiain and everyone fioin (he lop Io bottom in (he health establishment is getting some
perks. Who is bothered about the success or failure of the program.” -one functionary of
the consulting organization in one of the state.
15.
“ Do not raise the issue of resources for this program. If there is a good cause, the
resources can always be found by Government of India. So exorbitant expenses on this
program is a non-issue.” — One senior functionary in the Government
16.
“ Polio eradication is a good thing. Why should we pose other priorities against it.
If we have other pressing problems, we can solve those problems also”- one common
man on the street
17.
One view from Wl IO-SEARO region:
Box:
Polio-2 wiped out, polio 3 nearly; identified lineages from western UP that arc spreading
to other places- So (here is a clearly geographical area identified where if the virus is
contained, the success is possible.
In the yearl970, when the routine immunization was low, trials by one leading Indian
Expert used multiple rounds of the pulse polio to reduce the immunity gap and this
formed the basis for 1PP1 in 1999. The multiple rounds had their success in 2000 when
the number of cases came down substantially- 260 in 2000 and 2001. But after that the
number of rounds were reduced and that created the immunity gap in a background of
low routine coverage and also there was loss of natural immunity .
Vaccine implementation is poor in other areas too e,g one district in Kerala- case in 2000
and Ganjam and Bhadrak district in in Orissa- cases in 1999 and again in 2002 . So even
where Routine Immunization coverage overall is good there is problem in specific areas.
It has persisted through the years but in intervening periods, they did not have the virus
because circulation had got wiped out. Once the circulation again became widespread in
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
40
2002 cases again appeared but did not turn into a major outbreak States like Rajasthan
and MP were always at high risk for polio transmission because of poor RI coverage in
the background of decreasing IP PI rounds. There was an accumulation of susceptible and
once the virus crossed over in the high season, outbreak followed.
In the past also outbreaks occurred at intervals of 5-6 years because of build up of
susceptible, 1 similar situation has occurred in 2002. - Fewer rounds in previous year
with poor implementation in High Risk States, poor Routine Immunization, natural
immunity also declined with most of the genotypes getting wiped out.
The states that had better health systems implemented the program better and followed it
up with good routine immunization coverage have continued to be polio free.
But where there is a chance for virus to establish itself, it docs.
18. One view from a worker of Rotary International
Your technical objections on the desirability and feasibility of the polio eradication
initiatives may be correct. However, Rotary International Hq may not have been aware of
these dimensions. It was only trying to do a good job, moved by the very high motive of
making this world polio-free.”
i
19. Sckliar Bairn ct a! Despite high profile given to 1’1*1, and steadfast political and bureaucratic commitment,
the impact of PPI on coverage and sustainability of polio and non-polio EPl vaccination
is less than satisfactory. Findings of the study highlight the limitations of the “campaign”
approach to disease eradication in backward regions of India and elsewhere where weak
health systems operate in challenging social, cultural and physical environment.
As the global polio ciadication effort narrows down to lew geogiaphical regions of (he
world with poliovirus transmission, geographical regions that also share some of the most
challenging social and health systems barriers to public health, it may be essential to
strengthen health systems and address social challenges in addition to ongoing polio
campaign. A multidisciplinary understanding of social, cultural and health system related
realities in these areas may be essential to resolve the remaining challenges to polio
eradication.
Questions reinain about the other consequences of globally mandated disease eradication
program on floundering health systems in the most backward regions of the world. What
had been the opportunity” costs of global disease eradication program for poor societies
that had committed scarce resources to fulfill a global mandate? How can a disease
eradication program ensure efficiencies and effectiveness in reducing overall disease
burden by strengthening the routine immunization systems, while also succeeding in
eradication ol a disease? Unfortunately we do not have convincing answers. Further
health system operational research to evaluate difficrcnt aspects of global disease
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
41
eradication program implementation- including polio - can contribute to make health
systems more cflective and efficient.
20. Box — View from WHO-Europe:
Achieving a polio-free Europe
The WHO European Region has been polio-free for more than three years thanks to the
hard work of public health workers and volunteers in its Member States, with the
additional financial support of bilateral agencies and international partners.
In addition to (he substantial domestic polio eradication costs borne by the European
Region Member States, many European governments (including the governments of
Denmark, Finland, France, Germany, Italy, tlie Netherlands, Norway, Switzerland and
the Umted Kingdom) have supported other countries in the region to protect their
children against polio.
Rotary International and the United States government (through US CDC and USAID)
have funded considerable vaccine and operational costs; and the United Nations
Foundation has also funded over USS 1.3 million of operational costs to help the polio
eradication effort in the region.
Global progress
European governments and institutions have also made significant contributions to the
Global I oho Eradication Initiative, funding vital activities in over 100 polio-endemic and
high-risk countries.
loos)0" tk>n°,S 10 thC Gk,l>al l>Oli° li,adicatio,1 ''’ilialivc since 1985:(includes pledges to
Top ten donors Donations since 1985 in USS millions
United
Slates'
(CDC,
USAID)
598
Rotary
International
462
United
Kingdom
341
Japan
200
Netherlands
1 10
Germany
65
Bill
and
Melinda
Gates
Foundation
50
Denmark
36
Canada
35
United Nations Foundation 31
Of the European governments, the Umted Kingdom has contributed the most funding to
helmt.at.veto date: over USS 341 million since 1985. In 2002, the UK's DepartmenHbr
ntemational Development (DFID) set in motion more than USS 100 million for polio
eradication activities in India over the next four years
The Netherlands has donated USS 110 m.ll.on since 2000, to support v.tal disease
I surveillance systems.
Lessons Innn Global Polio Eradication Initiative in India- draft pa|>er-(l4/2J/03
42
Germany has been a long-standing partner to the polio eradication program in India,
providing USS 65 million for oral polio vaccine since 1997.
Denmark was also one of the earliest partners to the program in India, providing support
since 1997 for vaccine, cold chain, and surveillance support.
In 2001 Luxembourg, with its first contribution to the Initiative, showed how the impact
of a donation can be maximized by strategic directing of funds. Luxembourg made a USS
3.2 million contribution to fully fund the gaps in six of its priority countries. Burkina
Faso, Cape Verde, Mali, Namibia, Niger and Senegal.
Italy has provided USS 1 million each year over the past three years for India’s polio
eradication efforts.
In 2001, Norway provided USS 3.1 million to the Initiative, both globally and to support
activities in Nepal and Ethiopia.
In 2001, Ireland signed a three-year USS 2.3 million global pledge, in addition to
supporting activities in Ethiopia.
In 2001, the European Commission provided USS 17.4 million to the governments of
Nigeria for its polio Eradication efforts.
Private sector partners including Aventis Pasteur, British Airways (through the 'Change
for Good Appeal) and De Beers have made significant contributions.
This support has helped Io bring polio to its lowest levels in history. Today there are just
ten polio-endemic countries. The number of polio cases was down by 99.8 percent from
1988 to only 480 cases last year. Disease surveillance systems have been strengthened,
lealth workers have been trained to ensure rapid reporting of polio cases and other
epidemic-prone diseases. It is critical that wc build on these achievements to stop
transmission of poliovirus globally and avoid any re-establishment of poliovims
transmission in polio-free areas. Until all children are immunized against polio, children
remain at risk from this crippling disease.
Protecting our investment
loday, the greatest risk to (he polio-free status of Europe is a rcintroduction of the virus
from the remaining polio-endemic countries - such as the importation to Bulgaria and
Georgia from south Asia in 2001. Helping to finish the job in south Asia and Africa is
perhaps the most important step in protecting our investment in a polio-free Europe.
Lessons Irom Globa! Polio Eradication Initiative in India- draft paper-04/23/03
43
Annex-2
A-2.1 WHAT IS THE PROBLEM THAT WE ARE TRYING TO SOLVE AND
WHY DO WE WANT TO SOLVE THIS PROBLEM
Background
In the 1960s it became clear that smallpox was non-existent in the North
American continent 'and routine small pox vaccination was discontinued in the
USA. If one large continent could be free of small pox, obviously the whole world
could be free of small pox. In 1966 the 19th World Health Assembly adopted a
resolution to intensify efforts for the global eradication of small pox. At that time
small pox was considered to be endemic in 33 countries; India was one of them,
accounting for 65% of the global cases. The last case of small pox in India was in
1975 and in Somalia in 1976. In 1978, two years later, the WHO declared the
world free of small pox.
It was this success story that led to the idea that poliomyelitis could also be
eradicated. In 1976, it became apparent that there was no circulation of wild
polioviruses in USA. If a continent could be free of wild poliovirus, the whole
world could also be made free of wild polioviruses. Poliovirus is an exclusively
human infection (just as small pox was) without any extra-human reservoir. Safe
and effective vaccines are available against poliomyelitis, as was the case with
small pox. In 1984, the Rotary International (Rl) constituted a consultative
committee to consider the potential of a global effort against poliomyelitis.
Accepting the committee’s report, the Rl declared the goal of eradication of
poliomyelitis by 2005, the centenary year of Rl, giving itself a 20 year interval for
achievement. Stimulated by this development, the Pan American Health
Organization (PAHO) resolved in 1985 to eliminate poliomyelitis from the South
American continent, by the year 1990. Then in 1988, the World Health Assembly
resolved to commit the WHO and the member nations to eradicate global
poliomyelitis by the year 2000. ( T. Jacob John- Can wc eradicate
Poliomyelitis? -1996)
Are we targeting the correct problem?
It is obvious that under the guidance of WHO, the MoH&FW have are targeting
the polio virus. They have no concern with the other polio-like illnesses that have
been clubbed together under the AFP. Considering that new cases of AFP will
continue and virus may be present in sewerage and other places for a long time,
it would be important to have a proper case definition and understand the
underlying etio-pathology.
Box. Paralytic Poliomyelitis- Conditions causing muscular weakness
include:
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
44
1.Infectious neuronitis (Guillain-Barre Syndrome) - most common disease; most
difficult to distinguish from poliomyelitis
1. Peripheral Neuritis- Post-injeciional; Toxic-lead; avitaminosis; paralytic-cranial
hepeszoster; post-diphtheritic neuropathy
2. Arthropod borne viral encephalitis; rabies and tetanus;
3. Botulism
4. Demyelinating types of encephalomyelitis
5. Tic bite paralyses-uncommon
6. Neoplasms
7. Familial periodic paralyses, myasthenia gravis and acute porphyriauncommon causes
8. Hysteria and malingering-rare in children
Conditions causing pseudo-paralysis do not present with nuchal-spinal rigidity or
paralysis
1-Unrcogniscd trauma- from contusions, sprains, fractures and epiphyseal
separations- common causes of diagnostic confusion
2. Non-specific (toxic) synovitis
2. Acute osteomyelitis
3. Acute rheumatic fever
4. Scurvy
5. Congenital syphilitic osteomyelitis
An alternative approach could be understand paralytic poliomyelitis as an end
point of multiple and competing causes child morbidity and mortality; treat all
cases of AFPs as one syndromic category and apply a case management
approach with focus on the rehabilitation of cases with residual paralyses. This
can be made an essential component of the Integrated Management of Child
Illnesses or IMCI.
Another strategy could be based on tackling the water borne diseases. This will
address other all picoma viruses together. E.g. polio, hepatitis A and also- enteric
fever, diarrhea and gastroenteritis - the cluster of water borne diseases
Malnutrition and vulnerable child are also an important dimension of the
vulnerability to polio infection and paralytic poliomyelitis. Can we really address
the problem without addressing the underlying causes?
We will have no net gain by passing the issue of strengthening the health
systems for achieving results through vertical approaches and programs. A weak
health system will pursue all these vertical health programs like a ‘Bhasmasur.
Lessons (n>ni Global Polio Eradication Initiative in India- draft papcr-04/23/03
45
TO WILD POLIO VIRUSUAL CASES °F RES,DUAL PARALYTIC POLIO DUE
Issues
i
What data has been quoted by GOl/donor agencies of the baseline in 199495
Relationship of reported cases and estimated cases -is it justified - cases of
res'dual paralyses due to infection with poliomyelitis virus and cases of nonpolio AFP.
It is interesting to note that the magnitude of the
problem is being magnified
beyond all measures through manipulative use
of language to justify the massive
expenditures on this program. For example:
http://wbln1018.worldbank.orq/sar/sa.nsf ..
11/20/2002- Today India Makes Final Assault
on Polio - Bank Assits with $50
million
''With its annual nationwide
Pulse Polio
Immunization
Campaign getting
"resulting
adTm6 disease throu9h a fast track approach for polio eradication". ( emphasis
auueci)
'
r
Lancet May 20 1994- Hull, Ward and others
Before the advent of polio virus vaccine
1978 officially reported figures
1988 “
1989
1991
1992
“
“
Estimated 600000 new cases of
paralytic polio occurred worldwide
every year
50,000
--------------35,000 ( estimated cases 3,5'0,000)
---------- ( |ndia 13866)
r:“Tz±lQdia6020)
15406—( India 8756)
~
? d°''vnwarci. trend occurred despite improvements in surveillance
vertheless poliomyelitis surveillance remains inadequate in many areas of the
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
46
740dQ00d WH° estimales that the true figure for Paralytic polio in 1992 was
Same paper reports,
!
9 /o Immunization coverage in 1990 and incidence of poliomyelitis
fell to 6020 cases in 1991 from 13866 in 1989. The number of polio cases
increased by 46/□ in 1992 to 8756 ( 56% of the global total). While this is partly
ue to improved case detection, there is some evidence of real increase
C^cemS?ave been raised in lndia about the risin9 percentage of cases among
™ QneoX ° aVe received three doses of OPV. However with a vaccine efficacy
Of 80-85/o, a rising proportion of cases will be vaccinated as immunization
coverage rises and absolute number of cases decline.
National Medical Journal of India 1997 - Varghese, Qadeer, Mohan Paralytic poliomyelitis in rural areas of north India - based on house to house
survey conducted in 1990-91 in rural area of north India -Results- Thirty-seven
cases of paralytic poliomyelitis were identified indicating a prevalence rate of 1 6
per thousand populations. Of these 97 % were paralyzed before they were 2
Sses OnlvG'LP°rC<in' |,ad, 3 "i5l°r’ Of
-Son p'roeSng
had reCei''ed e“her partial or oomP|alo
immunization
Conclus'on amongst others- Injection given for treatment of fevers in rural
paper a™ysla!es mat0"5
preCi|”,a,inS "aral‘'"c PoHomyeilfc. The same
ntTnnn3'
conducted bV G01 showed a prevalence rate of 1.05
innn popu a ,on The estimated poliomyelitis infection works out to be 2 12
n3rJ?00 p°pulatl°n- ln our stuc*y population of 22883, 2-3 cases of fresh
paralytic poliomyehtis were seen every year. The WHO status reports on
poiomyehtis estimates that surveillance systems are still reporting only ? case in
10. - Quoted from Bulletin of WHO -1980”
Y
7 i'nnaHed °n
prevalence of lameness in school age children the annual
estimated °fhSymp^omatlc poll° in low and middle income countries was
estimated to be in the range of 20-40 per lakh population- source??? "
One of the documents states -
Lessons from Global Polio Eradication Initiative in India- draft paper-(U/23/03
47
It is primarily a disease of very young. 90 percent of the people who
become infdeted are less than three years old. It affects the poor
hardest, with most cases found in urban slums.
“The disease burden from polio has fallen sharply in India and rest of the
world since 1980 because the routine immunization program has been
effective in controlling the disease. Routine polio immunization in India has
boosted polio immunity levels in under-3s to a reported 90 percent, which
leaves just under 8 million children at risk from polio. The reported number
of cases in India fell sharply from around 40,000 per annum in 1980 to
30,000 in 1982 to 6000 in 1991 and to some 9000 in 1994.
But experience has shown that routine immunization alone will neither
continue to reduce the incidence nor lead to polio eradication. Based on
slowed rate of reduction in 1990s and on the experience of other
countries, India will probably continue to have 3,500 to 4,500 reported
cases a year if the NIDs are not implemented. The unreported cases of
polio are likely to be 3-10 times higher, i.e. around 10,500 to 45,000
per year. Further having made gain in reducing incidence, the danger of
epidemic is increased because of a lower level of natural immunity in the
population.”
The document also states that“At present polio is clinically diagnosed on the basis of acute flaccid
paralyses (AFP). AFP can be caused by several illnesses besides
polio, and only laboratory analyses of a patient’s stool can determine
whether the cause is polio. India has four national laboratories which
can undertake relevant tests (but which cover only a small proportion of
polio cases) and this is soon to be extended to seven. More needs to be
known about the skill levels of the laboratory staff and the budgetary
situation of the laboratories in order to judge how effective they are likely
to be in their viral diagnosis work. And it is likely that system for ensuring
the prompt collection and dispatch of stool specimens for laboratory
diagnosis also needs strengthening.
Other important links in the surveillance chain that needs to become more
effective are the hospital based and community mechanisms to trace
patients with AFP to enable follow up examinations to be undertaken on
all suspected polio cases. (This needs to be done 60 days after the
disease). More than half the children taken to hospital cannot be traced
once they leave. The polio monitoring capacity within MOHFW also needs
to be strengthened.”
Lcssons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
48
A-2.3 COST BENEFIT ANALYSES OF PULSE POLIO PROGRAM GLOBALLY
AND IN INDIA
Box-WHO-1997 - Benefits of Polio Eradication
Over the years polio has taken a heavy toll on the lives of both children and
adults. Before the advent of polio vaccines, about five lakh people a year were
paralyzed or died after contracting the disease. While the humanitarian benefits
of global polio eradication will be immeasurable, efforts have been made to
quantify financial savings that can be anticipated. WHO estimates that once polio
is eradicated and immunization halted, global savings from immunization,
treatment costs, and rehabilitation will amount to over US$1.5 billion a year
But there is no way of knowing how much of that money will be redirected
to other health programs.
The reduction in human suffering and death will be felt most in the poorest and
least developed countries, where disease is still endemic. But many of these
countnes are now paying an increasing share of cost of NIDs- representing a
higher proportion of GDP than in richer industrial countries. At face value
financial savings would be greatest in countries where the costs of polio
immunization, treatment and long term rehabilitation are greatest.
The United States will be a major beneficiary once the disease has been
eradicated globally and polio immunization can be stopped. And there is a
precedent for this. It has been estimated that, ever since the global eradication of
small pox was certified in 1979, the United States, the largest donor- has
recouped its entire contribution every 26 days.
In 1993 World Bank Development Report, Investing in Health, estimated that in
one year alone, 1968- the global amount spent on smallpox immunization,
quarantine, and treatment was over US$300 million- more than direct financial
contribution during entire 12-year eradication program. The eradication program
had saved hundreds of millions of dollars a year in direct, measurable costs, as
well as unquantifiable amounts of human suffering. Few investments of any kind
generate human and financial benefits on that scale.
In addition to human and financial benefits, polio eradication is having a positive
impact on health services and on development of health infrastructure throughout
the world. In 1988 when World health assembly resolved to eradicate polio by the
year 2000, Member states were determined to ensure that health service
provision was strengthened and not ignored at the expense of a " vertical"
program focused on a single disease. The resolution emphasizes that “
eradication efforts should be pursued in ways which strengthen the development
of the Expanded program on Immunization as a whole, fostering its contribution
in turn, to the development of health infrastructure and of primary health care.”
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
49
I
I
Box: Following is a summary view of the justification for polio eradication
program in India by one of the donor agency
Technical Justification: “Experience has shown that routine immunization alone
will neither continue to reduce the incidence nor lead to polio eradication. The
only way to eradicate polio virus is to build up immunity in the entire human
population. The PPI approach has proved that this can be achieved. It was used
successfully in Americas in the late eighties and in China in early nineties. It is
the WHO recommended strategy for global polio eradication. If India can
eradicate its remaining polio virus reservoirs, there is a very good chance that it
can be eradicated globally. Economic Justification
The economic case for investing 135 million sterling pounds (over five years) in
eradicating polio in India rested on two main groundsEliminating the distress and loss of income due to death and disability
Reducing and eventually eliminating the costs of treatment and immunization
programs
These benefits would be extended to a significant but nevertheless relatively
smal proportion of the population of India, and to potentially very large numbers
in other countries where polio has already been eradicated but where
immunization and other measures were still required.
If the project eradicates polio it would save all the DALYs associated with the
cases that would otherwise have arisen. In the present value terms the cost per
DALY averted is in the range of pound 90-350 based on an average life
expectancy of 55 years, which corresponds to range of possible cases that would
arise in the absence of the project. The data are too limited to indicate where in
this range the true value lies, because of the difficulty in predicting the number of
unrecorded cases. However we judge it unlikely that figure is below 100
pounds and it may be considerably greater.
In addition India would <eventually
'
benefit from reduced expenditure on
vaccines and patient care (upto pounds 7 million
i after 8 years). These
benefits are quite small.
Health interventions are onen
often juogeo
judged cost-effective
cost-effective ifif the
the cost per DALY
Pr,everit's within the Per capita GNP of the country covered. India’s per capita
GNP
pouns.
India
i
7 .. is 210 p— In '"‘■3 more
common benchmark is 66 pounds. The project
is
thus
relatively
expensive
but
not totally
■ .
n_■
------ j out of range of cost effective
^TeT/?n.Su There Wl be Other interver|tions in India ( to tackle other health
problems) that are more cost effective.
------------ On the other hand many current
Lessons from Global Polio Eradication Initiative in India-draft papcr-04/23/03
50
interventions cost considerably more 9 for example many forms of hospital based
care)
Much larger benefits would accrue worldwide. India remains a large reservoir of
polio virus imposing high costs on other countries when the virus is exported.
WHO has informed that Netherlands spent more than US $19 m in 1992/93 to
control an outbreak of more than 60 cases of poliomyelitis caused by wild polio
virus imported from South India. This was significant drain on Netherlands
national health resources.
The most impressive gain from polio eradication would be achieved when polio
immunization can be stopped globally. This would be most likely to occur three
years after the last reported case. It has been estimated that the cost of
protecting the world's children against polio is approximately US$ 3 billion per
year. No one country can stop immunizing unless all countries have achieved
polio eradication. Every year’s delay translates into another US$ 3 billion
that otherwise could have been saved. The economic benefits of
eradicating polio therefore enormously outweigh those of indefinitely
controlling the disease at a lower level of incidence.
The benefits will only be secured if India successfully completes the 5 year
program and eradicates polio.
Financial
The PPI program cannot be justified on financial grounds alone, as the additional
budgetary costs of eradicating polio are an estimated pound 30 million a year for
five years. While budgetary saving of pound 7 million will not be realized until
eight or nine years from now. But these savings do provide further justification for
eradication of polio on top of significant economic and social benefits expected.
The annual budgetary saving to MOHFW on vaccine alone on ceasing to have to
undertake the routine polio immunization program would be 34 crore (pound 6.6.
™l||on). There would be some delivery cost saving, but since polio is a part of
EPI, these are expected to be small. These savings should start some eight or
nine years from starting the pulse polio ( India will not be certified polio free until
there have been no reported cases of polio nation-wide for three years).
Smaller budgetary saving will arise from not having to meet the costs of acute
care and subsequent rehabilitation for polio patients in government hospitals An
estimated one third of polio victims seek treatment in hospitals at an estimated
average cost of around $ 250 ( both statistics taken from a forthcoming WHO
article on the cost benefit analyses of global eradication of polio). On these
figures the annual budgetary saving would be of the order of 216000 pounds.
Lessons from Global Polio Eradication Initiative in India- draft papcr-04/23/03
51
Social
Reduction in number of children suffering from polio-induced paralysis will have
significant social benefits. The children who otherwise would have been
paralyzed will be free of the anxieties, pain and social stigma attached to
disability and the additional obstacles disabled people have in finding
employment and participating in public life in India. Second the burden placed on
women to care for the polio disabled will be reduced.
World Bank Justification for the program:
“ Using standard public finance criteria, it is not difficult to justify public
involvement in, and financing of, strengthening the capacity to deliver and
monitor immunization and for the campaign to eradicate polio. Hammerf
Economic Analysis for Health Projects, May 1996) finds that infectious diseases
provide a prima facie case for government intervention on three grounds: (a)
externalities ( spread and incomplete course of treatment); (b) some options are
pure public goods ( vector control, information); and they disproportionately affect
the poor. While most non-information service are private in nature (rival and
exclusionary), there are substantial social externalities. The case of polio
vaccination is unique, however, in that it exhibits both characteristics of a public
good. When the vaccine is administered to many children orally in the
community, the virus multiplies in their intestines and released in much larger
quantity in excreta. This attenuated virus competes in the environment with the
circulating wild virus, which is responsible for polio. As a result benefits are non
rival and non-exclusionary and therefore public goods. Furthermore all the
elements of the behavioral change communication are pure public goods.”
Other issues discussed are
Equity: with the burden of vaccine preventable diseases falling on the poorest
and most vulnerable households, investments in vaccination program should
benefit the poor.
cost effectiveness- routine immunization in India is highly cost effective- cost per
DALY gained ranging from $5 to $37, while cost per death averted ranged
between $514 and 1233. Simulation for improvements in efficacy and
program coverage demonstrated a higher return to increase in coverage
lessons from Global Polio l.railication Initiative in India- draft paper-(M/2J/()J
I
i
52
and public- private roles—1997-98 less than 10 percent of immunization were
done in private sector and most of these were in urban setting
Sector issues
Despite the progress achieved, India's immunization program has the potential to
significantly increase its performance. First both human resources and the
physical infrastructure have declined since early nineties.
Technical and
program management competencies have gradually eroded in last several years.
Similarly cold chain and transport systems have weakened due to aging and
inadequate financing. Monitoring of cold chain functioning and vaccine supply
and logistics are inadequate. Second state level performances are highly varied,
with low coverage in Bihar and Eastern UP and six other states. Third in weaker
performing states regularity and/or geographic access to immunization sessions
is limited, and injection safety and client counseling is inadequate. And fourth
reporting of disease outbreak is weak, with the exception of polio, and the
capacity to respond to such outbreaks is almost universally inadequate.
19932 Intervention Characteristics and Cost effectiveness - Jamison and
others
$ 25 per DALY averted — for diphtheria, pertussis, tetanus
immunization
polio
other ranges
25-75 e.g. ORS
75-250- Schizophrenia treatment
;250-1000 e.g. antibiotic prophylaxis for rheumatic fever
1000 - COPD, surgery for rheumatic heart disease
— 95 --Cost benefit analyses by one donor agency based on WHO paper
If the project eradicates polio, cost per DALY averted is in the range of 90350 sterling pounds on average lige expectancy of 55 years ( based on
the presumption of 10,000-90,0000 cases averted.
1999 -Cost Benefit Analyses BY The same agency
Scenario
30,000 cases averted
50,000 cases averted
Base Case
128
73
Lessons from Global Polio Eradication Initiative in India- draft papcr-(M/23/O3
53
I
No Global eradication
151
87
NIDS upto 2003-04
220
125
NIDs upto 2003/04 NO
Global Eradication
246
140
These figures are higher than many other health interventions (i.e.
HIV/AIDS prevention cost estimated at $18 per DALY) but well below GDP
per capita ( US $ 440-1999) . The case for eradication is made more
broadly than national cost effectiveness but as part of global effort.
“Overall, the economic case for eradicating polio in India looks
reasonable provided program goes well. There are however
significant risks involved, so the case is not very robust. Thus the
main argument for proceeding with the project is on the basis of its
contribution to the global eradication program rather than because
of benefits that will accrue to India. “
Cost Estimates for the remaining countries for the Global Polio eradication -$ 12 billion
Projected savings? $ 1.6 billion poryQ^r
ITEM
DEVELOPED COUNTRIES
COUNTRIES
Vaccine
Saving
Delivery
Saving
$ 25 per child
$55m
$20 per child
$ 380 m
DEVELOPING
$ 0.48 per child
$460m
$ 6 per child
$ 700 m
Lessons fnim Global P9I10 Eradication Initiative in India- draft papcr-04/23/03
54
A2.4 IS POLIO ERADICATION A PRIORITY FOR INDIA
Tabic: Years lived with disability in India (YLDs) in thousands —year 1994
Total
Childhood Cluster
Pertussis
Poliomyelitis
Diphtheria
Measles
Tetanus
92,070
1738
199
1484 ( polio and non polio included)
35
19
1
Polio is a preventable and eradicable disease because it spreads from one
human to another and no other vector animal or insect is involved. It is primarily a
disease of very young. 90 percent of the people who become infected do so
when they are less than 3 years old. It affects the poor hardest with most cases
found in urban slums.
Although India has ono of the highest incidoncos of polio in the world, it
represents a small proportion of the total burden of disease. In 1990 it accounted
for just 1% of women’s infectious disease burden (DALYs) and 1.5% of men’s
burden. However, because it affects the very young, it represents some 10
percent of the disease burden among children suffering from the most common
childhood ailments in India (the so called childhood cluster of diseases) - check
the data and source
WHR-2001- SEARO region
High Child high adult morbidly population -1.24 billion see the table below for
contribution of paralytic poliomyelitis to DALYs in the SEARO region:
Ia'SSOHS from Global Polio Eradication Initiative in India- draft papcr-O-t/lJ/IIJ
55
Table: Co
C ntribution of paralytic poliomyelitis to the total DALYs
Total DALY
---------- —
3,64,581
1,63, 137
Communicable diseases, Maternal and Peri-natal
Conditions and nutritional deficiencies
Infectious and Parasitic diseases
Tuberculosis
STD excluding HIV
HIV/AIDS
Childhood diseases
Meningitis, Hepatitis Malaria
Tropical diseases- Trypanosomiasis, Chagas Disease,
Schistosomiasis,
ILeishmaniasis,
Lymphatic Filariasis',
Onchocerciasis
Leprosy, Dengue, JE, Trachoma
Intestinal Nematodes, Ascariasis, Trichuriasis, Hookworm
disease
Respiratory infections-Acute lower Acute upper, Otitis
media
Respiratory Infections
Maternal Conditions
Perinatal conditions
Non Communicable Diseases
----------Malignant Neoplasm :Mouth and Oro-pharynx, esophagus,
stomach, colon/rectum, pancreas, trachea/bronchus/linq’
breast, cervix, corpus luteum, ovary, prostate Bladder'
lymphoma, leukemia
1,55,306
Other Neoplasm
Diabetes Mellitus
I
Nutritional /endocrine disorders
Neuropsychiatry disorders-Uni-po|ar major depressionbipolar affective disorders; psychoses; epilepsy alcoholic
dependence; Alzheimer and other dementia; Parkinson's
disease; Multiple sclerosis; Drug dependence- PostTraumabc
stress
_disorders^_Obsessive-Compulsive
Ia-sxoiis fmm Global Polio lliadieation Initiative in India- draft papcr-(M/23/03
56
disorders; panic disorders
Sense Organ Disorder-Glaucoma: Cataract
Cardiovascular Diseases: Rheumatic heart disease;
Ischaemic heart disease; inflammatory cardiac disease.
Respiratory diseases:
disease; Asthma
Chronic
pulmonary
obstructive
Digestive Diseases: Peptic Ulcer Disease; Cirrhosis of Liver;
Appendicitis
Diseases of the genitourinary system-Nephritis/Nephroses;
Benign Prostatic hypertrophy;
Skin Diseases
Musculoskeletal
Osteoarthritis
diseases-
Rheumatoid
Arthritis;
Congenital Abnormalities
Oral Diseases:
Edentulisms
Dental
Caries;
Periodontal
disease;
Injuries
Unintentional: Road Traffic accidents; Poisoning: Falls;
Fires; Drowning; Other Unintentional Injuries
,
46,138
Intentional: Self Inflicted; Homicide, Violence; War
_______________
Out of these polio
i
Only62
lessons from Global Polio Eradication Initiative in India- draft papcr-O-l/23/OJ
57
ANNEX-3 LESSONS FOR
COOPERATION IN HEALTH
HEALTH
POLICY
AND
INTERNATIONAL
A-3.1 Evidence Based Policy Making
In Most areas in public health interventions the links between evidence and the
policy decisions, between before and after impact of the interventions
are either
tenuous or may not exist at all. There are several reasons for this:
The baseline or benchmark data may not be available. In fact the program
inten/entions invariably have as one of their objectives to create such a data
for the first time.
The nature of change in the specific health area may be amenable to a
vanety of influences and not just the proposed intervention
Z The sppropnate indicator for the proposed change in the health status may
not be available.
7
J The impact may appear not immediately but some years after the
cl'angTs'0115
hGnCe ear1y assessment may not demonstrate the desired
I
The changes may be present but may not be measurable.
Stly undertaking meaSurement and demonstrating impact may be a very
Therefore health policy decisions are more determined by the political influences
or compromise between different technical experts and the evidence-based
policy making cannot be taken absolutely literally. While process indicators are
mostly selected as proxy measures for monitoring the success of the program
interventions, these do not really solve the riddle. Good evaluation studies in the
long term can provide the only answer.
In the case of paralytic poliomyelitis we have already raised the following issues:
✓ The estimation of actual number of cases in the past from the reported
cases that came from very inadequate surveillance. We have tried to
question the multiplication factor of ten for this purpose. However this is
open to further discussion.
More importantly we have demonstrated that the case definition has now
changed and only,the virologically confirmed cases are being reported.
This could be one reason for decline in cases of poliovirus paralyses and
we might be overestimating the impact of the pulse polio immunization
lessons from Global Polio Eradication Initiative in India- draft |>a|ier-()4/23/03
58
activities. (Reference- Vaccines and Biologicals; WHO vaccinepreventable diseases: monitoring system; 2002 global summary-paqe 20poliomyelitis).
J Even more important is the issue raised by us of extrapolating this new
information to estimation of the actual number of paralytic polio cases in
the past due to poliovirus. This is important to assess the public health
priority of this intervention. If large number of reported polio cases in the
past were not due to poliovirus (which was not possible to detect at that
time due to non-availability of laboratories), then the justification for this
gigantic effort becomes even more questionable. It should be kept in sight
here that polio eradication program is targeted on the polio-virus only and
not on the acute flaccid paralyses of children or all cases of residual polio
paralyses of children which may be just ten to twenty percent of the toal
cases.
It will be useful to give a list of number of public health programs that face this
measurement problem:
Public Health Program
Measurement Problem
Water and sanitation programs
Difficult to measure improvement in
waterborne
and
water
washed
diseases. The improvement in hygienic
practices is used as one of the proxy
measure.
Difficult to demonstrate actual impact
on disease prevalence. The condom
uses has been used as proxies
measure in the past. New indicators
have been added in recent years.
Difficult to measure the rmpact onlhe”
prevalence of disease and reduction of
multi-drug
resistance
TB.
The
treatment completion rates have been
used as a proxy measure
Difficult to measure impact on the
reduction of infant and child mortality.
Service use data have been used as ■
proxy measures.
•
I
Difficult to measure the impact on the i
actual change in practices. The change ;
in knowledge and attitudes have been
used as proxy measures
HIV/AIDS prevention program
Tuberculosis Control Program
Primary health care programs
Reproductive Health Programs
Lessons fnmi Global Polio Eradication Initiative in India- draft papcr-04723/03
59
A-3.2 Role of WHO other UN organizations and Global Public Private
Partnerships
One may wonder why a reputed organization like WHO should not render wise
counsel to India on its health program priorities and the feasible ways of
achieving it. WHO and UNICEF enjoy universal respect as being the custodians
of the international expertise on the technical health issues and also the
neutrality of the UN organizations. However it is also a fact that many UN
institutions including WHO have come under increasing criticism for being
monster bureaucracies who have been unable to perform to the desired
standards and mandate. The failure of WHO in Roll Back Malaria Program and
dubious success in RNTCP is well known. In the case of Global Polio Eradication
Program also launched since the year 1988, its reputation is completely at stake.
It is natural, therefore, for WHO to push India to further intensify the pulse
polio program and strategy rather than admitting limited gains and
withdraw honorably from it. The G-8 nations are also providing liberal grants to
the WHO and developing countries for the Global Polio Eradication on the
recommendation of WHO to enable it to salvage its reputation. However they are
doing it year by year and reserving the option to withdraw if they do not see the
desired results. In that eventuality India will have no option but to withdraw from
this very expensive strategy which it cannot afford to spend from its meager
health budget.
It is difficult to find out whether the multinational vaccine Industry is playing any
role .in influencing these recommendations of WHO and UNICEF. It is a known
fact that UNICEF has the monopoly on the procurement of the vaccine and gets
twenty- percent commission from this. Therefore it has a vested interest in the
entire program and has no right to render technical advice on it.
Another dimension is added to the entire situation by the introduction of the
newer expensive vaccines for many other diseases by the multinational
vaccination Industry and marriage of WHO with this industry. Hepatitis B vaccine
has already been accepted in India for part-introduction in the selected districts of
he country under the general vaccination program for the children. Several
newer vaccines are already on the table. These so called national programs are
now being promoted by the liberal grants offered by Gates Foundation in Andhra
Pradesh in India and globally through the GAVI initiative in WHO chaired by Bill
Gates. It is expected that after initial phase of grant funding by these foundations
the national government and the state governments will bear these costs from
their own budgets. Whether these expensive vaccines are required as per the
epidemiological profile of the country and the financial priorities for the disease
control programs and health systems development is open to debate.
It is not our intention to here to find fault with any organization. It is natural to
WHO' was emboldened by the success of the strategy in Latin
believe that WHO
lessons fnmi Global Polio Eradiation loi(ia(i\ r in India- dral( papcr-0-4/23/03
60
America in early nineties and the new success in Western Pacific Region
including China in late nineties. It had therefore a strong ground to believe that
the same performance could be repeated in India given the sufficient resources
and efforts and despite the fact that India had poorly performing general health
systems. That is the kind of fundamental logic with which WHO and donors have
been working since nineteen eighties and this is not the place to question this
logic. However acceptance of good intentions of WHO does not help us here. We
have to scrutinize whether WHO has the capacity to render sound technical and
policy advice to us in this difficult situation and how we should apply our own
wisdom to sift through the options placed before us by the WHO technical
experts in the field and choose the best option for us and not follow the WHO
dictate in this matter. In this context we would like to highlight that there was
substantial shift between 1994 and 1999 when WHO proposed a IPPI instead of
shifting to localized campaigns and strengthening routine immunization as was
envisaged originally in 1995-96, after the polio cases drop significantly due to the
NIDs . The cases did drop but WHO insisted on the intensification of the
campaign on the plea that routine immunization was poor in some states and in
order to build sufficient resistance, number of SIA should increase. This has
costed the country dearly.
Child vaccination project (Andhra Pradesh) funded by the Gates Foundation
does envisage the cost to be met from the budgetary resources of the state
government or the grants from the central government. Therefore the sustenance
of the financial resources by grant mechanism is not possible and we have to
take into account our priorities before taking any program for implementation. »
There is no free lunch in the world. Even if there is one, we need to see whether
we really need it?
Public-private health partnerships: a strategy for WHO
Ln 1993 the World Health Assembly called on WHO to mobilize and encourage the
support of all partners in health development, including non-governmental organizations
and institutions in private sector, in the implementation of national health strategies for
health for all. Subsequently the interaction with commercial sector has broadened and
deepened. WHO participates in a number of global public private pailncrships. These
collaboiative relationships transcend the national boundaries and bring toeelher al least
tow parties, a corporation (or industry association) and an intergovernmental
organization, in order to achieve a health creating goal on the basis of mutually agreed
and explicitly defined division of labor. Nearly 70 global partnerships have been
identified.
Table: List of WHO Public Private Partnerships
_______________ ____________________ i___________________
European Partnership Project on Tobacco Dependence
Global Alliance for TB Drug development
Lessons from Global Polio Eradication Initiative in India- draft paper-04/23/03
61
Global Alliance to eliminate Lymphatic Filariasis
Global Alliance to eliminate Leprosy
Global Alliance for Vaccines and Immunization
Global Elimination of Blinding Trachoma
Global Fire Fighting Partnership
Global Partnership for healthy aging
Global Polio Eradication Initiative
Global School Health Initiative
Multilateral Initiative on Malaria
Medicines tor malaria ventures
Partnership for parasite control
Roll Back Malaria
Stop TB Initiative
UNAIDS/lndustry Drug access initiative
Views on Public private partnerships
Kent Buse
kriifhiisr
Amalia Waxman
ale • :
Public-private health partnerships : a strategy lor WHO
Public-private partnerships have elicited strenuous objections. The types of questions
that have arisen include: are partnerships desirable, and under what circumstances, from a
societal point of \iew? What are the appiopiiale criteria foi sekctiun of candidate
companies, industries and activities, and how are such criteria de\clnped'5 I low can
intciactions be stiucluied and monitored in oidt-i to avmd m dc.il wnh conlhci ol
interest? I low can partnership be made to function in accordance wnh principles ofeood
governance0
Lchsuns from Global Polio Eradication Initiath e in India- dr aft papcr-04/23/03
62
In relation to WHO, critics believe that some of their fears arc materializing. For
example, it is charged that the independent setting of standards was jeopardized during
elaboration of guidelines for the management of hypertension because of influence of a
firm that stood to benefits from them. Similarly, is ahs been asserted that deliberations on
unj^feCdln8 Were subj.ccl t0 ‘censorship’ because of consideration of sensibilities of
WHO s new commercial constituencies. Others argue that WHO’s emphasis on
marginalized will be displaced as resource rich partnerships dictate organizational
priorities and strategics. It has been suggested that WHO’s involvement in Global
lance for Vaccines and Immunization has derailed its commitment to equity in relation
to the goal of universal vaccination with traditional vaccines, as it joins its partners in
ringing new vaccines to relatively less hard to reach. Moreover for understandable
reasons, partnerships sometimes focus, at least initially on countries and activities that
offer reasonable chance of success. Thus they usually concentrate on relatively affluent
countries rather than on those that are very poor, and on drug donations and development
instead of the more difficult challenges of capacity development for service delivery and
research in low-income countries. Yet even relatively non-controversial initiatives such
as donation programs, may have considerable and unintended consequences linked for
C°S^ 10 rec'l)icH,s’ sustainability and equity, which could damage
WHO s reputation by association^.
Robert G. Ridley-( e-mail- rid leyr6'/)jnin v.org)
Chief Scientific Officer, Medicine for Malaria Venture,
It is vitally important that public and private sector discussion, engagement and
partnership are raised to a global level. Despite the competitive environment in which the
pharmaceutical industry operates, there ought to be mechanisms whereby an increased
amount of its huge resources and expertise can be targeted towards tackling the diseases
of the poor. Similarly if the public sector is to take lead in this whole area it has to
commit resources that can realistically incentivize private sector partnership and
investment. One ol (he biggest incentive for companies, private foundations and other
non-governmental organizations to commit (hemselves (i.e.provide resources) to a
partncrslup is hawng the confidence that public sector is serious about developing
appropriate infrastructure and capacities necessary to use partnership outputs for
e',l,ancing global health. 1 he increase in resources that have been made available by
both public and private sectors in recent years, complimented and m manv cases
stimulated by philanthropic donations, suggests that sufficient political will is developing
to make an impact. Both public and private sectors in recent years stand an improved
chance ol delivering on their objectives if they can find better ways of collaborating”.
James Grbmnski- ( e-mail- jani^mJunski^ii^^
1)^ |.or l1cg|cclcd
Canada^ W0I^in^ ^roup- Munl< Centre for International studies. University of Toronto,
Lessons rrom Global Polio Eradicalion Initial!
ivc in India- (h alt |)a|)cr-()4/24/()3
63
“ Charity and philanthropy have been key and welcome driving force behind most publicpi ivate partnerships. IVhile helpful and catalytic, tliouyli, they are not a substitute for
good and responsible government in the North and South. Even within a clear vision and
mission, public-private partnerships cannot displace the responsibility of government to
ensure and promote people right to equitable access to health care, and to set the health
agenda both nationally and globally. Public-private partnerships, their stakeholders and
national citizens must insist that government and intergovernmental institutions fulfill
their responsibilities in properly funding and directing need based K&D. Governments
stdl have a duty to ensure that appropriate resources and capacity exist in independent
national and intergovernmental institutions to set, drive, monitor and critically
evaluate the national and global health agenda. This is a minimum requirement and
goes far beyond the disease specific initiatives which typify most new public-private
partnerships”.
Public Private Initiatives in Health at the Global Level
Woikslmp organize.
ring (lie World Social Forum in Porto Alegre, 25 .lamian-
2003
'
J
Background paper
1. Position
As a result of globalization, the influence of the multinational corporations at the global
level has increased enormously. This influence has stretched out into the social sphere
and also in the international political ambits, like UN-system.
In 1999 Kofi Annan said to the World Economic Forum that the UN once only dealt with
governments but that by now he knows that peace and prosperity cannot be achieved
without partnerships involving the business community. Also the director of the WHO,
Gro Harlem Brundtland, has affirmed several limes that today’s health problems arc so
vast and complex that tackling these problems requires (he participation of all sectors,
including the business sector.
these statements reflect the recent trend of mushrooming of' initiatives, especially in
health, whereby UN institutions like WHO and Uniccf collaborate with pharmaceutical
companies and foundations such as the Bill and Melinda Oates Foundation. They tackle
health problems like the vaccination of children, the lowering of prices of patented
dings, the development ol new medicines and drugs for tropical diseases, etc. These
so-called global public private initiatives allow the UN institutions to access financial
icsourccs (hey could not access before and proc ides the business sector cc ith
opportunities to influence health policies as they never could before. For example:
Lessons from Global Polio Eradication Initiative in India-draft paper-04/24/03
64
one of the conditions of the industry in the Accelerating Access Initiative1 was that
countries that wanted reduced prices for anti-retroviral medicines would not allow
import or production of cheaper generic versions produced in Brazil or India. In
addition the industries involved, which often arc pharmaceutical companies, can and do
use these initiatives to raise (heir public profile.
From our perspective as civil society organizations working on the right to health, this
new phenomenon raises many questions. The most fundamental question is whether
public interests and values like equity and universality can ever be compatible with
private interests and values of free entrepreneurship, raising profits and rewarding
shareholders. Therefore it is of critical importance to know -apart from the goals- how
decisions are taken, how accountability is arranged for, how the operative systems
aic oiganizcd and how sustainability is assured. All these points involve many risks.
1 hese aspects have important consequences in public health and development terms.
So far little information is available about the real benefits these initiatives have delivered
for especially vulnerable and excluded populations, and for the strengthening of
comprehensive health systems. The information that wc do have is not very
promising. Until now only a few thousand 1HV/AIDS patients in Africa benefited form
the drugs that have been made available through the Accelerating Access programme,
while millions of people suffer from the disease. And it was the countries themselves that
had to take care of transportation and distribution of the drugs, which meant that they had
to divert funds and manpower from other health activities. The worst of it all was that the
prices negotiated were even higher than (he prices of generic drugs coining from
India.
2. Historical Background
Going back in history it appears that until the 1970’s, international cooperation in health
was driven by the notions of basic needs, participation and social justice. In 1978 the
international community adopted the Alma Ata declaration in which health for all by the
year 2000 was proclaimed. Important principles of the Alma Ala declaration arc: integral
approach to health, comprehensive health care, prevention, primary health care and
community participation.
However, in the 1980’s the world was hit by an economic crisis and the financial support
for health and health care decreased very quickly. At the end of the decade, the World
Bank and IMF introduced their Structural Adjustment Programs. What was left of Alma
Ata was a selective Primary Health (’arc approach, whereby vertical vaccination and
programmes were carried out.
In the Accelerating Access Initiative 5 UN organisations and 5 pharmaceutical companies
work together to lower the price of patented retrovirals. Price negotiations take place with
individual countries and are secret.
Lessons from Global Polio Eradication Initiative in India- draft papcr-0-4/24/03
65
In the 1990’s after'the falling down of the Berlin Wall a change started. In line with neo
liberal thinking, health is promoted as a private asset in stead of a human right and a
public good. Increasing participation of the private sector, less governmental
involvement, privatization, the introduction of user fees and so on arc the main features
of health policies. In international health, this tendency has had a critical point with the
publication of the World Development report 1993 of (he World Bank, ‘Investing in
health’ that was the start point for the I lealth Sector Reform policies. The need to invest
cost-effective interventions was elaborated and developing countries
in selected, cost-clIcctivc
were seen as markets.
I his tendency of less government involvement and (he introduction of' market
mechanisms were promoted in many social sectors. Health was considered a commodity,
Although already in the 80’s vertical vaccination programs were introduced whereby the
public and the private sector collaborated, we see more and more initiatives with a topdown, narrow approach of health problems in which technologies and
pharmaceutical producers (pharmaceutical transnational companies) play a
dominant role. Consequently the number of this kind of programs increased steadily.
At the present time we face a situation whereby some transnational corporations are
financially bigger than many small Southern countries. In the international arena, they
have become major players and influential actors that make use of the fact that their
conduct is essentially regulated on a national level. At the international level they lobby
for rules and regulations that protect their patents, their investments and their market
access.
We see that due to the increasing gaps between rich and poor countries and between
social groups within countries, several communicable diseases related to poverty and
the lack of fulfdlment of basic needs have taken astonishing proportions (AIDS,
Malaria, TB and others). New Public Private Initiatives are expected to play a role
attacking these problems. But the proposed approaches seem emergency actions (top
down, non integral approach, without strengthening local structures, magic bullets, etc)
that respond more to the immediate interests of the partners involved than to the real
needs of the affected populations.
3. Issues to be debated
Since the mushrooming of Public Private Initiatives at the global level is a very new
phenomenon, the analysis of this trend encounters difficulties. The first problem is the
number and the diversity of these initiatives. Today more than 80 have been identified,
all having their own goals, structures, ways of operation, funding mechanisms etc.
A second major pioblem is the definition of what Public Private Initiatives exactly are:
who are the partners, what is partnership. A critical aspect is: What is private? Does it
include NGO s and other civil society organizations? 1 low should the big foundations
like the Gales Foundation be classified?
Lessons from Global.Polio Eradication Initiative in India- draft papcr-04/24/03
66
Next to this, other fundamental questions arise like: Who decides in a partnership and
who should decide? What is the desired governance structure? Another crucial issue is
accountability. Most of these initiatives have autonomous secretariats and boards. At the
same time, they are closely related to the UN'-syslem: in fact, the UN is part of these
initiatives. In this way, situations arc created that could pul al risk the independence and
legitimacy of the UN itself.
It is very clear that the values and motives of the actors differ. A fundamental
question is whether the motives and values of a public body can al all be joined to the
values and motives of a business entity without losing its critical functions. It is of
critical importance to know how a specific PPI was established and whose interests
predominate when decisions arc taken. The issue of accountability is also a very
crucial one, since many these initiatives have their own secretariat outside the UNsystem.
Due to the complexity and magnitude of some health problems, PPI’s in health at the
international level can offer some opportunities like: additional financial resources for
health, increasing attention and political support for health, the involvement of new social
actors, etc. But we must also be aware of the considerable risks involved: conditionality
of financial support, pulling resources from donors, lack of attention for equity and
non-discrimination, establishment of parallel systems, the weakening of the already
feeble health systems in developing countries and lack of sustainability.
/
We feel it is very opportune time that a public debate lakes place on:
Arc these PPI’s desirable and appropriate to solve major health problems of
poor countries? Which alternatives do exist to tackle these problems?
Since they became so frequent: criteria are needed to assess their impact in terms
of: outcomes for public health, outcomes for poor and excluded groups, outcomes
in terms of outputs, outcomes related to the objectives of the partners.
- The need to have more public information on the effects of PPIs on public
health, health systems and the realization of the right to health for all. How
equitable arc these initiatives?
- The interrelation with WHO: Clear guidelines for interaction are needed to avoid
the risk of fragmentation and the loss of credibility of the international
regulatory system.
The real motivations and interests of pharmaceutical companies involved in
these initiatives. What are the effects of these partnerships in terms of increasing
the power and influence of these transnational corporations at the national
and international level?
We would like to start that debate today.
Wemos, the Netherlands.
Lessons from Global Polio Lradicalion Initiative in India- dealt pa|)er-0 l/24/03
67
q
’H I -
DRAFT REPORT
ON
CASE STUDY ON PULSE POLIO INITIATIVE
IN
MURSHIDABAD DISTRICT
WEST BENGAL
INDIA
BY
SUBHANKAR, SANGHAMITGRA, D.P.PODDAR, DR. U.K.BHADRA
SUPPORTED BY
WEMOS, HOLLAND
i4
CHAPTER
No.
Particulars
Page No.
1.
Introduction
3
2.
Objective of the Study
3
3.
Area of the Study
3
4.
Methodology
4
5.
Logistics
6.
Findings on the Polio Programme - Coverage Study
5
7.
Profile of the Respondents
6
8.
Findings on Health Determinants- Drinking Water and Sanitation
facilities
8
9.
Findings on the Polio Programme - Household Study
9
10.
Findings on the Health Infrastructure
15
11.
Cold Chain Maintenance
17
12.
A Note on Rights to Health
18
13.
Conclusion and Recommendation
19
5
ANNEXURE
I
List of Samples
II
Health Infrastructure in Murshidabad District
III
Achievement of Universal Immunisation Programme, Murshidabad
IV
Field Visit Report
21
23
24
25
1.
INTRODUCTION
This Report is places the salient findings of a Survey conducted in selected Blocks in the
district of Murshidabad district, West Bengal focusing on Pulse Polio initiative and some
selected issues pertaining to rights to health of the marginalized section of the society
2.
OBJECTIVE OF THE STUDY____________________
A survey of Pulse Polio Immunisation Initiative at the local level
To explore the health infrastructure at the local level in order to assess in
what manner the rights to health of the marginalized people are protected.
3.
AREA OF THE STUDY
3.1
General
The Study was conducted in selected Districts in Murshidabad. Murshidabad has
indelible place in the history of India. It was in the battle of Plassey that the then Nawab
of Murshidabad, Siraj-ud-dowlah lost to Robert Clive of East India Company and The
English East India Company made entry into India.
?KOm.'u9 ‘2 the present context, a part of the district has Bangladesh on one side and
Jharkhand on the other. The main river of the land Bhagirathi runs through the district.
Proximity to national and international border makes a part of the district accessible to
migrants with associated problems. The following table gives brief introduction to the
district.
Table I
Brief Profile of Murshidabad District
Area
5324 Sq. Km.
Population (as per Census 2001)
58,66,569
Sex Ratio
51.22:48.78
Density of Population (Per sq. Km.)
1101
Literacy Percentage
55.07
No. of Sub divisions
5
No. of Blocks
26
3.2
Area under focus
The area where the Study was carried out was divided into two virtual zones:
1.
Zone H : consisting of sampling units that are ‘High Risk’
2.
Zone L : consisting of sampling units that are ‘Low Risk’
The risk factor assigned to the areas has been as per perception of the District Health
Administration.
The Zone H Consists of sampling units in Dhulian town, Farakka, Samsherganj block,
Suit-I block, Suti-ll block, Raghunathganj-I block, Raghunathganj-ll block.
The Zone L consists of sampling units in Murshidabad Jiaganj, Murshidabad town,
Berhampore block, Beldanga-I block, Beldanga-ll block.
The zones are demarcated in the map enclosed.
4.
METHODOLOGY
The study was based on Cluster Sampling as per WHO guidelines.
In the context of this study, Cluster means Village Units or Wards in Urban
Municipalities.
30 Clusters were selected in each zone.
Clusters were selected purely on random basis.
7 Households were selected in each cluster.
The sample size in each Zone is 210
The rural-urban mix of the sampling units in two clusters was almost equal.
The Total sample size for two zones combined together is 420.
The List of samples are furnished in Annexure I
The Study has been carried out in two parts.
The first part seeks to assess the Coverage of the Pulse Polio Immunisation
Drive for three National Immunisation Days; February 22, 2004, January 4
2004 and November 9, 2003.
This particular survey is conducted on the basis of randomly selected 7
consecutive children in each cluster.
The second part of the study concentrated on 7 families, each one havinq at
least 1 eligible child.
The household were selected on the basis of two eligibility criteria;
The household is required to have a child aged equal to or below 5 years.
The child was to live in the area continuously for at least six months.
5.
LOGISTICS
The study was carried out for three days on March 27, 28 and 29, 2004.
40 Investigators and 10 Supervisors were employed for data collection. A One-day
Training session was organised for the Trainers and Supervisors by the Research Team
and Experts.
The total distance covered to reach the villages and town, selected randomly was
approximately 3500 km.
Two sets of questionnaires were specifically framed to assess in what manner rights to
health are protected in the context of the IPPI Programme. One was o assess Coverage
and the other was intended for the Household-level study. Therefore, the scope of the
study goes beyond a mere case study of Pulse Polio.
Apart from the Questionnaire Survey, viewpoints and opinions were solicited from senior
theCRep a^S0C'ated with Pulse Polio Pr°gramme- Their inputs have been incorporated in
The Research Team also visited the Pulse Polio Booth on the NID dated February 22,
2004 the details of which are also included in this Report.
6.
FINDINGS OF THE POLIO PROGRAMME - COVERAGE STUDY
The following two tables give the findings of the Coverage Survey in two Zones.
Table II
February 22, 2004
Participated
Did not
Participate
(%)
(%)
98.09
Pulse Polio Coverage - Zone H
January 4, 2004
Participated
Did not
Participate
(%)
(%)
November 3, 2003
Participated
Did not
Participate
(%)
(%)
1.91
92.86
Table III
Pulse Polio Coverage - Zone L
February 22, 2004
Participated
Did not
Participate
(%)
(%)
7.14
January 4, 2004
Participated
Did not
Participate
(%)
(%)
90.95
9.05
November 3, 2003
Participated
Did not
Participate
(%)
(%)
99.52
0.48
98.57
1.43
97.14
2.86
It is evident from the above findings that the Coverage Ratio is quite high and for the
people under the sample the coverage ratio seems to increase with every NID.
According Dr. B.R. Manna, Joint Director of Health Services, Department of Health
& Family Welfare, Government of West Bengal, ‘the coverage for the Pulse Polio has
touched 98% in the recent NIDs. Still, there exists some loopholes in the system which
prevents cent per cent coverage. Around 0.15 to .20 million children fall outside the
Pulse Polio Net for every NID. Efforts have been intensified, in many cases in
collaboration with the NGOs to close this gap.’
7.
PROFILE OF THE RESPONDENTS
This section deals with the profile of the people under the Household Survey.
ZONE H
7.1
Income Status
Table IV
Income Status of the Respondents
ZONE
Below the Poverty Line (BPL) (%)
Above Poverty Line (APL) (%)
H
71.43
28.57
L
71.04
28.96
It is evident from the above data
The sample consists predominanatly of economically marginalized people
7.2
Occupation Profile
Table V. Occupation Profile of the Respondents
Occupation
H
L
%
%
Daily wage earner
70.48
72.38
Service
7.14
6.67
Self Employed
17.15
17.14
Uemployed
1.90
1.90
Other
3.33
1.91
It is evident that the occupation structure of the respondents of the two zones is almost
similar.
7.3
Education Status
Table VI
ZONE
H
L
Education Level of the Respondents
Education Level of Mother
Attended
Not Attended Illiterate
School
School but
able To Read
(%)
(%)
(%)
26
22
52
51
16
33
Education Level of Father
Attended
Not Attended
Illiterate
School
School but
(%)
able To Read
(%)
(%)
36
33
31
50
20
30
It is evident from the above table that
The percentage of illiterates are more among women for Zone H
Also for Zone H, general level of education is higher among men. Percentage
figures are higher for both level of formal education and literates for men.
Zone L has much better literacy and general education indicators for women.
The respondents were asked to tell the date of birth of their child. The findings revealed
O/o °f the respondents in Zone H failed to inform the exact date of birth of
the child, either according to English or Bengali Calender.
Si?”16 L’ tt!i! fi9Ure 'S considerably lower at 35%. Relatively high literacy
rate among mothers may be one of the factors.
entitemtents for^eehlw^Lture.^ ft16 Ch"'S ‘’aS i"’POr,an' tain9 °n health a"d 0,her
7.4
Religion Profile
Th erespondents of the Survey in the Zone H has twi
ro religious groups. The break-up is
given as follows:
Table VII
Religion Profile of the Respondents
Religion Group
Muslims
H
L
%
%
64
33
Hindus
7.5
36
67
Caste Profile of the Respondents
Table VIII
Caste Profile of the Respondents
H
L
%
%
Scheduled caste
16.00
26.00
Scheduled Tribe
0.50
16.00
Other Backward Classes
6.00
6.00
General
77.50
42.00
Caste
Muslims have been assumed to belong to General Caste.
8.
FINDINGS ON HEALTH
SANITATION FACILITIES
DETERMINANTS - DRINKING WATER AND
Drinking water and sanitation facilities are two of the most important health determinants
^“^'^nx9^yheal,h- ™8 SMi°"seeks to
8.1
Drinking Water
In Zone H, out of the households surveyed, 99% have Tubewell as the source of
Drinking water. However, 1% of the respondents still use pond water as the
source of drinking water.
J" Z°n® L, 96% of the respondents reported Tubewell as the source of Drinkinq
Water, 2% reported Pond/River and 2% others, mainly Tap water.
Perception on Arsenic contamination among the respondents was investigated. The
findings are summarised in Table IX.
Table IX
Perception on Arsenic Contamination
Perception on Arsenic Contamination
H
L
%
%
Think water to be Arsenic Free
Think water to be Arsenic contaminated
29
23
25
11
Do not know
48
64
8.2
Sanitation Facilities
The quality of Sanitation facility is generally poor and this is evident from the following
table.
Table X
Nature of Sanitation Facilities
H
L
%
%
Do not have Sanitation facilities
76
56
Have Sanitation facilities
34
44
Type of Sanitation Facilities
Although the situation somewhat better in Zone L, still sanitation Coverage is generally
poor.
9.
FINDINGS ON THE POLIO PROGRAMME - HOUSEHOLD STUDY
The results of the Survey conducted in Zone H gives the following results.
9.1
Participation
In Zone H, children in the 91% of the Households participated in the three
consecutive Pulse Polio NIDs in November, 2003, January 2004 and Februarv
2004.
7
This figure is 95% for Zone L.
The Survey brings out wide coverage of the Programme, which is tandem with the
claims of the Government.
How the Jola Community was won over
The Jola community, by religion Muslim, in the Suti-ll Block of the Murshidabad district
showed resistance to Pulse polio Programme for two years. According to Mr. Amitabha
Mukherjee, former District Governor, District 3290, Rotary International, innovative
approaches were adopted to bring this community in the fold. Majority of these people
work in the local tobacco (bin) industry. Almost all of them are regular visitors to a local
red light area and the Commercial Sex Workers seemed to have considerable influence
on them. The Commercial Sex Workers were sensitised about the utility of the
Programme so that they could transmit this message to these people. Additionally the
owner of the factory with which these people are associated either as employee or as
daily labourer was also sensitised and was made a Rotarian. He issued instruction to
these people to participate in the Programme. After this, the participation has been
almost universal.
/
z/k. f t < zr
4 /4
9.2
Place for Vaccination
In Zone H, 82% of the children went to PP Booth for Immunisation, while 18%
took vaccination at home.
This figure is 96% for Zone L.
Table XI
Proximity of the Polio Booth from Residence
H
L
%
%
Within Walking Distance
70
52
Not very far
27
43
Too far
2
1
Dn Not Know / Cannot Say
1
4
Proximity of the Pulse Polio Booth
from Home
Those who took the vaccination at home expected the Health workers to come
home for vaccination.
9.3
Reasons for Non-participation
The figures for non-participation is low and the figure is gradually on the decline.
However, since the Pulse Polio Programme has Complete Eradication of Polio as the
sole objective, every reasons for non-participation, even by a handful people deserves
special look.
The reasons for non participation on fthe basis
\ of replies rerceived from the respondents
who did not participate in the Programme are as follows:
Table XII Reasons for Non-participation
H
L
%
%
Never heard
10
60
Not aware of time & day
5
No visit by service providers
15
The child was travelling to other place
25
Reasons narrated for non-participation
9.4
The child was sick
20
No one to take the child to the Booth
20
Inconvenient day/time/venue
10
Session not held
5
Advised by doctor
5
Rumour on side effect
5
Fear of getting polio after vaccination
5
Community boycott
15
Type and Level of Awareness on Pulse Polio Programme
The Government machinery, along with the partner organisations make elaborate
arrangements to inform the people about the Pulse Polio Programme. The study sought
to capture which form/s of messages are received by people on the Pulse Polio
Programme. The findings are given in Table XIII.
Table XIII
Source of Knowledge on the Pulse Polio Programme
Source of Knowledge
H
%__
Loudspeaker / Drumbeating
Health Worker
31.28
"18.21
TV
Radio
Anganwadi Worker
11.79
8.97
7.69
13.00
8.50
9.50
Wall Painting / Posters / Hoarding
5.64
’ 8.00
People’s Representative
Nobody / Never heard of IPPI
4.36
4.10
1.00
0.00
Newspaper / Magazine
2.82
Too
Relative / Friend
T?9
1.00
Religious / Community Leader
"1.03
Teacher
Private Doctor (General)
0.77
0.51
Govt. Paed(Splst)
0J51
0^26
0^26
Tso
Tso
o.oo
Too
Too
Too
Govt. Doctor (General)
Pvt Paed (Splst)
L__
%__
25.00
30.00
Opinion was solicited from the respondents to ascertain their perception on the necessity
of the Pulse Polio Programme and whether they feel Polio as a major threat.
Around 85% of the Respondents in Zone H, feel this Programme as
‘necessary’.
In Zone L, 95% of the respondents feel this Programme to be necessary.
64% of the respondents in Zone Hsee Polio as a major threat
The same figure for Zone L is 73%
9.5
Level of Awareness on Polio the Disease
The respondents were asked to inform how Polio occurs, what are their symptoms and
where they take their children in case pf Paralysis. The findings are as follows.
Table XIV
Awareness on how Polio Occurs
Awareness on Polio
Occurrence
H
L
%
%
Know how Polio Occurs
16
10
Do not know how Polio occurs
84
90
Table XV
Awareness on Symptom of Polio
H
L
%
%
Weakness in the limbs
15
25
Fever followed by sudden weakness of the limbs
6
1
Paralysis since birth
0
0
Sudden weakness of limbs followed by fever
5
3
Do not Know / Cannot Say
72
70
Others
2
1
Symptoms
Table XVI
Knowledge on where to take the child in case of Paralysis
H
L
%
%
Govt. Hospital
28
45
Primary Health Centre
19
22
Subcentre
6
9
Pvt. Hospital / Pvt. Clinic
7
11
Anganwadi Centre (AWC)
0
0
Do not Know / Cannot Say
29
10
Other (Specify)
11
Nature of Facility
It is noticeable from the findings in Table XV that a considerable portion, around 30% for
Zone H and 10% for Zone L are still unaware where to take the children in case of
Paralysis.
9.6
Advice on Regular Immunisation on NID
The respondents were asked to inform whether they are communicated about the need
for regular immunisation on the Pulse Polio day.
For Respondents in Zone H, 56% respondents reported that they were not
communicated to take vaccines other than polio.
The same figure for Zone L is 69%
9.7
Proper Maintenance of Cards
The Respondents were asked whether they maintain cards for Regular Immunisation as
well as for Pulse Polio. The findings are as follows:
Table XVII
Maintenance of Cards
Yes (%)
No (%)
56
76
44
24
46
68
54
32
Maintain Regular Immunisation Card
ZONEH
’
ZONE L
Maintain Pulse Polio Card
ZONE H
ZONE L
9.8
Perception on Adverse Effect of Polio Vaccine
25 % of the Respondents in Zone H feel that there are adverse effects of Polio
Vaccine with Fever as the most common adverse effect.
The figure for Zone L is 22% with fever as cited as the most common side effect
9.9
Perception on Safety Factors associated with Polio Vaccination
Table XVIIIa
Safety Factors associated with Polio Vaccination - Zone H
Factors
Yes
No
(%)
(%)
Do
Not
Know
(%)
Safe to administer Vaccine to neo-natals
74
5
Safe to administer Vaccine to children with diarrhoea
32
38
56
40
38
21
28
24
30
14
Safe to administer Vaccine to children with fever
Safe to breast feed the child after Vaccination
Table XVII lb Safety Factors associated with Polio Vaccination - Zone L
Factors
Yes
No
(%)
(%)
Do
Not
Know
(%)
Safe to administer Vaccine to neo-natals
Safe to administer Vaccine to children with diarrhoea
Safe to administer Vaccine to children with fever
Safe to breast feed the child after Vaccination
74
42
42
43
10
34
39
34
16
24
29
23
It is evident from the above table that the level of awareness on various issues is quite
considerable.
10
FINDINGS ON THE HEALTH INFRASTRUCTURE
In order to assess the manner in which the rights to health are protected, the
respondents were posed various questions on the health system under.
10.1
Physical Accessibility
The respondents were asked how far the nearest health facility from their home and the
replies are as follows.
Table XIX
Distance of Medical Facility from the residence of the respondents
H
L
%
%
Within 4 Km
70
83
Between 4-8 Km
14
11
Beyond 8 km
16
6
Distance
10.2
Quality of Service
The quality of the services depends crucially on the type of the health centre and in what
manner the health centre is equipped to handle the health dysfunction. Table XX below
traces the responses of the respondents of the quality of the Health Infrastructure that is
nearest to the residence of the respondents.
The answer varies because the Survey was conducted over a wide area covering
around 1500 kilometers.
Table XX
Nature of Health Facility
H
L
%
(%)
Sub-centre
37
54
PHC
39
37
BPHC
15
4
Rural Hosp
7
4
Higher Grade Hospital
2
1
Nature of Health Facility
Table XXI
Facilities sought at the time of Illness
H
L
%
%
Non-Govt. Facility
73
47
Govt Facility
37
53
Nature of Services sought
The reason why non-Govt. facilities are chosen by people were investigated and the
replies are given in Table XXI
Table XXII
Resons for Preference for non-Government Facilities
Reasons
H
L
%
%
Government Facility is too far from home
38
32
Non-availability of Medicine
29
34
Misbehaviour of staff
11
14
Too long wait
11
14
No doctor
3
4
Ineffective medicines
3
2
Don’t know where
1
Other
4
If the findings of Table XXI are placed together with the findings of Table XVIII, there
may be an apparent contradiction. One possible explanation could be that the Health
infrastructure that are near to the homes of the respondents are not equipped enough to
handle the medical needs of the people.
11.
COLD CHAIN MAINTENANCE
Cold Chain is one of the most crucial aspect of the Pulse Polio Immunisation Drive and
elaborate arrangements are organised to maintain Cold chain for the Polio Vaccine.
In the context of Pulse Polio Immunisation Drive in Murshidabad, the manner in which
the Cold Chain is maintained has been examined.
The central storing place for the vaccine in Kolkata is at Family Welfare Store in
Bagbazar. The vaccined are packed in vaccine carriers and transported to Baharampur
and stored in Walk-in-Coolers (WIC). From WIC, Baharampur, the vaccines are
transported to BPHC and PHCs one Day before Day I of the Pulse Polio Drive. On the
day of the vaccination, the health workers collect the vaccines from PHC/BPHC and
carry them to venue.
For instance, the vaccines for the Baharampur Block is carried to the Karnasubama
BPHC and from there the health workers carry the vaccine to the venue.
For Suti II Block, the vaccines are stored in Maheshail BPHC,
According to Mr. S.S. Chowdhury, Cold Chain Officer, Department of Health & Family
Welfare, Govt, of West Bengal, there has been improvement in cold chain maintenace in
the recent years.
There are two crucial aspects to Cold-chain maintenance. One is technical aspect. This
relates to the equipment and other arrangements. Equipment can be divided into
electrical and non-electrical. Electrical process is resorted to when there are
infrastructures for Refrigerators and Coolers. The places where electrical arrangements
are absent, cold-chain is maintained through ice.
Another aspect is human aspect. This relates to the manner in which the cold-chain
system is handled by various health workers involved in the process of cold-chain
maintenance.
On the technical side, efforts are made to smoothen the process. However, a few
problem areas still remain. One problem area is the wiring system in many centres that
are not suitable and requires repair.
On the human side, Training is provided to all the personnel at the Block level involved
in Cold chain maintenance, transportation of the vaccines and administering vaccines.lt
was noticed that most of the health workers involved in transportation and administration
of vaccines are aware of the Expiry label on the vaccine vial. They were also aware of
the manner in which vaccine are to be handled at the time of vaccination.
However, the Cold Chain Officer feels that, there is scope to augment the Training
aspects of the Health workers and he has suggested Training by means of Audio-visual
Aid to the Health Workers.
12.
NOTES ON THE PROTECTION OF RIGHTS OF HEALTH OF THE
MARGINALISED POPULATION
This section seeks to explore Protection to Rights of Health in the context of IPPI and
the Genral Health Infrastructure in the context of selected parameters.
12.1
Availability
IPPI
Pulse Polio services are available. In fact special efforts are undertaken by the
Government machinery to make the services available at the doorsteps. This is the
reason why the coverage of the programme is wide and is increasing with every NID
This has been corroborated in the present study as well.
General Health Infrastructure
In respect of the general health services in, the availability is not guaranteed. In fact, it is
the common refrain of the people that it is the Polio Drops that they receive without even
asking. However, in case of services for serious and even common ailments, they fail to
get the services in many instances. This is reflected in Table XXI.
12.2
Accessibility
andlnformat onA6 l00kbTtint° 'n termS °f Physical Accessibility. Economic Accessibility
12.2a Physical Accessibility
IPPI
In majority of the cases Physical accessibility is not a problem. As per Table XI majority
of the respondents have reported that the Polio Booth is either at walking distance or not
very far. Even if the respondents do not turn up at the Booth, the Health workers visit
home and administer the drops.
General Health Services
Physical inaccessibility of the Government Health services is one of the findings that
emerge from this study. Although 70% of the respondents report that they have a Health
centre within 4 Km from their home, still a majority opt for non-Govt services when their
child fall sick. This implies that the properly equipped health infrastructure is not within
the reach of the majority of the population, a substantial portion of which is
marginialised.
12.2b Economic Accessibility
IPPI
Since the Pulse Polio services are obtained for free, no health right is violated in this
context.
General Health Services
The health rights of marginalized population is likely to be violated when they opt for
private health facilities instead of Govt, facilities. This is because, the private facilities are
much more expensive than what is offered by the Government Infrastructure.
12.2c Information Accessibility
IPPI
Violation of Information accessibility was noticed in case of IPPI. This is evident from
Tables XIV, XV, XVI and XVIII.
As per findings summarized in Table XIV, majority of the respondents are unaware of
how polio occurs.
As per Table XV, a sizeable proportion of the respondents are ignorant of the symptoms
of polio.
Table XVI reveals that around 30% of the respondents do not know where to take their
children in case of Paralysis.
Table XVIII reveals that the safety factors in the context of the Polio vaccine is unknown
to a sizeable proportion.
General Health Services
Information inaccessibility in the context of health determinant is evident from Table IX
where it is evident that 48% of the respondents are unaware of the fact whether the
water they drink is Arsenic-contaminated or not.
13
CONCLUSION AND RECOMMENDATION
The conclusions of The Report are:
Pulse Polio Immunisation Programme has achieved wide coverage, although full
coverage is still not possible
Although a sizeable proportion of the respondents perceive this programme as
‘necessary’ and consider this disease as a ‘major threat’, majority of the
respondents in both the zones are unaware of how Polio Occurs and what are
the symptoms of the disease.
A sizeable proportion also do not have clear idea about the health seeking
behaviour in case of Paralysis.
The nature of sanitation facilities is generally poor and that has direct bearing on
the management of the disease, because, Polio is a water-borne disease.
The technical aspect of the Programme, the Cold Chain system in particular
requires upgradation.
The general health infrastructure requires upgradation in order that the rights to
health of the marginalized people are protected.
RECOMMENDATIONS
Vertical Polio implementation programme should be seen in the context of
Primary health Care approach and necessary policy decision required to be
made for integrated health approach to ensure health and well being of people
Awareness Generation with holistic approach. This would mean generating
awareness on importance of sanitation habits, making them aware of the
symptoms etc.
Training Peer Groups in the society who can take lead in Awareness Generation
Programme.
Research on Health Management, both relevant issues including the health
determinants
Lobbying in the relevant fora
Advocacy with appropriate authorities
Sensitization of Press and Media
PLANS FOR LOBBY/ADVOCACY
The thrust of the Lobby/Advocacy efforts would be to ensure that health determinants do
not have adverse impact. Besides other, two main determinants may be brought under
focus: Safe Drinking Water and Proper Sanitation Facilities.
The target for Lobby / Advocacy initiatives may include
Decision Makers
Government Officials
Corporate Houses
Industry Associations
Peer Leaders of the Society
ANNEXUREI
LIST OF CLUSTER SAMPLE
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
ZONE H_________________
'NAME__________________
LEVEL
' Dhulian (M)______________
TOWN
WARD
Dhulian (M) - Ward No.4
WARD
Dhulian (M) - Ward No. 15
WARD
Dhulian (M) - Ward No. 19
WARD
Jangipur(M) - Ward No,8
WARD
Jangipur(M) - Ward No. 19
C.D.BLOCK Farakka_________________
VILLAGE
Bewa (P)________________
VILLAGE
Ballalpur
VILLAGE
Kuli_____________________
VILLAGE
Mahadeb Nagar_______
WARD
Frka Barr. Tnshp (CT) - Wrd
No.1________________
C.D.BLOCK Samserganj________
VILLAGE
Bhasaipaikar_____________
VILLAGE
Balbalpara_______________
VILLAGE
Jafrabad_________________
WARD
Dhusaripara (CT) - Ward No.1
WARD
Chachanda (CT) - Ward No.1
C.D.BLOCK Suti -1___________ _
VILLAGE
Panchigachhi_____________
VILLAGE
Ramakantapur______
VILLAGE
Ahiron
C.D.BLOCK Suti - II__________________
VILLAGE
Bahagalpur_______________
VILLAGE
Amuha__________________
VILLAGE
Ichhlampur_______________
TOWN
Aurangabad (CT)__________
WARD
Paschim Punropara (CT) Ward No.1________________
C.D.BLOCK Raghunathganj -1__________
VILLAGE
Dafarpur_________________
VILLAGE
Kankaria_________________
VILLAGE
Brindabanpur_____________
WARD
Srikantabati (CT) - Ward No.1
C.D.BLOCK Raghunathganj - II_________
VILLAGE
Pananagar(P)____________
VILLAGE
Bara Jumla_______________
VILLAGE
Kul Gachhi____________ ___
VILLAGE
Fraser^Nagar
Urban
Urban
Urban
Urban
Urban
Urban
Rural
Rural
Rural
Rural
Urban
Total
Rural
Rural
Rural
Urban
Urban
Total
Rural
Rural
Rural
Total
Rural
Rural
Rural
Urban
Urban
Total
Rural
Rural
Rural
Urban
Total
Rural
Rural
Rural
Rural
ZONE L____________
Murshidabad Jiaganj
1_
Budhra_____________
Rural
2
Bali________________
Rural
3
Sashidharpur________
Rural
4
Banamalipur_________
Rural
5
Beliapukur__________
Rural
6
Satlakshmi
Rural
Murshidabad (M)______
Urban
7
Murshidabad (M) - Ward
Urban
No. 15______________
C. D. B LOG iBerhampore
Total
K______
8
VILLAGE Sahara_____________
Rural
9
VILLAGE Andar Manik____________ Rural
10 VILLAGE Kodla ________ 2Z
Rural
11 VILLAGE Fate Singdiar____________ Rural
12 VILLAGE Kharsadanga
Rural
13 VILLAGE Chaltia______
Rural
14IVILLAGE Sibpur
Rural
15 VILLAGE Usta_____________
Rural
16 VILLAGE Selamatpur
Rural
17 VILLAGE Baradaha__________
Rural
18 WARD
__________
Gora Bazar (CT) - Ward No.1 Urban
C.D.BLOClBeldanga -1
Total
__ K_______
19 VILLAGE Gopinathpur
Rural
20 VILLAGE Dalua_____
Rural
21 VILLAGE Jhunka
Rural
22 VILLAGE Bishannagar
Rural
23 VILLAGE Begunbari
Rural
24 VILLAGE Mirzapur
Rural
25 VILLAGE
______ Kapasdanga
Rural
C.D.BLOC Beldanga - II
Total
__ K______
26 VILLAGE Saktipur________
Rural
27 VILLAGE Mahammadpur
Rural
28 VILLAGE _________
Rampara Faridpur
Rural
29 VILLAGE
vn-i_nkji_ |Bikal
|L->ir\ai Nagar
iNagqf________
Rural
30|\/ILLAGE Kashipur
Rural
BLOCK
VILLAGE
VILLAGE
VILLAGE
VILLAGE
VILLAGE
VILLAGE
TOWN
WARD
ANNEXURE II
HEALTH INFRASTRUCTURE IN MURSHIDABAD DISTRICT
1
GRADE OF HOSPITAL
SUBDIVISION
SADAR
LALBAGH
DOMKAL
JANGIPUR
KANDI
District Hospital
1
0
0
0
0
State General (SG)
Hospital
1
0
0
0
0
Sub-divisional (SD)
Hospital
0
1
1
1
1
Rural Hospital
2
2
2
1
2
Block Primary Health
Centre (BPHC)
4
3
2
6
3
Primary Health Centre
(PHC)
14
14
9
15
18
Sub-Centre
167
122
110
175
140
State Special Hospital
1
0
0
0
0
(Under
Construction)
(Mental)
ANNEXURE III
Achievement of Universal Immunisation Programme,
Murshidabad, 2001-02 & 2002-03
TT(PW)
2001-02
2002-03
DPT
2001-02 I 2002-03
_____ POLIO
2001-02
2002-03
BCG
2001-02
MEASLES
2001-02
2002
2002-03
-03
MURSHIDABAD
119034
114799
120656
118621
117188
116803
138219
129480
WEST BENGAL
1668396 1557094
14428
9
1157
69
1687953
1572646
1697922
158325
9
1845802
17816
56
1633552
1545
399
INTENSIFIED PULSE POLIO IMMUNISATION PROGRAMME
ROUND APRIL 2003
Area
Estimated
(0-5)
children
population
Number of
Booths
established
Total No.
of
houses
visited
by the
team
No. of Children Immunised
Rural
Urban
Total
Murshidabad
847849
3340
1003772
752776
50876
803652
94.79
West Bengal
8427652
33654
12145296
6464351
1592680
8057031
95.60
%
Immunised
ROUND JUNE 2003
Murshidabad
847849
3340
1050095
763803
48768
812571
95.84
West Bengal
8427652
33647
12588962
6520111
1579148
8099259
96.10
ROUND SEPTEMBER 2003
Murshidabad
847849
3340
984961
749903
45203
795106
93.78
West Bengal
9444317
37806
14330016
7296288
1686921
8983209
95.12
Source: Health on the March, West Bengal, 2002-03
ANNEXURE IV
FIELD VISIT REPORT ON THE PREPARATIONS FOR NATIONAL IMMUNISATION
DAY (NID)
and
IMMUNISATION DRIVE ON FEEBRUARY 22, 2004 IN SELECTED VILLAGES OF
MURSHIDABAD
21/02/2004
Selected areas were visited to observe the preparations undertaken for the Pulse Polio
Immunisation Drive to be held on 22/02/2004. The places visited were on advice of the
CMOH, Murshidabad.
Th efirst place visited was Maheshail BPHC that falls in Suti II Block. Discussions were
held with Dr. Balaram Sarkar, BMOH, Maheshail BPHC. It was understood from
discussions with him that the coverage of Pulse Polio is not satisfactory. The reasons for
less than satisfactory coverage are:
Misconceptions among people
Physical inaccessibility of some areas within the Block
Other places visited were Kanchantala Gram Panchayat Office and Udyan Club, which
is adjacent to the Kanchantala Gram Panchayat.
The Panchayat falls within Shamsherganj Block. The Block is one of the problems areas
within the district where Polio Boycott and non-compliance.
It was found out that the residents of the area have high level of dissatisfaction against
the Govt. Health Infrastructure. The nearest BPHC is at Anupnagar. The approach road
to the Health centre is inaccessible and according to the inhabitants of the area, the
behaviour of the Medical and non-medical personnel of the area is rude.
However, the Govt. Health worker, named Jahanara, is committed in her job. She visits
the villages regularly, conducts awareness programme, organises Immunisation Camp.
Quality of Drinking water is very poor with high Iron content.
There is no Awareness on presence of Arsenic Contamination in the area.
The Sanitation facilities in the villages are almost non-existent.
Most of the people in the area are engaged in the Biri manufacturing.
22/02/2004
Selected Pulse Polio Booth was visited on NID to get first hand experience of the polio
immunisation . The booths visited were.
1. Gurudaspur Primary school
2. Beuchitala High school
3. Chuadanga.
4. Kalopur primary school.
5. Kalopur Mathapara.
6. Nawdapara
7. Abhiramhpur
8. Gopinathpur Health Sub-centre.
9. Khuniapukur
10. Ghordaur (100%Tribal village)
11. Kulberia Adibasi Para (100% Tibal Village)
General findings
Drinking water
Almost all people visited use the Tube-well as the sole source of Drinking water The
depth of the tube-well range from 80-100ft. The area is generally prone to Arsenic
Poisoning, although people have limited awareness on the issue. Tests have carried in
some areas but people are unaware of the Test Report. In some areas, notably
Gurudaspur, specially designed Arsenic preventive Tube-well have been installed but
most of the Tubewells are non-functioning. Iron content in the water seems to be high.
In the tribal village of Kulberia, one Tubewell cater to 185 families in the entire village.
In some villages, Tube-wells have been installed by Zilla Parishad.Although, there are
tap system in all the tube-wells, no tap works and that leads to considerable wasteage of
water.
Sanitation
Proper sanitation facilities are almost non-existent in the entire area. There is a scheme
of Installation of Latrine (non-sanitary type without water seal) at a cost of Rs. 385.00 by
the local Panchayat. There is also a system of a subsidy of Rs.200/- for Below Poverty
Line (BPL)-notified people. However, there has been limited response to this scheme for
a number of reasons:
People are unwilling to pay the amount and expect full subsidy .
Even when people pay in some instances the panchayat is unable to supply
the equipment . Which dampen the enthusiasm to install the system people
have little or no awareness on necessity of a proper sanitation facility
NID
Pulse Polio programme
Personnel
The Pulse Polio (PP) Programme is predominantly manned by ICDS workers and
volunteers from the Community (also termed as Social Workers) and Community Health
Guides (CHG). In some cases Govt Health Workers are also involved. .In most of the
villages, prior publicity is carried out by Miking and Door-to-door publicity.
The time-schedule that is mentioned in all publicity programmes is not adhered to I the
remote areas. The reasons are:
Delay in supplying the vaccines in the venue
Delay in arrival of the personnel
Coverage of more than one booth by same set of personnel
Response to the Immunisation Drive varies from place to place.
In some cases, the enthusiasm is perceptible. On hearing that Booth has
started functioning, mothers accompany their children to the booth for the
'two drops' of vaccine.
In some instances, although there is no adverse opinion about the
Immunisation drive itself, people choose to stay at home because of the
reason that even after the activities on the National Immunisation Day (NID),
follow-up operations take place for next two consecutive days where the
Health workers and Volunteers visit the household and carry on the
Immunisation Drive. People take this as an excuse for not visiting the booths
on the NID. In some centres, e.g. Gopinathpur Sub-centre, attendance on the
particular NID was 70-75% as compared to 90-95% on the previous NIDs.
In some areas, inadequacy in other areas affect the PP Drive. In Kalopur for
instance, people expressed the feeling that it is only the Polio vaccine that
they get for free. However, the facilities that they receive for other ailments
and for regular vaccination are grossly inadequate. They feel that these
should attract urgent attention.
People in some areas, e.g. Khuniapukur have expressed adverse opinion
about the Pulse Polio Programme. There is a feeling that administration of
the PP vaccine curbs the reproductive power and this programme is nothing
but a well-planned government ploy to restrict population growth.
In all the villages visited, there have been instances of some families who
have boycotted the PP Drive. However, the Health workers and the ICDS
workers have claimed that they have been able to allay the fears and
misconceptions of these people and ultimately they have participated in the
Immunisation Drive.
There are some areas, Ghordaur Tribal village for instance, where people are
in complete dark about the PP Drive. There have been no publicity drive, nor
there had been any visit from the health workers to inform about the PP
Programme. The regular Immunisatio Drive is also non-existent in these
areas. In the neighbouring tribal village of Kulberia, which is relatively more
developed, the regular Immunisation Programme is almost non-existent,
although there have been participation in the PP Programme.
On the technical side, the maintenance of the cold-chain was found to be
improper. The vaccine vial, once taken out of the Pack is not put into the cold
pack. The medicine is administered from the vial until it is exhausted.
Finding on the Health Infrastructure
The health infrastructure is generally poor.
The nearest accessible centre is Health sub-centre. These centres are usually open
thrice a week. These are manned by Health workers. The main activities of these
centres are
Birth Registration
Regular Immunisation
Distribution of some specific medicines.
The Health workers are supposed to visit the villages once a week. In many cases,
Health workers do not perform this duty. The Immunisation status is better in places
where the Health workers take a pro-active role.
The recording system for Immunisation, Awareness generation and monitoring is more
organised in places where ICDS programmes are operational.
BPHCs, in most of the cases are physically inaccessible. The condition of the roads
adds to the woes of the people.
BPHCs do not have the wherewithal to take care of urgent or critical are diseases.
The patients are referred to the State General or Sub-divisional hospitals.
Instances of Discrimination
Instances of Discrimination have been noticed in two places
This is a case of indirect discrimination that had affected the PP drive. In
Kalopara, 14 pregnant women were shortlisted for a government grant of Rs.
500/-. However, only two women were given this grant. This had evoked a
sharp response from the women and their families who were omitted. These
people showed their dissatisfaction on the personnel who were involved in
the PP Drive.
35 families from the tribal village of Ghordaur were completely omitted from
the PP Drive, although all facilities were given to the neighbouring tribal
village.
Position: 2286 (3 views)