RF_COM_H_91_A_SUDHA.pdf
Media
- extracted text
-
RF_COM_H_91_A_SUDHA
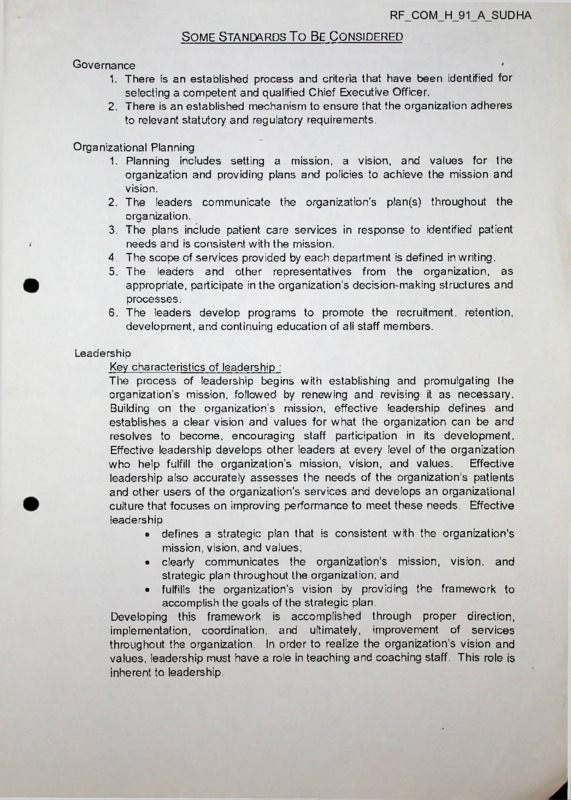
Some Standards To Be Considered
Governance
1. There is an established process and criteria that have been identified for
selecting a competent and qualified Chief Executive Officer.
2. There is an established mechanism to ensure that the organization adheres
to relevant statutory and regulatory requirements.
Organizational Planning
1. Planning includes setting a mission, a vision, and values for the
organization and providing plans and policies to achieve the mission and
vision.
2. The leaders communicate the organization’s plan(s) throughout the
organization.
3. The plans include patient care services in response to identified patient
needs and is consistent with the mission.
4. The scope of services provided by each department is defined in writing.
5. The leaders and other representatives from the organization, as
appropriate, participate in the organization’s decision-making structures and
processes.
6. The leaders develop programs to promote the recruitment, retention,
development, and continuing education of all staff members.
Leadership
Key characteristics of leadership :
The process of leadership begins with establishing and promulgating the
organization’s mission, followed by renewing and revising it as necessary.
Building on the organization’s mission, effective leadership defines and
establishes a clear vision and values for what the organization can be and
resolves to become, encouraging staff participation in its development.
Effective leadership develops other leaders at every level of the organization
who help fulfill the organization’s mission, vision, and values.
Effective
leadership also accurately assesses the needs of the organization's patients
and other users of the organization’s services and develops an organizational
culture that focuses on improving performance to meet these needs. Effective
leadership
• defines a strategic plan that is consistent with the organization's
mission, vision, and values;
• clearly communicates the organization’s mission, vision, and
strategic plan throughout the organization; and
• fulfills the organization’s vision by providing the framework to
accomplish the goals of the strategic plan.
Developing this framework is accomplished through proper direction,
implementation, coordination, and ultimately, improvement of services
throughout the organization. In order to realize the organization's vision and
values, leadership must have a role in teaching and coaching staff. This role is
inherent to leadership.
Directing Departments
1. Each department of the organization has effective leadership.
2. Department directors or supervisors are responsible, either personally‘or
through delegation for
• integrating the service into the organization's primary function;
• coordinating and integrating interdepartmental and intradepartmental
services;
• developing and implementing policies and procedures that guide and
support the provision of services;
• recommending a sufficient number of qualified and competent
persons to provide care, including treatment;
• continuously assessing and improving the performance of care and
services provided;
• maintaining quality control programs, as appropriate;
• orienting and providing in-service training and continuing education
of all persons in the department;
o recommending space and other resources needed by the
department.
Information Management
1. The information management processes provide for information
confidentiality, security, and integrity.
2. The organization reviews the completeness, accuracy and timely
completion of information in medical records at least quarterly.
3. There is a policy regarding the retention time of medical record information
determined by law or by its use for patient care, legal, research, and/or
educational purposes.
4. A medical record is maintained for every individual assessed or treated.
5. Medical record contains sufficient information to identify the patient, support
the diagnosis, justify the treatment, document the course and results
accurately and facilitate continuity of care among health care providers.
6. At discharge from patient care, a clinical summary gives reason for
hospitalization, significant findings, procedures performed, treatment
rendered, condition on discharge, and any specific instructions given to
patient or family.
7. Written operative reports are included in the medical record of patients
undergoing operative or other invasive procedures.
Human Resources Management
1. The organization’s leaders define for their respective areas the
qualifications and job expectations of staff and a system to evaluate how
well the expectations are met.
2. The organization provides an adequate number of staff whose qualifications
are commensurate with defined job responsibilities.
3. The organization has established methods and practices that encourage
self development and learning for all staff.
4. A staff orientation process provides initial job training and information.
5. Ongoing inservice or other education and training maintain and improve
staff competence.
Environment of Care
1. The organization has a documented management plan(s) for the
environment of care that considers the following functions:
Safety
Security
Hazardous materials and wastes
Utility systems
Emergency preparedness
2. All areas of the facility are surveyed at least twice annually to identify
environmental hazards and unsafe practices.
3. All incidents involving property damage, occupational illness, or patient,
personnel or visitor irj ury are investigated and reported.
4. Written policies and procedures are strictly followed in regards to Infection
Control.
5. Cleanliness is maintained in all areas with set standards to be achieved.
Dietary
1. Responsibility for preparing, storing, distributing, and administering food
and nutrition products is defined and assigned.
2. Food and nutrition products are administered in a safe, timely, and
acceptable manner to the patient.
3. Diet counselling and education by trained personnel is available and
provided to patients.
4. Quality control measures are practiced in regard to therapeutic diets.
Pharmacy
1. Availability of appropriate medicines as determined by the medical staff
2. Availability of pharmacy services at all hours
3. Emergency medication systems
4. Formulary available to staff who use drugs
5. Pharmacy and therapeutic committee
6. Appropriate policies and procedures that support prescribing or ordering
practices
7. Adherence to applicable law regulation, licensure, and professional
standards of practice.
Laboratory
1. Clinical laboratory services and consultation are available at all times in a
prompt manner to meet the needs of patients served by the hospital as
determined by the medical staff.
2. Current written policies and procedures are readily available and address
Specimen Collection
Specimen Preservation
Instrument Calibration
Quality Control and Remedial Action
Equipment Performance Evaluation
Test Performance
3. Staff performing tests have adequate specific training and orientation to
perform the tests.
4. Quality control checks are conducted on each procedure as defined by the
organization.
X-Ray
1. Radio-Diagnostic services and consultation are available at all times in a
prompt manner to meet the needs of patients served by the hospital as
determined by the medical staff.
2. Current written policies and procedures are readily available and address
Patient preparation for special procedures
Radiation protection
Equipment performance evaluation
Quality control and remedial action
3. Staff performing tests have adequate specific training and orientation to
perform tests.
4. Quality control checks are conducted as defined by the organization.
J
Spiritual Care
1. Spiritual care and counselling is available to all patients and families at all
hours
2. Chaplains visit in all wards daily
3. The Christian nature of the hospital and its mission is communicated to
patients, staff, and students.
4. Spiritual care is available to staff and students
5. Activities to encourage growth and meet spiritual needs of staff and
students are planned regularly.
ST. MARTHA’S HOSPITAL—EVALUATION
SECTION: 1 .NURSING EDUCATION
•Faculty
•Ancillary Staff
•Students
NURSING SERVICE
2.
•Ward-in charges
•Nursing Staff
METHOD OF EVALUATION:
•Questionairre
*7Focuspd Group Interview
Note: AJ1 members of each category will not asked to take part in the evaluation process. Only a
selected representative number will be included depending on the following criteria:
The staff be it in the Nursing Education or Service should •have worked in the institution for a continous period of nix months.
•be willing to take part in the evaluation.
PERSONAL DATA
Department:
Designation:
Status (F.eligiouu/Layperson):
Duration of service/Stay in the institution:
Educational Qualification:
Institution where Nursing was completed:
Date of completion of Nursing course:
Have you undergone an Inservice Education
Programme after joining St.Martha’s hospital ?
Given below are certain aspects of the institution you are expected to be aware
of. Please indicate your awareness , by encircling ‘ Y’ if your awareness of each aspect listed is YES and
‘N’ if it is NO.
1 The vision of the Good Shepherd Congregation:
Y/N
2.The philosophy of the institution :
Y/N
3.The objectives and goals of the institution:
Y/N
4.The policies regarding :
•Work
Y/N
•Beneftts/Salaries
Y/N
•Promotions
Y/N
•Recruitment of staff
Y/N
•Selection of students
Y/N
•Disciplinary action
Y/N
5.1he welfare facilities/schemes:
Y/N
6.The worker’s union:
Y/N
7.Performance appraisal:
Y/N
Given below are I i at of objectives /goals of your institution. Give your opinion to the extent to
which you think the objective /goal should be fulfilled under column A & under column B thecxtent. to
which each of them are presently fulfilled .Please give your answer in the form of a number ranging
fromONE to FIVE in the blank provided under each column.
1
Not fulfilled
at all.
2
3
4
5
Fulfilled completely
COLUMN-A
1 The hospital provides to the the sick irrespective of
caste/creed/race/social status.
The hospital strives to provide high quality care al a
2.
cost affordable for the common man.
3.The hospital focuses its services on health concerns
of women and children mainly.
4.Hie hospital endeavours to provide competent and
comprehensive health care Oro' recent yet cost
effective technology.
The hospital fosters a sense of dedication, moral &
5.
ethical integrity among its employees.
The professional skills of the employees are
6.
enhanced thro’ continuing education programs
7.
The hospital strives to develop in its employees
a desire to serve the poor & weak sections of
society.
ij. An awareness of the social problems & injustices
is developed in the employees, keeping in mind
the National Health pricrities
9.
The hospital provides spiritual cere to the sick
respecting the individual’s religious beliefs
10.
The hospital provides subsidised care to those
individuals in need
11.
The hospital attempts to develop Urban & Rural
centres of Health care for the underprivileged &
oppressed women and children.
12.
The hospital strives to expand its department &
education programs as per the need of society.
COLUMN-B
13.
The hospital constantly Ines to improve the
quality of tic health care.
14.
The hopital creates awareness of a clean &
healthy environment to die public.
15.
The hospital serves as a model of efficient health
health care.
16.
The hospital fosters in all its employees a respect
for respect fcr human life at all stages of life.
17.
The hospital tries to develop in its employees a
Learn spirit & a family atmosphere.
18.
Rules ®ulations of the institution are reasonable
19.
The hospital sliows concern for the welfare of its
employees.
20 Giveariy THREE POSITIVE aspects of the hospital:
21. Give any THREE NEGATIVE aspects of the hospital which you have experienced:
22. Give any THREE suggestions for improving the hospital functioning:
1 o what extent are you able to accomplish the following tasks . Give your answer honest ly by encircling a
number ranging from ONE to FIVE where 1 means you arc ‘not able to do the task at all’ and 5 means
you are * able to do the task to tlic best of your ability’Given below is space provided for comment- -Please
give your '.unsnents if you liave faced any problems /difficulties to do these t usks.
I am able to provide care to all patients irrespective of
theircaste/creed/social status.
1
2
3
4
5
I am able to provide the best possible care to all patients
at all times.
1
2
3
4
5
3.
I am able to ophold my moral/ethical values in dealing
with all the patients /co-workers.
12
3
4
5
4.
I am able to meet the spiritual needs of the patients
daily respecting their own religious views.
-1
2 3
4
5
5.
I arn able to participate in activities which will enhance
my skills/professional ablities.
1
2
3
4
5
1-
Given below are list of statements relating to various aspects of your education in St. Martha's School of
Nursing Give the extent to which you arc satisfied with each aiipect ,in the form of a number ranging from
ONE to FIVE in the blank provided against each statemenL
5
Fully
satisfied
4
moderately
satisfied
3
partially
satisfied
2
minimally
satisfied
1.
The encouragement you get from home to perform well in your studies.
2.
The encouragement you get from teachers to do well in your studies.
3.
The encouragement you get from the staff in the hospital to do well.
4.
The encouragement you get from the warden to do well in studies.
5.
The facilities on the campus for your personal/professional/spiritual
development:
■"classroom
♦chapel
♦canteen
♦hospital services
♦hostel
♦library
•mess
♦recreation
♦sick room
6.
The facilities for your social development:
♦interaction with fuculty/stalf
♦interaction with peers/seniora
♦involvement in the campus activities
♦S.N.A activities
♦C N.G.L activities
•sports
7.
The faculty/staff who are directly involved in your education
♦show genuine interest in your welfare
♦show respect to all of you
♦are available whenever needed by you
♦discipline you when appropriate reasonably
♦provide you with appropriate supervision
♦are firm yet concerned with your welfare
♦demonstrate fairness in dealing with you
♦are competent in various teaching methods
•use appropriate evaluation methods fairly
♦demonstrate moral/ethical values in dealing with you
♦possess good personal skills &are confident in selves
1.
least
satisfied
ST. MARTHA’S HOSPITAL—EVALUATION
SECTION: 1 .NURSING EDUCATION
♦Faculty
'__^3
♦Ancillary Staff
♦Students
, ,
NURSINC- SERVICE
2.
♦Ward-in charges
♦Nursing Staff
I
14ETHOD OF EVALUATION:
♦Questionairre
*?Focused Group Interview
Note All rner/ibwaol cwh r utx-yiry will not naked to hike pint in Ila-cvuluul ion pro< cua Only n
aclcclcd representative number will be included depending on the following crilei in
Tlic utaff be it in the Nursing Education
Service ulioiild -
♦have worked in the institution for a continouu period of six rnunthu.
♦be willing to take part in the evaluation .
PERSONAL DATA
Department:
Designation:
Status (Religious/Laypcrson):
Duration of service/Stay in the institution:
Educational Qualification:
Institution where Nursing was completed:
Date of completion of Nursing cotrse:
Have you undergone an Inservice Education
Programme after joining St.Martha’s hospital ?
Given below are certain aspects of the institution you are expected to be aware
of. Please indicate your awareness , by encircling * Y’ if your awareness of each aspect listed is YES and
‘N1 if it is NO.
1 .Hie vision of the Good Shepherd Congregation:
Y/N
2.The philosophy of tile institution :
Y/N
3.The objectives end goals of Die institution:
Y/N
d.llie policies regarding :
•Work
Y/N
•Eenefits/Ualarics
Y/N
•Promotions
Y/N
•Recruitment of staff
Y/N
•Selection of students
Y/N
•Disciplinary action
Y/N
5.The welfare facilities/schemes:
Y/N
6.The worker’s union:
Y/N
7.Performance appraisal:
Y/N
CJivcn below iu'<* list of oljjcdivcB Z^oiilu of /old inulilutioii < live your opinion Io lhe extent Io
whidi you Oank the objective /goal should be fulfilled under column A .ft under column B theextent to
which each of them are presently fulfilled .Please give your answer in the form of a number ranging
IromONE to FIVE in the blank provided under each column.
1
Not fulfilled
at all.
2
3
4
5
Fulfilled completely
COLUMN-A
The hospital provides to the lhe sick irrespective of
l.
caste/creed'race /social status.
The
2.
hospital strives to provide high quality care at a
cost affordable for the common man.
The hospital focuses its services on health concerns
3.
of women arid children mainly.
4.The hospital endeavours to provide competent and
comprehensive liealtli care Uro’ recent yet cost
effective technology.
The
5.
hospital fosters a sense of dedication, moral &
ethical integrity among its employees.
6.1he professional skills of the employees are
enhanced thro’ continuing education programs
7.
The hospital strives to develop in its employees
a desire to save the poor & weak sections of
society.
8.
An awareness of the social problems & injustices
is developed in the employees, keeping in mind
the National Health priorities
9.
The hospital provides spiritual ctre to the sick
respecting the individual’s religious beliefs
10.
The hospital provides subsidised care to those
individuals in need
11.
The hospital attempts to develop Urban & Rural
centres of Health care for the underprivileged &
oppressed women and children.
12.
The hospital strives to expand its department &
education programs as per the need of society.
COLUMN-B
13.
'flie hospital constantly tries to improve the
quality of tl«e health care.
14.
The hopital creates awareness of a clean &
healthy environment to the public.
15.
The hospital serves as a model of efficient health
health care.
16.
The hospital fosters in all its employees a respect
for respect for human life at all stages of life.
17.
The hospital tries to develop in its employees a
Learn spirit & a family atmosphere.
18.
Rules ^regulations of the institution are reasonable
19.
The hospital shows concern for the welfare of its
employees.
20.
Giveany THREE POSITIVE aspects of the hospital:
21.
Give any THREE NEGATIVE aspects of the hospital which you have experienced:
22.
Give any THREE suggestions for improving the hospital functioning:
To what extent are you able to accomplish the following tasks , Give your answer honestly by encircling a
number ranging from ONE to FIVE where 1 means you are ‘not able to do the task at all’ and 5 means
you are ‘ able to do foe task to the best of your ability’Given below is space provided for comment .Please
give your comments if you have faced any problems /difficulties to do these tasks.
I-
I am able to provide care to all patients irrespective of
foeir caste/creed/social status.
1
2
3
4
5
2.
I am able to provide foe best possible care to all patients
at all times.
1
2
3 4
5
3.
I am able to ophold my moral/ethical values in dealing
with all the patients /co-workers.
1
2
3
4
5
4.
I am able to meet the spiritual needs of the patients
daily respecting their own religious views.
-1
2
3
4
5
5.
I am able to participate in activities which will enhance
my skills/professional ablities.
1
2
3
4
5
Given below are list of statements relating to various aspects of your education in St. Martha's School of
Nursing. Give the extent to which you are satisfied with each aspect ,in the form of a number ranging from
ONE to FIVE in the blank provided against each statement.
5
Fully
satisfied
4
moderately
satisfied
3
partially
satisfied
2
minimally
satisfied
I.
The encoiragement you get from home to perform well in your studies.
2.
The encouragement you get from teachers to do well in your studies.
3.
The encouragement you get from the staff in the hospital to do well.
4.
The encoiragement you get from the warden to do well in studies.
5.
The facilities on the campus for your personal/professional/spiritual
development:
•classroom
♦chapel
♦canteen
♦hospital services
♦hostel
♦library
♦mess
♦recreation
♦sick room
6.
The facilities for your social development.
♦interaction with faculty/staff
♦interaction with peers/seniors
•involvement in the campus activities
•3.N.A activities
•C.N.G.L activities
♦sports
7.
The faculty/staff who are directly involved in your education
♦show genuine interest in your welfare
•snow respect to all of you
•are available whenever needed by you
♦discipline you when appropriate reasonably
•provide you with appropriate supervision
♦are firm yet concerned with your welfare
•demonstrate fairness in dealing with you
♦are competent in various teaching methods
♦use appropriate evaluation methods fairly
•demonstrate moral/ethical values in dealing with you
•possess good personal skills &are confident in selves
1.
least
satisfied
Questionnaire for out-patients / casualty
3.
Occupation
1. Age
2.
Sex
4. Family Income
a)
b)
c)
d)
Less than Rs. 2,000/- P M
Rs. 2,000/- to Rs. 4,000/- P M.
Rs. 4,000/- to Rs. 6,000/- P.M
Over Rs 6,000/- P.M.
5. Your House
a) - Rented
- Owned
b) - No. of rooms _______
c) - roof
- Thatch
- Tile
- RCC
d) - Floor
- Earth
- Cement
- Mosaic tile
- Marble granite
6. Do you own
Cycle
TV set
2 wheeler
Refrigerator
Car
___________________
(specify)
7.
Religion
8.
Education (tick any one)
9.
Through whom did you come to know of St. Martha’s (tick any one)
Family doctor
Friends
Relatives
Neighbours
Other _____________
(specify)
10.
Why did you come to St. Martha’s Hospital (tick any one)
- close to your home/office
- doctor recommended it
- friends/relatives recommended it
- mission hospital
- reputation of the doctors
- other
(specify)
No formal education
Class VII or less
Class VIII to X
Pre degree
Degree
Post graduate / professional
Ills this the first visit to St. Martha’s
- Yes
-No
12. Which department did you visit today
(specify)
13 . Do you like to see only one particular doctor or any doctor (tick any one)
- One particular doctor
- Any doctor
14.
If particular doctor
a) If he/she is not available (tick any one)
- will you go back & return another day
- see another available doctor
b) If he/she leaves the hospital service (tick any one)
- will you continue coming to St. Martha’s Hospital
- change the hospital
15.
How long did you have to wait to see the doctor (tick any one)
- less than one hour
- one - two hours
- more than 2 hours
16.
Do you feel that the time you had to wait was acceptable ?
- Yes
- No
17.
What diagnostic tests did you have today (tick one or more)
- None
- Laboratory (blood, urine, stool, sputum)
- X-ray
-ECG
- Ultrasound
- Endoscopy
- Others
(specify)
18.
Give your impressions of the services you received
- the doctor who treated you was
knowledgeable and good
- the nursing care is caring and efficient
- the staff in general are courteous and helpful
- were you overall satisfied with the care given
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Give your impressions of OPD / Casualty amenities
- general cleanliness is good
- toilets and water supply are satisfactory
- seats, fans and lights were adequate
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
19.
Did you have any problem with getting your record from the Medical Record
Department
- Yes
- No
If Yes, specify
20.
21. Please tell us your opinion of the following
- The hospital is meant mainly for
those who can pay
- The hospital serves the poor sections of the
population even if they cannot pay for services
- The hospital & its staff care for all patients
with love and care
- The religious sentiments of all patients are
respected
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
22.
Do you think the hospital charges are (tick any one)
- correct
- too high
- too low
23.
Name 3 things in the hospital you appreciate most
24.
Name 3 things in the hospital that need improvement most
25.
You must be aware that St. Martha’s Hospital tries not to refuse treatment to any
patient, no matter how poor. Can you suggest how the hospital can raise funds to
treat more poor patients
26.
Any other suggestions or comments
Questionnaire for In-patients
(at discharge)
1. Age
2.
Sex
4. Family Income
a)
b)
c)
d)
Less than Rs 2,000/- P.M.
Rs. 2,000/- to Rs. 4,000/- P.M.
Rs. 4,000/- to Rs. 6,000/- P.M.
Over Rs 6,000/-P M.
5. Your House
a) - Rented
- Owned
b) - No. of room
c) - roof
- Thatch
- Tile
- RCC
d) - Floor
- Earth
- Cement
- Mosaic tile
- Marble granite
6. Do you own
Cycle
TV set
7. Religion
_______________________
3.
2 wheeler
Refrigerator
Occupation
Car
(specify)
8.
Education (tick any one)
No formal education
Class VII or less
Class VIII to X
Pre degree
Degree
Post graduate / professional
9.
Through whom did you come to know of St. Martha’s (tick any one)
Family doctor
Friends
Relatives
Neighbours
Other
(specify)
10.
Why did you come to St, Martha’s Hospital (tick any one)
- close to your home/office
- doctor recommended it
- friends/relatives recommended it
- mission hospital
- reputation of the doctors
- other
(specify)
11 Is this the first time you have been admitted in St, Martha’s Hospital ?
-Yes
-No
12. For how many days were you admitted ?
(specify)
13. Under which department have you been admitted ?
(specify)
14. What ward were you treated in
- General ward
- Shared private room
- Single private room
15. Did you choose to be admitted in this hospital for treatment mainly because (tick
any one)
- of a particular doctor
- the reputation of the hospital
16. If for a particular doctor, if he/she leaves the hospital service (tick any one)
- would you still have been admitted in St. Martha’s Hospital
- changed the hospital
17. Which of the tests below did you undergo while you were admitted : (tick one or
more)
None
Laboratory (blood, urine, stool, sputum)
X-ray
ECG
Ultrasound
Endoscopy
(specify)
Others
18 Give your impressions of the services you received
- the doctor who treated you was
knowledgeable and good
- the nursing care is caring and efficient
- the staff in general are courteous and helpful
- were you overall satisfied with the care given
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
19. Give your impression of ward amenities
- general cleanliness is good
- toilets and water supply are satisfactory
- fans and lights worked well
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
20. Did you take diet from the hospital
- Yes
- No
21. If Yes, was it satisfactory
Yes/Somewhat/No
22. Did a chaplain visit you while you were admitted
- Yes
- No
23. If Yes, was his visit helpful
24. Please tell us your opinion of the following
- The hospital is meant mainly for
those who can pay
- The hospital serves the poor sections of the
population even if they cannot pay for services
- The hospital & its staff care for all patients
with love and care
- The religious sentiments of all patients are
respected
25. What is your opinion of the cost of
- Room bed charges
- Investigations
- Doctors fees (if any)
- Surgery/procedure charges
- Medicines
Yes/Somewhat/No
Y es/Somewhat/No
Yes/S omewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Too low/Correct/Too high
Too low/Correct/Too high
Too low/Correct/Too high
Too low/Correct/Too high
Too low/Correct/Too high
26. Name 3 things in the hospital you appreciate most
27. Name 3 tilings in the hospital that need improvement most
28. You must be aware that St. Martha’s Hospital tries not to refuse treatment to any
patient, no matter how poor. Can you suggest how the hospital can raise funds to
treat more poor patients
29. Any other suggestions or comments
EVALUATION OF ST, MARTHA’S HOSPITAL
^KEAS ASSIGNED : NURSING SERI'ICE DEET. A SCHOOL OE NURSING
Sample Nursing Service Dept -* Ward in Charges
* Staff Nurses
School of Nursing
- * Faculty
* Student nurses
(n/cj
c -s'/.n)
f e)
Description of the Sample:
Ward tn Charges \ There were totally 19 Ward in Charges in the hospital All of them were included
in the evaluation All (100% ) were lay persons The mean duration of years of service was 10.4 years
(n = 13), with a range of 1& 1/2 years to 32 years (X>^six of them did not respond to the duration of
their service in the institution , they hence were not included for computation of the mean duration of
service All ( 100%) had done the General Nursing Course , and only 2 (10.5%) had some additional
qualification out of whom one had done a course on Administration Twelve (63 .2%) of them had
there training from St. Martha’s School of Nursing . One (5 3%) had completed her course as early as
in the 1950s , 4(21.0%) in the 1960s , 5(26.3%) in the 1970s , 6(31.5%) in the 1980s and 2(10.5%) in
the 1990s . Most 15 (78.9%) had In Service Education after having joined St. Martha’s hospital
Staff Nurses: The staff nurses were sampled from the total list of all categories , using the simple
random sampling technique . Hence a total of 50 staff were selected ,of which 47 were accepted for
analysis. Most of them were junior staff 37 (78 7%), with just two or three years of service and 10
(21.3%) were interns with less than a years service . Only 3 (6.4%) were religious and the rest 44
(93 6%) were lay persons Most 31(66.0%) of the staff were alumnae of St. Martha’s School of
Nursing ,while 16 (34.0%) were from other institutions, of which 7 (43.7 %) were from institutions
within Bangalore city itself and the rest from out of Karnataka state . The mean duration of service for
the staff was 2.09 years with a range of 2 months to 10 years. Only 3 (4.3%) had not received any in
service education after having joined the institution . Majority 45 (95.7%) had done there G.N.M
course , 2 (4.3%) had done their Basic B.Sc.
faculty The total number of faculty in the School of Nursing were 15 . All were taken for the
evaluation . Ten (66.6%) were tutors, 3 (20.0%) were clinical instructors and 2 (13.3$%) were senior
tutors Only 1(6 7%) was a religious while the rest ,14 (93.3%) were lay persons The mean duration
of years of service was 3 87 years with a range of 10 months to 16 years . Most 10 (66.6%) had a
basic B.Sc qualification , 4 (26 6%) had done their P.C.BSc and 1(6 7%) had done her General
Nursing after which she had done her Diploma in Nursing Education .Eleven (73.3%) had their nursing
training in Karnataka of which 9 (81 1%) were trained within Bangalore itself Eleven (73.3%) had
inservice education after joining the institution .
Student Nurses : The students were selected from the 2nd, 3rd and the 4th year, although those in
their 4lh year have completed their training in the institution they were selected in the category of
students since they considered to be under the School of Nursing . The Is* year students were not
selected since it was assumed that it would be too early to get a valid opinion from them . The students
were selected through simple random technique , and comprised a total number of 45 , (i.e. 15 per
batch Only 4 (8 8%) were religious and the rest were laypersons. Most 42 (93.3%) were Christians
while 3 (6.6%) were Non Christians
Methodology :
The evaluation of these assigned areas was performed primarily from information provided by the
selected sample through a questionnaire The questionnaires were prepared based on the selected
functions of the hospital or the School of Nursing , the individual functions of each category , their
expectations and suggestions All the members of the review committee had accepted the format
proposed and a copy of the questionnaires for each category is attached
Results
1 Awareness of Nursing Personnel in relation to —
a Vision of the hospital .
b. Philosophy
c. Objectives / Goals
d Policy regarding
work
benefits
promotion
recruitment
student selection
discipline
e. Welfare Facilities
f. Workers Union
g Performance Appraisal:
W/S
S/N
F
St/N
19(100.0%)
18( 94.7%)
19(100 0%)
32(68 7%)
32(68.7%)
37(78.7%)
14( 93.3%)
15(100.0%)
15(100 0%)
42( 93.3%)
—
—
19(100 0%)
16( 84.2%)
17( 89.5%)
16( 84 2%)
15( 78.9%)
16( 84 2%)
14( 73.7%)
15( 78.9%)
17( 89.5%)
44(78.7%)
35(74.5%)
34(72.3%)
41(87.2%)
43(91.5%)
43(91.5%)
26(55.3%)
15(31.9%)
21(44.7%)
15(100.0%)
15(100.0%)
15(100.0%)
12( 80.0%)
14( 93.3%)
14( 93.3%)
1 1( 73.3%)
8( 53.3%)
9( 60.0%)
—
—
—
—
——
—
—
—
It is obvious from the above data that most (more than 75%) of the nursing personnel from all
categories were aware of the objectives and goals of the institution ; of the policies regarding work ,
benefits recruitment of staff, selection of students and disciplinary action . Among the three categories
of nursing personnel the staff nurses seemed least aware of the philosophy of the institution , welfare
facilities workers union and performance appraisal . The only question that student nurses were asked
was in relation to their awareness of the vision and mission of the hospital Majority ( 90% & > ) said
they were aware of the vision
Extent to which the objectives / Koa/s /functions of the hospital are met presently
The ward in charges , staff nurses and the faculty were given a list of statements pertaining to the
above mentioned aspects They were asked to rate each of the statements on a 5 -point scale
according to the extent to which they believed these aspects were presently fulfilled and also to
the extent to which they thought these aspects should be fulfilled However most of them did not
answer to the latter part
T he results of the extent to which the above aspects are met are presented in percentages .
5
1
Service given to the sick
irrespective of any factor
4
17(89 5) 2(10 5)
(W/S)
23(48 9) 18(38 2)
(S/N)
10(66.7) 3(20.0)
( F)
2 Quality care affordable to the common man
12(63.2) 5(26.3)
(W/S)
17(29 8) 14(29.8)
(S/N)
3(20.0) 6(40.0)
( F )
3 Main beneficiaries - women I children
8(42.1) 4(21.0)
(W/S )
10(21 3)
7(15.0)
(S/N)
—
3(20 0)
( F )
4. Provides cost effective competent care
8(42.1) 7(36.8)
(W/S )
3(
6.3) 4( 8.5)
(S/N )
K
6.7) 4(26.7)
( F )
5. Fosters dedication and ethical values
14(73.7) 4(21.0)
(W/S )
13(27.7) 17(36.2)
(S/N )
6(40^0)
7(46.6)
(F )
6 Enhances skills through CE programs
4(21 0) 7(36.8)
(W/S )
7(14.9) 12(25.5)
(S/N )
K 6 7) 6(40 0)
( F )
7 Fosters a desire to serve the poor
11(57.9) 7( 6.8)
( W/S)
14(29.8) 16(34.0)
( S/N )
6(40.0) 4(26.7)
( F )
8 Builds social awareness among its staff
3(15.8) 9(47.4)
( W /S )
17(36.2)
6(12.8)
( S/N )
—
2( 4.3)
( F )
3
1
2
—
4( 8.5)
2(13 3)
—
1(21)
—
2(10.5)
15(31.9)
6(40.0)
—
1(2.1)
—
5(31.6) 1(5.3)
15(31.6) 10(21.3)
8(53 3) 3(20.0)
1(2.1)
—
3(6.3)
5(10.7)
1( 6.7)
2(10.5) 2(10.5)
17(36.2) 11(23.4) 12(25.5)
8(53.3) 2(13 3)
K 5.3) —
6(12.8) 6(12.8)
K 6.7)
6(12.8)
1( 6.7)
6(31.6) 2(10.5)
17(36.2) 10(21.3) 1( 2.1)
1( 6.7)
7(46.6)
1( 5.3) —
13(27.7) 3(6.4)
5(33 3) —
—
1(2.1)
—
5(26.3) 1(10.5)
18(38.3) 3( 8.5)
10(66.7) 4(26.7)
1( 4.2)
9. Meets spiritual needs of all patients
( W/S)
—
17(63.1) 5(26.3) 2(10.5)
( S/N )
23(48.9) 16(34.0) 7(14.9)
1( 2.1)
6(40.0) 5(33.3) 2(13.3)
( F )
2(13.3)
10. Provides care at subsidised cost to those in need
( W/S)
—
15(73.7) 2(10.5) 2(15.8)
11(23.4) 23(48.9) 12(25.5) 2( 2.1)
( S/N )
6(40.0)
5(33.3) 4( 6.7)
( F )
11. Develops community centres for those in need
( W/S)
14(73.7) 5(21 0)
1( 5 3)
14(29.8) 14(29.8) 14(29.8) 4( 8.5)
( S/N)
5(33.3) 4 (26.7) 6(40.0)
( F )
12 Expands depts & education programs as per need
—
12(63.2) 4(21.0) 3(15.8)
( W/S )
9(19.1)
3( 6.4) 12(25.5) 19(40.4)
( S/N )
—
1( 6.7)
6(40.0) 8(53.3)
( F )
13. Attempts to improve quality of care
—
—
14(73.7) 5(26.3)
( W/S )
1(
2.1)
16(34.0) 22(46.8) 8(17.0)
( S/N )
1(
6.7)
2(13.3) 10(66.7) 2(13.3)
( F )
14 Creates cleanliness awareness in public
—
13(68.4) 4(21.0) 2(10.5)
( W/S )
3(
6.4)
14(29.8)
2(
4.3)
28(59.5)
( S/N )
—
5(33.3)
9(60.0)
1(
6.7)
( F
)
15. Serves as a model of efficient health care
—
—
14(78.9) 4(21.0)
( W/S )
—
3(
6.4)
22(46.8)
20(42.6)
( S/N )
—
3(20.0)
7(46.7)
5(33.3)
( F
)
Fosters
respect
for
life
in
all
its
staff
16
—
—
15(78 9) 4(21.0)
( W/S )
14(29.8) 25(53.2) 6(12.8)
2( 4.3)
( S/N )
—
5(33.3) 6(40.0) 2(13.3)
( F
)
17 Fosters a team spirit and family atmosphere
—
1( 5.3)
( W/S )
14(73.7) 5(26.3)
11(23.4) 19(40.4) 10 (21.2) 4( 8.5)
( S/N )
—
5(46.7) 4(26.7) 4 (26.7)
( F
)
18. Has reasonable rules and regulations
—
11(57.9) 7(36.8)
1( 5.3)
( W/S )
12(25.5) 19(40.4) 11(23.4) 4( 8.5)
( S/N )
—
3(20.0) 5(33.3) 7(46.7)
( F
)
19. Shows concern for its staff s welfare
—13(68.4) 3(15.8) 3(15.8)
( W/S )
5(10.6) 19(40.4) 16(34.0)
5(10.6)
( S/N )
—
4(26.7)
8(53.3) 3(20.0)
( F
)
—
—
1( 6.7)
1( 2.1)
—
4( 8.5)
;-—
—
—
—
—
—
—
2( 4.2)
—
—
—
—
3( 6.4)
1( 2.1)
2( 4 3)
—
It is obvious that most (80% & > )of the ward in charges believed I were of the opinion
that the objectives / goals / functions of the hospital are met presently They(36.8%) however
felt that women I children were not the main beneficiaries and social awareness wasn’t built
amongst the staff. Only 57 8% felt that CE programs were planned to enhance the skill of the
employees.
Most(80% & >) of the staff nurses felt that service was provided to the sick irrespective to any
factor, the spiritual needs of the patients were met , that attempts were made to improve the
quality of care always , to serve as a model for efficient health care , and create an awareness
of cleanliness in the public.
The faculty(80% & > ) also felt that the service was provided to all irrespective of any factor,
a sense of dedication and ethical values was fostered , an awareness of cleanliness in the public
was built , that the hospital served as a model of efficient health care
The aspects that possibly need to be reviewed by the management are obviously in relation to
the following objectives I goals:
e Who are its main beneficiaries 7
• What is the role of CE_ programmes in enhancing the skill of the staff and
thus the quality of care7
• Should the hospital build a social awareness amongst its staff7
• Is the institution responsible for providing community health centres,
expanding departments and educational programmes as per the need7
• Should there be concern for the welfare of the staff7
e Does the hospital employees and the management really strive to provide high
quality care at a rate affordable to the common man 7
• Is there any effort made to ensure that comprehensive and cost effective care
is provided ?
• Are the rules and regulations fair for and reasonable to all the employees 7
5. The extent to which the Nursing personnel from the Nursing Service were able to
perform certain tasks:
The ward in charges and the staff nurses were given an additional five statements relating
to
their functions or tasks They were asked to rate these statements on a 5-point scale depending
on their ability to perform the said functions The results are presented below in percentages
They were also asked to comment if they were unable to perform these functions to the best of
their abilities The reasons provided are also summarised below this data .
5
4
3
Provides care to all irrespective of
caste /creed /social status
17 (89.5) 2(10.5)
( W/S )
37
(78.7) 6(12 8) 4( 8.5)
( S/N )
2 Provides best possible care at all
times
7 (36 8) 7(36 8) 4(21.0)
( W/S )
4( 8.5) 26(53 3) 15(31.9)
( S/N )
3. Upholds moral & ethical values
4(21.0) —
15 (78.9)
( W/S )
27 (57.4) 17(36 2) 2( 4.3)
( S/N )
4. Meets spiritual needs of all patients
1( 5.3)
11 (57.9) 6(31.6)
( W/S )
5(10.6)
28 (59.6) 11(23.4)
( S/N )
5. Participates in activities to improve
2(10.5)
10 (52 6) 4(21.0)
self
( W/S )
20 (42.6) 14(29 8) 7(14.9)
( S/N )
2
1
1
—
2( 4.3)
1( 5.3)
-
—
1(2.1)
—
-
2(4.3)
1( 5 3)
1(2.1)
3(15.3)
6(12.7)
—
—
Majority of the Ward Sisters and Staff Nurses said that due to lack of sufficient staff and overload in
their work , they were unable to provide the best possible care to all patients. In relation to the ability
to uphold their moral and ethical values, only the staff nurses responded that they were unable to do so
at all times due to misunderstanding with their co-workers None of them gave any reasons regarding
their ability to meet the spiritual needs of the patients and their participation in activities which would
enhance their skills and professional abilities.
Points to be considered from this data which is available :
• Is there a definite lack of staff 9
• Is the environmental climate of the staff conducive for upholding ones ethical & moral
values ?
• Should the management look into the cultural activities of the staff?
l^sitive aspects of St. Martha’s Hospital and School of Nursing
1 he Ward in charges , staff nurses and the faculty were asked to give THREE positive aspects of
the institution . These aspects were scrutinised and are categorised under headings such as
Objectives
* Administration
* Satisfaction with the working environment.
(i ) Objectives :
a) Helping the poor & neglected
b) Care for all irrespective of caste
c) Respect for life & spiritual care
d) Giving work opportunities for
the poor
e) Low cost & high quality care
f) Spiritual care
(ii) Administration :
a) Administrators are approachable
b) Good Supervision
c) Good Management
d) Good co-ordination between
nursing service & education
e) Conducting Continuing
Education programs
W/S
n = 19
S/N
n = 47
Faculty
n= 15
7 (36.8 )
4(21.0)
4 (21 0 )
41 (87.2)
5 (10 6)
11 (23 4)
2(13.3)
4(26 7)
3(20 0)
2 (10.5 )
—
1( 5.3 )
—
11 (23 4)
7 (14 8)
—
3(20.0)
—
5 (26.3 )
1(53)
___
—
16 (34.0)
—
—
3(20.0)
—
—
K 6.7)
—
—
K 6.7)
38 (80 9)
2( 4.3)
—
10(66 7)
—
6(40.0)
—
2(13.3)
—
—
(iii) Satisfaction with the Working Environment:
8 (42 1 )
a) Care provided is appreciated
7 (36 8 )
Family
and
friendly
atmosphere
b)
6(31.6)
Safety
c)
3 (15 8 )
d) Hygienic working environment
1 ( 5.3)
Welfare
of
Staff
considered
e)
—
Freedom
to
work
f)
—
g) Rules & Regulations are fair
1 ( 5.3 )
h) Dedicated staff
—
9 (19 1)
2( 4.3)
3(64)
1 ( 2.1)
Negative aspects of the Institution :
The nursing personnel were asked to give THREE negative aspects of the
institution the comments were then categorised under specific headings such as :
*Communication , * staffing and
* administrative aspects
5.
S/N
n=47 .
F
n=l 5
2(4.3)
2(10.6)
3( 6.4)
—
1(2 1)
1(2 1)
2(10.6)
7(46 7)
K 5 3)
2(10.6)
3(15.8)
1( 2.1)
4(26.6)
—
—
3(15.8)
—
3(15.8)
9(47.4)
—
4( 8.7)
11(23.0)
—
1( 2 1)
34 (74.4)
20 (43.0)
3( 6.3)
5(33.3)
1( 5.3)
—
2(10.6)
—
—
—
3(15.8)
—
3(15.9)
—
1( 5.3)
2( 4.3)
1( 2.1)
___
9(47.4)
3(15.8)
4(21.0)
—
3(15.8)
—
—
9(17.1)
3( 6.4)
1( 2.1)
1( 2.1)
2( 4.3)
2( 4.3)
16(34.4)
—
1( 5.3)
—
—
—
—
—
W/S
n=19
i) Communication ;
___
a) Rules very rigid for ICUs
b) Inter departmental communication
—
is poor
c) Enquiry is not satisfactory
2(10 5 )
d) Nonavailability of 24 hrs STD booth K 5.3 )
—
e) Communication gap
ii) Staffing Problems :
a ) Lack of supervision
b) Indiscipline of security /class iv
workers
c) Night duty for one month
d) Lack of promotional avenues
e) Lack of concern for all staff
f) Lack of adequate staff
g) Inadequate pay
h) Health of staff not considered
i) Continuing education not planned
regularly
Hi) A dm in istrative A spects :
a) Lack of an isolation ward
b) Need for a waiting area for relatives
c) Salary is not adequate for the cost of
living in the city
d) Equipment and articles inadequate
e) Repair work and maintenance slow
f) Repairs allotted to outside agencies
g) Lack of promotional opportunities
h) Cash counter not available for 24 hrs
i) Lack of pharmacy & lab. for 24 hrs.
___
6
Sugf’estions for improvement: The nursing personnel were asked to give THREE
suggestions which they felt would help in the functioning of the hospital and the
School of Nursing After scrutinising the points given by the nursing personnel
the points were categorised under headings such as: Administrative , Equipment
and facilities, Staff welfare Three ward in charges and faculty did not give any
suggestions All the staff nurses gave suggestions
W/S
i) Administrative
a) Supervision of staff nurses to
improve
2(10 5)
b) Night supervision essential
1( 5.3)
c) Appreciation of work done
1( 53)
d) Maintenance dept to improve
1( 5 3)
e) Clerks in the ward for clerical
work to increase staff time with
—
patient
f) Communication between service
—
and education
4(21.0)
g) Increase the number of staff
h) Ambulance availability for
—
transport of dead
i) 24 hr lab and pharmacy services
j) Atleast one relative to be allowed
with an 1CU patient
S/N
F
2( 4 3)
1( 2 1)
--1( 2.1)
2(12.3)
—
1( 6 7)
___
15(32.0)
2(12 3)
1( 6 7)
2( 4 3)
15(32.0)
—
—
—
K 6 7)
K 67)
—
—
iijNeed for more Facilities and Equipment
___
—
1( 5.3)
a) Separate OT for Obstetrics
b) Ventilators for new-borns and
1( 2.1)
children to avoid referrals
U 5 3)
5(33.3)
15(32.0)
3(15
8)
c) More advanced technology
—
___
1( 5.3)
d) Need for a geriatric ward
—
1( 5 3)
4( 8.7)
e) Need for an isolation ward
—19(40.4)
K 5 3)
f) Waiting room for relatives
g) Ambulance with emergency
___
—
10(20 6)
facilities
h) Security to be trained to be
—
10(20.6)
—
courteous to all .
iii) Staff Welfare:
a) Need for CE programs regularly 3(15.8)
b) Staff health services to be
___
improved
c) Leave to be granted in emergencies —
—
3(10 9)
7(14.8)
4( 8.7)
—
-—
NURSING STUDENTS ( N= 45 ; 15/Batch of 2nd , 3 rd & 4,h year)
The nursing students were selected from the 2nd and 3rd year on a random basis Those who had
completed their training and who in this institution are considered to be in their 4,h year were also
selected randomly using the table of random numbers, The I s* years were excluded from the
evaluation since the committee felt that it would be too early to be able to get a valid opinion from
them . These students were given a set of four statements relating to the encouragement they receive
from various individuals , facilities available , facilities for their social development and characteristics
of the faculty Each of these statements had several items under them The students had to rate each
of these statements on a 5 - point scale reflecting the level of their satisfaction on each of the aspects
This tool was prepared based on a study conducted by
1
Encouragement received from
home
0(- )
1(2.2)
teachers
staff
1(2.2)
warden
1(2.2)
2
3
4
5
0( - )
0( - )
8(17 7)
4( 8.8)
0( - )
6(13.3)
12(26.7)
10(22.2)
4( 8.8)
14(31.1)
20(44.4)
19(42 2)
41(91 1)
24(53.3)
4( 8.8)
11(24.4)
It is obvious that the students are satisfied with the encouragement they receive from their
parents , teachers and the warden to do well in their studies The staff however do not seem to play a
major role encouraging their juniors to perform well in their studies
2. Facilities available :
classroom (n=44)
chapel (n=44)
canteen (n=44)
hospital services (n=45)
hostel (n=45)
library (n=45)
mess (n=44)
recreation (n=45)
sick room (n=45)
0( - )
0(- )
6(13.6)
2( 4.4)
1( 2.2)
0(- )
5(H.l)
3( 6.6)
6(13.3)
1( 2.2)
0( - )
7(15.9)
4( 8.8)
3( 6.6)
2( 4.4)
11(25.0)
6(13.3)
6(13.3)
5(H 1)
0( - )
11(25.0)
14(31.1) '
8(17.7)
5(11.1)
12(27.3)
10(22.2)
14(31 1)
15(33.3)
10(22.7)
15(34.1)
14(31.1)
17(37.8)
14(31 I)
13(18.2)
15(33.3)
15(33.3)
23(51.1)
34(77.3)
5(H.4)
11(24.4)
16(35.6)
24(53.3)
3( 6.8) W
11(24.4)
4( 8.8)
Most of the students again seem satisfied with their classroom , chapel , hostel, library
facilities They seem most dissatisfied in relation to canteen , mess , and sickroom facilities . They
appear to be moderately satisfied with the hospital services and recreation facilities .
Activities required for their social development
interaction with faculty 1( 2.2)
6(13 3)
interaction with peers
& seniors
2( 4 4)
K 2.2)
campus activities( n=44) 0( -)
3( 6.8)
SNA activities
0( - )
K 2 2)
CNG1 activities (n=44)
5(11.3)
K 2.2)
sports activities
2( 4.4)
K 2.2)
14(31 1)
14(31 1)
10(22 2)
12(26.7)
8(18.2)
6(13.3)
17(38 6)
4( 8 8)
17(37 8)
26(590)
17(37 8)
11(25 0)
26(57 8)
13(28 9)
7(15.9)
21(46.7)
10(22.7)
12(26.7)
The only area were the students appear to be quite satisfied is in relation to the SNA activities . The
rest of the activities relating to their social development would have to be scrutinised more deeply for
the overall development of the students
4
Characteristics of their faculty
shows genuine interest
1( 2.2)
shows respect
K 2 2)
is available
1( 2.2)
disciplines fairly (n=44) 0( -)
supervision good (n=44) 0( -)
firm yet concerned (n=44) 0( -)
fair in dealings (n=44)
1( 2.3)
competent (n=44)
0( -)
evaluation fair (n=44)
1( 2.3)
shows moral values
in dealings (n=44)
1( 2.3)
has good personal skills
(n=44)
0( -)
3( 6.7)
4( 8 8)
2( 4 4)
0( - )
0( - )
K 2.3)
5(H.4)
4( 9.0)
4( 9.0)
8(17.6)
15(33 3)
8(17.8)
6(13.6)
6(13.6)
10(22.7)
11(25.0)
14(31.8)
13(29.6)
16(35 5)
16(35 6)
18(40.0)
19(43 1)
16(36.4)
17(38.6)
18(40.9)
15(34.1)
20(45 5)
17(37.8)
9(20.0)
15(33.3)
19(43.1)
22(50.0)
16(36.3)
9(20.5)
11(25.0)
6(13.6)
4( 9 0)
9(20.5)
17(38 6)
13(29.5)
3( 6.8)
10(22.7)
16(36.3)
15(34.0)
In relation to the characteristics of the faculty the students again appear to be satisfied with most
aspects except in relation to their ability to show genuine interest in the welfare of the student, being
fair in their dealing with student, being competent in various teaching methodologies and being fair in
their evaluation methods
The students were also given a set of questions relating to the goals and functions of the institution
They were expected to either answer ‘yes’ or ‘no’ to the questions . No clarifications were made in
relation to their answers.
1.
2
3
4.
5
6
Knows vision and mission
Feels part of the hospital
Opportunities for spiritual growth
Availability of guidance & counselling
Remain as staff in the same hospital
Stress on care of poor during training
YES
42 ( 93.3 )
45 (100.0 )
43 ( 95.6)
29 ( 64 4 )
34 ( 75 6 )
37 ( 82.2 )
NO
3 (6.3 )
0( - )
2( 44)
16(35.6 )
1 1 (24.4 )
8 (17.8 )
It is evident from the above findings that majority (more than 80.0% ) of the students who were
selected to participate in the evaluation were aware of the vision of the hospital, felt a part of the
hospital, felt that there were opportunities for their spiritual growth and that a stress on the care of the
poor was made during their training The need for personnel trained in guidance and counselling was.
evident in that atleast 36% of the students responded that this was not available . The fact that at leas^
76% of the students responded that they would like to remain as staff in the hospital is credible .
Points to possibly review
•
•
•
•
•
•
•
•
Encouragement to be given to the students by the staff and the warden , to perform well in their
studies
Canteen and mess facilities may have to be improved
Hospital services for the students seem to be inadequate
Recreational facilities for the students could be increased
Interaction with the faculty / seniors at informal settings
C.N.G.I. activities could help foster their spiritual development It could also help to improve their
interaction with other students
Faculty characteristics such as ability to have respect for the students, to be firm yet concerned, to
be fair and ethical in their dealings & to be skilful need to be enhanced
Availability of guidance and counselling for the students
4
general functions of the management
The ward in charges ( W/S), faculty (F) and staff nurses (S/N) were also given a set of questions to
which they had to respond 'Yes’ or ‘No’ . These questions were relating to the general functions of
the management Flere again they were neither asked to provide details or clarify their answer
Yes
No
N/A
1. Someone available to communicate problems (W/S)
( F )
(S/N)
19(100.0)
14 ( 93.3)
43 ( 91.5)
0( - )
1(67)
4( 8.5)
0(- )
0(- )
0(- )
2. Complaints are heard
(W/S)
( F )
(S/N)
18 ( 94.7)
13 ( 86.6)
36 ( 77.0)
1(5.3)
1 (5.3)
11 (23 0)
0(- )
1 (6.7)
0( - )
3. Feel part of a team
(W/S)
( F )
(S/N)
19(100.0)
14 ( 93.3)
47(100.0)
0( - )
0( - )
0( - )
0(- )
1 (6.7)
0(- )
4. Knows the mission of the hospital
(W/S)
( F )
(S/N)
19(100.0)
15 (100.0)
47(100.0)
0( - )
0( - )
0( - )
0(- )
0(- )
o(- )
5. Promotional avenues available
(W/S)
( F )
(S/N)
9( 47.4)
10 ( 66.7)
30 ( 63.8)
10(52.6)
3 (20.6)
17(36.2)
0(- )
2 (13.7)
0(- )
6. Orientation received when joining institution (W/S)
( F )
(S/N)
17 ( 89.4)
14 ( 93.3)
45 ( 95.7)
2 (10.5)
1 ( 6.7)
2( 4.3)
0(- )
0(- )
0(- )
7. Feels appreciated
(W/S)
( F )
(S/N)
18 ( 94.7)
14 ( 93.3)
42 ( 89 4)
1 ( 5.3)
I ( 5.3)
5 (10.6)
0(- )
0(- )
0(- )
8. Feels policies/ rules are fair
(W/S)
( F )
(S/N)
18 ( 94.7)
14 ( 93.3)
42 ( 89.4)
1 ( 5.3)
1 ( 5.3)
5(106)
0(- )
0(- )
0(- )
9. Knows employee service rules
(W/S)
( F )
(S/N)
18 ( 94.7)
15(100.0)
40 ( 85.1)
0( --)
0( - )
7 (14 9)
1 (5.3)
0(- )
0(- )
10 Opportunities to give suggestions
(W/S)
( F )
(S/N)
14 ( 73.7)
13 ( 86.6)
30 ( 63.8)
4 (21.0)
2(13.3)
17(36 2)
1 (5.3)
0(- )
0(- )
11 Availability of personnel for guidance
(W/S)
( F )
(S/N)
19(100.0)
13 ( 86.6)
22 ( 46 8)
0( --)
2(13.3)
25(53.2)
0(- )
0(- )
0( - )
12. Work area comfortable and safe
(W/S)
( F )
(S/N)
17 ( 89.4)
15 (100.0)
45 ( 95.7)
2(10.5)
0( - )
2( 4.3)
0( - )
0( - )
0( - )
13. New skill training received
(W/S)
( F )
(S/N)
12 ( 63.2)
13 ( 86.6)
40 ( 89.4)
7 (36.8)
2(13.3)
7(14.9)
0( - )
0( - )
0( - )
14 Has a job description
(W/S)
( F )
(S/N)
17 ( 89.4)
15 (100.0)
44 ( 93.6)
2 (10.5)
0( - )
3 ( 6.4)
0(- )
0(- )
0( - )
15. Participates in special functions
(W/S)
( F )
(S/N)
9( 47.4)
13 ( 86.6)
35 ( 74.5)
10(52.6)
2(13.3)
12 (25.5)
0( - )
0( - )
0( - )
In relation to the functions of the management majority of the nursing personnel (80% & > ) were
satisfied . The only aspects to be possibly looked into are as given below:
• Avenues for promotion
• Opportunities to give suggestions for improvement
• Need for in- service education programmes
• Participation in special functions
WARD IN CHARGES ( N = 19 )
The ward in charges were given 18 questions regarding their functions to which they had to either
respond ‘Yes’ or ‘No’. No clarification of their answers were sought .
YES
11 (57.9)
Conducts regular meetings
Has good communication with
17 (89.4)
management
3. Involved with plan of annual budget
5 (26.3)
4 Involved in selection of staff
1 ( 5.3)
4(21 0)
5. Informed of financial process
17 (89 4)
6. Evaluates staff performance
11 (57.9)
7. Dept, has written policies
9 (47.4)
8 Sets goals each year for dept.
9. Feels part of planning &decision-making 7(36.8)
10. Knows vision & mission of hospital
18 (94.7)
18 (94.7)
11. Communicates above to staff
12. Orients new employees
17 (89.4)
13. Provides ISE or on- the-job training
12(63.2)
14 Attended CE- program on management 12(63.2)
15. Written standards are there to guide
11 (57.9)
work
14 (73.7)
16. Enough qualified staff available
17. All Staff have job description
15 (78.9)
18. Knows organisational plan
12(63.2)
1
2
NO
NA
6(31 6)
2(10.5)
1 ( 5.3)
13 (68 4)
17 (89 4)
13 (68 4)
1 ( 5.3)
7(36.8)
9(47.4)
10(52 6)
0( - )
0( - )
1 ( 5.3)
6(31.6)
6 (31 6)
l( 5.3)
1( 5.3)
1 ( 5.3)
2(10.5)
1( 5.3)
1 ( 5.3)
1(53)
2 (10.5)
1( 5.3)
1 ( 5.3)
1 ( 5.3)
1 ( 5.3)
1 ( 5.3)
7 (36.8)
4(21.0)
2 (10.5)
5 (26.3)
1 ( 5.3)
1 ( 5.3)
2(10.5)
2(10.5)
From the data available regarding the functioning of the ward in charges it is obvious that the
following functions would have to be reinforced to them:
•
•
•
•
The need to conduct regular meetings with their staff
To have written policies and standards in the department
To set goals each year for the department
To see to their own and their staffs professional development by organising in-service education
programmes and attending CE programmes
The management need to possibly get the ward in charges involved in the following aspects:
•
•
•
Plan for the annual budget
Selection of staff
Financial process
- Ms. Mary Ann Charles,
School of Nursing,
St.John' Medical College,
Bangalore.
SURVEY OF DOCTORS
SUMMARY ANALYSIS
A survey of the opinion of full time doctors working for at least 1 year in St. Martha’s
Hospital was conducted. Of 67 staff who received the survey questionnaire, 41
responded.
Based on an analysis of the survey issues have been placed under one of three categories 1. Issues that need urgent attention based on strongly negative assessment. 2. Issues of
concern where a significant number of responses were negative. 3. Issues that seem
satisfactory based on a generally positive response.
Responses were analysed from the questionnaire as follows:
Goals - the gap perceived by the respondent between the importance a goal should be
given and is actually given by the hospital.
2. Hospital functioning - respondents scoring on a 5 point scale of various aspects of
hospital functioning A score of 3 or less was considered a negative response.
3. Comments and suggestions - The number of positive and negative responses by
respondents in different areas.
1
It is strongly recommended that besides this summary the detailed evaluation report and
especially individual comments and suggestions be studied for more complete and
empathic understanding of the doctors’ views.
I.
Issues that need urgent attention
1. Inefficiency in health care delivery and planning
2. Ignoring national priorities and programmes
3. Resistance to ideas and innovation to improve quality of health care
4. Failure to modernise equipment and technology
5. Not motivating staff to work in a caring manner
6. Not consulting concerned department heads when planning and budgeting
7 Applying different rules and regulations for different people
8. Lack of concern for welfare of staff
9. Poor levels of salaries and remuneration.
11 Issues of concern
1. Should foster concern for respect for life among staff
2. Should emphasize health care of women and children
3. Should subsidize services for the poor
4. Should provide spiritual care to sick irrespective of their religious belief
5. Should foster moral and ethical integrity among staff
6. Should consider ways to generate additional income
7. Should encourage an atmosphere among doctors condusive to work
8. Should improve continuing education programmes.
III. Issues that seem satisfactory
1. Care provided to all irrespective of caste and creed
2. Providing low cost care
3. Cleanliness
4. Spirit of dedication
5. Past reputation
- Dr. Prem Pais,
Vice-Principal,
St. John's Medical College,
Bangalore.
EVALUATION BY DOCTORS
The evaluation instrument for doctors has 2 types of responses
a)
A scored response which is to evaluate
Hospital goals - a list of goals has been specified. The respondent has been
asked to grade them in a score of increasing importance from 1 -5 in ascending
order.
The respondent first grades the goals as he/she views them and secondly as
he/she feels the hospital views them.
ii. Hospital functioning - a number of statements regarding hospital functioning
have been given. The respondent has been asked to score them from 1 to 5 in
ascending order of agreement.
i.
b)
Open ended questions.
The respondents have been given the opportunity to give open ended responses in
the following areas.
□ Hospital goals
n Major strenghths of the hospital
□ Major weakness of the hospital
□ Hospital rules
□ Suggestions
Responses have been received from 41 of 67 full time medical staff
Analysis:
a)
Hospital Goals: Under each goal in part A of the questionnaire, the number (percentage)
of respondents giving various scores are tabulated. Score have been grouped as lowest
priority (1 or 2), highest priority (4 or 5) and intermediate priority (3). Responses have
been scored in two rows - “should be” indicates the importance and respondent feels the
stated goal should be given. “Is” gives the respondents perception of the importance the
hospital gives the goal. In general a score of 3 or less will indicate a negative perception.
Hospital Functioning: Tabulation has been done in a manner similar to Hospital Goals.
However in this section only the respondents perception of hospital functioning is called
for. Once again a score of 3 or less will indicate a negative perception.
It may be noted that due to an error in cyclostyling the questionnaire the scoring system
was not fully clarified. It is being assumed that the respondents have correctly understood
the system.
HOSPITAL GOALS
1. The hospital should foster among all staff respect for human life from conception to its
natural end.
Should be
Is
2.
Hospital should provide medical care to the public irrespective of caste, creed and
social status.
Should be
Is
3.
3
7(17.1)
4 or 5
38 (92.7)
32(78.1)
No response
3 (7.3)
2(4.9)
1 or 2
2(4 9)
3
7(17.1)
4 or 5
38 (92.7)
30 (73.1)
No response 1 or 2
3(7.3)
2(4.9)
7(17.1)
3
1(2.4)
18(43.9)
4 or 5
37(90.2)
14(34.2)
The hospital should treat all patients with human care and compassion .
Should be
Is
6.
1 or 2
The hospital should serve as a model of efficient health care.
Should be
Is
5.
No response
3(7.3)
2(4.9)
While providing high quality medical care the hospital should ensure use of
appropriate, low cost yet effective care where ever possible.
Should be
Is
4.
3
4 or 5
37(90.2)
(1 (2.4)
(13(31.7) 24(58.6)
No response 1 or 2
3(7.3)
2(4 9)
2(4.9)
No response 1 or 2______ 3_________4 or 5
3(7.3)
_
_
38(92.7)
2(4.9)
2(4.9)
11(26.8)
26(63.4)
The hospital should emphasize especially the health concerns of women and children.
Should be
Is
No response
3(7.3)
2(4.9)
1 or 2
1(2.4)
3
4 or 5
3(4.9)
35(85.3)
17(41.5) 21(51.2)
7.
The hospital should subsidise services for the poor.
Should be
Is
8.
No response
3(7.3)
2(4.9)
1 or 2
1(2.4)
10(24.4)
3
6(14 6)
15(36.6)
4 or 5
31(75.6)
14(34.1)
No response
3(7.3)
2(4.9)
1 or 2
3
3(7 3)
12(29.3)
4 or 5
38(92.7)
24(58.6)
The hospital should keep the national health priorities in mind when planning its
services.
Should be
Is
11.
6(14.6)
3
4 or 5
2(4.9) 36(87.8)
12(29.3) 21(51.2)
The hospital should serve as training institution where trainer doctors and nurses will
learn to deliver competent health care ethically and compassionately.
Should be
Is
10.
1 or 2
The hospital should provide spiritual care to the sick respecting the individual’s
religious beliefs.
Should be
Is
9.
No response
3(7 3)
2(4.9)
No response
3(7.3)
2(4.9)
1 or 2
12(29.3)
3
4(9.8)
15(36.6)
4 or 5
34(82.9)
12(29.3)
The hospital should foster a sense of moral and ethical integrity among all its staff.
Should be
Is
No response
3(7.3)
2(4.9)
1 or 2
12(29.3)
3
1(2.4)
10(24.4)
Hospital functioning
1. The hospital constantly tries to improve quality of health care.
No response
1 or 2
4(9.8)
3
20(48.8)
4 or 5
17(41.4)
4 or 5
37(90.2)
17(41.5)
2. The hospital innovates to find means of reducing the cost of health care to make it
more affordable.
No response
1(2.4)
3
4 or 5
17(41.4)
1 or 2
2(4.9)
3
4(9.8)
4 or 5
35(85.4)
The hospital functioning is such as to the efficient and reduce waste.
No response
5.
3
12(29.3)
The hospital is kept clean
No response
4.
1 or 2
11(26.8)
1 or 2
4(9.7)
3
11(26.8)
4 or 5
26(63.4)
The hospital functioning is such as to provide prompt attention to patients.
No response_________ 1 or 2____________ 3_____________ 4 or 5
2(4.8)
4(9.8)
13(31.7)
22(53.6)
6.
The hospital motivates all its staff to work in a caring and compassionate manner.
No response
7.
4 or 5
21(41.2)
1 or 2
12(29.2)
3
12(29.2)
4 or 5
14(34.1)
The hospital is concerned about ways to generate additional income.
No response
1(12.4)
9.
3
12(29.3)
The hospital involves each department in preparing the department’s budget.
No response
3(7.3)
8.
1 or 2
8(19.5)
1 or 2
10(24.4)
3
9(22.0)
4 or 5
21(51.2)
The hospital charges are reasonable compared to charges by other similar hospitals in
the city.
No response__________ 1 or 2____________ 3_______________ 4 or 5
3(7.3)
9(22.0)
29(70.8)
10.
The hospital has reasonable rules and regulations.
No response
7(17.1)
11
3
9(22.0)
4 or 5
17(41.5)
The hospital is ready to accept innovations and new and better ways to do things
No response
2(2.4)
12.
1 or 2
8(19.5)
1 or 2
16(39.1)
3
14(34.1)
4 or 5
10(24.4)
Relationship among staff is friendly and conducive to work
No response
1(2.4)
1 or 2
6(14.6)
3
10(24.4)
4 or 5
24(58.5)
13. The hospital shows concern for the staff and workers
No response
1(2.4)
1 or 2
12(29.3)
3
16(39.0)
4 or 5
12(29.3)
b) Open ended responses have great value as these may reflect opinions, emotions and
feelings of respondents more accurately than scored responses. In view of this all
responses have been reproduced below. They have been grouped under the five heads
under which they were collected
Under each head the responses pertaining to key areas have been grouped together. The
number given against each statement is to identify the questionnaire from which is has
been taken. Thus comments from the same questionnaire under different heads will all
bear the same number.
It will be seen that generally respondents see the strength of the hospital in dedication of
the sisters of the Good Shepherd, doctors and nurses and to the non-commercial nature of
the hospital.
At same time a sense of frustration seems to come through the comments. The negative
feelings lie mainly in the following areas:I. The hospital resists modernising and investing in newer technologies.
2. Poor salary structure for doctors. A repeated suggestion is to introduce an incentive
scheme for private ward admissions and start special paying O P. clinics.
3. “Unprofessional” management with inadequate communication with doctors. Doctors
feel they are rarely consulted or made part of management decisions.
4. Different rules seem to apply for different people
OTHER GOALS / COMMENTS:
Questionnaire No.
Comments:
A
Issues related to modernising:
3
Provide modern treatment at reasonable cost
6
Improve MICU
10
Get dialysis unit so that poor patients can benefit
11
Improve equipment in MICU and CCU
32
Keep up with technical advances
33
Should have basic infrastructure for investigations
36
Accept specialization as an integral part of health care
B.
Issues related to treatment policies.
6
7
15
18
22
23
35
37
40
C.
Introduce sterilization proceedures but not MTP
Discourage alcoholic patients - do not give them concessions
- More stress on preventive medicine
- Educate women about FP / immunisation
- Create awareness about nutrition and diet
- Adopt slum/village to create a model system
Introduce sterilization procedures as per National
Family Planning Scheme.
Follow national family planning policies
Land was gifted to sisters to care for all sick
people not only women and children
Should pursue national goals irrespective of religious
beliefs.
Provide spiritual support for those whose loved ones die
in hospital.
Improve maternal and child health facilities
Staff benefits:
11
33
Provide transport to staff
Provide benefits to staff dependants eg. Educational loan
Reward hard working staff
D.
Management issues:
19
32
33
36
40
E.
Educational Matters.
9
18
32
36
F.
Junior doctors are not given respect
Improve staff discipline in certain departments
Have a good maintainance department
Modernise record keeping
Should be able to give a feeling of belonging to the staff
Foster the old family spirit that St. Martha’s was famous for.
Send Drs to other institutions for training
- Encourage Drs to attend conferences and pay costs for this
Encourage Drs to develop specialised skills
Raise academic standards
Use company sponsorship for CME programmes for Drs, nurses
and technical staff
Miscellaneous:
19
All religions should be equally respected
MAJOR STRENGTHS
Questionnaire No
A.
Comments
Dedication and Spirit of Service
1
3
4
5
6
10
11
16
17
18
19
20
23
Dedication of workers
Dedication of Drs and nurses
Dedication
Consistent commitment to the down trodden
Dedicated Drs and nurses
Dedicated compassionate service
Service to the poor
Commitment and dedication of sisters of the Good Shepherd
Sacrifice and Service
Dedication
Dedication
Missionary zeal
Strong faith
Warmth kindness and concern
29
30
31
32
34
36
39
B
Dedication and hard work of staff
Good nursing care, dedicated Drs
Dedication of sisters, Drs, nursing staff
Sincerity and dedication
Showing compassion without consideration to cast or creed
Care and compassion of original IRISH nuns
Christian institution
Technical competence.
4
7
12
26
Competent staff
- Efficiency
Good nursing care
Skilled doctors and competent nurses
Prompt service at admission time
C.
Non commercial reputation:
D.
6
No corruption
7
Subsidised service to the poor
13
Optimal care at reasonable cost
16
Not being overtly commercial
27
Cheap yet good care
33
Poor patients
39
Non profit organisation
Reputation past and present:
7
12
20
40
E.
Following old rules and regulations
Past reputation
100 years experience
Past glory and dedication of people in the past
Others:
12
36
37
Location
Help from St. John’s Medical College in 60s and 70s
Location and facilities available
trainees & students eg. DNBE, nursing
MAJOR WEAKNESS
Questionnaire No.Comments
A.
Doctors Remuneration and Financial aspects
2
4
6
7
13
15
18
20
27
32
33
35
B.
Lack of modern technology:
5
10
12
18
19
29
31
32
C.
No incentive scheme
Financial constraints
Low wages of doctors
Unaffordability of newer modes of therapy
Difficulty in getting competent doctors without incentive payment
Finances
Low morale among doctors
Economic factor
Lack of finances to upgrade
Frustration of staff because of low income
Monetary factors
Cost factors
Technology update is slow
Lack of equipment
Delay in accepting new technology
Inflexible to suggestions for developing, tertiary care facilities
No interest in upgrading hospital
Lack of initiative to upgrade facilities
Notion that “high tech” care detracts from care of poor people
Hospital has not kept up with other institutions technically
Administration & Management.
1
3
5
6
11
17
30
36
39
40
Inefficient administration
Unprofessional interference by authorities
No long terms vision
- impersonal approach to staff
Rigid policies
Hierarchy
No long term plans
Absence of doctors in the administration
Lack of vision
Poor interpersonal relations of present Indian nuns
Active labour union
Large number of patients and less number of staff
Lack of vision
Unprofessionalism of the management
D. Other factors:
12
13
22
26
29
35
37
Poor standard of private ward accommodation
Unrealistic expectation of patient s
Religious
Uncertain availability of 2nd level consultant - delay in
getting specialist
Unhealthy competition
Religious factors
Some doctors and nurses are without commitment.
RULES AND REGULATIONS
Questionnaire No
Comments
A. Different rules for different people:
3
22
26
30
35
36
B.
Impersonal and inefficient administration:
22
35
C.
Different rules for different people
Favouritism
Rules vary with different departments and persons
Some get incentives, most dont
Disparity in rules depending on influence with administration
Different rules for different people
- Visiting doctors allowed to earn more than in-house
dedicated doctor
Administration is very poor
Senior specialists not given respect
Unconcerned about doctors welfare
Service expected even if doctors have to starve
Other issues:
5
12
15
35
Leave rules
Give incentives for doctors from private wards
Medical care should be free for all employees
Rules for doctors are unreasonable
SUGGESTIONS:
Questionnaire No.
Comments
A. Issues related to doctor’s income :
2
7
9
10
11
12
13
17
31
35
36
Incentives for doctors
Provide adequate income for all staff
Increase pay scales & introduce incentive scheme
Increase pay of junior staff
- introduce incentive scheme
- start evening speciality pay clinics
Give staff better pay
Incentive from private wards
Impossible to get senior doctors with present pay
find ways to pay reasonable salary to doctors and
nurses
Private OP clinics
Allow incentives to improve employees income
Allow pay clinics; staff should be better paid
Not allowing incentives for admitted patients
encourages doctors to go to nursing homes
B. Issues related to modernising the hospital
2
5
7
9
11
13
16
17
19
20
29
32
Improve equipment
Do not avoid technological growth
Open dialysis, neurosurgery a paediatric intensive
care units
- improve nursing care which has deteriorated of late
- improve casualty facilities for tackling emergencies
CT scanner is a must
Better and more modern equipment
Give up fear of high tech. Equipment
Better equipment
CT scanner
Lab and ultrasound facilities round the clock
CT, MRI, isotope scans
Replace old equipment with new
Ultrasound facilities should be available round the
clock
- Upgrade facilities including CT scanner
Buy new equipment and raise charges if necessary
33
34
35
Modernise; replace old equipment; computerise
Enhance standard of care of sick people
Facilities (technical) should be better
C. Issues related to administration and Management
3
5
8
9
10
11
15
16
17
22
23
26
32
33
36
40
Uniform rules, pay scales and promotional avenues
for all staff
- forum to hear and discuss staff grievances
Give doctors greater role in administration and
policy making
Department / unit head should be given powers to
give concession
Need to employee more SHOs and junior doctors
More flexibility with leave rules
Do not overwork staff
Categorise patients by economic status
- create more special ward, ITU and graded care beds
More interaction between doctors and administration
- consult doctors in matters of medicine, administration
and police
- better promotional avenues for doctors
Provide transport for staff using hospital vehicles/ BTS
Welfare of the staff should be looked after
Regular meetings between management and staff of
each department for better exchange of ideas
Doctors to have more say in areas like admissions, transfers
- Administration should work more quickly
- More junior staff
Doctors or heads of departments should be given more
power in the functioning of their department
- improve private wards
Improve inter departmental relations
- increase number of doctors and nurses
Too much “arm-chair” administration. Administrative
staff should move out and see the problems of departments
- sisters should be united. Their ego problems cause
problems between departments
More fairness in dealing with staff
- Less interference in medical matters by non medical
people
- management should show more care for the staff
D
Issues related to academic matters
4
5
7
36
Increase teaching programmes
Welcome commercial sponsorship of academic
meeting
Improve library and get Medline services
- start a clinical newsletter
Authorities have blinkers with respect to sponsorship
of CME programmes
E. Other issues
7
34
35
Generate additional funds-philanthropies and
increased OPD charges
Professionals and doctors should show more dedication
Goals should be based on national policies irrespective
of religious beliefs
ANNEXURES
Questionnaires used in Review
To:
Department:
St Martha’s Hospital Review -1998
The Health Commission
Chapter
the
of
set up by the
Good Shepherd
Provincial
Sisters,
have
requested a team of resource persons to review
the
YOUR
OPINION IS
Ministry
Health
Hospital
st.Martha’s
of
through a participatory, interactive and reflective
As
PROCESS.
PART
OF
THIS
PROCESS,
STAFF
OF
St.Martha’s Hospital and a sample of students of
CRUCIAL
JOIN
THE NURSING COLLEGE AND PATIENTS ARE BEING INVITED
TO PARTICIPATE, BY FILLING IN SPECIAL QUESTIONNAIRES
PREPARED BY THE REVIEW COMMITTEE.
THESE WILL BE
CIRCULATED / ADMINISTERED IN JULY 1 998. APART FROM
THE
SPECIFIC
QUESTIONS ASKED
IN
SPECIAL
FORMAT,
PLEASE FEEL FREE TO OFFER ANY OTHER SUGGESTIONS
FOR
CONSIDERATION
BY
THE
REVIEW
TEAM.
YOUR
PARTICIPATION IN THIS REVIEW IS CRUCIAL TO HELP US
IDENTIFY THE FUTURE DIRECTIONS AND THRUSTS AND ALSO
MEASURES
TO
MEANINGFUL.
MAKE
THE
HEALTH
MINISTRY
MORE
ALL YOUR RESPONSES AND SUGGESTIONS
WILL BE CONFIDENTIAL. WE INVITE YOU TO JOIN US IN THE
TASK AND MAKE THE REVIEW, A SUCCESS.
Dr. Reivi Narayan
Mr. Thomas Kandasami
Ms. Mary Ann Charles
1 5th July 1998
Dr. Prem Pais
Dr.Rebekah naylor
S.M.H. BANGALORE
[All completed questionnaires must be returned to the Medical / Nursing
Superintendents offices latest by 28th July 1998 and put in the box
specifically provided for them]
Please detach this page from the proforma before submitting.
THE
REVIEW
Questionnaire for Doctors
Part A
Hospital goals
Given below are a list of objectives/goals for an institution like St. Martha’s Hospital.
We would like you to indicate for each objective/goal, your impression on a) How
important the objective/goal should be and enter your answer under the first column
(“should be”) and b) How much the hospital is fulfilling it at present Enter this
impression under the second column (“is”). For your answer choose a score ranging
from 1 to 5 as shown below.
Score
12
Not important at all
or
Not fulfilling it at all
3
4
5
Of great importance
or
Fulfilling it completely
(For first column)
(For second column)
Should be
1.
The hospital should foster among all staff
respect for human life from conception to its
natural end
2.
Hospital should provide medical care to the
public irrespective of caste, creed and social
status.
3.
While providing high quality medical care the
hospital should ensure use of appropriate, low
cost yet effective care whenever possible
4.
The hospital should serve as a model of efficient
health care.
5.
The hospital should treat all patients with human
concern, compassion.
6.
The hospital should emphasise especially the
health concerns of women and children
7.
The hospital should subsidise services for the
poor.
8.
The hospital should provide spiritual care to the
sick respecting the individuals religious beliefs
Is
Should be
9.
The hospital should serve as a training institution
where trainee doctors and nurses will learn to
deliver competent health care ethically and
compassionately
10.
The hospital should keep the national health
priorities in mind when planning its services.
11.
The hospital should foster a sense of moral and
ethical integrity among all its staff.
12.
Any other goals you think the hospital should / is
pursuing
a)
b)
_________________________
c)
i_______________________
13.
What major factors have helped the hospital realise its goals ?
14.
What major factors have hindered the hospital from realising its goals ?
Part B
Hospital Functioning:
Given below are different aspects of the functioning of St. Martha’s Hospital. Please
indicate against each to what extent you agree or disagree that the hospital follows
these aspects. For your answer choose a score ranging 1 to 5 as shown below and
enter it in the column (“Score”)
Score:
12
3
Completely Disagree
4
5
Completely Agree
Score
1.
The hospital constantly tries to improve the
quality of health care
2.
The hospital innovates to find means of reducing
the cost of health care to make it more affordable
3.
The hospital is kept clean
4.
The hospital functioning is such as to be efficient,
and reduce waste.
5.
The hospital functioning is such as to provide
prompt attention to patients.
6
The hospital motivates all its staff to work in a
caring and compassionate manner.
7.
The hospital involves each department
preparing the departments budget
8.
The hospital is concerned about ways to generate
additional income
9.
The hospital charges are reasonable compared to
charges by other similar hospitals in the city
10.
The hospital has reasonable rules and regulations
If you score 1 or 2, specify unreasonable rules
in
Score
11.
The hospital is ready to accept innovations and
new and better ways to do things
12.
Relationship among
conducive to work
13.
The hospital shows concern for the staff anti
workers
14.
Any suggestions to improve the functioning of
the hospital
a)
b)
c)
staff
is
friendly
and
Questionnaire for Doctors
Part C
QUESTIONNAIRE FOR ALL STAFF
For each item please circle Yes or No
Is there someone in the organization to whom you can communicate
your problems ?
Yes / No
2.
Do you feel that your complaints or grievances are heard ?
. Yes / No
3.
Do you feel a part of the health care team ?
Yes / No
4
Do you know what is the mission of the hospital ?
Yes / No
5. Do you have promotional avenues open to you ?
Yes I No
1.
6.
Did you undergo orientation when you joined the hospital ?
Yes / No
7.
Do you feel appreciated in your work ?
Yes / No
8.
Do you think the rules and policies are fair ?
Yes / No
9.
Have you read and understood and Employee Service Rules ?
Yes/No
10.
Do you have opportunity to suggest ways that your department’s
work or function could improve ?
Yes I No
If you have a personal or family problem, is there someone in the
hospital who can guide or help you ?
Yes/No
12.
Is the area where you work comfortable and safe ?
Yes / No
13.
Since joining work, have you received any training or new skills ?
Yes I No
14.
Do you have a job description ?
Yes I No
15.
Do you participate in any special events or extra curricular activities
in the hospital ?
Yes / No
11.
ATTACHMENT II A
Questionnaire For Assistant! administrator
1. Please attach a list of supervisory and technical staff with their qualifications and
experience.
2. Please attach a list of major equipments in these departments such as vehicles,
generators, incinerators, etc.
3. Does the hospital provide ambulance service for patients to and
from hospital ?
Yes / No
4. Are ambulance equipped with life saving items such a s oxygen ?
Yes / No
5. Is ambulance service available all 24 hours ?
Yes / No
6. Does the transport department provide service for other departments
such as purchase and administration ?
Yes / No
Are there written procedures regarding :
maintenance of vehicles
logging of trips
accidents
Yes/No
Yes / No
Yes/No
8. Are security services given over to a contractor ?
Yes / No
9. Does the hospital maintain a security service ?
Yes / No
10. Is there a procedure for investigation of security lapses or problems ?
Yes / No
11. Do staff express any security concerns ?
Yes / No
12. Is there adequate control of visitors in the patient care areas ?
Yes / No
13.Are there written procedures regarding disposal of hazardous wastes,
Yes / No
contaminated materials, tissues, food wastes ?
14.Are legal requirements met regarding pollution control ?
Yes / No
15. Does the hospital have one or more incinerators ?
Yes / No
16. Is survey made of all areas at least annually to identify environmental
hazards and unsafe practices ?
Yes / No
17.Are essential services supported by generators during power outages ?Yes / No
18. Is there adequate planning to meet present and future needs for
water and electricity ?
Yes / No
19.Are measures enforced to conserve water and electricity ?
Yes / No
20. Is there a preventive maintenance program for all hospital and
biomedical equipments ?
Yes I No
21. Is there timely response to complaints from departments regarding
building and equipment maintenance ?
Yes / No
22. Is there procedure for disposal of scrap materials ?
Yes / No
23.Are there plans developed in case of disaster ?
Yes / No
ATTACHMENT
II B
Questionnaire for Personnel Officer
1. Please attach a list of staff in the Personnel department and their qualifications
and experience.
2. What is the title of the person with responsibility for Personnel?
3. How many total employees are there ?
Medical staff
Nursing staff
Clerical staff
Technicians
Others
------------------------------------------------------------------
4. Is there a Policy Manual containing personnel policies ?
( Please enclose)
Yes / No
5. Does each department have a Head of the Department or
Supervisor through which personnel administration is carried out ?
Yes / No
6. Are there prescribed procedures for recruitment and selection
of employees ?
Yes / No
7. Does every employee receive an appointment letter and sign an
appointment order ?
Yes / No
8. Are all employee personnel files maintained in one place for the
entire organization ?
Yes / No
9. Are current health files kept on each employee ?
Yes / No
10. Do all employees havejob descriptions in a standardized form ? Yes / No
11.Are employee performance evaluations performed regularly ?
Yes / No
12. Is there a written policy regarding promotions ?
Yes / No
13. Is an exit interview conducted when an employee resigns ?
Yes / No
14.Are employee records and files computerized ?
Yes / No
15. Is payroll computerized ?
Yes / No
16.Are salary scales revised at regular intervals ?
Yes / No
17.Are salaries and compensation comparable to similar positions
within the community ?
Yes / No
18. is there a formal orientation for new staff ?
Yes / No
19. Is the Personnel Department responsible for enquiries and
disciplinary procedures ?
Yes / No
20.Are there prescribed cadre positions in each department ?
Yes / No
21. Is there a superannuation or pension plan for all staff ?
Yes / No
22. Is there a recognized union in the hospital ?
Yes / No
23 Is there a Labour settlement in force at present ?
Yes / No
24.Are medical staff and first level management staff subject to
Employee Service Rules and Leave Rules as for other employees ?
Yes / No
25. Is the Personnel Department responsible for staff welfare activities ?
Yes / No
26. Does the hospital have a plan for human resource development at
all levels ?
Yes/No
27.Are programs in place to develop existing staff ?
Yes / No
28. Are there “cross training” opportunities within the organization ?
Yes / No
Questionnaire for Head of Departments (Ancillary)
I low long have you been Head of the Department ?
2
Do you conduct regular meetings of employees whom you supervise •? Yes / No
3. Do you feel that there is good communication with management ?
Yes / No
4. Are you involved in selection of staff for your department ?
Yes / No
5. Are you involved in the annual budget process for your department ?
Yes / No
6. Are you informed about the financial performance of your department ? Yes I No
7. Do you regularly evaluate the performance of the employees you
supervise ?
Yes / No
8, Do you know and understand the vision and mission of the hospital ?
Yes / No
9. Do you communicate the vision and mission to your employees ?
Yes / No
10 Does your department have written policies and procedures ?
Yes / No
11. Do you set goals each year for your department ?
Yes / No
12. Do you feel a part of planning and decision making in the
organization?
Yes / No
13 Do you orient new employees in your department ?
Yes / No
14. Do you provide any inservice or on the job training for your
employees ?
Yes / No
15. Have you attended any seminar, program or course on
management training ?
Yes / No
16. Do you have written standards that guide the work of your
deoartment ?
Yes / No
17 Do you have enough qualified staff to do the required work ?
Yes / No
18. Do all of your employees have job description ?
Yes / No
’9 Do you know the organization olan or structure of the hosoital 7
Yes / No
Questionnaire for Staff (Ancillary Department)
1.
Is there someone in the organization to whom you can communicate
your problems ?
Yes / No
2. Do you feel that your complaints or grievances are heard ?
Yes / No
3. Do you feel a part of thehealth care team ?
Yes / No
4. Do you know what is the mission of the hospital ?
"■r
Yes / No
5. Do you have promotional avenues open to you ?
Yes / No
6. Did you undergo orientation when you joined the hospital ?
Yes / No
7. Do you feel appreciated in yourwork ?
Yes / No
8. De you think the rules• and policies are fair ?
Yes / No
9. Have you read and understood the Employee Service Rules ?
Yes / No
10. Do you have opportunity to suggest ways that your department's
work or function could improve ?
Yes / No
11. If you have a personal or family problem, is there someone in the
hospital who can guide or help you ?
Yes / No
12. Is the area wheje you work comfortable and safe ?
Yes / No
13 Since joining work, have you received any training or new skills ?
Yes / No
14 Do you have a job description ?
Yes / No
15 Do you participate in any special events or extra curricular activities
in the hospital ?
Yes / No
t
16.
Any suggestions:
PROVINCIAL DIRECTIVES
These can be mod ifled by the
p5PXZ
OUR_GOAL
copter
'
■
Responding to the call of Jesus the Good Shepherd and
experiencing the merciful love of the: Father, we, the
Contemplative and Active sisters mediate this love to all,.
in the Spirit of,' our Foundress,.
i
'
We make real the incarnation of Christ in the India of
today through an authentic religious life.
, We share in the Church's mission of Evangelisation through
our special ministry of reconciliation by praying for and
working with girls and women deprived of hope and love and
by responding to the crying needs of the poor, exploited and
oppressed.".
OUR THRUST
We work with the poor, exploited,.oppressed and socially
discriminated, especially girls and y/ornen- in personnel,
family 'and social difficulties,1 through institutionalised
and non-institutionalised efforts in urban and rural areas.
OUR APOSTOLATE
.
in keeping with the Goal and Thrust of our province we set
our priorities as follows:
Services to Children, girls
and women through prevention
protection, rehabilitation
and crisis intervention We
extend our services to
commercial sex workers,
.twilight girls, persons with'
aids, working children (child
labour) and domestic women
workers.
PROGRAMS towards social
change:
faith formation
Non-formal education
- Conscientisation
- legal education
- community organisation
. - proTlife programmes
study, research and'publication
- pro-cana, net working
- ecological & environmental
protection, gender and
human rights issued,
■ - hospital chaplaincy/
pastoral care/
School counselling.
We make us of our existing institutions, land and property
to maet the needs of our new ministries.
2
ATTACHMENT
II C
Questionnaire For Medical Records Department Head
1. Please attach a list of Medical Records Officers and their qualification and
experience .
2. Please attach a list of other staff positions in the departments.
3. Are inpatient and outpatient records maintained in the same
department ?
Yes / No
4. Is a medical record maintained forever/ patient treated or assessed ? Yes / No
5. Are any department functions computerized ?
Yes / No
b. Is confidentiality, security, and integrity of information maintained ?
Yes / No
7.
Is there a policy regarding retention time of medical records ?
Yes / No
8. Is there regular review of completeness of medical records with
feedback to the concerned staff ?
Yes / No
9. Are written operative reports included in the medical record of patients
undergoing operative or other invasive procedures ?
Yes / No
10. Is coding system used for inpatient diagnosis ?
Yes / No
11. Is coding system used for outpatient diagnosis ?
Yes / No
12. Is a discharge summary written for every patient admitted for
48 hours or more ?
Yes / No
13.Are medicolegal charts kept separately and secured ?
Yes / No
14. Is there a medical records committee ?
Yes / No
ATTACHMENT
II D
Questionnaire For Head of Pharmacy
1. Please attach a list of staff and their qualifications.
2. What hours is the pharmacy open ?
3. Is there one central pharmacy ?
Yes / No
4. Does the pharmacy serve both outpatient and inpatients ?
Yes / No
5. Is the pharmacy located so that it is easily accessible ?
Yes / No
6. Is pharmacy stores adjacent to the pharmacy ?
Yes / No
7. Is a licensed pharmacist incharge of the stores ?
Yes / No
8. Is the pharmacy license upto date ?
Yes / No
9. Does the hospital have a Pharmacy and Therapeutic Committee ?
Yes / No
10. Is there a hospital formulary or drug list available to all who prescribe
Yes / No
and use drugs ?
11. Is the pharmacy computerized ?
Yes I No
12. Is the inventory in the pharmacy checked regularly ?
Yes / No
13.Are emergency drugs in the patient care areas maintained by the
pharmacist ?
Yes / No
14.Are there written appropriate policies and procedures regarding
prescribing and ordering practices ?
Yes / No
15.Are any preparations manufactured by the pharmacy ?
Yes I No
16. Is cost to the patient considered in the selection of drugs and brands ?Yes / No
17. Are inservice or continuing education programs conducted for staff ? Yes I No
18. Are books and journals available for staff ?
Yes / No
19. Do drug representatives deal directly with the pharmacists ?
Yes / No
20. Do you consider your space adequate ?
Yes / No
ATTACHMENT
II E
Questionnaire For Head Of X-ray Department
1. Please attach a list of staff and their qualifications.
2. Please attach list of equipments and date of purchase.
3. Please attach list of procedures and X-rays available.
4. What hours are the services of the department available ?
5. Are there written procedures which are followed fro preparation of
patients for special procedures ?
Yes / No
6. Can emergency portable films be done in casualty and crucial care
areas at all hours ?
Yes / No
7. Are Quality Control procedures in place ?
Yes I No
8. Are radiation protection procedures written and followed ?
Yes / No
9. Are radiation badges worn by all staff ?
Yes/No
10.Are inservice and continuing education programs available for staff ?
Yes / No
11. Does the department have a recognized training program ?
Yes / No
12. Is there an area for developing films in the operation theatre ?
Yes / No
13.Are X-rays read and reported within 24 hours ?
Yes / No
14. Do you consider space adequate ?
Yes / No
15. Do you perform X-rays and procedures on patients referred from
outside?
Yes/No
ATTACHMENT
II F
Questionnaire For Head of Laboratory
1. Please attach a list of staff and their qualifications.
2. Please attach a list of equipment available and when purchased.
3. During what hours are laboratory services available ?
4. Are the following services provided ?
Haematology
Yes 1 No
Yes / No
Serology
Yes / No
Biochemistry
Microbiology
Yes / No
Yes / No
Histopathology
Yes / No
Cytology
Yes / No
Blood Gases
5. Does the hospital have a licensed blood bank ?
Yes / No
6. Do you have an internal Quality Control Program ?
Yes/No
7. Do you participate in an external Quality Control Program ?
Yes/No
8. Do you use disposable needles and syringes ?
Yes / No
9. Do you have written policies and procedures that address : (please enclose)
Yes / No
Specimen Collection
Yes / No
Specimen Preservation
Yes / No
Instrument Calibration
Yes / No
Quality Control & Remedial Action
Yes / No
Equipment Performance Evaluation
Yes / No
Test Performance
Yes / No
Disposable Needles & Syringes
10.Are there inservice and continuing education programs available
for staff ?
Yes / No
11. Does the laboratory have a recognized training program ?
Yes / No
12. Do you consider your space adequate ?
Yes / No
13.Are universal precautions followed by laboratory staff ?
Yes / No
14. Do you have a licensed blood bank ?
Yes / No
15. Do you perform tests for patients referred from outside ?
Yes / No
ATTACHMENT
II G
Questionnaire For Head of Physiotherapy
1, Please attach a list of staff and their qualifications.
2. Please attach a list of equipments and date of purchase.
3. What are the hours for the laboratory ?
4. Does the department serve inpatients and outpatients ?
Yes/No
5. Is it easily accessible to the patients ?
Yes/No
6. Do you consider the space adequate ?
Yes/No
7. Do you also visit the wards to assess and treat patients ?
Yes/No
8. Do you interact with medical and nursing staff to plan rehabilitation
and treatment for the patient ?
Yes / No
9. Do you make progress notes in the patient record ?
Yes / No
10. Do all clinical units fully know and utilize the services of your
department ?
Yes / No
11.
Are
inservice and continuing education programs available for staff ?
Yes I No
12. Does your department have a recognized training program ?
Yes / No
13. Do you have written policies and procedures followed by the
department ?
Yes / No
14. Is an occupational therapist available in the department ?
Yes / No
15. Does your department treat patients from outside not referred by
the hospital ?
'
Yes / No
ATTACHMENT
II H
Questionnaire For Head Of Prosthetic And Orthotic Centre
1. Please attach a list of staff and their qualifications.
2. Please attach a list of equipments and date of purchase.
3. Please attach list of services and appliances provided.
4. Are goals set and treatment plans formulated for each patient ?
Yes / No
5. Does the department receive patients referred from outside as well
as St. Martha’s patients ?
Yes / No
6. Are funds or other resources available so that poor patients can be
treated?
Yes/No
7. Do you consider your space to be adequate ?
Yes I No
8. Does the Centre have a training program ?
Yes/No
9. Do you have written policies or procedures fro your department ?
( Please enclose )
Yes / No
ATTACHMENT
II I
Questionnaire For Head Of CSSD
1. Please attach a list of staff and their qualifications.
2. Please attach list of equipments and date of purchase.
3. What are the hours of the department ?
4. Does the department have written policies and procedures ?
( Please enclose)
Yes / No
5. Are Quality Control procedures followed ?
Yes / No
6. Is there Infection Control surveillance in the department regularly ?
Yes / No
7. Does the department serve all areas of the hospital including
operation theatre ?
Yes / No
8. Are inservice training programs available to staff ?
Yes / No
9. Is the space adequate for the department ?
Yes / No
10.Are there additional autoclaves in theatre or in other departments ?
Yes / No
ATTACHMENT II J
Questionnaire For Head of Laundry
1. Please attach a list of all equipments in the laundry and date of purchase.
2. How many pieces or items are handled daily in the laundry ?
3. How may staff are employed in the laundry ?
4. What are the working hours of the laundry ?
5. Are there written policies and procedures which address :
Collection of linen
Disinfection of contaminated linen
Washing of linen
Equipment performance
Distribution of linen to patient care areas
Yes I No
Yes / No
Yes / No
Yes/No
Yes / No
6. Is there a central store for linen ?
Yes/No
7. Is the supply of linen considered adequate in all patient areas ? Yes / No
8. Are universal precautions followed by staff in handling
contaminated linen ?
Yes / No
9. Is the rate of loss or damage of linen monitored ?
Yes / No
10.Are there targets or standards set regarding rate of loss ?
Yes / No
ATTACHMENT
II K
Questionnaire For Head Of Dietary Department
1. Please attach a list of staff and their qualifications.
2. At what hours is food service available ?
3. Is food service available to patients ?
Yes / No
4. Is food service available to staff and students ?
Yes / No
5. Is food service available to attenders and visitors ?
Yes / No
6. Does a Contractor provide part or all of the service ?
Yes / No
7. Are patients on therapeutic diets required to take food from the
hospital ?
Yes / No
8. Is the kitchen regularly inspected regarding cleanliness ?
Yes / No
9. Do kitchen staff have health checkups ?
Yes / No
10. Do kitchen staff follow procedures for safe handling of food ?
Yes / No
11. Is there a Quality Control procedure or program fro therapeutic diets ? Yes / No
12. Does a dietitian counsel and educate all inpatient department ?
Yes / No
13. Is diet counselling available in the outpatient department ?
Yes / No
14. Does the department have a recognized training program ?
Yes / No
15.Are inservice and continuing education programs available to
the staff ?
Yes / No
ATTACHMENT
II L
Questionnaire For Chaplains
1. Please attach a list of staff and their qualifications.
2. Number of Christian staff or employees :
Professional staff (medical & nursing ) :
Administration :
Class III & IV :
---------------------------------------------------
3. How many nuns or sisters of the order are working regularly in the hospital ?
4. How many services perweek are conducted with ;
Patients :
Staff:
Students :
5. How many visits or contacts are made with patients daily ?
6. In hiring or appointing employees, is preference or weightage given
to Christian applicants ?
Yes / No
7. Does the Chaplain have an adequate office where he can counsel
patients orfamilies ?
Yes / No
8. Is there an adequate budget for the Chaplain’s office ?
Yes / No
9. Does the organization allow the Chaplain the freedom to minister and
communicate the Christian faith ?
Yes / No
10. Do hospital staff refer patients or families to you for help and
counselling?
Yes/No
11. Do you pray with patients, especially in crisis or before surgery ?
Yes / No
12. Is Christian literature available to patients in all areas of the hospital ? Yes / No
13. Is there adequate place fro private prayer and public worship ?
Yes / No
14. Have there been any special emphases, or retreats for staff and
students in the past one year ?
Yes / No
15. Has there been improvement in the attitude of the community
towards Christianity as a result of the hospital ?
Yes / No
ATTACHMENT
Ill
Questionnaire For Staff
1. Is there someone in the organization to whom you can communicate
your problems ?
Yes I No
2. Do you feel that your complaints or grievances are heard ?
Yes / No
3. Do you feel a part of the health care team ?
Yes / No
4. Do you know what is themnssiun or the hospital ?
Yes / No
5. Do you have promotional avenues open to you ?
Yes / No
6. Did you undergo orientation when you joined the hospital ?
Yes / No
7. Do you feel appreciated in yourwork ?
Yes I No
8. Do you think the rules and policies are fair ?
Yes / No
9. Have you read and understood the Employee Service Rules ?
Yes / No
10. Do you have opportunity to suggest ways that your department’s
work or function could improve ?
Yes I No
11. If you have a personal or family problem, is there someone in the
hospital who can guide or help you ?
Yes / No
12. Is the area where you work comfortable and safe ?
Yes / No
13. Since joining work, have you received any training or new skills ?
Yes I No
14. Do you have a job description ?
Yes I No
15. Do you participate in any special events or extra curricular activities
in the hospital ?
Yes / No
ATTACHMENT
IV
Questionnaire For Students
1. Do you know the vision and mission of the hospital ?
Yes / No
2. Do you feel a part of the hospital and its work ?
Yes/No
3. Do you have any opportunities for spiritual development ?
Yes / No
4. If you have a personal or family problem, is there someone to guide
you or counsel you ?
Yes / No
5. Is the hospital a place you would like to remain as an employee ?
Yes / No
6. During your training do faculty and staff stress care of the poor ?
Yes/No
ATTACHMENT
'
V
Questionnaire For Head of departments
1. How long have you been Head of the Department ?
2. Do you conduct regular meetings of employees whom you supervise ? Yes/No
3. Do you feel that there is good communication with management ?
Yes/No
4. Are you involved in selection of staff for your department ?
Yes/No
5. Are you involved in the annual budget process for your department ?
Yes/No
6. Are you informed about the financial performance of your department ? Yes / No
7. Do you regularly evaluate the performance of the employees you
supervise?
Yes/No
8. Do you know and understand the vision and mission of the hospital ?
Yes/No
9. Do you communicate the vision and mission to your employees ?
Yes/No
10. Does your department have written policies and procedures ?
Yes / No
11. Do you set goals each year for your department ?
Yes / No
12. Do you feel a part of planning and decision making in the
organization?
Yes / No
13. Do you orient new employees in your department ?
Yes / No
14. Do you provide any inservice or on the job training for your
employees ?
Yes / No
15. Have you attended any seminar, program or course on
management training ?
Yes / No
16. Do you have written standards that guide the work of your
department ?
Yes / No
17. Do you have enough qualified staff to do the required work ?
Yes / No
18. Do all of your employees havejob description ?
Yes / No
19. Do you know the organization plan or structure of the hospital ?
Yes / No
)
Lt IG
11 'Oc.c ki ric.lc^
^/>CxrxaC^
pe^Cs-jd
_uxz>_e_- e^LiWi-cvp
_________
~
/cro/i
/oal-sc~cUl$......
Z2«=«x..e-C
..........
_..
xr>^-.^>^zs
______ —
___________________
---->
Z'cTr--'
_______________________________________
r^//' I
3 1
54.___ ©
i J.
£>v^?c(
?kJ<
/->‘'2j2^.z1
vr/ SL< t
/fc,'
3*7
_a
•/<?
16.
r-1 <2 c
/ft
/-<e7ae^_<r C<1
_
____ &£sf2k^.=>_ 9-1^-^____ ,Ub4 > cer__________________________________________________
/?-2._ /<L“3- S1ls2*=.__________________ ________________________________________________________ ________ ___ _
Z2.
‘Se^>l^c
t^c-b^
2q.
CJ Ho 'S-eppa
2^
^cbzJ' 3os
pp f M
■■
‘.C £r
P-^excA-f
/
x/ c
^JLz
...3
. ^__
^.IO
F)
d-3Z)1f\i o ~<>H
^7!' J
7/-'
Ph P £PbPc_ ttec ill
—/2’^/ oi.^e
-^fo ic’-^/'-e
O>4e-\ pcJ^c-o.
|__ 12XiJsaC3s»:a l4l_-^
2- 77ftis
/2fi-O flP ;z
-z Tr&A-c ______
P
onjICGG
<-t,
~7~/~e,
;-y > ,. G<_. •.. i
.5c
P)
^'5£lvofe.-o
^ ..
(L
glens' r f) i—1 •—'‘^j)
p(
PLe.__ /'4sG<37~<vc^^<?-<vc^ _^<l.
U>P I C.1SP
(^"7 PL-P- <P
4-iix^
/L Ped^
.
G<s.-^e.L^Lc^
^LeJ v
~7Z5—kol4. 7-v^e 1/7
____________________
'■ f^lc l
<3
Ccr>>^
6.
f)cr.
~r~
-
-o
^'c Hl- Se-_c^-
/to /SJfe r/^.£<- *c. _c^>__cl
__________________________________ ______
-v -
r^~> .
J^C>1.J5>.
J^- '
1-.
^>y.
T
V.
Ax ->-rc?
___
L‘..
_
eV.
itt- ct-,c peck ^/-)5S//?
i/&
____ Vj /-LyC C
— /^ CO rj J
~~fYcO
_ 'iCp c'-’_____ c-'npJ.cdL^c^
Ke^
r^~) c
GROUP-ffl
VENUE - TAGORE - B
Mr. Sinulingga
Mrs. Parera
Dr. Neeraj Sethi
Dr. Mohammad Asri
Mr. Seshu Dabu
_Dr. Ranjini Saxena
Dr. Keyword
Mr. David Peters
GROUP - III
Management of Partnerships, Private sectors, NGOs,
Media and Communication, maximising the benefits.
—
v
S ee Z c.
i
S u puJ
___________ 2Z_____
iYlLxxzt -CLzx&CjSs*._—..l&>__ co-uz^Y . ^o^-ruo^ctczi/^___ &3_Z^e
c o'Y - io _^>
/.
/cf'
C
2^2^
— Of fcix-i CH-^J
|JZ
C_^//u.c[
<r il
C
D.
M60
C-
........ 6 CCP k
y
’\_3 -
?
cLc
Some Standards To Be Considered
Governance
<
1. There is an established process and criteria that have been identified for
selecting a competent and qualified Chief Executive Officer.
2. There is an established mechanism to ensure that the organization adheres
to relevant statutory and regulatory requirements.
Organizational Planning
1. Planning includes setting a mission, a vision, and values for the
organization and providing plans and policies to achieve the mission and
vision.
2. The leaders communicate the organization’s plan(s) throughout the
organization.
3. The plans include patient care services in response to identified patient
needs and is consistent with the mission.
4. The scope of services provided by each department is defined in writing.
5. The leaders and other representatives from the organization, as
appropriate, participate in the organization ’s decision-making structures and
processes.
6. The leaders develop programs to promote the recruitment, retention,
development, and continuing education of all staff members.
Leadership
Key characteristics of leadership ;
The process of leadership begins with establishing and promulgating the
organization’s mission, followed by renewing and revising it as necessary.
Building on the organization's mission, effective leadership defines and
establishes a clear vision and values for what the organization can be and
resolves to become, encouraging staff participation in its development.
Effective leadership develops other leaders at every level of the organization
who help fulfill the organization’s mission, vision, and values.
Effective
leadership also accurately assesses the needs of the organization's patients
and other users of the organization's services and develops an organizational
culture that focuses on improving performance to meet these needs. Effective
leadership
• defines a strategic plan that is consistent with the organization's
mission, vision, and values;
• clearly communicates the organization ’s mission, vision, and
strategic plan throughout the organization; and
• fulfills the organization’s vision by providing the framework to
accomplish the goals of the strategic plan.
Developing this framework is accomplished through proper direction,
implementation, coordination, and ultimately, improvement of services
throughout the organization. In order to realize the organization's vision and
values, leadership must have a role in teaching and coaching staff. This role is
inherent to leadership.
Directing Departments
1. Each department of the organization has effective leadership.
2 Department directors or supervisors ate responsible, either personally'or
through delegation for
• integrating the service Into the organization ’s primary function:
• coordinating and integrating interdepartmental and intradepartmental
services:
• developing and implementing policies and procedures that guide and
support the provision of services;
• recommending a sufficient number of qualified and competent
persons to provide care, including treatment;
• continuously assessing and improving the performance of care and
services provided:
• maintaining quality control programs, as appropriate:
• orienting and providing in-service training and continuing education
of all persons in the department;
• recommending space and other resources needed by the
department.
Information Management
1. The information management processes provide for information
confidentiality, security, and integrity.
2. The organization reviews the completeness, accuracy and timely
completion of information in medical records at least quarterly.
3. There is a policy regarding the retention time of medical record information
determined by law or by its use for patient care, legal, research, and/or
educational purposes.
4. A medical record is maintained for every individual assessed or treated.
5. Medical record contains sufficient information to identify the patient, support
the diagnosis, justify the treatment, document the course and results
accurately and facilitate continuity of care among health care providers.
6. At discharge from patient care, a clinical summary gives reason for
hospitalization, significant findings, procedures performed, treatment
rendered, condition on discharge, and any specific instructions given to
patient or family.
7. Written operative reports are included in the medical record of patients
undergoing operative or other invasive procedures.
Human Resources Management
1. The organization's leaders define for their respective areas the
qualifications and job expectations of staff and a system to evaluate how
well the expectations are met.
2. The organization provides an adequate number of staff whose qualifications
are commensurate with defined job responsibilities.
3. The organization has established methods and practices that encourage
self development and learning for all staff.
4. A staff orientation process provides initialjob training and information.
5. Ongoing inservice or other education and training maintain and improve
staff competence.
Environment of Care
1. The organization has a documented management plan(s) for the
environment of care that considers the following functions:
Safety
Security
Hazardous materials and wastes
Utility systems
Emergency preparedness
2. All areas of the facility are surveyed at least twice annually to Identify
environmental hazards and unsafe practices.
3. All incidents involving property damage, occupational illness, or patient,
personnel or visitor injury are investigated and reported.
4. Written policies and procedures are strictly followed in regards to Infection
Control.
5. Cleanliness is maintained in all areas with set standards to be achieved.
Dietary
Responsibility for preparing, storing, distributing, and administering food
and nutrition products is defined and assigned.
2. Food and nutrition products are administered in a safe, timely, and
acceptable manner to the patient.
3. Diet counselling and education by trained personnel is available and
provided to patients.
4. Quality control measures are practiced in regard to therapeutic diets.
1.
Pharmacy
1. Availability of appropriate medicines as determined by the medical staff
2. Availability of pharmacy services at ail hours
3. Emergency medication systems
4. Formulary available to staff who use drugs
5. Pharmacy and therapeutic committee
6. Appropriate policies and procedures that support prescribing or ordering
practices
7. Adherence to applicable law regulation, licensure, and professional
standards of practice.
Laboratory
1. Clinical laboratory services and consultation are available at all times in a
prompt manner to meet the needs of patients served by the hospital as
determined by the medical staff.
2. Current written policies and procedures are readily available and address
Specimen Collection
Specimen Preservation
Instrument Calibration
Quality Control and Remedial Action
Equipment Performance Evaluation
Test Performance
3. Staff performing tests have adequate specific training and orientation to
perform the tests.
4. Quality control checks are conducted on each procedure as defined by the
organization.
X-Ray
1. Radio-Diagnostic services and consultation are available at all times in a
prompt manner to meet the needs of patients served by the hospital as
determined by the medical staff.
2. Current written policies and procedures are readily available and address
Patient preparation for special procedures
Radiation protection
Equipment performance evaluation
Quality control and remedial action
3. Staff performing tests have adequate specific training and orientation to
perform tests.
4. Quality control checks are conducted as defined by the organization.
4
Spiritual Care
1. Spiritual care and counselling is available to all patients and families at all
hours
2. Chaplains visit in all wards daily
3. The Christian nature of the hospital and its mission is communicated to
patients, staff, and students.
4. Spiritual care is available to staff and students
5. Activities to encourage growth and meet spiritual needs of staff and
students are planned regularly.
Evaluation of St. Martha’s Hospital
Evaluation of Clinical departments functioning
1. This will involve questionnaire for in-patients, out-patients, residents and staff
doctors. In-patients may be further classified by speciality and as general or private
ward cases and doctors by their departments.
2.
When questionnaires are prepared, a single questionnaire should be prepared for
each category to include elements of management, finance, ethical issues etc.
3.
Some interviews may also be required.
Draft questionnaires are enclosed.
Dr. Prem Pais,
Professor of Medicine & Vice Principal,
St. John’s Medical College.
Questionnaire for out-patients / casualty
1. Age
2.
Sex
4. Family Income
a)
b)
c)
d)
Less than Rs. 2,000/- P.M.
Rs. 2,000/- to Rs. 4,000/- P.M.
Rs. 4,000/- to Rs. 6,000/- P.M
Over Rs. 6,000/-P.M.
5. Your House
- Rented
- Owned
6. Do you own
Cycle
TV set
3.
Occupation
- No. of room
- roof - Thatch
- Tile
- RCC
- Floor - Earth
- Cement
- Mosaic tile
- Marble granite
2 wheeler
Refrigerator
7. Religion
8
Education
9.
Through whom did you come to know of St. Martha’s
Family doctor
Friends
Relatives
Neighbours
Other
10.
Why did you come to St. Martha’s Hospital
- close to your home/office
- doctor recommended it
- friends/relatives recommended it
- mission hospital
- reputation of the doctors
- other
11.
Is this the first visit to St. Martha’s
-Yes
-No
No formal education
Class VII or less
Class VIII to X
Pre degree
Degree
Post graduate / professional
Car
12.
Which department did you visit today
13.
Do you like to see only one particular doctor or any doctor
14.
If particular doctor
a) If he/she is not available
- will you go back & return another day
- see another available doctor
b) If he/she leaves the hospital
- will you continue coming to St. Martha’s Hospital
- change the hospital
15.
How long did you have to wait to see the doctor
- less than one hour
- one - two hours
- more than 2 hours
16.
What diagnostic tests did you have today
- None
- Laboratory (blood, urine, stool, sputum)
- X-ray
-ECG
- Ultrasound
- Endoscopy
- Others
17.
Give your impressions of the service you received
- Doctors know their job and are good
- All staff are courteous & helpful
- OPD amenities
(seats, fans, toilets, water)
- Were you satisfied with care given
18.Please tell us your opinion of the following
- The hospital is meant mainly for
those who can pay
- The hospital serves the poor sections of the
population even if they cannot pay for services
- The hospital & its staff care for all patients
with love and care
- The religious sentiments of all patients are
respected
19.
Do you think the hospital charges
- are correct
- too high
- too low
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
20.
Name 3 things in the hospital you appreciate most
21.
Name 3 things in the hospital that need improvement most
22.
You must be aware that St. Martha’s Hospital tries not to refuse treatment to any
patient, no matter how poor. Can you suggest how the hospital can raise funds to
treat more poor patients
23.
Any other suggestions or comments
Questionnaire for In-patients
(at discharge)
Occupation
1. Age
2.
Sex
4. Family Income
a)
b)
c)
d)
Less than Rs. 2,000/- P.M.
Rs 2,000/- to Rs. 4,000/- P.M.
Rs. 4,000/- to Rs. 6,000/- P.M.
Over Rs. 6,000/- P.M.
5. Your House
- Rented
- Owned
6. Do you own
Cycle
TV set
3.
- No. of room
- roof - Thatch
- Tile
- RCC
- Floor - Earth
- Cement
- Mosaic tile
- Marble granite
2 wheeler
Refrigerator
7. Religion
8. Education
No formal education
Class VII or less
Class VIII to X
Pre degree
Degree
Post graduate / professional
9.
Through whom did you come to know of St. Martha’s
Family doctor
Friends
Relatives
Neighbours
Other
________
10.
Why did you come to St. Martha’s Hospital
- close to your home/office
- doctor recommended it
- friends/relatives recommended it
- mission hospital
- reputation of the doctors
- Other
Car
11.
Is this the first time you have been admitted in St. Martha’s Hospital ?
-Yes
-No
12.
For how many days were you admitted ?
13.
Under which department have you been admitted ?
14.
Did you choose to be admitted in this hospital for treatment mainly because
- of a particular doctor
- the reputation of the hospital
15.
If for a particular doctor, if he/she leaves the hospital
- will you still have been admitted in St. Martha’s Hospital
- changed the hospital
16.
Which of the tests below did you undergo while you were admitted :
- None
- Laboratory (blood, urine, stool, sputum)
- X-ray
-ECG
- Ultrasound
- Endoscopy
- Others
17.
Give your impression of the care you received
- generally satisfied with the care given
- Doctors know their job & are good
- good nursing care is given
- wards and rooms are clean
- ward room facilities (lights fans, etc.)
18.
19.
Please tell us your opinion of the following
- The hospital is meant mainly for
those who can pay
- The hospital serves the poor sections of the
population even if they cannot pay for services
- The hospital & its staff care for all patients
with love and care
- The religious sentiments of all patients are
respected
What ward were you treated in
- General ward
- Shared private room
- Single private room
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
Yes/Somewhat/No
20. What is your opinion of the cost of
- Room bed charges
- Investigations
- Doctors fees (if any)
- Surgery/procedure drugs
Too low/Correct/Too high
Too low/Correct/Too high
Too low/Correct/Too high
Too low/Correct/Too high
21. Name 3 things in the hospital you appreciate most
22 Name 3 things in the hospital that need improvement most
23.
You must be aware that St. Martha’s Hospital tries not to refuse treatment to any
patient, no matter how poor. Can you suggest how the hospital can raise funds to
treat more poor patients
24.
Any other suggestions or comments
Questionnaire for Doctors
Department:
Status:
Resident / Permanent staff
Years of service:
Hospital goals
Score
1
Not at all
2
3
4
5
Very much
Should be
1. Hospital should provide the public irrespective
of caste, creed and social status high quality
medical care at reasonable cost
2. While providing high quality medical care the
hospital should ensure use of appropriate, low
cost yet effective care whenever possible
3.
The hospital should serve as a model of efficient
health care, cleanliness, human concern,
compassion and ethical and spiritual values
4.
The hospital should emphasise especially the
health concerns of women and children
5,
The hospital should ensure that the poor benefit
from hospital services by concessions.
6.
The hospital should provide spiritual care to the
sick respecting the individuals religious beliefs
7.
The hospital should serve as a training institution
where trainee doctors and nurses will learn to
deliver competent health care ethically and
compassionately
8.
The hospital should keep the national health
priorities in mind when planning its services.
9.
The hospital should foster a sense of dedication
and moral and ethical integrity among all its
staff.
Is
Should be
10.
The hospital should foster among all staff
respect for human life from conception to its
natural end
11.
Any other goals you think the hospital should / is
pursuing
a)
.
b)
c)
__________________
12.
What major factor have helped the hospital realise its goals ?
13.
What major factor have hindered the hospital from realising its goals ?
Is
Hospital Functioning:
1
2
3
Completely Disagree
4
5
Completely Agree
Score
14.
The hospital constantly tries to improve the
quality of health care
15.
The hospital innovates to find means of reducing
the cost of health care to make it more affordable
16.
The hospital is kept clean
17.
The hospital functioning is such as to be efficient;
reduce waste and provide patients prompt care
18.
The hospital motivates all its staff to work in a
caring and compassionate manner.
19.
The hospital involves each department
preparing the departments budged
20.
The hospital is concerned about ways to generate
additional income
21.
The hospital charges are reasonable compared to
charges by other similar hospitals in the city
22.
The hospital has reasonable rules and regulations
23.
The hospital is ready to accept innovations and
new and better ways to do things
24.
Relationship among
conducive to work
25.
The hospital shows concern for the staff and
workers
staff
is
friendly
in
and
26.
Any suggestions to improve the functioning of
the hospital
a)
b)
c)
SURVEY OF PATIENTS
Methodology: An administered questionnaire was used to obtain the views of patients
attending St, Martha’s Hospital on different aspects of hospital functioning. The
questionnaire was administered by interviewers who had been given some training. Since
the instrument was in English, the interviewer had to interpret the questions to the patient
as well as interpret open ended comments. This process may have vitiated the latter.
Open end comments were often missing or unsatisfactorily expressed. The present
analysis has therefore been restricted to scored questions which are less likely to be biased
by the interviewer.
Subjects The questionnaire was administered to both inpatients (on the day of
discharge) and out patients. The subjects were selected by the interviewers to generally
represent various areas and departments and is thus not strictly random.
I.
Patient Profile
a)
No. of proformae filled 159, 60 (38%) from inpatients and 96(60%) from out
patients. In 3 this data was not filled
b)
65 (41%) of the patients were male and 91 (57%) were female. In 3 data was not
filled.
c)
Income of patients per month
< Rs. 2000
Rs.2000-3999
Rs.4000-5999
> Rs. 6000
Missing data
30
44
30
29
26
19%
28%
19%
18%
16%
20
19
45
38
24
10
3
13%
12%
28%
24%
15%
6%
2%
Educational status
No formal education
7th Std or less
S.S.L.C.
P.U.C.
Degree
PG/Professional
Missing data
e) Religion of respondents
Hindu
Christian
Muslim
Missing data
107
33
12
7
67%
21%
8%
4%
f) Of the inpatients (60 respondents) 46 (77%) were from general ward and
13(22%) from private wards In 1 case the data was missing.
This data suggests that the sample has a representative socio-economic mix. . and is
probably representative of the hospital patient population.
II. Reasons for coming for treatment to St. Martha’s Hospital.
a)
Who referred the patient to SMH?
Relative
Friend
Neighbours
Family doctor
Others
Missing data
b)
55
46
23
13
18
4
35%
29%
15%
8%
11%
2%
Why did the patient come to SMH7
Recommended by relative / friend
Reputation of hospital doctors
Near home / office
Because it is a mission hospital
Recommended by doctor
Other
Missing data
67
27
23
14
12
12
4
42%
17%
15%
9%
8%
8%
2%
Both a) and b) provide consistent data that the reputation of the hospital and its
doctors among the general public is good. It is, however, noteworthy that few
patients are referred to SMH by their doctors. Since family doctors form an
important source of patient referrals for a secondary hospital, this area needs to be
corrected.
III.
Outpatient services
a)
Do patients visiting the OP come to see a particular doctor or are they willing
to see any doctor?
(n = 96)
Any doctor
Specific doctor
b)
66%
34%
How long did the patient have to wait in OP to see the doctor?
(n = 96)
< 1 Hour
1-2 Hours
> 2 hours
c)
37
33
70
40
19
39%
42%
19%
Was this waiting time acceptable?
(n = 96)
Yes
No
Missing data
70
25
1
73%
26%
1%
Two points emerge 1. That 61% of patients had to wait over an hour to see a
doctor and 26% felt that the delay was too long. Given that patients visiting a
general hospital are resigned to wait, these figures suggest that action is required
to reduce waiting time. 2. From a) and c) it would appear that about 30% of
patients may be ready to pay a fee to see a doctor of their choice with less waiting
time.
IV Staff Quality
a)
Doctors are knowledgeable and good
Yes
Somewhat
No
Missing data
147
8
0
4
92%
5%
0%
3%
b)
Nurses are caring and efficient
Yes
Somewhat
No
Missing data
c)
85.5%
11.0%
0.5%
3%
Staff in general are courteous and helpful
Yes
Somewhat
No
Missing data
d)
136
17
1
5
144
7
1
7
90.5%
4.5%
0.5%
4.5%
Overall satisfied with care given
Yes
Somewhat
No
Missing data
134
16
1
8
84%
10%
0.5%
4.5%
A fairly satisfactory picture on the whole
V. Amenities
a)
General cleanliness is good
Yes
Somewhat
No
Missing data
b)
142
12
2
3
89%
8%
1%
2%
Toilets and water supply are satisfactory
Yes
Somewhat
No
Missing data
125
24
3
7
79%
15%
2%
4%
c)
Fans and lights function adequately
Yes
Somewhat
No
Missing data
d)
137
15
2
5
86%
10%
1%
3%
Hospital diet taken (IP only)
n=60
No
Yes
58
2
97%
3%'
Water, toilets, lights and fans are generally judged satisfactory
although not as unequivocally as was the case for personnel.
Bangalore residents are accustomed to water and electricity shortages
yet 17% are not entirely happy with water and toilets and 11% with
electricity. The dietary service is conspicuous by its disuse.
VI. Some special services
a)
Medical records - any problem in getting records out (OPD only)
n = 96
No
84
87%
Yes
12
13%
b)
Chaplaincy services
- Did the chaplain visit you (IP only)
n = 60
Yes
No
Missing date
16
43
1
27%
71.5%
0.5%
- If yes, were his visits helpful
n = 16
Yes
No
14
2
88%
12%
Considering the mission of the hospital, visits by the chaplain are inadequate.
However, those who were visited seem satisfied.
VIII Perception of hospital mission
a) The hospital is mainly meant for those who can pay.
No
Somewhat
Yes
Missing data
104
28
22
5
65%
18%
14%
3%
b) The hospital serves the poor even if they cannot pay.
Yes
Somewhat
No
Missing data
c)
62%
22%
8%
8%
All patients are loved and cared for by the hospital staff.
Yes
Somewhat
No
Missing data
d)
99
35
12
13
134
16
2
6
84%
10%
2%
4%
Religious sentiments of all patients are respected.
Yes
Somewhat
No
Missing date
145
7
2
5
91%
5%
1%
3%
On the whole a satisfactory image. In view of the current controversy in the
political world, the last question and response could well be sent to the VHP!
VIII Hospital charges
a) Out patient charges and costs
n = 96
Correct
Too high
Too low
Missing data
61
16
15
4
64%
17%
16%
4%
b) In patient bed charges
n = 60
Correct
Too high
Too low
Missing data
c)
40
10
1
9
67%
16%
2%
15%
In patient (investigation costs in bill)
n = 60
Correct
Too high
Too low
Missing data
46
6
0
8
77%
10%
0%
13%
d) In patients (doctors fees, if any)
n = 60
Correct
Too high
Too low
Missing data
e)
62%
12%
0%
26%
In patient (surgery / procedure costs)
n = 60
Correct
Too high
Too low
Missing data
f)
37
7
0
16
35
5
0
20
59%
8%
0%
33%
In patients (medicine charges)
n = 60
Correct
Too high
Too low
Missing data
42
12
0
6
70%
20%
0%
10%
On the whole more patients seem to feel that the charge are reasonable. Among
inpatients a significant minority of patients (15 - 20%) feel that bed charges and
medication costs are too high. Similarly 17% of out patients felt that out patient
charges were too high.
Summary: The 159 patients interviewed seem to be fairly representative of a
cross-section of those who attend the hospital. It must be recognised that a survey of
this nature is presently biased as only patients who come to the hospital (and hence
approve of the hospital) have been included Keeping this in mind, the survey shows:
1. Patients are not often being referred to the hospital by the medical practitioners.
They come because of its reputation with the lay public.
2.
Waiting time in the out patient department is too long.
3.
About 30% of out patients may be ready to pay for services if these can be
stream-lined.
4.
Patients are generally satisfied about the medical and non medical staff.
5.
Dietary department services are grossly under used and could be stopped.
6.
There is scope to improve water and electricity supply.
7.
Chaplaincy services cover only a small proportion of patients.
8.
Hospital has good image among patients attending it.
»
•
... . .
-
,
i r-i i
.. .■ .
Lc.->
....
J
-------------- :------
CHAPTER.6
)
--------- —L____________________ _ '-J-------------------------------- -
Survey of Governance, Hospital Management, Personnel Management,
Associated and Ancillary Departments
As a member of the Review Committee which was formed to evaluate St. Martha’s
Hospital through a reflective process, I was assigned the following specific areas
for review:
1. Governance I Advisory' Board
2. Hospital Organisation / Administration
3. Personnel Management Policy
4. Departments including prosthetic and orthotic centre, physiotherapy,
pharmacy, radiology, laboratory', CSSD, medical records, laundry, and
dietary'
5. Ancillary services including security, telephone, water, electricity,
maintenance, transport
6. Spiritual care of patients
Evaluation was undertaken in such a way that the questions posed in the terms of
reference could be answered.
The goal is to gather information and propose
recommendations which could further strengthen the institution as it moves into a
new century'.
The methodology adopted was as follows:
1. Standards for evaluation in the assigned areas were proposed and accepted by
the review committee (attachment I) (Appendix 10(viii))
2. Documents obtained for review included the 1996 - 97 annual report, employee
service rules, organisation chart, list of members of Governing Body, current
salary' scales, list of employee benefits, sample job description, performance
evaluation form, sample appointment letter and appointment order.
3. An interview was conducted with the Administrator, Mr. A.C. Saldhana.
4. Questionnaires were completed by the heads of the departments and services
assigned to me for review (attachment II) (see Annexures)
5. Questionnaires were given to staff
I),students (attachment IV),
and all department heads / supeivisors (attachment V). (see Annexures)
6. Questionnaires were also given to patients (not yet completed).
Data collected are presented in attachment VI (staff), attachment VII (students),
attachment VIII (department heads / supervisors). The staff and department heads
were asked to give their suggestions.
This report summarises the information which was gathered and then makes
conclusions and recommendations in each assigned area.
Vision and Mission
The entire review committee was given the responsibility to reflect on the vision
and mission of the hospital and its expression in all activities and functions of the
hospital.
The vision and mission as stated in the stated papers given to the committee is that
of the sisters of the Good Shepherd and it is assumed that these statements also
apply to the hospital. There are statements of belief, objectives, and strategies
that arise from this vision and mission.
Among heads of departments, 94.3% said that they understood the mission of the
hospital and 82.9% communicate it to their employees. Among the 200 staff
questioned, 91.5% indicated that they know the mission of the hospital. These
figures are not verified in the sense that no one was asked to state the mission.
65
Summary of Evaluation Report
Page 2
it was observed that the hospital does not have immediate goals or a five or a ten
year plan. Only 34.3% of department heads set goals for their departments each
year. Reasons given by Administration for lack of planning include age of the
instltutionrchanginggovernment policies, and unpredictable economic conditions'.'
The recommendations suggested are as follows:
1. Based on the vision and mission statement of the order, the hospital
management should prepare a specific vision and mission statement and submit
it to the Governing Body and the Sisters of Good Shepherd for approval.
2. Based on this vision, organisational planning should take place. Departments
should be required to set annua) goals that are measurable. The organisation
should have annual goals as well as longer term goals. The five year plan can
be reviewed and modified on a regular basis as required by internal and
external circumstances.
Governance / Advisory Board
Tire hospital is owned by the Good Shepherd Sisters. The order is represented in
the hospital by the Sister Superior. The Chief Executive Officer of the hospital
(Administrator) is appointed by the order. The Administrator is accountable to the
Sister Superior.
There is a Governing Body which meets usually twice annually. The majority of this
Board are from within the hospital or order. Only six members, a minority, are
from outside. The Governing Body does approve the annual budget. The Board
has a wide range of power for review and supervision. They approve major
policies and new projects. It is assumed that this group along with the Chief
Officer ensure that the organisation adheres to relevant statutory and regulatory'
requirements.
It is recommended that there be more voice in the Governing Body from outside
including the community, experts Injipspital management and experts in finance.
There should~be an established process and criteria identified for selection of the
Chief Executive Officer, perhaps including a recommendation from the Governing
Body to the order on the selection.
Hospital Organisation and Administration
An organisational structure is in place and most management and supervisory
personnel are aware of it. The channels of communication are clear.
The Planning and Executive Committee, chaired by the Administrator, consists of
the”top officers“and' meets on regular basis. All decisions that affect the whole of
the organisation or all employees are taken by this group. This represents a good
participative management style.
'
In the area of finance, middle management seems less involved. Of the 35 heads
of departments / supervisors who responded, only 31% were involved in the annual
budgeting process for their departments, and only 28.6% were informed about the
financial performance of the department. Just over half (54.3%) have regular
department meetings with their employees. Only 28.6% were involved in selection
of staff. These data suggest that the organisation would be stronger if_middle
management was strengthened and participated in decision making.
An administrative policy manua£is needed in jorder that decisions _will be consistent,
fair and objective.
55
Summary of Evaluation Report
Page 3
Human Resources (Personnel Management)
The personnel department of the hospital seems adequately staffed, records are
maintained for all employees. There are cadre positions determined by the
Governing Body in al) areas of the hospital. This results in adequate but not
excessive staffing.
Salaries are similar or higher in all categories when compared to other non-profit
voluntary hospitals in the city of Bangalore. It is noted that in each major job
category there are only two, or at most three grades limiting avenues for
promotion. For class four staff, there appears to be only one grade. Other
employee benefits are available including adequate leave, uniforms, festival
advance, education advance, salary advance, and medical benefits.
The Employee Service Rules are proper and are printed in booklet form.
indicated that most are aware of these rules and have read part or all.
Staff
Job descriptions are prepared for many employees. Performance evaluations in
various formats are used during probation and for consideration for promotion.
No administrative or personnel policy manual is available.
promotion policy.
There is no written
There is a recognised labour union in the hospital. There are regular settlements
between the management and the union. Union dues are paid by salary deduction.
Most decisions involve the union, /^ministration believes that this situation has
resulted in a more relaxed attitudejoward work, some avoidable indiscipline, and
increasing demands resulting in financial pressures that must be met by increased
charges to patients.
The Administration has an “open door” policy towards employees. There is effort
to remedy grievances quickly as well as to resolve discipline matters quickly.
Many staff indicated that they did not undergo orientation when they joined. Many
stated that they had not received any further training or developed any new .skills
while employed.
Some recommendations regarding personnel management are as follows:
1. Have a standard job description format for all departments and staff. Ensure
that all employees have a job description and fully understand what is expected
from them.
2. Develop a promotion policy and more avenues for promotion in each job
category. Promotions should be based on merit and longevity.
3. Have a common performance appraisal form for all employees throughout the
hospital. This could be completed by the supervisors quarterly during probation
and annually after confirmation.
4. Appointment letters and appointment orders should be standardised and made
common for all employees.
5. All personnel policies and other administrative policies should be written and
organised into a policy manual. These may be written in a standard format and
be available with supervisors for reference.
6. There should be a standard organised orientation program for all new
employees.
7. Supervisors should participate in the selection of staff for their departments.
8. The management as a whole along with supervisors should have human
resource development plans, both to enhance performance of existing staff as
v./pll as tn nlan for future needs
Summary of Evaluation Report
Page 4
Specific Departments Reviewed
Generally the departments assigned to me for review seem to be functioning
adequately. For the purpose of report, I will comment on each one briefly.
The Prosthetic and Orthotic Centre treats poor patients including outside referrals.
They have adequate staff and space to manage a busy workload. They have a
treatment plan for each patient. They do not have any written polices and
procedures for the department.
Physiotherapy is well integrated into the patient care team contributing to good
patient care for both inpatients and outpatients. The level of staffing, equipment,
patient load, hours and record keeping are good. They have no written policies
and procedures. The department has been without a department head for nine
months at the time of this evaluation.
The clinical laboratory is well staffed, providing 24 hour service to patients. The
tests available are wide-ranging and internal and external quality control procedures
are in place. The question regarding space was not answered. Disposable
syringes are not being used though they stated that universal precautions are being
followed. They have no written policies or procedures
The radiology department provides 24 hour service to patients with good equipment
and staff. Reports are given in a timely manner. They have written policies
regarding patient preparation and radiation protection.
In the medical records department the basic standards for information management
are being met. Staff are not technically trained and_th_e. number of.staff appears to
be less when the patient load is considered.
The pharmacy also is meeting the basic standards. The department does not have
written policies and procedures. Adequate staff are in place to provide service to
inpatients and outpatients. They state that their space is not adequate. The staff
do not have any continuing education or inservice training opportunities.
The CSSD has good written procedures for their functions. They follow quality
control and infection control procedures. They state that their space is not
adequate. Safety of staff as well as patients is of concern especially with needles
that are beingjeused. Service is not available on Sundays and holidays, but it is
not known from data obtained whether there is any supply problem.
The laundry is fully mechanised. The department has written policies and
procedures. They are apparently not following universal precautions.Jn^e handling
of dirty or contaminated linen. With only one dryer, it is not clear if their hours are
adequate to supply needed linen.
The dietary service to patients apparently supplies very few diets per day. Diet
counselling is available to patients on request. There is no quality control on their
diets. Food service for staff is on contract.
Recommendations regarding these areas are as follows:
1. In those departments which see their space as inadequate (pharmacy, CSSD),
the management should assess this-and identify solutions if indicated.
2. All departments should develop. written policies and procedures relating to their
function.
3. Universal precautions, including use of disposable needles and syringes and
disposat’drsharps, should be strictly followed in all areas.
68
Summary of Evaluation Report
Page 5
4. Staffing in medical records department should be reviewed. As vacancies
occur, trained medical record officers or medical record technicians can be
appointed.
5. Inservice education and continuing education opportunities should be provided
for staff at all levels.
6. Adequacy of supply of linen and sterile items on weekends and holidays can be
reviewed by the management.
7. Professional staff in dietary department may be increased to provide more
patient education. Daily rounds by dietetians in the wards will allow them to
identify all patients needing special diets as a part of their long term treatment.
8. Laundry should set standards for rate of loss of linen with targets to decrease
present losses.
Ancillary Services
The transport department provides ambulance service for patients as well as
transportation for administrative services of the hospital. Staff and vehicles are
apparently adequate for needs. There are no written policies or procedures for
maintenance of vehicles or accidents.
Security services are provided by an outside contractor. Considering the size of
the property as well as buildings, staffing may not be adequate.
Surveys are made regularly to identify hazards in the hospital. Bore wells and
generators ensure adequate supply of water and electricity. There is also a plan to
meet these needs in future. A disaster plan is in place. The hospital has an
incinerator. There are no written procedures for disposal of various kinds of
wastes.
The hospital has a program of preventive maintenance for buildings and equipment.
There is timely response to complaints from departments regarding building and
equipment maintenance.
Recommendations regarding these areas are as follows:
1. All departments should have written policies and procedures.
2. Management should review adequacy of staffing in security,
including
frequency of complaints and thefts, control of visitors, and maintenance of order
within the property
3. Particularly in regard to waste disposal there should be written policies. Not
only is this important for the institution, but it is also important in case of further
legal requirements.
Spiritual Care
The hospital includes in its objectives provision of competent and comprehensive
care of the whole person with love and compassion as taught by Jesus Christ.
Spiritual needs are to be met even while respecting the religion of the individual
patient or family member. A commitment has been made to provide counselling
and support to people in crisis.
&
Summary of Evaluation Report
Page 6
Standards by which spiritual care is evaluated were accepted by the review
committee. A questionnaire was submitted to the chaplaincy department which
was returned in a very incomplete form. Therefore it is assumed that answers to
the many questions are unknown or are negative. There appears to be only one
chaplain on the staff. There is no report on how many employees are Christian or
whether preference is given to Christian applicants when hiring new staff. There
was no reply to the question regarding improvement in the attitude of the
community towards Christianity as a result of the hospital. It is not clear whether
patients have opportunity to hear about Jesus and His peace while in the hospital.
Thirty-eight percent of the staff questioned felt that there was no one to whom they
could go to share their problems or personal needs. One staff expressed need for
help with an alcohol problem. There has been no special programs or retreats for
staff and students in the past year.
One could conclude from this that there is not an emphasis on spiritual care.
Rather it is perhaps viewed as incidental. As a Christian institution, this emphasis
would be essential in order to justify fully the existence of the hospital In the face of
competition and costs of health care in today’s world. Feedback from patients is
still awaited.
However, it is recommended that the basic purpose and reason for existence be
reviewed. If affirmed it should be reflected in a strong Christian attitude and
activity from spiritual development of students to hiring and nurturing of staff to
spiritual care of patients Such an emphasis will require human and material
resources. But it could be the key to the future of the institution.
Responses from Staff
The majority of staff (94.5%)felt that they were a part of the health care team.
Eighty percent felt appreciated in their work. Over 75% felt there was someone in
the organisation to whom they could communicate their problems. These are
positive points on which further good will and spirit can be developed.
The staff responded with a wide variety of requests, suggestions, and comments.
Some did express concern that love and compassion are less evident than before,
that care of the poor has decreased, and that quality of care and caring has
declined. Many made requests regarding salary, increments, more loan facilities,
promotion avenues, resting room, better uniform, easier access to care when sick,
more free drugs and crepe bandages, and jobs for staff children. Several
requested retreats, staff get togethers, and restoration of Christmas lunch.
There were suggestions regarding their work situation including improved
procedures to control infection and protect staff, better availability of supplies like
adex and bleach, aprons in lab, improved brooms and rubber gloves for handling
contaminated linen. Some felt there was partiality with some staff allowed to work
less while others carried a heavier load.
There were numerous suggestions to improve hospital services:
1. Special fund to care for poor people
2. 24 hour reception and enquiry
3. 24 hour pharmacy
4. More security In OPD
5. Drinking water in OPD
6. Improved casualty care
7. Buildings and facilities to be modernised
8. More tertiary care services to be initiated
70
Summary of Evaluation Report
Page 7
9. Day care centre for mentally ill
10. Family counselling service
11. Guest rooms for patient relatives
12. Linen to be returned to the ward from which it came
13. Rats to be controiled
Some of these may already exist. Feasibility studies would be required for others.
No specific recommendations are made in this section of the report. These
responses are included in the report for the information of the management and
their consideration as indicated.
Summary
In conclusion, the overall function of the areas of the hospital evaluated is
satisfactory. There are many strengths in the institution including its long history of
service and good reputation in the city of Bangalore, certain weaknesses have
been identified which may suggest actions to be taken in order that the future will
be bright and contribution to the community great in the years ahead.
- Dr. Rebekah Naylor,
Baptist Hospital,
Bangalore.
SUMMARY
OF
STAFF
SAMPLE
TOTAL
RESPONSES
=
200
1
r(-- 03
35
I 5
DOCTORS
1
Yes
No
NA
(No.%) (No.%) (No.%)
1.Someone availble to communicate 27(65.8) 14(34.1)0
problems
FACULTY
STAFF NURSES
WARD INCHARGES
Yes
No
NA
YES
NO
NA
YES
NO
NA
(No. %) (No. %) (No. %)
(No. %)
(No. %) (No. %) (No.%) (No.%) (No.%)
14(93.3) 1(6 7) 0
43(91.5) 4(8.5)
0
19(100.0) 0
0
2.Complaints are heard
21(51.2) 18(43.9)2(4.9)
36(77.0)
3.Feel part of team
38(92.7) 3(7.3)
0
4.Know mission of hospital
37(90.2) 3(7.3)
1(2.4)
5.Promotion avenues available
11(26.8) 28(68.3) 2(4.9)
30(63 8)
6.Orientation received when joining
institution
14(34.1) 25(61 0) 2(4.9)
45(95.7)
7.Feels appreciated
21(51.2) 18(44.0)2(4.9)
QUESTION
ANCILLARY STAFF
YES
NO
NA
(No. %) (No. %) (No. 7.)
27(77.1) 8(22.9) 0
CLASS (V
YES
NO
NA
(No.%) (No.%) (No.%)
24(55.8) 19(44.2) 0
TOTAL
NO
NA
YES ,
(No.%)
(No.%)
(No.%)
154(77.0) 46(23.0) 0
11(23.4) 0
18(94.8)
1(5.3)
0
13(86.7)
1(6.7)
1(6.7)
27(771) 7(20.0) 1(2.9)
17(39.5) 24(55.8) 2(4.7)
132(66.0) 62(31.0)
6(3.0)
47(100.0) 0
0
19(100.0)
0
0
14(93.3)
0
1(6.7)
29(82.9) 5(14.3)
1(2.9)
42(97.7) 1(2.3)
0
189(94.5) 9(4.5)
2(1-0)
47(100.0) 0
0
19(100.0)
0
0
15(100.0) 0
0
29(82.9) 4(11.4) 2(5.7)
36(83.7) 6(14.0)
1(2.3)
183(91.5) 13(6.5)
4(2.0)
17(36 2) 0
9(47 4)
10(52.6) 0
10(66.7)
3(20.0) 2(13.3)
13((37.1) 21(60.0) 1(29)
6(14 0)
36(83.7) 1(23)
79(39.5)
2(4 3)
0
17(89.5)
2(10.5)
0
14(93.3)
1(6.7)
0
9(25.7)
8(18.6)
35(81.4) 0
107(53.5) 91(45.5)
2(1.0)
42(89.4)
5(10 6)
0
18(94.7)
1(5.3)
0
14(93.3)
1(6.7)
0
24(68.6) 11(31.4)0
41(95.3) 2(4.7)
0
160(80.0)
38(19.0)
2(1.0)
23(56.1) 15(36.6)3(7.3)
42(89.4)
5(10.6)
0
18(94.7)
1(5.3)
0
14(93.3)
1(6.7)
0
29(82.9) 6(17.1) 0
33((76.7) 5(11.6)
5(11.6)
159(79.5)
33(16.5)
8(4.0)
Knows Employee Service Rules
34(83.0) 5(12.2) 2(4.9)
40(85.1)
7(14.9)
0
18(94.7)
0
1(5-3)
15(100.0) 0
0
33(94.3) 2(5.7)
38(88.4) 5(11.6)
0
178(89.0)
19(9.5)
3(1.5)
10.Opportunity to give suggestion
30(73.2) 9(220) 2(4.9)
30(63.8)
17(36.2) 0
14(73.7)
4(21.1)
1(5.3)
13(86.7)
2(13.3) 0
17(48.6) 17(48 6) 1(2.9)
31(72.1) 12(27.9) 0
135(67.5)
51(30.5)
4(2.0)
11 .Availability of personnel for
guidance
14(34.1) 21(51.2)6(14 6)
22(46.8)
25(53.2) 0
19(100.0) 0
0
13(86 7)
2(13.3) 0
23(65.7) 12(34 3)0
23(53.5) 17(39.5) 3(7.0)
114(57.0) 77(38.5) 9(4.5)
12.Work area comfortable and safe
29(70.7)
11(26.8)1(2.4)
45(95.7)
2(4.3)
0
17(89.5)
2(10.5)
0
15(100.0) 0
0
30(85.7) 5(14.3) 0
38(88.4) 5(11.6)
13.New skill/training received
17(41.5)
17(41.5)7(17.1) 40(85 1)
7(14.9)
0
12((63.2)
7(36.8)
0
13(86.7)
2(13.3) 0
23(65.7) 12(34.3)0
9(21.0)
14.Have job description •
26(63.4) 15(36.6)0
44(93.6)
3(6.4)
0
17(89.5)
2(10.5)
0
15(100.0) 0
0
25(71.4) 10(28.6)0
40(93.0) 3(7.0)
15.Participates in special/
extracurricular functions
27(65.6) 14(34.1)0
35(74.5)
12(25.5) 0
9(47.4)
10(52 6) 0
2(13.3) 0
16(45.7) 19(54.3)0
1((2.3)
l
8.Feels policies/rules fair
0
0
174(87.0) 25(12.5)
1(.5)
34(79.1) 0
114((57.0) 79(39.5)
7(3.5)
0
167(83.5) 33(16.5)
0
42(97.7) 0
101(50.5) 99(49.5)
0
72
ATTACHMENT
13(86.7)
26(74.3) 0
115(57.5) 6(3.0)
SecK'<
Eaapier -
the ibllowirig, background papers, many of which were
The Review drew
circulated to all the members ofthe Teain.
1. St Martha's Hospital - Objectives (Mimeographed Handout)*
2. Provincial Directives - January 1998*
3. Guidelines and Terms of Reference for Reflective Process drawn up by Hospital
Commision - January 1998*
4. Framework of Review - approved by Review Committee and Hospital Commission
- March 1998*
•5. Survey-of psfcnis. ■<
6. Mission, Philosophy, Objectives and Strategies of St. Martha's Hospital (Revised
Document 1998)*
7. Memorandum of Association of St. Martha's Hospital - September 1965*
8. A Framework for die Establishment/maintenance of a Community Health Department
at St Martha's Hospital - Bangalore, August 1992.
9. Summary of the Discernment of St Martha's Hospital from November 1988 to
November 1986 and its follow up procedures,
10. Working draft of proposed Handing over of SMH to another Church Society
(Proposal to CBCI Society of Medical Education).
11. SMH Hospital - 6 options post Discernment with reasons for and against
(Handout).
12. New orientation of St Martha's Hospital - (handout) 21” November, 1986.
13. Some Standards to be considered for the Hospital (Rebekah Naylor)*
14. Annual Report 1997-98, ST. Martha's Hospital, Bangalore - 560 009.
15. Annual Report 1996-97.
16. Annual Report 1995-96.
n
17. Annual Report 1994-95.
18. Annual Report 1993-94.
19. Annual Report 1992-93,
20. Annual Report 1991-92.
21. Annual Report 1990-91.
22. Seeking the Signs of the times - A Discussion Document for Study and Action
arising out of the CHAI Golden Jubilee Evaluation Stuthj October 1992
u
Report from Dr. Naylor to the Evaluation Committee
14 September, 1998
Much data has been obtained relative to the areas assigned to me for review. The following work
has so far been completed:
1. Documents obtained: Employee Service Rules, organization chart, list of members of
the Governing Body, current salary scales, list of employee benefits, sample job description,
performance evaluation form, sample appointment letter and appointment order.
2. Some standards for evaluation written and circulated to the committee.
3. Interview with the Administrator, Mr. Saldhana.
4. Questionnaires from departments assigned to me for review: personnel, chaplaincy,
Assistant Administrator, dietary, laundry, Prosthetic and Orthotic Center, physiotherapy,
laboratory, pharmacy, X-ray, medical records, CSSD
5. General questionnaires from ancillary staff (35) and heads of ancillary departments
(initial analysis attached)
The work still to be done is as follows:
1. General questionnaire from other staff - nurses, doctors, and Class IV
2. General questionnaires from other heads of departments
3. Student questionnaires
4. Patient questionnaires
5. If time permits, a visit to some of the departments assigned to me for review.
Any conclusions becoming apparent are actually not valid since so much data is not yet in.
Having only seen questionnaires from ancillary staff, I would make the following observations:
1. At all levels, there is very little setting of goals, either long or short term
2. Most have an idea of the mission of the hospital but there is little communication
regarding it
3. There is no administrative policy manual available
4. Most departments have no written standards or procedures
5. Orientation of new staff is weak
6. Promotional avenues and policies need review.
It remains to be seen if these observations apply to the rest of the hospital.
Generally the departments which I am requested to evaluate seem to be functioning adequately.
Some stated that they have space problems. Several do not have written procedures or standards.
Staffing generally seems adequate. I will prepare a detailed summary of each department in view
of standards agreed upon.
It would seem that the spiritual ministry is generally not emphasized or is not a priority with the
administration. This may not be correct and I will pursue with more questions before making a
final report.
Questionnaire For Staff
1. Is there someone in the organization to whom you can communicate
your problems ?
j£>|a,nt
Yes / No
3-3
3
2. Do you feel that your complaints or grievances are heard ?
Yes / No
3. Do you feel a part of the health care team ?
Yes / No
• 5
I
4. Do you know what is the«niissiun or the hospital ?
Yes / No
Acl M
Yes / No
i 3> 2.)
I
5. Do you have promotional avenues open to you ?
6. Did you undergo orientation when you joined the hospital ?
Yes / No
7. Do you feel appreciated in yourwork ?
Yes / No
2.4 I I
8. Do you think the,rules and policies are fair ?
Yes / No
9. Have you read and understood the Employee Service Rules ?
Yes / No
&
33 zz.
10. Do you have opportunity to suggest ways that your department’s
work or function could improve ?
11. If you have a personal or family problem, is there someone in the
hospital who can guide or help you ?
Yes / No
l‘~l
Yes / No
.2 3 i2.
12. Is the area where you work comfortable and safe ?
Yes / No
30 5
13. Since joining work, have you received any training or new skills ?
Yes / No
■2.-3 J2.
14. Do you have a job description ?
Yes / No
/0
15. Do you participate in any special events or extra curricular activities
in the hospital ?
Yes / No
)
I
Questionnaire For Head of Departments
1. How long have you been Head of the Department ?
2. Do you conduct regular meetings of employees whom you supervise ? Yes / No
4 3>
3. Do you feel that there is good communication with management ?
Yes / No
4. Are you involved in selection of staff for your department ?
'■7
5Yes / No
5
4
5. Are you involved in the annual budget process for your department ?
Yes / No
3
3
6. Are you informed about the financial performance of your department ? Yes / No
4
7. Do you regularly evaluate the performance of the employees you
supervise ?
8. Do you know and understand the vision and mission of the hospital ?
5~
Yes / No
4
3
Yes / No
4
J
9. Do you communicate the vision and mission to your employees ?
Yes / No
5
3
10. Does your department have written policies and procedures ?
Yes / No
11. Do you set goals each year for your department ?
Yes / No
4
i
G?
12. Do you feel a part of planning and decision making in the
organization?
Yes / No
13. Do you orient new employees in your department ?
Yes / No
5
4
1
14. Do you provide any inservice or on the job training for your
employees ?
15. Have you attended any seminar, program or course on
management training ?
16. Do you have written standards that guide the work of your
department ?
Yes / No
3 4
Yes / No
H- s
Yes / No
3
H
17. Do you have enough qualified staff to do the required work ?
Yes / No
(C
72-
18. Do all of your employees have job description ?
Yes / No
tp -2Yes / No
19. Do you know the organization plan or structure of the hospital ?
8. CHALLENGES AND TASK AHEAD
This chapter will try to answer the seven questions which was included in the Framework
of the Review during the Review committees first discussion with the Hospital
Commission on 18th March, 1998 {See Appendix 10(ix)}
It will then enumerate some challenges and tasks before the Hospital sisters and
management as they reflect and evolve the vision-mission-growth-developmentmanagement plan of the Hospital into 2000 AD
Finally a short reflection will try to provide a glimpse of the future scenario if the review
committee suggestions are internalised by the management. This is hypothetical and
perhaps reflects some of the many options the 'hospital sisters' can seek to choose as
components of the vision-mission-structure of the fture. The Review can only provide
some ideas about the 'existing realities' and some ideas about 'future options'. Ultimately
the choices and the options must come from within
(This Chapter will be the focus of the final meeting on 16,h June, 1999. The
key suggestions from the remaining chapters have been highlighted and
integrated. At the time of action however the previous chapters must be read
in context and as complementary / supplementary to the final chapter.)
uestion One : Is the Hospital Apostolate in tune/consistent
Q
with the charism; mission, vision and philosophy of the Good
Shepherd Sisters?
NO
The hospital is a relatively well managed, secondary care oriented mission hospital trying
to survive with some difficulty and constraints - many internal; in an increasingly
complex 'market economy' and changing external environment and challenges with its
own vision and mission.
Not in consonance with the Good Shepherd Sisters modified directives of 1995.
1
.. BBBB'BI IB B B Bi Bii B BBBBBBii BBfBBit
r*- Il is not focussed on poor women (exploited, oppressed and socially:
discriminated) and children though they form apart of the clientele?
•*- Its not adequately prevention, protection, rehabilitation, and crisis
intervention oriented as it could: be and all the? initiatives be it
community health, family welfare, orthotic and rehabilitation: unit
etc., which add to this dimension are marginal/peripheral to the
central focus of 'acute care for sick and ailing',
w- Its hospital, based .and outreach programmes are not adequately
linked or supportive off the outreach: programmes and initiatives of
the other sisters of the Congregation in Bangalore, iKamataka or
South India - so that it could be sachihat-it-was supportive of more
charism oriented initiatives of the others.
YES? But....
w In its training policy and staff recruitment policy there is some focus
on women and some effort in some grades e.g., nursing students and
aides to give selective advantage to those from more disadvantaged
or difficult backgrounds but this seems more incidental rather than
the result of clearly stated policy supported by management
guidelines.
(The sisters by taking up professional responsibilities and supported by a large
team of committed nurses and some female professional and ancillary staff at
all levels are a good role model for women in today's society. This role could
be enhanced by clearly stated policy and enhancing the focus towards
charismal directive).
2
uestion Two :
Q
Does the hospital reach out to the less
affluent sections /poor in the population of Bangalore?
NO (in hospital care) not adequately
Inspite of an expressed keenness to reach out to less affluent section / poor in Bangalore
and some commitment to policies of low cost care (keeping cost of investigation
procedures and hospitalisation down), the hospital is able to invest less and less of its
funds and income for free and subsidised care over the last few years since its overall
position is fast moving into deficit financing further compunded by increasing cost of
medical care.
♦
Has not at governing body dr management level seriously addressed; this
issue recently to evolve any fund raising schemes or initiatives/to
subsidise this vision to reach, the poor.
♦
While this is marginally compensated for by the very slowly increasing
’outreach efforts' of the newly established CH Department : which is
establishing 'Primary Health Care' contact with urban slums in Bangalore even this has not been adequately supported by subsidised referral support
which could: allow poor in the urban slums served by the hospital to avail
of secondary'care facilities.
(This is particularly significant because inspite of the development of many
corporate hospitals/modern hospitals in Bangalore with sophisticated technology
and gadgets and highly professional staff; the mushrooming of small nursing
homes and 'specialist' private practitioners; the declining quality of services in
government hospitals there is, still urgent need in the presence of'plenty' for low
cost quality secondary care for the poor and marginalised who are increasing in
the slums of Bangalore. So a Hospital with a mission for the poor and that too
poor and exploited women and children (who form the bulk of the poor in
Bangalore is still relevant.')
3
YES (in training) But
There is some policy in selection of nursing students to increase the
number of students from disadvantaged backgrounds and for the tutors
to help these students catch up and be equal to the others. However
this policy needs to be sharpened; faculty need clear direction and
more motivation / encouragement to facilitate this policy; and the
numbers in this category must be increased gradually so that its
'central to the training challenge' not marginal to it.
Also it seems well established that most of the nursing students after
graduation and after the bond-phase serve in big city hospitals or go to
the gulf to carry on their profession as nurses. Serious consideration
must be given to more from just 'excellence in Nursing education'
which makes Nurses advantaged in an emerging market economy for
trained nurses - to a conscious Social and Community Orientation of
the course at all levels and by all faculty so that more are motivated to
serve those which the Congregations seek to serve'.
uestion
Q
Three :
Are
the Hospital policies
in
various
departments spiritually sound?
Yes, but
The overall consensus among patients, nurses, doctors, ancillary staff and reviewers are
that the hospital has by and large a committed / dedicated b/nd of sisters of Good
Shepherd and a committed I dedicated bifid of doctors I nurses and ancillary staff who are
competent and compassionate, courteous and committed to patient care providing this to
4
CKex,
all irrespective of caste, creed or income level but....
1.
There seemed to be no clearly stated policy statement on ethics, pastoral
care and teachings of the church promoted and upheld by the hospital in
its work including the justice dimension.
2.
There was no emphasis on spiritual or pastoral care for all the patients.
3.
Many staff expressed that there was no one to whom they could go to
share their problems or personal needs. Many felt that staff welfare was a
low priority concern. This is particularly crucial because those who need
to minister a 'value concern' must experience strongly this concern in their
working relationship with the institution!
4.
There were no special reflections, group discussions, retreats or vision
mission reflections with the staff at the time of joining, or on an ongoing
basis to keep up their motivation and commitment to ethics, and a 'pastoral
approach to patient care'.
5.
While all religions were respected and patients and staff from all religious
groups felt accepted there was no pro-active policy or other initiative to
enhance the multi religious I multi cultural ethos of the Hospital.
6.
There was also a challenge to involve the progressionals more pro-actively
in developing a secular (multi religious) humanist autonomous ethical
code for hospital practice and not have just a heteronomous ethical code
that is thrust on a top-down basis by management. This would need a
much stronger chaplaincy and a more proactive pastoral care policy for
the institution including pro-active introduction of the teaching of ethics
in all the training programmes of the institutions.
5
uestion Four : Is the hospital technically well administered/
Q
managed?
YES (technically)
Overall from all sections of stake holders there seemed an overall consensus that the
technical quality of the services provided by the hospital was good though there were
some concerns that
♦
The hospital was failing to modernise some of its equipment and
technology
Was resistant some times to ideas, innovations to improve quality
of health care,
♦
Was ignoring some of the national priorities and programmes
However these can be addressed by a more proactive, dialogue and participation of the
professional resource persons on the hospital staff with the technical policy planning.
NO with regard to Hospital management / administration
At present there seems to be many lacunae inspite of committed and overworked
Medical Superintendent; a busy Administrator; and a hospital Planning and Executive
Committee supported by a Governing Body.
a.
The Survey ofgovernance / management identified
o No immediate goals or short or long term plans
o Inadequate involvement and participation of heads of department and
middle management in the decision making processes and planning
o No administrative or personnel policy manual and no written
promotion policy
6
o No orientation to staff at the time of joining or on a continuous basis
regarding hospital policy and goals
o No written policies or procedures for many departments that provide
crucial and important services. Also for hospital waste disposal
procedures
o No staff continuing education, inservice training opportunities or
policies
o No staff safety policy and inadequate attention to staff welfare.
This has resulted in lowering staff morale and staff initiative and creativity.
b. The 'Doctors Survey' has identified key issues for urgent attention as
o inefficiency in health care delivery and planning
o not consulting concerned department heads when planning and
budgeting
o not motivating staff to work in a caring manner
o applying different rules and regulations for different people
c.
The Nurses Survey has identified some others as
<........................ .......... .......................................................... .............................. ;
o are rules and regulations fair for an reasonable to all the employees?
o to have regular meetings with staff?
o to set goals each year for the departments
o to have written policies and standards in the department
o> to see to staff professional development and inservice education
(Many individual respondents have given comments and suggestions which are a very
good check list for reflection and policy action - see earlier chp^ters)
7
uestion Five
Q
:
Does the running of the hospital faithfully
reflect the philosophy objectives, strategies as laid out in
the papers prepared for the Review?
(with reference to Appendix 10 (iv))
Suggestion I Response
A.
Objectives
I.
Promote, respect and
dignity of all human
life.
proactive
By and large as reported by Better
staff
counselling services are
required to further this
respect.
2.
Serve all irrespective
of caste, creed or race
Good record in this.
3.
Case of high quality at Trying to do this in many Needs much more attention
a cost that common ways
by all staff.
Creative /
people can afford
socially relevant low cost
options to be further
explored.
4.
Develop a team spirit
and
collaborative
ethos.
5.
and
Provide competent / Care is competent but not Communication
pastoral
skills
to
be
comprehensive health wholistic.
enhanced among all staff.
care for whole person.
6.
Provide care with
honesty and integrity.
7.
To
conduct Competence of all courses Need greater social and
level
skill
educational / teaching except perhaps the aides community
competence in all cadres.
programmes
with course is very high.
higher standards of
competence.
Findings / Comment
Keep it up }
Very weak in this aspect Needs more active efforts
even among the hospital to build team spirit and
sisters though staff have common
vision
ethos
reported that this spirit was among sisters and all
'56'> with the Irish Sisters grades of staff.
-phase.
Good record in this.
8
Keep it up I
A.
Objectives
Findings / Comment
Suggestion / Response
Siddha
system Need much more attention
alternative Except
of Health doctors in CH team this is a to low cost plural health
major blind spot.
systems,' care
building
dialogue
between
practitioners and systems.
8.
Provide
systems
Care.
9.
Participate
in CH Department work still This
needs
a
more
improvement
of strongly bio-medical.
comprehensive
planning
quality of life of
and
support for
CH
people in community.
Department
to
evolve
initiatives in the slums.
10.
Provide
counselling Very little is done by a few.
and support to people No proactive policy.
in crisis.
Could
be
a
strong
component of a more
proactive / comprehensive
pastoral care policy.
11.
Create awareness of No action on this as yet.
importance
of
preserving
ecologically
sound
environment.
Could start with effective
hospital waste management
strategy followed by more
eco-sensitive management
initiatives.
Findings / Comment
Suggestion / Response
B.
Strategies
1.
Promote good and
high quality services
2.
Rational use of drugs / Past contribution to CHAI - Of late this has become
formulary more adhoc / routinised.
therapeutics
and CMA1
methods of treatment supplemented by hospital A
more
proactive
drug policy well known.
and care.
rationalising
policy
is
needed going beyond drugs
to technology use and
'procedures' indication.
3.
Selectively
upgrade Have been relatively slow
medical technology to in keeping pace not always
keep
pace
with due to 'secondary care'
vision constraint.
advancement.
Relatively good and quality Need to evolve inhouse
quality control measures
service.
and indicators.
9
Needs
to
evolve
a
selection
/
updating
procedure in consonance
with evolving vision.
B.
Strategies
Findings / Comment
Suggestion / Response
Keep it up - and evolve
proactive
staff
sensitization.
4.
Courteous
and Generally good record in
considerate to patients this matter.
/ visitors and general
public.
5.
Create
a
climate
conducive to a pursuit
of excellence.
This strategy needs greater Excellenece without social
/ community relevance is
clarity.
not enough.
6.
Motivate
all
in
hospital
to
be
dedicated / committed
and give off their best.
No strategy as yet how to
do this.
7.
Promote health care This
is
still
rather What Health Care? Who is
rhetorical. Needs greater the 'all'?
for all.
clarity and focus.
8.
Lay strong emphasis This strategy needs further Values cannot be taught
on value education of clarity on what values? easily but need to be
'caught'. These need to be
patients, public, staff, How value education?
gradually internalised into
and students.
ethos of institution. So all
staff
absorb
it
by
experience and example.
9.
Readily accessible to While the first strategy is What crisis?
those suffering from well developed, the second
What type of access to be
sickness or those in one needs further clarity provided?
and policy evolution.
crisis.
10.
Create awareness of
sound health and evils
of smoking / drinking /
addiction.
Laudable objective but
strategy
needs
greater
clarity and commitment.
Health
education
in
hospital is still somewhat
adhoc.
11.
Create awareness of
clean
and
healthy
environment
and
living in harmony with
nature.
Laudable objective but at Clarify context of clean /
present
seems
mostly healthy
environment.
rhetorical. Needs greater Where? For Whom?
clarity and framework.
Living in harmony with
nature - how?
10
Dialogue and continuing
motivation / orientation
sessions must be part of
ongoing staff development
and inhouse training.
Health
education
in
Hospital situation needs
much greater emphasis
than at present. o»~> exit
Aeses c.
'-*f
'
e,L
uestion Six : Does the financial management of the hospital
Q
Q
reflect the objectives and strategies of the hospital?
uestion Seven : Is the Hospital Sustainable and financially
viable?
NO
The comprehensive financial management review which had to function within the
constraint of the data that was made available has shown
♦ Decreasing occupancy rate
♦ Deficit finances
:
♦ Ability to serve poor as target decreasing over the year
♦ Need for better control and monitoring systems to .keep costs down,
avoid waste or inefficient expenditure and enhance better resource
mobil ization and more effective utilization.
<
A'...,.,:U
'.N
/ .
(hurt her.details in report)
t
;
<
n
- . .
There is urgent need for proactive, professional financial management ■ to enhance
financial viability of the hospital which is itself critical to sustain its vision / mission.
d) C. c
Co
cu Lj
LAyO
Cc^-> 1-, C <sy~> kxe 1
Co
c.
cLe ca-a c. ^<s
c4.<s>xe
co
0
..
■
TASKS AHEAD
The Hospital sisters and the Hospital Management have some important tasks ahead
which need urgent, policy consideration and action. Atleast Five become somewhat
crucial.
1.
Multidisciplinary Advisory Committee
The Governing Body and Hospital Management need the advise and support of a
larger body of experts to help them evolve guidelines and strategic responses to the
emerging challenges. This must include atleast experts in Hospital Management,
Finances; Law; Community Health, Pastoral Care and representatives of the
community / civic society especially Women's Organisations, Social Scientists /
Social workers and community organisers.
2.
Fostering Participatory Management and Lay leadership
In addition to evolving a more responsive and multi disciplinary advisory structure
the hospital should urgently widen the scope of dialogue with and involve more
proactively the professional leadership among its doctors and the committed lay
leadership among the nurses and other categories of staff especially those who have
shown long standing commitment. They should be involved proactively in the vision,
mission, objective setting.planning exercises and in the development of strategies to
address the dilemmas and‘challenges that face the hospital.
3.
Translating Vision/Mission to Hospital Policy guidelines
The Vision / Mission / Objectives of the hospital need to be translated into guidelines
and hospital policies that are communicated to all concerned and are reviewed from
time to time - so that there is consistent experimentation and evolution of policies I
action in keeping with the goals. The discernment process at the time of the
centenary and the reviews / dialogue since then have thrown up large number of ideas
and thrusts. Somewhere along the line the translation of these ideas into specific
hospital policy has been a casualty.,. The present review could meet same fate if
commitment to this translation is not strong.
ec-r Ii'e-r
■
el.? > j...
e4..<
■ e z->
w
12
-
Some areas where this needs to be addressed urgently are
i)
ii)
iii)
iv)
v)
vi)
Financial management towards sustainability
Pastoral Care
Staff development and inservice training including Continuing Education
Quality control of services (standards and benchmarks to be evolved)
Long term and short term planning including annual plan at departmental level
Ethical and social I community orientation of all training programmes in
consonance with hospital vision.
Strengthening Management / Administration Capacity
4.
A more professional approach to Hospital Management particularly1' personal
management and financial management are urgently required. Adhoc p
c--. i.-. ■■ ■' « 1
■'
-<~r
Identification of full time resource persons including lay / religious trained in hospital
management or health care administration with experience in similar hospitals with
similar vision / mission is imperative.
,
;7
Terr de
,' 7
Alternatively suitable candidates from existing staff I sisters could be identified and
sent for suitable training as a long-term investment.
,
Financial management skills which must include ability for short term and long term
planning and commitment / especially to ensuring sustainability of the hospital must
be developed. . .. •
•
- 7
-7.
Towards further integration of 'Hospital' and 'Congregational' charism
5.
The most important challenge for the Hospital Sisters' and management is to
'proactively' and 'confidently' work towards the reduction of the dissonance between
the 'Congregational Charism1 and the hospital missions, thrusts and existing realities
by continuous inhouse participatory discernment and dialogue in active collaboration
with the Congregation and all those who share the same vision.
At least five component action initiatives are crucial for meeting this challenge.
a.
Serious efforts to strengthen the Community Health Department and the Hospital
outreach I extension work as an institutional mandate involving all faculty a.nd
departments supported by strong policy commitments and not the 'adhoc
amateurism' that is the reality today.
13
J
<.
*
\ 7. if'
■7 '
b.
Exploring and establishing links with all the 'charismal initiatives of the sisters of
the congregation so that all their institutional and non institution work with poor
women and children (particularly those marginalised and exploited is supported
socio-medically as much as possible.)
c.
Establishing meaningful linkages with women's groups and other voluntary
agencies who are working with women focussing on poor / oppressed / marginal /
exploited and evolving concrete support strategies and collaborative projects e.g,
An AIDS ward and AIDS care and counselling centre is an urgent need in
Bangalore.
ii. A Burns ward with an associated counselling service to handle the increasing
phenomenon of dowry deaths and suicides and violence against women.
iii. Providing 'training' facilities and space for women's groups in Bangalore with
some involvement of socially sensitive sisters and faculty.
iv. A more proactive family life education centre which is committed to more
than just NFP and skilled to tackle a wider range of family problems.
v An active 'Women's Health' initiative with women's colleges in Bangalore that
could help prepare women students for greater autonomy in Health through
active health education and counselling services.
i.
d.
Serious efforts to share vision / mission with all staff and students not as top
down directives but through creative dialogue and collective action at all levels
encouraging their involvement in a, b and c.
•••
e
There is need for greater unity of purpose and team work and collectivity among
the hospital sisters themselves since they form the 'Core' of the human resource
team of the hospital that has to constantly and consciously outline and
operationalise the hospitals vision / mission in consonance with the
congregational charism. Any compartmentalisation; competition; problems of
communication; strong divergence of views and styles; lack of coordination; and |e<elc
of constant commitment to group decision making over individuality can be
detrimental to the whole process and affect staff enthusisasm and morale and
'divert' or distract the hospital team from its commitment to quality action. While
this many often be inadvertent or accidental or even incidental to job
responsibilities and demands of specific roles - taking the onus for a 'charismatic
collectivity' is a crucial responsibility.
In the final analysis St. Martha's Hospital is a hospital today with its strengths far
outweighing its weaknesses and its opportunities far outweighing its threats. With a
Core group of experienced and committed sisters and a large number of very
conscientous, committed and quality docotrs, nurses and staff - whose creativity and
14
potential is waiting to be harnessed by a more proactive Hospital Management policy
that is strengthened in some of the directions identified by the multidisciplinary
review committee, the hospital can look forward to becoming a role model of a
Mission Hospital with a Vision / Mission to reach out to "poor exploited, oppressed
and socially discriminated especially girls and women in personal family and social
difficulties .... Working with girls and women deprived of hope and,., love
prevention, protection, rehabilitation and crisis intervention".,.,
SMH
15
ST. MARTHA S HOSPITAL - 2000 A.D.
A Scenario
._______________ -
■’
Jkx)
~~
The St. Martha's Institute of Women and Childrens Health is a Centre dedicated to
providing clinical and counselling support to a growing network of initiatives in
Women and Children's Health in Bangalore City, which is now one of the twenty
largest metropolitan cities of the world.. . .
W
The Institute includes under its jurisdictionthe old St. Martha's Hospital which phased
out some of its older departments and focussed all the remaining department on
Women and Children's health; the college of nursingf/the institute of allied health
professionals (now located in the old Priests quarters) and which trains methbers of the
health team - nursing aids, laboratory technicians, CBR workers, lay counsellors,
community health organisers and Family life educators through a wide range of short
courses.
Some at certificate and diploma level recognised by the Karnataka
Government and the three national Health Coordinating agencies - VHAI, CHAI and
CMAI and their member hospitals; the Uttarahalli Rural health centre, now a key field
practice area of the insitute extending its outreach services to a 100 villages on the
periurban fringe of Bangalore;’'the Integrated Community Health Department which
has a Netyvork of eight urban primary health care units of which three are centres built
with full participation of urban slum committees where the hospital worked in the
later 1990s; three are centre run by Women's organisations in Bangalore with a
memorandum of understanding with the institute and two are IPP-8 urban MCH units
that have memorandum of understanding between corporation and the Institute.
The Institute has a multidisciplinary advisory committee consisting of well known
yvomen professionals from Social Sciences, Psychology, Management, Law, Pastoral
Care and Theology and Community Health and representatives of eight women's
organisations who work focussed on groups similar to the Institutes charism. This
committee meets once a quarter and helps the Instiutte's planning and advisory
Committee and Academic committee to sharpen its focus on women's health issues and
supports all the institutes service, training and research initiatives in other ways.
»T
The staff of the Institute are professionally qualjified and highly dedicated group of
women resource persons both lay and religious who are inspiring role models for
studfyts, trainess and all the beneficiaries of the Institutes initiatives. The institute
has a strong yvomen focussed policy and the campus is yvomen friendly providing a yvell
run creche for yvorking mothers, a yvomen’s health insurance scheme, a yvomen's
16
counselling service that caters to women particularly of the poor and low income
groups from all over the city.
,
e-'
The clinical work of the hsppital has some distinctive features. There is a 30 bed Burns
unit which offers a wholistic care and counselling programme and is actively involved
in supporting women through this crisis and working in other ways to redupe violence
against women at family level; there is ,13bed HIV/AIDS ward that caters to women
with an HIV problem and provides all types of clincial support and procedures;"lhe
fiedicine and OBG department are working specially on women’s health issues such as
cervical cancer, and 'women and drugs' issues; the psychiatry department spcialises in
Family Counselling and works closely with Child Health world on care of girl children
and adolescent girls at community level.
" All these departments run extension clinics and contact centres for education and
counselling services especially in the urban network of centres and support self help
groups among women in this areas.
The Institute is affiliated to the Women's Study programme of the Bangalore
University and closely collaborates with various faculty from different departments of
the university in providing socio-medical support to thei: research and training
initatives.
'■ '/The Community Health Department of the Institute is also the affiliated Urban
Primary Health Care training centre for the Catholic Health Association of Indiaflthe
Nursing College is the founder facilitator of a network of community oriented and
socially relevant nurse trainers in Karnataka; 'the Pastoral Care unit specialises in
women's couselling and has a collaborative training with Christian Medical
Association of India in training female chaplains and pastoral care wpj-kersplthe
^alternative tfiedicine unit is part of a network of holistic health centres in the CHAI
network and also works closely with the Foundation for Revitalization of Local Health
Traditions on evaluation and then endorsing local herbal remedies and local home
remedies (including grandmother recipes). » 'As part of the support to the health
movement the institute has also provided space on its campus on long term lease $)f the
CHAI-Karnataka health office; the Voluntary Health Association of Karnataka and
two Women's support group NGO's. Staff of these centres also support many of the
initiatives of the Institute. The relationship is mutually supportive/ The cbdre of the
Institute include some of the senior / experienced sisters of SMH and some younger
ones who have had special training in pastoral care, management including personnel
and financial management, social welfare, alternative systems of medicine,
Counselling, which are some of the newer policy thrusts of the institute. They are
supported by experienced 'religious' from other congregations and an increasing team
of lay women professionals who form an essential component of the emerging
generation of women in Health and Development. The institute has manyynen on its
17
,
staff at various positions who are gender sensitive and supportive of the new thrust and
agenda.
The institute is supported by/j) A corpus or endowment fund that emerged from an
active fund raising drive that included approaching all the alumni, nurses, doctors and
well wishes of SMH.
ii)
Hi)
iv)
The training and research activities are funded by a range of governmental and
non-governmental funding agencies and trusts both local and foreign who are
keen to support the women's health thrust of the institute.
Three nationalised banks, and two public sector units and three private sector
units also support the institute under their corporate social responsibility
initiative.
Finally the Core group of sisters have believed in providence and grace for
more than a century and that source has never let them down!!
18
Appendix IV
FRAMEWORK OF REVIEW
{For consideration of Review Committee and Health Commission on 18th March, 1998}
Review of St. Martha’s Hospital through a reflective process (March - September
1998).
A.
Some Key Questions / Issues to be considered by Review Committee in the context of
the TOR, the background papers and Annual Report of 1996-97 provided by the
Health Commission.
1)
Is the Hospital Apostolate in tune/consistent with charism, mission, vision,
and philosophy of the Good Shepherd Sisters? Which is:
i)
“Poor, exploited, oppressed and socially discriminated, especially girls
and women, in personal, family and social difficulties through
institutionalised and non-institutionalised efforts in urban and rural
areas ” (January 1995)
ii) “Children, girls and women....including commercial sex workers,
twilight girls, persons with AIDS, working children (child labour) and
domestic women workers ” (January 1995)
a How does this ‘charism 'figure in the:
a) Focus of the work of the hospitals?
b) Focus of the type of staff/team members in the
institution?
c) Focus of the nurses training institution?
a Does the charism mean the hospital should focus on
women, women's ill health and women’s problems ?
Ifyes, then how ?
If No, then why not ?
2)
Does the hospital reach out to the less affluent sections/poor in the population
of Bangalore?
What percentage of outpatient/inpatient are provided free/subsidised
care?
b) Is this trend increasing, status quo or decreasing?
a)
What other measures are being taken to make the services of the
hospital, become more accessible or utilised by the poor and
marginalised?
d) What problems have been faced to increase the percentage of free and
subsidised care?
c)
3)
Are the hospital policies in various departments spiritually sound?
Are all practices, rules, mode of functioning ethical?
Are all religions respected?
Is adequate compassion shown to patients through pastoral care?
Is care taken to avoid negligence? I dehumanization?
.Are the teachings of the Church promoted and or upheld by the hospitals
work?
f) Is the justice dimension in Health and health care addressed by the
hospital?
g) Any others?
a)
b)
c)
d)
e)
4)
Is the hospital technically well administered / managed?
a)
b)
c)
d)
e)
f)
5)
Are the policies/programmes/activities rational?
Are the policies/programmes/activities logical?
Are the policies/programmes/activities efficiently managed?
Are the programmes/activities adequately utilized by the public?
How are the policies/programmes planned, monitored, evaluated?
Are there any weaknesses in the functioning of the hospital services? If
so, what can be identified as specific remedial measures7
Does the running of the hospital faithfully reflect the philosophy,
objectives, strategies as laid out in the papers prepared for the
review?
(Issues not covered above)
Objectives
Promote, respect and dignity of all human life
Serve all irrespective of caste, creed or race
Care of high quality at a cost that common people can afford
Develop a team spirit and collaborative ethos
Provide competent/comprehensive health care for whole person
Provide care with honesty and integrity
To conduct educational/teaching programmes with high
standard of competence
h) Provide alternative systems of health care (!)
a)
b)
c)
d)
e)
f)
g)
2
i) Participate in improvement of quality of life of people m Ac. cwr-irr-.^.n-tj ■
j) Provide counselling and support to people in crisis
k) Create awareness of importance of preserving ecologically
sound environment
Strategies
a) Promote good and high quality service
b) Rational use of drugs/therapeutics and methods of treatment
and care
c) Selectively upgrade medical technology to keep pace with
advancements
d) Courteous and considerate to patients, visitors and general
public
e) Create a climate conducive to a pursuit of excellence
f) Motivate all in hospital to be dedicated/committed and give off
their best.
g) Promote health care for all.
h) Lay strong emphasis on value education of patients, public, staff
and students
i) Readily accessible to those suffering from sickness/or those in
crisis
j) Create awareness of sound health and evils of smoking,
drinking and addiction
k) Create awareness of clean and healthy environment and living in
harmony with nature
{Please note there is some overlap between objectives and strategies as
enunciated in the background note}
6)
Does the Financial Management of the hospital reflect the objectives and
strategies of the hospital?
a) The budget
b) The income and expenditure of the hospital
c) The processes of financial management (Accounting - Auditing)
d) Is the hospital financially sound?
1o
■
7)
Is the hospital sustainable and financially viable?
{Note: All members of the Review team will consider these questions and
issues extractedfrom the TOR and background papers, and contextualise them
to the areas/sectors of the hospital which they are studying}
3
B.
Areas/Sectors for Review (identified from Annual Report 1996-97)
1) Vision / Mission
2) Governance / Advisory Board
3) Hospital organisation/Administration
4) Income / Expenditure
5) Financial Management policy
6) Concessional care
7) Capital Investments
8) Donations
9) Personnel Management policy
10) Endowment fund
11) Community Health Department
12)Nursing/Midwifery Training
13) Community Health Nursing
14) National Board of Examination
15) Radiographers Training
16) Clinical laboratory Technician course
17) Hospital Aids
18) Professional Meetings - Clinical Societies
19) Infection control Committee
20) Drugs/Therapeutics Committee
21) Medicine Department
22) Coronary Care Unit
23) Intensive Therapy Unit
24) Graded care unit
25) Paediatrics
26) Premature Unit
27) Sick Nursery
28) Dermatology
29) Psychiatry
30) General Surgery
31) Surgical ICU
32) Paediatric surgery
33) Plastic Surgery
34) Opthalmology
3 5) ENT
36) Orthopaedics
37)OBG
38) Day care ward
39) Anaesthesiology
40) Family Welfare Centre
41) Prosthetic and Orthotic Centre
42) Physiotherapy Department
43) Medico Social Unit
p
Rl-i
/ J V;
•T
2./- 3% O'?
•
i/O/ L' i’‘ 'jC
|2Z <3,55,57
, ■'/■>/
9
G’/ 0/.■
KMy-53 , *3 C.
>, 99 • 9 7
4
44) Pharmacy
CSSD
45)
46) Central Clinical Laboratory
47) Radiology
48) Dental/Oral Surgery
49) Casualty Department
50) Staff Health Service
51) Medical Records Department
52) Laundry
53) Dietary Department/Canteens
54) Library
55) Perpetual Help Health Centre - Uttarahalli
56) Ancillary Services - Security, Telephone, Fpr/Water/Maintenance
57) Nursing College
58) Future/Ongoing Plans
Others
59) Linkages - Church
60) Linkages - Non-Church
61) Congregational expectations
62) Women’s Groups expectations
5
Time Framework & Schedule of Review
C.
1.
Preliminary Meetings {March 1998}:
TOR: Objectives / Issues / Questions
Distribution of Responsibilities
Planning
2.
Preliminary Data Collection: Two Months (April - May 1998)
Each member will review the areas allotted to them and do their own data collection in
coordination with Sr. Mercy/Sr. Ann Marie of the Health Commission
3.
First Interactive Dialogue of Review Committee and Health Commission (June
1998)
Focus on key questions and gather ideas/datas for each question from different reviews
conducted by members of the review committee
4.
Next round of Data Collection / Analysis / Preliminary Reports (June - July 1998)
5.
Second Interactive Dialogue of Review Committee & Health Commission (August
1998)
Draft Report in sections to be circulated for perusal before dialogue
6
Final Meeting of Review Committee to finalise report and recommendations
(Early September 1998).
{The Chairperson of the Review Committee will keep in touch with all the
members, and the members should also keep him informed about the progress
of the review Dialogue and ongoing clarification will go on through the
process
through informal meetings and telephonic and postal
communications}
6
To:
Department:
St. Martha’s Hospital Review -1998
The Health Commission
Chapter
the
of
set up by the
Good
Provincial
Sisters,
Shepherd
have
REQUESTED A TEAM OF RESOURCE PERSONS TO REVIEW
the
YOUR
OPINION IS
Health
Ministry
St.Martha’s
of
Hospital
PROCESS.
AS
PART
OF
THIS
PROCESS,
STAFF
OF
St.Martha’s Hospital and a sample of students of
Crucial
JOIN
THROUGH A PARTICIPATORY, INTERACTIVE AND REFLECTIVE
THE NURSING COLLEGE AND PATIENTS ARE BEING INVITED
TO PARTICIPATE, BY FILLING IN SPECIAL QUESTIONNAIRES
PREPARED BY THE REVIEW COMMITTEE.
THESE WILL BE
CIRCULATED / ADMINISTERED IN JULY 1 998. APART FROM
THE
QUESTIONS ASKED
SPECIFIC
IN
SPECIAL FORMAT,
PLEASE FEEL FREE TO OFFER ANY OTHER SUGGESTIONS
FOR
CONSIDERATION
BY
THE
REVIEW
TEAM.
YOUR
PARTICIPATION IN THIS REVIEW IS CRUCIAL TO HELP US
IDENTIFY THE FUTURE DIRECTIONS AND THRUSTS AND ALSO
MEASURES
TO
MEANINGFUL.
MAKE
THE
HEALTH
MINISTRY
MORE
ALL YOUR RESPONSES AND SUGGESTIONS
WILL BE CONFIDENTIAL. WE INVITE YOU TO JOIN US IN THE
TASK AND MAKE THE REVIEW, A SUCCESS.
Dr. Ravi Narayan
Mr. Thomas Kandasami
Ms. Mary Ann Charles
15™ July 1998
Dr. Prem Pais
Dr. Rebekah naylor
S.M.H. Bangalore
[All completed questionnaires must be returned to the Medical I Nursing
Superintendents offices latest by 28th July 1998 and put in the box
specifically provided for them]
Please detach this page from the proforma before submitting.
THE
REVIEW
CHAPTER - 6
>
!
Survey of Governance, Hospital Management, Personnel Management,
Associated and Ancillary Departments
As a member of the Review Committee which was formed to evaluate St. Martha’s
Hospital through a reflective process, I was assigned the following specific areas
for review:
1. Governance / Advisory Board
2. Hospital Organisation / Administration
3. Personnel Management Policy
4. Departments including prosthetic and orthotic centre, physiotherapy,
pharmacy, radiology, laboratory, CSSD, medical records, laundry, and
dietary
5. Ancillary services including security, telephone, water, electricity,
maintenance, transport
6. Spiritual care of patients
Evaluation was undertaken in such a way that the questions posed in the terms of
reference could be answered.
The goal is to gather information and propose
recommendations which could further strengthen the institution as it moves into a
new century.
The methodology adopted was as follows:
1. Standards for evaluation in the assigned areas were proposed and accepted by
the review committee (attachment I)
2. Documents obtained for review included the 1996 - 97 annual report, employee
service rules, organisation chart, list of members of Governing Body, current
salary scales, list of employee benefits, sample job description, performance
evaluation form, sample appointment letter and appointment order.
3. An interview was conducted with the Administrator, Mr. A.C. Saidhana.
4. Questionnaires were completed by the heads of the departments and services
assigned to me for review (attachment 11)
5. Questionnaires were given to staff (attachment HI),students (attachment IV),
and al! department heads ! supervisors (attachment V).
6. Questionnaires were also given to patients (not yet completed).
Data collected are presented in attachment VI (staff), attachment VII (students),
attachment VIII (department heads / supervisors). The staff and department heads
were asked to give their suggestions.
This report summarises the information which was gathered and then makes
conclusions and recommendations in each assigned area.
Vision and Mission
The entire review committee was given the responsibility to reflect on the vision
and mission of the hospital and its expression in all activities and functions of the
hospital.
The vision and mission as stated in the stated papers given to the committee is that
of the sisters of the Good Shepherd and it is assumed that these statements also
apply to the hospital. There are statements of belief, objectives, and strategies
that arise from this vision and mission.
Among heads of departments, 94.3% said that they understood the mission of the
hospital and 82.9% communicate it to their employees. Among the 200 staff
questioned, 91.5% indicated that they know the mission of the hospital. These
figures are not verified in the sense that no one was asked to state the mission.
Summary of Evaluation Report
Page 2
vsa_s /sen.-ed that the hospital does not have immediate goals or a five or a ten
plan Only 34.3% of department heads set goals for their departments each
year. Reasons given by Administration for lack of planning include age of the
institution; changing government policies, and unpredictable economic conditions.
The recommendations suggested are as follows:
I Rased on the vision and mission statement of the order, the hospital
management should prepare a specific vision and mission statement and submit
it to the Governing Body and the Sisters of Good Shepherd for approval.
2. Based on this vision, organisational planning should take place. Departments
should be required to set annual goals that are measurable. The organisation
should have annual goals as well as longer term goals. The five year plan can
be reviewed and modified on a regular basis as required by interna! and
external circumstances.
Governance / Advisory Board
The hospital is owned by the Good Shepherd Sisters. The order is represented in
the hospital by the Sister Superior. The Chief Executive Officer of the hospital
(Administrator) is appointed by the order. The Administrator is accountable to the
Sister Superior.
There is a Governing Body which meets usually twice annually. The majority of this
Board are from within the hospital or order. Only six members, a minority, are
from outside. The Governing Body does approve the annual budget. The Board
has a wide range of power for review and supervision. They approve major
policies and new projects, it is assumed that this group along with the Chief
Officer ensure that the organisation adheres to relevant statutory and regulatory'
requirements.
itjs recommended that there be more voice in the Governing Body from outside
including the community, experts in hospital management and experts in finance.
There should be an established process and criteria identified for selection of the
Chief Executive Officer, perhaps including a recommendation from the Governing
Body to the order on the selection.
Hospit.aS Organisation and Administration
An organisational structure is in place and most management and supervisory
personnel are aware of it. The channels of communication are clear.
The Planning and Executive Committee, chaired by the Administrator, consists of
tfielbp officers and meets on regular basis. AH decisions that affect the whole of
the organisation or ail employees are taken by this group. This represents a good
participative management style.
In the area of finance, middle management seems less involved. Of the 35 heads
of departments / supervisors who responded, only 31% were involved in the annual
budgeting process for their departments, and only 28.6% were informed about the
financial performance of the department. Just over half (54.3%) have regular
department meetings with their employees. Only 28.6% were involved in selection
of staff. These data suggest that the organisation would be stronger if middle
management was strengthened anti participated in decision making.
An administrative policy manual is needed in order that decisions will be consistent,
fair and objective.
Summary of Evaluation Report
Page 3
Human Resources {Personnel Management)
fhe personnel department of the hospital seems adequately staffed, records are
maintained for all employees. There are cadre positions determined by the
Governing Body in al) areas of the hospital. This results in adequate but not
excessive staffing.
Salaries are similar or higher in all categories when compared to other non-profit
voluntary hospitals in the city of Bangalore. It is noted that in each major job
category there are only two, or at most three grades limiting avenues for
promotion. For class four staff, there appears to be only otie grade. Other
employee benefits are available including adequate leave, uniforms, festival
advance, education advance, salary advance, and medical benefits.
The Employee Service Rules are proper and are printed in booklet form.
indicated that most are aware of these rules and have read part or ail.
Staff
Job descriptions are prepared for many employees. Performance evaluations in
various formats are used during probation and for consideration for promotion.
No administrative or personnel policy manual is available.
promotion policy.
There is no written
There is a recognised labour union in the hospital. There are regular settlements
between fhe management and tire union. Union dues are paid by salary deduction.
Most decisions involve the union. Administration believes that this situation has
resulted in a more relaxed attitude toward work, some avoidable indiscipline, and
increasing demands resulting in financial pressures that must be met by increased
charges to patients.
The Administration has an “open door’ policy towards employees. There is effort
to remedy grievances quickly as well as to resolve discipline matters quickly.
Many_staf£ indicated that they did not undergo orientation when they joined. Many
stated that they had not received any further training or developed any new skills
while employed.
.
Some recommendations regarding personnel management are as foilows:
1. Have a standard job description format for ail departments and staff. Ensure
that all employees have a job description and fully understand what is expected
from them.
2. Develop a promotion policy and more avenues for promotion in each job
category. Promotions should be based on merit and longevity.
3 Have a common performance appraisal form for all employees throughout the
hospital. This could be completed by the supervisors quarterly during probation
and annually after confirmation.
4. Appointment letters and appointment orders should be standardised and made
common for all employees.
5 All personnel policies and other administrative policies should be written and
organised into a policy manual. These may be written in a standard format and
be available with supervisors for reference.
6 There should be a standard organised orientation program for all new
employees.
7. Supervisors should participate in the selection of staff for their departments.
8. The management as a whole along with supervisors should have human
resource development plans, both to enhance performance of existing staff as
well as to nlan for future needs
Summary of Evaluation Report
Page 4
FCl';11ie Departments Reviewed
ally the departments assigned to me for review seem to be functioning
adequately. For the purpose of report, I will comment on each one briefly.
he Prosthetic and Orthotic Centre treats poor patients including outside referrals.
Paey have adequate staff and space to manage a busy workload. They have a
treatment plan for each patient. They do not have any written polices and
procedures for the department.
Physiotherapy is well integrated into the patient care team contributing to good
patient care for both inpatients and outpatients. The level of staffing, equipment,
patient load, hours and record keeping are good. They have no written policies
and procedures. The department has been without a department head for nine
months at the time of this evaluation.
The clinical laboratory is well staffed, providing 24 hour service to patients. The
tests available are wide-ranging and internal arid external quality control procedures
are in place. The question regarding space was not answered. Disposable
syringes are not being used though they stated that universal precautions are being
followed. They have no written policies or procedures.
The radiology department provides 24 hour service to patients with good equipment
and staff. Reports are given in a timely manner. They have written policies
regarding patient preparation and radiation protection.
In the medical records department the basic standards for information management
are being met. Staff are not technically trained and the number of staff appears to
be less when the patient load is considered.
Tiie pharmacy also is meeting the basic standards. The department does not have
written policies and procedures. Adequate staff are in place to provide service to
inpatients and outpatients. They state that their space is not adequate. The staff
do not have any continuing education or inservice training opportunities.
The CSSD has good written procedures for their functions. They follow quality
control and infection control procedures. They state that their space is not
adequate. Safety of staff as well as patients is of concern especially with needles
that are being reused. Service is not available on Sundays and holidays, but it is
not known from data obtained whether there is any supply problem.
The laundry is fully mechanised. The department has written policies and
procedures. They are apparently not following universal precautions in the handling
of dirty or contaminated linen. With only one dryer, it is not clear if their hours are
adequate to supply needed linen.
The dietary service to patients apparently supplies very few diets per day. Diet
counselling is available to patients on request. There is no quality control on their
diets. Food service for staff is on contract.
Recommendations regarding these areas are as follows:
1. in those departments which see their space as inadequate (pharmacy, CSSD),
the management should assess this and identify solutions if indicated.
2. Al£departments should develop written policies and procedures relating to their
function.
3. Universal precautions, including use of disposable needles and syringes and
disposal of sharps, should be strictly followed in all areas.
Summary of Evaluation Report
Page 5
■i
5.
6.
7.
8.
Starling in medical records department should be reviewed. As vacancies
occur, trained medical record officers or medical record technicians can be
appointed.
Inservice education and continuing education opportunities should be provided
for staff at al! levels.
Adequacy of supply of linen and sterile items on weekends and holidays can be
reviewed by the management.
Professional staff in dietary department may be increased to provide more
patient education. Daily rounds by dietetians in the wards will allow them to
identify all patients needing special diets as a part of their long term treatment.
Laundry should set standards for rate of loss of linen with targets to decrease
present losses.
Ancillary Services
Phe transport department provides ambulance service for patients as well as
transportation for administrative services of the hospital. Staff and vehicles are
apparently adequate for needs. There are no written policies or procedures for
maintenance of vehicles or accidents.
Security services are provided by an outside contractor. Considering the size of
the property as well as buildings, staffing may not be adequate.
Surveys are made regularly to identify hazards in the hospital. Bore wells and
generators ensure adequate supply of 'water and electricity. There is also a plan to
meet these needs in future. A disaster plan is in place. The hospital has an
incinerator. There are no written procedures for disposal of various kinds of
wastes.
The hospital has a program of preventive maintenance for buildings and equipment.
There is timely response to complaints from departments regarding building and
equipment maintenance.
Recommendations regarding these areas are as follows:
I. Aii departments should have written policies and procedures.
2. Management should review adequacy of staffing in security,
including
frequency of complaints and thefts, control of visitors, and maintenance of order
within the property
3. Particularly in regard to waste disposal there should be written policies. Not
only is this important for the institution, but it is also important in case of further
legal requirements.
Spiritual Care
The hospital includes in its objectives provision of competent and comprehensive
care of the whole person with love and compassion as taught by Jesus Christ.
Spiritual needs are to be met even while respecting the religion of the individual
patient or family member. A commitment has been made to provide counselling
and support to people in crisis.
Summary of Evaluation Report
Page 6
'dards by which spiritual care is evaluated were accepted by the review
committee. A questionnaire was submitted to the chaplaincy department which
was returned in a very incomplete form. Therefore it is assumed that answers to
the many questions are unknown or are negative. There appears to be only one
chapimn on the staff. There is no report on how many employees are Christian or
whether preference is given to Christian applicants when hiring new staff. There
was no reply to the question regarding improvement in the attitude of the
community towards Christianity as a result of the hospital. It is not clear whether
patients have opportunity to hear about Jesus and His peace 'while in the hospital.
Thirty-eight percent of the staff questioned felt that there was no one to whom they
could go to share their problems or persona! needs. One staff expressed need for
help with an alcohol problem. There has been no special programs or retreats for
staff and students in the past year.
One, could conpJii.de from this that there is not an emphasis on spiritual ..care.
Tamer it is perhaps viewed as incidental. As a Christian institution, this emphasis
would be essential in order to justify fully the existence of the hospital in the face of
competition arsd costs of health care in today’s world. Feedback from patients is
still awaited.
However, it is recommended that the basic purpose and reason for existence be
reviewed. If affirmed it should be reflected in a strong Christian attitude and
activity from spiritual development of students to hiring and nurturing of staff to
spiritual care of patients. Such an emphasis will require human and material
resources. But it could be the key to the future of the institution.
Ramonses from Staff
The majority of staff (94.5%)felt that they were a part of the health care team.
Eighty percent felt appreciated in their work. Over 75% felt there was someone in
the organisation to whom they could communicate their problems. These are
positive points on which further good will and spirit can be developed.
The staff responded with a wide variety of requests, suggestions, and comments.
Some did express concern that love and compassion are less evident than before,
that care of the poor has decreased, and that quality of care and caring has
declined. Many made requests regarding salary, increments, more loan facilities,
promotion avenues, resting room, better uniform, easier access to care when sick,
more free drugs arid crepe bandages, and jobs for staff children. Several
requested retreats, staff get togethers, and restoration of Christmas lunch.
There were suggestions regarding their -work situation including improved
procedures to control infection and protect staff, better availability of supplies like
adex and bleach, aprons in lab, improved brooms and rubber gloves for handling
contaminated linen. Some felt there was partiality with some staff allowed to work
less while others carried a heavier toad.
there were numerous suggestions to improve hospital services:
1. Special fund to care for poor people
2. 24 hour reception and enquiry
3. 24 hour pharmacy
4 More security in OPD
5. Drinking water in OPD
6. Improved casualty care
7. Buildings and facilities to be modernised
8. More tertiary care services to be initiated
Summary of Evaluation Report
Page 7
9 Day care centre for mentally ill
10. Family counselling service
i 1 Guest rooms for patient relatives
; 2. i:nen to be returned to the ward from which it came
13. Rats to be controlled
Some of these may already exist. Feasibility studies would be required for others.
No specific recommendations are made in this section of the report. These
responses are included in the report for the information of the management and
their consideration as indicated.
Summary
In conclusion, the overall function of the areas of the hospital evaluated is
satisfactory. There are many strengths in the institution including its long history of
service and good reputation in the city of Bangalore. (Contain) weaknesses have
been identified which may suggest actions to be taken in order that the future will
be bright and contribution to the community great in the years ahead.
KM
5wb
SUMMARY
OF
STAFF
RESPONSES
SAMPLE
TOTAL
200
DOCTORS
Yes ■
No
NA
(No.%) (No.%) (No.%)
1.Someone availble to communicate 27(65.8) 14(34.1)0
problems
I FACULTY
STAFF NURSES
WARD INCHARGES
Yes
No
NA
YES
NO
NA
YES
NO
NA
(No.%) (No.%)
(No. %) (No. %) (No. %)
(No. %)
(No. %) (No. %) (No.%)
14(93.3) 1(6.7) 0
43(91.5) 4(8.5)
0
19(100 0) 0
0
2.Complaints are heard
21(51.2) 18(43.9)2(4.9)
36(77.0)
3.Feel part of team
38(92.7) 3(7.3)
0
47(100.0) 0
4. Know mission of hospital
37(90.2) 3(7.3)
1(2.4)
47(100.0) 0
5. Promotion avenues available
11(26 8) 28(68.3) 2(4.9)
30(63 8)
17(36.2) 0
9(47.4)
10(52.6) 0
6.Orientation received when joining
institution
14(34.1) 25(61.0) 2(4.9)
45(95.7)
2(4 3)
0
17(89.5)
2(10.5)
7.Feels appreciated
21(51.2) 18(44.0)2(4.9)
42(89.4)
5(10.6)
0
18(94.7)
8. Feels policies/rules fair
23(56.1) 15(36.6)3(7.3)
42(89.4)
5(10.6)
0
Sj. Knows Employee Service Rules
34(83.0) 5(12.2) 2(4.9)
40(85.1)
7(14 9)
lO.Opportunity to give suggestion
30(73.2) 9(22.0) 2(4.9)
11 .Availability of personnel for
guidance
QUESTION
4- if 3
bh 35
'. ■ 1 S>
h’. '
ANCILLARY STAFF
YES
NO
NA
(No. %) (No. %) (No. ■/,)
27(77.1) 8(22.9) 0
CLASS IV
NA
YES
NO
(No.%) (No.%) (No.%)
24(55.8) 19(44.2) 0
TOTAL
NA
NO
YES,
(No.%)
(No.%)
(No.%)
154(77.0) 46(23.0) 0
132(66.0) 62(31.0) 6(3.0)
1(5.3)
0
13(86.7)
1(6.7)
1(6.7)
27(77.1) 7(20.0) 1(2.9)
17(39.5) 24(55.8) 2(4.7)
0
19(100.0)
0
0
14(93.3)
0
1(6.7)
29(82.9) 5(14.3) 1(2.9)
42(97.7) 1(2 3)
0
189(94.5) 9(4.5)
2(1-0)
0
19(100.0) 0
0
15(100.0) 0
0
29(82.9) 4(11.4) 2(5.7)
36(83.7) 6(14.0)
1(2.3)
183(91.5)
13(6.5)
4(2.0)
10(66.7)
3(20.0) 2(13.3)
13((37.1) 21(60.0) 1(2.9)
6(14 0)
36(83.7) 1(2.3)
79(39.5)
115(57,5) 6(3.0)
0
14(93.3)
1(6.7)
0
9(25.7)
8(18.6)
35(81.4) 0
107(53.5) 91(45.5)
2(1.0)
1(5.3)
0
14(93.3)
1(6.7)
0
24(68.6) 11(31.4)0
41(95.3) 2(4.7)
0
160(80.0) 38(19.0)
2(1.0)
18(94.7)
1(5.3)
0
14(93.3)
1(6.7)
0
29(82.9) 6(17.1) 0
33((76.7) 5(11.6)
5(11.6)
159(79.5) 33(16.5)
8(4.0)
0
18(94 7)
0
1(5.3)
15(100 0) 0
0
33(94.3) 2(5.7)
38(88.4) 5(11.6)
0
178(89.0) 19(9.5)
3(1.5)
30(63.8)
17(36.2) 0
14(73.7)
4(21.1)
1(5-3)
13(86.7)
2(13.3) 0
17(48.6) 17(48.6) 1(2.9)
31(72.1) 12(27.9) 0
135(67.5) 61(30.5)
4(2.0)
14(34.1) 21(51.2)6(14.6)
22(46.8)
25(53.2) 0
19(100.0)
0
0
13(86.7)
2(13.3) 0
23(65.7) 12(34.3) 0
23(53.5) 17(39.5) 3(7.0)
114(57.0) 77(38.5) 9(4.5)
12.Work area comfortable and safe
29(70.7) 11(26.8)1(2.4)
45(95.7)
2(4.3)
0
17(89.5)
2(10.5)
0
15(100.0) 0
0
30(85.7) 5(14.3) 0
38(88.4) 5(11.6)
13.Newskill/training received
17(41.5) 17(41.5)7(17.1) 40(85.1)
7(14 9)
0
12((63.2)
7(36.8)
0
13(86.7)
2(13.3) 0
23(65.7) 12(34.3) 0
9(21.0)
14. Have job description •
26(63.4) 15(36.6)0
44(93.6)
3(6.4)
0
17(89.5)
2(10.5)
0
15(100.0) 0
0
25(71.4) 10(28.6) 0
40(93.0) 3(7.0)
15.Participates in special/
extracurricular functions
27(55.6) 14(34.1)0
35(74.5)
12(25.5) 0
9(47.4)
10(52.6) 0
2(13.3) 0
16(45.7) 19(54.3) 0
1((2.3)
13(86.7)
26(74.3) 0
0
0
174(87.0) 25(12.5)
1(.5)
34(79.1) 0
114((57.0) 79(39.5)
7(3.5)
0
167(83.5) 33(16.5)
0
42(97.7) 0
101(50.5) 99(49.5)
0
ATTACHMENT
18(94.8)
11(23.4) 0
ATTACHMENT VII
Responses From Students
SAMPLE__ No_.__ 45
YES
No. (%)
NO
No. (%)
1. Do you know the vision and mission of the hospital ?
42(93.3)
3(6.7)
2. Do you feel a part of the hospital and its work ?
45(100)
0
3. Do you have any opportunities for spiritual development ?
43(95.6)
2(4.4)
4. If you have a personal or family problem, is there someone to
guide you or counsel you ?
29(64.9)
16(35.6)
5. Is the hospital a place you would like to remain as an
employee?
34(75.6)
11(24.4)
6. During your training do faculty and staff stress care of the
poor?
37(82.2)
8(17.8)
ATTACHMENT VIII
Responses From Heads of Departments
SAMPLE__ Nor__ =____ 35
YES
NO
N/A
No.(%) No.(%) No.(%)
1. Do you conduct regular meetings of employees whom you
supervise ?
19(54.2) 11(31.4) 5(14.2)
2. Do you feel that there is good communication with
management ?
26(74.2)
3. Are you involved in selection of staff for your department ?
10(28.5) 23(65.7) 2(5.7)
4. Are you involved in the annual budget process for your
department ?
11(31.4) 22(62.8) 2(5.7)
5. Are you informed about the financial performance of your
department ?
10(28.5) 22(62.8) 3(8.6)
6. Do you regularly evaluate the performance of the employees
you supervise ?
26(74.2) 5(14.3)4(11.4)
7. Do you know and understand the vision and mission of the
hospital ?
33(94.2)
1(2.8)
8. Do you communicate the vision and mission to your
employees ?
29(82.8)
3(8.6) 3(8.6)
9. Does your department have written policies and procedures ?
17(48.6) 16(45.7) 2(5.7)
10. Do you set goals each year for your department ?
12(34.3) 18(51.4) 5(14.3)
11. Do you feel a part of planning and decision making in the
organization?
15(42.8) 17(48.6) 3(8.6)
12. Do you orient new employees in your department ?
29(82.8) 2(5.7) 4(11.4)
13. Do you provide any inservice or on the job training for your
employees ?
20(57.1) 10(28.6) 5(14.3)
14. Have you attended any seminar, program or course on
management training ?
18(51.4) 15(42.8)2(5.7)
15. Do you have written standards that guide the work of your
department ?
16(45.7) 18(51.4) 1(2.8)
16. Do you have enough qualified staff to do the required work ?
23(65.7) 9(25.7) 3(8.6)
17. Do all of your employees have job description ?
25(71.4) 6(17.1)4(11.4)
6(17.1) 3(8.6)
1(2.8)
18. Do you know the organization plan or structure of the hospital ? 24(68.6) 8(22.8)3(8.6)
CHAPTER - 5
SURVEY OF PATIENTS
Methodology: An administered questionnaire was used to obtain the views of patients
attending St. Martha’s Hospital on different aspects of hospital functioning. The
questionnaire was administered by interviewers who had been given some training. Since
the instrument was in English, the interviewer had to interpret the questions to the patient
as well as interpret open ended comments. This process may have vitiated the latter.
Open end comments were often
missing or unsatisfactorily expressed. The present
analysis has therefore been restricted to scored questions which are less likely to be biased
by the interviewer.
Subjects: The questionnaire was administered to both inpatients (on the day of
discharge) and out patients. The subjects were selected by the interviewers to generally
represent various areas and departments and is thus not strictly random.
I.
Patient Profile
a)
No. of proformae filled 159, 60 (38%) from inpatients and 96(60%) from out
patients. In 3 this data was not filled
b)
65 (41%) of the patients were male and 91 (57%) were female. In 3 data was not
filled.
c)
Income of patients per month
< Rs. 2000
Rs2000-3999
Rs.4000-5999
> Rs. 6000
Missing data
30
44
30
29
26
19%
28%
19%
18%
16%
20
19
45
38
24
10
3
13%
12%
28%
24%
15%
6%
2%
Educational status
No formal education
7th Std. or less
S.S.L.C.
P.U.C.
Degree
PG/Professional
Missing data
e) Religion of respondents
Hindu
Christian
Muslim
Missing data
107
33
12
7
67%
21%
8%
4%
f) Of the inpatients (60 respondents) 46 (77%) were from general ward and
13(22%) from private wards. In 1 case the data was missing.
This data suggests that the sample has a representative socio-economic mix... and is
probably representative of the hospital patient population.
II. Reasons for coming for treatment to St. Martha’s Hospital.
a)
Who referred the patient to SMH?
Relative
Friend
Neighbours
Family doctor
Others
Missing data
b)
55
46
23
13
18
4
35%
29%
15%
8%
11%
2%
Why did the patient come to SMH?
Recommended by relative / friend
Reputation of hospital doctors
Near home / office
Because it is a mission hospital
Recommended by doctor
Other
Missing data
67
27
23
14
12
12
4
42%
17%
15%
9%
8%
8%
2%
Both a) and b) provide consistent data that the reputation of the hospital and its
doctors among the general public is good. It is, however, noteworthy that few
patients are referred to SMH by their doctors. Since family doctors form an
important source of patient referrals for a secondary hospital, this area needs to be
corrected.
111.
Outpatient services
a)
Do patients visiting the OP come to see a particular doctor or are they willing
to see any doctor?
(n = 96)
Any doctor
Specific doctor
b)
37
33
66%
34%
How long did the patient have to wait in OP to see the doctor?
(n = 96)
< 1 Hour
1-2 Hours
> 2 hours
70
40
19
39%
42%
19%
c) Was this waiting time acceptable?
(n = 96)
1
Yes
No
70
25
Missing data
1
73%
26%
1%
Two points emerge 1. That 61% of patients had to wait over an hour to see a
doctor and 26% felt that the delay was too long. Given that patients visiting a
general hospital are resigned to wait, these figures suggest that action is required
to reduce waiting time. 2 From a) and c) it would appear that about 30% of
patients may be ready to pay a fee to see a doctor of their choice with less waiting
time.
IV Staff Quality
a)
Doctors are knowledgeable and good
Yes
Somewhat
No
Missing data
147
8
0
92%
5%
0%
3%
b)
Nurses are caring and efficient
136
17
1
5
Yes
Somewhat
No
Missing data
c)
Staff in general are courteous and helpful
Yes
Somewhat
No
Missing data
d)
85.5%
11.0%
0.5%
3%
144
7
1
7
90.5%
4.5%
0.5%
4.5%
Overall satisfied with care given
Yes
Somewhat
No
Missing data
134
16
1
8
84%
10%
0.5%
4.5%
A fairly satisfactory picture on the whole
V. Amenities
I
a) General cleanliness is good
Yes
Somewhat
No
Missing data
142
12
2
3
89%
8%
1%
2%
b) Toilets and water supply are satisfactory
Yes
Somewhat
No
Missing data
125
24
3
7
79%
15%
2%
4%
c)
Fans and lights function adequately
Yes
Somewhat
No
Missing data .
d)
137
15
2
5
86%
10%
1%
3%
Hospital diet taken (IP only)
n = 60
No
Yes
58
2
97%
3%'
Water, toilets, lights and fans are generally judged satisfactory
although not as unequivocally as was the case for personnel.
Bangalore residents are accustomed to water and electricity shortages
yet 17% are not entirely happy with water and toilets and 11% with
electricity. The dietary service is conspicuous by its disuse.
■
VI. Some special services
a) Medical records - any problem in getting records out (OPD only)
n = 96
84
87%
No
12
Yes
13%
b) Chaplaincy services
- Did the chaplain visit you (IP only)
n = 60
Yes
No
Missing date
16
43
1
27%
71.5%
0.5%
- If yes, were his visits helpful
n = 16
Yes
No
14
2
88%
12%
Considering the mission of the hospital, visits by the chaplain are inadequate.
However, those who were visited seem satisfied.
VI11 Perception of hospital mission
a) The hospital is mainly meant for those who can pay.
No
Somewhat
Yes
Missing data
104
28
22
5
65%
18%
14%
3%
b) The hospital serves the poor even if they cannot pay.
Yes
Somewhat
No
Missing data
c)
62%
22%
8%
8%
All patients are loved and cared for by the hospital staff.
Yes
Somewhat
No
Missing data
d)
99
35
12
13
134
16
2
6
84%
10%
2%
4%
Religious sentiments of all patients are respected.
Yes
Somewhat
No
Missing date
145
7
2
5
91%
5%
1%
3%
On the whole a satisfactory image. In view of the current controversy in the
political world, the last question and response could well be sent to the VHP!
VIII Hospital charges
a) Out patient charges and costs
n = 96
Correct
Too high
Too low
Missing data
61
16
15
4
64%
17%
16%
4%
b) In patient bed charges
n = 60
Correct
Too high
Too low
Missing data
40
10
1
9
67%
16%
2%
15%
c) In patient (investigation costs in bill)
n = 60
Correct
Too high
Too low
Missing data
46
6
0
8
77%
10%
0%
13%
d) In patients (doctors fees, if any)
n = 60
Correct
Too high
Too low
Missing data
37
7
0
16
62%
12%
0%
26%
e) In patient (surgery / procedure costs)
n = 60
Correct
Too high
Too low
Missing data
35
5
0
20
59%
8%
0%
33%
f) In patients (medicine charges)
n = 60
Correct
Too high
Too low
Missing data
42
12
0
6
70%
20%
0%
10%
On the whole more patients seem to feel that the charge are reasonable Among
inpatients a significant minority of patients (15 - 20%) feel that bed charges and
medication costs are too high. Similarly 17% of out patients felt that out patient
charges were too high.
Surnilljiry: The 159 patients interviewed seem to he (airly representative of a
cross-section of those who attend the hospital. It must be recognised that a survey of
this nature is presently biased as only patients who come to the hospital (and hence
approve of the hospital) have been included Keeping this in mind, the survey shows:
1. Patients are not often being referred to the hospital by the medical practitioners.
They come because of its reputation with the lay public.
2.
Waiting time in the out patient department is too long.
3.
About 30% of out patients may be ready to pay for services if these can be
stream-lined.
4.
Patients are generally satisfied about the medical and non medical staff.
5.
Dietary department services are grossly under used and could be stopped.
6.
There is scope to improve water and electricity supply.
7.
Chaplaincy services cover only a small proportion of patients.
8
Hospital has good image among patients attending it.
J>R Z?AV/ NSV
CHAPTER - 4
SURVEY OF NURSES, NURSING SERVICES & NURSING COLLEGE
AREAS ASSIGNED : NURSING SERVICE DEPT. & SCHOOL OF NURSING
Sample : Nursing Service Dept - * Ward in Charges
* Staff Nurses
C-s/.mj
School of Nursing
- * Faculty
Q p)
* Student nurses
Description of the Sample:
Ward in Charges There were totally 19 Ward in Charges in the hospital. All of them were included
in the evaluation All (100% ) were lay persons. The mean duration of years of service was 10.4 years
(n = 13), with a range of 1&1/2 years to 32 years . tV^six of them did not respond to the duration of
their service in the institution , they hence were not included for computation of the mean duration of
service. All ( 100%) had done the General Nursing Course , and only 2 (10.5%) had some additional
qualification out of whom one had done a course on Administration Twelve (63.2%) of them had
there training from St. Martha’s School of Nursing . One (5.3%) had completed her course as early as
in the 1950s , 4(21.0%) in the 1960s , 5(26.3%) in the 1970s , 6(31.5%) in the 1980s and 2(10.5%) in
the 1990s . Most 15 (78.9%) had In Service Education after having joined St. Martha’s hospital.
Staff Nurses: The staff nurses were sampled from the total list of all categories, using the simple
random sampling technique . Hence a total of 50 staff were selected ,of which 47 were accepted for
analysis. Most of them were junior staff 37 (78 7%), with just two or three years of service and 10
(21.3%) were interns with less than a years service . Only 3 (6.4%) were religious and the rest 44
(93.6%) were lay persons Most 31(66.0%) of the staff were alumnae of St Martha’s School of
Nursing ,while 16 (34.0%) were from other institutions, of which 7 (43.7 %) were from institutions
within Bangalore city itself and the rest from out of Karnataka state . The mean duration of service for
the staff was 2.09 years with a range of 2 months to 10 years. Only 3 (4.3%) had not received any in
service education after having joined the institution . Majority 45 (95.7%) had done there G.N.M.
course , 2 (4.3%) had done their Basic B.Sc.
Faculty : The total number of faculty in the School of Nursing were 15 . All were taken for the
evaluation . Ten (66.6%) were tutors , 3 (20.0%) were clinical instructors and 2 (13.3$%) were senior
tutors . Only 1(6.7%) was a religious while the rest ,14 (93.3%) were lay persons . The mean duration
of years of service was 3 87 years with a range of 10 months to 16 years . Most 10 (66.6%) had a
basic B.Sc. qualification , 4 (26.6%) had done their P.C.BSc. and 1(6.7%) had done her General
Nursing after which she had done her Diploma in Nursing Education .Eleven (73.3%) had their nursing
training in Karnataka of which 9 (81.1%) were trained within Bangalore itself. Eleven (73.3%) had
inservice education after joining the institution .
Student Nurses : The students were selected from the 2nd, 3rd and the 4th year, although those in
their 4th year have completed their training in the institution they were selected in the category of
students since they considered to be under the School of Nursing . The 1st year students were not
selected since it was assumed that it would be too early to get a valid opinion from them . The students
were selected through simple random technique , and comprised a total number of 45 , (i.e. 15 per
batch . Only 4 (8.8%) were religious and the rest were laypersons . Most 42 (93.3%) were Christians
while 3 (6.6%) were Non Christians
Methodology :
The evaluation of these assigned areas was performed primarily from information provided by the
selected sample through a questionnaire . The questionnaires were prepared based on the selected
functions of the hospital or the School of Nursing , the individual functions of each category, their
expectations and suggestions . All the members of the review committee had accepted the format
proposed and a copy of the questionnaires for each category is attached
Results :
1. Awareness of Nursing Personnel in relation to —
a Vision of the hospital
b. Philosophy
c. Objectives / Goals
:
d. Policy regarding
work
benefits
promotion
recruitment
student selection
discipline
e. Welfare Facilities
f. Workers Union
g- Performance Appraisal
W/S
S/N
F
St/N
19(100.0%)
18( 94.7%)
19(100.0%)
32(68.7%)
32(68.7%)
37(78.7%)
14( 93.3%)
15(100.0%)
15(100.0%)
42( 93.3%)
19(100.0%)
16( 84.2%)
17( 89.5%)
16( 84.2%)
15( 78.9%)
16( 84 2%)
14( 73.7%)
15( 78.9%)
17( 89.5%)
44(78.7%)
35(74.5%)
34(72.3%)
41(87.2%)
43(91.5%)
43(91.5%)
26(55.3%)
15(31.9%)
21(44.7%)
15(100.0%)
15(100.0%)
15(100.0%)
12( 80.0%)
14( 93.3%)
14( 93.3%)
11( 73.3%)
8( 53.3%)
9( 60.0%)
—
—
—
—
—
—
—
It is obvious from the above data that most (more than 75%) of the nursing personnel from all
categories were aware of the objectives and goals of the institution ; of the policies regarding work,
benefits recruitment of staff, selection of students and disciplinary action . Among the three categories
of nursing personnel the staff nurses seemed least aware of the philosophy of the institution, welfare
facilities workers union and performance appraisal. The only question that student nurses were asked
was in relation to their awareness of the vision and mission of the hospital. Majority ( 90% & > ) said
they were aware of the vision .
2. Extent to which the objectives /goals /functions of the hospital are met presently :
The ward in charges , staff nurses and the faculty were given a list of statements pertaining to the
above mentioned aspects They were asked to rate each of the statements on a 5 -point scale
according to the extent to which they believed these aspects were presently fulfilled and also to
the extent to which they thought these aspects should be fulfilled. However most of them did not
answer to the latter part .
The results of the extent to which the above aspects are met are presented in percentages .
5
1. Service given to the sick
irrespective of any factor
(W/S)
(S/N)
( F)
2. Quality care affordable to the common man
(W/S)
(S/N)
( F )
3. Main beneficiaries - women / children
(W/S)
(S/N)
( F )
4. Provides cost effective competent care
(W/S )
(S/N )
( F )
5. Fosters dedication and ethical values
(W/S)
(S/N )
(F )
6. Enhances skills through CE programs
(W/S )
(S/N )
( F )
7. Fosters a desire to serve the poor
( W/S)
( S/N )
( F )
8. Builds social awareness among its staff
(W/S)
( S/N )
( F )
4
2
3
1
17(89.5) 2(10.5)
23(48.9) 18(38.2)
10(66.7) 3(20.0)
4( 8.5)
2(13.3)
__
1(2.1)
—
__
1(2.1)
—
5(26.3)
14(29.8)
6(40.0)
2(10.5)
15(31.9)
6(40.0)
—
1(2.1)'
—
3(6.3)
—
8(42.1) 4(21.0)
7(15.0) 10(21.3)
—
3(20.0)
5(31.6) 1(5.3)
15(31.6) 10(21.3)
8(53.3) 3(20.0)
—
5(10.7)
1( 6.7)
8(42.1)
3( 6.3)
1( 6.7)
—
2(10.5) 2(10.5)
17(36.2) 11(23.4) 12(25.5)
—
8(53.3) 2(13.3)
12(63.2)
17(29.8)
3(20.0)
7(36.8)
4( 8.5)
4(26.7)
—
14(73.7) 4(21.0)
13(27.7) 17(36.2)
7(46.6)
6(40.0)
1( 5.3) —
6(12.8) 6(12.8)
1( 6.7) —
—
6(12.8)
1( 6.7)
4(21.0) 7(36.8)
7(14.9) 12(25.5)
1( 6.7) 6(40.0)
—
6(31.6) 2(10.5)
17(36.2) 10(21.3) 1( 2.1)
7(46.6) —
1( 6.7)
11(57.9) 7( 6.8)
14(29.8) 16(34.0)
6(40.0) 4(26.7)
1( 5.3) —
13(27.7) 3( 6.4)
5(33.3) —
—
1( 2.1)
—
3(15.8) 9(47.4)
6(12.8) 17(36.2)
—
2( 4.3)
5(26.3) 1(10.5)
18(38.3) 3( 8.5)
10(66.7) 4(26.7)
—
1( 4.2)
—
9. Meets spiritual needs of all patients
—
17(63.1) 5(26.3) 2(10.5)
( W/S)
7(14.9)
1(
2.1)
23(48.9)
16(34.0)
( S/N )
5(33.3)
2(13.3)
2(13.3)
6(40.0)
( F )
10. Provides care at subsidised cost to those in need
—
15(73.7) 2(10.5) 2(15.8)
( W/S)
11(23.4) 23(48.9) 12(25.5) 2( 2.1)
( S/N )
—
6(40.0) 5(33.3) 4( 6.7)
( F )
11. Develops community centres for those in need
—
( W/S)
14(73.7) 5(21.0)
1( 5.3)
14(29.8) 14(29 8) 14(29 8) 4( 8.5)
( S/N)
—
5(33.3) 4 (26.7) 6(40.0)
( F )
12. Expands depts. & education programs as per need
—
( W/S )
12(63.2) 4(21.0) 3(15.8)
( S/N )
3( 6.4) 12(25.5) 19(40.4)
9(19.1)
...
6(40.0) 8(53.3)
1( 6.7)
( F )
13. Attempts to improve quality of care
—
—
( W/S )
14(73.7) 5(26.3)
( S/N )
16(34.0) 22(46.8) 8(17.0)
1( 2.1)
2(13.3) 10(66.7) 2(13.3)
1( 6.7)
( F )
14. Creates cleanliness awareness in public
___
13(68.4) 4(21.0) 2(10.5)
( W/S )
28(59.5) 14(29.8) 2( 4.3)
3( 6.4)
( S/N )
—
5(33.3) 9(60 0)
1( 6.7)
( F
)
15. Serves as a model of efficient health care
—
—
( W/S )
14(78 9) 4(21.0)
—
22(46.8) 20(42.6) 3( 6.4)
( S/N )
—
7(46.7)
3(20.0)
5(33.3)
( F
)
16. Fosters respect for life in all its staff
—
—
15(78.9) 4(21.0)
( W/S )
14(29.8)
25(53.2)
6(12.8)
2(
4.3)
( S/N )
—
6(40.0)
2(13.3)
5(33.3)
( F
)
17. Fosters a team spirit and family atmosphere
—
14(73.7) 5(26.3)
1( 5.3)
( W/S )
11(23.4) 19(40.4) 10(21.2) 4( 8.5)
( S/N )
—
5(46.7) 4(26.7) 4 (26.7)
( F
)
18. Has reasonable rules and regulations
—
1( 5.3)
11(57.9) 7(36.8)
( W/S )
12(25.5) 19(40.4) 11(23.4) 4( 8.5)
( S/N )
—
3(20.0) 5(33.3) 7(46.7)
( F
)
19. Shows concern for its staff’s welfare
—
13(68.4) 3(15.8) 3(15.8)
( W/S )
5(10.6) 19(40.4) 16(34.0)
5(10.6)
( S/N )
—
4(26.7)
8(53.3) 3(20.0)
( F
)
—
—
—
—
—
1( 6.7)
___
1( 2.1)
—
—
4( 8.5)
—
—
—
___
—
—
—
—
2( 4.2)
—
—
—
<0(13 O
—
3( 6.4)
1( 2.1)
2( 4.3)
—
It is obvious that most (80% & > )of the ward in charges believed / were of the opinion
that the objectives / goals / functions of the hospital are met presently . They(36,8%) however
felt that women / children were not the main beneficiaries and social awareness wasn’t built
amongst the staff. Only 57 8% felt that CE programs were planned to enhance the skill of the
employees.
Most(80% & >) of the staff nurses felt that service was provided to the sick irrespective to any
factor, the spiritual needs of the patients were met, that attempts were made to improve the
quality of care always , to serve as a model for efficient health care , and create an awareness
of cleanliness in the public.
The faculty(80% & > ) also felt that the service was provided to all irrespective of any factor,
a sense of dedication and ethical values was fostered , an awareness of cleanliness in the public
was built, that the hospital served as a model of efficient health care.
The aspects that possibly need to be reviewed by the management are obviously in relation to
the following objectives / goals :
o Who are its main beneficiaries ?
o What is the role of CE_ programmes in enhancing the skill of the staff and
thus the quality of care?
o Should the hospital build a social awareness amongst its staff?
o Is the institution responsible for providing community health centres,
expanding departments and educational programmes as per the need"7
o Should there be concern for the welfare of the staff?
o Does the hospital employees and the management really strive to provide high
quality care at a rate affordable to the common man ?
o Is there any effort made to ensure that comprehensive and cost effective care
is provided ?
o Are the rules and regulations fair for and reasonable to all the employees ?
3. The extent to which the Nursing personnel from the Nursing Service were able to
perform certain tasks:
The ward in charges and the staff nurses were given an additional five statements relating
to
their functions or tasks . They were asked to rate these statements on a 5-point scale depending
on their ability to perform the said functions . The results are presented below in percentages .
They were also asked to comment if they were unable to perform these functions to the best of
their abilities The reasons provided are also summarised below this data .
5
4
3
2
1
1. Provides care to all irrespective of
caste /creed /social status .
—
—
—
( W/S )
17(89.5) 2(10.5)
—
37 (78.7) 6(12.8) 4( 8.5) —
( S/N )
2. Provides best possible care at all
times
7(36.8) 7(36.8) 4(21.0) —
( W/S )
1( 5.3)
—
4( 8.5) 26(53.3) 15(31.9) 2(4.3)
( S/N )
3. Upholds moral & ethical values
—
—
( W/S )
15 (78.9)
4(21.0) ...
—
27 (57.4) 17(36.2) 2( 4.3) 1(2.1)
( S/N )
4. Meets spiritual needs of all patients
( W/S )
11 (57.9) 6(31.6)
1( 5.3) —
1( 5.3)
28 (59.6) 11(23.4)
5(10.6) 2( 4.3) 1( 2.1)
( S/N )
5. Participates in activities to improve
self
( W/S )
10(52.6) 4(21.0)
2(10.5) 3(15.3) —
20 (42.6) 14(29.8) 7(14.9) 6(12.7) —
( S/N )
Majority of the Ward Sisters and Staff Nurses said that due to lack of sufficient staff and overload in
their work , they were unable to provide the best possible care to all patients. In relation to the ability
to uphold their moral and ethical values, only the staff nurses responded that they were unable to do so
at all times due to misunderstanding with their co-workers. None of them gave any reasons regarding
their ability to meet the spiritual needs of the patients and their participation in activities which would
enhance their skills and professional abilities.
Points to be considered from this data which is available :
• Is there a definite lack of staff ?
• Is the environmental climate of the staff conducive for upholding ones ethical & moral
values ?
• Should the management look into the cultural activities of the staff?
1
4.
Positive aspects of St. Martha’s Hospital and School of Nursing :
The Ward in charges , staff nurses and the faculty were asked to give THREE positive aspects of
the institution . These aspects were scrutinised and are categorised under headings such as:
* Objectives
* Administration
* Satisfaction with the working environment.
(i) Objectives :
a) Helping the poor & neglected
b) Care for all irrespective of caste
c) Respect for life & spiritual care
d) Giving work opportunities for
the poor
e) Low cost & high quality care
f) Spiritual care
(ii) Administration :
a) Administrators are approachable
b) Good Supervision
c) Good Management
d) Good co-ordination between
nursing service & education
e) Conducting Continuing
Education programs
W/S
n= 19
S/N
n= 47
Faculty
n= 15
7(36.8)
4(21.0)
4(21.0)
41 (87.2)
5 (10.6)
11 (23.4)
2(13.3)
4(26.7)
3(20.0)
2(10.5)
—
1( 5.3 )
—
11 (23.4)
7(14.8)
—
3(20.0)
—
5 (26.3 )
1 ( 5.3)
—
—
___
16(34.0)
___
—
3(20.0)
—
—
1( 6.7)
—
—
1( 6.7)
38 (80.9)
2( 4.3)
—
9(19.1)
2( 4.3)
—
—
10(66.7)
—
6(40.0)
—
2(13.3)
—
—
(iii) Satisfaction with the Working Environment:
8 (42.1 )
a) Care provided is appreciated
b) Family and friendly atmosphere
7(36.8)
6(31.6)
c) Safety
3 (15.8)
d) Hygienic working environment
e) Welfare of Staff considered
1( 5.3)
f) Freedom to work
—
g) Rules & Regulations are fair
1( 5.3)
h) Dedicated staff
3 ( 6.4)
1( 2.1)
Negative aspects of the Institution :
The nursing personnel were asked to give THREE negative aspects of the
institution . the comments were then categorised under specific headings such as .
""Communication , * staffing and * administrative aspects .
5.
S/N
n=47
F
n=15
2(4.3)
2(10 6)
3( 6.4)
—
1(2 1)
1(2.1)
2(10.6)
7(46.7)
1( 5.3)
2(10.6)
3(15.8)
1( 2.1)
4(26.6)
—
—
3(15.8)
—
3(15 8)
9(47.4)
—
4( 8.7)
11(23.0)
—
1( 2.1)
34 (74.4)
20 (43.0)
3 ( 6.3)
5(33.3)
1( 5.3)
—
2(10.6)
—
—
—
3(15.8)
—
3(15.9)
1( 5.3)
2( 4.3)
1( 2.1)
__
—
9(47.4)
3(15.8)
4(21.0)
—
3(15.8)
—
—
9(17.1)
3( 6.4)
1( 2.1)
1( 2.1)
2( 4.3)
2( 4.3)
16(34.4)
—
1( 5.3)
—
—
—
—
—
W/S
n=19
i) Communication :
__
a) Rules very rigid for ICUs
b) Inter departmental communication
—
is poor
2(10.5 )
c) Enquiry is not satisfactory
d) Nonavailability of 24 hrs STD booth 1( 5.3)
—
e) Communication gap
ii) Staffing Problems :
a ) Lack of supervision
b) Indiscipline of security /class iv
workers
c) Night duty for one month
d) Lack of promotional avenues
e) Lack of concern for all staff
f) Lack of adequate staff
g) Inadequate pay
h) Health of staff not considered
i) Continuing education not planned
regularly
Hi) Administrative Aspects:
a) Lack of an isolation ward
b) Need for a waiting area for relatives
c) Salary is not adequate for the cost of
living in the city
d) Equipment and articles inadequate
e) Repair work and maintenance slow
f) Repairs allotted to outside agencies
g) Lack of promotional opportunities
h) Cash counter not available for 24 hrs.
i) Lack of pharmacy & lab. for 24 hrs.
6. Suggestions for improvement: The nursing personnel were asked to give THREE
suggestions which they felt would help in the functioning of the hospital and the
School of Nursing . After scrutinising the points given by the nursing personnel
the points were categorised under headings such as : Administrative , Equipment
and facilities , Staff welfare . Three ward in charges and faculty did not give any
suggestions . All the staff nurses gave suggestions.
W/S
i) Administrative
a) Supervision of staff nurses to
improve
2(10.5)
b) Night supervision essential
1( 5.3)
c) Appreciation of work done
1( 5.3)
d) Maintenance dept, to improve
1( 5.3)
e) Clerks in the ward for clerical
work to increase staff time with
—
patient
f) Communication between service
—
and education
g) Increase the number of staff
4(21.0)
h) Ambulance availability for
—
transport of dead
—
i) 24 hr lab and pharmacy services
j) Atleast one relative to be allowed
—
with an ICU patient
S/N
F
2( 4.3)
1( 2.1)
—
1( 2.1)
2(12.3)
1( 6.7)
—
—
—
1( 6.7)
—
15(32.0)
2(12.3)
1( 6.7)
2( 4.3)
15(32.0)
___
—
—
1( 6.7)
iijNeed for more Facilities and Equipment
—
—
1( 5.3)
a) Separate OT for Obstetrics
b) Ventilators for new-borns and
1( 5.3)
11( 2.1)
children to avoid referrals
15(32.0)
5(33.3)
c) More advanced technology
3(15.8)
—
—
1( 5.3)
d) Need for a geriatric ward
___
4( 8.7)
1( 5.3)
e) Need for an isolation ward
—
1( 5.3)
19(40.4)
f) Waiting room for relatives
g) Ambulance with emergency
—
—
10(20.6)
facilities
h) Security to be trained to be
—
10(20.6)
—
courteous to all.
iii) Staff Welfare:
a) Need for CE programs regularly 3(15.8)
b) Staff health services to be
—
improved
c) Leave to be granted in emergencies
—
3(10.9)
7(14.8)
4( 8.7)
—
—
NURSING STUDENTS (N= 45 ; 15/ Batch of 2nd , 3rd & 4th year)
The nursing students were selected from the 2nd and 3rd year on a random basis . Those who had
completed their training and who in this institution are considered to be in their 4th year were also
selected randomly using the table of random numbers The 1st years were excluded from the
evaluation since the committee felt that it would be too early to be able to get a valid opinion from
them . These students were given a set of four statements relating to the encouragement they receive
from various individuals ; facilities available , facilities for their social development and characteristics
of the faculty . Each of these statements had several items under them . The students had to rate each
of these statements on a 5 - point scale reflecting the level of their satisfaction on each of the aspects ,
This tool was prepared based on a study conducted by
1
Encouragement received from :
home
0(- )
teachers
1( 2.2)
staff
1(2.2)
warden
1( 2.2)
2
3
4
5
0( - )
0( - )
8(17.7)
4( 8.8)
0( - )
6(13.3)
12(26.7)
10(22.2)
4( 8.8)
14(31.1)
20(44.4)
19(42.2)
41(91.1)
24(53.3)
4( 8.8)
11(24.4)
It is obvious that the students are satisfied with the encouragement they receive from their
parents , teachers and the warden to do well in their studies . The staff however do not seem to play a
major role encouraging their juniors to perform well in their studies .
2. Facilities available:
classroom (n=44)
chapel (n=44)
canteen (n=44)
hospital services (n=45)
hostel (n=45)
library (n=45)
mess (n=44)
recreation (n=45)
sick room (n=45)
0(- )
0(- )
6(13.6)
2( 4.4)
1( 2.2)
0( - )
5(H.l)
3( 6.6)
6(13.3)
1( 2.2)
0( - )
7(15.9)
4( 8.8)
3( 6.6)
2( 4.4)
11(25.0)
6(13.3)
6(13.3)
5(11.1)
0( - )
11(25.0)
14(31.1)
8(17.7)
5(H.l)
12(27.3)
10(22.2)
14(31.1)
15(33.3)
10(22.7)
15(34.1)
14(31.1)
17(37.8)
14(31.1)
13(18.2)
15(33.3)
15(33.3)
23(51.1)
34(77.3)
5(11.4)
11(24.4)
16(35.6)
24(53.3)
3( 6.8)
11(24.4)
4( 8.8)
Most of the students again seem satisfied with their classroom , chapel, hostel, library
facilities. They seem most dissatisfied in relation to canteen , mess, and sickroom facilities . They
appear to be moderately satisfied with the hospital services and recreation facilities .
3. Activities required for their social development
interaction with faculty 1( 2.2)
6(13.3)
interaction with peers
& seniors
1( 2.2)
2( 4.4)
campus activities( n=44) 0( - )
3( 6.8)
SNA activities
1( 2.2)
0( - )
1( 2.2)
CNGI activities (n=44)
5(11.3)
1( 2.2)
2( 4.4)
sports activities
14(31.1)
14(31.1)
10(22.2)
12(26.7)
8(18.2)
6(13.3)
17(38.6)
4( 8.8)
17(37.8)
26(59.0)
17(37.8)
11(25.0)
26(57.8)
13(28.9)
7(15.9)
21(46.7)
10(22.7)
12(26.7)
The only area were the students appear to be quite satisfied is in relation to the SNA activities . The
rest of the activities relating to their social development would have to be scrutinised more deeply for
the overall development of the students
4. Characteristics of their faculty
shows genuine interest
1( 2.2)
shows respect
1( 2.2)
is available
K 2.2)
disciplines fairly (n=44)
0( --)
supervision good (n=44) 0( --)
firm yet concerned (n=44) 0( — )
fair in dealings (n=44)
1( 2.3)
competent (n=44)
0( -)
evaluation fair (n=44)
1( 2.3)
shows moral values
1( 2.3)
in dealings (n=44)
has good personal skills
0( - )
(n=44)
3( 6.7)
4( 8.8)
2( 4.4)
0( - )
0( - )
1( 2.3)
5(11.4)
4( 9.0)
4( 9.0)
8(17.6)
15(33.3)
8(17.8)
6(13.6)
6(13.6)
10(22.7)
11(25.0)
14(31.8)
13(29.6)
16(35.5)
16(35.6)
18(40.0)
19(43.1)
16(36.4)
17(38.6)
18(40.9)
15(34.1)
20(45.5)
17(37.8)
9(20.0)
15(33.3)
19(43.1)
22(50.0)
16(36.3)
9(20.5)
11(25.0)
6(13.6)
4( 9.0)
9(20.5)
17(38.6)
13(29.5)
3( 6.8)
10(22.7)
16(36.3)
15(34.0)
In relation to the characteristics of the faculty the students again appear to be satisfied with most
aspects except in relation to their ability to show genuine interest in the welfare of the student, being
fair in their dealing with student, being competent in various teaching methodologies and being fair in
their evaluation methods
The students were also given a set of questions relating to the goals and functions of the institution .
They were expected to either answer ‘yes’ or ‘no’ to the questions . No clarifications were made in
relation to their answers.
1.
2.
3.
4.
5.
6.
Knows vision and mission
Feels part of the hospital
Opportunities for spiritual growth
Availability of guidance & counselling
Remain as staff in the same hospital
Stress on care of poor during training
YES
42 ( 93.3 )
45 (100.0)
43 ( 95.6 )
29 ( 64.4 )
34 ( 75.6 )
37 ( 82.2)
NO
3 (6.3 )
0( - )
2( 4.4)
16(35.6)
11 (24.4 )
8 (17.8 )
It is evident from the above findings that majority (more than 80.0% ) of the students who were
selected to participate in the evaluation were aware of the vision of the hospital, felt a part of the
hospital, felt that there were opportunities for their spiritual growth and that a stress on the care of the
poor was made during their training . The need for personnel trained in guidance and counselling was
evident in that atleast 36% of the students responded that this was not available . The fact that at least
76% of the students responded that they would like to remain as staff in the hospital is credible .
Points to possibly review :
•
»
•
o
o
•
•
•
Encouragement to be given to the students by the staff and the warden , to perform well in their
studies
Canteen and mess facilities may have to be improved
Hospital services for the students seem to be inadequate
Recreational facilities for the students could be increased
Interaction with the faculty / seniors at informal settings
C.N.G.I. activities could help foster their spiritual development. It could also help to improve their
interaction with other students
Faculty characteristics such as ability to have respect for the students, to be firm yet concerned, to
be fair and ethical in their dealings & to be skilful need to be enhanced.
Availability of guidance and counselling for the students
GENERAL FUNCTIONS OF THE MANAGEMENT :
The ward in charges ( W/S), faculty (F) and staff nurses (S/N) were also given a set of questions to
which they had to respond ‘Yes’ or ‘No’ . These questions were relating to the general functions of
the management . Here again they were neither asked to provide details or clarify their answer.
Yes
No
N/A
1. Someone available to communicate problems (W/S)
( F )
(S/N)
19(100.0)
14 ( 93.3)
43 ( 91.5)
0( - )
1 ( 6.7)
4( 8.5)
0(- )
0(- )
0(- )
2. Complaints are heard
(W/S)
( F )
(S/N)
18 ( 94.7)
13 ( 86.6)
36 ( 77.0)
1(5.3)
1(53)
11 (23.0)
0( - )
1 (6.7 )
0(- )
3. Feel part of a team
(W/S)
( F )
(S/N)
19(100.0)
14 ( 93.3)
47 (100.0)
0( - )
0( - )
0( - )
0(- )
1(6.7)
0(- )
4. Knows the mission of the hospital
(W/S)
( F )
( S/N)
19(100.0)
15 (100.0)
47(100.0)
0( - )
0( - )
0( - )
0(- )
0(- )
0(- )
5. Promotional avenues available
(W/S)
( F )
(S/N)
9 ( 47.4)
10 ( 66.7)
30 ( 63.8)
10(52.6)
3 (20.6)
17(36.2)
0(- )
2(13.7)
0(- )
6. Orientation received when joining institution (W/S)
( F )
(S/N)
17 ( 89.4)
14 ( 93.3)
45 ( 95.7)
2(10.5)
1 ( 6.7)
2( 4.3)
o(- )
0(- )
0(- )
7. Feels appreciated
(W/S)
( F )
(S/N)
18 ( 94.7)
14 ( 93.3)
42 ( 89.4)
1 ( 5.3)
1 ( 5.3)
5 (10.6)
0(- )
0( — )
0(- )
8. Feels policies/ rules are fair
(W/S)
( F )
(S/N)
18 ( 94.7)
14 ( 93.3)
42 ( 89.4)
1 ( 5.3)
1 ( 5.3)
5 (10.6)
0( - )
0(- )
o( — )
9. Knows employee service rules
(W/S)
( F )
(S/N)
18 ( 94.7)
15 (100.0)
40 ( 85.1)
0( -)
0( - )
7(14.9)
1 (5.3 )
0(- )
0(- )
10. Opportunities to give suggestions
(W/S)
( F )
(S/N)
14 ( 73.7)
13 ( 86.6)
30 ( 63.8)
4(21.0)
2(13.3)
17(36.2)
1(5.3)
0(- )
0(- )
11. Availability of personnel for guidance
(W/S)
( F )
(S/N)
19(100.0)
13 ( 86.6)
22 ( 46.8)
0( -)
2(13.3)
25(53.2)
0(- )
0(- )
0( - )
12. Work area comfortable and safe
(W/S)
( F )
(S/N)
17 ( 89.4)
15 (100.0)
45 ( 95.7)
2(10.5)
o( - )
2( 4.3)
0(- )
0(- )
0(- )
13. New skill training received
(W/S)
( F )
(S/N)
12 ( 63.2)
13 ( 86.6)
40 ( 89.4)
7 (36.8)
2(13.3)
7(14.9)
0(- )
0( - )
0( - )
14. Has a job description
(W/S)
( F )
(S/N)
17 ( 89.4)
15 (100.0)
44 ( 93 .6)
2(10.5)
0( - )
3 ( 6.4)
0( - )
0( - )
0(- )
15. Participates in special functions
(W/S)
( F )
(S/N)
9( 47.4)
13 ( 86.6)
35 ( 74.5)
10(52.6)
2(13.3)
12(25.5)
0( - )
0(- )
0(- )
In relation to the functions of the management majority of the nursing personnel (80% & > ) were
satisfied . The only aspects to be possibly looked into are as given below:
• Avenues for promotion
• Opportunities to give suggestions for improvement
• Need for in- service education programmes
• Participation in special functions
WARD TN CHARGES (N=19)
The ward in charges were given 18 questions regarding their functions to which they had to either
respond ‘Yes’ or ‘No’. No clarification of their answers were sought.
YES
1. Conducts regular meetings
11 (57.9)
2. Has good communication with
management
17(89.4)
3. Involved with plan of annual budget
5 (26.3)
4. Involved in selection of staff
1 ( 5.3)
4(21.0)
5. Informed of financial process
17 (89.4)
6. Evaluates staff performance
11 (57.9)
7. Dept, has written policies
8 Sets goals each year for dept.
9 (47.4)
9. Feels part of planning &decision-making 7(36.8)
10. Knows vision & mission of hospital
18 (94.7)
18 (94.7)
11. Communicates above to staff
12 Orients new employees
17(89.4)
13. Provides ISE or on- the-job training
12 (63.2)
14. Attended CE- program on management 12(63.2)
15. Written standards are there to guide
work
11 (57.9)
16. Enough qualified staff available
14(73.7)
17. All Staff have job description
15 (78.9)
18. Knows organisational plan
12(63.2)
NO
NA
6(31.6)
2(10.5)
1 ( 5.3)
13 (68 4)
17 (89.4)
13 (68.4)
1 ( 5.3)
7 (36.8)
9 (47.4)
10 (52.6)
o( - )
0( - )
1 ( 5.3)
6(31.6)
6 (31.6)
1 ( 5.3)
1 ( 5.3)
1 ( 5.3)
2(10.5)
1( 5.3)
1 ( 5.3)
1( 5.3)
2(10.5)
1( 5.3)
1( 5.3)
1 ( 5.3)
1( 5.3)
1 ( 5.3)
7(36.8)
4(21.0)
2(10.5)
5 (26.3)
1 ( 5.3)
1 ( 5.3)
2(10.5)
2(10.5)
From the data available regarding the functioning of the ward in charges it is obvious that the
following functions would have to be reinforced to them:
•
•
•
The need to conduct regular meetings with their staff
To have written policies and standards in the department
To set goals each year for the department
J To see to their own and their staffs professional development by organising in-service education
programmes and attending CE programmes
The management need to possibly get the ward in charges involved in the following aspects:
•
•
•
Plan for the annual budget
Selection of staff
Financial process
- Ms. Mary Ann Charles,
School of Nursing,
St.John1 Medical College,
Bangalore.
HEALTH
CARE B
° U T
•
WITHOUT
HARM
The campaign for
health care
HCWH’s Mission
To transform the health care industry so it is no longer a source of
environmental harm by eliminating pollution in health care practices
without compromising safety or care. We will accomplish this mission
■
.
•- -
■
•>
Promoting comprehensive
dilution prevention practices.
^Supporting the development and use of
f environmentally sate materials, technology
Educating and informing health care institutions,
providers, workers, consumers, and all affected
constituencies about the environmental and public
health impacts of the health care industry and solutions
to these problems.
Health care professionals and the institutions in which they work are the
ultimate defense against illness. Nurses, physicians and other health care prac
titioners strive to provide this protection for our families and our communi
ties. Yet, unknown to many of us, rhe purchasing and waste disposal practices
of health care institutions often undermine their own purpose, and our ex
pectations of them, by contributing to sickness.
WHEN HEALTH CARE DOES HARM
The 1994 draft Dioxin Reassessment done by the United States Envi
ronmental Protection Agency (USEPA) brought this to light. At the time of
its release, the draft Reassessment identified the incineration of medical waste
as the single largest source of dioxin air pollution. Dioxin is a carcinogen
which has been linked to birth defects, decreased fertility, immune system
suppression and other hormonal dysfunction. Responding to this serious prob
lem, several organizations formed the Health Care Without Harm campaign
in 1996.
Looking further, Health Care Without Harm campaign members found
that hospitals are not only a major source of dioxin, but a significant source of
HEALTH CARE
mercury as well. Mercury is a dangerous and potent neurotoxin and repro
ductive toxin. Mercury can interfere with the development of the fetal brain
PRACTITIONERS HAVE
and is directly toxic to the central nervous system, kidneys and liver.
A RESPONSIBLITY TO
Cost-effective solutions are available for the health care industry’s
WORK TOWARD THE
dioxin and mercury problems. Just as the Hippocratic Oath promises to
ELIMINATION OF
“first, do no harm,” the Health Care Without Harm campaign is based on
the premise that health care practitioners have a responsibility to work to
ward the elimination of environmental harm resulting from health care practices.
ENVIRONMENTAL HARM
In September 1996, representatives of 28 organizations met and created a
campaign to provide a remedy for the pollution from health care practices. By
April 1999, 178 organizations in nine different countries, including 41
hospitals, joined Health Care Without Harm (HCWH). The coalition has
already had a significant impact on large health care systems, government
regulatory bodies and industry leaders.
The Health Care Without Harm coalition is a broad-based international
campaign to reform rhe environmental practices of the health care industry.
HCWH advocates for policies chat eliminate the indiscriminate incineration
of medical waste, and calls for change in purchasing and materials management
W ?-
:
WE
A. / A
practices of hospitals and purchasing groups. In communities, HCWH
supports local campaigns against medical waste incinerators and works toward
improvements in the purchasing and waste disposal practices of local hospitals
and other health care institutions.
Health Care Without Harm researches and advocates for safer waste
disposal alternatives, and educates the broader public about dioxin, mercury
and other endocrine-disrupting chemicals and the health care industry’s
contribution to these problems. HCWH works with religious organizations,
HCWH IS A BROAD
BASED INTERNATIONAL
labor unions, health issue groups and other constituencies ready to join a
campaign that makes explicit links between environmental contamination
and public health.
CAMPAIGN TO REFORM
The campaign’s organizers believe that as health care professionals learn
THE ENVIRONMENTAL
PRACTICES OF THE
to “clean up their own house,” they will increasingly become advocates for
stronger environmental health policies and programs in society at large.
The work of Health Care Without Harm affects the health of every
HEALTH CARE INDUSTRY
person and every community. We welcome your support and involvement.
a
Io work with a wide range of con
To develop health-based standards
stituencies for an ecologically sus
for medical waste management
tainable health care system;
and to recognize and implement
the public’s right to know about
o
" o « I
*
WORK WITH A WIDE
To eliminate the nonessential incin
chemical use in the health care
eration of medical waste and to pro
industry;
RANGE OF CONSTITUENCIES
mote safe materials use and treat
ment practices;
FOR AN ECOLOGICALLY
To develop just siting and transpor
tation guidelines that conform to
To phase out the use of PVC (poly
the principles of environmental jus
vinyl chloride) plastics and persistent
tice: No communities should be
toxic chemicals in health care and
poisoned by medical waste treat
to build momentum for a broader
ment and disposal;
SUSTAINABLE
HEALTH CARE SYSTEM
PVC phase out campaign;
To develop an effective collabora
To phase out die use of mercury in ail
tion and communication structure
aspects of the health care industry;
among campaign allies.
H C W H ;
OUR
For more information or to join the campaign, contact one of the campaigns
three coordinators: Charlotte Brody at the Center for Health, Environment
and Justice at 703-237-2249 or cbrody@cssential.org; Jackie Hunt
Christensen at the Institute for Agriculture and Trade Policy at 612-870-3424
or jchristensen@iatp.org; or Gary Cohen at rhe Environmental Health Fund
at 617-524-6018 or gcohen@igc.apc.org. You can also e-mail rhe campaign
at noharm@iatp.org or visit our website at www.noharm.org. Our website
contains a library of HCWH educational materials as well as recent press
releases and information on upcoming events.
GOALS
HARMFUL HEALTH CARE:
How We Got Here and What
We Can Do About It
HOSPITAL WASTE PILES UP
Since 1955, the amount of waste
generated per hospital patient has more
than doubled. Changes in technology
and increased use of plastics and
disposable products have substantially
increased waste amounts, as have the
indiscriminate use of “red bags” for
non-infectious waste and inefficiencies
in hospital waste management and
purchasing programs.
Medical waste on the beaches of
New Jersey and Long Island and the
increased incidence of hepatitis and
HIV/AIDS led to a universal precau
tions concept that all body fluids were
potentially infectious. Thus, massive
amounts of what was believed to be
infectious waste were “red-bagged”.
(“Red-bagging” is the practice of
discarding infectious medical waste in
red garbage bags earmarked for disposal
as “regulated” medical waste, most often
in medical waste incinerators.) Yet
detailed analyses of red bag contents
show this disposal method has been
overused in most health care institu
tions, and surveys show that most
hospitals do little to monitor the
contents of the bags or educate workers
on proper waste disposal.
bag” material. The rest is solid waste
made up of paper and paperboard,
plastics, food waste, metal, glass, wood
and other non-infectious materials. While
health care facilities vary widely, most
medical waste can be reduced by using
the same waste minimization techniques
increasingly found in our homes and
offices.
According to the Centers for
Disease Control, no more than two
percent of a typical hospital’s waste stream
must be incinerated to protect public
health and safety. That two percent is
primarily pathological waste (mostly body
parts). Yet many hospitals routinely burn
75 to 100 percent of their waste. The
unnecessary burning of polyvinyl chloride
(PVC) plastic, paper, batteries, discarded
equipment and other non-infectious
materials leads to emissions of dioxins
and mercury, as well as other toxins such
as furans, arsenic, lead and cadmium —
and it creates toxic ash.
USEPA currently cites medical
waste incinerators as the second largest
source of dioxin and the fourth largest
source of mercury pollution of our
environment and food supply.
DIOXIN - TOXIC, PERSISTENT,
AND WIDESPREAD
<5
RED BAG REALITIES
The Society for Hospital Epidemiology
of America has found that “household
waste contains more microorganisms on
average than medical waste.” Only ten to
fifteen percent of hospital waste is
properly described as “infectious” or “red
Dioxin is the common name for a class of
75 chemicals. Dioxin has no commercial
use. It is a toxic waste by product formed
when waste that contains chlorine is
burned—or when products containing
chlorine arc manufactured. PVC plastic is
a major source of the chlorine in medical
waste. The primary medical use of PVC is
in intravenous (IV) bags and tubing.
Dioxin is atmospherically trans
ported and enters the food chain long
distances from its point of origin. Dietary
sources of dioxin, which account for 90%
of human exposure, include meat, dairy
products, eggs, and fish. Dioxin
bioaccumulates, building up in fatty
tissues and concentrating in organisms as
it moves up the food chain. According to
the USEPA, adults eating an average diet
are consuming 300 to 500 times the daily
"safe” dose of dioxin. Because of the high
fat content of breast milk, nursing infants
are exposed to about 50 times the average
adult dose and may receive more than
10% of their total lifetime exposure
during rhe nursing period, a time when
they are extremely vulnerable to dioxin’s
toxic effects.
ability, hearing deficits, cognitive defects
and behavioral alterations in infants.
iivii'ne effects. In animals, dioxin
causes decreases in testosterone at
relatively high doses and decreases in
thyroid hormones following perinatal
exposure. In humans, testosterone levels
were slightly decreased in exposed
workers. In infants exposed prenatally,
thyroid hormone levels were decreased.
Immune system effects. In animals,
dioxin suppresses the immune system
making animals more susceptible to
bacterial, viral, and parasitic disease. In
humans, dioxin has been found to slightly
suppress the immune system in adults and
to cause more marked suppression in
infants exposed prenatally.
Dioxin can cause:
POLYVINYL CHLORIDE (PVC)
PLASTIC: PRECURSOR TO DIOXIN
Cancer. Dioxin is a known human
carcinogen according to the International
Agency for Research on Cancer (IARC)
and a probable human carcinogen
according to the USEPA. Liver, lung,
stomach and connective tissue cancers as
well as non-Hodgkin’s lymphoma have all
been associated with dioxin.
To stop the production of dioxin, health
care institutions can minimize the
amount of waste from their facilities that
is incinerated and eliminate the purchase,
and disposal by incineration, of chlorinecontaining substances that create dioxin.
In hospital waste, polyvinyl chloride
plastic (PVC) is a major source of
chlorine.
Commonly used PVC items in
health care include IV bags, tubing, blood
bags, endotracheal tubes, oxygen tents,
mattress covers, packaging and office
supplies such as binders.
Dioxin is released both when PVC
is manufactured and incinerated. The
production of PVC plastic involves many
toxic feedstocks, additives or by-products,
resulting in a product that is 57% chlorine
by weight. When PVC is incinerated, the
chlorine is released and combines with
organic matter to produce dioxin.
Even while it is in use, PVC may
be dangerous to patients. The plasticizer
Reproductive and developmental
effects. In animals, dioxin causes de
creased sperm count, congenital malforma
tions (cleft palate, kidney disorders),
decreased testis size, premature onset of
puberty, feminization of behavior and
endometriosis. In humans, dioxin has been
shown to cause altered sex ratio, small
penis size and endometriosis. Birth defects
(spina bifida) have also been found in
children of Vietnam veterans exposed to
dioxin-contaminated Agent Orange.
Developmental neurotoxic effects.
Dioxin causes decreased psychomotor
SINCE I9S5.THE
AMOUNT OF WASTE
GENERATED PER
HOSPITAL PATIENT
HAS MORE THAN
DOUBLED
HEALTH CARE
DECISION-MAKERS
SHOULD CONSIDER
THE ENVIRONMENTAL
HEALTH IMPACTS OF
THE PRODUCTS THEY
CHOOSE
di-ethylhexyl phthalate, or DEHP, is
added to PVC to make it more flexible
for applications such as IV bags and
tubing. DEHP has been identified by the
USEPA as a probable human carcinogen.
Scientific studies have shown that DEHP
may also damage the heart, liver, testes
and kidneys, and interfere with sperm
production. PVC IV bag manufacturers
Abbott Laboratories and Baxter
Healthcare International both include
labels on their flexible plastic (PVC)
containers warning patients of the
possibility of the leaching of small
amounts of the plastics chemical compo
nents into the solutions being adminis
tered intravenously.
SOLUTIONS:
NEW PURCHASING PRACTICES
Health care decision-makers, including
hospital materials managers and purchas
ing directors, should consider the envi
ronmental health impacts of the products
they choose as part of their health care
mission. Chlorine- and DEHP-free
alternatives exist for many of the uses of
PVC in health care. Easily replaced items
include patient identification bracelets
and cards, IV bags, compression stockings
and fluid collection devices. IV containers
made of non-chlorinated plastics such as
polyethylene or other polyolefins are
currently available. These plastics do not
produce dioxin when burned or manufac
tured. In addition, plasticizers are not
used in the formulation of these plastics.
Rigid PVC products often have alterna
tives made of metal or non-chlorinated
plastic such as polypropylene and
polycarbonate. New non-chlorinated
plastic polymers are being developed that
will provide even more alternatives for
current manufacturers of PVC products.
Health Care Without Harm has
issued a health alert on PVC IV bags and
is working with hospitals, group purchas
ing organizations and health care profes
sional organizations to encourage the
development of alternatives to products
made with polyvinyl chloride.
MERCURY:
POLLUTING PREGNANCIES
Mercury can be found throughout many
hospitals in patient and laboratory
thermometers, blood pressure devices
(sphygmomanometers), dilation and
feeding tubes, batteries, and fluorescent
lamps. Because of the significant use of
these items in many hospitals, medical
waste may account for 20 percent of the
mercury in the solid waste stream. The
USEPA estimates that medical waste
incinerators are responsible for ten
percent of mercury air emissions.
Mercury cannot be destroyed
through incineration. Following release
through an incinerator smokestack,
mercury is deposited back to land or to
surface waters where it can remain
indefinitely, either in an inorganic form
(elemental mercury) or in an organic
form (methyl mercury). Microorganisms
can convert elemental mercury to methyl
mercury, which is more biologically
available or more able to interact with
cells and damage them. Methyl mercury
accumulates in the muscle tissues of
animals, especially fish, and through
consumption of mercury-contaminated
foods, it bioaccumulates in humans.
Mercury pollution is already
widespread. Both the United States and
Canada have targeted mercury for virtual
elimination of human uses and releases.
According to the USEPA's 1997 Report to
Congress, 39 states have determined that
all or some of their lakes, streams and
rivers are too contaminated with mercury
to allow people to eat fish and seafood
from those bodies of water.
Mercury is a potent neurotoxin,
which means it attacks the body’s central
nervous system. Neurotoxic risks to
developing fetuses and young children are
the primary reasons for fish consumption
advisories, which aim to discourage
pregnant women, women of child-bearing
age, and young children from eating too
much fish. Studies done on women who are
methyl mercury-contaminated fish or grain
showed that even when the mothers showed
few effects of exposure, their infants
demonstrated nervous-svstem damage.
Mercury not only attacks the
body’s central nervous system; it can also
harm the brain, kidneys and lungs. It can
cross rhe blood-brain barrier as well as the
placenta. Methyl mercury from contami
nated fish easily crosses the placenta and
enters the brain of the developing fetus.
The critical effect from prenatal exposure
to methyl mercury is mental retardation.
SOLUTIONS: ELIMINATING
MERCURY FROM HOSPITALS
Mercury has many properties that have
made it useful. It responds to temperature
and pressure changes (making it useful for
thermometers and blood pressure
devices), conducts electricity and forms
alloys with other metals. However,
alternative products have emerged for
most commonly used mercury-containing
medical equipment. Mercury' thermom
eters and blood pressure gauges can be
replaced with electronic devices. Tungsten
can replace mercury in feeding tubes and
dilators. Instead of mercury batteries,
rechargeable batteries can be used.
In 1998, HCWH participated in
the process which led to the American
Hospital Association’s decision to sign a
memorandum of understanding with the
USEPA. This memorandum, which
pledges to reduce waste within the
hospital system by half by the year 2010,
also calls for phasing out the use of
mercury' in hospitals by rhe year 2005.
Working within this agreement, HCWH,
the AHA and USEPA seek to help
hospitals achieve these goals.
Other HCWH mercury-related
activities include a mercury-free pledge for
hospitals and health care providers, and an
educational booklet entitled “Mercury
Thermometers and Your Family’s
Health,’ which discusses household use of
mercury in thermometers, explains how to
clean up mercury spills and advocates
non-mercury alternatives.
NEW RULES FOR MEDICAL
WASTE INCINERATION
In August 1997, the USEPA released the
first federal standards and guidelines (the
“MACT Rule”) regulating hospital and
medical waste incinerators. New facilities
have approximately six months after
startup to comply with the rule. Existing
facilities will have three to five years to
comply. Crematoria and incinerators that
burn only pathological waste, expired
pharmaceuticals, or radioactive medical
waste are not covered by this rule.
Health Care Without Harm
advocated for stricter, more protective
emission limits than were in the final rule,
and urged USEPA to focus on waste
reduction and waste segregation in health
care facilities rather than on pollution
control equipment — which protects us
less at a higher cost. States must now
create rules that are at least as protective
as the federal standard. Health Care
Without Harm is working with states to
adopt regulations that provide more
protection for people and wildlife than
the federal rule.
SOLUTIONS: REDUCE, SEGREGATE,
RECYCLE AND REUSE
USEPA’s medical waste incinerator rule
offers advanced and expensive technology
as the solution to pollution from medical
waste incinerators. Wet and dry scrubbers
and emission control monitoring equip
ment do make air emissions less toxic. But
such solutions cost more and accomplish
less than a “preventive medicine” approach
that integrates purchasing and disposal
decisions and emphasizes non-toxic,
recyclable, and reusable materials.
Reduce
The most important part of waste
management is waste reduction, which
begins with procurement. Purchasing
professionals can work with vendors to
buy items that decrease the amount of
waste generated, especially toxic waste.
More durable products and products with
less packaging also help to reduce the
waste stream.
Segregate
Waste segregation, already widely prac
ticed with our household waste, is crucial
to reducing the volume and toxicity of
the medical waste stream. Paper and
cardboard products, glass, some plastics,
and metals can readily be recycled in
existing markets. Waste segregation
requires commitment and education up
front, but little additional time if systems
are properly designed. For example,
strategically locating red bags only in the
necessary areas and liberally offering
non-red bag options where possible will
substantially reduce red bag volume.
Hospitals can post signs clearly designat
ing certain types of waste for the red bag.
But staff are not likely to change current
behavior without education, persuasion
and a regulatory “stick.”
For hospital administrators, the
ethical and public relations value of being
“green” can be substantially enhanced by
the data that shows that waste reduction
saves money. There are many examples of
institutions saving money by saving the
environment, including Beth Israel
Medical Center in New York which saves
$900,000 per year through product
purchasing and disposal modifications,
including reducing, reusing and recycling.
Assess Your Waste
Each hospital facility has a mix of solid
waste much like that in any institution, as
well as waste generated specifically as a
result of its patient care. A waste assess
ment can identify the waste types and
generation patterns in all areas of the
hospital, and thus areas for potential
improvement. A waste assessment can
range from looking in trash receptacles
and compactors or taking a trip to the
landfill with the hospital’s hauler, up to a
more comprehensive waste assessment
procedure, conducted in-house or with an
outside consultant. Such a comprehensive
waste assessment will give hospital staff a
clear idea of how their waste is managed
on a daily basis.
Recycle
Recycling (and buying products made
with recycled materials) reduces the
pollution from resource extraction
(mining, forestry) and manufacturing
products, and reduces the pollution
associated with incineration, landfills and
other waste disposal methods.
Health care facilities can use
mostly conventional recycling methods.
Health care waste is not primarily
needles, body parts, blood and bandages.
1 he dominant materials are paper and
cardboard, followed by plastics, metals,
glass and other materials which are
commonly recycled by other entities such
as hotels, restaurants and office buildings.
Recycling can save institutions thousands
of dollars in waste disposal costs.
Reuse
Hospitals can also reduce their waste
stream, cut costs, and reduce their negative
impact on the environment through a
conscious procurement preference for
reusable products that meet the needs of
health care workers and their patients.
Many common single-use disposable
products have safe, reusable alternatives
including underpads (chux), eggcrate
mattresses, dishware, sharps containers,
gowns, wash cloths, pillows, bedpans and
urinals. Single-use cardboard packaging
can be replaced with reusable tubs.
Alternatives to Incineration
Even the hospital with the best waste
reduction, segregation, recycling and
reuse program will still produce waste
that is potentially infectious. But most of
this “true” infectious waste does not need
to be incinerated to be made harmless
and unidentifiable. Various technologies
have been developed to sterilize and
reduce the volume of medical waste
without incineration. Note: HCWH does
not specifically endorse any of these
technologies.
Autoclaves are the most commonly
used medical waste treatment alternative
in tire United States. Like most disinfec
tion techniques, an autoclave destroys
infectious agents through the use of steam
heat, like a high technology dishwasher.
Unlike incineration, however, the
materials are not burned, reducing the
risk of dioxin production. Frequently,
wastes are shredded prior to autoclaving,
in order to facilitate the process. Another
alternative, microwaves, use radiant
energy to heat water that is sprayed onto
waste. Once the water reaches its boiling
point, it boils the microbes, rendering
most of them harmless.
Microwaves, autoclaves and other
alternative waste treatment technologies
must be independently evaluated for
safety and effectiveness. Any medical
waste treatment technology approved by a
state or federal agency should be subject
to stringent regulations, which have .been
developed with worker safety, public
health and environmental considerations
in mind.
SOLUTIONS: NINE STEPS TOWARDS
ENVIRONMENTALLY RESPONSIBLE
HEALTH CARE
Every health care facility can take imme
diate steps to reduce rhe environmental
harm that results from its purchasing and
waste disposal practices. By doing sb, it
can benefit financially, improve staff
morale, increase worker safety, avoid
liability costs, improve regulatory
compliance and strengthen its relation
ship with the community.
STEP ONE: Establish a “green team.”
Convene a task force of administrators,
housekeepers and others who are cur
rently responsible for waste handling.
Authorize this team to:
1. Identify the percentage and content of
your facility’s waste stream that is cur
rently being incinerated and what is
currently being recycled.
2. Conduct a waste audit with either
in-house staff or an outside consultant to
identify wasteful practices and design a
waste management strategy that incorpo
rates waste reduction, reuse, and recycling
measures.
STEP TWO: Put someone in charge.
Assign or hire staff for the full time
responsibility of developing and imple
menting a new and more environmentally
thorough waste management program.
This program should integrate
materials-purchasing with waste segrega
tion and recycling to reduce the waste
stream volume and toxicity through
environmentally sensitive work practices.
EVERY HEALTH CARE
FACILITY CAN TAKE
IMMEDIATE STEPS
TO REDUCE THE
STEP THREE: Train staff about the
environmental consequences of medical
waste incineration. Waste handlers,
nurses, purchasing staff, boards of
directors, medical ethicists, physicians,
medical assistants, administrative staff
and food service personnel all need to be
aware of the problems and costs of
ENVIRONMENTAL HARM
THAT RESULTS FROM ITS
PURCHASING AND WASTE
DISPOSAL PRACTICES
unnecessary red-bagging and the avail
ability of less expensive and more protec
tive waste disposal alternatives.
STEP FOUR: Don’t throw out what you
BEGIN A PROGRAM
TO ELIMINATE THE USE
OF MERCURY-CONTAIN-
ING PRODUCTS WITHIN
THE INSTITUTION AND
BECOME A MERCURY-
FREE FACILITY
can recycle. Implement or expand your
recycling program. Cardboard, glass,
office paper, drink cans, newspapers and
magazines, and PETE (#1) and HDPE
(#2) plastic have nationwide recycling
markets. Implement a purchasing
program that favors products made of
recycled paper that has not been
bleached with chlorine. Communicate
with suppliers about the need for totally
recyclable or reusable packaging materi
als.
STEP FIVE: Don’t throw out what you
can reuse. Create a plan to assess, on an
ongoing basis, the availability of reusable
products, and when feasible, substitute
them for disposable items.
STEP SIX: Don’t incinerate what you can
safely dispose of by other methods. The
small percentage of hospital waste that is
infectious can be made harmless and
unidentifiable by autoclaving,
microwaving or other alternatives to
incineration.
these. Where they do not — for example
in energy efficient fluorescent light bulbs
—■ engage in recycling to avoid releasing
mercury into the environment. You can
refer to the University of Massachusetts
at Lowell’s Sustainable Hospitals Project
for a list of mercury alternatives. The
web address is wwxv.uml.edu/centcrs/
LCSP/hospitals.
STEP EIGHT: Create a plan to reduce the
use of chlorinated plastics, such as
polyvinyl chloride (PVC), with the fiveyear goal of its near-complete phase-out
from your institution. PVC may be
present in ventilator and oxygen therapy
tubing, endotracheal rubes, ambu bags,
facemasks and oral airways, IV bags and
tubing, dialysis equipment, patient ID
bracelets, gloves, protective covers, record
binders and mattress covers.
STEP NINE: Assign materials manage
ment staff to research and communicate
with suppliers concerning the substitution
of materials (sterilizing solution, floor
cleaners, cooling unit biocides) to reduce
toxic chemical inputs, protect the health
and safety of health care employees and
reduce environmental pollution emissions
and impacts.
STEP SEVEN: Begin a program to
eliminate the use of mercury-containing
products within rhe institution and
become a mercury-free facility by the
year 2003. Mercury is present in batter
ies, thermometers, Miller-Abbott tubes,
Cantor tubes, sphygmomanometers,
electrical equipment, fluorescent lamps,
laboratory reagents and disinfectants.
Alternatives already exist for most of
Health Care Without Hann strives to help
hospitals and other health care facilities
achieve these nine steps. We can provide
educational materials, refer experts, suggest
speakers, and identify health care facilities
willing to share their experience in becoming
environmentally responsible. Our web site is
www. noharm. org.
Action for Women's Health, Albuquerque NM
St. John's Regional Medical Center, Oxnard CA
AFL-CIO, Washington DC
St. Joseph's Hospital 6 Med. Center, Phoenix AZ
American Indian Health, Dearborn Ml
St. Joseph's Medical Center, Stockton CA
American Nurses Association, Washington DC
St. Mary Medical Center, Long Beach CA
American Public Health Association, Washington DC
St. Mary's Medical Center, San Francisco CA
Asia Pacific Environmental Exchange, Seattle WA
St. Rose Dominican Hospital, Henderson NV
Bangladesh Environmental Lawyers Association
(BELA), Bangladesh
St. Vincent Medical Center, Los Angeles CA
Beth Israel Medical Center, New York NY
Blue Ridge Environmental Defense League,
Wadesboro NC
Woodland Healthcare, Woodland CA
Cebu Environmental Initiatives for Development
Center, Inc., Cebu City Philippines
Breast Cancer Action, San Francisco CA
Center for a Livable Future, Johns Hopkins University
School of Hygiene & Public Health, Baltimore MD
The Breast Cancer Fund, San Francisco CA
Center for Environmental Health, San Francisco CA
HCWH PARTICIPATING ORGANIZATIONS
(AS OF MAY 1999)
California Communities Against Toxics, Rosamond CA
California Nurses Association, Sacramento CA
Center for Health, Environment and Justice,
Falls Church VA
California, Nevada Board of Church & Society,
United Methodist Church, Santa Cruz CA
Center for the Biology of Natural Systems, Flushing NY
Canadian Association of Physicians for the
Environment, Kleinburg, ON Canada
Centre national d'information independante sur les
dechets (CNIID), Paris France
Central Conference of American Rabbis, New York NY
Cathedral of Saint John the Divine, New York NY
Centro Ecologista Renacer, Santa Fe Argentina
Catholic Healthcare West, San Francisco CA
CGH Environmental Strategies, Burlington VT
Bakersfield Memorial Hospital, Bakersfield CA
Chemical Impact Project, Kentfield CA
Dominican Hospital, Santa Cruz CA
Citizens Environmental Coalition, Albany NY
Marian Medical Center, Santa Maria CA
Citizens for a Better Environment, Chicago IL
Mark Twain St. Joseph's Hospital, San Andreas CA
Citizens for a Better Environment, Madison, Wl
Mercy American River Hospital/Mercy San Juan
Hospital Carmichael CA
Mercy General Hospital, Sacramento CA
Citizens for a Better Environment, Minneapolis MN
Citizens for a Healthy and Safe Environment,
Colchester VT
Mercy Hospital, Bakersfield CA
Clean North, Sault St. Mane ON
Mercy Hospital and Health Services, Merced CA
Cleanup Coalition, Baltimore MD
Mercy Hospital of Folsom, Folsom CA
Committee of Interns and Residents, New York NY
Mercy Medical Center Mt. Shasta, Mt. Shasta CA
Commonweal, Bolinas CA
Community Coalition for Environmental Justice,
Seattle WA
Connecticut Coalition for Environmental Justice,
Hartford CT
Mercy Medical Center Redding, Redding CA
Mercy Southwest Hospital, Bakersfield CA
Mercy Westside Hospital, Taft CA
Methodist Hospital of Sacramento, Sacramento CA
O'Connor Hospital, San Jose CA
Robert F. Kennedy Medical Center, Hawthorne CA
Saint Francis Memorial Hospital, San Francisco CA
Deti Zeme- Children of the Earth, Praha,
Czech Republic
Department of Environmental Health, Boston
University School of Public Health, Boston MA
Saint Louise Hospital, Morgan Hill CA
DES Cancer Network, Washington DC
San Bernadino Community Hospital,
San Bernadino CA
Sequoia Hospital, Redwood City CA
Seton Medical Center Coastside, Moss Beach CA
Detroiters Working for Environmental Justice,
Detroit Ml
Earth Day Coalition, Cleveland OH
Seton Medical Center, Daly City CA
Sierra Nevada Memorial Hospital, Grass Valley CA
Ecology Center, Ann Arbor Ml
Endometriosis Association, Milwaukee Wl
St. Bernardine Medical Center, San Bernardino CA
Environmental Association for Great Lakes Education,
Duluth MN
Environmental Stewardship Concepts, Richmond VA
St. Dominic's Hospital, Manteca CA
St. Elizabeth Community Hospital, Red Bluff CA
St. Francis Medical Center, Lynwood CA
St. Francis Medical Center, Santa Barbara CA
St. John's Pleasant Valley Hospital, Camarillo CA
EarthSave, Louisville KY
Environmental Working Group, Washington DC
Equis, Langley WA
Essential Action, Washington DC
Farm-Verified Organic, Medina ND
New Girl Times, New York NY
Fletcher Allen Health Care, Burlington VT
New Hampshire Nurses Association, Concord NH
Galveston-Houston Association for Smog Prevention,
Houston TX
New York State Nurses Association, Latham NY
Gateway Green Alliance, St. Louis MO
North Carolina Waste Awareness & Reduction
Network, Durham NC
General Board of Church & Society, United Methodist
Church, Washington DC
The Nightingale Institute for Health & the
Environment, Essex Jet. VT
Government Purchasing Project, Washington DC
Ohio Network for the Chemically Injured, Parma OH
Grass Roots Environmental Organization, Rahway NJ
Oil, Chemical and Atomic Workers Union,
Lakewood CO
Great Lakes Center for Occupational & Environmental
Safety & Health, Chicago IL
Oncology Nursing Society, Washington DC
Great Lakes United, Buffalo NY
Oregon Center for Environmental Health, Portland OR
Greater Boston Physicians for Social Responsibility,
Boston MA
People United for a Better Oakland (PUEBLO), Oakland
CA
Physicians for Social Responsibility, Washington DC
Greater Cleveland Coalition for a Clean Environment,
Cleveland OH
Greenaction, San Francisco CA
Physicians for Social Responsibility — Bay Area
Chapter, San Francisco CA
Greenpeace, Washington DC
Pollution Probe, Toronto ONT
Hamtramck Environmental Action Team,
Hamtramck Ml
Reconstructranist Rabbinical Association,
Philadelphia PA
Human Action Community Organization, Harvey IL
Reduce Recidivism by Industrial Development, Inc.,
Chicago IL
Illinois Student Environmental Network, Champaign IL
Indigenous Environmental Network, Bemidji MN
International Society for Doctors for the Environment
IISOE), Santa Fe Argentina
Institute for Agriculture & Trade Policy,
Minneapolis MN
Intravenous Nursing Society, Cambridge MA
Jenifer Altman Foundation, Bolinas CA
Judith Helfand Productions, New York NY
The Katahdin Center for Education and Research,
Brunswick ME
Kirschenmann Family Farms, Windsor ND
Lawrence Environmental Justice Council,
Lawrence MA
Learning Disabilities Association, Pittsburgh PA
Legal Environmental Assistance Foundation,
Tallahassee FL
Lightning Environmental Systems, Shrewsbury MA
Save Our County, East Liverpool OH
Science and Environmental Health Network,
Windsor ND
Sierra Club, Washington DC
Society for Conservation and Protection of the
Environment, Karachi Pakistan
South Bronx Clean Air Coalition, Bronx NY
South Carolina Nurses Association, Columbia SC
Southeast Michigan Sierra Club, Detroit Ml
Srishti, New Delhi India
Stanly Citizens Opposed to Toxic Chemical Hazards
(SCOTCH), Albemarle NC
Student Environmental Action Coalition,
Philadelphia PA
Students for a Healthy Hospital, Ann Arbor Ml
Students for a Healthy Hospital, Eugene OR
Student Physicians for Social Responsibility, Urbana IL
Li vmg/Dy ing Project, Fairfax CA
Surfer's Medical Association, San Francisco CA
Lone Star Chapter of the Sierra Club, Austin TX
Massachusetts Breast Cancer Coalition, Waltham MA
Toronto Environmental Alliance, Toronto ONT Canada
Toxics Action Center, Boston MA
Massachusetts Nurses Association, Canton MA
Toxics Action Center, West Hartford CT
Massachusetts Public Interest Research Group
(MASSPIRG), Boston MA
Unidad Ecologica Salvadorena, San Salvador
El Salvador
Methodist Federation for Social Action, Mason City IL
Vermont Public Interest Research Group,
Montpelier VT
Michigan Nurses Association, Okemos Ml
Mid-Michigan Environmental Action Council,
E. Lansing Ml
Minnesota Center for Environmental Advocacy,
St. Paul MN
Mt. Sinai School of Medicine, New York NY
Multinationals Resource Center, Washington DC
Mumbai Med-Waste Action Group, Mumbai India
National Environmental Law Center, Boston MA
National Medical Waste Resource Center, Iowa City IA
Vietnam Veterans of America- Michigan Chapter,
Saline Ml
Washington Toxics Coalition, Seattle WA
West Michigan Environmental Action Council,
Grand Rapids Ml
White Lung Association, Baltimore MD
Women's Cancer Resource Center, Berkeley CA
Women's Cancer Resource Center, Minneapolis MN
Women’s Community Cancer Project, Cambridge MA
National Women's Health Network, Moretown VT
Women's Environment and Development
Organization (WEDO), New York NY
National Wildlife Federation, Washington DC
Work on Waste, Canton MA
Natural Resources Defense Council, Washington DC
1199, the National Health & Human Services
Employees Union, New York NY
New England Medical Center, Boston MA
■ . .
HEALTH. CARE WITHOUT HARM
P.O. BOX 6806
<
FALLS-CHURCH, VA 22040
T: 703.237..2249 .<
F: 7 03.237.83 89
EMAIL: NOHARM@IATP.ORG. .< WWW.NOHARM.ORG
11
Barriers to the Quality of Care:
The Experience of Auxiliary
Nurse-Midwives
in Rural Maharashtra
AD1TI IYER & AMARJESANI
The notion of quality in the public health system is becoming increas
ingly an issue for policymakers and planners in India. The Eighth
Five-Year Plan identified the poor quality of family welfare services
as one of the factors hindering the achievement of a lower birth rate
(COI, Planning Commission 1992, p. 333). More recently, the Indian
government has outlined elements of a quality-oriented, or qualityfocused, approach in the Reproductive and Child Health Programme
(GOI, MOHFW 1996).
As a concept, quality is attuned to the needs and satisfaction of
the users o: health services. By that token, a quality approach lends
itself easily to the fulfillment of desired outcomes, whether these are
measured by better health status or improved demographic indica
tors. Such a result is possible only when quality efforts arc sufficiently
backed up by adequate and rationally distributed infrastructure and
material resources. The relationship between quantity and quality is
best expressed at the ground level. This chapter reflects these ground
realities from the perspective of auxiliary nurse-midwives (ANMs)
in Maharashtra.
ANMs are auxiliary
kers employed by the district adminis
tration to occuoy the low<._, rung of the'public health bureaucracy.
The World Health Organization has broadly defined auxiliary work
ers as technical workers in a particular field who have less than full
210
qualifications (WHO 1961, p. 4). India's Second Five-Year Plan de
scribed the role of auxiliary health workers as supplementing the con
tributions made by doctors and other highly trained personnel for
promoting preventive and curative health activities (GOI, Planning
Commission 1956, p. 540). In their capacity as technicians, vaccina
tors, and assistant midwives, auxiliary’ workers support both the medi
cal and the nursing professions. Therefore, auxiliary workers derive
their legitimacy from their interactive relationship with profession
ally trained personnel, and they derive their effectiveness from the
network of physical and professional support structures to which they
belong.
The role of AN.Ms in India has changed markedly over the past
four decades. ANMs were initially seen as assistants to midwives in
maternal and child, health (MCH) centers. All of this changed during
the 1960s and 1970s. Family planning was integrated with MCH ac
tivities and projected as a program deserving the highest priority
(GOI, Planning Commission 196S). The committee appointed to re
view the staffing pattern and financial provision of the Family Plan
ning Programme, now called the Family Welfare Programme, recom
mended a system of targets and incentives and identified ANMs and
other village-level workers as agents for the popularization of the pro
gram (Mukherjee Committee 1966).
Further discussions on integrating the functions of the primary
health centers (PHCs) and of village-level health workers led to the
formation of a full-fledged Committee on Multipurpose Workers in
1972 at the initiative of the Executive Committee of the Central Fam
ily Planning Council. The committee transformed ANMs and the host
of malaria workers into multipurpose workers (MPWs). ANMs were
now required to provide child health services and primary curative
care to villagers. Thus ANMs have long ceased to play the peripheral
role conceived for them at the time of national independence. Their
heightened accountability and increasing visibility in the community
have transformed them into key workers at the interface of health
services and ‘
-ommunity. The realization of this potential, how
ever, is depenu-iit upon support systems such as preparatory train
ing, ongoing professional and interpersonal support, facilities, and
equipment. This chapter reviews and evaluates the adequacy and
quality of these systems.
212
Experience of /Xuxiliary Nurse-Midwives in Rural Maharashtra
According to national norms, a PHC should serve a population
inumbering 30.CO0 under the leadership of a medical officer (doctor).
Even if a PHC has two medical officers, it still has only one doctor
for 15,000 people. 1 view of the demands of their work, these doc
tors arc hardly in .
ition to provide constant supervision to ANMs
and male health workers posted at the subcenters. The problem is
exacerbated by vacancies in the post of medical officer. This absence
of a team leader effectively forces the ANMs to carry out the day-today work of the subcenter in an independent fashion. Thus, contrary
to their status as auxiliaries, ANMs become de facto independent work
ers—quasi doctors—with neither the recognition nor the wherewithal
necessary to play such a role in the health service and the community.
The situation of ANMs is rendered more complex because it in
corporates a social dimension. Although both ANMs and male work
ers work under the jurisdiction of the district health administration,
ANMs have several inherent disadvantages, first, although they are
registered with the Nursing Council and their affiliation with the nurs
ing profession provides them with a better legal status than male
workers (who arc unregistered), ANMs are only paraprofessionals
by training. Therefore they do not enjoy the same status as fully
trained nurses and find themselves marginalized within the council.
Second, the cadre of ANMs is composed exclusively of women, un
like the nursing profession, which allows the participation of males,
however marginal that participation might be (in 1990, only 4 per
cent of nurses registered with the Maharashtra Nursing Council were
men). The inequalities rooted in ANMs' gender thus add another di
mension to their subordinate status. Their affiliation to nursing car
ries a negative social image, in view of the specific requirements of
their work. ANMs bear the additional burden of a reputation—a ster
eotype—that portrays them as immoral women, and this represents a
major handicap when they work with rural communities (Jesani 1990).
Tire gender differential is also manifested in a division of labor
between male d female workers. Whereas male workers are ex
pected to asst . an active role in controlling malaria, tuberculosis,
and other communicable diseases, ANMs are principally responsible
for MCH activities. One reason for this division of labor is undoubt
edly the carryover effect of their previous functions. Its outcome,
which draws its ultimate justification from the "natural functions"
argument, is striking. On the one hand, the sex of the male health
,
Aditi Iyer • Amar Jesani
213
worker and his use of laboratory slides and other "clinical" devices
conspire to project his image in the community as a malaria "doctor"
Jesani 1990); on the other hand, the female worker is regarded merely
as a
'rsc bni" (but being a common form of addressing women in the
are;.. ' ne difference is not merely a matter of semantics; the associa
tions suggest that the male worker is more competent than his female
counterpart.
In addition, unlike her male counterpart, an A.NM is expected
to maintain the subcenter. In fact, the female worker's responsibility
with regard to the subcenter goes beyond hygiene. She is expected to
stay there and run it on a day-to-day basis. This responsibility, how
ever, which is not entrusted to the male worker, is not matched with
administrative authority over the subcenter. As a result, the male
worker does not report his activities to the female worker or even
necessarily feel accountable to the subcenter.
We recognize that the axes around which ANMs' experiences
revolve arc the quality of their relationship with the community, their
positioning in the occupational hierarchy of the health services, the
nature and location of their health work (whether in a PHC or
subcentcr, a developed or underdeveloped district, an accessible or
remote area), and their support mechanisms (professional, infra
structural, and personal). An examination of how these diverse ele
ments interact with one another and how they influence the quality
of care rendered by ANMs forms the core of this chanter.
Methodology and Sample
Our study is designed to generate an understanding of the socioeco
nomic background of ANMs, their role expectations, performance,
satisfaction, and problems from the health system and the commu
nity. It focuses on ANMs not as an operational category, but as women
in the hierarchical structure of the health services, and attempts to
■' -iment the many ways in which the health system affects their
I. _s and experiences.
The study is set in the four districts of Maharashtra that repre
sent its major geographic divisions: Ratnagiri District in Konkan, Pune
District in western Maharashtra, Deed District in Marathwada, and
Wardha District in Vidarbha. These districts are also representative
of particular levels of socioeconomic development as measured by
7i.r.■.?
£
214
!.,;■& ■;
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
the Centre for Monitoring the Indian Economy’s (CMIE's) index of
socioeconomic development.’ In the mid-1950s, Pune District, with
an above-average index of 175, was considered to be an industrially
advanced district; Wardha and Becd Districts, with average figures
of S5 and 50, respectively, were moderately developed; and Ratnagiri
District, with a below-average index of 35, was classified as a back
ward district (CM1E 1987).
With the purposive selection of three talui-is (subdistricts) in each
of these districts and two talukas in the tribal belt of Pune, and with
the random selection of two PHCs per taluka from a list provided by
the Directorate of Health Services, we identified 27 PHCs for partici
pation in the study. Using an open-ended interview schedule, we in
terviewed all ANMs working at the PHC and each of the subccntcrs.
The interview schedule was designed to generate qualitative data and
to provide respondents with the opportunity to express themselves
freely. In addition, we selected five ANMs in each district for in-depth
interaction over a maximum period of three cays. This enabled the
female researcher, who accompanied ANMs on their rounds, to en
gage in lengthy discussions and witness health activities undertaken
at the village level. She was aided by an interview guidebook designed
to help generate the same range of information as the interview sched
ule but in greater depth. Data collection commenced in the winter of
1990 and lasted until midsummer of the following year.
The total sample listing consisted of 210 ANMs; however, only
183 ANMs could be interviewed. The remaining 27 were on leave
(maternity or extended leave), in training, simply unavailable, or their
posts were vacant. Among the 1S3 respondents, 68 were from Pune
(-12 from six Pl ICs in nontribal areas and 26 from three PHCs in tribal
areas), 50 from six PI ICs in Wardha, 36 from six PHCs in Becd, and
29 from six PI ICs in Ratnagiri. Of these 183 ANMs, 41 were posted at
their PHCs, 140 were in subcenters, and two were enrolled in train
ing courses at the district headquarters
Findings
Our analysis focuses first on the social and economic backgrounds of
the ANMs, their training as health providers, and their professional
and interpersonal support within the health care system. Subsequent
sections examine the political and social conditions at the PHCs and
Aditi Iyer • Amar Jesani
215
TABLE 11.1
Profile of ANMs: Rural Maharashtra, 1990—91
Socioeconomic indicators
Mean age at beginning of training (years)
20.5
Mean age at first posting (years)
22.7
Marital status at first posting (°,o)
Unmarned
69
Married
25
Separated, deserted, or divorced, widowed
6
Location of current posting (%)
In native district
72
Outside native district
28
Rural versus urban background (%)
Rural
65
Semiurban or urban
34
Community of origin (%)
High caste
Middle caste
Scheduled caste or tribo
Christian or Muslim
Education (%)
34
3g
jg
’•
\
\g
\
Somo secondary or high school
10
Matriculation
67
Intermediate hconso. junior college, or graduation
(No. Of ANMs)
24
(183)
Note f’ciccni.iacs may not add 10 100 because ol rounj.nq
r.iunh.vy nurse ttudwilo
subcenters, the quality of their facilities, deficiencies in the performance
of the ANMs, and problems caused by family planning targets.
Socioeconomic Btickgrouml of the ANMs
ANMs arc accepted into training schools at a young age (an average
of only 20.5 years in our study) (Table 11.1). Dy the time they gradu
ate from the training schools and receive their first posting in PHCs
and subccntcrs, they are two years older (the mean age in our study
was 22.7 years). More thai
>lhirds of all ANMs in our sample were
single when they began working in the rural health system. Instead
of using place of birth as the sole criterion for determining their back
grounds, we sought information on the places where they had stud
ied to understand their exposure to rural or urban life. Accordingly,
we classified ANMs who were born in rural areas and had their pri
mary and secondary education in rural areas as having rural back
grounds. The rest, by default, were considered Io have urban I- ■■ I
216
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
grounds. Two-thirds of the ANMs had rural backgrounds, and a third
were from scmiurban or urban areas. The one-third of ANMs with
urban backgrounds—mainly Christians and Muslims—had had little
exposure to • il life before their recruitment.Therefore, the ANMs
brought wit.
.m youth and inexperience, which made working in
conservative and patriarchal social settings an especially daunting
challenge.
To be effective, ANMs must establish a strong, credible presence
in the community. Because they are seldom posted in their native vil
lages (although nearly three-fourths of those in our sample were
posted within their native districts), they ore expected to build rap
port with strangers. Nor is this a one-time expectation. Transfers,
which occur every four years on average, ensure that ANMs spend a
large part of their career attempting to establish amicable relations
with largely unfamiliar communities.
Nearly three-fourths of the ANMs in our sample belonged to
upper and middle castes, nearly one-fifth belonged to lower castes
'■eduled castes and tribes), and fewer than one-tenth were Chrisi or Muslim. Middle-caste Hindus dominated our sample, account: for 38 percent. Scheduled castes were overrepresented (nearly 18
-ent as compared with 11 percent in the state, according to the
1991 census), and scheduled tribes were underrepresented (at nearly
2 percent as against 9 percent in the state). Similarly, within the group
of minorities, Muslims were underrepresented (nearly 2 percent as
against the 1981 census figure of 9 percent) and Christians overrepre
sented (nearly S percent as against the 1981 census figure of 1 percent).
The representation of lower castes (chiefly scheduled castes) and up
per castes, as evidenced by the caste variation among ANMs of differ
ent ages, has increased since 1980; the percentages of minorities (Chris
tians and Muslims) and middle castes has correspondingly declined.
Two-thirds of the ANMs in our sample had completed their sec
ondary education, a fourth had earned an intermediate certi'. e or
attended a junior college, and the remainder had received some sec
ondaryeducation. Nearly a third of the sample had acquired additional
training, mostly in clerical skills such as typing and stenography.
Although a majority of the ANMs came from middle- and up
per-caste families, many came from somewhat precarious socioeco
nomic situations. At the time of recruitment, 64 percent of the ANMs
TABLE 11.2
ANMs’ current economic role: Rural Maharashtra, 1990-91
Unmarried
Ever-married
All
ANMs
ANMs
ANMs
ill
Holo
%
(No.)
%
(No.)
%
(No.)
Sole earner
8
(3)
22
(32)
13
(35)
Earning more than husband or father
37
(14)
32
(46)
33
(60)
Earning as much as husband or father
3
(1)
7
(10)
6
(11)
!>
■f
1
ill
Ono ol two earners
Earning fess than husband or father
16
(6)
26
(37)
24
(43)
No knowledge or cash income not earned
37
(14)
14
(20)
19
(34)
(No. of ANMs)
100
(38)
100
(145)
100
(183)
rroies Per cemagcs Oo net add 10 100 beeaxe of rounding Bfomcf s
■t
i
rcomo consider cd d lamer rzw oed
ANM = auxiliary nursc-m.o^iffl
•/<!
^j|
'll
from rural areas belonged to landless and poor peasant families. Furthcr, the monthly cash income of the ANMs' fathers averaged Rs738,
the amount varying only slightly across the four study sites. Worsening the precarious financial position of the family were economic dependencies in the household at the time of the ANMs' recruitment:
on average, three to four dependents per earner or productive family
member. This was due in part to the fact that at the time of recruitmcnl, one in four of the ANMs came from households in which the
father cither had died or was economically inactive.
Consequently, the ANMs' wages contributed important economic stability to their households. One-fifth were the sole earners
in their families, and one-third of all ANMs commanded higher wages
than their husbands, fathers, or brothers (in the absence of a father)
(Table 11.2). The ability to alleviate the economic hardship of their
households motivated many of these women to join the government
service. Over time, the ANMs encountered numerous obstacles in
their work but could not dare to contemplate a job switch. Their de
pendence on their current employers was heig' ned by a realiza
tion that avenues of alternative employment wei. .united.
ANMs did not find many options in the labor market prior to
their employment in the Family Welfare Programme. Indeed, the role
of choice in their decision to work as ANMs was small. The most favored occupation—one with fixed hours of duty, an attractive sal
ary, job permanence, and a reassuringly large female representation—
was teaching, which nearly three out of four perceived as a concrete
,11
•:]
•'»
:1
j
2
j
!
t
;
;
21S
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
'i option after their matriculation but were unable to achieve. Morc' over, four-fifths would have liked to pursue higher studies but were
prevented from doing so by the fragile c amics of their households.
All these factors contributed to the vulr. oility of ANMs and, con
sequently, their bargaining power vis-h-vis the health bureaucracy
and the community.
Training
In the 1950s and 1960s, training courses for ANMs focused on mid
wifery and MCH, with 9 out of 24 months earmarked for those sub
jects. in 1973 the government integrated the various functions of the
health services, changing the ANMs' role (Kartar Singh Committee
1973) Two years later, a government committee called for an expan
sion of their training to prepare them for multipurpose health work
(Srivastav.i Committee 1975). In response, the Indian Nursing Coun
cil approved an expanded syllabus in 1977 (Indian Nursing Council
• 1977). However, the expansion in training requirements was not
matched by a longer period of training. On the contrary, with the new
syllabus came the decision to reduce the training period from 24 to
18 months, which some nurse trainers consider inadequate to pre
pare ANMs for work at the village level (Dcodhar 1994). Compro
mises in the length and quality of training affect recruits' confidence
and efficiency (Prakasamma 19S9).
. In Maharashtra the training standards received another setback
in the 19S0s, when vacancies in the public health system in rural ar
eas generated an urgent demand for ANMs there. A frenzied attempt
to recruit women for the job ensued. By the end of the decade, with
7,471 additional .ANMs pressed into service, the cadre had swollen
to twice its earlier size. This came about not by a redistribution of the
3,797 fully trained ANMs from the nongovernmental sector (who represente
arly cne-half of all registered ANMs), but rather by ex
panded ...rollments in training schools and by the induction of un
registered personnel. The unregistered ANMs accounted for 71
percent of all recruits during the 19S0s (Iyer and Jesani 1995). This
trend is reflected in our data. Three out of four ANMs currently em
ployed were recruited during the period 1981-91. Among that group,
42 percent were still unregistered with the Nursing Council at the
time of our interviews.
Ailili Iyer • Amar Jesani
219
The chief architect of this trend was the state government. In 1982
it introduced a so-called Sinn Ladder Course, which further reduced
the training period from >8 la 12 months and located nearly all its
instruction in the field instead of the training school. Given the re
duced standards of this course, it failed to win the immediate approval
of the Maharashtra Nursing Council. Eventually the Nursing Coun
cil and the state government worked out a compromise: the Council
agreed to register probationary workers provided they were put
through another six months of training and examinations at the end
of it, and the state instituted Step Ladder Promotional Courses at sev
eral (raining centers and began sending its workers to them.
This reduction in minimal training standards and its subsequent
legitimization has had several far-reaching implications. First, by not
providing enough time for students to assimilate the course mate
rial, it inadequately prepares young and inexperienced women for
their jobs. Most ANMs trained under the Step Ladder Course com
plained to us that too much information had been imparted in too
short a time. Second, ANMs' registration is now controlled by two agen
cies, the state bureaucracy and the Nursing Council. For ANMs, who
are considered to be temporary workers until they are registered, the
politics surrounding their formal acceptance by the health system only
intensifies the insecurity that their deficient training has engendered.
Their temporary status prevents them from receiving wages commen
surate with their full-time work, and their eligibility for basic employee
benefits is subject to the whims of the district-level administration.
Although the 18-month MPW course is superior to the Step Lad
der Course, it places an unwarranted emphasis on hospital-based and
nonnursing activities, even though ANMs' role requires an orienta
tion to outreach work. A radical reorientation of the content and peda
gogy of training is needed not only in the Step Ladder Course but
also in the IS-month MPW course.
In sum, young and vulnerable women who aspire to bccom
ANMs receive an unrealistic preview of their future career in the train
ing schools. In shielding them from responsibilities, nursing schools
fail to build trainees' confidence, a vital asset in unassisted health
work, which requires independent decisionmaking. Moreover, their
cloistered existence in the school does little to prepare them for work
in unfamiliar, often uninviting, village communities. The threat of
sexual harassment and abuse mars the careers of most ANMs, but
Ad 111 Iyer •
220
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
trainees arc not informed of their legal rights or channels of redress.
In the end, ANMs learn their lessons of village-level health work not
in training schools, but while negotiating the numerous hurdles they
encounter in everyday life.
Professional and Supervisory Support
Once ANMs are out of training schools, they need professional sup
port to help them carry out the tasks assigned to them. This need is
particularly acute in subccntcrs, where ANMs arc deprived of the re
assuring environment of a health campus. ANMs need to go through
periodic retraining programs and ongoing, continuous supervision
In the IT IC setup, the medical officer and health assistants (male
and female) arc responsible for supervising ANMs as well as male
Mi’iVs, dais (traditional birth attendants), and community health vol
unteers (CHVs). Lady health visitors (LU Vs), the female supervisors
of ANMs, arc no more than experienced paramedical staff who arc
given additional training for six months. Besides supervising ANMs,
'.heir duties include providing guidance to ANMs, strengthening their
knowledge and skills, helping them to plan and organize their activi
ties, making weekly visits to subcenters, and making, home visits to
observe and guide them in their day-to-day activities. Medical offic
ers arc also expected to make weekly visits to the subccntcrs and at
tend clinics organized there to examine and treat difficult cases. They
are also expected to hold monthly staff meetings at the PHC to evalu
ate workers' progress and suggest improvements. During those meet
ings. they convey information from their meetings with the district .
health officer, inform staff about campaigns and surveys proposed
by the district-level administration, monitor existing activities, and
outline work schedules for the next month. Sometimes they accom
pany this with a short lecture on a health activity of their PHC.
Supervision should consist no’ ■’rely of technical guidance but
also of moral support and encoun^ .nent. In reality, this docs not
happen. In one of the PHCs, for example, ANMs belonging to the
same caste as the medical officer were given preferential treatment;
in another, the medical officer's wife, who was an ANM, did no work,
but was not reprimanded. An ANM in VVardha was convinced that
her medical officer was penalizing her for her assertiveness by refus
ing to cooperate with her. Once, she told us, he kept putting off per-
Amar Jcsani
221
forming a tubcctomy for a woman she had recruited. Another time,
when there were no empty beds in the ward, he ordered her to bring
a cot from home for one of her sterilization cases and after the operation refused to let her take ■
k home in the Pl lC's jeep. His behavior made her job especially difficult.
The hierarchical relationship between medical officers and ANMs
erects barriers between the two functionaries that reduce whatever
bargaining power ANMs might otherwise muster. An authoritarian
medical officer in VVardha required his staff tosland at attention while
addressing him. He discouraged staff unity by inviting tattling, which
created an atmosphere of mistrust. ANMs were sometimes expected
to help the medical officer in his private practice or to manage the
clinic for outpatients with the compounder (medicine dispenser) in
the medical officer's absence. An ANM who was separated from her
husband reported the medical officer made sexual advances toward
her, suggesting that they "have fun" at a lodge in the town. When
she refused, he retaliated by issuing a memorandum critical of her
performance. Countering these reports of harassment, however, were
reports by other ANMs who gratefully acknowledged interventions
by their medical officers that helped resolve difficult confrontations
with community leaders. One of the medical officers even reduced
an ANM's work load when she was undergoing a personal crisis.
Another criticism voiced by our informants was that their su
pervision consisted of little more than monitoring contraceptivc-acccptor targets and making perfunctory inspections. Their supervisors
treated the achievement of targets as the only indicators of performance, zealously emphasizing them in individual interactions and in
monthly meetings at the PHC. This finding is echoed in other studies
(Durgaprasad et al. 19S9; IIHMR1991; Nichter 19S6). Indeed, monthly
meetings often became trials at which ANMs were publicly repri
manded for not completing targets assigned to them. This pressure
intensified toward th. 'nd of the fiscal year (in March). As a result,
the ANMs were somi ues driven to falsifying their records to exag
gerate their accomplishments. They expected to gain little useful in
formation from the monthly meetings; in fact, few looked forward to
them, and many set aside their routine health activities for one or
two days before those encounters to complete their records.
The content of supervision ranged from active encouragement
to indifference, non-cooperation, and even antagonism, depending
d i
l.i i
i !
■■
i
•
Ijj:
• :
‘
1
j:
i
;
j’
‘:
i
I
•1
222
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
on the medical officer's attitude to nurses in genera! and individual
ANMs in particular. Most medical officers issued reprimands more
often than praise. Some ANMs received no supervision at all. Those
in the more remote subcenters complained that the LHVs rarely vis
ited them because they were put off by the prospect of walking long
distances on their own. We came across some instances in which
ANMs worked in close association with their health assistants, but
these were the exception. In general, the intent, consistency, and qual
ity of supervision left much to be desired.
Aditi her • Amar Jesani
223
TABLE 11.3
Time utilization of ANMs on the last working day prior to Interview:
Rural Maharashtra, 1990-91
Average
ANMs
Location and activity
%
(No.)
duration
Percentage
of activity
of average
(hoursiminutes)
workday
PHCs
Home vxits
24
(10)
3 47
52
Travel
10
0)
1 49
25
Outpatient departments or clinics
73
(30)
4.56
68
Rocorc anting
22
(9)
1 40
23
12
(5)
Univorsa. immunization
Proq'a.mmo camps
Social Conditions anil Vulnerability ofANMs
AXMs are posted either at a 1’1 IC or at any of the subcenters under
its jurisdiction. Some 77 percent of the ANMs in our study were posted
at subcenters, while 23 percent were working in PI ICs, a distribution
not markedly different from the average for the state of Maharashtra
as a whole. PHCs tend to be located in more developed villages,
whereas subccntcrs are located in remote villages or in outlying ar-eas of larger villages. At the PI ICs, ANMs work within the structure
of a health campus or at least have a visible backdrop for their work
in the community. This includes the presence of the health team,
headed by a doctor, and health infrastructure with facilities fora daily
outpatient department. In contrast, ANMs posted to subcenters work
unassisted, receiving only transient professional guidance from the
medical officer or female health assistant. The presence of a medical
officer at a weekly clinic organized by the ANM at the subccntcr,
though mandatory, is a rarity. Therefore, rather than operate clinics
at the subcenter building, ANMs tend to deliver health care to their
communities through house-to-house visits. While taking stock of the
activities conducted by ANMs on the day of our interview and the
time spent on each activity, we found that slightly more than onehalf (55 percent) of the .ANMs posted at subccntcrs made b ? vis
its, compared with only one-quarter of those posted at PHC. , Fable
11.3). Both groups of workers spent an average of four hours, er threefifths of their working day, on house-to-house visits.
The mandated population size of an ANM's territory is 5,000
(3,000 in tribal and hilly areas). Among the ANMs in our study it was
4,565, somewhat less than the average of 5,163 for the state in 1991.
However, most ANMs were without transport and had to walk long
3.18
46
Deliveries
20
(8)
3 11
44
Mootings
7
(3)
4,50
67
Transporting family planning cases
—
(0)
—
Other axmt.os
15
(6)
4 00
Not opposable or on leave
2
(No. cl A?.Ms) and average workday
(1)
—
(■’1)
7.13
55
Gubconlo's
Homo vt$.ts
55
(77)
4.10
62
Travel
41
(57)
2 03
31
Outpabe"’ departments or clinics
15
(21)
4 05
61
Record u-.?,ng
30
(12)
2.21
35
Univorsa immunization
Prog.-a-mo camps
16
(22)
3 58
60
Deliveries
6
(8)
4 09
62
Mootings
9
(13)
5 01
75
Transporting family planning cases
3
(1)
2 45
41
Othor actvwos
17
(21)
2.34
38
Not applicable or on leave
5
(7)
__
No rosptrse
1
(’)
__
(110)
6.40
(No. of ANMs) and average workday
__
All locations
Homo vista
48
(87)
4 08
GO
Travel
34
(61)
2.02
30
Outpatie— departments or clinics
28
(51)
4:35
67
Record wting
28
(51)
2.17
33
Universa’ -immunization
Progra~me camps
15
(27)
351
56
Oelivenes
9
(16)
3.40
54
Meetings
9
(16)
4:59
73
Transport _g family planning cases
2
(1)
2 45
40
Other acv.xes
17
(30)
2.51
42
Not applipibie or on leave
4
(8)
—
No respo' se
1
(No. of ANMs) and average workday
(1)
(181)
6.50
r.’oies Humpe-. -J ANMs exclude those m training The average duration ol individual ax.tts in
each of the subgroups does not add up to the average work day because of multiple responses
Af.'M = auxJia'. *i;rse mtdwde. PHC=primary health center.
I xpcrn-nie of Auxiliary Nilrsc-Midwives in Rural Maharashlra
TABLE 11.4
Provision of government accommodation: Rural Maharshtra, 1990-91
Type of accommodation
PHC
Subccntcr
All
ANMs
ANMs
ANMs
26
Government quarters
58
17
No government quarters
42
83
74
100
100
100
(41)
(140)
(181)
Total
(No of ANMs)
m
Pj 1C primary health cen’Cf
distances under the blazing sun, sometimes through desolate and dan
gerous terrain. One-third of all ANMs spent an average of two hours,
ora third of their workday, commuting between their workplace and
the villages tinder their charge. Among those assigned to subccntcrs,
41 percent spent that much time commuting, as compared with 10
percent among those posted at 1’HCs. This travel time was in addi
tion to the time it took ANMs who lived outside the village where
they were posted to reach the.subcenter.
ANMs have numerous reasons for preferring not to live in their
subcenters. I’ersonal safety is a major concern, especially for unmar
ried and separated women, who are most vulnerable to sexual ha
rassment. All ANMs, particularly those living in subcenter villages,
require secure living quarters. However, a distinct bias favors ANMs
posted at 1’IiCs: 58 percent of ANMs posted at I’HCs, as compared
with only 17 percent of those posted at subccntcrs, were provided
with government quarters, whether they occupied them or not (Table
11.4). Despite the shortage of living quarters, 59 percent of all
subcenter ANMs were residing in the villages to which they were
posted (data not shown), and three out of four of them were doing so
without being provided with quarters.
In the course of their health work, ANMs are exposed to com
munity politics and prejudices. As we have mentioned, the disadvan
tages already imposed on women by a patriarchal and
e-based
social system arc compounded in their case by the association, in many
Indians' minds, of the nursing profession with pollution and disre
pute. Because ANMs' work requires them to speak openly about con
traceptives, to interact with men as well as with women, and to keep
itinerant schedules, they are viewed as women of loose morals. This
negative social image and their low status within the health system
Adili Iyer •
Amar Jcs.ini
22S
make them easy prey to sexual harassment—a prospect that plagues
them throughout their careers.
Unmarried or maritally disrupted w mien, who are believed to
be unspoken for or who do not visibly disp.ay the protection of their
families, are particularly vulnerable to sexual harassment. A number
of the ANMs in our sample recalled how their social position in the
community changed after their marriage. The lewd propositions and
taunts that came their way before marriage stopped as soon as they
had the protection of their husbands. This was particularly the case
in Wardha District, where social relationships tended to be more feu
dal. One of the ANMs in Pune District, a young divorcee, also re
called an unpleasant incident involving a man who approached her
late one evening for a medical certificate. It soon became apparent
that he had an ulterior motive; had she not slammed the door shut
against him, she believed he would have molested her.
Another kind of harassment emanates from village leaders, who
demand special services, such as immunizations, at their homes. In
one village, a sar/vinch (elected village head person) kept a close eye
on the ANM; another insisted that he be allowed to inspect her
records; yet a third badgered the ANM because she did not dispense
vitamin tablets (a difficult task since she had no supplies); and a fourth
made unjustified complaints to the district health officer before or
dering the ANM to leave the village and never return.
A third pretext for mistreating ANMs is their caste affiliation. In
Wardha several ANMs from lower castes mentioned that they faced
overt discrimination. One of them, a 36-year-o!d nco-Buddhist, re
ported that higher-caste groups who were dominant in the area gave
her tea in broken cups, made her sit on a sack on the floor, did not
allow her to touch them, and before her own eyes would throw away
the medicines she gave them. Conversely, a few of the ANMs from
higher castes in Ratnagiri were visibly uncomfortable dealing when
people of lower castes.
When an ANM arrives in a new viL..oe, she usually undergoes
a period of testing by certain groups in the community (often youths),
who accost, tease, or even sexually harass her. One of the older ANMs
in Ratnagiri recalled the problems she had in her first posting. Her
clients would become agitated over the onset of fever after an immu
nization. When she approached them with family planning informa
tion and contraceptives, they would say: "Why are you bringing us
Ad Hl Iyer ■
what you have left over?" or "Why don't you use them yourself?"
An ANM in Wardha described the early days of her stay in the
subccntcr village to which she was currently posted. People would
stone her house in a bid to drive her out, so that the previous ANM
would return. Young boys would drive to the steps of the subcenter
on their bicycles and frighten her and her young daughter. The ha
rassment lasted for a year and a half.
227
Amar Jcssni
TABLE 11.5
\
Subccntcr facilities, essential furniture, and basic equipment:
Rural Maharashtra, 1990-91
Percentage
ol ANMs reporting
Facilities and equipment
Facilities
Rented room/other government premises
46
Specially conslructed building
24
16
No subcenlor space
14
No separate building; run from ANM s house
The Quality of PIIC anti Subccntcr Facilities
Dasic equipment or furniture
79
Stove
Ideally, PFICs should be staffed with two ANMs, one handling work
within the I’HC itself, and the other conducting outreach activities in
the community. Disguised understaffing exists, however, the magni
tude of which can be gauged from state-level statistics compiled by
the Directorate General of Health Services. In 1991, Maharashtra's
1,650 I’HCs, which should have had 3,300 ANMs, had a shortfall of
1,376. a figure more than 14 times higher than the number of vacan
cies imported in official statistics that year. Under such circumstances,
ANMs, many of whom arc forced to handle the jobs of two individu
als, naturally feel overburdened.
Despite an increase in the number of I’HCs during the 19S0s,
the provision of buildings to house the new centers came only later.
In 19S7 fewer than one-half of the PHCs had regular buildings, but
by late 1993 nearly ail of them did (GOI, CBHI 1988-94; GOI, DGHS
1988-94; GOI, MOHFW 1988-94). In contrast, only about one-half of
the state's subcenters had regular buildings by late 1993. The PHCs
and subcenters remain inadequately equipped and supplied. These
problems affect the system's capacity to provide health care services
of satisfactory quality, and ANMs bear the brunt of those problems.
To perform their work, tire ANMs assigned to subcenters require
not only secure living quarters but also a well-constructed building
and essential equipment and supplies. Their physical working conditi' fall far short of that ideal. Fewer than one-fourth (24 percent)
of t
iNMs posted at subcenters in our study had a specially con
structed building. Thirty percent cither had no subcenter space at all
or had to conduct health activities from their homes, and the remain
der worked in a rented room or in space provided by the panchayat
(village council) or local government (Table 11.5). Of the 118 struc
tures used for subcenter activities, one-third were poorly constructed.
Fetoscope
64
Weighing machine
64
45
Chair/stools
39
Table
35
Autoclave
Cupboard
32
Dolivory/oxamination table
31
Bench
29
Stethoscope
21
16
Blood pressure instrument
(140)
(No ol ANMs posted at subcontor villages)
Noto Percentages do not odd to 100 UcCJuso ot mr: ok) rctocnics
ANM < auxiliary nurso mid*><c
\
More than a quarter of them lacked electricity, and as many as 70
percent did not have a piped water supply (data not shown).
Although subcenters constructed by the government were bet
ter than makeshift rental arrangements, they were usually located at
the village periphery or outside the protection of the main village dus
ter. ANMs were afraid to live in those structures unless they had their
families with them. Rented rooms that served as subcenters were lo
cated within the villages but were often dark and dingy, and most
offered no privacy to the ANM or her patients.
The subcenters were not adequately er uniformly equipped. For
example, a common item is the stove, because it has many general as
well as health uses. Yet, out of the 140 ANMs posted at thesu1
'tors,
one in five lacked this basic amenity. Apart from the stove, . only
other instruments we found in most of the subcenters were a
fetoscope, either as part or independent of a delivery kit (64 percent),
and a weighing machine (64 percent). Certain essential instruments
for preventive and curative care were found in fewer than half of
subcenters. These included the autoclave (35 percent), stethoscope (2!
percent), and instrument for measuring blood pressure (16 percent).
223
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
Essential items of furniture such as chairs or stools (45 percent), cup
boards (32 percent), a dclivcry/cxamination table (31 percent), and a
bench (29 percent) were also found in a minority of instances.
These inadequacies affected the ability of ANMs to work with
degree of confidence in the community. Three-fourths of all
ANMs in our study had multiple complaints about their working
conditions. Besides being overburdened, they cited the inadequacy of
facilities, equipment, and medicine stocks. They also complained about
the lack of proper accommodation and inadequate transport facilities.
ANMs are expected to conduct at least half of the deliveries in
their areas; but, by our estimates, ANMs based at I’HCs and subccntcrs
conducted no more than 19 and 13 percent of deliveries, respectively.
They attributed their inability not only to their sense of inadequacy,
due in part to their deficient training in this area, but also to the lim
ited facilities available to them and their having to function in isola
tion. That is why two-thirds of the deliveries they attended took place
in the women's homes, in most cases under far from ideal conditions.
Having to leave their subccntcrs for this work exposed them to
sexual harassment. Stories of the experiences of ANMs who had been
drawn out of their homes at night under false pretenses, only to be
molested or raped, spread among ANMs and were lodged in their
collective experience. As a result, the ANMs tended either to shun
health work after 8.00 p.m. or to live outside their assigned villages
so that they would not be expected to make night visits. Many ANMs
refused to budge after dark unless their attendants or CHVs could
accompany them.
Divergent Health Priorities
The ANMs in our study, including those posted at PHCs, conducted
an estimated 15 percent of all deliveries in their areas, fulfilled 64 per
cent of their targets for sterilization and 65 percent of their targets for
intrauterine device insertions, z ■ eported that they were providing
curative services to 68 percent of all those who approached them. If
ANMs could do all the work expected of them, they would indeed be
regarded as important workers at the village level. The reasons why they
cannot do this lie in their assigned priorities, their resulting allocation of
time, and the highly deficient support mechanisms available to them.
Adtli Iyer • Anur Jesani
229
The Family Welfare Programme has steadily overshad; ved all
other programs and services of the primary health care /stem.
Changes in health policy affect ANMs directly. They are expected to
implement health policies through their activities at the village level.
By virtue of their position in the community, however. ANMs are
faced also with demands for other health services by the people they
arc supposed to help. The government and villagers do not always
share the same priorities, and, in trying to accommodate both, ANMs
often end up caught in the middle.
We asked the ANMs we surveyed to rank eight health activities
from the perspective of the government and the people. Their com
bined ranking reveals a conflict between the community members,
whose highest priority is curative services, and the government,
whose perceived priority remains family planning.
Government priorities directly affect budgetary and financial al
locations, which in turn affect the provision of equipment and sup
plies. As a result, PHCs may experience gross deficiencies in essen
tial drugs but are invariably well-stocked with contraceptives (ICMR
1991). This deficiency not only limits the ANMs' ability to provide
tangible services at the point of contact with the community but also
reduces their credibility. "You don't give us medicines when we need
them; why should we listen to you when you tell us about family
planning?" was a refrain that the ANMs in our study were obliged to
hear over and over again. To rectify the communities' perception of
their role as superfluous and self-serving, they placed great emphasis
on their curative work and less emphasis on their function as midwives.
ANMs attempted to honor as many requests for medicines as
possible in an effort to gain acceptance in the community, a practice
that has also been documented elsewhere (Paul, Singh, and Sharma
1988). Every year subcenters in Maharashtra receive an annual pro
vision of dru ■ nd supplies valued at only Rs3,000. Despite that in
adequate lew. of support, ANMs posted at subccntcrs and PHCs in
our study reported that they were able to provide curative care to an
average of two-thirds of all clients who approached them.
Pressed for medications, the ANMs referred patients to the PHC,
rationed their stocks by giving patients medicines in smaller doses
than indicated, or simply turned them down. A few were driven to
dispensing innocuous drugs or placebos to satisfy clients. Others pur-
ti
A'
W
■I
...I
ij
U
A
.4
231
Adili Iyer • Am.ir Jcsani
chased and dispensed medicines in a private capacity. Inadequacies
in drug provision—and ANMs’ deficient training in drug use—thus
threaten the rationality and quality of health care available from I’HCs
and especially from subcenters. This conclusion is reinforced by find
ings reported by 1’hadke and colleagues (1995) in Maharashtra and
by Paul, Singh, and Sharma (19SS) in Uttar Pradesh
ANMs told us they hoped that their curative activities would
have a positive effect on their family planning performance. To in
crease their credibility, most (64 percent) conducted antenatal care,
deliveries, postnatal care, and immunizations (Table 11 6). And
through all of this, ANMs continued to promote the economic ben
efits of small families (mentioned by 52 percent of the ANMs) or the
health benefits to the women and their children of limiting their fam
ily size (mentioned by 39 percent). Accompanying these strategies
were a host of monetary and material incentives they offered clients,
including the provision of meals and snacks to the women and the
relatives who accompanied them to the Pl IC, medicines ami injec
tions during and after sterilization, and a personal monetary contri
bution to augment the government's monetary incentive of Rsl30 for
each sterilization.
Interestingly, ANMs were reluctant to admit that they relied on
incentives; a mere 16 percent did so at first. It was only when we asked
them to outline the motivational strategy they had employed in their
last case that they admitted having offered incentives. Nearly twothirds had given their last client food,57 percent had bought her medi
cine or an injection, 37 percent had topped up the regular motivation
fee offered by the government with their own contribution of approxi
mately Rs200, and nearly a third had reimbursed the woman for her
travel expenses.
T1:c Burden of Family Planning Targets
Since their institution, family planning targets have b me yardsticks
by which ANMs are judged and accordingly rewaru ,u or punished.
The rewards consist of praise at monthly meetings of PHC staff, a
cash, prize, or a certificate from the district health officer. Punishment
includes the withholding of an ANM's salary (sometimes for three
months at a stretch), a reprimand in the presence of other staff al a
monthly PHC meeting, a memorandum criticizing the worker's per-
TABLE 11.6
Strategies and material Incentives employed by ANMs to motivate women
to use family planning methods: Rural Maharashtra, 1990-91
Strategies and incentives
PHC
Subcentcr
All
ANMs
ANMs
ANMs
63
64
64
46
54
52
37
Motivational strategy (% ol ANMs using)
Budding credibility through other health services
Promoting the ideal ol a small family lor
nation’s development
Advising women to have lower children
39
39
42
34
35
Providing monetary and other material incentives
7
19
16
Promoting the ideal ol gender equality
5
9
8
Excluding men, targeting only women lor motivation
5
5
5
Other methods
2
1
1
Motivation not required
5
0
1
Not stated
7
0
2
to protect lheir health
Building rapport, explaining things in identiliabe terms
Incentives given tor sterilization (% ol ANMs ottenng)
Moats or snacks lor patient and relatives during stay
62
66
65
Medicines or tonics before, during, or alter acceptance
57
57
57
Augmentation ol sterilization incentive loo
29
39
37
Reimbursement ol travel expenses
33
30
30
Other
10
7
7
(No. ol ANMs offering incentives)
(21)
(74)
(95)
(Total no. ol ANMs)
(41)
(140)
(181)
Holo Percentages do not add io 100 because* ol mult
responses
ANM = auxiliary nurse rmdwilc. Pl <C * primary health CCT "Cr
formancc, and on rare occasions, termination of employment. ANMs
tend to receive more punishments than rewards.
Targets, we were informed, worked wonders for some workers
in more remote districts. Recruitment of one or two family planning
acceptors often resulted in a desired transfer or extraordinary favor
from the district administration. This saw several government ser
vants—teachers, gram sei’aks (village clerks), and talahs (revenue settle
ment officers) joining the fray and competing with ANMs for clients.
Because they had no quotas to fulfill, however, they could afford to
be extravagant. Some offered wom»n as much as Rs400 to agree to
have a tubectomy. This set up a m.
t economy at the village level,
and women began demanding a proper price for their impending ster
ilization. ANMs were now expected to make more out-of-pocket pay
ments. They offered travel expenses for the women and their accom
panying relatives in addition to food during the women's stay at the
PHC. Some offered a six-month course of vitamin B complex injec
tions following the operation. The most extraordinary request came
232
I ' per irnvc «'l Auxiliary Nur\r«Mii!wivrs in Rural Maha^^fetra
from one woman’s husband, who asked the ANM Io take his wife's
place while she was away at the PI 1C.
Targets distort what might otherwise become mutually benefi
cial relationships between ANMs and women in the community. Tliis
problem is particularly acute in areas ridden with compc!;,:on for fam
ily planning acceptors. Many of the ANMs in our stuc
tulcated a
narrow perspective on women's health, regarding women primarily
as reproducers and targets for acceptance. This view often contrib
uted to the alienation of ANMs from the community.
Male leaders and youths used the ANMs' anxiety about meet
ing targets as leverage to establish political control over them or as a
pretext for sexual exploitation. In one area, a gram sevak promised
to recruit acceptors for an ANM if she would accompany him to a
lodge in town. In another instance, the police />nlil (village official ap
pointed to oversee law and order) wanted her to provide his sexual
partner, an unmarried woman who had no children, with a CopperT. When the ANM refused, he complained about her to the district
health officer. An unmarried ANM recounted how the village
sarpanch had approached her for an injection that would cause his
pregnant sexual partner to abort the fetus. Since ANMs were not sup
posed to conduct abortions, she refused. He then complained to her
supervisor. Instead of supporting her, the supervisor explained her
behavior by saying that because she was unmarried, she did not know
about such an injection. The supervisor even offered to administer
the injection herself. Tire sarpanch decided that the village should
henceforth have a married ANM and demanded that the ANM who
had refused his request be transferred.
Despite many negative experiences, caused in part by their as
sociation with family planning targets, many ANMs were unwilling
to denounce the system of targets. One-third of them believed that
removing targets would harm other aspects of their work (Table 11.7).
An equal proportion, however, favored the removal of targets, and
one-fifth thought that the removal of *’ "gets would have no effect,
either negative or positive, on their we
The reason mentioned by most of those who took a negative view
of removing targets was that workers would be tempted to neglect
other health-related duties, because many ANMs tend to earn' cut
non-family-planning tasks with the expectation that they will have a
positive impact on their family-planning performance (that is, target
Adili Iyer • Amar Jrsani
233
TABLE 11.7
ANMs’ views on the effect of removing family planning targets:
Rural Maharashtra, 1990-91 !
■----------------
’
Percentage having
specified view
Effect of target removal
positive effect
33
Negative effect
33
No effect
20
Positive and negative
7
Cannot say
2
Other response
1
Not applicable (targets not given)
2
3
No response
Total
too
(No. of ANMs)
(iai)
Note Percentages as net add io 103 because c’ rounding
ANM = au»tliary nurse <Tud-vito
TABLE 11.a
ANMs' views on the hypothesized effects on health work of the removal
of targets, Rural Maharashtra, 1990-91
1
Percentage of ANMs
having specified view
Hypothesized effects
Negative
\
\
Other health activities will suffer
44
ANMs will suffer from a lack of direction
30
Family planning work will suffer or population will increase
18
There will bo no substantial difference
23
Positive
Quality of family planning work will improve
21
Harassment, tension, expenses will diminish
20
Other health activities will improve
17
Relationship witn community will improve
10
Relationship with colleagues will improve
2
Not applicable or no response
(No. of ANMs)
5
(181)
Note Percentages do net add to 100 because c! muTok? responses
ANM=auxiliary nurse -cr.dAilc
fulfillment); 44 percent or me ANMs gave this reason (Table 11.8). This
argument found ideological resonance among 30 percent who believed
that they would lose a sense of purpose and direction. About 18 per
cent thought that the removal of targets would lead to large increases
in the population. One-fifth of the ANMs, on the other hand, felt that
the quality of their family planning work would improve. Nearly as many
234
Experience of Auxiliary Nurse-Midwives in Rural Maharashtra
believed that the removal of targets would reduce the harassment aimed
at them, alleviate their tension, or lower their expenses. Seventeen per
cent felt optimistic that their other work would improve. One in 10 men
tioned that their relationship with the community would improve.
Thus, although activities related to family planning were an oner
ous burden for many ANMs, not all of them were willing to criticize
the program. Nor were all of them willing to discard acceptor tar
gets, despite the problems they created in their working lives. Their
induction and subsequent socialization into the existing health serv
ice program had given them a narrow view of their role and respon
sibilities in the health of rural communities.
Conclusion
The achievement of a high standard of care presupposes a concern
for quality assurance. Integral to quality assurance is the setting of
optimal standards for service delivery and outcomes. These concerns
have never been adequately emphasized in India's public health sys
tem. Instead, the achievement of targets has, until recently, been an
obsession at all levels of the health bureaucracy. The removal of tar
gets may be seen as a first step in the establishment of a quality frame
work. However, this will have to be backed up by uniformly avail
able and accessible health institutions and practitioners. Some of these
preconditions have not been achieved in India.
First, the quantitative expansion of the health system has been a
bureaucratic exercise; it has been created on paper and only later pro
vided with personnel and infrastructure. By the time the expanded
infrastructure attains an optimal level of performance, it is thoroughly
discredited among the people whom it is meant to benefit. Health
workers then require years to change people's negative opinion about
the services provided.
Second, selective health care has been the single most impc ‘-mt
cause of the low utilization and negative image of the health can.
vices. In rural areas, where people have few alternatives, selective
health care has meant ignoring people's basic health needs. The In
dian program's overemphasis on family planning, coupled with the
neglect of basic curative care, has created the impression among the
populace that the government is interested in little more than meet
Adill Iyer ■ Amar Jcsanl
235
ing its family planning targets. Paradoxically, the extremely high pri
ority assigned to those targets has worked to the detriment ol the pub
lic health system as a whole.
Third, it is difficult, if not impossible, to achieve a high quality
of health care without having basic facilities for delivering it. Unfor
tunately, the government's rural health care system is woefully defi
cient in basic physical standards of care, even though its own depart
ments and agencies have laid out guidelines for them. This is one of
the reasons why the government has no moral authority to enforce
minimal standards of care in the unregulated and often irrational pri
vate sector. The deplorable conditions that exist in many PHCs and
subcenters require tremendous effort on the part of the health work
ers to provide even minimal care.
A fallout of poor public health service.- has been the increasing
dependence on home-based care. In contrast with the situation in de
veloped countries, home-based care in India does not complement highquality institutional services th.it can be relied upon in emergencies.
Rather, those who arc driven to home-based care have hardly any sup
port systems—such as transport and communication—that they can
call upon in emergencies or when they need specialized referral care.
Fourth, ANMs are currently expected to function without close
and continuous supervision from medical and nursing profession
als. it is ironic that whereas institution-based paramedical workers
and auxiliaries in urban areas arc precluded from an independent
role in health care delivery, rural auxiliaries, with virtually no medi
cal supervision, hospital facilities, or means for transporting patients
during emergencies, arc expected to perform above their level of train
ing and without the assistance of medical professionals. The role of
auxiliary workers in health care and the quality of care expected from
them need to be carefully reconsidered and possibly redefined.
Finally, no health worker, let alone an AN''. can meet work ex
pectations in an atmosphere ridden with inse
y and anxiety. The
fact that the health care system is insensitive to concerns about their
security, and that some superiors contribute immeasurably to such in
security, undermines their ability to perform at optimal levels. An un
safe and inhospitable workplace does little to promote qualitvassurance.
The emerging concern among policymakers about the quality of
health care at PHCs and subcenters, though welcome, is belated.
237
Adil* ly vr • Amar Jcsar.i
Experience c» f Auxiliary Nurse-Mid wives in Rural N^WTarashtra
236
Health workers have complained in various ways about the prob
lems they face in the workplace. The present concern for quality must
now be translated into practical programs to alleviate their problems
Otherwise, the objective of making quality an integral part of the pub
lic system is likely to remain a distant goal rather than be»
2 a con
crete reality.
Government of India (GO»’i, Ministry of J lealth and Family Welfare (MOI IFW).
1996. Manual on Target Free Approach in Family Welfare Programme. New
Delhi: MOI IFW.
-------—. Various years. Family Planning Year Book. New Delhi: MOI IFW.
Government of India (GOIl. Planning Commission. 1956 Second Five Year Plan,
1956-61. New Delhi Planning Commission.
------- —. 1968 Fourth Five-}ear Plan, 1969-74. New’ IX. . Planning Commission.
--------- . 1992. Eighth Five-Year Plan, 1992-97, vol. 2. New Delhi: Planning Com
mission.
Indian
Council of Medic?.'. Research (ICMR). 1991. Evaluation ofQuality of Family
Welfare Services at Fmm.iry Health Centre Level: An ICMR Ta>k Force Study.
Acknowledgments
The study on which this chapter is based was conducted at the foundation for
Research in Community 1 lealth, Mumbai, with financial assistance from the Dan
ish International Development Agency (DANIDA). We are grateful to Audrey
Fernandes, Secma Hirani, and Sandeep Khanvilkar, fellow researchers, not just
for participating in the study but for shaping its contours. We are also thankful
to our colleague Sunil Nandraj at the Centre for Enquiry into I lealth and Allied
Themes (CEHAT) and to Michael Koenig for their valuable comments on an
earlier draft of the chapter.
Note
1
The CM1E index, which is a rough proxy indicator of the gross national
product, is a weighted average of indicators for three sectors of the
economy- the agricultural sector (per capita value of output of 26 major
crops and per capita bank credit for agriculture); the mining and manufac
turing sector (number of mining and factory workers per lakh (100,000)
population, number of household manufacturing workers per lakh popula
tion, and per capita bank credit for the manufacturing sector); and the serv
ice sector (per capita bank deposit, per capita bank credit to sen-ices, per
centage of the population literate, and percentage of the population urban).
References
Centre for Monitoring.Indian Economy (CMIE). 1987. District Level Data for Key
Economic Indicators with 70 Maps. Bombay (Mumbai): CMIE.
Deodhar, S. 1994. "Training of ANMs: An assessment," FRCH (The Foundation
for Research in Community Health/ Newsletter: 8(5): 1-3.
Durgaprasad, P., S Srinivasan, N.G. Reddy, and P.K. Bhowmick. 19S9. Health
Cr.r< Delivery System in Rural Areas: A Study of the Multipurpose Health Worker
S
e. Hyderabad: National Institute of Rural Development.
Cover: .nt of India (GOI), Central Bureau of Health Intelligence (CBHI). Vari
ous years Health Information of India. New Delhi: Ministry of Health and
Family Welfare.
Government of India (GOI), Directorate General of Health Services (DGHS). Vari
ous years. Bulletin on Rural Health Statistics in India. New Delhi: Ministry of
Health and Family Welfare.
New
Delhi ofICMR.
Indian
Institute
Health Management Research (IIH.MR) 1991. Training Needs
of Health System Fur.:::ananes in the Slate of Maharashtra. Jaipur.Ill IMR.
Indian Nursing Council. 1977. Syllabi and Regulations for the Courses of Studies for
Auxiliary Nurse Midwife. New Delhi Indian Nursing Council.
Iyer, A. and A. Jesani. 1^5. Women in Health Care: Auxiliary Nurse Midwives.
Bombay (Mumbai) Foundation for Research in Community I lealth.
Jesani, Amar. 19l,0. "Lim::< of empowerment: Women in rural health care," Fconomic and Political Weekly 25(20): 1098-1103.
Kartar Singh Committee 1973. Report of the Committee on Multipurpose Worker
Under Health and Family Planning. New Delhi: Government of India.
Mukherjee Committee, l^ro. Rqiort of the Committee Appointed to Review Staffing
Pattern and Financial Provision under Family Planning Programme New Delhi:
Government of India.
Nichtcr, M A. 1986. "The primary health centre as a social system. PI IC. social
status and the issue of team-work in South Asia," Social Science and Medi
cine 23(4): 317-355.
Paul,.D., J.V. Singh, and A.K. Sharma. 1988. "Qualitative and quantitative as
sessment of medication of sick persons provided by ANMs in a primary
health centre," in National Seminar on Essential Drugs m Primary Health Care
in India: A Report. New Delhi: National Institute of Public Cooperation and
Child
Phadke,
A.,Development
A. Fernandes. L. Sharda, and A. Jesani. 1995. A Study of Supply and
Use of Pharmaceuticals in Satara District. Bombay (Mumbai): Foundation for
Research in Community Health.
Prakasamma, M. 1989. Analysis of Factors Influencing Performance of ANMs in ........
Nizamabad District. Fh.D. thesis, Jawaharlal Nehru University, New Delhi.
Srivastava Committee. 1975. Report of the Group on Medical Education and Support
Manpower. New Delhi: Government of India.
World Health Organization (WHO). 1961. The Use and Training of Auxiliary Per
sonnel in Medicine, Nursing, Midwifery, and Sanitation. Technical Report Se- . ..
ries, No. 212. Geneva: WHO.
CHAPTER - 3
SURVEY OF DOCTORS
SUMMARY ANALYSIS
A survey of the opinion of full time doctors working for at least 1 year in St. Martha’s
Hospital was conducted. Of 67 staff who received the survey questionnaire, 41
responded
Based on an analysis of the survey issues have been placed under one of three categories 1. Issues that need urgent attention based on strongly negative assessment. 2. Issues of
concern where a significant number of responses were negative. 3. Issues that seem
satisfactory' based on a generally positive response.
Responses were analysed from the questionnaire as follows.
Goals - the gap perceived by the respondent between the importance a goal should be
given and is actually given by the hospital.
2. Hospital functioning - respondents scoring on a 5 point scale of various aspects of
hospital functioning. A score of 3 or less was considered a negative response.
3. Comments and suggestions - The number of positive and negative responses by
respondents in different areas.
1
It is strongly recommended that besides this summary the detailed evaluation report and
especially individual comments and suggestions be studied for more complete and
empathic understanding of the doctors’ views.
I
Issues that need urgent attention.
1. Inefficiency in health care delivery and planning
2. Ignoring national priorities and programmes
3. Resistance to ideas and innovation to improve quality of health care
4 Failure to modernise equipment and technology
5. Not motivating staff to work in a caring manner
6. Not consulting concerned department heads when planning and budgeting
7 Applying different rules and regulations for different people
8. Lack of concern for welfare of staff
9 Poor levels of salaries and remuneration
II.
Issues of concern.
1. Should foster concern for respect for life among staff
2. Should emphasize health care of women and children
3. Should subsidize services for the poor
4. Should provide spiritual care to sick irrespective of their religious belief
5. Should foster moral and ethical integrity among staff
6. Should consider ways to generate additional income
7. Should encourage an atmosphere among doctors condusive to work
8. Should improve continuing education programmes.
III.
Issues that seem satisfactory
1. Care provided to all irrespective of caste and creed
2. Providing low cost care
3. Cleanliness
4. Spirit of dedication
5. Past reputation
- Dr. Prem Pais,
Vice-principal,
St. John's Medical College,
Bangalore.
EVALUATION BY DOCTORS
The evaluation instrument for doctors has 2 types of responses
a) A scored response which is to evaluate
i
Hospital goals - a list of goals has been specified. The respondent has been
asked to grade them in a score of increasing importance from 1-5 in ascending
order
The respondent first grades the goals as he/she views them and secondly as
he/she feels the hospital views them
ii Hospital functioning - a number of statements regarding hospital functioning
have been given The respondent has been asked to score them from 1 to 5 in
ascending order of agreement
b) Open ended questions
The respondents have been given the opportunity to give open ended responses in
the following areas
□ Hospital goals
s Major strenghths of the hospital
a Major weakness of the hospital
□ Hospital rules
n Suggestions
Responses have been received from 41 of 67 full time medical staff
Analysis:
a)
Hospital Goals Under each goal in part A of the questionnaire, the number (percentage)
of respondents giving various scores are tabulated Score have been grouped as lowest
priority (1 or 2), highest priority (4 or 5) and intermediate priority (3). Responses have
been scored in two rows - “should be” indicates the importance and respondent feels the
stated goal should be given “Is” gives the respondents perception of the importance the
hospital gives the goal In general a score of 3 or less will indicate a negative perception
Hospital Functioning Tabulation has been done in a manner similar to Hospital Goals.
However in this section only the respondents perception of hospital functioning is called
for. Once again a score of 3 or less will indicate a negative perception.
It may be noted that due to an error in cyclostyling the questionnaire the scoring system
was not fully clarified. It is being assumed that the respondents have correctly understood
the system.
HOSPITAL GOALS
1
The hospital should foster among all staff respect for human life from conception to its
natural end
Should be
Is
No response 1 or 2_______ 3_____ 4 or 5
3(7.3)
(1(2.4)
37(90.2)
2(4.9)
2(4 9)
(13(31.7) 24(58.6)
2. Hospital should provide medical care to the public irrespective of caste, creed and
social status
Should be
Is
3.
4 or 5
38 (92.7)
32 (78.1)
No response
3 (7.3)
2 (4.9)
1 or 2_____ 3________ 4 or 5
38 (92.7)
2(4.9) 7(17.1)
30 (73 1)
No response
1 or 2______ 3_______ 4 or 5
3(7.3)
1(2.4)
37(90.2)
2 (4.9)
7(17.1)
18(43.9)
14(34.2)
The hospital should treat all patients with human care and compassion .
Should be
Is
6.
3
7(17.1)
The hospital should serve as a model of efficient health care.
Should be
Is
5.
1 or 2
While providing high quality medical care the hospital should ensure use of
appropriate, low cost yet effective care where ever possible.
Should be
Is
4
No response
3(7.3)
2(4.9)
No response 1 or 2______ 3_________4 or 5
3(7.3)
_
_
38(92.7)
2(4.9)
2(4.9)
11(26.8)
26(63.4)
The hospital should emphasize especially the health concerns of women and children
Should be
Is
No response
3(7.3)
2(4.9)
1 or 2_______ 3_____ 4 or 5
_
3(4.9)
35(85.3)
1(2.4)
17(41.5) 21(51.2)
7 The hospital should subsidise services for the poor.
Should be
Is
8
1 or 2
6(14.6)
3
4 or 5
2(4.9) 36(87 8)
12(29 3) 21(51 2)
The hospital should provide spiritual care to the sick respecting the individual’s
religious beliefs
Should be
Is
9
No response
3(7 3)
2(4 9)
No response
3(7.3)
2(4 9)
1 or 2
1(2.4)
10(24 4)
3
6(14 6)
15(36.6)
4 or 5
31(75.6)
14(34 1)
The hospital should serve as training institution where trainer doctors and nurses will
learn to deliver competent health care ethically and compassionately
Should be
Is
No response_____ 1 or 2__________ 3______ 4 or 5
3(7.3)
38(92.7)
2(4.9)
3(7 3)
12(29.3) 24(58.6)
10. The hospital should keep the national health priorities in mind when planning its
services
Should be
Is
No response
3(7 3)
2(49)
1 or 2
12(29.3)
3
4(9 8)
15(36.6)
4 or 5
34(82.9)
12(29 3)
11. The hospital should foster a sense of moral and ethical integrity among all its staff.
Should be
Is
No response_______ 1 or 2_________3________ 4 or 5
3(7 3)
1(2.4)
37(90.2)
2(4.9)
12(29.3)
10(24.4)
17(41.5)
Hospital functioning
1
The hospital constantly tries to improve quality of health care
No response_______ I or 2___________ 3__________ ' 4 or 5
17(41.4)
20(48.8)
4(9.8)
2
The hospital innovates to find means of reducing the cost of health care to make it
more affordable.
No response
1(2 4)
1 or 2
11(26 8)
3
12(29 3)
4 or 5
17(41 4)
3
4(9.8)
4 or 5
35(85.4)
3. The hospital is kept clean.
No response
4.
The hospital functioning is such as to the efficient and reduce waste.
No response
5.
1 or 2
2(4 9)
1 or 2
4(9.7)
3
11(26.8)
4 or 5
26(63.4)
The hospital functioning is such as to provide prompt attention to patients
No response_________ 1 or 2____________ 3______________ 4 or 5
2(4.8)
4(9.8)
13(31.7)
22(53.6)
6.
The hospital motivates all its staff to work in a caring and compassionate manner.
No response_________ 1 or 2____________ 3_________ ______ 4 or 5
8(19.5)
12(29.3)
21(412)
7
The hospital involves each department in preparing the department’s budget.
No response_________ 1 or 2____________ 3_______________ 4 or 5
3(7.3)
12(29.2)
12(29.2)
14(34.1)
8
The hospital is concerned about ways to generate additional income.
No response__________ 1 or 2___________ 3_______________ 4 or 5
1(12.4)
10(24.4)
9(22.0)
21(51.2)
9
The hospital charges are reasonable compared to charges by other similar hospitals in
the city.
No response__________ 1 or 2__________ 3_______________ 4 or 5
29(70.8)
9(22.0)
3(7.3)
10
The hospital has reasonable rules and regulations
No response__________ 1 or 2____________ 3______________ 4 or 5
7(17.1)
8(19 5)
9(22.0)
17(415)
11
The hospital is ready to accept innovations and new and better ways to dp things
No response__________ 1 or 2____________ 3____________ 4 or 5
2(2.4)
16(39 1)
14(34.1)
10(24 4)
12
Relationship among staff is friendly and conducive to work
No response
1(2.4)
1 or 2
6(14 6)
3
10(24 4)
4 or 5
24(58 5)
13. The hospital shows concern for the staff and workers
No response
1(24)
1 or 2
12(29.3)
3
16(39.0)
4 or 5
12(29 3)
b) Open ended responses have great value as these may reflect opinions, emotions and
feelings of respondents more accurately than scored responses. In view of this all
responses have been reproduced below They have been grouped under the five heads
under which they were collected
Under each head the responses pertaining to key areas have been grouped together. The
number given against each statement is to identify the questionnaire from which is has
been taken. Thus comments from the same questionnaire under different heads will all
bear the same number
It will be seen that generally respondents see the strength of the hospital in dedication of
the sisters of the Good Shepherd, doctors and nurses and to the non-commercial nature of
the hospital.
At same time a sense of frustration seems to come through the comments. The negative
feelings lie mainly in the following areas:I. The hospital resists modernising and investing in newer technologies
2 Poor salary structure for doctors. A repeated suggestion is to introduce an incentive
scheme for private ward admissions and start special paying O P clinics.
3. “Unprofessional” management with inadequate communication with doctors Doctors
feel they are rarely consulted or made part of management decisions.
4 Different rules seem to apply for different people
OTHER GOALS / COMMENTS:
Questionnaire No
A
Comments
Issues related to modernising:
3
Provide modern treatment at reasonable cost
6
Improve MICU
10
Get dialysis unit so that poor patients can benefit
11
Improve equipment in MICU and CCU
32
Keep up with technical advances
33
Should have basic infrastructure for investigations
36
Accept specialization as an integral part of health care
B Issues related to treatment policies
6
7
15
18
22
23
35
37
40
C
Introduce sterilization proceedures but not MTP
Discourage alcoholic patients - do not give them concessions
- More stress on preventive medicine
- Educate women about FP / immunisation
- Create awareness about nutrition and diet
- Adopt slum/village to create a model system
Introduce sterilization procedures as per National
Family Planning Scheme.
Follow national family planning policies
Land was gifted to sisters to care for all sick
people not only women and children
Should pursue national goals irrespective of religious
beliefs.
Provide spiritual support for those whose loved ones die
in hospital
Improve maternal and child health facilities
Staff benefits:
11
33
Provide transport to staff
Provide benefits to staff dependants eg. Educational loan
Reward hard working staff
D
Management issues
19
32
33
36
40
E
Educational Matters
9
18
32
36
F
Junior doctors are not given respect
Improve staff discipline in certain departments
Have a good maintainance department
Modernise record keeping
Should be able to give a feeling of belonging to the staff
Foster the old family spirit that St Martha’s was famous for
Send Drs to other institutions for training
- Encourage Drs to attend conferences and pay costs for this
Encourage Drs to develop specialised skills
Raise academic standards
Use company sponsorship for CME programmes for Drs, nurses
and technical staff.
Miscellaneous
19
All religions should be equally respected
MAJOR STRENGTHS
Questionnaire No__________ Comments
A. Dedication and Spirit of Service
1
3
4
5
6
10
11
16
17
18
19
20
23
Dedication of workers
Dedication of Drs and nurses
Dedication
Consistent commitment to the down trodden
Dedicated Drs and nurses
Dedicated compassionate service
Service to the poor
Commitment and dedication of sisters of the Good Shepherd
Sacrifice and Service
Dedication
Dedication
Missionary zeal
Strong faith
Warmth kindness and concern
29
30
31
32
34
36
39
B
Technical competence
4
7
12
26
C
Dedication and hard work of staff
Good nursing care; dedicated Drs
Dedication of sisters, Drs, nursing staff
Sincerity and dedication
Showing compassion without consideration to cast or creed
Care and compassion of original IRISH nuns
Christian institution
Competent staff
- Efficiency
Good nursing care
Skilled doctors and competent nurses
Prompt service at admission time
Non commercial reputation.
6
No corruption
7
Subsidised service to the poor
13
Optimal care at reasonable cost
16
Not being overtly commercial
27
Cheap yet good care
33
Poor patients
39
Non profit organisation
D. Reputation past and present:
7
12
20
40
Following old rules and regulations
Past reputation
100 years experience
Past glory and dedication of people in the past
E. Others.
12
36
37
Location
Help from St. John’s Medical College in 60s and 70s
Location and facilities available
trainees & students eg. DNBE, nursing
MAJOR WEAKNESS
Questionnaire No
Comments
A Doctors Remuneration and Financial aspects
2
4
6
7
13
15
18
20
27
32
33
35
B
Lack of modern technology
5
10
12
18
19
29
31
32
C
No incentive scheme
Financial constraints
Low wages of doctors
Unaffbrdability of newer modes of therapy
Difficulty in getting competent doctors without incentive payment
Finances
Low morale among doctors
Economic factor
Lack of finances to upgrade
Frustration of staff because of low income
Monetary factors
Cost factors
Technology update is slow
Lack of equipment
Delay in accepting new technology
Inflexible to suggestions for developing, tertiary care facilities
No interest in upgrading hospital
Lack of initiative to upgrade facilities
Notion that “high tech” care detracts from care of poor people
Hospital has not kept up with other institutions technically
Administration & Management :
1
3
5
6
11
17
30
36
39
40
Inefficient administration
Unprofessional interference by authorities
No long terms vision
- impersonal approach to staff
Rigid policies
Hierarchy
No long term plans
Absence of doctors in the administration
Lack of vision
Poor interpersonal relations of present Indian nuns
Active labour union
Large number of patients and less number of staff
Lack of vision
Unprofessionalism of the management
D Other factors
12
13
22
26
29
35
37
Poor standard of private ward accommodation
Unrealistic expectation of patient s
Religious
Uncertain availability of 2nd level consultant - delay in
getting specialist
Unhealthy competition
Religious factors
Some doctors and nurses are without commitment
RULES AND REGULATIONS
Questionnaire No.
Comments
A. Different rules for different people:
3
22
26
30
35
36
Different rules for different people
Favouritism
Rules vary with different departments and persons
Some get incentives, most dont
Disparity in rules depending on influence with administration
Different rules for different people
- Visiting doctors allowed to earn more than in-house
dedicated doctor
B. Impersonal and inefficient administration.
22
35
Administration is very poor
Senior specialists not given respect
Unconcerned about doctors welfare
Service expected even if doctors have to starve
C. Other issues
5
12
15
35
Leave rules
Give incentives for doctors from private wards
Medical care should be free for all employees
Rules for doctors are unreasonable
SUGGESTIONS:
Questionnaire No
A
Comments
Issues related to doctor's income_
9
7
9
10
11
12
13
17
31
35
36
B
__ __
Incentives for doctors
Provide adequate income for all stall'
Increase pay scales & introduce incentive scheme
Increase pay of junior staff
- introduce incentive scheme
- start evening speciality pay clinics
Give staff'better pay
Incentive from private wards
Impossible to get senior doctors with present pay
find ways to pay reasonable salary' to doctors and
nurses
Private OP clinics
Allow incentives to improve employees income
Allow pay clinics; staff should be better paid
Not allowing incentives for admitted patients
encourages doctors to go to nursing homes
Issues related to modernising the hospital
2
5
7
9
11
13
16
17
19
20
29
32
Improve equipment
Do not avoid technological growth
Open dialysis, neurosurgery a paediatric intensive
care units
- improve nursing care which has deteriorated of late
- improve casualty facilities for tackling emergencies
CT scanner is a must
Better and more modern equipment
Give up fear of high tech. Equipment
Better equipment
CT scanner
Lab and ultrasound facilities round the clock
CT, MR1, isotope scans
Replace old equipment with new
Ultrasound facilities should be available round the
clock
- Upgrade facilities including CT scanner
Buy new equipment and raise charges if necessary'
33
34
35
Modernise; replace old equipment, computerise
Enhance standard of care of sick people
Facilities (technical) should be better
C. Issues related to administration and Management
3
5
8
9
10
11
15
16
17
22
23
26
32
33
36
40
Uniform rules, pay scales and promotional avenues
for all staff
- forum to hear and discuss staff grievances
Give doctors greater role in administration and
policy making
Department / unit head should be given powers to
give concession
Need to employee more SHOs and junior doctors
More flexibility with leave rules
Do not overwork staff
Categorise patients by economic status
- create more special ward, ITU and graded care beds
More interaction between doctors and administration
- consult doctors in matters of medicine, administration
and police
- better promotional avenues for doctors
Provide transport for staff using hospital vehicles/ BTS
Welfare of the staff should be looked after
Regular meetings between management and staff of
each department for better exchange of ideas
Doctors to have more say in areas like admissions, transfers
- Administration should work more quickly
- More junior staff
Doctors or heads of departments should be given more
power in the functioning of their department
- improve private wards
Improve inter departmental relations
- increase number of doctors and nurses
>
Too much “arm-chair” administration. Administrative
staff should move out and see the problems of departments
- sisters should be united. Their ego problems cause
problems between departments
More fairness in dealing with staff
- Less interference in medical matters by non medical
people
- management should show more care for the staff
D
Issues related to academic matters
4
5
7
36
E
Increase teaching programmes
Welcome commercial sponsorship of academic
meeting
Improve library and get Medline services
- start a clinical newsletter
Authorities have blinkers with respect to sponsorship
of CME programmes
Other issues
7
34
35
Generate additional funds-philanthropies and
increased OPD charges
Professionals and doctors should show more dedication
Goals should be based on national policies irrespective
of religious beliefs
Position: 1215 (6 views)