15134.pdf
Media
- extracted text
-
TOWARDS UNIVERSAL HEALTH COVERAGE:
An operational manual for states in India
Intermediate
situation - SOME
services for ALL the
people
Universal Health
Coverage ALL services to
ALL the people
• Current situation ALL services only for SOME
people
TOWARDS UNIVERSAL HEALTH COVERAGE
An operational manual for states in India
CONTRIBUTORS
Cite as:
IPH UHC team. Towards universal health coverage: An operational manual for
states in India. Institute of Public Health, Bangalore. 2012.
Towards Universal Health Coverage: An Operational
Manual for States in India by Institute of Public Health,
Bangalore is licensed under a Creative Commons
Attribution-NonCcmmercial-NoDerivs 3.0 Unported
License.
1
PREFACE
There has been much talk about Universal Health Coverage (UHC), both internationally as well as
nationally. Presently, there is a major emphasis on moving towards universal coverage, a goal that is laudable
and must be encouraged at all cost. So it is heartening that the Planning Commission has taken the lead in
commissioning a high level expert group (HLEG) to initiate the debate and discussions on UHC in India.
In India the debates and discussions about Universal Health Coverage have tended to remain at a
policy and macro level coupled with inadequate information and much less clarity on the steps required to
operationalise the concept of UHC. It becomes more crucial in the context of health being a state subject in
India, with the State governments having the responsibilities to implement polices to achieve UHC. Further
there is confusion with regard to UHC and its linkages with current health systems and programmes like the
NRHM.
In this context some of us felt the need to go beyond broad policy recommendations and come up with
steps to operationalise UHC. The Institute of Public Health, Bengaluru undertook this task. The key guiding
principles in preparation ofthe document were that
•
Health care services should be accessible and affordable to all sections of Indian society, especially the
vulnerable section ofthe population.
t
•
Health care services should be equitably distributed between urban and rural India, between men and
women, between rich and poor, between the castes and among the States.
•
Health care services should be aimed at maximizing health gain.
This document attempts to provide an understanding of the concept of UHC, explain in detail the
critical aspects with reference to population and services to be covered, financing and the method of delivery.
It is specifically targeted for the State level policy makers and implementers, so that they are able to diagnose
where their state is vis-a-vis UHC, identify the necessary steps they need to take to prepare a roadmap
towards achieving UHC.
This document is not a blueprint, but provides some options for policy makers and those in the
decision making process to consider. The document draws from the various discussions held by various
stakeholders in the past and several documents and experiences of several countries in achieving UHC. The
document brings together a few practical tools (including an excel sheet) necessary to understand how UHC
may be planned at the state level. That said, there is no ONE way or the ONLY way in planning for UHC. Any
manual on UHC is never likely to be the one-stop-shop for EVERYTHING on UHC. The document is a "work in
progress" that may benefit greatly from experiences of policymakers and other stakeholders. We welcome
3
any discussion around shortcomings and critiques of the document, as long as alternatives are provided.
These could be included in subsequent editions of the document to improve its relevance and applicability.
This document does not take any positions regarding, "Public Vs Private"; "Biomedical Vs Social
determinants”; "Health Vs Health Services”; "Purchasing Vs Providing"; "BPL list Vs Actual Poor"; etc.
Similarly, we are silent on AYUSH services, not because we are pro-Allopathic, but because we are not clear on
how to include them in our design of UHC. We would really appreciate experts in this field to give us
suggestions to incorporate AYUSH services as well. This document was drafted with the premise that there
are existing health services and programmes with its own infrastructure, organisation, governance
mechanisms and information systems. Rather than ignore this and start on a clean slate, we decided to build
on these see how best to dovetail our suggestions into the existing system.
The document has been written with the assumptions that the State governments are keen on
moving towards UHC and are willing to allocate necessary resources (financial and others] to achieve
UHC. Each chapter of the document is linked to the preceding and subsequent ones, and so we would
request the reader to go through the entire document. To reiterate, this manual is a humble attempt by the
Institute of Public Health, Bengaluru, India to assist the governments increase the access to quality health
care for all residents (and especially the vulnerable] while protecting them from high medical costs and
subsequent indebtedness and impoverishment.
The authors
September 2012
4
Table of Contents
PREFACE..........................................................................................................................................3
BACKGROUND................................................................................................................................ 6
WHAT IS UNIVERSAL HEALTH COVERAGE?............................................................................ 8
WHAT IS POPULATION COVERAGE?...................................................................................... 13
WHAT ARE THE SERVICES TO BE COVERED?...................................................................... 16
HOW WILL THE SERVICES BE FINANCED?.......................................................................... 20
WHERE IS MY STATE ON THE PATH TO UHC?..................................................................... 23
HOW ARE THE SERVICES TO BE DELIVERED?.................................................................... 25
WHAT ELSE IS REQUIRED TO ACHIEVE UHC?..................................................................... 30
Governance........................................................................................................................ 30
Monitoring....................................................................................................................... 30
Support Services.............................................................................................................. 30
Quality and equity............................................................................................................ 30
CONCLUSIONS..............................................................................................................................31
References.................................................................................................................................... 32
Annex 1 - Health indicators in India, vis-a-vis the MDG goals........................................... 33
Annex 2 - Estimating the cost of UHC..................................................................................... 35
Annex 3 - Tool monitor the status of UHC............................................................................. 37
Annex 4 - Provider payment mechanisms to procure private provider services
38
5
BACKGROUND
It is now 65 years since India became independent and the health sector has achieved much from the pre
independence era. Currently, we have a three-tier government health service providing the spectrum of
promotive, preventive and curative health services. National health programmes focus on priority diseases
like tuberculosis and malaria. There is also a strong private health sector providing mainly curative services
at all levels. Some key milestones in the Indian context are:
1947
Acceptance of the Bhore Committee Report
1978
Acceptance of the Alma Ata declaration of 'Health for all'
1983
The first National Health Policy
2002
The new National Health Policy and the National Population Policy
2005
Launch of the National Rural Health Mission (NRHM)
2008
Launch of the Rashtriya Swasthya Bima Yojana (RSBY)
2011
Presentation of the HLEG report to the Planning Commission on Universal Health
Coverage (UHC)
Health services are provided by a mixture of government and private providers, practitioners of Allopathy,
AYUSH and herbal medicine, qualified and less than qualified health workers. Given this plurality, there is
very little coordination or synergy between them. According to a recent government report , there are
only 231 human resources for health (HRH) per 100,000 population; the desirable ratio needs to be 450.
So it is clear that we need to produce many more health workers and ensure that they are retained at the
desirable places.
Health financing by the government has been abysmally low. Most of health care in India is financed by
individual households at the point of care. This in turn leads to barriers to access, catastrophic health
expenditure and impoverishment due to medical expenses. Government has tried to infuse resources
through various mechanisms, ranging from the NRHM to the RSBY, but even then, the latest figures suggest
that the allocation on health has increased from 0.9% to 1.06% of the GDP.
Medicines and consumables are in short supply and there is evidence that most government health
facilities suffer from frequent stockouts. This leads patients to purchase medicines from private pharmacies,
increasing their out-of-pocket expenses. Articles have suggested that expenses on medicines have been an
important reason for impoverishment.
The NRHM tried to provide a voice for the community by creating institutions like the village health and
sanitation committees (VHSC), the Accredited Social Health Worker (ASHA), the patient welfare committees
at each facility (RKS) and independent health societies with civil society and panchayat representatives in
them. However, at the end of the first phase of the NRHM, there is unanimity that these bodies have not
fulfilled their roles.
Governance was decentralised and bottom up planning was encouraged through the NRHM. Facilities were
given the financial powers to receive and use untied funds. Quality was strengthened by developing Indian
public health standards (IPHS) and infrastructure was revamped using the additional funds.
However, in-spite of all this, the health status of Indians did not improve drastically (Annex 1). Infants and
mothers continued to die, we were home to the largest number of malnourished children, infectious diseases
6
still remained out of control and the health services had begun feeling the burden of non-communicable
diseases.
It is a matter of shame for India that many of our neighbouring countries, with much less resources, have
caught up with our health indicators. Admittedly, India is a large country compared to our neighbours, but
we forget that most of the Indian states are similar in size to these countries
It is in this context that the country decided to move towards UHC. Many middle-income countries like
Thailand, South Korea, Philippines, Brazil and South Africa are well on the way to achieve UHC. In the next
section, we describe what UHC is and give examples of how some countries have achieved it in the recent
past.
Iatrogenic poverty: the effect of no UHC.
S~ was the wife of a middle class businessman in Anand. She owned a
three storeyed house with the vegetable business in the ground floor. Her
two sons assisted her husband, while her two daughters-in-law helped her
in the upkeep of the house.
Her world was turned upside down when her husband met with a traffic
accident. He was admitted to a nearby hospital and lived for 40+ days
before giving up the struggle. S~'s struggle started only after this. She and
her sons had to sell their house to pay the hospital bills. They also had to
mortgage all the jewellery in the house to buy medicines.
When I met S~, they were living in a kuchha house and her two sons had
gone to vend vegetables in a push cart. Her grandson was removed from
school because they could not afford the fees and books.
7
WHAT IS UNIVERSAL HEALTH COVERAGE?
UHC is actually part of the WHO mandate to promote health for all (HFA). Unfortunately, the HFA
movement did not materialize due to various reasons. In 2005, the World Health Assembly passed a
resolution urging all countries to achieve UHC for their citizens as soon as possible. The Commission
on Social Determinants of Health (SDH) and two World Health Reports (2008 and 2010) further
reiterated the conceptof UHC.
Many of the high-income countries have achieved UHC, but over time and with a lot of resources.
Germany took nearly 118 years to achieve UHC, while Belgium took 64 years to ensure that 99% of
its citizens were protected against both major and minor health risks. Others like Thailand and
Korea used a big-bang approach to cover most of its population within a short period of time. There
are many examples of countries that have achieved UHC at the global level. An analysis of these
country case studies tells us that UHC is not a prerogative of only rich countries. Several middle
income countries such as Mexico and Thailand have been able to achieve UHC. On the other hand,
there are several high-income countries that have not been able to achieve UHC in spite of spending
a lot of money on health care. The classic example of this latter is the United States of America.
Hence, achieving UHC is not merely about resources, but also about "how” these resources are used
and the arrangements through which these resources are used to provide healthcare. And, more
important, it is about the political will.
UHC has been defined by the WHO as "access to key promotive, preventive, curative and rehabilitative
health interventions for all at an affordable cost". On the other hand, the Commission on SDH
states "Universal coverage requires that everyone within a country can access the same range of(good
quality) services according to needs and preferences, regardless of income level, social status, or
residency, and that people are empowered to use these services". In this manual we use the definition
as stated by the Steering Committee of the Planning Commission (7).
"Ensuring equitable accessfor all Indian citizens, resident
in any part of the country, regardless of income level, social
status, gender, caste or religion, to affordable, accountable,
appropriate health services of assured quality
(promotive, preventive, curative and rehabilitative) as well
as public health services addressing the wider
determinants of health delivered to individuals and
populations, with the government being the guarantor
and enabler, although not necessarily the only provider, of
health and related services.
Steering Committee, 12^ Five Year Plan, Planning Commission 2012.
8
What does this mean in reality? It basically means that should anybody in India fall sick, he/she
should be able to seek health care at enlisted health facilities at a cost that is affordable to the
patient. To expand this further, be it a manual labourer or a software engineer, if both suffers from
diabetes; they should be able to get their treatment at nearby facilities without having to pay for it at
the time of illness. So the key words in UHC are
• All citizens should be able to access
• Most of the health services at reasonable quality with
• Minimal direct payments because
•
Government guarantees these services
In moving towards universal health coverage three dimensions have to be considered namely;
a population dimension - who is to be covered, populations to be reached, with priority to be given
to the poor and vulnerable; a health service dimension - which services are covered and how
services are to be delivered; and a financing dimension - how to reduce OOP expenditures by
converting direct payments into pre-payments. The famous WHO cube elucidates this very well.
Figure 1: Universal health coverage - the three dimensions
Which population is covered?
Adapted from the World Health Report 2008.
In a country where there is UHC, this figure resembles a different picture, with most of the cube
beingfilled (Figure 2).
There is increasing interest in UHC because governments have realized that one of the drivers for
economic growth is a healthy population. The Commission on Macroeconomics and health [CMH]
has clearly identified the financial losses to a country because of illness and has requested countries
to invest more resources into the health sector. In India, the UHC dialogue was initiated only in 2011.
The Planning Commission constituted a HLEG to submita report on how India can achieve UHC, as a
prelude to the 12th Five Year Plan. The HLEG submitted its report in Oct 2011 which was met with
mixed feelings. While many have applauded it for bringing health to the centre of the development
debate, others have criticized it for being a wish list. Based on the HLEG, the Planning commission
clearly identifies UHC as the way forward for India (1).
Figure 2 : The WHO cube in a country with UHC
Which population is covered?
Narin's experience after head injury
The accident happened on 7 October 2006. Narin came off his motorcycle going into a bend. He struck
a tree, his unprotected head taking the full force of the impact. Passing motorists found him some time
later and took him to a nearby hospital. Doctors diagnosed severe head injury and referred him to the
trauma centre, 65 km away, where the diagnosis was confirmed. A scan showed subdural haematoma
with subfalcine and uncal herniation.
He needed an immediate neurosurgical intervention. He was wheeled into an emergency department
where a surgeon removed part of his skull to relieve pressure. A blood clot was also removed. Five
hours later, Narin was put on a respirator and taken to the intensive care unit (ICU) where he stayed
for 21 days. Thirty- nine days after being admitted to hospital, he had recovered sufficiently to be
discharged.
What is remarkable about this story is that the episode took place not in a high income country where
annual per capita expenditure on health averages close to US$ 4000, but in Thailand, a country that
spends US$ 136 per capita, just 3.7% of its gross domestic product (GDP). Nor did the patient belong
to the ruling elite, the type of person who - as this report shall show - tends to get good treatment
wherever they live. Narin was a casual labourer, earning only US$ 5 a day!
- 2010 World Health Report
10
While most state governments will aver that they provide 'free health services' to the poor
population, the reality is otherwise. Many health services are not available at the government
facility and even if they are available, patients may have to pay for it. Some examples are used to
illustrate this:
•
Immunisation services are available free to all children in India. This is easily available and
accessible in rural areas. However, the lack of facilities in urban areas forces parents to go to
the private sector and pay for the immunisation of their children. So while immunisation
services are available free to most rural children, it is not so for the urban children.
•
Outpatient services are supposed to be free in all the PHCs in the country. However, most
PHCs do not have enough medicines, so patients are forced to purchase medicines from the
private pharmacies . Thus once again, an assured service is not provided to the citizen,
resultingin deficiency of UHC.
•
TB treatment is provided free to all patients suffering from the disease. The network of TB
clinics and microscopy centres ensures that these patients have the potential to get free
treatment. However, this service is only limited to the TB patients and not to patients with
appendicitis or diabetes or pneumonia.
•
Employees of the Indian Railway services get comprehensive care for all conditions, be it
preventive, promotive, ambulatory or inpatient care. Even catastrophic events are covered
by the employer. However, this luxury is limited only to the employees of the railways and
their family members. It does not apply to people outside this exclusive circle.
So in reality, governments currently provide
1. Some services free of charge to all of the population (e.g. immunisation for children,
treatment for leprosy, TB, malaria, etc).
2. Some services free of charge to some of the population (e.g. inpatient services for BPL
population groups).
3. All services free of charge to some of the population(e.g. employees of the Indian
railways or the beneficiaries of the Central government health services).
4. All services free of charge to all the population (currently not provided by any state).
No state has achieved universal health coverage. The important point is to identify where the state is
and progress from #1 or #2 or #3 toward #4. More important, it is not enough for a government to
say -we are providing XXX services. The government HAS TO guarantee that the population
actually benefits from these services. This can be achieved either by the government providing the
services itself or by purchasing services from the private health sector. A tentative stepwise
approach is provided in figure 3.
Other than this, the government should also consider how this entire process should be
governed / managed / administered and from where it will mobilize extra resources to finance
UHC. In the next sections we take the reader through some of the key steps to achieve UHC.
11
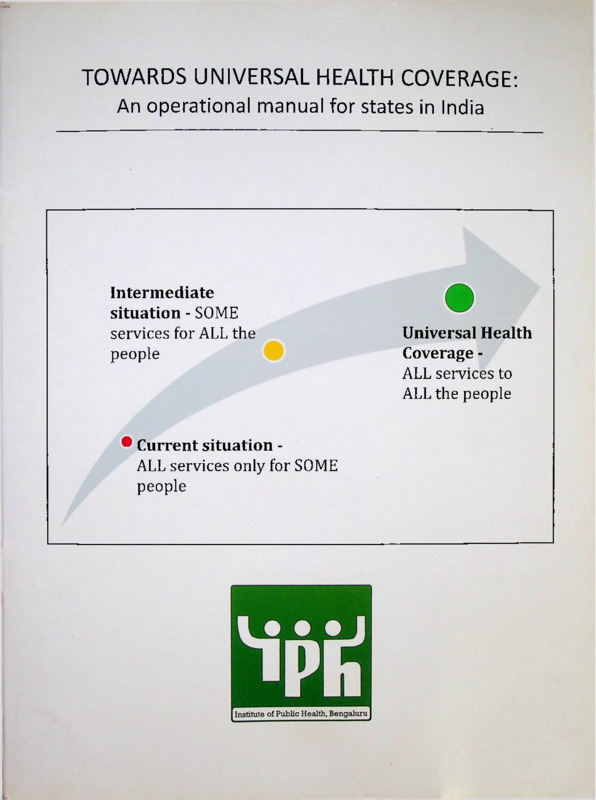
Figure 3 : Potential path to Universal Health Coverage in India.
Intermediate situation where SOME services are
provided free of charge to ALL
the population
Universal Health
Coverage where MOST of the
services are provided
free of charge to ALL the
population
Current situation most services are paid for by
individual households through direct
out-of-pocket payments
Adapted from: Carrins G; James C; Evans D. Achieving Universal Health Coverage: Developing the health financing system.
WHO: Geneva; 2005.
Some people in our country enjoy total and comprehensive health
care without paying money at the point of care. Examples are
employees of the Indian Railways, the troops of the defence forces, the
members of the CGHS scheme, etc.
India will achieve UNIVERSAL HEALTH COVERAGE the day each
Indian benefits from similar complete and comprehensive care that is
free at the time of use.
12
WHAT IS POPULATION COVERAGE ?
The first dimension of UHC is population - who should be covered under the universal health
coverage system? Ideally (see definition), all residents in the state should be covered under the UHC
system. This means that irrespective of the social, economic, cultural and political background of the
household, they are eligible to receive free health care. Currently, the existing government health
services do try to provide care to all the population. However, the reality is different. For example, a
tribal patient with an acute appendicitis may have to travel all the way to the district hospital to get
the necessary treatment. On the other hand, a white collared employee in a private firm can get the
treatment in a nearby hospital. Under UHC, ideally both these sets of people should get health care
as near as possible to their house, so that patients face the minimal barriers to care. In a health
system that has achieved universal coverage, the services must be provided to one and all,
irrespective of where they stay (in the state) or who they are.
Studies and surveys clearly show that currently, there are vast numbers of people who cannot access
health care because of barriers like money, distance, availability, acceptability, etc. Who are these
population groups who are excluded? In India, these could be the indigent, the SC / ST households,
those living in border districts, families belonging to certain religious minorities and of course those
who reside in rural areas. Politically and epidemiologically, the highest priority is to identify and
cover the most vulnerable people who are at risk of suffering due to lack of coverage. Therefore, any
UHC plan at the state must ideally seek to identify and cover the most vulnerable at the first instance.
Once this population is covered, then the government should move onto the next population group.
In the long-term, the goal is to cover everybody in the state under the defined services.
How does one identify the various groups? One simple way is to look at them from economic
parameters, e.g. BPL and APL. All those with BPL cards will be provided the services initially and
then those with the APL cards. This is a simple except that when one comes to APL, then the numbers
are large and a state government may not be able to provide to this entire group in one step. So we
may need to break down the APL group further. A simple way for this is to use occupational groups;
e.g. formal sector and informal sector. While the former is easy to cover, as their details are available
with the employers, the latter is once again a nebulous group. To cover the informal sector in
instalments, one can use existing natural groups like "unions," "cooperative societies,""societies,"
"associations," "welfare boards," etc. These usually have most of the individuals of that occupational
group as members. It may be argued that this will not cover the landless agricultural farmers; but
ideally this group should be covered under the BPL category. And, remember that this is a process,
once people realise that there is an economic benefit in joining a group, the chances of more such
individuals joining these groups become a reality.
13
The figure below depicts the mosaic that forms India. There are many groups and sub groups and
we can create similar mosaics along religious lines or caste lines or linguistic lines or
geographic lines. For the sake of this document, we have used a combination of economic and
occupational subgroups as they are easier to identify. Most important is that whatever the
mechanism of grouping, it should be easy to identify the subgroups using existing documents and
processes. For example, SC / ST populations usually have caste certificates, the poor have BPL cards,
domestic workers have union cards, farmers have cooperative society membership cards, drivers
have union cards, shop owners have their own association membership cards, Self Help Groups
have a list of members, construction workers and beedi workers are enrolled in their respective
boards, etc. In this manner, each sub group can be identified by existing documents and
systematically brought under the umbrella of UHC.
Figure 4 : The various groups within India's population
Members of
occupational unions
e.g. domestic workers
union, beedi workers
Employees in
Entrepreneurs shops and
establishments
Government
sector
employees
Thailand is a good example of a country that went about covering its population systematically.
In 1991, about 32% of the population had access to free health care (both ambulatory as well as
inpatient, preventive as well as curative). Most ofthese were either the government employees (10%)
through a civil servants medical benefitscheme or the poor (17%) through a welfare scheme. Over the
next ten years, they brought the private sector employees under health cover through a compulsory
health insurance and the informal sector through the Universal coverage plan.
While, theoretically all Indians can access 'free' health care, the reality is otherwise. Only 5% of
patients seeking ambulatory care do not have to make OOP payments. The situation is worse when it
comes to inpatient care. If we dis-aggregate populations in India along occupational lines (Table 1),
we note that 77 million I ndians have access to complete health care without having to pay at the time
of treatment. Another 195 million are protected against hospitalisation expenses for secondary
care, either under RSBY or by private health insurance. A hundred and forty five million Indians are
protected against hospitalisations for tertiary care because of the catastrophic social assistance
schemes in three southern states.
14
Figure 5 : Progress towards universal health coverage: example from Thailand
So the challenge is to identify sub-groups within the uncovered and partially covered population,
prioritise based on vulnerability, ease of coverage and financial resources and cover these
populations incrementally or totally.
Table 1 : Categories of Indians and the health services that they receive. (Population in millions)
Category of population
Benefits received
Number of
individuals
Central government
employees, MPs judges, etc
3
Free and compl ete care under CGHS
Formal sector but earning
<Rs 15,000 pm
56
Free and complete cover under ESIS
Defence troops
11
Free and complete care under AFMS
Indian Railway staff
7
Free and complete care under Railway health services
Formal sector and earning
>Rs 15,000 pm
55
Free hospitalisation services for secondary care under
private health Ins.
Informal sector - BPL
140
Free hospitalisation services for secondary care - RSBY
Informal sector - BPL (in
Andhra Pradesh]
70
Free hospitalisation services for tertiary care under
Aarogyasri.
Informal sector- BPL (in
Tamil Nadu)
40
Free hospitalisation services for tertiary care under CM's
Health Insurance.
Informal sector - BPL (in
Karnataka)
35
Free hospitalisation services for tertiary care under
Vajpayee Arogyashree Suraksha
Informal sector - Farmers
(in Karnataka)
3
Free hospitalisation services for surgical care under
Yeshasvirri
Formal and Informal sector
- who are partially covered
1,123
They receive free hospitalisation services or free
preventive services or free ambulatory care ....
NB: These are estimates based on data from multiple sources including the planning commission chapter on health.
It is not to be taken as the final figure.
Each state needs to first identify those populations that are not covered
by outpatient I inpatient services. If the numbers of this population are
high, then the state can further prioritise depending on the vulnerability
and target them first and later expand to other population sections.
15
WHAT ARE THE SERVICES TO BE COVERED ?
The World Health Organisation defines health services as all the services that deal with the
diagnosis and treatment of disease, or the promotion, maintenance and restoration of health. Health
services are the most visible part of any health system, both to users and the general public. Delivery
of health services is an important function and a building block of the health system.
Ideally, all the health services should be available to all the population at a negligible cost.
However, that is often not a reality, given various constraints within and outside the health systems.
As discussed in the earlier section (Population), there are inequities in access to health services
across the population groups. This could be due to various reasons, including non-availability of the
required services. For example, pregnant women need access to Comprehensive Emergency
Obstetric Care (CEmOC), but if blood is not available at the CHC, then CEmOC services will not be
easily accessible for a poor rural pregnant woman. Similarly, if common antibiotics are not available
at the PHCs, then children cannot access to treatment for pneumonia or other infectious diseases.
Another example is of a government medical college that provides cardiac surgery, but this service is
available only in the state capital. And, most who need valve replacement for rheumatic heart
disease may not be able to reach this college. So though the services are provided 'free' to all the
state's citizens, in reality it is accessible to only those who have the resources. All these examples
clearly show how in our country, access to health services is not universal in the government sector.
This means that the patients turn to the private sector for their needs, but end up paying high OOP
payments to get the benefits. Thus the extent of service coverage in our country is partial.
So one important step, in the path to UHC, is to list all the possible health services that a population
needs. This then can be prioritised according to the local demand, the technical needs, the
community's demands and the availability of resources. Some examples of a list of health services
are provided in table 2 for the readers' benefit. However, this is not exhaustive and is only indicative.
What is important is to first make a list of all the services and then highlight the priority services that
the government wants to provide at all its citizens.
Table 2 : Tentative list of health services that may be required by a population in India
Preventive Services
Provided
(Yes / No)
Curative Services
provided TAI'!
Provided
(Yes / No)
Promotive
Services
Antenatal care
Outpatient care
Safe drinking water
Immunisation
Emergency services
Nutrition services
Growth monitoring
Inpatient services
1EC services
Screening for cancer
Delivery services
Tobacco control
Screening for DM
CEmOC services
Yoga
Screeni ng for HT
ICU services
Counselling
Ambulance services
Surgical services
Anti vector measures
Yes/
No
16
Yet another way of making a list is to follow the existing national health programmes; e.g.
reproductive health
services, child health
services, malaria
control services, TB
control services,
blindness control
services, NCD control
In recent years, many low- and middle-income countries have gone
through exercises to define the package of benefits they feel should be
available to all their citizens. This has been one of the key strategies in
improving the effectiveness of health systems and the equitable
services, etc. The
distribution of resources. It is supposed to make priority setting, rationing
advantage is that
of care, and trade-offs between breadth and depth of coverage explicit. On
these services are
the whole, attempts ervfce delivery by defining packages have not been
already being
particularly successful. In most cases, their scope has been limited to
provided by most
maternal and child health care, and to health problems considered as
government health
global health priorities. The lack of attention, for example, to chronic and
non-communicable diseases confirms the under-valuation of the
services to a certain
demographic and epidemiological transitions and the lack of
extent. The
consideration for perceived needs and demand. The packages rarely give
government would
guidance on the division of tasks and responsibilities, or on the defining
then need to invest in
features of primary care, such as comprehensiveness, continuity or
them systematically so
person-centredness. A more sophisticated approach is required to make
that these services are
provided to all the
population in the
the definition of benefit packages more relevant. The way Chile has
provided a detailed specification of the health rights of its citizens
suggests a number of principles of good practice.
•
region or state. For
example, a
should look at demand as well as at the full range of health needs.
•
It should specify what should be provided at primary and secondary
•
The implementation of the package should be costed so that political
levels.
government may state
that it will ensure that
decision-makers are aware of what will not be included if health care
ALL children of the
state will have access
remains under-funded.
•
to free immunisation
services (including
children in the urban
The exercise should not be limited to a set of predefined priorities: it
There have to be institutionalized mechanisms for evidence-based
review of the package of benefits.
•
People need to be informed about the benefits they can claim, with
mechanisms of mediation when claims are being denied.
World Health Report 2008. Primary Health Care - Now more than ever
areas). Then, it puts
the various
mechanisms in place
to ensure this. Once
this service is assured,
the government can proceed to the next programme. The drawback of this approach is that
ambulatory care and inpatient care are usually not part of most of the national health
programmes. And, these are the basic demands of the community. Without them, the credibility
17
of the government health service suffers, affecting the performance of all other health
programmes. So if a woman is not assured of 24/7 delivery services, the chances are that she will
go to a private practitioner for antenatal checkup and subsequent delivery. Similarly, if 24/7
ambulatory services are not available, a labourer with cough will return from his work and go to
a private practitioner. The latter will then prescribe a serious of cough syrups and unnecessary
antibiotics and never screen for TB. The patient will ultimately end up in the DOTS programme,
but only after spending considerable amounts of money and spreading the disease to all near and
dear ones.
Yet another list that has been developed is as per the NCMH report (Table 3). The advantage of
this list is that it is costed, so when one wants to estimate the cost of choosing a service, one can
just follow the NCMH formula.
Table 3 : Examples of services that need to be provided, as per the NCMH report
Treatment of ARTI
Childhood conditions
Treatment of Diarrhoea
Immunisation
Antenatal checkups
Maternal health conditions
Insertion of 1UCD
Normal delivery
Treatment of TB
Other disease conditions
Treatment of uncomplicated malaria
Treatment of snake bite
Other examples of benefit packages can be from existing good practices, e.g. the CGHS
scheme, the ESIS, the Indian Railways' health services, the Armed Forces Medical Services, etc.
We (the authors] would prefer the checklist as shown in Table 2 as it has certain advantages.
For example, if one says that a government will assure free outpatient and emergency care to all the
patients and this service is available 24/7; then many disease conditions will be taken care of. Such
an assurance will ensure that pregnant women get antenatal checkups, patients with cough will be
screened for TB, patients with fever will be screened for malaria, typhoid and even dengue; children
with diarrhoea get their ORS, diabetic and hypertensive patients get their medicines and patients
with cataract are detected and sent for surgery. So there is a convergence of all the national health
programmes at the level of the PHC. However, for this to happen, the PHC must be strengthened by
ensuring physicians, nurses, medicines and diagnostics round the clock. This may not be possible
with our current staffing and vacancy patterns.
18
Once the services have been prioritised and a consensus arrived on the universality
of the services, then the next step is to decide how these services can be guaranteed
to the population. What is required to ensure that these services are provided to all the population
with minimal Financial barrier? More human resources? More medicines? More health
facilities? Specific equipment? This is dealt in more detail in the chapter on delivery of health
services.
So to conclude this section, the state needs to define the services that they will
guarantee to the population, and then ensure that this is provided to the population. In the
case of curative services, this would require provision of the services round the clock.
It is important to define a comprehensive benefit package, which is
the ultimate goal. And then move towards it systematically.
19
HOW WILL THE SERVICES BE FINANCED ?
Health financing systems have three basic functions: collecting funds, pooling them and then
purchasing care. Funds can be collected either through direct fees or through prepayments. Direct
fees are those charges paid by the individual patient at the point of care, and when the patient is sick.
This is currently not recommended by most health financing
experts. This direct payment has the propensity to act as a
barrier to accessing health care. It can also lead to
catastrophic health expenditure, indebtedness and
impoverishment. Nearly all experts recommend prepayments
to finance health care. This could be in the form of taxes, or
health insurance premiums or deposits into a medical savings
account.
Pre-payment is any expenditure
made for a future benefit (like
health care). People pay a small
amount when they are not sick, so
that when they are sick, they will be
compensated their medical
expenses from this fund.
The advantage of both taxes and health insurance is that there is pooling of funds. This means that
both the rich and the poor contribute towards a health care fund. To give some examples, the rich
pay direct taxes through income tax, wealth tax, capital gain tax, etc. On the other hand, the poor
usually do not pay direct taxes, but contribute through indirect taxes like sales tax, excise tax, octroi,
etc. Thus both contribute to a common pool, which can then be used for providing health services to
both groups of patients when they fall sick.
One of the cornerstones of UHC is to convert direct payments into prepayments. This reduces the
OOP payments and increases financial coverage. Currently, direct payments form the mainstay of
health expenditure in India. In 2008, individual households shouldered 72% of total health
expenditure [THE] through direct payments at the time of illness (Figure 6). Government finances
contributed only 20% of THE, the per capita expenditure on health by the government was one of
the lowest in the world (only INR 540). Health insurance was a negligible amount. In other
countries, the ratios are usually reversed. The majority of health expenditure is met through
prepayments like taxes and / or insurance and the individual households meet only a small
proportion of THE through direct payments. In India we have a long and uphill task to shift from
direct payments to prepayments.
So how much money do we need to achieve UHC? There are many guesstimates. A recent article in a
journal mentions that we need to spend INR 1,713 per person per year to achieve UHC .The NCMH
report way back in 2005 estimated that we would need about INR 1,160 per person per year to
provide the essential package of services. The HLEG report estimates that by 2022, we would have
achieved UHC, but at a cost of INR 5,145 per person per year (at current costs). Of this, the
government would have to spend 3,450 and the rest would be by the private sector. As stated, these
are estimates as there are many gaps in the data available to make such calculations. Some attempts
at calculating the total cost for achieving UHC is provided in Annex 2. Keeping in view, the range of
estimates that one is receiving and also that patients will still use the private sector for services in
the immediate future, INR 1500 per person per year will be a safe amount to start with. With time,
this amount will increase as the population coverage increases and as the services coverage
increases.
20
How does a state raise this amount? One must remember that the state is already spending
an average of about INR 500 per person per year on health services. So the state needs to increase
this by another 1000 rupees per person.
There are two options possible for a state. One is to allocate more money from taxes for
health care and then spend it effectively on the public health facilities. By strengthening the
government health services and providing better quality free health care, patients may shift from
the private sector to the government sector. This will reduce their OOP payments considerably
and protect them from financial catastrophe due to medical causes. NRHM tried this by infusing
more funds into the health system. The union health budget increased from Rs 8,086 crores
in 2004-05 to 21,680 crores in 2009-10 . The 12lh five year plan has also promised a substantial
increase in tax based funds. According to their calculation, the central government’s
contribution on health is expected to cross 300,000 crores while the state government v
also contribute about 700,000 crores for health services. The total contribution to healrh
expenditure from government sources is expected to cross 2% of GDP by 2017 and will be in the
range of INR 1,500 per person peryear.
Figure 6 : Health expenditure in India (2008) by source of financing.
One main challenge for the state will be toraiseits allocation to health care. Given that
most state governments have a deficit budget, and the tax: GDP ratio is only 17%, this may be
a valid objection. However, the health secretary can suggest some options to raise these
extra funds:
•
One obvious strategy is to allocate taxes from demerit goods (on alcohol and tobacco) for health care.
This will raise substantial funds to achieve UHC. While usually taxes on these goods are part of the
central excise and are collected by the central government, many states have started introducing entry
taxes on tobacco products.
21
•
The other option is to introduce a health cess, similarto the education cess. This can also raise substantial
resources for UHC.
•
There are many other (more radical) measures like transaction costs (for all financial transactions), etc.
The other option is to increase health insurance coverage among the populations. The important
point to note here is that schemes like RSBY, Rajeev Aarogyasri, Vajpayee Arogyashree and CM's
health insurance scheme are all financed by tax revenues. So they should be considered in that light.
Health insurance should be used to extend coverage rather than generate extra funds. For example,
by extending RSBY to the APL families, it is possible to increase the population coverage. Similarly,
by making health insurance mandatory for all the formal sector, one ensures that the population as
well as financial coverage is enhanced. So in our march towards UHC, we should use health
insurance not to raise funds, but to use people's contributions into a prepayment mechanism and
thereby increasing the coverage of UHC.
Some suggestions for such expansion are:
1.
Expand RSBY to APL populations through existing groups like trade union members, cooperative
society members; self-help group members, resident welfare associations, school children, etc.
The government can collect the premiums from the APL and thereby enhance the financing of
health care.
2.
Expand ESIS to cover the formal sector. Raise the salary limit from Rs 15,000 pm to Rs 150,000 pm.
This way most of the formal sector will have to contribute towards this ESIS fund and this fund
can be used to finance their health care as well asco-financethe RSBY scheme.
3.
Include outpatient services and tertiary health care to RSBY, so that patients get access to
comprehensive cover through one single scheme, rather than having multiple schemes and identity
cards.
To summarise, UHC should be financed using prepayment mechanisms along with pooling of the
collected funds. Direct payments at the time of illness should be converted to prepayments at all
cost. The amount required will depend on the services and the population coverage. We share two
potentially simple tools to arrive at the actual cost and the cost per capita for this expansion.
People will be protected from catastrophic health
expenditure if health care is financed by prepayments.
22
WHERE IS MY STATE ON THE PATH TO UHC?
One must visualize UHC as a goal towards which our society is moving. As stated earlier, there could
be many paths to the same goal, but what is important is that we start moving towards the goal. In
today’s environment, it is unacceptable that people are denied even basic health care because they
cannot afford it or households are impoverished because of high medical expenses for common
ailments.
To begin with, one needs to know where one is on the path to UHC. Is one's state nearing the goal or
is it far away from the goal. There have been many attempts to assess this, but most of these tools
are very complex and only not user-friendly. We propose a simple tool that may not capture the
minute details, but can give the policy maker a broad idea of where the state is. This tool uses
existing data that is easily available and gives a visual depiction of the position of health coverage
in a state. We have used this tool to depict the status of health coverage in India in this manual,
and the same can be used for each state.
We use six indicators to assess coverage, two for each of the dimensions. For the population
coverage, we assess the outpatient contact rate per capita per year and the admission rate per 1000
population per year. For the services coverage, we assess to what extent women are able to deliver
in institutions and what proportion of children are fully immunized by the 2nd year. For the financial
coverage, we calculate the amount of OOP payments made at the time of illness and also
the proportion of patients who did not have to make OOP payments when they sought health care.
All this is depicted in a spider diagram, where if one has achieved universal coverage, then all the
spokes will show 100%. And, to bring in the dimension of equity, we have two lines, one for the
riches quintile and the other for the poorest quintile.
23
If one uses this to analyse the status of UHC for India, we find that:
•
% of children (12 - 23 months) who have completed primary immunisation ideally should be 100%.
However, while children in the richest quintile have achieved 76% coverage, children among the poorest
families have only achieved 47%. This means that there is a gap in immunisation for the poorer segments
of the population. The same is the status for institutional deliveries. From this we can say that while service
coverage is good forthe rich, and affluent, there is a lot to be done for the poor.
•
When one looks at population coverage, one notes that people (both rich and poor) seem to have access
to outpatient services. However, when it comes to admissions, then the story is very different. Rich
patients have a higher chance of getting admitted compared to the poor patients.
•
And, the main reason for this is the OOP payments for health care. We have used "surgical care" just
because we had the data readily with us. NSSO data should give the researcher data on how many patients
received free treatment (for both outpatient and inpatient care) and how many had to pay OOP. This
clearly shows that this is the place that one needs to work on if we went to achieve UHC.
The template for filling up this data and creating a graph is provided in Annex 2. This is a good
starting point to identify gaps in the UHC that need immediate correction and also is a useful tool
to monitor the progress towards UHC.
24
HOW ARE THE SERVICES TO BE DELIVERED ?
India's health care delivery is a mix of public & private health sector practising diverse
systems of medicine. The provision of comprehensive health care by the public sector is a
responsibility shared by the state, central and local governments. More recently, under the NRHM,
the central government has emerged as an important financier of state health systems, while
encouraging the state governments to strengthen the provision of care.
It is clear from the previous chapter that while there are some populations who are not
receiving some services, the immediate issue to tackle is how to convert OOP payments into pre
payments. As stated earlier, it could be either by increasing the allocation for health services or
through a health insurance mechanism. While financing UHC may be easy, providing the necessary
services maybe more difficult. An example of this is given in the box below:
The current norms provide a PHC for 30,000 population. If all the outpatients had to be
seen by the PHC MO, then it would mean an average of 7 00 patients per day. Obviously
one MO cannot provide quality care to these patients AND conduct 1 - 2 deliveries a day,
supervise the ANMs, conduct school health visits, monitor the malnourished children in
the anganwadis, attend meetings at Block, District and Panchayat levels as well as
administer the PHC and manage the programmes. Especially ifone wants the PHC to be
providing 24x7 services. One would need at least three MOs at each PHC. In a state like
Karnataka, that would mean 4,000 new MOs, which may be difficult to find. Even with
reasonable salary and perquisites, Karnataka still has a high vacancy rate at the level of
PHCsMOs.
If one goes to the FRU level, the situation is even worse. Assuming that all normal
deliveries will happen at the PHC and only 15% that need specialized attention are
referred to the FRU, one can easily expect about 450 to 500 'complicated' deliveries in a
year. This has to be managed by a single obstetrician and is very difficult, especially if
one expects this obstetrician to also manage the outpatients, conduct tubectomy camps
and do night duties. Which means that one needs to recruit more obstetricians [and
anaesthetists) to the FRUs. Again, taking the example of Karnataka, in a recent drive to
fill up 600 specialist posts, the government advertised widely. Only about 120 came for
the interviews and 60 joined. If this is the situation in a doctor surplus state like
Karnataka, what will be the situation in otherstates?
Ifthe government wants to remain both the financier and the provider of health care, then it
can adopt various reforms like task shifting (introducing Rural Medical Assistants in place of MBBS
doctors; training MBBS MOs for providing CEmOC and LSAS, etc). This can be a short to medium
term solution, provided the state governments have the strength to counter the powerful IMA and
other medical lobbies.
One another option in terms of providing health care could be to use the existing private
health providers. They are available and it may make more sense to co-opt them rather than
confront them. The private sector practitioners range from General Practitioners (GPs) to the super
specialists, various types of Consultants, Nurses and Paramedics, Licentiates, Registered Medical
25
Practitioners (RMPs) and a variety of unqualified persons (quacks). The practitioners not having
any formal qualifications constitute the 'informal' sector. The above practitioners may practice
different systems of medicine, ranging from Allopathy to yoga. The institutions range from single
bed hospitals to large corporate hospitals, and medical centers, medical colleges, dispensaries,
clinics, polyclinics, physiotherapy and diagnostic centers, blood banks, etc. The private sector in
India has a dominant presence in the provisioning of medical care among other areas. Over 75 per
cent of the human resources, 68 per cent of an estimated 15,097 hospitals and 37 per cent of
623,819 total beds in the country are in the private sector. In such circumstances, no policy maker
can afford to ignore this rich resource.
One feasible option that has been tried in many countries is for the government to purchase
care from the private providers, especially for those services that are not provided by the
government. One little known example is the case of the National Health Service in the UK. While the
government finances the entire health care through tax revenues, it purchases care from the famous
general practitioners who are actually private practitioners. Similarly, the German government uses
social health insurance to finance health care in the country. It collects payroll contributions from
employees and employers, pools the funds together and then purchases care from both private GPs
as well as private hospitals. There are no or very few government facilities, the majority of providers
in this socialist country is from the private sector. In both the above examples, the main difference
between them and India is the strong regulatory framework that exists and is implemented
diligently. Thus there are rules on who can practice, where they can practice and what they can
practice. There are bodies that oversee the practice to ensure that the providers follow the
standards. And if providers do not comply with any of the rules and regulations, there are bodies
that take action. Hence the private sector in these countries is made to act for the public good.
Provi sion of care
Private
Public
Financing of care
Totally
government
provided. This requires:
Public
•
•
•
•
Private
funded
and
Enough revenue from taxes
Enough
resources
(human,
infrastructure,
medicine
and
consumables)
Reforms, especially vis-a-vis human
resources, medicines,
A good governance structure that
can make the staff accountable to
deliver the desired outputs and
outcomes.
Not desirable
Purchasing care from the private sector.
This requires:
•
•
Adequate private sector
Capacity of the government to
actually
purchase
care
and
implement
the
necessary
conditions.
•
Strong regulatory mechanisms to
ensure that the private sector
provides the required services
Current status - not desirable at all.
From the above table, it is clear that the financing of health care should be by the government,
either through taxes or through insurance premiums. There is no doubt about that. Financing by
individual households is not acceptable in today's environment. Then the debate is about provision
of care. This can be provided by the government, or by the private ora mix of the two.
26
The important question that the state needs to answer is - do we expect the government
health services to provide all the services? Does it have the resources in terms of qualified
professionals? Or do we need to purchase services from the private sector? In many instances, there
may be enough resources within the government to provide the services. However, in other
instances, in the short to medium term, it may be more efficient to purchase care from the private
sector. A good example of this is immunisation services in urban areas. It may take a lot of resources
and time to establish a network of primary health centres to cover the entire city. However, the
government can identify select private practitioners and provide them with the necessary
equipment (refrigerator, 1LR and UPS backup) so that they can store the vaccines and provide
immunisation services to the children in their catchment area.
The assumption here is that all state governments have its own health services in place with
a primary health centre, a community health centre and a hospital for defined populations. And that
there is a thriving private health sector whose services can be purchased.
For the sake ofclarity, we would like to define some terms that will be used in the coming sections.
Government health providers mean the Primary Health Centres, the Community Health Centres,
the Taluk Hospitals, the District hospitals, the Government medical colleges, the government
maternity centres, the Urban Health Centres, etc.
Private health providers mean the formal (Allopathic orAYUSH) practitioners like single doctor
clinics, nursing homes, polyclinics, multi-speciality hospitals, single speciality hospitals, private
medical college hospitals, corporate hospitals, etc.
Purchaser of care is the government health directorate (or department) who purchases care from
either the government or the private health providers. One may debate the artificial divide between
government health providers and the purchasers of care, but this is necessary as they have two
different roles.
However, purchasing care is not easy and requires a lot of skills and knowledge. We have
tried to equip the reader with some information about various ways of purchasing care. Details on
howto purchase care is provided in Table 4 and Annex 3.
27
Table 4 : Various mechanisms for purchasing health care from the private sector
Purchasing
mechanism
Ideal for purchasing
Remarks
From
The following
services
Through salaries
Government health
providers
l*/2* / 3*
This is the usual mechanism
used by most governments
Payment for
performance
Government health
providers
1* / 2* / 3*
This incentivises
performance in government
health facilities
Capitation method
Government /
Private health
providers
1*
Requi res the provider to
take responsibility of a
population and the
purchaser to calculate the
cost of the services to be
purchased
Diagnosis related
groups (DRG)
Government /
Private health
providers
2* / 3*
Requires the purchaser to
calculate the cost of the
services to be purchased
Per diems
Government /
Private health
providers
2* /3* usually medical
care
Requires the purchaser to
calculate the cost per day of
the services to be purchased
Fee for service
Government /
Private health
providers
l*/2*/3*
Not recommended as it has
the potential for escalating
costs
Vouchers
Government /
Private health
providers
1* / 2* / 3*
Health equity funds Government /
Private health
providers
2* / 3*
Contracting in of
clinical services
Government health
providers
1* /2* /3*
Contracting out of
facilities (PHC /
CHC)
Government health
providers
1* / 2* / 3*
Useful way of channelizing
social assistance funds
1* / 2* / 3* = primary, secondary and tertiary care respectively.
As one notes from the above table, the moment that the private sector is involved, it is
imperative that the cost of the service is obtained. This will prevent frauds and cost escalations.
Also one can mix and match these methods; for example a government can decide to
purchase primary care services from existing government providers through a salary mechanism
and secondary care services from private providers through a DRG mechanism.
28
Table 5 : Some examples of how other countries purchase care
Hospital care
Primary health care
Name of country
Provider
Payment
mechanism
Provider
Payment
mechanism
Thailand
Government
Capitation
Government
Capitation
Indonesia
Government
Salary + Capitation
Government
Fee for service
Canada
Private
Fee for service
Government
Salary
Taiwan
Private
Fee for service
Private
Fee for service
United Kingdom
Private
Capitation
Government
Salary
Germany
Private
Capitation
Private
Salary
However, it is important that the department has a separate cell to prepare the contracts
with the private sector, to monitor the utilisation of the scheme and also to ensure that it remains
cashless.
To conclude, financing and provision of care by the government has its advantages and
disadvantages. Also, given the epidemiological and demographic transition, the challenges of
provision may be too many to be handled by the government alone. Instead, it would be more
efficient to purchase care from the private sector, so that services reach the needy and vulnerable
as soon as possible.
If India wants to achieve UHC by 2022, it would be advisable to use the existing
private health providers to supplement the government efforts. The government trying
to provide all the services may not be feasible in the short to medium term.
29
WHAT ELSE IS REQUIRED TO ACHIEVE UHC?
While most of the debate and discussion on UHC has been limited to financing UHC and also
on the WHO cube, one should not ignore certain important steps that are required to ensure that
UHC is achieved.
Governance
Most countries that started on the path to UHC introduced enabling legislation that ensured
that the government could move ahead without too many obstacles. For example, Mexico
introduced a series of regulatory acts during the SSPH reforms. These varied from regulation of drug
safety to certification of providers. These laws enabled the government to ensure that the measures
that they introduced were effective.
Monitoring
This is a crucial activity if a country wants to achieve UHC. Monitoring can be through routine
data or from special studies. Thailand's research unit regularly conducted studies to monitor access
and utilisation of services and the extent to which patients incurred out-of-pocket payments. This
body of knowledge helped the government introduce a watertight plan for UHC soon after Mr.
Thaksin was elected in 2001. Also, what is important, especially in a country like India is the shift
from input based monitoring to outcome oriented information system and performance based
monitoring.
Support services
It is not enough to provide resources for UHC, this should be accompanied by expansion
of the support services like supply of medicines, use of technology and production of allied
health staff.
Quality and equity
In the rush to achieve UHC, it is easy to lose sight of quality and equity. To prevent this,
indicators to measure these should be part of the information system and should be monitored
incisively. The policy makers should monitor to ensure that the poorest are not the ones falling
through the safety net. In an effort to cut cost and be more efficient, quality is not compromised.
30
CONCLUSIONS
It is not acceptable that lakhs of mothers and children die every year because of
inadequate health services in a country like India. It is a shame that millions of Indians are
impoverished every year because of medical expenses. It is a matter of concern that every year
lakhs of young hypertensive patients end up with a stroke and become economically unproductive.
It is time that we come together and put an end to this unnecessary suffering.
The tools are there, the resources are available, it is a question of bringing all this
together for a vision where every single Indian will have affordable and equitable access to quality
health services. And, in this journey, we cannot afford to delay any further.
If we decide to move towards UHC, then there are certain basic changes we need to bring
into the existing health systems. The most important is the way of thinking. We need to go beyond
disease control programmes and tailor our services to the needs of the people. And, the people
(like all of us] want assured ambulatory, emergency and inpatient care that is affordable. The
second change that we need to bring is to infuse more resources into the health services. And, finally
we need to stop ignoring a huge resource that exists within our country and needs to be
used, the private sector. Having said that, we need to introduce important legislation to regulate
the private sector before using them, so that they perform for the public good rather than for
profit. One legislation that needs to be introduced into all the states immediately is the
Clinical Establishment Act. Until and unless we define the private sector, it will be difficult for us to
work with them.
We have been guilty of focussing on the poor in this manual. We have not come up
with possibilities for the middle class or the rich. We have neglected them purposely to keep
this manual short. However, they are important stakeholders, and needs to be considered when we
make plans for UHC in our state.
This manual is a work in progress. It is not the ultimate document on how India can
achieve UHC. It is the outcome from years of experience in the field and from observing the way
the Indian health system functions. We recognise that much of this experience may be different
in different contexts and if seen by different lens. Hence, we welcome suggestions, comments,
advise, opinions from our learned and experienced colleagues so that we can improve on the
second edition. Please do write to us atmail@iphindia.org
31
References
1.
Planning Commission. Health Chapter®: 12th Plan. 12th Five Year Plan. New Delhi:
Governmentof India; 2012. p. 1-71.
2.
Carrin G, James C, Evans D. Achieving universal health coverage: developing the health
financing system. World Health.Geneva; 2005 p. 1-11.
3.
Commission on Social Determinants of Health. Closing the gap in a generation: Health
equity through action on the social determinants of health.Geneva; 2008 p. 1-256.
4.
World Health Organization. The World Health Report 2008. Primary Health Care: Now
more than ever. Geneva: WHO; 2008. p. 1-148.
5.
World Health Organization. The World Health Report: health systems financing: the path
to universal coverage. Geneva; 2010 p. 1-128.
6.
Barnighausen T, Sauerborn R. One hundred and eighteen years of the German health
insurance system: are there any lessons for mi. Social Science and Medicine. Department
of Tropical Hygiene and Public Health, Medical School, University of Heidelberg, Germany
till_baernighausen@yahoocom; 2002 May;54:1559-87.
7.
Bang A, Chatterjee M, Dasgupta J, Garg A, Jain Y, Shiva kumar A, et al. High level expert
group report on Universal Health Coverage for India. Bangalore; 2012 p. 1-343.
8.
Ministry of Health and Family Welfare. Report of the National Commission on
Macroeconomics and Health.Health (San Francisco]. New Delhi: Government of India;
2005.p. 1-192.
9.
National sample survey organisation. Morbidity, Health Care and the condition of the
aged.Health Care. New Delhi: Ministry of Statistics and Programme Implementation;
2006. p. 1-482.
10.
World Health Organization. Definition of health services [Internet], Available from:
(http://www.who.int/topics/health_services/en/ )
11.
World Health Organization. The World Health Report 2000. Health systems: Improving
performance. The World Health Report 2000. Geneva: WHO; 2000. p. 1-215.
12.
Prinja S, Bahuguna P, Pinto AD, Sharma A, Bharaj G, Kumar V, et al. The cost of universal
health care in India; a model based estimate. PloS one [Internet]. 2012 Jan [cited 2012
Apr 21];7(l):l-9.
13.
Ministry of Health and Family Welfare; Annual report to the people on health. New Delhi;
2010p. 1-55.
/, A,/ Lrnc. ■
(p(
Koramanga
32
Annex 1-Health indicators in India, vis-a-vis the MDG goals
Initiatives, like the NRHM and the RSBY are efforts by the government of India to provide health care
to its citizens with minimal financial burden for the beneficiary. However, even today, inspite of all
these measures, the health status of Indians is disappointing. Results from various studies show
that we are still far away from the Millennium Development Goals (MDG). This is depicted in the
figures below. These aggregate figures hide vast disparities between states; between social,
geographical and economic sub-groups within states and between programmes.
33
Eighty per cent of Indians still use the private health sector for outpatient care, many still
spend money even for 'free' government health services and more than 60 million are impoverished
every year because of high medical expenses. While BPL families are benefitting from the RSBY
to some extent, they still need to make out-of-pocket (OOP) payments for outpatient care. On the
other hand, there is no such protection for the near poor or for the low and middle-income families.
Even basic services like safe drinking water, sanitary toilets and primary immunization are
not available for the 'bottom of the pyramid'. A recent UNICEF report states that only 50% of
tribal children are fully immunized and that only 40% of pregnant women in the poorest quintile
could deliver in a facility.
Figure 9 : Maternal mortality ratio in India
Source: SRS bulletins.
MDG target for India for 2015 is 1.1.
34
Annex 2 - Estimating the cost of UHC
How much will these services cost? This is the million-dollar question that the finance department
will ask and which the health secretary needs to answer. This will depend on the services that need
to be strengthened and the extra population that needs to be covered. In the following table, we
share some of the calculations made by the National Commission on Macro-economics and health
(NCMH). While these figures are of 2005, the process of calculation can help each state to estimate
the costs for extending services to new population groups, or for introducing new services into
existing populations. Note that Table 5 has only a few conditions; the NCMH Report has a more
extensive list. The states can use this format, with the caveat that the disease burden estimations
and the cost calculations are based on 2005 figures. This (especially the cost) may have changed
over time, so the element of inflation needs to be factored in. Also the disease burden estimations
were done on a national level, it will vary from state to state. For example, the burden of malaria will
be higher among the eastern and north-eastern states as compared to southern and western states.
So each state needs to calculate its own burden from the existing data that is available. The purpose
of this is to permit policy makers come up with figures to answer the finance ministry queries.
Snake bite
treating a
population of
100,000* (3)
treating one
patient' (2)
202,824
32%
21%
12%
12%
35%
141.49
424,500
12%
0%
4%
4%
84%
209.82
630,000
51%
0%
5%
5%
44%
278.46
667,200
11%
0%
56%
56%
34%
86.89
52,200
30%
2%
0%
0%
68%
840.98
302,760
38%
0%
28%
28%
30%
150.60
10,542
19%
0%
13A
6%
62%
462.65
166,554
49%
0%
0%
27%
24%
Human
resources
84.51
Cost of
Cost of
(1)
System cost
Antenatal
care
IUCD
Insertion
TB (sputum
+ve)
Malaria (pf)
Medicines
Diarrhoea
Diagnostics
ARTI
~ 2.4% of
population
~ 3% of
population
~ 3% of
population
- 2.4% of
population
~ 0.6% of
population
~ 0.36% of
population
~ 0.07% of
population
~ 0.36% of
population
Cost according to components
Equipment
Immunisation
Estimation of
disease load
/
Diseases
health
conditions
Table 6 : Cost estimation of select health / disease conditions (2005)
Source: NCMH: 2005 (http://www.who.int/macrohealth/action/en/ )
1 The cost is calculated based on cost of the medicines, the time spent by individual staff members for that activity and
finally on the equipment and infrastructure required.
’ The total cost of treatment for a population of 100,000 will be [(1) x (2) x 100,000]/100
35
A simpler and cruder method to assess the total cost is given in the table below. It is based on NSSO
(6O'h round) data. We have used the price in the private sector as a proxy for the cost of that service.
Similarly, we have calculated, using the 2004 figures in terms of price as well as incidence. Matters
would have definitely changed in the interim 8 years, but again, this rough and dirty method gives us
a clue about the amount of finances that the state will require to expand coverage, both of services
and of population. From this calculation, one arrives at an expenditure of about Rs. 1,284 per person
per year for primary and secondary care. This is substantially lower than the amount that WHO
recommends (US$ 35) for covering the total population with comprehensive care. The reason is that
many other health services are not covered, e.g. TB care, many other preventive services, etc.
While there are no exact estimates, these calculations give the policy makers some idea about the
amount required to achieve UHC. He /she can estimate that it will cost about INR 1500 per person
per year on providing comprehensive care. This can be a safe estimate as at least 40 - 50% of the
people anyway go to the private sector for seeking care.
Table 7 : Cost estimations based on NSSO (60“ round) data for a state with a population of 6crores
Incidence rate (1)
Unit cost (2)
Population (Crores)
(3)
Total cost(crores)
(4 = 1X2X3)
OP
1.17
300
6
2,106
Chronic disease
1.43
300
6
2,574
Inpatient
0.03
11550
6
2,079
Tertiary care
0.001
150
6
0.9
Immunisation
0.9
113
6
610
ANC
0.02
300
6
36
Delivery
0.02
2500
6
300
Total cost
7,706
Cost per capita
1,284
Disclaimer: Note that many other services are not covered in this calculation. The state can add as per their
requirements, but use the existing formula to arrive at the requirements.
36
Annex 3 -Tool to monitor the status of UHC
This template is useful to document where each of the states are in their march towards
UHC. This template should be copy pasted onto an excel sheet and the data entered
accordingly
Indicators
QI (poor)
Q5 (rich)
% of women who have delivered in a facility3
% of children (between 12 and 23 months] who have
received full immunisation4
Outpatient contact rate per population per year5
Inpatient admission rate per 1000 population per
year6
Corrected out-of-pocket payment’
% of patients who received free inpatient services8
’Formula = (number of women who delivered in a year in a facility x 100)
Total number of women who have delivered in that year
The source for this information is from NFHS or DLHS or from UNICEF’s coverage evaluation survey
‘ Formula = (number of children between 12 and 23 months who have received full immunisation x 100)
Total number of children between 12 and 23 months
The source for this information is from NFHS or DLHS or from UNICEF's coverage evaluation survey
’Formula = Number of outpatients seen in the entire state in a year
Total rural population in the state
The source for this information is from the routine HMIS that the health department collects.
’Formula = Number of inpatients seen in the entire state in a year x 1000
Total rural population in the state
The source for this information is from the routine HMIS that the health department collects.
'Formula =1 x 1000
Median (average) out of pocket expenditure spent by patients for any direct health care {op + ip+ ..)
The source for this information is from the NSSO 60lh round
’Formula =
Number of inpatients who did not have to pay any money for inpatient care
Total number of inpatients
The source for this information is from the NSSO 60,h round
37
Annex 4 - Provider payment mechanisms to procure private
provider services
Salaries
Salaries are an administratively simple remuneration method, but can only of course cover the
costs of personnel (and not other provider costs, such as drugs and medical equipment).
Salaries have performance-related aspects related to underproduction. It requires strong
monitoring mechanisms and supportive supervision to overcome this problem.
Performance based funding
One of the ways of overcoming the problems of salaries is to provide incentives based on
performance. Health providers are paid a basic amount and any further increase in funding is
paid on the performance of the provider who may be an individual or institutional provider. The
main strength of this method is that the provider has an incentive to provide more services to the
individuals to increase the performance and would also lead to competition. However in an effort
to increase performance, the quality of care (in terms of over performance and performing
unnecessary treatment) may suffer if adequate monitoring is notin place.
Budgets
Budgets can be set for providers, (usually in the government health services) which if strictly
fixed, help contain costs. As with capitation, this is because there is no link between the quantity
and mix of health services given to the individual and the amount received by providers. Their
ability to contain overall costs, though, is limited if the budget is insufficient and results in others
having to provide the necessary care. Further, when budgets are not entirely strict, and as they
are often based on historical costs, there is no incentive for providers to minimize costs, and even
an incentive to exceed the budget ceiling. Transfer of cases is also likely, along with
underproduction and waiting lists.
Capitation
Many states have problems with providing primary health care for vulnerable populations.
Especially in remote areas. Usually there is a shortage of staff, especially medical officers. One way is
to use private sector providers. However, one weakness is that monitoring of the services provided
by these private practitioners can be difficult. One potential solution for this is to purchase care from
the private practitioner using capitation method.
What is capitation method?
It is a way of purchasing care from a provider for specific services on a per capita
basis. The steps are as follows:
38
Step 1: Identify the services that need to be provided by the private practitioner. It
could range from just immunisation services to antenatal care to the entire package
of primary health services. Capitation is useful for primary care services, but very
complex for hospitalisation services.
Step 2: Once the services have been decided, then the cost of delivering these services
should be calculated. This will include the cost of medicines, diagnostics, provider
fees and overheads. Assume that this is Rs X per person
Step 3: Identify private practitioners who are willing to partner with the government
in providing the above-mentioned services.
Step 4: Inform the population that henceforth the specific services will be provided
by Dr Q or Dr Z who are private providers. If they desire to receive care from Dr Q, then
they will have to register with Dr Q at the beginning of the year. This may involve going
to the clinic and receiving a card, by paying a token amount of Rs 5 per family. Or this
can be decentralised to the HSC / ASHA level, who will issue the card and receive Rs 5
per family.
Step 5: Once the list of registered households are submitted to the government
(District / Block / PHC RKS) by Dr Q and by Dr Z; then they pay the provider upfront
Rs X times the number of families (or individuals] registered with the practitioner.
Step 6: In turn, the providers are now expected to provide 'free' services to all those
who come to him/her with the card.
Thus, the services are provided by the private practitioners and are reimbursed by
the government through an administratively simple method. There is no need to
monitor bills, or the number of patients, etc.
Advantages of capitation method of purchasing care:
1.
Minimum structural changes in the health department.
2.
Monitoring requirements are minimal
3.
People can vote with their feet. If a practitioner's performance is inadequate,
they can shift over to the competition the next year.
4.
It can be used both in private as well as public facilities.
Disadvantages of capitation method
1.
There must be some expertise within the state to cost the package of services.
2.
Providers (either government or private) must be available.
3.
a
Chances of providers providing inferior quality of services (to maximise profits) are
possibility. E.g. if providers are asked to provide antenatal services through a
capitation method; they may not do ultrasound scans for the patient, thereby saving
on that cost. This can of course be countered with proper IEC to the community.
4.
Providers may unnecessarily refer patients to higher levels to minimise their
expenses. Monitoring the referrals and/or placing charges on the provider for each
referral can curtail this.
39
Case based payments
Of late, many government sponsored health insurance schemes have been using private hospitals to
provide inpatient care. This is to improve access to hospital care for the population. One unique
aspect about these schemes is the way of reimbursing the hospitals. Instead of paying the hospitals
on a fee-for-service basis, they pay on a diagnosis related group (DRG) basis.
DRG basis of reimbursement is to pay hospitals a fixed rate for common procedures. For example, if a
hernia operation has to be done, then the insurance company will reimburse the hospital a flat rate
of Rs 10,000; irrespective of the costs involved for that particular case. It is in the interest of the
hospital to provide this surgery at less than Rs 10,000 so that they do not make a loss. The
Yeshasvini health insurance scheme in Karnataka was the one who pioneered it, but now this is
being used by various schemes like the RSBY, the Vajpayee Aarogyashree Suraksha, the Rajeev
Aarogyashree and the CM's health insurance scheme, etc.
The main advantage of this way of purchasing care is that there is minimal administrative burden.
The hospital has just to inform that they have conducted the specific surgery and they get
reimbursed for that. There is no need for anybody to check the bills, etc.
The disadvantage of DRG, which is being seen in many of the above mentioned schemes is the
tendency of hospitals to charge the patients as well as the insurance company. Patients, especially
those who are not aware will be asked to buy medicines and consumables (though this is covered
under the package]. This has to be monitored closely and can easily be done today through a simple
phone call on the patient's mobile. Further, there is an incentive for providers to diagnose more
severe - and thus lucrative - cases, and/or to transfer the more complicated cases towards other
providers (especially government providers).
To introduce such a way of reimbursing private hospitals; one requires that packages need to be
costed. While this is a laborious and difficult task, we have the advantage that a lot of secondary care
is already priced under the RSBY and most tertiary care is priced under the CGHS, the VAS, the RAS
and CM H1 schemes. So there is no need to reinvent the wheel.
Per diem
This is yet another easy method to reimburse hospitalisation expenses. It has been used in RSBY
wherein the scheme reimburses hospitals a fixed amount (Rs 500) per day of hospitalisation for
a medical condition, e.g. pneumonia. So all that the purchaser of care has to do is confirm
whether the patient indeed has been admitted for the stated number of days. This can be
through document checks or through a simple telephone call to the patient. If validated, then the
purchaser has to reimburse the hospital Rs 500 x the number of days hospitalised. To minimise
abuse of the system, maximum days for hospitalisation can be fixed for each medical condition.
Its main strength is in its simplicity. However, there is evidence to suggest that it can be abused
by hospitals who admit a patient for 1 day and then claim bills for 10 days of hospitalisation. Or
actually keep the patient unnecessarily for many days, to increase their income. However, these
40
are not insurmountable problems and can be managed. One issue that however needs to be
addressed is to fix the price per day. It needs to be an average of the costs of medical conditions
that are common to that area. For example, in some states, malaria may be the main problem; but
in others diabetes and hypertension maybe the main problem.
Fee for service
Fee-for-service for both ambulatory and inpatient care is a mechanism whereby providers are
paid for each service or act provided to a patient. Its perceived strength is in terms of quality: by
encouraging providers to provide health services. However, this incentive effect is also its main
source of criticism: fee-for-service is often criticized for encouraging an overproduction of health
services (supplier-induced demand), as providers are paid for each service given. Fee-forservice payments also encourage doctors to increase their volume of services rendered, most
often by decreasing the quality of each service. Further, administrative costs are likely to be high,
because of billing costs, reimbursing fees and monitoring/adjusting fee schedules.
This is the traditional manner in which insurance companies have been purchasing care from
private providers. It is a process that is understood by hospitals but has many disadvantages:
1.
It encourages the hospitals to perform unnecessary investigations and provide unnecessary
treatment, so that they can maximise their income.
2.
It is administratively very difficult as the company has to go through each item in the consolidated
bill-will have check if there are documents for the 6 IV fluids, if there are prescriptions for the 20
paracetamol tablets, etc.
Most health economists do not encourage Fee for service as a mechanism to reimburse health
care as it encourages cost escalation and unnecessary treatment to maximise profits.
Contracting in of services
Many times government health services may not have the required skilled professionals to provide
the necessary services. A classic example is the dearth of obstetricians and anaesthetists at the FRU.
On the other hand, there may be many obstetricians in the private sector, working in nearby private
hospitals. One possibility is to acquire the services of the required professional through a
"contracting in" mechanism. This has been tried out under NRHM with varying success. In some
states, it has proved successful, in others, specialists have been reluctant to join the services even
after being promised reasonably high salaries. There are many reasons for this, ranging from
inadequate compensation, to the work culture in a government facility to the lack of technical and
administrative support. To overcome some of these obstacles to contracting in, one may need to take
the following steps:
1.
In blocks I taluks / districts where the government has not been able to fill up the vacancies of
essential specialists like obstetricians, paediatricians, anaesthetists, the district health society
should be given the permission to contract in of these services.
2.
The district health society then should be able to negotiate with the concerned specialists for
the services. This may range from one specialist providing the entire service or a group of
41
specialists agreeing to a rota system, wherein the specialist who is free arrives to provide
the service. To give an example, there may be 3 anaesthetists in the district who are working
in the private sector. While ideally, one of them should be contracted in, it may happen that
none of them may be willing to provide full time services to the district hospital. One way
out of this is to use a rota system, wherein the anaesthetists are contacted in turn and
whoever is free at that time is invited to help out with the surgery. The District Health Society
needs of course to negotiate a mutually acceptable price for the service, either by the
numbers or by the time required, etc. And most important, the payment should be made
as soon as possible and with minimumadministrative work. Also it must be made very clear
who takes the responsibility of the patient after the departure of the specialist.
The main advantage is that the government is optimising the use of scarce human resources
by using available manpower. The disadvantage is that it is difficult for the contracted in specialist
to take on the responsibility, without being given the powers to execute.
To contract in services, one requires that financial and administrative powers be delegated to the
district level. Without this, it is difficult to manage contracts from the state level. Second, there must
be enough private practitioners who are willing to partner with the government health services.
And finally, the district health society should have the capacity to draw up a contract and also
monitor its implementation. This would require that the society review the performance of the
contracted in staff in terms of number of services provided, the time required to reimburse the
staff and sort out any problems that may have risen during that month.
42
No. 250, Masters Cottage,
2nd ’C Cross, 2nd 'C Main,
Girinagar, 1st Phase, Bangalore -560 085
Tele-Fax no: +91 80 26421929
Phone no: +91 08 264121929
E-Mail ID: mail(5)iphindia.org
Website: www.iphindia.org
Position: 3090 (2 views)