KARNATAKA HEALTH CARE SYSTEM.pdf
Media
- extracted text
-
»> *>
*» *» < *» *> *> *♦ *> •’
< *»
* F’ * > * »
•>?
>
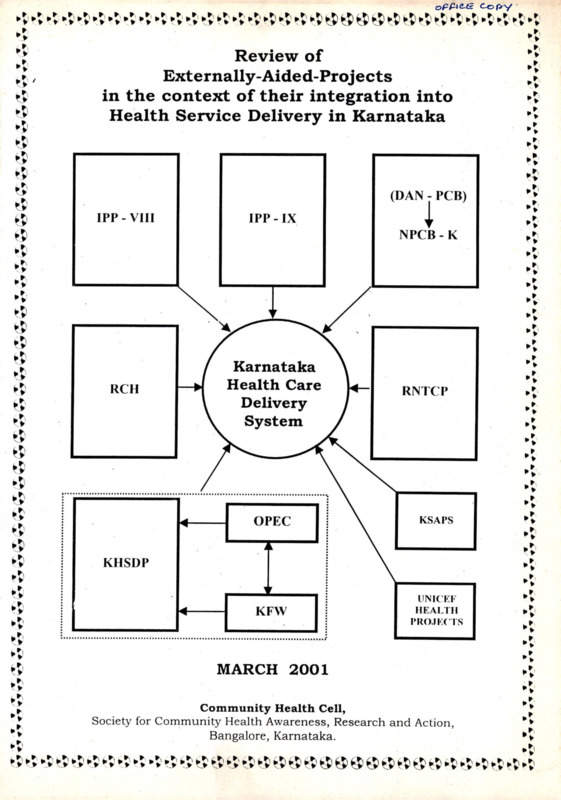
Review of
Externally-Aided-Projects
in the context of their integration into
Health Service Delivery in Karnataka
*»
$
(DAN - PCB)
IPP -VIII
*>
IPP - IX
NPCB - K
Karnataka
Health Care
Delivery
System
RCH
RNTCP
»>
*»
OPEC
KSAPS
KFW
UNICEF
HEALTH
PROJECTS
KHSDP
*>
4
*v
MARCH 2001
Community Health Cell,
Society for Community Health Awareness, Research and Action,
Bangalore, Karnataka.
*5 •-.>
»»*»' < >X' >5 t’P
>>'
®
®
W & €S
**
Content List
f-
A - Introduction
1
B - General Description of Externally Aided Projects (EAP’s)
4
C - Project Goals, Focus and Distribution
7
D - Overview of Programmes and Activities
15
E - Overall Strengths and Weaknesses of EAP's
17
F - Lessons from some Case Studies
26
G - Some Policy Imperatives Including Integration and
Sustainability
30
II - Some Reflections on Financial / Economic Implication of
EAP’s
38
I - General policy concerns : Are we reinventing the wheel ?
41
J - Final Conclusions and Recommendations from a future
policy point of view
44
K - Limitations of the Review Exercise
48
L - Acknowledgements
49
M -Bibliography
50
N - Tables
I Externally Aided Projects - General Description
II Objectives / Focus / Regional Distribution
III Programmes and Activities by - Review of Budget Heading
IV Some Strengths and Weaknesses
5
8
15a
19
O - Case Studies
A. Training Experience in a Northern District
B. An Urban Health Centre
27
29
P - Appendices
i)
ii)
Project Proposal
Some issues and questions addressed in the review
A conceptual framework for review - Diagrammatic presentation.
PROJECT REPORT: Review of Externally - Aided - Projects (EAPs) in the
context of their integration into Health Service Delivery
in Karnataka.
A: Introduction
Since the early 1970’s the Karnataka Government has negotiated and received
various grants and loans from international funding agencies, including the World
Bank, for health related projects that supported the growth and strengthening of
primary and secondary health care services in the state. These externally aided
projects have had their own particular focus; objectives; framework; operational
strategies; and management information systems geared to support and or enhance
both quantitatively and qualitatively, different aspects of Health Sector
Development in the state. Each of them has their own cycles of mid-tenn reviews
and concurrent reviews. The Human Development in Karnataka Report 1999
described five of these (see box).
Currently there arc however atleast ten major externally aided health projects in the
state- IPP VIII, IPP IX, KHSDP, OPEC, KfW, RCH, RNTCP, NACO, NLEP,
DAN-PCB being implemented through the Government and Directorate of Health
and Family Welfare Services. In addition UNICEF has provided project support to
different health related sectors including Child Development and Nutrition; Water
and Environmental Sanitation; Education; Child Protection; Communications and
Strategic Monitoring. For the purpose of this Review all UNICEF Projects have
been taken together as one and NLEP has been left out for unavoidable reasons.
Health related externally aided projects, e.g. for nutrition, water supply and
sanitation, implemented through other departments are not included under the scope
of this review.
The Karnataka Task Force in Health, while reviewing these projects in their
interactive and informal discussions and deliberations have raised some important
questions for review and enquiry:
i)
ii)
iii)
What are the learning points from each of these projects?
How can they be integrated into the health system incorporating beneficial
points and avoiding distortions.
What has been their experience concerning issues of sustainability,
accountability and transparency.
In the late 1990’s, policy researchers, academicians and decision-makers have also
begun to seriously review the “piecemeal pursuit of separately financed projects” as
against ‘the evolving options of more appropriate sector wide approaches*. This is
linked to the growing recognition of some of the problems associated with single
-1 -
Important externally assisted health projects
Karnataka Health Systems
Development Project
(KHSDP)
Kreditanstalt fur
Wiederaufbau (KfW)
India Population project
(IPP) VIII
India Population project
(IPP) IX
Reproductive and Child
Health Services (RCH)
Project
The Karnataka Health System Development Project is proposed to be
implemented over five years (1996-2001) with assistance from the
World Bank.
Its main objectives are improvement in the
performance and quality of health care services at the subdistrict and
district levels, narrowing current coverage gaps and improving
efficiency.
Major components include improvement of the
institutional policy framework, strengthening implementation
capacity, development of a surveillance system, extension and
renovation of all secondary level hospitals, improvement of their
clinical effectiveness and establishment of a properly functioning
referral system. The project outlay is Rs. 546 crores.______________
The KfW of Germany is financially assisting a project in the four
districts of Gulbarga division with objectives similar to those of the
KHSDP. The project outlay is Rs.59 crores of which 90% is being
provided by KfW as a grant. The project was launched in 1998.
IPP VIII is being implemented in the slums of Bangalore since 199394 with World Bank assistance. Major objectives are improvement in
maternal and child health and reduction of fertility among the urban
poor.
Strategies adopted include involving the community,
improving the quality of services provided by the City Corporation,
strengthening existing delivery services, establishing new facilities
and providing services at the doorsteps of the urban poor. The
project cost is Rs.39 crores.
This is the fourth in the series of India Population projects following
IPP I and IPP III. The project is under implementation since 1994 in
13 districts. The main objectives are reduction in the crude birth and
death rates as well as the infant and maternal mortality rates and
increase in the couple protection rate. Strategies adopted include the
promotion, strengthening and delivery of services through the
involvement of the community and improvement in the quality of
services by providing training and strengthening the monitoring and
evaluation systems. The project outlay is Rs, 122 crores.
The Reproductive and child Health Services Project marks a change
in the existing culture of achieving targets by shifting to a policy of
provision of quality services. The project helps clients meet their
own health and family planning needs through the full range of
family planning services. It is a natural expansion of the earlier child
survival and safe motherhood programme which was under
implementation till 1996.
It also includes the treatment of
reproductive tract infections, sexually transmitted infections and the
prevention of AIDS. All the districts of the state are-proposed to be
covered under the project.
The budget for RCH project for five years (1997-98 to 2002-03) is
Rs. 190 crores.
Source : Human Development in Karnataka - 1999
-2-
focus sector project assistance, which include:
• Fragmentation;
• Conflict and or duplication;
• Donor driven agendas;
• Recurrent operational costs;
• Undermining of national capacities,
• Lack of flexibility,
• Varying standards of provisions, and
• Issues of ownership.
This short-term interactive review has been undertaken to explore some of these
issues and address these concerns in the context of the Task Force recommendations
for the Health Sector development policy for the state.
Within the time constraints, the researchers have tried to achieve the following:
a)
Review all the externally aided projects not just individually but in their
collective context reviewing available documentation as well as interacting
with programme managers.
b)
Using a SWOT approach, trying to identify the key strengths, weaknesses as
well as opportunities and threats (distortions) from all these projects.
c)
Trying to do this review in such a way so that the stakes of programme
managers and hopefully the Health Directorate to learn from project
experience and address seriously the concerns and issues of sustainability
and integration are enhanced especially by improving in-house capacity and
system development.
(See Appendix "A" for Project protocol and issues and questions to be addressed.)
-3-
<r
c Cz)
-------
f
y
p,
Co C
--------
J PP Sx y Kf
!/- HSP P,
B: General Description of EAP's
Table I shows the 10 EAPS included in the review. From the table the following
key general observations on EAP's in Karnataka can be made.
1. Number
•
3
•
There are ten EAP's which contribute to the Health Service Delivery in the state.
(NLEP has not been included in the review fully).
World Bank ; Main player
While UNICEF and DANIDA have been long standing partners since 1970’s the
World Bank has become the key partner now supporting six out of the ten
projects (this is particularly so since the 1990’s) and there is reason to believe
that since the World Bank takes over as the key player the other funding partners
are getting some what sidelined or ignored.
Grant to Loans in the 1990,s
•
•
While the earlier bilateral donors were providing grants like UNICEF and
DANIP^, the trend in the 1990's has increasingly moved towards maMy loans
rather than grants with varied interest rates and associated conditionalities. The
World Bank support being mainly in this category it is therefore even more
important today to ensure that these loans are utilized efficiently with greater
accountability and transparency since if they were misutilised then we would
have the double problem of ineffective utilization coupled with a debt burden.
/
The German government (KfW) and the Organisation for Petroleum Exporting
Countries through the OPEC fund have joined World Bank in supporting
primarily infrastructure development. The former is a grant and the latter is a
soft loan to be paid over a twelve year period after a five year initial gap.
Stand alone
• Each of these projects are relatively distinct entities with clear cut objectives,
framework, programmes and though they have to be complementary or
supplementary to each other due to overlap at the field level (similar districts,
health centres, health teams) this is not at all emphasized in the project reports or
built into their outlines. There is a fair degree of compartmentalization and
hence they mostly stand alone with little dialogue between projects and seldom
visualized as smaller components of a larger strategic plan.
.V\ I - z-^ o
ICHSp^p
^C>F
ZP
Z-P
<^f-C ce
o
/
-4 -
r-C
^-<4.
J
e: C. ’VM-M
<rlee
c C-
u/
rt
SienW
TABLE -1
Externally Aided Projects in Health Service Delivery in Karnataka
GENERAL DESCRIPTION
S.No / Name
India Population
Project
IPP VIII
(Family welfare - urban
slums project)
1.
Year of
Starting
1993-94
^y^Aipoupt
of GraptA
'loans iff Rs.
World Bank
39 Crores
f y Improvement in MCH & (387.2million)
Fertility Reduction in
Loan
Bangalore's urban slums
.
2.
India Population
Project
IPP IX
1994
(Strengthening of Family
welfare and MCH services)
3. Karnataka Health
Systems Development
Project (KHSDP)
7^6^
* Short Description
tftxxr Ko SfV'
1993-2001
(in phases)
J
' :
’/c
) ferrCf
World Bank
122 Crores
Reduction in CDR/ CBR (1220.9million)
& IMR in Rural areas
Loan
through PHC Strategy.
Lere^f
(13 Districts)
-4
'
1996
Period
Launched in
1994
V
World Bank
Improvement of Quality
and Performances of
Health care at District
and subdistrict level
546 Crores
(109 per year)
Lean y
f
1996 -2001
5 yrs
y I
4. Kreditanstalt fur
Wiederaufbau(KfW)
1998
KfW of Germany
Improvement of Quality
and Performance of
Health care at District
and subdistrict level
(Gulbarga Division 5
backward districts)
59 Crores
( 0.38 million
DM)
Grant
Launched in
1998
5. Organisation of
Petroleum Exporting
Countries Fund for
International Development
(OPEC)________________
6. Reproductive and Child
Health Services (RCH)
Project
1991
OPEC Fund
350 Bed Multi specialty
hospital in Raichur.
29.25 Crores
(OPEC - 90%
25.7 crores)
Soft loan
Agreement
in 1991
1997
World Bank
Improving Quality of
Family Welfare Services
190 crores
38 crores/year.
1997- 98 2003
7 Crores
(2000-01)
Loan
1999- 2004
7. Karnataka States AIDS
Control
(Karnataka State AIDS
Prevention society)
1999
X^'orld Bank
Reducing the rate of
growth of HIV infection
in the state and in
strengthening the states
capacity to respond to
HIV/AIDS
-5-
feak/P^K
' J\ 1
Year of
Starting
S.No / Name
1994
8. Revised National TB
control programme
(RNTCP)
9. National Programme for
control of blindness
(DANPCB) now NPCB - K
10. UNICEF-GOK
Programme of Cooperation
in 2001.
1990
1970’s
Short Description
vf
World Bank
Supporting new
approaches to effective
TB control in state using
SCC/ DOTS and other
components.
DAN IDA
To reduce prevention
of blindness from 1.4%
to 0.3% by 2000 AD
UNICEF
To promote
comprehensive and
holistic survival,growth
and development of
children in the state
CX
A? //
r*-
-6-
Ampumt
of ranf/
loan^ihRs.
Phase III
18.3 Crores
Loan
P^L crgA..^
3 Crores
30 million
Loan
Period
1994Neelasandra
1998
Entire
Bangalore
corporation
1996Chitradurga
Bcllary
Raichur
Bijapur
1999 Davangere
Koppal
Bagalkote
7il/
C^rcz / )
6.3383 Crores
(2001)
Grant
e O'roV'sr-'.
unx* I ' ■
try-)
enr^
C: Project Goals, Focus and Distribution of EAP’s
A perusal of Table II on the project goals, focus and distribution helps to identify
certain significant trends.
1. Primary Vs Secondary
7
_
1 € vC 1
•
out of 10 projects support Primary Health care^while 3 out of 10 projects
support secondary care (one of three also support Tertiary care).
•
If the project costs / budgets are taken into account as a sign of priority or
emphasis th^n only thirty three percent is on primary care and sixty six
percent focussed on secondary and tertiary care. (Using project outlays as a
general indicator)
2. Comprehensive Vs Selective
•
Within the Primary Health Care group three of the projects IPP VIII, IPP IX
and UNICEF are more comprehensive in their design focussed on ’Urban
and Rural' primary health care and child health (and social development)
respectively, but the remaining fiv^Carc more selective primary health care
strategies with RCH being a slightly more composite package and the
remaining three being focussed vertically on single disease problem of
AIDS, TB, and Cataract Blindness.
3. Population agenda
Even IPP VIII and IPP IX which-ar-e-more comprehensive than the others are
strongly driven by the Family planning or population agenda with health needs
other than fertility related, getting much less focus.
4. Diversity and overlap
When the objectives and goals of these EAP’s are reviewed collectively then the
following observations can be made (refer Table II)
Each project is relatively multidimensional with different components
and strategies. At the implementation level some components get more
emphasized than others.
The objectives vary from very general ones to very specific outcome
oriented ones as seen in AIDS, TB, and Blindness control.
-7-
TABLE - II
Externally Aided Projects in Health Service Delivery Karnataka
OBJECTIVES/ FOCUS / REGIONAL DISTRIBUTION
S.No/ Name
LIPP VIII
Regional Distribution
Objectives/ Goals
_________ Focus
• Delivery of FW & ”• Urban Poor /Primary
Bangalore urban slums.
MCH to urban poor
Health Care
■'1 ■ ■ ■
cj r
and promote CS & SM. |(FW+MCH+CSSM+ $
• 0.851 million
• Reduce Fertility
population of urban poor in
rate and promote late
about 500 slums in an area
marriages.
of 225 sq. kms.
• Promote male
participation in FP.
• Awareness and
action for personal
hygiene, better
environment and
prevention of diseases
• Non Formal
Education (NFE) and
vocational training for
women
• Promote Female
Education
2. IPP IX
• Implement a
program sustainable at
village level to reduce
CBR, IMR and MMR
and increase CPR
(Couple protection rate)
through
• Involve community
in promoting delivery of
family welfare services.
• Strengthen delivery
of services by support
to drugs, kits, supplies
to TBA’s SC and PHC,
mobility of ANM's;
buildings of center and
residential
accommodation.
• Training to
Personnel and TBA's,
Community leaders and
voluntary workers.
•
• Rural
(Family welfare
and MCI!)
Primary Health care
Focus
• Civil works Focus
Bellary, Chickmaglur,
Dakshina kannada, Hassan,
Kodagu, Mandya, Mysore,
Uttar kannada, Shimoga,
Chitradurga, Belgaum,
Bijapur, Gulbarga
• IEC/M1ES Focus
In all districts
Strengthen
Monitoring and
evaluation by MIES
(from district to state
level)
-8-
S.No/ Name
3. KHSDP
Objectives/ Goals
• Improvement
in performance and
Quality of Health
Care services at District
and- Subdistrict level
• Narrowing
the current
coverage gaps by
facilitating access
to health care delivery.
• Achievement of
better efficiency in
the allocation and use of
health resources.
Focus
• Secondary level
health care
- To provide critical
support to PHC Networks
- Establish essential
linkages with tertiary
level.
Regional Distribution
• 31, District General
Hospitals ‘\
A
15, Hospital^ for specific
disease and special
problems.
165 Taluk hospitals,\
(24, hospital upgrading
casualty^ wards) \
Totally - 211 hospitals
<r-<l
i
=
7o
C-H c - I Lf
2$'I
TcuIuIk
By
-Strengthening
implementation
capacity.
- Strengthening delivery
of service.
- Improving
functioning of referral.
- Establishing effective
surveillance system.
- Improvement
of cost recovery
mechanisms.
- Improving access to
disadvantaged
sections SC/ST/women
Ck
DCo
b
mp -
l__ V Ch i le*
/Oi'
I-~ /3/
CW L - 2^1
fc^k
~ 71
—/b
C A t It*HrV ’
♦ cl Ct vt* e D 'iC
-9-
]
1
S.No/ Name
4. KfW
5. OPEC
6. RCH
Objectives/ Goals
• Significant
Improvement in the
Health status of socio
economic backward
region / state.
• Setting up a
Comprehensive referral
system in the division
through strengthening
and
revamping
secondary hospital
network.
• Sustainability of
Infrastructure and
Equipment.
• Increase
Sustainability of
Health care.
Focus
• Secondary level
Gulbarga district.
(Northern disadvantaged
districts)
• To build a 350 bed
multi speciality hospital
which will cater to
Raichur District and
four districts around.
(Med/Surg/ENT/ortho
Physiotherapy,
Cardiology /
Cardiothoracic,
Ophthal, Dental,
Nephrology, Urology,
Burns wards.
Gastroenterology,
Biochcm, Path,
Microbiology
Radiology and CSSD).
• Secondary and
Tertiary health care
• To meet individual
client health and family
planning needs and to
provide high quality
services through a
gender sensitive and
responsive client based
approach.
• Aim to reduce the
burden of unplanned
and unwanted child
bearing and related
mortality and morbidity
• Reducing 'unmet
need' increasing 'sendee
coverage' ensuring
quality of care.
Renovation
and upgradation of
facility.
Improvement
Maintenance
Regional Distribution
• Gulbarga Division
Bidar
- 6 hospitals
Bellary - 10
Gulbarga - 18
Raichur - 13
47 hospitals
26 in Phase One
21 in Phase Two
of
Improving
Sustainability through
fee collection.
• Old District hospital
will remain as a women
and children hospital with
skin, psychiatry, Leprosy
and TB (250 beds)
• Selective Primary
Health Care with focus on
Reproductive and child
health.
• Prevention and
Management of unwanted
pregnancies.
• Maternal care
- Antenatal
- Natal
- Post natal
- Child survival
- Treatment of
Reproductive tract
infections and STDs.
- 10-
• Raichur - / Gulbarga,
Bidar, Gadag, Bijapur (and
some neighbouring districts
of AP will be benefited.
•
•
All districts in 3 years.
Districts categorized
into A, B, C category
A = better off
B = average
C = weaker
I51 year = 9 District
A2, B1,C3
2nd year = 8 Districts
A1,B4, C3
3rd year = 3 Districts
B3
(Rationale of selecting
districts not clear).
S.No/ Name
7. KSAPS
Objectives/ Goals
• To assist state in
deducing the rate of
growth of HIV infection
and strengthen capacity
to respond to HIV /
AIDS on a long term
basis.
This includes:
- Delivering cost
effective prevention
against HIV/AIDS
- Promotive intervention
for general community.
- Low cost AIDS care.
- Institutional
strengthening.
- Intersectoral
coordination.
Focus
• Selective Primary
Health Care /AIDS / HIV
Control
- Surveillance and clinical
Management.
- Sentinel Surveillance
- Blood safety
programme.
- STD control
-IEC
- NGO coordination
- Training programmes
Regional Distribution
• 14 sentinel sites in 10
districts
• 25 NGO's in 9 districts
(15/25 in Bangalore)
• 30 STD clinics in 21
districts.
8. RNTCP
• Detect atleast 70%
of estimated incidence
of smear - positive
cases through quality
sputum microscopy.
• Administer
standardized SCC
under DOT during
intensive phase and
quality supervision
during continuation
phase.
• Achieve 85% cure
rate among all newly
detected sputum
positive cases.
Selective Primary Health
Care including
• Strengthening and
reorganizing state TB
control unit.
• Rigorous method for
detection treatment and
monitoring.
• Strengthening
training research capacity
• Targeting smear
Positive cases.
• SCC with DOT
• Decentralizing
service delivery to
Periphery
•
Rigorous system of
patient recording and
Monitoring.
• Initially Bangalore
Urban only Now 7 districts
of Chitradurga, Bellary,
Raichur, Bijapur, Mandya,
Bangalore urban (excluding
BCC area)
-II-
S.No/ Name
9. DANPCB
Now NPCB-K
10. UNICEFGOK
Objectives/ Goals
Reduction in the
prevalence of cataract
blindness from 1.4% to
0.3% by 2000 AD
• To promote
comprehensive and
holistic survival, growth
and development of
children in state through
- Improved new born
care.
- Development
protection and early
stimulation of
vulnerable 0-3 years.
- Enjoyable and quality
education for pre
school and primary
level.
- Access to clean water
and sanitary
environment.
- Protection from child
labour.
- Improved Nutritional
status.
- Better child care
practices.
Focus
- Selective Primary
Health Care and
Secondary care.
- State Opthalmic Cell
- LJpgradation of Medical
colleges. District
hospitals, Taluk
hospitals, mobile units
and PHC’s
- Eye Bank
- Training of surgeons and
ophth assistants.
- District Blindness
control societies.
- Cataract surgeries
- Microplanning
IEC, MIS, SES
Regional Distribution
Focus on all districts in all
divisions.
- Multidimensional child
health care and social
development. (Primary
Health care)
• Community,
convergent action (CCA)
• Health Action
• Child Development
and Nutrition.
• Water and
Environmental Sanitation.
• Education
• Child Protection
(Sericulture and Bonded
labour)
• Communication and
strategic planning.
• Different Districts
• CCA - Mysore,
Chitradurga, Gulbarga
and Raichur.
• Health - Bidar, Raichur,
Gulbarga and Bijapur.
• School sanitation
Mysore, Tumkur,
Chitradurga. and Raichur
• Other Activities
In all districts
- 12-
(Performance very good in
Bangalore urban Udupi,
Bagalkot, Dharwar,
Gulbarga.
Very poor in Chitradurga,
Chamrajnagar, Kodagu,
Gadag, Haveri, Belgaum,
Bijapur, Davangere).
There is overlap between projects in different areas e.g
• IPP IX and RCH have fair degree of overlap
• Training overlaps in many of them, (see also case study)
• Also IEC and MIS
• Surveillance and Health Management Systems especially since
they often focus on same districts, same categories and same
health centres and teams. (This will be considered again later).
5. Equity Focus
•
The focus on disadvantaged or marginal groups in the community varies from
explicit to ambiguous. In IPP VIII (Urban poor) and KHSDP (disadvantaged
sections /ST/SC/women) it is more explicit while in all the others it is
ambiguous, mostly with a sort of'reaching all’ focus. In RCH there is specific
reference to ’Gender sensitivity’ and in UNICEF's programmes focus on 'child
labour’ is emphasized, which are significant.
•
In terms of addressing Regional disparities in health structures and systems in
the state, EAP’s have a very varied contribution
KfW and OPEC are specifically focussed on the disadvantaged
Northern Karnataka (Gulbarga Division), though the donor decided
this focus in the latter loan, not the state.
IPP VIII is focussed on urban poor in Bangalore being the largest
urban conglomeration in the state though in the next phase other
cities and towns are being covered.
KHSDP, KSAPS, NPCB-K focus more widely.
Others like IPP IX, RCH, RNTCP and UNICEF do focus selectively
on some districts more than others for different components, but
while the disadvantaged Northern Districts of Karnataka do get
included quite often, the focus is not based on data for regional
disparities or need, but seem more adhoc, responding to more
extraneous pulls and pushes for selection including districts
patronized by politicians or other ‘lobbies’ or other such non
technical reasons.
6. Local and National Agendas
• Finally except OPEC and KfW which are only Karnataka determined and
focussed; and KHSDP which is Karnataka focussed but has counter parts in
Punjab, West Bengal and now Orissa; all the other projects are similar to those
promoted by the funding agencies in other states as well. Many like RNTCP,
- 13 -
AIDS, NPCB-K, perhaps even RCH and IPP IX are evolved as framework /
packages at National level and then offered to the state as a ‘fixed package deal’.
Sometimes the state directorate and experts have tried to modify or review these
national level prescriptions and tried to adapt them to state level realities but by
and large this process of adaptation is rather weak and adhoc.
• However while the sense of ownership by the state was very strong in KHSDP /
OPEC / IPP VIII it was relatively much less in the others and very little perhaps
in RCH which showed absence of stakes in planning and formulation.
•
Incidentally in IPP VIII especially in the sector of innovative schemes there are
different approaches and schemes being tried out in Bangalore, Hyderabad,
Delhi and Calcutta - a diversity which was both welcome and significantly
different from the usual ‘central top down’ prescribed packages.
Regional disparities between states and within states are so stark that greater
emphasis on District level planning in the context of local socio
epidemiological evidence and situation analysis is an important policy
imperative. EAP’s could well be an instrument to experiment with such diversity
of approaches.
•
Status of Bank Group Operations in India (Marek 31,1999)
__________ Original Amount with USS (Millions)
SI.
No
.....
Fiscal ilBRD: IDA
Project
year i
PopuTatTon V
" '
2 National Leprosy Elimination
(INPE-10424) *
3 Karnataka Water Supply and
Environment Sanitation
(IN-PE-10418)*
4 Population (IN-PE-i6457) *
5 Blindness Control (IN-PE-16455)"
*
79760" "
1992
■f993'
.... 85700
‘1993
■■■"' 92.00
9.07
Un
disbursed
Develop Implemental
Obj
Projects
■55786 '"
S
S
24.71
8
HS
31764
"8
S
1994"
88760"’
50.16
S
S
1994"
^17780 '
81.38
S
S
356760
263.11
8
S
■■"248730
233.16
8
8
164.80
152.45
8
U
142.40
128.63
8
U
6 State Health System II
"T996
(INPE-35825) *
7 Reproductive Health "
.....1997
(IN-PE-10531) *_
8 Malaria Control (IN-PE-i05f 17)”* '1997
9 Tuberculosis Control (IN-PE_10473)*
'
Cancel
1 1997 [
i
S - Satisfactory, U - Unsatisfactory and HS - Highly Unsatisfactory
Note: This table is not specific to Karnataka but is an overview of the All India situation. Projects
which are relevant to Karnataka are shown by an asterisk.
Source: Report No. 18918-1 N Project Appraisal Document May 13 1999.
- 14-
I
D: Overview of Programmes and Activities
•
Table III provides an overview of the overall focus of the programmes and
activities using budget headings including special programmes and allotments.
About 34 components were identified of which 13 were the commonest in all
the 9 projects (UNICEF was excluded in this table). These were
6 and more than 6 out of 9
Construction;
Furniture;
Equipments;
Drugs and supplies;
Local training;
Local Consultancies;
Maintenance of Vehicles and Equipment;
Contingencies.
4 and less than 6 out of 9
Staff salaries
Vehicles
Management Information System (MIS)
Information - Education - Communication (IEC)
Project management
NGO support.
Hardware over Software
The main focus of most of these have been hardcore infrastructure development
(Buildings, Equipment, Vehicles etc) and though software- like training, IEC, MIS
and NGO support were included and envisaged, at the operational level, hardware
always got greater focus than software. Also hardware was seen as absolute
necessity so often as in IPP IX and KHSDP, constructions were focussed upon
rather than initiating some of the software using locally available facilities and
resources concurrently. Also hardware investment was substantial and needed
greater supervision and control distracting from software development which
however is probably more important if long term sustainability is to be thought off.
•
Inadequate quality improvement focus
Another feature of the overview findings are that some elements which contribute to
improving quality especially at operational or performance level were not always
included in the project design and cost allotments.
These included
Provision for books and training materials;
- 15-
TABLE III
Externally Aided Projects in Health Service Delivery in Karnataka
COMPONENTS OF PROJECT PROGRAMMES AND ACTIVITIES FOCUS
(Review of Budget Headings)
KfW OPEC RCH KSAPS RNTCP | NPCB-K Score
IPP-8 IPP-9 KHSDP
Component
SI
No
1
Land Purchase / prepn
2
Construction
+
3
Furniture / Equipment
+
4
Drugs and supplies
+
i
j
+
i
+
5
Vehicles
6
Training (Local)
7
Consultancy (Local)
8
Training (Foreign)
+
+
+
+
+
I
+
!
+
1
+
+
i
i
+
+
9
Consultancy (Foreign)
10
Books / Training Mtrls
11
12
13
14
Innovative schemes
+
+
■
I
+
Additional staff-salaries
IEC Materials prodn
I
Revolving Fund
+
*
+
+
I
l
+
15
Maint Vehicles & Eqpt
16
17
18
19
Training Material
Video / Media
20
Waste Handling
+
21
22
Surveillance
+
i
Evaluation studies
+
i
Kits
+
+
■
23
I—
Safety Net for Disadvan
L__
Improving women health
24
MIS
25
Design and Engineering
26
r-.
•
. a «
.
Project Management
+
1-
+
I
+
- I
I
I
t
T
I
+
+
+
+
i
27
Sustainability
28
29
Contingencies
30
Blood safety
31
Voluntary testing
32
Adolescent Health
I
33
Remunerations
j
34
School Health
NGO support
+
+
+
j
+
I + .
i
i
!
I
i
15a
+
■
+
I
+
2
7
9
6
5
7
6
2
1
2
2
4
5
1
5
2
2
2
1
1
2
1
2
4
1
4
1
6
5
1
1
1
1
1
Training material development;
Innovative schemes;
Revolving funds;
Evaluation studies;
Documentation.
Very few projects had them as special allotments. No doubt some may have spent
on these items under other budget heads but allotment of a budget need for any
programme activity is definitely a sign of priority or significance.
•
Equity focus
Finally special focus on poor, disadvantaged and on women was mentioned in many
projects but only in IPP VIII and KHSDP were their specific programmatic
allotments for women orientation and involvement (IPP VIII and KHSDP) and for
safety net for the disadvantaged (KHSDP). Only a special allotment can ensure that
the thrust is part of operational policy.
•
Additional items
However since there were variations in the focus of the health problems addressed
by different projects specific allotments for specific additional themes were
observed. These included waste handling (KHSDP); Blood safety and voluntary
testing and counseling (KSAPS); Adolescent Health (RCH); School Health
(NPCB-K) all very important and significant. Some elements like school as a focus
of health activity should be a compulsory component of all health projects because
preparing / orienting future citizens is a policy imperative.
•
Learning from previous experience and each other
While UNICEF schemes were not included in the table their allotment to a range of
themes around child health exemplified a much more holistic; practical and
operational approach. The programme highlights included convergent community
action; border cluster strategy for MCH and ICMI (Integrated Management of
Childhood Illness); Child development and nutrition; Water and environmental
sanitation; Janashala, programme child labour protection; HIV / AIDS prevention
activities, etc.
NB: It is unfortunate that UNICEF’s longer experience of moving from
‘biomedically defined technological approaches’ to more ’holistic initiatives
responding to broader socio-economic cultural realities' has been totally ignored and
World Bank's 'selective prescriptions and initiatives' allowed to distort health
planning and in many cases leading to a reinventing of the wheel. Dialogue
between project funders and building on past experiences is crucial otherwise EAP’s
could be a wasteful distortion and also being ‘loans’ rather than 'grants' could be
wastefully counter productive.
-16-
E : Overall Strengths and Weaknesses of EAP’s
Table IV lists out the key strengths and weaknesses of different programmes as
identified by literature review and endorsed by interactive discussions. They vary
from programme to programme and cover wide range of sectors and issues.
Strengths
Taken as a composite group the key strengths of these projects are:
1. Infrastructure development
They have focussed primarily on infrastructure development, which includes
buildings for hospitals and health centres, operation theatres, staff quarters etc.
While these were necessary since the directorate had not invested in adequate
maintenance of existing infrastructure nor invested in adequate construction to fill
up the lacunae in the past, the demands of infrastructure often have tended to
overshadow all aspects of the project.
2. Support field action
In the situation when programme action budgets are shrinking with salaries taking
over greater and greater percentage these projects help to promote specific action
components and field activities.
3. Framework of strategy ; planning capacity enhanced
Conceptually whether primary or secondary, comprehensive or selective, many of
these projects have led to generation of some framework of strategy and action and
have been supported by a degree of background homework. Though the data base is
often patchy it is better than some of the adhoc decisions in the past which were
often repetitive without adequate evidence or data. Project formulation including
setting objectives; outlining strategies; identifying action plans; identifying outcome
and impact indicators and benchmarks all have helped build planning capacity even
though the compartmentalization causes overlap and some distortions.
4. Innovations
Project autonomy, which is relative has allowed many innovations to be
experimented with, which is a change from the routine generalized top down
prescriptions thrust on the whole system in different districts uniformly and at all
levels in the past. All the innovations cannot be listed out here but from the table
some of them need to be highlighted. These are
a. Link workers (1PPVIII)
b. Women’s clubs (SHE clubs) - IPP VIII
c. Gender sensitivity and women’s orientation - IPP VIII
- 17-
d.
e.
f.
gh.
i.
jk.
Herbal gardens - IPP VIII
Help desks and Boards of visitors - IPP VIII
Tribal ANM training - IPP IX
Partnership with NGOs to run centres, (IPP VIII, IPP IX, RCH and KSAPs)
Special interventions for disadvantaged - yellow card, KHSDP
Comprehensive MIS being evolved - KHSDP
Improvement of referral links - KHSDP
Good mechanisms for construction and supervision - KHSDP
l. Efforts at quality improvement (IPP VIII, KHSDP)
m. Focus on women specific and budget heading (KHSDP)
n. Decentralization of accounts (KfW)
o. Focus on Northern disadvantaged districts (KfW, OPEC, RCH, UNICEF)
P- Links with Literacy campaign (RCH)
q- Focus on adolescent age group (RCH)
r. Partnership with private sector - some contract services (KHSDP)
s. Involvement of Medical colleges (RCH, UNICEF)
t. Newsletters (KHSDP)
Many more may be there but these arc a representative sample. However there
seemed little effort at documenting these ‘innovations’ and even less on monitoring
or evaluating them in any sort of methodical or rigorous way. It is important to
ensure that they add value in quality and efficiency to the existing PHC option
programme before they get adopted by the whole system as an added innovation..
This element of operational research was significantly absent.
Weaknesses
The key overall weaknesses of EAPs were
1. Overemphasis on infrastructure
While focus on infrastructural development was a strength as pointed out earlier, it
also tended to overshadow all the so called ‘software’ or action / programmatic
components.
t
Inadequate operational management capacity
Overall there were inordinate delays between launch of the projects and getting
operational strategies of the ground. These seemed to be lack of capacity at all
levels to convert ‘good project objectives’ into ground level strategics. While these
improved over time at the state level as seen in KHSDP, IPP IX, at the ground level
i.e., the District level; the PHC level and Panchayati Raj Institutions (PRI) level
j these remained a weak chain in the link.
C>
..J
/o /Ao
A-o. I
//A
TABLE - IV
Externally Aided Projects in Health Service Delivery in Karnataka
SOME STRENGTHS AND WEAKNESSES
S.No/EAP
LIPP VIII
Strengths
Comprehensive Conceptual
Framework
(Family Welfare, MCH, CSSM
Water supply and sanitation
Education, Community
Development).
•- Link Workers
Women's clubs (SHE clubs)
(Social Health and Environment)
• Establishing creches, NFE and
Vocational training.
• Involvement of NGOs
• Involvement of Community
• Gender sensitivity and women
orientation
• Flexibility e.g. different
innovative schemes in Bangalore,
Calcutta, Delhi and Hyderabad.
• Social paradigm awareness
stronger at all levels.
• Operational guidelines for
most aspects of project quite good.
• Some good practices:
- Help desks in centres.
- Herbal gardens in all
- Overall morale and
discipline of staff good.
- Contract for cleaning /
security efficient
- Board of visitors.
- NGO participation.
•
• Citizens charter
• Slum based centre (more
accessible)
• Human Resource Development.
- 19-
Weaknesses
• Focus on Family Welfare
predominant other programmes present
but adhoc and not adequately integrated
perhaps even inconsistent. (Need to
actively convert from FWC to urban
Primary Health care centre).
• Long term sustainability especially
regularization of centre staff not
adequately addressed.
• Partnership and Liaison of project
team with Corporation Health Centres
problematic (ownership by corporation
inadequate)
• IEC more material preparation than
field use.
• Orientation and motivation of
Doctors not maintained after initial
training (need for more problem solving
sessions)
• Many innovative schemes built upon
but not in a sustained way.
• Involvement of NGO's and
community and G Ps patchy. Not
adequately evaluated or monitored.
• Lab facilities and services to be
improved.
S.No/EAP
2. IPP IX
3. KHSDP
Strengths
• Focus on rural Primary Health
care - Filling gaps.
• Flexibility in project formulation
and utilization across financial years
without lapsing of funds.
• Software inputs like IEC,
Training included in project
components
• Innovations like
- Tribal ANMs for tribal area (relaxed
requirements strengthened training)
- NGO take over of PHCs
(two
experiments)
- In some activities like IEC focus on
Northern Karnataka based on regional
disparities has been project emphasis
(at proposal level only)
- Short listing of NGO's done through
a planned / realistic procedure
though time consuming.
_____________ Weaknesses
• Hardware(civil works)
Moved better than software.
• Overall implementation
delays with complacency in the initial
stages and some lack of clarity/ capacity.
• Ownership by District Health officers
Inadequate.
• Centralized implementation except
for building aspects.
• Operational guidelines for many
aspects were not initially catered for e.g.
Fund flow mechanism to ZPs.
• More than just secondary
Care. Conceptually also focuses on:
- Special interventions for
Disadvantaged (Yellow card scheme).
- Comprehensive Surveillance system
- Trauma centre
- Hospital Waste Management.
- Blood Bank modernization.
- Improvement of Referral links.
• KHSDP, OPEC, KfW
share capacity building initiatives.
• Good mechanisms for
Construction and infrastructure
development has been organised that
can be used by other projects as well.
• Some areas of focus relevant for
Quality development - Equipment
maintenance, Quality, Women and
disadvantaged. Drug procurement
policy. Medical waste management.
• Delay in construction
and civil works continue and 'local
problem solving' to get over constraints
not yet adequately decentralised.
'^ost over runs affecting planning and
process.
® Contracting out and partnerships with
NGO's and others not being adequately
monitored (Are the effects really better?)
• Strategic planning cell has not been
developed adequately at capacity level
and from the point of sustainability of
planning process it is adhoc, marginal.
• Ownership problems especially for
long term sustainability not adequately
addressed. DHS or ZP who will
maintain?
-20-
•
Monitoring mechanism
not adequate to support effective
implementation.
• Community involvement of village
committees - not adequately
implemented. Involvement of NGO
equivocal.
• Lack of continuity of
key personnel in the project handicapped the project.
• IEC virtually a non
starter
• Training process direction given to
NIHFW (National) rather than SIFHW
(State) which led to delays.
• Government level
decision making bureaucratic - 3 standing
committees delay decision
S.No/EAP
4. KfW
Strengths
• Focus on a disadvantaged
Region.
• Linked to K.HSDP for most
of software development.
• Account in Gulbarga
(helped decentralised utilisation by
Additional director for project
stationed there.
• Improve Administrative facilities
at hospital level as well as for District
Health officers and Taluk Medical
officers.
• Strengthen referral.
• Additional staff.
• Project conceptually includes focus
on disadvantaged and women.
• Epidemic preparedness.
5. OPEC
• Focus on a disadvantaged
region of the state (but the choice
seems to have been by the donor).
Weaknesses
• Only lip service for
Software components (Training,
referral, MIS, support services not
adequately addressed inspite of
availability of KHSDP support system).
• Slow fund release /
Utilization.
• Seems mostly brick and mortar
project.
• Decentralised utilisation of funds
without close monitoring led to
problems of leakage, poor quality
control, 'thoughtless payments'
(Dilemma of centralization Vs
decentralization)
•
• Foreign consultants (SANI Plan)
from Germany were not very effective in
their coordination with local consultants.
hence inordinate delays.
Affected by Indo - German relations.
Scaled down after the nuclear bomb!
• Not a comprehensive
plan. Very focussed on just a hospital
and not need based.
• Inadequate local planning and
ownership.
• Delays and adhoc action.
• In the planning no clarity on how to
implement or actually go about running
the institution.
• No clarity on how government will
raise minimum Rs. 10 crores per annum
to run the hospital (Now approaching
Private sector for partnership!)
• No clarity on how tertiary,
secondary input would link or support
PHC through referral system.
•
_
;
b-e t
-21 -
I'-C'|
cl
•
• c. ,r .
h cop
b tf’sC.
S.No/EAP
6. RCH
Strengths
• Attempt to adopt Community
Needs Assessment approach (in
principle).
• Adolescent Health priority.
• Links with literacy campaign
• Financial envelope idea:
- Focus on disadvantaged.
- States free to choose intervention.
- Flexibility etc.
• Focus on Northern districts
- Gulbarga, Bidar, Raichur, Koppal,
Bijapur, Bagalkote.
• Bellary sub project which involved
NGOs.
• Partnerships with NGOs.
Professional bodies and medical
colleges initiated.
-22-
Weaknesses
• The work of UNICEF support in the
earlier phase of RCH not acknowledged.
Programme not learning from earlier
experience and strategies.
• Civil works preoccupation like
• Other WB projects with delays and
cost over runs.
• Software components like IEC,
Training, moving very slowly or not
at all.
• Too much Family planning oriented
not integrated with health adequately
(Population agenda strong).
• Delays in basic training / delivery
kits etc.
® Focus on Secondary care more than
primary care - institutional services more
than field services.
• Top down Package deals oriented
rather than 'process' and local planning
and empowerment oriented.
• Overall progress of RCH project
which is high priority is very slow and
financial utilization seems quite
sluggish.
• Nutrition neglected in programme.
• Consultants not clear about actual
roles.
o Not adequately integrated at project
planning level (left to adhoc decisions).
• Too women oriented need to retain
balance and involve men as well.
• Personal Hygiene kits pushed by ST
manufacturers and other lobbies without
adequate planning.
•- Sustainability not addressed
Community Needs Assessment on
paper.
Pe
S.No/EAP
7. UNICEF
Strengths
• Complementarity of initiatives like
CSSM, RCH, and immunization.
• Using fixed day session and
campaign approaches.
• Pilot schemes tried out in some
districts or towns and then expanded /
replicated in other areas.
• Generation of training materials
and training programmes more local
and relevant.
• Involvement of Medical colleges,
research centres in MICES survey and
other projects.
• Learning from experience and
responding to local needs and demands
good.
• Policies, guidelines manuals
evolved with local expertise.
• Policy to focus on Northern
Karnataka and districts with weakest
child development indicators.
Weaknesses
• High vacancy rates of ANMs in
disadvantaged Northern districts.
• Logistics of cold chain Drugs, kits
not adequately tackled delays etc.
• Orientation / training of Programme
managers to deal with many departments
network, sustain partnership is still not
adequately developed.
• Complementary of UNICEF and
• RCH (WB) programmes not
adequately tackled due to project
compartmentalization.
Inspite of attempts to promote intef
sectorality UNICEF support programmes
still get listed to one department or the
other.
8. RNTCP
Very important priority problem.
Hence selective strategy still required
and emphasized.
• Many DTC's do not still have
District TB officers (9)
• Laboratory technicians posts vacant.
• Abrupt transfer of trained personnel.
• Some DTC's have no building (9).
• Complex procurement procedures.
• Lack of cooperation from medical
colleges / major hospitals.
• Inadequate budgetary support at state
I district level.
• RNTCP districts Vs short course
chemotherapy districts of SCC continuing ambiguity.
• Overall TB still low priority.
-23-
S.No/EAP
9. KSAPS
Phase I
Strengths
• Zonal blood testing centres
established.
• Modernisation of Blood banks.
• Surveillance centres set up (8 + 5
hew)
• NGO involvement good leading to
development of AIDS Forum
Karnataka - mostly Bangalore
(includes work with sex workers,
truckers and care and support for
PLWHA’s)
• Strengthening of STD clinics.
• IEC activities at many levels.
• Training activities on a regular
basis.
• State AIDS prevention society set
up.
-24 -
Weaknesses
• Supply of drugs delayed and
continuity of care and treatment (due to
complicated procurement procedures)
• Lab diagnostic facilities for voluntary
testing in all districts still inadequate.
• Lack of full or sustained partnership
with NGO’s in other parts of Karnataka.
• Lack of counseling facilities in
District and major Hospitals.
• Inadequate policy guidelines on HIV
testing.
IK c-n
rYi
I- & c-C c •, c (<■
rO
IEC non starter
$
IEC was an overall weakness - w ith preparation of materials often overshadowing
actual efficient use in the field, Often materials did get printed / produced but
logistics of distribution were not
i
adequately planned and operational use by health
workers and others at the field- ---level1 were most inadequate with a few exceptions.
G
HMIS, Monitoring and Evaluation weak
The monitoring and evaluation of the projects seemed weak inspite of efforts at
building up M and E strategies and lots of effort in some projects to evolve HMIS
systems. Most of the HMIS seemed to be used only by higher levels to help the
central planning process or monitor the programme. At the field level or base the
quality of HMIS data was often poor since the ‘collector of data’ did not see himself
or herself as a user of the data for their own planning purposes and was collecting it
disinterestedly for someone else at a higher level
Sustaining innovative ideas was inadequate
Many innovative ideas were being tried out ,i)ut their long term integration or
sustainability was not properly planned for. Many schemes started but were
discontinued without proper evaluation; while many others were continued just for
the sake of continuity without monitoring evidence of value addition, if any.
Some other issues are included in the next chapter as policy imperatives.
An Innovative Scheme
“Under an innovative scheme the IPP IX project has provided funds to the
Vivekananda Trust to train girls from the tribal hamlets and post them as ANMs in
those hamlets. This training is a one-ycar course following the governmentapproved ANM curriculum with an added component of tribal medicine. The
training has not been recognized by the Nusing Council, and the trained tribal
ANMs are working through the NGOs working in these areas. Following
discussions with the MOHFW, the trained ANMs have been accepted as trainees in
the ANM training centers at the completion of which they will also be eligible for
employment in the non-tribal areas. An evaluation of the first batch of 40 tribal
girls trained as ANMs indicated a satisfactory knowledge of MCH, herbal medicine,
nutrition, and personal hygiene. However, their knowledge of the reproductive
system and human anatomy needed strengthening, and this will be rectified through
training in the government ANM training schools. This scheme ensures access to
MCH services in the remote and underserved tribal areas, and the presence of a
female service provider at the SCs. Another important benefit is the opening up of
job opportunities to tribal women within and outside of the tribal areas”.
Source IPP IX World Bank Review Mission Aide Memoire
-25-
F. Lessons from Case studies
In spite of the time constraint the researchers felt that it would be a good idea to add
a few case studies of the situation on the ground vis a vis some operational aspects
of these EAP’s. Using two strategic opportunities - a quick assessment of ‘training’
opportunities experienced by a group of medical officers in a Northern district was
included as case study A and a surprise visit to an urban health centre covered by an
EAP was included as case study B. Both case studies focus on some learning
experiences from ground level realities and are not meant to be taken as any sort of
rigorous evaluation.
1. Lessons from case study - A
An interview of 6 doctors in a surprise visit to a Northern district showed the
quantity and quality of training inputs from a wide variety of EAP’s (around five
EAP’s) These are described in case study A. They show the following important
trends:
i.
ii.
iii.
iv.
V.
vi.
vii.
Five out of the 6 doctors had undergone some training or the other with three
of them having attended 5-6 training programmes,
The EAP’s supporting these training programme included IPP IX, RCH,
NACO, DAN-PCB AND CSSM (UNICEF)
The programmes ranged from 4 days to 18 days.
Most of them were in the Rural Health and Family welfare training centre
though one was at Hubli and other at Bangalore Medical college.
Most of them wanted CME’s atleast once or twice a year.
They suggested better skill orientation in training programmes and more
comprehensive induction training when they first join as PHC medical
officers.
Have suggested better resource persons and better centres than at present.
On the whole the case study shows that the EAP’s have managed to support training
of project mangers at field level even in the disadvantaged Northern districts which
is very creditable. However since these are done by different project administrations
there is overlap in themes and focus and the selection of courses do not fit in to any
available training schedule or CME of a local PHC. The selection and deputation
seems adhoc and opportunistic. Very often the MO gets transferred after a special
training programme so he is not able to add value after training to his ongoing work.
- 26-
<3*^ -
♦ooV
CL
e.
crppef
r* »
cun
CASE STUDY - A :
Training Experience in Northern district
A few Doctors with Government service varying from 6 months to 20 years were interviewed
regarding their training under various projects / programmes. Some details about the training of
these doctors are given below:
1.
Dr. A with about 7 1/2 years of government service had undergone the following training
RHFWTC
1 week
1995
CSSM
MCH Training_______
a.
1 week
1997
RCH
FP & MCH Training
b?
2 weeks
1998
CSSM
FP Training
c.
1999
2
weeks
IFF
IX
Management
Training
d?
Nauzad
1
week
1999
MO
Administrator Training
e.
Ahmed, Rural
Training
Development
Training
Centre
Inspite of all the regular training feels necessity for skill based training in MTF, tubectomy (learnt
tubectomy himself) and CME’s (atleast twice a year). Also felt that quality of training at RFWTC
could be improved by getting trained resource persons from private / professional institutions.
If
fl
II
Dr. (Mrs.) B with about 5 1/2 years service underwent the following:
TrhfwTc
"CSSM
CSSM Training___________
a.
18 days
IFF IX
b7 Combined Medical Education
DANFCB
Blindness Training_________
c.
4 days
d? Leprosy Training__________
Atlkibli
4 days
NACO
AIDS / STD Training
e.
RHFWTC
5 days_____________
RCH Management Training
RCI1
Had not been given any training in MTF or tubectomy. Felt that such skill based training would
enable to cater to the female population. Felt the need for CME's (1-2 per year).
2.
If
•I
tl
r
Dr. C with 1 year service (excluding 4 years contract service). Very capable, efficient
young MO, underwent the following training:2 weeks
1996
RHFWTC
IFF IX
Reorientation Training
a.
fl
2 weeks
1997
MCH Training
RCH
b.
1 week
1998
Leprosy Training
c.
2000
1 week
d7 Management Training
2000
1 week
STD/AIDS Training
NACO
e.
2000
2 weeks
Bangalore
T Medico-legal Training
Medical College.
Is able to assist in tubectomy only. Feels the requirement of better training courses and skill based
training in MTF and tubectomy. Also feels that he could benefit from CME's.
3.
fl
If
4. Dr. D having 6 1/2 years service has underwent only Orientation training and Management
training under IFF IX. Has assisted in tubectomies. Feels the necessity for more comprehensive
induction training and training in Administration and Medico-legal aspects.
5. Dr. (Mrs) E also serving in the District with 5 months service has had no training whatsoever
(regular KHSDP appointment). Feels the requirement of rigorous training in all aspects to
effectively perform the job responsibilities of a PHC doctor.
6. Dr. F serving in the District with 5 years Government service underwent only 3 weeks continued
Medical Education Training under IFF IX on induction (1995 October) and no other training. Assists
in practical training of ANM's at the co-locatcd ANM Training Centre. Feels the requirement of
regular training especially skill based and activity based training. Training needs identified include
MTF, tubectomy (including laprascopic). anesthesia and Medico-legal training (including post
mortem is a must), as he has performed 30-35 autopsies in his short service.
-27-
2. Lessons from Case Study - B:
A visit to an urban Family Welfare (Health centre) supported by an EAP showed
some interesting features described in the observations listed out in case study B.
The case study emphasizes that inspite of quite a good level of conceptual
framework generation and the evolution of a large number of guidelines the gaps
between concept and practice can be wide.
Various local adhoc, modifications of programmes: temporary or permanent short
cuts: lack of continuing education: supportive supervision and motivation of field
staff: poor logistical support to supplies: and lack of sustained efforts to maintain an
innovation can lead to discontinuation of innovations; closure of certain functions;
modifications of strategies which can be wasteful or counterproductive; or result in
glaring mismatches and distortions as exemplified by the observations.
While some functions go on fairly well and as per the objectives, some get distorted
or modified. The case study exemplifies the need for continuous monitoring and
evaluation; efficient supplies and logistic support; constant problem solving
supportive supervision; and good team work and continuing education to ensure the
quality of the implemented programme and to reduce what is often called in policy
circles ‘the implementation gap’.
-28-
CASE STUDY B- An Urban Health Centre
SEC TOR OF WORK
1. Family Planning Oriented
2. Referral Oriented
3- Laboratory services not available
4. Family Planning services
5. Drugs Inadequate
6. SHE clubs defunct
7. Link workers a strong asset
8. LHV / ANMs from corporation
9. Immunization
10. Health Education IEC activities
discontinued.
11 ■ ISO 9002 Certification
12. Fall in activities / performance
OBSERVATIONS
No male patients seen;
No well baby clinic;
No well women clinic;
No screening for Breast Cancer or Cancer of the Cervix;
Only IUD insertion carried out, CCs and OPs distributed_______
No normal deliveries conducted even in day time.
All deliveries referred to Maternity Centres (MCs)
Referral card not well designed and common to all categories.
ANC card not given to the patient.
Laparoscopic Tubectomy or Tubectomy at MCs only.
Only Haemoglobinomcter available cases usually referred to MCs,
long queue;
Tests sometimes done at UHC by visiting Lab technician's;
Lab tests -VDRL Hb, Blood group, Urine Albumin.
Only where LMO trained, only Menstrual Regulation
Conditional i.e., only if patient willing for tubectomy / IUD.
Inadequate quantity to routinely treat OPD patients.
Very limited antibiotics.
No pediatric preparations/ syrups, no eye/ ear drops
(except chloroapplicaps) or skin ointments.
Definitely not Rs.50,000/- p.a. worth of drugs.
LMOs give prescriptions for purchase from outside.
Earlier vocational training - now discontinued.
Only serve as community feedback group.
From community, dedicated.
Low honorarium so frequent turnover.
Bring ANC cases early as well as children immunization.
Experienced, competent (could be corrupt)?
Cold chain maintained.
Vaccines available.
Outreach immunization also.
Twice a week, so load less.
Do not put posters in slums as destroyed by children.
A-V van discontinued due to corruption.
Mainly printing - less lecture demos.
Purely technical assessment.
Based on parameters like cleanliness, record keeping, waste
disposal, sterilization of OT and equipment etc.
Would not significantly improve quality of care.
False sense of perfection.
Since start of centre all activities have reduced significantly.
Assessment required of reasons for this.
Glossary IUD - Intrauterine devices
MC - Maternity Centres
OPD - Outpatients department
CC - Conventional contraceptive
(Condom)
LMO - Lady Medical officer
ANC - Antenatal card
UHC - Urban Health centre
OP - Oral Pills
-29-
G : Some Policy Imperatives Including Integration and Sustainability
The previous chapters provide an overall framework of the 10 EAP’s in Karnataka
and some of the quantifiable or qualitatively describable indicators and features of
these projects to help the project overview. As indicated in the project protocol this
exercise was primarily a critical policy review and not an evaluation exercise of
each of the EAP’s per se. Some of the finding in the previous chapters and tables
have addressed some of the questions that were included in our original list. In this
chapter we try to address those which have not been adequately covered by the
earlier one as well as provide some additional critical comments even on those that
have been covered, drawing primarily from the very candid and frank interactive
discussions we had with a wide variety of project directors. These policy issues and
imperatives are as follows:
1- Scone of Projects
All the projects focus on Health System Development with varying degrees of
emphasis on Primary Health care. While some focus on secondary level (c.g.
KHSDP) there is a built in assumption that the secondary care support is with a
view to support through efficient referral systems - the primary health care network.
While in practice the links may not be so well established the conceptual framework
is well directed to this issue. It is at the ‘Public Health’ context level however that
the projects show a general weakness inspite of the fact that unlike other states in
the country ‘public health expertise’ is available even among the senior leadership
of the state. One can only surmise that in the changing financial situation perhaps
financial management contingencies and bio-mcdically defined management
framework are inadvertently distorting public health concepts and priorities. The
focus on basic determinants of health is weak (nutrition, water supply, sanitation,
environment) both at content level, emphasis and linkages; key public health
components like surveillance and health promotion are inadequate; and the ‘new
public health’ emphasis on empowerment of the community and public at large in
health decision making is totally overshadowed by top down provision of specific
packages euphemistically called social marketing. This lacunae / weakness needs to
be seriously addressed.
2. Project Planning
In the absence of a strong Strategic Planning Cell in the Directorate (inspite of a
provision in KHSDP for this) problems of project flexibility, design, long lead times
and delays, in preparation, complications in procedures and various ongoing
management and operational problems, all of which have been experienced in one
EAP or another - are a symptom of lack of adequate attention to building in-house
Capacity for more realistic project planning and management. This has led to
compartmentalized planning, inadequate collection of field based data or evidence,
and adhocism in decision making further compounding the problem. Lessons are
not learnt from positive and negative experiences of a particular EAP or its success
-30-
at some form of system development so the ‘wheel is reinvented’ each time by each
project and the system is not enriched by the collective experience. E.g. Different
EAP’s have had different experiences of dealing with the ‘NGO sector’ or the
private sector - some positive; some not so positive; some even disastrous in tenns
of unreliable partners or even ‘fly by night’ operators but the whole system does not
learn from this to evolve a Directorates policy for NGO or Private sector
partnership. This situation may change with the Task Force recommendation on
state policy directives but for the present this is a lacunae to be urgently addressed.
3. Who drives the projects?
This was a very difficult policy issue to address. On the face of it, the State
Government / State Health Directorate drives the project not the funding partners or
their external consultants and all sorts of mutual consultations / reviews are
organised. However two factors do affect the ‘driving’ of the project.
Absence of local homework
In the absence of rigorous ‘policy’ and evidence based homework on the
governments / directorate side due to a lack of strategic planning capacity as
mentioned earlier, external consultants of funding partners are often able to drive
the decision by just providing more options, more evidence based on data
marshalled from experience elsewhere and the state policy makers are then more
easily influenced or ready to accept them. e.g. During the study period an external
funding agency resource person provided more data and perspective on private
sector in Karnataka, than could be marshalled by local expertise thus inadvertently
pushing the private sector agenda. The reliability of this data or whether it was
extrapolated from quite different sources could not be commented upon, adequately
without local homework.
•
Conditionalities of funding partners
World Bank loans more than other agencies are also usually supported by some
conditionalities that are clearly stated in their documents.
i.
The need for economic reforms.
ii.
The need to engage the private sector.
iii.
The need to promote user fees as a means of cost recovery.
iv.
The need to follow certain forms offender’ or ‘consultancy ‘laid down
by bank’ etc.
There does not seem to be adequate home work in-house on these and
implications especially long term options, before loan agreements are signed.
-31 -
their
Some World Bank conditions
“The Country Approach Strategy (CAS) recommends focussing Bank-group
financed investments on states that are undertaking economic restructuring
programmes and supporting sectoral policy reforms. Karnataka is one of the state
that has initiated important fiscal, sectoral and governance reforms. Further more it
supports the CAS objectives by strengthening institutional capacity
engaging the private sector
,
“Each project state
shall levy user charges in district and subdivisional
hospitals in accordance with a program and time schedule acceptable to the
Association(IDA)”.
“Goods and works shall be procured in accordance with provisions of section I of
the guidelines for procurement under IBRD loans and IDA credits” (International
competitive bidding, bid packages etc).
“Consultants services shall be procured under contracts awarded in accordance with
the provision of the Guidelines for the use of consultants by World Bank borrowers
and by the World Bank as executing agency - published by the Bank in August
1981”.
Source : Various reports of the Bank and Project Agreements
Both these factors lead to the continuing perception and the fact that indeed the
‘external agent’ does drive the project intentionally through general conditionalities
or ‘inadvertently through inadequate borrowers homework’. This needs to be
addressed urgently, j
,v r ,
c xoc5
\
4. Are thefre areas of overlap / duplication ?
•
Compartmentalized projects by the very fact of being developed independently
as ‘stand alone’ projects and not as components of a larger wholistic integrated
project are bound to produce overlap and duplication.
•
Not surprisingly the chairperson of the Task Force during one of his reefent
inspection visits found ‘three operation theatres in a PHC compound’ built by
different EAP's with no evidence from the MIS of local needs that warranted
such investment. In HMIS, IEC, and Training there are many overlaps and
duplications .
- So different projects produce manuals and teaching aids or audio visual
aids for Health Education which are quite similar in content;
- Health functionaries are expected to maintain a wide variety of registers
that cater to the needs of different HMIS of different EAP's ; and
-32 -
r '5<’
Doctors go for different training programmes organised by a wide
variety of EAP’s that add to variety but not to a coordinated training plan
at district or PHC level (see case study A)
•
An^ integratmg planning exercise is therefore urgently required. At the
directorate / state level there are efforts to prevent this duplication of input and
efforts but systematic change to streamline this process and prevent even
accidental or inadvertent duplication is required since the health sector functions
under a constant financial resource constraint and any effort to ensure more
I *
efficient deployment of available resources is welcome.
d'l
d
\S
p
5. Ownership and Leadership
r
f7
r
•
In most projects the state level ownership is strong except perhaps in those
projects which are ‘package deals’ decided at the centre.
•
Because some of the EAP's have established independent structural identities
e.g. KHSDP, IPP VIII, IPP IX, the links and feeling of shared ownership by the
parent directorate (in the case of KHSDP and IPP IX) and the parent Municipal
Corporation (in the case of IPP VIII) is weak. E.g. no serious consideration
regarding sustainability issues and integration challenges relevant to KHSDP or
IPP IX projects have been addressed at the directorate or Health secretarial. Nor
is the Municipal Corporation adequately concerned about the very same issues
vis a vis IPP VIII project.
•
Another significant lacunae seen in the EAP’s as they are presently structured, is
that ownership at District level - at the point of implementation is quite weak vis
a vis District Health Officers and PHC MOs; and perhaps non-existent vis a vis
PRI institutions. All these three groups arc crucial to ensure the integration and
projects.O
long term sustainability of all these projects.
•
>cch .
Leadership of the project directors has'been good tis long as there have not been
frequent changes of leadership or the burdening of project directors by multiple
and additional responsibilities.
•
However the leadership and ownership are particularly crucial if EAP’s have to
become more complementary or supplementary to each other and the whole
health care delivery system. Leadership that coordinates, networks and
promotes linkages is crucial.
•
Public Health orientation and socio-epidemiological orientation of the leadership
- whether generalist administrator or medical / technical leadership is an
important necessity to prevent inadvertent distortions due to extraneous lobbies
or market forces. This will also enhance capacity to negotiate with external
consultants and others as well.
-33 -
/
6. Intersectorality
While in many EAP’s the importance of this factor is mentioned, the intersectoral
coordination between departments and programme managers and decision makers
of different concerned ministries is still not given adequate priority. At the heart of
good ‘public health strategies’ is the emphasis on intersectoral coordination and
while EAP’s may have not seized the opportunity in this aspect so far, the evolving
Integrated Health, Nutrition and Population project (HNP) must focus on this aspect
urgently and significantly. Even at the grassroots level a better coordination
between PHC, ICDS centre, local schools, women credit cooperatives and
development workers would strongly strengthen programme performance and
outreach.
7. Integration
There is urgent need to integrate Health with Family welfare; public health , primary
health care and the population agenda with each other to avoid not only duplication
by compartmentalization but also to reach the community and tackle the health
problems of people especially the poor in a more integrated way. Much lip service
has been paid to the issue of integration but the stand alone EAP’s have not tackled
this issue adequately. In fact different EAP’s focussed on different problems even
further disintegrate the work of the directorate.
DHO’s and MO’s are constantly preoccupied or distracted at ground level by
frequent visits of consultants, review teams, project teams asking for this and that
data or feed back; the more EAP’s the more such distraction from the normal
planning and management routine.
At the directorate level different EAP’s require different protocols to be filled,
(different MIS mechanisms) so quite a bit of directorate staff time is spent in filling
up questionnaires, schedules enhancing paper work but not necessarily enhancing
efficiency of planning and management.
•
Consultants for each EAP provide their own framework of ideas and decision
making. These do not allow for any inter-EAP consultant communication. One
EAP may appoint a consultant that suggests one type of ideas, another EAP another
type and all these have to function at the same PHC level or the same district level
or have to be operationalised by the same health functionary. This situation
necessarily leads to adhocism and anarchy especially in the absence of state policy
guidelines. Integration and coordinated communication is urgently required.
Another urgent area for integration to avoid wasteful duplication of time and
procedure is the need for integrating all the single project related district level and
state level societies into one Health society at both levels to receive and disburse the
funds. Serious policy reflection also needs to be done to ensure that the District
society’s work under the purview of the Zilla Parishad and PRI.
-34-
8. Equity
While overall the EAP’s do not have a well planned Equity focus some emphasis on
Northern disadvantaged districts and on women and SC/ST have been identified and
noted. HMIS of all EAP’s as well as the Directorate must begin to focus on Equity
in a more concerted way in the years to come. This ‘equity imperative’ must include
i.
ii.
iii.
iv.
Geographical - Within districts and between districts.
Gender - between male and female sections of the population and
especially focus on girl child.
Class / Caste - Between rich, middle class and poor or the so called
haves and have - nots or ‘landed’ and ‘landless’ etc.
Marginalisation - SC / ST or special groups such as child labour or rural
migrants to urban areas, street child, elderly, people with disabilities etc.
Unless the HMIS focusses on disaggregated data the equity principle cannot be
furthered by active policy or programmatic intervention. EAP’s could build this in
to their framework more concretely so that they go beyond policy rhetoric.
9. Partnerships
All EAP’s have built some form of partnerships with the voluntary sector, NGO’s,
private sector, academic institutions or research institutions. But these do not build
on a larger policy framework of the state since guidelines on such partnerships are
not available. They tend to be some what adhoc. The directorate should actively
move towards some form of Resource Directory; Accreditation system; or
reviewing and registering system for such partners so that EAP’s and different
health departments can draw from pooled experience and pooled resource lists. A
partnership cell in the Directorate like the erstwhile Society for Coordination of
Voluntary Agencies (SCOVA) idea could build such directories, framework of
guidelines and linkages, of use to all departments and projects.
10. Community Partnership and Empowerment
• £•
The resistance of the Health department to work with Panchayati Raj Institutions is
well known and though some of the reservations of the health leadership may be
very genuine and based on difficult or awkward situations of ‘interference’ or
extraneous push / pull factors in decision making - there is urgent need to review
this and get over the problem rather than ignore it. With increasing political
decentralization, PRIs will play an important part in local planning and
administration in the future and EAPs should promote this process and not distort it.
The district level societies which leave decision making in the hands of the
bureaucracy may be good for efficient disbursement of EAP funds but they
definitely mitigate against active community participation. EAP’s in particular must
-35-
begin to focus on human development more than infrastructure; and in this human
development component strengthening of community based organizations like PRI
institutions to contribute to local planning and ensure accountability and
transparency through capacity building will become as crucial as building health
teams to deliver the programmes efficiently and effectively.
11. Accountability / Transparency
EAP’s may develop their own monitoring system and evaluation systems, even
audit systems but they are not accountable to the people, the political system, the
legal system in the same way as the directorate and its regular programmes. While
bureaucrats and technocrats may be closely involved with the development of these
projects and the evolution of their frameworks of action there is still the danger of
creation of a parallel system of decision making and programme management which
may be seen as relevant in the short term but could become problematic in the long
term.
However it was noted that overall some of the guidelines and procedures of the
projects were able to immunize the project from the corruption and political
interference which affect the larger system all the time since it does prevent the
influence of extraneous ‘push’ and ‘pull’ factors due to clear cut guidelines that are
not easy to circumvent.
In the short term review we were not able to make clear cut judgement whether
extraneous interference’s were making any sort of affect on programme formulation
or implementation. The use of retired government personnel as consultants was
common (a sort of ‘old boy’ network) which affected the dynamics of the
programme and subsequently its performance in some cases but not necessarily to
integrity. On the whole it may be surmised that EAP’s are as subject to outside
interference as the rest of the system not necessarily more.
•
However in the matter of construction costs and delays and whether some
contractors were favoured rather than others - These areas were difficult to explore
in the time constraint. There was hearsay evidence of this type all the time
including architects inflating designs / and enhancing profit margins in other
ways, etc.
12. Sustainability
This was one area on which there was very little real focus or policy discussion or
planning in the projects at any level - project plans, project dialogue, project
implementation mechanisms and so on.
irv'-yOcxTio
4 ct b»h’ it'y
J co
I errvty
•36-
't_z»
7
The overall assumptions which ignored this imperative and the trends seen were as
follows:
1.
The projects were seen as filling lacunae in the existing system and not
creating additional structures or functions.
ii.
The parent unit or department like the BMP in the case of IPP VIII and
Health Directorate in the case of IPP IX, KHSDP etc were expected to take
over the project when the period of the project was over. There seemed to
be no contingency plans being evolved for this inevitable reality.
in.
In some project documents there was mention of cost recovery usually
through user fees mechanism; or sustainability was to be made possible by
NGO - or private sector partnership or take over but this was not followed
up by serious operational guidelines or planning with the concerned parties.
iv.
Sustainability as an issue seemed to be considered in the last year of the
project as a knee-jerk reaction rather than as a serious plan evolved from the
very beginning.
v.
Unless the directorate estimates recurrent costs, running costs, maintenance
costs and other such definable entities seriously as the time for phasing out
of the project nears and unless these costs are budgeted for or recovery
planned in some sort of methodical way - Sustainability like cost recovery
will remain rhetorical and ultimately ignored or considered as someone
else’s problem at a later date.
vi.
In some cases there seemed to be a confidence that some project donor
would always step in to fill the lacunae if one donor phased out - so again
this complacency led to a fatalistic non-planning situation which was not at
all uncommon.
Sustainability of these relatively large EAP’s is a very serious policy issue that
needs urgent attention at the highest level and the active involvement of the finance
ministry as well.
-37-
H. Some Reflections on the Financial / Economic implications of EAP's
Understanding the financial / economic implications of the increasing reliance on
EAP’s to support the health care delivery system in the state and the gradual shift
from grant giving funding partners to becoming ‘borrowers’ of loans, was not an
easy policy issue to review due to atleast two constraints.
• The financial management of the EAP’s are separate systems not easily listed to
the states own health budgeting / accounting system.
• The loan implications and the debt burden and debt servicing implications are
not easy to explore in a short time constraint under which the project functioned.
The reviewers studied some earlier analysis particularly the review document
(Analysis of Expenditure Medical and Public Health, Family welfare by
S.Subramanya) and the more recent study of Dr. Vinod Vyasulu and group and also
studied the credit agreements of various projects and the budget and account
statements as well as status of project tables from World Bank and other sources.
From a review of all these secondary sources of data the following conclusions and
policy concerns are listed out: (Sec also box items which are extracts from authentic
source and support our conclusions)
1. While the overall expenditure on health and family welfare is gradually
decreasing and hovering between 1.1 and 1.4 of net state domestic product
which is itself an overall low investment (ICSSR / ICMR recommend 8%), the
reliance on EAP's is increasing which means Non-plan expenditure is coming
down and Plan allocations are increasing. This is not a very healthy trend.
2. Most of the expenditure in non-plan is now directed to salaries with less and less
available for programme / action components. EAP’s are tending to take over
more and more of this programme component - again not a healthy trend.
3. Considering that EAP’s are now more and more loans rather than grants or long
term soft loans this is a worrisome development. If these loans are not utilized
with efficiency then we have the double burden of continuing ill health and a
‘debt burden’.
4. Though all the projects talk about sustainability and cost recovery and user fees
mechanism is often mentioned as a long - term option there is no indication that
this mechanism is effective in reality.
While some recovery has been
demonstrated; and some efforts to identify those who cannot pay etc is being
experimented; and the decision to let the amount / revenue collected be kept at
the institutional level for local use rather than transferred to the general account
or treasury - none of the mid-term reviews show that this could be a major
option for sustainability even though in the short term they may help to improve
quality by enhancing consumer participation. Researchers and programme
evaluators are not unjustified in their concern that ‘user fees’ may ultimately
-38-
Health Financing - An Analysis
1. “State Finances, Health Finances and Efficiency: Three key issues, with regard
to public sector finances at the state level need to be addressed. First the overall
fiscal situation in many states has deteriorated sharply since the early 1990s,
with a rise in the fiscal deficit, an increase in interest payments as a share of
total revenues, and an increase in debt outstanding as a share of state domestic
product. The deterioration in the overall financial situation faced by the states
has had a deleterious effect on the health sector. The share of health and family
welfare in the total state revenue budget has declined since the early 1990s
suggesting that past declining trends of health sector’s share in the budget has
been exacerbated, rather than reversed. The decline in the health sector’s share
occurred despite a rise in real per capita expenditures in all states up to 1991,
indicating that total government expenditures rose faster than health
expenditures. Total government spending is about USS 2-3 per capita for health
services and is inadequate to meet the government’s stated objectives. To
achieve the government’s objective of funding a basic package of health
services, substantially more resources for health care are required, but the
overall state finances noted above pose a serious problem. Second, within the
health sector in most states, resource allocation in the public sector is skewed in
favour of tertiary care sendees relative to needs at the primary and secondary
levels, particularly rural and community hospitals. Third, much of the resources
are absorbed by salary costs. The recurrent budget for operations and
maintenance is chronically under-funded and the programs are not fully
effective’’.
2. “Alternative Methods of Health Care Financing : The resource constraints faced
in the health sector will required alternative methods of health care financing to
supplement budgetary allocations. Alternative methods of financing health care,
such as cost recovery, social and private insurance, and participatory schemes,
are limited. Reported revenue data indicate that cost recovery in the health
sector is about 3% on an average in India, although there are problems in
estimating the level. Some of the problems faced with cost recovery include:
a. Lack of an appropriate mechanism within the government to review user
charges;
b. Weak administrative mechanism for collecting user fees;
c. Difficulty in targeting the poor for exemption from user fees; and
d. Constraints to greater retention of funds generated through user charges at
the point of collection.
Based on international experience it should be noted, however, that a cost
recovery rate of 15-20% in the health sector is about the most that can be
expected in the public sector. In the long run, issues such as private insurance
and managed health care will need to be addressed, as the industrial and urban
sectors in India expand, and cost containment becomes increasingly important’’.
I Source : Analysis of Expenditure on Medical & Public Health. Family Welfare
-39-
State Health Finances
“Non Plan expenditure, which is met from resources raised internally by the state,
accounted for 63-69 percent of the total expenditure on health and family welfare
between 1990-91 and 1994-95; this came down to 57 percent in 1995-96.
Reduction in the proportion of non-Plan expenditure in 1995-96 is because of
increase in Plan allocations and capital outlays. One reason for this increase could
be the availability of funds from externally assisted population and health projects
and Central government aided projects such as the AIDS control programme”.
“With expenditure on health and family welfare accounting for only 1.21 percent of
the net State Domestic Product down to 1.14 percent in 1991-92, but up to 1.24
percent in 1992-93, decreasing again to 1.22 percent in 1993-94 before increasing to
1.37 percent in 1994-95. It is clear that fluctuations of this nature are undesirable
for the growth of the health sector as also that expenditure on health and family
welfare is, by any reckoning, inadequate. A study group on Health for Aik set up
jointly by the Indian Council of Social Science Research and Indian Council of
Medical Research, recommended ‘a substantial increase in public expenditure on
health at about 8 or 9 percent per year (at constant prices) over the next 20 years”.
Source . Human Development in Karnataka - 1999
de-emphasize the need to focus on the marginalised. Other problems with this
mechanism are highlighted in the box items as well.
5. There is a danger that increasing reliance on EAP’s will ensure that programme
costs in the regular non-plan health budgets will be ignored with a long - term
distortion in budgeting creeping in. (This will perpetuate long standing
budgetary imbalances with long term implications for health budgets).
6. There seems also a tendency to be more extravagant with issues like
constructions, consultancies, equipment, vehicles, etc because EAP’s promote
unwittingly a more ‘private sector’ ethos so thrift, careful planning, basic
simplicity and other such values that would ensure ‘quality’ at low cost or a
more judicious use of resources so that more is available for grassroot needs is
being affected.
7. Finally it may be important to caution that reliance on EAP’s should only be a
short term plan. Ultimately health budgets like the investment on education and
welfare (social sector) should be increased as a long term investment in quality
human development. Enough economic analysis and theory - including the
more recent endorsement by the work of economists like Amartya Sen and
others show this direction as the way ahead. This needs political will and
commitment and some courageous state development policy planning. Let short
term solutions like EAP’s not come in the way of concerted, action for sustained
development and higher investment in health.
-40-
J. General Policy Concerns; Are we reinventing the wheel?
The key researcher for this study and some of his colleagues had reviewed the
World Bank activities in the Health Sector in India based on a case study on “The
World Bank’s role in the Health system in India” facilitated by the Sector and
Thematics Evaluation Group of the Operations Evaluation Department of World
Bank in August 1999.
That review had raised seven sets of questions / findings for a policy meeting
organised by the Bank with Planning Commission, Ministry of Health and Family
Welfare and others. The review of EAP’s in Karnataka was a good opportunity to
look at these propositions in a wider variety of project initiatives and with
partnerships beyond the one with the bank. Our findings suggest that many of these
concerns are very real ones even in the context of the current EAP’s in the state and
need to be given serious consideration by policy makers and project directors within
the state before these distortions and concerns become too systemic. They are
equally important for the funding partners. These concerns are enumerated as a set
of policy questions that project directors and partners should reflect upon as they
review their projects for long-term sustainability and integration within the larger
system.
1
Is Public Health not being adequately emphasised in problem analysis
project planning and formulation?
Is there a confusion in understanding public health?
Is economic or techno-managerial context taking precedence over socioepidemiological analysis?
Are the w ider determinants of health like nutrition, water supply, sanitation,
and pollution not adequately addressed?
Is the focus on poor, indigent, marginalised not central?
Are regional diversities and differentials not central to decisions on focus of
programme?
2. Is Primary Health Care being given adequate emphasis and priority ?
Is there focus on selective ‘cost effective treatment strategies’ rather than
enabling / empowering processes?
Is there focus on first referral units rather than primary health centres,
subcentres and home based care?
Is community involvement in planning and organisation mostly
rhetorical with community capacity building made subservient to
exigencies of top down management systems.
Are Panchayati Raj institutions generally ignored and registered societies
promoted as an instrument of decentralization but under bureaucratic
control?
-41 -
3. Are these partnerships adequately transparent and accountable ?
Are the partners willing to share the costs of failure and distortions due
to poor programme design or planning which ultimately affects the poor?
Is long term sustainability or integration into existing health care system
being adequately addressed or followed up as an end of project after
thought?
Is there unhealthy competition between projects rather then collaboration
and sharing of expertise and experience?
Are accountability and transparency systems not clearly defined and
hence not actively monitored?
4. Some ethical issues and dilemmas ?
What is the ethics of promoting NGO-private sector partnership in the
absence of solid evidence that these arc more efficient operational
options?
What is the ethics of taking credit when an initiative is successful and
yield positive results while pointing a finger to the directorate or ministry
when the initiative is problematic?
What is the ethics of expanding quality at the cost of or absence of
adequate and operational quality control?
What is the ethics of promoting infrastructure and ‘hardware’ at the cost
of‘software ‘ that can more easily focus and reach the poor?
5 Some management issues and dilemmas?
In spite of marshalling lots of expertise both local and foreign is there a
tendency to;
-
-
6
Develop ‘hardware’ rather than ‘software’?
Expect ‘training’ to get over needs for serious management reforms?
Little thought to social accountability and transparency?
Inadequate attention to building ownership among different stake holders
particularly district level players?
Focussing on ‘user fees’ as the only primary fund enhancing option
rather than looking at diverse options?
Overall neglect of health human power issues like continuity, skill
development and promoting team concept?
Is the political economy adequately addressed?
Are the health projects adequately located in a broader, political, social,
institutional analysis and adequately based on evidence of how projects
run or do not run?
-42 -
Are issues such as political will; corruption and influence of lobbies
political interference; market economy; being given adequate emphasis
in the strategic planning exercises?
Without developing a strong ‘public health policy resource group’ within
the directorate is the free lancing, free floating, adhoc Consultancies and
commissioned studies not allowing the means of change to become
systemic?
7. Is cultural context being disregarded?
Inspite of a rich and diverse tradition of Indian and alternative systems of
medicine, including promotion and investment in health humanpower
development in these systems by government and private initiative; are
the EAP’s ignoring the local cultural context and these alternatives in
their formulation?
All these issues are relevant today and it was surprising to find that most of them
were applicable to all the EAPs in the state and not only for those supported by
World Bank. However it must be noted that the current health leadership both
bureaucratic and technocratic seemed much more alive to these policy issues. That
was a positive finding, symbolizing future potential. However as was brought out
again and again in the interactive discussions local holistic problem analysis and
policy homework was inadequate in all these aspects. Strengthening of
strategic policy analysis and development was an urgent action imperative.
Policy makers and project managers need urgent orientation to Public Health
aspects of decision making and socio-economic politico - cultural aspects of
health situation analysis. Any strategic planning exercise in the future for the
continuation of the existing projects or the evolution of newer one must take these
crucial questions into account so that the projects can be implemented more
effectively and in a more realistic context with reduction in the implementation
gaps.
-43-
J- Final Conclusion and Recommendations from a future Policy point of view.
The previous sections highlight the key findings and trends that emerged from the
review process. However taken as a whole set of project experiences the key issues
and conclusions that have emerged as significant for a concerted policy response are
the following
1. While the EAP’s do focus on a large number of health problems and health
sector development issues, addressing various lacunae in the existing Health
care delivery system in the state at both primary and secondary level, they do
evolve, exist and function in relatively compartmentalized ways without
fitting cogently into a comprehensive, integrated strategic larger state
health policy / plan evidenced by •
The absence of any state health policy document that includes serious reviews or
details of all of them.
•
Any coordinating mechanism at directorate level that addresses them in a
collective context.
•
Any consistent and rigorous strategic planning exercise / document that was
used by programme designers when these EAPs were evolved.
Some
congruence / complementarity between / across projects has evolved since the
members of the project committees overlap with senior policy makers common
to all, but this is ‘adhoc’ and not always intentional.
[Probably the HDR Report, Karnataka Task Force in Health and the recently
evolving HNP project are fore-runners for this much needed paradigm shift from
selective compartmentalized programme planning to more comprehensive
integrated Health sector planning processes].
2. On the other hand while compartmentalized evolution may have lead to some
problems of duplication and integration, especially in IEC and training, but also
sometimes
in
infrastructure development, the very
feature of
compartmentalization has also lead to a certain degree of project autonomy that
has lead to many interesting initiatives and innovations in structure, framework,
operational mechanisms, evaluation and monitoring, some of which have been
identified by this short-term review. These need to be rigorously documented,
objectively evaluated further and adopted / adapted by the whole system as the
projects phase out and get taken over and integrated by the ongoing larger
systems.
-44-
3. Overall the Directorate / EAP’s have shown
•
An ability to evolve laudable objectives for each EAP.
•
General lack of competence in the evidence based homework required to
translate objectives into implementable strategies leading to delays in starting up
times.
•
Diffidence in guidelines and systems development leading to operational and
execution delays.
•
While ability to handle the hardware (infrastructure construction - civil works,
equipment and transport) has been established, effective software development
(training, IEC and Quality Assurance) has remained a weak skill / capacity.
Also cost over runs have been many compounded with poor utilisation in other
areas showing in-different financial management capacity as well.
4. Like the general health care services development, the projects have not shown
any evidence-based focus on equity, gender, regional disparity or other
policy imperatives like impact assessment, community partnership and
ownership, partnership building and decentralization and hence though there
are some successes and some failures as well, in none of these areas can EAP’s
be shown to have used their own programme / project autonomy to enhance the
health sector experience in these areas. This is partly a reflection also that at
the Ministry level there are no clearly circulated policies or programme
guidelines on these policy imperatives and hence project managers have had to
explore these dimensions if at all with diffidence rather than confidence and
clarity. Similarly the issues of corruption, political interference, transparency
and accountability seem to effect them just as much as they affect the larger
public health system- no less, no more though perhaps in the tendering /
purchase policies sometimes as conditionalities of the funding agencies, there
seems to be an overall feeling among programme managers that outside or local
interference is less!
5. Lack of continuity of key personnel has been an important handicap and lack
of systems to monitor quality of care and responsiveness to local needs had
handicapped the establishing or the enhancement of effectiveness. In addition
selection of consultants and senior project consultant need to be critically
reviewed and made more competence based and transparent. Apart from an oldboy network phenomena selection is not always focussed on skills for the job.
-45-
6. While the general impression of the programme managers seemed to be that
these EAPs were not consciously donor driven and there was space and
opportunity for local technical opinion to evolve project formulation, the
impression of donor driven agenda was often attributed to lack of local
homework and evidence generation and hence a tendency to accept the
suggestions / frame work / ideas of working external consultants as an easy
option. This aspect again underlines the urgent need to develop and enhance the
strategic planning capacities of the Ministry / Directorate and making it multi
disciplinary as well [The KfW and OPEC experiences have however been good
examples of the need To look at gift horses in the mouth’ seriously which could
have avoided all the problems that have followed. They have also shown the
absence of long term planning capacities especially in human resource
development for the hospitals being upgraded].
7. Integration as an issue does not seem to have been seriously considered by any
of the projects since many projects were seen as stand alone or focusing on
infrastructure not process. [The absence of clarity in development of a referral
system complex between primary and secondary care (for example: IPP VIII,
IPP IX and KHSDP) is a case in point. Similarly IPP VIII, IPP IX and RCH
could have been more complementary, etc.] This leads to wasteful duplication
at the ground - level.
8. Sustainability is another policy imperative that does not seem to have been
taken seriously by the whole system since in many ways this should be a long
term concern of the Directorate and not just of the EAPs. KfW project had some
serious options outlined in the project part which were not adequately
experimented with. [Efforts to evolve systems of user fees; efforts to identify
and hand-over (contract) out services to NGO’s and or private sector etc. are
being experimented with in KHSDP, IPP VIII, RCH but these experiments seem
adhoc and not within a clear-cut policy framework. Nor are they being
evaluated objectively to establish relevance or effectivity]. Overall the human
power development experience that is crucial for sustainability has often been
ignored or inadequately addressed.
9. Overall EAPs do not seem to be adequately drawing upon the Public Health /
Community Medicine capacities of the state in any concerted or formal way
nor for that matter on the phenomenal inter-disciplinary capacities of institutions
such as IIM, ISEC, NLSUI and other resource centers of health, social
development or strategic planning expertise- many of which are also available in
other districts and regions. In fact there seems to be an overall lack of public
health / sociological orientation in problem identification, situation analysis
or programme planning in the EAPs evidenced by a sense the researchers got
of the dominance of:
Infrastructure over human resource development.
Bio medicine over socio-epidemiology.
-46-
Secondary care over primary health care (especially preventive
public health).
Centralization over decentralization.
Provision of services over enabling / empowerment strategies.
10. Finally a review of EAPs undertaken by us, inspite of the time and
methodological constraints, lead us to suggest that there is urgent need to:-
a)
Develop strategic planning capacities in the Health sector of the
State to handle the complexities of Health sector development as
well as the challenges of negotiating sustainable projects with
external agencies and funding partners that develop not distort /
enhance capacities all round/ and integrate not disintegrate.
This capacity should be multi-disciplinary, directorate-based and as
an immediate starting point should also become the integrated
evidence based monitoring unit for all the health programmes of the
state including EAPs.
b)
Develop mechanisms of integrated planning that would start as a
first step of all programme managers and programme implementers
being networked into a coordinated planning mechanism that from
time to time focuses on integration and sustainability issues beyond
the dynamics of compartmentalized projects / program. [The project
preparatory committee of the current HNP project could well become
the starting point of such a mechanism].
c)
Both these mechanisms should draw on multidisciplinary
professional expertise in the state especially public health and the
behavioral sciences from all the resource centres both public, NGO,
private and the professional colleges. (The HNP project is trying to
do this by involving a multi disciplinary group like Community
Health Cell (an NGO) but this needs to be done with greater clarity
and flexibility.
c)
A more detailed internal review and analysis of current EAPs
should be undertaken as an in-house exercise by both (a) and (b)
supported by (c) so that the positive lessons from EAP experience is
integrated into health sector development in the state and
distortions /problems handled by a more decentralized programme
implementation mechanism or countered through more effective
evidence based long term strategic programme planning.
-47-
K. Limitations of the Review Exercise
•
The task of reviewing ten Externally aided projects in Health in the state in a
short term framework of 4-5 months was a very stupendous and exhaustive task
and perhaps quite unrealistic as well.
•
Hundreds of pages of reports, reviews and other documents had to be perused
and interactive interviews had to be arranged with a large number of very busy
government officials and project managers within this short term framework by
researchers who also had to work within a framework of complementary
demand and deadlines.
•
In two cases RNTCP and KSAPS interactive discussions with programme
directors could not be completed so we used reported information monthly both presentations at KTFH meetings and documents and one other programme
due to time constraint. NLEP (Leprosy control) was not included. Since this
review was trying to identify the broader policy issues relevant to Externally
aided projects in general all the nitty gritty’s of all the projects were not
focussed upon.
•
The study was also focussing on many issues that are neither easy to measure
nor always easy to elicit because qualitative judgements on qualitative issues
are often not easy to collect especially if the judgements are negative or critical.
We must record however that most of the people interviewed showed a
phenomenal degree of openness, frankness and willingness to discuss even
‘sensitive’ areas and this candidness is really appreciated.
•
We have tried to do our best integrating the rich, response and feedback that was
received in the interactive discussions supported by background notes and
papers and our own reading and critical analysis of all the documents that we
were able to access. The effort has been made to make this review a learning
experience as a partner not as a critical external reviewer.
•
We hope we have been able to collate and highlight the salient features - both
strengths and weaknesses of EAP’s when taken collectively. Much more needs
to be done to address all the questions originally listed out, some have been
answered, others only just considered. More time would definitely have helped.
However the experience has shown that full justification can only be done if this
review, both
in-house and external becomes part of the ongoing Strategic
Planning Cell of the Directorate / Ministry. If our study has helped to get this
message across we would have felt fully complimented by our efforts.
-48-
L. Acknowledgements
To the Karnataka Task Force in Health for the opportunity to make an overview of
the externally aided Health projects of the state.
To all the project directors particularly Mr. Arvind Risbud (KHSDP, OPEC, KfW),
Mr. Krishna Rao (IPP VIII and IPP IX), Dr. G.V.Nagaraj (RCH) and Dr.
Jayachandra Rao (IPP VIII) Dr. Shamanna (NPCB-K) and all their consultants and
supportive staff for the frankness and openness with which they participated in the
review and made available reports and other documents.
To Dr. Thelma Narayan and Dr. C.M. Francis who shared insights as the Task Force
process continued; and all the CHC team members who encouraged and supported
the project framework.
Finally to Mr. Anil Kumar (Secretarial cum Account Assistant) who typed the
manuscript, Mr. M.Kumar (Administrative Officer) and the rest of the CHC office
team, who particularly helped with all the operational aspects of the short term
project.
Dr. Ravi Narayan,
Community Health Adviser,
Commurffty Health Cell,
Bangalore.
Dr
path. K. Krishnan,
Policy Fellow &
Research Associate,
Community Health Cell,
Bangalore.
Dated: 28,h March 2001.
- 49 -
M. Bibliography
(This is a partial bibliography which includes the main document / reports. It doesn’t include all the
aide Memoir’s, review mission notes, newsletters, credit agreements, project partnership documents,
submissions by project directors and other formal and informal documents).
General:
h
2.
3.
4.
5.
6.
7.
8.
Human Development in Karnataka, 1999. Planning Department, Government of Karnataka.
Analysis of Expenditure on Medical and Public Health, Family Welfare (Dr. S. Subramanya,
KHSDP)
Case study of World Bank Activities in the Health Sector in India, May 1999 (Sector and
Thematic Evaluations Group, Operations Evaluation Department, The World Bank).
Comments on ‘Case study of World Bank Activities in the Health Sector in India', Ravi Narayan
et al in Health and Equity - Effecting change, IIIVOS Technical Report series 1.8 (2000).
A guide to sector - wide approaches for health development - concepts, issues and working
arrangements, Andrew Cassels. (WHO, DANIDA, DFID, European Commission), WHO, 1997.
Towards Equity with Quality in Health (Karnataka), Interim Report of Task Force on Health and
Family Welfare Karnataka.
Health Budget in Karnataka - Vinod Vyasulu ( a report presented to Task Force on Health and
Family Welfare, Karnataka).
Handbook of Health and Family Welfare Sector investment programme Department of Family
Welfare, GOI and EC Health and FW programme office, March 2000.
IPP VIII;
9. Family Welfare (Urban slums project) Brochure of IPP VIII, Bangalore.
10. Staff Appraisal Report, India, Family Welfare (urban slums) project, May 1992, The World
Bank (India county operations department (10548-IN)
IPP IX;
11. Strengthening of Family Welfare and Maternal and Child Health services India Population
Project-IX Proposal, Department of Health and Family Welfare, Karnataka June, 1994.
12. IPP IX Background notes for World Bank Review Mission November 1999.
13. IPP IX Project Review and implementation status Report for World Bank Review Mission May
2000.
14. India: Family welfare project (Population IX) World Bank Review Mission Aide Memoire (May
2000).
15. IPP IX - Project implementation status, September 2000.
16. IPP IX World Bank Review Mission, Aide Memoire, September 2000.
17. Evaluation of ANM training for Tribal girls under India Population Project -IX - Innovative
scheme (P.J. Bhattacharjee and R. Venugopala Raju), Population Centre, Bangalore, March
1999.
KHSDP:
18. Karnataka Health Systems Development, Project proposal Department of Health and Family
Welfare, GOK, May 1995.
19. KHSDP project proposal - January 1996.
20. KHSDP Referral system manual. June 1999.
21. Staff Appraisal Report, February 1996, The World Bank, (State Health Systems Development
project II).
22. Procurement Workshop Manual, Second State Health Systems project (Karnataka, Punjab, and
West Bengal) September 1996.
-50-
23. Status Report of Manpower position in Karnataka Hospitals, KHSDP, Apiil 2000.
24. Overview of Training programmes under KHSDP and KfW project, KHSDP, June 1999.
25. Newsletters of the Strategic Planning Cell, KHSDP.
KfW;
■
26. Upgrading secondary
level Healthi care facilities in the state of Karnataka, Final project proposal
for KfW, Germany, Department of Health and Family Welfare, GOK, July 1995.
27. KfW project - Progress Reports numbers 8 to 12.
OPEC;
28. Project Proposal for OPEC Assisted Hospital at Raichur, Department of Health and Family
Welfare, GOK, May 1996.
RCH;
29. Reproductive and Child Health services. Programme. District level Implementation Guidelines,
RCH project Bureau, April 1999.
30. A brief note on Reproductive and Child Health, GOK, November 2000.
31. Reproductive and Child Health Project - status report, sub project Bellary, October 2000.
UNICEF:
32. Approach paper for 2000 - Karnataka, Hyderabad Field office, UNICEF.
33. Border Cluster Districts Project, A strategy paper (Sanjiv Kumar)
34. Reproductive and Child Health - UNICEF Cooperation - Achievements, Impact, Constraints - a
hand out.
RNTCP:
35. Project Report for Revised National TB control programme, Department of Health and Family
Welfare, GOK, 1997.
36. RNTCP - Project implementation plan, DOHFW / GOK April 2000.
DANPCB / NPCB-K;
37. National Programme for control of Blindness, Karnataka State profile. August 2000, State
Ophthalmic Cell, GOK.
38. NPCB - Schemes for implementation during IX plan, 1997-2000 Ophthalmology / Blindness
control section, DGHS, MOHFW, GOI.
39. NPCB - Guidelines for District Blindness control society, GOI.
40. NPCB - Course material for training in District programme GOI.
41. NPCB - Schemes for participation of voluntary organizations GOI.
42. DANPCB - Eye care through Primary Health centres.
43. DANPCB - Creating awareness and demand generation for cataract surgery.
44. DANPCB - Rapid Assessment of cataract Blindness, February 1997.
NACO / KSAPS:
45. The Karnataka Strategy on Management of HIV / AIDS - The way forward, KSAPS, September
2000.
46. NACO, Scheme for prevention and control of AIDS - Phase II.
47. KSAPS Project implementation plan, - Phase II - December 1998.
-51 -
APPENDIX -1
Pirojjecit Proposal
Review of externally Aided Projects
in the context of their integration into the
Health Services Delivery in
Karnataka.
Content List
1. Introduction
2. Objectives
3. Methodology
4. Budget
5. Project Outcome
6. References
7. Appendices
Submitted by
Dr. Ravi Narayan, M.D. (AIIMS), D.T.P.H, (London), D.I.H. (U.K.)
Community Health Adviser
Community Health Cell
367, 'Srinivasa Nilaya', Jakkasandra 1st Main,
Koramangala 1st Block, Bangalore - 560 034.
Tel/Fax: 5525372
Email: socharafrz \ snl.com
i. Introduction
Since mid 1990's, Karnataka Government has negotiated and received grants / loans from
International Funding Agencies for an increasing number of Health related projects.
These have included IPP - 8, IPP-9, KHSDP, KFW, RCH, Prevention of Blindness,
RNTCP and other projects. These externally aided projects have their particular focus
and framework and operational strategies to support and enhance both quantitatively and
qualitatively different aspects of the Health Sector development. Each of them has had
various mid term and concurrent reviews and some of them are currently reaching the end
of specific phases. The Karnataka Task Force in Health while reviewing these projects
informally in their discussions and deliberations have raised some important questions for
review.
i. "What are the learning points from each of these projects"
ii. How can they be integrated into the health system incorporating beneficial
points and avoiding distortions?
iii. What arc the issues for consideration of sustainability, accountability and
transparency" (1)
This project proposal is a short-term initiative to explore some of these issues
qualitatively as a preliminary to perhaps a larger study at a later date.
Community Health Cell is a technical Community Health and Public Health oriented
policy research and training group that has reviewed external aided projects in the past.
Four policy initiatives are relevant to this study.
1)
2)
3)
4)
Review of health projects in India supported by Misercor / Germany. (7)
Review of Health Partnership ofMemisa in Netherlands.
(6)
Review of partnership in Health (Cebemor Netherlands Government) (5)
Policy reflections on World Bank Activities in India - (see references) (3)
2. Objectives of Study
I. The study will review all the externally aided projects not just individually but in their
collective context and relation to the Primary Health Care and Public Health system
development in the state using a SWOT approach.
More specifically it will look at
a. The Strengths of each project and the positive learning experiences.
b. The If eaknesses or difficulties encountered in each project.
c. The Opportunities that have been created or exist to enhance primary and
public health care system development in the state.
d. The Threats or distortions that may have been inadvertently caused by the
project assistance to the health sector or that may be caused during the process
of integration.
Some specific questions are in Appendix one, though a more structured approach will
emerge after the literature, review.
3. Methodology
The time frame work of three months is too short to evolve a rigorous data based,
quantitative approach to project design and therefore a more qualitative approach that
will focus on a participation, interactive process is being suggested rather than an expert
external review the method suggested will try to make it a collective learning experience
for all concerned. Each project will be requested to allot atleast one project staff to be
part of an evidence collecting, evidence sifting; and evidence collecting exercise.
The steps of the process will be
A. Phase one 15th September - 15th October 2000
i.
ii.
Literature Review of all project proposals and mid term/ concurrent reviews and
aide memoirs.
Informal discussions with all project leaders and support team to clarify the
nature and process of review and seek required support and participation (As a
halfday interactive workshop together, tentative date 10th October 2000.)
B. Phase Two - 15,h October - 30,h November 2000
i
Qualifafivc interviews with Directors and staff of each of these projects and with
a small representative sample of other stake holders including medical officers
and other staff. (Some visits outside Bangalore will be required)
ii. Interactive participation workshop with representatives of all the projects to
address the issues of sustainability accountability etc. and all those issues, which
are common to all projects and derive from phase one review, (atleast two, to be
discussed at A. ii)
iii. A questionnaire survey of some key aspects relevant to the study to be filled up
by each project as ’evidence contribution’ to the review.
C. Phase Three - IS11’ November - 15,h December 2000
Integration of all the data/evidence from phase one and phase two processes into
a project analysis document.
ii. Circulation of this document to all concerned with a weeks time framework for
replies.
iii. Incorporation of all comments / suggestions and final editing of a document to be
submitted to KTFH hopefully not later than 15th October 2000.
i.
4. Budget
A budget proposal to support the study and including costs of Researchers, other
assistance, office support including photocopying, computer facilities, postage,
stationery, travel of research assistant and co-ordinator of study and some supportive
costs for three interactive workshops is included in Appendix Two.
The study will be undertaken by Dr. Ravi Narayan of CHC supported by a full time
research associate for 3 months and drawing upon short-term research assistance from
some other members of CHC team on a flexi-time basis.
Some elements of the study / review are complementary to the project proposals of
Mr. Vinod Vyasulu of Centre for Budget and Policy Studies, Dr. Ramesh Kanbargi of
ISEC; Mr. As. Mohamed of SJMC and Dr. Pankaj Mehta of Manipal Hospital and so
their involvement in some aspects of the study will be operationalised through informal
interaction at no additional cost.
Finally to make the short term process more cost effective and efficient under the
circumstances - close co-ordination with the project leaders will be established so that
some aspects of the study including the interactive aspects can be linked to any ongoing
schedule of meeting/training programmes or midterm/concurrent reviews so that
opportunity costs are enhanced.
5. Project Outcome
A project report highlighting a SWOT review of the External Aided Projects and Policy
guidelines for integration, sustainability and future projects of this type.
6. References
1. Topics for Action Research Studies identified by Task Force ( a KTFH handout)
2. Comprehensive Health, Nutrition and Population services development initiative in
Karnataka (An idea draft from CHC)
3. Comments on Case Study of World Bank Activities in the Health Sector in India (A
CHC policy reflection)
4. A Guide to sector-wide approaches for Health development - concepts, issues and
working arrangements (Andrew Cassels) A WHO/DANIDA/DFID publication.
5. Programme Evaluation-Basic Health Services India (cebcmo / icco/DGIS), October
1994. (CHC)
6.
Partners in Health - Challenges for the next decade: A process renew of the Indian
Partnership of Mcmisa - 1989-1994, (October 1994. Cl IC)
7. Promoting Health in India: A process review of the Indian Partnership of Misereor,
December 1994. (CHC)
APPENDIX -II
Integration of Externally Aided Projects in Health Services Delivery
(Karnataka)
Some Issues and Questions to be addressed in the Review Project by
Literature Review and Interactive discussions.
A Check List
1. Descriptions of each project including year of starting, period, focus, objectives,
components, programmes, budgets, reviews, etc.
2. Was the ‘problem analysis’ and the ‘problem solution’ comprehensive or selective?
If selective then factors used for prioritization? or selection of strategies?
3. How does the project support,
a) Health System Development ?
b) Primary Health Care?
c) Public Health?
4. How is the project funded?
a)
Direct or indirect
b) Loan agreemcnt/conditionality
c) Repayment
d) Budget components etc.
5. What has been the experience of
a) financial management
b) disbursement
c) expenditure
d) delays
e) shortfalls, etc.
6. Is the project funding leading to distortions in spending priorities?
7. Are a reliance on projects perpetuating long-standing budgetary imbalances;
implications on existing state health budget etc.?
8. Are there diversities in accounting/auditing procedures?
9. Strengths, Weaknesses, Opportunities, Threats of each project including those
identified by niid-tcmi reviews.
10. Are there problems of
a) Project flexibility
b)
c)
d)
e)
0
Overdesigned
unnecessary long lead time, preparation delays
Slow rates of disbursement
Complicated procedures
Any other managerial/operational problems.
11. Are there areas of overlap / duplication with other projects?
a) HMIS
b) IEC
c) Training
d) Staffing
e) Others
12. Are projects creating islands of excellence in an otherwise under funded sector?
13. Who drives the project?
a) State Health Directorate
b) Funding partners
c) External consultants
d) Others
14. Are there problems of:
i) Ownership
ii) Leadership
iii) Intersectorality
iv) Implementation
v) Monitoring and Evaluation
vi) Any other areas
15. How do the projects perform in the context of some policy imperatives:
a) Equity
b) Gender sensitivity
c) Regional disparties
d) Partnerships
i.
NGOs
ii. Private sector
iii. Academics-Research
iv. Others
e) Accountability including corruption and political interference
f) Community involvement and partnership
g) Decentralization and Panchayatiraj
16. Do multiple projects make it difficult for the government to develop and implement a
coherent health policy for the health sector as a whole?
17. What has the project done in the context of sustainability?
18. Any other cross cutting themes that emerge in the discussion between researchers and
the project leaderships.
Integration of EAP's in Health Service Delivery
Karnataka
CONCEPTUAL FRAME WORK (2)
Objectives ?
Focus ?
Regions ?
Complementarity,
Processes
or
programmes
Budgets
Supplementarity,
Overlap,
Ownership /
Leadership
Duplication
Partnerships /
Linkages
Evaluating /
Monitoring
Integration of EAR'S in Health Service Delivery
Karnataka
CONCEPTUAL FRAMEWORK (3)
Add
Quantity
Add Quality
Add Value
(Improve /
Diversity)
Relationship
Innovations
to Existing
Health Care
System
- ve
Distort
" ve
Undermine
System
Development
- ve
Confuse or
complicate
Integration of EAR'S in Health Service Delivery
Karnataka
CONCEPTUAL FRAMEWORK (4)
Whose Agenda ?
Who Drives?
a) State need
b) Funding partners
c) External Consultants
Sustainability
a) System
b) Financial
Some
Issues
for Integration
Duplication
a) HMIS
b) IEC
c) Training / CME
Financial Issues
a) Budgets
b) Financial System
Accountability
a) Corruption
b) Political
Interference
Position: 2286 (3 views)