Radical Journal of Health 1988 Vol. 3, Nos. 2-3, Sep. – Dec. Health and Human Rights.pdf
Media
- extracted text
-
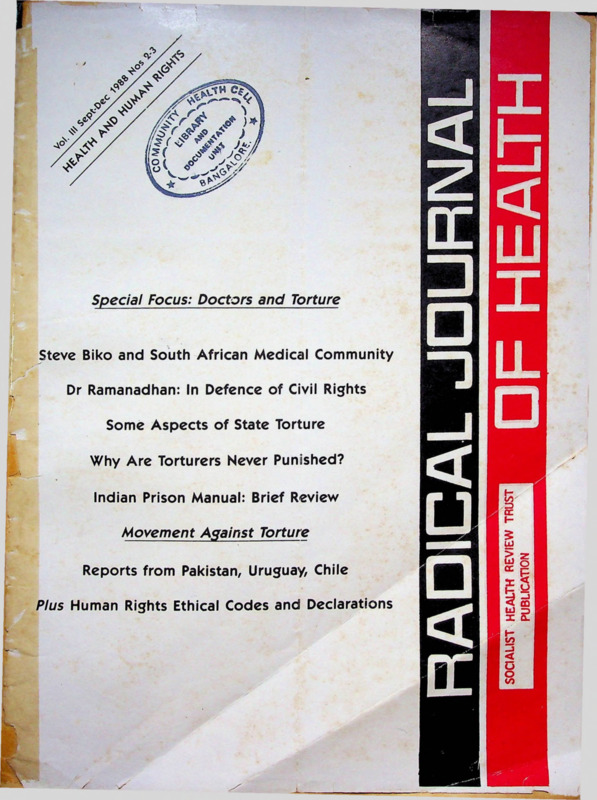
Special Focus: Doctors and Torture
Steve Biko and South African Medical Community
Dr Ramanadhan: In Defence of Civil Rights
Some Aspects of State Torture
Why Are Torturers Never Punished?
Indian Prison Manual: Brief Review
Movement Against Torture
■ ■'
Reports from Pakistan, Uruguay, Chile
Plus Human Rights Ethical Codes and Declarations
B
VX
L \
Volume III
September-December 1988
Nos 2-3
HEALTH AND HUMAN RIGHTS
<u
SPECIAL FOCUS ON DOCTORS AND TORTURE
33
Editorial Perspective
DOCTORS AND TORTURE
35
MEDICINE AT RISK
DOCTORS AS HUMAN RIGHTS ABUSERS AND VICTIM
AMNESTY INTERNATIONAL
40
Working Editors:
STEVE BIKO AND SOUTH AFRICAN MEDICAL COMMUNITY
Mary Rayner
Amar Jesani, Padma Prakash,
Ravi Duggal
50
IN DEFENCE OF CIVIL RIGHTS
A BIOGRAPHICAL SKETCH OF DR RAMANADHAN
Editorial Collective.Ramana Dhara, Vimal Balasubrahmanyan (AP)}lmrana
Quadeer, Sathyamala C (Delhi), Dhruv Mankad
(Karnataka), Binayak Sen, Mira Sadgopal (M P), Anant
Padke, Anjum Rajabali, Bharat Patankar, Manisha
Gupte, Srilatha Batliwala (Maharashtra) Amar Singh
Azad (Punjab), Smarajit Jana and Sujit Das (West
Bengal)
Editorial Correspondence:
53
WHY ARE TORTURES NEVER PUNISHED?
CASE OF ARCHANA GUHA
Peter Vesti
56
STATE TORTURE: SOME GENERAL PSYCHOLOGICAL AND
PARTICULAR ASPECTS
Fernando Bendfeldt-Aachrisson
62
Radical Journal of Health
C/0 19 June Blossom Society,
60 A, Pali Road, Bandra (West)
Bombay- 400 050 India.
Mehboob Mehdi
Printed and Published by
INDIAN PRISON MANUAL
PARTICIPATION OF DOCTORS IN TORTURE
REPORT FROM PAKISTAN
64
DOCTOR AND PRISONER
Dr. Amar Jesani for
Socialist Health Review Trust from C-6 Balaka
Swastik Park, Chembur, Bombay 400 071.
Colin Gonsalves
65
IMPLICATIONS OF PHYSICIANS IN ACTS OF TORTURE IN URUGL
Gregorio Martirena
Printed at;
68
Bharat Printers, Shivshakti,
Worli, Bombay.
MISSION TO CHILE
REPORT OF WORLD MEDICAL ASSOCIATION
Andre Wynen
Annual Subscription Rates:
70
30/- for individuals
Rs. 45/ for institutions
Rs. 500/- life subscription (individual)
US dollars 20 for the US, Europe and Japan US
dollars 15 for othgr countries.
We have special rates for developing countries.
ACTION AGAINST DOCTORS INVOLVED IN TORTURE
Francisco Rivas Larrain
Rs.
SINGLE COPY: Rs. 8/(All remittance to be made out ih'favour of Radical
Journal of Health. Add Rs 5/- on outstation cheques).
72
PRESS REPORTS ON HUMAN RIGHTS VIOLATION IN INDIA
Book Review
73
TORTURE, PSYCHIATRIC ABUSE AND HEALTH PROFESSIONALS
R Raghav
76
HUMAN RIGHTS ETHICAL CODES AND DECLARATIONS
Editorial Perspective
Doctors and Torture
TORTURE is condemned universally as inhuman and as
a calculatedly cruel practice. As such it should not find
any place in any civilised society. Yet its widespread use
is a truth that cannot be denied. To a greater or lesser
extent it is resorted to in all countries. Why is this so? Why
do countries which apparently place a high value on
human rights routinely practise and condone physical and
mental abuse of its opponents both in times of war and
in peace?
Torture has been recorded in history since the ancient
times and there have been references to torture in the 12th
and 13th centuries, and even earlier. The TUdor and Stuart
monarchs made frequent use of torture. But it was dur
ing the religious and political struggles of the 16th and
17th centuries in European countries that there was more
open discussion of the subject. Indian history also is
replete with references of torture of political prisoners.
It was in the 18th century that a movement against this
cruel inhuman practice was initiated with the hope that
by the end of the 19th century this practice would be
abolished altogether. But the reality of concentration
camps in Germany under Nazi rule, with their largescale
use of torture wiped off this optimistic belief. However,
it was in the aftermath of the war and the end of Nazi
rule that serious attempts were first made to set out norms
of conduct for medical people participating in torture.
Torture is among the most reprehensible aspects of state
repression. Unlike other forms of repression, it can be car
ried out in private and in such a manner that none but
those against whom it is used come to know of it. So it
can be practised with impunity within smiling democracies
professing to be ‘open’ societies ensuring freedom of
speech, expression etc. to its citizens.
Torture is used to suppress dissent against the state and
its ideology in various ways. It is used extensively to ex
tract infqrmation—and this use is often protrayed as be
ing justified in order to maintain ‘law and order’. But more
importantly, it is used to strike terror in the hearts of those
who oppose it. A torture victim becomes a warning to
others who may follow his/her path for much the same
reason that feudal barabaric societies displayed severed
heads or conducted public hangings.
The Indian state has consistently and widely used tor
ture to quell rebellion and protest whether it is to supress
movements of minorities for autonomy or those which
pose an ideological challenge to the state. In Telengana
in the 40s and Naxalbari in the 60s and fOs and Bihar,
Punjab and Andhra Pradesh in the 80s the state’s police
have systematically and routinely used torture on political
prisoners so much so that they have perfected methods
which cause pain and suffering to the individual but leave
September-December 1988
no mark which can be displayed to monitoring authorities,
such as they are. And in all this at some level or other—
whether in diagnosing and treating a victim of torture or
in issuing death certificates of those who have succumb
ed to it or in many other numerous small ways—is involv
ed a health worker most often a medical professional, who
ironically enough is pledged to preserve life and reduce
suffering.
Here there are two aspects which must be touched upon.
Usually torture in most codes is defined to mean the abuse
of person in the custody of the authority. In a larger sense
and increasingly, it includes the physical and mental abuse
meted out to the friends, relatives and others close to the
victim. Again the evidence of torture becomes valid only
with the involvement of the medical profession. Second
ly, sexual abuse and assault on women held in custody
or held for ‘questioning’ is becoming increasingly fre
quent. And in most cases, it is medical evidence which
will help in bringing the victimisers to book. The medical
profession thus plays a crucial role in protecting human
rights.
The United Nations, in 1975, in its Declaration, has
defined torture as: “Torture means any act by which severe
pain or suffering, whether physical or mental, is intentially inflicted by or at the instigation of a public official
on a person for such purposes as obtaining from or a third
person information or confession, punishing him for an
act he has committed or is suspected of having commit
ted, or intimidating him or other persons. It does not in
clude pain or suffering arising only from, inherent in or
incedental to, lawful sanctions to the extent consistent with
the Standard Minimum Rules for the Treatment of Priso
ners. Torture constitues an aggravated and deliberate form
of cruel, inhuman or degrading treatment or punishment”
(see Health and Human Rights, ICHP/cinpros 1986, p 25).
As Paul Sieghart states (p 95) the “prohibition against
torture contains no limitations or exceptions of any kind
and allows no derogation in any circumstances—not even
in times of war or public emergency treating the life of
the Nation” (Emphasis added).
Doctors As Victimisers and As Victims
It is an irony that the “protectors of law and order”—
the police themselves employ the method of torture which
is so universally condemned but what is unthinkable is
the involvement of doctors (actively or passively) in tor
ture, particularly when they happen to be police, prison
or military doctors. The conflict between the ethical posi
tions of the prison doctors and national laws are real and
superficially bewildering but certainly not unresolvable
33
As Dr. Wyner of the World Medical Association clarifies
“that if a certain legislation is criminal and contrary to
ethics, the doctor has the deontological duty to ignore it
and in some cases, even oppose it when practicing his pro
fession”. It is thus gratifying to learn and in Switzerland,
the prison doctors and subordinate medical authorities
alone are responsible for the prisoners’ health and thus
find it easy to maintain the patient-doctor relationship.
Such a trend must spread to other countries as well.
So far as the ethical codes on the subject are concern
ed, there need be no ambiguity in the mind of the medical
practfoner. The UN Declarations and codes relating to
Principles of Medical Ethics, the Declaration on the Pro
tection of All Persons from Torture and Other Cruel, In
human or Degrading Treatment or Punishment and (iii)
Standard Minimum Rules for the treatment of Prisoners
and related recommendations are amply clear and con
cise to permit any grey areas. Furthermore, the statements
by various orofessional associations viz. that of (i) physi
cians, (ii) psychiatrists, (iii) nurses and (iv) psychologists,
also leave no stone unturned in respect of the ethical posi
tions. [Elsewhere in the issue we carry the full text of some
of there codes and statements]
Even so, there are reports revealing medical practioners
attending the interrogation of punishment centres for examing the detainees to certify on their health and later
administering treatment for the victims* injuries. Some
of them are even reported to be active in torture. How
else could one explain some of the more modern and
sophisticated methods of torture which could not have
been devised without the active participation of experts
(forensic) having a high degree of knowledge in the area?
To the exteqt that many of its members contribute to tor
ture, the whole medical fraternity must also share his guilt
and it is for the respective medical councils to pull up its
members. Medical fraternity must do all that is in its col
lective power towards eliminating this obscene, cruel, in
human practice that is internationally outlawed.
The doctor compounding or assisting torture discar
ding the ethical norms is obviously only one facet of the
situation existing today, but consider the scene where (and
this*is known to take place more after in some countries
under some dictatorial regimes) the doctor has had to pay
heavy penalties including his life for having listened to
his consciense and abiding with ethical codes laid down.
Often a doctor is penalised for helping the victim of state
repression or for supporting movements for justice. One
such victim of police brutality was Dr. Ramanadhan who
was shot dead the state police in September 3, 1985. We
publish in this issue a short biographical sketch of the
doctor-activist. Undoubtedly, health workers who use their
professional skills to help those who protest against the
state are themselves vulnerable. Particularly under the dictitorial regimes the reality is such that people’s protest
34
against such actions cannot be expected to operate. In
ternational pressures need to be applied and the Human
Rights wing of United Nations have a pertinent role in
this.
What about the repurcussions of torture on physical
and mental health of the tortured? On the family? And
the responsibilities of medical and social scientists in this
matter? It is clearly imminent that torture would both
physically and more importantly mentally wreck the vic
tims’ and ruin them and their families but sadly there are
not enough studies on this important issue in our coun
try [see the case of Archana Guha in this issue]. Such
studies, if nothing else, could serve well towards
eliminating the apathy towards this distantly occuring
nonetheless sensitive issue. Surely it must be remembered
that until empathy towards the tortured does not percolate
through vast multitude of peoples, elimination of this in
human practice will keep eluding us time and again.
Why have we chosen to highlight the issue of the role
of the health worker in preserving human rights, especially
in state torture? Firstly, because as we have seen, the
medical profession plays a crucial role both in perpetrating
torture but also in publicising its use and bringing the vic
timises to book. In doing so, the health workers
themselves become vulnerable to attack. It is therefore
necessary that a strict code of conduct be implemented.
Also, doctors who are placed in vulnerable situations must
be ensured safety. In times of war, for instance, medical
help is always ensured safe conduct. In times of peace too,
it should be possible to safeguard the life of people who
give medical aid.
Secondly, there nas been an increasing incidence of
police torture and inhumanity. With the growth of
political awareness, mass movements are on the upswing.
The state is bound to become more repressive and if this
repression is to be effective while maintaining the facade
of democratic functioning, it has to use such instruments
which focus on the individual and are hidden from the
public eye. There is a tendency to legitimise torture (say,
by branding the victims as ‘terrorists’). Again there is need
to create an awareness of where, how and in what cir
cumstances torture takes place and the role the health
worker plays in this. It is also necessary to empower them
with information on how they can be coerced into abet
ting torture and what they can do about it.
While we highlight some of the major issues in the field
and how the international community of health workers
have tackled it this is certainly not the last word on the
subject. There is a particular lacuna about information
on India. We hope the issue will generate discussion on
the issue and lead to documentation of the Indian
situation.
Anil Pilgaokar
September-December 1988
Medicine at Risk
Doctor as Human Rights Abuser and Victim
Amnesty International
For over a decade now, the Amnesty International has been working to eradicate the use of torture. In this
effort, it has paid special attention to the role of health workers in human rights violations as well as the violation
of the human rights of people working in health.
[This paper was prepared by the Internationa! Secretariat of the Amnesty International and circulated as a background paper
for the International Seminar on the same subject at Pans from January 19 to 21, 1989.]
IN 1978, Amnesty International convened an international
meeting in Athens which brought together some 100
health professionals from 13 countries to discuss ‘medical
detection and effects of torture, the need for treatment,
rehabilitation and compensation of torture victims, and
other work of the medical profession against violations
of human right’. Among the many conclusions and recom
mendations made by the participants, three themes were
identified for continuing study and campaigning. T\vo of
these particularly relevant to the subject of ‘medicine at
risk’ were strategies for the prevention of torture, and the
elaboration of medical ethics codes against torture [1].
Despite continued widespread human rights violations,
there have been since 1978 a number of positive
developments with regard to prevention of medical in
volvement in torture and two in particular might be men
tioned here. The first was the adoption by the United
Nations General Assembly on 18 December 1982 of the
Principles of Medical Ethics Relevant to Health Profe
ssionals, Particularly Physicians, in the Protection of
Prisoners from Torture and other Cruel, Inhuman or
Degrading Treatment or Punishment. These, together with
the World Medical Association’s Declaration of Tokyo of
1975, offer the clearest ethical guidance to the health pro
fessional confronted with the problem of torture.
The second encouraging development has been the
active public opposition of some medical and other
associations to torture and their commitment to disciplin
ing those health professionals who participate in it.
However in the face of continuing human rights viola
tions and despite committed work by human rights groups
and professional bodies [2], a wider degree of engagement
by health professionals in supporting colleagues at risk
would make a significant contribution to the fight for
human rights.
This paper reviews some of the issues implicit in the
theme ‘medicine at risk’: that is, participation of health
workers in human rights violations, the violation of the
human rights of those working in health care; and the
role of professional associations in dealing with these
abuses.
Human Rights Standards
Human rights violations are contrary to the principles
of all the healing disciplines. Ethical standards of a wide
September-December 1988
relationship of the practitioner and his or her client should
be based, inter alia, on principles of beneficience and
respect for the client’s autonomy.
However, dealing with prisoners poses certain dif
ficulties to medical and other personnel since prisoners
have lost their freedom with concomitant restrictions on
their autonomy; secondly, the health professional has
obligations with regard to the detaining authority which
they may see as threatening the concept of medical confidentality, in practice if not in principle. Nevertheless, the
ethical standards have been clearly set out.
The World Medical Association, at its assembly in
Tokyo in 1975 adopted a declaration which stated that it
was prohibited for a doctor to “countenance, condone or
participate in the practice of torture or other forms of
cruel, inhuman or degrading procedures, whatever the of
fense of which the victim to such procedures is suspected,
accused or guilty.. .” [3] The World Psychiatric Associa
tion, in its Declaration of Hawaii [1977] stated, inter alia,
that “no procedure shall be performed nor treatment given
against or independent of a patient’s own will...” and
“the psychiatrist must never use his professional
possibilities to violate the dignity or human rights of any
individual or group...”.
Nurses’ and psychologists’ associations have also set
out the responsibilities of these particular professions with
regard to the care of those in detention.
An international code applying to all health
professionals— The Principles of Medical Ethics—which
embodied many of the elements of the Declaration of
Tokyo, was adopted by the United Nations on December
18, 1982. This states categorically inter alia that it is a con
travention of medical ethics for “health personnel, par
ticularly physicians, to engage... sub acts [of] torture or
other cruel inhuman or degrading treatment or
punishment”.
Unfortunately, in spite of the elaboration of these com
prehensive standards, there is irrefutable evidence that in
many countries professional expertise continues to con
tribute to human rights violations.
These breaches of professional ethics are manifested in
a number of ways, including participation in the practice
of torture. Direct involvement takes a number of forms:
Examination of prisoners before interrogation to en
sure that the prisoner can survive torture or to find sen
35
sitive fpci for exploitation during torture.
lb monitor the torture process: to stop the torture if
it threatens the prisoner’s survival or to resuscitate the vic
tim where necessary.
lb ‘patch up’ the victim after torture, possibility to
undergo further sessions or to make the prisoner presen
table for appearance in court or after release.
To provide the police or other authorities—under
pressure or by free will—with false certificates stating that
the prisoner is in good health or, in event of their death,
certifying a false and misleading cause of death.
lb advise the torturers or to directly use medical or
psychological techniques during interrogation eg. giving
sensitive information obtained during the interview or
helping administer drugs [4].
Other abuses of medical expertise constituting infr
ingements of medical ethics and human rights include:
Falsely certifying that an individual is seriously men
tally iU in order to have them committed forcibly to a men
tal hospital so as to curtail their political activities.
Advising executioners of the progress of an execution
to enable them to continue or to modify whatever techni
que they are using.
Using medical skills to mutilate an individual as a
punishment or advising others in the application of such
skills. [5]
Reasons for participation by health professionals in
behaviour of the kind cited above can, for the most part,
be the subject of speculation only; most of those who take
part in torture do not set out their reasons for doing so
[6]. However there is enough evidence to suggest that the
motives [or rationalisations] include some of the
following:
Fear of consequences of refusal or seeing open opposi
tion to abuses as an impossibility for whatever reason.*
Doctors under military discipline may feel, like others, that
they are under irresistable pressure to participate. In his
study of the behaviour of Uruguayan physicians during
the period of military rule [1973-1985], Bloche could iden
tify only one health professional working with political
prisoners who openly refused to collaborate in abuses [7].
Identification with the cause of the torturers and a
belief that serious measures are justified by what are seen
as serious threats to national security. The Chilean Physi
cian Alfredo Jadresic cited a young doctor explaining his
collaboration in military abuses at the Chile stadium after
the 1973 coup in these terms: “What do you expect? We
are at war?’[8]
Defining the doctor’s function as essentially a
bureaucratic one. A female Uruguayan prisoner testified
to pleading with a doctor to obey his physician’s oath;
she said that he replied; “I’qi just doing my job” [9].
Inadequate understanding of professional ethics: for ex
ample. to see it as the health professional’s job to minimise
36
suffering resulting from torture or ill treatment through
participation in the interrogation process.
The psychological mechanisms and ideological analysis
by which doctors have justified participation in systematic
human rights violations have been examined in depth by
Lifton [10] with respect to doctors in Nazi Germany, and
more briefly with respect to Uruguay during the military
government of 1973 to 1985, by Bloche [II].
Lifton suggested the concept of “doubling”—ie. the
creation of a second self who could participate in a life
style and professional conduct which might ordinarily be
seen as in conflict with the individual’s underlying moral
and professional values. He refers to the ‘technicalisation’of the medical role [dissociating the technical aspects
of their function from the moral values associated with
it] and a related psychological distancing. [Lifton points,
for example, to doctors’participation in selection of vic
lims for the gas chambers, noting that “by not quite see
ing it, they could distance themselves from the very kill
ing they were supervising; selections could be accepted as
an established activity and seem less onerous than special
ly brutal tasks [such as medical collusion in torture to pro
duce confessions]...”; pp. 199-200]. He suggests [p. 200]
that such a view could also be interpreted that selection
for killing was so onerous “that Nazi doctors called forth
every possible mechanism to avoid taking in
psychologically what they were doing [emphasis in
original]. Other authors have dealt more generally which
the motivation of tortures [12].
Participation in
Violations of Human Rights
Evidence of the participation of health professionals
in abuses of human rights is, unfortunately, readily found
but perhaps not widely discussed or acknowledged. The
report by the British Medical Association on doctors and
torture, published in 1986, concluded that “the evidence
given to the [BMA] leaves no room for doubt that doc
tors are involved in many pans of the world in the physical
and psychological torture of prisoners?’[13].
Documents published by Al both before and since the
publication of the BMA report as well as reports from
other medical associations [Chile, Uruguay, Turkey] and
organisations [such at the American Association for the
Advancement of Science] all confirm this phenomenon.
Abuses of psychiatry for political reasons have been
documented in the USSR, Czechoslovakia, Romania and
Yugoslavia, though the role of psychiatrists in these abuses
probably varies from those who knowingly falsify a
psychiatric diagnosis with the express purpose of colluding
in the imprisonment of a political or social non
conformist to those whose role is more passive and who
fail to protest at the failure of the legal system and their
September-December 1988
own colleagues and superiors to protect individuals from
such abuses. The motivations of psychiatrists involved in
these practices probably include genuine belief in the
diagnoses such as ‘sluggish schizophrenia’ [14] as well as
conformist, bureaucratic and ideological reasons 115].
With regard to the death penalty, the role of the health
professional is not well documented apart from the case
of the LISA where there has been a vigorous debate on
the ethics of professional participation. Physicians have
argued against [16] and for [17] physician involvement in
execution by lethal injection, though the American
Medical Association has made clear that any involvement
would be unethical.
The American Psychiatric Association and the
American Nurses Association have both ruled participa
tion unethical though some psychiatrists still present
evidence based on hypothetical questions relating to the
defendant’s “future dangerousness” in death penalty cases
[where their evidence can be highly influential in secur
ing the death penalty] despite the view of the APA that
such testimony has no value a$ expert testimony since
psychiatrists are no more accurate in such predictions than
non-psychiatrists [18]. The ethics of such behaviour has
yet to be ruled upon by the APA.
The involvement of health professionals in certain other
humartgights violations—flogging, amputations, prolong
ed solitary confinement—is more contentious since these
abuses are provided for by a law in some countries and
doctors’ presence at their infliction may be specified in
law. However, some individual doctors and some medical
associations have nevertheless protested at such punish
ments being carried out in their country. For example, the
Mauritanian Association of Doctors, Pharmacists and
Dentists expressed ‘deep concern’ at the involvement of
physicians in the punitive amputation carried out on three
convicted thieves in September 1980. Another amputation
took place in June 1981 and again a doctor was involved
though it was reported that two amputations carried out
in 1982 were executed by a medical auxiliary following
refusal by doctors to assist. In Pakistan, both the Karachi
branch of the Pakistan Medical Association and the
Pakistan Junior Doctors, Association voiced their con
cern about flogging of political prisoners.
“The problem with torture”, concludes the BMA report,
'“is not whether it is right or wrong. It is how to detect
nthe subtle changes in relationships which lead to the doc-tior’s acquiescence in torture.” It continues:
The experience of those who gave information to the [BMA]
demonstrates that a refusal to compromise is effective in the early
stages, firstly because the doctor himself is less likely to be compromis
ed and secondly because the apparatus of the state is likely to be
vulnerable to concerted public opposition. Once these early stages have
been allowed to pass unchallenged, it may be too late to avoid serious
abuse. [19]
September-December 1988
Violation Against Health Professionals
Reasons for repressive measures being taken against
health professionals include: (i) their real or perceived
peaceful or violent political activities against the govern
ment; (ii> their activities in human rights groups; (iii) their
professional activities or criticisms of government health
policy; (iv) their giving treatment to injured armed op
position; (v) the perceived deterrence value of making an
example of the health professional; (vi) accidental reasons
[for example, being in the wrong place at the wrong time].
In many, perhaps most cases, persecution cannot be
simply attributed to one unique reason. Doctors who are
active in political opposition groups may also be engag
ed in human rights activities. Similarly, those who criticise
health standards or government policy on health may also
be seen as politically active, or involved in human rights
action and so on. While the rights of doctors to participate
in political activity must be protected in the same way that
any citizen’s political rights should be protected, the par
ticular focus of this paper is the risk of doctors being vic
timised because of their professional or human rights
activities.
The actions which precipitate repressive measures can,
in some cases, be substantially attributed to human rights
activities: the attacks are focussed and concern individuals
whose prominence owes a lot to their position as a human
rights activist.
In Colombia for example, two doctors active in the
Committee for the Defence of Human Rights [CCDHM]
were the victims of political killings in 1988. On 25 August
1988, Dr Hector Abad, aged 65, and Dr Leonardo
Betancur, aged 41, were shot as they were leaving a ser
vice for the president of a teachers’ union who had been
killed that morning. Dr Abad, who was a former Dean
of the Medical School, reported receiving death threats
shortly before his murder.
In the USSR, those involved in the work of the un
official Moscow Working Commission to Investigate the
Use of Psychiatry for Political Purpose were detained in
connection with their work in documenting the practice
of internment of prisoners of conscience on spurious
psychiatric grounds. Dr Leonard Ternovsky [b. 1933], a
radiologist, was arrested on April 10, 1^80 in Moscow and
was charged under Article 190-1 of the RSFSR Criminal
Code with “anti-Soviet slander”. He was subsequently
convicted and sentenced to three years’ imprisonment.
Other members of the Working Commission were also im
prisoned in the period 1980 to 1981, culminating in the
sentence of 12 years’ imprisonment and internal exile for
Dr Anatoly Koryagin, the psychiatric consultant to the
Working Commission, following the publication in the
British journal The Lancet [20] of a paper describing his
experiences of the misuse of psychiatry for political
purpose.
37
More widespread and indiscriminate repression occur
red in Syria during the period 1978 to 1980, when there
was pressure on the Syrian government from lawyers and
other professionals to implement measures included lif
ting the State of Emergency in force since 1963. In early
March 1980, meetings of dentists, pharmacists, engineers,
lawyers, teachers and medical association representatives
in different Syrian cities urged the introduction of reforms.
On March 21 1980, a general conference of the Syrian
Medical Association met in Damascus and passed a reso
lution which included the following demands:
Re-affirmation of the principle of the citizens’ rights to freedom
of expression, thought and belief;
Denunciation of any kind of violence, terror, sabotage and armed
demonstration, whatever the reasons and justifications;
Abolition of exceptional courts;
Release or trial of all detainees
On March 31 1980 a one-day strike was called by lawyers
in Damascus and this was supported by other branches
of the Bar Association and by other professipnal associa
tions including members of the Syrian Medical Associa
tion. Shortly after the strike, the national congress and
regional assemblies of the Medical, Engineers and Bar
Associations were dissolved by the Syrian Ministerial
Cabinet. In the days that followed the dissolution,
numerous lawyers, doctors and engineers were arrested
and held without charge or trial. At least two doctors were
later executed and some 100 doctors remain imprisoned
still without charge or trial more than eight years after
their arrest.
In Central America, a wide range of health profes
sionals were subjected to intense repression in El Salvador
and Guatemala in the period 1980-1982 and in a less in
tense way in subsequent years. Some of the victims of the
torturers and ‘death squads’ were active government op
ponents but the institutionalised nature of the abuses and
the impunity with which those perpetrating the human
rights violations could act meant that those with little or
po political engagement were also victimised.
In July 1980 a United States Public Health Associa
tion Commission visited El Salvador and reported an
alarming pattern of military incursions into hospitals and
abduction and murder directed against health personnel.
Their report listed 23 health professionals who were kill
ed or had disappeared in the period January to June 1980.
Many were tortured before their murder.
In Guatemala, an equally disturbing pattern of attack
directed against health workers was occurring. On April
23 1981, a 32-year-old doctor, Dr Otto Raul Letona, was
shot 12 times in the torso by unidentified gunmen as he
stood in the emergency ward of a hospital in Antigua,
talking to a patient. Another 13 medical personnel were
reported killed during the first half of 1981 alone.
In both El Salvador and Guatemala, being involved in
providing health care to the rural poor appeared to be
38
linked—in the view of the military—with subversion and
opposition. The widespread and indiscriminate nature of
the repression particularly in the early 1980s suggests that
the definition of subversion was very loose and could be
applied to anyone working to improve the situation of the
peasants. In some cases, doctors did treat members of
armed opposition groups or individuals who had sustain
ed bullet wounds; occasionally doctors were detained for
giving this help though it was much more common that
a doctor suspected of ‘aiding the opposition’ would be
dealt with extra-judicially.
Where torture, ‘disappearance’ and political killings are
everyday realities [as in El Salvador and Guatemala dur
ing the period under consideration], the options for a
health professional appear rather limited. Even if they
wish to remain outside politics they are obliged to ensure
that anyone with injuries should-receive medical care and
must, as a consequence, evaluate the best way to ensure
the physical security of their patient. A number of cases
have been documented where medical personnel have not
reported patients with bullet wounds as required by law
in circumstances where they could reasonably fear that
reporting would lead to their patient being tortured or kill
ed. This action in itself may make the doctor a target for
human rights violations.
Since 1980, Amnesty International has issued medical
appeals on behalf of health professionals in the follow
ing 30 countries: Afghanistan, Algeria, Argentina, Benin,
Chile, Colombia, Cuba, Czechoslovakia, El Salvador,
German Democratic Republic, Guatamala, Iran, Laos,
Nepal, Paraguay, Republic of Korea, Romania, Singapore,
Somalia, South Africa, Sri Lanka, Sudan, Taiwan, Turkey,
Uganda, USSR, Uruguay, Vietnam, Yugoslavia, Zaire.
Role of Professional and other Associations
The central role of professional associations in assisting
health personnel at risk of being pressured into col
laborating in, or remaining silent about, human rights
violations is alluded to in the last article of the WMA’s
Declaration of Tokyo, this states that:
The [WMA] will support, and should encourage the international com
munity, the national medical associations and fellow doctors, to sup
port the doctor and his or her family in the face of threats or reprisals
resulting from a refusal to condone the uses of torture or other forms
of cruel, inhuman or degrading treatment.
Unfortunately, in many cases the associations
themselves are under severe threat or acute repression. As
noted above the Syrian Medical Association was dissolv
ed after calling for human rights reforms in 1980;
members of the Turkish Medical Association were pro
secuted in 1986 for calling for an end to the death penal
ty in Turkey; the Chilean Medical Association was raid
ed by security agents in 1986 at the time it was organis
ing a meeting with international participation on the
September-December 1988
theme of the role of medical associations in the protec
tion of human rights.
However, it is striking that medical associations and
other professional bodies in countries where abuses occur
systematically have frequently not spoken out against
them nor taken any apparent action against health pro
fessionals collaborating in torture, covering up deaths
following ill-treatment or carrying out other unethical
acts. Individuals doctors seeking support from their
association or an obvious body to whom to complain,
may interpret the silence of the professional association
[sometimes correctly] as a disinterest in the issue or an
unwillingness to speak out. If the professional leadership
will not speak out, the pressure on individuals to remain
silent is all that greater [21].
Recently, the Uruguayan Medical Association has been
active in promoting the idea of an international medical
forum for the hearing of evidence of medical abuses
against human rights. This idea was recently supported
at a meeting in Geneva in October 1988 of the Inter
national Council of Health Professionals. Some specialist
groups of professionals have looked at ways of using their
own expertise to counter human rights violations. For ex
ample, forensic scientists have contributed to the drafting
of a protocol for the investment of deaths in detention
or.in order circumstances where a proper investigation of
the cause of death should be instituted [22], and have par
ticipated in a number of investigations which have had
the objective of clarifying the fate of persons whose deaths
have been the subject of deliberate cover-ups.
While professional associations have a major role to
play in disciplining their members who assist human rights
violations and protecting members who are active in pro
moting human rights or who resist pressure to collaborate
in torture, other bodies also have an important role.
Human rights bodies can help translate and circulate
information, endeavour to break down isolation and give
support to both opponents and victims of torture and
other bodies; they can press governments to fulfil their
international treaty obligations; and they can offer inter
national solidarity—something which has been remarked
on as being of great support to those facing repressive
governments.
Notes
[ 1] The third was the rehabilitation of torture victims. See Viola
tions of Human Rights: Torture and the Medical Profession.
Report of an Amnesty International Medical Semianr, Athens
Mach 10-11 1987. Al Index: CAT 62/03/78.
[ 2] One of the associations which reversed a previous quiescent
stand on human rights was the Colegio Medico de Chile which,
after being permitted by the government to elect its own officers
for the first time since 1972, embarked on a programme of
medical ethical awareness, including the novel initiative of
publishing, in November 1983, the WMA’s Declaration of Tokyo
September-December 1988
as a paid advertisement in a major Santiago daily newspaper.
This reflected the Colegio’s belief in the importance of a public
and professional understanding of ethical standards particular
ly with regard to torture. See, Stover E. The Open Secret: Tor
ture and the Medical Profession m Chile. Wahsington: AAAS,
1987.
[ 3] For this and the codes cited below sec Amnesty International.
Ethical Codes and Declarations Relevant to the Health Profes
sions. Al Index ACT 75/01/85, 1985.
[ 4] Information on these abuses can be found in a number of
Amnesty International reports [see, for example. Recent Torture
Testimonies Implicating Doctors in Abuse of Medical Ethics in
Chile. Al Index AMR 22/29/84, May 31 1984] and also British
Medical Association. The Torture Report, London: BMA, 1986;
Stover E Nightingale. The Breaking of Bodies and Minds. New
York: Freeman, 1985.
[ 5] In Sudan in 1983, a surgeon was included in a delegation sent
to Saudi Arabia to learn amputation techniques; he later par
ticipated in the carrying out of the first amputations in Sudan.
In Iran, a new amputation device was apparently designed in
1985 with the advice of medical personnel in Teheran.
[ 6] Occasionally some talk to the press; see a series of press ar
ticles about a Brazilian doctor who, in 1988, was disciplined by
the Regional Medical Council of Rio de Janerio for assisting
torture in the 1970s: Istoe, April 1, 8 and 15 1987.
[ 7] Bloche MG. Uruguay's Military Physicians: Cogs in a System
of State Terror. Washington: AAAS, 1987.
[ 8] Jadresic A. ‘Doctors and Torture: An Experience as a Prisoner’.
Journal of Medical Ethics, 1980, 6:124-7.
[ 9] [‘Yo solo cumplo con mi trabajo’.] Testimonies on detention
procedures, torture and prison conditions in Uruguay. Al In
dex: AMR 52/18/79, June 25, 1979.
[10] Lifton RJ. The Nazi Doctors. London: Papermac, 1987.
[II] Bloche, op cit.
[12] Ruthven M. Torture: the Grand Conspiracy. London:
Weidenfeld and Nicolson, 1978; Peters E. Torture. Oxford:
Blackwell, 1985.
[13] BMA, op cit. p. 22.
[14] Reich W. ‘The World of Soviet Psychiatry’. In Stover and
Nighingale [eds], op cit.
[15] See Bloch S, Reddaway P. Russia’s Political Hospitals London:
Gollancz, 1977.
{16] Curran WJ, Casscells W. ‘The Ethics of Medical Participation
in Capital Punishment by Intravenous Drug Injection’. New
England Journal of Medicine, 1980, 302:226-30.
[17] Kevorkian J. Medicine, ‘Ethics and Execution by Lethal Injec
tion’. Medicine and Law, 1985, 4:307-13.
[18] Cited in Al. The death penalty in the [C/S>4 ].• an issue for health
professionals. Al Index: AMR 51/40/86, 1986.
[19] BMA report, op cit, p. 22.
[20] Koryagin A. ‘Unwilling patients’. The Lancet, 1981, z:821-4.
[21 ] Individual doctors can nevertheless speak out. The ease of Dr
Wendy Orr in South Africa is illuminating. On commencing
work as a district surgeon in the Port Elizabeth area in 1985,
she was struck by the number of prisoners alleging assault most
of whom had injuries consistent with their allegations; she noted
the complaints on the medical record cards, adding that these
should be investigated. When her efforts to have some action
taken on the persisting compalints of police brutality and tor
ture had no effect she sought an urgent ruling from the Supreme
Court restraining police from assaulting prisoners. An interim
injuction was made See Rayner M. Turning a Blind Eye?
Washington: AAAS, 1987.
[22] The Minnesota protocol: Preventing arbitrary killing through
an adequate death investigation and autopsy. A report of the
Minnesota International Lawyers Human Rights Committee.
Minneapolis, 1987.
39
September 7 and had attempted to assault an officer with
a chair.15
On the issu£ of proper hospitalisation, Dr. Lang told
the court that neither he nor Dr. TUcker had any option
but to acquiesce in security police demands. Dr. Lang
stated that he had the ‘impression’ that Mr. Biko could
not be transferred to a non-prison hospital because he was
regarded as “a security risk? Dr. Lang buttressed his
defence by claiming that “we [district surgeons] are
restricted in the sense that we cannot tell them where we
wanted a detainee. .. You cannot buck the security
branch?16
The effect of this particular line of defense was vitiated
when Dr. Lang later admitted to the court that he had
not really pressed the issue of hospitalisation with Col.
Goosen. Goosen, Dr. Lang said, could have interpreted
his reference to hospitalisation as necessary for diagnostic
rather than treatment purposes. When asked if he at any
stage suggested to Goosen that Biko was a sick man in
need of treatment in a hospital, Dr. Lang acknowledged:
“No, I did not?17
The two most egregious instances of questionable
behaviour raised against Dr. Lang during the inquest con
cerned his medical certificate and his final entry in the
bed letter. Col Goosen told the court that his request for
a medical certificate on September 7 was ‘plain logic’.
Dr. Lang’s certificate was, he added, completely satisfac
tory for his purposes. In the certificate. Dr. Lang had
recorded as the reason for holding the medical examina
tion that Biko “would not speak”. Yet, in his later report
to the pathologist conducting the post mortem, Dr. Lang
wrote: “The detainee had refused water and food and
displayed a weakness of all four limbs and it was feared
that he had suffered a stroke.” But, when asked to explain
the discrepancy between these two statements, Dr. Lang
could only reply: “I cannot explain it. It is inexplicable!’18
In the second part of Dr. Lang’s certificate of
September 7, he noted that he had found no evidence of
any abnormality or pathology. Dr. Lang admitted that this
claim was “highly inaccurate” as he had found evidence
of bruising, a lip injury, and edematous swelling of the
hands, feet and ankles. Counsel Sydney Kentridge then
asked Dr. Lang if it hadn’t occurred to him that, “if, at
some later stage, Biko might appear in court and com
plain about the way he was treated while in security police
custody, [his] medical certificate would be a most impor
tant piece of evidence”? The doctor agreed that it would
be but added that the possibility had not occurred to him
on the morning of September 7.19
Dr. Lang had similar difficulty in explaining the con
tents of the entry in the Sydenham Prison Hospital bed
letter, dated 10 September. He admitted that the statement
regarding the lack of evidence of pathology was false, he
knew that the cerebrospinal fluid was blood-stained, and
42
Excert From the Inquest
Kent
ridge: Why didn’t you stand up for the interests of your
(Counsel for patient? Biko family)
Lang: I didn’t know that in this particular situation one
could override the decisions made b\ a responsible
police officer.
Gord
on : Why didn’t you say that unless Biko goes to
hospital you would wipe your hands of it?
Lang: I did not think at that stage that Biko’s condition
would become so serious. There was still the ques
tion of a possible shamming.
Kent
ridge: Did you think the plantar reflex could be feigned?
Lang: No.
Kent
ridge: Did you think a man could feign red blood cels in
his cerebral spinal fluid?
Lang: No
Kent
ridge: In terms of the Hippocratic Oath are not the in
terests of your patients paramount?
Lang: Yes.
Kent
ridge: But in this instance they wer subordinated to the
interests of security?
Lang: Yes.
(Inquest into the death of Steve Biko,
Proceedings, in Bernstein, Biko, p. 94).
that Dr. Hersch had reconfirmed the extensor plantar res
ponse. Nevertheless, Dr. Lang argued that the misstate
ment arose from the inadvertent omission of the word
“gross” infron of “pathology”.20
In his testimony, Dr. Tucker, the chief district surgeon
in Port Elizabeth, attempted to explain his behaviour
towards the patient, both claiming that he had accepted
Col. Goosen’s theory of feigned illness and by alluding
to constraints affecting district surgeons’ activities in
relation to political detainees. At one point Professor
Gorden pressed Dr. Tucker to explain why he did not tell
Col. Goosen that he would disclaim all responsibility as
a doctor if Biko was not taken to a proper hospital.
Dr. Tucker replied that he did not consider the patient’s
condition as serious, as “there was still this question of
a possible shamming on his [Biko’s] part.” He did con
cede, however, that no one could feign an extensor plan
tar reflex or red blood cells in the cerebrospinal fluid, he
also accepted that, in terms of the Hippocratic Oath, the
interests of his patients should always be paramount. But
in this instance, Tucker admitted, as had Dr. Lang, that
rhey were subordinated to the interests of security. ‘‘I
didn’t knowj’ he said, “that in this particular situation one
September-December 1988
could override the decisions made by a responsible police
officer?’21
On several occasions during the inquest porceedings,
Dr. Tucker contradicted himself. Although stating at one
point his belief that Biko may have been feigning illness.
Tucker claimed elsewhere in his evidence that the though
of head injury had occurred to him. yet he failed to ask
the detainee the source of his lip injury or the police if
Biko had received a blow on the head. Dr. Tucker initial
ly denied that his reticence came from dealing with the
security plice. When Kentridge pressed him on this issue,
however, Tucker reponded. “I would say no, you don’t [ask
questions in that situation]?’ After a five minute court ad
journment, Dr. Tucker, in resuming his evidence, retracted
his statement. “Questions asked by the district surgeon,”
he said, “are not banned in the security offices?’ He fur
ther claimed that, “at all times I have always had all the
co-operation necessary from the security police. When we
require information and when we require things to be
done, then they are done.”22
If Dr. Tucker’s assertion about the co-operativeness of
the police was correct, then it threw on onus of respon
sibility for the fatal pretoria journey directly on to his
shoulders. Tucker’s evidence shows that he deferred
without protest to Col. Goosen’s refusal to allow the de
tainee local hospitalisation. Dr. Tucker consented to
Goosen’s alternative proposal tht the patient be
transported to Pretoria by motor vehicle. The only aspect
the arrangements he claimed to have insisted upon was
the need for a soft mattress. Tucker stated later, however,
theat he neither saw it as his responsibility to check the
vehicle used nor reassure himself that there was infact a
mattress, blankets, and a pillow for the patient. Further
more, he did not consider it part of his responsibility to
insist that Biko be accompanied by a medical attendent
or his medical records.23
On the crucial matter of the state of Steve Biko’s health
the day before his death, Dr. Tucker had written that he
found no positive sign of organic disease and that the pa
tent’s condition was satisfactory. Under questioning
Tucker admitted that he had found the patient lying on
the floor with forth at his mouth and hyperventilating.
He had found the patient weak in the left arm and
apathetic. He admitted that he knew of the extensor plan
tar reflex. Nevertheless, when challenged to admit that “in
this situation no honest doctor could have advised that
Biko’s condition was satisfactory?’ Dr. Tucker persisted.
“In the circumstances, [I] though it was,” he said.24
In his final submission made to the court on behalf of
the Biko family, Counsel Sydney Kentridge strongly
criticised the indifference displayed by Drs. Lang and
Tucker towards the patient. Their relationship to
Col. Goosen, he charged, “was one of subservience
bordering on collusion?’ And their behaviour carried a
September-December 1988
Excert From the Inquest
Kentridge : Why did you not ask the obvious question,
whether the man received a bump on the
head?
Tucker
: I did not ask it and that is all I can say.
Prins
: Did you ask Biko?
(magistrate)
TUcker
: No.
Kentridge : Was it not possible you were reluctant to em
barrass Goosen?
TUcker
: No.
Kentridge : Either from reading about it or from your
own experience have you no knowledge that
the police assault people in custody?
TUcker
: I have. (Further answer inaudible).
Kentridge : But on that occasion you did not ask?
Tucker
: No, I did not. Where persons are brought to
me for examination my report is completed
on a special form. This is all I am required
to do. This history was given to Dr. Lang...
The restraint [on the morning of 7
September] could have resulted in the
damage.
Kentridge : You accept it as a fact, what Goosen told
you?
Tucker
: May I put it this way? If am called to see a
patient and he has a cut onhis head, then I
am interested in treating him and not in how
he got the cut.
(Inquest into the death of Steve Biko,
Proceedings, in Bernstein, Biko, p. 85)
significance beyond the present case. For “the medical pro
fession’s general reputation has led couts in the past,
whenever an issue arose as to whether a prisoner seen by
a doctor had been assaulted or not, to place great if not
absolute reliance on the district surgeon’s findings?’ Ken
tridge submitted that in this case “the proved facts show
that not only can the court not rely on the evidence of
Drs. Ivor Lang and Benjamin Tucker, but that an analysis
of the evidence show that they joined with the security
police in a conspiracy of silence?’ The very best that could
be said, he argued, was that “they turned a blind eye?’ Ken
tridge concluded that the doctors’ neglect of the patient’s
interests in deference to the requirements of the security
police “was a breach of their professional duty, which may
have contributed to the final result?’25
Response of South African Medical Dental
Councils
The South African Medical and Dentral Council
(hereafter referred to as the Medical and Dental Council)
is South Africa’s principal regulatory body controlling the
medical and dental professions. The thirty-four member
43
statutory body has the power, under the 1974 Medical,
Dental, and Supplementary Health Service Professions
Act, to license and control the trainings of the members
of the medical and dental professions and to uphold
ethical medical standards. The Medical and Dental Coun
cil is vested with quasi-judicial powers to regulate the con
duct of the medical and dental professions, including the
authority to institute an inquiry into any complaint,
charge, or allegation of improper or disgraceful conduct
against any person licensed as a practitioner by the coun
cil. The Medical and Dental Council has the power to im
pose penalties, including striking the person off the
register of licensed practitioners.26
The 1974 Act does not define improper or disgraceful
conduct. The Medical and Dental Council has the discre
tion to define such conduct, and, periodically, the coun
cil makes rules specifying the acts and omissions for which
it may take disciplinary steps against a registered member
of the medical or dental professions. For instance, in 1976,
the year prior to Steve Biko’s death, the Minister of Health
approved, infer alia, a rule prohibiting a practitioner from
issuing a medical certificate unless he or she is satisfied
from personal observation that the facts are correctly
stated therein, or has qualified the certificate with the
words “as 1 am informed by the patient!’27 In a 1985
Supreme Court review of the powers and duties of the
Medical and Dental Council, the presiding judge describ
ed the council as “truly a statutory custosmorum of the
medical profession, the guardian of the prestige, status,
and dignity of the profession and the public interest, in
so far as members of the public are affected by the con
duct of members of the profession.. .”28
Despite its clearly crucial disciplinary role, the Medical
and Dental Council was to prove wholly inadequate for
the task before it. In January 1978 the council received
from Magistrate Prins a copy of the inquest proceedings
involving Lang and Tucker’s evidence. At the same time,
the Medical and Dental Council was set a formal “com
plaint” by Mr. Eugene Roelofse, ombudsman for the
South African Council of Churches. Mr. Roelofse’s com
plaint posed a series of questions regarding the ethical
conduct of Drs. Lang and TUcker.29 Though Mr. Roelofse
did not formulate specific charges against the physicians,
the Medical and Dentral Council’s president treated the
matter as a complaint within the meaning of the Act. He
directed the council registrar to refer the complaint, with
the portion of the inquest record, to the council’s Medical
Committee of Preliminary Inquiry (hereafter referred to
as the inquiry committee).30 He also directed the registrar
to send copies of these documents to Drs. Lang and
TUcker and to ask them for an explanation.
In response the state attorney, acting on behalf of
Drs. Lang and TUcker, requested a postponement of the
inquiry, pending the outcome of civil proceedings laun
ched by members of the Biko family.31 When the Medical
and Dental Council’s registrar insisted on an explanation
from the doctors, the state attorney replied that the com
plaint lacked the specificity necessary to initiate action
by the inquiry committee and that it was defective in cer
tain respects. The two doctors then applied to the Supreme
Court for a ruling to this effect. The presiding judge
dismissed the doctor’s application.'2
On April 24, 1980 the five-member inquiry committee
met to consider the inquest record and other materials.
The inquiry committee resolved that the contents of the
documents be noted and, in a highly unusual move, the
committee released its findings to the press before the full
council had met to consider the resolution. In the South
African Medical Journal of May 17, 1989, the inquiry
committee announced that it had found no prima facie
evidence of improper or disgraceful conduct on the part
of the practitioners and that it had resolved that no fur
ther action be taken in the matter. Professor Gordon, one
of the medical assessors at the inquest, later described this
premature public release of the inquiry committee’s fin
dings as unprecedented in his 25 years of service as a coun
cil member.33
The Medical and Dental Council met on June 17, 1980
to consider the inquiry committee’s.resolution. At the
meeting two members, Professors Shapiro and Carlton,
attempted to convince the council that it should not con
firm the inquiry committee’s resolution; that there was
prima facie evidence of improper or disgraceful conduct
on the part of Drs. Lang and Tucker; and that a second
inquiry into their conduct should be held.34 Their mo
tion was put to the vote and defeated. The resolution of
the inquiry committee was confirmed by a majority of
eighteen votes to nine.35
The Medical and Dental Council’s decision provoked
an uproar in the medical community.36 The medical
faculties of the Universities of Cape Town and the Witwatersrand disassociated themselves from the position
adopted by the council. The Board of tne Witwatersrand
Medical Faculty in Johannesburg unanimously adopted
a resolution expressing their deep disquiet at the coun
cil’s finding. The Witwatersrand faculty felt that there was
sufficient prima facie evidence to warrant a disciplinary
hearing, and warned that “the South African Medical and
Dental Council might have called into question its own
credibility as an objective and unbiased guardian of the
high standards of the medical profession in South Africa.’’
In addition the medical faculty expressed concern as “to
the possible effects of the decision of the Medical Coun
cil on the future treatment of prisoners and detainees by
the authorities!’ The faculty went on to endorse the
Guidelines for Medical Doctors Concerning Detainees and
Prisoners, adopted by the World Medical Association
(WMA) in Tokyo in 1975.37
September-December 1988
The Witwatersrand medical faculty noted in its resolu
tion that the Medical and Dental Council, as the pur
ported watch-dog of the ethics of the profession, had been
zealous, even over-zealous, in the severity of the
punishments meted out in the past for even minor infr
ingements of medical ethics. Yet, in the present case, they
found it difficult to accept “that the council [had] ap
plied its collective mind to the problem of the Biko doc
tors in a purely objective and dispassionate way?38
Despite these protests and the indications that medical
associations in other countries were beginning to review
their ties with South African medical organisations, the
Medical and Dentral Council announced in October 1980
that its dismissal of the complaints against the Biko doc
tors was final and irreversible.39
The Medical and Dental Council’s controversial deci
sion forced critics to turn to the Medical Association of
South Africa (MASA), a non-statutory professional
organisation whose membership is purely voluntary.40
On June 18, 1980 Dr. Jonathan Gluckman, a pathologist
who had attended the post mortem on Biko on behalf of
the deceased’s family and a member of MASA’s Federal
Council, presented the association’s secretary general, Dr.
C. Viljoen, with a letter signed by 38 association members.
The signatories called for an inquiry to determine whether
Dr. Benjamin TUcker “... is a fit and proper person to
continue to be a member of this Association.” (Dr. Lang
was not a member of MASA.)41
In accordance with MASA’s Articles of Association,
Dr. Wiljeon referred the letter with copies of a portion
of the inquest record to the Cape Midlands Branch of the
association where Dr. Tucker held membership. Unlike the
Medical and Dentral Council, MASA lacked wide powers
of inquiry and punishment. Its powers of censure ov6r
its members were limited to that of expulsion, with the
initiative for this lying at the branch level and not at the
national level. In this instance, the Cape Midlands Branch
notified the MASA’s Federal Council two weeks later “that
a charge of unethical conduct against Dr. TUcker could
not be sustained” and advised that “the case now be closed?
The executive committee of MASA’s Federal Council
met in August 1980 and accepted this recommendation.
The committee also resolved that the findings of the
Medical and Dental Council and its inquiry committee
“be noted? Even so, the Federal Council’s executive com
mittee did raise questions concerning the conformity of
the medical care received by Biko with the WMA guide
lines in the Declaration of Tokyo. The executive commit
tee acknowledged that the lack of conformity probably
contributed to the “subsequent unfortunate course of
events? Nevertheless, the executive committee shifted the
focus of its questioning away from the conduct of the doc
tors to the possibly restrictive effects of existing laws and
regulations upon doctors operating within the prisons.42
September-December 1988
Two additional resolutions adopted by the Federal
Council’s executive, committee alluded to the growing
domestic and international controversy surrounding the
response of the medical establishment to the charges
against the Biko doctors. The committee defended the ‘in
tegrity and bona Tides’ of the members of the Medical
and Dental Council and its inquiry committee, and
MASA’s Cape Midlands Branch. They also expressed
MASA’s satisfaction that the decisions of these bodies
“had in no way been subject to outside influence and that
there had not been any attempt at a ‘cover-up’ with regard
to the conduct of the practitioners concerned?
In contrast, the Federal Council’s executive committee
viewed the critics of these bodies as proceeding on the
basis of flawed newspaper reports, “which were frequently
incomplete, biased, or based on political rather than
ethical or humane considerations? The executive commit
tee concluded that if evidence of improper or disgraceful
conduct could not be found by the Medical and Dental
Council’s inquiry committee, the members of the MASA
executive committee “could not be expected to submit to
pressure or to violate their own consciences by laying a
charge simply to satisfy the demands being made!’43
To members of the South African medical community
anxious to investigate fully the conduct of the Biko doc
tors, it appeared That the medical establishment had closed
ranks. This impression was strengthened by statements
published in September 1980 in the South African Medical
Journal, the official journal of MASA.44 The journal
contained a statement by the Federal Council’s executive
committee recapitulating the discussion and resolutions
passed at its August meeting. The chairman of the Federal
Council, Dr. J. N. de Klerk, pointed out in the journal
that three separate medical bodes independently had
reached the same conclusion, namely, “that in light of the
evidence available to them, and taking into consideration
the particular circumstances surrounding this whole mat
ter, the doctors were not guilty of negligence or of im
proper or disgraceful conduct!’ For those colleagues who
still disagreed with these findings, de Klerk had only cold
comfort. “Manifestly!’ he concluded, “the [Medical and
Dental] Council itself is not able to reopen the matter,
while the ethical committees of the MASA are substan
tially in agreement with its findings!’45
MASA’s stance provoked a spate of resignations among
its members most prominently that of Professor Stuart
Saunders, then principal-designate of the University of
Cape Town, and Professor Frances Ames, head of the
Department of Neurology at the same university. In a Tet
ter to the editor’ of the South African Medical Journal,
Professor Saunders challenged MASA’s Federal Council
to state openly the implications of its position: namely,
that medical doctors should acquiesce in decisions taken
by the police and accept that there are considerations other
45
than the patient’s welfare to be taken into account in
treating a prisoner. Professor Gordon, in announcing his
decision not to stand for re-election for the executive com
mittee of the Federal Council after 25 years of service,
characterised the actions of the Medical and Dental Coun
cil and the MASA executive committee in exculpating the
doctors as “an act of impertinence and arrogance!’46
The resignations and negative publicity eventually
produced a response from MASA’s Federal Council.
Dr. Jonathan Gulckman persuaded it to form a commit
tee to inquire into the ethical issues raised by the medical
treatment of Biko. The Federal Council also agreed to ap
proach the government on the matter of the medical treat
ment of prisoners, especially those detained under the
security laws, and to establish a code of conduct for
medical practitioners working under these circumstances.
In a statement to the press announcing these decisions,
Dr. Gluckman expressed his personal distress at the posi
tion adopted by the Medical and Dental Council. He
acknowledged, as a member of MASA’s Federal Coun
cil, “that mistakes have been made by us in MASA in the
handling of the Biko matter!’ Dr. Gluckman said that it
was essential “in the public interest and in the interests
of the reputation and the good standing of the medical
profession as well as in the interests of the prisoners that
these mistakes be rectified!’47
The Ad Hoc Committee appointed to consider certain
ethical issues (hereafter referred to as the ad hoc commit
tee) reported to MASA in June 1981. Investigations by the
ad hoc committee were limited by its lack of subpoena
powers and the fact that Dr. Lang and Dr. Tucker did not
participate in any of the committee’s proceedings.48 In
addition, the police denied the ad hoc committee permis
sion to examine the Walmer police station cells where Steve
Biko had been held. The ad hoc committee’s report,
however, critically reviewed the available evidence concer
ning the doctors’ conduct and openly disagreed with the
findings of the Medical and Dental Council.49
The report of the ad hoc committee encouraged those
doctors who were dissatisfied with the Medical and Den
tal Council’s decisions. Five doctors subsequently lodg
ed with the council a detailed series of charges and com
plaints concerning the conduct of Drs. Lang. Tucker,
Hersch, and Keeley. Appended to the document was a list
of sixteen cases, dating from 1974 through 1980, involv
ing similar instances of improper or disgraceful conduct
by medical practitioners, along with the sentences imposed
by the council’s disciplinary committees.50 A month later,
in March 1982, five other doctors, together with the
Transvaal Medical Society (now the Health Workers’
Association), a voluntary organisation of mostly black
doctors and allied personnel, lodged a separate list of
complaints against Dr. Lang and 'Ricker.51 Both sets of
complainants referred extensively to the full record of the
46
inquest proceedings in detailing and motivating the
charges against the doctors.
In March 1983 the Medical and Dental Council’s in
quiry committee met to consider the allegations. The in
quirycommittee resolved “that all material evidence which
had been submitted in support of the present complaint
had also been considered by the committee and the council
previously, and that no new material evidence had emerg
ed such as warranted the rescission of the council’s
previous resolution’’. Accordingly the inquiry committee
resolved that no further action should be taken against
the doctors. A month later the Medical and Dental Coun
cil confirmed this resolution, once again rejecting a mo
tion proposed by Drs. Shapiro and Carlton to the
contrary.52
Faced with this rebuff, the complainants were forced
to seek Supreme Court review of the matter. They peti
tioned the Court to set aside the resolutions of the Medical
and Dental Council and its inquiry committee, and to
direct the council to hold a new inquiry into the allega
tions of improper or disgraceful conduct on the part of
Drs. Lang and Tuckty. The petitioners argued that it was
in the public interest and in the interest of South Africa
that the applicants* complaint be properly heard. “The
international reputation... of medical practitioners
within the Republic,” they noted, “has been tarnished by
the fact that the [council] had failed properly to get to
grips with an inquiry' into the conduct of the medical prac
titioners whose conduct is in issue!’53
In January' 1985 the Court ruled in the petitioners’favor. It found that the inquest proceedings did support
the charges and complaints of the applicants, and that
there wasprima facie evidence of improper or disgraceful
conduct on the part of Drs. Lang and Tucker. The
presiding judge referred, inter alia, to Dr. Lang’s false
medical certificate which represented an apparent breach
of one of the Medical and Dental Council’s rules of ethics.
The inquiry council and its inquiry committee, in con
cluding otherwise, had misdirected themselves. The Court
also found that the applicants, as medical practitioners,
did have locus standi to approach the Court, because the
purpose of the 1974 Act governing the activities of the
council was intended not only to protect the public vis-avis the medical profession but also the reputation of the
medical profession itself.
The Court then issued an order repudiating the resolu
tions adopted by the Medical and Dental Council and its
inquiry committee in 1983. It directed the inquiry com
mittee to resolve “that the evidence furnished in support
of the aforementioned complaints discloses prima facie
evidence of improper or disgraceful conduct, or conduct
which when regard is had to the respective professions of
[Drs. Lang and TUcker] is improper or disgraceful!’ It fur
ther directed the council to establish a disciplinary com
mittee to investigate the conduct of the doctors.54
After seven years of evading its statutory respon
sibilities, the Medical and Dental Council was now forc
ed to hold disciplinary proceedings against the doctors.
In July 1985 a disciplinary committee, chaired by the presi
dent of the council, held hearings for four days. The
committee found Dr. Lang guilty of improper conduct
on 5 counts in that it (1) had issued an incorrect medical
certificate and a misleading letter; (2) had failed to ex
amine the patient properly; (3) had failed to inquire into
and ascertain the possibilities of a head injury; (4) had
failed to obtain a proper medical history of the patient;
and (5) had failed to observe him and keep proper notes.
Dr. Lang, who intended to continue practicing for a fur
ther five years, was given a caution and a reprimand.
The disciplinary committee found Dr. Tucker guilty of
improper and disgraceful conduct on 3 counts: (1) he had
failed to object to the patient’s transportation by a Land
Rover to Pretoria; (2) he should have insisted upon
transportation by ambulance with proper medical atten
dants and the patient’s medical records; and (3) he failed
to make a proper medical check before stating that the
patient’s central nervous system had shown changes bet
ween examinations. The committee suspended Dr. Tucker,
who was due to retire shortly, for three months from the
medical rolls, but recommended that the enactment of the
penalty should be suspended for two years conditional
on his not being found guilty by the council or any other
contravention during this period.
MASA’s secretary general Dr. Viljoen issued a statement
welcoming the committee’s judgment. Dr. Viljoen added
that “as in the past the findings of the Medical and Den
tal Council were accepted by the MASA? The sentences,
however, were strongly criticised by others as being
“pathetically inadequate’’ Several months later, in October
1985, the council stripped Dr. Tucker of his medical
qualifications.55
The failure of the Medical and Dental Council and
MASA to respond quickly and appropriately to the allega
tions against the Biko doctors had resulted in a bitter in
ternational controversy concerning MASA’s membership
within the World Medical Association. In 1981 a number
of national medical associations, including the British
Medical Association, withdrew from the world body in
protest over MASA’s continuing membership. Throughout
1985, international pressure on the WMA, combined with
a campaign inside South Africa by a broad range of
medical and health groups, led the WMA to alter its plans
to hold its next annual meeting in Cape Town.56
Amid this controversy over its international standing,
MASA acknowledged that the “Biko case” had done ir
reparable harm to the South African medical profession.
The association, however, maintains a defensive posture
on the matter in its correspondence in professional jour
September-December 1988
nals, which has only deepened the growing polarisation
within the South Africa medical community. During an
interview in 1985, Professor Frances Ames, one of the
petitioners in the Supreme Court case against the Medical
and Dental Council, expressed her concern about “this
polarisation amongst medical doctors? The formation of
an alternative professional .association, the National
Medical and Dental Association* (NAMDA), in 1982 con
cretely expressed the dissension within the medical
community.57
During part of an exchange with MASA on ethical
issues which was published in the South African Journal
of Human Rights, Professor Trefor Jenkins, one of the
applicants in the Supreme Court suit, urged MASA to ad
mit that it had made errors of judgment in the Biko case.
Professor Jenkins argued that doctors, like other members
of the society, have been initimifiated by the police and
the repressive measures used to implement and maintain
apartheid. It was his firm belief that “the Council (and
to some extent the MASA) [had] allowed itself to be in
fluenced by irrelevant considerations when discussing the
case of the Biko doctors? The case was, he felt, “one of
straightforward and relatively simple medical ethics but
the two bodies in question [had] allowed political (and,
perhaps, what they perceived to be state security) con
siderations to cloud the issue? No good would be served,
he said, by MASA persisting in the view that it did all
it possibly could to ensure that justice was done in deal
ing with the unprofessional and even disgraceful conduct
of the doctors who cared for Biko? Professor Jenkins sug
gested that MASA intensify its efforts to restore the im
age of the profession to one in which all doctors could
feel'proud and in which the public could feel confidence
again. In a situation of deepening conflict in the coun
try, the medical profession, Professor Jenkins urged, must
be prepared to censure unequivocally any doctor who fails
to expose police brutality or torture, lest irreparable harm
be done to the trust relationship existing between doctor
and patient, and the practice of medicine become
impossible.58
Notes
1
District surgeons and general practitioners employed by the
Department of Health. Their responsibilities include the pro
vision of medical care to prisoners under regulation 6 of the
prison regulations promulgated in 1965 under Prisons Act
8 of 1959. About 26 localities in South Africa have full time
district surgeons. Part-time district surgeons operate
elsewhere. Interview with Mr. Filmalter, acting registrar of
the South African Medical and Dental Council, by Eric
Stover in Pretoria in December 1985; Gilbert Marcus,
‘‘Safeguarding the Health of Detainees? unpublished paper,
Center for Applied Legal Studies, University of the WitwaterSrand, April 1987, pp 6-9.
2 Biko had been detained on a number of occasions, including
for a period of 137 days in 1975. He had also been subjected
47
to a five-year banning order. Concerning his life and political
activities, see Hilda Bernstein, No 46—Steve Biko (London:
International Defense and Aid Fund, 1978); Milard Arnold,
ed, Steve Biko, Black Consciousness in South Africa (New
York: Vintage Books, 1979); Gail M Gerhart, Black Power
in South Africa: The Evolution of an Ideology (Berkeley:
Unversity of California Press, 1978).
3 Quoted in Bernstein, Biko, pp 76-78; Complaint by the
Transvaal Medical Society Against Doctors Ivor Lang and
Benjamin tucker in terms of Section 41 of the Medical, Den
tal, and Supplementary Health Services Act, 1975, made io
the South African Medical and Dental Council, March 18,
1982, pp 3-5.
4 An abnormal reflex after infancy characterised by extension
of the great toe with fanning of the other toes on sharply
stroking the lateral aspect of the sole, Blackiston’s Gould
Medical Dictionary (New York: McGraw-Hill, 1972). 3rd ed
p 168.
5 Bernstein, Biko, pp 87-90; Complaint by Dr. Frances Ames
and others involving allegation of improper or disgraceful
conduct made to the South African Medical and Dental
Council, February 17, 1982, pp 21-22, 31: Report to the
Medical Association of South Africa by the Ad Hoc Com
mittee appointed to consider certain ethical issues, June 1981,
pp 3-4.
6 Complaint by Dr. Frances Ames and others, p 26.
7 Bernstein, Biko, pp 33, 90-96; Report to the Medical Associa
tion of South Africa, p 4; Lawrence Baxter, ‘Doctors on Trial:
Steve Biko, Medical Ethics and the Courts’, South African
Journal on Human Rights, Vol 1, Pt 2 (August 1985), p 139.
8 Bernstein, Biko, pp 62-63.
9 Report to the Association of Law Societies in South Africa
by Sir David Napley, former president, British Law Society,
in Bernstein, Biko, pp 137-147.
10 Quoted in Complaint by Dr. Frances Ames and others, p 2.
Following the inquest verdict, the ^Attorney General declin
ed to pursue criminal proceedings and the Minister of Justice
announced that the appointment of a Police Board of In
quiry was not warranted. Baxter, ‘Doctors On Trial’, p 149.
11 Veriava and Others v. President, South African Medical and
Dental Council and Others, 1985 2 (SA) 293 (TPD), p 297.
12 Letter addressed to the Natal Coastal Branch of the Medi
cal Association of South Africa, quoted in Complaint by
Dr. Frances Ames and others, Annexure C, p 3. (The letter
was also reported in The Cape Times, November 26, 1989.)
Professor Gordon supplied an affidavit to the same effect
in a Supreme Court action in 1984 (discussed below).
13 Report by Dean Louis H. Pollack on behalf of the Lawyers’
Committee for Civil Rights Under Law, in Arnold, ed, Steve
Biko, pp 344-346.
14 Complaint by Dr. Frances Ames and others, pp 18-38; Com
plaint by the TYansvaal Medical Society, p 2-13; Bernstein,
Biko, pp 76-95, evidence of Dr. Lang.
15 Bernstein, Biko, pp 76-79, evidence of Dr. Lang.
16 Complaint by Dr. Frances Ames and others, p 23, evidence
of Dr. Lang.
17 Ibid, pp 22, 24, evidence of Dr. Lang.
18 Ibid, pp 25-26, evidence of Col. Goosen; Bernstein, Biko,
pp 76-78. evidence of Dr. Lang.
19 Bernstein, Biko, pp 76-78, evidence of Dr. Lang.
20 Ibid, p 88.
21 Ibid, pp 92-93, evidence of Dr. Ticker.
22 Ibid, pp 83-85; Complaint by Dr. Frances Ames and others,
p 49.
23 Bernstein, Biko, pp 95-96; Complaint by Dr. Frances Ames
48
and others, pp 40, 54-55, evidence of Dr. Ticker.
Complaint by the Transvaal Medical Society, pp 22-26; Bern
stein, Biko, pp 92-93; Complaint by Dr. Frances Ames and
others, pp 43--16, evidence of Dr. Ticker.
25 Counsel’s submission on behalf of the Biko family, in Bern
stein, Biko, pp 110-114.
26 Established in terms of Act No. 56 of 1974, the Medical and
Dental Council’s members include: i) The Secretary of
Health; ii) Ten members appointed by the Minister of Health
who has the power to overrule any of the council’s decisions,
iii) Nine designated members, including the Director of
Hospital Services, five medical and dental practitioners from
university faculties of medicine and dentistry and designated
by the principles of those universities, and three persons
designated by the College of Medicine of South Africa, the
South African Nursing Council, and the South African Phar
macy Board; and iv) Fourteen members elected by medical
practitioners and dentists.
27 South African Government Notice R2278 published in
Government Gazzettee 5349 of December 3, 1976. Rule 25(2)
prohibited the performance by medical practitioners and den
tists of professional acts under impropre conditions and/or
surroundings, except in an emergency.
28 Veriava, p 307.
29 Baxter, “Doctors in Trial” pp 140-141; Veriava, pp 297, 298.
30 The inquiry committee, created under Section 61 (1 )(a) of the
1974 Act, is appointed at the beginning of each year from
the members of the Medical and Dental Council and is charg
ed with the duty of conducting a preliminary inquiry into
complaints.
31 The plaintiffs^brought an action for R90.000 damages against
the security policy Drs. Lang and Ticker, and the Ministers
of Health and Police. In July the Biko family accepted an
out-of-court settlement of R65.OOO from the State. The
Minister of Police denied that the settlement amountd to an
admission of liability. Lawyers’ Committee for Civil Rights
under Law, Deaths in Detention, pp 67-68.
32 Judgment in Tucker & Another v. South African Medical
and Dental Council & Others,, 1980(2) SA 207 (TPD), pp
298, 213; Baxter, “Doctors on Trial,’’ p 151. Judgment was
rendered in December 1979.
33 The Cape Times, November 26, 1980; Veriava, p 299.
34 Quoted in Veriava, p 299.
35 Professor Gordon withdrew from the proceedings because
of his involvement in the inquest. A number of other coun
cil members were absent when the final vote was taken.
Veriava, p 299; Baxter, “Doctors on Trial,” p 142.
36 Interview with Professor Phillip Tobias by Eric Stover in
Johannesburg on December II, 1985.
37 Reported in Nature, Vol 286, No 5770 (July 1980), p 200;
The Lancet, No 8205 (November 29, 1980), pp 1184-1185. See
Appendix A for Declaration of Tokyo text.
38 Reported in Nature (July 17, 1989); Trefor Jenkins, “The
MASA Letter: A Rejoinder, The Organised Medical Profes
sion on Trial” South African Journal on Human Rights, Vol
2, Pt. 2 (July 1986), p 236; “Biko Saga: The Ethics of Suppressionr in Critical Health (Johannesburg), No 3 (July
1980), p 48; Survey of Race Relations 1980 (Johannesburg:
SAIRA, 1981), pp 570-572. In contrast to its response to the
charge against the Biko doctors, the Medical and Dental
Council moved quickly to organise disciplinary proceedings
against Dr. Aubrey Mokoape, after he had served six years
in prison for contravening the 1967 Terrorism Act. Accor
ding to Amnesty International, Dr. Mokoape was inter
rogated, beaten, and held in solitary confinement during his
24
September-December 1988
detention in 1974. He was convicted of two counts under the
Terrosim Act, after a long trial in which the State attempted
to proye a link between the Black Consciousness movement
and political violence. Not a single act of violence was prov
ed against any of the defendants. Tvo years after his release
from prison Dr. Mokoape was informed that the Council’s
Medical Committee of Preliminary Inquiry had resolved that
there was a prima facie case of improper or disgraceful con
duct against him. The charge against him, relating solelv to
his conviction under the 1967 Act, represented the first oc
casion in which the council used a political conviction as
ground for a disciplinary inquiry. One of the applicants in
the Supreme Court suit initiated in 1984 against the council
and the Biko doctors. Dr. Yosuf Veriava, attended the initial
council hearing which he later described as making the coun
cil appear to be “an extension of the South African repressive
machinery!’ The council eventually dropped the case after
Dr. Mokoape’s lawyers challenged the proceedings on
technical grounds. Amnesty International, Political Imprison-
iviuKoape by Mr. in. M. Prinsioo, Council Registrar,
November 6, 1984; Sunday Express, January 13, 1985; Sun
day Tribune, January 13, 1985; interview with Dr. Jerry
Coovadia by author in Washington, DC. on Ju$e 23, 1987.
39 The Argus (Cape Town), October 1, 1980.
40 According to Dr. Stuart Saunders of the University of Cape
Tbwn, about 70 per cent of the country’s medical doctors
are members of MASA. Dr. Jonathan Gluckman put the
membership of MASA at between 10,00 and 11,000. Inter
view with Dr. Stuart Saunders by Eric Stover in Cape Town
on December 14, 1985; interview with Dr. Jonathan
Gluckman by Eric Stover in Johannesburg on December 9,
1985. Of 16,815 medical doctors in South Africa in 1983,
15,251 were white, 60 2343 ‘colored’, 1,255 were Indian, and
249 were African (Department of Manpower figures for April
1983, quoted in Dr. M. Ramphele, ‘Health and Social Welfare
in South Africa Today’, unpublished paper presented at
AAAS annual meeting, Philadelphia, May 25, 1986, p 6).
41 Baxter, ‘Doctors on TYial’, p 142; private correspondence.
Dr. Viljoen to Prof. S. J. Saunders, November 27, 1980.
42 Private Correspondence, Dr. Viljoen to Prof. S. J. Saunders,
November 26, 1980; Report to the Medical Association of
South Africa, 1981, pp 7-8; South Arican Medical Journal
(September 13, 1980), p 433.
43 Statement by the executive committee of the Federal Coun
cil, MASA, regarding the conduct of the doctors responsi
ble for the treatment of the late Mr. S. B. Biko, in South
African Medical Journal, (September 13, 1980), p 433.
45 The chairman of MASA’s Federal Council, Prof. J. N. de
Klerk, described the SAMJ as the “official organ and
mouthpiece of MASA’’ which “must reflect the Association’s
policies” in a letter to Professor Stuart Saunders, November
27, 1980.
45 South African Medical Journal, (September 13, 1980),
pp 432-433.
46 Letter to the editor of the South African Medical Journal,
(September 17, 1980). Professor Saunder’s letter was neither
published nor acknowledged by the editor, although it ap
peared in full, without author’s permission, as an agenda
document for the Federal Council meeting of November 12,
1980. Private correspondence, Prof. Saunders to chairman
of the Federal Council of MASA, November 14, 1980. Com
plaint lodged by Dr. Frances Ames and others, Annexure C.
Apparently the journal editors also refused to publish the
Witwatersrand Medical School statement on the case. Inter
September-December 1988
view with Prof. Phillip Tobias by Eric Stover in Johannesburg
on December 11, 1985. In the interview, Prof. Tobias criticised
the then leadership of MASA for “dragging its heels in
subservience to the government.’’
47 Press statement by Dr. Jonathan Gluckman, November
19, 1980.
48 The authors of the ad hoc committee report claimed that
the Deputy Director of Health Services forbade the doctors’
involvement in the proceedings. The Assistant Secretary of
Health Services, according to Prof. Saunders, argued “why
should my district surgeons take up rap for the police.’’ In
terview with Professor Stuart Saunders by Eric Stover in Cape
Town on December 14, 1985.
40 Report to the Medical Association of South Africa by the
Ad Hoc Committee appointed to consider certain ethical
issues, June 1981; Baxter, ‘Doctors on Trial’, p 142.
50 Complaint by Dr. Frances Ames and others (see note 39).
The complainants were Dr. Frances Ames; Dr. Edward
Barker, senior surgeon, University of Natal Medical School;
Dr. TYefor Jenkins, head of the Department of Human
Genetics at the University of the Witwatersrand; Dr. Leslie
Robertson, a medical general practitioner; and Dr. Phillip
Tobias, dean of the Faculty of~M^^ine-atthe-LIiUY£rsity of
the Witwatersrand. Baxter, ‘Doctors on Trial! p 142; Veriava,
p 299.
51 Complaint by the Transvaal Medical Society and others (see
note 37). The individual complainants were Dr. Dumisani
Miamane, head of the Renal Unit at Baragwanath Hospital;
Dr. Yosuf Veriava, a senior physician at Coronation Hospital;
Dr. Rasik Gopal, neurosurgical registrar at Baragwanath
Hospital; Dr. T Wilson, a pediatrician; and Dr. E. Holland.
Veriava, p 30.
52 Baxter, ‘Doctors on Trial’, p 143; Veriava, pp 301-303.
53 Court papers in Veriava', Baxter, ‘Doctors on Trial’, p 143.
54 Veriava, pp 311-318.
55 Baxter, ‘Doctors on Trial’, pp 150-151; South African Medical
Journal, Vol 63 (August 3, 1985) p 131; The Lancet, No 8447
(July 20, 1985), p 136; The New York Times, July 6, 1985;
The New York Times, October 17, 1985.
56 Baxter, ‘Doctors on Trial’, pp 150-151; Survey of Race Rela
tions 1985 (Johannesburg: SAIRR publication, 1986), pp
454-455; The Lancet, No 8462 (November 2, 1985), pp
1000-1001; The Lancet, No 8424 (February 9, 1985), pp
342-343; Canadian Medical Association Journal, Vol 130
(June 15, 1985), pp 1623-1624; Memorandum submitted to
the World Medical Association by the National Committee
of Health Organisations, South Africa, June 1985.
57 The Lancet, No 8462 (November 2, 1985), pp 1000-1001; The
Lancet, No 8430 (March 23, 1985); British Medical Journal,
Vol 292 (February 22, 1986), p 506; Z4A£4, Vol 254, No 22
(June 12, 1987), pp 3066-3067; interview with Professor
Frances Ames by Eric Stover in Cape Tbwn on December 17,
1985. Some 60 per cent of NAMDA’s current membership
of 1,000 doctors and dentists are black. The new association
was created partly in reaction to MASA’s behaviour over the
Biko case and partly as an expression of concern about broader
health issues which NAMDa members felt MASA was not
properly addressing. Dr. Diliza Mji, ‘The struggle for Health:
The Struggle for Democracy’, unpublished paper presented
at the Institute of Social Studies, Amsterdam, December
1986; Memorandum submitted to the WMA by the National
Committee of Health Organisations (including NAMDA),
June 1985; interview with Dr. Jerry Coovadia by the author
in Washington, D.C. on June 23, 1987.
58 Jenkins, ‘The MASA letter*, pp 234-240.
49
In Defence of Civil Rights
A Biographical Sketch of Dr Ramanadhan
A doctor who renders help to political activists often comes into conflict with oppressive state apparatus and
is himself a target of repression. Dr Ramanadhan’s life and death exemplifies this. He was a civil liberties* activist,
a human and rational doctor’s who fell to a police bullet in Warangal in September 1985. This sketch is reprinted
from an anniversarv tribute to him published by the P U D R New Delhi.
MUSTIKUNTALA is a village in Mahira taluq,
adjust himself to worK in this kind of framework.
Khamamam district that separates the Telengana from the
Husnabad became his last job.
Andhra region. In the thirties the village had a small
Husnabad, a taluq centre, is a big village with around
population of about three hundred, subsisting on cultiva a population of 10,000. If Health Centre serves a number
tion of dry and barren land. But now the village has
of the neighbouring villages. The earlier doctors and com
become prosperous thanks to canal irrigation and even
pounders had established a routine pattern of corruption.
has a high school.
They did not attend the centre, but used the medicines
It was in the village that Dr. Ramanadhan was bom
and equipment of the centre to run their own private
_______ on October 16. 1933. third son of Anatarama Rao and
clinics. When Ramanadhan took charge, he put an end
Rajyalaxmi. me launiy nau auuui
oi
ju*at
io i.riis practice. ims camcu
land. Ramanadhan was the first person in the family to
pounder, the Block Development Officer, and the Samiti
insist on higher education and had to struggle his way to
president who all used to share the booty. But
become a doctor. He completed his primary education
Ramanadhan struggled against these forces and became
in the village and did.his secondary school is nearby
a very popular doctor. Eventually things came to a head
Khammam. Despite family oppostion he went to
when he was asked to issue a death certificate for an
C.R. Reddy College, Eluru for his intermediate, and then
unidentified young girl in the house of the Samiti presi
to the famous Nizam College, Hyderabad, for his B Sc.
dent. The doctor refused. And soon after, he resigned
degree. During his Nizam College days he become pan
from government service.
of a group of students who were peripherally associated
He set up his own children’s clinic on Jayaprakash
with the All Hyderabad Students Union. The house of
Narayan Road, Warangal, in 1968. He was the first
Dr. Balachandra Paranjpaye, well-known veteran of the
pediatrician in the town and soon became very popular.
Telengana struggle, was the cenre for all young men in
It was from- this period that he consciously engaged
those days. Dr. Paranjpaye remained a source of guidance
himself in social activities outside his profession.
to Ramanadhan all his life.
In the early seventies, before the APCLC was formed,
After his B.Sc he took up a number of irregular jobs
he became a kind of supportive centre for a number of
for more than a year, which included teaching and a job
people involved in a variety of problems and issues. He
as a medical representative. Around this time he also got
helped his friends run a monthly that became a well
married. Then he got admission in M.B.B.S. in the newlyknown non-commercial journal inTelegu, Srjana. In fact,
established Gandhi Medical College, Hyderabad. Finan
be it a writers’ organisation wanting to hold its first
cially, these were his bad days, having to live on the limited
meeting in Warangal or a young couple facing family
amount sent by father and his house surgeonship. He join
opposition to their marriage every one sought his help and
ed Osmania College for his Diploma in Child Health. It
received it. In a dramatic incident he rescued a young girl
and conducted her marriage. The girl’s parents were in
was during this period that he became a student of the
famous left wing intellecual, Dr. Rajagopalan. Both were
fluential people with powerfull connections. In the midst
of the marriage function, the police arrived and arrested
to work together, twenty years later, in the APCLC.
the bridegroom and his friends, on charges of abduction.
Throughout his student career he remained on the
Eventually the girl won her battle in court.
periphery of then student movement. In fact, later on too
In early 1974, along with another well-known doctor
he never became part of any organised political group.
of
Warangal, Dr. Amjad Ali Khan, he became a founder
After completing his studies he joined government ser
member
of APCLC in Warangal. Around the same time,
vice. First he taught in Kakatiya Medical College and
he also organised a polyclinic in Warangal. When
worked in Mahatma Gandhi Memorial Hospital where
emergency was declared in 1975 all activities ceased. The
he was to die later. Then for over four years he worked
General Secretary of the APCLC, advocate Prattipati
in the listless primary health centers at Chityala, Vangara
Venketewarli was among the first to be arrested.
and Husnabad in the Warangal and Khammam districts.
Ramanadhan was also arrested, which led to the closure
Primary health centres then and now are private clinics
of
the people’s clinic, virtually the only democratic activity
for those who weild social power in the village and not
in
the
town at that time. He was taken to the illegal camp
clinics for the people. Invariably Ramanadhan could not
September-December 1988
I
maintained by the police at Pakala reserve forest.
Pakala is a wild life sanctuary where two bungalows
meant for tourists were turned into police camps during
the emergency. A number of young people arrested during
the emergency were detained here and tortured. Among
them was the sole eye-witness to the Girapalli encounters
in which four young men were shot dead in cold blood
by the police Dr. Ram an ad han, who was a fellow detainee
of the eyewitness._as to_ be of crucial assistance to the
Ikrkunde Committee which brought out its famous report
on these encounters after the emergency. He was shifted
after, three weeks detention at the Pakala camp to
Warangal Central Prison, which serves as the main prison
for five north-western district of Telengana.
After the lifting of emergency, the central government
appointed the Shah Commission of Enquiry which
managed to submit its report, although no action was
taken on it. But anyone who has gone through the reports
of the Commission can see that the largest number of
crucial affidavits to the Commission from Andhra came
from the Warangal region. Again, the aborted Bhargava
Commission, which was appointed to enquire into en
counter killings in Andhra, was helped by the mobilisation
of crucial witnesses. In both instances, Dr. Ramanadhan
played an unobtrusive but significance role.
In November 1977, a tidal wave hit Divi Seema in the
Krishna district on the east coast. It led to hundreds of
villages being marooned and to the death of thousands
of people. Ramanadhan and his team was the first team
of doctors to enter the inundated areas, before any govern
ment organisations or voluntary agencies. Later tjie team
came back, raised funds, medicines and material neces
sities and went back to the flood affected areas and held
a mobile medical camp for a month.
In late 1979, the junior doctors in Warangal along with
their colleagues in the rest of the state went on a strike
for over seventy days. The government attempted to sup
press the strike at one level by repression and at another
level by generating a mass hysteria against the striking doc
tors. Dr. Ramanadhan took the initiative and organsied
a people’s clinic opposite to the government hospital with
the help of the doctors on strike. The clinic became a cen
tre for both the medical service and the strike. The ram
shackle pandal outside the hospital became so popular
that poor people requested the dcotors to continue the
clinic even after the eventual withdrawal of the strike.
In an unusual incident, Dr. Ramanadhan assited a
Brahmin widow whose husband had been the priest of
a temple. After his death the widow managed the temple.
But the trustes rejected her, presumably because of the
land value of the temple, on the ground that a woman
cannot be a priest. APCLC Warangal, under Ramanadhan,
took up her case and eventually won the battle for her
and also set a precedent.
September-December 1988
What earned him the wrath of the Warangal police was
systematic efforts by the APCLC to expose the lawlessness
of the police. Hundreds of illegal arrests, torture, setting
up of armed police camps in villages and colleges alike
have become routine in past years. Since 1983 at least 12
people were killed in either police lock-up or in so-called
encounters. In Warangal district, the APCLC investigated
each of these instances and brought police violence to the
noticeof the public. In a number of cases it orovided leaal
help to the victims of police harrassment. It challenged
the constitutional validity of the armed camps in the col
leges and villages of Warangal. As the APCLC steppted
up its campaign, it has become a fetter on the arbitrary
behaviour of the Warrangal police establishment.
Initially the police began with a systematic campaign
that APCLC was a extremist front organisation. APCLC’s
own diversified activities was projeetd as an organisation
that is working in the interests of extremists. Later,
APCLC activities began to be implicated in false cases.
In 1984, two of the activists were implicated in a case of
obstructing police from discharging their duty. The case
was later dismissed.
In January 1985, Dr. Ramanadhan was arrested along
with Dr. K. Balagopal and K. Seetarama Rao. They were
charged with, among other things, distributing arms to
the extremists. The doctor was released on bail a week
later. While he was in police lock-up, in a telling incident,
the policemen who had arrested him brought his child for
treatment to the doctor. The incident indicates the extent
to which he had become popular, even among the
policemen of Warangal.
Dr. Ramanadhan’s social awareness helped him to
understand the social origins of the diseaes of his patients.
He did not confine himself to giving medicines but tried
to spread a scientific outlook. It was in this process that
he wrote the famous book Medical Guide (in Telugu)
which was addressed to the people and not to the health
workers. The book became very popular. A second edi
tion came out within an year and now, after his death,
a third edition has been printed. Even after establishing
himself as a popular doctor, his interests in studies remain
ed. He took part in different seminars and meetings of
the profession. A few weeks before his death he par
ticipated in a conference held at Nizam Orthopedics In
stitute. This professionalism was to remain with him till
the very end. In the last twenty minutes of his life en route
to the hospital, he kept discussing with the young doctor,
who took him in his car, the diagnosis of his injuries and
suggesting treatment.
In a sense his involvement with his profession helped
the civil rights movement which in turn made him a bet
ter doctor. He was a doctor not only to rickshaw pullers,
hawkers, and slum-dwellers but also to the policemen and
their children. A few days before his death, an SI who
51
In Defence of Civil Rights
A Biographical Sketch of Dr Ramanadhan
A doctor who renders help to political activists often comes into conflict with oppressive state apparatus and
is himself a target of repression. Dr Ramanadhan’s life and death exemplifies this. He was a civil liberties' activist,
a human and rational doctor’s who fell to a police bullet in Warangal in September 1985. This sketch is reprinted
from an anniversarv tribute to him published by the PUDR New Delhi.
MUSTIKUNTALA is a village in Mahira taluq,
adjust himself to worK in this kind of framework.
Khamamam district that separates the Telengana from the
Husnabad became his last job.
Andhra region. In the thirties the village had a small
Husnabad, a taluq centre, is a big village with around
population of about three hundred, subsisting on cultiva a population of 10,000. If Health Centre serves a number
tion of dry and barren land. But now the village has
of the neighbouring villages. The earlier doctors and com
become prosperous thanks to canal irrigation and even pounders had established a routine pattern of corruption.
has a high school.
They did not attend the centre, but used the medicines
It was in the village that Dr. Ramanadhan was born
and equipment of the centre to run their own private
on October 16. 1933. third son of Anatarama Rao and
clinics. When Ramanadhan took charge, he put an end
Rajyalaxmi. ine tauuiy nau aouui Ju aue*
juauJ
to this practice. This vui'iku ’:•••
t’
land. Ramanadhan was the first person in the family to
pounder, the Block Development Officer, and the Samiti
.jasist on higher education and had to struggle his way to
president who all used to share the booty. But
become a doctor. He completed his primary education
Ramanadhan struggled against these forces and became
in the village and did.his secondary school is nearby
a very popular doctor. Eventually things came to a head
Khammam. Despite family oppostion he went to
when he was asked to issue a death certificate for an
C.R. Reddy College, Eluru for his intermediate, and then
unidentified young girl in the house of the Samiti presi
to the famous Nizam College, Hyderabad, for his B Sc.
dent. The doctor refused. And soon after, he resigned
degree. During his Nizam College days he become pan
from government service.
of a group of students who were peripherally associated
He set up his own children’s clinic on Jayaprakash
with the All Hyderabad Students Union. The house of
Narayan Road, Warangal, in 1968. He was the first
Dr. Balachandra Paranjpaye, well-known veteran of the
pediatrician in the town and soon became very popular.
Telengana struggle, was the cenre for all ydung men in
It was from- this period that he consciously engaged
those days. Dr. Paranjpaye remained a Source of guidance
himself in social activities outside his profession.
to Ramanadhan all his life.
In the early seventies, before the APCLC was formed,
After his B.Sc he took up a number of irregular jobs
he became a kind of supportive centre for a number of
for more than a year, which included teaching and a job
people involved in a variety of problems and issues. He
as a medical representative. Around this time he also got
helped his friends run a monthly that became a well
married. Then he got admission in M.B.B.S. in the newlyknown non-commercial journal in Telegu, Srjana. In fact,
established Gandhi Medical College, Hyderabad. Finan
be it a writers’ organisation wanting to hold its first
cially, these were his bad days, having to live on the limited
meeting in Warangal or a young couple facing family
amount sent by father and his house surgeonship. He join opposition to their marriage every one sought his help and
ed Osmania College for his Diploma in Child Health. It
received it. In a dramatic incident he rescued a young girl
was during this period that he became a student of the
and conducted her marriage. The girl’s parents were in
famous left wing intellecual, Dr. Rajagopalan. Both were
fluential people with powerfull connections. In the midst
of the marriage function, the police arrived and arrested
to work together, twenty years later, in the APCLC.
the bridegroom and his friends, on charges of abduction.
Throughout his student career he remained on the
Eventually the girl won her battle in court.
periphery of then student movement. In fact, later on too
In early 1974, along with another well-known doctor
he never became part of any organised political group.
of
Warangal, Dr. Amjad Ali Khan, he became a founder
After completing his studies he joined government ser
member of APCLC in Warangal. Aroupd the same time,
vice. First he taught in Kakatiya Medical College and
he also organised a polyclinic in Warangal. When
worked in Mahatma Gandhi Memorial Hospital where
emergency was declared in 1975 all activities ceased. The
he was to die later. Then for over four years he worked
General Secretary of the APCLC, advocate Prattipati
in the listless primary health centers at Chityala, Vangara
Venketewarli was among the first to be arrested.
and Husnabad in the Warangal and Khammam districts.
Ramanadhan was also arrested, which led to the closure
Primary health centres then and now are private clinics
of
the people’s clinic, virtually the only democratic activity
for those who weild social power in the village and not
in
the
town at that time. He was taken to the illegal camp
clinics for the people. Invariably Ramanadhan could not
50
September-December 1988
maintained by the police at Pakala reserve forest.
Pakala is a wild life sanctuary where two bungalows
meant for tourists were turned into police camps during
the emergency. A number of young people arrested during
the emergency were detained here and tortured. Among
them was the sole eye-witness to the Girapalli encounters
in which four young men were shot dead in cold blood
by the police. Dr. Ramanadhan, who was a fellow detainee
of the eyewitness. as_to_be of crucial, assistance to the
Tkrkunde Committee which brought out its famous report
on these encounters after the emergency. He was shifted
after three weeks detention at the Pakala camp to
Warangal Central Prison, which serves as the main prison
for five north-western district of Telengana.
After the lifting of emergency, the central government
appointed the Shah Commission of Enquiry which
managed to submit its report, although no action was
taken on it. But anyone who has gone through the reports
of the Commission can see that the largest number of
crucial affidavits to the Commission from Andhra came
from the Warangal region. Again, the aborted Bhargava
Commission, which was appointed to enquire into en
counter killings in Andhra, was helped by the mobilisation
of crucial witnesses. In both instances, Dr. Ramanadhan
played an unobtrusive but significance role.
In November 1977, a tidal wave hit Divi Seema in the
Krishna district on the east coast. It led to hundreds of
villages being marooned and to the death of thousands
of people. Ramanadhan and his team was the first team
of doctors to enter the inundated areas, before any govern
ment organisations or voluntary agencies. Later the team
came back, raised funds, medicines and material neces
sities and went back to the flood affected areas and held
a mobile medical camp for a month.
In late 1979, the junior doctors in Warangal along with
their colleagues in the rest of the state went on a strike
for over seventy days. The government attempted to sup
press the strike at one level by repression and at another
level by generating a mass hysteria against the striking doc
tors. Dr. Ramanadhan took the initiative and organsied
a people’s clinic opposite to the government hospital with
the help of the doctors on strike. The clinic became a cen
tre for both the medical service and the strike. The ram
shackle pandal outside the hospital became so popular
that poor people requested the dcotors to continue the
clinic even after the eventual withdrawal of the strike.
In an unusual incident, Dr. Ramanadhan assited a
Brahmin widow whose husband had been the priest of
a temple. After his death the widow managed the temple.
But the trustes rejected her, presumably because of the
land value of the temple, on the ground that a woman
cannot be a priest. APCLC Warangal, under Ramanadhan,
took up her case and eventually won the battle for her
and also set a precedent.
September-December 1988
What earned him the wrath of the Warangal police was
systematic efforts by the APCLC to expose the lawlessness
of the police. Hundreds of illegal arrests, torture, setting
up of armed police camps in villages and colleges alike
have become routine in past years. Sjnce 1983 at least 12
people were killed in either police lock-up or in so-called
encounters. In Warangal district, the APCLC investigated
each of these instances and brought police violence to the
notice of the.public. In a.number of cases it orovided leaal
help to the victims of police harrassment. It challenged
the constitutional validity of the armed camps in the col
leges and villages of Warangal. As the APCLC steppted
up its campaign, it has become a fetter on the arbitrary
behaviour of the Warrangal police establishment.
Initially the police began with a systematic campaign
that APCLC was a extremist front organisation. APCLC’s
own diversified activities was projeetd as an organisation
that is working in the interests of extremists. Later,
APCLC activities began to be implicated in false cases.
In 1984, two of the activists were implicated in a case of
obstructing police from discharging their duty. The case
was later dismissed.
In January 1985, Dr. Ramanadhan was arrested along
with Dr. K. Balagopal and K. Seetarama Rao. They were
charged with, among other things, distributing arms to
the extremists. The doctor was released on bail a week
later. While he was in police lock-up, in a telling incident,
the policemen who had arrested him brought his child for
treatment to the doctor. The incident indicates the extent
to which he had become popular, even among the
policemen of Warangal.
Dr. Ramanadhan’s social awareness helped him to
understand the social origins of the diseaes of his patients.
He did not confine himself to giving medicines but tried
to spread a scientific outlook. It was in this process that
he wrote the famous book Medical Guide (in Telugu)
which was addressed to the people and not to the health
workers. The book became very popular. A second edi
tion came out within an year and now, after his death,
a third edition has been printed. Even after establishing
himself as a popular doctor, his interests in studies remain
ed. He took part in different seminars and meetings of
the profession. A few weeks before his death he par
ticipated in a conference held at Nizam Orthopedics In
stitute. This professionalism was to remain with him till
the very end. In the last twenty minutes of his life en route
to the hospital, he kept discussing with the young doctor,
who took him in his car, the diagnosis of his injuries and
suggesting treatment.
In a sense his involvement with his profession helped
the civil rights movement which in turn made him a bel
ter doctor. He was a doctor not only to rickshaw pullers,
hawkers, and slum-dwellers but also to the policemen and
their children. A few days before his death, an SI who
5\
was leaving the town on promotion came to him and gave
him sweets by way of farewell. The SI is believed to have
said that for Warangal police he is not only a civil rights
activists but also a doctor. Ramanadhan accepted the
sweets with the confidence in human relationships which
he had built over sixteen years of service to his patients
and to the people of Warangal. Evidently the policemen
who killed him did not share such values.
But perhaps his patients, people for whose lives he had
“Tought ana wnose rights he had defended shared them.
That is why on September 4, defying Section 144 and
undeterred by the presence of armed police, they came
in their thousands and paid their respects to the man who
fought for them. His life and death will remain a defiant
celebration of human values and a never ending source
of inspiration for the democratic movement.
Aftermath
The news of Dr. Ramanadhan’s death reached Delhi on
the morning of September 14, 1985. Tvo prominent Delhi
dailies carried a report, field by a national news agency,
that Dr. Ramanadhan, vice president of the APCLC was
killed by ‘extremists’ in his clinic on the previous day. In
fact no correspondents of this news agency, which does
not have a Warangal office, were present in Warangal on
September.3. The report was filed from Hyderabad, within
two hours of the incident. All. other stae-level and local
dailies carried reports by their Warangal correspondents
saying that the doctor was killed by armed policemen
accompanying the dead body of SI Yadagiri Reddy.
Next day, the superintendent of police, Warangal, contradicated the local newspaper accounts and stated that
Dr. Ramanadhan was possibly killed by some extremists.
When eye-witness journalists pointed out that uniform
ed policemen were seen entering Dr. Ramanadhan’s clinic,
he stated that they had gone to the rescue of the doctor.
On the same day, Vasant Nageswara Rao, home minister,
made a statement on the incident in response to a notice
under rule 329, tabled by 23 memebrs in the state
assembly. The home minister maintained that the sugges
tion that the police were behind the incident was ‘baseless.
He added that the incident took place long after the
funeral procession of armed police had left the place. He
also indicated the involvement of extremists factions in
the murder. Meanwhile APCLC had released its own
report on the incident.
The postmortem report, quoted by the APCLC, states
that the death was caused by a service revolver fired at
point blank range. On that basis and other corroborative
evidence APCLC demanded the immediate susupension
of the senior police officials and ordering of a judicial
enquiry. The government refused to hold a judicial
enquiry. Instead a CBI CID enquiry was ordered. A few
weeks later the government suddently discovered that two
52
policemen were guilty-of dereliction of duty. They had
let their sendee revolvers be stolen from them two months
prior to the incident! Presumably the stolen revolvers were
to be traced to the ‘extremists’ who somehow became part
of an armed police procession and killed the doctor
without anyone ever noticing it.
Meanwhile police- claimed to have identified the six
people who were involved in the Yadagiri Reddy murder
case. The case itself was brought under the Terrorist and
Disruptive Activities (Prevention) Act, 1985 which came
into effect in Andhra Pradesh from August, W85. This
was the first and the only murder case so far under the
act in the state. Two of the accused, Nageswara Rao and
Ramakrishna, were killed in a so-called encounter in April
this year. The other accused include Dr. K. Balagopal
general secretary, APCLC, who was let out on bail and
Dr. P. Varavara Rao, general secretary of the Revolutionary
Writers Association, who is still in jail.
Eventually the CB CID enquiry did take place An SP
who was till recently in the Andhra police was deputed
for the enquiry. He visited Warangal in late October for
three days and submitted the report to the government.
It has not been released to the public or even to the
assembly so far. But we understand that the report came
to the conclusion that the “assailants remain unidentified”.
SUBSCRIPTION RENEWALS
Is this your last subscribed issue? A prompt renewal from
you will ensure that your copy is mailed directly from the
Press. Many of our issues have sold out fast! So book your
copies by renewing your subscription now!
Our new subscription rates:
For individuals—Rs. 30/- (four issues)
For institutions—Rs. 45/- (four issues)
Foreign subscriptions: US $ 20 for US, Europe ?nd Japan
US S 15 for all other countries
(special rates for developing
countries)
Life subscription: Rs. 500/-
D.D.s, cheques, IPOs to be made out to Radical Journal
of Health. Bbay. Please write your full name and correct
address legibly. And please don’t forget to add Rs. 5/- on
outstation cheques.
September-December 1988
Why Are Torturers Never Punished?
,
Case of Archana Guha
peter vesti
Archana Guha was arrested in July 1974 and subjected to 27 days of torture in the hands of the police. She was
not charged formally but was made to believe that the arrest was because of her association with the Naxalite
movement. AJter her release a physically shattered Archana filed a case against her torturers which has yet to
be decided upon. This article was first published in the Danish Medical Bulletin, 1988.
UNTIL recently, little was known about the various
aspects of symptomatology or about treatment of torture
victims. At the Rehabilitation Centre for Torture Victims
in Copenhagen (RCT), over the past five years we have
treated torture victims and compiled information about
the essential aspects of treatment of these most unfor
tunate human beings.
These experiences have made it increasingly clear that
the.end-purpose of torture is to ‘break’ the person, i.e.
to transform a formerly healthy member of society into
an individual broken in spirit and unable to function ef
ficiently in any aspect of personal or public life. An ap
palling insight by the torture victims is that the vast ma
jority of people are indifferent about what has happened
to them; even more horrifying is the undrstanding that
the torturers continue to perform whatever duties they are
assigned (perhaps including torture) and are never brought
to justice, often in spite of a change of national regime
or the election of new political parties.
This has been seen in various places and at various
times in the world. International attention has focused
on the very limited trials of only a few of the accused tor
turers in Greece after the fall of the military government
,
[1]
the strange circumstances surrounding the death of
Steve Biko in South Africa [2], and the impotence of the
newly elected government in Argentina to deal with
criminals who were torturers under the former military
junta [3].
A case that will illustrate such occurrences is the story
of Archana.
In 1980, an Indian national by the name of Archana
Guha was flown to Copenhagen to receive treatment at
Rigshospitalet, one of our University Hospitals. Thritynine years old, she arrived on a stretcher, had years before
been tourtured, and was now suffering the consequences.
With the help of Amnesty International, she was transfer
red to Denmark to receive treatment at the centre later
to be developed into the Rehabilitation Centre for Tor
ture Victims (RCT). Following is a review of the cir
cumstances of the case and the sad recognition that now,
many years later, Archana’s case against her tortures is
still pending before the court in Calcutta.
The early 1970s were a violent time in West Bengal. A
militant Marxist grouop, the Naxalities, were ravaging the
September-December J988
countryside, and many people were caught inthe crossfire
between it and a government using all means to fight it.
One such person was Archana Guha. Educated as a school
teacher, in 1967 she was appointed, head mistress of
Kolorah Girls Junior High School outside Calcutta.
Arrest and Torture
On July 17, 1974, Archana was arrested in the middle
of the night together with her sister-in-law and a friend
staying in the house. No formal charges were brought
against them, but they were made to believe that their ar
rests were due to some connection with the Naxalite move
ment. The matter was never brought to court.
IWenty-seven days of torture followed at Lalbazar, head
quarters. of the Calcutta police. First, Archana was made
to witness the assault on and torture of her sister-in law
and her friend. She was then tied, hands and feet, slung
upon a pole, head down, and severely beaten on the feet
(falanga). The five policemen involved took turns hitting
her and kicking her*on the hips, and later they burned
her toenails with cigars. She was threatened with rape and
made to understand that her family would also be tor
tured if she did not cooperate. When she was not in the
torture chamber, she was kept in a small, dark isolation
cell. During the torture she was forced to sign several blank
papers. She was suspended by her hair and, later, ‘brain
washed—a term used by torturers for a procedure in which
they begin a movement to bang her head against the wall,
but at the very last moment before her head struck the
wall, pull her back.This was done 10-20 times.
It seems likely that the three women were arrested
because of Archana’s brother Saumen. He was also ac
cused of involvement with the Naxalite movement. He was
arrested on the August 6, 1975, and when Archana’s tor
turers learned of his arrest, they stopped torturing her.
Saumen, himself, was allegedly on two occasions sub
jected to torture for periods of six and 14 days.
Archana never came before a judge, even though the
law specifically states that this must take place within
24 hours of the arrest. On August 13,1974, Archana was
brought to the Presidency Jail. In September 1974 she was
released, but immediately after was again detained under
the Maintenance of Internal Security Act (MISA). She was
53
released on parole in November 1976 and on May 3, 1977
was also released from MISA detention. The Left From
(a Coalition of left wing parties) was now in power in West
Bengal.
After the torture, Archana had multiple symptoms. She
suffered headache, swelling around the left eye, a burn
ing sensation in the head, difficulty breathing, irregular
periods as well as bleeding from the rectum. She suffered
several infections in the urogenital system. She also suf
fered difficultly sleeping, had no appetite, and poor
concentration.
Her condition deteriorated, and gradually she lost mus
cle strength in her arms and legs, grew weak and also lost
sensation. She was confined to bed and to a wheelchair.
From December 1975 to February 1976, she was hospita
lised in the SSKM Hospital—was under round-the-clock
police guard—but did not improve. She was later transfererred to the Medical College Hospital, still under police
guard, still paralysed, and was told that she could expect
no major improvement. An X-ray at that time showed a
fracture of the seventh cervical vertebra.
Upon arrival in Denmark four or five years later,
Archana was still suffering from a number of symptoms.
She had constant headache, nausea, and muscualar pain
in the neck and shoulders. She was constipated and slept
poorly, suffered tremous, and was still unable to concen
trate. She was mostly confined to bed, being unable to
walk without human support.
Neurological examination showed a decrease in strength
in the arms which were also somewhat atrophic. Her legs
showed a decrease in strength bilaterally, both for flex
ion and for extension. Both legs were atrophic. The pa
tient was unable to walk unless supported by two persons.
The reflexes could not be elicited.
Examination of the skin revealed several scars and
pigmentation changes compatible with the history’ of com
bustion and subsequent ulceration. The size of the scars
were in accordance with the size of a scar caused by the
glow of a small cigar. The patient also described pustulations and alopecia as well as discoloration after being
suspended by her hair. This is also in accordamce with
known sequelae to traction alopecia.
Beyond doubt, most of the patient’s symptoms and
signs are the result of torture. It is equally clear that poor
conditions in the prison (possibly a deficiency iin protein)
as well as the depressing effect of prison conditions in
general and uncertainty about the future, sustained and
possibly aggravated Archana’s condition.
In August 1977, soon after she was released, Archana
filed a petition accusing five policemen of having violated
relevant sections of the Indian Penal Code. At that time,
she was unable to walk and had to be carried to the cour
troom to make a personal appearance. The accused were:
Ranjiit Guha Neogi (Runu), officer in-charge of the in
54
vestigation; Santosh De; Aditya Karriaka; Arun Baner
jee; and Kamal Das, alias ‘the golden hand’, known for
being able to make most people talk under torutre.
Archana also requested a reasonable compensation for
almost three years in jail and was offered a few hundred
rupees. The authorities would not even bear the expenses
for her treatment at a major private clinic in Calcutta.
With the help of Amnesty International and human rights
groups as well as women’s groups in India, attention was
focused onthe case. Finally, the government in West
Bengal agreed to pay the expenses involved in transferr
ing Archana to Rigshospitalet in Copenhagen.
After intensive treatment, rehabilitation, and
physiotherapy, Archana’s health improved and gradually
she was able to walk again. She later returned to India.
While under treatment, she became painfully aware that
her torturers in no way were affected by her petition and
that the authorities apparently did not believe her and
wanted the whole thing to be forgotton. We believe this
influenced her rehabilitation negatively. During her stay
in Denmark, she had made the acquaintance of an emplo
yee at Rigshospitalet, and Archana later moved back to
Copenhagen to settle permanantly.
And what happened about the court case submitted in
August 1977? Nothing much, I regret to say. None of the
accused officers have been suspended. Death certificates
have been produced for two of the accused (Aditya and
Arun). Kamal Das (the golden hand) has disappeared and
records seem not to indicate that he was employed by the
Calcutta police in the first place. Every legal loophole has
been used and abused to prolong the proceedings at the
court. The accused have claimed that Archana’s lawyer
(A. P. Chatterjee) could not represent Archana because
he was also the government’s standing council. This was
put to the high court as well as the Supreme Court twice
before the legitimacy of his representing the client was
confirmed. It appears that the evidence was misrepre
sented and the court misled the first time.
During the 1980s several human rights organisations
and women’s organisations followed the case and even
demonstrated outside the court room—not,for a verdict
of guilt, but only for a speedy trial. Because of this, the
accused filed a petition asking that these organisations
be tried for contempt of court and that reportage of the
trial be prohibited. The local magistrate did bar the
newspapers from publishing the evidence of the witnesses.
However, this was not abided by and was rejected by a
higher court.
Aggrieved by the above-mentioned decision of the local
judge, a new petition was filed by the accused requesting
the transfer of the case to a new magistrate. And finally
it appears that a new petition has been filed asking for
change of judge as well as the place of trial. In addition
to these obstacles, the accused have repeatedly requested
September-December 1988
stay orders for various reasons, making it almost impossi
ble for Archana to go on with the cse, considering that
she is living abroad.
Conclusion
Ten years have lapsed, the case lingers on and still no
verdict is insight. At the end of the 1970s many cases were
brought against the police for torture; however, all other
cases have been dropped. Very few people can keep a court
case going for years; the legal expenses involved are
astronomical. A very storng personality is needed to go
through these ordeals with so little hope of success.
Archana’s lawyer has taken on the case on a humanita
rian basis. He, himself, has been threatened on many oc
casions, and threats have also been made against his fami
ly. The whole court case seems to be a clash of interests.
However, it is difficult to see who the accused party
represents. Very expensive lawyers have been helping the
accused (and prolonging the court case) all these years,
and a question has been raised as to who pays their fees.
In whose interest can it be to suppress a court case like
this, to keep it from reaching a verdict?
If it had not been for support from intematioinal
organisations, local human rights groups, and women’s
organisations as well as the press and television, this case
might also have been dropped years ago. This would not
be in the interest of a democratic country like India, where
torture is prohibited by law.
In this context, we must also consider the Convention
against Torture and Other Cruel, Inhuman or Degrading
Treatment and Punishment (4), the United Nations con
vention prohibiting torture and setting up rules and
regulations concerning international aspects of torture.
So far, 43 states have signed the document, and of those,
as of December 1987, 17 have ratified it. India has not
yet signed this document, whose aim is to help progressive
authorities bring about justice.
Archana was forced to spend three years of her life in
prison, was brutally tortured, and only after intensive
rehabilitation has been able to begin to live a reasonable
life again. Three years of a lifetime is a long time. Cases
of tortures being convicted and punished are virtually non
existent as are cases of compensation paid out to the vic
tims. More than three weeks of torture cannot be undone;
three years of a life cannot be given back. The duty of
society must be to compensate at a realistic level as well
as to use such occasions to better it control over and in
sight into various services in our society, including the
police. We must remember that the police force reflects
that society in general. The time has come to recognise
torturers as the criminals they are.
September-December 1988
References
[1] Amnesty International. Tbrture in Greece: The first torturers*
trial 1975. London: Amnesty International Publications,
1977.
[2] Mertz, J. Steve Biko. Ugeskr Laeger 1980; 142: 2638-40.
[3] Simpson J, Bennett J. The Disappeared, London: Sphere
Books Ltd., 1986.
[4] ‘Convention Against Torture and Other Cruel, Inhuman or
Degrading Treatment or Punishment.’ In: Outlawing an an
cient evil: Torture. New York: UN Department of Public In
formation, 1985.
Dr. Peter Vesti
Rehabiliterings Center for Torturofre
Juliane maries Vej 34,
DK-2100, Copenhagen (Denmark)
If your're wondering
what happened to
the civil rights movement
If you want to keep track
of civil rights groups
all over India
Read
Adhikar Raksha
(Quarterly)
the voice of the civil rights movement since 1977.
Subscribe to ADHIKAR RAKSHA
Bulletin of the Committee for the Protection of
Democratic Rights (CPDR),
C/o Super Book Hose,
Sind Chambers,
Colaba Causeway,
Bombay 400 005.
Annual Subscription: Rs 10/- only
October-December 88 issue out
(Send MO only)
Includes.-—Special Articles on Punjab—Human
Rights Tribunals Judgement on Chintapalli
Arson Case
State Torture: Some General, Psychological and
Particular Aspects
femando bendfeldt-zachrisson
State political torture has be$n practised in Latin American countries and is well-documented. What are the par
ticular aspects of this practice? What are the elements which contribute to a person participating in torture? Who
is the real torturer?
WE may describe torture as that extreme and deliberate
form of violence inflicted upon a victim who experiences
it consciously, and who has no control over its form or
duration. It produces pain and mental or psychologial
stress and is intended to destroy the victim’s will in an
attempt to perpetrate a determined order of power rela
tionships. When such practice is structured into the ways
state governs over the people of a nation, we may refer
to it as state torture; but when the primary target is the
citizens who oppose, or are believed to oppose, the order
of relationships established by that state, we may talk of
state political torture. In the American continent the use
of torture as an identifiable administrative policy has been
recognised in several countries [1-4], but the cases of Chile,
Uruguay, Argentina, Paraguay, El Salvador, and
Guatemala have become exemplary over the past ten years
[1, 5-9]. In these countries thousands of citizens who op
pose their governments have been (and are being) tortured
in semi-clandestine torture centers, where similar methods
and techniques of suffering are implemented. The sub
jects for torture are identified and selected by branches
of the military and then kidnapped by “heavily armed
men dressed in civilian clothes” who operate with impu
dent legal immunity. The victims are then taken to
camouflaged jails where a minority of those who enter
are able to come out alive to tell the story.
What is the purpose of such torture? On first hand it
may seem that the answer is information. But if we review
the methods and understand that in these countries tor
ture has been made a stable semiclandestine institution
of the state, its primary purpose can no longer be con
sidered simply to secure information or a confession. How
could we believe information is the aim when pregnant
women are burned in the nipples and genitals and then
receive electric shocks in the uterus producing either abor
tion or brain lesions in the fetus [3]? Or when splinters
are inserted into the eardrums? And besides the cruelty
per set how valid could a confession be under those cir
cumstances or under the effects of stupefacients? No, here
the specific purpose served by such brutality seems to be
primarily the destruction of the individual in his/her most
basic humanity, while the general objective seems to be
the attempt to preventing dissidence—a way of exercis
ing and maintaining power by terror.
56
By definition, torture assumes the involvement of at
least two subjects: the torturer, who applying torture
strives for maximal submission of the victim under his
physical control, and the victim, whose actual cir
cumstance makes an immediate defensive counterviolence
impossible. In the following sections, I will examine some
aspect of the methods of torture, the torturer and the ef
fects of this practice.
Methods of Torture
When torture is part of the state policy, the methods for
destroying the morale and physical integrity of the victims
are ample. Breaking down the victim, whether by produc
ing an organic impairment of the mental functions [10] or
by the effects of stress [11, 12], is achieved by the use of both
rustic and sophisticated methods and techniques. What,
when and how to torture is something established by ac
cumulated local and international experience. Not infre
quently, it is assisted by modem medicine and research fin
dings, even with direct participation of physicians [13-21]:
There are testimonial reports of medical doctors supervis
ing the process of torturing, or monitoring the procedures
so that unconsciousness and death are avoided while max
imum stress is applied [1].
The scientific approach to torture has been taken seriously
by some. In a recent article published in the Journal of
Medical Ethics, ‘On the Permissibility of Torture’, G. E. Jones
argues in support of torture [22]. Justifying it on utilitarian
grounds he states:
It (torture) cannot involve death, and must utilize the most advanced
medical techniques available so as not cause needless psychological
or physical harm. Only the minimal amount of pain necessary to ob
tain information would be inflicted (italics added).
And further, in a clearly marketing way, while discuss
ing the cost-benefit ratio of torture (which he compares
with solar energy: it pays in the long run) and under what
he calls humane (sic) torture, he goes on saying that:
The state of technology is such that we can stimulate certain centers
of the brain such that we can inflict pain without physical abuse or
physical side effects, (italics added)
The mode of torture that Jones proposes, which ap
parently includes electro stimulation or microsurgery to
affect brain centers, selectively ignores that torture is terri
ble as an experience and not only for its visible sequelae.
What Jones seems to be concerned with is the public or
September-December 1988
observable evidence that torture had taken place, rather
than what it represents, or the damaged self and relation
ships the torture victims are rendered with. Torture is a
devastating experience that accompanies the surviving vic
tim the rest of his/her life, affecting, as I will explain later,
more than the physical or physiological aspects. Jones’
statement that, “Only the minimal amount of pain
necessary to obtain information would be inflicted” is
naive. Would’t a torturer ever accept having inflicted pain
in excess of that necessary to his victims?
The pain and the stress caused by different methods
of torture need to be multiple, variable and unpredictable.
This way the victim’s attempts at behaving in consistent
ways or developing personal behaviour patterns to better
sustain the suffering are frustrated. The methods and
techniques of torture are often the same in the six Latin
and Central American countries (Thble 1), even to the
point that many types of torture receive the same name
(Table 2)—a case of internatioinal cooperation.
The catastrophic existential event that torture represents
for the victim will certainly leave a permanent stigma in
the survivor and his/her basic social nucleus. How, and
to what extent, the terror, humiliation, loss of dignity and
physical suffering will mark the victim is something that
cannot be generalised. The structural characteristics of
the victim’s personality are important: the victim’s clari
ty and strength of morale, sense of purpose and com
radeship and even hatred of the system that brings the
suffering [21]. But the effects of torture on the victim will
also depend upon the dose of experienced violence, that
is, the duration and intensity of the stressor.
The extent of the injury should be measured not ony
by the bodily deformity or loss, or impairment, but by
the emotional significance attached to the experience
which often leads to a radical alteration of the person’s
whole life [23, 24]. Torture results in anxiety, difficulty
in thinking, loss of self-esteem, social withdrawal, decrease
in productivity and abandonment of goals [1, 14, 23]. For
those who can no longer resist and who broke down, ad
ditional guilt and despair awaits.
From a psychiatric point of view, torture represents a
situation of massive stress which unequivocably provokes
anxiety, brought about not only by pain and mortifica
tions, but also by uncertainty. Under torture, the threat
of destruction is more than an imminent possibility—it
has already started. Yet what the victim lacks is access
to
knowing
how,
when
or if the destruction is going to be completed. In
psychiatric language, the symptomatic post-effects of tor
ture, together with other psychological traumatic events
of inordinate nature and outside the usual human -ex
perience, fall in what are called post-traumatic stress
disorders [25]. Briefly, these disorders constitute a con
dition that results in the contraction and disorganisation
September-December 1988
of the ego [26], hence to a symptom complex, acute or
chronic characterised by: 1) recurrent and intrusive
recolections of the traumatic event and nightmares in
which the event is re-experienced as it was or in a represen
tational way; 2) dissociative states that last from minutes
to days, in which the individual behaves as if the trauma
were recurring, because of an association with an en
vironmental or ideational stimulus that elicits them;
3) constriction of affect, reduced responsiveness to the
surroundings, and feelings of estrangement from others;
4) hyperalertness, exaggerated startle response, sleep
disturbances, memory impairment, etc. Yet, as has been
observed, the symptoms brought forth by deliberate man
made disasters, such as torture, often exceed other
stressors in severity and consequences and may even
precipitate premature death [27].
Table 1: Methods of Torture®
1.
2.
3.
4.
5.
Environmental Manipulation:
Social deprivation (isolation from family and friends)
Isolation (restrictionof company, sex, work, relaxation, food)
Sensory deprivation or overload
(solitary cells, noises, reflectors, etc.)
Sleep deprivation
Pharmacological Manipulation:
Parenteral barbiturates and stupefacients
LSD and related drugs
Apomorphine
Corrosive chemicals
Cyclophos phamide
Muscle-paralyzing drugs (e.g., curare)
Coercive Methods:
Forced seeing or hearing others being tortured
(friends, relatives, spouse, children)
False accusations
Occasional indulgences
Somatic Methods:
Forced standing: prolonged standing in a required position,
usually undressed.
Cold water: irrigation or submersion in cold water
Beating: with iron rods, rubber truncheons, whips, batons,
sticks, etc.
Starvation: deprivation of water or food
Mutilation: dismembering of various parts of the body
Breaking bones
Sexual molestation: stripping, touching, attempted rape
Rape: homosexual or heterosexual
Electricity: electric shocks applied specially to eyes, teeth,
head, genitals, rectum; “electric bed”
Fire: e.g., welding torches applied to head, eyes, genitals, etc.
Psychological Methods6
Denigration with insults, false accusations, use of brutal and
threatening language, threats of execution
Sham execution
Execution of family members or friends in front of the victim
Video or audiotapes of the torture of other victims, including
torutre of relatives, spouse and children
Witnessing homosexual or heterosexual rape performed on
friends, relatives, etc.
a See references 1, 3, 5, 6, 7, 49.
b The separation of psychological from somatic is ony made
for clarity sake. Any form of torture encompasses both
psychological and somatic effects.
57
State Torture: Some General, Psychological and
Particular Aspects
fernando bendfeldt-zachrisson
State political torture has be^n practised in Latin American countries and is well-documented. What are the par
ticular aspects of this practice? What are the elements which contribute to a person participating in torture? Who
is the real torturer?
WE may describe torture as that extreme and deliberate
form of violence inflicted upon a victim who experiences
it consciously, and who has no control over its form or
duration. It produces pain and mental or psychologial
stress and is intended to destroy the victim’s will in an
attempt to perpetrate a determined order of power rela
tionships. When such practice is structured into the ways
a state governs over the people of a nation, we may refer
to it as state torture; but when the primary target is the
citizens who oppose, or are believed to oppose, the order
of relationships established by that state, we may talk of
state political torture. In the American continent the use
of torture as an identifiable administrative policy has been
recognised in several countries [1-4], but the cases of Chile,
Uruguay, Argentina, Paraguay, El Salvador, and
Guatemala have become exemplary over the past ten years
[1, 5-9]. In these countries thousands of citizens who op
pose their governments have been (and are being) tortured
in semi-clandestine torture centers, where similar methods
and techniques of suffering are implemented. The sub
jects for torture are identified and selected by branches
of the military and then kidnapped by “heavily armed
men dressed in civilian clothes” who operate with impu
dent legal immunity. The victims are then taken to
camouflaged jails where a minority of those who enter
are able to come out alive to tell the story.
What is the purpose of such torture? On first hand it
may seem that the answer is information. But if we review
the methods and understand that in these countries tor
ture has been made a stable semiclandestine institution
of the state, its primary purpose can no longer be con
sidered simply to secure information or a confession. How
could we believe information is the aim when pregnant
women are burned in the nipples and genitals and then
receive electric shocks in the uterus producing either abor
tion or brain lesions in the fetus [3]? Or when splinters
are inserted into the eardrums? And besides the cruelty
per se, how valid could a confession be under those cir
cumstances or under the effects of stupefacients? No, here
the specific purpose served by such brutality seems to be
primarily the destruction of the individual in his/her most
basic humanity, while the general objective seems to be
the attempt to preventing dissidence—a way of exercis
ing and maintaining power by terror.
>6
By definition, torture assumes the involvement of at
least two subjects: the torturer, who applying torture
strives for maximal submission of the victim under his
physical control, and the victim, whose actual cir
cumstance makes an immediate defensive counterviolence
impossible. In the following sections, I will examine some
aspect of the methods of torture, the torturer and the ef
fects of this practice.
Methods of Torture
When torture is part of the state policy, the methods for
destroying the morale and physical integrity of the victims
are ample. Breaking down the victim, whether by produc
ing an organic impairment of the mental functions [10] or
by the effects of stress [11, 12], is achieved by the use of both
rustic and sophisticated methods and techniques. What,
when and how to torture is something established by ac
cumulated local and international experience. Not infre
quently, it is assisted by modem medicine and research fin
dings, even with direct participation of physicians [13-21]:
There are testimonial reports of medical doctors supervis
ing the process of torturing, or monitoring the procedures
so that unconsciousness and death are avoided while max
imum stress is applied [1].
The scientific approach to torture has been taken seriously
by some. In a recent article published in the Journal of
Medical Ethics, ‘On the Permissibility of Torture’, G. E. Jones
argues in support of torture [22], Justifying it on utilitarian
grounds he states:
It (torture) cannot involve death, and must utilize the most advanced
medical techniques available so as not cause needless psychological
or physical harm. Only the minimal amount of pain necessary to ob
tain information would be inflicted (italics added).
And further, in a clearly marketing way, while discuss
ing the cost-benefit ratio of torture (which he compares
with solar energy: it pays in the long run) and under what
he calls humane (sic) torture, he goes on saying that:
The state of technology is such that we can stimulate certain centers
of the brain such that we can inflict pain without physical abuse or
physical side effects, (italics added)
The mode of torture that Jones proposes, which ap
parently includes electro stimulation or microsurgery to
affect brain centers, selectively ignores that torture is terri
ble as an experience and not only for its visible sequelae.
What Jones seems to be concerned with is the public or
September-December 1988
observable evidence that torture had taken place, rather
than what it represents, or the damaged self and relation
ships the torture victims are rendered with. Torture is a
devastating experience that accompanies the surviving vic
tim the rest of his/her life, affecting, as I will explain later,
more than the physical or physiological aspects. Jones’
statement that, “Only the minimal amount of pain
necessary to obtain information would be inflicted” is
naive. Would’t a torturer ever accept having inflicted pain
in excess of that necessary to his victims?
The pain and the stress caused by different methods
of torture need to be multiple, variable and unpredictable.
This way the victim’s attempts at behaving in consistent
ways or developing personal behaviour patterns to better
sustain the suffering are frustrated. The methods and
techniques of torture are often the same in the six Latin
and Central American countries (Thble 1), even to the
point that many types of torture receive the same name
(Thble 2)—a case of international cooperation.
The catastrophic existential event that torture represents
for the victim will certainly leave a permanent stigma in
the survivor and his/her basic social nucleus. How, and
to what extent, the terror, humiliation, loss of dignity and
physical suffering will mark the victim is something that
cannot be generalised. The structural characteristics of
the victim’s personality are important: the victim’s clari
ty and strength of morale, sense of purpose and com
radeship and even hatred of the system that brings the
suffering [21]. But the effects of torture on the victim will
also depend upon the dose of experienced violence, that
is, the duration and intensity of the stressor.
The extent of the injury should be measured not ony
by the bodily deformity or loss, or impairment, but by
the emotional significance attached to the experience
which often leads to a radical alteration of the person’s
whole life [23, 24]. Torture results in anxiety, difficulty
in thinking, loss of self-esteem, social withdrawal, decrease
in productivity and abandonment of goals [1, 14, 23]. For
those who can no longer resist and who broke down, ad
ditional guilt and despair awaits.
From a psychiatric point of view, torture represents a
situation of massive stress which unequivocably provokes
anxiety, brought about not only by pain and mortifica
tions, but also by uncertainty. Under torture, the threat
of destruction is more than an imminent possibility—it
has already started. Yet what the victim lacks is access
to
knowing
how,
when
or if the destruction is going to be completed. In
psychiatric language, the symptomatic post-effects of tor
ture, together with other psychological traumatic events
of inordinate nature and outside the usual human -ex
perience, fall in what are called post-traumatic stress
disorders [25]. Briefly, these disorders constitute a con
dition that results in the contraction and disorganisation
September-December 1988
of the ego [26], hence to a symptom complex, acute or
chronic characterised by: 1) recurrent and intrusive
recolections of the traumatic event and nightmares in
which the event is re-experienced as it was or in a represen
tational way; 2) dissociative states that last from minutes
to days, in which the individual behaves as if the trauma
were recurring, because of an association with an en
vironmental or ideational stimulus that elicits them;
3) constriction of affect, reduced responsiveness to the
surroundings, and feelings of estrangement from others;
4) hyperalertness, exaggerated startle response, sleep
disturbances, memory impairment, etc. Yet, as has been
observed, the symptoms brought forth by deliberate man
made disasters, such as torture, often exceed other
stressors in severity and consequences and may even
precipitate premature death [27].
Table 1: Methods of Torture*
1.
2.
3.
4.
5.
Environmental Manipulation:
Social deprivation (isolation from family and friends)
Isolation (restrictionof company, sex, work, relaxation, food)
Sensory deprivation or overload
(solitary cells, noises, reflectors, etc.)
Sleep deprivation
Pharmacological Manipulation:
Parenteral barbiturates and stupefacients
LSD and related drugs
Apomorphine
Corrosive chemicals
Cyclophos phamide
Muscle-paralyzing drugs (e.g., curare)
Coercive Methods:
Forced seeing or hearing others being tortured
(friends, relatives, spouse, children)
False accusations
Occasional indulgences
Somatic Methods:
Forced standing: prolonged standing in a required position,
usually undressed.
Cold water: irrigation or submersion in cold water
Beating: with iron rods, rubber truncheons, whips, batons,
sticks, etc.
Starvation: deprivation of water or food
Mutilation: dismembering of various parts of the body
Breaking bones
Sexual molestation: stripping, touching, attempted rape
Rape: homosexual or heterosexual
Electricity: electric shocks applied specially to eyes, teeth,
head, genitals, rectum; “electric bed”
Fire: e.g., welding torches applied to head, eyes, genitals, etc.
Psychological Methods*5
Denigration with insults, false accusations, use of brutal and
threatening language, threats of execution
Sham execution
Execution of family members or friends in front of the victim
Video or audiotapes of the torture of other victims, including
torutre of relatives, spouse and children
Witnessing homosexual or heterosexual rape performed on
friends, relatives, eta
a See references 1, 3, 5, 6, 7, 49.
b The separation of psychological from somatic is ony made
for clarity sake. Any form of torture encompasses both
psychological and somatic effects.
57
Although not all researchers agree [4], some studies
have found that the psychological effects of torture are
sufficiently characteristic to constitute a ‘torture syn
drome’ [28, 29]. However, we still know little about what
occurs to the human body and mind as the result of tor
ture, notwithstanding the psychic and somatic changes
observed. In general, the investigations of long-term
psychological effects of torture are rare. However, a re
cent Danish study [4] sponsored by Amnesty I ntemational
in which 135 victims of torture were examined medically
and psychiatrically gives us an idea. The study showed
that at the time of the examination, conducted between
six months and a year after torture had taken place, 90 per
cent of the victims complained of various symptoms
which arose in conjunction with or following torture. Of
those, 75 per cent presented psychiatric symptoms which
included impaired memory, impaired concentration, men
tal changes and sleep and sexual disturbances. All the sub
jects had been healthy prior to their arrest. On the other
hand, Allodi and Cowgil [28] investigated 41 cases of tor
ture among the thousands of refugees from especially one
Latin American country, who had migrated to Canada.
The victims studied were 32 males and nine females,
whose ages ranged from less than ten to 46 years of age
(mean age 26.9). Twenty-five per cent of them had some
university training, and except two females, they had ex
perienced a total of 112 incarcerations ranging from weeks
to a year (one victim had been imprisoned 11 times in five
years). All were subjected to physical and psychological
abuse. Allodi and Cowgill concluded that all suffered from
a homogenous psychological disorder marked by severe
anxiety, insomnia with nightmares about persecution, vio
lence or their own torture experience, somatic symptoms,
phobias, suspiciousness and fearfulness. In the case
analysis they found that there seemed to exist a positive
relationship between the individual ideological prepara
tion, commitment and group support and psychological
recovery from torture.
The sequelae at times could lead also to lesions in
organs of functions not directly subjected to torture. For
instance, Lunde, Rasmussow and collaborators (30) stu
died the sexual function of 17 men exposed to torture.
They found that independently of cranial or genital
trauma or severity of torture, 19 per cent of the studied
victims presented sexual dysfunctions manifested as
decrease in libido and/or erectile dysfunctions, in absence
of abnormal pituitary or gondal hormones. In another
study, Jensen Genefke and collaborators reported cortical
or central cerebral atrophy, as determined by computerised
axial tomography, in five non-alcoholic, previously healthy
men ages 24 to 39 [31]. These men had been exposed to
severe and prolonged tortures (mean of four years), and
all had symptoms consisting of inability to concentrate,
headaches, anxiety, depression, asthenia, sleep distur
58
bances, cerebral asthenopia and sexual dysfunctions for
several yars. A suggested possible mechanism, assuming
that the atrophic changes cannot be attributed to head
trauma, has been the possibility of high levels of cortisol
secondary to the chronic severe stress of torture[32].
We did not dare to kill them all (the political prisoners) when
we could have done so and one day we shall have to release
them. We must take advantage of the available time in order
to make them go mad.
Major Arguimides Maciel
Director of Libertad Prison
Uruguay
When confronting human behaviour, especially if it is
deemed highly negative in quality, psychiatrists and fieldrelated professionals tend to seek the roots of such
behaviours primarily in the individual, or. at best, in
his/her immediate surroundings. In such a narrow view,
the torturer’s behaviour could be easily conceptualised as
one of a sadistic sociopath, brought about by defective
parental discipline resentment over emotional deprivation,
or more reductionistic, by congenital deficits or neuro
chemical imbalances in the brain. The problem with this
intrasystemic orientation is that it selectively assigns
causality intensively to one or a few individual elements,
while disregarding or simply enumerating socio-economic
conditions as aggregate factors in a multidetermined
causality. The socio-economic system and the culture that
derives from it is a basic element that shapes (and is
shaped by) history, that dictates priorities and modifies
environments.
Table 2: Specific Methods
‘Submarine or
‘Underwater
treatment’
‘The Hood:’
‘Telephone:*
‘Parrot Perch’or
‘Pau de Arrara’
‘Dogs Pit:’
‘Hook’ or
‘Hanging:’
‘Mitrione’s
vest:’1
‘Picada:’
The victim is forced io submerge the
head in a sink or bucket full of
excrement, urine and water.
The victim’s head is forced into a plastic bag,
usually containing insecticide, until
suffocation.
Beating from behind simultaneously on both
ears.
The victim’s wrists and ankles are
tied together and the whole body is suspend
ed from an iron bar under the knees, leaving
the naked body doubled over and defenseless.
In this position electro-shocks are applied
and filthy water forced into the mouth.
The victim is kept a few feet above the
ground as (s)he is hanged from the hands
which are kept tied together on the back.
The victim is hanged from a rope
which is hooked to a strap around the waist,
while the hands are tied to the back.
The garment is gradually inflated
until it crushes the victim’s ribs and makes
breathing impossible.
A straight pin inserted most commonly under
the victim’s fingernails._____________ _____
a Named after Dan Mitrione, a North American AID official, c8
ly an advisor to the Urguayan police in counter insurgency techniques,
including methods of torture (3, 9].
September-December 1988
By focusing on (he individual or his/her immediate
family as the source of aggression, this theory avoids a
critical examination of the problem. It ignores the history
of societies which value highly certain types of aggressive
behaviours, which glorifies the aggressive war hero, and
which pretend that amassing destructive power is a deter
rence of war and a preserver of peace. In other words,
for the study of the individual that concerns us here we
must look beyond the individual and his/her family, into
(he conditions that typically prevail in society which
favours—and benefits—from such practices. The political
torturer works in the name of the society, the army, the
interest of the nation, etc. He is not the isolated
maleficarum that our conscience would like us to believe;
he is a member of an organised group that operates semiautonomously, but does so under the direction of bran
ches of the government—an element of a network devis
ed to preserve power and facilitate domination. Does this
mean that anyone could become a torturer? The answer
is not black or white. Perhaps a now classical experiment
better illustrates the dilemma. Some years ago S. Milgram
conducted an experiment, ‘Behavioral Study of Obedien cy’ in a laboratory at Yale University [33]. The ex
periment consisted of 40 volunteers who were led to
believe that they were to take part in an experimental
design on memory and learning. Each volunteer was in
structed to administer electric shocks to a learner-victim
whenever (s)he gave an incorrect answer to a question.
Although the victims never actually received an electric
discharge, they had been instructed to pretend as if the
shock had been experienced. The experiment was designed
so that when the punitive shock had reached certain
voltage, the teacher-volunteer had the option of stopping
the procedure, but was verbally encouraged, and even
firmly ordered to proceed administering shocks at higher
voltage if the learner-victim failed to complete the task.
In the experiment none of the 40 subjects stopped prior
to shock level 300, at which the victim began kicking the
wall and no longer provided answers to the multiple choice
questions. At the end of the experiment 26 of the 40 sub
jects completed the series by administering 520 volts.
This experiment tells us about human potentialities, and
how given the manipulation of certain variables, one can
end up doing something contrary to one’s expectations.
Certainly, there are many aspects of the experiment that
one can question, eg., who were the real victims here. But
besides that, let us not forget that this experiment was con
ducted in one of the most prestigious universities in the
United States, in the name of sHence, and in a contem
porary industrial society wuere science is highly regard
ed. Therefore, the setting was one in which the average
person would have difficulty believing that such an ex
periment could be wrong [34]. Many of the participants
continued to shock the victims under much stress and
September-December 1988
pain, fighting the contradictoms and trying to justify the
scientists’ recommendations.
The point of this experiment is that ascribing to the
individual torturer a particular psychopathology reveals
nothing, unless there is interest in maintaining that if there
were no sadistic-sociopaths, or that if they all received
some sort of psychotherapy, this type of practice would
stop.
How does the torturer become a professional in tor
turing? First, the external and material circumstances of
his background must be such that will accommodate his
nefarious occupation with relative ease. Second, he must
be educated to be efficient and perform his work with
determination. This eduction, given in schools of torture
[1,35], sometimes with “instructors” from other countries
[3, 35], aims not only at providing the torturer with the
techniques for torment, but also at preparing him
psychologically and ideologically for his labour. How is
this mental preparation achieved? First, it is done by em
phasising the non-humanness of target groups. The vic
tim needs to be perceived as a thing, as something con
trary to what the state, and the social class it serves,
regards as the communal good—by educating this way
the propitious condet is motivated and targeted. Second
ly, training is done by conditioning the prospective tor
turers that they are to act for the good of the nation, the
good of the country. Therefore, even the most brutal ac
tions do not constitute a violation of the high moral prin
ciples under which they allegedly operate. Third, by educa
tion that emphasises loyalty to an organisation that will
protect the individuals involved and maintain secrecy. This
services to exculpate residues of personal responsibility
while subordinating individual will to that of the organisa
tion. Fourth, instructors simulate an aura of mysticism
aimed at encouraging a long-term commitment and group
cohesiveness. Torturers are frequently called by
pseudonyms that stress certain personal characteristics,
and some are even referred to as doctors [1, 36].
Despite these training and accommodating personali
ty traits, it is likely that the torturer experiences some men
tal stress by tormenting his victims, and realizes that he
is also the object of exploitation. He is usually a lowranking employee likely belonging to a social class ex
ploited by those whose interests he serves, and the mean
for ends that ar- not truly his. This situation not only
places him in s .ere contradiction that resonate in his
practice, but also demands attempts at resolution on the
personal level.
According to Festinger [37, 38], if an individual holds
two ideas of mental sets that are not psychologically con
sistent with each other, he will experience discomfort pro
duced by such inconsistency (or dissonance). In order to
resolve the conflict the individual will either change both
ideas or add a third one that will bring about less incon-
59
sistency. In other words, he will have to come up with
something that will convince him that one of the ideas
or sets is worth pursuing, especially if the ideas have
already been transformed into acts. What is characteristic
here is that the arousal of dissonance always contains per
sonal involvement, and, in order to reduce the dissonance
created, self-justification is the rule.
If we extrapolate this to the situation facing the tor
turer, then we can see that he finds himself in a dilemma:
he needs to rationalise, to deny, to protect himself from
the perception of his own doing. He needs to obtain some
(subjective) gains, or else, due to the nature of his prac
tice, he runs the serious risk of being flooded with
unbearable stress that would break into his psyche and
probably make him collapse (testimonies of victims of tor
ture and agencies for human rights indicate that frequently
the torturers torment their victims in a state of alcohol
intoxication or under the effects of drugs [39]). The
literature reviewed does not contain interviews or direct
‘studies’ on the psychology of the torturer, but by the
nature of his practice and the accounts given by some tor
ture victims one can infer some of the major psychological
response mechanisms assisting the torturer. First, the tor
turer, not blind to the perceptions of his own doing, needs
to distort reality, to exculpate himself from what and how
he does, and to come up with maneuvers that would
obscure the relationship between his actions and the ef
fect they cause. Here the basic mechanism is projection:
the victim is he’d responsible for his/her own suffering,
a “you’re getting what you looked for?’ But that transfer
of blame is probably not sufficient, for the torturer knows
he himself is the victimiser. Something more is needed:
the torturer needs to dissociate himself from the victim,
create distance, and he does it by ascribing a derogatory
status to the victim (something he has been taught to do)
which is, in a deeper level, a projected hatred of his prac
tice and of his ultimate sponsors, and that that he will
destroy in the victim. The contention here is not that the
torturer is the victim, but rather that the problem is, we
may say, dialectical. The torturer is the victimiser, but he
has within himself the victim which he denies. That is,
he conjures out his condition of (also) victim, by projec
ting it onto the tortured, and proceeds to destroy it. Thus,
by torturing his victim, the torturer obtians three victories:
one that comes from the triumph of having projectively
annihilated his own feelings of victimisation by tortur
ing others. Another victory is from avenging in the vic
tim, his own displaced hatred toward those for whom he
works and who are the real beneficiaries of his necrofiliac
activity. But also, at another level, by torturing the vic
tim, the torturer obtains a triumph over his own fear of
retaliation and death, by being in absolute control over
the lives of others.
60
Conclusions
To know and not to act is as if not knowing at all.
Old Japanese Proverb
Torture, as a structured apparatus used by nations to
structure and maintain a given order of power relations,
constitutes part of the daily experience suffered by
thousands throughout the world. The case of several Latin
American countries, whose governments not only declare
themselves democratic, but which are also referred to as
democracies by other governments, is a crude and typical
example.
Here, I have described some aspects of that particular
kind of torture, its known short-term and long-term ef
fects, and its purposes, and elaborated on some psycho
dynamic elements under which the man who carries on
with torturing probably operates. Of course, these elabora
tions do not pretend to be exhaustive, nor are they intend
ed to be an apology for the men who actually do the tor
turing. Rather, the point is that these men should be
understood in the historical and social context in which
they operate, without forgetting who pays, who supports
and who benefits from their practice. Fortunately, there
exists throughout the world agencies and organisations
concerned and vigilant of human rights which have brave
ly denounced torture, but unfortunately, those who are
in the position of strength to exert necessary effective
pressure over nations which indulge in such practice give
lip-service criticism, or plainly ignore it.
Finally, I want to briefly mention another type of state
torture that should concern us, but which due to its nature
and implications will require a separate study. I am refer
ring to the systematic, well-orchestrated and ‘dosed’
psychological and physical violence that a country, by vir
tue of its economic and military might, exerts over smaller
nations and their people. Such smaller nations, due to
their own historical and concrete existing conditions, lack
the effective means to prevent such violence, or to respond
with a likewise effective (defensive) counterforce.
[I want to express my appreciation to Dr. Kathy Blee for review
ing this manuscript and helping to make it more legible. My ap
preciation also to Virginia L Gift who patiently typed and
retyped the manuscript.]
References
Amnesty International. Report on Torture. Farrar, Strauss
and Giroux, San Francisco, 1973.
[2] Ibdeschi, L. G. Amnesty International and the forgotten
prisoner. Am. J Forensic Med and Path 1(3): 277-219,
September 1980.
[3] Pilsuk, M. and Ober, M. Torture and genocide as public
health problems. Amer. J Ortho-Psychit. 436(3): 388-392.
July. 1980.
[4] Rasmussen, O. V., and Lunde, I. Evaluation of Investiga
tion of 200 torture victims. Danish Med. Bull. 30: 241-243,
November 1980.
[1]
September-December 1988
Cienfuegos, A. J., and Monelli, C. The testimony of
political tepresion as a therapeutic instrument. Amer. J. Orthopsychaitry. 53(1): 43-51, January 1983.
[6] Sagan, L. A., and Jonson, A. Medical ethics and torture.
New Eng. J. Med. 294: 1426-1430, June 24, 1976.
[7] Treibunal Permanente de los Pueblos: Sesion sobrc
Gautemak* Madrid, Espana, 27-31, encro, 1983.
[8] Paraguay Power Game. Latin American Bureau Special
Brief, 1980.
[9] Uruguay: Genera! Rules. Latin Americn Bureau Special
Brief, 1980.
[10] Hinkle. L. E., Jr., and Wolf, H. G. Communist interroga
tion and indoctrination of the enemies of the state. Arch.
Neurol. Psychiat. 76: 115-174, 195t
ill:
for :!.e I'ir.d. London, 1257._______
[12] Aarr.es. H. Ike uau.ii-.uc
Canad. Psy\rtuitr.
Assn. J. 17: 391-395, 1972.
[13] Gault, J. E. Doctors’ involvement in torture. The Med. J.
of Australia 2(2): 101, July 26, 1980.
[14] Gel’.horn, A. Violations of human rights: torture and the
medical profession. New Eng. J. Med. 299(7): 358-359,
August 17, 1978.
[15] Peters, J., and Sullivan, M. Torture and Amnesty Interna
tional (letters tot he editor). New Zealand Med. J. 96(736):
584-585, July 27, 1983.
[16] Burges, S. H. Doctors and torture: the police surgeon:
J. Med. Ethics 6: 120-123, 1980.
[17] The Declaration of Tokyo. New Zealand Med. J. 83: 280,
April 28, 1976.
[J8] Berger, P Medicine and torture: the struggle for human
rights. CMA Journal 124: 839-840, April, 1981.
[19] Clavel, J. P. Doctors who torture. World Medicine 9(4):
18-25, 1983.
[20] Weinstein, M. Psychiatrists and political torture (letters to
the editor). Am. J. Psychat. 131(6): 721-722, June, 1974.
[21] Medical aspects of torture: report of a medical group tinder
the auspices of Amnesty International Lancet 2(834):
900-901, October 20, 1983.
[22] Jones, G. E. On the permissiblity of torture. J. Med. Ethics
6: 11-15, 1980.
[23] Riss, P. The many faces of inhumanity—and the few faces
of its psychic and somatic sequelae Danish Med. Bull. 27(5):
•213-214, November 1980.
[24] Colodron Alvarez, A. Psicologia y tortura. Clinica y
Anahsis Grupal 2(7): 7-13, Diciembre, 1977.
[25] Diagnostic and Statistical Manual of Mental Disorders, 3rd
Edition (DSM III). American Psychiatric Association, 1980,
pp 236-238.
[26] Kardiner, A. Traumatic Neurosis of War. In American
Handbook of Psychiary, edited by S. Aneti, Vol 1,
pp. 245-257. Basic Books, Ina, New York, 1959.
[27] Kieler, J. Immediate reactions to capture and deportation.
Danish Med. Bull. 27: 217-220, 1980.
[28] Allodi, F., and Cowgill, G. Ethical and psychiatric aspects
of torture: a Canadian study: Can. J. Psychiat. 27(2): 98-102,
March, 1982.
[29] Nowland, D. Measuring man’s inhumanity, J. of the Irish
Med. Assn. 70(13): 375, September 1977.
[30] Lunde, I, et al. Sexual and pituitary-testicular functions in
torture victims. Arch, of Sexual Beh. 19(1): 25-32, 1981.
[31] Jensen, TG. S., et al. Cerebral atrophy in young torture vic
tims. New Eng. J. Med. (Correspondence), 307(21): 1341,
November 18, 1982.
[32] Kellner, C. H., et al. New Eng. J. Med. (Correspondence)
308(15): 903-904, April 14, 1983.
[5]
September-December 1988
[33]
Milgram, S. Some conditions of obedience and disobedience
to authority. Human Relations 18: 57-74, 1965.
[34] Fromm, E. The Anatomy of Human Destructiveness p. 77
ff, Fawcet Crest Publications, Ina, 1973.
[35] Clavel, J. P. Return of torture Human Context 6(2): 409-414,
1974.
[36] Cooperman, E. M. Doctors, torture and the abuse of
doctor-patient relationship. CMA Journal 116: 707-710,
April 9, 1977.
[37] Festinger, L. Cognitive Dissonance In Science, Conflict and
Society, Reading from scientific American. W. II. Freeman
and Co., Fransisco, 1969.
[38] Aronson, E. Persuasion via self-justification: large com
mitments for small rewards. In Retrospections on Social
ntychNozI. r^siingeajQrford University Press,
lyoU.
[39]
Information Bulletin: Comision de Derechos Humanos de
Gautamela, U.S. October 14,
---------
REPRODUCTIVE AND GENETIC
ENGINEERING
[Journal of International Feminist Analy
sis] [(published three times in a year)] RGE
is designed to facilitate the development of
feminist multi-disciplinary and interna
tional analysis on the new reproductive
technologies and genetic engineering and
their impact on women worldwide. The
policy of the journal is to recognise the use
and abuse of women as central to the
development of reproductive technologies
and genetic engineering and to highlight the
relevance of the application of these tech
nologies to the past, present and emerging
social and political conditions of women.
RCE is edited by International Editorial
Collective and Editorial Advisory Board.
Subscription: One year (institution) $ 75
Two year (institution) $ 142.5
One year (individual) $ 25
Send International Demand Draft or Money
Order to:
Reproductive and Genetic Engineering Pergamon Journals Limited ,Headington Hill
Hall, Oxford 0x3 OBW England.
Participation of Doctors in Torture
Report from Pakistan
inahboob mehdi
Under the dictatorship of the late Zia ul Haq, the state legalised and actively used torture as a form of punish
ment in Pakistan. Invoking Islam and its so-called laws, ’the medieval practices offlogging, amputation, stoning
and so on were put to widespread use. Although the government has changed, these laws have not been repealed,
nor have those who practised them, including the medical profession who colluded in these acts been punished.
This paper was circulated at the at the ATs conference on 'Medicine at Risk ’.
TORTURE has never been taken seriously in the official
medical circles of Pakistan. The teaching of health pro-
(5) If the court orders amputation of a hand or a foot
as punishment then according to the law it will be-car—
bring into consideration the question of torture and how
-beedi! 1 professionals should react to it. The code of
medical ethics of the Pakistan Medical and Dental Coun
cil does not mention any thing about torture. Doctors who
take part in torture do not face any disciplinary action
by the Pakistan Medical and Dental Council. In Pakistan
the participation of doctors in the process of torture is
usually legal and has been made part of the duties of the
doctors.
(6) I have interviewed men and women who were tor
tured in different torture chambers and prisons of
Pakistan. These victims have given evidences about the
participation of doctors in the process of torture. One of
the victims interviewed is a doctors and he faced his own
class fellow-doctor in the torture chamber.
Usally the doctors:
(a) Advice the tortures about the actual condition of
the victim’s health.
(b) Revive the victims sufficiently to undergo further
torture.
For the first time in the history of Pakistan, we in the
Voice Against Torture (VAT) have systematically raised the
question of medical ethics in relation to torture. In a threeday seminar held in Islamabad one full session was
devoted to medical ethics in relation to torture, corporal
punishment and other forms of cruel, inhuman or
degrading punishments. We appealed to the Pakistan
Medical and Dental Council to incorporate in its ethirn’
code a clause against torture in line with the Declaration
of Tokyo. In this session we declared that nobody in the
world is medically fit for flogging. So doctors must not
declare anyone fit for flogging. After the intervention of
VAT in the medical scene of Pakistan more and more doc
tors have responded to the problem of torture. Thus
recently at the 7th International Psychiatric Conference
held in Karachi, different aspects of torture were discuss
ed in a seminar attended by a good number of doctors.
VAT fully coorpcrates in all such activities with its ex
perience and documentary resources.
r>iir jantv hv nn mxinnrivrrj tnpnird n ffieef-persona 11-)’.
The following types of the medical participation in the
process of torture is seen in Pakistan.
(1) Under the execution of the punishment of the whip
ping ordinance of 1979—before the execution of the
punishment commences, the convict shall be medically
examined by the authorised medical officer so as to en
sure that the execution of punishment will not cause the
death of the convict. If the convict is ill the execution of
the punishment shall be postponed until the convict is cer
tified by the authorised medical officer to be physically
fit to undergo the punishment. The punishment shall be
executed in the presence of the authorised medical officer
at such public places as the Provincial Government may
appoint for the purpose. If after the punishment has com
menced the authorised medical officer is of the opinion
that there is apprehension of the death of the convict, the
execution of the punishment shall be postponed until the
authorised medicci officer certifies him physically fit to
undergo the remainder of the punishment.
(2) In many interrogation centres, the person to be in
terrogated is examined by the doctor and declared fit for
Torture was always endemic in Pakistan but during the
interrogation.
(3) The conduct of the prison medical officer in most last decade it reached epidemic proportions. Authorities
often try to legitimise many crimes of torture by taking
of the cases is very unethical and falls very short of the
cover under religion. Due to this reason we are using the
United Nation’s declarations and codes of conduct. In
Declaration ol Kuwait along with the Declaration ot
stead of providing the standard and best available treat
Tokyo.
The Declaration of Kuwait is a good document
ment to the prisoners, the prison medical officers usual
relevant to the Muslim societies. It says:
ly behave as part of the prison administration and take
The medical profession shall not permit its technical, scien
part in torture.
tific or other resources to be utilised in any sort of harm or
(4) Cover-up activities by some doctors such as pro
destruction or infliction upon man of physical, psychological*
viding false death certificates or false clinical records of
moral or other damage... regardless of all political or milhaD
the victims of torture is very common.
considerations.
62
September-December 1988
Voice Against Torture has been organised to achieve the
following aims iri Pakistan:
and methods of treatment including rehabilitation.
(12) To provide free medical facilities for the treatment
of
victims of torture.
(1) To disseminate information among the people about
(13) To provide necessary specialised professional in
the methods and purposes of all forms of torture prevalent
formation to doctors who are treating, victims of torture.
here.
(14) To establish a specialised centre where victims of
(2) To mobilise public opinion for the eradication of torture of any type could be referred from anywhere for
all forms of torture.
treatment and rehabilitation.
(3) To make the doctors realise that torture is a serious
challenge to the medical profession.
(4) To make efforts that knowledge of torture and
knowledge of the methods of treatment of people who
have been tortured is incorporated in the teaching courses
of doctors, physiotherapists, nurses, psychologists and
social workers.
- ---------------------- -
(15) To keep cordial relationship with other anti-groups
in the world. To exchange experiences with them and to
participate in joint activities and seminars etc., with them.
(16) To cooperate with other human rights organisa
tions nationally and internationally. To join hands with
them for the struggle to eradicate torture throughout the
Unc important point to consider is that it is tortuic
"which has produced the struggle against torture.
ui the 1975 World Medical Association’s Declaration of
Geographically torture is not limited to few' places. Ir
Tokyo.
respective of faith and ideology torturers are united in
ternationally.
They cooperate with one another. They ex
(6) To make representation to Pakistan Medical and
change experience and technology. They do not like the
Dental Council to put the clauses against torture in it’s
struggle against torture. Those struggling against torture
code of medical ethics.
are in danger of becoming their victims themselves. It is,
(7) To ensure that doctors do not participate in any pro therefore, very important that those struggling against tor
cedure of torture, i e,
ture must also unite internationally irrespective of faith
(a) They do not take part in cover-up activities such as providing and learn from one another. They should exchange ex
false death certificates or false clinical records of victims of
periences and technology of the struggle against torture.
torture.
They should plan measures for the protection of persons
(b) They do not monitor torture by remaining present during involved in anti-torture work in high risk areas.
any act of torture or by declaring any person fit for torture
Those involved in the struggle against torture and
or by advising how far the tortures may proceed or by reviv
engaged in the task of treatment and rehabilitation of tor
ing victims sufficiently to undergo another bout of torture.
(c) They should not use their professional skill to extract infor ture victims in high risk areas like Pakistan and many
other third world countries need protection to ensure
mation, control the prisoner or simply on punishment.
(d) They should strive to provide the best quality treatment to smooth, efficient and safe functioning. The following
prisoners and people in detention; and should not have a bias steps may serve this purpose:
ed attitude with them.
(1) Recognition by the U.N. and relevant affiliated
(8) To give all the support to the doctors who refuse organisatons.
to participate in the acts of torture, so that they and their
(2) Support by Amnesty International.
families are not victimised by the different agencies of the
state.
(3) Support by different anti-torture organisations of the
--------- L3J------hx,
I nr- < 1F>1 riixAii. ^11—ill;/
(9) To collect evidences against the doctors who have
choosen to become instruments in the procedure of tor
ture. To present these cases to the Pakistan Medical and
Dental Council for necessary action; and to take these
cases to the court so that the doctors may be tried for
their criminal acts; and to expose them widely in the public
and media.
world.
(4) Support by different human rights organisations of
the w-orld.
(5)
Participation in international seminars etc.
(6)
Wide coverage in the international media.
(10) To mobilise opinion among the community of
scientists in such a way that they should refuse to make
Dr. Mahboob Mehdi,
instruments which could be used in the process of inflic
Voice Against Torture,
ting torture.
Po. Box No: 2428,
(11) To do research on all forms of torture, their effects Islamabad (Pakistan).
September-December 1988
63
Participation of Doctors in Torture
Report from Pakistan
mahboob niehdi
Under the dictatorship of the late Zia id Haq, the state legalised and actively used torture as a form of punish
ment in Pakistan. Invoking Islam and its so-called laws, 'the medieval practices offlogging, amputation, stoning
and so on were put to widespread use. Although the government has changed, these laws have not been repealed,
nor have those who practised them, including the medical profession who colluded in these acts been punished.
This paper was circulated at the at the ATs conference on ‘Medicine at Risk ’.
TORTURE has never been taken seriously in the official
medical circles of Pakistan. The teaching of health pro------ 'VMX.-i ft QI invent?
—DnVictan
(5) If the court orders amputation of a hand or a foot
as punishment then according to the law it will bc-car-
rinar -r>-p.r-------------------------------------------------------ruin nnt^niV hv nn -JHtnnnvw;
11 y.
bring into consideration the question of torture and how
(6) 1 have interviewed men and women who were tor
tured in different torture chambers and prisons of
medical ethics of the Pakistan Medical and Dental Coun
Pakistan. These victims have given evidences about the
cil does not mention any thing about torture. Doctors who
participation of doctors in the process of torture. One of
take part in torture do not face any disciplinary action
the victims interviewed is a doctors and he faced his own
class fellow-doctor in the torture chamber.
by the Pakistan Medical and Dental Council. In Pakistan
Usally the doctors:
the participation of doctors in the process of torture is
(a) Advice the tortures about the actual condition of
usually legal and has been made part of the duties of the
the victim’s health.
doctors.
(b) Revive the victims sufficiently to undergo further
The following types of the medical participation in the
torture.
process of torture is seen in Pakistan.
For the first time in the history of Pakistan, we in the
(1) Under the execution of the punishment of the whip
Voice Against Torture (VAT) have systematically raised the
ping ordinance of 1979—before the execution of the
question of medical ethics in relation to torture. In a threepunishment commences, the convict shall be medically
day seminar held in Islamabad one full session was
examined by the authorised medical officer so as to en
devoted to medical ethics in relation io torture, corporal
sure that the execution of punishment will not cause the
punishment and other forms of cruel, inhuman or
death of the convict. If the convict is ill the execution of
degrading punishments. We appealed to the Pakistan
the punishment shall be postponed until the convict is cer
Medical and Dental Council to incorporate in its ethics’
tified by the authorised medical officer to be physically
code a clause against torture in line with the Declaration
fit to undergo the punishment. The punishment shall be
of Tokyo. In this session we declared that nobody in the
executed in the presence of the authorised medical officer
world is medically fit for flogging. So doctors must not
at such public places as the Provincial Government may
declare anyone fit for flogging. After the intervention ot
appoint for the purpose. If after the punishment has com
VAT in the medical scene of Pakistan more and more doc
menced the authorised medical officer is of the opinion
tors have responded to the problem of torture. Thus
that there is apprehension of the death of the convict, the
recently at the 7th International Psychiatric Conference
execution of the punishment shall be postponed until the
held in Karachi, different aspects of torture were discuss
authorised medical officer certifies him physically fit to
ed
in a seminar attended by a good number of doctors.
undergo the remainder of the punishment.
VAT
fully coorpcrates in all such activities with its ex
(2) In many interrogation centres, the person to be in
perience
and documentary resources.
terrogated is examined by the doctor and declared fit for
Torture was always endemic in Pakistan but during the
interrogation.
(3) The conduct of the prison medical officer in most last decade it reached epidemic proportions. Authorities
often try to legitimise many crimes of torture by taking
of the cases is very unethical and falls very short of the
cover under religion. Due to this reason we arc using the
United Nation’s declarations and codes of conduct. In
Declaration of Kuwait along with the Declaration ol
stead of providing the standard and best available treat
Tokyo. The Declaration of Kuwait is a good document
ment to the prisoners, the prison medical officers usual
relevant to the Muslim societies. It says:
ly behave as part of the prison administration and take
The medical profession shall not permit its technical, scien
part in torture.
tific or other resources to be utilised in any sort of harm or
(4) Cover-up activities by some doctors such as pro
destruction or infliction upon man of physical, psychological.
viding false death certificates or false clinical records of
moral or other damage... regardless of all political or military
the victims of torture is very common.
considerations.
-kgahh professionals-should react to it. The code of
September-December 1988
Voice Against Torture has been organised to achieve the
following aims in Pakistan:
and methods of treatment including rehabilitation.
(12) To provide free medical facilities for the treatment •
of
victims of torture.
(1) To disseminate information among the people about
(13) To provide necessary specialised professional in
the methods and purposes of all forms of torture prevalent
formation to doctors who are treating, victims of torture.
here.
(14) To establish a specialised centre where victims of
(2) To mobilise public opinion for the eradication of torture of any type could be referred from anywhere for
all forms of torture.
treatment and rehabilitation.
(3) To make the doctors realise that torture is a serious
challenge to the medical profession.
(4) To make efforts that knowledge of torture and
knowledge of the methods of treatment of people who
have been tortured is incorporated in the teaching courses
of doctors, physiotherapists, nurses, psychologists and
social workers.
- --------------------------
(15) To keep cordial relationship with other anti-groups
in the world. To exchange experiences with them and to
participate in joint activities and seminars etc., with them.
(16) To cooperate with other human rights organisa
tions nationally and internationally. To join hands with
them for the struggle to eradicate torture throughout the
WO: id,-.
---------------------------------- --------
Urie important point to consider is that it is torture
»>»
------ hl tx->—J Iir nmnwjn q*
TvFuch has produced the struggle against torture.
oi the 1975 World Metrical Association’s Declaration of
Geographically torture is not limited to few places. Ir
Tokyo.
respective of faith and ideology torturers are united in
ternationally. They cooperate with one another. They ex
(6) To make representation to Pakistan Medical and
change experience and technology. They do not like the
Denial Council to put the clauses against torture in it’s
struggle against torture. Those struggling against torture
code of medical ethics.
are in danger of becoming their victims themselves. It is,
(7) To ensure that doctors do not participate in any pro therefore, very important that those struggling against tor
cedure of torture, i e,
ture must also unite internationally irrespective of faith
and learn from one another. They should exchange ex
(a) They do not take part in cover-up activities such as providing
false death certificates or false clinical records of victims of
periences and technology of the struggle against torture.
torture.
They should plan measures for the protection of persons
involved in anti-torture work in high risk areas.
(b) They do not monitor torture by remaining present during
any act of torture or by declaring any person fit for torture
Those involved in the struggle against torture and
or by advising how far the tortures may proceed or by reviv
engaged in the task of treatment and rehabilitation of tor
ing victims sufficiently to undergo another bout of torture.
(c) They should not use their professional skill to extract infor ture victims in high risk areas like Pakistan and many
other third world countries need protection to ensure
mation, control the prisoner or simply on punishment.
(d) They should strive to provide the best quality treatment to smooth, efficient and safe functioning. The following
prisoners and people in detention; and should not have a bias steps may serve this purpose:
ed attitude with them.
(1) Recognition by the U.N. and relevant affiliated
(8) To give all the support to the doctors who refuse organisat ons.
to participate in (he acts of torture, so that they and their
(2) Support by Amnesty International.
families are not victimised by the different agencies of the
state.
(3) Support by different anti-torture organisations of the
(9) To collect evidences against the doctors who have world.
choosen to become instruments in (he procedure of tor
ture. To present these cases to the Pakistan Medical and (4) Support by different human rights organisations of
Dental Council for necessary action; and to take these the world.
cases to the court so that the doctors may be tried for (5) Participation in international seminars etc.
their criminal acts; and to expose them widely in the public
(6) Wide coverage in the international media.
and media.
(10) To mobilise opinion among the community of
scientists in such a way (hat they should refuse to make
Dr. M ah boob Mehdi,
instruments which could be used in the process of inflic
Voice Against Torture,
ting torture.
Po. Box No: 2428,
(11) To do research on all forms of torture, their effects Islamabad (Pakistan).
September-December 1988
63
Doctor and Prisoner
Indian Prison Manual
colin gonsalves
THE Prison Manual contains several provisions relating
to the health and well being of the prisoner. The duties
of the Medical Officer are set out in Chapter IV. He has
to keep a check on the medicine and the water supply.
He shall oversee general sanitation. He shall examine and
treat prisoners.
Under the provisions of Chapter XXXVI, when a priso
ner dies, a report is to be made and submitted and the
doctor plays an important role in this. If the prisoner is
n;. j di"? lb?
rpucf *■»<* ’’r^orrned. If
•.ne death oi the prisoner is "unuer circumstances raising
a reasonable suspicion that some other person had com
mitted an offence” this has to be reported to court in order
that an inquest be held. Notices of death must also be
sent to the municipal officer of health.
Immediately on the death of the prisoner the medical
officer must be informed. The body must be left in the
position found until the doctor examines the body. The
medical officer is to prepare a report relating to the
background of the prisoner and the circumstances of his
death. This report along with the history of each prisoner
is preserved for two years. Chapter XLV is titled ‘Lunatics’.
Normally most sick persons are to be sent to mental
asylums. The provision most often relied on however, is
the one which permits the government to keep the prisoner
in a jail if no mental hospital is available for treatment
of the prisoner. The exception to the rule has become the
rule itself. Records are required to be maintained of the
condition of the patient and the treatment given for a
period of two years.
Criminal Procedure Code
Section 53 of the Code is as follows:
‘When a person is arrested on a charge of committing an of
fence. .. that there are reasonable grounds for believing that
an examination of his person will afford evidence as to the
commission of an offence, it shall be lawful for a registered
medical practitioner, acting at the request of the police.. . .and
for any other person acting in good faith in his aid (emphasis
added)..., to make such an examination of the person...
Often this section is misused by the police. After torture
the accused is sent to a doctor specially known to the
police and co-operating with them for a medical report
that the person was fit or for a report that injuries were
found but they were inflicted by fellow prisoners.
Section 54 of the Code provides for medical examina
tion of the arrested person at the request of the accused.
When a person who is arrested alleges... at the time when
he is produced before a magistrate or at any time during the
period of his detention in custody, that the examination of
his body will afford evidence... which will establish the com
mission by any person of an offence against his body, the
magistrate shall, if requested by the arrest person. . . direct
the examination of the body. . . by a registered medical
practitioner. .
Section 174 relates to the mode of inquiry to be con
ducted by the police in the case of deaths.
When the officer-in-charge of the police station. . . receives
information that a person has committed suicide, or has been
killed by another. ... or by accident, or has died under cir
cumstances raising a reasonable suspicion that some other per
sons has committed an offence. he shall make an investiga
tion, and draw up a report of the apparent cause of death,
descri^:n5? SUfh ’VAnnHc.
bruise.: 27.2?
m.qrV<;
oi injury as indy w >uuiio w».
bcJj. • ■ .
Note that the medical officer is not involved at any stage
in this investigation. A complete medical examination is
expected to be done by a lay person.
In the case of the death of a woman however, the sec
tion provides for an examination by the “nearest civil
surgeon or other qualified medical men appointed in this
behalf by the state government (emphasis)”.
It would be interesting to study the background and
performance of the doctors appointed by the government.
In many cases it appears that these persons appointed
must ‘qualify’ in that, they must be willing write reports
and conduct examinations according to the bidding of the
police. The need for an independent body of doctors free
from the intrusive forays of government is most necessary.
Some Cases
Veena Sethi’s Case (AIR, 1983, SC. 339) drew the atten
tion of the Supreme Court to the atrocious conditions of
the prisoners in the Hazaribaug Central Jail rendering
them insane. The prisoners were detained in jail for very
long periods of time though they were declared insane
because “there were no adequate institutions for treatment
of the mentally sick”. The judge’s were told that there was
only one institution in the state of Bihar, for the treat
ment of the mentally sick and that was the Mansik
Arogyashala but that was overcrowded. The judges said
“we have had occasion to see lunatic asylums in one or
two states and we find that the conditions in these is whol
ly revolting and one wonders whether they are placed for
making insane persons sane or sane persons insane”.
The court then took up the case of Gomia-Ho. He was
convicted in 1945 and sentenced to three years in prison.
In 1948 he was found to be of unsound mind and directed
to be kept in the Hazaribaug Central Jail since there was
no place in the mental hospital. Half yearly reports regar
ding his mental conditions were required to be submitted
(Cont. on page 72)
September-December 1988
Implication of Physicians in Acts of Torture in Uruguay
gregorio martirena
In 1984, prompted by public protest against the widespread use of torture against political prisoners, a National
Committee on Medical Ethics comprising doctors, medical students and lawyers was set up. Its findings have
led to the drawing up of a Code of Procedures for trying the numerous complaints against the doctors participating
in torture. (Reprinted from the Danish Medical Bulletin, August 1987)
FOR us physicians who have had the sad privilege of liv
ing for over a decade under totalitarian regimes that prac
tise terror and torture and which, in turn, are supported
by multinational expansionist economic interests, there
is a pressing need to develop and refine international
medical initiatives against torture. For those who govern
by applying the National Security Doctrine, torture is a
basic was fundamental element. In the words of my
Chilean colleague, Dr. Serio Pesutic, there is no better way
to defining torture than as a dehumanised use of power.
Torture is implemented by those who are dominant,
especially against those who threaten to undermine Sub
mission to their rule.
Torture has a Dante-esque etiology. It is the only man
made disease whose intention is here and now. In it, the
first sick factor is neither the victim nor the torture, but
rather the society which provides the opportunity and in
centive to use torture. In all its degrees and expressions
torture is nowadays deeply selective. Those who suffer it
are those who are able to organise large crowds of people
and who follow their own conscience. Torture tends to
damage individuals without causing them to die, rather
than obtaining information from them. This has led to
the need for physicians to participate in implementing and
sophisticating it. Among other things, means are sought
to torture without leaving marks in order to make any de
nouncement lose legal validity, since such complaints are
exclusively based on the testimony of the victims which
is met with the cynical denials of those responsible in the
security services.
Today, we are able to single out these points as the cor
nerstone of torture in the Third World. This, then, is the
time when the figure of the military doctor assumes a cen
tral role as protagonist in his functions, his practice, and
his aims.
Until the beginning of the early 1970s, the great ma
jority of medical doctors who served the health units of
the Uruguayan Armed Forces did so as civilians practis
ing their profession. The Armed Forces Function Act (No.
14,157) along with Article 50 of Decree No. 783/73 or
dained that the practice of their rights and the fulfilment
of their professional duties be subordinated to military
regulation. Likewise, their professional tasks were subor
dinated to the military authorities in direct opposition to
the universal values of medical ethics.
The adoption of the National Security Doctrine meant
September-December 1988
an ideological purge of the armed forces, since anyone
considered a danger to that ideology was dismissed from
his post. Undoubtedly, this fact along with the abovementioned decrees make it absolutely valid to say that the
military doctors were the medical part of the repressive
apparatus which committed innimaginable gross viola
tions of human rights. To many people, such affirmation
may seem too simplistic; but here we are not talking about
the ordinary man in the street or about those who had
no other job opportunity than to enter a military garrison.
We are talking rather about physicians trained culturally
and scientifically at a free university. This is why we can
not understand that they have collaborated with those who
directly oppressed our entire people.
The University of the Republic and the Uruguayan
medical profession have been the primary pillars of our
social gains for more than 40 years. For these institutions,
every medical doctor owes respect and, above all, the doc
tor’s respect is owed to a professional condition that iden
tifies him or her with the health of others. Impositions
from the established hierarchies can only alienate them
from carrying out their professional duty, resulting -n a
serious disregard of medical ethics.
Consequently, a military doctor is not released 1r, •-»
his ethical responsibilities if he enters service in the arm
ed forces, since this only constitutes a minor addition to
his fundamental condition of being human and being a
physician—conditions from which he can never be return
ed. The implementation of an alienating training system
with the imposition of a discipline aimed at estranging
him from his humanity and his moral conscience as a doc
tor is impermissible. It is also incompatible with real
medical training and with responsibility for the training
of other doctors, because for these situations the greatest
measure of freedom of conscience is required.
Although this is an affront to medical life in Uruguay,
it is an historical fact that certain military doctors par
ticipated actively or passively in tenure or violated ethical
norms they ought to have abided by when carrying out
orders from their superiors. In addition, we find a col
lective responsibility on the part of military doctors for
neglecting to issue denouncements when such acts
occurred—even today, a year and a half after democracy
has been restored. This happens despite the fact that they
belong to an institution which unquestionably has im
plemented measures that violated human rights on such
65
a wide scale and with so ample evidence that no one could
ignore it.
In July 1984, the 7th National Medical Convention took
place. On this occasion, public denouncements were
reiterated of the systematic torture used against political
prisoners as well as the violation of basic human rights
on the part of the dictatorial government in Uruguay. Fac
ed with these facts, a National Committee on Medical
Ethics was set up. Its task-was to study the denouncements
and make decisions on them. Moreover, it was to prepare
the elaborate a preliminary bill of compulsory medical
association membership with its corresponding ethical
code. These are long-standing aspirations of the
Uruguayan medical profession that even today have not
yet been achieved.
As a precedent, there is the decision made by the
Uruguayan medical profession on October 27, 1984 to ex
pel Dr. Eduardo Saiz Pedrini. Before that, an extraor
dinary tribunal set up by the Medical Federation of the
Provinces found him guilty of violating the principles of
medical ethics of the United Nations by giving perjured
evidence in the certification of death and by covering up
the torture suffered by Dr. Vladimir Roslik, who died on
April 16, 1984, at Fray Bentos Military Garrison.
On March 4, 1985, the National Committee on Medical
Ethics commenced functioning. It was made up of physi
cians representing the Uruguayan Medical Union and the
Medical Federation of the Provinces along with the
Association of Medical Students; in addition, it includ
ed members representing the Uruguayan Bar Association
and its Human Rights Committee.
From the outset, and as the denouncements from releas
ed political prisoners began to pile up, those who had the
honor to be designated members were faced with an in
credible range of horrors. The constant factor in them all
was that physicians played an active or passive part. There
were the doctors who took down data on the prisoner’s
entrance record. This enabled those who were directly in
charge of the torture procedures to know the person’s
physical or mental weakness or disability, enabling them
to act with a maximum of ferocity on those points. There
were the doctors who were unconcerned about giving
direct care to sick prisoners, who delayed consultations,
refused medication and specified diets, etc; the doctor who
stepped in when the torture victim’s life was at stake, thus
succeeding in returning him to consciousness, only to send
him back into the torture machine; the doctor who
falsified the death cause of prisoners, performing in
complete autopsies or issuing death certificates many
times without directly examining the bodies concerned;
and the doctors who directly participated in torturing
those interrogated or conducted a constant mental harass
ment of the prisoners, seeking ways to break down their
personalities.
66
In (his notes on Reflexiones Para un Judicio EticoMedico (Reflections for an Ethical/Medical Judgment),
Dr. Rodolfo Schurmann P., expert in criminal law and
member of the National Committee on Medical Ethics,
writes: “Many of these practices can be comprised within
criminal offenses such as injuries, abuse against detainees,
private violence, covering up, and failure to offer medical
care. This does not mean that they are not reproachable
from an ethical/professional viewpoint; on the contrary.
Taking into account the seriousness of the malpractice,
this goes beyond the strictly ethical field and falls into
that of criminal law. Thus, two negative judgments can
be passed which may coincide in the sentences, but where
each is independent. It is true that, as a rule, all criminal
acts involve an ethical depreciation, but not all ethical
deprecation involves crime. The principle of legality
underlying criminal law eliminates in this regard the
elasticity or fluctuation-of ethical norms (nullum crimen
sine lege)?'
In our country, there has been neither a regular organ
specifically for ‘trying’ unethical conduct nor an ap
plicable code. Thus, the new committee faced the need
to study the existing principles for it to act upon:
A Internationally Approved Principles
Global:
—The Universal Declartion of Human Rights, 1948.
—The Declaration of Geneva, 1949.
—International Agreement on Civil and Political Rights,
1966.
—Declaration on the Protection of All Persons from Tor
ture and Other Cruel, Inhuman or Degrading Treatment
or Punishment, 1975.
Regional:
—The Pan-American Convention on Human Rights, 1969.
B National Regulations
—Act No. 1088 of 1870 (concerning the Army: abolition
of flogging and other punishments involving torture).
—Present constitutional precepts in force: Articles 26-72
and 332 of the Magna Charta of 1967.
—Act No. 15737 on Nonreciprocal Amnesty, issued on
March 22, 1985.
C Special Regulations and Codes of Ethics
—The Declaration on Tokyo, adopted by the 29th World
Medical Assembly, 1975.
—Principles of Medical Ethics, United Nations, 1982.
According to Dr. Schurmann, the fundamental
guidelines—one could almost say the cornerstone—in the
worldwide system of ethical responsibility in this field are
those adopted by the United Nations General Assembly
on December 18, 1982.
Principle 1
Health personnel, particularly physicians, charged with
the medical care of prisoners and detainees have a duty
September-December 1988
to provide them with protection of their physical and men
tai health and treatment of disease of the same quality
and standard as is afforded to those who are not imprison
ed or detained.
Principle 2
It is gross contravention of medical ethics, as well as
an offense under applicable international instruments, for
health personnel, particularly physicians, to engage, ac
tively or passively, in acts which constitute pariticipation
in, complicity in, incitement to or attempts to commit tor
ture or other cruel, inhuman or degrading treatment or
punishment.
This is a clear affirmation of the concepts dealt with
stating that without exception of any kind the supreme
duty of all medical doctors is to prevent and cure disease
for the patients who are entrusted to their care and to help
them avoid suffering. The specific duty of military or
police doctors is to offer the imprisoned persons the same
health protection and the same treatment as they would
give to nondetainess. Correlatively speaking, their highest
duty is not to inflict on the people who are deprived of
their liberty any sort of cruel, inhuman, or degrading
treatment. By virtue of the profession they exercise, physi
cians hold unimpeachable duties vis-a-vis mankind which
extend beyond considerations of interest in the personal,
economic, admnistrative, political, or ‘national security’
spheres.
Furthermore, it became necessary for the committee to
draw up a Code of Procedures for dealing with and try
ing the numerous denouncements ft received. In this man
ner, the accused physicians will enjoy the widest possible
guarantees for their defense and discretion about the alleg
ed offeness.
In each case, at the committee’s plenary session, an in
quiry team is set up consisting of a physician and profes
sional aspects while the lawyer ensures that the correct
procedure is abided by. After studying the case in depth,
including a justification from the alleged offender, who
has a right to legal advice and may call witnesses, the team
writes its final report. Subsequently, this is submitted to
the full committee for approval, amendment or rejection.
If it is approved, the accused doctor is informed. He is
then offered a chance to present an apology; if this is ac
cepted by the full committee, a new trial is stipulated.
Should the concerned doctor not wish to respond, the rul
ing is put on record.
After the ruling is official, the next step is up to the
medical doctor’s professional associations (Sindicato
Medico del Uruguay and Federation Medica del Interior).
They decide on professional disciplinary sanctions accor
ding to the details of each case and bring relevant legal
action when necessary.
The National Committee on Medical Ethics has now
been functioning for a year and a half, and we can show
September-December 1988
the world only three verdicts on the participation of physi
cians in torture, despite the fact that we arc looking into
more than a hundred specific denouncements.
Today, a year and a half after the democratic govern
ment was installed—and despite the official mission of
the Uruguayan government, which led the United Nations
to lift its sanctions against the country for violations of
human rights during the years of dictatorial
government—we can show the world only a small total
of publicly established violations of human rights despite
the fact that the whole nation is convinced that such viola
tions took place; a completely intact army with its in
telligence and security systems still in force and constantly
pressuring the government’s political decisions; a state
which has not yet determined whether a civilian or a
military court is to be in charge of prosecuting those
responsible for the misdeeds of the past; and only one
bill of Regulations for the protection of Human Rights,
namely No. 433 of December 1985, proposed by Senators
Alberto Zumaran and Hugo Batalla on behalf of the
political opposition parties and which has not yet been
dealt with in any depth.
Facing the reality of obstacles imposed by the govern
ment, we as physicians feel proud of the few, but unben
ding penalties and denouncements made against those
who violated the universal ethical principles while carry
ing out their functions as military doctors. Now, once
again we turn to the worldwide medical community for
solidarity and to propose some joint course of action:
—A set of rules adopted by medical organisations
everywhere which shall be binding for physicians when
exercising their profession, for their relationship with the
society they live in and with the government they are at
tached to.
In her study on ‘Deontology and Repression’ Dr.
Susana Eirin, a lawyer and member of the National Com
mittee on Medical Ethics, says that in times of moral
decay, when a society enters a crisis, all its members are
affected by such “memoral shakeup!’ Before learning to
become a physician, one has to learn to become a human
being. It may not be possible to lay down exact^guidelines
for the behaviour of individuals in an environment that
is becoming difficult; but it certainly is important for
those who start practising a profession to be given norms
of conduct in the face of the social crises which our
societies in transition have to endure.
—It is necessary to define and implement universal
teaching norms on human ethical and professional stan
dards. In particular, the concept of due obedience, or obe
dience to superiors, should be defined as restrictively as
necessary in order to avoid its use as a justification fpr
any conduct violating human rights.
ICont. on page 75)
61
Mission to Chile
Report of World Medical Association
andre wynen
Since 1984 the Chilean Medical Association has been actively campaigning against the use of torture and against
the physicians who participate in it. In July 1986 during a general protest strike two office holders of the associa
tion Were arrested and taken to prison. The association invited the secretary general of the World Medical Association
to help free them. This is d report of that visit.
DR. J. L. ONZALEZ REUES and Dr. E Rivas Larrain,
president and secretary general of the Chilean Medical
Association, were arrested on July 10, 1986 and taken to
Capucinos, an annex of the public prison in Santiago. In
the last three years, the Chilean Medical Association has
been campaigning vigorously against the use of torture
and against physicians who participate in it. I had been
to Santiago, Chile, in February 1984 to hold a press con
ference in which I expressed the WMA’s full support of
the actions taken by the Chilean physicians.
Last year, the Chilean Medical Association joined other
professional groups (lawyers, engineers, arthitects, etc.) to
create a national civic assembly. Dr. Gonzalez was elected
its president. The purpose is to unite all groups opposed
to the regime. The Chilean Medical Association’s main
cause is to defend the rights of the patient and medical
ethics, which is directly linked with the defense of human
rights.
The National Civic Assembly called a two-day general
protest strike (July 2-3), during which violent confronta
tions between civilians and military patrols led to three
deaths and several injuries. Two young demonstrators were
seriously burned, their bodie were found near the airport.
The version given by the opposition—based on testi
mony by witnesses, including that published by the
Catholic Church—affirmed that an army patrol had
poured gasoline over the victims. On the other hand, the
government version stated reports by their witness that
the accident had been caused by the victims themselves
while handling Molotov cocktails. One of them died from
the severe burns received.
Fourteen leaders of the National Civic Assembly—
including Dr. Gonzalez and Dr. Rivas—were detained on
charges of inciting to riot and violence during the
demonstrations.
Alerted by the Chilean Medical Association, the WMA
secretary general issued a press release to international
press agencies informing them about the situation and
sent letters and telegrams to the Chilean government and
the judiciary appealing on behalf of the two collegues de
tained. These measures were taken in concert with Amnes
ty International and the American Association for the Ad
vancement of Science (AAS), among others. On July 24,
the Chilean Medical Association telephoned and asked
me to travel to Chile to help them in the effort to free
68
their president and secretary general.
Contacts were made with the Belgian Minister of
Foreign affairs and the Chilean ambassador in Brussels
to discuss the feasility of an urgent mission to the Chilean
government and the judiciary. Several meetings were ar
ranged in Santiago with the help of the Belgian ambassa
dor in that capital. In August, I arrived in Santiago to
meet with the Belgian ambassador and with represen
tatives of the Chilean Medical Association, thanks to
Dr. Jorge Jimenez de la Jara who assisted and interpreted
during my stay in Santiago.
On Sunday, August 3, the first visit to Drs. Gonzalez
and Rivas took place and preparations were made for the
forth-coming meetings with government authorities and
the judiciary. My last day in Chile, August 6, a second
visit with the imprisoned colleagues was allowed and prior
to my departure for the airport, a press conference was
held at the headquarters of the Chilean Medical
Association.
I wish to stress that at all times I was received with
deference and kindness by all those with whom I met.
Perhaps this can be attributed to the fact that I was an
nounced as the representative of more than two million
free and independent doctors not connected with any
communist country and to the excellent liaison work done
by the Belgian Foreign Affairs department, the Belgian
ambassador in Santiago, and the Chilean ambassador in
Brussels.
In Chile 1 met with:
—Alberto Cardemil, under-secretary of Internal Affairs,
known as the Government’s key man in repression
activities against the opposition;
—Hugo Rosende, Minister of Justice and personal friend
of Dr. L Gonzalez;
—Dr. Winston Chinchon, Minister of Health, and his
chief of staff, Dr. Ricardo Caram;
—Rafael Retamal, president of the Supreme Court;
—Judge German Valenzuela Erazo, President of the court
in charge of the affair and responsible for the final
ruling;
—Professor Amador Neghme, President of the Academy
of Medicine;
r
—Monsignor Sergio Valech, Ausxiliary Bishop, lea er 0
Catholic action in the country.
From these meetings, I gathered that the lawyers had
September-December 1988
not petitioned for the prisoners to be released on bail.
Therefore, during my meeting with Judge Valenzuela, I
officially presented a request for the release of Drs. Gon
zalez and Rivas, pledging the moral guarantee and sup
port of the two million physicians represented in the
WMA.
1 was authorised to inform the Chilean government that
in the event these two collegues were convicted, Belgium
and 1, myself—as well as the University of Louvain,
represented by its Rector, Monsignor Massaux—were
ready to grant them asylum if their sentence were com
muted to exile, which the Chilean government would be
willing to consider. If so, the Belgian government would
permit them to practise in Belgium during their exile and
under the same conditions as Belgian physicians.
Advised of this possibility, Drs. Gonzalez and Rivas
were reluctant on account of their solidarity with the
15 other people arrested for the same reasons. Their
lawyers, in the meantime, confirmed their intention of re
questing, within the next 48 hours, that the prisoners be
released on bail.
A meeting was also held with Dr. Alvaro Reyes and
Dr. Ramon Rojas who had spent three months in the same
prison as Dr. Gonzalez and Dr. Rivas for failing to report
to the police a wounded man they had treated at the
Chilce clinic. They had been released on bail the week
before. Two other colleagues, Ramiro Olivares and Juan
Macaya, are still in prison on the same charges. They work
for Vicaria de la Solidaridad, a Catholic Church human
rights organistion in Santiago.
I had the opportunity of visiting las Condes private
clinic and LI Salvador University Hospital, where 1 was
received by Professor Umberto Reyes, Head of the Internal.Mcdicinc Service. There is an indescribable contrast
between the luxury of the clinic and the meagerness of
the hospital, which is so deprived of the most essential
equipment and personnel that it has been forced to close
some of its departments for lack of resources.
The enormous discrimination between medical care
available to the rich and to the poor raises a serious ethical
problem and is unquestionably conducive to considera
tions of euthanasia motivated by a total lack of medical
care for the poor.
All physicians encountered, from heads of departments
to medical students and residents, unanimously denounc
ed this situation which they consider an unacceptable
breach of human rights. They expressed their moral
discontent by actively supporting the opposition and by
their solidarity with Dr. Gonzalez and Dr. Rivas and the
National Civic Assembly they had helped to create and
which they diligently direct.
As mentioned, the visit ended with a press conference
during which an objective report was presented on what
had been done in Santiago. Special emphasis was gives
to the total independence and apolitical attitude with
which the assignment had been accomplished. The sup
September-December 1988
port received in Belgium and the assistance given by
Belgian diplomatic circles, the Chilean Medical Associa
tion, temporarily presided over by Dr. Acuna, the Chilean
Academy of Medicine, the Universities, and the Catholic
Church were duly acknowledged and appreciated. Recog
nition was given to the Chilean authorities and judiciary
for their understanding. Obviously, they were impressed
by the World Medical Association’s moral prestige and
the strength it represents. I said that I hoped Chilean
justice would take into consideration the detainees’ moral
and professional values, which no one I met questioned
at any time. In conclusion, I would like to note how im
pressed I was by the enormous contrast in Chile between,
on the one hand, the serious government action against
the basic principles of medical ethics and human rights—
the latter now under review by a commission headed by
the department of the interior and a group of jurists and
lawyers—and, on the other hand, the great freedom en
joyed by a vigorous opposition press, the freedom of op
ponents to express themselves against the regime, and the
absence of border control mesures.
No entry or exit visa was required, and luggage was not
searched at any time. Neither was this an exception
because of the special nature of my trip. The rules are
identical for all travellers, and this was confirmed by col
leagues in the Chilean Medical Association. Nobody was
able to explain whether this contrast should be interpreted
as a strength or weakness of the government.
On August 19, I was informed that Drs. J. L. Gonzalez
and F. Rivas had been released on bail that day and
authorised to stay in Chile. Drs. Ramiro Olivares and Juan
Macaya were also released for days after my visit to San
tiago. The Minister of Health, Dr. Chinchon, was dismiss
ed from his functions in the government a few days after
my visit.
Correction
In the June 1988 issue please note the following cor
rection in Health Care, Health Policy and Underdevelop
ment in India by Ravi Duggal. On page 17 the sentence
beginning ‘The fact is that Britain’s. .. should read: The
fact is that Britain’s and USA’s state health expenditure
was equivalent to India’s national income and their health
care facilities between 30 to 40 times more than India. This
gap is even worse today. In 1984 health expenditure in the
USA was $ 1,580 per capita per year out of which state
expenditure accounted for 41 per cent.
On page 20, the sentence beginning ‘The budget
skyrocketed’ should read. The budget skyrocketed from
a mere Rs 2.2 crore to Rs 25 crore in the third plan.
The title of table 1 should read Growth of Health In
frastructure and Investment in India. The figures in
brackets in column 2 refer to private hospitals and in col
umn 5, rural beds.
69
Action Against Doctors Involved in Torture
francisco rivas larrain
In 1982 with the institution offree elections to the Colegio Medico de Chile which was charged with ethical super
vision of the profession, there has been much reorganisation and a new code of ethics has been prepared and
is implemented vigorously despite opposition from the political authorities.
TORTURE has been practised in Chile systematically and
continuously since the coup of 1973. There is sufficient
evidence that those responsible for torture in Chile are
the security institutions of the armed forces, the police,
and the government security agencies: first Direction de
Inteligencia Nacional (DINA), followed by Central Na
tional de Informaciones (CNI) to the present time.
Thousands of cases of torture perpetrated by the above
institutions have been documented and denounced by
Church and human rights organisations, professional col
leges, and international institutions.
In Chile, the armed forces have always included physi
cians, civilians as well as those with military rank. Until
1973, however, military* doctors were shown the same
respect as other doctors and were not burdened with the
suspicions which are now cast upon them.
During the dictatorship, over 80 physicians directly or
indirectly participated in acts of all-treatment, humilia
tion, or torture; the great majority of these physicians
belonged to the armed forces and were attached to the
security agencies.
From 1973 to 1982, the officers of Colegio Medico de
Chile were appointed by the military authorities. Servile
and obedient, these officers heard reports of physicians
participating in acts of torture but did nothing to in
vestigate or denounce them.
In 1982, the government enacted a new law on profes
sional colleges, whereby the organisation of more than
one college was permitted and authority of the Colegio
Medical de Chile for ethical supervision of its members
was revoked. Simultaneously, the law allowed free elec
tions to be held in the Coliegio. The pro-Pinochet, pro
dictatorship position was defeated at these elections,’and
the officers elected fully represented the opposition.
The Colegio’s new authorities set themselves three ma
jor lines of action:
(1) Defense and protection of physicians against abuse
from the Ministry of Health and optimisation of the
Solidarity and Welfare of Departments of the Colegio
Medico.
(2) Defence of Chilean public health. Criticism of and
mobilisation against those health laws which the govern
ment seeks to impose which are arbitratry and elitist,
beneficial to higher- income sectors. Report of poor con
ditions for medical service and near-irreparable
deterioration of the Chilean hospital system, which until
70
1973 was a model of high quality and efficiency.
(3) Struggle to defend, protect, and encourage human,
social, and political rights of physicians and all citizens
of this country.
This last item has evoked the vigorous, undeviating will
of the Colegio Medico to investigate the part played by
doctors in all forms of violation of human rights, especial
ly torture.
Since the democratic election of its officers, the General
Council of the Colegio Medico has reorganised its Depart
ment of Medical Ethics and set up a Human Rights
Committee.
From their inception, these departments began to
receive reports of the participation of doctors in acts of
torture. These reports have bfeen divided into cases where
evidence is obtainable and cases which, though un
doubtedly true, lack conclusive proof for an investigation.
All these reports have been received by the General Coun
cil of the Colegio Medico through the regional councils
across the country’, channelled by the Ethics Department
and the Human Rights Committee.
To date, two cases involving four physicians have been
investigated and tried; two of the doctors were suspend
ed from the Colegio for one year, the other two were ex
pelled. In addition a trial of another three doctors respon
sible for the death from torture inflicted by members of
the security agencies in a northern city is reaching its final
stage.
In the first two cases, the accused were found guilty
of negligence in the medical examination of individuals
under arrest who were subsequently tortured; various ex
tenuating circumstances were taken into account. In the
other two cases, most serious breaches of ethics including
negligence in medical examination, wilful omission in
reporting lesions, insufficient and unreported treatment
of torture victims, issuing false health certificates, together
with the absence of extenuating circumstances, deserved
the sentence of expulsion from the Colegio Medico.
The above trials were conducted impartially and im
peccably by the General Council of the Colegio Medico
which is its highest court with renowned counsel acting
for the defence of the accused. All counsel, including
counsel for the defense of the doctors expelled from the
college, agreed that the medical court had shown ex
emplary fairness and impartiality. Furthermore, not on
ly have the Chilean public opinion and the international
September-December 1988
medical community (World Medical Association) acknow
ledged the same ments, but also the entire body of Chilean
physicians have recognised the fair-mindedness of the
General Council in dealing out justice and in its generosity
towards the culprits.
However, the efforts of the Colegio Medico in this area
did not stop there. A new code of ethics was prepared and
drafted. At the preliminary meeting held recently in
Montevideo to restore the Federation of Medical Associa
tions of Latin America, this code was taken as a model
for a continental Code of Medical Ethics.
Our efforts are known beyond our frontiers; we have
reported on them before, as we are doing today, with both
pride and shame: With pride, because in the midst of cruel
dictatorship we have been able to denounce and punish
the henchmen of terror and death; with shame, because
the men we have tried are physicians, Chilean physicians
who had taken the Hippocratic oath and made a commit
ment to life, not death. Neither is our fight for human
rights framed within the bounds of medical ethics. Since
we know that we are citizens before being doctors and that
human and political rights are best nrotected in a
democracy, we are also involved in the political struggle
against the regime.
We say this with pride. The Colegio Medico de Chile
penalises physicians who practice torture and strives ac
tively to put an end to Pinochet’s dictatorship. We are
members of the Asamblee de la Civilidad de Chile, which
embodies the 22 most representative social organisations
in the country (blue-collar workers, rural workers, slum
dwellers, professional men and women, students, women.
university academics, ethnic minorities, and others), and
we are part of the plan for progressive civil disobedience
designed to put an end to dictatorship. We have been jailed
for it, and this we also declare with pride.
In Chile, physicians who practise torture are promoted
in the armed forces; we doctors who denounce torture
within the military circle of dictatorship are thrown into
the jails of Pinochet. Unamuno spoke of peoples with a
tragic sense of life. Of men who share this tragic feeling—
the feeling that leads a man or a people to folly in the
pursuit of freedom. Such folly is ours. To try a torturer
under a regime with torture as its policy is folly. To foster
civil disobedience under a regime that believes in sterlie
order and vertical authoritarianism is further folly. To be
jailed under a dictatorship that tortures and murders
unhindered is folly, too.
We love such folly. It is the folly of Bolriar, < arrera,
Manuel Rodriquez, and Salvador Allende: The sublime,
heroic folly that made our peoples free. The heritage that
allows us to know we are free and to continue struggling
for final liberation of our country. We Chilean physicians
know that the solidarity of Danish physicians and physi
cians all over the world is behind us. That is one of the
strongest support in our struggle. We will put an end to
torture when we recover democracy. Our victory will be
your victory too.
[This presentation was made at the International Meeting on
Doctors, Ethics and Torture in Copenhagen by Professor Bent
Sorensen on behalf of Dr. Francisco Rivas Larrain, who had
been imprisoned by the authorities in Chile on unspecified
charges.]
Economic and Political Weekly
A journal of current affairs, economics and other social sciences
Every week it brings you incisive and independent comments and reports on current problems plus a number
of well-researched, scholarly articles on all aspects of social science including health and medicine, environment,
science and technology, etc.
Some recent articles:
Mortality Toll of Cities—Emerging Pattern of Disease in Bombay: Radhika Ramsubban and Nigel Crook
Famine, Epidemics and Mortality in India—A Reappraisal of the Demographic Crisis of 1976-78: Ronald Lardinois
Malnutrition of Rural Children and Sex Bias: Amartya Sen and Sunil Sengupta
Family Planning and the Emergency—An Unanticipated Consequence: Alaka M Basu
Ecological Crisis and Ecological Movements: A Bourgeois Deviation?: Ramachandra Guha
Environment Conflict and Public Interest Science: Vandana Shiva and J Bandhyopadhyay
Geography of Secular Change in Sex Ratio in 1981: Ilina. Sen
Occupational Health Hazards at Indian Rare Earths Plant: T V Padmanabhan
Inland Subscription Rates
Institutions/Companies one year Rs 325, Two years Rs 625, Three years Rs 925
Individuals Only:One year Rs 250, Two years Rs 475, Three yeafs Rs 700
Concessional Rates (One year): Students Rs 150; Teachers and Researchers Rs 200
(Please enclose certificate from relevant academic institution)
[All remittances to Economic and Political Weekly, 284, Hitkari House, Shahid Bhagatsingh Road, Bombay 400
038. Payment by bank draft or money order preferred, Please add Rs 14 to outstation cheques for collection charges.]
A cyclostyled list of selected articles In EPW on health and related subjects Is available on request.
September-December 1988
Press Reports on Human Rights Violations in India
A Tiny Sample Study
ALERT citizen’s groups in many places over the world
have contributed much to exposing human rights abuses
by state organs and to biases in reporting through form
ing ‘media watch’ groups. The idea is to carefully scan
media reports and, (as somewhat we have done here)
classify the data collected. Such scanning also clearly
highlights policy biases in reportage by governmentcontrolled or other partisan media.
In order to make a small random study of press-reports
on human rights violations, we turned to two files main
tained by the Centre for Education and Documentation
Bombay, one on police atrocities/encounters/combing
operations/brutality and the other on ‘civil liberties/democratic rights/ihfringements/organisations/enquirics etc. There were no direct reports on specific in
stances of violation in the second category for the period
we looked up: July-September 1988. The first file yielded
32 items from nine major dailies and five magazines. We
did an exercise on classifying these reports in two ways
i)statewise and ii)by type of human rights violation—an
arbitrary but marginally useful exercise.
What we drew from our classification is as follows:
8 reports from Maharashtra (2 from Bombay but most
others also from areas nearby), 3: from Orissa, 2 from
Bihar and UP and 1 each from Dglhi, Gujarat, Karnataka,
Nagaland, Punjab, Rajasthan and West Bengal. (4 items
were ‘repeat’ reports qot counted here and 3 not clear).
Three reports covered the whole country. (Of course, it
must be pointed out that at CED we receive more dailies
(Cont. from page 64)
but were not. He was, however, examined in 1966 and
found to be sane. Yet he rotted jn jail. In 1981 after news
of his detention was published in a newspaper he was once
again mentally examined and found to be sane. He was
released in 1983 almost 35 years too late.
Like Gomia-Ho there were cases of many other
prisoners who were kept in jail as the mental hospitals
were full.
In Charles Sobhraj’s case (1978, 4.SCC.494) the
prisoner was kept day and night under bar fetters. The
doctor examining the prisoner had noted:
09.2.1977: Multiple infected wounds on right ankles. Bar
fetters be removed from right leg for 15 days (Sd) Dr. Mittal
R.M.O.
12.2.1977: Bar fetters also to be removed from left foot. (Sd)
Dr Bokra.
The supreme court severely restricted the use of bar tet
ters and condemned their generalised and indiscriminate
use. Case of torture in police lock-ups and prisons are
routine and endemic. The role of doctors in this is
dubious. They are mainly used for cover up purposes.
Irom Bombay than anywhere else. Hence perhaps the large
number of instances reported for Maharashtra).
Tne ‘type of human right violation’ exercise yielded the
following results:
1.
2.
3.
4.
5.
6.
7.
8.
9.
Torture/death in lockup
Police beatings/assault
Illegal arrests/detention,'seizure
Marauding, terrorisation, oppression of
depressed sections
Direct killing/shooting
False encounters
Sexual abuse (including gangrape)
Framing false charges
General reports on human rights abuse on
state/nation basis.
6
5
4
3
2
3
3
2
5
(one report has been counted under both 3 and 7).
Scanning these reports, there seem to be two major
categories of ‘motives’ for these acts. In half the cases,
the victims have clearly been earmarked for political
repression through the use of violence (and abuse of
machinery that is supposedly meant to protect the rights
of common citizens). Roughly another half are simply vic
tims of the police machinery blatantly overstepping its
brief: either out on a drunken, marauding spree or
unleashing calculated brutality against weak, marginalised
sections and/or person(s) who have, in some way (some
times unwittingly) exposed the weaknesses in the state
machinery.
R R
Appeal to Subscribers/Readers
We regret that the last few issues of the Radical Journal
of Health have been delayed. This has been because of
printing and other difficulties, none of which fortunately
are insurmountable. We hope to bring the publication
up-to-date in the next couple of months. Please bear
with us!
The RJH is for you and is sustained mainly by the sup
port of regular readers like you. So far the journal is being
subsidised by donations from concerned individuals. We
would not like to pass on the burden of the extra cost to
our readers by increasing the subscription rates. The
Socialist Health Review Trust, the publisher of RJH has
started a campaign for creating a corpus fund which can
continue to absorb the extra cost as far as possible.
We appeal to you and your friends to generously con
tribute to this fund. AU donations may be made payable
to the Socialist Health Review Trust and are exempted
from Income Tax under Section 80G of the Income
Tax Act.
September-December 1988
Book Review
Torture, Psychiatric Abuse and Health Professionals
r raghav
The Breaking of Bodies and Minds: Torture, Psychiatric Abuse and the Health Professioanals Edited by Eric
Stover and Elena Nightingale, The American Association for the Advancement of Science/WH Freeman and Co.,
New York, 19855; pp 320.
THE book is a result of a symposium sponsored by the
Committee on Scientific Freedom and Responsibility
(CSFR) of the American Association for Advancement
of Science (AAAS) in January 1981 on the subject.
Through case history and analysis, the contributors ex
amine the role of health professionals, (HPs) in the use
and prevention of torture and psychiatric abuse (TPA) “in
the context of the political, social and ethical forces that
guide their actions’*. It addresses itself to such questions
as—how and why HPs participate in serious violations
of human right; what are-the conditions under which Such
violations occur; and what can organisations of HPs,
scientists and others do to check the trend.
As the book notes, “violations of human rights have
become so well-organised, so systematic, so efficient, that
it is now a kind of industry’’. Through careful documen
tation of abuse and lucid insights into the dilemmas of
HPs and others working under repressive governments the
book presents a clear delineation of the ethical issues in
volved. In the final chapter, the editors suggest organised
monitoring, protest and action through professional
associations to counter state-sanctioned routinisation of
TPA for political purposes. To quote from the foreward,
“It is now more urgent than ever that we use the extraor
dinary human capacity for learning, communications, and
attachment to one another to foster the bonds of mutual
respect”.
Apart from sporadic misuse of authority or isolated
abuses resulting from poor practice/lack of proper
resources, TPA as a systematic means of political control
are prevalent in at least 66 (nearly one-third) of the world’s
nations, notes the book. In this, HPs are collaborators
in misuse of medicine, mis-certification of victims and
other forms of flagrant and deliberate abuse of profes
sional ethics. Alarmingly, “These collaborators in abuse
are not simply mad doctors... satisfying their own
sadistic desires; they include apparently normal HPs”.
Extent definitions of torture are reviewed and their com
mon features noted. In essence, torture is the deliberate
infliction of pain by one person on another to break down
the will of the victim. The degree of abuse that constitutes
‘torture’ sometimes needs clarification—for example,
solitary confinement, in itself, is not torture under inter
national law. TPA may include physical, psychological and
September-December 1988
pharmacological and psychiatric abuse forms. However,
all torture invariably produces psychological distress in
the victim.
Some Testimonies
“I realised that pain can always increase without end.
To have that feeling is devasting for the mind. Absolute
loneliness and endless time are abstract ideas... but when
experiencing them, the desperation is hard to describe”.
“The entire affective world... collapses with a kick in
the father’s genitals, a smack on the mother’s face, an
obscene insult of the sister, or the sexual violation of a
daughter. Suddenly an entire culture based on familial
love, devotion, the capacity for mutual sacrifice, collapses.
Nothing is possible in such a universe, and that is precisely
what the tortures know”.
“It is hard to be a survivor. It is hard to remember and
tell this story, but I reappeared because people worked...
Now I cannot let the others down”.
Widespread Prevalence
Apart from its routine employment in war, torture is
now being increasingly sanctioned by governments against
peacetime ‘subversion’. This form of official sanction is
often combined with suspension of basic human rights
and legal procedures; or else executed through quasigovernmental ‘intelligence’ groups over which direct
government responsibility is disclaimed. Another alarm
ing factor is the emergence of clear military/police train
ing programmes on ‘interrogation techniques’, such as at
the International Police Academy of the Agency for In
ternational Development at Washington, DC.
The book mentions cases of torture reported from the
Algerian War (French), Vietnam War (by all parties),
El Salvador, Guatemala, Indonesia; ‘disappearances’ and
torture are reported from Afghanistan, Argentina, Bolivia,
Burundi, Cambodia, Central African Empire, Chile, East
Timor, Ethiopia, Iran, Peru, Philippines, Syria and Ugan
da. References to psychiatric abuse (PA) in Rumania,
Uruguay, USA, Japan and USSR (which has been par
ticularly indiated) are included; as well as documented in
volvement of HPs in abuse in Rome, Japan, Chile,
Mauritania, Portugal, Sudan, Iran, Greece, USA and
_
13
USSR. Cases of conflict between HPs and governments
and the issue of putting to practice codes of medical ethics
have been considered from Chile, Uruguay, Brazil and
South Africa. The book, however, distinctly focuses on
physical abuse in Latin America and psychiatric abuse in
USSR... because abuse is particularly widespread,
systematic and well-documented in them”.
Compiled evidence indicates that the role of HPs may
include: Medical examinations at various stages: Atten
dance at torture sessions to intervene when the victim’s
life is threatened; treatment and ‘patch-up* of injuries;
development/refining of torture techniques and some
times, administration of torture; and false certification
of subjects for various reasons.
The participation of HPs in TPA clearly violates three
basic tenets of medical ethics: (1) To do more good than
harm; (2) lb intervene only when the patient is willing
and (3) To render treatment regardless of political or other
considerations. This disregard of medical ethics cannot
be justified in moral terms as serving any higher social
purpose, as the book clearly shows through consideration
of the commonly applied principles of justice, benevolence
and autonomy.
The utilitarian argument for torture sanctions its limited
use if it produces more good than evil; such as, say, against
terrorists who may destroy hundreds of innocent lives.
Such a position is difficult to achieve in practise, as its
inefficiency and inefficacy have been regularly remarked
up on. The ‘good’ result is a hypothetical probability,
often not realised. More importantly, the applicability of
such a rule is not clear. Known terrorists must be tortured.
Can we torture their family, friends, neighbours, uncer
tain acquaintances? Clearly, the good that may be achiev
ed is dwarfed by the evils imposed by a state-sanctioned
system, which brutalises many ordinary people wielding
some power—army, police, ‘intelligence’ people; asso
ciated medical and legal people, administrators—and cor
rodes the roots of civilised society.
One argument the book seems to have missed is regar
ding the context in which such a utilitarian argument is
propounded—as a dubious means towards unworthy ends.
‘Subversion’, ‘dissent’, ‘terrorism’, ‘war—these are usual
ly the result of an unsatisfactory political system—and
the right thing to address would be the correction of this
cause, rather than the sanction of a new evil in support
of the one existing.
Research indicates that some torture victims suffer
symptoms similar to concentration camp survivors and
prisoners of war ((POWs): long-term physical and emo
tional trauma-heightened anxiety, recurrent nightmares,
phobias that sometimes require counseling and treatment.
It is also apparent that emotional problems increase on
the torture victims emigrating to a new country and
culture Accounts of torture victims remind us that brutali
74
ty can never be comprehended or measured in the abstract.
It is a succession of personal tragedies, disabling to the
individuals involved and destructive to humankind.
HPs, employers and other persons who interact with
victims of torture need to be aware of and understand the
consequences of TPA on the life of victims who will other
wise continue to be victims of misdiagnosis, inappropriate
medical and psychiatric care, of preventable job stress and
discrimination, of marital and family disruption, and of
avoidable suicide.
The book outlines two studies on former torture
victims—one covering 44 perSons now settled in seven
cities of the USA, the other 41 people in Toronto. Standard
research protocols for physical and psychological evaluation
were established. Those, and other similar studies, indicate
a broadly consistent range of after effects in the majority
of victims; objective evidence of physical damage in in
verse proportion to the period of time elapsed; more
widespread long-term psychological disturbances ranging
from nervousness to post-traumatic stress disorder.
Therefore, many psychologists argue for the establishment
of specific diagnostic criteria for a ‘torture syndrome’.
While this will prevent the overlooking of the psycholo
gical difficulties of the victims, other psychologists argue
that this might also result in labelling and stigmatisation
of victims, particularly those who have come to terms with
their experiences.
The book outlines criteria for provision of appropriate
psychiatric service—underscoring the importance of
rebuilding trust in human values, expunging ‘situational
guilt’, assisting.in the victims ‘struggle for meaning’, and
cushioning the effects of rehabilitation into a new socie
ty and culture.
Psychiatric Abuse in USSR
Doubtless, PA is employed by intelligence agencies, par
ticularly military, the world over. The book examines in
detail the various factors (and the capability of HPs) that
have led to the existence of a seemingly institutionalised
system in the USSR.
Psychiatric internment for political purposes in Russia
started somewhere in the 1930s. It gathered political sanc
tion during the Khruschev period. A series of scandals
in the 1970s resulted in worldwide concern and debate,
culminating in the bowing out of the Soviet body, the All
union Society, from the World Psychiatric Association
(WPA) in January 1983. (The society has recently been
re-admitted to the WPA). However, there has been con
cern that while admitting maladministration of psychiatric
care, the USSR has detracted attention from its political
misuse, which is probably bound to continue. While many
political victims have been freed from psychiatric prisons
and there has been an announcement that all other
political prisoners would be released from jail (Indian Post
September-December 1988
October 27 1988, p 1) there is evidence of new cases of
internment during the past two years.
Some psychologically healthy dissenters and human
rights (HR) activists in the USSR are labelled mentally
ill and subject to compulsory hospitalisation and ‘treat
ment’. It is argued that the Soviet approach to psychiatric
diagnosis, particularly the concept of schizophrenia, is a
critical factor in labelling dissent as mental illness. Such
activity is not simply conformance to the prevailing
political system by one sympathetic part of the health
bureaucracy. It would appear that psychiatric theory and
practise have been systematically bent in the USSR for
this purpose—a large-scale, cross-cultural WHO study
showed that Soviet psychiatrists have a broader concept
of schizophrenia and a unique system of categorisation
that differs from that of other psychiatrists worldwide.
The Sovieztinevsley school which dominates Soviet
psychiatry is
characterised by extremely broad
diagnostic criteria, extreme schematism in classification
and overwhelming pessimism in prognosis”. It postulates
that schizophrenia is genetic in origin, irreversible and
deep-seated.
The forensic (legal) implications of the Soviet view are
also far-reaching. It states that “schizophrenia is a disease
in which patients are, with rare exceptions, deemed not
responsible (for their behaviour)”. Further, with the ex
tremely broad conception of the disease, it is possible that
the defendant, who is normal on examination, is still har
bouring severe illness.
State-sanctioned torture can become a malignancy of
the body-politic. The political system, professional group,
public opinion and individual values—these establish
norms of conduct, and normally these norms do not con
flict. The fact that professionals face dilemmas when con
flict occurs underscores the importance of developing
ethical standards. An epidemiolocal approach, such as ex
ists in the form of a national network in the US to study
the social ‘causation’ and medico-social implications of
murder, is suggested.
Since the people who stand to benefit from TPA are
usually those in political positions to sustain it; preven
tive strategies must be aimed at those in power..Protec
tion of human right is based on three methods: pressure
by the international community; actions by national
judicial system; and enforcement by international or
regional bodies (such as the UNHCR).
Governments bear the ‘shame of exposure’. Systematic
collection of information by national groups is important.
The International Committee of the Red Cross (ICRC)
has probably the most detailed information worldwide;
visiting prisoners worldwide to check on detention con
ditions as specified in the Geneva Convention. The In
ternational Medical Commission for Health in Human
Rights (Geneva) could probably coordinate a data network
September-December 1988
on epidemiology, suggest the editors in their concluding
chapter.
Research on how and wfiy reasonably normal people
get co-opted into perverse practises is also important.
R.J. Lifton has suggested that one of the key concepts
underlying Nazi medical killings was belief in the
legitimacy of destroying ‘life unworthy of life’. Lifton sug
gests that the Auschwitz doctors sometimes experienced
ethical conflicts but were able to resolve them through a
process of ‘doubling’—creating an ‘Auschwitz self as well
as a humance-husband father self—even as they killed,
they held on to the idea that they were healers.
Medicine has become part of society’s explicit political
response to the general predicament of humans. Medicine
is now an institutionalised social instrument employed for
the general political purposes of the community—
regulating birth and mortality rates, controlling epidemics,
etc. In the circumstances, HPs have a positive duty to pro
tect its ethical tenets. As the book states—we are now
technically capable of treating bodies and minds effec
tively on a large scale. To put Orwell’s fears of 1984 behind
us, we must put medical ethics and internationally defin
ed hum’an right in front of us.
R. Raghav
12/379B, TPS III,
15th Road, Bandra W.
Bombay-400 050
(Cont. from page 67)
Concerning the erroneous demand of ‘loyalty*, in Rpfael
Bielsa’s book Lafuncion publica, (Ed, Depalma, Buenos
Aires, 1960, p. 34.) (Public duties) we read as follows: “The
meaning of collaborating in public administration is not
that of a partnership where everything must be accepted
and legitimised. On the country, it implies checking, revi
sion, objections, observations, and even well-founded op
position to any illegal or inappropriate act contrary to
public interest” All professions should have a certain
autonomy enabling them to resist pressures from the
political systems in which they operate.
Finally, let us be united in our intentions and as physi
cians recall this statement from the Declaration of Geneva:
“I will maintain the utmost respect for human life from
its beginning even under threat and I will not use my
medical knowledge contrary to the laws of humanity?’
Let this be poignantly rooted in our consitences so that
society and all its institutions and organs can not accept
the practice of torture in their midst ever to happen again.
Likewise, let it no longer be allowed that physicians
alienated from their medical standards act as unconscious
robots for the military in prower. Let us under no cir
cumstances whatsoever permit the existence of statutes,
enclaves, or hierarchies that engender posibilities for such
barbarity.
75
Human Rights Ethical Codes and Declarations
A. Statements by Professional Associations
(i) The World Medical Association (WMA)
Resolution on Physician Participation
in Capital Punishment
Following concern about the introduction of an execution method
(lethal injection) which threatened to involve doctors directly in the
process of execution, the WMA Secretary-General issued a press
statement opposing any involvement of doctors in Capital punish
ment. The 34th Assembly of the WMA. meeting in Libson some
weeks after the issuing of the press statement, endorsed the SecretaryGeneral’s statement in the following terms:
Resolved, that the Assembly of the World Medical Association
endorses the action of the Secretary General in issuing the attach
ed press release on behalf of the World Medical Association con
demning physician participation in capital punishment.
Further resolved, that it is unethical for physicians to participate
in capital punishment, although this does not preclude physicians
certifying death.
Further resolved, that the Medical Ethics Committee keep this
matter under active consideration.
Secretary General's Press Release
The first capital punishment by intravenous injection of lethal
dose of drugs was decided to be carried out next week by the court
of the state of Oklahoma, USA.
Regardless of the method of capital punishment a state imposes,
no physician should be required to be an active participant. Physi
cians are dedicated to preserving life.
Acting as an executioner is not the practice of medicine and physi
cian services are not required to carry dut capital punishment even
if the methodology utilizes pharmaeological agents or equipment
that might otherwise be used in the practice of medicine.
A physician’s only role would be to certify death once the State
had carried out the capital punishment.
September 11, 1981
Regulations in Time of Armed Conflict
care impartially and without consideration of sex, race, nationali
ty, religion, political affiliation or any other similar criterion. Such
medical assistance must be continued for as long as necessary and
practicable.
5. Medical confidentiality must be preserved by the physician in
the practice of his profession.
6. Privileges and facilities afforded the physician must never be
used for other than professional purposes.
Rules governing the care of sick and wounded, particularly in
time of conflict
1. Under all circumstances, every person, military or civilian
must receive promptly the care he needs without considera
tion of sex, race, nationality, religion, political affiliation or
any other similar criterion.
2. Any emergencies, physicians and associated medical person
nel are required to render immediate service to the best of
their ability. No distinction shall be made between patients
except those justified by medical urgency.
B. 1. In emergencies, physicians and associated medical person
nel are required to render immediate service to the best of
their ability. No distinction shall be made between patients
except those justified by medical urgency.
2. The members of medical and auxiliary professions must be
granted the protection needed to carry out their professional
activities freely. The assistance necessary should be given to
them in fulfilling their responsibilities. Free passage should
be granted whenever their assistance is required. They should
be afforded complete professional independence.
3. The fulfillment of medical duties and responsibilities shall
in no circumstances be considered an offence. The physician
must never be prosecuted for observing professional secrecy.
In fulfilling their professional duties, the medical and aux
iliary professions will be identified by the distinctive emblem
of a red serpeht and staff on a white field. The use of this
emblem is governed by special regulation.
Declaration of Tokyo
The Declaration of Tokyo has, since its adoption in 1975, been
These regulations or guidelines set out the WMA’s standards on
.the most comprehensive statement produced by the medical pro
the medical ethical position of the physician during a period of war
fession on the question of the torture and cruel, inhuman or
or other armed conflict. The statement was approved by the 10th
degrading treatment of detainees. It was adopted by the 29th World
World Medical Assembly in Havana in 1956, was edited by the 11th
Medical Assembly, Tokyo, Japan.
Assembly meeting in Istanbul the following year and was amended
The rest is as follows:
by the 35th World Medical Assembly in 1983.
It is the privilege of the medical doctor to practise medicine in
The ameded text reads as follows:
the service of humanity, to preserve and restore bodily and mental
1. Medical ethics in time of armed conflict is identical to medical health without distinction as to persons, to comfort and to ease the
ethics in time of peace, as established in the International Code of
suffering of his on her patients. The utmost respect for human life
Medical Ethics of the World Medical Association. The primary
is to be maintained even under threat, and no use made of any
obligation of the physician is his professional duty; in performing
medical knowledge contrary to the laws of humanity.
his professional duty, the physician’s supreme guide is his conscience.
For the purpose of this Declaration, torture is defined as the
2. The primary task of the medical profession is to preserve health deliberate, systematic or wanton infliction of physical or mental suf
and save life. Hence it is deemed unethical for physicians to:
fering by one or more persons acting alone or on the orders of any
A. Give advice or perform prophylactic, diagnostic or therapeutic authority, to force another person to yield information, to make
procedures that are not justifiable in the patient’s interest.
a confession, or for any other reason.
B. Weaken the physical or mental strength of a human being
1. The doctor shall not countenance, condone or participate in
without therapeutic justification.
the practice of torture or other forms of cruel, inhuman or degrading
C. Employ scientific knowledge to imperil health or destroy life. procedures, whatever the offence of which the victim of such pro
3. Human experimentation in time of armed conflict is govern cedures is suspected, accused or guilty, and whatever the victim’s
beliefs or motives, and in all situations, including armed conflict
ed by the same code as in time of peace; it is strictly forbidden on
and civil strife.
all persons deprived of their liberty, especially civilian and military
2. The doctor shall not provide any premises, instruments,
prisoners and the population of occupied countries.
4. In emergencies, the physician must always give the required substances or knowledge to facilitate the practice of torture or other
September-December 1988
for the common good and a just allocation of health resources. To
forms of cruel, inhuman or degrading treatment or to diminish the
fulfil these aims requires continuous research and continual educa
ability of the victim to resist such treatment.
3. The doctor shall not be present during any procedure during tion of health care personnel, patients and the public.
2. Every psychiatrist should offer to the patient the best available
which torture or other forms of cruel, inhuman or degrading treat
therapy to his knowledge and if accepted must treat him or her with
ment is used or threatened.
4. A doctor must have complete clinical independence in deciding the solicitude and respect due to the dignity of all human beings.
upon the care of a person for whom he or she is medically respon When the psychiatrist is responsible for treatment given by others
sible. The doctor’s fundamental role is io alleviate the distress of he owes them competent supervision and education. Whenever there
his or her fellow men, and no motive whether presonal, collective is a need, or whenever a reasonable request is forthcoming from
the patient, the psychiatrist should seek the help of another
or political shall prevail against this higher purpose.
5. Where a prisoner refuses nourishment and is considered by colleague.
3. The psychiatrist aspires for a therapeutic relationship that is
the doctor as capable of forming an unimpaired and rational judg
ment concerning the consequences of such a voluntary refusal of
founded on mutual agreement. At its optimum it requires trust, con
nourishment, he or she shall not be fed artificially. The decision
fidentiality, co-operation and mutual responsibility. Such a relation
as to the capacity of the prisoner to form such a judgment should
ship may not be possible to establish with some patients. In that
be confirmed by at least one other independent doctor. The conse case, contact should be established with a relative or other person
quences of the refusal of nourishment shall be explained by the doc close to the patient. If and when a relationship is established for
purposes other than therapeutic such as in forensic psychiatry, iu
tor to the prisoner.
6. The World Medical Association will support, and should en nature must be thoroughly explained to the person concerned.
courage the international community, the national medical associa
4. The psychiatrist should inform the patient of the nature of
tions and fellow doctors, to support the doctor and his or her family
the condition, therapeutic procedures, including possible alternatives,
in the face of threats or reprisals resulting from a refusal to con and of the possible outcome. This information must be offered in
done the use of torture or other forms of cruel, inhuman or
a considerate way and the patient must be given the opportunity
degrading treatment.
to choose between appropriate and available methods.
5. No procedure shall be performed nor treatment given against
or independent of a patient’s own will, unless, because of mental
(ii) World Psychiatric Association (WPA)
illness, the patient cannot form a judgement as to what is in his
or her best interest and without which treatment serious impair
Declaration of Hawaii
ment is likely to occur to the patient or others.
In early 1976 work commenced on the drafting of an interna
6. As soon as the conditions for compulsory treatment no longer
tional code of thics for psychiatrists which was subsequently adopted
apply, the psychiatrist should release the patient from the com
in 1977 at the VI World Congress of Psychiatry in Honolulu, Hawaii.
pulsory nature of the treatment and if further therapy is necessary
At the same meeting the WPA committed itself to receive and in should obtain voluntary consent. The psychiatrist should inform
vestigate allegations of the abuse of psychiatry for political pur the patient and/or relatives or meaningful others, of the existence
poses; in 1979 the establishment of the Review Committee was
of mechanisms of appeal for the detention and for any other com
finalised and it first met in Paris in February 1980.
plains related to his or her well-being.
The constitutional status of the Review Committee was changed
7. The psychiatrist must never use his professional possibilities
at the VII Congress in Vienna in July 1983 when it was made per to violate the dignity or human rights of any individual or group
manent and had its remit widened.
and should never let inappropriate personal desires, feelings, pre
Minor amendments to the text of the Declaration were agreed
judices or beliefs interfere with the treatment. The psychiatrist must
at the July 1983 Congress. The text, as amended, reads as follows:
on no account utilize the tools of his profession, once the absence
Ever since the dawn of culture, ethics has been an essential part
of psychiatric illness has been established. If a patient or some third
of the healing art. It is the view of the World Psychiatric Associa
party demands actions contrary to scientific knowledge or ethical
tion that due to conflicting loyalties and expectations of both physi
principles the psychiatrist must refuse to cooperate
cians and patients in contemporary society and the delicate nature
8. Whatever the psychiatrist has been told by the patient, or has
of the therapist-patient relationship, high ethical standards are
noted during examination or treatment, must be kept confidential
especially important for those involved in the science and practice
unless the patient relieves the psychiatrist from this obligation, or
of psychiarty as a medical specialty. These guidelines have been
to prevent serious harm to self or others makes disclosure necessary.
delineated in order to promote close adherence to those standards
In these cases, however, the patient should be informed of the breach
and to prevent misuse of psychiatric concepts, knowledge and
of confidentiality.
technology.
9. To increase and propagate psychiatric knowledge and skill re
Since the psychiatrist is a member of society as well as a practi
quires participation of the patients. Informed consent must, however,
tioner of medicine, he or she must consider the ethical implications
be obtained before presenting a patient to a class and, if possible,
specific to psychiatry as well as ethical demands on all physicians
also when a case-history is released for scientific publication,
and the social responsibility of every man and woman.
whereby all reasonable measures must be taken to preserve the digni
Even though ethical behaviour is based on the individual
ty and anonymity of the patient and to safeguard the personal
psychiatrist’s conscience and personal judgment, written guidelines
reputation of the subject. The patient’s participation must be volun
are needed to clarify the profession’s ethical implications.
tary, after full information has been given of the aim, procedures,
Therefore, the General Assembly of the World Psychiatric
risks and inconveniences of a research project and there must always
Association has approved these ethical guidelines for psychiatrists,
be a reasonable relationship between calculated risks or incon
having in mind the great differences in cultural background, and
veniences and the benefit of the study. In clinical research, every
in legal, social and economic conditions which exist in the various
subject must retain and exert all his rights as a patient. For children
countries of the world. It should be understod that the World
and other patients who cannot themselves given informed consent,
Psychiatric Association views these guidelines to be requirements
this should be obtained from the legal next-of-kin. Every patient
for ethical standards of the psychiatric profession.
1. The aim of psychiatry is to treat mental illness and to promote or research subject is free to withdraw for any reason at any time
from any voluntary treatment and from any teaching or research
mental health. To the best of his or her ability, consistent with ac
programme in which he or she participates. This withdrawal, as well
cepted scientific knowledge and ethical principles, the psychiatrist
as any refusal to enter a programme, must never influence the
shall serve the best interests of the patient and be also concerned
September-December 1988
11
psychiatrist’s efforts to help the patient or subject.
10. The psychiatrist should stop all therapeutic, teaching or
research programmes that may evolve contrary to the principles of
this Declaration.
(Hi) The International Council of Nurses (ICN)
Role of Nurse in Care of Detainees and Prisoners
At the meeting of the Council of National Representatives of the
International Council of Nurses in Singapore in August 1975, the
following statement was adopted:
Whereas the ICN Code for Nurses specifically states that:
1. “The fundamental responsibility of the nurse is fourfold: to promote
health, to prevent illness, to restore health and to alleviate suffering.
2. “The nurse’s primary responsibility is to those people who require
nursing care.
3. “The nurse when acting in a professional capacity should at all times
maintain standards of personal conduct which reflect credit upon the
profession.
4. “The nurse takes appropriate action to safeguard the individual when
his care is endangered by a co-worker or any other persons,”
and
WHEREAS in 1973 ICN reaffirmed support for the Red Cross
Rights and Duties of Nurses under the Geneva Conventions of 1949,
which specifically state that, in case of armed conflict of interna
tional as well as national character (i.e. internal disorders, civil wars,
armed rebellions):
1. Members of the armed forces, prisoners and persons taking
no active part in the hostilities
(a) Shall be entitled to protection and care if wounded or sick,
(b) Shall be treated humanely, that is:
— they may not be subjected to physical mutilation, or to medical or
scientific experiments of any kind which are not justified by the
medical, dental or hospital treatment of the prisoner concerned and
carried out in his interest,
— they shall not be wilfully left without medical assistance and care,
nor shall conditions exposing then>to contagion or infection be
created,
— they shall be treated humanely and cared for by the Party in con
flict in whose power they may be, without adverse in conflict in
whose power they may be, without adverse distinction founded on
sex, nationality, religion, political opinion, or any other similar
criteria.
2. The following acts are and shall remain prohibited at any time
and in any place whatsoever with respect to the above mentioned
persons:
(a) violence to life and person, in particular murder of all kinds, mutila
tion, cruel treatment and torture;
(b) outrages upon personal dignity, in particular humiliating, and
degrading treatment.
WHEREAS in 1971 ICN endorsed the United Nations Univer
sal Declaration of Human Rights and, hence, accepted that:
I. “Everyone is entitled to all the rights and freedoms, set forth in this
Declaration, without distinction of any kind, such as race, colour,
sex, language, religion, political or other opinion, national or social
origin, property, birth or other status (Art.2).
2. “No one shall be subjected to torture or to cruel, inhuman or
degrading treatment or punishment (Art.5)”; and
WHEREAS in relation to detainees and prisoners of conscience,
interrogation procedures are increasingly being employed which
result in ill effects, often permanent, on the person’s mental and
physical health;
THEREFORE BE IT RESOLVED that ICN condemns the use
of all such procedures harmful to the mental and physical health
of prisoners and detainees; and
FURTHER BE IT RESOLVED that nurses having knowledge of
physical or mental ill-treatment of detainess and prisoners take ap
propriate action including reporting the matter to appropriate na
78
tional and/or international bodies; and
FURTHER BE IT RESOLVED that nurses participate in clinical
research out on prisoners, only if the freely given consent of the
patient has been secured after a complete explanation and understan
ding by the patient of the nature and risk of the research; and
FINALLY BE IT RESOLVED that the nurse’s first responsibili
ty is towards her patients, notwithstanding considerations of na
tional security and interest.
Nurse’s Role in Safeguarding Human Rights
Responding to requests from national member associations for
guidance on the protection of human rights of both nurses and those
for whom they care, the Council of National Representatives of the
International Council of Nurses adopted the statement given below
at its meeting in Brasilia in June 1983.
This document has been developed in response to the requests
of national nurses assosiations for guidance is assisting nurses to
safegurads their own human rights and those for whom they have
professional responsibility. It is meant to be used in conjunction
with the ICN Code for Nurses and resolution relevant to human
rights. Nurses should also be familiar with the Geneva Conventions
and the additional protocols as they relate to the responsibilities
of nurses.
The current world situation is such that there are innumerable
circumstances in which a nurse may become involved that require
action on her/his part to safeguard human rights. Nurses are ac
countable for their own professional actions and must therefore be
clear as to what is expected of them in such situations.
Also conflict situations have increased in number and often in
clude internal political upheaval, and strife, or international war.
The nature of war is changing. Increasingly nurses find themselves
having to act or respond in complex situations to which there seems
to be no clear cut solution.
Changes in the field of communications also have increased the
awareness and sensitivity of all groups to those conflict situations^
The need for nursing actions to safeguard human rights is not
restricted to times of political upheaval and war. It can also arise
in prisons or in the normal work situation of any nurse where abuse
of patients, nurses, or others is witnessed or suspected. Nurses have
a responsibility in each of these situations to take action to safeguard
the rights of those involved. Physical abuse and mental abuse are
equally of concern to the nurse. Over or under treatment is another
area to watched. There may be pressures applied to use one’s
knowledge and skills in ways that are not beneficial to patients or
others.
Scientific discoveries have brought about more sophisticated forms
of torture and methods of resuscitation so that those being tortured
can be kept alive for repealed sessions. It is in such circumstances
that nurses must be clear about what actions they must take as in
no way can they participate in such torture, or torture techniques.
Nurses have individual responsibility but often they can be more
effective if they approach human rights issues as a group. The na
tional nurses associations need to ensure that their structure pro
vides a realistic mechanism through which nurses can seek confiden
tial advice, counsel, support and assistance in dealing with these
difficult situations. Verification of the facts reported will be an im
portant first step in any particular situation.
At times it will be appropriate for the NNA to become a
spokesman for the nurses involved. They may also be required to
negotiate for them. It is essential that confidentality be maintain
ed. In rare cases the personal judgment of the nurse may be such
that other actions seem more appropriate than approaching the
association.
The nurse initiating the actions requires knowledge of her own
and other’s human rights, moral courage, a well thought through
plan of action and commitment and determination to see that the
September-December 1988
ncessary follow-up does occur. Personal risk is a factor that has
to be considered and each person must be use her/his best judg
ment in the situation.
Rights of Those in Need of Care
Health care is a right of all individuals. Everyone should have
access to health care regardless of financial, political, geographic,
racial or religious considerations. The nurse should seek to ensure
such impartial treatment.
Nurses must ensure that adequate treatment is provided—within
available resources—and in accord with nursing ethics (ICN Code)
to all those in need of care.
A patient/prisoner has the right to refuse to eat or to refuse
treatments. The nurse may need to verify mat the patient/prisoner
understands the implications of such action but she should not par
ticipate in the administration of food or medications to such
patients.
Rights and Duties of Nurses
When considering the rights and duties of nursing personnel it
needs to be remembered that both action and lack of action can
have a detrimental effect and the nursing personnel must be con
sidered accountable on both counts.
Nurses have a right to practise within the code of ethics and nur
sing legislation of the country in which they' practice. Personal
safety—freedom from abuse, threat or intimation—are the rights
of every nurse.
National nurses assosiations have a responsibility to participate
in development of health and social legislation relative to patient’s
rights and all related topics.
It is a duty to have informed consent of patients relative to hav
ing research done on them and in receiving treatments such as bloodtransfusions, anesthesia, grafts etc. Such informed consent is a
patient’s right and must be ensured.
(iv) Psychologist:
Statement by International Union of Psychological
Science
In July 1976, the Assembly of the International Union of
Psychological Science unanimously approved the statement of the
Executive Committee of the International Union of Psychological
Science made in July 1974.
The text is as follows:
The International Union of Psychological Science
which includes national psychological societies of 42 nations from
all oyer the world;
which thus speaks in the name of over 70,000 professional
psychologists who, because the subject of their science is behaviour,
are particularly concerned with any acts by which individuals in
a systematic and deliberate way infringe upon the inviolable rights
of human beings, regardless of race, religion on ideology, these rights
being guaranteed by the Charter of the United Nations;
and which is concerned with strict observance of professional stan
dards of ethics in the practice of psychology,
therefore makes the following declarations:
It proclaims that no psychologist, in the exercise of his or her
professional functions, should accept instructions or motivations
that are inspired by considerations that are foreign to the profes
sion; It protests solemnly against any use of scientific data or of
professional methods of psychology that impair the abovementioned rights;
It formally condemns any collaboration by psychologists—
whether actively or passively, directly or indirectly—with the abovementioned aubses, and it urges its members to oppose any abuses
of this sort;
It requests each member-society to make certain that it has enacted
a code of ethics and to take those actions required by its code against
any member guilty of such abuses against human rights; It declares
September-December 1988
that the Executive Committee of IPUS is ready to support, with
all.means at its disposal, any action undertaken by a member-society
in order to carry out the terms of the present resolution; It recalls
the following statement made by its Executive Committee on July 27
1974: “The Executive Committee wishes to make clear that the Inter
national Union of Psychological Science denounces vigorously all
practices that are contrary to the high level of morality that must
regulate the scientific and professional roles assumed by
psychologists in modem society!’
It welcomes the United Nation’s Resolution, adopted by the
General Assembly (Third Committee: A/10408; 243rd plenary
meeting, December 9, 1975) on the Protection of All Persons from
being subjected to Inhuman Treatment.
B. United Nations Declarations and Codes
Principles of Medical Ethics
The principles are elaborated within the text of Resolution 37/194
adopted by the United Nations General Assembly, 18 December
1982.
The General Assembly...
Desirous of setting further standards in this field which ought
to be implemented by health personnel, particularly physicians, and
by government officials,
1. ADOPTS the Principles of Medical Ethics relevant to the role
of health personnel, particularly physicians, in the protection
of prisoners and detainees against torture and other cruel, in
human or degrading treatment on punishment set forth in the
annex to the present resolution;
2. CALLS UPON all governments to give the Principles of Medical
Ethics, together with the present resolution, the widest possible
distribution, in particular among medical and paramedical
associations and institutions of detention or imprisonment in
an official language of the State;
3. INVITES all relevant inter-governmental organisations, in par
ticular the World Health Organisation, and non-governmental
organisations concerned to bring the Principles of Medical Ethics
to the attention of the widest possible group of individuals,
especially those active in the medical and paramedical field.
Principles of Medical Ethics Relevant to Role of
Health Personnel, Particularly Physicians, in Protection
of Prisoners and Detainees Against Torture and Other
Cruel, Inhuman or Degrading Treatment or Punishment
Principle 1
Health personnel, particularly physicians, charged with the
medical care of prisoners and detainees have a duty to provide
them with protection of their physical and mental health and
treatment of disease of the same quality and standard as is af
forded to those who are not imprisoned or detained.
Principle 2
It is a gross contravention cf medical ethics, as well as an of
fence under applicable international instruments, for health per
sonnel, particularly physicians, to engage, actively or passively,
in acts which constitute participation in, complicity in, incite
ment to or attempts to commit torture or other cruel, inhuman
or degrading treatment or punishment.1
Principle 3
It is a contravention of medical ethics for health personnel, par
ticularly physicians, to be involved in any professional relation
ship with prisoners or detainees the purpose of which is not solely
to evaluate, protect or improve their physical and mental health.
Principle 4
It is a contravention of medical ethics for health personnel, par
ticularly physicians:.
79
a; io apply their knowledge and skills in order to assist in the
interrogation of prisoners and detainees in a manner that may
adversely affect the physical or mental health or condition of
sucn prisoners or detainees and which is not in accordance
with the relevant international instruments;2
b) lb certify, or to participate in the certification of, the fitness
of prisoners or detainees for any form of treatment or punish
ment that may adversely affect their physical or mental health
and which is not in accordance with the relevant international
instruments, or to participate in any way in the infliction of
any such treatment or punishment which is not in accordance
with the relevant international instruments.
.Prihciple 5
It is a contravention of medical ethics for health personnel, par
ticularly physicians, to participate in any procedure for restraining
a prisoner or detainee unless such a procedure is determined in ac
cordance with purely medical criteria as being necessary for the pro
tection of the physical or mental health or the safety of the prisoner
or detainee himself, or his fellow prisoners or detainees, or of his
guardians, and present no hazard to his physical or mental health.
Principle 6
There may be no derogation from the foregoing principles on any
grounds whatsoever, including public emergency.
Notes
1) See the Declaration on the Protection ofAll Persons from Being Sub
jected to Tbrture and Other Cruel, Inhuman on Degrading Treat
ment or Punishment (General Assembly Resolution 3452 (XXX), an
nex), article 1 of which states:
IfFor the purpose of this declaration, torture means any act by which
severe pain or suffering, whether physical or mental, is international
ly inflicted by or at the instigation of a public official on a person
for such purposes as obtaining from him on a third person infor
mation or confession, punishing him for an act he has committed
or is suspected of having committed, or intimidating him or other
persons. It does not include pain or suffering arising only from,
inherent in or incidental to, lawful sanctions to the extent consis
tent with the Standard Minimum Rules for the Treatment of
Prisoners.
2. “Tbrture constitutes an aggravated and deliberate form of cruel,
inhuman or degrading treatment or punishment."
Article 7 of the Declaration States:
“Each State shall ensure that all acts of torture ns defined in article
1 are offences under its criminal law. The sale shall apply in regard
to acts which constitute participation in, complicity in, incitement
to or an attempt to commit torture."
2) Particularly the Universal Declaration of Human Rights (General
Assembly resolution 217 A (III), the International Convenants on
Human Rights (General Assembly resolution 2200 A (XXI), annex),
the Declaration on the Protection of all Persons from Being Sub
jected to Tbrture and Other Cruel, Inhuman or Degrading Treatment
or Punishment (General Assembly resolution 3452 (XXX), annex)
and the Standard Minimum Rules for the Treatment of Prisoners
(First United Nations Congress on the Prevention of Crime and the
Deatment of Offenders: report by the Secretariat (United Nations
publication, Sales Na 1956, IVA), annex I.A).
C. Amnesty International Declarations
Declaration on Participation of Doctors
in Death Penalty 1981
Amnesty International,
Recalling
that the spirit of the Hippocratic Oath enjoins doctors to prac
tise for the good of their patients and never to do harm,
Considering
that the Declaration of Tokyo of the World Medical Association
provides that “the utmost respect for human life is to be maintain
ed even under threat, and no use made of any medical knowledge
contrary to the laws of humanity”,
Further Considering That
the same Declaration forbids the participation of doctors in tor
ture or other cruel, inhuman or degrading treatments,
Noting
the the United Nations Secretariat has stated that the death penal
ty violates the right to life and that it constitutes cruel, inhuman
or degrading treatment,
Mindful
that doctors can be called on to participate in executions by, in
ter alia,
—determining mental and physical fitness for execution,
—giving technical advice,
—prescribing, preparing, administering and supervising doses of
poison in jurisdictions where this method is used,
—making medical examinations during executions, so that an ex
ecution can continue if the prisoner is not yet dead,
Declares
that the participation of doctors in executions is a violation of
medical ethics;
Calls Upon
medical doctors not to participate in executions;
Further Calls Upon
medical organisations to protect doctors who refuse to participate
in executions, and to adopt resolutions to these ends.
This declaration was formulated by the Medical Advisory Board
cf Amnesty International and was adopted by Amnesty Interna
tional’s International Executive Committee on March 12, 1981.
Conference on Abolition of Death Penalty Declaration
of Stockholm
The Stockholm Conference on the Abolition of the Death Penalty,
composed of more than 200 delegates and participants from Africa,
Asia, Europe, the Middle East, North and South America and the
Caribbean region,
Recalls That:
The death penalty is the ultimate cruel, inhuman and degrading
punishment and violates the right to life.
Considers that:
—The death penalty is frequently used as an instrument of repres
sion against opposition, racial, ethnic religious and underprivileg
ed groups,
—Execution is an act of violence, and violence tends to provoke
violence,
—The imposition and infliction of the death penalty is brutalis
ing to all who are involved in the process,
—The death penalty has never been shown to have a special deter
rent effect,
—The death penalty is increasingly taking the form of unexplained
disappearances, extra-judicial executions and political murders,
—Execution is irrevocable and can be inflicted on the innocent.
Affirms that:
—It is the duty of the state to protect the life of all persons within
its jurisdiction without exception,
—Executions for the purposes of political coercion, whether by
government agencies or others, are equally unacceptable,
—Abolition of the death penalty is imperative for the achieve
ment of declared international standards.
Declares:
—Its total and unconditional opposition to the death penalty,
Its condemnation of all executions, in whatever form, com
mitted or condoned by government,
.u
Its commitment to work for the universal abolition of the dea
penalty.
Calls upon:
—Non-governmental organisations, both national and
ticnal, to work collectively and individually to provide Pu .
formation materials directed towards the abolition of
penalty,
..
—All governments to bring about the immediate and total a
tion of the death penalty,
death
—The United Nations unambiguously to declare that the
penalty is contrary to international law.
80
September-December
Declaration Against Torture
The Declaration on the Protection of all Persons from Toiture
and other Cruel, Inhuman or Degrading Treatment or Punishment
(Declaration against Torture) was adopted without a vote by the
United-Nations General Assembly on 9 December 1975. It calls upon
states to takfe effective measures to prevent torture and lists some
of the mpst important safeguards and remedies to be provided. It
is one of'the most important international documents on torture.
Declaration on Protection of All Persons From Torture
and Other Cruel, inhuman or Degrading Treatment
or Punishment
The United Nations General Assembly adoj
December 9,
1975 a declaration condemning any act of torture or other cruel,
inhuman or degrading treatment as “an offence to human digni
ty”. Under its terms, no state may permit or tolerate torture or other
inhuman or degrading treatment, and each state is requested to take
effective measures to prevent such treatment from being practised
within its jurisdiction.
The Declaration was first adopted and referred to the Assembly
by the Fifth United Nations Congress on the Prevention of Crime
and Treatment of Offenders, held in Geneva in September 1975.
In adopting the Declaration without a vote, the Assembly noted
that the Universal Declaration of Human Rights and the Inter
national Covenant on Civil Political Rights provide that no one may
be subjected to torture or to cruel, inhuman or degrading treatment
or punishment.
The Assembly has recommended that the Declaration serve as
a guideline for all states and other entities exercising effective power.
The text of the Declaration follows:
Article 1
1. For the purpose of this Declaration, torture means any act by
which severe pain or suffering, whether physical or mental, is in
tentionally inflicted by or at the instigation of a public official on
a person for such purposes^ obtaining from him or a third per
son information or confession, punishing him for an act he has com
mitted or is suspected of having committed, or intimidating him
or other persons. It does not include pain or suffering arising only
from, inherent in or incidental to, lawful sanctions to teh extent con
sistent with the Standard Minimum Rules for the Treatment of
Prisoners.
2. Torture constitutes an aggravated and deliberate form of ctuel,
inhuman or degrading treatment or punishment.
Article 2
Any act of torture or other cruel, inhuman or degrading treat
ment or punishment is an offence to human dignity and shall be
condemned as a denial of the purposes of the Charter of the United
Nations and as a violation of the human rights and fundamental
freedoms proclaimed in the Universal Declaration of Human Rights.
Article 3
No state may permit or tolerate torture or other cruel, inhuman
or degrading treatment or punishment. Exceptional circumstances
such as a state of war or a threat of war, internal political instabili
ty or any other public emergency may not be invoked as a justificanon of torture or other cruel, inhuman or degrading treatment Or
punishment.
Article 4
m accordance with the provisions of this Declara
tion, take effective measures to prevent torture and other cruel, ined
ZZ t®
“ PUniShment fr°m bC'n£
Article 5
The training of law enforcement personnel and ofothci public
officials who may be responsible for persons deprived of their liberty
shall ensure that full account is taken of the prohibition against
torture and other cruel, inhuman or degrading treatment or punish
ment. This prohibition shall also, where appropriate, be included
in such general rules or instructions as arc issued in regard to the
duties and functions of anyone who may be involved in the custody
or treatment of such persons.
Article 6
Each state shall keep under systematic review interrogation
methods and practices as well as arrangements for the custody and
treatment of persons deprived of their liberty in its territory, with
a view to preventing any cases of torture or other cruel, inhuman
or degrading treatment or punishment.
Article ''
Each state shall ensure that all acts of torture as defined in arti
cle 1 are offences under its criminal law. The same shall apply in
regard to acts which constitute participation in, complicity in, in
citement to or an attempt to commit torture.
Article 8
Any person who alleges that he has been subjected to torture
other cruel, inhuman or degrading treatment or punishment by
the instigation of a public official shall have the right to complain
to, and to have his case impartially examined by, the competent
authorities of the state concerned.
Article 9
Wherever there is reasonable ground to believe that an act of tor
ture as defined in article 1 has been committed, the competent
authorities of the state concerned shall promptly proceed to an im
partial investigation even if there has been no formal complaint.
Article 10
If an investigation under article 8 or article 9 establishes that an
act of torture as defined in article 1 appears to have been commit
ted, criminal proceedings shall be instituted against ‘the alleged of
fender or offenders in accordance with national law?If an allega
tion of other forms of cruel, inhuman or degrading treatment or
punishment is considered to be well founded, the alleged offender
or offenders shall be subject to criminal, disciplinary or other ap
propriate proceedings.
Article 11
Where it is proved that an act of torture or other cruel, inhuman
or degrading treatment or punishment has been committed by or
at the instigationof a public official, the victim shall be afforded
redress and compensation in accordance with national law.
Article 12
Any statement which is established to have been made as a result
of torture or other cruel inhuman or degrading treatment may n
be invoked as evidence against the person concerned or against at
other person in any proceedings.
Why don't you write for us ?
This periodical is a collective effort of many individuals active or interested in the
field of health or interested in health issues. The chief aim of the journal is to provide a
forum for exchange of ideas and for generating a debate on practical and theoretical
issues in health from a radical or Marxist perspective. We believe that only through
such interaction can a coherent radical and marxist critique of health and health care be
evolved.
Each issue of the journal highlights one theme, but it also publishes (i) Discussions
on articles published in earlier issues (:i) Commentaries, leports, shorter contributions
outside the main theme.
Our forthcoming issues will focus on : Medical Technology, Agricultural Develop
ment and Health, Health in People s Movements.
If you wish to wiite on any of these issues do let us know immediately. We have
to work three months ahead of the date of publication which means that the issue on
Medical Technology is already being worked on. A full length article should not exceed
6.000 words and the number of references in the article should not exceed 50. Unless
otherwise stated author's names in the case of joint authorship will be printed in
dlphabetical order. You will appreciate that we have a broad editorial policy on the
basis of which articles will be accepted.
We have an author's style-sheet and will send it to you on request. Please note that
the spellings and referencing of reprint articles are as in the original and are NOT as per
our style
We would also like to receive shorter articles, commentaries, views or reports. This
need not be on the themes we have mentioned. These articles should not exceed 2,000
words. Please do write and tell us what you think of this issue.
i
All articles should be sent in duplicate. They should be neatly typed in double
spacing on one side of the sheet. This is necessary because we do not have office
facilities here and the press requires all material to be typed. But if it’is impossible for
you to get the material typed, do not let it stop you from sending us your contributions
in a neat handwriting on one side of the paper. Send us two copies of the article
written in a legible handwriting with words and sentences liberally spaced.
The best way to crystallise and clarify ideas is to put them down in writing. Here's
your opportunity to interact through your writing and forge links with others who are,
working on issues of interest to you.
WORKING EDITORS
Please send me Radical Journal of Health for one year (four issues). I am
sending Rs.
as subscription and/or donation by Demand
Draft/Cheque. (D D and cheque in favour of Radical Journal of Health and
for cheque add Rs. 5, if outside Bombay).
Name
Address
_
Position: 3092 (2 views)