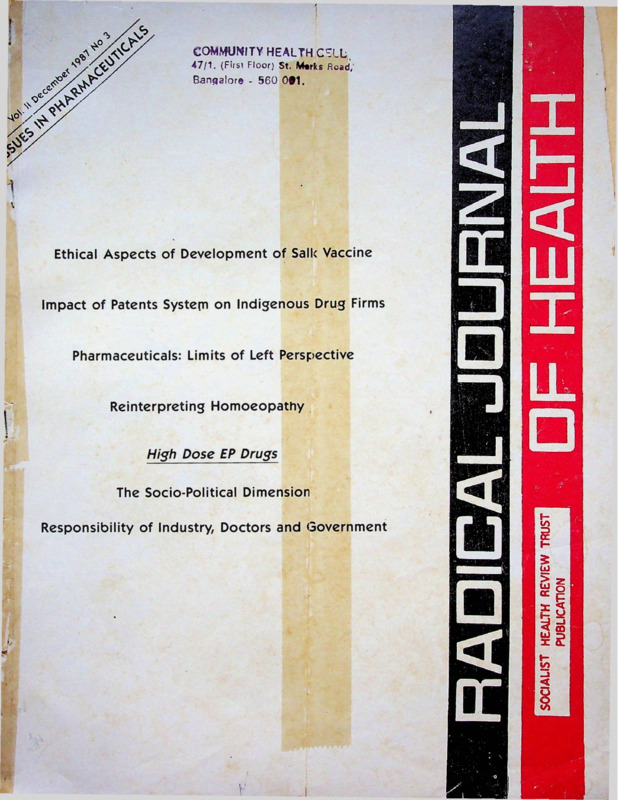
Radical Journal of Health 1987 Vol. 2, No. 3, Dec. Issues in Pharmaceuticals.pdf
Media
- extracted text
-
COMMUNITY HEALTH CELL,
47/1. (First Floor) St. Merks Road,'
Bangalore - 560 001.
Ethical Aspects of Development of Salk Vaccine
Impact of Patents System on Indigenous Drug Firms
Pharmaceuticals: Limits of Left Perspective
Reinterpreting Homoeopathy
High Dose EP Drugs
The Socio-Political Dimension
Responsibility of Industry, Doctors and Government
Working Editors:
Volume II
Amar Jesani, Manisha Gupte,
Padma Prakash, Ravi Duggal
ISSUES IN PHARMACEUTICALS
Editorial Collective:
Ramana Dhara, Vimal Balasubrahmanyan (A P), Imrana Quadeer,Sathyamala C (Delhi), Dhruv Mankad
(Karnataka), Binayak Sen, Mira Sadgopal (M P), Anant
Phadke, Anjum Rajabali, Bharat Patankar, Srilatha
Batliwala (Maharashtra) Amar Singh Azad (Punjab),
Smaraiit Jana and Sujit Das (West Bengal)
All Correspondence:
Radical Journal of Health
C/o 19 June Blossom Society,
60 A, Pali Road, Bandra (West)
Bombay-400 050 India.
December 1987
No 3
49
Editorial Perspective
PHARMACEUTICALS- LIMITATIONS OF LEFT PERSPECTIVE
Anant R S
52
IMPACT OF PATENT SYSTEM IN INDIA ON INDIGENOUS DRUG FIRM?
Sudip Chaudhun
55
High Dose EP Drugs I
RESPONSIBILITY OF INDUSTRY, .DOCTORS AND GOVERNMENT
Amitava Guha
60
High Dose EP Drugs II
THE SOCIO-POLITICAL DIMENSION
Imrana Qadeer
63
Printed and Published by
Amar Jesani for
Socialist Health Review Trust.
Registered Address: C-6 Balaka, Swastik Park,
Chembur, Bombay 400 071.
POLIO, POLITICS, PUBLICITY AND DUPLICITY
ETHICAL ASPECTS OF DEVELOPMENT OF SALK VACCINE
Allan M Brandt
Printed at:
Bharat Printers, Shiv Shakti,
Worli, Bombay.
BEYOND MEDICAL SOLUTIONS
Guy Poitevin
Book Review
70
Dialogue
75
Annual Subscription Rates.Rs.. 30/- for individuals
Rs.. 45/- for institutions
Rs. 500/- life subscription (individual)
US dollars 20 for the US, Europe and Japan US
dollars 15 for other countries.
We have special rates for developing countries.
SINGLE COPY: Rs. 8/-
(All remittance to be made out in favour of Radical
Journal of Health. Add Rs 5/- on outstation cheques)
REINTERPRETING HOMOEOPATHY __
Ch V Subba Rao
Editorial Perspective
Pharmaceuticals: Limitations of Left Perspective
WHAT are the issues that arise when we are discussing the
relationship between pharmaceuticals and health? There are
three types of issues. First, the issue of the general relation
ship between pharmaceuticals and health. Second the role
of pharmaceuticals in capitalism, and especially monopoly
capitalism, as well as that in state socialism and revolutionary
socialism. Third, the objective and the standpoint of the Left
movement in India as regards this issue of pharmaceuticals
and health. Let us take a brief overview of the various sub
issues involved in these three aspects of this problem.
Contrary to what the drug industry or the technocratic
ideology would like us to believe, drugs have played a
marginal role in improving or maintaining the health of the
people. In a way this is obvious because it is clear that health
status basically depends upon food, water, sanitation, en
vironment, working-conditions and cultural atmosphere.
Moreover, until recently, therapeutic efficacy of medicines
was very low. In ayurveda, the ancient Indian approach to
health and disease, what is notable, (given the primitive tools
of enquiry available in those days and given the dominance
of idealist tradition), is its materialist outlook—not much
scope for spirits and the like. It is however a controversial
issue as to what extent ayurvedic medicines have been effec
tive and safe. That they have been used for hundreds of years
does not necessarily mean that they have been effective and
safe. In the west things were probably worse. Medical pro
fessionals had very few useful medicines to offer to the
patients (less than the folk-people had) till as late as late 19th
century. Many of the remedies were of the nature of blood
letting, branding and the like or use of corrossives or other
drastic and harmful substances as medicines.
The era of safe and effective antimicrobials, anti-biotics,
started from 1930s and most of the antibiotics and other
‘wonder drugs* came after the second world war as a part
of the third industrial revolution and post-war restructuring
of the imperialist system and its boom. By this time, however,
most of the major infectious diseases in the west had already
declined substantially. Now it is well-known in informed
circles that modern drugs have thus not played an impor
tant role in the improvement of the health-status in the west.
It is basically the improvement in the general living standards
(food, sanitation, housing, work, education, etc.) which did
the job. In the developing capitalist societies, these power
ful catalytic agents—the modern pharmaceuticals including
most importantly the vaccines—have hardly realised their
potential because the socio-economic conditions are inimical.
This can be seen from the case of megapolis like Bombay.
Here we have drugs and doctors (including specialists)
available in every lane, but tuberculosis, leprosy, venereal
diseases and even polio show to sign of the respite. China,
which is a quite comparable out of the capitalist straight
jacket has shown how modern drugs can be a powerful aide
in the rapid control over the scourge of infectious diseases
when social cpnditions are favourable for such a control.
The so-called ‘diseases of industrialisation’ (which are the
diseases of monopoly capitalism and the culture it breeds—
cardiovascular diseases, injuries due to accidents, cancers,
December 1987
diseases due to obesity and psychiatric problems—cannot be
cured with drugs. On the contrary, the overuse of drugs in
such disorders lead to a number of iatrogenic health
problems.
It may be argued that the above is a rather simplistic state
ment. Yes, indeed, it is; it being a brief statement of a stand
point about a historical phenomenon or trend. There are
some phenomenon which do not quite fit into this scheme.
But that does not alter the overall picture. Secondly, to point
out the marginal role of medicines in improving health status
of population is not a criticism of modern medicines but
of technocratic, self-servicing ideologues who overplay the
role of medicines. There is no doubt that modern medicines
have a tremendous catalytic potential and even in absence
of favourable social conditions, they have made human life
more tolerable that what it could otherwise be. But its wrong
to attribute more than this to medicines.
The question of the role of non-allopathic medicines is
a perplexing one. Homeopathic and allopathic medicines
have entirely different presuppositions, are of entirely dif
ferent nature, both qualitatively and quantitatively; yet both
help in different .degrees and instances the human body in
its recovery from illness. It is a theoretical puzzle as to how
this can happen. This discussion cannot, however, be
separated from the one about different disciplines of medical
care—homeopathy, ayurveda, unani and others. Secondly,
this question is also related to the question of the very
method of science. Statistical criteria are used to decide the
efficacy of medicines in allopathy. How can this be done in
homeopathy and ayuveda when their basis is that of indi
vidualisation? Is there a way out? Is the very notion of scien
tific criteria as used in allopathic science open to question?
Is there any alternative scientific method? Can there be?
There are a long list of such questions which do not seem
to lead us anywhere.
One thing is, however, definite. Research into these systems
needs to be given more resources—financial and otherwise.
At the same time, unless the efficacy and safety of the nonallopathic medicines have been proved through research, by
some intelligible criteria proposed by the authorities in these
systems, these drugs should not be allowed to be commer
cially produced.
Capitalism and Pharmaceuticals
Drug technology was one of the branches of technology,
which stagnated for quite sometime even after the advent
of the industrial revolution in Europe. The knowledge of
human body in health and disease and the development of
chemistry was too meagre for quite some time. It is only in
monopoly capitalism—the advanced stage of capitalism—
that enough resources could be pumped into research in these
complicated sciences and it is only then that diagnosis and
treatment of diseases could flower into a discipline solidly
based on modern science. Modern pharmaceuticals is essen
tially a product of monopoly capitalism. This same mono
poly capitalism has, however, at the same time, become an
49
oostacle in (he path of the full and proper use of modern
pharmaceuticals. Monopoly drug companies restrict produc
tion and jack-up prices to ensure monopoly profits by using
methods characteristic of monopoly capitalism, a lot of
irrational and even harmful drugs are pushed onto the con
sumers. In India and other peripheral countries, this occurs
in a very crude manner wherein the market abounds in
useless, irrational, harmful products which fetch higher rates
of profits. This is at the expense of essential drugs which
are at least under some price-control. In the rest, this
phenomenon takes place in a more subtle form through a
technocratic consumerist ideology of ‘pill for every ill’.
The full flowering of the science of pharmaco-therapeutics
is also adversely affected by monopoly capitalism. A lot of
resources are wasted in inventing ‘me-too’ drugs which have
no significant advantage over the existing ones, but which
can be marketed as ‘new and better’ through aggressive
monopolistic marketing techniques. Social resources are also
wasted in attempts to prove through ‘scientific research’, really
harmful drugs as safe, or useless drugs as very effective.
•Monopoly multinational drug companies represent a
classic case of how modern imperialism operates. These
monopoly MNCs have on the one hand introduced the fruits
of the development of modern science of pharmacotherapeutics into the third world countries. On the other
hand, their monopoly, imperialist interests demand that a
part of the surplus value created in the drug industry be
pumped off to the imperialist centre; that the drug industry
in the peripheral countries be dependent on the imperialist
centre so that this sector remains one of the channels of more
profitable investments and easier markets. The methods
employed to achieve this aim are scandalously bad-produc
tion and marketing of the most irrational, irrelevant, and
even harmful products at rapaciously high prices through
blatantly unethical marketing practices; and the suppression
of development of indigenous technology by recourse to ‘fair’
and foul methods characteristic of monopoly capitalism. The
results are more disastrous than they are in the west, since
the wastage of and suppression of resources means too much
pressure on a weak economy and the impact of cheating and
exploitation is much more significant for the poor people
who constitute the majority in these peripheral capitalist
countries. The contrast between the potentiality of using
modern science and technology for the betterment of
humankind and the reality of a stunted, distorted develop
ment is much more poignantly seen in case of the drug in
dustry in the peripheral capitalist countries.
Contraceptives as a group of drugs need a special men
tion. The invention of the birth-control pill is regarded by
many as one of the important milestones in the path of
women’s liberation. In reality it is only a defence mechanism
for women in the world of patriarchal capitalism in which
safe, effective male contraceptives are neither developed nor
used adequately. Contraception is considered as the woman’s
responsibility. The availability of the effective pill in a society
wherein women are seen as objects of sexual gratification
for men has also meant women’s bodies being available
‘anytime’ without the fear of them getting pregnant. This
is convenient for patriarchal men since they can achieve the
twin benefit of free sex, and small number of children,
without any responsibility or botheration of use of
contraceptives.
50
For the women in peripheral countries and of the ethnic
minorities in the imperialist centres, hormonal contracep
tives are becoming in addition, a burden on their already
poor health. Patently unsafe injectable contraceptives and
subdermal implements have given the capitalists, patriarchal
state a powerful instrument to enforce its programme of
population-control in these countries—at the expense of
health of the poor women. Pharmaceuticals which are sup
posed to enhance feminity are another example of the crude
sexism practised by the drug industry.
Pharmaceuticals in Socialism
Human beings would of course continue to fall ill under
socialism and communism. The pattern of diseases would,
however, be quite different from those in undeveloped
capitalism or in monopoly capitalism since this pattern is
decided primarily by the nature of social production and the
set of relations encompassing it. It would be an idle specula
tion as to what kind of health problems would exist then
and which drugs would be used. All that we can say with
certainly is that in socialism and communism, there will be
less and less of illnesses and hence less and less necessity of
use of drugs in diseases.
In ‘existing socialisms’ alias state socialist societies (USSR,
China, etc.) conditions are, of course, quite removed from
this ideal. But the use of pharmaceuticals in these countries
is not vitiated by the narrow needs of a profit-hungry drug
industry and hence is quiteTational. But there are some pro
blems. For example, the widespread use of the injectable contraceptive,-Net-En in People’s Republic of China shows that
patriarchal relations are present there to quite a substantial
extent. In more developed societies—USSR and countries in
the eastern block, the disease pattern is not qualitatively dif
ferent from that in the capitalist west. This, however, does
not mean that drugs are overused and misused like in the
west since there is no profit-mongering drug industry in these
societies. It would be interesting to study the precise nature
of use of pharmaceutical in these societies, whether, and to
what extent there is any irrationality in the production and
use of drugs and why.
Standpoint of Left Movement in India
The Left parlies and groups have criticised foreign drug
companies as part of their anti-imperialist standpoint.
During last six or seven years a lot of concrete work has been
done to demonstrate how specifically MNC drug companies
exploit and cheat the Indian people and how they thwart the
Indian sector. There are, however, two problems in these
criticisms—firstly, most of this work has been done by Left
intellectuals as part of their research project or by Left acti
vists, as part of the broader ‘democratic’ science or healthgroups to which we belong. This has put certain limitations
on the standpoint that is expressed in these analyses and has
even put limitations on the very thinking of Left activists.
There is a need to a pause and think about these limitations.
In certain academic institutions, financed by the govern
ment, there exists a liberalism among decision-makers and
hence it is easier to get a research-project to study the impact
of MNCs on the Indian drug industry. This liberalism is in
tune with the interests of the Indian state; because such
Radical Journal of Health
studies fall within the limited anti-imperialist standpoint of
the Indian state. The interests of the Indian bourgeoisie
demand that MNCs be pressurised into allowing more and
more leeway to Indian capital to exploit the Indian people.
Studies focussing on the negative role of MNCs are, therefore,
even encouraged by the Indian state. Such studies unearth
a lot of valuable anti-imperialist material which can be used
by people’s movements in their thorough-going, revolutionary
anti-imperialist struggle.
But a more or less exclusive focus in these studies on the
role of MNCs by omitting a critique of the Indian sector
is more helpful to the non-revolutionary anti-imperialist
struggle of the Indian bourgeoisie. There is comparatively
less concrete research in such studies on the anti-people role
of Indian companies—and of the public sector. A critique
of the Indian sector does not necessarily mean neglecting
the distinction between MNCs, Indian private companies—
(monopoly and non-monopoly) and the public sector. But
a comprehensive critique is perhaps not encouraged. It is no
accident that a majority of these studies directly or indirectly
financed by the Indian state omit the Indian sector from their
critique.
Popular education and propaganda, based on these studies
have an ideological, political role of limiting the critique to
only the MNCs. The fact that many Left analysts have a
limited, anti-imperialist (understood in a narrow sense)
political perspective which excludes an important role of a
critique of the Indian sector, also helps to sustain this un
necessarily narrow focus. In terms of demands also, the focus
of most of Left analysts is limited to -the demand for na
tionalisation of MNCs. In our strategic demands, we should
ask for*nationalisation without any compensation and with
workers’ control/democratisation in the nationalised in
dustry. These strategic demands are for the public education
of what is possible in the coming stage of the revolution;
and hence the fact that the health movement is too weak
today, is no argument including this strategic perspective in
our study and propaganda.
Criticisms mounted as part of a health or science or con
sumer group have an advantage in that such criticisms bring
into focus the question of irrational and hazardous drugs,
SUBSCRIPTION RENEWALS
misleading propaganda by the drug companies about the
efficacy and safety of their drugs and so on. Here again,
misdeeds of Indian companies are generally not mentioned.
But the demand for banning of irrational and hazardous pro
ducts, is such that no concession can be given to the Indian
sector whose performance on this score has been no better.
As a part of the ‘democratic* health/science/consumer
movements, Left activists have participated in bringing
forward the medical (sometimes feminist) issues and
demands. But many such groups do not take a political stand
against even imperialism; leave aside Indian capital even
though the concrete demands made by such groups and their
implications are many times anti-imperialist, anti-capitalist.
But a lack of a clear political anti-imperialist, anti-capitalist
stand sometimes becomes a hinderance in the progress of
analysis in such groups. Part of this problem is due to the
fact that people’s movements and hence the political culture
in such anti-establishment groups has not advanced enough.
But part of the problem is also due to the fact that the
perspective of the Left activists working in such groups is
limited to a purely anti-imperialist standpoint, (understood
in a narrow sense). That is why even among Left-journalist,
analyses about the drug industry from a comprehensive
standpoint are a rarity; most of the writings being from
purely anti-MNC viewpoint.
The editorial perspective in RJH is meant to delineate
various issues (in a somewhat comprehensive fashion)
germane to the theme chosen for the current number of RJH
and to make editorial comments on some of them. In the
foregoing, I have merged this two-step operation into a single
step by making a summary-statement of a certain viewpoint
on the three types of major issues which were thought to be
central to the theme of this current issues of RJH. There are,
of course, viewpoints different from the one outlined above.
It is hoped that there will be further discussion and debate
on these issues. Obviously, in this number of RJH it has been
possible to cover only some of the issues.
Anant R. S.
50, LIC Quarters,
University Road,
PUNE - 411 016.
MEDICO FRIEND CIRCLE PUBLICATIONS
Is this your last subscribed issue? A prompt renewal from
you will ensure that your copy is mailed directly from the
Press. Many of our issues have sold out fast! So book your
copies by renewing your subscription now!
Medico Friend Circle Bulletin (Monthly):
Annual Subscription: Rs 20
Our new subscription rates:
Anthologies:
For individuals—Rs. 30/- (four issues)
For institutions-Rs. 45/- (four issues)
Foreign subscriptions: US $ 20 for US, Europe and Japan
US $ 15 for all other countries
(special rates for developing
countries)
Life subscription: Rs. 500/-____________________ _____
D.D.s, cheques, IPOs to be made out to RADICAL JOURNAL
OF HEALTH. Please write your full name and correct
address legibly. And please'don’t forget to add Rs. 5/- on
outstation cheques.
December 1987
In Search of Diagnosis
Health Care: Which Way to Go
Under the Lense
Rs 12
Rs 12
Rs 15
Bulletin subscriptions to be sent to C Sathyamala,
F-20 (GF), Jangpura Extension, New Delhi 110 014.
Orders for the anthologies to Dhruv Mankad,
1877 Joshi Galli, Nipani, Belgaum Dist, Karnataka.
51
Impact of Patent System in India on Indigenous Drug Firms
sudip chaudhuri
A demand is often made by certain quarters to modify the Patents Act of 1970 to make its provisions less restrictive
for the patentees. This paper examines the experience under the Patent and Designs Act of 1911 to argue that
such a change will go against indigenous efforts to develop processes and manufacture drugs.
THE objective of this article is to briefly relate the experience
of the indigenous drug firms with the Patents and Designs
Act. 1911 in the context of the Patent Act, 1970 which replac
ed the former in 1972.
The Patent and Designs Act, 1911 did not categorically
state what was patentable.1 The interpretation followed by
the Patent Office was that any new process for manufacturing
a drug (whether old or new) was patentable. A new drug was
also patentable provided the process of manufacture was
described in the patent. The process, however, in such a case
was not required to be new.2 Under the Act of 1911, the in
digenous firms have been legally prevented from manufac
turing most of the new drugs introduced by the transnational
corporations, during the life of the patent secured by the lat
ter, i c, for 16 years, which could be extended to a maximum
of another 10 years if the working of the patent had not
hitherto been sufficiently remunerative to the patentee3 This
had been possible because, as N R Ayyangar who was ap
pointed by the Government of India to examine the patent
law in India observed, the patentee, while patenting a new
drug, could describe all the known and possible porcesses.4
Actually the TNCs did so, as the experience of the indigenous
firms suggests.5 Even an old process, so specified by the
TNCs, could not be used by the indigenous firms for at least
16 years. The latter were also forbidden from processing a
patented drug into formulations or importing it.
The TNCs asserted their patent rights to proceed legally
against firms which tried to manufacture or import the
patented drug. Thus, Hindusthan Antibiotics Ltd (HAL),
a public sector firm, e g, claimed that it has developed an
indigenous process for manufacturing oxytetracyline Hcl. A
plant, in fact, was set up and production began in 1961
without any external technical help. In the same year a TNC,
viz, Pfizer too started manufacturing the same drug. HAL
had to suspend production as Pfizer took legal action alleg
ing infringement of patent rights.6 A TNC was importing
a drug at Rs 8 per 20 tablets. It sued an indigenous firm,
CIPLA, when the latter started importing it at Rs 2 per 40
tablets.7 Chloramphenicol and metronidazole are among the
other drugs for which the TNCs took legal action to pre
vent the indigenous firms from formulating.8
The manufacturing activities of the indigenous firms were
restricted to the old drugs or those new drugs for which it
could develop new processes of manufacture. We will now
discuss two cases which will give an idea about how the TNCs
could prevent or delay the use of these new- processes,
developed through indigenous efforts even w'hen these were
not specifically covered in the patents of the TNCs.
Haffkine Institute, a public sector firm, worked out a pro
cess for manufacturing tolbutamide from locally available
raw materials. A patent was also obtained. Unichem
Laboratories, an indigenous firm obtained a licence from it
and started manufacturing from 1961. Hoechst, a TNC,
52
however filed a suit claiming that tolbutamide had been
manufactured by Unichem on the basis of one of the for
mulas as mentioned in the former's patent granted earlier
in 1956. The judgement of the Bombay High Court delivered
in 1968 went in favour of Hoechst.9 What is important to
note here is that Hoechst won the case despite the fact that
its patent did not specifically mention Haffkine’s process.
What clinched the issue was that Hoechst’s description was
open-ended. One of the claims of Hoechst was, in the inter
pretation of the judge:
"Wide enough io cover all methods of eliminating sulphur from
thioureas (to manufacture Tolbutamide) whether desulphurisation
is effected by means of Hydrogen peroxide (as specifically mentioned
by Haffkine) or by the use of any other substance113 (phrases within
brackets ours).
Strange as it may appear, such widely worded claims were
permissible under the Act of 1911.
The same patent was also sought to be used for preventing
Bengal Chemical and Pharmaceutical Works (BCPW), an
indigenous firm, from manufacturing another drug, chlor
propamide. BCPW developed a new process for manufac
turing it and obtained a patent in 1959. But in 1961, BCPW
received a letter from Hoechst, alleging that the former had
infringed upon the latter’s patent under which Pfizer had
been given a licence to produce it. Denying the allegation,
BCPW sought legal action when it continued to receive such
threats. Hoechst and Pfizer, on their part, filed a suit in 1962
in the Calcutta High Court against BCPW.11 This time the
judgement went in favour of the indigenous firm. The judge
concluded that BCPW’s patent was an independent one, not
in any way influenced by Hoechst’s patent which, in fact,
did not relate to manufacture of chlorpropamide at all!
The case is quite revealing so far as the development of
indigenous technology and the role of patent legislation are
concerned. Hoechst’s patent did not refer to any specific
drug. It was for the broad group of sulphonyl Ureas. Forty
examples were given, but it was claimed that other com
pounds could be obtained easily from tKe general formula
and chlorpropamide was one of them. Hoechst, however, fail
ed to establish in the court that chlorpropamide could be
or had been produced on the basis of the process described
in their patent. Even an expert witness appearing for Hoechst
admitted that the information disclosed in the patent was
not enough to carry out the experiment. But Hoechst could
not give specific directions as to how to proceed. One of the
specifications, in fact, was found to be chemically incor
rect.12 Significantly, out of the 40 examples provided, none
referred to chlorpropamide.
One of the objectives behind the patent laws is to induce
the inventors to disclose the inventions (in return for the ex
clusive right of using the invention for a specified period)
so that knowledge may be diffused to facilitate further
technological progress. The above-mentioned case illustrates
Radical Journal of Health
how the TNCs used the Indian patent law existing then to
licence, but the foreign patentee offered to give (he licence
suppress indigenous growth. It is not only that Hoechst’s pa voluntarily on the basis of royalties to be fixed through
tent contained inadequate and misleading information which
negotiations. They demanded an absurdly high rate of royalty
prevents and distorts the diffusion of knowledge. The pa of 25 per cent. It took more than four years to reduce it to
tent was of a general type, supposed to cover a large and
10 per cent, which however was still higher than the limit
unspecified number of products/processes. Thus, other firms
of 5 per cent stipulated by the Reserve Bank of India. By
could be threatened with legal consequences even when their
that time the Haffkine Institute decided to abandon the
product was not at all connected with the patent. All the
scheme.-1 Again, another indigenous firm Neo Pharma In
patent disputes are not fought out in a court of law. A mere
dustries entered into a technical collaboration agreement with
threat may be enough deterrant in many cases. Significantly
an Italian firm for the technology to manufacture
enough, in 1968, before the court hearing started, Hoechst
chloramphenicol.
approached BCPW to settle the dispute ouside the court,
A licence was sought from Parke Davis, which held the
which however the latter refused.13
relevant patent in India. But whereas the subsidiary com
pany in India pointed out that the matter was beyond its
Compulsory licence: An indigenous firm intending to
manufacture a drug is required to obtain a licence from the jurisdiction, the parent company in the USA insisted that
Neo Pharma should first discuss with the local company, h
patentee concerned, if the process of manufacture to be used
took more than two years to decide as to who would
is covered by the patent. Under the Act of 1911, this was the
negotiate. At last when the negotiations started with the
requirement even if the process in question was well known
parent company, they did not formally refuse to grant a
(but even so had been mentioned in the patent as in the case
licence but simply sat over the proposal. Finally, when a com
of new drugs discussed above) or additional technical data
pulsory licence was sought for and was granted, Parke Davis
were necessary to implement the process and these had been
went to the court and obtained a stay order.-2
developed by, or obtained from, other sources. Obviously,
In fact, going to the court is a simple device the foreign
a patentee may grant a licence voluntarily to anyone on
patentees could employ. Even if ultimately the judgement
mutually acceptable terms. Compulsory licence is a licence
goes against the patentee, the applicant would normally be
granted by the Controller of Patents (or by the patentee as
directed by the Controller) or a non-patentee to use a pa prevented from using the compulsory licence during the
period of the court case. The longer the time taken to settle
tent on payment of royalties to the patentee. The Act of 1911
a case, the smaller will be the relative benefit to the appli
provided for the grant of compulsory licence in case of
cant for compulsory licence, because in any case after the
misuse or abuse of patent rights.14
expiry of the patent (normally 16 years) anybody was free
The Patents Enquiry Committee reported in 1950 that the
to use the patent. The hazards of obtaining a compulsory
foreign patentees did misuse or abuse their rights, e g, by
licence, which include legal battles, perhaps explain why so
importing the patented product rather than manufacturing
few applications for compulsory licence were made under
it here, fixing the prices at high levels, not allowing others
to manufacture the product even when it was not itself engag Section 23 CC. Till 1972. i c. when a new Act came into force,
there were only five applications for compulsory licence,
ed in manufacture.15 But, as the Committee observed, the
made by Hindustan Antibiotics Ltd (in 1959), Alembic
provisions regarding compulsory licences were “wholly
inadequate to prevent misuse or abuse of patent rights, par Chemical Works (1963). Dey’s Medical Stores (Manufactur
ing) (1960), Raptakos Brett and Co (1957) and Neo Pharma
ticularly by foreigners”.16 The Panel on Fine Chemicals,
Industries (1961).2’ The applications were ultimately
Drugs and Pharmaceuticals, appointed by the government
withdrawn in the first two cases. Compulsory licence was
also reported earlier in 1946 that not a single compulsory
refused by the Controller of Patents in the third case.24 The
licence could be obtained because of the wording of the rele
vant provisions.17 For example, under Section 22, a com controller granted compulsory licences in the last two cases.
pulsory licence could be claimed if “the demand for a
Patent System under Act of 1970
patented article is not being met to an adequate extent and
An important feature of the new Act, 197O25 is (he special
on reasonable terms”. As the Patents Enquiry Committee
commented, the Section unnecessarily also demanded that
provisions regarding drugs and a few other products. The
it has to be proved that as a result any trade or industry had
life of the drug (and food) patents has been reduced from
at least 16 years in (he previous Act to five years from the
been ‘unfairly prejudiced’. Obviously, in practice it appeared
very difficult to establish such a link.18
date of scaling.,26 or seven years from the date of filing of
complete specifications, whichever is shorter (sections 45 and
The provisions regarding compulsory licence (Sections 22
53), i e, for a maximum period of seven years. For other
and 23) were amended in 1950, following the recommenda
patents, the duration is 14 years. The new Act categorically
tions made by the Patents Enquiry Committee in its interim
states that drugs (and food and those manufactured by
report submitted in 1949.19 In 1952, an entirely new Section
chemical processes) can now be patented only for a new
(23 CC) dealing specifically with drugs (and food, insecticide,
germicide, fungicide, surgical or curative devices) was added.
method or process of manufacture, not for the products as
such (section 5). Hence in contrast to the previous situation,
Under this section, the Controller of Patents was empowered
to grant a compulsory licence to any applicant at any time
the indigenous firms can manufacture new drugs by old pro
cesses without violating the Act. Obviously, as before it can
unless there are ‘good reasons’ for refusing. The foreign
patentees, however, were still in a position to effectively pre continue to manufacture old drugs. Even in cases where new
drugs cannot be manufactured by known processes, and so
vent or delay the use of compulsory licence.
a new process is required, the indigenous firms are expected
The Haffkine Institute, e g, applied for a complusory
December 1987
53
to face less restrictions in developing such new processes. This
is because the firm discovering/inventing a drug can no
longer patent all the processes known to it even if these arc
new. For a particular drug, only one method or process—
the best known to the applicant—can be patented (Sections
5 and 10).27
Under Section 87 of the Patents Act, 1970. every patent
relating to processes for manufacturing drugs (or food or
chemical substances) has to be endorsed with the words
“Licences of right" after three years of the date of sealing.
This implies that anyone is automatically entitled to a licence
from the patentee for using the patent on payment of
royalties, the maximum rate being fixed at four per cent of
the ex-factory sales (Section 88). Even before expiry of three
years from the date of scaling, the controller is empowered
to grant a compulsory licence (and fix the rate of royalties)
if “it is necessary or expedient in the public interest" (Sec
tion 97). There is also a special provision in the Act of 1970
regarding the use of patents by the government. Any lime,
a patent may be used for official purposes, including those
of public undertakings. The maximum royally payable for
such a use, in case of drugs (and food) has been fixed at 4
per cent of the ex-factory sales (Sections 99 and 100).
It must be pointed out, however, that the actual use of a
patent by a non-patentee still remains hazardous. For exam
ple, under Section 87, as mentioned above, while the right
to obtain a licence automatically accrues after three years
from the date of scaling of a patent, it cannot actually be
used till the royalties are fixed either mutually or at the in
tervention of the controller. As before, the patentees can con
tinue to prevent or delay the use of their patents by others
by refusing to negotiate and then proceeding to the court
in case of any intervening action by the controller. This has,
in fact, happened in the case of each of the applications made
to the controller till now by three firms for fixation of
royalties. Incidentally, all these cases relate to products other
than drugs. In the case of the application made in March
1976 by Catalyst and Chemical India (West Asia), the con
troller fixed the rate of royally tentatively as per Section 88(4).
The patentee (1CI), however, went to the court and by the
lime the case came up for final hearing (July 1977) the pa
tent was about to expire (in August 1977). In the remaining
two cases, as the patentees approached the court, interim in
junction was granted and the Patent Office was directed not
to proceed with the applications of Titanium Equipment and
Anode Manufacturing Co and Coromandel Indag Products
made in September 1980 and July 1981 respectively. The two
patents in which Titanium was interested expired in February
1983 while the court case was still pending. Regarding
Coromandel, too, while the case is yet to be settled, one of
the patents has already expired in March 1982, w hile the other
is due to expire in February 1986.28
Despite such hazards, the Patents Act, 1970 appears, on
the whole, to be an improvement from the point of view of
the development of indigenous science and technology, com
pared to the previous situation. A demand is often made by
certain quarters to modify the present Act and make the pro
visions less restrictive for the patentees. If the experience
under the Act of 1911 is any guide, then such a change will
go against the indigenous efforts to develop processes and
manufacturing drugs.
54
Noles
[This paper was written in 1984 and hence does not contain any references
to later events.]
I. Report of rhe Patents Enquiry Committee (1948-50) (Delhi, GOI,
Ministry of Industry and Supply, 1950), p 64; N Rajagopala
Av yangar. Report on the Revision of the Patents Law (Delhi, GOI,
1959). p 20.
2. Av yangar. Report, pp 20. 34. 36.
3. See Section 14 and 15. "The Indian Patent and Designs Act 1911”,
reproduced in Patent Office Hand Book (Delhi. GOI. 13th ed, 1966).
4 A\yangar. Report, pp 34. 36.
5. See the evidence of K A Hamied of Chemical, Industrial and Phar
maceutical Laboratories (Cl PL A). Joint Committee on the Patents
Bill. 1965: Evidence (New Delhi, Lok Sabha Secretariat, 1966), Vol
1. p 154 and of S G Somani of All India Manufacturers Associa
tion, Joint Committee on the Patents Bill, 1967: Evidence (New
Delhi. Lok Sabha Secretariat. 1969), Vol 1, p 294.
6. HAL. Annual Report, 1961.
7. Evidence of K A Hamied of CIPLA, Joint Committee on the Patents
BUI, 1965: Evidence, Vol 1, pp 149-50.
8 Report of the Committee on Drugs and Pharmaceutical Industry
(Hathi Committee) (New Delhi. GOI, Ministry of Petroleum and
Chemicals. 1975), p 92.
9 For the text of the judgement, which also provides the background
of the case. see. The All India Reporter (Nagpur, AIR Ltd, 1969),
Bombay Section, Vo) 56, pp 258-73.
10 Ibid p 264.
II. Information on this Patent case has been obtained from the judge
ment of the Calcutta High Court (Suit No 1124 of 1962); the plaint;
the written Statement submitted by BCPW (all available at the
Calcutta High Court) and the BCPW Assistant Secretary’s Note
placed at the BCPW Board of Directors meeting held on 27 July,
1970.
12. Hoechst’s patent mentions alkalation with primary amides which
is chemically impossible See Ibid.
13. Minutes of the meeting of the directors of BCPW, Calcutta, 5
December, 1968
14. Report of the Patents Enquiry Committee (1948-50), p 71.
15. Ibid, p 162.
16. Ibid, p 172.
17. Report of the Panel on Fine Chemicals, Drugs and Pharmaceuticals
(New Delhi, GOI, Department of Industries and Supplies, 1947),
P 15.
18. Report of the Patents Enquiry Committee (1948-50), p 168.
19. Ayyangar, Report, p 1.
20.
21.
Patent Office Hand Book, p 32.
Evidence of C V Deliwala of the Haffkine Institute, Joint Com
mittee on the Patents Bill, 1967: Evidence, Vol I, pp 451-52.
22.
Evidence of,N L 1 Mathias and A C Mitra of Neo Pharma Industries,
Joint Committee on the Patents Bill, 1965: Evidence, Vol II, PP
487-88. 493-94.
Information obtained from the Patent Office, Calcutta. Apparent
ly. the application by the Haffkine Institute, referred to earlier in
the text, was made before Section 23 CC was added in 1952.
24. According to Rule 32B (inserted in 1953) of the Indian Patent and
Design Rules, 1933. the Controller shall refuse the application, if
"the Controller is not satisfied that a prima facie case has been made
out for the making of an Order" (Patent Office Hand Book, pp
71-72)
25. For the provisions, see The Patents Act, 1970 (New Delhi, GOI,
Ministry of Law, Justice and Company Affairs, 1973).
26. A patent is sealed after it is granted.
27. For a discussion of the important provisions regarding drugs in the
Act of 1970 vis-a-vis the Act of 1911, see S K Borkar, “Patent Act,
1970 and Its Effect on Drug Industry in the Country”, in Annual
Publication (Bombay, Indian Drug Manufacturers Association,
1974).
28. "Applications Filed for Licences of Right under Section 88(2) and
88(4) of the Patents Act, 1970", in Journal of Patent Office Technical
Society. Vol 16. 1982, pp 80-81.
23.
Radical Journal of Health
Responsibility of Industry, Doctors and Government
amitava gnha
The proliferation of irrational and dangerous drugs in India has generated a well-informed and dynamic drug
consumer's movement. Of the several issues that it has taken up the issue of banning high dose oestrogen pro
gesterone drugs illustrates best its capability. On the other hand, the issue has also revealed inefficiency of the
drug control authorities, their inability to implement the rules in the book designed to protect the consumer.
This inefficiency on the part of government institutions is compounded by their close collusion with the drug
industry. The medical profession has also played a crucial role in opposing the ban oj these drugs. The article
highlights the unethical practices and actions of (he different sections who have been involved in pressing for
(he continued marketing of high dose EP drugs.
IN 1982, the Indian Council of Medical Research
recommended:
“Fixed dose combination of oestrogens and progesterone may be
totally banned m the country, even for the treatment of secondary
amenorrhoea as other substitute are available in the market for
management of secondary amenorrhoea”
Based on this recommendation, the ministry of health and
family welfare banned HDEP in June 1982. Today five and
half years after, the drug is freely available in India! The in
dustry, medical profession, courts of law even the govern
ment departments played their role in undoing the govt’s ban
order.
For the first time in India the question of banning of a
drug is being discussed and debated; consequently it has ex
posed the low level of ethics followed by the people involved
in the medico-technical establishment.
It must be pointed out that the issue of harmful effect of
a drug and therefore, its banning had never been raised by
the medical profession. Even the issue of harmful effect of
‘thalidomide’ was taken up by the journalists and the ripple
created in the so-called ‘lay press’ raised a wave which not
only washed away any effort to defend the crime made by
Gruanthal (its manufacturer) but exposed the menace of the
industry in collusion with certain famous opinion maker
medical personnels. In India similarly nothing is being said
or no action had been taken by the famous doctors or opi
nion makers against the horde of drugs banned in developed
countries but freely and legally available in India. It is again
the ‘lay press’ Onlooker which raised the issue through the
write up—“Pregnancy Test Drugs can Detorm Babies—Ban
them’’. The issue, thereafter was widely taken up by the press
and excepting one or two write ups till date none of them
had spoken against the ban of HDPE.
Role of Industry
Harmful effect of the drug on pregnant women was
delected as back as 1967 for. Pioneering task in this area had
been taken by Dr. Isabel Gal. She writes:
“The unfavourable effect of synthetic sex hormones on animal
reproduction was known long before the introduction of HPT pro
ducts in 1958. Despite this the manufacturers recommended HPT pro
ducts as a safe and reliable method of pregnancy diagnosis and gave
assurance that it does not interfere with the physiological course of
pregnancy”
Following the reports of adverse drug reaction with HDEP,
Rousel in 1970, Schering in 1971 and Organon in 1970 did
not refer to use of the drug for pregnancy lest in UK. The
government of India issued order that this drug should not
be used for pregnancy testing and the order be printed on
the labels of the drugs marketed. The drug was established
in India as an abortificient. It was promoted widely for in
ducing abortion. Even after the said order issued by the
December 1987
government, the companies promoted the drug through
marketing staff as an abortificient.
Immediately after the ban order was issed, Organon India
Ltd., (now Infar) placed a writ petition in Calcutta High
Court and was interested to see that the writ was not con
tested by the Drug Controller of India during its hearing.
It happened exactly as desired by the company and the case
was heard and injunction was passed exparte against the ban
order. It is interesting to note that neither M/s. Organon nor
M/s. Unichem and M/s. Nicholas contested the finding of
ICMR on the potential hazard of the drug but simply
challenged that the ban order was not issued in accordance
with the provisions of law. It was submitted that Sec. 18 of
Drugs and Cosmetics Act allows the state govts only to ban
a drug after issuing official Gazette Notification. That too
the Act only provides banning of misbranded, sub-standard
or adulterated drugs. This was an eye opener for the
legislators, who after much shouting from the consumers and
by some Members of the Parliament amended the law later
giving the same power to the Central Govt also. Even now
the question remains that HDPE or any harmful drug, if
banned, should be done according to which law?
The industry did a lot to utilise medical profession in their
favour. In the submission to the Supreme Court and high
courts, the company placed letters written by a number of
general practitioners and gynaeocologists stating that HDEP
should not be banned. In reality this was again done with
the help of the marketing staff who went to the doctors with
the draft of such letters and requested them to write accor
ding to the draft, a letter on their own letterheads. There
fore, it was found that the letters are not only the matically
similar but, so is the language and text of the letters. In some
cases the marketing staff of the companies wrote the letters
on the doctor’s letter pad and asked the doctors to sign them.
The text of these letters more or less read:
“1 support the order of the government in banning the use of high
dose E. P. Drugs in pregnancy' testing.
The drug is highly needed for treating secondary amenorrhoea,
dysfunctional uterine bleeding, endometriosis and dysmenorrhoea.
I have used this drug for a long lime and never seen any adverse effect.
I recommend that this drug should not be banned”.
The industry made another attempt to mislead the courts
on the information regarding the status of the drugs in dif
ferent countries. Organon (I) Ltd stateu that
“It’s not a fact that many countries have banned these preparations.
These preparations are available in countries like UK, West Germany,
France, most of the Western European countries a.id many South West
Asian and African countries” (Infar, 1987).
One can easily find out how far this is a fact. Table 1 will
clarify the position (UN List, 1986).
Infar (I) Ltd had no reply when asked at the public hear
ing why HDEP was not allowed to be marketed in their
55
parent country, Netherlands. Similarly, the company could
not say why the drug was not allowed to be introduced in
many other developed countries. The company’s honesty was
again questioned when Hermann Schulte-Sasse of the In
stitute for Clinical Pharmacology, Hamburg confirmed that.
“l\vo German pharmaceuticals marketed such drugs in
Germany but withdrew them at the end of 1979”.
Was the company confident that Indian consumers did not
have any access to information from 'civilised European
countries’? In fact Dr N N Roy Chowdhury, the president
of Federation of Obstetrics and Gynaecological Societies of
India (FOGSI) wrote to DCI to the same tune of Infar Co
that the drug was available in most of the developed coun
tries. He had also submitted a list although he did not care
to mention any reference. From this list it appears that ‘Shering’ (he does not know that the real name of the company
is Schering Aktiengesellschaft) market HDEP in West
Germany, UK, TUrkey, Japan, Argentina, Mexico, Belgium,
Denmark, Australia. The drug is not enlisted in the ‘Red List’
(Rote Liste) 1984, 1985, 1986, 1987, a list of drugs approved
by the government of FRG. Corroborative statement from
Schering issued by Dr H Richter informs that only one brand
of HDEP was marketed by them in third world countries
that two had been withdrawn from October, 1986.
In the absence of any system of dissemination of unbiased
information to the medical profession, the industry takes the
fullest advantage to misinform the profession to mislead
them with the help of their own tailored and distorted facts.
As regards high dose EP drugs, the industry had taken the
fullest advantage of this situation. The Voluntary Code of
Marketing Practices adopted by International Federation of
Pharmaceutical Manufacturers Association (IFPMA)
suggests that
“Scientific and technical information shall fully disclose the proper
ties of pharmaceutical products as approved in the country in ques
tion based on current scientific information..
“Information on Pharmaceutical Products should be accurate, fair
and objective, and presented in such a way as to confirm not only
to legal requirements but also to ethical standards and standard of
good taste.’’ (IFPMA)
Classical example can be sited from the promotional
literatures of Infar(I) Ltd as to how they have violated all
such codes of ethics. Even the Guidelines of Introduction
of New Drugs by Government of India say that ‘‘the pro
duct monograph should comprise the full prescribing infor
mation necessary to enable a physician to use the drug pro
perly. It should include description, actions, indications,
dosage, precautions, warnings, and adverse reactions.”
A product monograph of Orgalutin, a high dose of EP
Table 1: Status of EP Drugs Worldwide
Countries
1. Norway
2. Sweden
3. Finland
4. Federal Republic of Germany
5. USA
6. UK
7. Australia
8. Austria
9. Belgium
10. Italy
11. Greece
12. New Zealand
13. tfenmark
14. Bangladesh
15. Venezuela
56
Status
Year
Withdrawn
Banned
Banned
Withdrawn
Banned
Withdrawn
Withdrawn
Withdrawn
Withdrawn
Withdrawn
Withdrawn
Withdrawn
Banned
Banned
Banned
1970
1970
1971
1979
1975
1977
1978
1978
1978
1978
1980
1974
1982
1975
used to promote the drug to the doctors is captioned as—A
Woman’s Strength Is a Woman’s Weakness’.
On page three of the monograph to emphasise that the
drug is ‘safe for the patients’ the following lines arc men
tioned quoting a write up of two doctors Dr Choudhury and
Dr Mitra that with the use of the drug there was—
“No alteration in blood pressure.
No alteration in blood-sugar level.
No hepato-toxic effect observed”.
The said monograph had given-indications of composition
and dosage only but nothing was mentioned about precau
tions, warnings and adverse reactions.
If the warnings and precautions circulated by the company
a few years back are consulted, one can find the following
facts in the Therapeutic Index of the company and judge
how safe the product could be,
"Since such preparations may cause an increase in blood pressure in
predisposed women, this should be checked regularly. In case of serious
hypertension the use of the preparation should be stopped immediately!’
“Since the glucose tolerance may diminish during the use of
oestrogen/progestogen preparation, diabetic patients should be kept
under strict control.”
“Hepatic adenomas have been reported in women on oestrogenprogestogen combinations!’
This gives us an opportunity to question the standard of
ethics maintained by the company and of the two doctors
who had shamelessly concealed the facts.
It is also interesting to note that the manufacturers of
HDEP were really’ frightened of the ban order issued by the
governments. In.the Therapeutic Index printed by Infar(I)
Ltd at the time the ban order was issued, the company deleted
all HDEP drugs namely, Menstrogen, Menstrogen Forte and
Orgalutin. But their effort to promote the drug in the market
remained unhindered. The company has never forgotten to
mention these drugs in their price list!
Role of Statutes
Important statute applicable to import, manufacturing,
etc of any drug is the Drugs and Cosmetics Act, 1940 and
the Drugs and Cosmetics Rules, 1945. This is not only an
cient but highly inadequate also. Although it is a central
statute but it has given authority to the State Drug Con
trollers for approval of a drug for registration and sale.
Because of such inadequacy of law, the Central Drug Stan
dard Control Organisation has prepared ‘Guidelines on In
troduction of New Drugs’. We shall see how even the scanty
restrictions under the said Acts and Guidelines have been
violated by the industry.
Organon (India) Ltd, now Infar (India) Ltd had introduced
the HDEP about 20 years before. Earlier, these hormones
had been marketed separately as single ingredients or in com
bination as oral contraceptives. The drug was imported and
the definition of a ‘New Drug’ under Rule 30A of the Drugs
and Cosmetics Rules (DCR) says:
“The importer of a new drug when applying for permission shall pro
duce before the licensiong authority all documentary and other
evidences, relating to its standards of quality, purity and strength and
such other information as may be required by the licensing authority
including the results of therapeutic trials carried out with it!’ (Drugs
and Cosmetics Rules)
At the time of introduction of the drug it could be defined
as a Fixed Dose Combination (FDC) of the third group ac
cording to the Guidelines on Introduction of New Drugs.
This Guideline requires:
“(c) the third group of FDC includes those which arc already marketed,
but in which it is proposed either to change the ratio of active ingre
dients or to make a new therapeutic claim.
For such FDC, the appropriate rationale should be submitted to ob
tain a permission for clinical trials and reports ot trial should be
Radical Journal of Health
from the Country of Origin’. It would be almost impossible
The clinical trials required to be carried out in India before for Infar to submit such a ‘free sale certificate* as it was never
a new FDC is approved for marketing depend on the status allowed to be manufactured and marketed in Netherlands,
of the drug in other countries. If the drug is approved/ their country of origin.
Not only question of ethics but the failure of the regulatory
marketed, phase III trial is usually required to be conducted
in India. If it is not approved/marketed, trials are generally authorities and the lacuna in the laws are exposed when we
allowed to be initiated at one phase earlier to the phase of consider that the manufacturers have not cared to submit
to the minimum requirements of law and the government
trials made in other countries.
On going through the records one can easily find out that guidelines and have developed a large market of Rs 6.18 crore
the company never obtained any permission to initiate clinical yearly.
trials in India as required by Drugs & Cosmetics Rules
(through form 11 and form 12) for a test licence. No pro
Role of Doctors and Professional Bodies
tocols for any trials were ever submitted by the company—
A famous gyaenocologist C S Dawn has written in his
this is required according to the Guidelines for Introduction
of New Drugs. No case report forms were ever submitted. widely used text book.
Secondary amenorrhoea has had spontaneous cure rate in more than
As required in the Appendix III of the said guidelines the
50% cases where any treatment becomes empirical. New therapies
following reports on the studies are to be submitted by the
of pituitary gonadotropin, clomiphene and bromocryptine showed
company. (1) Human/clinical pharmacology (2) Exploratory
promising results in the treatment of selected cases where these are
Trials. (3) Confirmatory Trials. This was never done. Neither
indicated. Longer the secondary amaneorrhoea persists poorer
the company nor the Director of Drugs Control, Government
becomes the prognosis.
of West Bengal, who allowed the company to sell the drugs
He, as a professor, never vouched for the use of HDEP
in India can produce the following records relating to trials in secondary amenorrhoea in the classrooms and thus hid
supposed to have been conducted by the company ajid ap his other face. For, as a member of the Federation of
proved by the government authority.
Obstetrics and Gynaecological Societies of India (FOGSI)
Title of the Trial
he says exactly the opposite. He attended the public hear
Name of investigator and Institution
ings held at Madras, Delhi and Calcutta just to say that as
Objective of Tribals
Design of Study: open, single-blind, or double blind, non an eminent teacher and famous gynaecologist he had never
seen any adverse reaction with HDEP, and the drug was very
comparative or comparative, parallel group or cross over.
much needed for treating secondary ameneorrhoea.
Number of patients, with criteria for selection and exclusion,
whether written informed consent was taken.
His notoriety had not stopped here. After the Delhi public
Treatments given, drugs and dosage forms, dosage regiments method
hearing, he had submitted a study report on May 10, 1987
of allocation of patients to the treatment;
of a purported trial as a chairman of the family welfare com
Observations made before, during, and at the end of treatment,
mittee of FOGSI. The report was titled as ‘Use of Common
for efficacy and safety, with methods used.
Drugs in Pregnancy—Indian Experience’. It is only two-page
Results; exclusions and dropouts, if any, with reasons, description
monograph
but the dimension of the study is enormous as
of patients, with initial comparability of groups where appropriate,
clinical and laboratory observations on efficacy and safety, adverse the first paragraph of this report says:
submitted to obtain marketing permission.”
drug reactions.
Discussion of results: relevance to objectives, correlation with other
report/data, if any guideance for further study if necessary.
Summary and conclusions.
In order to maintain a minimum standard of ethics, trials
should be conducted with any drugs prior to their introduc
tion in the country. For the purpos. ‘licence for examination,
test or analysis’ has to be procured under Rule 21(c) which
was never done by Infar in this case. While applying for
manufacture of ‘New Drugs’ as per Rule 75-B of the DCR
one needs to supply “informations as may be required in
cluding the results of therapeutic trials carried out with it’’
(sub sec ii). This was never done cither bv the manufacturers
of HDEP.
// is strikim* to note that a controversial drug iv</y in
troduced in our country at the time when enough controver
sy was raised elsewhere. The manufacturers never cared to
conduct any trials in India. They were not only given licence
to manufacture such a drug but it was periodically renewed
by the drug control authority.
The guidelines for the introduction of new drugs per sec
9.2 under the title ‘Regulatory status in other countries’ state.
“It is important to state if any restriction have been placed
on the use of the drug in any other country, e g, dosage
limits, exclusion of certain age groups, warning about adverse
drug reaction”.
This was not done at any time—either at the time of in
troduction of the drug nor any time thereafter by Infar. On
the contrary, as discussed before, the manufacturers have at
tempted to misguide authorities with false information that
the drug is in use in many developed countries.
The guidelines also require (sec 9.3) a ‘Free sale Certificate
December 1987
“An all-India multicentric study was conducted during 1982 and
1983 by the Food, Drugs and Medicosurgical Committee of FOGSI
by the author as the chairman of the committee. Fourteen teaching
and rural centres participated in this study. Statistically controlled
protocol was prepared in consultations with Department of Hygiene
and Public Health, Calcutta. The protocol covers 78 factors”.
No further methodology and materials used in the study
was mentioned. The result was:
“There were 245 congenitally malformed newborns in this study.
The incidence of congenitally malformed newborns at various cen
tres varied from 2 to 10 per 1000 births”.
The report never mentioned directly as to how many preg
nant women were covered in the study. If the average in
cidence of malformation of newborn babies are considered,
according to the study, say five per 1000 and a total number
of malformed newborn babies reportedly were 245 then we
arrive at the fact that’in order to get such result, the trial
covered 49,000 pregnant women. That such a phenomenally
high number of patients were covered in only one year from
“14 teaching and rural centres” is noteworthy as this type
of trial is impossible even in developed countries.
In the Calcutta public hearing Dr. Dawn was asked that
in order to prove that his trial was not fake, he should sub
mit papers relating to the ten protocols as required by the
government. Dawn is yet to prove that it is not fake Obvious
ly the sole objective of producing such a report, which has
never been published in any professional journal was to prove
that no congenital malformation could be found with the
use of hormonal drugs during pregnancy'. When the govern
ment had banned the use of HDEP during pregnancy' and
the manufacturers have accepted it, the eminent doctors like
Dawn, C L Jhaveri, P K Khan, Sharma are all rejecting it.
57
Dr. Sharma of Delhi and Khan of Calcutta had without any
hesitation said at the public hearings that they would con
tinue to use HDEP for pregnancy testing. We are yet to see
the Medical Council of India react to such violations by
cancelling the registration of these doctors.
Dr. Jhaveri of Bombay, seniormost and famous gyaenocologist and many times president of FOGSI went even further
that estoprogin (HDEP) drug came as a blessing. It had
helped—in the second world war women who had been
assaulted by the soldiers had used HDEP drugs to abort
unwanted feluses! He stated in the Delhi and Bombay hear
ings that in his 40 years’ of gynaecological practice he had
used the drugs for inducing abortion and had not found a
single case of malformation of babies. His statements were
recorded by the Drug Controller of India during the public
hearings.
One may conclude that Jhaveri had committed punishable
offences in two cases. First, he had practiced MTP when it
was not legalised. Second, that he had violated the govern
ment order in using the drug on pregnant women. We are
yet to see that DCI take any action against Jhaveri. This sertugenarian doctor was so loyal to the arguments put by the
industry that he rushed to the dias at the Bombay hearing
to assault one speaker who was dissecting a point of law
placed by the industry.
A good number of famous gynaecologists have attend
almost all the public hearings leaving their generally over
crowded chambers and have said the same things repeatedly.
They had not cared to place any pharmacological and clinical
evidence in support of their statement that the drug is safe
and necessary.
In the Delhi and Calcutta hearing N N Roy Chowdhury,
president of FOGSI stated that the Federation had
unanimously adopted a resolution that the government
should not ban HDEP as they were safe and needed to treat
secondary amenorrhoea, dysfunctional uterine bleeding, en
dometriosis, menopausal symptoms, etc. and there was no
substitute for this drug. This statement was challenged by
a professor of gynaecology at Calcutta who as a member
of FOGSI wanted to know where and when such
‘unanimous’ resolution was taken. He also produced a state
ment by Dr J Mitra, Honorary Joint Secretary of FOGSI
which stales
“I am of opinion that high dose combination of oestrogen
progesterone should not be used during pregnancy.
I also feel that it is not essential to use this high dose combination
for treating gynaecological condition like dysfunctional uterine
bleeding, menopausal syndrome, etc. These combinations should not
be used indiscriminately as there are potential hazards”
Roy Chowdhury could not provide any proof to substantiate
his statement which was openly challenged.
Another instance of violation of minimum standards of
ethics can be cited with reference to the activities of P K
Banerjee, Honorary Treasurer of the Indian Medical Associa
tion. There are complaints by his professional colleagues that
he is an obedient supporter of Infar (India) and defended
the company’s interest in using anabolic sterioid for pro
moting growth in children. Banerjee wrote a letter to DCI
dated April 6, 1987 in the capacity of honorary treasurer,
IMA stating that the drug is much needed and harmless. On
inquiry, it was found that he had misused the good name
of the IMA. As the President of IMA stated that
I would like to mention that the letter issued by Dr Banerjee is his
own view and he is not authorised to communicate the views of IMA.
It is unfortunate that he has used IMA stationary for expressing his
personal views”.
It is necessary to mention here the role of the two doctors
who were involved with banning the drug—P Das Gupta,
Deputy Drug Controller and P K Dutta of World Health
58
Organisation. The Deputy DCI had no scruples about
favouring the industry openly. He tried to dilute the issue.
The Supreme Court had clearly asked the DCI to conduct
public hearings on banning of high dose combinations of
E P drugs. The Deputy DCI. at the Calcutta hearing, attemp
ted quite something else. He stated that the question of ban
ning HDEP should not be taken as an ego fight. Although
the Drugs Controller’s office had once banned it, it did not
mean that they should stick to such decision for- ever. He
also appealed to the gynaecologists that they should come
forward and suggest a ‘cut off1 dose for estrogen-progestogen
combinations. He wanted to confuse the issue on the ques
tion of high dose and low dose EP. He wrote letters without
the knowledge of DCI to FOGSI and Indian Associations
of Fertility and Sterility asking them to give their views on
a questionnaire on estrogen progestogen combinations, dated
March 23, 1987. He carefully dropped words ‘high dose’ in
the questionnaire. The questions are tailored in the follow
ing way which is suggestive of the desired answers.
I W hether fixed dose oestrogen and progestogen is necessary i
the management of secondary amenorrhoea?
2. What are the possible side effects of fixed dose oestrogen and
progestogen combination?
3 Do you feel that with a suitable cautionary label the use of fixed
dose of oestrogen and progestogen combination in pregnancy be
prevented?
4. Whether fixed dose oestrogen and progestogen combinations are
marketed in other countries?
5. Whether fixed dose oestrogen and progestogen drugs should be
banned9
6. Do you have any other suggestions on this issue?”
Nowhere in the above questionnaire had Das Gupta men
tioned 'high dose estrogen and progestogen’. It can be noted
that oral contraceptives are also fixed dose oestrogen and
progestogen combination. The president of these two
organisations C L Jhaveri and N N Roy Chowdhury made
full use of such questionnaires and pumped the arguments
of the industry in their reply which was considered by Das
Gupta as an important document at the public hearing held
at Bombay where Prem K Gupta, DCI who was absent at
the Calcutta public hearing said that this was done without
his knowledge and offered an apology for the action of the
Deputy DCI.
At the Calcutta hearing Das Gupta was openly suppor
ting the manufacturers of HDEP. He, along with Dr P K
Dutta helped the management of Infar to create a stir at the
public hearing and cancelled the hearing with a plea that they
may be physically assaulted when there was no valid reasons
to do so.
It is necessary to mention the role of other doctors and
professional organisations. The reactions of famous
gynaecologists and pharmacologists of UK on the need of
HDEP were different. Some of these doctors are members
of the Committee on Safety of Medicines. Some of the
responses are as follows;
I “I feel strongly that there is no justification for (he use of these
drugs, in amenorrhoea, menstrual irregularities and other
"gynaecological disorders”. Amenorrhoea and menstrual irregularities
require investigation and specific causes identified and, if necessary,
treated. If menstrual regulation is required in patients who have no
periods and who have irregular (and perhaps heavy and painful) period
then the treatment of choice is either the conventional low dose
estrogen-progesterone oral contraceptive pill, or progestogen alone.
1 think it would be irresponsible and dangerous to encourage the
use of high dose estrogen-progestogen combinations in management
of these gynaecological symptoms”. (Dr. Stephen Franks, Reproduc
tive Endocrinology; St Mary's Medical School, London).
2 ”1 was alarmed and disturbed to learn that high dose combina
tions of oestrogen and progestogens are still marketed, and used in
the Indian sub-continent. I understood that steps had been taken in
1983, to withdraw- these productsand 1 find it extraordinary that four
Radical Journal of Health
years later it is still possible to promote, prescribe and purchase such industry than on the harm to consumers. They forgot that
medicines.
(his hearing was most important because for the first time
They arc associated with significant risks to the factus, if ad merits and demerits of a drug were being publicly heard.
ministered during pregnancy. The Committee on Safety of Medicines They also forgot that their counterparts in developed coun
(of which I am a member) issued warnings to all doctors about these
tries have forced the companies to obey a minimum code
hazards in 1975 and 1977. The British Medical Journal drew atten
of
conduct and Infar was admonished by the International
tion to the problem in an editorial in 1974. As a result of these publica
tions, and of professional opinion, pharmaceutical companies in the Federation of Pharmaceutical Manufacturers Association for
UK voluntarily withdrew their products containing high dose oestrogen violation of its voluntary code however biased, weak and in
and progestogen from the market.’ (M D Rawlins, Professar of Phar effective that may be.
macology, University of Newcastle upon Tyne).
It has also true that the trade unions had palyed different
3. “I find that I am in complete agreement with the opinions ex role in different places. While at Madras and Delhi there was
pressed by Dr Steven Franks and Professor Rawlins and I have no no scope for their intervention they responded remarkably
reason to change my own views, as expressed therein. Perhaps the only positively at Calcutta. Unions of medical representatives, the
thing I could add is that now, with four years experience as a member Federation of Medical and Sales Representatives Associations
of the United Kingdom’s Committee on Safety of Medicines, I’d like
to emphasise Professor Rawlin’s point—that is, that these drugs would of India (FMRAI) and the Organon(I) Ltd Workers Union
be unacceptable in the United Kingdom, that our attitude is that the organised a demonstration in front of the gate of the Infar
obligation is on the pharmaceutical company to prove quality, safety factory. The workers attended it and the president of their
and efficacy of preparation and not on the drug regulatory agency union announced that if the company failed to convince them
Me they would
to prove the converse and that, while those drugs are certainly not that the drug cannot cause any harm tn thf*
banned in the United Kingdom, were any attempt to be made to in refuse to produce it. The represer/itivca ot ;mkAI appeared
troduce them I have very little doubt they would fail to secure a licence”.
before the public hearing and narrated how they were being
(Dr H S Jacobs, professor of Reproductive Endocrinology, The Mid directed by their employers to misguide the medical profes
dlesex Hospital Medical School and University College, London).
The Public H earings
Thus, famous professors of the medical institutions did
not hide their surprise and disgust at the use of the drug and
role of government regulatory authority, nor did a large
number of the specialists in Calcutta and Bombay hearing.
The DCI initially decided to close the public hearing after
Delhi. About 150 doctors including professors of
gynaecology and pharmacology wrote to the DCI to hold
the hearing at Calcutta as well. Initially there was no res
pond from the DCI. This gave raise to such a reaction that
at the instance of the Association of Health Service Doc
tors, West Bengal about 200 doctors assembled in a conven
tion condemned the activities of the DCI and resolved to
start a campaign against the drug manufacturer and the
government of India for not banning the hazardous drugs.
This compelled the DCI to announce public hearings at
Calcutta and Bombay four months after the Delhi hearing.
During the Calcutta hearing, a large mass action for ban
ning the drug took place. For the first time the trade unions,
doctors, consumers and health activists demonstrated before
a drug company and condemned them for production of
banned drugs. It was encouraging to see that for the first
time, famous doctors who had been vouching for the industry
were challenged by other well-known professors,
gynaecologists, pharmacologists.
At the Bombay hearing it was also quite amazing to see
that when Jhaveri said, that he would give an award to
anyone who could place any evidence of foetal malforma
tion by HDEP, it was accepted by other group of doctors.
The real drama took place at the Bombay public hearing
when this group of doctors placed a little girl and her mother
as evidence of the foetal abnormality and placed a letter
which had congratulated them for their effort to delect such
drug induced malformation of the baby. The.author of the
letter was none other than Dr. Jhaveri himself.
Koh* of People
Long back, after the publication of the write up in
Onlooker, certain health activists tried to take up the issue
but it could not spread Even when the issue reached the
Supreme Court, Vincent Panikulangara a lawyer from Kerala
had to fight for a ban quite alone.
In Madras. Delhi and Calcutta hearing some people ap
peared as ‘consumer activists'. Their expressed concern was
more on ‘illegal’ and ‘unjust* blames being attributed to the
December 1987
sion with partially or totally false information. They also
exposed how the Infar and Unichem had been entertaining
and spending money for providing travelling expenses of a
particular group of famous doctors who had been appear
ing before the public hearing on repeated occasions. They
also stated that the drug was sold by the companies without
any promotional effort. The companies are manufacturing
the drug and through their distributioin channel it is reaching
the outlets where it is automatically sold. The margin of pro
fit in this drug is among the highest.
In contrast to this, the role of the Shiv Sena Union of
Unichem at their Bombay factory not only favoured the in
dustry but workers openly threatened the audience that if
anyone spoke against their management, they Would be forc
ed to take drastic actions. There was a large number of Shiv
Sena activists at the Bombay hearing who had been booing
and shouting at the women’s grodp whenever they express
ed their concern which was often tinged with emotion. This
shows the difference in level of consciousness among the
workers of the two places.
There was remarkable response from womens groups. In
1979 some women’s groups of northern and western India
look up the issue. The issue of banning a drug cannot be
solely seen in terms of exploitation of female by male. It is
also not because Dr Isabel Gal was a women that she first
explored the hazards of the drug. The question of banning
a drug concerns the profit motive of industry and the low
standards of ethics of some eminent opinion-makers of the
medical profession in India. During the public hearings. Most
of the women’s groups identified the crux of the issue—that
the existing condition in our country is conducive to industry
government clique. Some of them asked a pertinent ques
tion: Why had the court not first banned the drug in the in
terim which is said to be causing danger. Who would be held
responsible for any damages which are being caused even
now (if at all) the drug is officially banned in future? They
have also declared that they would file litigations against any
future malformation of newborns and would ask for com
pensations from the Drugs Controller and the industry.
However the question remains that when there is dearth of
ethics among all levels of the decision/opinion-making in
the establishment can the judiciary remain un affected?
[While preparing (his paper help had been sought from the excellent
compilation of documents and different monographs prepared by Mira
Shiva. Coordinator, All India Drug Action Network.1
59
High Dose EP Drugs—II
The Socio-Political Dimension
imrana qadeer
The EP drugs issue has brought into focus the sickness not only of the legal system, but of the medical system
as well. How is it mat we are Jightmg a case which should not have arisen al all in a sane society? In reality
the very need for pregnancy testing is rooted in the maladies in the social situation and the inadequacies of the
health system. Thus the movement against EP drugs and other such technologies must be woven into the wider
political movement against a system which breeds, and protects such oppressive developments.
THE addition of high dose oesterogen and progesterone
combinations to the long list of oppressive technologies for
women is not recent. These drugs have been freely sold in
the market for some time now, even though scientifically
speaking—their use is not indicated. Its use however, has
created such havoc that the victims, that is some of the
women, could not bear it any longer. Their protests led to
the banning of the drug. The ICMR had already recommend
ed its ban as a drug for pregnancy testing and the court pas
sed a judgment banning its sale. These steps by the authorities
were brought to naught by the companies which used the
loopholes in the legal system. They obtained the right to con
tinue their business not because they proved the drug safe
but because they argued that the Drugs and Cosmetics Act
had no provisions to ban a drug (however lethal it might be)!
Their victory over the petitioners (women), the referral of
the case to the Drug Controller of India and the public hear
ings in the major cities have revealed a lot more about the
sicknesses of not only the legal system but also the medical
system.
This compels one to ask, how is it that we are fighting
a case which should not have been there at all in a sane
society? How is it that while life saving drugs are scarce,
dangerous drugs are so easily available over the counter?
How is it that the majority of those who flaunt the Hippo
cratic oath as a mark of their superior-professional ethics,
preferred to stay out of the controversy when the health of
their clients was being jeopardised? How is it that for the
sake of so called scientific advancement and the doctors’
right to chose treatment for their patients, needy people are
treated as guinea pigs whose lives seem to be of very little
value?
When we ask ourselves these questions, it is not difficult
to see that the issue is not confined to EP drugs but relates
to the very nature of technology which is being propagated
today in the area of population control. To give it scientific
neutrality this area of research is called ‘reproductive biology’
and constitutes a part of the larger field of ‘biotechnologies’,
all meant to intervene in natural biological and not social
processes. They do however, become tools in the hands of
some and thereby influence the social process in a way desired
by only those sections who are in control. One, therefore,
has to ask a very basic question, do the majority really need
these technologies? And if they do, what should be the limits
of their use?
In this age of modernity and high technology, such ques
tions might sound backward, even anti-technology, but they
are neither. Let us aSk ourselves why do we need pregnancy
tests? The reasons are simple enough.
60
1. These couples/women for some reason either do not
want to have a baby or on medical grounds need to know
their status so that adequate care may be given to them as
in the case of pregnancy in diabetic or heart patients or in
case of high risk mothers with high probability of con
genitally malformed or diseased foetus.
2. Apart from these medical reason yet another reason for
pregnancy testing is to make a timely choice for abortion
if the sex of the baby is undesirable.
If the right of a women to avoid a pregnancy is accepted,
then, why is it that despite years of research, in reproduc
tive biology and contraceptive technology, despite millions
of dollars that have gone into this research, we still do not
have a contraceptive which is safe for the user, sure and
cheap? The researchers have in fact sacrificed safety for
surety and costs have never really mattered. A good example,
is the use of NET-EN despite adequate evidence of its
dangers, and the free distribution of oral pills despite their
exhorbitant prices. Oral pills were accepted by the planners
of the National Family Planning Programme for use in pilot
projects for the benefit of rural women and Net-En was
approved for marketing in India. All this because the focus
had all through been, not on discovering or inventing safe
technologies but on pushing those which fulfilled certain
targets. Similarly, if we were serious about providing contra
ceptive or abortion services to women, these should have been
an integral pan of the most basic health services. This
however, is not the case. Despite all the glib talk about health
for all by 2000 AD and about full coverage of populations
with minimum health services (Primary Health Care), the
majority, specially the poor, still have no access to health
services (GOI, 1983). People are much more familiar with
targets, force, paycuts and withholding of increments for not
getting ‘cases’ rather than with choices in family planning
methods. They don’t seem to know that the country’s
health services were in fact meant to provide these choices
to them and all that goes along with making such a choice.
Yet another related issue is that a large number of women
cannot avail even such services as are available, even if they
want to. This is primarily because of the pressures exerted
by the family and their own insecurity within that structure.
Despite voluminous reports on the status of women, national
celebrations of the international womens’ year and huge
amounts of money going down the drain into the so-called
women’s upliftment schemes, the status of women remains
at a level where the majority have little say in matters as inti
mate as their own selves.
l^he problem of women who need the test for medical
reasons or for failure of contraception is not very different.
Radical Journal of Health
Haa they been given access to a good health service, the ques
tion of their becoming a prey to the greedy private practi
tioner, or the ill informed doctor would not arise. There are
any number of safe and equally cheap pregnancy tests that
the health service ought to be ] roviding to women who really
need it (EPfT, 1987).
It is not difficult to see then that the medical establishment
is not interested in safety for the user but in surety of con
traception. It is not concerned with making services acces
sible to people but wants to catch them as targets for surer
methods like sterilisation. It is not bothered about the poverty
or backwardness of the people but is geared to control them.
The second reason for using pregnancy tests was the need
to be selective about the baby’s sex. A couple detects pregnan
cy, goes for amniocentesis and then opts for abortion if it
is a female foetus. In Maharashtra alone, between 1982 to
1986 the number of clinics performing amniocentesis has in
creased from 10 to about 600. The estimated numbers of
abortions done for expelling female fetuses in 1985 has been
40,000 (GOI, 1986). This pattern, frighteningly prevalent in
most parts of the country, is yet another reflection of a social
malady. Instead of provoking its professional ethics and
fighting the evil openly, the medical profession chooses to
keep quiet or fights against restrictions over the use of am
niocentesis, in the name of freedom of the medical practi
tioners to choose the best for their clients. The medical
researcher on the other hand continues to add to the list of
oppressive technologies, techniques such as those used for
sex pre-selection which promotes the practice of discrimina
tion against female foetuses. At the same time they also make
the obstetrician the complete controller who now diagnoses
as well as dispenses and thus acquires godly powers!
These questions lead us to the reality that the very need
for pregnancy testing in the majority of the cases, largely
arises out of maladies located in the social situation as well
as the inefficiency and inadequacy of the health service
system. Focussing on this need and not its causes, finding
technologies for satisfying this need without touching its
causes, can at best be called a symptomatic approach to
tackling deeprooted problems. Such technologies in fact not
only divert attention from the real nature of the problem but
also provide cover for the system’s wider failures. Accepting
them and using them for controlling female fertility amounts
to accepting an out-right neo-malthusian strategy for the pro
blems of population.
EP Forte is not the only drug which falls under this group
of reactionary technologies. When in 1984 women protested
against amniocentesis the government had expressed much
concern at the loss of female foetuses and the exploitation
of women by “clandestine private practioners”. In a seminar
organised by the Additional Secretary and Commissioner of
Family Welfare in December 1986 at Nirman Bhavan, the
steps suggested to tackle the problem included (1) Legal
reforms, specially in the Medical Termination of Pregnancy
Act 1971, (2) Social awareness through educational program
mes and upliftment of women (3) Restricted permission for
doing amniocentesis to public institutions (4) More than one
doctor’s recommendation for such a test. The government’s
representatives were very sympathetic to these ideas but they
argued that the legal system could not be changed. This was
perhaps because the MTP Act provides for abortion in a
December 1987
cases where contraceptions has failed and there is no way
in which this could be disproved. It is well known that MTP
has become a technology in use for the family planning pro
gramme and it is no wonder that the government is not
inclined towards making this explicit. At the same time it
is impossible to introduce stringent measures within the legal
system without making the conditions under which abortions
take place more restricted and explicit. The government’s
reluctance to change the law is projected as the ‘helplessness’
of its legal system. It is ironical that a government which
passed the Muslim Women’s Bill despite all the opposition
and social presures should plead helplessness and invoke
‘social awareness’ to put an end to the misuse of amnio
centesis.
Yet another example is the wide range of technologies used
in Family Planing Programme starting from IUD, tubectomy,
oral contraceptives, abortions and laparoscopy. All of these
were considered for family planning and within the pro
gramme, acceptance and desire for family planning were
simply taken as issues of availability of technology. The pro
gramme for a long time refused to take into account the
major socio-economic dimensions of family. This very
narrow approach to the problems of population is obviously
not an un-intended accident. The waxing and waning attrac
tion towards compulsion at one time and incentives at
another time is in itself an indication of the limited range
of options within which given technologies are expected to
be effective. It also reflects the direction and nature of the
overall developmental policies.
The latest in the barrage of technology is the case of Indo
US Vaccination Action Programme (EPW, 1987, corres
pondence). In the health programmes for mothers and
children as well as the general population, vaccines have been
in use since independence. Despite the availability of these
well known technologies, the diseases against which they are
effective continue to kill and maim. The-only exception is
smallpox, a disease that continued for decades despite the
use of vaccines in this country. Finally, when it was con
tained, it was not only because there was a vaccine, but
because a better understanding of the epidemiology of
smallpox developed over time and provided an alternative
strategy.
Suddenly, however, the faith of a set of experts in vaccines
has been revived and they have signed a collaborative scheme
with the US. Will they now test better vaccines on the Indian
population? Even if we believe the argument that only
vaccines needed in India will be tested like the cholera vaccine
(or rabies and pneumonia vaccines etc.), we have to answer
a very basic set of question. Firstly, what is the use of giving
effective cholera vaccine to a people who are to perish in
drought, without food and drinking water? Even if cholera
is to be fought, have we shown that it is possible with the
use of vaccines alone, rather than together with the provi
sion of drinking water, food rations and sanitation? Over
and above all this, do we have an understanding of the
dynamics of morbidity and mortality caused by these diseases
and their load and extent to be able to predict costs, set
priorities and do some kind of monitoring? With obvious
contempt for even the rhetorics of ‘scientific rationality’
vaccine technology is being glorified. This is not because
what it prevents is our priority health problem but because
61
there is a technology which creates the aura of action and
concern for the suffering of people without really touching
the cause of that suffering.
These examples illustrate that again and again the system
clutches at technologies which promise relief from suffer
ing without really changing some of the social constraints.
Therefore, in the case of EP Forte and its widespread
usage, it would be wrong to blame the lack of continuing
education on non-availability of information to doctors.
These may be peripheral reasons, the main reason being the
underlying ideological bias of the ‘scientific rationality’
which is taught, accepted and propagated within the medical
establishment. It is because of this ideological regimentation
(where all technology available must be accepted and used
and ill health should be seen as a medical problem alone),
that the medical profession at large has failed to stand up
together and speak in the interest of its clients. A good
number in the profession have in fact taken advantage of
the trend to make their own profits in the shape of money,
position and security. This has been possible because they
have been backed by those interested in actively or passively
propagating technologies like EP Forte. The drug companeis
who use these doctors, also paralyse the legal system which
invariably finds itself ‘helpless and incapable’ of banning
killer drugs. The control machinery has become ineffective
and is listening to the ‘impressions’ and ‘personal experien
ces’ of the so called scientists (the senior medical practioners)
rather than to the meticulously collected objective evidence
presented by those who are demanding a ban on the use of
EP Forte.
Where the inappropriate usage of EP Forte (and othei
medical technologies) can be traced to maladies at so many
levels, then the issue is not of fighting against just one drug,
one test or one technique. The issue is of weaving this pro
test into the wider political movement against a system that
breeds, nurtures and protects oppressive technologies and
ignores those technologies which could be better utilised in
the interest of the people.
References
EPW, 1987: Why Ban High Dose EP Drugs? August 1, vol 21,
p 1274.
EPW, 1987: Correspondences “Why High Dose EP Drugs? vol 21, No. 31
p 1274.
GOI, 1983: Govt of India Ministry of Health and Family Welfare (1983):
National Health Policy, New Delhi Ministry of Health and Family
Welfare.
GOI, 1986: Report of a conference on sex determination Test and Amnio
centesis” Nirman Bhawan, Sponspred by Government of India,
Ministry of Health and EW Dept, of F.W. 19th Dec. 1980.
Economic and Political Weekly
A journal of current affairs, economics and other social sciences
Every week it brings you incisive and independent comments and reports on current problems plus a number
of well-researched, scholarly articles on all aspects of social science including health and medicine, environ
ment, science and technology, etc.
Some recent articles:
Mortality Toll of Cities—Emerging Pattern of Disease in Bombay- Radhika Ramsubban and Nigel Crook
Famine, Epidemics and Mortality in India—A Reappraisal of the Democraphic Crisis of 1976-78: Ronald Lardmois
Malnutrition of Rural Children and Sex Bias.- Amartya Sen and Sunil Sengupta
Family Planning and the Emergency—An Unanticipated Consequence: Alaka M Basu
Ecological Crisis and Ecological Movements.- A Bourgeois Deviation?: Ramachandra Guha
Environment Conflict and Public Interest Science: Vandana Shiva and J Bandhyopadhyay
i
(
Geography of Secular Change in Sex Ratio in 1981: Ilina Sen
Occupational Health Hazards at Indian Rare Earths Plant: T V Padmanabhan
Inland Subscription Rates
Institutions/Companies one year Rs 300, Two years Rs 575, Three years Rs 850
Individuals Only One year Rs 225, Two years Rs 425, Three years Rs 625
Concessional Rates (One year): Students Rs 125; Teachers and Researchers Rs 175
(Please enclose certificate from relevant academic institution)
[All remittances to Economic arid Political Weekly, 284, Hitkari House, Shahid Bhagatsingh Road,
Bombay 400 038. Payment by bank draft or money order preferred, Please add Rs 14 to outstation
cheques for collection charges.]
A cyclostyled list of selected articles in EPW on health and related subjects is available on
request.
62
Radical Journal of Health
Folio, Politics, Publicity, and Duplicity
Ethical Aspects of Development of Salk Vaccine
allan m branch
This paper is an historical account of the discovery, testing, and early distribution of the Salk polio vaccine.
The discovery posed fundamental dilemmas of medical research, pharmaceutical production and public health.
This paper assesses the ethical problems which arose, and examines critically their resolution.
The great public demand which the discovery of the vaccine generated created a need for federal control which
was only partly met. The federal government did not have sufficient institutional and legal mechanisms to assure
the safety of the vaccine and protect the public. This discussion illustrates the failure of the government to keep
pace with medical technology.
Reprinted from International Journal of Health Services, vol 8, no 2, 1978.
THE introduction of a new biological pharmaceutical
presents a host of medico ethical dilemmas. The debate
surrounding the nationwide influenza vaccination pro
gramme suggests only a few of the multifarious difficulties
involved. Each step in the process—from the initial funding
for research to the testing, licensing, commercial production,
and distribution of the drug—is wrought with serious
judgmental considerations of both a medical and moral
nature. If one accepts the public welfare as the preeminent
value in the discovery and distribution of a new drug, the
role of the government is of primary importance.
The history of the Salk polio vaccine is revealing in this
regard. The discovery marks an important episode not only
in the growth of immunology, but, most significantly, in the
history of public health. The demands made upon the
government and the government’s response to these demands
provide critical insights into the recent course of public health
in America. This paper will examine the history of the Salk
vaccine in light of the ethical judgments involved.1
The vaccine discovered by Salk in 1952 marked the
culmination of the efforts of the National Foundation for
Infantile Paralysis to secure an immunological agent against
polio. The Foundation had grown out of efforts to raise funds
for Franklin D. Roosevelt’s Warm Springs retreat during the
Depression. In consultation with public relations firms,
Roosevelt’s former law partner, Basil O’Connor, organised
a series of “President’s Birthday Balls” in 1934 with the
slogan: “Dance so that others may walk” (3, p. 16). In 1937
Roosevelt announced the formation of the National Foun
dation for Infantile Paralysis (NFIP) for the purpose of en
suring “that every responsible research agency in this coun
try is adequately financed to carry out investigations into
the cause of infantile paralysis and the methods by which
it may be prevented” (5). Basil O’Connor became the presi
dent of the new organisation. The creation of the Founda
tion signaled a major new direction in the history of
American medical philanthropy. The appeal for funds now
utilised sophisticated public relations techniques (6). Of
significance was the dramatic extension of the traditional
concept of philanthropy, as the National Foundation now
sought funds from everyone, not just the affluent. Radio
spots requested that dimes be sent directly to FDR in honor
of his birthday on January 30, 1938. More than 2,600,000
dimes “marched” into the White House, inundating the mail
room (3, p. 18). Thus was coined the title “March of Dimes?
The Foundation pioneered in the techniques of modern
December 1987
fund raising with its mass appeals, use of media, public rela
tions, and a corps of volunteers. The unprecedented doorbell
campaign—the “Mothers’ March on Polio”—began in
earnest; the Foundation put its cadres into the sheets. Their
ability to raise funds, even during the most trying economic
circumstances, must be rated remarkable. By the 1950s the
National Foundation had developed the perfect form of
philinthropy for the burgeoning consumer culture.2 The
concept of philanthropy as consummerism—with donors
promised personal benefits—was to a great degree the con
tribution of the March of Dimes.
Why did poliomyelitis become the rallying point for
millions of Americans? One logical answer is, of course,
Franklin Roosevelt’s personal battle with the disease. Despite
FDR’s attempts to conceal his infirmity, a new media age
made polio the most prominent of diseases. But Roosevelt
merely symbolised a more general perception that polio was
a peculiarly American malady. More dangerous in affluent
nations, polio became America’s target although other
diseases and medical afflictions were really more common.3
An increasingly child-oriented society could not tolerate a
disease which crippled its young.4 In addition, the National
Foundation had a remarkably powerful influence on the
whole direction of American medical research and health
care priorities, a topic that demands more attention than is
possible here.
There can be little doubt that the Foundation put its funds
into the right hands. Through the use of long-term, substan
tive grants awarded to eminent researchers and institutions,
the NFIP insured the continuity of polio research. By 1948
a series of important epidemiological studies had been made
under the Foundation’s auspices. Most important was the
discovery of Drs. John Enders, Thomas Weller, and Frederic
Robbins, all of Harvard University, that poliovirus could be
cultivated in nonnervous tissue (4, pp. 369-381; 9). This Nobel
Prize-winning discovery virtually assured that a polio vac
cine could be produced. A race, with bitter political and per
sonal overtones, ensued.
Development of Salk Vaccine
Dr. Jonas Salk began his research on polio immunisation
in 1951 under a grant from the National Foundation. Within
a year he had successfully immunised monkeys in his
laboratory at the University of Pittsburgh. Confident that
he had found the key to immunisation in a killed virus vac
cine, Salk proceeded to test his discovery on human subjects.
63
The first of these experiments was conducted on children
from the D. T. Watson Home for Crippled Children. Risk
was reduced by vaccinating these children, who had already
had polio and were thus immune prior to injection. Salk in
oculated 43 children with no adverse reactions. He later com
mented, “When you inoculate children with a polio vaccine,
you don’t sleep well for two or three months” (1. p. 139).
Salk continued his experiments at the Polk State School,
where he again inoculated children with his test vaccine.
Unlike the polio victims at the Watson Home, these children,
who were mental defectives, had no history of polio and thus
much lower antibody titer, significantly increasing the danger
of the test. The ethical standards applied here, though in no
way unusual in the 1950s, must be questioned. Dr. Tom
Rivers, one of the most eminent virologists in the history
of modern immunology, in reviewing an experiment similar
to Salk’s, voiced concern about the morality of such a test
(10, pp. 466-467):
I think that if someone wants to use adults as volunteers to try out
a new drug or vaccine, that is perfectly all right, provided that the
adult has been told about the nature of the disease he is exposing
himself to, has been completely informed about the nature of the agent
he is to receive, and has been told the chances for success or failure
. .. An adult can do what he wants, but the same does not hold true
for a mentally defective child. Many of these children did not have
mommas or poppas, or if they did their mommas didn’t give a damn
about them.
Fortunately, Salk’s confidence in the vaccine was borne
out by the results of these initial human tests. But Dr. John
R. Paul, in his definitive history of poliomyelitis, pointed
out what failure may have entailed (4, p. 418):
Had the experiments gone wrong at this point there might have
been a tremendous outcry. Some would have called it unnecessarily
hasty to use so many subjects all at once. . . And others would have
called it a crime to subject helpless children and adults to this sort
of experimentation.
It would seem from this analysis that an experiment on
human subjects is ethical if successful, unethical if a
failure—a dubious formulation. No government guidelines
or requirements for human testing existed at that time.
Salk’s success buoyed his faith in the vaccine. In presen
ting his findings to the medical community, he was, however,
more cautious (11):
Although the results obtained in these studies can be regarded as
encouraging, they should not be interpreted to indicate that a prac
tical vaccine is now at hand. .. .It will now be necessary' to establish
precisely the limits within which the effects here described can be
reproduced with certainty.
The task of establishing the effectiveness and consistency' of
the new vaccine would not be Salk’s alone.
Planning Field Trials
By the middle of 1953 the National Foundation had begun
devising plans for a mass nationwide trial, the largest of its
kind ever attempted. The Foundation established a Vaccine
Advisory Committee (VAC) of eminent physicians and
researchers headed by Tom Rivers to oversee the field trials.
The NFIP’s decision to conduct such a field trial meant that
serious consideration of other forms of immunisation, par
ticularly the attenuated vaccine, no longer was possible
(4, pp. 423-425). The Foundation’s position, though clearly
understandable in light of the embryonic nature of attenuated
vaccine research, sparked controversy and aroused bitterness.
64
From this time onward, criticism of the Salk vaccine would
be an indeterminate mixture of scientific judgment and per
sonal animosity.5
The National Foundation conducted affairs on a grand
scale; the field trials slated for early 1945 were to be no ex
ception. The NFIP with its newly created Vaccine Advisory
Committee proceeded to design the trials in a direct, almost
autocratic manner. After his initial discovery, Salk found his
influence diminishing over subsequent decisions concerning
testing, as did a host of other scientific advisers to the Foun
dation. Basil O’Connor, anxious to move forward with all
possible speed within the bounds of safety, pushed the VAC
in the singular direction of conducting a definitive test (10,
pp. 495-500).
Scientific advisers dashed over the design of the trials.
Originally, the Foundation planned to vaccinate volunteers
and compare the rate of paralytic polio among this group
to a control group of nonvaccinated children. This formal
had the advantage of being easy to administer and evaluate,
and in addition gave all volunteers the potential benefit of
the vaccine. The Vaccine Advisory Committee insisted,
however, that a “double-blind” test was necessary to eliminate
the socioeconomic bias of the volunteer group and thus pro
vide a scientifically unassailable evaluation. Under this test,
half the volunteers would receive vaccine, half placebo.
This decision infuriated the increasingly confident Salk
who called the double-blind test a “fetish of orthodoxy. .
Salk clearly exposed the ethical dilemma of using a placebo
in an impassioned letter to O’Connor (1, pp. 191-192):
. .if we are aware of the fact that the presence of antibody is
effective in preventing the experimental disease in animals and in man,
then what moral justification can there be for the purpose of deter
mining whether or not a procedure that produces antibody forma
tion is effective. [?] I would feel that every child who is injected
with a placebo and becomes paralysed will do so at my hands.
Such an experiment, argued Salk, “would make Hippocrates
turn over in his grave.”
It is not difficult to sympathise with Salk’s viewpoint. With
a double-blind test the effectiveness of his vaccine would
essentially be proven by the contraction of polio among those
children who received placebo. But the emotional content
of Salk’s plea would also seem to indicate the importance
of removing the test from the hands of the discoverer. In a
sense, Salk favored an early limited distribution of his vac
cine as a test for efficiency, not a carefully controlled, scien
tifically conducted examination. Sure of the safety and ef
fectiveness of his vaccine, he actually jeopardised its full ac
ceptance in the medical community. This is not to question
Salk’s scientific ethics or his personal morality, but rather
to suggest the difficulties of participating in the evaluation
of one’s own researches.
Though the National Foundation took full responsibility
for the field trials, the VAC commissioned Dr. Thomas Fran
cis of the University of Michigan to evaluate the trials. Fran
cis, a pioneer in the fields of microbiology and immunology,
commanded unquestioned respect in the scientific communi
ty. The Foundation assured the University of Michigan am
ple funds to assist in Francis’ evaluation. He demanded com
plete control of the evaluation—with no outside pressure,
timetable, or supervision—and O’Connor agreed to these
stipulations. Francis also insisted on an injected control
Radical Journal of Health
group in at least some states. The decision to have Francis
assess the vaccine insured an irreproachable trial.
Before a trial could be attempted, however, the difficult
transition from an experimental, laboratory-produced vac
cine to a consistent, commercially manufactured vaccine had
to be negotiated. Until commercial laboratories could pro
duce vaccine, all talk of a field trial was really premature.
Although the National Foundation contacted five major
pharmaceutical companies to produce vaccine for the field
trials, a complete draft of the requirement for production
did not evolve until early 1954, only several months before
the trials began (1, pp. 207-211). The Vaccine Advisory Com
mittee supervised the shift to commercial production, mak
ing two critically important recommendations. First, the
Committee required that Salk conduct an initial trial on at
least 5,000 children using commercially produced vaccine
before undertaking nationwide trials. And secondly, 67//com
mercial vaccine for the field trials had to undergo safety tests
in three laboratories—the producers’, Salk’s and the U. S.
Public Health Service’s Division of Biological Control (12).
The decision to test commercial vaccine in the federally
operated lab represents the difficulty of the government’s
position. The government had no legal role in the trial; no
licence was required for such an experiment. The Food and
Drug Administration only required that the test drug be safe,
not necessarily effective(13). A major medical advance was
in the making, with the government’s only capacity an essen
tially extralegal one. Moreover, when it came time for the
licensing of the vaccine, the Public Health Service would be
in the dark. “We wouldn’t know enough about the vaccine
and the ins and outs of its manufacture”, remarked a Public
Health Service official. “We would not be able to act on
licence applications for months. But the public would want
action in hours” (1, p. 209).
With no official role in the testing of the vaccine but badly
needing most information, the Public Health Service gladly
accepted the functions allocated by the Vaccine Advisory
Committee of the National Foundation. Indeed, the Divi
sion of Biological Control, under the direction of Dr. William
Workman, scrutinised procedures to the point of threaten
ing the trials. Workman and other government officials
realised that, although they had no legal sanctions, they had
the responsibility of insuring a safe, effective vaccine (1, p.
208). Moreover, the National Foundation recognised the im
portance of having the blessing of the Public Health Ser
vice before conducting its trials.
Opposition to Trials
Scientific opposition to Salk’s vaccine remained for
midable as the trials approached. Some scientists had dif
ficulty duplicating Salk’s inactivation process in their own
labs, while others questioned the viability of a killed virus
vaccine. Dr. Albert Milzer had been unable to reproduce the
Salk vaccine in his laboratory at the University of Chicago.
He repeatedly found live virus in the vaccine—an ominous
result. Dr. Albert Sabin, at work on an oral, attenuated vac
cine, became Salk’s chief antagonist. Only one month before
the field trial was set to begin, Sabin called the test
“premature”. Salk and the National Foundation attempted
to combat the criticism: “I give every possible assurance I
can and that medical science can that the antipolio vaccine
December 1987
will be safe. I will personally be responsible for the vaccine”,
declared Salk (14, 15).
More troublesome than this criticism, however, were the
continued difficulties of the commercial producers in their
attempts to replicate Salk’s vaccine en masse. Scientists at
the Public Health Service’s Division of Biological Control
harbored serious doubts about the abilities of the manufac
turers to produce consistently safe vaccine. This reflected,
in part, inexperience in the histopathology of polio (10, p.
513). But it also revealed a very real production problem. In
March 1954, Dr. William Workman suggested that the field
trials be postponed:
I again come to the conclusion that the specifications and minimum
requirements. . .arc inadequate to assure the reasonable regularity of
production of a vaccine of acceptable safely to be used in the field
study. Under the circumstances, I cannot escape the feeling that an
occasional lot.. .which does pass the test, may actually contain liv
ing virus and be unsafe for use. My recommendation is that the pro
posed field studies be postponed until—(1) specifications and
minimum requirements can be revised to give greater assurance of
the safety of the final product; (2) it has been shown that the vaccine
prepared in accordance with such specifications meets acceptable
criteria for safety (1, p. 221).
It should be emphasised, however, that the government had
no legal means of postponing the trials. The National In
stitutes of Health and the National Foundation agreed that,
rather than revising the safety tests themselves, companies
must produce eleven consecutive lots of safe vaccine for any
to be acceptable for use. With this agreement, plans pro
ceeded for the field trials.
Despite the persistent opposition within the scientific com
munity, the National Foundation and the press stimulated
public optimism for the vaccine’s success. The dual role of
the National Foundation—philanthropic and scientific—
created tensions. The profusion of positive press release,
essential to fill the Foundation’s coffers, jeopardised scien
tific judgments (3, pp. 82-85). The National Foundation an
nounced publicly the plans for a mass field trial months
before a commercial laboratory had produced any vaccine
(16).
The press played upon the drama of the situation; no
medical discovery before or since has been covered as intense
ly. Beginning in 1953, progress in the vaccine’s development
was regularly front-page news in the New York Times. Press
reports were often filled with speculation (17):
If the vaccine fulfills the hope that at last a way has been found
to cope with poliomyelitis as effectively as public health officers cope
with smallpox or typhus, Dr. Salk will have scored one of the greatest
triumphs in the history of medicine.
Although Salk and the National Foundation attempted to
discourage such optimistic conjecture, Basil O’Connor’s
euphoria could not be contained. He declared that the
development of the vaccine had brought the fight against
polio to the “verge of victory” (18). The New York Times
Magazine called the trials the “climax of a stirring medical
drama” (19).
The vaccine’s notoriety undermined the control of the
scientific community. The public now clamored for the vac
cine, making it increasingly difficult for scientists with reser
vations to resist the demand for mass testing. Sabin’s attacks
on the vaccine, became more personal in nature: “Let us not
confuse justifiable optimism with achievement” (20). And
Salk’s defence became less scientific: “I have the courage of
65
my convictions. 1 couldn’t do it unless 1 was more critical
of myself than others are of me. It is courage based on con
fidence, not daring, and it’s confidence based on experience”
(21). Salk continued to announce that he would take “per
sonal responsibility” for the safety of the inoculation—a
courageous, if ill-advised stand (22). The New York Times
felt qualified to endorse the trials, remarking (23):
No matter how important a medical discovery may be. there are
always skeptics who try to strip it of importance. We need these skep
tics, but sometimes they may be nuisances.
At this point the skeptics were threatening the test. Several
states withdrew, from cooperation in the trials after Walter
Winchell announced on national television and radio that
the vaccine “may be a killer” (24).
This is not to argue that the press and public should have
no role in a medical discovery, but rather that, in this kind
of atmosphere, where public demands and expectations are
great, sound scientific judgment may be jeopardised. The
Sa/k vaccine was sold to the public before its safety and ef
ficacy were proven.
The National Foundation must bear some of the respon
sibility for the public fervor which surrounded the field trials.
Perhaps the most objectionable of all the Foundation’s pro
nouncements was that the test was exclusively designed to
test the efficiency of the vaccine. According to the Founda
tion, safety had already been conclusively demonstrated. In
light of the production difficulties, this was a particularly
bold assertion. The NF1P struck the word “experiment” from
its literature; this was a “trial” vaccine, not an “experimen
tal” vaccine. Although the test was conducted on a volun
tary basis, the quality of informed consent is thus highly
questionable.6
On April 25, 1954 the Vaccine Advisory Committee set
up final guidelines, giving its approval for the trials. The
United States Public Health Service issued the following
statement (26):
We believe (hat the judgment of (he Vaccine Advisory Committee
is sound and that the National Foundation for Infantile Paralysis is
justified in proceeding according to the Committees recommendation.
The next day the field trials began. With more than 1,800,000
children participating, the trials mark the largest clinical test
using human subjects in the history' of medical science. No
medical experiment ever held such public attention. Accor
ding to a Gallup Poll conducted in May 1954, 90 per cent
of the American people knew of the field trials, more than
could identify the full name of the President of the United
States (1, p. 268).
The test, conducted in 45 states, used placebo controls in
84 areas and observed, nonvaccinated controls in 127 areas.
More than 400,000 children received three injections; about
200,000 of these actually received salt-water placebo injec
tions rather than the test vaccine. Along with blood samples
to test antibody titer, Dr. Thomas Francis now had the in
formation needed for a conclusive evaluation of the vaccine
(1, pp. 238-261).
Speculation was rampant concerning the results of the field
trials, but Francis promised no annuoncements until the
spring of 1955. He had more than 144 million pieces of in
formation to assemble and review. Some days the Evalua
tion Center’s morning mail filled an entire elevator (1, p. 255).
A critical problem faced the National Foundation during
66
this interim penoa while awaiting Francis’ report. Without
a federal licence (which could not be obtained until the vac
cine was finally evaluated) and without advance orders, the
pharmaceutical companies could not afford to continue to
produce vaccine. It was not difficult to foresee a situation
in which the vaccine would be found to be safe and effec
tive, and yet there would be no vaccine available for the 1956
polio season. Basil O’Connor, with typical boldness, ordered
S 9 million worth of vaccine from six pharmaceutical
companies—an expensive gamble on the vaccine’s approval.
Of course, if the Congress had been willing to allocate funds,
this risk could have been avoided. But the government seem
ed content to let the National Foundation carry the ball.
On April 12. 1955, the tenth anniversay of Franklin
Roosevelt's death, Francis released his evaluation, one of the
most comprehensive epidemiological studies ever conducted.
According to Francis, the safety of the vaccine was “power
fully affirmed” (27, 28). This is an interesting observation
in view of the National Foundation’s reluctance to consider
the trials a test of safety. Francis found the vaccine 80 to
90 per cent effective in placebo-controlled areas, slightly less
in observed controlled districts (28, pp. 15-19). In short, the
vaccine appeared to be a tremendous success. The nation
celebrated; for many parents, it seemed, the anxious sum
mers were over.
The successful development of the polio shot characteris
ed the Eisenhower years as the moon shot did a later era.
The image of the scientist-hero, unhampered by government
intervention, held great appeal. The press proclaimed Salk
a national demigod, while some colleagues, resentful of all
the attention he received, suspected him a demagogue. The
vaccine became a perfect cause for an age in which ideology
was suspect.' The scientific atmosphere of the 1950s was
wrought with Cold War overtones. The vaccine, an affirma
tion of American scientific and technological progress, was
viewed as a triumph of the American system. American
science, pragmatic and purposeful, demonstrated the con
tinued viability of the promise of American life.
In Washington, Ms Olveta Culp Hobby, Eisenhower’s
Secretary of Department of Health, Education, and Welfare,
signed licences for six companies to produce vaccine. These
companies had, of course, been producing vaccine all along;
the licences gave them authority to distribute it.8 The Na
tional Foundation’s vaccination programme for school
children began immediately, with youngsters who had receiv
ed placebo during the field trials given top priority. For all
intents and purposes this should have been the dramatic con
clusion to the conquest of polio. Unfortunately, it was not.
The Cutter Crisis
On April 26, 1955, two weeks after Francis’ Ann Arbor
proclamation of safety, five cases of paralytic polio were
reported among children who had just received vaccine. All
five victims, it was found, had received vaccine from the Cut
ter Laboratories in California. Surgeon General Leonard
Scheele requested that Cutter recall all its vaccine pending
an investigation. Remarkably, the government had no power
to order the Cutter Labs to withdraw the vaccine, but Cut
ter readily complied. The infamous “Cutter Incident” would,
however, eventually encompass 25 states and Hawaii, 260
cases of polio, and 11 deaths (1, p. 316).
Radical Journal of H:a!th
These cases of polio cast an ominous cloud over the Salk
vaccine, the National Foundation, the pharmaceutical com
panies, and the National Institutes of Health. What had gone
wrong with the most rigorously tested drug in medical
history? The most obvious cause of the problems was that
the careful triplicate testing of the field trials had not been
continued for the licensed vaccine (12, pp. 329-331). Writ
ten protocols submitted by the manufacturers to the Divi
sion of Biological Control were the only legal requirement.
The Division had the right to make spot checks, but did not
exercise this option. Moreover, the consistency standards of
repeated safe batches which had been devised for the field
trials were not required of licensed vaccine. In brief, safety
precautions for commercially produced, licensed vaccine fell
far short of the guidelines used for the field trials.
During a series of meetings of top virologists and advisers
called together by Surgeon General Scheele, it was decided
to let the vaccination programme continue. But this consen
sus began to erode quickly. Dr. John Enders, regretting his
approval for continuing the programme, wrote to Dr. William
Sebrell, the Director of the National Institutes of Health (32):
1 am forced to conclude that active virus might be present in cer
tain finished lots of vaccine prepared by any or all of the manufac
turers concerned. I cannot, therefore, longer assert my confidence that
the poliomyelitis vaccine now being distributed and injected consists
solely of inactivated vaccine and in consequence, of harmless virus.
On May 7, Scheele requested that the national vaccination
programme be suspended pending further studies.
Scientific criticism of the Salk vaccine intensified. In June,
Enders and Sabin testified before a House subcommittee in
vestigating the crisis that the vaccination programme should
be stopped and the licences withdrawn until safety could be
conclusively proven. But they were overruled by an equally
eminent group of scientists who expressed confidence in the
quality of the vaccine if properly produced (33).
On June 9, Scheele released a Public Health Service
“Technical Report’’ on the Salk vaccine, an attempt to ex
plain and correct the problems which produced the Cutter
crisis. The “white paper”, though not a complete whitewash,
was carefully written to avoid directing blame (34).
The Salk vaccine applies new principles in the production of vital
vaccines. The speed of its development, which reflected the increas
ed tempo of all medical research, created problems in biologies con
trol amenable to solution only with the accumulation of knowledge
and experience. It is likely that problems of equal complexity will be
raised by the development of other new vital vaccines.
This analysis obscured the inadequate preparations made by
the Public Health Service for testing the vaccine. Despite the
easily predictable demand for the vaccine, the Bureau of
Biologies staff remained at only 35, insufficient to carefully
scrutinise the commercial production process. Moreover, the
protocols required of manufacturers did not provide enough
information for proper safety-evaluation. The contrast bet
ween the careful tripartite testing of the trial vaccine and the
tesung of the commercial product is a remarkable example
of the lackadaisical attitude of the government toward
biological control.
The irresponsibility of the Cutter Laboratories must not
be overlooked in evaluating the crisis. Repeated difficulties
in producing safe vaccine were experienced by the Cutter
Labs; 9 out of 27 lots produced had contained live virus and
were discarded. Yet Cutter failed to report this inconsisten
cy to the Bureau of Biologies; the company only submitted
December 1987
protocols for batches which passed their safety test (34). Cut
ter officials never asked for assistance from NIH or Salk.
Their ethical commitment to produce safe vaccine must thus
be seriously questioned. But it must also be remembered!hat
they acted entirely within the letter of the law. The NIH had
no consistency requirement and did not require reports on
discarded vaccine or production difficulties.
The Public Health Service’s “white paper” explained the
manufacturing problems in terms of inadequate sensitivity
of the safety tests (34, p. 17):
Each producer had had difficulties in processing and testing
materials at various stages of production. Because some lots were ob
viously unsatisfactory they were not submitted for release, and
therefore no protocols on them were submitted by the manufacturers.
These experiences showed the need for more sensitive and better con
trolled testing methods, and for greater attention to the history of
consecutive lots.
The Public Health Service revised the minimum requirements
for production in light of the Cutter incident, making them
mandatory standards. The Division of Biological Control
was reorganised, becoming the Division of Biologies Stan
dards with larger facilities and a fourfold increase in staff.
The relationship between the commercial producers and
the federal government lay at the heart of the Cutter inci
dent. This association became the target of serious investiga
tions in the days following the tragedy. Victor Haas, the
Director of the National Microbiological Institute, a divi
sion of NIH, evaluated the government-pharmaceutical con
nection in a series of memos to Sebrell in May 1955.9 Haas
argued that the responsibility for safety must ultimately rest
w'ith the manufacturers, and that the government could not
(and should not) participate intensively in the safety testing
of biologic products (35):
It has been lhe principle of operation that (his intensive panicipation in what is essentially a part of the manufacturing process, pro
perly should be only a temporary activity for the Laboratory of
Biologies Control. Once it has been established that manufacturers
can produce safe material (and production experience and field trials
of last summer formed the basis for licensing manufacturers for polio
vaccine), this principle of operation would assume that periodic plant
inspection, knowledge of the capabilities of supervisory personnel,
review of protocols, and spot-testing of materials would suffice to
assure us of continuing acceptability of any product within the limits
imposed by available knowledge and human acceptability to error.
Intensive and continuous testing in government laboratories,
Haas believed, would destroy industrial initiative and respon
sibility. According to his evaluation, more testing and inspec
tion would not have prevented the Cutter incident. This is
a dubious assertion, for certainly the manufacturing dif
ficulties experienced by Cutter and the other pharmaceutical
companies would have been revealed, raising questions of
safety.
Finally, Haas suggested that it would be improper to over
react to the Cutter incident by revising existing standards of
control. He ascribed the current fervor to the tremendous
publicity which the polio vaccine had generated (35):
Had the poliomyelitis vaccine been used on the same quantitative
scale that applies to other biologicals and had an incident occurred,
there would have been very little attention given it other than by the
constituted authorities. The many factors which have gone into creating
a demand for a safe and effective poliomyelitis vaccine, which would
be available at the earliest possible time, should not force us to aban
don careful and sound judgment as to what is the best method for
the operation of biological control over the years.
The Cutler incident exposed the inherent weakness in the
67
argument for governmental laissez-faire with regard to
biologies control and pharmaceutical production. The
limited role of the federal government clearly reflected the
Eisenhower political philosophy. Olveta Culp Hobby even
tually lost her job, largely because of the vociferous criticism
of her handling of the vaccine programme. In addition, the
government’s action was circumscribed by the miniscule legal
powers of the Public Health Service, essentially unrevised
since 1902, a time of relatively primitive pharmaceutical pro
duction. The government continued to assume that industrial
interest in producing a safe product would ensure the public’s
safety.
In view of the federal government’s minor role, the
National Foundation assumed massive responsibilities in the
development and distribution of the vaccine. Combining the
functions of fund-raising, research, testing, and distribution,
the National Foundation often found its multiple roles con
flicting. Although well-intentioned, the publicity mill created
an atmosphere in which demand threatened to outstrip sound
scientific decision making. In such an environment, ethical
questions can become obscured. The field trial, for exam
ple, though brilliantly engineered and promoted, and
meticulously evaluated, lacked truly informed consent.
The ethical aspects involved in the development and
distribution of the Salk vaccine are varied and complex, and
the historian must be leery of second-guessed, overarched
generalisations. But three key issues which demand continued
attention emerge. First, testing with human subjects presents
a series of problematic considerations, from the suspect use
of mentally defective children to the use of healthy, parentvolunteerd youngsters. High ethical standards for defining
risk-benefit ratios must be exercised in such investigations;
use of placebos complicates such assessment. Moreover, in
formed consent is liable to compromise (36). Second, the
obligation of pharmaceutical companies to manufacture safe
products cannot be assumed, especially when pressures to
market a new drug become intense. The third point is most
striking: the federal government’s minimal role in a major
scientific advance. Although the government cannot be the
final arbiter of ethical medical judgment, it is the only body
which can provide a central direction and standard for these
practices. By abdicating a more active role, the government
invited the possibility for crisis. The Salk episode seems to
indicate a less than complete commitment by the government
to the public welfare.
In the years since the discovery of the Salk vaccine, the
problems of pharmaceutical control have expanded rather
than diminished. The capacity of the government has remain
ed limited in overseeing industry. The Government Accoun
ting Office, Congress’ investigative arm, recently attacked
the lax attitude of the Food and Drug Administration’s drug
testing (37, 38). According to the GAO’s report, human sub
jects are exposed to unnecessary risks and the FDA has ap
proved new drugs for public use on the basis of highly ques
tionable data. FDA attempts at self-investigation have pro
ven largely useless (39). The FDA has failed to enforce its
standards and, according to many reports, has served as a
lackey to the major pharmaceutical companies (40). In its
mission of public protection, the FDA, by any standards, has
proven to be grossly inefficient.
The history of the Salk vaccine, from the initial research
68
through testing and production, speaks clearly to the pre
sent. The institutional connections through which a new drug
is channelled from laboratory to market remain uncertain,
subject to frequent short-circuit. The time between discovery
and production has steadily decreased, augmenting the dif
ficulties implicit in regulation. Most importantly, the federal
government has tailed to keep pace with the rapid innova
tions in medical and pharmaceutical practice, at great cost
to the public welfare.
[Acknowledgements— I should like to thank Harold
Fruchtbaum and Alan Gardner for critiques of earlier drafts
of this paper.]
Notes
1.
Several studies of the development of the Salk vaccine have been
written, although none is definitive. The most comprehensive of
these is Breakthrough: The Saga of Jonas Salk by Richard Carter
(1). Rich m detail, though weak in analysis, this book was par
ticularly helpful in my study Also recommended are John R.
Wilson’s Margin of Safety (2) and Aaron K. Klein’s Trial By Fury:
The Polio Vaccine Controversy (3). The definitive medical history
of poliomyelitis is A History of Poliomyelitis by John R. Paul (4).
The archives of the National Foundation have unfortunately
been closed to researchers. This rich collection of materials con
tains valuable information pertaining to the development and
distribution of the Salk vaccine.
2. For a more extended analysis of the implications of consumer
culture, see reference 7.
3. Nations with high standards of sanitation and personal hygiene
actually prove to be more susceptible to enteric viral infections
such as poliomyelitis (4, pp. 364-365).
4. For an explanation of attitudes toward children in the postwar
era, see reference 8.
5. See references 1 and 2 for extended discussions of the bitter rela
tionship between Salk and Dr. Albert Sabin of the University
of Cincinnati.
6. Parental consent was required for a child to participate in the
trial. Excellent essays on informed consent and human testing
are contained in reference 25.
7. Excellent discussions of political and cultural life in the 1950s
are contained in references 2 and 30.
8. One of the six companies was the Cutter Laboratories of Berkeley,
California. The Region Oral History Office of the University of
California at Berkeley recently completed an oral history memoir
with individuals from this organisation, documenting its involve
ment with the vaccine (31).
9. These memoranda, marked “confidential” have only recently
been opened to researchers as a result of a Freedom of Informa
tion suit. They are a highly valuable source for deciphering the
government's view of its role in the development of the vaccine
(35).
References
Carter. R. Breakthrough: The Saga of Jonas Salk. Trident Press,
New York, 1966.
2. Wilson. J. R. Margin of Safety. Doubleday. New York. 1963.
3. Klein, A. E. Trial By Fury: The Polio Vaccine Controversy.
Charles Scribner’s Sons, New York, 1972.
4. Paul, J. R. A History of Poliomyelitis. Yale University Press,
New Haven, 1971.
5. New York Times, September 23, 1937, p. 3.
6. Sills, D. L. The Volunteers: Means and Ends in a National
1.
Radical Journal of Health
Organisation, pp. 149-175. Free Press, Glencoe, III.. 1957.
G. Braziller, New York, 1970.
Leuchtenburg. W. E. A Troubled Feast: American Society Since 26. Poliomyelitis vaccine types 1, 2, and 3: Recommendations of
1945, pp. 55-69. Little, Brown and Company, Boston, 1973.
the Vaccine Advisory Committee. National Foundation Pam
phlet, New York, April 25, 1954.
8 Zuckerman, M. Dr. Spock: The confidence man. In The Fami
27. New York Times, April 13, 1955, p. I.
ly in History, edited by C. Rosenberg, pp. 179-209. University
28. Francis, T. J. Evaluation of the 1954 Poliomyelitis Vaccine.
of Pennsylvania Press, Philadelphia, 1975.
9. Enders, J. F., Weller, T. H., and Robbins, F. C. Cultivation of
University of Michigan, Ann Arbor, 1956.
the Lasing strain of poliomyelitis virus in cultures of various
Whitficld,
29.
S. J. The 1950’s: The era of no hard feelings. South
human embryonic tissues. Science 109: 85-87, 1949.
Atlantic Quarterly 74: 289-307, 1975.
10. Benison, S. Tom Rivers: Reflections on a Life in Medicine and 30. Solberg, C. Riding High: America in the Cold War. Mason and
Science. MIT Press, Cambridge, 1967.
Lipscomb Publishers, New York, 1973.
il. Salk, J. E. Studies in human subjects on active immunisation 31. Culler Laboratories: 1897-1972: A Dual Trust, Vol. I, p. 227.
Regional Oral History Office, The Bancroft Library, Universi
against poliomyelitis, I, A preliminary report on experiments
in progress. JAMA 151: 1098, 1953.
ty of California, Berkeley, 1975.
12. Benison, S. The history of polio research in the United States: 32. John F. Enders to William H. Sebrell, May 2, 1955. Poliomyelitis
Appraisal and lessons, In The Twentieth Century Sciences:
Vaccine File (10-535), Bureau of Biologies, Washington, D.C.
33. House of Reprcsentatises, Interstate and Foreign Commerce
Studies in the Biography of Ideas, edited by G. Holton, p. 330.
Committee, 84th Congress, 1st Session. Hearing on Poliomyelitis
W. W. Norton, New York, 1970.
13. Lasagna, L. 1938-1968: The FDA, the drug industry, the medical
Vaccine, June 22-23, 1955.
profession, and the public. In Safeguarding the Public Historical
34. U.S.Public Health Service. Technical Report on Salk
Aspects of Medicinal Control, edited by J. B. Blake, pp. 171-179.
Poliomyelitis Vaccine, p. 87. Unpublished mimeograph. Library
of Congress, Washington, D.C., June 1955.
Johns Hopkins University Press, Baltimore, 1970.
14. New York Times, November 11, 1953, p. 28.
35. Victor H. Haas to W. H. Sebrell and James Shannon, May 10,
1955. Poliomyelitis Vaccine File (10-535), Bureau of Biologies,
15. New York Times, November 13, 1953, p. 16.
Washington, D.C.
16. New York Times, October 11, 1953, p. 66.
36. Barber, B. The ethics of experimentation with human subjects.
17. New York Times, November 22, 1953, Section IV, p. 9.
18. New York Times, January 2, 1954, p. 1.
Scientific American 234: 25-31, 1976.
19. Engel, L. Climax of a stirring medical drama. In The New York 37. Federal control of new drug testing is not adequately protec
Times Magazine VI: pp. 7, 53, January 10., 1954.
ting human test subjects and the public. Report to Congress,
Government Accounting Office, July 15, 1976.
20. New York Times, March 12, 1954, p. 1: March 15, 1954, p. 15.
21. New York Times, October 11, 1953, p. 66; April 6, 1954, p. 33. 38. New York Times, July 20, 1976, p. 1.
39. Greenberg, D. S. FDA: Poor marks for its self-investigation.
22. New York Times, November 13, 1953, p. 16.
N. Engel. J. Med. 294: 1465, 1976.
23. New York Times, November 27, 1953, Section IV, p. 9.
24. New York Times, April 6, 1954, p. 33.
40. Mintz, M By Prescription Only. Houghton Mifflin Company,
Boston. 1967.
25. Freund, P. A., editor. Experimentation with Human Subjects.
7.
Pharmaceutical Industry in Latin America
BOTH the transnationalisation and oligopolisation of
the pharmaceutical industry is well known. A few com
panies occupy a large percentage of the worldwide
market. In 1985, the fifteen largest companies in the
world were responsible for 37 per cent of the total pharmaceutial sales (US S 79.8 billion).
This same phenomenon can be witnessed in Latin
America, which accounts for 7 per cent of the world
pharmaceutical market, or approximately US $ 5.5
billion. In 1985, the 10 leading companies in Latin
America—all transnationals—captured 30.5 per cent
of the pharmaceutical market in the seven countries
studied (Argentina, Brazil, Columbia, Chile, Mexico,
Peru and Venezuela). Sales in these countries reached
US S 4.13 billion that year.
The largest markets for pharmaceuticals in Latin
America are Brazil, Mexico and Argentina, which are
also the countries with'the largest populations. In 1985,
the total market in Latin America was valued at US
$ 5.5 billion; 69.3 per cent of these products were sold
in these three countries.
The most frequenfly sold products in the region are
antibiotics, cough preparations, antirheumatics,
December 1987
analgesics and vitamins. This illustrates well the pat
tern of pharmaceutical consumption in this part of the
world. On the one hand, while it is true that there is
a high incidence of infectious illnesses justifying the
use of antibiotics, these products are often used in
discriminately. Of more concern, however, is the fact
that “cough and cold preparations”, many of which
are simply useless for the purpose intended, occupy
second place on the list of sales. Analgesics and
antirheumatics—symptomatic drugs—also occupy a
preferential place, while products containing vitamins
represent a considerable proportion of the sales, thanks
to promotional campaigns which try to present them
as a solution to the nutritional problems of the Latin
American population.
The most startling fact, however, may be that
“Novalgina”, produced by HOECHST, occupies first
place in the sales list, in spite of the fact that its prin
cipal active ingredient—Dipirona or Metamizole—has
been withdrawn from the markets of many countries
because it can produce agranulocytosis, a sometimes
fatal blood condition.
[From ISIS Women’s Health Journal, no 3].
69
Book Review
Beyond Medical Solutions
guy poitevin
TAKING SIDES. The Choices Before the Health Worker by C. Sathyamala, Nirmala Sundharam and Nalini
Bhanoi. ANITRA, 1986, pp 320, copies available at B-7, 88/1 Safdarjung Enclave, New Delhi 110 029. Rs 7u.
THE authors address this sort of committed rural health
handbook written in English to middle level health workers’
engaged all over the country in rural health services. They
take as a starting point, on the one hand, the arguments rais
ed in’the last 10 to 15 years against the effectiveness of
modern medicine, and the other hand, the failure of the alter
native tried out to substantially improve the health situation
in rural India. The reason for both is assumed to be the ex
ploitative nature of a society of which the social, political
and economic forces by shaping the way of life of the people
produce the disascs affecting by and large the population.
Those who immediately and hopelessly confront this social
and economic reality of the people they work with, are the
middle level health workers upon whom the health services
actually rest. Yet, “it is these workers who are least involved
in a critical examination of their work”. Firstly, being located
in the lower rungs of the hierarchy of medical services, they
are just expected to follow’ orders. Secondly, their training
does not prepare them to conceive, let alone to suggest, ap
propriate alternatives. Frustration, insensitiveness or despair
eventually overcome them. Even so, out of their experience
of training programmes, the authors are convinced that those
scattered and isolated health workers could and should
achieve a lot once helped to develop the proper perspective
required with regard to rural health care. The four sections
of the book make, therefore, an attempt to help middle level
health agents to learn from their disillusion, and instead of
relapsing into the apathy or the self-complacently irrespon
sible stands of public health employees, lead them towards
attitudes and practices of social health activism.
The first section describes the baffling experience of
Radha, a woman health worker who happens to leave her
city hospital to work in a rural dispensary. Absolutely
unprepared for this by her training and previous experience,
she is progressively confronted with a series of puzzling ques
tions regarding unexpected attitudes and behaviour of the
villagers. She painfully realises that her medical knowledge
and skill prove of little use. Unable to cope with too many
doubts, she feels out of place, she is frustrated: she comes
back to her city hopsital.
Around eight common incidents which helplessly bewilder
her in the course of ther work, are structured eight chapters
which discuss the issues involved. They clarify the health rid
dles that Radha could not solve on account of her inability
to understand the nature of the constraints which inexorably
bear upon people’s lives. She had only medical answers of
a curative type to issues and needs which required first of
all a social and psychological analytical insight. The inade
quacies of her technological responses lead her to experience
that as a pure medical agent she is unfit to meet the health
problems of a common man. The following are the ques
tions which pushed her to the limit and that the book, in
a second part of the section, helps the health w'orker to firstly
70
come to terms with while embarking in tasks of rural health
care:
Why don’t people rush to get treated early?
Why do people have faith in local healers?
Why don't common people have satisfactory access to
health services?
Why are rural areas wanting in good medical
practitioners?
Why do people not implement even simple health
messages?
Why should a health worker know whether and to what
extent people are poor or rich, influential or looked down
upon? Aren’t diseases independent of any other
consideration?
Why do people prefer to impoverish themselves with too
many children?
Why is it that a few people avail of so many health
facilities and so many have so little of them?
The first section shows how the health care system as a
development asset, no more no less than land, waler, credit
system, etc., obtains the status of a commodity socially ap
propriated by those who can afford it or snatch it in pro
portion to their social, economic and political position of
power. As a consequence, ill-health is an unequal access to
health commodities when these latter are made unavailable
to some—actually many—by others—a few'. Ill-health, there
fore, mirrors and measures the state of deprivation of the
subaltern. Ill-health is injustice and no simple natural
disorder, no less than deforestation, unemployment, hunger
and malnutrition, starvation wages, etc. The survival
strategies of the deprived sections do not bear witness to their
ignorance and backwardness but to the sway of iniquitous
social forces. Once socially unaware and naively wellintentioned health workers like Radha understand this, they
may hopefully realise that they had better feel anything but
frustrated, if they really mean to avail the common man of
their professional capabilities. But then, a second stumbling
block threatens them.
Limitations of Established Modern Medicine
The second section deals with the inadequacies of the
health workers which should not necessarily be ascribed to
personal failure or inability. They are largely due to the in
herent limitations of established modern medicine itself, the
assumptions of which need questioning. Its development is
as much based on scientific and rational principles as shaped
by powerful economic and political groups. The second sec
tion expounds how the interests of doctors and big business
men while contributing to the development of modern
medicine, created also a limited view of health, diseases and
healing process. New theories shifted the focus of disease
causation from the social conditions that bred disease to the
Radical Journal of Health
immediate cause which was the germ, and the attention was
diverted from poor nutrition, bad living and working con
ditions, exploitative labour and sex relations, etc. Disease
became a physical event within an individual’s body and care
focussed on drugs, surgery and hospitals. Preventive
measures dealt with immediate environment and diseases at
the individual level. Health became a neutral and purely
technical subject with its experts wielding absolute authority
and monopoly on medical research management and health
care policies. Big industrialists prompted modern medicine
in order to increase the productivity of their workers through
control of diseases by therapeutic techniques dealing with
the immediate cause rather than the primary reason of
illhealth, i e, the exploitative social relations of production.
Modern medicine served the interests of those in power and
developed to the extent it served these interests. Medical
theories justified even the inferior roles of women.
As a matter of fact, the potent remedies and techniques
developed with the support of businessmen had a very small
part in reducing morbidity and mortality in the western coun
tries. Their major decline had already taken place before
specific medical technology was introduced. Death rates for
measles, scarlet fever, tuberculosis and typhoid were already
negligible by the time effective medical interventions were
discovered. This tremendous achievement was not the effect
of drugs nor doctors. It was due to improvement in living
standards and public health measures. Biomedical technology
once introduced had a very limited impact in improving the
health status of the population and was responsible for no
sharp decrease (except for polio) in mortality rates due to
infectious diseases. Only 3.5 per cent of this decline took
place because of medical interventions.
Ill-health in Independent India
The third section looks at the development of health ser
vices based on modern medicine in independent India with
regard to the activities commonly undertaken by health
workers in rural areas. Their limitations are pointed out and
explained by the fact that they have not been planned keep
ing in mind the social and economic constraints of the ma
jority of the villagers. As a result, health workers fail to meet
the people’s needs and by-pass the major causes of ill-health.
Examining the policies of the government regarding these
rural health programmes it is shown how health needs are
actually used as a cover for serving the interests of the
wealther sections of the rural population. A comprehensive
review of the following rural health problems provides the
essential results of the studies in the matter together with
an analysis of the inter-related factors: a health-worker can
afford to ignore neither of them. In each case the inade
quacies of the government health policies are exposed and
shown as basically due to the narrow health concepts of a
purely curative medicine system absolutely blind, to the
structural-social dimensions of health issues.
Health of children’. Data on high mortality and diseases
occurrences are related to structural constraints such as low
nutritional status, low education status of women, inade
quate access to medical care at birth and clean water, switch
over to tinned food, sex discriminations etc.
Health of women: Sex-ratio, life expectancy, mortality
patterns and causes of death, maternal mortality, nutritional
December 1987
status, access to medical services, amniocentesis, infanticide
arc determined by the discriminatory effect of the social
and/or economic degraded status of women on the one hand
and on the other hand, by the medical profession being con
cerned not with women’s health but with their (male) child’s
issue.
„ .
c , .
Health of adults: Given the over-all importance of their
undernutrition, the reasons for this and the inadequacies ot
the nutritional programmes are exposed at length. No health
worker may fail to be conversant with the misleading debates
and approaches in the matter, with the deceitful talks on the
so-called minimum wage, with the criminal exports of high
protein food, with the decrease of acreage under cheaper
coarse grains, with the export of rice, with the wasted buffer
stocks of cereals, etc. In such circumstances, “feeding pro
grammes and minimum wages themselves become oppressive
strategies in the long run”.
Health education: Some examples show how the official
health education as much as health advertising, resembles
a harmful brainwashing by its explicitly or implicitly false
or socio-culturally repressive messages, and by its conceal
ment of important aspects. The demystification through a
critical reading of all health messages may indeed prove a
skill difficult to acquire when everybody takes for granted
that education is merely a useful transfer of necessar ily ob
jective information. Actually, the assumptions of* health
education as commonly practiced should be denounced as
often biased in such a way as to prove in the long rur.i to
actually impair the health status of the majority of people.
The emphasis on individual responsibility and fault, the
theory that health problems cannot be solved without a 1 ot
of money, the persuasion that the poor being ignorant,
illiterate, superstitious and backward cannot but turn a deaf
ear to health advice, the greater importance of men’s health,
the dependence on modern, medicines and the knowledge of
doctor’s who alone know best, etc are message which con
veniently remove the responsibility for ill-health from th ose
who create and maintain “the exploitative practices” con
ducive to the poor’s helplessness.
Family Planning Policy, (FPP): The theoretical and u seeffectiveness of the commonly used contraceptive methi ids
are examined and advice in given to make them helpfu':. in
improving women’s health, as they are a meaningful way • to
this effect. The present failures are shown to be due to the
implementing strategies and false assumptions such as the
primary interest for population control at all costs, the be lief
that population growth is the cause of poverty and unc lerdevelopment, etc. Family planning methods will succeed c nly
if they are accompanied by an overall improvement in the
socio-economic conditions of everybody. Failing this, the
failure of the FPP can be considered an effective ‘resistat ice’
by the poor against the detrimental effects in their every day
life of government agricultural, social and economic polk ies:
a survival strategy in front of socio-political mechanism: > of
deprivation.
The Village Health Worker's Scheme (1977): It isdiset-.ss ed and evaluated in relation to one basic principle, viz, the
selection of the workers by the village community.
Curative services: Overuse and misuse of drugs, harmful
role of drug companies, cost of drugs, etc. such problems
are discussed and suggestions are made to help health
workers overcome them.
71
Setting Off Again on the Right Foot
The fourth section takes stock of the principles for an ade
quate practice on the part of health workers: focus on chang
ing the social environment for long term improvement in the
health status of the most affected groups among local com
munities; understanding of and dealing with, the root causes
of ill-health; choice of identifying oneself with those who
are the most likely to fall sick; decision to operate with all
of them as a collective; will to develop their insight into the
reasons of their ill-health and foster their collective strength
to act against them; attempt to make use of all resources
available at the village and block level in a self-help spirit
and with the firm conviction of one’s own right to health
vis-a-vis the government health services, etc. Then, an alter
native model of health practices and health education is
chalked out for the guidance of a middle level health worker
already working in a rural hospital, dispensary or health cen
tre but willing to spare time and resources to operate along
the above guidelines although deprived of any experience of
village work. Criteria are suggested regarding the selection
of two or three villages to work in/around her centre; direc
tives are given to help her develop a proper understanding
of those villages through a close relation with people and
renewed patterns of communication; the necessity is stressed
of bringing people together for them to consider collectively
their own needs, find out the reasons of their ill-health and
seek solutions; the modalities of selection and training of
a voluntary village health worker are clarified; explaining
how to keep a diary, conduct a survey or a group discussion
on health, from a permanent group of concerned people, deal
with problems in a manner really conductive to the group’s
collective initiative and ability to act on its own, organise
people to get due services from the government.
We thought proper to give this rather extensive account
of the contents of the book under review to convince the
health workers it is addressing of the many practical advan
tages they cannot fail to draw from it: well-researched
statistical information compiling the most relevant data on
each topic, didactic synthesis summing up studies otherwise
scattered and lengthy, eight pages of referential documenta
tion, a glossary. Considering the alarming and relentlessly
resilient extent of ill-health of this country, one cannot but
expect many health workers to make choices and definitely
take sides along lines expounded in this reference and guide
book. Every medical practitioner should hopefully have the
opportunity of getting through this book and honestly ques
tioning his practices and the methods of his/her institution
in the light of the critical insights provided by this challeng
ing appraisal of rural health problems.
The approach rightly avoids two pit falls. The first one is
to simply ask for multiplying the rural health services
(doctors, drugs, dispensaries, injections, surgical equipment,
etc) as others agitate for more dams only to bring more health
and irrigation facilities to those who can lay hands upon
them, with the same result in both cases: the majority of the
needy is kept deprived of the means to meet its primary needs
of health care and of the water required for irrigating its
staple food crops. An unflinching sociological insight only
may. preserve us from short-sightedly lapsing into this trap.
The most commendable quality of this review of rural health
problems is its permanent claim to refer health issues to
72
related structural-social factors and (he overall marginalis
ing dynamics engineered by them. Disparities in health status
measure the extent of social discrimination and unequal ap
propriation of the means of health. There is no health nor
ill-health as such: this approach has been the treachery of
the purely curative or biomedical modern medicine for
reasons known to its promoters. Both of them are outcomes
and symptoms of a given social structuring on the one hand.
and socio-cultural/anthropological systems of representa
tions on the other hand.
The two critical questions to be raised concern, firstly, the
exploitative social relations of health based on the present
system of established modern medicine, and, secondly, the
system of cultural-anthropological health representations. If
the first question, focus of the book, is methodically dealt
with, the second dimension, although occasionally and com
mendably tackled (for instance, illness seen as the result of
falling out of harmony with the universe, p 14-17, or the
women’s inferior value as an explanation for women’s lower
health status, p 148, 151), would yet deserve a wider and in
dependent consideration that the somehow narrow socio
economic perspective of the authors overshadows.
Let us stress the importance of this second aspect with the
example of the exorcism practices performed by religious
healers. Around these latter, symbolic sets wave together in
ritualistic health practices, the sick, the sacred power, the
departed, the go-between-the holy man, the enemy, the
genders, etc. (Poitevin). Especially in a traditional agrarian
community, health, death, disease, injury, wound, infection,
healing are no natural events. Body, blood, hair, sex, menses,
birth, injections, etc, are invested with far-reaching and inter
connected meanings. They are socio-cultural constructs
before being subject to the specific and restricted medical
constructs, outcome of the particular and alien assumptions
of modern medicine. We cannot lake for granted that these
latter will easily erase the previous constructs. On the con
trary, the traditional meanings are likely to turn up the new
speech in such a way as to give it a fitting place in their midst.
The point at issue is here that the working of the “exploitative
forces” so often rightly referred to, would still be better
understood once are discovered both the autonomy and the
interdependence of those two levels of analysis. (Althusser,
1970). They overlap in reality as two aggregate dimensions
the cumulative effect of w-hich is to be understood in each
given social formation under consideration.
A common and easy example may illustrate this interplay.
Why do rural people feel a deep and pressing urge for injec
tions? Some traditional unconscious drives and representa
tions (for instance, expectation of a sudden and miraculous
recovery through some mysterious device: pricking and pain
may act here as a substitute to the ritualistic cutting the throat
of a cock) have to be explored and brought out under con
scious light. Why do medical practitioners not try to scien
tifically demystify and reveal to their trustful clients, the
quasi-religious nature of their demand, instead of promptly
complying with the peoole’s expectations, if not anticipating
them, often without any medical necessity? And why do they
not, as a principle, entrust this task only to the nurse care?
The reasons are known. In doing so, male doctors invest
themselves with this very power otherwise attributed to the
local healers whose practices are no less mysterious and
Radical Journal of Health
knowledge no more transcending their reach and consequent
ly calling for the same complete trust (an important message
conveyed by the health education programmes, as ap
propriately stressed by the authors, p 185). One difference:
instead of accepting free gifts, the modern practitioner will
claim substantial fees taking advantage of the anxiety and
faith of his client—biting again into the starvation income
of the needy. In short, in the process, the traditional set of
feelings and representations as well as the passive, helpless
and submissive relations of health woven around the sacred
healers’ practice provides the rationale for the acceptance
and social sanction of the exploitative practices and the
overall male domination of the modern class of medical prac
titioners. This acquires a specific gender dimension when we
remember that it is mainly women who resort to the ritualistic
healers (Herzlich and Picrset, 1984).
The book keeps clear also of a second pit fall which usually
consists in resorting to health services offered by voluntary
agencies with technical qualities and appropriateness of
which the public health care system is deprived. The main
concern is here for professional performance. This is short
of the political will and thrust required to cope with the
remote and determinant causes of ill-health as well as with
the public dimension of a national service. Each citizen,
especially the deprived one, is entitled to health as a right
and not as a commodity to be made available even at a lesser
cost and served wrapped in humanitarian feelings.
Strategically speaking, it follows from this that health for
all cannot be achieved unless it is health by all, i e, obtained
as a right by the majority of all those who are kept deprived
of it. As neither the public health care system as it operates
nowadays nor the troups of NGOs in rural health care can
be expected to secure health for all in no century, those con
cerned with obtaining their right share of health facilities
are left with one single alternative, viz, to fight and vindicate
their right. This is the right perception which upholds the
whole approach.
Need for Tactical Model of Action
To the tactical question “How to go about it?”, the answer
is that the proposed alternative approach is firstly to be
monitored from within the low ranks of the health care
system, by the middle level health professionals transform
ing from within their concept of health and practice of health
care. They are staged as the sensitive category through which
defiance and innovation will arise. Why we may ask, do the
authors assume that this category is potentially fit for
spearheading the envisaged radical changes which will
reconstruct the established health system? From their own
experience? From the fact that this category of workers re
maining close to the common people while being technical!}
trained, may prove immediately operative, provided they only
shift their socio-cultural allegiance from the class interests
of the medical profession towards the lower sections of the
rural population? But then, why do the same authors, from
the last chapter, characterise these middle level workers as
short of experience of village work, deprived of proper train
ing, used only to follow orders and the least involved in a
critical examination of their work?
In the fourth section, the}' are snown a plan of action, and
equipped with pedagogical skills enabling them to raise.
December 1987
mobilise and train village health workers in two or three
villages around their dispensaries. From where and how do
they become all of a sudden motivated for investing their
time, energy and thinking capacity in tasks for which, as a
professional category, they could only feel shy or have aver
sion? And we know that as a rule such is actually the case.
Before showing how motivated health workers might
motivate village health workers, we would also like to know
how the low-rung health workers as a category could
themselves become enthused in a proportion sufficiently
significan as to make them a category and not only a few
individuals, initiators pioneering the envisaged alternative
methodology of health practice.
Barring exceptional cases which make no use of tactical
model of action for social change, one fails to realise how'
an individual woman from the middle rung health workers
may embark alone in such attempts without at least two
minimal pre-requisites. The first one is institutional backing,
however loose or informal it may be, not only to support
her after she has started but to secure since the inception
precisely what is taken for granted, viz. the means of a radical
reappraisal of her whole training ana practices. To put in
her hands Helping Health Workers Learn (Werner and
Bower) is no sufficient answer: a book does not offer a sup
portive group. In their final inset (p 307), the authors have
themselves raised the question to leave it open: does the
health worker continue to spend most of her time in her
dispensary or in the village? Does she want to radically
transform her role? Can she do it within her present institu
tion or should she work with another group? How can she
build up support for her w'ork and herself? Unable to
visualise a definite plan for mobilising the category they
address, the authors satisfy themselves with calling those con
cerned to chalk out for themselves their course of action.
Here comes the second prerequisite. Irrespective of the
forms and nature of the ‘institutional’ framework, the health
worker will not be able to act according to the new role she
wishes to assume unless groups of villagers either raised by
her or anyone else, organise themselves and through a sus
tained effort of cultural action develop among themselves
and the population that dynamics from the bottom required
to put them on the way towards what we have labelled health
by the people. Following the catalytic effect of the health
worker, it is this organised strength, embryo and basic ele
ment of a wider health movement, which may come to ef
fectively bear upon the health system to force it to change
in the long run. One may finally wonder whether in the
scenario imagined by the book under review and the course
of action to be chalked out, the leading role is not to be more
plausible ascribed to the villagers’ organisation. Without this
organisational prerequisite, an isolated female health worker
in rural areas cannot achieve much whatever the clarity of
her choices; but as a health professional taking sides with
such organised groups of villagers she may, for sure, work
wonders. To this effect, the chapters 3 and 4 of the 4th section
deserve a careful attention.
Many paramedics trained by or working in, Christian
institutions especially in southern states, may be able to take
advantage of this book directly in English. For the many
others, let us hope that translation will appear in vernacular
languages to make this precious handbook actually available
73
to all those whom it addresses.
The authors have made a successful attempt to wirte in
a clear and accessible language without compromising the
necessity for health workers and health activists to master
the relevant terms and facts. The presentation of the tables
and graphs deserves a special mention for its clarity, careful
selection, relevance and attractiveness. Many graphs may not
fail to impress even illiterate readers, such as the set show
ing the decrease in mortality due to infectious diseases for
the USA, 1900-1973, in relation to specific medical measures
(p 1’10): one is immediately, visually convinced of the very
low significance of the medical interventions in the matter.
No professionally competent health activist may afford to
do without this handbook. We even consider that no health
worker worth the name may go without the basic knowledge
imparted by this book. We wish all institutions dealing with
rural health care adopt it as a basic vade-mecum for all their
workers. A didactic style and the arrangement of the con
tents in about 35 more or less self-sufficient units, make the
book easy to be used as a reference book, to be read
piecemeal or utilised a la carte, according to one’s daily
requirements.
The authors deserve felicitations too for enlivening their
technical expositions with pictures and drawings which try
to give a graphic visualisation of abstract ideas and often
carry the appropriate emotional import. The big size of the
book (21.5 cm x 25 cm) was skillfully taken advantage of
to devices well-spaced out disposition of the drawing and
matter, each page being divided into two parts with short
lines: this facilitates the reading and helps to grasp and
memorise (he matter of each paragraph.
References
Althusser, 1970: See in this respect the theoretical frame work propound
ed by L Althusser, in For Marx, London, 1969 and Reading Capital,
London 1970.
Herzlich and Pierret, 19S4: Sant'e er Maladie, analyse d’une
repre sentation sociale, Mouton. Paris, 1984 and Malades d’hier,
tnalades d’aujourd’hui, Pa\ot, Pans, 1984, Herzlich C. Pierret J.
Poitevin, Guy: The anthropological issue of primary health care as a
gender issue, in Health in People’s Hand, to be published by The
Foundation for Research in Community Health. Bombay.
Daikon Shield Battle Continues
IN late January 1986, a former Daikon Shield user sug
gested that the Women’s Health Information Center
(WHIG) was the appropriate body in Israel to organise
a campaign to notify Daikon Shield users of their right
to apply for compensation for damages. The WHIG,
a project of the Israeli feminist movement, consists of
small group of volunteers who for several years have
provided health information and education to women
through a weekly open phone line, health fairs, lectures
and other activities. We knew that the manufacturer
of the Shield had been required by the Court in
America to notify users of their right to sue, but that
the company had made little or no effort to do so here.
We decided, in February, to take on the job of locating
Shield users. We also decided to work with an
American lawyer, who could give us information and
guidance and could later represent the women we
located, if they so chose.
We knew that Robins claimed to have sold the Shield
in Israel, but had no idea of how many were actually
inserted in Israeli women. The Ministry of Health told
a reporter from a local newspaper that there were none
in Israel. However, in mid-February we placed a small
ad in the same newspaper and over 100 women
responded immediately! Some of them definitely used
the Shield; others strongly suspected that this was the
IUD they had once used. Daily calls poured in, and,
helped by volunteers from the Feminist Center and the
Rape Crisis Center, we responded by sending out in
formation and forms, and listening to the horrifying
stories of complications women experienced with the
IUD.
.In February and March the WHIC sent information
to the press and some ten articles were published about
our campaign in Hebrew, Arabic and English
newspapers. We also spoke on radio and placed
74
another small ad in a women’s magazine. Women from
every corner of the country-cities, villages, kibbutzimrequested help filing claims. In April we held a meeting
to give potential claimants an opportunity to meet with
the lawyer, ask questions and discuss problems they
were having getting medical records.
Among the claimants was one who had already
verified that the IUD she received at Kalpan Hospital
was indeed a Daikon Shield, and that she had been one
of 500 to get a Shield as part of an experimental pro
gram. After several weeks of negotiation with officials
of the Health Ministry, Kalpan Hospital and the
General Health Insurance authorities, we received per
mission to notify these 500 women. Unfortunately half
of the addresses had been lost in the hospital archives,
so we were able to write to only 250, and we lost many
of these women due to lack of forwarding addresses
from their previous homes.
After the April 30th deadline, Kalpan Hospital sud
denly FOUND the misplaced list of the other 250
women—but now it was too late to put in claims!
Meanwhile, women continued to call us even after
the April 30th deadline passed. There is a definite
possibility that not all Daikon Shield users in Israel
were located, due to the limited time and money that
were available to us.
When women began to request their medical records
they discovered: that many files had been destroyed
(they seem to save files for only 7 years here); the
hospitals would not cooperate with them; details were
not carefully listed—only the word IUD appeared;
most private doctors had no files; and some doctors
were no longer alive.
[Information from WHIC, Israel from Womens
Global Network].
Radical Journal of Health
Dialogue
Reinterpreting Homoeopathy
ch v subha rao
IF homoeopathy is to take its rightful place in the health
care systems of the 21st century, it must be re-interpreted
from the standpoint of dialectical materialism. Samuel
Hahnemann, the celebrated founder of homoeopathy, was
never so dogmatic as to rule out new interpretations. He says
that natural laws cannot be capitalised or kept under the seal
of human authority. People may utilise natural laws and yet
may not be able to understand the crux thereof. Thus
Hahnemann indirectly admits that natural laws may be more
fully understood by future generations. He terms as probably
correct his explanation of the mode of action of
homoeopathic medicines. He expressly states that others can
form their opinions in the matter. He prepared six editions
of his magnumopus The Organon in his lifetime and he was
constantly innovating. Nearly 150 years have elapsed since
the deathof Hahnemann. It is high time somebody reinter
preted homoeopathy and surveyed medical science in general
in the light of subsequent developments in philosophy and
science.
In his book Principles and Art of Cure by Homoeopathy,
Herbert Roberts tried to demonstrate that homoeopathy was
based on the bedrock of natural laws. More effort on those
lines is required now. In the Soviet Union, philosophers and
medical scientists are trying to develop modern marxist con
cepts of life, health and disease. Hahnemann’s role in
medicine may be compared to that of Hegel in philosophy.
Both were philosophical idealists. The rational kernel of their
teaching was enveloped by a mystical shell. Marx accepted
Hegelian dialectics but rejected idealism. Similarly, it should
’)e possible to separate homoeopathic therapeutics from its
idealist shell.
During Hahnemann’s lifetime (1755-1843) there were hard
ly any scientists who were consciously and consistently
materialistic in their world-outlook. It is, therefore, not sur
prising that Hahnemann was deeply influenced by and deeply
dissatisfatied with idealist philosophers. He was a deist and
a religious free-thinker. He wrote: “The ever-beneficent
Godhead animating the infinite universe dwells in us also”.1
He felt attracted by philosophy, but the philosophers and
their works offered him little satisfaction. He said:
“Philosophy is not only the highest of all sciences, it is also
the basis and the fundamentals of all others. No science can
exist without philosophy, for without its help it falls to the
level of a handicraft or at any rate of a subsidiary subject.
This is true above all of medicine” (Haehl).
Hahnemann’s biographer Richard Haehl says: “What par
ticular philosophic system he supported is not discernible
from his writings or his letters. It seems very questionable
whether he definitely accepted any special system. He should
rather be regarded as an eclectic who selected from each
system the best for his own view of life and the world. From
his schooldays onwards he had followed Descartes, Spinoza
and Leibnitz (whose systems dominated the schools of the
lime) and then proceeded to vitalism and to the naturalism
of Schelling and Hegel. He advanced beyond this to
Dece;;..,.r 1987
spiritualism and for a time lost his way in occultism. In
temperment and development, both as man and as physi
cian, he was a strong opponent of materialism. With all his
emphasis on scientific exactitude and empiric certainty as
the starting point of his therapeutic reform he rejected
materialism equally as an outlook on life and as a funda
ment of his new theory:.. . But, on the other hand, he took
for his own purposes the basic thoughts of doubt from
materialism. He took up a definitely conscious standpoint
from facts of experience and rejected every philosophic
speculation which did not agree with the latter. For this
reason Kant was too impracticably abstract for him and not
clear enough in his manner of presentation. Of Plato he com
plains that he is only valuable when he speaks intelligibly
and expressively. His criticism of the philosophers after Kant
is that they wrote ‘even more mystically’ than Kant, that they'
composed too freely in fancy and that that they had therefore
not kept to the bounds of experience” (Haehl).
For Hahnemann, theory' was of minor importance (Haehl).
Engels, on the other hand, attaches great importance to
theory. “However great one’s contempt for all 'theoretical
thought, nevertheless one cannot bring two natural facts in
to relation with each other, or understand the connection
existing between them, without theoretical thought. The only
question is whether one’s thinking is correct or not, and con
tempt of theory is evidently the most certain way to think
naturalistically, and therefore incorrectly. But, according to
an old and well-known dialectical law, incorrect thinking,
carried to its logical conclusion, inevitably arrives at the op
posite of its point of departure. Hence, the empirical con
tempt for dialectics is punished by some of the most sober
empiricists being led into the most barren of all superstitions,
into modern spiritualism” (Engels, 1982).
Let us now turn to Hahnemann’s concept of vital force.
“In the healthy condition of man, the spiritual vital force
(autocracy) the Dynamis that animates the material body
(organism), rules with unbounded sway, and retains all parts
of the organism in admirable, harmonious, vital operation
as regards both sensations and functions.. . The material
organism without the vital force is capable of no sensation,
no function, no self-preservation; it derives all sensations and
performs all the functions of life solely by means of.the im
material being (the vital principle) which animates the
material organism in health and in disease” (Haehl).
On the concept of vital force Engels says: “If by this (vital
force) is meant that the form of motion in the organic body
is different from the mechanical, physical, or chemical form
and contains them all sublated in itself, then it is a very lax
manner of expression, and especially so because the force
presupposing transference of motion appears here as
something pumped into the organism from outside, not as
inherent in it and inseparable from it, and therefore this vital
force has been the last refuge of all supematuralists” (Engels,
1982). And again: “The Organism is certainly the higher uni
ty which with'm itself unites mechanics, physics, and
75
chemistry into a whole (emphasis original) where the trinity
can no longer be separated. In the organism, mechanical mo
tion is effected directly by physical and chemical change, in
the form of nutrition, respiration, secretion, etc., just as much
as pure muscular movement.” Thus it may be necessary to
modify or even altogether abandon some of the concepts of
Hahnemann.
All this, however, should not detract from the merits of
homoeopathy which are many and solid. The patient is
treated on the basis of ‘totality of symptoms’. The uniqueness
of each patient is recognised. Permanent cures are ac
complished in the gentlest manner possible. The pills are
sweet and incredibly cheap. The efficacy of homoeopathic
remedies is beyond question. Indeed, allopathic treatment
is said to be absolutely necessary only in a new cases.
Homoeopathy provides prophylactics as it did when
encephalities was taking a heavy toll of lives of children in
our country.
We are chasing the mirage of Health for All by 2000 AD.
In a rational world there will of course be great emphasis
on prevention of disease. It will be a non-violent, nuclearweapon-free world. It will be free from pollution. People will
consume unadulterated and uncontaminated foods free from
toxic food additives. There will be excellent sanitary ar
rangements. Everyone will get food, clothing and housing.
Occupational hazards will be minimised. Consumption of
narcotics, alcoholic liquors, cigarettes etc, will be drastical
ly reduced. There will be less stress and fewer deaths due to
accidents. Nowadays goods are being produced, advertised
and sold without the slightest regard for their harmful ef
fects on the consumers. The elimination of profit motive in
production is a pre-condition to achieve the goal of Health
for All.
If the masses are the real makers of history, it follows that
the above goal cannot be reached without a people’s move
ment. In India, progressive forces have been demanding the
nationalisation of drug industry’ and rationalisation of drug
policy. They have not met with much success. Drugs con
stitute one important area of multinational swindling. Our
dependence on transnational drug manufactures and on
drugs themselves must be reduced. Right now state aid to
systems like homoeopathy, ayurveda, and unani is just
nominal. It is nobody’s case that the baby should be thrown
away along with bathwater. The dialectical method should
be applied to the facts of medical science and health care.
Such a comprehensive critique will enable us to see things
in proper perspective and to assign to each system the role
it deserves. The quest for truth and for cures must be the
motive of such an inquiry and neither passion nor prejudice
nor private profit should be allowed to hinder it. The reinter
pretation of homoeopathy will form part of such a critique.
Much basic research has to be done if homoeopathy is to
gain wider acceptability. For instance the mode of action of
homoeopathic remedies has not been satisfactorily explain
ed so far. The materia medica can and must be enriched.
Potentisation of drugs can perhaps be explained in terms of
the law of transformation of quantity into quality. The law
of cure ‘Similia Similibus Curantur’ may have something to
do with the law of negation of negation. If sufficient funds
and talents are pumped into homoeopathy, it may develop
into the healing system par excellence of the future.
Bibliography
Haehl, Ruchard: Samuel Hahnemann—His Life and Works, Vol
I, B Jain Publishers, Delhi.
Engels: Dialectics of Nature, Moscow, 1982.
Ch. V. Subha Rao
LIC City Branch 1
Visakhapatnam
530 004
Adverse Effects
Women and the Pharmaceutical Industry
Edited by Kathleen McDonnell
Medical remedies which are inappropriate, wasteful and sometimes simply
downright dangerous, overload the world. Many are targetted specifically at women.
ADVERSE EFFECTS sets out to examine, in a global context, how women are fre
quently exploited and injured by drugs. Articles from India, the Philippines,
Canada, the Netherlands and USA illustrate how women are successfully organising
themselves to fight this ill-treatment and manipulation.
Part I
- WOMEN AS DRUG CONSUMERS
Articles on EP drugs, hormone treatments,
modifiers.
Part II
DES and mood
- PHARMACEUTICALS AND FAMILY PLANNING
Articles on Depo-Provera, the rise and fall of the IUD, and the fight
to keep injectables out of India.
Part III - TAKING BACK CONTROL
Two articles examine some of the efforts being made to-challenge the
power of the multinational pharmaceutical industry.
■
International Organization of Consumers Unions
IUCU Regional Office P.O. Box 1045,10830 Penang, Malaysia.
--------------------- Central Office 2595 EG The Hague, Netherlands.
ADVERSE EFFECTS: ISBN 967-9973-17-4 1986
76
1OCU 217 pages 5ki” *
US$7.95 pb.
Radical Journal of Health
Why don't you write for us ?
This periodical is a collective effort of many individuals active or interested in the
field of health or interested in health issues. The chief aim of the joiHnal is to provide a
foru n for exchange of ideas and for generating a debate on practical and theoretical
issues in health from a radical or Marxist perspective. We believe that only through
such interaction can a coherent radical and marxist critique of health and health care be
evolved
Eac'n issue of the journal highlights one theme, but it also publishes (i) Discussions
on articles published in earlier issues (ii) Commentaries, reports, shorter contributions
outside the main theme.
A full length article should not exceed 6,000 words and the number of references In the article
should not exceed 50. Unless otherwise stated author’s names In the case or joint authorship will
be printed In alphabetical order. You will appreciate that we have a broad editorial policy on the
basis of which articles will be accepted.
We have an author's style-sheet and will send it to you on request. Please note that
the spellings and referencing of reprint articles are as in the original and are N.OT as per
our style.
We would also like to receive shorter articles, commentaries, views or reports. This
need not be on the themes we have mentioned. These articles should not exceed 2,000
words Please do write and tell us what you think of this issue.
All articles should be sent in duplicate. They should be neatly typed in double
spacing, on one side of the sheet: This is necessary because we do not have office
facilities here and the press requires all material to be typed. But if it is impossible for
you to get the material typed, do not let it stop you from sending us your contributions
in a neat handwriting on one side of the paper. Send us two copies of the article
written in a legible handwriting with words and sentences liberally spaced.
The best way to crystallise and clarify ideas is to put them down in writing. Here's
your opportunity to interact tniough your writing and forge links with others who are,
working on issues of interest to you.
WORKING EDITORS
Please send me Radical Journal of Health for one year (for issues). I am sending
Rs
as subscription and/or donation, by Demand Draft/Cheque. (D D
and cheque in favour of Radical Journal of Health and for cheque add Rs. 5, if outside
Bombay).
Name
Add r e ss
PIN
____
The Hungry Sparrow
The hungry sparrow
flew about in search of grain.
The grain wa* trapped in the wood of the grinder.
The sparrow said to the carpenter:
Brother carpenter, brother carpenter, (he grain
is locked in the grinder.
What shall I eat?
How shall I cope with my hunger?
What shall I carry to another clime?
The carpenter split the grinder;
Out flew the grain.
and the sparrow after the grain.
But the wicked grain lodged in the royal
granary, guarded by a sentry.
Said the sparrow to the sentry:
Brother sentry, brother sentry, the grain
is lodged in the granary.
What shall I eat?
What shall 1 eat?
The sentry took the matter to the minister.
The minister to the monarch.
The monarch summoned the commander-in-chief
Who appointed a magistrate to study the case.
The magistrate read through reams of law,
and argued back and forth:*
Why, in the first place, the magistrate wondered,
did the sparrow have to be hungry?
At any rate, if hungry she was,
Why did she have to pursue the grain?
The grain that of its own desire lodged
in the royal granary.
News spread rapidly.
The papers carried it end to end:
•Sparrow versus the grain’ was the cry everywhere.
It was plain that
the sparrow was hungry without rhyme or reason.
Her guilt was beyond doubt.
The hungry sparrow' was shot.
Gorakh Pandey
(Hindi)
[From: Thenia Book of Naxalile Poetry edited by Sumanta
Banerjee. Calcutta 1987]
Position: 1463 (5 views)