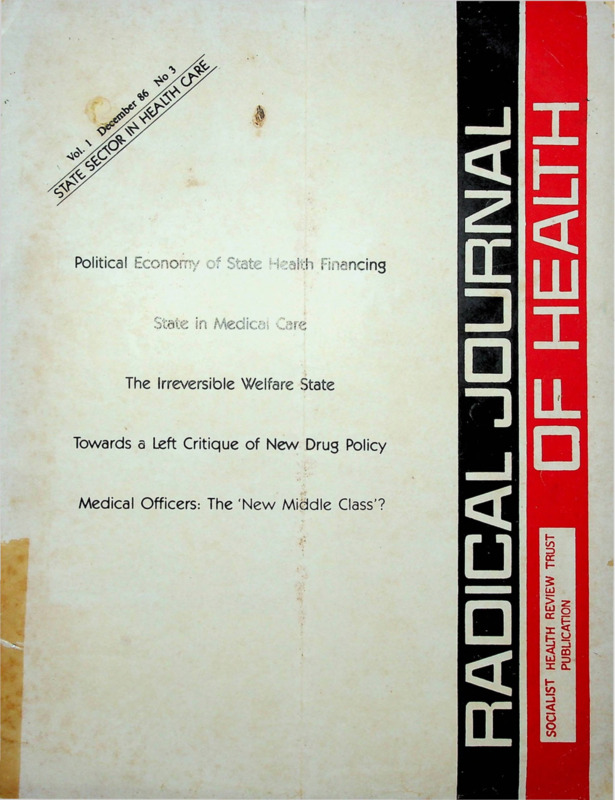
Radical Journal of Health 1986 Vol. 1, No. 3, Dec. State Sector in Health Care.pdf
Media
- extracted text
-
Political tconon-y
. •;
financing
State in Medica Care
The Irreversible Welfare State
Towards a Left Critique of New Drug Policy
Medical Officers: The 'New Middle Class'?
Vol I
Working Editors:
•Amar Jesani, Manisha Gupte,
Padma Prakash, Ravi Duggal
Editorial Collective:
Ramana Dhara, Vimal Balasubrahmanyan (A P), Im-
rana Quadeer,Sathyamala C (Delhi), Dhruv Mankad
(Karnataka), Binayak Sen, Mira Sadgopal (M P), Anant
Phadke, Anjum Rajabali, Bharat Patankar, Srilatha
Batliwala (Maharashtra) Amar Singh Azad (Punjab),
Smarajit Jana and Sujit Das (West Bengal)
Editorial Correspondence:
Radical Journal of Health
C/0 19 June Blossom Society,
60 A, Pali Road, Bandra (West)
Bombay- 400 050 India.
December 1986
No 3
STATE SECTOR IN HEALTH CARE
77
Editorial Perspective
STATE IN HEALTH CARE
Smarajit Jana
79
POLITICAL ECONOMY OF STATE HEALTH
FINANCING
Ravi Duggal
86
STATE IN MEDICAL CARE
Sujit Das
Printed and Published by
91
Dr. Amar Jesani for
THE IRREVERSIBLE WELFARE STATE
Socialist Health Review Trust from C-6 Balaka
Goran Therborn and Joop Roebroek
Swastik Park, Chembur, Bombay 400 071.
Printed at:
99
UPDATE—News and Notes
Omega Printers, 316, Dr. S.P. Mukherjee Road,
Belgaum 590 001 Karnataka.
102
Annual Subscription Rates:
TOWARDS A LEFT CRITIQUE OF NEW DRUG
POLICY
Rs.
30/- for individuals
Rs. 45/ for institutions
Rs. 500/- life subscription (individual)
US dollars 20 for the US, Europe and Japan US
Anant R. S.
dollars 15 for other countries.
We have special rates for developing countries.
Dialogue
MEDICAL
107
OFFICERS-THE ^NEW MIDDLE
CLASS ?
SINGLE COPY: Rs. 8/-
(All remittance to be made out in favour of Radical
The views expressed in the signed articles do not
Journal of Health. Add Rs 5/- on outstation cheques).
necessarily reflect the views of the editors.
Editorial Perspective
State in Health Care
THE Indian tradition of state intervention in health care municable diseases from one state to another and vital
is quite old. During the reign of Asoka in 3rd century BC, statistics have been placed under the Concurrent list, while
besides other social welfare measures, the state established the Union list mentions only Port Quarantine, and deter
medical centres for man and animals, undertook planting mination of standard in ‘scientific and technical institutions’
of medicinal herbs and trees, and supply of potable water meaning perhaps also medical institutions. In actual prac
through wells along the highways. Similar medical centres tice, however, the Union Government deals with international
were claimed to have been established in the neighbouring health relations, promotion and conduction of medical
countries at Asoka’s instance (Thapar, 1973). In modern research, regulation of production, quality control and trade
times, a major role of the state in health care service has of drugs, regulation of standard of medical education, vital
universally been recognised and accepted. Politics of each statistics, and medical care of employees. National disease
country determines the nature of intervention and quantum control/eradication programmes, family planning, MCH,
of contribution by the state. For instance, in the socialist drinking water supply, etc, are financed by the Union Govern
countries the state has assumed the entire responsibility; UK ment and operated through provincial health organisations.
operates the unique National Health Service; in Canada and Moreover, there are several other spheres where the Union
New Zealand, the state bears almost the entire expenditure; Government makes some contributions, e g, medical educa
in many European countries the allocation by the state is tion, health education, health information, dissemination,
ever increasing; and in the third world a similar feature is drug production, development and promotion of other
discernible. In India pressure on the government to spend systems of medicine, rehabilitative medicine, paramedical
more on health care is quite strong. The state’s role varies training, etc. Provincial Governments, on the other hand, not
ranging from the direct and absolute state administration to only enjoy almost absolute autonomy in health care opera
tions both at the policy and implementation levels, but are
indirect and partial intervention.
In India, the situation is^omewhat peculiar. The state has supposed to exclusively provide for medical care and public
undertaken the entire responsibility of health care of the per health services. Juridically therefore, it may be argued that
sonnel of the army, parliament and the railways; partial the Union Government contirbutes more than, its share in
responsibility of the other employees of the government and health care services.
But then one fundamental aspect is missing in such
public undertakings, and a dubious responsibility of the mass
of people. Historically, modern health service owes its begin analysis. Health care includes, as is now widely known, ade
ning to the British presence. Although the first legislation quate nutrition, safe water and sanitation, healthy environ
in this respect, the Quarantine Act, had been introduced in ment, education, employment, etc. Solution of these pro
1825, real concern for a state operated health service ap blems is necessarily dependant on the economic system and
peared after the ‘Indian Mutiny’ or 1857 in the context of political programme, i e, the conduct of the Union Govern
the over-riding political necessity to safeguard the health of ment. It may therefore be held that the basic determinants
the troops and the European civilians. All health interven of health necessary for the protection, maintenance and im
tion were geared to achieve this objective. However, endemic provement of health of the people are to be provided by the
and often epidemic prevalence of communicable diseases as Union Government and the Provincial Governments are
well as political compulsions put sustained pressure upon and responsible for the provision of universal medical care which
eventually forced the government to do something for the is no less an important determinant, if not .the most.
Till now the health of a community of people or that of
native civil population which relied largely on traditional in
digenous system (see SHR, Vol II, No 3). Montague- country is measured and appraised by certain parameters,
Chelmsford Constitutional Reforms of 1919 and later the e g, infant mortality rate, death rate, expectation of life at
Government of India Act, 1935 decentralised the respon birth, sanitation, per capita consumption of food and safe
sibilities which devolved almost entirely on the provincial and water, etc. In the context of such parameters, India has made
local authorities. This constitutional framework and the steady progress in the post-independence period. But in the
policy outlined in the report of the Health Survey and context of desirable goals and international standards the
Development Committee (1946) had been the basis of policy Union Government admitted that such progress brought little
benefit to the Indian masses and the health situation of the
guidelines for the national governments.
Article 47 of the Indian Constitution clearly avows, under country was still precarious and alarming (GOI 1982).
In the background of this reality the Government of India
the Directive Principles of state Policy, the state’s responsibili
ty to raise, “the level of nutrition and the standard of living endorsed the WHO target of “Health For All By The Year
of its people and the improvement of public health as among 2000 AD” which called for the following intermediate goals:
1985—Providing.right king of food for all;
its primary duties”. Here, the ‘state* actually means the seat
1986—Providing essential drugs for all;
of the Union Government. But the VII Schedule allocates
1990—(a) providing adequate basic sanitation for all;
almost all responsibilities to the provincial governments, e
(b) providing adequate supply of drinking water for
g, public health, sanitation, hospitals and dispensaries, drugs,
- all;
family planning and population control, medical education,
(c) immunisation of children against six common
medical profession, prevention of the extension of com
December 1986
77
diseases, viz, measles, whooping cough, tetanus, diphtheria, distinct feature of capitalist society and it is explained in
various ways. It is argued that state health care expenditure
polio and TB.
Needless to say, the targets for 1985 and 1986 remain is a form of social wage to the labouring class and it serves
unrealised. But the point is—food for all’ has already been the need of capital for the steady flow and reproduction of
a declared goal of the Indian State since the adoption of the labour power and to maintain/increase productivity. This
constitution. A period of three and half decades has made view is also discounted by the argument that historically the
it obvious tKat the Indian State has neither the means nor technological changes or a relative scarcity of labour have
the political will to achieve that goal. Hence, the endorse been found to be more effective than higher rates of medical
ment of the targets set up by the WHO appears to be either expenditure in obtaining increased productivity (Doyal an
Pennel, 1979). While there is positive evidence that public
a mere formality or an exercise in duplicity.
TUrning to the matter of medical intervention which is health legislation of the 1840s in UK resulted in improving
dominated almost exclusively by the provincial government, the productivity of labour, in India, fluctuating state expen
diture on health does not appear to bear any corresponding
we need to face certain facts:
(1) State medicare is practically free to all without relationship with availability of labour in the market. There
discrimination from millionaire to pauper; though in respect is broad agreement among the marxist commentators that
of finance and administration there are provincial boundaries the ruling class meets the social needs of capital through the
services are available to all transcending such boundaries; state invervention in health care or for that matter through
those who enjoy guaranteed medicare through certain agen all social welfare measures. It provides a benevolent image
cies are also welcome to the state’s free medicare; and even for the state maintaining support for the existing system, and
foreigners are not put to any restraint in obtaining free developing the dependency on the state. It legitimises
medicare from the state institutions.
bourgeois ideological underpinnings. On the other hand, it
(2) There exists a strong and evergrowing private sector is asserted that increasing state intervention is the product
of medicare consisting of hospitals, nursing homes, clinics, of the social demands of labour, achieved through class strug
diagnostic set-ups and dispensaries, which constitute 3/4th gle. Fluctuation of the magnitude of intervention generally
of the medicare field.
corresponds with the differing intensity of class struggle.
(3) Overall superiority in specialisation, sophistication, Then again it is argued that there is actually no contradic
modernisation and excellence is still attributed to the state tion between the two explanations and there is no single
sector for various reasons.
factor explanation of social policy. Social demands of labour
(4) State medicare institutions are disproportionately con seek increase in-social wages and public ownership of means
centrated in the urban areas, and the rural institutions, meant of production. Social needs of capital are served by employ
ostensibly for comprehensive health care, have mostly turn ment absorption of surplus population and provision of
ed into curative agencies.
social services pre-empting conflict and unrest from
Conceptually therefore, state medicare is delivered more unemployment, uncertainty and physical distress. The nature
on the principle of charity and not obligation or welfare. It and number of the combination of factors depend on the
is not then surprising that the resulting situation is historical situation, level of development of productive forces
disorganisation, deterioration in quality, unscientific prac and relations of production and the level of class struggle.
tice, corruption, chaos and frequent break-down of law and “There is no clear-cut dichotomy between the social needs
order. In the ensuing ‘free for all’ for the cost-free medicare, of capital and social demands of labour. Any given policy
the weaker sections are deprived of health care.
can serve both. Indeed, social policies that serve the interests
Medicare is provided to the industrial workers through the of the working class can be subsequently adapted to benefit
unique Employees State Insurance (Medical Benefit) Scheme, the interests of the dominant class... Indeed history shows
financed jointly by the workers and the employers, regulated that concessions won by labour in the class struggle become,
by the joint body of employees, employers, Union and Pro in the absence of further struggle, modified to serve the in
vincial Governments and medical profession, and operated terests of the capitalist class” (Navarro, 1976).
by the provincial governments. Services are rendered for
What role of the state do we then envisage for an
sickness, maternity and employment injury. This scheme egalitarian health system? The distorted nature of medicine
could be viewed as a forerunner of national health service under capitalism and the discriminatory delivery of health
but there is a big difference in the matter of financing com care haVe produced diverse reactions. Total state control or
pared to the similar schemes in other countries.
nationalised health care, integrated health care meaning in
Financing of health services in India presents an interesting tegration of other relevent state services with health service,
story. While the share of the allocation on health care has decentralised health care calling for peoples participation and
steadily been reduced in the Union budget in the successive sharing of power in planning and administration, de5-Year Plans, that on family planning increased with a sharp bureaucratisation, i e, replacement of generalists’ control by
upward jump in the 4th Plan. In terms of GNP it has not professionals, people’s health in people’s hands signifying
exceeded 0.5 per cent compared to 5-10 per cent in several vague assertion of self care and self-contained community
developed countries—(GOI, 1975, 78, 79, 80-81). In terms management—are some of the prescriptions. The reactions
of the state’s share in the total health expenditure of the coun seem to ignore the determinist nature of state intervention.
try, India (24 per cent) is way behind not only the developed With the growing magnitude of socialisation of the produc
countries but even Sri Lanka (50 per cent) (Roemer, 1984). tion process, the state inevitably assumes more and more
Steady increase of state intervention in health care is a
(Continued on page 108)
78
Radical Journal of Health
Political Economy of State Health Financing
ravi dugga 1
In a capitalist state the government is a functionary of capitalism—its role is to protect and strengthen it.
Thus the state’s behaviour even with regard to the health sector programmes, is a function of private capital.
The health sector started with a very low priority and has gradually gained an increased share of the state’s
expenditure, the growth rate of health and family planning expenditures has been much greater than both the
growth of government expenditure and the gross domestic product. But this does not reflect an improvement
in health care services provided by the state. Why this is so and what role state financing of health care has
played is examined in this article with specific reference to two states, Gujarat and Maharashtra.
THE health sector is popularly perceived as being part
of the social services sector. The corollary to this being
that it automatically becomes largely a responsibility
of the state. This perception is common even among
the most advanced capitalist states.
Health and education (besides unemployment
insurance in a few countries) are the ‘classical’ sectors
within the umbrella of state welfare. Over the years,
all over the world, these two sectors have increasingly
been supported through public finance for various
reasons. The most important being the predominance
of the view that they are a social service and therefore,
not in the direct interest of private capital. Nevertheless,
they being an important social need had to be met,
and therefore public finance became the provider
increasingly.
The historical consequence of this development has
been a greater role for the state in meeting the needs
of the people. Since state finances come largely from
taxes the household and corporate sectors have
gradually begun to feel the brunt of letting the state
take care of the social sector. Given the nature of the
capitalist state there comes a point beyond which tax
ing private capital becomes a threat to capitalism itself.
Thus emerges a “fiscal crisis of the state” and there
is talk of cuts in welfare and social expenditures. The
pressures of capitalism in its pursuit of surplus ap
propriation is responsible for this.
Advanced capitalism, especially monopoly capital,
and the state have a love-hate relationship. Love,
because the survival of capitalism is dependent on state
protection and support, and hate because increased
state expenditures mean enhanced taxes and public
debt that may terrfiinate in a fiscal crisis, or worse a
social one.
Of late this realisation has hit capitalism, which sees
the dangers inherent in an increased burden of state
welfarism. The result is increased “corporate welfare”.
This is happening in the USA in a large way and the
health sector is the best illustration. Expansion of
private health care (especially corporate) in the last
three or four years in the USA has been phenomenal.
What is more is that it has also been realised that the
sdcial sector, especially health, can be a highly pro
fitable one. This is largely facilitated by modern
technological advances in health care. For instance in
the USA between 1980 and 1984 corporate revenues
in health care grew from $ 25 billion to $ 118 billion,
along with increased monopolisation through mergers
December 1986
and takeovers (in spite of anti-trust suits). And in the
same period, of the 37 largest health and welfare cor
porations only two lost money, whereas 13 more than
doubled their revenues and 11 more than quadrupled
their revenues (Stoesz, 1986).
This trend is true for most advanced capitalist coun
tries and is fast emerging in backward capitalist coun
tries too. In the last two years in India over Rs 200 crore
have been spent by the corporate sector in setting up
60 diagnostic centres (CT scan etc.) all over the coun
try, of which 46 were set up by the United Group alone
(Business India, Dec 29, 1986).
This, however, does not mean that the state health
care sector is on the decline. Historically the state
health sector as well as other state welfare and develop
ment programmes have served the needs of private
capital (see Galper, 1975). We will return to this later.
The state financed health care sector in India is
‘patronised’ by only about one-third of the country’s
population, of this roughly 80 per cent being urban.
That is two-thirds of India’s population utilise private
services for health care; and the state’s health services
are concentrated disproportionately in urban/industrial areas. It may also be noted that municipal
health services, railway, defence and mining health ser
vices, as also those services provided by public sector
undertakings are not accounted for under ‘state health
expenditure’.
Health is a state (provincial) subject and therefore
the responsibility of providing health care vests with
the concerned state. However, the union government
does make a substantial contribution to the states
through grants and centrally sponsored health pro
grammes. Besides, policy making and planning for the
health sector has largely been determined by the centre.
The state health sector in India incorporates three
components (a) Medical Services including CGHS and
ESIS, (b) Public health (including water supply and
sanitation) and (c) Family Planning (including MCH).
Family Planning is almost entirely a centrally funded
programme (it falls under the concurrent list). In this
paper we will look at the health sector as including only
the first two components, treating family planning
independently.
The major sources of data for state spending on
health care are (a) The Combined Finance and Revenue
Accounts (CFRA) of the Union and State governments
compiled by the Comptroller and Auditor General of
India, (b) Summarised Accounts 'in the Indian
79
diseases, viz, measles, whooping cough, tetanus, diphtheria, distinct feature of capitalist society and it is explained in
polio and TB.
various ways. It is argued that state health care expenditure
Needless to say, the targets for 1985 and 1986 remain is a form of social wage to the labouring class and it serves
unrealised. But the point is—food for all’ has already been the need of capital for the steady flow and reproduction of
a declared goal of the Indian State since the adoption of the labour power and to maintain/increase productivity. This
constitution. A period of three and half decades has made view is also discounted by the argument that historically the
it obvious ttiat the Indian State has neither the means nor technological changes or a relative scarcity of labour have
the political will to achieve that goal. Hence, the endorse been found to be more effective than higher rates of medical
ment of the targets set up by the WHO appears to be either expenditure in obtaining increased productivity (Doyal an
Pennel, 1979). While there is positive evidence that public
a mere formality or an exercise in duplicity.
TUrning to the matter of medical intervention which is health legislation of the 1840s in UK resulted in improving
dominated almost exclusively by the provincial government, the productivity of labour, in India, fluctuating state expen
diture on health does not appear to bear any corresponding
we need to face certain facts:
(1) State medicare is practically free to all without relationship with availability of labour in the market. There
discrimination from millionaire to pauper; though in respect is broad agreement among the marxist commentators that
of finance and administration there are provincial boundaries the ruling class meets the social needs of capital through the
services are available to all transcending such boundaries; state invervention in health care or for that matter through
those who enjoy guaranteed medicare through certain agen all social welfare measures. It provides a benevolent image
cies are also welcome to the state’s free medicare; and even for the state maintaining support for the existing system, and
foreigners are not put to any restraint in obtaining free developing the dependency on the state. It legitimises
medicare from the state institutions.
bourgeois ideological underpinnings. On the other hand, it
(2) There exists a strong and evergrowing private sector is asserted that increasing state intervention is the product
of medicare consisting of hospitals, nursing homes, clinics, of the social demands of labour, achieved through class strug
diagnostic set-ups and dispensaries, which constitute 3/th gle. Fluctuation of the magnitude of intervention generally
of the medicare field.
corresponds with the differing intensity of class struggle.
(3) Overall superiority in specialisation, sophistication, Then again it is argued that there is actually no contradic
modernisation and excellence is still attributed to the state tion between the two explanations and there is no single
sector for various reasons.
factor explanation of social policy. Social demands of labour
(4) State medicare institutions are disproportionately con seek increase in-social wages and public ownership of means
centrated in the urban areas, and the rural institutions, meant of production. Social needs of capital are served by employ
ostensibly for comprehensive health care, have mostly turn ment absorption of surplus population and provision of
ed into curative agencies.
social services pre-empting conflict and unrest from
Conceptually therefore, state medicare is delivered more unemployment, uncertainty and physical distress. The nature
on the principle of charity and not obligation or welfare. It and number of the combination of factors depend on the
is not then surprising that the resulting situation is historical situation, level of development of productive forces
disorganisation, deterioration in quality, unscientific prac and relations of production and the level of class struggle.
tice, corruption, chaos and frequent break-down of law and “There is no clear-cut dichotomy between the social needs
order. In the ensuing ‘free for all’ for the cost-free medicare, of capital and social demands of labour. Any given policy
the weaker sections are deprived of health care.
can serve both. Indeed, social policies that serve the interests
Medicare is provided to the industrial workers through the of the working class can be subsequently adapted to benefit
unique Employees State Insurance (Medical Benefit) Scheme, the interests of the dominant class... Indeed history shows
financed jointly by the workers and the employers, regulated that concessions won by labour in the class struggle become,
by the joint body of employees, employers, Union and Pro in the absence of further struggle, modified to serve the in
vincial Governments and medical profession, and operated terests of the capitalist class” (Navarro, 1976).
by the provincial governments. Services are rendered for
What role of the state do we then envisage for an
sickness, maternity and employment injury. This scheme egalitarian health system? The distorted nature of medicine
could be viewed as a forerunner of national health service under capitalism and the discriminatory delivery of health
but there is a big difference in the matter of financing com care haVe produced diverse reactions. Total state control or
pared to the similar schemes in other countries.
nationalised health care, integrated health care meaning in
Financing of health services in India presents an interesting tegration of other relevent state services with health service,
story. While the share of the allocation on health care has decentralised health care calling for peoples participation and
steadily been reduced in the Union budget in the successive sharing of power in planning and administration, de5-Year Plans, that on family planning increased with a sharp bureaucratisation, i e, replacement of generalists’ control by
upward jump in the 4th Plan. In terms of GNP it has not professionals, people’s health in people’s hands signifying
exceeded 0.5 per cent compared to 5-10 per cent in several vague assertion of self care and self-contained community
developed countries—(GOI, 1975, 78, 79, 80-81). In terms management—are some of the prescriptions. The reactions
of the state’s share in the total health expenditure of the coun seem to ignore the determinist nature of state intervention.
try, India (24 per cent) is way behind not only the developed With the growing magnitude of socialisation of the produc
countries but even Sri Lanka (50 per cent) (Roemer, 1984). tion process, the state inevitably assumes more and more
Steady increase of state intervention in health care is a
(Continued on page 108)
78
Radical Journal of Health
Political Economy of State Health Financing
ravi duggal
In a capitalist state the government is a functionary of capitalism—its role is to protect and strengthen it.
Thus the state’s behaviour even with regard to the health sector programmes, is a function of private capital.
The health sector started with a very low priority and has gradually gained an increased share of the state’s
expenditure, the growth rate of health and family planning expenditures has been much greater than both the
growth of government expenditure and the gross domestic product. But this does not reflect an improvement
in health care services provided by the state. Why this is so and what role state financing of health care has
played is examined in this article with specific reference to two states, Gujarat and Maharashtra.
THE health sector is popularly perceived as being part
of the social services sector. The corollary to this being
that it automatically becomes largely a responsibility
of the state. This perception is common even among
the most advanced capitalist states.
Health and education (besides unemployment
insurance in a few countries) are the ‘classical’ sectors
within the umbrella of state welfare. Over the years,
all over the world, these two sectors have increasingly
been supported through public finance for various
reasons. The most important being the predominance
of the view that they are a social service and therefore,
not in the direct interest of private capital. Nevertheless,
they being an important social need had to be met,
and therefore public finance became the provider
increasingly.
The historical consequence of this development has
been a greater role for the state in meeting the needs
of the people. Since state finances come largely from
taxes the household and corporate sectors have
gradually begun to feel the brunt of letting the state
take care of the social sector. Given the nature of the
capitalist state there comes a point beyond which tax
ing private capital becomes a threat to capitalism itself.
Thus emerges a “fiscal crisis of the state” and there
is talk of cuts in welfare and social expenditures. The
pressures of capitalism in its pursuit of surplus ap
propriation is responsible for this.
Advanced capitalism, especially monopoly capital,
and the state have a love-hate relationship. Love,
because the survival of capitalism is dependent on state
protection and support, and hate because increased
state expenditures mean enhanced taxes and public
debt that may terrfiinate in a fiscal crisis, or worse a
social one.
Of late this realisation has hit capitalism, which sees
the dangers inherent in an increased burden of state
welfarism. The result is increased “corporate welfare”.
This is happening in the USA in a large way and the
health sector is the best illustration. Expansion of
private health care (especially corporate) in the last
three or four years in the USA has been phenomenal.
What is more is that it has also been realised that the
social sector, especially health, can be a highly pro
fitable one. This is largely facilitated by modern
technological advances in health care. For instance in
the USA between 1980 and 1984 corporate revenues
in health care grew from $ 25 billion to $ 118 billion,
along with increased monopolisation through mergers
December 1986
and takeovers (in spite of anti-trust suits). And in the
same period, of the 37 largest health and welfare cor
porations only two lost money, whereas 13 more than
doubled their revenues and 11 more than quadrupled
their revenues (Stoesz, 1986).
This trend is true for most advanced capitalist coun
tries and is fast emerging in backward capitalist coun
tries too. In the last two years in India over Rs 200 crore
have been spent by the corporate sector in setting up
60 diagnostic centres (CT scan etc.) all over the coun
try, of which 46 were set up by the United Group alone
(Business India, Dec 29, 1986).
This, however, does not mean that the state health
care sector is on the decline. Historically the state
health sector as well as other state welfare and develop
ment programmes have served the needs of private
capital (see Galper, 1975). We will return to this later.
The state financed health care sector in India is
‘patronised’ by only about one-third of the country’s
population, of this roughly 80 per cent being urban.
That is two-thirds of India’s population utilise private
services for health care; and the state’s health services
are concentrated disproportionately in urban/industrial areas. It may also be noted that municipal
health services, railway, defence and mining health ser
vices, as also those services provided by public sector
undertakings are not accounted for under ‘state health
expenditure’.
Health is a state (provincial) subject and therefore
the responsibility of providing health care vests with
the concerned state. However, the union government
does make a substantial contribution to the states
through grants and centrally sponsored health pro
grammes. Besides, policy making and planning for the
health sector has largely been determined by the centre.
The state health sector in India incorporates three
components (a) Medical Services including CGHS and
ESIS, (b) Public health (including water supply and
sanitation) and (c) Family Planning (including MCH).
Family Planning is almost entirely a centrally funded
programme (it falls under the concurrent list). In this
paper we will look at the health sector as including only
the first two components, treating family planning
independently.
The major sources of data for state spending on
health care are (a) The Combined Finance and Revenue
Accounts (CFRA) of the Union and State governments
compiled by the Comptroller and Auditor General of
India, (b) Summarised Accounts in the Indian
79
Economic Statistics: Public Finance, compiled by the
Department of Economic Affairs of the Ministry of
Finance, and (c) The Performance Budgets of health
ministries of the respective states.
In the CFRA data is available state-wise but the
disaggregation is of little use because the categories
ised are administrative ones like ‘establishment’, ‘direc
ion’, ‘grants’ etc. However, the state’s Performance
Budgets give programmewise expenditures but these
locuments are not easily available; and if available are
too voluminous for a time-series analysis. Therefore,
in this paper national aggregate figures will be used
for an overall analysis, and a case study of programme
based analysis will be done for Maharashtra and
Gujarat states.
State Financing of Health in India
The Indian constitution in its ‘Directive Principles
of State Policy’ has vested the state with responsibility
for providing free health care services to all citizens.
TABLE 1 A: HEALTH EXPENDITURE. GDP AND GOVERNMENT EXPENDITURE IN INDIA BY PLAN PERIOD
(Rs Crores)
State Health Expenditure (a)
Medical
Family
Total
Per Cent
Health
and Public Planning
Plan <b)
Health*
Expendi
ture
Plan Period
11
111
5 Years
annual average
1
3 years
Plan
annual average
Holiday
5 years
IV
annual average
5 years
annual average
V
1979-80
VI”
annual
5 years
annual average
(c)
GDP at
Current
Market
Prices
2
3
4
5
6
7
8
197
39.40
420.8
84.16
(113.6)
939.1
187.82
(123.1)
723
241
(28.31)
1954
390.8
(62.15)
4201.1
840.22
(115)
1320.9
11152.4
2230.48
(165.46)
0.15
0.03
2.2
0.44
(1366.67)
24.9
4.98
(1031.81)
70.4
23.47
(371.28)
284.5
56.9
(142.43)
538.2
107.64
(89.17)
121.8
1626.2
325.24
(202.15)
197.15
39.4
423
84.6
(114.55)
964
192.8
(127.89)
793.4
264.5
37.18
2238.5
447.7
(69.26)
4739.3
947.9
(11L7)
1442.7
12778.6
2555.7
(169.6)
38.7
NA
51.3
NA
37.1
2227
445.4
39.5
2237
745.7
(67.4)
5629
1125.8
(50.97)
6578
1315.6
(16.85)
1567
11479** *
2295.8
(74.5)
8915
1783
13520
2704
(51.65)
23080
4616
(70.7)
21213
7071
(53.18)
53255
10651
(50.6)
103305
20661
(93.98)
31670
262150
52430
(153.7)
50175
10035
66235
13247
(32.0)
9989C
19978
(50.8)
155390
31078
(55.56)
227395
45479
(46.34)
411810
82362
(81.1)
107444
846670
169334
(105.6)
1
5 years
annual average
5 years
annual average
(c)
(c)
Private Total Govt.
Medical
Expendi
Expendi
ture
ture
47.9
49.5
50.5
52.8
(c)
Population
in crore (plan
period
average)
9
?S
42
Af't
SI
55
62
66
71
(Figures in parenthesis are average percentage growth rates over the previous period)
• Includes water supply and sanitation, CGHS, ESIS, ICMR, Medical Education and Research.
•• Last two years of the Vlth plan are budget estimates/allocations.
•**4 years as reported in ‘National Accounts’ and fifth year estimated by the author at Rs 2930 crores.
TABLE 1 B: RATIOS
Per Capita Per Annum Health
Expenditure
(Rupees)
State (Col. 4)
Private
10
1.04
2.01
4.20
5.20
8.14
15.29
21.86
36.0
—
—
9.68
14.62
20.47
21.22
23.74
32.33
Ratio FP: Medical Ratio Pvt Medical
and Public Health State Medical and:
(Per Cent)
Public Health
(Col. 2)
(Per Cent)
11
12
0.08
0.52
2.65
9.74
14.56
12.81
9.22
14.58
_
_
237.14
309.40
288.07
156.58
118.63
102.92
Per Cent State
Health (Col 4) of
Total Govt.
Expenditure
Per Cent State
Health (Col. 4) of
GDP
13
14
2.2
3.13
4.18
3.74
4.20
4.59
4.55
4.87
0.39
0.64
0.96
0.85
0.98
1.15
1.34
1.51
Table ‘A’ Complied from', a) Comptroller and Auditor General of India: Combined Finance and Revenue Accounts, GOI, years
1951-52 through 1981-82 and Department of Economic Affairs: Indian Economic Statistics: Public
Finance, Ministry of Finance, GOI, 1982.
b) CBH1: Health Statistics in India 1984, Ministry of Health, GOI, 1985.
c) CSO. National Accounts Statistics, Ministry of Planning, GOI, Years 1965 through 1986.
to
Radical Journal of Health
Where does the state stand on this issue?
Analysis of finances of the state reveals that the
health sector started with a very low priority and has
gradually gained an increased share of the state’s
expenditure, stabilising between four and five per cent
of the government’s total expenditure. Similarly state
expenditure on health care has shown marginal
increases over the years with regard to proportion of
the Gross Domestic Product. Table 1 ‘A’ and *B’
presents data in this regard by various plan periods.
The most interesting finding that emerges from this
data is that the growth rate of both health and family
planning expenditures have been much greater than
both the growth of government expenditure and the
gross domestic product. Further, as per the estimates
of ‘National Accounts’ wc see that the gap between
state health expenditure and private medical expen
diture is narrowing. These facts are indicative of high
investment in the state health sector, but, unfortunately,
the results of health programmes do not corroborate
this. Why is this so?
Firstly, the level of investment and expenditure in
the state health sector, though experiencing a growth
rate higher than total government expenditure, is at a
fairly low level. For the year 1984-85 the allocated
expenditure for the entire state health sector was
. 3,287.8 crore, working out to a meagre Rs 43.84 per
. cpi.ta per annum (1.54 per cent GDP and 5 per cent
;»f government expenditure). This includes expenditure
g»; medical services and national disease programmes,
public health and PHC, water supply and sanitation,
CGHS, ESIS, MCH, family planning, medical educa
tion and research, health bureaucracy, construction of
new health centres and hospitals. At today’s market
prices providing the above services adequately to the
entire population free of cost requires much more
expenditure than is earmarked presently.
Secondly, a large proportion of health expenditure
in the III, V and VI Plan periods, when the growth
rate of health expenditure had been the highest, went
into infrastructure development i e, water supply
schemes and construction of health centres. In fac
more than one-half of the medical and public health
expenditure since the III Plan period is spent on water
supply and sanitation. The plan holiday period and
IV Plan, when capital expenditure was very little, show
low growth rate in health expenditure. And, in spite
of this the health infrastructure remains poor. Even
today the government is nowhere near the level of
infrastructure and facilities recommended by the Bhore
Committee in 1946.
Thirdly, between 70 and 80 per cent of the invest
ment and expenditure in the state health sector goes
to the 30 per cent population in urban areas. This
mismatch (of rural-urban disparity) by the state is in
spite of the fact that urban areas also have access to
other public and quasi-public health care facilities such
as municipal and other local body hospitals and
dispensaries, municipal protected water supply and
sanitation, municipal funded medical education, ESIS
and CGHS for industrial and government workers and
so on. For instance in 1983 in Maharashtra, of the total
478 state-owned (central and state government)
hospitals and dispensaries 432 (90 per cent) were in
urban areas and of all the state owned beds 97 per cent
were in urban areas. And of all the beds in
Maharashtra (public and private) 30 per cent were in
Bombay city alone (SBHI, 1983).
Fourthly, leaving aside the preventive and promotive
services, the curative services provided by the state,
especially in the rural areas, are grossly inadequate.
That curative services are the priority demand of the
people vis-a-vis health is evident from various studies
that have shown that even in rural areas the private
medical practitioner provides services for between twothirds and three-fourths of illness episodes in the
population.
Following from the above, the private medical sector
becomes a strong adversary to the state sector because
the former is totally curative-oriented, because it is
‘efficient’ and non-bureaucratic, because it is ‘effective’
and most importantly because it is easily accessible
TABLE 2: HEALTH FACILITIES IN INDIA
(selected years)
Year
No of
Popula
Hospitals
tion
Per
Hospital
(In lakhs)
No of
PHCs
Rural
Popula
tion Per
PHC
(In lakhs)
No of
Beds
Popula Percent
tion Per of Rural
Bed
Beds
Percent
of Hos
pitals
Owned
by4the
State
Percent
of Beds
Owned
by the
State
NA
NA
NA
NA
NA
62.6
(16.0)
50.8
(44.3)
49.3
(45.3)
NA
NA
NA
NA
1951
1956
1961
1966
1971
1974
2694
3307
3094
4147
3976
4014
1.3
1.2
1.4
1.2
1.4
1.5
—
725
2565
4631
5112
5283
4.4
1.4
0.8
0.8
0.8
117000
157000
230000
304000
331000
355461
3192
2554
1930
1628
1673
1668
NA
25.0
NA
NA
NA
13.7
1982
6805
1
5739
0.9
504538
1405
17.2
1984
7181
I
7210
0.8
536370
1378
17.43
NA
69.5
(16.2)
68.1
(26.7)
68.1
(*6.7)
No of Percent of
Dispen Dispen
saries
saries
Owned by
the State
6515
7100
9406
1023<j
10897
10200
16754
21780
NA
NA
NA
NA
NA
N^
60.9
(14.1)
51.8
(29.6)
(Figures in brackets are percentages in private sector; the remainder is facilities’ owned by local bodies)
Compiled from: CBHI: Health Statistics in India/Pocket Book of Health Statistics, Ministry of Health, GOI, respective years.
December 1986
81
when needed.
And finally, the credibility of the state’s rural health
services is very low. This is largely due to its obsession
with family planning targets. Over 60 per cent of the
PHC staffs time is spent on family planning work.
Thus, the high growth rate of health expenditure is
a deceptive feature, because disaggregated it reveals the
unhealthy direction of growth. In the following para
graphs the data in each column in Thble I is analysed
in detail.
Medical and Public Health
In the health sector the Britishers did not leave any
significant legacy of an infrastructure. Therefore,
a beginning from scratch had to be made after
Independence. What was left by the British was an
exhaustive Plan called the Bhore Committee Report,
a small network of civil hospitals, a few medical col
leges in premier cities and a network of military and
TABLE 3: MEDICAL EXPENDITURE BY SELECTED
CORPORATE AGENCIES
Organisation
TELCO (b)
National Rayon (b)
Ashok Leyland (b)
BHEL (a)
Railways (a)
SAIL (a)
Air India (a)
CGHS (c)
ESIC (c)*
Bombay Municipal
Corporation (d)
Per Employee
Family Annual
Expenditure (Rs)
Reference Year,
J106
860
717
830.47
310.45
677.93
725.00
271.90
80.99
1982-83
1982-83
1982-83
1980-81
1980-81
1980-81
1980-81
1980-81
1979-80
70.08
1983-84
Source: a Lok Sabha Estimates Committe, 22nd report, Ministry
of Health, GOI, 1982.
b ORG, Health Financing in India, ORG, Baroda, 1985.
c CBHI, Health Statistics in India, Ministry of Health,
GOI, 1983.
d BMC, Performance Budget Estimates 1985-86, BMC,
Bombay, 1985.
railway hospitals. No rural health infrastructure of any
significance existed at the time of Independence. The
expenditure by the British state was meagre (see
Appendix 1).
However, even after Independence the Indian state
did not deem the health sector to be a priority. In the
First Plan period the state spent an average of Rs 39.40
crore per year which was only 2.2 per cent of total
government expenditure and only 0.39 per cent of the
GDP; much less than what the British government had
been spending. At the end of the First Plan, besides
725 PHCs there were 3307 hospitals, and 7100 dispen
saries in India, the majority of hospitals belonging to
the state (breakup of ownership for this period is ot
available).
In the Second Plan period the expendii
medical and public health more than double !
pattern continued in each subsequent plao •
during the ‘plan holiday’ and the IV Plan w’.
rate of health expenditure showed a dra
Health facilities too increased but •
heavily skewed in favour of urban areas.
ching of the Minimum Needs -Progra; 7
Plan onwards rural health infrastru*
-.an to
receive some significant attention
Table 2 lists health care facilities in In?• t is evident
from this table that the health infrastructure is very
poor even today, especially so in rural areas. The best
indicator of health care facilities is the number of
hospital beds available to the population. The earliest
year for which this break-up is available is 1956 when
25 per cent of all hospital beds (government, local body
and private) were located in rural areas that had 80 per
cent of the country’s population. This declined to 13.7
per cent in 1974, clearly indicating that the rural areas
had been neglected grossly where investment in the
health sector was concerned. Even where PHCs are
concerned it is clear that the number of PHCs added
over the years has not been adequate for the rural
population as between 1966 and 1984 the PHC:
Population ratio has remained constant at one PHC
TABLE 4: PLAN OUTLAYS IN THE HEALTH SECTOR—INDIA
(Rs crores)
Health Programme
1. Control of communicable
diseases
2. Primary Health Centres,
Hospitals & Dispensaries
3. Education, Training and
Research
4. Minimum Needs
Programme (Health)
5. Indigenous Systems of
Medicine
6. Family Planning
7. Water Supply & Sanitation
8. Other Schemes
Plan Period (Plan Holiday Period Excluded)
IV
V
III
VI
VII
70.5
127.01
168.61
524.0
1012.67
36.0
61.7
164.78
155.62
•720.1
•1283.87
21.6
36.0
56.3
98.22
111.76
—
—
—
—
29.47
576.96
1096.35
0.70
0.40
49.0
20.2
4.0
3.0
76.0
6.0
9.8
27.0
105.3
11.2
15.83
315.00
407.00
27.69
27.72
516.0
1022.0
40.81
•
1010.0
3922'02
•
•
3296.26
6522.47
•
I
II
23.10
64.0
25.0
• Included in Health Programme 2 and 3.
Sources: 1. CBHI: Pocket Book of Health Statistics of India, Ministry of Health, GOI, 1976.
2. Planning Commission, Sixth Five Year Plan 1980-85, GOI, 1980.
3. Planning Commission, Seventh Five Year Plan 1985-90, GOI 1985
82
Radical Journal of Health
lor 80,000 population. This stability (sic) is also true
of the hospital/population ratio.
However, the point that emerges most significantly
from Thble 2 is the fact that since mid-seventies there
has been a sharp rise in the proportion of health
facilities in the private sector as compared to the state
sector. Thus, in 1974 the private sector accounted for
only 16 per cent of hospitals in the country but within
a decade the private sector’s share of hospitals rose 2.83
times to 45.3 per cent, and that of the state sector
declined from 62.6 per cent in 1974 to 49.3 per cent
in 1984. The change in the proportion of hospital beds
in either sector was not as sharp.
Therefore, it becomes very clear that both the “high”
growth rate of the state health sector and the narrow
ing gap between state and private health sector expen
ditures is only an illusion created by aggregated data.
Family Planning
Expenditure on family planning (now including
MCH, CHG scheme and the EPI program) is almost
entirely financed by the central government through
plan’ funds. Allocations to FP have increased at a
;’ienomenal rate in each plan period. Between the First
the Sixth Plan periods the allocation increased
m ■ ■’ 0.65 crore to Rs 1010 crore i.e. 1554 times, and
o:>‘
coundingly FP expenditure increased from
Rs 0.15 crore to Rs 1626 crore or 10840 times, whereas
total plan expenditures in the same period increased
only 50-fold and health expenditure (plan and non
plan) only 57 times. Computing this growth rate may
sound unfair because FP started with a very insignifi
cant allocation in the First Plan period but the fact
remains that the growth of family planning expenditure
has been at the cost of expenditure on health care ser
vices. In the VII plan for the first time plan alloca
tions (revised) to FP are higher than that for health.
Further, in each plan period we see a decline in
growth rate of family planning expenditure and the
growth has been the lowest, ironically, in the Emergency
period (Vth Plan). Therefore, this computation too is
unfair. This is the illusion that aggregate statistics
project!.
Notwithstanding this, the growth of family planning
expenditure remains higher than that of health expen
diture. And further, it may be noted that at the im
plementation level a large proportion of resources and
personnel-time allocated to health is used for family
planning work because the latter ranks as priority
number one in state policy making. (For details on
Ramily Planning financing see Duggal, 1986).
Private Medical Expenditure
It has already been pointed out earlier that over two-
‘ J-.E 5: DISAGGREGATED STATE HEALTH EXPENDITURE FOR MAHARASHTRA AND GUJARAT—VI PLAN PERIOD
(Rs million)
Programme
Maharashtra
Annual
Average
Per cent
Plan
1980-85
174.0
9.1
354.56
7.5
1.82
0
132.22
32.2
260.58
61.8
120.56
93.1
48.32
3.5
240.64
2.8
70.14
(1-1)
1216.30
(19.17)
34.38
(0.54)
262.42
(4.13)
746.03
(11.76)
457.93
(7.22)
170.32
(2.68)
558.59
(8.81)
248.1
(1.56)
NA
49.62
6.1
NA
NA
11. School Health
NA
NA
NA
12. Family Planning
1435.4
(9.04)
7536*
(47.45)
15883
(100)
287.08
99.5
1507.2
50*
1980-85
1. Direction and Administration
2. Medical Relief
3. Training
4. Medical Education
5. Control of Common Diseases
6. MNP
7. ISM
8. ESIS
9. Other Expenditure/Services/
Loans
10. Nutrition Programme
13. Water Supply & Sewerage
Total
870
(5.48)
1772.8
(11.16)
9.1
(0.06)
661.1
(4.16)
1302.9
(8.2)
602.8
(3.8)
241.6
(1.52)
1203.2
(7.58)
3176.6
138.74
(2.18)
324.86
(5.12)
2.05
(0.03)
927.81
(14.62)
1434.3
(22.6)
6343.87
(100)
Gujarat
Annual
Average
Per Cent
Plan
14.03
16
243.26
7
6.87
34
52.48
12
149.2
35
91.58
13
34.06
9
111.72
0.67
27.75
24
64.97
20
0.41
87
185.56
NA
286.86
67.3
1268.77
(Figures in brackets are percentages to total)
Source: ORG, Health Financing in India, ORG, Baroda, 1985.
• Plan expenditure was Rs 3768 million. Since the non-plan figure was not available the author has estimated it to be half each.
December 1986
83
when needed.
And finally, the credibility of the state’s rural health
services is very low. This is largely due to its obsession
with family planning targets. Over 60 per cent of the
PHC staff’s time is spent on family planning work.
Thus, the high growth rate of health expenditure is
a deceptive feature, because disaggregated it reveals the
unhealthy direction of growth. In the following para
graphs the data in each column in Thble 1 is analysed
in detail.
Medical and Public Health
In the health sector the Britishers did not leave any
significant legacy of an infrastructure. Therefore,
a beginning from scratch had to be made after
Independence. What was left by the British was an
exhaustive Plan called the Bhore Committee Report,
a small network of civil hospitals, a few medical col
leges in premier cities and a network of military and
TABLE 3: MEDICAL EXPENDITURE BY SELECTED
CORPORATE AGENCIES
Organisation
TELCO (b)
National Rayon (b)
Ashok Levland (b)
BHEL (a)
Railways (a)
SAIL (a)
Air India (a)
CGHS (c)
ES1C (c)*
Bombay Municipal
Corporation (d)
Per Employee
Family Annual
Expenditure (Rs)
Reference Year,
J106
860
717
830.47
310.45
677.93
725.00
271.90
80.99
1982-83
1982-83
1982-83
1980-81
1980-81
1980-81
1980-81
1980-81
1979-80
70.08
1983-84
Source-, a Lok Sabha Estimates Committe, 22nd report, Ministry
of Health, GOI, 1982.
b ORG, Health Financing in India, ORG, Baroda, 1985.
c CBHI, Health Statistics in India, Ministry' of Health,
GOI, 1983.
d BMC, Performance Budget Estimates 1985-86, BMC,
Bombay, 1985.
railway hospitals. No rural health infrastructure of any
significance existed at the time of Independence. The
expenditure by the British state was meagre (see
Appendix 1).
However, even after Independence the Indian state
did not deem the health sector to be a priority. In the
First Plan period the state spent an average of Rs 39.40
crore per year which was only 2.2 per cent of total
government expenditure and only 0.39 per cent of the
GDP; much less than what the British government had
been spending. At the end of the First Plan, besides
725 PHCs there were 3307 hospitals, and 7100 dispen
saries in India, the majority of hospitals belonging to
the state (breakup of ownership for this period is not
available).
In the Second Plan period the expenditure on
medical and public health more than doubled and this
pattern continued in each subsequent plan, except
during the ‘plan holiday’ and the IV Plan when growth
rate of health expenditure showed a drastic decline
Health facilities too increased but they remained
heavily skewed in favour of urban areas. With the laun
ching of the Minimum Needs-Program, from the IV
Plan onwards rural health infrastructure began to
receive some significant attention.
Table 2 lists health care facilities in India. It is evident
from this table that the health infrastructure is very
poor even today, especially so in rural areas. The best
indicator of health care facilities is the number of
hospital beds available to the population. The earliest
year for which this break-up is available is 1956 when
25 per cent of all hospital beds (government, local body
and private) were located in rural areas that had 80 per
cent of the country’s population. This declined to 13.7
per cent in 1974, clearly indicating that the rural areas
had been neglected grossly where investment in the
health sector was concerned. Even where PHCs are
concerned it is clear that the number of PHCs added
over the years has not been adequate for the rural
population as between 1966 and 1984 the PHC:
Population ratio has remained constant at one PHC
TABLE 4: PLAN OUTLAYS IN THE HEALTH SECTOR—INDIA
(Rs crores)
Health Programme
1. Control of communicable
diseases
2. Primary Health Centres,
Hospitals & Dispensaries
3. Education, Training and
Research
4. Minimum Needs
Programme (Health)
5. Indigenous Systems of
Medicine
6. Family Planning
7. Water Supply & Sanitation
8. Other Schemes
Plan Period (Plan Holiday Period Excluded)
V
IV
III
VI
VII
524.0
1012.67
•720.1
•1283.87
29.47
576.96
1096.35
27.72
516.0
1022.0
40.81
•
1010.0
3922x02
•
•
3296.26
6522.47
•
I
II
23.10
64.0
70.5
127.01
168.61
25.0
36.0
61.7
164.78
155.62
21.6
36.0
56.3
98.22
111.76
—
—
—
—
0.70
0.40
49.0
20.2
4.0
3.0
76.0
6.0
9.8
27.0
105.3
11.2
15.83
315.00
407.00
27.69
• Included in Health Programme 2 and 3.
Sources: 1. CBHI: Pocket Book of Health Statistics of India, Ministry of Health, GOI, 1976.
2. Planning Commission, Sixth Five Year Plan 1980-85, GOI, 1980.
3. Planning Commission, Seventh Five Year Plan 1985-90, GOI, 1985.
82
Radical Journal of Health
for 80,000 population. This stability (sic) is also true
of the hospital/population ratio.
However, the point that emerges most significantly
from Thble 2 is the fact that since mid-seventies there
has been a sharp rise in the proportion of health
facilities in the private sector as compared to the state
sector. Thus, in 1974 the private sector accounted for
only 16 per cent of hospitals in the country but within
a decade the private sector’s share of hospitals rose 2.83
times to 45.3 per cent, and that of the state sector
declined from 62.6 per cent in 1974 to 49.3 per cent
in 1984. The change in the proportion of hospital beds
in either sector was not as sharp.
Therefore, it becomes very clear that both the “high”
growth rate of the state health sector and the narrow
ing gap between state and private health sector expen
ditures is only an illusion created by aggregated data.
Family Planning
Expenditure on family planning (now including
MCH, CHG scheme and the EPI program) is almost
entirely financed by the central government through
‘plan’ funds. Allocations to FP have increased at a
phenomenal rate in each plan period. Between the First
and the Sixth Plan periods the allocation increased
from Rs 0.65 crore to Rs 1010 crore i.e. 1554 times, and
more astoundingly FP expenditure increased from
Rs 0.15 crore to Rs 1626 crore or 10840 times, whereas
total plan expenditures in the same period increased
only 50-fold and health expenditure (plan and non
plan) only 57 times. Computing this growth rate may
sound unfair because FP started with a very insignifi
cant allocation in the First Plan period but the fact
remains that the growth of family planning expenditure
has been at rhe cost of expenditure on health care ser
vices. In the VII plan for the first time plan alloca
tions (revised) to FP are higher than that for health.
Further, in each plan period we see a decline in
growth rate of family planning expenditure and the
growth has been the lowest, ironically, in the Emergency
period (Vth Plan). Therefore, this computation too is
unfair. This is the illusion that aggregate statistics
project!.
Notwithstanding this, the growth of family planning
expenditure remains higher than that of health expen
diture. And further, it may be noted that at the im
plementation level a large proportion of resources and
personnel-time allocated to health is used for family
planning work because the latter ranks as priority
number one in state policy making. (For details on
Family Planning financing see Duggal, 1986).
Private Medical Expenditure
It has already been pointed out earlier that over two-
TABLE 5: DISAGGREGATED STATE HEALTH EXPENDITURE FOR MAHARASHTRA AND GUJARAT—VI PLAN PERIOD
(Rs million)
Programme
Maharashtra
Annual
Average
Per cent
Plan
1980-85
174.0
9.1
354.56
7.5
1.82
0
132.22
32.2
260.58
61.8
120.56
93.1
48.32
3.5
240.64
2.8
70.14
(1.1)
1216.30
(19.17)
34.38
(0.54)
262.42
(4.13)
746.03
(11.76)
457.93
(7.22)
170.32
(2.68)
558.59
(8.81)
248.1
(1.56)
NA
49.62
6.1
NA
NA
11. School Health
NA
NA
NA
12. Family Planning
1435.4
(9.04)
7536’
(47.45)
15883
(100)
287.08
99.5
1507.2
50*
1980-85
1. Direction and Administration
2. Medical Relief
3. Thaining
4. Medical Education
5. Control of Common Diseases
6. MNP
7. ISM
8. ESIS
9. Other Expenditure/Services/
Loans
10. Nutrition Programme
13. Water Supply & Sewerage
Total
870
(5.48)
1772.8
(11.16)
9.1
(0.06)
661.1
(4.16)
1302.9
(8.2)
602.8
(3.8)
241.6
(L52)
1203.2
(7.58)
3176.6
138.74
(2.18)
324.86
(5.12)
2.05
(0.03)
927.81
(14.62)
1434.3
(22.6)
6343.87
(100)
Gujarat
Annual
Average
Per Cent
Plan
14.03
16
243.26
7
6.87
34
52.48
12
149.2
35
91.58
13
34.06
9
111.72
0.67
27.75
24
64.97
20
0.41
87
185.56
NA
286.86
67.3
1268.77
(Figures in brackets are percentages to total)
Source: ORG, Health Financing in India, ORG, Baroda, 1985.
* Plan expenditure was Rs 3768 million. Since the non-plan figure was not available the author has estimated it to be half each.
December 1986
83
thirds of health care services utilisation is in the private
sector and the remaining is divided between the state
sector and other public and quasi-public institutions.
In Thble 1 we see that the growth of private medical
expenditure has been much slower than the state health
sector. As a result the gap between the two has nar
rowed down to almost unity during the VI plan period.
This is contradictory to two facts indicated in earlier
sections. Firstly, that between two-thirds and threefourths of health care utilisation is in the private sec
tor. And second, that the growth rate of the private
health sector after mid-seventies has been very high (see
Table 2).
Therefore, this data on private medical expenditure
computed by the CSO in ‘National Accounts Statistics’
is highly questionable. Studies carried out by the Foun
dation for Research in Community Health indicates
much higher estimates of private medical expenditure.
For the year 1983-84 it has been estimated that the total
health expenditure in India was Rs 16,386.41 crore or
8.33 per cent of the GDP. Out of this only 11.7 per
cent was spent by the state, 60.4 per cent was spent by
private households, 22.7 per cent by the corporate sec
tor (private and public) for its employees and 5.2 per
cent by local bodies. Also, with regard to private
household health expenditure a gross rural-urban
disparity is seen—in rural areas an astonishing 94 per
cent of health expenditure was borne privately by
households whereas in urban areas this burden was
only 35 per cent of their health expenditure (FRCH,
1981). This is mainly because urban areas have access
to better state and other public (such as municipal)
health care facilities as also to employer or insurance
sponsored health care programmes. Expenditure of
selected agencies is presented in Table 3. Ratios: A few
selected ratios have been computed from Table I and
are presented in Table I ‘B’. The data in this Table
speaks for itself and it has also been referred to in
earlier sections. Therefore, we leave it at that.
State Health Expenditure on Health
Programmes
As mentioned earlier disaggregated data for state
health expenditure for the nation is not available on
a programme-wise basis, except for plan expenditure.
Therefore, we will look at the state (provincial) level
to get a detailed breakdown.
Where plan expenditure is concerned consolidated
data is available for eight categories. Thble 4 presents
this data. It is clear from this table that water supply
and sanitation leads as expenditure number one
grossing between 30 per cent and 50 per cent of the
health sector Plan—it has. grown in each plan period
taking a larger proportion each time.
Family planning on the other hand started by being
the lowest funded programme in the first plan (0.3 per
cent) to gaining second position (27.56 per cent) after
water supply, by the V Five Year Plan. As a conse
quence all the other programmes have suffered and
have had a smaller share in each subsequent health
84
plan since family planning took over the second posi
tion in the IV Plan. Thus the priority of the state in
the health sector is fairly clear—strongly in favour of
FP at the cost of other crucial health programmes.
Unfortunately such a breakup is not, available for
state health expenditure outside the plan. But at the
state-level detailed disaggregation is available. Table 5
gives a breakup of various health programmes for
Maharashtra and Gujarat during the VI Plan period.
Water supply and sewerage is the largest single category
of expenditure in each sate—as a percentage it is as
high as 47.45 per cent in Maharashtra and only 22. 6
per cent in Gujarat.
If one leaves aside water supply, then medical relief
accounts for the largest category’ of expenditure in both
Maharashtra and Gujarat. This is followed by family
planning, control of communicable diseases and ESIS.
The other programmes follow a different sequence of
priority in each state. The per capita per annum state
health expenditure (inclusive of water supply) for
Maharashtra and Gujarat works out to Rs 48 and
Rs 35 respectively.
Thus the priority and pattern of expenditure for
various health programmes is not very different from
that we have seen for ‘plan expenditure’ for the coun
try. Of course, it must be noted that Maharashtra and
to some extent Gujarat are the better performing states
vis-a-vis the health sector.
Role of State Health Sector
In the foregoing analysis we have seen that within
the health sector two programmes stand out pro
minently—water supply and sanitation and family
planning. Ironically both these programmes are not
perceived by the people as health programmes. For the
general population health care is synonymous with
curative services and this does not have a very high
priority with the state.
Why do water supply and sanitation and family
planning feature as high priority programmes? Water
supply itself has high priority with people, may be even
greater than medical services, but this is not the reason
why it is so heavily funded.
The role played by imperialist agencies is very crucial
in understanding this. If one lays threadbare the
development programme expenditures of the state it
is clear that those programmes which receive financial
support through various imperialist agencies, such as
bilateral (USAID, ODA, DANIDA, etc), multilateral
(World Bank, WHO, etc) or private (Ford, Rockefeller,
Population Council, etc), get into the state’s priority
list. The Indian state, being part of the world capitalist
system (though backward), is greatly influenced by it
in its policy and programme making. Thus water
supply and family planning and a few selected com
municable diseases (malaria, earlier small pox, now
measles and even AIDS) get. top billing in the state’s
resource allocation. If one goes through the CFRA or
RBI Finance Repons of any year and looks up the sec
tion on international debt the correlation between plan
Radical Journal of Health
priorities and public finances and foreign debt becomes
clear. Power projects, transport and communication,
industrial infrastructure, mining projects, irrigation
projects, water supply schemes and population con
trol projects are the major areas of international debt
financing. These areas also happen to be the ones that
take the cream of our plan public finances. These are
the very areas in which India lacks technological skills
and has to rely on multinational corporations. This is
too good to be a mere coincidence. If one were to list
all the significant water supply schemes and the
population control projects in India there would not
be a singie project that did not receive foreign finances
(see RBI, 1984).
This nexus does not exist only at the international
level but also within the country between the state and
private capital. In a capitalist state the government
(the functional form of state) is a functionary of
capitalism—its role is to protect and strengthen it. Tnus
the state’s behaviour, even with regard to the health sec
tor programmes, is a function of private capital. The
state’s financing patterns of various health sector pro
grammes are primarily the fulfilment of the needs of
private capital. At the time of Independence the Indian
state lacked any significant health structure. The Indian
bourgeoisie was not prepared to enter this ‘social sec
tor’ and therefore it allowed the state to develop this
sector. And today when a bare minimum of health in
frastructure has been developed and is functional the
bourgeoisie, following the footsteps of its western
allies, has stepped in a large way in the health sector.
In fact, in the next three or four years large financial
investments by the corporate sector in health care have
been planned.
Further the curative health care sector, which has
priority with the people and which forms the raison
d'etre of the entire pharmaceutical and medical equip
ment industry (overwhelmingly controlled by the
private sector, especially MNCs), has received a very
lukewarm attention from the state. This is because the
entire private practice of medicine thrives on curative
services. It is the life-line of the private health sector.
Private practice of medicine, which looks after threefourths of the population falling ill, has never been
controlled by the state. It has been given a completely
free hand to operate and amass surplus.
Most of the doctors who get into private practice
are trained at public institutions run entirely through
public finances. Thus the state is directly responsible
for creating an exploitative private health sector. The
state is also a very large buyer of drugs from the private
drug companies. The state provides tax concessions for
running private hospitals under the grab of-‘public
trusts* that are referred to as ‘voluntary hospitals’.
(According to the Directory of Hospitals in India
Maharashtra state does not have a single private
hospital. Jaslok, Breach Candy, etc are listed as ‘voluntary^ hospitals!).
Thus we may conclude that the state’s health expen
diture Which has been gradually increasing over the
years, grows in an unhealthy direction, is urban-biased,
anti-poor and above all is invested for the health of
private capital.
References
Duggal, Ravi (1986): Financing Family Planning, XIII Annual
Meet of Medico Friends Circle, Background Paper II.
2 FRCH (1986): Health Expenditure in India by Ravi Duggal.
FRCH Newsletter, Vol.I, No.l, FRCH, Bombay.
3 Galper, J (1975): The Politics of Social Service, Prentice Hall,
Engelwood Cliff, N.J.
4 RBI (1984): Report on Currency and Finance, Vol II, RBI,
Bombay.
5 Stoesz, David (1986): Corporate Welfare: The Third State of
Welfare in the United States, Social Work, July,August 1986.
1
Appendix-1
Health Expenditure During British Rule 1870-1939
(Rs million - annual average)
Category of Health
Expenditure
Central & Provincial Govt.
Medical and Sanitary
Military Medical
Municipal Water Supply
Conservancy, Drainage,
Hospital, etc
District and Local Boards
Sanitation & Hospitals
Total Health
Expenditure
Total Govt. Municipal,
District, etc. Expenditure
Per Cent Health Expenditure
of Total Expenditure
1870-79
1880-89
1890-99
Decade
1900-09
1910-19
1920-29
1930-39
6.2
(0.03)4.2
7.3
(0.04)’
5.5
11.6
(0.05)7.1
14.1
(0.06)’
8.2
23.0
(0.10)6.3
52.1
(0.22)NA
57.0
(0.21)’
NA
8.1
(0.04)
—
—
18.5
(0.07)
10.5
(0.05)
—
—
23.3
(0.09)
17.3
(0.08)
2.8
(0.01)
38.8
(0.14)
26.9
(0.12)
4.3
(0.02)
53.5
(0.20)
40.3
(0.18)
6.7
(0.03)
76.3
(0.31)
75.5
(0.32)
15.8
(0.06)
143.4
(0.60)
67.7
(0.25)
20.6
(0.08)
145.3
(0.54)
589.7
798.8
1026.7
1265.2
1679.6
2677.9
2651.4
3.14
2.92
3.78
4.23
4.54
5.35
5.47
(Figures in brackets are Rs per capita per annum expenditure on health at current prices).
• includes military medical expenditure.
Source: Statistical Abstract of British India, relevant years: quoted in “The Politics of Health in India” by Roger Jeffery. C alifornia
University Press, Berkeley, 1987 (forthcoming).
-
December 1986
85
State in Medical Care
V
• ;•/
The nature of state intervention in medicare has been determined by t'--. o factors . «•;. .r.and of rhe people
on the one hand, and the ruling classes' urge to acquire legitimacy and credibility on the other. Often enough
policies which have been a consequence of the pressures brought to bear by the
ciass, have subse
quently adapted to benefit the interest of the dominant class effective medical care to rhe poor, can never,
the article contends, be provide by a state geared to the interests of capital accumulation.
MODERN societies, without exception, view certain
?asic health care services as commodities to which
ivery member of the society should be gauranteed
recess, regardless of their ability to pay. This general
proposition seems widely shared among nations,
whatever their cultural and political complexions;
vastly different approaches, however, have been
adopted for acting on that precept” (Reinhardt, 1982).
Reinhardt’s statement reflects a somewhat univer
sal value; but, besides approaches, the understanding
and interpretations of the general proposition he men
tions also differ widely. Though it has long been
established that ‘basic health care’ includes food-clothshelter-safc water-sanitation, etc, as popularly
understood in India it actually means medical care.
i e, medical intervention to prevent and treat diseases.
That is why the Indian slate maintains a large number
of institutions where a citizen, dying from some
disease, may claim free life-saving medical aid. There
is no state agency which provides free food to a citizen
dying from hunger or for that matter clothing, shelter,
etc, to the similarly deprived. Neither is there any de
mand on the state from any quarter to arrange for such
provisions. In fact, conceptually it is yet to be accepted
that the basic elements of health care should be pro
vided free to the pauperised people; to each according
to his ability—is the motto; one should earn his
living—is the precept. Emergency situations,
e g, disasters like Hoods, earthquakes, accidents, etc,
of course, make exceptions. In contrast, universal free
medical care by the state is not only welcome but such
provision is actually there and more is being demanded.
The endeavour to provide medical care for its
members by human society is as old as any other social
activity, state, religious institutions, voluntary collec
tive efforts—ail have played their pari. Modern
societies, enriched by modern scientific knowledge.
have turned their attention to basic health care with,
as Reinhardt says, vastly different approaches. In the
socialist countries, state intervention is almost com
prehensive in all aspects though the citizens contribute
in varying proportions to its financing. In the
developed capitalist countries state intervention in the
matter of safe water supply, education and sanitation
is quite significant and, though food-clothing-shelter
remains as yet an individual responsibility, various
social security schemes help the pauperised citizens and
guard agains' death from deprivation. As regards
medical care, approaches are different. In the US there
is no direct state intervention and the semblance of a
free market is sought to be preserved, but with the
86
introduction of medicare (for aged) and medicaid (for
poor) programmes and financial support to other agen
cies, the financial contribution of the state has, steadily
in the last two decades, come to bear the largest share
in the national health care expenditure. United
Kingdom’s National Health Service is somewhat
unique and rather incomparable among the capitalist
countries as it is run entirely with slate revenue. Other
countries heavily depend on different kinds of
insurance systems with heavy state and employer con
tributions. In Canada medical care is almost totally
state care.
Among the developing and under-developed coun
tries, the trend is similar. Pressure on the slate to pro
vide for more and more health care is put from all
corners—deprived classes, liberal section, political
forces and international community—albeit from dif
ferent motives. Accordingly state health care is expan
ding more rapidly than private sector health care. The
Indian scene may be reviewed in two categories—non
medical health care and medical care.
The debate in the wake of WHO’s call ‘Health For
AH' has brought about a change in the concept of non
medical health care. It not only includes food-cloihingshelter-safe water-sanitation-poliution-free environ
ment, etc, but is also held to be dependent on educa
tion, economic security or effective employment,
women’s equality, social justice, political control over
economy, etc. For all these factors, the supreme role
of the economy is indisputable. The market economy
does not care for the achievement of all these health
determinants for the broad masses. Clearly, the private
sector of the economy cannot be induced to work for
equitable distribution of non-medical health care, nor
can such health care be achieved through individual
efforts. Its realisation depends entirely on the political
direction of state policy and its effective implementa
tion. In other words, non-medical health care for the
masses depends entirely on state intervention for the
development of new economic relations conducive to
equitable distribution.
Why Stale Medical Care?
State intervention in medical care depends not so
much on the economic structure of the social forma
tion; all societies appear to agree on the state’s increas
ing role in providing universal medical care. The extent
and magnitude of state intervention depend primarily
on political commitment and then on the level of
development of the state as an institution and on the
degree of its dominance over social activities. In India,
Radical Journal of Health
the operation of preventive medical intervention,
e g, national disease control and eradication pro
gramme, routine immunisation, etc, is almost exclu
sively in the hands of the state. Free curative services
operated by the state effectively reach only a few
selected target groups, e g, government employees,
including the armed forces, organised labour force
(ESI), and the socially powerful minority in both urban
and rural areas. The rest of the population depends
upon various kinds of private and corporate services.
All concerned people agree that the services are inade
quate and effective curative services do not reach the
largest section of the people in need. A variety of
prescriptions have been offered as remedial measures
and these should be considered in their political and
economic dimensions.
It is often argued that liberal philanthropic
welfare has given way to capitalist welfare measures,
e g, medical care which is intended to contribute
towards maintaining reproduction of labour; state
medical care, like education, is actually a part of the
social wage of the labouring class. This argument ap
pears to be relevant in the context of an advanced
capitalist economy where the role of skilled and highly
skilled labour is significant and capital’s stake in
developing that kind of labour is high enough to justify
large state allocations to medical care in order to main
tain the health of the labour force. In the drive for ac
celerated industrialisation in USSR and China, state
policy accorded priority to maintaining the health of
the labouring force by organising medical clinics in
each factory complex (Deacon, 1984; Wilenski, 1979).
But this argument is not sufficient to explain the Indjan
situation. Labour in Indian industry and agriculture
is mostly low-skilled and unskilled and the reserve force
is so abundant that its continuing health and quality
cause the least worry to the capitalists. There is as yet
no evidence to suggest a linear co-relation between pro
ductivity and improvement of the health status of the
people. Even in the case of the ESI, the apathy and
neglect of the state as well as of the employers indicate
that they are more interested in something other than
the protection of the workers’ health. On the other
hand, the argument that the entire state
service is entended to earn legitimacy for the ruling
classes and the cx.hting'social order and to secure
credibility for the state as the beneypjpnt fr-enti of the
poor appears to be more plausible. It will be evident
if the rtal state of affairs prevailing in the operation
of the state health service is reviewed.
State authorities never tire of proclaiming that the
state service is free and is meant for the poor. Actually,
both the principle and practice are otherwise. In
principle—legal, constitutional and otherwise—state
medicare is not meant foj the poor alone. By policy
the access is universal. Both the millionaire and pauper
have equal rights to claim free state service. Not only
that, the population groups who enjoy exclusive access
to reserved medicare schemes, e g, CGHS, ESI, railway,
armed forces, public undertakings, big industries, etc,
December 1986
also receive free treatment from state hospitals without
restriction. Even foreigners are freely entertained as a
routine. What happens really is that the larger portion
of effective state medicare is cornered by the sociallyeconomically-politically powerful sections who, in ad
dition, are exclusive recipients of other medicare pro
jects not accessible to the poor. That the real objec
tives of state policy are compatible with this situation
is evident from the fact that state medicare infrastruc
ture is concentrated in the urban areas; that provision
of high cost medical technology, e g, C T Scanner,
Echodiagnostics, cancer-therapy, intensive care,
surgical super-specialities, etc, which have little
relevance to the major medical needs of the poor
(TB, leprosy, enteric disease, bacterial and parasitic
infections, etc), is rapidly increasing; and that the state
frequently spends large amounts for high cost treat
ment of dubious outcome for the VIPs. An example:
state medicare in West Bengal is fairly well developed
compared to other provinces. But even after the
devastating experience of the enteric disease epidemic
in 1984, the government is unable to provide for cheap
oral rehydration salt packages to the chronically af
flicted population on account of stringency of funds
which does not impose any constraint, however, on the
expansion of high cost technology proceeding as per
schedule in the metropolitan hospitals frequented by
affluent clientele. Secondly, state service is far from
free for the poor. Supply of the needed essential drugs
is grossly inadequate and people have to purchase these
as a routine. In the urban and semi-urban hospitals
it is now customary to engage at the patient’s own cost
an additional care-taker in order to obtain minimum
necessary caring services. The practice of some form
of payment as premium to the doctor or hospital
worker for the privilege of admission in a free bed is
still rampant in most of the provinces. Quite frequently
such premiums ae obligatory for investigative, surgical
and similar services. It should however be kept in mind
that even with the premium, state service, on the whole,
is much cheaper than the market product both for the
poor and the affluent.
Medical Care vs Non-Medical Care
Ofiiciai vcir5’Pns °f state policy, expert commen
tators and the WHO su^tegy for Health For All-all
in quest of better health for trie people emphasise
nori-medical health care and preventive intervention
and underplay medical care. As a long-term strategic
approach this cannot be disputed. But a good deal of
ambivalence and many contradictions appear in the
field of practice. The strategic approach takes into con
sideration only the conventional measurable indices of
health, e g, mortality, morbidity, disability, water
supply, sanitation, etc, on the one hand and the pro
portion of doctors, paramedics, beds, drug consump
tion, etc, per unit of population on the other, in deter
mining the efficacy of health care service. BUt?medical
care serves a prime need which cannot be quantified
or statistically measured.
87
Healers have been venerated and honoured since the
infancy of human society for the vital function they
perform both at the individual and social levels; they
respond to human distress. Most of minor illnesses
treat themselves; people learn to tackle a good number
of everyday physical ailments themselves; when people
seek a healer it is a response to more than the mere
physical illness but includes added factors of apprehen
sion, fear and helplessness which compound the
distress. The healer propounds an explanation of the
causation of ailment (however weird), prognosticates,
takes charge of the battle, relieves the patients of their
helplessness, applies his technology (however primitive
and absurdly ritualistic) of diagnosis and treatment and
emerges triumphant when the self-healing ailment
heals itself. The entire episode restores confidence and
balance to the sufferer and his kinfolk, enabling
them to again face the adverse world with renewed
courage—the unknown enemy is now known and con
quered and the healer, the weapon to tackle the enemy,
is there. Even when the healer fails, he allays distress,
offers comfort and finally legitimises death, the most
fearful enemy, by performing rituals intended to ensure
a comfortable after-life for the dead. This is one of
the most vital psycho-social functions for mankind to
adjust to environmental adversity in the struggle for
survival and progress. Biologically potent therapy came
much later, only recently. In fact, as late as in 1980,
Oliver Wendell Holmes wrote that, except for opium
and wine, “if the whole materia medico, as now used,
could be sunk to the bottom of the sea, it would be
all the better for mankind—and all the worse for the
Tishes’’. Modern doctors also perform the same psycho
social function, only they are immensely more suc
cessful owing to the remarkable development of potent
preventive, life-saving, curing and relief-producing
technology of medical science. But distortions of this
very achievement have developed, influenced by
economic and socio-cultural transformations. Modern
medical care generated tremendous mass demand and
was rapidly transformed into a commodity attaining
its characteristic features. Doctors rely more and more
on the infallibility of technology and are at the same
time getting enamoured more and more of its commer
cial return. Time for consultation is now priced and
cannot be wasted for demystifying, caring and personal
attention. Drug industry, flooding the market with
useless drugs, makes skyhigh profit so that access to
essential drugs becomes dear for the poor. The very
expansion of medicare services gave birth to bureaucraiisation and de-personalisation. In short, while the
demand for more and better medical care is increas
ing, escalating prices are pushing it out of the reach
of most people.
Medical care continues to be one of the most press
ing fcit-needs of all societies. Medical care renders
credibility to any health care service and ensure people’s
acceptance of it. China’s post-revolutionary health
policy is a case in point. Policy makers understood that
ip order to ensure mass participation in the puolic
health programmes, the people’s felt-need of medical
88
care must somehow be met and they rapidly set up a
comprehensive organisation to serve even the people
in remote, inaccessible areas. To improvise, they requisi
tioned the services of the indigenous system of
medicine. The point is to provide for some form of
medical care to all regardless of standard and quality
which could come later. The Chinese health system is
now so organised that a citizen of a remote village is
assured of the most sophisticated treatment, if needed,
in an urban centre.
In our own society, preaching and practice differ.
While almost everyone harps on the priority need for
non-medical health care, in practice expansion of
medicare service goes on unabated. Government health
centres, established to provide comprehensive health
care, have over the years turned into centres of curative
service. People, who persistently deprecate the grow
ing trend of setting up sophisticated diagnostic and
curative centres, never fail to rush there for their own
needs. The reason for this is not far to seek. Medicare
needs of Indian people are so urgent and enormous
that they overshadow all other needs. And their priority
cannot be over-emphasised. Though it is well-known
that availability of safe water is the final answer to the
massive problem of diarrhoeal diseases, the instant
need of the diarrhoea-stricken dying child is curative
intervention and not safe water. To save the life of their
dear ones, the poor risk further pauperisation, the
extremely poor risk destitution. Medical care is a com
modity which never fails to find consumers who can
not afford it.
To sum up, medical care is the most important felt
health need of the people; medical care is the pivot of
health care service; medical care adds credibility to
health care programmes and ensures people’s interest;
medical care meets needs of the people which, though
not quantifiable, are indispensable in acquiring
strength to fight against adversities. And whatever role
is assigned, on paper, to medical care, it will continue
to play the dominant one in health care service.
People’s demand for more and better medical care will
never diminish.
Medical Care Delivery
How then to ensure a certain standard of effective
medical care to the people? At present the delivery of
medical care is operated through three channels with
some overlapping. Firstly, free care—through govern
ment and non-government hospitals and clinics.
Secondly, indirectly paid care—through various
medicare schemes for employed people, e g, ESI,
government employees’ medicare, corporate employees’
medicare and insurance schemes. Thirdly, directly paid
care—through open market which includes a few
voluntary institutions. The system, as underlined
earlier, has failed to provide medical care to the poor.
That is why pressure on the state to provide for the
deprived is mounting. The state, on the one hand, is
not in a position to disclaim such responsibility for
obvious political compulsions; on the other, it cannot
really provide for a minimum standard of effective
Radical Journal of Health
medicare for the deprived population without jeopar
dising the existing exploitative economic order. To find
the way out, several prescriptions have been offered as
remedies. The ICSSR — ICMR report recommends a
6-tier organisation from the smallest unit at the lower
level covering 1,000 persons operated by two part-time
voluntary health workers. The required cost has been
worked out to be very low, e g, Rs 30 per capita per
annum. The entire scheme appears to be not only
simplistic but idealistic as well. It also offers univer
sal access for affluent and poor alike; allows private
market to thrive; does not provide for guaranteed
emergency care and rests on the premise that both the
higher echelons of administration and the providers
are imbibed with the spirit of selfless public service.
Several other prescriptions include (a) people should
be taught and trained in demystified principles of
medical care so that they can take health in their own
hands, (b) indigenous and non-allopathic systems
should be adopted to develop an alternative cheaper
culturally acceptable medicare for the poor. None of
the alternative schemes suggests dismantling of the
sophisticated modern medicare merrily operating in the
market. Parallel existence of inaccessible and costly
high grade and free low grade services devalues the
latter and breeds demand for the high grade one. The
poor are already aware of the virtue of modern
medicine. TYue, owing to poverty, they have to go for
the cheaper alternatives most of the time, but that is
no indication that they love these alternatives or have
reconciled themselves to using them for ever. Govern
ment experiment in West Bengal illustrates the point
clearly. Government appointed homeopath and
ayurved practitioners are in a few health centres. It is
a common scene in those centres that they spend their
days without patients while people throng to the
allopathic counter even when the latter is attended by
only a pharmacist. The most repugnant feature of the
alternative prescriptions is the common objective that
each is aimed at lightening the burden of the state.
People should be made to realise that they are respon
sible for their own ill health and therefore must learn
to take care of health hazards by themselves. Hence
the slogan “people’s health in people’s hands”. Or they
ought to remain satisfied with traditionally superior,
culturally compatible indigenous medicine with a few
doses of cheaper but holistic homeopathy here and
there. In any case, they should not bother the state for
more costly modem medicare. The modern medicare
system will be there but only for the privileged and af
fluent as usual. The alternative schemes have a com
mon virtue. They spare the state large expenditure and
at the same time see to it that its image is not tarnished.
For this purpose, a number of issues, e g, cultural
compatibility, self-sufficiency, demystification, etc,
have been broached in order to confuse the problem
which is essentially economic. In fact, the chief con
tribution of modern science is to demystify the secrets
of the universe—natural and biological. At the present
level of knowledge, the ancient medicines stand almost
totally mystified, while modem medical science has
December 1986
been able to demystify the phenomenon of ill health
and health care to such an extent that even illiterate
people now can acquire an insight into the socio
economic and biological dynamics of physical disease
and its management. Self-help is another utopia. It has
long been abandoned by humankind since the intro
duction of division of labour in social production. By
no stretch of imagination does it seem advisable to con
sider creation of self-sufficient human beings produc
ing their own material, biological and cultural
necessities by themselves or immediate communities.
The development of state intervention in medicare
has two driving forces behind it. Demand of the people
on the one hand and the ruling classes’ urge to acquire
legitimacy' and credibility on the other. V Navarro
describes the relationship precisely. ‘Social demands
of labour’ include increase of social wages, the com
prehensiveness and levels of which depend on the
strength of working class pressure; ‘social demands of
capital’ include measures to smooth down and cushion
the dislocation, uncertainty and dis-welfare created by
the process of capital accumulation, e g, social security
and health care. Navarro explains, “there is no single
factor explanation of social policy... there is no clear
cut dichotomy between the social needs of capital and
the social demands of labour. Any given policy can
serve both. Indeed, the social policies that serve the
interests of the working class can be subsequently
adapted to benefit the interests of the dominant
class... the ‘bias of the system’ has always insured that
these policies can be deflected to suit the capitalist
class. Indeed, history shows that concessions won by
labour in the class struggle become, in the absence of
further struggle, modified to serve the interests of the
capitalist class” (Navarro, 1976). Several spanners have
been thrown into this convenient process of conces
sion and legitimacy—fast rising cost of modern
medicare, increased demands from all sections of
population, increased awareness of the discriminatory
distribution of state services, effect of the international
slogan of Health For All, increased trade unionism
among the employees of the state health services, etc,
to name a few. Mere slogans and superficial measures
now fail to contain dissatisfaction. It is now realised
that provision for a minimum standard of medicare
for all entails a magnitude of expenditure sure to
undermine other state priorities determined by the
ruling classes. Henc^ the urge and campaign for
cheaper alternatives. Noteworthy is the fact that the
alternatives are prescribed for only the poor. The state
cannot afford to alienate the privileged classes.
What the Poor Must Demand
Underplaying of the role of medical care should
stop. Such underplaying ignores the felt-need of the
people. Rakku’s story revealingly demonstrates that
Rakku risked further pauperisation for the elusive life
saving medicare for her child; seeing the government
auxiliary-nurse-midwife on her way to the city hospital,
“she suddenly felt resentment towards this woman. She
wondered why as a health worker she did not have
89
medicines for helping sick children. Why did she only
have injections [vaccines] for healthy children and ad
vice to mothers to stop having more children! Here was
her child dying and this woman could not help her”
(Zurbrigg, 1984). Valuable scientific advice about safe
water, personal hygiene, immunisation, balanced diet,
etc, do not cut much ice with the Rakkus.
Effective medical care to the poor will never be and
cannot be provided for by a state geared to the interest
of capital accumulation; nor can it be provided by col
lective humanitarian urge. India has a long tradition
of philanthropic, charitable, humanitarian effort to
provide medicare to the poor and such efforts have
increased through the recent spurt in voluntary agen
cies’ activities in the health field, but this has hardly
made any ripple on the health scene. The deprived
people will have to earn medical care; it must be
demanded from the state.
A. State medicare should be exclusively reserved for
the large indigent population, i e, people living below
a predetermined income level. Other existing schemes
of medicare be similarly reserved for the existing
beneficiaries. Affluent people be left to fend for
themselves. Semi-affluent people be assisted to develop
their own medicare facilities through insurance system,
as is prevalent in the developed countries.
B. To operate this schefne, the population will
necessarily be divided into economic categories as has
been for the rural rationing system. In marginal situa
tions and in the case of exigencies persons from
unauthorised categories may be entertained in the state
institutions but in exchange of a price, not free.
C. Eventually other related functions will have to
be modified and rationalised. For example, state
expenditure on medical education will be steadily
reduced to that optimum level necessary to train per
sonnel destined for state service.
A host of objections and problems will come up in
the course of implementation of this scheme. It has
been argued that such a scheme is discriminatory, is
not fesible and works against humanitarian principles.
Surely it is discriminatory but it is a reverse discrimina
tion in favour of the poor aiming to abolish the pre
sent discrimination and introduce equitable distribu
tion. The feasibility of such compartmentalised ser
vice has already been established. Several such
medicare services, e g, ESI, armed forces, railway, etc,
have long been functioning. In Andhra Pradesh such
compartmentalised public distribution service for
foodgrains is being operated for the entire state. About
humanitarian principles, the less said the better.
Is this scheme another alternative to meet the
medicare needs of the poor? Will the state concede this
demand if only its rationality and feasibility are
established? The prudent answer is NO. This scheme
is founded on the premise that no scheme of equitable
distribution and social justice is implemented by the
state in an exploitative, class divided society. A few
sporadic benefits may be realised from time to time
through class struggle to produce only some palliative
effect. The demand under this scheme is entirely dif
90
ferent. It does not call for some concession for a pair
ticular group. It is not only a demand exclusively for
the deprived classes so that they have a concrete slogan
to struggle for and organise, but also calls for restruc
turing of the entire medical care system of the society.
Moreover, the prospect of earning an exclusive right
will provide the necessary urge to struggle for it and,
once achieved, the poor will be equally zealous in guar
ding it. Likewise, the danger of exclusive control of a
state apparatus by the poor is apt to invite strong
opposition and resistance. The present beneficiaries of
state service will oppose it as they stand to loose an
existing privilege. The controllers of the state exche
quer will oppose it as it only entails increased alloca
tion for the poor but opens up a possibility of
establishing a system of accountability of the providers
to the recipients. When- this inevitable opposition
comes, it instantly identifies the real beneficiaries,
exposes the nature and utter inadequacy of the pre
sent system; it shatters the humanitaring camouflage
of the state; it makes a dent in the legitimacy of the
present order. In other words, this scheme envisages
conLiCt and polarisation of the contending forces. It
may act as a nexus for class struggle.
Then again, what happens in the unlikely event of
the state conceding this demand? An exclusive state
medicare service will necessarily render the situation
conducive for the deprived classes to exercise control
over it. The essence is control. Without control there
is no participation. They only participate meaningfully
who weild power and authority. The very exclusiveness
will generate demands for guaranteed service, accoun
tability of the providers, uniform and better standards,
more state allocation for medicare—in other words,
struggle for control. Struggle for control will soon
make it apparent that without eventual control over
the state itself, nothing could be achieved or sustained.
It will soon be apparent that the fundamental pro
blematic is political and economic. Without political
control no change in the economic order is possible.
Without economic change, provision of non-medical
health care will remain elusive. This situation is-not
peculiar to health care. The same situation prevails in
the other sectors of state policy, e g, education, hous
ing, agriculture, etc. The same discriminatory practice
operates under cover of universal eligibility. It cannot
be reversed without political control. The way to
achieve political control is struggle. It may also begin
in medical care.
References
Deacon, B: ‘Medical Care and Health under State Socialism’,
reprinted in Radical Journal of Health (1,1, 1985) from In
ternational Journal of Health Services, 14, 3, 1984.
Navarro, V: Medicine under Capitalism, Prodist, New York, 1976,
pp 220-221.
Reinhardt, U E: ‘Health Insurance and Health Policy in Federal
Republic of Germany’ in National Health Policy (ed Erlich
Isaac), Stanford University, California,’ 1982.
Wilenski, P: The Delivery of Health Services in the Peoples
Republic of China, International Development Research Cen
tre, Canada, 1979.
Zurbrigg, S: Rakku's Story: Structures of Ill-Health and the
Source of Change, 1984!
Radical Journal of Health
irreversible Welfare State: Its Recent Maturation,
Its Encounter with the Economic Crisis,
and Future Prospects
Goran Therborn and Joop Roebroek
This article describes the influence of the current economic crisis on the welfare state in the advanced capitalist
countries. The authors discuss how, under the surface of welfare state growth, the political relations offorce
have changed in favour of (hose social forces advocating fundamental reappraisal of the welfare state over
those supporting its maintenance or extention. it is argued that, as long as democracy prevails, the welfare
state is an irreversible major institution of advanced capitalist countries. While the building of a majoritarian
anti-welfare state coalition seems impossible for the forseeable future, the authors do not rule out significant
cuts in welfare expenditure in some countries and specify some of the economic and political preconditions
for such cuts.
(This article wes originally prepared for the conference on 'The Future of the Welfare Stale's held in Maastricht,
Netherlands, in December 1984 and is reprinted here from the International Journal of Health Services, Volume
16, No 3, 1986.)
RARELY in the modem history of advanced capitalism
has there been a major institution that is so much
talked and argued about with so little knowledge as
the welfare state. Very little is known—in the sense of
being digested by prevailing social scientific as well as
political knowledge—of (a) the recent developments
of the welfare state, (.6) its part in the current inter
national crisis, and, consequently (c) the future pro
spects of the welfare state. Given the severe space
limitations of this paper, what will be attempted here
can be no more than a modest contribution toward
some enlightenment in these three problem areas.
brought an increase in public expenditure of 16 percen
tage points between 1913 and. 1949. In the 1950s, dur
ing the unprecedented boom, the average increase was
1.4 points, compared with 8.4 in the 1960s, and no less
than 14 percentage points between 1970 and 1981.
The accelerated growth of Western states after 1960
has mainly been due to welfare state growth. In other
words, the welfare state has been the major factor in
the growth of state involvement in the life of the peo
ple it governs. No other force is comparable to it. The
rather limited proportion of welfare commitments in
the growth of the Danish and Swedish states is most
probably in part a statistical artifact, hiding an increase
Welfare State in Contemporary History
in the number of public employees working in the
History is the mother and teacher of the future. Any welfare administrations of the ordinary state apparatus'.
attempt at an analytical understanding of future op
This silent change has also meant a major internal
tions and possibilities, therefore, has to start from a transformation of advanced capitalist states. In their
historical grasp of the present. Here we will concen everyday activities, Western states have changed from
trate on two aspects: the location of contemporary being mainly apparatuses of armed forces, bureaucratic
welfare states in stale history, and the socio-economic ordering, and public transport and communication in
size and ramifications of current welfare stales.
to predominantly institutions of transfer payments to
Public social insurance, public health, and social care households, public education, and public caring and
have at least a century-old history. The major inter social services. In short advanced capitalist states have
national theoretician and architect of public welfare in their everyday routines become welfare states. In
arrangements, William Beveridge, made his epochal Belgium and the Netherlands, welfare expenditure in
contribution in the 1940s, and the accompanying the sense above occupied mere than half of all public
economic theory got its major statement in 1936 wth expenditure by i960 (1, pp 88, 93). In Sweden this jump
Keynes' General Theory. This is common knowledge, occurred between 1966 and 1968 (2,3). By 1981, all ad
but for an understanding of the present—and of the vanced capitalist states devoted more than half of their
future—it is quite inadequate.
public expenditures for welfare state purposes, even the
In fact, the welfare state as we experience it today United States and Japan (I, pp 70). With regard to
is an outcome of the 1960s and the 1970s. In a long terms of public employment, in the Scandinavian states
time perspective, the extraordinary changes, little employees in education, health care, and social care
theorised and little even noticed, of the sixties and now comprise between two-thirds and three-quarters
seventies stand out.
of all public employment (4). (The actual figures are
In the relatively uneventful years of 1960-1982, 62 per cent in Sweden <1981), 68 per cent in Denmark
overall public expenditure on the average grew by 24 (1981), and 76 per cent in Norway (I9S0). All figures
percentage points in.our ten selected countries. The except employees in public enterprises .operating on
combined effects of the two World Wars and the 1930s competitive markets.) In the Netherlands in 1977.
with its. sooner or later, ensuing turn of economic about 57 per cent of all government and governmentpolicy orientation (the arrival of Keynesianism) subsidised para-statal personnel were occupied with
December 1986
91
teaching, caring, and other social and medical services
(5). (From the total of the “kwartajre sector” (5) have
been subtracted private practitioners of medicine, den
tistry, and physiotherapy as well as personnel in privajc
child care,) In brief Western states have (largely)
become post-bureaucratic welfare states.
Socio-Economic Ramifications of
Welfare State
We have seen that the contemporary welfare state
is not an elderly institution, susceptible to the ailings
of old age. On the contrary, the developed welfare state
is a very recent phenomenon, better characterised by
the sometimes extravagant vitality of youth. In our
time, the welfare state has also become a major institu
tion of advanced capitalist societies. One expression
thereof is the significance of the welfare slate as a
source of income. Between one-fifth (Japan) and onethird (Netherlands and Sweden) of the sum of the
household income derives directly from the state.
Calculated in terms of income recipients, the
significance of the welfare state is even greater. By the
late 1970s, old age pensioners and public employees
together made up more than half of the voting-age
population in Britain and Sweden, and close to half
in Germany. In the United States, public employees
plus recipients of social security and of social
assistance constituted about 35 per cent of the adult
US population in 1975 (6).
In the Netherlands, old age pensioners and public
employees are not so many—roughly 30 per cent of
the electorate in 1981 (7,8). On the other hand, given
the massive failure of Dutch capitalism to provide
employment the total number of people receiving their
main income from the state is huge. In 1983, 49 per
cent of all income recipients below the general pen
sion age of 65 got their income from the welfare state,
27 per cent as receivers of social benefits and 22 per
cent as public or para-public employees (9, p 320).
Welfare State and Economic Crisis
The current, * now ten-year old, international
economic crisis has, of course, affected the parameters
pf the welfare state. However, from the discrepancy
noted earlier between the dramatic growth to maturity
of the welfare state and the relative lack of attention
to and comprehension of it, we should expect another
lack of fit between real developments and the foci of
prevailing public discourse. This is in fact the case.
Ideologically and politically, the welfare state is cur
rently under heavy attack. This phenomenon is most
briefly summarised in the election of the militantly
right-wing liberal regimes of Thatcher and Reagan,
seconded by several other governments, most
wholeheartedly by the Lubbers Cabinet in the
Netherlands, and in the retreating positions of the
Mitterrand government, of the US Democrats, the
Dutch and the Danish Social Democrats, and the disar
ray of the British Labour Party. In social science, the
way the wind is currently blowing is, most directly left
92
from the strongly increased influence .-n 1
_■ dwnc.'S
of a mi-Keynesian economics. But major
institu
tions can hardly be knocked down by rhetoric alone,
either from electoral platforms or from academic
chairs. Let us take a look at a few facts about actual
developments.
Developed capitalist welfare states remain subor
dinated to the business cycles and the structural crises
of the international capitalist economy. The current
crisis has shown that generous systems of social
security in themselves provide no security agamst
unemployment. But anti-welfare .statists cannot ‘‘have
their grain ground” here; there is no inverse relation
ship between social policy extension and unemploy
ment. The evidence is contradictory (Table 1).
Economic growth has become a weak predictor of
unemployment, only a quarter of the variation in
unemployment at the end of 1983 can be accounted
for by the economic growth between 197$ and 1983
(rJ = 0.25). Between the size of social expenditure
(from which education has been excluded here in order
to accentuate the more controversial social security
aspect) and low unemployment there is a small negative
relationship
(r2
=
0.11),
as
there is
between social expenditure and economic growth (r2
= 0.12). In other words, only one-njnth and one-eight,
respectively, of variations in unemployment and in
economic growth may be statistically accounted for by
the extension of public social commitments.
Briefly and crudely summarising a long argument
(which is developed and sustained empirically at some
liength in reference 10), contrary to the McCracken
Report (11) and other conventional wisdom, states can
maintain a low level of unemployment even in the face
of a deep international crisis, provided there is a deeply
institutionalised commitment to high employment. But
general Keynesian demand management is not enough;
a compatible monetary policy and/or an extensive
selective labour market policy is also required. And a
crucial factor is non-market control oyer employment,
whether through extensive public works and retrain
ing as in Sweden, public subsidies as in Norway, public
industrial employment as in Austria, publicly sup
ported paternalism as in Japan, or public control of
immigration in an immigrant-dependent economy such
as that of Switzerland.
Combining the extension of social security com
mitments and institutionalised full employment com
mitment, Scheme I shows the typology of welfare states
with regard to both employment and social security.
Commitments to social security and commitments to
full employment thus vary independently of each other,
something that must be brought into the centre of the
welfare debate and analysis. We may give our
typologised countries descriptive labels:
1. The strong welfare state (Sweden), highly com
mitted to social security and capable of preventing
mass unemployment, even in the face of a deep
worldwide economic crisis and a low rate of national
economic growth (12).
Radical Journal pf Health
2. The soft welfare states (Belgium, Denmark,
Netherlands), generously committed to social security,
but unable to control their labour market.
Table!: Unemployment. Economic Growth, and Social
Expenditure4
Unemploy
ment
Economic
Growth0
Social
Expenditure^
Australia
9.5
1.8
Austria
4.2C
1.8
Belgium
Canada
Denmark
Finland
14.9
11.1
(10.6/
6.2
1.5
1.6
1.6
3.8
France
Germany
Italy
Japan
Netherlands
Norway
Sweden
Switzerland.
8.8
7.8
10.0
2.6
14.0
2.8
3.4
(0.4)h
1.8
1.5
2.1
4.3
0.7
2.5
1.5
1.5
United Kingdom
United States
13.1
8.4
1.1
1.8
12.8
(1980)
24.1
(1980)
32.6
15.5
29'0
23.3
(1980)
23.8
26.4
22.7
12.5
29.1
21.0
(31.9)?
9.4
(1979)
19.0
15.0
Correlations-. Spearman’s rank order correlation
between unemployment and economic growth,
r = 0.50
between unemployment and social expenditure,
r = 0.35
between economic growth and social expenditure,
r « 0.34
Because of the less than perfect comparability, of the data, dif
ferences in unemployment rate of 0.5 per cent or less and of social
expenditure of 1 per cent or less have been left out of considera
tion. Since the Swedish figure was lower in 1980 than 1981,
Belgium alone is topranking in social expenditure.
Notes-, a The selected countries are meant to be exhaustive of
all advanced capitalist countries, except the smallest—
Iceland and Luxembourg. New Zealand has been left
out for lack of reliable employment data.
b Standardised rate of unemployment as percentage of
the labour force in the fourth quarter of 1983. Data
for Denmark, from Det Okonomiske Rad Dansk
Okonoihi December 1983, p 52 Direktoratet for Statens
Indkob, Copenhagen 1983. For Switzerland, from
OECD Observer 127, March 1984. The remaining coun
tries from OECD Quarterly Labour Force Statistics
1984, p 76, Paris 1984.
c Average annual growth of GDP 1978-1983, in per cent.
Data for 1982-1983 from OECD Observer 127, March
1984. For 1978-1981, from OECD Economic Outlook
33, July 1983, p 160.
d Public expenditure for health, social and welfare ser
vices (transfers, public consumption, capital expen
diture, exclusive of education) as percentage of GDP
in 1981 prices. From OECD Statistical and Technical
Annex, Report No SME/SA1R/SE 83.02, pp 31-69.
OECD, Paris, 1983 (unpublished).
e Third quarter of 1983.
f Non-standardised rate for 1983.
g The original data source had no final consumption and
capital expenditure for social and welfare services. The
latter have been assumed to be of the same size in rela
tion to social transfer payments as those in Denmark.
This will be seen as a conservative estimate.
h Non-standardised rate for 1982.
December 1986
3. The full-employment oriented medium welfare
states (Austria, Norway), giving priority to employ
ment policy.
4. The states of socio-economic mediocrity (Finland,
France, Italy, United Kingdom), distinguishing
themselves neither in social nor in employment policy.
5. The full-employment oriented market states
(Japan, Switzerland), dedicated to maintaining full
employment but with limited commitments to social
security.
6. The market-oriented states (Australia, Canada,
United States) where, in spite of significant welfare
state developments in recent years, the market is une
quivocally given the upper hand in income as well as
in employment determination.
The world of advanced capitalism is a world of wide
variations in public and in individual life chances (1).
Real Impact of the Crisis
Table 2 shows that the average yearly growth of
social security expenditure declined in almost all
western countries under review (except in France) bet
ween 1975 and 1981. However, up to and including
1981, social security expenditure continued to grow at
a respectable pace. There were considerable yearly
variations, but with the exception of Italy in 1977, the
United Kingdom in 1977 and 1980, Australia in 1979,
New Zealand in 1980, and Sweden in 1984, in no coun
try was there in any year an overall absolute decline,
although there were declines in individual programmes,
most often in family benefits (1).
For developments after 1981 we will hav^ to resort
to national data of various kinds. The Reagan ad
ministration has concentrated its cuts on the meanstested programmes for the poor, but social security (old
age, disability, and survivors) benefits grew- in real
Scheme 1: A Typology of Contemporary
Welfare States3
Social Security
Commitment13
Full-Employment Commitment
Institutionalised Non
institutionalised
Major
Sweden
Medium
Austria
Norway
Minor
Japan
Switzerland
Belgium
Denmark
Netherland
Finland
France
Germany
Italy
United
Kingdom
Australia
Canada
United
States
Notes-, a Data from Table 4 (social expenditure) and the analysis
of economic and labour market policies in reference 10;
b The procedure of trichotomisation of social security
commitments has been guided by a search for signifi
cant break points such that the difference between the
lowest scoring country of one group and the highest
scoring country of the group below should be larger
than the difference between the lowest and the second
lowest country of the same group.
93
terms by 15 per cent between 1980 and 1983. .’.nd
hospital insurance (for the aged) grew bv 25 ner cent
(13. 14). In Britain under Thatcher, public expenditures
on social security and personal benefits grew from
£ 25.336 million in fiscal year 1978/79 (under Labour)
to £ 28.444 million (in 1978 prices) in fiscal year
1982/83 (15, 16). In the Netherlands, net public
transfers to households (net insurance premiums naid)
grew from an average of .3.3 per cent of national
income in 1976-1980 and 4.6 per cent in 1981 (when
the Social Democrats took part in the government) to
5.0 per cent in 1984. exclusive of the growth caused
by the rise of unemployment (and of unemployment
compensation) (9, p 157).
But figures do not always tell tac whole truth. The
welfare state expenditures arc still growing, but t hi is
not to deny that painful cuts and redistribution
measures from labour to capital and from the poor to
the well-to-do are being made by governments. *1 his
is true not only for right-wing liberal regimes, but also
for coalition governments with social-democrat par
ticipation. The measures arc nearly the same in most
Western countries: (a) changes in indexation of
benefits, implying less, than full compensation for price
increase; (b) more strict entitlements to benefits, such
as unemployment insurance and taxed paid services:
(c) certain tendencies toward privatisation, e g, a
relative increase in number of beds in private hospitals
compared with public hospitals, and accommodation
of public-controlled services, especially in the sector
of health services, to the private sector; (d) a tendency
toward de-individuaiisation of rights on social
insurance and resirengthening of the “family bread
winner principle’’ in entitlements to social insurance;
(e) iationalisation, especially in the health services; and
Tab? e 2: Annua- Growth of the
E XPFNDJ rUP.FS ON Sc< 1AI Sf.CURi I Y *
1965-70
Percentage Growth
1975-81
1970-75
Australia
Austria
Belgium
5 3
64
9.1
15.6
< V
10.5
Canada
Denmark
Finland
France
Germany
Italy
Japan
Netherlands
Norway
Sweden
Switzerland
J 1.5
9.0
10.7
5.0
5.5
8.2
10.4
11.6
15.3
10.2
8.9
12.9
6.6
9.5
6.6
8.6
6.5
12.3
8.3
8.0
9.6
10.4
United
Kingdom
United States
Average
5.3
9.3
9.4
6.3
9.9
9.2.
2.8
4.6
5.1
(1975-80)
3.3
4.5
5.5
7.4
2.0
3.9
8.6
■
6.2
4.4
2.7
(1975-79)
3.9
3.7
4.6
A;ore: a Calculated from reference 1. in constant J'-’-O prices
Expenditure', on health, temporary sickness, pensions,
unemployment, family benefits, and other transfers.
94
budgt
phs is m Erect pa n ent rot serices nd insii
' P -................
Netherlands, and the United Kingdom these inec ures
are accompanied by a discussion about a more fun
damental reappraisal of the system of social security
on the basis
actions taken bv the government.
With regard to the welfare state as a whole, the real
impact of crisis policies has so far been marginal and
unable to break the trend of growth.. But it is worihw'd-c to investigate if these policies reveal recent
changes in the political relations of force.
Welfare State and Political Relations of Force
1 he explosive growth of the welfare state in the six
ties and early severities is accompanied on the political
plane by a strengthening of the position of labour visa-vis capital. This is the effect of wide-ranging social
processes that have undermined partriarchy and the
family control over production, challenged clientclist
and religious forms of social control of production and
class division, increased the scarcity of labour on the
market, and diminished the dependence of the proper
ryless upon the labour market for their support (17).
This development resulted In a compromise of the main
political actors, wherein the welfare state provisions oc
cupied an important place.
What happened to rhe political relations of force
from 1975 onward? In most countries the crisis policies
cracked the existing compromise. To answer the ques
tion more carefully, we have made, for a selected group
of Western countries, a more thorough analysis of
government social policy in the crisis.6 (The analysis
is based on materials from the project The Political
Future of Social Sectin y: Political Demands and Social
Relations of Force, financed by The Commission for
Research on Social Security (COSZ) of the Dutch
Ministry of Social Affairs and Employment.) As a first
result, we present two schemes. Scheme 2 contains an
overview of the points in time at which a “crisis state
ment” is given, the “first significant cuts” are carried
out. and the discussion about a more “fundamental
reappraisal” of an important pan of the welfare state,
the system of social security, begins. Scheme 3 reveals
the composition of the government at thsse points in
lime.
At the time of a “crisis statement” (a.*ad also of the
“first significant cuts”), with one or t wo exceptions
(Net: ter lands and Sweden) the sociaFden iocrats formed
a coalition government (in Belgium with the confes
sional and liberal parties) or took a dominant posi
tion within the government. Second, discussion about
a more “fundamental reappraisal” of -he system of
social security and the launching of plans in that direc
tion took place exclusively under right wing govern
ments. in the two countries where .he discussion was
advanced and the governments proposed plans for the
reappraisal, the right was, in a relative sense, best
represented >r>. the governments that announced the
“crisis statement” and carried through the first “signifi
Radical Journal of Health
cant cuts.” In the three countries where the discussion
was started by conservatives and liberals (Denmark,
Germany, and the United Kingdom), social democrats
were defeated in an election after a (long) period of
governmental power and were sent back to the opposi
tion. These developments indicate that under the sur
face of a relatively unbroken growth of the welfare
state, a change of the political relations of force has
taken place: a development that needs more attention
with regard to the future of the welfare state.
This shift in the relations of power should not be
understood as an exclusive effect of changes in elec
toral favour. It is a more structural development not
only of social and political relations, but also of social
and political moods. It is a field of forces in which
Scheme 2- The Policy of Welfare: A Sequence of Actions
Austria
Belgium
Denmark
France
Germany
Netherlands
Sweden
United Kingdom
Crisis
Statement3
First Signi
ficant Cutsb
Fundamental
Reappraisal
1983
1976
1980
1982
1975
1978
1980d
1976
—
1980
1980
—
1977
1980
—
1977
—
1983
—
—
—
1983
—
1983
Notes: a "Crisis statement” refers to the moment that the govern
ment announces that the policy of welfare cannot be
continued without changes.
b As a criterion for “first significant cuts” we use three
standards First, two quantitative standards: an annual
growth of expenditures on social security of less than
2 per cent and/or a decline in the annual growth rate
of more than 3 per cent. Also a qualitative standard:
the changes in a quantitative sense are the result of ob
vious alterations in policy. This estimation is based on
materials up to and including 1983.
c “Fundamental reappraisal” refers to the statement by
which the government takes the initiative for a possi
ble fundamental change of the social security system
as a whole. This is usually done through the setting up
of a public commission of investigation with farreaching tasks.
d In Sweden the “crisis statement” was made by the in
cumbent bourgeois government in 1980. After the reelec
tion into office of the social democrats in September
1982, the social cuts that followed the “crisis statement”
were redrawn and did not take effect.
Scheme 3: The Policy of Welfare and the Composition3 of
the Government
Austria
Belgium
Denmark
France
Germany
Netherlands
Sweden
United Kingdom
Crisis
Statement
First Signi
ficant Cuts
Fundamental
Reappraisal
left
coalition
left
left
left
right
right
left
—
coalition
left
—
left
right
—
left
—
right
—
—
—
right
right
right
Note', a Here we use a threefold distinction: “right” (conservalivcliberal-confessional), “coalition” (social democrats in a
balanced coalition with one of the right-wing parties).
and “left" (a government dominated by social democrats).
December 1986
political parties, labour unions, employees orgamsa
lions, and other organisations try to influence deci
sions that arc made within the government, the parlia
ment, and other organs. In this field one can. in
general, distinguish two fronts’ with regard to the
welfare state: on the one hand the organisations and
forces that advocate a fundamental reappraisal of the
welfare state, and on the other hand the organisations
and forces that stand for maintenance and, where
necessary, further extension of the welfare state. The
first front is composed mainly of the conservative, the
liberal, and larger or smaller parts of the confessional
panics, the employers’ organisations, and sometimes
middle-class organisations. The other front is made up
of the social democratic, communist, and other pro
gressive parties, the labour unions, and organisations
of consumers of services and recipients of benefits. The
development in the relations of force since 1976 in
dicates a shift in the direction of domination from the
“maintenance front” to the “rcapparaisal front”
(Scheme 4).
We can come to the more general conclusion that
the resistance to significant changes within the welfare
state, even when there is domination by the “reap
praisal front”, is so strong that a fundamental
reconstruction of the welfare state is.excluded. Even
in the Netherlands, it is not obvious that the defeat
of the trade unions in December 1983 weakened the
position of the “maintenance front” to such an extent
that the announced reconstruction of the social securi
ty system will be carried through.
Future of the Welfare State
On the basis of the evidence given earlier on the
socio-economic ramifications of the welfare state, and
further sustained by the record of the effects of the
welfare state upon the economic crisis, we conclude
that the welfare state is an irreversible major institu
tion of advanced capitalist countries. Or, to be more
precise. It is irreversible by democratic means. The size
of the population benefiting from the welfare state en
sures that as long as democracy accompanies advanc
ed capitalism, the core of the welfare state is safe. This
goes against a great deal of hopes on the right and fears
on the left. Bui it is not enough. We have seen above
that lhe welfare state is a variable, not a fixed, entity:
an assessment of its passible future will have to pay
attention to possible variations. Our general analytical
perspective involves two fundamental causes of welfare
developments: socio-economic tendencies and socio
political relations of force.
The major push ahead of the welfare state is the ag
ing of the population of advanced capitalist countries,
except that of Belgium. The aging of the population
means not only more pensions and more old-age ser
vices, it also means a great increase in health care. For
the Netherlands, ii has been calculated that for the
period between 1981 and 2000, a growth of expenditure
(for pension benefits, nursing homes, old people's
homes, old people's welfare work, and medicines) of
95
more than 20 per cent is needed to maintain existing
standards (18).
A second push for welfare state expenditure derives
from unemployment. Currently, almost all predictions
point to an enduring rate of massive unemployment
among two-thirds of advanced capitalist countries,
which have failed since 1975-76 to maintain more or
less full employment. This means the establishment of
a virtually permanent pool of unemployed. Except in
Belgium, existing unemployment insurance is not
geared to handling long-term and permanent
unemployment. Under existing political conditions,
permanent mass unemployment is likely to produce
mounting pressure for economic provision for the long
term unemployed at a level above that of social
assistance.
A third major pressure for increased public social
commitments may be expected from population con
cerns. In most Western European countries the cur
rent rate of reproduction is negative, and it may be ex
pected that procreation-stimulating social policies will
be adopted. The Sweden, this is already a consensual
issue.
Fourth, the number of single mothers is likely to in
crease. Particularly in countries with current high
unemployment and low rates of female participation
in the labour force, this implies an increasing demand
for social assistance.
One significant alleviation of the pressure is the visi
ble tendency of expenditure for public education to
decline because of demographic changes in Western
populations. For the Netherlands, this means a possi
ble decline of expenditures between 1981 and 2000 of
20 per cent while maintaining the existing level of
education (18, p 86).
The fiscal constraints of social policy are not ab
solute givens. They are to a large extent politically
defined and affected by policy outcomes. The endur
ing crisis does not mean a permanent depression, as
shown by the current upturn in which a growth rate
of 2.5 pr cent is forecast in 1984 for the European
Community and 4.5 per cent for the.OECD as a whole
(9, p 19). A provisional calculation by the OECD
Scheme 4: Changes in the Relations of Force Between the
“Maintenance-Front- and
the “Reappraisal Front”3
Austria
Belgium
Denmark
France
Germany
Netherlands
Sweden
Domination
Maintenance
Front
Balanced
Relations
1975-1982
1983-present
1975-present
1980-1982
1982-present
1977-persent
1977-1982
1980-1982
1975-1980
1975-1982
1975-1977
1975-1977
1975-1980
1982-persent
United Kingdom 1975-1976
1976-1979
Domination
by Reappraisal
Front
1983-present
1982-present
1979-present
Note-, a This overview has been made on the basis of electoral
results, changes in the composition of governments,
actions to economise, and the results of confrontation
between both fronts.
96
Secretariat for the seven major Western countries
estimates that, because of declining needs for educa
tion expenditure, a constant GDP share of welfare state
expenditure could ensure a 0.7 per cent annual growth
in real social benefits till 1990 (I). One the whole, and
by and large, there seems to be little reason for doubt
that the current level, or even a moderately higher one,
of social welfare commitments is payable.
However, there are at least two qualifications to be
made here. Pensions insurance schemes in many coun
tries are very sensitive to lower rates of growth and/or
to high rates of employment. In some countries revi
sions have already been made, and further ones are not
unlikely. Second, some countries have already incur
red large financial deficits in their public sector. The
mounting interest burden of this debt and the
narrowed policy margins of big structural deficits are
most likely to constrain furture social policy. This
holds, above all, for Italy and Belgium, but also to a
lesser extent for Denmark, the Netherlands, Canada,
and Sweden (16, p 27).
Socio-Political Forces of Welfare State Demands
and Defence
At least one major social force behind the welfare
state is growing and is likely to become more active
and demanding in the future: that is old people, the
“senior citizens.” They are growing in numbers, and
they are becoming more vital and active because of the
combination of increased longevity and reduced retire
ment age. The aged are also by far the most impor
tant beneficiares of the welfare state. Pensions and
health care of the aged make up the bulk of social
security expenditures in all countries. As the French
specialist Anne-Marie Guillemard has said: “The
welfare state is, first and foremost, a ‘welfare state-forthe-aged’” (19). The demands of the aged are likely
to grow for social, cultural, and recreational services,
and the aged are likely to be vigilant with regard to
their pension rights and level.
Another interested welfare state defender is the
group of welfare State employees. Their number is
unlikely to grow in the near future, but it is quite
significant already, between a quarter (in Sweden) and
a tenth (United States, Germany, and Italy) of the
economically active population (20). This is a well
organised and highly articulate category of people.
Welfare state employment has been especially impor
tant for the emancipation of women, who usually oc
cupy most of these jobs. Large-scale attacks on the
welfare state are therefore likely to meet with resistance
from articulate women, even those outside welfare-state
employment.
Finally, the labour movement is in modern times the
major political protagonist of the welfare state. In
countries with high unemployment, the labour move
ment is currently being weakened, and tendencies to
division between private and public employees are ap
pearing. However, even after some recent setbacks, the
labour movement in most advanced capitalist states is
Radical Journal of Health
located on a historically high plateau of strength and
acquired rights (17).
Precondition of a Right-Wing a Roll-Back
We have given a number of reason for our convic
tion that the welfare state is irreversible by democratic
means, and also for our belief that in the foreseeable
future even successful cuts and restrictions will not
change its fundamental base. However, countries
already vary in their line-up for or against the existing
welfare state and further variation cannot be excluded.
On the contrary, there are strong grounds to expect a
further divergence among advanced capitalist states
over the coming five to ten years. This divergence
derives mainly from the divergent impact of the cur
rent economic crisis, in particular with regard to
unemployment. The enormous differences in the rate
of unemployment (shown by Table 1) are likely to have
an enduring, diverging impact for two reasons. First,
all OECD estimates indicate that these differences will
remain for the rest of the 1980s (21). Second, and also
an explanation in part for the first reason, contrary
to pre-crisis predictions or fears, mass unemployment
has not led to massive socio-political upheaval. Mass
unemployment Netherlands remains as calm as lowunemployment Sweden.
Before going fuither, however, a major qualification
has to be made. Politics and policy are not amenable
to scientific prediction. Rather than expecting their
specific predictions to come true, political scientists
would do well to adopt as a major law of politics the
title of a book of stories by Andre Maurois, Tbujours
rinattendu arrive (always the unexpected happens). We
should formulate all of our predictions as conditionals:
“if a, then (probably) b'.'
The fundamental precondition for a significant
right-wing roll-back of the welfare state is a division,
a demoralisation, a decomposition, and an at least par
tial political marginalisation of the broad coalition of
socio-political forces that supported and sustained the
welfare state expansion in the 1960s and 1970s. The
building of a socially majoritarian anti-welfare state
coalition, dedicated to capital accumulation and to
private business ideology seems impossible in the
foreseeable future. The best evidence for the latter
assertion is given by the comparative class analysis of
Erik Olin Wright. Wright combines the scientific com
mitment of Althusscrian Marxism with post-orthodox
theoretical sophistication and the large-scale empirical
surveys of American Big Science. His results indicate
that even in the United States, about 60 per cent of
the labour force has at least a minimum of pro-labour
or working class consciousness. In Sweden the cor
responding figure is 90 per cent (22, 23).
W'hat then are the preconditions for a division,
demoralisation, decomposition, and partial
marginalisation of the welfare coalition? First, high
unemployment and/or other kinds of worsening in the
condition of labour, incurred under a government in
which the major left-of-center party lakes a significant
part. The record of the successful low-unemployment
December 1986
countries strongly suggests that such a major policy
failure is not primarily due to the openness to and force
of the international economic system, but to half
hearted, contradictory, or adverse policies. The elec
toral defeats of British Labour (in 1979), of the US
Democrats (in 1980), of the Danish Social Democrats
(in 1982), and the Dutch center-left (in 1982) fit into
this pattern, as does the current defensive of the
Mitterand regime. However, the original division and
demoralisation of the forces of the left and the center
left have to be reproduced for the right to be able to
make significant inroads into the welfare state. There
are a number of possibilities for this reproduction,
which are not mutually exclusive.
Second in our list of preconditions, and the strongest
and most reliable mechanism for reproducing division,
demoralisation, and decomposition of the left, is a
dualistic scoio-economic development. A dualistic
economy and society—a dynamic, well-off sector and
a stagnating or declining sector of low-wage or
unemployed misery—is the medium-term goal of the
new right, consciously or unconsciously. And the fact
is that some advanced capitalist societies are beginning
to take on those features earlier held to be characteristic
only of Third World societies. Thus in Britain, an in
crease of unemployment from 5 per cent in 1979 to
12 per cent in 1982 was accompanied by a slight in
crease of consumer expenditure, measured in constant
prices (24). The US economy grew by 7.6 per cent bet
ween June 30, 1983 and June 30, 1984, but unemploy
ment was still 7.1 per cent at the latter date (25). The
more a dualistic economy and society is created, the
stronger the roll-back pressure on the welfare state The
current upturn of the international business cycle’is
likely to produce significant dualistic effects even in
societies and politics not so extreme as those of Bri
tain and the United States. The economy is also begin
ning to grow again in Belgium, Canada, Denmark, and
the Netherlands, but mass unemployment and the
misery of the unemployed remains.
Managing a dualistic economy and society by
democratic means is largely dependent, however, on
the character of the political system. This is our third
variable: the more elitist the political system, the easier
a right-wing attack on the welfare state. One impor
tant measure of elitism is the prevailing electoral tur
nout. In this respect, the Western democracies currently
fall into three groups (26).
1 The exclusive democracies, with an electoral tur
nout of about 50 per cent of eligible voters: Switzerland
and the United States.
2 The reduced participation democracies, with a
70-85 per cent participation rate: the United Kingdom,
Japan, the Netherlands, Finland, Denmark, Norway.
3 The full participation democracies: the remaining
countries.
Elitist politics, reinforced by first-past-the-post elec
toral systems, mean that Thatcher and Reagan were
elected into office by less than a third of the electorate.
Finally, there are policies reproducing left-wing
97
anti-welfare state forces.
defeat. We began our list of variables conducive to
right-wing attacks on the welfare state by indicating
The welfare state has become a major and irreversi
ble (by democratic means) feature of advanced
the fateful effects of anything less than whole-hearted
capitalist societies. The current discussion of the
commitment to full employment in the period
welfare state crisis is little more than an ideological fad,
1975-1982. We will end it by listing a set of policies
which serious researchers cannot take seriously. On the
most likely to ensure the reproduction of the
other hand, a divergence of Western welfare states is
dominance of the right. From the point of view of the
likely to take place in the foreseeable future. The failure
right, the policies may be read as goal targets.
1 Disunity between trade unions and the political to maintain full employment that began in 1975 is likely
to have enduring effects. Further, the reactions to
parties representing labour. The gieater the disunity,
the earlier failures diverge. The West German labour
the greater the chances of a right-wing roll-back. This
movement seems to have learnt from its past, whereas
is partly a question of institutional structure—the ex
in the Netherlands, for example, we see strong left-of
tent of elitist middie-class character of the party, which
is thereby starkly distinguished from the unions. The
center forces heading for further defeats. However, we
would rather end by saying that the future remains
US, British, Dutch, and French cases indicate this. But
open. As political human beings, we are committed to
it is also something that is affected by policy, as ex
emplified by the Schulterschluss between the Social
full employment and to social security.
Democratic Party and the unions in Germany after the
Reference**
eviction of the Schmidt government.
1 OECD, Social Expenditure 1960-1990. Problems of Growth
2 Concessions from a weak position in the hope of
and Control, OECD, Paris, 1985.
2 Forsman, A, En teori om staten de offentliga utgifterna, p
reciprocity. Givebaeks of collective-bargained wages
133. Almquist and Wiksell, Uppsala, 1980.
and other benefits in a weakened position are likely
3 OECD National Accounts, 1963-1980, p 209, OECD, Paris
to produce mainly internal division and demoralisa
1982
tion, and unlikely to bring forth equivalent concessions
4 Nordisk Ministerrad.^efl offentliga sektorns sysselasttningfrom the counterpart. This tactic has been pursued by
sutveckhng i Norden Under 1970-talet, p 6, Oslo, 1983.
5 De kwartair*' sector in de jaren taching, pp 147, 241.
some US unions—that of the steelworkers above all—
Staatsuitgeverji, The Hague. 1980
and, en masse, by the Dutch unions, seconded by the
6 Rose, R, Changes in Public Employment, p 91. Centre for
Dutch Labour Party. The main effect of this is likely
lhe Study of Public Policy. University of Strathclyde, Glasgow.
to be a strengthening of the self-confidence and asser
1980.
7 Ministcrie van Binnenlandse Zaken/Sociaal en Cultured Plan
tiveness of the political right and of the employers. The
bureau, Over voorzieningengebruik en personeel in de kwarWest German unions and Social Democrats have, after
taire sector 1983-1987. pp 14. 67, 69, 71, 77. The Hague, 1983.
losing office, opted for another tactic, the result of
8 CBS. Statisrisch Zakbock 1982, pp 23-75. The Hague, 1982.
which is more respect for the concerns of labour.
9 Central Planbureau, Centraal economischplan 1984. The
Hague, 1984.
3 Selective social policies. There is a dilemma in
10 Therborn, G, H hy Some People Are More Unemployed Than
social policy between general and selective policies. In
Others, Verso. London, 1986
order to be effective and truly general, general policies
11 McCracken. P. et al. Towards Full Employment and Price
have to be high in transfer payment and in quality of
Stability, OECD, Paris, 1977.
services. This makes them very costly and also tends
12 Schmidt,M Arbeitslosigkeit und VoHbeschaftigungspolitik,
Leviathan, No 4, 1983.
to reduce their redistributive effects. On the other hand,
13 OECD. Economic Surveys 1983-1984; United States, p 15,
selective social services tend to be or become of lower
Paris, December 1983.
quality, and selective social policies are or become very
14 Stockman, D. Fortune, February 6, 1984, p 35.
vulnerable to political attacks, since the set of 15 Central Statistical Office, Social Trends, No 13, p 90, Lon
beneficiaries is restricted. Therefore, the more selec
don 1983.
16 OECD. Economic Outlook, July 1984.
tive (geared only to the poorest) the social transfers
and social services, the more likely they are to be sub 17 Therborn. G. The prospects of labour and the transforma
tion of advanced capitalism. New Left Review, No 145.
ject to roll-back attempts. Thus, to the extent that leftMay/June 1984, p 37.
of-center parties and trade unions adopt selective social
18 Sociaal cn Cultured Planbureau, Collectieve uitgaven en
demogrqftWie ontwikkeling Raijswijk, 1984.
policies, e g, in the form ot “basic*’ services and
transfers plus optional superstructures, the more like 19 Guillemard, A M, Old Age and lhe Welfare foge, p 97. Sage.
London 1983.
ly it is that the level ot the “basic” provisions will
20 Rose. R, Understanding Big Government, pp*132-139, Sage,
become the object of attack.
London 1984.
4 Decentralised, labour policies. The strength of the 21 1LO Report, Into the Twenty-First Century: The Development
of Social Security, pp 11. 102, Geneva 1984.
labour movement, and of the welfare coalition as a
whole, rests on its numbers and its unity. To the ex 22 Wright. E O, What is middle about’middle class? Tables 2,
Prokla, in press 1985.
tent that policies are adopted that are not based on 23 5,Wlight
E O, Class: Theoretical and Empirical Problems in
those assets, the right and the anti-welfare state coali
Marxist Class Analysis, NLB/Verso, London (in press), 1985.
tion will gain. This implies that the more collective 24 C ent; al Statistical Office. Economic Trends. March 1983. pp
10, 36.
bargaining is decentralised, and the more specificities
25 The Economist, July 28—August 3. 1984. p 83.
of private and public sectors, of industrial branches,
26 European Management Forum. Report on International In
and of enterprises are opted for in the current period,
dustrial Competitiveness 1984, Table 10.03. EMF. Geneva
the stronger will be the position of capital, and of the
1984.
98
News
Notes
Ij?etermmatlon Tests
Zl Surve fi eport
THE practice of prenatal sex determination followed study. Some o‘ (her important findings of the ->tudy
by selective female foetus abortion is one of the most
I Eighty-four per cent of tne gynecologists perform
striking examples of how advances in science and
technology are employed for the furtherance of amniocentesis for the purpose of sex determination.
women’s oppression. Although this inhuman practice These doctors together perform on an average 270
has been in existence in India for many years, it is only aminocentesis tests per month.
last year that anything like an organised and sustained 2 Some doctors have been per forming aminocentesis
mass campaign against it oecame a reality. While for the past 10-12 years. But a majority of the doctors
Bombay has been a principal centre of the campaign, (over 85 per cent) nave started performing these tests
it has now also spread to other cities, including some in the last five years. On the one hand, this shows that
small towns. A concrete manifestation of this positive Bombay is one of the first urban centres where SD tests
change has been the formation of the Forum Against and female foeticide started. On the other hand, it is
evident that the del ate that took place in the early 80s
Sex Determination and Sex Fre Selection.
Thu collective el forts ol several women’s groups and had a significant a.ui-pubiiuity effect.
3 Only very few (upto 5 per cent) of the
other voluntary organisations, spearheaded to some
extent by the Forum Against Sex Determination and aminocentesis tests conducted are done for the detec
Sex Pic-Selection, have yielded some notable results. tion of genetic defects.
4 Seventy-five per cent of the doctors interviewed
Two private bills concerning this issue were introduced
last year—one in Parliament and the other one in he said that over 50 per cent of the women who come for
Maharashtra legislature. This goes io prove that both the tests belong to the middle class, whereas 85 per cent
the Union and the state governments were forced to of i he doctors said they do not get women from the
take note of the issue because oi the growing popular lower classes for SD tests.
protest. The bill in Parliament is yet to come up for
5 It is generally believed that it is only women with
discussion. Ncvertheles inc minister of state for health four or live daughters who go in for SD tests and
and family welfare did convene a meeting in New Delhi female foeticide. But the study showed that the pro
last Decembei to discuss the issue. I he Maharashtra portion of women going for SD tests when they have
government formed a committee in September last to four or more da .ghters is quite small and that a
study the problem ana suggest a set of corrective majority of me women coming to the SD clinics are
measures. The private member’s bill in me legislature motners of two or three daughters. Significantly
came up for discussion in the 198b winter session at enough, 24 pet cen. of trie doctors said that 20 per cent
Nagpur,, bur the same was withdrawn following an of their patients had only one daughter. Thus, it
assurance from the government that the committee was appeals to oe a growing trend among the public to go
still studying the problem and that, on the completion in for SD tests in the second pregnancy itself, if the
oi the study, the government would itself initiate first issue happens to be a girl.
appropriate action in the matter.
6 About 30 per cent of tne doctors said that in nearly
As part of its activities, the state • government- 10 per cent ot their cases, the women already had one
appointed committee commissioned me for the or moie sons when they came for SD tests. This
Foundation for Research in Community Health findings explodes one more myth that only those
(FRCH), Bombay, to conduct a short study of me women go for SD tests who have no sons and only
prenatal sex determination tests and female foeticide daughters. This trend moreover, appears to oe on the
in Bombay city. The study was conducted in November ascendancy.
1986 with the objective
7 A majority of the doctors contacted in the studya) Determining the extent of the spread oi sex deter see SD tests and female foeticide as a humane service to
mination tests and female foeticide in Bombay city; women who do not want to have any more daughters.
b) Finding out other related aspects of this practice; Some doctors also fee that SD tests and selective
and
abortion of fernale foetuses are a good method of pro
c) Knowing the views and perceptions of the doctors moting family planning and controlling population
growth in the country.
involved in this practice.
8 Six out of the 50 doctors said that they also per
Filly private gynecologists, chosen randomly but
with a view to covering the entire city and the suburbs. form chorion villus biopsy for sex determination.
were interviewed in person during the course of the
—Sanjeex Kulkarni
December 1986
99
Isolate Apartheid Health Care
THE Anti-Apartheid Movement in Britain has been
campaigning for the isolation of the racist apartheid
regime in all areas—political, economic, cultural and
sporting for 27 years now. It has been realised that the
policies of apartheid in segregating health care in South
Africa and the inaction of the authorities in the face
of rampant malnutrition and preventable disease
amount to state-directed genocide against the coun
try’s black majority.
Recognising this and that health is an emotive issue
which effects everyone and that everyone can therefore
relate to, in 1979 health workers within the Anti
Apartheid Movement joined together to form a Health
Committee. The mandate was to use health as an issue
to educate people about apartheid and to mobilise
health workers to support the international boycott.
Since then Health Committee members have researched
the health situation and produced campaigning
leaflets, documents and a newsletter on health in South
Africa. We have travelled up and down the country
speaking at meetings and mobilising people in the
struggle against apartheid.
Health and Liberation our newsletter is produced
quarterly and covers the latest update on health in
South Africa as well as news of our campaigns in
Britain.
Exchange of medical skills in knowledge between
Britain, South Africa has gone on for many years.
British nurses are recruited to work in South Africa,
lured by the prospects of sun, sea, sand and higher
wages. The need for them lies in the racist ruling that
black nurses may not care for white patients. Thus
whilst black nurses, unemployed are relegated to the
Bantustans, white British nurses are recruited to make
up the shortfall of staff for the whites-pnly hospitals.
Many medical students go to South Africa for three
months ‘elective’ period as. part of their training and
many doctors go to work there for short periods. These
people are attracted by the regime’s publicity that
pathology can be seen in South Africa at a more
advanced stage than elsewhere in the world. This is
true, but it shows the true callousness of the regime
that it can use the misery of the nation’s black
majority—created by their denial .of'facilities* for the
prevention and early detection of disease—as a way
of attracting people to break the international boycott
and make up the shortfall in doctors which has arisen
through the denial of adequate places for training
African people as doctors. To all these groups of health
workers we have directed specific campaigns not to go
to South Africa to work or on lecture tours.
Our international work to gain the expulsion of
South Africa from international medical bodies began
in 1981 when the Medical Association of South Africa
(Mi^SA) applied to be readmitted to the World Medical
Association. A major international campaign was con
ducted with extensive briefing documents circulated
covering the medical treatment of Steve biko and the
100
inability of MASA to address itself to the collabora
tion of doctors with the security police and the in
equalities in and fundamental issues behind health care
in South Africa. International opinion was mobilised
against MASA. The campaign culminated with
MASA’s readmission solely on the basis of the voting
system which is loaded towards the United States.
However all the African countries resigned, the WMA
lost its consultative status with the WHO and in 1983
the British Medical Association withdrew. The WMA
was thus left as an impotent and unrepresentative body.
A similar campaign was conducted at the Inter
national Planned Parenthood Federation which ended
with South Africa’s resigntion in July 1986, and
currently we are campaigning for South Africa’s
expulsion from the World Psychiatric Association and
the International Dental Federation.
Another important facet of the struggle against
apartheid is direct material solidarity with the libera.tion movements. With this in mind we established live
Medical Aid Campaign for Southern Africa to collect
money for medical supplies for the .\NC and SWAPO.
We have sent a large amounts of books and drugs to
the ANC hospital in Tanzania at the Solomon
Mahlangu Freedom College and to their clinics in
Zambia and Angola.
Over the coming few years, the struggle in South
Africa will be reaching its most crucial stage and with
this comes an ever more urgent need for concerted
international action to gain the total isolation of the
apartheid regime and the final victory against the
forces of racial and national oppression in South
Africa. Health workers throughout the world must
unite with this goal to contribute in a small way to the
final victory.
Rachel Jewkrs
Secretary AAM Health Committee
Towards Rational Therapy
THE Prescription Guidance and Information Services
(PGIS) of LOCOST is an educational effort to pro
mote awareness about the correct use of medicines.
PGIS is therefore for the benefit of both prescribers
as well as patients. Two main aspects of PGIS being
proposed are:
(1) Information dissemination to doctors who write
prescriptions and
(2) Guidance to the patients regarding the correctness
and use of medicines prescribed in a particular
condition.
The objective here, is to help the patient, the end
user of medicines to know the correctness of the
medicines prescribed, the PGIS will give comments on
following aspects of prescription: correct medicine for
a particular diagnosis, adequacy of the treatment, the
uselessness or harmful effects of any medicine, the side
effects of the medicines required, the dosage, alter
natives available both in terms of cost, quality and
nature of medicines, etc. Wherever possible, other
aspects of the therapy will also be explained. This will
Radical Journal of Health
help the patient by developing an understanding regar
ding the treatment given to him/her. This will also
equip the patient and relatives or friends to question
and to ask for more information from prescribers in
future Thus the ultimate aim is to build up consumer
awareness and initiative to bring about a change
towards more rational therapy.
LOCOST is aware of the limitations of PGIS: Per
sonal examination of the patient may not be feasible,
the scope of PGIS may not cover all diagnostic situa
tions as also the fact that a large number of ‘successful’
treatments may not be touched, and so on and so forth.
The service may not be useful for the patient as it will
take at least 10-15 days to give a balanced view on the
prescription. However, queries by doctors for informa
tion can be attended to faster. LOCOST is keen on not
encouraging legal battles between the patient and the
doctor. PG4S is a beginning, a collective effort to
facilitate awareness, education and action. Action
towards more rational therapy and towards conserv
ing scarce resources of patients as well as that of the
community.
LOCOST is also prepared to facilitate prescription
medical audits of hospitals, dispensaries and com
munity health projects, if so requested. You may be
a like minded doctor, a patient or a person simply
interested in social change. Contact: Prescription
Guidance and Information Service (PG 1LOCOST,
1st Floor, Prcmanand Sahitya Sabha Hall, Opp. Lakadi
Pool. Dandia Bazar, Baroda 390 001.
Miracles and Profits in Sickness
A NURSE who focussed a small research project for
a post-graduate university course on a private food
allergy clinic managed to achieve a relatively high mark
from the tutors involved, and it was also considered
worthy of publication in a scholarly journal. To her
amazement the doctor whose clinic had been studied
objected to the publication, not because of any feared
damage to his professional reputation, but because of
certain implications seen behind the student’s work—
especially the open discussion of the sordid subject of
money.
There are a number of diseases where medical
science has not discovered or developed a method of
entirely halting their progress and treatment is limited
to controlling or alleviating the symptoms, but not the
spread of the disease itself. These conditions typically
attract imaginative mirage “cures” which are difficult
to get, expensive, or both. The cure is often proclaimed
as some commonplace naturally occurring subs
tance—igonred by modern western technology—which,
according to anecdotal claims, has been used for years
in a remote part of the world. Sometimes the product
or treatment method is a secret which cannot be
disclosed to the general public, but you can always buy
bits of the magic. Whatever the story, evaluation by
independent scientific workers will prove fraught with
snares and delusions.
If some unfortunate person whose name has
December 1986
publicity value falls ill, (s)he may be treated with the
remedy and live happily ever after. Recently a former
pop singer, hitherto not widely known but nonetheless
of some public interest, fell ill,- and her symptoms were
attributed to multiple allergies. Personal friends and
a sympathetic section of the public expended much
good will, time and effort in what appeared to be a
good cause. The patient was flown to Dallas, USA to
Dr Rea’s Environmental Unit, but her luck did not con
tinue; voluntary funds of sympathisers at home dried
up and she was not shown returning home in triumph.
She returned as she had left—on a stretcher with an
oxygen mask attached to her face, as she inhaled the
only unpolluted vapour she eould tolerate.
It has been said that “A fool and his or her money
are easily parted”; sadly many patients would seem to
be fools, if judged by the large sums of money they
seem willing to pay for treatment of very doubtful
value. Maybe it doesn’t matter what treatment patients
have if their belief in it is enough to effect a cure, but
the long-term consequences of ‘miracles’ have also to
be considered.
What happens when the dream fades, when the
symptoms return or new ones come in their place? The
despair and frustration must be magnified, as the
patient has once again to struggle with a handicapped
identity. Having attended an unorthodox clinic the
patient may not only be financially broke but, more
difficult to repair, psychologically damaged by the
disappointed dreams offered by modern medical
messiahs.
It costs a lot of money to run private clinics, and
to pay attractive salaries to people who remove
themselves from incremental ladders in the NHS, and
need financial incentives to get involved in work that
is of doubtful validity within scientic medicine. It is
not difficult to find private practitioners from various
disciplines who will quite readily remove NHS equip
ment and surgical supplies to “get their clinic started?
When they are challenged about this exploitation of
the health service, one is reminded that the patients
who attend the private clinic cannot be treated by
orthodox methods and as they are paying their NHS
contributions it is all OK. While a hospital porter may
get taken to court for removing flowers from a tip
outside the hospital, the consultant who sends a junior
nurse down to surgical stores to collect an expensive
piece of equipment is able with impunity to ‘transfer’
the hospital instruments to the private clinic and reap
the benefits from the fee-paying customers.
Doctors and nurses who work in private clinics using
untested methods which are either innocuous or
dangeroqs, are prostituting themselves by capitalising
on the dignity and prestige afforded by their medical
or nursing qualifications. It is indefensible to.take
advantage of the trust patients place in health care
practitioners, and to make financial gain out of their
vulnerability.
.............. .
*
—Nixgixua e*cott
Reprinted from Radical Community Health, UK. Spring 1985
101
Towards a Left Critique
of
New Drug Policy
anant r 8
The long awaited new drug policy has prompted this piece so that RJH-readers may get some systematic idea about
this issue, especially its economico-political aspect, albeit in a summary form. For a detailed treatment of the basic
issues involved in the drug policy, readers may refer to some of the sources at the end. A special issue on Pharmaceuticals
and Health is being planned in December, 1987 and will carry a substantial left analysis of issues in drug policy.
THE NDP represents a typical example of the ‘new’ think
ing in the ruling class circle and the new method of func
tioning. First about the latter. A lot of show was made about
consulting various experts and of giving a hearing even to
the representatives of the All India Drug Action Network.
(AIDAN). But all this facade meant nothing in practical
terms; or perhaps the drug industry used ‘tonic-M’ much
more liberally this time. The NDP was suddenly announced
in a hurriedly convened press conference; bypassing the
Parliament. The ‘policy’ consisted of only a breif statement
amounting to about 1500 words—That’s all!-! When a lack
of a detailed draft was criticised by all analysts, the govern
ment came out with a somewhat detailed 19-page announce
ment. When one reads this pamphlet a little carefully, it is
clear that it was written after the ‘policy’ was announced.
The press statement of the December 18, 1986 was not a sum
mary of a policy document since no such document was
ready the then.
For example, the press statement of December 18 says that
“A National Drug and Pharmaceutical Authority will be
created. This authority will be an apex body which will have
representation from all the concerned agencies including
those from the industry. Among other things, it would go
into the question of rationalisation of existing fomulations’
in the market including the banning of formulations of harm
ful nature.. .” When one looks for an elaboration of this
point in the detailed policy announcement, to one’s utter
dismay and shock there is not even a mention of “represen
tation from all the concerned agencies” nor of “banning the
formulations of harmful nature?’!! To release a brief state
ment to the press and then to prepare the main text is a
mockery of the norms of even bourgeois democracy. The
deletion of these to small concessions (announced in the press
statement,) given to the movement for a Rational Drug Policy
was perhaps on account of bowing to the pressure exerted
by the drug industry to scrap these concessions. To silently
drop certain measures already announced is shocking indeed.
The earlier policy of 1978 was based on the report of the
famous Hathi Committee which Had at least a few Members
of Parliament (though there were no representatives of the
concerned trade unions and of consumers.) The policymaking was done this time entirely by bureaucrats and
technocrats. The Drug Consultative Committee of the Parlia
ment was not involved. The content of this NDP is therefore
as bad as its flimsy form. None of the issues central to the
Drug Policy have been seriously considered except the ones
related to profits and production increase. All the important
issues have been adequately highlighted by different science
102
and health groups, some of which were dealt with by the
famous Hathi Committee more than a decade back. Instead
of making progress beyond the Hathi Committee there has
been a regression right from the basic stage. It is, therefore,
not much of a surprise that the content of the policy is also
reactionary.
Freer Hand to Multinational Companies
The drug industry in India in under the domination of
the MNCs. The various ill-effects of these MNCs have been
adequately proved by different studies—commercial exploita
tion of Indian consumers through transfer-pricing; huge
outflow of capital through repatriation of profits in different
forms, drain on the foreign-exchange account; huge social
waste on account of extravagant selling expenses, disinfor
mation of doctors, insistence on brand-names, production
of irrational and hazardous drugs when the same drugs are
not allowed in their parent country, etc. It is because of these
ill-effects that the Hathi committee had recommended
nationalisation of these MNCs. The Hathi committee’s
recommendation did not include confiscation (i e, nationali
sation without compensation) or worker’s control along with
nationalisaton. But even this radical bourgeois recommen
dation was not accepted by the Indira government.
The New' Drug Policy’ has on the contrary given further
concessions to the MNCs. “For the production new bulk
drugs, and drugs produced for exports, there will not be any
restrictions on the MNCs, even though it is well known that
MNCs tend to import penultimate products from their
parent-companies at extravagant prices and hence are respon
sible for a drain on the Indian economy even for foreign
exchange account. Production of penicillin, amoxycillin,
cephalexin etc, has also been completely decontrolled except
for FERA companies.” But the hitch is, there are now only
3 FERA companies; the rest of the MNCs have now become
‘Indian’ because they have diluted their foreign-equity to less
than 40 per cent as per the FERA. Out of these eight a fur
ther six have announced their intention to dilute their foreignequity to less than 40 per cent, so that like in other ex-FERA
companies, the foreign share-holders would continue to take
all the policy-decisions but the company would now be legally
counted as Indian. Thus a couple of restrictions applicable
to the FERA companies would now be applicable to only
two companies. There has been a demand to put all the exFERA companies is a separate category and not to treat them
on par with the rest of the Indian companies. But under Rajiv
Gandhi’s leadership, such a demand has not been accepted.
Self-reliance is no more a serious slogan.
Radical Journal of Health
Increased Rates of Profit
Economic Research (NCEAR) but was funded by the drug
industry.
Let there be an independent study by a public body
Under the New Drug Policy, the drugs have been
to determine the real costs of manufacturing. It is only then
recategorised as category I and II. Category I would consist
the question whether the existing mark-up is genuinely in
of those drugs which are required for various national health
adequate can be meaningfully discussed.
programmes; and category II would consist of ‘other essen
b) It is true that the wholesaler stockist claims 8 per cent
tial has not been published. The whole aim of this exercise
of
the selling price as his commission and the retailer a
is to reduce the total number of drugs under price control.
minimum of 11 per cent. These selling costs are in addition
Only those drugs belonging to these two categories would
to transport and sales-promotion costs. This leaves com
be under price control. The prices of the rest would be
paratively limited profits for the manufacturers when the
‘monitored’; but they would be out of the price control
mark-up is 40 per cent (i e, when the selling price is to be
basket. Going by the list prepared by the National Drugs’and
upto 40 per cent higher than the manufacturing costs. This
Pharmaceutical Development Council (NDPDC), three years
calculation,
it may be noted, assumes that the manufactur
back, this list of “essential drugs” would consist of around
ing costs have not been fictitiously jacked up.) If this is the
one hundred drugs, instead of the required number of around
situation, the real solution in order to increase manufacturing
two hundred. Today, about 360 bulk drugs are under price
profits is to reduce the costs and profits of distribution and
control; the majority of these would now join the category
marketing. The wholesaler’s margin should be reduced to 3
of decontrolled drugs.
per cent as in the case of other sectors. Secondly, the pro
Even those which would continue to be under price con
trol, would fetch a higher profit-rate than hitherto. Accor motional expenses can be drastically reduced. Giving free
samples, gifts to doctors, dinners after ‘scientific seminars’,
ding to the Drug Price Control Order (DPCO) of 1979,
etc, etc, are huge social-wastes which need to be stopped. But
category I consisted of life-saving drugs which were allowed
the Indian state is not in a position today to control the pro
a 40 per cent ‘mark-up;’ category II consisted of ‘essential
fiteering of even a section of the commercial bourgeoisie (the
but not life-saving’ drugs with a permissible mark-up of 55
stockists). That is their problem. The left should ask why
per cent and category III consisted of ‘useful drugs, new
drugs’ with a 100 per cent mark-up. The rest, mainly con should the people pay the price for the timidity of the Indian
state? Similarly, high-promotional expenses are “necessary”
sisting largely of quite useless drugs could earn unlimited
for monopoly capitalism, but the left has to ask—‘ why
profits. The NDP has now two categories with a “Maximum
should
the people pay for these necessities of monopoly
Allowable Post-manufacturing Expenses” (MAPE) a new
forms
of
competition’? In case of the MNCs, these promo
term for ‘mark-up—prescribed as 75 per cent and 100 per
tional expenses were as much as 33 per cent of the costs as
cent respectively for these two categories. (Readers may note
per the data collected by the Lovraj Kumar Committee.
that ‘mark-up’ or MAPE includes manufacturer’s profit plus
c) Today drugs are costly because they are available mostly
costs and profits of transport, and sale.) This hike in mark
up would cause a pricerrise in life-saving and other essen in the form of drug combinations. Most of these drug com
tial drugs in these two categories by 12 per cent to 25 per binations consist of an essential drug and one or more un
cent according to the government’s own admission. Many necessary or useless or even harmful ingredients. For exam
essential drugs are not going to be included in these new ple, popular analgesic brands like Aspro, Anacin, Powerin
categories I and II and hence would be decontrolled. Their etc, etc, consist of aspirin as the essential ingredient and in
prices would increase ‘as much as the market can bear’. As addition one or two unnecessary ingredients. The price of
a result the prices of essential drugs would rise much more aspirin is 3 to 5 paise, whereas that of these irrational brands
than this official estimate. According to the Secretary of the two to four times as much! AIDAN has, therefore, demanded
Indian Medical Association, which is otherwise a conser that all such irrational drug combinations should be banned
vative body, the drug prices would rise by 60 to 300 per cent. and that only rational, essential drugs be made available
under generic names only. If there is a sufficiently strong
Unnecessary Price-rise
movement which makes the government accept this demand,
Many of the leading national dailies have refrained from then prices of a overwhelming majority of drugs would be
criticising head-on this increase in mark-up. Many of them drastically reduced. (Prices of single-ingredient drugs 'will not
have called it as a ‘sensible’ step. If one takes the arguments be reduced much.) A rise in mark-up if, and to an extent ge
of the drug industry, uncritically, this step appears sensible nuinely necessary, can be allowed only if this above demand
indeed. But this increased mark-up and consequent price is accepted. In such a case, the price of aspirin would be in
rise in unjustified on three accounts:
creased by one or two paise but since there would no more
a) The drug industry argues that the earlier mark-up of be any costlier irrational brands (Aspro, Anacin eta) available
40 per cent and 55 per cent was ‘unremunerative.’ This at all, the consumer’s expenses on analgesics would still be
assumes that the cost-price as given by the drug industry is much less. This demand of AIDAN has no been accepted
not fictitious. The cost calculations furnished by the industry by the government because the movement is not strong
to the Bureau of Industrial Costs and Prices (BICP) are con enough.
sidered as trade-secrets and are not available for scrutiny by
This demand is not a socialist demand in itself since it does
any other public body. Let these figures be published and not question the very existence of the capitalists in the drug
be verified by other experts in the field. The study quoted industry. All it Says is that “you earn a reasonable rate of
by industry sources to show that the earlier mark-up was not profit by selling really useful drugs and not a lot of junk
remunerative was done by the National Council of Applied in addition!’ The World Health Organisation and other such
December 1986
103
non-socialist bodies have also been advocating the sale of
only rational, essential drugs under generic names. The pro
blem is, the people’s movement, the health movement is not
strong enough today to force the government to discipline
and control the parasitic, antiquated interests like those of
the stockists, or the monopoly-interests in the drug industry.
Though monopoly capital as a whole is in the dominant posi
tion in India, a control over their reckless profiteering in one
sector is possible even within bourgeois bounds if the people’s
movement is strong enough. This has been achieved to a cer
tain extent in Bangladesh due to the combination of public
pressure, historical accident and populist initiative by the
government. A similar thing can happen in India also.
Delicensing and Indigenisation
According to the industry, licensing means a lot of un
necessary beaurocratic interference (which also breeds cor
ruption) with the “freedom of enterprise”. But this is an
antiquated, 19th century thinking. That “free-market
economy” leads to repeated small and big crises which are
too painful for the people and hence inconvenient to the
capitalist class as a whole and therefore, capitalism needs
to be regulated at least to a certain extent has been proved
in theory and in practice over and over again the world over.
It is true that some of the licensing procedures and other
governmental regulations are too cumbersome today and they
also create another parasitic layer of administrative
beaurocracy which sometimes harasses the individual
capitalists or other citizens for its own corrupt interests. Thus
a regulatory mechanism which has evolved historically to
smoothen to a certain extent, the anarchic function of
capitalism is not doing its job properly.
The solution to this is not to abolish the regulatory
mechanism itself; but to simplify it, to make it more effi
cient and functional. But under Rajiv Gandhi’s leadership,
there is not even a concern for overall planning in the interests
of the capitalist class as whole. The new ‘modern’ policy
makers have been yielding in an ad-hoc manner to the purely
sectional interests of the Indian and foreign monopolists or
sometimes to the purely sectional interests of other sections
of the capitalist class. This is at the expenses of the working
masses and also at the expense of the long-term interests of
the Indian capitalist class as a whole. The policy of delicensing
in the drug-industry by the Rajiv-regime is a case in point.
Before the announcement of the NDP, the Rajiv regime
had delicensed 82 drugs which means any company can pro
duce any of these 82 drugs to any extent without prior per
mission of the government. Now' according to the NDP, this
policy is to be ‘progressively extended’. The reasons given for
this policy are: to remove unnecessary hurdles in the way of
the industry, so that there will be abundant production of
those drugs which are in short-supply. But in reality the con
sequences would be quite different:
a) Many of the essential drugs have been in short-supply
today not because of the licensing system (a fevy exceptions
apart) but because they were under price-controls. The drug
industry could get a much more higher rate of profit in the
production of decontrolled drugs and hence it concentrated
its efforts on the production of these high-profit though
mostly useless drugs. Of the 94 drugs delicensed, 75 so far
104
(even before the announcement of the N3 have been open
for all sectors for production. But the MNCs and big com
panies by and large neglected their pi-oduction. In the NDP,
except for about a hundred drugs, all the rest would have
no price-controls and hence the drug industry would con
tinue to neglect these 100-odd priority essential drugs and
would continue to concentrate on the rest. The shortages of
priority essential drugs would continue so long as the nonessential, useless, irrational drugs are allowed to be produced
and moreover are allowed higher-profit rates.
In case of certain essential drugs the existing capacities
are today underutilised because the drug-companies have not
been interested in a 40 per cent or 55 per cent mark-up. But
now that the mark-up on these drugs has been increased to
75 per cent and 100 per cent, the drug-companies may now'
fully use their existing capacities. In the short-run'therefore,
there may be increased production of some of the essential
drugs. This should not be interpreted as “success of the
delicensing policy”. In the long run, newer capacities ’would
be developed for the decontrolled drugs more than those for
the priority essential drugs.
b) Whatever limited planning that exists in capitalism
requires that the planning authorities can intervene to
stop/reduce or encourage the production of certain drugs
or to intervene to balance the growth of different types of
companies in different areas. Delicensing would mean the
drug production would be entirely left to the chaotic market
forces. The government would not be able to do anything
about it, nor w'ould it be able to threaten the monopoly com
panies with the stick of the licensing authority if these com
panies indulge even in brazen malpractices to fleece the
consumers.
Delicensing would not be applicable to FERA and MRTP
companies. But now' legally there would be only two FERA
companies and only a couple of Indian drug companies
would be counted as MRTP companies since now the limit
for inclusion in the MRTP list has been raised to Rs 100 crore
by the Rajiv-regime.
The deleterious impact of delicensing can be congertly
visualised since 12 drugs in March, 1983 and 82 more in June,
1985 have already been delicensed. As a result, a number of
monopoly companies have registered capacities for produc
tion of many delicensed drugs in quantities which are 3 to
10 times the targets for the seventh Five Year Plan! Generally,
most of these capacities are not utilised by the MNCs.
Registrations are made primarily to preempt competition!
For example, Duphar Interfram had 39 registrations in
1980-81; but utilised only 18 of these; in 1984, it acquired
eight registrations but used none of these. The government
cannot do anything about the chaos thus produced.
The ex-FERA companies would now more easily push out
other companies and this w'ould, amongst other things, push
up the import-content of drug-production in India. A study
of production of 8 drugs by MNCs after delicensing has
shown that the import of these drugs has increased substan
tially. For example, Boots produced 20 tonnes of Ibuprofen
and imported 4 tonnes in 1980-81, whereas by 1984-85, the
imports of this drug by Boots increased to 62 tonnes but in
digenous production by Boots increased to only 51 tonnes.
Delicensing would, therefore, lead to a further control by
Radical Journal of Health
the monopolies over the Indian drug industry and a further
chaos with all the ill-effects for the people as well as for the
balanced development of the Indian capitalist class as a
whole.
Probably in order to stave off criticism on the forecasted
increased import of drugs due to further delicensing the
government has announced in the NDP, a scheme if ‘indigenisation’. The NDP lays down that in cases where the
import content of a product is more than 20 per cent, the
drug companies would be required to submit an annual plan
of how its production is going to be indigenised. This is a
very loose formulation. Suppose, a foreign company un
necessarily imports, say codene, and prepares a costly, irra
tional cough mixture by adding a number of unnecessary
ingredients to it so much so that the imported essential in
gredient comes to less than 20 per cent of the total cost then,
this new restriction of ‘indigenisation’ would not be ap
plicable to this product. Thus vital, essential ingredients can
continue to be imported in large guantities. Secondly, there
is no time-limit given for ‘indigenisation’ nor any punish
ment specified if the companies do not observe in practice
the plan of ‘indigenisation’.
What is in fact needed, and is technically, definitely possi
ble, given the developed technical capacity of the drug
industry in India, is more or less a complete indigenisation
in say three-five years and rapid, drastic reduction in the cur
rent rising drug-imports (Rs 198 crore in 1984-85!) Sudip
Chaudhury (see references) amongst others, in his detailed
study, has shown that this is technically very much possible.
The Indian state, because of its class-character is not able
to take this step even today. On the contrary, during the last
five-six years (even before the Rajiv regime), it has been forc
ed to give more and more leeway to MNCs. The NDP is yet
another example that Rajiv Gandhi’s leadership has con
siderably accelerated this proces.
Broad banding
This is another measure to “remove the unnecessary
hurdles in the growth of the industry!’ Broad-banding means
that if a drug-company gets a permission for the produc
tion of penicillin, then now it can produce all types of
penicillins and chemically related analogues like ampicillins
and the like. The companies would not be required to take
separate permission from the drug controller for a new for
mulation once the basic type has been allowed. If such broad
banding is done for single-ingredient bulk drug only, then
it is a sensible step within the chaotic capitalist economy
because companies can produce in the same plant, chemically
related products in changing quantities depending upon
orders they receive without asking for a licence each and every
time. This can enable them to fully utilise the production
capacities they have built.
But the NDP allows broad-banding of formulations also.
This means that if a company has a licence to produce a mix
ture of say three types of analgesics or vitamins, it can change
their proportion or change a bit the chemical structure of
one or more of its ingredients and sell the ‘new’ product
under a new brand name. Earlier, the companies had, at least,
to undergo the formality of applying and getting a permis
sion. Now there will be a totally uncontrolled growth of all
December 1986
sorts of irrational drug-combinations sold under a range of
newer brand-names. It would become more or less impossi
ble to monitor the prices of the new formulations in order
to check price-rise. Monitoring the quality of drugs would
also be a mammoth task for the government since it is im
possible to check the ingredients qualitatively and quan
titatively if we have over 50-60,000 formulations.
Quality Control
The NDP seeks to make Good Manufacturing Practices
a statutory requirement. This was quite an overdue step. But
the problem is, there is no mention of qualitatively improv
ing and strengthening the existing too weak, too ineffective
and corrupt drug-regulatory authority. The statutory re
quirements would, therefore, remain on paper.
The NDP is to make a compulsory certification system
for quality-control from ‘recognised institutions’. This means,
now there will be specified institutions for this purpose.
Whether such institutions would be private or public has not
been mentioned. Going by the Rajiv regime’s trend towards
privatisation, it is likely that privatisation will take place here
also. The data with private laboratories is considered trade
secrets and generally it is impossible to get these data to find
out whether a particular private company has been doing
its job honestly or whether like the notorious Chemical Labs
involved in the J J Hospital death-scandal, the private
laboratory is giving false reports. Though many public
authorities tend to be as secretive, public laboratories can
be more accountable with increased public pressure. In case
of private laboratories, it is their constitutional bourgeois
right to keep their trade-secrets confidential.
The government does not want to spend money on increas
ing the number of public laboratories upto the required
number whereas it is willing to squander money on all types
of useless or anti-people projects. Hence the move towards
privatisation. This must be stoutly opposed. At the same
time, as a measure of rational utilisation of existing resources,
public bodies like laboratories in research-institutions, univer
sities, etc, can be entrusted to a certain extent, this task by
fortifying these facility-centres with the needed extra
equipments and personnel. This would obviate to a certain
extent the need to build new facility-centres from scratch.
Whether the existing system can do this is a moot point even
if socially, it is quite a viable propositon.
Medical Issues
Health and science groups in India have identified the
following key-issues from a medical aspect as part of a ra
tional drug policy; none of which find a place in the NDP.
i) Preparation of a priority essential drug-list and a com
prehensive rational drug list for India. Production of drugs
to take place in accordance with only these lists and no other.
ii) To assess quantitatively the drug heeds of the Indian
people on the basis of a study of prevalence of the disease
pattern in the country and to plan the production
accordingly.
iii) To completely and immediately ban all the irrational
and hazardous drugs. Only drugs as specified in (i) to be
allowed.
iv) Complete abolition of brand-names and replacing them
105
with generic names, with the company’s name in the brackets; non-allopathic systems of medicine. There is no serious
for example, “Penicillin-V (Alembic)”.
research policy nor any attempt to curb production of irra
v) Stopping the ‘disinformation’ of doctors and consumers tional (may be hazardous also) medicines under the name
by drug companies. Continous compulsory reeducation of of ayurveda of the misuse of these medicines.
ix) All medical research on human beings must be
doctors and relevant education of consumers by state medical
statutorily required to confirm to the 1975 Helsinki (Mark
authorities.
vi) Strict check on the unethical marketing practices by II) Declaration. This should be strictly followed in case of
the drug companies; a ban on incentive-schemes and on giv contraceptive research also.
None of these medical demands have been accepted. One
ing samples and gifts .to doctors by drug companies.
vii) Adequate supply of drugs free of charge to poor peo may conclude that the NDP is only a pricing and ‘liberalisa
ple through the government set up. Rational utilisation of tion policy’ with no concern for rationally or people’s health
the existing budget and increasing it rapidly to the adequate needs. The foregoing account shows that as an industrial
policy also, it is clearly reactionary and anti-people.
level.
vii) To stop the continuing colonial heritage of step
Selected reference material
motherly treatment being given to the non-allopathic systems
of medicine; to encourage research in these systems with 1 A Rational Drug Policy—Problems Perspective, Recommendations,
All India Drug Action Network and Voluntary Health Association
financial and other support. At the same time to disallow
of India, March 1986, pp 165, Price Rs 20. Available from VHAI,
the commercial production of any drug by any company
Institutional Area, New Delhi 110 016.
unless it is accepted as scientifically proved (effective and 2 40Drug
Industry and the Indian People (Ed), Amit Sen Gupta, Delhi
safe) by appropriate bodies. Encouragement to ayurveda does
Science Forum and FMRAI, pp 333, Price Rs 40. Available at Delhi
not meant that Richardson-Hindustan be allowed to avoid
Science Forum, B-II, II floor, I Block, Saket, New Delhi 110 017.
taxation or to get other concessions by naming its Vicks 3 Issues involved in Drug Policy, Prepared by Pondicherry Science
Forum, pp 56, Price Rs 6.50, Chennai Books, 6, Thayar Sahib Street,
Vaporub as herbal medicine! To enact that medical practi
II Lane, Madras 600 022.
tioners would use only those medicines or therapies in which 4 'Manufacturing Drugs without TNCs\ Sudip Chaudhury, EPW, Vol
they have been adequately trained by recognised institutions.
XIX, Nos 31-33, August 1984.
The NDP talks about only the standardisation of non- 5 S Singh, Multinational Corporations and Indian Drug Industry,
Criterion Publications 1985.
allopathic drugs and preparation of standard formulary for
Economic and Political Weekly
A journal of current affairs, economics and other social sciences
Every week it brings you incisive and independent comments and reports on current problems plus a number
of well-researched, scholarly articles on all aspects of social science including health and medicine, environ
ment, science and technology, etc.
Some recent articles:
Mortality Toll of Cities—Emerging Pattern of Disease in Bombay: Radhika Ramsubban and Nigel Crook
Famine, Epidemics and Mortality in India—A Reappraisal of the Democraphic Crisis of 1976-78- Ronald Lardinois
Malnutrition of Rural Children and Sex Bias: Amartya Sen and Sunil Sengupta
Family Planning and the Emergency—An Unanticipated Consequence: Alaka M Basu
Ecological Crisis and Ecological Movements: A Bourgeois Deviation9: Ramachandra«Guha
Environment Conflict and Public Interest Science: Vandana Shiva and J Bandhyopadhyay
Geography of Secular Change in Sex Ratio in 1981: Ilina Sen
Occupational Health Hazards at Indian Rare Earths Plant: T V Padmanabhan
Inland Subscription Rates
Institutions/Companies one year Rs 250, Two years Rs 475, Three years Rs 700
Individuals Only One year Rs 200, Two years Rs 375, Three years Rs 550
Concessional Rates (One year): Students Rs 100; Teachers and Researchers Rs 150
(Please enclose certificate from relevant academic institution)
[All remittances to Economic and Political Weekly 284, Skylark, Shahid Bhagatsingh Road,
Bombay 400 038. Payment by bank draft or money order preferred, Please add Rs 14 to outstation
cheques for collection charges]
A cyclostyled list of selected articles in EPW on health and related subjects is available on
request.
106
Radical Journal of Health
Dialogue
Medical Officers—The ‘New Middle Class’?
I WAS a little bit surprised by Sujit Das’s rather sharp socialists have to be critical about their interests as officers.
response (Organising doctors: a difference in approach, RJH, There has to be an independent platform clamouring for a
Vol 1:2) to my critical comments (SHR, Vol 11:3) on his article
revolutionary-change in the ‘health-system’. Such a platform
and my separate piece on ‘Organising Doctors’ in the same will take a dialectical approach to the contradictory interests
issue.
of medical officers. It is not necessary that the majority of
Das feels that my remark that his article is a “shamefaced
the new middle-class comes to the side of the revolutionary
defence of the interests of the doctors” is a rude one. The programme. There is a more numerous other section of
dictionary-meaning of “shamefaced” is “bashful, shy, retir doctors (junior doctors) and much more numerous
ing, modest. ..” and has no rude connotations.
paramedics who are more likely to come to the side of a
I am not sure whether I should go into a detailed debate
revolutionary programme in the field of health. Those
about the questions of terminology raised in the second
medical officers who do not join such a platform today will
paragraph of his response. Some people including Das may have to accept and implement after the revolution, the pro
find it irrelevant. I would only point out that a mode of pro gramme chalked out by this platform. Das, however,
duction is a relatively stable set of relationship consisting disagrees basically with my characterisation of the medical
of a specific intertwining of productive forces and produc officers as part ot the new middle class. For two reasons—
tion relations and which reproduces itself over and over the first reason is rooted in his misunderstanding of the con
again. Petty-commodity relations by their very nature can cept of the new middle class. I have explained my under
not constitute a mode of production (a stable, self standing of this term at some length in my note ‘(Organis
reproducing mode) but must disintegrate over a period of ing Doctors; Towards What End?)’ and it should be clear
time; general practitioners would, over a period of time, more to anyone that I have not ‘adopted this formulation’ of iden
and more be replaced by hospital-owners-capitalist doctors tifying “the highly skilled wage-earners of advanced capitalist
on the one hand, and the wage-earning doctors on the other society as new middle class’’ For me, their position as new
hand.
middle class is not due to their “skills” but derives from their
Now about the central issues: The main difference in role as officers. Das’s second reason is that “by no stretch
approach according to Das is:of imagination could India be labelled as an advanced
1) “Phadke wants to organise doctors towards the end of capitalist society;” and the new middle class is a product of
fulfilling the tasks set by his own lofty ideal” Das, however, advanced capitalist society. India is, of course, not an ad
believes that “such idealistic approaches have never helped?. vanced capitalist society like the West, but yet we have
I plead guilty to his first charge; I would only hasten to monopolists like Tatas and Birlas. In certain sectors, we do
add that the “lofty ideal” is not my personal invention. All have signs of advanced, monopoly interests; and the new
those who believe in scientific socialism from the point of middle class (executive engineers, foremen, supervisors,
view of human liberation believe in a “lofty ideal” of a medical officers all those who perform the function of the
revolutinary charge. His second charge is however, a little labourer as well as that of capital as officers) is very much
off the mark. I have not taken any idealist approach. I have a reality in India.
started with a “materialist analysis of position of doctors”,
3) Das disagrees with me on empirical grounds also. (“I
and have then tried to point out the contradictory class have not found these doctors, as a class, performing the func
location of medical officers—medical officers being one im tion of capital, of supervising, extracting work from the
portant layer within the category of wage-earning doctors. paramedics...”) The problem is tht Das continues to talk
Based on this materialist dialectical analysis, I have ques about “doctors in service” as a homogenous category,
tioned the existing strategy of organising this new middle
class “mainly on the basis of their trade-union demands”
(emphasis added).
MEDICO FRIEND CIRCLE PUBLICATIONS
2) Das disagrees with my critical attitude towards doctors:
It is, of course, true that a socialist health system cannot be
Medico Friend Circle Bulletin (Monthly) :
run without doctors. But it is also true that a revolutionary
Annual Subscription: Rs 15
socialist transformation in the medical system cannot be
Anthologies:
initiated by a new middle class organised mainly on trade
union demands. Such a change can only come (as a part of
In Search of Diagnosis
Rs 12
a broader revolutionary transformation) through revolu
Health Care: Which Way to Go Rs 12
tionary coalition within and outside the health system in
Under the Lense
Rs 15
which medical officers as a social layer may or may not par
Bulletin
subscriptions
to
be
sent
to
C
Sathyamala,
ticipate. It should be the attempt of marxists to bring at least
F-20
(GF),
Jangpura
Extension,
New
Delhi
110 014.
a section of this new middle class to the side of the revolu
Orders for the anthologies to Dhruv Mankad,
tionary programme; and my contention is that this cannot
1877 Joshi Galli, Nipani, Belgaum Dist, Karnataka.
be done by organising them mainly on their trade union
demands. Upholding the interests of medical officers as
wage-earning health-workers is not enough. Scientific
December 1986
107
whereas I have distinguished between doctors with hardly
any administratively supervisory or executive function, e g,
the junior doctors on the one hand, and the medical officers
who have to perform these functions on the other. If one
goes to any Primary Health Centre, one would immediately
come across a series of executive, supervisory tasks over the
work of the paramedics that the medical officer has to do.
It is because of their status as ‘officer’ that the MOs at PHC
get well-built quarters or bungalows (though no such accom
modation has been built in many new PHCs;) whereas the
junior doctors share one room amongst 2-4 doctors. The
MOs get a salary which is higher compared to that of the
junior doctors though junior doctors are many a times
clinically more competent and are more overloaded with
work. The MOs can be compared with the parademics also.
The salary' and the facilities that the medical officers have,
are more than would be explained purely by their training
if we compare them with the paramedics (like the ANMs).
It is because of their dominant position as officers that many
medical officers illegally earn money’ with impunity through
private practice. Medica’ officers as wage-earners have many
problems and that is why they have been unionising. But
marxists, scientific socialists should not point out only to
their problems but also must bear in mind their status as
officers.
Contrary to Das’s assertion, I have not ‘discounted trade
unionism as such’, nor have I said that doctors should behave
as if the world around is not commercial. I only wanted to
point out the fact that Das has not given any class
characterisation of doctors though the title of his article
raises this expectation and though he raised this pufestion in
the text also. Instead, the article gives an account of the pro
blems faced by the doctors without looking at their con
tradictions and hence becomes a kind of a one-sided defence
of the interests of doctors.
—ARS
(Continued from page 77)
responsibilities to serve the needs of the dominant class. Total
state control is a hightened level in the process of socialisa
tion. On the other hand, at the present moment it is obvious
that total state control is not equivalent to people’s control.
Our conception of people’s state or proletarian state has
received a jolt from the experience of the socialist countries.
People’s participation also remain elusive without sharing
in power. A rethinking is perhaps in order to conceptualise
people’s control in political and organisational terms.
But then it is also on observable fact that total state con
trol or major state control, in whatever form, have brought
about more equitable distribution of health care among the
people. Its contribution in human values has proved to be
immense.
References
Doyal L and Pennel I, The Political Economy of Health, Pluto Press,
London, 1979, p 40.
Government of India: Pocket Book of Health Statistics, Ministry of
Health 1975 and 1978-1981.
Navarro, V: Medicine Under Capitalism, Bodist, New York, 1976, p 221
Thapar, Romila: Asoka and the Decline of the Mauryas, Oxford Univer
sity Press, Delhi 1973.
—Smarajit Jana
108
Radical Journal of Health
Why don't you write for us ?
This periodical is a collective effort of many individuals active or interested in the
field of health or interested in health issues. The chief aim of the journal is to provide a
forum for exchange of ideas and for generating a debate on practical and theoretical
issues in health from a radical or Marxist perspective. We believe that only through
such interaction can a coherent radical and marxist critique of health and health care be
evolved
Each issue of the journal highlights one theme, but it also publishes (i) Discussions
on articles published in earlier issues (ii) Commentaries, reports, shorter contributions
outside the main theme.
If you wish to write on any of these issues do let us know immediately. We have
to work three months ahead of the date of publication which means that the issue on
Primary Health Care is already being worked on. A full length article should not exceed
6,000 words and the number of references in the article should not exceed 50. Unless
otherwise stated^author's names in the case of joint authorship will be printed in
alphabetical order. You will appreciate that we have a broad editorial policy on the
basis of which articles will be accepted.
We have an author's style-sheet and will send it to you on request. Please note that
the spellings and referencing of reprint articles are as in the original and are N.0T as per
our style.
We would also like to receive shorter articles, commentaries, views or reports. This
need not be on the themes we have mentioned. These articles should not exceed 2,000
words. Please do write and tell us what you think of this issue.
All articles should be sent in duplicate. They should be neatly typed in double
spacing, on one side of the sheet. This is necessary because we do not have office
facilities here and the press requires all material to be typed. But if it is impossible for
you to get the material typed, do not let it stop you from sending us your contributions
in a neat handwriting on one side of the paper. Send us two copies of the article
written in a legible handwriting with words and sentences liberally spaced.
The best way to crystallise and clarify ideas is to put them down in writing. Here's
your opportunity to interact through your writing and forge links with others who are,
working on issues of interest to you.
WORKING EDITORS
Please send me Radical Journal of Health for one year (for issues). I am sending
Rs.
as subscription and/or donation, by Demand Draft/Cheque. (D D
and cheque in favour of Radical Journal of Health and for cheque add Rs. 5, if outside
Bombay).
Name
Address
PIN
"When one individual inflicts bodily injury upon another, such injury that
death results, we call the deed manslaughter; when the assailant knew in
advance that the injury would be fatal, we call his deed murder. But
when society places hundreds of proletarians in such a position that they
inevitably meet a too early and an unnatural death, one which is quite as
much a death by violence as that by the sword or bullet; when it
deprives thousands of the necessaries of life, places them under
conditions in which they cannot live—forces them through the strong arm
of the law, to remain in such conditions until that death ensues which is
the inevitable consequence—knows that these thousands of victims must
perish, and yet permits these conditions to remain, its deed is murder just
as surely as the deed of the single individual; disguised, malicious murder,
murder against which none can defend himself, which does not seem
that it is, because no man sees the murderer, because the death of the
victim seems a natural one, since the offence is more one of ommission
than of commission. But murder it remains."
— Frederick Engels
(From The Condition of the Working-Class in England, 1892)
Position: 1220 (6 views)