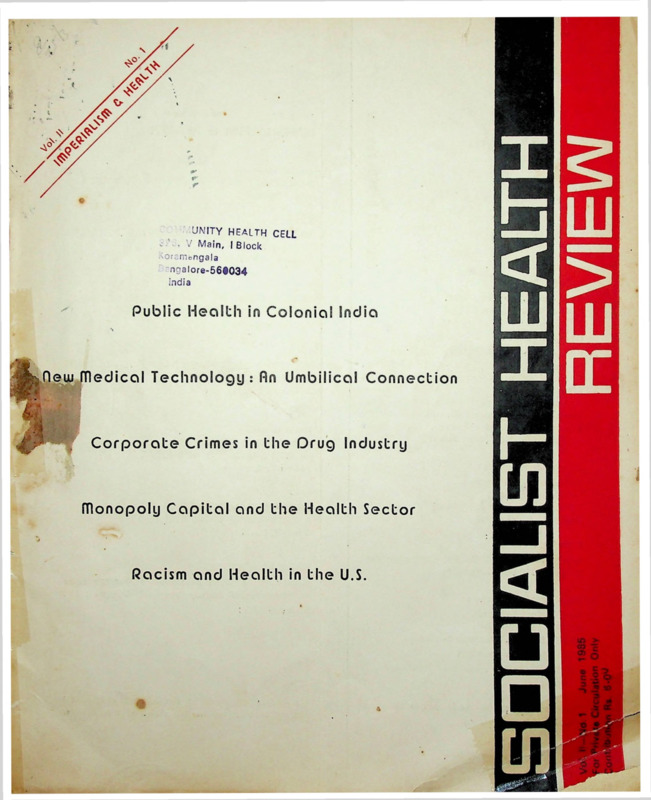
Socialist Health Review 1985 Vol. 2, No. 1, June Imperialism & Health.pdf
Media
- extracted text
-
UNITY HEALTH CELL
< • .7 Main, I Block
AOramongala
ngalore-56t034
India
Public Health in Colonial India
medical Technology: An Umbilical Connection
Corporate Crimes in the Drug Industry
monopoly Capital and the Health Sector
Racism and Health in the U.S.
Vol II
Number 1
IMPERIALISM a HEALTH
1
Editorial Perspective
HEALTH AND MEDICINE UNDER IMPERIALISM
Anant Phadke
6
00
THE COLONIAL LEGACY AND THE PUBLIC HEALTH
SYSTEM IN INDIA
Radhika Ramasubban
Working Editors :
17
Amar Jesani, Manisha Gupte,
Padma Prakash, Ravi Duggal
TRANSFERRING MEDICAL TECHNOLOGY:
REVIVING AN UMBILICAL CONNECTION ?
Meera Chatterjee
Editorial Collective :
Ramana Dhara, Vimal Balasubrahmanyan (A P),
Imrana
Quadeer, Sathyamala C (Delhi),
Dhruv Mankad (Karnataka), Binayak Sen,
Mira
Sadgopal
(M P),
Anant
Phadke,
Anjum Rajabali, Bharat Patankar, Jean D'Cunha,
Mona Daswani, Srilatha Batliwala (Maharashtra)
Amar Singh Azad (Punjab),
Ajoy Mitra
and Smarajit Jana (West Bengal)
Editorial Correspondence :
Socialist Health Review,
19 June Blossom Society,
60 A, Pali Road, Bandra (West)
Bombay - 400 050 India
23
MONOPOLY CAPITAL AND THE REORGANIZATION
OF THE HEALTH SECTOR
J. Warren Salmon
38
Bhopal Update
TRAGEDIES & TRIUMPHS :
HEALTH & MEDICINE IN BHOPAL
Padma Prakash
45
RACE AND HEALTH CARE :
A PERSPECTIVE FROM CHICAGO
Bindu T. Desai
Printed at:
Omega Printers, 316, Dr. S.P. Mukherjee Road,
Belgaum 590001 Karnataka
REGULAR FEATURES
Annual Contribution Rates :
Review Article : John Braithwaite's Corporate Crime
in Pharmaceutical Industry by Ravi Duggal : 31 ;
Rs. 20/- for individuals
Rs. 30/- for institutions
US$20 for the US, Europe and Japan
Dialogue : 43 ;
US $15 for other countries
We have
countries.
special
rates for
developing
(Contributions to be made out in favour of
Socialist Health Review.)
The views expressed in the signed articles do
not necessarily reflect the views of the editors.
Editorial Perspective
HEALTH AND MEDICINE UNDER IMPERIALISM
Jmperialism is
the
highest
stage
of
capitalism
wherein monopoly capital dominates the life of
society. Monopoly capital leads on the one hand,
to a tremendous development of the productive
capacity of human society, the spread of relations
of wage-labour and capital throughout the world;
but on the other hand, the private monopoly over
these productive forces leads to its underutilisation
its distorted development and the domination of
one country or a group of countries over others
either in the form of colonialism or otherwise. What
are the specific effects of this phase of capitalism on
health (the determinants, dynamics and the status
of health) and Medicine (medical knowledge and
medical profession) ? In general, the contradictions
of capitalism between development of productive
forces in society and the specific capitalist relations
of production get accentuated in the period of
imperialism. Thus the tremendous development of
productive forces in the period of imperialism makes
it more and more unnecessary for ill-health to
continue to prevail. Moreover this development
makes it more and more possible to improve health
in a positive sense. But at the same time, capitalist
relations of production in the imperialist phase do
not allow full utilisation of this possibility. This can
be seen from only a limited improvement in the
provision of food, water, sanitation, safe working
environment, medical care, to all the people in the
world Further, monopoly capitalism affects the
development of productive forces in such a manner
that they instead, foster ill-health by creating malnourishment all over the world (overnourishment
in the imperialist countries, and undernourishment
in the peripheral countries); pollution-creating and
accident-prone working environment, disease creating
medical interventions and so on.
This contradiction is also seen in medicine. On
the one hand there has been a fantastic development
in the medical knowledge leading to increased
possibility of preventing and treating diseases But
on the other hand, the character of medical service
as commodity (though often paid through social
insurance) continues to limit its usefulness and this
increasingly costly commodity is not adequately
available to vast sections of the population who
cannot afford to pay for it. Even the development
of medical knowledge and of the profession itself
June 1985
has been vitiated by the narrow interests of those
in charge of this knowledge and the services. Thus
for example there is comparatively less research on
the health problems of the people in the peripheral
countries; inspite of the rise of preventive medicine,
clinical medicine continues to dominate the scene;
sexism, racism, expertism continues to affect the
character of medicine. Medicine has also played an
increasingly important role as one of the ideological
supports of the ruling class (Ehrenreich. 1 978). For
example, medicine gives "scientific" credibility to
the ideas of the ruling class that diseases are caused
by germs, ignorance, bad habits and "ofcourse"
poverty for which people themselves are to be
blamed and that ill-health can be got rid of if people
become wiser, learn to live clean, give up bad habits
and listen to the advice of the medical experts.
Medical health care programmes have been used
to diffuse class tensions.
Imperialism has developed through two distinct
phases, from 1880's to 1945 is the colonial phase,
wherein
imperialist domination required direct
political rule. The post-war period has seen the
development of a new phase in imperialism with a
distinct change in the structure of imperialist centres
(rise of multinationals, of state intervention and so
on) in the international division of labour and rise of
politically independent bourgeois regimes in peri
pheral countries. We have to analyse health and
medicine in both these phases.
Health in the Imperialist Countries
After 1870, in countries like UK, the incidence
of infectious diseases and of diseases of malnourishment started a secular decline, thanks to the rising
living standards and some public sanitary measures.
But the mortality and morbidity declined much more
slowly among the working classes. A substantial
section of the population was still undernourished.
Thus as late as 1930, a study in UK showed that
out of six categories of population according to
their income, only the two most prosperous had
adequate diet (Doyal and Pennel, 1979). Even in
1970s and 80s some undernourishment continued
in some working class sections of the population.
But gradually food consumption had increased and
this along with better sanitation, housing, and
1
other facilities decreased the morbidity and mortality
due to infectious diseases. It needs to be noted that
the impact of cheap grains and other food products
from colonial countries enabled monopoly capital
to offer concessions to the working class through
an improved food basket, without much rise in the
money wages.
The secular decline in undernourishment in the
imperialist countries was, however, replaced by a
new form of malnourishment, overconsumption,
thanks to the rise of monopoly agri-business especi
ally after the second world war. Production of
concentrated foods stuffed with calories by reducing
its fibre content is the way of increase its value per
unit of weight and the surplus value
(profit)
contained in it. This low fibre, high caloric-density
food led to the problem of constipation and a host
of intestinal diseases related to it on the one hand,
and the diseases due to overweight, cardio-vascular
diseases on the other (Doyal 8- Pennel 1979).
Monopoly capital gave rise to a whole variety
of new industrial products and processes. The
technology to control pollution has,
however,
developed at a much slower rate since capitalists
are primarily interested in profits and not in the
health of the people. As a result, the workers and
people in the neighbourhood were exposed to a
new variety of pollutants, many of them being
carcinogens. A new set of "industrial diseases"
have sprung up.
Monopoly capitalism breeds consumerism. Even
those products which are harmful to health are
pushed onto the consumers through high pressure
salesmanship which is characteristic of monopoly
capitalism.
For example, cigarettes, individual
transport instead of efficient public transport, use
of drugs and medical equipment when not indicated,
and so on.
All the above tendencies are seen in a more
sharpened form in the post-war period. The hazards
of nuclear power reactors is an additional pheno
menon. Increased alienation, psychological stress
and strain has resulted in a higher incidence of
psychiatric disorders as indicated by the fact that
in England, 50 percent of the National Health
Scheme expenditure is now used to
provide
psychiatric care of one kind or another (Doyal &
Pennell, 1979). Massive state intervention in the
economy is the specific feature of post-war capitalism.
This has however not basically changed the process
of social production of ill-health; state intervention
has not been able to control the process of
2
overnourishment, pollution, accidents and psychol
ogical stresses, generated by the incessant drive
of the capitalist class for capital accumulation.
Two imperialist world wars figure as two dark
patches in this otherwise not so happy scenario
Millions and millions perished, crores got injured,
maimed, uprooted. Undernourishment, infections
raised their heads once again. These and other
effects turned the clock by decades.
Health in Peripheral Countries
What has been the effect of imperialism on the
health of the people in the peripheral countries ?
The deleterious effect has been manifold. Wars of
colonial conquest and inter-imperialist rivalry left
many natives dead, injured and maimed. The ravages
of war. the decline in availability of food, social
disruption also took their toll in health.
lhe impact of the policies of the colonial masters
have been studied by some researchers. Study of
Africa offers a typical example (Turshen 1977,
Doyal with Pennel 1979). Alongwith the conquest
by western imperialists came a host of infectious
diseases carried by the invaders from the pool of
infection in Western Europe (Doyal with Pennel,
1979) The imposition of high taxes in cash and
commercialisation of agriculture led to widespread
poverty and reduction of availability of food;
the migrant labour system, plantations, and the
filthy, newly-industrialised towns led to epidemics,
premature deaths, venereal diseases and alcoholism.
The extreme degree of exploitation with scant regard
to the health of the workers in the cities gave rise to
a high incidence of industrial diseases (Eiling 1981)
and high incidence of infectious diseases. In the
rural areas, indiscriminate tampering with the local
environment led to epidemics of sleeping sickness,
malaria and other diseases.
In the post colonial period, inspite of the faster
tempo of the development of productive forces in
the newly politically independent states the living
conditions of the labouring people did not improve,
except for a section of the working class in the
cities. Eradication of plague, small-pox; decline in
cholera, malaria (in other words, those problems
which are primarily amenable to technological soluti
ons) have increased the average longevity. But there
are medico-social and new health problems begging
solutions. Those polluting industries which cannot
now be tolerated in the West due to increased
popular resistance to pollution have been exported
Socialist Health Review
to the peripheral countries. Newly cheated irrigation
systems have led to malaria, filaria and Japanese
encephalitis in certain parts of India (PPST Bulletin,
1984). Unplanned use of pesticides in the strategy
of green revolution has increased the problem of
mosquito resistance to D.D.T. Dams have increased
the incidence of bilharziasis in places like Egypt. A
series of wars amongst peripheral countries have
benefited the imperialists at the expense of the
health of the people.
Concentration of world food production in the
imperialist countries after the second world war and
the dependence of peripheral countries on food
imports from abroad has converted the food situation
into a political issue. The sudden withdrawal of the
US food ''aid'' component in the seventies led to
wide spread hunger, death, malnourishment in
Sahel, Bangladesh and elsewhere. The health of the
people in those countries which are now dependent
on food imports is now at the mercy of the imperia
lists.
Medicine Under Imperialism
What have been the characteristics of Medicine
in the period of imperialism ? It is only after the
1870s that clinical medicine acquired some solid
scientific formulation. All the branches of scientific
clinical medicine have grown very rapidly during the
last 100 years. But at the same time, medicine
became more and more synonymous with clinical
medicine since the character of medical services
remained primarily in the form of sale and purchase
between individual doctor and the patient. Though
the sanitary and social reforms were almost solely
responsible for the improvement in the health status
of the population, clinical medicine and the "germ
theory of disease" usurped the pride of place in the
ideology of medicine since the vested interests of the
clinicians demanded this. With the establishment of
scientific clinical medicine a final, decisive onslaught
on the traditional medical system as well as homoeo
pathic system was made through the famous
Flexner report in the US which argued for allowing
only "scientific medicine "(meaning clinical medicine
with all the limitations imposed by the commercial
professionalism of male doctors) to
continue.
Scientific clinical medicine, however, arrived too
late on the European scene since most of the
infectious diseases had already declined substan
tially and medicine had hardly anything to offer on
the new health problems. The post-war period saw
a new explosion of scientific knowledge. In the
absence of a proper social perspective, and a
conducive structure of medical profession, this
June 1985
new knowledge led the ideology of supcrspecialisation and expertism.
The discipline of "public health" in the mid
nineteenth centrury grew into a modern science of
Preventive and Social Medicine (PSM) and still
further into Community Medicine in the twentieth
century. But firstly this all important approach has
been relegated to secondary importance by the
medical-industrial complex. Secondly, the established
discipline of PSM has neglected or rejected the
Marxian approach, is informed by bourgeois soci
ology and hence it has hardly any correct under
standing of the relation between health and the
process of capitalist development, of the changing
balance of class forces. Its scientific insights are
marred by its bourgeois paradigm/framework and
hence cannot challenge bourgeois social order. Nay
more — it tends to create illusions that ill-health can
be eliminated through technical interventions applied
on a social scale. Through concepts like "tropical
diseases", "diseases of industrialisation",
PSM
naturalises the cause of diseases which are primarily
of social origin. It has thus a kind of fetishistic
understanding of the diseases and hence has
become a part of bourgeois ideology.
The specific effect of monopoly capitalism has
been the rise of monopoly medical industrial
complex. The monopoly drug corporations, medical
equipment corporations and health insurance
corporations have joined hands together (with the
doctors acting as accomplices) to exploit the people,
to breed consumerism and help keep the labour
force docile and productive. Some medical insurance
companies like Metropolitan Life, Providential have
grown larger than General Motors and Standard
Oil. Unncessary medical interventions at each stage
of life; ("from womb to tomb") this medicalisation
of life (lllich 1976) is a specific feature of this stage
of capitalism.
Special mention needs to be made of the drug
companies. The explosion of antibiotics and other
"wonder" drugs after the second imperialist world
war is hailed as one of the greatest achievements of
n odern medicine. But these drugs which can con
tribute a great deal to relieve pain and sufferings, are
not available to the poor. Secondly, an illusion is
being created that medicine can solve the healthy
problems of society with the help of these "wonder"
drugs. The potential created by modern sciences
like chemistry and pharmacology is being used to
exploit people and create illusions. There is plenty
of literature available on this issue.
3
Thus the heightened capacity of medicine in
the period of monopoly capitalism has not only been
limitedly used, but the capacity itself has been
affected by monopoly capital.
Medicine and Imperialist Domination
What has been the role of Medicine in the
imperialist domination over the peripheral countries?
In the colonial peiiod, medicine helped the conquest
of colonies. Some of the infectious diseases like
yellow fever and malaria, took a heavy toll of the
imperialist army and hence made it impossible for
the army to win territories. Medicine solved this
problem by controlling these diseases (Brown 1978,
Doyal and Pennell 1979). But, those diseases which
exclusively affected the natives were not controlled
in this period. Secondly, effective curative services
offered by missionary dispensaries created a good
impression on the natives; and distracted their
attention from the ill effects of colonialism. In the
words of the then president of the Rockfeller Found
ation, "Dispensaries and Physicians have of late
been peacefully penetrating areas of Phillipines
Islands and demonstrating the fact that for the
purpose of placating primitive and suspicious
peoples, medicine has advantages over machine
guns." (Brown 1978).
Later, the imperialists initiated health progra
mmes for the natives to improve their health and
thereby their productivity. Increased productivity
meant increased profits for imperialists. For example,
the Rockfeller Foundation programme to control
hookworm infestation in Latin America (Brown 1 978).
Such health-programmes also offered them opport
unities to export drugs and equipment. Problems
like tuberculosis, leprosy, venereal diseases cannot
however, be eradicated by such techniques of social
engineering because they are much more deeply
rooted in the social structure of peripheral capitalist
countries. Colonialism has also led to the suppression
of indigenous systems of medicine.
In the post-colonial period, it is well known as
to how the imperialist domination in the field of
medicine over politically independent countries
continues in an indirect form through the multinati
onal drug companies, through population control
programmes and other 'health programmes". The
role of western dominated medical education is
also important. Western dominated medical education
in peripheral countries produces doctors suited to
work in imperialist countries. This enables imperialist
countries to import medical graduates from peripheral
countries and save money which would have
4
otherwise been spent on training doctors in their own
country. This "brain drain" is also a financial drain
since peripheral countries spend so much on training
these doctors here. Moreover, the illusion that
health problems of your society can be solved
through medical interventions carried with the help
of ' superior and benevolent" west, the ideology of
medical expertism percolates through this type of
medical education.
The period of rapid growth of peripheral
capitalist societies after political independence came
to an end in the late sixties. As a part of its response
to this crisis, the ruling class is changing its strategy
of medical care. The cost of medical care is sought
to be reduced through the scheme of village health
workers. New innovations in the management of
health problems are being used to create illusions
under the slogan of "Health for all by 2000 AD".
The talk about "indigenous" system being made
more suitable than "Western medicine" needs to be
understood in this context. There’s hardly an
adequate attempt to really find out and develop the
useful, rational aspect of indigenous systems of
medicine. The continued neglect of these systems
shows that the hollow praise bestowed on it is
only a part of the new strategy of dumping responsi
bility onto the people for their health.
A struggle to create a healthier society and an
appropriate system of medical care cannot be
separated from the struggle against imperialism. In
this struggle, the aim cannot only be taking over
the existing productive forces, the existing medical
system and using it in the people's interests How
can people in a socialist society be healthy if they
consume the same amount and type of food as is
being done in the US today or get their electricity
from nuclear reactors ? Likewise imperialism has
also vitiated the science of Medicine. How exactly
and to what extent this has happened is a matter of
further study. A word of caution is in order here.
Let us not fall into the opposite pitfall of rejecting
the relevant scientific advances made by medicine in
capitalism. One cannot talk in terms of modern
medicine as such and reject it. Rather its a question
of grasping the rational kernel of existing medicine
and developing it further Otherwise, we would
throw away the baby with the bath water.
anant phadke
References:
Brown E, Public health in imperialism: Early Rockfeller Programmes
at home and abroad, in Ehrenreich John (Ed) (see below).
Doyal Lesely with Pennel Imogen Political Economy of Health,
Pluto Press. London, 1970.
Socialist Health Review
References
INVITED :
Ehrenreich John (Ed), The Cultural Crisis of Modern Medicine
Monthly Review Press, New York-London, 1978
Eiling,
Ray H.
"Industrialisation
and Occupational
Health in
Underdeveloped Countfies", in Navarro Vicente (Ed).
Imperialism Health and Medicine, Pluto Press, London, 1981.
Illich, Ivan, Medical Nemesis. Pelican, 1976.
Navarro Vicente, Class Struggle, the State and Medicine,
Chapter-VIII, State intervention in NH , Martin Robertson,
Oxford, 1981.
Turshen Meredeth, "The impact of Colonia.ism on Health and
Health Service in Tanzania", International Journal of Health
Services, Vol 7, No. 1, 1977.
Waitzkin, Howard, "A Marxist View of Medical Care". Socialist
Health Review, Vol. I, No. 1,
Bombay-1984.
Author's address :
Requests for SHR First Issue
It's not really a collector's item, but
we do have queries and requests pending
for the inaugural issue now out of print I
We cannot, however reprint the issue unless
we have orders for a sufficient number. If
you would like a copy please write to us
urgently. If we receive orders for more than
200 copies we will be able to supply copies
at Rs. 10 each. If not, we can get the entire
issue photocopied at Rs. 25 per issue. Please
let us know if you would like a copy at
this latter rate or only if it is available at
Rs. 10 each.
50, LIC Quarters
University Road
PUNE 411 016
Centre for Education and
Documentation
In This Issue
Radhika Ramasubban
examines the
colonial
health policy in India and traces its legacy to the
present public health system LMeera Chatterjee high
lights the wide ranging implications of a new scheme
formulated by the American Association of Physicians
of Indian Origin in collaboration with the IMA to
transfer high technology in medicine to India.
Warren Salmon's reprinted article deals with the
increasing interest and involvement of large US
corporations in health issues in America and the
emerging class stand which will eventually restru
cture the health sector under monopoly control.
The article on racism and health in the US, a revealing
glimpse at health care in a country which spends
one billion a day on such care is by Bindu Desai a
neurologist working in the Cooke Country Hospital
in Chicago. The Bhopal Update which Is likely to be a
regular feature in future issues is a resumme of
health issues, health efforts and on-going medical
debates concerning the Bhopal disaster by Padma
Prakash. We feature a review article on John
Braithwaite's explosive new book on the drug,
industry. Corporate Crimes in the Pharmaceutical Industry
by Ravi Duggal. This book is a must for all con
cerned people — if one can afford the price I
SORRY :
Due to oversight the box requesting for
subscription renewals (1:4,p.144) quotes the new
subscription rates as Rs. 24. Here's some good
news! The subscription rate remains at Rs. 20
(for four issues). We have increased the price
of individual copies to Rs. 6. Do send your
renewals and PLEASE wri,te
your name and
address on the counterfoil of MOs --- we would
prefer cheques or demand drafts drawn in favour
of Socialist Health Review.
June 1985
The CED collects, collates, researches
and disseminates information on a wide
range of subjects of social importance.
The following publications are available
with us :
c/
1.
2.
3.
(CED Health Cell Feature)
Abuse of Female Hormone Drug — No. 1
Bleeding for Profit
— No. 2
Inj ectables: Immaculate Contraception ?
— No. 3
4 Health and the Work-place
— No. 4
5.
Asbestos -- The Dust that Kills
6.
Health Sans Multinationals : The Bangladesh
Crusade
7. Pills for All
8. ORT and the Credibility Gap
1.
Aspects of the
India
Drug
Industry
in
— Mukarram Bha gat
2.
Operation Flood : Development of
Dependence
— CED Research Team
3.
Land Degradations : Indian’s Silent
Crisis
— Mukarram Bhagat
For further details contact:
CED« 3 Suleman Chambers, 4 Battery Street.
Behind Regal Cinema, Bombay 400 039.
Tel : 202 0019
(Open 11 a.m to 7 p.m. Tuesday through Saturday)
5
THE COLONIAL LEGACY AND THE PUBLIC HEALTH SYSTEM IN INDIA
radhika ramasubban
Colonial health policy in India never really came to grips with the problem of public health. Through the
evolution of a ‘colonial mode of health care , the enclave sector — the army and the European civilian
population------ kept pace with the metropolitan developments in sanitary and medical sciences while attempts
to introduce epidemic control and public health measures remained abortive. In the last years of the nineteenth
century when the situation afforded a compelling basis for a far-reaching pubhc health policy, the colonial
government found an escape route in the new research possibilities. The contradictions of the health system in
India arise from its historical legacies. This article traces the various strands which evolved during the period
of colonial rule and the manner in which they continue to shape the present public health system.
This article is an abridged version of an earlier research report by the author. ‘ Public Health and Medical
Research in India. Their Origins under the Impact of Colonial Policy" (SAREC, 1982).
f | 1 he task of tackling widespread disease and of
raising the health status of the population requ
ires coming to grips with the conditions which cause
debility and disease. The three main instruments for
such a strategy in the Indian context are thorough
going public health measures, improvements in the
standard of living of the population through raising
incomes and providing employment and making
the health services available to those in need.
Obviously, the health system alone cannot cooe
with all these challenges and in a general sense the
contradictions of the Indian health system are a
reflection of the contradictions of the development
process itself. More specifically, the contradictions
of the health system in India arise from its historical
legacies and the overall framework which guides
its nature and functioning.
India missed going through the
period of
sanitary reform which swept through most of
Europe in the 19th and early 20th centuries.
Colonial health policy never really came to grips
with the problem of public health in India, whereas
through a policy of segregation and what evolved
into a 'colonial mode of health care', the enclave
sector — the army and the European civilian
population — kept pace with metropolitan develop
ments in sanitary and medical science. In the
absence of general public health measures, epide
mics of small pox, cholera, plague and influenza
continued to recur among the general population.
Some attempts made in the first quarter of the 20th
century to evolve epidemic control measures
remained abortive due to the administrative disrup
tions caused by the two world wars and the pre
occupation with the health of the army, particularly
the control of malaria in the eastern theatre of the
second world war.
6
The independent Indian State, although it
recognised public health as one of its main con
cerns, lacked the commitment to carry through a
public health revolution. Seen in the wider historical
perspective, the huge expenditure that public health
measures require have been incurred by the State in
the western countries for ensuring a steady supply
of the labour force and for raising its productivity.
The capitalist path of development launched in
India has remained distorted and slow. It could
neither impart dynamism to the public health system
as it had very little demands to make, nor could the
productive forces develop to the extent which
would improve the health status of the population
by meeting their nutritional and other basic needsAbout half the Indian population is still living below
the minimum nutritional standard for meeting the
energy requirements of the body and the incidence
of diseases preventible through public health
measures dominates the disease profile.
The problem with undertaking far reaching
public health measures such as protected and
adequate
water supply, sewerage systems and
better housing and nutrition is that it requires
massive public
expenditure. The independent
Indian State, however, has not been able to meet
these requirements (Ramasubban, 1984). It has,
instead, settled for softer options which are essent
ially a continuation of the colonial tradition. The
attempt here will be to trace the various strands
that evolved during the period of colonial rule and
the manner in which they continue to shape the
present public health system.
The Evolution of Colonial Health Policy
The main factors which shaped colonial health
policy in India were its concern for the troops and
the European civil official population. The response
Socialist Health Review
to this concern underwent a series of stages corres
ponding to the growth of knowledge in England
about the principles of disease causation. The old
climatic theory was that the Indian climate caused
diseases in the abdominal cavity' while that of
Europe caused disease in the 'thoracic cavity'
(Scott, 1939) This gave way to the theory of
miasma, resulting in a policy of segregation and
sanitation which began in the mid-nineteenth
century and continued tnrough until the end of the
century. The result was the evolution of a distinctly
colonial mode of health care. This policy also took
into account statistical patterns of mortality and
simple prediction of eoidemics. The general spread
of epidemics resulted, however, in the mobilisation
of international opinion and the perception of the
Indian population as a secondary source of infection
brought the general population into the ambit of
health policy. But the main concern remained the
army, and therefore, the evolution of colonial
health policy has to be necessarily placed within
the framework of the army. The shift in focus in
England and Western Europe from sanitation to
epidemiology and bacteriology, which began in the
1 880 s and gained revolutionary momentum in the
following decades, had significant implications for
India By the turn of the century, laboratory investi
gations were instituted in the four army commands,
to put army health on modern, scientific principles.
Although the direct link between health and
medical research remained confined within the
framework of the army, the growing interest in and
official patronage for the discipline or tropical
medicine in England integrated India, the largest
natural disease laboratory in the British empire,
into metropolitan scientific activities, and a few
laboratories for research were set up within the
country.
The army, the main instrument of the East
India Company's political
consolidation,
was
primarily composed of Indian soldiers, the European
component being outnumbered by roughly eight to
one (Imperial Gazetteer of India, 1909). The high
cost of transporting European soldiers to India and
of invaliding due to sickness, and the time taken in
further recruitment and replacement, were the
major factors responsible for the excessive reliance
on the Indian component.
Mortality, sickness and invaliding in the Euro
pean army was due mainly to four major diseases:
fevers, dysentery and diarrhoea, liver diseases and
epidemic cholera, in that order, all of which, parti
cularly the last-mentioned, assumed virulent form
June 1985
when the troops were on the march. And the troops
were almost constantly on the march in the prevail
ing unsettled state of the country.
As regards the European civil population, a large
section was concentrated in the three Presidency
towns of Calcutta, Bombay and Madras, which were
centres of government as well as the major ports.
Here European areas of residence were secluded
from the Indian areas and along with the canton
ments in these towns, were fully self-contained.
By the mid nineteenth century, these areas were
relatively well planned and drained and vaccination
against small pox (the only effective prophylactic
known), among the European civilian residents and
among the residents of the cantonments, was
almost universal
The ^events of 1857 — the 'Indian Mutiny' —
highlighted as never before, the importance of the
British soldier s health and efficiency. Army health
which became the primary concern of colonial health
policy remained an abiding concern as, with the
expansion of the British empire, the army in India
increased in importance as the largest single force
in the empire, and as a key instrument in the security
of Britain's eastern possession The 'Mutiny' of 1857
had highlighted the insecurity of British military
power in India. Reliance had hitherto been placed
on Indian soldiers and they had vastly outnumbered
the European component. Although the majority of
the Indian troops had remained loyal to the Com
pany and the 'Mutiny' had been successfully quelled.
it was decided that the defence of India would
henceforth have to be in British hands, and it was
resolved that the 'British army serving in India'
should form part of the Imperial British army. This
necessitated the transfer in 1858 of the European
troops of the East India Company to the Crown and
a Royal Commission was appointed to work out the
army's reorganisation. It recommended raising the
number of British troops, and that the ratio of Indian
and British soldiers should be of the order of 2 to 1.
The result was a 60 per cent increase in the number
of British troops. (Imperial Gazetteer of India, 1909)
The result of the increase in the strength of
British troops was that one-third of all British forces
came to be stationed in India. The problems in
acclimatising such large numbers to Indian condi
tions and ensuring their health, therefore, assumed
importance.
Along with the Indian Mutiny, the Crimean war,
too, played an active role in focusing discussion in
England on the health of the British army. The
7
Crimean experience had shown that mortality among
troops had been due primarily to epidemic ravages
and the insanitary state of barracks and hospitals
rather than to wounds of war. It highlighted the need
to apply the principles of modern sanitary science
currently championed in England by sanitarians like
Chadwick and John Simon, to the army. In 1857, a
Royal Commission was appointed to enquire into
the regulations affecting the sanitary conditions of
the army, the reorganisation of military hospitals and
the treatment of the sick and wounded. The enhanced
strength of the British army in India required a
similar enquiry into Indian conditions, and in 1859,
another Royal Commission was appointed to enquire
into the Sanitary State of the Army in India.
Of the total number of deaths in the period
examined by the Commission, i. e., 1817 to 1857,
only 6 per cent had been due to war. The rest were
caused by four major diseases : fevers, causing
about 40 per cent of all deaths and three-fourths of all
hospital admissions; and dysentery and diarrhoea,
liver diseases and cholera being the other killers.
Fevers, besides the suffering and immediate risk to
life, also had a tendency to relapse dangerously and
affect vital organs, resulting in considerable subse
quent illness, mortality and invaliding among
British troops. At this time 'fevers' was still a general
term for most forms of sickness. Clearly, therefore,
"the main enemy of the British soldier in India was
not the Indian enemy but disease". (Royal Sanitary
Commission Report, 1863).
a)
Sanitary principles and the policy of segre
gation.
The situation, however, was neither unfamiliar
nor irremediable. The old climatic theory had held
that the Indian climate produced diseases distinctly
different from those resulting from the English
climate. Now, the diseases which were fatal to the
British soldier in India were recognised as familiar,
as those which had until recently caused the highest
mortalities in Eng'and, and which had been brought
under control in that country through sanitary
programmes.
The keynote of metropolitan sanitary science,
which grew out of the compulsions of urbanisation
in England in the eighteenth and nineteenth centuries,
was environmental control. The means through
which this was accomplished were mainly town
planning, housing and sanitary engineering. These
measures required administrative and government
institutions embodied in 'local governments', which
were responsible for investigation of local insanitary
8
conditions and their control, and given the force
of legal sanction through public health legislations.
The physical placement of the European popula
tion in India was, as far as possible, based on the
principles of this sanitary science. Using criteria of
soil, water, air and elevation, the Royal Sanitary
Commission on the army in India laid down elabo
rate norms 'or the creation and development of
distinct areas of European
residence, and the
'cantonment', 'civil lines', 'civil station' and 'hill
station', regulated by legislations, developed into a
colonial mode of health care and sanitation based
on the principle of social and physical segregation.
From the time of the Royal Commission's Report of
1863, the location a.id layout of European civil and
military areas were determined by criteria of health
laid down by the prevailing medical scientific
theories of miasma and environmental control rather
than by political and strategic criteria. Most of the
troops were located at 'hill stations' or on elevated
ground In cases where strategic stations were
unhealthy, only small forces were posted there to be
reinforced at short notice. Earlier, the 'native lines',
i e., residential areas of Indian soldiers, had been
left outside the pale of colonial planning and con
struction activity for troops. European fears of
miasma emanating from them had even led to
construction of walls between Indian and European
troop locations to keep the miasma out. The Royal
Sanitary Commission voiced concern for the health
of the Indian troops and recommended that canton
ment planning should also be extended to the 'native
lines'.
b)
Public health machinery :
and disease control
vital statistics
Following the Royal Commission's
Report,
Cantonments Acts, Regulations and Codes were
issued modelled on public health acts in Britain.
While segregation was an effective tool, at least
in the three Presidency townscontact with the native
population was unavoidable. Native servants often
lived in the native areas, and native dealers and
tradesmen serviced the cantonments and civil lines.
Grossly insanitary conditions prevailed in these
large and unplanned urban centres and the native
population could well serve as secondary sources
of infection. An understanding of disease among
them was, therefore, considered essential. In his
despatch to the Government of India the Secretary
of State for India pointed out, "The determination
of the effects of local causes on the mortality of the
Socialist Health Review
native population, besides its intrinsic value in con
nection with the welfare of the people of India,
cannot fail to have an important bearing on the
health of the Europeans resident among them."
Gazette of India, 18G4).
Three Presidency Sanitary Commissions were
set up in 1864. The basis for the functioning of
these Commissions was to be the systematic genera
tion of facts about mortality, epidemics and sanita
tion, which would be embodied in an annual
sanitary report to be submitted io the Government
of India by the Sanitary Commissioner to the Gover
nment of India. This would in turn be summarised
in annual reports presented to parliament on the
progress of sanitary measures in India. This laid the
foundation for a public health machinery, parti
cularly in rhe field of vital statistics and disease
control.
The investigative tradition was an integral part
of the sanitary movement concurrently taking place
in England; in fact, the first stage of the public
health movement was that of governmental investi
gations on grand scale. Regular statistical reports
were also seen as essential to any systematic public
health control and since the establishment of the
office of the Registrar-General of Births, deaths and
Marriages in 1836, the steady accumulation of
statistical evidence had generated a demand for
further research into the causes of epidemic diseases.
(Shryock, 1 948)
In keeping with this tradition, the Government
of India appointed in 1861, the first systematic
enquiry into a major epidemic—the cholera epide
mic of 1861. The facts that it highlighted were
followed up in the annual sanitary reports, which
resulted in a steadily growing volume of statistics
and facts about the disease.
The significance of the 1861 epidemic was
that its impact was not confined to India alone; it
was followed by another epidemic in 1865 which
spread from Egypt across Europe to England.
Cholera had been the most important factor respon
sible for initiating the public health era in Britain in
the early nineteenth century. The 1861 epidemic
provided the final and most powerful spur to sani
tary legislation in England. This was the Sanitary
Act of 1866 embodying the important principle of
compulsion by the central authority if the local
sanitary authority failed in its duty.
This epidemic also gave rise to four international
sanitary conferences participated in by European
June 1985
countries in 1866, 1874. 1875 and 1885. They
devoted their deliberations specitically to this
disease and attempted to work out quarantine
measures acceptable to all participating countries;
systematise existing knowledge about the disease
and identify major questions for further investiga
tion; and, recommend measures for prevention. As
the 1861 epidemic had originated in India, the first
Conference at Constantinople discussed India as a
major topic.
The Constantinople Conference put the Imperial
government into a quandary by pronouncing India
the natural home of cholera. In the absence of any
breakthroughs in know edge about the cause and
mode of infection, the Conference stressed the need
for stricter implementaion of rigorous and lengthy
quarantine both in sea and land movements,
greater cleanliness and disinfection of ships, houses
and merchandise, and care to avoid overcrowding.
The central consensus of the Conference was that
the spread of cholera epidemics was due to rapid
movements of groups of people and their personal
effects, water and food supplies. It pronounced
that in the case of India the movement of pilgrims
and large congregations at fairs and festivals was
the single and ' most powerful of all the causes
which conduce to the development and propagation
of epidemics of cholera". (Cholera Committee
Report, 1867). In the opinion of the Conference
when the pilgrims congregated, the cholera spread
among them and when they dispersed they carried
the contagion with them over long distances. The
Conference recommended elaborate preventive,
sanitary and curative arrangements
at pilgrim
centres and on pilgrim routes.
The international arrangements outlined for
quarantine and the recommendation
proposed
regarding pilgrims, by the Constantinople Confere
nce, were particularly irksome to Great Britain which
had the largest international maritime trade as well
as the most frequent troop and naval movements to
and from its colonies. In the face of stricter quaran
tine restrictions imposed by the Constantinople
Conference and the international pressure to control
cholera within India and prevent its spread there
from, Great Britain responded by instituting its own
investigations into the authenticity of a quarantine
policy, i. e., whether it was local conditions of soil,
air and water rather than contagion carried through
people and their effects which caused the spread of
epidemics, and whether there was a possibility of
coping with cholera through
effecting sanitary
9
improvements rather than quarantine. Professional
medical opinion in England also provided support
to such a move and a special enquiry came to be
sanctioned by the Secretaries of State for War and
India in:o the mode of origin and transmission of
cholera
While the results of the scientific investigation
were being awaited, practical sanitary measures
were intensified in relation to all cantonments,
smaller military stations, troops on the march, jails,
hospitals and seaport towns. By 1872 local medical
officers in all the various military stations were
doing simple qualitative analysis of water. The
prohibitions upon soldieis going into the Indian
cities or cholera affected areas were more strictly
enforced and "sanitary cordons" (suggested by the
Constantinople Conference) were erected around
cantonments to prevent persons residing in nearby
villages and localities and those suspected of carry
ing cholera, from entering the area. Infected cases
in cantonments were isolated and barracks, jails and
hospitals fumigated.
Hitherto, troops on the march had been the
most vulnerable to cholera attacks. The new
sanitary rules governing the marches also included
rules regarding railway travel, such as provision of
good drinking water and wholesome meals at halting
stations, isolation of thetroops from the native towns
and bazaars en route and at destination, thirtyminute stops every four hours and travel for not
more than twelve hours at a stretch.
Systematic statistics about cholera were accu
mulating with the regular publication of annual
sanitary reports. These statistics pointed to direct
personal contact as an extremely unlikely cause of
infection Nor was land quarantine doing much
good; and nor did cholera appear to travel along
highways and major lines of communication. As
regards sea travel, however, stricter control was
instituted, mainly in deference to international
pressure.
Until the end of the 1880's, cholera of all dise
ases pressed most heavily on British soldiers in
India, being the most important cause of mortality
although not adding significantly to the sickness
rates. The investigations of Lewis and Cunningham,
by going into the question of sub-soil water levels,
had launched on a relatively fruitless line of enquiry
which failed to produce conclusive evidence on the
cause of cholera. But although their study (Lewis
and Cunningham, 1876) made little impact on the
10
control of cholera, it was valuable in that it stressed
the importance of looking elsewhere than into,
contagion through personal contact. But by the
period 1870-79, the combined effect of sanitary
measures and other reforms had brought average
mortality due to all diseases among European troops
down to 19.34 per 1030 of strength, of which cho
lera accounted for an average of 3.22 (calculated
from Annual Sanitary Report for relevant years). By
tne end of the century the severity of cholera came
down even further and after 1900 rarely one person
in 10,000 among the European troops came down
with cholera (Annual Sanitary Reports, 1899 1929).
The year 1883 was one of the major landmarks
in scientific investigation into disease causation.
A German Commission led by Robert Koch dis
covered the Cholera 'Comma' Bacillus in Egypt and
visited Calcutta in the same year to confirm the
discovery. Koch's discovery was a significant con
tribution to the germ theory of disease causation
which had emerged in Western Europe in the 1860's
and studies like his and those by Pasteur, which
linked a specific organism with a specific disease,
helped to firmly establish the theory in the 1870 s
and 1880's. This modern scientific revolution in
medicine challenged and ultimately triumphed over
the earlier miasmatic theories.
c)
General Population
The Constantinople Conference's declaration of
India as the source of epidemics, its condemnation
of the British government for failing to control these
epidemics and the latter's own recognition that the
Indian population constituted a secondary source of
infection, provided the compulsion for broadening
the scope of health policy and include the general
population in its purview.
In keeping with the theory of contagion, the
places of pilgrimage and pilgrim routes became the
starling point of health policy in relation to the
general population, and the formal motions of
attending to the problem were gone
through.
Committees were appointed and reports prepared.
But when it came to giving a concrete course to
the policy, however, the government's attitude
remained evasive.
While the suggestions of the Constantinople
Conference regarding the desirability of sanitary
precautions in relation to large groups of people
on the move was quickly given effect in the
case of troops on the march. In order to prevent
Socialist Health Review
the outbreak of epidemics among them, the ques
tion of epidemics at the pilgrim centres was treated
as a puzzle, and various other considerations such
as finance, religion and race clouded the issue.
However, at the 1867 Kumbh Mela, the govern
ment as a test case made some ad hoc sanitary and
hospital arrangements. These had proved success
ful in curbing cholera on the fair grounds. But no
sooner had the pilgrims dispersed, than the cholera
that they carried spread in the regions through
which they passed and in their ultimate destinations
even as for as 700 miles away. This seemed to
imply that not sanitation alone but land quarantine
measures were required. The official position was
to see this as an intractable problem, for quarantine
was not considered to be a feasible measure in the
case of people who would be dispersing over a
large area. The response of the Government of
India was to rest content with the prohibition of
pilgrims from entering military stations or even
their neighbourhood.
In fact, the whole question of pilgrims taking
cholera back with them to their towns and villages
raised the uncomfortable issue of an extensive
public health machinery for the general population
on a continuing basis, which would be the only
countervailing force against epidemic
cholera
emanating from pilgrim
movements and con
gregations.
But sanitary reforms were expensive and
unremunerative. The MacKenzie Committee appoi
nted to go into the pilgrim question recomm
ended
that the
government should under
take the responsibility for at least a few such
measures at pilgrim centres. If public health
measures for the general population at large could
not be adopted, at least the enforcement of con
servancy measures at fairs and pilgrim centres and
demonstration by the government thereby of the
desirability of sanitation would act as an incentive
for the general population to voluntarily adopt the
modern sanitary principles in townsand villages.
The Committee argued that such a step was also in
the interests of the European population. But the
government rejected the idea of expenditure on
conservancy measures and sanitary
police at
pilgrim centres, and policy floundered on the issue
of whether pilgrims should be made to pay for
sanitary
arrangement through a sanitary tax.
(MacKenzie Committee Report, 1868)
Progress on sanitary reforms concerning the
general population was blocked on the ground that
June 1985
no measures could be enforced, as any element of
compulsion would offend the people's religious
sensibilities and be construed as interference in
their customs. The bogey of interference in the
religion and customs of the people was not new,
but was more self consciously applied after the
'Mutiny.' Eighteenth century East India Company
officials many of whom recognised in India a
superior civilisation, had been replaced in the early
nineteenth century by administrators who saw their
mission as 'civilizing' and 'modernising' Indian
society. Indian socie'y was seen as a tabula rasa
waiting to be recast in the Western mould. The
civilising influence would be Western social and
economic institutions and Western religion, i e.,
Christianity. After the 'Mutiny', however, the enth
usiasm for remaking Indian society declined The
climatic and socio-religious theories gave way to
theories of racial exclusiveness, as Britain establi
shed itself as the supreme governing power and as
the European establishment in the country perfected
the mechanisms of physical and social segregation.
Indians now came to be seen as a distinctly inferior
race incapable of appreciating or successfully adop
ting British habits and institutions. That interference
in social and religious practices would offend Indian
sensibilities, was only the rhetoric, offered for
government inaction to bring into force a public
health machinery and sanitary reforms in India
along modern lines.
As far as the people themselves were concerned,
the MacKenzie Committee which sought Indian
opinion on the matter of sanitary measures at pilg
rim centres, found that the people were willing to
submit to any measures calculated to promote their
health. There was also evidence that the arrange
ments at Hardwar in 1867 had suitably impressed
the pilgrims.
While the government persisted in its evasive
ness the railway companies, realising that pilgrims
were good business, were cashing in on the age-old
enthusiasm of Indians for undertaking pilgrimages.
A large number of pilgrim centres existed across the
country, and it was the aspiration of every Indian
to visit at least one of these centres in his lifetime.
There were also certain specific religious festivals
which drew large numbers at certain times of the
year. In the old days the journey used to be lonq
and arduous and done on foot or by animal carriage.
There were accepted pilgrim routes and halting
places at villages en route where accommodation
and food or facilities for cooking were available
H
Most of these were free and maintained by philanth
ropists.
The introduction of railways offered a universal
opportunity for undertaking pilgrimages and the
possibility of a single person perhaps undertaking
several in his lifetime, and railway travel for this pur
pose became extremely popular. The railway compa
nies responded quickly to this source of profit, offer
ing return tickets and half fares for children. But the
facilities were appalling. Pilgrims were stuffed into
dirty goods wagons with no ventilation lighting,
drinking water and sanitary arrangements on board.
The doors used to be fastened from the outside and
not opened for hours at a stretch, as allowing the
pilgrims to climb in and out at stations en route
would cause delays. The few third class carriages
allotted for pilgrims were impossibly overcrowded.
And for a long time no provision existed for clean
accommodation, drinking water or meals at halting
stations. Death from suffocation and disease in the
goods wagons and cholera epidemics on railway
journeys and at pilgrim centres became more frequ
ent as the pilgrim traffic increased and the rapid
communications spread disease more rapidly. Pilgr
ims now poured into holy places in much larger
numbers than these places had been provided to
cope with and problems of sanitation were further
aggravated. Even as cholera had almost disappeared
among the troops, epidemics continued to rage
among the general population. The Committee
which investigated the matter recommended that
government move in to check the worst abuses of
railway travel and regulate the conditions of pilgrim
movements, conveying pilgrims in closed air-tight
wagons meant for goods should be discouraged,
eating houses at railway stations be licensed, and
provisions made for drinking water and toilets at
stations.
The salient feature of the pilgrim movement
now was that the congregations of people did not
take place only at certain times of the year; rather,
the pilgrim centres had a constant flow of people
round the year. Ad hoc measures, therefore, could
no longer be considered an effective solution to the
epidemic problem.
The last decade of the nineteenth century was
a period of significant landmarks in determining the
course of the colonial health policy. The two gove
rning landmarks were the plague epidemic which
broke out in Bombay in 1896 and the discovery in
India by Ronald Ross of the Indian Medical Service
of the mode of transmission in malaria in 1897. The
12
responses to these two events reflected the growing
complexity of Britain's international position and
rise of British imperialism, Britain's perception of
India's place within the Empire the internal changes
effected by the Government of India to adapt India
to its new role, and the contradictions within the
Government of India's policy.
The neglect of public health measures among
the general population; accompanied by
the
intensification of trade and commerce and the
growth of population in the seaport towns; as well
as the increasing impoverishment in the rural areas
and the flow of migrants into the towns and cities
in search of work; came to a head when the plague
epidemic which broke out in Bombay in 1895 was
followed by successive epidemics which spread
the disease to large parts of the country, and which
by 1918 had taken a toll of almost 10.5 million
lives. What was striking was that all the plague
deaths occurred only among the Indian population.
Plague was known to have been endemic to
Europe since early times but by the end of the
seventeenth century it had completely disappeared.
When the plague broke out in Bombay, the spread
of the epidemic within the city and to other parts of
the country combined with the movements of desti
tute people out of the rural areas and into the
towns due to the widespread famine, threw the
authorities into a flurry of confused activity. The
Bombay plague committee was set up on a crash
basis for the period 1897-1898. In the absence of
any scientific knowledge about what caused the
disease it was treated as contagious. House to
house searches were conducted with the aid of
police cordons to register deaths and remove sick
persons for isolation, dilapidated houses were
vacated and disinfected and the inmates removed to
camps, rural migrants to the city were detained in
camps to prevent disease conditions exacerbating in
the city, and at the railway stations passengers and
their baggage were disinfected.
But these ad hoc measures were no solution to
a situation which was rapidly getting out of hand.
The single most important cause of bubonic plague
was insanitation which created the conditions for a
large number of rats to live in and around human
dwellings, and poorly constructed, dark, ill-venti
lated houses where rat fleas could take refuse away
from air and sunlight which were their most effec
tive killers. As long as drainage, sewerage and
planned housing remained severally defective or
non-existent, the plague, once introduced, would
Socialist Health Review
continue to remain endemic. The transmission of
the disease from the rat to man through the rat flea
and not through human contact as in pneumonic
plague (familiar to England as the 'Black Death’)
rendered isolation and detention camps useless.
The plague epidemic could have provided a
take-off point for a more far reaching public health
policy. True, the unreformed sanitary conditions
among the general population exacerbated by the
impact of colonial economic policies and natural
calamities had worsened public health conditions.
While the urban centres were undergoing a hapha
zard development, the countryside was becoming
increasingly impoverished. But the result of the
plague innoculation drives, the first major attempt
at epidemic control, was the growing awareness of
and desire for sanitary reform among the general
population Representations were made by Indians
requesting the government to take the initiative in
maintaining the struggle against the plague, and in
widening the scope of sanitary reform. The need to
create an effective public health machinery had
also been unequivocally stressed by a body of
expert scientific opinion from England who, in
elucidating the mode of transmission of bubonic
plague, had pointed to insanitation as the single
most important cause, and had even drawn up a
tentative scheme for public health administration.
The scheme remained unimplemented by the
Government of India, and once again, the offi
cial response was the rhetoric of caution in qui
ckening the pace of sanitary reform for fear of
pressurising public opinion. In fact, as far as
the government was concerned, the living condi
tions of the general population were "beyond
the influence of sanitary effort..." (Annual Sanit
ary Report, 1900-01). Articulated public health
policy was growing into one of leavingthe Indians
to their own efforts.
The plague epidemic and Ronald Ross' malaria
breakthrough had been the thereshold for the
developments between 1900 and 1935. A step
could have been taken in the
direction of
focusing policy on evolving a public health machi
nery. However, the possibility of research also
presented itself at this moment and the colonial
government for its own reasons chose the latter
option.
In England, the public health system had
come into its own by the time of the scientific
advancements in medicine, and the new stream
June 1985
of scientific ideas while they revolutionised health
care, did not replace the public health machinery
which continued to enjoy a relative autonomy. In
India, the metropolitan sanitary science was addre
ssed only to the colonial population resulting in
what we had earlier referred to as a colonial mode
of health care. It, however, had a demonstration
effect on the general population, which began to
see its potential in the last few years of the nineteenth
century.
Public opinion was beginning to form the
basis for a potential sanitary movement in India.
The Indian elite showed eagerness to lay the
foundations in the country for the growth of
medical science in which Indians could participate
and benefit therefrom. The various international
sanitary
coneferences and the British Plague
Commission were an added source of pressure
upon the colonial government to pay attention
to public health.'
Just at a time when the situation afforded
the compelling basis for a far-reaching public health
policy, the colonial government found an escape route
in the new research possibilities, and public health
policy as in the past remained sporadic and ad
hoc. Tne Sanitary Department was most unpopular
with the colonial medical bureaucracy and by
the time sanitation and public health were made
a provincial subject in 1919, the Sanitary Depart
ment already lacking a coherent policy or substantial
financial provision, was depleted of most of its
supervisory personnel. In the remaining decades of
colonial rule nothing occurred to change this pattern.
No single authority responsible for the efficiency of
health measures throughout India came to exist,
and nor was there any single Public Health Act as
in England. The only concern of the Imperial
Government was port quarantine. Vital statistics
remained very defective due to the absence of a wide
deployment of medical personnel.
With the superceding of the era of active
sanitary reform by an era of emerging professionalisation in medicine in England, the consequ
ences for Indian public health in terms of the los*
historical possibilities were far-reaching. ^Medical
education had been
initiated
in
the Indian
Presidency towns by the mid-nineteenth century,
mainly to train hospital assistants for military and
civil hospitals. The medical colleges also received a
steady influx of Indians right from their inceptionWhen the bacteriological advances of the late
T3
nineteenth century put curative medicine on a
scientific basis and led to its increasing professionalisation this served as an argument for colonial
policy to encourage the expansion of the private
medical profession (ooth European and Indian)
— for a few medical colleges were a cheaper
alternative to expending goverernment resources
on sanitary reforms for the general population.
The growth of preventive and social medicine was
irremediably pre-empted and the rising medical
profession made its spoils from the ever expanding
disease market.
The Present Health System
and its Contradictions
The 'functional approach', which sees health
as 'fitness' to undertake one's work as a produc
tive member of society, and ill health as the
result of malfunctioning of one particular part of
the body which can be corrected through medical
interventions, arose out of the conditions of
maturing capitalist development in Europe in the
19th century, and achieved final consolidation
with the development of the germ theory in the
last two decades of the 19th century. (Doyal, 1979)
But the functional approach could come into its
own mainly on the strength of effective declines
in mortality and morbidity due to the control of
infectious diseases brought about by the State in
the pre-germ theory era thiough effective public
health measures which stressed the predominantly
environmental — 'filth' or miasma' — causes of
disease and death.
In India this functional approach, carried over
from the experiments during the colonial rule, has
remained partial and ineffective. In those spheres
where the regular supply of skilled and physically
fit manpower has been crucial, as for instance the
army and capital - and technology-intensive sectors
of the economy, the 'colonial mode has been
the preferred pattern : social and physical segre
gation of employees
and
their families into
exclusive residential areas or housing colonies
with clean and sanitary environments, access to
subsidised and good quality-medical and clinical
care, educational facilities, etc. To take care of
the possibility that the rampant infection, parti
cularly in the poorer urban areas given their
haphazard growth and insanitary environments
might break out in epidemic form, vaccinations,
hospitals and selective measures for improving
drinking water and sewage disposal have been
resorted to. Otherwise the rural areas and the
14
urban slums where most of the population lives,
remain by and large untouched by theexisting health
system. For the health system to reach them in any
significant way, within the functional approach,
requires heavy doses of public expenditure. In the
absence of effective preventive measures, the indivi
dual’s own approach towards health care has been
that of coping with repeated attacks of infectious
diseases only through medical interventions. The
private consumption expenditure on medical and
health care as estimated from the 28th round of
the NSS in 1973/74 was three times the public
expenditure on this activity (Lakdawala, 1978)
Since effecting public health measures through
environmental sanitation and provision of housing
and safe drinking water is an expensive proposition,
the Indian State, helped by advancing medical tech
nology and international assistance, resorted to the
easy alternative of tackling communicable diseases
through vertical programmes that involved the use
of known and tested technology such as vaccina
tion and DDT spraying in the case of small pox and
malaria respectively, and isolation and treatment as
in the case of the other major communicable diseases
such as TB and ’eprosy. With the exception of
vaccination and revaccination against small pox, all
the other known medical interventions presupposed
the existence of effective public health measures
and in a situation where the latter condition did not
exist, could be expected to have only limited
efficacy.
Next to small pox, the vertical programmes
showed some signs of success in the case of malaria,
supported through international aid for the import
of powerful insecticides and drugs which had proved
successful in malaria control in the second world
war. Between 1953 when the National Malaria
Control Programme started (it was stepped up to
'Eradication' in 1958) and 1965, the incidence
of the disease was brought down from around
100 million cases and 1 million deaths to 1
million cases and no reported deaths (Gol, 1977 64
Table 51). These achievements, as Cassen (1978:86)
has argued, must surely be recognised as the single
most important cause for the steep decline in
in mortality that India has been able to effect
after independence. The 1965 record, however,
regressed soon after, and the incidence of malaria
has been showing a sharp upward trend (Gol,
1977:64, Table 54). While the resurgence of
malaria may not have affected mortality so far
because of the dominance of the milder vivax
malaria, it has grave consequences for the population
Socialist Health Review
particularly
since
malaria
tends to
become
chronic and debilitates its victims leaving them
open to all other infections, and since malaria
has been demonstrated to be a major cause of
infant mortality. This regression in the case of
malaria demonstrates the floundering of the functi
onal approach. Apart from the 'human factor' —
premature acceptance of success and complacency
in sustaining the momentum of progress — and
organisational problems, the main reasons for its
failure structural in nature. They emphasise the
need for coming to grips with the problems of
disturbances in the ecology, centre state rela
tionships, crisis in the economy and the general
conditions for research and training. In the absence
of planned research even while the eradication
programme was in progress, full knowledge of
the epidemiology of malaria and the ecology of
the mosquito was lacking. Changes in the behaviour
of vector and parasite partly due to developed
resistance to insecticides and partly due to the
disturbances in the ecosystem — in the form of
population movements and congregation due to
war, floods and large scale public works projects,
clearing of forests for cultivation and refugee settle
ment and large scale use of insecticides in agricultu
ral production, without an integrated approach to
the environment — have contributed to the aggrava
tion of malaria in the country (Ramasubban, 1978).
The sluggishness on the part of the state govern
ments to commit necessary funds of Malaria
Eradication units, initially centrally sponsored and
subsequently handed over to the states for the
maintenance phase, represents the uneasiness in
financial equations between the centre and the
states. The shortage of insecticides for malaria
control in the wake of the oil price rise and com
petition from the agricultural sector further highlights
the interdependence of the communicable disease
control programmes with the rest of the economy.
Epidemic cholera, which alone among the
faecally related diseases has come under specific
control measures — innoculation and chemothera
peutic measures — has been far more difficult to
control, being food and water-borne rather than
contagious and finding fertile ground in the widely
prevailing unhygienic conditions of food and water
use. The incidence of cholera which came down
drastically from 176, 307 cases in 1E50 to 22,065
in 1954 steadily rose to 66,076 in the following
four years, came down briefly to 14,617 in 1959/60
but saw a sudden spurt again to the 1954-59 levels
(Gol, 1977). Here, again, the effectiveness of the
Jnne 1985
control measures was greatest in reducing mortality,
and the deaths due to cholera which accounted for
2.4 percent of all deaths towards the end of the
colonial rule came down to 0.4 per cent by 1966/67
(Cassen, 1978). But given the absence of protected
water supply and environmental sanitation, cholera
continues to pose a threat of epidemic outbreaks
during droughts, famines and floods.
The policy of vertical programmes for the
control of communicable diseases also included TB,
leprosy and filariasis. TB has remained more or less
firmly entrenched since 1958 (Cassen, 1978 : 90)
and nearly 2 per cent of the population is estimated
to be suffering from TB, of which 25 per cent are
infectious sputum positive cases (Gol, 1980 b). It
is significant that in spite of a National Programme
for domiciliary treatment launched in 1969, the total
number of cases detected as a percentage of total
estimated cases is only 30 per cent (Gol, 1980).
Although several “operational lapses" were identi
fied as reasons for failure in an assessment done by
the Indian Council of Medical Research (ICMR,
1976) the more fundamental problems are those of
poor nutrition and overcrowding. Moreover, the
chemotherapeutic domiciliary treatment is still too
long-drawn (18 months duration) for an average TB
patient to sustain, given the long distances to be
travelled to the health centres. The deceptive feeling
of improvement in the first phase of treatment may
also be responsible for discontinuation and relapse,
in the absence of regular supervision (Cassen 1978).
The growing evidence on the ineffectiveness of BCG
in several cases audits temporary naturein providing
immunity, points to the inevitability of taking cogni
sance of the structural factors. The National Leprosy
Control Programme which was launched in 1955
has also not made any headway. More than half the
population (Gol, 1974) is exposed to the risk of
contracting this disease which flourishes under
insanitary and overcrowded conditions. There are
3.2 million estimated cases of leprosy in the country
of which 20 per cent are infectious and another 20
per cent suffer from various deformities. The total
number of cases detected as a percentage of total
estimated cases is 60 per cent while disease arrested
cases is only 20 per cent, which goes to show that
the Control Programme has not really been effective
and there has to be a much more concerted effort in
controlling this disease. Much the same picture
holds for filariasis which came under a Control
Programme in 195j.
The control of communicable diseases through
vertical programmes poses difficulties because
15
these diseases have linkages with multiple factors
and dealing with them requires socio-economic
changes and a concerted action in the field of public
health measures. Accomplishment of this task within
the context of the health system would require
greater expenditure on health by the central and
state governments and/or effecting redistribution
within the health system in favour of public health
measures, and reorientation of health policy, backed
by determination to act in that direction, to tilt the
balance in favour of the rural areas. Here, again,
the main challenge lies in resolving the contradic
tions giving rise to the dominance of curative
services over preventive services, the urban-rurai
dichotomy and the lack of commitment on the part
of the State to provide necessary funds in the health
sector.
The Indian medical profession has a longstand
ing record of service, and in its development it
would rank quite high in comparison with many
developing countries and is recognised by the Indian
population as efficacious and functional in combat
ing disease.
Western medical education had its early origins
in colonial policy, when the first medical colleges
were set up in the mid-19th century. Right from
their inception these colleges received a steady
influx of Indians. Around the turn of the century
when the bacteriological advances of late 19th
century led to the increasing professionalisation of
curative medicine in the west, simultaneous with
the visible and rapid deterioration in India of the
health conditions among the general population,
the colonial authorities found it a cheaper alterna
tive to respond to the incidence of disease through
extension of medical education and encouraging
medical practitioners (both European and Indian)
rather than spend government resources on sanitary
reforms for the general population. The medical
professionals, however,
remained concentrated
mainly in the urban areas, which also meant con
stant contact with sources of power. The rural areas
remained by and large ignored and left in the
hands of the practitioners of the traditional systems
of medicine.
The concentration of health services in the urban
areas continues even thirty years after independence,
and it is only very recently that we are witnessing
an increase in the flow of practitioners in the
western system of medicine to the rural areas.
State action to provide health services to the rural
population was initiated through a network of
Primary Health Centres (PHCs). The PHCs, when
set up, were not meant to remain curative centres.
16
It was envisaged that an integrated preventive,
promotive and curative structure could be built
into the PHC system, and that this was just a matter
ot creating a team reflecting the three areas of work.
The concern of the PHC, therefore, was meant to
be mother and child welfare, control of communi
cable diseases, environmental sanitation, school
health, basic health education, collection of vital
statistics, immunisation and medical care services.
Obviously too much was being expected from the
PHCs and given the overall national bias towards
curative and family planning services, the PHCs,
too, in practice, soon turned into curative centres.
* This article is an abridged version of an earlier research report
by the author. Public Health and Medical Reserach in India : Their
Origins Under the Impact of British Colonial Policy (Stockholm,
Sarec, 1 982). This is also why the detailed reference to source
material has been kept to the barest minimum here. While the
above-mentioned research report is exclusively concerned with
the developments in the colonial period, in this article a section
has been added on the present public health system in order to
demonstrate the continuities and contradictions arising therefrom.
A fuller account of post-independence developments in health
policy, is contained in my paper "The Development of Health
Policy in India” in Tim Dyson and Nigel Crook (eds), India's
Demography : Essays on the Contemporary Population (New Delhi :
South Asian Publishers, 1984).
References
Annual Reports of the Sanitary Commissioner to the Government
of India.
Cassen, R H., India: Population.
MacMillan, pp. 84,89, 1978.
Economy,
Society,
London,
Doyal, L. with I. Pennell, The Political Economy of Health, London'
Pluto Press, 1979.
Gazette of India, March 2, 1864.
Government of India, Draft Fifth Five Year Plan 1974-79. Vols.
1 ft 2, Delhi, Planning Commission, p. 286, 1974.
Government of India, Pocket Book of Health Statistics of India,
P. 55 1977.
Government of India, Sixth Five Year Plan. 1980-85, Delhi,
ing Commission, p. 370, 1980.
Imperial Gazetteer of India, The Indian Empire, Vol.
strative, Oxford, The Clarendon Press, 1909.
Plann
IV: Admin 'r
Indian Council of Medical Research, Annual Report 1976, Delhi.
1976.
Lakdawala, D.T., Planning of Social Services in India, Tenth Lal
Bahadur Shastri Memorial Lecture, Delhi,'Indian Agricultural
Research Institute, 1978 (Mimeo).
Lewis, T.R., and D.D. Cunningham, Cholera in relation to certain
physical phenomena: a contribution to the special enquiry'
sanctioned by the Rt. Hon. The Secretaries of State for war
and India, Annual Sanitary Report, 1876, Appendix A
MacKenize Committee: Report and Order of the Madras Govern
ment regarding the control of pilgrims in the Madras Presi
dency, 1868.
Ramasubban, R., Encephalitis : There are no Short Cuts to Banish.
ing the Scourge, Indian Express, December 8, 1978.
(Contd. on page No. 22)
Socialist Health Review
TRANSFERRING MEDICAL TECHNOLOGY
Reviving an Umbilical Connection?
meera Chatterjee
The American Association of Physicians of Indian Origin and the Medical Council of India have recently
agreed to sponsor a new scheme for training Indian doctors in the latest medical techniques. This article
describes the elements of the scheme and discusses its implications especially in terms of its relevance to
the Indian health seen? and the dependency relationship it would reestablish and strengthen. The author
contends that government has devised an ideal plan to keep an important restless and fairly politicised group —
medical professionals — happy ct only a small financial outlay. Could this money not be better spent on
strengthening existing sources of medical knowledge such as professional foreign journals or available
medical equipment ? Or for that matter, could the money not be better spent on strengthening basic health care?
The scheme goes into operation sometime this year and needs urgent consideration. We invite readers to
critically examine the scheme and to generate debate around the issues it raises in SHR and in other forums
as well.
new scheme to "transfer high technology" in
the field of medicine has recently been announ
ced by the Health Ministry. The Ministry has joined
hands with the Medical Council of India (MCI) to
support a venture of the American Association of
Physicians of Indian Origin (AAPlO). We are told
that this scheme was cleared "at the highest levels"
last year, and will commence during the course of
this year (Statesman, 1985/
What is the proposed content and mode of
functioning of the scheme ? From the information
available, it appears that Indian doctors residing in
the USA will be invited by the Medical Council to
train their local counterparts in the latest medical
developments. Training will be "on the job ', using
demonstration techniques — "most probably" on
patients. "New" medical technology is to be used.
It is proposed to train doctors at 20 centres and in
20 different medical specialities in the next few
years. Each group of trainers is expected to consist
of 50 doctors. The first such group will travel to
the major cities of Bombay, Delhi, Jaipur, Madras
and Trivandrum by the end of this year. They will
undertake training in urology, neurology, cardiology,
etc., staying for "no more than three to seven days"
at each centre. The cost of the scheme is intended
to be borne by the individual doctors from the US—
an estimated 100,000 dollars this year — except for
their local transportation and stay costs which will
be met by the Indian Government. The scheme is
proposed on an "ongoing basis".
Several points need to be made about the
proposed scheme and some ques tions raised along
side. First, one must note that the programme is
June 1985
geared towards the training of local specialists in the
use of recently developed medical technologies
rather than to the transfer of manufacturing know
how. It would be interesting to know specifically
which medical technologies will receive attention,
and whether the equipment involved is manufactured
locally. The only clue we have is the emphasis
placed on "new" technologies and "specialist"
centres and personnel. This leads one to bel’eve
that the training might be in sophisticaied medical
techniques for which the equipment is not locally
manufactured. In the absence of specific plans for
the concurrent importation of blueprints to manu
facture the equipment indigenously, one can only
conclude that the government intends to import
ready-made equipment from abroad for use by the
trained specialists (or has already done so). Is it
the government's intention to enter into schemes
which provide a market in India for exogenously
manufactured equipment ? If this be the case, I
must opine that the government should not be
spending the very scarce resources of the health
sector - however little of them - on such an objective.
A second question that must be raised is : Is
t|ie scheme a good way to bring local medical
specialists up-to-date with the latest technological
developments ? To answer this question one can
compare the circumstances in which the trainers'
acquired their knowledge, and those in which they
seek to impart it The American medical practitioner
practices his speciality in a milieu replete with the la
test medical technology. The American doctor is in
undated with information on the latest developments
through literature, sales men, the media, access to
professional associations and speciality conferences
17
(where, incidentally, a prominent part is usually
played by the promoters of new drugs
and
equipment), not to mention his everyday work
environment. On top of all this, according to a
spokesman of the AAPIO, US-based doctors study
their speciality an extra 50 hours a year to bring
themselves abreast of the knowledge required to
pass th ir licensing exams.
In
contrast, the scheme proposes "three to
seven hours" of demonstrations for the local doctors
at specialist centres. The Indian medic, though
also exposed to a fair amount of promotional
literature from drug and equipment firms and some
of the other 'aids', does not have an easy access to
broad-based scientific literature which can assist him
in making reliable judgements on the use of new
materials. As a case in point one can cite the
rapidity with which private practitioners prescribe
the latest formulation of a drug. The culture of
"kickbacks" from company salesmen (calendars,
plastic knick knacks, tickets to dinner at a local
five-star, free samples,
support for travel to
conventions, and much more) has tended to sub
vert the spirit of scientific enquiry, and even clinical
ethics. On the other hand, practitioners may hesitate
to acquire even time-tested diagnostic equipment
at their private clinics, largely because they have
no shortage of clients, regardless how 'backward'
the service they deliver. (None of this is to say
that such abuses do not take place in the US
as well, but the points of check-and-balance
are considerably different.)
The situation of public medical personnel —
including those at specialist centres — is similarly
problematic. They work in intensely over-crowded
and poorly supplied circumstances. There are severe
bureaucratic and
financial constraints to
the
acquisition of new equipments. Adjunct medical
libraries are mostly in a sorry shape. Few pro
fessional associations bring out high quality journals,
and personal subscriptions to foreign ones are
prohibitive. There are few incentives or opportuni
ties to upgrade one's knowledge and skills. Thus.
the very different milieu of trainers and trainees will
make the transfer of knowledge extremely difficult.
One might suggest, provocatively, that the 100,000 dollars
the AAPIO proposese to spend annually on airfares to
India would be better spent on supporting journal
subscriptions for Indian institutions, or on schemes to
provide young Registrars and Senior Residents who are
anxious'jo upgrade their skills access to the "interest
ing' '/difficult cases and specialist equipment which are
usually nabbed by their seniors. Such efforts to fertilise
18
the soil before the specialist knowledge is trans
planted may result in a richer harvest.
It is in this context that the fact that the
proposed scheme does not mention the importation
of any equipment
or blueprints gains extra
significance. ' Three to seven hours" of demonstra
tion will not overcome the problem of short
supply of equipment extant at most centresDoes the government see this as a lesser constra
in’
to the proper functioning of
its health
institutions than a lack of training in the "latest
medical developments" of its doctors? Of course,
much sophisticated medical equipment is already
manufactured locally and therefore does not need
to, indeed shouid not be imparted. But the heavy
burden on specialist health centres, the lack of
adequate procedures and facilities for maintenance
and repair of equipment, the bureaucratic red-tape
which delays
or prevents the acquisition of
replacements, as well as the politics and mal
practices regarding the use of certain types of
equipment at public health institutions remain
major problems the government needs to tackle.
The third point then is that, even assuming that
the training programme is successful in transferring
the requisite specialist knowledge, it is difficult
to see how the specialists will be able to apply
their training given existing conditions.
A fourth and related question is: Are the
Indian doctors travelling home from the US the
most suitable trainers for our local specialists? We
must recall that most of these doctors would
have left India after their early medical education,
acquiring the bulk of their specialist expertise
abroad. Notwithstanding their Indian origins and
basic exposure to medical care in India, how
appropriate is
their
practical
expertise when
transplanted
from the
sterile, almost martial,
atmosphere of a US hospitaler clinic, to a local
centre where even the supply of gauze and
cottonwool, leave alone adequately aseptic instru
ments and operation theatres, is in doubt? The
main reason, however, to concede their suitability
(assuming —only momentarily— that attaining
scheme is necessary or desirable) is that it is difficult
to think of a better alternative. Non-lndians from
the West have the same handicap, perhaps without
the mitigating factor of cultural empathy. Sending
local specialists abroad for training is of course
a greater burden on the exchequer, and runs the
risk both of irrelevance and of further 'brain drain'
although this has worked in many instances in
the past.
Socialist Health Review
Returning to the proposed scheme, one is
compelled to ask, who are the intended bene
ficiaries? In view of the very short training that
will be given and the lack (to our knowledge)
of concurrent plans to overcome the bottlenecks
of inefficient management, poor logistics, highly
politicised working conditions, and low pav that
hamper the functioning even of our super-speciality
centres, it is doubtful that the local specialist train
ees have much to cain. The patients on whom
the techniques would be demonstrated would
merely be playing the roles of guinea pigs, ihe
likelihood of a spread of benefits to vast numbers
being most remote. Thus, one is forced to seek
the answer to this fifth question elsewhere, for
example, in the participating Association of Physici
ans or in the individual
physician trainers
themselves.
As the membership of the AAPIO currently
numbers some 25,000, it is worth investigating
whether the scheme passes muster on the ground
that a sizeable group of important people would be
benefited. Simple arithmetic, however, tells us that
over the next 16 years (until the year 2000 by which
time the world community is striving to achieve
"Health for All"), at the current rate of 50 doctors
per year, 800 may participate in the scheme. Alter
natively, if one allows for a five per cent per annum
rate of growth in numbers of participants in the
scheme, the total may rise to 1200. Even this
higher figure is less than five percent of the current
membership of the AAPIO (which will inevitably
increase over the years) —a figure so small that one
would not expect sizeable benefits to accrue to the
Association at large, especially as we hav.e not been
told of any mechanisms that the Association propo
ses to introduce to "spread" the effects of such a
scheme among its members We must remember too
that the AAPIO is ,an umbrella organisation compri
sed of 15 other associations of Indian physicians
resident in the US. The smaller organisations and
their members are scattered throughout the country,
a land two-and-a-half times the size of our own
vast one. Doctors in the US also work under most
rigourous, albeit better facilitated and more remun
erative, circumstances. So, how a 1000-odd fellows who
have participated in training their counterparts for "three
to seven days" on one occasion in India can benefit their
own larger community remains to be disclosed. How their
participation in such a scheme can help to bring
about the political clout that they aspire to within
the American medical fraternity and with the US
congress is certainly impossible to see.
June 1985
In the absence of the possibility of wider fallout
from this programme-either to the US-based or
indigenous professions, one can only conclude that
the main beneficiaries of the scheme would be the
participating doctor trainers. To put this into pers
pective, it must be realised that many of these
doctors moved away from the land of their birth and
early medical training with feelings of* despondency
and in search of better opportunity. Thus, we need
to consider their participation in the scheme at a
purely human level. The scheme provides a mech
anism through which they can make up in some
small part what they have taken from their homeland
and the government (and thereby "the Indian
people") in the way of a highly-subsidised and
western-oriented medical education. In my ten
years of residence in the US, I knew many Indians
including professionals in the health field, who felt
intense feelings of guilt on this score, and constantly
and earnestly searched for ways to assuage this
guilt. Another feeling was that of confusion about
cultural identity to which many emigres are subject
and Indians in the US — doctots included — are no
exception. This is manifest in a desire to have both
worlds—the better-heeled, more efficient working
and living environment of the west, as well as the
more "homely", colourful, and meaningful life of
India. Thus, the scheme at another level provides
an opportunity to bring this dream to fruition. If
nostalgia, aged parents, or the search for a
prospective son-in-law (a doctor who will quality
for a Green Card ?) draw participants to the scheme,
after the seven days of training will come the family
reunion, the shopping spree, the trip to Kashmir.
Given the groups of 50 or mora, the scheme may be
"development tourism" in its most disguised form
yet.
In sum it is possible that the doctors of the
AAPIO would benefit from this scheme, but as far
as I can see the benefits would be social and
psychological rather than professional.
Lest the reader misunderstand, let me be per
fectly clear. Both the sets of feelings mentioned
are perfectly human and one sympathises deeply
with those who experience them. But the question
here is: is it necessary or appropriate for the Indian
government to use its money and materials suppor
ting local transportation and stay costs, not to
mention the valuable time of the trainees and the
fanfare that will undoubtedly accompany the train
ing, to assist a few individuals (who are fairly
comfortably off) to overcome their pangs of con
science or estrangement ? I think there are more
pressing priorities for the very scarce resources of
the health sector.
19
If the scheme fails the test of its overt inten
tion — professional development — we must con
sider a sixth issue, its possible "hidden agenda".
The first item on this agenda could be the conduct
of collaborative research between the two groups of
doctors. India, as we well know, provides a huge
sea of human beings on which experiments could
be conducted, a vast range of pathologies which
pose real scientific problems or can be used as
"models”, and sufficient institutional facilities for
highly sophisticated experimentation. Similar material
is hard to come by in, say, a US situation while the
medical-scientific community there faces immense
pressures to do significant original research, "publish
or perish". Many Indian practitioners also would
welcome opportunities for collaborative research
because they may have insufficient funds of their
own, they may be devoid of ideas, or they may be
facing a problem "getting published" in reputable
international journals. These problems could be
overcome through collaborative efforts. The scheme
under discussion may well intend to foster such
'mutually beneficial' arrangements. As a young
doctor friend of mine put it, "in 'three to seven days'
there is little the US-based doctor can teach — but
much he can learn" and, I would add, arrange.
On the face of it, such collaborative efforts
should perhaps be welcomed if they further the
cause of science. But the point at issue is whether
this government appointed scheme will provide any
safeguards against the abuses with which we are
aware the system is already rife. While in the west,
human experiments and trials are rigidly controlled
by law, medical ethics review committees have been
widely established (particularly in large hospitals
affiliated with teaching or research institutions),
and wronged patients or unknowing individualshave
legal recourse through malpractice suits, in India
the field is almost wide open. We have no laws
expressly controlling human experiments, other than
torts. The potential of medical technology to be
misused in our social and economic context is
amply illustrated by the saga of amniocentesis and
fatal sex determination, and legal lacunae by the
governments inability to bring unscrupulous medical
practitioners to book in this case. Ethical guidelines
issued by the Indian Council of Medical Research
are at best applicable to its own institutions and
projects, and not binding on others, nor on private
practitioners. Although consent may be sought at
hospitals and clinics for various invasive procedures,
this is rarely "informed".
There is a second possible item on the scheme's
hidden agenda. It may simply be another way of
20
attracting investment from non-resident Indians.
Indian doctors in the US are certainly a group worth
enticing as the most successful among them would
have annual earnings of over 1 0,000, dollars and
considerable savings Their membeiship of associa
tions rrakes them easy to reach with investment pro
paganda. The doctors also enjoy prestige among
other non-resident Indians (NRIs), and so there
could be some 'snowball effects' on investment.
Without going into the pros and cons of NRI invest
ment I should like to take a close look at whether
the mechanics of this scheme would meet this
objective and, more importantly, at what the side
effects may be for the country's health system.
Regarding the mechanics, I have already pointed
out that the number of doctors the scheme can
reach is small. Although we do not know yet what
criteria would be used by the AAPIO to select
participants in the programme, if a good proportion
of them are to become investors, selection would
have to favour those who are 'commercial-minded'
and have large bank accounts. In the US, as in
India, wealthier doctors tend to be in private practice
rather than in public hospitals or academic institu
tions. They are likely to be the best participants in
the scheme from the investment point of view. But
they may not be the best candidates (even from
among the members of the AAPIO) from a profes
sional point of view, suggesting a diametral
contradiction between the scheme's overt and
possible covert aims.
There are also other possible negative "side
effects". In the hope of attracting financial invest
ment, are we potentially adding to the "brain drain"
of doctors out of the country ? We must not be
blind to the continued desire of many Indian doctors
to emigrate — and this scheme may provide a good
opportunity for the 'recruitment' they seek. There is a
growing disenchantment with emigration to Africa,
the Middle East and the Gulf, and a renewed effort
to get to the countries of the west is evident. There
may also be signs of a relaxation in the embargoes
placed by Western countries on immigration of
South Asian doctors five or seven years ago when
their health systems were saturated and when a
sense of international responsibility in the wake of
the Health-for-AII movement may have prevailed.
A demonstration that an emigrating doctor can have
his cake and roti too may act unconsciously to
motivate others to follow suit. Thus, while the scheme
may meet its unspoken investment objective, it may
obliquely harm the existing medical services. It is
worth recalling the Hippocratic oath - and hoping
that our policymakers and the doctors who propose
Socialist Health Review
to participate in the scheme will do the same:"First,
do no harm".
As an aside, it is possible of course that this
scheme is seen (at the same time as being invest
ment motivating) to be precisely an answer to the
brain drain issue By making specialist training
available locally, it may be hoped that the desire of
young doctors to go abroad, ostensibly in search of
such training, would diminish. Il is also easy to see
that by putting out a relativaly small amount of funds, the
government has devised a 'plum' to keep an important,
restless, and fairly politicised group of professionals —
medical specialists—happy and feeling that India will
enter the 21st medical century on time. Neither of these
situations is likely to obtain, however, in the conti
nued presence of the irritants discussed earlier,
which motivate both the outmigration phenomenon
as well as the political volatility of young doctors.
Another possibility that deserves some con
sideration is that the scheme has some actual or
potential connection with the programme of con
cessions to attract non-resident Indian professionals
to return to India — to reverse the brain drain, as it
were. All that needs to be said on this, in the light
of the foregoing discussion, is that concessional
strategies tend to gloss over the underlying causes
of the exodus. Thus, in lieu of them — if there is any
connection — the government would do better to
concentrate its attention on improving the working
conditions of those doctors who remain in India,
preventing not just legally but substantively, a
further drain.
Returning to the investment possibility, one
can further refine it. The government perhaps
hopes that the US-based doctors will invest not
just generally in Indian enterprises, but specifically
in the medical and health sector. It may be with
such prescience that the vice-president of the
AAPIO has expressed confidence "that this Scheme
will do a lot of good to the cause of the Indian
medical services" (for, as we have suggested, it is
unlikely that the training itself will achieve this
broadside.) The dual health economy is wellensconced in India. Many large hospitals and
specialist treatment centres have been established
by private investors including major industrial
houses such as the Mafatlal and Modi groups.
Privatisation is also being seen as the future mode.
The recently-framed National Health Policy speci
fically calls for .the encouragement of private
investment in speciality and super-speciality servi
ces, as well as 'for the government to "utilise
and assist" private voluntary organisations to
June 1985
participate in
health services.
At one leve’.
these are welcome suggestions because of the
innovation likely to be brought to the health
sector through these mechanisms, and more so
because they are intended to reduce government
expenditures for
sophisticated
medical
care.
thereby making more monies available for primary
health care and public health services. The pro
posed scheme may be seen as a step in this
direction, but there is also the grave possibility
that the cart has been put in front of the horse.
There is already
considerable investment
in
specialist health facilities in terms of their share
of the health pie. What is needed, first, for
"health for all" is a reallocation of funds (at
least plan funds) to rural health schemes. It is
also essential to enlarge the total allocation to
health. To
put further investment into the
sophisticated medical sector (however small the
amount) without such reallocation is to relegate
much of the National Health Po’icy to the status
of a lame duck. If the budget to the health
sector does not increase, both in real terms and
in terms of per cent of GNP, such skewed
investment may be tantamount to the government
opting out of health for all altogether. To attempt
to attract external investment through a scheme
"update*' specialised medical personnel in the
"latest developments in medical science" is to
give the lame duck a further kick in the pants.
This brings us the most crucial question of
all : is the proposed scheme relevant at all to the
country's needs? The National Health Policy itself
has called the existing system of sophisticated
health services ''inappropriate and irrelevant'' to
the country's needs. Is a scheme which proposes
to upgrade them any less so? The specialities
mentioned thus far are certainly not those requi
red to treat the major diseases or prevent the
untimely deaths in our country. In this respect,
the scheme is what Lewis Thomas has called
"halfway" technology rather than "real high
technology" which is addressed to significant pro
blems, is effective, inexpensive and inconspicuous.
In the latter category are many potential points
of collaboration between the government and the
AAPIO.
If the government is at all serious about its
commitment to primary health care, it should
perhaps encourage the AAPIO to 'invest' in
establishing clinics to supply basic health care
and medicines to the remotest rural areas, and
to "donate" personnel time to training trainers
21
response may shift attention away from medical
care institutions to contain the costs of the health
sector.
The drastic decline of U.S. power in the world
capitalist system has shaped an internctional situa
tion which has aggravated the acute domestic
stagnation. To cope with these conditions, the
capitalist class has been looking more and more at
the potential of the health services industry for
greater social efficiency. In the present economic
crisis, the containment of social consumption
expenses can provide funds for private investment
in the production sectors Health policy has been
encouraging attempts at general rationalization
(cost cutting, profit maximization, forcing higher
productivity).
At the same time, various segments of capital
are responding to opportunities for greater profits
to be derived from both the production of health
services10 and the circulation of commodities through
the health sector (e.g. drugs, hospital equipment
and supply, construction, systems and communi
cations, legal, accounting and management services,
etc;.11 As industrialisation proceeds in the health
sector (mass production, elaboration of the division
of labour, greater capital intensification, bureaucratisation, etc.), these industries will seek greater
capital flows toward the sector.
Renaud has demonstrated how capitalist growth,
while giving rise to disease patterns in society, also
institutionalises "'solutions" to disease which are
compatible with capitalism, in the form of a comm
odification of health services.12 With alienation and
disease
creating a greater dependency by the
working class on health (and other human) services,
these services must function more and more as
mechanisms for social control. 3 However, the
present structure of health care delivery has not
developed sufficiently for monopoly capitalism
today. A new organisational form is required, and
it will arise under conditions similar to those other
sectors where petty-bourgeois or pre-capitalist
forms historically were smashed or co-opted.11
It is surely not new for capitalists to be actively
restructuring the health sector. Berliner has detailed
how the Carnegie and Rockefeller Foundations in
the beginning of the century virtually rebuilt the
entire medical care system by endowing research
institutes and
selected medical schools.15 This
intervention strongly influenced the rise of the
presently-dominant organizational form in the health
24
sector, which has served through to the present
period.
Stagnation and crises necessitate a growing
awareness of monopoly capital's common interests
(as well as its conflicts). The coming together of
major capital segments to discuss and formulate
general policies in itself yields a greater measure of
class consciousness 16 Policy-planning organisa
tions, fsuch as the Trilateral Commission, Business
Council, Comittee for Economic Development,
Business Roundtable, etc.) have lately become the
arenas for working out programs for the capitalist
class as a whole. Their activities provide a system of
cooperative interpersonal and interorganisational
relationships based upon a commonly-held class
perspective. The role of these "consensus-seeking'
groups becomes critical, with the mounting con
tradictions of advanced capitalism and thecrescendo
of challenges to the American capitalist system on
both the international and domestic levels.17
Today the "class-conscious corporate direc
torate"18 is speaking directly to monopoly capital's
needs from the health sector in a number of
important publications and conferences. The follow
ing sections will review a few of the activities
of selected planning bodies, showing their ideolo
gical development as they educate the corporate
class. As yet, no definitive analysis on the nature
and function of the health sector has developed,
nor has a comprehensive strategy for the capitalist
class as a wnole emerged. Nevertheless, a class stand
is shaping as the problems for monopoly capital
are detailed and potential solutions are discussed.
In contrast to the last decade, Fortune, Forbes,
Business Week and the Wall Street Journal have
been devoting major amounts of space to health
care problems and editorializing for a changed
structure to favor capitalist interests.22 The National
Journal provides frequent indepth analyses of health
care issues to apprise business leaders of legislative
developments. All of this interest by the business
press (coupled with the popular media's attention
to health and health care inadequacies)19 is a
marked escalation over their coverage prior to
1970 — a change which parallels the new interest
by capitalist planning bodies
Committee for Economic Development
The
Committee
for
Economic
Development
(CED) is one of the central educational and
policy-making organisations of the corporate class,
Domhoff calls it the "major spokesman for the
Socialist Health Review
business viewpoint." Highly influential in state policy
formulation, it addresses their societal concerns in
lengthy policy statements.20 It represents a more
"progressive" capitalist perspective (generally the
longer view of reshaping society) and produces
studies that are somewhat broader and less detailed
than the issues analysed by the liberal Brookings
Institution21 or the right-wing American Enterprise
Institute for Public Policy Research (AEI).22
The CED provided a beginning outline of their
design for the health sector in a report entitled
Building a National Health Care System in April 1973.
It lecommended health maintenance organisations
(both profit-making and nonprofit) for restructuring
the delivery system. A health maintenance organi
sation brings together a comprehensive range of
medical services into a single organisation, provi
ding services in a benefit package for a fixed
contract fee which is paid in advance. A proposal
was made for health care providers to be financed
through prospective budgeting, with fees and char
ges fixed in advance. A national health insurance
program, providing a basic level of health benefits
for all Americans, would be administered by a
National Health Insurance Advisory Board. This basic
benefit package for all Americans, of course, would
be a phased and "practical program that does not
raise false hopes by promising services that cannot
be made available and does not lead to unwarranted
increases in costs with little benefit to people."23
Three categories of financing would be established:
1) employer-based insurance would be phased in
for all workers and their dependents; 2) Medicare
would be retained for the aged and disabled,
3) care for the poor, nearpoor, unemployed, and
others would be provided through federally-sponso
red community trusteeships. The policy statement
further recommended a control and planning mecha
nism — which has now been enacted in Public Law
93-641, The National Health Planning and Resources
Development Act of 1974.
In short the statement by the Committee for
Economic Development essentially endorsed the
health
policy of the Nixon Administration and
countered most of the stands taken by the American
Medical Association, which has fought all attempts at
restructuring and cost control.
The Business Roundtable
Perhaps the major capitalist lobbying group on
health care has become the Business Roundtable
(BR) and its associated Washington Business Group
on Health. Made up of the chief executive officers
June 1985
of the 160 largest corporations, BR was formed
in the early 1970's to develop class discussions
and to formulate corporate policy on labor problems.
in June 1974 the Business Roundtable con
vened a conference on health care legislation to
build a consensus among chief executive officers
about what business should be getting from the
health sector In an opening address, the chairman
of Eli Lilly Company, tne drug manufacturer, noted
that "at a recent meeting of the Business Roundtable there was complete agreement that the import
ance of the health issue to every company should
have a very high priority as an issue in future months
towards which we should devote our continued and
dedicated attention."24 The panel of speakers was
impressive. Chairman of the Business Roundtable's
Subcommittee on Health Policy; Chairman of the
CED Health Policy Committee; former Congressman
William Roy; who authored the Health Maintenace
Organisation Act of 1973; a representative from
the office of the HEW Assistant Secretary for Health
and Scientific Affairs; and Russell Long, Senate
Finance Committee Chairman and sponsor of a health
insurance bill. While endorsement was encouraged
for Senator Paul Fannin's National Health Standards
Act (the national health insurance bill of the Cham
ber of Commerce), what seemed to be emerging
was a firm conviction that restructuring the delivery
system was a necessity before legislation on the
national financing of health care. In the midst of
the recession, coupled with the state's fiscal pro
blems, capital was displaying its fear of increased
labor costs.
The Conference Board
The Conference Board based in New York
City, is a research organisation concerned with
"business economics and business management."
Its numerous studies address problems of the firm/
which it then relates in its published findings to
social policy issues. Their message promotes the
common interest of capital in the "efficient operation
and sound development of voluntary productive
enterprise."
The CB conducted several extensive studies
on health care funded by the U S. Department
of Health, Education and Welfare and a conso
rtium of large corporations and foundations. Top
Executives View Health Care Issues (1972), the first
product of this broad CB study in health, surveyed
118 executives about: 1) the nature of the nation's
major health problems, the need for new legisla
tion to deal with them, and the particular pending
25
legislation; 2) the ways in which health costs to
business might best be controlled; 3) the desirability
of companies creating or expanding their own in
house medical services; 4) a strong business role
in community efforts at health services planning,
controlling hospital and other health costs, and
developing prepaid group practice plans and other
new health delivery forms; 5) potential changes
over the next decade in corporate health care activi
ties; and 6) the order or priority that business should
assign to health care relative to other social issues
(e.g. environment, product safety, minority employ
ment and urban redevelopment).
A subsequent study on Industry Roles in Health
Care surveyed eight hundred large firms to provide
a statistical examination of present corporate health
care programs. The narrative description of these
programs and the suggestions on the "appropriate
management response" to the health sector delineate
specific policies and activities of corporations in
restructuring health care delivery arrangements for
their workers and surrounding communities.
Another publication. National Health Insurance and
Corporate Benefit Plans grew out of two surveys on
corporate health programs (a separate one on execu
tive health), which secured the cooperation of 1800
companies for their extensive detail. The national
health insurance bills before Congress were analyzed
for their effect on industry benefit plans, along with
an assessment of labor union attitudes and actionsThe report concluded that ''a substantive interventi
on by the federal Government would have a major
impact on the benefit planning, cost sharing, and
bargaining, but little direct effect on the benefit cov
erages to be provided to workers. Benefits to lowwage workers and unemployed wou’d increase
greatly "26
These reports provided a foundation to the
forward and sophisticated thinking presented by
the speakers in a CB-sponsored Health Care Issues
for Industry Conference in April 1974. Over 200
corporate executives and health and government
representatives met to discuss the "heavy healthrelated costs in the form of taxes, employee benefits,
workmen's compensation, absenteeism, impaired
productivity, and business stake in the allocation
of the nation's resources and the health of its
economy.'’27 Walter Hamilton, former Deputy Assis
tant Secretary of Commerce under the Nixon Admi
nistration and now a CB Vice President, began the
conference by observing that health care is "an
industry whose methods and structures the business
26
community has both the right and the obligation to
study and seek to improve."-”* Dr. Paul M Ellwood,
Jr., the ch ef architect of the Nixon Administration's
Health Maintenance Organization Strategy, decried
the lack of capitalist leadership in designing nati
onal health policy and suggested that.
"• . free enterprise solutions that have been
effective in solving the problems of conventional
business can be applied with similar effect within
the health industry, and that you are in the position
to apply them. In other words, I am suggesting that
you take certain active steps to make the health care
market work, by encouraging HMOs to compete
with the present system on the basis of prices and
benefits."-9
Dr. G H Collings, Medical Director of New
York Telephone Company, urged corporations to
become the "health care manager" for workers
through their industrial medicine departments. An
executive of Kaiser-Permanente, the largest HMO
in the country with over two million subscribers,
presented information on a cost benefit analysis of
occupational health measures to aid companies. A
corporate officer from Motorola discussed his
company's conflicts with hospitals in Phoenix,
Arizona and Motorola's attempts in the community
to contain their costs. A vicepresident of General
Mills spoke of the corporate-sponsored HMO effort
being designed and implemented in the Twin Cities
area Equitable, Prudential, Honeywell, General
Mills, 3M, Pillsbury, and Mutual of New York are
among the twenty corporations there reporting
attempts to centralize health services into health
maintenance organizations. With the information on
the nature and extent of corporate involvement
in health care activities from this conference and
the CB studies, monopoly capital has positioned
itself to initiate a more class-conscious analysis of the
health sector and itsrelation to capital accumulation.
The Health Manitenance Organisation
Strategy
Active state intervention to restructure the
health sector was taking place amidst these con
ferences and publications by capitalist planning
bodies and the upsurge in volume of health articles
in the business press. The HMO strategy initiated
by the Nixon Administration in 1970 had created an
awareness among monopoly capital firms of invest
ment possibilities in health care delivery. It was
designed for "using the forces of the private sector"
to "modify the entire system of health care."30 Dr.
Socialist Health Review
Paul Ellwood" of Interstudy, a health policy think
tank, has consulted extensively with large corpora
tions urging them to establish profit-making HMOs,
converting iheir industrial medical departments into
HMOs in order to "realize a susbstantial savings
over present health expenditures fcr employee
health care benefits.. 32" Through changing the
present "sickness-oriented, piece work basis" of
the delivery system, the HMO creates a profit
motive "to concentrate on keeping people healthy
and provide "greater efficiency."33 HMO patients
have a markedly lower rate of hospital admissions
and a shorter length of stay tnan those covered by
indemnity insurance plans of Blue Cross and the
commercial insurance companies. According to
Ellwood, HMOs would strengthen the role of com
petition by introducing economic incentives, and
minimize tne need for regulation by relying upon
market mechanisms. Ellwood's dream of a revamped
delivery system envisioned approximately WOO
HMOs across the country, organized similarly to
large corporations (possibly as their subsidiaries) to
serve up to serveral million persons each. One of his
latest suggestions, as an ideological entrepreneur
on health for the capitalist class, urges federal
government subsidies (up to one million per year)
for the nation-wide expansion of the 'superclinics"
(e.g. Mayo, Cleveland, Palo Alto, Marshfield,
Geisinger, etc) as models for a national network of
HMOs.31 The state's role in this redesign of the
delivery system would enhance monopolization
and assure a rationalized organizational form.
To stimulate corporate-controlled HMOs, HEW
under the Nixon Administration designed a program
to attract funds from venture capital and invest
ment banking firms, commercial insurance com
panies, and banks. Capitalist interest in HMO oper
ations, both as commercial ventures and as a more
efficient organization of present health care providers,
rose as they understood how HMOs could control
the runaway costs of the health sector and contain
their labour costs.35 A list of corporations who
have been involved in HMO activity reads like the
Fortune 500: Westinghouse, Texas Instruments,
Sun Oil, North American Rockwell, Zenith, General
Foods, DuPont, IBM, Kodak, Xerox, Upjohn, Mobil
Oil, Standard Oil of Indiana, and a few dozen
others. However, tight money over the past few
years and the lack of substantial financing of the
Health Maintenance Organization Act of 1973 (P.L.
9 3-222) by the Ford Administration have tempor
arily slowed this whole development.
June 1985
Both profit and non-profit HMO plans have
continued to expand, having doubled their enroll
ment (to approximately 8 million persons) over
the past three years in 178 HMOs across the
country.36
However,
new HMO
projects are
dependent on corporate and union support in their
"marketing'' activity (i e., acquiring enrollees) to
ensuie their existence and growth. With the eco
nomy on the upswing and several problems resolved
jn the new HMO law, corporations may reinstitute
their involvement in HMO activities and follow
the example of R.J. Reynolds, which this year
established its own HMO for its workers.37 The
National Association of Employers for HMOs, based
in Minneapolis, was just formed this year by several
corporations to guide firms in their HMO develop
ment.
Occupational Medicine Developments
While monopoly capital's investment in HMOs
has not reached levels predicted by the Nixon Admi
nistration corporate medical directors and emplo
yee benefits managers nevertheless have been
developing mechanisms within their firms to eventu
ally integrate industrial medicice and occupational
health programs with the medical care of workers'
families. Writing in a special issue on HMOs of the
Journal of Occupational Medicine, one corporate medical
director evoked the view that: "the scope of proper
concern of the occupational physician has expan
ded quite far beyond his involvement
with
occupational injuries and disease. It now extends
to the non-occupational health problems of the
worker and his dependents, and the ways in
which the health services they require are orga
nized, delivered, and paid for."38
Another corporate medical director has said, in
a speech entitled ''The Balance Sheet in Emplo
yee Health Conservation," that
the industrial
physician may become the primary care physician
of the future for the worker and the family.39
William Jend, Jr., Medical Director of Michigan
Bell Telephone Company, has argued that the
"workplace is probabiy the ideal locale to practice
real preventive medicine on a wide and effective
scale."40
This ideological thrust,41 coupled with actual
program formulation,42
by industrial
medicine
physicians, represents a slow but deliberate shift
which may lead to a personnel system in which
the firm will be able to provide health maintenance
services to assure the productivity of the indivi
dual worker. This implies a profound change in
27
the content and control of medicine
practiced today.13
from
that
to analytically grasp this beg’nning ruling class
coordination in the health sector also.
In a larger context, the employer as "health
care manager4' will deal with worker alienation
and disease, contain laborpower reproductive costs,
and promote greater social control in an attempt
to reduce the level of absenteeism and disability,
turnover rates, wildcat strikes, sabotage, and poor
quality products. The development of workplace
medicine is one more step in the transfer of
health services delivery to eventual monopoly
capital control.
J. Warren Salmon
Dept, of Community Medicine
and Environmental Healtn
Directions and Contradictions
While these conditions are shaped and shape
themselves from the outside, rapid change is
concurrently happening within the health sector.
Concentration and centralization in the production
of medical care services have been rearranging
patterns of control in the financing and delivery
of care. Health industry groups such as the
American Hospital
Association,
Group Health
Association of America and Blue Cross are be
coming more closely aligned with
monopoly
capital. Stimulated by increased efforts for bure
aucratization
and the
application
of
mana
gerial economics, the industrialization process in
the health sector is bringing forth fundamental
changes in its social relations of production.
Meanwhile, regional planning efforts by health
systems agencies and the forthcoming passage of
some form of national health insurance may help
create material conditions for further monopoliza
tion and a greater capitalist invasion.
As the rationalization of health services occurs
during the present period of economic crisis,
monopoly capital's class stand on health policy is
being developed. Discussions have been centering
around containing cost inflation in health care,
redirecting medical dollar flows through the mono
poly sphere, and eventual consolidation of health
services delivery by large corporations. Recognition
of their interest in more rational and precise social
investment may lead monopoly capital to mold an
organizational reflection of their need for human
capital maintenance.
As the larger crisis of accumulation is addre
ssed, the outlook of monopoly capital is becoming
more highly developed. How capital can assure
stability and predictability in the international and
domestic situations is certainly receiving more and
more class attention and action. It is crucial for us
28
Hahnemann Medical College
230 North Broad Street
Philadelphia, PA 19102
Notes and References
(Several persons offered some fine suggestions and critici
sms on an earlier draft. While not all were incorporated here,
special thanks is expressed to: Len Rodberg, Howard Berliner,
John Bradley, Evan Stark, Sander Kelman, Bill Lazonik, Diane
Flaherty, Lee Price, Dick Garfield and Kathy Miller. I am
particularly indebted to Audrey Colbert for her crucial assistance
in the preparation of the manuscript )
1. See both: Sander Kelman, "Adventure in
the Undialectical." Book review of Robert Alford's
Health Care Politics : Ideological and Interest Group
Barriers to Reform in Journal of Health Politics, Policy
and Law, 1:1 Spring 1 976, pp. 1 22-1 29; and Sander
Kelman, "Toward the Political Economy of Medical
Care” Inquiry 1:3, 1971, pp. 30-38.
2. A case example of corporate control over
health planning may be found in: Health Information
and Action Group, HSA's May Be Dangerous to Your
Health (Philadelphia: Medical Committee for Human
Rights, 1975).
3. For details on conflicts between monopoly
capital and smaller capitals see: James O'Connor,
The Corporations and the State (New York: Harper
Colophon, 1974).
4. For a capsule analysis of the cost problem,
see: Council on Wage and Price Stability, The Problem
of Rising Health Care Costs (Washington, D.C.:U.S.
Government Printing Office, April i976)
5. James O'Connor, The Fiscal Crisis of the
(New York: St. Martin's Press, 1973).
State
6. The federal government has adopted cost con
tainment measures through the economic stabiliza
tion program: utilization review of hospitalizations
under Medicare insurance for the aged and Medicaid
for the poor; monitoring hospital admissions and
length of stay by Professional Standards Review
Organization, federally-mandated organizations set
up by county medical societies; and authorities for
planning construction and equipment purchases
given to new regional health systems agencies.
Futher, state governments have regulated commer
cial and non-profit insurance firms, and enacted
certificate-of-need legislation for hospital and nurs
Socialist Health Review
ing home facilities construction, and hospital rate
setting legislation. See: Anthony R. Kover and
Edward J Husk, "State Regulation of Health Caie
Costs" Medical Care 13.8, August, 1975, pp. 619-629.
7. Victor Fuchs, Who Shall Live? Health, Economics
and Social Choice (New York; Basic Books, Inc , 'i 974)
8. Lee Benham and Alexandra Benham, ' The
Impact of Incremental Medical Services on Health
Status, 1963-1970' in Ronald Anderson, et al.
Equity in Health Services (Cambridge, Massachusetts:
Ballinger Publishing, 1975); and Victor R Fuchs,
Who Shall L/ve\ Health, Economics and Social Choice (New
York: Basic Books, 1974).
9. By no means has any consensus been reached
from outside or within the health sector; nevertheless,
the critiques of medicine are being given serious
attention. See Howard Berliners "Emerging Ideolo
gies in Medicine." Review of Radical Political Economics10 For detail on capitalist inroads in health care
delivery, see; J. Warren Salmon, "The Health Main
tenance Organization Strategy: A Corporate Take
over of Health Services Delivery", International
Journal of Health Services 5:4, 1975, pp. 605-623.
11. For a detailed description of the functions of
the health sector and the production and realization
of surplus value in health, see Leonard Rodberg and
Gelvin Stevenson, "Health Care Industry in Advanced
Capitalism," Review of Radical Political Economics (this
issue).
12. Marc Renaud, ''On The Structural Constraints
to State Intervention in Health, International Journal
of Health Setvices 5:4, 1975, pp. 559-572.
13. Gelvin Stevenson, "Social Relations of Pro
duction and
Consumption in Human Service
Occupations" Monthly Review July-August 1976,
pp. 78-87.
14. Maurice Dobb, Capitalism, Development and plann
ing (London : Routledge and Kegan Paul, 1967)
15. Howard Berliner, "A Larger Perspective on
the Flexner Report," International Journal of Health
Services 5:4, 1975, pp. 513-592.
16. See the entire issue of: G. William Domhoff
(ed). "New Directions in Power Structure Research*'
The Insurgent Sociologist 5:3, Spring 1975.
17. Notwithstanding the instrumentalist overtones
here the author is merely stating that Conditions
are propelling this development. Limitations, both
June 1985
on theoretical and empirical levels, exist in power
structure analysis of this sort and obviously the
varying theories of the state must be considered.
See John Mollenkapf, "Theories of the State and
Power Structure Research “Insurgent Sociologist 5:3
Spring 1975, pp. 245 - 264
18. James O’Connor, The Fiscal Crisis of the State,
p. Ill
19, Perhaps the first major indictment by mono
poly capital against the health sector was the
entire January, 1970 issue of Fortune 81:1 entitled,
"Our Ailing Medical System". The issue strongly
advocated health maintenance organizations as
did M. Rothfield, "Sensible Surgery for Swelling
Medical Costs" Fortune 88.4. 1973, pp. 110-119:
"Is There an HMO in Your Future? ' Forbes March
15, 1973, p. 21; "A Revolutionary Plan to Keep
People Healthy" Business Week, January 12,1974,
p. 58 "Still Waiting for that Revolutionary Health
Plan." BusinessWeek
January i3, 1975, p 53,
Dublin. "Unhealthy Start: Prepaid Medical Plans
Run Into Difficulties as Enrollment Falters," Wall
Street Journal February 11, 1975, p. I, plus num
erous other articles on aspects of the health
care crisis.
20. Every major television network ran specials
on the health care crisis. Today newspapers and
magazines follow health care developments quite
extensively often not missing opportunities to attack
the present medical care structure. For example,
see the week of front page articles in the New
York Times January 26-30, 1975.
21. On each of its policy statements the CED
writes that "by enabling businessmen to demonst
rate constructively their concern for the general
welfare, it is helping business to earn and main
tain the national and community respect essential
to the successful functioning of the free enterprise
capitalist system." It is not uncommon for a
CED policy statement to precede federal policy
or legislation on the issue.
22. The Brookings Institution in Washington, D.C.
has published the following studies related to
health care: Rashi Fein. The Doctor Shortage: An
Economic Diagnosis'. Herman Miles Somers and Anne
Ramsay Somers, Medicare and the Hospitals'. Issues and
Prospect: Karen Davis, National Health Insurance:
Benefits. Costs and Consequences : among others.
23. In 1973 the AEI established a Centre for
Health Policy
Research which has published:
29
C Stewart and C. Siddayao, Increasing the Supply of
Medical Personal Regulating Health Facilities Constructi
on proceedings of an AEI Conference; Judith R.
Lave and Lester B. Lave. The Hospital Construction
Act'. San Petlzman, Regulation of Pharmaceutical Innova tion. Rita R. Campbell, Food Safety Regulation', a
legislative analysis. National Health Insurance P.oposals:
David Schwartzman. The Expected Rate of Return From
Pharmaceutical Research'. William M. Wardell and
Louis Lasagna Regulation and Drug Development: Alex
R. Maurizi, Public Policy and the Dental Care Market.
Cotton M. Lindsay, Veteran: Administration Hospitals.
An Economic Analysis of Government Enterprise: Drug
Development and Marketing. Proceedings of an AEI Confe
rence, Health Insurance What Should Be The Federal Role?
proceedings of an AEI Roundtable television show:
and Robert Stewart Smith. The Occupational Safety
and Health Act. Its Goals and its Achievement Quite an
extensive undertaking for only three years work! See
also: David Pauly, "Celebration on the Right.'
Newsweek, May 17, 1976. p. 81.
24. Committee for Economic Development. Building
a National Health Care System, New York, 1974, p,. 66.
25. Business Roundtable, Washington Health Organi
zation Conference on Health Care Legislation, June 20
1974, Washington, D.C. pp. 3-4.
26. Commonwealth Fund, which has long been ac
tive in health: Rockefeller Brothers Foundation,
Andrew Mellon Foundation, as well as New York
Life insurance company, Johnson and Johnson
Company and medical supply firm and CIBA-Geigy
Company and Upjohn Company, both
drug
manufacturers.
27. David A Weeks, An Interim Report. National Health
Insurance and Corporate Benefit Plans (New York
Conference Board 1974). p. i.
28. Seymour Lustermann (ed.). Health Care Issues
for Industry. (N.Y. Conference Board, 1974) pj.
29. Walter A Hamilton, ''Conference Aims" in Ibid
p. 10.
30. Paul M. Ellwood. Jr , "Business and the Chan
ging Health Care Scene." in Ibid., p. 54.
31. U.S. Department of Health, Education and
Welfare, Towards a Comprehensive Health Policy for the
1970s: A White Paper (Washington, D.C. U.S. Govern
ment Printing Office, 1971).
32.
See Paul M. Ellwood, et al, ''Health Maintena
nce Strategy'' Medical Care May-June, 1971, p. 291,
30
Paul M. Ellwood. "implications of Recent Health
Legislation" American Journal of Public Health January
1972, p. z0. Paul M Ellwood. "Health Maintenance
Organizations: Concept and Strategy," Journal of
American Hospital Association 45:6 1971., pp. 53-15
Paul M. Ellwood "Sig Business Blows the Whistle
on Medical Care Costs" Prism. December 1974,
pp. 13-15; Paul M. Ellwood, "Models for Organ
izing Health Services and Implications of Legislative
Proposals" Mibank Memorial Fund Quarterly October
1972 among numerous others.
33. Paul M Ellwood and Michael Herbert, ''Health
Care: Should Industry Buy It or Sell It?" Harvard
Business Review July August 1973, pp. 99-107
4. Richard Nixon "Building a National Health Stra
tegy: Special Message to Congress.'' Washington
DC. February 18, 1971
35. "Spur 'Superclinics' Expansion to
National
Scale Ellwood Urges" Medical Group News 8:1. March
1976.
For a thorough assessment, see David Gaynor,
et al. "Implications of Corporate Involvement in
HMOs. HMOs in Historical Perspective" unpublished
paper. (Ithaca New York Cornell University 1 974).
36. See ref. 13. For a thorough assessment, see
David Gaynor, et al, "Implications of Corporate
Involvement in HM0s,HM0 in Historical Perspective"
unpublished paper
(Ithaca, New York Cornell
University 1974)
37. U. S. Department of Health Education and
Welfare, Forward Plan For Health F Y 1978-82
(Washington, D.C. U.S Government Printing Office.
1976). p. 50. and U. S. Department of Health,
Education and welfare. Health Maintenance Organizat
ions. Survey of F. Y. 1975 Annual Report
DHEW
Publication No (HSA) 76-13036.
38. "R.J. Reynolds to Open New HMO for Emplo
yees" Health Services Information April 2 ,1976, p. 6-7
39. Dean J Warshaw, "The Expanding Scope of
Occupational
Medicine" Journal of Occupations
Medicine 17:10, October 1975, p. 624.
40. Miles Colwell, "The Balance Sheet in Employee
Health Conservation," presentation to Annual Meet
ing of the Industrial Health Foundation, October
13,1970.
41. William Jend, "Where Do we Want To Be in
Occupational Medicine." Journal of Occupational
Medicine, 15:7 ; July 1973, pp. 517-579.
(Contd. on page 51)
Socialist Health Review
REVIEW ARTICLE
ILLS OF THE HEALTH INDUSTRY
ravi duggal
"Corporate Crime in the Pharmaceutical Industry" By John Braithwaite Routledge & Kegan Paul,
London 1984, £ 25.00
Illicit drug networks, contraband smuggling and
terrorist gangs constitute
popular international
crime syndicates against which most countries have
evolved elaborate and sophisticated means of
counter. Transnational Corporations (TNCs) also
operate an equally organised crime syndicate but
to which invariably the states'regulatory and enforce
ment machinery look the other way orare deliberately
kept as inadequate.
Pharmaceutical TNCs are probably the worst
of their kind. The pharmaceutical industry forms the
nucleus of the health industry. It determines the
nature of the health industry and controls the latter
completely. Pharmaceutical firms play a central role
in health (as well as general) policy making and
planning, education of doctors and other health
personnel, and of course socialisation of consumers
into a ' pill-popping'* culture
Pharmaceutical business is essentially transna
tional and therefore, its crimes acquire an even more
serious concern, especially because there is a gross
inadequacy of protection against the ills of the health
industry. For instance even in the USA, where the
consumer movement is probably the strongest in the
world, marketing a drug with dangerous side effects
is not even an offence unless the product is actually
banned or there has been criminal negligence.
Dr. John Braithwaite in Corporate Crime in the
Pharmaceutical Industry cites innumerable cases reveal
ing that the transnational pharmaceutical industry
has a worse record of international bribery and
corruption than any other industry, a history of fraud
in the safety testing of drugs, a disturbing record of
criminal negligence in the unsafe manufacture of
drugs, of unethical practices in pushing drug sales
including smuggling and of global law evasion and
financial fiddling whose worst victims are third
world countries.
Unlike the times and crimes of Hitler, the
brutalities of today s leading pharmaceutical corpora
tions have yet to find a prominent place in world
history. Many authors have documented in horrifying
details the brutalities of the drug TNCs that have
June 1985
built up an industrial
criminal undertakings.
empire
through inhuman
For example, Germany's I. G. Farben (today
divided into Hoechst, BASF and Bayer) which
operated a massive chemical plant at Auschwitz
with slave labour of 3C0,000 concentration camp
workers, tested drugs on a large number of workers
who died in the drug-testing programme. The
following extract from letters written to the camp at
Auschwitz by I. G. Farben indicates the grave nature
of the criminal offences indulged in by the pharma
ceutical companies to multiply their profits :
"In contemplation of experiments with a new soporofic drug,
we would appreciate your procuring for us a number of
women ... - we received your answer but consider the price
of 200 marks a woman excessive. We propose to pay not more
than 170 marks a head. If agreeable we will take possession of
the women. We need approximately 150........... Received the
order of 150 women. Despite their emaciated condition, they
were found satisfactory. We shall keep you posted on develop
ments concerning this experiment .... The tests were made.
All subjects died. We shall contact you shortly on the subject
of a new load."
Today Hoechst and Bayer are the largest and
third largest drug companies in the world. They
made capital through incriminating means; they
were criminals and twelve of their top executives
were sentenced to terms of imprisonment, for
slavery and mistreatment offences at the Nuremberg
war crime trials. (It must be noted, not for corpo
rate crimes in which allied forces were equally
involved). But once allied control loosened two of
the criminals, Friedrich Jaehne and Fitz ter Meer,
were appointed chairmen of Hoechst and Bayer,
respectively.
Braithwaite introduces his book on Corporate
Crime with this horror story and subsequently moves
on to expose the various areas and mechanics of
crime in the pharmaceutical industry with interestting but emotionally disturbing case-studies.
The Pharmaceutic Global Empire
The foundation for the transnational nature of
the drug industry was laid sometime at the turn of
31
the century but only consolidating itself in the
inter-war period. The modus operandi was invari
ably international traffic in illicit drugs. Bayer, at
the turn of the century, used the same mass marketting tactics for heroin as it uses for aspirin or
Baygon. the cockroach killer. Bayer even promoted
heroin as a panacea for infant respiratory ailments I
Parke Davis similarly promoted with great enthu
siasm the therapeutic virtues of cocaine, marketing
it as coca-cordial, cocaine cigarettes, hypodermic
capsules, ointments and sprays. Roche was heavily
involved in the supply of morphine to the under
world and theCanton Road smuggling case — Shan
ghai, 1925 — revealed extensive involvement of
Hoffman-La Roche in the illegal drug trade.
Thus "some of the great pharmaceutical com
panies of today owe their existence to profits from
the trade in heroin and morphine in an era which
laid the foundations for the self-perpetuating
cycles of addiction to these drugs in modern
societies. The next generation might look back on
the activities of Hoffman-La Roche in pushing
Valium and Librium with disgust equal to that we
feel today towards their heroin sales between the
wars".
The entire pharmaceutical industry is virtually
controlled and dominated by private firms from four
countries — USA accounting for 34 percent of world
production, Japan 20 percent, and West Germany 13
percent, Switzerland 10 percent, Hundred pharma
ceutical firms out of an estimated ten-thousand in
the world account for 90 percent of world shipments
of drugs; out of these the top 25 TNC's (half of them
from USA) account for 50 percent of this sales
(UNCTC, 1979).
In 1980, out of the 83530 million dollars produc
tion of drugs the developed countries (including East
Europe) accounted for 88.5 percent and the devel
oping countries only 11.5 percent (UNIDO, 1980).
And within the developing countries India, Egypt,
Brazil, Argentina and Mexico accounted for twothirds of the drug production (UNCTC, 1979). As
regards drug consumption the developed world
consumes 80 percent and the developing world
(including China) 20 percent of the world produc
tion (UNIDO, 1980) - an awesome irony when the
population ratio is just the other way around. To
quote Halfdan Mahler, "the public health services
of the 67 poorest developing countries, excluding
China, spend less in total than the rich countries
spend on tranquilisers" (Mahler, 1981).
32
On an average drug consumption in some of
the poorest countries works out to less than 50
pence per capita, whereas in some industrialised
nations it is35 pounds percapita (Faltorusso, 1 981).
These figures underline the lack of purchasing
power of the third world poor. Essentially, they
reveal more about wealth than health. It is, for
example, highly debatable whether the level of
drug consumption in much of the rich world
repiesents a particularly 'healthy' state of affairsBut one conclusion is inescapable : whereas rich
countries can afford to be extravagant with medi
cines without risking acute social consequences,
poor people and their governments cannot. Because
they have so little money, it is crucial that it is
spent only on essential drugs (Melrose, 1982).
Ironically, even the "little money'' in the third
world is largely spent on drugs which are not
necessary at all — this is because of the over
whelming control of drug production and trade in
these countries by the TNC's.
Thus as a consequence of this global oli
gopolistic control and domination (even in free
enterprise USA 20 firms account for 80 percent
of all drug sales) the pharmaceutical industry
has established a position through which any
amount of abuse may be hurled at the people
without any adverse consequences to the former.
Braithwaite's book consolidates most of the
earlier work since the early sixties and puts it to
gether into a comprehensive whole. He also draws
a great deal from the US Security and Exchange
Commission (SEC) files and rounds it off with
131 interviews with executives of 32 TNC's in
five countries. Braithwaite covers a whole range
of crimes from simple payoffs and kickbacks for
hastening administrative procedures to criminal
practices in drug-testing and manufacture, from
financial fiddling and oligopolistic practices to
malpractices in drug pushing, and from smuggling
and international law evasion to abuse of the
third world nations.
This survey of pharmaceutical criminal underta
kings is adequately supported by a wide range of
case-studies from most of the prominent drug
TNC's. Here is an overview of the crimes and
a few of the case-studies recorded in the book.
Bribery
Bribery is considered as normal and acceptable
business practice. "Almost every type of
person
Socialist Health Review
who can affect the interests of the industry has
been the subject of bribes by pharmaceutical com
panies : doctors, hospital administrators, cabinet
ministers, health inspectors, customs officers, tax
assesors, drug registration officials, factory inspec
tors, pricing officials and political parties'*.
Braithwaite, after a thorough search of SEC
files, lists 29 US pharmaceutical firms that have
disclosed substantial
amounts of questionable
payments. No other industry, he adds, has anything
approaching this record of documented corrupt
payments, sustaining the conclusion that the phar
maceutical industry is more prone to bribery than
any other international business. Possibly this is
because like aerospace, arms, petroleum
and
other heavy capital goods industry, pharmaceuti
cal firms deal with big win or lose situations —
the new billion dollar product to be approved
or the multi-million dollar supply contract to a
third world government.
Passing of a plain
envelope of currency notes under the table is
not the only method of bribing. In fact, most
often more sophisticated methods are used. Braith
waite points out for instance, that if the secretary
of a hospital board owns an architectural firm,
a law firm, or a public relations firm, then you
can hire his/her firm, perhaps even get some
genuine services from it, but pay extravagantly
for such services. You can even rent a property
from the person concerned at an unusual/y remu
nerative rental. The pharmaceutical disclosures show
that paying on an invoice to the company for
services not actually rendered, or overinvoicing
by the company so that an excess can be put
aside for the recipient of the bribe have been the
most commonly reported practices in the pharma
ceutical industry. What is most interesting is that
most questionable payments are treated as tax
deductible expenditures which means a substan
tial loss to the state exchequer. For instance Merck,
which reported 3.6 million dollars as qestionable
payments in 39 foreign countries claimed tax
deductions and after the disclosure agreed to pay
the US Internal Revenue Service additional tax
of 264000 dollars. Similarly Warner-Lambert had
an additional tax liability of 325839 dollars.
Corruption often reaches highest levels of
government as in the following incident reported
in the New York Times : In Italy a dozen manu
facturers, including some American companies,
once banded together to back an industry sponso
red bill in the Italian Parliament that would have
allowed manufacturers to sell their non-prescription
June 1985
products in supermarkets and other retail outlets.
There, they would no longer be subject to price
control. One million dollars ^80,000 dollars per
company) were paid into a war-chest of the ru
ling Christian Democratic Party.
There is an even more interesting case involving
Hoffman-La Roche, who bribed two Kenya govern
ment pharmaceutical buyers for favouring their
products. The two health officials were convicted and
imprisoned and it was revealed that they had brought
quantities of an anti-bacterial and a tranqui/iser from
Roche that would last the nation for a decade—not a hea
lthy situation with products having a shelf-lite of only
couple of years.
What has been done to curtail the menace of
bribery ? Nothing of consequence is Braithwaite's
conclusion. He cites the instance in Mexico when
Portillo came to power. Eight top executives of
pharmaceutical TNCs were arrested and jailed;
also a number of senior government officials were
dismissed. This raid was in reality aimed at launching
a moralising campaign to turn into reality the aims
set forth by the new government of the republic at
Inauguration Day, as also to remove officials who
would be a problem to the new government. Of
course, after a few days the defendants were
released on a bail of one million pesos each and
some months later even the charges were dropped !
But such dramatic gestures cannot be sustained for
long because once the international business com
munity recoils from the shock and regroups, it is a
worthy adversary to the state in instiutional power.
Similarly in the USA the SEC disclosures have been
firing blanks : who gets hurt in consent settlements ?
The SEC gets a notch in its gun. The law firm gets
money, the public is happy because they read
'fraud' in the newspaper and think criminality right
away. The company neither admits or denies any
thing. Its the perfect accomodation. And its all one
big charade.
Drug Testing
Bribery as a crime seems inconsequential when
one looks into the fraudulent practices in safety
testing of drugs and unsafe manufacturing practices
of the pharmaceutical industry. The crimes in these
two sectors have caused irrevocable human damage.
At one end there is gross manipulation and cheating
in drug research and on the other end cutting
corners on product quality in the manufacturing
process.
Morton Mintz's exposure of the frauds of the
drug industry was a pioneering effort and set in an
33
ora of greater vigilance towards illness-business.
In 1962 the FDA made multiple seizures of Regimen
tablets (phenylpropanolamine hydrochloride), mar
keted by the Drug Research Corporation as a
'reducing pill', on charges of misbranding. In
depositions by two doctors who had 'tested' the
drug it was revealed that the results were complete
fabrications. For instance one doctor reported that
her report was untrue in its entirely —57 of her 75
patients' charts were complete fabrications and of
the remainder only the patients' initials and starting
weights were correct ! (Mintz, 1967).
Two investigators in drug testing Dr. Bennett
Robin, who had tested 45 products for 22 reputable
pharmaceutical companies and Dr. Leo Cass, director
of Havard Law School Health Services, who had
undertaken 84 research projects for testing and 25
projects for product marketing applications were
identified for scrutiny by the FDA. It was revealed
that a substantial proportion of the 'testing' was
'graphited', that is, by invention of pencil, rather
than by actual testing.-The FDA revealed that many
of the patients on whom 'tests' were done had been
deceased earlier or were never hospitalised and
treated. Also, for those who were treated the state
ments made, including claims that treated patients
had certain medical conditions, were untrue. This
was in the early sixties.
Even in the late 'seventies, after substantial
tightening of regulations and monitoring by FDA,
graphiting and distortion of results in drug testing
were rampant. Between 1977 and 1980 FDA dis
covered at least 62 doctors who had submitted,
manipulated or downright falsified clinical data.
Add to this the fact that most fraud in clinical trials
is unlikely to even be detected; most cases which
come to public attention only do so because of
extraordinary carelessness by the criminal physician.
The 1978 hearings of the Kennedy Sub
committee on Health has catalogued a list of abuses
which are still of major concern : (1) Case reports
on fictitious subjects, and on subjects who were
never
administered
the
investigational
drug;
(2) Case reports containing the results of clinical
laboratory work which was not actually performed;
(3) False representation of Institutional Review Board
approval of a study; (4) Misrepresentation of patient
dagnosis and demographic data; (5) Consent (infor
med consent) of the clinical subject not obtained;
(6) Drug
doses given, farexceeding protocol
limitations. (7) Drugs given to inappropriate subjects
34
(especially pregnant women), (8) Serial use of inves
tigational drugs to the exclusion of accepted therapy;
(9; Administration to subjects of two or more
investigational drugs at the same time and the
administrat:on of other significant and perhaps
interfering drugs with the investigational drug ;
(10) Inadequate medical attention to the test
population through excessive delegation of authority,
lack of follow-up; and (11) Representation of
investigational drugs as marketed products and/or
the sale of such drugs.
This (researcher dishonesty) is indeed an alarm
ing situation but worse still is the situation in third
world countries where consumer protection is
almost totally absent. Drug companies opt to test
particularly dangerous drugs in the third world
because poor people are regarded as more dispens
able, and in some measure this is undoubtedly true,
concludes Braithwaite. But there are also other more
practical reasons for going to the third world first
with drugs for which fears of side-effects are great.
Peasants do no not sue global corporations for injury.
Informed consent regulations for drug testing do not exist
in tbe third world. Moreover, given that the patent
life of a new discovery is finite, and that monopoly
profits will only accrue while the patent lives, there
are incentives for companies to get a product regis
tered wherever they can as early as they can. And if the
product is found to be unsafe by subsequent, more
sophisticated, testing in a developed country, then
at least the company has made some money in the
third world while the going was good.
Unsafe Manufacturing Practices
Pharmaceutical transnationals
have a high
reputation, especially in the third world, as regards
their product quality and manufacturing practices.
But Braithwaite cites a number of cases even within
developed countries to prove that this is not wholly
true. Yes, it is a fact that manufacturing practices of
TNCs are relatively superior to those of other
industries but in the third world their standards are
very lax in part due to lack of well-defined standard
codes in most of the third world.
Many countries have legislations pertaining to
quality control such as Good Manufacturing Pract
ices (GMP), Good Laboratory Practices (GLP) and
Standard Operating Procedures (SOPs) but the
legislations provide adequate loopholes, and moni
toring and control is a fairly difficult process and
therefore a very constraining task for the state
Socialist Health Review
whose resources are limited. And as one qualit/
control manager put it 'government inspectors
ensure the quality of your records, not the quality
of your deeds'.
However, there is no doubt that the worst
quality standards are in the third world countries
where due to limited resources short-cuts are
invariably adopted In the drug industry cutting
corners on quality can have very serious consequ
ences for consumers and therefore ' bath-tub''
manufacturing which is extensively prevalent in the
third world, needs greater regulation In fact, in
many third world countries TNCs try to push up
quality control - GMP and SOP - Standards because
for manufacturers in the third world high quality
means cost constraint, which in turn pushes up
market prices and in a poor country high priced
products could mean loss in market share. Higher
quality standards puts the TNCs, who have virtual
monopoly of high quality technology, in a domineer
ing position, as well as assures them of a relatively
competition-free market.
Drug Peddling
Most countries have restrictions about what
claims are made about the products efficacy and
use as well as regulations pertaining to Indications
about side-effects about the drugs, and its contra
indications. However, as in the case of other areas
the scope of malpractice in advertising is also greater
in the third world revealing once more the double
standards of the drug TNCs. The cost of promotion
and consequences of criminal malpractices therein
are ultimately borne by consumers. The UNCTC
(1 979) indicates that approximately 23 percent of
all drug sales at the manufacturer's level goes for
promotion. In the US the drug industry is easily at
the top of league of the heaviest advertisers, with
the soap and detergent industry its only close rival;
even .tobacco, alcohol, food and soft drinks lag well
behind (Haslemere Group).
In the third world the expenditure is estimated
to be even higher. In. Columbia the money spent
each year by foreign, companies on marketing their
drugs adds-up. to, rnprq : .than half the country's
national healthsb}4dg^t..^ByjaLxn7 1980). The Concen
tration of sales re^^serjlatiyes to doctors in the
third world is ro.uct)3n^ate.r than in developed
countries. In Britain,..tf}p,ije is one medical represen
tative for 18 doctors,'whereas in Bangladesh the
ratio is 1:7; in Tanzania 1:4; in Nepal, Brazil and
Central American countries 1:3 (Melrose, 1982).
June 1985
The Kennedy Senate hearings have documen
ted gifts to doctors of freezers, tape recorders,
stethoscopes, golf balls with Pfizer stamped on
them; indeed, almost every type of consumer
product imaginable. Further, in 1973. 20 drug
companies in the USA gave 12.8 million gifts to
members of health care profession and over two
billion samples of (ree drugs. Drugs companies have
provided free to 80,000 doctors in 35 cities F M
radio sets tuned to the Physicians Radio Net
work that constantly churns out medical news
and features of interest to physicians.
The major consequence of such heavy pro
motion of drugs is that where people have access
to drugs there occurs a substantial amount of
over-medication especially of the non prescription
drugs that 'ease our ailing heads, noses, chests and
bowels' giving us fast action and rapid relief'.
Oligopoly and Price Fixing
High profitability is the lifeline of the drug
industry, contrary to what OPPI and IDMA would
like us to believe. Since World War II pharma
ceuticals has been the most profitable business.
The UNCTC observes that from 1953 to 1967
in the US, the equity capital in drugs increased
584 Percent whereas for the entire manufacturing
industry the increase was only 183 Percent in
the same period. Most American companies have
been recording on an average, net profit between
30 percent and 40 percent a year; SKF, CarterWallace, and Rohrer between 40 and 47 percent;
Syntex, A H. Robins and Marion Laboratories over
50 percent and Upjohn even during the depression
between 1930-35 recorded an average of 30 percent.
Braithwaite rightly argues that excessive profits
in the pharmaceutical industry arise in considerable
measure from the peculiar features of the market
which shelter producers from price competition.
Consumer sovereignty is absent in the prescription
drug market because it is not the consumer who
makes a decision to purchase, but the physician.
Doctors have no reason to be price-conscious.
Moreover, the need for effective medical care is
relatively price inelastic in affluent societies.
The Kefauver hearings before the US Senate
Sub-Committee on Anti-trust and Monopoly (1977)
found that the average production costs for 15
major drug firms were 32.3 percent of the whole
sale price at which the manufacturers sold their
product. Not one of the 50 companies compared
35
from other industries had production costs lower
than the highest product'on costs among the 15
drug companies; only Coca-Cola came somewhere
near with a production cost of 42.6 percent of
ex-manufacturer sales.
of the Anti-trust Law five massive mergers of
pharmaceutical TNC's have taken place in the last
decade or so: Mead Johnson and Bristol Myers;
Plough and Schering; Ciba and Geigy; Parke Davis
and Warner-Lambert; Dow and Richardson-Merrell.
Besides the drug market structure, the legal
back-up of patent holding for 16-17 years makes
the pharmaceutical industry oligopolistic. Patent
holding alongwith branding gives the pioneering
company an advantage because the brand name
becomes a habit and late-entrants to the market
find it difficult to break the original brand's
monopoly of the drug market. Thus the higher
price of the brand-leader is no threat to its market
share. As a result fortunes have been made
because of patenting and branding, and quite
often through direct oligopolistic deals as happened
in the case of tetracycline, quoted at length by
Braithwaite.
Then, as the markets and courts have failed to
regulate pharmaceutical prices effectively, and since
self-regulation of pricing would be to put Dracula
in charge of the blood bank, the only course,
argues Braithwaite, is for greater political admini
strative price control.
Pfizer and Cyanamid were dominating the
broad spectrum antibiotics market till 1953 with
their patents on chlorotetroncycline and oxytetra
cycline. This patent protection helped them main
tain high prices and massive profits. But in 1953
when the therapeutically superior tetracycline came
on to the scene their profits were threatened. Both
the firms wished to avoid this competitive market
structure and therefore manoeuvred a deal that
managed to restrict tetracycline sales to five firmsPfizer, Cyanamid, Bristol, Squibb and Upjohnall of whom recognised Pfizer as the patent holder.
Thus price-fixing was inevitable. Keauver's
investigations revealed a conspiracy that was in
violation of the Anti-trust law of USA (The first
charge was made in 1958 by the Federal Trade
Commission). A long drawn out legal battle began
which acquired an international dimension (includi
ng India). The various civil cases are still going
on but criminal charges have been inconclusive
So far damage worth 250 million dollars have been
paid by companies — the US government itself is
claiming overcharges of 376.5 million dollars.
However such price-fixing conspiracies are not
possible today because all governments (USA being
the only exception) have a price control policy. Of
course, this is no guarantee that the pharmaceutical
TNC's will not club together to influence what to
their understanding is a fair price. Oligopoly has
become the basic operating principle in the phar
maceutical industry. The most classic instance,
ironically, being free enterprise USA itself. Inspite
Financial Fiddling
Financial abuse is an area of crime that probably
has the worst consequences for the third woild
nations. Other areas of crime discussed earlier
affect health of consumers directly as individuals or
may be even as a class but financial fiddling can
cause irreparable damage to a third world nations'
economy.
For instance, a large proportion of transaction
on the books of an international company, writes
Braithwaite, are sales from parent to subsidiary,
subsidiary to parent, or one subsidiary to another.
Intracompany transfer prices can effectively shift
profits from one part of the world to another. For
example, drugs might be shipped from a high-tax
country to a low-tax country at below market
prices in order to shift profits to where they will
attract least tax. Transfer pricing is therefore a
classic law evasion strategy. Tax laws of the hightax country are not violated, they are evaded. In
one celebrated case vitamins were manufactured in
France at a cost of Fr. 50 per kilo, exported to West
Germany, from there sent to Switzerland, thence
Monaco, and eventually reimported to France at Fr.
250 per kilo under a different trade name. It some
times happens with such cases (especially in the
third word) that shunting around the circuit happens
only on paper without the corresponding physical
movement of materials.
The most important tax heaven in the pharma
ceutical industry is Puerto Rico. A large proportion
of transactions between the USA and other parts of
the world, comments Braithwaite, go through
Puerto Rico. Wall street analyst John Buttles II
calculates that Warner-Lambert had a 110 percent
return on its investment in Puerto Rico plant and
equipment in 1976. For Abbot the figure was 101
percent while for Schering it was a meagre 90
percent. In 1977, Schering recorded 59.2 percent of
its world-wide profits in Puerto Rico; Squibb 53*7
Socialist Health Review
percent; Abbot 48.4 percent; Smithkline 45.7 per
cent. But Searle outdid everyone: while Searle's
worldwide operations in 1976 and 1977 ran at a
loss (at least were shown as so) its Puerto Rico
subsidiary recorded over 100 percent of its world
wide profits.
A study of third world countries shows that
pharmaceutical imports into Columbia by foreign
owned companies were overpriced by 155 percent,
very much higher than the overpricing of other
imports. Vaitsos estimates that if Columbia had been
paying average world prices for its pharmaceutical
imports, the country would have saved a charge of
20 million dollers to the Columbian balance of
payment in 1 968. Approximately half of 20 million
dollars in excess profits repatriated by transfer pricing
would have gone to the Columbian government in
taxes (Vaitsos, 1974).
Besides fiddling books, repatriation of profits
from third world countries can be achieved by
fiddling packages. A European transnational was
found to be importing into South America sealed
packages of drugs which contained less than
30 percent of the declared contents. By paying
100 percent of the declared cost to the patent
company (through a tax haven) the subsidiary was
able to transfer 300 percent increased profits to the
parent.
There are many reasons apart from evading tax,
indicates Braithwaite, for a parent to charge high
prices for intracompany sales to an affiliate, and low
prices for sales from affiliate to parent. It might be
done to circumvent dividend repatriation restric
tions, reduce the affiliate's exposure to currency
devaluation and expropriation risks, lower apparent
profits when excessive profits might encourage
labour unions to escalate wage demands and local
customers (and governments) to demand price
reductions, or simply to allocate markets by making
the exports of a subsidiary noncompetitive.
Thus, if the control and domination of the drug
TNCs has to be broken, their abuse of human health
eliminated and their crimes in the manufacture and
marketing of health terminated, the fight necessarily
must be a political one and not one of improving the
market and legal situations as most countries are
resorting to today. The TNC power is derived from
their ability to control and manipulate political
affairs of both developed and developing countries.
Only a manifestation of power of an equal force
can offest the drug TNC's choking hold over people's
health and well being.
Case Studies
(1) Richardson-Merrell : In 1960, a subsidiary
in the USA began the marketing of a blood-cholestrol
reducing drug, MER/29 (triparanol). In its first 1 2
months 300,000 Americans used MER/29. Soon
reports flooded the market about its side-effects baldness, skin damage, changes in reproductive
organs and blood and serious eye damage including
cataracts. It was later revealed that the drug had
problems in the testing stage. On grounds of
integrity, Mrs. Benhah Jordan had quit Merrell.
There was gross manipulation of data in the animal
testing (monkeys) programme and gross misreporting
of facts to FDA, inspite of the fact that comparative
studies by Merck and Upjohn had reported severe
side effects. Even in the human testing stage doctors
reported severe side-effects but Merrell chose to
ignore them and fabricated the data for FDA appro
val. It was also revealed that the supervisor on the
project 'Dr* William King had not yet been awarded
his medical degree I In the criminal case that
followed the defendants pleaded 'no contest' and
after six month's probation and a paltry fine
(dollars 80.000) the three exceutives were let free.
In civil suits that followed Richardson-Merrell paid
200 million dollars, mostly in out-of-court settle
ments.
(2) Dawes Laboratories: In 1971, many
workers complained of sexual impotence — some
men had developed enlarged breasts, in one case
requiring surgical removal. Plant conditions were
bad - ventilation was practically non-existent and
the whole interior of the plant was covered with
dust containing as high as 10 percent DES (a hormonal
product) by weight. An enquiry by OSHA resulted
in a fine of only 21000 dollars.
(3) Hoffman-La Roche : In a patent hearing
in Canada it was revealed that the wholesale price
of Valium is 25 times thatof gold. It costs dollars 87
per kilo for the raw matrial for Valium (diazepam).
To put the raw material into final dosage form and
to label and package the tablets brings the cost
upto dollers 487 (high estimate). The final retail
price is dollars 11000 for that same original kilo
which has now produced 100000 ten milligram
tablets. The selling price is 140 times the original
cost of materials and twenty times the total
production cost. Roche sales of Valium in the USA
alone in 1972 was worth 200 million dollars. Roche
sells Valium in Germany at four timesits price in
Britain (both belong to EEC). In Sri Lanka Valium
was quoted by Roche
to the government as
70 times the price charged by an Indian company.
(Contd. on Page 42)
June 1985
37
BHOPAL UPDATE
TRAGEDIES AND TRIUMPHS
Health and Medicine in Bhopal
padma prakash
March 23, 1985 : A premature baby, born two
months too early died at the hospital at the DIG
bungalow after a nine-hour unequal struggle to live.
The mother was a gas victim and had brought the
baby to the hospital five hours after its delivery by
a dai. The child had been put on oxygen. The baby
and the mother lay uncared for on the floor of the
ward until 8 p.m. when a visiting pedaetrician just
happened to look in on the doctor-in-charge He
was directed to the child. By then it was too lateNo attempt had been made to clear mucous from
nose and throat of the child and although the suc
tion apparatus, dusty and rusted, did work, the
hospital had no stock of small-sized catheters The
heart had stopped, the hosptial had only coramine
which of course, was of no use. The child was
declared dead and a certificate was issued. There
was no post-mortem although it was actually a gasrelated death. The mother had attended the ante
natal clinic of the hospital three weeks before and
had been given an injection — presumably TT, but
had not been given any advice about her pregnancy
or the necessity of a hospital delivery especially if
premature.
March 24, 1985: A seminar on Pulmonary
Medicine was organised at the Gandhi Medical
College, (GMC) Bhopal. The afternoon session was
on effect of MIC on the lungs. There were several
eminent speakers — Dr. S R. Kamat of the K. E. M.
Hospital, Bombay rapidly projected innumerable
slidesand summarised his findings on treating 113
gas-hit patients who had been admitted to the
hospital. Prof. Heeresh Chandra, head of the Forensic
department of GMC talked of autopsy findings
screening slides which even his colleagues at the
college had not been allowed to see until then.
His findings, he said, pointed to cyanide poisoning
and vehemently advocated detoxification with Sodi
um Thiosulphate (NaTS). Dr. N. P. Mishra peppered
his presentation with long quotes from medical
researchers from UK and USA to whom he had
written. He declared that the gas victims had
died of carbon monoxide poisoning. His own
trials with NaTS showed that it caused a reaction—
two out of 200 patients developed gastrointestinal
38
symptoms and rashes — and so he was opposed
to NaTS. There were many others — all of them
taking great pains not to reveal the full details
of their studies. In the discussion that followed
everyone seemed to forget that the focus here was
not a scientific thesis but the future and death of
lakhs of people
Sitting in that lecture hall one could easily
forget the larger theatre of disaster across the city.
^hese two events illustrate the emerging situation
in Bhopal. In the gas-hit bastis the nightmare of
December 3rd continues to haunt the people —
their health is deteriorating, state-run medical relief
is almost at a standstill, equipment is inadequate,
•nformation supplied is nil, doctors are uncaring and
in any case, no medicines help. In the hallowed
halls of medical and scientific institutions resear
chers are engrossed in intricate debates to prove
their favourite hypothesis quite losing track of
immediate concerns. The macroworld of two lakh
suffering people has been reduced to the microcosm
hundred of odd hospital patients in the 'MIC wards'.
Typically the medical profession has transformed
the
stupendous medico-social situation into a
laboratory-based clinical/medical problem.
Reviewed here is the health picture in gas-hit
Bhopal as it has developed during these months and
the manner in which the medical community has
responded to it.
The Black days
The Bhopal disaster has been called the world's
worst industrial disaster, and with reason. The
number of dead mounted in terrifying proportions
— 350 by the end of December 3, 500 by the 4th,
over 1600 by the 5th December. One week after the
disaster a conservative estimate put the death toll
at 2,500. Unofficial estimates put the numbers
closer to 6,000. But the exact numbers will probably
never be known.
By the end of the third day over 20,000 people
were being treated in the city's seven hospitals.
They came with complaints of burning eyes, lacri
mation, cough, breathlessness, nausea and dizziness.
Socialist Health Review
That first c’ay alone saw over 1O,CCO patients in
one hospital showing signs of eye damage.
Bhopal's 350-400 doctors worked round-theclock
at numerous centres — make-shift tents,
medical aid posts and the wards. Hospitals ran out
of medicine and had to buy out stocks from the
city's shops, oxygen had to be obtained from other
cities. A hundred more doctors were brought in from
the near-by towns.
For a time no one knew for certain what the
killer gas was. Some said that it was methyl isocynate, others phosgene. None of the doctors knew
how to treat the victims.
It is now known that the Union Carbide (UC)
knew of the results of six animal studies initiated
by the company which provided enuogh evidence of
the chemical's high toxicity. (Three of these listed in
the Box) Moreover the Occupational Health Guide
lines for MIC states clearly that MIC might well
decompose into hydrogen cyanide, oxides of
nitrogen and caibon monoxide at high temperatures
(of over 200°C). UC's own standard line of treatment
prescribes intravenous
hydrocortisone,
oxygen
inhalation and if cyanide poisoning is suspected
then amyl nitrite. If there is no effect, sodium
nitrite and NaTS are to be administered. Yet, in the
first week when Bhopal's doctors desperately
needed information to save lives UC held back vital
information.
Many of the doctors of Hamidia were on the
Carbide plant's medical panel. Also UCIL had been
giving generous funds to the hospital and GMC and
had set up a respiratory research unit and ward. This
indicates a close enough association between at
least some of the hospital doctors and the plant's
medical personnel. It is curious that the former
did not know of the standard line of treatment for
such ‘accidents' which had apparently been long
established at UC.
By all accounts the efforts put in by hundreds
of people — the doctors, nurses and
medical
students, the army, the police, the NSS and the NCC
volunteers and voluntary groups — in that first
week was of heroic dimensions. (Many of them
later suffered from delayed exposure to MIC). But
the government machinery took time to dissociate
itself from the electioneering, recover from the shock
and coordinate relief measures.
Operation Cover-up
By December 6th it was, as one
June 1985
writer put it.
'back to business' for government doctors and
others. Private doctors and nursing homes were
also minting money and death and medical certific
ates were being sold at thousands of rupees.
Hordes of experts began to arrive in Bhopal and
everyone who was anyone began to make stateme
nts about the consequences of exposure to the gas.
Speculation about the real nature of the gas ran
rife. And the government put an embargo on infor
mation. Even the death toll was not revealed on the
grounds that it was not advisable in public interest'.
Autopsies were performed from the third day
but reports were not released. They showed fluidfilled lungs two-to-three times heavier than normal,
ulcerative changes, cherry red appearance of organs,
arterialisation of blood....... To Dr. Heeresh Chandra
the autopsy surgeon, they indicated
cyanide
poisoning.
Even as experts in the government and outside
it glibly began to assure people that there would be
no after-effects, many people who had earlier been
treated and discharged began to come to hospitals
with new symptoms — shivering, yellow appearance,
dryness of mouth, vomiting, nausea, stomach ache,
diarrhoea, skin irritation and headaches and more
seriously, conditions like cerebral palsy indicating
the involvement of the central nervous system.
More than 1,000 patients were on the critically ill
list and at least 50,000 had serious eye problems.
Some estimated that at least 500 of them would go
blind but others like Dr. N R. Bhandari, the superi
ntendent of Hamidia Hospital said that there was
no cause for anxiety and that the blurring of vision
was due to the administration of atropine. "The
worst is over" he stated and ruled out the possibi
lity of the gas affecting the brain. Dr. M. N. Nagu,
Madhya Pradesh's director of health services said
that there might be ulceration and appealed for eye
donations so that corneal grafting facilities could
be offerred.
Scientists from UC's Research and Develop
ment centre stated that the gas would be excreted
from the body in due course and only bronchodi
lators were necessary. Scientists at the Industrial Toxi
cological Research Centre (ITRC) Lucknow opined
on the basis of their study of literature that there
would be no further damage because of the gas.
And agricultural scientists were reassuring people
that there was no environmental damage and cauti
oning them to only make sure that vegetables were
washed, water and milk boiled before consumption.
39
With thousands still suffering from debilitating
symptoms the only treatment being meted continued
to be symptomatic — eye drops, antibiotics and cor
ticosteroids. Interestingly, the WHO toxicologists
approved of the then current of treatment and insi
sted that there was no known antidote for cyanate
poisoning. Two lone voices were hea.d to assert
that there was antidote which seemed to be effec
tive— NaTS. One of these supporters of NaTS
therapy was Dr. Max Donerer, a German toxicologist
who had arrived in Bhopal with ampoules of NaTS
and had started using it. The other was Dr. Heeresh
Chandra who on the basis of his autopsy findings
believed that NaTS would be effective and had taken
it himself. When two patients who had been given
NaTS died, the German was quietly packed off.
NaTS therapy was discontinued much to the relief of
UC's Dr. Loya and his supporters Dr. Mishra and
Dr. Bhandari Dr Chandra was methodically isolated
and ignored. Why was NaTS therapy discarded so
precipitously? The deaths it appeared, were merely
excuses, because
the real cause was never
investigated. Also curious is the fact that no one
seemed to have questioned why the second telex
from Union Carbide reversed the advice given in the
first to administer NaTS. One of the arguments
against using NaTS was that although there was
evidence that people who had been administered
NaTS seemed to recover there was no 'proof' that
it worked! The history of medicine has seen any
number of situations when a therapy which has been
found to be effective has been used because it is
needed and only years later has the mechanism of
its action in the body been worked out. The tragedy
of Bhopal is that it is now acknowledged that
thousands of lives could possibly have been saved
if detoxification with NaTS had been undertaken in
those first days.
By the end of the first week operation cover up
was well on its way. The panic-stricken state gove
rnment seemed more concerned about absolving
itself of any responsibility for the disaster than about
helping the victims. What is most shocking is that
a section of the medical community collaborated
with the government in keeping medical information
under wraps. There was deliberate falsification of
records, x-ray and pathological reports were refused
to patients, autopsy reports were not given to those
concerned. In normal times such a gross disregard
for ethical practice would have been soundly con
demned. But in Bhopal it was and is justified as
being in the interest of controlling public panic and
anxiety.
40
Expert vs Expert : While people suffer
A full eight weeks after the disaster the
deleterious effects of the gas were still eviden*.
New signs and symptoms were appearing — damage
o the liver, kidneys, gabrahat, anxiety, depression,
loss of memory, confusion and lack of co-ordination
deafness and impotency By the end of the second
week there had been 8u0 doctors working in
Bhopal's 64 round-the-clock medical centres. But
two months after the disaster most of the state-run
operations were winding down. Mobile hospitals
were still plying but people had generally realised
the ineffectiveness of medicines. Many had turned
vendors of antibiotics, antacids and vitamins. At
no time had any attempt been made by the govern
ment agencies to give medical and health informa
tion to the public. People were distraught and
confused. Controversies abounded and the situation
was made worse by the cloak of secrecy.
Earlier the team sent by the Royal Common
wealth Society for the Blind had asserted that no
permanent damage or blindness was likely to result.
American opthalmologists were of the opinion that
opacities were highly likely to develop in the centres
of the corneas thus affecting sight.
The ITRC team reported that the delayed effects
and neurological symptoms perhaps indicated the
presence of phosgene as well. They also reported
that pulmonary fibrosis was a possibility in the
survivors. American experts saw clinical evidence of
diffused lung damage. Others denied that there
could be any permanent damage — they attributed
the high incidence of lung complications to the
previously existing high rates of tuberculosis and
other chronic lung problems. In Bombay Dr. S.R.
Kamat was reported to have found evidence of
permanent pulmonary damage, of changes in
haemoglobin and neurological damage in gasaffected patients at the K.E.M. Hospital there. These
patients were put on levamesol (so far used as an
anti-helminthic) and the results were said to be
promising. But the full report is yet to be published
or presented.
Around this time another controversy which had
been brewing for some time erupted. And it reads
like a horror story. Since the second week there had
been reports of stillbirths and abortions among the
affected pregnant women. Some Hamidia doctors
had reported finding traces of phosgene in the
aborted foetuses. Abortions in gas-hit animals had
also been recorded. Defence Ministry sources were
quoted as saying that MIC was known to cause
Socialist
Health Review
damage to the foetus. Although the Sultania Zenana
hospital had set up a special antenatal unit, most
of the distressed and anxious women were turned
away with assurance that the babies were safe. A
survey in February / March of 1,900 households
showed 100 cases of abortions and 22 stillbirths.
Neither the government nor the medical pundits
were willing to concede that there just might be
some danger to the foetus either directly because
of the toxic gas or indirectly because of the mother's
health conditions. Given the state of knowledge at
that time all one could have done was to offer
facilities for amniocentesis examination and ultra
sonography and abortion services to those who
opted for it. This did not even necessitate a stand
being taken on whether MIC affected the foetus or
not. But the authorities consistently brushed away
these suggestions made by activist and health
groups. When the Medico Friend Circle fact-finding
team report in February suggested such a course of
action, the bigwigs of medicine came down heavily
on it for causing'unnecessary panic'. In February
two members of the Medico Freind Circle conducted
a clinic-based study of gynaecological problems
among the affected women in two bastis. They
found high rates of menstrual disturbances, non
specific white discharge and evidence of pelvic
inflammatory diseases. Up until then these conditions
had neither been recorded nor reported. But again,
no efforts have been made to set up special bastibased clinics or centres for women.
Medical Research in Bhopal
Not until January did the ICMR and other
research agencies meet to work out the strategy for
studying the impact of MIC. In the same month
irked by the heavy atmosphere of secrecy leading
newspapers had carried severe editorials criticising
the ICMR's unwillingness to divulge relevant infor
mation. Perhaps as a result of this or because the
lines of authority had now become clear, the ICMR
released a first report on Bhopal. Unfortunately the
report said little but listed out the various projects
which had been approved. Surprisingly no compre
hensive plan of research has been prepared nor
priorities
determined ! Research projects have
apparently been sanctioned on ad hoc basis. Despite
the Director General's earlier announcements there
was no large-scale epidemiological survey listed.
Earlier the MP government had instituted a detailed
medico-social survey by the Tata Institute of Social
Sciences in Bombay under strict surveillance and
superivsion of the government authorities. For some
unstated reason only a small portion of the survey
was reported to have been completed, the rest
June 1985
being taken over by the government. And so there
will never be a full-scale epidemiological survey of
the consequences of the world's worst industrial
disaster.
According to the ICMR's latest update, it has
funded twenty projects with a total budget of
over 156 lakhs. Only three of the projects are
of less than two years duration. ICMR's ad hoc
approach will certainly result in a series of research
monographs years from now, but how much will
it help the affected population ? In all likelihood
they will never even hear about the results. The
ICMR should have made it manadatory for all
projects which dealt directly with the affected
population to include a 'health education' comp
onent. If it had, we would not have the situation
existing today of people being prodded, poked/
examined x-rayed, and bleeded but never being
given any information or advice about their health,
their pregnancies. Bhopal's affected population is
being treated by researchers as a set of guineapigs
in a gigantic laboratory.
In the middle of February the ICMR finally
released the results of its NaTS double-blind
trial and issued a notification recommending NaTS
to those in whose families death had occurred;
those living within a radius of two km of the
factory and those with specified symptoms such
as nausea, tachycardia (high pulse rate), anorexia
(lack of appetite) and so on. But the state govern
ment took no action on this until April when
the ICMR issued a further set of guidelines. The
centre could undoubtedly have acted to get the
state to implement this decision. But it has conspi
cuously and distressingly kept out of the health
scene in Bhopal.
There are some in the scientific and medical
community who believe that debate on scientific
and medical
issues must be confined to the
pages of scientific journals or seminars. The
establishement's desire and its need for con
trolling information supports this archaic notion.
In Bhopal this combined stand of the state and the
professionals has had disastrous consequences for
the people.
( Most of this material has been drawn from articles in
newspapers and periodicals written by a number of people*
Some of them are Kannan Srinivasan and Kalpana Sharma*
Indian Express, Radhika Ramaseshan and Jyoti Punwani, Sunday
Observer, Praful Bidwai. Times of India, Darryl D'monte, Ill
ustrated Weekly and Arun Subramanyam, Business India. Other
material utilised : ICMR's Update on Bhopal, Rani Bang and
Mira Sadgopal's report of the study of gynaecological problems
MFC fact finding team's February report. ICMR's press rele
ases and minutes of the February meeting.)
4*1
Bhopal Disaster : Bibliography
Animal and human responses to MIC. U.C. Pozzoni and E.R. Kinkhead. Archiv Toxicologie, 1964 11 pages
2. Toxicity of MIC and how to determine its quantity in air. G. Kimmerle and A. Eben Union Carbide Chemicals. 1964. 8 pp
3. Range finding tests on MIC. Mellon Institute Special report. UCC Fellowship. Aug 12, 1963. Report 26-75. 6 pp
4. MIC — Acute Inhalation : Human response to low concentration, guinea pig sensitization and cross sensitization to
other isocyanates. E.R. Kinkhead U C. Pozzoni, L.J. Sullivan Mellon Institute. Chemical Hygiene Fellowship. Special report
33-19. 1970. 8pp
5. Congenital malformation induced by infusion of sodium cyanide in the golden hamster. P.A Doherty. V.H. Form and
R. P. Smith. Toxicology and Appld. Pharmacology 1982 9 pp
6. Long term toxicity and carcinogenecity studies with 2,472,6 Toluene diisocyanate (80/22) in rats and mice. E. Loeser.
Toxicology Letters 1983. 11 pp
7. Health effects of exposure to toxic gas at Bhopal : An Update on ICMR sponsored research. 10.3.1985. 31 pp
8. MIC : Chemistry, fate, pharmacological and effects. Serbjeet Singh. Drug Information Desk. Department of Pharmacology
Gandhi Medical College Bhopal, 24.3. 1985
9. Isocyanate induced pulmonary diseases : A current perspective. L. Bernstein J. Allergy. Clin Immunology. July 1982.8 pp
10. Disaster at Buffalo Creek. Am J. Psychiatry March 1976. 22 pp (Several papers describing studies on psychological
trauma after the Buffalo Creek disaster in the US)
If you would like to obtain copies of any of the above documents please write to us sending 0.50p per page, in advance. If the
number of pages exceeds 30 please add Rs. 5.00 postage (ordinary book post).
(For MFC fact finding team's February report and for information on its forthcoming report of the medico-social survey
in Bhopal, write to Dr. Ravi Narayan, 326 V Main, I Block, Koramangala, Bangalore 560 034)
(Contd. from page 37)
In Britain, Roche was sued for abusing monopoly
power by its pricing of Valium and Librium. In outof-court negotiations in 1975 Roche agreed to pay
3.7 million dollars for over-pricing their product in
the previous live years and also agreed to reduce
the price at half the level of 1970. The importance
of this case was that it focussed international atten
tion on overpricing and anticartel suits followed in
various countries.
(4) Upjohn and A. H.
Robins : Upjohn's
Depo-Provera, an injectable
contraceptive for
women, was found through early American research
to be associated with such a welter of side-effects
that the FDA has not only indicated that the product
is not approvable in the US, but has forbidden
human testing of the drug in the US. But huge
quantities are being dumped on the third world.
Throughout Central America one can walk into a
pharmacy and purchase Depo Provera without a
prescription. Earlier even most of the testing of the
drug was done in third world countries like Brazil,
Thailand, Chile, Philippines, Sri Lanka, Hong Kong,
Egypt, Honduras, Peru, Mexico and Pakistan. "When
research into its possible effect on the weight and
blood pressure of women taking the injections was
carried out in South Africa, the researchers saw fit
to examine these features by experimenting with
Negro (75 percent) and Asiatic (25 percent) women,
rather than on women with the same coloured skin
as the researchers".
Similarly A. H. Robins has dumped Daikon
Shields, an IUD, in some 40 third world countries.
42
It was recalled from the American market after
17 women were killed. In an enquiry later it was
revealed that in the teststage physicians had re
ported unfavourable effects like uterine perforation
and ectopic pregnancies.
The staggering thing about the dumping in
the third world in this case has been the invo
lvement of the US government's office of Popula
tion with the AID. USAlD purchased the contra
ceptive device at discount rates for assistance
to developing countries after the product was
banned in the US. Double standard for third world
consumers were even more remarkable when
Robins sold USAID unsterilised shields in bulk
packages at a 48 percent discount. USAID justi
fies the discount Daikon dump on the grounds
of getting more contraception for the dollar.
Ravi Duggal
D-3, Refinery View
62 63, Mahul Road,
Chembur, Bombay 400074
References
Braun, Dorit, Pharmaceutical Transnationals in Columbia, Ph.D,
thesis, quoted in Dianna Melrose, Bitter pills. 1980.
Faltorusso, V. Essential Drugs for the Third world World Health,
May 1981.
Haslemere Group, Who Needs the Drug Companies, London.
Mahler, Halfdan, World Health Forum 2 (i), 1981.
Melrose, Dianna. Bitter Pills, OXFAM, Oxford, 1982.
Mintz, Morton By Prescription Only (earlier Therapeutic Nightmare),
Houghton-Miffin, Boston, 1967.
United Nations Centre on Transnational Corporations (UNCTC),
Transnational Corporations and the Pharmaceutical Industry,
United Nations, New York, 1971.
UNIDO, Global Study of Pharmaceutical Industry, United Nations,
1980.
Vaitsos, Constantine, Inter Country Income Distribution and Trans
national Enterprises, Clarindon Press, Oxford, 1974.
Socialist Health Review
DIALOGUE
Whq The Scope of SHR Should Be Confined to Heolth & Medicine
Anant Phadke and Dhruv Mankad
The sharp yet substantive comments on the
first issue of SHR by Imrana Quadeer and Bharat
Patankar/Jogen Sengupta (in "Dialogue' SHR 1.3)
are welcome and raise hopes of SHR becoming a
forum for debate also.
We are responding to
Imrana Quadeer's criticism to clarify and defend the
standpoint taken by SHR to restrict the scope of
SHR to discussion on Health and Medicine. At the
same t:me we offer some critical comments on the
material published in the first two issues.
Though we agree with many of Imrana's points
of criticism and with her plea for greater analytical
rigor, we want to point out that the errors she has
pointed out do not flow from the decision of SHR to
restrict itself to health and medicine. Her criticism
on this point flows from her own confusion.
The dominant bourgeois ideology considers
Health and Medicine as primarily technical issues;
and if and when it considers social aspects, it glo
sses over, hides the role of the essential lelations
("economic base") and the class struggle flowing
from it. On the contrary in the first issue the Edi
torial Policy of SHR clearly states our standpoint
that "From a marxist standpoint, health can be
considered as a part and consequence of economic,
political and socio-cultural development of society.. "
(three more sentences on similar lines). Any
discussion on Health and Medicine within this pers
pective would necessarily be based on an under
standing of society in general. Within the left,
different individuals, organisations have differences
in their understanding of the society in general and
these differences would naturally reflect in their
analysis of issues in Health and Medicine. A rigo
rous, correct understanding of Health and Medicine
would not be possible with a superficial under
standing of society and hence Quadeer is mistaken
when she says that "It seems to me that a debate
concentrating on health and medicine alone, however
rigorous, tends to treat these general concepts
superficially." If somebody disagress with a particular
piece of analysis of Health published in SHR, one
can show how that analysis is wrong by discussing
that particular issue in Health and may also comment
upon the basic understanding of the person being
criticised but there is no point in having a debate
in SHR on the nature of the Indian State, or of
June 1985
imperialism. Debating on concrete levels is not
"an easy way out" as Quadeer thinks. Since a
discussion on health and medicine within the left is
relatively new, it is a more difficult path chosen by
SHR compared to the option of publishing in SHR
debates on general issues in
Marxism. Let us
illustrate our point by taking the same example of
Amar Jesani/Padma Prakash's article
The main weakness of this article is not that it
has focussed on "Health and Medicine alone", but
that, on the contrary, it has unnecessarily spent
about three pages on some of the details of quest
ions like the strength of the Indian bourgeoisie, the
strategy of economic development after Indepen
dence and so on. This exposition of strategy of
economic development is not organically integrated
in their analysis of health and medicine in post
colonial India. For example, for their discussion of
malaria and tuberculosis control programme, the
details about number of strikes on the morrow of
Independence, or evictions of tenants during the
agrarian transformation etc were not necessary.
The space devoted to these details could have been
better spent on arguing as to what exactly was
wrong with these health programmes, what were
their contradictions and so on. We are only told that
they are death-control programmes (is this bad?)
and that they have been used to divert the attention
of the people by equating disease eradication to
technical measures. It is not made clear as to what
exactly is wrong with these programmes. Would
not there be a malaria control programme or BCG
vaccination in a socialist society? Is it that the pro
gramme was correct but that its purpose and
ideological use is being criticised ? Or is it that the
theoretical basis and the very organisation of these
programmes is also being questioned? We need to
take community medicine much more seriously. We
need to study and identify how bourgeois ideology,
interests, seep into the existing discipline of com
munity medicine, and how a marxian approach can
remedy this discipline into a fully scientific discipline
which in turn would lead to appropriate health
interventions as an adjuvant part of socialist transfor
mation. If this is done, (and this is "not an easy
way out") our criticism of the existing health
system would be much more substantial and
concrete. (This is of course, a collective responsi
43
bility of all of us and hence it is not at all question
of merely pointing out mistakes of those who have
ventured to come forward with whatever analyses
they have.) However, we also believe that a rigorous
analysis of the concrete — Health and Medicine
keeping in mind its dialectical relationship with the
society at large should and can point to the general
direction of one's analysis of the society as well.
Amar-Padma's article fails to do so. Instead their
analysis of health and medicine is disjointed from
their analysis of Indian society. The two analyses
are merely juxtaposed without any obvious inter-
re’ationship having been established. It is a much
more demanding task since in India, such questions
have so far not been discussed within the left with
any depth.
What is the implication of Quadeer s suggestion
not to leave out issues of wider social order? To
continue to take the case of the article by Amar
Jesani/Padma Prakash; such a suggestion would
logically mean that if somebody does not agree
with (for example) the authors' analysis of the
strength and independence of Indian bourgeoisie he
would go into that question and put forward a
criticism and give an alternative. SHR would then
read like an EPW, or a Social Scientist; and not a
journal on Health and Medicine. On the other hand
she could concretely analyse the health issues from
one's political point of view and present an alter
native view on political economy of health, thereby
refuting at the same time the author's viewpoint
regarding e.g, the strength and independence of
Indian bourgeoisie.
the task ot SHR ''to develop an analysis of society
as well."
Articles in SHR need to be accurate on the
technical matters as well. We would only register
our strong reservations about C
Satyamala's
analysis of dysmenorrhea (painful menstruation)
See her incorrectly titled article: Is Medicine Inher
ently Sexist? SHR I : 2) At least our textbooks and
teachers did not teach it the way Satyamala has put
it. We also want to register our surprise about the
way Srilatha Batliwala (Rural Energv Situation) SHR
1:2 has arrived at the caloric intake of afamily(pp75)
and used it as a basis for her startling conclusion of
a daily deficit of 100 Calories for a woman and a
surplus of 800 Calories for a man. One can't take
up these questions in this short letter. We hope,
somebody else would take up these questions in
some detail.
Dhruv Mankad
877, Joshi Galli
Nipani-591 237
£ <2 E
Those "doctors and other health-workers who
were attracted to marxism because in it we found a
better approach to handle our own contradictions
and for relating ourselves to the wider society...”
would definitely find SHR very meaningful if it
contains analysis of their own field from a wider
perspective of historical materialism. The first three
issues of SHR have demonstrated this by analysing
different aspects of health and medicine on a wider
basis without however getting involved into a dis
cussion on the mode of proauction or the nature of
the Indian State. We very much believe that the
concepts of historical materialism need to be grasped
and used accurately, rigorously (otherwise one
makes statements like
since a mode of produc
tion is reproduced not only at the economic but
also at the political and ideological levels..." a
statement betraying confusion between "mode of
production” and "social formation.”) but it is not
44
Socialist Health Review
RACE AND HEALTH CARE
Perspective from Chicago
bindu t desai
In the past 30 years the US expenditure in health care has multiplied several times now amounting to
more than one billion dollars per day. This fantastic growth has not led to a dosing of black-and-white health
differentials The health care system mirrors the racism and inequalities in American society. This aft ide
begins with a ‘tour' of a medical centre complex in Chicago's financial and business district where the racial
divide from a white, privafe luxurious hospital to a non-white, public, run-down hospital is unashamedly
acknowledged It goes on to show how black health statistics which had improved are now undergoing a
reversal, and the Reagan administration's health budget cuts drastically affect the poor and the blacks. The
oppression and exploitation of racial minorities is not unique to the US. The status of blacks in the US and the
treatment meted out to them has obvious parallels to the situation of da Iits in India. This article, we hope wb!
motivate similar studies of casteism, communalism and sexism in the Indian health sector.
The United States and South Africa are the only
two industrialised countries in the world lacking a
system that guarantees medical care for all who
need it. The past 35 years have seen an exponential
growth in the United States both in the general
economy and in the expenditure on health care
which by itself now amounts to more than one billion
dollars per day (Blendon and Altman, 1984). This
growth has not led to equal access to health care
or to a closing of black-white health differentials.
This perspective will examine health care in
the US at different levels.
First we will tour the
conglomeration of hospitals and universities known
as the Medical Center on the west side of ChicagoThe outward differences noted on this tour will be
shown to accurately mirror the larger racism and
inequality in American society. We will then examine
population-based health statistics as they pertain to
race. After discussing medical education and
affirmative action (the rough US equivalent of a
reservation system in medical schools) we will
analyse future trends in US health care.
A Tour of the Medical Center
About a mile west of the Loop. Chicago's
financial and business district, lies the sprawling
Medical Center complex comprising two medical
schools, four major medical institutes and said to
contain, with typical American hyperbole, "the
largest collection of medical expertise in the world."
The apex of this medical pyramid is the Rush
Medical school with its Presbyterian-St. Luke's
Hospital (PSL).
This complex occupies six buildings, four of
which were built in the last 10 years, elegant
hulks of steel and aluminium, spacious, airy, the
newest resembling a Hyatt hotel, complete with an
June 1985
atrium and indoor plants. Across the street from
PSL is the bottom of the pyramid. Cook County
Hospital (CCH). Consisting of eight buildings, a
complex built at the turn of the century, CCH is the
only institution for the poor of the Chicago area.
Unlike PSL there are no carpets in the foyer of CCH,
no cushioned chairs either. When one crosses Harrison
street, one crosses the racial divide in the US from a
white, private, luxurious hospital, to a non-white, public,
run-down, hospital. A casual visitor cannot fail to
notice that something very fundamental has changed
in that short walk across a street.
A block away from CCH is the Abraham Lincoln
School of Medicine affiliated with the University
of Illinois (U of I) Hospitals. The medical school
and hospital are run by the state of Illinois. They
too have spanking new buildings, neat columns of
cement and glass that are centrally air-conditioned,
along with old red brick structures that house the
prestigious Neuropsychiatric Institute and the old
hospital. At the south-west edge of the Medical
Center is the West Side Veterans Administration
(VA) Hospital, an institution run by the federal
government. The U of I hospitals and the West Side
VA form the body of our pyramid.
These four institutions cover the different types
of hospitals in the US except for the newest and
fastest growing type of hospital — the for profit
hospital — a separate entity in itself which we will
discuss later. PSL dominates the area in terms of
the facilities offered to the patient, both those
providing physicial comfort and the latest in medical
Investigative technology. At PSL there are no long
waits in the Emergency Department^ED). The patient
is admitted to a private or semiprivate room with an
attached bathroom, each bed has a television set, a
45
telephone, and the hospital is centrally air-condi
tioned. A patient who requires an x-ray procedure
or a visit to a subspeciality clinic is seen without long
delay. The waiting rooms of these clinicsare cheerful,
provided with magazines, and so on.
In contrast, CCH patients often have to wait
eight to ten hours before being seen in the ED. As
the hospital has very few semiprivate rooms, most
of the patients are in a large general ward. The
wheel chairs could very easily be exhibited in the
Smithsonian's museums, patients share a common
bathroom, bring their own television set or radio
and may use the few pay telephones that are
available in each ward. Except for the Intensive
Care and Trauma units there is no airconditioning.
The many buildings of CCH are unsatisfactory both
in summer and winter. The wards are stuffy and hot
in summer and draughty and cold in winter. Leaky
ceilings and falling plaster are not uncommon. In
fact the author's office, which is on thethird floor of
an eightstory building, was flooded after a thunder
storm and many books and journals were damaged!
The patientsat CCH wait for nearly everything—wait
to be seen by a physician, wait for the diagnostic
tests to be performed, wait for their medicines, wait
in the corridors and hallways of the hospital No
magazines are provided for these patients.
gone up from 114,262 in the first quarter of 1981
to 150,146 in the same period in 1984, an increase
of 24 percent whilst transfers of patients, largely
because of lack of third-party payment whether by
private or governmental agencies, have gone up
from 110a month to 9C0 a month (Pharmacy News
letter, I 954). There is the typical capitalist picture
of smaller private hospitals closing units and laying
off or dismissing staff whilst CCH becomes more
and more overcrowded (Kotulak, 1984).
Let us now leave the Medical Center and survey
the larger issues that determine the architecture'
the distribution and the racial composition of the
complex.
A Portrait of the USA
a. Demographic : The black population, which
has risen from 9.9 percent of the total in 1950 to
11.7 percent in 1980, forms 26 5 million of the US
total of 226.5 million people. The Southern states of
the US account for more than half of the total
black population, 14 out of 26.5 million. Blacks
have moved from the rural areas to the centie of
cities and the suburbs, whereas whites have moved
out of the centre of cities to the suburbs. In the
past two decades the population of farm workers
who are black has dropped from 16 percent to 4
percent. In 1970 seven major cities had a black
majority compared to seventeen in 1980.In an
additional 13 cities blacks comprised 45 percent to
50 percent of the total population.
CCH patients also have to wait before a Health
Systems Agency grants a certificate of need for
expensive x-ray equipment. The hospital was
amongst the last in the Chicago area to obtain a
CT scanner and paid PSL nearly 500,000 dollars
per year to use PSL's scanner. Presently PSL already
has the equipment for Magnetic Resonance Imaging
so that the trend of an "underfunded public hospital
spending some of its scarce resources to enrich an
already wealthy private institution continues''
(Schlosser and Cohen, 1981). PSL and CCH are the
two ends of the pyramid - the apex rich and power
ful serving largely white patients, the base poor,
relatively powerless serving largely black and
Spanish-speaking patients, mostly from Mexico
and Puerto Rico (Latinos). The U of I and.:iWestside
VA fall somewhere in between these two extremes
in their facilities and equipment though in neither
hospital are the patients forced to wait long, hours
in crowded halls nor do they have to be in a large
general ward.
The seventies saw a decline in the number of mate
headed family households from 73 percent to 63percent and
an increase in the number of households headed by women.
for blacks it rose from 31 percent to 47 percent, for whites
from 8 percent to 13 5 percent. Fifty-five percent of
all black children were born to unmarried mothers
compared to 9.5 percent of white children. Fortytwo percent of all black children lived in two-parent
families compared to 83 percent of white childrenForty-four percent of black children were living only
with their mother compared to 13.5 percent of white
children. Moreover, the marital status of these
mothers differed considerably by race: 29 percent
of the black mothers were single, 37 percent separted, 9 percent widowed and 25 percent divorced,
whilst the figures for whites are 7 percent, 29 per
cent, 12 percent and 52 percent respectively.
Since 981 when President Reagan began cutt
ing back on health expenditures, CCH has seen a
phenomenal rise in outpatient visitsand transfer of
patients from other hospitals. Outpatient visits have
b. Income : In 1975, the peak of a 25-year
upward trend, median black family income was 62
percent of white family income. By 1982 it had
dropped to 55 percent. Black families with incomes
Socialist Health Review
46
ten,
1
under 10,000 dollars rose fiom 36.5 percent of the
black total in 1970 to 40.5 percent in 1 980, whilst
the figure for white families remained stable around
16 percent. In the past decade, the poverty rates
have gone up for all races, for blacks from 31.4
percent to 35.7 percent, for Latinos from 22 percent
to 28.4 percent and for whites from 8.4 percent to
1 2.1 percent (Pear 1984). The income gap between
black and white families varies with the composition
of the household and work experience. When a
family has two earners black median income is
dollars 20,000 compared to dollars 25,000 for
whites (81 percent of white income) whereas for a
family headed by a woman, black median income is
dollars 7,425 compared to dollars 12.000 for whites
(62 percent of white income) (Hacker, 1 983).
Seven-and-a-half percent of black families earned
more than 35,000 dollars compared to 17.5 percent
of white families. At the highest income levels in
excess of 75,000 dollarsthere were 548,000 white
men (0.6 percent), 11,000 white women (0.01 per
cent), 4,000 black men (0.03 percent) and less than
500 (0.004 percent) black women. The programs of
the past 20 years that were meant to aid minority
businesses have had little impact. The total assets of
all minority business amount to less than 1 percent of the
assets of the Bank of America alone. The top 100 black
business listed in Black Enterprise together have
assets less than that of the 500th corporation listed
in Fortune Magazine's top 500 corporations (Stok
es, 1981).
c. Employment : The overall unemployment
rate which was 7.1 percent in June 1984 is 18
percent for blacks and 4.3 percent for black teen
agers. The proportion of black males participating
in the labour force has declined from 83 percent
in 1960 to 71 percent in 1980; whereas that for
black women increased from 48 precent to 53 per
cent, and for white women from 37 percent to
51 percent. Black Americans are over-represented in poor
paying jobs such as garbage collectors (b5 percent) and
household servants (54), whereas they form fewer than 1
percent of all elected officials, engineers, lawyers and
2.6 percent of all university professors and physicians.
The public sector is. a relatively better source of
employment for black college graduates. Fifty
seven percent of black male college graduates
were employed by the government, compared to
27 percent of whites. The figures for women are
72 percent of blacks and 56 percent of whites res
pectively. Whilst blacks comprise 14 percent of
the federal civil service they form 30 percent of
the army and 20 percent of all US defense forces.
June 1985
These percentages have doubled in the last decade.
However only 5.6 percent of the officers are black.
Black employment in the public sector is a matter
of necessity. The US labour market is generally
manipulated by big business to keep blacks out of
private sector jobs. They are discriminated against
in hiring and are forced to cake lower paying jobs
regardless of their qualifications. For instance, black
women with education similar to white men earn
only half as much as white men, and earnings of
black men are 70 percent of an equivalently qualified
white worker. Blacks have Io tv seniority because
of past discrimination where certain trades did not
admit blacks to their rolls, and they have less work
experience because of unemployment and denial
of equal training and educational opportunities. If
there were equal opportunity in the labour market
the black-white ratio of per capita earning would be
89 percent instead of 58 percent. The estimated
losses due to employment discrimination exceed
by a factor of 11 the estimated excess welfare
payments to blacks ^Swinton, 1983).
d. Crime and punishment : Blacks formed
22 percent of the total number of arrests made in
1980 and 48.5 percent of a total state prison
population of 272,348 in 1981. The US black
imprisonment rate of 498/100,000 population for
1981, which can be compared with South Africa's
471/100,000 for 1976. (King and Whitman, 1981),
is the highest in the world. The US white imprison
ment rate is 75/100,000. Forty percent of the prisoners
on death row are black. Since 1930, when records
were first kept, 405 blacks have been executed
for rape compared to 48 whites. This figure does
not include the men lynched by white mobs.
e. Education : In the past 15 years black
enrollment in colleges has doubled from 5 to 10
percent. Although 70 percent of their parents had
never attended college and 45 percent had not fini
shed high school, these parents by working at two
jobs and so on have guaranteed their children higher
education which they themselves were deprived of.
Government programs have also played a role but
the Reagan administration has cut back aid and
reduced spending for disadvantaged students by
17 percent and on loans by 27 percent (Pear 1984).
Twenty five percent of black college graduates,
20 percent of high school graduates and 30 percent
of high school dropouts were unemployed compared
to 6.6 percent, 6.4 precent and 16.4 percent (respec
tively of whites). For black students 45 percent do
not complete high school, another 30 percent gra
duate from high school and 25 percent go on to
college, whilst among whites the figures are 14
percent, 30 percent, and 56 percent, respectively.
The State of Black Health: The life expectan
cy for blacks (68.3) is shorter than whites (74.4)
by 6 1 years. The infant mortality rate for blacks
is twice the white rate, 21.8 vs 11.4 deaths per
1000 live births, a phenomenon attributable to low
birth-weight, pneumonia, and influenza, and effect
of maternal disease upon the newborn. However,
as Sullivan points out, "These averages obscure
some apalling figures in some rural areas and
inner cities of our country. For example, in Georgia
(in the Southern US) today the average life expec
tancy of blacks is 8.4 years shorter than that
for whites. In six rural counties in Georgia, the
life expectancy for black males is only 49.6 to
51.5 years whereas the average life expectancy
for white males in the same counties is from
59.5 to 69.6 years. In Kenya, one of the less
developed and poorer countries of the world, the
average life expectancy of the male population is
51.3 years, exceeding that in some rural counties
in Georgia. In 1980 in 50 rural counties among
Georgia's 159 counties, the infant mortality rate
for blacks was higher than 30 per 1000 live births
and in 16 counties the rate was higher than 43
per 1000. Similar rates are found in many rural
areas and inner cities all over the United States’*
(Sullivan, 1983). A black mother is three times more
likely to die of complications of pregnancy, labour
and puerperium than a white mother. A black mother
is more likely to have had very little or no prenatal
care. In spite of the severe social and economic
stresses on black families the incidence of recognised
child abuse is similar for blacks and whites, around
11/1,000
The incidence and causes of head injury differ
for blacks and whites, the black incidence for both
inner-city and suburban blacks being twice that of
whites (400 vs. 196/100,000). Interpersonal attacks
were either the leading cause as in inner-city blacks
(176/100,000) or the second most common (100/
100,000) as in suburban blacks compared to the
fourth most common cause for suburban whites
18/100,000) (Whitman et al, 1984). These head injury
figures convey only the tip of the iceberg. For ex
ample, in 1979 murder was the leading cause of
death to men 15 to 44 years of age in New York
City and black men in this age group had "... a 1
in 20 chance of being murdered, a rate that is twice
the odds of an American soldier being killed in com
bat during World War I " (Chicago Sun-Times, 1980)
Homicide is the leading cause of years of life lost
48
Death Rates (per 100 000 Population) Homicide According
to
Race and
Sex
1960
1970
1979
Total
5.2
9.1
10.4
Black Males
44.9
82.1
71.3
White Males
3.9
7.3
10.1
Black Females
11.8
15.0
14.3
White Females
1.5
2.2
3.0
(Source : U S. Department of Health and Human
Services Health , United States, 1982. DHSS publication No. (PHS; 83-1232 Washington D.C. : US
Government Printing Office Dec. 1982)
for non-white men in the US. Age-adjusted death
for homicide have climbed steadily in the past 20
years (see Table). As the table indicates, the homi
cide rates for black men are seven times that for
white men, whose rates are lower than those for
black women. Blacks have a higher death rate than
whites for 13 of the 15 leading causes of death.
Other significant differences are in diabetes, nephri
tis, septicemia and chronic liver disease and cirrho
sis, where the death rate is twice that of whites.
Deaths from cirrhosis increased by 50 percent for
whites in the past 25 years whilst for blacks they
increased 20 percent.
Let us look at some other health statistics.
Regular dental health care is usually unaffordable
(APH, 1982). In 1978, 82 percent of rural Southern
blacks did not visit a dentist. For a white family a
perfect set of teeth with the ability to flash a brilliant
smile is a status symbol, and middle-class families,
of either race, can spend nearly 1500 dollars, per
child for orthodontia. Semi-annual dental visits for
regular cleaning of teeth are routine for them, while
dental care is out of reach for poor families, black
or white.
When asked in 1978 to rate their overall health
and "well being" as part of a Federal National
Health Interview Survey, black females reported the
lowest level of positive well-being of all groups
37 percent compared to 70 percent among white
males. Access to health care is dependent on income
level. This strongly affects families headed by black
women as 71 percent of them live below the poverty
level compared to 40 percent for white and 51
percents for Latinos.
Government — sponsored
programs — Medicare and Medicaid and tax subsidies
for private health care have spent a trillion dollars
Socialist Health Review
since 1965. Yet 34 million people remain without
health insurance of any kind. Only 33 percent of
people with income below the poverty level are
covered by Medicaid, 27 percent have no health
insurance of any kind.
Uninsured blacks have a 42
percent lower Physician visit rate compared to
whites, lower rates of elective surgery, are less
likely to have a regular source of care, and have to
travei further to obtain care It is estimated that one
out of every four black adults suffers from hyper
tension. which develops earlier in blacks, is frequ
ently more severe and results in higher mortality at
a younger age. For black women of all ages the
prevalence of hypertension is equal to or higher
than that of black men.
Let us now turn our attention to the delivery of
health care. Though forming 12 percent of the
population, less than 2 percent of the faculties
of medical schools are black.
The
percen
tage of black physicians in the
country has
increased only
marginally from 2.1 percent in
1950 to 2.6 percent in 1980 Further, the propo icn
of black medical graduates has decreased in the
past four years from 793 out of 14,393 graduates
(5.5 percent) in 1978 to 763 out of 15,985 (4.8
percent) in 1982. Six medical schools in the US
have no black enrollment and in 75 (61 percent of
all medical schools) the black enrollment is less
than 5 percent. Black physicians, who have always
faced difficulties in getting hospital privileges, are
likely to face more difficulties in obtaining these
privileges as hospital administrators try to keep
hospitals financially solvent amidst cost-cutting
measures initiated by government and private health
insurance agencies. Black physicians tend to have a
patient load which is predominantly poorer, sicker
and less likely to bring in revenues to the hospital.
Administrators are expected to try to eliminate the
physicians who admit those kinds of patients —
another example of economic racism (AM News,
1984).
Note that the percentage of black physicians
has increased only marginallyeven with the positive
impact of affirmative action programs. The changing
and increasingly right-wing political turn which
began in the late 70's can be further expected to
decrease black enrollment. Additional factors that
will contribute to the decrease are of equal impor
tance. Black students in high school and college are
victims of a pervasive inequality in education. A
survey of high school students in the Chicago area
(which contains 92 percent of all minority students
in the metropolitan greater Chicago area) showed
June 1985
that 56 percent had seldom or never worked in a
laboratory, the dropout rate at high school averaged
47.4 percent and abouthalf of the graduating seniors
from high school were deficient in the rigorous
academic subjects that are required for medical school
(Orfield, 1984). The costof medical education rises
each year; in 1984 the average medical student will
owe a debt of 50,000 dollars Financial assistance
is becoming increasingly short with a very grave
impact on black students, 80 percent of whom
come from families earning less than 25,000 dollars
a year. At other levels of the health industry blacks
become more commonly represented as one descends
in the hierarchy. In the nursing sector blacks form
1 1 4 percent of the registered nurses, but 30percent
of the aides and orderlies.
The American Health Care Industry
Between 1 950 and 1982 US health expenditures
increased more than 25 fold. The proportion of the
GNP accounted for by the health sector has incr
eased from 4.4 to 10.5 percent (Ninzburg, 1984).
In the past 10 years the number of people employed
in the health sector has increased from 4.2 to 7.5
million. In sharp contrast to other sectors of the
economy the health industry has expanded unaffec
ted by any of the recessions of the past 30 years.
Hospital room costs have gone up by 515 percent
in the last 15 years and physician services by 311
percent. In 1981 hospital costs accounted for 41
cents of each dollar spent on health, physicians,
services for 19, dentists services for 6, drugs 8,
appliances 2. Other costs included nursing-home
care 8, public health 3, research?, new construction
3, and administration and others, 8. Health care costs
average 1500 dollars per American of which dollars
g06 come from private funds and594 dollars from
public programs.
For profit hospital chains, a relatively new
phenomencn, have grown and are expected to
own 20 percent of all hospitals by 1990. In 1982
the largest chain. Hospital Corporation of America,
owned 351 hospitals with 50,000 beds with reve
nues of 3.5 billion dollars, up 47 percent from
the previous year. Humana, Inc, another chain,
had 14 billion dollars in revenues with stocks worth
18 dollars per share in 1968 now worth 336
dollars (Starr, 1982). The for-profit hospitals, which
are touted as being more cost-effective, have
actually charged more per patient than their notfor-profit counterparts, whilst generating a very high
net income for their owners (Reiman, 1983). These
chains are also moving into outpatient centres
49
called Emergicenters or Urgent Care Centers, which
are open 12-16 hours a day, resemble the fast-food
chains in their appearance, and have a potential
market of between 2—5 billion dollars a year.
Health expenses in the US are met in two major
ways, either by private health insurance or by
government programs like Medicare and Medicaid.
In 1974 the national average expenditure per
non-white beneficiary was 57 percent lower than
that for white (321 dollars vs 560 dollars). As we
mentioned earlier. 34 million Americans are without
any kind of health coverage, because they are too
poor to afford private health insurance and earn
more than the minimum requirements to qualify for
government assistance.
The Indian Connection
The relationship between race and health care has
obvious parallels for India, such as the hospitals based
on class and the use of affirmative action in medical
education, which if similar to the reservation system for
Scheduled Castes and Tribes in India. Both in India
and in the US there is yet another link, lhe Indian
medical graduate (better known as F.M.G. or Foreign
Medical Graduate), either in training or practising in
the US. There are presently about 14,000 FMGs of
Indian origin in the US, forming 10 percent of all
FMGs and 3 percent of all physiciansin the US. Note
that there are more FMGs of Indian origin alone than
the total number of black physicians in the US. A
relatively large number of Indian doctors work in
inner-city or county hospitals which serve the urban
poor who are largely black. There is a decreasing
number of Indians as one moves into the 10 most
prestigious medical schools, the so-called Ivy League.
Black and Indian relations within the medical
system have not been marred by overt conflicts,
which is heartening considering the generally racist
attitude of most Indian physicians. The federal
government has backed affirmative action in admis
sions to medical schools though this backing has
never been whole-hearted and can presently be said
to be nonexistent. White attitudes to affirmative action
parallel those of caste Hindus in India. The very same
arguments are used - selection should be on merit,' con
cern is expressed for lowered standards of medical care,
and so on.
The presence of large numbers of Indian doctors
also strengthens relations between the Indian elite
and the health care industry in the US. They have
already begun to play a role in creating Americanmodeled hospitals in India like the Apollo hospitals
in Madras and Hyderabad and the proposed Modi50
Hospital Corporation of America hospital in New
Delhi.
Conclusion
Black health statistics which improved in the
60s and 70s as a result of political changes
stemming from the civil rights movement which
stimulated government programme appear to have
peaked and a reversal may have begun. The
statistics of black health must be viewed in light
of the moneys poured into health care in the past
30 years. In that unprecedented period of economic
growth when real income doubled for most Ameri
cans, medicine was an "important ideological prop
for the ruling class in the maintenance of the
domestic tranquility and social stability needed for
production and profit . . . health care has been
used by the ruling class to cushion some of the
most savage aspects of capitalist industrialization
and forestall more radical working-class demands"
(Himmelstein and Woolhandler, 1984).
But the stagflation of the seventies has heralded
some fundamental changes in government policies.
lhe Reagan adminstration has cut the health budget
and reduced funding for education for poor and
handicapped people by 20 percent (Stokes, 1981).
Maternal and child health received 25 percent less
federal money in 1982. A rise in the overall foetal
death rate from 10 2 to 12.2 per 1000 from 1979 to
1981 maybe the first indication of the effects of
present cost-cutting measures (Pouissant, 1983).
The increase in the number of black people
below the poverty line, the general low income of
black people, the poor opportunities for advancement
in employment are not features that are unique to
the US. A recent
publication
from
England
(PSU, 1984) describes the black population as
occupying the same "precarious and unattractive"
position in society as in the50s The British National
Health Service encourages a "ghettostyle" employ
ment pattern with hospitals having British porters,
Spanish cooks and West Indian domestic staff
(Lancet, 1984). Doubtless the pattern can be
documented in other white nations with regard to
their racial minorities — Turkish in West Germany,
Algerian in France, Maoris in New Zealand and
Australia, leading to the conclusion that "Racism
is not a 'mistake' or a 'failure' of this society — it is
one of its great successes" (Cooper, 1983).
As the US changes to an hour-glass economy,
a large section of the population will be left in lowpaying dead-end jobs. In August 1984 the US
Socialist Health Review
Census Bureau showed that the number of Ameri
cans living in poverty had risen to its highest
level in 18 years. As a result of Reagan Admi
nistration tax policies, families earning less than
1 0,000 dollars annually suffered a net loss of dollars
400 or 4 percent of income, whereas those earning
over 80,000 dollars gained 8,270 dollars or about
10 percent. This will further limit the number of
blacks who can climb out of the poverty and
degradation they are born in'o. Increasingly large
US cities have a blask majority population. The
white exodus from the cities is matched by a loss
in jobs in the manufacturing, wholesale, retail and
service industries. In the past 10 years alone New
York, Chicago, Philade'phia and Detroit have lost a
million jobs with white unemployment levels staying
relatively static whilst black unemployment levels
have zoomed to nearly 55 percent for teenagers.
These trends are likely to continue.
"Profit has made A nerica what it is" is the proud
slogan of American capitalism, which wishes to be known
by its new, gleaming, dazzling, forprofit hospitals where
the birth of a baby is celebrated by the parents with cha
mpagne. In their shadow lies the decay of overstrained
public hospitals serving non white citizens and bearing
an uncanny resemblance to large municipal hospitals in
India. Their burden will be greater than before as
for profit hospitals both "cream" off capital and
resources and leave to them unprofitable diseases
and the care of minorities and poor people.
(This work was supported in part by the Epilepsy in the
Urban Environment Project, Centre for Urban Affairs and Policy
Research, Northwestern University Evanstan, IL)
References
American Medical News. Black MDs lambast Reagan policies.
August 17, 1 984 p.8.
American Public Health Association. Health of Minorities and
Women, August 1982
Blendon, R.J and Altman, D.E. Public attitudes about health
care costs. New England Journal of Medicine. 311:613-616,1984
Chicago Sun-Times. Murder top death cause to men 15 to 44 in
New York January 16, 1980
Cooper, R. Race and the social origins of disease. Radical
Community Medicine. 16: 5-19, 1983
Ginzburg, E. The modernization of medical care. New England
Journal of Medicine. 310:1162-1165, 1984
Hacker, A (ed). U.S. A statistical portrait of the American peopleViking/Penguin, New York, 1983
Himmelstein, D.N. and Woolhandler, S. Medicine as industry:
The health care sector in the United States. Monthly Review,
35:13-25, 1984
King L. N. and Whitman, S. Morbidity and mortality among
prisoners : an epidemiologic review. Journal of Prison Health
1 : 7-29, 1981
Kotulak, R. Hospitals face closings. Chicago Tribune. July 22,1984
Lancet. Black and White Health. Notes and News, 2:115, 1984
Orfield, G. Chicago Study on Access and Choice in Higher Education.
Report to the State Senate Committee on Higher Education.
Springfield II. 1984
Pear, R. Reagan has achieved many goals, but some stir
opposition. New York Times, August 20, 1954
Pear, R. Rate of poverty found to persist in face of gains
New York Times. August 3, 1984
Pharmacy Newsletter. Cook County Hospital, July 1984
Policy Studies Unit, Black and White Britain, London, 1984
Pouissant, A.F The mental health status of blacks in The state of
Black America 1983. Ed. Williams, J.D. National Urban League,
Inc.. Ny 1983
Reiman, A. Investor-owned hospitals and health-care costs. New
England Journal of Medicine, 309; 370-372, 1983
Schlosser, J and Cohen, R.L. Failure of CT Sharing. New
England Journal of Medicine, 305: 829, 1981
Starr, P. The Social Transformation of American Medicine. Basic
Books, New York, 1982
Stokes, L. Address to Training Institute for Special Programs {TRIO)
Projects Personnel, April 1981. Minneaplis.
Sullivan. L.W. The status of blacks in medicine. New England
Journal of Medicine. 309: 807-808, 1983
Swinton, D.H. The economic status of the black population, in
The State of Black America. 1983, p. 76-77.
Whitman, S, Coonley-Hoganson, R. Desai, B.T. Comparative
head trauma experiences in two socioeconmically different
Cnicago-area communities: A population study. American
Journal of Epidemiology. 119: 570-580, 1984
Dr. Bindu T. Desai
221
Oak
South Oak Park Ave
Park
Illinois-60302 (USA)
(Contd. from page 30)
42. Two particular issues of the Journal of Occupa
tiona! Medicine detail tasks for corporate medical
directors: a special section on "Cost Effectiveness
of Occupational Health Programs" In JGM 16:3,
March 1974: and a special issue on "HMOs and
Occupational Medicine" in JOM 17:10, October,
1 975. See also Jesse Steinfeld. "The Workplace as a
Health Care Resource," JOM 12 8. August 1970, pp
315-317: Robert O'Connor, "The Role of Industry
in the Health of the Nation." JOM 10:3, March 1968,
p. 379: and J. Williamson and M. van Nieuwenhuzea,
"Health Benefit Analysis: An Application in Industrial
Absenteeism. "JOM 16:4, April 1974. pp. 229-223.
43. For an excellent discussion, see: Sander Kelman
"The Social Nature of the Definition problem in
Health" IJHS 5:4, 1 975, pp. 625-642.
51
INDEX TO VOLUME I, 1984-85
Amniocentesis and female foeticide — Misuse of Medical Technology by Vibhuti
69
Patel
Assault at the Workplace by Ramana Dhara (Editorial Perspective)
The
Bhutali
93
Phenomenon — Why are Women Hunted down as Witches ?
88
by Kashtakari Sanghatana (Problems of Praxis)
A Bizarre Medley of Carrots by Vimal Balasubrahmanyan
179
The Black Lung Movement by L R (Loy Rego)
100
Campaign Against Long Acting Contraceptives (filler)
170
Contraceptive Research in India — Testing on Women by Kusha
166
A Cultural Critique of Modern Medicine by Anant Phadke (Review Article)
45
Death on the Job by A. D'mello (Review Article)
138
The Disaster by Anurag Mehra — A reaction to the tragedy at Bhopal
Give us an Answer by Bhaskar Jadhav (Poem)
146
2
Cover
Hazards of Agricultural Work — A case study from Punjab by People's Health
Group
126
Health Care in a Revolutionary Framework : Possibilities for an Alternative Praxis
by Binayak Sen and Ilina Sen
24
Health of Women in the 'Health' Industry by Sujata Gotoskar, Rohini Banaji and
Vijay Kanhere
78
Illness and Accident Reporting in Industry — A Review of Statistics and
1 10
Legi-
slation in India by Jean D'Cunha, Loy Rego, Mihir Desai and Vijay Kanhere
Is Medicine Inherently Sexist ? by C. Sathyamala
53
Marxist View of Health and Medicine — A Rejoinder
by Bharat Patankar and
130
Jogen Sen Gupta (Dialogue)
A Marxist View of Medical Care by Howard Waitzkin
4
Motivation for Family Planning A short critical review by Ilina Sen
173
Need for Analytical Rigour by Imrana Quadeer (Dialogue)
132
Orwell's Hints to Writers
(filler)
28
Politics of the Birth Control Programme in India by Sucha Singh Gill
Political
Economy
of
Health
Care
in
India -
An Outline
160
Amar Jesani and
29
Padma Prakash
Politics of Health and Safety by Anurag Mehra and Sandeep Agarwal
Population Control :
Perspective)
For or
Against
People ?
by
Manisha
102
Gupte (Editorial
141
The Price of Assistance — The Family Planning Programme in India by Ramala
148
Buxamusa
The Printed Word — Newsclippings on health and medicine
Protest Against Marxist
Male
chauvinism
96,145
68
(Response) by Ilina Sen and Reply
by Dhruv Mankad
Push Back the Catastrophes by Jayne Cortez (Poem)
Reply to Vasantha Kannabiran (Response) by Dhruv Mankad
Cover
3
171
Reply to Vasantha Kannabiran (Response) by Working Editors
172
Response (to Ilina Sen's letter) by Vasantha Kannabiran
171
52
Socialist Health Review
Response by Bruno Vitale
172
Roots of Women's III health by Padma Prakash (Editorial Perspective)
49
Rural Energy Situation — Consequences for Women's Health by Srilatha Batliwala
72
Rural Energy Situation : Consequences for Women's Health — A comment (Dialogue) 190
The Study of Women, Food and Health in Africa by Meredeth Turshen
82
Theories of Reproductive Behaviour — A Marxist Critique by Martha Gimenez
182
Towards a Revolutonary Approach to Health by Dhruv Mankad (Editorial Perspective)
1
Why don't we organise by N. Janakiramaiah (Response)
68
Women, Health and Medicine by Barbara Katz Rothman
58
"Women's Health is Women's Concern'' - A Brief Overview of Health Issues in
65
the Women's Movement by Nirmala Sathe
cover
A Worker's speech to a doctor (poems)
1
[Please note : Issue no. 1 (Politics B Health) covers pp. 1-48; Issue no. 2 (Women B
Health) pp. 49-92; Issue no. 3, (Work B Health) pp. 93-140; and Issue no. 4, (Politics of
Population Control) po. 141-192]
AUTHOR INDEX
Agarwal, Sandeep
Balasubrahmanyan, Vimal
Banaji, Rohini
Batliwala. Srilatha
Brecht, Bertolt
Buxamusa, Ramala
Cortez, Jayne
D' Cunha, Jean
Desai, Mihir
Dhara, Ramana
D'mello, A
Gill, Sucha Singh
Gimenez, Martha
Gotoskar, Sujatha
Gupta, Narendra
Gupte, Manisna
Jadhav, Bhaskar
Janakiramaiah, N
Jesani, Amar
Kanhere, Vijay
Kannabiran, Vasantha
Kashtakari Sanghatana
Kusha
Mankad, Dhruv
Mehra, Anurag
Patankar, Bharat
Patel, Vibhuti
People's Health Group
Phadke, Anant
Prakash, Padma
Quadeer, Imrana
Rao, Shobha
Rego, Loy (LR)
Rothman, Barbara Katz
Sathe, Nirmala
Sathyamala, C
Sen, Binayak
Sen Ilina
Turshen, Meredeth
Vitale, Bruno
Waitzkin, Howard
Working Editors
102
179
78
72
Cover no 1
148
Cover no 3
110
110
93
138
160
182
78
191
141
Cover no 2
68
29
78.110
171
88
166
1, 71, 171
102, 146
130
69
126
45
29,49
132
190
100,110
58
65
53
24
24, 68. 173
82
172
4
172
Voices of Silence
I’m nine years old
And I'll never die
One winter night
while I slept
and dreamt of
enchanted morns
piping hot jelebis
warm blankets
bright green kites
and blood red kurtas
a monstrous shroud
of sticky white fog
smothered me in a
terrifying embrace
endless, eternal.
In another time
and another place
I was nine years old
and did not die.
One August day
forty years ago
a mushroom cloud
rose from the earth
killed thousands
maimed millions
wiped out generations
embalmed me
for ever.
I'm nine years old
And I II never die
I'll haunt the ghouls
who thrive
on the blood of
men, women and children
I'll echo the
sobs, screams and gasps
of toilers in pain
the eerie
silence
of premature death
And I'll never die.
I'll sit on your
shoulder for generations
I'll goad you, worry you
anger you,
and never let you go
until you create a world
where Bhopals
and Hiroshimas
are mere nightmares
of a distant past
never to recur.
Until then.
I'm nine years old
And I'll never die.
—padma prakash
Position: 3092 (2 views)