RF_COM_H_5_PART_1_SUDHA..pdf
Media
- extracted text
-
H 5.4
RF_COM_H_5_PART_1_SUDHA.
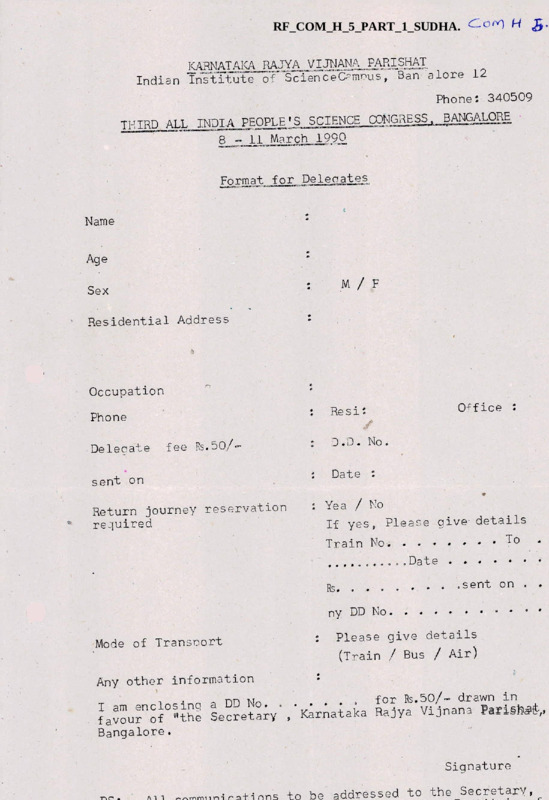
KARNATAKA RAJYA VIJ1JANA^.£ARISHAT
Indian Institute of ScienceCamnus, Ban a lore 12
Phone: 340509
BANGALORE
THIRD^ALLL INDIA PEOPLE'S SCIENCE CONGHESS
8^.±lJ^arch_1990
£ormat__for,..Deleoates
Name
Age
M / F
Sex
Residential Address
Occupation
Re si:
Phone
Defecate
Office :
/
D . D • No .
fee Rs.50/
Date :
sent on
: Yea / No
If yes9 Please give- details
Return journey reservation
required
Train No
....00.00..Date
Rs. .
..............
sent on . .
ny DD No
:
Mode of Transoort
Please give details
(Train / Bus / Air)
Any other information
for Rs.50/- drawn in
I am enclosing a DD No. . ’Karnataka Rajya Vijnana Parishat,
favour of "the Secretary
Bangalore.
9
Signature
addressed to the Secretary,
Coni
i
/
BEING HEALTHY
(or)
HEALTH FOR
INTRODUCTION
- NOW
:
The’ single most important need for all of us is good health
I
It is more important to us than all the wealth in the world,
is true that all of us living must eventually die-but while we
if we must be in a position to enjoy our lives and live, to the
fullest extent,
healthy.
we must be healthy.
Ill health and disease als
leads to premature deal th fo r drores of our people.
While in
many eountries of the world a child bom can .expect to live on
an average for 75 years or more an Indian child can expect to
live for only 57 years.
While in many countries of the world
for every 1000 children bom less than 10 will die in the firs
year of life.
in our country almost 100 will die within one ye
more than one in every ten.
Even this figure does;not tell the -cruth for it as an
<
average of the rich few and the ttiany who are poor,
The poor
have a for worse situation and die farmore easily than the ric
And more importaiat such figures hide the fact that while they
live, the poor suffer from repeated attacks of disease and the
grouwth and development is so stunded both physically and
mentally that they can never live fully.
WHAT IS HEALTH ?
’’Health is not the mere absence of disease.
Health is
a state of complete physical/ mental and social well-being”
(Definition of Health by World Health Crganisation)..
what
is it that our beigg healthy depends on?
Being Healthy depends essentially on our having adequate
food to eat, safe water to drink, a clean environment to live
in, proper employment and proper leisure,
components that are essential to health.
It is these five
*5
:
2
people who die of hunger are seen as dying of some disease or
the other.
A body weakened by hunger is a prey to every passin
i llness.
A mild diarrhoea,
an attack of measles,
a chest infec
a fever
tever - which in a normal healthy person would be only a few
inconvenience that would go away by itself, is enough to kill a
malnourished person especially children.
Thus it is that the
commonest cause of death of children are conditions like respir
(chest) infection, diarrhoeas, measles,
all of which need never
caused death at all but for the malnouri shment.
Malnouri shment also leads to a stunting of the physical
growth of the child,
so that it can never realize its potential
(The average weight of the Indian rural male is as low as 44 Kg
while of the female is only 40 Kg.).
The root causes of malnutrition lie in poverty - in the
inability of our people to purchase the food they need. There
i sz except on occasions/ no true scarcity of food.
Indeed our
country grows enough food - even to export if necessary.
And
if needed we have the capacity and the knowledge to produce
much, much more.
A BALANCED DIET:
Is malnutrition caused by lack of knowledge about the type
of food to be eaten?
Scientists say that a proper diet - a
balanced diet for an average Indian must include adequate stapl
grain like rice or wheat or jowar,
include about 170 gms.
and adequate pulses.
It mu
of vegetables, about 65 ml. of fats and
oil, 55 gms. of sugar and at least 250 ml. of milk or equivalen
value of meat,
fish or eggs.
If a person has all this he needs
no special health foods, no tonics to maintain his health.
Foo
is the best tonic.
Grains like rice or jowar or wheat is the main food,
chief supplier of energy for the body,
It is
The fats and oils are a
I
3
s
Other than these the body also need small amounts of
substances called vitamins.
Carrots, mangoes, leafy vegetables
and fish, meat especially the liver are good sources of Vitamixa substance essential for our eyes & skins.
major cause of blindness in India.
Fish,
Lack of this is a
fruits & vegetables
are a good source of Vitamin-C, especially lemons, guavas,
ami a
Even green chilies & other fresh vegetables & fruits contain th
A lack of this leeds to painfull bleeding into the skin and join
Milk,
eggs & meat provide Vitamin-D.
However a good exposu
to sunlight is by itself enough to provide enough Vitamin-D &
deficiency of this substance which is essential for strong bone
teeth is thus commoner in women who stay indoors ail the time.
Then there are minerals, like iron which is needed for the b
clacium that is needed for bones and iodine.
obtained from good,
Thesd too are
and the balanced diet suggested would provid
all of it.
I
However the average Indian finds such food far out of his re
His money is just enough to buy the staple grains that he needs
I some salt and perhaps a few chilles, and if money permits a bit
of dal.
An average Indian family of about 5 or 6 people would
require almost 3.5 Kg. of rice or lowar or wheat and about a
quarter kilo of pulse per dayo
This itself would cost at least
rupees twenty per day and even this is a great struggle to obta
And one has to remember that on many days there is no work to be
or there is sickness that prevents him from earning- a wage,
It
for these reasons basically that the poor do not have a balanced
diet.
They krow that milk is good for children,
that eggs are
etables are good,
that green ve
ve'etables
th=»t meat and
good for health,
fish make you strong - but they cannot but itw
There is nothing much that a doctor can do,
as a doctor to
remove this single most important cause of ill-health,
to prescribe a
Were ho
tonic or a milk powder or health food he i s
actually depriving the family of much needed food,
Such health
foods and toni os are frauds promoted by drugs companies to make
:
4
;
vegetables/ bananas,
guavas, orgnges and lemons are all healt
and more nutritious that any tonic and far cheaper too.
CCMBATTING HUNGER;
Then what indeed can be done to tackle hunger and ensure o
health.
The single most important measure i s to ensure employ—
ment that provides the minimum income necessary for a person to
live as a human being.
This would mean effective formulation
implementation of laws regarding land reform and of ensuring a
minimum wage for agricultural workers and indeed all other
categories of workers.
Whatever the circumstances
the minimum
wage cannot be less that the amount needed to provide the minim
food, clothing and shelter needed to sustain life and this can
determined by scientific calculations.
Ensuring employment must also in the present context mean
rural development programmes and technologies and industrial
development stratergies that are able to absorb the entire labo
force and provide gainful employment to all
•
NUTRITION EDUCATE ON:
However a proper programme of nutritional education may
be needed in addition to ensuring a minimum income,
especially
help parents make optimum use of the scarce resources available
provide proper nutrition to children.
Malnutrition in children
is often compounded by wrong feeding practices and ineffieicnt
use of available- resources.
Breafct feeding during the first 9 months of life is one
effective guarantee of good health,
The change to bottled milk
powders and infant formula is a major cause of preventable infa
deaths and in most cases should never be done,
Even where
bottles are to be used close attention need to be given to wash
the bottle and plastic nipple in boiling water for at least 5
minutes or better still feed the infant with a clean spoon and
avoid the bottle altogether.
*
s
5
3
cheap fruits like banana etc. should be given them as also a
greater content of fats and oils.
FOOD SUPPLEMENTATION SCHEMES:
4
Food subsidies are no long term solution as they are'diffic
to sustain due to high costs arid more important as they create
culture of dependency.
.However given the abyssmal poverty of s
sections of the population and the impact that^it has" on the fo
intake of the sections within these sections which are most
vulnerable to the ill effects of malnutrition namely ‘children a
p reg an ant women, food supplementation or subsidy schemes remain
an essential component of primary health care.
It is therefore
essential that the special nutriti'dn programmes, the I CDS
’ Anganwadi* based programme and mid-day school meal^s programme^
strengthened and expanded along with schemes like the 1 food for
work1 programme. Efforts need $lso be made to administer them
efficiently, and in a corruption free manner and to ensure that
these subsidies reach the sections that need them most.
SAFE DRINKING WATER:.
After food, the single me st ’importan t determinant <f health
is the availability ef safe, potable drinking water.
an essential* component of all life.
Water is
Today the efforts tb secur
adequate water for one1 s essential needs occupies the energies
and time ef most households,
especially of the wemen.
There ar
many districts especially in Punjab, Haryana, Andhra and Tamil
Nadu where the water so obtained had deleterious levels of
crippling'of a considerab
fluorides - a substance that leads
At other places high levels
section of the population.
iron
or salt makes th.e, water difficult to drink. Indiscriminate
dumping of factory effluents especially from chemical companies
and tanneries have also rendered water hazard>us for drinking in
many areas all over the country, as for example in and around
Madras, N^rth Arcet etc.
-s G
drinking water are therefore the two sides of the same coin.
Scientist^ estimate that almost ■'80% percent ef all preventable
incidence of sickness can* be eliminated by provision of.safe
drinking wat^r alone,
'The status of health in the .ountry sho
be measured’ not by the number of doctors it has but by the num
of water taps' - a very true quote indeed to which are may add
Qumber if water taps with water in them!
Provisi.n of safe drinking water and prtper sanitary facil
is. not an insunnountable problem even with already available
technoligy.
what wculd concretely need to be done for this in
your area? One may for exanple need a) proper construction of
wells taking all the necessary safety precautions to prevent
cntaimiaticn » chlorination .f wells c) filtration plants
in urban areas and larger rural habitats with a regular piped
water supply d) preventi.n of- defecation near tanks and streams
fr.ni which water is used for drinking purposes e) instruction
Jf l.cally appr^riate, cheap and culturally acceptable latrine
along with a proper sweage disposal system in urban and larger
rural habitats f) deflucridation techniques or identification o
safe drinking water sources in fluoride and ir.n affected areas
g) preventing factories and sweage disposal systems from dumping
untreated or hazardoues waste into river and other water source
inclining the sesj. If indeed this is such an. important, yet in m
places an‘easy measure, why has it not been done?.
There are m
reasons for it bu^. one major reascn we should n.te is because w
the people Have noc demanded it
despite the fact that^&Lsrrhoe
has killed and polio has crippled more of our children than any
• ther single cfisease!
Eventually rne we can ensure cur own
health and it is high time we organized and ensured safe
-drinking“'water in our own area.
®here are however many areas in the country where availabi
r f any water is a great problem, In such areas engineering work
•minor or major will ha\e to be taken up or new technologies like
desalination of aalt water adopted.
tit
ENVI ROJMENT :
I
7
to both industries and to the inefficient smoky chulhas are a
major cause of chronic cough and other respiratory problems.
Indiscriminate use of pesticides and unsafe unscientific dispo
■>
wf industrial wastes, poisons the land and water in isany area
Biological
envirement
:
Man as part of the living world,
i
I
and related by evolution
all living things, is also affected by a ny serious affection
Cutting down of trees and green plants dep
the living wor±d.
the air of oxygen sc essen’eial for life. The indiscriminate
killing off of so many plants and animals has alteredthe del
balance in nature on which all life depends.
This as well as
unplanned urban and rural development that leads to dirty ces
water in all our cities and towns have become ideal breeding
grounds for mosquitoes and flies and other cdrriere ef disease
The mosquitoe- al®ne is known to be’ a vector of 5 diseases in
India. Malaria, filaria, brainfever (viral encephalitis),
viral fever® (dengue), haemorrhagic fevers (fever with bleedin
the first three of which are major causes of death and diseas
Flies are the Carriers of diseasd like typhoid, cholera, worm
and dysentery and many other diseases. -The sand-fly causes
Kala-azar in many parts of Bengal, Assam, Bihar and Orissa.
Similarly pests on crops are also rapidly multiplying.
Contr
of such pests whether affecting man or crops is possible in th
long run only by ensuring a proper ecological balance and a
healthy environment.
Measures like pesticides may be needed
a limited and controlled manner but seldom will it by itself
t
a solution.
(The failure
programmes like the National Mala
Control Programmes are related to this).
SHELTER :
However by environment we need also include the social
environment. The provision of good shelter and clothing is o
major aspect, of this.
A person with adequate clothing hiving
in a well ventilated house which is not over crowded within
the house Or located in an over crowded area is far less like
8
Of the various respiratory Infections, by far the most
serious is tuberculosis.
Despite various programmes the
incidence of tub’erculosi s continues to rice and is more than
million• today.
°f there despite the fact that good drugs are
available 5,00, 000 die every year.
On the other hand, tubercul
which was a common disease in the West once is now almost
eradicated there. This is not prirarily due to drugs but to le
overcrowding, better shelter and nutrition.
Even in India,
tuberculosis is primarily a di seas of the poor and., ^a reflection
of their standard of living.
EMPLOYMENT g>
I
Another aspect of social -environment and a essentia^
pre-requisite for health is proper employment and leisure.
Proper employment is not only essential because an income
purchases food & clothing and shelter but it is essential
as an end in itself for mental and social well being. Indeed
man's prime want is to play a productive and useful role in.,
society and his satisfaction is most when his. employment ensure
this.
Abd his leisure he can use for rest and for developing
all the various aspects of his. self that all contribute to
being, a complete human. Indeed a social environment free of
•onfliets and tensions, meaningful employment and adequate s
leisure are the basis for mental and social well-bei*ng for
a truby healthy citizen.
(The basis of many a social disease
like suicides, alcoholism, drug addictions, crime5 are to be
found in the lack of satisfactry work and related social tensio
Just as only healthy individuals can make a healthy society, it
is also ttue .that a healthy society is needed for healthy
individuals.
:
.
HEALTH EDUCATION ;
To nearly all people much of this is common knowledge.
Medical science has only helped establish that most disease
result from a lack of these essential requirements. Medical
-I
i
1
This knowledge about how our body works and about how disease
are. caused is another essential pre-requisite of being health
It is necessary that not only doctors and nurses or health
workers know about-this but that every person has a ininimum
idea of it, so that, they can understand thpir own bodies and
keep it healthy*
( .
1
Health education should also include a minimum kixowledge
of diagnosis and treatment of simple diseases. Take for exam
.diarrhoea. If diarrhoea is watery and not associated with blo
$
I
or mucus the best and only correct treatment is to give the
patient’plenty of fluids.
The fluid adviced can be prepared
the home by mixing a scoOp of sugar and a pinch of salt in a
glass of boiled water* Alternatively rice water with some sa
a^ded is also good treatment. The majority of deaths due to
diarrhoea, especially in children can be prevented by this on
=1
measure alone.
Indeed more deaths have been prevented due to
this one advance than any other single advance in medical scie
in these last few decades.
Similarly colds, simple cuts & bruises, an occasional bo
ache or headache can all be treated with proper knowledge.
Health education should also be adequate for people to
identify certain serious diseases like polio, measles,
chickenpox/ tetanus etc. so that they seek medical help early
f
Measures to prevent diseases like tetanus & rabies, know
about immunization, knowledge about occupational health hazar
all are essential aspects, of being health.
EDUCATION :
Obviously a literate person has far greater access to suc
knowledge than an illiterate person. Literary is an essential
Component of health. But mere literacy is not enough*
The le
of general education is important.
1
General education increase
the ’health' literacy1 of the people. It enables them to und
stand their health problems and how to identify, prevent and
10
disseminate a lot of knowledge about health, and the. access to
", '■ -4
thi sin formation is directly related to literacy.
.Worneh* s literacy and schooling of girls peeds special
emptrasis for the impact of this;.on society & the family, is
much more.
Indeed just like food, water, shelter and worfor education
must be also considered an essential component of being healthy.
MATERNAL HEALTH CARE :
One area where medical science has led to a great benefit
is about pregnancy and childbirth.
There was a time when many
women and even more children died due to pregriancy and at
childbirth. Now we can in most cases detect problems of
pregnancy well in advance and take proper steps to save the
lives of the children, and mother. We know that a pregnant
women needs extra nourishment and should have more rest and
should be spared heavy work. We also know that if they have
many children top soon-and too frequently it endangers the
lives of the child a nd the mother. It is recommended that
the first child'should be after the age of* 21, the second child*
should be after a gap of 4 years at least and there should be
This is essential to safeguard her health.
no third child.
Suitably trained persons • both doctors and health worker §
can datect the .pregnancy cases; where natural delivery is not
possible or dangerous and in such cases the child can be safely
delivered by an operation or forceps.
When natural delivery; tak
place we can ensure by simple hygienfcc measures that any trained
nurse knows that the delivery is safe and that there are no
complications for the mother.
CHILD k CARE :
The newborn child fed on breast milk from a healthy mother
is likely to be healthy. Immunication prefects us against a
5
ft
<
•?
'A
11
*
-
JrLrth,^ and many more (about 40/1000) die in this age group
due to ca uses related to childbirth indirectly.The reason for this Ties in the poor health of our mothers
and the difficulty in getting or total 1 ack .of ..maternal and
Even if they are available
child care in most of our villages.
women are not adequately aware of why they need such help and
the vast difference such help, will make to their lives and that
4-
of their ^children1 s.
The children of illiterate women die far
more often, than those of literate mothers.
Studies have even
estabilished relationships between numbers of years of* schooling
A
of the mother^ and infant mortality.
This is not only related to. the proper socio-economic
background of the illiterate and the knowledge about health
that literacy contributes but also to a critical awareness of
their own reality and their attitude toward^ it.
51
■
’
The - inability of the illiterate woman to make the correct
choice - to ensure the health of their children, their own heajL
and of their children, their inability to plan for the future
security for th^ family leads her to reject the temendous pressu
that the government exerts today for the family welfare programm
and thereby she seriously endangers her own health.
a
♦
4
THE FAMILY PLANNING PROGRAMME :
India i^one of first countries in the world to have a maj
national family planning programme.
Enormous resources have bee
spent on it - *in the last five years plan period alone - more
than 3000 crores have beep spent-'on it. Nearly half the budgeta
allocation for health care goes*to family planning - yet the
programme has not succesded.
The crude birth rate over the
last H years has remained static at about 31/100r' as against
a 22/1000 that it was supposed to reach. Or in simpler words
despite 3000 crores spent there has been almost no change at
all in kirth '"rate. The measege of family planning has been
12
i s the only
tenI, Invent ,r 3avlngs
they are .la 4r elok it is only their ohilaron that they can fa
ac upon.
(In a better income gr.up in our ccuntry .r in more
developed c.untries savings is in the form of a home,
in a bank
pension, provident fund etc)
etc).. N.w when 10 ' aut
100 children
die the need
ensure a living child and that ioo ’ a male child
kedemes a matter of j----para mount importance.
The less of a child
for a mother is a matter of great r“arjeny and guilt, f<r the bein
she brought into the world and loved
-J so intensely is ±jst as th
was unable to protect it. But the millions of mothers are voic
and we do not hear, them
cry. And even as they cry they need to
through it again - to Jbear more children.
Only in s. society where there is social security and low
infant mortality will the birth rate erne down. And .nly in a
iety where the woman is literate and liberated en.ugh to mak
hex own cheiees will family welfare be realized.
There are
countries like Cuba where there is nr Family Planning Programme
at all yet the birth rate is low. There is no population problem
n any .f the developed countries .f the world. Indeed all of
them want more people.
Tha day dur women are educated, they day
they are able, tc ensure the survival of their children and becom
active participants of social development, that day family
planning will bec.me universal.
Till then all we can do it to
ensure easy access f.r every mither to health services which
include family planning and to inf.rmation ab^ut family planning
The money being wasted on many of the schemes be better spent in
educating women, providing, basic health care and .n development
pngrammes.
PREVENUCN OF ENDEMIC DISEASES :
Good knowledge .f the way diseases spread consequent to the
advancements of medical science have also helped us cmpletely
eradicate some diseases like small pox which once killed millions
of people every year. It has made it al so. possible fwr us to
eradicate ®r control may of others.
'
guinea women for examp
Take
1
v
15
w the district or taluk hospital.
Even here no mere than some 150
drugs are needed to take care of all the possible medical treatm
yen may ever need.
Unfortunately in most places .including these 25 primary hea
J
Even at taluk and
centres these 25 drugs are not available.
district level hospitals often there 25 drugs are not available
*
not to speak of the 15 0*. But at the same timeevery local drug
shop and even at villages there are freely available hundreds of
4
other tonics and injections and tablets which are of no use at a
Because people do not know the causes of their diseases they ofte
take tonics and $*ther tablets ’ f«r feeling better or stronger1.
Then why are they there at
But these medicines waste our money,
all?
Why do doctors prescribe them?
them?
Who' do companies make thefci?
Why do governments allow
Of all these questions only the last has an easy- answer.
T
companies make them because they get a lot of money by selling th
We need to ensure that our governments and doctors dch not encour
such useless drugs that waste o-ur money.
We also need to insist
that the drugs essential in that area are cheap and easily
accessible.
OF DOC^RSsLast of all, we need doctors/ too,
at least in every primary
health centre there must be two doctors
doctors who are intere
They can help when our own knowledge and
in serving the people.
training and that of the community health ^workers is inadequate
Doctors are also needed as scientists to find out more about the
causes of diseases so as to discover ways to prevent the disease
and to treat than. In every district there should be at least o
hospital where modern scientific instruments are available and
specialists in various fields are available to treat serious
They also need to provide training
Conditions or rare diseases.
to newer health personnel and educate people about the causes of
Ul, health and the way to be healthy.
5
HEALTH Pff&ICIES
If many doctors today to not do this it is also rbecause
9
-1G :-.
have proper, equitable access to' health or the other benefits
that advancements in medical science have made possible.
(
Goo 1 health needs far more,, than doctors and drugs.
The
struggle for being healthy is part of the struggld against cond
that make ill health possible. It is a struggle rftor good food,
good water; a clean environment, for good employment & for
leisure. It is a struggle for. a better quality of life.- Scienc
gives us the knowledge and the possibility of making good health
care available today but to^make thij? a reality, society must
*
be wil-uing to read stribute available ^resources so that these bas
needs for all are met.
This then is the true meaning of Health
for all ¥y 2T9J Ad.
*
J
Vf
&&&&&&&&
4
*
s
•#
4)
>
«
5
Com
SCIENTIFIC AWARENESS FOR PEOPLES^BENEFIT_-__CHAI^S_CONTRIBUTI
Catholic Hospital Association of India is a national
organization of 2,222 member hospitals, dispensaries, health
centres and social service societies spread throughout the
Country. Our member hospitals are noted for quality and
efficiency of services and utilization of latest technologie
and advancement in medical science.
Very often, missionary sisters and priests had started these
institutions in needy areas where suffering humanity had no
other option for health care. Some of them started in a ver
humble way and grew into impressive institutions. It was th
compassion and healing spirit of Jesus Christ that motivated
them to go to the extreme rural areas and to the peripherie
But as the years passed, critical evaluation makes us
realise that some of us have lost the original vision and
commitment to the people. Survival and maintenance of the
institution beceme the focus of attention. Sophistication
and incorporation of advanced medical technology turned out
to be the answer to survival. Some of these modern changes
are not affordable by the poor majority and the fact remains
that we fail to realise the additional burden we place on th
poor due to this.
CHAI,holding on to its original vision, endeavours a
critical analysis of the health situation in the country
in relation to the socio-economic and political situation.
Very often many of the health problems, in a detailed
analysis, ultimately are due to an unjust distribution of
land, unequal sharing of profits, exploitatory marketing
systems and unfair wages. This leads to poverty of many an
surplus for a minority. It is this poverty-stricken
majority that have malnutrition, recurrent illnesses and
chronic diseases unattended adequately. It is the weak wome
of this majority who will be doing hard labour inspite of
carrying a baby in an anaemic body. They will deliver a lo
birth-weight infant which will continue to have a poor
2
mosquitoes in plenty. They are fondled and cared for by
elders who cough out tuberculous bacilli. Their weaning food
are mixed with water drawn from the village pond which
r
carry any number of Rota Virus, Amoebic Cysts, Round Worm
Ova, Hepatitits Virus, Typhoid and even Cholera Bacilli.
Out of whatever little money their parents earn toiling
manyr.hours in the hot" sun, a good share is spent in the
local arrack shop which is run quite profitably by the rich
business class. This business class will see to it that no
saving schemes survive in the village as it will make the
poor villagers stronger in facing any financial crisis.
Only when such saving schemes collapse, the poorest of poor
will fall at the feet of the money lender and become more and
more chained to him.
Health can never be a reality in such a vicious circle.
No amount of medicines or efficient medical staff can ensure
the total well-being of that community.
0
In the light of the above analysis we realise that unless
people are made to take care of their own health, HEALTH
FOR ALL BY 2000 AD will be a "myth. It is this "enabling"
process that CHAI has been facilitating through many of
its programmes. Ultimately we want "empowered" communities
who can understand their health problems and take appropriate
remedial measures.
believe that the poor can do
"something" for themselves and they are "somebody" in
society. The poor man with a number of miseries, a great
deal of incapacities and innumerable needs, poses before us
as a man who has lost his dignity. We want people to
rediscover their dignity and self esteem. They should
also rediscover their potential in achieving remedial
changes.
Our awareness building programmes are aimed at raising a
critical consciousness' level of the community so that
3
insisted upon, based on a prioritization. Those health
activities which will bring about maximum desirable changes
in society and those activities which require minimum resourc
input., deserve a high priority. If people are involved in
health activities it becomes a people's movement. It is
chis movement we are facilitating through our orientation
sessions, training programmes, follow up and evaluation and
replanning < f various projects. Many of our hospitals are
getting reoriented in undertaking community based health
care programmes. Many institutions have taken up training
of local community health volunteers to increase the army of
community health movement. At a national level we organise ;
programmes for leaders of community health projects. We
also identify appropriate resource persons in various parts
of the country and strengthen regional resource team for trai
q
o
more workers.
CHAI has taken leadership in coordinating many of the isolate
health activists groups and promoting linkages among them.
We also facilitate exchange programmes between people based
health movements of other countries such as Philippines,SAARC
Countriesc Latin America etc.
Another attempt of ours is to influence the doner agencies
jn America, West Germany, Holland, Switzerland, etc to
direct more funds to ’people based’ health programmes rather
than sophistication of big institutions.
RATIONAL DRUG THERAPY: Drugs being one consumer item in
which the consumer has no say in the selection and use,
was our maj^r concern fox/nany years. This consumer item
.’as misused widely knowingly or unknowingly. The prescriber
has to apply maximum ethical principles considering
financial status of the patient, cost benefit ratio,
actual indication, side effects, availability of
alternative drugs etc. Through various conventions, training
programmes, our publication Health Action , we have promoted
the concept of essential drug and rational drug therapy.
4
hospital formulary. Still the pressurising marketing
technics of many drug companies are influencing our
institutions. In the field of quality control of available
drugs we do not have enough facilities to monitor and report
promptly to member institutions. Even at Government level
only lour states in India have adequately equipped drug .
testing labs and partial facilities in ten states,
states. 10
states do not have any equality control bust
test labs.
labs. To meet
this lacunae in service, and ensure the quality of the
drugs 9 CHAI is planning to start a central quality
control lab of its own.
on the
The necessity of public opinion andconsumer pressure
of
prescribing doctor, for the effective implementation
Our publications
rational drug therapy is quite significant.
continuously try to educate
including iHealth Action magazine
the masses; in this regard.
CHAI had initiated to bring together the producers »f
essential drugs who also believe in Rational Drug Therapy.
The plan is to form a cooperate body of these producers for
pooled procurement of bulk drugs and ensuring steady produc
of good quality essential drugs at reasonable prices.
MISUSE OR MEDICAL TECHNOLOGY : We are protesting against
misuse of any medical technology. The Amniocentesis for
sex determination and descrimination to girls are strongly
condemned. When Ultra Sound Scanning and CAT scanning becam
the fashion of the day an unhealthy trend to overuse them
was noticed. The Doctor-Medical Technology Axis was
unfavourable to the poor man. We also expressed our distres
in the growing commercial cooperate sector hospitals,
especially by the business groups and non-resident Indians.
The value system cultivated in these institutions is damagin
to the medical profession.
There are attempts to study mnd campaign against unnecessar
surgical procedures such as Caesarean, Appendicectomy and
5
which if explained to mothers can save millions of dying
children. We had organized 9 regional workshops for
Paediatricians and Paediatric nurses in reorienting them
in diarrhoea management. Each hospital is supposed to
start an Oral Rehydration Corner in their cut-patient
departments and in the paediatric wards. An innovative
attempt to expose ORT to the general public was done in
the twin cities of Secunderabad and Hyderabad by starting
demostration counters at Railway Stations, Bus Stands,
Post offices, Museums etc. during last summer.
Immunization is another scientific technology that, has to
reach e/ery common man for a safer future generation. Social
mobilization for immunization is one area to which CHAI had
given emphasis last year. There was overwhelming response
from our member institutions for taking this up seriously.
We believe many of the herbal and home remedies practiced
through generations in various parts of the country are
effective. It is cheap and affordable to the people.
Scientific bases of its action is yet to be discovered.
A lot of research if undertaken in due course might generate
many effective indegenous drugs eg. Reserpine, Vincristine
etc. We encourage the practice of herbal medicine.
CONCLUSION : CHAI believes in peoples’ welfare through
peoples’ power. This power of the people generates from
awareness. building and peoples’ organization. Science
movements contribute enormously to peoples’ awareness.
BACKGROUND PAPER ON HEALTH AND PSM'S
Presented at 2nd All India People's Science Congress,
Caleutta.
BY DELHI SCIENCE FORUM.
India was s signatory to the "Alma Ata Declaration"it a
adopted by the World Hea1th Assembly in 1978, which gave the
call "Health for all by 2000 AD". Today, 10 years after the
Alma Ata declaration, the state of health in India makes the
country one of the most backward in this respect. The faciliti
in some of our hospitals may be among the best in the world and
the same can be said about our doctors.
This, however, does
not determine the health ofnation. The only true index of a
nation's health is the state of health of the vast majority
of people, andnot that of a privileged few. In this regard the
Government's own "Statement on National Health Policy"
(1982)
states The hospital based disease, and cure-oriented approach
towards the establishment pf medical services has prodived
benefits to the upper crusts of societ specially those residin
in the turban areas. The proliferation of this approach has bee
at the cost of providing comprehensive primary health care
services to the entire population, whether residing in the urba
or the rural apeas".
POST-INDEPENl)ENCE expansion
in
health
services
However this should not detract from the fact that since
independence there has been improvement in many areas, both in
terms of growth in in restructure andinterms of their actual
impact on the health status of our people. The following table
gives an account of the progress made.
Table
1
IMPROVEMENT IN HEALTH FACI LITIES/CONDITIONS SINCE INDEPENDENCE
Year
Life expe
tancy at
1951
1961
32.1
Infantmort
ality rate
180
No. of
Populat ion No. Doct
hosptiaIs per bed
of
per
PHCs pop
2694
3199
725
16
-2
2
2-
It is however important to understand both the content
and the process involved into this progress made in the healt
sector, There is a tendency to cite the above figures to make
out a case for positing that this progress has been adequate,
hence no major policy interventions arenecessary. The health
services at the time of Independence were a function of the so
economic and political interests of the colonial rulers. Cons
quently they were highly centralised, urban-oriented and cater
to a small fraction of the population. Public health services
were provided only in times of outbreaks of epidemic diseases
like small pox, plague, cholera etc.
The post-independence er
witnessed a real effort at providing comprehensive health
care
and in extending the infrastructure of health service.
Even the West wemt through this rapid phase of improvemen
of health services, after a period of stagnation, at the turn
of the century, In the early days of the Industrial Revolution
the bulk of workers who came to work in factories from the
countryside suffered from malnutrition,
- communicalble diseases
an high rates of infant and maternal mortality. When it was
ed that the very suffering of the people was endangering
industrial production (and thereby profits), active steps were
publicshealth services. Economist
taken to dramatically imrpve publicchealth
who had considered medical
medical expenditure
expenditure as a mere consumption
item, realised that allocation on health care was actually
an
investment on increasing productivity of labour,
labour. Another
major thrust was provided in the aftermath of the Second World
War, when with the rise of organised workingclass movements and
democratic consciousness
consequent development
development of
the consequent
in many
of democratic
consciousness in
States" was mooted
uropean countries the concept of "Welfare States”
in Britain,
Britain, which is high
Scheme in
For example the National Health
Health Scheme
- shape
regarded even today, -took
under the Labour Government just
after World War II. A rough analogy can be drawn wkth this and
the Indian situation after Independence. Consequent to the
transfer of power in 1947 the character, amd as a result the
, - the ruling sections changed and conselong term interests, of
quently their intereest. and motivations were qualitatively
different from that of the British. Their own interests requi-
-s 3
At the same time major scientific discoveries revolutio
the treatment and prevention of many diseases. These hav
contributed greatly to the increase in life expectancy and
in reduction of mortality. The antibiotic era has made it
possible to control a larger number of infectious diseases
for which no cure was earlier possible. Rapid strides hav
been made in the field of immunisation, diagnostics, anaes
surgical techniques and pharmaceuticals. This has had a
dramatic impact on mortality and morbidity rates all over
world. There are pitfalls of an absolute dependence on te
nological solutions to health problems, but it is definite
true that in many instances newtechnologiqs have had a ma
impact. However the imporvements in ourhealth delivery sy
have not kept pace with the needs of a vast majority of ou
people.
So much so that the Government's "Statement on
National Health Policy" (1982) is forced to state "Inspite
such impressive progress, the demogfaphic and health pictu
of the country still constitutues a cause for serious and
urgent concern".
BALANCE SHEET OF HEALTH
The following statistics give a picture of the state of
health of our people:
— Only 20% of our people have access to modern medicine.
— 84% of health care costs is paid for privately.
— 40% of our child suffer from malnutrition. Even when
the foodgrain oroduction in India increased from 82
million tonnes in 1961 to 124 million tonnes in 1983,
the per capita intake decreased from 400gms. of cereals
and 69 gms.
of pulses to 392gms. and 38 gms. respectiv
Due to increasing economic burden on a majority of the •
people, they just cannot bujr the food that is theoreti
cally "available".
—Of the 23 million children born every year, 2.5 million
die within the first year. Of the rest, one out of nine
dies before the age of five and four out of ten suffer
-s 3 s-
At the same time1 major scientific discoveries revolutio
the treatment and iprevention of many diseases. These hav
contributed greatly to the increase in life expectancy and
in reduction of mortality. The antibiotic era has made it
possible to control a larger number of infectious diseases
for which no cure was earlier possible. Rapid strides hav
been made in the field of immunisation, diagnostics, anaes
surgical techniques and pharmaceuticals. This has had a
dramatic impact on mortality and morbidity rates all over
world. There are pitfalls of an absolute dependence on te
nological solutions to health problems, but it is definite
true that in many instances newtechnologigs have had a ma
impact. However the imporvements in ourhealth delivery sy
have not kept pace with the needs of a vast majority of ou
people.
So much so that the Government's "Statement on
National Health Policy" (1982) is forced to state "Inspite
such impressive progress, the demogfaphic and health pictur
of the country still constitutues a cause for serious and
urgent concern”.
BALANCE SHEET OF HEALTH
The following statistics give a picture of the state of
health of our people:
— Only 20% of our people have access to modern medicine.
— 84% of health care costs is paid for privately.
40% of our child suffer from malnutrition.
Even when
the foodgrain oroduction in India increased from 82
million tonnes in 1961 to 124 million tonnes in 1983,
the per capita intake decreased from 400gms. of cereals
and 69 gms.
of pulses to 392gms. and 38 gms. respective
Due to inceeasing economic burden on a majority of the ■
people, they just cannot bu$ the food that is theoreti
cally "available".
—Of the 23 million children born every year, 2.5 million
die within the first year. Of the rest, one out of nine
dies before the age of five and four out of ten
suffer
,4
0
—- 50% of children and 65% women suffer from iron defi—
ficiency, anaemia.
—— Only 25% of children are covered by the immunization
programme. 1,3 million children die of diseases whic
could have been prevented by immunization.
°f
total population of India is exposed to
Malaria, Filaria and Kalazar every year,
— 550,000 people die of TB every year.
About 900,000
people get infected by Tuberculosis every year.
—nAbout half a million people are affected with lepsor
which is 1/3 of the total number of leprosy patients
in the world.
— 70% of children are affected by some intestinal worm
infestation.
— 1.5 million children die due to diarrhoea every year.
A comparison of Infant Mortality Rates (i.e. number of
under the age of one month per thousand live births) of some
countries in 1960 and 1985 shows that many countries with a
poorer or comparable record 20 years back are today much ahea
of India.
TABLE
2
Country
I MR
in 1960
IMR
in 1985
Turkey
190
84
Egypt
Algeria
179
93
India
168
16 5
Vietnam
160
81
105
72
China
UAE
150
El Salvador
145
142
Jordan
135
36
35
661
49
Sources: *State of the World’s Children’ W87 - UNICEF.
•
5
TABLE - 3
Plan period
% share of Health
Budget
3.32
3.01
2.63
2V11
• 2.12
1.92
1.86
1.88 (esstimated
1951-56
1956-61
1961-66
1966-69
1969-74
1974-79
1980-85
1985-90
Sources GOI, Health Statistics of India, 1984..
The government spends just Rs.3/- per capita every month
on Health. ( This may be contrasted with the estimated averag
expenditure, incurred privately, of Rs.15/— per capita every
month) The following table gives a comparison of the percenta
of govt, allocation on health.
TABLE - 4
Country
India
Egypt
Bolivia
Zaire
Iran
Zimbabwe
Kenya
Brazil
Switzerland
FRG
% of central govt, expenditure
allocated to health (1|983)
‘
2.4
2.8
3.1
3.2
5.7
6.1
7.0
7^3
13.4
18.6
Source: The state of the World’s Children-1987.
Moreover, even these meager resources are not equitably
distributed, 80% of the resources is spent on.big hospitals and
research institutions which are situated in metropolitan cities
TABLE - 5
COMPARISION OF NO. OF HOSPITAL BEDS IN RURAL AND URBAN
AREAS (As on 1*1.1984)
No. of Hospitals % of total
Rural
1894
26.37%
Urban
Total
5287
7181
73.63%
100.00%
No.of Beds %of tot
68233
13.63%
432395
86.37%
100.00%
500628
Source: Health Status of The Indian People, FRCH, 1987.
Of the total number (just over 2 lakhs) of allopathic
physicians in the country, 72% are in urban areas.
Further, on
15.25% of all health personnel work in the rural primary health
sector of the government. As a result of the highly inadequate
Govt, intervention in the health sector people are forced to ta
recourse to the private sector in health care. By this kind of
an approach, health has been converted to a commodity to be
purchased in the market.
Only those who can afford it can avai
of the existing health facilities. It is thus clear that healt
perceived by the Govt, as a low priority area with grossly ina
quate resource allocation, and a skewed pattern of utilisation
his is afundamental problem in the he
these meager resources.
sector which calls for rethinking retarding the whole developme
process in this country.
Here another disturbing trend needs to be mentioned.
In
last few years there has been large scale investment by thepriiw
sector on curative services. With encouragement from the gover
for the first time in India big businesshouses are entering the
of health care.
In addition to the fact that they areexclusive
meant for the elite, the trend is also an indicator of a certai
of Philosophy within Goct. circles regafding health care. It
kind of thinking which draws inspiration from a World Bank repo
which says ’’present health financing policies in most developin
countries need to be substantially reoriented. Strategies favo
public provision of serv;ces at little or no fee to users and w
little encouragement of risk-sharing have been widely unsuccess
(de Ferranti, 1985). This, in other words, is a prescription f
-
in providing
O
7
health care to all.
Increased privatisation
in health can only serve to exclude the most impoverished
sections, pricisely the section who need health services the
most.1. The answer to theGovt*s inability to find sufficient
resources for health programmes certainly cannot lie in
taxing the community tot provision of health care.
LACK OF HOLISTIC APPROACH
Health services, in the traditional sense, are one of the
main but by no means the only factor which influence the healt
status of the people.
Today the concept of social medicine
recognished the role ofsuch social economic factord on health
nutrition, employment, income distribution, environmental sani
tion, water supply, housing etc. The Alma Ata declaration sta
"health, which is a state of complete physical, mental and soc
well bring, and not merely the absence of disease or informity,
a fundamental human right and that the attainment of the highe
possible by level ofhealth is a most important world-wide soci
goal whose realisation requires the action of many other socia
and econokic sectors in addition to the health sector". Flowi
from this understa ding, health is not considered any more a m
function of disease, doctor and drugs.
Yet even today the exi
public health infrastructure in India is loaded in favour of t
curative aspects of health.
For a country like India, it is possible to significantl
alter the health status of our people unless preventive and pr
motive aspects are giben due import a rate.
An overwhelming majo
of diseases can be prevented by the supply of clean drinking wa
by providing adequte nutrition to all, by immunizing children
prevalent diseases, by educating people about common ailments
by providing a clean andhygienic environment. It has been est
that water-borne diesases like diarrhoea, poliomyeilitis and
typoid account for the loss of .73 million work days every year.
The cost in terms of medical treatment and lost production, as
quence, is estimated to be Rs.900 crores-which is about 50% of
total plan allocation on health.’
8
OU of four Slums are the extremely insanitary environmental
an
ygeinic conditions in which the slum population is living".
Further, while India accounts for more than 35% (3000 deaths
ev
day) of all deaths taking place in developing coun ries due to
vaccine-preventable diseases, less than 25% of our children are
covered by the Expanded Programme of Immunization.
How prevent
measures can alter the course of diseases is typified by Tuber
culosis. Drugs for treating Tuberculosis were discovered after
Yet, 29 years earlier, the disease had been almost totally erad
from Britain due to improvement in conditions of living. But ev
today, when numerous drugs have been discovered for treatment of
d sease, more thanhalf a million die of its every year in India.
We have seen earlier that
resource allocation is heavily bi
in favour of urban areas,
Similarly the emphasis on curative se
vices also reflects a bias in
our planning process in favour of
services vis-a-vis preventive and
promotive services. As in oth
services are a function of the political s
walks of life, health
health services
T
of a community.
hey reflect
the needs
hey
reflect the
needs of the ruling sections,
terms of resource and manpower allocation andin regard to the ch
technology. A holistic approach towards health care, taking
technology.
to account the socio-economic factors influencing health, demands
a level of conciousness which is lacking in our planning process.
PRIMARY HEALTH CARE SYSTEM
II
The Alma Ata Conference defined Primary Health Care as
essential health care made universally accessible to individuals
and acceptable to them through their full participation and at
a cost the' community and country can affort". This concept was
mooted as <an alternative to the existing concept of comprehensive
health care, which vieweed the people as mere receivers of curati
seryees through doctors, health centres, dlspehsarles and hospit
It based itself on four broad principles:
1. equitable distribution of health services.
2. community involvement
3. multi-sectoral approach
4. appropriate technology
-s 9
3. Primary Health Centre Level-has a staff of 3 doctors (one
female and two male) and other auxiliary staff. PHCs have
facilities for laboratory tests, minor surgical procedures etc
They are also responsible for training of health workers, main
tenance of rec rds and for liaising .with various National Heal
Programmes.
While this 3 tier system is supposed to provide basic health
care, there are a number of "national health programmes".
The
cover areas requiring special attention and include areas like
Immunisation. Family Planning, Tuberculosis, Malaria, Leprosy,
Bliddness, ^hild helath (ICDS)programme) etc. Thes programmes,
also known as "Vertical Programmes" are technically not pert o
the Rural Health Scheme but areorganised along independent lin
with centrally administered control.
It is widely recognised that both the Rural Health Scheme
and the vertical progra,,es are plagued with problems of inadeq
facilities and resources. The annual report of the Ministry of
Health and Family Welfare (1987-88). very candidly states "becau
pf the resource constraints only 50% of the community Health Ce
would be established by the year 1990".
In other words the
targetted coverage of the PHC system by 1990 is just 50% Simila
.is the state of various vertical programmes. The Nutrition Fau
at ion of India in a study of the Integrated Child Development
Service (ICDS) says " Though ICDS has been extended to cover mo
blocks form time to time, the support it has received has been
gruding and halting" and often "extracted after much struggle".
The CAG report for the year ending March 31, 1987, has criticis
the functioning of three major programmes viz. Blindness gpntr
Programme, Tuberculosis control programme and Leprosy eradicati
programme.
/
These programmes have been pulled up fpr
improper
non utilisation of funds, non release of sanctioned funds and l
of planning andmonitoring of these programmes. The principal p
problem with all the health programmes in operation has been a
total lack of community participation and the consequent absens
of accountability of theseprogrammes to the local community,
-?10s-
I 50/6 of the total rural population.
these centres hsve be
set up, they are under staffed and suffer from lack of medicine
and equipment .
/another major drawback has been the difficulty in attracti
doctors to serve in the rural health scheme.
By and large doct
opt to work in rural centres only as a last resort, ^his refelc
on both the quaity and motivation of medical personnel manning
primary health centres.
Unwillingness of doctors to serve in t
rural sector is also an indictment of our medical education syst
The curriculum is heavily loaded in favour of curative medicine
and within this in favour of diseases (Conforming to themortality
and morbidity profile in the West. During their period of
training medical students are taught to rely on sophisticated
diagnostic aids. ^uch training ensures that medical graduates a
ill-equipped to work in conditions prevailing in the rural areas
Moreover the medical profession isinvesfed with an aura of glamo
which unfortunately is seen to be lacking in service in the rura
sectors•
It needs also to understood that entry into medical college
is by and large limited to those coming from a higher socio-econ
stratea, predominantly from urban areas, who consequently find
it difficult to conceive of working in rural areas. Even when
uneploument among doctors is not uncommonm doctors are unwilling
to take up jobs in PHCs. A two pronged strategy is required to
tackle the situation. Medical curriculum has to be reoriented
and entry into medical colleges needs to be regulated in a
manner which ensures amoreba lanced ’’mix" of students. bide by s
incentives have to beworked out to attract doctors to the rural
health schemes. After all its is impractical to believe that
doctors textkKXKxxxi:xh®x±thxxKkxxiK3#are natuitally fired by
altruistic motives and with feeling of "service to the poor".
At the same time, within the medical fraternity, there is a str
resitance in changingehthe age old concept of health as function
of doctors and drugs. Implementation of recent concept of prima
health care requi es a certain degree of demystification of
Medical Science. But within the established medical bureaucracy
-:11sever all theseprogrammes need tooperate
they arr6?
tbX is
and
but
through the rural
Separat? ^in^rative control
hSalth —• As a resu
needless duplication of administrative
verticarprr^10' regarding aims*
manpower, costs
the basic
aim behind
programmes of giving emphsis to problem
areas is lauda
ey need to be administratively integrated
with the rural heal
scheme. Otherwise, they will continue
-to wdrk .at oross<.purposes
e rural health scheme, often at
great cost to the available m
and human resources.
COMMUNITY PARTICIPATION
-^he slogan "Peoples"
health in people "hands has today
received universal support,
Diverse agencies cutting across all
kinds of ideological positions
| accept that community participati
is vital to the sustenance of .
any comprehensive health programme
The Govt's Statement
on Health Policy also recognises this posit
while statincr "Alqn
-tug z^iso, UVer
the years,
the planning process hasbec
over me
years, the
=rgely Qhifvious of the fact
ultimate ^ola of achievin
satisfactorv hea^
XXe
911
P“Ple
™
911
—t Ce
int the Identification of their
nvolvmg
l"9 the community
co""“"xty mt
"
health needs
needs andoriori
andpriorities
i--i oo as vsell
i i as in the
implementation and
management of the various health and related
P^ogT‘3mmes ”.. Unfort
of clarity on the
oasic lack
unately there is aa basic
lack of
ceoncept of commu
Participation. Often,
Often, especially in official
circles, it is take
O imply that the community participates in
collectively receivin
services.1
3’. * Strategy developed by the Govt, to
communir^^.!
bring about
Th
Y P3rcLC:LPation is the Community Health w'orker
(CHWf) schem
e scheme involves recruitment and traing of a
rkers from every village community. The CHW isCommunity Health
required to
in eract with the PHC system on hehalf of the village
a^ community
he rep. sents. The scheme ,was introduced
as part of the
SCheme' naSed 03 the recommendations of the
Srivasta^c1
onvastava Committee (1975)
Tho
- of
dandldates for the CHW schemes ere’ 1 " ""
perferhblld
community,
-:12sCandidates after selection are trained for a period of a
their training the CHWs are given
3 months. After completion of 1--an honorarium of Rs.50 and simple medicines worth Rs.50 per
free to continue in their earlier vocation, but
month. They are
2-3 hours every day to community health work.
expected to devote
As the CHWs scheme constitutes the Government s principal
effort in implementing the slogan of "Peoples" health in peoples
hands" it merits a closer look.
Under this scheme around 4 lak
CHWs have been trained. However the implementation and impact o
the scheme raises a number of questions related to the whole con
cept of community participation.
.
The CHWs scheme presupposes a degree of volunteerism
selected candidates. Otherwise a stipend of Rs.50 per motthis
is far short of an adequate remuneration for the CHWs whose
functions include - health education regarding preventive and
promotive measures; encouraging participation of community in
public health tasks; curative measures for treating simple disor
and referrals to the next level (sub-centre). In other words
CHWs is also required to play a leadership role in the community
However the methodology required to identi fy such personsis yer
In practice the contradiction between inadequate re
resalved in one of two w
neration and high expectations is often
performing the require
Either, after a short period of CHW stops
functions or dropts out of the scheme altogether, °r he sets hi
worked out.
(In shoirtd be real
up as a private practicioner in the village,
-- j than what a la
that the training imparted to them is often more
section of unqualified practitioners/quacks in villages have
received).
Moreover while the CHWs main functions are related to pro
motive andpre^entive aspects, the village community almost
in his curative abilities. Thus
invariably is more inter sted
in the village, albeit
the CHW ends up as another practitioner
partial Government support, The training programmes of CHWs ar
take into account regional and cast
also not flexible enough to
community based differences in perceptions towards health. Thu
perceptions (with are u
The tendency is to solicit support for any health programme from
the village 'sarpanch" or other infleuntial members of the village
which modtsareas means the "high" caste and landed sections. A
similar modus operand! is applied whle choosing the CHW "acceptab
to all sections" from the village community. This almost invariab
means excluding the landless and poor peasants, who form a bulk
of the population and are most in need of health services,
rom
decision making process.
The dificiencies enumerated above in CHW scheme are questions
if community participation is
which require to be faced squarely
theprobelem is the question
to be the desired goal. Central to
of acceptance by our village comm nities of the concept of
at intoruducing this concept
preventive medicine. Today attempts
' through curative servi
are carried out by initially gaining entry
offered as the “carrot” to
In other wdrds curative services are (---while preventive
esnure to be acceptability of the programme,
services are sought to be introduced through the "back door".
Such subterfuge, which starts by not takinc the local community i
confidence, cannot bring about any significant deg ee of communit
participation.
. .
It needs to be recognised that communities are priman y
of theutter inadequacy
interested in curative services because
ceived/ and rightly/ so
of these services. As result this is pe
Can the people befaulted for such a p
the immediate necessity;.
caption when majority of them are denied access to.even very rudi
Moreover the functioning of programmes. a
atproviding p reventive carehasnot shown to thepeople the advanta
It is only whe, from their own exper
ges of preventive medicine,
preventive servicesthat one can
people realise the advantages of
tary curative services.
expect a shift in perception.
.
Thus to sum UP, for any tangible changes to takeplace in th
field of health, radical redemarcation of priorities m the whol
health care delivery system ha e to be initiated.
Hard politica
decisionsto greatly increase spending on health care have to
be taken. for the Primary Health Care system to function adequa
ft has to be made answerable t
local bodies.
Tftis in turn woul
require steps to democratisethe functioning of panchayat system
14
leaps and bounds.
From a
meager 0.14 Crores in the First Plan
went up to 409 Crores in the
Fifth Plan, 1426 Crores in the Six
and finally to a
proposed 3256 Croees in the Seventh Plan. Yet
birth rate has remained static at
around 33 per 1000, for the l
decade.
How then is the
continued increase in expenditure on f
planning to be justified?
tually the basic problem
yiuDiem lies
in the
the inverted
lies in
inverted logic that
falling birth rate
development. The
rate preceds
preceds socio-economic
socio-economic development.
experience in countries all over
over the
world has
shown that exactl
has shown
the world
the reverse is true. The family planning programme as it stands
today, is another example of attempting to find technological
solutions to social problems which require societal measures.
Moreover, the family planning programme with its fetish for targ
Pieces an added burden on the health care delivery network, whic
it is ill equipped to carry. As a result there is a further
whittling down of the already meager relief that the primary hea
care system provides.
As noted in the case of other vertical
programmes, the family planning programme too needs to function
an integrated manner with the rural health scheme.
CRISIS IN PHARMACEUTICAL INDUSTRY;
Though there continues to be a greater emphasis on the curat
aspect of health even this area is plauged by a variety of proble
This is examplified by the total anarchy which prevails into the
production and supply of medicines.
Only 20% of the people have
accessto modern medicines. There are perennial shortages of
essential drugs, while useless and hazardous drugs flourish in th
market. There are 60,000 drug, formulations in the country, thou
it is widely accepted that about 250 drugs can take care of 95%
of our needs.
The market is flooded with useless formulations li
tonics, caugh syrups and vitamins while anti-TB drug production i
just 35% of the need. While 40,000 children go blind every year
due to Vitamin-A Deficiency, Vitamin-A production was just 50% of
the target in 1986-87.
The production of Chloroquine has shown
decline in recent years, at a time when 20% of the people are
a
15
s
turnover of the Pharmaceutical Industry has increased by leaps
and bounds and today, globally, it stands next only to the
Armaments Industry. The growth of the Industry has been
phenomenal in India too. From a turnover of Rs.10 crores in 1947
it rose to Rs.1050 crores in 1975-76 and today stands at
Rs.2350 crores.
In spite of the growth in Pharmaceutical production in the
country, however, morbidity and morality profiles for a large
number of diseases continue to be distressingly high. It is thus
clear that there is a dichotomy between the actual Health '’needs'
of the country and drug production.
It is also obvious that a me
arithmetic increase in Drug production cannot ensure any signific
shift in disease patterns. Hence, if this dichotomy between drug
production and disease patterns is to be resolved, some drastic
measures are called for to change the pattern.
The Pharma:eutica1 Industry in India has developed along the
lines followed '.n developed countries, The reasons for this are
First, the Industry in India being in the grip of MNCs,
drug production las naturally followed the pattern of production
in the parent ccn ntries of these MNCs. No attempt has been made
twofold.
Secondly, the India/Drug
assess to actuc'. needs of the country.
’ ‘
, who
Industry caters principally to the top 20% of our population,
have the purchasing power to buy medicines. ■Lhis is also the sec
which is amenable to manipulationsby the high power marketing str
of the drug cor panies. Moreover, in this section, disease patte
do roughtly cotrepondent to that in developed countries. The
industry ?*,s thuc able to ueglect the needs of 80% of the populati
andyet make subs tantial profits.
^t sees no ned to change its pa
of drug product! c n and thrust of its marketing strategu.
One is
unlikely to see <iny change ir. these areass unless the industry is
compleeled to cl.enge by stringent regulatory measures, by the ^ov
Government.
drugs differe f.rom other consumer goods, in that
while the co: turners have a direct say in the purchase of consumer
goofd, such !.,' not case for Irugs. Drugs are purchased on the
Further
16
large the curriculam has very limited relevance to the existin
situation in the country. On this the report of the Medical
Education Committee, Ministry of Health and Family Welfare say
’’The present system of medical education has had no real impac
medical care of the vast majority of the population of India”.
is thus the not suprrising that what doctors prescribe have li
relevance to the disease patterns in the country..
what is probably even worse is the fact that doctrs,
afte
passing out of teachinginstitutions, have almost no access to
unbiased dnnrg information. As a result their prescribing habit
moulded by information regularly supplied by drug companies.
his information for obvious reasons, is manipulated to support
production pattersn of the drug industry. ^o ulti tely what
medicines the patients gets is determined not by his actual nee
but by what the drug companies feel are necessary to maximise t
profits.
INCORRECT PRIORITIES OF GOVERNMENT
The problem is compounded by themanner in which the governm
^he most important crit
makes estimates for drug requirements. T.
used for this purpose is based on ’market needs *f Given the sc
related above, this can neveif reflected the actual drug needs o
country.
- Today, a need is created forvarious inessential dur
by salves prmotion campaigns conducted by drug companies. ^hus
ecample Vitamins and tonics in large doses are prescribed laon
antibiotics. This is a ’created need’, though vitamins and ton
are sameof thehighest selling products in themarket.
India accounts for about 18% of the world’s population, many
factures andmarkets only 2% of the total global drug production,
out of which barely 30% are essential, to meet the drug needs
to drug to treat 24% of the total global morbidity, '^hefollowir
table gives us some idea of the shortfall in essential drug prod
(Though the gravity of the situation ismore than waht the table
cates, as the demand estimategiven for 1982-83-based on governmer
figures are a gross under estimation. Moreover for 1986-87 the
Chemicals Ministry has even stopped giving gurues for demand est
ChlorampheniGol
Ampicillin
Vitamin-A
300
111.46
300
200
MMU 77
142.27
52.00
3 80
140
INB (anti Tuber
cular)
T
250
288.40
Chloroquine
T
200
194.57
325
410
177.61
Dapsone (Anti Leprosy)T
200
86.90
60
25.51
Diptheria Anti Texin MU
800
653.57
800
691.05
T
T
71.60
158.45
69.34
188.59
Sources Indian Drug Statistics, 1984-85 Ministry of Chemicals
Fertilizers, c-‘ Annual
"
GOI. &
Report Department of Chemic
GOT, 1987-88.
and PetrochemicaIs, GOI,
The Indian sector in the Pharmaceutical Industry(including
both private and public) has the capability to produce all
essential drugs. Yet the multinational sector continues to pl
a dominant role.
he mercenary attitude of drug multinationals
responsible for holding the health of the country to ransom. T
market drugs in this country which arebanned in their parent co
ries. They use the country to test new drugs with dangerious s
effects and in a variety of ways flout the law of the land with
inpunity. Health related industry has the second largest turno
owlr over, after the armaments industry. Today the predatory n
of thepharmaceuticaIs industry appears ready to outstrip even t
arnaments industry,
he conctol of drug multinational companie
the Indian market is alsmot complete. There are more than 50 M
in the drug market in India.
ifteen such companies control as
as 31.8/ if the total Indian market.
MNCs in theprocess have e
huge profits while charging exorbitant prices for their product
There have been persistant demands that the Multinational
companies should be nationalised. In fact this was one of the
recommendations of the Hathi committee set up in 1974 to go int
the problems of the Pharmaceutical Industry. MNCs are. still be
allowed to operate in this country on the plea that they bring
new technology. Yettheir record in the last decade shows that
contribution in this field has been less than the Smail Scale S
-sl8:TABLE-7
COMPARATIVE CONTRIBUTION OF MNCs AND NATIONAL Cos
.(Top 85 Cos.)
Class of Drug
ESSENTIAL
(Rs.in Crores)
Nationa1(45)
Total prod.
MNCs(40)
Antibiotics
Anti-T.B.
2 56.5
29.2
82.9
173.6
(6 7.7%)
Anti-T.B.
29.2
(32.3%)
4.0
Sera-Vaccines
1.5
0.5
(33.3%)
Ironies
32.0
Courtjh&Cold
55.7
20.1
(6 2.8%)
41.4
(74.3%)
11.9
(37.2%)
14.3
(25.7%)
12.3
(98.4%)
0.2
(1.6%)
25.2
1.0
(66.7%)
INESSENTIAL
SIMPLE REMEDIES
Preparations
Rubs &Ba1ms
12.5
Vitamin
98.0
78.8
19.2
(80.4%jD
(18.6%)
Source s ORG Retail Survey/ April 85 to March 86.
The new drug policy announced in December 1986, instead of
spelling out measures for control of MNCs has granted them even
i
more concessions.
It has allowed increased profitability on
drugs and has reduced production controls. 1he recent trends of
import liberalisation and peeduction and price decontrols are in
line with the present over ments attitude to industry as a whole.
However the drug industry is probably unique in that it has adirec
bearing on the lives of almost everyone,
^he government has never
while formulating its drug policy, takenitbo account this uniquenc
As a result ’’market”forces” are being allowed to determine the
availabilty andprices of drugs, In a situation w ere only one out
following a policy which is detrimental to the interests of an
overwhelming majority of people.
ROLE OF VOLUNTARY AGENCIES
/
Probably the single largest contingent of Voluntary agencies
are involved in work in thehealth sector.
Unfortunately thenet ou
.'V,'
19
•
are depedent on the quality of those heading such projects,
whi
1ely works as
a constraint in replication of pioneering
efforts in different
conditions. Moreoverthe need to develope
models for replication
are not recognised as a priority by most
These problems
are often compounded by the mt Itip licity of bun
agencies, each with differing perspectives.
This results/ at t
in agencies having
to modify their outputs to suit the needs of
funding agencies.
Compared to^Gpvernment services the
coverage by the.Volunta
sector in providing primary health
care is negligible and will
so indeed, the basic
responsibility forhealth care must rest on
with the state.
ence the contribution of the oluntary section
India needs to be assessed in terms.of the
kindof innovative ide
programmes it has been able to throw
up in thelight of its exper
h
voluntary sector three broad trends can be identified
broad trends can be ideni-i -f< oa
ThZ1^ aC*/n”rea
Prl
H
PotZL-t
providing Onratlve services.
®rS ”h° have att™Pted to imptnentea the concept of
h 2"
B1S0 ” = ldU1^ PW^es aimed ot co.mun
.«
1 sue
Z 7Z’*” “«• "
taken up hro
!
?,
reletions, egc cultural „a3ss„ po„er structures
villate communities etc. in addition to health issues.
The latter two t^nds. have come up with alternate models
for
primary health care. Unfortunately very f of them aresuch as
can be replicated under different conditions all overthecountry.
reasons for this are many, but some
may.be highlighted.
Most
a gencies depend heavily on the drive an<3 initiative of 2-3 indiv
7L 1S" As replicabinty is not seen as a priority little thinkin
as gone into formulating strate ies that do not depend on the
quality of a 2-3 project leaders. The costs involved, sources of
undmg and their i71pact on r.epiiCability ha-e also
worked out.
not been
Another notable trend is that, in looking for altern
modesl, emphsis has been on "parallel" structures andmechanisms
outside the state run PHC structures-!.* the outlook is to build
new^structures to by passor even run counter to the existing healt
delivery network. For nationwide impact, such an enterprise would
neither be successful nor desirable. further, such fundamentally
differently structures may in fact be envisaged only under alter
-;20s-
in the purely socio—economic political dokain> PSMorganisations
work both to promote greater consciousness about the issue and
creat working "models'1 -i.e. viable and replicable structures wi
the potential for becoming nationwide alternative policies and
implementation mechanisms. In the health sector9 as perhaps in
education too, this would necessarily involve working/ in a broa
sesnes, within existing institutionsl&other structures and look
for alternative modeIsSmechanisms for the State Health Delivery
System, with well-defined roles for PSM and other peoles1 organ
sations.
ROLE OF AIPSN
The AIPSM has the potential forintervening in a meanginful
way in the health sector. xt has thetwin advantage of having a
All India reach and a relative homogeneity of purpose and appro
There is also the in-built scope for exchange of views among
constitutent organisations. Moreover already existing linkages
with organisations of medical and para-medical personnal can be
strengthened. °uch advanta es confer on the AIPSN the necessar
impetus to overcome many of the shortcomin s of voluntary agenc
cited above. The broad direction of AIPSN’s involvement in hea
should be along the following lines;
4
__ Policy issues; Work out its perspective on Health Policy, D
Policy etc. A campaign aimed at the policy makers can be
planned based on this perspective.
—Mass campaigns; Based on the AIPSN's basic understanding
regarding health some fundamental demands need to be formula
These can be taken up as campaign issues among the general
public. Given the nascent stage of develppment of the Peopl
Science Movement in most stages, the campaign should be focusse
on a few key demands.
— Linkages with health delivery personnel; Lingages need to be
built with organisation of doctors, para-medical personnel,
medical representatives etv. Such linkages can work also to
attract these sections, involved in health care delivery, to
the Peoples Science Movement.
— Models ofor Primary Health Care; Initially in a few selected
-:21s-
The most problematic area in the Health Care Delivery
system in the country is the interface between the PHC system
and the users of this system i.e. village communities. The
AIPSN can have a major role to play in this area. *t can play
t e catalysing role in making the PHC systeip more answerable
to the community. It can also work towards sensitising communi
ties to issues to issues related to health, so that instead of
being passive receptents of Government serv±es they can involve
themselves in the decision making process. Such interventions
also require demooratisation of the political and administrative
set up, with much greater powers being reserved for local
b odies right down to the panchayat samities. ffere a^ain the
AIPSN can play a major role in association with local democratic
organisations of thepeople. Given such a perspecpective the AIP
t its All India reach, is in a position to work out models fo
cQuntry<
primary Health Care whlch can bg replicated gll
— Reference
Debabar Banerjee z Health and Family Planning Services
in India;
Pub, Lok Paksh, 1985 <
Health Care Which Way to Go: Medico Friends Circle.
Statement on National Health Policy:Government of india. Ministry
of HeaIth&Family Welfare, 1982.
Health for All, an Alternative Strategy; ICSSR&JCCMR, 1983.
Drug Industry And The Indian People: DSF&FMRAI, 1986.
H ealth Status of the Indian Peole: Foundation of Research in
Community Health, 1987.
State of the World's Children, UNICEF, 1987.
Meera Chaterjee, implementing Health Policy: Manohar, 1988.
J.E.Park, Text Book of Preventive and Social medicine; Pub.
Banarsidas Bhanot, 1986.
*****************
Gem M
A PSM APPROACH TO PRIMARY HEALTH CARE
The Declaration ^f Alma Ata marked a histories step in the
history of health.
it was the first clear international decla
ration that health which is a state of complete physical, menta
and social-wellbeing,
and not merely the absence of disease or
infirmity, is a fundamental human right and that the attainment
of the highest possible level of health is a most important wor
wide social goal whose realization requires the action of many
other social and economic sectors in addition to the health
sector'
The Alma-Ata declaration was a major step forward for it
was beased on an understanding
( a)
and implied that
’the main roots of poor health lie in the living
conditions and the environment in general,
and more
specifically in poverty, inequity and the unfair
redistribution of resources in relation to needs, both
inside individual countries and internationally.
(b)
That the people have the right and duty to participate
individually and collectively in the planning and
implementation of their health care.3
(c)
Primary health care,
defined as "essential health care,
based on practical,
scientifically sound and socially
acceptable method and technology...
at a cost that the
community and country can affort to maintain atevery
stage of their development in the spirit of,
self-reli-
ances & self determination., is the key to attain the
target of health for all by 2000 AD’4.
Unfortunately despite the brilliant polemic and sweep of th
declaration, its implementation lags far behind, and now 22 yea
since its adoption in practical terms, at least in India, this
great slogan has had little impact.
Unfortunately the World
Health Organization who gave this call, has its contacts limited
to the health ministries and to medical and allied professionals
and it is to these sections that the task of implementing
programme went.
this
One critic ruefully comments ’Handing over the
implementation of PHC to the medical establi shment was similar
to handing over the implementation of land reforms to landlords
O^e outcome was to attach ’health for all by 2000 AD'
as a sloga
2. s-
.J-
r.
The other major thrust of ftihe preserHt primary health
cave programme,
as.it is in India, is the establishment of
primary health centres and the deployment of community health
workors-both at subcentres
and at village level.
run into serious problems.
Not only is the number of’ health
This too has
workers that have been trained and deployed far short of what is
needed, but even those who are deployed yield only a limited
quality of health service.
The selection, training, monitoring
and motivation of the community health workers is so poor that m
tend to drop out & some even migrate and set up as quack medica
practioneers themselves.
‘Community participation’, one import
planned feature, is in most places completely absent.
Almost
no research, planning or training goes into identifying the
problems and working out the tactics of health care delivery.
i
For the medical establishment, it is business as usual.
The last 10 years have seen the mushrooming of corporate private
hospitals and -a number of private capi tati on-fee based medical
colleges.
A top few eminently ‘successful’
over medical
doctors preside
association, act on. medical councils,
governments on health policy,
advise
serve on its commitees and working
groups, influence governmental decisions by virtue of their
physician-level personal contacts with decision makers and in
many a case even dominate research and private practice.
The
entire primary health care campaign and the Health for all by
2000 AD slogans are seen as empty politician's slogans or at
best as the department of p g SM's responsibility.
Clearly
no major change is likely to be contributed by these sections.
It must be recognised that members of the medical profession
can do little in their professional capacities to achieve this
goal.
Medical & paramedical professionals are well positioned
to investigate the causes?and consequences of ill health.
However they can rarely tackle the root cause of ill-health
hunger, poverty,
shelter,
water,
sanitation, employment, leisure
etc., Without tackling these basic questions-primary healthcare
as spelt out by the Alma-Ata declaration is not realizable.
-
o
3 :-
It is possible with adequate political backing and administra
tive will to immediately achieve,
large areas of the country.
doctors,
such medical care at least in
It is possible for socially minded
helpted by donations or grants to provide such basic
medical services in remote rural areas or even in urban areas
where the poor have limited access to such health services.
Th
is a record of numerous doctrs from a wide variety of backgroun
the catholic hospitals associations,
the people* s polyclinics o
Andhra Predesh,
at Chikmagalur etc., who
the work at Nagapur,
have undertaken such work.
Such work is a valuable contribution
but in terms of the actual contribution to the health of the
community as measurable by indices the impact has only been
Impact on health itself can only take place by the
marginal.
implementation of primary health care in its broader concept.
Though provision of health services and essential drugs are a p
of the concept of primary 7 health care,
they are not the major p
or the focus of primary health care.
This should not however be interpreted to mean that health
professionals have no role in the implementation of primary hea
The word ’doctor ’ is itself the derrivative of the word
care.
1 to teach'
The doctor and other health professionals are looked
upon as a source of knowledge about health and disease.
Today
many of the ideas prevalent about disease, both right and wrong
and most of the health policies have been contributed by the me
professional.
To view disease as an affliction of an individua
by a germ! and lose its social dimensions is the result of a cur
bias,
that the PHC approach sets itself against.
The result of
such a bias in the sphere of health policy i s to search fortechn
logical or managerial solutions to what are essentially social
issues.
The doctor has contributed to such a bias and the doct
can contribute to its unmaking also.
The people’s Science Movement and indeed all other individu
group's & organisations desirous of realizing the goals enchriv
in the Alma Ata declaration need to plan for intervention to
prevent the demise of a powerful concept-He al th for All, by
2000 A.D. ”'A great concept should not be allowed to-'dissolve
-:
4
Health education has many limitations and pitfalls.
Much of the health education current today is technical,
fragmented and culturally in—appropri ate, other than being for
Thus a health worker may deliver a
that situation irrelvant.
one hour lecture on diarrhoea, without ever mentioning that the
water source in that village should be safe.
Instead she would
probably preach a sermon on cleanliness, suggest using boiled
for water all drinking purposes and finish with suggesting
oral vehydration therapy.
By the time she reaches the most
useful part, both sympathy and inevest would have been lost.
Or a class on nutrition may tell all mothers assembled that
they must give milk,
eggs,
fish,
fresh fruits & vegetables to
their children - when most of them are going hungry for want o
ability to purchase rise.
Even in many a people's Science
movement lecture we tend to leave out social causes and
possibilities of remedial collective action and instead stress
technical causes and individual solutions.
It would of course be of little use if health education
lectures were only polemical or philosophical in nature and
discussed and curative knowledge will need to be imparted.
Bu
where collective action is the only real solution and the basi
problem is a health determinant like water or nutrition or
sanitation, health education should be aimed at exposing such
causes and- appropriate remedical collective action.
The
health professional should provide the technical information,
if such is needed,
to justify,
a PSM effort to organising such
action.
Could health by itself serve as an entry point for
collective action? The health worker-can she become the agent
of social change?
Can oppressed people be organized around
and for health issues.
Though this debate is far from over
some Indian experiences have replied in the negative.
'Health
work they feel has only weak political implementation
and
without a proper political context not much of genuine people’
participation can be achieved in community health work done.
-s
e
5
The reception and popular response to proper health
education is also limited, by the dominent culture of seeking
a pill or an injection as an instant remedy instead of trying
fpr a more scientific understanding of the cause of disease.
They come to the health professional vfor a 'cure*
and not for
Many health education strategies therefore choose
knowledge.
to combine therapeutic services with oral education-both within
the governmental and in the non-governmental sections.
Thus
the women waiting to see a doctor in the gueue before a primary
health centre are given an half-hour lecture before he arrives^
or while they are waiting for their turn.
Or else after seekin
the doctor they have to see a social worker who spends a few
minutes talking to her about her disease.
Both these of course
and only in an occassional centre, usually
are rare events,
run by a socially concious doctor do they really occur?
Experiences in the pec-p]@’s science movement,
though
have foun? greatest success where the heal
undoubtedly limited,
education has been done in the form of a mass campaign.
media used has been popular lectures, slide shows,
The
street-theat
(the Kalajatha), posters and to a limited extent video.
The
popular response from the audience has been very positive but i
is difficult to evaluate the gains of such general health campa
Campaigns focussed on specific issues especially on pro
vision of essential drugs and tne drug policy have had a much
greater impact.
The KSSP in particular by its wide dissemi
nation of books on essential drugs and on hazardous or irrationa
drugs, have been able to make a mark on drug consumption end pr
cription patterns.
lectures
and
To this end they have held seminars and gue
for doctor^,
campaigned in the local press, used post
news papers and kalajathas to disseminate their views
drug policy.
Their successful efforts to expose multinationals
selling anabolic steroids by intervening in the usual 5 star ho
drug promotional campaign also won them popular suoport and med
coverage.
Such a wide variety of activities and on such a
scale needs a major organisational network and this the KSSP
had.
The KSSP organisational growth is a result of the wide
-s 6 sa broad-based organ! sation -has helped all PSMs in carrying ont
effective health campaigns.
The K.R.V.P.
the Loj< Vigyan
Sapgatana are some of theother PSMs who have held such campaign
he'al th.
Another factor in the success of many KSSP programme is
their educational campaigns not only on health but also on en
vironment, do not stop at awareness generation but go on to
mobilizing people for collective action.
The scope for such
health education campaigns which lead on to direct collective
interventions by the people have not been adequately explored
by other PSM groups & health activists maiinly due to their
organisational weaknessess.
But as the PSMs continue to expand the'scope for such ac
increases exponentially.
for total immunization
It is possible non to plan for campa
or control of diabotical diseases.
It
is also possible and needed to campaign for implementing iodize
salt distribution in the Terai & other iodine deficient areas
of the north while at the same time opposing the ill advised m
to ban
common salt/
commercialize salt production-handing
it o
to large monopoly houses all in the name of preventing a wide
incidence of goitre that-is far from established.
It is possible today to campaign extensively for ensuring
provision of the 25 essential drugs within 1 km of any habitati
and for banning hazardous drugs.
In select areas it may be eve
possible to launch health education combined with collective a
against diseases like gyineawcrm
infestations which are poten
tially easy to eradicate and even against di eases like leprosy
te measles which are potentially ers^Lcable even within the prese
system with exi ting medic-1 knolnledge.
Successful health education work however needs a lot of
careful planning
and knowledge of local conditions and culture.
It also needs an analysis and understanding of the health probl
involved.
Given the bi - s of the medical establishment and off
structures today/ one is seldom able to rely of official
documents and pronouncements alone to evolve a people’s unders
tanding *f the issue.
As a result one major area of people’s
7
There are many groups notably the groups associated., wi th
Medicos friends circule, A.I.D.A.N.
Helhi Science F»rum,
Karala Shastra Sahitya Parishat, F.M.R.A.I. who have made
major contributions in this regard.
Though due to their organis
tional structure most such groups have limited themselves to pre
critiques,
such critiques are essential for future action.
The8
critiques ceuld have formed the basis for collective action by
• ther groups J-ikg y^uth movements, women’s organizations eta. bu
in practice such a crcss-ferti zation has nvt wccurred to any
significant degree.
Most such analytical, thee re ti cal contributions are desk
work relying largely jn seeendary date or compilatiens frcm
various publis\ed sources.
There are however a number of >
significant health surveys and field studies by health activists
which has formed . the basis for critiques.
Health problems
com sequent tn the Bhopal gas tragedy, occupational disease in
selective areas & industries, the general health survey and the
study of primer; health centre facilities in Kerala are some
examples <^f such intervention.
needs be pointed eut that
the maj->r medical research institutes with elaborate re^narch
facilities seldom study such topics.
The marked reluctance of
such institutes to undertake study en areas of immediate
relevanc® to ,people,
especially if the topic is likely t» be
controversial an«j go against local vested interests in well
known.
Unless health, activists intervene, actively^in such ■
areas of research work,
the PSM’s and democratic groups wi ll be
unable to intervene in both the for .mulation of health policy
• r even identify the deleter?
3 effects of ill Concieved
health or developmental strategies.^
Even' theoretical work, based on analysis of published data
has a significant role to play.
The drug policy is one area,
where health activists in India can take pride as being the
sole force to have eppossed the government’s consistent pro
industry and anti-health policies.
And most of this inter
vention is based on study done by various health activists
themselves.
Similarly on patent law and on ioidi sation of salt,
8
critiques or ev >lve alternative strategies.
There i s an urgent
for health activists to widen its contacts amung trained and
sincere health professionals who. can help.*
4
A large number of
doctors, esperirajlly junior doctors and medical stMdents-and
many with good academic backgrounds are interested in a social
activity of the medical system and willing to contribute to it.
Their participation in the work f PSM should be ensured.
Can PSM s go beyond health education campaigns (both gener
health awareness and on specifie issues) and beyond presenting
critiqi/es and critical reviwes of health policy? Can it attemp
to tackle the concept of primary health care in its entirety?
Can it by ifs ..work raise the- level of health in a measurable
fashion or' o-'ntribute -to such a rise in health status?
One approach to these questions is to work
a mo^elto take up an area varying in size from a village to a taluk
or district-and in this area attempt to render primary health
Too • ften what is rendered is only basic medical service
care.
and then in the long run the results are not adequately rewardi
However ther^ are attempts to integrate in such a model, basic
medical services with major health educational campaigns,
introduction of scientific inputs to upgrade existing rural
technologies andlLaunching rural development schemes that
z
j
„
generate employment, provision\of better nutrition notionly
through income generation but by a more optimal \se of available
resources especially fo’r children, provision of safe drinking
water and elementary sanitation and above all literacy educatio
and scientific awareness.
The people1 s science movement is
better equipped th^y me st groups to implement such an approach.
It has within it folds considerable experience in rural technol
in literacy.
and non forfbal education, in running campaigns on
issues espei^Lly usiftg local art-farms as a vehicle for new
ideas, in drinking-water and sanitation woric - and in running
basic health services. It should be th©s possible fbr such '
a model to the buil't up with the available experience in the PS
a
When building such models one deeds remenlber the past PSM
experience, that success ful campaigns need a critical size for
9
automatically replicable all over the country, by virtue of
its being successful in one place.
Even for the model area to
succeed social inequ.dties will pose a problem but we need not
d-ssune they are insurmountable ones..
(Such a model cannot theref
be posed as the road to success of primary ' heal th care).
Then what would such a model contribute?
It co.uld by its
very presence and success help to pose the issue of an alternati
strat^/ to health care and development.
It could demonstrate
that health for all is possible - now, given the administrative
political will.
it would help bring, by virtue of its experienc
the issu'e of health on to the agenda-of national priorities -
where it is theie notionally but not in practical terms.
In
organizational terms it would mean mobilizing new sections into
PSM activities and adding a newer dimension to activi^i^; aimed
at social change.
What we should not do when the PSMs take up primary health
care work i s to confine i t to health services, and to health
professionals,
Thereby we would be going back to locating hqalt
i ssues as separate from other social problems and nurture the
belief that good health can be won by technological or manageria
inputs alone.
PSMs can organize people around health issues
only - if they link it up.
especially literacy,
with other issues of development -
education andemployment.
One area of expanding PSM activity that offers immediate
scope for linking with the health issue is literacy.
of functional literacy as understood by
understanding of health.
Literacy,
The concep
us, includes an
and education by themselves,,
independent of all otherfactors have been shown to. be major
oeterminant of health status.
Women’s literacy in particular
has been shown to affect, independent of other parameters, women
health,
attitudes to family planning, number of childfen born and
infant mortality.
The process of imparting literacy is a useful
vehicle for the generation of scientific awareness of which healt
awareness is an important aspect.
One major new area of contribution of PSMs is in adult
10
ny operation smiles - a project for 100% immunization in
Ernakulam district,
Diaorrheal deaths & mortality have come
down si gni fi can tly.
In Pondicherry too a health phase!s likely
to follow the total literacy campaign.
The coming Bharat Cyan Vidyan Jatha, being organized by the
people's science movements of India isone major avenue for health
activists to enlarge the oCOpe of thei r work.
The B.G. V.’7O aims
to organize one cultural groups of volunteers from all walks of
l
each
these
In
of
in each of the 500 odd districts of
India.
of Indian
districts the jatha will give performances at 120 to 150 centres,
Their performance is aimed at creating an
awareness of literacy
The basi c organizational task of the BGW i s to
and science.
organize 60,000 centres all over India to receive
thesetroupes,
Each centre will also identify a resource persons to give 10
cOne of- these topics is 'Being Healthy*
lectures each onetopic-.
a basic talk exp alining the? causes of diseases and the need and
nature of primary health c a r e.
The generation of such wide and diverse voluntary n e two rk
of activists by the people's science movement opens up vast
potentials for future action by the peOple.’sscience movement.
, literacy is ^finitely the major follow-up action envisaged -
and
definitely the issue we need to address ourselves j
to most urgently
But it is not possible to open up actual teaching work in
) all
these 60,000 centres as follow up, nor will we be able to
sustain even the
active centres with a single point programme
of literacy alone.
Health is definitely one major thrust area
for follow up work in these centres.
The follow-up work may
take the form of health education campaigns or even of interventio
in areas like immunization, guinea wbr; eradication etc.
Or there may be areas where we could attempt comprehensive
primary health care.
It
premature at this stage when the
60,000 centres exist only on paper to plan for a detailed follow-
up but we need to start thinking about it.
We can however state
confidently that the very attempt to train 60,000 voluntures
to djive a talk- on primary health c^be in
every village of India,
i s an unique attempt that is bound to throw
up a major manpower
’^Health for All by 2000 A.U.
Resources
Dr. C.M. Francis
President
Indian Society of Health Administrators
and
Dean
St. John’s Medical College
Bangalore - 560 034
Cor
Resources for ’’Health for All by 2000 AD”
If ’’Health for All by 2000 AD” is not to become
another slogan like the large number of ’’International
Years” and ’’International Decades”, we will have to
mobilise all our resources towards that objective,► Our
greatest resource in this regard'is our National
Commitment to attain r. Health for. All by 2000 AD1’ . That
commitment should
(i)
make each individual, family and community
become their own agents for health
(2)
enable us develop the needed health manpower
and provide the needed financial and material
resources. ■
The Government has to mobilise all resources to
these ends, with the full participation and active invol
vement of the community. All sectors must contribute
towards health, as it is a goal and a means for developme
There are sectors in agriculture, industry, public works,
education, etc, which have important contributions to mak
towards health. Our providing resources ’Will depend on
•whether we consider health as a consumer item or as a
means of increasing the productive capacity of the
factors, of production—labour, land and capital - that ma
result.in health care? If health care merely restores or
maintains the well-being of the people but does not add
to their productive capacity it has to be considered as
consumer goods, however it is clear that health care is
an investment; by improving the quality of life, persons
become more productive and hence adds to the economy of th
country.
jq ’
-
■
Health for All" should basically provide primary
health care for all. There should be a minimum programme
involving
(lj
(2)
(3)
(4)
promotion of health
prevention of disease
care of the sick and cure where possible, and
rehabilitation
These have to be achieved ^by
(!) hg.olth.e^cAtiorx. : This would involve all attempts
at making the individual, family and community assume
responsible roles for promotion of health, with greater
self-reliance - both formal and non-formal education can
be used. The mass media could be utilized, with a little
more imagination and not much mqre financial inputs.
./Il
2
During the school years, it is easy to inculcate the
principles and practices of good health. Well—planned
steps have to be taken at all levels of school and
University education. This would not only help the
school goers but also help in creating better health
awareness in their families and the social groups in
which they live. The National Council of Educational
Research and.Training has made some efforts in bringing
about some behavioural changes but not enough. The
concept of healthful living has to be included in the
different disciplines and with the use of all types of
educational materials. These do not involve any
additional expenditure over and above what is spent
in the educational sector.
(2) N^ptipn.! Activities, have to be directed towards t
production and supply of food and to improve the nutriti
status. We have seen that even though India has achieve
self-sufficiency in food production, the distribution ha
not been such that all can benefit; the purchasing powe
of large_numbers of people, especially the marginalised
people, is very low. The expenditure on food and drinks
in India.is about 63% of the income; this is one of the
highest in the world, next only to Sri Lanka, among the
43 countries surveyed this year by the World Bank. There
is no prospect of increasing this amount. In spite of s
a.proportionately enormous segment of the income, nutri
tional anaemia is common especially among pregnant women
and young children. Many women die during pregnancy or
childoirth because of anaemia; it is also responsible
for premature or still births. Measures have to be
undertaken.for greater distributive justice with respect
to availability of nutritious food and supplements to
vulnerable groups.
(3)
,Ve have still with us many
infectious diseases, which can be prevented by immuniza
tion programmes. The new expanded programme of immuni
zation should reduce the prevalence of these diseases.
The cost for.this programme has been worked out by World
Health Organization and the materials are being made
available .
(4) £radj.._c.ation and control programmes: The programmes o
eradication and control for the major diseases have to be
followed up vigorously. This would include attacks on
malaria, tuberculosis, blindness, leprosy and filariasis.
Measures will have to taken to reduce the incidence of
parasitic infestation, which takes a big toll as far as
morbidity is concerned.
(5) Water^ujDjDly and sanitation:
The Miinistry of Uorks and Housing have drawn up a
3
Tho regulfMents of funds for fulfini.uj the tarqets
set for 1990 are (in
. i crores of rupees)
--gers
J
Urban water supply
'Urban sewerage
- 3044 (100% coverage)
- 2432 (80% coverage)
Rural waiser supply
- 7057 (100% coverage)
Rural sanitation
- 3301 (25% coverage)
This has been studied again in an effort to reduce
and use
cost; with low unit costs
-i
local community
resources, th(. c .
Public Health and Environment
E ngineering Org ani s ation ~ha s
-; worked out the cost as
fil*££es_.ilL xrores
Urban water supply
2,475
Urban sewerage & Sanitation -
2,590
Rural water supply
Rural sanitation
4,288
1,584
l
Total
if the targets are to be achieved.
i — ibi
■rt_x
10,877
curing the deca
Many underdeveloped countries are making efforts to
iZ^eDS1hnkln9 777 ? 311 and sanitarV dispoSSof°wa
Bangla Deshis scheduled to achieve the target of orotor+o
drinking „at„ supply in every village within 200 Sef o
?«ido&7thin the ** 2 years' ““ “
4- £Ujnary,„He a It h Ce nt r e
_ The sheet anchor of our primary health care is the
primary health centre with the subcentres. While we starte
ell, our progress has been tar,dy. There ought to be at
?20S000inPhillvY heal^h centre for 50,000 population
(2U,uuo m hilly areas) and one subcentre for 5000 oooulat
(one subcentre for 3000 population in tribal and hill? are
7 ^Srl^T-T1" ^ablishing prls.aly^eiUh JeSI
to havVI^dSitiXJ°9000 jfiSSWt2TO1^ft”ha:1aisha''e
been decided t.o upgrade 1 in 4 PHCs as the fi“t ooint
of referrals; about 3700 PHCs will have to be upg?Id?d
A
these require enormous inputs by way of finances and mate-
4
and utilise locally available material and cheaper
bo able to reach our
methods of construction, we should be
targets.
These primary health centres and subcentres must
provide primary health care which should be comprehensive
to the extent possible. The priorities must be for promo
tion of health and prevention of disease. In whatever
way the Health Administrators may see the needs, the
immediate needs for the people are cure where possible
and care of all illness.
The Primary Health Care should address itself to the
cure and care of the commoner diseases.
Among these are
1.
2.
3.
4.
5.
6.
7.
5.
Respiratory diseases, including tuberculosis
Parasitic infections
Injuries and accidents
Infections of various kinds, fever, influenza
Gastro-enteritis/diarrhoeal diseases
Abdominal pain; back pain
Insect bites and stings
Laboratjjryi^cc^amary He a,1th.
A Laboratory Service usually exists only at the Hospita
with only rudiments of such a service at the Primary Healt
Centre and none at all at the subcentre. Provision of a
reasonably competent Laboratory at the Primary Health Leve
is a necessity. This can be managed with a trained tech
nician. Many of the underdeveloped countries like Indone
sia, Malaysia, Sudan and United Republic of Cameroon, have
Laboratory Services at their Health Centres. Without simp
reliable laboratory services at the primary level, health
cannot be improved. The techniques must be adapted to the
local possibilities- and resources. These could be
supervised by periodical visits by senior laboratory staff
from the referal centres. Quality control is necessary to
ensure that the results of the investigations arc reliable
6.
£omm^iy_p^J^pjtion
Community consists of all the families living in the
area without any reference to their occupation or social o
economic status. Community involvement would contribute
to a significant reduction in the costs of projects and al
ensure better management, It is also prudent to charge a
small charge to the beneficiaries (perhaps for every house
hold), as the services will be better appreciated and prop
erly utilized #
5
i
the people. This is particu
worR ^both inslde
y
pollution control
legislative protection of the p P
shouid be taken
the factory and outside the tactory;
’industry to avoid pollut
With incrcasiaginaustrraliZ'
ahead of the establishment of the in
ide
y
and, If there.
health hazards,th(j
to reduce their effects•
n+ed by the Ministry of
report of the
(under the chairmanship of
Housing and bocal Govcrnmcnt
tion of pollution whic
Sir Hugh Beaver) to
attributed to'smog in
resulted in about t.OQO d^ths attri^
Thure
December 1952, the clean Ai
•
ntnentai pollution
was a further report °2
composite Control of pollutio
(1971-73) which preceded the Comp
commissions- and the
Act. of 1974. The aPP01^^ep!nd to a very large extent
legislations following ^hem op
ssur0 groUps,
.
on the public opinion,
q
A report “A Blueprint
lobblesCr wdlvidusl
nraatad a lot.of
•
. n
for Survival by
governmental action,
interest in the. public and -d to
h meetings,
^s^r^io^Ktlo^orSher
-dia.
Legislation is also J^essa^to^rotucu^nCtC.vvlupnK
of industries including th<- p fimported displacing
Capital intensive.machinery is bping^impo
pollution.
the local labour intensive
<ieads to poorer. health
Teaislation must be aimed at
economic deprivation whic
of the marginalised people.
9
and alsQ the labour
providc employment
protecting the small scale ^dust
nS’of people and lead t aconcmc 9bp«
and Sottr9distribution of wealth.
Hot all’companies based in^developod^caunt
qo to developing countri
P i the developed
lame civic-mlndoonoas which they sho^^^^ of
countries. They usually •
porant countries; this
and occupational health in
r(ymDUlsion. When they,
may be either by c
developing countries these high
ranSr^not o^-eiibS^te ’ an^uSuii^S^o5of
irSsSkSludgeable Governments^ nd people ^a\ualth
hazards.»n^LegisIation%hould be^brou^ht^out^suc
a
these transnationals have tr
In India there a
as they have in the country of o 9
s Act, Tea planter
many Acts like the Fa<ctorie- .^A
have prc)Visions
Act, Dock Labourers c
ority of instances such
”u»ivalY or uuuliiotrvuly
■
■ already prese
Very often the legislations which are
of*fragmentation of
6
in Mines and Quarries by the Department of Industries
Oceupabional Health by the Department of Employment or
the be pa rtment of Agriculture, Hygiene in Food Handling
Institutions by the Department of Health and so on.
Such fragmentation and the multitude of departments will
not be dondusive to the effective control of the problem
which are allied and intertwined.
Heam^an_Po^r
.the resources for health care the most important
critical will be the human resources. It is necessary t
we make all ci-forts to develop their skills, knowledge,
and capacity for the betterment.of health. Health manpo
oevelopment could be. thought of in terms of the demand f
the health personnel and the need for them. It is
necessary to make a judicious decision as regards the
number and types of health personnel necessary for
delivering primary health care. Once such a decision is
we can proceed to the training of these personnel. Such
persons could be manning the hospitals, rural health
complexes including the peripheral centres, laboratories
and activities such as health education.
not OGa-L
deal W1bh
with man-power resources' development
.1 I shall nOr
anu the cjst of such development. Today, India has enoug
information on the cost of the training programmes
ano deployment of personnel of different categories, we
also know the availability of manpower; various targets
and projections have also been made to meet the needs of
health care. The cost-benefits and cost-effectiveness
have also been analysed. But till we know our options an
our readiness for substitution, if necessary, it will be
meaningless to forecast our requirements.
Financing
There is little accurate infomaticn available on the extent and
lands of sources of health care finance, excent for the direct Sources
such as that provided ty the Government, Centre or State. Jh India
where there is a mixed eoonoray, the biggest single source for health
care financing has/come from 'the general tax revenues. Tn view of the /t
low gross national product in India the allocation from State revenues
is limited. The per capita income is very low (India being one of the
poorest countries) and the amount available after meeting the immediate
direct necessities is small. A. recent study by Earthscan has sham that
the mean expenditure n food in India is 63%' of the income. Ifader the
circumstances increase in taxation and increase in allocation are both
difficult to achieve. With a lew priority for health ths budget allocayaas for health are usually small, and unfortunately has teen
slbccwing a tendency to.be reduced. Budget projections usually involve
overestimates of tax collections and underestimates of expenditures
Wnen unforseen expenditures become necessary lite increase in pay of
Government employees etc. , the funds actually available for disbursement
tor ate sectors fall short of expectations. The immediate priorities
have to be met. Hie health sector which often lacks strong*political
support and direct demand by the people may then receive proportionately
lower
tewer disbursements than had teen projGctecl in the national budget all
oca ti on: net result in this particular source of fin nee is stagnant
or oven receding.
allocation
tion varies from Shu
to to
• xt ,
lovols
State
levels of resource Q.lloca’
State bo'J
to State,
both
with respect to the amount per capita'and the osreentage of the State
revenue. It has produced disparities in the health
—i care available in
different parts of the country and therefore in the quality of life of
tho people c once mod.
Deficit Financing: This may be either a part of the entire budget
allocation or specifically for health care. It is dene by borrowing
both dcmostically and.internationally. Hie borrowing may be for spocic projects which directly or indirectly bring about health benefits
lite water supply, sewage and drainage systems or irrigation systems.
Domestic borrowing has an advantage in that it mops up domestic sav
ings. International borrowing could be from bi-lateral or multi-lateral
foreign aid m the form of long term,
interest loans. These loSf
are very often limited to the cost of imports required for develop
°£ thG aid P^o^ded ty the donors requires that
Ef JG ?SnSr r te madG lnr?hose countries. This is disadvantageous for a
numter of reasons. The mosu important is that it limits the flexibite.y of uhe recipient country to look for the more suitable imports.
so costs the recipient country to purchase relatively hteher*cost
goods .and seryicos which could have been procured at a cheaper price
e ocw-ere.
t -Iso produces dependence on the aid giving country for
the technology and service and maintenance later. Aid loans usually
T'*’'
advantage is that it nafes immediate progress possible at tho oxis t-inc'
costs and prices.
■
v ■ nx§agaaj. insurance finances; Social Insurance Finance mav cover
health care , invalidity and old age of employed workers (and" often of
?fF? sfeff.^datory insurance payments as a percentage
^eXfamnies)
of tnoir wages and tgr imposing on their employers a similar payment: in
some cases the GoTOrnmcnt is a contributor to the soheme. The test
example in.India of such financing is the Fmployoes State tesur-nco Schem
It is a m. jor. source ,ox tuiance for health care and locks after tee per
sons who are involve m production in Industry. Its principal shortartteln13 lfc^
coverage. The large majority of labour fofees,
fXteP^+? T ° Cn'Ot COTGK3d; ^tever coverage exists
is for the tetter paid anc tetcor organised sections of the society.
+0£,+ h(: forc®stUhcT Qiployccs ..State Insurance Scheme was started
wso that it could ultimately evolve itsolf into a national health ins-‘
urencc sysren with wurersal coverage. This hope has not materialised.
'and
!?orfelTf snd ?ublic sector workers derive many medical
and health.care. tenants ap$t from the Employees' State Insurance Scheme:
so also private sector industries give coverage for their employees who
S
v7 ?G Shp?5'ees
S^.
Shese^re
spitel-te.sed? doctor^centred programmes and their impact on the health
efre oftte tenl+h
laT‘ Rocontly shorts are being made to take
arTsick (i
\
rS ^d not nereU affo^ to them when they
are sick. One such effort is that of the Ross Institute Lhit of
Occupational Health of St. John's Madical College. There are complete
(1) pre-employmcnt chock-up
(2) periodical check-up and
(3) monitoring of the onvirenmont.
^Sioste
the
such ^at ^GpS cai} he .ta-W
tho
. Ig^teriGs.: Sono State Governments run lotteries for various -ru-mncno.
eSSS
xtaiMl
5P£!X™t
though tho ooohoos ot V^ing „„ oxtzonoly s„n.
“
i“iti* “»»■ our
-Wo hovo „rM out potato
industries and enterprises
It’is osneHa?^ icularly so m the largdr
graphical areas whew a^ssa^ty
these and other agencies in monitoring the health condit-J cns, idmtifying
factors which function central^ to positive health and take moasa
to
provide healthy living.
Private, Health Bsurcunce: Private Health Insurance has been carried
out only to a slight extent in India, unlike countries life the thited
The
States of America; it Usually covers only medical care of the sick
premiums are acturially determined and there could be individtial or
group insurance.
Charitable C cn tri but i on s ? The amount that is made available for
health care bycharitable contributicns is not fully Imam; 'thosecar.
be by contributions^in the countiy and contributions from abroad. It may
be - by. wealthy individuals, families, business enterprises, t msts or
religious bodies. These contributions often enjoy tax deductions which
work as incentives to give largo amounts as contributions. One of thdifficulties in these charitable contributions is that the den.o^s night
have priorities which do not coincide with the most crossing health needs
of the population involved. Very often these donors prefer to oroide
physical facilities aand largo equipments as visible evidence of their
Funds are provided for construction of buildings for hospitals
charity
and donation of sophisticated equipments. Other sources'have to
found
o provide for operating budgets; often it is very difficult to find
iunds to meet the recurring expenditure.
I
I
I
. In many parts of India religious organisations have been the first
to introduce modem medicine. Very often those health centres have ’
oi excellence in the quality of service provided because of
,
icir dedication to service. Some of the largest charitable contributions
come from.orcign organisations in the form of grant aid. Tn 1978 Z 7nn
ah?!FatXani 1
received 297 croros in foreign exchange from donors
abroad, mainlyor social services. A large chunk of those foreign donat
ions has gone into health related activities. One of the defects in those
large foreign aids is a dependency for funds, material and. technology and
c tendency not to use sufficient care in the utilization of funds.
jy°oufoholcl k?°nc!A maj’or Part of oxponditure on health
c re is a direct expenditure by the persons who wish to have the health
care Payments are made directly to the provider as fee for services and
p,
for fch® Produc^ purchased. Very largo amounts are spent in this
way and wc can hare only very crude estimates of amounts thus available.
gyunitv Help: Mth the dwafcnfeg of different sections of society
more ano more arc comre., foreard with solf-holp progrades. This is still
aTC nu^rous oxamplV Chc s^h is tfe
a X J, + A. Cc>-0PcratlTC >
which the members of the co-operative have
n " Uk °
programme. If such programmes can bo multiplied wheroovor feasible considerable finances can be mobilised to take up local
projects which improve the environmental sanitation. It can also take
Up spociiic disease eradication programmes.
_The consumer demand for health care varies from place to place,
H^zaseuticalg for Priraarv Health Ca-ro
>*.
feasible costs.
via
“““r °f drues
tality of essontial drugs at
in the cXtiy, India SdAXjJfhAteh‘S' 2e^a^0!u$ical industxy
^ho provasicn of phanaacouticals for the pc onio
Bio aT,r,1m+
of drugs and pha’nnaceubi^s“by'7 po^cnTr Andi - tSed f°r
Pu-nch.ase
/
Lf
18 Gxfcrone-V email
compared to what is used in th- do^i
the developing caatA
mL
™
?0Untne®
not to toXfor of Sto K ““X toSV't”?
I
sane of
18
IS available for the purchase of
minimum amount
the sick. A look at tho XS S: wdXXom?5e Cal-'tO Carc
■^mounts spent by
. oome countries is revealing,
ggtimatecl purchase .of human pharmacouticals (1975)
Per ec-pita
Average
West Gennany
W 53.35
Japan
38.45
35*05
19.50
U.S.A.
U.K*
India
0.75
.for tho io, XlXiX^^TdurtX^f 0^?1^13 X
adia bufc 0TOn
The financial roquirononts for SoX^laceuticais is not cnough>
estimated to bo fe.720 crores for I93^«f " .1 °f bul< drugs haTC teQn
of Ps.2,160 crores. Iho investmentpr°ductian of formulation
of the order of Rs. 150 crore- and Rs /nX Publlc £Lnd private sectors is
crores. We are still dependent XoS^nf
a ®aP of Hs. 1,610
those
thOr
dovcl°rod countries
for
products, hi tho ihtemati^ S ” °
there is a wide disparity totweon theXX 7 “ medicinal proiucts
h developed countries and the devol"
opmg countries.
Jht^erria.'ticaial. ~trado in nedicinal products 1969-197/.
i
--------- —
Unports
1969
Exports
1974 J 1969
1974
h
control the.production of drugs as regards the nature of the products
the priorities and the final prices. Modem drugs are mostly chemical
The
substances derived frefa potro-chemical or fermentation industries
Uonnan chemical indust©- was the only major international supplier
before World War I
T.-itop other developed countries joined them, especlally when ib w^s xound that the Ccinans witdrew their supply of some of
the more unportant drugs fren the international market; the countries in
volved also put large duties on tho imports discouraging the worts of
these drugs and thereby helping the indigenous production, of the drugs.
S^atc a?M as a facilitator in the growth of tho ph’rmacoutical
industries in thecountries and was mediator between interests of the
industry , the medicaj. profcssicaa and the densumihg public.
+.
capitals, modem technology, expertise and extensive promotion
*°?S- taeS.arC ncGQssa.ry in tho highly sophisticated phnmaceutical trade
So
+• C®centra31ai of those Metrics in the developed world,
r/' Phv^ " °utlcal “d^s'tnos are often a part of tho activities of the
wnXWhMh aS na:mly a chem-cal industiy. Hoechst which ranted 2nd in
world wide drugs was eno of the 8 largest companies in the world of
verail not sales in 1976. Bayers which was among the top 15 transrdrug sales was cne of tho most successful
he+W° ld,x“
to thc overall net sales in 1976. Most of
baling with pharmaceuticals have '
Sllv
Gd lntercsts’ A count© lite India has little chance to
PcTOlcw,nt .. Research and Development am often geared’
o the necdo ~f the more developed countries (because of the greater pur
chasing power) and carried out in the technologically forward countries^
c developed countries have different .prevalent disease patterns from ’
ableSGa^
is a chanS° ^cm ccmunicCTtr?GS‘
able ana parasitical illnesses to chronic and degenerative such as heart
+wa 2c 'v ’ can°er and various stress-related diseases. This would mean
th^t lan.es of research which could have yielded beneficial results 2
tacking health problems of countries lite India by developZt of Reaper
andefficacious drugs nay not bo followed up.
cneaper
up.
based^Sarch"
sect research.
13
rodistributiar of ^ustry
a
This is evident in some of the countries lite Mrxico and
0) CGrtain ^velopment costs part£Xri?for
fr“C4.L ' pc^^aol are lower in developed countries, (2) the roavircr-nts
for testing human subjects are less fomidable and 3 delays^n r-X
Son^flT Prcd"cts+aNevertheless this
iXtSXl
has
“Motel th.
-Liseu countries disease orientation of• the Transnationals.
Sloped
eountSfiX^
com drug products but tho' nrH
^Ien a oreat majority concountries am on3v’^' n-p
+^ionals within the group of doveloning
wore Toother StSes
are actually worked^ the dXte
often decide
b to So SeS 2
d
a 11 tho ^afedor
^.P^011*3 registered by foreigners
hoWrs
prevent others frrn develonW tho
develop them and also
i
in providing the eoisumor with ehoap3r,^fkSire^repShaS
Prcnoticn: Many of these drugs are given intense promotion by various
advertising moans when doctors become used to recommending the drug by its
brand name, ’ and not by the generic name. Che drug may be Imam by a very
large number of different brand names a&cr depending upon the capacity to
advertise and exploit, the same drug marketed by different firms may be
sold at different levels in different countries. There are certain countrie
which are now insisting on purchases being made by generic nares. Some of
the developed countries like Norway have national formularies and purchases
had to bo restricted to the drugs found in the formulary
The total
number of drugs in the Norwegian formulary comes to about two thousand
whereas in India there are over 15,000 products in the market, most of them
aas been estimated that marketing expenses
being duplicate products.
were .equivalent to 15 - 35%- of the sales and represent roughly 3 times the
expenditure on research ■uo 1 development.
I
Pricing arid Profitability: Only a small proportion of the selling
price of the drags represents direct cost of production. Wen whore the
substance has been produced by the same manufacturer, costs vaiy greatly’
between the various"distributors. The firms often get monopolies by var
ious methods and therefore are able to fix the price. The US Trade Comm
ission found that the first company to patent Tetracycline f Msssrs. Pfizer,
was directly responsible for "procurement by misrepresentation" of monopoly
control over tetracycline. It was found that Pfizer and Cynamid had con
cluded a secret agreement by which Cynamid withdrew its application for
■patent for tetracycline after accepting an offer from Pfizer to divide up
the market for the drug.
P-'ricihg pattern is often higher in the developing countries.
100 tablets of 10 mg librium the cost was
Mexico
0.^3 us<
4.^
Costa
Rica,
7o03
U. K.
For
The transnational companies have charged whatever the national market
would bear.
i
One of the ways in-which the prices arc irdlpulated is by transfer
pricing. The prices of intermediate chemicals which aro produced only by
a few firms are fixed at different levels and supplied at different costs to
imports by_subsidaries or joint ’ operations in developing countries.
U.K. has a system of negotiating profits with pharmaceutical firms.
Hoffman La-Roche, the biggest manufacturer of drugs in the world , included
the costs 1 of-act!vo-ingredient of Librium at £437/- per kilogram. When
Com H
cor«umTy
2
r’S,M"001k’^
bAr^
^^AtOaE-560
REGIONAL OFFICE FOR
SOUTH EAST
ASIA
WORLD HEALTH
organisation
POLE .OF. T?T?IDMATIONAL AGENCIES ...IN .PRIMARY HEALTH CAPE
DR.
1.
by
RO
KO
Introduction
Of late, we have been talking and hearing a lot on Primacy
Health Care and I believ^, the word ’FHC1 is quite well kno’-ra/yand
quite familrler to me st peoplOc
L
Though th.e practice and approach
of PHC will vary from situation to situation and country to country,
there are certain basic principles which can be applicable anywhere.
The two most striking features in PHC are the utilisation of some form
of volunteer workers and the predominant role placed on the community o
Since the PHC programme is conceived as an inter sectorial progr.amme
which is to be shaped around the life pattern of the people , in many
countries, PHO is understood or misunderstood as a simple and cheap
health care of the people which can be organised successfully by
lay people ignoring the importance of professional leadership.
I
like to stress the important role of the medical profession underlining
its leadership role in Primary Health Care, without of course, meaning
to undermine or challenge the overriding importance of community
participation.
I feel that at the sane time I should reiterate the
vital role of team approach, where, the professional 3, the para
professionals and the auxiliaries participate in their respective
part.
2e
definition
There are a number of ways of defining primary health cars,
but for the purpose of this discussion ’Primary Health care is taken
to mean a health approach which integrates at the community level
all the elements necessary to make an impact upon the health status
of the people.
Such an approach should be an integral part of the
national health care system.
It is an expression or response to the
- 2 in the acuions required to live a healthy life and where can a person
go if ho/she needs relief from pain or suffering» A response to such
needs must be a series of simple and effective measures in terms of
cost, technique and organisation, which are easily accessible to the
people in need and which assist in improving the living conditions of
individuals, families and communities®
These include preventive,
promotive, curative and reaabilitative health measures and community
development activities1®
3.
This approach can be sumarizc-d by the following general
pxu.nciples which should be adhered to if primary health care efforts
are to be successful:
i)
Primary health care should be shaped around the life
patterns of the population it should serve and should
meet the needs of the community-.,
ii)
Primary health care should be an integral part of the
national health system, and other echelons of services
should be designed in support of the needs of the
peripheral level, especially as this pertains to technical
supply, supervisory end referral supports
in)
Primary health care activities should be fully integrated
with the activities of the other sectors involved in
community development (agriculture, education, public works,
housing and communications)®
iv)
The local population should be actively involved in the
formulation and implementation of health care activities
so that health care can be brought into line with local
needs and priorities®
Decisions upon what are the community
needs requiring solution should be based upon a continuing
dialogue between the people and the services®
v) Health care offered should place a maximum reliance on
available community resources, especially those which have
- 5 stringent cost limitations that are present in each
country.
vi)
Primary health care should use an integrated approach of
preventive, promotive, curative and rehabilitative services
The balance
for the individual, family and community.
between these services should very according to com. .unity
needs and may well change over time.
vii)
The majority of health interventions should be undertaken
at the most peripheral practicable level of health services
1/ workers most suitably trained for performing these
activities.
4.
Role of International Agencies
In conformity with the principles of primary health care ,
primary health care approach is essentially a self-help approach
relying on the resources and efforts of the community itself.
However,
the programme needs a strong political commitment by the Government
with its full technical and administrative support.
UN and bilateral
agencies, which are always coordinating and assisting Member Governments
also have their role to play in the planning and implementation of
primary health care programme.
The respective role and area of
interest for individual agencies is given as follows:1.
UNDP:
From general development point of view.
PHC as a part of general development
2.
WHO:
PHC as a part of general development as well as integral
part of health delivery system.
3
UNICE?;
PHC with relation to basic services of the children.
4.
UNFPA:
PHC as an instrument in delivery of family planning.
5.
IBRD:
Socio-economic development as a basin of health
development and health as an important contribution
to general socio-economic development.
...a/-
- 4 6.
In recent trend of moving into field of population,
family planning and health, PHC found to be a feasible
area of support.
7.
ESCAP:
Interested in PHC in the context of the integrated
programme on rural development.
8.
9.
Bilateral Agencies:
1)
USAID
2)
sida /sasec
3)
IDliC/ciDA
4)
eorad
OTHERS
1)
League of Red Cross Societies
2)
International Union Against Tuberculosis
3)
4)
World Federation of Public Health Associations
International Union of Nutritional Sciences etc. etc.
* * * * * * *
banerji
/
Oc-m
■*1
lij
'I’
COMMUNITY HEALT
47/1,(First F!oor)St\ M
BZXNGAlORE SCO
I
t
> I
national
seminar
on primary
7TH & 8TH NOVEMBER 1977 f
f
*
AGENDA & PROGJUNME
!•
!•
2*
3«
4*
health
care
DELHI.___
Inaugural Meeting.
Alternate Approach on Primary Health Care (Countries Experience)~
Dr. V.N.Rau.
Role of International Agencies in primary health care- Dr. U. Ko
Health Planning Specially in relation to Primaiy Health Care - Shri C.R.Krishnajnurthy.
Proposed Rural Health Scheme, concept of primary health
care as an integral part of the national Health Service. - Dr. B.C. Ghoshal,
z
6<
Feasibility of utilizing-indigenous system of medicine
in primary health care delivery Dr. P.V. Kurup.
Principles and Practice of Primary Health Care - Dr. Pq Diesh.
7MONDAY THE 7TH NOVEMBER 1977
PROGRAMME
2.
i.
Registration.
Invocation -
a.
Welcome Speech - Shri C.R.Krishmanurth
3.
4.
Inaugural Address - Shri Rajeshwar Pra
President's Address - Dr. P.P.Goel.
5>
Vote of Thanks
11.00 Hrs.
—
Coffee Break.
11,3013.30 Hrs.
Plenary Session
Chairman - Shri K.P.Singh, Addl. Secretary(H
9.00 - 10.00 Hrs.
10.00 Hrs.
■
R.A.K.College Students
- Dr. B.C.Ghoshal.
Presentation of the following papers:
1.
Alternate approach on Primary Health-Care
— Dr. V.N.RaUf
(Country’s experience)
D.D.G.(l.C.M.R
2.
Health Planning specially in relation
to Primary Health care Shri C-R.Krishnamurthy, JS(k
3.
Proposed Rural Health Schemef concept
of primary health care as an integral
part of the National Health Services Dr, B.C.Ghoshal, ADG(HA)
r
/
-
4
2/ 67
- 2 Feasibility of utilising indigenous system
of medicine in primary health care delivery Dr. P.V. Kurup, Adv. (.ISM)*
4.
Discussion of the above papers presented .
-
Formation of groups.
Lunch Break.
13.^0-14.50 Hrs.
14.50—17*00 Hrs.
- Grour Discussions .
Divide into discussion group as follows:
Group I
Service Priorities within Primary
Health Care.
Group II
Role of Primary Health Worker*
Group III
Relationship between Primary Health
Workers and other hMUh workers in
the Block*.
Group 1\T
'Community Participation and Multi-sectoral-*
Appro ach.
Group V
Guidance/Supervision of Primary Health Wor
(Coffee will be served in the meeting)
WSDAY THE STH NOVEMBSR 1977
Plenary
9o50-10.00 Hrs*
Session
Review of Previous dayis Group Discussions.
-
Open Discussion.
Chairman 10*00-11.00 Hrs.
Dr. R.M.Varma, DoD.Ga(RH\
1.
Role of International Agencies in
Primary Health Care
Dr. U. Ko Ko7
Asstt. Director, W.H.O.
2.
Principles & Practice of Primary Health Care - Dr. P. Diesh.
11o00-11.15 Hrs.
Coffee Break.
11.15-j 5.OO Hrs.
Divide into group as follows:
Group
T
Group
Group
->Aeses«inenirdr requirements- of-Pri^a^p
- Critera for Selection
for training.
of—cotivi ties- and raining of tne
Primary Health Worker 4
^X^inihg and utilisation of‘_;“rkorz
-workers in
J
^xioting- indigenous systerns«'
3/“
1
- 3 -
13.00-14.00 Hrs.
14.00-15.00 Hrs.
Group
Development cf training materials.
Group V
Reorientation training for existing
Health Personnel/
I
Lunch Break*
Plenary 3ession.
Discussions on Group Reports.
Chairman
Shri C.R.Krishnamurthy, JS(k ).
Group Rapporteurs to prepare their reports
with conclusions and re. commend aliens.
15.00-15.30 Hrs.
Coffee Break.
15.30-17.GO Hrs.
Plan ary S e gs ir>n
Adoption of conclusions and recommendations
by Workshop - Rapporteurs.
Vote of Thanks - A representative of the
Participants.
Bwp.n;/
4.11.77
a
Com, h c
health
CELL
(First Fl
^
aimgalore
560 001
BANGALORE-
community
■PRIMARY
HEALTH CARE
A WHO STUDY
pRIMARY Health Care is essential health care
made accessible to everyone in the country ;
care given in a way acceptable to individuals,
families, and the community, since it requires
their full participation ; health care provided at a
r ‘’t the community and the country can afford.
The Primary Health Care approach forms an
integral part of the country’s health care system,
of which it is the keystone, and of the overall
social and economic development of the nation
and the community. Primary Health Care attacks
the main health problems facing the community,
and does so through promotive, preventive, cura
tive and rehabilitative actions as they are needed.
Since these actions grow out of the real-life condi
tions and social values of each country, they vary
from country to country. Since underdevelop
ment and poverty are major factors in causing
ill-health, national development can contribute
greatly to better health ; specially those compo
nents that raise the incomes of the poor, such as
rural development, agrarian reform, and the pro
motion of employment.
Actions taken to improve health will accelerate
economic development by building community
self-reliance, overcoming apathy, improving the
quality of labour, reducing the burden of illhealth, and expanding labour-intensive services.
The Primary Health Care approach draws largely
on community resources that otherwise would
remain untapped. At the same time. Primary
Health Care raises the standard of living of the
mass of the population by adding a component of
'‘health income”, thus contributing directly to
economic development goals.
Though no single model is applicable every
where, Primary Health Care should include the
following :
★ Promotion of proper nutrition
★ An adequate supply of safe water
★ Basic sanitation
★ Maternal and child care, including family
planning
★ Appropriate treatment for common diseases
and injuries
★ Immunization
diseases
against
major
infectious
★ Prevention and control of locally endemic
diseases
Education about common health problems
and what can be done to prevent and con
trol them
Primary Health Care : How it works
Primary Health Care seeks to bring about the
overall promotion of health :
★ by giving the individual, the family and the
community responsibility for Primary
Health Care, with support from the national
health care system ;
★ by the active participation of the commu
nity in defining its needs and finding ways
to satisfy them ;
★ by using community as well as national
resources ;
★ by using simpler and less costly technology ;
★ by mobilizing other sectors, such as educa
tion, agriculture, housing, public works,
information and communications and
industry.
Primary Health Care recognizes that in order
to achieve good health people must have the basic
necessities oj life : e.g. enough food to eat and
plenty of safe water. It emphasizes the need for
a safe environment and for people to understand
the role they themselves can play in improving
health and in promoting socio-economic develop
ment. This approach has evolved as a result of
the hard experience of countries in the promotion
of the health of their people.
medical systems PHIUPS
o
co
o
1
i. rtf
IS
EK
'i
KM
M
fff
h
A
I
I
I:
Now
go to the
villages!
*•
□
IIB:
Go with
the mobile
ODELCLINIC
for mass
chest survey
The need is urgent!
ODELCLINIC is ready to meet it now!
t
MSI
4*
liM
Ready to roll to remote rural areas,
to schools and industrial belts all over
the country.
The ODELCL1N1C is a complete mobile
x-ray clinic with everything'under one roof.
At the heart of this Chest Survey System
is the trusted ODELCA Camera with a
choice of 70 mm or 100 mm film format.
Mobile ODELCLINIC incorporates:
• Odelca camera.
• Battery-fed x-ray unit
• Petrol-operated power supply system
© X-ray film processing system
• And an office too
Write to: PHILIPS INDIA LTD. Medical Systems
Block 'A', Shivsagar Estate, Dr. Annie Besant Road, Worli, Bombay 400 018
PHILIPS
PRIMARY HEALTH CARE
Self-reliance and community participation
There is much that an active and self-reliant
people can do to improve their health. Indeed,
better health is not simply a commodity that can
be delivered to the people. Its attainment requires
their enlightened participation, as individuals,
families and communities, in measures to prevent,
to control and to treat disease.
The necessity for community participation has
often been overlooked in national development
and health programmes.
Communities have
important resources comprising human intelli
ce and ingenuity, labour, materials and money.
The creative use of these resources opens up
dramatic new possibilities for the improvement of
health.
Individuals and families cannot bocome real
agents of their own development unless they are
given the opportunity to identify their true health
needs, to assess the existing situation and to
suggest how problems may be solved, using all
available resources. Within a national strategy
of Primary Health Care, individuals and their
communities can help plan health care activities,
and participate in the process of providing services.
Individuals should accept a high degree of respon
sibility for their own health care, recognizing how
the health of each person and each family contri
butes to the development of the community. This
I jfllli
j
■
I ■y
i
includes adopting a healthy life style, ensuring
good nutrition and hygiene, and proper use of
immunization services. Mothers deserve particular
attention as they carry a major responsibility for
the health of infants and children, the most vulne
rable members of society. Within the community,
actions to improve health should provide visible
results and fulfil expectations in a short time.
This may range from building an irrigation ditch
or constructing a school, with community partici
pation, to promoting immunization and improved
nutrition.
In many countries, the process of community
participation may lead to the selection by the
community of one of their own people to serve
as a Primary Health Care work. After appropri
ate training and with continuing support from the
national health service, the Primary Health Care
work, who may be a volunteer or part-time, will
become the main agent for preventive and cura
tive action in the community, with the support of
conventional health services.
Just as a part-time Primary Health Care
worker cannot go it alone, the community too
needs continuous help in many forms. The health
system must provide education and information
about the causes and prevention of illnesses
about the implications of the solutions being
proposed and their costs.
An adequate and
continuing supply of basic drugs, and adequate
in
I
:
v;)^yiVA.?AWZ„..,..
1®
O’l
pi
811
Constellation to guide
the surgeons' hands
©
CTle
"SlB
5»
A. G. JOSHI & CO.
S. No. 49,1 PARVATI.POONA SATARA ROAD,POONA 411 009
J
PRIMARY HEALTH CARE
equipment for Primary Health Care workers is and within economic reach. Attempts to bring
health care and protection to people in need are
also required.
still hampered in many places by the absence of
Training of primary health workers
simple, low-cost materials, and techniques that
Training of primary health workers and the are designed for local conditions.
This technology must be in keeping with local
retraining of existing workers should be under
taken at the nearest point to their communities, customs and traditions. It should be easily under
and should address itself to the most urgent local stood and applied by community health workers
problems. Practical and non-formal approaches and be capable of adaptation or development as
The identification of such
can be used in continuing education, including conditions change.
learning by doing, in-service training during visits technology must be considered when formulating
by supervisors and frequent short courses. This a national strategy for Primary Health Care.
is essential because the demands on primary Such technologies now are available, for instance,
' alth workers will increase and because the to ensure safe cold storage of vaccines, to sterilize
_..alth situation will be changing. The training medical equipment in the field and diagnose
of primary health care workers is a formidable anaemia in villages. Medicinal drugs are an impor
task because of the large numbers and because of tant element in health technology. A model lists
the variety of education techniques involved. of some 200 essential drugs now is available, and
Hence, special preparation of trainers, who will can be used to select those drugs required locally
to deal with specific conditions. It is an advantage
also participate in supervision, is a prerequisite.
if both drugs and equipment can be manufactured
New challenges to the existing
locally.
health system
No community need wait for basic improve
Introducing Primary Health Care into all ments in such things as environmental sanitation
communities will greatly increase the demands on until large-scale, expensive means are brought to
existing services in terms of training, supervision, bear. Work on water supply and waste disposal,
logistical support and referral care. The redistri for example, is already underway. Sophisticated
bution of functions involved in the new approach technology may not be the most suitable, and it is
will also make for a more efficient use of health often the most expensive; the cost is high, even
personnel and health facilities.
Professional for industrialized countries. The important thing
personnel and hospitals will no longer be dealing to discover is what can do the job and what the
with minor ailments and problems but will direct community can afford.
eir resources to more complicated problems
beyond the competence of primary health workers. More equitable and more efficient
To assure the success of this approach to
Primary Health Care, all categories of existing
health personnel—professional and auxiliary—will
need to be reoriented so as to gain their under
standing and support. They will need to realize
that community level Primary Health Care is not
reducing their status and responsibilities; it is
enhancing them. In some situations, they will
need additional training in their supportive and
of all
The basic training
1
referral functions.
health personnel will also need to be reviewed and
adapted so as to fit them for different functions
at various levels of the health systems.
use of resources
In many countries today, 80 per cent of the
health budget is still spent on 20 per cent of the
population. As a result, rural people and the
urban poor are neglected and still have little
contact with conventional health systems. Only
through active community participation, and
equitable reallocation of growing national resour
ces can maximum impact on the health of the
total population be achieved.
Scarcity of resources can no longer serve as an
excuse for not providing better health care for all.
Better use of existing resources, fairer distribution
of what is available and the use of untapped
Appropriate technology
resources within the community can go a long way
Primary Health Care needs scientifically sound to improving the situation. But community, non
techniques that are acceptable to the community government and local governmental resources
21
With Lest compliments
from
*
Kalali Chemicals Limited
Registered Office S Works :
Kalali Road, Atladra, Vadodara-390005
Phone : 65854
22
Grams : 'KALACHEM' Vadodara
Telex : 0175-316
PRIMARY HEALTH CARE
In this new ordering of the health system, the
nation will be getting more for its money. For
one thing, there will be a reduction in preventable
diseases ; and this in itself will result in substantial
savings in supplies and staff time. Concurrently,
common illnesses which now take up so much of
the time and facilities of the health services will be
dealt with effectively and at much less cost in the
communities. Sophisticated and expensive health
resources will be used in more selective and
appropriate ways.
Food for health
- 1
Amust all be used, following an overall plan, for
any rapid advance can be made.
More rational use of the national resources
will also contribute to narrowing the resource gap.
More rational use means providing better referral
services, and the supplies and equipment the
community is unable to obtain for itself. If coun
tries are to develop Primary Health Care on a self
reliant basis, most of the resources must come
from within; and along with the growth of natio
nal resources, a process of reallocation and equile sharing becomes essential.
It has already been pointed out that commu
nity participation brings significant new resources
into improving health. Although the resources
of communities are limited, experience shows that
many communities are willing and able to pay
some part of the costs of basic health care, besid
es contributing labour and materials. These
community resources will go directly to the
support of Primary Health Care.
But community resources are not sufficient.
Government aid is required for training, supervi
sion, referral services and logistical support. In
most countries this means increasing the amount
and the proportion of funds in the national budget
supporting Primary Health Care. As the national
health budget gradually increases, the new money
will go to extending health to unserved commu
nities rather than, for example, constructing
hospitals in cities.
More than half of the deaths of children in
developing countries are directly related to poor
nutrition and a large proportion of those who
survive are physically stunted ; for many, mental
development is retarded. Thousands become
blind from an early age because of vitamin A
deficiency. Lack of food and iron-deficiency
limits the work capacity of the labour force.
Furthermore, these nutritional deficiencies increase
the risk at childbirth both for mother and baby,
and contribute to high maternal mortality and the
delivery of small, weak babies who are sus
ceptible to diseases and early death.
The first step in dealing with nutrition is seeing
that people get enough of the right food. Food
must be made more abundant and more accessible
to the millions who need it and cannot afford to
buy enough to keep their families healthy. This
may mean new ways of farming, new crops and
23
SANJEEVANI
97.
SANJEEVANI
POLYVALVE
It automatically operates by
the pressure variations
occuring during spontaneous
and controlled respiration.
I' ■' ■
IJ
SANJEEVANI
RE VI VALVE
Same as Sanjeevani Polyvalve
except that it has an inlet
for fresh air and extra oxygen
can be added to the inspired
air, both in spontaneous and
artificial respiration.
181
Lt,y
1
SANJEEVANI POSITIVE
PRESSURE VALVE
It permits one handed operation
squeezing the breathing bag
automatically closes the exhalation
opening. Functions as conventional
non-rebreathing valve when
positive pressure is not applied.
ANAESTHETICS
16, Vakharia Industrial Estate, Ram Mandir Road, ftoregaon-West
BOMBAY-400 062
ANAESTHETICS
Manufacturers of:
ANAESTHESIA & OXYGEN THERAPY EQUIPMENT
16, Vakharia Industrial Estate, Ram Mindir Road,
Goregaon-West, BOMBAY-4QO 062
Tel : 62 34 69
24
PRIMARY HEALTH CARE
changes in land tenure. In addition to an increase human waste is crucial. This waste can become
in quantity, sound education is needed to en valuable compost or a focal point for contami
courage people to make better use of locally nation and a breeding place for insects that carry
available foods. A handful of green vegetables a disease. The water in drains, rubbish, and the
weak can prevent vitamin A blindness. A little excreta of man and animals can either be used as a
iodine added to salt can prevent goitre. By careful resource or pose a dangerous threat to health.
mixed feeding and giving young children enough
solid food, serious nutritional diseases such as Prevention of disease
marasmus and kwashiorkor can be avoided. The
The Primary Health Care approach lays stress
danger of malnutrition in pregnancy can be pre on prevention, which is the first line of defence
vented by giving mothers a litte more of their against disease and ill-health. Most of the
accustomed diet.
measures required can be carried out within the
Just as food is needed, so are good eating community itself, using local people and local
b * its. Mother’s milk, for example, is the best resources, backed by support from the national
safest food for babies everywhere and breast health service and other agencies of government.
feeding should be encouraged. Young children’s
Improvements in the environment, provision of
foods can be prepared from locally available
adequate
water and proper nutrition, as outlined
resources. Cleanliness in the preparation and
go a long way in the prevention of
will
above,
storage of food goes a long way in preventing
diseases that are currently causing ill health and
infection.
death in the world.
It is essential that early in life children receive
Other programmes such as family health,
a diet that will ensure a healthy growth and an
family planning and
immunization against
effective immune response. Without the latter
several of the major killing diseases, can also
immunization programmes will be less effective.
reduce illness and suffering, particularly among
mothers and children. To make any real difference,
The environment as an ally : Enough safe
immunization must reach everyone who needs it.
water and a safe environment
Steps in this direction include simplified immuni
The importance of improving the environment zation techniques, firm administrative procedures
so that it promotes rather than undermines the and enlisting the help of the community, to see
health of the individual is fundamental to the that those who need protection receive it. In
Primary Health Care approach. Formal health many cases, better ways of producing and distri'>-*ivities and medical care cover only a very small buting the vaccine will be needed. These have
t of a person’s life, even for someone who is
repeatedly ill; most of one’s life is spent working
and living far from the walls of a clinic. Therefore
the way in which people lead their lives, and the
setting in which they do it affects their health and
that of others around them to a vast extent.
Water, for example, can help a community to
health in many ways or on the other hand it can
menace its well-being. Where water is abundant
and safe, a number of diseases will be greatly
reduced or eliminated. Where water is scarce and
polluted, nothing can prevent high infant mortality
and constant attacks by gastro-intestinal disease on
all members of the community. Malnutration can
result from infestations and worms and frequent
diarrhoea.
More is needed than greater quantities of
water. It is important to avoid polluting water
and its surroundings. The proper disposal of
25
Estd.
1920
BOLE BROTHERS
A HOUSE OF EVERYTHING OF
MEDICINE & SURGERY
S. Gandhi Marg (Princess Street)
BOMBAY- 400 002
Drugs, Medicines, Surgical and Veterinary Instruments
Hospital Furniture, Science Apparatuses etc.
Post Box No. 2072
26
Phone : 310316
Grams : 'BOLEBROS' Bombay-2
PRIMARY HEALTH CARE
allocating their resources to meet the real needs of
been worked out in many countries, using imagi
the people. This requires decentralization of ope
nation, local cooperation and hard work.
rational responsibilities and the coordination of
A national policy :
sectorial activities so that the overall goal of
health through development can be achieved.
Coordinated support at all levels
Implicit in this partnership is the involvement of
Although no single model of Primary Health
members of the community in identifying what
Care can be applicable everywhere, in all cases
thay feel are the most pressing problems they face
there must be a national policy and political will.
and
in determining priorities and solutions they
Furthermore, this approach should encourage the
will
work in their local setting. ,
feel
community to become actively involved from the
very first stages. Primary Health Care means a
4
close partnership between community and govern
ment in the development of resources and health
'-'"W
care, and involves a continuous dialogue between
a. The community must identify itself with
the purposes and activities that are called for.
Planning, shaping of specific activities, evaluation
and modification should all be carried out with
the participation of the people.
HI
"W
Ml
S'
llffl
s1
Health is not a separate entity. This is why
Primary Health Care has to be unequivocally sup
ported at the national level as part of the govern
ment’s overall national plan for total development.
A matter of will
Government activities should be oriented in
order to encourage and support community
actions. These should include intersectoral plan
ning and coordination, and the identification and
reallocation of resources to provide the personnel,
material and finances needed to support the
community.
Solutions to national and local health and
development problems can only be found through
mutual support and collaboration. All levels of
government—district, provincial and nationalmust commit themselves to coordinating and re-
The Primary Health Care involves a political
commitment to reorient national development, to
direct increase resources to the under-served
majority and often to increase health budgets
substantially.
For industrialized countries, a Primary Health
Care approach means rationalizing their health
systems and controlling and redirecting soaring
expenditures from
hospital-based, high-cost
technology towards basic care for all. It also
means a commitment to assist the developing
countries, and particularly the least developed, in
carrying out the Primary Health Care approach,
as an integral part of rural and urban development.
The world has the resources and know-how to
{Continued on page 31)
27
Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Rallifan
Supersur what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Supersiar
what ceiling fan should be Rallifan
Superstar
Rallifan Supersur what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Supersur
what ceiling fan should be Rallifan
Supersur what a ceiling fan should
be Rallifan Superstar whal a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Ralhfan
Superstar
Rallifan Supersiar what a ceiling
what ceiling fan should be Rallifan
Superstar what a ceiling faa should
be Rallifan Superstar what g ceiling
fan should be Rallifan Saperstar
what a ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Supersiar what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Rallifan
Superstar
Rallifan Supersiar what a ceiling
fan should be Rallifan Superstar
what ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Rallifan
Supersiar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifah Superstar
what ceiling fan should be Rallitaa
Supersiar what a ceiling fan should
be Rallifan Superstarwhat a ceiling
fan should be Rallifan Superstar
what a ceiling fan should ba Rallifan
Superstar what a ceiling fan ahould
be Rallifan Superstar what a celling
fan should be Rallifan Superstar
what ceiling fan should be Rallifan
S<>,RalUfan Supersur whal a ceiling
fan should be BaUifan Supersur
wbat a ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Supersiar
what ceiling fan should be Rallifan
Supersur what a ceiling fan should
be Rallifan Superstar what a ceiling
fen should' be Rallifan Superstar
wbM a ceiling fan should be Raliifaa
541 Rahiftn Superstar what a ceiling
'
tan ahould be Rallifan Superstar
whal ceiling fan should be Ralldaa
Superstar what a ceiling bn should
be Rallifan Supersur what a ceiling
fan should be Rallibn Superstar
what a ceiling fan should be Rallifan
Supersiar what a ceiling Can should
be Rallifan Supersur what a ceiling
fan should be Rallifan Superstar
what ceiling fan should be Rallifan
Superstar what a ceiling fan shouM
be Rallifan Superstar whal a ceiling
fan should be Rallifan Supersur
what a ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Supersur whal a ceiling
fan should be Rallifan Superstar
what ceiling fan should be Ralhfan
Superstar what a ceiling fan should
be Rallifan Supersur whal a ailing
fan should bo Rallifan Supersiar
whal a ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar
WithSmaior
competitors already
in the market,
we're introducing
thenewRallifan
Superstar.
Which could
mean only one thing.
V
k A regulator designed for a
I minimum of 40,000 on-off
I operations. Which means,
' it will be functioning just
as efficiently 10 years
from now I
Backed by the engineering
expertise that has gone into the
production of the Superstar.
Add to this, the Superstar's
good looks. The slim, classic
design. And superb finish.
A ceiling fan that is a couple of
notches above ell competition.
But we'd rather you discover
Superstar quality for yourself.
You'll be glad we asked you to.
We're confident of our
Offer. And for good reason;
The Superstar offers you
features few others can match.
For example, the motor.
Power balanced with double
heavy duty ball bearings.
So you have a ceiling fan that
runs many extra years
in peak condition.
Blades weight-matched to
within half a gram. With
specially designed contours to
ensure smooth, silent,
wobble-free operation. And
a wider, more even air cone
than any other.
Rallifan Supentar whrt * ceilii'I
tan ahould be RalliTan Supem. r
what a ceilint fan thou Id be Railif. ’
Supenlar what a ceiling fan shot I
be Rallifan Superstar what a ccili. :
fan should he Rallifan Supers!»r
what ceiling fan should be Railif--1
Superstar what a ceiling fan shot1 t
be Rallifan Superstar what a ceili :
fan should be Rallifan Supers' r
what a ceiling fan should be Ralhl. i
Superstar what a ceiling fan shoo I
be Rallifan Superstar what a ceilii e
fan should be Rallifan Supers! what ceiling fan should be Railif. i
Superstar what a ceiling fan shou I
be Rallifan Superstar what a ceilii •
fan ahould be Rallifan Supers! r
what a ceiling fan should be Rallifan
Superstar
Rallifan Superstar what a ceilir ?
fan should be Rallifan Supers! •
what ceiling fan should be Railif. ■
Superstar what a ceiling fan shot .1
be Rallifan Superstar what a ceili..g
fan should be Rallifan Supers: r
what a ceiling fan should be Railif n
Superstar what a ceiling fan shoe I
be Rallifan Superstar what a ceili g
fan should be Rallifan Supers- r
what ceiling fan should be Rallil n
Superstar
Rallifan Superstar what a ceiling
fan should be Rallifan Supers- r
what a ceiling fan should be Railif. n
Superstar what a ceiling fan should
be Rallifan Superstar what a ceili g
fan should be Rallifan Supers r
what ceiling fan should be Rallil t
Superstar what a ceiling fan shou d
be Rallifan Supersiar what a ceiling
fan should be Rallifan Supers!..r
what a ceiling fan should be R -llifan
Superstar what a ceiling fan s.tot id
be Rallifan Supersiar what a ceilii g
fan should be Rallifan Supers! r
what ceiling fan should be Rallif-.i
Superstar
Rallifan Superstar what a ceil ng
fan should be Rallifan Sutier-tar
what a ceiling fan should be Rallilan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what ceding fan should be Ralhun
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Supersiar
what a ceiling fan should be Rallifan
Supersiar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what ceding fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Rallifan
Superstar
<
Rallifan Superstar what a ceiling
fan should be Rallifan Supersiar
what ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Supersiar what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be Rallifan
Superstar
Rallifan Superstar what a ceiling ‘
fan should be Rallifan Superstar
what ceiling fan should be Rallifan
Supersiar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Supersur
what a ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Supersur what a ceiling
fan should be RaWfan Supersiar
what ceiling fan should be Rallifan
Superstar what a ceiling fan should
be Rallifan Superstar what a ceiling
fan should be Rallifan Superstar
what a ceiling fan should be RallifaaSuperstar what a ceiling fan should
be Rallifan Supersur
B
I
C
W
.
v •
-
What a ceiling fan should be
28
E3SSHIAL EmUMS FOR IEALTK
H S'-
You nay ask idiaty within any ran^ ©f elm<?nts> are tlose
that are escent/Lal to the cttainrwt of health for all« I
svfg’est that they indhrlo adequate fool and hoi;si.ng> with
j^otectdon of hcftiseo against Insects and roieirtaj water ade
quate to permit oleariliness and safte drilfcingj suite'le waste
disposal; eorvices for the provision of ante-mtel and post
natal care, including fhnily ^Laming; infant and o’ ildhood
care, including mitriticnal sir pert; i ranimtion against the
maior infectious diseases of ehlldhool; prevention aM control
of locally endcEdC diseases; ele^entery cart? of all age- ’pewps
for in,Jury and diseases; and easy access to samd and vseftl
infermtion on prevailing teelth prollerss and tho methods of
proventine ’
controllinf; them.
A IHOADEH lEAUHI SYSTEM
If w could succeed in providing rrir:;®^ health care to all,
we sMul 1 be well on the wy to enstrin;: Maith for all» Prirrry
health care, however, cannot le offcctive alone; it has to form
pert of a : render Maith system, and tlx- otlu^r ca^ omnts of that
system must te organised in such a wry as to support its mods#
This io anothor dirsension of ths filter-inmr-ls process to which
I referred earlier wiaareby problems of the peri^wy should
dotermina the content and organization of tho more central levels
of the Maith system - wMrcas I am cur© you will adMt it is
(F
vsn:ally jwt the or.?posit©#
ib /
IIWfilZ&TION CF /JI, CHIWRO EJ 1%o
w
Inuurd^tion a^inst the corjjon diseases of childhood is
another high priority pro Tarw. Again* the ‘HUrtdeth itarld
Health Assembly set the direction idw. it adopted a resdution
aimed at ensuring that by 199C all the children of the world
will be provided with such i:.wni2ation« Experience Ms shovm that
episodic mass ^npaigns have not been effective; pro.^rarws have
to be established on a per^nsient basis and for this it is again
neoessrry to have recourse to the prteKry health tssre services •
But in raost cwntrios these services will only bo a le to provide
i nmlsations if a r^mn^wit decision is taken to this effect,
2
pH k/E/Z
imsoa to Livii lira rsca dregs
Drugs • and I aza not reftering to nor cold cs-^re :lnsepm*all©
ftw health toclwolojy, tahtoh has tocme wH?ly dru, ^^openlenta
We wst learn to live with few? drugs if w are to raster tto
health situation, and I to'?rilr w haw shown ccrnrhncl ngly that
wc can# A resent sdentlflo conmilteticn in ’ W, based on
country visits, cr-rx to tbs ecndlrsion that seno 150 essential
drugs ca;ld met the vast mjority of health oar® needs. If
you taint to fHe y<n^Ek?lves from drug cdan'al^-sm, let is v>ork
to'-^tlw to rake sure that these essential drugs becone aw liable
to all wto seed ttom. To lo so will aBan fbraulatinn new national
pdieios scorning tJ e rarufbetere, quality and pr ce control,
import, and export of those drugs. Yor will arTTOCir.te the need
for .intcxr*coi2Ttx^ cdU^' ca-ation within tl-e Region, as well as with
other Redons, to enstre the orderly application of this new pdicy
of pre^res^ive rational uni regional- sdl£--relia;;ic© in dreg natters.
xamazzc’; acotitii
^ - a ccrr®
orumvinr .bam
’'%lrR,Ttr-ltion is prefcatty tto MnfAe nest ir^ortaat health
problem in ■'developing' ccR-mtries. The nattonel ©nd ■'ntcsrne.tioTiBl
health sectors wst now case to grips with their res* cr^-Hllities
in wtrition, identify t ear proper roliticol needs, leflre real
istic pcHales .ami strategies, •’Bnerate aprrorT'iate toc^wlo'ies,
end fcsTTulnto arpl.icable pragmaEBS. If we do not m-coeel in raking
effective and realistic mtritioral activities a c^Tieraton© of
primary health care, we are 1^2 lly worth orr spit as oalth rara'-ers.
Once meu’e we soe.i to haw the l^wvlcdge but neitlxxr the pttitlcal.
will rxxr the social iwdmtitoa to apply it*
BCCRAM^ KWG-rH?;G AT TIB COUl :®y LEVEL - A OOWEn CFKFTDlOT
As another aspect of
coritril.naticsi to health ■Imrl.crwnt
in countries, we arc, as you know, alout to introhiee a new system
of progm^ budgeting and mnagemnt of UOto rosovrees at tlie
country level. The min effects of th s new system slwli be to
ievclqp tlse Wi:i progreme budget in cowitries in term of broad health
-cue-
bjMC
cc ',.( h
I
WIMARY HEALTH CME
Prinairy Heal’th. Care is essential health care rjacle
universally accessible to individuals and families
in the connunity by means acceptable to them, through
their full participation and at a cost that the
Community and country can afford. It forms an
integral" part both of the country’s health system
of which it is the nucleus and of the overall,
social and economic development of the community.
Primary Health Care addresses the main health problems in
the connunity, providing promotive, preventive, curative and rehabili
tative services accordingly. Since these services reflect and evolve
from the economic conditions and social values of the country and i s
communities, they will vary by country and community, but wr^l includ
at least: promotion of proper nutrition and an adequate supply o±
safe water: basic sanitation; maternal and child care, including fami
■planning: immunization against the major infectious diseases; prevent
and control of locally endemic diseases; education concerning prevail
health problems and the methods of preventing and controlling them;
and appropriate treatment for common diseases and injuries.
In order to -make Primary Health Care universally accessible
in the community as quickly as possible, maximum community. and indivi
self-reliance for heth development are essential.’ -o attain such sel
reliance requires full community participation in the planning, organ
zation and management of Primary Health Care, Such participation is
best mobilized through appropriate education which enables communi -i
to deal with their real health problems in the most suitable ways.
They will thus be in a better posticn to take rational decisions
concerning Primary Health Care and to make sure that the right kind
of support is provided by the other levels of the national
system. These other levels have to be organized and strengthened
so as to support Pririary Health Care with technical knowledge,
training, guidance and supervision, logistic support,supplies, .
information) financing and referral facilities including insti
tutions to which unsolved problems and individual patients can be
referred.
Prinary Health Care is likely to be noSt effective if it
employs means that are understood and accepted by the community and
applied by community health workers at a cost the community, and the
country can afford. Those community health workers, including tradi
tional practitioners where applicable, will function best if hey
reside in the community they serve and are properly trained social y
and technically to respond to its expressed health needs.
Since Primary Health Care is an integral part both of
the country’s health system and of overall economic and social
Go
_ j m .. u.
'.r
-3*-*oad
001
'
®.. J
'
Health for
by the Year 2000 A»D.
Re c om ruend at i on s of t he
Involvement .
Grou p on Com-nunity
(Group 4)
The Group on Co:amunity Involvement met in New Delh
on r/'arch 18.
The f ol 1 o?:’ing were present.
( i ) Dr.K. S. San jivi,
11, Link Street, 1. ,
C. IcT. Colony,
Chairman
•<
Ifedras -6 0000’4.
*.<r: •
( i i ) Dr. (Mrs) B • J • Coy a j i
C • MO., K ing Dd’var d Memor ia 1
Hospital, 3?rd?r Elidliar Road,
Rast a Path, PJNZ-40^611.
Memebr.
(iii)Shri. R.R. Gupta,
Joint Secretary,
Ministry of Health & F.7.
Memebr.
( iv ) Dr. Vijay Ku ma. r,
5; Health Community iodic ins,
Post Graduate Institute of
1
Me d i c a 1 Education & Re s e a r c h,
Chaudigarh.
Member•
(v ) Dr. L. Ramachandran
Memebr.
(vi )Shri. V.N. Kakar,
Convenor
Member Se
Director, Gar db. ig ram Ins t itu e
of Rural Health,
Gandhigram. (District Madurai)
:I .
I’"
-.J.:
Dr. R.S. .A role, Director,
?
Comprehensive Rural
health Project, T^mkhad-413201 (Distt.a Ahmednagar ) could no
2.
The Group recommends that the concept that health is n
only a basic right of man but -'Iso one of his essential res
ponsibilities must be promoted vigorously in order to bring
about greater community involvement in health care programm
The comunity at present looks at health as the sole respons
bility of the State as something, to be administered by the
Gcvernment to the people.
Th.e tendency needs to be changed
The communityj should be given the feeling that promotion of
health is a joint responsibility to be shared by the Govern
ment and the people.
: 2 :
3.
There cannot be any uniform pattern for the involvemen
of the community in health care rr ograiishes for the country
as a whole or even for any single region.
Depending upon
needs of the situation and availability of infr@stazucture
other recourses, the pattern of coi: uaity involvement will
inevitably differ from place to place.
This important thin
is that all sectors of the com. unity should be associated
with health care programmes at -»11 stages-from planning to
utilisation of resources. The comunity should be encourage
to make monetary contributions to these programmes.
The Group feals that to bring .bout greater invovement
of the com unity in health care programmes, it is importan
that entry points, in tune with felt local needs^. should be
dice the community gets the confidence that h
identified.
programmes will help it in meeting its own needs, the part
pat ion of the community in these programmes can be achieved
with less difficulty.
4a
5.
The Group recommends that in relation, to community inv
□ent, health care should embrace all aspects of health and
family welfare, including maternal and child health program
nutr it ion programmes and family ’.volfa.re services.
6>
The Group feels that the community health volunteers in
in the rural scene in the recent, past can play an extremely
ful role in bringing about community participations in hea
programmes in villages. The weaknesses in the scheme as ha
of st
come to light must be removed quickly.
The Group is
view that there should be no compromise with the essential
principles of the scheme-viz. volunteers should not be Gov
ment f unct ?. 3nar is, they should command respect amongst the
people they seek to serve, they should live in the villages
where they work and they should be available to the commn
The Group recommends that the scheme
in all times of need.
community health volunteers should be strengthen d and enla
with modifications wherever considered necessary.
The Group feels that :*in ev ry village there should be t
7.
at least
community health volunteers. and
j one of them must
„ ------------“‘ *
be a woman. rThis
*
is
particularly essential from the point
of view of involving women in maternal
----- child
-------- 1 care as w
____ and
as family planning programmes*
8.
The Group feels that the importance of the mother for
promot ion of he a It h within the family and, through the fam
in the community as a whole has not received due recognitio
from health planners.
The^mother has a vital stage in the
The Gr
health of her children and cleanliness of her home.
feels that special programmes should be designed to encoura
mothers to emerge as leaders in community participation in
care.
/ -i
' to o; r.^'\ '
•
<1.
-■
: 3
:
and one does not find ^h"oFth^ir0 ^"t
v
i= mo o£
if he alt h is r__
health education oust receive
o du c a t i on s y s t e ei
its due place in the formal
10.
rThe
Group further recommends that health education sho
be inducted m all p—
— ----- programmes of non-formal education for
various sectors of the
—‘ society - Viz. agricultural extensio
workers, industrial workers,
, cooperative societies and orga
sations devoted to social welfare
> Particularly v/elfare of
women and childfen. —
also
ine
Group
rococmends thnt healt h
education should be
through the Nat
lro^rted
Srta^tiCa11^
nal ^udit Education
M-ogranrie
launched
by
Ministry of
the
Educat i on.
The C-r3up t ook
11 •
of the nedia explosion which
witne
the country 'aas been cognizance
f°r SQVeral years.
It note
with regret that even T *
though mass nedia provide innense scop
for the pronotion of health care
cipat ion of the community in such progracmes and for the oar
utilised only margin oily and not _ programmes, these hava'bee
Th
m a systematic manner.
Group feels that the Government
both at the Centre and in th
otates, should take the lead in
remoulding this situation.
There is dearth of fiins and other
audio-visual media mater
on health education. There
is not
nuch
n° /aUC^-eVid0nC
e of iarge sc
^on of\
and systematic utilisati
.-on of print media.
T
Drugs and cosnet
are advertised on la. massive scaled through all
Sedia\
-------------This
potential should beJ used m a planned and ,•
sy st enat ic r.ianne r
by the Government 1.*
m
J as aspects of
health and in achievinpromoting the positive'a
’
• ■’*lrv greater participationi of the people
in them.
intorparaon,,!'
pro8r^ Sri
'*
> (mtn uss of
hns 1™c!,cd •
leaders in vill?oeo
. r 10n tat 1On CaaP9 °f opinion
welfare. The
Group reconaends^thnt oen-r-1 or inciJG fa
should always find reflexion ? ? 1^GS '
°f health car*
of orientation £ind
campsreflection
should be utllls^ f^n^Jo^
canps should be utilised
---- -.1 all health
recoimeends that y------'• in the orientation
: 4 ;
13.
The Group feels that Government-sponsored programeies
for the involvement of the community in health care should
have an in-built mechanism of evaluation. The Group furth
suggests that those responsible for conducting these prog
mmes should be given refreshner courses from tine to time.
(Note:
The Group did not consider specific
the role of voluntary organisations
cor^unity participation programmes
ause this matter is being taken up
greater depth by another group).
(Dr. Ko 3. Sanjivi)
Chairman.
■:r . ■
! •
I
Health for All by the Year 2 000 ;:,D.
Recoaaondaticng_gf.thc Group on Connunity Involvement
^2a2-ix_±jliti.onal Note from the Chairman of the Group
ihe roconmendations of the group prepared by th
convenor and ap'roved by me contain all th.; point s on v/hich
there was unanimity during the discussions,
I had circulat
to the group a note on the subject containing ny viev's.
Th
.
following two points contained in my note are considered so
important that I am sending these additional recommendation
^althefornIil7ati°n °£the Gntil 'e National Committee on
In continuation of para 3 of the Groupfs recomm
Hon. ni
tions please add 'comminity consists of all the families li
in an area Witnout any reference to their occupation or eco
In ?yjscbelao f3r CCHCC2Cs and Min i Health Cen
it1Ch-!aJUS*
behSf of
1 ?r?:lded *hat aacb
should contribute, on
behalz of all its members, 0.5^ of its annual income subjec
a minimum of H.s.6/- per annum and a maximum of Rs. 180/■VHO HAro^ho Jn't 1Gt mt?UOte Dr‘ Fahler, Director General
0.5 to 7 "
amounts to
reasonable cost,
around a hundred
y Pny ftandai'd a
a reasonable
If L f
<
by
many
rich countries
fS ??ent ,Cn health
people
in
-I
health by people
hinder govermonts
-J nGt
not hinc'er
goverrnent s 1whon
*
•f
rrf a‘\°Uld
they cons
they should con it thenselves'to the
target of health for all by" thes yes.r ?,000”.
(’/arid Health,
November '79).
?juc<ap=er
r°::r?
cho„-M k
The National Service corps in the various colleg
health education
a big vav ^o ™
r?n"far^1 and
is a noth ’
S-V1Kg th3n SUCh j°bs as building roa
tE,lr
S!tLZ
r -
exr"1SG-
11 is “^rstood that nos£ Uni
h-, 11 r
ir'Q la haV° taken a firn decision that comunity ser
nctuallvV01'*^P 0^/01and that narks will
actually be alloted for the smae. More than the decision it
”,in? “:hod ai
«>» dOeisi„„e trs“eTa
fronth tbe entire connunity gets naxinun benefit, ouite ap
to the
do to
?
from the good it will do
the student’s motivation;
Co/
Extracts from
H e a It h for All
An Alternative Strategy
Major Recommendations
0 b j ec t i v e s:
The objective of the national health policy should be to
1.
provide health for all by 2000 AD. This implies the provision of a
good and adequate health care system for all citizens, and especially
for women and children and poor and underprivileged groups.
It also
implies a drastic reduction in the total morbidity and mortality.
In particular, it will mean a fall in infant mortality from 120 to
60 or less, and in the overall death rate from 15 to 9.
These ob
jectives and targets are realistic and feasible. But they cannot be
achieved by a linear expansion of the existing system and even by
tinkering with it through minor reforms. Nothing short of aradical
and for this it is necessary to develop a
change is called for;
comprehensive national policy on health.
Approac h:
2.
If this goal is to be realised, a major programme for the
development of health care services is necessary but not sufficient
Health is a function, not only cf medical care,but of the overall
integrated development of society - cultural, economic, educational,
Health also depends on a number of supportive
social and political.
services - nutrition, improvement in environment and health education.
During the next two decades, therefore, the three programmes of
1) integrated overall development including family planning,
( 2)improvement of nutrition, environment and health education, and
3) the provision of adequate health care services for all and
especially for the poor and underprivileged (through the creation
of an alternative model proposed here) will have to be pursued side
by side.
Integrated Devel opment
3,
The obj£?ctives of integrated development are to eliminate
poverty and inequality, to spread education, and to enable the poor
and underprivileged groups to assert themselves. This will include
the following programmes.
1) Rapid economic growth with the object of doubling the
national income per capita (at constant prices) by 2000 AD.
2) Full-scale employment, including a guarantee of work
on reasonable Wgges to every adult who offers to work for eight
hours a day;
creation of adequate opportunities of gainful employ
ment for women, with an emphasis on equity of remuneration and re
servations to make up for past neglect, so that women become
’vSsBble’ assets to their families.
Report of a study group set up jointly by the Indian Council of
Social Science Research and the Indian Council of Medi
2
3) Improvement in the status of women with a determination
to check ths adverse sex-ratio and to make it rise substantially
upwards, say to 927, the level it was in 1901.
4) Adult education w:*ith emphasis on health education and
vocational skills, the targets being to cover the entire illiterate
population in the age-group 15-35 by 1991 and liquidation of illiteracy by 2000 AD.
5) Universiil elementary education for all children (age
group 6-14) to be provided by 1991.
6) Welfare of Scheduled Castes and Scheduled Tribes
7) Creation of a democratic,
pat ory form of Government.
8)
decentralised and partici-
Rural electrification
9) Improvement inheusing with emphasis
on the provision of
houses for the landless and slum clearance.
10) organizing the poor and underprivileged
groups.
Family Planning
There should be a national Population Commission set up by
an Act of Parliament to formulate and implement an overall population
policy.
The objective should be to reduce the net reproduction rate
This will imply
from 1.67 to 1.00 and the birth rate from 33 to 21.
effective protection of 60^ of eligible couples against 22% at presen
It will dlso imply a reduction in the average size of the family from
4.3 to 2.3 children, and the eventual stabilization of the total
population at about 1200 million by 2050 AD.
The family planning pr o
gramme must be fully rehabilitated at an e-rly date-and converted
into a people’s movement closely linked to development.
The emphasis
should be on education and motivation, especially through interperson
communication and group action.
Incentives especially those of a com
pensatory character, should be widely used.
While work with women
willcontinue
through MCH services, intensive efforts should be made
to work with men also.
While the’ health services will have a role
to play in motivation also, their majn responsibility is to supply
the needed services and follow-up care.
The alternative model of
health services has been designed to meet these challenges fully
and squarely.
l\l utr iti on
on will
\
5*
Nutrition
have to be improved through adequate produc
proper organization
tion of food, reduction in post-harvest losses,
loss
of storage and distribution and increasing the
purchasing power of
th
the poor through generation of employment and organization of foodfor-work programmes.
Great emphasis should be placed on improving the
status of women and children and special programmes should be deve
loped for specific nutritional disorders like iron-deficiency,
In addition, supple
anemia, or vitamin A and iodine deficiencies.
: 3
Improvement of the Environment
Improvement of the environment will reduce infection, make
programmes of nutrition more effective, and htIp materially in re
Safe drinking water supply will hav
ducing morbidity .nd mortality.
to be provided to all urban and rural areas.
Coed sewage dispersal
tems should be established in all urban a teas where simultaneously,
massive programme of proper collection and disposal of solid wastes
and their conversion into compost will have to be developed.
Similarly, an intensive programme of improving sanitation, with s pecial emphasis on proper disposal of night soil, should be developed
in rural areas.
Greater attention will have to be paid to town and
village planning (with special emphasis on removing the segregation
of the Scheduled Castes), and
large scale programmes of housing
for the rural poor and clearance of urban slums will have to’ be
undertaken.
Urgent steps have to be tqken to prevent water and air
pollution, to control the ill-effects of industrialisation and to
provide better work-place environment.
Health
Education
7.
Health education should become an integral part of all gener
education and should receive adequate emphasis.
Health education
should also be an essential component of all health care; and the he
care services should assume special responsibility for the health ed
tion of the poor and underprivileged groups who need it most.
Alternative. Mod el of H e a It h Care 5 e rv i c e s
Within the health sect or, our most important recommendation
is that the existing exotic, top-down, elite-oriented, urban-biased,
centralized and bureaucratic system whichi over-emphasises the curativ
aspects, large urban hospitals, c‘
doctors and drugs should be replaced
by the alternative model of health care services described in detail
in a planned and phased mann r by 2000 AD.
This alternative model is
strongly rooted in the community, provides adequate, efficient and
equitable referral services, integrates promotive,, preventive and cu
tive aspects, and combines the valuable elements in our culture and
tradition with the bust elements of the Western system.
It is also
more economic and cost-effective.
MatEfnal and Child Health (MCH)
9 .
MCH services
<
■be expanded and improved.
should
There should
be attempt to cover all women and <children
’ * '
with basic services wi th
special attention to those ’at risk’ through an essentially domicilia
programme.
The dais should be trained and fully utilised.
The MCH
staff at each level should be adequate, have specific responsibilitie
(withan indication of priorities) and should receive job-specific
training. Health education of the mothers should be an important
component of MCH services.
: 4 :
Communicable Discsses
10.
Communicable diseases still form the largest cause of morbi
dity and mortality and the fight against them should be continued
with still gr ater vigour in the years ahead.
A good surveillance
system has to be set up and better coordinated efforts are needed.
By 2000 AO, our object should be to eradic tc or atleast effectively
control diarrhoeal diseases, tetanus, diphtheria, hydrophobia^,
poliomyletis, tuberculosis, guinea-worm, malaria, filariasis and
le prosy.
Training and Manpower
11.
.Under the new alternative model, the organization of the health
services will be radically different from that in the existing system
A new category of personnel, the Community Hi olth Volunteers will be
introduced and it will be the main bridge b. tween the community and
the services.
The middle level personnel will increase very substan
tially.
Very important decisions will have to be taken about nurses,
paramedicals, doctors, specialists and super specialists and these
relate to their numbers, quality and duration of training, and value
system.
There should be adequate arrangements for the continuous in
services education of all categories of health personnel.
The
Government of India should establish, under an Act of Parliament, a
Medical and H a.lth Education Commission, with comprehensive terms of
reference.
A continuing study of manpower and training and taking
effective action thereon should be a major responsibility of this
C ommission•
Drugs
and Pharmaceuticals
12.
There is need for clear-cut drug policy and a National Drug
The pattern of drug production should be
Agency to implement it.
oriented to the disease pattern, with an emphasis cn the production o
runs (especially tho'se needed by the poor and
basic and essential
urri erpriviliged groups) which should be produced in adequate quanti
ties and sold at cheapest possible prices.
The domination of the
foreign section in drug production should be reduced further and
price control made more effective by reducing overheads and packag
ing costs and adeption of generic names.
There should be strict
quality control, supply of adequate drugs to the rural sector, and a
move in the direction to make the clients pay for the cost of drugs.
Research:
13.
The priority areas obviously are primary health care, e’pidemioiogy^ communicable diseases with a special emphasis on diarrhoea, en
vironmental research, and research on drugs, problems of rural water
supply and sanitation, indigenous medicine, health implications of
It is also necessary to
industrial development, and family planning.
promote research on social aspects of medicine and especially on
economics of health, joitnly under the ICM^ and ICSSR.
Considerable
attention has tc be given to the development of appropriate technolog
Side by side, there should be an emphasis on the development of cli
nical and basic research, particularly in the field ofbiology, and a
bid ta
V build up high-level indigenous research capability
dttermin
: 5 :
Administ rat i on
14.
It is necessary to redefine the roles of the Central and State
Governments in view of the large powers delegated tc the local bodie
at the district level and below.
Voluntary agencies will have tc
function witKin the overall policy laid down by the State. But they
should receive encouragement .and aid, espec in lly-when fighting at
the frontiers and doing pioneer work. There will be considerable
tensions within the new health care services and need for redefiniti
of roles and mutual adjustment.
This is the responsibility of the
administration to secure through good leadership and proper training
A new and efficient national information system should be created an
adequate arrangem^n s made for morueffactive coordination at all lev
F inancial
__
15.
The total investment in health services should L_
be substantiall
raised and health expenditure should rise by 8 to 9 per pent; per yea
AD.
at constant prices and reach about 6 per cent of GNP by
Th
existing priorities should be radically altered and the bulk of the
additional resources will have tc go into promotive and preventive a
vities, in rural areas, in the development of supportive services li
nutrition, sanitation, w ater supply and education, and for providing
health care services to women and children and the poor and undurpr
leged groups. This will need taking of both positive and negative d
sions. While the ma jority of expenditure on health in the proposed
organization will be the responsibility of local bodies who will x
exercise financial control, basic responsibility of financing health
qtill continue to rest with the Centre and States,
An effort should
also be made to tap local taxes and individual payments to cover dru
c cst s.
National He ? al th Service
16 .
The altornati ve | model proposed here is a large step in thecrea
tion of a national health service, but it does not create it. In ou
o pinion, the time is not ripe for the purpose and the issue may be
examined in due course, say, ten years from now.
There is, however,
need to control private practice and it should not be allowed to
employees in the public
health care system.
Conditions Essential for Success
17.
The programme suggested here to realise the objectives of healt
for all is as existing and worthwhile as it is realistic and feasible
Its success will depend upon our capacity tocrcate a mass movement
and the ranks of millions ofyoung men and women to work for it.
It
will be proportional to the extent to which it is possible (i) to
reduce poverty and inequality and to spread education;;
(ii) tc organise the poor and underprivileged greups sc that they are able to
assert themselves; and (iii) to move away from the counter-productive
consumerist Western model of health care and tc replace -it by the
alternative model based in the community as is proposed in this
Report.
S;.
Report of the Working G-roup on the Role of Voluntary
Organisations for the goal of Health for All by 2QQO AD*
■'X: 7
10 The Working Group constituted for making recommendation
on the role of voluntary organisations in the context of th
.goal of health for all by 2000 AD met at Nirman Bhavan, New
Pelhi, on 20th March, .1980, under the Chairmanship of Dr. K
Rao. Th? list of participants is attached at annexure.
The. meeting generally considered drawing attention to t
viz,,
following aspects of the matter
(i) the functions that could be assigned to the volunt
organisations in replacement/reinforce*ment of the wor
of State and Central Government systems at the field l
and
(ii) the interaction and mutual relations between the
Governmental system and the voluntary organisationso
3.
After detailed deliberations, the foilwing suggestions
emerged:
(a) Voluntary organisations in this context could be de
fined as those organisations which are non-goverment non-pr
fit making in character, and not fully funded whether dire
ctly or indirectly only by the Government o V/hile private o
ganisations also fall in_the general category of non-govern
mental organisations, unless they fulfil the criterion of n
profit organisations, they could not be qualified for assistance from Government resources.
(b) There is a definite and important role for voluntary
and recognised private organisations in delivering health
care services as contemplated in the concept of health for
all by 2000 ADo The work in this field cannot be carried
our only by Government agencies £ the work of all organisa
tions in this field will requTe coordinated inter-meshing t
make optimum use of all available'resources - men, money
and materials - to the nation(c) Promotion of community participation to the largest
extent possible in order to generate demand for health
services as ’.'ell ^s utilisation of such services, should
be a common goal of all organisations in this regard.
(d) Voluntary or recognised private organisations will
have a role to play in all aspects of health services, such
as service delivery at different levels from the periphery
to the highest referral points - curative, preventive, prom
and rehabilatative, including prophylaxis coverage; educati
and motivation, including health education! training of
2
para-medical or other workers, such as CHVs, Dais, etc. 9
research into health care delivery system in all these aspe
including undertaking innovative approaches; field studies
to test out assumptions in accordance with their capacity.
(e) In all the functions mentioned above, the goal
of primary health care should be kept in the central focus,
oluntary organisations also should bear in mind cost effec
eness of ..their activities vis-a-vis governmental systems.
(f)
The need for coordination of activities of all
v° U-'1 ary organisations with those^of the Government is of
paramount importance. To achieve /dialogue between the
and the voluntary organisations it would be nece
local levels UPThP Stand mg Committees at the Central, Stat
se
should look into all aspect
of
yqlantary organisatiSs^
P hetween the Government and
dimi-iln+s Where yolnntary organisations have taken root,
benvoid/T
services from the. Government could
Tamil Nadu’ln the areas of raini-health centres of
amil Nadu or similar progammes in other States.
(h) Recognistion of voluntary organisations for their
work as well as for the purpose of Government al support to
would be a proper step, Procedures for this purpose may hav
to be worked out.
maximum fl The work of the voluntary organisations must have
capacity manpower avnilabilitv
suped to the capacity,
of operation, financial strength, and the gene
ril nCk +
1 Ves Of each orefnisation. While, therefore, ther
of assignee from the Government
to sichXXr^
standard n? ^satlGns there would be need to mde available s
organisation^ nS around whlch chaiges cm be made to suit ea
PPlies^fro^+h^rH orSanis2tion nUst be ^le to receive' su
^n!ral
vaoSZr oTn
purposes su
ns S
rial/ So 4 vaccines for immunization, health education mat
°UtSs S^- In ‘^ition, recognition by way
of
boost to theia n
ooqst
to
?
bOdiCS W°Uld
These organisations.
Z this and also to maintain close and continuous
30 8^6 3
- 3 -
(k) Only those organisations whiqh fulfil the criteria
and which have
voluntary
organisations9 as; defined
of
def ined . abave^
e.boveand
a secular outlook and provide free accessibility to all secti
of people j should be recognised and afforded ■assistance from
the Government,
(1)
In the field of providing financial assistance to
voluntary organisations? cstablishnicnt of an autonomous and
financial body like the Agricultural Finmce Corporation?
etCo could even be considered.Such a body could receive a mai
cor mis fund by way of support from the Government as also
private grants? including grants from foreign donors« It cou
also be provided with annual subventions» Such corporation
make available funds in turn to Voluntary organisations» For
purpose of raising funds? specially for health coverage? taxe
insurance? local cesses and people’s contribution for servic
rendered according to financial status of the individual ? cou
also be considered.
The need for vertical as well as horizontal linka
(m)
of all voluntary organisations with the ov■-•rail health infra
structure was repeatedly emphasizedo
- 4 - ■ -
Annexure;
LI ST OP PARTI CI PAJTTS
1
Dr. K.N. Rad,
Health Association of India
D.57, "Naf aina, '
New Delhio
2. Dr. M.G. Garg,
General Secretary
Indian Medical Association
I.M.A., Indraprastha Estate,
New Delhi.
3...Mro JoS.
Bali 9
Consultant
Voluntary Health Association of India .
C.66 D.efence Colony
New D.elhi.
4. Dr. Daleep S. Mukarji,
Drogrammo Director RUHSA
MELKAVANUR P.O.
Via. JC.V. Kuppsup
Dist. North Arcot, T?mil Nadu.
5
Director, Christian Medical
Association of India,
Bangalore.
6. President, Ramakrishna Mission,
R.K. Ashram Punjkuin Road,
New Delhi.
7. Shrio R. Natarajan 9
Joint Secretary?
Ministry of Health and F.W 0 9
Nirman Bhavan, Now Delhi.
8. Shri RR Gupta,
Joint Secretary , (FA)
Ministry of Health & FW
Nirman Bhavan, New Delhi.
9,
Shrio NoN. Vohra,
Joint Secretary
Ministry of Health and P.W. 9
Nirman Bhavan, New Delhi.
10.Dr. M.D. Saigal,
Deputy Director General (RHS)
Dte. Genl, of Health Services,
Nirman Bhavan, New Delhi.
c;
COM MU NI TY_£
-L E_f_-If
&GEmES_lN_MULTIzSECTDRAL_APPROACH
t>y
Dr. K.5.Sanj ivi
Ex-UNICEF Consultant
Health Care
on
Primary
Before any discussion of the topic assigned to me is comme
I wish to comment on the term ’’Community Participation” itself.
there in modern India the feeling, awareness of the community in
sense of ’’for a nighbourhood/body of people living in
same loc
not in the sense of ’’the antagonistic religious and racial comm
in a district”.
Both these quotations' are taken from the Concis
The politicians in India should be thanked
Oxford dictionary.
. will ’’blamed” be the correct term - for this position in which
’’community” has become a dirty word and not understood in the. sa
way as it should be in any modern society.
It is therefore e'ss
tial that we should as a first step restore a proper community
ing as an area, neighbourhood feeling that was part of our anci
culture.
Primary Health Care must necessrrily have its origin in the
It
will be bet
most remote villages where the problems arise,
action
with
about
by
community
participation
therefore to talk c
The programm
agencies.
Government or organised voluntary health agencies,
and executed by tfecommunity with whatever
should be conceived
conce:
technical and financial support may come from the Government ur
other agencies.
To reiterate that the organizations for Primary Health Car
start in the villages is in consonance with Sutton’s Law.
Sutto
an Australian Bank robber when asked why he was robbing banks in
particular, gave the simple reply ’’because the money is thei?e”$
likewise the problems of health care are in the villages, and u
slums
and not
in
New Delhi.
A distinction should be made between voluntary agencies wh
on par with the Government can be regarded as dohors, and the in
viduals in the community, the consumers of health services who
the recipients.
Our effort should be to alter the role of the
community from that of a passive recipient to that of an active
initiator.
Therefore I shall start with the illiterate citizen
who-to a large extent are the beneficiaries.
Here the mistake
often made in thinking that an illiterate person is un-intellige
God, or if you like nature, has endowed all human beings with a
basic intelligence and the villager who has not had the opportu
to go to a university is nevertheless very intelligent and capa
In 1973, th
of providing excellent support to the health team.
WHO World Health Day’s Theme on April 7th was ’’Health begins at
: 2 :
We conducted a number of meetings, to stress how the most imp
reliable and dedicated para-medical worker.in a health team,
the mother in the house.
Fiel cL experience since then has furt
given support to this concept that if only she can be properl
volved many of the targets can be achieved.
In our programme we have local action committees, who
have been told clearly that the health centre is theii? projec
to which the medical profession, with its auxilliaries, only
provided the technical skills.
It should not appear to be a
paternalistic condescending gift of better off persons to the
infe riors.
The Community Health Volunteer/Lay First /\ider is the. on
individual who can make maximum contribution to health educati
In her training, therefore, we emphasise environmental sanita
personal prophylactic methods, improved nutrition with locally
available products, mother and child care, and family planning
Talking of environmental sanitation, one notable area
in which community involvement has failed is in the in dividual
families putting up their own cheap latrines even when they c
afford it.
Taking another example, the resurgence of malaria is not
due so much to the resistance developed by the mosquitoes . to
pesticides or by the malarial parasites to chloroquine, as it
is due to the failure to build up the infrastructure.
The in
structure should require every householder to take care of the
mosquito breeding foci in his own surroundings and report ever
episode of fever to the MHC/CHV.
This is a clear example of
community involvement without which public health measures can
succee d.
We often talk of health care delivery,
It should be real
that health care cannot be delivered; it is essentially a "do
yourself" proposition.
For example, drug addiction, alcoholis
smoking and sex permissiveness are four, recent important addi
tional causes of disease. Nene of these can be controlled in
community unless the individuals involved are motivated to co
operate in their cure and prevention.
Likewise patients in ne
of prolonged treatment (e 9. pulmonary tuberculosis, leprosy)ca
obtain a cure even with modern, wonder drugs if they default i
taking the drugs.
Health Education therefore is of the utmost importance.
Health Education specialization is a profession practically no
It is questionable whethe r we can afford a
existent in India.
category; every health worker should therefore be a health
educator..-
Briefly t'he objects of health education are (a) to educat
people and alter the behaviour, where necessary, to promote an
maintain their health; (b) to impart the minimum knowledge
required for people to be aware of the factors that affect hea
and recognise the early symptoms of disease; (c) to assure the
3
It has been shown that it is comparatively easy to achieve
r
success in situations depending, on techniques eg. vaccinations,
But where techniques play only a minor part
mosquito control.
and people must be persuaded to change their habits, the situat
becomes much more difficult eg. choice cf correct food, smoking
family planning.
It will thus be seen that health education must adopt diff
erent approaches and must be continuous and simple.
Most authorities believe that mass media do not produce as
O
consistent and good results as personal man-to-man approach,
viously the latter will require many more teachers of health ed
cation; that is why health education is stress: d as the most im
ant functic.n of the CHV.
The ideal set-up for community health must provide for the
following essential requirements:
A health post manned by a lay first-aider/community health
volunteer for every 1000 population.
A male and a female multi-purpose worker for every 5000
population;
A doctor being available at the mini-- ntre for atleast
three hours a day on three days a. week;
The identification of, and liais'on with,
hospital within a reasonable distance.
a referral
The LFA at the Health Post is in fact the most effective v
teer in health work and all organised voluntary health agencies
The mother in the
only subordinate to these Queen Volunteers.
h ciw s e has been justly acclaimed as the most dependable medical
In view of her importance we ensure that the LFA is
xiliary.
selected 9 trained and supervised in the proper way.
”The effects of a world wide plan of action on behalf of
. Primary Health Care, extend well beyond the frontiers of health
itself and into the economic and social- fields” said Dr.Mahler
(Director General^WHO) at Alma Ata.
Of the many facets which one may consider in "integrated/t
rural development ” abolition of illiteracy, maximised through N
Formal Education, is very important and should be regarded as a
Among th
project that can be taken up even by health agencies.
reasons for the failure of community participation in health p
fer their own benefit is the lack of knowledge o
grammes set up for
the average citizen on the possibilities of modern medicine and
He now has consider
avai-lability of solutions to his problems,
fear and diffidence in reaching those who can deliver the goods
health services really arises out o
The inadeessibil lity too the health
illiteracy and, true democracy an’d illiteracy are incompatible
as much as the former demands on the part of its citizens a kno
ledge of all its institutions.
4
Here the National Service Corps in the various colleges
should be mobilised for non—formal and for health education i
To my mind giving them such jobs as building road
a big way.
is a rather futile exercise.
It is understood that most Uni
versities in India have taken a firm decision that community
service should be compulsory for every student and that marks
More than the decisi
will actually be allotted for the same.
itself is the exact method of implementing the decision in su
a way that the entire community gets maximum benefit, quite a
fram the good it will do to the s tudent’s motivation.
Next in importance is the production and utilisation, at
the local level, of nutritional needs -obtainable from agri
culture (staple carbohydrate); horticulture (vegetables and f
animal husbandry (milk) and poultry (e^gs).
Unorganised community/citizens/sharing an old traditiona
customs is not to be given up for the western models of centr
impersonal, official rid'den institutions.
CHARITY is to^rjno
as 5HARITY, the CH as in Chicago.
The poorest citizen in a w
state need not ask for charity; he is entitled to share the
available resci urce s/f acil it ies with the richest.
The challenge is tofind the solutions for poverty and ap
local community action, under proper guidance and leadership,
can cure the latter atleast and that will^an essential fore-r
Shultz (Royal College of
Medicine, I
for curing the former.
national Congress Symposium No. 24, P. 57) has underlined the
importance of stressing on self interest
which is a natural
and an intrinsic aspect of human nature.
Ergonomics is the management of people.
It is time one
forgets New Delhi, metropolitan elite and conce ntra s./
on the
poor people where they live and change their attitudes if
passible.
We have no doubt that a very effective way of involving
community,iis to get a monetary contribution from each family
The principle of obtaining such contributions from the commun
is no longer disputed.. No Government in the world can offer
provide all health services free, i.c. on its own general rev
Besides such a personal co ntt r ibu t io n will ensure the coopera
Any service wh
and wholesome participation of the community.
is entirely free at the point of consumption is bound to be
abused and is bound to enormously increase in cost year after
year, as has been demonstrated in UK National Health Service.
In our scheme of Medical Aid Plan and Mini Health Centre
it has been provided that each family should contribute, n i
behalf of all its members, 0.5$ of its annual income subject
200/- per
to a minimum of Rs 12/- per annum and a maximum of
annum.
Here let me quote Dr.Mahler, Director General of WHO'.
’’Are the costs exorbitant ?
Recent small scale studies have
shown that considerable improvements in people’s health can t
place for as little as 0.5 to 2% of the yearly gross national
5
This is by any standard a reasonable cost, around a hundredth
what is ppent on health by people in many rich ’countries.
So
factors should not hinder Governments when they consider if, an
to what extent, they should commit themselves to the target of
health for all by the year 2000"
(World Health, November ’79)
In addition, at the Health Posts manned by the Lay First
Aiders, which form an integral part of the Mini Health Centre
there is a provislion for? collection of 25 paise from the patien
for the symptomatic treatment given by the LFA.
Pat ients norm
seek curative trcatrrent only from the Mini Health Centre and th
go t □ the LFA only when a sudden symptom arises at odd hours an
she gives the symptomatic treatment, based on the complaint, fo
once o.nly after collecting the 25 paise.
She also tears off a
coupon, writes on the back, the name, the complaint and the tre
The LFA has been provided vjith a Hundi box in add
ment given,
to the kit bag.
The Hundi box has two slits, one for the co-in
the other for the coupon.
The supervisory staff open the box a
fortnightly intervals; the coupon provides both a financial and
technical check on the LFArs performance,
This charge is to
ensure that the LFA is not taxed without a real need. She has a
been empowered to waive this payment in a really poor patient a
enter the fact on the coupon.
The pre-payment plan is better than payment for each servi
A combination of both systems is effect d when 0.5% of the annu
income is charged for the community health prograrnrre and furthe
charge, if any, made when the need for referal arises.Of' cour
it is understood that while the family will contribute accordi
to its ability to pay, the services provided will depend on th
medical needs and will have no relation to the
quantum of the
family’s contribution.
It is therefore imperative that, on behalf of their employ
the Central and State Govornrrnts should offer 0.5% of the salar
of each employee, living in the MHC area.
This will be towards
individual’s/cemmunity’s contribution and will have nothing to
with the expected Governrrent grants (totalling 75^ from the Ce
and State Governments) to meet the annual recurring expenditure
Likewise the 0.5% contribution on behalf of i rail st rial work
covered by the ESI Corporation must be transferred to the MHC
entitled to it.
I began by saying the community initiates and the Governm
evalua
should participate; likewise at the end I wish to focus
not on the lowest level of the LFA/iCHV but on the highest leve
For example, will Governments and ESI Corporation contribute on
As regards the financing of health
behalf of their employees?
there are several methods which need to be urgently evaluated
These
particularly on their content of preventive services.
schemes like, the- Central Governrrent Health Scheme, The Employe
State Insurance scheme, the ’’awards” given by large employers l
the Life Insurance Corporation and the Nationalised Banks reall
provide very little for prevention of disease and maintenance o
6
Finally, let us consider organised voluntary associations
It is good to remember that voluntary health agencies have pla
a significant role in the development
f health care in India.
Their main assets are (a) in their capacity t. enlist the serv
of devoted workers, particularly doctors, (b) to tap private f
cial resources for the development of health and (c) to vcrk ou
operational cxpdriments due partly to the personnel they can
command and partly to the grater academic and administrative f
dom they ordinarily enjoy.
Their main handicap is the inadequ
of financial resources available and this inadequacy is increa
continuously because private charity is being spread too thinl
over an ever increasing number of voluntary organisations.
I
is obvious, therefore, that tte voluntary organisations can pl
a very vital part in the reconstruction of health care if the
three principal assets mentioned earlier are recognised and d
oped to the full and if their principal handicap is obviated
through special financial assistance.
By
c
i.
bLoOC)
frjy
o n t e n t s
Strategies for health for all by the
year 2000 - India
Report of the joint WHO/UNICEF
Meeting on fStrategies for
Health for all by the year 2000, New Delhi,
, 24.30 J une, ’80.
2.
3.
Community Participation
- Role of different agencies in
Multi-Sect oral approach - by Shri K. S. Sanjivi, Ex-UNICEF
Consultant on Primary Health Care.
Report of the Working group
on the roles of Voluntary
Organizations for the goals of Health for all by 2000 AD
Report of the Group on Voluntary Organization
health for all by 2000 AD.
4 .
to (achieve
Health for all by the year 2000
-------- AD. Recommendations
of the
Group on Community Involvement.
Report of the group on Community Involvement To
Ac hieve
Health for all by 2000.
5.
Extracts from: Health for all :
Major Recommendations.
An Alternative Strategy -
Report of a study
< '
group set up jointly by th
e I ndian Council
of Social Science Research and the Indian
Council of Medical
Research, New Delhi,, 1900.
6.
Extracts from: Health for all
Issues and Conclusions.
:
An alternative strategy -
ofPSOnci!? S StUdy
by the Indian Council
group Set
study pr0UP
set UP
of Social Science Research and the Indian Council of Medical
Research, New Delhi, 1980.
neaical
4
: 9
:
Every Primary Health Centre area has 2—3 cr even more dispe
3.3.5
saries of allopathic/ayurvedic/hcmoeopathic system.
More and mere
It is envisaged under the MPW
such dispensaries are being opened.
scheme to have one male and one female health assistant at one out
of every four sub—centres (one male and female assistant for 20,00
It is propsed that all the dispensaries functioning
pppulation).
in rural areas would be brought under the PHC Complex.
It is pro
posed to accept the concept of having a Subsidiary Health Centre
every 2500 rural population on uniform basis.
A subsidiary health
centre would consist of staff of present dispensaries, one health
assistant female, one health assistant male, and one male and one
These subsidiary health centres would
female multipurpose worker.
undertake all the functions for about 25,000 population, which at
present are being carried out from the PHCs.
The number of subsi
diary health centres required on the basis of one centre for about
25,000 population by 2000 A.D.would be about 26,960.
These sub
sidiary health centres in future would provide laboratory support
to Malaria, Tuberculosis and Leprosy programmes, services for
_j common mino
vasectomy operation and IUD insertion and to attend to
ubsidiary
health
It is envisaged that the s
obstetric emergencies.
properly
a
gua
centre would be the most peripheral unit manned by
fied doctor.
3.3.6
At present Primary Health Centres form the nucleus of prov
ing health services in rural areas.
These are about 5534 PHCs
functioning at present in the country, each covering a populatio
It has been found that these PHCs are
between 80,ODD to 1,25000.
unable to provide adequate health coverage to such a large segment
of population.
Additional PHCs woul’d be established onwards in
a phased manner so as to have one PHC for every 50,000 population
In particular, the PHCs would be equipped to provide basic labora
tory services, facilities of certain surgical procedures like vas
ectomy, tubectcmy MPP ‘ inor surgical interference required in ob
stetric cases and facilities for treatment of ailments of infancy
and childhood.
While the infrastructure, as detailed above, it is consi
3.3.7
dered adequate to provide primary health care to rural population
it would need to be backed up by proper referral services.
It
has already been decided to upgrade one out of every four PHCs, o
a sub-district-hospital into a rural hospital.
Next.referral po
would be district hospitals, which would provide services in all
major specialities and diagnostic facilities.
It is proposed tha
each district hospital should run a speial out-patient clinic to
provide consultancy and diagnostic services for cases referred fr
rural area and certain number of existing be ds in these hospital
may be reserved for these referral cases.
10
-RyRAL^ERVJCE^.DE5IGN^F0R^PHC_
RURAL-HOSPITAL
(200,000 population)
-y-----------
I
PRIMARY HE^LT H CENTRE
P.H.C
!
!
t
f
SUBSIDIARY’ HEALTH
CENTRE
t
—x
»
P.H.C
P.H.
i
t
!
!
SUBSIDIARY HEALTH
CENTRE
(25,000 Popula
t
i
i
!
t
i
swb Icentre
SUB
CENTRE
SUB
CENTRE
SUB-CfNTRE
i
t
t
!
t
CHv’+ DAI
CHV+DAI
CHV+DAI
!
CHV+DAI
SUB-CENT
______ xt
CHV+DAI
(1000 po
REHEBRAL_5Y5LEM
C.H.Vt DAI .
M.P.W. - JUB-CENTRE
P.H, C
i
t
t
t
f
i
!
t
UPGRADED f.H.C. 5. D. HOSP IT AL
Ii
DISTRICT;HOSPITAL
!
!
.
1
f
f
t
t
f
I
»
SPECIALITIES HOSPITALS
t
t
»
!
i
f
I
TEACHING HOSPITAL
11
In India about 21% of the total deaths are in the age group
3.3.0
0-1 year and another 10.4% among the age group 1-4 years.
Keeping
in view the major causes of deaths, the main health programmes to
achieve the long term objectives ares
The particular, emphasis in this, program
A Care:
Care:
i)
Maternal
' j against nutrition
would be to provide ante-natal care, prophylaxis
trained
personnel of natal
’naluna and tetanus, availability of a '
and post-natal care.
The infant and children care
ii)
lQfant_and_Child_Care :
programme consists of health education of the mothers, prophylax
against diphtheria, whooping cough, tetanus and tuberculosis,
extensive use of rehydraticn therapy in case of diarrhoeal disease
provision ofor the treatment of fevers and respiratory diseases
and special programmes to take care if nutritional deficiency
diseases.
comprehensive school health programme would be launc
which could cover regular health check up of school going childre
education about personal hygiene and prevision of the treatment o
sick children.
iii)
National Malaria Eradication Programme.
Intensification of the Tuberculosis programme for
detection and treatment of all effected cases, wider coverage wit
B.C.G.vaccination and health education.
iv)
’ '
Leprosy Eradication
programmej would include screening
of population 'for detection and bring under treatment all. cases
The Programme would cover the re habilit a
suffering from leprosy,»
and health education of the community to rem
of the leprosy cases u.
the social stigma associated with the disease.
v)
vi)
Diarrhoeal Disease Control Programme would include
vi)
education about personal hygiene, environmental sanitation, pro
vision of potable water and extensive use of oral rehydration
mixtures •
Prevention of Blindness Programme: the programme inclu
vii)
vii)
regular check up provision of Vitamin A prophylaxis and service,
mobile teams.
facilities in rural area through mobile
4.
Sup £o rt _Mg a su r e s
4.1
Technical, S u^ro rt
4.1.1
In order -to provide the nedessary trained man_powcr and
participate in continuing education of health personnel, there ar
390 training schools for the Multipurpose workers, with an annua
training capacity of over 13,000, 33 promotional schools fo- the
training of Health Assistants, 20 Nursing Colleges to train.
ub
Health Nurses and Sister-tutors, 44 Health and F.W.Training centr
provide refresher and orientation training to the P.H.C.Staff.
:
12
The country has adequate capacity to ’train required medi
4.1.2
and specialists through its 106 medical colleges.
man -power
The various professional organisations like Indian Medic
4.1.3
Association, Trained Nurses Association of Inc' ia and others arran
refresher training to their members.
4.1.4
In India, besides the government, large number of volun
tary organisations are engaged in providing health care to the
The full advantage would be taken of these organisations
people.
by fully co-ordinating t/heir work with the efforts of the Gover—
mant in providing health care to the people.
The spcialised U.N.Agencies like UNICEF, UNFPA, WHO,
4.1.5
UNDP are assisting India in various aspects of health programmes.
Full advantage is taken of their technical expertise in developin
the programmes for achieving Health for All.
Managerial Support
4.2
The managerial support to the primary health care programiie
4.2.1
at present is provided by the Central Institutes, particularly by
National Institute of Health and F.W., All India Institute of Hyg
and Public Health, Calcutta, Gandhigram Institute of Rural Healt
and F.W. , Gandhigram.
It is proposed to strengthen these Institu
further so that they may take up the following functions
i)
Review the training programmes of various health
functionaries;
ii)
Participate in planning, implementation and evalua. .
tion of primary health care programmes;
iii)
Undertake training of the trainers and
to the principal training institutes;
provide guidance
iv)
Develop training methodologies, training aids and
mate rial;
v)
Operational research studies on Primary Health Care
System and utilization of manpower and facilities.
vi)
Impact of the primary health care programmes on the
health status of the community.
In addition, the
the support is also available to the health
sector from the national institutes in the field of Management,
Public Administration, Communication,
Commii nicat ion , Man-power Development and
T raining•
4.2.2
The managerial support for the Primary Health Care deve
4.2.3
‘
;isalso derived from exchange of infor
lopment and‘ implementation
mation and observation visits by the planners and programme manag
to the other countries particularly the countries of the South
East Asia region, which have much in common in the field of heal
13
4.3
Research
and
Development
In India the research in the field of health is co-.ordina.te
by the Co-ordin at ion Committee constituted by the Ministry of
The Committee provide guidlines and identify the
Health &. F. W.
priority areas.
The research councils, Indian Council of Medic
Research, Indian Council ofResearch in Ayurveda, Research Counc
in Unani, Council of Research in Homoeopathy coordinate the
research work in their respective fields.
Besides this the op
erational research is being carried cut by the different univer
Priority is given for the operatio
sities and medical colleges.
research in the field of primary health care delivery system,
appropriate technology and management information system.
4.4
Inform atio n
In order to meet the
stators, a properly built
requirements of planners and adminis up information support is indispensab
. Cfrg... f. r_° qr am me
4.4.1
Date generated through medical care programme are useful
not only for efficient management, planning and evaluation of m
care programme but also for working out a morbidity and mortalit
pattern of the community and epidemiological studies as reasona
accurate diagnosis of diseases is available.
The requirements
medical certification of causes of deaths and uniform classifica
tion of diseases is not uniformly observed by all hospitals.
It is proposed to strengthen the medical record keeping
in hospitals and to admpt the Ninth Revision of Internati nal
Classificatirn of Diseases and new lists for tabulation.
4.4.2
He a11 h
M an-p owe r:
Formulation and implementation of a realistic National
Health Policy needs assessment of available health man-power and
At present registration of
training facilities are essen ial.
professional by the statutory councils in respect of doctors, n
dentists and pharmacists is the main source of information in
Council of Scientific and Incdust
respect of these categories.
Research undertakes voluntary registration of highly qualified
Indian doctors abroad and those returning to India.
Studies to
estimate the stock of health professionals and the extent of
brain-drain is undertaken by the Institute of Applied Man-power
Inspite of these efforts health Man-power data are
Research.
not quite satisfactory.
It is proposed to strengthen the present mechanisms and
to establish man-power units at the Central and State levels
to coordinate the collection of information and develop the
data collection on health man power, particularly in respect
of more categc.ries of health personnel, about whom no informatio
is collected at present.
: 14
4.4.3
Epide m.i c_ I_nt e 11 i^en ce :
National Diseases Control Programmes of Malaria, Filaria,
Tuberculosis, Leprosy, Cholera, Trachoma, E.P.K Disease and S.T.
have developed suveillance mechanism with a view to facilitate th
containment.
However epidemiological services are not yet wellIt is proposed to collect regularly statistics of cas
developed.
and deaths of about 20 communicable diseases on countrywide basis
4.4.4
It is proposed to strengthen the existing mechanism of
i)
collection of health information generated from rural communities
through basic
health
workers.
Community health survey registers and village or town
ii)
peoples to provide socio-economic and demographic situation of th
They would be further consolidated
community are being prepared.
provide useful summary data on distribution of population by imm
nisation status, family planning practices, nature of disabilitie
chronic ailments, occurance of communicable diseases, maternal an
child care, vital events, health education activities and many
other useful
4.4.5
informations.
Surve^s_and_studies:
order to meet’ the requirements, data from official hea
statistics would be supplemented by special surveys and studies,
particularly in the fields where the information is not being co
In
cted routinely.
5
5£ne r.at ion__a rdd
Mobi 1 izat ion.q u r ce s
5.1
Human. Re s ou r ce s/ De ye 1 o pme nt
Based on the health infrastructure required for the delive
of primary health care and back-up services required to support
a long term plan to meet the requirements of trained manpower ha
The country has developed the potential to train
been drawn up.
the required number of medical, paramedical, auxiliary and volun
workers and it is proposed to put them in position in a phased
during the next two five-year development plans (1980-85
manne r
Necessary training facilities have also been crea
and 1F85-90).
trained
trainers for manning the varioius training
to provide t he
5.1.1
in stitut ion s.
5.1.2
The programme of re-orientation of the. health workers and
primary health centres Medical Officers has been made an integra
part of the training programme in the new health plan.
It is
proposed to provide
even to ten days reorientation to all the h
personnel every year.
The re-oreient at ion to the health personn
would be provided by the Basic Training Institutions in collabor
with
the
district
level
health
personnel.
:
15:
5.1.3
In view of the. very large number of Community Health Vo
eers (CHVs) it is not proposed to provide -them institutionalised
The re-orientation training of the CH
re-orientation training.
is being carried out in batches in the periphery by the medical
officers and Health Assistants for one day every month. -This i
supported by a ’’correspondence course”, which deals with the he
problems indicated by the CHVs themselves.
This programme has
been launched from October 1979 and at present done on quarterl
basis, but it is proposed to make it monthly in future.
5.1.4
The programme of health education of the community is
carried cut through group and inter-personal communication by t
field staff.
In addition,over 50,000 orientation camps are hol
every year.
Each camp is attended by 40 community leaders who
in turn arc expected to pass on the knowledge to the community
In addition, full use is made of mass media like radi
members.
films, T.V. and print media to educate the public regarding the
The Mass Education and Media Division of the
health problems.
Ministry of Health & F..W. and C.H.E.B guide and provide technic
support to the similar units in the States to carry out the hea
and population education activities.
Financial
5.2
and Material
To meet the
resources in the
be
^g,sources
increased requirements of financial and mater
health sector following steps are proposed to
taken:
5.2.1
Higher budgetary
provisions
for health
sector.
5.2.2
Preferential allocation for tho-unserved areas and popu
tion and to the programmes specific to the needs of vulnerable
section of the community.
5.2.3
Maximising the available
appropriate technology.
resources
by
the
adoption
Involving the community and encouraging them to
5.2.4
and share some of the cost of primary health care.
Co-ordinating the
5.2.5
organizations e ngaged in
of
particip
programmes with the efforts of volunta
providing health care to the community
Utilising all the trained man-power and facilities avail
5.2.6
under the various Indian systems of medicine for the delivery o
primary health care.
5.2.7
Taking advantage of the assistance available from foreig
sources, international agencies and T.C.D.C. for the developme
and implementation of Primary Health Care Programme.
Budgetary allocations for IV, V and VI
well as preliminary projection of Resources
below :
Five-Year Plans as
Estimates are given
:
Table
I.
16
:
5howinq_Budqetar
duriri_g_t te__Year_
V Plan
VI Plan
(1974 -1978)
(1978 - 83)
(In Million of Rupees)
IV Plan
(1969-1974)
Item
(A)
Public Health
i) Rural Health
765(17.5%)
1203 (17.6%)
4900(36.8%
Communicable
Disc a sc s
Control
1270(29.3%)
2651
(38.9%)
4500(33.8%
T ot al
2035 (46.759
3854 (56.5%)
9400(70.6%
Others
(includin g
Urban insti
tutions etCj)
2304(53.3%)
2962 (43.5%)
3900(29.4%
Grand Total
4339(100%)
6816 (100%)
13300 (100%
ii)
(B)
Al1ocati□ns_for_Health_
Allocati n for Nutrition and Water Supply are shown in Tab
II below:
Table II Showing Plan Allocation_f or_Nutrition ’
and Water Supply Sanitation f .□ r_t he_£e rio d_L1.9,74-8
He
VI Plan
V Plan
(1978-83)
(1974-1978)
(in Million of Rupees)
(A)
Water Supply and
San it at io n
Rural
Urban
T ot al
(B)
III.
Nutrit ion
1940
3800
5740
3470
4060
7530
1 1 56
1 745
Gross approximations of resources needed for attainment
of HFA/2DDQ amount to 71B20 Million of Rupees over and abo
Thus,
the current level of allocations for 1980-2000.
there will be an average shortfall. of 1 7,955 million of
Rupees per each five-year plan period.
17
6.
_I nt.e,r-5e ct o ral__Coll ab£r ajti ve_Me c_h a_nism
The National meeting on India’s strategies for achieving Hea
for All appointed separate Working Groups to recommend the mechani
for i nt r a and inter-sectoral collaboration and they have recommend
Setting up of a’National Coordination Committee for Health
for All under the Chairmanship of the Prime Minister with minister
of all the economic and social welfare Ministries as its members.
6.1.1
6.1.2
A committee to review the progress of Revised Minimum needs
Programme (R.M.N.P) ^as already been constituted under the Chair
This committee would appraise the
manship of Cabinet Secretary.
implementation of the R. M.N.P in respect of health, housing, water
supply, sanitation and sodal welfare programmes.
6.1,3 To bring about meaningful coordination in the plan approach
and implementation of programmes by various concerned Ministries,
a Standing Coordination Committee under the Chairmanship of Advis
(Health) Planning Commission should be set up with Joint Secretari
of the concerned Ministries as members.
6.1 .4
at
Similar committees should be set up State and District lev
7.
In view of the high priority given to the rural health prog
the need for developing an efficient organization for monitoring
The steps to build up such an or
evaluation is well appreciated,
zation would involve:
7.1
Improvement of system of Maintenance of records and data
re porting from periphery.
7.1.1
Standardisation of definitions,
tabulation plans.
7.1.2
reporting procedures and
7.1.3
Improvement of system of storage, retrieval and data handl
7.1 .4
Providing in-service training to health statistical person
Establishing ma chinery and mechanisms for sample surveys
7.1.5
and special studies and programme evaluations.
7.2
The indicators to be used initially would:
7.2. 1
He alt h._5t at u s Indic at ors
Like Death Rate, Birth Rates, Infant Mortality Rate, Child
Mortality Rate, Maternal Mortality Rate and expectation of life a
Birt hs.
18
:
7*2.2 Health
would cover health organ
H e a It In, Organization
0 r g ani z at io n Indicators:
In die at or^.:
zations"'and health manpower in relation to population.
would be in particular relati
to the. hation allheal th programmes like-:
7.2.3
Healthier vice indicators :
- percentage population" covered by E.P.I
- percentage of expecta'nt mothers provided antinatal care prophylaxis against anaemia and tetanus
- percentage of deliveries conducted by trained per
sonnel
- percentage of couple using contraceptive methods
- number of fever cases inve st i gat e d
number of tuberculosis, leprosy cases
brought under treatment, and so on.
7.2.4
detected and
Health Impact Indicators
These would include disease specific morbidity and mortal
particularly in respect of prevalent communicable diseases.
peov ch
'
§lRATEGIE5^0R-HEALTH-FCR^L!_3Y-THE„YEAR 20g0 *
- INDIA
'■ r1,
1*
Mjgin_Health
and_Health
Related Problems
1.1
India is a vast country with a population of 646 millio
(estimated as.,on 1st
1 st March, 1979) and density of population of
about 196 sq.Km.
Though the rate of population growth in the l
decade has come down from 2.24% to 1:.95% per annum and is likel
to go down further to 1.64% per annum by 1991, the population
projection indicate that the country’s population would increas
about 799 millions by 1991 and to 917 millions by 2000 A.D.
Ov
78% of the country’s population is settled in’575936 villages,
pearly half of which have a population of 50.0 and less.
Even
amongst urban population, there are only 370 towns with popula
tion of 50,000 ’dnd over, remaining of the Urban population re
Children in the age group 0-14 constitute
side, in small towns.
little over 40% of the total population.
There is a vast dis
parity in dispersal of populat ion. from areas to areas.
While
density of. population in States of Kerala and West Bengal is
over 500 per. sq.km. , it is less than 50' per sq.km, in Miioram,
Arunachal Pradesh, Manipur, Meghalaya,■Nagaland, Sikkim and
Andaman and. Nicobar Islands.
Only 32.93% of the- total population constitute the wor
1 >2
ing population resulting in a higher dependancy rate.
Being p
dominantly agricultural country about 70% of the working popul
Employment
tion is either’cultivators or agricultural labour.
among woman is extremely low, only 17.36% of the working popula
tion is female.
Per Capita G.N.P for the year 1977-78 was onl
Rs 1163 and per capita availability of foodgrains only 472.6 g
Using caloric consumption as a norm it is estimated that 48%
of the rural and 41% of urban population is living below the
poverty line.
Unemployment is estimated to be 20.6 million
The concept of poverty is wider and
person years during 1978.
includes not only those unemployed and poor but also those who
are fully or partly employed and earn very little because of lo
productivity or low wages.
There are certain disadvantaged gro
in society like scheduled castes and scheduled tribes, which
continue to suffer from social disabilities and poor economic
status.
1.3
Inspitc of primary education being compulsory and con
certed national efforts, literary rate continue to be low- only
While literary
39.44% male and 18.69% female being literate.
percentage Kas increased appreciably in the tecent years, the
number of illiterates is estimated to around 387 millions,' '
majority of them belong to 304 group.
* Report of the Joint WHQ/UNICEF Meeting on.Strategies for Hea
For All By the Year 2000, New Delhi, 24ir30 June 1980.
Copies produced for discussion purposes at the
National Confere
r
xix)
7.' ' •
■
XX )
4
Encourage research on alternate appraches to health care
delivery systems and a discovery of simple lowvcost appropriate technology.
To provide legislation support wherever necessary.
”
2.2 Social and economic policies: The social and economic poli
of the Government are directed towards:
2.2-1
Launching of new economic programme through country’s Five
Year Development Plans to focus attention on twin objectives of
increasing production and promoting social justice.
2.2.2 To make the reduction of disparities of all kinds - socia
economic and regional - one of the central objective of developm
planning.
To direct the planning to solve over a period of time the
2.2.3
problems of the poor of all communities, expecially tribal, har
backward communities and regions.
2.2.4
Provision of fuller employment as a surest means of prom
greater social justice, by augmenting a gricultural productivity
vigorously implementing land reforms.
2.2.5
Vigorous efforts to implement the
programme launched by tte Government.
20 point socio-economic
2.2.6
Very high priority to the elementary education programme
increasing enrolment for secondary education with vocationalisa
the secondary stage, and additional facilities for weaker sectio
of society and in backward areas for university education; and
strengthening of national adult education programme.« of
Rur£i
Development programme with
Integrated
Launching
2.2.7
social services inputs.
2.2.0 Special development plans "Tribal sub-plans” for the dev
ment of tribal economy.
2.2.9
■
Special services for the welfare of backward classes.
5
3.
MAin Long-Term Programme
3.1
3.1.1
-
Objective
ne r al_0b je c_U_ve s :
‘ 'i care delivery system to make
i) To provide improved health
to all by 2000 A.D.
available
primary health care services i
ii) To make people conscious of their health needs and to
make them plan and participate in the health programme.
iii) To improve the standards of environmental sanitation
and personal hygiene leading to reduction in incidence of di
seases and healthier life.
iv) To improve maternal &, child health services.
v) To create. awareness about the need and advantages of
small family and encourage adoption of contraceptive practices.
vi) Cont rol/e radicate common communicable/and infectious
disease s.
vii) Bring down by about 50% death rate; and maternal and inf
mortality rates.
3.1.2
Af £ o^i b cti ve s
Showing targets of ’’Health for All by 2000 A. D. ”
Pre bent
2000.A.
Crjrle Death rate
14.1
9.0
Infant mortality rate
1 29
Perinatal mortality rate
60-109
35-40
Preschool (0-5 years)
death rate
Maternal Mortality Rate
(MMR)
Below 60
30-35
10
Below 2
5-8
52.6 M
64 yr
10%
Crude birth rate (per 1000)
30%
33.2
(1978)
21.0
% Effective couples protection
22.0
60.0
Life expectancy at birth
Birth-weight
below 2500 g.
Net reproduction rate
Natural growth rate
f.
1.67
1.9
(1978)
1.0
1.26
6
Pre ss nt
Family size
% pregnant mothers rural receiving
ante-natal care
4.3
--
2000 A.
2.3
46.3%
(estimate)
100%
10-15%
(estimate)
100
% population with protected water supply
R 10
U 80
100
100
% population with sound excreta disposal
R 10
U 34
50
100
% of deliveries by trained birth
atte ndant s
Immunisation status
(percentage coverage of pregnant
mother and infants)
a)
TT
21%
100
b)
DPT
51%
1 00
c)
Polio
1 8%
100
3.2
Approaches:
The main objective will be to provide better health care
3.2.1
services to the rural areas and poor -people.
3.3.2 People has the right and a duty individually and collect i
ly to participate in the development of health.
Governne nt and
the medical professions would help the jaeople in realisation of
their responsibility by providing a large band of health worker
from among the community itself to take care of basic health
needs of the community.
3.2.3 Government recognises the need for more equitable distri
bution of health resources, and in order to correct the past
imbalances, preferential allocations would be made for developi
Even while developing health
health facilities in rural areas.
services in rural areas, priority would be given to satisfy fir
and foremost the health needs of mothers and children and of we
er sections of the society.
The main emphasis would be on preventive, promotive and
3.2.4
rehabilitative aspect of health which would be integrated with
the functions and responsibilities of all those institutions,
which at present -are providing only curative services.
In providing primary health care to the people, full
3.2.5
advantages would be taken of the traditional methods and techn
ques which are scientifically sound, familiar and acceptable to
For this purpose, the facil
the community, and easy to adopt.
:
7
:
under different Indian system of medicire
in the delivery of primary health care.
would be fully, utilised
3.2.6
Primary Health care would form an integral part of the hea
system.
Proper linkage would be established so that the total he
system supports the primary health care programme by providing
consultation on health problems, referral of patients to local an
more specialised health institutions and supervision and guidance
3.2.7 The further expansion of health facilities under different
systems of medicine would be so planned and c oordinated that they
support and complement and not compete with each other in providin
health care.
3,2.8
The medical education would be restructured to give it a
positive bias towards community health.
The traiming programmes of health workers has been modifie
3.2.9
to give it a special orientation and technical training to meet th
health needs of the population, they are to serve.
Educat ion, motivation and provision of services for incre
Education,
3.2.10
sing the adaptation and practice of contraception would form an
integral part o
the primary health care system.
3.2.11 The pace of providing safe, adequate
supply to the villages would be accelerate d.
and
potable water
Appropriate technology would be developed for adoption fo
3.2.12
safe disposal of spent water and human-wates to improve the sanit ation•
3.2.13
Necessary guidance and support would'be provided to weake
sections of the community for construction and improvement of
housing facilities in villages.
In order to facilitate planning, evaluation and implement
3.2.14
of the national health plan and policies, the health information
system would be strengthened and streamlined.
3-2.15
The evaluation system would be Iguilt up,i'Q that the imple
tion of the policies, strategies and the plans of action can be m
tored and their impact in improvement of the health status of peo
can be assessed.
3.2.16
The Primary Health Care programme would be fully coordina
with other socio-economic programmes like Integrated Rural Devel
ment Programme, Nutrition Programme, Integrated Child Development
Scheme, National Adult Education Programme, which have been laun
ched by different Ministries/Departments of the Government.
Various social and voluntary organizations working in rur
3.2.17
areas would be encouraged to participate in the implementation of
the health plans and the delivery of the primary health care.
3.2.18
No linear expansion of curative services in urtjan areas
8
except in few cases where the need for such expansion is justifie
In such cases urban
on sound principles of need and. priority.
areas would be expected to meet a part of the cost of these facilitie s.
3.3
t e rri f
It is estimated that bjz the year 2000 A.D., the populati
3.3.1
of India would increase to 917 million - 674 million rural and 24
The subsequent five year development plans of the
million urban.
country would take into account the need of health infra—structur
required for the delivery of the primary health care to this incr
sed population.
The health infrastructure envisaged would be as
follows:
The Gcvcrnmentt has already accepted the policy of creati
3.3.2
a band of voluntary health workers by training persons selected b
It is
the community under the Community Health Workers Scheme.
proposed to train about 5.8 lakhs CHWs during the present plan pe
1980-85, so as to have cne CHW for every village.
Thereafter Go
nment propose to continue the training programmes for creating in
creasing number of health guids/health promoters in rural areas,
who can take up. preventive and promotive aspects of health care ’
on voluntary basis.
3.3.3 The' dais (indigenous birth attendants) training programme
has already been intensified and it is proposed to train 5.8 Ink
dais by March, 1 983 so as to have one trained dai for every villa
Realising that in large number of villages, there is more than on
dai functioning at present and each dai is traditionally attached
to only limited number of families, the dais training programme w
be continued beyond 1983, with the aim of training all the da'is
practising in rural areas.
There are certain parts of the countr
where indigenous dais do not function and their role is performed
by elderly women of the family.
A programme through village Wom
clubs would bo launched to educate them regarding the needs and c
of expectant mothers during ante-natal, pre-natal and post-natal
period.
3.3.4
It has been accepted to have a health sub—centre with one
male and one female multipurpose worker for every 5000 population
There are about 50000 sub-centres by the end of Year 1979-80.
It
is proposed to have additional 30,000 sub-centres during the plan
pe ried 1 9 8 5-90.
Based on the present norms, country would need
about 1,34,800 sub-centres by 2000 A.D which would mean establishm
These may be opened
of 23,000 additional sub —centres after 1990.
during the period of 1 990-1 995 , sc that the norms of having cne
subcentre for every 5000 rural population on 2000 A. 0. population
base is achieved.
At present the functions of a sub—centre are
limited, and it is nut able to meet even some basic health needs.
It is proposed that the facilities in future would be provided at
all the sub-centres for IUD insertion, and simple laboratory in
vestigations like routine examination of urine, for albumin and ‘
The MPWs would be trained for this purpose.
sugar.
Creation of
those facilities would undergo long way in greater acceptance of
IUD and detecticn of common complications of pregnancy.
Com h 3->3
0277-9536/84 S3.00 +
Copyright c 1984 Pergamon Press
Soo. Sei. Med. Vol. 19. No. 3. pp. 217-224, 1984
Printed in Great Britain. All rights reserved
WILL PRIMARY HEALTH CARE EFFORTS BE
ALLOWED TO SUCCEED?
H. K. Heggenhougen
*
Evaluation and Planning Centre, London School of Hygiene and Tropical Medicine, Keppel Street,
London WC1E 7HT, England
care includes a concern with such factors. PHC, if it .s to succeed, must ultimately lead tc i reduc ion
in the greater benefit for the few to the greater benefit for the many. This; wiU receive suong oppos
.
The situation of a PHC programme in Guatemala is presented as a case of PHC efforts which were
succeeding being violently opposed. This is compared with PHC development efforts in Tanzania where
unlike Guatemala, there has been a conscious effort at restructuring the soc.ety and where nat.onal
development policies are in tune with PHC principles. The future of PHC in Tanzania wd depend mor
on whether or not the organization and management of selection, training and imp
^2 t0
and the minimal available resources, will lead to success, than on whether or not it wdl be allowed to
SUIt1s concluded that the situation in most countries comes closer to that of Guatemala than of Tanzania
and that many people and institutions in hierarchial, non-egalitanan societies will spend a great deal ot
energy to prevent PHC programmes from succeeding. This forces us to consider the promotion of P
in a much more serious manner than we might wish.
It is my contention that the natural consequence of
accepting Primary Health Care (PHC) principles as
guidelines for health care development must be a
restructuring of the socio-economic conditions exist
ing in most countries of the world [1]. In the light of
this one must ask whether or not the implementation
of PHC concepts is really
QI
icauy possible.
pvaoiMiv. Will
mu *PHC efforts
be allowed to succeed? Most countries do, of course,
* ‘
profess a desire to improve the health status of"* their
populations. Much verbal support is given to the
PHC approach and many countries have formulated
national PHC plans. It is espoused as the most
appropriate means for achieving ‘Health for all by the
year 2000’ [2]. But the degree to which such efforts are
being allowed to be implemented depends on existing
national political, as well as socio-economic, charac
teristics.
PHC is not only a matter of curative medicine and
that which we have come to think of as preventive
medicine, but is concerned with active health pro
motion and development activities:
The practice of medicine is only a small part of the total
pattern which includes responding to total community need,
whether that be in the field of agriculture, marketing,
housing, home-crafts, nutrition, family planning, schooling,
transport...” [3].
It is by now a well established fact that such
improvements as clean water, enough food, a min
imal economic level, environmental sanitation and
the like, are the crucial factors affecting health status.
McKeown, in his review of health statistics from
♦The views expressed in this article are those of the author
and do not necessarily represent those of the institution
with which he is associated.
’ 5 over the last several hund
England and Wales
years has clearly shown this to be so [4]. It is
course, these ideas which are being restated in
various declarations of PHC.
The concern of any government advocating P
should be with making changes to improve the
situation of communities. Such improvements
quite often the consequences of basic changes in
social and economic situation of particular po
lation groups, and are related to issues of s
Jjustice, ^equal1 access to available resources and
return for one’s labour [5].
As such PHC is nothing new. We may recogni
PHC principles much of the philosophy expresse
Virchow more than a hundred years ago. “Medi
is a social science and politics is medicine on a
scale’’ [6], and more recently by Dubos [7] and o
[8],
„‘... health and illness are to a considerable e
determined by the existence of a particular mode of
and economic organization ...’’ [9].
The growing acceptance of the (renewed)
perspective is not only a challenge to medical
health professionals but to anthropologists and o
social scientists as well [10]. As Foster states.
“On the surface, at least, it looks as if the time is prop
for anthropologists to play an increasingly important r
international health programmes” [11].
Even if PHC is only a fad or a hopeless and im
sible dream, rather than the enduring enterpris
may wish it to be, social scientists must now tak
opportunity to have their voices heard and to
concrete contributions to the processes of h
development (in planning and implementation a
217
COMMUNITY HCALTH CELL
218
H. K. Heggenhougen
as in evaluation) which draw on the holistic perspec
tive for which there was only limited receptivity in the
past [12]. If social scientists, who attempt to under
stand the ‘human condition', are to participate in
these processes they must be concerned with issues of
justice and human rights—with analysis and exposi
tion of exploitation, and they must discuss (health)
development in terms of such analysis [13].
A few countries, such as China, have attempted
revolutionary restructuring of the total society. With
out necessarily holding these countries up as para
gons (the reality does not always mirror policy!) PHC
efforts related to such general development operate
within quite different parameters than health devel
opment efforts in countries which do not profess such
encompassing reconstruction policies [14],
Despite the common pronouncements of broth
erhood, equality and freedom, most countries are not
engaged in social reconstruction but are quite clearly
maintaining stratified socio-economic as well as po
litical structures which benefit the ‘haves’, not the
‘have nets’. In these societies, PHC, as ultimately a
social enterprise, may be seen as subversive and even
revolutionary.
A great deal of reliance has been made on the so
called barefoot doctor or Village Health Worker
(VHW) to provide PHC services to village commu
nities [15]. In all too many cases, however, such
services have consisted almost exclusively of simple
treatment for a few diseases. This does, of course,
constitute a real service as McKeown states:
The conclusion that medical intervention is often less
effective than has been thought in no way diminishes the
significance of the clinical function. When people are ill they
want all that is possible to be done for them and small
benefits are welcome when larger ones are not available [16].
Curative medicine is what people themselves want
and providing this is usually what official and
unofficial national and local decision makers see as
the rightful role of health workers. Provision of
curative medicine is also held out by the authorities
as a sign that they are concerned with, and are doing
something to improve, the health of the population.
But putting plasters on boils will not reduce the
number of sores which will fester. It does not attack
the underlying causes of disease prevalence. It does
little to improve the overall health status of the
community.
To bring about such improvement is a difficult
task. It is not achieved through the kind of health
care which can be delivered by a technically capable
health worker, at whatever level, through an injection
or other clinical treatment. It requires active engage
ment on the part of the people themselves and
changes within the structure of their community. One
of the functions of the PHC workers, therefore, is to
increase people’s awareness of their own situation, to
help them to recognize problems and to develop a
reasonable and jointly agreed upon plan of pro
cedure. Some have called it a process of ‘conscientization’ [17]. Health workers
“ ... must create in the people an iunderstanding that they
have the ability to solve most of their problems themselves,
that assistance is available when it is needed and that
occasionally public action is necessary... . The challenge is
to increase the people's control over their enviro
[18] .
We know well enough, however, that the sit
of rural communities is not entirely controlled
people in those communities themselves. Cer
what is necessary is self-help action and chan
health related behaviours. But there are other o
forces at work, such as the manipulation of m
prices and the control of resources by a rulin
[19] . Can or should VHWs also motivate their
neighbours to influence or to improve the re
ship which exists between the villagers and
forces?
If a VHW takes on the role of PHC worker
broadest sense he she may be seen, accordi
David Werner, as:
“ ... an internal agent of change, not only for heal
but for the awakening of his people to their human po
and ultimately to their human rights. In countries
social and land refonns are sorely needed where oppr
of the poor and gross disparity of wealth is tak
granted it is possible that the health worker knows an
and thinks too much. Such men are dangerous. They
germs of social change" [20].
Some may ask if we have the right to motivate V
to discuss and encourage changes outsid
confined arena of medical care. Should issues su
improved marketing mechanisms, buying co
atives and land tenure questions be include
many countries this will mean stepping on dang
ground. It may mean that VHWs, and the vil
they motivate, put themselves at risk—at ri
repression or even open violence and brutal rep
[21]. Such reprisals to health workers in
Bangladesh [22] and in Guatemala [23] testify
danger involved. Many have been killed, and o
intimidated and forced to abandon their work
answer is not simple.
Following the PHC approach does not neces
mean that VHWs should forcefully challenge ex
power structures nor that VHWs should be re
tionaries; much can be done conservatively. Bu
not always easy to anticipate what the reaction
be to a group of people which becomes more
reliant and less susceptible to manipulation
outside. This article addresses the question,
PHC efforts be allowed to succeed?” by descr
the fate of a project initiated in the Departme
Chimaltenango, Guatemala some twenty years
by a private voluntary agency. This progra
focused on the selection, training and use of VHW
promotores de salud—who worked on a part
basis in their own communities of Cakch
Indians. More than 85% of the population o
Department is Indian. But the programme
also involved with agricultural improvement
operatives, water development schemes, Mat
and Child Health services and additionally r
hospital for the Cakchiquel population [24],
The philosophy of this programme is summe
in the statement:
“... the service is for others, on their terms, at their le
understanding, in their language, and with their best m
always the important stake in the deal... nothing gen
will happen in the oflenng of total community me
services until such services are dispensed generally b
Will PHC efforts be allowed to succeed?
2
become seasonal migrant labourers on the lowla
plantations.
In one village a co-operative venture was starte
In another an agricultural improvement project.
This programme was controlled by a board made up still another a chicken project; several villages d
of the Indians themselves. Indian peasant men were wells and installed piped water. A few joined togeth
chosen by their own neighbours for training and and were able to buy a piece of land which w
returned to work on a part-time basis in their villages worked co-operatively. Here and there the spirit
as health workers. Once a week they participated in self-help and co-operation in bringing about sm
a half day continuing education session and once a development efforts blossomed and began to impro
month a skills evaluation exam was required for them the lives of those involved.
to be able to maintain their status as VHWs. The
Many of the health workers as well as other vill
training programme began and ended with a week of leaders and special ‘improvement committees’, w
classes, but the core of the instruction was carried out in the forefront of bringing about such projects
during one day per week for a year at the pro
their villages. Most still spent their time treating th
gramme’s hospital and clinic facilities in the town sick neighbours and dispensing medicine but as
centre. It was deemed important not to remove the philosophy of the programme was based on a holi
trainees from their villages for too long. The pro
view of health other activities were also seen by th
gramme does receive some funding for its various as central to their health work. It is after
activities but:
significant that these workers are called ‘promoto
de salud’—promoters of health.
. even if all costs must be borne by the patient,
At the end of the 1970s and during the first ye
the.programme demonstrates that many communities,
which could otherwise not afford a physician, can support
of the 1980s certain factions within Guatemala
medical services delivered by non-physicians [26].
came increasingly concerned and threatened by th
It was felt important that the service should be activities which seemed to improve the lot of
something the villagers themselves could control and Indians. The repression and sporadic violence wh
had been at a relatively low level throughout
support.
1960s and 70s started in earnest [28]. Those villag
Village people tended to trust, understand and rely
on the VHW because they identified with him as one attempting to make changes were called unpatrio
of their own. It was significant that health workers traitors and communists by those who benefited fr
were also peasant farmers dependent for their liveli maintaining a suppressed and dependant Indian p
hood on cultivation before they were practitioners ulation. Most villagers were quite ignorant ab
and as such were integral members of their commu such political theory, however, and were simply
nities. This understanding of the community and volved in bringing about some small improvemen
intimacy with the lives of its members, was crucial. the lives of their families and their neighbours. P
When treated by the VHW the villagers said they military gangs from the towns invaded the co
understood the treatment since it was administered tryside. Houses were destroyed. The incidence
by one of their own, in their own language, and in a torture and murder increased, reaching a new l
style and setting familiar to them, interspersed with during the Lucas regime of 1978-1982.
The VHWs were some of those particularly sou
the full range of gossip that occurs in ordinary
• • • * , Were ki
conversation. The VHWs practised a simple form of out in their villages for
Eleven of the 49~VHWs in the Chimaltenango
"
_ 'but it
’t was framed
Western, cosmopolitan medicine,
within the socio-cultural milieu of the patients the gramme were ‘eliminated’ and members of t
families were killed. Many went into hiding [29]. T
programme
—z~~?.—’^'3 serves.
The programme continuously impressed upon the were far from being revolutionaries in the true s
VHWs that although the importance of curative of the word. They were not involved in aggres
medicine should not be minimized, it could not by actions, either armed or unarmed, against the l
itself break the cycle of poverty and repeated ill lords or others with power and privilege outside
health [27]. Thus the involvement in agriculturejand villages. But in attempting to make changes in
villages and become more independent and
tenure, water, sanitation and other village efforts
beyond the narrow confines of medicine was con reliant they were seen as threatening the exis
stantly encouraged. This programme helped m mak- power structure.
Why were these self-help activities more th
ing the Indian population in this part of the Gua
temalan Highlands increasingly conscious of their ening now than before? The answer may be foun
own collective situation. And, with increased commu the fact that although Indians have been activ
.
' -a
in their villages
efforts to improve the situation
nication between different Indian communities
c-----long
time
it
is
only
recently
that a collective
<-------throughout the country, they recognized that their
own situation was quite similar to that of other national, consciousness has developed. Accordin
communities. A severe earthquake in 1976, in addi Shelton Davis, what had taken place was a:
tion to causing a great deal of destruction and killing “ ... transformation from a local, community based
more than 20.000. people, also seems to have in- iiuiuciivii
w a national political
___________
nomenon to
movement_ [and ..it ..i
creased communication between Indian groups, and
has ]e(j to the recent political violence against In
prompted various self-help activities. Villagers real communities” [30].
ised that they could take certain actions to improve
Until
recently Guatemalan Indiaijs drew their i
the situation within their own communities so that
-------------->
they would have less of a need, for example, to tity from their own village, or from the town to w
unsophisticated on the patient's terms, and not by the
sophisticated powerful who sell medicine as a commodity at
their price [25]”.
220
H. K. Heggenhougen
it related, and did not have substantial collaborative
ties with Indians elsewhere. Changes did, of course,
occur as a result of the revolution in 1944 and during
the more egalitarian governments of Arevalo and
Arbenz which recognized the rights of the Indians.
During this time a few Indians were elected to local
political office. This political participation, the activ
ities of the labour movements (e.g. the formation of
the National Peasant Federation of Guatemala) and
the agrarian reform bill which gave rise to local
co-operatives had significant impact on the Indian
population. But at the time of the coup in 1954,
which brought a return to a successive number of
repressive regimes, a national movement had not
been established among the Indian population.
It was not until the mid-1970s that co-operatives,
growing out of the Catholic Action movement—
originally an ‘anti-communist and anti-protestant’
movement—again flourished. Politically, Indians
made great strides through their participation in the
election of 1974 when they won a number of mayorial
seats. _More significant than municipal victories, how
ever, was the election of an Indian representative
from the Department of Chimaltenango to the na
tional congress, the first time that this had occurred.
This represented not only a ‘first’ in Indian represent
ation from Chimaltenango but “it marked the begin
nings of political co-operation among Indians across
municipal boundaries” [30].
The 1970s also saw a rejuvenation of the labour
movements and at this time these consciously at
tempted to establish bonds with the Indian popu
lation. In 1978 the Committee for Peasant Unity
(CUC) was established which was the first or
ganization to unite Indian and non-Indian peasants
alike.
Village improvement schemes throughout the
country were now no longer simply viewed within a
local context because:
“by the end of the 1970s a major political mobilization had
taken place among the Guatemalan Indian population. The
social and economic horizons of this population had not
only been expanded by the activities of foreign missionaries
and participation in rural co-operatives, but also new
alliances had been formed among socially conscious Indian
leaders, opposition political parties and an increasingly
militant labour movement” [30].
Such political participation and collaboration on the
part of the Indians were not tolerated and as a
consequence anyone promoting village improvement
projects, no matter what their nature, was suspect
and treated violently.
In March of 1982 Guatemala had a change of
government*. The Chimaltenango health programme
which had come to a stand-still in 1980 is beginning
to partially function again; at least the hospital and
clinic and some of the other activities are operating.
Many of the VHWs, however, are still inactive or in
hiding. They are fearful that they or their families
may come to harm should they again actively resume
their health work.
It is claimed by the Government and in the inter
national press that the rate of violence which charac
terized the Lucas regime has now been greatly
*This regime was in turn overthrown in a coup in 1983.
reduced and that there is a renewed sense of
in the country. Others are not so optimistic, ho
especially not with respect to the Indian pop
[31]. There are still reports of repression, killin
even village massacres [32]. Amnesty Intern
has claimed that at least 2600 people were
during the first six months of the new regime [3
number of Guatemalan Indians in the refugee
in Chiapas, Mexico, continues to increase dai
number of displaced people within the coun
been stated as numbering in the hundr
thousands [34]. The situation in Guatemala
fact it is in most of Central America, is critic
future is at best uncertain.
What the future will hold for this program
difficult to say. But it seems quite clear that s
the individual workers were killed, not becau
were political revolutionaries, but because they
begin to show some form of success in terms o
goals. I believe it was precisely because thes
efforts were succeeding that they were rep
They were not allowed to succeed! As Oscar G
one, has stated, “it is regrettable that in all too
countries the interests of the few are exce
destructive of the health needs of the many
Bryant, in 1973, raised the same issue:
Health is but one of a number of social benefits o
populations are deprived, and any inquiry into the
redistribution of those benefits should be concerned
basic structure of society, the way in which p
balanced, and the extent to which there is a late
ingness to share that power and those benefits [36]
One is justifiably sceptical about whether t
willingness to share such power and whethe
with power will come to see it as their interest t
more equitably available resources.
The socio-political background and the c
devastating situation in Guatemala can not
plored in detail here, but must be understood
considering the prospects for PHC in that c
(numerous sources exist for this purpose) [37]
temala is not unique, however. In any hiera
and non-egalitarian society PHC efforts, w
seen within a local or national context, w
repressed when they begin to succeed, since suc
necessity implies an attack on existing socid-p
and economic structures. The violent repress
the VHWs in the Chimaltenango Programme
course not a direct result of, nor proportional
threat their activities represented to local elite
these activities were associated with those of
throughout the country which at this point in
temala’s history could have succeeded, collectiv
restructuring the total society.
Some may well ask if the attempt at crea
successful PHC programme was worth it; if th
in terms of death and fear, which still remain
worth whatever advances were made. Was it
the slight (and temporary) improvements in th
of the people? Are the people really any bet
now than before? In many ways the situation
Indians today is immeasurably worse than itrw
years ago and only they themselves can a
whether whatever advances and-whatever new
sciousness and determination gained were ‘wo
2
Will PHC efforts be allowed to succeed?
In comparison, the development of a PHC pro
gramme in a country such as Tanzania is quite a
different matter [38]. It is true that there are many
problems to be faced in that country as well, and that
people with power are not eager to share it: the
‘Bwana Mkubwa’ (big man) syndrome still exists.
Nevertheless from Independence (1961) onwards,
Tanzania was concerned with restructuring the whole
society and, since the Arusha Declaration [39] m
1967, which formed the blueprint for Tanzania’s
development, an emphasis has been placed on selfreliance, on ‘sharing the little we have’ and on
extending social services to the rural sector. The
equitable distribution of health services was a major
concern and health was seen, already then, as an
integral part of an overall social and economic devel
opment process. It is quite a different matter to
develop a PHC approach within such an atmosphere.
Here the main problems are lack of drugs and
transportation—of limited resources and problems
in management and organization [40].
ln ;1974 the final stages of a ‘villagization’ pro
gramme was carried out with the objective of locating
the total rural population in villages [41] instead of
being dispersed in isolated settlements. The main
justification for this transformation included the pro
vision of educational, water and health care services.
It was stated that although every person had a right
Table I Development of rural health care infrastructure in T
zania 1961 1980
1961
22
975
200
380
400
150
1972
99
1501
335
578
700
290
Target
1980
300
2300
1200
2800
2500
1800
Actua
1980
239
2600
140
231
207
681
Health centres
Dispensaries
Medical assistants
Rural Medical Aides
MCH aides/village midwives
Health assistants
______
From: AFYA, United Republic of Tanzania. 1982. Country Rep
of Tanzania. Prepared for the WHO Workshop on Prim
Health Care, Ethiopia, 1982.
of a dispensary, let alone a health centre in ev
village within the foreseeable future. Attention
re-focusing on the selection, training and use
village health workers. These are the Wahuduma
Afya vijijini, now known as Community Health P
moters (CHPs). The newly re-formulated Natio
PHC Guidelines document, which was prepared
1980-1981, is centrally concerned with establish
CHPs in the villages without an official health faci
[45].
Community Health Promoters have existed in T
zania for some time with a substantial number
them being trained
since the late 1960s. Many
—
i • «i iwe
those trained m
'f™*
relatively
young
men
and
women
with at leas
to such services they could not be provided easily to relatively young
widely scattered populations living in settlements of standard seven education. They were not part of
only a few households each. Except for a relatively official health system but were voluntary work
small nomadic population rural Tanzanians now live who were to receive some financial support from
in 8300 villages and in more than 3000 of these there village in which they worked. In most villages
support was not forthcoming, or at least only irre
are government health units.
Hospital services continue to account for the larg larly so and in very small amounts. Supervis
est share of the health care budget but since the late support from within the village and perhaps m
1960s and throughout the 1970s, a definite shift has significantly,
--- ------ from health personnel within the off
1960s,
health
taken’place. Health resourcei allocation
system, was sporadic (or non-existent).
allocation for
the
rural
for the rural
sector was only 20% in 1971 but more than twice that, CHPs often felt isolated and as if no one particul
at 42% in 1981 [42]. From 1972 to 1980 the number cared what they did. Drugs were often in short sup
and even when transportation to the district hosp
of urban doctors increased by 43% (to 598) whereas
possible," sufficient drugs might not always h
the doctors in rural areas increased by 153% from 216 was possible,
been
obtainable there either. These and other p
to 547 during the same period. The number of Rural
________
_______ J‘
\ high drop
lems
were
the reasons
for. a relatively
Medical Aides (RMAs) increased five and a half
that
only
a
small
proportion
of those tra
,
.
times to 2800 in the rural areas and there was a rate so t
active
long.
remained
for
ten-fold growth of rural health centres and a near
national PHC Guidelines have attem
The new i--------trebling of rural dispensaries (Table 1). In 1979, it
'* some
seme of the problems of the C
to
overcome
was found that 92% of the population were within
10 km, and 70% were within 5 km, of a health facility, programmes of the past and of those existin
pivovuv. It
.v is now proposed that, allowing for regi
and 45% hadsuch a facility within their place (village) present.
differences and being sensitive to specific need
of residence.
individual communities, a relatively standardize
Despite the vast improvement in the rural PHC
infrastructure health statistics have not shown months curriculum be carried out for CHP trai
marked improvement in many areas [43]. It is recog in all parts of the country. The training should
nized that this is not simply related to the func place in health centres, dispensaries (and d
tioning, or non-functioning of curative services but is opment colleges/institutes) rather than primari
tied to a number of other factors such as the avail district hospitals, with a substantial portion o
■_ spent
r t in the trainees’ home villages. T
j
also
ability of food as well as inadequacies of preventive time
are preferably to be older, married and
and health promotive services. Attention is being selected
—
focused on the improved functioning of existing established than those trained in the past. A
health units and staff through special training pro deal of emphasis in the training programmes sh
be placed on ways in which to provide preve
grammes and operational research [44].
Even with improved functioning of existing units it services and means by which to motivate village
remains that these exist in only one third of the carry out health promotive activities. Some for
country’s villages and that time and limited economic payment of"an honorarium will be established b
and manpower resources make it unrealistic to think government without necessarily making the C
•
. 1
I*
a
* -A
1
222
H. K. Heggenhouges
full-time employees as such; the post is still seen to be
voluntary.
Recognizing the need for supervision, a great deal
of time is being spent in preparing PHC Coordinators
and in setting up a coordinated PHC system at
division, district and regional levels, within which
CHPs can function. Greater involvement of villagers
is also foreseen.
Training in how best to carry out preventive ser
vices is emphasized, as are methods for the provision
of regular supervision and support. The or
ganizational structure which can facilitate the various
aspects of supervision and support, continuing edu
cation and motivation, regular drug supply, record
keeping and monthly reports, planning and evalu
ation, is being readjusted. Although CHPs would
essentially remain voluntary and not official employ
ees of AFYA, such a structure would strengthen the
linkages between the village health posts and the
dispensaries and health centres.
Such linkages are extremely important as too often
the tendency in many countries has been to equate
PHC simply with CHPs; as if PHC is something they,
and they alone, should do, with the rest of the system
going on as before. Obviously, CHPs are, and should
be, carrying out PHC efforts on the village level, but
such efforts can best be carried out if they are
inter-linked with services guided by a PHC approach
at other levels within the health care system.
Tanzania has made a strong recommitment to a
PHC approach and has decided that as a part of this
approach, which implies providing health services
equitably to all the people, the training and use of
CHPs must continue to be central. A restructuring is
taking place and the PHC orientation is being
strengthened at all levels. What is important is that
the PHC plans are seen as part of the overall socio
economic development of the country and that there
is a national political will supporting the changes
necessary for making PHC successful.
This is not to idealize Tanzania. Tanzanians them
selves would no doubt think such a presentation of
their country foolish—the devastating economic situ
ation, for one, has had drastic repercussions through
out the whole structure of the society and in all
sectors. But it remains true that the existing devel
opment policy, despite its shortcomings, is one which
is very much in tune with the overall policy of PHC.
The question here becomes not so much whether or
not a PHC programme will be allowed to succeed, or
a successful programme will be allowed to continue,
but rather whether organization and management of
selection, training and implementation processes, and
the minimal available resources, will lead to success.
These are problems of a different order from those
prevailing in Guatemala.
Most developing countries in the world probably
fall somewhere between Guatemala and Tanzania.
Unfortunately there are probably more countries in
which PHC programmes will not be allowed to
succeed than those in which such programmes will be
slow in achieving success because of lack of resources
and organization. The implementation of PHC calls
for social change in village communities. If the
definition pronounced by the Alma Ata Declaration
is to be taken seriously, it must be tied to “... the
overall social and economic development of th
munity" and be a development process whi
pends on the people's .. full participation ...
spirit of self reliance and self determination" [4
we know well enough that many people and
tions in developing and developed countrie
expend a great deal of energy to prevent suc
grammes from succeeding.
But whether PHC efforts receive only mild
opposition or the kind of repression which took
in Guatemala we are now quite aware that th
be resisted in one form or another. The Guate
situation is but one example which forces us t
the promotion of PHC in a much more
manner than perhaps we would wish. The w
proceed should, of course, be distinct for par
situations but I believe we can only respond
affirmative to Ray Eiling who states:
“To look aghast at WHO, or smile wryly to one’s se
idea of truly supporting PHC would be to give in be
battle has been fought. Will we cooperate with tho
wish to avoid the kind of fundamental social and p
economic changes in the world system as well as n
changes which will be necessary to achieve health for
will we get in the act to bring about such change
Acknowledgements—I greatly appreciate the comm
colleagues and friends; they are not responsible, h
for the final version of this article.
REFERENCES
1. Doyal L. and Pennel I. The Political Economy of
Pluto Press, London, 1979. Especially pp. 2
. the demand for a healthier society is, in its
demand for a radically different socio-economic
(p. 297).
2. WHO/UNICEF. Alma Ata—Primary Health
Report of the International Conference on P
Health Care. Alma Ata, U.S.S.R., World
Organization, Geneva, 1978. Mahler H. Health
by the year 2000. Wld Hlth Org. Chron. 29, 45
1975.
3. Behrhorst C. Thoughts on community services
production physically deprived nations. Mimeo,
altenango. 1973.
4. McKeown T. The Role of Medicine, Dreams.
and Nemesis. Blackwell, Oxford, 1979. McKinla
Epidemiological and political determinants of
policies regarding public health. Soc. Sci. Med
541-558. 1979.
5. Gish O. The political economy of primary heal
and “Health by the people": an historical explo
Soc. Sci. Med. 13C, 203-211, 1979: “As long
remains essentially impossible to deal seriousl
existing social and property relations, so long
remain impossible to alter significantly the health
of the world’s poorest, say, one billion people” (p
Navarro V. Justice, social policy, and the p
health. Med. Care XV, 363-370, 1977.
6. Ackerknecht E. Rudolf Virchow. Johns Hopkins
Baltimore. MD, 1953.
7. Dubos R. Man Adapting. Yale University Press
Haven, CT. 1965. Dubos R. Mirage of Health. H
& Row. New York, 1959.
8. Engle G. L. The need for a new medical mo
challenge to biomedicine. Science 196, 129-136,
9. See Ref. [1]. p. 44.
10. National Council for International Health fN
Medical anthropolgy lends unique perspective to
national health. Int. Hlth News October, 8, 1982.
C. The anthropological contribution to primary
Will PHC efforts be allowed to succeed?
care research. Presentation to the Conference on Strate
gics for primary health care research in developing
countries. Copenhagen, 1983.
11. Foster G. M. Applied anthropology and international
health: retrospective and prospective. Hum. Org. 41,
189-197, 1982.
12. Heggenhougen H. K. The future of medical anthro
pology. In Technical Manual on Medical Anthropology
(Edited by Hill C. E.). AAA. Washington, DC, In press.
Heggenhougen H. K. and Mandara M. P. Primary
health care/villagc health worker programmes—the role
of anthropologists in planning and evaluation.
Presentation to IUAES Congress symposium: Anthro
pology and Primary Health Care, Amsterdam, 1981.
13. “Anthropology ... must give direction to change (away
from exploitation), it must define and show us how to
improve and how to progress. It must be employed to
combat self-righteous missionary conversion steeped in
ethnocentrism and the mindless progress of Icarus. It
must combat heavily against exploitation based on
greed that causes us to rob others while unwittingly
bankrupting ourselves. Based on its special focus of
attempting to understand ‘the human condi
tion', ..“.. Anthropology must help us understand
change and progress in terms of realistic, contemporary
needs of human beings”. Heggenhougen H. K. Health
care for the ‘Edge of the World'. Ph.D. Dissertation,
New School for Social Research, New York, 1976.
14. Sidel V. and Sidcl R. The delivery of medical care in
China. Scient Am. 230, No. 4, 19-27, 1974. Sidel V. and
Sidel R. Serve the People: Observations on Medicine in
the People's Republic of China. J. Macy Foundation,
New York, 1973.
15. Bibeau G. New doctors for new health care delivery
plans in Africa. Paper presented at AAA Meeting,
Cleveland, OH, 1979. Djukanowic V. and Mack E. P.
(Eds) Alternative Approach to Meeting Basic Health
Needs in Developing Countries. WHO, Geneva, 1975.
Drayton H. New types of health personnel for rural
areas; some experiences in the Caribbean and Ve
nezuela. Paper at the Pan American Conference on
Health Manpower Planning, Ottawa, Canada, 1973.
Storm D. M. Training and Use of Auxiliary Health
Workers—Lessons from Developing Countries. APHA,
Monograph Series no. 3, Washington, DC, 1979. Walt
G. and Vaughan P. An Introduction to the Primary
Health Care Approach in Developing Countries. Ross
Institute Publication Number 13, London, 1981.
16. See Ref. [4] p. 7.
17. See the writings of Paulo Freire, e.g. Pedagogy of the
Oppressed, Penguin Books, London, 1972. Werner D.
The village health worker—lackey or liberator. Paper
presented at the International Hospital Federation Con
gress, Tokyo, 1977, in which he states: “The role of the
village health worker, at his best, is that of a liberator.
This does not mean he is a revolutionary.. . the main
role of the primary health worker is to assist in the
humanization or, to use Paulo Freire s term, conscientizacio of his people” (p. 10). Sidel V. W. Public
health in international perspective: From ‘helping the
victim’ to ‘blaming the victim' to ‘organizing the vic
tims’. Can. J. publ. Hlth 70, 234-239, 1979. Werner D.
Helping Health Workers Learn. Hesperian Foundation,
Palo Alto, CA, 1982.
18. Storm D. M. op. cit., p. 4. Foster G. M. Abstract:
Section 12: “Community Mobilization”. In Ecological
Socioeconomic and Cultural Factors in Health. The
Institute of Medicine, Committee on International
Health in Foreign Assistance in Health, 1978.
19. See for example? Behm H.. Gutierrez H. and Requena
M. 1972. Demographic trends, health and medical care
in Latin America. Int. J. Hlth Serv. VII, 4, 1972.
“Health is a dialectical, biological and social process,
2
which is the result of the integration of the individu
and the environment, infiuenced by the relations
production in a given society and expressed in levels
well-being and physical, mental and social efficacy
Chenssudovsky M. Human rights, health, and capi
accumulation in the third world. Int. J. Hlth Serv.
61-75, 1979. Abel-Smith B. and Leiserson A. Pover
Development and Health Policy. WHO, Geneva, 197
20. Werner D. Health care and human dignity—a subje
tive look at community based rural health programm
in Latin America. Contact 57, 2-16, 1980.
21. But while we consider the possibility of violent repercu
sions and loss of life as consequences of encouragi
social change must we not also weigh this against t
misery and death associated with the prevalence
malnutrition and infectious diseases caused by the stat
quo'l To quote Rigoberta Manchu. a Quiche Indi
refugee: “They massacre us now with bombardmen
and torture, but they have always massacred us w
starvation. We are determined not to live another 5
years of oppression, exploitation, discrimination a
repression. We are determined that our children do n
face this life of total misery that we are living. W
Indians are alive today only because we know how
eat roots and leaves, because there is never even corn
last the year” From mimeographed publication of t
Committee of Solidarity with the People of Guatema
19 West 21st St, New York.
22. Islam K. In search of relevant health care, with a vi
from Gonoshasthaya Kendra. Paper for the symposiu
on Anthropology and Primary Health Care, Ro
Tropical Institute. Amsterdam, 1981.
23. Personal communication.
24. Heggenhougen H. K. Health care for the ‘Edge of
World’. Ph.D. Dissertation, New School for Soc
Research, New York, 1976. It is important to und
stand this project in terms of the particularly ha
socio-economic conditions of the Cackchiquel India
and of the Guatemalan Indians in general. It is pertin
to know that the per capita income is around $350
year but because of the significant difference betwe
population groups this is much lower for the India
Eighty-seven percent of the farms hold less than 20%
the farm area while 2.5% of the farms hold more th
60% of the land area. Ten years ago INCAP stated t
70% of all Guatemalan children were malnourished—
situation which has not improved. Approximately 5
of all deaths are children under five years old. In ma
communities the infant mortality rate is more than 50
The mortality rate for children between 1 and 4
the Department of Chimaltenango (mainly Ind
population) is more than six times greater than
Guatemala City. This was the situation prior to 19
since then the Indian population of the country
essentially been in a state of war resulting in
paralleled suffering. See publications of the No
American Congress on Latin America, Box
Cathedral Station, New York, NY 10025 for detai
information about Guatemala.
25. Behrhorst C. Alternatives in offering of commun
health services, some notes. A draft, mimeo, Ch
altenango, 1972.
26. Habicht J. P. Delivery of primary care by med
auxiliaries: techniques of use and analysis of bene
achieved in some rural villages in Guatemala. Paper
WHO, regional office. Guatemala, 1973.
27. Curative medicine could even have a detrimental ef
on health status if. by the availability of such serv
alone, villagers would believe that they were get
“good health” and activities which would improve
underlying social and economic causes maintaining
cycle of ill-health would be devalued and forgotten
28. The New York based Committee of Solidarity with
224
H. K. Heggenhougen
People of Guatemala estimated in 1982 “... that some
80,500 have been assassinated under bloody dicta
torships that have continued with U.S. support from
1954 to our day”. Violence and repression of the
Indians have been continuous occurrences in Gua
temala ever since 1524 when 3000 Quiche Indians were
massacred by Conquistador Pedro de Alvarado. Within
recent history this violence reached new heights during
the 1978-1982 regime of General Lucas Garcia.
29. “Te escribe esta carta con el corazon. Eche pedazo perdi
mi casa, mi negocio, mi ijo baron de 18 ano fue
capaturado por la policia ... el ano pasado, ya nunca
aparecio. Estamos excondido con el resto de mi familia
en un lugar de Guatemala. Por motive que yo soy un
lideres Indigena abierto y publico colabora alqualquer
programa que abla de desarrollo .. “I write this letter
with my heart. I lost my house, my small business, my
18 year old son was captured by the police on
the... last year, and was never seen again. We are
hiding with the rest of my family in some place in
Guatemala. (This happened) because I am one of the
indigenous leaders who openly and publicly collaborate
with whatever programme concerns itself with the develv opment (of our community)... ”. Letter from a village
health worker.
30. Davis S. The social roots of political violence in Gua
temala. Cult. Surv. Im. 7, No. 1, 4-11, 1983.
31. Guatemala: Indian Leaders report on the army’s geno
cidal war. IWG/A Newslett. 30, 39-44, 1982. Berryman
A. The terror continues—testimonies to the United
States Congress. Am. Friends Service Comm. Phil. 9,
1982. Update on Guatemala. Committee of Solidarity
with the people of Guatemala. 8, 15 November, 1982.
Information bulletins. Amnesty International. Urgent
action—Guatemala. 17, 24, 25 January, 3, 25 February,
4 March 1983 (information bulletins). Guatemala death
raid into Mexico. The London Times 31 January, 1983.
Pope lashes Montt regime. Guardian 8 March, 6, 1983.
Guatemala: ‘What is faith in the eyes of a Mayan
Indian’; ‘Pope denounces abuses against Indians'; ‘Gua
temalan Lives’. IWGIA Newslett. 33, 5-18, 1983. (Inter
national Work
Group for Indigenous Aff
airs—Copenhagen.) Paul B. Communication based on
visit to Guatemala in April, 1983. 24 April 1983.
32. Guatemalans tell of murder of 300. New York Times 12
October, 1982.
33. Report on Guatemala Killings. New York Times, 12
October, 1982.
34. Institute for Food and Development Policy. Gua
temala: hungry for change, (Food First Action Alert),
1983. Figures of more than 500,000 displaced persons
within Guatemala at the end of 1982 were repeatedly
mentioned in the international press. Also see Refs [30]
and [31] above.
35. Gish O. op cit.
36. Bryant J. Principles of distributive justice as a basis for
conceptualizing a health care system. Paper presented to
the Christian Medical Commission, Geneva, 1973.
37. Adams R. N. Crucifixion by Power. University of Texas
Press, Austin, 1970. Bossen L. Plantations and labor
force discrimination in Guatemala. Curr. Anthr. 23,
263-268, 1982. Concerned Guatemalan scholars. Dare
to struggle, dare to win, 1981. Death and disorder in
Guatemala. Cult. Surv. Q. 7, No. 1, 1983. Davis S. and
Hodson J. Witness to Political Violence in Guatemala:
The Suppression of a Rural Development Mo
Oxfam America, Boston, 1982. Jonas S. and To
GUATEMALA. North American Congress o
America, New York, 1974. Melville T. and Me
Guatemala—Another Vietnam? Penguin, Londo
Villagran K. F. The background to the current
crisis in Central America. In Central America
national Dimensions of the Crisis, pp. 15-35. H
Meier, New York, 1982. Warren K. The Symb
Subordination; Indian Identity in a Guatemala
University of Texas Press, Austin, 1978.
38. Heggenhougen H. K. and Mkumbwa Z. M.
health workers for primary health care in Ta
Nordisk Med. 97, 61-62, 1982.
39. Nyerere J. K. The Arusha Declaration, 5 F
1967. In Ujamaa, Essays on Socialism. Oxford
sity Press, Dar-es-Salaam, 1968.
40. Chagula W. K. and Tarimo E. Meeting basi
needs in Tanzania. In Health by the People (E
Newell K. W.), pp. 145-168. World Hea
ganization, Geneva, 1975. Stirling L. Primary
care—the Tanzanian experience. Tanzanian Mi
Health, 1978. van der Stoop A. Health in Tanza
USAID. Dar-es-Salaam, 1980. WHO. Country
Profile—United Republic of Tanzania -, prepared
rele, Challa and Qhobela. Dar-es-Salaam, 197
41. Mwapachu J. V. Operation planned villages
Tanzania: a revolutionary strategy for developm
Vries J. and Fortmann L. Large scale villag
Operation Sogeza in Iringa Region. Both in
Socialism in Practice—The Tanzanian Experien
ted by Coulson A.), pp. 114-127, 128-135. Spo
Press, Nottingham, 1979. Shivji I. G. Class Stru
Tanzania, pp. 103-120. Tanzania Publishing
Dar-es-Salaam, 1976. Von Freyhold M. Ujam
lages in Tanzania. Heinemann, London, 1979. M
D. E. M. Tanzania’s Ujamaa villages: the
mentation of a rural development strategy, 19
42. AFYA, United Republic of Tanzania. 1982.
Report on Tanzania preparedfor the WHO work
Primary Health Care, Ethiopia, 1982.
43. This is not to say that improvement has not tak
in the general health status of the populatio
expectancy has increased, for example, from 35
1961 to 52 in 1980 and infant mortality has d
from 160/1000 in 1967 to 135/1000 in 1978.
44. AFYA, United Republic of Tanzania. Guidel
the implementation of the primary health ca
gramme in Tanzania. Unpublished document,
Salaam, 1981.
45. WHO/UNICEF op. cit.
46. Eiling R. Perplexed. Comp. Hlth Syst. Newslett.
Newslei t.
1980. See also Sidel V. W. op. cit. 1979, who
“Within the poor countries the ‘organizing’ or “
nity’ model will have to be introduced internall
people themselves and in many countries t
require overthrow of oppressive, exploitive
groups. But that does not mean we in the rich c
can stand idly by. We must work both within
societies and try to direct resources to poorer so
(p. 238). According to Sidney Mintz, “It beco
longer a matter of what we shall do for them
what they must know, and have, in order to
themselves”, as quoted in Reinventing Anthr
(Edited by Hymes D.). Vintage Books, New Yor
Com
J
RADICAL JOURNAL OF HEALTH
C/O 19, June Blossom Society
60-A, Pali Road, Bandra,
Bombay. 400 005
■iii.w I— IRI i—
III
■ ■■ ■■!
«-• -r
-
EDITORIAL PERSPECTIVE FOR VOI IIQp.2 on PRIMARY HEALTH CAR
BY IMRANA QUADEER,
During the serventie$,in many national and Internationa
Circuts of Health Bureaucracies Primary Health Care (PHC) ha
become a panacea for all the evils of the. poorer nations. T
WHO has projected it with all its convictions and the member
nations have accepted it with equal vigour. As professed in
Alma Ata declaration, it means.
s,
-i
"Primary Health care is essential health care based on
practical, scientifically sound and socially acceptabl
methods and technology made Universally accessible to
to individuals and familiesin the community through th
full participation and at a cost that the community an
country can afford to maintain at every stage of their
development in the spirit of self reliance and selfdetermination. It forms an integral part both of the
country's health system'of which it is the central
function and main focus, and of the overall social and
economic development of the community".
Today when this strategy has been accepted by such a large
of countries, there is a need to examine it potential streng
and weaknesses.
The idea that health is closely related to people's li
and working conditions and that it is an outcome of their s
economic environment was vocalised by men.in different field
like John Snov Engels and later Virchow in the west. It
manifested itself in the sanitary movement of the 19th cent
In India and other parts of the east it had much deeper roo
visible in the method of ancient medical science itself and
the cultures of Harappa and Mohan Judaro. In India during
struggle for independence, a demand for comprehensive healt
was a part of the national movement. Why then this sudden
fervour for projecting PHC as a new concept by internationa
national official circles ?
Politics of PHC then becomes a crucial issue. To unde
this one has to understand the role that U.N. and WHO have
in the overall politics of the world. Always supporting th
interests of the imperialist nations, these organisations h
used the liberal tools of aid, support and providing consul
to diffuse, control and direct crisis situations. The effo
develop an alternative world economic order in the 70's was
such spurious exercise and as a part of it the notion of
alternative health care for the third world. The motives b
it were to check impending destructive and costly ,reactions
from and within third world nations whose poverty,
J-'-~ b
squallor were becoming threats to stability. PHC
PUT was the
of the liberals in the imperialist camp and WHO projectedIjf
2
At the national level the concept of PHC acquires multi
dimensions. Given the particular hue of the government, the
implications have varied from Africa to- South east Asia and
Eastern Mediterranean regions. The issue is what use does a
national government make of the concept. Does it use it as
concept is presented by the Alma Ata declaration, and makes
part of its effort to develop an integrated strategy for the
betterment of its people as in Angola, Tanzania and Mozambiq
or allows the concept to degenerate into a slogan behind whi
the same old strategies with some new features continue to b
implemented - at a faster rate perhaps with the additional i
from the international fund givers as in India and Pakistan
A grasp on the national politics of PHC requires an und
standing of the country’s socio-economic and political struc
and the nature of its government and health service structur
Only such an understanding allows one to assess the potenti
ies or limitations of the system to achieve PHC. An example
the interplay between PHC and Politics is the level at which
is integrated into the planning process of a country. Thus
Chiness and Vietnamese incorporated PHC in the very process
national planning right from the period of their independenc
without givinq it a name. In contrast, India made so much
and then relegated PHC to the care of the health ministry w
the overall planning processes took their own directions.
another example is the imp.'e-mentation an^ outcome of progra
introduced under the banner of PHC. These programmes which
may have a potential of providing much needed services are
overtaken by the local power elite through their links with
health and administrative bureaucracies. The nature of the
latter thus becomes the primary determinant of the outcome.
community healthguides scheme and the drinking water supply
through borehole hand pumps in India are two such example.
Another dimension of the PHC efforts at the national l
is the setting of priorities and selection of technology.
India despite the official acceptance of implimenting PHC b
2000 AD the heavy emphasis on urban based services and cura
approach in rural areas continues with heavy dependence on
expensive equipments and drugs. The drug policy needed to
provide PHC is still being avoided. Can issues of prioriti
and technology be then isolated from politics? A simple bu
revealing example is the supply of "Electrolyte" packets in
community Health Guide’s kits ! Does it show any links betw
the health administrators and the drug industry who know th
addition of so many salts to the basic mixture only increase
cost and not effectivity!
If the concept of PHC is getting distorted in the hand
the not so democratic government and is becoming a tool for
creating two types of services, one for the rich and the ot
for the poor, should it be criticised, rejected, accepted a
an unavoidable distortion or used to broaden the base of
democratic movements? These are some of the questions whic
need, to be answered by those who are working in the intere
of people’s health. Can PHC as a concept become an inspira
for those involved in peoples struggle for their rights? I
... 3
There are many small or regional projects experimentin
with implimentation of primary health care. What is the ro
of such projects in focussing upon the issue of PHC or in
diluting it?
In the academic circles, in the name of professionalis
the need to achieve results, a concept of ’’Selective PHC” h
been circulated which means let us not talk of comprehensiv
development but do what we can without disturbing the exist
balances* This is attractive to those who would like to go
back to singing praises to powers of technology and manager
competence* There is need to examine such concepts thread
bare to show their reactionary ideology as well as monfeasib
Are there any lessions that we can draw from the exper
of the socialist countries which have tried to provide heal
care not in isolation but as a part of their total developm
processes? These are the major questions which need to be
addressed when one is dealing with the bipronged weapon of
Primary Health Care.
Please send your comments to Imrana Quadeer f
/for Community Health & Social Medicine Centre,
I Jawaharlal Nehru University,
New Mehrauli Road,
NEW DELHI.
By the 1st Week of May, 1986.
/?/•
Sic %
w..
f \ i'
» '1J
'
"‘Qj
i?
-fcS'QO?^ 5'(5()7V'v )NVS
Y^^NVvy>!
■>X’°) a L
!\
5^ £
“TV^TryopJ
. 5^
•05^.^,
Hn«H
&
Com
z
H
The life and death of Primary
Health Care
The Alma-Ata Declaration of 1978 set out for hum .nkind the goal of Health for All by the year 2000. It also
declared that 'Economic and social development... is of basic importance to the fullest development of
health’. The truth of this observation was amply demonstrated by the fate that befell the concept of
Primary Health Care which had been adopted by the Conference as the means to realise the above goal.
David Werner
T
‘fl
I
Primary Health Care was conceived as a comprehensive strategy which would include a people-centred approach to health
services.
r M 1 D those of us committed to the
j
drcam of Health for All. in to
day’s troubled world one thing
becomes increasingly clear: The health
of people - as individuals, as commu
nities. anti as an endangered species on
this fragile planet is determined less
by health services than by the relative
fairness of social structures In last
analysis, the overall health ol the world's
be t wee n I o vc a n d g reed. To ga i n a c I earc r
understanding ol the fate of Primary
Health (’are oxer the last 15 years, we
therefore need ’ place it in that context.
I hc Alma
• i Declaration ol I97X
was seen by n
v as a breakthrough,
for it officially fcclared that the pursuit of health is inseparable from the
struggle for a fairer, more caring so
ciety. The Declaration drafted at a
Kazakhstan, and endorsed by the world’s
nations - was a response to the failure of
Western Medicine to meet the health
needs ol a large sector of the world's
people, especially those in the South.
Based on costly doctors and urban ’dis
case palaces’, the Western medical
model entered io a small, privileged
minority. It- high cost and limited
outreach m some ways did more to
erty.
The Alma-Ata Declaration declared
health as a basic human right. To ad
vance toward the ambitious goal of
Health for All by the Year 2000, it
proposed a radical and potentially revo
lutionary approach to meeting all peo
ple's basic needs. 'This was called Pri
mary Health Care.
Primary Health Care was conceived
as a comprehensive strategy that would
not only include a people-centred ap
proach to health services, but would
address the social and political factors,
that influence health. In recognition that
change comes from organised demand,
it calls for strong community participa
tion. accountability of health workers
and health ministries to (he people, and
social guarantees to make sure that the
basic needs - including food needs - of
all people are met.
Although Primary Health Care was
a radical new concept for most ministries
of health, for years many of its practices
had been implemented by non-govemment community-based groups and by a
few, exceptional governments that gave
high priority to people’s basic needs.
China's approach lo community health,
care, featuring ‘barefoot doctors’, had
provided much of the basis for the de
sign of Primary Health Care.
However, for most governments
and health professionals, comprehensixe Primary Health Care as conceived
at Alma-Ata xvas too revolutionary. To
those in positions of poxver. the idea of
giving ordinary people more control
over their health and lives sounded
dangerously leftist and subversive.
So very soon after the Alma-Ata
Declaration, high-level health ‘experts'
began to systematically extract the teeth
of Primary Health Care and to convert
it. at best, into a means for extending
conx entional. (op-doxvn health services
into underserved areas.
Strategically, there have been three
major watersheds that have under
mined and dissipated (he radical es
sence of Primary I Icalth Care. 'The first
was the introduction of Selective Pri
mary Health Care in (he early I98()s.
The second has been the push for Cost
Recovery or User-financed Health
Serx ices, introduced in the late I98()s.
And (he third is the take-over of Third
\\ orld health care policy by the \V<n ld
Bank in the 199()s.
All three of these monumental as
saulls on Primary Health (’arc Selec
tive Pl IC, user-final icing and the Bank's
socio-political and economic trends. So
to put these interventions into context,
let us first lake a brief look al the un
derlying macro-irends.
As we knox\ the decade of the
of global recession
1980s was a p
f conservative powandretrcnchm
ers. By the begt . i ng of the 1980s. high
level ‘-development’ strategics had be
gun to backfire. I he Big is Beautiful
model of development, pushed in the
1960sand 1970s by huge loans from the
North, had made poor countries more
dependent on the global market, with its
ruthless ups and downs. The rise of
large-scale indt y, by replacing la
bour-intensive p luction with energyhad intensified pre
intensive indust
existing inequities. In rural area.-., big
agribusiness concentrated farmland into
large holdings, causing a massive exo
dus of landless peasants into mush
rooming city slums. But in the cities, big
factories had replaced millions of work
ers with machines. Unemployment,
poverty, homel ^sness, hunger, and
crime increased \nd the growing un
rest brought more repressive measures
of social control. Fven in countries that
experienced so-called ‘economic mira
cles’, like Brazil, real earnings of work
ers drastically declined. While the rich
got richer, the poor got poorer. More
trickled up than trickled down. In sum.
for vast numbers of people, ‘develop
ment’really meai underdevelopment'.
It brought detci rating Fixing condi
tionsand denial • basic rights.
‘Structural Adjustment’ policies
But troubles were just beginning.
By the start of the 1980s, as a result of
the giant development loans from
Northern banks, poor countries were
faced with a st a? tiering foreign debt.
Huge interest payments offset any
benefits from economic growth, and
Third World economies began to falter.
Anticipating disaster, the banks got
scared and withheld new loans. As a
result, scores of countries went into a
fiscal tailspin. Some announced that
they simply could not pay. 'The North
ern hanks, with billions of dollars in
loans to poor countries, were worried
sick.
Then the W orld Bank and Interna
lional Monetan I und came to the res
cue. Thev ga\ e ‘hail ouT loan . lo allow
poor countries to keep scr\ icing their
debts, and lo promote economic recox
cry.
namely ‘Structural Adjustment'
cies. Adjustment measures wer
signed lo ‘stream-line' poor co
economics, and to bind them into
national trade accords that favou
business and free market' intere
the North.
Structural adjustment has u
included the following measures:
• cutbacks in public spendin
• privatisation of governme
terprises;
O freezing of wages and free
prices;
• increased taxation, espe
sales taxes
• increase of production - in
ing food - for export rather than
consumption.
As so often happens, these h
handed ‘austerity' strategies hit th
hardest. Budgets for health, educ
and food assistance were ruth
slashed, while bloated military e
ditures were left untouched. Lik
public hospitals and health centre
turned over to the private sector, p
their costs out of reach of the
Falling wages, higher prices, food
city, and increased unemployme
to government layoffs, all joined t
low-income families into wors
poverty.
The overall results of adjus
have been hotly debated. In some
dle-income countries it appears to
helped stabilise the economics, alt
the human and environmental co
main in question. But in many
poorest countries, adjustment ap
to have caused even greater eco
stagnation.
In spite of overwhelming evi
to the contrary, at First the World
flatly denied that structural adjus
has hurt the poor. More recent
Bank has conceded that ad justmen
have caused temporary hardshi
low-income families, but that
‘austerity' is necessary to restor
nomic growth. Ignoring the his
record, the Bank still seems to thi
by helping the rich get richer, th
efits will somehow trickle down
poor.
But the evidence is stron
structural adjustment, linked to th
conservalixc. nco-liberal trends
cent years, has caused lar-re
setbacks in the slate of world he
The World Bank in its public
mcnls consistently points out dia
the past 30 years Third World hea
ports shrewdly omit or downplay (he
fact that in many countries improve
ments in health have slowed down or
stopped since the beginning of the
gi
1980s. Indeed. id . sonic countries rales
I
s'
of tindv’ nutrition, tuberculosis, chol
ft
era. am: othei inJ.icalors of deteriorat
ing conditions, have been increasing.
And in a few countries, mortality rales
appear to be rising.
In 'pile of all the talk of develop
ment aid and pox erty relict , m the 1990s
more than $50 billion net
flows each
year from the poor countries to the rich.
Today. the income of the richest 20% of
the world’s inhabitants is I40 times as
great as that of the poorest 20‘ '<. And the
gap between rich and pot'r has grown
M)f/( w ider in the last 10 years. Accord
. A
ing to the UNDP, one quarter of the
world’s people do not get enough to eat.
BH • •T'
It is in this context of unfair global
economic policies and structures that
w e nniT look at the three major strate
gics that have contributed to the
disempowermeni of Primary Health
Care.
I. Selective Primary Health Care
No sooner had the dust settled from
the Alma-Ata Conference in 1978, than
top-ranking international health experts
in the North began to trim the wings of
Pri nuiry Health Care. They asserted that,
in view of the economic recession and
shrinking health budgets of poor coun
The disappointing impact of Oral Rehydration Therapy(ORT) could have been
avoided by teaching families to mix home-made drinks.
tries. a-comprehensive or holistic ap
proach was unrealistic. If any health
Buttechnoh
ical solutions-while
distribution of ORS packets. This meant,
statistics were to improve, they argued,
sometimes he I pl. i - can only go so far
in some countries, that poor families
high risk groups must be Targeted’ with
in combating health problems whose
with earnings of less than half a dollar a
a few carefully selected, cost- effective
roots are social and political. Not sur
day, were expected to spend up to a third
interventions. To implement this new
prisingly, therefore, the Child Survival
of their daily earnings on a single packet
of ORS.
strateg). called Selective Primary Health
initiative has had far less of an impact
Care, children underage five were Tar
than predicted. Between
!4
When we consider that under
geted' in what became known as the
million children still die each year, and
nutrition is the main predisposing
Child Survival Revolution.(Somecritics
most of their deaths are related to under
condition leading to death from diar
call it a counter-revoluiH ii .) Two Tow
nutrition and po\ erty.
rhoea, it is easy to see how the social
cost. low-resistance’ health technologies
The disappt
marketing campaigns that induce poor
12 and
iting impact of Oral
Immunisation and Oral Rehydration
Rehydration TT rapy (ORT) can be
families to spend their limited food
Therapy - became the Twin engines' of
traced, in part, to structural adjustment.
The damage might have been avoided if
money on commercial ORS packetscan
actually be counterproductive in terms
Child Survival quickly won enthu
siastic high-level support. For those in
ORT had been promoted by teaching
of lowering child mortality.
families to mix home-made drinks,
And if the commercialisation of
positions of privilege and power, it was
which would help foster self-reliance.
ORS is not enough, the hatchet job that
politically safe. Il prudently avoided
But unfortunately. WHO and UNICEF
structural adjustment has done on wages,
confronting the economic and political
causes of poor health, and left the slams
have strongly promoted factory-made
!1 ating dependency on
'ORS packets
health services, mid food subsidies pro
vides the final coup de {•race for mil
quo comfortabls in place No wonder
a manufactun
product outside the
lions of hungry children. And so, in
so many health professionals, govern
ments. I SAID.and I 'NK'l l . all jumped
on the Child Sun ival bandwagon. I''ven
the World Bank which had previously
pul little investment in health began to
control of I ami l
and communities. Al
poor countries today, one of every four
Child Survival.
first ORS pack 's were distributed at
child deaths is still caused by the vicious
health posts free But when health budg
cycle of under-nutrition and diarrhoea.
ets were sla-shcd through structural ad
justment. health ministries were pres
tinuing debt crisis and adjustment poli
Of course, in addition to (he con
i
I
is
1
6
contribute to the high incidence of death
from diarrhoea. Bottle feeding, forexample. is still unscrupulously promoted
by multinational producers of infant
lormula. despite the International ('ode
and IBFAM boxcoll. Studies in several
countries show that the death rate from
diarrhoea can be over 20 times as
great in bottle-fed as in breast-fed
babies. UNICEF estimates that the un
ethical promotion of bottle feeding
contributes to more than 1.5 million
infant deaths a year - up 50% from the
estimate five years ago.
medicines. they max . ;1|Ty inore than tally cut. In response to the grow
their share of cost for the health post.
rates of homelessness, desperation, str
While Bamako has prox isions to charge children, and crime, the governm
less to families who are \ cry poor, such docs not provide more public servi
‘safety nets’ work betier on paper than or a higher minimum wage, but rat
in practice.
more policemen and jails. In the gr
Reportedly, in
mc areas the
American spirit of ‘self-reliance’,
Bamako Initiative ha
1 ven good rc- disadvantaged must care forthemsclv
suits. But studiesinso
countries have
And so we see that the Bama
shown that when cust recovery has
Initiative and other cost-recove
been introduced, utilisation of health schemes in poor communities - wh
centres by high risk groups has perhaps the only alternative in face of
dropped. In some cases the incidence unjust social order - are consistent w
of illness - including sexually trans the neo-liberal ‘free market' forces th
mitted diseases - has increased.
arc trying to free the owners of
2. User-financing and cost-recovery
Whatever their immediate impact,
markets from their social and ethic
schemes
the introduction of thi .• cost- recovery
responsibility.
The next big set-back to Primary
schemes has disturb
implications,
Health Care has been growing pressure Placed in historical pc cclive, when a
3. The World Bank take-over of
to make disadvantaged people in poor health system begins to saddle the
health policy planning
countries pay for the cost of health poor w ith the burden of its costs, this
The World Bank tells us that it h
services.
is a great step backwards. It means that turned over a nexv leaf and has come
To make the conversion to user health care is no longer a basic right.
recognise that real development mu
financing or cost-recoxery schemes During most of this century society has
take direct measures to eliminate po
more palatable, often ibex arc promoted made gradual if halting progress toward
erty. But the way it is going about it. o
as a wax of fostering self-reliance and “human rights for all’. With a push from
wonders if the Bank would not pref
community participation.
the Left, people gradi 'iy accepted the simply to eliminate the poor... oral lea
One ot the biggest promoters of concept of proportion
axation: those the children of the poor. Certainly pop
these user-financed community health who have more pay .... re, so that the
lation control - or rather, ‘family pla
services has been UNICEF. Its so-called community as a who,, can guarantee
ning - is nigh on its agenda.
Bamako Initiative now functions in that the basic needs of all people are
The World Bank has so consis
many African countries. While UNICEF fairly andadequately met. In short, there ently financed policies that worsen th
has some reservations
about
....
, . uthe Initia- has been a gradual trend toward a spirit situation of disadvantaged people th
tive, it argues that in today s hard times of collective responsibility, toward recwe must question its ability to change i
it sees no Lbetter alternative. In the 1980s ognition that the well-being of each is
course. Perhaps the most effective ste
cutbacks in health budgets resulted in linked to the well-being of all, and that
the World Bank could take to elim
the closure of many rural health posts, sharing is more fulfil’ ng than greed.
nate poverty would, be to eliminat
largely for lack of medicines. UNICEF
In the epic strug* between equity itself.
recognised that people want medicines and greed, since the arly 1980s, hu
In recent years the World Bank ha
and are willing to pay for'them. So, manity has in some ways regressed. The
become increasingly involved in Thir
through Bamako, consumers are charged conspiracy between big government and
World health care and health policies
enough for medicines to keep the health big business has undermined democratic
The Bank’s 1993 World Developmen
post functioning. A positive feature of process, and given almost free reign to
Report is titled ‘Investing in Health’. A
the Bamako Initiative is that only essen powerful market forces. Main stream
better title might be’Turning Health int
tial drugs are used. Also, in some of the economists promote a so-called freeInvestment’, for the Bank takes
community-run health posts, participa market system-that is. a market system
dehumanisingly market-oriented view
tion is active and enthusiastic.
free of democratic controls - that seeks of both health and health care. Its chill
But 1many such user-financing unbridled economic i 'Wth, regardless
ing thesis is that the purpose of keeping
schemes have some serious - and per of the human and en\ onmental costs.
people healthy is to promote economic
haps life-threatening - drawbacks. Just The United States sucks to impose its
development., but I can’t help feeling
because poor families are wifling to pay Greed Centred Development model on
that the Bank has it backwards. Wouldn’
for medicines does not mean they are the entire world. Yet poor people in
it make more sense to say that the
able to pay for them. As with ORS USA have been trampled by the same
purpose of economic development is
packets (which are included as essential ,powerful market forces and adjustment
to promote health?.... What are we
medicine) poor families will often spend policies that have widened the gap be ants?
for medicine the money they need to tween rich and poor in the Third World.
The Bank has worked out an elabo
feed their sick children... And liicy may Progressive taxation is being system
rate scheme whereby it tries to measure
even pay for more medicines than arc atically undermined a 'he government
the value of each person (that is to say.
needed. When health posts arc largely gives bigger tax brea 10 the rich and
the dollar value) by what it calls Dis
financed through sale of medicines, the raises taxes for the rust, fen years ago,
ability Adjusted Idle Years' or
temptation for health workers to over one in seven children in the USA lived
DAEYs . But I can l discuss all that
prescribe is considerable.
in poverty; today it is one in five. And because it is so foreign to my xvay of
Because the poorest families gel since (he early 1980s. public services
thinking.
r
>VER
-
urgent need to overcome poverty and to
Through elaborate statistical studies, the Care, with remarkable improvements in
guarantee that the health needs of all
Bank has selected those interventions health. Cuba, since the Revolution, has
people arc met. It quite rightly criticises calculated to be most cost-effective in taken a very comprehensive approach
the persistent inequity and inefficiency increasing Disability Adjusted Life which guarantees to meet the basic needs
ol current Third World health systems.
Years' of productive work to advance of all people for housing, education
And it echoes much of the Alma.Ala call the national economy. How the com health care, and food. As a result. Cuba
lor community participation, self-reli munity - or even host country - is sup has health statistics equal Io that of the
Northern, industrialised countries.
ance. and health in the people's hands., posed Io panic >ate in (or even under
Unfortunately, however, many
so far so good.
stand) this extreme form of globally
countries that have opted for peopleBut on reading further, we discover computerised planning remains vague.
that under the guise of promoting an
What can I say, except that all this centred development, in defiance of the
equitable, cost-effective, and country- is very scary. And it is dangerous be development paradigm that favours big
appropriate health system, the World cause the World Bank, with its enormous business, have been subject to relentless
attacks and terrorism. For this reason
Bank’s key recommendations spring money-lending capacity, has almost
their health care programmes - and im
from the same sort of market-friendly, god-like clout. It can force poor coun
proved health of their people - have
structural adjustment paradigm that has tries to accept it health care blueprint
been hard to sustain.
exacerbated poverty and been so devas by tying it to Io; programmes, as it has
Nevertheless, hundreds of grass
tating to the health of the world’s neediest done with adju . nent.
roots groups and movements around the
people.
world have kept a liberating approach to
According to the World Bank’s
Dangerous implications
Primary Health Care alive, often against
prescription, in order to save ‘millions
great obstacles. Activists realise that, in
of lives and billions of dollars’ govern
The commercial medical estab the long run, the health of our planet and
ments must adopt ‘a three pronged policy lishment has celebrated the Bank's new its people depends on far-reaching so
approach of health reform:
World development Report as a ‘major cial change.
1. T’ostcran enabling environment breakthrough' toward a more cost effi
for households to improve health.
Conclusion
cient health c .hc strategy. But many
2. Improve govcrnmciH spending health activist' e the Report as a dis
1 have given this talk as a protest in health.
turbing docun t with dangerous im
3. Promote diversity and competi plications. The; are especially worried or ‘URGENT ACTION ALERT' tion in the promotion of health serv that the Bank will impose its recom warning that the global power structure,
ices.'
mendations on poor countries that can spearheaded by the World Bank, is
poised for the final death blow to Pri
These recommendations are said to least afford to implement them.
mary Health Care, so that the health
reflect new thinking. But stripped of
It is an ominous sign when a giant
their Good Samaritan facelift, and read financial institution with such strong systems of poor countries will fall in
line with what we might call the
ing the ‘fine print’ from the text of the ties to big government and big business
McDonaldisation of Global Develop
Report, we can restate the policy’s three bullies its way into health care. Yet ment.
prongs more clearly:
according to th British medical jour
On one thing the World Bank is
1. Put the responsibility of cover nal, Lancet, th World Bank is now certainly right: Achievement of a
ing health costs back on the shoulders of moving into first place as the global healthier society requires the reduc
the poor... in other words, fee for service agency most influencing health policy,
tion of poverty. But the changes needed
and cost recovery through user financ leaving the World Health Organisation to overcome poverty will never come
ing.
in a weaker second place.
from the Bank nor the powers it repre
2. Reduce government spending on
It is urgent that all of us con- sents. They can only come from the
health by drastically reducing services cerned with the health and rights of bottom up. In last analysis, the social
from a comprehensive to a very narrow, disadvantaged people become famil transformation needed to bring Health
selective approach... in other words, a iar with this World Bank Report, for All turns on the ability of a worldnew brand of Selective Primary Health wilh the harm •» unrealistic policies wide coalition of grassroots groups and
Care.
are likely to d and whose interests concerned world citizens to bring the
global power structure under control.
3. Turn over to private, profit they are real I) designed to serve.
I close with the conclusion of the
making doctors and businesses all those
International People’s Health Council:
government services that used to pro
Successful approaches to
Health for All can only be reached
Primary Health Care
vide fee or subsidised care... in other
through
a united grassroots struggle for
words, privatisation of most medical and
EQUITY, ACCOUNTABILITY,
health services.
As we have seen, Primary Health
Thus we find the new health policy Care as conceived at Alma-Ata has run and PARTICIPATORY DEMOC
RACY.
is little more than old wine in new bot into serious pi "Hems. This is no :surThe struggle for health is a struggle
tles: a rehash of the conservative strate prise. A revolt
ary approach to health for social justice.
♦
gies that have systematically derailed care requires;
olutionary process in
Comprehensive Primary Health (’are. society as a win
In that context, a few I he above talk \va\ilcliveretl in lieltfiuin on December
with elements of structural adjustment countries have been relatively success
/99< b\ David Werner at a seminar organised b\
Medit ine Jor the People, Medical Aid for the Third
to boot. It is a market-friendly version
ful in introducing Primary Healthcare.
World, and International People's Health Cornu il.
of Selective Primary Health Care com Nicaragua under the Sandinistas intro-
CO VI
I
;
■
r
F
i
J
t
I
!■
I
ft
The economic crisis, structural
adjustment and health care in Africa
When African governments turned to Structural Adjust ont Programmes to overcome the economic crisi
and recession facing their countries in the 1980s, one of the principal casualties was health care. These
policies resulted in severe cuts in government spending on the infrastructure that supports
improvements in health and nutrition. They also undermined women’s traditional support role in the
promotion of health care in society.
corresponding improvements in th
quality of life for survivors.
In the 1980s, this progress, pro
UNTIL recently the slate has been the
and uneven though it often wa
lematic
largest provider of medical care in Af
began to unravel. The early 1980s sa
rica. Slate involvement in health origi
large drops in the national incomes
nated during the colonial era. Originally
African countries as the prices of the
designed for the purpose of serving the
export
commodities fell to record lo
Idiropcan population, health care was
levels.
At the same lime, the demand
eventually extended, often through
on this income were increasing. Dr
forced therapy, to the indigenous popu
matic increases in international intere
lation to defend against the spread of
rales
made debt repayment
a problem
. .
infectious diseases. Some colonial gov
crisis
proportions
for
many
countrie
ernments provided maternal and child
Other pressures on this income cam
health services which they saw as a
from a variety of factors: military equi
Christian act of charity. Competing
ment to sustain local wars or participa
European churches of different de
in superpower conflicts, the person
of
the
gains:
effects
Reversing
nominations often ran these services,
greed of corrupt officials in governme
the economic crisis on health
sometimes with government support.
or international corporations. Anoth
Health services were mostly curative,
factor was the natural expectation
In the 1950s, ’60s and 1970s,
urban-based and available to Europeans
Africa's growing populations that th
African
countries
ade
substantial
and African elites. The health system
level of government services and ec
progress
in
health
caie
delivery.
In
the
was also dependent on personnel, sup
1970s, in particular, relatively high nomic development opportunities the
plies and technology from the various
prices for Africa’s export commodities experienced would continue to improv
colonial home countries.
This system, inherited by African and low international interest rates made to eventually match those of industria
ised countries in Europe and Nor
countries at. Independence, was rarely possible substantial increases in health
America.
spending
by
African
governments.
modi fled. The retention of colonial struc
This economic crisis triggered
tures has had important consequences Health-related projects were among the
many
development
projects
which
were
correspondi
ngI crisis in health care an
for the hopes of general improvements
health
in
Africa.
This crisis was exace
established
during
th
s
period,
and
inL
.........A
in social welfare. These hopes have
bated by the structures of underdeve
creases
in
the
numbe
of
health
profes
been thwarted as African elites (who
opment and the legacy of colonialism
stepped into the shoes of the colonialists) sionals on the government payroll also
African societies. These structures ma
cu 11 i vated pri vi leges for themsel ves. The occurred. With this development of
African health systems heavily depen
elites inherited the colonialists’ exclu health care infrastructure, rates of death ent on imported medicines and su
sive facilities, including their medical and illness declined and general gains plies. as well as medical technolog
facilities. These exclusive health care were made in the health of African popu
When foreign exchange became scar
privileges have been documented. In lation. However, while there were dra as a result of the economic crisis,
Zambia a complete renal unit was im matic improvements in some health care imports, including those needed to su
ported and installed al Lusaka Hospital indican < like the Infant Mortality Rale, tain the health care system, were s
to enable a permanent secretary to re it was’not always clear how evenly
verely reduced. In addition, the unequ
turn from England for continued treat distributed these improvements were distribulion of medical faciliti
wilhin countries, communities, or even regionally wilhin countries and betwe
ment al home. Overseas ircalmcnl foi
w ilhin households. Also, while signifi cities and rural areas, as well as i
African heads of slate and lop lune
nonaries is another dimension ol this cant improvements were made in (he privileged access of a limited few
expensive hospitals, have further exa
exclusivity. For example, in spile of trcaimenl of some diseases and the pre
Health care: I he colonial legacy
prove health service xigeria’s presi
dent General Babanv .ia went to Paris
fora full month of medical care in 1987.
The legacy of the colonial system
has pcrpetuaicd a serious maldistribution
in health care. Whereas 70% of the
African population is rural, health and
services and other amenities are avail
able mostly in urb. areas. ConscqucniE. lherearesign .ant differences
between urban and r 1 health condi
tions. infant mortalil} in rural areas is,
for instance, often 2 to 5 limes ashigh as
in urban areas, while life expectancy is
lower by 3 to 5 years.
>VER
Structural adjustment and
health care
In the !9<S()s African governments
were laced with economic crises and
recession.domestic political discontent
and tremendous international pressures
lo meet foreign debt obligations. As a
result, many African governments ei
ther chose or were forced to adopt struc
tural adjustment policies. These poli
cies. which were initially intended
mainly to improve the adjusting coun
try's international financial balances,
later grew in scope and complexity.
They were supposed to bring about the
restructuring of different sectors of the
economy, including that of health serv
ices. and to allow for a better approach
lo problems of poverty, as well as to
support political reforms which many
Western donor countries were simulta
neously encouraging. However, in the
areas of health and healthcare in Africa,
structural adjustment policies have not
had the hoped for positive effects. In
stead. African countries have experi
enced increasing numbers of babies with
low birth weights, increasing rates of
death among young children, an in
crease in the incidence of infectious and
poverty-related diseases and increases
in HIV infection and AIDS. Worse yet,
the severely eroded health care systems
in most African countries are increas
ingly ill-equipped to respond to these
problems.
naled health care system. In many Afri
can countries private sector delivery of
health care has often resulted in the
undermining and draining of resources
from the public sector.
Within the health care budget, it
has been politically much easier to cut
spending on sup; ncsand facilitiesralher
than salaries. S< mrses. doctors, medi
cal assistants ano nrth attendants found
themselves working in run-down build
ings without equipment or medicine,
and often without an adequate supply of
water or electrici I y. Where savi ngs were
made in salaries, this occurred mostly
because salary levels were not increased
to keep up with inflation, so that their
real value erock' . Frequent delays of
weeks or mom
in the payment of
these salaries als.. eroded their value in
situations of high inflation. These con
ditions contributed to the exodus of
health professionals to other countries.
Exacerbating poverty
Structural ad iiistment policies have
resuljcd in inci ses in poverty and a
reduction in fo. j security at both the
national and the household level. In its
recently released report Implementing
the World Bank '.s Strategy to Reduce
Poverty, the World Bank acknowledges
that, even using the most optimistic
projections for regional economic
growth, poverty in Sub-Saharan Africa
will continue to grow worse during the
1990s, as it has roughout the 1980s.
Eroding the health care system
The deepening o >overty in Sub-Saha
ran countries is an essential feature of
The effects of structural adjustment structural adjustment. As one of the
on health and health care has been to economists involved in the recently re
exacerbate rather than fix the problems leased Organisation for Economic Co
created by the economic crisis. This has operation and Development (OECD)
happened in several ways. First, through study'of structural adjustment and eqan erosion of the health care system. uity comments:
Structural adjustment has imposed strict
‘...it does not pro\ .optimal to alle
limits on government spending, and viate poverty dui g the first three years
many governments have seen little rea ofthe adjustmen eriod. Some redistri
son not to make the necessary savings bution does take place in years 2 and 3,
through cuts to the social sectors. As a but it is in favou> fthe rich or middle
result, government spending on health class... The poverty reduction policy
care has dropped dramatically in coun becomes optimal < mly when the econom v
tries adopting structural adjustment poli starts to recover in year 4... Optimality
cies. For example. Ghana’s expenditure is not achieved in redistributing to the
for health care dropped 47% between poor., either in current income or in
1978 and 1988. while that of Cole producti ve asst ' during the first three
d’Ivoire decreased by 43% over the years ofadjusti
t because of the very
same period.
large opport in
cost of investment
I hese cutbacks, combined with the during those yc
increased influence of private initia
Recent suggestions by the World
tives. has led lo an erosion of govern
Bank that properly designed structural
ments ability to implement a coordi- adjustment programmes can help io
alleviate poverty are misleading on sev
eral grounds. First, the recommended
changes to structural adjustment pro
grammes generally involve the addition
of a special programme to mitigate its
costs, both lor some groups of poor
people and for politically volatile groups
like laid-off civil servants. These pro
grammes require funds from other coun
tries, since resources within an adjust
ing country are desperately needed for
debt repayment and for investment.
However, in a climate of global reces
sion and political conservatism, there
have been reductions rather than in
creases in the foreign aid and loans
available to African countries.
Second, the process of structural
adjustments is taking longer than ex
pected in African countries, so the in
crease in poverty it generates is not a
temporary problem of transition which
can be easily fixed. In stead, adjust
ment-enhanced poverty is becoming a
serious long-term predicament in Afri
can societies where poverty was a sig
nificant problem even before the eco
nomic crisis and structural adjustment.
Third, the idea that a little additional
external money can be devoted to a
compensatory programme to help the
poor while no significant changes are
made to the process of structural adjust
ment itself, is a contradictory one. It
becomes an attempt to ‘eradicate pov
erty while, at the same time, working
within and often strengthening the very
structure of... relationships that gener
ate and reproduce it’ in the first place.
Undermining food security
Efforts to promote food security
are also undermined with the implementation of structural adjustment poli
cies. A recent study carried out by the
Organisation of Rural Associations for
Progress (ORAP) in Zimbabwe illus
trates how structural adjustment poli
cies exacerbated the agricultural prob
lems in the country which were already
severe due lo the drought.
As part of the drive to boost ex
ports, the government raised producer
prices for export crops such as tobacco,
cotton and cut flowers, inducing many
farmers to abandon maize production.
The government also sold off its surplus
grain as part of its adjustment pro
gramme. As late as February 1992, when
the extent of the drought and impending
crop failure was clear, the Grain Mar
keting Board was still exporting grain.
I
I
p
I
i
tural adjustment policies involve a
duction in real wages to increase
resources which can be devoted to
vestment for economic restructuring a
Gender relations denote the com
posite of ideas and practices concerning for debt repayment. Women, alrea
receiving lower and less regular incom
die relationship between men and
than men. have seen theirsmall incom
women. These ideas a* 1 practices have
further diminished. In cities and tow
an impact not only 1 1 the health of
Abandoning infrastructure
women but on the hea uh of families and l»rmai seetor employment Jor■ wom
is increasingly limited under structu
Structural adjustment policies have communities. Because historically
adjustment policies, so they are for
had a negative impact on health because women have been assigned the task of
into lower-paying and less product
they have involved extremely severe caring for the family, any policy which
informal work.
cuts in government spending on infra undermines women, undermines the
With reduced income. Afric
structure that supports health and nutri health of families.
women have to spend more time ea
For a long lime, women in Africa
tion improvements. This includesspending extra income for the family, hunt
ing on waler supply, sanitation, roads, have been placed under stress by the gap for bargains, making and mending
national and local food storage facili between their econot. ic responsibility home rather than buying. The increa
ties, as well as education and communi and their access to res trees. Structural demands on their lime limit that av
cations infrastructure that allows the adjustment exacerbate this gap further,
able for health and nutrition-related
spread of new information about health not only in terms of resources but also in
tivities. Moreover, women have incre
terms of
stress, time and health. As
and health care.
t------- -------ingly become responsible for taking c
Ingrid Palmer warns.
of
sick relatives thereby adding m
If the gender bias, the weakest link
Environmental degradation
responsibilities to their already he
in sub-Saharan economies, is not re
burden. This leaves them with littl
solved. these economics may have an
Structural adjustment policies di
no time to lake adequate care ot th
minish the possibilities for good health absolute advantage in no product and a
selves further diminishing their o
------because they hasten the deterioration of comparative adv
anta only in lines of
health and consequently of their fa
the natural environment in which peo- production based on 1 super-exploitalies.
ple must live and from which they ob lion of women and a demand for chil
The negative impact of struct
tain resources to provide for their well dren’s assistance.
adjustment on women is not an ea
Structural adjustment programmes
being. SAPs call for increased exports
remedied oversight, as is someti
also
seek to shift production from nonas a way of increasing foreign exchange
suggested. Women’s labour is actu
earnings. Many African countries de tradeables, which are goods and services an important factor in the adjustm
the'export derived from their produced and consumed withinnational
pend Oh t
process. It is women who are expe
.... j boundaries, to tradeables, which are
natural environment - timber, cash
to make up for the loss of governm
etc. The resulting accelera- ’ goods and services mtended for the incrops,
services in health and education thro
tion of commodity production is not ternational market.T ereisanunderly- the increased care of sick family m
‘ that
’ ni difference exists
ecologically sustainable. The destruc- ing assumption
bers and increased responsibility
tion to the environment associated with in the ability of m^i and women to children unable to attend school. In
this export-led growth strategy is not survive the transitional cost of making case, savings at the level of the nati
accounted for in GNP calculations and this switch, and that men and women budget are illusory ones, gained onl
the loss of future productivity is disre- have equal1 access to resources and to shifting costs from the monetise
garded. Reductions in government markets. But this is not the case. The non-monetised parts of the econ
switch from non-tradeable to tradeable
spending,
privatisation
SpVI
IM1I 111, Ml
• » Ull.iuuvi and liberalisation
- ----------------through unpaid and underpaid fem
also leads to the lack of enforcement of production invol ves a relocationor many
labour. Women arc also under incre
environmental laws and the removal of activities from the paid to the unpatd or
pressure to make up for losses to
regulations to protect the environment. underpaid econom; accomplished
family income by taking on additi
women. As a
By intensifying poverty, structural ad through the labour
paid work, by providing additiona
justment policies have also forced peo result, the ability of tructural adjust paid labour to income-generating
ment programmes to meet their objec
ple to move onto marginal lands to
tivities organised by male family m
tives, may be won at the cost of a longer
overuse scarce resources in order to
bers, or by carrying out their own
and harder working day for women.
come-generating activities. At the s
survive.
This cost will be invisible to the macroIn Ghana, timber exports were rap
time, women face greater difficulti
economic policy makers because it is
idly accelerated as part of its adjustment
their role as household managers,
unpaid time. But the cost will be re income and available time diminish
programme. As a result of these poli
vealed in statistics <1 the health and tive to the cost of obtaining goods
cies, Ghana’s tropical forest area is now
nutritional status of sih h women.
services necessary for the family, c
just 25% of its original size. Wide
Women’s abilit} 1 1 promote health ing daily crises of consumption.
spread deforestation is resulting in re
and nutrition for them wives and their
gional climatic change, soil erosion and
families is conditioned by income, ac
large-scale desertification. Women have
The above is an e.uerpi from lieyond Adjus
cess
to resources, and their level oF Responding to the Health Crisis in Africa tpa
lost an important source ol food, fuel
and medicines that they had harvested education. In Africa, adjustment pro 28) published by the Inter-Church Coalilion on
honouring the World Bank/IMl* re
quirement that it balance its books. Once
a surplus maize producer, Zimbabwe
ran a deficit of one million metric tonnes
in 1991. In 1992. more (han half the
population required lood-aid assistance.
•
a
• • ••
V •
• *
Women, health and structural
adjustment
The World Bank’s vision of health:
a critique
The model of health care for developing countries promoted by the World Bank in its World Development
Report 1993 is a deeply flawed one. The proposed system of health care is a two-tiered one, which is
commercial in inspirations and profit-motivated in orientations. As such, it constitutes a further assault on
the principles of universality and equal access.
THE World Development Report 1993
offers a model of health care for the
developing world. Since the health and
livelihood of citizens around the world
are very closely linked to the policies
which the World Bank promotes, a
critical analysis of the World Bank’s
health proposals s essential.
Investing in Health proposes a vi
sion of health care for developing coun
tries based on a set of assumptions about
the way health care is currently pro
vided. First, government spending in
developing countries is disproportion
ately skewed touard the more expen
sive tertiary sector, that is for hi-tech,
hospital-based, curative care. Second,
public health systems in poorer coun
tries are inefficient; private health care
delivery is of a higherquality. Third, the
pursuit of pro-poor adjustment policies
can help to maintain cost-effective health
expenditures.
The Bank’s specific policy propos
als include the following:
• Reduce public expenditures on
tertiary facilities, specialist training, and
interventions that are not cost-effective.
• Finance a set of public health
interventions dealing with infectious
disease control, environmental pollu
tion, etc.
• Ensure financing of a package of
essential clinical services for the poor.
• Promote private finance of all
clinical services outside the essential
package, with government regulation of
the private sector.
• Encourage private suppliers to
compete both to deliver clinical serv
ices and to provide inputs such as drugs
to both the public and private sectors
Domestic suppliers should be protected
from international competition.
The vision of health promoted in
the World Development Report 1993
falls far short of the most basic require
two-tiered syste of health care which
is commercial ii aspiration and is dis
torted by an undue emphasis on privati
sation and the profit motive. In essence,
the report urges poorer countries to cede
most health care to the private sector,
leaving governments to provide basic
primary health care for the poor and to
try to regulate the private sector.
T he World Jank’s vision of
wealth
There are several problems with
these assumptions and proposals. First,
the contents of the basic health care
package for the poor are extremely lim
ited. Since the poor are rfiore vulnerable
to disease and injury than the rich, and
are more likely
1”
already to be suffering
ill-health, they ; ■ trapped in a vicious
cycle. Their acc -s to adequate health
care depends on their ability to partici
pate in the economy, but their present
ill-health makes full participation diffi
cult, if not impossible. A second prob
lem relates to the World Bank’s as
sumption that in providing a basic health
care package for the poor, governments
will be committing themselves to a
modest expendi 1 e fora relatively small
part of the poj ation. In many subSaharan Africai; countries, more than
half of the population lives in poverty,
and the numbers of the poor are rising
rather than shrinking. In such a situation, a modest expenditure targeted at a
small, easily-defined group of people in
poverty is neither a realistic nor an ad
equate response m a crisis of health and
health care.
While the
’fid Bank's emphasis
on primary be 1- care is positive, it is
also selective, ii argets individuals for
immunisation or micro-nutrient supple
ments. but does not take adequate ac
count of the close relationship between
Targeted remedial programmes for
children such as immunisation or food
packages, as outlined in the World De
velopment Report, are not adequate be
cause they are not linked to the im
provement of peoples’ economic, po
litical, social and physical environments.
Ignoring the broader dimensions of illhealth and focusing instead on ad
dressing only their symptoms does not
embody a holistic and comprehensive
vision of health.
A two-tiered health care system
While the World Bank agrees that
health care is a basic human right, its
policy prescriptions treat it not as a right
but as a scarce commodity to be allocated according to ability to pay. This
assumption leads to a division of com
munities and societies into two classes
of people: the ‘haves’ who can afford to
pay for a privatised, profit-driven health
care system and the ‘have-nots’ who
will have to content themselves with a
bare minimum of treatment in the pub
lic health care system.
The World Bank’s vision also in
volves a division of rich and poor coun
tries. In the Bank’s view, the rich coun
tries are to do health research, develop
health care technologies and manufac
ture drugs, while the poor countries
must, as far as their means allow them,
remain consumers of these health prod
ucts.
In effect, the World Bank is pro
moting an international health care sys
tem based on the American model. And
yet, as the World Development Report
itself points out. the US has the most
inefficient health care system in the
world. It accounts for 42% of total glo
bal health care expenditures, while
making uponly 2% of the world’s popu
-—JEW
cov
Research and training
'AM’ ■
.. • •
As a result of Structural Adjustment Programmes, governments have been forced to
cut back on spending on health clinics.
The World Development
Report also argues for a shift
of poor countries’ priorities
away from health research
and the training of health
personnel in favour of pri
mary health care. While this
recommendation seems sen
sible, it masks a disturbing
reality. This reallocation of
expenditure will continue to
erode the fragile and impor
tant base of research and
training in poor countries. It
is estimated that during the
1980s more than 30,000 pro
fessionals have left Africa as
a direct result of the aban
donment of state support for
basic research and teaching.
Rather than abandoning
these people and their work,
it would be belter to consider
ways to support research and
training institutions appro
priate to the health and health
care needs of African coun
tries at either a national or
regional level. If such meas
ures are not taken, indigenous
■
research and training will
continue to be turned over to
' private, profit-driven North
ern health institutions. These
institutions are not account
able to anyone other than their
- shareholders or boards of
governors. They will thus be
likely to perpetuate current
biases in health care towards bio
medical definitions of health prob
lems, as well as toward the health
problems of white, well-to-do men.
guarantees minimum care for the poor
uealth care.
The World Bank’s prescriptions for and makes those who can afford it pay
_____________
for lhese services. What is sacrificed,
health ____
care constitute
a further assault
on the principleof universality and equal though, is the principle of universality,
access. Their report argues that, ‘The The result is a health care system which
Privatisation
main problem with universal govern will provide one leve' of health care to
ment financing is that it subsidises the those who can afford 1: and a far inferior
Rather than deal with the root
wealthy who could afford to pay for standard of health care to some, but
causes of ill-health, more money goes
r own services,
tin. u---------------, --and thus leaves fewer probably not all of the poor. The princifrom most African governments into
pie of universality is subverted in fa
government resources for the poor.’
private health care than to public and
Arguments like these form an inte- vour (of profit-driven schemes. This is
mission health care put together. Al
gral part of the neo-conservative doc- especially problematic: in countries
most half of the doctors, nearly all
trine which, over the past decade, have where those in poverty constitute a large . pharmacists and many nurses and mid
percentage of the population.
wives in African countries work in the
been used to dismantle social pro
There are proven alternatives tothe
profit-based sector and establish them
grammes around the world and replace
selves in large cities.
them with user-pay, privatised two- approach advocated b\ the World Bank,
In the scenario proposed by the
tiered systems. The premise for this such as ensuring that richer members of
World
Bank, with the private sector
society
pay
their
fair
share
of
taxes,
change is seductive: why should the
responsible
for individual cure and the
which
would
preserve
the
principle
of
rich receive the benefits ol universal
public
sector
responsible for collective
universality
and
ensure
an
adequate
level
programmes if they can al I ord to pay for
integration of preventative and curative
health care.
Privatisation and the shift of gov
ernment expenditure toward primary
health care also includes a call for non
governmental organisations and
churches to become more involved in
the provision of health care. This can
only be viewed as a short-term, stop
gap measure. It will lead to greater frag
mentation in health policy as well as
considerable variation in the quality and
availability of health care. It also results
in greater assymetry in the maintenance
of information systems which threatens
the ability to provide quality healthcare.
Long-term national health planning,
regulation and coordination become
extremely difficult, if not impossible.
Reduplication of services and the inef
ficiency of several bureaucracies are
another result of this approach
Bank’s claims, bor example, since the
introduction of user fees in Zimbabwe,
there has been a dramatic drop in the
number of hospital visits. Fewer babies
arc being deli vered in clinics and hospi
tals in the rural areas while the number
of women dying in childbirth in Harare
has doubled.sii ce the introduction of
the structural adiustment programme in
1990.
Women, girls pay dearly
The World Bank’s system of health
care not only pits richer against poorer
members of society, it also forces fami
lies to decide which of their members
are to receive i.eatment. It is in this
regard that the inequity of this system of
health care for women is clear. Since
women and girls presently receive fewer
resources in many families, they are
more likely to be further discriminated
Cost recovery and user fees
against if health care resources must be
rationed. As a result of declining in
The World Development Report comes and rising expenses for basic
/993 promotes the introduction of user necessities,man womenandgirlshave
fees for basic health services. User fees also been forces to reduce their intake
and cost recovery are the foundation of of food, which only increases their vul
the World Bank's proposal for health nerability to disease and accident. In
care financing in developing countries. addition, women are mostly likely to
The World Bank argues that, ‘since have to take on the additional work of
patients are already paying for suppos- caring for sick family members when
edly free or low cost health care, new professional care is unaffordable.
user fees, when accompanied by a re
The World Development Report
duction in indirect costs and improved does offer up the solution that better
services, may increase utilisation.’ In a education for girls will improve the
context of high unemployment, soaring general health ol families and commuprices and growing poverty this strat- nities. However, ibis recommendation
egy only increases inequities in access not only papers over the serious probto health services and effectively closes lem of gender inequality, it also overoff access to adequate health care for the looks the greatest threat to the health
poor.
and well-being of women, and of entire
According to the World Bank, the communities: poverty. The World De
justification for this trend lies in the fact velopment Report does, to its credit, af
that a developing country cannot afford firm the close link that obtains between
free health care and education. There poverty and health. It also recognises
fore, through user charges, the popula the appalling le' Is of violence against
tion should pay for a significant part of women throughout the world as a
the care with private enterprises playing dominant health issue. What the report
a much greater role. Governments im fails to do is make the link between
plementing structural adjustment pro poverty and the failure of the World
grammes are forced to cut back their Bank’s economic policies.
allocations to health care and seek
The proposals contained in the
compensation by giving more room to World Development Report do not ad
private initiatives and donors as well as dress the single greatest factor contrib
introducing large fees for patients.
uting to the health care crisis in the
The transformation of health care South. The debt isis remains the larg
into a privatised, user-pay system thus est single threat ; > health currently fac
constitutes another assault on both the ing the global 1 mmunity. In addition,
physical welfare and the basic human many countries have been compelled to
dignity of the poor. Evidence about the adopt structural adiustment programmes’
health care systems of a number of Af (SAPs), which have had a devastating
the majority of their citizens. Structural
adjustment undermines the ability o
states to allocate resources towards ei
ther health care or self-reliant develop
ment. and instead turns these resources
towards the export sector and debt serv
icing. How can poor countries possibly
give cither resources or attention to
healthcare when significant amounts o
their scarce capital continue to be si
phoned off by Northern banks, G-7 gov
ernments, the International Monetary
Fund and the World Bank? The reduc
tion of public investment due to SAPs
has also affected the ability of countries
to maintain and develop infrastructure
in watei and public sanitation. In its
1989 document entitled African Alter
native Framework for Socio-Economic
Recovery and Transformation, the
United Nations Economic Commission
for Africa warned against the cutbacks
in social spending as a debt-servicing
strategy: ‘Reductions in budget deficits
must not be accomplished at the ex
pense of expenditures on the social sec
tor, ie, education, health and other so
cial infrastructure.’
Promoting an unhealthy planet
Structural adjustment policies also
result in serious constraints on efforts to
promote better health through more
environmentally responsible develop
ment policies. The promotion of toxic
waste exports to poor African countries
by the former Chief Economist of Ithe
World Bank, Lawrence Summers is an
example of this. His recommendation
was not an aberration, but rather the
logical extension of a structural adjust
ment agenda which forces countries
desperate for foreign exchange to sacri
fice the health of their citizens by expos
ing them to the unwanted waste of
Northern countries:
The World Bank’s own internal
review of its project lending, conducted
by W Wapenhans in 1992, points to an
alarming 37.5% failure rate. The same
report notes that the worst-affected sec
tors were in water supply and sanitation
where 43% of the projects were said to
have ‘major problems’ and in agricul
ture, with a rate of 42%.
The World Bank continues to lend
money for projects which harm the en
vironment and which do not directly
involve the people who will be directly
affected by them al every step of the
^ **’•>*
R'fl
11
•f
■ ’
fact became the cause of further in
debtedness. The World Bank refuses
to accept its share of responsibility
for contributing to and exacerbating
the debt crisis. It could do so without
difficulty given that it has amassed
over $13 billion in profit over the
past decade.
As the world’s largest develop
ment institution, the World Bank
must take responsibility for its con
tribution to the growing poverty and
declining health of the majority of
the world’s people. /\ thorough re
view of the World Bank’s develop
ment, environment and lending
record is urgently required. The Bank
must be called to account for its
disturbing legacy of bad loans to
corrupt leaders, failed projects and
flawed development policies. The
World Bank must also accept its share
of responsibility for contributing to
and exacerbating the debt crisis by
cancelling the debts owed to it by the
poorest countries and channelling
these funds towards social sector
transformation and growth.
Ensuring universality and
equal access
As a result of privatisation, maternity wards in many African countries have
suffered a depletion of midwives, nurses and other staff.
Conflict of interest
It is the poor who ai • being forced
to pay, through cutbacks in health
spending and through reductions in their
living standards and physical well-being
for the irresponsible lending and bor
rowing that occurred during the 1960s
and 1970s. During the 1970s, World
Bank lending to developing countries
increased five-fold at the same time as it
was actively encouraging banks and
Northern governments to increase their
lending. In spile of very clear indica
tions that this lending was unsustainable,
the World Bank continued to increase
its lending as well as encourage North
ern banks and governments to do so.
During the 1980s, the World Bank
effect bailing out commercial banks,
Northern governments, the IMF and
itself by using funds earmarked for de
velopment assistance for debt servic
ing. The servicing of ne growing debts
owed to the World Bank and the IMF is
another problem. An average of 45% of
African countries’ debt servicing goes
for multi-lateral debt. The need to serv
ice this debt has directly contributed to
the dismantling of health care systems.
The solution advocated by the
World Bank in the 1980s has been to
encourage indebted conn tries to increase
exports of their primary commodities.
Rather than solve the debt problem, this
strategy only exacerbated it as the oversupply of commodities led to plummet
ing prices. The ‘solution’ to the debt
Comprehensive health care
should be seen as part of an overall
development strategy to combat
poverty and promote self-reliance.
The provision of adequate health care
depends upon a commitment of
public resources. This vision can be
realised only if governments, health
services and donors support a proc
ess that will ensure a democratic
system of health care which guaran
tees universality and equal access.
This vision cannot be seriously
considered in the context of diminish
ing resources for the social sector and
the privatisation of basic social serv
ices. At the heart of these trends is the
problem of international indebtedness
and the implementation, of orthodox
structural adjustment programmes.
These have been the most important
factors contributing to the deterioration
of health care systems not only in Africa
but as part of a global trend.
Efforts to address the HIV/Al DS
crisis in Africa must be part of a com
prehensive national plan al all levels ol
health care. An adequate response to the
HIV/AIDS crisis cannot be mounted in
the context of shrinking national budg
ets owing to debt servicing or a frag
system.
The failure of top-down develop
ment methods to eradicate poverty and
improve the living conditions of (he
poor in African nations has led to de
mands for and adoption of participatory
initiatives to strengthen the power and
welfare of people. Such initiatives rely
on the sharing of power and scarce re
sources. These include efforts by social
groups to control their own destinies
and the opening up of opportunities
from below. This approach has bolstered
community involvement in the design,
execution and management of develop
ment projects and resource management.
It has led to increased benefits and effi
ciency in the provision of social serv
ices, especially those related to health,
nutrition, education and income gen
eration. Included in this vision is the
reaffirmation and support for i ndigenous
healing systems and the integrity of
indigenous health knowledge and prac
tices.
These community-based efforts can
only succeed where health care is ac
corded primacy at the national level. A
comprehensive national health care
policy framework can only emerge
where there is continuous consultation
with patients, health-care practitioners
and policy-makers at all levels. This
entails a massive reshifting of resources
away from the private sector and towards
the public sector. The allocation of
secondary and tertiary care to the private
sector, as the World Bank proposes,
will only lead to a further skewing of
health care which favours the rich.
Secondary and tertiary health care have
to be integrated and become part of a
comprehensive basic package that is
made available to all citizens.
We favour a democratic, commu
nity-based, comprehensive vision of
health care where communities are given
the power and the tools to reduce prob
lems of ill-health, problems which are
intimately related to the econorpic and
social patterns of their society. Promot
ing democratic health practices would
mean placing the definition and control
of health care in the hands of those who
use the services. This will mean that
people, especially women, will not be
treated as the targets of health cam
paigns, but as members of society with
equal political rights, social status, and
economic value.
The basic elements of a democratic
health service would include:
• Equitable distribution of food,
services, and free curative medical care
to women, children and men of all so
cial classes in rural and urban areas.
• Support for community-based
health care initiatives which give all
members of a community control over
decisions involving their health and
livelihood.
• Affirmation of and concrete
support for indegenous health care
knowledge and practice.
• Support for and promotion of
food security. In particular, the produc
tion of food crops for domestic con
sumption must be given priority over
commercial production of export crops.
The redistribution of land is another
important component of food security,
as are a more equitable and appropriate
distribution of agricultural services and
inputs to small farmers, especially
women.
• Support programmes which
would enable groups to overcome
poverty such as housing development,
literacy training, improved education
and skills development programmes for
the poor.
• Programmes to combat family
violence and sexual inequality.
An integrated health
care system
There is a need to build health care
facilities to serve rural communities.
Such facilities must be intergrated into
the secondary ar tertiary care system
and must not be ci npromised by making
the poor carry an unfair burden of the
costs while enabling urban elites to avoid
sharing the benefit of advanced medical
technology.
In addition, medical education
which has tended to produce clinical
specialists needs to be revised to train
generalistsaswcll Such generalists must
be familiar will ural health problems
and prepared to >rk in teams of public
health professionals under conditions
of scarcity in rural areas. Community
rather than economic concerns should
be the motivating force behind the op
eration of these health care teams. Ide
ally, such teams should function within
a transformed political structure, but
realistically, the' would need to cope
with the limits
)osed by existing na
tional and local .. stitutions.
Transnational pharmaceutical cor
porations represent another area of ne
glect in health care strategies for poor
countries. These corporations operate
lowed to amass widfall profits through
monopoly pricing. For example, prices
for drugs can be lowered through leg
islation as Germany did when it reduced
the reference prices of drugs for health
plans to those of generic brands, using
pharmacological properties as the basis
for grouping and pricing drugs. This
forced transnational pharmaceuticals to
reduce the price of their drugs to the
level of generic brands.
Transnationals must be more
closely monitored in both rich and poor
countries, and made more accountable
to the customers they purport to serve.
This would include imposing higher
taxes on the profits made by pharma
ceutical corporations and channelling
these funds into national health care
systems. Stiff penalties should be im
posed on unscrupulous companies that
dump expired drugs and con duct dan
gerous tests of new medications in poorer
countries. Medicines which benefit all
people, and which arc derived from the
genetic stock which is the heritage of all
humanity, should not be controlled by
private interests. The shining example
of Dr Manuel Patarroyo's donation of a
malaria vaccine to the World Health
Organisation serves as a model of soli
darity and true concern for the well
being of the world's inhabitants.
Comprehensive health care should
be seen as part of an overall develop
ment strategy to combat poverty and
promote self-reliance. Th? provision of
adequate health care depends upon a
commitment of public resources. This
vision can realised only if the govern
ments, health services and aid donors
support this process of change.
What African countries need now
is a commitment from ouniovernments
and from development agencies like the
World Bank to support their efforts to
develop and implement their own
comprehensive health care programmes
where people not markets take priority,
Promoting democratic health prac
tices would mean placing the redefini
tion and control of health care in the
hands of those who use the services. By
doing so, the majority of people, especially women, will not be treated as
targets of health campaigns, but as
members of society with equal politi
cal rights, soial status, and economic
value.
♦
Hie iilMn'e is an excerpt Jmni Beyond Adjustment:
Responding to the Health Crisis in Africa (pa}>es .11)42) published by the Inier-Church Coalition on Africa
C.om
h
DOCUMENT
Declaration of Alma-Ata
The International Conference on Primary Health Care, meeting in Alma-Ata this twelfth day of
September in the year Nineteen hundred and seventy-eight, expressing the need for urgent
action by all governments, all health and development workers, and the world community to
protect and promote the health of all the people of the world, hereby makes the following
Declaration:
THE conference strongly reaffirms that
health, which is a state of complete
physical, mental and social wellbeing,
and not merely the absensc of disease or
infirmity, is a fundamental human right
and that the highest possible level of
health is a most important world-wide
ocial goal whose realisation requires
the action of many other social and
economic sectors in addition to the health
sector.
I 1
MilvO
-
I
.?.W!
;
*
H
II
'I’he existing gross inequality in the
health status of the people, particularly
between developed and developing
countries as well as within countries, is
politically, socially and economically
unacceptable and is. therefore, of com
mon concern to all countries. -
*
I-.' .
Ill
Economic and social development,
based on a New International Economic
Order, is of basic importance to the
fullest attainment of health forall and to
the reduction of the gap between the
health status of the developing and de
veloped countries. The promotion and
protection of the health of the people is
essential to sustained economic and so
cial development and contributes to a
bet ler qua 1 i ty of 1 i fe and to wor 1 d peace.
IV
The people have the right and duty
to participate individually and colleclively in the planning and implementa
tion of their health care.
V
Governments have a responsibility
for the health of their people which can
be fulfilled only by the provision of
adequate health and social measures. A
main social target of governments, in
?x
muoon
The Alma-Ata Conference in Kazakhstan in progress.
world community in the coming dec
ades should be the attainment by all
peoples of the world by the year 2000 of
a level of health that will permit them to
lead a socially and economically productive life. Primary healthcare is the
key to attaining this target as part of
development in the spirit of social jus
tice.
VI
I’rimary health care is essential
health care based on practical, scientifi
cally sound and socially acceptable
methods and technology made univer
lies in the community through their full
participation and at a cost that the com
munity and country can afford to main
tain at every stage of their development
in the spirit of self-reliance and selfdetermination. It forms an integral part
both of the country’s health system, of
which it is the central function and main
focus, and of the overall social and
economic development of the commu
nity. It is the Trst level of contact of
individuals, the family and community
with the national health system bring
ing health care as close as possible to
where people live and work, and consti
tutes the first element of a continuing
p
I
sure primary health care
for all people since the
attainment of health by
people in any one coun
try directly concerns and
benefits every other
country, in this context
the joint WH0/UN1CEF
report on primary health
care constitutes a solid
basis for the further de
velopment and operation
of primary health care
throughout the world.
An acceptable level
of health for all the peo
ple of the world by the
year2000 can be attai ned
through a fuller and
‘The people have the right and duty to participate... in the planning and implementation of their
better use of the world’s
health care’.
resources, a consider
VII
ganisation, operation and control of pri able part of which is now spent on
mary health care, making fullest use of armaments and military conflicts. A
Primary health care:
local, national ai.d other available re genuine policy of independence, peace,
sources, and to this end develops through detente and disarmament could and
1. reflects and evolves from the appropriate education the ability of should release additional resources that
economic conditions and socio-cultural communities to participate;
could well be devoted to peaceful aims
and political characteristics of the coun
6. should be sustained by integrated and in particular to the acceleration of
try and its communities, and is based on functional and mutually-supportive resocial and economic development of
the application of the relevant results of ferial systems, leading to the progresive which-primary health care, as an essen
social, biomedical and health services improvement of comprehensive health
tial part, should be allotted its proper
research and public health experience.
care for al k. and giving priority to those share.
2. addresses the main health prob most in need;
lems in the community, providing pro
7. relies, at b cal and referral lev
motive , preventive, curative, and reha els, on health woikers, including phy
bilitative services accordingly;
sicians, nurses, midwives, auxiliaries
The International Conference on
3. includes at least: education con and community workers as applicable,
Primary Health Care calls for urgent
cerning prevailing health problems and as well as traditional practitioners as
and effective national and international
the methods of preventing and control needed, suitably trained socially and
action to develop and implement pri
ling them; promotion of food supply technically to work as a health team and
mary health care throughout the world
and proper nutrition; an adequate sup to respond to the expressed health needs
and
particularly in developing countries
ply of safe water and basic sanitation; of the community.
in
a
spirit of technical cooperation and
maternal and child health care, includ
in
keeping
with a New International
ing family planning; immunisation
III
Economic
Order.
It urges governments,
against the major infectious diseases;
WHO and UNICEF, and other interna
prevention and control of locally en
All governments should formulate
demic diseases; appropriate treatment national policies, strategies and plans of tional organisations, as well as multilat
of common diseases and injuries; and action to launch and sustain primary eral and bilateral agencies, non-govern
mental organisations, funding agencies,
provision of essential drugs;
health care as part of a comprehensive
4. involves, in addition to the health national health system and in coordina all health workers and the whole world
sector, all related sectors and aspects of tion with other sectors. To this end, it community to support national and in
national and community development, wilt be necessary to exercise political ternational commitment to primary
in particular agriculture, animal hus will, to mobilise the country's resources health care and to channel increased
bandry, food, industry, education, and to use available external resources technical and financial support to it,
particularly in developing countries. The
housing, public works, communications rationally.
Conference calls on all the aforemen
and other sectors: and demands the co
tioned to collaborate in introducing,
ordinated efforts of all those sectors;
IX
developing and maintaining primary
5. requires and promotes maximum
community and individual self-reliance
All countries should cooperate in a health care in accordance with the spirit
f
Science and ethics in the
NORPLANT trials
Safety trials are being conducted in India on NORPLANT, the implantable hormone
contraceptive developed by the US Population Council. The way the trials are being
carried out, however, raises serious questions.
WALK in to the Family Plannning clinic
at the Safdarjung hospital and you are
greeted by two posters of NORPLANT,
the five-year implantable hormonal
contraceptive invented by the Populaion Council of the USA. The counsel
lor takes great pains to explain to you all
about this new contraceptive costing
Rs 1,800 received from the US. Six
white match-sized capsules comprising
this contraceptive are stuck on the poster
- so that women can sec it for them
selves. But neither the counsellor nor
the doctor on duty bother to inform
women of the minor hitch - NORPLANT
is not as yet an approved method for
contraception but is undergoing trials in
the country. Women who agree to use
NORPLANT will in fact be participat
ing in the Phase III trials of the Indian
Council for Medical Research which
will establish the safety and effective
ness or for that matter the lack of it for
Indian women.
While the inventor, namely, the
Population Council, lists out a number
of side effects which include spotting,
amcnorrhea,menorrhagia, metrorrhagia,
ovarian cysts, mastalgia, weight gain,
dermatitis, acne, hair loss, hirsutism,
headache, nervousness, nausea, dizzi
ness, change of appetite, depression
and other mood changes, infection,
itching or pain at the site of implanta
tion, our researchers reassure women
that NORPLANT is perfectly safe,
(‘You may suffer some bleeding dis
turbances but we can easily take care of
them') in complete disregard of the fact
that there is no treatment for these dis
turbances.
Of course this irrational therapy is
not confined to India alone but is ram
pant in almost all countries where this
miracle device is in use, ranging from
Finland to Indonesia. ‘Only a hundred
devices have been sent to us and even
our own staff is queueing up for them,’
Kalpana Mehta
fl
VT
NORPLANT capsules... designed to
prevent pregnancy for up to five years.
The doctor on duty first screens
two women based on their reproductive
status including age and parity and pos
sible inclination to seek a contraceptive
for full five years She then sends them
for routine exam i 1 tion and a pap smear.
It is a bit late in the lay and the concerned
doctor refuses to take the smear. The
women persist saying that they need to
get the test done on the same day be
cause they have been asked to get
NORPLANT inserted the next day. ‘But
the result of the smear will be available
only after two weeks,’ Says the doctor.
The women rush back to the Family
Planning clinic
1 bit confused. The
doctor on duly iu.. .sures them that it is
not necessary to wait for the results.
Now the unsuspecting volunteers arc
truly worried why all this testing if it
is not needed?
are dissuaded that ‘these contain hor
mones and will ruin your uterus. Why
don't you go for the Copper T?' by the
very doctors who promote NORPLANT
as being safe. IS THIS ETHICAL?
Ethics apart, what is the rationale
for all the promotional glossies that have
been printed already by the Ministry of
Health and Family Welfare or for that
matter the video on NORPLANT inser
tion. all of which make NORPLANT
seem like an ideal contraceptive? How
has the Ministry decided that
NORPLANT trials will prove to be a
safe and efficacious device for Indian
conditions? Are these trials being con
ducted to determine the side effects
among Indian women or are they a ritual
exercise meant to give a scientific fa
cade to a political decision? Or are the
trials meant to pacify the joint front of
women’s organisations which has de
manded that NORPLANT not be in
troduced in India.
Time and again NORPLANT ap
proval in the US is cited as a ground for
the safety of this device. But a cursory
look at the National Drug Approval
before the US informs the reader that
the US application was made so that it
would be easy to obtain approval from
drug authorities in the Third World.
In 1991 I happened to attend a
meeting called by the Indian Council of
Medical Research and the Ministry of
Health and Family Welfare where they
revealed their plans to go ahead with
NORPLANT introduction without car
rying out the Phase III trials. They
sought the support of women’s groups
to go ahead. This was not surprising
because at that stage only a few wom
en's groups like Saheli, Chingari and
Slree Shakti Sanghathana had raised
their voice against introduction of unsafe
contraceptives and the abuse potential
of contraceptive technology.
NORPLANT as a contraceptive
HEALTH MSAPETY
for that matter hear
tablishment ideally,
disease are absen
second only to sterili
from this protoco
sation. Once moti
even though they hav
vated a woman could
been reported to occu
be forgotten about for
with a fair regularit
five years. Not only
among NORPLANT
was the question of
users in other studies
safety being ignored
A recent evalua
but also the actual
tion
in Indonesi
proof of abuse from the
suggests
that as man
country of origin ie the
T
as 1 1% women re
<■ ■ ’ ■"?US.
ported symptoms o
In India the con
fi
heart disease whi Ie o
traceptive had not even
NORPLANT. Th
undergone the neces
Population Counci
f
sary clinical trials
suggests that ovaria
which would have an
I
cysts have occurre
swered the question of
among nearly 10% o
effectiveness, side ef
the users even though
fects and adverse re
it does not provide in
actions among Indian
formation on the per
women. NORPLANT
centage
which re
administration also re
quired surgery. Th
quires sophisticated
research protocol o
screening and moni
ICMR suggests tha
toring systems which
the
study could b
were then non-existent
discontinued if life
in the country or were
threatening side ef
fast being dismantled.
fects were discovered
This had already been
xx\ I //
but for most India
\V'//
proved in the case of
women heart attack
\WI//
version
of
another
would mean loss o
NORPLANT where
life given the low ac
for a large number of
The 5 year contZacepttve plan
cess
to health care
cases contact was lost
FAMILY PLAN
COUfiCll
fix/urffter infon-niiv.hlkh^urlcc-ICtPervit'^oarneornfu'-cor Healthcentre.
The
logic
of carryin
rtHyr
par
tore
tbr
a
bexr
UH
altogether. Non-reout research to fin
moval at the end of the
Promoting NORPLANT in Africa. The oove advertisement was used in
out what is alread
effective period could
Zimbabwe.
known escapes one.
subject these women
Medical research
to the life-threatening
cannot be done in dis
other methods. While the study aims to
condition of ectopic pregnancy.
On these premises a broad coali see the acceptability of the method regard of social and infrastructural real
tion of women’s organisations and health among young women, this is not even ity. Research is justified if there exist
groups came- forward to say a resolute built into the design of the study. Hos a possibility of finding a superior solu
‘no’ to NORPLANT. While their posi pitals are. in practice, putting pressure tion to an existing problem
NORPLANT fails to meet this require
tion on the suitability of this device for on women with two children to adopt
Indian conditions was not accepted there sterilisation or toopi for IUDs instead of nte -1 for women. Time and again fig
was no denying that Phase 111 trials were offering them a hoice including ures of maternal mortality are quoted a
NORPLANT. Woi ien who opt for a defence for introducing contracep
a must. The Indian Council of Medical
tives. But death rate from NORPLANT
Research thus admitted before the Na NORPLANT are to be provided with
tional Commission for Women that it health cards so that they can get good use sans medical facilities to treat fo
would carry out a Phase III trial instead medical care for all their problems - an side effects would itself surpass the ex
of the proposed post- marketing sur inducement which can hardly help if isting rate of maternal mortality
veillance of 20.000 women. A sample one of the objectives is to assess the NORPLANT has an effective life o
five years, is not recommended for lac
of 1,000 women was then drawn up and relative acceptability of the device.
tating
women and yet is being promote
this trial was initiated in July this year at Similarly targets have been set for
NORPLANT recruitment but not for an as a spacing method. Which woma
ten medical colleges.
There are a number of problems overall limit for the udy biasing coun would be advised to space her childre
with the way this study has been de sellors to push NORPLANT among by seven years?
NORPLANT the world over has
signed and also with its implementa eligible women. Similarly, the re
tion. First and foremost NORPLANT is searchers arc not full} informed of the record of abuse possibly surpassed onl
not being offered as an experimental side effects by the research protocol. by the vasectomy drive in India durin
method but as a choice among many Serious side effects which include ovar- the emergency. While in the US it ha
We have taken a Five Year
Insurance Plan...
'■
1
3
c
VJe have left no roon for Surprises
[WRPLANT
*
HEALTH
aulhorities such as judges
ated with injectables and
and welfare workers who
implants arc brushed aside
Caira eksklut»if
rnelestarikan mi Uses
want to ensure that women
as minor inconveniences
on parole and welfare do
without scientific basis and
not reproduce, in Indonesia
it has taken thirty years to
it has been used without
even initiate research on this
even informing women that
subject. Similarly while the
it can be removed before
stress is on the promotion of
five years are over.
spacing methods many
US approval at any rate
methods have not been
is no guarantee for safety.
tested sufficiently for return
There is no comparison
of fertility, return of the
between healthy North
ability to bear healthy chil
American women and their
dren and (he likely impact
■IMA '
■I
average Indian counter
of invasive methods on
parts. There is no compari
breastfed infants. Long
son between emergency
term follow-up of subjects
X'.
medical assistance or for
which is essential to deter
that mailer in product li
mine the carcinogenic po
ability laws. Or do we
tential of hormonal contra
propose to follow the ex
ceptives among women and
ample of Indonesia where
their children is absent. Is
this scientific?
insertion (and hence
screening and surgery) is
Medical researchers
carried out in facilities Promoting a positive image for NORPLANT in Indonesia.
never tire of talking about
which lack examination ta
the cafeteria approach. But
sessed. The abilii to deliver services what recourse is available to sexually
bles. running waler and electricity?
We are now aware that HIV virus safely depends 01 :ie quality and reach active women who are not living within
spreads also through heterosexual inter of the health cai system. Even if it the confines of marriage? Why does
course. Experts suggest that India is on were possible to deliver a particular research always model itself on a long
the verge of an AIDS epidemic. In this technology the costs arising out of the standing couple relationship where a
context it is important to note that cost of delivery, cost of screening and woman is constantly exposed to the risk
NORPLANT provides no protection monitoring, cost of training the per of pregnancy when this is akin to taking
against HIV and is likely to contribute sonnel and above al 1 the cost of morbidity a daily dose of aspirin to prevent a
to the spread of the virus because of the likely to result h orn the side effects headache? - It is well known to all, that
surgery involved. The Population must be weighed against the benefits of ever increasing migration from rural
Council makes a ludicrous suggestion providing additional choices to women areas would mean that even married
that NORPLANT should be used for ie, how many wi icn would have an women need contraception for sporadic
contraception but a condom should be unmet need satisfi- 1 and hence the con and spontaneous sexual intercourse. Yet
used against HIV. Why not dispense crete benefits from the method. These little research is aimed at this segment.
with the implant because a condom can estimates are invariably available be
It is equally well known that a large
cause most contraceptives undergoing proportion of Indian women are anae
ake care of both requirements?
Of course the side effects listed in trials in India are in use elsewhere. It is mic and yet no research is aimed at
the official literature occur among important to state that in a family plan
methods which do not entail increased
women who have been screened for ning programme like ours, the abuse bleeding losses, with the exception of
contraindications including pregnancy, potential of a contraceptive (which immunological contraceptives which
liver disease, hypertension, heart and means how it can be forced upon women) put more at stake than the present hor
clotting disorders, cancer etc. No one is a critical factor n approving contra monal methods.
knows how other women will respond. ceptive methods > cn for research.
In fact, it can safely be asserted that
In today’s context, only a method research on contraceptives is akin to
Not allowing research to take place
labels women's organisations as being which has the potential to serve contra endless packaging of old wine in new
anti science. But surely quest of ceptive needs of men or women better bottles - most of it is aimed at finding
knowledge cannot be at the expense of and costs the exchequer less than the new delivery system for synthetic hor
human beings. And al any rate what is other methods while providing protec
mones for continuous contraceptive
scientific about trying to do away with tion against HIV and with a lower po
protection while safety questions are
research before introducing a new drug? tential for abuse can be logically cleared left unanswered. And increasingly even
Or for that matter what is scientific for cI inical triaIs. B ut this logic couId be this research is being dispensed with as
about printing promotional literature in applied if the trial are meant to serve has been the case with the approval
advance of the research? Or for that the cause of scicir ‘ and humanity.
accorded to Depo Provera last year and
matter what is scientific about research
Not only doc'■ ’hequestion ol choice the promotional literature on
ing into products which will only in of new methods have to be answered
NORPLANT’ and Cyclofem.
♦
through research but some other enquir
crease human misery?
Before starling research the appro ies with respect to existing methods arc
1 IM®
■
%
I
!
HEALTH & ^SAFETY.
I
l
4
The case of the nuclear
human guinea pigs
Recent revelations that US government agencies, private corporations, hospitals and
universities have subjected pregnant women, newborn infants and mentally retarded
I
I
I
r
children to secret radiation experiments have sent shock waves throughout the world.
US OFFICIALS say they area long way
from compensating the thousands of
human guinea pigs subjected to secret
government radiation experiments fol
lowing World War II.
‘People don’t want to gel caught
with something that could be a multibillion-dollar thing.’ an administration
official told reporters. ‘There’s just not
loads of money to go around.'
The comments appear to contradict
those made by Energy Secretary lla/el
O'Leary, who has led the government's
inquiry into the experiments. She said
on television that victims should be
compensated.
‘Many have suggested, and I tend
to agree personally, that those people
who were wronged need to be com
pensated,’ O’Leary said in the 28 De
cember interview. ‘1 am appalled by
what was done.' she said. ‘Clearly
standards were used that should never
have been approved.’
800 people involved
I
The experiments involved expos
ing people to. and injecting them with,
doses of radiation without their informed
consent. The extent of the experiments
is still unknown and new reports surface
almost daily. O'Leary said some 8(H)
people were involved.
Government agencies, private cor
porations, hospitals and universities
conducted the experiments from the mid1940s to al least the mid-1970s on
pregnant women, newborn infants,
mentally retarded children, native
Americans, and prisoners, among oth
ers.
The Atomic Energy Commission,
the predecessor of the U.S Energy De
partment which oversees the country's
nuclear programme, managed most of
the experiments.
O'Leary's suggestion of compen
sation was the first time the government
has taken the lead in offering payments
to survivors of nuclear tests.
But the Bill Clinton administration
will not immediatel change course,
according to official Spokesman Jeff
Eller has said on 10 January 1994, that
the White House was still a ‘long way’
from committing to compensation.
High-level task force
The administration has, however,
announced the formal ion of a high-level
task force to investig . the scope of the
radiation experimen. including how
many people were us. I as guinea pigs
and i f they should receive compensation,
The scandal over the experiments
began in December 1993 when a New
Mexico newspaper reported that 18
hospital patients were injected with high
concentrations of plutonium between
1945 and 1947.
On& woman wa reportedly moni
tored for 35 years ' ithout being told
what had been done to her. The paper
said another subject’s body was ex
humed 31 years after burial and sent to
a government laboratory in Chicago for
further tests.
More revelations of the experiments
surfaced as researchers dug through
thousands of newly declassified docu
ments released by ll Energy Depart
ment. The media als< 11 vestigated local
reports of abuse.
The Boston Glohe reported in early
January that more than 30 meniallyretarded children were fed radioactive
foods as part of a l()-year study in the
1940s and 1950s. It said the experi
ments were performed at Harvard Uni
versity and the Massachusetts Institute
of Technology and upported by the
food company QuaL ■ Oats.
In another case in the late !940s.
hundreds of pregnant women in Nash
ville. Tennessee, were reportedly given
radioactive iron to study its effect on the
development of the child. The stud
found higher than normal cancer ral
among the children born.
Newborn infants were also su
jected to tests, hi one study. 235 we
reportedly injected with radioactive i
dine, apparently to see how the thyro
gland works. The results were publishe
in the 1950s and 1960s.
At the time of the experiment
officials acknowledged they riske
criticism for not telling people what wa
being done to them. One official likene
the experiments to those of Nazi doctor
at the Buchenwald concentration cam
during World War IL
Buchenwald touch
‘If this is to be done in humans
warned researcher Dr Joseph Hamilton
in a 1950 memo, T feel that those con
cerned in the Atomic Energy Commi
sion would be subject to considerabl
criticism as admittedly this would hav
a little of the Buchenwald touch.’
But the studies enjoyed the suppo
of government agencies, universities an
hospitals, including the National Aero
nautics and Space Administratio
(NASA), the US Public Health Service
Columbia University and the Universit
of California.
Government Researchers also con
ducted experiments in prisons. I
Washington and Oregon, reports sa
131 prisoners had their testicles expose
to radiation to see what effect it woul
have on sperm production and to fin
out how much radiation was necessar
to make them sterile.
The Clinton administration’s new
task force, comprised of representative
from all major government agencies
will seek to answer lingering question
and see if experiments involving
chemical and biological weapon
were also performed on unwitting sub
jects. - IPS
♦
Soc. Sci. Med. Vol. 22, No. 11, pp. 1235-1245, 1986
Printed in Great Britain
0277-9536/86 $3.00 + 0.00
Pergamon Journals Ltd
Coro H
SECTION T
CULTURAL COMPONENTS OF BEHAVIOURAL
EPIDEMIOLOGY: IMPLICATIONS FOR
PRIMARY HEALTH CARE
1 and L. Shore 2
H. K. Heggenhougen
‘Evaluation and Planning Centre, London School of Hygiene and Tropical Medicine, University of
London, Keppel Street, London WC1 and department of Health and Welfare Education, Institute
of Education, University of London, Bedford Way, London WC1, England
Abstract—In this article we discuss the association of culturally linked behaviour and epidemiology: that
patterns of disease are significantly related to cultural sets of normative beliefs and behaviour. The
literature on this is vast and includes much of what is written under the headings of Medical Anthropology
as well as, for example, Cross-cultural Psychiatry and Medical Geography. A comprehensive review is
obviously impossible, but as this is presented primarily as a background paper, basic issues are raised,
and related to examples from the literature, to stimulate discussion. The article is divided into four
subsections which give an indication of our focus: (1) culture, disease and illness causation; (2) utilization
and provision of health resources; (3) health, illness and normative socio-political and economic behaviour
and (4) primary health care, community participation and culture—implications for the future.
INTRODUCTION
li
We need only read Fabrega’s 1974 volume Disease
and Social Behavior [1] and scan its 30 pages of
references to be convinced that behaviour and disease
prevalence and incidence are interconnected. It is
clear that people’s behaviour affect agents, hosts and
environment to either increase or decrease the risk of
a whole range of diseases and ailments. It is this
which we understand as behavioural epidemiology,
the study of patterns of morbidity and mortality of
various groups which may be associated with par
ticular behaviour (e.g. it has been found that smok
ing behaviour is, epidemiologically, associated with
higher rates of lung cancer for smokers than for
non-smokers).
There are many reasons why we behave as we do,
but much of what we do, and how we do it, is
culturally determined. We may agree with Landy
that, “. .. almost every facet of human behavior
seems to be either modifiable or impressively
influenced by cultural factors” [2]. Culture has many
definitions, but most would agree that it is a set of
beliefs and behaviour shared by a specific group.
Thus by the very fact of our belonging to such a
group, as we all do, we all have been socialized to
accept certain values and behaviours as normative.
Even if we argue that no culture is static, with some
being particularly fluid, and that acculturation and
multiculturism, not to mention cultural imperialism,
have relevance in most parts of the world, we are
all undeniably influenced by cultural norms, be they
The views expressed in this article are those of the authors
and do not necessarily represent those of the institutions
with which they are associated.
those of dominant and/or of the sub-culture in which
we live. It may be that the culture of our youth is
different from the one we live in as adults both
because of change over time and because we may
have moved from one culture to another, but this
does not minimize the influence of culture, though it
does signify dissonance.
Since the publication of Benjamin Paul’s Health,
Culture and Community [3] in 1955 and Steven Polgar’s
major article, “Health and Human Behavior: areas of
interest common to the social and medical sciences”
[4] in Current Anthropology in 1962, the connection
between culture and epidemiology has been clearly
established. It is now widely accepted, not only by
social scientists but also by a substantial number of
health professionals that patterns of disease are
significantly related to cultural sets of normative
beliefs and behaviour. It is now no longer considered
strange that anthropologists work in medical schools
or with health services programmes as it was less than
10 years ago.
More recent volumes such as Tandy’s, 1977,
Culture, Disease and Healing [2] and those published
in the “Comparative Studies of Health Systems and
Medical Care” series edited by Leslie [5] since 1978
and those in the “Culture, Illness and Healing” series
edited by Kleinman [6] which began in 1981 are but
a few of the more well known of a vast literature
which convincingly makes the connection between
culture, behaviour and epidemiology (e.g. [7-14]). The
current prominence of this connection does not imply
that it is a new discovery. It has been recognized and
expressed by medical philosophers and practitioners
from Hippocrates [15] to Virchow [16] and, more re
cently, Dubos [17, 18] and Engel [19]. The rediscovery
is connected with a growing disillusionment with the
disproportionate prominence and pre-occupation
1235
COMMUNITY HEALTH CELL
47/1, (First Floor)St. Marks Road
BANGALORE-560 001
1236
H. K. Heggenhougen
and L. Shore
and other’s health. Although many practices linked
to ill health are a matter of personal choice or prefer
ence, for the most part they are socially condoned
within a given cultural context. Excessive alcohol
consumption, for example, with related morbidity
and mortality, is primarily a problem culturally
confined to non-Moslem societies.
In a broader context, industrial-technological
progress initiated in the Western world may be
regarded as health-hazardous behaviour, in which
environmental pollution, as well as direct contamin
ation by carcinogenic agents, is essentially condoned
by its very presence.
The crucial importance of diet to one’s health is
widely accepted; today, in the West, the concept of
‘you are what you eat’ has developed to the point of
fanatic fadism—in which specialized, exclusive diets
purported to be health promotive, compete with one
another for followers. There are, however, dietary
practices which can be directly associated with
various illnesses [20, 21]. This is in addition to those
associated with malnutrition caused by specific
deficits in food resources [22].
A number of practices, associated with specific
cultures, have been noted for their deleterious effects
on health; the practice of female circumcision [23],
particularly the practice of infibulation, is significant
for the attention it has received not only as a health
but also a feminist issue. Some practices are more
indirectly linked to ill-health; the performance of
uvulectomies on newborns in Northern Nigeria, for
example, has been linked to high incidence of early
childhood anaemia [24]. Another example is that of
unilateral breast-feeding, in which an increased risk
of cancer in the unsuckled breast has been evidenced
[25]. The occurrence of what has been called ‘culture
bound syndromes’ which are said to be culture
specific, should also be mentioned although their
etiology is not clearly established [26, 27]. In both
developed and developing countries, specific behav
iour as well as cultural context, are influential
in determining health status (see, for example
[28-34].
Hypothesizing that lifestyle—or culturally influ
enced behaviour—is a major determinant of com
munity health, a rural subsistence community (Papua
New Guinea) and an urban industrialized society
(Australia) have been contrasted regarding such
features as physical environment, social situation,
human relationships and parameters of health and
patterns of disease. The former community, seen as
self-reliant, socially cohesive, whose members are well
adapted to their physical and social environment,
were free from major degenerative cardiovascular
diseases, with little overt psychiatric illness, but with
a heavy burden of infectious disease and marginal
nutritional status.
On the other hand, the highly industrialized com
munity lacks social cohesion and depends heavily on
technologies of production and discourages direct
relationships between its members and their physical
environment. The price for containment of infectious
CULTURE, DISEASE AND ILLNESS—PATTERNS
disease, diminished infant mortality and extended
OF ILLNESS CAUSATION
life expectancy would seem to be increased levels of
It is widely acknowledged that a great deal of degenerative disease and disease from psychological
human behaviour is directly hazardous to one’s own stress. The authors conclude that health, in its fullest
with the technological and biomedical aspects—the
technological fix—of health and illness. This does not
imply a disregard for the value of biomedicine but
rather a recognition that it may be faulted for having
become but a partial healing process.
Most of what is known as medical anthropology
and much of the literature of such fields as crosscultural psychiatry, culture and personality, and medi
cal geography can be related to culture, behaviour
and epidemiology. It would be unrealistic to attempt
a comprehensive review of such literature. Rather, we
want to present a few examples of this relationship
and, as this is written as a background paper, to raise
some issues which may serve to stimulate discussion.
We have done this under four basic headings: (1)
culture, disease and illness causations; (2) utilization
and provision of health resources; (3) health, illness
and ‘normative’ socio-political and economic behav
iour and, in conclusion; (4) primary health care,
community participation and culture—implication
for the future.
First a word must be said about measurement,
however, and about the care which should be taken
in drawing conclusions from comparative crosscultural morbidity and mortality statistics. ‘Obvious’
differences may not be as obvious as they first seem.
The quality of health statistics is not uniform
throughout the world; the reliability of statistical
records varies considerably. In some countries
national health statistics are based upon reports from
less than 25% of the health facilities. Emphasis on
what is recorded and the categories used also vary
from country to country.
It must also be remembered that, especially in
developing countries, a significant proportion of ‘ill
ness events’, and causes of death, are not included in
the statistics at all since they are unknown to the
official health system. There are usually no records of
ailments receiving the attention of traditional prac
titioners, for example, or of those dealt with through
self care. Even where medical pluralism is practised,
as it is in most places throughout the world, where
health care is sought from the orthodox as well as
from a number of other health resources, the problem
persists. The complications arise both because of
multiple resource use for the same ailment as well as
from the tendency to use one rather than another
health resource because of the character of a
particular ailment.
The epidemiological pattern which emerges from
the morbidity and mortality statistics recorded by the
official health system, therefore, may be both mis
leading as well as incomplete. This is not to say that
cross-cultural epidemiological comparisons can not
be made but rather that specific comparative studies
which do not only rely on available (regional and
national) statistics may be needed before conclusions
can be pronounced about the associations between
cultural characteristics and specific epidemiological
configurations.
Cultural components of behavioural epidemiology
sense, is not the prerogative of any one type of society
[35].
The well being of a family may be influenced in
most societies by the degree to which the female
carries out the usually unpaid role of nurturer, and
provider of physical and emotional comfort. In the
industrialized West, the woman’s burden of a ‘double
workload’ when she is wife and mother as well as a
salaried worker is one she shares with most women
in rural developing societies. Common to both is the
lack of value placed on the non-paid work women
carry out. Paradoxically for cultures predominantly
defined by men, the concept of motherhood holds
high status, but the toil of mothering is largely un
acknowledged. Misogyny is perhaps not too harsh a
term to describe cultural attitudes in which not only
is little value placed on women’s work within the
home, but unequal value is placed on work outside
the home as well, by lower salaries, fewer opportun
ities for advancement, etc.
The preference for male babies has been docu
mented in several cultures, where property and status
are male sex linked. A most recent example of female
infanticide is seen in China, where the one-childfamily ruling has led families to sacrifice first born
daughters to allow them a ‘second chance’ for a son.
So concerned has the Chinese government become
that special allowances have now been made to
permit some families more than one offspring.
Cultural change and health
Culturally influenced psychological stress is not
only of concern to members of highly industrialized
Western societies, where stress related morbidity and
mortality have been well documented. Cultural trans
formation has also been studied as it has affected
patterns of illness in various groups. Coronary heart
disease, hypertension and cancer as well as a number
of other diseases have been found with greater inci
dence among people who have migrated from one
culture to another [36-38]. The patterns of illness
may change due to diet, physical environmental
factors as well as to socio-psychological phenomena
of cultural change and stress related to adaptation
[39-41].
Differing levels of physiological stress have been
related to cultural change and the extent to which
acculturation has been undertaken. Reaction to
culture change, either short-term or over generations,
has been noted to follow a (/-curve, with intermedi
ately acculturated immigrants exhibiting higher levels
of stress than either high or low contact groups [42].
Rapid socio-cultural transitions, brought about in
primarily subsistence economy societies by post-war
contact with Western culture, have caused trans
formations in economic structure and dependence, in
demographic shifts, as well as in traditional com
munal life styles. In Micronesia, this transition has
seen suicide rates among adolescent males increase
in epidemic proportions; the phenomenon has been
suggested attributable to the post-war social change
in Micronesia, in which the communal village level of
organization has largely disintegrated [43]. Also,
comparatively higher incidences of high blood pres
sure have been found among males in more modern,
urban areas in Micronesia [44].
SSM 22'11—J
1237
One hypothesis suggested by Cassel [44], based on
comparative studies of blood pressure levels, holds
that low pressures occur in societies with a coherent
value system which remains relatively unchallenged
in a generation, but migration to a society with a
different value system could lead to dissonance, re
sulting in sustained elevation of blood pressure. The
other hypothesis emphasizes physical factors, caloric
intake, physical activity, body build, salt intake
and the presence of parasites and diseases which
could influence blood pressure level. However, both
hypotheses could be associated with modernization
and migration [45].
High levels of modernity and acculturation have
similarly been found to influence higher rates of
coronary heart disease (CHO); in a study of
Japanese-Americans, the most traditional group had
a CHD prevalence as low as that observed in Japan,
whereas the group which was most acculturated to
American culture had a 3-5-fold excess in CHD
prevalence [46].
Implications of psychological stress on health
Although the mortality rate world wide is greater
due to disease, comparative rates of suicide may be
indicative of the level of psychological stress in a
society, as well as of the relative lack of sociopsychological support in situations of personal dis
tress. Compared with figures from the British Isles,
the real rate of suicide is twice as high in Denmark,
for example [47].
This difference is surprising, perhaps, due to the
latter country’s highly developed health and social
welfare system, which optimally provides security
from poverty and untreated illness. The security may
not provide support, however, but in fact may be
regarded as an alienating and patronizing safety net
of caretaking for those who have not met the high
standards of health and socio-economic status set.
State provisions of homes for the elderly have
expanded as the extended family has diminished,
leaving many elderly virtually alone; indeed the high
est rate of suicide in Denmark is among the older
citizens, although the rates among younger people,
and younger women especially, is increasing.
The alarming fact that younger people in many
societies today experience the ultimate breakdown of
psycho-social support networks and resort to suicide
may also be linked to a society’s lack of opportunities
for mobility—for changing environment, ‘starting
over’ and finding new inspiration or support. In the
United States the ‘go West young man’ phrase can
clearly be seen adhered to in its high level of mobility
and varied opportunities (we have already noted
some of the negative effects of this constant tran
sition, but it also has its advantages). As a side
comment, it is notable that the majority of those
committing suicide by falls from the Golden Gate
Bridge in San Francisco are reported to have jumped
off the West side.
UTILIZATION AND PROVISION OF
HEALTH RESOURCES
What do people do when they become sick? Obvi
ously, the reasons for the choices depend on the type
of ailment and on a great number of other factors.
1238
H. K. Heggenhougen
They are also related to, and influenced by, culture.
Specifically, they may be linked to beliefs about
etiology and to more general concepts of health,
illness and appropriate treatment which differ from
culture to culture (much has been written on this and
some of the more recent literature includes [2,4855]). The consequences of these choices, the different
processes, types and timing of treatment, can be
related to outcome and thus, epidemiologically to
prevailing patterns of disease. There are many
accounts, for example, of beliefs about appropriate
treatment for certain afflictions which contradict
what is considered medically sound by allopathic
practitioners—not that they have always been found
to be correct.
Definitions of disease and illness also vary from
culture to culture and if what ‘we’ think of as disease
is not considered as such (nor considered an illness)
but rather as a normal phenomenon [56], attempts to
combat it would also be expected to be non-existent
or minimal. In Malaysia, for example, Heggenhougen
was directly told by several villagers that it was
impossible for people not to have worms, and that if
they did not have them something would be wrong
with them. Numerous such examples can be found in
the literature which consider it normal to be afflicted
by a variety of, what we would call diseases. Klein
man et al. [53] among others [1] have clearly discussed
such differences in definitions and have emphasized
the distinctions between disease and illness. These
differences are relevant not only for decisions to
engage in, or seek, treatment or not, but are also
pertinent regarding the practitioner-patient inter
relationship, subsequent compliance and outcome.
Only a few years ago the World Health Organiz
ation’s estimate claimed that traditional medicine is
the primary health service resource available for up
to 80% of the population in the rural areas of many
countries [57]. Self care and the considerable knowl
edge and assistance of people themselves must of
course not be forgotten, be this in rural areas of
developing countries or elsewhere. Increasingly, how
ever, at least some form of alopathic health services
are available to most people; the value of allopathic
medicine is widely recognized, albeit more for certain
afflictions that for others. But this recognition does
not necessarily mean that allopathic medicine is
always the preferred choice of treatment. Quite often
medical pluralism is practised [58,59]. Different
resources are used either alternatively for different
ailments and/or multiple resources are used at the
same time, serially or intermittently, for one ailment.
Such treatment practices could have both positive
and negative outcomes.
The position of the afflicted within a particular
cultural group, the accepted sick role and the
relationship of the larger group and of health pro
fessional to the sick is significant to the health of
the individual and often to the group at large [60].
Included here are concepts of stigma and status and
accepted long- and short-term rehabilitation prac
tices. Types of illness behaviour and the behaviour of
others to the ill person obviously relate to choice
of treatment, to the quality of the immediate,
practitioner-patient therapeutic process, to compli
ance and to the overall rehabilitative process which
and L. Shore
can be significantly related to outcome (see, for
example [50, 61]).
The interaction between practitioner and patient is
crucial. It is a process which could be a positive
‘therapeutic alliance’ [62] but at least within the
Western medical paradigm, the interaction often
takes place between people of unequal power across
a considerable cultural gap. The quality of this inter
action—of the immediate treatment process—can be
related to rates of compliance to treatment regimen
[63-65]. This relationship and the consequent quality
of compliance and subsequent outcome can in turn be
related to culturally determined concepts of health
and illness which may be shared by, but which often
are different for, practitioner and patient.
Steffensen and Colker [66] have reported on a par
ticularly interesting study which “provides evidence
that absence of shared concepts between practitioner
and patient may impede even willing compliance”. In
other words, patients do not comply because they do
not understand what the practitioner is talking about.
The study involved a matched group of Australian
Aboriginal and North American women who heard
and recalled two stories incorporating Aboriginal and
Western conceptions of illness and treatment. Both
groups showed an equal ability in recalling the story
relevant to their own culture and an equal inability to
recall the story relevant for the other group’s culture.
Significant also are differences in manifestation,
presentation and description of symptoms including
response to, and admission of, pain by members of
different cultures [67-74].
Health education attempts to influence people to
do something they are not now doing or to make
others stop or change what they are doing. It is
recognized that it is necessary to promote cultural
change. The provision of health education, and its
impact as reflected by how people react to it, is a
factor concerning both disease incidence and preva
lence. The rigid, hierarchical approach of some health
education must be examined, as it assumes a medical
cultural imperialism in which the Western allopathic
medical model is superior.
Much of the technical and biomedical aspects of
allopathic medicine is effective and is clearly recog
nized as such by most. It is the character of the
treatment process and the lack of communication,
despite the conversations held, which constitute the
problem. And here, allopathic medicine may have
something to learn from traditional medicine [75-78].
This is another vast subject and Engel [19] is but one
of the most widely quoted critics of the prevailing
bio-medical model, suggesting that the character of
the medical system(s) itself should also be changed.
Reasons for choices
The decision to use, or not to use, a particular
treatment resource, or a multiple of resources, neces
sarily depends upon availability and accessibility. Of
equal importance is the acceptability of these re
sources. How does a system, and/or its practitioners,
relate to particular patients? Do patients and their
families have confidence in the practitioner? Are they
at ease within the therapeutic setting? Do they believe
the practitioners properly understand them? Do
patient and practitioner speak the same language
Cultural components of behavioural epidemiology
—both literally and figuratively? In short, do they
belong to the same culture, and if not, can they
overcome and communicate across the cultural
barriers?
Annis [79], for one, has argued that the reason
people—in this case Guatemalan Indian peasants—
do not use the available allopathic services is more
because they lack drugs and equipment than because
of any cultural barrier. We agree that this is a
significant reason and lack of drugs and equipment is
the norm in rural areas throughout much of the
developing world. As stated above, we further agree
that most people, be they peasants or nomads, recog
nize the significant efficacy of much of allopathic
medicine, but we still maintain that despite avail
ability of a well stocked health centre its use may be
considered unacceptable because they may be too
great a cultural distance between patient and prac
titioner and because of such factors as racism and
arrogance—this certainly is the case in Guatemala.
These factors, in addition to drugs and equipment,
are significant for quality of care.
Choice depends on culturally instilled normative
concepts of health and illness and on what is felt to
be appropriate treatment. It also depends on the
patient’s, and/or his family’s, etiological perception
about the particular ailment in question. Much of the
vast literature on this is well known and need not be
expanded on here (see, for example [2, 48, 80-82]).
Let us but mention two sets of binary concepts—the
hot/cold or yin/yang perceptions about illness, food
and medicines, and what we may call the how/why
perceptions about etiology—both of which may be
related to choice, treatment and to outcome.
The division of foods, illnesses and medicines into
hot/cold, or yin/yang categories is evident in a great
number of cultures and is well documented par
ticularly in the medical anthropological, but also in
the more general public health, literature. As illness
is often conceived of as dissonance, or imbalance,
between these binary forces within the body it is felt
important to restore harmony by reinforcing the
element (hor or cold) which has become depleted.
Thus a cold illness should be treated by what is
considered a hot medicine or aided by a hot food.
Many people are concerned not only with how they
became ill—the host/agent inter-relationship consid
ered biochemically—but also with why they became
ill. They are not only concerned with, for example,
the biomedical inter-relationship between agent and
host but also with the more spiritual or social aspects
of illness, many ailments are, of course, considered as
purely naturalistic, but others are also seen in a
different light. Most people are aware that they fell ill
because of, for example, a snake bite or even because
of a mosquito bite—what we refer to as the ‘how’ of
an affliction—but many are also often concerned with,
“why me?" And with “why me, at this particular
time?’’
Voodoo, charms and spiritual aspects of illness of
various kinds may be of utmost importance to many
patients. Illness may also be seen as a sign of wrong
doings or sins. The dissonance to be balanced is then
not only within the body, but also outside. The
relationship with others, or even with ‘the gods’ or
the ancestors may be seen as faulty, and if it is, then
1239
a treatment process which aims to restore harmony
within the family, the group, or between man and
the ancestors or gods may be considered of equal, or
greater, importance than the biomedical treatment
of the physical disease. And if such treatment does
not take place—if this ‘why’ aspect of an illness is
not attended to—stress will remain: the patient will
remain uneasy or dis-eased.
We know well enough the powerful inter-relationships between attitude and feelings and physical
health—the inter-relationship between mind and
body [83]—to recognize the deleterious effects of not
paying attention to this ‘why’, whether we believe it
to be ‘superstitious’ or not. In many ways, reality
becomes what we perceive it to be [61,84, 85]. In this
light the use of allopathic health resources may be
seen as a necessary, but not always as a sufficient,
treatment process. One reason for the frequent
preference for traditional over allopathic treatment
is precisely because traditional medicine tends to pay
greater attention to this aspect of healing. If an
ailment is considered to be predominantly of a super
natural nature, biomedical treatment whether by
allopathic or traditional herbalists, however, will be
secondary.
Consequences of choices
The choice of treatment we make, or are urged to
make, is usually, but not always, made in the ex
pectation that it will be to the benefit of ourselves or
an ailing relative. However, the choice of treatment
may have either positive or negative consequences, or
both. Leaving aside the positive for the moment, let
us concentrate on the negative consequences and
on how choices, and timing, of treatment may affect
patterns of diseases.
Before mentioning treatment choices for what we
would call actual disease and illness we must also
consider the consequences of a number of culturally
determined practices, or medical interventions, such
as infibulation, uvulectomies, cutting of so-called
plastic teeth and the like which are done both for
social and for their potentially disease preventive
effects (see, for example [23]). Similarly it should
be mentioned that the perhaps too frequent and
accepted practices of tonsillectomy and coronary
bypass surgery may be unnecessary and could have
negative medical as well as economic consequences.
A common complaint of allopathic practitioners
(and especially of the few who are ethnocentric and
who do not fully understand the concept of ‘accept
ability’) is that because patients first seek help from
traditional practitioners, or practice self-care, they
delay too long in finally arriving at a health centre or
a hospital. Many of these ‘cases’ which could have
been cured, die because they arrived too late. And
why do they arrive too late? In addition to the
reasons mentioned previously, another is that hospi
tals and even health centres have become known as
places people go to, to die. Because people hesitate as
long as possible before going, the chances that people
will die when they finally do go increase—it is a
vicious circle.
The capability of many traditional healers in treat
ing a number of ailments must be questioned; but it
is not always clear if the rate of iatragenesis is greater
1240
H. K. Heggenhougen
for traditional healers than for allopathic practi
tioners. The multiple use of different health resources
is also a cause for concern since these do not neces
sarily complement each other but may be in conflict
especially if a patient receives and takes medicines
from more than one source at the same time.
Rehabilitation and behaviour toward the afflicted
It is evident that the illness behaviour of the
afflicted—how s/he behaves and/or is allowed and
expected to behave by her/his cultural group—is
important relative to the choice of treatment, the
quality of the therapeutic process and to the eventual
outcome. How the family, the larger cultural group
and various health personnel treat the sick both in
terms of acute affliction and relative to rehabilitation
and degree of integration within the group for
chronic patients, is also important. The literature
point to a great deal of cultural divergence of such
behaviour which is epidemiologically relevant.
Do family and friends tend to isolate, ignore or
shun the sick or do they closely comfort and care for
and associate with the afflicted? Depending on the
ailment, both extremes of such behaviour could have
negative effects for either/or both the patient and
those with whom he is in contact. Does this depend
on the type of ailment? In many cultures in both
developing and developed countries leprosy and
STD, for example, carry a stigma. They are diseases
which are often considered the results of sins or
ethical and social misconduct. Will such ailments be
kept secret and treatment avoided or delayed? What
of those with other ailments such as polio, or the
mentally retarded, the neurotic and psychotic? How
are they treated or cared for by the communities in
which they live? Are some confined? Are others
ignored and left to suffer in poverty and starvation
for want of being able to support themselves? Are
boys better cared for than girls? The answers will vary
from culture to culture.
Two specific examples may be mentioned: studies
of psychological support in illness and rehabilitation
found that cultural attitudes regarding personal
responsibility for illness in Sweden influenced the
quality of care received by hospitalized patients.
Comparing Australian and Swedish health profes
sionals, it was found that differences in the quality of
patient care were attributable to the Swedish health
professionals’ stronger belief in personal responsi
bility for health. This belief was found to influence
the health workers’ perceptions of patients as less
attractive and less deserving of care. Conversely, the
Australian health workers, more highly trained in a
psycho-social approach to patient care, were found to
assume that their patients’ illnesses caused emotional
distress and that they were in need of support. The
study concludes that the cultural values of health
professionals may influence the outcomes of inter
actions between patients and practitioners [86].
Psychological support and maternal attitudes have
been found to critically influence the outcome of
rehabilitation efforts provided for children suffering
from malnutritional diseases. A study of Ugandan
children treated for kwashiorkor and marasmus
found a higher rate of successful rehabilitation
among those children whose mothers were actively
and L. Shore
engaged in stimulating, playing with and holding
their children during hospitalization. The children
whose mothers ignored their cries for attention and
cared fared much more poorly, and in many cases the
rehabilitation efforts were totally unsuccessful. The
fact that familial support and caring during illness
influences the outcome of rehabilitation is not
questioned. What is, is the extent to which cultural
factors determine the implementation of the psycho
logical resources necessary to provide for successful
rehabilitation.
The Western model and its accompanying cultural
norms have been accepted or enforced throughout
the world. In addition to economic constraints, the
character of this medical orientation is also inappro
priate in a great number of situations in both devel
oped and developing countries. It is not the optimal
approach required to achieve the stated goal of better
health for the total population. This inappropriate
ness is now widely recognized, at least in theory if not
in practice, and one reaction may be related to the
promotion of primary health care.
HEALTH AND ‘NORMATIVE ’ SOCIO-POLITICAL
AND ECONOMIC BEHAVIOUR
We have mentioned the potential consequences to
health for those individuals who by and large accept
and carry out their culture’s normative pattern of
behaviour. Here we intend to discuss culturally deter
mined behaviour on a slightly larger scale and the
consequences this may have both for the health of
members within as well as outside the boundaries
of a specific culture [87]. Related to this is cultural
imperialism—both within and across national bound
aries, which imposes the normative behaviour of one
cultural group onto another. Regarding both of these
concepts we recognize, though, that cultures are not
static and that because of cultural diffusion, trans
mission and international communication it is not
always easy to distinguish specific cultural bound
aries.
Our concern here is with political, social and
economic behaviour—policies and practices—which
are either accepted, or at least recognized by people
as the ‘normal’ socio-political and economic practices
of the cultural group to which they belong. This
concern includes such basic issues as racism, exploita
tion, the greed/profit motive where the end justifies
the means, aggression and war.
Development, business practices and health
The accepted behaviour by major cultural—
national or other corporate—groups of intervening in
the internal affairs of such countries as, for example,
Afghanistan and Chile, or in Central America,
certainly having dire consequences for the health of
the people in those countries [88]. Accepted industrial
and business practices can be directly linked to
the extermination of Amazonian Indians and to the
persecution and ostracism of indigenous fourth world
populations in all parts of the world. Also in Scan
dinavia, there have been infringements against the
same people—the so-called Lapps—which though
perhaps not as drastic as elsewhere in the world, may
certainly be linked to their state of well being. This
Cultural components of behavioural epidemiology
relationship has been amply documented by, for
example. Survival International and in the scores
of publications of the International Work Group
for Indigenous Affairs (IWGIA)—established by a
Scandinavian anthropologist—in Copenhagen [89].
The consequences of development, when pursued,
as it quite often is, in purely technical and economic
terms, are of utmost importance to the health of vast
numbers of people throughout the world. As well as
having positive consequences development can also
be associated with ill health which results from
poverty and life in urban slums, from migration and
from the stress of so-called modernization as men
tioned earlier. Their is also an enormous literature on
this and here we can do little more than allude to the
epidemiological significance. By mentioning these
issues within this article we may be accused of
including everything under the term ‘culture’. But,
perhaps because we agree with the earlier statement
by Tandy, we do believe that development policies
nd industrial and business practices reflect culturally
determined and accepted norms of behaviour and
should therefore be central to the consideration of
culture and behavioural epidemiology.
The magic of science, technology and so-called
development seem to have entirely won the day in
much of the world. Technicians are at a premium
with affect seen as a ‘commodity’ of little value. The
accomplishment of the possible, rather than of what
is considered valuable, has become a guiding prin
ciple. The creations of Daedalus have taken on a life
of their own and like Icarus, unmindful of the
warnings, we are borne away, riding ever onward, to
‘progress’ binging destruction to our environment, to
our fellow men, and ‘unwittingly’ (?) to ourselves.
Wordsworth’s poem is certainly much more apt now
than at the beginning of the last century.
The world is too much with us: late and soon
Getting and spending, we lay waste our powers;
Little we see in Nature that is ours;
We have given our hearts away, a sordid boon (1806).
Apartheid, racism and health
South Africa is unquestionably the most out
standing example of a country where the normative
socio cultural behaviour of one powerful group is
detrimental to the health of a significant number of
others. The recent WHO publication Apartheid and
Health [90] and the previous Apartheid and Mental
Health Care [91] clearly point to the detrimental
significance of the normative racist behaviour of the
dominant white cultural group for the health of
South African Blacks.
Racism is a fact of life not only in South Africa but
in countries throughout the world. It is inherent
in the cultural make-up and culturally transmitted
normative behaviour patterns of dominant and
subservient groups and sub-groups. The situation of
Sri Lanka is but one case in point. The ‘accepted’
behaviour of Ladinos towards Indians throughout
Latin America, of whites towards Aborigines in
Australia, and the covert, and often overt, racism in,
for example. North America and England are but a
few additional examples.
The health status of the United States is relatively
low compared to many other industrialized countries.
1241
A major reason is the considerably lower overall
health status of Blacks than of whites [92,93]. Racist
behaviour inescapably contributes to this difference.
Considering health in terms of psychological and
social as well as physical well being, we need not even
read the considerable literature on the effects of
racism, such as for example, Black Rage or the works
of Fanon [94, 95], to realize that racism is a health
hazard. Littlewood and Lipsedge’s [96] work on
racism and the behaviour toward, and of, aliens—
the outsider, the ‘different person’—and their health
consequences is most relevant.
Sadly, we must also admit, both in terms of econ
omic exploitation and of racism, that slavery and
the sale of people, particularly children [97], into
servitude, including prostitution, is not a thing of the
past but occurs in many places throughout the world
where it is an accepted way of life. The practice
may not be the ideal, or stated, cultural norm, but
it is certainly the actual and observed normative
behaviour which for various reasons exists largely
unchallenged.
Psychiatry as social control
Psychiatry, with its power to stigmatize, has been
blamed for maintaining the status quo for the elite in
dominant Western cultures. Those who are the out
siders, be they religiously, politically, racially or
socio-economically different, have been classified in
terms of psychiatric disorders, as a means by which
to contain them as separate, unequal and sick.
So-called deviant behaviour is essentially socially
defined, reflecting the balance of power in society; it
can be defined as anything which is considered a
problem by a group powerful enough to do some
thing about it. Medical labels have been assigned to
problems, which are essentially of a social origin. A
theory which maintains that deviant behaviour is the
result of mental disorders, together with a definition
of deviance which reflects the prejudices of the
socially powerful, forms a considerable weapon for
social control [98].
In the United States, the lower socio-economic
status groups predominate in psychiatric hospitaliz
ations and in being prescribed psychotropic drugs; do
the poor have greater mental disorders per se—or do
their problems arise from poverty, impotence and
fear, and is treatment of their deviant behaviour an
attempt to pacify, control and camouflage; rather
than attend to the social imbalances which lead to
‘deviant’ expressions of frustration and rage? An
historical example of how ‘deviant’ behaviour and
subsequent psychiatric labelling follows the norms or
prejudices of the predominant social group, is the
19th century mental disorder ‘drapetomania’, charac
terized by the ‘inexplicable’ and irresistable urge of
slaves to run away from their owners [96].
War and aggression—children of the nuclear age
Aggression and war are commonplace. The pre
dominance of the military-industrial complex is a
fact of life in most countries. The appropriations of
major portions of national budgets for military hard
ware is normal behaviour throughout the world.
Such expenditures leave less for other sectors which
more directly and immediately promote and support
1242
H. K. Heggenhougen
and L. Shore
health. We are all familiar with the comparisons of
how many days of required food could be supplied to
the total world's population from the funds used for
one day’s military expenditures. It is not always
convincing to be told that the considerable military
stockpiling is for defence, preservation of life and
maintenance of health. The argument that the pos
session of a gun leads to its eventual use is as coherent
as that which claims it prevents others from using
theirs [99].
The health consequences of an actual war are, of
course, obvious (see, for example [100]), but the
preparations for war, or the build-up of defences, also
have direct and indirect consequences for our health.
Yet, from generation to generation in most cultures
throughout the world we take it as a fact of life. And
now, the nuclear age. We can blow ourselves up
numerable times over. Yet we can not cry, “Stop the
world, I want to get off”. How do we stop the
treadmill; how do we stop the insanity of escalation?
How can we become, or remain, sane or healthy, in
an insane world [101]? How can health be achieved
when in so many cultures normative, accepted and
transmitted behaviour is in so many ways antithetical
to health? (Yet, to be abnormal in insane societies is
also not necessarily health promotive.)
In a nuclear holocaust there is no first aid, nor does
‘last aid’ [102] seem particularly pertinent. Whether it
makes sense or not to escalate nuclear stockpiling in
the name of maintaining peace through a sufficient
deterent, and ignoring for the moment the results of
the actual use of these weapons, the effects of growing
up in a world, in a culture, where expenditures on
nuclear weapons, and where their potential use, is a
reality is directly related to our health. Alienation,
fatalism, anomie and addictions of various kinds are
but a few of the associated consequences. Being
children of a nuclear age produces stress which,
whether acknowledged or suppressed, seriously affect
both our mental and physical state of health (see, for
example [103] concerning research which is beginning
to be carried out on this subject).
The issues we have attempted to raise here are akin
to the concerns expressed by Gellhorn, the keynote
speaker of the 1983 Social Science and Medicine
Conference [104].
influence the character and the kinds of efforts to
be undertaken to achieve the desired aims. It is
this second understanding of PHC which is more
pertinent to our discussion.
PHC implies a reaction against the limitations of
an exclusively high-tech, bio-medical orientation
(often arrogantly and ethnocentrically executed) and
accepts an encompassing definition of health. The
concept of PHC is one which quite clearly recognizes
the cultural behavioural determinants of health and
the significance of a culture’s prevailing economic
and socio-political normative behaviour.
We believe, that if taken seriously, PHC will
necessitate significant changes in the behaviour of
individuals, and overall changes in the cultural
make up of communities or nation states. These are
changes which go beyond those usually thought of as
falling within the health sector [107, 108]. The central
position of health education, as part of the specific
activities of PHC, is a concrete example of the
perceived need to bring about cultural change. We
feel, however, that most health education efforts are
considered in too limited a way—without denying the
positive effects this may have. We suggest that the
wider conceptualization of health education should
include proposed changes within the culture of the
dominant health professionals and of dominant
national groups.
Some of the reasons for this belief have already
been stated. Two additional examples may be men
tioned:
PRIMARY HEALTH CARE, COMMUNITY PARTICIPATION
AND CULTURE —IMPLICATIONS FOR THE FUTURE
Community participation is considered a corner
stone of PHC. This is, of course, translated in many
ways, from merely carrying out prescribed activities,
dictated from on high, to a truly equitable co
operation in the planning, implementation and
control of efforts which are believed to be of benefit
to an individual’s and a group’s physical, social and
psychological well being. At best, what could be
implied and attempted is the practice of democracy
and social justice.
The kind of changes which community partici
pation may call for, and which is implied by an en
compassing definition of health education, however,
may not be particularly appreciated by dominant
individuals or groups since it may call for changes in
their behaviour as well as in that of peasant and tribal
communities. One specific example of the rejection of
community participation health promotion efforts
It is clear that we believe that the sets of normative
behaviour of dominant socio-cultural—corporate/
national—groups influence not only patterns of
health of adherents of those cultural norms but the
health of sub-cultural groups within and of cultural
groups without.
If we are at least partially correct, what are the
implications for the future relative to efforts for
improving health? What are the implications for
primary health care (PHC) which, in theory at least,
is being universally accepted as the guiding concept
for improved ‘health for all by the year 2000'
(HFA/2000)? PHC is by now familiar to most and
need not be described in detail [105, 106] other than
that it is conceived of both as a set of specific
activities and as a general concept which should
(1) The 'Physical Quality of Life Index' [109] shows
that health status is not necessarily associated with
overall GNP or total wealth of a country, but rather
with the distribution of resources and benefits within
it. The examples of Kerala State in India and Sri
Lanka which have much higher PQLI ratings and
specific health status statistics than countries with
higher per capita GNPs are well known [110].
(2) Belmar’s recent findings, though apparently still
limited to Latin America, show a strong correlation
between level of democracy and health. “If this is
found to be generally true, it will have profound
implication for health policy and planning experts
who now tend to focus on technical medical care
and public health measures more than on societal
context” [111].
Cultural components of behavioural epidemiology
is that of Paulo Frcire's work in Brazil; originally
supported by USAID, finding was cut off and Freire
exiled as his conscientization programme with peas
ant groups heightened their socio-political awareness
to an extent found threatening to the existing regime.
The normative behaviour of dominant groups will
not be easy to change, yet if they remain as they are,
we maintain, they constitute a major obstacle to the
achievement of PHC goals.
PHC efforts may therefore face significant resist
ance which will impede its success [108]. This is quite
clearly pointed out by Werner [112, 113] and many
others. This is not to say that many non-threatening
changes can not take place which will have significant
positive health consequences, but this should not
blind us to the necessity for more basic changes to
attack the underlying causes responsible for the
perpetual occurrence of specific diseases. We should
also remember that the provision of certain curative
services (and the encouragement of only limited
changes) may even camouflage and divert attention
from the necessity to deal with these more basic
changes.
In closing, it must be said that it is impossible to
create a blueprint for a ‘new society’, or an Utopian
culture, where behaviour optimally supports and
promotes our own and other’s health. History is
full of accounts of the disastrous consequences of
dictatorial attempts to enforce ‘the ideal society’. We
believe dogma, no matter how comforting and health
preserving, is no solution. We agree with Audy and
Dunn that, “We do not know nearly enough to plan
societies; but we do know enough to see a number of
hazards and harmful processes and to plan construc
tively for improving the quality of the individual, a
process that starts well before birth or even concep
tion” [114], and we believe that the quality of the life
of the individual depends to a great extent on his
culture. But if it is culture which is the problem and
makes us sick, or at least contributes to our ill health,
then is not cultural, as well as individual therapy
required [115]?
We believe there are certain basic ideas which in
theory have legitimized societies for centuries,
namely, freedom, justice, equality and fraternity to
name but a few. It is appropriate to evaluate these
declared philosophies in the light of actual normative
behaviour. And since we do inevitably live in
Toeffler’s world of ‘future shock’, where ‘the only
constant is change’, the task becomes also to establish
harmony, balance and rootedness in spite of per
petual transition.
Acknowledgement—We gratefully appreciate the comments
of colleagues and friends; they are not responsible, however,
1243
common to the social and medical sciences. Curr.
Anthrop. 3, 159-205, 1962.
5. Leslie C. M. (Ed.) The volumes included in the series:
Comparative Studies of Health Systems and Medical
Care. University of California Press, 1978.
6. Kleinman A. M. (Ed.) The volumes included in the
series: Culture, Illness and Healing—Studies in Com
parative Cross Cultural Research. Reidel, Dordrecht,
1981.
7. Bibeau G. Current and future issues for medical social
scientists in less developed countries. Soc. Sci. Med.
ISA, 357-370, 1981.
8. Cassell J. T. Social science theory as a source of
hypotheses in epidemiological research. Am. J. publ.
Hlth 1482, 1964.
9. Dunn F. L. Human behavioural factors in the epi
demiology and control of Wuchereria and Brugia infec
tions. Bull. publ. Hlth Soc. Malaysia 10, 34—44, 1976.
10. Hughes C. C. Medical care: ethnomedicine. In Health
and the Human Condition (Edited by Logan M. and
Hunt E.). Wadsworth, Belmont, 1978.
11. Kleinman A. M. Toward a comparative study of
medical systems: an integrated approach to the study
of the relationship of medicine and culture. Sci. Med.
Man 1, 55-65, 1973.
12. Logan M. H. and Hunt E. E. (Eds) Health and the
Human Condition—Perspectives on Medical Anthro
pology. Wadsworth, Belmont, 1978.
13. Marmot M. Culture and illness: epidemiological
evidence. In Foundations of Psychosomatics (Edited by
Christie M. J. and Mellett P. G.), pp. 323-340. Wiley,
Chichester, 1981.
14. Vayda A. P. (Ed.) Environment and Cultural Behavior.
National History Press, New York, 1969.
15. Bulger R. J. (Ed.) Hippocrates Revisited—A Search for
Meaning. Medcom Press, New York, 1973.
16. Ackerknecht E. Rudolf Virchow. Johns Hopkins Press,
Baltimore, 1953.
17. Dubos R. Determinants of health and disease. In
Culture, Disease, and Healing (Edited by Landy D.),
pp. 31—41, Macmillan, New York, 1977.
18. Dubos R. Mirage of Health. Harper & Row, New
York, 1959.
19. Engle G. L. The need for a new medical model: a
challenge to biomedicine. Science 196, 129-136, 1977.
20. Cassel J. Social and cultural implications of food and
food habits. In Culture, Disease, and Healing (Edited
by Landy D.), pp. 236-242. Macmillan, New York,
1981.
21. Foulks E. and Katz S. H. Nutrition, behavior, and
culture. In Malnutrition, Behavior and Organization
(Edited by Greene L. S.), pp. 219-231. Academic
Press, New York, 1977.
22. Aaby P., Bukh J., Lisse I. M. and Smits A. J. Measles
mortality, state of nutrition, and family structure: a
community study from Guinea-Bissau. J. infect. Dis.
147, 693-701, 1983.
23. El Dareer A. Attitudes of Sudanese people to the
practice of female circumcision. Int. J. Epid. 12,
138-144, 1983.
24. Fleischer N. K. F. A study of traditional practices and
for the final version of this article.
early childhood anaemia in northern Nigeria. Trans.
R. Soc. trop. Med. Hyg. 69, 198-200, 1975.
REFERENCES
25. Ing R., Ho J. H. C. and Petrakis N. L. Unilateral
breast-feeding and breast cancer. Lancet 124-127, 16
July, 1977.
26. Jilek W. G. and Jilek-Aall L. The Methamorphosis
of‘culture-bound’ syndromes. Soc. Sci. Med. 21, 205210, 1985.
27. Yap P. M. The culture-bound reactive syndromes. In
Culture, Disease, and Healing (Edited by Landy D.),
pp. 340-349. Macmillan, New York, 1977.
28. Burkitt D. P. Some disease characteristic of modern
1. Fabrega H. Disease and Social Behavior. The MIT
Press, Cambridge, 1974.
2. Landy D. (Ed.) Culture, Disease, and Healing—Studies
in Medical Anthropology. Macmillan, New York, 1977.
3. Paul B. (Ed.) Health, Culture, and Community—Case
Studies of Public Reactions to Health Programs.
Russell Sage Foundation, New York, 1955.
4. Polgar S. Health and human behavior: areas of interest
1244
H. K. Heggenhougen
western civilization. In Health and the Human Condi
tion (Edited by Logan M. and Hunt E.). Wadsworth,
Belmont, 1978.
29. Dunn F. L. Behavioural aspects of the control of
parasitic diseases. Bull. Wld Hlth Org. 57, 499-512,
1979.
30. Gillett J. D. The behaviour of homo sapiens, the
forgotten factor in the transmission of tropical disease.
Trans. R. Soc. trap. Med. Hyg. 79, 1-11, 1985.
31. Khogali M. Epidemiology of heat illnesses during the
Makkah pilgrimages in Saudi Arabia. Int. J. Epid. 12,
267-273, 1983.
32. MacCormack C. P. Human ecology and behaviour in
malaria control in tropical Africa. Bull. Wld Hlth Org.
62, Suppl. 81-87, 1984.
33. Nations M. K. Illness of the child: the cultural context
of childhood diarrhea in northeast Brazil. Ph.D.
dissertation. University of California, Berkeley, 1982.
34. Zhang Y. Q.. MacLennan R. and Berry G. Mortality
of Chinese in New South Wales, 1969-1978. Int. J.
Epid. 13, 188-192, 1984.
35. Sinnett P. and Whyte M. Lifestyle, health and disease:
a comparison between Papua New Guinea and
Australia. Med. J. Aust. 1-6, 1978.
36. Hull D. Migration, adaptation, and illness: a review.
Soc. Sci. Med. 13B, 25-36, 1979.
37. Marmot M. G., Adelstein A. M. and Bulusu, L.
Lessons from the study of immigrant mortality. Lancet
1455-1457, 30 June, 1984.
38. Waldron I., Nowotarski M., Freimer M., Henry J. P.,
Post N. and Witten C. Cross-cultural variation in
blood pressure: a quantitative analysis of the relation
ships of blood pressure to cultural characteristics, salt
consumption and body weight. Soc. Sci. Med. 16,
419-430, 1982.
39. Boyce W. T. and Boyce J. C. Acculturation and
changes in health among Navajo boarding school
students. Soc. Sci. Med. 17, 219-226, 1983.
40. Pawson I. G. and Janes C. Biocultural risks in longev
ity: Samoans in California. Soc. Sci. Med. 16, 183-190,
1982.
41. Turnbull C. M. The Lonely African. Simon & Schuster,
New York, 1962.
42. Brown D. E. Physiological stress and culture change in
a group of Filipino-Americans: a preliminary investi
gation. Ann. Hum. Biol. 9, 553-563, 1982.
43. Rubinstein D. H. Epidemic suicide among Micro
nesian adolescents. Soc. Sci. Med. 17, 657-665, 1983.
44. Patrick R. C., Prior I. A. M., Smith J. C. and Smith
A. H. Relationship between blood pressure and mod
ernity among Ponapeans. Int. J. Epid. 12, 36-44, 1983.
45. Cassel J. and Tyroler H. Epidemiological studies of
cultural change. Archs envir. Hlth 3, 1961.
46. Marmot M. G. and Syme S. L. Acculturation and
coronary heart disease in Japanese Americans. Am. J.
Epid. 104, 225-247, 1976.
47. Walsh D. et al. Suicide and self-poisoning in three
countries—a study from Ireland, England and Wales,
and Denmark. Int. J. Epid. 13, 472-474, 1984.
48. Brownlee A. T. Community, Culture, and Care—
A Cross Cultural Guide for Health Workers. C. V.
Mosby, St Louis, 1978.
49. Chrisman N. J. and Maretski T. W. (Eds) Clinically
Applied Anthropology—Anthropologists in Health
Science Sellings. Reidel, Dordrecht, 1982.
50. Escobar G. J., Salazar E. and Chuy M. Beliefs regard
ing the etiology and treatment of infantile diarrhea in
Lima, Peru. Soc. Sci. Med. 17, 1257-1269, 1983.
51. Fabrega H. The ethnography of illness. Soc. Sci. Med.
13A, 565-576, 1979.
52. Helman C. Culture, Health and Illness. Wright, Bristol,
1984.
53. Kleinman A.. Eisenberg L. and Good B. Culture,
and L. Shore
illness, and care—clinical lessons from anthropologic
and cross-cultural research. Ann. intern. Med. 88, 251,
1978.
54. Moreman D. E. Anthropology of symbolic healing.
Curr. Anthrop. 20, 59, 1979.
55. Morley P. and Wallis R. (Eds) Culture and Curing—
Anthropological Perspectives on Traditional Medical
Beliefs and Practices. University of Pittsburgh Press,
Pittsburgh, 1980.
56. Kellert S. R. A sociocultural concept of health and
illness. J. med. Philos. 1, 222-228, 1976.
57. Bannerman R. H., Burton J. and Ch’en Wen-Chieh
(Eds) Traditional Medicine and Health Care Coverage
—A Reader for Health Administrators and Practi
tioners, pp. 9-13. WHO, Geneva, 1983.
58. Heggenhougen H. K. Bomohs, doctors and Sinsehs—
medical pluralism in Malaysia. Soc. Sci. Med. 14B,
235-244, 1980.
59. Leslie C. M. Pluralism and integration in the Indian
and Chinese medical systems. In Culture, Disease, and
Healing (Edited by Landy D.), pp. 511-517. Mac
millan, New York, 1977.
60. Sigerist H. E. The special position of the sick. In
Culture, Disease, and Healing (Edited by Landy D.),
pp. 388-394. Macmillan, New York, 1977.
61. Sharp P. T. Ghosts, witches, sickness and death: the
traditional interpretation of injury and disease in a
rural area of Papua New Guinea. PNG med. J. 25(2),
108-115, 1982.
62. Zola I. K. Structural constraints in the doctor-patient
relationship: the case of non-compliance. In The
Relevance of Social Science for Medicine (Edited by
Eisenberg L. and Kleinman A.), pp. 241-252. Reidel,
Dordrecht, 1981.
63. Crawford R. You are dangerous to your health: the
ideology and politics of victim blaming. Int. J. Hlth
Serv. 7, 663-680, 1977.
64. Helman C. The role of context in primary care. JI R.
Coll. gen. Pract. 34, 547-550, 1984.
65. Weidman H. H. The transcultural view: prerequisite to
interethnic (intercultural) communication in medicine.
Soc. Sci. Med. 13B, 85-87, 1979.
66. Steffensen M. S. and Colker L. Intercultural misunder
standings about health care—Recall of descriptions of
illness and treatment. Soc. Sci. Med. 16, 1949-1954,
1982.
67. Fabrega H. and Tyma S. Culture, language and the
shaping of illness: An illustration based on pain. J.
psychosom. Res. 20, 323-337, 1976.
68. Good B. J. and Good M. D. The meaning of
symptoms: a cultural hermeneutic model for clinical
practice. In The Relevance of Social Science for
Medicine (Edited by Eisenberg L. and Kleinman A.),
pp. 165-196. Reidel, Dordrecht, 1981.
69. Kleinman A. M. Medicine’s symbolic reality—on a
central problem in the philosophy of medicine. Inquiry
16, 206-213, 1973.
70. White G. M. The role of cultural explanations in
‘somatization’ and ‘psychologization’. Soc. Sci. Med.
16, 1519-1530, 1982.
71. Wolff B. B. and Langley S. Cultural factors and
the response to pain. In Culture, Disease, and Healing:
Studies in Medical Anthropology (Edited by Landy D.),
pp. 313-319. Macmillan, New York, 1977.
72. Wright A. L. A cross-cultural comparison of meno
pausal symptoms. Med. Anthrop. 7, 20-35, 1983.
73. Zborowski M. Cultural components in responses to
pain. J. soc. Issues 8, 16-30, 1952.
74. Zola I. K. Culture and symptoms: an analysis of
patients’ presenting complaints. Am. social. Rev. 31,
615-630, 1966.
75. Edgerton R. B. A traditional African psychiatrist. In
African Therapeutic Systems (Edited by Ademuwagun
Cultural components of behavioural epidemiology
Z. A. et al.), pp. 87-94. Cross Roads Press, Waltham,
1979.
76. Jelliffe D. B. and Jelliffe E. F. P. The cultural cul-desac of Western medicine (towards a curvilinear com
promise?). Trans. R. Soc. trop. Med. Hyg. 71, 331-335,
1977.
77. Torrey E. F. The Mind Game: Witchdoctors and
Psychiatrists. Bantam Books, New York, 1973.
78. Young A. The relevance of traditional medical cultures
to modern primary health care. Soc. Sci. Med. 17,
1205-1211, 1983.
79. Annis S. Physical access and utilization of health
services in rural Guatemala. Soc. Sci. Med. 15D,
515-523, 1981.
80. Eisenberg L. and Kleinman A. (Eds) The Relevance of
Social Science for Medicine. Reidel, Dordrecht, 1981.
81. Rubel A. J. The epidemiology of a folk illness: Susto
in Hispanic America. In Culture, Disease and Healing:
Studies in Medical Anthropology (Edited by Landy D.),
pp. 119-128. Macmillan, New York, 1977.
82. Young A. Some implications of medical beliefs and
practices for social anthropology. Am. Anthrop. 78,
5-24, 1976.
83. Pelletier K. R. Mind as Healer, Mind as Slayer: A
Holistic Approach to Preventing Stress Disorders.
Dell, New York, 1977.
84. Lex B. W. Voodoo Death: new thoughts on an old
explanation. In Culture, Disease, and Healing: Studies
in Medical Anthropology (Edited by Landy D.), pp.
327-331. Macmillan, New York, 1977.
85. Mumford M. Culture: Life perspectives and the social
meanings of illness. In Understanding Human Behavior
in Health and Illness (Edited by Simons R. S. and
Pardes H.), Chap. 16. Williams & Wilkins, Baltimore,
1985.
86. Westbrook M. T., Nordholm L. A. and McGee J. E.
Cultural differences in reactions to patient behaviour:
a comparison of Swedish and Australian health profes
sionals. Soc. Sci. Med. 19, 939-947, 1984.
87. McKinlay J. B. Epidemiological and political deter
minants of social policies regarding public health. Soc.
Sci. Med. 13A, 541-558, 1978.
88. Chomsky N. The little guys America fears. The
Guardian p. 7, 22 July, 1985.
89. International Work Group for Indigenous Affairs
(IWGIA), more than 50 volumes. Copenhagen.
90. WHO. Appartheid and Health. WHO, Geneva, 1983.
91. WHO. Appartheid and Mental Health Care. WHO,
Geneva, 1977.
92. U.S. Department of Health and Human Services,
National Center for Health Statistics. Vital and Health
Statistics—Health Indicators for Hispanic, Black and
White Americans. Data from the National Health Sur
vey Series 10, No. 148. DHHS Pub. No. (PHS)84-1576,
1984.
93. U.S. Department of Health and Human Services,
National Center for Health Statistics. Vital Statistics
1245
of the United States 1980, Volume //, Mortality Part B.
DHHS Pub. No. (PHS)85-1002, 1985.
94. Fanon F. Black Skin, White Masks. Grove Press, New
York, 1967.
95. Fanon F. The Wretched of the Earth. Grove Press,
New York, 1963.
96. Littlewood R. and Lipsedge M. Aliens and Alienists—
Ethnic Minorities and Psychiatry. Penguin Books,
Harmondsworth, 1982.
97. Das K. A Doll for the Child Prostitute. India Paper
backs, New Delhi, 1977.
98. Richards H. The mind managers. New Internationalist
146, 20-21, April, 1985.
99. Baker S. P. Without guns, do people kill people? Am.
J. publ. Hlth 75, 587-588, 1985.
100. Siegel D., Baron R. and Epstein P. The epidemiology
of aggression—health consequences ofwar in Nicaragua.
Lancet 1492-1493, 29 June, 1985.
101. Fromm E. The Sane Society. Fawcett, New York,
1967.
102. Chivian E. (Ed.) Last Aid. Freeman, New York, 1982.
103. Solantaus T., Rimpela M. and Rahkonen O. Social
epidemiology of the experience of threat of war among
Finnish youths. Soc. Sci. Med. 21, 145-151, 1985.
104. Gellhorn A. National Security and the health of
people: human needs and the allocation of scarce
resources. Soc. Sci. Med. 19, 307-332, 1984.
105. Walt G. and Vaughan P. An Introduction to the Prim
ary Health Care Approach in Developing Countries.
Ross Institute, Publication No. 13, London, 1981.
106. WHO/UNICEF. Alma Ata—Primary Health Care—
Report of the International Conference on Primary
Health Care. WHO, Geneva, 1978.
107. Doyal L. and Pennel I. The Political Economy of
Health. Pluto Press, London, 1979.
108. Heggenhougen H. K. Will primary health care efforts
be allowed to succeed? Soc. Sci. Med. 19, 217-224,
1984.
109. Morris M. D. and Liser F. B. The P.Q.L.I.: measuring
progress in meeting human needs. Urban Ecol. 3,
225-240, 1978.
110. Agbonifo P. O. The state of health as a reflection of
the level of development of a nation. Soc. Sci. Med. 17,
2003-2006, 1983.
111. Belmar R. Research statement on democracy and
other social variables as determinants of health. Comp.
Hlth Syst. Newslett. 5, 1-4, 1984.
112. Werner D. Helping Health Workers Learn. Hesparian
Foundation, Palo Alto, 1982.
113. Werner D. The village health worker: lackey or libe
rator. Wld Hlth Forum 2, 46-48, 1981.
114. Audy J. R. and Dunn F. L. Community Health. In
Human Ecology (Edited by Sargent F.), pp. 345-363.
Elsevier-North Holland, Amsterdam, 1974.
115. Heggenhougen H. K. Therapeutic anthropology:
response to Shiloh’s proposal. Am. Anthrop. 81, 647651, 1979.
Position: 3092 (2 views)