ROOL BACK MALARIA GUIDELINE.pdf
Media
- extracted text
-
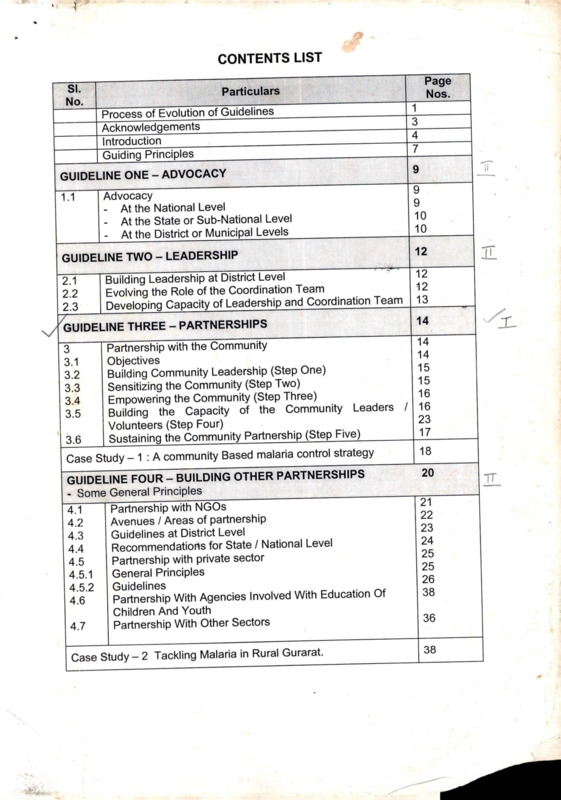
CONTENTS LIST
SI.
No.
Process of Evolution of Guidelines
Acknowledgements
____
Jntroduction_____________________
j~Guiding Principles
GUIDELINE ONE - ADVOCACY
1.1
Advocacy
- At the National Level
- At the State or Sub-National Level
- At the District or Municipal Levels
GUIDELINE TWO - LEADERSHIP
2.1
2.2
2.3
Building Leadership at District Level
Evolving the Role of the Coordination Team
Developing Capacity of Leadership and Coordination Team
GUIDELINE THREE - PARTNERSHIPS
3
3.1
3.2
3.3
3.4
3.5
i
Page
Nos.
Particulars
1
3
4
7
ii
9
9
9
10
10
12
12
12
13
14
14
Partnership with the Community
14
Objectives
15
Building Community Leadership (Step One)
15
Sensitizing the Community (Step Two)
16
Empowering the Community (Step Three)
Building the Capacity of the Community Leaders / 16
23
Volunteers (Step Four)
17
Sustaining the Community Partnership (Step Five)
3.6
Case Study - 1 : A community Based malaria control strategy
18
___
20
GUIDELINE FOUR - BUILDING OTHER PARTNERSHIPS
- Some General Principles__________
Partnership with NGOs
4.1
Avenues
/ Areas of partnership
4.2
Guidelines at District Level
4.3
Recommendations for State / National Level
4.4
Partnership with private sector
4.5
General Principles
4.5.1
Guidelines
4.5.2
Partnership With Agencies Involved With Education Of
4.6
Children And Youth
Partnership With Other Sectors
4.7
21
22
23
24
25
25
26
38
Case Study - 2 Tackling Malaria in Rural Gurarat.
38
36
IL
2
SI.
No.
Particulars
Page
Nos.
TT
GUIDELINE FIVE : COMMUNICATION FOR BEHAVIOR CHANGE
39
Organise I EC Strategy and Materials
40
Communication strategy - principles
41
Communication Methods
Innovations_______________________________________ 41
Case Study 3 Evolving a Community Strategy to keep
42
villages Malaria-free.
_____
GUIDELINE SIX : DIAGNOSIS, TREATMENT AND TRANSMISSION
CONTROL AT THE COMMUNITY LEVEL
43
Simple Ways for diagnosis and treatment of malaria
6.1
43
How to recognise malaria
6.2
43
What to do
6.3
44
What should be done at the Primary Centre
6.4
44
When to refer patients to a health centre/hospital
6.5
44
Laboratory Diagnosis
6.6
44
Rapid Diagnostic Tests
6.7
45
Treatment
and
follow
up
of
malaria
patients
home
care
6.8
45
Community level
6.9
45
At the Health Centre / Hospital
6.10
46
Malaria in pregnancy
6.11
46
Administrative Level
6.12
47
Medical Audit
6.13
5.1
5.2
5.3
5.4
.ILL
GUIDELINE SEVEN : MANAGEMENT OF SEVERE MALARIA
7.1
7.2
7.3
7.4
7.5
What is severe and complicated malaria?
Diagnosis and Clinical Features
Physical Examination
Investigations
Management
48
49
49
50
50
GUIDELINE EIGHT : REFERRAL SYSTEM FOR MALARIA
8.1
8.2
8.3
Who should be referred? Criteria for referring malaria cases
Who will and where to refer
What facilities should be available at the referral centre?
52
52
53
GUIDELINE NINE : PACKAGE DELIVERY FOR COMMON DISEASES
9.1
9.2
9.3
9.4
Definition of Common Diseases for Health Care Package
Package Kit
Preventive drugs / equipment:
Curative:
54
55
55
55
v 47
>
SI.
No.
Particulars
Page
Nos.
///
GUIDELINE TEN : DRUG SUPPLY AND MANAGEMENT
10.1
Management of Drug Supply
57
GUIDELINE ELEVEN : IMPROVEMENT OF HEALTH CARE AT HOME
THROUGH EMPOWERMENT OF WOMEN.
58
Identification of key persons
Tm
58
Methods that may be adopted
11.2
GUIDELINE TWELVE : INTER PROGRAMME LINKAGES WITH SAFE
MOTHERHOOD AND OTHER PROGRAMMES.
60
Malaria and Pregnancy
12J
Malaria in pregnancy as part of Reproductive and Child 60
12.2
Health (RCH) ~
Malaria as part of Integrated Management of Childhood 60
12.3
Illness (IMCI)
60
Links with existing health infrastructure
12.4
Malaria related to development projects
61
12.5
GUIDELINE THIRTEEN : MONITORING DRUG RESISTANCE
62
Identifying Sources of Information
137f
62
Information on Failure of Treatment with Anti-malarials
13.2
63
Testing for Resistance
13.3
63
Vigilance for Pv Resistance
13.4
GUIDELINE FOURTEEN : HEALTH MANAGEMENT INFORMATION SYSTEM
14
14.1
14.2
14.3
14.4
14.5
14.6
14.7
Health Management Information System
Data Collection System
Analysis of data
Who is responsible?
Coordination with other health sectors
Personnel
Public domain information
Implementation of Computerized HMIS
64
65
65
66
66
67
67
67
ITT
4
Page
Particulars
SI.
Nos.
No.
GUIDELINE FIFTEEN : MALARIA PREVENTION AT COMMUNITY
LEVEL
69
Ts- Malaria Prevention At Community Level
69
Personal protection against mosquito bites
15.1
69
Insecticide treated mosquito nets/curtains
15.2
69
Mosquito repellents
15.3
70
operationalisation
of
use
of
repellents/ITN
programme
in
15.4
different settings
Elimination of mosquito breeding places in and around 71
15.5
houses.
73
Larvae Control
15.6
74
House spraying and thermal fogging
15.7
74
Chemoprophylaxis
15.8
______________
I
74
Malaria vaccine
15.9
GUIDE JNE SIXTEEN : STRATEGY ON ELIMINATION OF BREEDING
PLACES THROUGH COMMUNITY ACTION______________________
Special Strategy On Elimination Of Breeding Places 75
16
Through Community Action
75
Concept
16.1
75
Guidelines
16.2
79
Case Study - 5
16.3
GUIDE JNE SEVENTEEN : EPIDEMIOLOGICAL SURVEILLANCE
17
17.1
17.2
17.3
17.4
Mapping Of Malaria And Geographic Reconaissance (Gr)
Entomological Surveillance
Forecasting and Early Detection of Epidemics
System Surveillance
Behavioural surveillance
80
81
81
82
82
GUIDELINE EIGHTEEN : EPIDEMIC PREPAREDNESS AND RESPONSE
18
18.1
18.2
18.3
18.4
18.5
18.6
18.7
Epidemic Preparedness And Response
Epidemic
Epidemic Forecasting
Parasite load
Vector Dynamics
Population Dynamics
Ecological Changes
Epidemic preparedness
J1L-.
84
84
84
84
84
84
85
85
—
111
5
GUIDELINE NINETEEN : MAPPING OF MALARIA AND GEOGRAPHIC
RECONAISSANCE (GR)___________________________________ _________
87
Mapping Of Malaria And Geographic Reconaissance (Gr)
19
87
Why Mapping and GR?
19.1
87
Mapping and GR
19.2
87
GR
in
Malaria
Control
19.3
GR to Map Basic Receptivity and for Formulation of Control 87
19.4
Studies
GUIDELINE TWENTY : RESEARCH AND DEVELOPMENT
20
20.1
20.2
20.3
20.4
20.5
Research And Development
Socio-economic studies
Vector Studies
Drug Studies
Epidemiological Studies
Control Strategies
Case Studies - 6
89
89
89
89
90
90
91
7
IL
14
Fo^
1 ■
tSCT I ON
in
GUIDELINE THREE:
PARTNERSHIP WITH THE COMMUNITY
3.1 Objectives
The objective of Roll Back Malaria is to promote the broad participation and
ownership of the community in malaria control. This will be done through the
active mobilization, involvement and participation of the community in
planning, implementation and monitoring of the health programme.
This can be evolved in five steps:
Step one:
Building community
leadership.
Step five'.
Sustaining the
community
partnership.
Step four:
Building community
capacity,
(leaders / volunteers)
I
Step two. Sensitising
the community.
4
>
Step three'.
Empowering the
community.
15
•3.2
BUILDING
COMMUNITY LEADERSHIP (STEP ONE)
1. Identify leadership in the community (this may be village, tribal hamlet
or township)
(a) These would include:
• Formal leaders
• Informal opinion leaders
• Community clubs and organisations - youth, women, farmers,
• Teachers
• Religious and community leaders
• Village health workers / local development workers
• Others in the community who could assume leadership roles.
(b) Proactively increase the participation of women members by involving
women’s groups1.
(c) Ensure adequate representation of marginalised/ minority groups.
2. Evolve the health committee at community level with the involvement of
the people
■
■
If there is a functional health committee or group already, integrate malaria
function with that group.
If a functional committee does not exist then evolve a malaria committee
which can take up other health programmes at a later stage.
3. A dialogue of the district administrator2 with the community leadership /
health committee should be initiated to elicit the participation in the
Malaria Programme.
4 Orient the leadership/committee to the malaria situation and malaria
control to get their help in sensitizing the community.
3.3 SENSITISING THE COMMUNITY (STEP TWO)
Through community level meetings, organised by the identified leadership and or
the health committee, sensitize the community to all aspects of malaria situation
and malaria control.
1. Create awareness of national malaria programme at village/township level and
define the expected role of all members of the community.
2. Emphasise community’s role by stressing:
a) that they are partners in the programme and have their roles and
responsibilities in malaria control, and
b) that their participation will ensure benefits to their community.
1 for example, mahila mandals in India; PKK in Indonesia; and MMCWA in Myanmar
2 for example. District Collector in India and Bhupathi in Indonesia
16
3.4 EMPOWERING THE COMMUNITY (STEP THREE)
1. Initiate a dialogue using participatory approaches to understand the existing
knowledge, attitudes and practices of the community in relation to the malaria
problem.
2. Assess the strengths and weaknesses from the KAP exercise against the
expected behaviour.
3. Create awareness in the community on the causes, signs and symptoms
of malaria and about the treatment and prevention of malaria.
4. Involve them in a planning exercise:
• to survey and identify the local situation.
• to identify the existing resources in the community including volunteers
who could be trained for the programme.
• to identify external resource inputs that will be required, and local
resources that can be mobilised.
• to develop a plan of action for malaria control that could include health
promotion, early diagnosis and treatment, and malaria prevention
activities(including vector control).
• to identify clearly the role of the community and the role of the Health /
Malaria programme team.
5. Facilitate the operationalisation of this plan by
• helping them to implement,
• helping them to monitor, and
• helping them to review and revise the plan of action.
3.5 BUILDING THE CAPACITY OF THE COMMUNITY
LEADERS / VOLUNTEERS (STEP FOUR)
Helping the community to build its capacity for malaria control activities will
essentially mean building the capacity of leaders and local volunteers in a
variety of tasks.
1. To understand all aspects essential for malaria control. These will
include all those aspects included in the box pV Malaria A to Z). The
training / orientation must address all these questions in a simple,
demystified way, using supportive health education and learning aids.
2. To further build the capacity of volunteers/leaders in:
• early diagnosis and treatment
• identification of serious cases and their suitable referral
• community surveillance of malaria morbidity and mortality.
• vector control activities at community level
• communication and mobilisation.
• monitoring and evaluation at community level.
Practical skill development in the context of the local situation will be the
key to success.
17
Malaria AtoZ
a) What is the current magnitude of malaria problem : National / State /
District/Local
b) What is malaria - its symptoms and characteristics for identification?
c) How is malaria caused?
d) Where do mosquitoes come from?
e) Where do they breed?
f) Who are at most risk of suffering from malaria?
g) How can we test for malaria?
h) Where can these tests be done?
i) What can be done to treat malaria?
j) Where is the treatment available?
k) How can we control the mosquitoes?
l) What are the complications of malaria?
m) What should be done in case of complications?
n) What are the protective measures against mosquito bites?
3.6 SUSTAINING THE COMMUNITY PARTNERSHIP (STEP FIVE)
Community partnership can be sustained by:
1. Frequent interaction with community, providing solutions to
the problems in carrying out control activities will also sustain
the interest of community in malaria control activities.
2. Ensure that supplies are constantly available (insecticides,
fish, nets, medicines, neem oil, equipment, microscopes,
stain, slides). This will also greatly help the sustainability of
the programme.
3. Encouragement of income generating vector control activities,
e.g., social forestry plantations will also help sustainability of
the community involvement.
4. Incentives for the community from the district administration in the form
of:
a) declaring malaria-free or healthy villages
b) developmental inputs.
“True partnership begins when the community
involved decides what needs to be doneand
particularly what needs to be done first.’*
18
Case Study -1
A community based malaria control strategy
Bissamcuttack, Orissa, 1996
[The Christian Mission hospital in Bissamcuttack, Orissa has been recently involved with tackling the
malaria problem by involving the community from the villages served by the hospital as follows:]
Step One
• We began with helping people to recognise their public health enemy No.1 - Malaria
by sharing with them the MIS data from the government PHC on Morbidity and
Mortality. This prepared the ground for step two.
• We also did an informal survey to ascertain sleep habits and patterns, according to
community, age and gender.
Step Two
•
If the village so desired they invited us to explain to them the basics of Malaria. This
involved almost a full day when we met with as many of them as could get organised
into groups according to gender, age and community. The classes were quite
intensive and based on 4 questions:
1. What is Malaria?
2. How does one get it?
3.
4.
What can we do if we get it?
What can we do to keep from getting it?
•
•
•
We used teaching aids, flashcards, photographs, Neem oil, mosquito nets, synthetic
pyrethroids, etc.
An Oriya pamphlet was also distributed to those who could read.
We stressed environmental methods, neem oil, clothing and nets - as alternatives.
Step Three
*
•
The villages chose the options they wished to pursue. Most opted for Neem oil and
impregnated nets.
• The village decided who will take charge - usually 2 or 3 respected people. They
would be incharge of finalising the order, supervising the distribution and collection of
money. Each village decided on different schedules and modes of payment.
• We supplied nets, taught the method of impregnation and taught 8 principles of using
the net. Our team members stayed over the first night to help sort out ‘teething
problems’.
• We got nets from Raipur and synthetic pyrethroids from Calcutta.
• More than 50% of our investment has been repaid already.
• Our investment had been in terms of time, energy and capital money. The approach
chosen was slow but encouraging.
• We have not raised the question of subsidy because most families spend around Rs.
800-00 a year on Malaria and our nets are cheaper than local shops - so they opt for
it.
To summarise:
Our strategy is an Alternative, people based, village level, sustainable strategy with 3 basic thrusts:
a) Malaria Education
b) Promotion of personal protection measures - all methods including IBNs
,c) Early clinical diagnosis and prompt treatment.
We then did a 2 day workshop for other NGOs to share our experience. The idea is that they will go
home and launch similar village level ‘wars’ against malaria!
Christian Hospital, Bissamcuttack, Orissa.
19
REMEMBER!
RBM is a social movement for better health and poverty alleviation
"RBM is a social movement for better health and will focus on providing access to the poor
who suffer from malaria the most. RBM actions would lead to poverty alleviation. The
community and the private sector would have the opportunity to play important roles in the
delivery of effective anti-malaria interventions, particularly in primary prevention and
treatment of malaria. National plans to roll back malaria should reflect diverse opportunities
and approaches."
Community mobilization
"The program should address health issues arising through enhanced community
awareness and knowledge about disease prevention, diagnosis and treatment, as well as
through local operational research activities. Bottom-up planning should be the core
principle where decision-making and planning capacity will be based at the level where the
problem occurs i.e., local-level planning, disease surveillance, monitoring of program
activities, resource allocation, IEC, training, vector control etc. Epidemiological information
would be analyzed at the local level and used in proactive action in developing evidence
based planning. However, national-level competence and coordinating function should be
retained or developed at the central level during the process of decentralization and
thereafter."
RBM promotes equity in health by focussing on disadvantaged populations
"Malaria primarily affects the poorest people. Children, women and migrants are the main
victims of malaria. RBM will promote health equity by strengthening interventions focussed
on disadvantaged populations and by developing acceptable standards of health care,
focussing not just on disease burden but also on the cost effective interventions."
Improving access to health care
"Because of poor quality public sector facilities and the lack of public confidence in
them, the private sector plays a dominant role in treatment. There is thus a need for
an effective regulatory function to protect public health interest and secure quality
service."
43
GUIDELINE SIX
DIAGNOSIS AND TREATMENT AT THE COMMUNITY LEVEL
6.1
Simple Ways for diagnosis and treatment of malaria
Recognition of signs and symptoms of malaria, especially the serious
forms of it and the actions expected in an episode of malaria of various
actors at home and at village or primary level should be as clear to the
lay people as to the technically trained people. It is this factor that will
make the Roll Back Malaria Initiative to survive the inadequacies of state
funding, collapses of health systems due to war / violence and the
vagaries that people of developing countries often have to face.
It is hence imperative that as many people as possible are trained in
each community who can learn to distinguish malaria from other
illnesses, can help to detect the serious forms of the disease and help
them to reach the nearest and appropriate treatment facility.
6.2
How to recognise malaria
• Every case of fever in highly endemic areas or in persons with a
history of travel to high endemicity area in the past four weeks, should
be presumed to be due to malaria, unless proved otherwise.
• In low risk areas, other causes of fever should be eliminated before
suspecting malaria.
• Classically a group of symptoms consisting of headache, myalgia,
malaise and nausea occur before the first episode of fever.
• Typical, fever due to malaria occurs in cycles occurring every 48
hours. The fever is accompanied with chills and rigors and ends with
profuse sweating. P.malariae fever recurs every 72 hours. This
classical pattern may not be observed in all cases, particularly so in
P. falciparum malaria and treatment failures.
• Atypical symptoms like abdominal pain, vomiting & dry cough may be
present in some patients. Particularly in children, there is no classical
pattern of fever, regardless of the infecting species.
6.3 What to do
• Patients with any of the above symptoms should visit the nearest
health facility centre for diagnosis and treatment of malaria. This
centre should ideally be situtated within a short distance for any
community: short enough that a lone woman with a sick child can
access easily.
44
6.4 What should be done at the Primary Centre
• If facilities for blood smear examination are available locally or
nearby, and results can be obtained within 2 hours, defer treatment
till results are available. Otherwise, treat presumptively for malaria as
per National guidelines.
• If facilities for blood smear examination are not available, treat
presumptively for malaria as per National guidelines. However if
possible, exclude other causes of fever before presumptively treating
for malaria.
6.5 When to refer patients to a health centre/hospital
The following criteria should be able to help a reasonably aware person
to make a judgement about referring a patient for better treatment
facilities.
• Pregnant women and children with high fever (above 39° C).
• Persistent and/or very high fever (fever over 7 days or above 39° C)
Restlessness/Refusal to take feed in children.
Severe pallor or Jaundice
Change in level of consciousness / Convulsions
Signs of shock (cold & clammy skin, thready pulse and rapid
respiration)
• Bleeding from any site / black or brown discoloration of urine (cola
colored urine) / fall in quantity of urine
• Failure to respond to previous antimalarial treatment (if symptoms of
malaria recur within 1 month of treatment)
• Persistent vomiting and inability to swallow antimalarials.
•
•
•
•
6.6 Laboratory Diagnosis
• Blood smear should always be taken or dipstick test done, wherever
possible, for identification of malaria parasite and its species, before
starting treatment. However, it does not mean that treatment should
be delayed for availability of the result of such a test.
6.7 Rapid Diagnostic Tests
• In high risk areas, where facilities for blood smear examinations are
not available, facility for dipstick test for P.falciparum should be
provided at the fever treatment depot for early diagnosis. In case of
limited availability of these kits, priority should be given to children
and pregnant women and seriously ill patients.
• Where dipsticks are made available but health workers are not
available, efforts should be made to train some responsible
45
community members, such as teachers and volunteer health workers,
to diagnose P.falciparum by the dipstick method. It may be noted that
the sensitivity of Dip stick test is about 95% and not 100%.
• Private practitioners should be encouraged to provide facilities for
laboratory diagnosis of malaria.
• In areas where health facilities are not available, NGOs may be
involved in the diagnosis of malaria, particularly by dipstick method.
• In high risk areas, if laboratory test for malaria is negative and fever
persists, the laboratory test should be repeated on 3 consecutive
days.
6.8 Treatment and Follow up of malaria patients Home care (by
family members)
•
Fever should be brought down as quickly as possible with cool
water sponging. Paracetamol, 500mg to 1gm for adults and
10mg/kg per dose for children may be used. Patient should be
given plenty of fluids.
•
Glucose or sugar solutions must be given to drink, particularly to
children and pregnant women.
•
In case of children, continue breast feeding.
•
Seek medical care as early as possible.
6.9 Primary level (community level/DDC/FTD/sub-centre)
• At the Basic Health Facility Centre in the village
• If a presumptive diagnosis of malaria is made, then the local fever
treatment depot (FTD) or other health facilities should be contacted
and patient treated with Chloroquine or other appropriate drugs
(depending on the drug policies already laid out by the malaria
control programme of individual countries).
• There is no benefit of giving Primaquine to all patients in hyper
endemic areas.
• Advise patient / care providers to look for signs of serious illness and
refer the patient to a health centre / hospital .
• Provide supportive therapy as required (Paracetamol for fever and
headache, plenty of fluids etc.)
• Advise patients / care providers about nutrition, home care, the need
for treatment adherence and when to report back.
• In high endimicity areas, where the probability of malaria is high,
algorithms as per national guidelines may be followed for diagnosis
and treatment, (see box at the end of Guidelines 6)
6.10 At the Health Centre/Hospital
. • Diagnosis of malaria should be confirmed and patient treated with
Chloroquine or other appropriate drugs as per the National policy.
• Patients of severe and complicated malaria should be treated with
intra venous (i/v) Quinine infusion or other appropriate drugs like
Quinine, Mefloquine, Sulfadoxine-Pyrimethamine and Sodium
Artisunate / Arteether as per the national malaria treatment
guidelines.
46
• Chloroquine and Quinine can safely be given during pregnancy
including the first trimester for the treatment of malaria. However
Quinine infusion should be given in dextrose solution to avoid
hypoglycemia.
• Sulfadoxine-pyrimethamine combination can be given after the first
trimester of pregnancy up to one month prior to delivery.
6.11 Malaria in pregnancy
During pregnancy, not only does malaria attack more frequently and
severely, but it also worsens women's anaemia and can cause a high
incidence of abortion, neonatal deaths and low birth weight. Effective chemo
prophylaxis in pregnancy effectively protects the women from malaria and
should be given for the entire duration of pregnancy (preferably avoided in the
first trimester because of nausea.
Approved doses of Chloroquine or Quinine may be given in any trimester
of pregnancy for curative treatment of malaria.
Sulfadoxine - Pyrimethamine combination may be given after the first
trimester of pregnancy and upto one month prior of delivery.
Primaquine should not be given during pregnancy (and to infants below
one year).
6.12 Administrative level
• Establish, where possible, a functional drug distribution centre (DDC)
or fever treatment depot (FTD) in each village and urban slum.
• Ensure timely replenishment of diagnostic supplies and antimalarial
drugs.
• Paediatric formulations of antimalarial drugs should be made
available.
• Evolve mechanisms to ensure quality control of antimalarial drugs.
• Training of health workers and volunteers in malaria diagnosis and
treatment.
• Coordination should be ensured between different partners (eg:
private practitioners, volunteers and NGOs) and different programmes
(eg: RCH, IMCI etc) in malaria diagnosis and treatment.
• Local patterns of drug resistance should be monitored by the
specialised teams in order to formulate the local drug policy.
• Development and maintenance of relevant surveillance and reporting
system for monitoring and evaluating malaria situation in the area.
Case definition for reporting should be followed as per the
recommendations of 20th Expert Committee on malaria (WHO).
• Provision of required drugs, preferably in age-group-wise packets,
with instructions in local language.
47
6.13
Medical Audit
To ensure a good quality of care provided to patients with malaria, each
member country in the region should develop a system of medical audit to
build effective mechanisms for ensuring the quality of patient care.
Medical audit is a systematic critical analysis of the quality of
medical care including the procedures used for diagnosis and
treatment, the use of resources and the resulting outcome for the
patient._________________________________
6.13.1 Medical Audit should be carried out in district hospitals with suspected
malaria deaths to begin with. Later it can be expanded to other institutions
and areas. An attempt must be made to introduce it as a necessary
component of good hospital practice in private clinics, nursing homes and
hospitals through professional bodies. Adherence to national treatment
guidelines on malaria and rational malaria care can be promoted through
medical audit and besides ensuring quality care to people, it also goes a long
way in preventing or delaying resistance to antimalarials.
6.13.2 At district level, a committee consisting of district health authority,
public health experts and clinicians not directly involved in the direct
management of the case. The report of the medical audit should be sent to
the concerned authorities for appropriate action. For hospitals, medical audit
committees can be formed by physicians and pharmacists not directly
involved in the case management.
Antimalarial drug policy for the country or region should be
reviewed periodically by an expert committee and changed
whenever required depending
on the sensitivity patterns of
Plasmodium species.
54
GUIDELINE NINE
PACKAGE DELIVERY FOR COMMON DISEASES
It is envisaged that by strengthening District Health System through Primary
Health Care Services we are indirectly strengthening the malaria control
operation in the district. It is in this context that PACKAGE DELIVERY CARE to common diseases is to be incorporated in Roll Back Malaria Program. As
the malaria control activities now are integrated with the general health
services, it would rather be useful to deliver a package of services to the
community related to the- communicable diseases as per the need “of the ’
community. However this packaging of essential care should be defined as
per existing disease prevalence and the felt-need of the community to be
served; availability of manpower (both from government and other sectors);
provision of static health facilities; and not the least, the least care-seeking
behavior of the community. The already existing “Essential Services Package
(ESP)” and the “Integrated Management of Childhood Illnesses (IMCI)” may
be considered wherever useful.
P'
9.1 Definition of Common Diseases for Health Care Package
Since the pattern of endemic diseases and morbidity varies from area
to area, the approach to select the diseases to be addressed for Health
Care Package should be based on area specific pattern of diseases.
Though communicable diseases are common in all parts of the
country, there are certain diseases which have high prevalence and
hence we need to have some criteria to selectsuch diseases for the
delivery of the package. The following criteriajehould be used for
prioritization of health care package.
~~
•
•
•
•
Quantum of morbidity
Complications/Disabilities
Epidemic potential
Amenability in Control , -
Methodology for Selection of Diseases is
• Study of existing records at District level and below
• Special Survey Reports, if available.
• Study of infrastructure including manpower institution.
• Study of the delivery system.
• ^Pattern of local administrative system and community system
It is suggested that about 5 to 6 such diseases may be selected by
following the above criteria.
55
9.2 Package Kit
There is a system of having Drug ^ with^e^ryQMPW^rid
list of the
MPW
drugs supposed to be kept in the kit are givenbelov^5^
Chloroquine tablets and microslides are invariably kept in the kit. This
kit may be revived to see whether it sen/es the purpose aimed for
prevention, control and cure of the disease. An indicative /ist of such •
drugs/ equipment may be:
9.3 Preventive drugs / equipment:
1. Tab Iron & Folic Acid
2. Tab. Chloroquine
3. Vit A solution/capsule
4. Chlorine tablets
5. Disposable pricking needle
6. Gauze /Bandage
8. Microslides
9. Sputum cup
10. Thermometer
9.4 Curative:
1. ORS packets
2. Cotrimoxazole tablets/syrup
3. Paracetamol tablets/syrup
4. Anthelminthics tab./syrup
5. Cough expectorant syrup
6. Amoxycillin tab./cap /syrup
7. Diazepam tab/syrup
8. Tab. Primaquine
9. Tab. Sulphadoxine/Pyrimethamine
10. Tab. Quinine Sulphate
11. Tab. Ergometrine
12. Antispasmodics
13. Anticoagulant tablets
14. Anti-emetic tablets, e.g., Prochlorperazine/Metoclopramide/
Drug information inserts detailing the indication, dosage, side effects and
expiry dates must accompany the drug kit written in easily
understandable language(in local language where possible)
58
GUIDELINE ELEVEN
IMPROVEMENT OF HEALTH CARE AT HOME THROUGH
EMPOWERMENT OF WOMEN
Empowerment of women means:
•
•
•
creating an awareness among women through basic knowledge for
prevention of malaria and other common diseases.
Providing adequate information for recognizing the seriousness of the
disease and identifying its possible complications and adopting simple
methods to undertake home care within the family.
This will directly result in early diagnosis and prompt treatment of common
illnesses including malaria.
11.1 Identification of key persons:
For the empowerment of women it is necessary to identify different
groups of women. Depending upon the physio-demographic
characteristics of the area, the women groups can be divided into the
following:
1. Rural
2. Urban slums / laboUr colonies
3. Urban areas
11.2 Methods that may be adopted
A. Rural areas:
• In rural areas women can be empowered through women
members of local bodies. The other organizations and situations
which hold significance in empowering women are
(i)
(ii)
(iii)
Women’s organizations
Religious organizations/social gathering
Weekly markets
IEC material will have to be developed. Street plays / puppet
shows / other sources of entertainment may be used as a vehicle
to provide the necessary education.
• Special groups of women interested and trained in health should
be identified as a trained resource. These groups may include lady
teachers and female members of local bodies, bank and post
offices and may be trained for early detection of malaria also.
•
59
A. Urban slums / labor colonies
•
Knowledge to women in urban slums may be imparted through NGOs /
voluntary organizations and cooperative societies.
A. Urban areas
B. Women in urban areas can be empowered through
♦ Welfare Associations
♦ Women’s development Councils
♦ Women's clubs
♦ Voluntary Organizations involving women (eg: Lions club etc.)
C. The member(s) of these organizations may be trained in imparting
knowledge regarding home care of malaria, who in-turn will train other
women at home. Their training shall include the following thrust areas:
1. Health education and awareness about common diseases
including malaria.
2. Cleanliness, in and around the house including water
management and disposal.
3. Use of preventive measures like use of bed-nets, repellents,
mosquito proofing etc
4. Knowledge and awareness about existing local health
infrastructure.
The home care package given to women may include the following:
1. Fever as a symptom to be taken seriously and presumptive
treatment for malaria to be given preferably after taking blood
smear for malarial parasite.
2. Symptomatic treatment like sponging, plenty of fluids,
antipyretics.
3. Identification of complications like drowsiness, vomiting, low
urine out put, convulsions, which need immediate referral to
the hospital.
4. Pregnant women / infants & children with fever to be dealt
with as a potential emergency and immediate treatment to be
given.
5. Prophylaxis for pregnant women especially in high endemic
areas.
Women involved in social development work including malaria control should be
recognized and honored by the local bodies / NGOs. This would act as an incentive for
involvement of more women.
69
GUIDELINE FIFTEEN
MALARIA PREVENTION AT COMMUNITY LEVEL
There are four main ways to prevent malaria
1. Prevent mosquitoes from biting people by personal protection.
2. Control mosquito breeding by elimination of breeding places
3. Kill adult mosquitoes by house spraying and thermal fogging.
4. Chemoprophylaxis by regular intake of drugs taken to prevent malaria.
Important preventive measures that can be adopted and applied by
individuals and the community are personal protection against mosquito
bites and elimination of mosquito breeding places.
15.1
Personal protection against mosquito bites
• Mosquito nets / insecticide treated mosquito nets and curtains
• Mosquito repellents
• Mosquito coils
• House screening
However, none of these measures can provide full protection against
mosquito bites and the diseases transmitted by them (Table 1).
15.2 Insecticide treated mosquito nets/curtains
A major impact on malaria incidence/mortality following the large-scale
application of insecticide treated mosquito nets (ITN) has been
demonstrated. From the experience gained in the usage of ITN, it has
been observed that to optimize the use of nets the following basic
information is essential:
• Mosquito biting times and site of contact
• Sleeping habits / socio-behavioral practices of the communities to
be
protected.
Unless this information is available and ITNs are found relevant in the control
of
malaria in the area, introduction of ITNs in the programme may not
have the desired results.
Operational aspects including delivery, cost sharing and social marketing of
nets should be investigated to look at feasibilty and self-sustainability.
15.3 Mosquito repellents
Mosquito repellents are effective against outdoor as well as indoor biting
vectors. They could supplement effects of mosquito nets and could be
used more frequently in some high-risk groups such as rubber-tappers
and night hunters.
70
Table 1
Personal Protection
Pleasures_________
Mats
Active Ingredient/
Principle_________
Synthetic Pyrethroids
Mosquito Coils
Herbal/synthetic
pyrethroids
Synthetic Pyrethroids
Insecticide Treated Nets
I Curtains
Vaporizers
Light Traps
Mosquito proofing/
window screening
Mosquito Repellent
Creams
Lotions (DEET)
Eucalyptus Oil
Citronella oil
Protective Clothing
Neem Oil
Synthetic pyrethroids
Light attraction
Mechanical barriers
Likely side-effects
Respiratory/eye problem
including asthma,
itching, rash, etc.
--- do--------■do
-do
Nil
Nil
Herbal /Chemical
Skin irritation or rash
Chemicals
Natural oil
Natural oil
Natural oil
Neem derivatives
Skin irritation
Nil
Nil
Nil
Nil
Note: Effective protection by the repellents (except treated mosquito
nets/curtains) varies from one to four hours in the field in different seasons.
The effectiveness also varies against different mosquito species. All repellents
are more effective against Anopheles (malaria vectors) than Culex (filariasis
and J.E. vectors) or Aedes (Dengue vectors).
15.4 Operationalization of use of repellents/ITN programme in different
settings
The strategy for the sustainable use of these methods at the community level
is as follows:
•
The manager of the malaria control programme, at the District Level will be
overall in charge, working under the purview and guidelines of District
Malaria Society. His/her responsibility will include the procurement and
distribution of repellents and ITNs, and providing back up support and
coordination of IEC and other promotional activities through media,
educational institutions, local government institutions, NGOs, etc.
•
It is recommended that the money received from the sale of the subsidized
items such as nets should be handled by a voluntary agency / NGO/
autonomous society created for the purpose.
•
The monitoring mechanism should be developed according to local
situation for which a committee could be set up, taking representatives
from the community and malaria society.
71
•
Annual evaluation of the programme be conducted by a small committee
with representatives of Malaria Control Programme, community, NGOs,
local Government and experts with social science background.
•
In the distribution and use of mosquito, the priority should be given to
pregnant women, infants and children. The significance of protecting this
vulnerable group should be highlighted through mass media and IEC
activities.
•
Type of insecticide for treating mosquito nets should be decided by the
National Program Managers as per insecticide policy of the country.
•
There is evidence in few countries that repellent formulations are of poor
quality or fake. Therefore quality control checks should be rigidly applied.
•
Herbal repellents like Citronella oil, Eucalyptus oil, Neem oil, etc. should
be encouraged.
15.5 Elimination of mosquito breeding places in and around houses.
A. In the Homes
Major mosquito breeding sites within the house, comprise water
storage container, animal drinking pans and flower vases, roof gutters
and pit latrines. Mosquito breeding in these habitats could be checked
by taking the following preventive measures that need to be made
public knowledge through IEC campaigns:
•
•
•
•
•
•
Water storage within the household should be reduced to a
minimum. However, this may not be possible in areas without a
piped water supply or with intermittent supply. In such cases,
mosquitoes must be mechanically excluded by keeping all domestic
water storage containers covered.
Unwanted standing water should be cleared and the containers
inverted. This is required because mosquito larvae dive to the
bottom of the container when disturbed, and may survive in the
residual water at the bottom of the container.
Choked roof gutters should be cleared of debris, so that rain water
does not stagnate.
Water in animal drinking pans, flower vases, etc., should be
replaced every day.
Sullage should be removed from the premises through properly
designed drains.
Breeding of mosquitoes in pit latrines could be controlled by treating
with malaria oil to cover the water. Another novel method is
placement of polystyrene balls to form a complete physical barrier
over the water to prevent oviposition. These balls are cheap, non
toxic, virtually indestructible and have little attraction or value for
72
people to steal them. Proper design and maintenance of sanitation
systems is essential for eliminating mosquito breeding in these
habitats.
Access of mosquitoes to the interior of the house could be
prevented by screening doors and windows with 18 inch guage wire
mesh screens.
B. Around the House
Mosquito breeding habitats around the house include rainy water
collected in waste articles dumped in vacant plots, underground
cisterns and water storage tanks, wastewater drains, cesspits, and
septic tanks. Mosquito breeding in these habitats could be eliminated
by adopting the following preventive measures.
•
•
•
•
•
•
A thorough search of yards and vacant plots must be made for
discarded articles and rain water collection sites.
Tree holes should be filled with mud or cement to prevent
accumulation of rain water. If solid waste disposal services are
inadequate, articles that may collect rain water could be dealt with,
in other ways, e.g., cans could be cut open and crushed, pans and
trays could be turned over, discarded tires could be cut and turned
over, etc.
Underground cisterns and water storage tanks should be covered
with 18-guage mesh screens. If possible these may be stocked with
mosquito-eating fish such as Gambusia affinis for clean water and
Poecilia reticulata for dirty water.
Drainage arrangements should be made.
Cesspits should be avoided completely and replaced with proper
soakage pits.
Septic tanks should be sealed properly and the vent pipes furnished
with screens. Effluent from the septic tank should be discharged
into a soak away and not into the open.
C. In the Community
In the community, major mosquito breeding habitats comprise spillage
around water supply sources, wastewater drains, storm water drains,
cesspools, ponds and other large water bodies, and low-lying vacant
plots. These habitats should be dealt with as follows:
•
Water spillage around community water supply sources such as
hand pumps, wells, public stand posts, etc., should be checked and
drainage arrangements made.
•
Wastewater and storm water drains should be maintained properly
and dumping of solid wastes into these areas should be forbidden.
73
e
Undesirable water collections in the community could be eliminated
by drainage or filling. Cesspools and low-lying vacant plots are best
dealt with by filling with rubble, earth or refuse. Ponds, borrow pits
and ditches could be filled or, alternatively, these could be drained.
However, small and temporary habitats such as small pools and
puddles, roadside ditches, water-filled vehicle tracks and cattle
hoof-prints may be too numerous and scattered to fill or drain.
•
Mosquito breeding in large water areas could be eliminated through
environmental modification e.g., construction of public irrigation
works that allow control of the water level and shore conditions
(impoundment).
Drainage, filling and impoundment are methods that usually give
long lasting effects. However, these may have other ecological
repercussions and therefore should be undertaken only with expert
advice.
•
•
Houses may be graded periodically on the basis of cleanliness and
action taken by the individual /family on points mentioned in Table
2.
•
Houses with Grade I (best) may be given some incentive,
recognition or free gifts.
15.6 Larvae Control
Larvae control can be carried out if breeding sites are within the flight
range of mosquitoes from the community and breeding sites are limited
and accessible.
The following options can be used:
•
•
• Chemical larvicides like Temephos
• Use of larvivorous fish
• Covering/screening of water tanks
Biolarvicides like toxin formulations from Bacillus thuringiensis
(BT)/Bacillus sphaericus (BS), and insect growth regulators (IGR).
Use of expanded polystyrene beads (EPB) to cover the water surface.
The following points may be considered in the application of the above
methods:
•
Temephos is useful for an instant larval kill and may be used even in
potable water.
•
•
Larvivorous fish are cheap, can be linked with edible fish production and
can provide long term control, if proper supervision is maintained.
Bt and Bs toxin preparations are specific for mosquito larvae, do not kill
predators and are not prone to illicit sale for other purposes. However
resistance develops against Bs.
74
o
®
•
Screening or sealing of tanks may be expensive but is long lasting.
EPS is long lasting in confined sites without wind and overflow.
IGRs are effective at very low doses (p.p.b.) but the effect is not
immediately visible.
15.7 House spraying and thermal fogging
House spraying and thermal fogging should be done by well-trained
health personnel.
Communities should assist in house spraying
operations and fogging by providing volunteers for spraying and
motivating people to accept house spraying.
15.8 Chemoprophylaxis
The community should be educated by the National authority, whether
or not to take Chemoprophylaxis and which drugs to be used for the
same. In special circumstances, Chemoprophylaxis should be offered
as per national guidelines to special groups such as pregnant women in
endemic areas and short-term non-immune travelers to endemic areas.
15.9 Malaria vaccine
An effective malaria vaccine is not yet available although various
candidate vaccines are being developed and tested.
75
GUIDELINE SIXTEEN
SPECIAL STRATEGY ON ELIMINATION OF BREEDING PLACES
THROUGH COMMUNITY ACTION
In the previous section, we have identified step of involving the community in the
Malaria Programme. A special effort must be made as part of the RBM strategy to
involve them in Elimination of breeding places through Community Action as a social
movement.
16.1 Concept:
Mosquito control can be done by eliminating breeding habitats as much as possible.
Community action is required to eliminate breeding places as most of the breeding
habitats are man made and hence it is the responsibility of the community at risk of
vector borne diseases to eliminate the source of breeding.
Methods of elimination of breeding places are:
■ source reduction by eliminating or changing the breeding places to make them
unsuitable for developing larvae.
■ Making the breeding places inaccessible to adult mosquitoes for laying egg.
■ Releasing fish / predators that feed on larvae and pupae.
Operational area principle:
In and around human settlements in an area with a radius greater than the flight range of the
target mosquito species (normally 1.5 -2 kms).
Elimination of breeding places can be on permanent (long term) basis through
environmental, modification or on a temporary basis through environmental manipulation and
release of bio-control agents.
16.2 GUIDELINES
1. Identify target community : rural, urban, development project area, and
stratify if there are diversities in the socio-epidemiological situation of
malaria in the area.
2. Motivate the community through awareness campaign using appropriate I EC
materials.
3. Carefully identify breeding places at community level and map them.
4. Evolve Guidelines for community action to eliminate breeding places
(depending on local mosquito species it and choice of methods for specific
breeding habitats identified locally (see point 13. Also Appendix 2 for further
guidelines for action for different types of situations in rural and urban
areas).
76
5. It is necessary to establish a committee with a chairperson. Active members
such as teachers, postmasters, retired employees, KDS workers, religious
leaders can be included and one person assuming the leadership role.
6. The activities of the committee should include
•
motivation of the community through - interactive meetings
•
identify solutions - including those from community experience
•
involve / motivate other depts and their field workers
> local administration
> sanitation / water supply
> agriculture.department
> fisheries
> PWD
> forestry
7. Small groups with active members can be formed to generate collective force
in filling low lying areas of public interest. Such reclaimed areas can be used for
public use such as playground, etc.
8. School children can be motivated in planting trees in the reclaimed marshy /
low
lying areas in the effort of developing social forestry.
9. Technical skill in masonary, plumbing and constructing of soakage pits need
to
be developed so as to make the community self reliant.
10. It is necessary to ensure the availability of materials such as larvivorous
fishes, EPS beeds, neem oil cake, etc. This can be achieved through
collaborative approach. Information management system will help in
monitoring activities for feedback..
11. Potential avenues can be explored for resource mobilization.
12. Community participation can be sustained some of the by following
measures in the programme:
Planning income generating programmes with vector control as a
byproduct.
■=> Advocating alternative methods
• drainage
• water supply
■=> Legislation and strict enforcement of law
Dynamic leadership and encouraging self reliance
77
|=>
Periodical meetings with the community - to assess the situation, listen to
local problems and be open to suggestions
Promoting socially acceptable and viable solutions that are
• Culturally acceptable
•
Low-cost - available / affordable by all
• Socio-epidemiological need
Involve community right from planning in all stages of programme
Increase popular awareness of the value and the benefits of a malaria
programme.
Minimize conflicts by keeping organizations small; restricting
memberships to persons with harmonious objectives; defining objectives;
in a focussed way and distributing benefits equally.
Facilitate incentive from District Collector for those who involve in
community action.
78
13. A checklist of methods for mosquito control through environmental management
identifying site of action and assigning ‘roles’ and responsibilities is given below in
Table 2.
Table 2
Methods for Mosquito Control through Environmental Management
(Individual / Family / Community / Government)
Action site in
The house
Action to be taken by
The individual, the family
The house
The house
The house
The individual, the family
The individual, the family
The individual, the family
The house
The family, the community, the
local government____________
The family, the community, the
local government
The house
The house
The family, the community
The house
The house
The family
The family
The house_____
The surroundings
The surroundings
The individual, the family
The individual, the family
The family
The surroundings
The surroundings
The surroundings
The family, the community, the
local government
The community, the local
government_____
The community, the local
government_____
The community, the local
government_____
The community, the local
government_____
The community, the local
government_____
The contractor; the building
laws by government__________
The vendor, community_______
The family, the housing society
The surroundings
The family, Community
The surroundings
The family, the community
The surroundings
The surroundings
The surroundings
The surroundings
The surroundings
The surroundings
Action_________________
Cover domestic water storage containers;
tight fitting lids; empty water once in 7 days
Clear unwanted standing water___________
Clean roof gutters/sun shades____________
Replace water once in 7 days in animal
drinking pans, flower vases, etc.__________
Ensure provision of properly designed
sullage drains_____________________
Ensure proper design and maintenance of
sanitation / cover vent pipes with mosquito
netting__________________________
Store used articles and other refuse in
closed containers ______
Screen doors and windows______________
Coolers / air conditioners may have water
changed once in 7 days or a dry day
observed each week___________________
Use mosquito nets and repellents_________
Clean yards and vacant lots_____________
Cover with lid tightly; screen underground
cisterns and water storage tanks, or stock
them with mosquito eating fish____________
Ensure proper drainage
Control water supply sources and ensure
proper drainage_______________________
Provide properly designed waste water
drains and storm water canals____________
Drain or fill undesirable water areas like
cesspools, puddles, ditches, etc, tap pits
Modify large water areas by impoundment
Ensure adequate solid waste collection and
disposal_____________________________
Construction site
Coconut shells to be cut in 4 pieces_______
Mosquito proofing of overhead tanks (OHT),
make OHT accessible for inspection,
demolish discarded tank completely._______
Unused wells may have water covered by
EPS beads, crude oil or larvivorous fishes
Used wells may be covered, screened with
net or use larvivorous fishes
Adapted from : The CAP guide for Insect and Rodent Control through Environmental Management (WHO/UNEP)
79
CASE STUDY- 5
THE PUDUKUPPAM INITIATIVE
!
“The Vector Control Research Centre (VCRC) demonstrated that vector control could be made into an income
generating programme, which is the only way to enlist and sustain community participation in such endeavours.
A success story of a research project, carried out froml980 tol985 in the coastal villages of Pondivherry in
which malaria control was made a by-product of income generating activities is given below:
•
Pudukuppam, a coastal village, in the Union Territory of Pondicherry, was meso-endemic for malaria. The
vector incriminated was Anopheles subpictus breeding in brackish water. The major source for mosquito
breeding was a backwater lagoon (approximately 3 to 5.5 sq. kms.) with the entire water surface covered
with Enteromorpha compressa a filamentous algae facilitating vector proliferation. Removal of algae was
the only practical solution to control the vector breeding. Vector Control Research Centre explored the
economic utility of this algae in paper industry and the technology developed was handed over to the hand
made paper unit of Sri. Aurobindo Ashram, Pondicherry. The art paper made by the unit using this algae
drawn world wide attention with an excellent export market. This resulted in the creation of a self
sustaining system for algae removal with economic incentives to the local populace. Total elimination of
malaria was thus demonstrated exclusively through community action.
Feasible vector control measures
Source reduction : By the removal of algae which promote vector breeding
Quantity of algae removed in one year: 130 tons
Practical permanent solution : Economic exploitation of algae for manufacturing paper, file
etc.
cover.
Technology developed by : Vector Control Research Centre
Technology transferred to : 1. Hand made paper unit of Sri. Aurobindo Ashram, the pioneers in art
paper manufacture. 2. Hand made paper unit of Mahatma Gandhi Leprosy Rehabilitation Centre.
Benefits to the Community
Total elimination of indigenous transmission of malaria from the village.
Additional regular income to the villagers.
Employment opportunities to the unemployed youths, who collect and sell algae.
Reduction in the cost of production or mottled art paper, file covers, etc
A clean environment”
VCRC project - Pudukuppam
GUIDELINES : Process of Evolution
WHAT?
Guidelines on Roll Back Malaria Programme for South East Asia
Region
WHY?
To develop guidelines that would enable various components of the
Roll Back Malaria Initiative to be understood in-depth and with clarity.
The guidelines deal with strategies and methodologies for involving the
community and civic society at large; with diagnosis, treatment and
referral of malaria patients; and with the systems required at District
level to implement, monitor and review the programme effectively.
FOR
WHOM?
The effort was to evolve simple, generic guidelines for Malaria
Programme officers and their partners primarily at district level.
(Some guidelines were found necessary for the state / national /
regional levels as well so that the programme at district level benefits
from support at higher levels as well, (e.g., structural inputs, human
and material resources inputs, and planning and management
backup). These have been indicated.)
HOW/
WHERE?
1. The guidelines on Advocacy and Community and Partner
Mobilisation were evolved through an interactive, participatory
workshop held in Bangalore, facilitated by the Community Health
Cell, Society for Community Health Awareness, Research and
Action, Bangalore (CHC) from 9-11th December 1999. (It also drew
up from an interactive, participatory process report entitled
“Towards an Appropriate Malaria Control Strategy" that was
facilitated by the Society and VHAI, New Delhi, in 1997).
I
2. The Guidelines on Strengthening of District Health System for
Implementation ^foLjmplementatiorb of the RBM Initiative were
evolved at a workshop of past and present experts conducted by
the Indian National Anti-Malaria Programme (NAMP) Directorate
from 27th to 29th December 2000 at NAMP Directorate, Delhi.
3. The Guidelines for Simple Ways for Diagnosis and Treatment of
Malaria were developed by experts invited by The Post-Graduate
Institute of Medical Education and Research, Chandigarh from 3r
to 5th Jan 2000.
All guidelines were finally reviewed and revised in the context of the
South Asian diversity and restructured in an informal consultation at
WHO-SEARO New Delhi on 18-21 Jan 2000.
The guidelines were then integrated, edited and standardised by a
team of three consultants at CHC, Bangalore in June - July 2000.
I
2
WHO?
1. The participants of the Bangalore Workshop included resource
persons from academic and research centres, field NGOs, NGO
support groups, and citizens groups.
The group was
multidisciplinary with multi level experience in health care and
control
of
communicable
disease
programmes
(See
Acknowledgements).
2. The participants of the New Delhi workshop were mainly past amd
present senior officials from the National Anti-Malaria Programme,
and also had representatives from the Railways, Armed Forces
Medical
Services,
Industry
and
from
NGOs.
(See
Acknowledgements).
3. The experts on malaria involved in the Chandigarh workshop were
mainly academics from various disciplines like parasitolgy,
medicine, public health and also had participants from the local
health authorities and NGOs. (See Acknowledgements).
4. A group of consultants from WHO-SEARO and the region revised
the three guidelines to suit the pan-South East Asian Region at the
Delhi Consultation. (See Acknowledgements).
3
ACKNOWLEDGEMENTS
0.^0
List of participants of the Bangalore workshop organised by CHC :
Dr. V.P. Sharma; Dr. Rajaratnam Abel; Dr. Sunil Kaul; Dr. C.M. Francis;
Dr. Thelma Narayan; Dr. Ravi Narayan; Dr. V. Benjamin; Mr. S.D. Rajendran;
Dr. Rakhal Gaitonde; Dr. M.V. Murugendrappa; Dr. P.N. Halagi; Prof. N.J. Shetty
Dr. T.R. Raghunatha Rao; Dr. P. Jambulingam; Dr. K. Krishnamoorthy; Dr. K.
D. Ramaiah; Dr. S.K. Ghosh; Dr. Sathyanarayana; Dr. S.N. Tiwari;
Dr. A.K. Kulshrestha; Mr. R.R. Sampath Dr.K. Ravi Kumar; Dr. Mira Shiva ;
Dr. Mani Kalliath; Dr. Pankaj Mehta ; Dr. B.S. Paresh Kumar; Dr. Daniel;
Dr. J. Fernando; Dr. V.R. Muraleedharan; Dr. Prabir Chatterjee; Dr. Rajan Patil;
Dr. Biswaroop Chatterjee; Dr. H. Sudarshan; Dr. Prakash Rao; Dr. Anton Isaacs;
Mr. Suresh Shetty;
List of partcipants of Delhi workshop held by NAMP at NAMP Directorate: |
Dr Shiv Lal; Dr N Dhingra; Dr PB Deobhankar ; Dr J P Gupta; Col Basappa;
Dr Amrish Gupta; Dr S Pattanayak; Mr Rajesh Gehlot; Dr R Sonal; Dr Aruna Srivastava;
Dr Neena Valecha; Dr S P Misra; Dr T Adak; Dr Nagraj; Dr S K Aggarwal;
Dr. JC Gandhi; Dr R S Sharma; Dr P K Phukan; Dr Rajaratnam Abel;
Dr G P S Dhillon; Dr Sunil Bhat; Dr D Sen Gupta; Dr Kiran Dambalkar;
Dr B N Nagpal; Dr NL Kalra; Dr Bossaiya; Dr Sunil Kaul; Dr Mohanti;
Shri. C Krishna Rao; Dr P N Sehgal; Dr Kuldeep Dogra; Dr B K Borgohain
List of participants of Chandigarh workshop held by PGI, Chandigarh:
Prof S C Varma; Prof N Malla; Dr V P Sharma; Dr R C Mahajan; Dr V K Monga;
Dr T Adak; Dr R M Joshi; Dr M L Dubey; Dr R Sehgal; Dr Sunil Kaul;
Dr Rajaratnam Abel; Dr Archana Sud; Dr S K Ghosh; Dr Khosla; Dr N Valecha; Dr
Bhatti; Dr V P Sharma;
The guidelines were reviewed in WHO-SEARO and further modified and edited
with the participation of Dr. V.P. Sharma - WHO-SEARO, Dr. Ravi Narayan Community Health Cell, Dr. Rajaratnam Abel - RUHSA Department, CMCVellore; Ms. Tavitian-Exley (Myanmar); Dr. B.N. Gultom (Indonesia), Ms.
Jyotsna Chikersal, Mrs. Harsaran Bir Kaur Pandey (Nepal); Mr. V. Alexeev, Mr.
Omaj M. Sutisnaputra, and Dr. Sunil Kaul - CHC Associate; Dr. Sawlwin; Dr. A.
Mannan BangaliTDr. P.B. Chand; Dr. G.P. Dhillon; Dr. Hadi M Abednego; Dr. N.
Kumara Rai; Dr. Harry D Caussy; Dr. MVH Gunaratne.
WE ACKNOWLEDGE THE CONTRIBUTIONS AND ACTIVE PARTICIPATION
OF ALL OF THEM.
Dr Ravi Narayan, Dr. Rajaratnam Abel, and Dr. Sunil Kaul specially helped with
the final editing and integrating of the guidelines. There support is specially
acknowledged.
'
4
GUIDELINES FOR THE IMPLEMENTATION OF ROLL BACK
MALARIA IN SOUTH EAST ASIA REGION
Introduction
Malaria. People of the world’s poor communities face many threats to their well
being. 40% of the world’s population is at risk of malaria and the disease is a
particular burden for the poorest countries.
There are as many as 500 million cases of acute malaria in the world each year - as
many as 5% of them causing severe illness associated with time away from work or
studies. The risk of malaria is a constraint to the economic development of
communities, regions and nations.
Roll Back Malaria Initiative. In 1998, Dr. Gro Harlem Brundtland, Director-General
of the WHO launched The Roll Back Malaria (RBM) Initiative against malaria. RBM
emphasises evidence-based strategies, community level action, partnership between
governments and development agencies, and a reformed response from all of WHO.
It recognizes that sustained success in rolling back malaria inevitably calls for
development of health sector so that they can address a range of priority health
problems. The RBM Initiative seeks to mainstream efforts to roll back malaria
throughout the range of community-level health activities being taken forward by
societies at risk of malaria and is expected to evolve into a social movement on a
global scale.
Within countries, the Roll Back Malaria movement will be backed by governments
and development agencies, NGOs and private sector groups, researchers and
media working in partnerships. The same partners will be organized as a global
partners.
The global Roll Back Malaria partnership has an overall goal of halving malariarelated deaths throughout the world by 2010; the strategy builds on the 1992
Amsterdam global malaria control strategy; with the following six elements:
1. Enhanced diagnosis and treatment of malaria (eg., new diagnostics test,
universal access to treatment, combination drugs);
2. Disease transmission control (cost effective integration of vector control tools eg.,
insecticide treated nets, selective vector control, bio-environmental methods);
3. Enhanced surveillance (rapid response, border malaria, and monitoring process);
4. Health sector development (eg., decentralization, health equity, package delivery
care, changing role from implementors of malaria control to leadership, regulation
and coordination);
5. Community mobilization (empowerment of communities,
planning and ownership); and
evidenced-based
6. Advocacy (forum for advocacy, strategic investments eg., mapping, new drugs
and vaccines, regional support networks eg., drug policy, rapid response, etc.,
health impact assessment, research on reform in health system).
5
Malaria in South East Asia. Malaria continues to be one of the most serious public
health problems in the South-East Asia region. 85% of the total population in
Southeast Asian countries is at risk of malaria, with 35% living in moderate to high
risk areas.
Malaria in South East Asia - Situation Analysis
❖ In South East Asia Region - there are about 3 million (25-26 million
clinically suspected) malaria cases annually.
❖ Malaria in Asia is unstable and causes epidemics and high morbidity.
❖ An estimated 1,202.5 million people or 85% of the total population of SEA
region are at risk of malaria. About 90% live in moderate to high risk of
malaria in India, Indonesia, Myanmar and Thailand.
❖ Chloroquine resistant P. falciparum is reported from all endemic countries
(except DPR Korea); nearly 400 million people live in areas with risk of
contracting drug resistant malaria. Sulfa-Pyrimethamine resistance is also
reported from all endemic countries except Sri Lanka and DPR Korea with
an estimated 140 million population at risk. Multi-drug resistance P.
falciparum is highly prevalent on the Thai-Cambodia and Thai-Myanmar
borders.
❖ Deteriorating epidemiological indices are associated with drug resistance
and operational problems.
❖ In this region 80-85% malaria cases are reported from India and bulk of the
malaria deaths (55-65%) from Myanmar.
❖ Malaria has adverse effects on economic and social development. Malaria
has been called the single biggest cause of poverty in some countries.
Morbidity caused by malaria reduces family earning by 12% and a
weakened workforce brings down productivity.
❖ The process of development itself contributes to the spread of malaria. As
roads are built, forests cut down, new mining areas opened, habitats which
favour the breeding of mosquitoes, expand. This is very common in the
SEA region.
6
Simple guidelines have been developed to implement the six elements of the Roll
Back Malaria. These guidelines address the health sector development leading to
advocacy and the community mobilization.
The RBM is different from previous efforts to fight the disease. While drawing on the
strengths of past experience in malaria control, it focuses on political commitment,'
community empowerment, inter sectoral linkages and partnerships with the
community; voluntary agencies and NGOs; and the private sector involving both
health and development related programmes.
The focus is on finding local solutions to local problems while drawing on potential
resources outside the health sector. With this aim in mind, The Roll Back Malaria
project emphasises decentralization and district level planning with the full
involvement of the community and other partners.
The National Malaria Control Programme then assumes a role of leadership,
facilitation, co-ordination, regulation and not of sole implementation.
RBM - the New Initiative - What is New?
1. RBM is a social movement for better health and poverty alleviation.
2. RBM plans are country driven, evidence based and adapted to local
realities.
3. RBM promotes health equity by focussing on disadvantaged
populations.
4. RBM solicits effective partnerships within and outside WHO.
5. RBM plays the role of leadership, regulation and coordination.
6. RBM activities mainstream into health sector development.
7. RBM is an integrated approach to address malaria and other
common diseases.
8. RBM is a pathfinder for health and human development.
9. RBM is for high level of advocacy for change.
10. RBM promotes research and development for new tools."
■
7
Guiding Principles
RBM draws on the Primary Health Care (PHC) strategy and aims to strengthen the
existing district health systemffor the sam^. It also identifies that early diagnosis and
treatment cannot be made unless common women and the community at largej
understands the basics of malaria and has access to medical aid for all kinds of
common ailments one of which is malaria.
Mobilisation and advocacy are therefore deeply embedded in the Primary Health
Care approach. This is done through the emphasis on
.
i. Community participation
I
ii. The use of appropriate technology .
j
iii. Intersectoral coordination
iv. Social equity - central to thq strategy of the control programme.
y
9 i
The following principlesjorm the blueprint to these Guidelines:
' 1
1. The 'comrYtenity^rn the urban slum, the rural or tribal area?must first be^- \
accepted at all levels of the control strategy as ‘active participants’"of the \
programme and not ‘passive beneficiaries’.
\j-^~
2rrtJi^Tforiimunity and/or its representatives botITTormal and informal leaders,
' should be involved in the planning and organisation of the activities at all
stages of the programme. A village health committee will operationalise this
further.
.-v,
3. The focus of the activities and strateqies^shouldj nodjust be on providing the
community - a package of servicesj^it on actively enabling and empowering
them to participate in decision making that helps them to make health,
including malaria control activities, their own responsibility, —
4. The large number of human resources that are available in any community must
be identified and mobilized to support the programme.
5. The Primary Health Care approach is a comprehensive approach.and therefore \
malaria control programmes should not become unipurpqse or selective in their
. .
orienTatidfCahcf whether it is the village committee, the health guide, or the~ Z v
strategy, there should be scope and openness to use the same structures and /»
resources for other disease and health problems in the community / / /
country.
6. A major thrust of suctrTprimary health care oriented programme will be the
approach of demystifying the problem at the community level; to build |
confidence and perspective to tackle that at the level itself; so that the health
team works in close partnership with the people and the programme becomes
identified by the people as their programme.
7. The Primary Health Care approach also calls for a certain ^umiljty in the health
team about not always wanting to ‘teach’ or tell the people something, but also a
willingness to learn from local experience, wisdom and health culture. The
?/
people, when provided the right forum and context will often share ideas, options,
/
alternatives that the health teams should consider. New approaches or
/
alternatives can emerge if this learning from the people and working ‘with them’
rather than ‘forthem’ becomes a team commitment.
"We need not only to persuade the people to accept the
professional's wisdom, but also the professional to understand
people's wisdom."
8
8. Building new partnerships is another challenge of the RBM initiativeJThese
concrete guidelines are intended for use by all partners involved in RBTvE They
identify the steps required at district level by the programme managaer leading the
anti-malaria operations to broaden the range of partners in the control of malari
(supported by national, state/division level):
•
•
•
•
•
/
With the communities
With non-govemment, civil society organisations
With the private sector (medical and non-medical)
With the educational sector
With other sectors in a spirit of intersectoral collaboration.
They are designed to be applicable and suitable for use in the field. They have been
arranged in logical and chronological sequence of activities. Case studies and a few
examples have been included to illustrate the possible applications.
9. While advocacy, leadership development and community mobilization, capacity
building of communities and building new partnerships@the main focus of the
RBM initiative, there is also a need to strengthen the whole District Health System
\and its capacity to respond to the malaria problem. The guidelines therefore also"^\
Y.y\
focus on strengthening of the District Health System through a wide range of | /v
activities.
s > CA
10. One of the challenges of evolving these guidelines was to keep them as generic■
as possible so that they could be adapted to each country situation in the region.
At the same time, there is a need to be specific and provide some details as well.
11. These guidelines are designed to be applicable and suitable for use in the field.
They have been arranged in logical and chronological sequence of activities.
Case studies and a few examples have been included to illustrate the possible
applications.
y
W
I'^z
r/
/
12. These guidelines are not complete. We have tried to look at as many aspects that )
the consultants who participated in the process of evolution of these guidelines'—^
Each country, each district in the region has its own distinct in-its ecology,
environment and requirements that need further guidelines. These will have to be
evolved locally.
Health is created and lived by people within the setting oi
their everyday life, where they learn, work, play and love."
.
JL
9
Bo
LE
5 H/
<HiCovA H
. tec
GUIDELINE ONE
ADVOCACY
1.1
ADVOCACY
As the causes of malaria lie outside the control of the health sector, obtaining
political will for malaria control is an essential first step. Intersectoral collaboration is
an important principle of RBM, and this will need advocacy at many levels.
AT THE NATIONAL LEVEL
•
Political commitment must be obtained at the highest level to ensure inter
ministerial collaboration, as well as sufficient budget allocations to fight malaria.
It is important that top leadership is convinced about the need for action across
various sectors, and makes the necessary commitment for this. It is also
important that the top leaders make public commitment to the cause.
•
WHO and the Health Ministry need to make a strong case, based >n evidence, of, /
the importance of such commitment and action.
, izz
advocacy materials need to be produced to present the case,
.x 6
•
Print and audio visual^ materials would clearly spell out the issues.
•
These would need to highlight the argument that malaria is (a net’drainj both on
the health of the people, and on the workforce, causirfglTnegative impact on the
economic productivity of a country.
•
National and state level data are needed so that the argument is based on y
evidence.
Different versions would target separate key stakeholders: eg: A
government/ other ministries/Chief Ministers of States/captains of industry/ the )
news media.
n
/
Role of media^_^y 7
•
•
•
Ar
At the national level, media need information to understand the scale of the
problem, in health and economic terms.
vXu ?
The link with environment degradation and unplanned urbanisation are issues
already under media scrutiny in most countries. The malaria issue’s linkage to
these developments needs to be highlighted.
The news media offer a good channel to set the agenda and make malaria
control an issue, particularly at the national level. They can ask questions, and
play a watchdog role.
!,
Ja
10
AT THE STATE or SUB-NATIONAL LEVEL
•
A similar high level commitment must be sought from the top political leadership.
•
This would translate into inter-department cooperation.
•
As different states would have varied situations, the malaria situation must be
spelt out for that state.
•
Health ministries/departments must obtain the health and economic data related
to malaria morbidity and mortality for that state. Advocacy materials at this level
would use this in the formulation of key arguments.
Role of media
At the state level too, the news media play an important role in setting the agenda, in
awareness creation among policy makers, creating public awareness, and in
following up on action taken or the lack of it.
AT THE DISTRICT or MUNICIPAL LEVELS
•
Activate the district/ municipal administration or mechanism
implementation and monitor the programme components.
•
The private sector/other departments/service organizations, and the media, are to
be targeted for advocacy.
to
ensure
Role of media ^
At the district level,
the media can be used increasingly for information
dissemination, about the problems related with malaria, possible community action,
role of service organizations and the private sector. Media has a greater role in
social mobilization and support to social marketing, at this level.
11
THE STEPS FOR ADVOCACY AT ALL THESE LEVELS INCLUDE
1. Analyse situation and problem
“Analysis is the first step to effective advocacy, just as it is the first step to any
effective action. Activities or advocacy efforts designed to have an impact on
public policy start with accurate information and in-depth understanding of the
problem, the people involved, the policies, the implementation or non
implementation of those policies, the organizations, and the channels of access
to influential people and decision-makers. The stronger the foundation of
knowledge on these elements, the more persuasive the advocacy can be”.
2. Design strategy (What are the messages to be communicated)
Every advocacy effort needs a strategy. The strategy phase builds upon the
analysis phase to direct, plan, and focus on specific goals and to position the
advocacy effort with clear paths to achieve those goals and objectives”.
3. Mobilise resources
Coalition-building strengthens advocacy. Events, activities, messages, and
materials must be designed with your objectives, audiences, partnerships', and
resources clearly in mind. They should have maximum positive impact on the
policy-makers and maximum participation by all coalition members, while
minimizing responses from the opposition"..
o
4. Implement action
“Keeping all partners together and persisting in making the case are both
essential in carrying out advocacy. Repeating the message and using the
credible materials developed over and over helps to keep attention and concern
on the issue"?'
'
5. Evaluate results
Advocacy efforts must be evaluated as carefully as any other communication
campaign. Since advocacy often provides partial results, an advocacy team
needs to measure regularly and objectively what has been accomplished and
what more remains to be done. Process evaluation may be more important and
more difficult than impact evaluation”.
5. Plan for continuity
“Advocacy like communication is an ongoing process rather than a single policy
or piece of legislation. Planning for continuity means articulating long-term goals,
keeping functional coalitions together, and keeping data and arguments in tune
with changing situations”.
“Public policy advocacy is the effort to influence public policy through
various forms of persuasive communication. Public policy includes
statements, policies, or prevailing practices imposed by those in
authority to guide or control institutional, community, and sometimes
individual behaviour.’’
12
GUIDELINE TWO
LEADERSHIP
2.1
BUILDING LEADERSHIP AT DISTRICT LEVEL
THE MALARIA CORE GROUP LEADERSHIP (COORDINATION TEAM)
The malaria programme activities at the district level needs the involvement of
atleast the following:
•
The District Administrator
•
District Health Officer
•
Health Officer designated for malaria, if available.
•
Education Officer
•
Agricultural Officer
•
Public Works engineer
•
Representative leaders of local / village self government
•
Selected NGOs
•
Representative of health care providers associations if any
•
Public / private industry if any
Officers in charge of:
❖ water and sewerage
❖ irrigation r
❖ rural and urban development
❖ social welfare
(The composition of this coordination committee will vary in each country
and state and will depend on the resource persons available at district
level)
•
2.2 EVOLVING THE ROLE OF THE COORDINATION TEAM
These will include the following steps:
Step One
A coordination committee chaired by the district administrator and
health/nTalariTofficer as secretary wilPbe the first step to develop leadership
at the district level. In keeping with the new philosophy of RBM,
representatives of leaders of the community, NGOs, private practitioners and
industry should also be included in, the committee so that the ownership and
■ the stakes of a much wider group are facilitated.
.
20
Guideline 4
BUILDING OTHER PARTNERSHIPS
General Principles
Partnerships for Health
“Partnerships for health bring together a set of actors for the common goal
o improving the health of populations based on mutually agreed roles and
principles.
a
Partnerships imply that a balance of power and influence is maintained
between the partners and that each .partner can maintain its core values and
identity. They are built on:
common interest
. ❖ mutual respect
\
a»a
clear manageable objectives
/
i
commitment
to
contribute
time,
resources
and
energy,
and/
> a’a
Recognising Partnership Diversity
To sustain the community level malaria control activities, there is a need to
build a relationship with a wide variety of partners. These’could be:
a»a
et%
NGO sector
Private sector
a»a
Educational sector
•’a
et»
Other developmental
construction,
industry, etc.
including
sectors
agriculture,
irrigation,
Evolving Partnership Process
Partnerships do not just come about. They need to be built with skill, care
and mutual trust. A partnership strategy needs to constantly keep in’mind
each of the following steps:
0,^0
a^a
a»a
etv
a^a
et«
a^a
identifying opportunities
identifying potential partners
selecting the most suitable partners
negotiating / reaching a clear partnership agreement
maintaining the partnership
regularly evaluating the partnership.”
Partnership Criteria
_
“Partnerships should meet three basic^criteria:
the partnership should lead to significant health gains
\
efla
the health gains should be worth the effort involved in establishing and
maintaining the partnership.
'
e't'o
the partnership should strengthen the programme’s role as a catalyst
for
health development.”
i
5^
$ .
I
21
‘‘Partnership is an alliance in which individuals,
groups or organisations agree to:
•
•
•
•
•
•
work together to fulfill an obligation,
undertake a specific task,
meet a shared objective,
share the risks as well as the benefits,
review the relationship regularly,
revise the agreements as necessary”
y
r
^PARTNERSHIP WITH NGOs
I - ---- ----- ------------i z 1
i
Context
i) The role of NGOs especially the voluntary agencies (not for profit NGOs) is being increasingly
recognised in planning and policy circles as an effective complementary/
supplementary
strategy.
ii) In the past, they have played this role without much governmental support In recent years a
greater degree of collaborative effort is emerging as a policy alternative.
iii) The Voluntary agencies (Volags) have their Strengths
a) They are closer to the people and usually more aware of grass root realities.
b) They often work in more interior and inaccessible areas or in accessible areas with
more marginalised groups and the underprivileged.
c)
They tend to be idealistic and committed to certain values and principles.
d) They often have a stronger development orientation and awareness building
commitment and skill.
iv) The Voluntary agencies (Volags) have their Weaknesses as well
a) They are very dispersed and individualistic and not woven into any integrated
network.
—-— ------- ---- ------ ---------------- ----b) They ire often aloof from governmental programme^ having their own programmes
and agenda^
- ------ -—
c) They are very diverse in their size, type, ideology, focus, distribution, lineages and
professional competence.
d) They are inadequately informed about governmental programmes and initiatives and
often lack adequate professional expertise being stronger in motivation rather than in
skills.
e) They often follow fund driven / donor driven agendas.
f) They are also not often present in areas where they are needed most.
v)
It is a very important development that the opportunities of government - non-governmental
collaboration are being increasingly promoted in recent years though involvement in malaria
care is still not significant The evolving process should build on NGO strengths but it is
necessary to be alive to NGO weaknesses as well. These vary in different countries of the region.
/
22
4.2 AVENUES / AREAS OF PARTNERSHIP
A. Community awareness
As the NGOs work with the local communities, they understand the community
dynamics and the local culture. Any community awareness programme should be
relevant to the local context and hence working with the NGOs as partners could
greatly enhance the efficacy in the community awareness programmes. Developing
IEC material relevant to the local context and carrying health messages through
indigenous and local methods will have greater acceptability and adoption and
could be a major role for NGOs.
B. Community planning
Most of the organisations promote participatory methods of problem identification
and planning. This favours bottom up planning and ownership of the programme by
the community. In the area of vector borne diseases, this will be a good strategy for
control mechanisms and the government could use this expertise available with the
NGOs-
,
C. Community mobilisation
As mentioned earlier this is one of the great strengths of the NGOs. A recent
example of this has been the pulse polio programme. Similar strategy could be
adopted for vector control and personal protection measures, and this should be
seen as a positive aspect in partnership.
D. Socio epidemiological research
Unfortunately there are very few good local and community based research studies^)
so essential to have policies on control of vector borne diseas^s^Studies like KAP^
community behavioural pattern, health seeking behaviour etc., could throw a lot of
light for effective strategy formulation. Here the NGOs could play a larger role and
this partnership will enhance efficacy of the work.
E. Diagnosis and treatment
As the NGOs are the first level contact in the community, access to diagnosis and
treatment could be made available nearer to the community. They also could be
involved not only in case finding but also on follow up of patients. (A few NGOs
could be trained in this direction as an approach to partnership).
F. Epidemic preparedness
A few NGOs could be built as resource centres for epidemic preparedness as they
are closer to the scene of action. Here the partnership will enhance the effective
control of the epidemics in epidemic prone areas.
rz'
23
4.3 GUIDELINES AT DISTRICT LEVEL
A. Identification of NGOs in the districts The State coordination cell will develop
tools for partner appraisal and accountability in choosing the right type of partner for
the control programme.
B. Setting up district coordination committee The district health malaria officer
will form this committee with some NGO representation. The basic function of this
committee would be to appraise the NGOs, proposal and budget screening, and
working out a time plan of activities.
C. Sensitisation and capacity building of the NGOs The committee will conduct
a workshop of the identified NGOs to sensitise them on the issues of vector borne
dis'eases'Shd do a need assessment to look at gaps in the skills. This committee
will also identify resource persp ns jn the district to build the skills of the NGOs, .*
especially in areas of diagnosis Treatment and vector control.
?j
D. Information dissemination The district committeeCwill develop appropriate^
'-*■ '
information and programme guidelines for various activitesTor the NGO partners,
on the health issues identified. This in turn will be further simplified by the NGOsfor community level dissemination.
7^ .*
< “ ° QInformation from the community also will be received, sometimes through the
NGO at the district level for follow-up. This may be documented systematically or
could be taken up for policy advocacy work.
E. IEC materials The committee will encourage production of community specific
IEC materials which can be used in the local context. This committee can over a
period of time review the impact in the community due to this IEC, which may then
be documented. Local artists, school teachers and school children can be
involved in generating local materials. Local folk arts and folk media may be used
to evolve themes relevant to the malaria programme.
F. District level action plan The district coordination cell will ensure that each
district has an action plan worked with the help of NGO partners. This may be
presented to the cell and queries clarified and approved.
G. Participatory planning and monitoring The committee will encourage the use
of participatory tools for programme planning and monitoring. Other than this, the
committee also will develop indicators as MIS for bringing out reports and to
measure outputs.
H. Monitoring and review The committee along with the partner and community
will conduct this review at regular intervals to give direction to the programme.
I. Advocacy The committee along with the partners and networks will take up local
issues for advocacy. This may be at the local government level or at the district
level
7
J. Documentation
This is usually the weakest area in the /NGO'sector.
Enhancing the
documentation skills of NGOs involved in the programime are an important adjunct
activity and should be promoted. Learning from field experiences both positive
and negative are an important adjunct to group learning.
24
4.4
RECOMMENDATIONS FOR STATE / NATIONAL LEVEL
A. Dialogue with key agencies
The government should have a meeting with the key NGO coordinating and resource
agencies whose priorities are on health and communicable diseases to work out
collaborative mechanisms. A clear terms of reference should emerge on the modes
operand!, roles and the financial commitment. Usually these agencies would work through
their partner organisations and the government should also work out a Terms of
Reference for working through them.
B. State level nodal NGO
The government should identify nodal agencies in each state as a “single window system”
for building up collaborative alliances, identification of NGO partners, mobilizing resources,
etc.
C. Database on NGOs
Government along with the nodal agency should develop a data base on NGO working in
the respective state and classify them according to their focus of work (like agencies
working on vector borne diseases, health care, etc).
Where a data base already exists this should be reviewed and constantly updated.
D. State level workshops with NGOs
The government along with the nodal agency should organize a workshop to discuss the
challenges in vector borne diseases and to appraise the key role the agencies have to
play in collaboration with the government.
E. Formation of a State coordination cell
Along with the nodal agency a coordination cell could be formed to appraise the NGO
partners, review and approve the proposals sent by them, approval of funds. This cell
could also play a role in taking up advocacy issues raised from the districts.
F. Approval procedures of proposals from partnersThe state coordination cell using
expertise of some coordinating national and international NGOs could evolve forms /
formats for proposals writing and develop guidelines for approval procedures.
G. Identify themes for social epidemiological research
This could be identified by the cell at the district level. The cell could identify experts to
conduct this study at the community level and facilitate / support them.
H. Policy advocacy
Issues raised from the district could be related to policies or policy implementation. The cell
would develop strategic alliances with agencies involved in advocacy work to take up the
issues for policy advocacy and policy reform.
25
------------------- ,
^PARTNERSHIP WITH PRIVATE SECTOR
vt
_________
Range and Diversity
Private sector at district level would consist of one or more of the following groups:
1. Health Care Providers:
•
•
•
•
General practitioners of all systems of medicine
Dispensaries, hospitals and nursing homes
Laboratories and diagnostic centres
Chemists and pharmacists
2. Health Product manufacturers of:
•
•
•
Pharmaceuticals
Insecticide
Bed nets and personal protection equipment.
3.Non-health private sector including corporate sector, small scale industry,
construction, engineering, etc.
\
4^.1 General Principles
o
All the above groups would need guidelines on Scientific Diagnosis,
Presumptive and Radical treatment, Prevention and Control measures.
(Emphasis on these components would vary depending on the activity of the
group. For example, the medical profession would focus on prophylactic
preventive measures and bio-environmental control measures whereas the
Architects and Building Contractors would focus more on designing and
constructing houses which would prevent mosquito breeding and entry.
Similarly overhead tank manufacturers would focus on manufacture of tanks
that deny entry to mosquitoes so as to prevent their breeding inside the tank).
" ''
........... J
Providers of care should adopt scientific diagnosis and treatment of malarial
cases. It was also recognized that there would be variation in the regimens
used in some parts specially where resistance is widespread or where
Plasmodium falciparum happens to be the predominant pathogen. However, ‘
in all regions guidelines on management of malaria cases as applicable in the
region have to be strictly followed.
All healthcare providers should also be aware of different types of malaria and
their presentations and when and where to refer if need arises. The
programme officer should properly instruct on the above and on the need for
notification of all proven cases. He should ensure that all private health care
providers are well versed with environment control measures of mosquito
borne diseases. The programme officer should also stimulate the private
sector in taking part in malaria control activities.
All guidelines should be made available widely and promoted at every
available opportunity. Private sector involvement in their publication and
distribution is possible.
i
t
/
26
4.5.2 Guidelines
1. Building a partnership with all the above would involve the followinasteps:
Step One
I
I
Identifying all'potential partnerd^from each of the groups above at the district level.
Step Two
Sensitising them and making them aware of various aspects of malaria control by
2
organising meetings with them.
2
Step Three
Helping them adopt malaria control initiatives in their own work places, and
Step Four
_ _
Identifying the role and the contribution they could make to the programme.
Each of the above groups could contribute to the programme in various This
would vary with different groups:
A. Health Care providers.
They should be encouraged to:
> adopt scientific and rational diagnosis and treatment of malaria.
# provide referral support wherever feasible.
< Support IEC at patient, family and community level in their area.
For this purpose CME (Continuing Medical Education) programmes, bulletins,
newsletters and handouts may have to be prepared in collaboration with
professional associations/institutions. The CMEs must update the health care
providers on all aspects of Rational Malaria Care and Control. They must also
counter irrational practices and approaches that are not uncommon (see Box
below).
27
CONTINUING MEDICAL EDUCATION PROGRAMMES
CMEs must specifically address the following trends in malaria control in the private
sector:
1.
A use of a wider diversity of irrational regimes and combinations often at a
high cost to the patient and totally at variance with the national malaria guidelines.
2.
A tendency to exploit the illness episodes by the use of injectable preparations
and other adjuncts not in consonance with the principles of rational malaria care.
3.
A tendency to see the ‘outbreak’ or ‘epidemic’ as an opportunity for gain rather
than as an opportunity to be actively involved in a national health programme and
national efforts to tackle a major public health programme.
4.
These trends are further complicated by an increasing fall in clinical diagnostic
standards and inadequate recourse to lab diagnostic facilities. The clinical
laboratories also have been showing a lack of quality and standardization even when
they are available and utilized.
5.
Further some degree of medical misinformation by medical representatives
pushing their company’s remedy against the other to enhance profit margins even
when low-cost generics are available is a growing problem.
6.
The obvious result of such continued, irrational medical practice is reflected in
the increasing problem of drug resistance, as well as the continuation of unnecessary
and avoidable suffering.
B\ Health Product manufacturers
Opportunities should be explored with all local manufacturing industries to
produce malaria control related products that are low-cost and appropriate to
the local needs;,
'
Nets
» Mosquito repellants
|gc materials—' ' ' ’
> Drugs
The private sector, specially the manufacturers and distributors should adopt
rational production, good manufacturing practices, fair pricing, ethical
marketing and sales of all malaria prevention and control products.
Pharmaceutical companies manufacturing and promoting anti malarial
compounds should provide rational formulations and produce single ingredient
products and drugs in the recommended dosages only.
C. Non-health private sector
They could be harnessed at district level for providing.the following:
® Financial resources for the programme
< Promotion and marketing skills.
> Taking steps to prevent mosquitogenic condition!
itiongjnjhejr^institution /
project areasrfe&^^^^X'
Support I EC F*i
..........
The private sector usually has very good marketing and retailing skills. These
could be fruitfully shared with Non Government Organizations and other
A
28
voluntary organizations working in the field of malaria specially those involved
in social marketing.
“Today more than ever public health
institutions world wide need to re
define their mission in the light of the
increasingly complex environment in
which they operate”
Julio Frenk
\
30
Recommendations at State / National level for Government - Private
Sector partnerships
2
■
The private sector specially the Corporate Sector should be approached for financial and other
resources for the control of vector borne diseases. Many corporate sectors have their own
townships. They should take all necessary steps to prevent malaria transmission in these"
towh^HipS'as well as all other vector borne diseases mainly through environmental and biological
control measures.
- --------------9
■
Prior to the sanctioning of manufacturing licenses, all new industries andpfojects should have a
health impact / malaria risk assessment. Drug industries should me^sT^oirns and standards for
their products used for malaria management and^all insecticide manufacfurers should follow WHO
guidelines. To facilitate this, collaboration wit^Ctfan^other bodies should be formed.
■
National, State and District data base specially on malaria morbidity and mortality, health
personnel and health care institutions of all systems, active players and groups from the private
sector and other sectors involved in malaria activities are required for proper programme
implementation. It is also important to have all demographic and resource data and plan for
adequate funding and obtain all necessary resources for successful partnership with the private
sector.
■
To prevent misuse of anti-malarials, second and third line of drugs should be made available at
tertiary care level centres and some identified institutions only. No sale of these drugs should be .
allowed at other centres/places and even in the identified centres these drugs are to be dispensed
to those having a proper prescription only.
■
Therapeutic guidelines for treatment for insurance purposes should be issued thereby making
insurance bodies effective regulators for care as per stated guidelines. Claims of those claimants
that have not had treatment as mentioned in the guidelines should not be honoured.
■
All private practitioners and institutional staff should be encouraged to implement national drug
regimens for all cases of malaria. To facilitate this, booklets on malaria with all necessary
information are to be widely distributed and also presented to all new graduates.
Undergraduate courses in all medical fields should ensure that students receive adequate training
in rnaTaria.arecompetent in its diagnosis and management and are able to provide correct advice
on prevention and control measures.
■
All professional organizations (Homeopathic, Ayurvedic, allopathic) are to be involved.
■
For those who have completed their courses continuous educational programmes should be
organized on a regular fashion and participants should be given recognition of having attended
these courses in the form of certificate of attendance and or competence.
■
To obtain cooperation from industry as well as in training various groups like traditional
practitioners, Registered Medical Practitioners, etc. Non Governmental Organizations with
requisite capacity should be identified and involved. Linkages between these organizations should
be encouraged so that they can utilize IEC capacity should be involved and requested to
contribute to IEC activities for malaria.
/
I
V
29
1
A Word of Caution
Partnership with Corporate sector
1.
“Partnership with the corporate sector at all levels from global to local are essential. The public health
sector has not and can not make sufficient health gains on its own. Developing partnerships with the
corporate sector is a matter of balancing the potential benefits to be gained against risks. The stakes are not
trivial”
2. “The risks in developing partnerships with the corporate sector include the possibilities that,
(a) the government / programme reputation willjje used to sell goojs and services for corporate gain, thus
diminishing government / programmes repufafion as’ an imp^artiaThoBer of hea’ith'vaTues,
(b) Government / programme’s judgment on a particular product, service, or corporate practice may be
compromised by financial support provided by the involved company or industry, and
(c) Government / programme involvement with an industry or company is perceived as acceptance by
government / programme of unhealthy products, services, or practices”.
"’~s'
3.
Government / Programme policy toward the industry involved
"The involved industry must be a suitable partner for government / programme. The following questions
which must be asked when developing a policy toward a specific industry:
❖
❖
❖
Are the major products or services of the industry harmful to health?
Does the industry engage on a large scale in practices which are detrimental to health?
Is the influence of government / programme’s role in the partnership likely to do more good than the damage
done by harmful practices, products or services?"
4.
❖
❖
❖
❖
❖
❖
“Health provider organizations, the pharmaceutical industry, health care technology industries and similar
organizations are generally quite spitable^partners. The tobacco and arms industries, which have
indisputably negative health impacts, are^ciearTy not suitable partners.
Many industries such as
transportation industry, fast food industry, and chemical indusfiyrtrave’both a positive and a negative impact
on health."
’
“Suitability of the individual company
Even when an individual industry is a suitable partner, individual companies may not be. Additional factors to
consider in evaluating partnerships with individual companies are:
the occupational health conditions on which products or services are produced
the environmental commitment of the company «•
the marketing and advertising practices of the company
the research and development policy and practice of the company
the regulatory adherence of the company —
but also the subsidiary / combine has to be looked at
no past activities (not to exceed 3 years) which might affect objectivity, credibility of government /
programme”.
5.
“Appropriateness of the individual activity
Partnerships often focus pn a specific activity or set of activities. Most categories of activities proposed in
the context of a government / programme partnership will be appreciate, since they will aim at specific health
policies or health practices. However, the following categories of activities are not appropriate within a
government/programme partnership:
❖
❖
activities which involve conflict of interest or perceived conflict of interest
activities which benefit the corporate partner, but provide no clear health benefit, benefit to government /
programme or benefit to Member States.
Conflict of interest is of particular concern for government / programmes involved in setting regulatory
standards and other norms which may affect product costs, market demand, or profitability of specific goods
and services”.
6.
“To avoid conflict of interest - real or perceived -the concerned government I programmes must
establish procedures which ensure that
(a) final normative decisions are free from undue influence,
(b) industry funding is not used for salaries of staff involved in normative decisions, and
(c) consultations and other normative activities never have their majority financing from the concerned industry.
In the context of an on-going partnership, some proposed activities may service public relations and other
interests of the external partners, but have no clear health benefit. In general, such activities should be
avoided.”
7
30
Recommendations at State / National level for Government - Private
\
Sector partnerships
■
The private sector specially the Corporate Sector should be approached for financial and other
resources for the control of vector borne diseases. Many corporate sectors have their own
townships. They should take a)^ necessary steps to prevent malaria transmission in these
townships as well as all other vector borne diseases mainly through environmental and biological
control measures.
\
/
■
Prior to the sanctioning of manufacturing licenses, all new industries and projects should have a
health impact / malaria risk assessment.\Drug industrie/should meet ISI norms and standards for
their products used for malaria management and all insecticide manufacturers should follow WHO
guidelines. To facilitate this, collaboration with Cl I ancfother bodies should be formed.
■
National, State and District data base specially on malaria morbidity and mortality, health
personnel and health care institutions of all sy^ terns, active players and groups from the private
sector and other sectors involved in malari; i/activities are required for proper programme
implementation. It is also important to have < ^ demographic and resource data and plan for
adequate funding and obtain all necessary res Durces for successful partnership with the private
sector.
/
■
To prevent misuse of anti-malarials, second/and third line of drugs should be made available at
tertiary care level centres and some identified institutions only. No sale of these drugs should be
allowed at other centres/places and even in the identified centres these drugs are to be dispensed
to those having a proper prescription only./
Therapeutic guidelines for treatment for insurance purposes should be issued thereby making
insurance bodies effective regulators for care as per stated guidelines. Claims of those claimants
that have not had treatment as mentioned in the guidelines should not be honoured.
■
All private practitioners and institutional staff should be encouraged to implement national drug
regimens for all cases of malaria. / To facilitate this, booklets on malaria with all necessary
information are to be widely distributed and also presented to all new graduates.
■
Undergraduate courses in all medical fields should ensure that students receive adequate training
in malaria, are competent in its diagnosis and management and are able to provide correct advice
on prevention and control measures.
■
All professional organizations (Homeopathic, Ayurvedic, allopathic) are to be involved.
■
For those who have completed their courses continuous educational programmes should be
organized on a regular fashion and participants should be given recognition of having attended
these courses in the form of certificate of attendance and or competence.
■
To obtain cooperation from industry as well as in training various groups like traditional
practitioners, Registered Medical Practitioners, etc. Non Governmental Organizations with
requisite capacity should be identified and involved. Linkages between these organizations should
be encouraged so that they can utilize IEC capacity should be involved and requested to
contribute to IEC activities for malaria.
31
4.5 PARTNERSHIP WITH AGENCIES INVOLVED WITH EDUCATION OF
CHILDREN AND YOUTH
A) Principles
1. Target for behavioural change
•
•
•
School and college going children (6-21 years)
School drop-outs
Children with no formal education.
2. Partners
•
•
•
Local schools - primary, middle and high schools.
Colleges
Non-formal education.
(to enhance these local partnerships, there should be dialogue between the
government / programme with directorates of school / college education, technical
education; medical and agricultural organisations etc.,)
\
3. What is expected from children and youth:
•
•
•
know cause and control of malaria, change attitude and practice preventive
measures
involve in health education campaigns to create awareness among corjnmunity
participate in mosquito breeding preventive measures (in and around educational
institution)
/
4. What is the role of partners?
•
•
•
•
inclusion of health education in school / college curriculum
motivate the students
mobilize their participation in preventing mosquito breeding
involve them in community awareness programmes.
B)
Guidelines for advocacy for partnership in school /
education
health
District level
i)
Involve the education department in celebrating malaria month by carrying out
anti-malaria activities on the occasion.
'
’
ii)
Involve science clubs and science networks in increasing awareness about
anti-mataria activities amongst children and youth.
32
iii)
Conduct seminars / guest lectures / demo-exhibitions / field trips / essay
competitions / debates appropriate to the level of schooling / education.
iv)
Explore the possibility of inputs by teachers and students into fairs and
festivals.
—-------
v)
Including the practice of vector-control_activities by students and youth in scout
movements, national defense and social service auxiliary corps.
vi)
Exposing students and youth to various aspects of malaria by including
malaria related activities and experiments as project work in the curriculum.
vii)
Initiating debates /competitions between schools, colleges, and universities on
malaria control and on vector control to create widespread awareness.
To sustain the above:
•
•
•
Have regular meetings with teachers and staff involved in education
Have capacity building/training sessions for volunteers, teachers and high
school students.
\
Organize events at regular intervals to maintain the interest and tempo of^V
awareness activities in the educators and the students / youth.
j
Guidelines For Advocacy With Agencies Involved In Non-Formal Sector
C)
Of Education
Agencies like NGOs, Slum Welfare Boards, Social Welfare Boards and tie
educational department that are involved with street children, child labour and schc ol
dropouts must also be encouraged to increase awareness about various issujs
regarding malaria through appropriate efforts from those mentioned in the guidelin 3S
above and those given in section on partnership with voluntary agencies.
Content Clarity
Some or all of the answers to the following questions must be included in the awareness /
education programme depending upon the target age. The content needs to be presented in
interesting, interactive forms whereby the children and youth can learn from participating in\
situations and role plays that make a lasting impression. The questions are:
'
a) What is malaria ? b) How is malaria transmitted? c) How do mosquitoes breed? d) Where do
mosquitoes breed? e )How can we stop mosquito breeding?
f) How can fishes be used to eliminate mosquito breeding? g) How can we protect
ourselves from mosquitoes? h) What are the disadvantages of insecticides?
\
j) What should we do in case of fever? k) What can we do at village / community level to tackle
the problem?
/
i'
/
■
33
D) To support advocacy for partnership in school I college health education at
loca|
leve
e partnership at State / National level are also useful
State / National Level
i)
Approach the education secretary or vice-chancellors through appropriate
forums to incorporate various aspects of malaria in the school or college
curricula respectively.
ii)
Prepare (or adapt and translate) audio / video / audio-visual / print material for
IEC appropriate to local needs and for the target audience, designed after
pre-testing them successfully.
iii)
Encourage the education department to train teachers and to prepare
educational material on malaria.
iv)
Approach polytechnics / engineering / architecture colleges and institutions to
promote and stress on designs that prevent vector breeding.
v)
Encourage medical colleges to appropriately enhance the scope and content
of malaria in the syllabus and in examinations.
vi)
Promote agricultural practices that use appropriate technology for water
management to prevent vector-breeding through Agricultural Colleges and
Krishi Vigyan Kendras.
Organize workshops for training health educators / health illustrators and
trainers in appropriate communication skills and for preparing communication
materials that attract and interest the children / youth.
vii)
viii)
Collect quantitative and qualitative data from the state / local area on morbidity
and mortality from malaria, and work out the impact of awareness /
educational programmes on the situation, in order to make more effective
advocacy materials.
ix)
Explore the options of using internet and other futuristic communication tools
to enhance the reach and update content of awareness / educational
programmes.
x)
Approach open universities and distance learning institutes for starting /
including courses on malaria and vector-borne disease control in their list of
courses.
xi)
Understand the educational process in order to identify and exploit every
opportunity to include malaria and vector-borne diseases in all curricula.
xii)
Send regular feedback to the agencies involved in education regarding the
progress of their efforts in combating malaria and their impact on malaria, to
generate a sense of true partnership with comments and suggestions.
34
•V
“
Case Study 3
School Health Education on Malaria in Goa - I
With an aim to make students in schools of Goa malaria literate, a systematic
education programme was devised and initiated in Goa, in 1992 by Malaria Research
Centre, Goa, in collaboration with Indian Red Cross Society, Goa. This programme
was implemented in phases starting 1992 when 81 schools were enrolled targeting
16211 students from 8th to 10th standard. In 1994, this programme was extended to
Higher Secondary classes up to 12th standard and by 1998, 227 schools participated
in the programme targeting 53,462 students throughout Goa.
The aims and objectives of the programme were us under:
1. To introduce teaching on Malaria in the entire state of Goa in school children
through Junior Red Cross (JRC) and Youth Red Cross (YRC) components in
Secondary and Higher Secondary classes.
2. To train JRC and YRC counsellors (Teachers) to impart malaria education to the
students.
5. To prepare curriculum on malaria and seek its ratification from Goa Board of
Secondary and Higher Secondary Education.
4. To reach community through these students and teachers so as to train and
involve people in the vector and disease control process.
5. To undertake field projects on malaria with the help of Red Cross counsellors and
volunteers (students) wherein the local community is exposed to the problem and
its remedial measures.
6. To prepare a cohesive force over a period of time in the community who would
practice the mosquito / vector control in their day to day life and also continue to
disseminate the self action idea to others in future.
Training of Red Cross Counsellors
Thirteen State Level Workshops have so far been organised by the MRC and Red
Cross for imparting Orientation training to 808 teachers with the understanding that
organisational and technical responsibility will be shared by the Red Cross and MRC
Goa Field Station respectively.
The technical aspects of training included lectures, preparing course material, hand
outs, audio visual aids, and films and exhibitions on malaria. 61 exhibitions were
organised for 24,133 students in 232 schools.
(contd
)
School Health Education on Malaria in Goa (contd)
35
The exhibitions on malaria included:
1. Immature and adults of Anopheles, Culex and Aedes mosquitoes explaining the
life-cycle and their distinguishing features.
2. Models of domestic and peridomestic breeding habitats. These focussed upon
man’s negligence and indifference which may support the growth of mosquito
populations.
.1
3. The control aspects demonstrated, consisted of:
i.
?
-|C<.
Larvivorous fish such^as^Aplocheilus blockii, Rasbora daniconius, Gambusia
affinis and Poecilia reticulata devouring mosquito larvae and pupae. -----------
ii. Bacillus thuringiensis and Bacillus sphaericus samples.------- >
iii. Expanded polystyrene beads (EPS) forming a top layer on the water in the model
of an unused well.
iv. Models of air-tight overhead tanks and sumps, highlighting the mosquito-proof
arrangements such as the lid assembly and the sieved overflow pipe opening.
v. Models showing efficient drainage of water from terraces and water channels to
avoid stagnations responsible for mosquito breeding.
vi. Personal protection methods such as mosquito nets and window screens.
vii. In addition, blood slides with P. vivax and P. falciparum parasites were shown
under the compound microscope. Charts showing the life-cycle of a malaria
parasite, the need for early detection and treatment of malaria cases and the
importance of species-specific treatment of malaria were also displayed.
viii.A set of panels highlighting various aspects of malaria
settings were also exhibited.
in the urban and rural
ix. Handbills containing tips on self-action for the prevention and control of malaria
were distributed.
Reference Text for the Training of Teachers
A book entitled “Elementary Malariology” has been published by the Goa Board of Secondary and
Higher Secondary Board authored by Dr. Ashwani Kumar, MRC, India.
o
36
4-7 PARTNERSHIP WITH OTHER SECTORS (Intersectoral Coordination)
A key feature of the RBM Initiative is the focus on inter-sectoral coordination
symbolizing that malaria should be everyone’s concern and not only the
responsibility of the health ministry / department. The coordination committee /
core group mentioned in the leadership guideline also reflects this inter
sectorality.
The coordjnalian-Qpmmittee and the district health / malaria programme officers
shou(daialogug^-with different departments and explore their supportive
involvement IrTmany different ways.
A) Agriculture
The agriculture department can be involved in:
• IEC activities for agricultural community
• Source reduction to decrease mosquitogenic conditions
• Promotion of larvivorous fish hatcheries
• Introduction of larvivorous fishes in water bodies in selective high risk
areas.
B) Urban Development
Urban development department can help in:
• Awareness of byelaws / legislation
• Source reduction drive
• IEC activities particularly for slum dweller and migrant labour
• Promoting guidelines for construction and maintenance of
- Roads
- Safe drinking water supplies
- Sewerage systems
• Orientation of engineers from different sectors for their involvement for the
malaria control activities.
y
p
Note
Similar partnerships can be evolved at local / district level supported by
National / State level partnerships with all the other ministries and
departments as well -including Forestry, Industry, Mining, Social
Welfare,Railways, Defence, Irrigation, Power, etc,, and so on. Specific
guidelines for thes have have not been outlined and these will vary from
country to country.
37
4^
REMEMBER!
The following strategic directions will mark the worl
of RBM over the next 5 years
• An integrated approach for health promotion and disease prevention, audressing
'dressing
the major communicable diseases that shares the same risk factor as the focus for
primary prevention initiatives.
• Promoting equity by strengthening interventions focusing on disadvantaged
populations and by developing acceptable standards of health care. Focusing not
just on disease burden but also on cost effective interventions.
• Primary preventive initiative will be incorporated into the primary health care in a
strategy that is based on community mobilization and intersectoral action.
• Expanding the role of the media through partnership in advocacy and
disseminating information on healthy lifestyles and primary prevention against
malaria.
• Strengthening advocacy and raising awareness in malaria control among policy
makers, health professionals and the general public.
• Enhancing the role of the health professionals in health promotion and disease
prevention as key strategy in prevention programmes.
• Effective approaches to support communities, families and homes in the
prevention of common health problems.
• Mainstreaming RBM into the health sector development, integrating health care
delivery and management of support system.
• Form new partnerships with other agencies and potential donors based on sector
approach to health development
7
38
Case Study - 2
Tackling Malaria in Rural Gujarat
[SEWA - Rural is a voluntary agency that has provided health and development services extending
from the nucleus of a small rural hospital in Jhagadia. This case study highlights the key features of
the experience with malaria control]
• As an NGO we had taken over a PHC and done mainly surveillance and
presumptive / radical treatment of fever just as any other PHC is supposed to
do.
• After four years we realised we were getting nowhere and malaria prevalence
was changing inspite of our efforts; so we decided to look at feasibility and
efficacy of introducing simple vector control measures.
j
JT
f" • We took a study and control population and monitored fever cases (smearsjj
~
round the year and vector density (standard procedures) fortnightly.
r • Interventions included simple engineering measures, fish, kerosene and very
rarely insecticide (for one-time use to curb exceptionally heavy breeding
sites).
• Interventions and Monitoring were done by Male Multipurpose workers and
?.
supervisor after due training and alongside routine ‘PHC work’. The female
?
health workers took on some extra load (of other work) from the male /
workers.
• We also took the community’s help, especially school children, informally.
• Ongoing informal health education was given to people about mosquitoes and O']
malaria.
'
Result
I
7
3
7
2
39
GUIDELINE FIVE
COMMUNICATION FOR BEHAVIOUR CHANGE
[Note : These guidelines are for National / State / District programme managers who
organise IEC activities. Different guidelines are more applicable to one level or the other.
Each country programme will have to decide at what leyeLthe_guideline will apply]
5.1 Organise IEC Strategy and Material
Ap darry'out a formative survey which cofisist^o
ie following
C<7
Situational analysis of the knowledge, attitude and practice (KAP) regarding
malaria and vector borne diseases
(if already available than that
information / survey may be used)
• Identify behavioural gaps against acceptable behaviour - promotive,
preventive and health seeking related.
B) Set an action plan for IEC strategy based on district level RBM strategy and
based on
----—■
assessment made in (1) above
•
•
•
•
Identify possible target groups to focus upon in the IEC strategy
Define media / channel / method to be used
Schedule the programme initiative^
s
Assign responsibility.
'
B) Prepare directory/inventory of all available educational materials and collect
them. This may be entrusted to one partner with appropriate experience and
may obtain information from all the potential sources .
—
C)
Develop IEC materials (as and when necessary, especially if not available or
are not adequate / relevant)
i) Design messages
Prepare a list of messages that are generic and applicable to all
populations; that are scientifically accurate; acceptable to or approved by
..PP1 malaria control; focusing on action points; structuring educational
7 (peers;
■materials correctly, such as minimum lines per poster^*-*
• Messages should be prepared for different groups.
• The messages relating to vectors should be area specific depending
on whether it is forest; border; revenue; tribal; construction site;
industrial; irrigation site; domestic - urban, overhead tanks, coolers,
water pots; drinking water for animals; coconut shell; car tyres.
• Messages should be region specific such as handling run off water
from hand pumps, covers for manholes, etc. (Picture of hand pump).
Simulation games may be developed for health workers and school
children to Nghlight messages/*
• There is a need for developing appropriate communication methods
for the illiterate populations.
.
i
40
ii) Pretest the messages
iii) Revise the messagespf required^after pretesting
iv) Produce IEC material
2
"—
Explore local, decentralised, low cost productionjO'
E) Distribute, disseminate and communicate the IEC materials antfepfeduet as
planned (Identify person/institution in-charge at all level)
The message dissemination will consist of
•
•
•
Product/Service distribution such as printing and electronic media
Using mass media such as local radio, television, news paper and
traditional media
Face to face communication (individual and group) such as training,
orientation seminars, workshop and field visits.
/
5.2 Communication strategy - principles
Communication strategy based on interactive participatory two-way ;
A)
approaches should be planned and some of the principles to be followed are:
• This is to be a two way process.
• Qualitative and participatory
methods which facilitate
communication are to be taught to health worker.
/c’
• Communications skills also need to be taught to health personnel by some
one who is committed and capable.
• Catchy events and events from the life of important people may be used for
communication.
• Communication should be simple, straightforward and direct.
• Communicators are encouraged to listen to what the community has to say
before they plan messages.
• Communication must be adapted to the four phases namely that of
awareness, knowledge, attitude and practices.
• Tools should be developed for each phase.
• Role plays should be utilised for attitude change, emphasizing how people
don’t do certain things in a particular way.
• Community should know where blood smear is carried out.
• Teaching the skills of blood slide-making is a high priority.
/
• Health education or behaviour modification strategies may be adopted,
analysed in a socio-political perspective
./
• Communication should use the curricular approach with observable,
measurable, feasible and relevant objectives.' These should be provided
after obtaining community feedback. It should be learner oriented rather
than teacher oriented.
• IEC materials are for self learning and group education: "
/
'
41
5.3 Communication Methods
A) Information materials could include:
J
J
J
J
J
J
Posters
Handbill
Flash card
Booklets
Video cassettes
Audio cassettes
\
\
Maintain quality of education with respect to the choice of a language that is
simple, unambiguous in mother tongue focusing on specific spoken dialect, with
emphasis on marginalised and tribals.
)
B)
The following methods of interactive education are to be utilised?^
v Role play;
J Street theatre;
Folk songs;
v Exhibitions;
■J Puppet shows;
J Jathas
Folk artistes should be treated as professional at their own level
and should be reasonably remunerated.
5.4 Innovations
New and innovative methods of communication should be evolved and
A)
experimented with
• Colouring books / sheet on mosquitoes and malaria control.
• Develop educational toys around the theme of malaria.
• Activity modules for science experiments
• Audio visual material on the human stories about malaria, for example
'why did Mr. Y die ?’ reflecting a death due to malaria should be
produced.
42
Case Study 3
Evolving a Community Strategy to keep villages Malaria-free
[The Uttari Rajasthan Milk Union Limited (URMUL) Trust is a farmers’ cooperative that
organises an integrated rural development programme with health care being an important
component of the diverse development package. They were actively involved during the
malaria epidemics in their area of operation in recent years and tried to evolve strategies to Ur \
keep their villages free of malaria deaths]
y [l\J
k /
Aim: To keep our villages free of deaths from Malaria
Our limitations
1.
One lab technician for our 30000 population scattered over 2500 kms. and also doubling
as Health Coordinator.
2.
3 PHCs and 1 CHC as referral support andnumerous RMPs and quacks - none of them
under our control.
3.
No data for 1994 but government data put API below 2 everywhere so no spraying could
be done.
4.
Literacy levels of women <5% and males below 20%.
Our Strategy
a)
Drug Distribution Centres with teachers who were trained for the purpose.
b) Chloroquine taken from government and replacement made every month.
c)
Modified Fever Treatment Depots with our own workers.
d) Presenting our findings on fortnightly basis to CHC, CM & HO, Dy. CM & HO - Malaria,
District Collector and Divisional Commissioner to galvanise action on behalf of district
authorities.
e)
Posters procured from government and pasted all over.
f)
Pamphlets in Hindi for all educated people and RMPs and quacks.
g) Street theatre and puppet shows by our communication team in each village.
h) Placing slides with RMPs etc., to help in monitor patients.
j) Introduced larvivorous fishes in own campus to help staff gain confidence in method and
effect.
k) Holding and referral facilities for the serious at our headquarters centre.
Results Succeded in our pledge to prevent malaria deaths.
URMUL TRUST, Rajasthan
j
48
jn
C* Ul DE LibJ £ 5
Fo^
N'T
M
GUIDELINE SEVEN
MANAGEMENT OF SEVERE MALARIA
Although it may not be possible for lay people to understand and distinguish
severe malaria from other types of fevers with complications, it is desirable
that some members of the community understand the effects of severe
malaria and the principles of treatment at various levels of care. This would
ensure reasonable expertise available at the community level to help select
the appropriate level for referring the patients of severe malaria for the
earliest treatment.
Needless-tcracra; |he information in the following paragraphs should form part
of the curriculum for frequent refresher trainings for all levels of health workers
- including nurses and doctors -- in malarious areas and as continuing
medical education for local practitioners.
7.1
What is severe and complicated malaria?
Any patient with asexual forms of P.falciparum in peripheral blood smear
showing one or more of the following complications is labeled as severe
and complicated malaria. (WHO criteria 1990)
Cerebral Malaria - Unrousable coma, after exclusion of other
causes of coma. At least 30 minutes or more after seizure the
coma must continue to distinguish it from post-ictal state.
Severe anaemia - Hb < 5 gm %
Acute renal failure - S. creatinine > 3mg/dl_
Acidosis - pH<7.2
Hypoglycaemia - Blood glucose < 40 mg/dL
Spontaneous Bleeding or DIG
Massive I.V. Haemolysis with Heamoglobinuria
Acute Pulmonary Oedema or Adult Respiratory Distress Syndrome
Malaria shock or algid malaria
Repeated generalised convulsion
Minor Criteria
The following minor criteria when present may also help the health worker
in tilting the diagnosis to severe malaria in case of doubt.
-
Hyperpyrexia - Core temp > 104° F OR 40° C
Jaundice - Bilirubin > 3mg/dl
■ Hyperparsatiaemia - > 5%
. However, health workers, auxiliary nurse midwives, community health
volunteers, FTD workers and community leaders must be made
Treatment of severe malaria must not be delayed by diagnostic
procedures.
49
aware that they must urgently refer any patient of fever with the following
features as they indicate severe malaria:
=> altered mental
=> blood in urine
state
=> severe pallor
=> convulsions/fits
=> high jaundice
=> unconsciousness
• Smear negative cases coming from endemic areas must be treated as
for malaria unless otherwise proved.
• Any fever should be treated as cerebral malaria whenever there is
little change in sensorium or change in behaviour.
7.2. Diagnosis and Clinical Features
Diagnosis needs to keep the clinical features listed above in mind, but
wherever possible, it should be supported by a laboratory diagnosis.
a) Peripheral blood smear for malarial parasite. Repeat if negative
b) Dipstick method (wherever available)- epecially useful in cases of
- Low parasitaemia
- Partially treated cases
Clinical Features
Patient enquiry
■ Travel history to /from malaria endemic area ust be taken.
■ Duration of illness, particularly coma as described earlier
■ Treatment history n£ds to be taken to prevent overdosage or correct
interpretation of lab results.
■ Pregnancy/delivery needs to be kept in mind for all women with
malaria for choice of drugs, esp., Primaquine.
7.3 Physical Examination
Look for
- Anaemia
! Look for features
- Jaundice
! of severemalaria
- CNS - (including meningeal signs)[/as described in 7.1
- Respiration
!
- B.P./Pulse
!
- Urine output
!
50
7.4 Investigations *
Different investigations may be carriaci-out-depending on theJevel of faciities
available^-ffbvvever, ifmust be reiterated that .treatment of a case of
fsevefemalaria may be started based on clinical suspicion without any
' laboratory investigations in the interest of the patient’s life.
A. Primary level (sub-centre 7 FTD / DCC/ community level)
Blood for malarial parasite - blood slide to be taken.
B. Secondary level
Blood glucose to check for hypoglycaemia.
Hb to identify severe anaemia.
Bleeding Time
1 To identify Algid Malaria
Clotting Time
! at the earliest.
C. Tertiary level (Hospital / District level)
Blood urea
) For severe malaria affecting
S. Creatinine
) the kidneys.
S. Bilirubin
! To confirm if jaundice is
Liver enzymes like ALT & AST ! due to haemolysis.
Lumbar puncture To rule out bacterial meninigitis.
7.5 Management
A. Primary level ( sub-centre / FTD / DCC/ community level)
♦ General Nursing care •—•>.
♦ Treatment of high fever. •
♦ Adjunctive therapy
;
♦ Chloroquine or other anti-malarial as per national guidelines.
Patients should be referred to the secondary level (PHC / sub-district
hospital) at tfie’earliest along with a note about previous treatment. 'J *
B.
Secondary Level (primary health centres /sub-district level)
♦ All available at primary level.
♦ Antibiotics/I.V. fluids/Oxygen/Anticonvulsants
♦ Parenteral Quinine or Parenteral Chloroquine
♦ Artemisinin 1/M - If 1/V line not possible.
♦ Supportive therapy
At this level the physician, gynaecologist and paediatrician should form
a team for management of severe malaria cases in pregnancy and
after childbirth.
51
C. Tertiary Levbl (Hospital / District level)
Few patients will require this level of support and the system needs
to gear up to the challenge of malaria at the end of the referral
chain.The following are considered essential for such a tertiary
referral. Appropriate specialists would also be required to be present
to carry out this level of care.
♦
All available at primary and secondary level
♦
Correction of severe anaemia.
♦
Hypoglycaemia to be corrected urgently and watched for.
♦
Peritoneal dialysis for renal failure.
Facilities for blood transfusion and for trained personnel to carry out simple
procedures like peritoneal dialysis need to be created.
T I
c
52
GUIDELINE EIGHT
REFERRAL SYSTEM FOR MALARIA
Each member country in the region needs to establish a good referral system
especially to manage the severe and complicated cases of falciparum
malaria. Malaria control programs in each country should identify the referral
health institutions at different levels of health care delivery system and these
institutions should be strengthened to take care of the referred patients. All
the health personnel involved in the management of malaria should be trained
in identifying the cases and institution to be referred and in the proper
management of malaria cases.
8.1 Who should be referred? Criteria for referring malaria cases
The type of the patients to be referred will depend on the available resources
at the institution. However, the following patients require special attention
therefore should be referred to the appropriate level of medical care.
• Severe and complicated cases of malaria.
• Malaria in children with very high temperature, convulsions,
dehydration or disorientation.
• Malaria in pregnant mothers with P. falciparum infection and /or
severe anemia.
• Cases of malaria — not responding to known available anti-malarials.
• Malaria cases with continuous vomiting and inability to retain oral
drugs.
8.2. Who will and where to refer?
7
Countr£es''should workout in detail about the type of malaria cases to be
'referred by health personnel at different level of health care delivery
system to appropriate institutions.
Symptomatic treatment as well as a loading dose of appropriate antimalarial should be administered to all suspected severe malaria cases
(depending upon the national anti-malarial drug policy) before referral.
A referral form should accompany the patients indicating history and
treatment given before referral. The referral centre must send a feedback
to the referring unit regarding the treatment and outcome of the case.
Referral centres should be identified at the District level. Inter-district
coordination may be necessary to facilitate the referral of such patients
to the closest appropriate level of treatment even if the facility falls in
the other district.
The life of patients is crucial and administrative mechanisms have
to be created to facilitate life-saving referrals across district
boundaries.
/
53
8.3. What facilities should be available at the referral centre?
The minimum facilities required in each referral centre should be:
- Tablets / syrups of basic antimalarials.
- Blood smear for examination.
- Hb estimation.
- Urine R/E.
- 1/V and oral Quinine.
-1/V fluids.
- Oxygen
- Oral and injectible antipyretics, anti-convulsants, diuretics and
antibiotics.
However, other specialized facilities will be required depending upon the level
of referral institution as discussed earlier.
4s the mortality due to severe and complicated malaria is highest
amongst poor and marginalised communities because of delay in
reaching the referral facilities, some mechanism must be worked out in
consultation with partners to allow reimbursements for transportation in
such cases (as has been permitted in the Reproductive and Child Health
Programme in India for pregnant women needing institutional delivery
^/intervention).
4
56
GUIDELINE TEN
DRUG SUPPLY AND MANAGEMENT
Uninterrupted and timely supply of essential anti-malarial drugs and other
equipment and supplies are critical needs of the malaria control Program.
The objective is to ensure supply of drugs to the user units, in the right
quantity, of right quality and at right time. A good drug supply management
will prevent either shortages or excess of supplies. Existing administrative
units and their procurement procedures for drug supply management should
be strengthened. Mg^ers-pertaining to drug supply management should be
discussed witlrconcefned authoritieg in the districts to apprise existing
bottlenecks and problems in the procurement, storage and supply of drugs.
Bottlenecks and problems will have to be remove^ U-
Countries should estimate their individual drug requirements as per the
existing Anti-malarial Drug Policy, and maintain adequate stock and ensure
proper distribution up to the users’ points. An indicative list of anti-malarial
drugs depending on the level of health facilities and provision of care may be:
a) Primary level (sub-centre/FTD /DDC)
\
4
I) . Tablet and syrup Chloroquine
II) . Tablet and syrup Paracetamol
\
III) . Tablet Anti-emetic Prochlorperazine/Metoclopnamide ! only for
IV) . Tablet Antacid
I
V) . Tablet Primaquine
b) Secondary Level (PHC/sub-district)
i) All above
ii) Tablet, syrup and Injection Chloroquine
iii) Tablet, syrup and Injection Paracetamol
iv) Tablet, syrup and and injection Quinine ( or as per national list)
v) Inj 25%/50% w/v Glucose.
A
vi) Tablet and Injection anti-emetic.
\
vii) 1/V Fluids
• \
viii) A combination of Sulpha and Pyrimethamine
c) Tertiary Level (Hospital / district)
i) All above
ii) Artemisinin and its derivatives
iii) Dipstick test kits for P.falciparum diagnosis.
■
57
}
10. 1
Management of Drug Supply
1. For effectively managing a regular and adequate availability of antimalarials at all levels, correct estimation of requirements/of different
drugs for different levels must be made. These estimates must be
made on the following information :
•
•
•
total number of malaria cases including severe malaria.
quantity of various tablets, syrups and injectibles used in
corresponding season / period of previous years.
average lag - time required for drug replenishment from source
and to peripheral levels.
2. An increased requirement during epidemics must be anticipated and
worked into the estimate.
3. A percentage of drug supplies must be held as reserve at the district
level that may be released as per the requirement of a Epidemic
Response Team during an epidemic. The same should be regularly
turned over to prevent expiration.
4. Regular visits must be made to Drug Distribution Centres / Fever
Treatment Depots, sub-centres and PHCs to discuss the problem
faced in drug supply and to ensure sufficient stocks of drug are
maintained.
5. Random samples of various drugs procured can be sent for quality
control to drug analysis laboratories to ensure quality. It must be
mandatory for the suppliers to enclose a copy of the batch analysis
report with every batch of drugs supplied along with the bill submitted
for payment.
-J
60
GUIDELINE TWELVE
INTER PROGRAMME LINKAGES WITH SAFE MOTHERHOOD
AND OTHER PROGRAMMES
p
12.1 Malaria and Pregnancy
Malaria is a disease that affects motherhood both directly and indirectly.
Malaria by itself can produce anemia, abortions particularly in the first
trimester, stillbirth, premature/ low birth weight babies and sometimes
even maternal mortality. Besides, deaths due to malaria among children
it causes insecurity in the family, thereby affecting family planning
behaviour. Integrating RBM and Safe Motherhood programmes would
increase programme effectiveness and efficiency.
12.2 Malaria in pregnancy as part of Reproductive and Child Health
(RCH)
Malaria in ppregnancy should be included as part of the RCH. This
should be incorporated into the syllabus' with specific emphasis’ on
x
.
i specific emphasis
antimalanal treatment schedule, chemoprophylaxis
i'
and personal
protection through use of ITNs and other methods. RCH programme
Js„°u_ alsojnvest in malaria control through purchase of antimalarial
drugs in emergency situations. Treatment of pregnant women and
children should follow the national drug policy on malaria.
12.3 Malaria as part of Integrated Management of Childhood Illness
(IMCI)
a
As is done in African countries, malaria among children should be
incorporated as one of the diseases under the IMCI programme This "I
will ensure that medical practitioners develop the skills L,,
for diagnosing
and treating malaria in children and in managing complications.
J
12.4 Links with existing health infrastructure
0^
RBM can establish links with the existing health infrastructure. For
example, peripheral^ health workersyipyolved in the safe motherhood
programme can be trained in diagnosis and treatment of malaria
Likewise, private practitioners and traditional healers can be involved in
the programme. They may also be used to'promote use of bed nets and
elimination of mosquito breeding sites and remove misconceptions and
false beliefs regarding malaria in the community.
'
The main thrust of training should be to diagnose malaria early in
patients with fever. If presumptive treatment is started, complete course
of treatment should be ensured. Complete drugs may be provided in
one strip. In case of severe fever with loss of sensorium and/ or loss of
Y
i*-
61
consciousness, patients should be referred to pre determined referral
centres.
12.5 Malaria^related to development projects
Majtff projects and construction works are providing migrant labour with
gainful employment. In addition, seasonal agriculture work supports
migrant labour. These categories of persons should be identified as
high-risk groups for malaria. Wherever feasible, assessments of malaria
impact should be conducted prior to the commencement of development
projects and malaria prevention strategies should be incorporated into
the projects.
The managers, supervisors of these projects and employers of migrant
labour should be educated about the problem of malaria, how it can be
handled and the available resources from the government. In this way
the management may be encouraged to take an interest in the welfare
of the migrant labour and provide support for safe motherhood and
control malaria among the labour.
62
GUIDELINE THIRTEEN
MONITORING DRUG RESISTANCE
With malaria not being adequately controlled and with inadequate or irregular
treatment with Chloroquine and/or other drugs, resistance to available drugs
is becoming an increasing problem. Therefore monitoring drug resistance
becomes important in the control of malaria.
For carrying out the activities of drug resistance monitoring, there is a need to
establish sentinel centres in different parts of the country situated in medical
colleges, hospitals or any other appropriate institution located in endemic
areas. These centres will regularly carry out drug resistance studies in their
own areas or by collecting material from different areas with the help of mobile
teams. These activities will generate sufficient data to enable the countries to
scientifically review and formulate their drug policies.
13.1 Identifying Sources of Information
The District Health Authority should identify all sources of information
relating to drug resistance. The following is the suggested list.
A. Medical practitioners treating large number of malaria
patients.
'
.
Q
B. Primary Health Centres
C. Sub-district Hospital
’
—
D. District Hospital
E. Teaching and Research Medical Institutions.
2
13.2 Information on Failure of Treatment with Anti-malarials
Whenever information on failure of anti-malarial drugs anywhere is
received, the District Health Authority should investigate other possible
factors such as
~
a
F. Adequacy of treatment, whether
Complete
Incomplete
Irregular
G. Whether drugs are substandard
H. Host factors - such as other concomitant diseases like diarrhea
which could limit absorption
63
13.3 Testing for Resistance
On receiving information of drug resistance and after ruling out failure
of treatment due to other causes, district health officer should pass on
this information to state health authorities to initiate activities for testing
ot drug resistance through sentinel centres.
Methodology to be followed for testing drug resistance may be \
conventional in vivo tests or by testing of the therapeutic efficacy of
anti-malaria drugs against clinically manifest infections with P. j
falciparum (WHO document WHO/MAL/96.1077)
13.4 Vigilance for Pv Resistance
Since resistance in Plasmodium vivax against Chloroquine has been
identified in localized foci in some countries, e.g., Indonesia,
Myanmar3, therefore malaria personnel must be on the look out to
identify earliest occurrence of resistance of P.vivax by following
therapeuticeTficacy fests as for P .falciparum.
3 WHO. Management of UncomplicatedMalaria and the Use ofAntimalarial Drugs for the Protection
ofTravelersfNmQfMkLI^A^^)
64
GUIDELINE FOURTEEN
HEALTH MANAGEMENT INFORMATION SYSTEM
The National Health Management Information Systems are operating in most
of the countries from the PHC level through the district/township and
state/region/province/division levels to the national level. From time to time
these have been modified. Most of these systems have certain weaknesses
mentioned below:
• Delayed information
• Inaccurate information
• Insufficient information
• Scattered information
For effective functioning of the information system it is necessary to build in
modifications that could bring about the needed improvement. The following
are some of the suggested guidelines.
/1.
Information Requirement (Indicators)
A"
The first step is to identify the essential information that is required for
decision making. This information may be used to identify the following in
order that appropriate action may be taken.
• outbreaks of disease so that these can be investigated and
containment measures implemented
• high-risk populations and areas that need special attention
• areas with poor programme performance so that corrective measures
can be taken.
The information to be analyzed and accessed
each level is indicated below
as a list of indicators.______
Indicators (o~be monitored
~
•
Administrative Level
Community Level Worker
• No. of fever cases treated.
No. of slides prepared and sent for microscopy
Primary Health Centre
No. of fever cases treated
(PHC)
No. of slides prepared and sent or examined
No. of slides positive for Pv
(These indicators will be
No. of slides positive for Pf
analyzed Village-wise4)
No. of villages sprayed
No. of malaria cases treated
No. of treatment failures
No. of Health Education programmes________
District/Township
Annual Parasite Incidence (API)
(These indicators will be • Annual Blood Examination Rate (ABER)
analyzed PHC-wise )
Slide Positivity Rate (SPR)
No. of Deaths due to malaria
4 That is the lowest level where health workers are available in a country.
65
c
14.1 Data Collection System
The information that is required determines what data should be collected.
The data collected or collated at each level should be in relation to the
information requirements. Periodicity of data collection may vary between one
week to three months. In addition to recording numbers for each indicator, the
date and the administrative area code should also be recorded. This might
require establishing some standard codes (E.g. coding each administrative
location) or modifying the existing standards (if necessary). All efforts must be
made to use^computers. at the district level. Existing system should be
improved and wherever possible district network should be enhanced using
Information Technology (IT).
Forms are generally used to record surveillance data. The existing forms
should be reviewed. The purpose of each set of data should be identified
along with its level of usage. Formats that could be combined should be
clubbed together. The forms should be modified to ensure that:
• all the data that is required to generate essential information is
included
• data not used for analysis is eliminated5
• it is easy to use
• has enough space for recording the values
• has no ambiguous text
• contains all the crucial instructions, etc.
It is recommended that a proposed / modified form be tested in the field
before implementation.
The anti-malaria programme should collect and analyze all essential
information at the national level. In addition it should provide selective
information as required by HMIS for national level planning.
In order to avoid further modifications to the formats necessary for
computerization, it may be essential to have discussion with MIS consultants
early in the development or adaptation of the system.
14.2 Analysis of data
The data collected should be analyzed at each level using computerized
or manual system to produce information—for 'action and monitoring
progress.
The PHC staff can utilize the analytical skills of MIS personnel at
district/township level. Neighboring districts could share a common
computer center facility. At the district and state levels also the analysis
may^edoneTjasSd on the information needed at these levels. Gradually,5 reduced amount of data collection from the field level generally results in more accurate information.
However, data collected should be sufficient to satisfy the information requirements.
66
computerization
should
be
completed
at
the
national,
state/region/province/division and district/township levels in a phased
manner.
It is important to highlight in each report deviations from the normal
occurrence at each level to the next higher level. Each higher level may
access information from lower level, that is necessary for analysis and
action. Each data collection site must report to the next higher level, even
if no cases of the disease under surveillance have been identified during
the given time period. This will provide distinction between “Zero
reporting” and “No reporting”. The analyzed reports must be disseminated
to the next higher and lower levels6.
Diagrammatically, the sharing of information is shown as below:
\
National
State/Region/Province/D
ivision
District/Township
PHC
Periodic Validation of data
To verify the accuracy of the data collected, officials from each higher
level should validate the data periodically in sample populations. Field
visit data should match the data reported. This further contributes to
accuracy of data. Similarly, quality control on analysis of data should
be implemented.
14.3 Who is responsible?
2
The MO’ PHC is ultimately responsible as the team leader for all the
data coming out of the PHC. However a senior PHC staff may be
designated to support in this responsibility, preferably the health
supervisor. District Medical Officers will be responsible for district level
analysis and quality control.
14.4 Coordination with other health sectors
Since the Government health system both at PHC and district/township
levels provides diagnosis and treatment of only a proportion of the
population, others such as the private practitioners, voluntary agencies,
private dispensaries, railways and armed forces should be involved to
participate in the malaria control by providing essential information.
6 Sending analyzed feedback to the lower levels highlights the importance of the reporting system to
the reporting centre.
67
The initiative should come from the government. Centers where
microscopy is done and where treatment is provided should also be
listed. Efforts should be made to collect information from private
practitioners, private hospitals, nursing homes, other governmental
organizations, armed forces, railways etc. All these should contribute
to the overall information.
14.5 Personnel
Even while the population has increased there has not been a
concomitant increase in personnel, and also many posts are lying
vacant. On the other hand, filling all posts will not necessary increase
timely and accurate information. It may be necessary to re-deploy
existing personnel so that some minimum predetermined levels are
maintained.
However, when personnel are short, then other
alternatives that are agreed earlier, should be adopted.
14.6 Public domain information
Once data have been collected, consolidated and analyzed at the district,
state and national levels, periodically, preferably each quarter
predetermined data should be made available as public domain
information through usual channels and wherever possible through
Internet/World Wide Web. This would provide opportunity to strengthen
mulfi-sectoral collaboration. Sensitive information should be disseminated i
only after appropriate authentication by"government authorities.
'
14.7 Implementation of Computerized
C ;
All efforts must be made to use computers at the district level. Existing system
should be improved and wherever possible district network should be
enhanced using information technology (IT). The following resources are
essential for implementation of Computerized Health Management
Information System.
Software: Integrated computer based Health Management Information
System should be implemented at different levels based on factors such as
availability, cost, local expertise etc. Sufficient user documentation and
technical documentation is essential.
•
Hardware: Hardware requirements are determined, to a large extent, by the
software that is to be used. The choice of hardware depends very much on
available finance, local support etc.
Human Resources: It is worthwhile
finding out about the availability of
manpower and training facility and other support locally before finalizing the
choice of software and hardware.
68
e
Communication Infrastructure: Modern communication facility such as Fax,
E-mail, other Internet services (\N\N\N, FTP etc.), should be made available to
whatever extend possible.
•
Data Flow: The data flow from the most peripheral level to the most central
level should be clearly established, taking into account the following factors:
*
Which forms are to be used at which level.
■
Which data items are to be forwarded to the next level, how often and in what
format.
If the data are to be sent in computer files, then standardized format should
be used compatible with the software.
80
GUIDELINE SEVENTEEN
EPIDEMIOLOGICAL SURVEILLANCE.
17.0 SURVEILLANCE : RURAL, URBAN/ PERI URBAN
Surveillance is an essential activity of anti-malarial programmes that must aim to,
provide early evidence for outbreaks and epidemics, besides indicating the efficacy
of anti-malaria programmes and effecting necessary changes in them. With the
change of malaria scenario, it is necessary for systems of surveillance to keef
pace with the changes in agent, vector, environment and the human host. Hence
surveillance must include:
•
•
•
•
•
OH
Routine Epidemiological surveillance.
Entomological Surveillance.
Surveillance For Forecasting And Early Detection Of Epidemic.
/
System Surveillance.
/
Behavioural Surveillance.
/
• Surveillance must be instituted with reference to urban and rurafi
areas. Special care must be taken to include peri-urban areas,
because of the temporary nature of residence of migratory and
labour populations, and the lack of effective outreach of health a
services in such areas.
, '
• In urban areas, surveillance must tilt towards passive case /
detection, although frequent active surveillance will be required/
for the respective peri-urban areas and priority groups like
migratory populations, seasonal workers’ groups, labour
aggregations at construction sites.
• Surveillance for rural areas that has been a feature of all
national malaria programmes including active and passive case
detection, mass surveillance will require further strengthening in
terms of human and material resources. Surveillance methods
must be suitably modified to prevent the higher morbidity and
mortality amongst infants, children and pregnant women.
Routine Epidemiological Surveillance
• Routine epidemiological surveillance that is part of the /national malaria_\
programmes needs to be strengthened. As many urban centres in the/SEA \
Region countries are contributing to the increasing malaria incidence^—<
wherever the routine systems of surveillance are deficient in urban centres,
they must be instituted to complement the rural epidemiological surveillance.
• All national programmes must evolve standards for monitoring the rates of
blood slides examined and of the proportion of active and passive case
detection so that the surveillance is effective and accurate.
/
81
• Personnel and equipment necessary to effect a good surveillance system ]
in tune with the requirements of the Roll Back Malaria programme must be /
placed at the disposal of the districts as a priority.
/
• The status of malaria and the anti-malaria operations in the districts
analysed out of regular and continued surveillance must be shared with the
6/.
district health committee at regular intervals to strengthen the spirit of/
partnership envisaged in the Roll Back Malaria Programme.
17.1
Entomological Surveillance
Continued entomological surveillance is necessary not just for predicting
outbreaks and epidemics, but also to guide the districts in selecting vector '1-'1
control measures, drafting IEC messages and propagating personal protection
measures.
This surveillance should include regufar monitoritrcf of-:
• Vector population dynamics, esp. at rural/urban and rural /peri-urban
interfaces..
• Vector bionomics.
• Vector density.
• Vector behaviour.
• Susceptibility of larvae and adult vectors to insecticides/biocides.
• Mosquitogenic conditions created by industrial or irrigation project
works.
The responsibility of such surveillance should rest with:
Urban / Peri-urban areas: Entomologist/Biologist or Local body health
officer.
Rural: Entomologist or other responsible authority.
17.2 Forecasting and Early Detection of Epidemics
The importance of epidemiological and entomological surveillance in forecasting
and early detection of epidemics cannot be overstated. It is necessary to
organise and analyse the data arising out of the routine epidemiological and
entomological surveillance to help forecast - or detect at the earliest - an
epidemic.
?
Changes as highlighted below may be picked up to initiate prompt corrective
action:
• Rapid increase of nos. of fever cases/clinical malaria cases/slide
positivity rate
• Change in Pv: Pf ratio in favor of the latter
• Spurt in vector density.
• Change in vector behaviour.
82
« Change in vector population dynamics.
o Change in susceptibility of larvae and adult vectors to
insecticides/biocides.
• Intermixing of vector populations at rural/urban and rural/peri-urban
interfaces.
• Natural calamities, mass influx.
• Disarrayed intervention programme schedule.
The responsibility of the surveillance should rest with :
Urban / Peri-urban areas: Entomologist/Biologist or Local body health officer.
Rural: Entomologist/Epidemiologist/MO PHC/DISTRICT HEALTH AUTHORITY
as appropriate.
17.3 System surveillance
A very important component of surveillance is “system surveillance," that must
be rigorously maintained. The entire onus of surveillance and preventive
activities depends on the system and hence any deficiencies if not corrected
immediately may have disastrous consequences.
Surveillance to monitor the system must be instituted to ensure:
procurement and distribution of anti-malaria supplies.
authorisation and placement of personnel.
coverage.
work quality.
adherence to time schedules (in respect of larviciding, spraying,
surveillance and EDPT).
• effective response to epidemic situations.
•
•
•
•
•
The responsibility to carry out such surveillance can be rested with the in-built
supervisory hierarchy, but involvement ofcommunity lea
ders -and . civc-society in
:3ders~and
such a surveillance will go a long way in empowering the partners of the RE
RBM
programme
\\ ,
z
17.4 Behavioural surveillance
Although conventional anti-malaria programmes have been strong on measures
responding to vector and parasite behaviour, the changes in the third angle of
the epidemiological triad,, namely human behaviour have not been adequately
studied. Social scientists .who study human behaviour and can guide the A
programme at various levels should be included in the surveillance for malaria )
programmes.
\
?
The input from such surveillance would form the basis of choosing appropriate
personal protection measures, spraying activities, and for making IEC messages
appropriate to the customs and traditions prevalent in the area or to implement
strategies to alter them.
2
83
Provision of social scientists can be made from local educational institutions or
by inclusion of such personnel as part of the programme resources at
appropriate levels.
Results of programme interventions are dependent on the behaviour of various
ethno-cultural commanitiQs and their sociological characteristics. The •
involvement of social scientists in the formulatjon and implementation of the
bl^rto positively influertce'tfie outcomes^of the programme,
programmes will
Social scientists can al^o help to smoothen the interface between the service
providers and the recipients, particularly in areas of doctor-client relationship
r
and the behavioural aspects of interventions in respect of active participation
and co-operation from the community.
<3
84
GUIDELINE EIGHTEEN
EPIDEMIC PREPAREDNESS AND RESPONSE
18.1 Epidemic
A malaria epidemic is defined as the occurrence of malaria in a community or
geographical area in excess of the normal (for the part of year) that is of public
health significance. For conditions where an accurate diagnosis of malaria is not
feasible, preparations to combat an epidemic must begin if an increase of fever
cases is reported to the PHO /Dispensaries by the community or are clinically
suspected to be suffering from malaria, or there are deaths reported in the media
that have followed fever episodes.
Epidemic preparedness must include forecasting and early detection of epidemics,
systems that can be mobilised at short notice for countering the epidemic, and
guidelines for effectively responding to the outbreak or epidemic.
18.2 Epidemic Forecasting
The importance of epidemic surveillance cannot be denied especially in light of the
number of malaria epidemics and fatalities that follow the epidemics in the region.
Epidemic forecasting relies heavily on the reliability of routine epidemiological
surveillance data, and on the analysis of reports generated regularly. District health
authorities and Medical Officers in-charge of PHCs should ensure that the
surveillance systems are functioning effectively. They must also make an
endeavour to involve and motivate other health agencies in the district like private
laboratories, private practitioners, medical associations, and hospitals/ NGOs
belonging to the voluntary sector in forecasting and early detection of epidemics.
There are a number of indicators that the District Health Authority must monitor to
forecast a malaria epidemic at the earliest. These are:
18.3 Parasite load
Rapid increase in number of fever cases/clinical malaria cases/ Slide positivity rate or
a change in P.v:P.f ratio in favour of the latter.
18.4 Vector Dynamics
Rapid increase in mosquito / Anopheles density. A simpler way may also be to monitor
the increase in number of vector breeding places.
18.5 Population Dynamics
Influx of migrants from non-endemic area to endemic area or vice versa for wages,
conflict, calamity; movement of labour to forests, for seasonal agriculture or for large
construction projects.
,
T‘
85
18.6 Ecological Changes
Early and heavy rains in pre-transmission period; intermittent heavy rains;
natural disasters like floods, cyclone and earthquake and large-scale
deforestation, etc. Also, large construction activities, like dams and irrigation
channels need to be kept in mind for their large and widespread malariogenrc
potential.
7
-) Z*. n
>
18.7
Epidemic preparedness:
A)Establishment of Epidemic Response Team
Because of the fact that malaria epidemics can kill swiftly and in large numbers,
it is felt that all epidemic-prone areas should provide for a Epidemic Response
Team (ERT) at the District level. The ERT must take physical shape at very
short notice from existing district resources and should be trained and be
available for other epidemic diseases as well.
'
Resources like personnel and drugs required for the ERT should be generated
from the existing district resources. A buffer stock of anti-malaria drugs,
insecticides and other essential supplies should be maintained for this purpose.
B) Response to an Epidemic
4)The District health authority should keep him/herself abreast of the formal and
informal health data arising in the district and monitor them for epidemic
surveillance. Eveg^if a high number of fever cases / deaths are reported to the
OPDs/ private p’ractitioirersANGO health facilities by members of the community
of which a majority are clinically suspected_to be of malarial origin, the first
^response to an epidemic must be started^^Pis necessary to investigate and
confirm(or denynfTe reports so that timerjrgction can be initiated.
• The District health authority should organise the investigation of
epidemic so that confirmation of the epidemic and mobilisation of the
. ERT can be effected within the shortest possible time. The mobile ERT
should quickly be able to delineate the affected population^oT
geographical area, and rapidly assess the extent of involvement by
-yfcapid Fever Survey or Mass Survey Methodology. Blood smears to
confirm mataria on the sp'ot must be made by "establishment of mobile
field laboratories and appropriate treatment provided to all cases. AntT
ve'ctor7~anti
parasitic and anti-larval measures "must also be
commenced starting from the identified foci of epidemic/outbreak. It is
important that the entire anti-malarial exercise is completed within ten,
Jo fifteen days so that secondary cases are prevented.
• Sample villages from the area must be randomly selected for a follow
up for rapid fever survey/mass survey at th6 end of three and six
weeks of completion of remedial measures.
*04
86
• The District health authority should ensure that prescribed malaria
activities should also be resumed at the earliest, and that the full
complement of health staff is kept posted to the area to prevent a
relapse.
• The malaria core group must be kept informed about the
developments and the District health authority must call for
reinforcements of personnel and material if required.
• IEC material based on area specific strategy like pamphlets, posters
and through PA systems and AV aids must be used for dissemination
of malaria specific information.
• Information on the epidemic should be disseminated through the
media so that speculative reporting that tends to create panic can be
avoided.
C)
Training
Training and refresher training of the health personnel in a district and others is
very important because of the changes that take place on account of transfer,
promotion and retirement. Hence it must form an integral part of the epidemic
preparedness of a district.
• District Health Authorities, MOs i/c PHCs, and other medical and
paramedical staff especially those earmarked for the ERT should undergo
initial and refresher training in responding to epidemics at regular intervals.
• Human resources that would need to be mobilised from within and outside
the district during an epidemic must be identified with the help of
appropriate authorities and training must5e~pr5vigecf for such personnel
also.
The training manuals and schedules must be developed by district health)
authorittesand ’must' include clearly laid out stepwise procedures that are/
rehearsed during the training.
/
~)
87
GUIDELINE NINETEEN
MAPPING OF MALARIA AND GEOGRAPHIC RECONA1SSANCE (GR)
19.1 Why Mapping and GR?
CountrieS/Of the region are beset with the problem of resurgence of malaria.
Major^onstraints include drug resistance, vector resistance and resistance of
the communities to insecticidal spray. Global Malaria Control Strategy
formulated by WHO has been adopted by the countries of the region. Among
other elements it emphasizes on selective and sustainable vector control. Vector
control strategy therefore does not follow umbrella approach but lays emphasis
on evidence based vector control strategies for properly mapped malaria foci
with active intersectoral and community participation.
19.2 Mapping and GR
Geographical Reconnaissance (GR) can be defined as a afield -survey for
collection of preliminary information required fo!L^cientific__studies3 or
implementation of a disease vector control programme. The scope of GR varies
with the objective(s) of the study or the control programme to be undertaken.
Before conducting GR,^inventory of the existing material such as maps, survey
reports, tabular information on entomological components, disease scenario and
control measures taken in past should be made. Preliminary interpretation
based on this data and the local "knowledge of the interpretation team can
optimize the data collection.
Mapping can be defined as the process and set of procedures for plotting
Disease surveillance case data at the appropriate geographical locations on
National Maps.
19.3. GR in Malaria Control
There are four objectives of GR:
•
•
•
•
For mapping basic receptivity
To serve as a guide for establishing control priorities
Cost effective control methods and
Monitoring and intervention schedule.
19.4 GR to Map Basic Receptivity and for Formulation of Control Studies
Rural Area
GR for mapping the basic receptivity of the area information regarding
topological and ecological parameters need to be collected both at macro and
micro levels as follows:
88
______________ Macro Levs!
________ Micro Level
Contour map/altitude
Soil type
Local temperature, relative humidity Surface water bodies
and rainfal
species and breeding sites
Drainage Social,
cultural
& Ground water
economic practices
Meteorological data
Major projects
Forest cover •
Irrigation pattern
Crop pattern
In general , district map showing PHC boundaries may be taken as amase map.
All the land marks, viz. roads, canals, villages, religious places, swamps, forest
areas etc. should be clearly marked.
All the geographic areas may then be classified into well-defined ecologicalgeographic areas viz. Forested areas, foothill areas, swampy areas, riverine
plains, etc. Data analysis collected at macro level will permit to identify the basic
receptivity of each geographic area.
Malaria foci, then in each geographic area can be explained by interactive
analysis of micro level data to define the dynamics of transmission and for
building up locally adopted vector control strategies for transmission centre.
Urban areas
In the urban areas, malaria is generally transmitted by An.stephensi, domestic
species using stored water for breeding. However same urban areas are also
under the influence of An. culicifacies in the peripheral areas. Therefore, a
complete GR needs to be carried out to map all breeding foci for planning an
integrated anti-larval programme for control of malaria.
Depending on the area for manual analysis, three to four important parameters
from the above list may be selected. Maps of these parameters may be
transferred to transparency sheets for overlaying and identifying receptive
areas.
Because of population growth and rapid urbanization, urban areas become
wider and peri-urban areas get less attention in all aspects. Health problems are
mainly contributed from peri-urban areas. Because of these reasons, GR should
emphasized on peri-urban area to delineate the foci of breeding places for
effective vector control.
Border areas
In border areas, health infrastructures are less developed and communication is
poor. Spread of drug resistance problem along with the uncontrolled population
migration is also seen in these areas. Above information should also be included
in GR for effective management of cases , prevention and control. This will help
synchronization of control measures across the border and strengthen inter
country collaboration.
*
89
GUIDELINE TWENTY
RESEARCH AND DEVELOPMENT
Malaria Research is restricted to a few institutions / organizations. Reasons are (a) Malaria
research underfunded, (b) At the university level, there is inadequate importance given to ■
communicable diseases, and (c) Research is disorganized.
Inadequate funding on research is hampering even the ongoing research project.
sufficient funding should be provided.
Hence
Under Roll Back Malaria initiative, the following areas are highlighted which need
proper research for better implementation of the ongoing control operations.
20.1 Socio-economic studies
1. Studies on sociological, behavioural (anthropological) and economic dimensions
KAP and how it can help IEC programmes
Prescription practices
Costing of malaria programme at regional / district level
HRD studies (health education courses at university level)
Policy studies to examine appropriateness of some on going health
care programmes (eg., the adaptability of society model in addressing
public health issues)
Policy studies to examine the relevance of market economy approach
in addressing public health issues.
Encourage universities / other research organizations to undertake
research on tropical diseases.
2. Studies to examine how we can restructure primary health care system for
strengthening RBM.
3. Demonstration of costs and benefits of control measures, eg., school attendance
increased, increased crop yield, hospitalization decreased, anaemia decreased, etc.
20.2 Vector Studies
4. Studies on impact of ecological changes on mosquito biology with specific reference to
weather changes, natural calamities viz., recent super cyclone of Orissa, epidemic
forecasting.
(Consolidate existing meteorological data base at local level for the
above mentioned studies).
5. Conduct studies on distribution of vector species, their biology in relation to
transmission dynamics in persistant malaria area.
20.3 Drug Studies
6. Conduct studies on combination drug and on efficacy of quinine and other alkaloids. It
must be emphasised that the knowledge existed in pre-synthetic era (pre 1930s)
should be brought to light in furthering research in the area.
7. Studies on monitoring of drug resistance both in P.vivax and P.falciparam.
8. Research into herbal remedies and natural insecticides.
9. Research on alternative personal protection methods
90
® evaluating side-effects of the existing personal protection should be researched.
Also studies on social marketing, of personal protection method should be
undertaken.
20.4 Epidemiologies! Studies
10. Studies on dry land rice farming to control vector breeding especially for JE.
11. Studies on wet land farming - uses of urea, neem cake, azoIla and other aquatic
fauna, eg., local fishes.
4- Establish demonstration sites of non-chemical control measures eg., good drainage
and engineering practices.
Their comparative cost-effectiveness can be
demonstrated.
12. To undertake risk assessment studies and develop appropriate methodologies for
conducting rapid assessment of malaria.
13. Developing a sound malaria information system for conducting studies at all levels.
14. Border malaria - highly neglected area of research
4- it is essential to take up a wide range of studies (all the above)
4- very little is known about the type of vectors in these areas.
20.5 Control Strategies
15. Studies to explore ways to involve community in adopting control strategies
4- link with income generation activities
-4 link with district malaria societies
4- special IEC measures should be designed to promote correct practices and de
promote wrong practices and beliefs in vector control.
16. Studies on why alternative malaria control strategies (eg., bio-environmental
measures) are not being tried adequately.
17. All these R & D activities should be encouraged in all local research institutions and
universities.
Strengthening the Socio-Cultural-Economic-Political Dimension of Problem
Analysis
❖ Behavioural
sciences
approaches
and
socio-anthropological
and
socioeconomic/health economic research competence must be urgently built into the
‘problem analysis’ and ‘problem solving’ structures at all levels - to ensure that these
dimensions are no longer ignored.
❖ Well planned, multidisciplinary action/operations research must be initiated and a more
holistic effort strongly rooted in the social sciences must be encouraged.
❖ From Action/Operations research practical, realistic operational guidelines can be
evolved on all the above areas and these then incorporated into the planning process,
the training process and the action process at all levels.
Source: Towards an Appropriate Malaria Control Strategy - VHAI/SOCHARA, 1997
91
wjrniff ■ iwfiwmra'mwwwpiampa;* \'Mi&i*c&naaaMa^-r»T*vjrauroMMHcirw
Case Study -6 /
Madras City Experience
I
J.
7 //
I
—-
A seven-point action plan was prepared for malaria control. An action committee was
constituted. Students made house-to-house visits and interacted with residents One of the
main misconceptions-that was addressed was that overhead tanks should not be closed - it
would make water stale, therefore the overhead tank should be only partially covered so that
air could enter and maintain the water fresh. A student action group was formed under Prof.
Swaminathan. The students were drawn from various schools and colleges. They also
monitored the status of the fish in overhead tanks after they were released. All the schools in
the city with grades 6th to 12th were targetted.
The handouts consisted of:
1.
2.
3.
4.
5.
Procedures for schools
Posters
Fac sheets for teachers
Har Jouts for the students
Pamphlets for the community
School principles were informed about the campaign through letters. One or two teachers per
school were oriented; they, in turn, oriented the students.
I
Position: 3092 (2 views)