RF_CH_7.1_SUDHA.pdf
Media
- extracted text
-
SURVIVAL
VANAJA RAMPRASAD
he recent announcement by
the Government of India to
intervene in five different
sensitive areas of people’s
lives through technology
missions, includes the programme
of immunisation. This echoes the
scale of enthusiasm pronounced at
the international level as a social
movement. The State of the
World’s Children 2986, a UNICEF
annual feature, begins its rhetoric
by claiming—‘Immunisation leads
the way’. It continues to pronounce
that several nations have doubled
and trebled their levels of immun
isation against the vaccine prevent
able diseases.
However, somewhere along the
line ^isolation, in which the prog. ramme of immunisation is envis
aged, the technology mission is
likely to miss the wood for the
trees. It appears that the task has
been given the misplaced honour
of playing the principal role in
child survival and health care
without taking into account the
fundamental biological and human
aspects of it.
What does the immunisation
package consist of? Four vac
cines—the DPT (diphtheria pertus
sis tetanus), BCG (bacillus calmette
guerin), polio and measles—
against six major diseases—
T
Aga
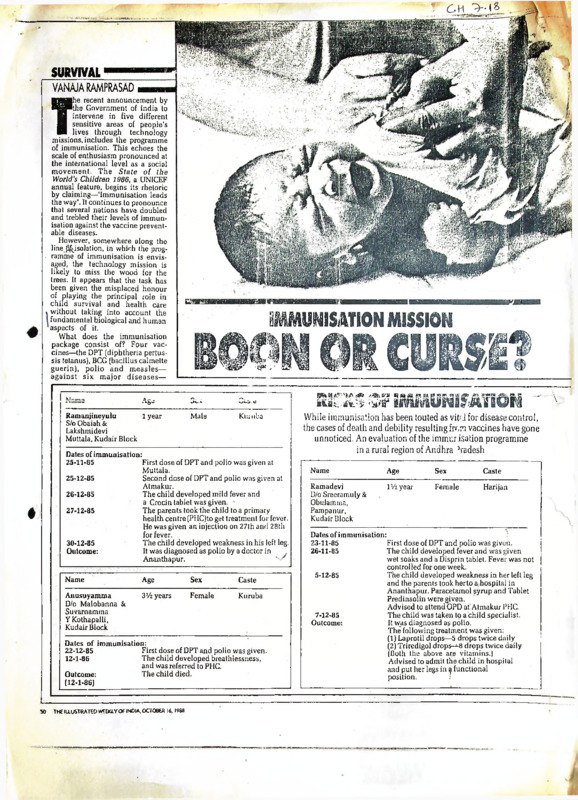
Ramanjineyulu
1 year
S/o Obaiah &
Lakshmidevi
Muttala, Kudair Block
IMMUNISATION MISSION
BOON OR CURSI?
tk.r
Cu. a
Male
Ktunba
Dates of immunisation:
25-11-85
First dose of DPT and polio was given at
Muttala.
25-12-85
Second dose of DPT and polio was given at
Atmakur.
26-12-85
The child developed mild fever and
a Crocin tablet was given. The parents took the child to a primary
27-12-85
health centre (PHC)to get treatment for fever.
He was given an injection on 27th and 28th
for fever.
The child developed weakness in his left leg.
30-12-85
It was diagnosed as polio by a doctor in
Outcome:
Ananthapur.
'
Name
Age
Sex
Caste
Anusuyamma
D/o Malobanna &
Suvarnamma
Y Kothapalli,
Kudair Block
3>/2 years
Female
Kuruba
Dates of immunisation:
22-12-85
First dose of DPT and polio was given.
12-1-86
The child developed breathlessness,
and was referred to PHC.
Outcome:
The child died.
(12-1-86)
SO
THEIU.USTRATCOWEEtU.YOftNOIA,OCTOe£R 16. 1988
^^^HMKUNISATION - V
While immunisation has been touted as vit-'J for disease control,
the cases of death and debility resulting from vaccines have gone
unnoticed. An evaluation of the immurisation programme
in a rural region of Andhra ,’radesh
Name
Age
Sex
Caste
Ramadevi
D/o Sreeramuly &
Obulamma,
Pampanur,
Kudair Block
iWyear
Female
Harijan
Dates of immunisation:
23-11-85
First dose of DPT and polio was given.
26-11-85
The child developed fever and was given
wet soaks and a Disprin tablet. Fever was not
controlled for one week.
5-12-85
The child developed weakness in her left leg
and the parents took herto a.hospital in
Ananthapur. Paracetamol syrup and Tablet
Predinsolin were given.
Advised to attend OPD at Atmakur PHC.
7-12-85
The child was taken to a child specialist.
Outcome:
It was diagnosed as polio.
The following treatment was given:
(1) Laprotil drops—5 drops twice daily
(2) Triredigol drops-^-8 drops twice daily
(Both the above are vitamins.)
Advised to admit the child in hospital
and put her legs in a functional
position.
'
J
diphtheria, pertussis (whooping lysis, when subsequently they are the 30 years since independence
has been much slower in the
cough), tetanus, tuberculosis, exposed to poliomyelitis virus.
The nutritional status of the host 30 years preceding independen
poliomyelitis and measles respec
tively—that .iffect a large per cent before' immunisation is also an ce.
It is evident from the poignant
of Third Wo Id children have been important factor. Immunocompe
advocated to form the package. tence is compromised by severe reports of death and debilitation
Each of these vaccines has to be malnutrition. The body’s ability to that the newly propagated strategy
administered under careful condi cope with infection is reduced for survival using such medical
tions to realise maximum efficien with poor nutritional status. In technology without the corres
cy.
•isolation, immunisation does not ponding efforts for socio-economic
The most important of the con take into account the importance of change and equitable distribution
ditions is s’orage of the vaccine these factors. Environmental mea of resources, has a close resemblance
and the cold chain that is main sures against disease transmission to the much criticised family plan
tained during the time of adminis and the reduction of exposure cus ning model that has been advo
tration of the vaccine. (Vaccine is tomarily involve the provision of cated to control the population of
an immuno-biological substance clean drinking water, institution of the country.
designed to produce specific pro safe disposal of excreta and im
tection against a given disease.)
proved personal and community Invisible benefits
The immune response is net hygiene besides ensuring adequate
entirely"Arrce~lrom~the risk o< nutrition. The huge resources set What has not been openly acknow
adverse reactions, especially those aside for the operationalisation of ledged by the international interest
resulting from septic conditions an immunisation programme are to thrust immunisation on the
due to faulty sterilisation of the- not without their opportunity Third World is that it is a lucrative
25 million dollar-a-year business
equipment and microbial contami costs.
for firms in the industrialised
nation. Use of improperly steril
countries. According to WHO’s
ised syringes and needles carry the
<#tsible Risks
own estimates, about 85 per cent of
hazard of hepatitis virus and
The poor information base in the ‘cold chain’ equipment and pro
staphylo and streptococcal infecWill the government’s
. tions. Medical researchers like country rarely documents the ducts used to keep vaccines safe
wlDr Sathyamsla have documented negative impacts of immunisation are produced in the industrialised
immunisation mission
facts to prove that the increasii g [ "ogrammeS on high risk children world, mainly in Denmark, Luxreally ensure greater
i incidence of polio in areas whe e ci poor and deprived families in umburg, the US, Sweden and
large amom.cS of polio-vaccine are rural areas. Vaccines have at times Japan.
protection against
Vaccines lose potency if exposed
administered annually is due o 1 .ft children debilitated. In some
disease?
the intramuscular injections which Li.es, they have even resulted in to heat and light and must be
death.
While
the
technology
mis
stored below 8’C while tetanus and
- predispose the children to parasion advertises immunisation as a DPT vaccines must not be allowed
new miracle for disease control, to freeze. The 3 M company of the..
u'S is the sole supplier of chc.nicaiName
Caste
Age
Sex
i. ;en'crippled or killed by immun-ii ly treated cards that warn whether
isation go unpubiicised. An eva- the vaccine is usable or not. Each
Nagar.iju
1 Year
Male
Boya
h ation of the universal immunisa- year it ships 1,50,000 cards nt a
S/o Na. asimhulu &
tTm programmehn a rural region of cost of three dollars each. Similar
Venkafalakshmanna
Andhfa~~Pradesh has recorded ly, one can name several firms
Madigubba,
cases of debility and death induced from Denmark, France, Sweden
Kuda;r Block
by vaccinations (see charts):
and Britain that will stand to be
While one is bombarded with nefit. In the next five years, India
Dates of immunisation:
tie rhetoric of guaranteed success expects to spend Rs 2300 million
25-11-85
1
First
dose of DPT and polio was given
of the mission and the internation for immunising 85 per cent of the
25-12-85
Second dose of DPT and polio was given.
al agencies in Delhi, the reality of children and 100 per cent of the
The child got high fever, and was given wet
26-12-85
rise lies in the invisible distant mothers. According to the ministry
soaks and a Disprin tablet: fever was not
viLages whereK children are ex of health, the estimated expendi
controlled.
posed to the hazards of being crip ture on syringes and needles alone
The child could not move both his legs.
27-12-85
pled or killed by the technocratic is Rs 325 million and Rs 820
The child was taken to a hospital.
28-12-85
ap. roach to health care. Technoc million on vaccines.
Outcome:
It was diagnosed as polio in both legs
ratic interventions have anyway
The technocratic approach of the
and left hand.
never been central to bringing technology mission will ensure
health care to people.
that the invisible costs to high-risk
I: may come as a surprise to children or, on the other hand, the
ma ly that in spite c. the fact that invisible benefits to international
Caste
Sex
Age .
Name
most medical technologies were economic interests will never
not available in India in the early reach the public in an open and
Boya
Female
14 months
S Anthamma
yea s of this century, death rates honest way. Hidden beneath the
D/o Verriswamy &
begin to decline from as early as technology mission’s preoccupa
Obulamma
1923.
tion with immunisation as an ex
Sheikshanapalli,
"he facilities and services of clusive panacea for child survival
Urvakonda Block
medical technology were extended lie the sad stories of many children I
to lha general population only after who are victims of technocratic 1
Dates of immunisation:
E3
India gained independence in insensitiveness.
First dose of DPTiand polio was given.
21-11-85
1947. If technology had made an
The child had mild diarrhoea.
impact on the health status of the This is one of a series of articles
Onset of fever, diarrhoea, vomiting,
22-11-85
population there should have been concerning Survival. Any queries
symptoms of malnourisnment
a sharper decline in t.ie death rate regarding these articles and the
Paracetamol, an anli-diacrhoea tablet
Treatment:
in li e period after independence. issues dealt with herein may be
and oral rehydration ih-iapy were given.
On tie contrary, the figures reveal addressed to Lokayan, 13 Alipur
that .he decline in the death rate in Road, Delhi 110 054
{
THE ILLUSTRATED WEEKLY OF INDIA, OCTOBER 16. 1988
St
iH-rui.zzATiOir
DMJBITY
12.1
When antigens arc introduced into tlx body by infection with
o disease or through immunization, the body responds by manufacturing
antibodies to protect itself against then. An individual becomes
immune or dovclopcs immunity when his body has a-, sufficiently high
level of antibodies against a specific disease or infection. Such
an individual lias developed a kind of resistance to the disease.
.
There arc two types of immunity: •
' :
1• Natural immunity: This is the type 'that a person lias from
birth and it is related to race, species and to individual inhiritancc
from, parents, o.g., tian is immune to some diseases tliat affect animals.
2. Acquired immunity: This can be developed by the individual
either through getting the diseases or through immunization against the
disease. It may be Required actively where the body is stimulated to
produce its own antibodies, or passively where the body is tonpcrai-ily
protected against disease by the adHn.isstration of already prepared'
un+.i bodicis Many
ol.p'll dio vicocl—
md childxon 3 ivirir in Ux.
lossly from a number of coct.-iunicablo disease..- such ns tuberculosis,
diphtheria, whooping cough and tetanus, which can be prevented by
innunization.
This situation persists because of the following Facts:
1. Parents end other adults often de not know that children
can be protected from many co; nunicablc diseases, by giving then the
necessary immunization.
2. The services for irirunization nay not be available in the
villages at a title and place that is convenient to the people.
fl
3« Individuals nay have religious or ether beliefs that inter
'f''. their accepting innunization.
4* Pregnant women do net get tetanus boxoid immunization and as
a result the newborn child is exposed to the iri.sk of tetanus.
Tlic immunizations -most commonly rood in India arc those
against the following diseases:
i.
Smallpox
ii.
Tuberculosis (BOG)
iii.
iv.
Diphtheria
Pertussis (whooping cough)
{
|
v.
Tetanus
J
vi.
Poliomyelitis
v,«’.
(DFT)
i
vii’. Cholera.
Typhoid (TAB)
Smallpox, BCG and JpT vaccines are administered routinely to .
infants and young children. Tetanus toxoid is administered to pregnant
women as part of prenatal health care. However, protection against
poliomyelitis, c clora and typhoid is usually limited to commnitics tint
have a high or frequent occurrence of these diseases, or where there
arc outbreaks of such. diseases.
• •Contd/2-
’
,
$
:2:
The protection that is possible through immunization docs
not last for a lifetime. The lenght of protection from various
diseases depends on the particular immunization, o.g., for cholera
it is six nonths and for snailpax three years. This is the reason
why the sane immunizations have to bo repeated regularly for the sane
individual over a period of tine. The immunizations that are adminis
tered after the initial dose or doses at regular tine intervals in
order to maintain a high level of protection are called booster doses.
12.2
RESPONSIBILITIES OF HEALTH WORKER (MALE)
RELATED TO IMMUNIZATION
In the intensive area
1. To administer DPT vaccine, BCG vaccine, and wherever
available, oral polinyclitis vaccine to children one to five years.
ii. To give primary vaccination agniist. smallpox to children
above one year and to adults.
iii. To revaccination all children and adults against smallpox
every three years -or earlier in the event of an Outbreak cf smallpox.
iv. To assist the Health Assistant (Malo) in conducting immuni
zation of school children against smallpox, diphtheria, tetanus, tuber
culosis,” and other diseases.
v. Tc give cholera, TAB or pclimyolitis vaccine in the ease
of.'”n wttowl
typhoid or poliomyelitis.
vi.
To educate the
-f-.lnr.. ^oeossniv for "jmnnrn *^^ti nn
vii. To plan your activities.related. tc immunization with the
Healtli Worker (Female).
viii.
To maintain the required records a.r'1 subrit reports.
In the twilight area ’
In addition to the eight activities listed above, your additional
tasks in the twilight area are as fellows:
ix. To administer DPT vaccine, BCG vaccine, and wherever
aval 1 nbl a, oral polimyolitis vaccine? tc chil Iren aged zero
year.
x. To give primary vaccination against small rex to all children
aged zero to one year.
7
xi.
12.3
To administer tetanus toxoid to pregnant women.
pWIHZATION SCHEDULES
In order to rake sure that the susccptibel groups within the
community arc well protected against preventable communicable
diseases, immunization schedules have boon developed. You will note
that sene i munizntions arete be given to newborn infants as well as
to infants during the first year of life and subsequently'booster
doses arc to be given or revaccination rust bo carried cut.
Schedule cf iarmizations for children.
Age
At birth or as seen ns
possible after birth
Irnunizntion
Smallpox vaccination BCG
Vaccination.
. .Contd/3-
: 3 :
4 to 9 months
DPT (Triple Vaccine):
2 doses at intervals of 8 to
12-weeks ■
Poliomyelitis (trivalent oral
vaccine):
3 doses at ir.turyals of 4 to 6
weeks
........
" .",
1 year
Smallpox rc/accination
5-6 years (school entry). Smallpox revaccination
or soon thereafter
. DT booster, 1 dose
TAB vaccine 2 doses at inter
vals of one month (Repeat every
year)
Every 3 to. 5 years
Smallpox rc'-r.ccinaticp '
During outbreaks, c..g.,
cholera, typhoid or
poliomyelitis
■ Cholera vaccine : 2 ,d< sos atl1Odr.y i ntcrvals
T/JB: 2 doses at 10-day intervals
Poliomyelitis (Trivalent oral
vaccine) : as above
Following injury
Tetanus toxoid booster
Schedule for tetanus i. nunization of pregnant women
Duration of pregnancy
Tota.nus toxoid
20-26 weeks
30-36 weeks
1st d JSc*
2nd dose
*Therc should be on interval, of 8-12 weeks between the first
and second dese-. The second dose should be given at least.
2 to 4 weeks before the expected. date of delivery.
CONTRAItOICATIONS TO IM-iUmZATIOI-I
12.4
;
a
■^0^*
Immunizations should not be administer d to individuals who
arc sick, because illness interferes with the production of a ntibodics
by the body. However, during cpidcidcs, this general rule may be
relaxed in order to protect as ’.’any as possible who arc exposed to
the disease.
. ■ ?,
.
Generally, the following symptoms in 'a.i individual ord considered
as contro-indicdtions for ad. ini st-., ring inainioatic-ns:
i.
ii.
iii.
Fevcris'l'’ncss, cough, running nose, lethargy.
Skin conditions, ■especially rashes.
Vomiting and diarrhoea if an oral v: ccino is to bo administered ■
DEI-FMBER THAT IMMUNIZATIONS SHOULD KQTdiAlY BE ADI1NISTERED
ONLY TO WELL INDIVIDUALS APB SHOULD BL BISTFOMED IF THEY ARE
ILL .
Malnutrition is not a contraindication for administering
immunizations to children. Such children fear:. a low level of resist
ance to infections and need the protection ti. t can-bo -given’be imCuizations. Their parents will have to be infer ud that additional pro
tein fods will have to be given 'for several d-.ys following, i munizati-on
....Contd/4-
to help tho body develop irunity. Such children will also need to
be given additional carbohydrates so that the bdy can utilize the
proteins properly.
12.5.
METHODS OF ADimJISTERilNG IMMUFIZATICN
To naxirizc thoir effectiveness, iv; vnizaticns are advinisterod by various routes. The routes that you will be using for giving
innunizations arc as follows:
By rzouth,. c.g., pclionyclitis vaccine.
On tho skin using multiple puncture, c.g., srallpcx
vaccination
iii. Into the upper layer, of tho skin (intruder:-al), c.g.,
BCG vaccination.
iv. Into the nctscle- (intro: uscular) c.g., DPT vaccination.
i.
ii.
. -■ --BEFORE GIVING A Y VACCINE, YOY MUST MAKE SUFE THAT YOU KNOW
' THE’ PROJER ROUTE FOR WMU'JISTERDJG IT.
CARE /ID STORAGE OF VACCINES
12.6
-The vaccines which you will use for iirunization certain
the following:
'
1.
Live organists that have been we.-honed or diluted so that
they arc no longer capable" Of preducing.the disease, but
are still capable of producing i: r.unity.
2.
Dead organises which can rise st:.Eulato tho production
of protective antilodies.
3.
Toxoids w ich arc toxins produced by or'-.-misns, tut which
have been treated so as tc cstry their toxicity without
destroying their ability tc stirlate the body tc produce
its own i:n unity.
ALL LIVE VACGEHES 1-iUST BE:
'
i.
STORED AT A TE'-WATURE WITHIN THE RANGE WESCETPER^gb
THE WJJUFACTURER.
n . JROTECTED FROM SUNLIGHT.
' iii. PREVENTED FROM CONTACT WE TH ANTISEPTIC SOLUTEOiJS SUCH
AS SHRIT OR SAVLON *
Form
Type-
Stere/refrigerate
. D7T, DT and
Tetanus toxoid
Lqpid
Toxoid
2° to 10°C
BCG
Freeze-dried
live
organist :s
2U tc 10uC
Smallpox _
Frcczo-dried
IdAO
orr^nis^s
to 10v'C
Cholera
liquid
Dor.d
cr^nis'is
to 6 %
Liquid
Do-d
or^'inis’.is
2° to 8 UC
liquid
Li.vo
cr‘7?.rAs:.:s
■ i-inus 20uC
(keep- frozen)
Vaccine
Typhoid and
paratyphoid
’ A" and B
M-ioryoli ti s
Contd/5-
: 5 : '
Since there is a lock of refrigeration facilities at the sub
centres, you will have to remember to order only what is needed each
week from the IriLr.ry Health Centre. Use care in transporting it
from tlio Primary Health Centro to the subccntro and improvise wa.ys
of keeping the vaccines as cool as possible. Vaccines should be
carried in a thermos flask packed with ioc or cold water. They
should be stored in tile coolest place in the subcentre, preferably
in an earthenware container which is covered with a wet cloth.
ALL VACCINES MUST BE STOPED LT TEMPERATURES RECOr MELDED BY THE
MANUFACTURER OTHERWISE THEY WILL DETERIORATE /J© EECOLE USELESS.
DISCARD ALL UNUSED LIVE VACCINE AT THE EID OF THE WORKIIIG DAY
BECAUSE ITS POTENCY DETERIORATES RAPIDLY WHEN NOT REFRIGERATED .
12.7
PREPARATION OF VACCINES. FOR ADlgLI STRATTON
The vaccines that you will be using to administer i:: unizations
to children and pregnant women arc avilablc either in liquid or in
powder fora.
It is important that both for.is are kept sterile during
preparation, recosntitution and administration. If tis is not done,
the results ray not be valid and there ray be infection.
The vaccines in liquid fora generally co: :c in ! ultiple-dose
vials with a sealed rubber cap at the top, in sealed ampoules, or in
small bottles with screwtops which hove attached calibrated or non
calibrated medicine droppers. The?-vac ci nos which come in powder fora
are pack*?'-1 in sealed glass a’, .poulcs. The diluents or liquid which
must be used for : ixing the into sc 1 tion arc usually packed in
either multiple-dose vials or in sealed glass ampoules.
...
....
i
Points to remember
Clean the rubl er cap ef tin vial with spirit before inserting
the needle.
2. Inject air into multiple-dose viols before withdrawing a dose
or doses in order to equalize pressure, and facilitate withdrawal of the solution.
3. Protect fingers when filing and opening glass ampoules so
that cuts are avoided.
Avoid •.aking bubbles when rocostituting vaccines because
this can interfere with accurate measure: ent.
1.
•
12.8
SITES USED FCT. ADMLIC STORING VACCINES
'
Because of the danger of injury to nerves and the need to avoid
injecting vaccines into largo blood vessels, certain sites bn the
body arc selected for administering injections. The core only used sites
are a s fellows:
1.
For intramuscular injections (DPT, DT, Tetanus Toxoid, TAB
Cholera):
i. The upper ara two to three finger widths below the point
of the shoulder on the outer asnoct (sec fig. 12.1).
Be careful to avoid the radial nerve which runs along
the inner aspect of the ar?..
•
Contd/6-
Fig. 12.1 Site for intr-.'mscular injection - ----upper arm.
ii. The buttocks can be divided with imaginary lines into
four parts and the injection given in the upper part
as shown in figure 12.2. Be careful to avoid the
sciatic nerve in the hip. Usually tills site is not
used for infants who ar. not yet walking since it is
not sufficiently well developed.
fig. 12.2: Site f'.r intramuscular inject!; n buttock
iii. The front of the thigh (see fig.12.3). This site doos ’
net lir.vc large nerves and is easily accessible. It is
commonly used in children
Discomfort of the injection
can be ; ini', ized b; slight flexion of the thigh and k
knee before injection
fig.12.3:Sitc for intra:xtscular injection
- front of thi.'fli
: 7 :
Fig .12.4:Site for intramuscular injection —
cut silo of thigh
Hie site used is dependent on whether CG and smallpox
vaccinations are administered at the sane tiro.
i.
If BCG and smallpox vaccinations arc given at the sane tine,
use the right upper am outer portion for BCG and the loft
upper am outer portion for smallpox. The use of different'
sites is necessary to reduce the possibility of complications.
ii.
If BCG is given after the smallpox scab has fallen off, use
the left upper am outer portion.
3.
Multiple-puncture method (smallpox v; ccination);
2.
For primary vaccination, tho loft upper am, outer aspect1
is used (sc.c fig. 12.6).
.......... .Contd/8-
Fig. 12.7 :Sito for S’.'alj.rox revaccination
- front of rr cam
12.9
POINTS TO BE KE IT IN iJIH JJ.CUT A;/flail iili-iG liMJNIZATIONS
Seiction of site should bo dene, by;
i. Inspecting the size of the : n.-jclc •
ii. Ascertaining th.-* the site i" free of bruises or any
sore areas.
iii. Avoiding an area t’>at ‘-'as any scratches, cuts or skin
disease.
iv. reviewing that t.nc area selected, is anatoiically correct.
1.
............... Contd/9-
q
2.
It is necessary to restrain cldldron while
administering irrunizatic ns • This can be'done
be a parent or othcradult so that accidents such
as the noodle breaking during injection can bo
avoided.
Health teaching is in- ortant for .ainiipg the confi
donee of parents- Unless they know about the kinds
of discomforts that can bo expected after im.unization and what action is tc "o taken, parents ray not all
allow i’.nuniz.ytion of their children.
Information
regarding the care of the site is especially important
after an -ind-iy-idnal has been vaccinated against
smallpox.
4- The vaccine rust bo prc'-'crly stored and an;, vaccine
that lias boon improperly kept er left over must,be
discarded.
5. Proper technique is necessary for ensuring go cd
results.
3.
12.10
SHALLFCK VACCINATION ■
.
Your responsibilitis with regard’ to st allpox vaccination
are of two kinds:
To give primary vaccination and revaccination to all
unprotected persons in the community.
2. To vaccinate all persons in the event of an cutbreak
of smallpox irrespective of then they were It. st vaccina
ted. ,
.
1.
CONTRAINDICATIONS FOR ADWKE STERIHG SI'f^LIOX VACCINE
12.10.1
In the absence of an epidemic or exposure to a case of,
grind 1 pox, the following individuals should not bo given, smallpox
vaccination-:
i.
ii.
If the person has a skin rash with discharge.
If the child is ralnaurrshod, c.g., if it has
kwashiorkor.
iii. If tlie child is just recovering from a serious disease.
iv. If the worxHi is pregnant.
12.1
STORING AND TRANSPORTING TH'- VACCINE
Ci2
Freeze-dried smallpox vaccine is used in India, and ■
this-vaccina must be stored between /fc and 10°C.
2. The vaccine should bo kept as codas possible by
keeping the ampoules in an earthenware pot covered
with a damp cloth.
3 • If tho vaccine lias boon out of the refrigerator for
for over four wpeks, it should be discarded.
1.
■
REMEMBER, OPDEI ONLY ENOUGH VACCINE FEQUU ED FOR A MAXIMUM OF
TWO WEEKS. AT A TH® TO AVOID WASTING IT BECAUSE OF LACK OF PRO
PER FEFREGEEATION FACILITIES
Use a thermos or other container tc carry the vaccine.
The container should bo packed with ice if possible
or insulated by wrapping it in wet cloths.
................. .Contd/10-
: 11 :
Steps to bo followed:
■ >• -.
Clean the site with cotton weclthat has been r.'.cistenod
with, water and allow it to dry. Do not scrub the skin
vigorously. Do not use .spirit er other antiseptic.
2. Insert a sterile, cold, bifurcated needle into the ampoule
of reconstituted vaccine. -.When it is withdrawn, a droplet
of vaccine, sufficient for vaccination is contained within
the fork of t he needle.
■ 3. a. Hold tile needle at ah angle 90 to the skin as in the
figure with your wrist resting against the am (see fig.
12.6).
■
b. Touch the points -<f the needle lightly to. the.skin so
that the droplot if vaccine is deposited’on the skin.
c. Males 15 up and down strikes cf the needle in an area
about 5 tn. across through the droplet of vaccine. The
strokes, should be hard enough sc that a. trace of blood
appears at the vaccination site.
4. Allow the vaccine to dry before the individual rolls down
his sleeve or goes away.
5. No dressing should be applied after the vaccination.
6. Focord the administration of vaccine in the individual
health card and in the infant an I child immunization
register.
1.
A VISIT SHOULD BE MADE TO THE HOME OF TIE CHILD BETiEEN THE
SIXTH AND NINTH DAY TO CHECK WIETHE! THE. VACCIIL-TION HAS BEEN
SUCCESSFUL .
STERLIZATIOrl OF BIFURCATED PEEPLES
12.10.5
it is
The needles can bo sterilized by fin’ ing er bciling. Howovrr
referable to boil father than flame needles to sterilize thorn..
1.
-----
Flaring: The needle is passed through the flare of a spirit
lamp. It should net remain in the flare’ fef more tian 3
seconds.
COOL THE NEEDLE BY EXPOSING TO THE AIR K.FORE INSETTING INTO
THE VACO NE AMPOULE. A HOT NEDLE FULL KILL THE’CRGANLSMS IN
THE VACCINE MAKING IT USELESS.
.
.
2.
Boiling: The needles can bo sterilized by bciling for
20 r.hnuts. They can be toil el in ’the plastic container
that holds, the bifurcated. no fibs (see fig. 12.8). Remove
the container from the water nrr’ stand it on its end to
drain out the water after first shaking it hard to remove
as much water as possible. Put the container in the stand
ing position to dry.
Ccntd/12-
Fig . 12.8:-Sterilizing b? furcated needles
THE FORK OF TH’ NEEDLE MUST NOT CONTAIN A DROP OF WATER WEAN IT
IS INSEITID INTO THE VACCINE AMFOUL. WATil WILL WEAKEN THE
STBENGHT OF THE Vl’CCINE ........
NEVER USE A NEEDLE MORE THAN ONCE WITHOUT STABILIZING IT BACAUSE
of the’ danger of shielding infection.
'
.. •.
12.10.6
REACTION TO VACCINATION
A prir.ia.ry vaccination is one that is.g;von to 'an individual
for the first tine. Any subsequent vaccinations arc called rcvaccintions
■When there has been a successful or posit j- f. reaction to a prirary va •
vaccination, it is called. a ’take1 . ■
Tire usual course of a successful take is os follows:
A blister forms at the vaccination site between three
to five days after vaccination. ■
ii. The clear fluid in the blister turns into pus and by the
Bthe and 9th day the blister becomes larger.
iii. By the 11th or 12th day it dri..s air’ forms a scab.
iv. Tire dry scab falls off about 14 to 21 days after the
vaeeinatior., leaving a -pear at the site.
i.
IF THERE IS NO JUS FORMATION .T THE SITE OF A HI. ARY VACCINATION
THE PROCEDURE AS BEEN DONE INCORj FCTLY OD ".’HF, VACCINE WAS NOT
lUTENT AND VACCINATION MUST BE FE HEATED .
12.10.7
HEALTH EDUCATION
It is inportant to emphasize certain facts about vaccina
tion.
z1. It is. harmless and practically painless.
2. It is important for every individual to be protected against
si allpox.
...........................Ccntd/13-
;13 :
3« After vaccination nothing sh-culd be applied on the
vaccination because water, bandages, tight sleeves,
ointnents, herbs or unclean tilings can interfere with
the action of the vaccine•'
4. If there is no reaction at the site between the 3rd
aril 5th days, 'he individual should return to the subcctre
to have the. vaccination repoatod;
'
12.11
BCG VACCINATION
In order to protect an individual fror. tuberculosis, BCG vaccine
trust, be administered before he is exposed tc the disease. It is for
this reason that a high priority is given to administering BCG to infants
as soon after birth as possible. Since children aid. young persons in
the community are also exposed to the disease and need protection, BCG
•is also g.ven to t hen up to the ago of 20 years.
ALL INFANTS AND CHILD; EN SHOTLD BE GIVEN I"G VACCINATION AS
EARLY AS POSSIBLE TO PROTECT THEM AGAINST TUBERCULOSIS.
12.11.1.
PERSONS ELIGIBLE TO ILIAAE gCG VACCINATION
Bic eligible groups in the co.npunity for BCG vaccination
include the following:
.
r
i.
ii.
iii.
All newborn infants.
All children between zero and’ five years of a go.
All persons between 5 and 20 years.of ago.
However, you will to responsible for adtri.nist0r3.ng BCG vaccine
. to the following groups I .
i.
All children between one and five years in the intensive
area. The. Health Worker (For ale) will ndrinistur BCG
Vaccination to infants aged zero to one year in the
intensive Area.
.
■
ii. All children from zero to f ve years in the twilight area.
iii. All school children. You will assist the Health Assist
ant (Male'’ in carrying out this programs.
12.11.2
CONTR/xINDICA^IGNS TC THE USE OF BCG VACCINE
Individuals with tie following characteristics should not
be given BCG vaccinations
1. A person who already has two or more BCG scars.
■ 2. A person who is a known case of tuberculosis (although
it, would not cause hart?. if the vaccinationis ' iven by
mistake).
BCG Vaccine should be postponed if:
1.
ii.
iii.
12.11.3
.
A person has a generalized skin disease.
h person has a high fever or is acutely ill.
A person i§ severely -.'alncuri.shcd unless additional
protein and energy-.giving foods can be started, right
away<
STORING AND TEA IJS PORTING THE VACCINE
BCG
1..
vaccine available in Indan is a freeze—drl cd
vaccine. which must bo stored. nt 2 to 10°C, but not
frozen.
Ccntd/l^-
2.
It can be kept in a refrigorc.tor for up to six months
or in an ice chest up to three months. ’ At room temp
erature it can be kept for two to four weeks. This
means that vaccine for usd at the subcentre rust be
obtained at least twice a month since refrigeration
is net available.
3.
An alternative to keeping the vaccine under re frigera
tion is the use of an cartheir-'are container which is
kept covered with a wet cloth and which is kept in the
ccolcst part of the building. The vaccine can thus
be stored for about feur weeks.
4« Carry the vaccine in a thermos packed with ice when
transporting ..it for any distance, e.g., from the IHC
to the subcontrc.
5.
Light rapidly destroys BCG vaccine either freeze-dried
or in the reconstituted form. The vaccine should be
protected against light throughout, during storage
as _woH_as during transport and use in the field.
ALWAYS REMEMBER Td PROTECT BCG VACCINE FROM HEAT AID LIGHT
TO ENSURE 'ITS FOijENCY. ..... ..
’
’
' :’
RECONSTITUTING BCG VACCINE
12.11.4
Equipment required:
i. Sterile 5 ml syringe
ii'. Sterilq 22 gauge neefj.es
iii. BCG Vaccine ampoules
iv. BCG diluent ampoules
v. Ampoule files
vi. Plastic sheet.
Proceed a» fellows:
1.
!
'
••
.
Examine thj ampoules .-nd discard them, if:'
.
i. There are colour changes;
11 . The powter appears to be wot;
There
iii,
a?e cracks or the ampoule is broken;
There
iv.
is no label on the ampoule;
The
v.
datq ofeepiry is over.
Follow stepfc 2 to 8 under the procedure for reconstituting
smallpox Vtccinc (see section 12.10.3) except substitute
the use of the plastic sheet instead of cotton swab.
9•
Follow -the uc.nufacturor’ s instructions regarding the
amount of ciluent to be added to the dry powder.
10.
Fix the 22 gauge needle into the 5 ml. syringe, withdraw
the requires a.r.'.cunt of diluent fpom the ampoule and gentry
—inject it into the ampoule containing the dry powder.
2-8.
THE USE OF TOO MUCH FGCE III INJECTING THE DILUENT WILL CAUSE B
BUBBLES TO FORM IN THE- SOLUTION. AVOID THIS BECAUSE IT WILL
INTERFERE WITH ACCURATE lE/SbTEMENT OF Till'CAVVI1E .
11. Withdraw and rc-injcct the vaccine into the ampoule at least 4
- tines to cake- -sure that it is thcrougld.y mixed.IF ANY OF TE DILUENT "IS LOST DURING IFCORSTITUTICD TIE STRENGTH OF
THE SOLUTION WILL NOT -3E ACCURATE SC YOU l.UST'OIEN ANOTHER AMPOULE
' OF POWER ’AND' DILUENT JND BEGIN THE ILCGEDUT E OVEI AGAIN.
Contd/lj-
.
: 15 :
12.
Keep the anpoulc of reconstituted vaccine in the anpculc holder
. ’ in a cool place protected free. light by wrapping black paper in
the shape a cone around it.
REMEMBER THAT BCG IS A LIVE VACCINE W1ICII C/JT EASILY LOSE ITS
POTENCY IF IT IS NOT iiANDLED 'IROEER1Y
12.11.5
TECHNIQUE FOR■ INTRALErdlAL ADl-iINI3Tr.ATI0N CF BCG VACCINE
An intradcrnal injection is given in the uppermost cr'superfi-cial layer of the skin. In order to be able to inject a vaccine or drug
intradermally, a special sized needle and a special syringe with fine
parkings (tuberculin syringe) arc needed (see fig. 12.9) and. the needle
trust be introduced at a part? ufLar angle to the skin.
o
Fig. 12.9. Tuberculin syringe and needle
Equipment and supplies required:
i. Sterile rtital box containing noodles and syringes .
ii. 'Sterile roadies 26 gauge, I cn
iii. Sterile tuberculin syrings (calibrated in 1/100 nl)
iv. Weeden I lock for holding opened ampcules
v. Spirit leap and bottle of spirit
vi. Metal shield for spirit lamp
vii. Blackpapcp for covering BCG vaccine
viii. Mantoux ruler for -ensuring intradermal weal.
■
‘
f
' ,
.
!
i
Proceed as fellows:
”
■
1. Assemble the tuberculin syringe us^ng the proper techni
que to avoid cental in ti on r-< attach the 26 gauge needle
to it.
2. Make sure that -the ’eye’ or opening of the needle and the
nr.rld.ngs qn th.: syringu are on the same plane. This isinpor+ant so tint the correct docs can be injected (see,
fig. 12.10).
;
•Contd/t°/-
: & :
Fig. 12 .'0: Intradcrcal noodle shewing tine I’oyo"
>
3.
1
Draw up tho Vaccine into the-syringe'talcing care net to
touch the needle with the fingers or other unstcrilc
objects.
'■ .
4. Ilacc the loaded, syrin o on a sterile surface. ■
5 • Select the ££to for vaccination. BCG vaccine is usually
given on the Loft, upper arc just -below the point of the
shoulder. (Daf-jr to section 12.8).
6. Cleaning the itc is not noco-sary unless it is grossly
dirty in whijii aaso wipe it with a clean, wet cloth.
7. Make tho slcii of the site taut by stretching it slightly
between the tiuub and -forefinger.
8. Keep-! the ’eye' of the needle up, hold the syringe parallel
er flat along tho skin and insert tho needle into tho
upper or superficial layer of the skin (see fig. 12.11).
LEfEEER, DElf liJECHCN GF BCG VACCINE CAbSE ABSCESSES AID
TAKE A LONG TIME TO HEA1.
Cbnd/1!?-
9« Irjcct the required dose which is:
i. 0.05 ul. for infants, under..four-weoks of ago.
ii. 0.10 rfL.' for all other children.
A weal or elevation of the skin should fom at the site
of vaccination. A proper intradcrdal injection of 0.10
ul. of vaccine will fora a weal of about 8 up.. in diauctor. This should be check using the Mantoux ruler for
every tenth person vaccinated.
10. Renovo the needle after administering the vaccine and do
not rub the site of vaccination. .
11. Replace tho used needle by a sterile needle or fierce it
between use.
• •
12. Administer the vaccine to time next individual using the
sane procedu:»■.
13. Record tho administration of vaccine in tho individual
'health card and in the infant and child immunization
register.
-........................
■
^gjBgG.
12.11
.6
IS NOT US!© WITHIN 4 HOURS OF RECONSTITUTION
WHAT TO EX7ECT AFTER BCG VACCINATION
Explain to parents the changes which they should expect
to see at the site where the vaccination has be n given and alert
then to those synptens which requires referral to the lYirnry Health
Centre for further at ten tic n.
Time, precess cf scare formation is as follows:
■4. The BCG veal or raised spot in the skin is. usually
absorbed and is net visible after 30 minutes.
2. After three tc four weeks, there is redness ana ,-^rc.i1ing
and a lunp appears at the . ita, of vaccination. This
is about 3 to 8
in dinretor.
3. By six t? eight woo! s, the area, increases in size to
6 tc 8 ra. in dirmmter. Crusting or pus my be present..
Deep abscess formation always indicates that the injection
was given incorrectly either.into the subcutaneous tissue
■ or into tho uusclj. ~cpending- on tho severity of the
abscess, refer t<. the RHC.
. By 12 weeks, there shoul-’ be a well-lealed scar at the
site of vaccination.
12.11.7
HEALTH EDUCTION
Points to emphasize should.include the following:
1. Rabies aid children need to t-_ im.-unized ns early as
possible with BCG so that they can be protected against
tuberculosis.
• .
■
2. BCG vaccination is a simlc, safe procedure which consi
sts in injecting vaccine into tho skin.
3« Within three m.onths after the vaccination, there will be
a scar showing that the individual is protected against
tuberculosis.
4- BCG vaccination can be taken at the subcentra or at
other convenient places in tho villa/.-, where groups
can bo ga'atcrcd together.
5. A. second vaccination will be required to be given to
the child during the school years.
..........Contd/l8-
: 18 :
DPT, DT, DiniTffiSK AND TETANUS TOXOID
12.12
Tlie vaccine used for itxiunizing -persons against diphtheria,
pertussis and tetanus is available either in a. combined fom, i.c. as
DPT er DT, or as a single vaccine which protects against diphteria or
tetanus. Every op-ortunity should be taken to- protect children under
five years of age against diphtheria, pertussis and tetanus, and pre
gnant women against tetanus.
PERSONS ELIGIBLE TO RECEIVE DPT, DT, DIPHTHERIA CP.
TETANUS TOXOID
12.12.1
Groups eligible for DPT arc-as .folios:
i. Infants from four to 12 noths of age.
ii. Children fro;.: one to five years cf age.
Groups eligible for DT are as follows:
i. Children from five to ten years of age (they nc longer need
pertussis vaccine).
Groups clcigible for tetanus toxoid arc as follows;
i. Pregnant woven.
ii. Others in the corr.unity who have not received PIT or DT as
children.
iii. Those who sustain an injury.
In the event of an epidevic cf diphtheria in tho oornunity, all
groups should bo_ immunized with diphtheria toxoid.
12.12.2*
CONTRAINDICATIONS FOPt ADIill'HSTERING DPT.DT A1--D TETANUS TOXOID
Those persons with the following character i.sitcs should not
be given DPT, Dt or tetanus toxoid:
Anyone who is ill or is just recovering from an illness.
History of convulsions.
History of allergies, i.e. inflaraa.tory skin conditions
with blisters, crusts or discharge, or weals with or with
out etching, or wheezing rcspirttion.
4* History of previous unexpected reactions to medicine or
1.
2.
3.
vaccine.
Innunizatitn of anyone who is ill shen Id be postponed and those
vhp have other contraindications should ba examined and screened by tho
doctor.
.
12.12.3
STORING AND TTJ^SIURTING THE VACCINE
.(Soq faction 12.6)
12.12.4
DOSAGE OF VAOffiE
Tho dose of tn vaccine Can vary according to -the manufacturer
and the type of vaccine t< be administered. For full protection child
ren under five years cf age should receive two doses of DPT at intervals
of eight to 12 weeks followed by a booster dose of DFT at one and a half
yar to two years of ago ;.nd a second’booster dose cf DT on entry to
School or soon after.
Pregnant women need to have tzo doses cf tetanus toxoid with
on interval of eight to ’2 weeks between oac' -lose. ■ The second dose
should bo administered tvo to four weeks before tho expected date of
delivery in order io protect the infant at birth against tetanus.
12»12.5
rROCEDUP.S FOR ADnCKISTRATION OF DPT, DT AJO TETANUS,TOXOID
Equipment required:
i. Sterile 2 uL. or 5 ml. syringe
.
'
.......... .....Cbntd/l9-
’ ■
. i.
i
: 19 :
ii.
iii.
iv.
v.
Sterile noodles 1.5 cn (for children) 23 gauge
3.5 cn (for .adults) 23 gEUgo
3.5 cn (for withdrawing vaccine
fren vials) 20 or 21 gauge
Vaccine (DPT, DT or tetanus toxoid) ..
Cotton swabs.
Antiseptic such as spirit or savlon.
Proceed as follows:•
.
Assor.blo the syringe.
Withdraw the required auount of vaccine into the
syringe.
iii. Clean the skin site selected.
iv. Inject the proscribed dose.
v. Record the date and arcunt of vaccine given on the
individual’s health card ant in the register.
vi. Tell tile nether what tc expect and advis^. fcr what to do.
(Pefer also to Chapter 28, 1 Sterilization and Disinfection’
and to section 30.8.4).
i.
ii.
-12.12.6
POINTS TO REISFiBER ABOUT ADrU-ilSTERIIIG PIT, DT HID TETANUS >.
TOXOID
1. Read the label of the vial to ■. akc sure that you have the
correct vaccine far the innunization to be given.
2. Measure each dose carefully when giving no re than one dose
fTon a single syringe.
3. '.Nover use a needle acre than once without first flaring
it or boiling it for 20 tiinutes.
4- The dose is the s-nc whether it is the first or second
injection or the booster dose. The de so tint is usually
prescribed is as follows:
DPT
- 0.5 r?l. for infants and chaldron up to
five years.
*
DT
- 0.5 r.l
for children over five pars.
Tetanus loxr id - 0.5 r.il. for pregnant wenen.
However, rale sure of the dose indicated by the nanufacturer
on the vial before adr.nnistoring the vaccine because this nay vary.
12-12.7
PJEACTIONS 10 DPT, DT AND TETANUS TOXOID
Expo ctod syupters
SLiglt fever, sore am and irritability fcr a day or two.
Trcatr’ent: '
i. Apply hot wet copross.
ii.. Give AJO (1/4 tablet under 1 year
1/2 tablet one to five years).
Unexpected synptons
1
i. Disco’curation or bruising of injoctioii site.
Troatront!
Apply hot -4et copress.
ii. High fever, abscess formation, convulsions.
Refer anyone with those con-licaticns to the Fritary
Health Centre.
12.12.8
HEALTH TELlyH NG ABOUT PIT, DT Ai'~ TETANUS TOXOID
Points for discussi n should include the following:
1. Infants and young children arc -vulnerable to diphtheria,
whooping cough and tetanus r.ni rany die each year from
the effects of such infccti'.ns. They need protection
fro:.’, all three diseases thr ugh. irrunization.
........................... Contd/23-
: 31 :
2,
At least 2 '■loses of DPT '-'.ven net mere than three
r.o: ths apart are needed t<< bi’-ild up protection,in
infants and young children. later, booster doses
arc needed. One infection in not enough to pr<+-oct
infants and ycv.n'’ children against diphtheria, whooping
cough and tetanus.
3« All pro'uant wo~.en need tc. got tetanus toxoid rhrri ng
pre;-nancy in order to protect the ba1 v at birth.
4« Children no. d a booster dose when they arc ready
to enter set. cl since there will bo orc exposure
to infection and they should' be protected'.
5- Immunizations are available bitter at tlx* subcentre
or in the hor.o«
'
6. After ii runia.- tion tte.ro cay be slight fever, sore
ness of the site and irritability for a day er two.
These synpters are expect.i reactions and should riot
be a cause for worry or ilr nc 11 ding the second
IT IS lETOI-TAr?TO EXILAIN THAT TWO C01-STC1 Tlv;; INJECTIONS ARE
NEEDED FOE' DEVELOTlIIG FULL liGTECTION AC.’INST THESE DISEASE ' * '
12.12.9
TETANUS TOXOID IN 1DEG1.ANCT
One cf your inportant tasks in the. villa.-cs of the twilight' '
area is to imnunizo as nany pregnant women as possible against tetanus.
Uiis is necessary because their newborn ha’.ies often contract the
disease as a result of being dcliv re 1 by untrained dais who do net care
properly for the umbilical cord. A large number cf babies die from
tetanus infection each year in India. Such deaths can be prevented
by immunizing pregnant women with tetanus toxcid luring the prenatla
period.
■
In order to bo able to do this, you will have.to develop
goed working relationships with village dais since they a re the only
ones who take care of pregnant women in t’ j twilight area. _ Sone of
the ways in which you can do this arc as .follows:
Sr.ok then out whenever y u rake a regular visit to the
village to show that you recognize their work.
ii. I’ blidy recognize their assistance in prenoting the use
of family planning and other health services by the people
in the village.
iii. Tutoress upon then the health benefits cf tetanus toxoid
f r the pregnant wcr.cn under their care.
iv. Inform the dai after you have given tie tetanus toxoid
to lie pregnant woman.
i.
The Health Worker (Ferric) nay else be able to offer
further suggestions fry approach! g dte's when she ; ay already know thro
through her work in assisting the R alt’-i Assistant (Fonelo) in the
training of dais. These a^it-ional sources of assistance should be
regularly used. since they nay often load to more effective ways of
working withwomen in the village.
One of the problems that you ray fin1 is that pre. pant
women ray n-1 allow you tc i/.mmizc then i.i their hones because cf
social custons. In order to get around this y. u ray have tc take
the following steps:
i.
Ask r number cf women to go.c.bcr in a convenient
place sc that the vaccine C"n bo administered to a
group -of women.
.................. .Ccntd/2l/-
: a, :
. ii. Hol?1, a combined clinic fcr adud nistering tetanus
toxoid to rrc ,-nnnt women a.il J1T fcr•pre-school
children on a rcgularly sc'icduled day in the
village.
iii. Ask the lais tc assist you in gathering together
women and children win liv. in the sane area, so
that innunizaticns can be administered io the
residents of every sector in.the village over a
period ,f months.
12.13
rOUOK ELITIS VACCINATION^ ■ ,T. SAC-IIT VACCIE1) .
In India, policmyo'' itis is adi ini’.tcred on a mass basis
only when there1 is an outbreak cf th- disease in a community, i.c. when
a high or unusual number of cases arc found in a locality.
12.13.1
ELIGIBILITY FO
VACCIH.’.TION
Wherever availaMe the vaccine is given to infante ' J'-ween
four tc six months since this is the period w on the body is able to
begin manufacturing its own antic Bodies. The vaccine can be given at
the same tine as DPT vaccine.
12.13.2
, couTFAiiDiciTicms to vaccination agaenst rcLii-gELiTis
Vaccination against ; clionyclitis should not be given
if the Allowing conditions are present:
i.. Acute infectious disease
ii. High fever
iii. Vomiting.
iv.
Dyseritory..............................-.........................
. —....
USUALLY rOLIOl.YELITlS VACCINE IS NOT AD’IlCJTEnED DUIING THE
SUM® AND MONSOCN SEASONS BECAUSE OF ?1HE HIGH INCIDENCE OF GASTFOINTESTINAL'DISEASES . ' ' "
' '
STORAGE OF VACCINE
Because .the poliomyelitis vaccin ■ that is used in India
is a live vaccine, certain precautions i.ust L>. folloi-cd in storing it
before it is administered.
12.13.3
Fig.12.12:Frocc^urc fcr adrdni.st ring'oral ■''reps to children.
: 22 :
Special facilities are made available for keeping it at minus 20° to 0°C to
ensure that the vaccine retains its potency.
Usually special containers and
ice are provided for this purpose. ,
12.13.4
ADMINISTERING ORAL POLIOMYELITIS VACCINE
Proceed as follows.
1. Note whether the vaccine comes in a container with an attached medici£lfidropper. If there is no dropper, a clean syringe will be needed for /
measuring the dose to be given.
2.
Examine the dropper provided to make sure that it is not cracked or
broken and discard it if this is so.
KEEP THE CONTAINER OF POLIOMYELITIS VACCINE JN A VESSEL CONTAINING ICE
WHILE YOU ARE ADMINISTERING IT. IF THIS IS NOT SCRUPULOUSLY FOLLOWED,
THE VACCINE WHICH YOU WILL BE DISPENSING WILL BE USELESS SINCE HEAT
DESTROYS ITS POTENCY
3.
Measure the dose to be given according to the manufacturer’s instr
uctions using either the medicine dropper or the syringe.
4.
Ask the parent or adult to hold up the head and shoulders of the
baby or child as the vaccine is dropped into his mouth slowly so that
he does not choke. If the child will not open his mouth press down
gently on his chin(see fig 12.12) or press the cheeks.
5.
If the child spits out most of the vaccine, repeat the dose
6.
After the vaccine has been given, instruct the mother or adult
with the child that no breast milk or hot(temperature) foods
should be given for four to six hours following the vaccine. Other
food and liquids can be given. This is important for ensuring
the effectivdness of the live oral vaccine.
7.
Record the dose and date on the child's health card.
8.
Give the second and third doses at intervals of four to
six weeks.
12.13.5. HEALTH EDUCATION
Points for emphasis should include the followings
1. Poliomyelitis is. a serious disease that can paralyse and cripple
arms and legs, but it can be prevented by oral poliomyelitis
vactlnc
2.
The vaccine is given in the form of oral drops
3.
In order to be protected, three doses given at four to six weeks •
intervals are needed by the child.
4.
Usually a booster dose is necessary after four to five pears.
............ Crntu/23—
ANTIBODIES IN BREAST MILK CAN ALSU INACTIVATE LIVE ORAL POLIOMYELITIS
VACCINE SO BREAST FEEDING MUST RE 'WITHHELD FOR FOUR TO SIX HOURS BEFORE
AND AFTER AN INFANT HAS BEEN GIVEN THE VACCINE.. HOWEVER,IT IS IMPORTANT
NOT TO STARVE INFANTS OR CHILDREN WHO HAVE RECEIVED THE VACCINE. THEY
CAN BE GIVEN OTHER FOOD AND LIQUIDS AS DESIRED AS LONG AS THEY IRE NOT
SERVED HOT.
12.14
CHOLERA VACCINATION
Vaccination against cholera is given to individuals on request and
mass programmes for administering the vaccine arc carried out in tho event of
.epidemics of the disease in the community.
You will need to bo alert to cases of cholera and gastro-enteritis in
each village as you make your house-to-house visits since prompt treatment may
be necessary to save life. You must immediately inform your supervisor,
whenever there is a sudden riso in the number of persons who have signs and
symptoms of cholera sc that a decision can be made whether a mass programme needs
to be organized for the community(see soction7.l)
12.14.1
STORING AND TRANSPORTING THE VACCINE
....
1. The vaccine should be stored in.a refrigerator at 2°to 9°C. When
a refrigerator is not available, keep the vaccine in an earthenware
pot covered with a wet- cloth and.in a cool place.
'
' ’’
2.
Transport the vaccine in a thermos flask from the Primary Honith
Centre to the subcentre
3.
Order only enough vaccine that can be used within seven to 14 days
since it will deteriorate whon kept at room temperature for longer
periods.
f"-.
.12.-14.2 DOSAGE OF CHOLERA VACCINE
j.
The dose for adults and children over five years is 0.5 ml. followed by
a second dose within ton days. The dose for children under five years is half
the adult dose. . In orddr to maintain protection against the disease, individuals
nded to be given re—vaccination every six months.
12.14.13 ADMINISTERING CHOLERA VACCINE
Equipment required?
Sterile needles both short and long(for withdrawing vaccine from
multiple—doso vials and administration of vaccine)
ii. Sterile 2 and 5 ml syringes
iii. Cotton swabs
-x
iv. Cholera vaccine vials
v. Antiseptic such as spirit or savlon
i.
Proceed as follows?
1. Remove the metpl disc covering the rubber cap of the vial and clean
the cap with a cotton swab moistened with antiseptic.
2.
Assemble the syringe and attach tho needle for withdrawing the
vaccine
3.
Withdraw the -required, a.miiunt of vaccina from the vial
4.
Change the needle for administering the vaccine
5.
Select the site for administering the vaccine which should be either:
the outer aspect of the upper arm about midway between the
shoulder and elbow, or
ii. the outer aspect of the thigh(see fig 12.4).
i.
............ Contd/24~
6.
Clean the skin site selected using a cotton swab moistened with
antiseptic ->nd allow to. dry.
7.
Inject the prescribed dose of the vaccine intramuscularly
8.
Record the date, name and amount of vaccinr. administered on the health
card of the individual
'
9.
Tell the person immunized or the person accjmpanying a child that after
the injection the following reactions may recur?
i. Soreness and swelling of the site
ii. Fever
iii. Headache
'
These symptoms may last for about two to tnrec days, but should not be a
cause for worry. Tell him to take APC tn reduce pain and fever and apply
warm compresses to the area. 'If the reactions arc more severe than expected tell
him to go to the Primary Health Centre. .
12.14.4. HEALTH EDUCATION
Points to be emphasized should include thi
following?
1. Cholera is a serious disease transmitted thv-ug?. contaminated water or
food and which can be fatal if teatment is not given ■ imc.-idiately.
To be protected against the disease, an individual needs to have two
doses bf vaccine ten days apart. 'Revaccination every six months is
necessary for maintaining n high leVel of protection.
A
,
TYPHOID, PARATYPHOID/AND PARATYPHOID-B Vi,CuINATION(TAB.) -■
2.
12.15
In India vaccination against typhoii! fever is carried out on a mass
scale only when the disease is highly endemic in an area. When there is an
epidemic, house-to-house vaccination is carried out.
You will need to be alert to cases of diarrhoea with abdominal .pain,
headache, skin rash and fever as you go about your work since these are the
signs and symptoms of typhoid fever. You must report any sudden increase in the
number of sych cases to your supervisor,' so that ine can decide whether a mass
programme needs to be organized. Your responsibility is to assist, the Health
Assistant(Male) to immunize the eligible population(refer to section 6.1.7),
H2.15.1 PERSONS ELIGIBLE TO RECEIVE TAB VACCINATION
{
The eligible groups in the;community for TAB vaccine in an-endemic
area are, in order of priority.
i. School-aged children■
ii. Adults up to 50 years of age
However, during an epidemic, all persons in the community should receive
the vaccine.
12.15.2
CONTRAINDICATIONS FOR ADMINISTERING ROUTINE TAB VACCINE
Individuals with the following conditions should not be given TAB
vaccine except during epidemics
1. Fever with running nose or cough
2.
Lethargy associated with illness
In such cases, the administration of the vaccine can be postponed and given
to them when these signs and symptoms have subsided.
. .............. Ccr-td/ 25-
: 25 :
12.15.3. STORING AND TRANSPORTING THE VACCINE
,r
’■
1. The vaccine should be stored in the refrigerator at 2° to 8°C. If a
refrigerator .is. not available, keep the vaq'cihe ip ah earthenware
'■ pot covered, with a.-wet clpttVand. kept- in a’’-cdol’‘(Sjlace.
::: „ ,
.-1&U.-1 nno
,..'.3
: ’r. ’.1“ 2*-%“should be transported.jnrfo.ithermos 'fOas^^ftbtn^Eh'e .Primary..Health
----Centre to the subcentre.l- i'o-i ni
dui'bc .. . , . . 37(. nrtd r.oai-iir.s 3’-- ?fii 6
*S
.en'.133-^?1J0i‘de^'.8rtiy. enoughIvaBcine t'baW’oh
"u^ec1 ,Witiii^',^.§von to 14 days since
it will deteriorat-e when/kept'.at'' rboni temp ■'rraturc-iA’’:'5 .■
- n'.f;
JriT
ej^'12.15:.4 BfJff«SE.’TQR...TflB. W&INAbj?; .•SrfdAhfife’
- n Ale
.....' f J;'rl i?t ;nci-dnRj;s!d'PV,-:
hnnJ
_
f . .
...-. This can vary according to the manufactu ?er of. t|nq;,v.a;ccin§i%..(!-,'Usually
the . dose Jorp .cbildrep jus; ha^f^;^heila(dulth.tto'sicf;1J-.•VVj?.^jjL^!’-vp^‘e|ctiqn, .ap
/J■■Jindiv/iciuai.’-1 hepds tp. 'r.e(?.ei.ve 2,;1,dqS'gbi;,of thbivacci
cfj) day..int ervals.
... “ '.‘ Annual .revnccifiatibri. is necessary for1 persons li Jihg in>cn(denij.c areas.
.
■
ridi:iadi2U15.5-'ABMiNIsfE^NG3TiBj)AeQiNEpil^'
ziuda
r:tJ?lSiPUh^ y4 nrn ibiooi Hose ph^avco
-. j-‘ W’-'■ t'<'ITA&-!9a'c.c£fie ’is ava^^^q.jb^rbres'ent'din'hf’y 'rrf’,; 100? dosp ..v^als^fTherefore
inJ order to .avoid wasting -vaccine, ybu 'should gasper’ tpg'pthot;.a .sufficient
x
7 number'of-p’ersons-.when planning'.tn: admxhist'er it in,the community.-; qp
“ '■
■'
- £ ..'J l a
jT“vf’
■miP.’S
t I
.1 ■• .’
tEquipment,..r,equij?ed.S:
*r
hn-Uhi-'ii-''
■ V •
'
' ’
<t‘.'-X-<’t ''-'; . sir.'j-'fi'H'.’rlj'.f. -:).H J
/ .
. -s-t •'«.I "
'
xx;JV/
8f>
'IIJ - ’’
_,t\d^v-St3j$le .2 or- 5-ml, syringes^ in :cteriie’ container/; A .-i .'-> .<S.Li
x-p'- ; 1 '• ii/'Sterile needles? '3.5 enh length/20 ’or 21 "gaugoCfor withdrawing
/accine from vial)
.
.
-r-1.,5' cm 'lengf ti/&5 ghuh^(?o'r''’'ft'5i&nfs't.erxp;g-r
'
iii« '.ottop-'swabs,
‘
c.nt -n-.
.1
? J /'
'iy'I 'A_8 vaccine,-.v,iai-sut tJy-'cS5 J’ '”’w
3
rx. ,,-,.r- eot'la
'tr/ n’
,;v.’ 'Antiseptic such as-'Spirit'or savlb'nf..
b.O
c
Proceed as ."'ollows
•fi
Step^l) to . 9) are the same as-for.-thc administration,'of''.’cholera vaccine
(see section. 12.1,4.3)
-.-A-'r':'I'ox'rr; ; > n-.
-
;l\
-■
'
■?- h-?' •
-.12.T5i6'HEAVh 'EDUCATION :
rHhn uh h’.; i'<"“
;
.
Pqir:g, Cor discussion,■shQult! xncl'jte bhl: Toliowipg?
'I ■'
if
'
"
•> ;
If
-r^-.'
r ■
,..<.4n ,,
3:.'.iji.b,!y--d: '.h.:..n a t
‘
...
■; _ <1 ,
’<■ nJ'-C-' •
.1
—
1. 'yphqicl is a serious'disease Which is transmitted through food and
rater contaminatedwith the typholu ‘ batilliial'7 J *5-\
..,3'.J.
\
,‘^r
-or
V .
t «•
s- : .»•.r .
. 4^.,;
o
1 Jr- 2. Individuals .can. benprotected-.against'5 sfib disease’.by obtaining
f
vaccination with TAB,vaccine. for ' f cfl 'prptect'ion. -'art, individual
• " .* heeds to have -2’ doses ■ erf vaccine t op days, apart ,;.f S4b.sequent.lyj
if- he is living-.in..............
an ...endemic
area,
ha should,
get
.a-booster3 ■■•’"■1 .
.. •
.'/■ ’rn-'fa
1
»
.. dose oach year* ' j.?---’ *• ' '
.1
• 1 *•
12.16
SCHOOL IMMUNIZATION PROGRAMME
You are assigned the task of assisting the Health Assistant .Male)
to immunize the school children in ths villages. .^Som(e...,qf-these children may
need initial immunizations': becauseI thdy' jerio'nSr protected as.-infanes' or '•
toddlejs, but others may only require Be'osters.ar’revaccination, for BCG or
' smallpox. Childr.ep. who att end’ school arn^'a l'passive' popi'.JjatiQ'n and cad ;'
easil' be reached fur administering immunizations in contrast.'to pre-s ohool
children and pregnant women in the villages' w.ho ,mus,t be identified In their
homes.
.
:
■
.
1'" .. ' h ■ ,-.
ontd/26
12.16.1.
SELECTION OF GROUPS TO BE
IMMUNIZED
Usually a few classes in the school are designated as the target
population for administering immunizations. The criteria used for the
selection of classes are as follows^
1. Protection of children as early as possible i.e. vaccination of
children entering the 1st standard and all new admissions
2; Maintenance of protection, i.c. perin-lic booster doses to children
in standards 4 and 8.
Protection of children before they leave school, i.e. .booster
doses to children in standard 101 When these groups are
immunized annually, together with all new admissions, the total
school population is protected within, n- few years.
3.
TYPES OF IMI.UNI7..1TIONS ADMINISTERED
12.16.2.
**
The types of immunizations that are administered in ;n school are
usually similar to the ones that are.ndministerec to pre-school children with
one important difference.
Instead of DPT, children in school are given DT
since they no longer need protection against
wir oping cough. ■ The immunizations,.
that are usually administered in school, ares
-
i. Diphtheria-Tetanus(DT) (primary and booster)
ii. Smallpox vaccination(primary and revaccination)
. iii. BCG vaccination (primary .and booster)
iv. Poliomyelitis oral vaccinc(primary and booster) given only
when there is a high incidence of the disease
When an unusatelly large number of cholera or typhoid fever cases occur in
the community, immunizations against these diseases shouldialso be administered
to children in schools.
■ •
12.16.3
ARRANGING AND CONDUCTING THE PROGRAMME
’
*.
-
'
•
1 r •
The dates for the immunization programme are usually set by the Health
Assistant(Malel after he has received the suggested dates from the principal of
the school. These dates may change from year to year depending bn the request
of the teachers, other programme responsibilities and special campaigns, as
well as the outbreak of particular diseases in the area. ■ •
'
Your specific activities related to‘the school immunization programme
will generally include the following”’
1. Identification of the target population for BCG and smallpox by
doing a scar survey. The toachers can also be shown how to look for
scars.so that, they can help to identify the unprotected in their
classrooms and in the homes.
■
'
.
Compiling a list of •hildron who are t ■ be given immunizations. This
shpuld be done classriecu
a
•
*
.
3. Informing the Health Assistant (Male)’ about the suggested dates
for the programme And the number of children to be given BCG, smallpox
and DT vaccination. ’•
'
■
2.
-
-
4.
Obtaining visual aids on immuhizat ion . from the Primary Health Centre
for health education programmes in th:, school
5.
Assisting the teachers in the school t> plan and carry out health
education activities related to immunization in their classrooms,
covering such topics as why immunization is necessary,how.it is
done, and what happens afterwards.
6.
Inferring children, teachers, and other school personnel
where iraunizntions can bo obtained for ether neribers of
their families.
7 • Assisting the Health Assistant (bfalo) in the adninistration of the innuni zatipns, preparing the equipment, recons
tituting the vaccine, and screening children to identify
those who arc -ill .
8. Making armngericnts for recording the icrunizcticns
adidnistered in each school. This t ay be in the fora of
a register.
9.
Sub, itting the required reports to the Health Assistant
(Iidle) and to the Primary Her 1th Center.
FEMEMBER, WELL-Il'ffORiiED TEACIF.TS AID CHIj.OMAT PAM BE iSLHHiL IN
FINDING OUT THE UFP’OTECTZD AND IN FEJ SUADING FIJEiiTS AID RELATTES TO OBTAIN IM UCTZATIONS F(T OIHlfr CHILDrEN AT HOiE.
12 .17
PROMOTING THE USE GF IllUNIZATIONS IN THE 03EUMTY
Instead of conducting a separate canpaign for inferring
the coraunity a bout the value of inmnizations, it would, be norc prac
tical and effective to incorporate tils topic with your other educat
ional activities pertaining to the prevention of communicable diseases
or fatdly planning as a part of family welfare.
-
IN TALKS SEVEN TO IIUEVIjUAIS AND GROUPS DURING ”TI( FEG’lLAR.
HOUSE-TO-HOUSE VISITS,- YOU SHOULD INCLUDE '.HE VALUE CF I..i UNI
ATION 107 ailLDTEN AND B'.RGIW WOMEN.
The usual orientation Sessions that you conduct for the
ccncrunity loaders and influential individuals regarding ether health
services should also inclu’e the subject of innrnizpticn. In this way,
you will be able to g t their support for this important health nca.sure
for preventing the spread of cor.runica.hle diseases. The help, of the
connunity centers may be taken for preparing suitable visual aids
for use in such sessions. Attractive aucic visual aids • ay also be
obatinod fron the Block Health Assistant.
Together with the Health Worker (Ferric) ;• cu should syste
matically teach- Ider children in schools, their teefhers, and Lalwadi
workers about the value of innniza.ticns since th ose raccps often have
close contact with young children’.-he comprise the targ./t population
for innurization. Educating lais with regard tc 'l.o need for adminis
tering tetanus toxoid to pregnant women is also an important part of
your health educational activities.
12.17.1
WOHITG WITH THE HEALTH W CEKEE (FEMALE; .
As you are aware, in the intensive -rea the Health Worker
(Female) will be administering iixiunizations to the newborn and to
pregnant women. Since you will both be visiting tho same families,
there is a possibility of duplicating y-v? efforts. It is, therefore,
necessary for ycu and the Health Worker (Female) to meet periodically
nd decide on your respective rcs-cnci’ ilitios regarding tire innuxiiaaa.
tion of the non’ ers of each family.
......................Contd/28-
12.18
RECORDS A?" PilR'ATS
You arc expected to submit ti the Primary Health Centre
a monthly report of your activities regarding immunizations given.
This should cover the following points;
1. Numbers and types of I eneficiarios .jivon various types
of immunizations, i.c. zero to one year, one to five
years, pregnant women, scl:-xl-going children, and' other
groups in the co; s unity given smallpox vaccination
(Primary and revaccination), DPT, IT, Tetanus toxoid,
BCG, Poliomyelitis, TAB, Cholera and any other vacci
nation.
2.
Eecoipt, issue and balance of stock of vaccine. IN
order to submit those reports you will 1x3 required to
maintain the: follrwing root rds:
i. Individual health c.
f~r ■chil'h’cn and mothers
to be kept in the family folder.
.ii. Health cards for school children.
iii. Register of individuals receiving immunization*
iv. Stock register of vaccines received and used.
o
Gh 3--K
GOVERNMENT OF, KARNATAKA •
Directorate of Health & F,.W.Service
NO,uiP.187/88-89
Bangalore-9.-Dated: 5th April 1'89.
■
CIRCULAR
'
Immunization Targest for the year
1989-90 and guidelines.
SUB:
Please find enclosed herewith the immunization targets and vac
cine allocation for the year .1989-90,
Following guidelines are Issued
for implementation of the programme,.
1•
TARGETS :
a)
‘
•
Targets for primary immunization
i)
:
1981 census population has been projected to
mid 1.989-90 based on the Expert Committee
report on. Population projections.
ii)
The pregnant women beneficiaries are calculated
taking 27.3 per thousand estimated population as.
. -
birth rate i.e. pregnant -woman = estimated popu
lation x .0273.
iii)
j'
Eligible infants are worked out based on the sur-
-
vivors at the age of one year taking 84 infant
mortality rate per thousand live births.
Margin
is given for the still births out of the total
The actual survivor rate'at the age'of
women.
one year works out to 911.66 per thousand live births.
iv)
All the estimated pregnant women and infant sur-
- , vivors at the age of one year are targetted for
full immunization coverages.
Efforts should be
made to achieve 100% of the estimated beneficiary.
However in case of infant coverages' upto atleast
85% may-be acceptable be'cause' of the' multiple an
tigen, multiple dose, drop outs .etc;,
and herd
immunity.
v)
Though estimates are made and communicated if the
enumeration is complete the local authorities may
adopt higher or lower targets'-based on the actuals
enumerated.
However the responsibility of defend- y
ing the altered targets rests with the local authorities.
/
TT ■
BOOSTER DOSE
:
'
'
The achievements of the booster dose and for the children
receiving three doses of DPT and Polio during the year 1987-88 in .
the year 1988-89 has been aroung 50% only.
All out efforts must be
made to give booster dose to all infants who had received third dose
of DPT and Polio in the year 1988-89.;
1989-90.
firing .the ensuing year of
2
III.
Targets for Secondary Immunization- :
Survivors at the different age groups (5,
10 and 16 years) has*
been worked out and the target is indicated'and 85% of the eligible
...estimated children at the particular age.
• *
IV.
Vaccine allocation :
The vaccine allocation is indicated for each antigen■for every
district.
Vaccine wastage provided is 25% for all vaccines except
ECG and Measles for whidh 50% wastage is allowed,. .
/ v» Vaccine indenting and procuring :
.The vaccine allocated are to be: procured from the concerned bulk
stores..
Vaccine balance as on 1.4r89 is to be. deducted out of the
total allocation for the year 1989-90.
The districts in turn should
store the vaccines for three months requirement but supply only one
months requirement to the Primary Health' Centres and other users.
If
the vaccine requirement for any particular month are more or less than
the average monthly allocation,
the bulk storage institutes must be
kept informed atleast one month ahead to take suitable measures.
This
will avoid unnecessary wastage of vaccines.
ALL VACCINES MUST BE STORED? TRANSPORTED AND MAINTAINING
PROPER COLD CHAIN.
VACCINES LIKE DPT, DT AND TT SHOULD
NOT EE FROZEN
VI.
IMMUNIZATION SCHEDULE
The following revised National Immunization schedule should be
adhered at all levels.
Benericiaries
A.
B.
INFANTS
Age
6 weeks, to
9 pion th s
.
Vaccine
No. of
,
doses
Route of
. . .
, .
administration
DPT,
POLIO
B.C.G.
3
3s
1*
Intramuscular
Oral
Intra-dermal
•
Subcutaneous
1
‘9-12 months
MEASLES
*For institutional deliveries B.C.G. may be given at Birth
CHILDREN
1*
Intramuscular
16 to 24
DPT
1*
Oral
months
POLIO
Booster Dose
DT
1*
Intramuscular
UjO years
TT
1*
-I.M’.
16 years
TT
1*
I.M.
1*
I.M.
5-6 years
C.-
PREGNANT
WOMEN
16-36
weeks of
pregnancy
TT
•
/
*dose to be given if not vaccinated earlier '
'
*-
4
ydar of birtn must be entered on data card against the child’s name.
Vaccination dates also must be entered,
mark should
putting a
be avoided.
Every month in addition to informing the antigen - wise dose-wise
performance, the number of children who ere fully immunized during the
month should be invariably reported.
X.
Calculation of Beneficiaries’ :
■
-
The following criteria are applied for considering beneficiaries
achievements.
i)
Primary Immu n i z at ion :
Fully immunized i.e. three doses of DPT,
3 doses of Polio,
1 dose
of BCG and one dose of Maeasles before the age of one year and a minimum
|interval of four weeks in between the multiple doses of antigens. ■
Tetanus Toxoid
(Pregnant women)
-
2 doses + Booster dose .
D. T.
-
2 doses
(10 years) '
—
2 doses -!•
(16 years)
-2 doses of T.T, only
T.T.
Booster dose
Booster dose
Surveillance s
XI.
Date of vaccine preventable diseases should be maintained in all
the institutions and reported monthly.
In each case of death, vacci
nation status should be clearly indicated.
Active surveillance of
diseases like Measles, Acute Paralytic Polio, Whooping cough and
^'eonatal Tetanus should also be given in the community through the
Health Workers in their regular .visits.
ALL DISTRICT HOSPITALS/ MEDICAL COLLEGE HOSPITALS, SUB! DIVISIO
NAL HOSPITALSANDTALUK LEVEL PRIMARY HEALTH CENTRES
WOULD ACT SENTINEL
AS SURVEILLANCE CENTRES AND THEY SHOULD REPORT THE VACCINE PREVENTABLE
DISEASES‘DATA TO THE CONCERNED DISTRICT HEALTH AND FAMILY WELFARE
OFFICER WITH A COPY MARLED TO THE DEPUTY DIRECTOR ( MCH&UIP ) DIRECTORATE
OF HEALTH & F'.W. SERVICES
BANGALORE.
/
XII.
Reporting ;
'
Monthly reports whether sent in MIES form or special UIP proform
the figures should tally to one another.
The report must reach before
7th of the succeeding month to the Assistant Commissioner (Immunization)
Government of India, Ministry of Health and Family Welfare, Nirman
Bhavan, Nev/ Delhi - 110 Oil.
Hie following information must be indicated.
i)
antigen-wise, dose-wise performance during the month and comulative
achievement,
.
.
S/—
. ''
VII.
3 , - s
VACCINATION SERVICES :
Vaccination services must be provided through out the year
' •
uniformly.
All tlie medical institutions (Primary■Health Centre,
Primary Health Unit, General Hospital etc.,) must provide vaccination
atleast once a week.
If the institutions do not possess a refrigera- -
the vaccine must be brought in a vaccine carrier on the -day of
tor,
’'-.ccination session.from the nearest refrigerator.
• Routine outreach sessionsmust be planned in the subcentes and
bigger villages.
The vaccine should be delivered in the vaccine
c arriorsand arranged to be returned the same evening or atleast by next
morning.
The doctor's participation in vaccination sessions go a long
way in creating demand for vaccine. . Routine vaccination outreach
sessions should be arranged in all the villages having one thousand or
more population every month.
However BCG and Measles can be given once
in two- three months.
Private practitioners wherever available should be motivated_tp
provide imijunization services.
Vaccines to these people, should be
given and the performance collected^ jat the end of every, month., ^Ib>-vbL
tioners who have a refrigerator han be given on month1s vaccines an< I
those who do not have a J^£.rfig_o_ra,tor _can be requested to collect the
vaccines from the local Government institutions on the date of the
ses_sion and return it/the next morning./(both used and unused vials).
VIII.
Technique of Vaccination :
One sterilized syringe and one sterilized needle per prick per
child should be ensured.
Auto-glaving the syringes and needle should
be the choice of sterilizing syringes and needles.
If this is not
feasible for some- local reasons on the spot- boiling in clean water for
atleast 20 minutes must be ensured.,
there many beneficiaries are
catered in a session and many syringes may not be available atleast
there should bo no compromise qin using separate sterilized needle for
every prick.
ONE VIAL OF I. CH ANTIGEN MU T BE OPEN ‘D AT A TIME
DO NOT C PRY
ND USI OPENED VI .LG
SESSIONS/DAYS.
'OR
IFT’SQU'.NT
DO NOT USE EXPIRED VACCINES.
DO
NOT USE FROZEN VACCINES;.'
IX.
Maintainence of records
s
Enumeration and updating of beneficiaries at the village level '
must be ensured.
A master register of immunization done in the areas'
of Primary Health Centres/Primary Health Units/Post Partum Centres/
Urban Family Welfare Centres should be maintained in the institutionsconcerned.
Vaccination card should be issued to all beneficiaries making
proper entries for each dose of vaccine.
Date or atleast month and
...4/-
5 ' ii)
Fully imnpnized children,
achievement during the month and cumu
Performance
iii)
'
■
lative achievement.
of primary immunization under one year and over one
year separately.
b)
.
;
Vaccine position ;
received during the month of report
Individual vaccines on hand,
utilised during the month of report and balance at the end of the month.
"H
c}
c)
■
’
•
Cold Chain Equipments position :
Item-wise cold chain equipment position should be indicated.
d■
Di.-case .wise surveillance :
No. of casesof each of the vaccine proventable disease during the
:..unth and cumulative indicating the immunization status.
W--1II.
Va ccine related accidents
;
All vaccines related accidents and reactions should be reported
to.the divisional Joint ^irector of Health and Family Welfare Services
'
of the concerned division who is the chairman for the Committee consti
tuted for investigation of such accidents and reactions.
F.IoR. is received,
Once the
the Divisional Joint Director of Health and Family
Seifare Servicesshould take up immediate action along with the Committee
Members to investigate and report :to this Directorate.
.
.
■.
■ ■'
.
r.’
W/’
A
'
?
ADDITIONAL DIRECTOR (FW&MCH)
'
/>
’
...6/-
/
GOVElJUuJNT Or' .lARi i.’.J.'AKA
DIRECTORATE OF HEALTH AND. FAMILY '-F3LFARE ’ SERVICES
No. UIF''187/88-89
VACCINE
B.C.G.
ALLOCATION
Measles
138200
138200
108500
43400
43400
43 200
216000
86400
86400
' 59800
54500
272500
109000
109000
32201
63600
58000’
290000
116000
116000
6. Shimcga
20421.
55700
"50800
254000
101600
101600
7. Tumkur
■24032
.65600
59800
299000
119600
119600
143449
3<316OO
357100
1785500
714200
714200
30200
27500
137500
55000
55000
Est.
PopIn.
ESTIMATED &' TARGET
Pre-Worn
Infants
27736
757.00
2. Bangalore (UD)
8713
23800
21700
3. Bangalore (RD)
'17353
47400
4, Chitradurg a
21893
5. Kolar
SI.
District
.NO.
1. Bangalore (c)
I
BANGALORE Dvm.
DPT & POL’:
69100
345500
■
■
r
8. Chickmagalur
■11051
9. D. Kanndda
28644
78200
71300
356500
142600
142600
10. Hassan
15456
44900
41000
205000
82000
82000
11. Kodagu
4821
13200
12000
60000
24000 I
24000
12. Mandya
17113
46700
.
42600
213000
85200
13. Mysore
29562
80700
■
73600
368000
147200
147200
268000
1340000
536000
536000
II
MYSORE Dvn.
107647'
■
-
293900
.
85200
-
s ■
7
4
2
1
5
1 — — — — —
6
/
•'
7
8
“ ....... - — —- •— — —
14.' Bel rjaum
35001
90300
89600
448000
179200
179200
15. Bij apur
28727
78400
71500
357500
143000
143000
16. Dharwad
36042
98400
89700
■ 448500
179400
179400
17. Uttara’Kannada
13148
35900
32700
163500
65400
65400
113918
311000
283500
1417500
567000 .
567000
18. Bellary
18773
51300
46700
233500
' 93400
93400
19. Bidar
11906
32500
29600
148000
59200
59200
■2 0. GuIbarga
24835
67800
61800
309000
123600
123600
21. Raichur ’
21851
59700
54400 .
272000
108800
108800 ’ .
_
_
■ 773’65
211300
192500
962500
—a »-—■ —a a.- »
385000
a—
»«.a
385000
1207800
1101100
5505500
2202200
... -
.
Ba —*
►—*
a—a
aw-a
BELGAUM Dvn. Total
a—■
•—
*-aa
— —
a.—.
a—-
«a_a
a
... .
a- —1
V--*
GUL/3 .R ?-A Dvn'
GRAND’ TOTAL
* *
To ta 1
-w —
442379
A.a>
wm.
a— a
•RMtf M.«*
W-a
2202200
8
•
GOVERNMENT OF KARNATAKA'
<■
TOP. ATE OF HEALTH AND FAMILY WELFARE ;5.
BNNGALORE
No. UIP/187/88-89
Q *1
„ ’
No.
District
\
A
1
* — — — —
j
2
Vaccine Alloce/cion
Target
T.T.
3
(P.W)
■
T .T.10 years
4
T.T.
16 years
5
D.T.
6
T.T.
7
D.T.
8
1. Bangalore (C)-
75700
56000
53200
57800
462250
2. Bangalore (UD)
23800
17540
16740
18160
145200
3. Bangalor-e (RD)
47400
34860
33290
36100
288875
90250
.113900
'
144500
-
45400'
59800
43980
41990
45560
364425
•Z 63600
46800
4:710
48500
387775
121250
6. Shimoga
55700
41040
39180
42500
339800
106250
7. Tumkur
65600
48260
46070
49980
BANGALORE Dvn. Total
391600
288430'
275180
298600
2383150
30200
22230
21200
23000.
184075
57500
78200
57570
54950
59620
476800
149050
10. Hassan-
.44900
33150
' 31650
3434C
274250
85850
11. Kodagu
13200
9700
9250
10040
80375
' 25100
4. Chitradurga
5. Kolar
8. Chickmagalur
'9. D. Kannada
’
'
■
399825 v . 124960
746500
12. Mandya
46700 _
34400
32800
35600
284750
89000
13. Mysore
80700
59550
56750
61600
492500
15400
MYSORE Dvn. Total
293900
216600
206600
224200
1792750
560500
G0V3RNH7.NT OF KARN7TX
otr-ctorz.t-X of *H3Ai?nr /-In ’ ‘f -^"ily
No. UIP/187/8S-89
~B.VK3aLO.rff
SL.
DISTRICT
1
2
"
VACCIND ALLOC/’.TICK
TARGET
T.T.(P.W) ,
3
T.T.16 Y3A.’’S
■5
T.T.10 YD-'-RS
4 ■
dt
6
T.T.
7
DT
a
1.
Bangalore (C)
75700
56000
53200
57800
462250
144500
2.
Bangalore- (UD)
23800
17540
16740
18160
145200
45400
3 .
Bangalore (RD)
47400
34860
33290
36100
288875
90250 .
439’80
41990
45560
36’425
113900
44710
48500
387775
121250
39180
42500
339300
106250
-.
Ch’itradurga
5.-
Kolar
5.9800
63600''
6.
Shimoga
55700
41040
7.
Turukur
48260
46070
.49980"
399825
124960
8.
Bangalore Dvn.,
65600 '
— — — — —
391600
283430
275180
298600
2333150
746500
23000
181075
57500
59620
476800
149050
35350
Total
46800
. ■
8.
Ch i ckrnaga lur
30200
22230
21200
9.
D.Kannada
78200
57570
5-1950
10.
x'16.3 sun
-44900
33150
31550
34340
27 4250
11.
Kodagu
13200
9700
9250
10040
80375
25100
•„
.
.
•
- .
12.
Mandya
46700
34400
32800
35600
284750
89000
13.
Mysore
80700
59550
56750
61600 '
492500
.154300
Mysore Dvn. Total
293900
215600
206600
224200
1792750
56050C
.
, -
-
;
1
2
14.
Belgaum
15.
10
:
4
5
6’
7
98300
7 2420
69100
74960
599550
137400
Bij apur
78400
57760
55100'
59830
47.8150
149575
16.
Dharwad
98400
7 2420
69100
74960
599800
137400
17.
Uttara Kannada
35900
• ' 26400
25 200
27350
218750
68375
229000
213500
237100
1896250
592725
37730'
36000
39050
312575
97625
Belgaum Dvn.Total
3
-4
311000
j
-
.
8
A
■?
Bellary-
51300
19.
Bidar
32500
23950
22820.
■ 24800
198175
62000
2’0.
Gulbarga
67800
499-40
47600
51600
413350
129000
21.
Raichur
5'9700
43900
41900
45 45 0
363750
113625
211300
155520
148320
160900
1237850
402250
1207800
889600
848600
920800
7305000
18.
2 2.--------------------------------------------
Gulbarga Dvn. Total -
GRAND TOTAL
-
'
2301975
■
SUBMITTED TO
-
The Secretary, health & FW Department, M.S. Buildings,
Bangalorr
for 'Kind information.
2.
The Additional Secretay (FW) Health’& Fw Department, M.S. Buildings
3.
Bangalore for kind information.
The ^iroctor of.Health & FW Services, Bangalore.
1.
The Commissioner, Bangalore City Corporation, Bangalore
Cp PY WITH, COMPLIMENTS TO£-
5.
The project Co-ordinator IPP-III,
5.
The Chief Secretaries,
Bangalore
Zill a Parishad.
with a request to arrange for all out efforts right from' the
ba.jining to a ihieve the targets.
7.
The Deputy Commit; s ions r (MCH), Ministry of Health & FW, Government
of India,
uirman Rhavan,
New Delhi - 110011.
The Assistant Cornmis ioner (Im1-unis at ion)/Assistant Director '
p>.
General (DPI) Nirman Shaven, Nov; Delhi - 110011.
The Principals and Post partum Centre,
Directors of Medical
.............................
College
.-'Y TO;
10.
11.
The Health Officer,
city corporation, Bangalore.
Tho Divisional Joint Director
...............................
.......
Division of Health & FW Cervices
12.
The Joint Director,. Public
Health Institute, Bangalore Vaccine
Institute, Bolgaum.'
13.
The Joint Directors HPEcP/CMD,. M&F/TB/lPP-IIl/Leprosy for inforr. ntio a - DHe/FHS,
Bangalore
14.
Deputy Directors MGH/FW/NUTRITIO’VdH&FWS, . Bangalore
15.
The Demographer, • Directorate of Health & FW Services,
16.'The District Health & FW Officer
17.
District
Tho professor and Head of Dcpartmenh/PDSM/Paad./Ohst.Gyn
Department
13.
..................
Bangalore
/
.Medical College
Th- District Surgeon, Cum Post Partum Centre Director,
District Hospital
19.
23.
s Di'trict lie unication Officer
Principal,
Health & Family Wolfar.
.,, ........ .District
Training Centre,
21. Cony with compliments to the Zona Ropr sentative, UNICEF
SOUTH INDIA OFFICE,20, Chitharanjan Road, Madras - 18.
ADDITIONAL DIRECTOR (FW & MCH) ,
Ch
ITIPLEMLN1 Al'IUN OF EXPANDED PROGRAMME OF IMMUN ISA FinN
FROM 1ST APRIL 1978 - IMMUNISATION SCHEDULE
X'
A child needs to be protected against infections through
' imiimnisation. Immunisation should be done early in life and repeated
periodically.
SCHEDULE OF VACCINATIONS
AGE
VACCINATION
I. PRE-NATAL;
16-20 weeks
20-24 weeks
36-38 weeks
Tetanus Toxoid
-------- do---------------- do—-----
1st dose
2nd dose
3rd dose
II. CHILDREN
3-9 months
-
Smallpox vaccine
B.C.G. Vaccine
Diphtheria— Pur fur, in—T stains (Triple Vaccine)
3-doses at
9-12 months
18 - 24 months
5-6 years
(School entry)
an interval of 1—2 months
— Measles vaccine? one dose
- Diphhhorin-Purl-1 is i n Tolioniis (Ti i pl.o Vaccine)
Booster dose
Polio(Trivalent oral vaccine) Booster dose'
— Diphtheria—Totnins(Rivh!snt vaccine) — Roostov dose
Typhoid(Monovalent or bivalent vaccine) one dose
after an interval of 1—2 months the typhoid vaccine
one dose
10
years
- Tetanus Toxoid - Booster dose
Typhoid(Monovalent or bivalent vaccine)
Booster dose
1'6'
years
- Tetanus Toxoid - Booster dose
Typhoid(Monovalent or bivalent vaccine)
Booster dose
/ .PRE-NA"AL : When mothers are registered late in pregnancy, at least two
doses of Tetanus toxoid should be given. 3 rd dose may be given after
dao interval after delivery. For a lady who has been .immunis ed as above
in childhood, one booster dose of Tetanus Toxoid should be given in
subsequent pregnancy, preferably four weeks before the expected date of
delivery.
v
CHILDREN ; Agos indicated are considered to be the best times. However,
if there is any delay in starting the first dose of Triple vaccine, the
ages may be adjusted accordingly. It should be the aim to ensure that a
child receives Smallpox, B.C.G.^ D.P.T. and polio vaccination where
available, before it reaches one year of age. The different vaccines
indicated- against the various age groups-can be given simultaneously; for
example, B.C.G., Triple vaccine and polio vaccine, Smallpox, Triple vaccine
and Polio etc. When typhoid vaccine is being given far the first time, two
dosos should be given at an interval of 1-2 ijnnths.
Sd/for DIRECTOR OF HEALTH & F.W. SERVICES
*Polio (t rivalent oral
vaccine)
doses at an interval of 1—2 months.
Introduction
The Government of India through its National Health Policy has expressed its
major concern for improving the health of women and children. The National
Immunisation Programme being implemented in this country is one such endeavour,
which has been accepted as a priority programme in this direction. Since 1978, the
efforts have been mainly concentrated on protecting more and more of the benefici
ary population through the Expanded Programme on Immunisation (EPI). For
achieving this, various policy changes as well as alternative operational strategies
have been tried out. Currently, with the world-wide emphasis on enhancement of
child survival programmes and schemes, the Immunisation Programme has attained
still higher priority. Dedicated to the memory of the late Prime Minister S mt. Indira
Gandhi, the Universal Immunisation Programme (UIP) was launched in 1985 with
accelerated efforts for universal coverage of immunisation of young children. The
anxiety of the Government to generate a sense of urgency and commitment towards
achieving the stated programme goals can be appreciated from the fact that this
programme has found a place, in the name of “Technology Mission on Vaccination
and Immunisation of the vulnerable population, specially children”, among the
seven Technology Missions taken up on priority basis by the Government of India.
It is imperative that programmes of this nature which are implemented with
clear objectives and specific time-bound goals and targets, be systematically re
viewed to examine whether the programme has been effective in achieving the set
goals. As an important means for assessing the programme achievements, a large
number of coverage evaluation surveys have been conducted in different parts of the
country which have shown varying extent of coverage of the beneficiary population
Such achievements though encouraging, have indicated that much needs to be
achieved for reaching the stated goals. However, output of a programme by way of
programme performance achievement alone will not suffice to enable programme
administrators to effectively and efficiently manage the programme For this
detailed review of the programme, with scope broad enough to include various
managerial facets of the programme, is essential. Thus, it requires a close examina
tion of the policies related to the programme, the relevance and feasibility of its
1
!
targets, the adequacy and appropriateness of the programme planning procedures and
the plan itself. Further, the operational strategies adopted and the implementation
processes, with particular reference to qualitative aspects of the programme and
results in terms of actual immunisation coverage achieved, and, ultimately, the
programme’s impact on the magnitude of the problem of vaccine preventable
diseases, also need to be looked into. Such indepth reviews would also enable the
reviewers to understand the strengths and weaknesses of the programme which, in
turn, can help in bringing about improvements in the programme.
It is in this context that the Ministry of Health and Family Welfare decided to
undertake a National Review of the Immunisation Programme at the end of about a
decade of its implementation.
It is important to appreciate that in a vast country like India, with diversities in
population characteristics, cultural features and socio-administrative milieu, no
single solution for improving the programme is likely to emerge after such a review.
There is need to view theStates as independent units and, thus, the scope of the review
would naturally be widened to cover the maximum number of States in the country.
The Ministry of Health and Family Welfare identified the National Institute of
Health and Family Welfare as the nodal institution and entrusted it with the
responsibility of coordination of this massive effort.
States were covered during this review. In addition, for obtaining information on
similar aspects related to the programme in urban areas, four major.urban metropoli
tan areas viz. Madras, Bombay, Calcutta and Delhi were also included in the review.
Thus, the total number of units studied was 29 i.e. 18 major States, seven small NorthEastern States and four urban metropolitan areas.
Four main aspects of the programme received emphasis in this review viz.
i. The programme inputs like policies, plans, resources etc.
ii. The details of processes of implementation, including operational strategies,
management of various resources, other programme management aspects
like monitoring, supervision, information system, etc.
iii. Programme output in terms of actual performance and extent of coverage of
iv.
specific vaccine preventable diseases.
METHODS OF DATA COLLECTION
2.
3.
4-
To review the policies, strategies and plans of action for the EPI/UIP at
different levels of health administration i.e. Central, State and district levels.
To measure the progress in implementation of the EPI/UIP in relation to
targets for acceleration of the programme accessibility, coverage, and mortality/morbidity reduction.
To identify the bottlenecks and constraints in die progress of the Immunisa
tion Programme at different levels of programme implementation.
Tomtike recommendations for overcoming the constraints and problems and
thereby improving the implementation of the programme qualitatively and
quantitatively, as well as for assessment of additional resources required for
this purpose.
METHODOLOGY
Study Area
t0 exist in terms of programme
Because of the inter-state variations llke y
s and, consequently, related
policies, strategies, achievements, managern unit jn this review. Thus, all the solutions,'the State’was considered as a stu y
2
■ ii.
Interviews/discussions with programme officials and staff at Central, State,
District, Primary Health Centre (PHC), subcentre and village levels.
Study of records, repons, guidelines, instructions and other relevant docu
iii.
ments.
Observation of immunisation activities, service premises, cold chain mainte
i.
OBJECTIVES
1.
the beneficiary population.
The programme impact in terms of disease occurrence with reference to
iv.
v.
vi.
nance, etc.
Vaccination coverage survey using the 30 clusters sampling method among
children aged 12-23 months and for pregnant women.
Conducting disease survey for lameness and neonatal tetanus.
Interview with community members, leaders and representatives of non
governmental agencies.
SAMPLING PROCEDURE
i.
For 18 Major States
From each major State, the Immunisation Programme operations and proce
dures were studied at the State headquarters and in two selected districts from the
State. Immunisation coverage and disease surveys (lameness and neonatal tetanus)
were conducted in these two districts.
Selection of Study Districts
For the purpose of selection, in each State, the total districts covered under UIP
were grouped into two categories viz. i. those which were included under UIP
3
duringl985-87; and ii. those covered during 1987-88.
From each group, one district each was chosen using the probability propor
tional to population size sampling (PPS). The list of districts covered within each
State is shown in Appendix I.
In each district, apart from coverage evaluation, operational details of the
programme were studied in selected PHCs, subcentres, urban health facilities and
cluster villages/ localities.
•it.
f
■
1
|
For Urban Metropolitan Areas
Since urban metropolitan areas are not divided into districts as in the States, the
units equivalent to districts were identified in the four metropolitan areas as follows:
a.
Delhi
The total area of Delhi was divided arbitrarily into two zones i.e.
Rural and Urban, and 30 clusters each were selected from the
two zones.
b.
Madras
The total area was divided into two zones i.e. North and South,
c.
d.
Calcutta
and 30 clusters each were selected from the two zones.
The total number of 100 urban wards were divided into two
Bombay
groups, 1-50 and 51-100, and 30 clusters each were selected
from the two groups.
'
The total of four zones in Bombay were grouped into two i.e.
1+2 and 3+4, and 30 clusters each were selected from the two
groups.
Apart from discussions with the programme officials in each district/State, the
following were also studied:
i. Selected urban health institutions functioning in the area of the urban clusters.
ii. Medical college located in the district headquarters, if any.
>ii. Selected private practitioners.
iv. Any Government institution run by agencies other than the State Government
like Central Government Health Services (CGHS), Employees’ State
Insurance Corporation (ESIC), Railways, Armed Forces, etc.
y- Sentinel centres in the district/S tate headquarters.
V1- Popular leaders identified from the cluster areas.
4
Anganwadi workers/health guides serving the cluster area.
The paramedical supervisory staff related to the cluster area.
.
Missed opportunity for immunisation in institutions from the se cc
areas
’
The
total
volume of work covered during the review is in rtcatc j ;n
Appendix II.
MANPOWER INVOLVED
In order to collect information about various facets of the programme from 22
For Seven Small North-Eastern States
units (as indicated above), 29 expen teams were identified whose members include
faculty from medical colleges and public health expens from various organisations.
Each team consisted of a team convenor, three supervisors and team members whose
numbers varied between 15 and 20. The names of the Team Convenors are shown in
Operational details of the Immunisation Programme were studied separately
from each State headquarters and at least in one district and sub-units viz. PHCs,
subcentres, urban institutions, etc. within this district, in each State. For Immunisa
tion Coverage Evaluation, all seven States were combined together as one unit, in
which the districts covered by UIP in 1985-87 and 1987-88 were grouped separately
and from these groups, 30 clusters each were selected and studied.
iii.
vii.
viii.
ix.
,
Appendix III.
A team of20-30 paramedical personnel of the rank of Health Supervisors were
deputed for each district for carrying out lameness and neonatal tetanus survey under
the supervision of district team members. In order to ensure independent appraisal of
the programme, officers and paramedical staff were selected from neighbouring
States/districts.
OPERATIONAL DETAILS
In order to advise the Coordinators at NIHFW at various stages of the
preparation of the project proposal and its implementation, a Task Force Group was
constituted with representatives from the Ministry of Health and Family Welfare,
ICMR, WHO, UNICEF and the Planning Commission as members. The list of
members of the Task Force Group is shown in Appendix IV.
In order to assist the coordinators in the implementation of the review project,
including preparation of data collection tools and in deciding an operational strategy,
a Planning and Implementation Group was constituted with faculty from NIHFW,
representatives from WHO, UNICEF and experts in the Immunisation Programme
from other institutions as its members. The list of members of the Planning and
Implementation Group is indicated in Appendix V.
In order to familiarise the State Health Officials with the details regarding the
objectives and methodology of the review and also to seek their support and
cooperation, a meeting was organised at NIHFW, New Delhi, on 6 and 7 April, 1989
for State Directors of Health Services and State EPI Officers.
A briefing for the 29 team convenors who were to coordinate the total review
in each State was arranged at NIHFW, New Delhi, on 16,17,18 April, 1989, and the
operational details, including study tools, were discussed in detail.
Before the actual start of the field survey, detailed briefing sessions were
5
conducted by the Team Convenors at State Headquarters, one for State level
supervisors and the other for district team members regarding the methodology and
collection of data from various agencies for the National Review.
Briefing of paramedical staff of the level of Health Supervisors for carrying out
lameness and neonatal tetanus survey was carried out at the district headquarters by
the respective State level supervisors.
At the end of the data collection, which lasted for about 2-3 weeks, the reports
for the selected study districts and the State were prepared by the team and the same
were discussed with the State officials for necessary clarifications. Based on the
findings from the different study units, at N1HFW, a national level report was
prepared.
Apart from the routine data collection in the 29 study units by expert teams, in
order to give a deeper look at the programme to examine its status and role in the
context of national goals of health for all by 2000 A.D. to be achieved through the
primary health care approach, a team of five expens was involved in conducting an
indepth study in selected States/districts. The main emphasis in this study was on
immunisation as a component of primary health care, perception about the pro
gramme among community and health functionaries, social mobilisation efforts,
innovative experiences, if any, etc.
In addition, a separate cost study of the programme was also undertaken in two
districts, one from Maharashtra and the other from Madhya Pradesh by a special
team. The report of the cost study is being submitted separately.
6.
Organisational Structure and
Programme Delivery System
There are 25 States and 6 Union Territories (UTs) in the country. According to
the Constitution of India, health is a State subject and, therefore, planning and
implementation of health programmes and provision of all health care services is the
State’s responsibility. In Union Territories, various programmes and services are
Centrally administered. However, even in the major States, some of the national
health programmes and schemes are centrally sponsored for which entire planning
along with resource provision in varying degrees is the Central Government’s
responsibility. The Immunisation Programme, being one of the important compo
nents of the national family welfare programme, is also a Centrally sponsored
programme. The three major divisions of health administration at the Centre and in
every State are:
a. the political leadership responsible for policy decisions under the Ministry of
Health and Family Welfare;
b. the executive leadership under the Health Secretary; and
c. the technical leadership under the Director General/ Director Health Services
supported by their respective subordinate divisions/officials.
Even though immunisation as a service was being given as a component of
Maternal and Child Health (MCH) care in the past, special emphasis on this service,
with a separate and exclusive programme, was accomplished in 1978, when the
Expanded Programme on Immunisation (EPI) was initiated in India. The main
objective of the programme was to reduce morbidity and mortality due to six vaccine
preventable diseases (VPD) by providing immunisation services to the eligible
population. The programme also aimed at achieving self-sufficiency in the produc
tion of vaccines required for the programme. Tetanus Toxoid (TT) Immunisation
initiated for pregnant mothers in 1975-76, was subsequently integrated with EPI in
1978. Immunisation against polio was included in EPI in 1979-80 (though, initially,
in selected urban areas and under the ICDS programme only, it was later integrated,
in 1982) and TT for school children was included in 1980-81. BCG was brought
under the purview of ErPI during 1981-82. Immunisation against measles was
initiated under EPI in 1985-86.
7
The Universal Immunisation Programme (UIP) was launched on 19 Novem
ber, 1985, to accelerate the immunisation coverage of the eligible population and to
ensure betterment of logistics and managerial aspects. Though initially only those
districts which had a potential to achieve the programme targets of universal
coverage ahead of schedule were included in the UIP, it was to be extended in a
systematic manner to cover all the districts in a phased manner by 1989-90, as given
below:
Appendix VI. Accordingly, the Mission Director is supported by technical experts
like the Deputy Commissioner (MCI!) and Assistant Commissioners who mam y
look into training, surveillance and the internal evaluation oi the mission aettvittes.
In addition, support is also available for managing the administration and accounts,
supply of vaccines and equipment, including the cold chain system, monitonn= an
independent evaluation, as well as media activities.
_
The current organisational set up of the mission on immunisation at the Centre
at the time of review is as follows:
Table I
Secretary Health & Family Welfare
Year-wise Phasing of Districts to be Taken up for UIP
Special Secretary (FW)
I
Joint Secretary (Mission Director)
No. of Districts
Year
taken for UIP
30
62
90
120
137
439
1985
1986
1987
1988
1989
TOTAL
The UIP targets are to cover 85% of eligible children and 100% of the pregnant
women by 1990. One could see that over a period, considering the epidemiological
features and the priority needs, there has been a shift in focus towards infants rather
than children under five years or under two years, unlike earlier.
Realising the tremendous impact this programme can have on the enhancement
of child survival, it has been recently included as an integral part of one of the
Technology Missions of the Government of India. The National Immunisation
Mission is, thus, a joint responsibility of the Ministry of Health and Family Welfare
and the Department of B iotechnology. Under the Mission, the responsibilities have
been divided between the two Ministries/departments as follows:
Under Ministry of Health and Family Welfare
Mini Mission I
Mini Mission II
-
Storage and distribution of vaccines
Administration of vaccines, monitoring and
evaluation.
Under Department of Biotechnology
Mini Mission III
Vaccine research and development '
Mini Mission IV
Vaccine production
The organisational structure of the Mission Directorate in the Ministry of
Health and Family Welfare as proposed by the Government of India, is shown in
Deputy Co mmissioncr
(DC) MCH
Assistant
Commissioner
(AC)
(Training)
—r~
Assistant
Commissioner
(AC)
(Immunisation
Surveillance)
Assistant
Director
(Statistics)
Deputy
Secretary
(Urban Immunisation)
(Cold chain supplies)
Under Secretary
(EPl)
Assistant
Commissioner
(AC) (EPI)
Training
& Vaccine
Supply
I
Deputy Assistant
Commissioner
(DAC)
(Immunisation)
The position of AC (Training) in the mission is vacant. The AC (EPI) is looking
after the coordination of supply of vaccines to different States and the training
programmes are also looked after by him. The AC(EPI) is assisted by the DAC(I).
The Mission Director also has technical support from the Directorate General of
Health Services (DGHS) and Indian Council of Medical Research (ICMR). In the
DGHS, the Immunisation Programme is being looked after alongwith other Public
Health Programmes by the Deputy Director General, DDG(P) who is overall incharge of all Public Health Programmes. The Assistant Director General, ADG(EPI)
looks after the EPI programme exclusively. The ADG(EPI) is supported by two
Deputy Assistant Directors General (DADG) and the main responsibility of this
8
9
section is currently related to the administration of the vaccine production institu
tions under the Ministry of Health and Family Welfare. By and large, a major share
of the management of the programme is with the Mission, and the bifurcation into the
Ministry and DGHS appears to be somewhat peculiar with a very marginal share of
responsibilities lying with DGHS. This could generate problems of coordination.
However, the same is being presently taken care of by the DC(MCH) who has a
horizontal relationship with the ADG(EPI) in technical matters. The ADG(EPI) was
stated to be responsible also for organising training activities on planning and
management of EPI, though here also, these activities need to be undertaken with
close liaison with the Mission in order to avoid duplication of efforts.
At the State level, in the Department of Health and Family Welfare, the
Immunisation Programme forms an important component of the Integrated Maternal
and Child Health and Family Welfare Programme. There has been variation between
States in regard to organisational structures. The organisational structure at the State
level is shown at Appendix VI(a). However, most of the time, one officer in the
Directorate of Health Services has been identified to look after EPI/UIP, either as a
sole responsibility or as one among many responsibilities. The State EPI officer is
responsible for the planning and management of the programme in the whole State
by ensuring coordination between the various implementing agencies. Districts are
the major administrative units responsible for the implementation of all health pro
grammes including EPI/UIP. The Chief Medical Officers (CMOs) are in direct line
command with the Director Health Services (DHS) and the State EPI officer is
functioning as staff officer to the Director Family Welfare and/or Director Health
Services.
With the involvement of medical colleges in UIP, the Directorate of Medical
Education also has a joint role in this programme. Moreover, the responsibility of
implementing UIP in the three PHCs adopted by Medical Colleges under the Reori
entation of Medical Education (ROME) scheme makes their involvement still more
essential. The state EPI officer is, therefore, required to maintain Faison with the
Medical Education Directorate and medical colleges also. Health services for
specific population groups are being provided by various agencies like the Railways,
Armed Forces, Public Sector Undertakings, ESIC, CGHS, etc. and proper coordina
tion with such agencies also is to be ensured by the state EPI officer with regard to
the Immunisation Programme. Large urban populations in major cities are provided
health care through major health institutions run by State and other health agencies,
and the preventive health care programmes are mainly to be provided'by the
Municipal authorities. In bigger cities, Municipal Corporations, within their avail
able resources, provide these services including immunisation. The state EPI officer
has to actin liaison with this agency also. At present, these relationships between the
10
State Health Directorate and other agencies mentioned above are not so well defined
all over the country.
At the district level, the District CMO or District Health Officer (DHO) is the
chief of all health programmes, including EPI/UIP. By and large, the basic organisa
tional structure at the district remains the same all over the country but minor
variations do exist in nomenclatures, numbers and categories of divislons/departments, etc. Till recently, the total responsibility of implementing EPI was with the
district officer in-charge of family welfare with delegated responsibility from the
CMO. However, under UIP, a new post of District Immunisation Officer (DIO) has
been sanctioned at the district level exclusively, for improving the management of
the Immunisation Programme and to function under the direct control of the CMO.
Below the district level, the Immunisation Programme is totally integrated
with primary health care and is being delivered at the rural health infrastructure
including the Community Health Centre (CHC), Primary Health Centre (PHC) and
subcentre through the available medical, nursing and para professional personnel.
While the female Multipurpose Health Worker (MPW) and Female Supervisor may
be identified as the key persons responsible for implementing the programme, every
functionary at this level has a definite share in this responsibility, though of varying
degrees. In addition, in the rural as well as urban areas where the Integrated Child
Development Services (ICDS) scheme has been operational, the functionaries like
Anganwadi Workers (AWWs) under this scheme also share a major pan of the
responsibility with theprimary health care personnel including Health Guides (HGs)
and Dais.
Thus, the administrative/functional units as well as the average population
covered at different levels in the hierarchy for the Immunisation Programme in the
States is as follows:
Community health centres have not been included in the diagram because these
are 30 bedded upgraded PI ICs mainly responsible to provide referral services to the
community.
The various responsibilities under the Immunisation Programme broadly
divided among Central and State Governments are as follows:
Central
1. Provide vaccines, supplies and equipments.
2. Preparation of prototypes of health education materials.
3. Training of senior health personnel.
4. Periodic evaluation.
State
1. Delivery of services.
2. Maintenance of cold chain.
3. Organisation of surveillance.
4. Training of junior level health personnel.
5. Monitoring of programme.
Policies and Issues
The National Health Policy for India has given high priority to health care of
women and children and has included immunisation as one of the priority program
mes requiring special attention in the immediate context for enhancement of child
'
survival. Moreover, according to the policy statement, primary health care, including
' immunisation as one of its essential components, has been accepted as the strategy
for achieving the policy goals.
Legitimisation for according such high priority was based on the morbidity,
mortality and complications following vaccine preventable tjiseases among children.
j In the absence of national epidemiological surveys conducted in the country on
■
VPDs, the main source of information was reported <fata from various health
institutions all over the country. In the memorandum of understanding of the
iGovernment of India with UNICEF, the prevalent situation on VPDs was described
as follows:
About two million children die or become disabled due to six VPDs annually.
About 500 children are paralysed daily by poliomyelitis, 2,50,000 new boms die
annually of neonatal tetanus (NNT), 2,00,000 children die of measles, some 4,00,000
children die of tuberculosis and 1,50,000 die due to whooping cough. The aftermath
of measles results in severe malnutrition, and bronchopneumonia. Tetanus also takes
a heavy toll of lives in older children.
Prevention of the occurrence of vaccine preventable disease will not only
reduce morbidity and mortality, but also prevent handicaps arising due to poliomyei1
litis. It has been reported that about 2/3 lameness amongst children is due to
!' poliomyelitis.
The true picture of the magnitude of the problem due to 2 major VPDs, NNT
I and poliomyelitis was made available in India in 1981 -82. Sample surveys conducted
■ in 1981 and 1982 in 11 States revealed the neonatal tetanus mortality rate to be 13.3/
■ - 1000 live births in rural areas and 3.2 in urban areas. The incidence rate of paralytic
poliomyelitis was estimated to be 1.6 and 1.7 per thousand children in the 0-4 year
age group in urban and rural areas respectively. It is projected that in the absence of
>
12
13
the Immunisation Programme, around 40 million eases with 1.5 million deaths occur
due to VPDs annually.
Against the goals specified for immunisation coverage in the National Health
Policy, EPI which was in operation since 1978 showed very slow progress, which
clearly indicated the need for accelerating the pace for improving coverage with
quality' services. Recognition of the potential of immunisation as a cost effective
technology for child survival had resulted in the extension of EPI with the aim of
providing universal immunisation by 1990 under UIP. Members of the Task Force
constituted by Government of India under the chairmanship of Shri R.P.Kapoor, to
prepare a plan of action to achieve the objectives of UIP, felt that successful
implementation of the project will:
1. greatly reduce the morbidity and mortality among children and will enhance
the child survival rate;
2. establish an active interaction between mothers and primary health care
functionaries;
3. constitute an important step in the journey towards health for all by 2000
A D; and
4. be the leading'edge of primary health care and could be the entry point for a
continuous system of delivery of a package of MCH services.
Policy planners believed that immunisation, prophylactic treatment against
nutritional deficiencies and oral rehydration therapy against childhood diarrhoea, are
the most simple, cost effective package of health services which will enhance child
survival and prevent avoidable disability long before significant improvement in the
level of economic development could be achieved. The high priority accorded to the
Immunisation Programme by the Government of India is reflected in the fact that it
has been included under one of the seven National Technology Missions.
According to the Government of India, the package of MCH services com
bined with simultaneous efforts in other related areas like sendees for aseptic and safe
delivery through trained birth attendants, improvement in nutritional standards,
provision of safe drinking water, etc. should make it possible to achieve reduction in
infant and child mortality.
Convinced about the benefits of universal immunisation, the National Health
Policy has set the following targets to: be achieved by 1990.
Though measles vaccine was not mentioned in the National Health Policy, the
Planning Commission’s steering group on health and family welfare has recom
mended the inclusion of measles vaccination.
As a policy, the programme will be implemented as a part of primary health
care through a network of female MPWs, supported by male MPWs and assisted by
VHGs and AWWs. The universal coverage of immunisation of infants and pregnant
14
women will be executed over a five-year period in a phased manner. Thus, about 18
million infants and 24 million mothers will be immunised every year.
Table 2
Expected Immunisation Status by 1990
DPT
Polio
BCG
Measles
T.T.
T.T.
D.T.
Typhoid
Infants
Infants
Infants
Infants '
Pregnant women
(for school children)
10 years
16 years
(New school entrants)
5-6 years
5-6 years
Immunisation Status: 1990
_____ (% population)_____
85
85
85
85
100
100
100
85
85
In the final analysis, the objectives of the mission for the Universal Immunisa
tion Programme are to:
1. Reduce morbidity and mortality due to diphtheria, pertussis, tetanus, polio
myelitis, tuberculosis, and measles among infants.
a. Reduce the incidence of residual polio paralysis to less than 0.5 per
1,00,000 population;
b. Reduce the neonatal tetanus mortality rate to less than 1 per 1000 live
births.
2. Reduce mortality due to tetanus amongst pregnant women.
3. Achieve self-sufficiency in vaccine production.
Policy planners may display a great deal of confidence and make believe that
the package is an 'opportunistic marvel'. Yet there are many issues raised by critics
of the programme who question the wisdom in launching such a costly mega venture.
They fear that the fanfare with which the programme has been launched may
ultimately misfire. They feel that UIP like the Family Planning Programme is
hijacking the space from various other programmes needing greater attention and
high order of prioritisation.
It has been argued by some that the premise on which the programme had been
built is totally untenable. There is no epidemiological evidence to support the
contention that control of six vaccine preventable diseases will make any dent in
infant mortality. Six VPDs form a very small proportion of diseases which cause
death and illness in children below five years of age. According to surveys of causes
of death in infants by the Registrar General of India, prematurity, respiratory
infections, and diarrhoea predominate and none of them are vaccine preventable.
15
According to them, 60-90% of deaths of children under five years are due,
diarrhoea and respiratory diseases and only 10-12% account for six vaccine prevcn(
able diseases and, thus, lack epidemiological justification for launching an ]ln
munisation Programme at the national level. To quote Dr. Debabar Banerjee "The-, ?
arc gaping holes in the knowledge of epidemiology of six vaccine preventabl» '
diseases to be attacked. This sounds incredible. This is like mobilising a huge army '
without even knowing who the enemy is; what are its strengths and weaknesses?” I
Thus, according to him, it is by far die most staggering flaw in the policy.
Forgetting for a moment tliat the six VPDs pale into insignificance when
looked at against the backdrop of total health problems viz. poverty, malnutrition,tu. ;
berculosis, leprosy, diarrhoea, dysentery, cholera, worm infestation, acute respira- ■
tory infections, anaemia, etc., the question has also been raised as to how and why im. ;
munisation is chosen as the most effective method in controlling the six VPDs. ,
Knowing fully well that causation of disease is multifactorial, relying totally on one |
single tool to control the disease has not been accepted as a sound policy. For 1
example, tuberculosis is best controlled by interrupting transmission in adults; yet, ■
the government, instead of revamping the national tuberculosis control programme, L
is relying on B.C.G. vaccination which gives very little protection.
i.
Similarly, the spread of measles is not only greater among the malnourished ’
population, but complications and mortality are also high in this group. Therefore, f;
doubts have been expressed regarding the usefulness of measles vaccination alone k
without tackling the problem of malnutrition among children.
|
Various questions have been raised regarding the immunisation schedules h
recommended for India also. There is a feeling that a large number of issues related jto the schedule of immunisation, doses, and type of vaccine should have been |
resolved before launching such a massive programme. Similarly, the number of
doses of polio vaccine has also been under debate - whether it is enough to give three I
doses or whether it should be five doses, or it should be started at birth, etc. There)
has been doubt expressed regarding the rationale of fixing of the age group fori
completion of primary immunisation under one year. The question raised is whether f
it is based on epidemiological observations or is it the acceptance of inability to cover [■
all the preschool children and, therefore, the target group has been scaled down to one!
year.
Another issue raised about the Immunisation Programme is regarding the;
fixation of target of coverage at 85% level. It is not understood as to how and on whal!
basis it has been assumed that 85% coverage of infants would provide adequate herd
immunity and help in interrupting disease transmission. It is also said that the phe-.
nomenon of herd immunity would only be effective when all potential suspects are ■
protected. The potential suspects for these six VPDs are children from the 0-5 years
16
:hou<’h there is a
-ne group whereas under DIP, only infants are being protect--1-.
=
provision for providing services to older children on demand
g.% coverage
Besides, several studies have shown that even with mom uk
st:]] been
and vaccine efficacy of more than 95%, cases of poliomyelms
to
occurring in those areas. Many are, therefore, recommending mat
.hou[d be
revise the policy regarding expected coverage level and suggesting that it s
extended to 100%.
■ Evenintheareasshowinganoveralloptimumcovcrage,thenumbero senou
outbreaks of measles have been reported in pockets with poor coverage scattere
within such areas due to lack of uniform coverage.
It is also pointed out that the natural process of immunity is altered in a
population which is dependent on immunisation. Therefore, mass campaigns Oi
immunisation, if not continuously maintained, can result in severe outbreaks. With
growing stress on immunisation coverage, it is feared that the tendency to organise
special camps would gradually increase, without proper attention to sustained efforts
to protect the new susceptibles.
■ It has been repeatedly stated by the authorities that the Immunisation Pro
gramme is an integral component of the MCH programme w’hich, in turn, is one
essential element of Primary Health Care. As per the existing set-up, this is to be run
by the existing infrastructure and the services under the ptogramme are to be
delivered to the community in an integrated manner by the field health functionaries.
However, the extra emphasis laid on target achievements under UIP as in the case of
the Family Planning Programme, makes one fear that all other components of MCH
or primary health care services are likely to be pushed aside by the functionaries.
Similarly, the present organisational set-up of the programme itself leads one to
suspect a strong element of vcrticality in the programme. At the Centre, State and
district levels, additional staff exclusively looking after different components of the
Immunisation Programme are being appointed, e.g. seven additional officers with
nine support staff at Central level; two additional officers with nine support staff at
State level; four additional staff at district level. Out of the four, one will be the
district programme officer.
Even at the Centre, though the mission on immunisation is within the
Department of Family Welfare, there are doubts regarding the extent of intemation
of the programme with other components of family welfare. Creation of an exclusive
organisational set-up, separate budget provision as well as independent handling of
the same and the formulation of a mission give credence to the argument that once
again a vertical programme has been thrust by the authorities.
Another issue raised by many regarding the programme is that, apart from
being a vertical programme, the total overall programme details including stratemes
operational details, norms of resource allocation, etc. follow a uniform pattern
throughout the country. No consideration has been given to epidemiological and
ecological profiles, organisational and managerial capabilities and preparedness or
limitations in terms of the general economic development status of different States. '
It is a well established tact that socio-economic variations between the States oreven
within the same State influence the implementation of the programme and achieve
ment of results. The poor performance in many States in the Hindi belt lends support
to such assumption. A universal Central pattern and the dependency on Central
assistance have failed to enthuse State Governments. According to the critics, most
of them have received it passively and branded it as a'Centre’s programme’. Such an
attitude interferes with the absorption of the programme in the total health services
of the State and raises questions regarding the sustainability of the programme once
the 100% assistance from the Centre is withdrawn.
To reach the target of immunisation coverage of 85% of infants and 100% of
pregnant women before 1990 is a very challenging and stupendous task. It is also
pointed out that the programme is not a one-time venture, but year after year, even
after 1990, around 18.5 million infants and 22 million pregnant women have to be
protected. Many experts believe that to achieve such goals is nearly impossibleand
requires a huge army of workers, massive input of resources and intensive efforts.
Current levels of achievement lend support to their criticism and seek an answer to
the question as to how it is expected that those districts included in the year 1989-90
will achieve such a high level of target when even the districts included in 1985-86
are still lagging behind.
Either by design or oversight, the rapidly increasing urban population has not
been included seriously under UIP. No specific policies have been adopted as to how
this group is to be protected. It may be argued that urban areas already have some
built-in facilities for providing immunisation services through their medical care
facilities, yet, it cannot be denied that they are not large enough to meet the challenges
of the evergrowing urban population, with mushrooming of slums; nor are they
prepared to assume areawide responsibilities in a coordinated manner. Therefore, the
immediate questions that arise are;
1. Ignoring such a laree part of the population how do we hope to achieve the
targets set for 1990 for protection of infants and pregnant women? This
would in itself jeopardise the phenomenon of herd immunity.
2. Do the existing facilities in urban area have the will or wherewithal to meet the
needs of the socially handicapped urban population?
Pushing the States to achieve targets will mean upsetting the rhythm of general
health services. Bavin" failed to achieve targets through routine services, the States
will be compelled to organise mass drives/campaigns. States with 'weak' health
services are more likely to default and consequently be singled out to launch special
'
drives resulting in diverting of their meagre resources. Loading the fragile health
infrastructure in many States with target oriented programmes will only hasten the
process of crippling the structure.
A number of national programmes like control of communicable and non
communicablediseases are transferred to the State Governments for implementation
by dangling thecarrot of 100% Central Government support. The States, in their own
wisdom, accept such programmes, utilise the assistance for creation of posts and de
velopment of infrastructure-mostly to work in a vertical fashion. In this process, the
States are constantly playing a balancing game of according priori t v and giving more
attention to one at the cost of the others. Once the assistance begins to dry up, the
programmes are allowed to languish and problems allowed to perpetuate.
Another apprehension about the programme is regarding the manner in which
the health staff will perceive their role in this programme. Introduction of any new
programme is likely to generate a feeling amongst peripheral workers that they are
being burdened with additional responsibility and, thus, create anger and disinterest
among them.
The Immunisation Programme is the single largest programme in terms of
financial allocation in thecurrent Five-Year Plan. The Ministry of Health and Family
Welfare has allocated Rs.240 crores -nd the Department of Biotechnology Rs. 100
crores. It is also suspected that besides the budget of Rs.340 crores, the programme
may use large chunk from the MCH programme budget also.
Integration of the Immunisation Programme in the general health services has
been ominous, and is proving to be worse than the vertical programme. Being targetoriented and time-bound, it has hijacked space from other health activities. Many feel
that the prohibitive costs and manner in which these programmes are run make one
believe that they are being nurtured at the cost of the provision of primary health care
along the lines envisaged by the Bhore Committee and that these programmes have
not only diverted material resources but have resulted in paralysing the primary
health care and rural administrative services.
Even international agencies like WHO and UNICEF have come under a cloud
of suspicion and are being accused of becoming conduits for the resurrection of the
utterly wasteful, discredited technocentric campaigns against selective diseases.
Contrary to the assertion of policy planners that UIP will be the leading edge
of Primary Health Care and constitute an important step in the journey toward health
for all by 2000 A.D., the policy of UIP is believed by some, to be an antithesis of the
statement of the national health policy. In their view, it is a technocentric programme
thrust upon the people, making them totally dependent, without promoting commu
nity self-reliance. It is an exercise of motivational manipulation by instilling a
psychosis of fear for six diseases and expounding the virtues of immunisation.
19
18
Critics ask, “Why a Mission on Immunisation”? How can die creation of
Mission, without removing planning flaws, could hcip in achieving the goals set? Itis also asked how loading the Mission with generalist administrators without
adequate technical support is going to help the programme. Besides, they cannot be
held accountable for their decisions because of their frequent transfers, a classical in
stance of authority without responsibility.
The objective of the Mission is to reduce mortality and morbidity due to the 6
VPDs. However critics feel that the programme's performance is monitored not by
measuring the impact on mortality or morbidity but by assessing the achievement of
the targets. Consequently, the programme has degenerated into a numbers game,'
bereft of its epidemiological and human dimensions.
Critics also question the wisdom of totally marginalising the DGHS from the
activities of the Mission. Moreover, it is an irony of fate that whereas other
components of the MCH programme are being looked after by the Department of
Family Welfare, immunisation of infants has been singled out to be looked after by
the Mission. It is also not clear, what role the Mission has in providing booster doses
and immunisation of older children and who acts in the event of outbreaks of vaccine
preventable diseases.
Though it is loudly claimed that all services should be integrated, it appears that
the total family welfare services have been severely fragmented and segmented.
Different components of activities are being looked after by different agencies, some
by the Department of Family Welfare, some by the Technology Mission and others
by DGHS, and IEC by various other agencies.
It is feared that such an expensive time-bound and target- oriented programme
without any epidemiological justification thrust upon the over-burdened infrastruc
ture in the States, will ultimately prove to be yet another misadventure without
making the tiniest dent in the total health problems of children.
The issues raised above draw a dismal picture of the entire programme.
However, it may not be entirely true. Therefore, it would be more appropriate to
review all the issues more objectively and pragmatically and put the matter in the
right perspective.
There is no disagreement on the fact that enough baseline data are not available
to justify the high prioritisation of the Immunisation Programme. There is also no
denying that major health problems influencing child survival are due to poverty,
poor sanitation and lack of adequate health facilities requiring greater efforts on the
socio-economic fronts through employment, better living conditions, nutrition,
improvement of sanitation, etc. Nevertheless, critics do admit that 10-12% of child
mortality is due to vaccine preventable diseases. Many of these diseases also cause
severe morbidity and, sometimes, permanent disability. Around 2.5% of measles
20
............. severe malnutrition
caSes die during the acute stage of the disease. Besides, it cau^ J f ber; n feet ions.
andaffects.theimmunesystem,thus,makingchildrcnvulnciaD.^
common
Measles is also known for its seriousness when associawO
in the
complications like respiratory infections and diarrhoea. AcC0"i'.‘“
non„ VPDs.
field of child health, neonatal tetanus and measles are the prime
f._st
hence, immunisation against these diseases should have beert .’
death>sets
instance. Whooping cough, an acute respiratory infection, besides ca
«
in encephalopathy and, in some children, severe brain damage. It is a
,
in<r
that pneumonia can be one of the serious complications associated wit i
. =
' cough. It has been agreed upon by many that the leading causes of morta i y
’ morbidity among pre-school children are diarrhoeal diseases and respiratory in c
tions. The causal relationship of acute respiratory infections with diseases t -c
measles and whooping cough also needs to be taken into account. Poliomyelitis, it is
well known, leaves its tell-tale stories. It is estimated that nearly 2,00,000 children
become lame due to poliomyelitis annually in India.
Therefore, it is untenable to allow these diseases to multiply and take a heavy
toll of life, (even though it may not be as high as due to other causes) particularly,
when technology is available to contain them, and which is stated to be a cost
effective one. It is true that vaccination may not be the only solution, but it is
immediately available. The success story of the eradication of smallpox by protect
ing potential suspects with a potent vaccine also needs to be remembered. Also, this
strategy has already been tried out and not only has it been found effective but has
been acceptable to the community too. With increasing awareness, people have
started appreciating the value of immunisation, though at a slow' pace. Moreover, one
cannot afford to wait for socio-economic and environmental development, which
will take long time to come about. One has to remember that for enhancement of child
survival, one would have to depend upon a mix of technology and development. It
cannot be either one or the other. It has to be both.
One may dispute the manner in which the programme has been launched, or the
cost input, but the validity of the programme is unassailable for the simple reason that
its impact, howsoever little, is going to influence child survival.
However, the caution sounded by experts that areas of low coverage or where
the natural process of immunity is altered are potentially prone to outbreaks of
diseases, is logical and merits respectful consideration.
Taking a cue from demographers, who are constantly predicting the number of
births prevented as a result of family planning procedures, experts in UIP have also
begun to predict the number of vaccine preventable disease cases prevented due to
the Immunisation Programme. The occurrence of disease is a biological phenome
non which does not follow the rules of birth but is governed by a number of variables
21
related to causative organisms, environmental factors favouring transmission, level
of immunity in the community, etc. Therefore, such predictions should be judged on
the anvils of epidemiological truth and accepted with caution.
It is, therefore, suggested that in disease control programmes, it is not sufficient
to know “what has been achieved”; it is important to know “what remains to be
achieved”. Instead ofjudging performance by target achievement, it is important to
know how many eligibles remain to be protected. Peripheral workers may be trained
to monitor their own progress through regular assessment of eligibles to be protected
in her/his area of coverage.
Our country is committed to accept the primary health care strategy of which
immunisation is one component. The Government of India has intensified efforts
simultaneously toaccelerateothercomponents of primary health care, viz. expansion
of infrastructure, maternity and perinatal care, diarrhoeal disease control, family
planning programme, prophylaxis programmes against nutritional deficiencies,
information education and communication for health and family welfare, provision
of safe drinking water and improvement of environmental sanitation, etc. It will
suffice to say that the Minimum Needs Programme, Integrated Rural Development
Programme, schemes for rural unemployed, massive allocation of funds for water
supply and improvement of sanitation in the current environmental sanitation decade
are directed towards total development of the common man. Therefore, it would be
incorrect to state that the Immunisation Programme is siphoning off precious
resources from other programmes. It is also true that the need for development of
expensive specific technical resources like the cold chain equipment is an essential
requirement for the implementation of this programme which may not be true with
some othercomponents of primary health care mentioned above. Further, the way the
programme is run today in a relatively vertical manner, forces the authorities to
deviate from the desired path of strengthening the total health care system with a
comprehensive MCH package which, in the long run, could have given better results
in terms of improved health status of women and children. Therefore, if at all a
Mission was to be formed, it should have been for MCH, rather than for immunisation
alone.
The Immunisation Programme run as a time-bound, target-oriented pro
gramme, is jettisoned with the existing health care system and is allowed to swim or
sail with it. Yet it would require certain essential inputs, so as to immunise children
with good quality and safe vaccines, given under aseptic condition by a trained
worker. Therefore, a good organised programme would require:
1. Good quality of vaccine
2. Scaling up of production of vaccine and supply
3. Maintaining quality of vaccine through a well organised cold chain system
from the production site to the remotest outreach.
A well organised distribution system.
Supply of equipment and material for sterilisation of syringes and needles, so
as to ensure services under aseptic conditions.
6. Retraining of the health workers to ensure better quality of services.
Though the Immunisation Programme has been going on in our country for a
long time, the efforts to develop the above facets of the programme have been rather
slow. It is only with the acceleration of the programme, under UIP, that serious
efforts have been made to ensure a well organised cold chain system, enhanced
production of vaccine and arrangement of an efficient distribution system. There
fore, the major portion of the budget had to be spent initially on establishing and
developing various essentials required for a good programme. Such expenditure was
inevitable and should not be considered a wasteful investment, in whatever manner
the programme had been launched. Of the total allocation of Rs.2400 million,
Rs.717.67 million is spent on walk-in-coolers, deep freezers, ILRs, vaccine carriers,
transport vans, loan for mopeds, etc. Another Rs. 826.20 million goes to meet the cost
of vaccine, Rs.328.5 million towards the cost of syringes and needles. Only a
minimum of 5% of the total budget has been allocated for expenditure on salaries.
It can be said without any hesitation that programme managers have meticu
lously gone into details and streamlined the distribution system of hardware, its
monitoring and its maintenance (and for vaccine too). By and large, short supply of
vaccines and other equipment does not remain a major cause of anxiety today.
It can be said that the above inputs have gone to a great extent to strengthen the
primary health care system and boosted the credibility of the institution and workers.
For example, increase in POL and allocation of Rs.2000 per PHC to meet contingent
expenditure like maintenance of the cold chain equipment, will go a long way in
meeting the shortage generally with which these institutions suffer.
It really goes to the credit of planners to have strengthened the system well
within the appointed time. However, it will be pertinent to remind the planners to
make provision for the maintenance of equipment and its replacement when required.
Therefore, the recurring cost though enormous, is essential to maintain high
4.
5.
standards of immunisation.
Health is a State subject and as per the Constitution, it is the responsibility of
the States to provide health care and launch preventive and promotive health
programmes. The national health policy has been accepted in 1983, and following
this, the S tates are expected to develop their own specific S tate Health Policies within
this broad framework and, at the same time, identifying their priority needs.
Similarly, regarding any decision to take up new programmes/schemcs at the
national level, there is a mechanism of coordination among the States through the
meetings of Central Councils of Health and Family Welfare. This forum is to be fully
22
23
utilised by each State to accept or reject programmes proposed to be taken by all the
States.
During the past four decades, not many States have shown leadership and
dynamism in ’lunching preventive and promotive programmes based on local needs
Scarce resources had always been given as the reason for not doing so. Consequently
since the inception of Five Year Plans, they have depended on Centrally assisted
health programmes related to control of diseases and on other promotional program
mes. Initially, because of the magnitude and national significance of the problems
and also due to the absence of a well organised basic health infrastructure in the
States, most of the national health programmes yere launched as vertical program
mes. The understanding was that with the achievement of a certain degree of control
of the problem and development of infrastructure, the programmes will be gradually
absorbed/integrated into the States’ health system and will be run by States them
selves. By and large, the States have continued to depend upon the Centre for
financial assistance for most of the health programmes. On the other hand, most
States spent most of their own resources for providing facilities for secondary and
tertiary care. With regard to the Immunisation Programme, the States have accepted
the programme giving it considerable priority attention, although with a reservation
in using Central resources by many, particularly for appointing mtytpower exclu
sively sanctioned under UIP, under the apprehension that it may become a liability
to them once the Central assistance is withdrawn.
Immunisation is not a new entrant. It was one of the important activities
required to be performed by peripheral health workers. With the introduction of the
MPW scheme, the female MPW is still required to perform the same activities that
she was performing as an ANM. Nothing new has been added. Therefore, expecting
her to immunise children cannot be considered as overburdening her. During the
review of immunisation, it was revealed that in more than 80% of subcentres,
immunisation services were being provided as an integrated component of MCH.
The ANM showed a greater sense of confidence and believed that some tangible
sendees are now being offered and she is getting more opportunities to establish good
rapport with the mothers. On the other hand, a well planned operational strategy for
organising sessions in her institution or area should be considered a help to her to
improve her functioning and image in the community.
Observarions of immunisations conducted by these workers, either at the
subcentre or outreach, bear testimony of the good quality of services provided. In
nearly 70% of the sessions observed, separate syringes and needles were used for
each immunisation. Likewise, during the sessions, the ANMs were commtinicating
with the parents of child beneficiaries about various aspects of immunisation. Also,
the. vaccine and diluent were kept in ice in more than 80% of the sessions observed.
24
Rather than considering the programme an additional burden on the health
svstem on the whole, and undoing the total benefits accrued thus far, our effort should
be to expand the coverage well beyond what has been already achieved and to utilise
the already established infrastructure and the systematic operational strategies
worked out, for incoiporating more effectively other components of the MCH
package to reach the community.
A system of logistics and supplies, maintenance of the cold chain, sterilisation
procedures for equipment, scheduling of activities, systematic and regular reporting
mechanism, etc. have been established under the programme and the health person
nel are increasingly getting oriented to this system through training and experience.
Even though it appears to be oriented to a single programme at this stage, this
experience can be extended to take care of other programmes also in a gradual
manner.
No doubt, as and when other components of MCH are included in the package,
simultaneous efforts to provide adequate and appropriate resources should also be
made. According to Dr. Ghosh, the view that UIP has interfered with heal tit delivery
may be an exaggeration since very little w: s being done and the utilisation of primary
health care services according to many reports, is rather poor.
. Setting specific targets under any programme should be considered an effec
tive management tool for achieving better and timely results. The Immunisation Programmehas been launched as a target-oriented and specific time-bound programme.
Unfortunately, the use of targets has been wrongly applied and resulted in over
playing it, resorting to strategies of special drives in many situations at the cost of
other programmes rather than a stable and regular service for achieving the targets.
The fault lies not in making the programme target oriented, but in the wrong methods
used in either target setting (without rational basis and/or involvement of function
aries) or its allocation, or its use in monitoring progress in the achievement of the
programme.
Clouds of misconception over international agencies like WHO and UNICEF
are misplaced and uncalled for given the circumstance prevalent immediately after
independence, when communicable diseases like smallpox, malaria, cholera and
many other diseases were taking a heavy toll of lives. With hardly any resources in
terms of trained manpower, infrastructure, materials and finances, the only alterna
tive available was to launch mass campaigns against some diseases coupled with
simultaneous development of resources. With the increasing numbers of health
manpower and vastly expanded health infrastructure, there is no longer any need for
continuing or launching new vertical programmes. Yet the results of the mass
campaigns launched then with the support of international agencies are clearly
perceptible. Smallpox is no longer killing or maiming our children. Malaria is still
25
/
a problem, but the magnitude has been greatly reduced. The physician of yore will
vividly remember the vast number of children, the young and old, suffering frOtri
malaria. Children are no longer found with enlarged spleens. Yaws is a forgotten
entity. Therefore, it will be uncharitable to ignore or minimise the gains made.
For our failure to reap the fruits of various programmes, instead of searching
for scapegoats, we should ask ourselves, “Why have we failed?" Unfortunately,
tinted vision dims the perception, obliterates the obvious, takes away the courage to
look at our own faults. Instead of searching for alibis for our failures, let us begin to
remedy our flaws.
One of the most important issues is to revamp the health infrastructure. Most
of the failures can be ascribed to poor implementation due to the gradually increasing
culture of no work. However, it would not suffice to blame the workers, and raise our
hands in despair. We have not faced this challenge squarely and boldly. It would be
suicidal to postpone tackling of the situation any further, because the success of any
programme, not of UIP alone, depends upon the interest, involvement and commit
ment of workers at all levels. Mere application of tiers of supervision is not going to
achieve results. Instead of humiliating and demeaning the workers, we should try to
build them up, instill in them a sense of pride and involvement and empower them
to take decisions and enable them to discharge their duties with a full sense of
responsibility.
Resources
HEALTH INFRASTRUCTURE
It had been planned that immunisation services will be delivered as an integral
component of primary health care. The gradually expanding rural network of CHC,
PHC and subcentres as well as urban family welfare centres, postpartum centres and
medical colleges do play a key role in the delivery of the immunisation services to
• the beneficiaries.
To meet the national goals of health for all, the infrastructure of health services
is being expanded. Under the minimum needs programme, it has been planned to
provide one subcentre for every 5,000 population and for 3,000 population in hilly
and tribal areas, manned by a trained maleand female worker; a primary health centre
headed by a qualified medical officer for 30,000 population and 20,000 population
in tribal and hilly areas; and a community health ccntre/upgradcd PHC which will
_ work as a referral centre for a population of 1,00,000.
A review of the existing facilities published in the Bulletin on Rural Health
Services in India for the quarter ending September, 1988, reveals that there are
16,535 PHCs in existence serving, on an average, a population of 28,941. These
PHCs have a back-up of 1,10,275 subcentres serving, on an average, a population of
5,518. Approximately 5,000 PHCs and 20,000 subcentres are yet to be established in
the current year, so as to reach the targets set by the end of the Seventh Five-Year
Plan.
1
A review of the existing subcentres vs expected number in different districts
revealed that in 15 districts out of 43, the number of subcentres was in accordance
with the expected number. In four districts, the number of existing subcentres
exceeded the expected number. However, in 13 districts, the number of existing
subcentres was less than expected. The deficiency ranged between 10% and a little
over 40%. In Dibrugarh district, in Assam, and Ganjam in Orissa, the deficiency was
more than 40%, whereas in the districts of Anantnag, Badgam, Kasargode and
Hissar, the gap ranged between 20-30%. In Warangal, Singhbhum, Hissar and
Bijapur districts the proportion of subcentres falling short of expectation ranged
between 10-20%, and in district Patiala, the gap was less than 10%. The results are
26
27
•he <?t?? afddltion to the above three approaches the detailed information collected oy
analvsed
COnstltutcd foraverage evaluation and review was also utilized and
analysed.
.,,pH
Study Costs have been simply defined as the value of resources
each
6 pTOgramme cost ha» been estimated as a sum of the monetary value of
Cost Analysis of UIP
each
resource category
for the
programme.
denendinA
[es°urceutilized
- monetary
value
was estimated and allocated to the UIP
The°fidl'V et
canitalmcfn
Keeping in view the requirements of the Central Government and donor
agencies, a scZy was undertaken with the aim of financial analysis of the programme
providing estrcates of total cost of the programme for an administrative area of
implementator, and the cost of sustaining the programme to the local and State
Government
The specific objectives of the study were:
1. to identify the cost composition of UIP at district level and below,
2. to esuntate total cost of the programme and the cost composition at district
level arZ below,
3. to esti.-zate unit cost of services provided under UIP, and
4. to estt.xate cost of sustaining the programme for future years.
The study was conducted in two districts namely, Nanded in Maharashtra and
West Nimar in Madhya Pradesh. A random sample from each category of institution
within each dut-ict was drawn to study the cost of running UIP at the institutional
level.
The study required dataon three different aspectsof Immunisation Programme
viz.
the data about various kinds of inputs available and utilized,
quantum of programme output in terms of services provided by various
nealth institutions in rural and urban areas, and
in. data on completed immunisations.
For this purpose various methods of data collection were adopted.
i. Interviews and discussions with the officials at State, district and institutional
level.
ii. Study of.secondary records for details about central budget and State budget
as well as expenditure for the UIP from State HQs.
in. Delphi technique and interviews with the functionaries at various levels were
conducted to estimate staff time allocation to the activities related to
immunisation.
i.
n.
154
d*rect cost component or indirect cost component.
° ProT'amme has been estimated in two components as
monetary value of(JlinnuKfr'he pr°sramme has ***" estimated by adding up the
other activities related to uip0^^
provision of s^ces and undertaking
details in these^XdnXrebconected7ldedhfOr
expenditure incurred, the
1988-89.
‘eCted from the Iwo diners under study for the year
COST OF UIP AT DISTRICT LEVEL
In order to estimate the cost of Universal Immunisation Programme at d istrict
level for one year period (1988-89) and to project the cost for future years, it was
thought essential to identify the cost components i.e direct/incremental cost and
indirect/obligatory cost with subdivision into capital and recurring costs and cost
composition at district level as well as at institutional level.
The total cost of UIP at district level and cost composition in two districts
(1988-89) are shown below:
Table 47
Total Cost of UIP at District Level and Cost Composition in Two Districts (19SS-S9)
West Nimar
Item of
Expenditure
Capital*
Recurring
Nanded
Obligatory/
Indirect cost
Incremental/
Direct cost
Total cost
62,337
(1.4%)
43.S6.04S
(9S.6%)
S6.0I6
(S.7%)
9,03.847
(91.3%)
1.43.353
(2.7%)
52.S9.S95
(97.3%)
Ts'^5
I’65848
H3.O6.16S
sV-T's
3.73,373
115,13,693
177TUI-------------------- :—•
9,5'1,353
54,38,245
’1.60,326
126,74,059
(”-8*>
(9.2C.1
(S1.S%)
(1S.2%)
(100.0%)
* : Capital cost includes only the annualised cost per year for the investment made and not the acluaTinvcsirnenif-------- ■--------- vehicles, etc.
equipments.
Total
44,45,385
_
O
~T~
V
155 s
It showed that the total cost of operating UIP at district level was Rs. 126.74
lakhs for district Nandcd and Rs. 54.38 lakhs for district West Nimar. It is seen that
the total cost for West Nimar was less than half compared to district Nandcd. This can
be explained that UIP was implemented one year prior in district Nanded and more
number of health infrastructure facilities and health functionaries available within
the district were involved in immunisation activities. This resulted in utilisation of
more resources of various types leading to higher cost
The composition of the total cost in capital and recurring cost was approxi
mately in the ratio 1:33 for both Nanded and West Nimar. Thus, the recurring cost
was the major component contributing to 97.0 per cent of the total cost in both the
districts.
COST COMPOSITION OF UIP AT DISTRICT LEVEL
Matrix of cost components into direct and indirect cost for both the districts
shows that the major element of indirect cost was the salary of health personnel
working in various institutions involved in immunisation activities and it accounted
for nearly 98 per cent of total indirect cost. The remaining indirect cost was incurred
on vehicles, their running cost and maintenance cost.
In regard to the direct cost of the programme, the percentage contribution was
different and it was observed that 8.7 per cent of total direct cost was incurred on
capital items in West Nimar whereas it was 14.3 per cent in Nanded. Among the direct
recurring expenditure items, major share was for vaccines and immunisation supplies
such as needles, syringes and immunisation cards. These elements accounted for 81.9
per cent of direct recurring expenditure in West Nimar district and 62.5 per cent in
Nanded district. The salary expenditure as percentage of direct recurring cost was
only 6.5 per cent and 19.8 per cent in West Nimar and Nanded respectively. The
production and supply of health education material such as pamphlets and posters
accounted for 4 to 5 per cent of total direct recurring expenditure whereas operating
cost for vehicles was about 3 to 4 per cent of total direct cost.
UNIT COST OF SERVICES FOR IMMUNISATION AT DISTRICT LEVEL
This was estimated for both the districts by dividing the total cost of the
programme by the output of services for the same period 1988-89.
The estimates derived for the unit cost of output of services in UIP indicated
that the average cost per dose of immunisation to child or pregnant woman was about
Rs. 10 to 11 in West Nimar and Rs. 26 to 27 in Nanded. The average incremental cost
per immunisation was Rs. 1.99 in West Nimar and Rs. 2.42 in Nanded.
The cost per fully immunised child for six VPDs was estimated by using the
denominator in terms of number of fully immunised children. For this, the norm
provided by WHO, i.e. 90 per cent of children immunised for measles to be
considered as fully immunised was utilised. From the estimates thus derived it was
observed that the average cost per fully immunised child was Rs.96.97 in West Nimar
and Rs. 270.25 in Nanded of which 20 per cent and 9.2 per cent respectively were the
incremental costs in the two districts.
COST OF UIP AT INSTITUTIONAL LEVEL
To assess the management of these resources and their utilisation for im
munisation services at various levels in the district health organisation and to idem i fy
the levels at which the cost incurred on immunisation is high, the operating 19
these services was estimated for each category of health unit for the year 1988-89. In
addition, the variation in health units of the same category were also explored for cost
profile and unit costs for immunisation services for two districts under study.
TOTAL COST
It was found that in urban area the average expenditure for immunisation
services was Rs.2,08,370 for the three hospitals and ICDS facilities available in
Nanded district and it was much higher than the average expenditure of Rs. 47,017
for two hospitals in West Nimar. The factors contributing to the variation were
availability and utilisation of infrastructural, equipment and manpower facilities at
institutional level as well as the output of services provided.
In rural areas, the average cost incurred for provision of immunisation services
at CHC and PHC level was about Rs. 1,64,168 in West Nimar and Rs. 1,96,172 in
Nanded. The Mini-PHCs and civil dispensaries fuentionirig in West Nimar spent
approximately same amount of Rs. 28,189 and Rs. 26,595 respectively for im
munisation activities. But in district Nanded the average expenditure incurred by
civil dispensary (Rs. 74,515) was nearly three times that in West Nimar. At the l^kst
peripheral unit, namely subcentre, the average expenditure on immunisation was Rs.
10,375 in West Nimar and Rs. 23,872 in Nanded. It is to point out that the range of
total expenditure was narrower for all categories of health units studied in West
Nimar district compared to those studied in Nanded district.
It was also seen that the percentage of incremental cost to the total cost of the
programme was comparatively more in higher level health institutions in West
Nimar.
UNIT COST
To explore the variation in efficiency with the level of health units, the unitcost
estimates were compared among different categories of health units within two
districts as well as between the two districts. The average cost per immunisation
156
157
provided by hospitals, CHC and PHC was observed to be around Rs.5 in West Nimar
district and it increased to more than Rs. 10 for lower level health units with wide
variations between health units ofthe same category in that district. On the other hand
in Nanded district, the average unit cost of immunisation services did not show any
consistency but unit costs varied with more or less same range in all categories of
health units except civil dispensaries where the variation was comparatively less. The
similar situation was observed for average cost per fully immunised child but higher
range of variation because of poor performance in measles immunisation in some
units.
Inspite of the variation in average cost per immunisation within and between
various categories of health units in two districts, the degree of variation in average
incremental cost per unit of service provided by these health units was much less.
COST COMPOSITION
In general, recurring cost, mainly the manpower salary and other benefits
component, made up a larger percentage of greater spending in all categories of
health institutions in both the districts. Its average contribution in urban units varied
from 63 to 80 per cent and 76 to 96 per cent in West Nimar and Nanded respectively.
In rural areas this component accounted for nearly same percentage of total cost upto
CHC and PHC level but it increased to more than 85 per cent in lower health units.
Conversely, vaccine and immunisation supplies for lower level health units repre
sented a smaller proportion of about 8 per cent of total cost compared to urban health
units and CHCs, PHCs where it was more than 20 per cent
COST OF SUSTAINING UIP AT DISTRICT LEVEL
The annual estimates of cost for sustaining the programme at district level with
the proposed norms of government of India for input facilities, se'vices and activities
at various levels within the districts under study were worked out
TOTAL COST
COST COMPOSITION
As expected, the vaccines, immunisation supplies and annualised capital cos..
of cold chain and immunisation equipments account for more than 65 per cen t oi 1.1incremental cost of which more than 50 per cent is for vaccines. The annua ise cost
of vehicles and their operation and maintenance account for nearly 5 per cent o tntotal direct cost of the district in both States. Though the Government of India as
provided funds for other activities such as surveys, meetings and training of new
entrants in a year it constitutes hardly 2.2 per cent of direct cost.
The major component of vaccine cost was estimated on the basis of quantum
of different vaccines required to immunize the expected number of infants and
pregnant women in a year and then this quantity was expanded to account for tne
quantities lost during transportation or due to cold chain failure etc., using the rate 25
per cent for DPT/TT/ OPV and 50 per cent for BCG/Measles. Thus, the major cost
for sustaining the programme needs to be incurred on vaccines, immunisation
supplies and salaries of the staff appointed under UIP, which are principal variable
costs of importance for overall lower unit costs and higher manpower productivity.
UNIT COST
For district West Nimar in M.P. the incremental cost per immunisation that
government has to incur will be Rs.2.25 whereas it will be Rs.3.01 for district Nanded
in Maharashtra. This cost of immunisation was nearly 50 per cent more for a child
compared to a pregnant woman. The incremental cost per fully immunized child is
estimated to be Rs.22.00 in West Nimar and Rs.28.81 in Nanded.
The incremental cost estimated with proposed health facilities, equipment and
staff when compared with the incremental cost incurred during 1988-89 by two
districts under study showed that there is an estimated increase of about 28.2 percent
in West Nimar and 18.6 per cent in Nanded. This indicates that there is a need to
provide additional inputs if these disricts are to sustain the programme and achieve
the objectives of 85 per cent immunisation coverage for children and 100 per cent
coverage for pregnant women.
Utilising the norms and assuming that the pattern of utilisation of the resources
remain same for future years as was observed during 1988-89, the total incremental
cost has been estimated for the two districts under study. Thus, it was found that the
total incremental cost per year for UIP in district West Nimar of M.P. would be Rs.
12,68,600 and in district Nanded of Maharashtra it would be Rs. 13,76,700. While
estimating the cost, fixed amount sanctioned to district by Govtemment of India for
specific activity of the programme was assumed to have been fully utilized for the
programme, e.g. contingency money of Rs.2000 per PHCper year or POLof Rs.9500
per year per diesel run jeep or van provided under the programme, etc.
158
159
OH
success depended heavily oh individual governments.-In the
early years few believed the 1974 resolution could be more
than a pipe dream. Improvement has been rapid, however,
and the current projection is that by 1990 four fifths of
children in the most populous countries—India, China,
Nigeria, Bangladesh, and Indonesia —will have received their
third dose of oral polio virus and diphtheria, pertussis, and
tetanus vaccines? This year there will be fewer than 30 cases
of paralysis from wild poliomyelitis in all the Americas, and
possibly both they and Europe will achieve eradication by the
end of 1990.
Saving children’s lives by
vaccination
Much achieved but > uch more could be done
Three quarters of the world's population lives in the develop
ing countries of the South. A decade ago, $40 billion flowed
every year from the North to the South: Now $20 billion flow
annually in the opposite direction. In the North at least four
fifths of all born are likely to enter retirement at the age of 65.
In the South there are still many communities where three
quarters will die before the age of 65 — and half of these deaths
will be in childhood. Ten years ago the median figure for
health expenditure per person in the North was $220, whereas
in the South it was just $4 each year. Over the past 10 years
Unicef has shown that in the poorest 36 countries this
spending on health has halved and that in some countries
infant mortality is rising.' Yet spending on armaments has
continued. Can we hope that the changes in Eastern Europe
lead to a worldwide decline in military expenditure? Just
fifteenth of the world’s military spending would provide
all basic health care needs for developing countries?
Not all is gloom, however, for health care in developing
countries. A quiet public health revolution has been taking
place, instigated by a resolution of the World Health Assembly
in 1974 to provide immunisation for all children of the world
by 1990. At that time less than 5% were immunised. The
expanded programme of immunisation now prevents around
2 million deaths from measles, pertussis, and neonatal tetanus
and almost a quarter of a million cases of paralytic poliomyelitis
each year.' There are still, however, nearly three million
children who die, 200000 who are paralysed, and 150000 who
are blinded by diseases that can be prevented through
immunisation.
Population growth
Preventing these child deaths has wider implications. No
country has reduced its population growth without first
reducing child deaths. In Africa, the current average family
Bbe is 6-7 children, and the World Bank has calculated that
mis must be cut to 3-4 to keep in step with growth in
agriculture? Demographers have shown that halving the
child mortality in the next 10 years would substantially reduce
the final stable world population.' Population growth in
relation to resources available remains the greatest ecological
threat for the future.
The eradication of smallpox fired the imagination of the
international community. Out of this arose the enthusiasm for
the programme of worldwide immunisation against six
diseases: diphtheria, pertussis, tetanus, poliomyelitis,
measles, and tuberculosis. With able guidance from the
World Health Organisation an effective cold chain and
training and management programmes were set up in every
country. Unicef played its part in funding and social mobilisa
tion. gaining political commitment through heads of states
and popular publications such as the yearly The State of the
World's Children. Many other organisations such as the
United Nations Development Programme, the Save the
Children Fund, and the Rotarians played their parts, but
Deaths from measles
Measles continues to kill at least 1-6 million children a year,
• and new research suggests that this is an underestimate. After
severe measles mortality is increased for many months from
other causes, particularly diarrhoea and respiratory infections.
The increased mortality is related to the size of the infecting
dose rather than malnutrition in the children." Vaccination
gives substantial protection, reducing child mortality from
the age of vaccination by at least 30%? A big difficulty in
many countries is that up to the present measles immunisation
cannot be given to children aged under 9 months. The World
Health Organisation recommends, however, that in 1990 a
high titre of the more immunogenic Edmonston-Zagreb
vaccine should be made available. This concentrated vaccine
will overcome residual maternal antibodies and may be used
at the age of 6 months? Unicef hopes to have supplies
available for sub-Saharan Africa by the middle of 1990.
What about other new vaccines? All the vaccines available
were already in use as long ago as 1974. There are many
exciting potentials for the improvement of existing vaccines
and new vaccines against major killer diseases, but resources
for the development of new vaccines are limited. Many
countries allot half of their research resources to the military.
Can we hope that a proponion of this could be deflected to
research on saving children’s lives? Even then, particularly at
this time of year, we need to consider the saying, “The
difference between children and adults is the size and
complexity of the toys they play with.” World wide there is an
unholy alliance between the developers of adult toys and their
manufacturers and the medical profession, and it is this that
absorbs so much research money. In Britain we suffer from
vociferous pressure groups wanting investment in a £10
million cyclotron, though there are grave doubts over its
medical value and a cost benefit analysis that would be
absurd? Such monetary resources could save the lives of
thousands of children.
DAVID MORLEY
Emeritus Professor of Tropical Child Health,
University of London,
Institute of Child Health,
London WC IN 1EH
Unicef. State of the world's children. Oxford: Oxford University Press, 1989.
Burki SJ, Voorhocve JJC, Layton R, et al. Global estimates far meeting basic needs. Washington DC:
World Bank, 1977.
3
World Health Organisation. Expanded programme of immunisation. Geneva: World Health Organisa
tion, 1989 (Progress and Evaluation Report A42/1O. )
4
World Bank. Sub-Saharan Africa from cnsis to sustainable growth. Washington DC: World Bank,
1989.
5
Unicef. State of the world's ihitdren. Oxford: Oxford University Press, 1985.
6
Morlev IX-. Aaby P. Severe measles a new understanding. Medical Digest 1970;14:4-6.
’ Aaby P, Pedersen IB, Knudsen K, et al. Child mortality related to seroconversion or lack of
seroconversion after measles vx'cmation. Paed'atr fnfea Dis 1989;8:197-200.
8 Khanum S, Uddin N. Carei: I H, Mann G, Tomkins A. Comparison of Edmondston-Zagreb and
Schwarz strains of measles vaccines given by aerosol or subcutaneous injection. Lancet |987;i;
1
2
9 Tobias JS fbccyclotron .<aga continues. Be MedJ 1989;299:1294-5.
4PROM BMJ VOL. 299 23 -30 DEC 1989, 1544-1545)
SELECTIONS FROM BMJ
vol 6
APRIL lW0
101
<LH 9
Pulse Polio Immunization (PPI) in India
Process EValuation
7 December 1996
7 DECEMBER, 1996
18 JANUARY, 1997
Name of interviewer: —-----------------------------------------------------------------------------------------------------
Designation:--------------------------------------------------------------------------------------------------------------------Date of Visit:------------------------- Time of Visit:---------------------- State :---------------------------------------
District:-------------------------------------------- City/Town/Village :-------------------------------------------- —----name of Post:---------------------------------------------------Post Coordinator:---------------------------------- —
Type of Post: Urban/Rural/Urban-slum/Re-settlement colony/Tribal transit points.
Contests:
Form I:
Interview of PPI Post Coordinator (person in-charge of post)
Form II:
Observation Check List (by independent obsrver)
Form III:
Exit Interview of People Leaving the Post (4 forms)
1
DEPARTMENT OF FAMILY WELFARE,
MINISTRY OF HEALTH & FAMILY WELFARE
GOVERNMENT OF INDIA, NEW DELHI
INSTRUCTIONS FOR FILLING UP THESE FORMS
As you are an experienced observer, the information you provide us with this evaluation is
extremely useful for the programme. Plese take time to fill out the attached forms according to the
instructions given below which may kindly be noted before filling out the forms. We value your
comments anf suggestions.
1.
Please fill up a complete set of forms including, one Form I, one Form II and four Four III (one
each for four children) for each PPI post visited by you.
2.
Please fill out one set of forms per post. If you visit more than one post, please copy this set as
needed.
3.
This is a qualitative survey. Please try to record the responses as they ar emade by the
respondents without changes. If mor ethan one response is made, record all.
4.
Please try to spend some time observing the working at the PPI post before filling up Form 2.
The post should have been open for at least two hours before the observations are made.
5.
Please tick the relevant answer.
6.
Whenever "other" is selected as a response to a question, pleaser try to specify what exactly
is meant by “other," using whenever posible the words of the respondent or your own description.
7.
An incorrect response (for instance a date other than 18/1/1997 for the next PPI or any other
vaccine) should be recorded as "doesn't know" indicating the respondent does not know the
correct answer.
8.
please try not to prompt the respondent. This is especially important for questions like No. 5
and 6 of Form III where the responses should be recorded as said by the repondent.
9.
Please be free to record your own observations in the spaces provided on Form II. Your valuable
observations will enable us to improve the second round on 18/1/1997.
10.
Kindly post these forms back latest by Monday, December 9,4997 so that they can be analyzed
in time to improve the second round of PPI on 18/1/1997, using the enclosed self addressed
envelope.
W
THANK YOU.
PLEASE POST ALL FORMS BY 9 DECEMBER TO :
Dr. Kaushik Banerjee
Assistant Commissioner (I)
Ministry of Health and Family Welfare
Post Box No. 5419
Nirman Bhavan
New Delhi -110 011.
2
Form I
INTERVIEW OF THE PPI POST COORDINATOR
1.
What is the total number of workers at this post ?
Health workers
Anganwadi workers
Teachers
Students
NGOs
Community vonteers
Armed Forces
Others (specify)
2.
What is the number of children 0-59 months (less than 5 years) of age expected ?
3.
How many ORV vaccine vials were received ?
4.
Did vaccines arrive :
5.
What cold chain equipment are available at this post ?
on time / delayed
Vaccine carriers Day carriers
6.
Others (specify)
What communication materials have been received?
Banner / Flag / Stickers / Posters / Others (specify)
7.
A)
Are there some localities within your catchment area from where children may not
come?
Yes / No
B)
If yes to part A, please describe these areas :
(C)
If yes to part A, what is your plan to reach these areas:
8.
Are any children being returned without vaccination?
9.
What suggestions do you have for change or improvements?
3
Yes/No If yes, give reasons:
Form II
OBSERVATION CHECKLIST
1.
Where FROZEN ice packs or ice present ?
Yes / No
2.
a) Did you find the Vaccine Vial Monitor (VVM) sticker on the vaccine vial?
Yes / No
b) If yes, the colour of the square changed
to-------------------- than the circle.
Lighter/Same /Darker
Yes I No
3.
Is the age of the child being checked ?
4.
Record maintained by: Tally sheets I Enumeration lists / Names being recorded /
Others (specify) ------------------------------------------------------------------------------------------- —--------
5.
Observe 4 children being given polio vaccine: Record the number of drops given to:
Child No. 1------------------------
Child No. 2---------------------------
Child No. 3------------------------
Child No. 4---------------------------
6.
Is the PPI site easily identifiable ?
7.
What are your additional comments or observations about the functioning of this PPI Post
(examples: description of physical facility, vaccination skills of person giving vaccine, adequacy
of materials, novel ways to identify post, etc.) ?
Yes / No
4
Form III
EXIT INTERVIEWS WITH PEOPLE LEAVING THE PPI POST (Fill out 4 forms)
Child No. 1
1.
How old is your child ?
2.
What vaccine did your child receive today ?
3.
How did you know where and when to come for the vaccine ?
------------------- Years ------------------- Months
Polio / None/Doesn't know
(do not prompt)
Check all the aapply :
Health staff
Anganwadi worker
Teacher
SchoOl students
Relative, friend or neighbour
Other volunteers
Radio
TV
Posters, leaflets
Loudspeaker/microphone
Others ------------------------------------------------------------------------------------------------------------------------
4.
When is the next Pulse Polio Immunization Day ?
18 January 1997
5.
------------------- Doesn't know
How will the programme today help your child ?
Prevent polio or eardicate polio / Others (specify):--------------------------------------------------
6.
What suggestions do you have for change or improvement of this programme ?
Thank respondent for participation and remind them about NEXT PPI on 18 January 1997.
5
Child No. 2
----------------- Years ------------------ Months
1.
How old is your child ?
2.
What vaccine did your child receive today?
3.
How did you know where and when to come for the vaccine ?
Polio / None /Doesn't know
(do not prompt)
Check all that apply :
Health staff
Anganwadi worker
-------------
Teacher
School students
-------------
Relative, friend or neighbour
Other valunteers
-------------
Radio
TV
-------------
Posters, leaflets
Loudspeaker/microphone
-------------
Others --------------------------------------------------------------------------------------------------------------------- -----4.
When is the next Pulse Polio Immunization Day ?
------------- 18 January 1997
5.
--------------- Doesn't know
How will the programme today help your child ?
Prevent polio or eradicate polio / Others (specify) :
6.
What suggestions do you have for change or improvement of this programme ?
Thank respondent for participationand remind them about NEXT PPI on 18 January 1997.
6
Child No. 3
1.
How old is your child ?
2.
What vaccine did your child receive today?
3.
How did you know where and when to come for the vaccine ?
---------------- Years ------------------ Months
Polio I None /Doesn't know
(do not prompt)
Check all that apply :
Health staff
Anganwadi worker
Teacher
School students
Relative, friend or neighbour
Other valunteers
Radio
TV
Posters, leaflets
Loudspeaker/microphone
Others -----------------------------------------------------------------------------------------------------------------------
4.
When is the next Pulse Polio Immunization Day ?
18 January 1997
5.
------------- Doesn't know
How will the programme today help your child ?
Prevent polio or eradicate polio / Others (specify) : -----------------------------------------------
6.
What suggestions do you have for change or improvement of this programme ?
Thank respondent for participationand remind them about NEXT PPI on 18 January 1997.
7
Child No. 4
1.
How old is your child ?
2.
What vaccine did your child receive today?
3.
How did you know where and when to come for the vaccine ?
Months
--------------- Years
Polio / None /Doesn't know
(do not prompt)
Check all that apply :
Health staff
------------
Anganwadi worker
Teacher
------------
School students
Relative, friend or neighbour
------------
Other valunteers
Radio
------------
TV
Posters, leaflets
------------
Loudspeaker/microphone
Others -------------------------------- —----- ------------------------------------------------------------------------4.
When is the next Pulse Polio Immunization Day ?
------------ 18 January 1997 ------------- Doesn't know
5.
How will the programme today help your child ?
Prevent polio or eradicate polio / Others (specify) : --------------------------------------------
6.
What suggestions do you have for change or improvement of this programme ?
Thank respondent for participationand remind them about NEXT PPI on 18 January 1997.
8
dH
.dispelling vaccination myths
Page I of 14
SUMERIA
Dispelling Vaccination Myths
A Documented Report
© by Alan Phillips
An introduction to the contradictions between
medical science and immunization policy.
Revised periodically. This Printing Revised July 14, 1996
INTRODUCTION
|
When my son began his routine vaccination series at age 2 months, I did not know there
were any risks associated with immunizations. But the clinic's literature contained a
contradiction: the chances of an adverse reaction to the DPT vaccine were J in 1750, while
his chances of dying from pertussis each year were one in several million. When I pointed
this out to the physician, he angrily disagreed, and stormed out oflhc room mumbling, "1
guess I should read that sometime..." Soon thereafter I learned of a child who had been
permanently disabled by a vaccine, so 1 decided to investigate for myself. My findings have
so alarmed me that I feel compelled to share them; hence, this report.
Health authorities credit vaccines for disease declines, and assure us of their safety and
effectiveness. Yet these seemingly rock-solid assumptions are directly contradicted by
health statistics, medical studies, Food and Drug Administration (FDA) and Centers for
Disease Control (CDC) reports, and reputable research scientists from around the world.
In fact, infectious diseases steadily declined for decades prior to vaccinations, U.S. doctors
report thousands of vaccine reactions each year'including hundreds of deaths and
permanent disabilities, many fully vaccinated populations have experienced epidemics, and
researchers attribute dozens of chronic immunological and neurological conditions to mass
" immunization programs.
Hundreds of published medical studies document vaccine failure and adverse effects;
several dozen books have been written expounding on these and related information
condemning vaccines. Yet, amazingly, most pediatricians and parents are completely
unaware of these findings. There is, however, a fast growing international movement of
doctors and parents who are questioning the use of widespread, mandatory vaccinations.
My point is not to tell anyone whether or not to vaccinate, 'nit rather, with the utmost
urgency, to point out some very good reasons why everyone should investigate the issue
before submitting to the procedure. As a new parent, I was shocked to discover the
absence of a legal mandate or professional ethic requiring pediatricians to be fully
informed, and to see firsthand the prevalence of physicians who are applying practices
based on incomplete - and in some cases, outright mis-information.
ittp://www. Iivelinks.com/sumeria/health/myth2.html
08/08/96
’At|-
DISPELLING VACCINATION MYTHS
Page 2 of 14
Though only a brief introduction, this report contains sufficient evidence to warrant further
investigation by all concerned, which I highly recommend. You will find that this is the
only way to get an objective view, as the controversy is a highly emotional one.
A note of caution: Be careful trying to discuss this subject with a pediatrician. Mo,st have
staked their identities and reputations on the presumed safety and effectiveness of vaccines,
and thus have difficulty acknowledging evidence to the contrary, regardless of the sources.
The fii ;.t pediatrician 1 ten.pled to share my findings with yelled angrily at me when 1
calmly brought up the subject. The misconceptions have very deep roots.
VACCINATION MYTH #1: "Vaccines are completely safe..."
... or are they?
The FDA's VAERS (Vaccine Adverse Effects Reporting System) receives about 11,000
reports of adverse vaccine reactions annually, some 1% (112+) of which are deaths from
vaccine reactions.[l] The majority of these reports are made by doctors, and the majority
of deaths are attributed to the pertussis (whooping cough) vaccine, the "P" in DPT. This
figure alone is alarming, yet it is only the "tip of the iceberg." The FDA estimates that only
about 10% of adverse reactions are reported,[2] a figure supported by two National
Vaccine Information Center (NVIC) investigations.[3] In fact, the NVIC reported that "In
New York, only one out of 40 doctor's offices [2.5%] confirmed that they report a death
or injury following vaccination," - 97.5% of vaccine related deaths and disabilities go
unreported there. Implications about the integrity of medical professionals aside (doctors
are legally required to report all adverse events), these findings suggest that vaccine deaths
actually occurring each year may be well over 1,000.
With pertussis, the number of vaccine-related deaths dwarfs the number of disease deaths,
which have been about 10 annually for recent years according to the CDC, and only 8 in
1993. the last peak-incidence year (pertussis runs in 3-4 year cycles, though vaccination
doesn't). Simply put, the vaccine is 100 times more deadly than the disease. If it were not
for the many instances in which highly vaccinated populations have contracted disease (see
Myth #2), and the fact that the vast majority of disease decline this century occurred before
compulsory vaccinations (pertussis deaths declined 79% prior to vaccines; see Myth //3),
this might be understandable, but given the complete story, it can hardly be considered a
necessary' sacrifice for the benefit of a disease-free society.
Unfortunately, the vaccine-rclated-deaths story doesn't end here. Both national and
international studies have shown vaccination to be a cause of SIDS [4,5] (SIDS is "Sudden
Infant Death Syndrome," a "catch-all" diagnosis for cases when the specific cause of death
is supposedly unknown; estimates range from 5 - 10,000 cases each year in the U.S.). One
study found the peak incidence of SIDS occurred at the ages of 2 and 4 months in the
U.S., precisely when the first two routine immunizations are given.[4]
There are also studies that claimed to find no SIDS-vaccine relationship. However, many
of these were invalidated by yet another study which found that "confounding" had skewed
http://www.livelinks.com/sumeria/healtli/myth2.hlml
08/08/96
^SPELLING VACCINATION MYTHS
'
Page 3 of 14
their results in favor of the vaccine.[6]
Shouldn't we err on the side of caution? Shouldn't any credible correlation between
vaccine’s'and infant deaths be just cause for meticulous, widespread monitoring of the •
vaccination status of all SIDS cases? In the mid 70’s Japan raised their vaccination age
from 2 months to 2 years; their incidence of SIDS dropped dramatically.
In spite of this, the U.S. medical community has chosen a posture of denial. Coroners
refuse to check the vaccination status of SIDS victims, and unsuspecting families continue
to pay the price, unaware of the dangers and deprived of the right to make a choice.
Low adverse event reporting also suggests that the total number of adverse reactions
actually occurring each year may be more than 100,000. Due to doctors' failure to report,
no one knows how many of these are permanent disabilities, but statistics suggest that it is
several times the number of deaths (see "petitions" below). This concern is reinforced by a
study which revealed that one in 175 children who completed the full DPT series suffered
•"severe reactions,"[7] and a Dr.'s report for attorneys which found that 1 in 300 DPT
immunizations resulted in seizures.[8]
England actually saw a drop in pertussis deaths when vaccination rates dropped from 80%
to 30% in the mid 70's. Swedish epidemiologist B. Trollfors' study of pertussis vaccine
efficacy and toxicity around the world found that "pertussis-associated mortality is
currently very low in industrialised countries and no difference can be discerned when
countries with high, low, and zero immunisation rates were compared." He also found that
England, Wales, and West Germany had more pertussis fatalities in 1970 when the
immunization rate was high than during the last half of 1980, when rates had fallen. [9]
Vaccinations cost us much more than just the lives and health of our children. The U.S.
Federal Government's National Vaccine Injury Compensation Program (NV1CP) has paid
out over S650 6 million to parents of vaccine injured and killed children, a rate of close to
S90 million per year in taxpayer dollars. The NVICP has received over 5,000 petitions
since 1988, including over 700 for vaccine-related deaths, and there are still some two
^housand total death and injury cases pending that may take years to resolve.[10]
'Meanwhile, pharmaceutical companies have a captive market: vaccines arc legally
mandated in all 50 U.S. states (though legally avoidable in most; see Myth #9), yet these
same companies are "immune" from accountability for the consequences of their products.
Furthermore, they have been allowed to use "gag orders" as a leverage tool in vaccine
damage legal settlements to prevent disclosure of information to the public about
vaccination dangers. Such arrangements are clearly unethical; they force a nonconsenting
American public to pay for vaccine manufacturer's liabilities, while attempting to ensure
that this same public will remain ignorant of the dangers of their products.
It is also interesting to note that insurance companies (who do the best liability studies)
refuse to cover vaccine adverse reactions. Profits appear to dictate both the pharmaceutical
and insurance companies' positions.
VACCINATION TRUTH #1: "Vaccination causes significant death and disability at an
>://www. Iivelinks.com/sumeria/health/myth2.html
08/08/96
DISPELLING VACCINATION MYTHS
Page 4 of 14
astounding personal and financial cost to families and taxpayers."
VACCINATION MYTH #2: "Vaccines are very effective..."
... aren't they?
The medical literature has a sui prising number of studies ducumcniing vaccine failure.
Measles, mumps, small pox, polio and Hib outbreaks have al! occurred in vaccinated
populations.[l 1,12,13,14,15] In 1989 the CDC reported: "Among school-aged children,
[measles] outbreaks have occurred in schools with vaccination levels of greater than 98
percent.[ 16] [They] have occurred in all parts of the country, including areas that had not
reported measles for years."[17] The CDC even reported a measles outbreak in a
documented 100 percent vaccinated population.[18] A study examining this phenomenon
concluded, "The apparent paradox is that as measles immunization rates rise to high levels
in a population, measles becomes a disease of immunized persons."[19] A more recent
study found that measles "produces immune suppression which contributes to an increased
susceptibility to other infections. "[19a] These studies suggests that the goal of complete
immunization is actually counterproductive, a notion underscored by instances in which
epidemics followed complete immunization of entire countries. Japan experienced yearly
increases in small pox following the introduction of compulsory vaccines in 1872. By 1892,
there were 29,979 deaths, and all had been vaccinated.[20] Early in this century, the
Philippines experienced their worst smallpox epidemic ever after 8 million people received
24.5 million vaccine doses; the death rate quadrupled as a result.[21] In 1989. the country
of Oman experienced a widespread polio outbreak six months after achieving complete
vaccination (98%).[22] In the U.S. in 1986, 90% of 1,300 pertussis cases in Kansas were
"adequately vaccinated."[23] 72% of pertussis cases in the 1993 Chicago outbreak were
fully up to date with their vaccinations.[24]
VACCINATION TRUTH #2: "Evidence suggests that vaccination is an unreliable means of
preventing disease."
VACCINATION MYTH #3: "Vaccines are the main reason for low disease rates in the U.S.
today..."
... or arc they?
According to the British Association for the Advancement of Science, childhood diseases
decreased 90% between 1850 and 1940, paralleling improved sanitation and hygienic
practices, well before mandatory vaccination programs. Infectious disease deaths in the
U.S. and England declined steadily by an average of about 80% during this century
(measics mortality declined over 97%) prior to vaccinations.[25] In Great Britain, the polio
epidemics peaked in 1950, and had declined 82% by the time the vaccine was introduced
there in 1956. Thus, at best, vaccinations can be credited with only a small percentage of
the overall decline in disease related deaths this century. Yet even this small portion is
questionable, as the rate of decline remained virtually the same after vaccines were
introduced. Furthermore, European countries that refused immunization for small pox and
http://www.livelinks.com/sumeria/healtli/m_Mh2.html
08/08/96
DISPELLING VACCINATION MYTHS
’
Page 5 of 14
polio saw the epidemics end along with those countries that mandated it. (In fact, both
small pox and polio immunization campaigns were followed initially by significant disease
increases; during smallpox campaigns, other infectious diseases continued their declines in
the absence of vaccines. In England and Wales, smallpox disease and vaccination rates
eventually declined simultaneously over a period of several decades.) [26] It is thus
impossible to say whether or not vaccinations contributed to the continuing decline, or if
the same forces which brought about the initial declines - improved sanitation, hygiene,
improvements in diet, natural disease cycles - were simply unaffected by the vaccination
programs. Underscoring this conclusion was a recent World Health Organization report
which found that the disease and mortality rates in third world countries have no direct
correlation with immunization procedures or medical treatment, but are closely related to
the standard of hygiene and diet. [27] Credit given to vaccinations for our current disease
incidence has simply been grossly exaggerated, if not outright misplaced.
Vaccine advocates point to incidence statistics rather than mortality as proof of vaccine
effectiveness. However, statisticians tell us that mortality statistics can be a better measure
of incidence than the incidence figures themselves, for the simple reason that the quality of
W reporting and record-keeping is much higher on fatalities.[28]
For instance, a recent survey in New York City revealed that only 3.2% of pediatricians
were actually reporting measles cases to the health department. In 1974, the CDC
determined that there were 36 cases of measles in Georgia, while the Georgia State
Surveillance System reported 660 cases.[29] In 1982, Maryland state health officials
blamed a pertussis epidemic on a television program, "D.P.T. - Vaccine Roulette," which
warned of the dangers of DPT; however, when former top virologist for the U.S. Division
of Biological Standards, Dr. J.. Anthony Morris, analyzed the 41 cases, only 5 were
confirmed, and all had been vaccinated. [30] Such instances as these demonstrate the
fallacy of incidence figures, yet vaccine advocates tend to rely on them indiscriminately.
VACCINATION TRUTH #3 "It is unclear what impact vaccines had on infectious disease
declines which occurred throughout this century."
VACCINATION MYTH #4: "Vaccination is based on sound immunization theory and
^ctice..."
... isn't it?
The clinical evidence for vaccinations is their ability to stimulate antibody production in the
recipient, a fact which is not disputed. What is not clear, however, is whether or not such
antibody production constitutes immunity. Agamma globulin-anemic children are incapable
of producing antibodies, yet they recover from infectious diseases almost as quickly as
other children.[31] Furthermore, a study published by the British Medical Council in 1950
during a diphtheria epidemic concluded that there was no relationship between antibody
count and disease incidence; researchers found resistant people with extremely low
antibody counts and sick people with high counts.[32] Natural immunization is a complex
phenomenon involving many organs and systems; it cannot be fully replicated by the
artificial stimulation of antibody production.
p://www. Iivelinks.com/sumeria/health/myt h2.html
08/08/96
DISPELLING VACCINATION MYTHS
•
Page 6 of 14
Research also indicates that vaccination commits immune cells to the specific antigens
involved in the vaccine, rendering them incapable of reacting to other infections. Our
immunological reserve may thus actually be reduced, causing a generally lowered
resistance.[33]
Another component of immunization theory is "herd immunity," which states that when
enough people in a community are immunized, all are protected. As Myths #2 revealed,
there are many documented instances showing just the opposite - fully vaccinated
populations have contracted diseases. With measles, this actually seems to be the direct
result of high vaccination rates. [19] A Minnesota state epidemiologist concluded that the
Hib vaccine increases the risk of illness when a study revealed that vaccinated children
were five times more likely to contract the disease than unvaccinated children.
Carefully selected epidemiological studies are yet another justification for vaccination
programs. However, many of these may not be legitimate sources from which to draw
conclusions about vaccine effectiveness: If 100 people are vaccinated and 5 contract the
disease, the vaccine is declared to be 95% effective. But if only 10 of the 100 were actually
exposed to the disease, then the vaccine was really only 50% effective. Since no one is
willing to directly expose an entire population to disease - even a fully vaccinated one vaccine effectiveness rates cannot be taken at face value.
Yet another concern about immunization practice is its assumption that all children,
regardless of age, are virtually the same. An S pound 2 month old receives the same dosage
as a 40 pound five year old. Infants with immature, undeveloped immune systems may
receive five or more times the dosage (rela'tive to body weight) as older children.
Furthermore, the number of "units" within doses has been found upon random testing to
range from 1/2 to 3 times what the label indicates; manufacturing quality controls appear to
tolerate a rather large margin of error. "Hot Lots" (vaccine lots with disproportionately
high death and disability rates) have been identified repeatedly by the NV1C, but the FDA
refuses to intervene to prevent unnecessary injury and loss of life. In fact, they have never
recalled a vaccine lot due to adverse reactions. Some would call this infanticide.
Finally, vaccination practice assumes that all recipients, regardless of race, culture, diet, or
any other circumstances, will respond the same. This was perhaps never more dramatically
disproved than an instance a few years ago in Australia's Northern Territory, where
stepped-up immunization campaigns resulted in an incredible 50% infant mortality rate in
the native aborigines.[34] Researcher A. Kalokerinos, M.D. discovered that the aborigine's
vitamin C deficient "junk food" diet was a critical factor (vaccination depletes vitamin C
reserves; children in shock or collapse often recovered in a matter of minutes when given
vitamin C iniections). He considered it amazing that as many survived as did. One must
wonder about the lives of the survivors, though, for if half died, surely the other half did
not escape unaffected.
Almost as troubling was a very'recent study in the New England Journal of Medicine
which revealed that a substantial number of Romanian children were contracting polio from
the vaccine, a less common phenomena in most'developed countries. Correlations with
http://www.livelinks.com/sumeria/health/myth2.html
08/08/96
DISPELLING VACCINATION MYTHS
•
Page 7 of 14
injections of antibiotics were found: a single injection within one month of vaccination
raised the risk of polio eight times, two to nine injections raised the risk 27-fold, and 10 or
more injections raised the risk 182 times [Washington Post, February 22, 1995],
What other factors not accounted for in vaccination theory will surface unexpectedly to
reveal unforeseen or previously overlooked consequences? We will not begin to fully
comprehend the scope of this danger until researchers begin looking and reporting in
earnest. In the meantime, entire countries' populations are unwitting gamblers in a game
that many might very well choose not to play if they were given all the "rules" in advance.
VACCINATION TRUTH #4: "Many of the assumptions upon which immunization theory
and practice are based have been proven false in their application."
VACCINATION MYTH #5: "Childhood diseases are extremely dangerous..."
... or are they, really?
Most childhood infectious diseases have few serious consequences in today's modern
world. Even conservative CDC statistics for pertussis during 1992-94 indicate a 99.8%
recovery rate. In fact, when hundreds of pertussis cases occurred in Ohio and Chicago in
the fall 1993 outbreak, an infectious disease expert from Cincinnati Children's Hospital
said, "The disease was very mild, no one died, and no one went to the intensive care unit."
The vast majority of the time, childhood infectious diseases are benign and self-limiting.
They also impart lifelong immunity, whereas vaccine-induced immunity is only temporary.
In fact, the temporary nature of vaccine immunity can create a more dangerous situation in
a child's future. For example, the new chicken pox vaccine has an effectiveness estimated at
10 years. If effective,it will postpone the child's vulnerability until adulthood, when death
6from the disease is 20 times more likely. (About half of measles cases in the late 1980’s
resurgence were in adolescents and adults, most of whom were vaccinated as children,[35]
and the recommended booster shots may provide protection for less than 6 months.) [36]
Furthermore, some healthcare professionals are concerned that the virus from the chicken
pox vaccine may "reactivate later in life in the form of herpes zoster (shingles) or other
immune system disorders."[37] Dr. A. Lavin of the Dept, of Pediatrics, St. Luke's Medical
Center in Cleveland, Ohio, strongly opposed licensing the new vaccine, "Until we actually
know...the risks involved in injecting mutated DNA [herpes virus] into the host genome
[children],"[38] The truth is, no one knows, but the vaccine is now licensed and
recommended by health authorities.
Not only are most infectious diseases rarely dangerous, but they can actually play a vital
role in the development of a strong, healthy immune system. Persons who have not had
measles have a higher incidence of certain skin diseases, degenerative diseases of bone and
cartilage, and certain tumors, while absence of mumps has been linked to higher risks of
ovarian cancer.
VACCINATION TRUTH #5: "Dangers of childhood diseases are greatly exaggerated in
order to scare parents into compliance with a questionable but profitable procedure."
http://www. livelinks.com/sumeria/heahh/myt h2.html
08/08/96
DISPELLING VACCINATION MYTHS
•
Page 8 of ;
VACCINATION MYTH #6: "Polio was one of the clearly great vaccination success
stories..."
... or was it?
Six New England states reported increases in polio one year after the Salk vaccine was
introduced, ranging from more than doubling in Vermont to Massachusetts’ astounding
increase of 642%. In 1959, 77.5% of Massachusetts' paralytic cases had received 3 doses
of 1PV (injected polio vaccine). During 1962 U.S. Congressional hearings, Dr. Bernard
Greenberg, head of the Dept, of Biostatistics for the University of North Carolina School
of Public Health, testified that not only did the cases of polio increase substantially after
mandatory vaccinations (50% increase from 1957 to 1958, 80% increase from 1958 to
1959). but that the statistics were manipulated by the Public Health Service to give the
opposite impression.[39] According to researcher-author Dr. Viera Scheibner, 90% of
polio cases were eliminated from statistics by health authorities' redefinition of the disease
which occurred when the vaccine was introduced, while in fact the Salk vaccine was
continuing to cause paralytic polio in several countries at a time when there were no
epidemics caused by the wild virus (thousands of cases of viral and aseptic meningitis are
Q
diagnosed each year in the U.S.; prior to the polio vaccine, these were diagnosed as polio).
In 1985, the CDC reported that 87% of the cases of polio in the U.S. between 1973 and
1983 were caused by the vaccine, and later declared that all but a few imported cases since
were caused by the vaccine (and most of the imported cases occurred in full}' immunized
individuals). Jonas Salk, inventor of the 1PV, testified before a Senate subcommittee that
nearly all polio outbreaks since 1961 were'caused by the oral polio vaccine. At a workshop
on polio vaccines sponsored by the Institute of Medicine and the Centers for Disease
Control and Prevention, Dr. Samuel Katz of Duke University cited the estimated 8-10
annua! U.S cases of vaccine-associated paralytic polio (VAPP) in people who have taken
the oral polio vaccine, and the [four year] absence of wild polio from the western
hemisphere. Jessica Scheer of the National Rehabilitation Hospital Research Center in
Washington, D.C., pointed out that most parents are unaware that polio vaccination in this
country entails "a small number of human sacrifices each year." Compounding this
contradiction arc low' adverse event reporting and the NVIC's experiences with confirming
and correcting misdiagnoses of vaccine reactions, which suggest that the actual number of
VAPP "sacrifices" may be much higher than the number cited by the CDC.
VACCINATION TRUTH //6: "Vaccines caused substantial increases in polio after years of
steady declines, and they are the sole cause of polio in the U.S. today."
VACCINATION MYTH #7- "My child had no short-term reaction to vaccination, so there is
nothing to worry about..."
... or is there?
The documented long term adverse effects of vaccines include chronic immunological and
neurological disorders such as autism, hyperactivity, attention deficit disorders, dyslexia,
allergies, cancer, and other conditions, many of which barely existed 30 years ago before
mass vaccination programs. Vaccine components include known carcinogens such as
http://www.livelinks.com/sumeria/healtli/myt h2.html
08/08/96
DISPELLING VACCINATION MYTHS
Page 9 of 14
thimersol, aluminum phosphate, and formaldehyde (the Poisons Information Centre in
Australia claims there is no acceptable safe amount of formaldehyde which can be injected
into a living human body). Medical historian, researcher and author Harris Coulter, Ph D.
explained that his extensive research revealed childhood immunization to be "...causing a
low-grade encephalitis in infants on a much wider scale than public health authorities were
willing to admit, about 15-20% of all children." He points out that the sequelae [conditions
known to result from a disease] of encephalitis [inflammation of the brain, a known
side-effect of vaccination]: autism, learning disabilities, minimal and not-so-minimal brain
damage, seizures, epilepsy, sleeping and eating disorders, sexual disorders, asthma, crib
death, diabetes, obesity, and impulsive violence are precisely the disorders which afflict
contemporary society. Many of these conditions were formerly relatively rare, but they
have become more common as childhood vaccination programs have expanded. Coulter
also points out that "...pertussis toxoid is used to create encephalitis in lab animals."
A German study found correlations between'vaccinations and 22 neurological conditions
including attention deficit and epilepsy. The dilemma is that viral elements in vaccines may
persist and mutate in the human body for years, with unknown consequences. Millions of
children are partaking in an enormous, crude experiment; and no sincere, organized effort
is being made by the medical community to track the negative side-effects or to determine
the long term consequences.
VACCINATION TRUTH #7: "The long term adverse effects of vaccinations have been
virtually ignored, in spite of strong correlations with many chronic conditions."
VACCINATION MYTH #8: "Vaccines are the only disease prevention option available..."
... or arc they?
Most parents feel compelled to take some disease-preventing action for their children.
While there is no 100% guarantee anywhere, there are viable alternatives. Historically,
homeopathy has been more effective than "allopathic mainstream" medicine in treating and
preventing disease. In a U.S. cholera outbreak in 1849, allopathic medicine saw a 48-60%
death rate, while homeopathic hospitals had a documented death rate of 3%.[40] Roughly
similar statistics still hold true for cholera today.[41] Recent epidemiological studies show
homeopathic remedies as equaling or surpassing standard vaccinations in preventing
disease. There are reports in which populations that were treated homeopathicahy after
exposure had a 100% success rate - none of the treated caught the disease. [42]
There are homeopathic kits available for disease prevention.[43] Homeopathic remedies
can also be taken only during times of increased risk (outbreaks, traveling, etc.), and have
proven highly effective in such instances. And since these remedies have no toxic
components, they have no side effects. In addition, homeopathy has been effective in
reversing some of the disability caused by vaccine reactions, as well as many other chronic
conditions with which allopathic medicine has had little success.
VACCINATION TRUTH #8: "Documented safe and effective alternatives to vaccination
have been available for decades but suppressed by the medical establishment."
http://www.livelinks.com/sumeria/health/myth2.html
08/08/96
DISPELLING VACCINATION MYTHS
Page 10 of 14
VACCINATION MYTH #9: "Vaccinations are legally mandated, and thus unavoidable..."
... aren't they?
There are three exemption possibilities in most U.S. states:
I.
Medical Exemption: All 50 states in the U.S. allow for a medical exemption. A few
states allow licensed naturopathic or chiropractic doctors to issue medical
exemptions in addition to medical doctors. However, few pediatricians check for
indications of increased risk before administering vaccines, so it is advisable for
parents to research this matter for themselves. Epilepsy, severe allergies, and
siblings' previous adverse reactions are but a few of the many conditions in child or
family history which may increase the chances of an adverse reaction, and thus
qualify for a medical exemption;
2
Religious Exemption: Nearly all states allow for a religious exemption. This may or
may not require membership in an established religious organization, as individual
state laws vary; and
■ 3. Philosophical Exemption: An increasing number of states allow philosophical
exemptions, in recognition of the controversy and/or violation of freedom that
mandated vaccination laws impose.
Generally, exempted children may not be banned from attending public schools and
colleges except during local outbreaks. It is best to contact local school officials in advance
to determine their particular procedure for handling exemptions.
The best source for a copy of your state's vaccination laws is state health officials. A phone
call to the state Department of Epidemiology may be all that it takes to get a copy mailed
to you.
VACCINATION TRUTH #9: "Legal exemptions from vaccinations are obtainable for most but not all - U.S. citizens."
VACCINATION MYTH #10: "Public health officials always place health above all other
concerns..."
... or do they?
Vaccination history is riddled with documented instances of deceit designed to portray
vaccines as mighty disease conquerors, when in fact many times they have actually delayed
and even reversed disease declines. The United Kingdom's Department of Health admitted
that vaccination status determined the diagnosis of subsequent diseases:
Those found in vaccinated patients received alternate diagnoses; hospital records and death
certificates were falsified. Today, many doctors are still reluctant to diagnose diseases in
vaccinated children, and so the "Myth" about vaccine success continues.
http://www.livelinks.com/sumeria/health/mvth2.html
08/08/96
/
/DISPELLING VACCINATION MYTHS
.
Page 11 of 14
However, individual doctors may not be wholly to blame. As medical students, few have
reason to question the information taught (which does not address the concerns presented
in this report). Ironically, medicine is a field which demands conformity; there is little
tolerance for opinions opposing the status quo. Doctors cannot warn you about what they
themselves do not know, and with little time for further education once they begin practice,
they are, in a sense, held captive by a system which discourages them from acquiring
information independently and forming their own opinions. Those few that dare to question
the status quo are frequently ostracized, and in any case, they are still legally bound to
adhere to the system's legal mandates.'
SUMMARY
W
In the December 1994 Medical Post, Canadian author of the best-seller Medical Mafia,
Guylaine Lanctot, M.D. stated, "The medical authorities keep lying. Vaccination has been a
disaster on the immune system. It actually causes a lot of illnesses. We are actually
changing our genetic code through vaccination... 10 years from now we will know that the
biggest crime against humanity was vaccines." After an extensivb study of the medical
literature on vaccination, Dr. Viera Scheibner concluded that "there is no evidence
whatsoever of the ability of vaccines to prevent any diseases. To the contrary, there is a
great wealth of evidence that they cause serious side effects." These would seem to be
radical positions, but they are not unfounded. The continued denial of the evidence against
vaccines only perpetuates the "Myths" and their negative consequences on our children and
society. Aggressive and comprehensive scientific investigation is clearly warranted, yet
immunization programs continue to expand in the absence of such research. Manufacturer
profits aie guaranteed, while accountability for the negative effects is conspicuously absent.
This is especially sad given the readily available safe and effective alternatives.
Meanwhile, the race is on. According to the NV1C, there are over 250 new vaccines being
developed for everything from earaches to birth control to diarrhea, with about 100 of
these already in clinical trials. Researchers are working on vaccine delivery through nasal
sprays, mosquitoes (yes, mosquitoes), and the fruits of "transgenic" plants in which vaccine
viruses are grown. With every child (and adult, for that matter) on the planet a potential
required recipient of multiple doses, and every healthcare system and government a
potential buyer, it is little wonder that countless millions of dollars are spent nurturing the
growing multi-billion dollar vaccine industry. Without public outers', we will see more and
more new vaccines required of us and our children. And while profits are readily calculable,
the real human costs are being ignored.
Whatever your personal vaccination decision, make it an informed one; you have that right
and responsibility. It is a difficult issue, but there is more than enough at stake to justify
whatever time and energy it takes.
I
Do not use this report alone to make your vaccination decision:
FIND OUT FOR YOURSELF!
’’This report is periodically revised. For the latest version, point your World Wide Web
http.7/ww wjivelinks.com/sumeria/healtli/myth2.html
0S/08/96
DISPELLING VACCINATION MYTHS
'
Page 12 of 14
browser to Sumeria's Home Page at: http://www.livelinks.com/sumeria/heahh/myth2.html ,
send email to intcrconi-gnandpjict, or write to the address below. For permission to
reprint, distribute or electronically post this report, write to the address below or send
email.
Dispelling Vaccination Myths and the Vaccination Resource Directory (publishers, books,
tapes, videos, newsletters, government agencies, nonprofits, vaccination alternatives,
internet and WWW sources, etc.) are available for $5 + $2 P/H from: Vaccine Awareness,
P.O Box 62282, Durham, NC 27715, U.S.A. Quantity discounts available.
ABOUT THE AUTHOR...
Alan Phillips is an independent investigator and writer on vaccine risks and alternatives.
This report appeared in the April 1996 edition of "Wildfire Magazine," as well as numerous
newsletters in the U.S. and around the world. It is being used by the Sheffield School of
Homeopathy, UK. Alan has written to the Australian Minister for Human Services and
Health for the Immunisation Investigation Group and the Campaign Against Fraudulent
Medical Research in NSW Australia.
Ak\'.i is also the founder of Human Development Services, Inc., an international nonprofit
conducting training and research in psychorientology; the designer of a national children's
literacy program and materials; and a singer-songwriter and composer with albums of
original songs and music in over two dozen countries on six continents. 1 lis academic
achievements include a B.A. Magna Cum Laude, and election to the Phi Kappa Phi
National Honor Society and The National Dean's List.
INFORMATION SOURCES:
I.
National Technical Infonnation Service. Springfield, VA 22161. 703-487-4650. 703-487-4600.
2.
Reported by KM Severyu,R.Ph..Pb.D. in the Dayton Daily News, May 28, 1993.
3.
National Vaccine Infonnation Center (NVIC), 512 Maple Ave. W. #206, Vienna, VA 22180,
703-938-0342; "Investigative Report on the Vaccine Adverse Event Reporting System.''
4.
Viera Scheibuer, Ph.D.. Vaccination: 100 Years of Orthodox Research Shows that Vaccines Represent a
Medical Assault on the Immune System.
5.
W.C. Torch. "Diptheria-pertussis-tetauus (DPT) immunization: A potential caouse of the sudden infant
death syndrome (SIDS)," (Amer. Adacemy of Neurology. 34th Annual Meeting. Apr 25 - May I. 1982).
Neurology 32(4). pl. 2.
6.
Confounding in studies of adverse reactions to vaccines [see comments). Fine PE, Chen RT, REVIEW
ARTICLE: 38 REFS. Comment in: Am J Epidemiol 1994 Jan 15; 139(2):229-3O.
Division of immunization. Centers for Disease Control, Atlanta. GA 30333.
7.
Nature and Rates of Adverse Reactions Associated with DIP and DT Immunizations in Infants and
Children" (Pediatrics. Nov. 1981. Vol. 68. No. 5)
X. The Fresno Bee. Community Relations. 1626 E. Street. Fresno. CA 93786, DP f Report, December 5.
1984.
http://www.livelinks.com/sumeria/health/myt h2.html
08/08/96
/DISPELLING VACCINATION MYTHS
.
Pagel3ofl4
9.
Trollfors B. Rabo. E. 1981. Whooping cough in adults. British Medical Journal (September 12). 696-97.
10.
National Vaccine Injury Compensation Program (NVICP). I leallh Resources and Services Administration.
Parklawn Building. Room 7-90. 5600 Fishers Lane. Rockville. Ml) 20857. 800-338-2382.
11.
Measles vaccine failures: lack of sustained measles specific immunoglobulin G responses in revaccinated
adolescents and young adults. Department of Pediatries. Georgetown University Medical Center.
Washington. DC 20007. Pediatric Infectious Disease Journal. 13(l):34-8. 1994 Jan.
12.
Measles outbreak in 31 schools: risk factors for vaccine failure and evaluation of a selective revaccination
strategy. Department of Preventive Medicine and Biostatislics. University of Toronto. Ont. Canadian
Medical Association Journal. 150(7): 1093-8, 1994 Apr 1.
13.
I lacmophilus b disease after vaccination with 1 lacmophilus b polysaccharide or conjugate vaccine.
Institution Division of Bacterial Products, Center for Biologies Evaluation and Research. Food and Drug
Administration. Bethesda, Md 20892. American Journal of Diseases of Children. 145(12): 1379-82. 1991
Dec.
14.
Sustained transmission of mumps in a highly vaccinated population: assessment of primary vaccine failure
and waning vaccine-induced immunity. Division of field Epidemiology. Centers for Disease Control and
Prevention. Atlanta. Georgia. Journal of Infectious Diseases. 169( l):77-82, 1994 Jan. I.
15.
Secondary measles vaccine failure in healthcare workers exposed to infected patients. Department of
Pediatrics. Children's Hospital of Philadelphia, PA 19104. Infection Control & Hospital Epidemiology.
14(2):81-6. 1993 Feb.
16.
MMWR, 38 (8-9). 12/29/89).
17.
MMWR (Morbidity and Mortality Weekly Report) "Measles." 1989; 38:329-330.
18.
Morbidity and Mortality Weekly Report (MMWR). 33(24),6/22/84.
19.
Failure to reach the goal of measles elimination. Apparent paradox of measles infections in immunized
persons. Review article: 50 REFS. Dept of Internal Medicine. Mayo Vaccine Research Group, Mayo Clinic
and Foundation. Rochester, MN. Archives of Internal Medicine. 154(16): 1815-20, 1994 Aug 22.
19a. Clinical Immunology and Immunopathology, May 1996; 79(2): 163-170.
20.
21.
22.
Trevor Gunn. Mass Immunization. A Point in Question, p 15 (E.D. 1 [time, Pasictn Exposed - The False
Foundations of Modem Medicine. Bookreal. Australia, 1989.)
Physician William I toward I lay's address of June 25. 1937: printed in the Congressional Record.
Outbreak of paralytic poliomyelitis in Oman; evidence for widespread transmission among fully vaccinated
children Lancet vol 338: Sept 21. 1991; 715-720.
23.
Neil Miller, Vaccines: Are They Safe and Effective? p 33.
24.
Chicago Dept, of Health.
25.
See Nole’23 pn 18-40.
26.
See Note 23 pp 45,46 [NVIC News, April 92, pl2],
27.
S. Curtis. A 1 landbook of Homeopathic Alternatives to Immunization.
28.
Darrell I luff. I low to Lie With Statistics, p 84.
Jttp://www. Iivelinks.com/sumeria/healtli/rnyth2.html
08/08/96
DISPELLING VACCINATION MYTHS
29.
Page 14 of 14
quoted from the internet, credited to Keith Block, M.D., a family physician from Evanston. Illinois, who has
spent years collecting data in the medical literature on inununizations.
30.
Sec Note 20, p 15.
31.
See Note 20 p 21.
32.
See Note 20. p 21 (British Medical Council Publication 272, May 1950)
33.
’
See Note 20, p 21; also Note 23 p 47 (Buttram. MD. Hoffman. "Mothering Magazine". Winter 1985 p 30;
Kalokerinos and Dettman, MDs, "The Dangers of Immunization," Biological Research Inst. (Australia].
1979. p 49).
34.
Archie Kalolerinos, MD, "Every Second Child", Keats Publishing. Inc. 1981
35.
Reported by KM Severyn,R.Ph,Ph.D. in the Dayton Daily News, June 3, 1995.
36.
("Vaccine Information and Awareness. Measles and Antibody Titre Levels,") from "Vaccine Weekly".
January 1996
37.
NVIC Press Release, "Consumer Group Warns use of New Chicken Pox Vaccine in all Healthy Children
May Cause More Serious Disease".
1
38.
Sec note 35 (quoted from The Lancet)
39.
1 learings before the Committee on Interstate and foreign Conuncrcc. 1 louse of Representatives. 87th
Congress. Second Session on H.R. 10541, May 1962, p.94.
40.
Ullman. Discovering Homeopathy, p 42 (Thomas L. Bradford, Logic figures, p68, 113-146: Coulter,
Divided Legacy, Vol 3. p268).
41.
See Note 27.
42.
See Note 27.
43.
Golden. Isaac, Vaccination? A Review of Risks and Alternatives.
[ 1 leallh 1[ SumenaJ
vww.livelinks.com/sumeria/health/niyth2.html
08/08/96
ME
. MEASLES
MtNZADCN
Introduction
National Mission on Immunization is a
societal mission and it is committed to the
goal of immunizing -
(a) atleast85% of all infants born, with one
dose of BCG, three doses of DPT and
OPV and one dose of measles
vaccinations. This prevents infants and
young children from contracting six
common, vaccine-preventable diseases,
namely, measles, neo-natal tetanus,
acute paralytic poliomyelitis, pertussis,
childhood tuberculosis and diphtheria.
(b) 100% of all pregnant women with
tetanus-toxoid.
These objectives are to be achieved by
the year 1990 and sustained year after
year thereon.
Measles immunization situation
The immunization coverage has been steadily increasing, but the coverage
levels remain far less than desired (see figures 1 & 2).
IMMUNIZATION PERFORMANCE (% )
100
90
80
70
60
50
40
30
20
10
0
BCG
DPT3
OPV3
MEASLES
■ 1981
El 1985
01986
□ 1987
011988
01989
TT2
Figure 1
IMMUNIZATION PERFORMANCE (% )
M Routine Statistics
from GOI (1988-89)
Figure 2
Nation-wide coverage evaluation surveys done in May ’89 with a
population of 72 million indicate that measles coverage ranges between
2.4% and 59.7%, as against 20% to 93% and 19% to 91% of DPT3 and
OPV3. The fully immunized coverage status fell down to the range of 2.4%
to 54.6% because of poor measles immunization coverage.
Facts about measles disease and immunization
Measles is such a common communicable disease in India that many
communities have accepted it as a normal milestone of growing up.
Measles is highly infectious. Rarely will an un-immunized child escape.
Measles is nearly always symptomatic. Diagnosis of measles is easy. The
main characteristic features would be:
• A cold, cough and running nose.
• Fever, 38 degrees C (100 4 degrees F) or more.
o Eyes are pink (even red), watery and sensitive to light.
o Within 3 to 7 days a characteristic blotchy rash appears, beginning on
the face and then spreading all over the body.
o The rash Fists for 4-7 days, and often ends with
desquamation (peeling of skin).
° The pigmentation due to the rash remains for 2 weeks or even longer
° Koplik’s spots (greyish-white spots with red borders) often appear on
the inside of the cheek at about the same time the rash begins These
spots are diagnostic, since they occur only in measles
Risk factors
0 Measles virus is transmitted through the air by respiratory droplets
from infected children even before the rash is seen. Therefore isolation
of a case has no relevance in the control of the disease.
o Measles is more rapidly transmitted in large families, crowded homes
and urban slums.
• With high population density, measles is apt to occur year-round,
sometimes with seasonal peaks.
• Without immunization, nearly ever}' child gets measles.
• Measles can occur at any age. In India, due to crowding and increased
contact among young children, effects are mostly seen before the third
birthday of the child.
° Secondary cases in homes tend to be more severe.
• Measles is severe among infants and malnourished children.
Post-measles complications are also more common in these children.
Post-measles complications
Immediate complications
Pneumonia
About 4% of the cases develop pneumonia.
Diarrhoea
The incidence of diarrhoea in children affected with measles will be twid
as much as in normal children.
Otitis media
About 2% of children develop otitis media following measles.
Encephalitis
One in 2000 cases has encephalitis. This is frequently associated with
brain damage and mental retardation.
Vitamin A deficiency
Many children develop acute deficiency of vitamin A, which may lead to
keratomalacia and blindness. In Tanzania 50% of blind children had
become so from corneal scarring following measles.
Deaths
Death strikes the malnourished, especially where multiple cases crowd
the home. In a country like India 2% to 3% of children die generally
following measles, but in a measles epidemic, case fatality as high as 30%
to 50% is reported.
Delayed complications
Measles has been shown to have an effect on mortality and morbidity
not only in the period immediately after the acute infection, but also
for a considerable period thereafter.
(
Mortality
An African study indicated that having measles increased the chance of
death over the next 9 months by fifteen times.
A Bangladesh study indicated that measles vaccination reduced mortality
by 35% over the next 12 months.
Morbidity
Several studies have examined delayed morbidity after measles infection.
Bhaskaran.et al. (J. Trop. Med. Hyg, 1984-87:21.5) have reported that
measles cases had 10 times more days of illness than controls
Magnitude of the problem in India
Mam cases of measles are not reported to the health institutions. As a result,
the complications that arise due to measles are often not associated with
measles itself Therefore no reliable data on the incidence of measles and
its complications is available in India.
It is estimated that, in India, ever}' year there are some 20 million cases of
measles.
Inspite of a case fatality rate of 1 % to 2%, a minimum of 2 lakh (and more
likely 5 lakh) measles-associated deaths occur each year in India.
Innumerable number of children suffer other infections like diarrhoea,
acute respiratory infections, malnutrition and vitamin A deficiency, as a
result of measles.
Measles immunization
Being a viral disease, measles cannot be cured by antibiotics and therefore
prevention is more important. Because measles has such a profound
influence on childhood mortality and morbidity, measles prevention
deserves to take the first place in UIP.
It may be possible to prevent many measles-associated deaths and diseases
by good medical care (ORT, antibiotics, vitamin A, supplementary
feeding), but the cost of taking proper care of all children ill with measles
alone is at least four times that of a complete UIP.
Preventing measles by immunization will have the multiple benefit of
preventing other diseases, particularly diarrhoea, dysentery, malnutrition,
blindness, pneumonia and acute respiratory infections.
Measles morbidity is influenced over the long term only by immunization
and is, therefore, a much better indicator of programme impact.
Monitoring measles immunization and disease
surveillance
By monitoring measles immunization and measles disease surveillance we
can double-check and evaluate the following:
Quality of immunization services
Strict compliance of not using reconstituted vaccine vials after 4 hours
is advised as any such use is likely to lead to vaccine-associated
reactions. All deaths following measles immunization reported in the
newspapers are attributable to incorrect handling of the vaccine and
compromise on aseptic precautions.
Cold-chain
Since cold chain requirements are nearly as rigorous as of any other
EPI vaccines, efficacy of the measles vaccine is directly related to
effective maintenance of the cold chain.
Fully immunized infant population
Measles is usually the last vaccine given. Tracking every infant till
measles vaccine is given will ensure improvement in full
immunization coverages.
,
Measles surveillance
Because of the relative simplicity, surveillance of measles cases and
demonstration of its reduction is the best single indicator of the
effectiveness of the immunization programme.
Immunization schedule
Vaccination against measles was inducted in the national immunization
schedule in 1985. Our national immunization schedule advocates measles
vaccination at 9-12 months of age. This is early enough to prevent most
cases and late enough to avoid most interference from maternal
antibodies.
THE IDEAL IMMUNIZATION SCHEDULE
FOR THE PREGNANT WOMAN :
Early in pregnancy
T.T.-l (injection)
One month after T.T.-l
T.T -2 or T.T. Booster (injection)
FOR THE INFANT :
At 1 '/z months
B.C.G. (injection)'
D PT 1 (injection) and O.P.V.-l (dose)
At 2 */2 months
D P.T.-2 (injection) and O.P.V -2 (dose)
At y/i months
D.P.T.-3 (injection) and 0 P.V.-3 (dose)
At 9 months
Measles (injection)
At 16 to 24 months
DPT. Booster (injection)
and O.P.V. Booster (dose)
•If the infant has been delivered in a hospital/clinic, she should be given
the B.C.G. injection at birth.
Some doctors feel that the measles vaccination should be given between
7-9 months since some measles cases occur before the age of 9 months
In India we do not have the data on the proportion of cases occuring before
the age of 9 months.
A study conducted in Kenya (1974-81) to show the impact of measles
vaccination at various ages (see figure 3) between 4 to 10 months showed
that at 9 months the percentage protected was the greatest because only
immunization
measles before
not protect due to maternal
immunization
antibodies
• Source AVER 1982; 12:89-91
Implementation of measles immunization at 9 months of age has
been successful in many areas in reducing measles morbidity and
mortality.
In some areas, however, measles morbidity and mortality among infants
less than 9 months of age may be substantial. There are four ways
suggested in which the failure to adequately protect these young infants
with the current vaccine might be overcome-.
(a)
Achieving a high enough vaccine coverage (85% and above) so thac
herd-immunity of the older children will protect the younger ones
(b)
Using seroconversion studies to determine the youngest possible age
at which the vaccine can be administered in a given population.
(c)
A two-dose strategy, at 6 months and 15-18 months.
(d)
Overcoming the problem of maternal antibodies by a different
route of administration or by the use of a different
vaccine (Edmonston-Zagreb, Strain).
Countries like India have to depend heavily on the first
alternative at present. The other ways are under trial and as yet
are of no relevance for field purposes.
Safety of measles vaccine
Measles vaccine is very safe if reconstituted vaccine is used within 4 hours,
and one sterilized syringe and sterilized needle is used per injection.
However, about 30% of those vaccinated develop malaise, mild fever
and/or a rash 4-10 days after the vaccination. The parents need to be
informed about this possibility.
Severe complications like convulsions have occurred in 0.02 to 190
per 1 lakh vaccinated individuals, compared with 500 to 1000 per 1 »
lakh measles cases. Similarly encephalitis has been observed in 1 per 10
lakh vaccinated individuals, against 500 to 4000 per 10 lakh measles cases.
Measles vaccination during epidemics
Measles vaccine can protect children who have been exposed to measles,
and prevent the disease from occurring. But this is only possible if the
children receive the vaccine within the first 72 hours after exposure The
vaccine given beyond 3 days after exposure will do absolutely no harm
but may not protect the children.
Thus mass measles vaccinations during epidemics are useful only if
vaccination can be completed within 3 days of the first case.
Measures to improve measles vaccination coverage
• Orient colleagues in the medical profession with requisite technical
update to stress the magnitude of the measles problem and the need
for measles immunization.
o Let doctors know that in the present situation, the country can derive
best results by administering measles immunization immediately after
9 months (270 days) of age.
• Promote measles immunization for all children in the age group of
9-12 months, even if they are malnourished.
• Promote community awareness through mass media, interpersonal
communication and action, to identify each child and to get her fully
immunized.
• Ensure that immunization card ( home-based) is issued to parents of
every child and counterfoil is kept with medical institution or
health worker.
• Ensure review of the card for immunization status (actively or
passively) until measles immunization is given. This will help in
achieving high coverages of full immunization.
• Ensure provision of measles vaccination services in all immunization
sessions.
• Let the institutions/sub-centres open a vial of measles vaccine even if
there is a single eligible child on the fixed day of the session. Also
immunize children above the age of 12 months if they have not already
been protected.
• If required, promote intensive measles immunization once every three
months to supplement routine services.
f)
How to give measles vaccination
• Measles vaccine is freeze dried.
• You must reconstitute it, using pyrogen-free double■ distilled water
(supplied as diluent with the vaccine) before you can use it. Cool the
diluent before using.
• Wait until at least one child of eligible age has arrived.
• Take a sterile 5 ml syringe and a sterile mixing needle (20 G).
"
• Open a cool ampoule of diluent.
• Draw 5 ml of distilled water for 10 dose vial.
• Check the label, for expiry date, and open the vial.
• Empty the diluent into the vaccine vial.
• Gently roll the vial between the palms of your hands for mixing. There
is no need to shake the vial.
• Do not leave the needle in the vial.
• Position the child.
• Load a 2 ml sterilized syringe with 0.5 ml of reconstituted vaccine. Use
23 G sterilized needle only.
• Pinch the skin on the outer part of the child’s upper arm (left or right)
with your fingers.
• Push the needle into the pinched skin - not straight in but sloping.
• Do not push the needle in too for.
• To control the needle, support the adaptor end of the syringe with
your thumb and finger while you push the needle in.
• Withdraw the plunger to check for blood.
£
• After ensuring that the needle is not in any vein, press the plunger with
your thumb and inject the vaccine.
• Withdraw the needle and keep syringe and needle in a separate tray for
sterilization.
• Ensure use of reconstituted vaccine within four hours.
NATIONAL IMMUNIZATION PROGRAMME
Government of India
ccu
V Main, I Block
Koramongala
8angalore-560Q34
India
VACCINATION COVERAGE EVALUATION SURVEYS:
INDIA,
1987
VACCINATION COVERAGE EVALUATION SURVEYS: INDIA, 1987
Jotna Sokhey, M.D., Ph.D.
Assistant Commissioner (I),
Ministry of Health & Family Welfare, New Delhi
Robert J. Kim-Farley, M.D., M.P.H.
Regional Adviser (EPI),
World Health Organization (SEARO), New Delhi
ABSTRACT
Vaccination coverage evaluation surveys are increasingly
being used as a management tool for monitoring and evaluating
immunization programme progress. Over 257 such surveys have
been conducted in India since 1979. The results of 93
surveys conducted in 1987 document increases in coverage,
especially in selected areas where serial survey data are
available,
and
the
feasibility
that
high
levels
of
immunization coverage can be achieved and sustained in the
Indian
context.
Immunization
programme
managers
are
encouraged to continue to expand the use immunization
coverage surveys in their areas.
KEYWORDS
Evaluation; Coverage surveys; Immunization Programme
Coverage Surveys
- 2 -
INTRODUCTION
The Universal Immunization Programme (UIP) was launched
in India in 1985 as a comprehensive immunization programme
designed to achieve immunization coverage of 100 percent of
pregnant women with 2 doses or a booster dose of tetanus
toxoid (TT) and at least 85 percent coverage of infants with
3 doses each of DPT and OPV and one dose each of BCG and
measles vaccines. UIP was started in selected districts in
1985-86 and is undergoing a carefully planned systematic
expansion to all the districts in the country by 1989-90
(1).
The accurate measurement of immunization coverage in
eligible population groups is essential in the monitoring and
evaluation of programme implementation. Vaccination coverage
evaluation surveys are an important management tool in
assessing programme achievement, determining reasons for
immunization failure and obtaining a better understanding of
the sources of immunization in the community. To date, 257
such surveys are known to have been conducted since 1979 to
determine immunization coverage levels of children and the
mothers of young children. The results of 93 surveys carried
out in 1987 are presented in this paper.
METHODOLOGY
The survey methodology used in India is the standard WHO
30 cluster sampling technique, adapted to suit the programme
needs of the country (2). The adaptation of this methodology
and its advantages and limitations have been discussed
separately (3). Briefly, 30 clusters (villages or urban
wards) were randomly selected by population in the geographic
area to be covered by the survey. House to house visits were
made in each of these clusters until seven children 12 to 23
months of age and their mothers, or seven mothers of children
under one year of age, were found. The selection of the first
house was done randomly and subsequent houses were selected
by going to the next nearest house.
The
immunization
status
of
children,
source
of
immunization and reasons for failure to initiate or complete
immunization were ascertained. Where possible, the dates of
immunization were determined by immunization
cards or
registers. For those who had no such documentation, the month
and year of vaccination were recorded only if convincing
verbal history was given. In addition to questions on
immunization status, mothers were asked about antenatal care,
place of delivery and persons conducting the delivery.
Questions were also asked to ascertain knowledge regarding
the names of the vaccine preventable diseases, number of
doses of DPT recommended and the source of information about
immunization.
O
COMMUNITY HEALTH CELL
326. V Main, I Block
Koramangala
Bangaloro-560034 •
Coverage Surveys
- 3 -
RESULTS OF SURVEYS CONDUCTED IN 1987
Number of surveys
The results of 257 surveys conducted since 1979 are
available. The surveys have been variably distributed among
the states (Table 1).
Prior to the launching of UIP the annual number of
surveys averaged 18 per year with a range of 9 to 28. The
number of surveys has now increased and at least forty two
and ninty three surveys were conducted in 1986 and 1987,
respectively.
Population size of the areas surveyed
Since the initiation of UIP, a generally increasing
trend of surveying larger areas is evident. The population of
the areas surveyed in 1987 ranged from 38,000 to 4,807,000
with a median population of 1,362,000 as compared to the
population of the areas sampled in 1983 which ranged from
20,000 to 1,575,000 with a median population of 113,000.
Over two-thirds of the surveys (62/88) covered entire
districts. Thirteen surveys were conducted in cities or
selected urban wards and 13 in rural blocks. Although the
total population covered in 5 surveys is not known, it
appears that 4 covered entire districts and 1 was conducted
in a rural block (Table 2).
Immunization coverage levels
Over a fifth of the surveyed areas (20/93) recorded
coverage levels of 75 percent and above for the third dose of
DPT and OPV. In 55 percent (51/93) of the other surveyed
areas, coverage levels between 50 and 74 percent for these
vaccines were noted. Only in 19 areas were these coverage
levels less than 50 percent,
including two areas with
coverage levels below 25 percent. Coverage with BCG and
measles vaccines were less than with DPT and OPV in many
areas (Table 2, Fig.l).
Coverage levels of above 75 percent with 2 doses or a
booster dose of TT during pregnancy were reported in 41
percent (32/78) of the surveyed areas reporting TT coverage.
Over three-fourths (61/78) of the areas recorded coverage
levels of 503, or more. However, there remain areas in the
country (5/78) with less than 253; coverage of pregnant women
with TT. In 15 of the surveys coverage with TT vaccine was
not reported (Table 2, Fig.l).
Immunization status of children
High coverage with individual vaccines correlates with a
higher percentage of fully vaccinated (FV) children receiving
Coverage Surveys
- 4 -
three doses each of DPT and OPV and one dose of BCG. Bharuch
district had the highest percentage of fully vaccinated
children (84X). Three areas in Delhi ari an urban and two
rural
blocks
in
Rohtak district al'.o recorded fully
vaccinated levels of above 80 percent. In more than a third
of the surveyed areas (27/76) 50 percent or more of the
children were found to be fully vaccinated (Table 2, Fig.l).
BCG scar rate
The BCG scar rate was recorded in 35 of the 93 surveys
conducted. In 80 percent (28/35) of these areas scar rates of
85 percent or above were documented (Table 2).
Serial surveys
Comparison of results with previous surveys in the same
geographic
area
convincingly
documents
improvement
in
immunization coverage for all vaccines in some areas.
Dropout rates were nearly halved during the period between
these surveys (Table 3).
Dropout rates
The median dropout from first to third dose for DPT and
OPV was 20 and 21 percent, respectively in 1987. More than a
third of the surveyed areas (31/90) recorded dropout rates of
15 percent or less for DPT. There are, however, still many
places in the country which continue to have high dropout
rates as reflected by the results in 20 percent (18/90) areas
surveyed showing dropout rates exceeding 30 percent for DPT
(Table 2, Fig.2).
Reasons for immunization failure
The reasons for failure to initiate or complete
immunization have been received for 37 percent (34/93) of the
surveys conducted in 1987. The specific areas and the reasons
for immunization failure, by percentage of the total number
of partially immunized (PI) or not immunized (NI) children,
are shown in Table 4. Percentage of fully vaccinated children
(FV), who had received 3 doses of DPT and OPV and ’ 1 dose of
BCG, as well as coverage by third dose of DPT are also shown
in Table 4.
Lack of adequate information, unavailability of vaccines
and absence of health workers were most frequently recorded
as
reasons
for
immunization
failure.
Postponement
of
immunization and the mother being busy were also noted us
important reasons. Contraindications to vaccination, minor
illnesses, fear of reactions and no faith in immunization
were cited as major reasons only in certain areas. Among the
miscellaneous reasons, the most common were illness of the
mother or long periods of absence of the family from their
place of residence. Rumours against immunization were not of
Coverage Surveys
significance in any of the areas surveyed.
Source of immunizat i on
Primary health centres (PHCs) and their subcentres
remain a major source of immunization (Table 5). Analysis of
the data available from 23 surveys on the source of DPT3
showed that in 43 percent (10/23) of the areas the greatest
percentage of the children had been vaccinated at such health
centres. Outreach services also serve as the major source of
immunization in 39 percent (9/23) of the areas. Hospital and
private sector rarely serve as
the major source
of
immunization, although the surveys show that in certain areas
they may be significant providers of immunization services.
DISCUSSION
Although many states have conducted a number of surveys,
the larger populated states of Andhra Pradesh, Bihar, Orissa
and Uttar Pradesh have conducted only a very few. The 7
surveys in Delhi, as well as some of the other surveys in
urban wards and rural blocks, were carried out as part of the
UIP training programme..
The results of the surveys indicate a wide variation in
immunization coverage levels in the country. A positive and
encouraging result is the documentation in selected areas of
the feasibility of achieving and maintaining high coverage
levels and the increase in immunization coverage levels from
those of previous years.
Because measles vaccine was
introduced in selected districts only starting in 1985-86,
coverage with this vaccine is currently much lower than the
other vaccines.
In general, areas with high coverage of DPT and OPV also
achieved high levels of BCG coverage. However, in several
areas with only moderate DPT and OPV
coverage,
BCG
vaccination
performance
was
significantly
lower.
BCG
vaccination services were previously provided as part of the
National Tuberculosis Control Programme by teams of BCG
technicians. BCG vaccine was integrated with the other
vaccines provided under the immunization programme in 1981■
82. Many districts have since conducted training of the
multi-purpose workers (MPWs) in BCG vaccine administration
which has resulted in improvements in BCG vaccination
coverage and increases in the percentage of fully vaccinated
children. The survey results, however, indicate a continuous
need to improve delivery of BCG services, especially in arcus
where low or only moderate levels of coverage with DPT and
OPV have been achieved.
Coverage Surveys
- 6 -
Almost all children should have a vaccination scar after
proper immunization with potent BCG vaccine. The BCG scar
rate can serve as one of the indicators of the quality of
immunization services. Since many of the health workers have
only been recently trained in BCG vaccine administration, it
is important that BCG scar rates are monitored in all future
vaccination coverage evaluation surveys to ensure that
corrective measures are taken where necessary.
Comparison of results of surveys in different years in
the same geographic areas clearly demonstrates the important
relationship of dropout rates to immunization coverage. In
selected areas where serial survey data are available,
dropout rates have been more than halved in the period
between the two surveys. Reduction in dropout rates and
increases in the percentage of fully vaccinated children
reflect
a
consolidation
of
programme
activities
and
improvement in planning and management of immunization
services.
The reasons for the failure to initiate or complete
immunization of children suggests that lack of adequate
information, unavailability of vaccines and absence of the
health workers at the time of immunization sessions may be
important factors in many areas. Minor illnesses still seem
to be taken as a contraindication to vaccination in some
areas and children are either not brought for immunization or
are turned away by the health workers. The fact that fear of
injections or side reactions and no faith in immunization
appear to be localized as major causes in only a few areas
may reflect the quality of the immunization services and
general credibility of the health services in these areas.
Experience gained over the years and feedback on the
reasons for immunization failure should provide a solid
foundation for further improving services. Results of the
serial surveys clearly demonstrate that dropout rates can be
reduced
and
immunization
coverage
levels
improved
substantially over a relatively short period of time.
CONCLUSIONS
The following conclusions can be drawn from the coverage
surveys conducted in India in 1987:
- Immunization coverage surveys are being increasingly
used as a management tool to monitor and evaluate programme
progress.
- 7 -
Coverage Surveys
Marked increases in coverage are documented
selected areas where serial survey data are available.
in
- It is feasible to achieve and maintain high levels of
immunization coverage in the Indian context.
- Reasons for failure to immunize can be elicited which
are important for planning of immunization strategies to
reduce dropout rates and to extend services to those who are
not yet being reached by the programme.
Immunization programme managers
are
encouraged to
continue to make increasing use of immunization coverage
surveys as a management tool to assess programme progress in
their areas. Results of surveys should be reported to the
Ministry of Health and Family Welfare in a timely manner so
that periodic updates on the use and results of coverage
surveys
can
be
disseminated.
When
possible,
training
programmes
on
immunization
should
include
practical
experience in the organization and implementation of a
coverage survey so that an increasing number of persons
knowledgeable of the techniques are available to actually
conduct them.
ACKNOWLEDGEMENTS
We are grateful for the cooperation of the state EPI
Officers who provided the information on the results of the
coverage surveys. We wish to thank Mr T.R. Toteja for his
assitance in typing the manuscript.
REFERENCES
1.
Towards Universal Immunization - 1990. Ministry of
Health and Family Welfare, Government of India, New Delhi
1985.
2.
Evaluate Vaccination Coverage - Module for training
under UIP. Ministry of Health and Family Welfare, Government
of India 1987.
3.
Sokhey Jotna & Kim-Farley R - Evaluation of Vaccination
Coverage through Sample Surveys. J.Comm. Dis. 1987, V 19,
No.l, 341-348
c/p.ind/13.4.88-7
Coverage Surveys
- 8 -
Table 1
VACCINATION COVERAGE EVALUATION SURVEYS, INDIA
1! ’79
’SO
A.P
Assai
Bihar
Gujarat
Haryana
1
1
i
i
1
1
H.P.
JiK
Karnataka
Kerala
N.P.
1
1
1
1
1
State
’82
’83
'84
1
1
7
1
3
1
2
1
2
1
3
1
1
2
11
1
1
11
SI1
1
11
’85
’86
'87
4
2
2
1
1
1
1
4
1
3
2
3
6
5
3
3
3
2
2
3
5
5
1
1
1
1
2
4
1
15
7
7
1
1
4
1
1
1
1
3
5
3
2
1
4
1
6
1
1
24
2
1
1
1
1
2
4
1
2
1
1
1
1
2
1
1
1
1
1
1
I
6
1
1
U.P.
1I1
N.B.
|1 1
Arun. Pr
1
AiH Islands
Delhi
1 1
Goa
1 1
Chandigarh I1
DIN Haveli
Lakshadweep 11
11
Nizorai
1
Pondicherry
1
India
1 9
2
1
2
1
1
2
1
2
1
2
2
1
19
14
28
1
7
1
1
21
; Total;
1
1
Maharashtra 1
Manipur
1
Meghalaya
i
Nagaland
1
Orissa
11
Punjab
Rajasthan
Sikkii
T.N.
Tripura
’81
16
15
42
93
1 i
31
3;
25 1
1 u i
;
;
! 20 1
: 13;
27 1
! 8 1
1 19 1
I
1
i 19;
i 5;
; i :
1 0 ;
1 4 1
11
11
1 12 1
1 8 1
1 2 1
1 34 1
1 1 1
1
1
i 3;
1 9 ;
1 3 1
1 0 1
: is i
! 5 !
1 1 !
! 0 1
: o;
! 2 I
1 0 !
____ 1
1 257 1
Coverage Surveys
- 9 -
Table 2
VACCINATION COVERAGE EVALUTAI'iN SURVEYS, INDIA I'-'ti?
AREA
ASSAM
01 Guahati City
GUJARAT
02 Aheedabad Dist.
03 Bharuch Dist.
04 Pancheahal Dist.
HARYANA
05 Gurgaon Dist.
06 Hissar Dist.
07 Bahadurgarh Bl.,Rohtak 1
08 Beri-Kathura Bl.,Rohtak 1
09 Non-ICDS Ward Rohtak(Urban)*
10 ICDS Ward, Rohtak (Urban) 1
HIMACHAL PRADESH
11 Chaiba Dist.
12 Kullu Dist.
13 Nandi Dist.
14 Solan Dist.
JAMMU I KASHMIR
15 Udhaipur
KARNATAKA
16 Hassan Dist. 1
17 Kolar Dist.
18 Chickiaglur Dist.
19 Tuikur Dist.
20 Chickiaglur Town
21 Karwar Town
22 Ullal PHC.Dakshina Kannada
23 Hubli Tehsi1,Dharwad Dist.
24 Raichur Tehsil.Raichur Dist.
25 Chelur PHC,Tuikur Dist.
26 Shivally PHC.Mandya Dist.
27 Turvekere PHC(ICDS)
28 Kunigal PHC(ICDS),Tuikur
29 Anekal PHC,Bangalore Dist.
30 Nelaeangla PHC,Bangalore
KERALA
31 Cannanore Dist.
32 PHC Pannoor, Cannanore
33 Kasargod Distr.(Chengala
4 Chennad panchayats) 1
34 Idukki Distr.
35 Kottayai Distr.
36 Trichur Distr.
37 Quilon Distr.,Kerala
MADHYA PRADESH
38 Sagar Dist.
39 Baruani Dist.
40 Bastar Dist.
41 Surguja Dist.
4? Bhind Distr.
43 Gwalior Distr.
44 Shivpuri Distr.
POPULATION TT(PW)
BCG SCAR DPT3 0PV3 MEA EV
RATE
DROPOUT
DPT OPV
600000
73
44
89
58
55
25
20
20
22
4435000
1400000
2596000
53
82
29
53
88
30
83
31
91
26
35
91
25
0
54
21
20
84
9
49
6
58
44
5
50
976300
1717000
166564
232949
115563
87349
55
61
...
...
44 . ..
49
76
98
98
91
54
61
66
95
97
89
53
61
67
96
97
89
5
8
39
89
96
72
35
39
34
87
92
68
21
18
24
2
2
8
21
20
24
2
2
8
358400
262500
748546
337000
47
39
55
63
33
46
47
66
9?
...
97
...
46
61
66
76
43
58
61
73
18
5
30
23
28
33
23
57
33
23
22
17
29
15
17
17
...
62
59
55
51
24
29
1487115
1905492
912000
1975907
68372
48000
168614
103391
166084
63170
46380
148301
94380
95530
98350
63
72
79
41
84
89
84
65
47
54
64
70
67
65
58
76 84
73
52 100
39 74
64 90
42 86
72 98
30 95
20 72
32
67 92
52 93
63 100
74 100
72 94
78
67
62
31
78
74
71
46
31
54
67
60
79
71
62
78
67
62
32
78
76
71
46
32
53
67
50
71
71
57
45
32
0
0
19
4
31
4
0
0
0
4
20
22
20
40
56
44
21
55
40
54
25
18
30
55
39
53
60
50
14
25
28
41
10
11
1
20
37
22
11
13
12
22
21
13
25
28
42
9
8
2
22
34
22
10
12
10
22
27
1930000
89
88
69
68
68
68
68
67
68
32
0
12
29
70207
47
21
41
16
15
11
13
17
12
78
74
68
76
6
19
12
45
14
4
97
78
74
68
72
11
20
12
15
50
61
35
22
35
62
48
51
64
29
19
32
62
49
8
25
24
43
46
35
24
25
23
43
52
38
23
31
2193630
94
75
60
41
87
1472100
1630000
1840000
1631000
1088000
1280000
993000
44
43
20
8
30
41
33
45
40
32
20
30
6b
38
86
1807000
72
94
87
88
4
30
16
10
...
39
38
32
20
9
21
53
36
70
10 -
Coverage Surveys
AREA
MAHARASHTRA
Akola Dist.
Aurangabad Dist.
Thane Dist.
Nagpur Dist.
Pune Dist
- MANIPUR
50 Iiphal Nunc.* 1
51 Iiphal Mest(R)
52 Thoubal Dist.
PUNJAB
53 Faridkot Dist.,(Rural)
54 Ferozepur Dist.,(Rural)
55 Hoshiarpur Dist.,(Rural)
56 Ludhiana Dist.,(Rural)
57 Ludhiana City,(Urban)
58 Patiala Dist..(Rural)
RAJASTHAN
59 Kota Dist.
SIKKIM
60 Sikkii East
TAMIL NADU
61 Chidaibaranar
62 Chingleput
63 Cuddalore
64 Tirunelveli
65 Dindigul(Anna)
66 Kallakurichi
67 Kaiarajar
68 Kancheepura*
69 Kanyakuiari
70 Madurai
71 Naiakkal
72 Nilgiris
73 Palayaikottai
74 Periyakulai
75 Periyar
76 PMR Lingai
77 Raianathapurai
78 Saidapet
79 Sale*
80 South Arcot
81 Thanjavur
82 Thiruvarur
83 Tiruchengode
84 Villupura*
ARUNACHAL PRADESH
85 Louer Subansiri Dist.
DELHI
86 Delhi Trilokpuri LCDS
87 Delhi,Paia* PHC
88 Delhi,Nizaiuddin ICDS
89 Delhi Khanpur, Madangir
90 Delhi Kalkaji, Malviya Ng
91 Delhi Mongolpuri
92 Delhi Paharganj ICDS
MIZORAM
93 Lunglei, Mizora*
45
46
4?
48
49
POPULATION TT(PW)
BCG SCAR DPT3 0PV3 MSL
RATE
FV
DROPOUT
DPT OPV
2009800
1751000
3952700
3010000
4807000
66
...
80
79
69
46
58
73
73
54
...
...
92
...
...
66
68
78
83
75
58 ...
74 26
78 44
74 19
71
6
35
17
62
12
16
20
126124
53523
...
...
23
16
51 98
41 89
13 ...
57
52
16
65
51
15
16
10
1
44
38
5
17
20
39
0
21
36
1610000
1469000
1362000
2064000
600000
1817000
55
71
85
79
84
85
19 ...
30
56
61
87
64
38
65
82
68
84
69
36
64
81
68
83
69
15
9
21
24
58
5
13
22
53
54
55
36
31
17
10
13
10
11
32
14
10
13
11
(2
1802300
49
31
94
47
49
22
23
20
17
157815
17
51
79
42
42
36
33
35
31
1451200
4292370
1628940
2388749
1716049
1459983
1483274
1986642
1572800
1946261
880330
741000
2388749
1313112
2268108
1065719
1140581
2305728
1481775
4635221
2094029
2344741
1429452
1546298
46
.. .
77
83
85
78
77
26
93
...
7
41
17
28
22
22
23
51
70
77
65
84
49
66
61
62
61
66
91
65
78
69
61
62
79
45
60
67
62
49
55
43
65
9
77 13
56
83 31
50 12
59
58
8
66 29
58 27
64 20
90 49
56 ...
77 48
69 40
59 29
53 ...
72 10
44 31
60 13
66 29
61 24
43 15
54 13
__
...
...
15 20
19 19
...
19 24
23
13 14
...
36 34
59
20 25
2
22 24
21
18 19
11
23 26
7
26 25
...
6
6
...
19 24
38
15 15
...
22 21
56
27 27
49
26 29
...
9 16
15
41 40
...
30 28
...
24 24
...
25 25
6
33 32
33 34
135000
...
39 ...
42
28 ...
11
41
51
110873
38000
87253
118000
84000
110000
104000
58
65
71
76
84
75
78
75
60
76
86
83
95
84
59 60
69 69 . . .
75 74
89 88 36
87 87 36
86 86 36
76 '78 32
51
51
70
81
82
83
73
29
20
15
10
8
13
17
29
20
16
11
8
13
13
88823
50
51
0
17
20
11
85
67
79
67
66
...
87
73
77
88
67
79
66
77
79
9
25
..55
2
...
11
68
37
23
31
.. ...
64
88
99
97
96
94
95
93
» - 28 clusters onlv
I FV includes 'children who received leasles vaccine also
. - information not received
63
33
24
10 12
11
14 . . .
Coverage Surveys
11
Table 3
Comparison of Results of Surveys at Different Times
in the same Geographic Areas
Gauhati
City
Vaccine 1987 1985
Bharuch
Kota
Sagar
1987 1985
91
j
51
1 91
50
|| 88
66
1| 54 ...
I|
1987 1983
22
i|
21
9
•••
I1
I|
1!
1987 1985
23
50
22
51
45
8
8
23
4
I|
38
7
20
17
42
41
;|
25
25
52
53
49
17
44
25
1
DPT3
0PV3
BCG
MSL
58
55
44
25
FV
DROPOUT
DPT
OPV
20
20
22
46
27
|1
|1
6
5
TT2/B
74
...
|I
82
35
28
10
•••
84
33
1
i|
|!
1(
1
1I
|1
Thane
47
49
31
22
1
33
32
53
|
|
J
I|
11
I1
I
FV - Fully vaccinated
AJ C-r-
!>
oi'^-G'2-
COMMUNITY HEALTH CELL
326, V Main, 1 Block
Koramongala
Bangalore-560034
India
z
1987 1986
1
j
1
j|
|
|
78
78
73
44
69
69
69
|
|
j
50
[
|I
I1
||
11
|1
62
46
io
12
20
19
|
1
|
1
|
I
80
69
|
11
12 -
Coverage Surveys
Table 4
REASONS FOR IMMUNIZATION FA1IIIRE
Percentage of Uninnunized or Partially Iwunized Children
AREA
1
Coverage
!
X Cov.
1DPT3
FV
I
... Inforiation ...
I... Inplenentation ...I ... Motivation ...
Child Contra! HJ-U
No. ! Unaware of
No Fear
No IHothar Post- Tine Placeluther
PI/III! Need Sch. Place• iil -indie! Abs. Vacc. Inj.l:aith ! Busy poned Inconv Far 1 Reasons
9 1
1 Faridkot (R)
1
38
13
222 1
49
5
5
5
2 Surguja Dist., M.P.
1
22
9
192 1
32
5
2
3
3 Lunglei Dist.,Mizorai
1
63
17
176 1
7
4 Bhind Distr.,M.P.
1
35
21
171 1
9
3
3
3
5 Bastar Dist., M.P.
1
35
20
169 ;
21
7
11
4
6 Mandi Dist., H.P.
1
66
23
165 1
38
16
5
3
7 Kota Dist.,Rajasthan
1
47
23
161 1
40
3
12
3
8 Chanba Dist.,H.P.
!
46
28
154 1
27
13
3
1
9 Cannanore Dist.,Kerala
1
68
29
149 1
16
2
5
15
10 Sikkia East, Sikkio
1
42
33
145 1
32
8
10
8
5 1
11 Patiala(R)
1
69
36
145 I
21
2
9
17
3 !
1
12 Barwani Dist., M.P.
1
61
32
143 1
15
8
2
4
10 ;
18
13
61
33
143 1
31
20
3
1
2 !
13
16
0
27
4
7
4
1 !
14
2
4
12
13 Kulu Dist.,H.P.
13
5
16
14 ;
n
34
8
7
;
3
1
8 1
33
35
7
1
5
!
4
20
17
4 !
4
1
20
1 !
28
19
1
1 !
3
1
!
3
i:
1
I
17
6
3 1
4
1
5 !
1
6
6
3
2 !
3
1
21
1 !
14
24
1
1 !
3
2
8 1
3
2 !
2
7
11
4 1
3
17
3
1 1
7
2
3
6 !
6
2
6
9 !
3
3
8
8 1
11
22
2
11 !
26
33 1
13
1 1
9
0 !
2
7
3 !
2
8
6 !
!
15
2
1
54
35
138 1
15 Shivpuri Distr.,M.P.
!
48
36
137 1
17
16 Rohtak (R)
...
50
136 1
32
17 Sagar Dist., M.P.
1
1
38
131 !
33
3
3
5
1
24
18 Hissar Dist..Haryrna
1
61
39
131 1
24
15
3
2
5 !
8
19 Ouilon Dist.,Kerala
1
72
39
129 1
13
3
3
20
6 !
2
13
23
17
1
14 Gurgaon Dist.,Hanau
18
1
20 Hassan Dist..Karnata! 1 1
78
40
126 1
26
3
3
3
3 !
21 Ferozepur(R)
65
53
113 !
49
4
34
7
8 !
1
I. Wise .1
1
6
1
15
2 1
31
1
6
7
11
4 1
7
32
14
;
6
8
20
5 :
is
18
4 !
7
6
3 !
5
6
4
15
1 1
10
10
2
6 1
3 1
15
18
21
. 4 !
3
42
6
12 1
12
27
7
20 !
35
5
3
6 ;
2
2
1
1 1
4
3
6
6
2
:
15
9
15 !
54
1 1
:
12
6 !
16
5
6
6
1
22 Guahati city, Assan
;
58
20
112 1
13
5
9
32
5 !
23 Ludhiana(U)
:
84
55
109 1
17
8
1
6
5 1
24 Hoshiarpur(R)
;
82
53
105
37
13
15
9
7 1
3
8
11
13 !
20
30
25 Delhi Trilokpuri ICDL
I
59
51
103 1
27
13
6
6
11 !
1
2
5
3 1
10
4
62
53
101
11
6
6
2
19
5
6
12 !
11
4
1
68
54
99
31
12
15
14
11 !
8
4
17
17 !
36
34
3
28 Kolar Dist.,Karnataka
1
67
56
91 !
23
1
4 )
11
2
2
4 ;
29 Solan Dist.,H.P.
1
76
57
90 1
24
6
8
1
2 !
1
30 Thane Dist.,Maharashtra 1
78
62
80 !
30
5
1
8
3
1
10
3
26 Gwalior Distr.,M.P.
27 Ludhiana(R)
31 Rohtak (0)
11
15
2
10
10
2 ;
ii
2 1
18
9
2 ;
7
10 '
4
1
5 !
5
23
i
36
12
!
4
6;
5
6
3
3 !
5
8
6
1 1
1
32
16
15
13
25 1
4
4
9
I
4
2
6
2 1
6
38
3
6:
6
12
1
29
78 1
23
32 Delhi,Nizaiuddin LCDS
1
75
70
63 ;
11
19
33 Delhi Paharganj ICDS
1
76
73
53 1
11
34 Bharuch Dist.,Gujarat
;
9i
84
34 1
FV - Fully vaccinated
i
19
- Fully vaccinated includes children who received neasles vaccine also
Note:
Due to lultiple reponses totals nay be ncre than 1001 in soae areas
Nunber of children surveyed in Punjab ranged frea 220 to 255
6
5
13 -
Coverage Surveys
Table 5
SOURCES OF OPTS IMMUNIZATION
AREA
y'!'
Tl 1 Bharuch Dist..Gujarat
0 2 Gurgaon Dist. .Haryana
G, r 3 Hissar Dist.,Haryana
^6- 4 Mandi Dist., H.P.
5 Hassan Dist.,Karnataka
7 6 tolar Dist.,Karnataka
66* 7 Cannanore Dist.,Kerala
?«- 8 uuilon Dist.,Kerala
7^9 Thane Dist.,Maharashtra
5-2-10 liphal Nest(R),Manipur
6 r H Barwani Dist., M.P.
—7
12 Bastar Dist., H.P.
J's 13 Sagar Dist., H.P.
—7 2 2 14 Surguja Dist., M.P.
3^15 Faridkot (R), Punjab
bS'U Ferozepur(R), Punjab
'-—VtYl Hoshiarpur(R), Punjab
6 s 18 1 udhiana(R), Punjab
47 19 Ludhiana(U), Punjab
Gi 20 Patiala(R), Punjab
97 21 Kota Dist.,Rajasthan
7 j. 22 Sikkii East, Sikkis
gy 23 Delhi Trilokpuri ICDS
1
! HOSPITAL
I
1
;
;
9
22
23
1
|
!
1
!
1
1
!
!
1
1
:
1
;
1
!
1
1
1
9
14
16
18
21
29
26
3
17
19
12
24
so
7
13
19
27
7
0
SOURCE
HEALTH OUTREACH PRIVATE
CENTRE
47
34
48
80
18
25
25
49
13
14
16
12
17
0
49
38
49
31
43
60
34
42
98
31
37
16
13
7
13
63
58
10
0
27
50
55
61
56
J4
0
13
6
28
0
0
26
50
0
10
6
49
33
39
5
2
1
10
6
35
24
16
27
44
13
1
2
1
NOT
KNOWN
1
1
■
1
20;
1
1
oi
0 1
1
2 !
i;
3 1
1
i;
4;
1 !
1
7 '
}
21 1
1
11
1
.
H i*
—
( o
—--------
3/
<6
'I1!
17
6
SO
Io
o
O
J £
2.
6
Coverage Surveys
- 14 -
N U M B E R OF SU R V E Y S
FIGURE 1
771 TT2/B
IV\]
DPTS
PERCENTAGE COVERAGE
Y///A om
bX\\j BCG
[XX msl
ES23 rv
- 15 ••
Coverage Surveys
FIGURE 2
N U M B K R OF SU R V E Y S
DROPOUT RATES FOR DPT AND OPV, INDIA
[771
DROPOUT RATES: FIRST TO TBIRD DOSE (M)
DPT1 to DPT3
F\X1 0PV1 to 0PV3
><<3o
THE CASE AGAINST IMMUNIZATIONS
By Richard Moskowitz, M.D.
'tyg ■ • Ok^t A6|AlM^T' /MMl'NIZATid<
■_’
•
'
-.''
. ■’
'
'
■;•
-
•>'.■•’•-• •.’ ’ '.•' J,’* •** '••,,'•• •'.•.•’••■'. '* $• '■■'■
.
' '
R/CtlAkXY'iL ^AoSU-uv'vl
I,
,
'
f^OO
?
.
-
Av^wvU-
lAz ^/>Ux\AAH'yv J> £-•
- „.r.
M ,<b
'
W- '
,
',
'>
«®9®tftlK?>*SwS
For the past ten years or so, I have felt a deep and growing compunction against
giving routine immunizations to children. It began with the fundamental belief that
people have the right to make that choice for themselves. Soon 1 discovered that I
could no longer bring myself to give the injections even when the parents wished
me to.
At bottom, I have always felt that the attempt to eradicate entire microbial
species from the biosphere must inevitably upset the balance of nature in fundamental
ways that we can as yet scarcely Imagine. Such concerns loom ever larger as new
vaccines continue to be developed, seemingly for no better reason than that we have
the technical capacity to make them, and thereby to demonstrate our power, as a
civilization, to manipulate the evolutionary process itself.
Purely from the viewpoint of our own species, even if we could be sure that
the vaccines were harmless, the fact remains that they arc ampullary, that al! children
arc required to undergo them, without any sensitive regard for basic differences In
Individual susceptibility, to say nothing of the wishes of the parents or the children
themselves.
Most people can readily accept the fact that, from time to time, certain laws
may be necessary for the public good that some of us strongly disagree with, cut the
Issue In this case Involves nothing less than the Introduction of foreign proteins or
even live viruses Into the bloodstream of entire populations.
For that reason alone, the public Is surely entitled to convincing proof, beyond
any reasonable doubt, that artificial Immunization Is In fact a safe and effective
procedure. In no way Injurious to health, and that the threat of the corresponding
natural diseases remains sufficiently dear and urgent to warrant mass inoculation of
everyone, even against their will If necessary.
Unfortunately, such proof has never been given; and, even If it could be.
continuing to employ vaccines against diseases that arc no longer prevalent or no
longer dangerous hardly qualifies as an emergency.
Finally, even if such an emergency did exist, and artificial immunization could
be shown to be an appropriate response to It. the decision would remain cr-cntlally
a prililital one. Involving Issues of public health and safety that arc far too important
to be settled by any purely scientific or technical criteria, or. indeed by a-v criteria
less authoritative than the clearly articulated sense of the community about to be
subjected to it.
.
•
'
For all of these reasons. I want to present the case against routine immunization
as clearly and forcefully as I can. What 1 have to say is not quite a formal theory
capable of rigorous proof or disproof. It Is simply an attempt to explain my own
experience, a nexus of interrelated facts, observations, reflections, and hypotheses
which, taken together, are more or less coherent and plausible and make intuitive
sense to me.
1 ofTcr them to the public In part because the growing refusal of parents to
vaccinate their children is so seldom articulated or taken seriously. The fact Is that
we have been taught to accept vaccination as a sort of Involuntary communion, a
sacrament of our own participation in the unrestricted growth of scientific and
industrial technology, utterly heedless of the long-term consequences to the health
of our own species, let alone to the balance of nature as a whole. For that reason
alone, the other side of the case urgently needs to be heard.
The principal evidence that the vaccines arc effective actually dates from the
more recent period, during which time the dreaded polio epidemics of the 1940’s
and 1950’5 have never reappeared in the developed countries, and measles, mumps,
and rubella, which even a generation ago were among the commonest diseases of
childhood, have become far less prevalent, at least In their classic acute forms, since
the triple MMR vaccine was Introduced Into common use.
Yet how the vaccines actually accomplish these changes is not nearly as well
understood as most people like to think It is. The disturbing possibility that they act
In some other way than by ptoduclng a genuine Immunity Is suggested by the fact
that the diseases In question have continued to break out even In highly immunized
populations, and that In such cases the observed differences in Incidence and severity
between immunized and unlmmunlzed persons have tended to be Ear less dramatic
than expected, and In some cases not measurably significant at all.
in a recent British outbreak of whooping cough, for example, even fully immu
nized children contracted the disease in fairly large numbers, and the rates of serious
complications and death were reduced only slightly (5). in another recent outbreak
of pertussis, 46 of the 85 fully immunized children studied eventually contracted the
disease (6).
In 1977, 34 new cases of measles were repotted on the campus of UCLA. In a
population that was supposedly 91 percent Immune, according to careful serological
testing [7). Another 20 cases of measles were reported In the Pecos, New Mexico area
within a period of a few months In 1981, and 75 percent of them had been fully
Immunized, some of them quite recently (8). A survey of sixth-graders In a wcllImmunlzcd urban community revealed that about 15 percent of this age group arc
still susceptible to rubella, a figure essentially Identical with that of the prcvaccine
era (9).
Finally, although the overall Incidence of typical acute measles In the U5. has
dropped sharply from about 400,000 cases annually In the early 1960 s to about 30,000
cases by 1974-76, the death rate remained exactly the same (10); and, with the peak
Incidence now occurring In adolescents and young adults, the risk of pneumonia and
demonstrable liver abnormalities has actually Increased substantially, according to one
recent study, to well over 3 percent and 2 percent, respectively (11).
The simplest way to explain these discrepancies would be to postulate that the
vaccines confer only partial or temporary Immunity, which sounds reasonable enough,
given the fact that they arc either live viruses rendered less virulent by serial passage
In tissue culture, or bacteria or bacterial proteins that have been killed or denatured
by heat, such that they can still elicit an antibody response but no longer Initiate the
full blown disease.
Because the vaccine Is a "trick," in the sense that it limulalrt the true or natural
immune response developed in the course of recovering from the actual disease, it is
certainly realistic co expect that such artificial Immunity will In fact "wear off’ quite
easily, and even require additional "booster" doses at regular intervals throughout
life to maintain peak effectiveness.
Such an explanation would be disturbing enough for most people. Indeed, the
basic fallacy inherent in It Is painfully evident in the fact that there is no way to know
how long this partial or temporary Immunity will last in any given individual, or how
often it will need to be restlmulatcd, because the answers to these questions dearly
depend on precisely the same Individual variables that would have determined
8
9
1. ARE THE VACCINES EFFECTIVE?
There is widespread agreement that the time period since the common vaccines
were Introduced has seen a remarkable decline In the incidence and severity of the
corresponding natural Infections. But the customary assumption that the decline is
altrifulafk to the vaccines remains unproven, and continues to be seriously questioned
by eminent authorities in the field. The Incidence and severity of whooping cough,
for example, had already begun to decline precipitously long before the pertussis
vaccine was Introduced (t). a fact which led the epidemiologist C. C. Daucr to remark,
as far back as 1943:
’ .
If mortality [from pertussis] continues to dedine at the same rate
during the next 15 years. Il will be extremely difficult to show statis
tically that [pertussis Immunization] had any effect in reducing mortality
horn whooping cough (2).
Much the same Is true not only of diphtheria and tetanus, but also of TB, cholera,
typhoid, and other common scourges of a bygone era, which began to disappear
toward the end of the nineteenth century, perhaps partly In response to improve
ments In public health and sanitation, but In any case long before antibiotics, vaccines,
or any specific medical measures designed to eradicate them (3).
Reflections such as these led the great microbiologist Rend Dubos to observe
that microbial diseases have their own natural history. Independent of drugs and
vaccines, In which asymptomatic Infection and symbiosis arc far more common than
overt disease:
v
It Is barely recognized, but nevertheless true, that animals and
plants, as well as men, can live peacefully with their most notorious
microbial enemies. The world Is-obsessed by the het that poliomyelitis
' can kill and malm several thousand unfortunate victims every year. But
more extraordinary is the Eact that millions upon millions of young '
people become Infected by polio viruses, yet suffer no harm from the
infection. The dramatic episodes of conflict between men and microbes
arc what strike the mind. What Is less readily apprehended Is the more
common het that Infection can occur without producing disease (4).
whether or how severely the same person, unvaccinated, would have contracted the
disease In the fust place.
In any ease, a number of other observations suggest equally strongly that this
simple explanation cannot be the correct one. In the first place, a number of
Investigators have shown that when a person vaccinated against the measles, for
example, again becomes susceptible to It, even repeated booster doses will have little
or no effect (12).
In the second place, the vaccines do not act merely by producing pale or mild
copies of the original disease; all of them also commonly produce a variety of symptoms
of their own. Moreover, In some cases, these illnesses may be considerably more
serious than the original disease, Involving deeper structures, more vital organs, and
less of a tendency to resolve spontaneously. Even more worrisome is the feet that
they are almost always more difficult to recognize.
Thus, In a recent outbreak of mumps in supposedly Immune school children,
several developed atypical symptoms, such as anorexia, vomiting, and erythematous
rashes, without any parotid Involvement, and the diagnosis required extensive serol
ogical testing to rule out other concurrent diseases (15). The snydrome of "atypical
measles" can be equally difficult to diagnose, even when It Is thought of (14). which
suggests that It Is often overlooked entirely. In some cases, atypical measles can be
much more severe than the regular kind, with pneumonia, petcchlac, edema, and
severe pain (15). and likewise often goes unsuspected.
In any case. It seems virtually certain that other vaccine-related syndromes will
be described and Identified, if only we take the trouble to look for them, and that
the ones we arc aware of so far represent only a very small part of the problem. But
even these few make It less and less plausible to assume that the vaccines produce a
normal, healthy Immunity that lasts for some time but then nwi off, leaving the
patient miraculously unharmed and unaffected by the experience.
2. SOME PERSONAL EXPERIENCES WITH VACCINE-RELATED
ILLNESS.
I would like now to present a few of my own vaccine cases, both to give a sense
of their variety and chronlcity, and to show how difficult It an be to trace them,
and also to begin to address the crucial question that Is too seldom even asked,
namely, how the vaccines actually u'srf, l.c, what effects they do in feet produce In
the human body.
My first case was that of an 8-month-old girl with recurrent fevers
of unknown origin. 1 first saw here In January of 1977. a few weeks
after her third such episode. These were brief, lasting 48 hours at most.
but very Intense, with the fever typically reaching 105° F. During the
second episode, she was hospitalized for diagnostic evaluation, but her
pediatrician found nothing out of the ordinary. Apart from these
episodes, the child felt quite well, and appeared to be growing and
developing normally.
I could get no further information bom the mother, except for
the feet that the episodes had occurred almost exactly one month
20
apart; and. upon consulting her calendar, we learned that the fust
episode had come exactly one month after the last of her DPT Injec
tions, which had also been given at monthly Intervals. At this point.
the mother remembered that the child had had similar febrile episodes
Immediately after each Injection, but that she had been Instructed to
ignore them, Inasmuch as they are "common reactions" to the vaccine.
1 therefore gave the child a single oral dose of dilute homoeopathic
DPT vaccine; and I am happy to report that die child has remained
well since, with no further episodes of any kind.
This ease illustrates how homoeopathic remedies prepared from vaednes an be
used for rhiijnauT as well as treatment of vaccine-related Illnesses, which, no matter
how strongly they are suspected, might otherwise be almost Impossible to substantiate.
Secondly, beause fever Is the commonest known compilation of the pertussis
vaccine, and Inasmuch as the child seemed quite well between the attacks, her
response to the vaccine appeared to be a relatively strong and healthy one, disturbing
beause of its recurrence and periodicity, but In any use relatively simple to cure, as
indeed It proved to be. But one annot help wondering what happens to rhe vaedne
In those tens of millions of children who show no obvious response to It at all.
Since that time, I have seen at least half a dozen ases of children with recurrent
fevers of unknown origin, associated with a variety of other chronic complaints,
chiefly Irritability, temper tantrums, and Increased susceptibility to colds, tonsillitis.
and car Infections, which were similarly traceable to the pertussis vaccine, and which
responded successfully to treatment with the homoeopathic DPT nosodc. Indeed, I
would have to say, on the basis of that experience, that the pertussis vaccine Is
probably one of the .major auses of recurrent fevers of unknown origin In small
children today.
My second ase was that of a 9/, month old gid. who presented
acutely with a fever of 105° F.. and very few other symptoms. Like the
first, this child had lud two similar episodes previously, but at Irregular
Intervals; and the parents, who felt ambivalent about vaccinations in
general, had given her only one dose of the DPT vaccine so fer, although
the fust episode occurred a few weeks afterwards,
I first saw the child In June of 1978. The fever remained high and
unremitting for 48 hours, despite rhe usual acute remedies and sup
portive measures. A CBC revealed a white count of ja.loo per cu. mm..
with 45 percent lymphocytes, 11 percent monocytes, 25 percent neu
trophils (many with toxic granulations). 20 percent bands (also with
toxic granulations), and 1 percent metamyelocytes and other Immature
forms. When I asked a pediatrician about these findings, "pertussis"
was his Immediate reply. After a single oral dose of homoeopathic DPT
vaccine, the fever came down abruptly within a few hours, and the
child has remained well since.
This ase was disturbing mainly beause of the hematological abnormalities,
which were in the leukemoid range, together with the absence of any cough or
distinctive respiratory symptoms, which suggested that Introdudng'the vaedne dircedy
Into the blood may actually promote deeper or more systemic' pathology than
11
allowing the pertussis organism to set up typical symptoms of local inflammation at
the nonml portal of entry.
The third ease was a j-ycar old boy with chronic lymphocytic
leukemia, whom I happened to sec In August of
while visiting an
old friend and teacher, a family physician with over 40 years’ experience.
Well out of carshot of either the boy or his parents, he told me that
the leukemia had fust appeared following a DPT vaccination, and that.
although he had treated the child successfully with natural remedies
on two previous occasions, with shrinking of the liver and spleen to
approximately normal size, and dramatic Improvement in the blood
picture, full relapse had occurred soon after each successive DPP booster.
The Idea dial vaccinations might also be Implicated In some cases of childhood
leukemia was shocking enough In Itself, but it also completed the line of reasoning
opened up by the previous case. For leukemia is a cancerous process of the blood and
the blood-forming organs, the living,.the spleen, the lymph nodes, and the bone
marrow, which arc also the basic anatomical units of the immune system, insofar as
the vaccines arc capable of producing serious complications at all, the blood and the
Immune organs would certainly be the logical place to begin looking for them.
But perhaps even more shocking to me is the fact that the boy’s own physician
dared not communicate his suspicion of vaccine-related Illness to the parents, let alone
to die general public. It was this ease, that convinced me, once and for all, of the
need for serious, public discussion of our collected experiences with vaccine-related
illness, precisely because rigorous experimental proof will require years of investigation
and a firm public commitment that has not even been made yet.
I will now present two eases from my limited experience with MMR vaccine.
In December of 19S0 I saw a j-ycar old boy with a 4 week history
of loss of appetite, stomach aches, indigestion, and swollen glands. The
stomach pains were quite severe, and often accompanied by belching,
flatulence, and explosive diarrhea. The nose was also congested, and
the lower eyelids were quite red. The mother also reported some
unusual behavior changes, such as extreme untidiness, "wild” and
"noisy" playing, and waking at 2 a.m. to get into bed with the parents.
The physical examination was unremarkable except for some
large, tender left posterior auricular and subocdpltalhodcs, and markedenlargement of the tonsils. I then learned that the child had received
the MMR vaccine In October, about 2 weeks before the onset of
symptoms, with no apparent reaction to It at the time. I gave the child
a single dose of the homoeopathic rubella vaccine, and the symptoms
promptly disappeared within 48 hours.
In April 1981, the parents brought him back for a slight fever, and
another ywcck history of Intermittent pain In and behind the right
car, stuffy nose, etc. On examination, the whole right side of the face
appeared to be swollen, especially the cheek and the angle of the jaw.
The right eye was red and injected. He responded well to acute
homoeopathic remedies, and has remained well since.
This boy was typical of my rubella vaccine cases. At an Interval of a few weeks
after the MMR vaccine, which is about the same as the normal incubation period of
rubella, a rather nondescript illness develops, which becomes subacute and rather
more severe than rubella in the same age group, with, c.g.. abdominal or joint pains
and marked adenopathy, but no rash. Usually the diagnosis Is suspected because of
the characteilstlc posterior auricular and suboccipital nodes, and confirmed by a
favorable response to the homoeopathic rubella nosode.
As I read over this ease, I am struck by the posssibility that his second illness,
and especially the parotid enlargement, may have represented continuing activity of
the mumps component of the vaccine, inasmuch as I did not have the triple MMR
nosode, but only those derived from the individual components. We must therefore
also consider the probability that a variety of "mixed” or composite syndromes may
occur, representing the patient’s responses to two or all three of the vaccine com
ponents, either simultaneously or over time.
In April of Jpsi I fust saw a 4 year-old boy for bilateral chronic
enlargement of the posterior auricular nodes, which were also occa
sionally tender. The mother had noticed the swelling for about one
year, during which time he had become more susceptible to various
upper respiratory Infections, none of them especially severe. The mother
had also noticed recurrent parotid swelling at Irregular intervals over
the same time period, which began shortly after the MMR vaccine was
given at the age of j.
At the time of the first visit, the child was not 111: and, because
the mother was about 2 months pregnant at the time, I elected to
observe the child and do nothing If possible until the pregnancy was
over. He did develop a mild laryngitis in thc last trimester, which
responded well to bed rest and simple homoeopathic remedies.
In April of 1982. he omc down with acute bronchitis. I noticed
that the posterior auricular nodes were once again swollen and tender.
and I decided to give him the homoeopathic rubella nosode at that
point. The cough promptly subsided, and the nodes regressed in size
and were no longer tender. Two weeks bter, however, he returned
with a noticeably hard, tender swelling on the outside of the right
cheek, near the angle of the jaw, and some pain on chewing or opening
the mouth. A single dose of the homoeopathic mumps nosode was
given, and the child has been well since.
In this ease also, we see the subacute pattern of, the disease, with a strong
tendency to chronldty and Increased susceptibility to weaker, low-grade responses,
In contrast to the vigorous, acute responses typically associated with diseases like the
measles and the mumps when acquired naturally.
3.
HOW DO THE VACCINES. WORK?
It is dangerously misleading, and, indeed, the exact opposite of the truth to
claim that a vaccine makes us "Immune” or protects us against an acute disease, if in
fact it only drives the disease deeper into the Interior and causes us to harbor it
(firwikully, with the result that our responses to It become progressively weaker, and
show less and less tendency to heal or resolve themselves spontaneously.
What I propose, then. Is simply to Investigate as thoroughly and objectively as
we can how the vaccines actually u’orf inside the human body, and to begin by paying
attention to the Implications of what we already know. In particular, 1 would like to
consider In detail the process of falling III with and recovering from a typical acute
disease, such as the measles, In contrast with what we an observe following the
administration of the measles vaccine.
We all know that measles Is primarily a virus of the respiratory tract, both
because It Is Inhaled by susceptible persons upon contact with infected droplets In
the air, and because these droplets arc produced,by the coughing and sneezing of a
person with the disease.
Once inhaled by a susceptible person, the measles virus then undergoes a long
period of silent multiplication, first In the tonsils, adenoids, and accessory lymphoid
tissues of the nasopharynx; later In the regional lymph nodes of the head and neck;
and eventually, several days later, it passes Into the blood and enters the spleen, the
liver, the thymus, and the bone marrow, the "visceral" organs of the Immune system
(16). Throughout this "incubation” period, which lasts from 10 to 14 days, the patient
usually feels quite well, and experiences few or no symptoms (17).
By the time that the first symptoms of measles appear, circulating antibodies arc
already detectable In the blood, and the height of the symptomatology coincides
with the peak of the antibody response (18). In other words, the "illness" Is simply
the definitive effort of the Immune system to clear the virus from the blood. Equally
noteworthy Is the fact that the virus Is eliminated by sneezing and coughing, l.c.. via
the same route through which It entered In the first place.
It Is evident that the process of mounting an acute illness like the measles, no less
than recovering from It, Involves a general mobilization of the entire Immune system.
Including Inflammation of the previously sensitized tissues at the portal of entry,
activation of leukocytes and macrophages, liberation of the scrum complement
system, and a host of other mechanisms, of which the production of circulating
antibody Is only one, and by no means the most Important.
Such a splendid outpouring leaves little doubt that such illnesses arc In fact the
decisive experiences In the normal physiologic maturation of the Immune system as
a whole In the life of a healthy child. For not only will the child who recovers from
the measles never again be susceptible to It (19); such an experience also cannot fall
to prepare the Individual to respond even more promptly and effectively to any
Infections he may acquire in the future. The ability to mount a vigorous acute
response to organisms of this type must therefore be rcckkoncd among the most
fundamental requirements of general health and well-being.
In contrast, when an artificially attenuated virus such as measles Is Injected
directly Into the blood, by-passing the normal portal of entry, at most a brief
Inflammatory reaction may be noted at the Injection site, or In the regional lymph
nodes; but there Is no "Incubation period" of local contact at the normal portal of
entry, and consequently very little possibility of eliminating the virus via the same
route.
Even more important is the fact that the virus has been artificially "attenuated,"
so that It will no longer Initiate a generalized inflammatory response, or indeed any
of the nonspecific defense mechanisms that help us to respond to infection generally.
By "tricking" the body In this fashion, we have accomplished what the entire immune
system seems to have evolved In order to prevent: we have placed the virus directly
Into the blood, and given It free and Immediate access to the major Immune organs
and tissues, without any obvious way of getting rid of It.
The result is, Indeed, the production of circulating antibodies against the virus,
which can be measured In the blood; but the antibody response now occurs as an
Isolated technical feat, without any generalized Inflammatory response, or any notice
able Improvement In the general health of the organism. Exactly the opposite. In
fact: the price that we have to pay for those antibodies Is the persistence of virus
elements In the blood for prolonged periods of time, perhaps permanently, which In
turn presupposes a systematic weakening of our ability to mount an effective response
not only to measles, but also to other acute Infections as well.
Far from producing a genuine Immunity, then, the vaccines may act by actually
Interfering with or tuppresting the Immune response as a whole, in much the same way
that radiation, chemotherapy, and corticosteroids and other anti-inflammatory drugs
do. Artificial Immunization focuses on anlifody predudion, a single aspect of the Immune
process, and disarticulates It and allows It to stand for the whole. In much the same
way as chemical suppression of an elevated blood pressure Is accepted as a valid
substitute for a genuine cure of the patient whose blood pressure has risen. Worst of
all, by making It difficult or Impossible to mount a vigorous, acute response to
Infection, artificial Immunization substitutes for It a much weaker, chronic response,
with little or no tendency to heal Itself spontaneously.
Moreover, adequate models already exist, for predicting and explaining what
sorts of chronic disease arc likely to result from the chronic, long term persistence of
viruses and other foreign proteins within the cells of the immune system. It has long
been known that live viruses, for example, arc capable of surviving or remaining
latent within the host cells for years, without continually provoking acute disease.
They do so simply by attaching their own genetic material as an extra particle or
"cplsomc" to the genome of the host cell, and replicating along with It, which allows
the host cell to continue Its own normal functions for the most part, but Imposes on
it additional Instructions for the synthesis of viral proteins (20).
Latent viruses of this type have already been Implicated In three distinct types
of chronic disease, namely, 1) rrcumnl or episodic aorlr diseases, such as herpes, shingles,
warts, etc. (21); 2) "Jtw-vlrui" diseases, l.c., subacute or chronic, progressive, often fatal
conditions, such as kuru, Crcuzfcldt-Jakob disease, subacute sclerosing panencephalitis
(SSPE), and possibly Guillain-Barre syndrome (22); and j) (umorj, both benign and malig
nant (2)).
In any case, the latent virus survives as a dearly "foreign" clement within the
cell, which means that the Immune system must continue to try to make antibodies
against It, insofar as It can still respond to It at all. Because the virus is now permanently
Incorporated within the genetic material of the cell, these antibodies will now have
to be directed against the cell Itself.
The persistence of live viruses or other foreign antigens within the cells of the
host therefore cannot fail to provoke rtitlo-immuttc phenomena, because destroying the
1$
Infected cells Is now the only possible way that this constant antigenic challenge an
be removed from the body. Since routine vaccination Introduces live viruses and
other highly antigenic material into the blood of virtually every living person, it Is
difficult to esapc the conclusion that a significant harvest of auto-immune diseases
normal restraints of "histocompatibility" within the architecture of the surrounding
cells, and begin to multiply autonomously at their expense.
A tumor could then be described as "benign" Insofar as the breakdown of
histocompatibility remains strictly loallzed to the tissue of origin, and "malignant,"
Insofar as It begins to spread to other cell types, tissues, and organs, even In more
remote areas. Malignancy might simply represent the reactivation of the virus horn
Its latent phase Into a more acute mode, albeit with less Inflammation and more tissue
destruction than the original wild-type Infection.
If what I am saying turns out to be true, then what we have done by artificial
Immunization Is essentially to trade off our acute, epidemic diseases of the past century
for the weaker and far less curable chronic diseases of the present, with their
amortizable suffering and disability. In doing so, we have also opened up llmldess
evolutionary possibilities for the future of ongoing lit niuo genetic recombination
within the cells of the race.
most automatically result.
Sir Macfarlanc Burnet has observed that the components of the Immune system
all function as If they were collectively designed to help the organism to discriminate
"self' horn "non-sclf." I.c., to help us to recognize and tolerate our own cells, and to
Identify and eliminate foreign or extraneous substances as completely as possible (a.|).
This concept is exemplified not only by the acute response to Infection, but also by
the rejection of transplanted tissues, or "homografts," both of which result in the
complete and petmanent removal of the offending substance from the body.
If Burnet Is correct, then latent viruses, auto immune phenomena, and cancer
would seem to represent different aspects of the same basic dilemma, which the
Immune system an neither esapc nor resolve. For all of them presuppose a certain
degree of chronic immune failure, a state In which It becomes difficult or Impossible for
the body either to recognize Its own cells as unambiguously Its own, or to eliminate
Its parasites as unequivocally foreign.
In the use of the attenuated measles virus, It Is not difficult to Imagine that
Introducing It directly Into the blood would continue to provoke an antibody response
for a considerable period of time, which Is doubtless the whole point of giving the
vaccine; but that eventually, as the virus succeeded In attaining a state of latency
within the cell, the antibody response would wane, both because circulating antibodies
annot normally cross the cell membrane, and because they arc also powerful Immu
nosuppressive agents In their own right (05).
The effect of circulating antibody will thereafter be mainly to keep the virus
witliin the cell, I.c., to continue to prevent any acute Inflammatory response, until
eventually, perhaps under circumstances of accumulated stress or emergency, this
prcarlous balance breaks down, antibodies begin to be produced In large quantitiesagainst the cells themselves, and frank auto-immune phenomena of necrosis and tissue
destruction supervene. Latent viruses. In this sense, arc like biological "time bombs,"
set to explode at an indeterminate time In the future (26).
Auto Immune diseases have always seemed obscure, aberrant, and bizarre, bcausc
It Is not Intuitively obvious why the body should suddenly begin to attack and
destroy Its own tissues. They'make a lot more sense, and. Indeed, must be reckoned
as "healthy," If destroying the chronically Infected cells is the only possible way of
eliminating an even more serious threat to life, namely, the persistence of the foreign
antigenic challenge within the cells of the host.
Tumor formation could then be understood as simply a more advanced stage
of chronic Immune failure, according to the same model. For. as long as the host Is
subjected to enormous and unremitting pressure.to make antibodies against itself,
that response will automatially tend to become less and las effective.
Eventually, under stress of this magnitude, the auto-immune mechanism could
easily break down to the point that the chronlally infected and genctlally trans
formed cells, no longer clearly "self' or "nonself," begin to free themselves from the
I want next to consider each of the vaccines on an Individual basis, In relation
to the Infectious diseases from which they are derived.
The MMR Is composed of attenuated live measles, mumps, and rubella viruses,
administered In a single intramuscular Injection at about 15 months of age. Subsequent
re-immunization Is no longer recommended, except for young women ofchlldbearlng
age, In whom the risk of congenital rubella syndrome (CRS) Is thought to warrant It,
even though the effectiveness of re Immunization Is questionable at best.
Prior to the vaccine era, measles, mumps, and rubella were reckoned among'
the "routine childhood diseases," which most school-children contracted before the
age of puberty, and from which nearly all recovered, with permanent, lifelong7
Immunity, and no compilations or sequelae.
But they were not always so harmless. Measles, In particular, can be a devastating
disease when a population encounters It for the first time. Its Importation from Spain,
for Instance, undoubtedly contributed to Cortez' conquest of the great Aztec Empire;
whole villages were arrled off by epidemics of measles and smallpox, leaving only a
small remnant of cowed, superstitious warriors to face the bearded corqulsladom from
across, the sea (27). In more recent outbreaks among Isolated, primitive peoples, the
ase fatality rate from measles averaged 20 to 30 percent (28).
In both these so allcd "virgin-soli" epidemics, not only measles but also polio
and many other similar diseases take their highest toll of death and serious compil
ations among adolescents and young adults, healthy and vigorous people In the
prime of life, and leave relatively unharmed the group of school-age children before
the age of puberty (29).
This means that the evolution of a disease such as measles from a dreaded killer
to an ordinary disease of childhood presupposes the development of nonspecific or
"herd" immunity In young children, such tint, when they arc finally exposed to the
disease. It activates defense mechanisms already prepared and In place, resulting In
the long Incubation period and the usually benign, self-limited course described above.
16
17
4.
TOE INDIVIDUAL VACCINES RECONSIDERED.
Under these circumstances, the rationale for wanting to vaccinate young childrcn
against measles Is limited to the fact that a very small number of deaths and serious
complications have continued to occur, chiefly pneumonia, encephalitis, and the rare
but dreaded subacute sclerosing panenccphalitis (SSPE), a slow-vlrus disease with a
reported Incidence of i per aoo.coo cases (50). Pneumonia, by for the commonest
complication, Is usually benign and self-limited, even without treatment (31); and,
even In those rare cases In which bacterial pneumonia supervenes, adequate treatment
Is currently available.
By all accounts, then, the death rate from wild-type measles Is very low, the
Incidence of serious sequelae Is insignificant, and the general benefit to the child who
recovers from the disease, and to his contacts and descendants, Is very great. Conse
quently, even if the measles vaccine could be shown to reduce the risk of death or
serious complications from the disease, It still could not justify the high probability of
auto-immune diseases, cancer, and whatever else may result bom the propagation of
latent measles virus In human tissue culture for life.
Ironically, what the measles vaccine certainly has done Is to reverse the historical
or evolutionary process to the extent that measles is once again a disease of adolescents
and young adults (32), with a correspondingly higher Incidence of pneumonia and
other complications, and a general tendency to be a more sedous and disabling disease
than It usually Is In younger children.
As for the claim that the vaccine has helped to eliminate measles encephalitis, I
myself, In my own relatively small general practice, have already seen two children
with major seizure disorders which the parents dearly ascribed to the measles vaccine,
although they would never have been able to prove the connection In a court of
law, and never even considered the possibility of compensation.
Such cases therefore never make the official statistics, and arc accordingly omitted
from conventional surveys of die problem. Merely Injecting the virus Into the blood
would naturally favor a higher incidence of deep or visceral complications affecting
the lungs, liver, and brain, for which the measles virus has a known affinity.
The case for Immunizing against mumps and rubella seems a farliarl even more
tenuous, for exactly the same reasons. Mumps is also essentially a benign, self-limited
., disease In children before the age of puberty, and recovery from a single attack
,j confers lifelong immunity. The prindpal complication is meningoencephalitis, mild
or subdinlcal forms of which arc relatively common, although the death rate is
extremely low (33), and sequelae arc rare.
The mumps vaccine Is prepared and administered in much the same way as the
measles, usually in the same Injection; and the dangers associated with it arc likewise
comparable. Again like thcmcaslcs, mumps too Is East becoming a disease of adoles
cents and young adults (33), age groups which tolerate the disease much less well. The
chief-complication Is acute cpldidymo-orchitis, which occurs in 30 to 40 percent of
the males affected past the age of puberty, and usually results in atrophy of the testicle
on the affected side (35); but It also shows a strong tendency to attack the ovary and
the pancreas.
For all of these reasons, the greatest favor we could do for our children would
be to expose them all to the measles and mumps when they arc young, which would
18
not only protect them against contracting more serious forms of these diseases when
they grow older, but would also greatly assist In their Immunological maturation with
minimal risk. I need hardly add that this Is very dose to the actual evolution of rhey
diseases before the MMR vaccine was introduced.
The same discrepancy Is evident In the case of rubella, or "German measles.”
which In young children Is a disease so mild that It frequently escapes detection (36),
but In older children and adults not Infrequently produces arthritis, purpura, and
other severe, systemic signs (37). The main Impetus for the development of the vaccine
was certainly the recognition of the "congenital rubella syndrome (CRS)," resulting
from damage to the developing embryo Ik utcro during the first trimester of pregnancy
(38), and the relatively high Incidence of CRS traceable to the rubella outbreak of
1964.
But here again, we have an almost entirely benign, self-limited disease trans
formed by the vaccine Into a considerably less benign disease of adolescents and young
adults of reproductive age, which Is, Ironically, the group that most needs to be
protected against It. Moreover, as with measles and mumps, the simplest and most
effective way to prevent CRS would be to expose everybody to rubella in elementary
school; re infection docs sometimes occur after recovery from rubella, but much less
commonly than after vaccination (39).
The equation looks somewhat different for the diphtheria and tetanus vaccines.
First of all, both diphtheria and tetanus arc serious, sometimes fatal diseases, even
under the best of treatment; this Is especially true of tetanus, which still carries a
mortality of dose to 50 perccht.
Furthermore, these vaccines arc not made from living diphtheria and tetanus
organisms, but only from certain "toxins" elaborated by them; these poisonous
substances arc still highly antigenic, even after being Inactivated by heat. Diphtheria
and tetanus "toxoids" therefore do not protect against Infection per k. but only against
the systemic action of the original poisons, In the absence of which both Infections
arc of minor Importance clinically.
Consequently, It Is easy to understand why parents might want their children
protected against diphtheria and tetanus, If safe and effective protection were avail
able. Moreover, both vaccines have been In use for a long time, and the reported
Incidence of serious problems has remained very low, so that there has never been
much public outcry against them.
On the other hand, both diseases are quite readily controlled by simple sanitary
measures and careful attention to wound hygiene; and, in any asc, both have been
steadily disappearing from the developing countries, since long before the vaccines
were Introduced.
Diphtheria now occurs sporadically in the United States, often In areas with
significant reservoirs of unvaednated children. But the claim that the vaccine Is
"protective" Is once again belled by the fact that, when the disease docs break out,
the supposedly "susceptible" children arc in fact no more likely to develop clinical
diphtheria than their fully Immunized contacts. In a 1969 outbreak in Chicazo, for
example, the Board of Health reported that 25 percent of the cases had been Fully
Immunized, and that another 12 percent had received one or more doses of the
19
vaccine and showed serological evidence of full immunity; another rS percent had
been partly Immunized, according to the same criteria (40).
So, once again, we arc faced with the probability that what the diphtheria
toxoid has produced Is not a genuine immunity to diphtheria at all, but rather some
sort of chronic Immune tulrraiuc to it. by harboring highly antigenic residues some
where within the cells of the Immune system, presumably with long-term suppressive
effects on the Immune mechanism generally.
This suspicion Is further aggravated by the fact that al! of the DPT vaccines arc
alum-precipitated and preserved with Thiomcrsal, an organomercury derivative, to
prevent them from being metabolized too rapidly, so that the antigenic challenge
will continue for as long as possible. The fact is that we do not know and have never
even attempted to discover what actually becomes of these foreign substances, once
they arc Inside the human body.
Exactly the same problems complicate the record of the tetanus vaccine, which
almost certainly has had at least some impact In redudng the Incidence of tetanus in
its classic acute form, yet presumably also survives for years or even deCades as a
potent foreign antigen within the body, with long-term effects on the immune
system and elsewhere that are literally Incalculable.
The power of the pertussis vaccine to damage the central nervous system, for
example, has received growing attention since Stewart and his colleagues repotted
an alannlngly high Incidence of encephalopathy and severe convulsive disorders In
British children that were traceable to the vaccine (qrJ-My own cases, a few of which
were reported above, suggest that hematological disturbances may be even more
prevalent, and that, in any case, the fawn compilations almost certainly represent a
small fraction of the total.
In any case, the pertussis vaccine has become controversial even In the United
States, where medical opinion has remained almost unanimous in favor of Immuni
zations generally; and several countries, such as West Germany, have discontinued
routine pertussis vaccination entirely (42)..
Pertussis Is also extremely variable dlnially, ranging In severity from asympto
matic. mild, or inapparent infections, which arc quite common actually, to very rare
eases In young infants less than 5 months of age, In whom the mortality Is said to
reach 40 percent (43). Indeed, the dlscasc'is rarely fatal or even that serious In children
over a year old, and antibiotics liavc very little to do with the outcome (44).
A good deal of the pressure to immunize at the present time thus seems to be
attributable to the higher death rate in very young Infants, which has led to the
terrifying practice of giving tills most clearly dangerous of the vaccines to infants at 2
months of age, when their mothers’ milk would normally have protected them from
all infections about as well as It an ever be done (45). and the effect on the still
developing blood and nervous system could be atastrophlc. ■
For all of these reasons, the practice of routine pertussis Immunization should
be discontinued as quickly as possible, and more studies done to assess and compensate
the damage that it has already done.
Poliomyelitis and the polio vaccines present an entirely different situation. The
standard Sabin vaccine Is trivalcnt, consisting of attenuated, live polioviruses of each
of the three strains associated with poliomyelitis; but It Is administered orally, In much
the same way as the Infection Is acquired In nature. The oral or non-lnjcctable route,
which leaves the recipient free to develop a natural Immunity at the normal porta!
of entry, l.c„ the Cl tract, would therefore appear to represent a considerable safety
factor.
On the other hand, the wild-type poliovirus produces no symptoms whatsoever
In other 90 percent of the people who contact It, even under epidemic conditions
(46); and, of those people who do come down with recognizable clinical disease,
perhaps only 1 or 2 percent ever progress to the full-blown neurological picture.of
"poliomyelitis," with Its characteristic lesions In the anterior horn cells of the spinal
cord or medulla oblongata (47).
Poliomyelitis thus presupposes peculiar conditions of susceptibility In the host,
even a specific anatomical susceptibility, since, even- under epidemic conditions, the
virulence of the poliovirus Is so low, and the number of ases resulting In death or
permanent disability was always remarkably small (48).
Given the fact that the poliovirus was ubiquitous before the vaccine was
Introduced, and could be found routinely In samples of city sewage whcrevcr.it was
looked for (49). it Is evident that effective, natural Immunity to poliovirus was already
as close to being universal as It an ever be', and a fatliarl no artificial substitute could
ever equal or even approximate that result. Indeed, because the virulence of the
poliovirus was so low to begin with. It Is difficult to see what further attenuation of
It could possibly accomplish, other than to abate as well the full vigor of the natural
Immune response to It. .
.
For the feet remains tint even the attenuated virus is still alive, and the people
who were anatomlally susceptible to It before arc still susceptible to It now. This
means, of course, that at least tome of these same people will develop paralytic polio
from the vaccine (50). and that the others may still be harboring the virus in latent
form, perhaps within those same cells.
.
The only obvious advantage of giving the vaccine, then, would be to Introduce
the population to the vims when they arc still Infants, and the virulence is normally
lowest anyway (5I); and even this benefit could be more than offset by the danger of
weakening the Immune response, as we have seen. In any ease, the whole matter is
clearly one of enormous complexity, and illustrates only too well the hidden dangers
and miscalculations that are Inherent in the virtually Irresistible attempt to beat nature
at-her own game, to eliminate a problem that cannot be eliminated. l.e„ the
susceptibility to disease Itself.
So even In the asc of the polio vaccine, which appears to be about as safe as
any vaccine ever can be, the same fundamental dilemma remains. Perhaps the day
will come when we can fece the consequences of deliberately feeding live polioviruses
to every living infant, and admit that we should have left well enough alone, and
20
21
"Whooping cough." much like diphtheria and tetanus, began to decline as a
serious epidemiological threat long before the vaedne was Introduced. Moreover,
the vaccine has not been particularly effective, even according to its proponents; and
the Incidence of known side-effects is disturbingly high.
addressed ourselves to the art of healing the sick when we have to. rather than to
tire tcdmology of eradicating the porsifililg of sickness, when we don't have to. and
can't possibly succeed In any case.
5.
VACCINATION AND THE PATH OF MEDICAL TECHNOLOGY.
In conclusion, 1 want to go back to the beginning, to the essentially political
aspects of vaccination, that oblige us all to reason and deliberate together about
matters of common concern, and to reach a dear decision about how we choose to
live. I have stated my own views regarding the safety and effectiveness of the vaccines.
and I hope that others of differing views will do the same.
That Is why 1 am deeply troubled by the atmosphere of fanaticism with which
the vaccines arc imposed on the public, and serious discussion of them Is ignored or
stifled by the medical authorities, as If the question had already been settled defini
tively and for all time. In the words of Sir Macfarlane Burnet,
It Is our pride that In a civilized country the only infectious diseases
which anyone b likely to suffer qrc cither trivial or easily cured by
‘ available drugs. The diseases that killed In the past have in one way or
another been rendered Impotent, and. In the precess, genera! principles
of control have been developed which should be applicable to any
unexpected outbreak In the future ($:).
Quite apart from the truth of these claims, they exemplify the smugness and
self-righteousness of a profession and a society that worships Its own ability to
manipulate and control the processes of nature itself. That is why. as Robert Men
delsohn has said, "we arc quick to pull the trigger, but slow to examine the conse
quences of our actions (53)."
Indeed, one would have to say, mclfioJicallg slow. In 1978. for example, the
American Academy of Pediatries, which had been charged by Congress with respon
sibility to formulate guidelines for Federal compensation of "vaccination-related
Injuries," issued the following eligibility restrictions:
1. Compensation should be made available to any child or young
person under the age of is yean, or a contact of such person
of any age. who suffers a major reaction to a vaccine mandated
for school entry or continuation in school In his or her state of
residence.
2. Such a reaction vdould Have ban prrvinu!^ rczsgnitril ar a pwiifIr riwqucitcr
of tfj vaccine given.
3. Such a reaction ifovld Have oavrred no mere [fan jo days following Ide
immvnitalion (5g).
These restrictions would automatically exclude all of the chronic diseases, or
Indeed anything other than the very few adverse reactions that have so far been
identified, which dearly represent only a tiny fraction of the problem.
22
Still less can cither the government or the medical establishment be considered
Ignorant of the possibility that lurks In every parent's mind and heart, namely, that
the vaccines cause cancer and other chronic diseases. Precisely that possibility was
raised by Prof. Robert Simpson of Rutgers in a 1976 seminar for sdcncc writers,
sponsored by the American Cancer Society:
Immunization programs against flu. measles, mumps, polio, and .
so forth, may actually be seeding humans with RNA to form latent
provlruses In cells throughout tire body. These brent provlruses could
be molecules In search of diseases: when activated, under proper con
ditions, they could cause a variety of diseases, Induding rheumatoid
arthritis, multiple sderosls, systemic lupus erythematosus, Parkinson's
disease, and perhaps oncer (55).
Unfortunately, this Is the sort of warning that very few people arc willing or
able to hear at this point, least of all the American Cancer Society or the American
Academy of Pediatrics. The fact Is, as Dubos points out, that all of us still want to
believe In the "mlrade,” regardless of the evidence.
The faith In the maglol power of drugs often blunts the aldol senses,
and comes dose at times to a mass hysteria. Involving scientists and
hymen alike. Men want mltades as much today as In the past. If they
do not |oln one of the newer cults, they satisfy this need by worshiping
at the altar of modern science. This faith In the maglol power of drugs
Is not new. It helped to give medicine the authority of a priesthood.
and to recreate the glamor of ancient mysteries (56).
The idea of eradicating measles or polio has come to seem attractive to us.
simply because the power of medical science makes It seem technically pouiflr; we
worship every victory of tcdmology over nature. Just as. the bullfight celebrates the
triumph of human Intelligence over the brute beast.
That Is why we do not begrudge the drug companies their enormous profits.
and gladly volunteer our own bodies and those of our children for their blest
experiments. Vaccination Is essentially a religious sacrament of our own participation
In the miracle, a veritable anto ela fd In the name of modern civilization Itself.
Nobody In his right mind would seriously entertain the Idea that. If we could
somehow eliminate, one by one, measles and polio and all the known diseases of
mankind, we would be any the healthier for It, or that other even more serious
diseases would not quickly take their place.
Still less would a rational being suppose that the Illnesses from which he suffered
were "entitles" somehow separable horn the patients who suffer them, and that,
with the appropriate chemical or surgical sacrament, this separation can literally be
carried out.
Yet these are precisely the "mltades" we are taught to believe in. and the
idolatries to which we aspire. We prefer to forget the older and simpler truths, that
the propensity or susceptibility to illness is deeply rooted In our biological nature,
and that the phenomena of disease arc the expression of our own life energy, trying
to overcome whatever It is trying to overcome, trying, in short, to fieal itself.
The myth that we can Find technical solutions for all human ailments seems
attractive at Fust, precisely because It bypasses the problem of healing, which Is a
genuine miracle in the sense that it can always foil to occur. We are all genuinely at
risk oF illness and death at every moment: no amount of technology can change that.
Yet the mission of technical medicine is precisely to try to change that: to stand at
al! times in t.hc front lines against disease, and to attack and destroy it whenever and
wherever it sl^ows itself.
That Is why. with all due respect, I cannot have fanli In the miracles or accept
tire sacraments of Merck, Sharp, and Dohme and the Center for Disease Control. I
prefer to stay with the miracle of life itself, which has given us illness and disease, but
also the arts of medicine and healing, through which we can acknowledge and
experience our pain and our vulnerability, and sometimes, with the grace of God
and the help of our fellow men, an awareness of health and well-being that transcends
all boundaries. That is my religion; and. while I would willingly share it. I would not
fora it on anyone.
NOTES.
i Moruner. E.. "reitunli tmmuniniion." ILr/ilal hxlMr, Oaobca !$&□. p >oj.
3. Quoted in Mortimer, if tU.. p. b?.
j. Dubes. R , Muap a( IlzaltA, Harper. 1959, p. )j.
4. IfU . h>. >4
5 Stewart C.. "Vaccination against Whooping Cough. Efficiency w. RbJx” Laerrt. 19,7. p. ap.
6 Mz/«al Tnhv, Jan. 10. 1979. p 1.
Cherry, J. ’The New FpxJcmwIc^y of Meadei ar*J Rubella.' Hry.uf frarlKc. July i>to. pp. $>•$<.
I Unfx.Hr.hcd data fiorn (lie New Mexico Health Department (private communtcation}.
9 law leu M , el al, "Rubella Suk.cptlbJiiy in Snili Olden." M-amnBf lUby-io&y. June 19M
to Cl^rty if ul.p n
>1. la/cilrAI tkuam. lUiiiaijt lyll.p JI.
II Cherry, if nt., p. ya
I). Fi-J| P>«Ikc N<*1. July if. ipRi. p. I.
14. Ferrante, "Atypical Symptoms! Il codd idl Be Mcasla." M4o»
Sept. y>. 19S0. p. ?4.
>$. Cher nr. if rtf.. p. 5).
16 Ft.nlrfx. C. "Meador In Vaughan, V, et al. Nzta«’i Trtfh4 if Pifuim, Dth fd. iaundm. iqn. p If),
i) lYa»u. B. et a!, Mxrafiafaff. jnd fj, Haij>er, 19; j. p.
il If J. p 1
>9 iM.p >H»
». IW p 141S.
at. Ibyfl*.k. L. "Slow Vlruscj," EutWirc Hza/di Rryot, February 19I1. p 4.
31. IM . pp 1-4.
ay Cbm. et al. if rtf. Ch 6). pp. 1411-1447.
24. Burnet. M . FAz latrprfj »f lAr My. Athencum. 1966. p tl
a$. Talar. N . “Autoimmunity,” in Fudcnberg, It. et J. Banit a«J Clued
yd Ed.Lange, ipM, p. an.
a6 (Uyn«k. if rtf , p 4.
ay MtNeifl. W . Ffi|wi aU Prryln. Anchor. 1916. p itf
il Brunei, M, ard White. D., TAz Na Ural I Intrrj if blitUiw C>wne. Cambridge, 1971. p. 16.
19 If J. pp qo. 1)1, et parslrn.
ya Srrignun. A .
Vlnit Infeitkma.” In Vaughan. V., if rtf. p Qp
|>. Ildl^*. rf tit, p Ko
p U/nlmx Dtvavs. Aptd 19)9, p )6.
I). rtuHtjt. C . "Mump.- in Vaughan, et J . 7
. p i-ji.
14 Hayden. C . ct al."Mump and Mumpa Vxctnc tn the U SC*>tfi**><7 E7w«.'im. Sept. >919. p 9).
Jg fh'Orjn. Mumfn.'/y nt. p Ip
)6 Fhul^n. I ulrlla." »y rtf.p. M|
W IM.p »a
yl Glasgow L . and Overall. |. "Congenital Rubella Syndrome," tn Vaughan. et al. ff. rtf., p. 4I).
W H-ill-fn. RulrUa. ry itf.p 26s
•'
fj Cited m Mci>lcl>*>hn. R . ’The Truth About Imrnunluttoni," TA< FrrylrT DmIx. April >9;!. p. 1.
41 Stewart. 7 n. p jp.
41 Mvttmiet ay (U . p ill,
4] Fc»gw. R . PtrtuBB. ‘ tn Vaughan, et al. 7 rtf, p. )<•>
<4 IM. p .<9.
45 Batrca. L. "Baeaxt Feeding." In Vaughan, et il. 7 (It., p. *91
46 Burnet and White. 7
p 9tR.
4; Davu et d . 7 («.. p 1 jrjuff.
4« IM.p u!n
49 Burnet ard White. 7 tU. p 91.
$0. Idgmatt. V,' holderra of Polkr.trus Immunlntlon." ILnydd P>xtk/. AuguX 19B0. pp 61-6).
$1. Burnet and White, ay rtf., p 94.
y Burnet. 7 (tf.p. Ul.
5) Mendehchn. if.ill. p. y.
$4 Quoted tn Wcl-ale.
"Vacctno. Rbka, and Compensations." Wali«a [><re>a. February 19SJ. p. 16.
Quoted n Mendelsohn. 7. dt. p. 1.
$6. Duben. 7 nt. p. ijy.
TOWARDS A NEW IMMUNIZATION STRATEGY
[In the seventh Annual Meet of the MFC at
RUHSA, we spent 1J days in discussing critical issues
in the care of under-fives— nutrition, inmunization,
diarrhea - as faced at the level of community work.
We had planned to publish the proceedings of this
discussion on all these three topics in the Bulletin.
But we have now decided to publish only the report
on immunization strategy - a discussion in which
Dr. Jacob John of the Christian Medical College,
Vellore, presented his path-breaking idea of a really
scientific strategy for mass-immunization of the underfives Editor.]
THE PROBLEM
Should immunization be performed on a mass scale
at a community level ? What strategy should be
adopted to get 100% coverage? What vaccines should
be used ? How to improve compliance of people with
an immunisation programme ? How to simplify the
procedure ? Should immunisation be voluntary or
compulsory ? These questions were raised in the minds
of many.
To immunise or not to immunise on a mass scale
was the basic question. Various views were expressed.
The extremists on one side adopted a nihilistic view :
the entire immunisation programme is futile. Their
reasons :
1.
2.
Within the present social structure and with the
available Government health structure, no signi
ficant immunisation coverage is possible. Immu
nisation is therfore no longer an epidemiological
tool to reduce disease, but a means of persona!
prophyhaxis for those with access to the health
system.
, H
The necessity for and efficacy under field condi
tions of available vaccines, have never been
tested on the basis of hard epidemiological data
in India.
3.
Especially with vaccines which cause some reac
tion e. g. DPT-people’s compliance in completing
the course of vaccination is poor.
4.
Lack of a proper “ cold chain ” i. e. a system to
keep vaccines which are sensitive to heat in a
cold environment from the point of production
to the point of delivery.
The result is that existing immunisation programmes
have little impact on the morbidity and mortality rates
in a community. They are a collosal waste of human
and material resources which can be diverted to basic
purposes.
The moderates wanted to stick to the present stra
tegy but improve coverage through a massive health
education programme and motivation of the people
for immunisation - a typical moderate remedy for all
ills relating to the social, political or health care
systems.
>
DECIDING PRIORITIES
SCIENTIFICALLY
Dr. Jacob John, a virologist at the Christian Medi
cal College, Vellore, provided what was perhaps a
happy mean. According to him, cne of the main pro
blems with the present Immunisation schedule and
system was that it was unscientific. Western schedules
had been taken over and tacked on to the Indian health
care delivery system. If properly followed, according
to the present schedule, an Indian child by the age of
five years, was expected to have 28 separate injections
all to be provided by the ANM at the doorstep.
According to Dr. John, in order to overcome these
difficulties, it is necessary to •
1.
Select vaccines according to need, efficacy and
safety.
2.
Simplify immunisation schedules.
.
:
3.
Concentrate on mothers for improving compli
ance.
A vaccine can be assigned approximate “ notional ”
scores according to its need, efficacy and safety. Need
is determined by the prevalence of the disease; morbi
dity and mortality due to that disease in the commu
nity. Efficacy is decided by the degree of protection
obtained after immunisation. Safety depends on the
incidence and severity of adverse reactions due to the
vaccines.
Even though accurate data regarding prevalence,
morbidity etc. are unavailable, rough scores can be
assigned on the basis of available data and common
experience. We went through this exercise at our
session. The scores we assigned, through consensus,
were as follows : (The scores were assigned on a scale
of 0-4 ’)
(6)
Vaccine
Against
Diphtheria
Whooping cough
Tetanus
Polio
T.B.
Small Pox
Measles
Typhoid
Cholera
Need
Efficacy
1
4
0
4
2
4
2
4
2 or 4
depending on
1 cold chain ’)
1 or 2
4
4
2
I
1
3
3
4
Safety
4
2
4
4
Product of
the three
16
12
48
vaccine) are also minimised.
Dr. Jacob John and his colleagues have tried this
64 or 32
new strategy in a village near Vellore.
To avoid adverse reaction of the vaccines and high
3
2
4
3
3
24 or 12
0
64
12
3
Dr. John’s experience was that the ranking of the
the vaccines, on the basis of the product scores, tended
to agree, no matter who went through the scoring
exercise. According to this ranking system, the priority
vaccines were against-
1 ) Measles,
5 ) Diphtheria,
is that the cluster schedule ■ uses available manpower
more efficiently, in order to acnieve wider coverage as
well as greater epidemiological impact. By this means
logistic problems (e.g. “ cold chain ” for oral polio
2} Polio, 3) Tetanus,
6 ) Whooping Cough.
4)
dropout rate at present, the strategy was modified to
give two safe vaccines like measles and polio.
Following
coverage :
to primary health centre and their mothers equate
coming to P.H.C. to sickness.
,
The most important innovation described by
Dr. Jacob John was his concept of “ cluster ” immu
should go from house to house distributing
immunisation cards and hand bills giving infor
mation about disease and benefit of its prevention
by immunisation. Idea being, though mothersmay not be able to read the information it can.
be transmitted to them by some literate person
in the surroundings. ANM should.talk to mother
and motivate, her for. immunisation. .,.In this
nisation.
We hope soon to carry ..an article by
Dr. John describing the (epidemiological , basis and
practical details.. So this is only a short account
strategy ANM. has to gp from .hqnse. , tQ , house
only once.
. .
3.
Give exact time at which mother .should bring
her child to the immunisation centre.
4.
Give all children below one year three doses of
oral polio vaccine at an interval of 4 weeks and
give single dose of measles vaccine to the children
above one year. '
<
..,
i
5.
well as about the specific time and place as. planned.
The propoganda is directed mainly at the mothers of
the target children.
to to eradicate small-pox 1. The programmatic basis
.3-4 days before the immunisation day, ANM
,2.
THE “ CLUSTER - APPROACH ”
. The epidemiologic basis of the ‘‘ cluster ” schedule
is that if a large proportion of the vulnerable popula-'
tion (children under five) are protected together, the
transmission of infection becomes much more diffi-'
cult, so that even unprotected children have less
chance of getting the disease. (Similar strategy was used
Keep immunisation centre separate from primary
health centre because sick children are brought
1.
TB
The idea is to reorder the immunisation schedule
and programme completely. Instead of ANMs immu
nising individual children in their homes right through
the year, health teams immunise all the children in a
community together, according to a simplified schedule
based on the ranked priorities,, at a time and place
fixed beforehand. The visit of the health team is.
preceded by one week “ propaganda blitz
which
aims at providing information about immunization, as
rules were followed to achieve 100 %
Collect immunisation cards that were given to
the mothers by ANM so that it becomes easier
to keep a record of the number of people who
attended the centre. .
.
Advantages of this strategy are :
-'
I.
Schedule is simpler
2.
It is necessary to go to particular village on three
days at an interval' of one month in a year.
Because of this storage and transport problems
'
are minimised. Vaccine can be stored at district
place throughout the year and can be brought to
the village only thrice.
■ ■ *1 ■ •
(3)
REDIRECTING
CONTRACEPTIVE RESEARCH
1; (
Research Priorities
First, as you may know, contraceptive research at
present focuses heavily on hormones, drugs and inva
sive devices, such as hormone-releasing IUDs, prosta
glandins, injectable progestogens, silastic hormonal
skin implants and antipregnancy vaccines. At the same
time, there is relatively little research on safer and
cheaper mechanical and barrier methods, on contra
ceptives which act locally rather than systemically, or on
methods which require no mechanical intervention
whatsoever. Examples of such safer methods include the
cervical cap, diaphragm, contraceptive sponge, ovula
tion method and thermal sperm control.
The safer contraceptive methods also tend not to
require physician’s intervention, thus providing low cost,
easily accessible birth control for more people. Parti
cularly good examples are the contraceptive sponge,
FROM THE EDITORS DESK.There is no question that world population is grow
ing at a rate not commensurate with availability of
material resources. The population growth rate in devel
oping countries is generally higher than in the developed
onse. There is therefore a .need to. evolve methods to
control this growth. The policies for and the methods
of population control, however,, need to be. critically
and continuously evaluated. In two of the early issues
of the Bulletin (Nos. 9 and 10), the population con
trol policy vis a vis the socio-economic Conditions
were discussed.. ■ •
■
... .
In this issue, we present a more technical aspect,
namely, contraceptive research and the hazards of the
“ pill. ", Mahtab Bamji, in her article,. discusses the
associated risks of steroidal coontraceptives and.
concludes that the benefits outweigh the risks. The
other viewpoint is from the Boston Women’s Group.
Much contraceptive research is directed towards
women. The woman ultimately has to bear the burden
of either pregnancy or contraception. The Group
feels that since all contraceptive research is dominated
by men, the drug companies are controlled by men and
the policy makers are men, there is no proper under
standing of women's problems. MFC is not directly
involved with feminist mavements. The question
which I, however, wish to raise is-when scientific
research is also dominated by men, to what extent are
women scintists and doctors influenced and perhaps,
“ brain-washed ” by male thinking ?
Kaniala Jayarao
By Judy Norsigian
which requires rid fitting,and the ovulation method,
which requires' no mechanical intervention.
Those of us active in the women’s health movement
are concerned that present funding is > too heavily
weighted toward drug and device research. Too often
such research has exposed human subjects,, mostly
women, to serious adverse consequences. In cases where
insufficient research has resulted in premature approval
of contraceptive methods, much larger female popula
tions have been exposed unnecessarily to dangers. The
sequential Pill and Daikon Shield . are two. well
publicized examples of this, although all Pills and IUDs
might well be classified as unjustifiably,- hazardous in
light of the extensive and increasing documentation of
Pill and IUD risks. lu addition, adverse consequences
of contraceptive drugs and devices account for a sur
prisingly large number of hospital admissions, which
are both expensive and traumatic for the women
irivolved.
...........
It is alarming to note that in 1976 out of 870 million
spent worldwide on contraceptive research outside of the
drug industry, only 50,000 dollars was spent on barrier.
method research. Safe birth control methods do not
receive priority by those who control the research dol
lars, while potentially dangerous methods do attract the
majority of funds. We urge a. major reordering of priori
ties, so that research on the safer birth control methods
mentioned above receive the greatest emphasis. New
priorities would also include research on better ways to
communicate information about birth control methods.
Male Researchers and policy makers :
.
It is interesting to note that most contraceptive
investigators are male and hence have little direct
understanding of the practical impact of their research
on women.- According to the inventory of population
research projects in the U.S. over 80 % of federally
funded investigators in the areas of contraceptive
development and contraceptive evaluation during 1976
were males. It is of no small significance that-, these
male investigators will never have to use the, methods
that they develop. Moreover, we believe that their
focus on the biological model and their fascination and
involvement in the research process sometimes over
(4)
shadows their concern for the well-being of research
subjects.
In our opinion, there needs to be more research
conducted by Community-based women’s health centers
which have worked directly with those who are intended
to benefit from this research. Furthermore, subjects
should play a major role in designing and/or approving
the research design. We believe that such an approach
would result in stricter adherence to research protocol.
Our third area of concern is policy-making. Private
organizations like the Population Council, Ford
Foundation, the Rockefeller Foundation, Planned
Parenthood, and drug companies, as well as the federal
government, sponsor practically all current contracep
tive research, setting priorities for this research as well.
Policy-makers for these organizations are also primarily
males, who make decisions with little or no input by the
many users of contraceptives, who supposedly benefit
from the research.
An example of policy recommendations that almost
totally ignore the areas of safer research we are ad
vocating may be found on page 40 of the Inventory
and Analysis of Federal Population Research.
1. Development of male contraceptive methods and
techniques, including studies of combinations of
known drugs and new delivery systems. .
,
. 2. Synthesis of new chemical agents for the regula
tion of female and male fertility.
3. Expanded screening capabilities as well as ac
celerated assessment Of new and old chemical entities.
4. Critical biological assessment of biodegradable
drug delivery systems.
5. Investigation of new methods for reversible and
permanent sterilization of both males and females.
6. Development of a long
ceptive method.
7.
acting female contra
Increased research on intrauterine devices.
8. Support of clinical studies required by FDA to
to expedite the availability of new methods.
9. Assessment of the mode of action of post
ovulatory contraceptives.
10.
Development of technology for the detection of
for
ovulation and utilization of such technology
family-planning purposes.
These recommendations were submitted
by the
ICPR Committee., composed of 17 men and one woman
We doubt if a committee composed primarily of women
-consumers as well as researchers and government administrators-would have presented a similar list of
recommendations.
It is our position that women should be creating
policy on behalf of women, at the very least, and that all
users of contraceptives should have a significant voice
in determining what kind of research is funded. To the
extent that birth control is still primarily the responsibil
ity of women, and that women are the ones who bear the
major consequences childbirth, as well as the risks
and serious complications of birth control, women
should have a major voice in determining which contra
ceptive research priorities will best meet their needs.
' Currently, the National Women’s Health Network
(NWHN) is conducting a nation-wide survey of over
100 women’s health centers and women’s health educa
tion groups to establish what women’s health organiza
tions see as their contraceptive research priorities. When
complete, this study will be a first-of-its-kind, revealing
what kind of research women want and expect the
government to fund.
The Network is particularly concerned that the
whole issue of contraceptive research be viewed in the '
context of the rising incidence of sterilization abuse. The
widespread absence of safe and effective birth-control
methods and the promotion of newer, more hazardous
contraceptives, coupled with the withdrawal of abortion
services, especially for poorer women, has forced more
and more people, both men and women, to submit to
sterilization as the solution to fertility control. At this
time, we urge a moratorium on all funding for new ex
periments with new sterilization methods and recom
mend further investigation into the consequences of cur
rent methods of sterilization.
The medical establishment, including government
and private organizations, universities, and industrial
supply corporations, presently promote research which
emphasizes patents, profits and the development of new
technologies. The NWHN recommends a shifting of
priorities so that safer contraceptives, for both men and
women, can be developed and marketed in a timely
manner.
Extractedfrom Science For The People.
•
COMPLEMENTING PLANS AND RESOURCES FOR
UNIVERSAL IMMUNIZATION
Operational guidelines to be followed by UNICEF programme staff when discussing and draw
ing up ajoint Plan of Action for an immunization programme.
General
Primary health care is defined in the De
claration of Alma Ata as essential health care
based on practical, scientifically sound and
socially acceptable methods and technology
made universally acceptable to individuals
and families in the community through their
full participation and at a cost that the com
munity and country can afford. The eight
essential elements of primary health care
are: education concerning prevailing health
problems and the methods of preventing and
controlling them; promotion of food supply
and proper nutrition; an adequate supply of
safe water and basic sanitation; maternal and
child health care, including family planning;
prevention and control of locally endemic
diseases; appropriate treatment of common
diseases and injuries; provision of essential
drugs; and immunization against the major
infectious diseases.
These guidelines should be read in light
of the Primary Health Care approach, in con
junction with the booklet “Immunizing More
Children" in which there is a comprehensive
statement on supporting and complementing
the immunization programmes of the Govern
ment of India, state governments and others.
Over many years, UNICEF has cooperated
extensively with the Ministry and Depart
ments of Health. Firm commitments have
been made to continue and augment that
co-operation in actions which will raise levels
of social awareness and participation, assure
the availability and quality of vaccines, bols
ter administrative support and explore prog
ramme design and management. These will
be elements of our programme of assistance
in the coming years.
It is evident that this involvement will
not be sufficient to meet the burgeoning de
mands created in India by the message of the
Child Survival and Development Revolution
and by the upsurge of political interest and
will, national and international. These call
for urgent extension and acceleration of im
munization programmes. While we continue
to build up our own knowledge and resour
ces, the claims upon them increase almost
daily. UNICEF is a strong advocate of univer
sal immunization and is prepared to join with
our major partners in governments, WHO, in
the medical profession and with others too.
Only if the resources of many armsof govern
ment, of non-governmental and voluntary
organizations and of communities are fully
mobilized can universalization of immuni
zation become a reality in 1990. Wherever
and whenever immunization is discussed,
UNICEF will evince an interest, share infor
mation and experience and strongly advo
cate planned action.
This is in accordance with the proc
laimed policy of our Executive Board and in
harmony with the current upsurge of inter
national interest and commitment to univer
sal immunization against the diseases of
childhood. However, in considering joint
actions with any of our partners, we must be
assured that the programmes envisaged are
comprehensive, immunologically effective,
operationally sustainable and socially accep
table.
At the present time UNICEF’s concern
is with the primary vaccinations: BCG, DPT,
polio, measles and with IT for women of
child bearing age, all of which are included
in the GOt schedule. UNICEF will cooperate
in programmes designed to immunize child
ren against the six major childhood diseases.
Resources and time cannot be diverted to
incomplete programmes which will offer
protection against only one or a few of the
six.
Coverage
In order that the limited resources may
not be dissipated and unnecessarily diluted,
UNICEF will direct its involvement to prog
rammes which cover at least one adminis
trative block or ward. And in all cases, a
minimum target coverage will be 85 per cent
of eligible children, under two years old. In
coming years, coverage will be of the age
group under one year.
Project Areas
The following are priority areas for
UNICEF collaboration, identified in order to
ensure a measure of cost-effectiveness and to
fully
utilize
existing
infrastructures:
—where ICDS is established and functioning;
-in GOI/state government intensive immuni
zation districts;
-at district rehabilitation centres;
—where there are UCD/SMTD projects;
—where there are DWCRA projects;
—where there are SIAD projects;
—in the “catchment” areas of medical col
leges.
[Areas which are identified as being specially
served by bilateral immunization programm^^
should be avoided.]
Planning
The average immunization programme
will take at least six months to prepare. Un
less there is adequate lead-time, no project
should be embarked upon.
“Immunizing More Children” describes
three case studies in which the strategies and
processes are carefully analyzed. Obviously,
negotiations, responsibilities and procedures
will vary in different situations but many of
them are common and in no case is it likely
that all planning and preparation will be com
pleted in less than six months. In brief, there
will be negotiations with appropriate indivi
duals and organizations; there will be a
check-list of resources and materials to go
through systematically; a plan of action wi(^)
be prepared in consultation between all invol
ved parties and appropriate sections of
ROSCA and based on the check-list and ini
tial surveys; vaccine availability will have to
be confirmed; so will other committed inputs;
evidence will be presented that the immuni
zation will not be a one-time affair. All of
these will be time-consuming and arduous—
but essential prerequisites to UNICEF par
ticipation.
Infrastructures
Programmes in which UNICEF will col
laborate will be effected through existing
infrastructures and resources in almost all
cases. First and foremost that will mean the
Health system, its extensions, and the facili
ties of other arms of government machinery.
There will also be State/ District/Municipal
Administration/Development Ministries and
Departments of Social Welfare (ICDS, SIAD,
etc.), Education (pre and primary schools,
female literacy centres, etc.), and other non
governmental organizations like the Family
Planning Association of India, Indian Coun
cil of Child Welfare, Indian Red Cross Society
and other similar voluntary organizations
which run MCH and Family Welfare Centres.
They may be actively involved and supplies
of vaccines and drugs may be made to them
(by GDI) on the condition that they are
administered properly to the beneficiaries
and proper accounting done in accordance
with government instructions. (Ministry of
Health & Family Welfare memorandum D.O.
No. M.12014/1/83-MCH of 13 April 1983.)
There are, in addition, the controlled
communities such as ESI, planters’ associa
tions, industrial and commercial enterprises,
the coal and other mining industries, rail
ways, etc. with whom UNICEF may coope
rate in training, exchange of information,
provision of promotional materials, and so
on.
UNICEF Commitments
UNICEF has already made significant
commitments to the GOI as mentioned in
“Immunizing More Children”. Amongst those
commitments is one to make good shortfalls
in vaccines which may occur while India’s
own production is stepped up to meet
national needs (as distinct from national tar
gets). In all cases, therefore, the GOI is res
ponsible for supply of vaccines in the
amounts specified in plans of action.
Other UNICEF commitments to specific
plans of action may be any of the following,
as occasions demand:
a) Direct Inputs
—Syringes and needles [not disposable].
—Reimbursement cost of HER.
-Autoclaves and sterilizers.
—Additional refrigerators, voltage stabi
lizers and cold chain equipment for
PHCs, where necessary.
—Thermocole boxes and carriers.
—Paper and printing, survey and recor
ded forms, ledgers and cards.
-2-wheeled vehicles for supervision.
b) Capacity Building
—Training for all cadres:
1) Mid-level management for DMOs
and managers (10 days);’
2) Orientation of non-medical super
visors, PHNs, PMAs, media officers
and officials, state functionaries,
etc. (3-5 days);
3) Orientation ofPHCstaff(2-3days);
4) Orientation of survey staff;
5) Technical aspects of Logistics and
Cold Chain Management for mana
gers and key personnel handlingvaccines (3-4 days);
6) Refrigerators repair technicians’
course (10 days);
7) Users’ course on preventive mainte
nance of refrigerators, cold boxes,
vaccine carriers, etc.;
Orientation of communication and
community participation for exten
sion educators, community workers
and volunteers, etc.;
9) Support for inclusion in curricula
of medical colleges and nursing
schools.
-Exchange between officials of partici
pating projects-but only after actual
involvement.
-Consultants and contractors for train
ing/monitoring/planning.
—Support for Health Education Bureaux,
state radio stations, regional TV, etc.
for training courses and production of
advocacy materials.
-Manuals, training materials and aids
for implementing individuals and teams
8)
Channels of communication may inc
lude the schools, mahila mandals, religious
associations, NGOs of all kinds as well as the
mass media (radio and TV spots—which, by
themselves, cannot be effective). Motiva
tional material will be germane to local
conditions and will require pretesting and
modification. Traditional and community
based advocacy may be supported, e.g.
“prabhat pheri” (morning procession), puij|
pet shows, street theatre, local fairs, exhifli
tions, etc.
d)
Planning, Monitoring and Evaluation
—Survey, baseline data collection, inven
tory, questionnaires, etc.;
-Record keeping and data processing;
-Coverage surveys by independent eva
luations;
—Consultants and contractors;
—Research of problems, constraints, cultural/social/economic factors;
—Analyses of reductions in prevalence,
IMR, CMR, morbidity and disability.
e)
Discretionary Funds
e. for conveyance costs, POL for vehi
g.
cles used in the project, ice, kerosene,
cotton, gauze, alcohol, analgesics, swe^^
loud-hailers, prizes, etc.
WP
c)
Advocacy
The major objectives in advocacy will be
to create political and administrative commit
ment at all levels; to motivate community
leaders; to build up awareness and demand
amongst the people. In a recent investigation
of the knowledge, attitudes and practices
related to immunization amongst mothers in
two areas of New Delhi, the variables studied
were: (a) awareness of the diseases of child
hood, (b) the symptoms, (c) the number of
doses required for immunization against each
of the diseases, (d) understanding that death
can possibly result if the child is not immu
nized. This last “message”—that death can
be the possible outcome of not immunizing
the child—appeared to be the most relevant
of all to the motivation of parents towards
having their children immunized.
UNICEF, ROSCA, New Delhi : 14 May 1984
■SBK‘
Overall cost to UNICEF
In no case should the per capita cost to
UNICEF exceed US$ 1.50. This is a generous
complement to existing resources which need
not necessarily be fully utilized. The cost will
be substantially lower in densely populated
urban areas.
Jan,
CRASH
OF THE IMMUNIZATION
15,
199®
PROGRAMME
Consequences of a Totalitarian Approach
DE BA BAR BANE R JI*
* Professor, Centre of Social Medicine and Community Health,
. School of Social Sciences, Jawaharlal Nehru University,
New Delhi
110 067.
RETREAT FROM ALMA.:.- ATA
The Alma Ata Declaration^ (WHO
all
the history of public health.
providing integrated health
population all ove-r the
advocating
1978), signed by virtually
important watershed in
of the world marks an
the countries
It called for a new approach to
to all sections
services
world.
Its distinction lies in its
formation of systems of health services
around the people,
the. sheet anchor of the health services;
community self-reliance;
and,
that are
built
rather than around predetermined packages of
problems -forms
People’s response tg. their health
technology.
of the
they a re
to promote
they should, be under social con trol ;
they should form a component of a wider intersectoral
action in health.
daring
the reaction
declaration
of self-reliance
sharp and swift.
technpcentrie,
with
of affluent countries to this
Expectedly,
Reverting to their old patronising,
dependence producing approach,
what they called
and Warren
by the poor countries was
1979)
- a
they came
"Selective Primary Health
contradiction in
terms.
1988 ;
forward
(Walsh
Even though this
idea clearly lacked a scientific basis (Banerji
St deBethune
Care"
1984;
Institute of Tropical Medicine
Grodos
1985),
it
received immediate support from UNICEF,’ which went to launch
what it
called .’’Child Survival Development Revolution"
(Grant 1983), selectively focussing on. Growth Monitoring,
Oral Rehydra tjspn,
tq
Breast Feeding and Immunization- GOBI,;later
be linked with Feeding Programmes,
Female Literacy,
Family Limitation and
1985).
from different parts of- the world
making it GOBI - FFF (Vittachi
.. Many eminent scholars
have expressed deep concern over this obvious attempt to retreat
from the commitments made at Alma Ata.
A
group of Scholars in
2
from different parts of the world?
public health
Antwerp (Institute of Tropical Medicine
meeting at
had declared in
1985),
1985s
.....in
developing countries,
in spite
of history and of past experience,
of the lessons
major national and
international donor agencies are diverting scarce
resources into a short term approach known as ^elective
primary health-care".
This approach•concentrates
exclusively on certain interventions claimed to be the
most efficient and aimed only at' sections of the
population.
This self-contradictory term should be
since at 'their^bes t,
considered as
principles underlying Primary Health Care.
Social Science in Medicine
Vol,
contradiction with the
deliberations at Antwerp and works
Eased on
26,
1988)
only be
such programmes cen
"selective health status interventions".
This approach is in total
fundamental
banned,
by other scholars,
brought put a Special Number (No.9?
on Selective Primary Health Care,
which raised
doubts about- the soundness of a J'selecti ve" approach*
serious
However,
undaunted,
"
WHO joined UNICEF in.becoming even more
"selective" in its approach by converting its earlier Expanded
Programme
Of Immunization into a global;
pro gramme
which was aime d "tec ensure that the six immunizable
diseases'- diphtheria,
tuberculosis,
1985;
adopted a
bound ( 1990)
tetanus,
childhood
poliomyelitis and measles-cease to be
health problems,
(Grant
whooping cough,
time
WHO
public
if not totally eradicated ^from .the ■ globe
1989).
Indeed,
the World Health Assembly
resolution fcommiting to. a programme of global
eradication of poliomyelities (WHO,
1987).
3
The Economic and Political Weekly (Editorial Comment
1 98 6)
first to draw attention
was among the
of launching the global
programme.
to the implications
It brought T .. ...
the large^r issue'of the role of public health
into focus
technologies and emphasised that health improvements
about
by immunization,
growth charts or nutrition supplements
by availability
of
food,
r’
can. only be sustained
water and shelter and the political
and economic power of the
people
to obtain
them<
rightly emphasised that these technologies are
the ruling
brought
use of Oral .Rehydration Therapy (ORT),
It had also
being used by
class in third world countries to achieve visible
and dramatic improvements in health to divert attention away
from the lack of basic survival needs*
opened up
the wider questions of motivations
efforts to impose
problems of child health in
conditions
prevailing in
the
third world, when it is
the
These
have revealed many serious
programme itself. ..... The most outstanding among
was, leave alone
problem
considerations,
ecological
such
them
was
finding out what
the .other important epidemiological
as incidence rates under different
conditions and time
addition*
flaws
very complicated programme had
been .re-co'mmEn de d for launching without even
In
well
the ecological
these countries.
that a massive^ e-kpsTnsive an d a
the
the
Subsequently, a number of articles have appeared in EPW„
Banerji 198'5) which also dealt with the narrower
' *
programmatic aspects.
in
behind these
technocentric approaches to deal with
known that these problems are rooted in
(e.g,
These observations
trends of the chosen
diseases.
there were other critical areas such as efficacy
of different strains of vaccines under different epidemiological.
and ecological conditions,
vaccine
dosage, mode of vaccine
administration, maintenance of the cold chain,
level of the
fixation of the
rtherd immunity’* needed for the programme,
ensuring
action
get the needed covc.ruge, impact of the time
to
bound,
target oriented programme bn other health services, including
to mothers and children, monitoring
those .pertu ining
of the
vaccine and. the ■ vc ccina tion
quality
the
procs du res and implications
of persistence of unfavourable ecological conditions
for the
health uf Vaccine .. protec te d children.Recognizing the importance of the issues raised in
these .publications,
Ass ucj-a tion
th e ■ Journal of the Indian Medical
ca me'out wi th an. Editorial ( 198 6)
(JIMA)
r.
under the
Behind the .Universal Child Immunization
caption,' "Hidden Menace
g
Programme",’drawing heavily from one of the EPW articles
the
In
19861
(Bonerji
turn,
the JIMA Editorial was reprinted in
(Sept -Oct 198 7) ..(I n v rnati onal
FDA D-jSsier
for Development Alternatives)' and in
of Health Services
IMPOSING THE
11 is
impression
ON
19 8 8.
THE PEQPIE
remarkable that such a strung and persistent
scientific analysis,
bused or
criticism
the In te rnational Journal
( Vol. 18) ’, ' pp . 29 3-99 ,
PROGRAMME
Foundation
on
the
failed to make any
decision makers,- ■ Some
respected physicians
'(’nb't necessa'rily e cientifically competent, at least in
'epidemio’lQgy and health administration) lent their support to .
the p'r up used global
techriicoi
thd
respe ctj, ve; general
(Grapt '1985'; Mandi. 198.4)
a massive publicity
child survival
hallmark
of the
the recommendations of
"expert©" and-.consultants in 'the secretariates :.of
UNICEF,
WhP
venture and on
drive
bodies of WHO and UNICEF
also,, jsn dors e d jit. ••
to "market1’ the
"social" product of
(Man of f 19,84), ’ Social Marketing bfcame a
of this programme'- (Duquijie et el
world were- involved in a marathon
extravaganza
UNICEF launched
1984),.
'
Top pop singers
tranSa tian tic . TV . p op
the World Aid of Bob Glldoff -■ to involve
the
1
5
affluent people in western
the needy children in
this task
countries in
poor countries,
of helping
Marathon races
were
held in all the major cities of the world wi. th a similar
purpose;Containing the largest number of needy children in
the
A
world,
Task
(GUI
Force
■ drew up
(UIP)
India reacted enthusiastically to the proposal.
the
which
1985),
details
was meant
generalist administrator,
headed by a
of ap Universal Immunization Programme
to our late
to become a ” living memorial
Prime Minister Indira Gandhil
at th e . in te rna ti onal ’ le vel,
Following the trend set
(p.ii),
the
Force also made
Task
unsubstantiated claims about 'the cost-effectiveness of UIP.
the Planning C.ommission.
It also received prompt support from
The Prime Minister's Science Advisory Committee set-up
special Technology Mission
on Immunization .(GUI
India wep t a s te p ' further in
the
setting up.the Indo~US. Vaccine Action
their zeal
to stress
technologists,
1988).
field of "vaccinology" by.
Project ’(GDI
1987a). ..In'
the importance of vaccines,.some bio-..,
who'had little knowledge and information
concerning epidemiological qi'tu'ation in India,
otherwiss^ went about literally to
diseases to create market
the vaccines- developed ip industrialised countries,
fc.
Without
they started' to claim primacy for such, problems
as infective Hepatitis,. Of Measles, Mumps and Rubella
It is
■
unwittingly or
"manufacture" or concoct
public health importance- of certain
any data base,
a
a matter "of deep nation'al 'concern that -things
manipulated tp this extent.
(MMR)
J
could be
It i-s.' a' grave danger signal. —
The UIP envisa-ged an expenditure of 250 crores, of
rupees '(GUI
1985),
over and abpve
the mobilisation o.f the needed
manpower and other resources at the
sub-centre levels in rural areas
urban area's)',
primary,health centre and
(and corresponding levels in
to va c cin a te . the children,'
principally meant to cover the
This sum was
cost of yapcines, equipment,
transport and some additional personnel needed.specifically
for
UIP,
"
'
/ '■ '
' '
6
1985,
from April,
task.
gigantic
was
It
the five years starting
than 575,000 villages,
living in more
towns and cities of the
(Sokhey
Within
than 90 million pregnant mothers and
more
83 million infants,
-
vast country, were to be immunized’
It required 300'0,000 vaccine carriers,
1988:9).
15.2
million syringes, b0 million needles: and over 1000 million
does of vaccines'and many other equipment and supplies (Sokhey Z
were,, in addition,
1988 :^5).
There
concerning
vaccine production, import of vaccines and equipment,
ensuring
timely supplies, .maintenance’ of the’ cold chain,
thr.ou-gh programmes of
promoting community participation
Information,
Education and Communication
(IEC), training and
monitoring,
valuation
• . ’
an d s urveillan ce ..
-It is astonishing
. '
■
the stupendous problems
that dt.spi te .such obvious indications
■■
■
to
the
contrary,
the’ Government of India should have
. that "vaccination is
claims
one of the most cost effective
to man" (GDI
interventions known
by responsible, officers
th e li tera ture
Sokhey 1988)
literature
( sae-,
1985:i).-
has
for ins tan ce,
been'a
claimed
health
Making os such’ wild.
recurrent
GDI • 198 5;
feature
1988 ;
GDI
brought out ..by th’e Government- of India,
GOT
in
1989 ;
Such
pro vide ..documentary e vidence of ign.orancfe of the
decision Inakers about basic epidemiological and administrative
aspects'of the immunization programme.
It is not only
unscientific to. make such irresponsible claims:
unethical and immoral.,
The
detailed activities
chalked out in the
Mini Mission. — I
4
it is
downright
,
,
for implementing the DIP
form of two Mini Missions
(GDI
1988 )
were
-
for storage and dis tri bu tion ' of va ccihes and
Mini Mission - II for administration of vaccines, monitoring and
evaluation.
The dominant, approach waq to’ adopt a "central
...
.
’' .'
. '.i1,
.j
, ■ j, r..
patteiri1’ and ■impierhSriti"lt-,'tiniforml:y. in',, different parts of the
..'j • -. I ’. ; • ■.
'
”*
country’tu obtain the- required coverage.. Those with even a
7
with health administration in
nodding acquaintance
parts
of the
country could have immediately pointed out that
task in many major states -
obviously impossible
this was an
e.g. Uttar Pradesh,
Bihar,
Rajasthan., Madhya Pradesh, .Orissa,
What is worse,
Assam and West Bengal.
time
imposition of the
target oriented programme on such'states created very
bound,
serious problems of "absorption" within
systems of' these- ver^ sta’tess
weak organizational structures,
by the UIP
damage done
other activities
particularly the network
even
these
critical issues
those
raising such
India,
purpose
was
Then,
should have
the
that the UIP had
regardless of the consequences,
of health administration had to be ignored:
had to be kept out of the.
issues
team and
actively shunned,
MANIPULATION AND
in
programme was much more extensive.
then^if the overriding
in
of
weaker management system,
(e.g. National Tuberculosis Programme)
to be pushed through
had
to ths’organisation and management of
process of absorption of the
Obviously,
the health service
precisely because such states
services at the. periphery, and an
the
different
'
CONTROL
OF INFORMATION
s
it should also became understandable why there
been so many vital
implementation of the
flaws in
"M on i to ring-®-,
the process of
Evaluation and Surveillance*
components of the Techrtology Mission
on Immunization.
the baseline epidemiological data on
the six- deseases were'
virtually non-existent,
of directly measuring the
the question
epidemiological impact of UIP was not even raised.
had
they had adequate
competence in epidemiology,
at least partially retrieved the situation
models.
as
Because
Incidentally^
they could haw.
by using epidemetric'
Instead, recourse was taken to conduct what is termed
"SentinaJ Surveillance'? in .some selected medical
centres in
the best of the
the^country (Sokhey 1988).’
Obviously,
circums tan ces,
obtained from such , centres is of
in forma tian
in
’
8
very limited value.
c-julo not
centres
even this limited information
However,
be. collected' sys tematically,
as a large number Qf the
did hot have a reliable, information system.
In de'pen dent evaluation has shewn (Banerji. 1989)
there were serious lapses in
internal evaluation^
in monitoring the
chain and in making
vacination assessment surveys.
Ministry of Health and Family Welfare
data oh 93 assessment surveys in
in
1988: 29),.
198 7 (Sokhey
(p,29),
because
surveye’d areas in
or more
with
areas
(51/93)
cent"
(p,
three
the
29).
The Union.
presented limited
selected areas
(not specified)
fifth
( 20/93)
1987 ie corded coverage levels
surveyed
of the
of 75 per cent
doeses of DPT and OPV and more
documented coverage levels
between
than
half the
50.to 74 per
How can.they claim impressive progress.with
selected
cats’cn
has
cold
fragile ground it has
than a
"in more
functioning of the
(unspecified)
On such
claimed "impressive progress in
areas"
that
carrying out systematic, concurrent
areas and when
figure of 85 per cent
(GDI
1988)
they themselves
have set a
to have "herd immunity" in
■’
the community?
Attempts-(p £. "cove r-up." routine performance in formation
was even more pathetic.'
Fo r~ in s tan ce ,
the Annual Report of the
Union Ministry of Health and Family Welfare
(GDI
1989 : 208-10)
gives
figures' for the entire
the
for 1988-89
year-wise performance and target
country
for TT (Tetanus
Polio,' BCG and measles, without caring to give
in terms
Toxoid),
DPT,
the break-up
the number of doses of DPT and Polio and in
states or districts.
<
terms of
Till he became a member of the
(Independent)' National Review Committee on Immunisation
(July 1989 ),' this author faced a blank wall- whenever he made
9
efforts
to get the
detailed break-up or the
internal National Review of 1987,
findings of the
conducted by th e Union
Ministry of Health and Family Welfare which covered the .districts
of Bharuch. (Gujarat)
(Sokhey 1987a),
(Sokhey 1987b), Kota
(Rajasthan)
(Maharasthra)
Sagar (Madhya Pradesh)
Sokhey
198 7c)
and Thane
(Sokhey 1987d).
POOR LEVELS OF PERFORMANCE
Ironically, fl much breadbased and systematic surveys'
organised by an Independent National Review Committee,
of study of 25 districts,
basis
in
revealed that the routine performance
data submitted
state governments . were .often highly exaggerated,
please
authorities in
the
ought not to come as a -surprise.
designed,
the
by the
presumably to
the Union Ministry.' Actually,
Performance
similarly concocted earlier when the Union
or without pressure
on
tweleve major stotes(and Goa)
this
■•
figures had been
Government had;
with
from abroad,' imposed ill-conceived an d' ill-
technocentric,
target oriented and time bound programmed
on the'people through un eh th usias tic and poorly performing state .
health
135)
departments
(e.g.
family planning
(GUI
1987b;
Bose.,1988 s
and the earlier attempts at smallpox eradication
(Basu et al
1979).
The Indian Council of Medical
Research
( 1989),
which
was asked to conduct external evaluation of UIP, limited
itself only to evaluation of availability of supplies and
equipment in
196 primary health centres which were
positioned near the district headquarters.
out by ICMR revealed serious flaws in
so concerned were the
call
authorities
favourably
A summary brought.
the UlPi
Apparently,
to cover-up such data,
which
into question their.,loud claims concerning "impressive
progress",
that the full report of the ICMR study has not br-.en
i
10
made available to an
the present author,
outsider like
inspite
of repeated requests.
the authorities did set up an Independent
However,
on DIP under the sponsorship of the
Review Committee
National
National Institute of Health and Family Welfare, nine months
before the programme was
due
to come to an
end (July,
1989).
The Independent National Review Committee has- brought out
to confirm
convincing data
several scholars made
1984;
(Banerji
way back in
for more
than a
1?85;
Banerji
(Banerji
198 6).
of the
deseases
did not reach
fully
the coverage, hit almost
was also included as the sixth
Even in
1 989 ).
;
the best performing, states,
accounted for a tiny fraction of the total population,
coverage
In
than half of the population
ruck'bottom when measles
desease
1985 and 1986
fifth of -the eligible children were
protected against the five
the
forebodings of
1964,
Grodos^et de Bethune
States accounting
country, less
the worst of the
whic
the
th e' pre scribe d 85. per cent. - it wavered
between 70 - 83 per cent.
Again,
these very s ta te s(e ,g
Kerala ,
Himachal Pradesh and Goa)' already had low mortality and morbidity
rates and therefore
very limited.
the impact of ths coverage will naturally be
The coverage was a byssmall y. 1 ow in
which are expected to have
incidence states,
literacy,
again,
□ nd in their levels
they got
for female
for health services
of management. . The Techn ology. Mission had
bj.upder Jn overlooking the glar^ing. differences
the organisation
pnd imposing a
allocation
very states
These high desease
have.very low figures
per' capita income,
mass a serious
in
high incidences.
the
and managemen t , of the
state
"central pptte.rn" op all of them.
health services ■
Probably,
dazzled by the -high pressure salesmanship of the
interna tiopal agencies, individual affluent countries and by
g
11
international voluntary organisations like the Rotary
International ano the Rockfellar Foundation.
India's experience with the DIP should provide enough
of the level of implementation of this
data to get a picture
ill—conceive d end unimaginative
global
large majority of other poor countries
venture in. by far the
of the world (
Bangladesh, Nepal,' Afghanistan, Sudan, Somalia,
Dominican Republic) 'which have even
Chad,
e.g-.
Haiti,
weaker political clout
and weaker infrastructure qf the health services.
It is
shuddering to find that even in ■ the eighth decade of the, current
century,
an
unholdy alliance of, national and international
power brokers could impose
their will on hundreds of millions
of human brings living in
the poor countries of world r and
make- them forget all
that ahppened at Alma Ata in
the pwc r the struggle
for health is.a long and a grinding one.
197S,
For
POLITICS . OF ] TECHNOLOGICAL TOTALITARIANISM
One can thus discern a' deeply disturbing - indeed
frightening
chain
of disinformation,
distortion and cheap
propagenqa irja bid to sell the imm uni z.a pi on
globally an d in India;
making a. case
selective .primary health
data;
care on the
programme,
both
for -copt- t effectiveness of
basis of highly questionable
making e xagge ra te ii assessmen t-o f load of mortality and
morbidity due
to
e fficcqy’ of the
the six diseases; mak in g -e xag ye ya te d '• cl aims
yagcipes;
ignoring vital Epidemiological,
biological and- administrative issuer in programme’s
and i mplemc-ri to tion ;
on
formulation
poor monitoring. and surveillance,
restricting or aqtiyely .pre venting access .t.o the- available
information; and indulging in
foy the
progr-mme-.'
fal $e 'propaganda claimin g success
The-s.c precisely form ip.q.ny of the key
elements of a. tdtalitu yi.a.n syteml.' ..This account pf "selling"
-
uf the immunization
12
programme in Indio provides an awe - inspiring
.instance of formation .of a syndicate medical scientists,
burs a ucia is ■ and p oli ti cal. le a ce rs end t.hf ir mentors
who invoked the emotional cause
of th*
in. pog-'r countries to build a closed,
There appears
programme.
rise ..and fall of the UIP.
to be
plight of the
monolithic,
children
"totalitarian1'
the
a deterministic streak in
It almost faithfully conformed to the
1 98.6 ( Bane rji
■forecast maos in
from abroad,
198 6)
;
"Global an d pa ticnal
■ power structures ordain that che oppressed people of the world
will have to. pay yet anuthr heavy instalment to-their tormentor^
•■ . . s The
•are
tormentprs have
to
be
proved wrong before
they
forced t p .a ban don. thpir ill-con pei vf d programmes.!?
11 may
:
one? eguin
stressed the? protection of phildren'is
be
a very
desirable health action ano it should form an important- element
of primary health care activities.
in yoking the c apse
of c hil dre n by
This is..quite
different from
ves ted,. marks t end political •
interests joining, some well meaning though' simplis tic
in affluent countiir. s • to impose a
technocen tric,
persons
high priority
targ-t oriented,
time- bgun o' immunization • programme .on - a country.
This is not the:
first time
’India
the
third world country like-
sp.ve.ral examples, of ’S uc h'mun.ippl...a tiv.e .‘in tf r ven cion s
There ore-
in
chat a
has' been a victim of spgh .a •"?Q:tbi4.tariann.: onslaught.
past
the
family planning ■ progr-aiumr (Vame.ro.th 1976)
the jn'el'eria program me ’ (pieia've r -19 76)
instances,’
The
and .
off*, r two glaruing
^orld H-eelth Assembly has- already given the
mandate to WHQ to launch a gl^Jbal'-programme- of e ra die a ti on of
ppliomyeiitis,
’The re? is alrea-'dy a move about promotion
of
similfsr poorly conceived and -designee' global programmes against
Acute ■ f^e’spir& tory In fec tions
Diseases
(WHO &- UNICtf 1985).
(WHO- 198 7)
'
'
and Diarr-hoea-1
-
13
the existing immoral i-nd unethical North-South
In
Divide, based on
programme
South
and,
on
rhe South,
by imposing such
back to the
rhe North seems to come
with a tiny fraction
of what it has plundered from
adding insult to injury, it serins
condescendingly s
We
unequal terms of exchange,
•? Hepp
to be
them
telling them,
we come with our technological magics.
have a magical Wand to remove your health problem^
What
does it matter if you ape force q to. live under degrading
conditions of'ppvi-rty,
illiteracy, exploitation and social
injustice?
you and your children are alive
Look,
After all,
how we
have raised your life expectancy JI*
people in the South musp learn to Sfee through the
The
machinations of the
suitable
them with
I
market any manipulative forces and take
correptiye steps.
Efforts will be made
the glamour of high
of re. jep ting all tpchn olqgyj
technology^
the
The
to dazzle
question is not
qu e s tian is t o s ee
th pa ugh
the dangers'of the marks| forces ip•both th e North an d' th e
Soyth apd ensure.that concerted efforts are made
self-reliance and to s q bq r di n'a te
the pe-ople,
to promote
technology to .the
needs of
as contained in,-the Alma Ata Declaration,
14
SUlMI-iAR Y
'-...
i
The reaction of the effluent countries
to
the daring
Alma Ata Declarutiin of self-^re li-apce in health fields
poor countries was sharp and Swift-.
the
by
They came forward,
without, producing a scientific basis,
with an alternative.
approach of Selective Primpry Health Care - s clear
contradiction, in terms/ 'Despite this,
it received support
from UNICEF apo WHO'apd'Soop■ they got together to. plead for a
global progro mmc of' immunisation in t.hi rd. world coup tries
that -such-, a .te.chn open trie,
target oriented programme,
contrary to the
that is- thrust on
time
I
bound,
the people,
was
basic postulates of the, Alma Ata Declaration.
It was also poiptE’d out,
programme
.
disease's.. • Scholars .from all ove r
against six communied titip
the world, pointe g out
-.
again ana agtin,
was launched without
even
that the
suggested
getting basic epidemilogica|
in fopna tipp about the six'diseasesanti oye r and above, there
were, serious- unanswered, questions concerning
their dosage and mode,
aoministrative
nil
' •
pf -adminis tra tiop ano logistics and
and ecological ’aspects ,o f .programme implemrntati.i®
these warnings
were'ignored by the authorities con cerned.
India also followed the
agencies
the' va pc in es ,
by launching
a
pa^h laid by vhe- international
250Tcrore rupees five year Universal
Immunization- Progru.rn.me against the -six diseases in
19 85 ,
It
also joine'e. them in launching a massive propeg<.ndd ■ drive and ir»
making puteptly un-s ufc>s to n tip te d claims in
only aid
the .administra tors
favour of DIP.
Not
fail ip setting up sound and'
reliable internal information sys.ee,m yp monitor the performance^
but they took,the next expected SV P
on
whatever information
that
imposing an embargo
they 'had with
them.
However,
“
1 5
towards
to end.,
they he d
co submit UIP
which seriously culled into question many
National Review,
hpart from pointing out serious
claims made earlier,
of the
to an In ds pen cent
flaws at th.e levels of policy,
strategy,
and implementation and evaluation, it
programme
formulation
was stated that
there
were serious shortfalls even in vaccination coverage and that
there
was a coverage of less
than one.
of the
eligible population^
where
expected to 0;
much
higher,
fifth in as much as half
the incidence rates are
The situation in . th? vast majority
of ocher third world countries is expect'd to be much worse.
than what 4-S
found in
India,
The DIP pre sen ts "an' awe-inspj.rin g instance of ,the power
of a syndicate, of vested market a n d: puli tical interests,
coopted certain well meaning but simplistic persons,
their will on the
Using
peoples
disin for ma tian ,
had succeeded in setting up a
system to carry out
to .impose
of the poor countries of the
distortion and cheap
propaganda,
closed, monolithic,
their pre-conceived mission,-
which
world.
they
totalitarian
In
the
existing immoral .-.nd unethical No^th-South Divide, North seems
to come
back
to
the South with 'a
plundered from it, here
too it insists
own terms and conditions which
unimaginative,
REFERENCES ;
tiny fraction of what it had.
are
on laying down its
blatantly unscientific,
ill-fated and counter-productive.
■ ■
' '
"
1.
barie^^i, D ( 1984) s Primary Heal ch Ceres Selective or
Compre.liensive, World Health Forum, Vol,5, pp.312-315,
2'.
Baqerji, p ( 198 6); Techn open trie-Approach to Health:
Western Hrs ponse i cAlrna- A ta, Economic an d. Pojitjcal .
Weekly, Vol.21, No,28, July 12, pp, 1233'-1234
16
1
3.
Banerji, D( 1989 ) : Un.JiubLish_e d...pata_.pn _ N ationai.
Eyalue _xjun of Immunization P_ru£l£‘-rnme, New Delhi,
CSM ii. CH’,~S5S,"JNU"." ~
.
■■■'■.'■ ■
4.
Basu,
5.
Bose, h, (1988): From Population
B,R, Publishing, Vols.2.
6.
Cleaver, H( 19 76) ; Political Economy of Malaria De con trol^
Econ om i c_en d_ P pl i ci.ca J._ We e.kl y ’ Vol. 11. No. 36, pp , 14 63- 14
7.
Deme rath, N,J( 19 76): Bi rth Con t rol .an d_.F_prg_ign__P.plicy.s
The Al ee pn-tiye s to Family Planning, New York,
Harper &, Row.
8.
Duque, L.F, e tai ( 1984) s The National Vaccination
Crusade in Colombia, Assignment Children, Vol, No. 65t%68
pp, 159-178.
9.
Editorial Comment ( 1986):
Vol.21, No.20, May 17.
0.»
R.N. e t al ( 19 79 ) ; The_E £a^j,.£a,tion._cif_§.!IleU-.XP54
1.011 isu, New Delhi, WHO South Bast Asia Regional
pp. 309-31 2, (WHO Regional Publications South East Asia
Sc ries No,5),
.
to People, ..Delhi,
.
Economic and Political Weekly, -
Government of India ( 1985) ; Universal Immuniza tion
■ Programme. by 1990;. Re ijor_t_ pf_a^Task . Fpjg^e, New De 1 hi ,
Minis try o f Health and Family Welfare.
11.
Government of Inaia ( 19 8 7s) ; Vaccine Action project.
New Delhi, Deptt. of oio-techn olo gy (Mimeo) .
12.
Government of India ( 1987b): India’s Population;
Demographic Scenario-, New Delhi, Ministry.. u f Health
and Fam il y v»el fa re .
■
12,
Government of India ( 1988J: National Mi ns si on on
Immunisation . New Delhi, Ministry of Health arid
Family. Welfare.
'
’
...
14.
Government of Inaia ( 19 89) s Annual Report 1988 -89 ,
New Delhi, Ministry o f Heal th "an- d Family Wei fare . .
15,
Grant, J.P, ( 1984); Marketing Child Survival,
Aqgiqnment Children, 65/6(J, ppT 3-9,
16.
Grant, J.P, ( 1985): Universal Child Immunization
by 19 90 , ' Assiqnme n t C'hxlciran, 69/72, pp.3-14.
X
-
,
17
-
17.
Grodos, D and de Bethune? X ( 1988): Les Interventions
Sanitairus Sei*-ctives: UN Pledge Pour Les Politiques
De Sante Du Tiers Monde, Social Science and Medicine
Vol. 26, No.9, pp. 879-889.
18'.
Indian Council of Medical Research ( 1989) : Evaluation.
of Quality of Maternal and Child Health and Family
Planning Services at Primary Health Ce n tre sand
5 uggs s te d S t ra tejgj.es_ fo r_ th e.i.r Improvement ; Summary
Report, New Delhi, ICMR.-
19.
Institute
20.
Mandi, P.E. ( 1984) Achieving Nation-wide Programme
Coverage? Innovative Strategies and Methods,
2.§.§.i.S£lK.Q.X Children, Nos, 65/68.
of Tropical Medipine, Antwerp ( 1985) :
Belgium, Institute of Tropical Medicine
21. ■
j
••-\1">
,v
Man of f,, R.K, ( 1984) : Social Marketing and Nutrition
Education : A Pilot Project in Indonesia, AssignemfntChildren,; 65/68 , pp.95-1-13,
-22...
. ■/
S ok hey,...J.,' ( e d) ( 1'987a) ' : (Jn jvej.sal.. I.mm un i..2a $j._on
Progrt-m'ins - Ma tian a]. Review,; Bharuch.__ Gu.ja ra t, 23 J un e
■ tv 3; J-uj?y, ■ .1 98 7 , N e. w •.Delhi ,<■ Ministry-^rif He-^lth.-and .
Family Wei fare
-
23.’
/ Sokhey, d (ed)- ( 1987b)« Uni ve.rs §1' I mm un j za tj on .
Prog runtm
Nation-al Rd vi ew , .Sa ga r , Ma dh ya . P ra de s h,
'■ ■rTjo-"24-Juiy, 1987, Ne w’.Delhi, Ministry of Health and
family Welfare." .
13
24,
'
Sdfjheyi J (cd) (I9ff7c) ; Universal Immunization
:.A'
Programme
National’ Review. Thane. Maharashtra , ?70j ul y toV- 11’August, 1987’, New Delhi, Ministry of Health and'
Family Welfare..
25.
Sokhey, J- (sd) T987d): Universal Immunization
Programme - National Review.' Thane, Maharashtra 1Q _^o
21 August, 1987, New Delhi, Ministry p f Heal th .an d
Family Welfare1*- v. •
. ’•
•
26.
Sokhey, J ( 19 8 8 )-.? * National Immunization Programne,
New Delhi, ■NIHFW-,'’"'.(NIHFW'National Health .Programme ■
Ss rie's N □. 1 ) «’
•
.
•x27.
•
'Vittachi, V.T ('1985) »■ CSDH? .The Dialectics of
Survival and Development, Assignment Children,
69/7.2,-. pp. 19-31.■
r
8 -
28.
Walsh, J.A and Warren, K .5 ( 1979): Selective
Primary Health Caret An Interim Strategy for Disease
Control in Developing Ccuntries, New England Journal.
of Medicine f Vol. 30, pp. 9,64-9 67.
29.
World Health Organization ( 19 78) ; Primary Health Care;
of the International Conference on Primary Health
Crjrq.., hlma Ata, USE rt, September 6-12, 19 70 , Gen e va', ■
World Health Organization.
•
,30. ■’
World Health Organization ( 1987); Programme of Acute
Respiratory Infccti on s ; Re port of the Third Meeting,
.Geneva, WHO fwH O/RSD/8 7. 37) .
31;
World Health Organization ( 1980): 41st World Health
Assembly, World Health Forum, Vol. 9, No. 3, pp,
4 70-480.
32.
World Health Organization (1589); Re port of th a
Expanded Programme on I mm unjzation, Global Advisor y
Group Meeting, Oct. 17-21, 1988 , Geneva, WHO. ■ ■
33,
World Health Organization and UN I CEF ( 1985): The
Management of Diarrhoea and Use of Oral Re h.ydrdti on
The ra j y,- 2nd ed, Geneva, WHO,-
*
I
j*
b.
(
PARENTING
Vaccine shots ca
W
hen my two-month-old
son began his routine
vaccination series, 1 did
not know
there were
risks
associated
with any
ini ■
munisations. But the clinics literature con
tained a contradiction: the chances of an
adverse reaction to the DPT vaccine were
1 in 1,750, while his chances of dying from
pertussis each year were one in several
million.
1 lealth authorities credit vaccines for
disease declines, yet their assumptions are
contradicted by health statistics, medical
studies, the Pood and Drug Administration
and Centers for Disease Control reports,
and research scientists from around the
world. In fact, infectious diseases steadi
ly declined for decades prior to vaccina
tions.
American doctors report thousands of
vaccine reactions each year, including
hundreds of deaths and disabilities. Many
fully vaccinated populations have expe
rienced epidemics.
Myth 1 Vaccines are completely safe
Truth Vaccination causes significant
death and disability
The FDA's Vaccine Adverse Effects
Reporting System receives 11,000 reports
(mostly from doctors) of adverse vaccine
reactions a year, one per cent of which in
clude deaths (the majority after the per
tussis or whooping cough vaccine, the P
in DPT). With pertussis, the number of
vaccine-related deaths dwarfs the num
ber of disease deaths: the vaccine is 100
times more deadly than the disease. In
many instances, highly vaccinated popu
lations have contracted disease. Besides,
pertussis deaths declined 79 per cent pri
or to vaccines.
Studies have shown vaccination to be
a cause of the Sudden Infant Death
Syndrome, a catch-all diagnosis for cas
es when the specific cause ofdeath is sup
posedly unknown. One study found the
peak incidence of the syndrome occurred
at the ages of two and four months in the
United States, precisely when the First two
routine immunisations are given.
Britain actually saw a mid-Seventies
drop in pertussis deaths when vaccination
rates dropped from 80 per cent to 30 per
cent.
Myth 2 Vaccines are very effective
Thu in Vaccination is an unreliable
means to prevent disease
Measles, mumps, smallpox and polio
outbreaks occurred in vaccinated popu
lations. In 1989, the CDC reported: "Among
school-aged children, (measles) outbreaks
occurred in schools with vaccination lev
els of 98 per cent. There was even a
measles outbreak in a 100 per cent vacci
nated population." A recent study con
cluded that measles "produces immune
suppression which contributes to an in
creased susceptibility to other infections."
Myth 3 Vaccines are the main reason
for low disease rates in the United
States today
Truth The impact of vaccines on infec
tious disease decline is unclear
Acco-ding to the British Association for
the Advancement of Science, childhood
diseases decreased 90 per cent between
1850 and 1940, paralleling improved san
itation and hygienic practices, well before
mandatory vaccination programmes.
Infectious disease deaths in the United
States and England declined steadily by
about 80 per cent during this century
(measles mortality declined 97 per cent)
prior to vaccinations.
In Britain, polio epidemics peaked in
1950, and declined 82 by the time the vac
cine was introduced there in 1956. Thus,
at best, vaccinations can be credited with
Vaccines have been sold as catch-all lifesavers.
But the hardsell is not all true, says Alan Phillips
only a small percentage of the overall de
cline in disease related deaths this century.
Yet even this small portion is questionable
as the rate of decline remained virtually
the same after vaccines were introduced.
Furthermore, European countries that
refused immunisation for smallpox and
polio saw the epidemics end — along with
those countries that mandated it. In fact,
both smallpox and polio immunisation
campaigns were followed initially by sig
nificant disease increases; during small
pox campaigns, other infectious diseases
continued their decline in the absence of
vaccines.
A recent World Health Organisation re
port found that disease and mortality rates
in Third World countries have no direct
correlation with immunisation proce
dures or medical-treatment but are close
ly related to hygiene and diet.
were actually exposed to the disease,
then the vaccine was really only 50 per
cent effective.
It is assumed that all children, re
gardless of age, are virtually the same. An
81b two-month-old receives the same
dosage as a 401b five-year-old. Infants with
immature, undeveloped immune sys
tems may receive five or more times the
dosage (relative to body weight) as older
children.
Finally, vaccination practice assumes
that all recipients, regardless of race, cul
ture, diet, or any other circumstances will
respond identically. But this was dramat
ically disproved a few years ago in
Australia's Northern Territory, where
stepped-up immunisation campaigns re
sulted in an incredibly high infant mor
tality rate in the native aborigines.
Researcher A Kalokerinos, MD, discovered
Myth 4 Vaccination is based on sound
immunnisation theory and practice
Truth Many of the assumptions upon
which immunisation theory and prac
tice are based have been proven false in
their application
The clinical evidence for vaccination
is its ability to stimulate antibody pro
duction in the recipient, which is not dis
puted. What is not clear, however, is
whether such antibody production con
stitutes immunity. Furthermore, a study
published by the British Medical Council
in 1950 during a diphtheria epidemic
concluded that there was no relationship
between antibody count and disease in
cidence; researchers found resistant peo
ple with extremely low antibody counts
and sick people with high qounts.
Another component of immunisa
tion theory is "herd immunity,” which
stales that when enough people in a com
munity are immunised, all are protected.
As Myth 2 revealed, fully vaccinated pop
ulations have contracted diseases.
There is a flaw in statistics given: If 100
people are vaccinated and five contract the
disease, the vaccine is declared to be 95
per cent effective. But if only 10 of the 100
that the aborigine’s vitamin C-deficient
"junk food” diet was a critical factor (vac
cination depletes vitamin C reserves.
Children in shock or collapse often recover
within minutes when given vitamin C in
jections).
Myth 5 Childhood diseases are ex
tremely dangerous
Truth Dangers of childhood diseases are
greatly exaggerated in order to scare par
ents into compliance with a question
able but profitable procedure
Mostly, childhood infectious diseases
are benign and self-limiting, and they im
part lifelong immunity, whereas vaccineinduced immunity is only temporary.
For example, the chickenpox vaccine has
an effectiveness estimated at 6-10 years.
If effective, it will postpone the child's vul
nerability until adulthood, when death
from the disease is 20 times more likely.
Some healthcare professionals are
concerned that the virus from the chick
en pox vaccine may "reactivate later in life
in the form of herpes tester (shingles) or
other immune system disorders."
Myth 6 Polio was one of the clearly
D70c- P
2,
14/01/97
an kill
OS
?ase,
• per
, reAn
ame
with
systhe
Ider
mes
culwill
latin
ere
reories.
red
—
;
I
great vaccination success stories
Truth Vaccines caused substantial increases in polio after years of steady de
clines and they are the sole cause of polio
in the United States today
Six New England stales reported in-'
creases in polio one year alter the Salk vac
cine was introduced.
It was reported that not only did the
cases of polio increase substantially after
mandatory vaccinations (50 per cent
from 1957 to 1958, 80 percent from 1958
to 1959), but statistics were manipulated
by the Public 1 lealth Service to give the opposite impression. Researcher-author Dr
Viera Scheibncr says 90 per cent of polio
cases were eliminated from the statistics
by the health authorities’ redefinition of
the disease when the vaccine was introduced, while in fact the Salk vaccine was
continuing to cause paralytic polio in sev
oral countries at a time when there were
no epidemics caused by the wild virus.
In 1985, the CDC reported that 87 per
cent of the cases of polio in the United
States between 1973 and 1983 were caused
by the vaccine, and later declared that all
but a few imported cases since were
caused by the vaccine. Jonas Salk, inven
tor of the IPV, testified before a Senate sub
committee that nearly all polio outbreaks
since 1961 were caused by the oral polio
vaccine. Jessica Scheer of the National
Rehabilitation Hospital Research Center
in Washington, DC, pointed out that
most parents are unaware that polio vac
cination in this country entails "a small
number of human sacrifices each year."
Myth 7 My child had no short-term re
action to vaccination, so there is noth
ing to worry about
Truth The longterm adverse effects of
vaccination have been virtually ignored,
in spite ofstronng correlations ivith
many chronic conditions
The documented longterm adverse ef
fects of vaccines include chronic immunological and neurological disorders
such as autism, hyperactivity, attention
deficit disorders, dyslexia, allergies, can
cer, and other conditions, many ofwhich
barely existed 30 years ago before mass
vaccination programmes. Vaccine components include known carcinogens such
as thimersol, aluminum phosphate, and
formaldehyde (the Poisons Information
Centre in Australia claims there is no ac
ceptable safe amount of formaldehyde
which can be injected into a living human
body). Medical historian, researcher and
author Harris Coulter, PhD explained his
expensive research revealed childhood im
munisation to be "causing a low-grade en
cephalitis in infants on a much wider scale
than public health authorities were will
ing to admit.”
Myth 8 Vaccines are the only disease
prevention option available
Truti i Documented safe and effective al
ternatives to vaccination have been
available Jin decades but suppressed by
the medical establishment
Most parents feel compelled to take
some disease-preventing action for their
children. While there is no guarantee any
where, there are viable alternatives.
Historically, homoeopathy has been more
effective than allopathic mainstream
medicine.
And since these remedies have no tox
ic components, they have no side effects.
In addition, homeopathy has beer, effec
tive in reversing some ofthe disability
caused by vaccine reactions, as well as
many other chronic conditions with
which allopathic medicine has had little
success.
From the Internet at:
http://iviviu.livelinks.com/sumeria/health
/myth2.html
I
NAT ONAL
REVSEW OF (IMMUNIZATION
PROGRAMME 8N INDIA
Ww
DR. J.P. GUPTA
DR.(MRS.) INDIRA MURALI
flrf:
MB
AT
on ■
INFORMATION AND DCCI’MENTATION
40. in
■■■'■’ < I India
n.’rl Ar-.-.i. \rv.tl> cl 11T,
i Qi.t.b Uriel)
11C016,
Introduction
The Government of India through its National Health Policy has expressed
its major concern lor improving health of women and children.The National
Immunisation Programme being implemented in this country is one such
endeavour which has been accepted as priority programme in the policy in this
direction. Dedicated to the memory of late Prime Minister Smt. Indira Gandhi, w
the Universal Immunisation Programme was launched in 1985 with accelerated
efforts for universal coverage of immunisation for young children well as to
improve the quality of services. This programme has been included in one of the
seven technology missions.
It is imperative that programmes of this nature which are implemented with
clear objectives and specific time-bound goals and targets need be systemati
cally reviewed to examine if the programme has been effective in achieving the
set goals.
It is in this context that the Ministry of Health and Family Welfare decided
to undertake a National Reviewof Immunisation Programme at the end of about
a decade of its implementation. The National Institute of Health and Family
Welfare was identified as the nodal institution and it was entrusted with the re
sponsibility of undertaking this massive effort.
~~
Objectives
1. To review the polices, strategies and plans of action for EPI/UIP at different
levels of health administration i.c. Central, State and District levels.
2. To measure the progress in implementation of the EPI/UIP in relation to
targets for acceleration of the programme, accessibility, coverage, mortality
and morbidity reduction.
3. 7 o identify the bottlenecks and constraints tor the progress of the immunisa
tion programme at different levels of programme implementation.
4. To make recommendations for overcoming the constraints and problems and
thereby improving the implementation of the programme qualitatively and
quantitatively including assessment of additional resources required for this
.7
purpose.
The State was considered as a study unit in this review and all the 25 States
were covered. In addition, for obtaining information on similar aspects related
to the programme in urban areas, four major urban metropolitan areas viz.
Madras, Bombay, Calcutta and Delhi were also included in the review. Thus, the
total number of units studied was 29 i.e. 18 major States, seven small North
Eastern States and four urban metropolitan areas.
The programme was viewed in its totality covering its different aspects in
terms of programme inputs like policies, strategies and resources, the details of
processes of programme implementation including operational strategies,
management of different resources, etc., programme performance in terms of
extent of coverage of beneficiary population and impact of the programme in
terms of disease occurrence with reference to paralytic poliomyelitis and
neonatal tetanus.
Methods of Data Collection
Various methods used for data collection were as follows:
Interview/discussions with programme officials and staff at Central, State,
District, Primary Health Centre (PHC), subcentre and village levels.
ii. Study of records, reports, guidelines, instructions and other relevant docu
ments.
iii. Observation of Immunisation activities, service premises, cold chain main
tenance etc.
iv. Vaccination coverage survey using the 30 cluster sampling method among
children aged 12-23 months and for pregnant women.
v. Conducting disease survey for lameness and neonatal tetanus.
vi. Interview with community members, leaders and representatives of non
governmental agencies.
i.
Sampling Procedure
i.
u.mig me 11 usability Propor
•_
ii. For Seven Small North-Eastern States
Operational details of Immunisation Programme were studied separately
from each State headquarters and at least in one district and sub units viz. PHCs,
subcentres, urban institutions etc.,within this district in each State. For im
munisation coverage and disease survey, all- seven States were combined
together as one unit, in which the districts covered under UIP in 1985-87 and
1987-88 were grouped separately "nd from each group, 30 clusters each were
selected and studied.
"
iii.
For Urban Metropolitan Areas '
1
Two units of 30 clusters in each of metropolitan town were included in
coverage evaluation and disease surveys.
From each district/smdy unit, apart from immunisation coverage evaluation
and disease survey, operational details of the’.pfogramme were studied from
selected PHCs, subcentres, urban health facilities,'sentinel centres, etc. through
interviews with health functionaries and record study.
Manpower Involved in the Review
In order to collect information about various facets of the programme from
29 units (as indicated above), 29 expert teams were identified whose members
included faculty from medical colleges and public health experts from various
organisations. Each team consisted of a team convenor, three supervisors and
team members whose number varied between 15 and 20.
About 20-30 paramedical personnel of the rank of Health Supervisors were
deputed for each district tor carrying out lameness and neonatal tetanus survey
under the supervision of district team members. In order to ensure independent
appraisal of the programme, officers and paramedical staff were selected from
neighbouring States/disiricts.
For 18 Major States
From each major State, Immunisation Programme operations and procedures
were studied at the State headquarters and in two selected districts from each
State. Immunisation coverage and disease surveys (lameness and neonatal
tetanus) were conducted in these two districts.
Selection of Study Districts:For purpose of selection, in each State, the
total districts covered under UIP were grouped into two categories viz.:
i. Those which were included under UIP during 1985-87, and
ii. Those covered during 1987-88.
2
l imn
vup, one juu uicu was
tional to Population size Sampling (PPS).
Major Observations
Policy Aspects
Sense of urgency andcommitincnt of national government is reflected from
the fact that Immunisation.Programme had been included in the 20 point pro
gramme and a technology mission for immunisation has been created to look
after the various aspects'of programme. Likewise, Slate■; have accepted to carry
out the programme and formed technology missions to look after the same.
3
^dilability- of subcentres W:
Nolof districts with subcentres as per
pt iiimry health care and immunisation services are to be provided through PHc
•2j^r^W<j^
exPectcd n.°rms
and its subcentres. Support manpower and like health guides and anganwadi
fNo of districts with more no. of
workers are expected to assist the heath workers in successful operation of the •WW&*...................
subcentres as per expected norms
programme.
■ No of districts with less no. of
For enhancement of the performance under the programme and to enable the
■ subcentres as per expected norms
States to meet special requirements of the immunisation programme, Govern
• Information not available
ment of India provided 100% financial support to States for creation of posts of
■ (The percentage deficiency in subcentres
. in the study districts ranged between 10-40%)
Cold Chain Officers and Technical Assistant at State level and District Im
munisation Officer, Refrigerator Mechanic, Statistical Assistant, Stenographers
2.'Availability of Female Worker at Subcentre
and Drivers etc. at district level. In addition, the Central Government has also •
.
% of subcentres with female staff residing
committed to provide vaccines, cold chain equipments, and other related
- ‘ i" ’ ~ '■ eitherwithin area or in subcentre building
supplies for effective implementation of the programme.
.; ’- % of subcentres with female staff residing
As a matter of policy, it has been already decided that all districts in the
y^'" The policy decision has been to integrate immunisation programme with
i
country would be included under UIP by 1990 in a phased manner.
Clear cut policies for implementing Immunisation Programme in urban areas
were found to be almost non-existent.
|
4
75.7%
7
‘1-4.. (range 10-100)
'100-200
’ : 201-300
9
301 +
14
Total number of districts
42
Approachability
With the exception of Aizwal district, distance between farthest PHC and
district headquarters required travel time upto eight hours.
In nine districts few PHCs/subcentres were cut off from the rest for few days
to three months either during winter or rainy season.
F
5.
Availability of Vehicle
All except four districts (Tura, Tripura, Bhiwani and West Nimar) had at least
one vehicle exclusively for UIP at headquarters.
All Block PHCs within study districts had vehicles though generally in one
district 1-4 vehicles of PHCs were off the road for want of repairs.
1. Infrastructure Facilities
Being a programme which has been integrated fu nationally at the peripheral
level, infrastructure facilities within the district could be a major influencing
factor for the success of Immunisation Programme.
Relevant data in this regard about 42 districts covered during review are
presented below:
13 (30.95%)
outsidearea
4.
Resource Availability
In the area of availability of various types of resources and their management
for the programme, the main items considered in the review were infrastructure
^Rilities, financial resources, material supplies like vaccines and equipments
and health manpower.
4 (9.52%)
35'population Density in Study Districts
^<100/sq.km.'
Organisational and Operational Aspects
From the organisational and operational point of view, it was found that the
programme was being implemented in an integrated manner involving almost all
types of health facilities/institutions. However, at the district level, the District
Immunisation Officer (DIO) who is expected to be responsible for the manage
ment of the programme had faced some problems like lack of adequate admin
istrative authority, ambiguity regarding relationship with other district health
officials etc.
15 (35.7%)
2. Manpower Resources
—
The Government of India provided 100%- financial support for creation of
certain posts like DIOs, Cold Chain Officers, Technical Assistants, etc. How-
I
r
5
ever,inmanyStateseithermanyoUh«epostswerestillvacantortheavaUab?^^^OBSi®te:“!;c
'
personnel were not adequately trained.
.
All States had designated one officia a tate irectorate level to look after'^^^^^.wjth1 reference towaccines, with the exception of polio vaccine, the epuntry, _
Immunisation Programme either exclusive y or alongwith some other pro-,^^?^%Quld'’be’cconsidered to have achieved self-sufficiency in production of other
""" in nl
. ^fe^.^
ccines> From the.
gramme. Cold Chain Officers were. in position
all| States and urban cities
Mvaccines.
the beginning of the current financial year 'Serum
‘Serum Institute of
Or^Piine
’
has
gone
into
production
of
measle
vaccine,
hence
there
will be no need
except in Delhi and Assam.
With regard to staff position at district level in 42 study districts the number
iSfor its imports in future. Steps are being taken for expanding the production of
and percentage of districts where vacancies existed among the various catego
!9,'BCG. OPV is still being imported. To meet requirement of vaccines UNICEF has
j^giyeh its full support in importing vaccines.
Sai'i/i.Cold chain system which is one of the mo t crucial elements of the proNumber and Percentage of
Category of Staff
$ gramme for ensuring potency of vaccines has been strengthened considerably
Districts with Vacancy
i/at’all levels, though the situation regarding availability of such equipment and
9 (21.4%)
DIO
■ a their maintenance in different States varied considerably.
.
Likewise, provision has been made for maintenance of cold chain equip-"
21 (50.0%)
Refrigerator Mechanic
I
14 (35.7%)
jinients; Rate contract with suppliers in each State has been entered into. Task
Statistical Assistants
?! •Force at each State has been set up to regularly review position of cold chain.
12 (28.5%)
Drivers
/Regular monitoring of cold chain equipment is expected to be done from
Other staff categories like MOs, Health Assistants (F) and Health Worker (F)
•
different levels and every effort is made to ensure to remedy the fault immedi
though were not exclusively posted for UIP were expected to play crucial role .'U
ately.',.:
in Immunisation Programme. Their postion in study districts was as follows:
’’’A contingent amount of Rs.2,000 has been sanctioned for each PHC for
Table 1
maintenance of cold chain equipment. It also covers the expenses for purchase
of ice, kerosene oil, etc.
Number of Districts with Percentage of Vacancies
-.
i'; To ensure good quality of vaccine, officials at all levels are required to pick
in Different Staff Categories
up samples of OPV and send them to different laboratories for potency testing.
% Vacancy
Category of staff
! Number of laboratories have been identified and are equipped to carryout the
HA(F)
MO
HW(F)
potency tests.
Nil
■ Observations regarding various aspects of logistics and cold chain mainte
12
7
13
<10
7
7
9
nance system at district headquarters and PHCs are shown below:
ries of staff is as follows:
10-20
21-30
31-40
41 +
No Information
9
5
3
5
6
6
3
1
7
6
8
3
2
1
6
Total no. of districts
42
42
42
Thus, to summarise:
’ i. MOs post vacancy was over 20% in 13/42 (30.9%) districts
ri. HA(F) post vacancy was over 20% in 11/42 (26.1%) districts _
■ 1‘1’ HW(F) post vacancy was over 20% in 6/42 (14.2%) districts
<5
. 1.
it
2.
3.
4.
5.
6.
The refrigerators and freezers
in working order
There is a thermometer in all the
refrigerators ■
The daily temperature record
pcroperly maintained in all the refrigerators
Irregular temperature recorded
There is thermometer in the ILR
Vaccine after expiry date found stock
District
%
PHC
%
97.6
81.5
88.0
73.0
78.57
71.0
97.6
67.2
16.4
74.1
3.7
»
jr
£
•
7. DPTorTT vaccine found frozen
8. Open vaccine vials found in the stock
9. Returned unopend vials are marked
10. Tirst-in first out’ principle is
observed
11. More than three months supply of
vaccine present
12. Less than one month supply of
vaccine present
13. Food or drinking water seen
alongwith vaccines in the refrigerator
14. Frozen ice packs available in the
freezer compartment
15. Vaccine stock register are
maintained
16. i. Stock book entries are
made properly
ii. Stock book entries are made
regularly
ill Stock entries correspond
to actual stock in hand
2.4
of the programme, ioformadon system fenMd
also covered.’i o .■
76.1
4.8
6.3
49.2
86.1
68.8
States, at different levels, though there was much scope
11.9
15.3
order to make them really operational.
Particulars about planning activities in different ois
7.2
52.1
2.6
6.9
96.0
61.9
97.6
85.2
90.0
79.4
90.0
80.4
90.0
77.2
The area which needed special attention with regard to supplies of all kinds
e.g. vaccines, cold chain equipments, syringes, needles, etc. was the distribution
system ensuring their availability at peripheral/institutional levels like PHCs
and subcentres.
,
i. Planning Activities
■
Detailed Action Plans worked out systematically were
............. .
. 1 '
n^ovement^n
P
are shown be]ow.
*
No. of Districts
33 (78.5%)
Action plans available
District officilas involved
actively in Action Plan Preparation
23 (54.7%)
Allocation of targets using
specific population criteria
29 (69.04%)
r
Correct information used for
33 (78.5%)
estimating vaccine required
Adhering to Scheduled Immunisation Sessions
' Out of 383 workers at subcentres, 54.2% stated to have experienced disrup-
tions in immunisation sessions.
for disruption is indiThe proportion of workers stating different reasons
cated below:
Table 2
Proportion of Heath Workers Expressing Various Reasons
of Disniption of Vaccination Sessions
Training of Health Personnel
Training of heath personnel of different categories in immunisation pro
gramme has become an ongoing programme in every State. Middle level
managers are being trained at national level. Medical officers and paraprofes
sionals are being trained at district and Primary Health Centres respectively.
Central Government is providing financial support to State Governments for
training programmes. However, backlog in training, poor quality of training
processes and inadequacy of training aids etc. were not uncommon.
””'
% Respondents
Reasons for Disruption
1.
2.
3.
4.
5.
6.
Shortage of vaccinc/dilucnt
Called for other duties
Absence of workers
Lack of transport
Shortage of syringes
Shortage of needles
.
50.6
37.3
28.8
23.2
7.4
6.8
Operational and Managerial Processes
Hi. Special Strategies
During the review, operational and managerial processes regarding the
programme like programme planning, supervision, monitoring and evaluation
In 20 (46.5%) districts special strategies were being adopted to achieve
immunisation coverage in inaccessible areas or in special population groups.
9
iv. Micro-planning in Immunisation
Further, it was encouraging to note that States have begun strategy of
\
• '^^wB^’^M.fl'upei^isory checklist practically did not exist in any districts
planning in a few districts to ensure more realistic planning with active in^r^i^^^^The' average number of supervisory visits per month by district officials to
ment of health functionaries at all levels.
V° V^OS^£neripheral institutions was four which ranged between 1-10.
'
/ v*-.'.'' > ■ .
,,'
v. Monitoring
,
'
"^^^Immunisation Coverage.
i
Similarly,
monitoring
of thereports
programme
at all levels has
bppn Strengthen^»^One of the major
. observations
,
•
. during
. . the review
.
through
review
of the various
on performances
a/wT
made
was related to the
regarding various resources i.e. availability, consumption etc. Ev"
coverage of beneficiaiy Population.
some States over-emphasis was found to be laid on nrooramm'
vi. Supervision
Supervision, by and large, was found to be one of rhp
programme management. Though supervisory visits were be’
officials in many States, they were more routine *nature
Immunised Children
...........................................................................
''
distribution of study
districts/units (43) and their names by immunisasW^tion status of children i.e. completely protected is presented in Table 3,4 and 5r
XBWlWithout measles, only 20 districts achieved more than 50% coverage.
$ ^•yV^j^With measles this number was brought down to only Two. No district had
‘he S gfe;achieved 85% coverage of immunisation.
• ■
ere
.
attention to documentation and follow-up of the observations marl
■ equate 'i
v>S!ts. Further, all aspects of the programme like re
consumption or use, quality of performance, diseaseZ7 d
!
adequately attended to in many States and districts wh71e
n°‘ '
visits Regular meetings in all States held at different levels So
'
monitoring and supervision.
aIso be,Ped in '
'g fX' Y.
Further details about supervisory practices i„ the district are shown be|ow;
No. of Districts
Supervisory visits by offcials
as per scheduled dates
Checking cold chain, vaccine
stocks and performance records
during visits
Checking disease surveillance
also during visit
Visit observations recorded
Monthly meeting records maintained
Reports on complications and
adverse reactions at district
District officials satisfied
with health workers performance
17 (40.4%)
&
I
Table 3
x•
Distribution of Districts/Units According to Percentaage of
Dully Immunised Children
i Percentage
26-50
..... 51.75
1 76-85
86 +
Total
Without Measles
With Measles
9
14 (2 urban)
16 (4 urban)
4 (2 urban)
16 (2 urban)
25 (5 urban)
2(1 urban)
“w.
-
43*
43
* 35 districts + 8 urban units «= 43
20 (47.6%)
14 (33.3%)
11 (26.19%
32 (76.19%)
38 (90.4%)
24 (57.1%)
IO
11
Table 4 .
(■individual groups of vaccines is shown in Table 6.
% Coverage
<25
Number
16
26-50
25
- o
51-75
2
76-85
Nil
85 +
Nil
No. of Districts
Cuddapah, Warangal, Nowgaon, Katihar, Singhbhum, Bijapur,
Nanded, Ganjam, Bharatpur, Jhalawar, South Arcot, Kanpur
Dchat, Burdwan, Murshidabad, Calcutta (District I), Calcutta
(District II)
Name of Districts/units
Cuddaph, Katihar, Bijapur, Warangal, Bharatpur, Nowgaon,
Singhbhum, Kanpur Dchat, Murshidabad
26-50
14
Dibrugarh, West Nimar, Nanded, Ganjam, Patiala, Meerut,
Burdwan, Hissar, Mandla, Sambalpur, Jhalawar, South
Arcot,Calcultla I and Calcutta II
4
Nil
Panchmahal, Rajkot, Bhiwani, Shimla, Bilaspur, Anantnag,
Coimbatore, Badgam, Kasargode, Tumkur, Pune, Sangrur,
Bombay (A)
North Goa, Ouilon, Bombay (B), Delhi (Urban),Delhi (Rural)
b) Immunisation Coverage for Different Groups of Vaccines
Distribution of districts/units according to immunisation coverage for
12
86+
43
opys
n
6
24
6
5
43
BCG
Measles
4
10
21
(2urban)
5
(4 urban)
3
(2 urban)
11
21
11
43_________ 43
Out of 43 districts/units 36 (83.72%) achieved over 50% coverage for DPT3.
Out of 43 districts/units 35 (81.3%) achieved over 50% coverage for OPV3.
■--------- —--------------------Out of 43 districts/units 29 (67.4%) achieved over 50% coverage for BCG.
Out of 43 districts/units 11 (25.5%) achieved over 50% coverage for measles.
9
76-85
86 +
76-85
Total
<25
16
2
5
25
(3 urban)
6
(3 urban)
5
(2 urban)
<25
26-50
51-75
North Goa, Dclhi-A
Distribution of Districts /Units According to Percentage of
Fully Immunised Children (without measles)
51-75
DPTs
% Coverage
Dibrugarh, Panchmahal, Rajkot, Bhiwani, Hissar, Bilaspur,
Shimla, Anantnag, Quilon, Kasargode, Badgam, Tumkur, West
Nimar, Mandla, Pune, Sambalpur, Sangrur, Coimbatore, Pa
tiala, Meerut, Bombay (District A), Bombay (District B), DclhiB, Madras (North), Madras (South)
J£
Number
'ib h'.
Districts/Units Showing Coverage of Four Different Groups of Vaccines
Name of Districts
Table 5
% Coverage
-•
Table 6
Distribution of Districts /Units According to Percentage of
Fully Immunised Children (with measles)
c.
Dropout Rates for DPT (1-3) and OPV (1-3)
Distribution of districts and urban units according to dropout rates for DPT
(1-3) and OPV (1-3) isshownin Table 7. Out of 43 districts/units, 14 (325.%) had
reported dropout rate of over 20% for DPT (1-3). Out of 35 districts, 18 (51.42%)
had reported dropout rate of over 20% for OPV (1-3).
Table 7
Dropout Rates for DPT (1-3) and OPV (1-3)
in Districts and Urban Units
% Dropout
<10
11-20 .
21-30
30+
Data not available
Total
Number of Districts
DPT
OPV
13
16
8
4
2
7
10
11
6
1
43
35*
* Excludes urban units.
13
Table 4 .
.
.
Distribution of Districts /Units According to Percentage of
Fully Immunised Children (with measles)
% Coverage
<25
Number
16
26-50
25
o
51-75
2
76-85
Nil
85 +
Nil
Name of Districts
Cuddapah, Warangal, Nowgaon, Katihar, Singlibhum, Bijapur,
Nanded, Ganjam, Bharatpur, JhaJawar, South Arcot, Kanpur
Dchat, Burdwan, Murshidabad, Calcutta (District I), Calcutta
(District II)
Dibrugarh, Panchmahal, Rajkot, Bhiwani, Hissar, Bilaspur,
Shimla, Anantnag, Quilon, Kasargodc, Badgam, Tumkur, West
Nimar, Mandla, Pune, Sambalpur, Sangrur, Coimbatore, Pa
tiala, Meerut, Bombay (District A), Bombay (District B), DclhiB, Madras (North), Madras (South)
Distribution of Districts /Units According to Percentage of
Fully Immunised Children (without measles)
Name of Districts/units
< 25
9
Cuddaph, Katihar, Bijapur, Warangal, Bharatpur, Nowgaon,
Singhbhum, Kanpur Dchat, Murshidabad
26-50
14
Dibrugarh, West Nimar, Nanded, Ganjam, Patiala, Meerut,
. Burdwan, Hissar, Mandla, Sambalpur, Jhalawar, South
Arcot.Calculttal and Calcutta II
•
51-75
76-85
86 +
16
4
Nil
Districts/Units Showing Coverage of Four Different Groups of Vaccines
—
% Coverage
< 25
26-50
51-75
76-85
86 +
No. of Districts
DPTs
OPVs
2
5
25
(3 urban)
6
(3 urban)
5
(2 urban)
2
43
Total
>---------------- —--------------------
Number
Table 6
24
6
5
North Goa, Dclhi-A
Table 5
% Coverage
individual groups of vaccines is shown in Table 6.
Panchmahal, Rajkot, Bhiwani, Shimla, Bilaspur, Anantnag,
Coimbatore, Badgam, Kasargodc, Tumkur, Pune, Sangrur,
Bombay (A)
North Goa, Quilon, Bombay (B), Delhi (Urban),Delhi (Rural)
b) Immunisation Coverage for Different Groups of Vaccines
Distribution of districts/units according to immunisation coverage for
43
BCG
Measles
4
10
21
(2 urban)
5
(4 urban)
3
(2 urban)
11
21
11
43
43
Out of 43 districts/units 36 (83.72%) achieved over 50% coverage for DPT3.
Out of 43 districts/units 35 (81.3%) achieved over 50% coverage for OPV3.
Out of 43 districts/units 29 (67.4%) achieved over 50% coverage for BCG.
Out of 43 districts/units 11 (25.5%) achieved over 50% coverage for measles.
c. Dropout Rates for DPT (1-3) and OPV (1-3)
Distribution of districts and urban units according to dropout rates for DPT
(1-3) and OPV (1-3) is shown in Table 7. Out of 43 districts/units, 14 (325.%) had
reported dropout rate of over 20% for DPT (1-3). Out of 35 districts, 18 (51.42%)
had reported dropout rate of over 20% for OPV (1-3).
Table 7
Dropout Rates for DPT (1-3) and OPV (1-3)
in Districts and Urban Units
% Dropout
<10
11-20 .
21-30
30+
Data not available
Total
Number of Districts
DPT
OPV
13
16
8
4
2
7
10
11
6
1
43
35 ‘
* Excludes urban units.
13
Names of dislrie.s and urban unils according !odropoulralesforPolio(l-3)
is shown in Table S.
Table 8
achieved over 50% coverage forTT. Of these 11 had achieved more than 85 %\^
coverage.
Table 10
Dropout Rates for Polio 1-3 in Districts/Urban Units
%Coverage
Number
7
< 10
,
---------------
Distribution of Districts/Units by % Coverage of Tetanus Toxoid •
Two doses/Booster to Pregnant Women
Name of Districts/Units
- North Goa, Panchmahal, Bhiwani, Quilon, Pune, Sangrur,
Madras (South)
Dibrugarh, Rajkot, Hissar, Bilaspur, Badgam, Kasargode,
Tumkur, Mandla, Ganjam, Sambalpur, Coimbatore, Calcutta
(District-I), Calcutta (District-11), Bombay (District A), Bom
bay (District-B), Dclhi-B, Madras (North), Madras (South).
11-20
IS
21-30
11
Cuddapah, Warangal, Shimla, Anantnag, Patiala, Jhalawar,
South Arcot, Meerut, Burdwan, Murshidabad, Delhi-A
31+
6
Data not available
1
Nowgaon, Kalihar, Singhbhum, Nanded, Kanpur Dchat,
Bharatpur
West Nimar
e.
% Coverage
No. of Units
<25
26-50
51-75
76-85
86 +
1
7
17
7
Total
43
o
Vaccination Coverage in North-Eastern States
Status of immunisation coverage among infants andrpregnant women in
North-Eastern States is shown in Table 11.
.v^
Name of districts and urban units according to dropout rates for DPT (1-3)
Table 11
is shown in Table 9.
Vaccination Coverage in NorthEEastem States
Table 9
Drop out Rates for DPT (1-3) and /Urban Units in Districts
Name of Districts/Units
Dropout rates
Number
< 10
13
North Goa, Panchmahal, Bhiwani, Bilaspur, Quilon, Pune,
Sambalpur, Sangrur, CalcuUa-I, Bombay A, Bombay B, Madras
(North), Madras (South)
11-20
16
Cuddapah, Dibrugarh, Nowgaon, Rajkot, Hissar, Shimla,
Badgam, Kasargode, Bijapur, Tumkur, Mandla, Ganjam,
Coimbatore,Calcutta-II, Delhi (urban), Delhi (rural)
21-30
S
Warangal, Anantnag, Nanded, Patiala, Jhalawar, South Arcot,
Meerut, Burdwan.
30 +
4
Kanpur Dchat, Bharatpur, Katihar, Singhbhum
Data not available
2
Murshidabad, West Nimar
_______________________ _
d. TT Coverage for Pregnant Women
Immunisation
Status
Fully Immunised
. DPT
OPV
BCG
Measles
TTII Pregnant women
Proportlon.of eliHbles
protected In districts by
year of initiation of UIP
1985-87
1987-88
30.9%
56.8%
49.7%
21.02%
44.3%
44.8%
51.1%
36.6%
59.9%
29.9%
20.0%
49.5%
£
’’
Percentage of coverage for all groups of vaccines was higher in the group of
districts where UIP was initiated in 1985-87 as compared to the group of districts
taken up in 1987-88.
Distribution of districts/urban units according to TT immunisation status of
pregnant women is shown in Table 10. Out of 43 districts/units, 35 (81.4%)
14
15
(b)
Obstacles
f. Recsons for Failure of Immunisation
Reasons fot failure of imn-unisation as reported by mothers in study districts/units are shown in Table 12.
Table 12
Causes
■-
■
Unaware of need
Number of units
reporting with
% range
. Number of units
reporting more
than 25 per cent
40
(18.99-52.66)
Unaware of need
Place and time
32
Time of immunisation
inconvenient
Vaccinator absent
27
(0.8-23.33)
Vaccine not
available
31
(0.5-23.2)
Mothers too busy
32
(2.6-19.2)
Child ill not brought
32
(1.8-32.0)
32
,
10 return
Number of units
reporting more
than 15 percent
34
(0.92-26.5)
Fear of side
33
reactions
(0.6-30)
Wrongideas about
18
^contra-indications
(0.95-8.8)
3
Nil
/
6
4
4
'
6
4
(c)
(0.5-27.1)
unknown
26
(0.5-48.9)
23
(0.8-13.33)
Place too far to go
Distribution of Districts/Urban Units by Dfferent Reasons
for Failure of Immunisation.
(a) Lack of Information
Number of units
reporting more
thanl5 per cent
Number of units
reporting with
% range
Causes
2
Causes
3
Nil
Lack of Motivation
Number of units
reporting with
% range
Number of units
reporting more*
than 15 per cent
Postponed till
another time
31
(10-24.1)
6
No faith in
immunisation
33
(0.5-28.5)
3
Rumours
18
(0.5-12.6)
Nil
Results of Observation of Immunisation Sessions
Immunisation sessions held at subcentres and outreach were observed
for selected quality aspects and findings are presented in Table 13.
17
Table 13
Disease Surveillance
Specified Condilions Satisfied
1.
2.
3.
-4.
.5.
6.
7.
Immunisation services integrated with other
' MCI! activities
. •
Immunisation cards filled correctly
Immunisation cards given to the mothers
Age screening done correctly
Following immunisations are being given
DPT
OPV
BOG
Measles
Vaccines within expiry date
Vaccine kept on ice at the time of immunisation
8.
Diluent also kept in the vaccine carrier
The dosage correct
X). Immunisation site correct
11. Immunisation technique correct
12. Number ofsyringes and needles adequate,
in proportion to the required number of
vaccinations to be given.
IS" Separate syringe and needle used for
each immunisation
14. Adequate number of frozen ice packs in
vaccine carriers
15. Partially used vials discarded at the
end of the session
16. Mothers properly informed about:
-Purposeof immunisation
-Number of doses
-Right age for immunisation
-Possibility of side effects
-When to come back for next dose
-Safe keeping of immunisation card
9.
&
5’SV‘X'
\
\
Results of Observation of Immunisation Sessions
Proportion of sessions
Subcentre
Outreach
84.6
80.5
81.3
88.6
76.6
70.2
60.4
82.0
97.2
94.4
77.6
94.3
84.1
78.8
83.9
97.0
94.0
83.8
80.0
86.0
98.2
94.6
92.9
85.0
94.0
92.2
88.0
70.5
70.0
73.0
75.6
79.1
72.7
87.0
83.1
87.0
94.0
86.2
88.6
93.1
82.8
77.1
88.8
80.8
78.5
90.4
74.4
JU.'
83.8
<.
Disease surveillance was another component of the programme examh^ ,
during the review. By and large, the surveillance system was found to be poor tns
most States even through the sentinel centres. Problems related to poor training
of staff involved, inadequate attention to record maintenance, insufficient
attention to investigation of reported diseases or outbreaks were common in
many States.
Special disease surveys for poliomyelitis and neonatal tetanus were con
ducted under the national review. In a total of 4,23,201 children below five years
surveyed for lameness, 1,149 were found to be lame due to paralytic polio and
after applying the correction factors for paralysis of upper limbs, migration and
death the prevalence rate came to 4.5 per 1000 children below five years. Wide
variation was seen in prevalence of lameness due to polio in different^tudy
districts ranging between 0.372 per 1000 in Dibrugarh in Assam and l‘WPer
1000 children under five years in Kanpur Dehat in U.P. (Table 14 and 15). One
important observation was that about 20-30% of children suffering from polio
myelitis were reported to be immunised against polio.
Table 14
Distribution of Districts/Urban Units According to Prevalence Rate of
Paralytic Poliomyelitis
Prevaience/1000 children
under five years
No. of Districts
<1
2
3
4
5
5r
Data not available
6
6
8
2
5
15
Total districts/units
A
V
43
11
«U.s
Table 15
Table 17
, Distribution of Districts/Urban Units According to Jr^alence
Rate of Paralytic Poliomyelitis
Prevalence
rate of Polio
Number
6
2
6
3
8
4
2
5
5
Si
15
Name
1
Name of Districts
Number
0
8
North Goa, Ouilon, Kasargode, Pune,Coimbatore,
Calcuttta-II, Madras North, Madras (South)
Nowgaon, Quilon, Kasargode, Bijtcx, Nandcd,
Cakutta-n
<1
10
Warangal, Rajkot, Bijapur, Shimla, Tumkur, Maidla,
fatiala, Sangrur, Calcutta-I, Bombay-B
Singhbhum,
Rajkot, , Buur,nt,
Sambalpur,
Murshidabad,CaJcutta-II, Delhi (trun), Coimbatore
1-2
5
Cuddapah,Nowgaon, Bijapur, Delhi (urban), Delhi (rural)
Marxfla, Madras (North)
2-3
3
Ganjam,Sambhalpur,South Arcot
+
Cuddapah, Panrhmah.il, Patiala, Lrnbay-B, Delhi (rural)
3-5
5
Murshidabad, Bombay-A, Dibrugarh, Bhiwani, Hissar
Tumkur, West Nimar, Sangrur, Kafnar, Hissar, Badgam,
Warangal, Ananlnag, Bijapur, Gtaam, Bharatpur, Jhalwar, South Arcot, Meerut. Kann,--_ ■
5-10
8
Katihar, Singhbhum, Panchthahal, Anantnag, Badgam,
West Nimar, Bharatpur, Meerut
10+
Data not
available
2
Jhalawar, Kanpur Dchat
2
Burdwan, Nandcd
Burch’.7m
Table 16
Distribution of Districts/Urban Units According to NUT Mortality Rates
No. ofDistricU/IJuot
1000 Live Births
0
8
l2
3
25
35-10
10 +
Data not
NNT Mortality
Rate per 1000 Live
Births
As regards neonatal tetanus mortality, in as many as 16 utits studied the
mortality rate was less than one perlOOO live births and infact in eight units no
case of neonatal tetanus was reported. The highest rate of 23,72 per 1000 live
births was reported from Kanpur Dehat (Table 16 and 17).
NXT Mortality rate
Distribution of Districts/Urban Units According to NNT Morality R es
Dibrugarh, North Goa, Shimla.ihne. Bombay A,
Madras (South)
Data not
available
‘ .I'i >.: it-f^
10
5
3
5
8
Another important observation made during the review was the existing
level of involvement of non-governmental agencies in the programme. We in
some States they were participating actively in the programme, the need for
expanding efforts for utilising this potential support in future was Clearly
brought out. Among the Govermental agencies also, need for expanding the role
and involvement of the medical colleges, ICDS and Central Government agen
cies with better coordination for success of the programme was highlighted
during the review.
In the light of various observations made during the review and considering
the urgency of achieving the targets set for the programme, a number of recom
mendations have been made. While alongwith individual State Review Report,
State specific recommendations have been given, in the national report recom
mendations of more general nature indicating action at national level are in
cluded. Details are shown in succeeding pages.
2
available
2
21
' PROBLEMS
Policies
Inspite of the fact that National
Government is fully committed to the
goal of providing immunisation to all
the target population, within stipu
lated timeframe, it appears that the
urgency of the programme is not un
derstood at all levels of the health
system. Consequently sense of com
mitment is lacking.
It would be pertinent to seek an
swer as to how the districts covered
under UIP in various years in phased
manner could reach the same cover
age level by 1990 because districts
included in the earlier period can be
assumedto have the obvious advan
tage over those included later in
terms of various resource inputs.
A major deficiency in terms of
lack of clearcut policies regarding
implementation of immunisation in
urban areas was observed.
.22
RECOMMENDATIONS
Policies
It may be considered worth while
to request Prime Minister to address a
conununique to all Chief Ministers of
States reiterating goals of UIP and
seeking their full and wholehearted
support. They may be further re
quested to assume responsibility to
ensure that all pregnant women and
eligible children in their States are
protected.
It is recommended to reconsider
the dates of achievements of the set
goals.
Role of Panchayat vis-a-vis
health programme should be rede
fined. More meaningful involvement
of Panchayats will not only boost the
programme but ensure universal
coverage.
It is recommended that there '
should be clear policies related to
implementation of immunisation
programme in urban areas in terms of
joint planning, resource allocation,
demarcation of area/population re
sponsibility between State health
administration, urban local selfGovemment etc.
Instead of generalised approach
to cover total urban area, it would be
appropriate to identify priority areas
based on load of disease, chances of
transmission of diseases, poor living
condition, poor sani tation and socio
economically handicapped areas for
special efforts for complete cover
age.
\
Sustainability
Sustainability
The Immunisation Programme
will have to be continued to maintain
the coverage level of 22 million
pregnant women and 18.5 million
year after year. The States generally
accept the programme so long as the
100% financial support from Central
Government is available. As soon as
this support is withdrawn the States
find it difficult to bear the burden of
the programme.
Central Government, before stis-. ’
pending the 100% support, should '■
ensure that the State Government are
fully prepared to assume responsi
bility to run the programme on their
own. In the absence of such prepar
edness it may not be a surprise to find
that programme has been pushed to
back seat
UIP as a Component of MCH
Services
UIP as a Component of MCH
Services
_
UIP is viewed in isolation from
other components of MCH services.
UIP needs to be developed as a
part of 1 arger MCH programme. The
service for infants (contacts with
health functionaries as well as sup
port system) need to include meas
ures for control of D-Diarrhoeal dis
ease (DD), Acute respiratory infec
tions (ARI), parasitic infections,
anaemia and Vitamin A deficiency,
etc. Similarly, for mothers, services
should include measures for. birth
spacing, safe motherhood and con
trol of anaemia. For this to be
operationalised the technical MCH
wings at national and State levels
need to be considerably augmente^
Programme Planning
Programme Planning
Though plans of action are pre
pared, generally they are target
oriented, and percolate from top to
bottom, hence these fail to generate
enthusiastic responses from periph
eral levels.
It is recommended that micro
planning process should be initiated
at subcentre and PHC levels in each
district. This would help in mobili
sing resources, identifying and enu
merating eligibles, organising ses-
23
priate measures to overcome the
siun auu toliowup ut dropouts, in
volvement of grassroot level work
ers wall make them responsible and
accountable to achieve what they
have planned. Sense of participation
will also boost the morale of workers.
Advance scheduling of im
munisation sessions on a fixed day
which is publicly known to staff and
community is important.
Strategy
Strategy
While formulating operational
strategies for immunisation, not
much consideration is given to
difficult areas or areas adversely af
fected by floods, landslide or ad
verse climatic factors and difficult
terrain. Similarly, not much attention
is given to the specific groups of
population like tribals or migrants.
Alternative approaches to cover
remote areas, difficult areas and spe
cial groups of population should be
searched - these could include mo
bile teams, intensified, campaigns
etc. Area specific operational strate
gies should be determined in consul
tation with officials. Additional fa
cilities for mobility during limited
periods in which teams will be work
ing should be provided. For flood
affected or water-logged areas boat
squads may be provided for running
immunisation sessions. States
should be given flexibility to decide
on strategies suited to local situ
ations.
Provision should be made for
meeting the extra expenditure to be
incurred for organising special cam
paigns, intensified drives, and spe
cial squads, so that the health budget
of States is not affected.
Districts or. regions performing
poorly should be identified and .in
tensified programme should be car
ried out in such districts with appro
Generally, same operational
strategy is followed for good performing'and poorly performing dis
tricts:
•
<
.
24'/:^'
’
■
.
.
While allocating the area of work
to the health personnel only popula
tion is taken into consideration
which has its own drawbacks be
cause of the low density of popula
tion and difficult terrain etc. in some
States.
During coverage evaluation it
was observed that in couple of dis
tricts children even below the age of
three months had been affected with
paralytic poliomyelitis. '
bottlenecks, and hurdles.
It is recommended that while al
locating the area to workers, popula
tion should not be the only criterion
but socio-geographical and commu
nication factors should also be taken
into consideration, so that the work
ers are able to reach the beneficiar
ies.
It is recommended that in'the
event of such situation, immunisation for poliomyelitis should be
takenimmediately after thebirthand
completed before completion of
three months of age. This will of
course necessitate more contacts
because poliomyelitis vaccination
will have to be given separately and
not alongwith the DPT. Government
has therefore, taken policy decision
to change immunisation schedule to
initiate the same as early as possible
ie. OPV at birth, DPT and OPV at6,10
and 14 week. BCG is to be combined'
It was reported that in some States
immunisation sessions were not held
on scheduled days or were cancelled
often without prior intimation to the
community. Credibility of function
aries get adversely affected in such
situations.
with any of these.
Immunisation session at all lev
els should be held on fixed day. It will
help people to remember the due day
for subsequent dose and reduce
dropouts. Except for reasons beyond
control, sessions should not be
cancelled.
Stencils as in malaria indicating
schedule of sessions at PHC should
be an annual feature. This should be
monitored in terms of number of
sessions held (as percentage) against .
the scheduled.
25
Villages at a distance from
subcentre are visited less frequently.
Reasons for not holding sessions
should be enquired into, so that ac
tion can be initiated (Panchayat
should be made responsible for
doing this).
In villages at a distance from
subcentre, MPW(M) should be as
signed the responsibility to give
vaccination on fixed day at fixed
place, as far as possible, e.g. Anganwadi or place identified by HG
for holding the sessions.
Organisation and
Infrastructure
Organisation and
Infrastructure
■ ■ The role relationship between the
Mission on immunisation and DGHS
at the central level in total immunisa
tion programme is unclear particu
larly since all districts have been
brought under UIP since beginning
of 1989-90. Problems are likely .to
arise in relation to the following:
i. Coverage and monitoring of
booster doses for DPT and Polio
vaccines.
ii.’ Coverage with complete im-
At the central level there is need
to specify the roles and inter-rela
tionship of the EPI Wing of the DGHS
and the Immunisation Mission in the
Ministry of Health and Family Wel
fare mainly concerned withUIP. This
is particularly important since the
immunisation programme is a con
tinued programme which is to be
sustained for many more years.
Being technical programme,
technical support at centre should be
strengthened.
■ munisation for those children
who could not be protected under
- _... one year of age.
,iii. Immunisation of older group of
i
.>■ children for DT, TT etc.
; Health facilities have expanded
but not become fully operational in
£1*:' many States for want of staff, equipinent etc.
•;'
■
Norms for supply should be re
vised for institutions including new
PHCs and urban institutions. State
government should ensure adequate
staff, transport facilities and equip
ments including cold chain equip
ments and other supplies for im
munisation. Areas of newly creau^
PHC should be' demarcated and\
subcentre should be attached to these \
health centres. In this regard, meas
ures initiated at Central Government
level need to be specially imple
posts of Cold Chain Officer, DIO,
Refrigerator Mechanics, Statistical
Assistants and Drivers were found to
be vacant in many States. In couple of
States these positions had not yet
been created.
mented.
Posts of Cold Chain Officer, DIO,
Refrigerator Mechanics and Drivers
should be filled up without delay.
Wherever posts have not been sanc
tioned the steps should be taken to
create and fill these up..
It is also recommended that jol^)
responsibilities of these categories
of staff be defined so that they func
tion effectively.
• •
DIOs should not be part-time
officials and adequate administra
tive authority should be given to
Similarly, large number of posts
of Medical Officers, Health assistant
(F), MPW (F) are lying vacant. In
some States the vacancies are more
than 30%.
At PHC even when accommoda
tion is available and all other facili
ties exist, MOs and other staff stay
outside the area and commute every
day from their residence to place of
work. Such practices are totally un
justified.
Lack of motivation with no sense
of commitment and gradually in
creasing culture of no work among
health manpower was reported from
them.
Vacant posts of medical officers,
HA(F) and MPW(F) should be imme
diately filled as they are the key func
tionaries, not only for imfhunsation
but also for providing health care
with special focus on mothers and
children.
Such situation should be seri
ously viewed. Effort to study reasons
for such practices be made aw
prompt action be taken to prevent
such situations.
Minor but easily soluble person
nel management issues like delay in
payment of salary, TA/D A, sanction
ing of leave etc. should be immedi-
27
every Sta,v
' ’
’^^strictunder review.
Thougi.
created and, J °f DIO have been
Q yet most of ./"/'have been posted,
quate adm,',j*
not have a^epowers. For //"dive or financial
depend up^/z'^hing they have to
find themse,’,. ^0-Therefore, they
not able to g<, f 6 be ineffective or
over in the ai, /'!red results. Moreauthority the
°f administrative
their relation^'. 75 felt uneasy about
.. • In some fz ,/''*’th MOsofPHCs.
, who are work/**’- medical officers
; tricians in he/ clinical paediaj signed resporl..,'/<!,|s have been as' \ sequently will,
of DIOs. Con•l-.they are not ab '°f clinical work,
•<,- nnmumsation J,''' do any justice to
Jly- Frequent /Mmme.
turnoverp/^'fcrs and large
eposes anm '^'t'ularly of trained
•v/|to successful
Serious problem
ijASfPgfunitne.
'//Ahientation of the
ately looked into and sorted out.
Awards, appreciation and recogni
tion of good work should go a long
way in boosting the morale of workers/staff. As a long-term measure,
serious efforts should be made for
human resource development
through a well defined national
manpower development policy in
cluding opportunities for career
development and continuing educa-'
tion.
Any responsibility without au
thority makes a bad manager. There
fore to make them more effective,
their specific roles, administrative
authorities, and financial relation
ship with other officials need to be
clearly spelt out.
The tendency of officers holdjng
additional charges of immunisation
should be discouraged as far as pos
sible.
Posting of medical officers work
ing as clinical paediatricians in hos
pitals as DIO should be discontinued.
Wherever such arrangements exist,
they should be remedied by posting
full time DIO.
Only under very exceptional cir
cumstances the staff should be trans
ferred. Moreover the trained staff
should be allowed to continue to
work for a reasonable time, so as to
reap the benefits of their training.
However, it is important to orient
everyone as far as possible through
massive training.
The HG and AWW were to play
key role as agent for change and
assist in providing services. In pur
suance to Government of India’s
decision that only females may be
employed as HG, the institution of
HG has become more or less non
operative in many States.
It is accepted generally that the
most effective organisational set up
at the district would be where the
implementation of different pro
grammes can be undertaken in an
integrated manner based on area
wide responsibilities rather than on
vertical programme basis. Therefore
instead of labelling officers as spe
cific programme'officer. they should
be identified as area officers and held
responsible to look after all activities
in their allocated area. Working in a
small area will not only ensure better
supervision but will also reduce the
burden of medical officer of PHC to
be answerable to several programme
officers.
The State may be clearly in
formed about the decision regarding
continuance of the HG scheme and if
it is to be continued it should be seen
that it is carried out both in letter and
spirit. It will also be necessary to
reconsider the amount of honorar
ium paid to HG.
Supplies
Supplies
System of supply of vaccines by
push system without taking into con
sideration the actual quantity of vac
cine consumed and the stock avail
able at State or district headquarters
has resulted in excess stock of vac
cines in a few places.
Vaccine should be supplied only
on monthly basis instead of quar
terly. This is important because if for
any reason one batch of vaccine is
found unsatisfactory, only small
quantity of vaccine would be re
quired to be destroyed. Utilisation of
vaccine should also be taken intoaccount while deciding quantities to
be supplied. Supplies should be
made by indenting system instead of
In some States, the areas/zones in
the districts have been allocated to
district officials on geographical ba
sis for supervision of all health pro
grammes. Even with such arrange
ments officers continue to be identi
fied as individual programme offi
cer, and many tend to lay more stress
on their own programme and pay less
stress on others during supervision
and monitoring. Creation of the post
of DIOs, however brings in the con
cept of verticality and make his role
ambiguous under such circum
stances.
. 29
Cold chain equipment and other
supplies related to immunisation
programme were found in short sup
ply in many places either due to delay
in despatch or failure in distribution
by the State to districts and from dis
trict to other peripheral institutions.
The workers were found to use
thermocole boxes to carry vaccines
in the field. They prefer to use them
because they are lighter in weight
. and easy to carry. However, they are
not adequate because ice melts very
soon in such boxes, hence, it is
difficult to maintain appropriate
temperature.
In some districts electric supply
is very erratic. Some times power is
. not available for number of days. In
some areas there is no electric sup
ply- '
In areas like Leh, Kargil, Lahaul
and Spiti where temperature goes be- • low 0°C. T group of vaccines gets
frozen.
push system.
Apart from ensuring availability
of adequate quantum of supplies at
district level, special care needs to be
taken to arrange for proper and
timely distribution of the same to the
peripheral institutions upto the
subcentre level.
Thermocole boxes used by MEW
should be withdrawn. They should be
compelled to use either vaccine car
rier or day carrier with required
number of frozen ice packs. This is
necessary to ensure safe transit of
vaccines from PHC to subcentre and
outreach villages..
Feasibility of supplying solar
refrigerator or kerosene/battery op
erated refrigerator be explored for
areas where there is no power, or
electric supply is very erratic.
In areas like Leh, Kargil, Lahaul
and Spiti where temperature goes
much below 0°C, equipment to pro
tect ‘T group of vaccines from ex
treme cold should be provided.
i'i&tji. safe is not maintained.
Gradually- number ’oft private
practitioners involved in giving im
munisation to their clients is multi
plying. Large number of them pur
chase vaccines from chemists and
druggists shop.
. During transit, many a time either
due to delay/cancellation of flights
delay in receipt of information
about despatch of vaccine, number
days elapse between date of des".Patch and actual receipt of vaccine
^■w^^byconsignee. Many airports at hold-
Monitoring of Vaccine Quality
Monitoring of Vaccine Quality
Number of samples lifted from
most of the States were grossly in
adequate. In the absence of labora
tory facilities within the State, it was
found too cumbersome to send vac
cines through couriers from every
district to the allocated laboratory.
There was significant time lag be
tween despatch of sample and re
ceipt of results.
To ensure the quality of vaccine
clear cut instructions should be is
sued for lifting the minimum number
of samples at different levels in each
State. Facilities should be provided
in each State for testing the OPV so as
to avoid problem in sending them
and preventing time lag. Number of
laboratories should also be increased
in phased manner.
Coloured monitors should be
standardised for checking quality of
vaccine. This will reduce the require
ment of vaccine .samples being sent
for potency test.
Nearly 30-40%
OPV sample®
or consignees end have no cold
j&^^ri^tprage facility. Consequently optitemperature for keeping vaccine
Cold Chain Maintenance
At all airports particularly at Cal
cutta and in North-Eastern sector
cold chain facilities should be imme
diately provided so that in event of
delay, vaccine can be stored under
optimal temperature. Specific strat
egy for supply of vaccine to NorthEastern States should be evolved, so
that vaccine reaches in time and
safely.
in optimal conditions. Drug ibspec- ■
tors should periodically inspect the
facilities available for keeping vac
cines and should regularly get
samples of vaccine tested for po
tency.
An orientation programmes for
private practitioners and chemists
and druggists may be organised to
familiarise them regarding require
ments for maintenance of cold chain.
£
Cold Chain Maintenance
should be ensured that shofc .
keepers who sell vaccines keep themX
After collection of sample, the
remaining vaccine is generally being
consumed without waiting for re
sults. There is no mechanism to reach
those children who have already
been immunised with the batch of
vaccine which was later found to be
unsatisfactory.
have been found unsatisfactory.
Therefore utilisation of vaccine
should be cycled in such a way that
no incoming vaccine is utilised be
fore its potency has been tested. It
should be arranged that results are
available within a. fortnight. If
31
Officials from national level to
district level during their visits have
found vaccine being kept at tempera
tures detrimental to quality of vac
cine. Sometimes vaccine has been
found to be kept in unsatisfactory
Conditions for number of days. Yet,
^^.erally excepting censuring the
defaulting officials no one issues in
structions not to use such vaccine or
see that it is destroyed in their pres
ence. Such a compromising attitude
raises questions about validity of
maintenance of temperature.
.
“ Many a times it has been observed that opened/used vials are
reused both in government institu. tions and by private practitioners.
'W.^Trairiinp ' ■!
samples of vaccine are-found unsat
isfactory, whole lot should be de
stroyed. This will obviate the
chances of vaccinating children with
unsatisfactory vaccine.
Whenever a vaccine is found to
be kept improperly or not under opti
mal temperatures, visiting officials
should immediately disallow the use
of vaccine, and get it destroyed. Al
ternatively samples from such lot
should be got examined before al
lowing use of such vaccine.
Defaulting officials should be held
responsible for such neglect.
Fact of such observations and
actions should be widely circulated
so as to keep others alert. Such mat
ters may be released to press, it will
increase the credibility of pro
gramme and sincerity of efforts for
giving good quality of vaccines.
It is recommended that manufac
turers should be persuaded to manu
facture small dose vials preferably
single dose. If it is not feasible no vial
should be of more than five doses.
Manufacturing single dose vials may
be expensive, but in long run it will
be cost effective for two reasons:
1. It will prevent wastage.
2. It will ensure that no child is
vaccinated from open or used
vials.
Training
Training programme should be
accelerated to meet requirement of
Assessment of knowledge and
skills among workers indicated in
adequacies which may be due to in
adequacy of training or lack of up
dating of knowledge.
In training provided to different
categories of workers, component
related to EEC for demand generation
is missing.
Middle level managers and PHC
doctors have to play role of trainers.
Training imparted to them at national
level does not prepare them as train
ers.
Training requires a team of train
ers. This concept has not been appre
ciated and no provision exists to train
team of trainers.
;,
DIO and MO (PHC) have to at
tend various administrative, respon
sibilities, and field supervision. Be
sides, MO (PHCs) are also involved
in clinical work. It is therefore
difficult for them to find adequate
time for organising or imparting
training to heath personnel.
training to update the backlog as well
as to train personnel in the new dis
tricts taken up for CUP. All MOs (and
not only the MO I/C) at PHG are to be
trained as per the new policy.
Refresher training courses of
short duration may be organised to
update knowledge and skills of the
workers. Monthly meeting provides
opportunity fur this.
The component of IEC should be
incorporated in the training schedule
of different category of health per
sonnel with special emphasis on
communication skills.
At national level instead of train
ing of middle level managers it
would be appropriate to train a team
of trainers dr^wn from each State. A
team may consist of teachers from
medical colleges, HFWTCs, nursing
colleges and health administrators
etc. The State level team will be re
sponsible for training of middle level
managers and medical officers-of
PHCs in the State.
Till such decisions on team train
ing is taken, there is need to incorpo
rate ’Training Component’ in the ex
isting DIO’s training curriculum.
It is recommended that a district
training team may be formed com
prising of a senior medical officer,
block extension educator and senior
paramedical- assistant drawn from
various programmes. Member of
district training team can also be
trained by the State level team.
District training team will be re-
33
■»
Doctors working in district hos
pitals, post partum centres and vari
ous health organisations in urban
areas are not being trained.
Supervision
” Supervision at all levels is one of
■>. the ■ most neglected management
functions. Supervisory visits are
: generally unplanned and unscheduled, without making any reports of
■ the. visit or informing the PHC/
' subcentre area where improvement
'speeded. No effort is made to ensure
sponsible for training of all para
professionals for both orientation
training to new entrants and re
fresher courses.
Teaching aids including audio
visuals in local languages may be
provided to State and district training
teams.
It will be appropriate to develop
curriculum for trainers at national
level. Curriculum should incorpo
rate the requirement of training of
different levels of functionaries.
State and district teams should have
the freedom to modify them accord
ing to their needs. Funds may be
provided to get them locally printed
and distributed.
Training inputs under Nursing
schools, paramedical training insti
tutions and ANM schools be
strengthened.
Crash courses for medical offi
cers working in district hospitals,
post partum centres in Central Gov
ernment institutions, private sector
and public sector organisations and
private practitioners should also be
organised.
that lacunae or deficiencies obser
ved on earlier visit, have been cor
rected.
Supervisory checklists are not
routinely used.
First level supervisory staff (HA)
are not being routinely supervised.
Transport facilities are not avail
able for enabling mobility of super
visory staff.
Delay in payment of TA/DA is
reported to be a major deterrant in
carrying out supervisory visits.
A checklist for supervision
should be used.
Immunisation sessions held at
different levels, should invariably
be supervised during supervisory
visits.
Non-availability of transport is
not a valid, excuse for cancellation
of visits. Alternate means of trarfi^
port should be used and TA
claimed.
It should be ensured that TA/
DA is regularly paid so that it may
not be used as an excuse for cancel
lation of visits.
Complaints or difficulties
brought out by the staff during visit
should not be brushed aside. Hon
est efforts should be made to find
reasonable solution. This-will pre
vent frustration and demoralisation
of the workers.
The first level supervisory staff
(HA) should also be supervised and
guided.
Supervision
Schedules for supervision
should be’ developed well in ad
vance and adhered to.
Observation made during super
visory visits should be recqrded
and problem identified should be
solved either locally or recom
mended to higher authorities. Feed-
back should, be obtained for action^
taken or suggestions made during
visits.
Monitoring
Monitoring
Monitoring is generally limited
to reviewing monthly reports and
comparing achievement against tar
gets. Generally no effort is made to
find out the utilisation of vaccine visa-vis number of immunisations per
In meeting held at State, district
and PHC level, monitoring should
■not be related to find out target
achievement only but all related is
sues should be discussed. For ex
ample number of immunisations
35
■ formed. Even at district level in re
view committee chaired by district
collectors, emphasis is mostly on
target achievement only. Generally
no enquiry is made about occurrence
of VPD or any untoward reaction
after vaccination.
&<f?t^ecords and Reports
A-.Maintenance of records is one of
neglected areas. Though
given against number of beneficiar
ies enlisted, utilisation of doses of
vaccine against number of im
munisations given, percentage of
children below one year of age pro
tected against vaccine preventable
diseases, adverse reactions and oc
currence of vaccine preventable
disease and regularity of scheduled
immunisation sessions etc.
System .of allocating targets and
measuring performance by target
achievements should be totally
stopped.
Unit of assessment for progress
should be village in rural areas and
ward in urban areas. List of eligibles village-wise should be ob
tained and coverage be checked.
This will help to assess the extent
of variation of performance in dif
ferent areas and help to remodify
the approach.
Monitoring checklist be pre
pared and used.
At national level Director of Im
munisation Mission conducts peri
odic meetings of State EPI Officers
which are found to be very useful.
However, these State EPI Officers
are not final decision makers.
Therefore, it is suggested that dur
ing such meetings, Directors of
health services may also be invited
at least once or twice in a year.
Records and Reports
Registers and reports should be
scrutinised for the completeness,
registers are maintained, they are
generally incomplete and not up
dated. Likewise reports are incom
plete and it is generally found
difficult to rely upon them. There is a
tendency to over-report perform
ance and under- report untoward re
actions.
Registers and reports are gener
ally not thoroughly scrutinised and
discussed during supervisory visits
or review meetings. Consequently
workers get away with the impres
sion that this exercise is of no signifi
cance.
Since Health Workers are in
volved in various health activities,
they have to prepare number of re
ports which takes away significant
portion of their time. It is further
observed that the formats of reports
are also changed frequently.
correctness and updatedness.
Immunisation card is to be used
as a home-based record.
Scrutiny should be made for
registration and • enumeration of
beneficiaries and should be tallied
with estimates and number pro
tected and action taken for reduc
tion of dropout should be verified.
If wide gaps are observed, cause
should be looked for and worker
explained. Need for completeness
should be repeatedly emphasised.
Standardised registers, report
forms and sufficient stationery
should be provided at all levels.
Formats of registers and reports
should not be frequently changed.
Minimum number of reports which
are to be really used should be
asked for. A comprehensive report
for all activities will facilitate the
grassroot worker. .Only monthly re
ports should be obtained from
subccntrcs, PHC and district.
System of quarterly or annual
reports should be suspended at
these levels. On the contrary all re
ports should be collated and
analysed by higher authorities and
the reporting agencies should be
fed back with results of the analysis
so as to enable them to improve
their performance.
37
Programme Evaluation
'From time to time coverage
evaluation is being conducted by in
dependent agencies. However, it is
found that it is notgcnerally repeated
in the same district and therefore the
change in performance is not
assessed.
Disease Surveillance
It was found to be one of the
Weakest links in the programme and
• the following constraints were rio. ticed:
- Sentinel centres have been identified,but many have not become
operational.
- Staff at sentinel centres have not
been adequately trained.
- Records about VPD are not main--- .tained by age, sex, residence and
. immunisation status etc.
• - Sentinel centres are generally not
h involved in investigation of outbreak of cases.
r,.;,.Records of untoward reactions
"ow'ng immunisation except
■qs'.^al.o are n°t maintained propxfy,? erlyrai’
Programme Evaluation
cases and to take appropriate ac
.
^.sSpecial survey for finding out
■
To assess the improvement or4|^
disease’ load or active surveilotherwise in performance, coverag$^j& j$t£-.lance are not adequately carried
evaluation should be repeated in atW>
least 25% of districts after a de-w$ fe’There is no periodic review of
fined period of time. District au-&v' ',:jq\;?,VPD cases and such cases are
thorities should on their own, con-ipfc’
generally not investigated.
duct evaluation to find out the ex--.^t|\
tent of coverage in their district at"<OV
least once a year.
It is further recommended that-ftl^
such evaluation surveys should^M:
also incorporate operational/mana-Ofe;;
gerial aspects of the programmers^
These surveys will be useful only if&
sincere efforts are made to take re-$
medial actions.
-id
Disease Surveillance
■)
F
All sub divisional, district and,
h. I
teaching hospitals identified as sen-/
tinel centres should be charged,} '
with the responsibility of recording ; 1and reporting all VPD cases. Differ
ent categories of staff like child
specialist, epidemiologist and '
medical record technician/officcr
should be trained to diagnose VPD
at the earliest and maintain all the
records according to age, sex. resi
dential address and immunisation
status. All VPD cases should be re
ported by sentinel centres to district
administration and State authorities
for appropriate action.
Monthly meeting between senti- ’
nel centres and administration
'
should be held to review the VPD
’'
tion.In addition to coverage evalu
ation surveys, UNICEF and Gov
ernment of India may consider
assisting medical colleges in carry
ing out annual disease surveys us
ing neonatal tetanus and polio *as
indicators, particularly in areas
with very high percentage of cover
age.
Pictures of VPD cases with ma
jor signs and symptoms may be dis
played at prominent places and
people requested to report to the
nearest health facility if they have
come across such cases. All such
reported cases be investigated.
Similarly, all neonatal deaths
should be investigated by the offi
cer incharge of health facility.
To strengthen disease surveil-_
lance systerm it is imperative that
the disease situation uncpverd
through surveys should result in
some action. ■
Practitioners of ISM, or dispen
saries of ISM, and registered medi
cal practitioners treat fairly large
segment of population including
children. Their involvement in re
porting vaccine preventable disease
should be seriously considered.
They may be provided with prepaid
postcards to be mailed giving de
tails of VPD cases whenever they
may come across in their clinic.
Reports provided by them should
not only be acknowledged, but they
39
About 20-30% of children suffer
ing from paralytic poliomyelitis
were reported to be fully immunised.
Cases of provocative paralytic
poliomyelitis have been reported
after receiving some injections or
even DPT during fever.
suits ot investigation and action
taken.
It is important that all adverse
reactions and deaths be thoroughly
investigated, public educated about
them and suitably compensated.
All such incidence should be
thoroughly investigated and results
reported. Public should be taken'
into confidence and without fear
the reSults should be communi
cated.
Low grade pyrexia is an impor
tant clinical symptom in pre-paralytic poliomyelitis. Therefore, to
avoid risk of inducing provocative
poliomyelitis, low grade fever
should be considered as a contrain
dication for giving DPT immunisa
tion.
Information, Education and Communication
IEC cells/media divisions have
been created at each State HQ/district HQ under family welfare pro
gramme. However, following bottle
necks were observed:
Inadequate number of positions of
IEC personnel at all levels.
Lack of trained manpower at dif
ferent levels.
' Lack of transport facilities.
•
Lack of funds resulting in inability
—to produce or procure IEC material
in adequate quantity so that it may
. reach every nook and corner of
State.
IEC staff is not fully conversant
40
IEC cells should be strength
ened by increasing number of posi
tions and posting trained persons.
IEC is a very specialised job in
volving team work and requiring
experts for media, for preparation
of publicity and educational
material and communication.
Hence, providing a single function
ary without sufficient back up will
not be sufficient to create any ef
fect.
Emphasis has been in the past
more on health education. Now it
should be given with more stress on
with UIP, hence, they find them
selves inadequate to produce
material suited for the programme.
Lack of coordination between
State Health Education Bureau
(SHEB) and media divisions has led
to the two to be working indepen
dently of each other.
Inadequate supply of hardware
and education material related to IEC
was noticed. In many States 16 mm
projectors and public address sys
tems are not working and have been
condemned. Replacement has not
been made.
Even though awareness regard
ing the programme is gradually
building up, people are not strongly
motivated to come forward for serv
ices on their own.
demand generation.
.
Personnel in IEC should be
trained in programmes related to
child survival including UIP.
Adequate funds should be pro
vided for procuring and producing
educational materials according to
needs of State.
State Health Education Bureau
and Media Divisions should coordi
nate their activities. This will avoid
duplication of efforts and maximise
the utilisation of resources.
Efforts to develop communicg|
tion skills among health personnel
at all levels is most essential and
therefore, be incorporated in all
training activities.
IEC material should be syn
chronised with training material.
Direct communication between
Directorate and PHC to be estab
lished (intra-organisational) par
ticularly regarding change in policy*
etc.
They should also be provided
with easy to carry education
material. Linkages should be estab
lished with literacy mission. Dis
semination of knowledge on health
related subjects including
munisation should be included m
adult education programme. Com
munity Need Assessment (CNA)
surveys should be carried out par
ticularly in special groups of popu
lation, so that programmes for edu
cation for these groups may be
more realistic.
41-
16 mm projector and other au
diovisual equipments which have
been condemned should be re
placed and more supply should be
ensured according to the needs of
State.
Since person to person commu
nication has been found to be more
effective, every opportunity for in
ter-personal communication should
be utilised for dissemination of
knowledge and to motivate people
to use service.
Linkage
Linkage
Though within the health sector,
different agencies are involved in the
Immunisation Programme, effective
functional linkage among them was
not established to the desired extent.
Iris recommended that linkages
within the health sector among dif
ferent components need to be
strengthened. Within health sector,
different agencies/bodies need to
be involved with proper coordina
tion in terms of joint planning and
sharing of targets, area responsi
bilities and resources e.g. State and
Central Government health agen
cies, ESI Corporation, Railways,
Armed Forces etc. Effective link
ages need to be developed with dif
ferent public sector undertakings
and voluntary organisations also.
• •; Medical Colleges
■j.^ Even though from the initiation
..ofUIP, medical colleges were ext0 play a very significant role
•.c,programme, in many States
seemed to be certain degree of
in terms of area responsi-
Medical Colleges
Since medical colleges in many
States do not come under health ad
ministration, linkages are not estab
lished between health department
and medical colleges. It is, there
fore, recommended that clear cut
bilities, distribution of targets and
.resources and coordination and su
pervision between State/district
administration and medical colleges.
Funds to medical colleges had not
been released by State Governments.
policy should' be laid down'and
money and material should be pro
vided directly to the medical col
leges and they should be account
able for the performance in the ar
eas under their coverage.
Medical colleges should also
demonstrate well organised Im*
munisation Programme by way of
better surveillance, coverage evalu
ation survey and training etc. in
their field practice areas.
Private Practitioners
Private Practitioners
The opportunities for involve
ment of private practitioners have
not been fully exploited.
It was found that administration
was hesitant to supply vaccines and
other supplies to them.
It is, therefore, suggested that
private practitioner’s support in
UIP should be maximised by quar
terly meetings to discuss various
aspects of the programme and
Government’s approach for child
survival including immunisation.
During these meetings VPD cases
reported in the quarter may also be
discussed.
Private practitioners should be
supplied with vaccine irrespective
of the fact that they charge fee for
service. It should not be forgotten
that the cost of vaccine is not more
than l/10th the cost of total time
and effort put in by private practi
tioners. This will spare Government
functionary’s time for involvement
in UIP for better contribution in
other areas.
Printed forms and cards may be
supplied for maintaining records
and reports.
43
Professional Bouies
Professional bodies Jiavc 1101
sumed responsibility >n 1 ® ™ ■
munisation Programme to the oesired level.
Professional Bodies”
Support from professional bod
ies like State branches of IMA, As
sociation of Paediatricians, Asso
ciation of Obstetricians and Gynae
cologists and Tuberculosis Asso
ciation etc. should be taken in mo
bilising their members to accept the
responsibility in a national pro
gramme of such vital importance.
Distribution of vaccine to pri
vate practitioners can be channel
ised through these bodies under the
guidance of State UIP Officers.
Their help can be sought in or
ganising special drives, or in
spreading the message through
popular talks in educational institu
tions.
Others
Others
Generally, at time of outbreaks'of
measles cases, health authorities re
sort to mass immunisation in and'
around the areas from where out
breaks are reported. Measles is infec
tious during incubation period,
therefore, long before sgins and
symptoms appear and health
department swings into action, large
number of children have been in
fected and may be in later stage of
incubation period.
Keeping in view of the epidemi
ological features of disease, the va
lidity of resorting to mass im
munisation during measles out
breaks should be thoroughly exam
ined and clear cut instructions is
sued with regard to action to be
taken during such situations.
44
REPORT
Cost Analysis of UIP
Kcepz'g ;n view the requirements of the Central Government and donor
—agencies, a ssiywas undertaken with the aim of financial analysis of the programme
providing es~ates of total cost of the programme for an administrative area of
implementatrzc and the cost of sustaining the programme to the local and State
Government’.
The specific objectives of the study were:
to idecdfy the cost composition of UIP at district level and below,
to esdnate total cost of the programme and the cost composition at district
level ar/J below,
3, to estimate unit cost of services provided under UIP, and
4. to estimate cost of sustaining the programme for future years.
The study was conducted in two districts namely, Nanded in Maharashtra and
West Nimar in .Madhya Pradesh. A random sample from each category of institution
within each dittrict was drawn to study the cost of running UIP at the institutional
1.
2.
level.
The study required data on three different aspects of Immunisation Programme
In addition to the above three approaches the detailed information collected b;.
the State team constituted for coverage evaluation and review was also utilized and
analysed.
In the present study costs have been simply defined as the value of resources
used and the programme cost has been estimated as a sum of the monetary value of
each resource category utilized for the programme.
For each resource, monetary value was estimated and allocated to the UIP
depending on whether it is direct cost component or indirect cost component.
The full cost of the programme has been estimated in two components as
capital cos t and recurring cost. The capital cost has been estimated by annualising the
value of the capital input. '
The recurring cost of the programme has been estimated by adding up the
monetary value of all inputs consumed for the provision of services and undertaking
other activities related to UIP.
For information on budget provided for UIP and expenditure incurred, the
details in these regard were collected from the two districts under study for the year
1988-89.
COST OF UIP AT DISTRICT LEVEL
In order to estimate the cost of Universal Immunisation Programme at district
level for one year period (1988-89) and to project the cost for future years, it was
thought essential to identify the cost components i.e direct/incremental cost and
indirect/obligatory cost with subdivision into capital and recurring.costs and cost
composition at district level as well as at institutional level.
The total cost of UIP at district level and cost composition in two districts
(1988-89) are shown below:
viz.
the data about various kinds of inputs available and utilized,
quantum of programme output in terms of services provided by various
health institutions in rural and urban areas, and
iii. data on completed immunisations.
For this purpose various methods of data collection were adopted.
i. Interviews and discussions with the officials at State, district and institutional
level.
ii. Study ofsecondary records for details about central budget and State budget
as well as expenditure for the UIP from State HQs.
iii. Delphi technique and interviews with the functionaries at various levels were
conducted to estimate staff time allocation to the activities related to
immunisation.
i.
ii.
154
Table 47
Total Cost of UIP at District Level and Cost Composition in Two Districts (19SS-S9)
Nanded
West Nimar
Item of
Expenditure
Capital’
Recurring
Total
Obligatory/
Indirect cost
Incremental/
Direct cost
Total cost
Obligatory/
Indirect cost
Incremental/
Direct cost
Total cost
62,337
(1.4%)
43,56,048
(98.6%)
86,016
(8.7%)
9.03.847
(91.3%)
1,48,353
(2.7%)
52,89,895
(97.3%)
2,07.525
(1.8%)
113,06,168
(98.2%)
1,65,848
(14.3%)
9.94.528
(85.7%)
3.73.373
(2.9%)
123.00.S5
(97.1%)
44,48,385
9,89,863
5438,243
115,13,693
11,60,326
126,74,069
(92%)
(90.8 %)
(100.0%)
(18.2%)
(81.8%)
* : Capital cost includcsonly the annualised cost per year for the investment made and not the actual investment for cquipme.-.H.
vehicles, etc.
155
It showed that the total cost of operating UIP at district level was Rs. 126.74
lakhs for district Nanded and Rs. 54.38 lakhs for district West Nimar. It is seen that
the total cost for West Nimar was less than half compared to district Nanded. This can
be explained that UIP was implemented one year prior in district Nanded and more
number of health infrastructure facilities and health functionaries available within
the district were involved in immunisation activities. This resulted in utilisation of
more resources of various types leading to higher cost.
The composition of the total cost in capital and recurring cost was approxi
mately in the ratio 1:33 for both Nanded and West Nimar. Thus, the recurring cost
was the major component contributing to 97.0 per cent of the total cost in both the
districts.
COST COMPOSITION OF UIP AT DISTRICT LEVEL
Matrix of cost components into direct and indirect cost for both the districts
shows that the major element of indirect cost was die salary of health personnel
working in various institutions involved in immunisation activities and it accounted
for nearly 98 per cent of total indirect cost. The remaining indirect cost was incurred
on vehicles, their running cost and maintenance cost.
In regard to the direct cost of the programme, the percentage contribution was
different and it was observed that 8.7 per cent of total direct cost was incurred on
capital items in West Nimar whereas it was 14.3 percent in Nanded. Among thcdircct
recurring expenditure items, major share was for vaccines and immunisation supplies
such as needles, syringes and immunisation cards. These elements accounted for 81.9
per cent of direct recurring expenditure in West Nimar district and 62.5 per cent in
Nanded district. The salary expenditure as percentage of direct recurring cost was
only 6.5 per cent and 19.8 per cent in West Nimar and Nanded respectively. The
production and supply of health education material such as pamphlets and posters
accounted for 4 to 5 per cent of total direct recurring expenditure whereas operating
cost for vehicles was about 3 to 4 per cent of total direct cost.
UNIT COST OF SERVICES FOR IMMUNISATION AT DISTRICT LEVEL
This was estimated for both the districts by dividing the total cost of the
programme by the output of services for the same period 1988-89.
The estimates derived for the unit cost of output of services in UIP indicated
that the average cost per dose of immunisation to child or pregnant woman was about
Rs. 10 to 11 in West Nimar and Rs. 26 to 27 in Nanded. The average increm'ental cost
per immunisation was Rs. 1.99 in West Nimar and Rs. 2.42 in Nanded.
The cost per fully immunised child for six VPDs was estimated by using the
denominator in terms of number of fully immunised children. For this, the norm
156
o
1-
’
provided by WHO, i.c. 90 per cent of children immunised for measles to be
considered as fully immunised was utilised. From the estimates thus derived it was
observed that the average cost per fully immunised child was Rs.96.97 in West Nimar
and Rs. 270.25 in Nanded of which 20 per cent and 9.2 percent respectively were the
incremental costs in the two districts.
COST OF UIP AT INSTITUTIONAL LEVEL
To assess the management of these resources and their utilisation for im
munisation services at various levels in the district health organisation and to identify
the levels at which the cost incurred on immunisation is high, the operating cost of
these services was estimated foreachcategory of health unit for the year 1988-89. In
addition, the variation in health units of the same category were also explored for cost
profile and unit costs for immunisation services for two districts under study.
TOTAL COST
It was found that in urban area the average expenditure for immunisation
services was Rs.2,08,370 for the three hospitals and ICDS facilities available in
Nanded district and it was much higher than the average expenditure of Rs. 47,017
for two hospitals in West Nimar. The factors contributing to the variation were
availability and utilisation of infrastructural, equipment and manpower facilities at
institutional level as well as the output of services provided.
In rural areas, the average cost incurred forprovision of immunisation services
at CHC and PHC level was about Rs. 1,64,168 in West Nimar and Rs. 1,96,172 in
Nanded. The Mini-PHCs and civil dispensaries fuentionirig in West Nimar spent
approximately same amount of Rs. 28,189 and Rs. 26,595 respectively for im
munisation activities. But in district Nanded the average expenditure incurred by
civil dispensary (Rs. 74,515) was nearly three times that in West Nimar. At the lowest
peripheral unit, namely subcentre, the average expenditure on immunisation was Rs.
10,375 in West Nimar and Rs. 23,872 in Nanded. It is to point out that the range of
total expenditure was narrower for all categories of health units studied in West
Nimar district compared to those studied in Nanded district.
It was also seen that the percentage of incremental cost to the total cost of the
programme was comparatively more in higher level health institutions in West
Nimar.
UNIT COST
To explore the variation in efficiency with the level of health units, the unit cost
estimates were compared among different categories of health units within two
districts as well as between the two districts. The average cost per immunisation
157
COST COMPOSITION
provided by hospitals, CHC and PHC was observed to be around Rs.5 in West Nimar
district and it increased to more than Rs. 10 for lower level health units with wide
variations between health units of the same category in that district. On the other hand
in Nanded district, the average unit cost of immunisation services did not show any
consistency but unit costs varied with more or less same range in all categories of
health units except civil dispensaries where the variation was comparatively less. The
similar situation was observed for average cost per fully immunised child but higher
range of variation because of poor performance in measles immunisation in some
units.
Inspite of the variation in average cost per immunisation within and between
various categories of health units in two districts, the degree of variation in average
incremental cost per unit of service provided by these health units was much less.
COST COMPOSITION
In general, recurring cost, mainly the manpower salary and other benefits
component, made up a larger percentage of greater spending in all categories of
health institutions in both the districts. Its average contribution in urban units varied
from 63 to 80 per cent and 76 to 96 per cent in West Nimar and Nanded respectively.
In rural areas this component accounted for nearly same percentage of total cost upto
CHC and PHC level but it increased to more than 85 per cent in lower health units.
Conversely, vaccine and immunisation supplies for lower level health units repre
sented a smaller proportion of about 8 percent of total cost compared to urban health
units and CHCs, PHCs where it was more than 20 per cent.
COST OF SUSTAINING UIP AT DISTRICT LEVEL
The annual estimates of cost for sustaining the programme at district level with
the proposed norms of government of India for input facilities, services and activities
at various levels within the districts under study were worked out.
TOTAL COST
-
As expected, the vaccines, immunisation supplies and annualised capital cost
of cold chain and immunisation equipments account for more than 65 per cent of the
incremental cost of which more titan 50 per cent is for vaccines. The annualised cost
of vehicles and their operation and maintenance account for nearly 5 per cent of the
total direct cost of the district in both States. Though the Government of India has
provided funds for other activities such as surveys, meetings and training of new
entrants in a year it constitutes hardly 2.2 per cent of direct cost.
The major component of vaccine cost was estimated on the basis of quantum
of different vaccines required to immunize the expected number of infants and
pregnant women in a year and then this quantity was expanded to account for the
quantities lost during transportation or due to cold chain failure etc., using the rate 25
per cent for DPT/TT/ OPV and 50 per cent for BCG/Measles. Thus, the major cost
for sustaining the programme needs to be incurred on vaccines, immunisauon
supplies and salaries of the staff appointed under UIP, which are principal variable
costs of importance for overall lower unit costs and higher manpower productivity.
UNIT COST
For district West Nimar in M.P. the incremental cost per immunisation that
government has to incur will be Rs.2.25 whereas it will be Rs.3.01 for district Nanded
in Maharashtra. This cost of immunisation was nearly 50 per cent more for a child
compared to a pregnant woman. The incremental cost per fully immunized child is
estimated to be Rs.22.00 in West Nimar and Rs.28.81 in Nanded.
The incremental cost estimated with proposed health facilities, equipment and
staff when compared with the incremental cost incurred during 1988-89 by two
districts under study showed that there is an estimated increase of about 28.2 percent
in West Nimar and 18.6 per cent in Nanded. This indicates that there is a need to
provide additional inputs if these disricts are to sustain the programme and achieve
the objectives of 85 per cent immunisation coverage for children and 100 per cent
coverage for pregnant women.
Utilising the norms and assuming that the pattern of utilisation of the resources
remain same for future years as was observed during 1988-89, the total incremental
cost has been estimated for the two districts under study. Thus, it was found that the
total incremental cost per year for UIP in district West Nimar of M.P. would be Rs.
12,68,600 and in district Nanded of Maharashtra it would be Rs. 13,76,700. While
estimating the cost, fixed amount sanctioned to district-by Govtemment of India for
specific activity of the programme was assumed to have been fully utilized for the
programme, e.g. contingency money of Rs.2000 per PHC per year or POLof Rs.9500
per year per diesel run jeep or van piovidcd under the programme, etc.
159
158
C-10.253
S:pt:18.2.'82
IM MUNI ZATION
In our country diarrhoea is the first'major cause of death in chi 1 dren.
Communicable diseases like diphtheria, whooping cough, tetanus, polio,
tuberculosis and measles form the second major cause of death. The
tragedy is that the illness and death due to communicable diseases can
be easily prevented. Immunization is a simple and an inexpensive way
of doing this.
A child gets whooping cough only once. When a child gets whooping cough
his body makes a substance called antibodies. These antibodies fight
against the germs of whooping cough and kill the germs. After these
germs die, the antibody remains in the body of the child for a long time.
Later at any time, if the germs of whooping cough enter this child is body
again, the antibodies that were produced earlier, fight against the new
germs and kill them. This child does not fall ill with whooping cough
again. In other words the child has developed immunity (resistance) for
whooping cough. In the same way, our bodies can develop immunity (specific
antibodies) for each of the communicable'diseases listed above.
There are different ways by which our bodies develop immunity:
1. Passive Immunity: The antibodies for a particular disease are supplied
ready made to the body. This can be done in two ways:
(a)
Natural passive immunity;
The mother passes'her antibodies to
the baby in her womb. The antibodies are also supplied to the
child through the breast milk of the mother. Eg: Antibodies
for Tetanus, Measles.
(b)
Artificial passive immunity:
The antibodies are taken from an
. immune person or immune animal and injected into the person who
needs it urgently. '
.
Passive immunity ia a quick way of transfering immunity from one
person to another. The effect of this kind of immunity does not
last for long in the person who receives the antibodies. This
is because the antibodies are destroyed quickly and the body
does not know how to produce its own.
2;
Active Immunity:
The body develops this immunity in two ways:
(a)
By getting the actual disease (infection): In the example of
whooping cough given earlier, we saw that a child gets a disease
and makes its own antibodies. A well nourished child will be able
to make the antibodies faster than an under nourished, child.
This is why the severity of the disease is less in a well nourished
child.
(b)
By Immunization : In this a small quantity of the germs of a
disease are injected purposely into a person. The body of the
person responds in the same way as it would to a disease i.e.
by producing antibodies. After this the body has enough anti
bodies to fight against the actual infection.
2/
C-10.253
S:pt:18.2.'82
2
The germs we inject for immunizing are called vaccines.
These germs can be
killed (dead vaccine) or made weak (live vaccine). The method of injecting
the vaccines is called vaccination or immunization.
Examples of live vaccines: (Germs that are made weak but are alive)
■ '
Polio
Measles
■ Tuberculosis
Examples of dead vaccines: (Germs that are killed).
Diphtheria
Whooping cough
Tetanus.
In active immunity the body takes a little longer to produce antibodies but
the antibodies last longer as compared to passive immunity.
POINTS TO REMEMBER ABOUT IMMUNIZATION
1
a.
Age: ’ We must try and immunize children before the usual age when they
have the disease. Eg: Maximum number of children get diphtheria between
the age of two and five years. So children should be immunized against
diphtheria before they reach the age of two. As a general rule we must
immunize all the children before the age of one. Very young children
below three months of age are not good at making antobadies and they
already have ready-made antibodies from the motheri; So one must not
immunize children too early. There is a-best age to give every vaccine
and we must try and immunize our village children at the right age.
(However, when we start an immunization programme we might find many
older children who have not received the vaccines at the right age.
We should still immunize them.) .
b.
The right number of doses: Each vaccine has to be given in the right
number of doses as recommended. If we reduce the number of doses of the
■ vaccine, its effect is lessened. Eg: BCG vaccine (for tuberculosis)
needs to be given in two doses whereas DPT vaccine has to be given in
four doses. . With each dose of the vaccine the amount of antibodies
produced increases and its effect lasts longer.
c.
The right interval between doses (Time between doses): For each vaccine
the right interval between doses is different.
If the doses of a vaccine
are given too soon then the child will not develop a strong immunity.
The interval between the first and second dose is most inportant. If the
gap between the first and the second dose is too long, then the first dose
is ineffective. This child should be considered as a new case for
■ immunization.
..5.
d.
Storing the vaccine: This is very important. If the vaccine is not stored
properly the vaccine will, get spoilt. Spoilt vaccines are useless.
A spoilt vaccine will not be able to stimulate the child’s body to make
antibodies.
ALL VACCINES MUST BE STORED- AT THE RECOMMENDED TEMPERATURE
Live vaccines get spoilt faster than dead vaccines because the live germs
in the live vaccine die quickly if the vaccine is not stored properly.
e.
Expiry date; Each bottle of vaccine has an expiry date written on the
• ■ label. This means that the vaccine should not be used after the expiry
date. Before both buying and using the vaccine CHECK THE EXPIRY DATE.
f. Preferably do not immunize children during the rainy season.
3/
C-10.253
S:pt-.18.2.'82
:
3
:
IMMUNIZATION IN CHILDHOOD
1.
BCG VACCINE:
This is to prevent the child from getting tuberculosis.
There are different opinions about its effectiveness. As there is
evidence that it is effective in children we still give it. It is a
live vaccine.
When should it be given: The first doss of BCG should be preferably
given at birth or soon after birth. The second dose is given at 5 years
of age (school-going age).
Preparation:
BCG vaccine comes in ampules as a freeze dried vaccine
in a powder form. The powder has to be dissolved in saline before it
can be used as a vaccine. In our local PHC we have vaccinators specially
trained for giving BCG vaccination. We must get the BCG vaccine and
the help of the vaccinator from our PHC.
Points to remember about BCG vaccination:
-
The powder and the solution must be kept in a refrigerator.
The vaccination should not be given in bright sunlight and should
he preferably given in a room or at least in shade.
The ampules and filled syringes should be covered with black paper
when not in use.
The vaccine must be used the same day it is dissolved in the saline.
At the ehd of the day, if any vaccine is left,this should be thrown
away. It should not be used for the next day evenif kept in a
refrigerator.
What happens when BCG vaccine is given:
When the vaccine is given a small lump is formed at the site of the
injection. This lump disappears after half an hour. About the 3rd
week after the injection has been given, the site of injection becomes
a little thickened and the place is painful to touch. This thickness
slowly increases to the size of a pea. By the 6th week the thickness
becomes soft and pus is formed. The pus then escapes leaving an ulcer.
The ulcer slowly heals and forms a scar.
We must inform the mother about the changes that occur at the site of
the injection and reassure her. Sometimes an absces^might form at the
site of the injection. This usually heals on its own. If the abscess
does not heal, remove pus with the help of a needle and syringe
(aspiration).
BCG Vaccine should not be given to:
-
children who are known to have tuberculosis
children who already have a scar on the arm
severely malnourished children
children with severe skin disease
acutely ill children
*’ Freeze dried means the live vaccine is frozen oo that the gnurvi--------------
stay alive. Thon it le dried and powdered for use..
.. V
C-10.253
S:pt:l8.2.'82
: 4 :
2.
COMBINED VACCINE FOR DIPHTHERIA, WHOOPING COUGH AMD TETANUS
(TRIPLE VACCINE OR iDPT VACCINE)
This vaccine is given to all the children below five years of age. It
contains killed germs and so can be kept for a longer period of time.
The advantages of the combined vaccine are:
-
more antibodies are produced
the effect lasts longer
the children are given less number of injections.
When should it be given:,
Four doses are given.
First dose
:
Second dose
:
Third dose
:
Fourth dose
()
(Booster dose)():
The best is if the doses are given as follows:
when the child is 3 months old
4 to 6 weeks after the first dose
4 to 6 weeks after the second dose
/
when the child is lj to 2 years old* •
(In rural areas it may not be possible to give all the four doses. In
such areas the first and second dose must atleast be given. The internal
between th.® first and second dose should be between 8 to 12 weeks. If
possible the booster dose should be given 1g years after the second dose./
Points to remember about DPT vaccine:
-
DPT vaccine must be kept in the refrigerator between 4°C to 10°C.
DO NOT FREEZE THEM SOLID (Don't keep in the freezer). Also DO NOT
KEEP IN THE DOOR OF THE REFRIGERATOR. This destroys DPT.
-
Shake the bottle before using and leave it for 3 minutes. If the
liquid is clear, then the vaccine is useless. Send it back.
-
At room temperature DPT loses its value in 4 days.
-
Keep the vaccine away from heat and light.
What happens when DPT is given;
Normal reaction:
In children there will be a slight to moderate pain
at the site of the injection. Some children also might develop a mild
fever. Mothers must be warned about this pain and fever. You can also
give some antipyretic (acetaminophen) to the children with fever. (For
dosage, see page 414 of 'Where There Is No Doctor')
Abnormal reaction: Some children might develop high fever and convulsions.
This is due to some unknown factor in the whooping cough vaccine. Those
children should not be given the next doses of DPT.
*
DPT is
1
-
D for Diphtheria
P for Pertussis or. Whooping cough
T for Tetanus
.
+ World Health Organization recommends that only 2 doses of DPT be given.
The first dose 4 weeks after birth and the second dose 10 weeks after birth.
....5/
C-10.253
S:pt:l8.2.'82
5
DPT vaccine should not be given to a child;
•
- with a history of convulsions or other nervous system disorder.
- with fever or infectious disease
- with allergic disease
- with skin disease
- getting steroid drugs
3.
COMBINED VACCINE FOR DIPHTHERIA AND TETANUS (DT VACCTNE);
Whooping cough does not affect children after the .age of 5 years. So
children above the age of 5 years should receive only DT vaccine.
This comes in bottles containing 10-20 doses. Only one dose of DT is
given at the age of 5-6 years.
Same precautions to be taken as for DPT vaccine.
4.
POLIO VACCINE:
This vaccine is given orqlly (by mouth).
therefore gets spoilt easily.
It is a live vaccine and
When should it be given:
Three doses are given.
- J ■
• ’
First dose
Second dose
Third dose
:
:
:
The best is if the doses are given as follows:
,
.
when the child is 3 months old
4 to 6 weeks after the first dose
4 to 6 weeks after the second dose
Children above the age of eight years normally do not require polio
vaccine.
(The latest dosage recommended by CMC Vellore is to give 5 doses of polio
vaccine at the interval of 4-6 weeks between each dose,)
Points to remember about Polio vaccine;
This is a live vaccine and has to be stored with extra care.
-
The vaccine must be kept at a temperature of -20°C. That means,
when the vaccine is transported from the institute wherte-At- is
manufactured, it should be kept on dry ice or a freezing mixture.
When it is in a centre, it should be kept in the freezing compart
ment of the refrigerator and when it is taken to the village it
should be kept in a flask containing a lot of ice.
-
The vaccine should not be frozen and thawed repeatedly.
That means that the vaccine must be taken to the village only when
.we are sure that we will get enough children to finish all the
doses in the bottle.
-
The vaccine must not be kept near the stove etc.
-
Polio vaccine must be preferably given in a room or in the shade
of a tree. (Do not give it in a hot humid, crowded room).
6/
C-10.253
S:pt:l8.2.'82
:
6
:
-
The vaccine can be given by a dropper or a spoon. The
dropper or spoon is sterilized by boiling in water for
20 minutes. It is then cooled by keeping in ice cold
water. The dropper or spoon should also be carried with
the vaccine in the flask to the village.
-
DO NOT’USE CHEMICAL DISINFECTANTS like lysol, dettol,
savalon etc. FOR STERILISING THE SPOON OR THE DROPPER.
-
The vaccine must not be diluted with water, milk or honey
before giving it to the child.
-
We must advise the mother not to breastfeed the chi 1d
atleast for 4 hours before and after the child has been
given polio vaccine.
-
The child can be given water and other food instead of
breast milk during this time.
■s
-
The 'child MUST NOT BE GIVEN HIT MILK, HOT WATER, OR HOT
COFFEE FOR ATLEAST HALF AN HOUR AFTER THE VACCINE HAS BEEN
GIVEN.
■
What happens when polio vaccine is given:
It is an oral vaccine and it does not have any effects like fever, pain etc.
Polio vaccine should not be given to children with:.
-
5.
high fever
vomiting
diarrhoea
who are on steroids x
MEASLES VACCINE:
It is a live vaccine like polio vaccine. Right now it is not widely
available in India. But we hope that in a few years time it will
become as common as DPT and Polio vaccine.
It comes in a powder form (just like BCG vaccine). This powder has
to be kept in the freezing compartment of the refrigerator. The .
solation to dissolve the vaccine comes in an ampule and has to be
kept inside the refrigerator but not in the freezing compartment.
To use the vaccine, take the cold solution and
the powder of the
measles vaccine to it. THIS LIQUID VACCINE MUST BE USED WITHIN
ONE HOUR.
When should it be given:
Only one dose is given. This is given between the age of 9 months
and one year. (Best time 9 months). It is given as subcutaneous
injection. One dose contains 0-5 ml of vaccine.
Points to remember about Measles Vaccine:
The same points in terms of storage for polio vaccine must be followed.
7/
C-10.253
S;pt:l8.2.'82
:
What, happens
-
7
:
when the vaccine is given:
The child might develop fever within 8 to 9 days.
The child might also get mild measles (rash).
Measles vaccine should not be given to children:
-
who
have already had measles.
CONCLUSION:
In this paper, so far we have discussed the different ways in which a
child's body can fight against communicable diseases by producing antibodies.
In order to effectively produce antibodies against infections, children
need to be immunized at the right age, given the right number of doses
of the vaccine and these must be given at the right intervals. Details
of using each vaccine have also been given.
Conmunicable diseases spread easily from one person to another. This means
that one child with a communicable disease can give the infection to many
other children in the village.
As our aim is to protect as many children
as possible from communicable diseases, it is important that we immunize .
as many children as possible at the same time. In most places children
are immunized as and when they come to the clinic. This practice does
prevent the individual child who has been immunized, but does not protect
the other children in the village. In such a village an epidemic of a
communicable disease could easily break out. TO PREVENT AN EPIDEMIC,
WE MUST IMMUNIZE ATLEAST 90% OF ALL CHILDREN UNDER FIVE YEARS OF AGE IN
THE VILLAGE.
We may find that there are many undernourished children in the village.
When a child is undernourished it is more likely to get a communicable
disease. These children also get a more severe attack of the disease.
In fact the child's life can be in danger because the disease will create
further undernutrition. Therefore undernourished children must be immunized.
=
.: oOo : =====
References:
Primary Child Care by King, King, Martodipoero
Manual for Immunization by Mass Mailing Unit.
* Epidemic means that an unusually large number of persons get the
same disease at the same period of time.
Prepared by
Community Health Team
Voluntary Health Association of
India, C-14> Community Centre
S.D.A., New Delhi 110 016.
dJofvM-l
IMMUNIZATION
CHILDREN fall an easy prey to many communicable diseases.
Widespread in India among these diseases are poliomyelitis,
tuberculosis, measles, diphtheria, whooping cough and tetanus.
Besides the unfortunate children who die of these diseases,
many are disabled for life with complications such as brain
damage, paralysis, chronic lung ailments, deafness and
blindness. All these diseases can be prevented by immunization!
The expanded Programme on Immunization (EPI) was launched in
January, 1978 with the objective of reducing the incidence of
these childhood diseases. Effective vaccines are available
against them.
Begin Immunization Early:
A child is at risk of getting a number of
infectious diseases soon after birth. Tetanus among new-borns
is common and is usually fatal. The disease begins so suddenly
after birth that there is no time to immunize and protect the
infant. But the infant can be saved from tetanus if the mother
receives three doses of anti-tetanus vaccine during pregnancy.
This is usually given at one-to-two month intervals. The
protection which the mother thus develops is passed on to the
infant and lasts during the first few weeks of life. However,
this protection does not last very long. Hence it is important
that the child gets immunization again.
A combined vaccine is available against three
diseases, namely, diphtheria, whooping cough and tetanus. Three
doses of this triple vaccine, otherwise known as DPT vaccine,
should be given at 3 months of age at 4 to 8 weeks’ interval
followed by a booster dose 12 to 18 months later. A booster dose
of diphtheria-tetanus vaccine (DT vaccine) should be given at
the time of entry to school (5 to 6 years) and a booster dose of
tetanus toxoid (TT) at 10 years and 16 years. '
Polio is an acute viral disease which may cause
paralysis to any part of the body. This can be prevented by
giving 3 doses of oral polio vaccine at intervals of 4 to 8
weeks followed by a booster dose 12 to 18 months later. Folio
vaccination can be started at 3 months of age DPT and polio
vaccines can be given at the same time.
...2
2
Children can be protected against tuberculosis by
giving one dose of BCG vaccine between 3 to 9 months of age.
Typhoid fever is a disease which leads to prolonged
ill-health. The disease can be prevented by 2 doses of typhoid
vaccine given at an interval of 4 to 8 weeks at school entry
(5-6 years) followed by booster doses at 10 years and 16 years of
age.
Children become very weak after an attack of
measles which may lead to secondary infection of the liings,
ears and eyes. Measles vaccine is effective in controlling
the disease in about 95 per cent of the vaccinated children.
One dose of measles vaccine, where available, is recommended
for children between 9 and 12 months of age.
Harmless;
All the vaccines are quite harmless. Some mild
reactions such as low grade fever, local pain and swelling
occur in a majority of the children. Such reactions subside
within a day or two. After BCG vaccination a small ulcer will
appear at the site of the injection after two weeks. It is
not necessary to use any ointment or give any other treatment.
The ulcer will disappear within a few weeks leaving a small scar.
Services :
Immunization services are available free of cost
at the Maternal anc Child Welfare (MCW) centres, Dispensaries,
hospitals and primary health centres. These centres or the
health workers will provide any additional information on the
immunization programme.
Follow the National Immunization Schedule and
protect your children against many diseases.
*tetanus toxoid (injection) to
the pregnant woman.
Prenatal
Child
Age 3 to 9 months
(a)
(b)
start with
♦first dose of DPT(ingection ).
♦first dose of polio (oral drops).
♦BCG (injection)
After an interval of 1-2 months,
give.
♦Second dose of DPT (injection).
♦Second dose of Polio (oral dropi).
♦Smallpox (vaccination).
.3
3
(c)
After an interval of 1-2 months, give DFT(injection)
anc’ polio vaccination (oral drops)
9 to 12 months
*Measles vaccine (injection)
one dose, where available.
13 to 24 months
*Booster DPT (injection).
♦Booster Folio Vaccine (oral drops)
*Booster D.T. (Diphtheria and tetanus}
(Injection).
♦first dose of typhoid monovalent or bivalent
vaccine (injection).
5 to 6 years (a)
(b)
10 years
16 years
*After an interval of 1-2 months, give second
dose of typhoid vaccine (injection).
*Booster tetanus toxoid (injection).
♦Booster typhoid monovalent or bivalent
vaccine (injection).
CR
first dose of typhoid monovalent or bivalent
(injection), if not given earlier, followed
by second dose of typhoid vaccine (injection),
after an interval of 1-2 months.
*Booster tetanus toxoid (injection).
♦Booster typhoid monovalept or bivalent vaccine
(injection).
CR
♦first dose of typhoid monovalent or bivalent
(injection), if not given earlier, followed
by second dose of typhoid vaccine (injection)
after an interval of 1-2 months.
Note (1) Pregnant woman: Since the history of a previous tetanus
immunization is normally not available, it is preferable
to give three doses <bf tetanus toxoid (tetanus vaccine),
at monthly intervals starting as early in pregnancy as
possible. This should be the aiml However, no pregnant
woman should be denied even one dose of tetanus toxoid
(tetanus vaccine) if she is seen late. This protects
both the mother and the new-born against tetanus.
Children(a): The ages shown for the various immunizations
are considered the best times. However, if there is any
delay in starting the first dose, the periods may be
adjusted accordingly. It should be the aim that a child
before reaching one year of age, should have received DPT?
BCG, smallpox and polio vaccine and if available, measles
vaccine.
4
4
(b) Where two or three vaccines are shown together,
e.g. ECG + DPT + Polio, these vaccines can be given
at the same time.
(3) (a) When Different vaccines, unless received as a mixed
vaccine should not be mixed together in the same syringe.
It is preferable to give the different injectable vaccines
at different sites.
(b) When typhoid vaccine is being given for the first time,
two doses at an interval of 1-2 months should be administered.
(c) If a child is immunized against DPT and injures himself
anti-tetanus serum should not be diiven. Instead one booster
dose sf tetanus toxoid may be given under the doctor's
advice. This booster dose (of tetanus toxoid) gives
protection for atleast five years.
-x-x-x-x-x-
4
A Classic Reprint
The case against immunizations
Dr. Richard Moskowitz
Editor's note:
In today's world it is taboo to speak out against vaccinations. Yet agro wing number of
dissenting voices have dared to do so. Moskowitz's article published a decade back has not
been properly appreciated and justifies a reprint, lie argues that an artificially attenuated virus
(used tn immunization) evokes an isolated antibody response minus the generalised
inflammatory response or any of the non-specijic defence mechanisms which occur naturally
in any infection. By 'tricking' the body in this way, we have pushed the disease into the body
and made it something like a 'biological time bomb'. Moskowitz reasserts Simpson 'sfear that
immunization programs may actually be seeding humans with ENA to form latent proviruses
which when activated could cause a variety ofdiseases - viz. rheumatoid arthritis, multiple
sclerosis, systemic lupus erythematosus, parkinson's disease and perhaps even cancer.
For the past ten years or so I have felt a deep
and growing compunction against giving
routine immunizations to children. It began
with the fundamental belief that people have
the right to make that choice for themselves.
Soon I discovered that I could no longer
bring myself to give the injections even when
the parents wished me to.
At bottom, I have always felt that the
attempt to eradicate entire microbial species
from the biosphere must inevitably upset the
balance of nature in fundamental ways that
we can as yet scarcely imagine. Such con
cerns loom ever larger as new vaccines
continue to be developed, seemingly for no
better reason than that we have the technical
capacity to make them, and thereby to
demonstrate our power, as a civilization, to
manipulate the evolutionary process itself.
Purely from the viewpoint of our own spe
cies, even if we could be sure that the
vaccines were harmless, the fact remains that
they are compulsory, that all children are
required to undergo them, without any
sensitive regard for basic differences in
individual susceptibility, to say nothing of
the wishes of the parents of the children
themselves.
Most people can readily accept the fact that,
from time to time, certain laws may be
necessary for the public good that some of us
27
-----------NoMok
strongly disagree with. But the issue in this
case involves nothing less than the introduc
tion of foreign proteins or even live viruses
into the bloodstream of entire populations.
For that reason alone, the public is surely
entitled to convincing proof, beyond any
reasonable doubt, that artificial immuniza
tion is in fact a safe and effective procedure,
in no way injurious to health, and that the
threat of the corresponding natural diseases
remains sufficiently clear and urgent to
warrant mass inoculation of everyone, even
against their will if necessary.
Unfortunately, such proof has never been
given; and, even if it could be, continuing to
employ vaccines against diseases that are no
longer prevalent or no longer dangerous
hardly qualifies as an emergency.
Finally, even if such an emergency did exist,
and artificial immunization could be shown
to be an appropriate response to it, the
decision would remain essentially a political
one, involving issues of public health and
safety that arc far too important to be settled
by any purely scientific or technical criteria,
or indeed by any criteria less authoritative
than the clearly articulated sense of the
community about to be subjected to it.
For all of these reasons, 1 want to present the
case against routine immunizations as clearly
and forcefully as I can. What I have to say is
not quite a formal theory capable of rigorous
proof or disproof. It is simply an attempt to
explain my own experience, a nexus of
interrelated facts, observations, reflections
and hypotheses which, taken together, are
more or less coherent and plausible and
make intuitive sense to me.
I offer them to the public in part because the
28
Vol. 3, Issue 2, 21st February 1996
growing refusal of parents to vaccinate their
children is so seldom articulated or taken
seriously. The fact is that we have been
taught to accept vaccination as a sort of
involuntary communion, a sacrament of our
own participation in the unrestricted growth
of scientific and industrial technology, ut
terly heedless of the long-term consequences
to the health of our own species, let alone to
the balance of nature as a whole. For that
reason alone, the other side of the case
urgently needs to be heard.
Are the vaccines effective?
There is widespread agreement that the time
period since the common vaccines were
introduced has seen a remarkable decline in
the incidence and severity of the correspond
ing natural infections. But the customary
assumption that the decline is attributable to
the vaccines remains unproven, and conti
nues to be seriously questioned by eminent
authorities in the field. The incidence and
severity of whooping cough, for example,
had already begun to decline precipitously
long before the pertussis vaccine was intro
duced (1), a fact which led the epidemiologist
C. C. Dauer to remark, as far back as 1943:
If mortality (from pertussis) continues to
decline at the same rate during the next 15
years, it will be extremely difficult to show
statistically that (pertussis immunization)
had any effect in reducing mortality from
whooping cough (2).
Much the same is true not only of diphtheria
and tetanus, but also of TB, cholera, ty
phoid, and other common scourges of a
bygone era, which began to disappear to
ward the end of the nineteenth century,
perhaps partly in response to improvements
in public health and sanitation, but in any
------------------------------
case long before antibiotics, vaccines, or any
specific medical measures designed to era
dicate them (3).
Reflections such as these led the great
microbiologist Rene Dubos to observe that
microbial diseases have their own natural
history, independent of drugs and vaccines,
in which asymptomatic infection and sym
biosis are far more common than overt
disease:
It is barely recognized, but nevertheless
true, that animals and plants, as well as
men, can live peacefully with their most
notorious microbial enemies. The world is
obsessed by the fact that poliomyelitis can
kill and maim several thousand unfortu
nate victims every year. But more extra
ordinary is the fact that millions upon
millions of young people become infected
by polio viruses, yet suffer no harm from
the infection. The dramatic episodes of
conflict between men and microbes are
what strike the mind. What is less readily
apprehended is the more common fact
that infection can occur without produ
cing disease (4).
The principal evidence that the vaccines are
effective actually dates from the more recent
period, during which time the dreaded polio
epidemics of the 1940s and 1950s have
never reappeared in the developed coun
tries, and measles, mumps, and rubella,
which even a generation ago were among the
commonest diseases of childhood, have
become far less prevalent, at least in their
classic acute forms, since the triple MMR
vaccine was introduced into common use.
Yet how the vaccines actually accomplish
these changes is not nearly as well under
stood as most people like to think it is. The
The case against immunizations
disturbing possibility that they act in some
other way than by producing a genuine
immunity is suggested by the fact that the
diseases in question have continued to break
out even in highly immunized populations,
and that in such cases the obscivcd differ
ences in incidence and severity between
immunized and nnimmunizcd persons have
tended to be far less dramatic than expected,
and in some cases not measurably significant
at all.
In a recent British outbreak of whooping
cough, for example, even fully immunized
children contracted the disease in fairly large
numbers, and the rates of serious complica
tions and death were reduced only slightly
(5). In another recent outbreak of pertussis,
46 of the 85 fully immunized children studied
eventually contracted the disease (6).
In 1977, 34 new cases of measles were
reported on the campus of UCLA, in a
population that was supposedly 91 percent
immune, according to careful serological
testing (7). Another 20 cases of measles were
reported in the Pecos, New Mexico area
within a period of a few months in 1981, and
75 percent of them had been fully immu
nized, some of them quite recently (8). A
survey of sixth-graders in a well-immunized
urban community revealed that about 15
percent of this age group are still susceptible
to rubella, a figure essentially identical with
that of the pre-vaccine era (9).
Finally, although the overall incidence of
typical acute measles in the U.S. has dropped
sharply from about 400,000 cases annually in
the early 1960s to about 30,000 cases by
1974-76, the death rate remained exactly the
same (10); and with the peak incidence now
occurring in adolescents and young adults,
the risk of pneumonia and demonstrable
------------Nm<l!
liver abnormalities has actually increased
substantially, according to one recent study,
to well over 3 percent and 2 percent, res
pectively (11).
The simplest way to explain these discre
pancies would be to postulate that the
vaccines confer only partial or temporary
immunity, which sounds reasonable enough,
given the fact that they arc either live viruses
rendered less virulent by serial passage in
tissue culture, or bacteria or bacterial pro
teins that have been killed or denatured by
heat, such that they can still elicit an antibody
response but no longer initiate the full-blown
disease.
Because the vaccine is a ‘trick,’ in the sense
that it simulates the true or natural immune
response developed in the course of recover
ing from the actual disease, it is certainly
realistic to expect that such artificial immu
nity will in fact ‘wear off quite easily, and
even require additional ‘booster’ doses at
regular intervalsthroughout life to maintain
peak effectiveness.
Such an explanation would be disturbing
enough fOr most people. Indeed, the basic
fallacy inherent in it is painfully evident in
the fact that there is no way to know how long
this partial or temporary immunity will last in
any given individual, or how often it will
need to be rcstimulated, because the answers
to these questions clearly depend on pre
cisely the same individual variables that
would have determined whether or how
severely the same person, unvaccinated,
would have contracted the disease in the first
place.
In any case, a number of other observations
suggest equally strongly that this simple
explanation cannot be the correct one. In the
30
Vol. 3, Issue 2, 21st February 1996
first place, a number of investigators have
shown that when a person vaccinated against
measles for example, again becomes suscep
tible to it, even repeated booster doses will
have little or no effect (12),
In the second place, the vaccines do not act
merely by producing pale or mild copies of
the original disease; all of them also com
monly produce a variety of symptoms of their
own. Moreover, in some cases, these ill
nesses may be considerably more serious
than the original disease, involving deeper
structures, more vital organs, and less of a
tendency to resolve spontaneously. Even
more worrisome is the fact that they are
almost always more difficult to recognize.
Thus, in a recent outbreak of mumps in
supposedly immune school-children, several
developed atypical symptoms, such as ano
rexia, vomiting, and erythematous rashes,
without any parotid involvement, and the
diagnosis required extensive serological test
ing to rule out other concurrent diseases (13).
The syndrome of ‘atypical measles’ can be
equally difficult to diagnose, even when it is
thought of (14), which suggests that it is often
overlooked entirely. In some cases, atypical
measles can be much more severe than the
regular kind, with pneumonia, petechiae,
edema, and severe pain (15), and likewise
often goes unsuspected.
In any case, it seems virtually certain that
other vaccine-related syndromes will be
described and identified, if only we take the
trouble to look for them, and that the ones
we are aware of so far represent only a very
small part of the problem. But even these few
make it less and less plausible to assume that
the vaccines produce a normal, healthy
immunity that lasts for some time but then
wears off, leaving the patient miraculously
The case against immunizations
--------------------------------------
unharmed and unaffected by the experience.
Some personal experiences with
vaccine-related illness
I would like now to present a few of my own
vaccine cases, both to give a sense of their
variety and chronicity, and to show how
difficult it can be to trace them, and also to
begin to address the crucial question that is
too seldom even asked, namely, how the
vaccines actually work, i.e., what effects they
do in fact produce in the human body.
My first case was that of an 8-month-old
girl with recurrent fevers of unknown
origin. I first saw her in January of 1977, a
few weeks after her third such episode.
These were brief, lasting 48 hours at most,
but very intense, with the fever typically
reaching 105° F. During the second epi
sode, she was hospitalized for diagnostic
evaluation, but her pediatrician found
nothing out of the ordinary. Apart from
these episodes, the child felt quite well,
and appeared to be growing and deve
loping normally.
I could get no further information from
the mother, except for the fact that the
episodes had occurred almost exactly one
month apart; and, upon consulting her
calendar, we learned that the first episode
had come exactly one month after the last
of her DPT injections, which had also
been given at monthly intervals. At this
point, the mother remembered that the
child had similar febrile episodes imme
diately after each injection, but that she
had been instructed to ignore them, in as
much as they arc “common reactions” to
the vaccine. 1 therefore gave the child a
single oral dose of dilute homoeopathic
DPT vaccine; and I am happy to report
that the child has remained well since,
with no further episodes of any kind.
This case illustrates how homoeopathic rem
edies prepared from vaccines can be used for
diagnosis as well as treatment of vaccinerelated illnesses, which, no matter how
strongly they are suspected, might otherwise
be almost impossible to substantiate.
Secondly, because fever is the commonest
known complication of the pertussis vaccine,
and in as much as the child seemed quite well
between the attacks, her response to the
vaccine appeared to be a relatively strong
and healthy one, disturbing because of its
recurrence and periodicity, but in any case
relatively simple to cure, as indeed it proved
to be. But one cannot help wondering what
happens to the vaccine in those tens of
millions of children who show no obvious
response to it at all.
Since that time, I have seen at least half a
dozen cases of children with recurrent fevers
of unknown origin, associated with a variety
of other chronic complaints, chiefly irrita
bility, temper tantrums, and increased sus
ceptibility to colds, tonsillitis, and ear infec
tions, which were similarly traceable to the
pertussis vaccine, and which responded
successfully to treatment with the homoeo
pathic DPT nosode. Indeed, 1 would have to
say, on the basis of that experience, that the
pertussis vaccine is probably one of the
major causes of recurrent fevers of unknown
origin in small children today.
My second case was that of a 9'/2-monthold girl, who presented acutely with a
fever of 105° F., and very few other
symptoms. Like the first, this child had
two similar episodes previously, but at
irregular intervals; and the parents, who
31
Nanult
felt ambivalent about vaccinations in
general, had given her only one dose of
the DPT vaccine so far, although the first
episode occurred a few weeks afterwards.
Vol. 3, Issue 2, 21st February 1996
of the liver and spleen to approximately
normal size, and dramatic improvement
in the blood picture, full relapse had
occurred soon after each successive DPT
booster.
I first saw the child in June of 1978. The
fever remained high and unremitting for
48 hours, despite the usual acute remedies
and supportive measures. A CBC revealed
a white count of 32,100 per cu. mm., with
43 percent lymphocytes, 11 percent mono
cytes. 25 percent neutrophils (many with
toxic granulations), 20 percent bands
(also with toxic granulations), and 1
percent metamyelocytes and other imma
ture forms. When I asked a pediatrician
about these findings, “pertussis" was his
immediate reply. After a single oral dose
of homoeopathic DPT vaccine, the fever
came down abruptly within a few hours,
and the child has remained well since.
The idea that vaccinations might also be
implicated in sonic cases of childhood leu
kemia was shocking enough in itself, but it
also completed the line of reasoning opened
up by the previous case. For leukemia is a
cancerous process of the blood and the
blood-forming organs, the liver, the spleen,
the lymph nodes, and the bone marrow,
which are also the basic anatomical units of
the immune system. Insofar as the vaccines
are capable of producing serious complica
tions at all. the blood and the immune organs
would certainly be the logical place to begin
looking for them.
This case was disturbing mainly because of
the hematological abnormalities, which were
in the leukeinoid range, together with the
absence of cough or distinctive respiratory
symptoms, which suggested that introducing
the vaccine directly into the blood may
actually promote deeper or more systemic
pathology than allowing the pertussis organ
ism to set up typical symptoms of local
inflammation at the normal portal of entry.
But perhaps even more shocking to me is the
fact that the boy’s own physician dared not
communicate his suspicion of vaccine-related
illness to the parents, let alone to the general
public. It was this case that convinced me,
once and for all, of the need for serious,
public discussion of our collected experi
ences with vaccine-related illness, precisely
because rigorous experimental proof will
require years of investigation and a firm
public commitment that has not even been
made yet.
The third case was a 5-year-old boy with
chronic lymphocytic leukemia, whom I
happened to sec in August of 1978. while
visiting an old friend and teacher, a family
physician with over 40 years’ experience.
Weil out of earshot of either the boy or his
parents, he told me that the leukemia had
first appeared following a DPT vaccina
tion, and that, although he had treated the
child successfully with natural remedies
on two previous occasions, with shrinking
32
I will now present two cases from my limited
experience with MMR vaccine.
In December of 1980 I saw a 3-ycar-oId
boy with a 4-wcek history of loss of
appetite, stomachaches, indigestion, and
' swollen glands. The stomach pains were
quite severe, and often accompanied by
belching, flatulence, and explosive diar
rhea. The nose was also congested, and
^/om!
the lower eyelids were quite red. The
mother also reported some unusual be
havior changes, such as extreme untidi
ness, ‘wild’ and ‘noisy’ playing, and
waking at 2 a.m. to get into bed with the
parents.
The physical examination was unremark
able except for some large, tender left
posterior auricular and suboccipital nodes,
and marked enlargement of the tonsils. I
then learned that the child had received
the MMR vaccine in October, about 2
weeks before the onset of symptoms, with
no apparent reaction to it at the time. 1
gave the child a single dose of the homoeo
pathic rubella vaccine, and the symptoms
promptly disappeared within 48 hours.
In April 1981, the parents brought him
back for a slight fever, and another 3week history of intermittent pain in and
behind the right ear, stuffy nose, etc. On
examination, the whole right side of the
face appeared to be swollen, especially
the cheek and the angle of the jaw. The
right eye was red and injected. He res
ponded well to acute homoeopathic reme
dies, and has remained well since.
The case against immunizations
possibility that his second illness, and espe
cially the parotid enlargement, may have
represented continuing activity of the mumps
component of the vaccine, inasmuch as I did
not have the triple MMR nosode, but only
those derived from the individual compo
nents. We must therefore also consider the
probability that a variety of “mixed” or
composite syndromes may occur, represent
ing the patient’s responses to two or all three
of the vaccine components, either simulta
neously or over time.
In April of 1981 1 first saw a 4-year-old boy
for bilateral chronic enlargement of the
posterior auricular nodes, which were also
occasionally tender. The mother had
noticed the swelling for about one year,
during which lime he had become more
susceptible to various upper respiratory
infections, none of them especially se
vere. The mother had also noticed a
recurrent parotid swelling at irregular
intervals over the same time period, which
began shortly after the MMR vaccine was
given at the age of three.
At the time of the first visit, the child was
not ill; and, because the mother was about
two months pregnant at the time, I elected
to observe the child and do nothing if
possible until the pregnancy was over. He
did develop a mild laryngitis in the last
trimester, which responded well to bed
rest and simple homoeopathic remedies.
This boy was typical of my rubella vaccine
cases. At an interval of a few weeks after the
MMR vaccine, which is about the same as the
normal incubation period of rubella, a rather
nondescript illness develops, which becomes
subacute and rather more severe than rubella
in the same age group, with, e.g., abdominal
or joint pains and marked adenopathy, but
no rash. Usually the diagnosis is suspected
because of the characteristic posterior auri
cular and suboccipital nodes, and confirmed
by a favorable response to the homoeopathic
rubella nosode.
In April of 1982, he came down with acute
bronchitis. I noticed that the posterior
auricular nodes were once again swollen
and tender, and I decided to give him the
homoeopathic rubella nosode at that
point. The cough promptly subsided, and
As I read over this case, I am struck by the
longer tender. Two weeks later, however,
the nodes regressed in size and were no
33
Vol. 3. Issue 2. 21st February 1996
he returned with a noticeably hard, tender
swelling on the outside of the right check,
near the angle of the jaw, and some pain
on chewing or opening the mouth. A
single dose of the homoeopathic mumps
nosode was given, and the child has been
well since.
In this case also, wc see the subacute pattern
of the disease, with a strong tendency to
chronicity and increased susceptibility to
weaker, low-grade responses, in contrast to
the vigorous, acute responses typically asso
ciated with diseases like measles and mumps
when acquired naturally.
How do the vaccines work?
It is dangerously misleading, and, indeed,
the exact opposite of the truth to claim that a
vaccine makes us “immune” or protects us
against an acute disease, in fact it only drives
the disease deeper into the interior and
causes us to harbor it chronically, with the
result that our responses to it become
progressively weaker, and show less and less
tendency to heal or resolve themselves
spontaneously.
What I propose, then, is simply to investigate
as thoroughly and objectively as we can how
the vaccines actually work inside the human
body, and to begin by paying attention to the
implications of what we already know. Jn
particular, I would like to consider in detail
the process of falling ill with and recovering
from a typical acute disease such as the
measles, in contrast with what wc can
observe following the administration of the
measles vaccine.
Wc all know that measles is primarily a virus
of the respiratory tract, both because it is
inhaled by susceptible persons upon contact
34
with infected droplets in the air, and because
these droplets are produced by the coughing
and sneezing of a person with the disease.
Once inhaled by a susceptible person, the
measles virus then undergoes a long period
of silent multiplication, first in the tonsils,
adenoids, and accessory lymphoid tissues of
the nasopharynx; later in the regional lymph
nodes of the head and neck; and eventually,
several days later, it passes into the blood
and enters the spleen, the liver, the thymus..
and the bone marrow, the ‘visceral’ organs of
the immune system (16). Throughout this
‘incubation’ period, which lasts from 10 to 14
days, the patient usually feels quite well, and
experiences few or no symptoms (17).
By the time that the first symptoms of
measles appear, circulating antibodies are
already detectable in the blood, and the
height of the symptomatology coincides with
the peak of the antibody response (18), In
other words, the ‘illness’, is simply the
definitive effort of the immune system to
clear the virus from the blood. Equally
noteworthy is the fact that the virus is
eliminated by sneezing and coughing, i.c.,
via the same route through which it entered
in the first place.
It is evident that the process of mounting an
acute illness like the measles, no less than
recovering from it, involves a general mobili
zation of the entire immune system, includ
ing inflammation of the previously sensitized
tissues at the portal of entry, activation of
leukocytes and macrophages, liberation of
the serum complement system, and a host of
other mechanisms, of which the production
of circulating antibody is only one, and by no
means the most important.
Such a splendid outpouring leaves little
The case against immunizations
doubt that such illnesses are in fact the
decisive experiences in the normal physio
logic maturation of the immune system as a
whole in the life of a healthy child. For not
only will the child who recovers from the
measles never again be susceptible to it (19);
such an experience also cannot fail to pre
pare the individual to respond even more
promptly and effectively to any infections he
may acquire in the future. The ability to
mount a vigorous acute response to organ
isms of this type must therefore be reckoned
among the most fundamental requirements
of general health and well-being.
In contrast, when an artificially attenuated
virus such as measles is injected directly into
the blood, by-passing the normal portal of
entry, at most a brief inflammatory reaction
may be noted at the injection site, or in the
regional lymph nodes; but there is no ‘incu
bation period’ of local contact at the normal
portal of entry, and consequently very little
possibility of eliminating the virus via the
same route.
Even more important is the fact that the virus
has been artificially ‘attenuated’ so that it will
no longer initiate a generalized response, or
indeed any of the nonspecific defense me
chanisms that help us to respond to infection
generally. By ‘tricking’ the body in this
fashion, we have accomplished what the
entire immune system seems to have evolved
in order to prevent. We have placed the virus
directly into the blood, and given it free and
immediate access to the major immune
organs and tissues, without any obvious way
of getting rid of it.
The result is, indeed, the production of
circulating antibodies against the virus,
which can be measured in the blood; but the
antibody response now occurs as an isolated
technical feat, without any generalized in
flammatory response, or any noticeable
improvement in the general health of the
organism. Exactly the opposite, in fact: the
price that we have to pay for those antibodies
is the persistence of viral elements in the
blood for prolonged periods of time, perhaps
permanently, which in turn presupposes a
systematic weakening of our ability to mount
an effective response not only to measles, but
also to other acute infections as well.
Far from producing a genuine immunity,
then, the vaccines may act by actually inter
fering with or suppressing the immune res
ponse as a whole, in much the same way that
radiation, chemotherapy, corticosteroids
and other anti-inflammatory drugs do.
Artificial immunization focuses on antibody
production, a single aspect of the immune
process, disarticulates it and allows it to
stand for the whole, in much the same way as
chemical suppression of an elevated blood
pressure is accepted as a valid substitute for a
genuine cure of the patient whose blood
pressure has risen. Worst of all, by making it
difficult or impossible to mount a vigorous,
acute response to infection, artificial immu
nization substitutes for it a much weaker,
chronic response, with little or no tendency
to heal itself spontaneously.
Moreover, adequate models already exist for
predicting and explaining what sorts of
chronic disease are likely to result from the
chronic, long-term persistence of viruses and
other foreign proteins within the cells of the
immune system. It has long been known that
live viruses, for example, are capable of
surviving or remaining latent within the host
cells for years, without continually provo
king acute disease. They do so simply by
attaching their own genetic material as an
extra particle or ‘episome’ to the genome of
35
----------- Momok
the host cell, and replicating along with it,
which allows the host cell to continue its own
normal functions for the most part, but
imposes on it additional instructions for the
synthesis of viral proteins (20).
Latent viruses of this type have already been
implicated in three distinct types of chronic
disease, namely, 1) recurrent or episodic
acute diseases, such as herpes, shingles,
warts, etc. (21); 2) 'slow-virus' diseases, i.e.,
subacute or chronic, progressive, often fatal
conditions, such as kuru, creuzfcldt-jakob
disease, subacute sclerosing panenccphalitis
(SSPE). and possibly guillain-barrtS syn
drome (22); and 3) tumors, both benign and
malignant (23).
In any case, the latent virus survives as a
clearly “foreign" element within the cell,
which means that the immune system must
continue to try to make antibodies against it,
insofar as it can still respond to it at all.
Because the virus is now permanently incor
porated within the genetic material of the
cell, these antibodies will now have to be
directed against the cell itself.
The persistence of live viruses or other
foreign antigens within the cells of the host
therefore cannot fail to provoke auto-im
mune phenomena, because destroying the
infected cells is now the only possible way
that this constant antigenic challenge can be
removed from the body. Since routine vacci
nation introduces live viruses and other
highly antigenic material into the blood of
virtually every living person, it is difficult to
escape the conclusion that a significant
harvest of auto-immune diseases must auto
matically result.
Sir Macfarlane Burnet has observed that the
components of the immune system all func
36
Vol. 3, Issue 2, 21st February 1996
tion as if they were collectively designed to
help the organism to discriminate ‘self’ from
‘non-sclf, i.e., to help us to recognize and
tolerate our own cells, and to identify and
eliminate foreign or extraneous substance^
as completely as possible (24). This concept
is exemplified not only by the acute response
to infection, but also by the rejection of
transplanted tissues, of “homografts,” both
of which result in the complete and perma
nent removal of the offending substance
from the body.
If Burnet is correct, then latent viruses, auto
immune phenomena, and cancer would seci,
to represent different aspects of the same
basic dilemma, which the immune system
can neither escape nor resolve. For all of
them presuppose a certain degree of chronic
immune failure, a state in which it becomes
difficult or impossible for the body either to
recognize its own cells as unambiguously its
own, or to eliminate its parasites as unequi
vocally foreign.
In the case of the attenuated measles virus, it
is not difficult to imagine that introducing it
directly into the blood would continue to
provoke an antibody response for a consi
derable period of time, which is doubtless the
whole point of giving the vaccine; but that
eventually, as the virus succeeded in attain
ing a state of latency within the cell, thj«
antibody response would wane, both b“
cause circulating antibodies cannot normally
cross the cell membrane, and because they
are also powerful immunosuppressive agents
in their own right (25).
The effect of circulating antibody will there
after be mainly to keep the virus within the
ceil. i.e.. to continue to prevent any acute
inflammatory response, until eventually, per
haps under circumstances of accumulated
The case against immunizations
stress or emergency, this precarious balance
breaks down, antibodies begin to be pro
duced in large quantities against the ceils
themselves, and frank auto-immune phe
nomena of necrosis and tissue destruction
supervene. Latent viruses, in this sense, are
like biological time bombs’, set to explode at
an indeterminate time in the future (26).
Auto-immune diseases have always seemed
obscure, aberrant, and bizarre, because it is
not intuitively obvious why the body should
suddenly begin to attack and destroy its own
tissues. They make a lot more sense, and,
indeed, must be reckoned as ‘healthy’, if
destroying the chronically infected cells is the
only possible way of eliminating an even
more serious threat to life, namely, the per
sistence of the foreign antigenic challenge
within the cells of the host.
spread to other cell types, tissues, and
organs, even in more remote areas. Malig
nancy might simply represent the reactiva
tion of the virus from its latent phase into a
more acute mode, albeit with less inflam
mation and more tissue destruction than the
original wild-type infection.
If what I am saying turns out to be true, then
what we have done by artificial immuniza
tion is essentially to trade off our acute,
epidemic diseases of the past century for the
weaker and far less curable chronic diseases
of the present, with their amortizable suf
fering and disability. In doing so, we have
also opened up limitless evolutionary possi
bilities for the future of ongoing in vivo
genetic recombination within the cells of the
race.
The individual vaccines reconsidered
Tumor formation could then be understood
as simply a more advanced stage of chronic
immune failure, according to the same
model, b'or, as long as the host is subjected to
enormous and unremitting pressure to make
antibodies against itself, that response will
automatically tend to become less and less
effective.
Eventually, under stress of this magnitude,
the auto-immune mechanism could easily
break down to the point that the chronically
infected and genetically transformed cells,
no longer clearly ‘self or ‘non-self, begin to
free themselves from the normal restraints of
‘histocompatibility’ within the architecture
of the surrounding cells, and begin to
multiply autonomously at their expense.
A tumor could then be described as ‘benign’
insofar as the breakdown of histocompati
bility remains strictly localized to the issue of
origin, and ‘malignant’, insofar as it begins to
I want next to consider each of the vaccines
on an individual basis, in relation to the
infectious diseases from which they are
derived.
The MMR is composed of attenuated live
measles, mumps, and rubella viruses, ad
ministered in a single intramuscular injection
at about 15 months of age. Subsequent reiminunization is no longer recommended,
except for young women of childbearing age,
in whom the risk of congenital rubella
syndrome (CRS) is thought to warrant it,
even though the effectiveness of re-immu
nization is questionable at best.
Prior to the vaccine era, measles, mumps,
and rubella were reckoned among the ‘rou
tine childhood diseases’, which most school
children contracted before the age of pu
berty, and from which nearly all recovered,
with permanent, lifelong immunity, and no
complications or sequelae.
37
----------- NomI
Buf they were not always so harmless.
Measles, in particular, can be a devastating
disease when a population encounters it for
the first time. Its importation from Spain, for
instance, undoubtedly contributed to Cor
tez’ conquest of the great Aztec Empire;
whole villages were carried off by epidemics
of measles and smallpox, leaving only a small
remnant of cowed, superstitious warriors to
face the bearded conquistadores from across
the sea (27). In more recent outbreaks
among isolated, primitive peoples, the case
fatality rate from measles averaged 20 to 30
percent (28).
In both these so-called ‘virgin-soil’ epide
mics. not only measles but also polio and
many other similar diseases take their high
est toll of death and serious complications
among adolescents and young adults, heal
thy and vigorous people in the prime of life,
and leave relatively unharmed the group of
school-age children before the age of puberty
(29).
This means that the evolution of a disease
such as measles from a dreaded killer to an
ordinary disease of childhood presupposes
the development of nonspecific or ‘herd’
immunity in young children, such that, when
they are finally exposed to the disease, it
activates defense mechanisms already pre
pared and in place, resulting in the long
incubation period and the usually benign,
self-limited course described above.
Under these circumstances, the rationale for
wanting to vaccinate young children against
measles is limited to the fact that a very small
number of deaths and serious complications
have continued to occur, chiefly pneumonia,
encephalitis, and the rare but dreaded sub
acute sclerosing panenccphalitis (SSPE), a
slow-virus disease with a reported incidence
38
Vol. 3, Issue 2, 21st February 1996
of 1 per 100,(X10 cases (30). Pneumonia, by
far the commonest complication, is usually
benign and self-limited, even without treat
ment (31); and even in those rare cases in
which bacterial pneumonia supervenes, ade
quate treatment is currently available.
By all accounts, then, the death rate from
wild-type measles is very low, the incidence
of serious sequelae is insignificant, and the
general benefit to the child who recovers
from the disease, and to his contacts and
descendants, is very great. Consequently,
even if the measles vaccine could be shown to
reduce the risk of death or serious compli
cations from the disease, it still could not
justify the high probability of auto-immune
diseases, cancer, and whatever else may
result from the propagation of latent measles
virus in human tissue culture for life.
Ironically, what the measles vaccine certain
ly has done is to reverse the historical or
evolutionary process to the extent that
measles is once again a disease of adolescents
and young adults (32), with a correspond
ingly higher incidence of pneumonia and
other complications, and a general tendency
to be a more serious and disabling disease
than it usually is in younger children.
As for the claim that the vaccine has helped
to eliminate measles encephalitis, 1 myself,
in my own relatively small general practice,
have already seen two children with major
seizure disorders which the parents clearly
ascribed to the measles vaccine, although
they would never have been able to prove the
connection in a court of law, and never even
considered the possibility of compensation.
Such cases therefore never make the official
statistics, and are accordingly omitted from
conventional surveys of the problem. Merely
---------- N(Mok
injecting the virus into the blood would
naturally favor a higher incidence of deep or
visceral complications affecting the lungs,
liver, and brain, for which the measles virus
has a known affinity.
The case of immunizing against mumps and
rubella seems a fortiori even more tenuous,
for exactly the same reasons. Mumps is also
essentially a benign, self-limited disease in
children before the age of puberty, and
recovery from a single attack confers lifelong
immunity. 1'he principal complication is
meningoencephalitis, mild or subclinical
forms of which are relatively common,
although the death rate is extremely low
(33), and sequelae are rare.
The mumps vaccine is prepared and adminis
tered in much the same way as the measles,
usually in the same injection; and the dan
gers associated with it are likewise com
parable. Again like the measles, mumps too
is fast becoming a disease of adolescents and
young adults (34), age groups which tolerate
the disease much less well. The chief com
plication is acute epididymo-orchitis, which
occurs in 30 to 40 percent of the males
affected past the age of puberty, and usually
results in atrophy of the testicle on the
affected side (35); but it also shows a strong
tendency to attack the ovary and the pan
creas.
For all of these reasons, the greatest favor
we could do for our children would be to
expose them all to the measles and mumps
when they are young, which would not only
protect them against contracting more se
rious forms of these diseases when they grow
older, but would also greatly assist in their
immunological maturation with minimal
risk. 1 need hardly add that this is very close
to the actual evolution of these diseases
The case against immunizations
before the MMR vaccine was introduced.
The same discrepancy is evident in the case
of rubella, or ‘German measles’, which in
young children is a disease so mild that it
frequently escapes detection (3(>), but in
older children and adults not infrequently
produces arthritis, purpura, and other se
vere, systemic signs (37). The main impetus
for the development of the vaccine was
certainly the recognition of the ‘congenital
rubella syndrome’ (CRS), resulting from
damage to the developing embryo in utero
during the first trimester of pregnancy (38),
and the relatively high incidence of CRS
traceable to the rubella outbreak of 1964.
But here again, we have an almost entirely
benign, sell-limited disease transformed by
the vaccine into a considerably less benign
disease of adolescents and young adults of
reproductive age, which is, ironically, the
group that most needs to be protected
against it. Moreover, as with measles and
mumps, the simplest and most effective way
to prevent CRS would be to expose every
body to rubella in elementary school; re
infection does sometimes occur after reco
very from rubella, but much less commonly
than after vaccination (39).
The equation looks somewhat different for
the diphtheria and tetanus vaccines. First of
all, both diphtheria and tetanus are serious,
sometimes fatal diseases, even under the best
of treatment; this is especially true of teta
nus, which still carries a mortality of close to
50 percent.
Furthermore, these vaccines are not made
from living diphtheria and tetanus organ
isms, but only from certain ‘toxins’ elabo
rated by them; these poisonous substances
are still highly antigenic, even after being
Vol. 3, Issue 2, 21st February 1996
inactivated by heat. Diphtheria and tetanus
‘toxoids’ therefore do not protect against
infection per.se, but only against the systemic
action of the original poisons, in the absence
of which both infections are of minor im
portance clinically.
Consequently, it is easy to understand why
parents might want their children protected
against diphtheria and tetanus, if safe and
effective protection were available. More
over, both vaccines have been in use for a
long time, and the reported incidence of
serious problems has remained very low, so
that there has never been much public outcry
against them.
On the other hand, both diseases are quite
readily controlled by simple sanitary mea
sures and careful attention to wound hy
giene; and, in any case, both have been
steadily disappearing from the developing
countries, since long before the vaccines
were introduced.
Diphtheria now occurs sporadically in the
United States, often in areas with significant
reservoirs of unvaccinatcd children. But the
claim that the vaccine is ‘protective’ is once
again belied by the fact that, when the
disease does break out, the supposedly
‘susceptible’ children are in fact no more
likely to develop clinical diphtheria than
their fully immunized contacts. In a 1969
outbreak in Chicago, for example, the Board
of Health reported that 25 percent of the
cases had been fully immunized, and that
another 12 percent had received one or more
doses of the vaccine and showed serological
evidence of full immunity; another 18 per
cent had been partly immunized, according
to the same criteria (40).
So. once again, we are faced with the pro
40
bability that what the diphtheria toxoid has
produced is not a genuine immunity to diph
theria at all, but rather some sort of chronic
immune tolerance to it, by harboring highly
antigenic residues somewhere within the
cells of the immune system, presumably with
long-term suppressive effects on the immune
mechanism generally.
This suspicion is further aggravated by the
fact that all of the DPT vaccines are alumprecipitated and preserved with Thiomersal,
an organomercury derivative, to prevent
them from being metabolized too rapidly, so
that the antigenic challenge will continue for
as long as possible. The fact is that we do not
know and have never even attempted to
discover what actually becomes of these
foreign substances, once they are inside the
human body.
Exactly the same problems complicate the
record of the tetanus vaccine, which almost
certainly has had at least some impact in
reducing the incidence of tetanus in its classic
acute form, yet presumably also survives for
years or even decades as a potent foreign
antigen within the body, with long-term
effects on the immune system and elsewhere
that are literally incalculable.
‘Whooping cough’, much like diphtheria and
tetanus, began to decline as a serious epi
demiological threat long before the vaccine
was introduced. Moreover, the vaccine has
not been particularly effective, even accord
ing to its proponents; and the incidence of
known side-effects is disturbingly high.
The power of the pertussis vaccine to damage
the central nervous system, for example, has
received growing attention since Stewart and
his colleagues reported an alarmingly high
incidence of encephalopathy and severe
---------- NoM.1
convulsive disorders in British children that
were traceable to the vaccine (41). My own
cases, a few of which were reported above,
suggest that hematological disturbances may
be even more prevalent, and that, in any
case, the known complications almost cer
tainly represent a small fraction of the total.
In any case, the pertussis vaccine has become
controversial even in the United States,
where medical opinion has remained almost
unanimous in favor of immunizations gene
rally; and several countries, such as West
Germany, have discontinued routine per
tussis vaccination entirely (42).
Pertussis is also extremely variable clinically,
ranging in severity from asymptomatic, mild,
or inapparent infections, which are quite
common actually, to very rare cases in young
infants less than 5 months of age, in whom
the mortality is said to reach 40 percent (43).
Indeed, the disease is rarely fatal or even that
serious in children over a year old, and
antibiotics have very little to do with the
outcome (44).
A good deal of the pressure to immunize at
the present time thus seems to be attri
butable to the higher death rate in very
young infants, which has led to the terrifying
practice of giving this most clearly dangerous
of the vaccines to infants at 2 months of age,
when their mothers’ milk would normally
have protected them from all infections
about as well as it can ever be done (45), and
the effect on the still developing blood and
nervous system could be catastrophic.
For all these reasons, the practice of routine
pertussis immunization should be disconti
nued as quickly as possible, and more studies
done to assess and compensate the damage
that it has already done.
The case against immunizations
Poliomyelitis and the polio vaccines present
an entirely different situation. The standard
Sabin vaccine is trivalent, consisting of
attenuated, live polioviruses of each of the
three strains associated with poliomyelitis;
but it is administered orally, in much the
same way as the infection is acquired in
nature. The oral or non-injectable route,
which leaves the recipient free to develop a
natural immunity at the normal portal of
entry, i.e., the GI tract, would therefore
appear to represent a considerable safety
factor.
On the other hand, the wild-type poliovirus
produces no symptoms whatsoever in over 90
percent of the people who contract it, even
under epidemic conditions (46); and, of
those people who do come down with re
cognizable clinical disease, perhaps only 1 or
2 percent ever progress to the full-blown
neurological picture of 'poliomyelitis’, with
its characteristic lesions in the anterior horn
cells of the spinal cord or medulla oblongata
(47).
Poliomyelitis thus presupposes peculiar con
ditions of susceptibility in the host, even a
specific anatomical susceptibility, since, even
under epidemic conditions, the virulence of
the poliovirus is so low, and the number of
cases resulting in death or permanent dis
ability was always remarkably small (48).
Given the fact that the poliovirus was ubi
quitous before the vaccine was introduced,
and could be found routinely in samples of
city sewage wherever it was looked for (49),
it is evident that effective, natural immunity
to poliovirus was already as close to being
universal as it can ever be, and a fortiori no
artificial substitute could ever equal or even
approximate that result. Indeed, because the
virulence of the poliovirus was so low to
41
Vol. 3, Issue 2, 21st February 1996
begin with, it is difficult to see what further
attenuation of it could possibly accomplish,
other than to abate as well the full vigor of
the natural immune response to it.
For the fact remains that even the attenuated
virus is still alive, and the people who were
anatomically susceptible to it before are still
susceptible to it now. This means, of course,
that at least some of these same people will
develop paralytic polio from the vaccine
(50), and that the others may still be har
boring the virus in latent form, perhaps
within those same cells.
The only obvious advantage of giving the
vaccine, then, would be to introduce the
population to the virus when they are still
infants, and the virulence is normally lowest
anyway (51); and even this benefit could be
more than offset by the danger of weakening
the immune response, as we have seen. In
any case, the woic matter is clearly one of
enormous complexity, and illustrates only
too well the hidden dangers and miscalcula
tions that arc inherent in the virtually irresis
tible attempt to beat nature at her own game,
to eliminate a problem that cannot be
eliminated, i.e., the susceptibility to disease
itself.
So even in the case of the polio vaccine,
which appears to be about as safe as any
vaccine ever can be, the same fundamental
dilemma remains. Perhaps the day will come
when we can face the consequences of
deliberately feeding live polioviruses to
every living infant, and admit that we should
have left well enough alone, and addressed
ourselves to the art of healing the sick when
we have to, rather than to the technology of
eradicating the possibility of sickness, when
we don't have to, and can’t possibly succeed
in any case.
42
Vaccination and the path of
medical technology
In conclusion, I want to go back to the
beginning, to the essentially political aspects
of vaccination, that oblige us all to reason
and deliberate together about matters of
common concern, and to reach a clear
decision about how we choose to live. I have
stated my own views regarding the safety and
effectiveness of the vaccines, and 1 hope that
others of differing views will do the same.
That is why I am deeply troubled by the
atmosphere of fanaticism with which the
vaccines are imposed on the public, and
serious discussion of them is ignored or
stifled by the medical authorities, as if the
question had already been settled definitely
and for all time. In the words of Sir
Macfarlanc Burnet,
It is our pride that in a civilized country
the only infectious diseases which anyone
is likely to suffer are either trivial or easily
cured by available drugs. The diseases
that killed in the past have in one way or
another been rendered impotent, and, in
the process, general principles of control
have been developed which should be
applicable to any unexpected outbreak in
the future (52).
Quite apart from the truth of these claims,
they exemplify the smugness and self-right
eousness of a profession and a society that
worships its own ability to manipulate and
control the processes of nature itself. That is
why, as Robert Mendelsohn has said, "we
are quick to pull the trigger, but slow to exa
mine the consequences of our actions (53).”
Indeed, one would have to say, methodically
slow. In 1978, for example, the American
case against immunizations
Academy of Pediatrics, which had been
charged by the Congress with the respon
sibility to formulate guidelines for Federal
compensation of “vaccinalion-related inju
ries,” issued the following eligibility restric
tions:
molecules in search of diseases; when
activated, under proper conditions, they
could cause a variety of diseases, inclu
ding rheumatoid arthritis, multiple scle
rosis, systemic lupus erythematosus, parkinson’s disease, and perhaps cancer (55).
1. Compensation should be made available
to any child or young person under the age of
18 years, or a contact of such person of any
age. who suffers a major reaction to a vaccine
mandated for school entry or continuation in
school in his or her state of residence.
Unfortunately, this is the sort of warning that
very few people are willing or able to hear at
this point, least of all the American Cancer
Society or the American Academy of Pedia
trics. The fact is, as Dubos points out, that all
of us still want to believe in the ’miracle’,
regardless of the evidence.
2. Such a reaction should have been pre
viously recognized as a possible consequence
of the vaccine given.
3. Such a reaction should have occurred no
more than 30 days following the immuni
zation (54).
These restrictions would automatically ex
clude all of the chronic diseases, or indeed
anything other than the very few adverse
reactions that have so far been identified,
which clearly represent only a tiny fraction of
the problem.
Still less can either the government or the
medical establishment be considered ignor
ant of the possibility that lurks in every
parent’s mind and heart, namely, that the
vaccines cause cancer and other chronic
diseases. Precisely that possibility was raised
by Prof. Robert Simpson of Rutgers in a 1976
seminar for science writers, sponsored by the
American Cancer Society.
Immunization programmes against flu,
measles, mumps, polio, and so forth may
actually be seeding humans with RNA to
form latent proviruses in cells throughout
the body. These latent proviruscs could be
The faith in the magical power of drugs
often blunts the critical senses, and comes
close at limes to a mass hysteria, involving
scientists and laymen alike. Men want
miracles as much today as in the past. 1,
they do not join one of the newer cults,
they satisfy this need by worshipping at
the altar of modern science. This faith in
the magical power of drugs is not new. It
helped to give medicine the authority of a
priesthood, and to recreate the glamour of
ancient mysteries (56).
The idea of eradicating measles or polio has
come to seem attractive to us, simply because
the power of medical science makes it seem
technically possible; we worship every vic
tory of technology over nature, just as the
bullfight celebrates the triumph of human
intelligence over the brute beast.
This is why we do not begrudge the drug
companies their enormous profits, and glad
ly volunteer our own bodies and those of ou
children for their latest experiments. Vacci
nation is essentially a religious sacrament of
our own participation in the miracle, a
veritable auto-da-fe in the name of modern
civilization itself.
43
-----------Now!
Nobody in his right mind would seriously
entertain the idea that, if we could somehow
eliminate, one by one, measles and polio and
all the known diseases of mankind, we would
be any the healthier for it, or that other even
. e serious diseases would not quickly take
their place.
Still less would a rational being suppose that
the illnesses from which he suffered were
‘entities’ somehow separable from the pa
th :ts who suffer them, and that, with the
appropriate chemical or,surgical sacrament,
this separation can literally be carried out.
Yet these are precisely the ‘miracles’ we arc
taught to believe in, and the idolatries to
which we aspire. We prefer to forget the
older and simpler truths, that the propensity
or susceptibility to illness is deeply rooted in
our biological nature, and that the pheno
mena of disease are the expression of our
own life energy, trying to overcome what
ever it is trying to overcome, trying, in short,
to heal itself.
The myth that we can find technical solutions
for all human ailments seems attractive at
first, precisely because it by-passes the
problem of healing, which is a genuine
miracle in the sense that it can always fail to
occur. We are all genuinely at risk of illness
and death at every moment; no amount of
technology can change that: to stand at all
times in the front lines against disease, and to
attack and destroy it whenever and wherever
it shows itself.
That is why, with all due respect, I cannot
have faith in the miracles or accept the
sacraments of Merck, Sharp, and Dohme
and the Center for Disease Control. I prefer
to stay with the miracle of life itself, which
has given us illness and disease, but also the
44
Vol. 3, Issue 2, 21st February 1996
arts of medicine and healing, through which
we can acknowledge and experience our pain
and our vulnerability, and sometimes, with
the grace of God and the help of our fellow
men, an awareness of health and well-being
that transcends all boundaries. That is my
religion; and, while I would willingly share it,
I would not force it on anyone.
References
1. Mortimer R. Pertussis Immunization. Hos
pital Practice, October 1980, p. 103.
2. Quoted in Mortimer. Op. cit., p. 105.
3. Dubos R. Mirage of Health. Harper, 1959,
p. 73.
4. Ibid. pp. 74-75.
5. Stewart G. Vaccination against Whooping
Cough: efficiency vs. risks. Lancet, 1977,
p. 234.
6. Medical tribune. January 10, 1979, p. 1.
7. Cherry J. The New Epidemiology of Measles
and Rubella. Hospital Practice, July 1980,
pp. 52-54.
8. Unpublished data from the New Mexico
I Icalth Department (private communication).
9. Lawless M. ctal. Rubella Susceptibility in
Sixth-graders. Pediatrics. 65: 1086-1089, June
1980.
10. Cherry. Op. cit., p. 49.
11. Infectious Diseases, January 1982, p. 21.
12. Cherry. Op. cit., p. 52.
13. Family practice news, July 15, 1980, p. I.
14. Ferrante J. Atypical Symptoms? It could still
be Measles. Modern Medicine, September
30, 1980, p. 76.
15. Cherry. Op. cit., p. 53.
16. Phillips C. Measles, in V. Vaughan, ct al.
Nelson's Text book of Pediatrics, 11th Ed.,
Saunders, 1979, p. 857.
17. Davis B. et al. Microbiology. Harper, 1973,
p. 1346.
18. Ibid.
19. Ibid. p. 1342.
---------- Najno.k
The case against immunizations
38. Glasgow L., Overall J. Congenital Rubella
Ibid. p. 1418.
Syndrome in V. Vaughan, et al. Op. cit.,
Hayflick L. Slow Viruses. Executive Health
Report, February 1981, p. 4.
p. 483.
22. Ibid. pp. 1-4.
39. Phillips. Rubella. Op. cit., p. 865.
23. Davis, et al. Op. cit., Ch. 63, pp. 1418-1449. 40. Mendelsohn R. The truth about immuniza
24. Burnet M. The Integrity of the Body. Athetions. The People’s Doctor, April 1978, p. 1.
neum, 1966, p. 68.
41. Stewart. Op. cit., p. 234.
25. Talai N. Autoimmunity in H. Fudenberg, et 42. Mortimer. Op. cit., p. 111.
al. Basic and clinical immunology 3rd Ed., 43. Feighin R. Pertussis, in Vaughan, etal., Op.
Lange, 1980, p. 222.
cit., p. 769.
26. Hayflick. Op. cit., p. 4.
44. Ibid. p. 769.
27. McNeill W. plagues and Peoples. Anchor, 45. BarnessL. Breastfeeding, in Vaughan, etal..
1976, p. 184.
Op. cit., p. 191.
28. Burnet M., White D. The Natural History of 46. Burnet and White. Op. cit., p. 91ff.
Infectious Disease. Cambridge, 1972, p. 16.
47. Davis, er al. Op. cit., p. 1290ff.
29. Ibid. pp. 90, 121, et passim.
48. Ibid. p. 1280.
30. Steigman A. Slow Virus Infections in V. 49. Burnet and White. Op. cit., p. 93.
Vaughan, et al. Op. cit., p. 937.
50. Fulginiti V. Problems of Poliovirus Immu
31. Phillips. Op. cit., p. 860.
nization . Hospital Practice, August 1980,
32. Infectious Diseases. April 1979, p. 26.
pp. 61-62.
33. Phillips C. Mumps in V. Vaughan, et al. Op. 51. Burnet and White. Op. cit., p. 95.
cit., p. 891.
52. Burnet. Op. cit., p. 128.
34. Hayden G., er al. Mumps and Mumps 53. Mendelsohn. Op. cit., p. 3.
Vaccine in the U.S. Continuing Education, 54. Quoted in Wehrle P. Vaccines, Risks, and
September 1979, p. 97.
Compensations. Infectious Diseases. Febru
35. Phillips. Mumps. Op. cit., p. 892.
ary 1982, p. 16.
36. Phillips. Rubella. Op. cit., p. 863.
55. Quoted in Mendelsohn. Op. cit., p. 1.
37. Ibid. p. 862.
56. Dubos. Op. cit., p. 157.
20.
21.
(Courtesy: Journal of the American Institute of Homoeopathy, 1983.)
45
Vol. 3, Issue 2, 21st February 1996
References
1. Shigeaki Baba. Quality of Life. Geneva;
World Health, No. 3, May-June 1993, p. 9-10.
2. Oliver, M.F.. Doubts about preventing coro
nary heart disease. BMT, Vol.304, 1992,
p. 393-394.
3. Sri Aurobindo. The Life Divine. Pondicher
ry, Sri Aurobindo Ashram Press, SABCL,
1972.
Dr. Alok Pandey is trying to live the concept of Integral Health.
26
re. .'
Jottings by the staff of the GPV's Expanded Programme on Immunization (EPI)
DTP coverage fell precipitously following
vaccine scares.The first group included
former East Germany, Hungary, Poland and
the United States; the latter, former West
Germany, Italy, Japan, Russia, Sweden and
the United Kingdom.
Freedom of expression is a human right.
A study, however, published in the British
journal Lancet at the end of January
suggests that exercising that right to attack
vaccines too hastily can have a dire, even
deadly, impact on health.The study found
that tne incidence of a disease can be up to
1 00 times higher in a country where
vaccination against the disease is disrupted
by anti-vaccine movements than in
countries where coverage of the population
with tne vaccine remains constantly high.
Artur Gaiazka.a member of the study
research team and former EPI medical
office: befeves'this is one of the first global
reviews to show clearly that a dramatic
impact can result from anti-vaccination
propaganda."
The study looked at the incidence of
pertussis (whooping cough) between 1940
and 1956 in two groups of countries; those
where vaccination with the diphtheriatetanus-pertussis combination vaccine (DTP)
was reaching a steady 90-100% of the
population for many years and those where
The study's comparison of neighbouring
countries - Sweden and Norway, Spain and
Portugal, Canada and the U.S., Greece and
Hungary - one with, the other without, an
anti-vaccination lobby, is particularly telling:
pertussis incidence rates were 10- to 100fold greater in the less protected neighbour.
The difference, in fact, could be much
greater, the study notes, since the research
group used numbers of reported cases to
calculate incidence, and these numbers
are notoriously well below the true
incidence of disease."And history tells us,"
notes Dr Galazka,"that it can take 10 to
20 years to reverse the damage wroughf.by
anti-vaccination movements."
’
Acaseinpoint..
i.. At the end of February, 4 weeks after
i publication of the study described here,
j. the Lancet ran 2 reports, one2 by
. .
; 13 scientists from London suggesting a
pcipossiblelink between the mumps~
- - measles-rubella (MMR) vaccine and
inflammatory disease of the bowel
(Crohn's disease) and autism, and calling
for further research to investigate the
possibility; the other providing scientific
evidence refuting such a link’. (A WHO
review, also published in February, of
9 reports of a link between measles
vaccine and Crohn's disease found none
to be "very convincing."4)
In the same issue of the Lancet, an
editorial’by Robert Chen and Frank ■
DeStefano of the U.S. Centers for Disease
Control and Prevention points to several
scientific flaws in the London study but
notes that“no vaccine is perfectly
safe...[However,] because vaccines are
given to millions of healthy people,
usually infants, extremely high
standards for vaccine safety are
demanded."
That damage can be considerable.'Cases '
(of pertussis] among children deprived of
vaccine may have exceeded hundreds of
thousands,' says the study report,“and
disease-related clinical complications (e.g.
pneumonia, encephalopathy and seizures)
may have numbered tens of thousands."
Although the ftudy focussed on disease
incidence rather than deaths,"other reports
indicate that pertussis mortality also
increased.[with'; excess (newborn) deaths
inversely related to vaccination coverage
during pertussis outbreaks." >
Meanwhile, parents'advocacy groups,
anti- and pro-vaccination activists, public
health officials and vaccine industry
officials are flooding the media with
conflicting, often partisan, statements
and calls for action. Whether or not there
is even a flickering flame beneath the
smoke, the damage to immunization
programmes - and to the children they
were set up to protect - may well
have begun.
Vaccines - not perfect but clearly effective, U.S. data show
Disease
Pre-vaccine
year’
No. of cases
in pre-vaccine year
% change
-99.99
Diphtheria
1921
206,939
5
Measles
1941
894,134
135
■99.98
Mumps
1968
152,209
612
-99.60
Pertussis
1934
265,269
5,519
-97.92
Polio (wild)
1952
21,269
0 .
-100.00
1969
57,686
20,000
■
Rubella
■.
,CRS’
Tetanus
1964-655
1948s
Hib3
1984s
1,639,066
Total
161
-99.98
4
-99.98
1,560
43
-97.24
20,000
165
-99.18
6,644
-99.59
Vaccine adverse events
1. Congenital rubella syndrome
2 Im asr/e Hsemophi inf..uenzae type b disease
3. Peak year for no. oi>cases
4. Prozsior.a! data
5. Estimated case numbers: no national reporting in pre-vaccine era
8
No. cases
in 19974
11,365
Courtesy Tr.e Lancet, from reference (5)
:. ...J
Notes
1.
EJ.Gangarosa et al.,Lancet, 351:356-61,1998
(31 January)
2.
AJ. Wakefield et al., Lancet, 351:637-41,1998
(28 February)
3.
M.A.Afzal et al.. Lancet, 351:646-47,1998
(28 February)
4.
Weekly Epidemiological Record, WHO, 73:33-40,1998
(6 February)
5.
R.T.Chen and F. DeStefano, Lancet, 351:611-'.2,1998
(28 February)
Vaccine & Immunization News & Number 6, March 1998
Immunization: Protection from diseases
SWASTH BHARAT
- A NATIONAL INITIATIVE
IEC Division
Ministry of Health and Family Welfare
Government of India
BACKGROUND
India's universal immunization program (UIP) is one of the
largest immunization program in the world in terms of
numberof children targeted.
Immunization is one of the most cost effective ways for
prevention of infectious diseases.
While the primary goal of UIP is to
reduce infant and child mortality, new
vaccines like the Hepatitis B vaccine
protects against cancer and liver
diseases.
contracting the full blown disease in future.
•
The idea of introducing vaccines (that is live or killed germ
particles which has lost ability to produce disease) into the
human body is to make the body's defense system believe that it
is under attack by the bacteria or the virus. Our defense
mechanism recognises this organism and start preparing for a
painless
Know which vaccine is to be given at what age
AGE
VACCINATION
fight by producing protective factors referred to as anti-bodies.
At Birth
BCG, Polio, Hepatits B
The first time such an interaction occurs, the body takes some
time to identify the foreign organism and then produce anti
bodies but subsequently, the anti-body formation is quicker
1 % month
DPT 1, Polio 1, Hepatitis B 1
2 % month
DPT 2, Polio 2, Hepatitis B 2
3 / month
DPT 3, Polio 3, Hepatitis B 3
9 months
Measles-1, Vitamin A
16-24 months
Booster shots of DPT and Polio, Vitamin A,
Measles-2, JE in selected areas
because the body tends to remember the offending organism
and accordingly act faster. This process, known
Under UIP, children are vaccinated
against 7 vaccine preventable
diseases i.e. Diphtheria, Pertussis,
Tetanus, Poliomyelitis, Hepatitis B,
Childhood Tuberculosis and Measles.
In addition, Pregnant mothers are
given tetanus toxid vaccination.
as immunological memory, enables the body
to produce the same kind of anti-bodies more
rapidly and in higher quantities on repeated
contacts with the disease causing agent.
JE vaccine is provided in 112 JE endemic
districts and pentavalent vaccine has been
introduced in (Tamilnadu and Kerala)
It offers protection against Tuberculosis.
BCG VACCINE
Special precautions
Do not rub the site of injection
RESEARCH FINDINGS
•
India has one of the highest number of un-immunized
children in the world. The District Household & Facility
Survey-3 (DLHS 2007-08) reveals that
53.5% children
(12-23 months) are fully immunized and that
children received no vaccination (~4 million) - Coverage
Evaluation Survey 2009 - Full Immunization - 61%, No
Immunization-7.6%
^b%
•
Latest figures from the CES 2009 show that while full
vaccination coverage for children has improved in 19 states,
it has dropped in the remaining 10 states
TECHNICAL DETAILS
Vaccination is deliberate introduction of the disease causing
agent in some form in a healthy child, to incite a special response
(known as immune response), which offers protection from
Occasionally a child may develop swelling of a lymph node
(gland) in the armpit after the vaccine. Nothing needs to be
done if it is small (size of a pea), not discharging pus and is
•
Initially there is a slight swelling followed usually by a small
scar.
DPTVACCINE
DPT protects against diphtheria or Galghontu , tetanus or Dhanu
ba and whooping cough or Kali Khansi. All three are serious
diseases. Diphtheria usually
manifests with sore throat and
quickly progresses to fever,
headache & loss of appetite. It
causes a thick gray coating
(membrane) at back of the
throat, over the tonsils, that
makes it hard to breathe and
swallow and can result in
suffocation and death.- There is
no definitive treatment
available except for supportive treatment.
Pertussis better known as Whooping cough, is a highly
contagious bacterial infection. It starts with features of a
common cold but quickly progresses to a severe exhausting
cough.
Tetanus : A Child can get tetanus by infection of a cut/wound by
Dust/Sand/Cowdung/Rusted material etc. It causes painful
tightening, severe stiffness and spasms of the muscles all over
the body and particularly of the jaw (lockjaw). This can lead to
convulsions, respiratory failure and death.
POLIOVACCINE
Polio Vaccine provides protection against Poliomyelitis. Polio is
an infectious disease caused by polio virus. It enters a child s (or
infection can occur at any age. Only when it has damaged the
liver considerably, do the symptoms become noticeable. And by
then, it becomes too late to undo the damage. After an infection,
some children may develop a severe liver failure leadingto death.
Signs & symptoms
•
There may not be any obvious signs & symptoms in a
majority of sufferers. Some patients develop symptoms like:
•
loss of appetite, nausea/vomiting
•
mild fever,tiredness, bodyache
•
there may be yellow discoloration of skin & eyes (jaundice),
dark urine & pale stools.
Whom to contact for further clarifications:
In case of any clarifications, ANM/Medical officer of the nearest
health facility should be contacted.
At district level, the District Immunization officer (DIO) should
be contacted.
adult's) body through the mouth. In some children the Polio
virus attacks the nervous system and can cause permanent
muscle paralysis (can't move leg or arm) or weakness.
Children infected with the virus excrete it in their stools, thereby
posing a dangerforthe unimmunized children around them.
MEASLES VACCINE
•
high fever, cough, running nose, watery eye
•
a characteristic rash appears on 4th day of illness, first
behind the ears, upper part of forehead, face and neck,
which later spreads to the trunk& limbs.
Infected children may develop complications - a serious form of
pneumonia.
HEPATITIS B VACCINE
Hepatitis B vaccine gives protection against disease caused by
Hepatitis B virus. Hepatitis B virus causes destruction of the liver
and is the leading cause of severe liver disease. Hepatitis B
vnfci
Pivh
IEC Division
Ministry of Health and Family Welfare
Government of India
Designed & Printed at Batra Art Press
Measles is a highly infectious viral disease. The disease is spread
by airborne droplet infection from secretions of nose and throat.
ClUal symptoms include:
Position: 1464 (5 views)