CHILD TO CHILD ACTIVITY
Item
- Title
- CHILD TO CHILD ACTIVITY
- extracted text
-
Child-to~Child
Activity Sheet 6.10
Chlld-to-Chlld Activity Sheets are a resource for teachers, and health and
community workers. They are designed to help children understand how to
Improve health in other children, their families, and their communities.
Topics chosen are Important for community health and suit the age, Interests
and experience of children. The text, ideas and activities may be freely
adapted to suit local conditions.
AIDS
THE IDEA
Every country has AIDS. In some countries the number of cases recognised so far are very few. In others
the disease is wide-spread and many people are dying. In all countries everybody, including children and
young people, must learn the facts about AIDS. Children everywhere in the next ten years of their lives
will be in danger of catching the AIDS virus. In countries where many young adults are infected, the future
’ of the society depends on their children’s knowledge, attitudes and practice.
This sheet gives explicit facts about how the AIDS virus is caught and how it can be prevented. It also looijs
at people’s attitudes and practices concerning AIDS. It aims to develop in children, their teachers and their
families an openness to discuss these sensitive issues, a confidence to take decisions for thehrselves, and
a sense of caring for people with AIDS.
WHAT DOES ‘AIDS’ MEAN?
A
Acquired
means ‘to get
*.
AIDS is acquired (or got) from other people who
have the AIDS virus.
I
Immune
means ‘protected’.
The body is normally immune (or protected)
against many diseases.
D
Deficiency
means ‘a lack of.
With AIDS, the body has a deficiency (or lack) of
immunity against many diseases.
S
Syndrome
means ‘a group of different signs of a disease’.
When people have AIDS they have a syndrome
or many different signs of disease.
WHAT IS AIDS?
AIDS is a disease which attacks the body’s protective
system. The body Is unable to protect itself properly
from other diseases such as diarrhoea, TB, coughs
and sores in the mouth. With AIDS, these diseases
make people very sick and they may even die.
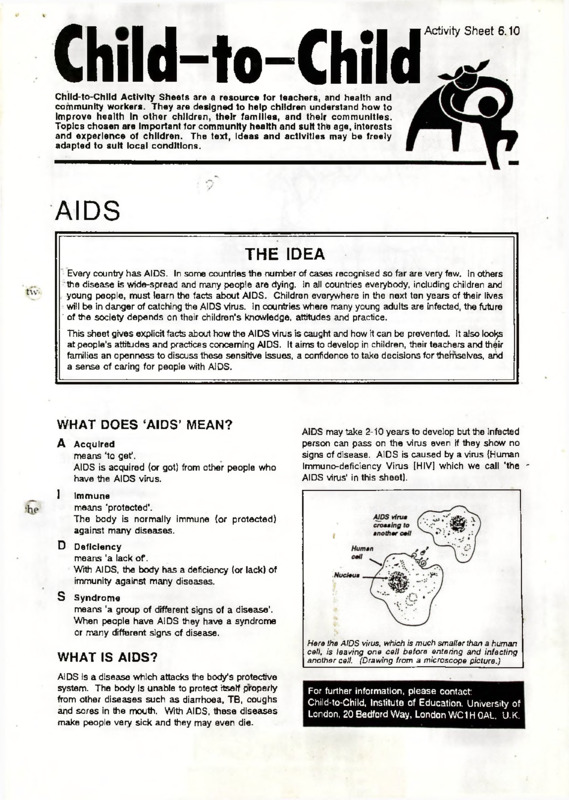
AIDS may take 2-10 years to develop but the infected
person can pass on the virus even if they show no
signs of disease. AIDS is caused by a virus (Human
Immuno-deficiency Virus [HIV] which we call 'the *
AIDS virus’ in this sheet).
Here the AIDS virus, which is much smaller than a human
cell, is leaving one cell before entering and infecting
another cell. (Drawing from a microscope picture.)
For further information, please contact:
Child-to-Child, Institute of Education. University of
London, 20 Bedford Way, London WC1H OAL, U.K.
The AIDS virus can be passed
from any infected to any healthy
person by UNPROTECTED sex
ual intercourse, EVEN ON ONE
OCCASION.
Although in some cases no
symptoms are noted for up to
10 years, any infected person
remains able to infect others
during this time.
Any time after 2 years from
infection, AIDS disease can
appear and the consequences
of common infections, such
as diarrhoea, cough, etc., can
become more serious and
lead to death
HOW IS AIDS SPREAD?
There are two main ways of getting AIDS. The AIDS
virus is transmitted:
•
By sexual intercourse (vaginal or anal) with any
infected person;
•
Blood-to-blood, if someone receives blood con
taining the AIDS virus from another person:
by sharing needles or using unsterilised
needles (for injections);
by transfusion in a hospital or clinic where the
blood has not been properly tested;
by using unsterilised instruments that cut the
skin (for circumcision, scarification, tattooing,
ear-piercing, etc);
However, unborn babies can also get the AIDS virus
from their mother’s blood during pregnancy.
AIDS IS NOT SPREAD BY
•
•
•
•
•
•
•
•
•
Shaking hands
Touching
Breathing
Kissing
Mosquitoes and bed bugs
Caring for those with AIDS
Cutlery and cooking utensils
Bedding and clothing
Toilets and latrines
MOTHERS WITH AIDS SHOULD CONTINUE
BREASTFEEDING. BREASTMILK IS STILL
THE BEST FOOD FOR BABIES.
J
PREVENTING THE SPREAD OF THE
AIDS VIRUS
The AIDS virus must be prevented from passing
between one person and another. It is impossible to
tell by looking at someone whether they carry the
AIDS virus. Therefore it is very important to protect
oneself against catching the virus.
HOW CAN THE AIDS
VIRUS BE PREVENTED
FROM SPREADING
BY.4SEX?
PEOPLE HAVE LIVED IN THE SAME HOUSE AS SOMEONE WITH THE
AIDS VIRUS FOr'mORE THAN 10 YEARS WITHOUT GETTING AIDS
•
By staying with one faithful
sexual partner.
The more
partners people have, the
greater the risk for both of
catching the AIDS virus.
••
By having safe sex. Kissing,
cuddling, touching are safe sex.
Penetration by the penis is not
•
By using a condom always.
Condoms, if used properly, will
do much to protect people from
AIDS and other sexually
transmitted diseases.
•
By drinking less alcohol. Alcohol
causes people to lose their
judgement about safe sex.
Drugs such as marijuana,
hashish, cocaine, heroin, etc.
can do the same thing.
•
By seeking early treatment for sores or unusual
discharge from the penis or vagina. People with
these sores or discharge are more likely to catch
and spread the AIDS virus.
.
HOW CAN THE AIDS VIRUS BE
PREVENTED FROM SPREADING BY
BLOOD?
•
By ensuring that needles, syringes and cutting
instruments are thoroughly washed after use and
sterilised by heat or chemicals. In national
immunisation programmes, health workers have
been specially trained in giving injections safely.
•
By asking for medicines which can be given by
mouth instead of by injection.
•
By avoiding contact with other people’s blood.
When giving first aid, it is important to cover cuts
and sores and wash hands well afterwards.
•
By reducing the number of blood transfusions.
Because blood can carry many diseases, doctors
now choose to give fewer blood transfusions.
School children are the future community and must
learn to be responsible for others as well as
themselves. Guided by school teachers, health
workers and community leaders, children can learn
how to protect their family, their partners and
themselves against AIDS. Children and young people
can make decisions about their own behaviour and
thereby offer safer patterns of sexual behaviour for
the community. For example, in Zambia there are
over 600 'Anti-AIDS Clubs’ organised by students in
schools throughout the country. The main aim of
these clubs is to give information on how AIDS is
spread and how to avoid it.
Here is part of a letter from a club member to the 'AntiAIDS Project in Lusaka which initiated the clubs:
/ received the things you
sent and I was very, very
glad.
I’ve signed on the
membership card and I’ve
kept the promises which I
must promise to follow as a
WHAT CHILDREN CAN DO
member of the Anti-AIDS
AIDS worldwide is a new problem and requires
changes in behaviour everywhere. Governments
can make some changes but families, communities
and schools play an important part
club. I’ve got questions for
you to help me.....
CARING FOR PEOPLE WITH AIDS
WHAT EVERY CHILD
SHOULD KNOW
We al! care for each other, In our families and
communities. Sick people, small children, old people
and orphans need our care. When a person has
AIDS, they may feel lonely and frightened. We need
to show that we care for them.
Schools should develop a policy that every
child should leave school knowing these
essential facts. Health workers and youth
group leaders can make a similar commitment
to pass on this vital knowledge.
People with AIDS need food, support, medical care,
physical help and particularly family and friends who
will accept them and listen to them. They can be
encouraged to live an active life wherever they are.
We can help them to lead a healthier life by encouraging
them to eat well, smoke less and drink less alcohol.
WHAT IS AIDS?
We cannot catch the AIDS virus by caring for someone
who is sick with AIDS. We must remember.
to protect the person with AIDS from infections;
to protect ourselves and others from the AIDS
virus.
AIDS is an infection. Al DS makes people
unable to protect themselves against many
kinds of diseases, such as diarrhoea, TB,
cough. Due to AIDS, these diseases can
make people become very sick and die.
We do this by following the usual hygiene principles:
HOW IS THE AIDS VIRUS SPREAD?
•
•
•
•
•
•
•
;
person:
•
•
•
By sexual intercourse with a person
carrying the AIDS virus;
By blood containing the AIDS virus getting
from one person’s body to another in
blood transfusions or on needles and sharp
instruments;
From an infected, pregnant mother to her
unborn child.
THE AIDS VIRUS IS NOT SPREAD BY
•
All teachers, not just the health education teacher,
have a responsibility to include teaching on AIDS in
their lessons. There are also many opportunities for
teaching about AIDS on other occasions where
children and young people gather together - in clubs,
religious meetings, youth and scout/guide groups.
The adults leading these sessions can choose the
appropriate activities. (In the following examples the
word 'teacher
*
can apply to all adults working with
children.)
|
The AIDS virus is spread from person to®
Covering open wounds on our hands;
Washing hands before and after caring for the
sick person;
Washing hands before handling food;
Keeping the sick person and surroundings clean.
ACTIVITIES FOR SCHOOL
AND YOUTH GROUPS
J
Insect bites, touching, and caring for
people with the AIDS virus.
WHEN AND WHERE TO DISCUSS ABOUT
AIDS
•
In health clubs or special anti-AIDS clubs, in
which the children learn about how AIDS is spread
and make a commitment to protect themselves
and teach others how to prevent AIDS.
•
Sometimes it is easier to talk about these sensitive
issues in single sex groups. The groups of girls
or boys can discuss issues about AIDS, share
their concerns openly, and support each other to
have confidence in the decisions they need to
make. It is easier if the adult involved is also of the
same sex.
|
|
GETTING THE FACTS RIGHT
years’ time. The teacher can ask questions like:
‘Who will you be living with?’; ‘Who will your
friends be?’; ‘How will you show your love and
friendship?’; ‘Might you try drugs, alcohol or
*;
smoking?
‘How might AIDS enter your lives or
the lives of your families and friends?’ The
children can then imagine their lives in 10 years’
time and answer the same questions. Finally
they can imagine that they are parents and have
children aged 13. What advice would they give
them?
Children can:
•
•
Play a true/false’ game. The teacher writes down
true or false statements about AIDS on separate
pieces of paper, e.g.: ‘You can catch the AIDS
virus from mosquitoes’ (false); ‘You can’t catch
the AIDS virus by shaking hands’ (true). On the
floor mark three areas - ‘TRUE’, ‘FALSE’ and
‘DON'T KNOW
*.
Each child takes one statement,
puts it on one of the three areas and explains the
reason for their choice. Anyone else can challenge
the decision.
•
Make a role play about different married couples
and how they treat each other. Which are the
happiest marriages?
•
Where possible, find out from newspapers or
government health departments the number of
AIDS cases in the country. Work out the
percentage of the total population this figure
represents.
Discuss situations when it is sometimes difficult
to say ‘No’ and list the reasons. In pairs, children
can role play different situations, imagine how
people might try to persuade them to do something
and how they could say, ‘No’ in a way which is
polite but firm, e.g. when asked:
to have a cigarette;
to go somewhere with a stranger;
to go out for the evening.
•
Visit a local health centre. Health workers can
talk about why they give injections and
demonstrate how needles and syringes are
sterilised.
Find out what guidance their religious books give
on sexual practices.
DISCUSSION AND ROLE PLAY ABOUT
ATTITUDES TO PEOPLE WHO HAVE AIDS
Write quiz questions about AIDS and discuss the
answers in pairs.
FINDING OUT ACTIVITIES
Children can:
•
•
DISCUSSION AND ROLE PLAY ABOUT
AVOIDING AIDS
Children can:
•
Imagine how AIDS might affect their lives. They
can shut their eyes and imagine their lives in two
Children can:
•
Collect newspaper cuttings concerning AIDS and
discuss the attitudes the articles suggest.
•
Write poems expressing their feelings about AIDS
and its effect upon their own or other people’s
lives.
•
Use pictures, e.g. of someone caring for a friend
with AIDS, to help them to imagine how they
would feel in the role of one person in the picture.
They can ask questions about what events led to
the scene shown and what might happen in the
future.
•
Create short plays, for example about caring at
home for a person with AIDS. They can first act
the play themselves, then each make a simple
puppet for their character and perform the play
with puppets to the rest of the school or the
community.
•
Collect and discuss stories from religious books
of people caring for the sick.
•
Fill in the details of a story, for example about an
imaginary school pupil thought to have AIDS.
The children divide into groups representing, in
this example, the pupil, other pupils, teachers
and parents. Each group separately considers:
*What do I feel?’, ‘What are the main effects on
me?**, and ’What do I want to happen?’. After 15
minutes the groups reassemble and share their
discussions.
•
PASSING ON THE MESSAGE
Children can:
•
make up and perform songs, plays and puppet
shows about AIDS;
•
design and make posters to display in class and
on open days;
•
join in the promotion of sports for better health of
people with AIDS.
Listen to the following stories:
A young woman returns to her village
from a neighbouring city. As she walks
across the square people shout at her
“AIDS! AIDS!” Her stepfather insists that
she gets an AIDS test before she lives in
the family home. The test is positive. ’
FOLLOW-UP
Teachers can:
•
A group of politicians see a video showing
a person dying of AIDS and make a policy
that everyone should be tested and those
carrying the virus should be locked up.’
ask children different questions to find out if they
know:
what spreads AIDS;
what does not spread AIDS.
•
ask children to write stories:
about people catching the AIDS virus;
about caring for people with AIDS.
Then look at the stories. What do they tell us
about children’s knowledge and about their
attitudes?
‘The colleagues of a woman whose
husband has AIDS refuse to work with her.
She is sacked.’
•
ask children to find out how many local schools or
youth groups have clubs and activities which look
at AIDS. What do they do? Have the children
joined them?
•
find out if children have:
Then try to answer these questions:
•
•
•
•
What do you think about these situations?
Why do people react in these ways?
Will these reactions help to control the spread of
AIDS?
What would you do If you were any of the
characters in these stories?
taken part in anti-AIDS campaigns;
helped anyone with AIDS;
warned other children about the risks of AIDS.
CHILD-TO-CHILD PUBLICATIONS
Available through
TALC (TEACHING-AIDS AT LOW COST)
DECEMBER 1993
ENGLISH
1.
Sample pack of Child-to-Child Activity Sheets
Free
2.
Complete pack of Child-to-Child Activity Sheets
£2.00
3.
Child-to-Child and Disability (2 Readers and 14 Activity Sheets concerning disability)
£4.20
4.
Child-to-Child Readers:
Dirty Water (level 1)
Accidents (level 1)
Not Just a Cold (level 1)
A Simple Cure (level 2)
Teaching Thomas (level 2)
Down with Fever (level 2)
Diseases Defeated (level 2)
Flies (level 2)
I Can Do It Too (level 2)
Deadly Habits (level 3)
£1.30
£1.30
£1.30
£1.45
£1.45
£1.45
£1.45
£1.45
£1.45
£1.45
5.
Health into Mathematics: William Gibbs and Peter Mutunga. The first in the Health Across the
Curriculum series, this volume teaches many basic concepts of mathematics while making them
relevant to everyday life by using health examples.
£4.50
6.
Primary Health Education: Beverley Young and Susan Durston. This successful and extremely
popular volume has been used by primary school teachers worldwide to help with health education
in schools.
£5.50
7.
Toys for Fun: June Carlile (Ed). A book of toys for pre-school children with multi-lingual text
(English. Arabic. French, Portuguese, Spanish and Swahili all in one volume).
£2.00
8.
Children, Health and Science: Hugh Hawes, John Nicholson and Grazyna Bonati. This book,
designed for science teachers in primary and secondary schools, contains an introduction and 20
specially selected Child-to-Child activity sheets. Certain groups can receive bulk orders free.
(French and Spanish versions are available directly from Unesco. Paris.)
£1.00
9.
Child-to-Child: A Resource Book: Grazyna Bonati and Hugh Hawes (Ed). This contains most
Child-to-Child activity sheets, sections on methodology, evaluation and running workshops, and
examples of action taken from round the world.
*
£5.00
10.
Education for Health in Schools and Teachers’ Colleges: This contains guidelines for the
introduction of Child-to-Child approaches in primary schools, teachers’ colleges and the curriculum.
based on experience from projects over many years.
£2.00
11.
We are on the Radio (book plus tape): Clare Hanbury and Sara McCrum. Introduces basic broad
casting techniques and skills for those who want to involve children in making effective broadcasts
about health.
£3.50
12.
Child-to-Child and Children Living in Camps: Clare Hanbury (Ed). Written for people working
with children in refugee camps or camps for displaced people, this volume contains specially adapted
Child-to-Child materials plus a section on these children’s special needs.
£2.50
13.
Children for Health: Hugh Hawes and Christine Scotchmer (Ed.) This book contains all the
messages in the 1993 version of Facts for Life together with sections to help children understand the
health ideas and act upon them both in and out of school. 25% discount available on orders of 100 or
more copies.
£2.00
Special price for overseas.
’
SPANISH
1.
Child-to-Child Activity Sheets
2.
Spanish versions of the Child-to-Child Readers:
*
£2.00
£1
Accidentes
£1
\gua Sucia
£1
Buena Alimentation
£1
Enseriandole a Tomas
£1
Un Remedio Sencillo
£1
8 8 8 8 8 8
A Bajar la Fiebre
Please send your orders with payment to TALC, P.O. Box 49, St Albans, Herts AL1 4AX, U.K. (Tel. (0727) 853869;
fax: (0727) 846852). Add 30% to the total cost of the books for surface or U.K. mail (minimum £2.00) OR 60% for
airmail (minimum £2.50).
Available from ARC, PO Box 7380, Nicosia, Cyprus:
ARABIC
Adaptations of Child-to-Child Readers:
Dirty Water
Teaching Thomas
I Can Do It Too
Diseases Defeated
Down with Fever
A Simple Cure
Good Food
Flies
Available from EDICEF, 26 rue des Fosses Saint-Jacques, 75005 Paris, France:
FRENCH
Child-to-Child Readers:
La Fievre du Lion (Le coup de chateur)
Le Vieux Roi et la Petite Fiancee (L’alimentation des bebes)
L’Hyene aux Yeux de Poulet (La vitamine A)
Halte aux Maladies! (Les vaccinations)
Fati n’est plus Triste (Les enfants handicap's)
La Revanche de Sonko-le-Ltevre (L’hygiene des puits)
Mon Petit Frere est Malade (La diarrhee)
Surveillons les Petits (Les accidents)
La Pernique Rouge de Bouki (Les poux)
Le Jeune Homme et le Dragon (Les vers)
Available from the Child-to-Child Trust, Institute of Education, 20 Bedford Way, London WC1H 0AL, U.K.:
A set of 4 Activity Sheets Helping Children in Difficult Circumstances:
Children who Live or Work on the Street
Children who Live in an Institution
Helping Children whose Friends or Relatives Die
Helping Children who Experience War or Disaster
Christian Responses to AIDS
A Bibliography
Caritas Internationalis: El SEDA. Un Desafio a la Iglesia.
Memoria del Coloquio de Santo Domingo, Iglesia y Enfermos de SIDA, Enero 7 al 12, 1990.
Secretariado Latinoamericano de Caritas (SELAC), Apartado Postal 1703 1389, Quito Ecuador.
Catholic Health Associaton of the United States (ed.): The Gospel Alive. Caring for
Persons with AIDS and Related Illnesses.
(1988). Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO
63134-0889/ USA. ISBN 0-87125-149-3.
This book addresses AIDS in relation to the special opportunity it provides all of us, as Church, to herald
Christ's message and care for others.
Cosstick, V.: AIDS. Meeting the Community Challenge.
(1987). St. Paul Publications, Middlegreen, Slough SL3 6BT/ United Kingdom. ISBN
0-85439-264-5.
This book brings together the precious experience ofprofessionals and concerned laity, of religious leaders,
priests and religious. And it makes abundantly clear that the solution to the moral problem which lies behind
the questions ofpublic health is not to be found in declarations by experts but in the perceptions and
spiritual renewal ofthe whole people ofGod.
Cullen, T.: AIDS. A Christian Response.
(1991).Montfort Missionaries, P.O.Box 280, Balaka, Malawi.
This pastoral book aims at improving our understanding of the AIDS disease by presenting it from four
different angles: the Spritual, Psychological, Moral and Cultural viewpoints. The book does not offer an
exhaustive analysis ofall these aspects; only a few are selected and reflected upon. The writers come from
different Christian denominations and they are concerned to present a Christian response to the present
AIDS crisis in Malawi.
Dorr, D.: Integral Spirituality. Resources for Community, Justice, Peace, and the Earth.
(1990).Gill and Macmillian Ltd., Goldenbridge, Dublin 8/ Ireland. ISBN 07171-1730-8.
Throughout the book there are guided meditations and other resource materials which can be used by groups
or individuals to put the spirituality into practice. Beginning with a study of "down-to-earth-spirituality"
which enables one to be "rooted" or "grounded", the author goes on to show how personalprayer plays a key
role in spirituality.
Joinet, B.A.: The Challenge of AIDS. Vol.l: Basic facts.; Vol.2: Prevention and
Survivors. (1992).Fr. Bernhard Joinet, W.F., P.O.Box 280, Dar es Salaam/ Tanzania.
These two volumes will give educators and pastors the information they need to help people make their own
decisions when faced with the AIDS pandemic.
Kelly, R.(S.J.): Calming the Storm. Christian Reflections on AIDS.
Mission Press, P.O.Box, 71581 Ndola/Zambia.
This book invites usfirst to make sure that we have some understanding ofthis new disease, how it spreads
and how it can be prevented. Then we will reflect on what the AIDS crisis is saying to us as people and as
Christians about modem society and the way we live and the values that influence our life-style.
Kirkpatrick, B.: AIDS. Sharing the Pain. A Guide for Caregivers.
(1990). Pilgrim Press, 475 Riverside Dr., New York, N.Y. 10115/ USA. ISBN
0-8298-0827-2.
The author offers practical and sensitive guidelines for the care of those infected by HIV. He explores the
pain and difficulties ofthose who are going through the various stages ofAIDSfrom initial to full-blown
AIDS.
MAP International (Ed.): The Church's Response to the Challenge of AIDS/HIV. A
Guideline for Education and Policy Development.
(1991). MAP International, P.O.Box 50, Brunswick, GA 31521-0050.
This document is not designed to be an exhaustive discussion of the issue, but rather a frameworkfor the
local church's approach to AIDS/HIV. It touches on the fears and the facts related to AIDS and HIV
infection, as well as ways to educate and involve a local congregation. Each local church will need to address
AIDS/HTV in its own specific community.
Me Cloughry,R., and C. Bebawi: AIDS: A Christian Response.
Grove Ethical Studies, No.64. (1990). Grove Books Ltd., Nottingham NG9 3 DS/ United
Kingdom.
In this small booklet there are two parallel lines ofthought. The first may be seen by some as pessimism about
the future. Even were it possible to find a vaccine for AIDS soon, many thousands ofpeople will still die. The
scale of the human tragedy to come is awesome, but farfrom bringing people to a new sense of their need of
God. The second arises out ofthe Christian calling to hope, faith and love and to enable those who may
otherwise choose despair to choose life.
Sandys, S.: Embracing the Mystery. Prayerful Responses to AIDS.
(1992). SPCK, Holy Trinity Church, Marylebone Road, London NW1 4DU/ United
Kingdom. ISBN 0-281-04574-7,
In this book there are prayers, readings and meditations - many ofthem written specially for this book - that
can be used by individuals or groups as part oftheir practical response to the tragedy ofHIV infection.
Tilleraas, P.: The Color of Light. Daily Meditations for All of us Living with AIDS.
Hazeldon Meditation Series. (1988). Hazeldon Press. Pleasent Valley Road, Box 176, Center
City, MN 55012-0176, USA. ISBN 0- 89486-511-0.
This book offers hope and comfort as we struggle to cope with AIDS in our lives and in our society. Here is
daily guidance on moving from isolation toward loving support, rediscovering spiritual rewards, and
reaching out with love and wisdom.
<
htlcrnnlioiinl {ouriml of STD & AIDS 1992; 3: 79-86
/A / ■
1/lJ W
EDITORIAL REVIEW
HIV and pregnancy
Frank D Johnstone MD FRCOG
Royal Infirmary of Edinburgh/Simpson Memorial Maternity Pavilion, and Department of
Obstetrics and Gynaecology, University of Edinburgh, Centre for Reproductive Biology,
Edinburgh, UK
Keywords: Human immunodeficiency virus, pregnancy, baby, transmission
In the United States and Europe, the number of
women with AIDS is increasing rapidly, both in
absolute terms and as a ratio to men1'2. Thus in the
55% of all AIDS cases in women in the
epidemic's first decade have occurred within the last
two years3. Although injection drug use was the
predominant mode of transmission initially, hetero
sexual transmission is becoming the dominant
route3, with all the potential this involves for much
wider dissemination. In a Paris study, 20% of
infections in women were attributed to heterosexual
intercourse in 19874. In 1989 the proportion was
58% and increasing.
In Africa, the scale of the problem and the
potentially devastating consequences of maternal
and childhood infection with HIV have long been
recognized5. New worries surround reported
increases in prevalence in South America6,
Thailand7 and India8.
In addition to the particularly harrowing problem
of children becoming ill and losing parents^ there
^^many unresolved scientific questions concerning
W-ie, timing and prevention of vertical transmission.
All these features combine to project pregnancy to
the forefront of current concern in HIV infection.
In this necessarily limited review I will leave aside
important issues such as testing and screening for
HIV in pregnancy9-11 and clinical management12-14.
Instead, I will restrict discussion to three areas
which are contentious, but of intense research and
clinical interest; the effect pregnancy has on HIV
disease progression; the effect HIV has on
pregnancy outcome; and vertical transmission.
EFFECTS OF PREGNANCY ON HIV DISEASE
Pregnancy is believed to be associated with a mild
impairment of the immune system, together with
an increased virulence of some infections. This has
fuelled concern that pregnancy may exacerbate the
progression of HIV disease.
Correspondence to: Dr F D Johnstone, Senior Lecturer,
Department of Obstetrics & Gynaecology, University of Edinburgh,
Centre for Reproductive Biology, 37 Chalmers Street, Edinburgh
EH3 9EW, UK
Pregnancy and susceptibility to infectious disease
The evidence for a decline in immune response in
pregnancy is conflicting. There is agreement that
antibody mediated immunity is unchanged, with no
alteration in B cell number15, satisfactory antibody
responses to vaccines in pregnancy16-18 and
unchanged or slightly increased complement
levels19'20. Most studies have found a reduction in
absolute T cell counts15'21-23 but this could simply be
a haemodilution effect, and there are differing reports
about a decrease in CD4 cells expressed as a
percentage of total lymphocytes or as a CD4/CD8
ratio22'23. T lymphocyte function does not appear
to be reduced23*24. Current opinion suggests that
systemic T cell function is maintained, but that there
is some depression of cell mediated immunity,
perhaps due to the raised levels of some steroid
hormones and/or plasma proteins in pregnancy25.
There are many studies which suggest increased
virulence of a number of infectious diseases in
pregnancy and these have been excellently
reviewed26-27. The methodology of many of these
studies has been criticized28 but the totality of
supporting evidence is impressive. Perhaps the best
example of increased susceptibility to infection is
falciparum malaria29 but there is also good evidence
of increased risk with hepatitis30-31, polio32-34>
influenza35'36 and general clinical recognition of
worsening of vulval papillomata26.
Progression of HIV disease
For the above reasons there have been persistent
concerns that pregnancy may adversely affect
progression of HIV disease. Initial reports tended to
confirm these concerns37'38. However, these studies
were based on identification of mothers of children
who had already developed AIDS, and who were
themselves at particularly high risk39.
Although several studies of the effect of pregnancy
on the natural history of HIV disease are in progress,
none have been reported in full. Two reports, one
from France40, the other from Haiti41, suggested
higher progression to CDCIV disease in women who
had completed a pregnancy compared to a non
pregnant control group. However, numbers were
SO
Inh*iIidlion.il lounidl et SID & AIDS Volume 3 March April IW?
small, and whether I he groups were comparable in
time since seroconversion is not known. Similar
studies from New York42, Bethesda'13, and Genoa1'1,
did not document any adverse clinical effect of
pregnancy on the progression of HIV.
A number of studies have examined prognostic
markers which may be taken as surrogates for
clinical progression. In Edinburgh, follow up of
152 women enrolled since 1985 has not shown
women who had a pregnancy to be disadvantaged
(compared with non-pregnant HIV infected women)
in terms of clinical, virological, or immunological
progression45 (and unpublished data). Similar
conclusions have been reached by Berrebi et al.46
from Toulouse, France.
The type of analysis used in all the above studies
has implicit methodological problems of ensuring
comparability of disease status between groups.
Indeed, systematic bias could occur if iller women
deliberately avoided pregnancy; if non-pregnant
drug users were more likely to continue to inject47;
or if the non-pregnant group were significantly
older. Another, and perhaps preferable, method is
to study the effect pregnancy has on each woman's
slope of fall in CD4 lymphocyte count with time.
She will thus be her own control, in terms of CD4
decline before and after pregnancy. An attempt to
do this was made by Biggar et al.48. The authors
believed their data were compatible with the
hypothesis that pregnancy may mildly accelerate
HIV induced depletion of CD4 lymphocytes, and
could therefore increase the rate of progression.
However, they had.no non-pregnant HIV sero
positive control group, and this conclusion does not
seem justified.
In short, conclusive evidence about the effect of
pregnancy on longer term progression of HIV
disease is lacking. Available studies have small
numbers, relatively short follow up, and methodo
logical problems. However, it seems unlikely
that pregnancy has any major adverse effect on
asymptomatic women.
AIDS in pregnancy
There are other possible ways in which pregnancy
could affect disease. In susceptible, immuno
compromised women, the additional pregnancyinduced fall could reduce CD4 lymphocyte count
below the threshold for opportunistic disease.
Pregnancy could also increase the probability of an
AIDS defining illness being fatal, or affect longer
term prognosis after a CDC 4CI defining event.
Published case reports suggest that the outcome
of AIDS in pregnancy is poor. In the United States,
the first 6 reported cases of Pneumocystis carinii
pneumonia (PCP) were fatal49"51 as was a case of
listeria bacteraemia where AIDS was assumed52.
Further reports of pregnancy-associated deaths from
AIDS have followed53-55.
In contrast to this? as late as 1990, Hicks et al.56
described a single case of a woman who developed
PCP during pregnancy but survived (his initial
episode. The authors claimed this was the first
reported case of survival from PCP in pregnancy.
This bias to mortality is strikingly different from
the situation in non-pregnant women. However, the
gloomy outlook may simply represent reporting
bias. Thus survival from PCP in pregnancy has been
reported by others57. Physicians are more likely to
report fatal cases, and perhaps journal editors are
more likely to publish such reports. Nothing is
known of non-fatal AIDS defining illness in the
population from which these women are drawn,
and there is no satisfactory information about
survival time after AIDS in pregnancy.
The only series which addresses these issues,
and has the advantage of being based on a total
geographical population, is from Edinburgh58.
Numbers are too small to provide reliable data, with
only 22 women with AIDS, four of whom were
pregnant. However, all three women who had PCP
for the first time in pregnancy survived this initial
episode, and survival time was not obviously
reduced by the conjunction of AIDS and pregnancy.
Whether the onset of AIDS in pregnancy does
carry a worse prognosis is not known. Because it
remains an uncommon event in the developed
world, and because the issue has not been
specifically studied in Africa, it will be some time
before this becomes clear.
EFFECT OF HIV INFECTION
ON PREGNANCY OUTCOME
There are several theoretical ways in which HIV
infection might affect pregnancy outcome59.
Abortion
Several studies have found an association between
HIV seropositivity and a history of spontaneous
abortion6®-62 but these studies have the problem
that the woman's HIV status during that pregnancy
was unknown. A case control study in Nairobi
showed HIV infection to be more common in
women admitted with a spontaneous abortion,
but the difference with control women whose
pregnancy was continuing was not statistically
significant63. A small prospective study64 did not
show an increase in spontaneous abortion. It is,
therefore, uncertain at present whether HIV is
directly associated.
Several studies have shown a higher HIV sero
prevalence in women having induced abortion than
in those continuing pregnancy65*66 and it might be
expected that women infected with HIV would
accept termination of pregnancy readily. Thus, 80%
of pregnant women in France67 and 83% of young
women in New York68 were in favour of abortion
for HIV infected women. Women actually infected,
behave differently however.
Studies from New York69 and Edinburgh70 have
not shown termination of pregnancy to be chosen
luhii.sienv
more commonly bv 11IV seropositive women
compared Io 111V seronegative drug using controls.
Eighty-five per cent ol women who tested HIV sero
positive were estimated in a survey of major obstetric
clinical centres to continue their pregnancy71.
Some of the reasons which underlie decision
making about pregnancy were discussed bv
Selwyn69. However, local perception of illness and
death due to HIV may influence choice, and in
Edinburgh, seropositive women now seek termi
nation of pregnancy significantly more often than
controls.
Powerful factors motivate an asymptomatic infected
woman to continue pregnancy, and counselling
must be sensitive to the extremely difficult issues
considered by her in making her decision.
Pregnancy complications K
Aarly studies reported a high incidence of pre-term
labour, caesarean section, syphylis and low birth
weight72-75. These studies were uncontrolled and
illicit drug use and poverty are known to be
associated with both HIV infection and poor
pregnancy outcome.
The first controlled study, in Edinburgh women,
most of whom had a history of drug use, showed
both case and control groups to have a high
incidence of pre-term labour, intrauterine growth
retardation, and low birth weight. However, there
were no differences according to HIV status74.
A prospective study of methadone clinic attenders
in New York64 did not show differences in
pregnancy complications and outcome, and nor did
a larger study from New York75. Similar findings
were reported from Milan76 and Toulouse77.
These data from the United States and Europe
^ontrast with much information from Africa. Several
wLrge studies from Zaire78-79, Congo80, Zambia81,
Kenya82, Uganda85 and Rwanda84-85 compared
pregnancy outcome in women who were, and were
not, infected with HIV. These studies include
1832 infected mothers and 3911 HIV seronegative
controls. HIV seropositivity was associated with;
pre-term delivery in some studies78"85 but not
others79-82-84-85; increased perinatal deaths in some
studies78-85-85 but no difference in others82-84. An
increase in chorioamnionitis in HIV positive
pregnancies was reported in one study78, bleeding
in the third trimester in another82, twinning in
another80. One large case control study from Kenya
focused on stillbirth and low birth weight86. Linear
logistic regression retained HIV status as a
significant association of these adverse outcomes
with odds ratios ranging from 2.0 to 2.9.
Although these reports on pregnancy compli
cations are somewhat inconsistent, all of the African
studies agree that birth weight is reduced in HIV
infected women. The difference from controls
ranges from 130 g84 to 232 g (calculated from ref 78).
There is evidence that decrease in fetal size at birth
is related to stage of maternal disease78. However,
11|\'.mJ prvgn.ui*y
S|
birth weight is unrelated to whether or not the baby
is itself infected'
Congenital abnormality is probably not more
common in HlV« infected women
*
5’. A dysmorphic
syndrome associated with 11IV was reported1’0-91
but subsequent reports have not confirmed this
finding92-95 and an HIV dysmorphic syndrome was
not seen in the large European Collaborative
Study89.
Reasons for the discrepancies between studies
The differences between African studies and those
from Europe and the United States may arise partly
from problems of methodology. Control groups in
the African studies are loosely matched and clearly
differ in other respects apart from HIV status. The
differences tend to be in a direction which would
favour the control groups as far as pregnancy
outcome is concerned. Attempts have been made
to allow for these differences using linear logistic
regression, but residual distinguishing features may
remain to confound the analysis.
There are other possible reasons for the dis
crepancies. The number of pregnancies studied in
Europe and the United States is very small in
comparison with the African studies and thus real
differences could be missed. In addition, the great
majority of women have been asymptomatic. In
contrast 18% of women had AIDS in one African
study78 while 53% and 17% were symptomatic in
others81-82. Finally, the difference in African popu
lations may be due to differential load of other
infectious diseases (particularly malaria) and to
differences in nutritional status. Basic data on
malarial parasites and maternal weight do not seem
to have been reported.
Conclusions
In asymptomatic women, HIV infection per se
may be associated with a modest reduction in birth
weight, but the effect on pregnancy appears to be
slight. Under African conditions, there may be
increased rates of spontaneous abortion, pre-term
labour and stillbirth. When a woman' becomes
clinically ill, it seems inevitable that there will be
a detrimental effect on pregnancy, and there is
evidence that this is so.
TRANSMISSION OF INFECTION TO THE BABY
Infection could be transmitted to the baby in utero,
at delivery, or by breast feeding. The relative
importance of these routes is still not certain,
although unlike other retroviruses breast feeding
does not seem to be the major mode of spread. The
outlook for infected children seems poor with one
third becoming ill with HIV disease within the first
year of life89., Th ere may be a bimodal pattern of
disease in perinatally-acquired infection94.
M2
h.»< rn.i!:oii.il bnirn.ii ■ .1 s| D - ,.\!i;S
Volume 3
M.iu.lvApnl |V»2
Timing and inode of transmission
The mode of transmission is uncertain. hi vitro
studicsshow that trophoblast is readily infected by
HlV-lM- ’ though there is dispute about whether
this is by a pathway mediated by CD/'5-96. Lewis
ct al.'
* 7 apparently located HIV-1 antigen in villus
trophoblast derivatives, villus mesenchymal cells,
and embryonic blood cell precursors in tissues from
3 out of 3 8-week fetuses, and claimed that there is
therefore a cytological pathway for transmission
established by 8 weeks.
Several early studies suggested that transmission
of HIV could occur in utero5*-™'™. Subsequently,
successful culture of HIV-1 was reported from 4 out
of 14 second trimester fetuses1(x)-101 and HIV DNA
sequence could be detected using polymerase chain
reaction in 12 of 41 fetuses101'104. In all these
studies, precautions were taken to minimize the
possibility of maternal cell contamination, but it is
difficult to exclude this beyond all doubt. One study
which seems to have done this used a polymorphic
DNA sequence adjacent to the cystic fibrosis
locus105. These authors examined only fetuses
where the mother was heterozygous, and the fetus
homozygous, for this sequence. In 9 such fetuses,
the maternal specific allele could not be detected,
thus excluding maternal cell contamination, but
HIV-1 DNA sequences were detected in 8. This
seems a surorisinglv high rate of HIV detection in
the light of known figures for transmission to the
child, and raises the possibility that defective
fragments of DNA are being identified rather than
true infection.
Even though infection can be transmitted early in
intrauterine life, it is not clear whether this is the
common or usual timing. The very early onset of
clinical and immunological features in some infected
children is suggestive. However, the fetus could be
infected late in pregnanev, during delivery bv
exposure to maternal blood or cervical mucous, or
postnatally through breast feeding. This timing is
of critical importance because if infection is usually
around delivery, the risk might be reduced by
prophylaxis (for example with large amounts of
soluble CD4 or zidovudine). Unfortunately, though
this is such a key issue, many uncertainties remain.
The risk of vertical transmission
Early reports suggested a transmission rate of at
least 50% but were biased by the inclusion of
children who presented ill. Prospective studies have
suggested rates of 13-39%78-81 -s~-89-106. The largest
study reported is the European Collaborative
Study89. Of 419 children born 18 months or more
before analysis, 372 were of known infection status,
48 were infected (12.9%). A further 4 had repeatedly
positive viral cultures, even though they had cleared
maternal antibody. Some of the differences in these
studies can be attributed to methodological problems,
as was discussed in the paper from the European
Collaborative Study89. Thus some studies included
younger children who were ill, hence inflating the
numerator artificially. Others had a low follow-up
rate, and one used virus culture on cord blood as
an end point for infection. Nevertheless, it seems
likely that much of the variation in transmission is
genuine and is related to population differences.
These include particularly stage of HIV disease, but
may also include other infections, and breast feeding.
Factors influencing vertical transmission
These are becoming clearer. There are maternal
features, probably mainly reflecting high viral load.
Placental abnormality and fetal genotype may also
be relevant.
There are accumulating, and convincing, data that
transmission is particularly likely late in the course
of disease107, when the woman is severely immuno
compromised. A French study108 reported that 66%
of 15 women with CD4 count in pregnancy
< 150/cm3, 50% of 24 women with P24 antigenaemia,
and 78% of 14 women who displayed a high viral
replication rate of HIV in culture, transmitted
infection to their babies. The significance of a low
maternal CD4 lymphocyte count was confirmed by
others39-109 while a Nairobi study110 claimed that
transmission correlated with maternal viral load as
assessed by quantitative polymerase chain reaction.
In addition to late disease being a risk factor, there
is evidence that vertical transmission is also likely
in the first year after seroconversion39. This
presumably also represents a time of higher viral
load, before relative protection from broadly
neutralizing antibody.
There is a search for more specific markers to
identify those individuals most likely to transmit
infection. This would help in counselling about
pregnancy and termination and also could select out
pregnancies at sufficiently high risk to justify trials
of drug prophylaxis. The levels of antibody to
epitopes on the hypervariable V3 loop of viral
gp 120, or the MN primary neutralizing domain,
have been found by some workers to be predictive
of fetal infection106111. This has not been confirmed
by others112"117 and certainly infection does seem to
have occurred despite high maternal levels of
antibodies. Nsvami et al.Ub may be correct when
they suggest that any protective effect of antibodies
against gp 120 neutralizing epitopes is type specific
rather than group specific.
As well as maternal factors, there are suggestions
that placental damage may be associated with
an increased rate of transmission. There is an
association with chorioamnionitis 78. The finding of
a high transmission rate with maternal anaemia
(though it could simply be a reflection of HIV
disease activity) could result from malaria, which
preferentially infects the placenta118. In addition,
fetal genotype may be important. One study reported
that susceptibility to HIV infection was related to
genetic variation in HLA immune response genes119.
h’hnstenv.
Finally, what obstetric factors could influence
transmission? Invasive fetal procedures, (cordocentesis, scalp sampling, application of scalp electrodes
etc) could result in micro-inoculation of the fetus
with maternal blood and hence cause infection.
Interestingly, the only fetal sample with maternal
blood contamination in one study was the one
where earlier cordocentesis had been performed101.
Such procedures should therefore be avoided where
the mother is infected. The role of caesarean section
is unclear. In theory elective caesarean section could
be protective by minimizing time spent by the baby
exposed to cervical mucus and blood from cervical
dilatation. A study of twins discordant for HIV
transmission could give support to this120. Of 15
discordant twin sets the first twin was infected in
13 cases, the second in only 2 (P = 0.01). Infection
of the baby has certainly occurred despite caesarean
^^ection being performed72'87'88'1061121. However,
wPaost studies do not clearly distinguish between
elective caesarean section, with intact membranes,
and caesarean section done after many hours in
labour with ruptured membranes, where it would
not be expected to be protective.
At present caesarean section should be performed
for standard obstetric reasons only, but this advice
may have to be revised as more evidence
accumulates.
The situation with zidovudine is unclear. In
the few cases reported so far, there have not been
major problems with use during pregnancy122'123.
However, infection of the infant has been
documented despite zidovudine treatment
throughout pregnancy124*125.
Breast feeding
^Dther retroviruses, such as Moloney murine
leukaemia virus126 or HTLV I in the human127 are
spread principally by breast feeding. HIV-1 occurs
in breast milk128 and there is no doubt that
infection has been transmitted to the baby postnatally by women infected by blood transfused for
post partum haemorrhage129"131. In addition, an
African study showed that 53% of women who were
seronegative at birth but who later seroconverted,
infected their babies132. In these situations, before
the development of neutralizing antibody, viral load
may be very high, and this may not parallel the
situation with an already infected woman. However,
one European study has reported significantly
higher infection rates in breast fed babies88.
It seems probable that breast feeding carries a risk
of infecting an otherwise non-infected baby. This
extra risk is probably small, and current belief is that
breast feeding is not a major route of transmission.
The avoidance of breast feeding itself carries risks,
particularly in developing countries but also to a
lesser extent in the industrialized world. Advice
about breast feeding is therefore dependent on an
assessment of these different risks in the population.
Mathematical models of the event frequencies
IIIV and prvgn.mcv
S3
which have to be taken into account have been
suggested133. In general terms, HIV infected
women in developed countries should be advised
to bottle feed. In countries where formula milk is
not readily available, and where poor standards of
hygiene are used in constituting milk powder,
breast feeding should continue to be promoted, as
offering infants the optimum chances for survival.
Conclusions
Progress is being made in several aspects of the
interaction between HIV and pregnancy. However,
many uncertainties remain. In particular, the timing
and mechanisms of vertical transmission are criticallv
important but poorly understood, and there is so
far no effective way of interrupting transmission to
the baby.
There is no reliable way of predicting early in
pregnancy which woman will transmit infection,
and no fully established method of early diagnosis
of infection status in the infant. The only certainty
about HIV and pregnancy is that the problem will
not disappear in the near future.
References
1 Centre for Disease Control: Update: Acquired immuno
deficiency syndrome—United States 1981-1990. M.MWR
1991;40:358-63
2 WHO Collaborating Centre on Aids—AIDS surveillance in
Europe Quarterly Report No. 24: 1989 December (Paris WHO)
3 Berkelman R, Fleming P, Chu S, Hanson D. Women and
AIDS: the increasing role of heterosexual transmission in the
United States. Vllth International Conference on /\IDS
1991—Florence, Abst. No WC 102
4 Henrion R, Henrion-Geant E. Mandelbrot L, et al. Trends
in HIV transmission in pregnancy. Lancet 1990;i: 1401(letter)
5 Piot P, Plummer F, Mhalu F, et al. AIDS: An international
perspective. Science 1988;239:573-9
6 Duart G, Mussi-Pinhata MM, Feres MC, et al. The ascendent
pattern of seropositivity for HIV antibody and the risk factors
associated to the HIV transmission in parturients cared at
a school hospital in Brazil. Vllth International Conference
on AIDS-Florence, 1991 Abst. No. WC 3257
7 Ung Chusak K, Thanprasertsuk S, Vichai C, et al. Trends
of HIV spreading in Thailand detected by National Sentinel
Surveillance. Vllth International Conference on AIDSFlorence, 1991 Abst. No. MC 3246
8 Kandaswami J, Ravinathan R, Padmarajan S, et al. Seroepidemiological study of HIV infection in two major centres
of South India. Vllth International Conference on AIDSFlorence, 1991 Abst. No. MC 3302
9 Johnstone FD. Ante-natal screening for HIV—review and case
for anonymysed unlinked studies. In: Templeton AA,
Cusine D, eds. Reproductive medicine and the law. Edinburgh:
Churchill Livingstone, 1990:123-39
10 Holman S, Sunderland A, Berthaud M, et al. Prenatal HIV
counselling and testing. Clin Obstet Gynecol 1989;32:445-55
11 Gillon R. Testing for HIV without permission. BM]
1987;294:821-3
12 Minkoff HL. AIDS in pregnancy. Curr Probl Obstet Gynecol
Fertil 1989;12:205-28
13 Johnstone FD. HIV infection in pregnancy. Curr Obstet
Gynecol 1991;1:78-83
J4
IT
|n‘ern.iti«<n.il Journal <>i STD
AIDS
Volume 3
M.irch/Apnl 1992
MacGregor SN. I Inman immunodeficiency virus infection
in pregnancy. Clin Perinatal 1991;18:33-50
15 Sridama V, Pacini F, Yang SI., Muawad A, Reilly M, De Groot
LJ. Decreased levels of helper T-cells—a possible cause of
immunodeficiency in pregnancy. N Engl J Med 1982;307:352-6
16 Carvalho AA, Giampaglia CMS, Kimura H, et al. Maternal
and infant antibody response to meningococcal vaccination
in pregnancy. hiucet 1977;ii:8G9-I1
17 Sumaya CV, Gibbs RS. Immunization of pregnant women
with influenza A/New Jersey'76 virus vaccine: reactogenicity
and immunogenicity in mother and infant. I Infect Dis
1979;140:141-6
18 Brabin BJ, Nagel I, Hagenaars AM, et al The influence of malaria
and gestation on the immune response to one and two doses of
adsorbed tetanus toxoid in pregnancy. Bull WHO 1984;62:919-30
19 Johnson U, Guslavii B. Complement components in normal
pregnancy. Acta Pathol Microbiol Immunol Scand 19S7;95c:97-9
20 Kovar IZ, Riches PG. C3 and C. complement components
and acute phase proteins in late pregnancy and parturition.
J Clin Pathol 1988,41.650-2
21 Castilla JA, Rueda R, Vargas ML, Gonzalez-Gomez F,
Garcia-Olivares E. Decreased levels of circulating CD, + T
lymphocytes during normal human pregnancy I Reprod
Immunol 1989;15:103-11
22 Tallon DF, Corcoran AJ, O'Dwyer EM, et al. Circulating
lymphocyte sub-populations in pregnancy: A longitudinal
study. / Immunol 1984;132:1784-87
23 Bailey K, Herrod HG, Younger R. et al. Functional aspects
of T-lymphocyte sub-sets in pregnancy. Obstet Gynecol
1985;66:211-15
24 Hawes CS, Kemp AS, Jones WR, et al. A longitudinal study
of cell-mediated immunity. / Reprod Immunol 1981;3:165-73
25 Weinberg ED. Pregnancy associated immune suppression:
risks and mechanisms. Microbiol Pathogenesis 1987;3:393-7
26 Weinberg ED. Pregnancy-associated depression of cellmediated immunity. Rev Infect Dis 1984;6:814-31
27 Brabin BJ. Epidemiology of infection in pregnancy. Rev Infect
Dis 1985;7:579-603
28 Falkoff R. Maternal immunologic changes during pregnancy:
a critical appraisal. Clin Rev Allergy 1987;5:287-300
29 Brabin BJ. An analysis of malaria in pregnancy in Africa. Bull
WHO 1983;61:1005-16
30 Khuroo MS, Teli MR. Skidmore S, et al. Incidence and
severity' of viral hepatitis in pregnancy. Am J Med 1981;70:252-5
31 Borhanmanesh F, Haghighi P, Hekmat K, et al. Viral hepatitis
during pregnancy. Gastroenterology 1973;64:304-13
32 Weinstein L, Aycock WL, Feemster RF. The relation of sex,
pregnancy and menstruation to susceptibility in poliomyelitis.
N Eng / Med 1951;245:54-8
33 Priddle HD, Lenz WR, Young DC, et al. Poliomyelitis in
pregnancy and the puerperium. Am / Obstet Gynecol
1952;63:408-13
34 Siegel M, Greenberg M. Incidence of poliomyelitis in
pregnancy. N Engl / Med 1955;253:841-7
35 Freeman DW, Barno A. Deaths from Asian influenza
associated with pregnancy. Am I Obstet Gynecol 1959;78:1172-5
36 Greenberg M, Jacobziner H, Pakter J, et al. Maternal mortality
in the epidemic of Asian influenza. New York City, 1957.
Am ] Obstet Gynecol 1958;76:897-902
37 Scott GB, Fischl MA, Klimas N, et al. Mothers of infants with
the acquired immunodeficiency syndrome. Evidence for both
symptomatic and asymptomatic carriers. JAMA 1985;253:363-6
38 Minkoff HL, Nanda D, Menez R. etal. Follow-up of mothers
of children with AIDS. Obstet Gynecol 1987;87:288-91
39 Hague RA, Mok JYQ, MacCallum L, et al. Do maternal factors
influence the risk of vertical transmission of HIV? Vllth
International Conference on AIDS, Florence, June 1991:
Abstract WC3237
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
Delfraissey |F, Pons JC, Sercni D, et id. Docs pregnancy
influence disease progression in HIV positive women. Vth
International Conference on AIDS, June 1989, Montreal,
Canada Abstract MBP 34
Deschamps M-M, Pape JW, Madhavan S, et al. Pregnancy and
acceleration of HIV related illness. Vth International Conference
on AIDS, June 1989, Montreal, Canada. Abstract MBP 6
Schoenbaum EE, Daverny K, Selwyn PA, et al. The effect
of pregnancy on progression of IIIV related disease. Vth
International Conference on AIDS, June 1989, Montreal,
Canada Abstract MBP 8
Bledsoe K, Olopoenia L, Barnes S, et al. Effect of pregnancy
on progression of HIV infection. Vlth International Conference
on AIDS, June 1990, San Francisco, USA. Abstract ThC 652
Mazz.arello G, Canessa A, Melica F, et al. Influence of
pregnancy on HIV disease progression. VII International
Conference on AIDS, Florence, June 1991. Abstract WC3235
MacCallum LR, Cowan FM, Whitelaw J, et al. Disease
progression following pregnancy in HIV seropositive women.
Vth International Conference on AIDS, June 1989, Montreal,
Canada. Abstract MBP 3
Berrebi A, Puel J, Tricoire J, et al. Influence of gestation on
HIV infection. Vlth International Conference on ?\IDS, June
1990, San Francisco, USA. Abstract ThC 651
Des Jarlais D, Friedman SR, Marmor M, et al. Development
of AIDS, HIV seroconversion, and potential co-factors for
T. cell loss in a cohort of intravenous drug users. AIDS I
1987:105-11
Biggar RJ, Pahwa S, Minkoff H, et al. Immunosuppression
in pregnant women infected with HIV. Am / Obstet Gynecol
1989;161:1239-44
Jensen LP, O'Sullivan MJ, Gomez-Del-Rio M, et al. Acquired
immunodeficiency (AIDS) in pregnancy. Am / Obstet Gynecol
1984;148:1145-6 '
Antoine C, Morris M, Douglas D. Maternal and fetal mortality
in acquired immunodeficiency syndrome. N Y State / Med
1986;86:443-5
Minkoff H, de Regt RH, Landesman S, Schwarz R.
Pneumocystis carinii pneumonia associated with acquired
immunodeficiency syndrome in pregnancy: a report of three
maternal deaths. Obstet Gynecol 1986;67:284-7
Wetli CV, Roldan EO, Fujaco RM. Listeriosis as a cause of
maternal death: an obstetric complication of the acquired
immunodeficiency syndrome (AIDS). Am / Obstet Gynecol
1983;147:7-9
Kell PD, Barton SE, Smith DE, et al. A maternal death caused
by AIDS. Case Report. Br / Obstet Gynaecol 1991;98:725-7
La Pointe N, Michaud J, Pekovic D, et al. Transplacental
transmission of HTLV-III virus. N Engl J Med 1985;312:1325-6
Koonin LM, Ellerbrock TV, Atrash HK, et al. Pregnancyassociated deaths due to AIDS in the United States. JAMA
1989:261:1306-9
Hicks ML, Nolan GH, Maxwell SL, Mickle C. Acquired
immunodeficiency syndrome and Pneumocystis carinii
infection in a pregnant woman. Obstet Gynecol 1990;76:480-1
Minkoff HL, Willoughby A, Mendez H, et al. Serious
infections during pregnancy among women with advanced
human immunodeficiency virus infection. Am J Obstet Gynecol
1990; 162:30-4
Johnstone FD, Willox L, Brettle RP. Survival time after AIDS
in pregnancy.
Johnstone FD, HIV and pregnancy outcome. Bailliere Clin
Obstet Gynaecol 1991 (in press)
Lasley-Bibbs V, Renzullo P, Goldenbaum M, et al. Patterns
of pregnancy and reproductive morbidity among HIV
infected women in the US Army: a retrospective cohort
study. Vlth International Conference on AIDS, June 1990,
San Francisco, USA: Abstract Th.C 655
JiihnMuiiv
Miolti PG, Dallabvlta G. Wlo\ i E, if al. HIV-l and
pregnant women: associated tailors, prosalencc. estimate of
incidence and role in ictal wastage in central Africa. AIDS
1990;4:733-6
62 LePage P, Dabis F, I lilimana DG. el til. Perinatal transmission
of HIV-1: lack of impact ot maternal HIV inteclion on
characteristics of livebirths and on neonatal mortality in
Kigali, Rwanda AIDS 1991;5:295-300
63 Lopitn MI, Temmerman M. Sinei SKF, et til. HIV infection
as a risk factor for spontaneous first trimester abortion. Vlth
Internationa! Conference on AIDS, June l°90, San Francisco,
USA: Abstract Th.C 653
64 Selwyn PA, Schoenbaum EE, Davcnny K. et al. Prospective
study of human immunodeficiency virus infection and
pregnancy outcomes in intraxenus drug users. JAM A
1989;261:1289-94
65 Johnstone FD, MacCallum LR, Brettle RP, et al. Testing for
HIV in pregnancy: 3 years experience in Edinburgh City. Scott
Med J 1989,34:561-3
66 Emanuelli F, Ermigha ML, Gabutti G, et al. Human
I
immunodeficiency virus infection among women attending
F
obstetric and gynaecology departments in Liguria, Italy. VII
International Conference on AIDS, Florence, June 1991.
Abstract WC 3275
67 Moatti JP, Gales C, Seror V, et al. Social acceptability of HIV
screening among pregnant women. AIDS Care 1990;2:213-22
68 Balanon A, Fordyce EJ, Stoneburner R. AIDS concerns and
women's reproductive intentions: HTV testing and pregnancy
choices. Vlth International Conference on AIDS, June 1990,
San Francisco, USA: Abstract Th.D 804
69 Selwyn P.A, Carter RJ, Schoenbaum EE, ct al. Knowledge
of HIV antibody status and decision to continue or terminate
pregnancy among intravenous drug users. JAMA 1989;261:
3567-71
70 Johnstone FD, Brettle RP, MacCallum LR, et al. Women's
knowledge of their HIV antibody state its effect on their
decision whether to continue the pregnancy. BMJ 1990;
300:23-4
71 Stratton P, Mofenson L, Willoughby A, et al. Prenatal
screening policies for HIV antibody at major obstetric clinical
centers in the United States. Vlth International Conference
i
on AIDS, June 1990, San Francisco, USA: Abstract SC 665
72 Minkoff H, Nanda D, Menez R, Fikrig S. Pregnancies
resulting in infants with acquired immunodeficiency syndrome
or AIDS related complex. Obstet Gynaecol 1989;69:285-7
73 Gloeb DJ, O'Sullivan MJ, Efantis J. Human immuno
deficiency virus infection in women 1. The effects of human
immunodeficiency virus on pregnancy. Am J Obstet Gynecol
1988;159:756-61
74 Johnstone FD, MacCallum L, Brettle R, et al. Does infection
with HIV affect the outcome of pregnancy? BMJ 1988,296:467
75 Minkoff HL, Henderson C, Mendez H, et al. Pregnancy
outcomes among mothers infected with human immuno
deficiency virus and uninfected control subjects. Am J Obstet
Gynecol 1990;163:1598-604
76 Semprini AE, Ravizza M, Bucceri A, ct al. Perinatal outcome
in HIV-infected pregnant women. Gynecol Obstet Invest
1990;30:15-18
77 Berrebi A, Lahlov M, Puel J, et al. Effects of HIV infection
on pregnancy. VII International Conference on AIDS,
Florence, June 1991. Abstract WB2042
78 Ryder RW, Nsa W, Hassig SE. el al. Perinatal transmission
of the human immunodeficiency virus type 1 to infants of
seropositive women in Zaire. N Engl J Med 1989;320:1637-42
79 Kamenga M, Manzila T, Behels F, et al. Maternal HIV
infection and other sexually transmitted diseases and low
birth weight in Zairian children. VII International Conference
on AIDS, Florence, June 1991. Abstract WC3244
bl
I !l\ ..mi pregnancy
8?
Lallcmanl M, 1 allemanl-LeC’ovur S, Cheynicr D, <7 al.
Mother-child transmission of IIIV-I and infant survival in
Brazzaville, Congo. A IDS F\Sl’;3 013-6
81 1 lira SK, Kamanga J, Bhat Gl, <7 al. Perinatal transmission
of HIV-1 in Zambia. BMJ 1°89:299:1250-2
82 Braddick MR, Krciss JK, Ernbrec IE. et al. Impact of maternal
HIV infection on obstetrical and early neonatal outcome.
AIDS 1990;4:1001-5
83 Guay L. Mmiro F, Ndugwa, et al Perinatal outcome in HIVinfected women in Uganda. VI International Conference on
AIDS, San Francisco, June 1990. Abstract ThC42
84 LePage P, Dabis F, Hitimana D-G, et al. Perinatal trans
mission of HIV-1: lack of impact ot maternal HIV infection
on characteristics of livebirths and on neonatal mortal it v in
Kigali, Rwanda. AIDS 1991;5:295-300
85 Bulterys M, Chao A, Kurawige IB, et al. Maternal HIV
infection and intrauterine growth: a prospective cohort
study in Butare, Rwanda. VII International Conference on
AIDS, Florence, June 1991. Abstract WC3234
86 Temmerman M, Plummer FA, Mirza NB, et al. Infection with
HIV as a risk factor for adverse obstetrical outcome. AIDS
1990;4:1087-93
87 Italian Multicentre Study. Epidemiology, clinical features,
and prognostic factors of paediatric HIV infection. Lancet
1988;ii:1043-5
88 Blanche S, Rouzioux C, Moscato M-L, et al. A prospective
study of infants born to women seropositive for human
immunodeficiency virus type 1. N Engl J Med 1989,-320:
1643-8
89 European Collaborative Study. Children born to women
with HIV-1 infection: natural history and risk of trans
mission. Lancet 1991;337:253-8
90 Marion RW, Wiznia AA, Hutcheon G, Rubinstein A. Human
T-cell lymphotrophic virus IH (HTLV-HI) embryopathy: a new
dysmorphic syndrome associated with intrauterine HTLVIII infection. Am J Dis Child 1986;140:638-40
91 Marion RW, Wiznia AA, Hutcheon RG, Rubinstein A. Fetal
AIDS syndrome score. Correlation between severity of
dysmorphism and age at diagnosis of immunodeficiency.
Am J Dis Child 1987;141:429-31
92 Nicolas S. Is there an HIV associated facial dysmorphism?
Pcdiatr Ann 1988;5:353
93 Qazi QH, Sheikh TM, Fikrig S. Lack of evidence for
craniofacial dysmorphism in perinatal HIV infection. J
Pcdiatr 1988;112:7-11
94 Auger I, Thomas P, de Gruttola V, et al. Incubation periods
for paediatric AIDS patients. Nature 1988;336:575-7
95 Maury W, Potts BJ and Rabson AB. HIV-1 infection of first
trimester and term human placental tissue: a possible mode
of maternal-fetal transmission. J Infect Dis 1989;160:583-8
96 Zachar V, Noskov-Lauritsen N, Juhl C, et al. Susceptibility
of cultured human trophoblast to infection with human
immunodeficiency virus type 1. J Gen Virol 1991;72:1253-60
97 Lewis SH, Reynolds-Kohler C, Fox HE, Nelson JA. HIV-1
in trophoblastic and villous Hofbauer cells, and haemato
logical precursors in eight-week fetuses. Lancet 1990;
335:565-8
98 Sprecher S, Soumenkoff G, Puissant F, Degueldre M.
Vertical transmission of HIV in 15 week fetus. Lancet
1986;ii:2S8-9
99 Jovaisas E, Koch MA, Schafer A, et al. LAV/HTLV HI in a
20 week fetus. Lancet 1985;ii:1129
100 Peutherer JF, Rebus S, Aw E, et al. Detection of HIV in the
fetus: A study of six cases. IV International Conference on
AIDS, Stockholm, June 1988; Abstract 7235
101 Mano H, Chermann J-C. Fetal human immunodeficiency
virus Type 1 infection of different organs in the second
trimester. AIDS Res Hum Retroviruses 1991;7:83-8
80
<6
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
International Journal of STD & AIDS
Volume 3
March/April 1992
Siegel G, Schafer A, Unger M, cl al. HIV-1 in fetal organs
and in embryonic placenta of HIV-1 positive mothers. VI
International Conference on AIDS, San Francisco, June
1990, Abstract FB 445
Soeiro LR, Rashbaum WK, Rubinstein LA, et al. The
incidence of human fetal 111V-I infection as determined by
the presence of HIV-1 infection as determined by the
presence of HIV-l DNA in abortus tissues. VII International
Conference on AIDS, Florence, June 1991 Abstract VVC3250
Ehrnst A, Lindgren S, Dictor M, cl al. HIV in pregnant
women and their offspring: Evidence for late transmission.
Lancet 1991,338.203-7
Courgnaud V, Laure F, Brossard A, et al. Frequent and early
in ulero HIV-1 infection AIDS Res Hum Retroviruses
1991;7:337-41
Coeder: JJ, Mendez H, Drummond JE, et al. Mother-toinfant transmission of human immunodeficiency virus type
1: association with prematurity or low anti-gp 120. Lancet
1989;ii:1351-4
D'Arminio M, Ravizza .A, Muggiasca M, et al. HIV infected
pregnant women: possible predictors of vertical trans
mission. VII International Conference in .AIDS, Florence,
June 1991. Abstract WC49
Boue F, Pons JC, Keros L, et al. Risk for HIV-1 perinatal
transmissions varies with the mother's stage of HIV
infection. VI International Conference on AIDS, San
Francisco, June 1990. .Abstract ThC44
St Louis ME, Kabagaho U, Brown C, et al. Maternal factors
associated with perinatal HIV transmission. VII International
Conference on AIDS, Florence, June 1991. Abstract MC 3027
KreissJ, Datta P, Willerford D, et al. Vertical transmission
of HIV in Nairobi: correlation with maternal viral burden.
VII International Conference on AIDS, Florence, June 1991.
Abstract MC3062
Rubinstein A, Calvelli T, Goldstein H, et al. Correlation of
maternofetal (abortus) HIV-1 transmission with high
affinity avidity antibodies to the primary neutralizing
domain (PND). VII International Conference on AIDS,
Florence, June 1991. Abstract MC3052
Attain JP, Mathews T, Coombs R, et al. Antibody to V3
loop peptide does not predict vertical transmission of HIV.
VII International Conference on AIDS, Florence, June 1991.
Abstract WC3263
Beyssen V, Meyohas MC, Gras G, et al. Neutralization titers
in sera from HIV-infected pregnant women, and their corre
lation with materno-fetal transmission. VII International
Conference on AIDS, Florence, June 1991. Abstract WA 1344
Shaffer N, Parekh BS, Pau CP, et al. Maternal antibodies
to V3 loop peptides of GP 120 are not associated with bulk
of perinatal HIV-1 transmission. VII International Conference
on AIDS, Florence, June 1991. Abstract WC48
Halsey NA, Markham R, Rossi P, et al. V3 loop peptide
antibodies in Haitian women and infant HIV-1 infections.
VII International Conference on AIDS, Florence, June 1991.
Abstract WA1311
Nsvami M, St Louis M, Geoge JR, et al. Low prevalence
in HIV-infected Zairian mothers of antibodies against GP
120 neutralizing epitopes of the MN HIV-1 isolate lack
of association with perinatal HIV transmission. VII
117
118
119
120
121
122
123
124
125
126
127
128
129
130
131
132
133
International Conference on AIDS, Florence, June 199L
Abstract MC 3065
Krasink.ski K, Cao Y-Z, Friedman KA, et al. Elevated
maternal total and neutralizing anti-HIV-1 antibody does
not prevent perinatal HIV-1. VI International Conference
on AIDS, San Francisco, June 1990; Abstract fhC 45
Diro M, Beydoun SN. Malaria in pregnancy. South Med /
1982;75:959-62
Just J, Louie L, Abrams E, et al. Genetic risk factors for
perinatally acquired HIV infection. VII International
Conference on AIDS, Florence, June 1991. Abstract MC3044
Goedert JJ, Duliege AM, Amos CI, et al. The International
Registry of HIV-exposed twins: a first report. VII
International Conference on AIDS, Florence, June 1991
Abstract MC3090
European Collaborative Study. Mother to child transmission
of HIV infection. Lancet 1988;ii: 1039-42
Carcassi C, Chiappe F, Lecca U, et al. A. study of 9 infants
born from HIV-1 positive mothers who continued treatment
with AZT during pregnancy. VII International Conference
on AIDS, Florence, June 1991. Abstract WC3228
Ferrazin A, Terragna A, Loy A, et al. Zidovudine (ZDV)
therapy on HIV infection during pregnancy: assessment of
the effect on the newborns. VII International Conference
on AIDS, Florence, June 1991. Abstract MC 3023
Crane L, Schuman P, Cohen F, et al. Failure of zidovudine
(ZDV) to prevent vertical transmission of HIV VII
International Conference on AIDS, Florence, June 1991.
Abstract MC3182
Crombleholme W, Wara D, Cambertoglio J. Perinatal HIV
transmission despite maternal/infant AZT therapy. VI
International Conference on AIDS, San Francisco, 1990.
Abstract ThC605
Sharpe AH, Hunter J, Ruprecht RM, et al. Maternal
transmission of retroviral disease and strategies for
preventing infection of the neonate. J Virol 1989;63:1049-53
Ando Y, Nakano S, Saito K, et al. Transmission of adult
T cell leukaemia retrovirus (HTLV-1) from mother to child:
Comparison of bottle with breast fed babies. Jpn I Cancer
Res 1987;78:322-4
Thiry L, Sprecher-Coldberger S, Jonckheer T, et al. Isolation
of AIDS virus from cell free breast milk of three healthy virus
carriers. Lancet 1985; ii:891—2
Ziegler JB, Cooper DA, Johnson RD, Gold J. Postnatal
transmission of AIDS-associated retrovirus from mother to
infant. Lancet 19S5;i:896-8
LePage P, Van de Pcrre P, Carael M, et al. Postnatal
transmission of HIV from mother to child. Lancet 1987; ii MOO
Weinbreck P, Loustaud V, Denis F, et al. Postnatal
transmission of HIV infection. Lancet 1988;i:482
Van De Perre P, Simonon A, Msellati P. Postnatal
transmission of human immunodeficiency virus type 1 from
mother to infant. N Eng! / Med 1991;325:593-8
Kennedy K, Visness C, Rogan WJ. Breastfeeding and AIDS:
A health policy analysis. VII International Conference on
AIDS, Florence, June 1991. Abstract VVC3223
(Accepted 2 October 1991)
Contents:
The changing face of AIDS................................................2
Resources for your congregation................................... 3
Terms defined....................................................................3
Discussion guide for adult group leaders...................... 4
AIDS and HTV infection: How much do you know?.....7
AIDS: What does the Bible say?.................................... 10
Resources......................................................................... 11
AIDS and HIV Infection
Throughout this guide we will be referring to both AIDS and HIV
infection. Since what we know about AIDS has increased and the
infection has spread, it has become important to focus on both HIV
infection and AIDS. Persons with HIV infection but not AIDS are
the main source of AIDS, so prevention efforts must focus on HIV
more than AIDS..
In this resource, those with AIDS will usually not be referred to as
AIDS “victims,” but “people with AIDS.”
The Changing Face of AIDS
Information about AIDS (Acquired Immune Deficiency
Sxndromc) has increased during recent years The
Christian church must now face how AIDS is changing
s< )cicty:
•
continues to spread quickly. About 195.000
cases of AIDS were reported by the end of 1991 and
125.000 deaths resulted.
• Current health care facilities have not been able to
keep up with the demand for AIDS care.
• The cost of AIDS w ill affect us all. AIDS care in the
U.S. will cost ten billion dollars a year by 199-l
Since Medicaid provides some money, taxes will
increase to pay for treatment.
• Insurance costs will also increase. Claims will rise as
people with AIDS turn in expenses and hospitals
raise fees to cover the costs of non-paying patients
• AIDS brings up several important issues which arcdifficult to deal with suffering, death, compassion.
and sexuality. AIDS causes discomfort because it
forces us to look at our understanding of Biblical
teaching in these areas.
• Education and changing behavior are the only
ways to prevent HIV infection. Sex education has
often been difficult. Today, however, education is a
matter of life and death. We need to learn how to
prevent HIV infection and also how to be caring.
The church’s challenge and opportunity
Today’s church is being forced to respond to AIDS. How will people in
your congregation:
• respond to the changing views of people who practice medical care?
• see the church as a place to provide care in kind and inexpensive
ways, especially for the terminally ill?
• respond with compassion to persons with AIDS as they prepare for
death and seek hope?
• openly discuss the issues of sexuality, suffering, and death?
• prevent the spread of HIV infection among children and youth by
helping them develop responsible behavior and appropriate views
of their sexuality?
• overcome fear and prejudice by living the hope and compassion
of Jesus?
Terms Defined
Resources for Your
Congregation
This resource booklet includes a variety of ideas and suggestions to
help you. There are basic facts about AHIS to help lessen fears and
correct misinformation. A discussion guide for adult small groups is
also included. The rest of the booklet directs you to other resources
available in the church and the community. These resources were
designed primarily for use with adults. We encourage you. how ever.
to include AIDS education in your children and youth programs to
supplement the secular education that occurs in schools.
Flexible options
Helping your congregation to w elcome people with AIDS will take
careful thought, much effort, and prayer. You may need to plan
different kinds of input to meet different needs among members—to
give facts, to encourage discussion, to further understanding and
action. All the resources listed here are recommended by the Educa
tional Resources staff of Mennonite Mutual Aid. but we strongly
recommend you preview them prior to use in your congregation.
Some public resources, such as those from county health departments
or the American Red Cross, do not emphasize strong religious values.
They can. however, provide helpful information to add to your
congregation's own reaching of a Christian response in sermons.
Sunday School classes, youth group meetings, fellowship group
discussions and other settings.
Preparing for ministry
Mennonite churches are already responding to members with HIV
infection or AIDS. Even if AIDS has nor yet touched your congrega
tion. ir is likely that it will. Soon, nearly all of us will know someone
with AIDS.
We will need the help of our congregations to face the suffering and
preparation for death that seem certain with this disease. As church
leaders and as disciples of Christ, we arc responsible to prepare
ourselves and our congregations for the challenges of IIIV infection
and KIDS. May wc. through study, prayer and discussion, be ready to
follow Jesus' model of compassion as we face the future.
AIDS:
Acquired Immune Deficiency
Syndrome. A physical condition
caused by the HIV virus which attacks
a person s immune systems, thus
damaging the body's ability to fight
diseases. There is no known cure.
HIV:
Abbreviation for the name of the virus
that causes AIDS. It is called the
Human Immunodeficiency Virus,
or HIV.
HIV positive (seropositivity):
When HIV enters the blood stream it
begins to attack certain white blood
cells. The body responds by
producing substances called •‘anti
bodies" to defend itself against
the infection. It is these antibodies
that signal the presence of HIV in
the body. People who test positive
for these antibodies are "HIV
positive" or "seropositive.”
NOTE: It can take several months
or even years, however, from the time
the virus enters the body until these
antibodies are produced. Therefore,
before blood tests show evidence, a
person may be infected and can
spread the infection to others. He or
she may experience few or no AIDS
symptoms or only several during this
time. Between the onset of infection
and becoming HIV positive is the
time of high risk because tests during
this time may not be reliable.
Opportunistic diseases:
Diseases which occur because resis
tance is lowered. When a person's
immune system becomes impaired
with HIV infection, bacteria, fungi,
parasites and viruses, or certain
cancers can cause "opportunistic
diseases. These diseases would not
ordinarily be devastating, but lowered
resistance gives them the opportunity
to infect and destroy. HIV may also
attach itself to the nervous system
and cause damage to the brain,
resulting in mental illness or dementia.
3
A Discussion Guide for Adult Group Leaders
Read the guide
MMA made the following discussion guide to help you
lead group discussions about HIV infection and AIDS.
Rc;A|ic guide carefully, thinking about lhe group you
will lead and the resources available to you.
Session I:
Facts about HIV infection and AIDS
1.
Plan your sessions
You. as leader, will plan the agenda. A small amount of
preparation time may be needed to arrange for the
resources you want to use. Please feel free to adapt or
adjust the materials in the guide as needed for your
congregation.
For more information about AIDS, consult the
resource listing later in this packet.
2.
Schedule adequate time for your group to deal with the
issue of AIDS. The guide was designed for three sessions.
Although it could be used for only one or two sessions.
you should allow the time for more, depending on the
group’s interest.
Drover your congregational issues
A week or two before you begin the session(s) on AIDS.
set up an anonymous question box to discover the issues
of greatest importance. This will give you time to get
information and prepare responses that will be most
helpful to your group.
Schedule resources
Schedule any video or film you want to use well in
advance. This will allow you time to see rhe material
before the session and determine how to lead the
discussion or add to the material with more input. It will
also unsure that you gut the audiovisual you want ar thu
rimu \ou want it.
Begin with the quiz. AIDS: How Much Do You
Know?" on page
Have people complete the quiz
and be sure to tell them they will not report or share
their answers. Use the answers in the booklet to
present facts about HIV infection, the AIDS
condition, what causes the spread of AIDS, and how
to prevent it.
Some people may be afraid of getting the disease
through casual contact or may not be informed about
it. so these facts are an important beginning point.
Help the group discuss how they understand HIX'
infection and AIDS. Help to relieve unnecessary fears
about infection, and also emphasize what behaviors
will put one at risk of HIV infection.
After understanding the facts, it is important to
examine our attitudes about and actions toward those
who are HIX’ positive or have AIDS. Encourage the
group to discuss these issues openly in the next
sessions.
"We do not believe
that the God of love,
wages germ warfare
on the human family,
including the unborn
and newborn. ”
Session 2:
Biblical perspective on AIDS
1.
Begin the session by contrasting responses of different 3. Choose a method of discussing these scriptures that
Christians to HIV infection and AIDS. Here are
fits your group. You may want to divide into smaller
examples:
groups and give each participant a different passage to
read and discuss; then have these clusters share with
• In a snn ey by the group Americans for Moral
the larger group the insights they have. Or you could
Integrity’, one pastor said a person with AIDS is
ask people in the larger group to read the verses aloud
“obviously being punished by God," that the
and invite responses in that group setting.
problem was in God’s hands and that there was
nothing he could do.
4. Invite group members to suggest other Bible passages
• A statement of the United Methodist Church
Council of Bishops says, “While the origin of the
virus is still in question in the medical commu
nity, we in the religious community are certain
that it is not sent as a curse from God upon those
whose lifestyle is called into question. We do
not believe that the God of love, revealed in
Jesus Christ, wages germ warfare on the human
family, including the unborn and newborn."
• A church member told the mother of a person
with AIDS that she should not come to church
until her son had died.
• A statement on AIDS adopted by the Church of
the Brethren Annual Conference in 1987,
recommends that “Congregations and individuals
become involved in direct care for persons with
AIDS, care for the affected families and friends,
and the giving of spiritual support through the
healing ministries of visitation, counseling.
anointing, and in other appropriate ways to
promote wholeness and acceptance."
2.
Lead the class in looking at scriptures which show
the kind of response we as Christians arc called
upon to give. Suggested passages from the Gospels
arc included in this booklet (page 10). along with
questions to start discussion.
that can give insights into a Christian response to
AIDS. However, guide the discussion so it does not
become focused on the issue of homosexuality’. Keep
in mind that AIDS is not a “male homosexual disease”;
it afflicts both sexes, including children, and many’
who are not homosexual. Worldwide. 75 percent of
those infected with HIV got the virus through hetero
sexual intercourse.
Move on to related issues if time allows. Here are
several suggestions:
AIDS and sin
Some people say those with .-VIDS "deserve it" because
of sinful behavior. However, we seldom blame a
person for heart disease, and it can. in some situations.
also result from "sinful behavior": overeating.
underexercising, not managing stress, or eating
excessive amounts of fat are also not being good
stewards of our bodies. Why are we more likely to
accept people with heart disease (or cancer) but
judge those with HIV infection? Tony Campolo.
Christian speaker and evangelist, has written. “If God
sent a disease like AIDS immediately upon every
human being who was participating in some sinful
act. it seems we would all be on our deathbeds at this
very moment."
Does our attitude
toward persons with
AIDS reveal that we
believe some per
sons “deserve” our
help while others
do not?
Session 3What can our congregation do?
AIDS and difficult issues
.VIDS raises questions about our understanding of
j^uality, illness, suffering, death and dying. How can
W Christian faith grow as we study these issues in
the context of HIV and AIDS? Does AIDS help us
understand these in a new way? Does AIDS reveal
issues w e need to study further in our own Christian
discipleship? For example: Does the fear of HIV
infection interfere with our readiness to care for the
person with .-VIDS? Does our attitude toward persons
with .-KIDS reveal that we believe some persons
‘deserve" our help while others do not?
AIDS, race and economics
.AIDS has had a disproportionate impact on non-wliites
and the poor. What does this imbalance say about the
racial and economic climate in our country? What is
our responsibility in the factors that contribute to drug
dependency and limited medical care for those at high
for AIDS?
Can we comprehend the hopelessness of those living
in the poverty of inner cities? How can we under
stand the mentality of unemployed young people in
violent areas who say. ‘Why worn- about safe sex or
contaminated needles when 1 11 be killed by age 50
anyway?"
1.
To concretely show what it means to care for some
one with AIDS, show' the video. ‘AIDS: A Family
Experience” available from MMA. Follow this w ith a
discussion from the guide provided with this video.
2.
If time allows, focus on one or more of the following
issues:
AIDS education in the church
What needs does the congregation have for AIDS
education? What needs do youth have? Parents?
How can these needs be met? How can we help
young people develop a healthy understanding and
appreciation of their sexuality as well as strong values
about the role of sexuality in their lives and commit
ment to family life?
Preparing to respond
Some congregations are adopting statements about
AIDS before the disease directly affects their members
or families. Then these congregations are prepared
(in a more objective way) to respond when AIDS does
affect them directly. How can your congregation
prepare to deal with AIDS? What study and discussion
will be helpful? What resources will you need?
Confidentiality is one of the primary issues as a
congregation helps someone with HIV infection.
How will your congregation protect confidentiality
while helping persons with AIDS? (For examples of
statements on AIDS, call MMA.)
AIDS and community opportunities
\\ hat are the current needs in the community related
to AIDS? Is there a hospice program needing volun
teers? Is there an education need that members of the
church can address? Can members help persons with
AIDS in tasks of daily living such as houscclcaning.
shopping, child care, etc.? Can members be a support
group to families of persons w ith AIDS?
(i
I m- (hf I'.U'di in^ quiz al the Ih'>ihuiu^ •,/ a .(•>, .it,11 >,n . ]f/)S and lll\ in/ci.linn H u ill
hrl]> i.n-alf inh-r<-\i in the i.vjhx and Ihe men vrs tehit.h /olbnr trill hcl[> u muter
nu .uijennaiuni ami mrth\ Phuhn <>!>v the fiane /hr each ^rtiup member and allan Unit'
in an jut ihc ifiii’\W>n\ th, not a.d‘ [>ft,{,lf i<> >hare or report (heir anstreix.
AIDS and HIV Infection:
How Much Do You Know?
Information about .AIDS is prevalent in the media.
But how much do we know? Try to answer these
questions. You will not be asked to share or report
vour answers.
6.
1. Should I be afraid of becoming HIX’ infected
from my dentist or physician?
2. Thanks to HIV antibody testing of blood and
blood donors, the nation's blood supply (for
transfusion purposes) is truly safe.
True or False?
5.
Because HIV has been found in saliva and tears.
kissing has become risky because it might be a
means of transmitting the virus.
True or False?
A person whose blood tests positive for HIV
can pass the virus on even when there are no
symptoms present. True or False?
5. On a university campus a student with AIDS
comes to school after a holiday to learn that 20
percent of returning students arc going to the
Health ('.enter for treatment—there is an
epidemic of bronchitis/flu. 'I'hc student refuses
to attend classes, gets back in his car and drives
home. \X hv?
A person applies for employment at a school
cafeteria. A blood test reveals that tills person
has HIX’. Considering the environment of
knives, meat slicers, and food preparation.
should this person be hired?
Compared to other viral diseases. AIDS is
regarded as higlily contagions. True or False?
8.
XXlio should be tested for HIV?
9.
"Safe sex" is achieved by the regular.
conscientious use of a condom. True or False?
10. An individual has tested positive for HIX'. How
likely is that person to develop symptoms
within the next ten vears?
11. XX'hy have the American Medical Association
and other public health authorities been so
reluctant to support widespread mandatory'
testing for HIV?
In what ways docs the use of alcohol increase
one s chances of getting AIDS?
•A >/>(•</ by U ilia i\ I K'i\ il nil. 11.1 >
7
How Much Do You Know?
Answers and Explanations about AIDS and HIV Infection
1
The chances arc low that your professional health
caregiver is infected and the chances of he or she
transmitting the virus to you in the course of
^klinary care are even more unlikely. All health
professionals are expected to take “universal
precautions" like wearing gloves. HIV infected
professionals are expected to avoid doing invasive
procedures.
Requiring all health professionals to be tested would
be to throw vast amounts of money at a problem
without giving us either assurance or protection (see
question -11). To determine public policy based on
isolated cases seems unwarranted.
Physicians are not making absolute statements about
the safety of our blood supply. The blood supply is
ven safe, but there is still a small window of risk.
After a person has become infected with HIV', it may
^ike several months or even years before the body
Bigins to produce antibodies. Testing for these
antibodies is currently the only way to detect the
presence of the vims. So there is a period of time
when a person could donate blood—after infection.
but before developing antibodies—and test negative
but be able to pass the virus to others.
It is because of this slight risk that people facing
elective surgery are encouraged to bank their own
blood ahead of time in case a transfusion is needed.
5.
8
False. There have been no cases of HIV infection in
which saliva or rears were found to be the means of
transmission. However, in practicing “safe sex.”
avoid deep, wet kissing. If a person has an open
lesion in the mouth and participates in deep, wet
kissing, the virus could be transmitted from one
person s blood stream to die other s. 'Hie transmis
sion is b\ wav of blood, not saliva.
4.
True. X person can be infected with HIV for many
years without developing AIDS. The vims can be
transmitted from anyone carry ing it to another
person through high risk sexual behaviors.
5.
A person with .AIDS has lessened immunity to other
infections and viruses. Thus, a cold or the flu which
is an Inconvenience to a healthy person can be life
threatening to a person with AIDS. We are more
dangerous to a person with z\J DS than he or she is
to us unless we are sharing needles or having sex
with them.
6.
We cannot acquire the virus through our digestive
tract. Also, the virus cannot live outside the human
body. For these reasons, we should not be
concerned about someone with .AIDS preparing or
serving food. However, a person with AIDS may
want to reconsider employment in the food industry
because of his or her own safety.
7.
False. AIDS is not highly contagious: other viruses.
such as hepatitis B. are more easily transmitted.
Many viral illnesses are much more contagious: you
can get them simply by being in the presence of an
Infected individual. But with AIDS, you must do
specific, defined actions (exchanging body fluids) to
become infected.
8.
Anyone who is at risk of having ever acquired HIV
infection. 'Illis includes anyone who:
• received a blood transfusion between
19~8-1985.
• injected illicit drugs or shared hypodermic needles.
• has hemophilia.
• has had sexual intercourse with gay or
bisexual men.
When someone
engages in inter
course, he or she has
sex with everyone
that person has ever
had intercourse with.
• hits had any sexually transmitted disease
(chlamydia, gonorrhea, syphilis, etc.). The
occurrence of other sexually transmitted diseases
puts one at greater risk for HIV infection.
• has had sexual intercourse with any person whose
sexual history is unknown or uncertain. When
someone engages in intercourse, he or she has sex
with everyone that person has ever had intercourse
with. Tlie facts about HIV transmission are power
ful support for the church's teaching that sexual
intercourse should be reserved for marriage and
for faithfulness within marriage on the part of
both partners.
Since it has been learned that drugs such as AZT can
help delay the onset of full blown AIDS, it is even
more important that everyone who carries the virus
should be identified. Because some people in our
congregations have had multiple sex partners,
voluntary confidential HIV testing should be chosen
by many people throughout our churches.
9.
Condoms mean safer sex, not safe sex. Condoms
are not 100 percent reliable: they only reduce the
risk of becoming infected with HIV and only if they
are used for even- sexual encounter. L'sing the
condom is the best preventive measure for those
who will not abstain from sexual activity or practice
monogamy. To call the use of the condom ‘safe” is
misleading. Recommendations for condom use
come after the preferable recommendation to
abstain or be monogamous. AIDS and all sexually
transmitted diseases are diseases of multiple
partnerships.
10.
'Hie average time from infection to the development
of symptomatic AIDS is currently about ten years.
Blood tests, however, can detect falling immunity
and the use of drugs such as AZT can, in some
persons, delay the onset of hill blown AIDS. Anyone
who is HIV positive should be closely monitored.
11.
'Hie HIV antibody test only reveals the HIX' status of
the person at that particular time, not next week.
next month, or next year. So how often would you
want to test? It is quickly apparent that a single test
can be misleading, and frequent testing would be
prohibitively expensive. Furthermore, mandatory
testing tends to drive “underground" those most
likely to be HIV positive.
Tlie millions of dollars required for mandatory’ testing
would be better spent on prevention strategies, on
education, and on selective confidential testing of
those at high risk.
12.
There are two ways alcohol increases one s possibil
ity of developing AIDS: a) people do things when
they have been drinking that they would not do
otherwise, such as being less selective in choosing
sexual partners, less careful about using condoms.
and less careful in using injectable drugs: and
b) alcohol depresses the immune system. .Alcohol
use and abuse is a known risk factor for HIV
infection.
'nun nit ilei'hil (Iffch
tiiid
h\ \\ ilhii'd Kmhtll. \l D . (,ushc»i /.\
.L'<//»/<
*«/
implied
9
What priority did
Jesus give to healing
those in need?
AIDS: What Does the Bible Say?
The Bible clous not address AIDS directly. But it docs
address related issues: healing, caring for others, the
relationship between spiritual brokenness and sickness.
and^-sponses to other serious illnesses. Examine these
Go^el passages in the current context of AIDS. What
docs the Bible say? What docs Jesus’ life show us?
Judging others
Matthew 7:1-5. Luke 6:37-42
Have you ever done anything tor which you were
afraid of being judged? Did you fuel judged b\ others?
What was that like? What did you want to do as a
result of feeling judged? How did you work through
that event? How did you experience Jesus reaching
out to you?
Healing a person with leprosy
Matthew 8:1-4
How do you see yourself as a leper? How does that
affect your Life and your relationships with others?
c you ever felt shunned, excluded, or on the
“outside?" Who reached out to you and what did they
do? Have you been healed of that leprosy? How did
the healing happen? Did Jesus touch you? Through
whom? What did that person do to help you experi
ence Jesus’ healing?
Healing and gathering food on the Sabbath
Matthew 12:1-13
What priority did Jesus give to healing and feeding
those in need? What risks did Jesus take to earn' out
th.it priority?
The parable of the good Samaritan
Luke 10:25-37
Is it possible that persons with AIDS have something
to teach us? \\ h\ did the Samaritan help the wounded
man? Manin Luther King said the priest and l.evitc
a>kcd."\\ hat will happen to us if we help?” The
Samaritan asked. “\\ hat will happen to him if I don’t
help?” Would \ou be willing under am circumstance
It)
to risk sour health tor the sake of helping another
person? Why'' Why not?
Parable of the prodigal son
Luke 15:11-31
With whom do you most identify ? Docs that change
from time to time? What urges you to lease the Father
at times? What draws you back? Are you ever resent
ful of those w ho think you have “wasted’ their lives?
What do you do w ith those feelings? How do you
respond to those who you think have taken advantage
of the Father s gifts of los e? Hosv do you feel about a
Father who will take someone back who you don’t
think deserves being taken back?
Healing the man by the pool
John 5:1-14
What did Jesus mean by his statement at the end of
tliis passage? What implications docs this have for
how we relate to persons with AIDS? (Note that Jesus
first healed the man. then told him to stop sinning.
Jesus did not make compassion and healing contin
gent on the man changing.)
Woman caught in adultery
John 8:1-11
Hoss' does this encounter apply to our attitudes to
persons with AIDS? What docs this encounter say to
persons who have contracted AIDS through high risk
behaviors?
Illness and spiritual brokenness
John 9:1-3
The New Testament seems to view illness in more
than one way. At times it is seen as resulting from
people’s wrong choices. But in this passage, what did
Jesus say about whether people’s illness or injury is
punishment? Do we ever identify ourselves to be
among those in need?. How arc we like the leper, the
prodigal, the older brother, the adulteress? Do we
hurt or help to heal?
Additional Resources for HIV and AIDS Education
Toll-free telephone numbers
•
Mennonite Mutual Aid: 1-800-348-7468
A oibliography of Mennonite church press articles
about HIV and AIDS can be obtained from the MMA
Educational Resources team.
•
Video resources
These videos provide reliable data about HIV infection and
AIDS, prevention and care. Preview these materials and
supplement them with teaching on Christian compassion,
commitment to strong family and moral values, and
understanding of sexuality.
U.S. Public Health Service hotlines:
AIDS information line: 1-800-342-AIDS
Spanish language; 1-800-222-SIDA
Hearing impaired: 1-800-553-AIDS
Brethren/Mennonite AIDS
information hotline
“AIDS: What Everyone Needs to Know.”
Rental: S60
Purchase: Video $275/Film $390
Order from
Churchill Films
662 North Robertson Boulevard
Los Angeles. CA 90069-5089
800-334-7830; (213)657-5110 in California
• Telephone number: 717-393-7140
Several Lancaster County, Pa., Mennonites and
Brethren started a hotline in 1990 for persons who
are HIV positive or living with AIDS. Any person who
feels isolated or wants additional church support in
dealing with AIDS can call. Though the hotline was
formed out of a local initiative, it is now open to
callers from all parts of North America. Callers
seeking basic information or supportive relationships
will be referred to the closest local resource if they
wish. All calls are strictly confidential: callers are not
required to give their names.
“AIDS: A Family Experience”
A family shares how they are dealing with a son/brother
with AIDS. Presents issues of feelings about homosexual
ity. fears of contracting the disease, reactions of friends.
and feelings about facing death. Also includes interviews
with a medical doctor and psychiatrist to give medical data
about AIDS.
33 minute video
S15 rental from Mennonite Mutual Aid
Discussion guide included
U.S. Department of Health and Human Services and local
County Health Departments:
“Teens. Questions and Answers,” video
by Dr. C. Everett Koop, former Surgeon General, with
discussion guide for teenage audiences.
"Epidemic of Fear: AIDS in the Workplace”
Includes video, discussion guide, and guidelines for writing
policies.
"Can I Get It?” Outlines sexual behaviors that increase
risk of HIV infection.
11
Printed materials
National Council of Churches Task Force on AIDS:
AIDS: A Resource Packet for Congregations.
k75 Riverside Drive. New York. NY 10115. $5.00.
AIDS, A Manual for Pastoral Care.
Ronaid H. Sunderland and Earl E. Shelp.
Philadelphia: The Westminster Press, 1987.
Includes medical facts, fears about AIDS, recognizing
and dealing with grief, ethical issues, and case studies.
When AIDS Comes to Church.
William E. Amos.Jr. Philadelphia:
The Westminster Press. 1988.
Excellent first-person account of a pastor’s
experiences in working with persons with AIDS. William
Amos is pastor of a Baptist congregation in a
Ft. Lauderdale, Fla., suburb
AIDS and the Church.
Earl E. Shelp and Ronald H. Sunderland.
Philadelphia: The Westminster Press. 1987.
Encourages the church to respond to AIDS; gives
medical information, considers the responsibility of the
church, and describes ways of ministering to those
with AIDS.
"Sex education has often been difficult. Today, however,
education is a matter of life and death."
•
12
— Willard Krabill, M. D.
/Il.
. X• 2 •
i
_ AID SN EW S«
/ jX
G L «B A L
The Newsletter of the W 3 r 1 d Health
WHO
accepts drug
donation
for AIDS
patients in
Africa
........
Organization Global Programme on AIDS
Belgian pharmaceutical firm has agreed to give the World
Health Organization a large quantity of drugs to treat people
in developing African countries for two common fungal infections
related to AIDS: oral and oesophageal candidiasis. WHO believes the
drugs donated by Janssen Pharmaceutica of Belgium will be enough
to treat 300 000 people over five years.
A
The agreement, signed on
25 November, is a result of GPA
collaboration with the pharmaceu
tical industry on improving HI\/
AIDS care in developing countries.
Dr Hiroshi Nakajima, DirectorGeneral of WHO, expressed his
thanks to Janssen for the donation.
“Our objective is to alleviate the
suffering of hundreds of thousands
of AIDS patients in Africa and to
improve the quality' of their life,”
he said. “I sincerely' hope that
others interested in helping
AIDS patients will make similar
donations.”
continued page 3
S€x education leads to
safer behaviour
Inside Global AIDSnews
NEWS ROUNDUP
Terrence Higgins Trust
marks 10 years
Health Secretary’s ABC
Ethiopian, 64 walks for AIDS
NGO campaign features
4
5
6
Kama Sutra
7
AIDSbriefs
8
GPA IN ACTION
Experts back microbicides 9
GPA publishes handbook
on AIDS care in the home 11
Bangladesh boosts prevention 13
Indian doctors learn AIDS skills 14
Tuvalu hopes to stay AIDS-free 16
RECENT PUBLICATIONS 17
DIARY 19
PLATFORM
Shivananda Khan 20
eaching young people about sexuality and contraception is often
thought to encourage early sexual experimentation. This belief,
which is a powerful barrier to the introduction of HIV/STD preven
tion programmes, has been conclusively disproved by
* a GPA review
of studies on the effects of sex education in schools. In fact, sex and
AIDS education often encourages young people to delay sexual
activity and to practise safer sex when they are sexually active.
T
Among rhe studies that evaluated
the sexual behaviour of students
exposed to sex education, 19
considered its effect on reported
age at first intercourse and re
ported levels of sexual activity.
■ No study revealed evidence of
sex education leading to earlier
or increased sexual activity in
young people.
3 In six studies, sex education
either delayed the onset of
sexual activity or caused a tall in
its overall extent.
35 Two studies showed that access
to counselling and contraceptive
services did not encourage
earlier or increased sexual
activity.
continued page 2
The Newsletter of the World Health Organization Global Programme on AIDS
GLOBAL
AIDSNEWS
Sex education leads to
safer behaviour
(continued from page I)
| Two public information
■ Ten studies showed that sex
: programmes on HIV/AI DS
education increased the adop
tion of safer practices by sexually • brought about a large rise in the
use of condoms and other contraactive vouth.
, ceptives, while causing no decrease
School programmes
i in age of first intercourse and no
which promoted
rise in the amount of sexual activity
both the postpone
among young people. ■
ment of sexual
intercourse and the
; The GPA review was conducted by Drs
use of condoms when
Peter Aggieton, Mariella Raldo and Gary
Slutkin of GPA’s Office of Intervention
sex occurs were more
Development Support, in collaboration
effective than those
with the National Centre for HIV Social
which promoted
Research, Macquarie University, Sydney,
abstinence alone.
Australia; the Institute of Population
They were also more
Studies, University of Exeter, UK; and the
Psychology Department, Rowling Green
effective when given
State University, Ohio, USA.
before young people
become sexually
active, and when
they emphasized skills and social
norms rather than knowledge.
Typical studies reviewed:
l.Two programmes, each of 15
modules lasting 50 minutes,
among 722 males and females
averaging 15 years old.
H Young people children - need to
learn about AIDS
prevention before
they become sexually
active, and school
based education
programmes
must make sure
they do. fl
likely to have sex, but were
more likely to use contracep
tion.
5.
FINDING: Programmes
delayed initiation of unpro
tected sex in those with no
sexual experience.
FINDING: Programme
caused postponement of sex
(particularly in girls), greater
contraceptive use and lower
pregnancy rates.
2. Cross-sectional survey of
1880 males aged 15-19.
FINDING: AIDS/sex
education was associated
with fewer sexual partners,
less frequent intercourse
and more condom use.
Dr Michael H. Merson,
Executive Director, GPA,
Third Pan American Conference
on AIDS and Ninth Latin American
Congress on Sexually Transmitted
Diseases, Cartagena, Colombia.
3 November 1993.
3.
4.
Survey of 3711 males and
females aged 15-19.
FINDING: Those who had
sex education were no more
2
i
6.
Intercountry comparison of
education, sexual behaviour,
•teenage pregnancy and
abortion.
FINDING: Information
and services did not boost
sexual activity.
1993-No. -I
Peer-led education programme
among 536 adolescents aged
13-14, focused on contracep
tion and postponement of sex.
Fifteen skills-based lessons
focused on contraception and
postponing sex among 758
males and females aged 15-18.
FINDING: Programme
delayed start of sexual inter
course and raised the use of
contraceptives among the
sexually active.
7.
Analysis of 14 separate sex
ed ucation program mes.
FINDING: No effect on
incidence of sexual inter
course.
Pain
Pain,
Perpetual pain,
Aching, slogging, grieving,
feeling,
piercing, future blinding
round embracing,
isolating,
oneness
loneness
weary sadness making.
Pain of watching,
waiting
nothing certain
one year, two years
time is breaking over
day by day
and holding in its grasp
our lives and loss
Pain of never winning
not improving
slowly waiting
for the end that will be no end
but start again of grieving
paining,
pining
further anger
sadness
Pain of being rendered helpless.
Nothing cures
though love can ease the time
of days and nights of
help me, turn me, lift me
feed me,
touch me softly, giving
hopeful love’s embrace.
Is this empty
PAIN of inner man?
Analgesics cannot touch
this deeper hurt.
Can it covered be by
alcohol’s soft dream
or drugs’ high lift?
Is there in the hurt
endured,
a glimpse of Christ
hanging, waiting, paining
on the tree.
Is this pain a part
of when our Lord
is crossing me?
No-answer have I
Only this I say
that when I look at him
He is with me.
Ivan Mann
Trust
Loving God, you show yourself to those who are vulner
able and make your home with the poor and weak of this
world;
Warm our hearts with the fire of your Spirit. Help us to
accept the challenges of AIDS.
Protect the healthy, calm the frightened, give courage to
those in pain, comfort the dying and give to the dead
eternal life;
Console the bereaved, strengthen those who care for the
sick.
May we your people, using all our energy and imagina
tion, and trusting in your steadfast love, be united with one
another in conquering all disease and fear.
Terrence Higgins Trust Interfaitb Group
Guilt
A Carer’s greatest fear
I have been guilty again —
Guilty of being tired
Guilty of possession
Did I do that right?
Guilty of pushing that fear down hard
Guilty of being hurt and hurting
Of making decisions
Guilty of crying
Did I try as hard as I should?
Guilty7 of keeping my emotions in check and not
succeeding
Of not communicating
Guilty of exploding with my frustration
Can I do better tomorrow. Guilty
And then my absolute exhaustion makes me feel guilty,
Can’t I have two more minutes to myself, on my own.
Guilty
But today I am much better, guilty of being
A good Carer
Guilty of loving and caring and knowing
I have got it right
And tomorrow I will be guilty again
Guilty of not feeling guilty
Till tomorrow I will feel alright
But then, I really must find a new guilt
I have used all these before
Ross Davis
AIDS CARE, VOL. 6, NO. I, 1994
L /■
5
Should wider HIV testing be encouraged on
the grounds of HIV prevention?
S. Bearjdsell
SZQVL4, Department of Sociology, University of Essex, UK
Abstract The issue of the role of HIV testing in HIV prevention is an important one. Some
commentators have argued that HIV testing should be encouraged more widely on the grounds that
it can stimulate behaviour change to safe sex and drug use. Testing has been advanced as an
important means to control the epidemic. There is, however, insufficient evidence to support this
contention at this time. The hypothesis of a link between HIV testing and behaviour change is based
on the assumption of a linear relationship. It is argued that this assumption is based on two others,
that the 'stimulus’ of testing and counselling is uniform, and that information will be perceived and
used by all recipients in an identical way. It is argued that there is currently insufficient research
evidence to encourage more widespread testing on prevention grounds. Issues which should be
considered in future research designs are discussed.
Introduction
The issue of HIV antibody testing and the balance of its advantages and disadvantages has
always been a contentious issue, and one which constantly needs to be re-examined. Whether
to take an HIV antibody test or not is a major decision and the individual must be aware of
and weigh the benefits against the drawbacks at any one point in time.
For those who test positive there is still no ‘magic bullet’ of a cure and they are faced
with terminal illness and the additional burdens of stigmatization and discrimination, social
isolation and rejection, even from partners, family and friends. Given this, an individual may
simply ‘not want to know’. On a practical level, even if the result is negative difficulties in
getting life insurance or a mortgage may be experienced (Came & Kapila, 1988).
On the other hand, testing can put the individuals’ mind at rest (BMRB, 1991; Bor et
al., 1991) and allow long-term plans to be made, including those regarding sexual practices,
contraception and pregnancy (Leen et al., 1989; Came & Kapila, 1988). Moreover, the major
advantage of testing is ongoing monitoring in order to identify clinical problems early on and
receive early prophylaxis and therapies:
... an anti-testing position is at best self-defeating and at worst dangerous. It is self
defeating since only from patients can we learn more about the natural history of
An earlier version of this paper was prepared for the Inter-Regional HIV/AIDS Forum Working Group on HIV
Testing while the author was Senior Research Officer at Nonh East Thames Regional Health Authority.
Address for correspondence: Dr Susan Beardsell, Project SIGMA, Unit 64, Eurolink Business Centre, 49 Effra
Road, London SW2 IBZ, UK.
6
S. BHARDSELL
HP/ infection so that we can plan for their care and treatment; it is potentially
dangerous because patients are denied the benefits of treatment that may prolong
life. (Bor et al., 1991)
There is increasing evidence that early treatment and prophylaxis may delay the progression
of HIV disease (for discussions see, for example, Miller & Pinching, 1989; Amo et al., 1989;
Friedland, 1990). Evidence from the US (Bennett et al., 1989) and the UK (Whitmore-Overton et al., 1993) suggests that early access into medical care may slow disease progression and
lead to improved survival. (Note that these conclusions are inferred since early referral is also
related to the experience of the treatment centre (Whitmore, personal communication)).
Thus, Friedland argues that HP/ testing provides a “powerful program for delaying the
progression of HP/ infection”.
Access to medical services may now well be the most crucial factor in individual decision
making around HP/ testing. The focus of this paper however is a public health advantage
that has been discussed extensively: whether HP/ testing can perform a health education role
and bring about behaviour change. It is argued that the experience of having an HP/
test leads to a reduction or cessation in behaviours likely to put the individual at risk of HP/
infection.
The proposed prevention component of HIV' testing has been discussed as an important
means of controlling the HP/ epidemic (see, for example Weiss & Thier, 1988; Rhame &
Maki, 1989). Testing has been held by some physicians and public health commentators to
be a necessary part of promoting behaviour change (see Bayer, 1989; Miller & Pinching,
.
1989)
Calls have therefore been made for routine HP/ testing of those at ‘high risk’ (e.g.
Brandon, 1988; Barbacci et al., 1991) or even of the whole adult population (e.g. Rhame &
Maki, 1989). Given that there is already mandatory testing of certain groups in the US and
elsewhere, these arguments are on a slippery slope to advocating mandatory testing (for a
discussion of the ethical issues see, for example, Gillon, 1987; Miller & Pinching, 1989;
Bayer, 1989; Rhame & Maki, 1989; Brandt, ei al., 1990).
In Britain, the Department of Health appears to be developing a more proactive policy
towards testing. In December 1990, Sir Donald Acheson, the Chief xMedical Officer stated
that “If people think they have been at risk they should seek a test” and in July 1991, Virginia
Bottomley, Minister for Health, said “I want to encourage people to come forward for a test.
There should be no stigma attached”. This developing policy [see, for example, Chief
Medical Officer’s press statement of 25 July 1991; Department of Health guidelines PL/CO
(92)5, 1992] appears to be based on two premises, the medical care available to those who
test positive and behaviour change:
A person who is unaware that he or she is HIV infected may unintentionally infect
sexual or drug misusing partners. Conversely, people who know that they are
infected have the opportunity to adopt behaviours that minimise the risk of trans
mitting the virus to others. Furthermore, evidence now suggest that an infected
person may benefit clinically from prophylactic treatments to delay the onset of HIV
related disease and from earlier treatment of any such conditions. [Department of
Health guidelines PUCO (92)5, 1992.]
In the great majority of cases people will be found to be negative but testing will still
be beneficial because it means they will have access to advice about how to protect
themselves and others from the risk of infection in the future. (The Chief Medical
Officer in a press statement of 25 July 1991.)
HIV TESTING AND PREVENTION
7
Demand for testing does seem to be increasing. In the North East Thames Regional
Health Authority, testing services experienced a significant increase in workload during
1990-1. This coincided with a national HIV prevention campaign but there was a particularly
large increase in requests for advice and testing following the statement by the Chief Medical
Officer in 1990. Demand declined after the initial impact but levelled at a higher point than
before (NETRHA, 1991). More recent figures indicate that this increased demand continued
in 1991-92 (O’Brien et al., 1992). In response to the preliminary findings of the anonymised
seroprevalence surveys, some centres (e.g. genito-urinary medicine and antenatal clinics) now
offer a more proactive testing service—that is, testing is offered to all clients instead of only
responding to their requests for a test. Recent Department of Health guidelines [PL/CO
(92)5, 1992] also encourage offering HIV testing more widely and the setting up of
alternative testing sites.
Would more testing help to control the spread of HIV? If testing is found to be
an effective prevention tool, this has serious ramifications. To change our current
strategy in Britain would have huge resource implications and care would have to be taken
to ensure that the quality of counselling services was not compromised. Moreover,
how would more people be encouraged to be tested? A survey commissioned by
the Department of Health and the Association of British Insurers (BxMRB, 1991)
found that 80% of HIV/AIDS specialists (doctors, health advisers, helpline workers,
charity workers, etc.) believed that the questions on HIV testing on life insurance
forms would put people off having a test. In Sweden, HIV testing is one of the
most important part of the authorities’ prevention policy and the government strongly
encourages voluntary testing—more people per million inhabitants have been tested
than in any other European country, despite comparatively low rates of HIV infection
(Henriksson, 1988). Between 1985 and 1989 the numbers of gay and bisexual men,
and injecting drug users coming forward for HIV testing decreased slightly while
the numbers of heterosexuals (mainly HIV negative) dramatically increased (MAnsson,
.
1990)
Thus, xMAnsson (1990) concludes that “people who are unlikely to be infected
are the ones who take the test, in droves”. Therefore, encouraging testing may not actually
help to identify those who are HIV positive. (From a prevention perspective, of course,
it could be argued that having many seronegative individuals coming for testing may
be no bad thing, since they will have access to HIV prevention counselling). HIV
testing may even be emphasized to the neglect of other prevention measures—
Watney (1990) has commented that "... culturally, antibody testing is still being promoted
as a form of technological solution to safer sex, largely by the mass media”. In the
worst instance, there is also the danger that calls for an increase in testing would lead to
calls for more coercive measures in order to ‘protect the public health’. We must
thus examine the assumptions around testing and prevention very carefully if testing
is to be adopted as an HIV prevention strategy. The present paper will critically examine
a number of assumptions made around this issues by commentators, policy makers
and researchers.
Since 1985 it has been the policy of the Department of Health and Social Services that
everybody seeking an HIV antibody test in Britain should receive pre- and post
test counselling. .Any proposed effect on behaviour will, therefore, be a result of the
combination of testing and counselling, and it is not possible to isolate the individual
contribution of each to any behaviour change. All discussions of the effect of HIV testing on
behaviour in this paper will relate only to situations similar to Britain where testing has been
accompanied by counselling. It is thus the effects of the whole testing process that is being
considered.
8
S. BEARDSELL
Assumption 1: There is a correlation between HIV testing/counselling and behaviour
change
Assumption 2: Behaviour change should be most marked in those who test positive
As discussed above, policy makers and commentators have claimed or implied that testing
can be of benefit to public health by leading to behaviour change (e.g. Department of Health
guidelines, PL/CO(92)5, 1992; see also discussions in Bayer, 1989; Miller & Pinching, 1989;
Brant et al.> 1990). That is, that the experience of HIV testing and associated counselling will
lead to a reduction or cessation in behaviour patterns likely to put the individual at risk
HIV infection and that “No-one would then spread the virus ignorant of the fact that thqB
were infected” (Brant et al.} 1990). This assumption has been tested by looking at data from
various studies, mainly from the US and Europe. Most of these studies have also tested the
hypothesis that there will be a difference between those who test HIV positive and those who
test seronegative. It has been suggested (Jacobsen et al.} 1990) that a negative result may
reinforce or even decrease the perceived threat of HIV and, therefore, limit motivations to
change behaviour. On the other hand, one could also hypothesize no difference between
seropositives (who change to protect others) and seronegatives (who change to protect
themselves).
Research has rarely been designed with the express purpose of evaluating the effects of
counselling and testing on behaviour, and studies which systematically evaluate the effect of
HIV counselling are absent, probably due to the crisis response of HIV counselling (Carballo
& Miller, 1989). However, a review of available research was published at the end of 1991
(Higgins et al.} 1991). The ‘effectiveness’ of counselling/testing was defined in terms of
self-reported behavioural indices such as condom use, number of sexual partners, frequency
of drug use and needle sharing, needle hygiene, etc., and participants were followed
longitudinally or compared cross-sectionally to assess any changes on these parameters.
Studies were organized into the following samples: gay men, intravenous drug users, pregnant
women and ‘other heterosexuals’. Readers are referred to the Higgins et al. paper for a fulU
review of the relevant studies. The purpose of this paper is not to replicate their work but to
*
consider some of the issues arising from their conclusions. For the readers convenience,
however, the following sections precis the findings for the above samples:
Gay men
Seventeen studies, predominantly from the US, were reviewed. Comparisons were mainly
done on those who knew their antibody status versus those who did not and, among those
who knew their status, those who were seropositive versus those who were seronegative. Over
the periods of research, all groups tended to report ‘dramatic reductions
*
in risk behaviour,
although it is clearly not possible to empirically establish that this was due to counselling and
testing alone. Cross-sectional comparisons indicated greater reductions among those who
knew their serostatus compared to those who did not but these results often disappeared
when longitudinal analyses were conducted, suggesting that changes in behaviour were
independent of knowledge of serostatus. Some studies indicated greater risk reduction among
known positives as opposed to negatives, but some contradictory evidence leaves this issue
unresolved.
Intravenous drug users
Twelve studies from the US, UK and the Netherlands were reviewed. Improvements were
made in needle-use behaviour and there was some sexual behaviour risk reduction. However,
HIV TESTING AND PREVENTION
9
all but one sampled their participants from methadone maintenance programmes, so it is
impossible to separate the effects of the programme from that of HIV counselling and testing.
No differences were reported between those who tested positive or negative and those who
were untested, indicating that any differences are not due to knowledge of HIV status.
Pregnant women
Eleven studies from the US, Scotland, France, Switzerland and Nairobi were discussed.
Prevention was defined in terms of seropositive women electing to abort. [This definition of
prevention is somewhat value laden and perhaps reflects the pressure on seropositive women
to terminate in order not to infect the foetus, despite more recent evidence from the
European Collaborative Study (1991) of a 13% perinatal transmission rate (in women who
were mainly asymptomatic).] Serostatus did not effect termination decisions. However, there
was no control for how much a baby was wanted in the first place—all the US women were
in antenatal programmes which may indicate commitment to the pregnancy. Only the
Nairobi study looked at condom use, but found no significant effect between seropositive and
seronegative women.
Other heterosexuals
Ten studies were banded under this heading. They include four studies of couples consisting
of one seropositive and one seronegative (seven European sites, Rwanda, New York, Los
.Angeles), one of women in Zaire, one of STD clinic clients (Los Angeles), one of couples
with an intravenous drug using history (New York), two of high risk women (New York,
Long Beach) and one of adolescents (New York). In contrast to the studies discussed above,
-here was a trend for counselling and testing to have an effect on safer sex. Only one study
provided tests of statistical significance.
Results are thus contradictory and as yet the relationship between testing and prevention
remains unproven. Even where changes in unsafe behaviour were observed over time, other
factors, such as the mass media and health promotion initiatives, were at work concurrently.
Clearly, methodologically, it is not possible to isolate the effects of each. Testing and
counselling may well have contributed to the behaviour changes, but it is not possible to say
to what extent. iMany studies shared the hypothesis that knowledge of serostatus would have
a significant effect (i.e. that it is not just the experience of testing and counselling that effects
behaviour, but knowing that one is HIV positive or not), but there was only evidence for this
in some of the studies of gay men. The conclusions that we can draw from the current
research into the behavioural effects of HIV testing are limited by methodological limitations
and there are also theoretical reasons why the predicted effects may not occur anyway. These
will now be discussed.
Methodological problems with available studies
The major methodological flaw in the available studies is the lack of any control or
comparison group (Higgins et al. 1991)—all participants receive counselling and testing, and
changes in behaviour are monitored over time. Given the plethora of other variables that can
10
S. BEARDSELL
effect sexual and drug-taking behaviour, we can never be sure that these changes were solei
due to the testing experience or what degree of contribution counselling and testing cou!
have. However, given the ethical problems of refusing counselling and testing to groups c
clients who want it, this problem is unlikely to be addressed. Hypotheses are often based or
the presumption that the effect of counselling and testing will be to decrease risky behaviour
However, a negative result may lead to a false sense of security that may sustain or ever
increase these behaviour patterns. Some commentators on intravenous drug users hav-.
expressed the view that testing may be counter-productive to prevention, with a positivresult leading to more chaotic drug using and sexual behaviours (Mulleady, 1989; see alsc
Bond, 1991). Thus, the process of counselling and testing could have the effect of changir.z
risk behaviours in either direction. It is possible that individual differences within samjf^^ma-.
lead to these effects cancelling themselves out in statistical analysis.
The time period between receiving counselling and testing and behavioural assessment:
is usually not reported (Higgins et al., 1991), but this may be a crucial factor. It may be, for
instance, that assessments taken very soon after testing show the largest effect which may
then quickly dissipate. Alternatively, later assessments may show a greater effect, reflecting
the time for intentions to be translated into behaviour. For individuals who test positive, it
is also likely that counselling will be ongoing, so that any behaviour changes are due not jus:
to pre- and post-testing sessions only. Tnere is a need for more longitudinal research with
assessments made at regular intervals.
Assessments of behaviour are often taken only at two points in time. Studies therefore
fail to take account of those individuals who are inconsistently safe by not considering
behaviour over a long enough period (Han et al., 1992) or negotiate unprotected sex or
needle sharing through knowledge of partners identical HIV status (Hart et al., 1992; Kippax
et al.j 1992). Behaviour change, moreover, is not irreversible.
Behavioural measures are self-reported retrospectively. Thus they rely on memory and
are subject to various intentional or unintentional errors (for instance, ‘social desirability’
responses may occur when an individual does not want to admit unsafe sex to a researcher
in the context of a study on HIV). iMeasures, moreover, vary across studies, making the^^ess
comparable. Wording of questions can be very important as shown, for example, in the work
of Project SIGMA on different interpretations of identical sexual terminology (e.g. Coxon,
1988; Hunt & Davies, 1991).
The studies under discussion are also biased by the self-selecting nature of the sample
(Higgins et aL> 1991). That is, participation in the study was dependent upon respondents
coming forward and wanting a test, and also upon them coming back for the results and
agreeing to take part in follow up. It could be hypothesized that they come forward because
they are more aware of their own risks and may, therefore, be more motivated to change their
behaviour. Similarly, the longer participants stay in the study, the more motivated they may
be around HIV issues. Well controlled studies tend to show that those who come forward to
be tested may have made greater changes in high risk behaviour before testing, and that while
counselling and testing may have hastened the behaviour change, it did not cause it (Miller
& Pinching, 1989; Cohen, 1991). Testing and counselling may not be the occurrence that
leads to behaviour change, but a mid-point in the change process. A current study of HIV
testing in women in Newhaven, USA, indicates that behaviour prior to testing is the best
predictor of behaviour after testing (Ickovics, personal communication).
The temptation, therefore, is to design studies which specifically address the hypothesis
of a relationship between counselling testing and behaviour change, and which take account
of these methodological issues. However, the hypothesis is still based on several assumptions
HIV TESTING AND PREVENTION
11
which can also be challenged and which also have serious methodological implications for any
studies chat are to be designed.
Assumption 3: The relationship between receiving testing and counselling, and
behavioural change is a linear one
Implicit in various discussions around the effects of HIV counselling and testing on preven
tion is the notion of a linear effect between exposure to the ‘stimulus’ (HIV testing and
counselling) and the ‘subject’ (the person being tested), the effect being a reduction or
cessation of risky practices. It will be argued that this assumption is erroneous and is, in fact,
based on two further assumptions which assume a simplistic notion of behaviour change:
Assumption 4: The ‘stimulus’ of testing and counselling is uniform
The nature and content of the counselling session itself are uncontrolled factors in the
available research. The content and methods of HIV test counselling may vary widely (Bond,
,
1991)
therefore, the studies may not even be evaluating the same thing and it would be
erroneous to hypothesize that they would have a uniform effect on behaviour. Why should
we, in any case, assume that all testing and counselling will work to similar ends?
There is limited research as to what actually goes on in HIV test counselling and whether
its content can reasonably be predicted to affect behaviour change, although it should include
information on risk reduction. The notable exception is the work of Silverman and colleagues
(e.g. Silverman, 1990; Silverman & Perakyla, 1990). Using discourse analysis of real life
counselling sessions, they have illustrated the degree of disparity in the content of sessions
and the way that counsellors
*
work:
... [some] ... faced with a heavy patient load for pre-test counselling, may concen
trate on conveying accurate information in order to obtain informed consent. Still
others, with lower patient loads, may manage pre-test counselling sessions of up to
45 minutes, based on theoretical models that may be fundamentally at variance with
individualised, psycho-pathological theories. (Silverman, 1990, p. 200.)
Initial analysis of pretest counselling identified four styles which are described in Silverman
(1990) as follows:
The information-giving model
This model is basically a paramedical one with a stress on getting informed consent for the
test. The emphasis is on understanding body functioning and on civil rights issues such as
confidentiality and insurance.
The medical model
Under this model history taking is followed by physical examination.
•Throughout this paper the term ‘counsellor’ does not necessarily refer to someone with a professional counselling
qualification, but to whoever conducts HIV test counselling, whatever their profcssion/discipline.
12
S. BEARDSELL
The systems model (e.g. Miller & Bor, 1988)
Information is tailored to the individual client and advice giving is avoided. Based on family
therapy, it seeks to identify patients’ understandings and practices in the context of their
support systems in community.
The psycho-pathological model
Many social workers defined HIV/AIDS counselling in terms of emotions and fears. Themes
of ‘empowerment’ and building up ‘self-esteem’ are central.
Individual counsellors may produce widely differing ‘prevention effects’. HIV test
counselling may be undertaken by a wide variety of health care professionals—doctors,
nurses, health advisors, psychologists, psychiatrists, social workers, etc., with a good deal of
disparity in terms of qualifications and training (Coyle & Sodin, 1992), counselling (in the!
British Association of Counselling’s meaning of the word) experience and time available. It
is understandable that this too will affect the nature of the counselling session although there
is no evidence that adherence to any particular philosophy of counselling affects outcome
(Aspy & Roebuck, 1977). What may be important, however, are the qualities of the
counsellor—empathy, positive regard, genuineness and concreteness (Rogers, 1958; Truax &
Carkhuff, 1967). The WHO Global Project on AIDS sees “a supportive and trusting
relationship on the basis of which crises and problems emerging from HIV awareness or
infection can be mutually addressed and overcome” (cited in Carballo & Miller, 1989) as
implicit in prevention counselling. In the limited time available (one or two sessions, if HIV
negative) some counsellors with some clients may find it difficult to develop this relationship,
which in turn will affect client ‘compliance’ to risk reduction advice. Many of the British
counsellors consulted by Bond (1991) thought that preventative work was unlikely to be
effective without such a counselling relationship. On a practical level, this lack of time also
makes it difficult to cover issues around having an HIV test, ensuring informed consent, etc.,
and prevention measures adequately, particularly in busy clinics where time is at a premium.
There is a plethora of work on the communication problems in doctor-patient interac
tions (see Pendleton & Hasler, 1983). Much non-compliance with doctor’s advice is due to
the patient not understanding what the doctor said and the fact that doctors use terminology
that even they themselves believe will not be understood by the patient. Difficulties iri(
doctor-patient communication also increase with social distance (e.g. social class, sexual
orientation, ethnicity, etc.) between the doctor and patient. In terms of information around
risk reduction, in some instances, similar processes may operate, which may act to decrease
the likelihood of behaviour change. iMoreover, clients may only be able to take in limited
information when worried about the possibility of a negative result (pre-test) or relieved by
a negative result (post-test), although, clearly, if positive and receiving ongoing counselling
there is more opportunity for risk reduction advice. Individual differences in comprehension
and retention of information received should be accounted for in any analysis of the effects
of counselling.
Assumption 5: Information will be received by all clients in an identical way
Even if the nature and content of testing and counselling is identical for all recipients, it
would still be erroneous to assume that effects would be the same. Individual differences
between clients in the way that risk reduction information is perceived and put into practice
must be taken into account—relevant studies utilize rather crude categorizations based on
HIV TESTING AND PREVENTION
13
transmission categories. Recent data (Ostrow, 1992) indicated that a ‘lapse’ from safe sex
prior to testing to unsafe sex after the test among a sample of self-identifying gay men was
associated with lower income, slightly lower education levels, higher rates of depression (as
assessed by standardized scales), lower social support, higher levels of social conflict and
isolation and higher denial/fatalism. HIV status had no effect. Data from a study of women
in Newhaven (Ickovics, personal communication), however, shows no effect of psycho-social
characteristics, so clearly more research is necessary in this area. There are clearly limitations
to these studies; Han et al. (1992) have produced an excellent critique of the concept of
•relapse’ and the variables studied were closed-ended, and did not explore fully the economic
and social bases of sexual interactions, but they do highlight the need for considering
psychological and social factors.
Motivation on the part of the person being tested to change risk behaviour is an
uncontrolled factor in all relevant studies. Tne transtheoretical approach to change, devel
oped from the work of Prochaska & DiClemente on addictive behaviours and processes of
change (e.g. Prochaska, 1979; Prochaska & DiClemente, 1982; DiClemente & Prochaska,
1982), is relevant here. They propose that in order to change an addictive behaviour there
must first exist motivation to change. They argue that without it change is not possible and
clients may in fact actively resist change by finding reasons to maintain the current behaviour.
Research with smokers (e.g. Prochaska & DiClemente 1983) and opiate users (e.g. Van
Bilsen & Ernst, 1986) supports this argument. Although I am not suggesting that sex is an
addictive behaviour and injecting drug use can occur without addiction, it is easy to see how
the basic tenets of the model can be translated to changing sexual or drug taking habits.
Motivation to change may thus vary in ±e samples who took part in the various studies,
which will influence behavioural outcomes. This has implications for widening HIV testing.
The effectiveness of counselling may vary depending on whether the client comes forward for
the test and asks for it, as opposed to being offered the test without any prior thought of the
issues (as in the case of routine antenatal testing, for instance). It is also a good argument
against calls for mandatory testing of certain groups, in that it may be useless without
motivation. A study in San Francisco (Watters et al., 1986) showed that 53% of intravenous
drug users contacted in the community would not enter treatment even if it were available
‘tomorrow’. Similarly, resistance to condom use among male heterosexuals may also work
against counselling success. There is also a need to consider existing attitudes and beliefs, and
the relative importance of HIV risk in an individual’s life—poverty and housing concerns may
make HIV a minimal concern, for instance.
Motivation to change is not enough, however. Much available research works within the
framework of the Health Belief Model (Becker, 1974; Rosenstock, 1974) or the Theory of
Reasoned Action (Fishbein & Azjen, 1975; Azjen & Fishbein, 1980). The former sees health
related decisions as based on rational evaluation of ‘facts’. The assumption is that knowing
how to protect yourself and knowing what the consequences of not protecting yourself are
will automatically lead to protection. The latter sees behavioural intentions (affected by
beliefs, knowledge and subjective norms) as the best predictor of behaviour.
There is increasing evidence, however, that this assumption of rationality is misplaced
(see Cohen, 1991; Ingham, et al., 1991). Simply providing health-related information is not
sufficient to produce and sustain behaviour change (see Gatherer et al., 1979). The social
science literature on social perception and cognitive processes conceptualizes the perception
of information as an active constructive process not a passive one (Bransford & Franks, 1971;
Shank & Ableson, 1977; Hamilton, 1981; Neisser, 1980; Miller & Tumbill, 1986). It is
argued that pre-existing schemata are confirmed through selective perceptions (Markus &
Zajonc, 1985). Echabe & Rovira (1989), for instance, have found that people have different
14
S. BEARDSELL
social representations of AIDS and that recall of information congruent with these schemata
was more likely than recall of incongruent information.
The Health Belief Model has been found to be a poor predictor of health-related
behaviour generally (e.g. Reid & Christensen, 1988; Rosenstock et al., 1988) and with
reference to HIV (e.g. Montgomery et al., 1989; Hingson et al., 1990; see also a review of
studies with gay men by Cohen, 1991).
Whatever the motivation or intent to change behaviour, there are external constraints on
behaviour change. There is a qualitative difference between deciding to be safe and actually
being safe (Salt, et al., 1990). The Health Belief Model focuses on individual perceptions
(Hart et al., 1992), but drug using may take place with others and sex, by definition, involves
more ±an one person. Thus, the behaviour and attitudes of others may intervene in thei
change process and affect the efficacy of counselling. One clear example is the difficulties
many women experience in negotiating sexual activity within the context of gender ideologies
and power relations (e.g. Holland et al., 1990a, 1990b; Ingham et al., 1991). Expecting
change is to neglect the significance of sexual or drug-taking behaviour in an individual’s life.
We cannot ignore the cultural meanings of certain behaviour patterns and beliefs. In his
evaluation of the Gay Men’s Health Crisis ‘800 men project’ in the US, Silin (1987) argues
that such projects "... are built on the belief that we can change our behaviour while ignoring
questions of the deeper meanings with which these may be charged by different elements of
society ...”.
There may also be positive reasons for not behaving in a ‘rational’ manner (Ingham et
al., 1991). For instance, as Cohen (1991) points out, condoms may not be used, despite
knowledge that they can protect against HIV, simply because they are not liked.
A rational intent to change behaviour may also be thwarted by other factors such as state
dependency effects. Sexual arousal, anxiety, alcohol or drug intoxication, etc., may all affect
‘rational’ cognitions, memory retrieval and behaviour (e.g. Birnbaum et al., 1978; Ostrow,
1990; Plant et al., 1989; Stall et al., 1986, but see also Weatherbum et al., 1992 for a
conflicting view on the effects of alcohol).
The linear model of behavioural change is rooted in stimulus-response psychology and
assumptions of a direct link between exposure to information, and attitude and behaviour
change. This approach has been supplanted by a more cognitive approach which sees
individuals as active, not passive, recipients of information (e.g. Bransford & Franks, 1971;
Shank & Ableson, 1977; Neisser, 1980) and change as a two (or more) way process. The
attitudes and beliefs an individual brings with them to the counselling session will interact
with information given to produce selective perceptions, not necessarily in line with the intent
of the counsellor. Changing attitudes and behaviour is a complex process unlikely to be
effected in just a couple of counselling sessions (which, it must be remembered, cover more
than just advice on safe sex and drug-using behaviour). Sexual and drug-taking behaviour
patterns are complex, adopted over a period of time and affected by a variety of beliefs and
experiences. Why should change be simple or quick? The emphasis on rational decision
making in behaviour change fails to account for the fact that ‘non-compliance’ to advice may
be unintentional and that human beings are often far from ‘rational’.
In the light of this, if we are investigating the effects of HIV test counselling, perhaps
instant behavioural changes are unrealistic outcome measures. The linear model also seems
in conflict with the wider goals and aims of counselling, as outlined in the psychological
literature. As discussed above, the counsellors consulted by Bond (1991) saw the counselling
relationship as a priority in prevention counselling. It was felt that counsellors should use
counselling methods and [resist] the temptation to switch to giving advice or general
HIV TESTING AND PREVENTION
15
information.” They believed that any information giving should be presented selectively and
in a personally relevant way:
This way of presenting information ensures that it takes the minimum time and can
be alternated with times when the counsellor uses reflective responses to elicit the
clients views and feelings and thus helps them to process this information. (Bond,
1991, p. 56.)
A focus on an ‘expert’ who ‘tells’ a client ‘what to do’ is a disempowering experience
(Homans & Aggieton, 1988), at odds with the philosophy of counselling although this
approach may, nonetheless, be used by some HIV counsellors before and after the HIV test
(Silverman, 1990).
Assumption 6: Prevention should be one of the aims of HIV testing
For many individuals, coming for an HIV test may be the only opportunity they may have for
personal HIV education. Many commentators see risk reduction as an important component
of the testing process as the following quotations illustrate:
[HIV counselling is] ... an on-going dialogue and relationship between client or
patient and counsellor with the aims of preventing HIV transmission and providing
psycho-social support for those affected, directly and indirectly, by HIV. (WHO’s
Global Project on AIDS, 1989.)
even internationally it is
... increasingly being proposed as a key component of HIV prevention programmes
which compliments other information, education and communication strategies.
(Carballo & Miller, 1989.)
In the UK, counselling is viewed as an important strategy in the prevention of the
transmission of HIV:
... we have been repeatedly told that the most effective means of providing
information and enabling individuals to understand that information and relate it to
their own life is through one to one counselling. (The House of Commons Social
Services Committee, 1986-87.)
At a policy level, therefore, there is some agreement that HIV test counselling should
include a prevention component. However, not all counsellors would concur with this view.
Bond’s (1991) survey found tensions between the role of the counsellor and an information
giving role:
[there was felt to be] ... incompatibility between counselling viewed as a client-cen
tred activity in which the client sets the agenda for the counselling sessions and
identifies their own goals, with the introduction of preventative strategies derived
from an externally created agenda and series of goals. One person summarised the
conflict she felt by asking “is the counsellor there for the client or to help the client
meet someone else’s agenda?” (Bond, 1991.)
Bond concludes that a significant minority of counsellors have thus avoided preventative
work although many could cite instances in which they may have contributed to prevention.
Thus, whether test counselling can have an effect may depend on the counsellors expecta
tions of the session. However, Bond recommends that “Contribution to HIV prevention is a
16
S. 3 EARDS ELL
new task for most counsellors which should be incorporated into the training of HIV
counsellors”. It is not clear, however, how this would work in practice given the wider agenda
of test counselling and time limitations.
Conclusion
This paper has examined the argument that HIV resting (and- associated counselling) will
lead to a reduction in risky practices, thus protecting the individual from future infection if
negative and protecting future sexual or intravenous drug using contacts if positive. The
wider implications of this argument is that testing is an important component of HIV
prevention activity and that by adopting a proactive policy towards testing we can help to halt
the epidemic.
The assumption that there is a positive relationship between testing and receiving
information on risk reduction during pre- or post-test counselling may have surface validity,!
but it is argued that the relationship between testing and counselling and behaviour change
is more complex than that and we currently have insufficient empirical evidence for a clear
statement on the effects of testing and counselling. Moreover, the hypothesis of a linear
relationship is rooted in an outdated model of human behaviour. Individuals may move
between safe and unsafe behaviour depending on a variety of situational and personal factors
and there is no reason to suppose that an HIV test will lead to irreversible changes in
established behaviour. For some counsellors with some clients in certain circumstances,
testing for HIV may, indeed, have an effect, but it is difficult to draw generalizable
conclusions.
It is argued that if a more proactive policy towards testing is adopted, this should not,
at this stage, be on prevention grounds alone. This does not mean that testing should not be
encouraged on other grounds, such as the advantages of early treatment. It must be
remembered, however, that a wider programme of testing has serious resource implications.
There is a danger that wider testing will lead to a cutback in counselling and more emphasis
on information giving and advice. This type of counselling seems problematic for some
counsellors and may be less likely to produce any behavioural changes than pre- and post-test
counselling founded in more therapeutic approaches.
Clearly, the issue of prevention and testing is an issue that will continue to be debated
and will no doubt be the focus of future research. Hopefully, this discussion has highlighteq
some of the important issues that any rigorous methodology will need to consider.
Acknowledgements
I would like to thank Rita O’Brien of NE Thames Regional Health Authority and the
members of the Inter-Regional HIV/AIDS Forum Working Group on HIV Testing: Peter
Exon, Simon Hall, Andrea Kelmanson, Edward King and Nicola Woodward for informative
discussions around this issue and comments on an earlier version of this paper. Thanks also
to Hazel Belfield-Smith for kindly proof reading the final version.
References
Arno, P.S., Shenson, D., Seigel, N.F., Franks, P. & Lee, P.R. (1989) Economic and policy implications of early
intervention in HD/ disease, Journal of the American Medical Association, 262, pp. 1493-1498.
ASPY, D.N. & Roebuck, F.N. (1977) Kids don't Learn from People they Don't Like (Amhunt, Mass, Human Resource
Development Press).
HIV TESTING AND PREVENTION
17
AzjEN, I. & FlSHBEiN, M. (1980) Understanding Attitudes and Predicting Social Behaviour (Milton Keynes, Open
University Press).
BaRBACCI, M., Repke, J.T. & Channon, R.E, (1991) Routine prenatal screening for HIV infection, Lancet, 337,
pp. 709-711.
Bayer, R. <1989) Ethical and social policy issues raised by HIV screening: the epidemic evolves and so do the
challenges, AIDS, 3, pp. 119-124.
Becker, M. (1974) The health belief model and personal health behaviour, Cognitive Therapy & Research, 8,
pp. 231-255.
Bennett, C.L., Garfunkel, J.B., Greenfield, S. et al., (1989) The relation between hospital experiences and
inpatient mortality for patients with AIDS related PCP, Journal of the American Medical Association, 261,
pp. 2975-2979.
Birnbaum, I. et aL, (1978) Alcohol and memory retrieval processes, Journal of Verbal Learning & Verbal Behaviour, 17,
pp 325-335.
BOND, T. (1991) HIV Counselling: Report on National Survey & Consultation 1990. (Rugby, BAC).
Bor. R., Miller, R., Murray, D. & Johnson, M. (1991) HIV counselling in the 1990s, Lancet, pp. 337-950.
BMRB '1991) AIDS and Life Insurance (London, HMSO).
Brandon, S. (1988) HIV testing Without permission, Lancet, July 9, p. 109.
BRANSFORD, J. & Franks, J. (1971) The abstraction of linguistic ideas, Cognitive Psychology, 2, pp. 331-350.
Brandt, A M., Cleary, P.D. & Gostin, L. (1990) Routine hospital testing for HIV: Health policy considerations, in:
L. O. Gostin (Ed.) AIDS and the Health Care System (New Haven, Yale University Press).
Carballo, M. & Miller, D. (1989) HIV counselling: problems & opportunities in defining the new agenda for the
1990s, AIDS Care, I, pp. 117-123.
Carne, C. & Kapila, M. (1988) Testing and Screening for HIV Infection, AIDS Programme Paper 2 (London, HEA).
Cohen, M. (1991) Changing to safer sex: personality, logic and habit, in: P. Aggleton, G. Hart <3c P. Davies (Eds)
AIDS: Responses, Interventions and Care (London, Falmer Press).
Coxon, A. (1988) Tne numbers game—gay lifestyles, epidemiology of AIDS & social science, in: P. AGGLETON, G.
Hart & P. Davies (Eds) Social Aspects of AIDS (Lewes, Falmer Press).
COYLE, A.G. & SODIN, C.M. (1992) Training, workload & stress among a sample of HIV counsellors, AIDS Care, 4,
pp. 233-237.
DEPARTMENT of Health (1992) Department of Health Guidance: Additional sites for HIV antibody testing/Offering
voluntary named HIV antibody testing to women receiving antenatal care/Partner notification for HIV infection
(PL/CO(92)5) (London, DoH).
Dl Clemente, C.C. & Prochaska, J.O. (1982) Self change and therapy change of smoking behaviour: A comparison
of processes of change in cessation and maintenance, Addictive Behaviour, 7, pp. 133-142.
Echabe, A.E. & Rovtra, D.P. (1989) Social representations and memory: The case of AIDS, European Journal of
Social Psychology, 19, pp. 543-551.
European Collaborative Study (1991) Children bora to women with HIV-1 infection: Natural history and risk of
transmission, Lancet, 337 pp. 225-260.
F1SH3EIN, M. & AzjEN, I. (1975) Belief, Attitude, Intention and Behaviour: An Introduction to Theory and Research
(Reading, Mass., Addison-Wesley).
Friedland, G.H. (1990) Early treatment for HIV: The time has come, New England Journal of Medicine, 322,
pp.1000-1002.
Gatherer, A., Parftt, J., Porter, E. & Vessey, M. (1979) Is Health Education Effective? (London, HEC).
Gillon, R. (1987) Testing for HIV without permission, British Medical Journal, 294, pp. 821-823.
Hamilton, D.L. (1981) Cognitive representations of persons, in: E. T. Higgins, C. P. Herman & M. P. Zanna (Eds)
Social Cognition: The Ontario Symposium (Hillsdale, Lawrence Erlbaum).
Hart, G., Boulton, M., Fitzpatrick, R., McClean, J. & Dawson, J. (1992) ‘Relapse’ to unsafe sex behaviour
among gay men: a critique of recent behavioural HIV/AIDS research, Sociology of Health & Illness, 14,
pp. 216-232.
Henriksson, B. (1988) Social Democracy or Societal Control. A critical analysis of Swedish AIDS policy (Stockholm,
Glacio Bokfdrlag).
Higgins, D.L. et al (1991) Evidence for the effects of HIV antibody counselling and testing on risk behaviours, Journal
of the American Medical Association, 226, pp. 2419-2429.
Hingson, R.W., Strunin, L_, Berlin, B.M. & Heeren,T. (1990) Beliefs about AIDS, use of alcohol and drugs, and
unprotected sex among Massachusetts adolescents, American Journal of Public Health, 80, pp. 295-299.
Holland, J., Ramazanoglu, C. St Scott, S. (1990a) Managing risk and experiencing danger: Tensions between
government AIDS education policy and young people’s sexuality, Gender & Education, 2, pp. 125-146.
Holland, J., Ramazanoglu, C., Scott, S., Sharp.S. & Thomson, R. (1990b) ‘Don’t die of ignorance—I nearly died
18
S. BEARDSELL
of embarrassment’—condoms in context. Paper delivered at the 4th Social Aspects of AIDS Conference, South Bank
Polytechnic, London, 7 April.
Homans, H. & Aggleton, P. (1988) Health education, HP/ infection and AIDS, in: P. Aggleton & H. Homans
(Eds) Social Aspects of AIDS (London, Falmer Press).
Hunt, A. & Davies, P. (1991) What is a sexual encounter? in: P. Aggleton, G. Hart & P. Davies (Eds) AIDS:
Responses, Interventions and Care (London, Falmer Press).
INGHAM, R., Woodcock, A. & Stenner, K. (1991) The limitations of rational decision making models as applied to
young people’s sexual behaviour. Paper presented at the Sth Social Aspects of AIDS Conference, South Bank
Polytechnic, London, 23 March.
Jacobsen, P.B., Perry, S.W. & Hirsch, D.A. (1990) Behaviorial and psychological responses to HIV antibody testing,
Journal of Consulting and Clinical Psychology, 58, pp. 31-37.
Kippax, S., DowsetC, Q.W., Davis, M., Rodden, P. & Crawford, J. (1992) Sustaining safe sex or relapse: gay men’s
response to HIV. Paper presented at the VII International Conference on AIDS/III STD World Congress, Amsterdam
[Abstract TuD 0545J.
Leen, C.S., Brettle, R.P. & Bird, A.G. (1989) Benefits of HIV testing in symptom-free risk groups, Lancet, 2,
pp. 512-513.
MANSSON, S.A. (1990) Psycho-social aspects of HIV testing—the Swedish case, AIDS Care, 2, pp. 5-16.
Markus, H. & Zajonc, R.B. (1985) The cognitive perspective in social psychology, in: G. Lindsey ic E. Aronson
(Eds) Handbook of Personality & Social Psychology (New York, Random House).
Marlatt, G.A. & Floyd, J.D. (1985) Relapse Prevention (New York, Guilford Press).
Mn_LER, R. & Bor, R. (1988) AIDS: A Guide to Clinical Counselling (London, Science Press).
Miller, D. & Pinching, A.J. (1989) HIV tests & counselling: Current issues, AIDS, 3 (Supp 1), pp. si87—193.
Miller, D.T., & TURNBILL, W. (1986) Expectancies and interpersonal processes, Annual Review of Psychology, 16,
pp. 89-130.
Montgomery, S.B., Joseph, J.G., Becker, M.H., Ostrow, D.G., Kessler, R.C. & Kirscht, J.P. (1989) The Health
Belief Model in understanding compliance with preventative recommendations for AIDS: how useful? AIDS
Education & Prevention, 1, pp. 303-323.
MULLEADY, G. (1989) Drug abuse and HIV, in: J. Green & A. McC REARER (Eds) Counselling in HIV Infection and
AIDS (Oxford Blackwell).
Neisser, U. (1980) On social knowing, Personality & Social Psychology Bulletin, 6, pp. 601-605.
Netrha (1991) AIDS (Control) Act Report for April 1st 1990-1991 (London, NE Thames Regional Health Authority).
O’Brien, R., Batliwala, Y., Belfield-Smith, H. & Beardsell, S. (1992) AIDS (Control) Act Report for April 1st
1991-1992. (London, NE Thames Regional Health Authority).
Ostrow, D.G. (1990) Recreational drug use and sexual behaviour change in a cohort of homosexual men, The Journal
of Acquired Immunodeficiency Syndrome, 4, pp. 759-765.
Ostrow, D. (1992) Untitled paper presented at VII International Conference on AIDS/III STD World Congress,
Amsterdam.
Pendleton, D. & Hasler, J. (Eds) (1983) Doctor Patient Communication (London, Academic Press).
Plant, M.L. et al. (1989) The sex industry, alcohol and illicit drugs: Implications for the spread of AIDS, British
Journal of Addiction, 84, 53-59.
Prochaska, J.O. (1989) What causes people to change from unhealthy to health enhancing behaviour? In: C. C.
CUMMINGS & J. D. Floyd (Eds) Human Behaviour & Cancer Risk Reduction (Atlanta, American Cancer Society).
PROCHASK.A, J.O. (1979) Systems of Psychotherapy: A Transtheoretical Analysis (Homewood Ill., Dorsey Press).
Prochaska, J.O. & DiClemente, C.C. (1982) Transtheoretical therapy: Toward a more integrative model of change,
Psychotherapy: Theory, Research & Practice, 19, pp. 276-288.
Prochaska, J.O. & DiClemente, C.C. (1983) Stages 3c processes of self-change of smoking: Toward an integrative
model of change. Journal of Consulting & Clinical Psychology, 51, pp. 390-395.
Raymond, J.S. & Wood, D.W. (1989) Social context phenomena influencing developmental aspects of health
behaviour, in: C. C. Cummings & J.D. FLOYD (Eds) Human Behaviour & Cancer Risk Reduction (Adanta,
American Cancer Society).
Reid, LD. & Christensen, D.B. (1988) Norwegian gay men: reasons for continued practice of unsafe sex, AIDS
Education & Prevention, 2, pp. 109—115Rhame, F.S. & Maki, D.G. (1989) The case for wider use of testing for HIV infection, Neto England Journal of
Medicine, 320, pp. 1248-1254.
Rogers, C.R. (1958) The characteristics of a helping relationship, Personnel & Guidance Journal, 31, pp. 6-16.
Rosenstock, I.M. (1974) Historical origins of the health belief model, Health Education Monograph, 2, pp. 354-386.
Rosenstock, I.M., Strecker, V.J. & Becker, M.H. (1988) Social learning theory and the Health Belief Model,
Health Education Monograph, 2, pp. 354-386.
HIV TESTING AND PREVENTION
19
Rosenstock, I.M., Strecher, VJ. & Becker, M.H. (1988) Social learning theory and the Health Belief Model,
Health Education Quarterly}. 5, pp. 175-183.
Salt, H., Boyle, M. & Ives, J. (1990) HIV prevention: Current health promoting behaviour models for understanding
psycho-social determinants of condom use, AIDS Cart, 2, pp. 69-75.
Shank, R. & Asleson, R. (1977) Scripts, Plans, Goals & Understanding (Hillsdale, NJ, Erlbaum).
Silin,/. (1987) Dangerous Knowledge, Christopher Strut, 113, pp. 34—40.
Silverman, D. (1990) The social organisation of HIV counselling, in: P. Aggleton, P. Davies & G. Hart (Eds)
AIDS—Individual, Cultural & Policy Dimensions (Basingstoke, Falmer Press).
Silverman, D.& Perakyla, A. (1990) AIDS counselling: the interactional organisation of talk about ‘delicate’ issues,
Sociology of Health & Illness, 12, pp. 293-318.
Social Services Committee Session Report (1986-87) Problems associated with AIDS. House of Commons, 13 May
1986, p. 46, para 71.
Stall, R-, McKltsick, L, Wiley, J., Coates, T. & Ostrow, D. (1986) Alcohol and drug use during sexual activity
and compliance with safe sex guidelines for AIDS: The .AIDS Behavioral Research Project, Health Education
Quarterly, 13, pp. 359-371.
TRUAX, C.B. i Carkhuff, R.R. (1967) Toward Effective Counselling & Psychotherapy: Training & Practice (Chicago,
Aldine).
Van BlLSEN, H.P.J.G. & Emst, A.J. (1986) Heroin addiction & motivational milieu therapy, International Journal of the
Addictions, 21, pp. 707-713.
WaTTERS, J.K, LURA, D.M. & Lura, K.W. (1986) AIDS prevention & education services to intravenous drug users through
the Mid City Consortium to Combat AIDS: Administrative Report of the 1st 6 months. (Unpublished document,
Institute for Health Policy Studies, University of California, San Francisco).
WaTNEY, S. (1990) cited in V. George (Ed.) Voluntary HIV Testing: Should we be Encouraging it? (London, Hampstead
Health Promotion Department).
Weatherburn, P., Davies, P.M., Hunt, A J., Hickson, F., Coxon, A.P.M. & McManus, T.J. (1992) There is no
relationship between alcohol and ‘unsafe’ sex. Paper presented at VII International Conference an AIDS/III STD
World Congress, Amsterdam.
Wass, R. & Thier, S.O. (1988) HIV testing is the question—what’s the answer? Hew England Journal of Medicine,
319, pp. 1010-1012.
Whitmore-Overton, E., Tulett, H.E., Evans, B.G. & Allardice, M. (1993) Improved survival from diagnosis of
AIDS in adult cases in the UK and bias due to reporting delays. AIDS, 7, pp. 415-420.
f994, 69, :V/-.76
No. 26
Organisation mondiale de la Sante, Genove
World Health Organization, Geneva
CONTENTS
x•
SIDA - Donnees mondiales
La situation actuelle de !o pondemie de VIH/SIDA dons le monde
189
• AIDS — Global daro
I
The current global situation of the HIV/AIDS pandemic
191
189
191
Index des Nos 1 d 26
1 Index to Nos. 1 to 26
)
Subjects
192
Sujets
192
195
Pays et territoires
Notifications de maladies soumises au Reglement
195
1
Countries and territories
Notifications of diseases subject to the Regulations
195
195
196
Maladies soumises ou Reglement
196
■ Diseases subject to rhe Regulations
ACQUIRED IMMUNODEFICIENCY SYNDROME (AIDS) — DATA AS AT 30 JUNE 1994
SYNDROME DIMMUNODEFICIENCE ACQUISE (SIDA) — DONNEES AU 30 JUIN1994
• Counrry/Arec — Pc'/s'/Terrircire
Number
Date of report
of cases
Dare
Nombre de cos
de notification
.
Benin — Benin
Date of report
of cases
Dote
Nombre de cos
de notification
Seychelles...........................................................................
2
10.12.93
138
08.08.93
Sierra Leone.......................................................................
95
07.07.93
...................... ...
703
31.12.93
Somalia — Somalie........................................................
13
01.01.91
..................
742
09.05.94
South Africa — Afrique du Sud.....................................
3210
28.02.94
Africa — Afrique
Algeria — Algerie
Angola
Number
Counhy/Areo — Pays/Ter ritoire
Botswana
...........
1415
31.12.93
Sudan — Soudan.............................................................
904
17.04.94
Burkina Faso
___ ...................
4 193
31.12.93
Swaziland...........................................................................
413
28.02.94
7 225
10.12.93
Togo.....................................................................................
3 472
23.02.94
.........................
3 072
13.12.93
Tunisia — Tunisie.............................................................
136
21.05.93
143
10.12.93
Uganda — Ouganda........................................................
43 875
31.12.93
Central African Republic — Republique centrafricoine
3 730
30.11.92
United Republic of Tanzania — Republique-Unie de
Chad — Tchad
1523
08.12.93
Tanzanie.......................................................................
38 719
07.01.93
4
12.04.94
Zaire — Zaire...................................................................
22 747
26.04.94
6 393
23.03.94
Zambia — Zombie..........................................................
29 734
20.10.93
18 670
24.02.94
Zimbabwe...........................................................................
27 905
31.12.93
490
19.04.94
91
07.02.94
43
02.12.93
Burundi
______
Cameroon — Cameroon
.................. :
Cape Verde — Cap-Vert
......................................
Comoros — Comores
....... ..
:
Congo
Cote d'Ivoire
____________
Djibouti
Egypt — Egypfe
........................................
...
Equatorial Guinea — Guinee equatorial
Eritrea — Er/riiree
_____ ...
Ethiopia — Eitiiopie
Gabon
..............................................
.........
Total
.............. .................................................................
331 376
372
31.12.92
Americas — Ameriques
12 958
03.06.94
Anguilla................................................................................
5
472
10.12.93
Antigua and Barbuda — Anrigua-er-8arbuda..............
34
30.09.93
31.12.93
.........................................
277
31.12.93
Argentina — Argentine...................................................
3 904
31.03.94
..... .......................................
11629
03.03.94
Bahamas.............................................................................
1 389
31.12.93
........
976
31.12.93
Barbados — Barbade.....................................................
418
31.12.93
.......................
380
11.06.93
Belize..................................................................................
82
31.12.93
Kenya
„
...
Lesotho--------------------- --------- .---------------------------------
30126
31.12.93
Bermuda — Bermudes...................................................
223
30.06.93
479
10.12.93
Bolivia — Bolivie............................................................
87
31.03.94
Libeno — Liberia
191
10.12.93
Brazil — Bresil................................................................
49 312
28.02.94
Libyan Arab Jamahiriya — Jamahiriya arabe libyenne
10
01.02.93
British Virgin Islands — Iles Vierges britanniques......
6
31.03.94
Madagascar
9
14.03.94
Canada.................................................................................
9511
31.03.94
31857
10.02.94
Cayman Islands — Iles CaTmanes................................
15
31.03.94
1874
25.11.93
Chile — Chili....................................................................
831
31.12.93
Mauritania — Mauritania
50
01 12.93
Colombia — Colombie....................................................
4 583
31.03.94
Mauritius — Maurice
13
31.01.94
Costa Rica..........................................................................
587
31.03.94
Morocco — Maroc
196
20.05.94
Cuba....................................................................................
245
31.12.93
...........................................
826
31.12.93
26
31.12.93
..........~.................................
5101
31.12.93
Dominica — Dominique..................................................
Dominican Republic — Republique dominicome........
2 353
31.03.94
..................................................................
921
15.06.93
Ecuador — Equateur.......................................................
381
31.03.94
1 148
04 04.94
El Salvador.........................................................................
630
31.03 94
65
20.03.92
French Guiana — Guyone francaise..............................
232
30.09.90
10 706
30.06.93
Grenada — Grenade........................................................
58
31.03.94
Soo fame and Principe — Soo foine-et-Principe
24
1012.93
Guadeloupe........................................................................
353
31.03.93
Senegal — Senegal ......
911
31.05.93
Guatemala...........................................................................
499
31 03.94
Gambia — Gambie
Ghana
Guinea — Guinee
Guinea-Bissau — Guinee-Bissau
Malawi
.......................................................
..
_____________
..................................................
Mali
Mozambique
Namibia — Namibie
Niger
Nigeria — Nigeria
...........................................
Reunion — Reunion
Rwanda
189
WEEKIY [PlDfMIOlOGKAl RECORO, N«. 24, 1 JULY 1994
Country/Area — Pays/Temtoire
•
Number
Dote of report
of cases
Dole
Nombre de cos
de notification
REUVE EPIDEMIOLOGIQUE HEBDOMADAIRE, N
* 26, I
*
JUILIET 1994
Number
Country/Areo — Pays/Territoire
Guyana......................................................................... ....
465
31.03 94
Haiti — Haiti....................................................................
4 967
31.12.92
Honduras........................................................... .................
3 473
31.03.94
Jamaica — Jamoique.....................................................
669
31.12.93
Martinique................... ............. .............. ..........................
266
30.09.93
Mexico — Mexique.........................................................
18 353
Montserrat............. ............................................................
7
Viet Nam
.
Yemen — Yemen
Dole
Nombre de cos
de notification
107
15.04.94
8
19.0194
...............................................................................
8 968
31.03.94
Europe
31.03.94
Albania — Albanie..........................................................
1
Austria — Autriche..........................................................
Netherlands Antilles and Aruba —
Total
Date of report
of cases
I
1 150
31.03.94
31.03.94
•
1
1
Antilles neerlondoises er Aruba.................................
157
30.06.93
Belarus — Belarus..........................................................
10
31.03.94
Nicaragua................... -.....................................................
66
31.03.94
Belgium — Belgique......................................................
1603
31.03.94
Panama................................... ...........................................
644
31.03.94
Bulgaria — Bulgarie........................................................
24
31.12.93
Paraguay................... ....................... .................................
77
23.05.94
66
31.03.94
■
Peru — Perou.................................. ...................... _.......
1068
31.03.94
Croatia — Croatie...........................................................
Czech Republicb— Republique tchequeb.................
48
31.03.94
’
Saint Kins and Nevis — Saint-Kitts-et-Nevis...............
41
31.03.94
Denmark — Danemark...................................................
1 411
31.03.94
Saint Lucio — Sain te-lucie...........................................
56
31.03.94
Estonia — Estonie...........................................................
3
31.03.94
Finland — Finlande.........................................................
158
31.03.94
Saint '/incent and the Grenadines—Sain t-Vincent-etGrenadines......... .........................................................
56
31.03.94
France..................................................................................
30 003
Suriname...............................................................„...........
177
31.03.94
Germany — Altemogne...................................................
11 179
3103.94
31.03.94
‘
Trinidad and Tobago — Trinite-et-Tobogo...................
1 545
31.03.94
Greece — Grece..............................................................
916
31.03.94
•
Turks and Caicos Islands — Iles Turques et Caiques
39
30.09.93
149
31.03.94
United Stores of Amenco — Etats-Unis d’Amerique..
411 907
31.12.93
Hungary — Honqrie.......................................................
Iceland — Islande...........................................................
31
31.12.93
469
31.03.94
Ireland — Irlande...........................................................
392
31.03.94
Uruguay....................... ........... ....... ..................................
Venezuela........................................ -....... ~.....................
3511
31.03.94
Italy — Italic....................................................................
21 770
Latvia — Lettonie...........................................................
8
31.03.94^|
31.03.941
Lithuania — Lituame......................................................
5
31.12.93
Luxembourg........................................................................
79
31.03.94
Total
......................... ........................................ ............
523 777
Asia — Asie
Afghanistan.........................................................................
Armenia — Armenie.................................................
Malta — Malte................................................................
29
30.09.93
—
15.02.92
Monaco...............................................................................
24
2
30.04.93
Netherlands — Pays-Bas................................................
3 055
30.09.93
31.03.94
31.03.94
Norway — Norvege.........................................................
375
31.03.94
31.03.94
Azerbaijan—AzerbaTdjan.............. „...........................
Bahrain — Bahrein.......... ...............................................
13
21.03.94
Poland — Pologne..........................................................
201
Bangladesh................... ........................ ............................
1
14.06.94
Portugal..............................................................................
1811
31.03.94
14.06.94
Republic of Moldova — Republique de Moldova.......
4
31.03.94
Bhutan — Bhoutcn..................... ..................................
Brunei Darussalam — Brunei Darussalam..................
3
17.05.93
Romania — Roumanie....................................................
2 736
31.03.94
Cambodia — Cambodge..... ......................................
—
31.03.94
Russian Federation — Federation de Russie..............
136
31.03.94
Chino0 — Chine0
36
31.12.93
1
30.09.92
31
19.05.94
San Marino — Saint-Marin............................................
Slovak Republic0 — Republique slovoque6 ._______
7
31.03.94
Slovenia — Slovenie......................................................
32
31.03.94
_________ -.
Cyprus — Chypre..... ......................................................
Democratic People's Republic of Korea —
14.06.94
Spain — Espagne...........................................................
24 202
31.03.94
Georgia — Georgie......... ................... ...........................
2
30.04.93
Sweden — Suede...........................................................
1 001
31.03.94
Hong Kong.......... ........................ ........ ~...........................
99
28.02.94
Switzerland — Suisse....................................................
3 662
31.03.94
Indio — Inde.......................... ........................................
713
14.06.94
Ukraine...............................................................................
27
31.03.94
Indonesia — Indonesia..................................................
49
14.06.94
United Kingdom — Rovoume-Uni.................................
9 025
31.03.94
......................................
334
31.03.94
................................................................................
1 15 668
Republique populcire democratique de Coree .......
Yugoslaviac—Yougoslaviec
Iran (Islamic Republic of) — Iran (Republique
isfomique d')......... .....................................................
92
15.03.94
Total
Iraq................ .....................................................................
26
28.04.94
Israel — Israel................... ........ ................................. ...
279
31.03.94
Oceania — Oceanie
Japan — Jopon___ _________ ________ _________
713
30.04.94
American Samoa — Samoa americaines...................
Jordan — Jordanie..... „.................................................
31
03.02.94
Australia — Australia......................................................
4 727
Kazakhstan................... .....................................................
4
31.03.94
Cook Islands — Iles Cook..............................................
—
15.04.94
Kuwait — Koweit....................................... ......... ...........
10
17.04.94
Fiji — Fidji........................................................................
6
31.12.93
Kyrgyzstan — Kirghizistan............................................
—
30.04.93
French Polynesia — Polynesia franjoise.....................
33
13.10.93
Guam...................................................................................
20
31.03.94
Kiribati.................................................................................
1
31.03.94
Mariana Islands — Iles Mariannes..............................
4
12.04.94
Marshall Islands — Iles Marshall.................................
2
30.04.94
federes de)................................... ............................
2
09.09.93
Nauru...................................................................................
New Caledonia and Dependencies —
—
26.08.93
Loo People's Democratic Republic —
Republique democratique populaire loo..................
14
30.04.94
Lebanon — Liban............................................................
72
24.05.94
Macao..................................................................................
7
15.04.94
Malaysia — Moloisie.................... .. ..................... ........
107
28.02.94
Maldives......................................... ........ ...........................
—
14.06.94
Mongolia — Mongolie...................................................
—
14.06.94
Myanmar............................................................................
261
14.06.94
Nepal — Nepal...... _................................ .....................
24
14.06.94
Oman............................. ................................... -..............
33
10.05.94
Pakistan.............................................................................
41
09.05.94
Philippines.................... ................................... .................
136
31.03.94
Qatar................................................... ..............................
Republic of Korea — Republique de Coree................
41
20.03.94
19
31.03.94
Saudi Arabia — Arabic sooudite...................................
61
29.04.94
Singapore — Singapour.............. ..................................
75
31.12.93
Sri Lanka............................................................................
37
14.06.94
Syrian Arab Republic — Republique orabe syrienne..
26
30.04.94
Tajikistan — Tadjikistan......... _....................................
—-•
31.03.94
5 654
14.06.94
Turkey — Turquie................................... .. ....................
130
31.03.94
Turkmenistan — Turkmenistan....................................
1
30.04.93
United Arab Emiro res — Emir ots orabes unis.............
8
12.02.93
Uzbekistan — Ouzbekisfon...........................................
2
30.06.93
Thailand — Thailande...................................................
Nouvelle-Caledonie et Dependances........................
32
15.04.94
New Zealand — Nouvelle-Zelande..............................
431
31.12.93
Niue.................................................. ..................................
—
20.04.94
Palau...................................................................................
Papua New Guinea — Popouosie-NouvellfrGuinee...
1
19.07.93
64
19.04.94
Samoa.................................................................................
1
18.04.94
Solomon Islands — Iles Solomon................................
—
25,04.94
Tokelau...............................................................................
—
31.04.94
Tonga...................................................................................
6
31.12.93
Tuvalu..................................................................................
—
—
26.07.93
—
24.05.93
Total
...............................................................................
World total — Total mondial
..........................
06 05.94
5 330
985 119
3 Does nor include rhe Province of Tomon which has reporred -18 cases. — A I’exdusion de la Province de Taiwan qui a nolifie 48 cos.
‘
5 Previously reported under Chechoslovakia — Notifies onieneurcmenr sous khdcoslovnquie.
1 Refers to steres, ureas oi .’he former Sonofisf federal Republic ul Yugoslavia not otherwise listed separately- — Conterne les flots/termoires de I'lincrenne Republique fhterale sociaiiste Je Youqoslovie qui tie sonl pas cites sepurcment.
190
1
;
.
31.08.93 31.12.93f
Micronesia (Federated States of) — Micronesia (Etats
Vanuatu..............................................................................
Wallis and Futuna Islands — lies Wallis et Futuna...
.
WEEKLY EPIDEMIOLOGICAL RECORD, No. 26, I JULY 1994
The current global situation of the HIV/AIDS
pandemic
/
As of 30 June 1994, 985 119 AIDS cases have been
reported to WHO since the onset of the pandemic. This
represents a 37% increase since 30 June 1993.
The accompanying table provides the number of re
ported AIDS cases to date, by year of diagnosis.
Fig. 1 compares the global distribution of reported
and estimated AIDS cases to mid-1994. Allowing for
under-diagnosis, incomplete reporting, and reporting de
lay, and based on the available data on HIV infections
around the world, it is estimated that around 4 million
AIDS cases in adults and children have occurred world
wide since the pandemic began. This represents a 60%
increase over the estimated 2.5 million cases as of July
1993. The proportion of AIDS cases estimated to have
occurred in Asia has increased from 1% in mid-1993 to
6% in mid-1994, due primarily to the rapid evolution of
the epidemic in South and South-East Asia.
Fig. 1 Total number of AIDS cases in adults and children from late
•
RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE, N* 26, I" JUILLET 1994
La situation actuelle de la pandemie de VIH/SIDA dans le
monde
|
I
Au 30 juin 1994, 985 119 cas de SIDA avaient etc signales a ;
1’OMS depuis 1c debut de la pandemic. Ccla represente unc >
augmentation de 37% depuis le 30 juin 1993.
Le tableau ci-contre donne le nombre de cas signales jus- I
qu’ici, par annee de diagnostic.
La Fig. I etablit unc comparaison entre la repartition au ;
niveau mondial du nombre de cas signales et du nombre cstime ;
de cas de SIDA au milieu de 1’annee 1994. Compte tenu du sous- i
diagnostic, ainsi que des lacunes et des retards dans la declaration *
des cas, on cstime, en s’appuyant sur les donnees disponibles
concemant les infections a VIH dans le monde, qu’environ !
4 millions de cas de SIDA se sont produits chez les adultes et les 1
enfants a 1’echelon mondial depuis le debut de la pandemie. Cela :
represente une augmentation de 60% par rapport a 1’estimation :
de 2,5 millions de cas en juillet 1993. On estime que la proportion :
de cas de SIDA qui se sont declares en Asie est passee de 1% a la
mi-1993 a 6% a la mi-1994, en raison principalement de I’evolu- :
tion rapide de 1’cpidemie en Asie du Sud et en Asie du Sud-Est. '
Fig. 1
1970s/early 1980s until mid-1994
Nombre total de cas de SIDA chez les adultes et les enfants depuis la fin
des annees 70/debut des annees 80 jusqu'a la mi-1994
Li'-ared 4 0Q0CC0
=5:.-es 4 000 000
Afr.ca - A“ aue
Map 1
Estimated distribution of total adult HIV infections from late
Carte 1
Repartition estimee du total des infections d VIH chez les adultes
depuis la fin des annees 70/debut des annees 80 jusqu'a la mi-1994
1970s/early 1980s until mid-1994
A la mi-1994, on estime que plus de 16 millions d'adultes er
plus d'un million d'enfants ont contracte I'infection a VIH depuis
le debut de la pandemic (de la fin des annees 70 au debut des
annees 80). La Carte I donne la repartition regionale actuelle de
I'ensemble des infections a VIH chez 1’adulte; I’OMS estime que
As of mid-1094, it is estimated that over 16 million
adults, and over I million children, have been infected
with HIV since the beginning of the pandemic (late 1970s
to early 1980s). Afap / presents the regional distribution
of total HIV infections in adults to date; WHO estimates
191
RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE, N* 26, 1" JUILLET 1994
WEEKLY EPIDEMIOLOGICAL RECORD, No. 26, I JULY 1994
80 a 90% des infections touchant les enfants se sont produitcs en
Afnque subsaharicnne.
La Cane 2 indique la repartition regionale des adultes infectcs
par 1c VIH (y compris les cas de SIDA) encore vivants a la mi1994. Comme le nombrc des infections a VIH a continue a
s’accroitre, en particulier en Afrique subsaharicnne de meme
qu’en Asie du Sud et en Asie du Sud-Est, la disproportion de
1’impact du VIH/SIDA s’est accentuee au detriment des pays en
developpement. Malgrc le nombrc rclativement restreint d’etudcs fiables, les donnees dont on dispose incitent egalement a
penser que, chez les populations a risque, il y a une transmission
non negligeable du VIH dans certaines regions d’Afrique du
Nord et du Moyen-Orient, ainsi qu’en Asie de 1’Est et dans le
Pacifiquc. Le nombre estime d’adultcs porteurs du VIH encore
vivants a la mi-1994 dans les pays industrialises n’a guere change
depuis la mi-1993, ce qui indique que le nombre de deces du
SIDA au cours de 1’annee ecoulee a etc sensiblement egal au
nombre de nouvelles infections.
that 80-90% of the infections in children have occurred in
sub-Saharan Africa.
Map 2 shows the regional distribution of HIV-infected
adults (including AIDS cases) alive as of mid-1994. The
continued increase in HIV infections, particularly in subSaharan Africa and South and South-East Asia, has ac
centuated the disproportionate impact of HIV/AIDS in
developing countries. Although reliable studies arc rela
tively few, the available data also suggest significant HIV
transmission in populations at risk, in certain parts of
North Africa and the Middle East, as well as in East Asia
and the Pacific. The estimated number of HIV-infected
adults alive as of mid-1994 in industrialized countries
remains more or less unchanged since mid-1993, indicat
ing that the number of deaths from .AIDS over the last
year has approximately equalled the number of new HIV
infections.
Mcd 2 Estimated distribution of HIV-infected adults alive as of mid-
Carte 2
1994
Repartition estimee des adultes infectes par le VIH encore vivants d la
mi-1994
Index, Volume 69, 1994, Nos. 1 to 26
Index, volume 69, 1994, Nos 1 d 26
Subject index •
Index des sujets
Acquired immunodeficiency syndrome (AIDS):
AIDS: Images of the Epidemic, new WHO publication,
141; current global situation of the HIV/AIDS pan
demic, 7, 189; global data, 5, 191; interpretation of
dually seroreactive HIV-1 and HIV-2 blood samples,
37; study of the effect of blood transfusion on survival
among children in a Kenyan hospital, 69
Alcool voir Toxicomanies
Aliments voir Salubrite des aliments
Anatoxine tetanique voir Programme elargi de vaccination
(PEV)
Brucellose voir Sante publique veterinaire
Cancer: deces par cancer du sein, Etats-Unis d’Amerique, 185;
tendances de la monalite pour certains cancers lies au tabagisme et pour le cancer du sein, 1950-1990, Etats-Unis
d’Amerique, 107
Acute respiratory infections see Diarrhoeal and
Acute Respiratory Disease Control Programme
(CDR)
Alcohol see Substance abuse
Cecite, prevention de la: prevalence et causes de la cecite et de
la baisse de vision, Maroc, 129
Anthrax see Veterinary public health
Centres de vaccination centre la fievre jaune pour les voya
ges internationaux: amendements a la publication de 1991,
28, 44, 92, 136, 144, 176, 188
Blindness, prevention of: prevalence and causes of
blindness and low vision, Morocco, 129
Blood transfusion see Acquired immunodeficiency
syndrome (AIDS)
Chagas, maladie de: elimination de la transmission, Uruguay,
38
Bovine tuberculosis see Veterinary public health
Charbon voir Sante publique veterinaire
Brucellosis see Veterinary public health
Cholera: mise a jour, fin 1993, 13; surveillance du cholera du a
Cancer: deaths from breast cancer, 1991, United States
Vibno cholerae 0139, 52
of America, 185; mortality trends for selected smokingCoqueluche:
resurgence de la coqueluche, 1993, Etats-Unis
related cancers and breast cancer, 1950-1990, United j
d’Amerique, 95
States of America, 107
I
192
.
’
WEEKLY EPIDEMIOLOGICAL RECORD, No. 26, I JULY 1994
•
RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE, N« 26, I” JUILLET 1994
Chagas disease: elimination of transmission, Uruguay,
38
Creutzfeldt-Jakob, maladie de voir Sante publique veterinaire el Sante mentale
Cholera: surveillance of cholera due to Vibrio cholerae
0139, 52; update, end of 1993, 13
Dengue: la dengue dans les Ameriqucs, mise a jour, 177; flambee
de dengue elassique, Costa Rica, 85; Panama, 43
Dracunculose: bilan de la surveillance mondiale, 1993, 121;
eradication de la dracunculose, mise a jour, 1993, Mali et
Niger, 71, Ghana et Nigeria, 161
Enccphalitc a tiques: flambec d'encephalitc a tiques, probablement transmise par le lait, Slovaquie, 140
Enccphalitc japonaise: vaccin inactive contrc le virus de
1’encephalite japonaise, 113
Creutzfeldt-Jakob disease see Veterinary public
health and Mental health
Dengue fever: dengue in the Americas, an update, 177;
outbreak of classic dengue, Costa Rica, 85; Panama, 43
Diarrhoeal and Acute Respiratory Disease Control i
Programme (CDR): CDR and EPI technical brief- I
ings at WHO Headquarters, I; Diarrhoeal Disease
Control f'CDD) Programme, health facility survey,
Jordan, 132
Dracunculiasis:
dracunculiasis eradication, update,
Mali and Niger, 1993, 71, Ghana and Nigeria, 161;
global surveillance summary, 1993, 121
Epidemiology: .Annual Summer Programme in Epidemiology and Biostatistics, Montreal, Canada, 12;
epidemiological surveillance and control of communi
cable diseases, International Training Course in
French, September-December 1994, Paris, 59; epide
miology and intervention in public health, Diploma in
Applied Research, October 1994-September 1995,
Bordeaux-Tours, France, 82
Expanded Programme on Immunization (EPI):
CDR and EPI technical briefings at WHO Headquarters, 1; epidemiological situation of vaccine-prevent
able diseases, Croatia, 163 (corrigendum, 184); Global
Advisory Group, Pan I, 21, Part II, 29; measles elimination programme, Puerto Rico, 157; poliomyelitis in
1993, 169; poliomyelitis eradication, China, 45, Philippines. 47; poliomyelitis outbreak, Azerbaijan, 101; programme review, Bangladesh, 87; tetanus toxoid quality
assessment: an update, 137
see also Immunization programmes, national
Food safety: conference announcement, Bangkok, Thai
land. 103; document available, 103; food microbiology,
course announcement, France, 91, United Kingdom,
100; foods produced by biotechnology. WHO Work
shop. Copenhagen, Denmark, Sept. 1993, 67
see also Veterinary public health
Foxes see Veterinary public health
;
j
j
■
|
1
'
1
:
i
Hajj see Vaccination requirements
Immunization programmes, national: Iceland, 42
see also Expanded Programme on Immunization
(EPI)
Influenza: recommended composition of influenza virus
vaccines for use in the 1994-1995 season, 53
Influenza (notes): Austria, 3, 17, 35; Belgium, 3, 17;
Bulgaria, 43; Canada, 11, 27; China, 11: Croatia, 27,
43; Czech Republic, 11, 35, 51, 67; Denmark, 11;
Finland, 11; France, 3, 76; Germany, 59; Greece, 35;
Hong Kong, 4, 59, 104; Hungary, 35, 67; Iceland, 27;
Iran (Islamic Republic of), 76; Israel, 81; Italy, 4, 17,
67; Japan, 4, 51, 112, 152; Kazakhstan. 51; Nether
lands, 4, 17; New Zealand, 152; Norway, 4, 17;
Romania, 17, 43, 51, 76; Russian Federation, 43, 51,
67, 82, 99; Slovakia, 4, 43; Spain, 4, 17, 51; Sweden,
11, 17; Switzerland, 11, 43; Thailand, 11; Ukraine, 51;
United States of America, 11, 17, 59; Uzbekistan, 51;
Yugoslavia, 51; Zambia, 11
Injury prevention: violence-related attitudes and be
haviours of high school students. New York City, 1992,
United States of America, 56
International Health Regulations: position of WHO
Member States, 32
Japanese encephalitis: inactivated Japanese encephali
tis virus vaccine, 11J
Leprosy: progress towards eliminating leprosy as a pub
lic health problem. Part I, 145. Part IL 15 3
193
biostatistique, Montreal, Canada, 12; epidemiologie et inter- j
vention en sante publique - Diplome d’Etudes appliquees, j
octobre 1994-septembre 1995, Bordeaux-Tours, France, 82; I
surveillance epidemiologique et lutte centre les maladies trans- j
missibles, Cours international en langue franchise, septembre- '
decembre 1994, Paris, 59
Fasciitc necrosante: Royaume-Uni, 165
Fievre jaune: Ghana, 44 (rectificatif, 76); surveillance du virus
amaril en Afrique occidentale, 93
voir aussi Centres de vaccination contre la fievre jaune ,
pour les voyages internationaux
Grippe: composition recommandee des vaccins antigrippaux ;
pour la saison 1994-1995, 53
Grippe (notes): Allemagne, 59; Autriche, 3, 17, 35; Belgique, 3, j
17; Bulgarie, 43; Canada, 11, 27; Chine, 11; Croatie, 27, 43; i
Danemark, 11; Espagne, 4, 17, 51; Etats-Unis d'Amerique, 11, i
17, 59; Federation de Russie, 43, 51, 67, 82, 99; Finlande, 11; :
France, 3, 76; Grece, 35; Hong Kong, 4, 59, 104; Hongrie, 35, I
67; Iran (Republique islamique d’), 76; Islande, 27; Israel, 81; !
Italie, 4, 17, 67; Japon, 4, 51, 112, 152; Kazakhstan, 51; |
Norvege, 4, 17; Nouvelle-Zelande, 152; ©Uzbekistan, 51; Pays- I
Bas, 4, 17; Republique tcheque, 11, 35, 51, 67; Roumanie, 17, ;
43, 51, 76; Slovaquie, 4, 43; Suede, 11, 17; Suisse, 11, 43; •
Thailande, 11; Ukraine, 51; Yougoslavie, 51; Zambie, 11
Hadj voir Vaccinations exigees
Infections respiratoires aigues voir Programme de lutte I
contre les maladies diarrheiques et les infections respira- !
toires aigues (CDR)
I
Lait voir Encephalite a tiques
i
Lepre: progres de 1’elimination de la lepre en tant que probleme '
de sante publique, Partie I, 145, Partie II, 153
Leptospirose voir Sante publique veterinaire
Maladies diarrheiques voir Programme de lutte contre les
maladies diarrheiques et les infections respiratoires
aigues (CDR)
Meningite: flambee de meningite meningococcique, Chili, 35 ;
Microbiologie des aliments voir Salubrite des aliments
Mycobacterium bovis voir Sante publique veterinaire
Pelerinage a La Mecque (Hadj) voir Vaccinations exigees
Peste: la peste humaine en 1992, 8 (additif, 67)
Poliomyelite voir Programme elargi de vaccination (PEV)
Programme de lutte contre les maladies diarrheiques et les
infections respiratoires aiguSs (CDR): programme de lutte
contre les maladies diarrheiques, enquete sur les etablissements <
sanitaires, Jordanie, 132; reunions d’information technique de •
CDR et du PEV au Siege de POMS, 1
Programme elargi de vaccination (PEV): eradication de la I
poliomyelite, Chine, 45, Philippines, 47; evaluation de la qua- j
lite de 1’anatoxine tetanique: mise a jour, 137; examen •
du programme, Bangladesh, 87; flambee de poliomyelite,
Azerbaijan, 101; Groupe consultant’ mondial. Panic I, 21, |
Partie II, 29; la poliomyelite en 1993, 169; programme d’elimi- I
nation de la rougeole, Porto Rico, 157; reunions d’information '
technique de CDR et du PEV au Siege de l’OMS, I; situation '
epidemiologique des maladies evitables par la vaccination,
Croatie, lo3 lrectificatif (anglais seulcment], 184)
voir aitssi(Vaccination, programmes nationaux de
WEEKLY EPIDEMIOLOGICAL RECORD, N<». 26, 1 JULY 1994
•
Leptospirosis see Veterinary public health
RELEVE EPIDEMIOLOGIQUE HEBOOMADAIRE, N* 26, I" JUILLET 1994
Rage voir Sante publique veterinaire
: Measles see Expanded Programme on Immunization
■
(EPI)
Riiglement sanitaire international: position des Etats Membres de 1’OMS, 33
I Meningitis:
:
Chile, 35
Renards voir Sante publique vdterinaire
outbreak of meningococcal meningitis,
i Mental health: possible Creutzfeldt-Jakob disease in an
>
adolescent, United Kingdom, 105
Ross River, virus: infection due au virus Ross River, Australie,
98
• Milk see Tick-borne encephalitis
Rougeole voir Programme Glargi de vaccination (PEV)
• Mycobacterium bovis see Veterinary public health
Salmonellose voir Sante publique veterinaire
: Necrotizing fasciitis: United Kingdom, 165
Salubrite des aliments: aliments obtenus par biotechnologie,
atelier OMS, Copenhague, Danemark, sept. 1993, 67; annonce
de conference, Bangkok, Thailande, 103; document disponible, 103; microbiologie des aliments, annonce de cours,
France, 91, Royaume-Uni, 100
• Pertussis: resurgence of pertussis, 1993, United States
of America, 95
1 Pilgrimage to Mecca (Hajj) see Vaccination require!
ments
voir aussi Sante publique veterinaire
Plague: human plague in 1992, 8 (addendum, 67)
Sante mentale: cas suspect de maladie de Creutzfeldt-Jakob
chez une adolescente, Royaume-Uni, 105
Poliomyelitis see Expanded Programme on Immu!
nization (EPI)
Sante publique veterinaire: cas suspect de maladie de Creutz
feldt-Jakob chez une adolescente, Royaume-Uni, 105 (rectificatif, 120); consultation OMS sur la lutte centre les zoonoses
Rift Valley fever: Egypt, 74
■
dans les pays d’Europe orientale, 90; la leptospirose en 1993,
Ross River virus: Ross River virus infection, Australia,
France, 182; lutte centre les infections a Salmonella, 187; lutte
98
centre les zoonoses: brucellose, tuberculose bovine, salmonelSalmonellosis see Veterinary public health
lose, trichinose, rage et charbon, Bulgarie, 118; projet EUROPE/OMS-Telematics sur la salubrite des aliments, 91; rage
' Smoking-related cancers see Cancer
humaine, New York, 1993, 80; reunion OMS sur la coopera
j Substance abuse: frequent alcohol consumption among
tion en Europe pour la vaccination orale des renards contre la
;
women of childbearing age, United States of America,
rage, 64; trichinose, 61; tuberculose zoonosique {Mycobacte
180
rium bovis), 139; vaccination orale des renards, Autriche, 40;
vaccination orale des renards en Europe - logiciel, 159
i Tetanus toxoid see Expanded Programme on Immu|
nization (EPI)
Syndrome d’immunodeficience acquise (SIDA): donnees
i
mondiales, 5, 189; etude des effets de la transfusion sanguine
i Tick-borne encephalitis: outbreak of tick-bome en
sur les chances de survie d’enfants hospitalises au Kenya, 69;
cephalitis, presumably milk-bome, Slovakia, 140
interpretation de la double seroreactivite vis-a-vis du VIH-1 et
i Travel and health: International Travel and Health, 1994
du VIH-2, 37; Le SIDA: Images de I’epidemie, nouvelle publica
i
Edition, 60; amendments to 1994 Edition (Bahrain and
tion de 1’OiMS, 141; situation actueile de la pandemie de VIH/
!
Croatia), 68
SIDA dans le monde, 7, 191
i Trichinellosis see Veterinary public health
Tabagisme, cancers lies au voir Cancer
Rabies see Veterinary public health
I Tuberculosis: tuberculosis in the Caribbean, 19831992, 73; tuberculosis notifications, 77; United States
•
of America, 65
i Vaccination , requirements:
■
(Hajj), Saudi Arabia, 17
•
pilgrimage
to
Tiques voir Encephalite a tiques
Toxicomanies: frequence de la consommation d’alcool chez les
femmes en age de procreer, Etats-Unis d’Amerique, 180
Mecca
Transfusion sanguine voir Syndrome d’immunodeficience
acquise (SIDA)
see also Travel and health
i
Traumatismes, prevention des: attitudes et comportements
des lyceens face a la violence, New York, 1992, Etats-Unis
d’Amerique, 56
• Veterinary public health: control of Salmonella infec■
tions, 187; control of zoonoses: brucellosis, bovine tu!
berculosis, salmonellosis, trichinellosis, rabies and an!
thrax, Bulgaria, 118; EU/WHO CARE-Telematics
project on food safety, 91; human rabies, New York,
i
1993, United States of America, 80; leptospirosis,
1993, France, 182; oral immunization of foxes, Austria,
>
40; oral immunization of foxes in Europe - computer
'
software, 159; possible Creutzfeldt-Jakob disease in an
adolescent, United Kingdom, 105 (corrigendum
[French only], 120); trichinellosis, 61; WHO Consulta•
tion on Zoonoses Control in Eastern European Coun!
tries, 90; WHO Meeting on European Cooperation on
i
Oral Vaccination of Foxes against Rabies, 64; zoonotic
.
tuberculosis {.Mycobacterium bovis), 139
Trichinose voir Sante publique veterinaire
Tuberculose: Etats-Unis d’Amerique, 65; la tuberculose dans
les Caraibes, 1983-1992, 73; notifications, 77
Tuberculose bovine voir Sante publique veterinaire
Vaccination, programmes nationaux de: Islande, 42
voir aussi Programme riargi de vaccination (PEV)
Vaccinations exigees: pelerinage a La Mecque (Hadj), Arabie
saoudite, 17
voir aussi Voyages et santd
. Violence see Injury prevention
Vallee du Rift, fi&vre de la: Egypte, 74
Yellow fever: Ghana, 44 (corrigendum, 76); yellow fever
I
virus surveillance in Western Africa, 93
I
! Yellow-fever vaccinating centres for international
!
travel: amendments to 1991 publication, 28, 44, 92,
•
13o, 144, 17o, 188
Violence voir Traumatismes, prevention des
Voyages et sante: P’tn'dtfCJ intemationaux et sante, edition 1994,
60; amendements a {’edition 1994 (Bahrein et Croatie), 68
Zoonoses voir Sante publique veterinaire
Zoonoses see Veterinary public health
194
WEEKLY EPIDEMIOLOGICAL RECORD, No. 26, 1 JULY 1994
•
RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE, N* 26, 1« JUILLET 1994
Index of countries and territories1
Index des pays et temtoires1
Australia, 98 ?
Austria, 40
Azerbaijan, 101
Bahrain, 68
Bangladesh, 87
Bulgaria, 118
Canada, 12
Chile, 35
China, 45
Costa Rica, 85
Croatia, 68, 163, 184
Denmark, 67
Egypt, 74
France, 59, 82, 91, 182
Ghana, 44, 76, 161
Iceland, 42
Jordan, 132
Kenya, 69
Mali, 71
Morocco, 129
Niger, 71
Nigeria, 161
Panama, 43
Philippines, 47
Puerto Rico, 157
Saudi Arabia, 17
Senegal, 93
Slovakia, 140
Thailand, 103
United Kingdom, 100, 105, 165
United States of America, 56, 65, 80, 95, 107, 180, 185
Uruguay, 38
Arabie saoudite, 17
Australie, 98
Autriche, 40
Azerbaijan, 101
Bahrein, 68
Bangladesh, 87
Bulgarie, 118
Canada, 12
Chili, 35
Chine, 45
Costa Rica, 85
Croatie, 68, 163, 184
Danemark, 67
Egypte, 74
Etats-Unis d’Amerique, 56, 65, 80, 95, 107, 180, 185
France, 59, 82, 91, 182
Ghana, 44, 76, 161
Islande, 42
Jordanie, 132
Kenya, 69
Mali, 71
Maroc, 129
Niger, 71
Nigeria, 161
Panama, 43
Philippines, 47
Porto Rico, 157
Royaume-Uni, 100, 105, 165
Senegal, 93
Slovaquie, 140
Thailande, 103
Uruguay, 38
: This index relates only to articles concerning specific countries. Articles
which contain general information are not indexed by country, but by
subject (see above). Moreover, the notes on influenza are not included in
this index, but appear in the subject index.
1 Cct index ne couvre que les articles concemant des pays specifiques. Les articles
contenant des informations generates ne sont pas indexes par pays, mais par sujet (voir
ci-dessus). En outre, les notes sur la grippe ne sont pas comprises dans cet index, mais
se trouvent dans 1’index des sujets.
Notifications of diseases subject to the Regulations
Notifications de maladies soumises au Reglement
PLAGUE
PESTE
Africa
Madagascar, 12, 20, 28, 36, 76, 100, 120, 176, 184
Zaire, 60
Afrique
Madagascar, 12, 20, 28, 36, 76, 100, 120, 176, 184
Zaire, 60
America
United States of
America,
*
Amerique
Etats-Unis d’Amerique, 120, 168, 176
120, 168, 176, 184
CHOLERA
CHOLERA
Africa
Benin, 44
Burundi, 52, 160
Cote d’Ivoire, 76
Djibouti, 4, 12
Ghana, 60, 184
Mozambique, 20, 52, 60, 92, 160
Nigeria, 76
Rwanda, 4, 136
Somalia, 68, 76, 112, 128, 168, 188
Zaire, 4
Zimbabwe, 44
Afrique
Benin, 44
Burundi, 52, 160
Cote d’Ivoire, 76
Djibouti, 4, 12
Ghana, 60, 184
Mozambique, 20, 52, 60, 92, 160
Nigeria, 76
Rwanda, 4, 136
Somalie, 68, 76, 112, 128, 168, 188
Zaire, 4
Zimbabwe, 44
America
Argentina, 36, 84
Belize, 36
Bolivia, 36, 84, 100
Brazil, 12, 28, 36, 52, 60, 76, 92, 112, 184
Canada, 52
Colombia, 84
Costa Rica, 20, 188
Ecuador, 36, 60, 84
El Salvador, 4, 20, 28, 36, 44, 52, 60, 68, 76, 84, 100,
104, 112, 128, 144, 152, loO. 168, I7o, 184
Amerique
Argentine, 36, 84
Belize, 36
Bolivie, 36, 84, 100
Bresil, 12, 28, 36, 52, 60, 76, 92, 112, 184
Canada, 52
Colombie, 84
Costa Rica, 20, 188
Equateur, 36, 60, 84
El Salvador, 4, 20, 28, 36, 44, 52, 60, 68, 76, 84, 100, 104, 112,
128, 144, 152, 160, 168, 176, 184
195
WEEKLY EPIDEMIOLOGICAL RECORD, Me. 26, I JULY 1994
•
RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE, N« 26, I" JUILLET 1994
Guatemala, 36, 84
Honduras, 84
Mexico, 36
Nicaragua, 36, 84
Peru, 36, 84
United States of America, 84, 92, 120, 136, 152
Venezuela, 36
Etats-Unis d’Amerique, 84, 92, 120, 136, 152
Guatemala, 36, 84
Honduras, 84
Mexique, 36
Nicaragua, 36, 84
Perou, 36, 84
Venezuela, 36
Asia
China, 12
Hong Kong, 12, 60, 152, 196
India, 12, 52, 76, 84, 112, 152, 176, 196
Iran, Islamic Rep. of, 4
Iraq, 4
Lao People’s Dem. Rep., 152, 160, 168, 196
Lebanon, 36, 76
Myanmar, 120, 136
Pakistan, 76
Singapore, 12, 68, 104, 136
Asie
Chine, 12
Hong Kong, 12, 60, 152, 196
Inde, 12, 52, 76, 84, 112, 152, 176, 196
Iran, Rep. islamique d’, 4
Iraq, 4
Liban, 36, 76
Myanmar, 120, 136
Pakistan, 76
Republique dem. pop. lao, 152, 160, 168, 196
Singapour, 12, 68, 104, 136
Europe
Denmark, 84
Poland, 160
United Kingdom, 4, 84, 100
Europe
Danemark, 84
Pologne, 160
Royaume-Uni, 4, 84, 100
Oceania
Australia, 92, 120, 144
New Zealand, 84
Oceanie
Australie, 92, 120, 144
Nouvelle-Zelande, 84
YELLOW FEVER
FIEVRE JAUNE
Africa
Ghana, 44
Afrique
Ghana, 44
America
Brazil, 12, 44
Amerique
Bresil, 12, 44
Articles oppearing in the Weekly Epidemiological Record may be reproduced
Les articles paraissont dans le Releve epidemiologique hebdomadaire peuvent etre reproduits
without prior authorization, provided due credit is given to the source.
sons outorisotion preolable, sous reserve d'indication de la source.
Note on geographical areas
Note sur les unites geographiques
The form of presentation in rhe Weekly Epidemiological Record does not imply
II ne foudrait pas condure de fa presentation adoptee dons le Releve epidemiologique
official endorsement or acceptance by the World Health Organization of the
hebdomadaire que I’Organisation mondiole de la Sonte admet ou reconnoit officiellement le
: status or boundaries of the territories as listed or described. It has been adopted
stotut ou les limites des territoires mentionnes. Ce mode de presentation n'o d1 outre objet
: solely for the purpose of providing a convenient geographical basis for the
que de donner un cadre geographique aux renseignements publies. Io meme reserve vout
information herein. The same qualification applies to all notes and explanations
egalement pour routes les notes et explications relatives aux pays el territoires qui figurent
j concerning the geographical units for which data ore provided.
dons les tableaux.
DISEASES SUBJECTfOTHEREGULATIONS'^
NotifRations received from 24 to 30 June 1994
Notifications recues du 24 au 30 juin 1994
C - cases, D - deaths, ... - data not yet received,
i - imported, r - revised, s - suspect
C - cas, D - deces, ... - donnees non encore disponibles,
i - importe, r - reuse, s - suspect
Cholera • Cholera
C
D
195
1-31.V
0
India - Inde
Asia • Asie
C
D
3(h)
20-23.VI
0
Hong Kong
Telex: 415416
Lao People's Dem. Rep.
Rep. dem. pop. lao
Telex: 415416
Fox: 788 00 11
8.IV-26.V
2 009
78
Fax: 788 00 11
(A I'allenlion d'EPIDN ATIONS cancer nont les notifications des maladies soumises au Regiemen t)
(Attention EPIDNATIONS for notifications of diseases subject Io the Regulations)
Automatic telex reply service:
Service automatique de reponse par telex:
Telex 415768 Geneva followed by ZCZC ENGL for reply in English
Telex 415768 Geneve suivi de ZCZC FRAN pour une reponse en Francois
Price of the Weakly Epidemiological Record
Prix du Releve epidemiologique hebdomadaire
Annual subscription Sw. fr. 190.-
Abonnement annuel Fr. s. 190.-
’600 7 94
ISSN 0049 8114
196
_
Printed m Switzerland
‘
A.2.
Young Women: Silence, Susceptibility
and the HIV Epidemic
Young Women: Silence, Susceptibility
and the HIV Epidemic
Gender as an independent variable for HIV
infection
There is a critical reality about the HIV epidemic
which is yet to be grasped. It can be glimpsed through the
following three assertions.
First, women are increasingly becoming infected with
HIV. In most of the third world, there are as many, or
more, infected women as there are infected men1. These
women are wives and other partners, daughters and
grandmothers, sisters, aunts and nieces.
Second, women are becoming infected at a signifi
cantly younger age than men. In areas where the epi
demic is newly emerging and in areas where it is deeper,
the same pattern is recorded: on average, women become
infected five to ten years earlier than men.
Third, proportionally more girls and young women
in their teens and early twenties are becoming infected
than women in any other age group. A possible exception
is post-menopausal women who also seem to be particu
larly susceptible to HIV infection.
The response to each of these assertions must be to
ask why this is occurring.
The implications are that it is plausible that women
become infected more easily than men, possibly at all ages
and most definitely when they are in their teens and early
twenties and after menopause. There appears to be a
biological, immunological and/or virological suscepti
bility in women which changes with age.
In 1986 two critical studies, disaggregated by gender
and age, became available. One from the University
Teaching Hospital in Lusaka, Zambia, showed one in ten
women attending the ante-natal clinic infected with HIV
and, amongst the hospital patients:
• one in three men aged 30 to 35 were infected;
• one in four women aged 20 to 25 were infected.
The other study reported the first 500 cases of AIDS
diagnosed in Mama Yemo Hospital, Zaire (Figure I)2.
This data set was also remarkable in showing:
• as many women as men were diagnosed with
AIDS;
• the diagnosed women were on average ten years
younger than the men;
• there was a sharp peak in AIDS cases in younger
women, 20 to 29 years old.
These data were deeply disturbing yet they did not
elicit a particular concern about women and HIV at the
international level nor did they challenge and change
the dominant discourse on the epidemic and thus the
responses3.
First 500 cases of AIDS, Mama Yemo Hospital,
Kinshasa, Zaire, 1986
Silence
The first diagnosed case of AIDS in a woman was
recorded as early as 1982, in the first year of the known
epidemic. In 1984, the first joint US/Belgian mission to
Zaire clinically diagnosed virtually as many women with
AIDS as men. Nevertheless the characterization of the
epidemic by gender (male) and sexual orientation (homo
sexual) remained dominant.
1
Now, ten years after the first woman was diagnosed,
an estimated three and a half million women are infected,
the vast majority through sexual transmission. For most
women, the major risk factor for HIV infection is being
married4'5*6. Each day a further three thousand women
become infected and five hundred infected women die.
Most infected women are between 15 and 35 years old.
Age as an independent variable for HIV infection
The profile of extremely high rates of HIV infection
or AIDS in young women, first seen in the 1986 Kinshasa
data set, reappears time and again in later data sets, in
newly emerging epidemics, Thailand and Myanmar for
04
These data sets dramatically indicate that the pat
terns are everywhere and over time similar:
• the prevalence of HIV infection is highest in
young women aged 15 to 25 and peaks in men
five to ten years later in the 25 to 35 age groups;
and
• among women, the infection profile by age has a
precipitous peak in the age group 15'to 20 and
declines for older pre-menopausal age groups.
Thailand
Myanmar
Age and gender disaggregation of rates of
HIV infection cumulative to 1990
Age and gender disaggregation of people
with HIV infection
5-9 1014 15-19 2024 25-29 3034 35-39 40-44 45-49 50-54 55-59 6O+-
i jure 2
2
example (Figures 2 and 3), in established epidemics,
Uganda for example (Figure 4) and in industrialized coun
tries, Europe for example (Figure 5)7.
Age In years
Uganda
Europe
Age and gender disaggregation of people diagnosed
with AIDS (to June 1991)
AIDS cases disaggregated by age and gender
Cumulative 31 European countries to 1991
Other studies8,9'10 are providing dramatic illustration
of the vulnerability of young women when they become
sexually active early in life. Anne Chao's data from
Rwanda (Figure 6) show that the younger the age of first
pregnancy or first sexual intercourse the higher the inci
dence of HIV infection: over 25 percent of young women
pregnant at age 17 or younger are infected and about
17percent of those 17 or younger at first sexual inter
course are infected. Infection rates decrease sharply in
both categories in later age groups.
11 is our contention that the extent of HIV infection in
young girls in their teens or early twenties shown in these
data sets wili be affected by all the contributory factors
currently identified in the literature as increasing the
rates of infection in women and men but cannot be
adequately accounted for by these factors, even in the
aggregate. Tn the case of young women there would
seem to be other influential factors. These need to be
identified.
The factors identified in the literature include the
incidence of sexually transmitted infections (STIs)11'12,
frequency of intercourse13, sexual practice^14, and male/
female age differences in sexual relationships15'16.
To these may also be added women's nutritional status17,
and the presence of lesions, inflammation and scarifica
tion in the female genital tract from causes other than
STIs18 as well as women's socio-economic status16.
These may well be contributing factors but cannot
be the complete explanation. Individually they are as
true or more true of older, pre-menopausal women or
young men in the same age group. However, these
Risk of HIV in Rwandese women
groups do not exhibit the same extent of infection. Fre
quency of intercourse is not adequate as an explanatory
variable since young women have become infected with
HIV during their first act of intercourse19 and with infre
quent sexual activity20. Infected young women have not
been shown to be more sexually active than uninfected
young women in their age group, than older women or
than young men20.
Similarly, sexual practices which cause lesions or
inflammations of the genital tract are not usually prac
tised by young women. These are more prevalent after the
birth of the first child21.
Nutritional status is not a sufficient variable since it
is poor in all women of childbearing age. Furthermore,
thesocialand economic conditions through which women
enter sex work apply as much or more to women in the age
group 20 to 29 as in the age group 10 to 19.
When social explanations are offered for this pattern
of high infection rates in young women, they are usually
offered in terms of older men having sexual intercourse,
consensually or otherwise, with younger women15. Whilst
this and all the above are clearly contributory factors, we
contend that they are insufficient, even in the aggregate,
to explain the steepness of the infection profile in girls and
young women.
Anatomy as destiny?
The extent of the early and easy infection of young
women, exhibited in the figures above, indicates a par
ticular susceptibility to infection in this group. This
susceptibility cannot be adequately explained by the cul
tural, social or economic conditions under which young
women have intercourse, nor by the presence of infections
and lesions, frequency of intercourse or nutritional status.
The possibility of physiological vulnerability as a con
tributory factor must be explored urgently.
A series of questions can be posed.
Is the intact female genital tract in young women less
efficient as a barrier to virus penetration than that of
older women, and if so, why?
Figure 6
Ag« in years
Anne Chao, 1991
A young woman's genital tract is not mature at the
time she begins to menstruate. The mucous membrane
changes from being a thin single layer of ceils to a thick
multi-layer wall. This transition is often not completed
until late teens or early twenties. It is conceivable there-
3
fore that the intact but immature genital tract surface in
young women is less efficient as a barrier to HIV than the
mature genital tract of older women. In post-menopausal
women, the mucous membrane becomes thinner and so it
is also possible that the genital tract wall, even when
intact, is less efficient as a barrier.
Is mucous production in young women less proficient
than in older women?
Mucus in the female genital tract has four relevant
roles. It acts as a physical barrier, separating semen and
other material from the vaginal and cervical walls. It is a
lubricant, protecting the surface of the vagina from abra
sion during intercourse. It flushes the cervix and vagina
in the same way that mucus flushes the respiratory tract,
removing foreign material. It has an immune function22,
that is, mucus contains ceils of a separate immune system
whose function is to activate the immune responses of the
cells in 'be "actinal and cervical surfaces.
If mucus production in young women, and post
menopausal women, is less proficient than in older pre
menopausal women, so too will these protective roles be
less effective. There will be less of a barrier to viral
penetration. It will provide less assistance in minimizing
irritation and tearing of the genital membranes and so
facilitate viral entry23.
It is known that the hormonal fluctuations of the
menstrual cycle influence the production of vaginal and
cervical secretions24. Secretion is most prolific at midmenstrual cycle and so at other times of the cycle of young
women whose mucus secretion is not fully developed,
may be inadequate. This could also be true of young
women whose menstrual cycle is irregular.
Does the presence of cervical ectopy in young
sexually-active women make them more prone to HIV
infection?
The cervix has been postulated as the most likely site
of HIV infection in women25. Any erosion of the cervix or
damage to it would increase the likelihood of virus entry.
An association between HIV infection and the incidence
of cervical ectopy has been reported2026 but the causal
relationships need to be clarified26. In particular it ur
gently needs to be determined whether the presence of
cervical ectopy disposes women to HIV infection. There
is already considerable evidence that disproportionately
more young sexually active women contract human
4
papilloma virus and herpes simplex virus infections and
that human papilloma virus infection of the cervix is a
major cause of the cellular changes which lead to cervical
ectopy and to cervical cancer. Furthermore, it has been
known since at least 1950 that the incidence of cervical
cancer is higher in young women who began sexual
activity or were married before the age of 1727.
Do the hormonal and physiological changes at
menopause increase the vulnerability of older women
to infection?
There is some case evidence that the efficacy of
transmission in post-menopausal women is higher than
in pre-menopausal women21*. However, epidemiological
evidence is lacking since the female population most
usually tested (commercial sex workers and pregnant
women) do not include them, it could be anticipated that
post-menopausal infected women would usually die with
out diagnosis or treatment.
The biology of a woman's genital tract is poorly
understood. We know more about the increased protec
tion from HIV infection offered by intact genital mucosae
in monkeys29. The above analysis, however, does show
the urgency of developing an international commitment
to providing answers to these questions.
Situational factors
The influence on vulnerability to infection of these
biologically based differences may be amplified by the
circumstances and situations in which young women
have sexual intercourse.
Non-consensual, hurried or frequeii
*
i:.tercourse
may inhibit mucus production and the relaxation of the
vaginal musculature both of which would increase the
likelihood of genital trauma. A lack of control over the
circumstances in which intercourse occurs may increase
the frequency of intercourse and lower the age at which
sexual activity begins. A lack of access to acceptable
health services may leave infections and lesions untreated.
Malnutrition not only inhibits the production of mucus
but also slows the healing process and depresses the
immune system-1*’. Cultural norms may favour early
pregnancy, i-.scourage the use of condoms or facilitate
intercourse with older men who are more likely to be
infected
The unheard scream
An action agenda
These data show that girls and young women are
excessively vulnerable to HIV infection. When will the
agony of these young infected women press upon us?
Anecdotal evidence from one geographic area suggests
that one half of all young women there aged 15 to 19 years
are infected. In other areas, the figure is one in three or
one in four8.
We must respond to this tragedy. There are two
essential elements in the immediate strategy. First, the
silence around the infection of young women must be
challenged at every level: individuals, families, commu
nities and organizations, nations and internationally.
Second, a new research agenda must be established. The
established hypotheses and assumptions about the na
ture of the epidemic, about research priorities and about
gender must be set aside so that the research agenda can
be reconceptualized. To do ^his, those responsible for the
agenda must also change. The critically important and
insightful works of Nancy *’exander25, Bruce Forrest22,
Elizabeth Duncan23, Zena Stein34 and others must be ac
knowledged, valued and acted upc...
When will the pain and anger of these young women
goad us to action7 Or will we be capable of ignoring this
too? There is the possibility of a disturbing parallel in the
krceptance throughout the world of the loss of women's
lives during pregnancy and childbirth. In Africa, as many
as one woman in 21 die in the process of bearing a child.
In Asia, it is one in 54; in Latin America and the Carib
bean, one in 73. The tragedy and suffering of these women
is too often unremarked and their deaths unmarked31.
These deaths are needless32.
The prophetic voice
The growing numbers of women infected and dying
bri ng a deep sadness bu t must sound an urgent alarm. We
must be aware of what the world will lose through the
deaths of so many young, and older, women.
Because we live in sharply gender-divided worlds,
the impact of women's deaths is different from that of
men. Most, if not all, cultures raise girls differently from
ys and treat women differently from men. As a result,
women bring to daily life different qualities from men.
Women tend to be the guardians of compassion rather
than ambition, of connectedness rather than control, of
healing rather than harming, of closeness rather than
conquest, of mercy rather than judgement. They make
possible the circle of the dance as an alternative to the ladder.
Women are the creators of new life, the caretakers of
daily life and the custodians and transmitters of commu
nity norms and social values. However, in some parts of
the world, one third or one half or more of all women are
infected. How will the loss be bome?
Cabbage soup, writes Helene Cixous, can only warm
us passingly. To live, we need the presence of women
who pav attention to life33. Yet even soup is usually
prepared by women. It is not solely a matter of appeasing
hunger, of providing shelter, of resolving conflict, of
raising children, of tending fields. Women bn ng much
more to life.
These two elements are necessary but not sufficient
conditions for an effective strategy to protect girls and
young women from being infected through their sexual
and reproductive activities. An effective strategy will
need to add ress all the factors which directly contribute to
their susceptibility to infection. It must also address, in
the short term wherever possible but certainly in the
longer term, the indirect contributory factors35. There will
be many elements in such an action agendi. Here we
identify only a few to stimulate thought and o’iscussion.
Neither the immediate strategy nor the broader re
sponse will be effective without political will and pres
sure for change. Politicians, community leaders and
parents will need the courage to speak out to save these
lives, to save the continuity of life. We are all responsible.
Breaking the silence
The silence surrounding the infection of young
women must be broken. Girls and young women must be
able to speak out, to cease to feel silenced or powerless to
change what happens to them. Others, too, must speak out.
It is critical that parents, communities and nations
realize that, unless they face this issue urgei. Jy, not only
will many young women be lost but so, too, will their
children and their chi’d~en's children. Clansand commu
nities will cease to exist and, with them, their ancestors.
Pregnancy, birth and nurturing, the cor ? luity of life will
all be placed in jeopardy.
If the silence is broken and young infected women
begin to speak out and tell their stories, we must have
already in place effective programmes to prevent their
5
younger sisters from also becoming infected. If not, the
breaki ng of the silence will add the agony of younger girls
who will now know that they face a future of possible,
perhaps almost certain, infection, to the agony of the
young women already infected. Young girls will feel
po werless to avoid the fate of their mothers and older sisters.
Safe havens must also be found or created which
would allow social and emotional interactions between
girls and boys, young women and young men, and in
which they can discuss and set aside the peer pressures,
cultural norms and gender archetypes which increase
their vulnerability to infection.
The psychological trauma of such a situation is virtu:
ally beyond comprehension. If we do not succeed in
developing an effective, timely agenda for action, the
insight and analysis which demand that the silence be
broken will become a curse.
The family should be the foremost of these sanctu
aries. Young girls should leave their families uninfected
and should be able to return to them when in fear of
infection. The silence around incest must be broken,
above all by mothers and those who minister to and
provide service to such families. The direct price of incest"
is higher than ever now. The collusion of families, whether
from greed or acceptance, in customs and practices which
threaten the lives of their daughters must cease. Neither
young women nor young men should be pressured into
child or early marriages or into early pregnancies. Dowry
payments or pa trilocality should not prevent the possibil
ity of a young woman returning to her family home when
in fear of being infected.
Changing the operational research agenda
The mere possibility of a physiological basis to the
susceptibility of infection in young women should pro
vide the impetus for an urgent and significant research
effort. Answers to questions about the femalegenital tract
identified here, as well as others, must be found so that
protective programmes can be developed.
Those who are undertaking relevant research on the
female, and male, genital tracts must be supported and
their findings widely and quickly disseminated. A fo
cused effort must be made to bring together the observers
of the reality and those undertaking such research and
analyses together with research funders so that priorities
in the bioscientific research agenda can be reset and
financial support be immediately available. Doctors,
nurses and social workers who are observant and under
standing of the relationship between the condition of
y.»ung women's genital tracts and their life situations are
essential partners ir. the process of determining the re
seardi agenda.
Sanctuaries
Strategies must be found that lengthen the time be
fore the onset of sexual intercourse in young women,
increase the age at first pregnancy, and which increase
the ability of young girls to control the situations in
which they are sexually active.
Spaces must be created within which young girls can
be free, and feel free, from the threat of HIV infection,
within which they can pass more time before leaving to
enter the world of sexual relationships and procreation
and within which they can talk to one another about their
coping and survival strategies, their difficulties and their
successes.
6
Families alone cannot change cultural norms, values
and practices36. Thus, advocating families as sanctuaries
requires a complementary strategy of cultural change.
Such a strategy must be led by the guardians and enfor
cers of culture, influential community leaders, older
women, the elders, as well as by those who are now
demanding such change, young men and women and
their parents.
The school should also be a sanctuary from infection.
However, the school is a site of non-consensual sexual
activities and of HIV infection. Rape, sexual abuse and
coercion by male staff and pupils combined with the
exchange of sex with older men for school fees currently
make the school a feared and fearful place. Community
acceptance of this as normal must change. A policy of
providing scholarships would obviate the need for young
girls to find older men to finance their schooling. Sanctions
enforced by local communities would change entrenched
patterns of sexual exploitation of young girls by teachers or
male students. These sarctions are now beginning to be
imposed in some seriousi / affected areas as communities
strive to keep some of their young girls uninfected.
Organizations and clubs for young women create
sanctuaries where young girls can spend time without the
threat of infection. They break the isolation of individual
women and can lead to the creation of social support
networks where young women can seek counsel and be
given support to change their behaviour and to create
change in their communities.
Groups working amongst street children in Brazil
have opened safe houses where the girls can escape from
the pressures of the street and regain a feeling of security
and control over their lives. One such house is the Casa de
Passagen (Passage house) in Recife, Brazil37.
Such gn
dnd organizations can also provide a
refuge where inrtxuC'1 girls and young women can come
jether and provide one another with support, exchange
ormation on care and treatment and discuss issues of
basic concern such as disclosure, sexuality, discrimina
tion, pregnancy and their children's futures.
t
It is critical that religious organizations also create
such sanctuaries for women and for men, separately and
together. This would lend their moral authority to a
recognition of the importance and value of young women
and would help families and communities to find the
courage to change and to provide sanctuary themselves.
These safe havens are critical for young girls to reach
the physical maturity and the emotional and social matu
rity necessary to have greater control over their lives and
the situations in which they have sexual intercourse.
Sanctions
The urgency of the situation may well necessitate the
use of sanctions. In this respect the law can be used as an
agent of social change. For example, the introduction and
enforcement of laws in Southern Africa requiring men to
provide financial support to all children they father,
whether within marriage or outside it, have led to a
significant decrease in the number of such children.
V
Laws against rape and incest and family law relating
to the age of marriage or divorce have been less successful
where there have not been concurrent changes in social
and cultural values. Communities must therefore accept
and decide to enforce such laws and place pressure on
their members to change.
In Uganda, recent changes in governmental and com
munity attitudes brought about by the epidemic have led
to military courts trying soldiers for rape, legal services
being expanded for women who have been sexually
abused, vigorous reporting by the media of sexual abuse
in schools and teachers being sacked for unacceptable
sexual behaviour
.
*
Safety
For women throughout the world, safety, that is,
freedom from physical, sexual, verbal, psychological and
other forms of violence, is an issue that dominates all others
in their lives. The data on the extent of violence to women is
quite appalling39 but little known or acknowledged.
Abuse in the childhood or early adult lives of young
women leads to low self-esteem, little ability for selfassertion and the probability of increased abuse by others,
all factors which have been shown to increase the likeli
hood of HIV infection. In men, childhood abuse also
leads to low self-esteem and to an increased likelihood of
their abusing others39.
New women's crisis initiatives exist in at least 35
developing countries
*
0. All of these are dependent on
external support agencies for their financing. It is vitally
important to support and expand programmes to lessen
violence to women and to provide refuges for abused
women. This can become a significant role for external
support agencies.
Restructuring gender
The ability of young women to protect themselves
from infection becomes a direct function of power
relations between men and women and, in particular,
of men's sexual identity. Gender is formed in families
but constructed by societies36. Changing accepted
patterns of male behaviour and expected patterns of
female behaviour requires community organizing and
collective action.
Individual families and societies must change how
they value girls. The more women are valued, the better
they will be fed and nurtured, given access to health
services and education, provided with the skills re
quired for economic autonomy and have their rights *
honoured, in particular to land and property, especially
through inheritance.
This valuing of women will make it possible for
women to value their own bodies, to improve their genital
health and to have their genital infections and conditions
diagnosed and treated, for cultural practices such as
infibulation which increase women's likelihood of infec
tion to be changed and for women to live through preg
nancy and childbirth with minimal risk of death or lifelong
disability32.
7
Families must also change what they value in boys
and men so that men will be less likely to place themselves
and others at risk of infection. Boys and men, not only
girls and women, must become the guardians of compas
sion, of respect for others, of healing, connectedness and
of mercy.
The circle of the dance
For young women to be able to remain uninfected,
men and women, their communities and nations must
want this to happen and be committed to work urgently
towards it. Only then will there be hope. The priorities of
the bioscientific research agenda must be changed and
knowledge of all the factors which contribute to the
susceptibility of young women to HIV infection deep
ened. Agendas for action must be drawn up locally and
nationally. This will best be achieved through the cre
ation of consultative processes which involve all those
implicated in the required changes. These processes must
be such that men feel able to pa Hcipate, that women's
insights and analyses are valued and listened to and that
the external factors, the socio-economic and political cli
mate which creates theconditions which increase women's
and men's vulnerability to infection, can be addressed.
Such processes are already occurring either spontane
ously41 or set in motion by concerned individuals as in the
case of the Women and AIDS Support Network in Zimba
bwe. They are critical if the lives of young women are to
be saved. The resulting agenda for action will provide the
basis' >• >r hope.
References'
1. Chin, James L. "The increasing impact of the
HIV/AIDS Pandemic on Women and Children." Paper
presented at the American Public Health Association
meeting. Atlanta. November 1991.
2. Quinn, Thomas C., Jonathan M. Mann, James
Curran, Peter Piot. "AIDS in Africa, an Epidemiologic
Paradigm." Science. Vol. 234, No. 957.1986.
3. Reid, Elizabeth. "Gender Knowledge and Re
sponsibility." AIDS in the World. Harvard University
Press. Forthcoming 1992.
4. Jacob, May. "STDs among seropositive patients
of a referral hospital in India and their role in the transmis
sion of HIV." VIHlntemational Conference on A1DS/III
8
STD World Congress. Amsterdam. July 1992. [Poster
Abstract PoC 4334].
5. Hunter, D., S. Kapiga, G. Lwihula et al. "Risk
factors for HTV-1 infection among family planning clinic
clients in Dar-es-Salaam, Tanzania." VIII International
Conference on AIDS/III STD World Congress.
Amsterdam. July 1992. [Poster Abstract PoC 4158].
6. Allen, Susan et al. "Human Immunodeficiency
Virus Infection in Rwanda." Journal of the American Medi
cal Association. Vol. 266. No. 12:1657-1663. 1991.
7. Sources are respectively: Figure 2, Thailand Na
tional Al DS Control Programme. 1991. Figure 3, Myanmar
AIDS Control Programme. 1991. Figure 4, Uganda Na
tional AIDS Control Programme. 1991. Figure 5, Euro
pean AIDS surveillance. 1991.
8. Wawer, Maria J. et al. "Dynamics of spread of
HIV-1 Infection in a Rural District of Uganda". British
Medical Journal Vol. 303:1303-1306. 1991.
9. Holt, Elizabeth. "HIV seroconversion in Haitian
Women." Poster No. MC3010 presented at VII Interna
tional Conference on AIDS. Florence. 1991.
10. Chao, Anne et al. "Risk factors for HIV-1 Among
Pregnant Women in Rwanda." Poster No. MC3097
presented at VII International Conference on AIDS.
Florence. 1991.
11. Wasserheit, J. "Epidemiological Synergy: Inter
relationships between Human Immunodeficiency Virus
Infection and Other Sexually Transmitted Diseases." Sexu
ally Transmitted Diseases, 19 (No. 2): 61-77. 1992.
12. VandePerre, Phillipe et al. "Risk factors for HIV
seropositivity in selected urban-based Rwandese adults."
AIDS Vol. 1:207-211. 1987.
13. Melbye, Mads, et al. "Evidence for Heterosexual
Transmission and Clinical Manifestations of Human Im
munodeficiency Virus Infection and Related Conditions
in Lusaka, Zambia." Lancet. :1113-1115. 15 November
1986.
14. Padian, Nancy et al. "Male-to-Female Transmis
sion of Human Immunodeficiency Virus." Journal of the
American Medical Associu ion. Vol. 258, No. 6: 788-790.
1987.
15. Decosas, Josef and Violette Pedenault. "The
Demographic AIDS Trap for Women in Africa." Paper
presented at the VII International Conference on AIDS.
Florence. 19Q1
16. De Bruyn, Maria. "Women and AIDS in Devel
oping Countries. Social Science and Medicine. Vol. 34 No.
3:249-262. 1992.
30. Chandra, R.K. Nutrition, Immunity and Infec
tion: Present Knowledge and Future Directions. Lancet.
Vol.: 688-691. 26 March 1983.
17. Bailey, Mike. Report for Save the Children Fund
of V International Conference on AIDS in Africa.
Kinshasa. 1990.
31. Diallo, A. Boubacar. "A Tora Mousso Kele La: A
call beyond duty; often omitted root causes of maternal
mortality in West Africa. UNDP HIV and Development
Issues Paper No. 5. Forthcoming 1992.
18. McNamara, Regina. Female genital health and
the risk of HIV » ansmission. UNDP HTV and Develop
ment Issues Paper No. 4. Forthcoming 1992.
19. Bouvet, E. "Defloration as risk factor for heteroiRual Hlv *
ransmission." Lancei: 615. 18 March 1992.
20. O'Farrell, Nigel and Isobel Windsor. "Sexual
Behaviour in HIV-1 Seropositive Zulu Men and Women
in Durban, South Africa." Letter to the Editor, Journal of
Acquired Immune Deficiency Syndromes. 4:1258-59. 1991.
32. UNDP. "Safe Motherhood Priorities and Next
Steps: A Forward-Looking Assessment on the Reduction
of Maternal Mortality and Morbidity Within the Frame
work of the Safe Motherhood Initiatives (SMI). April
1991.
33. Cixous, Heldne. From "Vivre 1'Orange". Ex
cerpted in Love Poems By Women, Wendy Mulford (ed).
Fawcett Columbine. NY. 1991.
21. Nyirenda, Meya. Oral presentation at VIII inter
national Conference on AIDS/III STD World Congress.
Amsterdam. 1992.
34. Stein, Zena. "HIV Prevention: The Need for
Methods Women Can Use". American Journal of Public
Health. Vol. 80: 460462. 1990.
22. Forrest, Bruce. Women, HIV and Mucosal Immu
nity. Lancei. Vol. 337: 835-836. 1991.
35. Hamblin, Julie and Elizabeth Reid. "Women, the
HIV Epidemic and Humaji Rights: A Tragic Imperative."
Paper prepared for International Workshop on AIDS: A
Question of Rights and Humanity. International Court of
Justice. The Hague. May 1991.
23. Duncan, M. Elizabeth et al. First coitus before
menarche and the risk of sexually transmitted disease.
Lancet. Vol. 335:338-340. 1990.
24.
Forrest, Bruce. Personal Communication. 1991.
25. Alexander, Nancy J. "Sexual Transmission of
Human Immunodeficiency Virus: Virus Entry into the
Male and Female Genital Tract." Fertility and sterility. Vol
54, No. 1:1-18.1990.
26. Mandelblatt, Jeanne S. et al. "Association Be
tween HIV Infection and Cervical Neoplasia; Implica
tions for Clinical Care of Women at Risk for Both
Conditions." AIDS. Vol. 6:173-178. 1992
27. Terris, Milton and Margaret C.Oalmann. "Carci
noma of the Cervix: an Epidemiologic Study." Journal of
the American Medical Association. Vol. 174. No. 4: 18471851. 1960
28.
Dwyer, John. Personal Communication. 1992.
29. Miller, Christopher and Murray Gardner. "AIDS
and Mucosal Immunity ; Usefulness of the SIV Macaque
Model of Genital Mucosal Transmission." Journal of Ac
quired Immune Deficiency Syndromes. Vol. 4: 1169-1192,
1991.
36. Reid, Elizabeth. "Women and HD.; " Editorial in
AIDS Health Promotion Exchange. Forthcoming 1992.
37. Baker, G. Felicia Knaul and Ana Vasconcelos.
"Development as Empowerment: Brazilian Project Of
fers Passage to a Better Life for Street Girls." Passages.
Vol. 10. No. 4: 3-6. International Center on Adolescent
Fertility. 1991.
38. Slutkin, G. "What has been Learned in HIV
Prevention Programmes." Presentation made at VIII
International Conference on AIDS. Amsterdam. 1992.
39. Heise, Lori. "Violence Against Women: The
Missing Agenda." in Woman s Health: a Global Perspective.
Marge Koblinsky, Judith Timyan and Jill Gay (Eds).
Westview press, 1992.
40.
Heise, Lori. Personal Communication. 1992.
41. Orick, George. Interview with Margaret
Mwangola and Rose Mulama. Kenya. UNDP HIV and
Development Programme. Reflections on the Impact of
the HIV Epidemic Project. Taped 1991.
United Nations Development Programme
This is one of a series of publications by
the HIV and Development Programme in
tended to raise issues of importance to the
global understanding of the HIV epidemic
and the required responses.
For further information, please contact:
The Director
HIV and Development Programme
United Nations Development Programme
304 East 45th Street, Room FF1094
New York, N.Y. 10017, USA
Tel: (212) 90&6976
Fax: (212) 906-6336
C>3q-o]
CHILD-to-child
programme
c/o Institute of Child Health, 30 Guilford Street, London WC1N 1EH.
Telephone 01-242 9789
NEWSL
57
NOVEMBER 1986
"
Two years have passed since the last CHILD-to-child Newsletter. During this time much has
been happening. The aim of this Newsletter is to let you know about some CHILD-to-child
activities in different parts of the world.
z
Amongst the developments which we will be looking at are the Workshops, the opening
of a French CHILD-to-child office in Paris, and the Readers.
WORKSHOPS
The fifth edition of the Newsletter looked at the planning of
workshops. Since then workshops have become an important
CHILD-to-child activity. In 1986 workshops have been held in India,
Uganda, Benin, Somalia, Botswana and Zambia. At some of these
workshops, CHILD-to-child booklets and Activity Sheets written
in London have been translated into local languages; at others, new
booklets and activity sheets have been written on topics which have
not previously been covered but which are particularly important to
local situations. For example, at a workshop in Ahmedabad held in
May 1985, several new Activity Sheets were produced including
one on the control of intestinal worms and another on the treatment
of Malaria. There are plans for workshops next year in Burkina Fasso,
Lesotho, and Guatemala.
If you wish to run a local or national workshop PLEASE WRITE TO US, we may be able
to offer some help.
1
30- o j
ADDRESS BY PRESIDENT KENNETH KAUNDA TO THE
CHILD-to-child WORKSHOP IN ZAMBIA, JULY 1986
Last year CHILD-to-child Zambia held a successful workshop in Lusaka which was opened
by President Kaunda. In his speech the President said:
“It really gives me great pleasure to officially open this CHILD-to-child Seminar. I want
you to know that I am speaking straight from the heart of my deep concern for children.
Children are. after all, the most helpless members of any society. One of the reasons for their
helplessness is the fact that they have no voice. This is true not only in a physical sense, but is
true also in any other area of Human endeavour including of course the political. Children have
no spokesman. They are the weakest and most vulnerable members of our society.”
“My fundamental concern is to make Zambia a healthy nation; a peaceful nation; and a
happy nation. Children are sacred. They are lent to us by God our Creator. Was it not our Lord
Jesus Christ who said: ‘Suffer not the little children for theirs is the Kingdom of Heaven. See
that you do not despise one of these little ones . . ‘Let the children come to me, do not hinder;
for to such belongs the Kingdom of God.’ “Of course we find similar wise instruction from other
faiths.”
“And yet, the health and lives of children in many countries are ravaged by preventable
sickness and premature death. Some three hundred and fifty million children in developing
countries remain beyond the reach of even a minimum of essential services in health, nutrition
and education. Worse still it is estimated that within the next year, five million children will die
in Africa. These deaths are not inevitable. They are not ‘acts of God’. Almost without exception
they are the result of man’s lack of concern. They are the result of man’s inhumanity to man.
Let us draw our attention to this fact. It is in our power to let this situation remain as it is or to
change it for the better. We should quite seriously reflect upon problems that our sons and
daughters, and our younger brothers and sisters are facing.”
“Childhood problems are common to the whole of mankind. But there are problems which
are particularly acute in countries such as Zambia which lack the material resources of the
so-called industrialised nations. When looking at problems which confront us in these difficult
times, it is easy to be discouraged'. Many of the problems appear to be far beyond our ability
to control, let alone to solve.”
“My great delight in opening this seminar comes with the realisation that much of the
suffering which afflicts our children can be prevented, lessened or overcome altogether. I am
also pleased by the fact that this can be done in a way which does not entail foreign exchange,
but also no currency at all save the currency of human kindness combined with enlightenment.”
2
“I understand that this CHILD-to-child Programme has already started in a small way and
in certain districts of the Northern Province. It is my heartfelt wish that the spark which has
already been kindled will fan into a bush fire as a result of this seminar.”
“We all know that prevention is better than cure. This age-old axiom has acquired increased
importance since the emphasis in medical care has shifted from curative to preventive care. It
therefore pleases me that the CHILD-to-child Programme aims at making children themselves
the principal agents of this campaign.”
“It aims at making the children help themselves. This is something marvellous. It is a unique
example of self-reliance which is the corner-stone of our national Philosophy of Humanism. It
equips children with knowledge with which to tackle the sufferings of their younger brothers
and sisters. One of the wonderful traits of children is their trust. When an adult tells them
something, they believe it.”
“We adults become cynical. We hesitate to accept new ideas and programmes. We are
easily suspicious of a programme that claims that children can become the most useful health
workers in society. Let us acquire some of that child-like trust in embarking on this CHILD-tochild Programme. 1 guarantee that you will be amazed at the results. Children work without
counting the cost. If they have the encouragement of kind and skilled adults, they work even
harder and more fruitfully.”
“I sincerely hope that the launching of the CHILD-to-child Programme is the beginning of
something really great in our country. I want to see this concern for involving children in
improving the health of their younger brothers and sisters really take root in Zambia. I want to
see it in every school in the Republic, teachers, health workers, agricultural workers, church
personnel, all helping each other to help children to help themselves.”
“LONG LIVE THE CHILD-to-child PROGRAMME.”
Illustrations from a book on how children can make toys for younger children, “Toys for Fun —
A Toybook for Preschool Children.” To be published in 1987.
3
IT ENFANT pour 1'enfant jffig
CHILD-to-child
JEb'-rf
SECRETARIAT : 137, BD. MALESHERBES, 75017 PARIS - TEL. : (1) 47 63 98 40
”
®
1 4
Last year the International Catholic Children’s Bureau generously offered office facilities
to CHILD-to-child. ICCB in both Paris and Geneva through Dr. Lucien Michon and Stefan
Vanistendael has supported CHILD-to-child activity for a number of years. French material and
advice are now available from the address given above. We in London have difficulty in providing
our material, the “basket of ideas” in English, and maintaining material in other languages is
difficult. We are delighted with this French initiative and with Dr. Lucien Michon’s drive we are
discovering many new ideas. We hope this will lead to similar initiatives in many other language
areas.
Ma
EVERYONE LOVES A GOOD STORY AND STORIES REPRESENT ONE OF THE MOST
EFFECTIVE WAYS OF PASSING ON HEALTH EDUCATION MESSAGES
Language teaching enjoys higher status in the school than health education. Education
authorities and individual parents may be more willing to pay for language books than for health
education books, especially if they serve a double purpose by helping develop language skills as
well as passing on health messages.
CHILD-to-child has produced a set of six stories, in graded English. These stories are clearly
and simply written so they are easy to translate into another language if necessary. There are two
levels, Grade One and Grade Two.
Boys and girls are the heroes and heroines in the Readers. In one story, for example, a girl
saves her younger brother from being scalded, while in another, a boy helps his brother to
become bright and alert. (Accidents and Teaching Thomas). The Readers thus convey to young
people the idea that they too can take an active part in promoting food health practices. The
stories are attractively presented, with illustrations on each page, and each Reader ends with
puzzles and games. The stories and illustrations are based on African situations.
TITLES
Grade One
Grade Two
Good Food
Down with Fever
Accidents
Teaching Thomas
Dirty Water
A Simple Cure
These Readers have been adopted as Supplementary Readers in Zimbabwe and are under
consideration in a number of other countries. Some have already been translated into French,
Chinese and Nepali.
HOW TO GET THE STORIES
The Stories are published by Longman and sold at the subsidised price of 65p for Grade One
Readers and 80p for Grade Two Readers. They are available through TALC, P.O. Box 49,
St. Albans, Herts AL1 4AX. United Kingdom. The pack of six titles costs £5.85 including post &
packing by surface mail.
The books are published by Longmans and are available from local bookshops.
4
OTHER CHILD-to-child TEACHING MATERIAL
The organisation TALC, which sends out the Readers and the CHILD-to-child book, also
produce other materials which may help adults to organise activity. TALC have many slide sets
which can be used in classes. There is a set called “Schools — a resource for primary health care:”
which shows how school children become involved in practical health and in the local village
programmes in South India.
TALC also stock a book called “Happy Healthy Children” by Janie Hampton. This is a
resource book for teachers and health workers which includes ideas for activities for the children
to learn about health topics as well as reference information for adults.
YCW
&/£££>
Finally, Sue and Gill Gordon have recently produced a book on
“Puppets for Better Health.” The book gives information on how and
why puppets can be used to convey health information, with detail on
making the puppets and how to make up puppet show stories and
shows. The book is published by Macmillans.
c&w. rcb 'tecz.
School-children put on a puppet play at a vaccination centre session
“Primary Health Education” is a new book written by Dr. Bev Young and Sue Durston,
published by Longmans. To most of us teaching primary science conjures up a picture of students
in a laboratory, but this is not the case of the authors of this book. Bev Young shows how
teaching can be very practical using material which is readily available. He particularly emphasised
the CHILD-to-child approach and how this can be used in schools. Practical ideas have spread
in his family, when he asked his son how he could show children in a classroom to measure salt
and sugar for making up the oral rehydration solution his son came back with an answer in half
an hour. Origami - the art of folding paper. We strongly recommend this practical book.
5
REVIEW OF CHILD-to-child ACTIVITIES
WE NEED YOUR HELP
CHILD-to-child was started in 1979, for the International Year of the Child, so it has now been
running for eight years. In 1981 a survey of early activities was undertaken but we now feel it is
time for a more detailed review. On the files in London we have numerous letters describing
CHILD-to-child activities in many countries. We are sure that there are many other programmes
using CHILD-to-child materials, for example Activity Sheets or Readers, or involving
child approaches which we have not heard of. Will you please help us to find out about these?
If you are involved in a programme using CHILD-to-child approaches or materials we should
be most grateful if you would write to us describing the programme. It would be useful if you
could tell us what the main activities are, and what groups of people take part.
If you know of programmes but are not personally involved with them, would you please
drop us a note giving us names and addresses of people we can contact?
If you would be interested to receive a pack of recent CHILD-to-child Activity Sheets,
please tell us when you write and we will send you one.
Please write to:
GEORGINA PAGE
CHILD-to-child
Institute of Child Health
30 Guilford Street,
London WC1 1EH
United Kingdom
THANK YOU IN ADVANCE FOR YOUR HELP
6
- Media
 3401.pdf
3401.pdf
Position: 6251 (1 views)