Christian Medical Journal of India
Item
- Title
- Christian Medical Journal of India
- extracted text
-
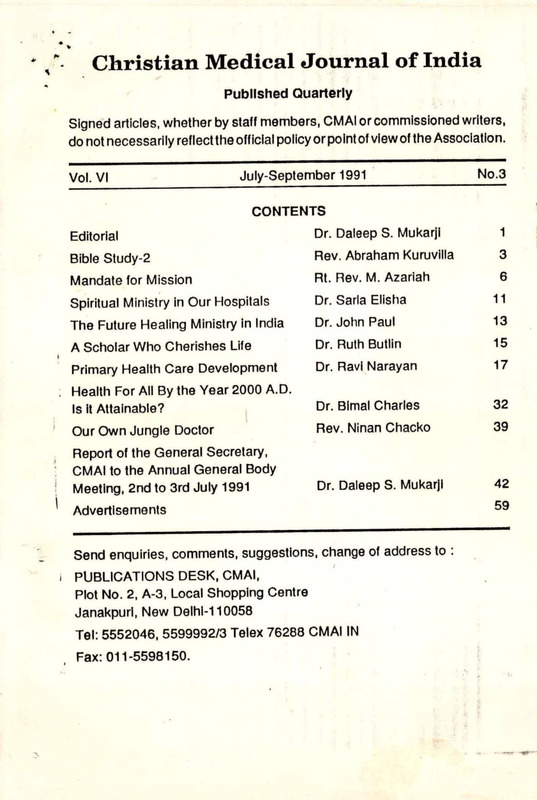
Christian Medical Journal of India
*
Published Quarterly
Signed articles, whether by staff members, CM Al or commissioned writers,
do not necessarily reflect the official policy or point of view of the Association.
Vol. VI
July-September 1991
No.3
CONTENTS
i
I'
Editorial
Dr. Daleep S. Mukarjl
1
Bible Study-2
Rev. Abraham Kuruvilla
3
Mandate for Mission
Rt. Rev. M. Azariah
6
Spiritual Ministry in Our Hospitals
Dr. Sarla Elisha
11
The Future Healing Ministry in India
Dr. John Paul
13
A Scholar Who Cherishes Life
Dr. Ruth Butlin
15
Primary Health Care Development
Dr. Ravi Narayan
17
. Health For All By the Year 2000 A.D.
Is it Attainable?
Dr. Blmal Charles
32
Our Own Jungle Doctor
Rev. Ninan Chacko
39
Report of the General Secretary,
CMAI to the Annual General Body
Meeting, 2nd to 3rd July 1991
Advertisements
Dr. Daleep S. Mukarjl
42
Send enquiries, comments, suggestions, change of address to :
I PUBLICATIONS DESK, CMAI,
Plot No. 2, A-3, Local Shopping Centre
Janakpurl, New Delhi-110058
Tel: 5552046, 5599992/3 Telex 76288 CMAI IN
Fax:011-5598150.
59
c^-i-
Primary Health Care
System Development
Learning from the NGO Experience
in Community Health
1. THE HEALTH POLICY EXHORTATION — RECOGNISING
THE NGO
The National Health Policy 1982-84 is a comprehensive statement
on the goals and intent of the Government on all aspects of health care
delivery and manpower education in the light of the national commitment
to Health For All by 2000 A.D.
One of the significant departures In this policy statement from the
planning process and framework of previous decades is the recognition
and importance given to the ‘Voluntary Organisations’—a large network
of health and development organisations working all over the country at
the grass-roots level.
The policy emphasises this 'new partnership’ In at least four different
paragraphs.
The recognition and the comprehensive dimensions of collaboration
are unambigously worded (Ref. National Health Policy, 1983).
To reiterate, they Include :
i)
Utilising the services of NGOs
ii)
Intermeshing NGO services with governmental efforts
Hi)
Encouraging increased Investment by NGOs
lv)
Offering financial, logistical and technical support to NGOs
V)
Assist in enlarger ent of services by NGOs.
17
ft
I
O
1
2.
AN OVERVIEW OF THE NGOs IN HEALTH CARE
There are estimated to be over 5000 NGOs involved in Health Care
all over the country (recent estimates are much higher). Quite a large
percentage of these are situated in the six states of Gujarat, Maharashtra,
Tamilnadu, Andhra, Kerala and Karnataka. A smaller number are available
in most other states.
The hallmark of the Indian NGO Health Action Initiators are the
diversity of approaches, structure, methodology and ideology. A special
issue of Health Action (a magazine of HAFA Trust. Secunderabad)
highlights some of this diversity and presents an overview of the situation
in the NGO sector.
exploring certain social dimensions of health work which are grossly
neglected or unrecognised in governmental efforts. In fact it is this
contribution that can be considered most significant to the Primary Health
Care movement.
I
These dimensions are :
£ The links with a socio-political process.
]
* The commitment to individual and community awareness building
and generation of greater autonomy.
i
* The commitment to a participatory decision making process within
the health team, and within the community & health team interactions.
The process of ‘community building’, including increasing the participa
tion of those who do not/cannot participate at present.
The NGO health project ranges from alternative service provider at
micro level to alternative trainer, developer, issue raiser, awareness builder,
social activist, networker, health educator and community organiser.
The acceptance of conflicts of interests within the community.
The confrontation of various factors in the ‘medical model’ of health
care including the over medicalisation of health, over professionalisation of skill and knowledge, and the over emphasis on the ‘physical
dimension’ of health.
Due to the special nature and peculiar history c. their development
in the country, the NGO health project is marked by their diversity of
approaches and flexibility of options at the micro level.
I
The quest for medical pluralism.
Most of them however provide a combination of two or more of the
following types of services:
The reorientation process required to modify the existing super
structure of health services and training institutions to meet the larger
social goals of health care.
Appropriate Technology for Health.
Community Organisation and Participation in Health of Mahila Mandal,
Youth and Farmer Clubs.
I
The increasing commitment to accountability and medical audit.
The NGOs are brought together by various coordinating and
networking organisations like Voluntary Health Association of India (New
Delhi and state leve branches), Catholic Hospital Association of India
(Secunderabad), Christian Medical Association of India (New Delhi), All
India Drug Action Network (New Delhi), Medico Friend Circle (Bombay)
and so on. Through meetings and their bulletins/journals they maintain
constant interaction and dialogue between these groups.
& Community Based Village Health Workers.
Involvement of Traditional Healers, Dais and Indigenous Systems.
A
Education for Health.
Health with Integrated Development.
& Community Support to ? -alth Care—financia?,resources.
While these describe the technical and m. ;agerial aspects of the
NGO action they are increasingly characterised by their commitment to
1
19
18
1
?
5
3.
SOME CRITICAL ISSUES
The Community Health Cell is a study reflection action experiment
that has been learning from the micro level NGO experience In India
to evolve and explore macro level contributions to Health Policy and
PHC System Development.
I would like to present seven key policy formulations that the macro
health care delivery system, mostly under the Government of India,
can consider adopting for the next decade so that Health for All
becomes a much closer reality.
A. People as Participants and not as Beneficiaries
People do not mean only the formal leaders but a host of other
Informal sections including women, youth, children, local healers,
farmers, teachers and so on.
Care should be taken to focus on those marginalised,
underprivileged groups who do not participate in decision making
in the present social structure.
More than anything else, this attitudinal shift calls for a courageous
shift In present day beaurocratic/technocratic planning.
r
Informal awareness building, discussions, non-formal education,
community organisation and mobilisation, community building
activities and mobilisation of local skills, resources, Ideas and
Initiatives must take precedence over top-down centrally managed
distribution systems.
In concrete terms this will mean a change In emphasis from e.g.,
— providing taps or tube wells to ensuring their maintenance;
The NGO experience has shown time and again, that people can
participate as planners in programme development and
organisation and should not continue to be considered as
beneficiaries of a top down, centrally planned and heirarchically,
compartmentalised, health programme—be it from the national
or state level.
I
There has to be a shift in emphasis to enabllng/empowering
people to make decisions and carry them out in matters of health,
be they at an individual or collective/communlty level.
B. Focus of Service on Enabling and Empowering rather than
Just Providing and Distributing
For too long health programmes have been seen as distribution
programmes of food, vitamins, vaccines, contraceptives or drugs.
The focus has been on providing, distributing, record keeping,
accounting, supplying etc.
20
— from providing vitamin supplements to encouraging vegetable
gardens and low cost local nutrition mixes;
— from antidiarhoeals to home based ORT mixtures;
— from medical check ups to child to child, and child to home
school based health programmes and so on.
Training ‘tap turners off’ and not ‘floor moppers’
Much of present day focus and training of health manpower is on
curative skills—drugs, dispensing and diagnosing and not on
community awareness building or mobilisation.
The NGO community health trainers have made a significant
contribution to preparing manuals and organising courses that
shift emphasis so that health action begins to explore and support
action at the deeper roots of ill health—at the community and
societal level and not on a superficial, individual, physical level.
The shift In skills is not only from curative to preventive and
promotlve but from Individual to collective, from providing to
enabling and so on.
Case studies, field experiences, simulation games, small group
discussions and aliernatlve pedagogy have been developed to
21
-W-
11
bring this change in the trainee's attitudes and prepare him for
more meaningful roles.
The overall pedagogical shift is from working for people to working
with and through people.
Most health care delivery systems today are hierarchical,
authoritarian with lot of ideas, decisions, targets, going down the
system but little feedback going upwards. Unless these top down
authoritarian systems change to a more participatory management
process, giving all team members due importance and share in
decision making and credit, PHC systems will just not deliver the
goods. The medicalised hospital system with the glorified role of
the specialist is at the heart of this problem and since most
health workers including doctors and nurses continue to be trained
in this setting—team work concept at the community level has a
long way to go. But change it must.
II
!
D. Supervision — From Fault Finding to Problem Solving
Any meaningful action programme at the field level needs an
effective supervision process. However, this has today become,
especially in the government health system a target setting, fault
finding system amounting to a sort of rigorous policing by superiors
over their juniors, all the way down the ladder. The average
monthly Primary Health Care meeting is typical of this situation.
F.
Supervision can be a very creative exercise and from the NGO
experience we know that to bo effective it should be supportive
and basically a problem solving exercise. Team members get
together regularly to look at their actions and results in a mutually
supportive way with the more senior members of the team
exploring ways of getting over problems encountered by junior
staff. The ethos is one of dialogue and the supervision process
looks at strengths and weaknesses as well as identifies
opportunities and threats.
There has been a preoccupation in all our education and
monitoring programmes with quantitative indicators and measures
of service distribution e.g. no. of vaccines given, no. of condoms
or contraceptives distributed, etc.
Apart from the fact that these have been consistently subjected
to inflation, and cooking up’ due to the stresses and pressures
of top down targets, these do not give any indication of the
processes and qualitative changes that need to take place if the
Health For All goal has to be reached.
This attitudinal change is an urgent necessity in the present
system.
E. Management
Management
Monitoring and Evaluation — From Quantitative Project
Indicators to Qi.?alitative Process Indicators
There is a need to shift to qualitative and quality indicators as
well as indications of equity and social processes e.g.
From Authoritarianism to Participatory
— From immunizations given to fully immunized children.
— From condoms distributed to couples seeking advice.
Building a Primary Health Care System which is responsive to
the needs of the large majority of people, with their participation,
is basically a democratic process which needs patience, faith
and enthusiasm. If health, workers at all levels ha j to develop
these basic attitudes, they need to function
a system that
considers them as ‘participants’ and ‘key components’ and not
just as ‘cogs in a wheel’.
22
— From health talks given to the extent of ideas and suggestions
given by the people in programme development.
I
!
— From numbers of materials distributed to numbers of people
made aware or enabled to make decisions regarding health.
— From what the Primary Health Care doctors, statisticians
23
or professional programme evaluators feel about the programme
to what people and grassroot level health workers feel about
the programme and so on.
THE PARADIGM SHIFT
PEOPLE
BENEFICIARIES
PARTICIPANTS
SERVICES
PROVIDING
ENABLING/EMPOWERING
The present focus of much of our research is at the Intracellular,
moleculor, biological level with the hope that we will discover
new drugs or vaccines that will cure or prevent some of our
health problems.
HEALTH WORKER
FLOOR MOPPERS -♦TAP TURNERS OFF
SUPERVISION
FAULT FINDING
PROBLEM SOLVING
MANAGEMENT
AUTHORITARIAN
PARTICIPATORY
There Is need to shift this emphasis to ‘societal or community’
research that will seek to determine, describe and understand
the larger societal forces that make ‘health’ an Impossible goal
for most people.
EVALUATION/
QUANTITATIVE/
QUALITATIVE/
MONITORING
PROJECT
PROCESS
RESEARCH
INTRACELLULAR -♦
COMMUNITY/SOCIETAL
What are these factors that prevent large majorities of our people
from getting the knowledge, skills, attitudes, means, opportunities
or services that make health possible?
All health planners, policy makers, administrators, educators, service
providers and evaluators need to appreciate this shift.
G. From Intracellular Research to Baloonlst/Socletal Research
We now know that Inadequate water supply is at the root of the
diarrhoea problem; inadequate land reform at the root of the
malnutrition problem; caste and corrimunal consideration prevent
access of large numbers of people to health services; class
determines access to education and wage Income; Indebtedness
as well as government liquor policy at the root of the alcohol
problem and so on.
4.
The entire group of regional review meetings and the previous
meetings of the past decade have seen Primary Health Care System
Development In a very myopic fashion.
|
As these deeper links are understood, action plans will emerge
which will strike at the larger issues and not focus only on
superficial programmes.
I '
They have focussed all along on infrastructure, manpower, materials,
logistics and educational materials and rightly so because they are the
basis of public health programmes.
But they have missed an Important dimension of Primary Health
Care System Development. Primary Health Care can never be a reality
In this country If PHC is provided by professionals, technical/beaurocratlo—
from the top.
The Paradigm Shift
These seven dimensions represent a major paradigm shift in our
understanding of Health and Primary Health Care and these are crucial
to the goals of Health For All 2000.
FROM SYSTEM DEVELOPMENT TO AWARENESS BUILDING
(DEMAND/CREATION)
!
Primary Health Care has to be a demand from the grassroots—a
demand from an aware and health conscious people. We have failed In
our understanding of the need and necessity of planning for this dimension.
Unless health Is seen as a right and a responsibility, unless people and
24
25
communities begin to have a vested interest in Health and unless Health
becomes a demand for the common people, all our efforts will fail.
Health Education to Education for Health
II
Awareness building in Health or the term Education for Health used
in this paper is very different from what we know as. Health Education,
which has become a euphemism for telling people the dos and don’ts of
Health in a sort of passive, one way, top down process. Education for
Health is a more creative, liberating process exploring the roots of ill
health with people through informal group discussions and a host of two-
It is therefore necessary to recognise that Primary Health Care System
Development means both
Services
Provision
V o
(Supply)
[
Education for
Health
I
This will mean that we will need to face up to some new questions:
Are we ready to discuss how to make health and health care
important on this country’s political agenda?
iii) Are we willing to plan.to generate health as a people’s science
movement involving science educators, teachers, youth groups
media people, folk and modern communicators and so on?
z-><4i<-»
_ —i —
puippoii y , oiicci iiicdiic, u ckjuioi icil ikJirx dl IO
I
More than any other action I think the NGOs in Health Care and
Development have skills, resources, ideas and initiative in this direction.
If only health planners and health policy makers are willing to see this
V4I 11-i more and more wr
IVUIlll NGOs see this
UIIO CiO
UH WiyClll
need and
of the Health
as an
urgent
1 necessity, a major break-through could be made.
■
IIUWV*
IIIWIIZ
iriv'ikz
iiivr
I
M
Awareness building is not new. It has been mentioned differently in
policy statements. (Ref. National Health Policy, 1982, and National
Education Policy, 1986).
iv) Are we willing to plan how to generate health as a mass move
ment from below, involving all sections of the people—their
leaders, political parties, health, social & development activists,
trade unions, women’s groups, dalit and marginalised groups,
workers and so on?
The 1990s call for a major shift in our efforts and deliberations to this
important aspect of system development, otherwise our efforts will remain
as unimportant, peripheral, anaemic and ineffective as they continue to
be, inspite of all our efforts.
inTArnr’Iii ir\
, nnuiuuii»<. i>n.uia
and jathas so that, not only are people able to understand what causes
or maintains their ill health, but what means, processes and initiatives’are
available or need to be sought to build health, both individually and
collectively. For example, while teaching about water borne diseases, the
stress on the need to have good personal hygiene and to drink boiled
water is an example ol orthodox health education. On the other hand,
i initiating a discovery process by which water availability and access are
explored in a community and the group is motivated to take collective
action to improve the situation in the community through village based
action or pressure on the authorities is an example of the new emphasis.
(Demand)
ii) Are we willing to discuss how to infiltrate the entire educational
system of this country—formal and informal, professional,
technical or vocational with the message of individual and
community health?
urow
The emphasis has, however, unfortunately been on a passive, top
down education process thrust on people rather than an active grass
roots and upward extending process.
1
The purpose to highlight it here is to emphasise that this new emphasis
.1 on education for health must be given, and that this crucial area must
I receive concerted attention and action.
■»
27
26
?
■
<
will continue to be the main service In quantitative terms. This cannot
and should not be Ignored.
5. GOVERNMENT — NGO COLLABORATION IN THE 1990s
Having recognised the Health NGO as a potential partner In the
health policy statement In 1982, the experience of the last 8 years has
shown some important but disturbing trends In the area of Govt.—NGO
collaboration in Health Care. I would like to highlight them, raise some
points of caution and explore some alternative approaches.
4.
Linked to the above, there is an Increasing tendency to belittle or
denigrate the government system and plead about its inabilities or
built In problem or hs resistance to change. This leads to two problems
at the planning level. The first is, that reforming the government
system is not adequately worked upon. The second Is that under the
garb of NGO Involvement there is a definite move towards privatisation
and involvement of the profit oriented corporate sector In health care.
Trends
1.
Recognition as service providers only
The government continues to see NGOs as only alternative service
providers and at best, alternative family planners or Immunises. Their
skills in providing other aspects of the package of health programmes
are still not seen. Their additional abilities as trainers, evaluators,
issue raisers, awareness builders Is still unrecognised. In many states,for planners, NGOs still mean Rotary or Lions Clubs or at best the
Family Planning Association of India or a Mission Hospital. The Indian
NGO today Is a much more diverse and creative species and needs
to be understood as such.
2.
Government systems can change if all those at the helm of affairs
are committed and rightly oriented. There are innumerable.examples
all over the country and these need to be highlighted.
■-
Pressures on scaling up
There is a tendency to expect NGOs who have shown their abilities
at the micro level to scale up their efforts to larger and larger levels
to make up for the deficiencies and Inadequacies of government 5.,
programmes at the periphery. The NGO’s strength Iles In its creative
abilities at the micro level, allowing for qualitative Inputs and processes.
Pressures to expand will often make them as ineffective or :
bureaucratic as the larger system.
’I
3.
Glorifying NGO & denigrating Govt, sector
Due to the inadequacies and failures of the existing health care
delivery system and the large unmet needs, there Is a growing
tendency to 'glorify' or 'romanticise' the NGO and have unrealistic
expectations of this sector. This sector Is small and primarily qualitative ;
in Its contribution. For a long time to come, the government service
i-
28
Privatisation under the garb of NGO Involvement
i1
While the private sector may have Its role in providing some aspects
of health care—health services are basically a state responsibility
and the tax payer must get basic health care for his contribution.
Profit orientation of the private sector means that the consumer Is
always paying more than Is necessary and this must be recognised.
It is at least Important not to confuse the NGO voluntary sector with
the private sector to begin with, and to deal with them rather differently
on policy Issues.
Community participation
Synonyms
and NGO Involvement
are
not
Finally, at all levels community participation is often seen as being
equivalent to Involving NGOs. This is neither synonymous nor realistic.
NGOs are definitely closer to people, more responsive to the local
situation and function under lesser, top down controls and are hence
more creative. But they too are trying to explore real Involvement of
people In their own initiatives and processes and are meeting with
varying degrees of success. Not all NGOs have succeeded In eliciting
meaningful participation. If these terms are not confused, then we ■
29
will at least see community participation as a process that can be
Primary Health Care System Development Is the backbone of this
Initiated In any system, Government or NGO.
planning and management exercise.
What is most crucially required is the development of a new culture |
The 1980s have seen a preoccupation with infrastructure development,
in health services and planning and this Is highlighted by the following logistics, supplies and manpower development and statistical exercises,
aspects:
valid and Invalid, Interspersed with a large dose of populist rhetoric
I) Information transfer and awareness building programmes for the ancJ P°,,cy statements.
PeoP,e|
The 1990s must see a paradigm shift In attitudes and efforts so that
li) Reorientation programmes for government staff at all levels about Primary Health Care Is an enabling, empowering process and not Just a
the concept of people as ‘participants’ rather than as ‘beneficiaries’. Jmere provision of services and Infrastructure. A new spirit and a qualitative
ill) Monitoring and record keeping systems that are Interactive and change In all our efforts are required. The NGO experience In the country
qualitative and build on feedback from people and grass roots Is diverse and creative. Major lessons can be learnt from studying this
wealth of micro level experience. There Is need to Incorporate these
level staff who are closer to them.
[Ideas and processes into all our efforts In Primary Health Care System
iv) Increasing involvement of voluntary agencies/NGOs in the role of
■Development—governmental or non-governmental. This Is the challenge
monitors, evaluators, Issue raisers, demand creators and trainers,
ibefore us.
not just as programme implementors.
v) Positive discrimination towards those groups who do not partici- ^pr. Ravi Narayan, Coordinator, Community Health Cell, Bangalore.
pate In local decision making processes.
fThe original article has 6 pages of cartoons, references and
vl) Health/Educatlon efforts to strengthen the community building
appendices. All those Interested could request these from the
aspects.
Community Health Cell, 326, V main, I Block, Koramangala,
vli) A move away from top down, centralised models to regional lBangalor^S60034.
planning that reflects local soclo-economlc-politlcal-cultural |
realities.
I
viii) Increasing acceptance of diversity of options and flexibility of |
approaches.
Many of these have been highlighted earlier. Concerted political will and
professional will Is necessary in the 1990s to bring this major attitudinal
change.
11
CONCLUSION—THE CHALLENGES AHEAD
There are hardly 110 months ahead to reach the goal of HFA 2000,
whether comprehensively or selectively.
i
31
30
i
T-
- Media
 CH-10.pdf
CH-10.pdf
Position: 259 (40 views)