MEDICINE MEDIA AND CONSUMER EDUCATION
Item
- Title
- MEDICINE MEDIA AND CONSUMER EDUCATION
- extracted text
-
RF_DR_21_SUDHA
□>2-- □-'-l
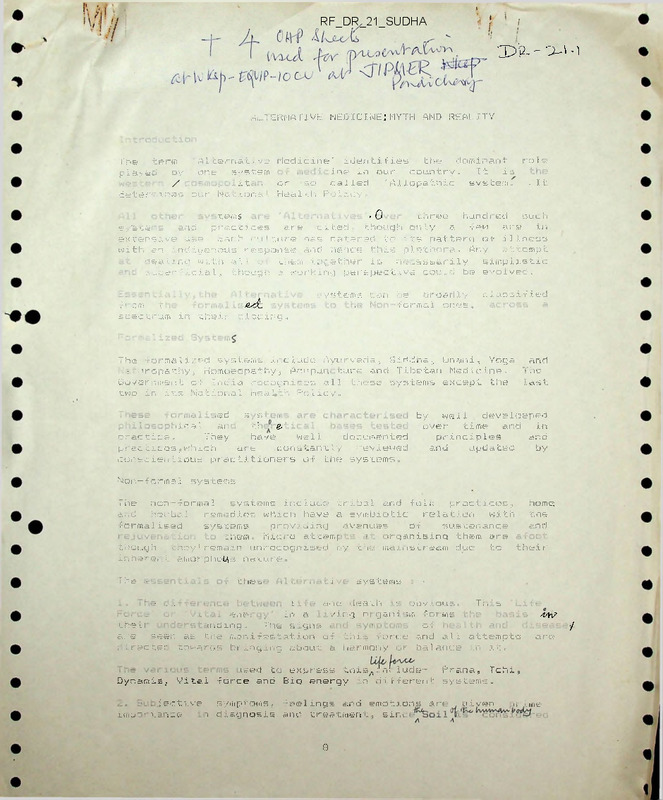
ALT ernative medicine: myth and reality
the
dominant
role
A1 c e rn a t i v e Medicine' identifies
The
term
ine in our country.
It is
played
by
one
system
/ .
.
i t,
or
so
called
'Allopathic
system.
. It
determines our National Health Policy.
■ terns
>0
three
hundi ed
such
Systems
and
practices
are
cited, though only
a
re.w
are
in
exlfensive use. Each culture has catered tn its pattern of illness
with an indigenous response and hence this plethora. Any
attempt
dealing with al* c- tnern together is
necessarily
simplistic
superficial, though: a working perspective could be evolved.
?! om
t
edc
systems can be
broadly
■ ■
formal ones,
classified
spectrum in t he ir pl acing ..
The -formalized systems include Ayurveda-, Siddha, Unani, Yoga
and
= :uropathy, Homoeopathy, Acupun tune and Tibetan Medicine.
The
Government of India recognises all these systems except the
last
two in its National Health Policy.
>ed
s s .. i ..
by
well
develoeped
ij ca 1
ai
tle.
oyer
time
and
in
practice.
They
have
well
documented
principles
and
and
updated
by
practices,which
are
constantly
reviewed
conscientious practitioners of the systems.
Non-fo rma1
systeiiis
The
non-formal
systems induct- tribal and folk
practices,
home.
ar.d
herbal
remedies which have a symbiotic
relation
with
the
formalised
systems
providing
avenues
of
sustenance
and
them
Micro attemf
:■
Organising them are
though
easy1remain unrecognised by the mainstream due
to
their
interact amor photf,-: nature.
I he ■-
11>e =
■. i
systems
- .. .
L
and death
'
sbvious.
TI, ' s
.
enei
in a
/ing oi gani ;m foi ms
.
theii
inding.
The signs
of
■ . ..
are
seen as the manifestation of this force and all attempts
clrectet cowards bringing about a harmony or balance in it...
Dynamis,
Vital
44V
/
are
ised to express this.lnclude
Rrana, Tchi,
force and Bio energy :.n different systems.
jective
symptoms, Feelings and emotions art
Kiio-"’ v.sjxcg
\ diagnosis and treatment, sirr
8
given
irime
Alternative medicine;
MYTH # REALITY
ALTERNATIVES
GojMopolLtav\
Modem
'AlLopafruc'
MEDICINE
§ 4A
these
Now, to look at the myths and enhance our understanding of
systems.
MYTH
:
ALTERNATIVE MEDICINE IS NOT
■
the
oriental
■.
io;
thoifeht, like
Samkhya
one of the six schools al-
Vaisheshika
— the system o-f
propositions; and
'SCIENTIFIC'
Alternative systems originated
-from
Indian Philosophy.;
logic used
to
explain
Yoga.
the science or shastra explaining the working
mind and its relationship to the body..
The
Chinese
systems
have absorbed Taoism,
t h o u g h t i n t h e i r p h i 1 o s o p h i e s.
' Zen
and
Ayurvedic
of
the ■
Confucian
Logic,
experimental
methods,
measurement
and
quantification
exist in these systems., providing a frame work to validate their
theory and practice.
The
fundamental
differences between these
and
Western
science
makes unintelligible any comparison between systems, as
no exact
equivalents exist, or can be made.
MYTH :
v.'
,
ALTERNATIVE MEDICINE IS OBSOLETE
The
survival
of
medical/heal th
practices
have
always
been
dictated
by
the patronage of the state. Factors
of
political
expediency
in
the
history
of colonialism
in
our
past
have
suspended
and even supressed progress of these systems with
the
.
times. Evidence in archeology and history supports their
ahi Id ’:
u to meet the needs of the day from water and sanitation
measures
U
1
,
to plastic surgery and inoculation against small
pox.
' fhe
Acupuncture during the Chinese
Revolution
under
-AYURVEDA
-SIDPHA
~ Re-cogni^ai
by
I .
Cj.O.
I.
' * ”
-UNANI
-yotjA*
NATUROPATH/
-Homoeopath/]
-acupuncture
- TIBETAN MED.
S
\
-Tribal
-FolX
- Herbal
- Howe
Remedies
ESSENTIALS ,'
1. 'LIFE FORCE' is recognised - Prana/Tobi/Dynamis
Bio-e+xenjy .
2. I^porhwce to SU&JfCTIVE -
« SOfu
3. HOLISTIC approach/^MtYHaL,
AlUtd di'ccipUwes recmibeJ.
5". BEHAVIOUR modi^'cah'cm procedures.
fe. LOCAL *He-«ck h\et - rwdfvidvAdl & Fawuly
the patronage of Mao-ze-dong
MYTH
:
ALTERNATIVE MEDICINE SYSTEMS ARE
People have
always
recognised
the
ensuring their survival to this day.
'RECOGNISED'
NOT
worth
of
these
systems,
"The W H.O has been promoting Traditional Medicine as part of
its
Policy
since
1'175.
e
Government
of
India
recognises
the
formalised
systems in its National Health Policy
Document
1981.
These
expressions
of 'recognition' have a paternalisitic
(as
opposed to fraternal) tone on paper and in practice, while their
perplexity
is evident in their equating all these
systems
with
mystical practices.
Luckily,
or otherwise, we have
all .these
systems,
including
the very advanced formalised systems
in
our
country, unlike the African and American continents which
typify
t r * s n o : ■■ -for: ■ ■, as y s t e ms, a 4—i-u-e—trt-rte r—end—&f-—fete spectrum-?
MYTH :
THERE ARE NOT ENOUGH TRAINING/RESEARCH CENTRES,
TRAINED PERSONNEL IN THESE SYSTEMS
OR
WELL
Figures
from the document “Health Information of India 1991“
published
by
the
Central
Bureau
of
Health
Intelligence,
DGHS, Ministry of Health and Family Welfare, G.O.I. should suffice
in this context.
No of colleges of l.S.M
and Homoeopathy ( 1989)
with admission capacity
Ayurveda
Unan i
Siddha
Homoeopathy
Total
98
17
214
No.
of Medical
No.
of Students admitted/
Colleges/
No. of students passed out
in M.B.B.S.
128
10,021
13,262
12,29
egistered ISM and
Homaeopathic practitioners
No.
Ayurveda
Unani
Siddha
Naturopathy
Homoeopathy
Total
c)
315,719
34,888
11,644
146
1,48,866
of Doctors registered
Under
IMC Act with -State
Medi ca 1 Counci 1 s
,11,261
Summary of Medical care (1989)
facilities under ISM and
Homoeopathy
10
'CHAOS' , 'FRACTALS', '4AIA'....
THE 'ART7 OF MEO/CINE RETURNS
THRU7
SCIENCE
T.he survivial of these systems to this day has been mainly due to
people
using
them
-for their needs. The common
man
does
not
differentiate
between
systems
as we
professionals
do.
Their
utilization
of
any
system depends on ■considerations
of
easy
availability
in terms of economics and consonance
with
her/his
belief systems.
The
W.H.C.
"World Drug Situation" places India among
countries
where less than 307. population have access to modern medicine,
the vast majority depend on al ternatives■in our country.
MYTH
:
ALTERNAlIVE MEDICINE IS SAFE
demands on
dltcicaative medical
products,/^
increasing
production and marretina methods have invaded these systems.
ty control ahd supervising capabilities being stretched, the
T he
ills
of industry and lack of ethical practices a r e e v i d e n t.
recent 'SURA' tragedy in New Delhi is a pointer to this trend.
MYTH
:
ALTERNATIVE MEDICINE IS CHEAP
Trends cited above have added to the cost of medicine instead
of
reducing
i t,
especia11y the private sector
and
Trtan s-nationa1
companies
having
entered this market for
profit
making..
The
pper
crust
have
added
to
their
quest
for
the
best - ouviously is the costliest.
MYTH
ALTERNATIVE MEDICINE IS USEFUL ONLY
DOES NOT WORK
11
WHEN
'ALLOPATHY'
‘'T'4' 1
ALTERNATIVE
MEDICINE I MYTHS
1. hot 'scientific/
ySav^kkya
— Shadm r VairkeskiXa
'Yoga
+ Tao
ZCK
ConJwciani.W
2. OBSOLETE
- Stale patronage / Mao ge dong.
5. not reco^nizep
WHO 1973 / ^or-NHP
INADEQUATE TR^./RBS./ PERSONNEL
VKl|ealt^ Iv\jo. o|
- 1^1"
Altern^ Med.
No. o| colleges AdwiSSioh 030Regd. Practiticm*
Hosptfols
bispenscuries
-
214.
10,021
^Uz26l
(z 963
19,791
Modern A^ed.
128 413,262/12,292
3Z52J9G
II, 2^4
27,997
9. NOT PEOPLES CHOICE
(
f
-NHO - "INorld brug
6. SAFEf
,
- morleehng / bad e^UicS - SURA .
7. CHEAP
- Trans-Konels / ^iacsI' ^oy B8ST?
g.
USEFUL
3.
0NLV 'PLACEBO^
ONLY
?F MODERN MED. PAILS.
- creative ia$e * ‘nocebo7
'heal/n^' zs a
wide concept.
From
i>;nor
ailments to chronic diseases, many
people
adopt
alternative medicine as a fad. a reaction to the ills of
'modern
medicine’, aecause they can afford to shop around, or, because they
can:;ct
afford the cost of modern medicine.
i"he
truth is that many illnesses are treatable by any
of
these
systems,
and
the
individuals/community
do
not
have
the
information to make logics., choices suitable to themselves.
This
leads to a potentially exploitable situation for a profit maker.
MYTH :
ALTERNATIVE MEDICINE IS ONLY
'PLACEBO'
HEALTH/Dgf/g CO.l/PAW.
Drug doctors under fire
Pharmaceutical
companies who spend
millions of dollars
each year to seduce
medicos into
prescribing their
products are causing
serious concern.
David O’Reilly
reports
he Keating government is tinder
pressure to crack down on multi
national pharmaceutical companies
which stand accused of manipulating the
$2 billion-a-year trade in doctor-pres
cribed drugs for the ill and aged.
Concern is growing in Canberra at
methods employed by drag companies
which spend an estimated $150 million.$200 million a year in promotions to con
vince doctors to prescribe their products.
The concern springs from the taxpayer
picking up a big part of the tab through
the Pharmaceutical Benefits Scheme
(PBS) when drug companies induce doc
tors to endorse an ever-spiralling array of
new brands. Monies spent on advertising
and promotion are also tax-deductible.
Yet recent research suggests that be
tween 16% and 31% of these company promot ions - possibly costing as much as $60
million - are misleading.
Code of silence: The behind-the-scenes
battle has become highly sensitive, with
various government and private agencies
complaining the industry is a law unto it
self and companies refusing to divulge key
information about their activities.
The industry umbrella body, the Aus
tralian Pharmaceutical Manufacturers
Association (Al’MA), denies there is evi
dence of wrongdoing in Australia al
though it is not uncommon overseas.
The pharmaceutical ding trade is one
of the fastest-growing components of
Australia's $26 billion-a-year health bill three-quarters of the $2 billion pre
sent ssl-dnigs business is listed on PBS.
Another worry is that Australians are on
T
Dr Ken Hervey with part of the pharmacopeia: are Australians on a drug binge?
a drug binge, consuming twice as many
antibiotics per capita as Sweden and far
more than the US and Britain.
Last year, the Hawke government
moved to try to rein in the zooming bill by
imposing the ill-fated Medicare co-pay
ment. But that just sparked the question,
why should the consumer be hit when it is
the doctor who pens the prescription?
Within weeks, two pertinent reports
will be released - one, by the Trade Prac
tices Commission, into drug promotion
and advertising; tile other, by the House
of Representatives Standing Committee
on Community Affairs, inlo'prescription
and supply. Both will reeommend tighten
ing the industry’s self-regulatory code of
behaviour which is overseen by the Al'MA.
This is despite complaints that self
regulation is a toothless tiger, allowing
ding companies basically to do whatever
they want. Ear tougher action is being
urged on the Minister for Aged, Family
and Health Services, Peter Staples. He is
considering a law to encompass the indus
try code, but he is also under pressure to
establish an industry council to consider
complaints and impose penalties, the
details of which would be made public.
Staples is also being urged to consider
steps which would prevent companies of
fering inducements to prescribers of
drugs. This goes to the heart of the con
cern among healt h administrators - for, as
rm: uri.i.KTix. maiu a ci. ivirt
officials chip away at the citadel, what drugs should slow down because germs times the computers, without fear or fav
emerges is a none-too-flattering picture of are becoming resistant and many now our from any company.
“They argue it all balances out and
companies scrambling for greater market cornel's have been either too powerful or
share as they load the market with new had as yet unclear side effects. Companies they are not biased. But I say back, ‘It’s
products, irrespective of wider commun often were pushing a new product be the patient who is paying for it all in the
cause the old one had come off patent, end.’ In teaching our medical students, I
ity health considerations.
ask them do they think our patients would
In short, companies are spending a for making it available to others.
Campaigns: A disparity had opened pp
tune each year "getting" to doctors. An
be impressed if they realised the forces
estimated 40% of the .$150 million-$200 in recent years between what drugs the that work on the hand that pens the script
million promotions bill is spent on the scientific, medical and educational instit are worth about $10,000 a year in pads,
small army of “detailers", as they are utions were recommending and what doc pens, gifts, giveaways, hospitality, all
known - the foot soldiers who travel the tors were prescribing. “It
emblazoned with brand
country talking their way into surgeries became apparent to us that
name products.
to try to influence doctors to prescribe the doctors seemed to
“The students concede
reflect promotional pres
certain brands.
concern. The problem is,
The Bulletin has talked to detailers sures and campaigns of the
after five years out in prac
in Melbourne who admit they are trained industry rather more than
tice, with six drug reps a
in “psychological techniques” to get doc the messages from edu
week coming in, they have
tors on-side. A key aspect is the assump cators in the teaching hos
gone away from prescrib
tion that, once doctors agree to try a pro pitals and universities.”
ing sensibly and by scien
duct, a certain percentage will feel obliged
Medical educators such
tific name to prescribing
to follow up.
as Harvey and the instit
the brand promoted by the
Millions of dollars api>ear to be spent utions began to fight back
last rep who walked in."
on “duchessing". Detailers say they can by producing guides on
Experts such as Har
have near-unlimited budgets to wine and appropriate drug use and
vey suggest restrictions
dine medical practitioners, either at one- touring the nation trying
of, say, 10% of sales should
to-one lunches or at functions for up to 150 to convince medical practitioners to look be put on promotion, as occurs in Britain;
guests at quality city hotels.
for independent advice. But Australia or a levy on the industry to fund a founda
Free trips: Accommodation and travel
does not yet have anything to match, say, tion to provide independent advice.
packages are also offered to doctors (and Worst Pills-Best Pills, the 500-page
However, Al’MA executive officer
sometimes their spouses) to attend con “bible” of drug use for older people pro Kerry Bell points out that the industry
ferences. seminars and workshops, local duced by a US consumer lobby.
has to abide by various laws such as TYade
ly and overseas. These are hosted by drug
Harvey and his colleagues conducted Practices as well as the voluntary code.
companies and. while they may ostensibly an experiment in which they put a trained He denies challenges that promotion is
he examining some medical issue, often pharmacist on the road as adetailer. Some manipulative, arguing that drugs require
they are just thinly veiled promotions.
500 of Australia’s 15,001) medical prac rigorous pre-market approval. “The claim
Then there are the handouts: every titioner were selected and the detailer of manipulation also doesn’t acknowledge
thing from samples of drugs to pens and talked to 250 of them. It was found the the role of doctors. They are highly qual
pads and expensive gifts such as com prescribing rate for the drugs she pushed ified people and, like most technical
puter equipment, all designed to help climbed from 110% to 85% after her visit.
people, are pretty analytical.”
detailers establish rapport.
Harvey confirms that ull-expensesEvidence: Bell is not aware of any evi
It could be argued this is simply com paid trips are offered to places like the dence suggesting that increased use of
mercial reality. However, people such as Gold Coast where "you are wined and prescription pharmaceuticals results
Staples are uneasy because of claims that dined ostensibly to learn about a new drug from promotion. “There is a lot of anecdo
doctors’ prescription practices are being ... But the view that comes across is tal evidence, but I haven’t seen any defini
driven by this kind of promotion.
maybe not as balanced as it would be ifyou tive evidence ...”
Dr Ken Harvey, senior lecturer in got independent experts to look at it."
Bell says the cost of the PBS is increas
He said doctors could he offered trips ing because of the aging of the population
health administration and education at La
Trobe University, be
to overseas conferences and the "provision of new ding entities
came an expert on
with "no questions which the profession considers are more
society's drug usage
asked”. This wus accept appropriate than some older products".
after growing concern
able if the doctor was
Al’MA regarded promotional activities
ed, in the '80s, at the re
going there to work. as generally appropriate. "Our reviews
sistance germs were
“But to be flown over indicate the process is under control and
developing to anti
seas to a conference that there is a high level of compliance
biotics. A member of the
sponsored by a company with the code-that's something the draft
government Pharma
is essentially a form of Trade Practices report confirms.”
ceutical Health and Ra
bribery. That’s my view,
Despite the industry's protests, other
tional Use of Medicines
though not everyone research to be released soon will throw
Working Party, Harvey
would agree with it."
horrifying new light on the drug problem.
says doctors too often
Harvey says doctors A paper by Roy Harvey, head of the
prescribe the latest and
are happy to he wooed. Health Services Division at the Austra
most expensive drugs
"Some of my colleagues lian Institute of Health, will reveal that up
even though well-estab
say they like to receive to 40,000 hospital admissions a year are
lished ones would do the
all this hospitality plus caused by the prescription of wronger in
job and sometimes with
the giveaways, like the adequate drugs. The study goes so far as
out side effects,
tape recorders, the digi to claim this could be leading directly to
The flow of new Health Services Minister Staples
tal docks and some the deaths of up to 000 people a year. ■
THE HI I.I.ETI N. M MU’ll
21
"OlZ - S2-I - 3
01
__________
____£\v. ■^•&,fcvvwtAAw HOLISTIC
CTlpME^,
MaWt ftgg;-
cou^&t^
fa Lz.
M<wW^
(TyPt^/kJ.
^ovt.
foucy/ a cvm
fflfcyAtjJU
Paw/a
tx> cr
^c
.
-j^v^v&wU
fewv^WwviL
•] /^tVOW^
Lc«t>j £z
'
A^(/\> Ia/uXa
f<V/w7U/)
/
ZocmJu, ^co-waaA^z
CvvL^Aiixl.,
SX) (XC'tvj
. J
JA'sxAziZ/
®
^Azlfl/Vvv’A-
- ICt'VV^^O
^vw^L/ JD-AzSXiVJ-^--AvwCt/
fe (Xvs,.
Io
■2^
l'h^Mc)
lA-C
—------
.P-W^x
/]y^
Pcrt^i
<
(co tfV ^Izbrfc .
COkgVMcRS
R&ppWl g/(JTy
~ 'TH 5 OT/fe^ -^/Dg
__________________ RE
/RES P0Mr / illEpT/
Sil)£
o^P
— "Tfre
7^ co/M
•
In/
dry
PM
01
— PdzticiX p^^C££wi4/
AxxV) kfr Zkzz<
P1A ■
SQSNAR.I o
LMblAh/
' fZ/VtzU/V L(/V\A
j
OcoS&roetdA
—
ZbtXVWl^Ci .
/j <wtv Pa © LEia
AX- ZaZaC
IA/QA7
,
17 ?
MW
2'4
W^'tvCAZ'
COvqCmaz
lwoc/7-
— Qaws..
WCV\7 pA%vv<^- ''----------- -—<~~
---------- l^lA.LZK>LX-
HI
(BFv<?Vw(>7S 7\t^wv^T‘~^=-
V
_ PouT/C^ f____________
Y^iJViZy /^w^iPCot^Z
Xzvv£-(ZU>a€ C/ZxtUd. "''
- vf>
_________________ [Q(oJ _AaXX/0z4z Ps-ir/'ZAZZ/
/i
Mjoi-oovo ---- }4&aCc/-
UhrkP e^c^>-
-
- S'/t^l^^. r^\tsvA,o^(A
------------ LO---------- 1--------------------- Tfe-^PztX^-----------
'&WC2>
^ecmx^ Tic/w W QKy/vg^
Pft&W l_
CAT-'^c^w —> Ccm^t/vwvW byofzciwvt —'AVu^cLj P^vix^ wxia
People
h./g w
E . c
iLtAA^a^MK^A.
AaZZj^x -Vl/jV Uo /vviVYMeEtz). azZ«
E-Cor
Zz/MA z? 6^v0vvf/vy
—■
(Vp AA CAA/E
A^r^Q, cwx- Up -------- >
-A/
p^zCUv vxZct^z,
^iwvb I
Z?
^(\/\A~
.
h^fa.cd' -^'l^vt^L'
' l^T US 5&T GUI^ HOW£ /M OfcbeP
Dw^pX^p &
/j^cLopvvvfl cz>vmbiA/^ ---- ?
L^'T W GA kQo\J& fG(M^>
AM7ZWA
- I^Fh/^ P^eACWAJ
GAS
WvvvU-s
—5>
pA'tM/vvO'fa/vt/^
A^ CvCz&AA <AW^
'■^xLc D(aJ^a-z^Mz-
St^-efa'j {
pov-s.
—
Cl-vCV^tj
—
S’at/VMz/
^O'\aj[ Si%via£a
o
.77-tZiJ)
^127 Pvj:
p^po^ s
■^CU7JSa\Aa)AJIA.
fi~L
^XAaIaJOXAAA S<^V\A/IVC> -
] Az/V^GvGvauAAi/i
zvz
C^Wtz^yCoy 'H/XZ^L. /MzO'IG/zvmZ
Wvcctv
9vjU-mv </r€^frkcz(,
-j-
Go c^., J^-a/ tGvS- cxw2A>?rv
I
(^A
izs^o/ww Gv l/v Kzz
0
,.
0/7)2&N'A
,Giz!y2/l
4/Y^ ■
z/,
.
9!
4\
4\
j
aaaJa
k'
■
vmiuTy
— CA-t/tllzb C-
V'OyvWc-' •
I
/
r
■■'■ '
( (^g/VVZAVCz
—■ ■
•— ^oW~- S)^)£z/Uz^vv^>
•—■^'vO^/Vv Co?t^ —
L/ ^aHT),
■ • -.^ ~ <^(z>_^zx_ ■
-^V'4',
^kz^v-M/
d53) smaWvim, f^TU^ys ^(ASs.
— zX^ov<^)
GA//.
,
M0~ I NT) 7C^-. ~
K)07
€7)’
p£/C WMW/2J>
7p'7toAl77gJ>
/NJ O'P.b. ^ITUA7/O/J •
AW
ZW£e
--m
ho CvQSIrWie
70
7//14B 47
^47^//V^
d^
.
6
2
itfQJtjkv
/
t\j
iM^ziA^fAx^
ztLo'C/t^
2v
[/xjuqJJA'^ A^SaaIA .
5ka4 z
0^(J^
2v\i<V\/vy^C<lrv^ !<-—
5\
/
/^jVWiAAZ^vvksAZ/ k>
^%v^^vt/C'^vvj/' Aa^c ■ Z-u)
6.
^Iazv?)
•etez .
^^^^X/vk>W
/\JU^[a2aa CaaaCaa/^ .
7.- 12^,
------ f--------- -------------- -----------------------
---- ■_
^(MU^vuUx/ /2>/vx2ao X€mA^
j^Cyw^T^
"
fit -
JzvJ^KTrx 6-^
htoV^o
2-o
U/vuMaM
(C/-»
^^vvtvgVAX :
AMxlaX- EaawC
(Tw
CwM^jtu/c
?
~„
(7y> gW"(Mtwv\ /^4-
■
—X)
Ma
^Mr/v -
7T
"Ti .
(
ovvk
' ^vWv (c^
P/\/\a^
______________
i
i oCv^j^L
k-f/zv
0\^y\
zu4>Cv^vk^- £t>
_____
0
o
V]^y -
f/J
(DU',9^)
/J)
lAj-lc^p Ow ^W/.eW 'A&VtfZ - JTtt. (p
I
/ yty •---- ^3<v
C-D'GOM ^acxXvCiyi — CaaV t-e- HzKzt- ^/oZlsy”- t?Or £c<az4_-
b&zm-
K?-^vtA>PcA^<
'
. ^Vvu^vt^ CAa<£z, ~
^tOv
(^VTA2/l/VW'«AV
-y
—'-----
t
A^tTviA/^L^vV-^-^i
z zkv/c/(^
-FmOil
SoU
/
fU( yS\y(- ' (qC>0 C> 3-S
—
C
6
DoC'K;
_
PiM/xz-Z/
Z^vS^Oiz-i^v C^Vb ■
■I
CcriAA/p/vv&-(zvv^6<^y
^-. C-,(^----
Vj^T A&g '&5T<>
ZX5S^g~
KJ&C&S.
C/A/2)^_
O\JW rc^c^AAju^ ~(h/^
P&)CZbURj?$z
<
- KJei- £aJ^, //^rf'
/
i a a x y. //
^i/i /aJ^
/^/Q-zy-rr
^bt'CAllONS
-wvSi
bCo OaxU-
(AA OwS4 .
C/ROUP- 2
(AAZs \>CA^^\yV\^ (A ^IZv^^bvUZx Po
sz'z/zjz'tzr
^WVt^.
zAwS/lciXx
\2/Pj^ p'zt^><zz
u^V/VL-Z^AZ^^. t
20
IaJ
i/VAAz(jC
CArAAA
_. _______________________
P-b , AJ-Ji V'\Z<’ V^--C^-
P/tcxYy, ■
IZy-oC jr1_
~^-£zvi^/i/iW/lz
> i.
.A. -CA-V-fe,
Z2-)
znAZXx2<4^zS
^A.'V\ji/->~
U
Z|M
_ J^^VA-VtCt^z &O1a4&\.
Clui/l/ ity pt fl-w
IJ
2£
t'C^A.C-tv CV1S-V3
d^i
tLAA
v>^^>
,.'l c T&.i^ ■- WVvty1 h?.kj I
^f-e
I V'luU-'h'Mt'.
’^H/vxJ^v^Xz ’—
C^Ov^jp^''
CO C^CoCyed^i^ si^vwo/y
xr(
lop^r^^- 1
/lA.i't-- C'L'l^T-<i P lip'pt
h^d - &d loi^:..
..
oi-zr
P^L^7~y<
" 7k^ .
SdoL - i/>
fyl/lW &
'I'vvvuty' A-A^vvit-UA/t^
^TTV^L
pc(.l/
/{'VI1
tA,V\T^>CCX2-<7
I'KfivxJ (jyCA
mo
'^-1-4-
ALTERNATIVE MEDICINE : MYTH AND REALITY
by
DR. SHIRDI PRASAD TEKUR,
M.B.B.S., D.C.H.
Coordinator,
Community Health Cell,
Society for Community Health Awareness, Research & Action,
No.326, 5th Main,
Koramangala, I Block,
Bangalore - 560 034.
ALTERNATIVE MEDICINE
MYTH AND REALITY
INTRODUCTION
The term 'Alternative Medicine' identifies the dominant role
played by one system of medicine in our country.
It is the
western / cosmopolitan or so called 'Allopathic system'.
It
determines our National Health Policy.
All other systems are 'Alternatives'.
Over three hundred such
systems and practices are cited, though only a few are in
extensive use. Each culture has catered to its pattern of illness
with an indigenous response and hence this plethora. Any attempt
at dealing with all of them together is necessarily simplistic
and superficial, though a working perspective could be evolved.
Essentially,the Alternative systems can be broadly classified
from the formalised systems to the Non-formal ones,
across a
spectrum in their placing.
Formalised Systems
The formalised systems include Ayurveda, Siddha,
Unani, Yoga
and Naturopathy, Homoeopathy, Acupuncture and Tibetan Medicine.
The Government of India recognises all these systems except the
last two in its National Health Policy.
These formalised systems are characterised by well developed
philosophical and theoretical bases tested over time and in
practice.
They
have
well
documented
principles
and
practices,which
are constantly reviewed and
updated
by
conscientious practitioners of the systems.
Non-formal systems
The non-formal systems include tribal and folk practices,
home
and herbal remedies which have a symbiotic relation with the
formalised
systems providing avenues of
sustenance
and
rejuvenation to them. Micro attempts at organising them are
afoot though they remain unrecognised by the mainstream due to
their inherent amorphous nature.
The essentials of these Alternative Systems
1.
The difference between life and death is obvious.
This
'Life Force' or 'Vital energy' in a living organism forms
the basis in their understanding.
The signs and symptoms
of health and disease are seen as the manifestation of this
force and all attempts are directed towards bringing about a
harmony or balance in it.
\
2
The various terms used to express this life force includePrana, Tchi, Dynamis, Vital force and Bio energy
in
different systems.
Subjective symptoms, feelings and emotions are given prime
importance in diagnosis and treatment, since the Soil of the
human body is considered to be more important than the Seed
of disease
3.
Ail factors which could affect rhe soil and life force
whether external,
internal,
tangible or otherwise
are
considered for change and manipulation in these systems.
In
short, the mental,
social and spiritual dimensions are
adequately recognised.
4.
The
canvas being wide, other allied practices
Astrology, Palmistry, etc., are utilised to help in
systems.
5.
Health promotion and maintenance with prescribed patterns
for behaviour modification across diet, exercise, sleep and
rituals form part of their procedures.
6.
All practices are adapted to local need, local resources and
attempt to focus on the individual or family, with a global
spiritual perspective.
Now,
to look at the myths and enhance
these systems.
MYTH :
our
like
these
understanding
of
ALTERNATIVE MEDICINE IS NOT 'SCIENTIFIC'
Most of the philosophies of Alternative systems originated from
oriental thought, like the
Samkhya - one of the six schools of Indian Philosophy;
Vaisheshika - the system of logic used to
propositions; and
explain
Yoga - the science or shastra explaining the working
mind and its relationship to the body.
The Chinese systems have absorbed Taoism, Zen
thought in .their philosophies.
and
Ayurvedic
of
the
Confucian
Logic, experimental methods, measurement and quantification
exist in these systems, providing a frame work to validate
their theory and practice.
. . 3
: 3 :
The fundamental differences between these and Western
makes unintelligible any comparison between systems,
exact equivalents exist, or can be made.
MYTH :
science
as
no
ALTERNATIVE MEDICINE IS OBSOLETE
The survival of medical/health practices have always been
dictated by the patronage of the state. Factors of political
expediency in the history of colonialism in our past have
suspended and even suppressed progress of these systems wit?:
the times. Evidence in archaeology and history supports their
ability to meet the needs of the day from water and sanitation
adopted, to plastic surgery and inoculation against small pox.
The revival of Acupuncture during the Chinese Revolution under
the patronage of Mao-ze-dong is a recent example of revival of
a useful system.
MYTH :
ALTERNATIVE MEDICINE SYSTEMS ARE
NOT 'RECOGNISED'
People have always recognised the worth
ensuring their survival to this day.
of
these
systems,
The W.H.O has been promoting Traditional Medicine as part of
its Policy since 1975.
The Government of India recognises the
formalised systems in its National Health Policy Document 1981.
These expressions of 'recognition' have a paternalistic (asopposed to fraternal) tone on paper and in practice, while
their perplexity is evident in their equating all these systems
with mystical practices. Luckily, or otherwise, we have all
these systems, including the very advanced formalised systems
in our country, unlike the African and American continents
which typify the non-formal systems.
MYTH :
THERE ARE NOT ENOUGH TRAINING/RESEARCH CENTRES, OR WELL
TRAINED PERSONNEL IN THESE SYSTEMS
Figures from the document "Health Information of India 1991"
published by the Central Bureau of Health Intelligence, DGHS,
Ministry of Health and Family Welfare, G.O.I. should suffice in
this context.
a) No of colleges of I.S.M.
and Homoeopathy ( 1989)
with admission capacity
No. of Medical Colleges/'
No. of Students admitted/
Ayurveda
Unani
Siddha
Homoeopathy
98
17
2
27
3947
665
150
5259
Total
214
10,021
No. of students passed out
in M.B.B.S.
128
13,262 .
12,292
4
4
b)
No. of registered ISM and
Homoeopathic practitioners
No. of Doctors registered
c)
Ayurveda
Unani
Siddha
Naturopathy
Homoeopathy
315,719
34,336
11,644
146
1,43,866
Total
5,11,261
Under IMC Act with State
Medical Councils
Summary of Medical care (1939)
facilities under ISM and
Homoeopathy
Ayurveda
Unani
Siddha
Naturopathy
Yoga
Homoeopathy
Total
1527
109
105
11
6
205
12,339
953
306
1963
19791
No. of Hospitals/
Dispensaries
7
567 0
11,254 / 27,99
The urban/rural,
Sex-wise details of personnel etc., are
available for the 'Allopathic' system, while no such details
are available for the 'Alternatives'.
Also,
the Alternative
medicine details are disposed off in three tables of 1989
vintage,
while those of the Allopathic system spreads across
forty pages, and that too, well up-dated! The bias is evident
despite the comparable figures listed above.
The Directorate for the Indian systems
of Medicine and
Homoeopathy ensure standards and curricular requirements for
the training of personnel, as well as medical facilities
available to, people within the constraints they operate- in.
MYTH :
ALTERNATIVE MEDICINE IS NOT THE PEOPLES' CHOICE
The survival of these systems to this day has been mainly due
to people using them for their needs. The common man does not
differentiate between systems as we professionals do. Their
utilization of any system depends on considerations of easy
availability in terms of economics and consonance with her/his
belief systems.
The W.H.O.
"World Drug Situation" places India among countries
where less than 30% population have access to modern medicine.
So, the vast majority depend on alternatives in our country.
5
ALTERNATIVE MEDICINE IS SAFE
MYTH :
With increasing demands on medical products of alternative
systems, mass production and marketing methods have invaded
these systems. Quality control and supervising capabilities
being stretched,
the ills of industry and lack of ethical
practices are evident. The recent 'SURA' tragedy in New Delhi
is a pointer to this trend.
ALTERNATIVE MEDICINE IS CHEAP
MYTH :
Trends cited above have added to the cost of medicine instead
of reducing it,
especially the private sector and Trans
national companies having entered this market for profit
making.
The upper crust have added to the problem in
their quest for the best - obviously is the costliest.
MYTH
:
ALTERNATIVE MEDICINE IS USEFUL ONLY
DOES NOT WORK
WHEN
'ALLOPATHY'
From minor ailments to chronic diseases, many people adopt
alternative medicine as a fad, a reaction to the ills of
'modern medicine', because they can afford to shop around,
or,
because they cannot afford the cost of modern medicine.
The truth is that many illnesses are treatable by any of these
systems,
and the individuals/community do not have
the
information to make logical choices suitable to themselves.
This leads to a potentially exploitable situation for a profit
maker.
MYTH :
ALTERNATIVE MEDICINE IS ONLY 'PLACEBO'
This blanket proposition equates all alternative methods to
each other,
and detracts from our ability to understand and
utilize any particular system for its merits.
Also, the concept of placebo as a derogatory, hood-winking
effort is strengthened.
It fails to mobilize the innate
healing capabilities of an individual and recruit all available
forces for a positive outcome.
The placebo
systems.
effect
is very creatively
used
in
alternative
The Nocebo effect (negative placebo effect)
is increasingly
being
recognized now by us,
a factor
incorporated
in
Alternative Medical System Practice.
. . 6
6
CONCLUSION :
In conclusion,
we need to understand in all humility that
"Healing" is a wide concept which can be learned with an open
mind towards all practices, and not necessarily through our
limited perspective.
Serendipity has been the hall-mark of all major medical
advances, considering the complexity of the human organism and
its relation to all life.
Spin-offs from the space age are
eulogised while our heritage begs for recognition.
We have been marshaling ideas from the theories of "Chaos",
"Fractals",
"Gaia Principle",
"Spirituality" and other so
called frontiers of sciences, cowards a holistic approach.
We
recognize
"patterns" and "multi dimensional" and
"multi
factorial" aspects of Health and Disease.
The
'ART' of
Medicine is coming alive again through science.
We need to explore these possibilities and understand them from
our fraternity who explored human health and disease over rhe
ages, albeit in a different framework.
We would be foolish co
ignore this "Established Medicine." which had successfully
exploited the ART of medicine in an age where its Science was
not what it is today.
REFERENCES AND FURTHER READING
Health Information of India 1991 - CBHI, DGHS - G.O.I.
State of India's Health - V.H.A.I. - 1992
Local Health Traditions - an introduction - L.S.P.S.S. June 1989
4. Herbal Medicine for Human Health - W.H.O. SEARO Regional
Publications No. 20 - 1992.
5. The Use of Traditional Medicine in Primary Health Care SEARO - Regional Health Papers No. 19 - 1992.
6.
Home Remedies - C.H.A.I. - 1992
7.
'Alternative Health Care Systems - Another Point of View' MADHYAM - April 1991.
8.
'The Philosophy of Homoeopathy' - Health Action - March 1991
9.
Acupuncture, Acupressure and Related Drugless Therapies Health Action - March 1991
10. 'What is Traditional Medicine' - Background paper to
FEVORD-K AGBM - May 1990.
11. The Promotion and Development of Traditional Medicine W.H.9. - T.R.S. No. 622
7
1.
2.
3.
12.
13.
14.
15.
16.
Traditional Medicine and Primary Health Care - E.P.C.
Publication No. 18
National Health Policy Document - 1981
LOVE, MEDICINE and MIRACLES - Bervie S. Siegel - Arrow
Books - 1988
'QUANTUM HEALING' - Deepak Chopra - Bantam Books 1990
Super Nature I & II - Lyall Watson - 1976.
********
******
****
**
13 U' Xi •
THE PATIENT’S CHARTER
PATIENT’S RIGHTS
I.
RIGHT TO HEALTH CARE AND HUMANE TREATMENT
' 1. Every individual shall have access to competent health care and treatment
regardless of age, sex, ethnic origin, religion, political affiliation, economic
status or social class.
2.
Health care services shall be available on the basis of clinical need regardless
of the ability to pay and it shall be the responsibility of the Government to
ensure that every person has access to essential health services.
3.
Every patient shall be treated with care, consideration, respect and dignity
without discrimination of any kind.
4.
All drugs dispensed shall be of acceptable standards in terms of quality,
efficacy and safety.
5.
Every individual shall have the right to prompt emergency treatment from the
nearest government or private medical and health facility.
6.
Patients shall be interviewed and examined in surroundings designed to
ensure reasonable privacy and shall have the right to be chaperoned during
any physical examination or treatment.
A child admitted to hospital shall, whenever possible, have the right to the
company of a parent or guardian.
II.
RIGHT TO CHOICE OF CARE
1.
A patient shall have the right to a second opinion at any time.
2.
A patient shall have the right to a copy of his or her case history and medical
records and have them explained. The patient shall also have the right to
authorise in writing another health professional to obtain a copy of the same
and to inform him or her of what they contain.
3.
A patient shall, whenever possible, have the right to be treated at a hospital of
choice and to be referred to a consultant of choice.
4.
A patient who has received adequate information about his or her condition
during consultation shall have the right to accept or to refuse treatment.
THE PATIENTS' CHARTER
If a patient's health professional refuses to allow another health professional
to be called in, or breaches any other provisions of this charter, the patient shall
have the right to discharge that health professional and seek the services of
another.
5.
III.
RIGHT TO ACCEPTABLE SAFETY
Before any treatment or investigation, a patient shall have the right to a clear,
concise explanation in lay terms of the proposed procedure and of any
available alternative procedure. Where applicable the explanation shall incor
porate information on risks, side-effects, or after-effects, problems relating to
recuperation, likelihood of success, risk of death, and whether the proposed
procedure is to be administered by or in the presence of students. A patient may
refuse any treatment dr investigation.
1.
IV.
RIGHT TO ADEQUATE INFORMATION AND CONSENT
1.
A patient shall have the right to know the identity and professional status of
the individuals providing service to the patient and to know which health
professional is primarily responsible for the patient's care.
2.
A patient shall have the right to information regarding all aspects of medica
tion, including:
• The right to adequate and understandable information on prescribed and
purchased medicines.
3.
•
The right to the most effective and safe medicines. Safety must be ensured
by the manufacturers and by legislative control.
•
The right to convenient access to medicines.
•
The right to choose among competitive products.
All medicines shall be labeled, and shall include the pharmacologic name of
the medicine, the dosage and how often the medicine has to be taken.
In addition, the patient shall be informed about the medication, including the
following:•
The purpose of the medicine
•
The possible side effects
•
The avoidance of any food, alcoholic beverages or other drugs
•
The duration necessary for any medication prescribed
•
The measures to be taken if a dose is forgotten or if an overdose is taken.
THE PATIENTS' CHAPTER
4.
A patient shall have the right to an itemized account after any treatment or
consultation and to have this explained.
5.
If a patient is in hospital or any health care facility, the patient shall, unless
incapacitated, be consulted about any decision to discharge or transfer the
patient to another facility.
6.
Where it is appropriate to a patient's condition or treatment, the patient shall
be given advice about self-care, drug administration, special precautions
which may be necessary or desirable, and the existence of special associations,
facilities, aids or appliances which may be of assistance.
7.
A patient's consent shall be required before any procedure is carried out. No
patient shall be treated or examined without his or her consent. In the case of
a minor the consent shall first be obtained from the parent or guardian. If a
patient is incapacitated and delay would be dangerous, a doctor is entitled to
carry out any necessary treatment or operation.
8.
A patient's writtenconsent shall be required for the inclusionof a patient in any
research. The patient shall be adequately informed of the aims, methods,
anticipated benefits and potential hazards of the study and the discomfort ft
may entail. The patient shall be informed that he or she is at liberty to abstain
from participation in the study and that he or she is free to withdraw his or her
consent to participation at any time. To ensure that the informed consent is not
obtained under duress or from a patient in a dependent relationship to the
health professional, the informed "onsent shall be obtained by a health
professional who is not engaged in the investigation and who is completely
independent of the official relationship between the patient and the health
professional. In the case of a child the informed consent shall be obtained from
the parent or guardian.
9.
A patient shall have the right to have the details of the patient's condition,
treatment, prognosis and all communication and other records relating to the
patient's care to be treated as confidential, unless:
•
authorised in writing by the patient
•
it is undesirable on medical grounds to seek a patient's consent but it is in
the patient's own interest that confidentiality should be broken
•
the information is required by due legal process.
V.
1.
2.
RIGHT TO REDRESS OF GRIEVANCES
A patient shall have access to appropriate redressal procedures.
A patient shall have the right to legal advice as regards any malpractice by the
hospital, the hospital staff or by a doctor or other health professional.
3
THE PATIENTS' CHARTER
3.
A patient shall have the right to recover damages for injury or illness incurred
or aggravated as a result of the failure of the health professional to exercise the
duty and standard of care required of him or her while treating the patient.
VI.
1.
RIGHT TO PARTICIPATION AND REPRESENTATION
A patient shall have the right to participate in decision-making affecting the
patient's health:
o
with the health professionals and personnel involved in direct health care;
and
®
through consumer representation in planning and evaluating the system
of health services, the types and qualities of service and the conditions
under which health services are or were delivered.
VII.
1.
Every individual shall have the right to seek and obtain advice with regard to
preventive and curative medicine, after care and good health.
VIII.
1.
RIGHT TO HEALTH EDUCATION
RIGHT TO A HEALTHY ENVIRONMENT
Every individual shall have the right to an environment that is conducive to
good health. This includes and extends to a health professional's office, health
centre, hospital room and/or ward and other treatment facilities.
PATIENT’S RESPONSIBILITIES
1.
The patient shall ensure that he or she knows and understands what a patient's
rights are and shall exercise those rights responsibly and reasonably.
2.
The patient shall ensure that he or she understands the purpose and cost of any
proposed investigation or treatment before deciding to accept it. The patient
shall insist upon explanations until adequately informed and consult with all
relevant persons before reaching the decision.
3.
The patient shall accept all the consequences of the patient's own informed
decisions.
4.
The patient shall provide accurate and complete information which the health
professional requires about his or her health and ability to pay for health
services.
4
THE PATIENTS' CHARTER
5.
The patient shall follow the treatment determined by the health professional
primarily responsible for the patient's care.
6.
The patient shall keep appointments and shall inform the health professional
if unable to do so.
7.
The patient shall inform the health professional if he or she is currently
consulting with or under the care of another health professional in connection
with the same complaint or any other complaint.
8.
The patient shall so conduct himself or herself so as not to interfere with the well
being or rights of other patients or providers of health care.
9.
Every individual has a responsibility to maintain his or her own health and that
of society by refraining from indulging in:-
10.
®
unhealthy consumption;
o
addiction forming substances such as dadah, tobacco and alcohol;
»
life styles thatha ve an adverse impact on health such as sexual promiscuity,
reckless activities and physical inactivity; and
•
contamination of the environment.
Every individual has a responsibility' to accept all preventive measure sanc
tioned by law.
A A" k
5
PONDICHERRY DECLARATION ON HEALTH RIGHTS AND
RESPONSIBILITIES
This consensus statement was adopted by the participants attending a workshop on "Medicine, Media and
Consumer Education" held in Pondicherry , India December 1-4, 1993. Thirty participants from 3
countries attended the workshop organised by the Educators for Quality Update of Indian Physicians with
the support of the International Organisation of Consumers Unions.
THIS WORKSHOP EVOLVED THE FOLLOWING GUIDING PRINCIPLES;
the work of rational drug use groups should be expanded to include diagnostics and non-drug
therapy
the concept of continuity of care through the family physician should be encouraged by consumer
education and medical education
a Charter of Patients' Rights and Responsibilities should be widely adopted by professional and
consumer groups.
•
*
«
We call on CENTRAL AND STATE GOVERNMENTS to:
bring all issues pertaining to drugs under the purview of Ministry of Health and Family
Welfare;
1.2
enunciate and effectively implement rational drug policy;
1.3
promote the concept of essential drugs and ensure their availability at affordable cost;
1.4
promote use of generic names of drugs;
1.5
regulate and monitor all promotional measures and advertising materials;
1.6
establish a National Drug Authority of India consisting of governmental, non
governmental organisations as well as professionals bodies;
1.7
establish and support a drug information and usage monitoring system to facilitate and
implement an effective rational drug policy. This should include systems for
monitoring adverse drug reactions;
1.8
integrate the concept of rational drug use, including drug information into health and
medical education;
1.9
introduce within the formal and non-formal educational system information on healthrelated issues;
1.10 promulgate the charter of patients rights and responsibilities and physicians' rights and
responsibilities.
1.
1.1
2.
2.1
2.2
2.3
2.4
2.5
2.6
We call on HEALTH PROFESSIONALS to:
adopt an holistic approach to health care;
develop two way linkages between different levels of health care;
promote prudent use of diagnostic aids and therapy;
endorse and respect the charter of patients rights;
acquire communication skills to interact with patients, the mass media and the public;
periodically update their professional knowledge and improve their skills.
3.
We call on PROFESSIONAL GROUPS, NON-GOVERNMENTAL AND
VOLUNTARY ORGANISATIONS to:
promote the adoption of a charter of patients rights and responsibilities;
establish networks at all levels in orderto facilitate health information, communication
and education;
encourage multi- and inter-disciplinary researchon health related issues;
facilitate periodic .updates for health knowledge.
3.1
3.2
3.3
3.4
4.
4.1
4.2
4.3
We call on the MASS MEDIA to:
recognise their far-reaching influence on the level of public awareness and assume a
more active and responsible role in informing the public on health issues;
use a resource network of competent health experts to ensure objective and balanced
reporting of health issues;
establish regular communication with health professionals and consumer groups;
1
4.4
participate in the screening of advertisements on health-related issues for unsubstantiated
claims and unethical promotion;
5.
5.1
We call on the HEALTH AND PHARMACEUTICAL INDUSTRY to:
develop and enforce code of marketing, promotion and dissemination of information in
participation with governmental and non-governmental organisations;
recognise their social responsibility to the public with regard not only to the safety and
efficacy of their products and services but also to their cost and societal impact and
to devise and to disseminate health information accordingly.
5.2
PATIENTS RIGHTS AND RESPONSIBILITIES
This charter was adopted by the participants attending a workshop on "Medicine, Media and
Consumer Education" held in Pondicherry, India December 1-4, 1993. Thirty participants
from 3 countries attended the workshop organised by the Educators for Quality Update of
Indian Physicians (EQUIP) with the support of the International Organisation of Consumer
Unions (IOCU).
PART 1:
PATIENT RIGHTS
Section 1: Right to health care and humane treatment
1.
Every individual shall have access to adequate and appropriate health care and
treatment.
2.
Every patient shall be treated with care, consideration, respect and dignity without
discrimination of any kind.
3.
A patient has the right to be treated by fully qualified health care professionals in
private or public health care facilities.
4.
A patient has, wherever possible, the right to be treated at a hospital of his choice and
to be referred to a consultant of his choice.
5.
Every individual shall have the right to prompt emergency treatment from the
nearest government or private medical and health facility.
6.
Patients have the right to humane terminal care and to die in dignity.
7.
A patient can be transferred to another health care establishment only after an
explanation of the need for thic transfer and after the other establishment has
accepted the patient.
8.
A patient has the right to have all identifying information, results of investigations,
details of his condition and his treatment kept confidential and not made available to
anyone else without his consent.
Section 2: Consent
1.
Before any treatment or investigation, a patient shall have the right to a clear,
concise explanation in lay terms of the proposed procedure and of any available
alternative procedure. Where applicable, the explanation shall include information
on risks, side effects, or after-effects, problems relating to recuperation, likelihood
of success, and risk of death. Informed consent of the patient must be obtained prior
to the conduct of a treatment or a procedure. In the case of a minor, consent has to be
obtained from the parent or guardian. If a patient is incapacitated and any delay would
be dangerous, a doctor is entitled to carry out any necessary treatment or operation
after a second opinion is obtained.
2.
A patient has the right to refuse treatment to the extent permitted by law and to be
informed of the medical consequences of his decision.
3.
Explicit, informed consent is a prerequisite for participation in scientific
experimentation. Experimentation must not be carried out on a patient who is unable
to express his will.
Section 3:
Right to information
1
Information about health services (including recent developments In the field) and
how best to use them is to be made available to the public in order to benefit all those
concerned.
2.
Information may be withheld from patients in cases where there is good reason to
believe that this information would affect the patient's health adversely but, however,
the information must be given to a responsible relative.
3
A patient has.he right to know the identity and the professional status of the
individuals providing service to the patient and to know which professional is
primarily responsible for the patient's care.
4.
Patients should have the right to seek a second opinion from another physician.
5,
Patients should upon request, be able to obtain a copy of a summary of their diagnosis,
treatment and care including diagnostic results on discharge from a hospital or other
establishment. They shall also have the right to authorise another medical
professional to obtain a copy of the same and to inform the patient of the contents.
6.
A patient shall have the right to examine and receive an explanation of his bill after
any treatment and consultation.
Section 4:
1.
The right to adequate prescribing information
While prescribing medication, the patient shall be informed about the following:
expected outcome, adverse and after-effects, chances of success, risks, cost and
availability.
2.
All drugs dispensed shall be of acceptable standards in terms of quality, efficacy and
safety.
3.
All medicines shall be labelled and shall include the pharmacological name of he
medicine.
Section 5: Right to health education
Every individual shall have the right to seek and obtain advice with regard to
preventive and curative medicine, after-care and good health.
PART 2:
PATIENT'S RESPONSIBILITIES
1.
The patient shall ensure that he or she knows and understands what a patient's rights
are and shall exercise those rights responsibly and reasonably.
2.
The patient shall ensure that he or she understands the purpose and cost of any
proposed investigation or treatment before deciding to accept it.
3.
The patient shall accept all the consequences of the his/her own informed decisions.
4.
The patient shall provide accurate and complete information which the health
professional requires about his or her health and ability to pay for health services.
3
5.
The patient shall establish a stable relationship with and follow the treatment
determined by the health professional primarily responsible for the patient's care.
6.
The patient shall inform the health professional if he or she is currently consulting
with or under the care of another health professional in connection with the same
complaint or any other complaint.
7.
The patient shall so conduct himself or herself so as not to interfere with the well
being or rights of other patients or providers of health care.
8.
Every individual has a responsibility to maintain his or her own health and that of
society by refraining from indulging in high risk behaviour detrimental to health.
9.
Every individual has a responsibility to accept all preventive measures sanctioned by
law.
For 'he' or 'his' in this document, please read "he or she', and 'his or her'.
PATIENTS RIGHTS AND RESPONSIBILITIES
—
.
This charter was adopted by the participants attending a workshop on "Medicine, Media and
Consumer Education" held in Pondicherry, India December 1-4, 1993. Thirty participants
from 3 countries attended the workshop organised by the Educators for Quality Update of
Indian Physicians (EQUIP) with the support of the International Organisation of Consumer
Unions (IOCU).
PART 1:
PATIENT RIGHTS
Section 1: Right to health care and humane treatment
1
Every individual shall have access to adequate and appropriate health care and
treatment.
2.
Every patient shall be treated with care, consideration, respect and dignity without
discrimination of any kind.
3.
A patient has the right to be treated by fully qualified health care professionals in
private or public health care facilities.
4.
A patient has, wherever possible, the right to be treated at a hospital of his choice and
to be referred to a consultant of his choice.
5.
Every individual shall have the right to prompt emergency treatment from the
nearest government or private medical and health facility.
6.
Patients have the right to humane terminal care and to die in dignity.
7.
A patient can be transferred to another health care establishment only after an
explanation of the need for this transfer and after the other establishment has
accepted the patient.
8.
A patient has the right to have all identifying information, results of investigations,
details of his condition and his treatment kept confidential and not made available to
anyone else without his consent.
Section 2: Consent
1.
Before any treatment or investigation, a patient shall have the right to a clear,
concise explanation in lay terms of the proposed procedure and of any available
alternative procedure. Where applicable, the explanation shall include informationon risks, side effects, or after-effects, problems relating to recuperation, likelihood
of success, and risk of death. Informed consent of the patient must be obtained prior
to the conduct of a treatment ora procedure. In the case of a minor, consent has to be
obtained from the parent or guardian. If a patient is incapacitated and any delay would
be dangerous, a doctor is entitled to carry out any necessary treatment or operation
after a second opinion is obtained.
2.
A patient has the right to refuse treatment to the extent permitted by law and to be
informed of the medical consequences of his decision.
3.
Explicit, informed consent is a prerequisite for participation in scientific
experimentation. Experimentation must not be carried out on a patient who is unable.
to express his will.
Section 3:
Right to information
1.
Information about health services (including recent developments In the field) and
how best to use them is to be made available to the public in order to benefit all thosaconcerned.
2.
Information may be withheld from patients in cases where there is good leason to
believe that this information would affect the patient's health adversely but, however,
the information must be given to a responsible relative.
3.
A patient has'he right to know the identity and the professional status of the
individuals providing service to the patient and to know which professional is
primarily responsible for the patient's care.
4.
Patients should have the right to seek a second opinion from another physician.
5.
Patients should upon request, be able to obtain a copy of a summary of their diagnosis,
treatment and care including diagnostic results on discharge from a hospital or other
establishment. They shall also have the right to authorise another medical
professional to obtain a copy of the same and to inform the patient of the contents.
6.
A patient shall have the right to examine and receive an explanation of his bill after
any treatment and consultation.
Section 4:
1
The right to adequate prescribing information
While prescribing medication, the patient shall be informed about the following:
expected outcome, adverse and after-effects, chances of success, risks, costand
availability.
2.
All drugs dispensed shall be of acceptable standards in terms of quality, efficacy and
safety.
3.
All medicines shall be labelled and shall include the pharmacological name of he
medicine.
Section 5: Right to health education
Every individual shall have the right to seek and obtain advice with regard to
preventive and curative medicine, after-care and good health.
PART 2:
PATIENT'S RESPONSIBILITIES
1.
The patient shall ensure that he or she knows and understands what a patient's rights
are and shall exercise those rights responsibly and reasonably.
2.
The patient shall ensure that he or she understands the purpose and cost of any
proposed investigation or treatment before deciding to accept it.
3.
The patient shall accept all the consequences of the his/her own informed decisions.
4.
The patient shall provide accurate and complete information which the health
professional requires about his or her health and ability to pay for health services.
3
5.
The patient shall establish a stable relationship with and follow the treatment
determined by the health professional primarily responsible for the patient's care.
6.
The patient shall inform the health professional if he or she is currently consulting
with or under the care of another health professional in connection with the same
complaint or any other complaint.
7.
The patient shall so conduct himself or herself so as not to interfere with the well
being or rights of other patients or providers of health care.
8.
Every individual has a responsibility to maintain his or her own health and that of
society by refraining from indulging in high risk behaviour detrimental to health.
9.
Every individual has a responsibility to accept all preventive measures sanctioned by
law.
For 'he' or 'his' in this document, please read "he or she', and 'his or her'.
PONDICHERRY DECLARATION ON HEALTH RIGHTS AND
RESPONSIBILITIES
This consensus statement was adopted by the participants attending a workshop on "Medicine, Media and
Consumer Education" held in Pondicherry , India December 1-4. 1993. Thirty participants from 3
countries attended the workshop organised by the Educators for Quality Update of Indian Physicians with
die support of die International Organisation of Consumers Unions.
THIS WORKSHOP EVOLVED THE FOLLOWING GUIDING PRINCIPLES:
die work of radonal drug use groups should be expanded to include diagnostics and non-drug
therapy
the concept of continuity of care through the family physician should be encouraged by consumer
educauon and medical education
a Charier of Patients' Rights and Responsibilities should be widely adopted by professional and
consumer groups.
•
♦
•
We call on CENTRA!. AND STATE GOVERNMENTS to:
bring all issues pertaining to drugs under the purview of Ministry of Health and Family
Welfare;
1.2
enunciate and effectively implement rational drug policy;
1.3
promote the concept of essential drugs and ensure their availability al affordable cost;
1.4
promote use of generic names of drugs;
1.5
regulate and monitor all promotional measures and advertising materials;
1.6
establish a National Drug Authority of India consisting of governmental, non
governmental organisations as well as professionals bodies;
1.7
establish and support a drug information and usage monitoring system to facilitate and
implement an effective rational drug policy. This should include systems for
monitoring adverse drug reactions;
1.8
integrate the concept of rational drug use, including drug information into health and
medical education;
1.9
introduce within the formal and non-formal educational system information on healthrelated issues;
1.10 promulgate the charter of patients rights and responsibilities and physicians' rights and
responsibilities.
1.
1.1
2.
2.1
2.2
2.3
2.4
2.5
2.6
We call on HEALTH PROFESSIONALS to:
adopt an holistic approach to health care;
develop two way linkages between different levels of health care;
promote prudent use of diagnostic aids and therapy;
endorse and respect the charter of patients rights;
acquire communication skills to interact with patients, the mass media and the public;
periodically update their professional knowledge and improve their skills.
3.
We call on PROFESSIONAL GROUPS, NON-GOVERNMENTAL AND
VOLUNTARY ORGANISATIONS to:
promote the adoption of a charter of patients rights and responsibilities;
establish networks at all levels in orderto facilitate health information, communication
and education;
encourage multi- and inter-disciplinaty research on health related issues;
facilitate periodic .updates for health knowledge.
3.1
3.2
3.3
3.4
4.
4.1
4.2
4.3
We call on the MASS MEDIA to:
recognise their far-reaching influence on the level of public awareness and assume a
more active and responsible role in informing the public on health issues;
use a resource network of competent health experts to ensure objective and balanced
reporting of health issues;
establish regular communication with health professionals and consumer groups;
1
4.4
participate in the screening of advertisements on health-related issues for unsubstantiated
claims and unethical promotion;
5.
5.1
We call on the 1 IEALTH AND PHARMACEUTICAL INDUSTRY to:
develop and enforce code of marketing, promotion and dissemination of information in
participation with governmental and non-governmental organisations;
recognise their social responsibility to the public with regard not only to the safety and
efficacy of their products and services but also to their cost and societal impact and
to devise and to disseminate health information accordingly.
5.2
I4AI
news
NUMBER 70, APRIL 1993
Health for all now
HAI News presents the happenings in the international campaign for more rational and fairer
health policies The organ of Health Action International is an informal network of non
governmental organisations and individuals committed to stnve for ‘health for all now'. This
newsletter aJso carries matcnal supportive of the participants’ work.
Historic Day for Patients’ Rights
By Shila Rani Kaur
INTRODUCTION
On March 1, 1993, Malaysia joined the ranks of those
nations in the world, which recognise that essential
health care is a right for all and not a privilege to be
conferred on those who can afford to pay for it. A
memorandum of understanding on a Patients’ Charter
was signed by the Malaysian Medical Association
(MMA), the Malaysian Dental Association (MDA), the
Malaysian Pharmaceutical Society (MPS) and the
Federation of Malaysian Consumer Associations
(FOMCA).
With the signing of the memorandum by the various
professional bodies. Malaysia becomes the second
country in Asia, after South Korea, to have drawn up a
Patients’ Charter. Similar initiatives have been taken by
the United Kingdom and the European Community.
It also addresses a patient's right to request a second
opinion, to have access to his or her own medical
records, to receive prior explanation on any medical
treatment and the risks involved, as well as the right to
take part in the decision-making for his or her own
health.
Other rights of a patient covered by the Charter are the
right to redress of grievances in case of negligence, the
right to adequate information such as advice on
prescribed and purchased medicines and the right to an
itemised bill.
AN UNEQUAL RELATIONSHIP
Recent years have seen the relationship between a doc
tor and patient changing; today this relationship is in-
Initiated in 1989 by the Selangor and Federal Territory
Consumers Association and later taken up by FOMCA,
the Charter is timely as it reflects consumer demand for
better quality services.
The document, which outlines the rights of anyone who
seeks medical services in either the public or private
sectors, also requires of patients, their cooperation in ex
ercising these rights responsively and reasonably.
Among the rights of a patient covered by the charter is
the right to quality care, treatment and medication
regardless of race, religion, social status and ability to
pay.
MMA President, Dr Tibbs Fernandez signing the Memorandum of
Understanding on the Patients' Charter. Looking on. is die Minister of
Domestic Trade and Consumer Attairs. Malaysia. Datuk Abu Hassan Omar.
HAI NEWS. APRIL 1993
creasingly becoming a contractual relation entailing
legal rights and responsibilities. Because the contents of
this contractual relation arc unclear, and because the
doctor-patient relationship is essentially unequal, the
patient is frequently al an emotional and physical disad
vantage.
For instance, in practice, distinctions are made between
patients, based on social status, on personal relations
with doctors, on opportunities, due Io urban-rural dis
parities .etc. There is a clear disregard for the elderly,
for the uneducated, for the rural poor especially women
and children and for the mentally-handicapped and incnlally-ill who are unable to exercise or insist on their
rights.
Patients also feel out of depth when faced with the im
personal service provided at large hospitals and clinics.
They are at a loss and do not know where to go or whom
to ask about their condition. In such a health facility, it
is almost impossible for a patient to know the doctor or
staff who will be treating him or her; in fact in such
cases the patient has no choice but to implicitly trust the
medical staff in charge of his or her treatment.
status, professional associations, domination of registra
tion and disciplinary bodies, clinical privileges and peer
review.
This unequal relationship between the patient and the
health care provider will be corrected by the Patients'
Charter which sets down the rights of patients in
Malaysia.
MALAYSIA'S PATIENTS' CHARTER
The Patients Charter is built on several fundamental
premises including:
I.
The consumer has rights that are not automatically
forfeited on entering a doctor-patient relationship
or a health care facility.
2.
A doctor-patient partnership in which patients
rights and personhood are respected is the most
beneficial model for medical decision-making for
both patients and doctors.
3.
The provision of health care in Malaysia is no
longer the sole responsibility of the government
and family doctor, dentist or pharmacist. The
patient must also play a major role in the decision
making regarding his/her health and well being.
4.
The Charter is not a document of confrontation, it
is one that encourages cooperation. It is meant to
establish a meaningful partnership. It is carefully
worded so as to effectively guide the relationship
between health care provider and patient.
Malaysia's Patients' Charier represents a major step
towards raising consumer awareness of their rights in
the Malaysian health system as well as a means of seek
ing legal recognition of common health rights in
Malaysia.
While consumer responsibilities have long been known
and are entrenched in existing law and practices, the
same cannot lie said for their rights. The situation is
clearly unequal because the rights of health providers
are already well entrenched in law and practice reflected
in the existence ami influence of their 'professional'
is pi o du cod 6 times a year by the Regional
Office tor Asia and tho Pacific of the International Organization of Consumers Unions
■
(IOCU) to support the work of Health Action
International (HAI). HAI is an Informal
cooperating network of consumer, develop
ment action and other public interest groups worldwide. It works to
further the safe, rational and economic use of pharmaceuticals
throughout the world, to promote the full implementation of the
World Health Organization s Action Programme on Essential Drugs
and to look for nondrug solutions to the problems created by
impure water and poor sanitation and nutrition, HAI Nows Is a
means of communication within the network.
m
■ m
•
n
news
Information requests or enquiries:
Please quote the reference number following each item and direct
to The HAI Clearinghouse, IOCU, PO Box 1045, 10830 Penang,
Malaysia Phono: (GO 4) 371396 Fax: (60-4) 366506.
Information about HAI Is also obtainable from:
HAI-Europe, Jacob van Lennepkade 334T, 1053 NJ Amsterdam,
Netherlands. Phone: (31-20) 6833684, Telex: Luxembourg
6105915 GMA LU. Fax: (31-20) 6855002.
t See Page 11
| ]
New subscription
[ ]
Renewal
This publication Is a service for IOCU members and participants in
the HAI network. It Is also available to others outside Malaysia at
tho following rates:
Poriod/Ratos
Nonprofit
groups and
Individuals
in the Third
world
Non profit
groups and
individuals
in industria
lised coun
tries
|| 3 years(18 issues)
[J 2 years(12 issues)
[~] US$24
US$18
["] US$48
US$36
[’j US$120
US$ 90
|_ | 1 year ( 6 issues)
US$10
US$20
us$ so
Others
[ | Payment enclosed, international money order or bank draft
drawn on any US bank for US$
. made in favour of
IOCU. The rates include postage by airmail.
Just check ( V) the appropriate boxes and fill In the form below:
Name:
Organisation:
Address:
IOCU Regional Office for Latin America and the Caribbean, Casilla
9635. Santiago. Chile. Phone: (56-2) 2234172/2234763. Fax:
(56-2) 2234638.
Cou ntry:
Mail to: HAI News. IOCU, PO Box 1045, 10830 Penang. Malaysia.
HAI t.EV.'S APRIL 1993
« From Page 2
Historic Day for Malaysian Consumers
5.
Rights come with responsibilities. The patient's
responsibilities are also spelled out in the Charter.
6.
The Charter is a dynamic one. allowing for peri
odic review, refinement and improvement so as to
better serve the needs of all parties concerned.
The 28 patients' rights in the Charter can be summarised
in the principles of right to: health care and humane
treatment, choice of care, acceptable safety, adequate in
formation and consent, redress of grievances, participa
tion and representation, health education and a healthy
environment.
Right to Health Care and Humane Treatment
Every patient has the right of access to competent health
care and appropriate treatment without any discrimina
tion. This right must be ensured regardless of age. sex,
ethnic origin, religion, political affiliation, economic
status or social class. Health care services should be
made available on the basis of clinical need and not
based on ability to pay or socioeconomic status.
The United Nation's Universal Declaration of Human
Rights, affirms the right to human dignity. Consequent
ly, every patient has the right to be treated with care,
consideration, respect and dignity without discrimina
tion of any kind.
Every person also has the right to privacy without undue
exposure of personal facts. Those who suffer from any
illness do not usually wish to reveal their personal suf
fering or living environment to the public. Because the
patient and doctor relationship is based on the premise
of confidentiality, the doctor should keep personal facts
from others, including other staff not directly involved
in the patient’s treatment. This information should only
be divulged if:
• authorised in writing by the patient;
• it is undesirable on medical grounds to seek a patient’s
consent but it is in the patient’s own interest that con
fidentiality should be broken;
• the information is required by due legal process.
Right to Choice of Care
A patient has the right to be treated at a hospital of
choice and to be referred to a consultant of choice. This
includes the right to accept or refuse treatment and to
choose or switch medical institutions or doctors. Since
illness can strike at any time and place, a patient has the
right to seek the help of medical staff any time,
anywhere and to choose the medical institution or doctor
he/she prefers.
In all cases, therefore a patient should have the right to a
copy of his/her own history and medical records and
have them explained. If undecided or unsure about the
quality of the treatment or care received, the patient
should have the right to a second opinion any time.
Right to Acceptable Safety
Everyone wants to have accurate information about the
state of his/her health. It is a fundamental right of all
patients to have knowledge about their health condition
or disease so that they can seek appropriate treatment.
Because medical information is in the control of doctors
and health care providers, the choice or treatment or
practice is often made without considering the patient’s
needs.
Before any treatment or investigation, a patient should
have the right to a clear and concise explanation in lay
terms of the proposed procedure or treatment and of any
available alternative procedure. Where applicable, this
explanation should include information on risks, side-ef
fects, or after-effects, problems relating to recuperation,
likelihood of success, risk of death, and whether the
proposed procedure is to be administered by or in the
presence of students.
Right To Adequate Information And Consent
An important factor in ensuring the best medical service
is good advice and cooperation from medical staff along
with informed decisions made by the patient.
A patient alone, aided by medical advice, can judge
what is best for him/her, according to his/her own
reasons or need.
A patient therefore has the right to receive sufficient ex
planation of the contents of any document he/she is re
quired to sign before any treatment or at the time of
admission or discharge. A patient’s written consent
should be required if the patient is to be included in any
research. Possible complications of operations or tests
must be explained to the patient by the medical staff,
and the written informed consent of the patient received
before any procedure is carried out. At the present time,
a patient is not provided sufficient time to read and un
derstand the contents of such documents.
A patient also has the right to know the identity and
professional status of the individuals providing service
to the patient and to know which health professional is
primarily responsible for the patient's care.
A patient’s right to an itemised account for any- treat
ment or consultation received, is an essential component
of his/her right to information. The patient has the right
to question and raise' objections if be/she feels this is
necessary and to understand the contents of the bill.
Medical bills should be very specific, clearly stating the
various treatments, tests, operations, medicines, etc and
their individual costs. A patient should be ensured the
Page 11
HAI NEWS, APRIL 1993___________________________________________________________________________
right Io pay only alter he/she has received any explana
tion asked for.
Information regarding all aspects of medication includ
ing advice on prescribed and purchased medicines, drug
efficacy and safely, and choice among competitive
products should be provided to the patient.
A patient needs to know the dosage to be consumed and
fiequency of consumption. A patient must also know
the purpose for which the medicine is luting prescribed,
its ixissible side effects, ftxids and drugs to avoid when
taking a certain medicine and measures to be taken if a
dose is forgotten or an overdose taken.
after care and good health.
Every individual also has the right to an environment
that is conducive to good health. This includes and ex
tends to a health professional's office, health centre,
hospital room and/or ward and other treatment facilities.
WHAT LIES AHEAD
In Malaysia, the tremendous socioeconomic changes of
the past 35 years including improvement in personal in
come, a higher level of education, and rapid change in
disease patterns have resulted in higher public expecta
tions for quality health care. Malaysia has also attained
Right to Redress of Grievances
a much belter health care coverage than most developing
countries as a result of
strong public revenue sup
A patient should have
port. In many developing
the right to legal advice
countries, studies have
with regards to any
"There will be those who assert that
shown that private health
malpractice
by
the
patients should concentrate on getting
spending has typically been
hospital, the hospital
better and that doctors should con
much greater than public.
staff or by a doctor or
However,
even
in
centrate on making them better.
other health profes
Malaysia, the extensive
sional.
Neither should focus on rights. Their
development
of
health
argument is that 'patients have needs,
facilities in the public sec
A patient should also
not rights'. The fact is that they have
tor and a reasonably gtxid
have the right to recover
both."
and
attractive reward sys
damages for injury or
tem for government doctors
illness incurred or ag
- Dr. Sothi Rachagan, Associate Professor
hits not stopped the growth
gravated as a result of
at the Law Faculty, University of Malaya
of a lucrative private sector.
the failure of the health
The
challenge for Malaysia
and main author of the Charter, at the sign
professional to exercise
is to achieve a realistic
ing of the Memorandum of Understanding,
the duty and standard of
balance between public and
care required of him or
March 1, 1993.
private health care services.
her while treating the
patient.
In the meantime, safe
guards must be put into place to protect the rights of the
Right to Participation and Representation
patient who seeks ettre from the medical sector, be it
A patient shall have the right to participate in decision public or private. Malaysians today have the Patients'
making affecting his/her health with the health profes Charter to back'them if they feel they have been 'short
sionals and personnel involved in direct health care.
changed' while seeking medical treatment. Although
the Malaysian Charter is not enforceable in court, it is
A patient can only do (his if he/she has accurate infor expected to inform both doctor and patient of their rights
mation on his/her health condition and the appropriate and responsibilities, and it sets out the duty and standard
treatment or procedure necessary. The patient therefore, of care a patient shall be provided.
must be provided with sufficient, and adequate informa
tion. in an understandable language, so that he/she can The battle for better quality health care is far from over.
The challenge for Malaysians will be to ensure that the
paiticipatc in decision-making.
principles of the Charter are incorporated within the na
tional health policy.
A patient, must also be ensured the right to participate in
decision-making through consumer representation in
planning and evaluating the system of health services,
the types and quality of services and the conditions
under which health services are delivered.
*
-it
*
*
*
Right to Health Education and Right to a Healthy
Environment
It is the right of every individual to seek and obtain ad
vice with regard to preventive and curative medicine.
Editors: Dr K Bala and Shila Rani Kaur
Production: Lin Min Min
MAI NEWS. APRIL 1992
' Jomtien Consensus on Essential Drug Information
This consensus was adopted by the participants attending a workshop, ‘Society and Medicine: Essential
Drug Information', held in Jomtien, Thailand, December 1-13, 1991. Thirty participants from eight Asian
countries and 10 resource persons attended the workshop organized by the Department of International
Health Care Research, Karolinska Institute!, Box 60400, S-104 01 Stockholm, Sweden.
1.
1.1
1.2
1.3
1.4
1.5
1.6
1.7
1.8
1.9
We call on GOVERNMENTS to:
consistently implement a rational drug policy;
promote the concept of essential drugs;
require generic names for prescribing and both brand and generic name for labelling;
establish mechanisms, e.g. a national code, to regulate all promotional and advertising materials;
consult non-governmental and other people’s organizations as well as professional bodies in policy and
decision-making processes;
establish and support a drug information system to facilitate and implement an effective rational drug
policy, including research;
integrate the concept of rational drug use, including drug information into health and medical education;
introduce within the formal and non-formal educational system information on rational drug use,
particularly for children at an early age;
establish systems for monitoring adverse drug reactions, including cooperation with international
agencies.
We call HEALTH WORKERS INCLUDING PHARMACISTS AND OTHER DRUG
DISPENSERS to:
2.1 respect the sensibilities of the patients and their relevant expectations as well as their information needs;
2.2 acquire communication skills to interact with patients, the mass media and the general public;
2.3 recognize the problem of misuse, overuse and irrational use of drugs and promote rational drug use.
2.
3.
3.1
3.2
3.3
3.4
We call on UNIVERSITIES, PROFESSIONAL GROUPS AND NON-GOVERNMENTAL
ORGANIZATIONS to:
establish networks at all levels in order to facilitate drug information, communication and education;
encourage multi-and interdisciplinary research on drug information and drug use;
update their knowledge of drugs and information technologies;
enhance their communication skills, particularly regarding the dissemination of drug information to
patients and the general public.
We call on the MASS MEDIA to:
recognize their far-reaching influence on the level of public awareness and assume a more active role in
informing the public on drug issues;
4.2 acquire a deeper understanding of the scientific aspects of drug issues;
4.3 establish regular communication with health workers and consumer groups;
4.4 participate in the screening of drug advertisements for unsubstantiated claims and unethical promotion
in collaboration with experts and other interested groups.
4.
4.1
We call on the PHARMACEUTICAL INDUSTRY to:
develop a revised code of marketing, promotion and dissemination of drug information in consultation
with governmental and non-governmental organizations as well as concerned UN agencies, and to
enforce such a code in all nations:
5.2 recognize their social responsibility to the public with regard not only to the safety and efficacy of their
products but also to their cost and societal impact and to devise and disseminate drug information
accordingly.
5.
5.1
6. We call on the WORLD HEALTH ORGANIZATION (WHO) to:
6.1 develop a global drug information policy, disclose and disseminate all information on drugs.
7. We call on WHO, WORLD BANK, UNICEF AND OTHER AGENCIES, to:
7.1 support governmental and non-governmental organizational efforts to make drug Information
programmes, including their research component, a priority.
Printed by Jutaprint. Malaysia - ISSN 0128 1321
Sdlcs of Irrational Jbrugs in 1992
'tfank,
6
10
16
Salas '% c??
.Drug
BeaosuUz
2.3 92.
Dexorange Plus
l’iv 52-
20.H
Elcctral
B evitdA
Corax
Benadryl
Ampoxi*1
'Baralga-n-
2A
26.
’ 20
30
_ 32
35
36
i5.d£.
(obadejc. fexrVc
pken$<2dyl
4l
44
40
56
G3
^teWs-iV MPS
Nlovalgin
Coxian.
Vics Veporwb
0^\o C^lol u.V*A
Ha «m - u^?
Enlrd^ai »iol
I'Aaczvl viV
GG
7i
72
77
0.5
. . •
IQ.0
(3.83 . . . 12-2
24
13.^6 t_. .
»3.3fl • ■ • 0.3
13.17 . . . 10.2
I2.0G - • • 3<l«8
12.70 • • ‘ 23-412-49 • • • 10.6
1.1
H.96 • •
10.72 • * 11.0
153
I0.S3
6-0
t-fl
17.6
8 67
6-1
».^0
1«1
843
16-6
3-0*1
Co mH flam
Voy-'Hon
.’3g
Cirovittt ,'4
. • • 17-0
17-80 . . • 15.2
15.80 . • 3t0
16.83 • • 244
FleurobiOrt-
‘7
20
. .
S'c?'ArQa: QR6 J^n'32> -^Conp* devat id 1
<ut* * J
‘ No
J'm tte
«** j*ls
it is
c 1
Tes^siUe
Table 1
Retail prices of 100 units (capsules/tablets) of selected essential drugs, three common food items
and two economic indicators in eleven countries in-mid-1992 (all values in US dollars)
Australia
Bangladesh1
Bolivia
Brazil
India
Indonesia
Malaysia
Pakistan
Sri Lanka
Tanzania
UK
Per capita GNP - US' (1989)
15.940.00
180.00
620.00
2.540.00
340.00
500.00
370 00
430.00
130.00
14,610.00
Minimum monthly wages USS
1,020.00
31.00
75.00
80.14
12-30.00
45.00
2,160.00
125.OO2
n.a.
60.00
11.60
1,428.00
3229
42.13
5.13
5.64’
10.00
23.60
6.80
10 00
3.87
4.00
3.66
3.50
6.70
Penbritin 250 mg
13.00
n.a.
n.a.
25.00
14.50
5 00
14.02
6.60
14.60
Cimetidine 200 mg
18.93
3.59
10.00
22.20
3.20
6.00
15.60
8.60
5.98
23.20
29.40
Tagamet 200 mg
18.93
n.a.
39.00
27.10
3.80
37 00
39.90
13.00
28.59
63.00
29.50
Cotrimoxazole 400-80 mg
6.44
6.44
3.59
3.59'
10.00
n.a.
1.90
10.00
2.10
5.60
1.83
5.00
9.70
26.00
23.85
2.40
17.50
13.90
6.80
9.76
7.00
24.90
28.92
28.92
n.a.
11.90’
21.00
19.55
11.40
10.00
3.95
5.20
4.88
4.80
8.60
26.00
n.a.
12.30
37.50
9.00
6.80
7.93
13.30
21.30
10.24
10.62
n.a.
4.23’
Flagyl 400 mg
41.62
41.90
Zantac 150 mg
52.00
Average
Name of drug & strength
Ampicillin 250 mg
Bactrim 400+80 mg
Erythromycin 250 mg
Erythrocin 250 mg
Methyldopa 250 mg
Aldomet 250 mg
Metronidazole 400 mg
13.00
11.10
11.20
n.a.
5.40
2.80
2.80
2.00
6 80
21.00
12.06
12.00
10.00
12.40
2.80
4.88
4.00
11.90
2.31
2.4l'
6.00
15.35
2.40
5.00
1.60
3.20
0.61
0.90
14.50
7.00
n.a.
20.00
4 00
10.85
3.30
44.40
26.00
n.a.
2.90
4.903
50.00
5.511
110.00
85.90
38.90
60.98
124.40
99.20
26.11
4.79
17.54
19.39
6.27
27.33
17.55
8.21
12.06
20.08
25.84
0.61 generic
o.31
0.73
0.55
0.36
0.35
0.47
0.88
0.46
0.66
1.74
*
'
Food prices
Rice 1 kg
1.06 brand
Sugar 1 kg
0.66
0.77
0.47
0.45
0.56
0.51
0.47
0.46
0.63
0.66
1.26
Eggs 1 dozen
1.36
0.92
0.78
0.66
0.48
0.75
0.85
0.52
0.76
1.19
4.40
World prices: Rice 1 kg « 0.31; Sugar 1 kg • 0.18
1 The brand forms listed are not available in Bangladesh. The prices given are for popular and well selling brand forms.
2 $125 is the poverty line lor a family of five.
3 Glaxo manufactures and markets ranitidine in India as Zinetac. n.a. - not available.
Source
(i)
Drug i food prices I minimum wage - personal communication from HAI partners.
(ii)
World p'ices for rice and sugar. Prices for remediate delivery as traded in Bangkok for rice and New York for sugar in May Quoted in Asiaweek. May 1992
(iii)
Per capita GNP - Stare of the World's Children. UNICEP. 1992
Dd- T-i-8
PEDDLING 'HEALTH' TO THE PUBLIC
Sakuntala Nnrasimhan
Sakuntala Narasimhan, a journalist anti author with a special interest in women's issues ami consumer rix’/i/s.
also teaches post graduate students of journalism.
"For health and strength and happiness we pray to
Thee" goes the popular prayer. Good health takes
precedence over everything else, for even the most
abundant riches cannot compensate for the pain and
suffering that ill-health means. Naturally,anything that
promises healthy living becomes attractive. Cashing in
on this pervasive preference, advertisements fora wide
range of goods and services rake in profits for the smart
seller, without always delivering the promised returns,
and sometimes even causing harm by inveigling the
gullible buyer.
On Bombay’s suburban trains, a particular brand of
gripe water is advertised as Pushli kc hue (for g<x>d
health); the truth is that gripe water is not a nourishing
product, it merely helps relieve gas and is supposed to
assist digestion. And yet, thanks to sly advertising
copy, mothers will assiduously buy gripe water, believ
ing that it can make their babies healthy and robust.
Remember the ad with a picture of a man-on-the-go
who declared he had "Copper for breakfast?" Vitamin
pillsand iron tablets arc touted as a panacea and sure
fire health-givers; millions of persons, voting and old.
swallow vitamin pills every day in pursuit of health.
Baby foods, for instance. The decade of the '80s saw
The truth, however, is that only naturally balanced
increasing world wide awareness of the fact that multi
national manufacturers of in
foods provide all the neces
fant formulas were resorting to
sary nutrients in a form that
advertising tactics of a kind
the body can assimilate
A very common advertising trick is to
fully; extra amounts of one
that actually endangered the
make the buyer feel that a medical specialist
vitamin or the other in
lives of vulnerable newborn
has endorsed a particularproduct and that it
babies in Third World
manufactured preparations
can, therefore, only be "good for you.”
cannot increase one's well
countries.
By using
being, but will only be ex
photographs of chubby and
creted in the absence of the
cute babies on the tins and in
necessary supportive sup
ads, and by distributing free
plements. For the gullible lay person, however,
tins to new mothers in hospitals and nursing homes, the
"vitamin" spells health and, therefore, the more the bet
manufacturers managed to persuade tens of thousands
ter4.
of mothers to believe that tinned baby food was better
— and more nourishing - than mother's milk. In the
Even when a formulation boasts of a combination of
absence of clean water with which to mix the formula,
nutrients, very often thcrc-arc unnecessary ingredients
and lack of facilities for proper sterilisation of the bottle,
that only add to the seller's profit without offering any
babies ended up succumbing to infections; in addition,
benefits to the consumer. The unassimilated nutrients
among poorer sections, the formula was often diluted
go
literally down the drain; but the seller has made his
in order to stretch each tin further and cut down costs,
profits nonetheless.
with the result that the babies grew undernourished.
The widespread outcry against the promotion of bottle
feeding in such conditions led to a global boycott of
Claims about Health Benefits
some multinationals like Nestle', and a World Health
A very common advertising trick is to make the
Organisation (WHO) code on baby food advertising
buyer feel that a medical specialist has endorsed a par
which required that ads should make it clear that breast
ticular product and that it can, therefore, only be "good
feeding was best.
for you." Toothpaste ads use the devise of showing a
man
in a doctor's whitecoat, with a stethoscope draped
Advertising Gimmicks
around his neck, extolling the virtues of a particular
brand. Whatever the doctor recommends must be
The ingenuity of corporate cleverness is such that
good, right? Except that this "doctor" is merely dressed
even while observing this code, the words "There is no
up to look like one for the ad. For centuries people who
substitute for mother's milk" is printed in very small
did not have the good fortune of using that brand of
letters, in a comer, while the brand name of the tin is
toothpaste had good teeth all the same - because they
splashed prominently, in very large letters.
kept their mouths clean!
Paediatricians in Bombay have produced photographs
of emaciated babies who died due to dehydration
Endorsement by "doctors" is a tactic that slimming
caused by diarrhoea brought on by the use of con
ads, too, use. A real doctor's name might even be
taminated water for mixing the formula, but health
printed in the endorsement - but lay readers will not
activists face a stiff fight from multinationals that dump
know that the doctor who extols the product is himself
milk powder on hungry and malnourished populations
in the pay of the manufacturer. Sheri Louise, for in
in poorer countries. The battle is still on.
10
stance, promoted their slimming regimen with the use
of a doctor's recommendation which turned out to be
not quite above board because the doctor was found to
be an employee of the same company.
I lealthand slimness is an area where ads have really
cashed in on public vulnerability, especially women's
subconscious association of slimness with health,
beauty, desirability and glamour, thanks to deeply
entrenched, hard to break social and cultural condi
tinning. While olx’sity does cause health problems, the
inordi nate emphasis on slimness has, in fact, led to
problems like anorexia nervosa, where the person
literally starves herself to death unless treated in time.
< aven the pervasive obsession with "dieting" and "slim
ming" among women, several ads promote products
that promise to help shed weight "without pain" and
with speed, and few victims realise that these weight
loss claims are often either illusory or dangerous unless
undertaken under care fill medical supervision.
"The healthy way to lose weight and look
glamorous," gush the ads for slimming devices or
preparations that suppress one's appetite. On testing,
some ol these have lx-en found to contain harmful am
phetamines; one person who undertook a much-touted
slimming course died recently.
The latest into the 'health' market, a toothpaste
brand-named Calcium, is another example of how ads
< apitalise on the health business — calcium is doubtless
important for good teeth, but rubbing a paste, even
literally consisting of calcium, on the teeth is hardly
going to 'stick on' extra strength to the molars and
canines! One does not cat toothpaste, so the "calcium"
is not even ingested or assimilated internally. Nonethe
less, thanks to the association of ideas in the buyers'
minds, the assumption is that the product is "good for
you."
Similarly, shampoo ads claiming that the brand has
"added proteins" mislead because, although protein is
vital for healthy hair, there is no way protein can be
pasted on to hair, much less through occasional contact
during washing. The lay buyer, not aware of this fact,
gets conned into choosing a product on the basis of the
claims made by the advertiser that It has protein and is,
therefore, better than competing brands that do not
make such a claim.
Selling 'Instant' Beauty
A survey done by nutrition experts some time ago
showed howcommercial preparationsof beverages that
claim to be "full of nourishing vitamins and proteins"
work out much costlier than natural products (or con
ventional Items of our normal diet) that provide the
same nutrients at a fraction of the cost -- groundnuts,
sesame seeds and sprouted beans, for instance, have
been proved to be sources of essential nutrients at a
quarter of the price of commercial preparations like
"protein biscuits" or beverages. And yet, the public gets
misled because the lowly groundnut, chana and mixing
do not advertise themselves while the commercial
producer has an advertising budget running to a few
lakh rupees. The power of advertising copy is so
awesome that it brushes aside even scientific facts.
The beauty business is another aspect of the health
issue —you only need to pick up a tube of such-and-such
cream, says the hype, to become a beauty queen; con
veniently bypassed is the possibility that masking with
medication is not the same as curing the skin internally
to ensure a healthy glow. Fancy anti-wrinkle creams
and vitamin E preparations have all been touted with
hyperbole, while experts prove that the claims made for
such products can never be substantiated.
effective in the altered parameters of modern living
conditions. In such situations, products claiming to be
"healthful" only mislead.
"Herbal" and "natural" have similarly become
mantras of the modem scam, following the prolifera
tion of reports on the adverse effects of synthetic in
gredients, preservatives and additives in the last 25
years, there has been a widespread shift towards
products that are "natural" -- herbal medication, for
instance, in preference to allopathic formulations. For
that very reason, ads have been know to add the word
"herbal" even to products that ought not to make such
claims. Many so called ayurvedic or herbal prepara
tions fall in this category (at least one 'ayurvedic'
product, when tested, turned out to contain cortisone,
which could actually harm the user). For one thing, by
their very nature these products fall outside the purview
of the mandatory product-testing requirements, with
the result that unscrupulous quacks can - and do -exploit the buyer and cause harm, instead of doing
good. Foranother, indigenous formulations were effec
tive within the framework of a particular regimen, life
style and diet, and may not necessarily always be
The role of the media in such a scenario is, therefore,
not only pivotal but powerful. When ads make use of
the media to put across their hardsell messages with a
plethora of techniques and tricks, the same media must
be enlisted to spread the messages of awareness (of the
kinds of tall claims that ads make, both overtly and
covcrtly)and caution (against unscrupulousor mislead
ing claims). The message that "the more, the better" is
not necessarily true in the case of synthetic vitamin
preparations needs to be put across through the media,
just as the message that "more costly docs not always
mean better" in terms of health, needs to be publicised.
This is particularly important in a country that is snug
gling to pull up millions from the subsistence level to a
higher standard ofliving,asin India. Both conventional
and non-conventional and media — print,
radio,telcvision^udiovisual and variations thereof -have a vital role to play, and it is for media activists to
apply their minds, explore the possibilities and deliver
the goods. |
Media and the Girl Child: Strategies to Effect Change
Madhyam organised this Workshop On December 20,1990 at Bangalore,in collaboration
with UNICEF and the Department of Women and Child Development. The specific purpose
of this exercise was to enable mediapersons, with their technical know-how and the potential
to be powerful agents of social change, to gain a better understanding of the situation of the
girl child and create programmes which could be valuable tools in working towards social
change and a better deal for the girl child.
Copies of the Report of this workshop are available on request.
12
. ■ ,..R. SETHUiiniwr.«,M D..
PROFESSOR OF MEDICINE
.’IJ>KFR. ?OMDY-<J.
4. - element
multi- DI
SlONfiL
MODEL. oP HE^^rW CfiKE
sysrsM
HEALTH
c
5-1
roO
m3
••
»
Ul
The Medical Prot^^pn and the Law
<3>
Examples of huatile pattenia:
8
Chronically dissatisfied with treatment given.
0
Expert in producing guilt in other*.
8
Change endlessly from one doctor to another, often expecting
that each new doctor will be the “right one". Sooner or later, they
become invoked with useless treatment procedures rendered by
quacks.
(41
Examplea ofmalingering patienta:
0
Feigning illnesses like acute abdominal pain to obtain drugs like
pethidine.
8
Criminals seeking transfer from prison to a hospital.
0
Persons seeking benefits through litigation in iryury rases.
In dealing with 'difficult''patienta (except malingerer?:, it is good to
introspect whether then- are the products of ‘difficult doctor?'■ Lack of
concern, tactlessness, rudeness and brusqueness on the part ofdoctor? and
their teams may change goodpatienta into 'difficult' ones.
Difficult patients are among the most costly group* in the health cars
field. They often insist upon expensive and useless diagnostic and treat
ment efforts. Direct focus on the relationship between the doctor and the
difficult patients is the mast economical way oftreating these patienta.
PATIENTS’ RIGHTS AND RESPONSIBILITIES
The Rights ofa Patient
TO GET
(1)
Proper medical attention as and when required and at the
earliest possible moment.
(2)
Humane and compassionate treatment from the doctor.
(3)
Courteous and considerate behaviour from the attending staff.
<41
I r&rmetion and explanation in a simple language about diag
nosis, investigation, traatment and prognosis of illness (what is
wrong, what is being done and why, what outcome ia expected).
The Uedlcal Pro'ession a-d me L»i
(5)
Proper follow-up and necessary instruct::?.* :n a clear, simple
and definite way.
<6>
Information from attending medical personnel about the cause
and various ways to avoid recurrence (prevention!
(7l
An explanation, if the patient is required to be referred to a
proper centre where better treatment of the is ease can be had.
(8)
Attention and hearing from proper authority if he she has any
complaints about the treatment being g-ven
(9)
Right to refuse treatment or to participate in any research project
such as a dimes] trial for a new drug or a new operation.
The Med^l Profession and the Law
DOCTORS' RIGHTS AND RESPONSIBILITIES
There is no legal obligation on a doctor to accept any and every
patient that happens to go to him. Tne only exception is an emergency
situation wherein he has a legal obkgation to render help if he happens
to be approached on the spot (see Supreme Court judgement reproduced
on page 2 Parmanand Katara vs. The Union of India, 19S9. Supreme
Court p. 2029).
The ethics of the medical profession enjoins upon the doctor
not to turn away any patient arbitrarily, or capriciously. But in
some situations he can decline:
(1)
If the doctor himself is not welL or free to attend.
(2)
If the doctor already has bad blood and strained relation* with
die patient.
(3)
If a doctor has declared and earmarked bouts of professional
wutk. he ranntt be compelled tn treat a patient outside these
hours.
(4)
To take medicines regularly and follow meticulously any other
instructions given by the medical staff regarding diet, everr-ise
smoking and drinking, stress-coping and so on.
There is no legal obligation to answer a cal to visit the patient
at the latter's place of residence. If the physician does only office
practice, he is not held negligent in refusing home visits.
(5)
He can turn down a visit during night hours on the grounds of
incidents of robbing doctors at night, or kidnapping.
Preserve medical case papers and records given by the doctor or
the hospitaL
(6)
If the patient declines to give written consent to a p:creedure or
treatment involving known risk to life and safety of the patient,
but which is essential to be done in the best interest of the
patient.
(7)
Ifhe finds that the patient and his relatives are not co-operative.
(8)
Aymti^r practitioner is consulted without his knowledge.
(9)
If his fees are not paid. If the patient does not pay, it is illegal to
detain or confine a patient (under Section 342 of the IPC). Hence
the only safe approach ■ to insist on payment in advance of the
consultation or procedure, or for hospitals and nursing homes to
insist on an advance or deposit to cover future bills. (Please see
comments at the lisgiisiiug of this Cheparr regarding payment
The Dirtier of a Patient
(1)
To be sober and polite to the medical staff.
(2>
The patient and persons accompanying him her to give truthfuh
correct and relevant answers to the queries put bv rhe medical
personnel. This is particularly difficult in patients admitted
under a Mediriaim policy, because in order to be eligible for the
policy they might have suppressed «ome infhrmarrin that thev
are now required to reveal to the treating doctor.
(3)
(4J
(5)
To be neat and dean and maintain cleanliness Anting his/her
stay in the hospitaL
(6)
To report promptly far follow-up as and when required and also
to promptly report any adverse reactions to the medications
twingtalwn
CT)
To Rave confidence a: the treatment given and remember that
everything done is m bnsfaer intarest.
(8)
Ifnot satisfied, tn apeak ehnnt it to the msdiesl perwamy] without
abusing or insultingthsm.
(9)
Srould be patient and remember that medical staff are also
human harr^a have fimttatioiB arvi mini and vthrv! valve
The Medical Prof
|on and the Law
Tbs Medical Profession and the Law
35
Consent of the Patient
DOCTOR’S OBLIGATIONS
As far as “consent of the patient" is concerned, the fclltw.r.g Sections
of the Indian Penal Code need to be noted carefully:
I1)
To keep himself abreast of progress ;n his profession and utilise
accepted and recognised methods :r. diagnosis and treatment.
The doctor-patient relationship is fiducial I baaed on trust I, hence
the doctor must maintain his professional knowledge, skills and
competence to desen e the trust reposed by the patient in him.
(2i
He must set towards the patient with the utmost good faith, and
act with the best interest of the patient in m:nd. He ahould
exerase his best judgement in his decaions, always remember
ing the dictum, primum non nocere — "Ar least do no harm to
the patient".
<31
He should not accept a case which is beyond his skill and
competence. He should frankly tell his patient about this and
suggest appropriate alternatives keeping in mind the best inter
est of the patient. Undertaking an assignment beyond one's
competence is a gross case of rashness or negligence. Hence
doctors should take care to see that they do not do anything for
u-hich thes are not technically qualified and have not acquired
sufficient experience.
(4)
He has a duty to disclose immediately to the patient if some
injury has been caused to him/her by inadvertence. Fraudulent
concealment offsets violates the trusting relationship.
(5)
Once be accepts responsibility for the care of a patient, he should
be available until the treatment is no longer required, or until the
understanding to treat is dissolved by mutual assent, or
reasonable notice is given so that the patient may obtain another
doctor's services. This is particularly important when attending
upon patients an a critical condition.
Section 88: ".Act not intended to cause death, done by consent in good
fa.th for the person's benefit"
— Nothing which is not intended to cause death is an offence by reason
of any harm which it may cause, or be intended by the doer to cause, or
be known by the doer to be likely to cause, to any person for whose benefit
it :* done in good faith, and who has given a consent whether express or
implied, to suffer that harm, or to take the risk of that harm.
Section 89: "Act done in good faith for benefit of child or insane
person, by consent of guardian"
"
— Nothing which is done in good faith for the benefitof a person under
twelve years of age. or of unsound mind, by oonsent. either express or
implied, of the guardian or any other person having lawful charge of that
person, is an offence by reason of any harm which it may cause, or be
intended by the doer to cause, or be known by the doer to be likely to cause
harm to that person.
Section 92: “Act done in good faith for benefit of a person without
consent"
— Nothing is an offence by reason of any harm which it may cause to
a person for whose benefit it is done in good faith, even without that
person’s consent, if the circumstances are such that it is impossible for
that person to signify- consent, or if that person is incapable of giving
consent, and has no guardian or other person in lawful charge of him from
whom it is possible to obtain consent in time for the thing to be done with
benefit.
Ifa situation is so urgent and imperious that it can brook no delay. and
the doctor honeatly feels that in order to save the patient's life or to avoid
grate complications his treatment ofthe patient is indispensable, he has a
right to tackle that case, even though consent (normally insisted upon to be
obtained) cannot be obtained without inviting grave risk to the unconscious
patient's life, or to save him from otherwise irreparable harm in the form
ofgrievous hurt.
The physician's refusal to accept a patient (except ih an emergency
situation as specified by the Supreme Court)prevents the imposition ofany
duty upon him.
A doctor who leaves or abandons his patient in o critical stage of
disease, without a reasonable notice to enable the patient to secure another
medical attendant when giving such a notice is reasonably possible, is
guilty of culpable dereliction of duty, and if damages are occasioned
thereby, he is liable therefor.
A surgeon undertaking an operation on a patient is not justified i«
ceasing to attend on the patient after the operation while further care and
treatment are nemsary. It is his duty to give the patient such attention
after the operation as the necessity of the case demands, in the absence of
cmy special agreement limiting the services or reasonable notice to the
patient.
MEDICINE, MEDIA & CONSUMER EDUCATION
PRUDENT USE (MANAGEMENT) - SURGERY
PROBLEMS
SOLUTIONS
Legal aspects
Education of
Neg 1 igence
professionals St
Consent
media and consumers.
ACTION PLAN
The LEGAL ASPECTS of medical practice are dealt in depth
neither in medical profession
nor in
legal
profession.
Medical and surgical books prescribe only certain norms and
prevention of infections and medical complications, which some
times result
in death. In such cases, the question generally
arises is as to whether negligence could be attributed to the
medical
professionals
associated with
treatment of
the
deceased patient.
NEGLIGENCE: The meaning of the word "negligence", as derived
from observations made in decided cases is, the omission to do
which a reasonable person, guided upon
the instructions, which
ordinarily regulate the conduct of human affairs, would do or
doing something which a reasonable and prudent person would
not do.
Negligence is not a question of evidence. It
is an inference
drawn from proved facts. Negligence
is not an absolute
term
but a relative or rather a comparative term.
In surgical context, it is to be inferred as, wh ere there is a
duty to exercise care, reasonable care must be taken to avoid
acts or omissions ( which could be reasonably foreseen)
that
are likely to cause physical
injury to persons. The degree of
care required depends upon the facts
in each case. There are
three basic elements of this tort —
1) An act or omission on the part of the defendant
2) Intention or negligence ar breach of duty "
3) Damage resulting to plaintiff from the wrongful act
of the defendant.
Proof of Negligence: The Supreme Court has held that proof of
negligence
is necessary
before any compensation can
be
claimed. The normal
rule is that it is for the plaintiff to
prove negligence
but in surgical cases considerable hardship
is caused to the plaintiff as the true cause is not known to
him but is solely within the knowledge of the defendant, under
criminal
jurisprudence a person is presumed to be' innocent
till he is found to be guilty.
MEDICAL SEGLICENCE: means failure to act in accordance with
the standard of reasonably competent medical professional
at
that time. The medical
professionals are
assumed to possess
and professed to use proper skill and care.
However, it has
been held that medical professionals are not answerable merely
because same other more experienced colleagues might possibly
have shown greater skill and knowledge. Medical negligence is
considered to be committed
- drugs overdosage, wrong usage or
misuse, experimental surgery,
carelessly fails to remove a
swab or instrument during operation etc.
?
?
?
?
in the event of mass casualties surgeon
attends to one
successful but the other patients succumbs to injuries
due to non performance of operation.
non- availability of suture materials
"
"
of essential investigation facilities
surgeon or the hospital management or government or
society
The general rule of LAW is that if the medical professional
has taken all necessary precautionary measures and does his
best for the treatment of the patient in
accordance with the
recognised
medical
technology,
no
negligence
can
be
attributed.
The basic question in judging
a mishap is whether the medical
professional personally or the hospital
administration
in
general are guilty of culpable negligence. The relevant
legal
provisions are in Sections 81, 87,
88, 89 and of the Indian
Penal Code.
STATUTORY PROVISIONS
Section EL
: Nothing
is an offence merely by reason of
its
being done with the knowledge that it is likely to cause harm,
if it
be done without any criminal intention to cause harm
and ' in good faith for the purpose of preventing or avoiding
other ham. The explanation
to the section states that it is a
question of fact in each case whether the harm to be prevented
or avoided was of such nature and so imminent as to justify or
excuse iije risk of doing the
act with the
knowledge that it
was likely to cause harm.
Section
(Consent) The section states that nothing which is
not intended to cause death, or grievous injury and unknown to
the inflicting person, is an offence by reason of any harm
which it nay cause to any person,
above 18 years of age, who
has given consent,
whether expressed or implied, to suffer
that han.
PROTECTIVE PROVISIONS
Section BS: Nothing which is not intended to cause death is an
offence by reason of any harm which it may cause to any person
for whose benefit it is done in good faith and who has given a
consent, whether expressed or implied,
to suffer that harm or
to take the risk of that harm. The
illustration under this
section is - A surgeon knowing that a particular operation is
likely to cause the death of a patient suffering
from painful
complaint,
but not
intending to cause patient death and
performs an
intending in good faith and patient benefit,
operation with consent, has committed NO OFFENCE.
This covers Acts done in good
Section 89:
faith for the
benef it af a c hild or insan e person by guardian's consent.
Section 92:
Act done
in good faith of a person without
consent. Nothing is an offence by reason of any harm which it
may cause to a person for whose benefit
it is done in good
faith,
even
without
that
person's
consent,
if
the
circumstances are such
that
it
is impossible
to for that
person tn sign the consent or if that person is
incapable of
giving consent and has not guardian or other person
in lawful
charge of him from whom it is not possible to obtain consent
in time for the thing to be done with benefit; provided —
1) that
this exception
shall not
extend
intentional or attempted causing of death; ■
to
the
2) that
this exception shall not extend to the doing of
anything which the person doing
it knows to be
likely to
cause death, for any purpose other than preventing death
or grievous injury,
or treatment of any grievous disease
or infirmity;
3) that this exception shall not extend to the voluntary
causing of injury or any attempt to cause injury for any
purpose other than the preventing of death or injury;
4) that this exception shall not extend
to the abetment
of any offence,
to the committing of which offence it
would not extend.
How to Spot Possible Health Fraud and Quackery
Here are guidelines for spotting health fraud compiled by Emory
University history professor James Harvey Young, who has studied
and written about the field for more than thirty years:
Exploitation of fear
Promise of painless treatment and good results
3. Claims of a miraculous scientific breakthrough
4. Simpleton science: disease has but one cause, and one
treatment is all that is needed to fight it. For example, bad
nutrition causes all disease) good nutrition cures it.
5. The "Galileo ploy": like Galileo, we cult gurus are misun
derstood by blind scientists, but are destined to be heroes
to future generations
6. The conspiracy theory, also known as "The establishment
is out to get us"
7. The moving target: shifts in theory to adjust to circum
stances. Laetrile went from drug to "vitamin," from cure
to palliative to preventive, from low to high dosages, from
working alone to never working alone, from one chemical
formula to another, and so forth. "B-i$" ("pangamatc") is
any chemical or combination of chemicals the seller
chooser to put in the bottle.
H. Reliance on anecdotes and testimonials. They don't sepa
rate fact from fiction, or cause and effect from coincidence.
9. Distortion of the idea of "freedom." By distorting "free
dom of informed choice" to "freedom of choice," snake-oil
salesmen acquire freedom to defraud, and their victims
can lose their money, their health, and their lives.
to. Large sums of money
i.
i.
Adapted from guidelines presented at an American Association for tin- Advance
ment of Science panel on fact rile. The complete version is found in Gerald E. Markle
and James C. Peterson, cds., I’ohtlcs, Science nnd C.iiuccr The Lnclrile I’hennnieiuui
(Boulder, Colo.: Weatvlcw, lyHo).
Health fraud and quackery
No parent wants to jeopardize his or her child's chances of a
cure. But when the child's life is at stake and the pressure is
on to "do something" and not leave a stone unturned, it may
be tempting to try the unproven, treatment—either in addi
tion to or instead of the treatment your child's doctor recom
mends.
Not all alternative treatments are harmful. But many are
—either because they are inherently dangerous (e.g., highly
toxic drugs) or because they promise cures they cannot de
liver, cost a fortune, and distract patients from getting proper
care. Health quackery is big business, and typically such
fraud relies on several common elements which you can
quickly learn to spot, using the accompanying list of tips.
Clues you're not getting the care you
should
There are twelve warning signs that should raise a red flag in
alerting you to the fact that you may not be getting proper
health care or may be seeing a doctor who's not right for you.
Your doctor:
i. Doesn't seem to be listening to what you're saying.
2. Doesn't answer your questions or take time to ask if you
have any. When there is an answer, it's in words you don't
understand.
3. Fails to take an adequate medical history or give you a
complete physical examination when it's called for. (Over
a period of time, of course, your doctor gets to know your
health history, and for certain types of illness, say a cold or
"flu bug," may forgo a total-body-system physical and ex
amine only those areas where you have symptoms.)
4. Doesn't help you learn more about your condition and
what you can do about it, or explain why the recom
mended tests, treatment, or medications are necessary.
5. Neglects to inform you of potential risks, benefits, and
side effects of prescribed drugs or suggested procedures and
tests. (Beware if you've said you're "allergic" to a certain
medication and your doctor prescribes it anyway.)
6. Doesn't respect your modesty and makes suggestive re
marks while doing a pelvic examination or examining
your breasts.
7. Doesn't make a follow-up appointment for you or urge you
to call the office to report how you're doing.
8. Seems forgetful, peculiar,.or belligerent at times, and may
even have alcohol on the breath.
9. Is hard to reach, doesn't return phone calls, and, when
away, fails to arrange for a replacement.
10. Is not on the staff of any community hospital or medical
center.
11. Is rigid, a know-it-all, and insists on an "only" way to treat
your condition.
12. Reacts defensively when you suggest a second opinion.
MAKING MEDICAL DI CISIONS
If you have doubts about the surgery your doctor recom
mends, don't hesitate to get a second opinion. A glance at the
following chart shows why. In a 1983 study, doctors disagreed
with each other an average of 17 percent of the time over
whether a patient should have surgery ns follows:’
Operation
Varicose vein
Breast
Back
Bunion
Knee
Prostate
Hysterectomy
Gall bladder
Tbnslls and
adenoids
Dilatation and
curettage
Cataract
Hernia
Nose
TOTAL
Number
of times
surgery
proposed
Surgery
opposed
by and
physician
6
*3
19
12
58
«7
53
15
3
9
11
8
16
3
9
3
50
39
3«
3<>
28
18
>7
11
43
5
12
43
5*
39
15
435
3
3
7
6 .
5
4
«7
2
1
7<>
% of
disagreement
Results of mandatory second opinions (or insored employees of Owens Illinois Inc.
In 1983.
(For more on second opinions in medical and surgical mat
ters, see Chapter 2. But don't forget, if the consulting physi
cian examining you goes over your report and then says, "I'll
get back to your doctor with my opinion," you're right back
at square one — with only one opinion. You don't want the
consultant's opinion relayed through your surgeon, you want
it given directly to you.)
Questions to ask for informed consent
i.
2.
3.
4.
What's wrong with me? What's the diagnosis?
How serious is this condition/illness?
What tcst(s) do you plan to do?
Why are you doing this test? How will the information
affect the way you plan to treat me?
5. What are the risks of this procedure or test? How accurate
is the test, and what are the percentages of false negative
or false positive results?*
6. What kind of treatment do you recommend—surgery, ra
diation, drugs?
7. What's the purpose of this treatment? Will it cure my con
dition? Is it going to relieve pain or help to rehabilitate
me?
8. What are the risks of such treatment?
What are the chances that the proposed treatment will be
successful in my case?
10. Will this be a long-term or short-term benefit?
11. What will happen to me if 1 refuse all treatment?
12. What alternative treatments are available?
13. How do they compare to the one you're recommending in
terms of risks and benefits?
14. Of these other treatment methods, which do you think
would be best for me?
15. li you were in my situation, which treatment would you
choose for yourself or a family member? Why?
16. Do you have any information on this test or procedure
which 1 could take home with me to read? Is there a pa
tient information center here (or at the hospital, office,
clinic, etc.) where I can get more information, see a film,
or review other materials?
9
’A false negative result means the test has indicated the absence of a given dis
ease or condition which, in fact, the patient has. a false positive result means the
test has indicated the patient has a certain disease or abnormality which, actually,
he docs not have.
Questions to ask in evaluating a fertility
program
i. How many women have gone through your program?
2.
What percentage of your patients get pregnant? (Is this
based on ultrasound confirmation at five weeks, or simply
a "chemical" pregnancy confirmed by blood tests?)
3.
What is the miscarriage rate of women in your program?
4.
What percentage of women have given birth to a live in
fant? (For example, in two and a half years, seventy-one
babies have been bom to couples in the Northern Nevada
Fertility Clinic program, which claims that 35 percent of
women who undergo IVF there become pregnant. Since
some miscarry, however, there is only 325 percent chance
per each IVF that a woman will have a baby.)
5.
What are the criteria for admission to your program?
6.
What can I expect if I enter your program?
7.
What are the costs? Does your quote include any hidden
costs for extras?
H What arc the ethical standards of your clinic-'
9 Do you participate in any experimental programs' Would
my eggs or embryos be used without my consent?
10.
Do you have a psychological support system? If so, what
does this entail?
11.
Is staff available seven days a week, twenty-four hours a
day? (You don't want to go there Monday through Friday,
and be on your own over the weekend!)
12.
What kind of rooms or facilities do you have for patients
during the twenty-four-hour period of bed rest following
the embryo transfers?
13.
If I become pregnant, where do I go for prenatal care?
Where do I have my baby — in my hometown or at your
clinic?
Will I be expected to take part in any'public relations or
publicity efforts for your clinic?
15.
Could you put me in touch with some of your patients
who have had in vitro babies...and some who haven't
been successful in your program?
14.
Exercising Your Rights as a Patient
In America today, dll institutions which carry out legiti
mate human-subjects research follow these guidelines.
More to the point, all institutions in which research is car
ried on must have an Institutional Review Board (1HB) or sim
ilar committee responsible for reviewing and approving all
human subject research proposals, consent forms, and proto
cols. (A protocol is a document which specifies in detail how
patients will be selected for research projects and how the
procedure or testing will be carried out.)
Here's what this means to you. As stated in the revised
U.S. Guidelines on Human Experimentation (1974), you
should receive the following:
■ A fair explanation of the procedures to be followed, and their
purposes, including identification of any procedures which
are experimental
■ A description of any attendant discomforts and risks reason
ably to be expected
■ A description of any benefits reasonably to be expected
• A disclosure of any appropriate alternative procedures that
might be advantageous for you
■ An offer to answer any inquiries concerning the procedures
• An instruction that you are free to withdraw your consent
and to discontinue participation in the project or activity at
any time without piejudice to you
hi other words, you can leave the program whenever you
want and can't be "punished" or penalized in some way for
dropping out. (But don't forget the Schroeders' experience.
Consider signing a Durable Power of Attorney for Health
Care Decisions, explained in Chapter 4, so that your spouse
or other proxy can remove you from a research program if
you become incapacitated and are unable to express your
own wishes.)
In addition, you should be neither required nor requested
to give up any of your legal rights or to release the institution
or its agents from liability for negligence.
M A KIN(; MF.DICA 1,1 >ECISit)NS
mother to deliver vaginally. The use of x-rays (hiring pregnancy has
generally been replaced by ultrasound, which poses fewer risks to
the mother and fetus.
Ff.TOSCOI’Y
A procedure in which a hollow tube is inserted into
the uterus to observe the fetus, its placenta, and the amniotic fluid.
blood samples and biopsy of fetal tissues, such as muscle or skin,
can be taken for analysis. This procedure carries the highest risk of
miscarriage, but may be critical in diagnosing certain structural ab
normalities in the fetus ns well as rare fetal blood disorders, such ns
hemophilia.
The newest of the intrauter
ine diagnostic tests, CVS involves the insertion of a catheter
through the woman's vagina and cervix to remove a sample of the
chorionic membrane, which surrounds the fetus. Cells from this
membrane, which arc genetically identical to the fetus, can be stud
ied in the laboratory for certain genetic defects, such as Down syn
drome.
Chorionic Villus Sampling (CVS)
(AFP)
This relatively new blood test ana
lyzes the alpha-fetoprotein circulating in the mother's blood as a
result of neural-tube defects in the fetus. AFP levels arc useful in
detecting major nervous system disorders, such as spina bifida and
hydrocephalus. Because of false-positive results (see Chapter t) this
screening procedure, if positive, must be confirmed by amniocen
tesis and ultrasound.
At.rHA-FETOrROlT.IN
Hormonal J ests
Measurement of hormones produced by the
placenta and found in the mother's blood often provides data which
arc useful in evaluating placental function and maturity.
Questions to ask before undergoing a
prenatal tes.L
i.
Why are you doing this test or procedure? Is it to get infor
mation which will help me and/or my fetus, or is it simply
for research purposes?
i. Will the results reveal something that can be treated!
3- I low will the results affect the way you treat or care for me
and/or my fetus during the pregnancy? During labor and
delivery! After I give birth!
4.
What arc the risks to me and/or to my fetus?
5.
Will the results lead to a consideration of abortion?
6.
How soon should the tests be done! When will you have
the results!
If any of these prenatal tests or procedures indicates that
you or your fetus has a significant problem, you will face
some difficult choices—whether to consent to surgery or
other treatments in utero; whether to confront a difficult
labor, delivery, and postnatal period, or whether to end your
pregnancy through abortion.
Fetal testing, fetal surgery
Good prenatal care often includes fetal testing and genetic
counseling. Only a woman's doctor, who knows her medical
and obstetrical history and physical condition, can tell her
what the risks and benefits are of specific tests designed to
reveal whether her baby is healthy and developing normally.
These tests include ultrasound, x-rays, amniocentesis, fetoscopy, blood hormone levels and alpha-fetoprotein (Aid’)
screening, and a new technique known as chorionic villus
sampling (CVS).
Prenatal Tests
Amniocentesis
A procedure by which amniotic fluid is with
drawn through a needle inserted through the pregnant woman's ab
domen directly through her uterus into the amniotic sac
surrounding her baby. This fluid and the cells container! in it can be
analyzer! for various chromosomal and other fetal abnormalities. It
is usually done at around fifteen to sixteen weeks to detect fetal
defects and late in pregnancy to evaluate fetal maturity anti the
likelihood of the child's being born without developing respiratory
distress.
Ultrasound isonogrami
Ultrasonography refers-to the direct
ing of high-fiequency sound waves painlessly through the mother's
abdomen to produce images of the fetus on a screen or photograph.
Because of the different'densities of various parts of the developing
fetus, the deflected sound waves allow doctors to "see" the size,
shape, anti position of the fetus, to evaluate many of its organs, anti
to determine its sex. Ultrasound is most useful in detecting multi
ple pregnancies, major abnormalities, and treatable conditions of
the fetus ami, near the end of the pregnancy, the size of the infant's
head relative to the mother's pelvis.
X-ray
Although all x-rays should be avoided whenever possible
and especially in the first trimester of pregnancy, they are some
times used to determine the age of- the fetus anil the ability of the
Questions to ask about experimental
treatment for your child
What new research methods are available for treating my
child's condition?
2.
Why should my child participate in this research program?
3.
Will there be any benefit to my child, or is this primarily a
research project to obtain new information which might
help other children in the future?
4.
What are the risks to my child? Will he or she die sooner, or
be in more pain or discomfort?
5.
Will we be free to withdraw our child from the research
program at any time that either we or our child wants out!
(If the answer is "no," don't enter your child in the experi
mental program!]
6.
Do some researchers have more experience than others in
using this experimental approach?
7.
How can we contact these researchers for a second opinion
and advice on whether to put our child in an experimental
program?
i.
8.
Will taking part in the program require travel to another
medical center? Will we have to live away from home or
move to a n$w area!
9.
Who pays for the care of my child in this experimental pro
gram— the government, a foundation, the researchers, or
our insurance company? Do we pay anything?
Yon have a right to know what the
abortion procedure entails, what its
potential benefits and risks to yon and
the fetus are, what yon can expect during
the recovery period, what total fees will
be, and what signs of conipl ' ations yon
should look for.
In getting this information, you should not be harassed or
intimidated into making a decision for or against the proce
dure. Friends, family, and others you consult may try t" per
suade you one way or another, but your informed consent
must be free and not coerced.
California investigators, for example, are following up on
reports that a pregnant 14-ycar-old who went for help to a
"free pregnancy center" in San Francisco was talked out of
having an abortion by counselors who tried to get her to
leave home under a reportedly false pretext, to continue the
pregnancy without telling her parents, and then put the baby
up for adoption through the center — although it is not li
censed by state adoption agencies.1''
You have a right to know what your
prenatal, childbirth, and support options
are.
Questions to ask your doctors about
alternative therapies
What alternative methods of treatment are available’
What are the benefits and risks of these methods;
What are the chances of cure or remission if we choose one
of these methods'
4.
Will one enhance or inhibit the benefits oi the other:
5.
Will you continue to see my child even if we seek alterna
tive treatment elsewhere?
6.
Will vou refer us to an expert in alternative treatment
methods?
1.
2.
3.
ANNEXURE.2
QUESTIONS TO ASK BEFORE AGREEING FOR A DIAGNOSTIC TEST
1.
Uhy are you doing thia test or procedure?
Is it for research purpose or to get information that
will help me?
2.
Will the teat results reveal something that can be treated?
3.
Hou will the results affect the way you treat me?
4.
Uhat are the risks involved?
5.
Mill the results lead to any treatment option that I am not
prepared to accept?
6-
fa)
(b)
(c)
7.
Is there a better 'more foolproof - less painful - less
harmful) alternative available?
How soon should the tests be done?
Uhen -•ill you have the results?
How reliable are the test reports?
PATIENTS RIGHTS AND RESPONSIBILITIESt
A paper on patients' rights is never complete without an
enumera
tion of
patients’ responsibilities and hence I would like to give
emphasis to both. The concept of patients rights and responsibili
ties
is now being discussed with reference to a
charter
setting
out
these rights and responsibilities. Therefore I shall
present
this
paper
with a description of a model charter. But
first,
a
background on this!
World over, starting with the UN declaration on Human Rights,
the
rights
of people to security in medical care has come to
be
ac
knowledged.
Several countries such as The United
Kingdom,
other
European
countries and more recently, Malaysia, have taken
steps
to
incorporate a charter of patients rights and
responsibilities
into
their
health care policies. A European declaration
on
the
Rights Of Patients is being drafted by the WHO.
In India too, the scenario is much different from what it was even
a decade ago. There is an increased awareness about health
care,
higher public expectations about services delivered, and
mounting
claims
being
filed by patients
against
medical
practitioners .
While patients rigtits are only now receiving the recognition
they
deserve,
the rights of health care providers have long
been
en
trenched in Indian Law and reinforced by professional associations
and clinical privileges.
Fortunately,
doctor-patient relationships have been changing
for
the
better. However, it is also true that this
relationship
re
mains
largely unequal, and patients often find themselves
at
an
emotional
and
physical
disadvantage. Hence the
need
for
such
c h a r t e r s has never been stronger.
What is a patients charter?
The
Charter
adopted
in Malaysia for example,
is
an
agreement
between consumers organisations and medical,den tai and
pharmaceu
tical associations and sets out the standard of care to. patients.
This
charter will be displayed by medical practitioners at
their
place of practice.
The charter that I am about to describe is an attempt to formulate
a set oP patients' rights and responsibilities which reflects
the
evolving concepts and is relevant to health care systems in India.
ft is essentially a set of guidelines to be used in discussions to
formulate
laws,
and policy statements. It seeks to
reflect
and
express peoples aspirations not only for the improvement of
their
health
care, but also for the fuller recognition of their
rights
as
patients. In doing so, it keeps in mind the interests of
both
health
care providers and patients. It makes a
basic
assumption
that
the
articulaton of patients’rights will
rrlake
people
more
conscious
of their responsibilities
when receiving
health
care
•1
and
that this will ensure that patient/doctor
marked by mutual respect and support.
are
relationships
in drawing up this charter, 1 have taken into account the views of
about
125 doctors and students of medicine. Briefly, they are
as
•follows:
I.
647. of doctors felt that a charter
sometimes very highly effective.
would be quite effective and
Only a very low percentage i.e. 37. of doctors felt that a
would be totally ineffective.
charter
2. 667. of doctors felt that a charter would reduce the number
cases before the courts.
of
3. On
the question of giving adequate information
to
patients,
doctors expressed some practical difficulties. These are:
a. Some medical
problems are too complex to be explained fully.
b. There are many illiterate people in India.
4. Several
doctors
agreed that the code of
doctors had lost its significance.
adopted
ethics
5. The question of medical records and patients’rights
regard when addressed threw up the following answers:
in
by
thsis
a) 497. of doctors said that lack of patient awareness
contributed
to the practice of not giving the patient all/relevant records.
b)
257. agreed that there was no legal
maintaining patients records.
obligation for
and
giving
6.There
was
near unanimous opinion that adequate
disclosure
information will improve relationships to a great extent.
of
CONCEPTUAL. FOUNDATIONS:
In the prepration of this draft,
been taken into account:
the following declarations
A)
Draft
European Declaration on the rights
document has been framed in turn, based on
patients.
This
The International Covenant on Civil and Political Rights
(1966)
The Universal Declaration of Human Rights
-
of
have
The
International Covenant on Economic,
Rights (1966)
(1940)
Social
and
Cultural
The European Convention on Human Rights and Fundamental
Free-
dome
<19*50)
The European Social Charter
(1961)
The Targets in support of the European Regional
Health for All.
Strategy
for
E<) The Patient's Charter adopted by the National Helath Service of
the United Kingdom.
C)
The Patient's Charter adopted in
D)
A Patient's Bill of Rights
Association, 1973).
Malaysia.
(Adopted by the .American
Hospital
Part 1
Section Is
RIGH'I
TO HEALTH CARE AND HUMANE
HUMAN RIGHTS IN HEALTH CARE)
TREATMENT:(THE
APPLICATION
OF
1. Every individual shall have access to health care and treatment
regardless
of age,sex,ethnic
origin,religion , political
affilia
tion , economi c status or social class, and according to the
finan
cial, human and material resources available in a society.
2.Every patient shall be treated with care, consideration,
and dignity without discrimination of any kind.
3. Every
individual
treatment
from
the
health facility.
shall have the right
nearest government or
to
prompt
emergency
private
medical
and
Note:
There
is a Supreme Court ruling on this for
accident victims.
4.
respect
treatment
of
Patients have the right to humane terminal care and to die
in
dignity.
5. A patient has, wherever possible, the right to be treated at
a
hospital
of his choice and to be referred to a consultant of
his
choice.
6. A patient can be transferred to another health care
establish
ment
only after an explanation of the need for this transfer
and
the other establishment has accepted the patient.
7. A patient has the right to be treated by fully gualified health
care professionals in private or public health care facilities.
3
Section 2:
RIGHT TO INFORMATION:
1.
Information about health services (including
recent
develop-ments in the field) and how best to use them is to be made
avail
able to the public in order to benefit all those concerned.
2.
Before any treatment or investigation, a patient shall have the
right to a clear, concise explanation in lay terms of the proposed
procedure
and of any available alternative procedure.
Where
ap
plicable, the explanation shall include information on risks, side
effects,
or
after-effects, problems
relating
to
recuperation,
likelihood of success, and risk of death.
3. Information may be withheld from patients in cases where
there
is
good reason to believe that this information would affect
the
patient’s health adversely.
4.
Information must, as far as possible, be communicated
to
patient in a way appropriate to his capacity to understand.
the
5.
A patient has the right to know the identity and
the
profes
sional status of the individuals providing service to the
patient
and
to know which professional is primarily responsible
for
the
patient's care.
6.
Patients should have access to more than one opinion.
/.Patients
should
upon request, be able to obtain a
copy
of
a
summary of their diagnosis, treatment and care including
diagnos
tic results on discharge from a hospital or other establishment.
They
shall also have the right to authorise another medical
pro
fessional
to obtain a copy of the same and to inform the •patient
of the contents.
8. Patients have the right of access
to their medical
file
and
technical
records and any other files and records
pertaining
to
their diagnosis, treatment and care and to receive upon request, a
copy of their own medical files and records or parts thereof.
Note:
This
provision
may need to consider whether
practical to give copies for a charge.
it
is
9.
While
prescribing medication,
about the following:
-be
informed
*
*
*
*
The
The
The
The
the patient shall
purpose of the medicine
possible side effects
avoidance of any food, alcoholic beverage or other
duration necessary for any prescribed medication.
drugs
10. A
patient
shall have the right to examine
and
receive
explanation of his bill after any treatment and consultation.
4
more
an
Section 3s
THE RIGHT TO ADEQUATE PRESCRIBING INFORMATION:
1 . This provision is applicable to manufacturers and dispensers of
drugs.
Patinets shall have the right to:
*
Adequate and understandable information on prescribed and
pur
chased medicines.
* Convenient access to medicines.
* choose among competing products.
2. All drugs dispensed shall be of acceptable standards in
of quality, efficacy and safety.
3. All medicines shall be labeled and shall
logical name of the medicine.
include the
terms
pharmaco
CONSENT:
'1 . A prerequisite of any treatment is the informed consent of
the
patient.
In the case of a minor, consent has to be obtained
from
the
parent
or guardian. If a patient is
incapacitated
and
any
delay
would be dangerous, a doctor is entitled to carry
out
any
necessary treatment or operation.
Note:
This
provision has to be reviewed/modified
to
take
into
account an illiterate patient.
to
the
extent
2.
A
patient
has the right to refuse treatment
permitted by law and to be informed of the medical consequences of
his decision.
partici pa3. The informed consent of the patient is required for
t i on in clinical teaching.
4. Explicit, informed consent is a prerequisite for
participation
in scientific experimentation. Experimentation must not be carried
out on a patient who is unable to express his will.
Section 4:
RIGHT TO REDRESS OF GRIEVANCES:
1. A
patient
procedures.
shall have access
to
appropriate
redressal
2. A patient shall have the right to legal advice as
regards
any- malpractice by the hospital, the hospital staff or by a
doctor or other health professional.
RIGHT TO HEALTH EDUCATION:
1.
Every individual shall have the right to seek arid
obtain
advice with regard to preventive and curative medicine, after
care and good health.
Having dealt with patients’rights at
responsibilities.
length,
let me now move on to
Part 2:
PATIENT’S RESPONSIBILITIES
■1 .
The patient shall ensure that he or she knows and
under
stands
what a patient’s rights are and shall exercise
those
rights responsibly and reasonably.
2.
The patient shall ensure that, he or she understands
the
purpose
and cost of any proposed investigation or
treatment
before deciding to.accept it.
The patient shall insist
upon
explanations
until adequately informed and consult with
all
relevant persons before reaching the decision.
3.
The
patient shall accept all the
his/her own informed decisions.
consequences
of
the
4.
The patient shall provide accurate and complete
informa
tion which the health professional requires about his or
her
health and ability to pay for health services.
5.The patient shall establish a stable relationship with
and
follow
the treatment determined by the
health
professional
primarily responsible for the patient’s care.
6.
The patient shall keep appointments and shall
health professional if unable to do so.
inform
the
7.
The patient shall inform the health professional if he or
she is currently consulting with or under the care of another
health professional in connection with the same complaint
or
any other complaint.
8.
The patient shall so conduct himself or herself so as not
to interfere with the well being or rights of other
patients
or providers of health care.
9.
Every individual has a responsibility to maintain his
or
her own health and that of society by refraining from indulg—
i ng ins
*
unhealthy consumption;
*
addiction forming substances such as tobacco, alcohol
and
narcotic d r u g s;
•it
life styles that have an adverse impact on health such
as
sexual promiscuity, reckless activities and physical inactiv
ity; and
*
contamination of the environment.
6
10.
Every
individual has a responsibility
to
accept
preventive measures sanctioned by law.
Eg.The Tamilnadu Public Health Act provisions on malaria
overing of open wells and tanks.
al 1
control -
DEFINITIONS
For the purpose of this Declaration:
"Discrimination"
means
any
distinction
exclusion
or
preference
made
on the basis
of
other
impairing
equal
than
medical
criteria
of
access
to
treatment
and
equality
health care.
"Health care
includes
medical
intervention,
nursing
anil
allied services by health care
pro
viders and health care establishments.
"Health care
providers"
"Medical
Intervention"
includes
physicians,
nurses,
dentists,
and other health professionals.
includes
all
kinds
of
examinations,
treatment
or other acts, having
preven
tive,
diagnostic,
therapeutic
or
rehabilitative aims, and which are admin
istered by a physician or by other health
7
EQUIP-IOCU WORKSHOP ON MEDICINE, MEDIA AND CONSUMER EDUCATION
1-4 DECEMBER 1993 : AT HOTEL SURGURU, PONDICHERRY.
/ '•/
PROGRAMME
1-12-1993
08.45 hrs Registration
09.00 hrs Inaugural function
10.00 hrs Getting acquainted
11.00 hrs Holistic view of health care .. Dr. K.R. SETHURAMAN
11.45 hrs Public policy issues in
health care
12.30 hrs LUNCH
14.00 hrs The current Indian scenario
- symposium
moderator
Ms. MARY MURRAY HODGE
- Medical profession at crossroads .. Dr. S. CHANDRASEKAR
- Consumers' responsibilities other side of the coin
.. Ms. ANJANA DAS
- Women's health
.. Ms. SAKUNTALA N.
- The drug industry & the consumer .. Dr. I.S. GANDHI
2-12-1993
09.00 hrs Promoting consumer education the Australian experience
.. Ms. MARY MURRAY HODGE
10.00 hrs Co-ordination & co-operatioii Group game
.. Dr. N. ANANTHAKRISHNAN
hrs Group work on 'Issues in child : Dr. ASHA OUMACHIGUI &
and women's health'
Dr. S. SRINIVASAN
Group I & II - Child Health
| Problems, possible soluGroup III&IV - Women's health jtions and plan of action
13.00 hrs LUNCH
14.00 hrs Plenary presentations
10.30
3-12-1993
09.00 hrs Alternative medicine:
.. Dr. S.P. TEKUR
myth and reality
09.30 hrs Role of media in health education
- Panel forum
moderator . Dr. S. CHANDRASEKAR
10.30 hrs Group work on "Prudent use of
modern medical amenities :
diagnostics, drugs & surgical
therapies)
*■
..Dr. K.R. SETHURAMAN
13.00 hrs LUNCH
14.00 hrs Plenary presentation (Problems, possible solutions
and plan of action)
Group I
Diagnostics
Group II Drugs (a) Macro [NHP, NDP, Drug Industry]
Group III
(b) Micro [Dr., Pt., Retailer etc.]
Group IV Surgery
4-12-93
09.00 hrs Consolidation of Action Plan.
11.00 hrs Release of the Pondicherry Declaration.
12.00 hrs Valedictory function.
2
"TH I -S
S u
5
(jj? fe Pfc I oR it i£J
4 MRBpipHS
Towards the wiser use of medicines
rime
(jyuiPj '
pha-moc ,
Support E>
ingredients of o suppon-ve health system include.
◄ Educate
• Access to health services for all regardless o; ability, age gender cd\.'e
o' economic status
cJ-
.•e'o?
on should strive to
• C'Oice of practitioners and choice of treatments
• Good teamwork between health providers and the consumer
• Good teamwork between health providers including doctors pha'mocis’s.
r.u'ses and allied health workers
• health core plans tailored to the needs of the individual
Educative processes should:
• be developed with target group
be considerate of literacy
• r.eguiar reviews
• 5a’-ent held medication records
• research into the effects of medications
inform participants of the bigger
picture
recognise religious and cultural
acknowledge family, community
Inform >
and religious authority
Info'maiion is necessary. Its provision should empower the consumer.
too into and support existing
Attention needs to be paid to making it appropriate to the person, the?
community networks
abilities and their culture.
pay special attention to the
Peoo>e should be able to hove information on the safety of the medicine, its
iong ie-m effects, realistic alternatives, other treatment options and how to
use the medicine appropriately.
Inro-matioa should be:
• uo-ro-do’e
• to'geted to different audiences
• inclusive
◄ Equip
People need tools to heip them
• derailed
• realistic
• available for medical as well as surgical conditions
Tools include:
oral information
• usaole
• disributed widely
• relevant to particular conditions as well as to particula' medications
graphics, posters,
talks, discussions.
• hero-tested prior to production
• consistent
words from opinion leaders
Info-motion should be provided to:
• ass»s* with informed decision-making
• engende' trust between provider and consumer
A continuing cyde of planning,
• p'cMde balance between fear, expectation and reality
implementation, evaluation,
• heip people prepare for a medication regimen, if necessary
modification and replanning is
• heip with short term and long term implications
imperative.
Adopt an
holistic
Pondicherry Declaration on
Health Rights Responsibilities
approach to
health care.
This consensus statement and Charter on Patients
Rights and Responsibilities was adopted by the partici
pants attending a workshop on “Medicine, Media and
Consumer Education" held in Pondicherry, December
1-4, 1993. Thirty participants from three countries
attended the workshop, organised by the Educators for
Quality Update of Indian Physicians (EQUIP) with the
support of the International Organisation for Consum
ers Unions (IOCU).
This Workshops Evolved the Following Guiding
Principles :
o
The work of rational drug use groups should be
expanded to include diagnostics and non-drug
therapy.
2.
We call on Health Professionals to:
♦
Adopt an holistic approach to health care.
♦
Develop two way linkages between different levels
of health care.
♦
Promote prudent use of diagnostic aids and
therapy.
♦
Endorse and respect die Charter of Patients Rights.
♦
Acquire communication skills to interact with
patients, the mass media and the public.
♦
Periodically update their professional knowledge
and improve their skills.
3.
We call on Professional Groups, Non-Governincntal and Voluntary Organisations to :
♦
Promote the adoption of a Charter of Patients
Rights and Responsibilities.
o
The concept of continuity of care through the
family physician should be encouraged by con
sumer education and medical education.
♦
❖
A Charter of Patient’s Rights and Responsibilities
should be widely adopted by professional and
consumer groups.
Establish networks at all levels in order to facilitate
health information, communication and education.
♦
Encourage multi-and inter-disciplinary research on
health related issues.
1.
We call on Central and State Governments to :
♦
Facilitate periodic updates for health knowledge.
❖
Bring all issues pertaining to drugs under the
purview of Ministry of Health & Family Welfare.
4.
We call on the Mass Media to :
♦
Recognize their far-reaching influence on the level
or public awareness and assume a more active and
responsible role in informing the public on health
issues.
♦
Use a resource network of competent health
experts to ensure objective and balanced reporting
of health issues.
o
Enunciate and effectively implement a rational
drug policy.
♦
Promote the concept of essential drugs and ensure
their availability at affordable cost.
«
Promote use of generic names of drugs.
♦
Regulate, and monitor all promotional measures
and advertising materials.
♦
♦
Establish a National Drug Authority of India
consisting of governmental, non-governmental
organisations as well as professionals bodies.
Establish regular communication with health pro
fessional and consumer groups.
♦
Establish and support a drug information and usage
monitoring system to facilitate and implement an
effective rational drug policy. This should include
systems for monitoring adverse drug reactions.
Participate in the screening of advertisements on
health- related issues of unsubstantiated claims and
unethical promotion.
5.
We call on the Health and Pharmaceutical
Industry to :
♦
Develop and enforce a code of marketing, promo
tion and dissemination of information, in partici
pation with governmental and non-governmental
organisations.
♦
Recognize their social responsibility to the public '
with regard, not only to the safety and efficacy of
their products and services but also to their cost
and societal impact; to devise and to disseminule
health information accordingly.
♦
♦ ' Integrate the concept of rational drug use, includ
ing drug information into health and medical
education.
♦
♦
Introduce within the formal and non-formal edu
cational system information on health related
issues.
Promulgate the Charter of Patients Rights and
Responsibilities and Physicians’ Rights and Re
sponsibilities.
Health for the millions
Patients Rights
in lay terms of the proposed procedure and of
any available alternative procedure. Where appli
cable, the explanation shall include information on
risks, side effects, or after-effects, problems
relating to recuperation, likelihood of success,
and risk of death. Informed consent of the patient
must be obtained prior to the conduct of a treatment
or a procedure. In the case of a minor, consent has
to be obtained from the parent or guardian. If a
patient is incapacitated and any delay would be
dangerous, a doctor is entitled to carry! out any
necessary treatment or operation after a second
opinion is obtained.
PART 1 : PATIENTS RIGHTS
Section-1: Right to Health Care and Humane
Treatment
I.
Every individual shall have access to adequate and
appropriate health care and treatment.
2.
Every patient shall be treated with care, consider
ation, respect and dignity without discrimination of
any kind.
3.
A patient has the right to be treated by fully
qualified health care professional in private or
public health care facilities.
4.
A patient has, wherever possible, the right to be
treated at a hospital of his choice and to be referred
to a consultant of his choice.
2.
Every individual shall have the right to prompt
emergency treatment from the nearest government
or private medical and health facility.
A patient has the right to refuse treatment to the
extent permitted by law and to be informed of the
medical consequences of his decision.
3.
Explicit, informed consent is a prerequisite for
participation in scientific experimentation. Experi
mentation must not be carried out on a patient who
is unable to express his will.
5.
6.
Patients have the right to humane terminal care and
to die in dignity.
7.
A patient can be transferred to another health care
establishment, only after an explanation of the
need for this transfer and after the other establish
ment has accepted the patient.
8.
A patient has the right to have all identifying
information, results of investigations, details of his
condition and his treatment kept confidential and
not made available to anyone else without his
consent.
Section-3 : Right to Information
1.
Information may be withheld from patients in cases
where there is good reason to believe that this
, information would affect the patient’s health ad
versely but, however, the information must be given
to a responsible relative.
2.
Section-2 : Consent
1.
Before any treatment or investigation, a patient
shall have the right to a clear, concise explanation
Information about health services (including recent
developments in the field) and how best to use them
is to be made available to the public in order to
benefit all those concerned.
3.
A patient has the right to know the identity and the
professional status of the individuals providing
and Responsibilities
stands what a patient's rights arc and shall exercise
those rights responsibly and reasonably.
service to the patient and to know which professional
is primarily responsible for the patient’s care.
,
4. : Patients should have the right to seek a second
opinion from another physician.
5.
: ■,
Patients should upon request, be able to obtain a copy
of a summary of their diagnosis, treatment and care
including diagnostic results on discharge from a
hospital or other establishment. They shall also have
the right to authorize another medical professional to
obtain a copy of the same and to inform the patient
of the contents.
j
;
A patient shall have the right to examine and receive
an explanation of his bill after any treatment and
. consultation.
:
Section-4 : The Right to Adequate Prescribing
Information
f-
1:
While prescribing medication, the patient shall be
informed about the following : expected outcome,
adverse and after- effects, chances of success, risks,
cost and availability.
, 2.
All drugs dispensed shall be of acceptable standards
in terms of quality, efficacy and safety.
3.
All medicines shall be labelled and shall include Lire
pharmacological name of the medicine.
6.
2.
The patient shall ensure that she understands the
purpose and cost of any proposed investigation or
treatment before deciding to accept it.
3.
The patient shall accept all the consequences of the
his own informed decisions.
4.
The patient shall provide accurate and complete
information which the healdr professional requires,
about his health and ability to pay for health
services.
5.
The patient shall. establish a stable relationship
with and follow the treatment determined by the
health professional primarily responsible for the
patient’s care.
6.
The patient shall inform the health professional if
he is currently consulting with or under the care of
another health professional, in connection with the
same complaint or any other complaint.
7.
The patient shall so conduct himself or herself so
as not to interfere with the well being or rights of
other patients or providers of health care.
8.
Every individual has a responsibility to maintain
his own health and that of society by refraining
from indulging in high risk behaviour, detrimental
to health.
9.
Every individual has a responsibility to accept all
preventive measures sanctioned by law.
Section 5: Right to Health Education
Every individual shall have the right to seek and obtain
advice with regard to preventive and curative medicine,
after-care and good health.
PART 2 : PATIENT’S RESPONSIBILITIES
1.
The patient shall ensure that she knows and under
Note: (For 'he' or 'his' in this document, please read "he
or she", and 'his or her'.)
W -2-1-1
Consumer
o Health
Oughts
A summary of your health
rights and responsibilities.
Consumers’ Health Forum
of Australia
The Consumers’ Health
Forum
The Consumers’ Health Forum is an inde
pendent national organisation that com
menced its work in 1987 to represeig|
community and consumer groups at er
national level on health related issues.
The Forum aims:
Principles
A We are entitled to a healthy and safe
environment in which to live and work.
V That is:
• our basic needs are met;
• the physical environment enhances
our quality of life;
• we are protected from health hazards.
» to create a network of Australia’s
community and consumer groups
with interests in health and to identify
areas of common interest;
B We are entitled to adequate, accurate
information and education enabling us
to make informed decisions which
promote health and prevent ill health
and disability.
• to develop policy positions and
actively pursue their adoption and
implementation; and
• to increase access by community
and consumer groups to decision
making on policy, research priorities,
budget allocation and regulator^
and legislative change.
Consumer Health
Rights
The Consumers’ Health Forum of Australia
promotes the following set of principles,
rights and responsibilities to enhance the
health rights of consumers individually and
collectively within Australia.
C We are entitled to participate in the
development, monitoringand implemen
tation of social and economic policies
and programs.
flh
D We are entitled to equal access to health
services which:
• promote health;
• prevent and alleviate ill health and
disability; and
• provide health care.
E We are entitled to determine whether
or not to seek assistance from health
workers.
RIGHTS
The Consumers’ Health Forum of Australia
supports the rights outlined below for all
consumers. These rights are not all currently
enforceable by law in Australia. The Forum
recognises that, in exceptional circumstances, 4|,
individuals may be unable to exercise theirw
rights. In some cases a person independent
of the care giver and institution may be
required to act on an individual’s behalf.
1 I have a rightto appropriate, quality health
care, when I need it.
2. I have the right to determine what
happens to me, including:
» to choose to leave my condition un
treated;
• to give my explicit consent before any
procedure can be carried out;
• to withdraw my consent to a proce
dure;
• to refuse to allow a procedure to be
carried out;
• to refuse health care from a particular
health worker (including medical prac- w
titioners, allied health professionals
and alternative health practitioners);
• to refuse health care from students;
• to refuse to participate in research and
experiments.
3 I have the right to an adequate ex
planation, in terms and language I can
understand, of:
• the nature of my ill health and likeli
hood of my return to good health;
|
4
|
a
• the details of any proposed procedures
and therapies (eg consultations, tests,
examinations, treatment) as well as
possible alternatives including
— expected outcome,
— adverse and after effects,
— chances of success,
— risks,
— costs and availability,
— whether the procedure is experi
mental or to be used in research;
• the results of any procedures which
have been carried out and the implica
tion of those results;
° the possible consequences of not
taking the advice of the health worker;
• the name, position, qualifications and
experience of health workers who are
carrying out the procedures.
I have the right to receive health care in
privacy and to be treated with respect and
dignity.
I have the right to decide who will be
present when I receive health care.
• I can require the presence of other
people, including a friend, family
member, advocate, interpreter, etc.
• I can refuse the presence of:
— health workers not directly
involved in my care
— students
— researchers, and
— others including family members
RESPONSIBILITIES
6
I have the right to seek information and
advice from other sources.
7 I have the right to seek treatment from
other health workers of my choice.
8 I have the right to have all identifying W
personal information kept confidential.
Thus no identifying information about
me, my condition or treatment will be
made available to anyone else without my
consent.
9 I have the right of access, and to seek
amendment or additions, to all in
formation relating to my health care and
condition, either personally or through
another person I nominate.
10 I have the right to comment on, or com
plain about, my health care.
11 I have the right to receive compensation
for injuries or illness caused, or aggra
vated by, health care or health care advice
provided by a health care worker.
12 I have the rightto refuse admission to, and
to leave, a health care facility regardless of W
my physical condition or against medical
advice, and regardless of whether I have
paid the bill.
Exercising responsibilities in the health
system can be as important as exercising
rights.
however, there are many areas of life in
Which people find it difficult to exert control.
I n many instances consumers find it difficult
to make an informed choice.
Nevertheless, it is in our best interests to
assume as much responsibilityfor our health
as possible.
After all, it is our health at stake!
In orderto promote partnership between the
consumer and health workers, the Consum
ers' Health Forum of Australia recommends
that consumers:
• provide information that enables
the health care worker to provide
adequate advice and care;
• actively seek health care information;
• treat seriously any agreement to
W
action chosen in partnership with a
health worker;
• acknowledge responsibility for the
consequences of their decision to
accept or reject advice;
• recognise that choices concerning
their lifestyle affect their health;
• advise the appropriate authority of
any complaint they may have
concerning their health care so that
corrective action can be taken.
CONSUMERS’ HEALTH FORUM
P.O. Box 52, Lyons ACT 2606
67 Launceston St., Lyons 2606
Phone (06) 281 0811 Fax (06) 281 0959
PoNDICHERBV
P
ECLARATION ON
Health Rights
AMD
Responsibilities
EQUIP-IOCU WORKSHOP ON
MEDICINE, MEDIA and
CONSUMER EDUCATION'
DEC1-4, 1993, PONDICHERRY, INDIA
Pondicherry Declaration
on Health Rights and
Responsibilities
This consensus statement was adopted by the
participants attending a workshop on "Medicine.
Media and Consumer Education" held in Pondi
cherry, India December 1-4. 1993. Thirty partici
pants from 3 countries .attended the workshop
organised by the Educators for Quality Update of
Indian Physicians with the support of the Inter
national Organisation of Consumers Unions.
THIS WORKSHOP EVOLVED THE
FOLLOWING GUIDING PRINCIPLES
B the work of rational drug use groups should
be expanded to include diagnostics and non
drug therapy.
o the concept of continuity of care through the
family physician should be encouraged by
consumer education and medical education.
• a Charter of Patients' Rights and Responsi
bilities should be widely adopted by profes
sional and consumer groups.
1.
1.1
12
1.3
1.4
1.5
We call on CENTRAL AND STATE
GOVERNMENTS to:
bring all the issues pertaining to drugs under
the purview of Ministry of Health and Family
Welfare;
enunciate and effectively implement rational
drug policy;
promote the concept of essential drugs and
ensure their availability at affordable cost;
promote the use of generic names of drugs;
regulate and monitor all promotional measures
and advertising materials;
establish a National Drug Authority of India
consisting of governmental, non-govemmental
organisations as well as professionals bodies;
1.7 establish and support a drug information and
usage monitoring system to facilitate and
implement an effective rational drug policy.
This should include systems for monitoring
adverse drug reactions;
1.8 integrate the concept of rational drug use.
»
including drug information into health and
medical education;
1.9 introduce within the formal and non-formal
educational system information on healthrelated issues;
1.10 promulgate the charter of patients rights and
responsibilities and physicians' rights and
responsibilities.
1.6
P
We call on HEALTH PROFESSIONALS to:
adopt an holistic approach to health care;
develop two way linkages between different
levels of health care;
2.3 promote prudent use of diagnostic aids and
therapy;
2.4 endorse and respect the charter of patients
rights;
2 5 acquire communication skills to interact with
patients: the mass media and the public;
2.6 periodically update their professional knowl
edge and improve their skills.
2.
2.1
2.2
B
3.1
3.2
3.3
3.4
We call on PROFESSIONAL GROUPS. NON
GOVERNMENTAL and
VOLUNTARY ORGANISATIONS to:
promote the adoption of a charter of patients'
rights and responsibilities;
establish networks at all levels in order to
facilitate health information, communication
and education;
encourage multi- and inter-disciplinary research
on health related issues:
facilitate periodic updates for health knowl
edge.
4.
41
4.2
4.3
4.4
We call on the MASS MEDIA to:
recognise their far-reaching influence on the'
level of public awareness and assume a more
active and responsible role in informing -the
public on health issues;
use a resource network of competent health
experts to ensure objective and balanced
reporting of health issues;
establish regular communication with health
professionals and consumer groups;
participate in the screening of advertisement™
on health-related issues for unsubstantiated
claims and unethical promotion;
We call on the HEALTH AND
PHARMACEUTICAL INDUSTRY to:
develop and enforce code of marketing, pro
motion and dissemination of information in
participation with governmental and non
governmental organisations;
recognise their social responsibility to the
public with regard not only to the safety and
efficacy of their products and services but
also to their cost and societal impact and to
devise and to disseminate health information
accordingly.
5.
5.1
5.2
PATIENT’S RIGHTS AND
RESPONSIBILITIES
I
PART 1: PATIENT’S RIGHTS:
■
1.
2.
Section 1: RIGHT TO HEALTH CARE AND
HUMANE TREATMENT:—
Every individual shall have access to adequate
and appropriate health care and treatment.
Every patient shall be treated with care, con
sideration, respect and dignity without discri
mination of any kind.
A patient has the right to be treated by fully
qualified health care professionals in private or
public health care facilities.
4 A patient has. wherever possible, the right to be
treated at a hospital of his choice and to be
referred to a consultant of his choice.
5 Every individual shall have the right to prompt
emergency treatment from the nearest govern
ment or private medical and health facility.
6. Patients have the right to humane terminal care
and to die in dignity.
.7. A patient can be transferred to another health
care establishment only after an explanation of
the need for this transfer and after the other
establishment has accepted the patient.
8. A patient has the right to have all identifying
information, results of investigations, details of
his condition and his treatment kept confidential
and not made available to anyone else without
his consent.
3.
Section 2: CONSENT: —
1.
Before any treatment or investigation, a patient
shall have the right to a clear, concise explana
tion in lay terms of the proposed procedure and
of any available alternative procedure. Where
applicable, the explanation shall include informa
tion on risks, side effects, or after-effects.
problems relating to recuperation, likelihood of
success, and risk of death. Informed consent of
’ the patient must be obtained prior to the con
duct of a treatment or a procedure. In the case
of a minor, consent has to be obtained from the
parent or guardian. If a patient is incapacitated
and any delay would be dangerous, a doctor is
entitled to carry out any necessary treatment or
operation after a second opinion is obtained.
2. A patient has the right to refuse treatment to the
extent permitted by law and to be informed of
the medical consequences of his decision.
3. Explicit, informed consent is a prerequisite for
participation in scientific experimentation. Experi
mentation must not be carried out on’ any
patient who is unable to express his will.
Section 3: RIGHT TO
INFORMATION:—
Section 5: RIGHT TO REDRESS
GRIEVANCES:—
Information about health services (including
recent developments in the field) and how best
to use them is to be made available to the public
in order to benefit all those concerned.
2.
Information may be withheld from patients in
cases where there is good reason to believe that
this information would affect the patient's health
adversely but, however, the information
be given to a responsible relative.
3.
A patient has the right to know the identity and
the professional status of the individuals provid
ing service to the patient and to know which
professional is primarily responsible for the
patient's care.
4.
Patients should have the right to seek a second
opinion from another physician.
5.
Patients should upon request, be able to obtain
a . copy of a summary of their diagnosis, treat
ment and care including diagnostic results on
discharge from a hospital or other establish
ment. They shall also have the right to authorise
another medical professional to obtain a copy of
the same and to inform the patient of the
contents.
6.
A patient shall have the right to examine and
receive an explanation of his bill after any treat
ment and consultation
1.
Section 4: THE RIGHT TO ADEQUATE
®
PRESCRIBING INFORMATION:—
While prescribing medication, the patient shall
be informed about the following: —
Expected outcome, adverse and after effects,
chances of success, risks, cost and availability.
2.
All drugs dispensed shall be of acceptable
standards in terms of quality, efficacy and safety.
3.
All medicines shall be labelled and shall include
the pharmacological name of the medicine.
1.
A patient shall have access to appropriate
redressal procedures.
2. A patient shall have the right to legal advice as
regards any malpractice by the hospital, the
hospital staff or by a doctor or other health
professional.
1.
I
Section 6: RIGHT TO HEALTH
EDUCATION: —
1. Every individual shall have the right to seek and
obtain advice with regard to preventive and
curative medicine, after care and good health.
PART 2: PATIENT'S RESPONSIBILITIES:
1. The patient shall ensure that he or she knows and
understands what a patient’s rights are and shall
exercise those rights responsibly and reason
ably.
2. The patient shall ensure that he or she under
stands the purpose and cost of any proposed
investigation or treatment before deciding to
accept it.
3. The patient shall accept all the consequences of
the his/her own informed decisions.
4. The patient shall provide accurate and complete
information which the health professional requires
about his or her health and ability to pay for
health services.
5. The patient Shall establish a stable relationship
with and follow the treatment determined by
the health professional primarily responsible for
the patient's care.
6. The patient shall inform the health professional
if he or she is currently consulting with or under
the care of another health professional in con
nection with the same complaint or any other
complaint.
7.
The patient shall so conduct himself or herself
so as not to interfere with the well being or
rights of other patients or providers of health
care.
8.
Every individual has a responsibility to maintain
his or her own health and that of society by
refraining from indulging in high risk behaviour
detrimental to health.
9.
Every individual has a responsibility to accept all
preventive measures sanctioned by law.
*
Educators for Quality Update of
Indian Physicians (EQUIP)
Address: Dr. S. CHANDRASEKAR, M.D.
Chairman
Society of EQUIP, 5, RUE SUFFREN,
PONDICHERRY-605 001, INDIA.
TEL: (0413) 36252
FAX: (0413) 38132
(AttmC.H.SHASHINDRAN)
CAG Reports
NOVEMBER 1993
CONSUMER
ACTION
GROUP
44 Venkatakrishna Road, Mandaveli, Madras 600 028.
Phone: 839984
For Private Circulation Only
HIGHLIG
HTS
Medical Profession And Self-Regulation
Guidelines For TNC (Transnational Companies) Conduct
Time Share Agreements
Metrowater’s Call Does Not Hold Water
All is not bright with bulbs
East Coast Road Project
It is extremely disturbing to know that products
bearing the ISI mark of quality and safety may not
always conform to the standard specifications
stipulated by the Bureau of Indian Standards(BIS).This startling fact has come to light fol
lowing the direction by BIS to manufacturers of
two widely advertised and aggressively marketed
brands of bulbs. They have been given 3 months
to tighten up their quality control systems. This
direction came as a result of the submission of
laboratory test findings to BIS by Consumer
Education and Research Centre (CERC).Ahmedabad.The tests were done for 40 watt bulbs.
Only strict monitoring by random testing and con
stant vigil can ensure that lax manufacturers are
brought to book. Incidentally, the price difference
between conforming and non-conforming bulbs is
marginal,varying from 70p.to 1 Rupee.
Readers may recall that we had reported in our
February ‘ 92 issue about the East Coast Road
Project.We had then obtained interim injunction
only against the cutting of the trees on the land
demarcated for the East Coast Road.Now a stay has
been obtained on further construction of the high
way itself till the Project gets environmental
clearance from the Ministry of Environment and
Forests.
Reminder
We would like to remind our Associates to renew
their subscription to CAG Reports for the year
January - December 1994. The remittance of
Rs. 100/- should be sent in the form of cash/cheque
favouring Consumer Action Group, payable at
Madras. Please specify your Associateship Num
ber and any change of address.
The Medical Profession And Self-Regulation
In September the medical fraternity went on strike
demanding that they should not come under the Con
sumer Protection Act. One of the arguments they ad
vanced against their inclusion in the Act was that they
had their own internal regulatory mechanisms in the
form of the Medical Council of India and the various
State Medical Councils, to take disciplinary action
against erring members of their profession.
Medical Councils
The Medical Council of India has been set up under
the Indian Medical Council Act to regulate the medical
profession. Doctors practising in India should be
registered with the Medical Council of the State , in
which they practisc.Thcsc councils have been set up
by the acts passed by the respective State Legislatures.
The State Councils maintain registers of the medical
practitioners. These lists arc collected and con
solidated by the Medical Council of India at the
Centre.
The State Medical Councils consist of members
elected from the medical profession and nominees of
the State Government. The functioning of the Medical
Councils has been far from satisfactory. Elections to
these bodies arc not conducted regularly and properly.
Every State has a set of Medical Council rules and
the State Medical Councils are empowered to inves
tigate complaints of professional misconduct. A com
plaint must be in writing, signed by the complainant
and must set down the relevant facts. The State
Medical Council through its disciplinary committee
can take action against erring doctors.
Following are the circumstances under which Medical
Councils may take disciplinary action:
1. Improper or indecent conduct towards the patient.
2. Conviction in a court of law.
Failure or dereliction of duty in giving professional
certificates, reports and other documents.
4. Contravening the Drugs and Cosmetics Act.
3.
5.
Selling schedule poison.
6.
Performing or abetting an illegal operation.
7.
Receiving or giving commission or using touts.
8.
Employing unqualified persons.
9.
Associations with manufacturers of drugs and medical
equipment.
10.
Advertising professional services.
11.
Running medical shops, etc.
12.
Failure to give professional service on
grounds.
religious
All this, however, remains only on paper. In practice,
erring members of the profession are rarely brought
to book, because of a false sense of solidarity and of
professional camaraderie. Unfortunately, the ex
perience of consumer groups has been that complaints
referred to the Medical Councils are rarely acknow
ledged, let alone acted upon.
Currently, we have with us the complaint of a patient
who suffered injury to his right knee in an accident
and was advised conservative (non-surgical) treatment f
by a doctor he consulted. Since his pain persisted,
he consulted another doctor who had claimed to be
qualified in orthopaedic surgery. This doctor advised
him to go in for surgery, which would enable him to
walk without pain. The patient underwent the recom
mended surgery but to no avail. He was then advised
corrective surgery by the same doctor. At this point,
the patient started entertaining doubts about the
doctor’s professional qualifications. On checking
with the Medical Council's records, he discovered
that the doctor concerned had no post-graduate degree
in orthopaedics. He then wrote a formal letter to the
Council demanding that suitable action be taken
against the doctor. That letter was sent on 8th Sep
tember,1993. We received a copy of his complaint
on 28th September,1993. The complaint has been
forwarded to the Secretary of the Health Department "
and to the Tamil Nadu Medical Council on 1st Oc
tober, 1993, with a request for their comments. To
date we have not received even an acknowledgement
of our letter from the Council.
With so much protest going on for exclusion of doctors
from the ambit of the Consumer Protection Act, one
would expect Medical Councils to take prompt note
of complaints, institute enquiries where necessary and
take disciplinary action, if professional misconduct
or negligence is proved. Surely that is the way to
reassure the patients and consumer groups alike that
the self-regulatory mechanism they boast about is
alive and functioning? No wonder the public has no
contidence in the Councils when they do not even
acknowledge receipt of complaints.
Patients’ Charter
Self regulation world over has been tried and found
wanting as an effective mechanism to control violation
of laws,malpractices,etc.."There are some who will
assert that those in the professions and in particular
those in the medical profession are noble and capable
of self-regulation" said Dr.Solhi Rachagan, University
of Malaya Law Professor, in a speech delivered at
the signing of a Memorandum of Understanding on
the Paticnts’Chartcr."The fact is that there is no
group,be it lawyers,academics,the clergy,rulers or
even Knights of the Round Table,that has shown that
ethical standards can be maintained by self- regulation
alone..... This is where the Patients’Charter,which sets
down the rights of patients in Malaysia,can play a
role."
'j The Malaysian Patients’Charter is an agreement be
tween consumer organisations and medical,dental and
pharmaceutical associations to be displayed by medi
cal practitioners in their clinics.However, it is not
enforceable as a statutory right.
The doctor-patient relationship remains largely une
qual and patients often find themselves at an emotional
and physical disadvantage.Thus the need for such a
charter has never been stronger.
One of the initiatives discussed in the I0CU- CAG
National Seminar on Consumer Redress held in
February this year was the drafting of a Patients’
Charter after the Malaysian model (Participants got
an opportunity to study the draft copy of the Charter).
The need for such a move has become greater now
in view of the increasingly confrontational stances
adopted both by consumer groups and doctors fol
lowing the enactment of the Consumer Protection Act
and the debate it has started about the inclusion of
doctors in it.
Other rights of patients covered by the Charter are
the right to redress any grievance in case of
negligence,the right to adequate information such as
prescribed and purchased medicines and the right to
an itemised bill.
As a follow-up of the I0CU-CAG National Seminar,
CAG designed a questionnaire to find out how medical
practitioners and medical students feel about these
trends in health care and specifically about a Charier
for Patients, which sets forth both the rights and
responsibilities of patients.The questionnaire, circu
lated to 250 doctors and 50 medical students in Tamil
Nadu, tried to draw from them responses to questions
on information to patients, failure to give medical
records and the usefulness of the Charter in reducing
the number of cases of alleged medical negligence
before the courts.lt also listed the broad categories
of rights and responsibilities of patients for possible
inclusion in the Charter and invited the respondents’
comments. 61 doctors and 22 students responded.We
give below the results.
The Malaysian Charter is not a document of confron
tation, but one that encourages coop.cration.lt is care
fully worded so as to effectively guide the relationship
between the health care provider and the patient.The
patients’ responsibilities are also spelled out in this
Charter,which is dynamic in allowing for periodic
reviews,refinement and improvement so as to better
serve the needs of all the parties concerned.
Only a very low percentage i.e. 3% of doctors felt
that a Charter is totally ineffective. 28% felt that it
would be moderately effective. 20% gave a highly
effective rating. 16% gave a rating of 4 on a scale
of 5. In summary, this implies that 64% of doctors
felt that a Charter is quite effective and sometimes
very highly effective.
This Charter covers the patients’ rights to quality
care, treatment and medication.lt also addresses the
patienls’right to request a second opinion,to have
access to one’s own medical records,to receive prior
explanation on any medical treatment and the risks
involved, as well as the right to take part in the
decision- making for one’s own health.
)
law and reinforced by professional associations and
clinical privileges.
In India too, the medical scenario is much different
from what it was even a decade ago.There is an
increased awareness about health care, higher public
expectations about services delivered and mounting
claims being filed by patients against medical prac
titioners. While patients’rights arc only now beginning
to receive the recognition they deserve,the rights of
health care providers have long been entrenched in
Doctors
66% ot doctors felt that a Charter would reduce the
number of cases before the courts.
Only 38% of doctors were emphatic (this means that
they specifically said ‘yes’, while others did not
answer) about the fact that patients were not being
given information adequately and hence were ag
grieved. The most common reason for the above
grievance is that medical problems are too complex
to be explained fully (51%). The second reason was
illiteracy (46%) Unfortunately, 10% of doctors felt
that the responsibility for getting the information lies
with the patient or his relative. 28% emphatically
agreed that the practice of holding back medical
records could aggrieve patients.21% emphatically dis
agreed.49% said that lack of patient awareness con
tributed to the practice. 25% agreed that there was
no legal obligation to provide information. An over
whelming 84% of doctors agreed that adequate dis
closure of information will remove fear of malpractice.
It is significant to note that 36% of doctors felt that
the code of ethics adopted by doctors had lost its
significance.
Medical Students
Only a very low percentage i.e. 5% of students felt
that a Charter would be totally ineffective. 55% felt
that it would be moderately effective. 14% gave a
highly effective rating. 14% gave a rating of 4 on a
scale of 5. In summary, this implies that 83% of
students felt that a Charter is quite effective and
sometimes very highly effective.
68% felt that it will reduce litigation.
On the question of reasons for poor information flow
between doctors and patients, the reasons attributed
were illiteracy and complexity of medical problems
(50% of respondents). It is significant to note that
36% were emphatic that records were being given to
patients and this could not be a reason for patients
to be aggrieved. 36% cited low patient awareness as
a reason for the practice of records not being given
to patients. 73% affirmed that adequate disclosure
helped to remove fear of malpractice.
25% agreed that codes of ethics had lost their impor
tance.
Since by and large the response towards a Patients’Charter is positive,we propose to draft one to be
circulated to the concerned people,namely,Medical
Associations,individual doctors and consumer groups
inviting their suggestions and recommendations.
Guidelines ForTNC (Transnational Companies) Conduct
Every morning the newspapers talk of some new
foreign company coming into India - be it in the
sphere of food or machine tools or information tech
nology or financial services or just anything. The
recent liberalisation moves have thrown open the
doors to foreign direct investment. The value of
foreign equity in joint ventures approved in the first
7 months of 1992 was almost 3 times greater than
the value approved in the whole of 1991, and already
1993 has seen much more. What is happening in
India is happening all over the world, especially in
developing countries. Today, some 35,000 Transna
tional Companies (TNCs) operate in every economic
sector, dominate key industries, and control 70% of
all international trade. Enormously wealthy and
powerful, their strength and influence will grow even
more in the future, as major structural changes take
place in the world economy.
in all major corporate functions - research and
development, procurement, manufacturing, marketing,
linance, accounting and human resource development.
However, while all this is highly commendable, there
is no denying the fact that there are some serious
problems with TNCs.
For developing countries, TNCs hold the great promise
of bringing in highly desired investment, capital
goods and new technologies. They can stimulate
domestic production and improve export performance.
TNCs promote worldwide economic interaction, in
volving the cross-national coordination of activities
- o promote the good conduct of TNCs, to ensure
the.r fair treatment by host countries, to preserve
TNCs do not always deal honestly with government, *)
communities or competitors. They can exploit na
tional laws and economic policies. They can export
to developing countries ‘dirty’, outdated technologies
and substandard or even hazardous products, which
have been banned or restricted in their home countries.
They can be less strict in enforcing safety and anti
pollution standards. Bhopal is a classic example.
It is increasingly being recognized that there is the
need for more clear, fair rules and minimum standards
to be established - both nationally and internationally
’nd 10 pro,ec' ",c h“nh
A number „ L “
•»« consume,,.
A numbe, or code, o, guideline, for TNCs h„e bec„
developed by various international organizations over
the past few years.
The UN has been working, since the 1970s, on a
code of conduct for TNCs, but has so far been unable
to arrive at a consensus due to vested interests.
Recently, it has been proposed that the UN start on
a new agenda to frame global ‘guidelines’ (the word
code has been generally thought to signify light
regulations) for TNCs, drawing upon existing inter
national standards such as the UN Guidelines for
Consumer Protection, UNCED’s Agenda 21, the
OECD Multilateral Guidelines for Foreign Direct In
vestment and the UNCTAD Guidelines for Multina
tional Enterprises. The new document should put
forth an "internationally agreed set of ethical prin
ciples dealing with issues such as environmental
protection, consumer protection, restrictive business
practices, financial behaviour and the treatment of
global business".
Consumer involvement is vital in research and cam
paigns on TNC issues. Consumer organisations can
take positive action by highlighting and encouraging
examples of good TNC practice, for other companies
to follow
suit. They will, of course, be invaluable in forcefully
communicating key consumer concerns to govern
ments and businesses. They can press for strong
action, when needed, to curb serious abuses by TNCs
operating in their countries. Consumer groups can
look into prices of basic TNC products to determine
how affordable they arc for low income groups and
also detect any excessive price increases over time.
Consumer campaigns should raise awareness about
the need for TNC manufacturing facilities in in
dustrialised countries and their subsidiaries in
developing countries to have the very same health
and safety standards. There should be no compromise
on this issue. The view expressed by the World
Bank’s chief economist, Laurence Summers, that more
migration of the dirty industries to the least developed
countries should be encouraged ("I’ve always thought
that underpopulated countries in Africa are vastly
undcrpolluted") is very shocking indeed. The false
perception among the very poor developing countries
that they must choose between economic growth or
environmental and consumer protection is exploited
by unethical TNCs who take full advantage of their
opportunities to deplete natural resources and
encroach on local communities.
The UN has published, and is regularly revising and
updating, a ‘Consolidated List of Products Whose
Consumption And/Or Sale Have Been Banned,
Withdrawn, Severely Restricted or Not Approved by
Governments’. This list is the only document that
presents, in one comprehensive source, all known
regulatory decisions taken by governments on a range
of products and chemicals including pesticides, phar
maceuticals and industrial chemicals. This is a very
effective tool for use by consumer groups to raise
public awareness on international trade in hazardous
products and to push for government attention and
legislative change to ban such products in their
countries.
The world is a shrinking market today and for
‘globalisation’ in industry and trade to become strong
and viable in every aspect in every country - developed
and developing - the conduct of TNCs is the key
issue. The vigilance and campaigning of consumer
organisations and other public interest groups can be
decisive factors in ensuring good TNC conduct.
(With acknowledgements to IOCU)
Time Share Agreements
The number of advertisements for lime share holidays
have been on the increase in India. This is a review
of time share agreements and the clauses which are
against the interests of the consumers in the Standard
Form Contracts formulated by companies floating
time shares.
Although time sharing is a new concept in India, time
share contracts have been the subject of much dis
cussion in other countries. Recently the Consumer
Affairs Council in Europe made a detailed study of
this which was presented by the European Parliament
for declaring a policy directive to its member states.
The consumer organisations in Europe have called
for :
1)
Improved requirements for the information to be sup
plied on the rights and obligations of the time share
contract.
Compulsory escape clause in the contract giving the
purchaser the right to withdraw within a specified
deadline. (The Economic and Social Committee of the
European Parliament has prescribed 28 days as a time
limit for withdrawal of the contract by purchasers).
3)
Guarantees required from the vendor and the penalties
that should be imposed for breach of guarantees.
2)
4)
Right of cancellation of loan contract.
High pressure selling techniques, special offers, mis
leading statements about the discounted price and
non-disclosure of withdrawal performance are all
grounds for challenging time share contracts.
The peculiar nature of time share agreements in India
is that :
(a)
The terms are not clearly laid down.
An ordinary person is not able to comprehend the
fact that what he is buying is a share in the company
for which the company grants the right to stay for a
certain period in a specific apartment and not real
estate in some form. The company code requires a
prospectus of the company be available to the pur
chaser. However, all that the time-share purchaser
gets is promotional literature and the time share con
tract.
(b)
The company reserves the right to change the
terms of contract.
The time share agreement calls for payment of an
advance subscription running to thousands of rupees
from consumers towards facilities promised but the
definition clause of the facilities itself contains a
catch, which is a provision declaring that the schedule
specifications may be changed from time to time. For
example, the company reserves the right to change
the location of the property, the facilities and even
the description of the premises offered.
show the accounts and, in our experience, most of
the inflated charges are collected in the name of taxes.
(e)
The company collects huge amounts of money
towards advance subscription. Yet, the company also
has a right to demand chargcs/fces/priccs of
electricity, telephone, gas, oil, water, etc. There is no
clarification on what can fall under the ‘ etcetera.
(f)
Although a transfer facility is given, the time share
contract subjects this transfer facility to a written
permission from the company and the company only
guarantees that it will not refuse unreasonably. But
this clause gives the company the widest power to
decide what is reasonable and what is un
reasonable.For effecting the transfer an administrative
charge of Rs.250/ -is collected.
(g)
No escape clause has been given in this agreement
for the consumer to get out of the contract. Moreover,
an amount equivalent to 25% of the amount paid by
the time share holder is to be retained by the company
when it terminates this agreement due to default in
payment of the instalments. The catch provision in
the agreement is that an alienation will call for a new
agreement with the company on new terms i.e more
money and different terms of contract in line with
the demand and supply position.
,
(h)
The deductions for breach of agreement by the
time share holder arc higher than what the company
chooses to pay for breach of agreement, which is a
liquidated damage of 55% of the money collected by
it from renting to others for that particular week.
Obviously, the time share holder will have no mode
of verifying the rentals charged by the company.
| )
The company agrees to pay a liquidated damage
equivalent to 55% of the rent/tariff that may be
charged by the company to other persons for stay in
the apartment. In the event of it committing a breach
(c)
The time share week is cut down by nearly half of the agreement the contract also excludes the en
a day, as ten hours arc reserved for cleaning the
titlement of time share holder for specific perfor
apartment between two consecutive occupations,
mance. In the event of a breach being committed by
while the advertisements cry hoarse about a whole
the lime share holder, the amount equivalent to 25%
week being available.
of the amount paid subject to a minimum of Rs. 1000/(d)
The company reserves the right to collect all is to be collected by the company.
levies/taxes/chargcs/dutics/fecs imposed by any
(i)
The company also reserves to itself the discretion
government or local body or public body (there is no
to offer a generally equivalent place to stay during
clear explanation about what is a public body) or
the time share week if it is not able to offer its
authority in respect of the agreement. But there is no
apartments. It also reserves the right to change the
clause in the agreement requiring the company to
definitions of the facilities offered by it.
In the circumstances, we would suggest that con
sumers be on the look out for the clauses in fine
print. If there are any defects with the agreement
relating to the general points raised above, the contract
can be challenged.
Metrowater’s Call Does Not Hold Water
The recent call given by Metrowater to harvest rain
water is, no doubt, commendable, but is totally
lacking in credibility. While individual householders
are being asked to save rain water, Metrowater itself
has not cared io harvest nearly one year’s supply of
rain water that falls into the sea every rainy season.
Madras, a water starved city, has a very low per
capita water consumption of 70 litres per day, when
compared to other cities in India, which have a per
capita consumption of not less than 140 litres per
day.
Madras gets nearly 110 mm of rain every rainy
season and, if the rain water failing on the ground is
conserved and stored, it can recharge the aquifers
and the ground water in the neighbouring areas thus
ensuring supply of a year’s water. But, unfortunately,
till today, development agencies have failed to
preserve the storage spaces which were available
earlier in Madras by way of temple tanks and lakes
called ‘eris’.
I
The population explosion in the city has created
demands which the city’s waler supply system is not
able to fulfil. But, according to many experts, the
situation would not have deteriorated to the current
state, if only the development agencies involved had
made a scientific study of the existing resources of
water supply and of the projected demand. Till 1947
Madras had an abundant supply of water, not only
because of its limited population, but also because
the storage spaces of water were in good repair.
Madras has pipeline waler supply which is drawn
from the surface water available in the lakes and tanks
around the city. The condition of the rivers flowing
through the city are such that they cannot be used
for drinking water purposes because they arc polluted
and heavily silted.
The rivers flowing into the city of Madras flow
through Chengai MGR District and all the rivers have
an interconnected eri system in their basins. These
eris, called system eris, exchange their surpluses
within themselves and also with the river thus acting
as micro flood regulators. They also act as percolation
ponds collecting the rainwater and allowing it to
percolate into the ground enriching the ground water
in the neighbourhood. It is, therefore, very important
to preserve these storage spaces. But, unfortunately,
development agencies have failed to control encroach
ment in these eris. In fact they have contributed to
the closing of these eris. For example, the Nungambakkam Eri was converted into a rubbish dump by
the Corporation and we have irretrievably lost this
freshwater resource. Temple tanks have become com
pletely non-functional, because of the choking up of
their catchment points by buildings. Many eris like
the Chctput Eri have also been lost because private
builders have filled them and converted them into
building sites.To top it all, the Tamil Nadu Housing
Board (TNHB) is trying to provide housing for higher
income groups filling up huge eris around Madras
and offering the land at low cost under Ministers’
discretionary quotas.
On receipt of this information, Consumer Action
Group (CAG) visited the TNHB sites at Vclachery,
Ambatlur, Kakkalur and Nolambur, where huge eris
have been filled up by soil upto 7 feet resulting in
an expenditure of Rs 14 to 15 lakh. On examination
we found lhat the ground water resources in the
neighbouring areas are drying up and all these housing
projects arc dependent only on whatever ground waler
is available in the eri sites. Excessive drawal of
ground water leads to cracking of walls and sinking
of houses which is called shrinkage settlement. We
fear that this will be the ultimate fate of these houses
built on the eri sites. Moreover, constricting the
natural inclination of rain water to collect into this
area will lead to flooding of the roads, affecting the
already stretched civic services.
Disturbed by these findings, CAG has gone to Court
asking for an injunction against all these projects as
well as the restoration of the lakes mentioned above.
Since we found this phenomenon not only in Madras,
but also all over Tamil Nadu, we have filed a writ
petition in the Madras High Court asking for an
injunction against the wiping out of lakes and catch
ment areas of lakes all over Tamil Nadu. The Court
has admitted this writ petition and has ordered notice.
Solved Complaints
Name of the
complainant
Nature
Adversary
Remarks
Mr. Srirain
Visweswaran
Damage to watch
given for repair
Lalitha Jewellery,
Madras.
Repairs done
to the satisfaction of
the complainant.
Mr. Hanumantha Rao
Non-refund of school
admission fee - Rs. 700/-
Venkatasubba Rao
Matriculation School,
Madras.
Refund given.
Dr. Khurshccd
Non-functioning
of telephones
Madras Telephones
Defects rectified.
Students of
‘F’ Batch -Exteriors &
Interiors Course
No proper coaching
Exteriors and
Interiors P.Ltd. Madras
Some administrative
changes made.
Mr.M.V.Subra nianiam
Refund of
money - Rs. 1355/collectcd towards
interest.
Tamil Nadu Housing
Board, Madras
Refund given.
Happenings
06/10/93 Ms. Kavitha, M attended the quarterly meeting of the Civil Supplies and Consumer Protection Department.
13/10/93 Mr. Sriram Panchu gave a talk on the ‘Changing Face of Consumer Action’ to the'members of the Madras
Management Association.
Consumer Quiz
Banks are responsible in all circumstances for the
safety of valuables and important documents lodged in
their keeping in safe deposit boxes. True or false?
2.
Once an airline has issued you with a boarding pass it
is obliged to carry you. True or false?
3.
If you buy something on the basis of a false or mislead
ing advertisement, even if the statement was made
innocently, you are entitled to demand your money
back. True or false?
1.
4.
A case can be filed in the redrcssal machinery set up
under the Consumer Protection Act, 1986 against a
private medical practitioner if the treatment he
provides fails to bring the desired result. True or
false?
Answers
FALSE. The relationship between the bank and the
customer in this case is more or less like that between
a lessor and a lessee. Unless the bank is unduly care
less, it will not be liable for the loss or destruction of
the safe deposit box in which valuables are kept
through fire or robbery and the customer should ar
range his own insurance.
2. FALSE. An airline is not obliged to carry you if you
are unfit to travel - for example, possessing arms and
ammunition, or if you are drunk and behave indecent
ly1.
TRUE. You arc entitled to claim damages in such a
ease vide section 36A (1) of the MRTP Act.
4.
FALSE. Only when it is proved that the treatment he
gave loll below the standard of a reasonably competent
practitioner in his field, can a case be lodged in the
redrcssal machinery set up under the Consumer
Protection Act, 1986.
3.
Courtesy: Upabhokta Jagaran
HEALTH IN THE MOVIES
Mailhili Rao
Maithili Rao is a freelance writer and film critic who contributes to The Sunday Observer, Bombay, Cinema
in India and The Independent, among others.
The health of the box office depends on upholding —
overtly or covertly -- the status quo as it exists in practli ally every aspect of society. This is true of mainstream
cinema the world over. Naturally we feel the manipula
tions, cop-outs and insult to our collective intelligence
more keenly as it applies to our own commercial
cinema. The guiding principle of commercial cinema
then is not to seriously upset its mass viewers with
unpleasant reality. If the story does compel such depic
tion, viewers have to be given the placebo of wish-ful
filling, easy answers to relieve the dose of anxiety
measured out with such calculated cunning.
It goes without saying that problems of health —
physical and menial - come under the category of un
pleasant truths Io be administered with utmost care.
,\nv illness shown in .1 run of the mill film is planted
l hei e lo tugat our collective heartstrings, to manipulate
our sympathy and encourage us to identify with the
hero. I he solutions are equally easy and ridiculous to
anvone who has even a nodding acquaintance with the
methods of scientific medical care.
The antidote to most ailments is prayer — preferably
musical,, with wailing sarangis or frenzied tablas to suit
the music director's current mood. Or it could be to
propitiate a particular deity: a Sherowali Ma ensconced
in a temple preferring dandiya and drums, while an
enigmatically smiling Krishna adorning a domestic puja
room might be cajoled by the strains of a wishful flute.
The obverse of this is the instant fatality conferred by
dreaded diseases. Earlier, our filmi favourite was tuber
culosis, no doubt our legacy from Devdas, an ar
chetypal hero whose self- destructive genius is
reincarnated over and over again. The coughing fits, the
handkerchief stained with blood... and the audience is
clued in. Hardly ever does any filmic character survive
tuberculosis, never mind that medical science has found
effective treatment once the disease hasbeen diagnosed
in its early stages.
Of late, though, cancer has displaced tuberculosis as
filmdom's favourite scourge. Blame it on the sob epic.
Love Story, if one must. Anand was the sensitive ex
ception in its prognosis of the disease but its purpose
was to deify the stricken man who smiles through his
I o give one outstanding example which rings a col
pain and brings joy to the troubled living. In Mill, by
lective bell: the blood transfusion scene in Amar Akbar
the same director, again it was an inspiring love story of
Anthony, where the separated brothers lie in adjoining
a vivacious, intensely alive
hospital bedsand their blood
girl stricken with pernicious
is simultaneously transfused
anaemia and a brooding,
into the long-lost mother's
' '
I'-.-'- .
■ >,
wounded young man who
runs! The intention was to
The health of the box office depends on
finds a reason to live through
underline the irony and
upholding — overtly or covertly •• the
her. The medical scenes gave
pathos -- to hell with the
status quo as it exists in practically every
us enough details that spelt
tedious routine of collecting
aspect of society. This is true of
out the course of the illness
(he donor's blood, testing
mainstream cinema the world over,
and its fatality.Mili spawned
and storing it alter it hasbeen
a numberof imitators in other
pul into a centrifuge. In
languages and at a later
Manmohan Desai's world -period: Suhasini in Manchu
and ours tor the magical
Pallaki, playing a smiling
three hours of entertainment
martyr who reforms a cynical artist and his layabout
-- blood flows directly from the donor sons to the
friends and, most recently, Girija and Nagaijuna in
recipient mother. This film also staged a miracle — a
Gitanjaii, with the difference that each is under a sen
catchy hhaian addressed lo Shirdi Saibaba -- lo cure the
tence of death, lie from chronic myeloid leukaemia and
mother's blindness!
she from a congenital heart block. To be fair to Mani
Ratnam, the diagnosis of Nagarjuna comes after a series
Contrived Cases, Sentimentalist Purpose
of tests, spelt out in detail by the doctor, conducted
when he was hospitalised for broken bones. What the
Such situations are the norm in most of our films. It
film glosses over is the abundant energy a young man
is on par with the practice of showing a physician
is
left with when he apparently has only a few months
pronouncing a woman pregnant — and, to add to the
to live. The reaction of the tough hero rings psychologi
drama, it is normally an unmarried girl - after rumi
cally true wanting to be away from a weepy mother
nating over her pulse. And mind you, he is a proper,
and an anguished, if silent, father. Girija's sudden
stethoscope-flaunting M BBS - not a vaidya initiated into
deterioration is also medically credible.
the arcane mysteries of ancient Nadi Sastra.
ting portrayal of the appal ling conditions in many of our
hospitals where mentally ill patients -- women and men
— are sexually abused with impunity? Somehow, one
doesn't get the impression that this was Bhagyaraj's
intention at all.
"Dard ka Rishta" — an Exception
Hut the most detailed -- if pardonably sentimen
talised - jxirtrayal of leukaemia and its treatment came
in Sunil Dutt's Dard ka Rishta, subtitled 'Pain is a Many
Splendoured Thing.' The personal pain of watching a
beloved wife die despite the best medical care comes
through in the film. It is also made part of the doctor's
commitment. Smita Patil is dedicated to fighting a dis
ease that snatches the young, even if it means a painful
divorce from a man she loves. And for Sunil Dutt, it is
a patriotic commitment to give the best he can to his own
[M’ople, after the experience he has gained in the USA.
It is when his own young daughter is stricken by
leukemia that he can understand his ex-wlfe's pass
ionate, single-minded dedication. Though the film
makes concessions to matters of faith and uses the
child's illness to bring a diehard Brahmin and a pious
Pathan together in prayer, it shows us that doctors, too,
are human beings first.
A favoured affliction of our film writers is amnesia
— so convenient to add all sorts of twists to a story,
making it resemble a corkscrew. An exception was Balu
Mahendra's Sadma, where Sridevi's regression to a sixyear-old state was believable. The memory wipe-out
ranged beyond the immediate events preceding the
injury. Her sensory memory is not affected. The film
capitalises on the appeal of her sexual provocation com
bined with a child's trust to underline Kamal I lassan's
pain of unrequited adult love.
Dard ka Rishta lakes care to explain In easy terms
the process of bone marrow transplant and how the
donor's blood and genetic make-up have to match the
patient's. It also gives you reason to hope that early
diagnosis and a matching donor — siblings arc often
found to lx.1 the best — can save life. Tire conditions of
our hospitals — lack of enough affordable drugs, over
crowding and the sheer poverty which makes nutritive
food during convalescence a cruel mockery - arc con
trasted with the hi-tech efficiency of America, as well as
the willingness of donors there to come forward. The
doctor in the film fervently hopes that our people, too,
can have such facilities within reach. And it doesn't
sound like a politician's pitch, for once.
Menial Illness — a Source of Fun
If theslateof physical health is so dismal inourfilms,
the depiction of mental illness is abysmal, because It is
so cruel. Physical handicaps and mental illness - the
latter stigmatised as madness - arc usually held up for
ridicule.
1
Take the Tamil film, Araro Ariraro. The setting is a
mental hospital and the hero is an upright, compas
sionate warden who sings and dances with the inmates
as a matter of therapy. The vaunted compassion doesn't
extend to the patients, who arc all shown to be
stereotyped "mad peoplc"--a thumb-sucking,obcscgirl
sidling up to men, a stick (gun to him) toting ex-army
captain forever on the lookout for enemies and sundry
other characters put there to prance and prattle. Worse
is the so- called discipline enforced in the hospital by a
kindly Church- fathcr-cum-doctor. The hero,
Bhagyaraj, is allowed all sorts of physical intimacies —
all purportedly innocent — with a beautiful young girl
who Is apparently from an affluent and educated back
ground. It is a different matter that (he runaway girl is
pretending madness. The hospital authorities believe
that Bhagyaraj has taken sexual advantage of
Bhanupriya, the heroine. After the discovery of her
pregnancy, they let him go with nothing more than a
reprimand. And a bride! Could the film be an unwit
Misinformation on Sex
As expected of a repressive, prudish society when it
concerns matters sexual, our films positively revel in all
kinds of sexual misinformation and superstition to
seriously injure our collective emotional health.
To cite a telling example, Akarshan was a tortuous
love story set in the glitzy glasshouse world of Hindi
films. Sonu Walia and Akbar Khan arc stars who have
to marry in stealth because Khan's older sister — and
surrogate mother for the suggestion of Ocdipal fixation
- forbids the marriage. The explanation is offered later.
Khan had meningitis as a boy and the sister is afraid
8
th.it any child bom to him would inherit the brain
damage. The heroine, who is already pregnant, forces
herself to have an abortion, with disastrous consequen
ces, not to herself but the man, who goes into a catatonic
state w hen he learns of what he thinks as love’s betrayal.
And the film-maker has a simple solution to bring the
man out of a wheelchair - a song and a visit to the scenic
spot (bv the Niagara) where they had first made love.
A repeat performance. And presto! He is cured.
An even more recent film, Kamama, built its emo
tional drama around the involuntary vasectomy suf
fered by the hero, Vinod Khanna, a rampaging and
insouciant stud who sows wild oats carelessly. No, it
was not the dreaded Emergency that made the stud
virile vet stenle - unbeknownst to him, of course. It was
a fall that injured his groin without impairing his sexual
prowess but preventing him from spawning sons in his
image.
^'he Rare Film Intelligently Made
One of the few intelligent films dealing frankly with
the sexual roots of hysteria was Amol Palekar's
Ankahee. The fearful, hysterical reaction that is set off
in a charming, talented Dipti Naval is worsened by the
usual tantrik tortures the villagers subject her to. They
believe she is possessed by the devil and torment her
with exorcist rituals. It is in the city that a psychiatrist
correctly diagnoses her malady as a mild form of curable
hysteria. After marriage and sexual fulfilment, her con
dition is normalised. The film's theme was to lay bare
the hold of superstition on even educated people who
believe in predictive astrology. Such faith makes moral
monsters of even educated, charming men nurtured on
stncl ethical principles.
The trauma of having to accept and care for a hand
icapped child is the heart of Anjali. The film is faithful
to the behaviour and likely life span of a severely hand
icapped littlegiri who was not expected to survive even
^for weeks after birth. It shows how patient care and
selfless love can help such a child overcome insur
mountable odds. The prejudice of "normal" society and
the unwitting cruelty of children are factsof our nation
al life that the film brings out. And of course, it also
sugarcoats the pain with extended sentimentality and
Hollywood-style show biz. But the film does raise our
awareness and the need for empathy.
The threat to the collective health of society is nor
mally nota theme thatattracts mainstream cinema. You
have tc go to our one master for that. Satyajit Ray's
Canashatru was not in the master's lyrical manner or
the period perfection of a Charulatha The Indianisation of Ibsen's Enemy of the People squarely confronts
the possibility of an epidemic from contaminated water
and a small town's faith in the efficacy of godly
charanamril. It is not merely faith versus science. The
small town's flourishing economy depends on devotees
thronging the new Devi temple. The prosperous temple
is situated in the most crowded area of the town, where
the water supply is contaminated with the jaundice
virus.
Soumitra Chatterji is the gentle, humanist doctor
committed to scientific truth even if it means uttering
what is blasphemy to the pious townsfolk — the
charanamril of the temple contains polluted water and
neither the chanting mantras, the presence of tulsi nor
the fact that it washes the Dem's divine feet can contra
dict laboratory findings.
A scientist dedicated to truth in a society caught in
the fever of religious revivalism becomes a victim of
abuse and ostracism. Ray pulls no punches about this
confrontation and it is an act of political and moral
integrity in an air filled with religious hatred and fanatic
faith.
Perhaps only a society that can accept unpalatable
truths — whether of contaminated charanamril or bad
medical services - can find the way to health: physical
mental and moral health. ■
Madhyatn welcomes articles, reviews,
alternate viewpoints and rejoinders. Please
write in to us ensuring that your entries are
typed in double space.
- Media
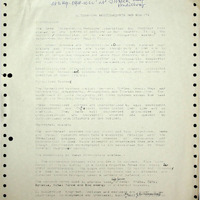 RF_DR_21_SUDHA.pdf
RF_DR_21_SUDHA.pdf
Position: 721 (17 views)