DRUG ISSUES-GENERAL POLICY MATTERS
Item
- Title
- DRUG ISSUES-GENERAL POLICY MATTERS
- extracted text
-
RF_DR_1_PART_1_SUDHA
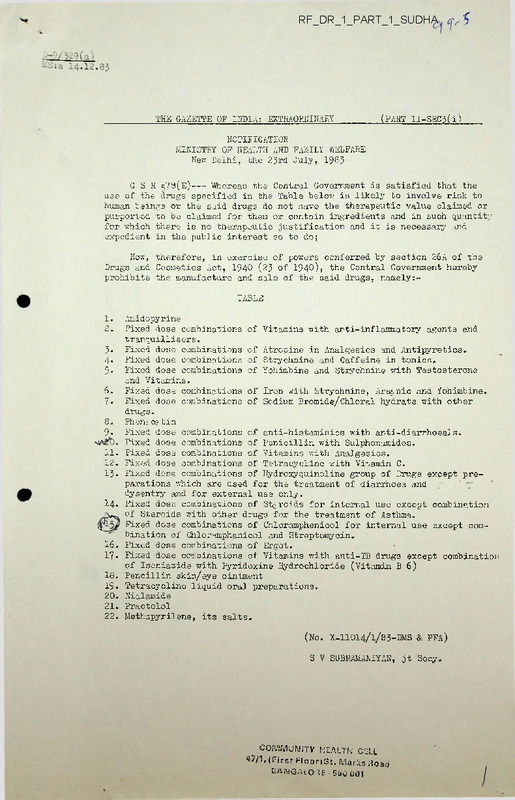
THS GAZETTE OF INDIA; EXTRAORDINARY
(PART II~SEC'5(i)
NOTIFICATION
MINISTRY OF HEALTH AND FAMILY WELFARE
New Delhi, the 2Jrd July, 198?
GSR 579(E)---- Whereas the Central Government is satisfied that the
use of the cirugs specified in the Table below is likely to involve risk to
human beings or the said drugs do not have the therapeutic value claimed or
purported to be claimed for them or contain ingredients and in such quantity
for which there is no therapeutic justification and it is necessary and
expedient in the public interest so to do;
Now, therefore, in exercise of powers conferred by section 26A of the
Drugs and Cosmetics Act, 1940 (2J of 1940), the Central Government hereby
prohibits the manufacture and sale of the said drugs, namely:-
TABLE
1.
2.
Amidopyrine
Fixed dose combinations of Vitamins with anti-inflammatory agents and
tranquillisers.
J. Fixed dose combinations of Atropine in Analgesics and Antipyretics.
4. Fixed dose combinations of Strychnine and Caffeine in tonics.
5. Fixed dose combinations of Yohimbine and Strychnine with Testosterone
and Vitamins.
6. Fixed dose combinations of Iron with Strychnine, Arsenic and Yohimbine.
7- Fixed dose combinations of Sodium Bromide/Chloral hydrate with other
drugs.
8. Phen: os tin
9. Fixed dose combinations of anti-histaminics with anti-diarrhoeals.
Fixed dose combinations of Penicillin with Sulphonamides.
11. Fixed dose combinations of Vitamins with Analgesics.
12. Fixed dose combinations of Tetracycline with Vitamin C.
IJ. Fixed dose combinations of Hydroxyquinoline group of Drugs except pre
parations which are used for the treatment of diarrhoea and
'
dysentry and for external use only.
14. Fixed dose combinations of Steroids for internal use except combination
of Steroids with other drugs for the treatment of Asthma.
$-5/ Fixed dose combinations of Chloramphenicol for internal use except com
bination of Chloramphanicol and Streptomycin.
16. Fixed dose combinations of Ergot.
17. Fixed dose combinations of Vitamins with anti-TB drugs except combination
of Isoniaside with Pyridoxine Hydrochloride (Vitamin B 6)
18. Pencillin skin/eye ointment
19. Tetracycline liquid oral preparations.
20. Nialamide
21. Practolol
22. Methapyrilene, its salts.
(No. X-11O14/1/85-DMS & PFA)
S V SDBRAMANIYAN, jt Secy.
community health cell
47/1, (First Floor)St. Marks Road
CAAiG.HO IE ■ 560 001
D-9/329(a)
MS;a-14-12.S3
THE GAZETTE OF INDIA; EXTRAORDINARY (PART II-SEC.3(i)
PUBLISHED BY THE CONTROLLER OF PUBLICATIONS, DELHI-]1OO54, 198J.
NOTIFICATION
MINISTRY OJ' HEALTH & FAMILY WELFARE.
New Delhi, the 2Jrd July, 198$.
GSR 577(E)— Whereas the Central Government is satisfied that the use of
the drugs specified in the Table below is likely to involve risk to human
beings or animals and it is necessary and expedient in the public interest
so to do;
Now, therefore, in exercise of powers conferred by section 10A of the
Drugs and Cosmetics Act, 1940 (23 of 1940), the Central Government hereby
prohibits the import into India of the said drugs, namely
table
1 - Nialamide
2. ’ practolol
3- Amidopyrine
4- Phenacetin
5. Methapyrilene, and its salts.
(No. X X1O14/1/83-DMS Q PFA)
S V STBRaMANIYAN, jt Secy.
„./■
’’r T JP'’jTV
y (f- ■ r st FI o or) 31. Marks Hoau
DAIMGAlOKE - 560 001
97.
HEALTH FOR ALL. - Al ALTERNATIVE STRATEGY
report o£ a* "s’tuSy’ 'group set up JoTatly ty^thT"’
INDIAN COUNCIL OF SOCIAL SCI! NCI- RESEARCH (ICSSR)
and the
INDIAN COUNCIL OF MEDICAL RESEARCH (ICMR)
13ol
TZraSjCngs bn drug's’ ~anct' ph’agTnace'ut'i'c^l's
THE INDUSTRy
THE TOTAL output of the industry increased a
hundredfold - from Rs.lOO million in 1947 to Rs.lu,50O
million in 1970-79. '.(his was due to expanded production,
especially of an ever-increasing number of sophisticated
drugs, and rising prices...
THE DRUG industry has enjoyed a higher man-average
profitability so that investment therein has increased
substantially from Rs.240 million in 1952 to Rs.4,50o million
in 1977.
THERE ARE about 125 large and medium factories and
nearly 3,000
small scale sector units engaged in this
industry which provides employment to about loo,GOO workers.
(11.0?)
PATTERN OF DRUG PROTECTION
THERE: IS now an overproduction of drugs (oftenvery costly)
meant for the rich and the well-to-do while the drugs
needed by the poor people (and these must be cheap) are
not adequately available. This skewed pattern of drug
production is in keeping with our ineauitous social
structure which stresses the production of luxury goods
for the rich at the cost of the basic needs of the poor.
(11.05)
c'-'
COL
.660°°'
• >.2
ad
2
OUT OF a total production of R9.700 crores in
1976, 25 percent is taken away by vitamins, tonics,
health restor tivts and enzyme digestants, mostly
consumed by the relatively well-fed urban population
*
Twenty percent is covered by antibiotics, only 1.3 percent
by sulphonamides (a very cheap and useful anti-infective)
?nd 1.4 percent by anti-tuberculosis drugs.....
(11.07).
PATTERN OF PRESCRIBING
ONI OF the most distressing aspects of the present
health situation in India is the habit of doctors
to over-prescribe glamorous and costly drugs with limited
medical potential. It is also unfortunate that the drug
producers alvays try to push doctors into using their
products by all means—fair or foul. These basic facts
are more responsible for distortions in drug production
and consumption than anything else.
STRUCTURE OF THE IMDUSTRy
THE EXISTING drug policy rightly emphasises the
attainment of self-sufficiency in the production of
drugs, in increasing the share of the Indian producers
and in giving a more significant role to public sector.
(11.14)
THE FOREIGN companies account for about 40 percent
of the total dtug production in the country; their
share in the production of basic drugs was about 2d percent
and that in formulations, 44 percent (197b-79). This
is still high A
(11.15)
PEICE CONTROL
THE DRUG prices are high and continue to rise. In
some instances, Indian prices are even higher than
the international ones
(11.les)
PACKAGING increases the cost of drugs very
gr atly because the trend is to mike it attractive
anc highly elegant anc to add cosmetic embellishments
to promote sales..■
(11.19)
THERI MAY indeed be a glut of applications for
the introduction of *Me- ’Jbo Drugs 1 which will
not attract new legislation for another five years
in regard to price control.••
(11.19)
GENUINE ‘BREAKTHROUGH
*
research has declined
in recent times.
(11.19)
EXISTING PPJC.S of drugs including those of
essential drugs of everyday use is highly
inflated. Far example, the cost of analgin sold
over the counter is 30 times the cost of production.
(11.19)
PRICES ARE often inflated by the use of brand
names. • • (11.19)
VERY OiTEN, prolonged controversy over the price
of a drug has resulted in stopping its production.
(11.19)
THE BII
l
*
for import of bulk drugs, intermediates,
solvents etc., has jumped from Rs.53.77 crores
in 1976-77 to about Rs.119 crores in 1979-bO.
4
4
DUALITY CONTROL
THE STANDARDS prescribed arc unrealistic
,
*
are
mechanically copied from books. ....and not unformly
enforced in all parts of the country.
CONSUMPTION OF DRUGS
AT PR. SENT the supplies of drugs to urban and
rural institutions within the health care system
is very uneven. In an urban hospital, for Instance,
the drug cost is rs.6 rerepatient per year while in
a Primary Health Centre, it is about 40 pais
,
*
per
patient per year.•.
(11.22)
STATEMENT SHOWING THE CATEGORIES OF FIXED-DOSE
COMBINATIONS RECOMMENDED BY THE SUB-COMMITTEE
OF THE DRUGS CONSULTATIVE COMMITTEE FOR BEING
WEEDED OUT
Categories of Fixed-Dose combinations to be weeded, out immediately.
CATEGORY
1- Fixed dose combinations
of Steroids
REASONS FOR WEEDING OUT
Fixed dose combinations of
Steroids with any other category
of drugs should not be allowed
as they are considered harmful
for the following reasons:(a) T^e adrenal suppression
accompanying steroid therapy
leads to symptoms and signs
of adrenal insufficiency, if
the steroid is abruptly
with-dr awn.
(b) It is difficult to titrate
the dose of the steroid
when it is present in fixed
dose combinations with other
drugs.
2. Fixed Dose Combinations
of Ami-dopyrine
Ami-dopyrine is considered toxic
because:-
(a) It causes high incidence of
agranulocytosis.
(b) In some individuals, it may
cause a sharp fall of total
leueocyte count associated
with chill, fever, headache
and pain in muscles and
joints following the administra
tion of drug.
3. Fixed Dose Combinations
of Chloramphenicol
Fixed Dose combinations of
Chloramphenicol with any other
category of drug is considered
harmful for the following
reasons and should not be allowed-
(a) Chloramphenicol is the
commonest drug which causes
pancytopenia and peripheral
blood changes including
Leucopenia, Thrombocytopenia
and aplasia of the bone
marrow. This reaction is not
related to dose and when done.
marrow aplasia is complete;
the fatality rate is almost 100%.
(b) Patients receiving chloramphenicol
must be checked repeatedly for
blood studies which is however
generally done in the case of
patients receiving fixed dose
combinations of Chloramphenicol.
2
4»
Fixed Dose combinations
of Ergot
Fixed dose combinations of Ergot
with Quinine, Ethinyl estradial,etc.
should not be allowed. Such
combinations are considered harmful
for the following reasons:
(a) They may cause uncontrollable
bleeding and may lead to
serious consequences.
(b) They may cause many harmful
s ide effects.
5•
Fixed Dose combinations
of Fits, with anti
inflammatory Agents &
Tranquilizers.
Fixed dose combinations of Vits.
with anti-inflammatory agents and
tranquilizers should not be allowed.
Such corabinations are considered
irrational for the following reasons:
(a) There is no definite role of
Vitamins in the management of
inflammatory disorders and
therefore a fixed dose addition
of vitamins in such preparations
will be irrationals
(b) Similarly there is no rationale
for adding Vitamins to
tranquilizers.
6. . Fixed Dose combinations
of Atropine in Analgesic
Anti-pyretics-
Fixed dose combinations of atropine
in analgesic antipyretic should not
be allowed as atropine may reduce
efficacy of antipyretics by block
ing sweating response.
7-
Fixed Dose combinations
of Analgin
Fixed dose combinations of any
category of drug with analgin in
oral dosage form are considered
generally harmful as analgin is
potentially a toxic drug and may
cause agranulocytosis except for
some combinations which may have
therapeutic rationale e.g. with
neurdvitanins. However, fixed dose
combinations with analgin in
injectable form may be continued to
be allowed as these are generally
meant to combat an acute attack of
pain, and injectables are less
likely to be misused.
8.
Fixed Dose combinations
of Yohimbine and
Strychnine with
Testosterone and Vit
amins.
Fixed dose combinations of
Yohimbine and Strychnine in a form
ula containing Testosterone and
Vit.B.12 should not be allowed. Such
combinations are considered harmful
and irrational for the following
reasons:
(a) Yohimbine easily penetrates the
Ol'TS and can cause central
excitation including rise of
B.P. and heart rate, hyper
excitability and tremour.
3/-
5
(t>) There is no convincing evidence
regarding the aphrodisiac
effect of Yohimbine and the
drug has no proven therapeutic
value(c) There is no rational basis for
the use of strychnine in
therapy and therefore no justi
fication for the use of it in
any proprietory medicine.
( d) There is a very narrow margin
between the therapeutic dose
and the toxic dose of
Strychnine.
9• Fixed dose combinations of
Iron with Strychnine,
Arsenic, Yohimbine
Fixed dose combinations of Iron
vrith Strychnine, Arsenic and
Yohimbine should not be allowed as
there is no rationale of such
combinations and such a combination
can cause harmful side effects.
10. Fixed dose combination of
Sodium Bromide/Chloral
Hydrate with other drugs
Fixed dose combinations of sodium
Bromide/chloral Hydrate with any
category of drug are considered
irrational and harmful for the
following reasons:
Use of both Sodium Bromide and
Chloral Hydrate have become obsolete,
as there safer hypnotic drugs
available today and their therapeutic
concentration in blood is very close
to their toxic levels.
Fixed Dose combinations of
Tetracycline, Analgin with
Vitamin 0.
Fixed dose combinations of Tetra
cycline, Analgin, etc. vrith Vit. C
should not be allowed as there is
no rationale of such combinations.
1 2. Fixed dose combinations of
Ayurvedic drugs vrith modern
drugs*
Fixed dose combinations of
Ayurvedic drugs and potent allo
pathic drugs like Stilboestrol
could be very harmful and there is
no adequate evidence of safety of
the interaction of drugs of these
two systems of medicine.
1 3. Fixed dose combinations
of Phenacetin
Fixed dose combinations of any
category of drugs with Phenacetin
should not be allowed, as the
question of banning Phenacetin
because of its potential toxicity
(nephropathy, methemoglobinemea,
hemolytic anemia as a consequence
of chronic over dosage) is under
active consideration of the
Government.
1 1.
•4-/-
4
14« Fixed dose combinations of
Chloramphenicol with
Streptomycin
Fixed dose combinations of
Chloramphenicol with Streptomycin
should not be allowed as Chloram
phenicol being potentially a
toxic drug its use should be kept
restricted to enteric fever only.
15- Fixed dose combination of
Penicillin with Strepto mycin.
Fixed dose combination of
penicillin with streptomycin should
not be allowed-
16. Fixed dose combinations of
more than one anti-hista
minics
Fixed dose combinations of more
than one anti-histaminics in oral
dosage form should not be allowed
as the differences between their
action is "out marginal.
B.
Categories of fixed dose combinations to be weeded out over a
specified time.
Category
Reasons for weeding out
1. Fixed dose combinations of
Anti-histaminics in antidiarrhoeal s.
Fixed dose combinations Of'sedative
anti-histaminics in antidiarrhoeal preparations may be
permitted provided all ingredients
are in adequate therapeutic doses.
2. Fixed dose combinations of
Penicillin with Sulphonamides.
Fixed dose combinations of
penicillin with sulphonamides are
irrational for the following
reasons:
(a) T-ne combination of penicillin a
bactericidal drug and sulphon
amide, a bacteriostatic drug may
cause antagonism.
(b) T^ere is risk of development of
bacterial resistance to both
the drugs.
•
5. Fixed dose combinations of
anti-histaminic with
tranquilizer.
Fixed dose combinations of antihistaminics having patent sadative
preparations(for example, diphen
hydramine dimenhydrinate, tripelennamines, pyrelamine, Antazolin
methapyrilline etc. ) with ranquilizers are considered irrational for
the following reasons:
Such combinations may cause enhanced
sedation, which may interfere with
the patient's day time activity
and dull the mind and slow the
reflex activity.
5/-
5
4»
Fixed dose combinations of
Tranquilizers with anti-histaminics
and analgesics in oral dosage form
are considered irrational for the
following reasons:-
Fixed, dose combinations of
tranquilizers, Anti,
Histaminics and Analgesics.
(a) Such combinations may car";
lot of unwanted sedation, which
may interfere with the patient's
day time activity and dull the
mind and slow reflexes.
(b) There may not be many clinical
situations which would need a
fixed dose combination of
these
■ 3 categories of drugs &
there will be unnecessary drug
ging. However, fixed dose
combinations of these drugs in
injectable form may be allowed
as injectables are not likely
to be misused.
5•
Fixed dose combinations of
Vitamins with Analgesics
Fixed dose combinations of high
dose vitamins with analgesics
should not be allowed unless there
is adequate evidence in support
of the rationale of such combination.
6.
Fixed dose combinations of
Paracetamol with Anti histaminics and tranquilizers
Fixed dose combinations of Para
cetamol with anti-histaminics and
tranquilizers should not be allowed
as there is hardly any clinical
situation which should demand a
fixed dose combination ofanti
pyretic, an anti-histaminic and
tranquilizer. However, fixed dose
combinations of paracetamol with
anti-histaminics and paracetamol
with tranquilizers may be allowed
provided the formula contains an
adequate dose of such ingredient.
7«
Fixed dose combinations
Fixed dose combinations of Vit
amins in prophylactic doses in
anti-TB drugs should not be allowed
as such combinations lack rationale.
However, combinations having a
therapeutic rationale such as IMH+ Bb
may be allowed.
*
*#
notification to implement this policy was issued only in January 1981.
Hoechst and
Pfizer, two of the 'affected' MNC, went to the Delhi High Court and obtained a stay
order.
At present the Government is still debating whether this stay order should be
contested.
3 jor
y to
ting
ugs
oad
una!
(2) MNC continued to produce several non-essential drugs far in excess of the
licensed capacity.
In 1978, the Government decided that in such cases the capacities
had to be 'regularised' and it was declared that the new licensed capacity would be
fixed as the maximum production achieved in any one year during the 3 years preceding
1977. This effectively condoned and in fact provided legal approval for the unauthorised
excess production. The MNC drug lobby which tried to extract further concessions has
been demanding that the 'regularisation' should be at the level of production achieved in
1980. The Government has bowed to this demand and recently, in 1981, the Government
has decided to regularise all capacities'liberally'as of September 1981. Significantly,
there has been no attempt on the part of the Government to force drug companies to
produce at least the licensed capacity of essential drugs many of which are produced in
quantities well below the licensed capacity
*.
sale
ired
tart.
■d in
up a
uirethe
t did
merit
lures
(3) Foreign companies were directed to reduce their foreign equity to 40%.
But
they were eligible to retain more than 40% foreign equity if they produced 'high
technology' basic drugs or intermediates for the production of high technology basic
drugs. To identify companies eligible for this concession, the Government appointed a
High Technology Committee which submitted its report in 1979,
The criteria for
eligibility have been so broadly defined that almost any drug company can claim itself to
be one employing 'High Technology'. For example, some of the criteria used are—use of
toxic materials in production, use of different kinds of sophisticated purification and
seperation techniques, etc.
Based on such criteria the Government has permitted
Hoechst, a leading MNC to manufacture drugs which are already being produced in the
small scale sector. The Government has not only ignored the report of the 'High
Technology Committee' but also stated recently that 'The need and scope for review of
the findings of the Committee
will be considered in the light of representations
received from individual companies concerned'. This is only likely to enlarge the list
of companies eligible for concessional treatment.
I
J
-lathi
ficial
I me of
icreses
brand
>ver in
there
aedical
variety'
f drugs
among
about
.
|
i
|
;
.
■
(4) The Drug Price Control Order of 1979 has resulted in a number of foreign
companies reducing the production of vital drugs whose prices have been fixed by the
.
**
orders
Simultaneously, the production and prices of drugs not covered by the Drug
Price Control Order have increased constantly. In fact diversification of production into
areas of low technology, low priority consumer goods has been one of the routine
* For example, the production of the anti-tubeicular drug PAS- has declined from 482 tonnes in 1979-80
to 405 tonnes in 1980-81 due to under-utilisation of capacity.
The demand for the drug continues to
be much in excess of 482 tonnes
** The production of the anti-malarial drug Amodiaquin, anti-tubercular drug Thiacetazone and the antifilarial drug DEC have all shown a decline in the year 1980-81 in comparison with the year 1979-80.
One foreign drug company has closed down an entire department making a group of 6 formulations
used in the treatment of TB, citing 'continued losses'.
15
responses of the MNC to any drug price control order. Thus, even earlier, Warner
Hindustan had commenced production of chicklet chewing gum and Johnson &
Johnson had started producing baby shampoo and baby powder.
The magnitude of the problem
To-day, nearly 7 years after the Hathi Committee produced its report, none of its
major recommendations have been translated into practice. The feeble attempts towards
a reform, represented by the Drug Policy of 1978 have been largely ineffective, thanks
to subsequent reversal of policy by the Government itself and due to the manipulation
of legal loop holes by MNC.
Recent years have in fact seen a further deterioration of
the situation with steep increases in drug prices and the dumping of hundreds of harmful
drugs banned for use abroad, into India and several Third World countries.
The Third World countries have not succeeded in their attempts to control their drug
industries and make them truly responsive to their people's needs.
A striking recent
example is the case of Sri Lanka. The Sri Lanka Government in 1971 set up a State
Pharmaceutical Corporation (SPC) and implemented a new drug policy. The number of
marketed drugs was slashed from 2100 to 600 and brand names were almost entirely
(though not totally) abolished. The State Pharmaceutical Corporation took over the
import of drugs and achieved 40% savings in just the first 6 months alone. When one
of the multinationals, Pfizer, refused to fall in line with the new drug policy, it was
threatened with nationalization. The United States ambassador intervened with the
Government of Sri Lanka and, in turn, threatened to withdraw the U.S. aid. As a result,
the Chairman of the State Pharmaceutical Corporation was asked to 'continue
negotiating' with Pfizer and no action was taken against it. Later, when there was
an epidemic of cholera, Pfizer was asked to make Tetracycline tablets but it delayed it
for so long that the state had to purchase it from abroad at an enormous expense.
Finally, the new government in 1977 once again allowed the private sector to
import drugs and effectively neutralized the benefits of State Pharmaceutical
Corporation.
Third World countries have also failed to support each other in their efforts
to fight MNC. For example; India and other Third World countries have been
silent on the recent Bangladesh ban order. Even the World Health Organisation
has maintained a silence at the current efforts of Bangladesh Government to
translate its (WHO's) own recommendations into action. Past efforts have shown
that the MNC can bring several sorts of pressure to bear upon even the most
committed Government. They can use threats and persuasions from abroad, get
their home Governments, to support them, restrict future investments and,
above
all, use their powerful alliance with local doctors who are used to a powerful
drug promotion system. In fact, the doctors and the local elite have accepted
radical reforms only in response to popular movements or mass pressure, such as
that which had installed a socialist Government in Sri Lanka in the election of
1970. In the case of Bangladesh, the demand for reform was spearheaded by the
Gonoshasthya Kendra (Peoples’ Health Centre), which in 1981 set up Gonoshas-
16
<rner
n &
thya Pharmaceuticals Ltd. (GPL) and started production, of 2 of the 32 essential
drugs, and by 1982, of 6 more drugs. GPL could sell these drugs at 50 - 65%
of the prices charged by the MNC and still make a profit of 10-15%, The MNC
responded by forming a cartel to undercut the GPL in its efforts to secure con
tracts to supply essential drugs to Government hospitals and clinics. By its new
drug policy the Bangladesh Government has provided strong support to the Peoples'
Health Centre and GPL. The policy contains provisions to protect local manufac
turers and instructs MNC to "...concentrate their efforts and resources, on those
items not easily produced by smaller national companies’'.
!
I
)f its
ards
anks
ation
?n of
mful
drug
hcent
State
ter of
itirely
r the
n one
t was
th the
esult,
itinue
e was
/ed it
rense.
tor to
;u tical
’
i
;
!
■
'
I
efforts
been
"ation
ent to
shown
most
, get
above
jwerful
cepted
uch as
:ion of
by the
ioshas-
The Third World people are faced with a situation where, all the studies by
their own Governments as well as the WHO, clearly point to a need for a drastic
change in the drug industry. Nevertheless, the MNC still continue to impose, on
the Third World a pattern of drug production and consumption that is irrational,
irrelevant and harmful. Any serious attempt at remedying this situation will have
to address itself to the question as to what exactly is making us so totally dependent
on the MNC, in the first place.
One is then likely to be led to the discovery
that the root of the problem lies in the fact of our having based the entire
health-care system on the capital-intensive, high-technology, chemical-based modern
Western approach towards medicine and health-care. As long as we are obsessed
with such an approach, it is unlikely that we will ever be able to free ourselves
completely from the tentacles of the MNC. And that could be realised only when
we take a completely different approach to the entire philosophy and practice of
medicine and health-care delivery—an approach that may have to learn much from
our traditional systems of medicine. Even though this may be the only long-term
solution to the menace of the MNC, a definite need nevertheless exists to initiate
some immediate steps to curb the loot of health and wealth of our people by
the MNC. Firstly, legislative action is crucial and needs to be fought for. How
ever, this alone will not be effective, unless it is backed by a Peoples' Movement
that can launch an educational campaign among the consumers and, more so,
the doctors.
—Madras Group
[
17
Voluntary Health Association of India
C-14, Community Centre
Safdarjung Development Area.
New Delhi-110016
Telegrams : VOLHEALTH
New Delhi-110016
Phone : 652007, 652008
MS-cb/HCA-18/
24th March,1982
Dear Friend.,
SUB;
LOW COST DRUGS
Ensuring availability of low cost essential drugs to all those who need
is part of our responsibility as individuals and groups involved in
’peoples' health movement1.
Ensuring enactment of a Code of Conduct aimed at discouraging unethical
marketing practices by profit oriented drug companies is part of this job.
Persuading the Government to enforce legislation to safeguard the consumers'
rights to safe and low cost drugs is crucial for the efforts made in this
direction.
Your participation is needed at this hour, to join in to demand an effective
Code of Conduct for the Pharmaceutical Companies.
Please study the material being sent to you,with your colleagues and send
in your responses and comments immediately , i.a. before 10th April 1982,
so that it can be sent to Health Action International to deal with it,
when they meet on the 15th April 1982.
On behalf of your friends in VHAI involved in Low Cost Drugs.
JDr Mira Shiva J
Coordinator
Low Cost Drugs & Rational Therapeutics
. ——-------
Encl: [ 'Low Cost Drugs and Rational Drug Therapy , JI andjfou.'
'Code of Pharmaceutical Marketing Practices'
CONIW1L)N11 Y
47/1,(First '
BANGA’-D-'"-
llth cell
,.iarks Road
International Codes
-
IFPMA
Voluntary Health Association of India
C-14, Community Centre
Safdarjung Development Area
New Delhi-110016
Telegrams : VOLHEALTH
New Delhi-110016
Phone : 652007, 652008
D-10/545
LOW COST DRUGS AND RATIONAL DRUG THERAPY
INTERNATIONAL CODES AND TYOU J
Last year the WHO was instrumental in passing an International Code of
Conduct of Marketing Practice of Baby foods.
This not only focussed the attention of the public, the health professionals
on the baby food issue, but placed the concept of breast feeding from
a 'rustic, old fashioned practice1 to scientifically sound and recommended
one. What this will do to the commercial interests of the milk food
industry is anybody's guess? It is up to the aware public, the consumer
associations, the journalists to ensure that the code of conduct of which
India was a signatury - is firmly adhered to.
The contents of this code are being circulated for awareness and action
of the health personnel and the public.
Along with it is a copy of the International 'Code of Pharmaceutical
Marketing Practice, proposed by IFPMA (international Federation of
Pharmaceutical Manufacturers Associations).
A copy of this provisional code was given to the participants of our
Drug Workshop at Poona, for discussion and comments.
The code is being circulated along with extracts from the discussion
document prepared by Health Action International on the code.
You are requested to read it carefully, share it with your colleagues
and pass it on. Your comments and suggestions regarding the international
code of pharmaceutical marketing practice are requested.
You are request,d also to bring to our notice, cases of malpractice by
drug companies which may be,by way of misinformation, selling of spurious
drugs, unethical marketing practices, commissions for prescriptions, cut
backs etc. Your participation is not only requested but is NEEDED for
us and other groups and organisations to take any legal action, for
malpractices to be curtailed before it is too late.
What is IFPMA ?
IFPMA is an International Federation of Pharmaceutical Manufacturers
Association, a Zurich-based trade organisation, set up and supported by
a number of national associations of manufacturers of prescription drugs.
Altogether there are JO affiliated national associations plus 12
affiliated through the Latin American Association of the Pharmaceutical
Industry.
Why the IFPMA Code was introduced and what it aims to be?
"The Paris-based International Chamber of Commerce has published codes of
advertising and marketing practice - which are meant to apply to business
of all kinds. However, the IPJWIA Code (which makes no reference to the
requirements of the International Chamber of Commerce) is believed to be
the first ever attempt to introduce an international code of marketing
practice for pharmaceutical companies.
D-10/343
MS-cb/23.3.82
- 5 -
2.
to discuss "briefly its significance in relation to controls that are
needed and which might be applied; and
5.
to suggest options for action by HAI participating groups. 11
According to the discussion document, what are the three essential
ingredients of any code of practice omitted in this IFMA's Code?
1.
Need for interpretation.
Reference to the need to ensure that the industry makes products which
have full regard to the needs of public health - appears a statement
so vague that it is hard to accept it as anything much more than an
advertising or public relations slogan.
2.
Need for monitoring
The question raised is 'what assurance is there,that the code will be
adhered to?' Is the Code to operate on the basis of a complaints
procedure? The mechanism for complaints handling and monitoring,
which are fundamental to a code have not been referred to.
J.
Need for enforcement
VThat happens if the Code is violated?
-
who Judges? industry (through its association or otherwise) or
truly independent bodies.
-
whether enforcement decisions are published - or this is kept
a secret? Could it be possible to establish, on the basis of past
decisions, what practices are acceptable or unacceptable? And what
is the record of individual companies- where complying with the
Code is concerned.
-
what sactions would be applied if companies break the provisions
of the Code?
-
what incentive is there for firms to observe the requirement of
the Code?
What are the implications and significance of this for the HAI groups?
This is useful to iefer to the obligations of the industry identified
by IFEMA;
Individual groups may think alternative or additional requirements which
might be needed to control abuse in pharmaceutical marketing, and to
consider how such requirements mi^it effectively be enforced at both
national and international level;
...4/-
10.341
:k/31.12.81
international federation of pharmaceutical
MANUFACTURERS
SOCIATIONS (IFPMA)
CODE OF PHARMACEUTICAL MARKETING PRACTICES
Preamble
The Statute of the Federation article 3 states that one of the
objects of the Federation is "to promote and support continuous
development throughout the pharmaceutical industry of ethical
principles and practices voluntary agreed on and "to coordinate
the efforts of its members towards the realization of the above
obj ects".
It is believed that in keeping with the pharmaceutical industry's
international responsibilities, the members of the Federation
will be prepared to accept certain obligations, insofar as their
marketing practices are concerned, and to ensure respect for
them.
IFPMA recommends a Code of Marketing Practices to its member
associations, recognizing the difficulty of setting out a simple
Code which will be applicable in all parts of the world. It
seems clear that national and regional conditions and legal
restrictions will continue to vary to such an extent as to make
a simple world Code impractical. Nevertheless, the Federation
believes that it has a duty to encourage its member associations
to either introduce such Codes of Practices or where such Codes
already exist, to continually re-examine and where necessary
revise them so that a voluntary system based on such a Code
keeps pace with modern medical knowledge and changing health
services and conditions.
It is recognized that many individual member associations of
IFPMA have laid down their own Codes of Marketing Practices and
this recommended Code is not intended to replace similar Codes
or instruments already in force by members of the Federation.
The following voluntary Code is therefore put forward as a
model for IFPMA's member associations.
A Code of Marketing Practices of this sort should be the res
ponsibility of member associations who should also provide
guidance to their members on matters of compliance and inter
pretation .
Obligations of the industry
The obligations of the industry may be identified as follows:
The pharmaceutical industry, conscious of its special position
arising from its involvement in public health, and justifiably
eager to fulfil its obligations in a free and fully responsible
manner, undertakes:
-
to ensure that all products it makes available for
prescription purposes to the public are backed by
the fullest technological service and have full
regard to the needs of public health;
to produce pharmaceutical products under adequate
procedures and strict quality assurance;
to base the claims for substances and formulations
on valid scientific evidence, thus determining the
therapeutic indications and conditions of use;
P-10.341
ss:k/31.12.81
3
7.
jlI.
Promotional communications should have medical
clearance, or where appropriate, clearance by the
responsible pharmacist, before their release.
Medical Reoresentat.i ve
Medical representatives must be adequately trained
and possess sufficient medical and technical knowledge
to present information on their company's products in
an accurate and responsible manner.
III.
Symposia, Congresses and other Means of Verbal Communi
cation .
Symposia, congresses and the like are indispensable
for the dissemination of knowledge and experience.
Scientific objectives should be the principal focus
in arranging such meetings, and entertainment and
other hospitality shall not be inconsistent with
such objectives.
IV.
Printed Promotional Material
Scientific and technical information shall fully dis
close the
properties of the pharmaceutical product as
approved in the country in question based on current
scientific knowledge including:
The active ingredients, using the approved
names where such names exist.
At least one approved indication for use
together with the dosage and method of use.
-
A succinct statement of the side-effects,
precautions and contraindications.
Except for pharmaceutical products where use entails
specific precautionary measures, reminders need not
necessarily contain all the above information providing
that a form of words is used which indicates clearly
that further information is available on request.
Promotional material, such as mailings and medical
journal advertisements, must not be designed to dis
guise their real nature and the frequency and volume
of such mailings should not be offensive to the health
care professionals.
V.
Samples
Samples may be supplied to the medical and allied
professions to familiarize them with the products, to
enable them to gain experience with the product in
their practice, or upon request.
<?<?•
COMMUNITY HEALTH CELL
47/1, (First FloorjSt. Marks Koad
BANGAlOJE - 560 001
MULTINATIONALS IN DRUG INDUSTRY :
A RETROSPECT OF THE HATHI COMMITTEE REPORT
On June 12th this year the Bangladesh Government promulgated an ordinance
that prohibited the sale of over 1700 drugs. The drugs banned fell into 3 cate
gories: (1) those deemed harmful and to be banned immediately by September;
(2) those requiring reformulation in accordance with new criteria and (3) those
classed as being useless or of little therapeutic value, which are 'to be removed
from the market at the end of 9 months. The decision was based on the report
of an expert committee appointed by the Government of Bangladesh to evaluate
the drugs currently in the market and to formulate a new drug-policy replacing
the old one of 1940. The drug sales in Bangladesh are worth over $100 million
a year and 75% of this is shared by 8 Multinational Corporations (MNC). (Pfizer
dominates the market with over $ 10 million sales in 1981). This new drug policy
has been a significant blow to the exploitative drug market in Bangladesh and the
multinational drug corporations are bringing a considerable amount of pressure on
the Bangladesh Government in an attempt to revoke the ban. The U.S. Govern
ment has urged the Bangladesh Government to reconsider its new drug policy
and the U.S. State Department has admitted that this was in response to a
request from the Pharmaceutical Manufacturers Association of USA. The Pharma
ceutical Manufacturers Association has argued that blocking the flow of drugs
from its member companies could open the market in Bangladesh to potentially
'impure' drugs from other sources.
This should be viewed in the light of the
fact that 70% of the drugs in the banned list are either banned in USA, or consi
dered worthless—that is, described as being 'therapeutically useless' by the Federal
Drug Administration of USA and the British National Formulary. The Bangladesh
Government has already made some concessions in the face of mounting pressure
and, in July 1982, it appointed a panel of military doctors to 'review' the ban.
Multinationals in the Indian Drug Industry.
The foreign investment policy of the Government of India
was extremely
'liberal' right from its inception in 1949.
This was being justified by the argu
ment that such a policy would: (1) provide the technology for the production
of basic essential goods ; (2) attract foreign investors and thus bring in foreign capital
and (3) stimulate the transfer and growth of advanced technology in various industrial
sectors. As a result, the first 25 years after independence saw the phenomenal
growth of foreign companies in the Indian drug industry.
The colossal profits
repatriated by foreign companies and the inability of the Government to control
drug prices was subject to heavy criticism in the Parliament
and there was a
demand fora thorough reform of the Indian drug industry.
Hence, in 1974, the
Government appointed a committee headed by Shri. Jaisukhlal Hathi to study
various aspects of the Indian drugs and pharmaceutical industry.
12
nee
ste
er ;
ose
ved
jort
sate
•ing
lion
rizer
licy
the
on
The Hathi Committee pointed out in its report that the Indian drug industry
was heavily dominated by the Multinational Corporations (MNC). In 1973 they accoun
ted for about 80% of the total drug market in India and held 85 - 90% of all
drug patents. However, 80 - 90% of the production of several MNC consisted of
simple household remedies like cough syrups, formulations with vitamins, tonics,
etc. On the other hand, about 90% of the basic drugs
*
manufactured in the
country were from the Indian sector (including small scale industries). In the
case of many basic drugs-MNC, production was well below the licensed capacity
.
**
However, the production by MNC of non-essential drugs like tonics and vitamins
often far exceeded the licensed capacity
.
***
In many cases where MNC did market
basic or life-saving drugs, it was merely the packaging of the basic drugs imported
from their own principals or subsidiaries, or the importation of the intermediate or
penultimate product from abroad, with just the last stages being completed in India.
;
erh■ I icy
o a
marugs
tally
the
>nsiieral
Jesh
sure
ban.
"ely
.rgu:tion
pital
atrial
senal
ofits
ntrol
as a
the
■tudy
I
.
;
I
MNC spent a bare 1% of their annual turnover in R & D, in contrast to 1215% spent on R&D in industrialised Western countries.
This figure includes
money spent on marketing-research and also sometimes the money spent on
quality control. Of the 'new' drugs introduced by the MNC in the market 87%
were imitation drugs (such as the sale of an already marketed drug under a new
brand name by a different company) and 10% were improvements on the existing
products ; only about 3% represented new drugs as such, i.e., containing new active
ingredients. The Hathi Committee also noted that the MNC actively discouraged
research by their Indian subsidiaries.
MNC were repatriating colossal amounts of foreign exchange by way of royalties,
technical fees and dividends, often after paltry initial investment. Additional remi
ttances were also made in the form of purchases of basic drugs and intermediates
at prices dictated by their foreign principals. 'These prices', the Hathi Committee notes
bear no relation to either the cost of production or the international prices of the
products.
Thus the MNC were making no significant contribution to the production of basic
essential drugs and in fact chose to concentrate in the area of low technology, low
priority consumer goods and formulations. Their contribution was negligible in terms
of introducing new basic drugs. All the MNC were enjoying a privileged treatment
under FERA (Foreign Exchange Regulation Act).
#
Basic drugs’ is used to refer ro essential drugs, such as those used in the treatment of Leprosy, Mala
ria, Tuberculosis etc.
'Formulations’ are those such as cough syrups, vitamin tonics, mineral tonics,
digestion aids, etc. These are not essential drugs and in fact a vast majority of these are of little or
no theraputic value.
*
«
For example, the production of Dapsone, a drug used in the treatment of leprosy, was less than 50% of
the licensed capacity in 1976-77 and this drug was unavailable in the market over a 6 month period
due to shortage,
*«
♦
Between 1952 and 1965, 364 'Permission Letters' were issued to 15 leading foreign units. Only 4 of
them were for basic drugs and the remaining were for formulations which included ointments, cough
mixtures, etc.
It was in this context that the Hathi Committee made the following
recommendations about the drug industry.
major
(1) The MNC should be directed to reduce their foreign equity immediately to
40% and in course of time, to 26% . Those foreign companies that were marketing
imported basic drugs should be directed to commence production of basic drugs
by themselves. Further, any raw materials or intermediates required from abroad
should be imported and distributed by the Government through a proposed 'National
Drug Authority'.
(2) The Committee decided that there was a strong case for restricting the sale
by generic name alone instead of by the brand name
*.
However it was considered
'inadvisable' to achieve this transition immediately. Hence, it proposed that as a start,
the sale of 13 drugs could be restricted to sale by generic name. It was also suggested
that the generic name could be displayed prominently on all drugs sold with the brand
names also marked less conspicuously, if necessary.
(3) The Committee noted that, there were several thousands of drugs marketed in
India, a vast majority of which were formulations sold by brand names. It drew up a
list of 117 drugs, which were considered sufficient to meet the essential drug require
ments of the country and suggested that the Government should concentrate on the
production and distribution of these drugs
.
**
New drug policy of 1978 and the current position
For about 3 years after Hathi Committee submitted its report, the Government did
not initiate any action on its recommendations.
It was in 1978 that the Government
announced its new drug policy and the following is a summary of some of the features
of this policy and its current status.
(1) A list of 5 drugs was drawn up (out of the 13 recommended by the Hathi
Committee) which could no longer be sold under brand names.
However, the official
* 'Brand' name is the commercial name under which a drug is sold, while 'generic’ name is the common
chemical name of the active ingredient in any drug. For example, a variety of headache 'remedies’ such
as Aspro, Aspirin, Anacin etc., have Aspirin as the active ingredient; thus Aspirin is the generic name of
all these drugs. When a single active ingredient is marketed under a number of brand names, it increses
the price of the drug considerably. Each company spends a fortune in trying to promote its own brand
among doctors and consumers. It has been estimated that MNC spend about 17% of their turnover in
marketing and advertisement (approximately 17 times the amount spent on 'Research'). In India, there
is one medical representative for every 4 doctors while in most Western countries there is one medical
representative for every 15-30 doctors. Doctors are 'encouraged' to prescribe specific brands by a variety
of means such as giving commissions, gifts, handing out of free samples, etc. Hence, the sale of drugs
by brand names was considered not in the best national interest and one that causes confusion among
doctors and consumers.
** A World Health Organisation expert Committee in 1977 (and again in 1979) recommended that about
200 drugs are sufficient to meet the drug needs of the developing countries and suggested that it is
advisable to market these drugs under their generic names.
14
D-10:343
MS : k : 5.1.82
2)
: 3 :
Production of all new single ingredient drugs to be
under generic names.
On what were these recommendations regarding generic drugs
based?
The Committee found that 1)
use of brand names led to
unnecessary increase in cost because of costly promotional
activities; 2) medical students were taught pharmacology
using generic names.
What are the. Drug Industry's objections against abolishing of.
brand names?
1.
It is illegal and discriminatory because it contravened the
protection afforded by the Trade and Merchandise Marks Act
1958 and there was no provision in the Drugs and Cosmetic Act
1945 to empower the government to abolish brand name^f:r
drugs.
2.
Since prices are fixed under clearly defined formulae by
the DPCO (Drug price Control Order 1979), generic names will
not reduce prices.
3.
Standard medical text books use both brand names and generic
names.
4.
Trade marks guarantee ethics in manufacture and in the absence
of brand names, customers cannot be sure of quality.
5.
Generic names will lead to wrong dispensing of drugs with
different pharmacological effects and harm patients 1 health.
6.
The ban on brand names for single ingredient new drugs will
completely stop introduction of new drugs in the market.
7.
Drugs sold under brand names often have superior bid- avail
ability than those marketed under generic names.
8.
The use of generic names takes aw.-.y the choice from the
doctor to the chemist.
9.
The general prescription is difficult to remember and repro
duce, lengthy and cumbersome.
10.
The' Hathi Committee recommendations would have been quite
different had it observed the results of the Pakistan
experiment.
(Source: S. Viswanathan:
Business India - Sept.28
Oc tobe r 11)
What advantages are seen in having a planned generic policy?
1)'
It will eliminate monopolization because of brand names,
and it will encourage healthy competition.
2)
It will curb production of non-essential combination drugs
which only add to the increase in price and have no
additional benefit.
For example-: Aspirin is marketed unde^two generic names:
- acetyl salycilic acid and aspirin
- 8 different brand names
- 7 brands marketing ASA and Caffeine
- 19 brands of ASA and Phenac-..'tin and Caffeine
D-10:343
MS : k: 5.1.82
: 4
Effect on Costs
Content
Manufacturer
Name under
j
which drug is
marketed ____
Price per
unit( Paise)
Hoechst
Analgin (.5gm)
Novalgin
20.00
IDPL
Analgin (0.5gm)
Analgin
18.27
Haffkine
Analgin (.5gm)
Analgin
18.24
Nicholas
Aspirin (350 mg.)
+Caffeine 30 mg.
As pro
7.75
Sarabhai
Aspirin 350mg.
Kenalgesic
22.00
Boots
Aspirin 3'00 mg.
Aspirin
3.60
Haffkine
2.84
Aspirin
Aspirin 300 mg.
Source: Indian Pharmaceutical Guide 1980
Some more examples:
Anacin
Aspirin 389mg.
Anacin
Caffeine 16.2mg.
8
Quinine sulfate 8 mg.
Avedanplus
Aspirin 350 mg.
8
Acetyl Aminophenol 125mg.
-
Powerin
Caffeine 30 mg.
Aspirin 350 mg.
•.
20
Caffeine 65 mg.
Codeine 8.125 mg.
Paracetamol 65 mg.
'
Salicylamide 65 mg.
(Analysis 'of Painkillers done by Dr. Anant Phadke
in his paper) Scientific Scrutiny of ©ver the
Counter drugs)
\
What does WHO Expert Committee on selection of essential drugs
( 1st Report Technical series 615, 1977) recommend? 11 recommends
Acetyl Salicyclic acid amongst the analgesics because besides
being the cheapest it was therapeutically as effective as analgin
(aspirin is 1/6) APC and multiple other combinations.
What are the loopholes being made use of in this generic policy
by profit-motivated drug industry’'?
Since the use of generic named drugs applies only to the 5 single
ingredient drugs it does not touch the COMBINATION DRUGS
which anyway form the majority.
Drug companies will try avoiding the issue by producing more
combination drugs and less single ingredient generic drugs.
Since BRAND NAMES is to be ABOLISHED for ALL NEW SINGLE INGREDIENT
drugs, the drug industry will try introducing new drugs under
BRAND NAMES with more than-two ingredients. So not only the cost
will go up because of the use of brand, but also because of
addition of often unnecessary ingredients.
Since the government had emphasised that generic drug names should
be displayed more prominently than:brand names with effect from
1st August 1981, the drug companies complain of difficulties in
making a long chemical name more prominent on small vials, ampoules
and pleaded of accumulation of stocks inspite of 7 months' notice.
0-10 343
MS : k: 5.1.82
What are the Drug Companies doing about this?
On 13th March, the industry's delegation met Mr. P.C. Sethi,
Minister ofChemicals and Petroleum, under which the drugs come,
having failed, Hoechst, Cynamid and Pfizer sued the Government
in the Delhi. High Court against abolishing of brand names and
have got a stay order.
What is the New Drug Policy?
Three years' debate following the Hathi Committee's recommenda
tion ended with the New Drug Policy.
(Presented in Parliament
on the 29th March 1978 by Mr. Bahuguna, the former Minister for
Petroleum, Chemicals and Fertilizers).
The NDP, the primary objectives were "to develop self-reliance
in drug technology;" to provide leadership role to the public
sector,"to foster and encourage the growth of the Indian sector”,
under NDP several limitations were imposed upon foreign sector
drug companies. These included -
the gradual reduction of the foreign share holdings of
Multinational Corporations,
- no further expansion of capacity to foreign companies
"engaged in the manufacture of household remedies".
the grant of licences to manufacture formulations to
foreign sector companies to be "linked with the production
of high technology bulk drugs from the basic stage".
- the grant of licences for the manufacture of high technology
bulk drugs to be conditional upon foreign sector companies
supplying 50% of their production to "non-associated
formulators".
(Source: Dilip Thakore - The Ethics of
the Drug Industry Pg. 27
Business India : July 7-20, '-80jf
Page 29.30)
If a multinational produced, say, Rs.100/- worth of bulk drugs,
half of it had to be sold to the Indian sector and the regaining
half used for formulating drugs under its own brand. The total
turnover of drugs could not exceed three tim^s the worth of bulk
drugs, if produced, i.e., 100 x 3 = 300 lakhs.
What is the DPCO?
Drug Frice Control °rder, an offshoot of the.New Drug Policy
passed in 1979 is aimed to restrict prices of the bulk drug and
formulations produced by any pharmaceutical company in the
organised sector.
What are the stipulations under the DPCO?
Bulk or generic drug manufacturing companies are entitled to
12-14% return on net worth (capital + reserves) depending upon
the complexity of the technology utilized in the production
process.
Formulations (i.e. branded drugs) are divided into 4 categories'
Category
I
Category II
Category III
Category IV
- Life Saving Drugs
- )
- ) in between
- Over the Counter Drugs.
__
.
—’
"Mark ups" above the cost of production to the extent of 40%,55%,
100% are pe mittfl by “he Ministry of Pc.rcoterm, Chemicals and
D-10:343
MS:k:5.1.82
production costs to be submitted by the manufacturing company.
What d_oes the Drug industry have to say about it?
According to Dr. S.K. Bhattacharya recently elected President of
the Organization of Pharmaceutical Producers of India (OPPI)
(which constitutes of 62 big and 54 medium firms and produces
60% of that total bulk.drugs and formulations in the country),
the present drug shortage of commonly prescribed drugs is because
of the New Drug Policy and the rigid price control and it will
definitely get worse.
Which are the drugs which have had problems regarding availability
*
Newsreports and A survey done by Medical Times (Glaxo's) Aug.
has revealed a shortage of painkillers
- antiepileptics
- anti-diabetics
anti TB drugs
- sera vaccines
'81
- Cardiac glycosides
- anti' hypertensive
*Regarding prescription practices - surveyed by Medical Times
(Glaxo's) use of brand and generic was concerned. Almost all
the doctors seemed to use brand drugs.
Reasons:
1)
2)
3)
confidence in the brands
less chance of substitution by chemist
convenience in remembering
Any info what guides prescription practices?
A study done by NIN Hyderabad on drug utilization revealed that
14% of.the population surveyed (1800 urban education population)
was taking drugs on the basis of advertisements alone.
Only
1.72% gave satisfactory replies on the proper use of drugs.
48% allopathy
18% homeopathy
14% naturopathy
11% ayurvedic
2% Unani
63% had erroneous idea about dosage schedules and mode of adminis
tration which could result in bioavailability and therapeutic
problems.
What is OPPI paying to build up public opinion against the
Government policies? OPPI has launched a Rs.24 lakh MEDIA CAMPAIGN
in what is says is a bid to help avert more serious shortages in
the future.
(Source: Vanishing Drugs: Hindustan Times April 27, 1980)
What is the situation regarding Drug-Control?
The Drug Control situation in India is pretty bad. Only 3
(Maharashtra, Gujarat, West Bengal) our of 22 States in India
have machinery to regulate the manufacture, distribution and
sale of pharmaceuticals.
D-10:343
MS : k : 5.1.82
: 7 :
In Maharashtra, acknowledged to have the most effective drug
control administration, there are only 96 drug inspectors and
1 drug testing laboratory for over 2000 manufacturers and 15, 000
shops.
(Source: Dr. S.K. Bhattacharya of OPPI in
Medical Times - August 1981)
In Delhi for 5 million population there are 20 drug inspectors.
In Uttar Pradesh for 100 million population there are only 24 drug
inspectors.
'Source: Rajender Rainer : Efelhi Repordvr
July 1981 ".Spurious Drugs dealing in
Death)
At the time of the Hath! Committee Report ( 1975) the- Total drugs
Inspectors in the whole of India was 305 . Current estimates are
5 °*
(Source: The Ethics of Drug Industry: Business
India, July 7-20, 1980 - Pg. 33)
What percentage of drugs are considered sub-standard in the Indian
Market?
Conservative estimates arc 25-30%.
The Drug Control authori
ties accept this figure.
(Source: Spurious Drugs: Delhi Recorder,
July 8)
52% drugs are substandard according to a survey quoted by Anil
Aggarwal in Drugs and the Third World.
2% drugs are spurious
(According to the drug control authorities).
Wb_a.t. a re. ...t.he__re^s_Qn.s__ojf.._suc.h._a_h igh....percen page...of _s_ubs.tan.dard_
drugs?
1)
Inadequate drug control.
The centre can only lay down policies, state governments have
control over manufacturers, sale and distribution (the inter
state barriers are fully exploited by trade in spurious drgs).
Control, if any, is at. the earlier stage of production into)6
bulk form or later formulations, improper storage, etc. are not
given that importance.
Shortage of certain brands of popular drugs gives an opportunity
to spurious and substandard drug producers to take advantage
of the situation. Linked to this is high demand of life saving
and other common drugs.
-
easy availability of drugs over the counter without
prescription from a qualified doctor
easier availability of drug selling licence
ignorance about drug adulteration and substitution
- the increasingly prevailing habit of chemists to stock drugs
of a company giving them commission in some areas
the desire of the consumer to buy cheaper drugs because of
the high cost of drugs (and his poverty in many cases)
- the buying of drugs by chemists without any bill to avoid
payment of taxes
- only drug control authorities have been associated with
checks and control unlike food adlteration where the consumer
can play a role.
D-10.-343
MS:k:5.1.82
What can consumers do to deal with this problem of substandard and
spurious drugs?
1)
Buy drugs only from licensed chemists.
2)
Read the drug label carefully, verfy expiry date, price
and-seal before mrchasirig. Check with the price lists of
manufacturers available with the chemists.
Ask for a cash memp-give the chemist enough time to fill
entries of drugs bought, your address, etc.
Don't swallow all the claims made by the advertisers of the
various drugs.
3)
4)
5)
Avoid self medication by use of patent drugs.
yourself witl>Any drug you do not know about.
6)
Follow instructions given by your doctor, pharmacist or on
the medicine label regarding mode of administration of the
drug dosage, frequency, etc., and duration. Check if in
doubt specially if deasling with patent drugs.
7)
Avoid using left-over drugs or drugs that change colour,
taste, or look different. Keep drugs as advised - in a dark
and cool place.
8)
Keep drugs away from children's reach.
separate ly.
9)
Destroy old cartons, labels, containers to prevent misuse of
spurious drug manufacturers.
10)
If you feel doubtful abouc the quality of any medicine, contact
the Erug Control Department.
11)
If in Delhi, ring up 22 60 18 be4ween 9 A.M. - 6 P.M..
After office hours and on holidays ring up 63 33 00, 63 40 73
and 63 11 16.
~
'
Don't medicate
<
Keep poisonous drugs
The punishment provided in Sec. -27 and 27A of the 1940 Drugs and
Cosmetics Act to safeguard the consumer is maximum imprisonment
of 10 years, increased to life imprisonment by West Bengal.
What’constitutes the public sector and how are they faring?
The public sector constitutes of -
IDPL
-
Indian Drugs & Pharmaceuticals Limited
HAL
-
Hindustan Antibiotics Limited
SSPL
-
Smith Stanistreet Pharmaceuticals Limited
BEPL
-
Bengal Chemicals & Pharmaceuticals Limited
IDPL and HAL incurred losses of almost 2 ccores in 1979. Monthly
losses of IDPL and HAL are 2 crores and 45 lakhs respectively.
(Source: Policy Pitfalls: ^anjana Kaul:
Hindustan Times, April 27, 1980)
Why are they running at a loss?
The reasons given are mismanagement, inefficiency, poor coordina
tion, undu.r-utiliza'tion of capacity, corruption, frequent machine
breakdowns.
Probably, one acceptable reason is the refusal of the MNC and
othvr private companies to go into production of essential and
life-saving drugs of Category I & II which allow mark-up of only
40 and 55% r ,s ctivc ly (ns they cm make up to 100% profit on
no"- s.~" -
t •
...“.t-r
rt
tid - - ■ . p .blic sector
W
0-10:343
MS;k;5.1.82
/
According to Mr. D.B. Telang, Financial Manager of the company
for every kilo of streptomycin produced, a loss of Ps.25 is
incurred. The more esssential dHigs are produced the more are
the losses incurred.
Losses are due to increase in the price of
raw materials, inflation - 35-40%; packaging 30%, power 30%, cost
of transportation. A,, this in the presence of fixed drug prices
apparently has caused the ever increasing losses in the public
drug sector. IDPL, HAL, IDRI were instituted to break foreign
monopolization and produce a reasonably cost essential drugs for
the Indian public. But even today, 33 years we still import drugs
for Kalazar, malaria, leprosy, diphtheria, TB. Losses can be made
up by raising production or by asking government to alter the
pricing structure.
How self sufficient are we regarding production of drugs? What
do the MNC's and OPPI have to say about production of essential
'drugs?
/
Dr. Bhattacharya of OPPI says "We are business concerns. Why
Witt actgSS^c^ri^sI profits)CaUSG incurrence of ^s.
What is S.P.C.?
Chemicals & Pharmaceuticals Corporation is for channelizing drugs
and regulating their availability in the country. The Corpora
tion has had problems regarding availability and prices of
imported ingredients. There are reports of essential bulk drugs
not being lifted from the C.P.C. by the drug company on account
of low profitability.
On December 1, 1979, CPC had 4 crore worth
of canalized bulk drugs in stock. These included essential drugs
like tetracycline, streptomycin. doxycyclin.
Drug
Company
Licensed capacity
in million^ tons
Actual produc
tion in mil
lion tons
56.06
135.82
PAS
a) Biological Evans
b)’-Warner Hindustan
120
300
INH
a) Biological Evans
b) Ghas. Pfizer
c) Warner Hindustan
10
1.6
90
0.13
0.06
6.08
What are the objectives of C.P.C.?
The basic objectives of CPC in canalizing import of drugs is as
follows:.
1.
Bulk purchase for all manufacturing units gave bargaining
power in world market so that concessional or low prices
could be secured.
2.
To prevent disturbance of indigenous production of drugs with
a certain therapeutic value - introduce and regulate imports
of. newer, sophisticated drugs in a planned manner.
3.
To protect the indigenous production of drugs, especially when
the production is inadequate to meet-internal demand.
4.
Tg ensure the equitable supply of raw materials at uniform
prices, eliminating middleman's profits,, so that formulations
from this are priced at a fixed uniform level.
£-10:343
MS;k:5.1.82
.
10:
5.
To help the small scale sector of the industry whose require
ments are small and who would otherwise find it uneconomic
and impractical to import.
6.
To regulate the import of drugs whose- indigenous production
is substantial enough to warrant their being given protection
so that their growth and utility are ensured with a view to
achieving ultimate self-sufficiency.
7.
To secure those drugs which have very few world manufacturers
and monopolies at reasonable prices.
8.
To regulate the import of drugs whose imports can cause public
health problems, eg., addiction forming drugs, etc.
Loopholes points. 4. and.5 were., to avoid middlemen but unfortunately
since small-units have, to give their..REQUIREMENTS AND ADVANCE
PAYMENT several months prior to time of supply (promptness, of which
is not assured), the small scale agencies are unable to take full
advantage and it is the MIDDLEMEN who lift the STOCK, HOARD it and
sell it at 25-3074 higher than the usual rate.
10% foreign firms have not utilized 3 industrial licences and
7 letters of intent for the manufacture of 16 bulk drugs.
40 firms in the Indian private sector failed to implement the
investment proposals with 31 industrial licenses and 27 letters
of intent. ■
Of 32 items of bulk drugs covered by 13 licenses, 21 items were not
produced by Glaxo laboratories for the last 5 years.
(Source: J.S. Mazumdar: Drug Industry
Instruments of Policy)
And with all this, useless non-essential drugs are pumped into the
market while essential drugs are not produced. Very obviously,
profit is the motive of the drug production industry and not ful
filling of the country's need as is often alleged.
The small scale sector feels itself financially ill-equipeed to
undertake any undue losses or profits and therefore also opts for
non-essential drugs.
What does the 6th Five Year Plan require regarding drug production?
From Present
By 1984-85
Bulk 226 crores
to
665 crores
Formulation Rs. 1150 crores
2450 crores.
VIth PLAN aims at:
1)
Developing self-reliance in technology,
2)
Ensuring availability of drugs with reasonable prices and
inadequate amount
3)
Dominant role of the public sector in the industry.
What's the situation?
Growth rate of bulk drugs has fallen from 13% to 6% and for formula
tions from 10% to 4%.
D-10:343
MS :k.5.1.82
: 11
IN THE FIRST YEAR OF THE PLAN, the foreign and big Indian
companies are not interested in manufacturing the 'drugs that yield
low profit margin.
In fact, by cornering the already sanctioned
licenses and letters of intent they are .out to blackmail the
government-in order to secure substantial price rise - by starving
the market of these drugs.
(Source: MNC's Fatten, Indian Die:
Dr. Pankaj Shah: Link, Aug. 2, 1981,Pg.10)
The Multinationals give the high prices because of the 'research'
they apparently finance. What all constitutes research?
It includes
- basic research
- product development
- toxicity tests
- research on formulations
- mass production methods
- clinical trials, etc.
it also includes studies on colour design of product, its packaging
to promote sales, general market studies, purchase of international
patents, solely to extend the company's monopoly position abroad.
(Source:
Link, Aug. 2, 1981, Pg.11
Dr. Pankaj Shah)
What percentage of their sales do they put into research?
what percentage in publicity?
and
Glaxo in 1979-8Q spent Rs.1.52 crores on publicity - . . percent
on tropical diseases.
Amount MNC's spend on research is <^3% of their sales turnover
compart to 14-15% in Developed countries. Even so research acti
vities are seldom in tropical diseases but in diseases like cancer
hypertension etc.
What are the country's health requirements based on priorities set
by Alternative Strategy: ICMR/ICSSR Study
Measures against
-
Communicable Diseases
-
Nutritional deficiencies
-
Family Planning, Fertility rate,
-
Basic health care
Some of the figures that indicate the seriousness of the problem
*IMR in 1976 129/1000 live births (when Sri Lanka's is 45:1 in'72
(pg.129) )
*Maternal mortality 163 in 1976 (Percentage Distribution
(pg. 125)
*Birth rate - 33.3%per thousand per annum in 1978 (Pg.13'
Health Budget set'aside for the VIth Five Year Plan - 1823-05
Crores
50% of the Health budget earlier has been spent on curative care ...
40% in construction and capital expenditure
and only 10% on preventive health care(Health Staiisticsl
Intelligence Report)
50% of under fives and pregnant mothers are found to te anaemic.
6.0.-.80..% are clinically malnourished.
50% of Indian children get
the calories .that they Tegtir'5 -
40,000 children b^com- ■ blind each year b^co-usc of Vitamin A ,
D-10:343
MS:k:5.1.82
:
12
:
*27,08,222 get malaria every year and 147 die of malaria in 1979
4. (pg-82)
Incidence of T.B. is . 2%, i.e., 8 million people. About
2 million have open TB.
*Incidence of leorosy is 25,59,566 cases on Record - Mar. '80 1
21,58,822 cases under treatment
SPg.89)
on Record - Mar. '80 J
(India harbours 1/3 of the world's leprosy, malaria cases).
(■★Source: Pocket Book of Health Statistics
’80,.CBHI, New Delhi)
The incidence of malaria - even Falciparum - Filaria, polio,
Kalazar, Japanese ‘Becephalitis has shown an increasing trend.
The above becomes extra significant when, we focus on the percentage
of people below or bordering the poverty level - a figure that is
also showing a rising trend. 60% Indians are below poverty line
(assessed in relation to average caloric requirement).
What is the production of drugs like in relation to these health
requirements:
Out of Rs.636.9 crores of drugs sold in 1980
19% were anti-biotics
10.21% vitamins
4.41% tonics
/
4.241% anti-anaemic preparations
4.71% cough and cold (increase in growth within
the last 5 years has been
70%) .
Talking in absolute figures 137 crores worth of vitamins were sold
in the year 1980.
Break-up of the above available in Dr. A. Patwardhan's paper
1,2, and 3.
All modern drugs are available to economically well off 5%.
Dasic drugs available to another 20%.
Percentage of people denied availability of essential modern drugs
is 75%.
This is when our population is 65 million.
With annual expenditure of 636.9 crores.
By 2001 the po-ulation will be 950 millions.
Amount required for drugs with inflation, increasing prices of
raw material, etc, etc., will be
Our National Formulary has over 60,000 drugs and chemicals.
(15,000 brand drugs)
68% are obsolete, and useless (only about 5000 are useful and 2500'
of marginal use)
The Hathi Committee has identified 117 as essential drugs and WHO
about 200- drugs which would take care of the 90% of the EXISTING
HEALTH PROBLEMS .
----------- —
’ ^-10:343
MS: k: 5.1.82
: 13 :
Regarding essential drugs production what is happening?
Out of Rs.1260 crores worth of drugs manufactured in 1979-80
essential and life saving drugs accounted for Rs.350 crores only the rest were tonics, digestive enzymes, formulations of medicines
with marginal benefit.
MANY VITAL BULK DRUGS IN HUGE QUANTITY HAVE BEEN WASTED WHICH
COULD HAVE BEEN UTILIZED FOR MANUFACTURE OF ESSENTIAL DRUGS.
(Source: Drugs : Industry Instruments of Policy
- J.S. Majumdar)
1977
1978
Installed ProducProduction
Installed
Anti-T.B. Drugs
capacity
capacity
tion
Tonnes
'•£' onnes
ronnes
tonnes
INH
509
57
5 39
94
PAS and its salts
1170
56
1290
558
Theacetapone
15 3
25
153
13
S treptomycin
257
194
257
225
DDS and its derivatives
26
17
38
17
Anti-filaria
DEC citrate
56
18
S6
23
Anti-typhoid
Chloramphinicol
128
95
128
95
Halogenated
Quinolines
5 87
157
590
Metronidazole
137
16
170
156
34
176
Anti-Leprosy
Anti-Dysentery
195
•
55
Anti-malariaIs
Chloroquin
45
Pfizer Ltd.
Production during
1979
1978
Products
Licensed capacity
INH
80 metric tonnes
45 MT
52 MT
110
90 MT
54 MT
PAS and its salts
Terramycin
14
5 3 MT
54 MT
Protienex
110
269 MT
290 MT
Burrouqh's Welcome
Licensed annual capacity
Production 1980-81
26 million tablets
187 million tablets
Septran
.
Similarly, Glaxo's production of Betamethazone has been increasing
while production of antibiotics - penicillin, streptomycin, serra
and vaccines is much below licensed capacity.
Make-up of Drug Industry at a glance?
*5000 pharmaceutical units
3500 manufacuring units
*
*1500 units based on loan
* 118 companies in the organised
license system
sector
*45 Multinational drug companies
*
Of the 20,000 formulations in th®
which have foreign equity
market - 7 8% formulations irj the
more than 40%
hands of Multinationals, 16%
-IO:343
S:k:5.1.82
VOLUNTARY HEALTH ASSOCIATION OF
C-14 Community Centre, S.D.A.
New Delhi - 110016
COMMUNITY
326, V Main, 1 Block
INDIA
°R-
THE DRUG SITUATION IN INpfA ‘^zgs
------------------------------------------- ' ■^'■I'onal n.
Korambngala
Bangalore-560034
India
■■
c‘’
Nc«,
The causes of the problems and the solutions Of the present day
drug situation differs markedly when seen from the eyes of the
drug industry especially OPPI, the Drug Controller, WHO, IMA,
groups and organizations who see everything in terms of what is
socially just or not, and the consumer.
Many significant changes have occurred in the past few years
which are bound to have far reaching effects.
It is important
for all of us to be familiar with the problem, with the loop
holes, with the different versions of the various groups involved.
THE FACT THAT THE SOLUTION OF THE MAJORITY OF THE HEALTH PROBLEMS
IN INDIA DOES NOT LIE IN MORE PILLS, MORE DOCTORS, MORE .HOSPITALS,
KOT IN SCCIO DCOiK'MlC & POLITICAL POWER RELATIONS IN KTu-.T IS W,
7- ACCEti-FD
MOST OP US HERE.
The need for greater social awareness is not only relevant for
the villager who gets deprived of his right to the least basic
needs, basic health care, but also for those involved in health
work (whether it is in a community health programme, a dispensary,
hospital or even a teaching hospital).
to be
Knowing about dr?gs is not/limited to their brand names, dosages,
side effects, but also their COST and their AVAILABILITY.
The various factors influencing these need to be analysed.
We will highlight some of the more important aspects which will
strongly .influence our search for solutions.
Here are some questions that arise and need answers. How much
is our health budget for the 6th Five Year Plan? and how much of
it goes on drugs as a total percentage and what is the per capita
expenditure on health? (Medical & Public Health & Family Welfare)
a)
1821.05 Crores (1980-85) Centre/State &/Union Territory
Source :
(6th Five Year Plan - Pg.382)
b)
Traditional System of Medicine - Centre 29 Crores
Source: (Planning Commission - N.D.)
c)
Rs.15.05 ( + Rs.1.51 for Family Welfare) in 1977-173
Source:
(Pocket Book of Health Statistics of India 1980 Pg.37)
What percentage of the Indian population utilizes the benefits
of modern drugs:
- about 20%; according to some estimates only 10%
How self-sufficient are we in producing this?
We rtill import 50% of the raw material at stupendous rates inspite
of our Pharmaceutical industry being 33 years old and the biggest
in the Third World.What is happening to drug imports?
Our imports tripled'between 1963-64 to 1973-74 from Rs. 13-1.7.-crores .
to Rs. 37.50 crores ---- within next year it increased to 'g. 4 7 crores
this constituted 35% 'of the-bulk drugs utilized in formulations.
According to Dr. S. 8. Gothoskar, the Drug Controller of India ''
"The last 3 yrs have witnessed a steady increase in the requirements
of’imported raw materials by nearly 100 percent.
Thus while our
: 2 :
D-10:343
MS : k : 5.1.81
production increased by only 50% from 1976-77 to 1978-79 the expenditure incurred on import of bulk drugs, intermediates,
solvents etc. rose by nearly 80%.
The break-up of the drugs in the market is :Foreign Multinationals
. . 78%
Public Sector
..
6%
.. 16% (Source: Dr. Pankaj
Shah:Link - Aug. '81)
Pg. 12.
Indian Private Sector
In 1978-79 MNC's produced
.. 28% Bulk drugs (Basic drugs)
.. 44% Formulations
(Source: Dr. Thakor - Businss
India, July 1980,Pg.26)
What are the allegations against Multinationals?
According to the Hathi Committee Report in 1975 the Multinationals:
'•i block others from producing drugs for a period of 16-20
years by invoking patent production,
- din the brand names into the minds of the medical
profession by employing a large force of medical detailers,
- resort to high pressure sales techniques, and,
- rig up prices to levels which have no relation to the cost
of manufacture of products or international prices.
What were the Hathi Committee's
major recommendations?
1)
Nationalise the Drug Industry,
2)
Foreign undertakings operating in the country should be
directed to bring down their equity to 40% with
progressive reduction to 26%
**
(Under the New Drug Policy it was added that Multinationals
maintain a ratio of 1:5 for production of bulk dru^to
formulations)
**In the US more than 10% share by a foreign undertaking
classifies the company as foreign.
What were the Hathi Committee's recommendation regarding generic
drugs?
1)
Abolition of brand names in a phased manner, beginning
to be made with 13 single ingredient drugs:
- analgin
- aspirin
- piperazine
- ferrous sulfate
- chlorpromazine
- chlorampheniol
- streptomycin
- Tetracycline
- reserpine
- tolbutamide
- INH
- INH & thiacetazone
Recommendations made in 1975.
In Jan. 17th 1981 decision was
taken to abolish brand names for
5 classes of drugs:
- analgin
- asprin
- chlorpromazine
- ferrous sulfate
- piperazine
qr!2.
Voluntry Wealth Awociatlen of
C-14, Community Centre,
Sardarjung Development Area,
New Delhi-110016,
July 17, 1984.
ESSENTIAL DRUGS
A DEMAND FOR PRIORITIZATION
Prepared for
V H A I members,
Drug Action Networkers
and all. those who believe
in the concept
and implementation
of Rational Drug and Health Policy
Background paper
for
Drug Action Network
Core Group Meeting
Wardha
30 - 31st JULY 1984.
CELL
!-,s .-load
Dr. Mira Shiva
Coordinator
Low Cost Drugs
and Rational Therapeutics
V.H.A.I.
rrLZ:pt:-|9.7.'84
ESSENTIAL DRUGS - A DEMAND FOR PRIORITIZATION
- Dr. Mira Shiva, VHAI.
Content Outline
I.
Essential Drugs - An Introduction
II.
Courageous Efforts - Brief Review
Chile
Srilanka
Pakistan
Mozambique
Bangladesh
W H 0
India
w
III.
Our Efforts in the area of essential drugs
IV.
The Selection of essential drugs -and the essential drug programme
w H 0 Recommendations.
"
V.
The Rationale of Essential Drugs
Drug List?
or Why do wo noed an Essential
A.
Existing low priority to essential drugs; needed for the
priority health needs; and the deteriorating trends in output,
B.
DPCO The Drug Price Control Order and its negative impact on
Production of Essential and life saving drugs i.e. Category I
and II drugs.
C.
Poor performance of multinationals in production of essential drugs.
D.
Dilution of EERA companies - an invitation to more formulations.
E.
The need for rational use of scarce resources: Controlling Cost
by: ■
1. preventing wastage of scarce foreign exchange by net
importing excess inessentials.
2.
ensuring prevontivo hoalbh measures before promoting
inessential drugs.
" ■
3.
ensuring placing essential drugs before inessential drugs
4.
increasing production of essential drugs, decreasing
drug costs through economy of scale.
5.
ensuring bulk purchase of selected essential drugs and
thus cutting costs.
....2/
2-4/37S(o) LCD & RT
VH/I:pt19.7.'84
'JI.
2
:
F.
Subsidizing costs of essential drugs
G.
Need for influencing market demand and thus the drug
production pattern in favour of essential drugs
H.
Need to decrease drug misuse and overuse .
I.
Need for efforts in preventing Iatrogenesis
J.
Need for ensuring unbiased drug information for health
personnel and consumers.
K.
Need for ensuring better quality control
L.
Need for ensuring generic prescribing
Graded Essential Drug List
I.
ESSENTIAL DRUGS
INTRODUCTION
The concept of essential drugs is the focal point of the drugs
issue and of the rational drug policy.
Our focussing on essential drugs does not mean that by ensuring
production and supply of essential drugs., the health care status of
our people -will dramatically improve. Wc arc focussing on it to high
light the fact that majority of our people are not merely deprived of
health care facilities, but whatever they are given by way of health
care does not necessarily .have thoir interest in mind. The kind of
health caro facilities, medical technologies and drugs being promoted
under the garb of "sciontificity" and "modern advances" and as "latest
break through" usually servo the interest of the "medical industry" i.c-.
the drug industry and the medical establishment, Some of these modern
myths and superstitions have to bo demolished. Eg. Myth I - medicine
is a noble profession brimming with selflessness, putting patients
interest and welfare, above self interest.
Myth II - The drug industry
produces 'pills for every ill1 and is fighting an unselfish battle
against death and disease. If it wasn't for them, lots of us would be
sick and suffering if not dead.
Myth III - India is. a welfare state,
signatory of the Alma Ata Charter giving priority to Primary Health Care
and that our health policies arc people oriented and are' guided by reco
mmendations of Committees like the BJjore Committee, 1946, Hath! Committe
1975. Alternative strategy Health for Jill "ICMR-ICSSR Report 198l"and
even the last year-.the'National Health Policy Statement'all of which
emphasise that the health needs of the majority, have to take priority
over sophisticated,centralised,costly, high technology medical services
meant for the minority with the purchasing power.
■4Z?7S(c) LCD & RT
The concept of essential drugs, questions the health personnel
who are supposed, to safeguard, the health of the people; it. questions why •
their prescriptions include irrational, inessential, costly combinations
and often'hazardous drugs. It questions the mpdical establishment for
not demanding bans on bannable drugs, noi’ attempting to ensure and
implement such bans. It. focusses the attention oh the present‘day medical
services- private and government; tho proscription patterns; the gross
lack of accountability to the public or to any medical council. The
doctors bask in the prestige that comes, with tho practice of ’white
man's' medicine.
It is the public that pets them on
* a pedestal (not
far below the one meant, for tho Almighty). In reality, they, like the
drug manufacturers and their representatives arc no better than salesmen;
and medical care is debased into a 'commercial service'and it sells,
even if? the people needing it have to beg, borrow, or steal.
If tho proscription patterns have to bo.based unmodified.
blindly, unchallenged.on the medical text book written by and for the
West - then wo should also ensure that their controls go with them.
There should be registration with the medical council, need to pass
board exams after certain years of practice, medical audit and withdrawal
of medical license for unethical medical practice. If cur . state mechanism
is meant to ensure anything, it is to ensure total safeguard against
those who in the name of medicine, believe in making quick money, and
use their medical license, to exploit the people.
Not merely are such
medical practitioners whoso number is fast increasing an insult to
medical practice, but they set examples for others, so that medicine
has become a "Dhanda" (business) for many. Youngsters bribe, fudge
mark sheets, pay lakhs of capitation fees to .get admission in medical
colleges to join their ranks - while Primary Health Centres lib unstuffed,
unequipped and disfunctions!. Rarely do the prestigious medical establish
ments raise a hue and cry over tho ever increasing medical swindles;
against the decreasing health budget of tho 5 year plans; against
tho drug bans that never como or are never implemented; against health
and drug policies that arc not in the interest of the people.
Myth .II - The drug industry is there not to serve, but safeguard its
own interests. The performance of multinationals in decreasing product
ion of essential and life,.saving drugs, and the double dealing ii giving
biased drug information; their ensuring tho purchase of drug prescript
ions for ones company by gratifying doctors with samples, gifts and
sponsored medical conferences. With loan licensing, products of many •
of the big name companies arc produced by small scale drug outfits
with as much quality control as most other small scale drug companies.
All commercial enterprises serve a purpose, but a few like
drug industry start sharing the role of a healer, server, educator,
benefactor, having touched the dizzy heights of highly technical
mystified science.
M?/th III — The third myth of course is that our heal th policy is
geared to. fulfil the health needs of the majority.
The ^health budget has steadily decreased. It may have been
broken up under different heads but with increasing population and
increased need for health services, health budget should be going up
much more rapidly.
■ ......... -V
Hew has the money boon spent? What are the disparities existing?
What has been the role of the policy makers? • What has happened to the
various recommendations mentioned earlier? The perspective should have
been set when wo attained independence. The direction being pursued now
hasn't changed very. much from the pre-independence period.
The public
has had no.say ip'deciding the kind of doctors it wants trained with its
nonoy and what kind of health facilities.and drugs it needs. ; Such an
intervention by the consumers remained impossible inspite of the numbers
because sc far they have remained unorganized and fragmented.
Focussing public attention on the issue, of essential drugs provides
a platform for organizing the consumers for focussing attention on our
health care services, on our legislations, policies, education and
legal systems.
It is to focus on the role the experts, the committees and policy
makers have played in the past (many of whom are known to have been
bought and sold). It focusses on tho role of consumers and on their
demand for participation in decision making as a majority, for the benefit
of tho majority.
Demand for essential and life saving drugs as a priority is an
exercise in demystifying medicine; it is an exercise in public education,
an exercise in ensuring that public needs guide and influence decision
making. This demand is also an exercise in learning to boycott drug
decisions and policies which are thrust down peoples throats against
their will and against the interest of tho majority.
It is part of a slowly emerging consumer movement, peoples science
movemeict and also peoples health movement. It is an integral part of a
larger process and not a piece-meal demand of a minor rectification.
The politics of health at the concrete level can only be based on
peoples action. As Fritjof Capra points out in the Schumachpr Lectures
'Refusal to take even a single pill is such a political act'. On this
political philosopjsy is based the mobilization for essential and life
saving drugs as a priority.
Just as manufacture, sale and prescriptions of hazardous and irrational
drugs is a oppressive political actj refusal to become victims of this
oppression is a political response.
II.
COURAGEOUS EFFORTS - A Brief Review
The concept of essential .drugs list is nothing new nor did it have
its origins in WHO's Technical Report Series No. 615 (1977) as many believe.
Many efforts had been made prior to this. We just mention few.
CHILE:
As far back as 1973> the Chilian Medical Commission comprising cf
Dr. Salvador Allende had believed in limiting the drugs to those that had
demonstrable therapeutic value and thus 'scale down the pharmacopea'.
.-.11 ends during his short tenure as President quite successfully compelled
the medical profession to servo "basic" rather than profitable needs.
He proposed to ban drugs not proscribed for clients in North America
or Europe.
5/
~=li/378(a) LCD & RT
VJl'I:pt:19.7.'84
5
:
.Within- one week after the taking over of tho military junta on
'ith September 1973 the Chilian doctors who participated in this
. rcvclutionization of medicine, these outspoken proponents of Chilian
medicine based on community action rather than oil drug imports and
drug consumption word'assassinated. Men with much" courageous ideas
oven though they arc for the benefit of tho people, aro seldom
appreciated.
—:-
Sil LANKA:
In 1971 under the guidance of Soneka Bibile, Sri Lanka had formed
the State Pharmaceutical Committee.to launch-its people oriented new
Drug Policy. The number of drugs in the market were slashed down from
2100 to 600 and made available mostly under generic names and obtained
by calling international tenders. Within 6 months there were savings
of about 2rC^ in relation to expenditure incurred earlier.
It is absolutely essential for those of us involved in drug work,
to know how the resistance from multinationals, their governnssnts, v/ith
support from Sri Lanka's own medical establishment forced the Sri Lanka
government, to give into vested interests and revert some cf itsown
brave and correct decisions.
PAKISTAN:
Pakistan's attempts at restricting the drug list to essentials,
with rejection cf unessentials-met with similar resistance from, tho
2 most powerful lobbies in the medical industry 'the drug industry
and tho medical establishment'.
INDIA:
In 1975, the Hath! Committee in India recommended a restricted
essential drug list of 116 drugs which were to be sold under their
generic names. There was no dramatic opposition to the recommenda
tions. They were just very effectively ignored. So much so that
today for interested health and consumer groups no copies of the.
Hatlii Committee recommendations aro available, from the health ministry.
Those recommendations are shrouded in cob-webs. The difference between
tho Indian experience with essential drugs and. that of others is that
the demand for them did not omorgc from enlightened medical profess
ionals arid has till recently remained an official exorcise.
It was
net from people like Dr. Sonck?. Bibile(of Sri Lanka, br, ^afrullah.
Chowdhry and Dr. Nurul Islam of Bangladesh, Dr. Salvador Allende o*
Chile.
MOZAMBIQUE:
-
After its liberation from. Portuguese rule in 1975 the Mozambique
government took some drastic decisions regarding its health and drug
policy. Health was nationalized and private practice banned within
eno month of independence.
Tho number of drugs were decreased from
to 430 medicines in 1977. Essential'<drug31ist was revised
in 1980 and contained only 343 drugs. ONLY THESE DRUGS COULD BE
PRESCRIBED.
.
, .
........... 6/
p-4/378(e) LCD & RT
VH.l;pt; 19-7. ’84
6
The result of streamlined contracts was that the drug prices of many
esscntialjbn^s_cjrn©_j.oi<i to 1/3 of their original prices.
The essenti
drugs became available, to more people in remote areas, net just to the
privileged few. This could be done with the drug import costs th© same
as they were 10 years ago because the selection was more sensible,
li H 0:
The WHO Expert Committee on essential drugs in Technical Report Seri
615 gave the criteria for selection of essential drugs and a model of
such a list. Another report in 1979 was followed by.the Technical Repor
Series 685 which dealt with the 'use of Essential Drugs' and gave the
essential drug list for emergency situations and primary health care.
BANGLADESH;
In June 1982 Bangladesh's Military regime under General Ershad,
promulgated a Drug Policy based;on WHO recommendations. '742 drugs
were banned because of their hazardous and irrational nature. This
of course had been preceded by educational campaigns about rational
drug use by some of the individuals involved in pushing the National
Drug Policy. The January 1982 international conference on Health and
Pharmaceutical Policies was one such attempt organized by Gcnoshasthya
Kendra. Through its monthly magazine"Gonoshasthya Patrika" dealt
with this and other issues systematically. Dr
*
Zafrullah Chowdhury
admits that the Hathi Committee and its recommendations hold great
inspiration for evolving and for implementation of the Bangladesh drug
policy.
In Bangladesh the resected drug list constitutes of 150
drugs. The grading of 15'0 selected essential drugs has also been done
based on location of utilization and level of potential users.
I
II
Ill
12 Essential drugs have been selected for vi 11 age level health
workers.
- Additional 33 essential drugs for Primary Health Care up to
Thana Health complex level.
- Additional 105 essential drugs for use up to tertiary level.
-
There is also a list of 7° supplement ary drugs for restricted use which
after discussion will be compiled to 100.
The heavy pressure being applied to dilute or just scrap this
courageous pro people drug policy, which is ironically very much based
on tre WHO guidelines for Rational Drug use ~ has come from the multi
national drug lobby and the medical lobby. The loudest voice being
from the US based multinationals and from B H A (Bangladesh Medical
Association).
It is openly stated by the lattor that if India can
Allow unrestricted sales of drugs banned in Bangladesh, the drugs must
be safe and wonderful. .After all Indian Medical Establishment with
all its brains and advanced technology can't be wrong - (any way wo
Allow continued manufacture and sales of drugs banned by our Drug
Controller of India and recommended for withdrawal by our export
committees.)
Efforts to gather support for Bangladesh's brave drug policy had
boon made by us right from the beginning aid our efforts continue;
since survival of Bangladesh drug policy is crucial for the people of
Bangladesh and other third world countries including India.
7/
±h£/378(o) LCD & RT
VH/I;pt:l9j7.'S4
ZIMBABWE;
. Zimbabwe's Government has selected 376 essential drugs to be
Public health system. Government will not make foreign
exchange available for importing drugs outside this list.
•'■'uy is tills concept of essential drugs seen as such a bi? threat b^
medical establishment and the drug lobby? The reason is"very obvious
It interferes with the drug companies profit making even though in
reality it benefits more people.
HI •
OUR INITIATIVES IN PROMOTING AWARENESS OF
ESSENTIAL DRUGS
By the end of 1980, tine drug issue,the rational use of drugs and
the.role of non-drug therapy and of systems of medicine etc. had become
an important component of our training programmes• whether it was up
grading- of diagnostic and therapeutic skills of middle level health
workers, holistic health workshops, community health or health care
management training programmes.
By January 1930 a clearly defined strategy of drug work was drawn
up. Tliis was later presented to VHAI's general body for ensuring organi
sational support. This work strategy figures in the special issue of
Health for the Millions - April-June 1981 and indicates the various
levels at which it was felt that intervention was required. (Right from
village hospital to health personnel and -their trainers; policy makers,
drug companies, multinationals and international drug and health action
groups).
In April-Juno 1981 issue of our bi-monthly wo informed our VHAI
members and HEM readers of the concept of essential drugs and gave the
essential drug List meant for Primary Health Caro. The list of irra
tional and ■ hazardous drugs wliich was at that time recommended for being
wooded out, was also disseminated to warn, the health personnel and
health institutions about them.
By 1981 end a serious attempt to draw up an essential drug list
of 50 drugs and recommended management of 10 commonest health problems
was made, based on the invited views and opinions of selected academi
cians, health personnel in the field or hospitals and pharmacologists
etc. (There wore too many disparities in the responses and effort
to comp2! 1 e a very unanimous and coherent result based on these responses
was abandoned. It was found that most health personnel were not
familiar with ths concept of essential drugs and NEC's essential drug List,.
In January 1982, the first drugs workshop 'Drugs Issues and
Feasible Alternatives' was-organized in Pune to bring socially
conscious health personnel, consumer group activists for drug action
together. The Hathi Committee and'WI-D essential drug, lists were
made available to the participants of the first Drug Workshop in Pune
as well to the participants of various training workshops and.organi
zation Development (0D) seminars etc. conducted by VHAI and dissemina
ted amongst various levels of health and. non-healih personnel..
A sub group constituted of doctors and pharmacologists mot during
the course of the workshop to compile a mutually acceptable essential
drug list. (The Pune workshop list - in the comparative drug list
was an outcome of this effort). Soo Annoxuro I.
3-4/378(o) LCD & RT
Vffil:pt; 19.7.'84
:
8
:
Ry August 1982 it was fully realized that an essential drug list
drawn up by us even as a group would not necessarily be acceptable to
health personnel, /nd if while attempts to influence government autho
rities wont on side by side in the voluntary health sector, the accept
ance and implementation of this had to be ensured.
The exercise to draw up a comparative essential drug list was
undertaken for 3 reasons:
1.
To demonstrate that any rational drug policy formulated
had a lot in common,no matter from which country.
2.
That it was not a handful of concerned persons but expert
committees that had drawn up these lists. The fact that
these experts believed in the concept of essential drugs,
we felt would have greater convincing and educational value.
3.
The rationale in making the comparative drug list available
to the individuals in the field and solicit a response from
those informed individuals was to give a better guidelineas well as to involve them in the evolution of a process.
The comparative essential drug list prepared incorporated the
following drug lists:
-
WHD
Hath! Committee
PGI (Fest Graduate Institute list) Dr. V.S, Mafahur
Pune Workshop list
Sri Lanka list
Restricted lists used by ECHO UK and Action Kedeor (both
agencies are involved in bulk purchase of essential drugs for
third world countries).
It was obvious that those essential drug lists would provide gwide—
lines for drug selection for larger medical institutions. But for smaller
health programmes with which I was mainly involved in the course of ny
work, there was a need for a graded essential drug list, based on the
experience, qualifications of the health personnel
- the availability or non availability of other health facilities
specially referrals
— availability of supervision, consultation and on going education
- the gamut of health problems dealt with and the workload
- resources available in terms of finances, manpower, diagnostic
facilities, transport etc.
Effort to obtain graded essential drug lists from Bangladesh,
Sri Lanle, Mozambique and EMRO have been made.
Dealing with Resistance:
The most vocal argument against the concent of essential drus list
by the drug lobby and its supporters is that it is relevant onJXr
the extremely poor countries and not for developed countries nor country like India with the most developed pharmaceutical industry in
tho third world. Thus is far from true since drug lists of many developed
countries are highly rationalized and limited. Prolification of non- ‘
essential drugs is no indicator of development.
•9/
j!-4/378(o) LCD & RT
VHAI:pt: 19.7.'84
In 1982 a request to tie Editor MUIS was made? to:
1) delate the drugs that wore recommended forbeing weeded out by
the Drug Consultative Committee
2) indicate clearly the drugs included in WHO essential drug list,
so as to give a guideline for the readers to help them in their
selection process - by underlining or writing these drugs in capitals
or italics.
This evoked besides a personal response, an editorial in MIMS
where the relevance of the essentia], drug list only for the struggling
poor countries was emphasised. Dr. Halfdcn Mahler, Secretary General
WHO was quoted as saying "that a consignment of antimalarials was
received in a certain country with as much celebration and gaity as
demonstrated at that country's independenco". This was an attempt to
show that the concept of essential drug list is meant only for extremely
poverty stricken and not countries like ours.
This is totally untrue.
Developed countries have made more serious efforts to restrict drugs.
In UK, the 6500 preparations is considered too many by the Rational .
Health Campaigners and^&harles Medawar of Social Audit in his latest
book 'The Wrong Kind of Medicine'. Norway has about 1900 preparations.
The Norwegian authorities have licensed a total of 730 active ingredients.
An attempt to have less of irrational and non-sensical drugs is not
limited to the third world countries but developed countries thcaseives.
Hew long in tne name of 'free enterprise' and so called 'clinical freedom'
will irrational and hazardous drugs continue to be inflicted upon the
people spacially when they are ill, affordable by them at tlie cost of
their actual health care needs being met? -
Today the question is not whether to include or delete a particular
drug, but for health personnel ana people alike to be exposed to and
to internalize the concept of essential drugs, so that they can mala? an
informed choice about essential and unessential drugs.
"The benefits of our huge drugs list are essentially to do with
trade, not health. The advantages of a restricted drug list include
having fewer bad drugs and a reduction in drug induced disease, and
better information about drug use and less confusion about which drugs
to use". (Charles Medawar 'The Wrong Kind of Medicine' page 15).
Dr. John Yudkin who has long been concerned about third world
drug policies says 'the drug companies must not bo permitted to becomo
a hazard to health in the underdeveloped world by f a-iling to provide
information or by drawing scarce resources, away from more effective
projects'.
......... 10/
B-4/373(o) LCD & RT
’ VHAI:pt:l9.7.*S4
IV.
10
:
SELECTION OF ESSENTIAL DRUGS AW CT-EPS FOR
mPLEMENflNG an'essential drugs programme
- WP RECOMMENDATIONS
In order to ensure that an essential drugs programme is adequately
instituted at the National level, several steps are advised:
1. Establishment of a list of essential drugs, based on recommend
tions of a local committee constituted of individuals competent in the
fields of medicine, pharmacology, and pharmacy ns well as peripheral
health yprkers.
2. The international non-proprietary (generic) names for drugs
or pharmaceutical substances should be used whenever possible and
prescribcrs should be used whenever possible and prescribers should be
provided with a cross index on noproprietary and proprietary names.
3. Concise, accurate, and comprehensive drug information should
be prepared to accompany the list of essential drugs.
4, Quality, including stability and bio-availability should
be assured through testing or regulation.
5. The success of the programme is dependent on. efficient
administration of supply, storage and distribution at every point from
the manufacturer to the end user.
Government intervention may be
necessary to ensure the availability of some drugs.in the formulations
listed,and special arrangements may need to be instituted for the
storage and distribution of drugs that have a short shelf life or
require refrigeration.
..
.
6. Efficient management of stocks is necessary. To elinrinate
waste and to ensure continuity of supplies, a Procurement Policy should
be based upon detailed, records of turnover. In some instances- drug
utilization studies- may contribute to a better understanding of true
r equirements.
7. Need for both clinical and pharmaceutical research under
local conditions.
Criteria for selection of essential drugs:
ESSENTIAL DRUGS 'ARE THOSE THAT SATISFY THS
HEALTH CARE NEEDS OF TIE MAJORITY OF TIE
PEOPLE. THEY SHOULD-THEREFORE, BE AVAILABLE
/fl1 ALL TIMES IN ADEQUATE AMOUNTS AND IN THE
APPROPRIATE DOSACS FORMS.
O-^Y..f-.tose _drugs should to,selected for which sound and-adequate
Jta on efficacy and safety are available. And from adequate clinical
studies and for which evidence of performance in general use in a variety
of medical settings has been obtained.
?~4/37-3(o) LCD & RT
VHAI:pt:l9.7.'84
11
:
Each selected drug must be available in a form in which adequate
quality, including bio-availability can be assured. Its stability under
tho anticipated conditions of storage and use must be established.
The choice between 2 or mono drugs which are similar in all tho
above respects, should be'based on careful evaluation of their relative
efficacy, safety, quality, price (of the cost of taking a full course
and not merely tho unit cost) and availability.
Other criteria to be kept in mind are pharmacokinetic properties
and availability of facilities for manufacture or storage.
Formulations should be single ingredient drugs. Fixed dose
combinations should be acceptable only when a combination provides a
provon advantage over single compounds administered separately in
therapeutic effect, safety or compliance.
Selection of Dosage forms;
' Tablets are usually loss expensive than capsules, but wliilc
the cost factor should be taken into account, the selection should also
be based on a consideration of pharmacokinetics, bioavailability,
stability under ambient climatic conditions, availability of excipients
and established local preferance.
- A range of dosage strengths is provided from which suitable
strengths should be selected on the basis of local availability and need.
- The use of scored tablets is recommended as a simple method
of making dosage more flexible.
- There is a need to periodically revise and update tho list.
But frequent and extensive cliangos are clearly undesirable since they
result in disruption of channels of procurement and distribution and may
have implications for the training of health personnel.
Provision of information on essential drugs:
•Concise, accurate and comprehensive information on tho use of
essential drugs should be available to all proscribors in a format that
is appropriate to their responsibilities and levels of training.'
Drug information sheets for the doctors by WPD's Export Committee
on tho selection of essential drugs has been compiled in the following
format:
1. International Nonpropriotary Name(INN) of each active
substance, and recommended dosage form.
2. Pharmacological information: brief description of pharma
cological effects and mechanism of action.
3.
Clinical information:
3.1
3.2
Indications: whenever, it is.thought appropriate, simple
diagnostic criteria should be provided.
Dosage regimen and relevant pharmacokinetic data;
12/
^-4/3?8(-) LCD & RT
VHAI:pt:l9.7.'S4
12
:
Average dosage and range for adults and children
Dosing interval
Average duration of treatment
Special situations, eg. ronal, hepatic, cardiac
or nutritional insufficiencies vzliich require either
upward or downward dosage adjustments.
3.3
Contraindications
3.4
Precautions (reference to pregnancy, lactation etc.)
3.5
Adverse effects (quantitate by category, if possible.
3.6
Drug interactions (to be mentioned only if
clinically relevant: drugs used for self-medication
should be included)
3.7
Overdosage:
3.7.1 Brief clinical description of symptoms
3.7.2 Non drug treatment and supportive therapy
3.7.3 Specific antidotes
3.2.1
3.2.2
3.2.3
3.2.4
4.
V.
Pharmaceutical information.
TIE RATIONALE OF ESSENTIAL DRUGS
Tho concept of essential drugs is the backbone of any Rational
Drug Policy. Tho repercussions of acceptance and non-acccptanco of an
essential drug list arc too many. If there is one unanimous demand which
has to come from us people it has to bo tho selection of an essential
drugs list based on the health needs of majority, for priority to bo
given to
- ensuring their production
- ensuring their efficient distribution
— ensuring appropriate stocking of pharmacies with those drugs
- ensuring appropriate drug prescription and practices to be
based ch.those accepted drugs.
Since 46% of tho drugs marketed are obtained ever the- counter without
a prescription (according to WIN Drug Utilization study) it is obvious that
altered or improved 'proscription practices' alone cannot alter tho drug
consumption patterns. With tho degree of self prescription of drugs,
selection of essential over unessential drugs can have a groat impart T
Specially if this is associated with a total boycott by tho consumers
and health personnel, of highly irrational and .hazardous drugs-as was
done by Swedish doctors.
The boycott led by Dr. Oils Hansson, Paediatric
Neurologist in the international campaign against clioquinol, moxaform
related drugs was later joined by doctors of Norway, Denmark - totally
by over 3000 doctors and veterans.
The implementation of essential
drugs list needs to be done urgently and the reason why it is so crucial
are given below:
A.
Existing low priority to essential drugs needed for' tho priority
health needs and the deteriorating trend:
The myth of 'pill for every ill' detracts from tho real health
issues being dealt appropriately. Tho majority of drugs manufactured
arc unessential and not based on the health neods of our people. Of the
1260 croros worth of drugs manufactured in India in 1979-'80,only Rs. 350
crores worth of drugs wero'essential and life saving drugs, the rest wore
mainly non-essential drugs.
13/
S-4/378(o) LCD & RT
Vfu'J:pt: 19.7.’84
13
:
The following figures speak for themselves:
Table
Category
I
1978
1980
4.5$
3.6$
II
16.7$
13.2$
III
67.1/c
68.6$
IV
11.7/
14.6$
Source:
FMRAI News
July 1984.
The production of category I drugs i.e. essential and life
saving drugs and Category II drugs (essential drugs) is showing a
declining trend according to Ministry of Petroleum and Chemicals and
Fertilizers.
Production of antimalarial, anti-TB, antifilarial and anti
leprosy drugs have been trailing far behind the estimated demand and
while demand has increased the actual production has been falling.
In fact, production of the antimalarial Chlorcquin, and tho anti tuber
culosis PAS, INH and thiacetazone fell short of estimated demand by
about 84, 50, 44 and 70$ respectively in 1979- '30, except for a small
increase in INH production for all those drugs decreased further in
198O-'81.
Estimated demand Production in tonns MT Estimated Production
1979-80
79-80
81-82
80-81
82-83
Antinalarial
Chlcroquin
Amodiaquin
250
40
35.16
38.49
34.62
23.15
58.96
26.02
70.00
33.00
Antitubercular
PAS & Salts
INH
Thiacetazone
Streptomycin
600
200
40
300
481.78
112.43
12.55
220.16
405.46
129.20
8.44227.33
261.97
110.40
13.98
255.45
290.00
128.00
25.00
266.00
Antifilarial
DEC
30
21.57
18.99
16.43
13.00
Antileprosy
DDS
28
16,20
21.05
25.61
30.00
Ref:
Dr. W.Y. Pane - Why don't our drugs match our diseases Scioncc Today■ - October 1982.
....14/
S-4/378(c) LCD & RT
VHj'J:pb:19.7.'84
14
:
Demand Projection for Bulk drugs for the period. .19722^2-^.2—Lr:4~'A5_.
E sij unzxt ed. R c cjiiix* cmcix c
B 3.s o
79-80
80-81
81-82
82-83
83-84
81-85
250
40
275
46
300
53
335
61
365
70
400
SO
Anti Tubercular
PAS
INH
Thiacctazone
Streptomycin
600
200
40
300
630
240
42
330
660
290
44
363
700
360
400
730
415
4£>
440
770
poo
50
485
Ant ifi larial
DSC
30
33
36
40
45
50
Anti leprosy
DDS
28
32
37
45
50
5o
Antima!aria!
Chloroquin
Amdiaquin
■
&
The Indian Pharmaceutical Industry Problems ani Prospects.
P.L. Narayan, NCAER Study
National Council of jjrolied Economic
Research - January 1984.
Ref:
- IGMR and ICSSR study on Alternative Strategy had indicated the
grossly inadequate drug production for IB and. leprosy which happen
to be our priority health problems.
With half of the TB patients
of the world in India our production of IN® was less than 1 /3 of the
minimum requirement.
- Tha Malaria deaths in Rajasthan-were not merely due to drug
resistance and cerebral malaria, but due to non-availability of
chlorcquin even at certain government PHCs. The estimated require
ment and the actual production are getting further apart and reliance
on imports is resulting for drugs that aro so routinely noedod.
Chloroquin imports in tons
1979-'80
1980 - '81
1981 - >82
Production
Imports
Production
Imports
Production
Imports
35.2
52.8-
34.6
71.8
59
166.3
Ref:
5K4BR Report - The Indian Pharmaceutical Industry.
SJ'Jpl^d’^c^nomic Research.
15/
S-4/378(e) LCD & RT
VIVI: pt: 19.7.'84
:
15
- There are an estimated 60 million iodine deficiency cases
of goitre in India, It is known that children of' iodine
deficient mothers are known to bo born as cretins, deaf,
mutes and mental, subnormality.
■The simple technology of production of iodized salt is known.
Merely 50 paisa worth of iodized salt can make all the diffcronc
between a child being normal and subnormal,■
We still produce only 20$ of the iodized salt required.
Required amount of iodized salt is - 7 lakh tons
Amount produced
- 2 lakh tons
Amount sent to Nepal
- 1 lakh tons
Amount left for utilization for
tho 60 million goitre cases
- 1 lakh tons
When adequate production of an essential low cost item'like
iodizod salt for a National Goitre Programme cannot be assured,what
happens to production of the essential drugs for non priority national
programmes can very well be imagined.
In Konya, in a pilot project funded by D/iNIDA and SID A, supplies
of drug kits containing 39 drugs in 15 rural districts has increa. ed the
accessibility of essential medicines for the rural population from
1Qb to 4$.
B.
DPCO and its negative impact on Production of Category I and II ckpu
Under D, CO (Drug Price Control Order) the mark up on Category I
drugs is limited to 4<$ and that on Category II is 60/. Producing category
IV drugs because of tte high mark up allowed are therefore definitely most
profitable.
For the decreasing priority being given to essential and life saving
drugs DPCO is therefore blamed. With the decontrol of prices of 75/ of
the drugs as is being recommended by the drug lobby and its supports, a
further switch bto production of mere profitable unessential drugs is
imminent. If government is serious about ensuring that essential drugs
are sold at a reasonable price - this can be done by doing away with taxes,
C•
Poor performance of multinationals in production of essential drugs:
The'outright, calculated neglect of the priority drug, needs of
the majority is well known. The following table speaks volumes. (See
Annoxuro II r- Production of Essential Drugs by Multinat ionals and Organised
Sector)
D.
Dilution of FERA Companies - an invitation to more formulations:
With the dilution of foreign equity shares to 40/, various
concessions arc being granted to the FERA companies so that bulk to
formulations ratio will be increased from 1:5 to 1:10. With the drug
production pattern as it is, we can look forward to more formulations
and more unessential drugs irrelevant to our <apcoplos health need.
Bulk production by foreign sector for 1982-'S3 was Rs. 55 croros worth;
the formulation turnover according to 1:5 ratio should not have exceeded
Rs. 275 croros, however, Rs. 515 crores worth of formulations ’were
produced, i.e. more than 1:10 ratio when only 1:5 was allowed.
16/
5-4/378(0) LCD & RT
VHAI:pt: 19.7.'84“’
16
E.
Rational uso of scarce resources:
i) Wastage of scarce foreign exchange: India with its level of
indebtedness to IMF World Bank, IDA etc., can hardly afford to sqandcr
its scarce foreign exchange for importing inessential drugs.
ii) Inessential vs basic health needs: Worse still is the
enforced wastage of scarce resources of the poor on useless nonsensical
drugs, when they can hardly afford adequate food and clothing and bare
essentials. When the percentage: of people, below or around the poverty
1 1 no happen to be around 60 — 70
*
of a country's population - the very
production and heavy promotional- of costly irrational and hazardous drugs
is criminal.
A strong public opinion alone can ensure withdrawal of
such drugs, with priority being given to essential and life saving drugs.
iii) Inessential vs essential drugs: Often inessential drugs
arc bought at the cost of specifically needed essential drugs. For the
ignorant majority, the difference between the therapeutic value of a
costly tonic, vitamin, digestive ensymes, antipyretic and much needed
specific drug eg. antiasthmatic, antibiotics etc.
all written in the
same proscription - does not exist. This was shown by Veena Shatrughana1 s
study of Prescription writing and drug consumption. By ensuring
priority availability and prescription of essential drugs, we woulu. be
contributing to preventing the wastage.
iv) Economics of scale increased: If essential drugs wore given
priority in production, through sheer economics of scale, the production
cost wuld decrease for the manufacturer and thus the consumer.
v) Bulk purchase: An essential drug list can ensure bulk purchase
of selected essential drugs, which can cut down drug costs.
F.
Influencing market demand and thus the Drug Production pattern in
favour of essential drugs:
If the concept oi essential drug list was widely propagated, accented
by choice.cr by legislation, this would necessarily influence the
prescription pattern and hence the drug demand in the market. This would
definitely alter the drug production pattern towards essential drugs.
G.
Decrease drug misuse and over use:
This can bo done with identification of• drugs which arc - thera
peutically effective, safe, easy to administer, and of appropriate cost
preferably single ingredient well tried drugs. The use of drugs vrhich
are of doubtful value, costly, irrational and hazardous drugs should bo
avoided. Majority of the drugs available aro combinationidrgga. This
increases costs as these drugs are often in subtherapeutic’and irrational
dosages. According to Halfden Mahler, 9<$ of drugs in the developing
countries are non essential.
H.
Preventing Iatrogenesis (Drugs induced health hazard):
As long as potentially hazardous drugs with very'high risk
(compared to) benefits ratio are misused and overused, unwarranted high
incidence of iatrogenesis1 is bound to occur.
■ ;
'
■ " .
’
.17/
E-4/378(c) LCD & RT
VHAIjpt: 19.7.'84
17
:
In USA where the drug control and the prescription practices
are much bettor controlled, the incidence of iatrogonesis is very high.
One in 5 hospital admissions are known to be due to iatrogenesis. In
India we have such a high degree of self prescription, prescription
writing by unqualified health personnel and by qu.nl i f-i ed personnel who
are made highly biased by drug representatives. This along with poor
drug controls ensures drug misuse, overuse and iatrogenesis. Most
cases of iatrogenesis are not diagnosed in India. This of course docs
not imply that they don't exist.
Most of the combination drugs have 2 or more ingredients. _ It is
known that with consumption of over 6 drugs compared to 2, chances of
drug interaction increase by 40/ as compared to 5'/^ •
I.
Drug Information for health personnel and consumers possible:
With 30,000 drugs in the market it is impossible not to be
confused about them. A doctor may be familiar with the drugs he or she
uses routinely. Unfortunately ho or she cannot be so with the various
brands used by others. Their prescriptions are often taken from one doctor
to another by critically or chronically sick patients.
Confusion abounds, sinco majority of the health personnel have no
access to pharmaceutical index to figure out what drug lias been given.
Majority of the drugs in the market, are combination drugs. Lack of
familiarity with the contents and their dosages makes matters worse.
If prescription practices for the majority of the health problems could
be based on essential drugs? Relevant drug information about their
relative cost, dosages, indications, contraindications, side effects and
toxicity could be made available to health personnel and consumer
caution be ensured?
Studies also indicate that it is impossible to remember details
of even 1C0 drugs in routine practice. Ensuring that these prescribed
drugs are the ones that people need and not what aro'most heavily pushed
by the drug companies because of their profitability, is our responsibility..
Focussing on all aspects of essential drugs and rational drug use in
medical education wopld ensurelheir bettor use which would be bettor
for the nation and the patients.
J.
Ensuring better quality control:
There are 30,000 formulations in tho market. Most of them arc
combination drugs and one in 5 drugs in the market is substandard. With
a lesser number of drugs in the market which are single ingrocient drugs
quality control can bo better streamlined.
Making profits by promoting
unessential drugs is crazy, but to make inadequate number of essential
drugs available, with even these being substandard, is really unacceptable.
K.
Ensuring generic proscribing:
Generic prescribing is recommended by WHO itself as it cuts down
drug costs.
Pharmacology input during medical education, nomenclature used
in medical literature and medical journals is based entirely on generic
names.
18/
u/^/b(e) LCD oc i-.T
VHAIipt: 19.7.*34
:
18
:
With a restricted essential drug list generic prescribing can
definitely be ensured. The pharmaceutical industry and government drug
control authorities would have to take greater responsibility to ensure
quality control AT ALL LEVELS. Brand, name prescribing is no solution
for substandard drugs. Brand names do not prevent spurious drugs enter
ing the market as most spurious drugs arc imitations of well known
brands. Name of the specific drug house can bo -written if it is felt
absolutely necessary. Generic prescribing is possible with single ingre
dient essential drugs which arc quality controlled.
L• ■
Subsidizing costs of essential drugs:
With restricted list of drugs meant for the health needs of
the majority, subsidizing is possible by removing sales tax, excise duty
and octroi for these. Any loss in the taxes can be compensated by
increasing taxes on cigarettes, alcohol and other such anti-health
products or more so on luxury items meant for the rich. In conclusion,
demanding an essential drug programme is aimed at focussing attention
and giving priority to health needs of the majority.
CONCLUSION/SUI^/RY'
Demanding priority production and distribution for essential
■ drugs is accompanied by demand for a just health care delivery system.
We know that a just health care delivery system cannot exist in isolat
ion in a socially unjust system.
Demand for essential'drugs before un
essential drugs is accompanied by demand for employment, fair wages}
food, water, sanitation and all that goes to ensure good health. Our
fight for essential drugs and health care as a fundamental right of
every Indian, specially the deprived sections is a fight against the
injustice of the present socio-political system, which in reality
accepts this deprivation of health and basic health care as a normal
phenomenon.
Sj—3 /Oy O /
Id
-’-x
VH;i: pt: 19.7.134 ' ’'
Annoxuro III
PRODUCTION OF ESSENTIAL DRUGS BY 1RRTINATI0NALS /ND ORGANIZED SECTOR
Name of the firms
IN
PAS
T CT ACIT AZONE
ETH/MBUTOL
RIF/MPICIN
STREPTOMYCIN
Abbott
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil.
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
ACCT
Hoechst
Nil
S.K. & F.
Nil
Nil
Nil
Nil
Searle
Nil
Nil
Nil
Nil
Nil
Nil
Sandoz
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Roche
Parke-4) avis
Nil
Nil
Nil
Nil
Nil
Sarabhai
Yes
Nil
Yes
Yes
Nil
Beohringor Knoll
Nil
Nil
Nil
Nil
Nil
Glaxo
Nil
Nil
Nil
Nil
Nil
Yes
3, Marek
Nil
Nil
Nil
Nil
Nil
Nil
Ciba-Giegy
Nil
Nil
Nil.
Nil
Nil
Nil
Pfizer
Yes
Yes
Yes
Nil
Nil
Yes
Warner
Yes
Nil
Nil
Nil
Nil
Nil
Burrough Wellcome
Nil
Nil
Nil
Nil
Nil
Nil
German Remedies
Cynamid
Ethnor
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Yes
Nil
Nil
Nil
Nil
Nil
Yes
Nil
in India, by J.S. Majumdar; prepared for the Drug Workshop in Jaipur, organized by V
For sharing this endeavour, we are grateful to the following
for thoir help and moral support in compiling the Essential
Drug List,. ■
— -Prof,-M M S 'Ahu-.ja./Hepd Departinent of Medicine, ..A- -I- T M 3.
(Tem'pOral’y-Advisor)- The use of Essential Drugs,Technic.al
Report Series 685, WHO.
Dr V S Mathur,PGI Chandigarh, Editor Drug Bulletin
for i) providing the graded EMRO list for which he was
a consultant
ii) for providing the PG I drug formulary
iii) for b^ing with us at Pune Workshop -January 1982
where Pune Drug List was finalized.
Dr Qasem of Gohosasthya Kendra, for having kindly complied
to our request to send the graded Bangladesh drug list.
Dr Joel Fernando, Medical School, Sri Lanka for providing
the Sri Lanka drug list.
Friends in Echo and Action Medeor who sent thoir li
-ts.
*
Late Mr John Agacy, Secretary Low Cost Drugs and Rational
Therapeutics, who tediously typed the first draft of the
Comparative Essential Drug list in alphabetical order.
Alphonse our Secretary of Low Cost Drugs and Rational
Therapeutics for typing this comparative drug list based
on WHO format.
77 /-?
Voluntty Health Association of I«di»,
C-14, Community Centre,
Safdarjung Development Area,
New Delhi-1 IWlf.
7.84
?Y HEALTH CEI&
47/i.b-irst . iou.
Marks Road
BANGALORE ■ EGO 001
Graded ZEssential Drug List
3 xp 1 a n a t o ry Note:
These are the guidelines to help Community health progra
mmes and health institutions draw up their own essential drug
list.
This is a compilation of various drug lists and it empha
sises the concept of Essential drugs. For those believing in
and for those involved in alternative health care, the concept
of Essential drugs is an integral part of health work.
The format used for this compiled list is based on WHO's
Essential drugs list , Technical Report Series 685. An outline
of it is given. It should^be noted that certain drugs are
repeated as they are used more than one. disease entity.
The various drug lisle as they appear in the compiled form
are as follows:
EMRO(Eastern Mediteranean Regional Office)- WHO
List A - for Sth class passed
List B - for that are class 10 passed and have had training
Bangladesh drug list;
Category I - for village level workers
Category II - for Primary Health Cure.up to Thana complex lev<al
CMC Christian Medical Council list - Contact He.63,August
1981, "Getting Essential Drugs to the People"- Stuart
Locost;- Low cost standard therapeutics a collective volun^a&y
enterprise for rational therapeutics
C/0 Amr.l, G P 0 Dox No.7, Vadodara 390001.
PC:Essential drug list drawn up by sub-group dealing with.
this at VHAI's Pune Workshop "The Drugs Issues seeking feasible alternatives".
PG I? Formulary of Post Graduate Institute of Medical
Education and Research.
SL:Sri Lanka graded Drug list included here is list of
drugs recommended for doctors incharge of Peripheral
health centre.
G:.Gambia restricted drug list based on their national
formulary.
E^ho
An English NGO supply equipment and drugs to Charity
Hospitals overseas.
AM:-t ’
Action Medecr. Qur humble recommendations
A >
for trained village health worker level
B )
for trained Paramedic or middle level workers
c
)
for doctors involved in primary health care
Those drugs included in the Hath! Committee have been
underlined. This drug list is meant i'o ’be a guideline to help
health care institutions in the voluntary health sector to
select their own essential drug list. It is up to us to show
it to the government aX Our medical colleagues who believe in
commercialisation of medical care that good health care does
not necessarily depend upon the length and variety of the
d rug s us ed .
It is extremely difficult to go against the current created
by the market forces. It is a true test of our conviction and
our capability to eonviaice others.
* - Alternative substitute from the same therapeutic group
can be selected based on comparative dost and availability of
equivalent products, eg. Hydrochlorothiazide: any other thia
zide type diuretic currently in broad clinical use.
lumbers in the Paren thesis following the drug names indicat
1) Drugs subject to international control under the Single
Convention on Narcotic Drugs(1961) and the Convention on
Psychotropic substances(1971)
2) Specific, expertise, diagnostic precision or special equip
ment required for proper use
3) Greater potency
4) In renal insufficiency, contraindicated or dosage adjust
ments necessary.
5) To improve compliance
6) Special pharmacokinetic properties for purpose
7) Adverse effects diminish benefit/risk ratio
8) Limited indications or narrow spectrum of activity
9) For epidural anaesthesia
Letters in the parentheses following the drug names indi
cated the reasons for the inclusion of compelementary drug
When
A.
drugs in the main list cannot be made available
When
B.
drugs in the main list are known to be ineffective or
inappropriate for a given individual
For
C.
use in rare disorders or in exceptional circumstances.
The criteria of selection of essential drugs,
Steps to be taken bo implement such a programme.Provision of
information on essential drugs as recommended by WHO have been
dealt with earlier. In the text of the paper the format of the
drug list is as follows:
Revised model list of Bssential Drugs - a WHO Expert Committee
Report - Technical Report Series
635
1. anaesthetics
1.1 general anaesthetics and oxygen
1.2'Local anaesthetics
2. Analgesics, antipyretics', nonsteroidal antiinflammatory
drugs and drugs used to treat Gout.
2.1 non - opioids
2.2 Opioid analgesics and antagonists
5. Antiallergics
4. Antidotes and other substances used in poisonings ■
4.1 general
4.2 specific
5. Antiepileptics
6. Antiinfective drugs 6. 1 anthelmintic drugs
6.2 antiamoebic drugs
6.3 antibacterial drugs
6.3.1 penicillins
6.3.2 other antibacterial drugs
6.3.3 'entileprosy drugs
6.3.4 antitub c-rc.ul os is drtigs
6.4 antifilarial drug's
6.5 antifungal drugs
6.6 antileishmaniasis drugs
6.7 antimalarial drugs
6.8 antischist os omal drugs
6. 9-antitrypanosomal drugs.
7. Antimigraine drugs
8. Antine©plastic and immunosuppressive drugs
9. Antiparkinsonism drugs
10. Bleed,,drugs affecting the
10.1' antianaemia drugs
10.2 anticoagulants and antagonists
11. Blood products and blood, substitutes
11.1 nlasma substitute
11.2 plasma fractions for specific
11.5 plasma substitute.
uses.
12. Cardiovascular drugs
12.1 antianginal drugs
12.1 antiarrhythmic drugs
12.5 antihypertensive dru,gs
12.4 cardiac glycosides
12.5 drugs used in shock or anaphylaxis.
15. Dermatological drugs
15.1 antifungal drugs
15.2 antiinf ective drugs
15.5 antiinflammatory and ant ipruri.„ .
...
. ..
tic d rue s
15.4 astringent drugs
15.5 keratoplastic and. keratolytic
15.6 scabicides and pedi-r- ‘ ’'.drugs.
culicides
14. Diagnostic agents
14.1 ophthalmic drugs
14.2 radiocontrast media
15. Disinfectants
16. Diuretics'
17. Gastrointestinal drugs 17-1 anacids and other ahtiulcer <
17.2 anti era et ic d rug s
ru° s
17.5 antihaemorrhoidal drugs
17.4 antispasmodic drugs
17.5 cat hart ic d rug s
17.6 diarrhoea,-drugs used in
17.6.1 ant id Larrhoeal(sympt ornat ic
17.6.2 replacement solution, drugs.
18. Hormones
18.1 adrenal hormones and synthetic
18.2 androgens.
substitutes.
18.5 estrogens
.. ...
18.4 insulins and other antidiabetic
18.5 oral contraceptives.
agents
18.6 ovulation inducers
1§.7 progestogens
18.8 thyroid hormones and antithyj&id-'
13. Immunologicals
19.1 Sera and immunoglobulins
19.2 vaccines
1V9.2.1 for universal immunization
19.2.2 for specific groups o'. indivi20. Muscle relaxants(peripherally acting) and choline- duals.
st erase inhibitors.
21. Ophthalmological preparations. 21.1 anti infective agents
21.2 antiinflammatory agents
21 .5 local anaesthetics
21.. 4 mi ot ic s
■ 21.5 mydriatics
22. Oxytocics
21.6 systemic preparations
25. Peritoneal dialysis solution
24. Psychotherapeutic drugs
25. Respiratory tract,drugs acting on the 25.1 antiasthmatic 7 .
25.2 antitussives
drugs
26. Solutions correcting water electrolyte and acid-base distui26.1 oral
bonces.
27. Vitamins and minerals. ^6.2 parenteral
0oraparative Essent ial Drug List
Ljs1 Ljs t JLow PU PG I SL G
Main List
Complementary List
Route of administration dosage
...___ _ ______________________ ______ ________forms and strengths
Emi 0 INC Cos 5
1. Anaesthetics
1.1 General anaesthetics and Oxygen
ether,anaesthetic(2)
inhalation
thiopental(2)
powder for injection,0.5g,1.Og
(Sodium salt) in ampoule
1.2 Local anaesthetics
.
*Lidocaine
.5% inj, 1,2(hydrochloride)in via L
inj.1%, 2% + epinephrine 1:100000
topical forms 2-4 (hydrochlol-ide^3 1
2. Analgesics,antipyretics, Nonsteroidal anti infl animator Z
Drugs and drugs used to treat Gout.___
2.1 Non- op i o id s
acetylsalicylic
tablet 100-500mg, suppository,
5O-15Omg poed Aspirin
* ibuprofen
tablet 200mg
indometacin
capsule or tablet 25 mg
paracetamol
tablet 100-5OOmg,suppository 100m □*
_
+ Syp
3 AM £
c
I II
c
c
B
A
•
A
•
2. 2. 0Pio.id analg esic s .and _ ant agonists
(phenylbutazone)/Oxyphenbutazone
morphine(l)
inj 10mg(sulfate or hydrochloride )
in 1 ml ampoule
pethidine Hcl 5ml/ml
3. Antiallergics
*chlorphenamine
—...........
eoiaiephrine
x
■
tablet 4mg(maleate)
inj 10rng in 1ml ampoule
inj 1mg(as hydrochloride in 1ml
ampoule
*
i
i
A
*
1
.
•A
•
Main List
■
■
't
Complementary List
Boujbsr'Qfiadiiiinistration dosage
forms and strengths
Lis Lis'
A B
Ee ro
4. Antidotes and other substances used in poisonings
4 . T Cr'e neral
charcoal, activated
Powder
4.2 specific
atropine
.
'
inj' 1 mg(sulfate)in 1ml ampoule
diazepam
inj 5mg/ml in 2mT ampoule
5 . Ant iep ileot ic s '
phenobarbital (1)
tablet 5Omg,1OOmg,syp 15mg/5ml
capsule or tablet 2.5mg, 10Omg (sodium,
,
inj 50mg.(sodium salt/ml in 5ml v?atT )
rphenyt .in
lnx..Eaxalfi.sdiyda.LH?t hi_)
6.
drugs
1 b. • ,
•
' ■' Antiinfective
--- —
J J -- ■ X
6.1 Ant»helmint.ic drugs
? ; m^lendhzole
tablet lOOmg
.piperazine
.
.
tablet 500mg(citrate or adipate)
senna .tablet Xlevamisol)'II tablet elexir,
.
_
Elexir or syp(as citrate)equivalent!
t pt rachl or el'iyl in e (Hat hi)
to 500mg hydrate/5ml
6.2 Antianio& ic drugs
•
.. chloroquine '
"■
tablet 200mg(as phosphate or sulfate
dilbxand.de
tablet 5OOmg(furoate)
metronidazole
tablet 2OO-5OOmg
...
.. £.eiiyr0 emetine(B) v 1 ,7) inj 60mg(hydrochloride)in 1ml ampot Le
furazolidine
_
Pt.hg.lyl. smluhathiazole</M.4:>}
r
1°’'' PUI GI
C0£ t
§
SL G E ] AM A I II1
A
A
B
B
*
C
c
•
.
A
•
B
•
•
•
B
B
•
•
B
inj 60mg
i .
1
1
Route of administration dosage
forms and strengths •
A
ID
.Emro
6.5,
*ampleillin(4)
b enzathine b enzyIpenici11in(5)
f ortified • b.erizyl penicillin
-bensy.loer
phenoxymethyl p.ehic ill in
procaine benzyl penicillin( 7)
Capsule or tablet 25Omg,5OOmg
(annydrous)I
powder for oral suspension 1 25mg
(anhyd rous)/ 5ml
powder for inj 500mg(as sodium
.It) I in vial
inj 1.44mg benzylpehcillin
procaine benzyl penicillin 30000
u/ml + benzyl
pencillin 10000 u/ml
powd.er for inj 0.6g
IziLlion IU) 3.0g(=5millionIU^(as
sodium or potassium salt)in vial
tablet 250mg(as potassium sa.lt) I
powder for oral suspension 250mg
(as potassium salt)/5ml
powder for inj 1g(=1million IU)
3g(=3 million IU)
6._ Antiinfective drugs
6.3.2 other antibacterial drugs
*chlo-rajnphenic ol (7)
capsule 250mg
powder for inj 1g(as sodium succilnati)
in vial
erythromycin
capsule ortablet 250mg(as lactobionate)/5ml
powder for inj 500mg(as lactobio-|
nate) in vial
inj 10mg,40mg(as sulfate)/ml in
2ml vial
tablet 2OO-5OOrag
PGIiSL
Main list
' 'Complementary list
-Route Of administration-dosage
forms and strengths
jist nisi CMC Low
B
A
( ost PUJ GI
.Sil 12_
zi
B
SJ G E AM C I
' ,
'
,
*Su1 -fad imi d ine(4) (sulphad-iazine)
inj 500rng in 100ml
Suppository 500mg, 1g
tablet 500mg,oral suspension
inj 1g (sodium salt)in Jml ampoule
sulfapethoxazole+t.ricethoprim(4)
*
■.
tablet 100mg+20mg,400mg+80mg
tet racycline(4)
*
■
, b,
■" capsule or tablet 250mg(hydrochior .de)
doxycyline(i) (5>6)
capsule or tablet -100mg(as hydroch
loride)
inj 100mg;(as hydrochloride )/5ml in
nitrodurantoil.(A. B) (4.7) tablet 100mg
ampoule
Hydroxyquinolines :
,
Furazqlidine
100mg tablet
> ■
“6-! 3 • 3 Antileor ^sy c rugs
clofazimine
. capsule 100mg
dapsone ■
tablet 50mg,100mg
rifampicin'
;
.
capsule or tablet 150mg,300mg
■' ■"
6.3.4 Antituberculosis drugs
ethamt^utol
. •
tablet 100-5 00mg( hydrochloride)
isoniazid
pyrazinamid'e
rifampicin
streptomycin ,;(4)
thidacetazone^isoniazid
.
II
A
B
8
■
C
A,
•
•
•
c
!
tablet 100-30Omg
B
tablet 500>jig
capsule or tablet 150mg,300mg
powder for inj 1g(as sulfate) in vial
tablet 50rag+1 OOing, 150mg+300ng
C
c
•
i
i
B
Thiac eta zone' '
'
6 i4 -.nt if ilari aid rug s
dietbylcarbamazing tablet 5Or.ig(citrate)
6.5 Ant if ary, al drugs
nystatin
'
.................................... tablet 500000 IU
n
i
*0
i
Cor.pl e... ent ary list
6.6 Rnt ileishaanias.is
s od iun st ib ogluc onat e
'■pent amid i ne
. .. p. ..
Rout e”"of’ adai'nTst’rat' 1'on~1 osdffe
forms and strengths
L i stjL 1st SMClow'
W
Gos: PU?GI SL
inj 33% equivalent of 10% antimony
in 30nl
powder for inj 200mg in vial
tablet 150i~g(as phosphate or
. syrup 50mg(as phosphate or sulfate)
. ~
/5ml
tablet
^nb(§alg'ho§?hSte^
pri .aquino
;quinjne
;
•
tablet 300mg(as bnsulfate or
inj 300rng(as diSy^r‘3cfiloride)/
ml in 2„:1 ampoule
pyran. et ha—ine
sulfadO7rine+pyri."ietha.~ine(B) tablet 5OOrag+25ng
7. Antimigraine drugs
ergotamine(5,7)
■
' '
tablet 2„'.g(as tartrate)
10. Blood ,drugs affecting the blood
10.1 An-uianaemia drugs
ferrous salt .1
tablet equivalent to 60ng.iron
""
----(as sulfate or fumarate)
oral solution equivalent to 15mg
iron(as sulfate)in 0.6ml
tablet 1mg
folic acid(2)
inj 1ng(as sodium salt)in 1:?.l a.ujoul
*hyd roxoc obala:..in(2),
inj 1r.g in 1nl ampoule
• *
iron d ertran'(.8) (5)
inj equivalent to 50ng iron/ml
in 2:.'il a.-poule
' '
12. Cardiov .-gscular drugs
12.1 .'jTUinag inal drugs
'Izcoxyl- trinit rat;
tablet, (sublingual )0.5mg
td W
6.7 ,.ntr~'.a.larial d.rugs
^lSil^prp£.uinQ.
6,
ientary list
. Route of administration dosage
List IL;
List CMC.low
forms and st engths
B |
C os'
Er:ir<
ro
t ablet(s ub1ingual)5og
tablet 1Oog,40mg(hydrochloride)
inj 1 mg (hydrochloride) in 1ml aopoiie
tablet 4Ong,80ng(hydrochloride)
inj 2.5ng/nl(hydrochloride)in
amp2ml-,
ouj ,e
1 2. 2 Antiarrh., thrnj c drugs
"procainamide
“
"tablet 250mg,500ng(hydrochloride)
inj 100mg(hydrochloride)/ml in
10nl ampoule '
12.3
TiSblet 5Ong(hud rochlorid e)11
*hydrochloroth.’.azine
tablet 5 Ong
tablet 40ng,80ng(hydrochioride)
.^propranolol
tablet 0.1mg,0.25mg
’pine(A) (7)
inj log in 1al
ipoule
'.
12,4 Cardiac
-rcosides
d jj5axin(4)’
-------------------------------------- tablet 0.0625 ng,O.25ng
• ,
oral solution 0.25 ng/ml
inj O.25og/nl in 1r.il ampoule
; - ‘ • 12.5 Drugs usc^ in shock or anaphylaxis
epinephrine
inj • 1ng(as hydrochloride) in 1-nlamp )ule
■propranolol
•
15mg/ml
1ng/nl
. inj nophenteraoine sulohate
1 •*- nj n.oracbnal in (Hathi)'
B
O'
3
C
1 3_._ Dermatological drugs
acid + salicyli
Whitfield o'i. 4th
td w
t
;C.
drugs
itra.
|
ointment 5>-g neomycin sulfate+50011
b a c i t r a c i n z in 3/ <
Main list
Co ip leuent ar y list
'
—
OW
Route of administration dosage 1 1 jpS’t I^st CMC' j!ost
?PL PG I SI G E 714 B
forms and strengths
C
EL-rc
tetracycline ointment
chloramphenicol
1-3.3. Antiinflammatory and antipruriti c drugs
*betanethasone(3) ■
ointment or cream 0.1%(as' valer, ite)
*calamine lotion
lotion
*hydrocort'isone
ointment or cream 1%(acetate)
•
'
13..5 Keratoplactic and keratqlyt.ic_agents
salicylic acid
,
"" 'solution t op real 5%
13.5 Scabicides and p cdiculicides
^.benzyl benzoate
lotion 25%
’
14, D iaxn 0 st i c ag e nt s
tuberculin'; purified:'p’rbtien'"’
derivative (BPD)
injection
fluroescein
14.1 Ophthalmic drugs eye drops 1%(sod-ium salt)
15. -Disinfectants
*chlorhexidine
solution 5%(gloonate)for diluti< m.
*iodine
solution 2.5%
16. Diuretics
*£uiLQamrxLd.e
tablet 4Ong
inj 10mg/nl in 1ml ampoule'
^hydrochlorothiazide
tablet 5 Ong
17x Gastrointestinal drugs
aluminium hydroxidFCaT5^
tablet 500mg
oral suspension 320mg/5nl
magnesium hydroxide
oral suspension equivalent to
. 550mg magnesium oxide/lOr 1
tab . ant ac id ( mat hi )
*prohethaziae(^.) 17.2 Anti emetic'drugs tablet 10mg, 25ng(' hydrochi oride)? fcl.
chi
elixir or syrup/5ni
5ng'(hydrochloric e)
.......... .
- --
I
B
B
B
B
A
B
C
B
B
B
•
_ J
,8
Route of adi.ifni
forms and stren
-riEhoide 1
:nt
*loca:l
: c.ru
ointment or suppository
0 xyp lie n on i u: I
*at ropin s(Hat
17.6.1
*codeine(l)
,
oral rehyd rat i oh
salts(for gluons
.rii
inj 1mg(sulfate in 1ml ampoule
1 syapt Qhaiic )d rugs
tablet 30m (phosphate.)
nt solution
act iy.at ed charc oal
solut ion
18
and synthetic substitutes
t .ablet 0.5mg, 4ng
inj 4ng(sddiuxn phosphate)in 1
ampoule
tablet 5mg
tablet 0.05mg
01 .es
. *dexarethaso>:
*pr edn_ig^l on e
*ethinyl est rad i ol 18
nd other antidabetic agents
*glib on.
Tolubuta:
13.5 Or
• * cti1jjLKl
il'i- i bl
’ *
iov on ora er i;rol
injection
tablet 0.05ng+15ng+0.25-~g
tJliC Cow
...9...
lessen
levothyroxine
Route of administration dasage
orris and strengths.
Xist
’iL'isl
•I CiTC "[Il
dw ; ”
A
I
T5
!
iCost; pu?c-i
a nd a nt i h yd r o id d rug s
tablet 0.05ng,0.1 mg (sodium salt)
tablet 5Ong
ant iveno
intheria ant it
ssnit
nlasma fractions should
with WHO requirements
) ccomply
on
inj' for the collection,processir
and quality control of hunar
blood and blood product
in j 10000 IU
20000 IU in vial
inj 50000 IU in vial
1 9• 2* 1. .for universal _inii.unizat i on.
BCG vaccine(dried)
.
inj )all vaccines should comply ;
diplltjiaj;ia^_'p.^lHfU.s-j'Q.tanus_Ci>cc,.xie.inj) the WHO requirements’ for
. . \ biological substances.
in 3)
light her is
inj)
p.ql’i?- ye] itis vaccine(liveattenuatec )inj/oral solution
t e tan’us vaccine(WHO, Hath!)
i©-?j
19. 2. 2 cholera TABC, snail pox
21 • OpthaliiQlog:.cal preparations
silver hitrate. 21.1 antiinfectivc agents solution(eye drops) 1%
eye ointment 10%(sodium salt)
Lcol
solution(eye drops) 10% sodium
eye- ointment 1:/ (hydrochloride)
ifInn ; at cry.atent s
21.2
iB
(B
3i
10
T.Hin last
■
'
21.1
•pilocarpine
C.pnnler.entary
21.4 liiotics
’
'
21.5_ 21 yd rt«£t io s
' houa^rop'£npliTU/’<Ju',,^~'
list
Route of administration dosage
forms and strengths.
iist; ^isi CMC Low
solution(eye drops)2%,4%(hydroclc
ride or nitrate)
solution(eye drops)2%(hydrobro±Ld
c)
22. Oxytocics
”
'" ’
In^S?2°gf“alealefuP 1ml ampoule
imj 10 IU in 1ml ampoule
24. Psychotherapeutic drugs
chlorpromazi tie
*
<
..... ..
tablet 100mg(hydrochloride)
'
syrup 25mg(hydrochioride)/5Eil
! • ; ’
■
■
inj 25ng(hydrochioride)ml in 2 cl
*diazepan
tablet 5 mg
,
ampoui e
25. Respiratory tract, drugs acting on
*aminophylline25 (T antiastnmat ic 3^lets 200ag
*erga:ietrine
oxytocin
epinephrine
*salbutamol.
c o si PU
-A !
Erir
•
inj '25mg/ml in 10ml ampoule
in3 1mg(as hydrochloride)in
le
tablet 4mg(sulfate)
oral inhalation(?erosol)0-1mg per
syrup 2mg(sulfate)/5ml
doe e
adrenalin tartarate maliate in 1000
PET- phen^bard'5mg, ephedrine 10mg,
..... ... taeophyline,.1_252(Hathi)
r.o3oaplr.S(oOTihhSgpr|s,ant)
hytlrochloride,
•
i
Drugs in Small _Ru_rjatl Hoc .ital
“ A repliminary study
Note: Tick where indicated
A.
General Description of hospital
1. State in which, hospital located;
—
2. DPd strength;
<.25
”50
"’25
3. Staff position (specify number and grades
a. Medical Officer
b. Nurses
c. Others
4 o Facilities available
a. Laboratory
b. X-ray
c. Pharmacy
d. C.T.
5. Patient load - numbers seen in last year.
a. Out-patients;
b. In-patients;
6. Commonest disorders seen (top 5 only)
Medical
Obst &. Gynae
Paediatric
Surgical
OPD
IPD
B.
Drug Availability (range and type)
7.
How many drugs are available in your pharmacy?
a.
tablets/capsules;
b.
Injections;
c.
Syrups/liquids;
d.
Skin/eye/ear;
e.
Total
p.t.o....2
2
8.
>
Kt
7^’
,
1
What are the brands you stock in the following categories?
(Mention brand names (company names in brackets) eg.,
Baralgan (Hoechst))
a.
Antibiotics
b.
AnaIges ic/antipyretic
c.
Anti-inflammatory
d.
Antidi a rrh oeals
e.
Steroids
f.
Hormonal preparations
g.
Psychotropic drugs
h•
Anti-histaminics
i•
Cough syrups
j•
Tonics/Vitamins
k.
Skin preparations •
1.
Non-allopathic drugs
Tor combinations)
m.
Food substitutes•
n.
Eye/ear preparations
9. What fixed-drug combination drugs do you stock in the
following categories?
a.
Antibiotics
b.
Vitamins with other drugs
c.
Steroids with other drugs
d.
Antihistaminics with others
3
C.
Drug selection/Purchase/Pricino
10.
Who selects drtigs in your hospital?
11.
What are all the criteria for selection?
12.
D.
Do you purchase -
a.
whole sale?
b.
by generic names
retail;
or
through medical representative
brand names?
13.
Do you purchase any drugs in bulk? Specify.
14.
Do you prepare any medicines/mixtures/ointments in
the hospital? Specify.
15.
Do you get drugs donated from abroad?
(Mention names and sources).
16.
How do you price your medicines?
(What percentage formula over wholesale-retail price)
a.
Injections?
b.
Tablets/capsules?
c.
Vaccines?
d.
Samples?
e.
Foreign drugs;
Dispensinq/Prescribing
17.
What categories of staff in your hospital -
a.
prescribe,?
1' . dispense?
4
18.Do you have a trained pharmacist?
Does your hospital dispense drugs in any of the following
situation? If so, in each one (a) who prescribes? (b) who
dispenses?
(c) is there a standardised list for each level?
19.
a.
Mobile clinics
(a)
(b)
(c)
b.
Village Health Centre/Sub-Centre
(a)
(b)
(c)
c.
School/Hostel/infirmary
(a)
(b)
(c)
d.
Rehabilitation Centre
(a)
(b)
(c)
What is the regime you follow in your hospital for the
treatment of (specify brand names of drugs) -
20.
a.
Malaria
b.
Tuberculosis
c.
Diarrhoea in children
aDo
21.
you have any policy about use of expired drugs?
some beyond the expiry date, which are these?
b.
If you use.
c.
For how long beyond expiry date do you use them?
5
22.
Do you use any drugs as Placebos?
Yes/No
If yes, which are the' commonest and
for what situation?
23.
Are you . awar
July 1983?
of
drugs han. :ed by th'? Government in
Do you have a b?.nn. ’d brand list?
Have you weeded these drugs out of your hospital?
D ruq information
E.
24.
25.
F.
Hbw do you/your S'.aff get 'information on .drug indications/
doses/s.ide. effects.
1
a.
Product literature
- Yes/No
b.
Drug company handouts
- Yes/No
c.
Any other sources
. '
Do you have in your hospital -
a.
formulary;
b.
list of minimum/essential drugs; and
c.
standardised drug regimes?
Adverse Reactions
26.
G.
'
Have you had any adverse reactions with drugs in your
practice in the last one year?
YES/NO
If yes, specify;
Drug Budget
26.1
What is the annual expenditureon drugs in the last
financial year?
26.2
Did the pharmacy run at a lossor a profit?
If so, how much during that year?
LOSS/PROFIT
6
H.
Additional Information
27.
Have you taken any initiatives in recent times to
rationalise the prescribing/dispensing practices
in your institution?
What arc they?
How successful have you been?
28.
If there are any other problems/issues that you
have come across with your hospital, please
mention them here.
29.
Have you identified any forms of irrational prescribing,
over-prescribing, under-prescribing or wrong prescribing
of the medical practitioners in your area through
prescriptions your patients may have brought with them?
Give details.
.7
7
30.
Are there any pressing drugs issues on which you would
like reliable information?
31.
Do you have any suggestions for issues/problems that
should be discussed/considered at the workshop? Mention.
Small i;ura1 Hc.ita 1
° A repliminary study
Note: Tick where indicated
A•
■A- c s; '• i t a ]
General Descript ion
1.
State in_vdai'-l* hp/.y tel__located:
2. Bed strength:
3.
-it
50
25
Staff position (•p-< i.fy number and oracles);
a.
Medical Offi-
b.
Nurses
c.
Others
r
4• Facilities available
a.
Laboratory
b. X-ray
c.
Pharmacy
d. O.T.
5. Patient load - numbers seen in last year.
a.
Out-patients:
b. In-patients:
6. Commonest disorders seen (top 5 only)
Medical
_
_
—
Obst & Gynae
Paediatric-
Surgical
OPD
IPD
. .
B.
Drug Availability (rance and type)
7. How many drugs are available in your pharmacy?
a.
tablets/capsules:
b.
Injections:
c.
Syrups/liquids:
d.
Skin/eye/ear:
a.
Total
p.t.o.. .. 2
2
8. What are the brands you stock in the following categories?
(Mention brane names (company names in brackets) eg.,
Baralgan (Hoechst))
9.
a.
Antibiotics
b.
Analgcs: ?/e r hi- .yret ic
c.
Anti-i.
d.
Antidiarrhpeals
e.
Steroids
f.
Ho rmon al preparations
9•
Psychotropic drugs
h.
Anti-histaminics
i.
Cough syrups
j.
Tonics/Vitamins
k.
Skin preparations
.1.
Non-allopathic drugs
Tor combinations)
m.
Food substitutes
n.
Eye/ear preparations
1
tor
What fixed-drug combination drugs do you stock in the
following categories?
a.
Antibiotics
b.
Vitamins with other drugs
c.
Steroids with other drugs
d.
Antihistaminics with others
3
3
C.
D.
Drug selection/Pi1rchase/Pricino
"rugs in your hospital"
10.
Who selects
11.
What are all the criteria for selection?
12.
Do you purchase -
a.
whole sale;
b.
by generic names
retail;
or
through medical representative
brand names?
13.
Do you purchase any drugs in bulk? Specify.
'14.
Do you prepare any medicines/mixtures/ointments in
the hospital? Specify.
15.
Do you get drugs donated from abroad?
(Mention names and sources).
16.
How do you price your medicines?
(What percentage formula over wholesale-retail price)
a.
Injections;
b.
Tablets/capsules;
c.
Vaccines;
d.
Samples;
e.
Foreign drugs;
Dispensinq/Prescribing
17.
What categories of staff in your hospital -
a. prescribe?
b. dispense?
4
18.Do.you have a trained pharmacist?
Does your hospital dispense drugs in any of the following
situation? If so, in each one (a) who prescribes? (b) who
dispenses?
(c) is there a standardised list for each level?
19.
a. Mobile clinics
(a)
(b)
(c)
b.
Village Health Centre/Sub-Centre
(a)
(b)
(c)
c.
School/Hostel/infirmary
(a)
(b)
(c)
d.
Rehabilitation Centre
(a)
(b)
(c)
What is the regime you follow in your hospital for the
treatment of (specify brand names of drugs) -
20.
a. Malaria
b.
Tuberculosis
c.
Diarrhoea in children
aDo
21.
b.
you have any policy about use of expired drugs?
If you use
some beyond the expiry date, which are these?
ct For how long beyond expiry date do you use them?
5
22.
Do you use any drugs as Placebos?
Yes/No
If yes, which are the commonest and
for what situation?
23.
Are you aware ? : tr ? d.-jrs banned by the Government in
July 1983?
Do you have a banned brand list?
Have you weeded these drugs out of your hospital?
E.Drug information
24.
25.
How do you/your staff get information on drug indications/
doses/side effects.
a.
Product literature
- Yes/No
b.
Drug company handouts
- Yes/No
c.
Any other sources
Do you have in your hospital -
a. formulary;
b. list of minimum/essential drugs; and
c.
F.
Adverse Reactions
26.
G.
standardised drug regimes?
Have you had any adverse reactions with drugs in your
practice in the last one year?
YES/NO
If yes, specify;
Drug Budget
26.1
What is the annual expenditure on drugs in the last
financial year?
26.2
Did the pharmacy run at a loss or a profit?
If so, how much during that year?
LOSS/PROFIT
6
H.
Additional Information
27.
Have you taken any initiatives in recent times to
rationalise the prescribing/dispensing practices
in your institution?
What are they?
How successful have you been?
28.
If there are any other problems/issues that you
have come across with your hospital, please
mention them here.
29.
Have you identified any forms of irrational prescribing,
over-prescribing, under-prescribing or wrong prescribing
of the medical practitioners in your area through
prescriptions your patients may have brought with them?
Give details.
7
7
30. Are there any pressing drugs issues on which you would
like reliable information?
31. Do you have any suggestions for issues/problems that
should be discussed/considered at the workshop? Mention.
.
*
COM
’'-
MS-cb/D-10:3 43 /
Some Instances of 'Drug Dumping1
For any drug promotion FDA in USA insists on four requirements
1- There must be enough information in the advertisement to enable the patient
to use the product properly with side effects, precautions, contraindications etc.
included in the information.
2. All such information must also be on the product label.
3-
Good and bad aspects of the label should be given equal emphasis.
4- Brand name should be followed immediately by generic names.
Medical professionals can atleast demand compliance with the above in India too.
They can point out outrageous nonsensical bombastic claims.
They can check-out the references to so called medical authorities which give a
positively biased picture of the product.
They can share valuable information with others.
Kefanver Commttee was set up in States one decade ago to deal with the problem
of unethical practices of pharmaceutical industry. The Committee concluded that:
'The high margin and proflits in the drug industry result from monopoly control of
the market excercised by larger firms through monopoly grants that come from
patients, through extraordinary high expenditure on promotion and advertising and
their success in brainwashing doctors into writing prescriptions in terms of brand
names, rather than generic names.'
-
What is happening to drug imports?
These tripled between 1965-64 to 197 -74 from 15.17 crores to Rs,37
50
*
crores within next year it increased to Rs. 47 crores this constituted 35$ of the
bulk drugs utilized in formulations.
According to Dr S S Gothoskar, the Drug Controller of India, "The last three years
have witnessed a steady increase in the requirements of imported raw materials by
nearly .100$. Thus while our production increased by only 50$ from 1976=77 to
1978-79 the expenditure incurred on import of bulk drugs, intermediates, solvents
etc. rose by nearly 80$
Theqquestion is with this dependence on foreign imports in which the multinationals
have the trump card can one really expect them to comply with drug legislations
which may have the interest of common nan in mind but which may curtail their’
high profits.
Double Standards,
1. Ancoloxin marketed by Glaxo, information is altered according to the strictness
of regulatoiy agency.
In America doctors are warned not to prescribe te pregnant women as exper-irannta
with rats have shown to endanger-the-unborn child■
In Britain whilst drug therapy is undesirable during the first trimester of
pregnancy the administration of Ancoloxin may be warmed if vomiting is severe.
In U.K. M.I.M.S. there are no warnings against the use of drugs in pregnancy.
In Africa, India and other Third World Countries - Ancoloxin specifically recomm
recommended for treatment of morning sickness during pregnancy as assessed from
information material issued to doctors chemists and in the prescribing guides
used in the Third World.
...2/-
YPAI;
„ 2 -
MS-cb/D-10:343/
2.
Melsedin (a hypnotic) produced by Boots.
Dest Reference 1977
According to Physicians
'PREGNANT WOKEN AND CHILDREN SHOULD NOT USE THIS DRUG1
But two out of three, Third World prescribing guides had 'DOSES
SPECIFICALLY SUGGESTED FOR BABIES.’
(Boots were under the impression it had been withdrawn worldwide in 1973 - 74
Social Audit purchased a sample from India in 1978
*
Boots subsequently
confirmed it was being made in India)
J.
Migrel (for Migraine) produced by Englands Wellcome.
In U.S.A, maximum dose set by Wellcome five tablets (10 mg) A WEEK with
adequate warnings about side effects.
England maximum dose - six/weeks.
I-'.
(
India - maximum 12 tablets per week. One serious side effect m like
headache, for which they may take more MIGRIL.
Wellcome aware of these discrepencies says that differences reflect
"current medical opinion" in the countries concerned.
Hydroxyquinolines (vioform lioquinol) available in India as Mexaform,
entero Vioform has been banned in Japan as it was associated with
numerous cases of neurological toxicity causing partial or severe
blindness which left 10,000 patients with permanent disability. This drug
is sold freely over the counter with'warning of ocular toxicity, written
nucroscopily in English which, anyway very small percentage of population
can read.
4.
5.(Metronidazole)^Flagyl too has been under severe attack in the West, g&oauee
of
association of cancer in rats when given in large doses. In India with
so much amoeibiasis its use has continued.
8.
Bismuth Salts used for digestive upsets haee been found to be connected
with more than 1,000 cases of encephalitis in France.
Lomotil (Diphen o^ylate/atro pine)
LomotilBanned abr'dad for infants is used indiscreminately in India
for paediatric age groups.
7.
.
Selected Drugs banned in the US >ut marketed in the Third World.
(Continued on the next sheet)
’
x/ti/ll.
MS-cb/D-10:343/
Selected Drugs Banned In The U.S. But Marketed In The Third World
Drug
Drug Company and
FDA Status
Reason for banning or special warning
Dipyrone
Alginodia
Beserol
Conmel
Not marketed in the U.S. A.M.A. has
justified it only as a last resort
Upjohn
Winthrop/Sterling
Winthrop/Sterling
Drugs containing Dipyrone can cause a fatal blood disease
known as agranulocytosis (a disease in which a sharp drop
in bacteria fighting white blood cells leads to drastic decrease
in immunity to infection.
Coricidin s/a
Schering
Corilin
Diprona MK
Dolopirona
Dorflex
Schering
McKesscn/F McK
Winthrop/Sterling
Merrel/Richardson-M
A paper published in 1980 by the Regional Office of the
International Organisation of Consumers Unions in Penang
Malaysia reported 20 preparations containing Dipyrone and
related compounds on the uarket in 28 similar preparations
are listed in the amain prescribing guide with little or no
mention of the dangerous side effects.
Genservet
Stegalgina
Valprione
ICN
Searle
Endo/lbpont
Op talidon
Do1on eurobion
Sandoz
Merck
Novalgin
Cibalgin
Hoechst
Ciba-Cei’y
Pepo Provera
Upjohn
Not Approved by FDA
Sources: Multinational Monitor, 8/80 and Interfaith Centre
on Corporate Responsibility in New York
Upjohn has been trying for more than ten years to get FDA approval
for this 3 month injectable contraceptive. Reported side effects
include: breast nodules, cancer of the reproductive organs of test
animals, irregular te bleeding, reduced resistance to infection, long
term or permanent sterility.
If injected into a pregnant woman, it can cause birth defects,
especially congenital heart defects. The drug should not be used
in lactating women.
Source: AFSC Women's Newsletter Summer, 1980
..4/-
VH Aj
MS-cb/D-10:343/
I-------------------------------------- “--------- 7
Clinoquinil
two Ciba brands sold
in Southeast Asia:
Entero-Vioform and
Mexaform
Chloramphenicol
(Chloromycetin)
Wintetil
Chlora&fenicoli
Ciba-Geigy
US ai d several countries
have banned the drug
Clinoquinil and its derivatives have been associated with sub
acute nyelooptic neuropathy, a crippling, sometimes fatal
disease of the nervous system. The directions given for these
drugs in Malaysis and Thailand suggest their use for"non-specific
diarrheal disorders and also as a prophylactic".
Parke Davis
Parke Davis
Winthrop/Sterling
While Chloramphenicol is clinically useful, it should be
reserved ONLY for those serious or life-thfgatening infections
caused by susceptible organisms for which less potentially
hazardous therapeutic agents are ineffective or contraindicated
*
McKesson
Chloroptic
Allergan
Ambra-Sinto
Dow
Chloroptic
Allergan
I.S.O.P.
Econochlor
Opthochlor
Alcon
Parke Davis
Opthocort
Parke Davis
Status: should carry
warning regarding severe
and cften fatal occurence
of ajlastic anemia.
Both the Physician's Desk Reference in the U.S. and the
British text, Martindale's Extra Pharmacopeia provide
warnings about the drug causing severe irreversible aplastic
anemia. This warning is often not provided in the drug
inserts in the developing countries.
Sources: Multinational Monitor, 8/80, Physician's Desk
Reference, 1980, and Intergaith Center on Corporate
Responsibility New York.
VH/U
MS-cb/5-10:343/
1
Tetracyclines
Bristacycline
Tetrex
Bristacin
Achromycin
..chrostati
Cyclopar
Kesso-Tetra
Panmycin
Comycin
Robitet
2
5
BristolMyers
Bristol/BM
.
Bristol/BM
Lederle/AmCy
Lederle/AmCy
Pirke Davis/WL
As a group, Tetracyclines have relatively low toxicity
but can have potentially very sgrious side effects that
can also become life-threatening. Liver damage can occur
with certain people. The drug should not be used in
children under eight years or in women during the first
half of pregnancy due to the drug's tendency to permanently
stain children's teeth $nd to retard fetal bone development.
^cKesson/PMC
n . .
pa
Upjohn
According to the International Organisation of Consumer
Unions, of the 42 tetracycline preparations in the 1979
^g Index for Malaysia and Singapore, only two contained
a caution nbtation.
SK Tetracycline
Robins
Smith Kline
Sumycin
Squibb
Tetracycline?
Tetracycline
Tetracyn
Tetrastatin
Topicycline
Mysteclin
Aueromycin
Ledernicin
Vibramicin
Philips Roxanne
Wyeth/AHP
Pfipharmccs/Pfizer
Pf iph arraec s/Pfi zer
Proctor and Gamble
Squibb
uedeile/AmCyan
Lederle/Am Cyan
Pfizer
Terramicin
Pfizer
Status: All of the above
tetracyclines should provide
a caution in the drug insert
thpnd^ ti?e Physician not to use
the drug m women who are in the
’
Sources:
unSer eig£t°f eg^ncy^ in children
.....
^Multinational Monitor, 8/80, and ICCR, New York
VH Al
MS-cb/D-10:343/
-
1
’’<5 -
2
3
Lincocin
Upjohn
Cleocin
Upjohn
In 1973, the British medical joirnaj. Lancet published an article linking
Lincocin and Cleocin with a high incidence of intestinal disorders, diarrhea,
and occasional deaths. The cur.’ent U.S. PDR does offer sa ’warning regarding
these side effpcts, however, this warning may not be present in the third
world countries.
MER-29
Richardson/Merre11 Inc.
This is an anticholesterol drug which was taken'off the U.S. market in the
mid 1960s after it was found to catse cataracts, baldness and impotence.
Si nt ex
Richardson/Merrel Inc.
Status:
banned in U.S.
Source: Everybody's Business, The Irreverent Guide to Corporate America,
Moskowitz, Milton,, et.al., 1980, Nev/ York.
/
Selacryn
In 1978 the company had to recall and reformulate their Sintex nasal spray
after the company found that in contained resistant bacteria.
According to a report by Dr Wolfe of the Public Citizen Health Research
Group, as of November, 1980, the FDA had received 1,100 adverse reports
Status: U.S. Justice
including 600 cases of liver toxicity and over 60 deaths, as a result
Dept, is -investigating
of Selacryn's eight month tenure on the U.S. market as a antihypertensive.
the company and may bring
criminal charges against the
Source: Multinational Monitor, July, 1981
company for failing to report
adverse reactions to the FDA.
Smith Kline
Banned in West Germany, Mexico, the
Philippines, and Switzerland
..." 1:
vi-l '''I
2
-Stanozolol
(Winstrol)
V.i nt hr op/ St c r li ng
FDA Status: 1980 PDR states,
“Final classification of less
than effective indications
requires further investigation
Indomethacin
(indocin)
Merck, Sharp and Dohme
“3
~
~
~
~
~
------ ------ ----------------
Stanozolol is a steroid hormone chemically and pharmacologically
related to methyltestosterone. The actions of this drug are similar
to those of the male sex hormones with the possibility of causing
serious disturbances of growth and sexual development.
Source:
Interfaith Center for Corporate Responsibility, Nev; York.
Indocinig, precise mode of action is not known. It relieves symptoms,
but does/1,’not alter the progressive underlying disease. Careful
instruction to the / patient is essential.
Source: II ICCR, New York
Res-^-Aire
resuscitator
Daikon Shi eld, I UP
Banned in the U.S but
exported to Africa
Ineffective as a respirator; failed to revive the Kenyan politician
Tom Mboya when he was shot some 12 years ago.
This device has geen linked with the deaths of 17 women in the U.S.,
however hundreds of thousands of Daikon Shields have been sent to
third World countries.
Source:
Mother Jones, May 1981
-
vjpn.
8
-
MS-cb/D-10:343/
RESOURCES
Interfaith Center on Corporate Responsibility
C/o Father Michael Crosby, OFMCap
3900 North Third Street
Milwaukee, Wisconsin, USA 53212
New York
Depo-Provera Campaign to block FDA approval:
Judy Norsigian
Boston Women's Health
Book Collective
Box 192
West Somerville Massachusetts, 02144
Multinational Monitor
p 0 Bo- 19312
Washington, D.C. 20036
Circle of Poison, Pesticides and People in a Hungry World,
David Weir and Mark Schapiro, published by the Institute for Food
and Development Policy, J.981
Institute for Food and Qevelopr .nt Policy
2588 Mission Street
San Francisco, California, 94H0
<?r
XLOat.5.0001
MULTI-NATIONALS IN THE INDIAN DRUG INDUSTRY
*
- An ant Phadke
**
'in trod uct’.ijo n
THE Pharmaceutical industry all over the capitalist
world is controlled by a fw giant multi-national
corporations (MNC). These corporations can apply the
latest fruits of scientific and technical research
because they have the resources to do so. They can also
set aside large sums of money to do the research required
for identifying newer and better drugs. However, since
their primary motive is to maximise their profits, this
potential is not realised adequately. Instead their
strength is used mainly to manipulate the system to
serve their narrow profit-interests. This is clearly
seen in their role in a developing country like India.
* This article is modified from the original which
appeared in the medico friend circle bulletin in
January-February 1982.
** Anant Phadke is the Convenor of the medico friend circle—
a socially conscious group of individuals which is working
to evolve a pattern of medical education and methodology
of health care relevant co Indian needs and conditions.
Also actively involved with the Lok Vidyan Sangachana,
Maharashtra, Anant has been writing on health related
issues in English and Marathi
2
i2i
The follow!' g facts highlight the monopolistic structure
of tiie MNCs in the world and in India
*
* In 1974, the top 30 multi-national firms accounted
for 52 percent of the total sale of pharmaceutical
products in the world
* In 1973, the top 20 firms accountedfor over 75
percent of the total ethical drug sales in the
USA and the UK (2).
* In 1973, according to Roche Company *s own estimates,
their two main tranquilizer formulations—LIBRIUM
and VALIUM—held more than a third of the entire
world tranquilizer market^.
* In India, while the value of drug production has
increased from Rs.lo crores in 194b, to Rs.445 crores
in 1973 and Rs.1376 crores in 1979-bO, the share of
MNC subsidiaries and minority ventures still remains
substantial
* In India in 1973-74, 60 firms with foreign shares
accounted for 70 percent of the country *s total
drug sales. The remaining 30 percent was shared
by 116 large and 2500 small manufacturing companies^.
THE pharmaceutical industry in India has been dominated
by the giant foreign companies in the 30 years after
independence, since most of the research in Pharmaceuticals
in the commercial sector of the capitalist world is
undertaken by MNCs and since the industry is protected by
....3
S3:
patent laws, 90 percent of patents in the pharmaceutical
industry in India are also held by these foreign controlled
corporations. What is the role and the effects of this
commercial, profit-oriented, giant monopolistic sector?
(1)
Emphasis on Drug Formulations
and its social cost
PRODUCTION of bulk drugs requir. s setting up complex
manufacturing units here in India. However, foreign
companies, which started here as marketing subsidiaries
of their giant parents are not interested in this. They have
beenforced by circumstances into manufacturing activity. This
mainly consists of importing bulk drugs from parent companies
and merely mixing them together in various proportions to
make various formulations with particular brand names
*
* In 197&-79 out of a total production of Rs.220 crores
of bulk drugs in India, the foreign sector accounted
for 16.7 percent, whereas out of Rs.1050 crores of drug
formulations, it accounted for 43.d percent worth of
formulations
.
This affinity for formulations exists
because formulations means more profit.
* The average profitability (pre-tax) of four
foreign companies during 1974-77 was 7 percent
for bulk drugs and 21.a percent for formulations
4
«4<
ONE of the main reasons given for allowing the foreign
companies to operate in India is that these companies
will bring their complex technology with them and thereby
help setting up a modern manufacturing drug industry in
India. Though this has happened to a certain extent, the
main effect has been to thwart the development of a modern
drug industry in India. Since the foreign companies are
the prime movers in the drug industry in India, private
companies of Indian origin also indulge mainly in production
of formulations.
* In 1973-79, private Indian companies accountedfor
22«3 percent of bulk drug production and 32.4 percent
of formulations. The public sector, however, produced
14.6
percent of bulk drugs and only 5.7 percent of
d r ug fo rmulations
•
IT is well known that many of the formulations in the
market are not useful on account of one or more of the
following factors—unnecessary Ingredients, wrong ingredients,
sub-therapeutic dosages and wrong combinations. The WHO, the
Indian Medical Association and the Hath! Committee have
recommended respectively 200, 156 and 116 essential active
substances as essential drugs. The WHO has, in addition,
recommended 30 complementary drugs for treating rare disorders.
To this list could be added a few more rational drug combinations.
As opposed to the fact chat we need about 250 or so drugs
as calculated above,the situation in India is very different.
....5
:5s
About 15000 formulations are being marketed under different
brand names—-most of these being repetitive.
* Out of Rs. 1260 crores worth of drugs manufactured in
our country in 1979-80, essential and life saving drugs
accounted for Rs.350 crores only; the rest were pick-ups,
tonics and formulations of marginal value(4).
* An analysis of 289 manufacturing units (accounting
for over 65 percent of drug production) showed that
in 1972, these units were marketing 244 multi-vitamin C
preparations9 262 Vitamin-B complex tonics and 126 cough
syrups
1.
Most of these formulations and brand ,
products arc not
very different from one
another and therefore the main technique of selling
them is through high-pressure advertising and
marketing. Tnis advertising pushes up the price to
be paid by the consumer.
* As much as 18 percent of turn over on an average is spent
/o)
by Pharmaceutical firms on sales promotion in India'
".
*
* In a study of 24 foreign drug companies over heed costs
(including sales promotion expenditure) amounted to
33.32 percent during 1974-77 as opposed to an average
of 20 percent in other industries
These expenses are a huge social waste. They
are, however, necessary for the drug companies
....6
if> S
formonopolistic competition among themselves.
(2)
Irrational combinations
TO justify a different brand name, drug companies
many times add some ingredients to the essential drug.
Most of the times these additions are irrational
*
A sub-commitcec
under the Drugs Consultative Committee stated that of the
34 categories of fixed combinations examined, 23 categories
were to be weeded out. The medical profession are aware of
many examples of irrational combinations but it would not be
out of place to quote examples of a couple of scandalous
combinations.
* Analgin causes serious blood dyscrasias as well as
gastric ulcers. Phenylbutazone and O2<yphenbut azone
arc equally hazardous drugs. But a combination of
Analgin and Phenylbutazone achieves a record sale of
over Rs. 2 crores within a year of its introduction^^.
*Amidopyrine is a very toxic drug that is banned the
world over; but most of our antispasmodic combinations
contain Amidopyrine. In 1979-ao, we imported 95 tonnes
of Amidopyrine\
Because of their monopoly-control leading
manufacturers can dump these products into
the consumer’s body; the doctors virtually
acting as agents of these companies
*
7
(3)
Drugs--Not for the Poor
MOST of the combinations and formulations of drugs in
India are too costly for the vast majority of our
population because of the brand-names, advertising,
unnecessary ingredients and high-profit margins.
The drugs that the poor need - drugs against tuberculosis,
leprosy, malaria etc., and also vaccines are under-produced
because those who need these do not have the money to buy
them. Tables (1) and
(2) show the discrepancy between installed
capacity and actual production of some of these drugs in 1978
and between targetted and actual production of vaccines in
1980-81.
Table
1978
Name of drug
Installed
capacity
(tonnes)
1. Isonex
539
94
2. PAS and its salts
1290
558
3. Thiaceta^one
153
13
4. streptomycin
257
225
5. Chloroquin
176
45
38
17
6. DDS and its derivatives
ms——as —s; —
=
sr”:
Production
(tonnes)
—=—-;j—~—=—=—x:
8
8
Table (2)
(7 )
1980-81
= —33 — 3s“SS“S3 “E5“S3 “S3“S3 “33 “S3 “S3 “33 “S3 “33 “S3 “S3 “SS“= “= “= “= — — “S3 “S3 “S3 “S3“S3 “S3 “p
*
Vaccine against
Target
(lac tonnes)
Production
(lac doses)
1. Diphtheria, Pertussis
Tetanus
400
145
2. Diphtheria-Tetanus
250
120
3. Tetanus
11O
70
4. Poliomyelitis
60
20
-=
—
~= -=—=-=-= —»-= -= ~= —x.—= -=
—=-= -j-
EVEN amongst the same class of drugs: for example - the
Vitamins, a similar pattern is seen between what the poor
need .-nd what the rich can afford.
* Vitamin B Complex
preparations of various sorts consisting
mainly of irrational combinations consumed by the rich
account for 5.5 percent of total drug production. Fbwever,
Vitamin-A (the deficiency of which is extremely widespread
amongst che poor and turns 12000 children blind every year)
accounts for mere 0.3 percent of total drug production^.
As against this, the drugs consumed mainly by thewell-to-do,
eg., high protein concentrates and drugs prescribed by doctors
for their own interests: eg., injection terramycin are produced
much beyond their licensed capacities. Table (3) highlights the
discrepancy between such products and much-needed anti-tuberculosis
drugs.
.9
9
Table (3)
—as —gr—~ —xs—-3—sz —st —as —53—=2 —as —=s —ss
Licensed capacity
(metric tonnes)
Product
—53 —y— —— —~ —r-
Production during
1979 (metric tonnes)
1. I N.H
80
52
2. PAS and its salts
110
94
3. Terramycin
14
54
4. Protinex
110
290
1
DRUG firms obtain licenses and letters of intent for
bulk drugs and formulations but do not use them when
they find that the profitability is less.
* Of 32 bulk items covered by 13 licenses, that 21 items
were not produced by Glaxo Laboratories for a period
of five years has been reported^).
(4)
Very little research for the poor
OUT of a total world production of drugs of 50 billions,
the developing countries in 1974, imported about 2.1 billions
worth ie., about 4.2 percent. But out of an estimated annual
research bill of 2 billion only 30 million ie., 1.5 percent was
spent by the companies on the tropical diseases which constitute
one of the most pressing health problems in developing countries.
This amount according to W.H.O. is equivalent to the cost of
building a few miles of motorway and less than one fiftieth of
the annual expenditure on cancer research (D. whatever research
1O
IO
is done toy western agencies on tropical diseases, takes
place in developed countries and is focussed mainly on
problems which they are concerned with. For example, the
U.S. walten Reed Army Research Institute is the only
Western agency doing systematic research in Malaria. It
got interested in malaria because of the U.S. involvement
in Vietnam where malaria caused more American casualties
than did the vietcong army^.
MNCs and their subsidiaries in India show the same
pattern in research.
* In India out of 45 foreign companies identified
by the Hath! committee, under the Foreign Exchange
Regulation Act, FERA, only 7 companies performed
R & D in the manufacture of basic drugs
* An analysis of 20 MNCs in India showed that during
1974-75, the R & D expenditure of these firms ranged
between 1.5 to 2.5 percent of their sales turn over,
Whereas their parent companies in the West spend
typically between 5 to 15 percent of their annual
turn over on R &
* The Sandoz group as a whole spends nearly 9 percent
of its world wide turnover on R & D while its Indian
subsidiary spent only 1.4 percent of its turn over on
(3)
R & D in 1975' .
11
11
THE reasons for this pattern is obvious. The MNCs cannot
afford to spend on research on drugs to be used by the poor,
the poor being unable to pay for this research through higher
prices for new drugs. This state of affairs will not change
unless human needs take a priority over the profit-motive of
the drug industry. It costs around 50 million to develop a new
drug . In case of drugs for tropical diseases it may even be more,
since a lot of ground work needs to be done initially. The MNCs
are not going to change their research strategy unless strong
to
public pressure forces them/do so.
(5)
Are MNCs needed on Technological
grounds?
ONE of the important arguments in favour of allowing the
MNCs to continue their operations in India is that they
bring new and better drugs into the country. Recent studies
and reported facts show this to be no longer a valid supposition.
* A study on MNCs in India showed that the time-lag between
years of production of a drug abroad and in India was 7-16
years showing that fruits of research done in the West
do not percolate quickly through MNC subsidiaries in India
(9 )
,
* Out of 138 drugs listed as major pharmaceutical innovations
from 1950 to 1967 in the west, only 20 were being manufactured
in India in 1973^.
12
12
Now in the West in spite of growing expenditure on
drug research, less and less genuinely new drugs
are being innovated since the scope for newer drugs
is becoming less and less for the developed societies.
* Out of the 1500 drug patents field in 1972, only 45 (3 percent)
were genuine new drugs, 150 (10 percent) were major
modifications and the remaining 1305 (87 percent) were purely
imitative drugs
This means that the post-war period of explosion of
new better drugs is over.
THE second argument usually presented is that the Indian drug
industry is not yet tecnnically competent to produce most of
the drugs needed in the country. The situation in recent years
makes this argument equally untenable.
IN 1977, there were 64 foreign controlled firms of which only
38 produced bulk drugs, numbering 207
*
Out of these 207 bulk
drugs, 93 were exclusively produced by foreign companies, the rest
being also produced by the Indian sector—both public and private
included. Out of these 9 3 drugs only 29 drugs were high technology
drugs, the production of which could probably not be taken up by
the Indian sector for lack of know-how
The Indian sector had
the technology to produce the remaining 64 drugs being produced
exclusively by the foreign sector at that time. Among the 29
high technology drugs, some may be chemical analogues that are
closely related and hence the total number of drugs that the Indian
13
13
industry could not produce because of lack of know-how would
be a very small number. Even in the case of such drugs Indian
companies could enter into technological collaborations (as
they have been doing currently) with foreign companies.
THUS on technological grounds it is not at all necessary
to allow foreign companies (MNCs) to operate here.
(6)
Economic effect on Industry
GUITE apart from the above mentioned facts of the MNC
operations in India, a very crucial problem is the long-term
deleterious effects they have on our industrial economy—through
the practices of pumping money out of India through repatriation
of profits and
’transfer pricing ’•
* A case study of 42 foreign drug companies showed that
during the period 1968-69 to 1977-78, these companies
repatriated Rs.45.11 crores out of India in the form of
(3)
profits, dividends, royalties, office expenses etc
•
IT is clear that though most of the MNCs operating in India
earn huge profits by exploiting ch^ ap labour in India, they
do not re-invest all of it here.
REPATRIATION of profits is only one of the mechanisms. The
other mccnanism is ’transfer pricing
The subsidiaries of
multi-nationals import raw materials from parent companies
at rates higher than the prices in the international market.
This raises the prices of the final products andthereby pumps
off money from the pockets of our people into the coffers of
14
14
the parent companies.
* A systematic study of 29 foreign companies showed that
in .1.977 the out-flow through transfer pricing was an
estimated 20 to 40 percent more than the out-flow through
repatriations'
,
* A foreign subsidiary charged Rs.6OOOO/kg for dexamethasone
(steroid) which was later reduced to Rs.l6OOO/kg at the
intervention of the Controller of Imports'
.
* Gentamycin (ar. antibiotic) was being imported into India
by a multi-national subsidiary at the rate of Rs.450bo/kg.
When import of some drugs was channelised through a government
agency j the price was lowered to Rs. lGOUO/ltg. similarly the
price of Doxycycline (another antibiotic) was brought
down from Rs.3000 to Rs.15OO/kgf
‘BahVluslon
MULTI-NATIONALS in India, because of their profit-motive,
monopolistic form, inter-company competition especially
product differentiation through brand names, high-pressure
advertising and other such characteristics, are primarily
inter.sted in manufacture of fancy formulations for the
well-to-do at the expense of essential drugs for the vast
majority. For the same reasons they are not interested in
research areas vital for our people’s health. Their presence
15
15
in our country cannot be justified on technological groundsMoreover they have been responsible for exploiting the cheap
Indian labour and pumping out large sums of money into the
coffers of their parent companies. By their own performance
in the last few decade they have demonstrated their irrelevance
to the Indian drug Industry and the Indian people
*
A foot note
,
The functioning of the Indian private and public sector also
need to be analysed, in order to get a better understanding
of the important obstacles to the evolution of a rational
drug policy. Even at a glance, however, the Indian private
sector will show that it is dominated by monopoly profit
motives while the public sector has been unable to reverse
the basic trends towards irrelevance in the drug industry in
India. Both of these, however, are outside the scope of this article
16
16
'Revererices
1.
ANIL AGARWAL, Drugs and the Third world, Earth-scan Document,
London, 1978.
2.
NAGESH KUMAR & KAMAL MITRA CHENOY, MNCs in the Indian Drugs
and Pharmaceutical Industry.
3.
CHANDRASHEKAR & PURKAYASTHA, Multinational investment, Profit
repatriation and the Production of Drugs in India.
4.
NARESH BANERJEE, Common diseases of the Indian People and
their requirements of basic and bulk drugs •
5.
MAJUMDAR, J.S. Drug Industry-Instruments of Policy.
6.
RANE & PATWARDHAN, Priorities in Drug Manufacture.
7.
GHOSH, Pattern of Diseases and Drug Production in India.
8.
MANOHAR RAO, J., Research and Development in Private pharmaceutical
firms in India.
2-8 are papers presented at the seminar
VH/IzptiiS.V.'Si'
Name of the firms
rRODiCTIOil OF
INH
Abbott
3331.TI AL DRUGS BY MULTINATIONALS AND ORGANIZED SECTOR
PAS
T HE ACIT AZONE
ETHAI4BUTOL
RIFAMPICIN
STREPTOMYCIN
Nil
Nil
Nil
Nil
Nil
ACCI
ail
Nil
Nil
Nil
Nil
Nil
Hoechst
Nil
Nil
Nil
Nil
Nil
Nil
S.K. & F.
Nil
Nil
Nil
Nil
Nil
Nil
Searle
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Sandoz
Nil
Nil
Nil
Roche
Nil
Nil
Nil
Nil
Nil
Nil
Parke-Davis
Nil
Nil
Nil
Nil
Nil
Nil
Sarabhai
Yes
Nil
Yes
Yes
Nil
Yes
Beohringor Knoll
Nil
Nil
Nil
Nil
Mil
Nil
Glaxo
Nil
Nil
Nil
Nil
Nil
Yes
3t Merck
Nil
Nil
Nil
Nil
Nil
Nil
Ciba-Gicgy
Nil
Nil
Nil
Nil
Nil
Nil
Pfizer
Yos
Yos
Yes
Nil
Nil
Yes
?
g
Warner
Yes
Nil
Nil
Nil
Nil
Nil
Burrough Wellcome
Nil
Nil
Nil
Nil.
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
German Remedies
Cynamid
Ethnor
SO
Nil
Nil
Nil
Nil
Nil
Nil
Nil
Nil
■
i.;.
Nil
Yes
Nil
*
Annazuro III
b--j.s. ’^jumdar; prepared for the Drug ’
/;
§
'
:
■
in Jaipur, organized by Vil’I.
THE
MEDICINE
MEN
Following the tricky footwork of the multinational drug com
panies calls for an eye skilled in pharmaceutical and financial
choreography-even the most sophisticated health services have been
confused into paying exorbitant prices.
So what chance do the deve
loping countries stand ? Not much according to a forth coming
*
report
by the Haslemere Group. Gross overpricing inadequate label
ling and the restrictive use of patents are just some of the distur
bing features of the drugs trade revealed in the extract below.
If there is one industry that's given multinational companies
a bad name it's the pharmaceutical business. The subject of constant
investigations in both Europe and North America.on.charas of every
thing from selling useless drugs to unethical/€riais - the industry
continues nevertheless to increase its profits resist its critics
and even to counter-attack with its own propaganda. Indeed, UK judge
Lord Justice Diplock has remarked, "We are might be pardoned for
supposing that we were witnessing a contest between rival philanthr
opists, as to which of them might be permitted to confer great
benefit on the public".
The industry is strength which has enabled it to escape most
government attempts it to control drives from two facets of its
operations which are closely related its multinational character and
its monopoly trading position. Since the 1950's the pattern of
development has been increasingly that of mergers and takeovers so
that the larger national companies rapidly grew into multinational
giants and smaller companies were gradually swallowed up or beaten
out of the market.
OBSCURE ACCOUNTS
The swiss drug companies keep the economics of their operati
ons a tightly guarded secret, under the protection of swiss law they
are■financially answerable to no one save their shareholders. The
published accounts of most British companies give little more useful
information, profits from drug sales are carefully concealed among
those from their other diverse interest in foods, drinks, fertilisers
and cosmetics.
American law, however forces all publicly owned drug companies
to disclose their accounts in some detail. From these it is evident
that profitability of the drug companies is nothing short of stagg
ering. The average return on capital around 18% compared with only
11% for all other types of manufacturing industry. The situation has
been so throughout the history of the drug industry, and the high
returns have only been topped by the soap and cosmetics industry
which in many cases is linked with pharmaceuticals.
When considering the giant nationals, however even these
average figures make the true enormity of their profits. Merck,
Sharpe and Dohme, for example, the second largest drug maker in the
USA, showed a 5o% return on capital in 1973, and other manufactures
all show well above average returns.
Such high returns are not less true for operations in the
developing countries. In India for example, the 33 foreign controlled
drug firms supplying 65-75% of the total maker showed’returns on
capital of 30% in 1970, and recorded profits of over 2o% in every
single year between 1968 and 1970. There is no doubt that in India
the foreign drug companies are not only the most profitable of
manufacturers, but also of all the foreign controlled businesses
generally.
HEALTH cell
a?/!, (First Floor)St. Marks Road
BA f0 ■' t. O i E - 560 0£^
2
HIGH PRICES
In view of the enormous profits, it will come as no surprise
that the pricing of individual drugs relates less to the cost deve
lopment production and promotion than to what the market will bear.
In 1960, Scherings anti-inflamatory drug, predisolone cost
them 1.6$ per tablet to produce. It was sold to the pharmacist for
17.9$, who sold it-to the patient for 28.8$ a' mark-up of 1,118%. On
a drug for which this firm did not even have to do the research,
profits were even more astronomical. Schering purchased oestradiol,
a sex hormone, from the french firm Roussel, and sold it under the
Schering lable at a mark-up of 7,079%.
But if prices are high in the developed world, when we come
to consider Third World countries, they are, as David warburton,
General Secretary of the General and Municipal Workers 1 Union put
it near criminal1. This view was recently endorsed in a confidential
report of the WHO in Geneva. Fo'r, whereas Britian pays American
firms $2.40 per kilo for vitamin 'C'. India has to pay nearly $10 _•
per kilo. The tetracycline antibiotics, costing $24.30 in Europe
>
are being sold to India, Pakistan and Colombia for between $100 and
$270 and one of the most popular semi-synthetic penicilline,
Bristol's Polycillin, has been sold for $41.95 per hundred tablets
in Brazil, when the same product in the US was only $21;84.
Although it is American prices which have been most closely
scrutinised through senate comittee hearings, it is clear that some
European drug multinationals operate equally exploitative in the
absence of effective policies in the absence of effective machinery
for price control in most developing countries. A particularly
disturbing feature of pricing in the Third World is that the cost
of well established drugs. Whose patients ran out years ago, conti
nues to rise, whereas in the developed countries it typically
declines. In India a survey of 8 long established drugs showed that
their price had risen by 42% between 1961 and 1970.
RESEARCH COSTS
Drug companies are always quick to point out that the unparalled profitability of the pharmaceutical industry is offset by
the cost of research and development, which in this filed is uniq
uely high and unduly risky.
There is no doubt that the fundamental research necessary
for real innovation, the safety testing of new drugs and the
development of formulations suitable for marketing, is a costly
business. But on average, research and development expenditure
comprise only 10% of income, while advertising and promoting take
up more than 2o%. And even the term 'research1 may be deceptive.
It not includes fundamental research in’to formulations and
methods of production. And therapeutic research (clinicaltrial in
man). But may also includes such items as development of more
pleasing colours, tastes and packing for drugs, expenses for
employees to attend conferences at home and abroad, as well as
general market research aimed at improving sales and profits,
and the purchasing of international patents whose purpose is
merely to extend the monopoly position of the firms.
A "HIGH RISK" INDUSTRY
And what are the risks we are always hearing about ? At
first sight, the cost of developing individual drugs in relation
to possible risks, seems quite high: for example, in the field
of contradiction, so extensive are the requirements for safety
evaluation that it has been estimated that the cost of develop
ing a new type of pill would be of the order of £1q million.
. .3.
3
However,’ very- few drugs will be. .ma jor.-innovations, 'Estimated at only
•4 to 7 a year from the whole industry. Most of these potential
drugs already inexistencethat require no major development in such
chemical synthesising techniques, or in subsequent screening proce
dures .
The industry certainly seems to have few qualms about mark
ing useless drugs. In 1971, an investigation of 2,000 products by
a panel of the American Food and Drug Administration, found 6o%
lacked evidence for their therapeutic claims, some of these were
ordered off the US market, but most have found ready market else
where, in Third World Countries, where regulations governing toxi
city and efficacy of drugs may be non-existent or rudimentary. The
drug dithiazanine iodide (netocyd) active against certain types of
worms was voluntarily taken off the market by one US manufacturer,
Eli-Lilly, because of toxic effects that emerged with its use,
Pfizer, however continued to market the drug in areas not under the
control of the American FDA, and in 1973 it could still be brought
in Panama with a package insert discribing the drug as a "significa
nt" advance in the treatment of the most common kinds of parasitic
infestation", with no attempt to restrict its use.
NEGLECTED AREAS
It is clear that the industry does not invest in what would
seem to be genuine high-risk areas. There is almost no research into
drugs for rare disease, where there is little prospect of things
high returns. Ronald Edwards, former chairman of Beecham, recently
suggested that the government should finance such research. Presum
ably the industry should continue to reap its high profits on more
commercial enterprises, vastely over-priced to cover those 'high
risks 1.
The drug industry is equally neglectful of research into
drugs for tropical disease, many of which are wide spread through
out the developing world, and would lend themselves to international
co-operation in research. The multinational pharmaceutical industry
with its highly developed research and production facilities spread
throughout the world, is ideally placed to tackle such problems,
but chooses not to. For although the potential sales at first sort
of money the drug companies would want them to pay in neglect of
Third World health problems, the pharmaceutical industry not alone;
only 1% of all money spent by industry government and charities, on
medical research is devoted to the major disease problems of the
developing countries;.
Because the pharmaceutical industry is geared not only to
the needs, but also to the petro-chemical resources of the indust
rial world, there is no research done into the possible alternative
resources for pharmaceuticals within Third World countries themselv
es. It has been suggested for example that agricultural by-product
should be utilized for the manufacture of pharmaceuticals in
Tanzania. And a group of Chinese experts have identified some fifty
species of plant growing in Tanzania, extracts of which are used in
current Chinese medical practice. Not only does the western phar
maceutical industry not investigate these possibilities it actively
discourages them, preferring to sellintermodiate ingredients to
subsidiary companies.
UNUSED PATENTS
Pharmaceutical companies maintain their position of their
power through a patent system designed originally to ensure remune
ration for the time, physical and intellectual energies, and
costs that were put into the development of the idea. Drugs, however
are patented not by industries, giving manufacturers of new drugs
sole rights over production, and in the absence of any competition,
save that from drugs already market for the same therapeutic indic
ations, the right to name its price,
.
4 In developing nations generally, 90% or more of the patents
are held by foreign ownership is increasing
Chile for example,
98.4% of chemicals and drugs, patents are foreign owned, concentra
tion of these patents in the hands of very f<b>i is also evident;
in Colombia in 197q, 60% of drugs patents were held by only 10% of
all the foreign patent owners. In effect, there is a ruthless exer
cise in monopoly power by.the multinational pharmaceutical companies
for once a patent is registered neither a- na-tidnal nor a foreign
competitor can enter the production market it-covers, even if it
is not being exploited by the patent holders.
The fact is that foreign-owned patents are almost totally
un-exploited. In Colombia and Peru less than 1% of drugs patented
are actually produced in-those, countries the function of the patent
is to preserve secure import markets.for foreign companies, without
necessitating investment, and to block potential competition from
other close substitutes.
,,
DANGEROUS LABELLING
The fact that drugs available only on prescription in the1
west, are obtainable over the counter in developing countries' makes
adequate labelling and warnings all the more' important. A recent
survey of the situation in Latin America showed that companies fre
quently minimise risks and exaggerate claims for their own drugs in
the way they are not permitted to do in the U.S. Drugs are recomm
ended for a wider variety of conditions than allowed in the n.s.,
and warnings on restrictions of use and adverse reactions are
incomplete or entirely absent. According to one drug company spoke
man, "Product documentation will sometimes vary in individual coun
tries to reflect local needs economics, health conditions and
government regulations". Clearly, for some companies, absence of
government regulations on the inclusion of warnings moans that such
for warnings become unnecessary.
One drug which may have caused unnecessary death is Raudixin,
originally introduced as a major tranquilliser and still to reduce
high blood pressure. The frequent tendency of this drug to cause
severe depression, occasionally resulting in suicide, led to aband
onment of its use as a tranquilliser some years ago in the west
however, a package insert obtained in Brazil in 1974 still descri
bed the drug as "the ideal medicine, for the treatment of emotional
disturbances" and the drug of choice in daily practice". A spoke-man for the manufacture squibbs, said that the package insert had
been written twenty years ago, but that it still conformed with
Brazil's present drug regulatory requirements, as of last autumn
it had still not changed the package insert, once again we see
that it is sales, and the letter of the law, which concern the
drug companies.
Along with the rest of western medical practice, we have
exported to third world countries our own mistaken believes in
efficacy of chemical intervention in individual sufferers for
endimic disease. Third World countries continue to deploy large
amounts of their scarce resources on buying drug from Western
countries, often as we have seen at higher absolute cost than in
industrialised countries where health and social welfare bedgets
are low, the high cost of medicines puts them well out of reach
of the much of the population. Where governments do pay for
drugs, the cost takes up a dis-proportionatoly high amount of
the total money available for health, to the detriment of pre-.
ventative medicine schemes.—
....5.
5
PROPOSALS FOR CHANGE
The particularly vulnerable position of third world countries
in their relationship to the international pharmaceutical industry
has been noted in a recent -report published by the UN conference on
Trade and Development.
'
•
• ■
The report proposes certain immediate measures that poor
draw up a list of essential drugs, that brand names used, and that
drugs be purchased through a centralised distribution agency,
supplied by small producers in both developed and developing count
ries. It also.advocates the third world countries should co-operate
in the manufacture on pharmaceuticals and the setting .of technology
centres' to conduct research and development and diseminate informa
tion on drugs, thereby facilitating the transfer of pharmaceutical
technology to the developing countries.
Many of these ideas have been advocated before. The reduction
of the national pharmacopeia to a few dozen items was advocated in
Chile by its late president Dr. salador Allende, himself a physician,
but the majority of Chilean doctors were opposed to his ideas.
It
remains, to be seen whether a co-operative effort on the part of
third world countries, both to restrict the import of non-essential
drugs and to establish their new pharmaceutical manufacturing indus
try, can succeed in breaking the monopoly power of the multinational
pharmaceutical companies.
■Gor)3i. •'-.arks float
SIC- NAT URB CAMPAIG- N
A note to demand for a People"Oriented Drug Policy.
Dear Friend,
This signature campaign is against misuse of drugs. It is
against continued sales of hazardous, irrational and banned
drugs, against allowing sales of substandard and spurious drugs
It is a demand for streamlining production, distribution
of drugs that are needed for the health problems of the
majority. More than that_.it is a demand for dealing with those
conditions that ensure ill health.
Please go through the text of the memorandum which summa
rises the basic demands of the organizations mentioned below
it.
{
Name
Address
) four Organizations [ four jobIf possible j
j Name
1
iplease give
the capacitji
in which you
are working ’
there
|
1
j
1
i
1
i
i
I
1
1
|
i
I
i
j
i
j
If you feel strongly about the injustice in the healthand
drug scene, circulate this to others and obtain signature of
others supporting the demands.
If you wish to be involved in the Drug Campaign join the
Drug Action network which is part of an emerging 'People's
Health Movement
.
*
If you would like the name of your organiza
tion included in the list of organizations who are taking a
strong stand against the drug misuse, let me know. Please also
specify the responsibilities you would be willing to take
and contributions you would like to make in Drug'Action.
Within two months' the New Drug Policy would have been
passed. The time to express our concerns/to make our demands
and suggestions is now. Probably what the most important need
of the
moment is to be-- ■ able to organize ourselves around
...2. ..
this issue, whether we are health groups, Consumer groups,
legal aid groups or involved in Community Organization or
People's Science movement. Public pressure is crucial to
prevent vested interest from getting away unchecked with anti
people, policies, stands.
The signature campaign is to
- urge you for your support
- it is to build a network of groups to act as the watch
dogs on behalf of the people
- it is to build
pressure to demand public accountabi
lity from our drug industry : ' health personnel and
policy makers.
Only a very small minority feels concerned about issues
of social justice. To demand any People Oriented policy
whether it is related to human rights, enviornmental issues
or health we have to support each other. Since health and
survival are everybody's concern and not the pregorative of
those involved in health work alone, we hope you will join
ha ids with us.
Looking forward to your support, and solidarity.
C oorclir
Low Cost Drugs & Rat: onal The
V. H A I
b-10.341
SS:k/31.12.81
INTERNATIONAL FEDERATION OF PHARMACEUTICAL,
MANUFACTURERS ASSOCIATIONS (IFPMA)
CODE OF PHARMACEUTICAL MARKETING PRACTICES
Preamble
The Statute of the Federation article 3 states that one of the
objects of the Federation is "to promote and support continuous
development throughout the pharmaceutical industry of ethical
principles and practices voluntary agreed on and "to coordinate
the efforts of its members towards the realization of the above
obj ects".
It is believed that in keeping with the pharmaceutical industry's
international responsibilities, the members of the Federation
will be prepared to accept certain obligations, insofar as their
marketing practices are concerned, and to ensure respect for
them •
IFPMA recommends a Code of Marketing Practices to its member
associations, recognizing the difficulty of setting out a simple
Code which will be applicable in all parts of the world.
It
seems clear that national and regional conditions and legal
restrictions will continue to vary to such an extent as to make
a simple world Code impractical. Nevertheless, the Federation
believes that it has a duty to encourage its member associations
to either introduce such Codes of Practices or where such Codes
already exist, to continually re-examine and where necessary
revise them so that a voluntary system based on such a Code
keeps pace with modern medical knowledge and changing health
services and conditions.
It is recognized that many individual member associations of
IFPMA have laid down their own Codes of Marketing Practices and
this recommended Code is not intended to replace similar Codes
or instruments already in force by members of the Federation.
The following voluntary Code is therefore put forward as a
model for IFPMA's member associations.
_j °
V’j
A Code of Marketing Practices of this sort should be the responsibility of member associations who should also provide
guidance to their members on matters of compliance and interpretation.
Obligations of the industry
The obligations of the industry may be identified as follows:
The pharmaceutical industry, conscious of its special position
arising from its involvement in public health, and justifiably
eager to fulfil its obligations in a free and fully responsible
manner, undertakes:
to ensure that all products it makes available for
prescription purposes to the public are backed by
the fullest technological service and have full
regard to the needs of public health;
to produce pharmaceutical products under adequate
procedures and. strict quality assurance;
to base the claims for substances and formulations
on valid scientific evidence, thus determining the
therapeutic indications and conditions of use;
0 •£ ?
P5 1
u u?’
X
> o 3
fe 2
o 2
o “
0 ~
D-10.341
SS:k/31.12.81
: 2 :
—
to provide scientific information with objectivity
and good taste, with scrupulous regard fortruth,
and with clear statements with respect to indications,
contra-indications, tolerance and toxicity;
-
to use complete candour in dealings with public health
officials, health care professionals and the public.,
Suggested Code of Marketing Practices
We hereby declare our intention to voluntarily conform to the
following Code of Marketing Practices :
I.
General Princinles
1.
The term "pharmaceutical product" in this concept
means any pharmaceutical or biological product
intended for use in the diagnosis, cure, mitiga£
tion, treatment or prevention of disease in humans,
or to affect the structure or any function of the
human body, which is promoted and advertised to
the medical profession rather than directly to the
lay public.
2.
Information on pharmaceutical products should be
accurate, fair and objective, and presented in
such a way as to conform not only to legal require
ments but also to ethical standards and to
standards of good taste.
3.
Information shou.-.l be based on an up to date
evaluation of all the available scientific evidence,
and should reflect this evidence clearly.
4.
No public communication shall be made with the
intent of promoting a pharmaceutical product as
safe and effective for any use before the required
approval of the pharmaceutical product for market
ing for such use is obtained. However, this pro
vision is not intended to abridge the right of the
scientific community and the public to be fully
informed concerning scientific and medical
progress.
It is not intended to restrict a full
and proper exchange of scientific information
concerning a pharmaceutical product, including
appropriate dissemination of investigational find
ings in scientific or lay communications media,
nor to restrict public disclosure to stockholders
and others concerning any pharmaceutical product
as may be required or desirable under law, rule
or regulation.
5.
Statements in promotional communications should be
based upon substantial scientific evidence or
other responsible medical opinion. Claims should
not be stronger than such evidence warrants.
Every effort should be made to avoid ambiguity.
6.
Particular care should be taken that essential
information as to pharmaceutical products' safety,
contradictions and side effects or toxic hazards is
appropriately and consistently communicated subject
to the legal, regulatory and medical practices of
each nation. The word-"safe" must not be used
without qualification.
P-10.341
SS:k/31.12.81
3
7.
II.
Promotional communications should have medical
clearance, or where appropriate, clearance by the
responsible pharmacist, before their release.
Medical Reordsentative
Medical representatives must be adequately trained
and possess sufficient medical and technical knowledge
to present information on their company's products in
an accurate and responsible manner.
<
III.
Symposia, Congresses and other Means of Verbal Communi
cation .
Symposia, congresses and the like are indispensable
for the dissemination of knowledge and experience.
Scientific objectives should be the principal focus
in arranging such meetings, and entertainment and
other hospitality shall not be inconsistent with
such objectives.
IV.
Printed Promotional Material
Scientific and technical information shall fully dis
close the
properti.s of the pharmaceutical product as
approved in the country in question based on current
scientific knowledge including:
The active ingredients, using the approved
names where such names exist.
At least one approved indication for use
together with the dosage and method of use.
-
A succinct statement of the side-effects,
precautions and contraindications.
E.xcept for pharmaceutical products where use entails
specific precautionary measures, reminders need not
necessarily contain all the above information providing
that a form of words is used which indicates clearly
that further information is available on request.
Promotional material, such as mailings and medical
journal advertisements, must not be designed to dis
guise their real nature and the frequency and volume
of such mailings should not be offensive to the health
care professionals.
V.
Samples
Samples may be supplied to the medical and allied
professions to familiarize them with the products, to
enable them to gain experience with the product in
their practice, or upon request.
mfc ms
THE DRUG INDUSTRY IN INDIA
What our experts say.
-njty
,;.th ceil
51 Ho;>:
Marks Hoad
BAL<GAl.Qag - 560 001
THE INDUSTRY
The total output of the industry increased hundredfold - from
Rs.100 million in 1947 to Rs.10,500 million in 1978-79. This was
due to expanded production, especially of an ever-increasing number of
sophisticated drugs, and rising prices
The drug industry has enjoyed a higher man-average profitability
so that investment therein has increased substantially from Rs.240 milb®
j
1
in 1952 to Rs.4,500 million in 1977.
There are about 125 large and medium factories and nearly 3,000
small scale sector units engaged in this industry which provides
employment to about 100,000 workers.
PATTERN OF DRUG PRODUCTION
I
There is now an overproduction of drugs (often very costly)
j
meant for the rich and the well-to-do while the drugs needed by
the poor people (and these must be cheap) are not adequately
available. This skewed pattern of drug production is in keeping
with our inequitous social structure which stresses the production
of luxury goods for the rich at the cost of the basic needs of the poor.
Out of a total production of Rs.700 crores in 1976, 25 percent is
taken away by vitamins, tonics, health restoratives and enzyme digestant
mostly consumed by the relatively well-fed urban population. Twent
percent is covered by antibiotics, only 1.3 percent by sulphonamid
.2
2
(a very cheap and useful anti-infective) and 1.4 percent by
anti-tuberculosis drugs
PATTERN OF PRESCRIBING
One of the most distressing aspects of the present health
situation in India is the habit of doctors to over-prescribe
glamorous and costly drugs with limited medical potential. It is
also unfortunate that the drug producers always try to push doctors
into using their products by all means—fair or foul. These basic
facts are more responsible for distortions in drug production and
consumption than anything else.
STRUCTURE OF THE INDUSTRY
The existing drug policy rightly emphasises the attainment
of self-sufficiency in the production of drugs, in increasing the share
of the Indian producers and in giving a more significant role to
public sector.
The foreign companies account for about 40 percent of the total
drug production in the country; their share in the production of
basic drugs was about 28 percent and that in formulations, 44 percent
(1978-79). This is still high.
PRICE CONTROL
The drug prices are high and continue to rise. In some instances,
Indian prices are even higher than the international ones.
Packaging increases the cost of drugs very greatly because the
trend is to make it attractive and highly elegant and to add cosmetic
embellishments to promote sales....
There may indeed be a glut of applications for the introduction
of 'Me-too Drugs' which will not attract new legislation for
3
another five years in regard to price control
Genuine 'breakthrough
*
research has declined in recent
times.
Existing prices of drugs including those of essential drugs
of everyday use is highly inflated. For example, the cost of analgin
sold over the counter is 30 times the cost of production.
Prices are often inflated by the use of brand names
Very often, prolonged controversy over the price of a
drug has resulted in stopping its production.
The bill for import of bulk drugs, intermediates, solvents
etc., has h'-hU jumped from Rs.53.77 crores in 1976-77 to about
Rs.119 crores in 1979-80.
QUALITY CONTROL
The standards prescribed are unrealistic...are mechanically
copied from books... . and not uniformly enforced in all parts of
the country.
CONSUMPTION OF DRUGS
At present the supplies of drugs to urban and rural institutions
M within the health care system is very uneven. In an urban
hospital, for instance, the drug cost is Rs.6 per patient per year
while in a Primary Health Centre, it is about 40 paise per patient
per year
4
AN OVERVIEW
We recognise the value and significance of drugs in the
health care system. We fully support the policy that all the
essential drugs should be produced in the country, preferably
in the Indian sector,- and that they should be made available
to the people at reasonable prices. To realize these objectives,
it is essential to lay down and vigorously implement a national drug
policy which will ensure that the pattern of drug production in the
country (barring drugs meant for export) should be geared to its
actual needs. While the supply of drugs should be adequate, eternal
vigilance is required to ensure that the health care system does not
get medicalized, that the doctor-drug-producer axis does not exploit the
people, and that the 'abundance' of drugs does not become a vested
interest in ill-health.
Source;
Health for All - An alternative Strategy
:;
report of a study
group set up jointly by the Indian Council of Social Science Research
(ICSSR) and the Indian Council of Medical Research (ICMR).
drug colonialism
A new type of colonialism—drug colonialism
is oppressing us. Long after the other type of
colonialism had left the stage, the poor countries
of the world continue to be oppressed by the
exploitative practices of multinational drug com
panies. In this game of drug colonialism, the
privately owned Indian companies also join in.
For both are in search of quick profits with little
concern for the real drug needs of the country.
Consider the facts:
*
80-90% of the output of some major foreign
owned drug companies in India consists of
simple household remedies like cough syrups
and vitamin preparations. But life-saving drugs
account for only 30% of the total value of the
formulations sold by the major foreign com
panies.
on the assumption that we are endeavouring to
treat all patients of TB and leprosy and giving
them a complete course of treatment. Even if
we put a conservative estimate of half the requi
rement against what is calculated in the box,
our industry still remains far behind the target.
Because of this a drug like dapsone is difficult to
obtain and there was a period of six months when
none was available due to stoppage of produc
tion.
*
For many important drugs, installed capa
cities are far below licensed capacities. Even in
the case of insulin, only 50% of Installed capacity
is being used in the country.
For nonessential items like vitamins and
tonics, production in several firms exceeds licen
sed capacity. Much of drug promotion money,
goes into convincing the doctor to prescribe
and the patient to buy such socially useless
drugs.
*
Although malaria is a major disease in India,
primaquin and trimethoprim are not produced
locally at all and imports of chloroquine exceed
production. The production of cholera vaccines
in India cannot meet needs in times of epidemic,
even though production was started 40 years
ago. Vaccines against influenza, mumps, measles
and poliomyelitis are not produced in India at
all.
*
Although India has the third world's most
sophisticated drug industry, out of 51 major
drugs sold against infections and parastic
diseases, respiratory ailments and diseases of
the central nervous system, 28 are being im
ported.
[*
In 1976, the total production of drugs was
;
Rs. 700 crores. Out of that amount, 25 percent
!
was taken by vitamins, tonics, health restoratives
and enzyme digestants, 20% by antibiotics and
only 1.3% by sulphonamides and 1.4%byantijt TB drugs. Obviously, the pattern of the drug
J
production is irrational and irrelevent to our
I
health needs.
:■
*
Look at the box item on INH and dapsone.
i The estimations calculated in the box are based
ig HEALTH FOR THE MILLIONS/APRIL-JUNE 1981
*
There is a marked resistance from the
drug industry and the medical profession against
using generic names instead of brand names,
and against having an essential drugs list for the
country (See other articles in this issue).
*
A variety of sharp marketing practices and
false advertisements have been used by drug
companies to increase the drug dependency,
and promote fancy formulations and costly
drugs (see article on advertisements and mar
keting in this issue of Health for the Millions).
.
7
Estimated Requirement of Two Essential Drugs
Drug
Licensed
capacity
in MT
Production
1976-77
in MT
No of
cases
Daily dose
for one
patient
Total requirement
for all patients in
a year in MT
INH
538.56
79.21
2.2 million
Sputum
positive
300 mg drug
regimes
240.1
Dapsone
37.8
16.42
2.5 million
(detected)
75 mg in
all types
68.45
* 85-90% of drug patents in developing coun
tries are estimated to be held by foreign com
panies. Only 5-10% of foreign held patents are
ever used in local production. Patents are used
to secure import monopolies and more to prevent
Both health professionals and the public are also
responsible for giving in to this hard-sell.
brute power
The major accusation against the multinational
drug companies is their misuse of their brute
market power. They sell drugs to especially third
world countries at terms very unfavourable and
suicidal to the buyer. Tied purchase clauses
force the local company to import its raw
materials, intermediate products, equipment and
spare parts from a specific foreign company
usually the parent company. And these are
usually priced at a highly inflated rate. An
UNCTAD survey in 1975 reported 30-500% over
pricing of imported inputs for pharmaceutical
firms in Chile, 20-300% in Peru, 40-1600% in
Mexico and 100-800% in Spain. In the case of
diazepam, Colombia imported from the parent
company paying to the extent of 6,478% over
pricing (See box below).
In the Columbian case, the actual returns by
the subsidiary to the parent company 100%
= Reported Profits for Tax Purposes 3.4% +
Royalties 14% Overpricing 82.6%. This figure
is an average. The case gives an idea of how
repatriation of profits occur directly and in
directly. There is enough other evidence to
indicate that such overpricing and tied purchase
clauses are damaging to the development of
countries like India, for they occur with Indian
imports too.
* In India, the 33 leading foreign controlled
drug firms were always more profitable than the
6 main local ones. They also make more profits
than all other types of foreign controlled enter
prises.
8
Product .
Multinational Range of
price of im
other quo
portation to
tations to
Colombia
more deve
(FOB) US§ loped counttries in the
world market
(FOB) USS
Percen
tage
over
pricing
1,250.00
Chlordiazepoxide
18.90-20.00
6,155
Diazepam
2,500.00
30.00-45.55
6,478
420.00
Ampicillin
162.50-200
136.5
Tetracycline base
250 00
23.5
948.0
Erythromycin
132.00
275.56
108.7
31.75
Oxytetracycline
147.00
387.5
19.70
Promethazine
140.00
654.3
Triamcinolone
24.000.00
6,600 00
233.3
53.00
37.7
Neomycin
40.6
29.00
. Dihydrostreptomycin
27.50
5.4
Chloramphenicol
27.00
13.5
100.0
27.50
7.10
Dexamethasone
267.0
Methyldopa
80.00
18.48
333.0
640.00
72.5
Indomethacin
611.0
Hydrochlorothiazide
90.00
5.20
1,530.7
Guanethidine
920.00
190.80
382.0
Metronidazole
390.00
11.15
3,398 0
Penicillin G
0.03MU
0.018MU
66.7
local production rather than protect their own
local
manufacture (as happened
in Latin
American countries when they attempted to begin
manufacturing their low-cost antibiotics).
*
The
expecation
of
the
country from the
HEALTH FOR THE MILLIONS/APRIL-JUNE 1981
table-A
Im ports of selected pharmaceuticals by the State Pharmaceuticals Corporation (SPC)
of Sri Lanka, 1974. Comparison of actual cost with cost of traditional supplier.
(Dollars)
Drug
1.
Traditiona I
supplier
Cost
Hoechst
Carlo Erba
New
supplier
Cost
Savings
45 999
Sarabhai
33 166
12 833
27.9
926
Ranbaxy
555
371
40.1
15 208
Medimpex
Medimpex
10 866
6 871
' 4 342
9 072
2 201
28.6
24.3
Savings as
percentage
of original
cost
2.
Benzyl penicillin
Chloramphenicol inj.
3.
Melhyldopa
4.
Nalidixic acid
5.
Nitrofurantoin
Smith, Kline and
French
7 611
Unique
1 485
6 126
80.5
6.
Phenylbutazone
Ciba-Geigy
30 088
Ranbaxy
1 710
28 378
94.3
7.
Benzhexol
Cyanamid
5 433
Aktielskabet
1 503
3 930
72.3
8.
Balladonna a phenobar
bitone
Sandoz
23 126
Wockhardt
1 997
21 129
91.4
Merck, Sharp and
Dohme
Sterling
9.
Chlorpromazine
M and B
16 179
Unique
1 521
14 658
90.6
10.
Diazepam
Roche
Total
19 583
1 73 225
Ranbaxy
790
60 464
18 793
1 12 761
96.0
65.1
Source: S. Bibile, The Stale Pharmaceuticals Corporation of Sri Lanka, Colombo, 1976
what is transfer pricing
In 1973, the Sri Lanka, SPC took over the
purchase of some of the raw materials required
by privately owned drug factories. The following
table shows the prices paid by the SPC in 1973,
ro
0)
co
E
£
co
O <N
o CD
•it
HEALTH FOR THE MILLIONS/APRIL-JUNE 1981
V)
U 9?
Q- o
W t-
cc
compared to the prices paid in 1972 by multina
tional subsidiaries for the same supplies bought
from their parent companies. This illustrates the
widespread phenomenon of “transfer pricing".
o
Q.
Q.
° 8
w
<y a>
CO V)
> c
w
co
o
3 “
Q.
Q 8
V) Q.
o
07
co
m
Tolbutamide
Hoeschst
W Germany
Hoeschst
W Germany 40.62 19.24 47
Polfa Poland 40.62 2.52 6
Paracetamol
Sterling
UK
R. Poulenc
France
3.24
2.76
85
Chloropropamide
Pfizer
USA
Pliva
Yugoslavia
126.21
9.46
8
Tetracycline
Pfizer
USA
Hoeschst
W Germany
98.87 19.72 20
Aspirin
Glaxo
UK
Polla Poland
1.16
Ampicillin
Beecham
Singapore
Beecham
Singapore
0.99 85
569.90 95.11
17
27
The Joint Mission Hospitals Equipment Board
Limited (ECHO) in England, whose sales have
grown tenfold in the last ten years, services more
than 1000 mission and charity hospitals in 80
developing countries. “Manufacturers come
running to us because of our large orders’’, says
Dr James Burton of ECHO.
drugs to India," says Mr Beckers the Managing
Director, who is also the mayor of the .town,
Spokesmen of both ECHO and IDA, the
Netherlands-based
International
Dispensary
Association, claim that their prices are generally
30-40% cheaper than their individual clients
would be able to obtain for themselves.
Action Medeor would welcome if an organiza
tion could unify and systematize their supply in
India.
(1) The Indian institutions cannot make pay
ments in dollars or Deutsch Marks
(2) Difficulties at customs in spite of the fact
these drugs are imported under the Indo
German Agreement.
At the request of WHO, ECHO has recently
prepared a list of standard equipment required
for a rural health centre (which would include
accommodation for minor operations and lab
work) and for a small village clinic. By bulk pur
chasing drugs and other items, ECHO is now
providing a completely pre-packed kit for a rural
health centre and for a small village clinic. ECHO
recently supplied prepacked kits for 10 rural
health centres and 50 village clinics to Vietnam.
medeojAction Medeor is Europe's largest mail order
dispensary solely and exclusively intended for
the developing countries. They supply medicines
to nearly 4,000 institutions in the Third World.
The brain child of Dr Ernst Boekels “a country
doctor"—who continues to be the chairman of
its Board of Directors, MEDEOR has an assort
ment of 95 medicines which can be ordered at
the cost price.
Medeor buys the basic ingredients for the
medicines needed in the Third World from the
pharmaceutical industry. These ingredients are
used to manufacture, under medical supervision,
medicines according to the standards set by the
scientific community against cholera, scabies,
leprosy, malaria, tuberculosis and other prevalent
diseases existing in tropical and subtropical
countries.
The pharmacy stocks about 100 million tablets
and has an yearly turn over of 2 million dollars.
"There are two kinds of difficulties in supplying
28
medeor in action
The UN Children's Fund (UNICEF) is another
organisation that bulk-buys drugs for developing
countries. It buys all its drugs as generics. As
its orders are quite large, manufacturers are
willing to label these drugs in the way UNICEF
asks them.
UNICEF drug prices are often half the market
prices and sometimes as low as one quarter.
Even some rich countries like Iran order certain
drugs through UNICEF. In 1977, UNICEF distri
buted drugs and vaccines worth about 315 million,
most of them as gifts.
What does this mean? It is obvious that even
if groups of voluntary institutions in India get
together, and do bulk purchasing of formulations
and/or bulk drugs, enormous savings can be
effected. Who will bell this cat?
HEALTH FOR THE MILLIONS/APRIL-JUNE 1981
Council on International and Public Affairs
(Formerly Conference on World Affairs, Inc.)
777 United Nations Plaza
New York, New York 10017
(212)972-9877
Cable: COUNINTERP NEW YORK
March 29, 1982
Please reply to above address
unless otherwise noted.
MEMORANDUM
TO:
Coordinating Committee on Toxics and Drugs
FROM:
Ward Morehouse
SUBJECT:
Pharmaceuticals in India
Dr. C. Sathyamala of Health Action India (and VHAI) will,
working with other concerned health care professionals,
pick some drugs (such as the Oestrogens mentioned in the
attachments to the note) which they consider to be high
priority and gather documentation on labeling practices,
content and distribution of explanatory literature, how
sold (i.e., over-the-counter or through prescription),
etc.
This documentation can then be forwarded to us, so
that those on the Committee working especially on pharma
ceutical questions can take up specific products with
individual U.S.-based multinationals.
Office of Secretary: 15th Floor, 522 Fifth Avenue, New York, New York 10036
Policy Studies Associates: P.O. Box 337, Croton-on-Hudson, New York 10520
Accounting Office: P. O. Box 337, Croton-on-Hudson, New York 10520
DANv. uO .t ECuOOl
1.
COMMUNITY HEALTH CELL
I discussed with several persons the concerns of our Committee
and how we might work most effectively with similarly concerned
groups in India and have the following suggestions to put before
the Committee for its consideration:
4 7 /1 , (F irs t F lo o rfS t. M arks Road
As most of you know, I have been for the last six weeks in
India, where I was in contact with a number of environmental,
consumer, public health, and other voluntary social action groups.
I enclose a brief note on health care and drug companies in India,
growing out of discussions with these groups.
I hope shortly to
prepare a similar note on pesticides and industrial chemicals,
where the problems and what can be done about them are somewhat
different.
Memo/Pharmaceuticals
in India
- 2 -
March 29, 1982
2.
Both Dr. C. Sathyamala of Health Action India/Voluntary
Health Association of India and Dr. Anant Phadke of
Medico Friends Circle need the latest version of the U.S.
Physician's Desk Reference.
(Dr. Phadke has the 1981 PDR.)
I took it upon myself to promise that one way or another
we would see that they received the latest PDR edition.
3.
I think we should make an effort to bring someone from
Medico Friends Circle or Health Action India to educate us
on the nature of health care problems in India and what
needs to be done about them.
By "us", I mean not just the
Coordinating Committee but also our respective constituencies.
4.
If we really mean what we say about avoiding a "top-down"
approach in working at the international level with NGOs
in the Third World, I think we need the benefit of an
external observer undertaking a critical examination of
who we are, what we do, and how responsive we are to Third
World concerns.
(The reverse occurs all the time - witness
my recent trip to India.)
My candidate is Anil Agarwal,
the founder of the Centre on Science and the Environment,
former Assistant Editor of Earthscan in London, and a
well-known, serious, and careful investigative science
journalist.
I am sharing copies of this memorandum and the attached note
with some of the people with whom I discussed these matters in
India by way of keeping them informed.
I hope we can give some
serious attention to these suggestions at our next meeting.
WM/mbi
cc: Anil Agarwal
Dr. C. Sathyamala
Dr. Anant Phadke
Attachment: Note on Health Care and Drug Companies in India
March 26, 1982
A Note on Health Care and Drug Companies in India
Some Key Actors
Among the groups involved in the struggle for more socially
relevant health care in India are:
Voluntary Health Association of India, an organization of
doctors, hospital administrators, and others engaged in
community health work, which grew out of the joining to
gether of two associations of Christian hospitals m India.
Medico Friends Circle, a small but strongly committed
group of doctors, mostly young, who are working in a variety
of rural and urban community health projects around the
country.
Centre for Science and Environment, a non-profit "public
interest" research agency which conducts investigative
reporting of economic and social issues which are science
and technology-related.
Health Action India, not a formal organization as such but
simply those individual health care professionals willing
to engage in common action on specific health care issues.
A list of addresses and contact persons is attached.
The Problem
Drugs are not the main issue in working toward a more socially
responsive health care system in India, let alone pharmaceutical
multinationals.
The main issue would appear to be the Indian medical
profession, which is maldistributed in relation to the population
(80% of the doctors are in the cities while 80% of the people are
in rural areas), socially irrelevant in terms of much of the technique
they use, and motivated more by their own greed rather than their
patients' need.
Chemists or druggists certainly aid and abet a health care system
largely irrelevant to the health care needs of most of the people
but they are not the prime problem.
Indeed, most of the population
has no contact with chemists, who are overwhelmingly concentrated
in urban areas - thereby suggesting that one pharmaceutical MNC
argument is spurious, at least in India (i.e., in poor countries,
chemists frequently substitute for doctors).
To the extent that drug companies are a significant part of the
problem, India may be atypical among Third World countries because
2
a substantial part of that problem is Indian, not foreign - i.e.,
Indian drug companies producing and marketing drugs for the domestic
market.
(A glance at the "Dear Doctor/Chemist" letter attached
indicates, using the case of Oestrogen-Progesterone drugs, that a
significant proportion of the companies making and marketing the
offending product are Indian companies, not Indian subsidiaries of
MNCs (although the latter are involved as well).)
There is some government regulatory machinery, including a
Government of India Controller of Drugs. While this machinery is
not totally ineffective, it is far from being as efficacious as it
should be.
Of course, at a more fundamental level, the problem of inadequate
and misdirected health care is both a manifestation and a cause of
widespread poverty, illiteracy, infant mortality, malnutrition, and
the other social ills of Indian society.
The Remedy
There is, naturally, no single remedy for such a deep-rooted and
pervasive problem.
But if the foregoing summary of the nature of
the problem is near the mark, much of what needs to be done must be
done by concerned individuals, including health care professionals,
and groups within India.
Concerned persons and organizations in the
North, can at best be helpful at the margins of the problem and should
tailor their efforts so as to be responsive to priorities determined
by those working toward a more socially responsive health care system
within India.
The most essential need is obvious but, because it is so massive,
elusive—greater public awareness and understanding of patterns of
morbidity which afflict them and what can be done about them.
Steps
are being taken through a number of community health projects at
the local level throughout the country. At the national level, one
of the more important has been to bring out an Indian edition of
Where There is No Doctor, first in English and Hindi, and in time,
in other Indian languages.
The need for educating, and ultimately changing the behavior
patterns, of health care professionals is obvious.
One small step
in that direction is reflected in the Oestrogen/Progesterone campaign
described in the attachments ("Dear Doctor/Chemist" and "Dear Sister").
Drugs are a small part of the total problem in India but not an
unimportant one.
Some action is beginning to move forward by groups
such as those mentioned above.
The Oestrogen/Progesterone campaign
is one example.
The Medico Friends Circle recently held a workshop
3
on drugs.
And the VHAI has produced a special issue of its bimonthly
magazine, Health for the Millions on the subject.
Ward Morehouse
Council on International and
Public Affairs, Inc.
777 United Nations Plaza
New York, NY 10017
(212) 972-9877
Attachments:
List of health care organizations and points
of contact in India; "Dear Doctor/Chemist,"
and "Dear Sister" (letters on misuse of
Oestrogen/Progesterone combination drugs);
Counterfact Health Cell Feature ("Abuse of
Female Hormone Drugs," Centre for Education
and Documentation, March 8, 1982),'
description of Medico Friend Circle of India; subject
index of back issues of MFC Bulletin.
March 29, 1982
List of Health Care Organizations
and Points of Contact in India
Voluntary Health Association of India
C-14, Community Centre
SDA, New Delhi 110 016
INDIA
(Dr. C. Sathyamala)
Health Action India
C-14, Community Centre
SDA, New Delhi 110 016
India
(Dr. C. Sathyamala)
Centre for Science and Environment
807, Vishal Bhawan
95, Nehru Place
New Delhi 110 019
INDIA
(Dr. Anil Agarwal, Director)
Medico Friends Circle
50 LIC Quarters
University Road
Pune 411 016
INDIA
(Dr. Anant Phadke)
Pune Journal of Continuing Health Education
1913 Sadashiv Peth
Pune 411 030
INDIA
(Dr. A.R. Patwardhan)
q9 ?
Alternative Drug Policy — Some Criteria
Amitava Guha
Profit cannot be’ the only motive force for the
development of Drugs & Pharmaceutical Industry.
11 Committee on Drugs & Pharmaceuticals"
In the recommendations of'the Hathi Committee .are-"'
-the first ever attempt was done to-wards a real development
of drug industry in our country. Almost all recommendations
of the committee including the nationalisation of multina
tional drug companies (TNCs) are vitally required for our
country. Few relevant issues needs to be taken up afresh. The
Committee did not considered distribution system in their report.
Dilution of foreign equity s
Recommendation of the Committee in this respect is
to taper down the foreign equity to 26%. In fact it should be
brought down to 10% within a span of 3 years and no company
having any amount of foreign equity should be considered as
'Indian Company'. No company should be given the status of
Indian company unless the plant and machinaries are installed
on turn-key basis and no stipulation is put for import of
raw materials from the parent company.'
Transfer technology should be guided under UNIDO
recommendations. Only latest technology can be imported on
the basis of global tender from all the developed countries.
Preference should be given to the countries whoever accept
"Rupee" as transfer currency and indegenous plant and machi
neries are accepted.
Petrochemical industry in our country is mainly ori
ented for heavy chemicals/ detergent/ paints' synthetic fibres/
etc. There should be adequate stress for orientation of Petro
chemicals‘for production of raw materials for fine chemicals
and phyto-c hemic als.
&■
Production capacity of the plants' producing basic
drugs of essential nature should be increased. No intermidi aries for essential drugs should bo imported.
Export of r® harbs and alkalids should be banned.
"Committee for Rational Drugs"
There has been various development after the report
of the Hathi Committee was published. Patem of the industry
has been changed and large scale manufacturers have made up
le£ ways to make the recommendations futile. Therefore it has '
become most important to constitute another Committee for ra
tional drugs where doctors from research centres/ people from
health institutions and drug action groups should be included
(and none‘from the manufacturers). Objective of the committee
shall be 1.
To prepare a ’List of Essential Drugs 1 (WHO guideline) /
including the drugs needed for tropical diseases.
2.
To prepare an overall study report on the production of
drugs and pharmaceuticals/ requirement and production
pattern for essential drugs.
CONTD. . . 2
alth cell
coninwnhy HC
J. Marks Road
47/1,(First Floor)J
BANGA<-Oat . 560 001
2
3.
National survey on disease pattern and drugs needed thereto.
4.
Weeding out of the harmf ul/bannec/habit "forminef
drugs
and drugs having doubtful action.. Survey for substandard
drugs and their sources.
5.
To judge the applicability of the drug policies of diffe
rent countries including the countries under socialist
block.
6.
Reduction of the number of formulation and intrriductio-n-of
brand names.
7.
To bring effective check, on the expensive and tunethical
sales promotion.
. ■>.
8.
Develop drug distribution system- under total, government
control. ,
-- 9*
Develop drug information machinery.
— 1 ' Fo r -the consideration of the. said’ Committee. the
following-notes., may.be.placed...
.....
M clTItlf clC IS'UXX HQ o
-r
.......
.- *
TNCs
-■ _
......
—--------- • ■ - -
'
— ...
--
....
should not be'hllowedr-to manufacture.common-formations
. (essential drugs) household remedies
*
..cosmetics.:
' -
- a Suitable .change in. -thcr Drugs
Cosmetics- Act’
Rules..so--—
that small .scale, industries do. not,suffer .(schedule *M ’ -of
- ....... the. Rules
*
etc..),
x
" Stringent laws on-qn-ality-control-is. required,. Quality
’ ------ control laboratories are to established by the Government
in all manufacturing-centres all over the country
*
to'
'facilitate'tdstes^at cheaper cost and to maintain uniform
standard.
,
- ,
* No import of machineries directly or without the guaran
tee from the end-users,
- -
-No import of machineries/ if the similar machines are
-indeg.enously available. Import of the machines for filling
*
*
sealing
■ labelling
*
*
caping
*
packing
etc. should be banned.
... * 'Open General Licence system is to be abolished. There
------ should be raw materials pool in .each state for inform pri
cing of- raw-mat erials, A Bulletin is to be published : infor
ming availability and prices of the raw-materials every
months Prices of raw materials should.be uniform all over
the country.
* A-standard has to be fixed for packing of fixed dosage
.--forms - uniformity in.bottle size
*
strips# shippers
*
etc.
■ 'No. fashionable packs like tonic bottles
*
blister pack
*
etc.
_ '
should-be. allowed.
■'.........
0'^
. -All taxes should be abolished! ■ Subsidy should be provided
.. ..
—for-transport of essential drugs and raw .materials.1
- - Deader price system is-' to. be -ch-anged/and maximum price
■ "'of each drugs is to be calculated on the basis pf BICP data.
The basis of this calculation and., all BICP data-about drugs
and pharmaceuticals should become...public document.
'
'
CONTD...
3
’
*Loan Licence system is to be totally withdrawn.
* Product-mix and production capacity has to be determined
by the Committee and it should be distributed to the manu
facturers for essential drugs vzhich should form the minimum
base line for capacity utilisation.
* No COB licence or production over the licenced capacity
should be allowed.
Quality Control;
■ T $s t d L abo rato ri es are to be established in each districts
0.1%’surcharge can generate adequate finance for the purpose.
- All complaints regarding harmful effects of druqs are to
be entertained" Analysis should be conducted at least in
three taste labs, on the basis of double blind study.
Regular sample survey throughout-the nation should be done.
Special statute and judicial set-up should be made to check
production and sales of harmful and substandard drugs. Com
pensation should be ext acted from the convicted producers.
-- In arrangement with the leading institutions in four
.
zones of tie country trial and study has to be made for
- each nevi druqs before its introduction.
- Informations regarding banning/ withdrawal of drugs from
the market has to be published in news papers and mailing
to the retailersk
Drugs should be immediately replaced to the buyers if any
doubt is expressed even if a Part of the .pack is used.
Cosmetics? OTC drugs? household, remedies cannot be sold
from the shop where pharmaceuticals are sold in the cities
and towns.
Sales promotion ;
There should be a permanent National Organisation for
information on druqs and therupy. Informations are to be circula
ted by the organisation every month through a journal. A full
fledged machinery has to be established by the Govt.
In sales promotion activity only scientific information can
be circulated by the manufacturers. All sales promotion informa
tions/advertisements has to be checked by the national net work
of information education-and communication on medicines.
Physician sample of now medicines can be given for three
years after introduction. For all other druqs? samples required
to treat one patient for a particular drug can he provided on
written request from toe physician.
No literature‘can be published without mentioning full
indications? contra-indications? side effects? drug interaction
and anti do te s.
No gifts of any form shall be allowed to be given to the
medical profession/^
No seminar? scientific session can be held without written
permission from the national Het-work.
Conus/incentive system on sales of the products by toe dis
tributors or retailers,, has to be abolished.
All manufacturers shall inform their yearly sales promotion
strategy to the National Net work for approval. Expenses equal to
the sales promotion has to be contributed for research by toe
MRTP companies. All research and development centres are to be
run jointly by th 3 private and Govt, .sectors.
Each pack of neutri^hts and food products should bear the
mark "it is not a substitute to normal food".
MK-iOHANDUi'I
We, the health personnel and citizens of India recognize health as a
fundamental right of the people in this, our welfare state. We recognize
and strongly believe that the health status of our people is more dependent
on their access to adequate food, safe and adequate water, proper sanitation
and clean environment.
While we support the overall perspective and approach of the new
National Health Policy Statement and demand its proper implementation, we
believe that a 'Rational Drug Policy1 is an integral part of a good National
Health Policy.
We therefore, demand the following:
We have a right to safe, essential, quality drugs which arc- in keeping
with the health needs of tho people, at costs which the majority can
afford.
2. We urge our government to accept and implement the Hath! Canmittee
Recanmendations -which are also in keeping with the WHO Guidelines for
a Rational Drug Policy.
3. Further the national drug formulary should be revised and compiled by
an export multi diciplinary committee keeping the following criteria in
mind;
Essentiality
Efficacy
Safety
Cost
Ease of administration
Availability
Potential for misuse.
Such evaluation of the drugs in the market and revision of the lists
should be done periodically.
4. The Essential Drugs Policy should be adopted for all health services,
government and private, and priority in production, distribution and
dispensing should be given to these essential drugs.
5. The public sector should produce essential and life saving drugs on a
priority basis at the national level.
6. Drug production by multinationals and private manufacturers in India
should also be aligned with national health priorities.
7. Bulk procurement of essential and needed drugs should be through world
wide competitive tenders and rationalization of drug purchases should
govern both the public sector as well as private health sector.
8. Imports and production of non essential, specially hazardous drugs,
should be strictly curtailed.
9. Drugs which have been banned from sale after being marketed for some
time in one country may net be submitted for clinical trial or marketing
in India. The onus of proving ’why a non-essential drug should be intro
duced or allowed to continue on the market should be with the manufact
urer and such introduction should be proceded by adequate trials and
evaluation by Drug Control Authorities.
10, Ccmprchensivc drug legislation which covers areas such as price control
at different levels, patents, and marketing practices should be incor
porated to servo the objectives of the national drug policy and there
should be no levies, sales tax or excise duty on any pharmaceutical pro
duct in the essential drugs list by the Central or State governments.
11. No techno logs’- transfer agreement shall be legal, and binding which cont
ains restrictive practices, disproportionate and unnecessary use of
imported intermediaries n-r obsolete technologies or unfair arrangements
with respect to prices, payments or repatriation of profits.
12. The National Drug Policy should state clearly the steps towards a
complete abolition of brand names and as a first step use of generic
names should ba made compulsory in medical education, prescribing and
labelling of drugs. Generic names should appear more prominently on all
packagings
•„ ..
1.
It shall be the primary responsibility of the manufacturer to ensure the
quality cf drug products. However, it shall be the statutory responsibi
lity of the Drug Control Authorities to monitor the standards-and ensure
a minimum uniform level of government control. Consequently, the govern
ment shall take all necessary measures to enable the Drug Control Autho
rities to function in an. effective manner and discharge the statutory
duties cast upon them.
14. It shall bo the statutory duty of the drug control authorities to inform
health personnel and jccnsumers cf the essential drugs lists, policies,
categories or brands0 drugs banned for manufacture or sale, through pub
lication in the national newspapers, magazines, medical journals with
adequate explanations and details.
15. Availability of drugs required in the Governments National Programmes
should be ensured on a priority basis to the government as well as
voluntary and private health institutions. Quotas for anti TB, anti
leprosy, anti malarial drugs, iodized salt etc should be made easily
available with regularity of supply to the voluntary health institute'-ns
whereever possible, specially when their performance, in health care
delivery is known tc be effective.
16. In all review canmittecs, statutory bodies and other such bodies, there
should be adequate representation of consumer groups and voluntary health
sector.
1?. Drug companies should follow ethical marketing practices, and this should
be ensured by their own organizations like OPPI,1DMA, IFPMA. We deplore
the tendency of those companies and associations to get around every
progressive measure of the government through reccurse^technicalities of
the law and through the courts.
18. The marketing cede drawn up by HAI(Health Action International) should
form the basis for a National Cede for Marketing Practices. This should
be accepted by our government and should be suitable implemented through
legislation.
19. The government of India should take a lead and endeavour to influence
the WHA and WHO to adopt tile Code in the interests of the other develo
ping countries and their peoples.
13.
(IFPMA and HAI Code attached).
- Voluntary Health Association of India
- Centre.for Science and Environment
- Centre of Social Medicine and Ccminunity Health-Jawaharlal Nehru Univer-
- Kerala Sahitya Shastra Parishad
.
- Medico Friends Circle
- Arogya Dakshata Mandal
- Lok Vigyan Sanghatana
- Consumer Guidance Health Services
- Consumer Education Research Centre
- Federation of Medical Representatives Association of India.
Alternative Drug Policy — Some Criteria
Amitava Goha
Profit cannot be the only motive force for the
development of Drugs & Pharmaceutical Industry.
“Committee on Drugs & Pharmaceuticals'1
In the recommendations of'the Hath! Committee'-are^he'first ever attempt was done to-wards a real development
of drug industry in our country. Almost all recommendations
of the committee including the nationalisation of multina
tional drug companies (TNCs) are vitally required for our
country. Few relevant issues needs to be taken up afresh. The
Committee did not considered--distribution system in their report.
Dilution of foreign equity :
Recommendation of the Committee in this respect is
to taper down the foreign equity to 26%. In fact it should be
brought down to 10% within a span of 3 years and no company
having any amount of foreign equity should be considered as
'Indian Company'. No company should be given the status of
Indian company unless the plant and machina.ries are installed
on turn-key basis and no stipulation is put for import of
raw materials from the parent company.1
Transfer technology should be guided under UNIDO
recommendations. Only latest technology can be imported on
the basis of global tender from all the developed countries.
Preference should be given to the countries whoever accept
"Rupee" as transfer currency and indegenous plant and machinaries are accepted.
Petrochemical industry in our country is mainly ori
ented for heavy chemicals/ detergent/ paints' synthetic fibres/
etc. There should be adequate stress for orientation of Petro
chemicals‘for production of raw materials for fine chemicals
and phyto-chemic als.
Production capasity of the plants/ producing basic
drugs of essential nature should be increased. No intermicliarics for essential drugs should be imported.
Export of raw harbs and aLkalids should be banned.
"Committee for Rational Drugs"
There has been various development after the report
of the Hathi Committee was published. Patem of the industry
has been changed and large scale manufacturers have made up
led ways to maize the recommendations futile. Therefore it has ’
become most important to constitute another Committee for ra
tional drugs where doctors from research centres/ people from
health institutions and drug action groups should be included
(and none'from the manufacturers). Objective of the committee
shall be 1.
To prepare a 'List of Essential Drugs'(WHO guideline)/
including the drugs needed for tropical diseases.
2.
To prepare an overall study report on the production of
drugs and pharmaceuticals/ requirement and production
pattern for essential drugs.
CONTD. .. 2
2
3.
National survey on disease patem and drugs needed thereto,
4,
Weeding out of the harmful/banned/habit forming -, drugs
and drugs having doubtful action.. Survey for substandard
drugs and their sources.
5.
To judge the applicability-of the drug policies of diffe
rent countries including the countries under socialist
block.
6.
Reduction of the number of formulation and Lnt-reduet-io n of
brand names.
7.
To bring effective check.-pn the expensive and i unethical
sales promotion.
’
.8,
Develop drug distribution system- under total, government
control. . .
9,
Develop drug inforrfta-bicm machine-ry.
—For-the consideration of the. said"Committee, .the
-followi ng-notes, may .be. placed.-
■'Manufacturing's
’• --- • .
■
-
...
.
■
—■ -—
'
-
"
- . . .
uZ
*TNCs should not" be allowed--to manufacture, common formations
. (essential drugs) household remedies
*
.cosmetics.:■ ■
■ * Suitable...change i-n.-the-Drugs -crCosmetics- Act ■&'Rules..sox —•
that small scale..industries do not..suffer.Cschedule ’M
* of
- ........ the. Rules
*
etc..)„._
J
"Stringent laws on-quality-control-is. required.. Quality
------ control laboratories are to established by the Government
in all manufacturing-centres all over the *
country
to
facilitate' t^st^s<fet cheaper cost and to maintain uniform
standard.
- .
- ...
* 'No import of machineries directly or without the guaran
tee from the end-users.
- -
* No import of machinaries
*
if the similar machines are
Indegenously available. Import of the machines for filling
*
*
sealing
*
labelling
*
aaping
,
*
packing
etc, should be banned.
.... *
"Open General Licence system is to be abolished. There
----- should be raw materials pool in each state for inform pri-’
cing of- raw-materials. A Bulletin is to be published infor
ming availability and prices of the raw-materials every
"month-. Prices of raw materials shoul-d.be uniform all over
the.-country.
A-standard has to be fixed for packing of fixed dosage
... -forms - uniformity in.bottle- size
*
*
strips
*
shippers
etc.
No. fashionable packs like tonic bottles
*
.blister pack
*
etc.
should-be. allowed.
...
*'All taxes 'should be abolished^ - Subsidy should be-provided
■—-'■for transport of essential drugs and raw materials.1
* '- -’-Leader price' system' is to. be.chang-eet and maximum price
' of each drugs is to be calculated on the basis pf BICP data.
The basis of this calculation and. all BICP -data .about drugs
and pharmaceuticals should become...public document.
---
.'f..CONTD... 3
- 3
■•‘Loan Licence system is to be totally withdrawn.
* Product-mix and production capacity has to be determined
by the Qommittee and it should be distributed to the manu
facturers for essential drugs which should form the minimum
base line for capacity utilisation.
* No COR licence or production over the licenced capacity
should be allowed.
Quality Controls
• • T^ste Laboratories are to be established in each districts
0.1% surcharge can generate adequate finance for the pur'.nse.
- All complaints regarding harmful effects of drugs are to
be entertained- Analysis should be conducted at least in
throe taste labs, on the oasis of double blind study.
Regular sample survey throughout-the nation should be done.
■ • Special st tout to and judicial set-up should be made to check
production and sales of harmful and substandard drugs. Com. pensation should be ext acted from the convicted producers.
• • In arrangement with the leading institutions in four
zones of the country trial and study has to be made for
- each new drugs before its introduction.
- Informations regarding banning/ withdrawal of drugs from
the market has to be published in news papers and mailing
to the retailers^ jvuustvcw-4
- Drugs should be immediately replaced to the buyers if any
doubt is expressed even if a part of the pack is used.
-- Cosmetics/ OTC drugs/ household remedies cannot be sold
from the shop where pharmaceuticals are sold in the cities
and towns.
Sales. Promotion t
There should be a permanent’ National Organisation for
information on drugs and therupy. Informations are to be circula
ted by the organisation every month through a. journal. A full
fledged mechinary has to be established by the Govt.
In sales promotion activity only scientific information can
be circulated by the manufacturers. All sales promotion informa
tions/'advertisements has to be checked by the national net work
of information education and communication on medicines.
Physician sample of now medicines can be given for throe
years after introduction. For all other drugs/ samples required
to treat one patient for a particular drug can be provided on
written request from the physician.
No literature can be published without mentioning full
indications/ contra-indications/ side effects/ drug interaction
and antidotes.
No gifts of any form shall be allowed to be given to the
medical profession^
No seminar/ scientific session can be held without written
permission from the national Het-work.'
Conus/incentive system on sales of the products by the dis
tributors or retailers., has to be abolished.
All manufacturers shall inform their yearly sales promotion
strategy to the National Net work for approval. Expenses equal to
the sales promotion has to be contributed for research by -the
MRTP companies. All research and development centres are to be
run jointly by til; private and Govt, sectors.
Each pack of neutri^ats and food products should bear" the
mark "it is not a substitute to normal food".
Who's winni ig this war?
With the increasing
use — and abuse—of
antibiotics, bacteria are
learning to fight back against
the deadly drugs
0 blame the GP
alone for
increasing
antibiotic
resistance?
1 Patients
should be
educated
agai nst selfmedication -
Did yOU know?
Antibiotic
resistance
t goes back a little to the days when Alexander Fle
ming discovered penicillin, which led finally to
the use of the first antibiotics in the Forties. Mass
production of the first antibiotics, penicillin and
streptomycin, began during World War II. Penicil
lin opened the flood gates to a variety of antibiotics
that worked very effectively against disease
causing bacteria.
Since it was relatively cheap and easy to admi
nister, and since they worked miraculously on the
then life-threatening diseases like tuberculosis,
typhoid and venereal disease, the use of antibiotics
spread like wild fire.
Even today, newer antibacterials (for the pur
poses of this article, antibacterials and antibiotics
are being used synonymously in terms of their
fiction, i.e. inhibiting bacteria) are being created
regularly by drug designers with a little tinkering of
the organic chains of older drugs, or with other che
mical jugglery. The potential for new drugs seems
limitless.
Except for one thing. Even five decades after the
first antibiotics were introduced, bacterial diseases
remain a major cause of illness, and even death.
I
ou have the sniffles, you are running a
Y
temperature and your headache won't
let you think. Your doctor sympathises
with your desire to be back to normal
for tomorrow’s crucial event and pre
scribes an antibiotic. You wince at the price, but the
next day, there is good news because you are
already feeling fine. Good doctor, you think indul
gently and spread the word to your friends.
Now for the bad news: the antibiotic could not
have made you better. An antibiotic takes more than
a day to even begin to effectively cure you — at
least for most common infections.
Perhaps you didn't need the antibiotic anyway as
you probably had a viral infection. And though doc
tors never bother to explain this to patients, antibio
tics have no effect on viruses.
The truth is that antibiotics are among the most
used and most abused of drugs today. By some esti
mates, more than ten per cent of all drugs prescribed
in India are antibiotics. And because they
are
expensive; they account for almost half
the value of all drugs sold in the market.
So what, you shrug, perhaps I took the
wrong medicine. But 1 got better, didn’t
I?
Maybe you did. But maybe you also
helped create m°re antibiotic resistant
germs (pathi°8ens) within your body.
That could imean that someday, when
your body
needs an antibiotic
drug to fight a serious illness, the drug
won’t have t?16 desired effect.
i And now...
Suffer the little ones
Mass production of the
first antibiotics began
during World War II,
when penicillin was
found to have reduced a
great number of
amputations and
casualties.
Take a look at these
figures. Incredible as it
may sound, today, the
Indian drug market has
70.000 formulations
available to doctors and
patients —even though
the World Health
Organisation lists only
250 essential drugs.
With so many
'■ antibiotics in the market
today with so many
The overuse of
antibiotics is
particularly shocking
when it is extended to
children, who can
develop resistant strains
of bacteria in their
'i systems which they pass
on to other children.
These children can then
develop diseases tor
spread like wildfire.
’, Bacteria ? >
i evolve much' ’
faster than ,
humanbemgs.i
t’TI s only way .
out against
ie^tep ahead;]
Some little-known facts about antibiotics
The beginning
Then, since it was
relatively cheap
the use of antibiotics
Ram Shah, pharmacist
The more you take, the less it works
„
On the mai
: we need
more than
variation!’-lbis ,catls
tothedar|gerous;,buse
of drugs l’y an
unsuspecl,n® Publ,c’
. which commonly
j prescribed antibiotics
i provide no cure.
■ Good news for the
manufacturer
The economic problem
• has not stopped
pharmaceutical
companies from
pumping a lot of money i
into the antibiotics
research market.
Cynics would say it is ;
with good reason. The
53
52
SUNOAV *-,)»«««
SUNDAY 7-13Mo
*.
-nriev 1993
MEDICINE
Although this has something to do with
poverty and the lack of medical care, it
also has a lot to do with the problem of
resislance.
As bacteria are bombarded with the
antimicrobials (another term covering
antibiotics) designed to kill them, they
do their best to fight back, to develop
armour against the deadly drug. And
they use formidable and cunning
methods to do so. The bacteria, micro
scopic as they arc, are diabolically
clever. Their very simplicity allows
them to evolve easily to win the war
against the enemy.
Among the many methods used by
micro-organisms to develop resistance
a drug is genetic mutation. The gene
the bacteria Which is supposed to be
sensitive to the antimicrobial factor
mutates and the antibiotic proves use
less in attacking the micro-organism.
Worse (for us, not for the bacteria),
they can transmit the acquired resistan
ce. called the R-factor, to other bacteria.
And worst of all, there is then a selective
multiplication of antibiotic-resistant
strains. These are the supergerms, which
can laugh into the face of the doctor's
prescription and continue to wreak
havoc in your body, in defiance of many
of the multi-coloured tablets in the
market.
K
When
in doubt,
prescribe
-
leads to an overusage of antibiotics.
which then makes bacteria more quickly
resistant. Doctors sometimes also pre
scribe the wrong doses.
If a patient is underdosed, some bacte
ria in the body could remain active or
through some method of mutation could
actively thrive. Equally, overdoses have
theirown problems: they make the bacte
ria more aggressive.
All doctors are well-acquinted with
these facts. So why is there so much
abuse of antibiotics?
Well, there are many reasons. One,
doctors have a mandate to give the pati
ent relief. And they cannot wait for the
sensitivity tests (which tell you which
antibiotic will work on your infection)
to start medicating a patient because that
will push recovery further away.
What is the impact of these malpracti
ces on the community as a whole? The
frightening truth, as a handbook on anti
biotics says. "One clinician's bad pre
scribing can directly affect patients of
colleagues via selection of the cross
infection by antibiotic-resistant micro
organisms. Furthermore, the profligate
use of antimicrobials in one locality may
result in resistant organisms with the
potential to spread widely and rapidly."
o all of us it means that if your friends
Sheela and Ramesh take their chil
dren regularly to a physician who often
and wrongly prescribe antibiotics for
every small ailment like upper respirato
ry viral infection or fever, then the bacte
ria in the kids' bodies may become resist
ant to the drug. And when you meet
T
those cherubic kids at the next neigh
bourhood party, it is just possible that
your kids could bring home the
antibiotic-resistant infection. And you,
model parent as you are, with little or no
antibiotic exposure for your kids, will
still find that the commonly prescribed
antibiotic does little to cure your chil
dren quickly. Individual abuse leads
directly to collective resistance.
tian doctors love antibiotics
Did you know? o Some little-known facts about
g^esistance to antibiotics develops
■ Cmainly because of their inappropria
spiralling prices of
te and irrational use. Survey after survey
reveals that antibiotics are being widely
newer drugs that are
misused, especially in India, where drug
entering the market each
laws even if stringent, are rarely
day also mean better
implemented.
One survey conducted by the Christi bottom lines for the drug
an Medical College and Hospital at Vel industry.
lore found that in common infections
like fevers of short durations, antibiotics The doctor isn’t God
are not indicated in 7S per cent ot the
cases in which they are prescribed.
Don't be afraid to
What do these specialists mean when
question your doctor
1 they say that your trusted family doctor
1 ls responsible for widespread resistance when he prescribes
antibiotics. They will
I ro antibiotics?
I
General practioners can prescribe not cure you if, for
antibiotics for relatively minor ailments
instance, you have a
,, by prescribing them when they are
not required at all. Such shotgut.
.apy_
A pill for every ill: doctors dare too much
viral infection. Ideally, antibiotics should
only be given after a culture/sensitivity test
determines what will be effective.
SUNDAY 7—13Novemoer 1993
I.
■
MEDICINE
afford, or as many as their husband
bought," says Dr Nalini Shcnoy, a pedi
atrician
in Bangalore.
There is no
Given this patent misuse among the
need for any
general public, DrTilak Kumar, a fami
ly physician, thinks it is unfair to blame
knee-jerk
the GP alone for increasing antibiotic
resistance. "If we abolish quackery,
reaction to
where allied medicine doctors wrongly
prescribe antibiotics, if we get druggists
antibiotics
to dispense antibiotics strictly against
either. Modem prescriptions only, and if we educate
patients against self-medication or
societies could . incomplete medication, there will defi1 nitely be less of a problem," he says.
not survive
Even if there was no misuse on the
I part of doctor or patient, however, bacte
without
ria would still someday beat the drugs
meant to destroy them. Says Ram Shah.
antibiotics,
proprietor, Tilrode Chem. with a PH.D
which are
in pharmacy from Belgium, "It is a pure
ly evolutionary process. Bacteria evolve
marvellous
so much faster than human beings.
Some bacteria could have a life span of
agents of
half a day. So the evolution time scale is
much smaller. In a matter of time, a
recovery
strain of bacteria would develop natural
resistance to a drug."
So how do mere human beings win
the war against deadly bacteria? Ram
bacteria to remain within your body. Shah displays the same i nsouciance shar
But in fact, it is often patients them
And the bacteria need just that opportuni ed by many others in the pharmaceutical
selves w ho are responsible for misusing
ty to develop mechanisms to resist the industry. He keeps faith in the endless
antibiotics. Two days into an antibiotic
drug next time around.
course, when one of the milder side
innovation of medical technology. "The
Sometimes, however, it is also the eco • only way out is to keep one step ahead
effects c>f the antibiotics are becoming
nomic factor which precents a patient through technical innovation," he says.
bothcrso'me (perhaps gastro-intestinal
from completing his antibiotic course.
problem^) and you are otherwise recove
One of the ways of tackling resistan
"Often, my patients, especially the poo ce, for instance, is to develop missiles
red, you tmay be tempted to stop the medi
rer mothers, say they gave their children that penetrate the shields that bacteria
cine. Thd' s when you are tempting fate.
only as many tablets as they could develop around them.
Because You have allowed some active
This brings up the question: Is it infi
nitely possible to create new antimicro
bials? Can we have newer and newer
generations of cephalosporins etc.?
medication —and keep
Technically, the answer is yes. "We
would
hate to think that there could be a
to them.
limitation," says K.S. Chandraprakash,
Never self-medicate,
senior product managerat the Bangalore
re-use old prescriptions
Pharmaceutical and Research Laborato
ry (P) Ltd (BPRL).
or old antibiotics lying
Even so. it still begs the next question.
around the house. It may
At what cost? And there's the nib. "The
tempt you to take
future is limitless so long as money is
limitless." explains Ram Shah. "With
non-optimal doses.
faster obsolescence of drugs, more and
Remember that
more money has to be pumped in all the
prevention is better than
time (to create newer generation antibac
cure. Antibiotics arc no
terials) and then you get into an econo- I
mic problem." So far. the economic pro
substitute for good
Oner y°u are conv'nced of the need to
blem has not stopped pharmaceutical
sanitation and personal i comptimes from pumping a lot of money
,„i.,
antibiotic, inform yourself about
IclKL dll
i >
•
ci
hygiene.
I into the antibiotics research market.
the con
*
ecl t*osa^e anc* tlural,on o* lhe
|
Cynics would say it is with good
antibiotics
------------------------ ■----- lovomber 1993
SUNDAY 7 13 b
son. The spiralling prices of newer
drugs that are entering the market each
day also mean better bottom lines for the
drug industry
*.
And the obsolesence of
older, cheaper antibiotics is only good
news tor pharmaceutical companies. As
doctors prefer to, or are forced to use
higher order antibiotics to kill simple ail
ments. the bills that go up are the
patients’.
Take a look at these figures. The Indi’ an drug market has 70.000 formulations
I available to doctors and patients when
, WHO lists only 250 essential drugs and
even the Hathi committee which went
into the issue found only 116 drugs
essential for India. The mind-boggling
figure of 70,000 preparations includes
many unessential and sometimes dangerdrugs that are in fact banned in many
other countries.
At what price?
The bill that goes up is the
patient's
he problem with overusing antibio
tics of course, is quite special, due to
the resi'i "ice factor. But theie are other
related | ■ blems as well. Price becomes
a big factor in the ..nroduction of newer
T
56
antibiotics. Millions of dollars are spent
to research, produce and market each
new-gencration antibiotic drug. And the
pharmaceutical companies have to pass
on the cost to the consumer. Which they
do. That is why a newer antibiotic, such
as Ceftum (which is a new antibiotic
drug called cefuroxime) from Allenbury’s costs around Rs 4! for one 500 mg
tablet, whereas the middle-range anti
microbials like cephalexin costs Rs 9.50
for a 500 mg tablet. Compare that to sulphonomides, or cotrimoxazoles like
Septran. which costs between 75 paise
to Rs 1.50 per tablet depending on its
strength.
And these are only the more common
antibiotics. Some of the higher-order
injectable antibiotics can cost upto Rs
350 per dose, whereas the higher-order
tablets can reach upto Rs 90 per tablet.
One of [he ways of
tackling resistance is
to develop missiles
that penetrate the
shields that bacteria
develop around
them
And if the Dunkel draft agreement goes
through, you can expect drug prices to
go through the roof.
It is not just the price factor, however.
There is also the question of side effects.
While they have undoubtedly played a
crucially important role in human health
in the last 50 years, antibiotics have also
been guilty of generating problematic
side effects, most of which are common
ly known, but some of which can even
be deadly. For instance, the known side
effects of the relatively new antibiotic,
gentamicin, (available only as an injecta
ble) are nephrotoxicity (which can lead
to kidney damage) and ototoxicity,
(which can cause deafness).
The rapid obsolesence of old drugs
and the corresponding manufacture of
new drugs also brings a sort of consumer
culture into the drug industry. It only
increases the misuse of medicine. Dr S.
P. Tekur, an active member ofjhe_Drug
Action Forum and of the Bangalore
based Community Health Cell, who him
self runs a child health clinic, is very dis
turbed about the widespread irrational
use of drugs.
There arc so many antibiotics in the
market today, with so many variations
in side effects, half life and site
effectiveness that it is understandable
that doctors themselves arc confused.
But sometimes, this leads to the danger
ous abuse of drugs on an unsuspecting,
ill-informed and apathetic public. Doc
tor Tekur cites the instance of Nor
floxacin and Ciprofloxacin, which
belong to the family of the recently intro
duced quinolones. "The recommended
dosage per day is 400 mgs twice a day."
he says. "They are not meant for
children.”
Quinolones are contra-indicated for
children under 14 because they have
been reported to cause damage to the
joints of immature animals. "And yet."
says Dr Tekur. "this antibiotic is availa
ble in 100 mg tablets, which tempt pedi
atricians to try them on children."
Shocking instances of antibiotic
abuse like this expose the complete lack I
of coordination and implementation of
the government's drug policy. But con
sumer awareness is the only really effec
tive means to stop the misuse of drugs.
and especially antibiotics. Because the
vested interests of the manufacturer, the
preseriber and the dispenser combine to
perpetuate this misuse. And it is left to
each individual to say. IT'S MY BODY
AFTER ALL. •
Uohlnl Nilekanl/Bangalore
SUNDAY!- nNovsmw.. 1993
'Eternal vigilance is required to
ensure that the health system
does not get medicalised, that the
doctor-drug producer .axis does.
not;exploit the people and that
the abundance of drugs does: not
become a vested interest in•ill-health1.
----- ICMR/ICSSR Health for All Report.
Venue; ST JOHN'S MEDICAL COLLEGE, BANGALORE 560034
SIGNIFICANCE .OF THE THEME
2
THE Workshop is to help participants understand the
issues relevant to drug prescribing, drug distribution
and pharmacy policy in our institutions in the context
of the ICMR/ICSSR warning and to challenge them to
participate in the growing national response to
the problem.
WHAT does the 'abundance of drugs' mean to the millions
of the poor in our country who struggle in life to
make both ends meet? Can they ever have access to the
modern health care system which has become a business
today, rather than remaining at the service of humanity
at large? Do they have essential and life saving drugs
at their reach within a price range they can afford?
IS our drug policy today more profession-oriented, drug
industry-oriented rather than patient-oriented? Whose
interests are we serving in our institutions?
HOW can we move towards a more people and patient-oriented
drug policy?
THESE are some of the QUESTIONS which we -shall respond to
in our Workshop.
ooooooooooooooooooooooooooo^oooooooo
"Community Health is a process
of enabling people to exercise
collectively their responsibi
lities to maintain their health
and to demand health as their
right. Thus it is beyond mere
distribution of medicines,
prevention of sickness, and
income generating programmes".
—CHAI new-vision
oooooooogoooooooc-ooc.
000000000000000
OBJECTIVES
1.
3
TO CREATE AN AWARENESS OS'sthe health situation in India, the role of drugs
in health care, the pattern of drug production
in India vis-a-vis the people's health needs, the
dynamics of the drug industry, the pattern of drug
distribution and availability in the health system,
the national drug policies and laws.
2.
TO CREATE AN AWARENESS OFs=
irrational use, over use and misuse of drugs by
health personnel.
3.
TO DISCOVER
the social, economic, political, cultural and
other factors responsible for this problem.
4.
TO DISCOVER
how all of us are part of the problem at a.
personal level.
5.
TO CONSIDER
the various responses at national/regional levels.
in the areas of s— consumer av/areness and people's
movements," continuing professional education;
pressure group on policy makers; search for low cost
alternatives; individual/group action; institutional
policy changes.
6.
TO DISCOVER
ways and means by which we can respond to this
situation at individual, institutional and
regional/national levels.
4
PROGRAM! IE_ HIGHLIGHTS
HiSesFions on:
■
Understanding the problem
Drugs and the healing ministry
Towards rational therapeutics
What to do to tackle the problem
Some initiatives in the country
The people's medicine
;::Group discussions on■>
What/why the problem in our health institutions?
What can we do to tackle this problem?
:jjLiturqy
Reflecting on our calling and the faith dimension
of our response
;ijExhibition on::
Socio-political dimensions of Health and Drugs
Rational Drug Therapy
Home remedies and Herbal medicines
;;^Studies ons
Drugs for a Community Health Center
Understanding the injection/tonic culture
Use/misuse of drugs in surgery
Drug situation in small rural hospitals
Cost of treatment
^Cultural Programme
Understanding the problem from the poor man's
point of view.
5
SYNOPSIS OF PAPERS
Drugs for Primary Health Care (C M Francis)
An integral part of our commitment to primary health care is
the provision of essential drugs to all those who need
them, in adequate quantity and quality and at affordable
prices wherever the person is. The various aspects of
the drug problem needing our attention include production,
what drugs are required, choice of drugs, National Drug
Policy, selection of drugs, drug production and procurement,
logistics of supply, quality control, regulating the drug
trade, drugs for immunization, drugs for cure, drugs for
symptomatic relief, search for new drugs, drug information
and the need for evaluation of the efficacy of primary
health care including drugs.
The Ten Commandments of the Drug Industry (Augustine Veliath)
1.
Thou shalt have tens of thousands of drugs
2.
Thou shalt not question the price of a drug
3.
Thou shalt not tamper with nature's garden
4.
Thou shalt respect they doctor more than thyself
5.
Thou shalt betray thy people and thy nation for petty rewards
6.
Thou shalt not covet, court, or subscribe to any other
system of medicine
7.
Thou shalt never reveal company secrets
8.
Thou shall first seek remedies for fashionable ailments
9.
Thou rhalt be a dumping ground for banned drugs
10.Thou shalt be a guinea pig for new and untried drugs.
6
The Ethics of Prescribing (George Lobo, sj)
Discusses reasons for the unfortunate situation related to
drugs prevalent today, viz., technological model of
health care leading to manipulation of the patient,
search and demand for instantaneous cure of symptoips,
mystification of medicine, profit motive and 'free
enterprise' of the pharmaceutical industry, a deep
rooted cultural alienation from the people, exploitation
of dependent developing countries, decreasing emphasis
being given to preventive medicine and other systems
of medicine.
The use of drugs should be regulated by the principles 'of
totality (overall good of the patient) and of double
effect (the good effect overriding any harmful effect).
It suggests remedies for the development of a personcentred and holistic approach to health care.
Professionals in the Church - an introspection (George Joseph)
Serious questions have been raised about the institutional
witness of the church in India, particularly its
relevance in the social context of today. In the case of
the Healing Ministry there is urgent need to critically
look at our priorities and commitment and our style,of
functioning in the light of the gospel. The role of the
professionals have to be reassessed as part of an
overall effort to bring back the true spirit of 'Diakonia'
into this ministry.
The whole issue regarding the need 'for evolving a 1 rational
drug policy' has to be seen in this perspective.
7
What is Rational Drug Therapy? (Mira Shiva)
Rational drug therapy means practice of socially
conscious, relevant, concerned and yet scientifically
sound medicine. It recognizes the non-role of drugs
in certain conditions, the role of alternative systems
of medicine and recognizes the limitations of Western
Medicine in our social context.
It emphasises selective use of drugs based on essentiality,
efficacy, safety, easy availability, easy administration,
quality drugs preferably of indigenous production.
Rational Drug Therapy recognizes the concept of essential
drugs and the concept of graded essential drug lists for
different levels of health personnel. It recognizes the
right of health personnel and consumers to drug information
and its effective communication.
x
It is taking of a conscious decision to boycott certain
drugs and use others only when needed. It means
prescription with awareness, to avoid as far as possible
— iatrogenesis (drug induced problems, drug 'interactions,
adverse drug reactions and emerging drug resistance).
It is understanding the role of drugs and rational drug
therapy in the emerging health movement.
What can be done at a pharmacy level (Alan Cranmer)
(a) Management of Pharmacy Services include involving the
users of the service; the Pharmacy Committee - its
constitution and functions, viz., implementation of
hospital policy, selection of medicines, sources of
medicines, cost versus quality, basic drugs and formula
tions, medicines banned in India and abroad, medicines
from other systems; stock control," prescribing
discipline and pharmacy discipline.
(b) Good dispensing services involve need for good
professional service to patients, proper presentation
of patient's medicines, preparation of medicines in
the pharmacy compared to purchase, medicines in the
pharmacy and at clinic level.
contd..
9
INITIATIVES IN THE COUNTRY
(1)
Arogya Dakshata Mandal, Pune has been raising awareness
about drug related issues among medical professionals
and the lay public since the past 3 years. They publish
a monthly—'Pune Journal of Continuing Health Education'—
on drug issues and are also bringing out a book
'Rational Drug Therapy' in December 1984.
They launched a ircvaient called 'Operation Medicine' in
1977 against irrational prescription cf vitamins, tonics
and tinned foods.
(2)
All India Drug Action Network; A number of groups have
been working in the field of drug related issues at
various levels during the past 3-4 years. They have
been in contact with each other and have been working
informally together sharing information, putting forward
a memorandum (demanding a Rational Drug Policy),
participating in campaigns, lobbying with government etc.
In August 1984, they felt the need to have a more organized
base and have formed the All India Drug Action Network.
CHAI is also a member of the Network.
(3)
Lok Vjgyan Sanghatans, Maharashtra, or the People's Science
Movement have launched campaigns about anaemia and
irrational anti-anaemia drug preparations and also about
over the counter drugs. They organize jathas, hold district/
town seminars, write in the mass media etc.
(4)
Kerala Sastra Sahitya Parishad is a voluntary non-government
organization consisting of sei- ntists, doctors, engineers,
social scientists, teachers, students, workers, peasants,
technicians who arc committed to popularising science and
channelising it for social revolution. The KSSP has recently
decided, to cake up the Drug issue and initiate a big campaign
to expose the anti-people and exploitative tactics of the
Multinational Drug Companies. The questions of essential
versus non-essential and dangerous drugs, the inadequacy
of drug safety control measures, the rising prices of
life saving drugs and the non-implementation of the Hathi
Committee recommendations are the highlights of the
programme.
11
(10)
State Forums; During the past year drug action forums
have been active in Andhra Pradesh and West Bengal.
Drug Action forums are also being initiated in Gujarat
and Orissa.
(11)
The Pharmacology Department of the Post-Graduate Institute
of Medical. Education and Research, Chandigarh, provide
unbiased technical information on drugs and therapeutics
through a monthly publication 'The Drugs Bulletin'.
Others?
The following organizations have also been
involved in drug related issues and are part of the
All India Drug Action Network?
Consumer guidance Society of India, Bombay
Consumer Education Research Centre, Ahmedabad
Federation of Medical Representatives
Association of India
Health Services Association, Calcutta
Delhi Science Forum, New Delhi
People's Participation in Science and Technology,
Madras/Bangalore
Centre for Science and Environment, Delhi
Centre of Social Medicine and Community Health,
J N University, Nev; Delhi
W h a t
vz e
can
do ?
— Support them
— Join them
— Keep them informed about what you are doing
AN INSPIRATION
13
Reading
The story of the sickman
at the. pool of Bethsaida
John 5? 1-9
Reflection
The action of Jesus in bypassing the pool is an
Invitation to us to look more critically at
our own health care system. Thanks to our
emphasis on curative health care, we have grown
accustomed to thinking solely in terms of the
health needs of the individual rather than addressing
ourselves to the community as a whole. While
concentrating on the symptoms, we have failed
to take into account the environment and other
social factors. Poor sanitation, polluted water
supply, the superstitious beliefs and taboos
of the community are also related to sickness and
disease.
Further, the miraculous pool in its ineffectiveness is
a symbol of our own ineffective health care system
despite the highly qualified doctors and nurses,
well equipped private and public hospitals, medical
research centres and multinational drug industry.
The poor man in the gospel story lived very close to
the pool, yet he was helpless because of his
poverty. In like manner the poor in our midst
remain helpless in the shadow of an expensive,
curative health care system that is geared
exclusively to the service of the rich.
Source: The Bibles Aspirin or Dynamite
by Cedric Rebello s.j.
"The greatest danger to Health in India is the over
medicalising of our Health Care System. Eternal vigilance
is required that the Doctor-drug producer axis docs not
exploit the people and that the 'abundance ' of drugs does
not become a vested interest in health".
- ICTB/ICSSR study on 'Health for All '
-an alternative strategy
The problem of Drug Policy and low cost drugs encompasses
a very wide spectrum of issues-multinationalism, industrial
policy, medical advertising, research, drug production,
medical education, price control and so on. The recent
upsurge in interest in this important area of health policy
has led to the publication of numerous reports, books and
papers and many seminars and workshops have and are being
organised.
In the final analysis any collective action in
the form of policy, analysis, research or education can only
result from an individual understanding of the related issues
translated into a prescribing policy to be accepted volunta
rily by doctors, nurses, para-professionals and others in
their attempt to contribute to a solution of the problem.
Readers of this bulletin are requested to think over
the following facts, observations, conclusions taken from
V.HO, ICf/R, ICSSR, Earthscan, VHAI, Govt, of India and other
sources of information. Can we collectively accept as many
of these gf-points as possible?
(1) 15000 branded drugs are on sale in India but a
Government Committee believes that Health needs would be
met by only 116 drugs.z»3
There is now an overproduction of drugs (often very
costly) meant for the rich and well to do, while the drugs
needed by the poor people (and these must be cheap) are not
adequately available!
WHO in its report on selection of essential drups has
prepared a list of 200 drugs, needed for health care.
*
The real purpose of an essential drug list must be seen
as taking drugs to those who need them most, not as reduc
ing the drugs bill.2
Could v/e accept an essential drug list for our
practice in which cost would be an important criteria in
selection in addition to efficacy, safety and quality?
(?) All UN agencies and governments involved in pre
paring a list of essential drugs are convinced that pres
criptions should be through the generic names of drugs
only.6
Generic name is not chemical name but official,
international, non-proprietary name e.g., not
Acetylsalicylic acid but Aspirin.z
Trended named products cost higher because they
include promotional costs and cost of claims of additional
ingredients in formulation e.g., Librium by Roche is
available for ft.16/- per JOG tablets but generic equi
valents are available for ft. 1.50.6
A study of UNCIAL has shown that bio-availability
argument for branded drugs i.e., therapeutic difference
based on formulation is not very valid for most drugs.6
Could we accept Generic prescribing? i.e., Ry Aspirin
not Flusprin, lisprin, etc.
(3) In India 60 firms with Foreign shares accounted
for 70% of the country's total drug sales in 1973-74. The
remaining 30% was shared by 116 large and 2,500 small manu
facturing companies.2
Drug industry in India is an offshoot of dc-velooment
of the industry in the Western World
is in private
hands which produces mainly for profit.
IC?.R/ICSSR and the Hathi Commission have recommended
that the small scale sector, cooperative sector should be
encouraged. Hospital and dispensary based formulations
should be promoted.
Can we prescribe drugs which arc- Indian rather than
foreign, Government rather than private industry, small
scale and cooperative sector rather than large sector?
(4) One of the most distressing aspects of the present
health situation in India is the habit of doctors to pres
cribe glamorous and costly drugs with limited medical
potential.'
The drugs required by the poor are not produced on the
main grounds that there is no profitable market and adequate
demand for them, while the country continues to be flooded
by plethora of costly and wasteful drugs meant for the
minor illnesses of the rich and well to do.'
l/ultiple drug combinations often containing drugs in
amounts far in excess of what is required are presently
marketed in India. There is a collosal national wastage
of drugs because of such combinations.3
Packaging increases the cost of drugs very greatly
because the trend is to make it attractive and highly ele
gant and to add cosmetic embellishments to promote sales.
*
The drugs Consultative Committee examined 34 categories
of fixed dose combinations and concluded that in the case
of 23 categories of these formulations, there was no thera
peutic rationale for their marketing.6
Could we stop prescribing drugs whose only additional
advertised values are a ) cosmetic embellishment
b) Elegant packing
c ) Irrational combination
d ) Imitative drugs
e) Inadequate evidence of greater value?
(5) 25% of a total production of Fa.700 crores in
1976 as analysed by a Task force of the Planning Commission
was on vitamins, tonics, health restoratives and digestive
enzymes.’
An ICMl/ICSSR study observed that production of INH
and Dapsomc are a third and a quarter respectively, of the
....3.
-3minimal requirements of the country. On the other hand,
tonics and vitamins which are mostly alcoholic preparation
and spin money are produced in wasteful abundance.'!
A NIK study on tonics has shown that mist of the high
potency or 'Forte ' preparations of multi-vitamins are a
sheer economic waste.4 These arc- not only a drain on the
patients ' purse but also help only to vitaminise our sewage
systems.
Can we stop this
'tonic ' practice?
(6) A 'AHO report notes that drug advertising and con
tacts with representatives of pharmaceutical firms are
often the main sources of information for a physician on
drugs and sometimes the only one. Cuch information is
largely Influenced by commercial interest.6
Drugs arc often being prescribed by doctors not
because they think a particular one is best suited for the
situation but because the company which produced it gives
the maximum monetary and material advantages and inducements
to them. These range from fiee samples (often sold in
practice), pens, calendars, diaries, teas, lunches, travel
and conference attendance costs.1,6
Medical training In Colleges docs not train future
physicians to judge a preparation critically ............... nor
docs it include conscious immunization against the half
truths of persuasive industrial advertising.^
Can we stop accepting physicians samples and other
forms of inducements from Medical Companies?
(7) Many medicinal herbs and roots that are usee' by
grandmothers, local dais and village medicine men have
been scientifically tested and researched and known to have
therapeutic value. Their descriptions in journals collect
dust in reference libraries.2.6
Herbal medicines and home remedies are not only low
cost and easily available but their popularisation will
help in breaking the doctor-drug producer axis for over
80% of the common minor ailments which are now being over
treated .
China has integrated over DO herbal medicine and home
remedies in their armamentariums not only as a drug policy
but as an expression of local participation in health care.^»6
Can we propagate simple home remedies and locally
available herbal medicine after studying their efficacy?
(8) A very large number of techniques of healing are
leing researched today in which diseases are tackled and
cured without drugs. Non-drug therapies include Yoga,
Pranayama, Meditation, Accupuncture, Acupressure and
Chiropractice among others. Traditional systems of Medicine
such as Ayurveda, Unani, Homeopathy which use drugs hut of
a different sort are being researched in various places and
the therapeutic effectiveness of many of their products are
being discovered and documented.
Can we adopt a more open policy of enquiry and use of
traditional medicine and non-drug therapies?
4.
(9) Health Care is becoming increasingly a quest for
priorities. "Clean water before antibiotics, food before
vitamin pills, vaccination before kidney machines, mothers
milk before powdered baby foods mixed with dirty water,
health for villager"- and slum"- before more hospitals for the
affluent suburbs of capital cities".2
Inspite of our preoccupation with Drug Prescribing
policy could we commit outselves to other more important
Health Care Priorities?
- ravi narayan
Deferences :
1.
Health for All -as alternative strategy
ICMJ1/ICSSR Report (£'980 J
2.
Drugs and the Third b'orld, Anil Aggarwal
Earthscan publication, 10 Percy Street,
London Wirorr. (1978)
3• Hsthi Committeerort of the Committee on Drugs
and Pharmaceutical Industry, Ministry of Petroleum
and Chemicals, Govt, of India (1975)
4.
fg Search of g Diagnosis MFC book containing
reprints from bulletin
-• The Selection of Essential Prues, ’AHO Expert Committee,
WIO IRS h=o.615(1977nand 641 (1979 )
6. Medicines as if people mattered - Health for the
Millions (VHAI bimonthly) Vol.VII No.2P,3, April-June 1981.
ZD-7
nuig pushers or healers?
"The greatest danger to Health in India is the over
medicalising of our Health Care System. Eternal vigilance
is required that the L'octor-c’rug producer axis does not
exploit the people and that the 'abundance ' of drugs does
not become a vested interest in health".
- ICtTR/ICSSR study on 'Health for All '
-an alternative strategy
The problem of Erug Tolley and low cost drugs encompasses
a very wide spectrum of issues-multinationalism, industrial
policy, medical advertising, research, drug production,
medical education, price control and so on. The recent
upsurge in interest in this important area of health policy
has led to the publication of numerous reports, books and
papers and many seminars and workshops have and are being
organised.
In the final analysis any collective action in
the form of policy, analysis, research or education can only
result from an individual understanding of the related issues
translated into a prescribing policy to be accepted volunta
rily by doctors, nurses, para-professionals and others in
their attempt to contribute to a solution of the problem.
Readers of this bulletin are requested to think over
the following facts, observations, conclusions taken from
V.HO, ICM\, ICSSR, Earthscan, VHAI, Covt. of India and other
sources of information. Can we collectively accept as many
of these gi-points as possible?
(1) 15000 branded drugs are on sale in India but a
Government Committee believes that Health needs would be
met by only 116 drugs.
'
*
»3
There is now an overproduction of drugs (often very
costly) meant for the rich and well to do, while the drugs
needed by the poor people (and these must be cheap) are not
adequately available!
HO in its report on selection of essential drops has
v.
pre-pared a list of 200 drugs needed for health care.3
The real purpose of an essential drug list must be seen
as taking drugs to Jhose who need them most, not as reduc
ing the drugs bill.^
Could we accept an essential drug list for our
practice in which cost would be an important criteria in
selection in addition to efficacy, safety and quality?
(2) All UN agencies and governments involved in pre
paring a list of essential drugs are convinced that pres
criptions should be through the generic names of drugs
only.6
Generic name is not chemical name but official,
international, non-proprietary name c-.g., not
Acetylsalicylic acid but Aspirin.2
branded named products cost higher because they
include promotional costs and cost of claims of additional
ingredients in formulation e.g., Librium by Roche is
available for Rs.16/- per 100 tablets but generic equi
valents are available for Rs. 1.50.6
A study of UNCIAL' has shown that bio-availability
argument for branded drugs i.e., therapeutic difference
based on formulation is not very valid for most drugs.6
Could we accept Generic prescribing? i.e., Ry Aspirin
not Plusprin, 1 isprin, etc.
(3) In India 60 firms with Foreign shares accounted
for 70% of the country's total drug sales in 1973-74. The
remaining 30% was shared by 116 large and 2,500 small manu
facturing companies.^
Drug industry in India is an offshoot of development
of the industry in the Western World
is in private
hands which produces mainly for profit.
ICkR/ICSSR and the Hathi Commission have recommended
that the small scale sector, cooperative sector should be
encouraged. Hospital and dispensary based formulations
should be promoted.
Can we prescribe drugs which are Indian rather than
foreign, Government rather than private industry, small
scale and cooperative sector rather than large sector?
(4) One of the most distressing aspects of the present
health situation in India is the habit of doctors to pres
cribe glamorous and costly drugs with limited medical
potential.'
The drugs required by the poor are not produced on the
main grounds that there is no profitable market and adequate
demand for them, while the country continues to be flooded
by plethora of costly and wasteful drugs meant for the
minor illnesses of the rich and well to do!
Multiple drug combinations often containing drugs in
amounts far in excess of what is required are presently
marketed in India. There is a collosal national wastage
of drugs because of such combinations.3
Packaging increases the cost of drugs very greatly
because the trend is to make it attractive and highly ele
gant and to add cosmetic embellishments to promote sales.'
The drugs Consultative Committee examined 34 categories
of fixed dose combinations and concluded that in the case
of 23 categories of these formulations, there was no thera
peutic rationale for their marketing.“
Could we stop prescribing drugs whose only additional
advertised values are a) cosmetic embellishment
b) Elegant packing
c) Irrational combination
d ) Imitative drugs
e) Inadequate evidence of greater value?
(5) 25',/. of a total production of Fa. 700 crores in
1976 as analysed by a Task force of the Planning Commission
was on vitamins, tonics, health restoratives and digestive
enzymes.'
An ICM1/ICSSR study observed that production of INH
and Dapsome arc a third and a quarter respectively, of the
....3.
-3-
minimal requirements of the country. On the other hand,
tonics ano vitamins which are mostly alcoholic preparation
and spin money are produced in wasteful abundance.'l
A NIN study on tonics has shown that most of the high
potency or 'Forte ' preparations of multi-vitamins are a
sheer economic waste.4 These arc- not only a drain on the
patients ’ purse but also help only to vitaminise our sewage
systems.
Can we stop this
'tonic ' practice?
(6) A -HO report notes that drug advertising and con
tacts with representatives of pharmaceutical firms are
often the main sources of information for a physician on
drugs and sometimes the only one. Such information is
largely influencer by commercial interest.6
Drugs are often being prescribed by doctors not
because they think a particular one is best suited for the
situation but because the- company which produced it gives
the maximum monetary and material advantages and inducements
to them. These- range from free samples (often sold in
practice), pens, calendars, diaries, teas, lunches, travc-1
and conference attc-nc
Pedicel training in Colleges docs not train future
physicians to judge a preparation critically ............... nor
docs it include conscious immunization against the half
truths of persuasive industrial advertising.°
Can we stop accepting physicians samples and other
forms of inducements from Medical Companies?
(7) Many medicinal herbs and roots that are usee! by
grandmothers, local dais and village medicine mon have
been scientifically tested and researched and known to have
therapeutic value. Their descriptions in journals collect
dust in reference libraries.2.6
Herbal medicines and home remedies are not only low
cost and easily available but their popularisatfon will
help in breaking the doctor-drug producer axis for over
80% of the common minor ailments which are now being over
treated.
China has integrated over 50 herbal medicine and home
remedies in their armamentariums not only as a drug policy
but as an expression of local participation in health care.2,6
Can we prorogate simple home remedies and locally
available herbal medicine after studying their efficacy?
(8) A very large number of techniques of healing are
leing researched today in which diseases are tackled and
cured without drugs.
Non-drug therapies include Yoga,
Pranayama, Meditation, Accupuncture, Acupressure and
Chiropractice among others. Traditional systems of Medicine
such as /.yurveda, Unani, Homeopathy which use drugs hut of
a different sort are being researched in various places and
the therapeutic effectiveness of many of their products are
being discovered and documented.
Can we adopt a more open col icy of enquiry and use of
traditional medicine and non-drug therapies?
4.
-4-
(9 ) Health Care is becoming increasingly a quest for
priorities. "Clean water before antibiotics, food before
vitamin pills, vaccination before kidney machines, mothers
milk before powdered baby foods mixed with dirty water,
health for villagers and slums before more hospitals for the
affluent suburbs of capital cities".?
Inspite of our preoccupation with Drug Prescribing
policy could wo commit outselves to other more important
Health Care Priorities?
- ravi narayan
Pefercnccs :
1.
’Health for dll - as alternative strategy
ICW/ICSSR Report (1980)
2.
Drugs and the Third b'orld, Anil Aggarwal
Earthscan publication, 10 Percy Street,
London WIPOEF. (1978)
/
3.
H-athi Committee rFgnort of the Committee on Crugs
and Pharmaceutical Industry, Ministry of Petroleum
and Chemicals, Govt, of India (1975)
4.
In Search of a Diagnosis MFC book containing'
re-prints from bulletin
5.
The Selection of Essential Prues, V-HO Expert Committee,
WP IBS to.61571977y~<3nd 641. (1979 )
6.
Medicines as if people mattered - Health for the
Millions (VHAI bimonthly) Vol. VII No.2P.3, April-June 1981.
ZD-7
PRUG HIGHERS OR HEALERS?
"The greatest danger to Health in India is the over
mericalising of our Health Care System. Eternal vigilance
is required that the Doctor-drug producer axis docs not
exploit the people and that the 'abundance ' of drugs does
not become a vested interest in health".
- IC.7R/ICSSR study on 'Health for All '
-an alternative strategy
The problem of Drug Policy and low cost drugs encompasses
a very wide spectrum of issues-multinationalism, industrial
policy, medical advertising, research, drug production,
medical education, price control and so on. The recent
upsurge in interest in this important area of health policy
has led to the publication of numerous reports, books and
papers and many seminars and workshops have and arc- being
organised.
In the final analysis any collective action in
the form of policy, analysis, research or education can only
result from an individual understanding of the related issues
translated into a prescribing policy to be accepted volunta
rily by doctors, nurses, para-professionals and others in
their attempt to contribute to a solution of the problem.
Readers of this bulletin are requested to think over
the following facts, observations, conclusions taken from
V.HO, ICiVR, ICSSR, Earthscan, VHAI, Covt. of India and other
sources of information. Can we collectively accept as many
of these cp-points as possible?
(1) 15000 branded drugs are on sale in India but a
Government Committee believes that Health needs would be
met by only 116 drugs.2,3
There is now an overproduction of drugs (often very
costly) meant for the rich and well to do, while the drugs
needed by the poor people (and these must be cheap) are not
adequately available!
V>HO in its report on selection of essential drugs has
prepared a list of 200 drugs needed for health care."
The real purpose of an essential drug list must be seen
as taking drugs to those who need them most, not as reduc
ing the drugs bill.2
Could we accept an essential drug list for our
practice in which cost would be an important criteria in
selection in addition to efficacy, safety and quality?
(?) All UN agencies and governments involved in pre
paring a list of essential drugs are convinced that pres
criptions should be through the generic names of drugs
only.6
Generic name is not chemical name but official,
international, non-proprietary name c.g., not
Acetylsalicylic acid 1 ut Aspirin.2
branded named products cost higher because they
include promotional costs and cost of claims of additional
ingredients in formulation e.g., Librium by Roche is
available for Rs.16/- per 100 tablets but generic equi
valents are available for Rs. 1.50.6
A study of UNCTAD has shown that bio-availability
argument for branded drugs i.e., therapeutic difference
based on formulation is not very valid for most drugs.6
Could we accept Generic prescribing? i.e., Ry Aspirin
not Plusprin, lisprin, etc.
(3) In India 60 firms with Foreign shares accounted
for 70% of the country's total drug sales in 1973-74. The
remaining 39% was shared by 116 large and 2,509 small manu
facturing companies.-
Drug industry in India is an offshoot of develooment
of the industry in the Western World
is in private
hands which produces mainly for profit.
ICftfl/ICSSR and the Hath! Commission have recommended
that the small scale sector, cooperative sector should be
encouraged. Hospital and dispensary based formulations
should be promoted.
Can we prescribe drugs which are Indian rather than
foreign, Government rather than private industry, small
scale and cooperative sector rather than large sector?
(4) One of the most distressing aspects of the present
health situation in India is the habit of doctors to pres
cribe glamorous and costly drugs with limited medical
potential.'
The drugs required by the poor are not produced on the
main grounds that there is no profitable market and adequate
demand for them, while the country continues to be flooded
by plethora of costly and wasteful drugs meant for the
minor illnesses of the rich and well to doJ
f/ul+iple drug combinations often containing drugs in
amounts far in excess of what is required are presently
marketed in India. There is a collosal national wastage
of drugs because of such combinations.3
Packaging increases the cost of drugs very greatly
because the trend is to make it attractive and highly ele
gant and to add cosmetic embellishments to promote sales.'
The drugs Consultative Committee examined 34 categories
of fixed dose combinations and concluded that in the case
of 23 categories of these formulations, there was no thera
peutic rationale for their marketing.“
Could we stop prescribing drugs whose only additional
advertised values are a ) cosmetic embellishment
b) Elegant packing
c ) Irrational combination
d ) Imitative drugs
e) Inadequate evidence of greater value?
(5) 25% of a total production of E-..700 crores in
1976 as analysed by a Task force of the Planning Commission
was on vitamins, tonics, health restoratives and digestive
enzymes.'
An IC’-R/ICSSR study observed that production of INH
and Dapsome are a third and a quarter respectively, of the
....3.
-3minimal requirements of the country. On the other hand,
tonics and vitamins which are mostly .alcoholic preparation
and spin money arc produced in wasteful abundance.'
*
A NIN study on tonics has shown that mist of the high
potency or 'Forte ' preparations of multi-vitamins are a
sheer economic waste.These are not only a drain on the
patients ' nurse but also help only to vitaminise our sewage
systems.
Can we stop this
'tonic ' practice?
(6) A V.'HO report notes that drug advertising and con
tacts with representatives of pharmaceutical firms are
often the main sources of information for a physician on
drugs and sometimes the only one. Such information is
largely influenced by commercial interest.6
Drugs are- often being prescribed by doctors not
because they think a particular one is best suited for the
situation but because the company which produced it gives
the maximum monetary and material advantages and inducements
to them. These range from free samples (often sold in
practice), pens, calendars, diaries, teas, lunches, travel
and conference attendance costs.1,6
Medical training in Colleges docs not train future
physicians to judge a preparation critically
nor
docs it include conscious immunization against the half
truths of persuasive industrial advertising.°
Can we stop accepting physicians samples,and other
forms of inducements from Medical Companies?
(7) Many medicinal herbs and roots that are usee’ by
grandmothers, local dais and village medicine men have
been scientifically tested and researched and known to have
therapeutic value. Their descriptions in journals collect
dust in reference libraries.2.6
Herbal medicines and home remedies are not only low
cost and easily available but their popularisation will
help in breaking the doctor-drug producer axis for over
80% of the common minor ailments which are now being over
treated.
China has integrated over DO herbal medicine and home
remedies in their armamentariums not only as a drug policy
but as an expression of local participation in health care.^,6
Can we propogete simple home remedies and locally
available herbal medicine after studying their efficacy?
(8) A very large number of techniques of healing are
being researched today in which diseases are tackled and
cured without drugs, Non-drug therapies include Yoga,
Pranayama, Meditation, Accupuncture, Acupressure anc
Chiropractice among others. Traditional systems of Medicine
such as Ayurveda, Unani, Homeopathy which use drugs hut of
a different sort are being researched in various places and
the therapeutic effectiveness of many of their products are
being discovered and documented.
Can wo adopt a more open policy of enquiry and use of
traditional medicine and non-drug therapies?
4.
-4(9) Health Care is becoming increasingly a quest for
priorities. "Clean water before antibiotics, food before
vitamin pills, vaccination before kidney machines, mothers
milk before powdered baby foods mixed with dirty water,
health for villagers and slums before more hospitals for the
affluent suburbs of capital cities".2
Inspite of our preoccupation with Drug Prescribing
policy could we commit, outselves to other more important
Health Care Priorities?
- ravi narayan
Deferences :
1.
Health for Pll, - as alternative strategy
ICM1/ICSSR Deport (1980)
2.
Drugs and the Third World, Anil Aggarwal
'Earthscan publication, 10 Percy Street,
London WirOPP. (1978)
3.
H=thi Committee r^pnort of the Committee on Drugs
and Pharmaceutical Industry. Ministry of Petroleum
and Chemicals, Govt, of India (1975)
4.
In Search of j pianpo^i? MFC book containing
reprints from bulletin
5.
The Selection of Essential Prues, WHO Expert Committee,
WHO TRS hkj.61571977T~<and 641(1979 )
6.
Medicines as if people mattered - Health for the
Millions (VHAI bimonthly) Vol. VII Nb.2R3, April-June 1981.
A handout prepared as guidelines for exploration of the theme.. wijhi_thje
participants of the Health Care Administration Course at St. John's
hidical College Hospital, Bangalore.
A Rational Drug Policy (issues and prospects)
1 .
"Menial vigilance is required to ensure that the health care system
does not get-medicalised, that the doctor-drug producer axis does not
exploit the people and that the abundance of drugs does not become
a vested interest in ill-health".
- ICMR/lCSSR
2.
Health for All Report, 1981
Understanding Irrationalities of the present situation
i.
45000 formulations available in India while WHO says 200 are
essential and Hathic Committee in India says 116 are essential.
ii.
Twenty percent of drugs are substandard and spurious.
iii.
The formulations available include:
- irrational combinations
- hazardous drugs
- banned drugs and bannable drugs
- costly drugs
iv.
Inadequate drug legislation and drug control
v.
Shortages and non-availability of essential drugs and life
saving drugs
vi.
Non-availability
vii.
Unethical medical advertising and drug company sponsored mis
information.
viii.
Irrational prescribing practices of medical profession induced
by doctor-drug producer axis
of unbiassed drug information.
ix.
Tonics, vitamins and enzymes are in excess whereas anti-TB
and anti-leprosy drugs and Vit. A are in short supply.
x.
Drug policy is an industrial policy not a health policy.
xi.
Increasing prices or inadequate price control.
xii.
Drugs as a substitute for caring - new medical culture.
2
2 :-
Sene issues
a.
Brand vs. Generic names
Drug/business - dumping
transfer pricing
profit orientation
mis-information
corrupting control systems
doctor-drug producer axis
(one of the biggest and most profitable business in the world
today)
c,
Inadequacies in Medical/Nursing education and health team training
do
Consumer Awareness/consumer protection forums
e.
Absence of health personnel’s continuing education
f.
Bloor poppers to Tap turners off
- the increasing role of preventive/promotive health care.
Components of a Rational Drug Policy
i.
Drug availability/roduction in consonance with health needs of
the people.
ii.
Elimination of irrational, useless and hazardous drugs
iii.
Low cost drugs in adequate quantities particularly essential/
priority drugs.
iv.
Adequate quality control and drug control.
v.
Availability of unbiassed drug information and ethical market
ing of drugs.
Vi.
Drug legislation reform
vii.
Generic prescribing.
viii.
Technological self reliance.
ix„
Increase drug availability through fair price shops
ment health infrastructure.
x.
Training of health personnel in Rational therapeutics and
rational drug policy.
and govern
What_can Managers of_Hospitals_do?
i.
Educate yourselves on rational drug policy and rational thera
peutic issues.
ii.
Share and disseminate information to all staff and colleagues
in hospital and associated centres.
3
5 :iii.
Adopt essential drug list using cost, efficacy, safety and
Quality as criteria. Evolve a hospital formulary and purchase
and stock drugs in accordance with this.
iv.
Adopt 'generic' concept during purchasing, prescribing and
dispensing drugs.
v.
Weed out the following types of drugs from the hospital
pharmacy:
a.
banned and bannable drugs
b.
irrational combinations
c.
imitative or me-too
d,
costly drugs with cosmetic embellishments and elegant
packaging.
e,
drugs with inadequate evidence of greater value.
drugs
vi.
Avoid injection and tonic practice.
vii.
Avoid drug industry linkages - gifts, sponsorship, unethical
trade discounts and other forms of inducement.
viii.
Adopt bulk purchasing and or supports co-operative purchasing
and production ventures.
ix.
Evolve a system of health education on drugs (use, misuse and
overuse) for patients and also a continuing education for
hospital personnel.
x.
Join and participate in groups at local/regional/state/
national level who are interested in rational therapeutical/
rational drug policy/consumer awareness issues.
Seek information on other forms of treatment. Adopt open
policy to rationally tested non-allopathic systems and non-drug
therapies and incorporate in work.
xii.
6.
Promote 'Health for All' priorities:
a.
simple home remedies;
b.
health education;
c.
community health initiatives;
d.
development programme;
e.
community organization and awareness pro
Suggestions for Reading
1.
A Rational Drug Policy (All India Drug Action Network and Volunt
ary Health Association of India publication, Rs. 20)
2.
banned and Bannable drugs, Health Action Scries 2, VHAI publi
cation, lis.10.
J.
Towards a People Oriented Drug Policy (Medical Service, Vol. 41,
No. 9, Oct.-Nov. 1984 and Vol. 42, No. 1, January 1985, CHAl)
...4
4.
Drugs-Fact, Fallacy and Fraud, (The Journal of Christian Medical
Association of India, Vol. LX, September 1983, No. 9)
5.
Getting Essential Drugs to People (CONTACT, No. 63, August 1981 )
6.
Strengthening & Regulating the Supply, Distribution and Production
of Basic Pharmaceutical Products (CONTACT, No. 73, June 1983)
7.
Tho Use of Essential Drugs, WHO
8.
Tonics, How Much an Economic Waste, Kamala Jaya Rao, Medico Friend
circle bulletin, November 1976.
9.
Tho Dangerous Drug List, Claude Alvares, Illustrated Weekly of
India, 12 July 1987.
10.
Formulary and Therapeutic Guide, kurji Holy Family Hospital,
January 1 983.
Tech Report Series 722 (1 988)
Items 1,2, 7, 8, 10 available from VHAI, 40 Institutional Area, South
of IIT, New Delhi 110016.
******
COMMUNITY HEALTH CELL'
47/1, (First Floor) St. Marks Road
BANGAIOSE- 560 001
LG1N - A
1.
.TU-Y FOR u HJG
>CTZ
-
..^T KA
Thejlrug
A class of chenlc-’.ls c lied PY.';
*
.’3L0KCS have Deen used
as msdicinos for over ninety yw.’srs. dyrazolonas inc uda
drugs liks Anti Pyrlno
*
Atninaoyrine, Phenyl Sutazone,
*
SxyphBnbutazons
Sulf Inpyrazar.e and a derivative af Assincpyrine called Dipyrane nr Analgin
*
The pyrszolonss share
similar pain-kllling»Fnvsr-r?ducingt inflamsMtion reducing
end also toxic properties. Analgin being mor w.tsr soluble
is amenable to uso in in jscti-.ns eno lit.-uid oral prep ra
tions (for children).
They are rapidly absorbed in the
stomach and intestine ano spread in various tis ;ues of the
body In proportion to their water c ntant. While 33 to 43:5
of the drug is altsrsd in -.ha liver end eliminated in the
*
urine
S'£ is eliminated unaltered.
The fate of a signi
ficant fraction is not noun.
The range of actions of ^yrnzalones is similar to tef Salicylates (Aspiri.^) except in reducing Favor in
t
discjaes like Hodgkins disease and ^eriartsritis nodosa
*
uhe^e aspirins arc not ccmol-rtsly nff^civE.
The post important and aotentially fatal adverse
effect of Pyraz lenes (Analgin) is Agranulocytosis.
This
is a c’edition whore the Granulocytes which form tha major
part of the White Blood Cell population ond arc the? first
11ns of the ‘jady’s defines agoinst inf cti«n ar? destroyed.
It is an allergic reaction and c ;n occur suddenly even
aftsr st fraction of a dase in any person uho has i-sen
pr-vleusly taking Analgin with no cad Qffacte. Uithin
6 tp 24 h-urs, the uhi(i blood cell c&unt fall end
granulocytes disappear from the tlogd. The.
*
start reapse -irlng 5 to
days aftsr tr-a drug Is :i tscontinuad md
r pid recovery occurs. Ths incidence of agranulocytosis
has bt's?n variously ssti^atod froa C.DT
*
to 0.36>. If
infaction occurs n«u# it starts as « sore threat nF sudden
2
2
an-c-t, high fev&r find prostr .-ticn
*
c.xrins ■:. mortality of 20 to 5Q/>.
which oven on oroper treatment
Ths other adverse effects of Analgin documented in a
study -.rs, skin re^hoe
*
*
Dyspepsia
*
Fever
-naphylsctic shock
■.nd ^ranchoapas>n. Analgin can aggravate a bleedin? tendency
and produces a saricue fall in body tempo rat xs when given along
with Chlorpromazine.
Liver cancer in
ice has also t-.een reported
by licensee.
Cyan nnu
a* the «sdde of action is not <not
n$
*
b. which ire th® metabolites wretch c -.uae agranulocytosis
and haw is noKknownj
o*
9aslc pharmecslo'- ic- ; data
*
causing Ctncnr
*
and Live.
**
like potential for
c-or.gsnital naifarsaotitsns
*
kidney
d;imge •■nd damage in elderly patients
are not known;
d» Interactions with other drugs for diabstas
*
hypertension ate.
*
hsva not been investigated
because Pyro? riorsea uere introduced in ths
pra^Thalidorddo ere whan registration was assy.
2. «History
-*i
<«aia o<" end
-M o» ont
aw» vo S-.-U;o
«.«• «»..
»
**
«x- w
1897 - •ninnpyx-ins usa i irst introduced and fcseasae ver y popular
in 1129s for psinkikiil®g and fever.
wa;> world wide
Sy 1930s it’s uss
1922 - -IgrnnulDcytcwis u-ns f irst Gsscrifcsd hy !.J Schulz
1922 - Olpyrans or An-dgin was introduced by Hoechst
*
Hot
being “ec^jniaed as a derivative of ^minopyrlne, it
gained popular uso.
1933 - Hrtdlscn find Squier a stab 4 iahsd a causal relation
uatween Anidopyrlne and agranulocytosis
1935 - Kracke and Parker ®s:t»blished its relstirnship to
agranulocytosis beyond d-ubt
1938 - O.T.C. sale in U.S.A u>s prohibited
3
Batuesn 1955-59 - The Amarican Medical Association Registry
on Advarse Reactions recorded only 10
reports of leucopenia (fall in W.B.C count)
and none in children
1960-64 - 19 cases reported (7 in children)
An increase in ths import into U.S.A
of dipyrona from Nil in 1958 to 18,879 lbs
in 1962 was noticed.
1964
- AmoricaB council of drugs - section one
adverse reactions studied the case of
Dipyrone (Analgin) and questioned the
justification of continued use of this drug.
1960
- Great Britian and Canada revoked the licence
1965
1974
~ Australia and Nau Zealand issued an import
ban on dipyrone
«. Sweden revoked Dioyrone licence
1976
1977
- Norway revoked Oipyrcne licence
- U.S.A revoked Dipyrone licence
of Dipyrone
1977
- Japan banned free C.T.C sals
1970
- Ireland and Singapore revoked licence of
1979
Dipyrone
- Denmark revoked licence of Dipyrone
1930-84 - An intern.'tional study for Agranulocytosis and
ApJj&stic Anaemia was done in Europe - called
ths Boston Study, since coordination and
data analysis was done at tha Drug epidemi
ology unit at Boston, This was primarily
financed by Hoechst, and the results
published in the JAflA of Oct 1986.
1983
- The G.3.I banned the manufacture and sale
1986
of Amidopyrine.
- Malaysia banned dipyrone
1986
— F.R.G banned O.T.C sale
In Netherlands, Dipyrone use is only allowed
for uncontrollable favor.
4
4
Fslleuing raparts of anaphylactic shock, Italy, Egypt .and
inudi Arabia have prohibited manufacture of injectlble
prapr.ratlsna
Th F.3, A of U.S.A regards that "true risk associated with
*
this drug far autuaigh any benefit derived from its use,
including use in Hodgkins and similar malignant diseases".
30 The I«;ucs
i.
According tc Hoechst, approximate!y 25 tonnes or
IS.5
million c’osos of Novalgin ar? used world wide
Everyday. With moat of the developed nations banning
or restricting its use, it is obvious that it is sold
mainly in third world countries,
Th<- countries which have- banned Oipyrcnc have been
managing csin without Oipyrone by using equally
effective and s-njfa analgesics.
ii.
The ’Boston *
Study gsnorstsd a lot of controversy,
sines Hcachst used the results aven bafora publication
fur s misleading advertit^snt campaign showing the
occursnce to fos 1 per millinn. The Hearing of the
German Federal Health Office finally confirmed the
assumption of 1 par 3-J,333 to SO,003 to bo nearer t’-e
nark, or one tablat per 70,SOO cunsumsd could cause
\\ '
sgranulrr^ytnsis bssad ?n this sano study.
The iiaiietiohs of this study are, that
®. it excludes all patisnte
i.
who die of agranulocytosis without receiving
madias! aid}
ii. uhc die without having a uhita cell cuunt, and
Hi who hove up'biaynosBd agranulocytosis and
rac war frpm it.
b. The study dess not look into othsr ®ida effects
of ilipyrona, Ilk® shock, fall in 3.P., Urticaria ate
5
5
Co Th® data presented in th© intarciediate and
final reports arc incpnsistont.
do *
Jher®a.? 400 case# of agranulocytosis ware
registered to assess risk properly, only
221 cases ware analysed in th® final report, and
®. There is extreme variability in data batuern
different countries and even within th? s ae
country.
f. So®® data were seen to
■?» cleerly unrollabl®.
Sii» The findings of ths controversial ’Boston Study
*
is
being utilised by Hoechst ths largest manufacturar of
Analgin for ealas promotion in Germany, Eastern Sloe
countries and th® Third Uarld. Unethical propaganda
practices with different types of promotional liter
*
Eture in different countries is being practiced.Evan
claims of -intl-tipasmadic action which is net
sclentifIcally substantiated is being wade. Any
source of detailed scientific litorature is virtually
nan-axiatant beyond the literoturs supplied by the dru
cowoanies.
iv. Since 1965, Uipyrone (Analgin) has not found mention
in eny standard medical text b.oks, except for nanIng
it a® a drug which can cause ©granulocytosis.
v. Even in our country, Medical students de net learn
about Analgin uhile doing their Pharmacology.
4. In,Indie
1.
In 1983, the G.O.I bannod the manufsecure end gala ef
Amidopyrine but not dlpyrons. The Crugs Consultative
Carnalt-tan had reco®i»andsd ban on fCCs of dipyrons olso,
but this saens to have slipped Ftor.' ths banned list.
2.
The Government is the largest
thia country
*
manufacturer of Dipyrona in
&
6
3.
Analgin la a^ong the largest sailing annlgaaice in the
country with solos Figures accounting for ft. 70 million.
Thare ar?t approainataly 200 formulations containing
'nalgin, including injectablsE, and droos far new?. roe
rid infant® For colic.
4.
Analgin la available as D.T.C inspite of its being a
Schedule H drug in our country and the attitude of the
p?; a scribing doctors as per •• study (Lancet 8d) w; a " if
I prescribe it 30 tifiies a day and it is available over th®
counter it sust ba saFa”.
In e fisld study (Lancet cfi)
it use Hen that the pyrazolones made up
h? majority of
Loth S.P prescriptions and 8.T.C sales nF Analgesics.
□ne .r,or•■• aF thesa drugs worn given to aver 50% of patients
re westing sn anelrjwsic.
5.
2-rug .'iii'.r’i groups have inlti^tad ?■ c .r?
r. on Analqin
esaecially it
*»oBb.ay 9 OAF
b.sng.-..l and
Nau Galhi.
6.
An’Viyir: InducKd agranulocytosis dcea occur in Indi-.s»
aapecially If one looka for it sy»t.?r>i:<iically as
a
i-n-sb&y h.?.8r’iafcolo jist ■',C."'whl-i; has dans, bs? rsnsrto
12—tS cas^s of egrsnulocytssls a y®ar4 of which 13-12
ar;® caused by Olpyrone ar Dijjyrone g ntaining drugs.
F.von
by the risk cstiniotinn of th® Session Studyt in Indi.^,
one parson develop® An^l^in induced a§ranuloeyto®i®
per day by othar reasonsbl's ssxtiraates, it could bs 13
tiflss this figure.
5. Mid&g issues
Developing enuntri;.-® like ours sr^ ill placed to nfforrj
axpenslv© and useless hsalth care roducts end cfaf.initely
not ths frankly rangsraus ones.
U» have unsophletic-»trid e ^nautnsr^ ana poorly ••cv<.>lon«d
regulatory and advisory eyatens© - this is fartila ground
?
7
for pharmaceutical companiaa to indulge in unacceptable
practices.
The vest majority of rural doctors working in ?:rof-j&sional
isolation have no access tn independent InforsiEtion on drugs
they prescribe,
Hsr®f the reprssentstive of the pharmacauticel
company uno is ill-infer-sed himself and paid by commission
on drug sales becomes an ideal tool to promote the interests
of th® Pharmaceutical company.
1234567
Thus, it up-.ears that ths ccnsusar is at th® mercy of drug
manufacturers, Dther than an appeal to tha Food and Drugs
Administration, th® Central jovernmsnt and ths ’1RTP Commission
the consumer is virtually without recourse to any indepsndent
body such as th® judiciary. Ths 3,3 Hospital Commission (Luntin
Commission) enquiry reveals the ineffectiveness " those
agencies. The consumer protection Act of 1936 is expected
to offer some htspn.
In effect, only a public: outcry by ths con^umor can force
Voluntary withdrawal by or reform by drug cosipeniss,
— 5P ’
1, The Pharmacological Oasis of Therapeutics
- Goodman ^nd Gillman Sth Edition, 1975
2. Kevicu of Medics! i"’hartnacelo^y
- Msyprs, 3«uotz, Goldfien, 6th Edition 1579
3, Agranulocytosis inauced by Dipyrane, a Hazardous
antipyretic and Analgesic
— Ch.-jrlcE M Huguley 3r, 3/U’A 21 "aetamber 1964
4. Rieke of Agranulocytosis and Ajisetic Anaemia - A
first Report of the International Agpanulocytoaig^nd
Aplastic Hnaefaia study • 3AMA 03 October 138G
5, Analgin — Pain killers ar nan killers?
«■ Indian Express 34 October 1987
6, Why Analgin should be banned - A it of history
» Anant Phsdke
7, Countsrfact an Analgin (An untold story)
Drug Disaa;..® Doctor Vol 3, No 4 1983
- Arun 8»1 and Anil dilgoankar
I -cJaLluV
3
Jlnyrane, Honchst and the Boston Study, <t'C Sullstln Sac 96
«• Gilbert Benncnbt’r^
>» uru-.; ri-.rkoting In tht? Third World t Sene ..th the
cosmscIc r»farr>s, L'ncet 07 January 138S
- Trisha Gretmtaalgh
.
*
V
Seng®raws, and Inaoorapri i>to drugs
Inftcat 28 3uns 13SS6
“ ‘<»3»S
*
Langsan
11. A 6Ea-.pslgn <• A Crug Campaign ^©wslattar
fsFe 'iuti'-nal Syug Policy Cell, 1965
12.
Ths Hoschst
Sul.! ptin « issue Mo 8«
HARRIS’ L. COL’L’TC/<
Several comments may be made on the homoeopathic
dilutions. In the first place, their value has been proven
by much clinical experience. Thousands of homoeopaths
have used them and are using them today. I hese dilu
tions have been found highly effective when used ac
cording to the correct indications. In the second place,
a series of biological, chemical, and physical experiments
have uniformly demonstrated the existence of some
physico-chemical, or other, force in the ultra-molecular
dilutions. In 1928, II. Junker added various substances,
in dilutions up to IO-27, to bacterial cultures and found
that they affected the growth of the bacteria. J. Patterson
and W. Boyd in Scotland found that the Schick test for
diptheria was changed from positive to negative by oral
administration of alum-precipitated toxc-id in a dilution of
10-60 or of Diphtherinum (a homoeopathic preparation of
throat swabs from diphtheria patients) in a dilution of
10~02. W. Persson in Leningrad investigated the effects of
dilutions up to 1CH20 on the rate of fermentation of starch
by ptyalin and on the lysis of fibrin by pepsin and trypsin;
in 1954 W. Boyd announced positive results from a retest
of Persson’s findings with respect to the effect of dilutions
of mercuric chloride up to 10-61 on the rate of hydrolysis
of starch by diastase.23 These findings appear to be strong
evidence against any suggestion that the homoeopathic
infinitesimal doses are mere placebos.24
Furthermore, it is worth noting that orthodox medicine
has never made an effort to test this aspect of homoe
opathy under controlled conditions. Criticism of the ultra23See James Stephenson, M.D., “A Review of Investigations into the Action
of Substances in Dilutions Greater than I x IO-24 (Microdilutions),” Journal
oj the American Institute of Homoeopathy XLVIII (1955), 327-355.
24Some results of research on the physical basis of the action of microdilu
tions are reported in James Stephenson. M.D. and G. P. Barnard, “Fresh
Evidence for a Biophysical Field,” Journal of the American Institute of
Homoeopathy LXII (1969), 73-85.
36
7972.
910
A/.w /
oL L&Wj'vC-X
OCvcA. /V 0 , ’/£ -j
molecular dose has been strictly a priori—with vague
references to common sense which is a notoriously un
reliable guide in medical matters.
Use of the ultra-molecular dose, in any case, is not an
essential principle of homoeopathy. Hahnemann insisted
on the “minimum dose”, which is an ambiguous concept in
view of the associated doctrine that increased dilution of
the substance actually enhances its power. Homoeopathic
physicians, like Hahnemann himself, make use of the
whole range of dilutions, from the lowest to the highest.
3.) The Single Remedy. Hahnemann’s third rule re
quires the physician to administer one remedy at a time.
Here again his rule contrasts with orthodox practice
which permits the use of several drugs at once or in
combination.
The homoeopathic principle is not arbitrary but stems
logically from the other elements of the homoeopathic
system. The physician may give only one drug at a time
because the provings are only of a single substance. The
physician may not give two remedies at once (i.c., on the
ground that their combined symptoms match all of the
symptoms of the patient) because, when two remedies are
administered at the same time, they yield additional
symptoms which arc neither those of substance A nor of
substance B, but of A and B combined. Administration of
two remedies at the same time introduces an unknown
into the picture, and the purpose of Hahnemann’s new
method was to eliminate just such speculative and un
reliable procedures from medicine.
Homoeopathy is in no way averse to the use of chemi
cal compounds provided they have been proved as such.
Thus, Ferrum metallicum yields one set of symptoms,
and Phosphorus yields another set. Phosphate of iron
{Ferrum phosphoricum) yields symptoms of both Ferrum
metallicum and Phosphorus, but, in addition, has a
2o'ooC
Q 2g )
ALTERNATIVE HEALTH CARE SYSTEMS
ANOTHER POINT OF VIEW
Dr. Shirdi Prasad Tekur
I >r. Shirdi Prasad 7 ekur is with the Communitv / leallh Cell, Pangalore. A practising paediatrician, he is
interested in allopathic and other [onns of medicine and in community health.
The western system of medicine, also called
Allopathy' or 'Cosmopolitan Medicine,' dominates the
medical and health care systems of our country. The
Bhore Committee, charged with laying down the blue
print for health care systems in India, based its 1946
recommendations on the allopathic system. This
dominance continues today, with a few cosmetic chan
ges to keep up with the times and rhetorical references
to the Indian systems of medicine. The reason could be
that the allopathic system has kept pace with other
tronliersof scienlilic research. The backing required for
such efforts can only come from the developed, Western
countries, which look primarily for solutions to their
own problems.
evolving a holistic approach to problem-solving seem
to be contributory factors. Other, more immediate
reasons could be because traditional systems are
Allopathy came to our country with the British, as a
system of medical care for themselves. It flourished with
the patronage of the ruling and elite classes of India and
evolved into a system sponsored by the state for all
people. The Indian systems lost the patronage of the
rulers and were thus unable to interact dynamically
with larger issues of public health — both of which were
needed for their further development. They remained
static in some areas while decaying in others and were
left behind as 'native medicine.' The national move
ment for Independence saw a resurgence of interest in
Indian systemsand a I tempts at reviving them marginal
ly improved their status.
It calls for the promotion of traditional medicine
because of its intrinsic utility, unique and holistic ap
proach and operational feasibility in the drive to
achieve health for all by 2(XX) A.D.
a)
A valuable resource
The World Health Organisation (WHO) refers to
traditional medicine as "the sum total of all the
knowledge and practices, whether explicable or not,
used in diagnosis, prevention and elimination of physi
cal, mental or social imbalance, relying exclusively on
practical experience and observation handed down
from generation to generation, whether verbally or in
writing.”
The National Health Policy statement of 1989 clearly
states : 'The country has a large slock of health man
power comprising private practitioners in various sys
tems -- for example, ayurveda, unani, siddha,
homoeopathy, yoga, naturopathy etc. This resource has
not so far been adequately utilized."
The table on page 27 provides an idea of health
resources in our country :
Interest in Alternatives
Unis, the terms 'alternative systems’ or 'traditional
medicine' usually refer to a group of systems other than
the 'allopathic.' Traditional medicine does not define a
unified, homogeneous practice. Formalised medical
systems exist, along with informal folk practices. The
Government of India officially recognises formalised
svstems like ayurveda, siddha, unani, yoga, naturopa
thy and homoeopathy in addition to allopathy. Tibetan
medicine (the amchi system) is gaining popularity in
areas contiguous with Tibet and in and around the
Tibetan refugee settlements in our country. Acupunc
ture a nd acupressure (Chinese systems) arc increasingly
accepted in urban India and are also prevalent in the
rural areas of north-eastern India. Other non-formalised systems, such as tribal medical practices, arc
being documented and studied in tribal areas.
The resurgence of interest in alternatives and tradi
tions is a worldwide phenomenon, probably linked to
crowing awareness of the limitations of present-day
science in explaining nature. Increasing consciousness
iboul the environment, pollution and attempts towards
26
1
Ayurveda
Unani
Siddha
Yoga
Naturo
pathy
Allopathy
1,08,085
7,912
1,183
-
43
3,30,755
2,72,800
28,711
11,581
108
3,30,755
1,469
101
106
6
10
9,831
15,913
1,267
885
40
190
5,85,889
12,109
871
316
4
43
1,18,806
100
18
2
34
3
125
No. ofinsti
tutionally
qualified
practitioners
2
Total no. of
registered
practitioners
3
No. of hospitals
4
Total beds
provided
5
No. of
dispensaries
6. No. of colleges /
institutions
Source : Health Information India - 1988
b)
Accessible to people
An awareness of allopathic medicine's limitations,
the economic ability to shop around, and a fad for
everything 'natural/ 'ethnic,' 'non-synthetic,' and 'non
chemical' promotes traditional medicine among af
fluent groups. A cause for concern is that rationality is
a casualty in this keeping up with Joneses, and that
patronage by the elite results in the hiking up of costs
which takes traditional medicine, too, out of the reach
of those who need, but now can't afford these services.
The focus on curative medicine, rare and exotic, trueand
imaginary illnesses and thelureof lucre di verts valuable
health resources needed by the majority. At the same
time, it is a fact that this patronage docs help promote
traditional medicine.
The WHO document, "The World Drug Situation,"
classifies India among countries where less than 30 per
cent of the population has access to allopathic drugs.
This lack of access is applicable in different degrees, to
health facilities, whether government-run or private,
because of costs, distances and non-functional health
structures. Scarce health resources meant to be used for
preventive and health promotive measures for the
l^hy are gobbled up by the costly diagnostic and cura
tive services accessible to the few.
I raditional medicine is used by a significant number
of people as the only health resource available, or as a
substitute for or complement to allopathic services.
c)
e) Of interest to pharmaceutical producers
I lolistic in approach
The drug manufacturing industry has very good
reasons to promote traditional medicine if one considers
the potential for profits. With the avowed aim of look
ing for safer, cheaper and better drugs,, big companies
have entered this unorganized market of small
producers. Government restrictions on manufacture
and sale are less stringent, while the clientele need no
selling of these products! With hardly any standards
laid down, or measures for quality control, it is a market
open to the unscrupulous, small or big. To the common
man, it means that he pays for a bottled remedy instead
of learning to use the herb in his backyard.
The traditional practitioner often depends more on
his or her ability to mobilise the patients' hopes, restore
their morale, and gain re-acceptance by their group,
than on pharmacoepia.
Traditional medical practices arc concerned with the
totality of human functions in society and represent a
more holistic approach. Illness is seen not only in terms
of biochemical and supernatural disharmony, but also
as a breakdown in the interaction of the patient with
others in his or her social environment. The psycho
logical /psychosomatic value of traditional medicincis
widely recognised.
d)
f) The field of community health activists
In their efforts to preserve tradition and culture, and
make communities self-sufficient in tackling health
needs, health activists revive and promote useful tradi-
A fad among the elite
27
1
Safety status of commonly used drugs in pregnancy
Doctors
are many times confused about or even
ignorant
of
the
precise relative risk of using different types of
drugs
in
pregnancy.There
is no readymade, detailed source of
information
available
on
this
aspect.
The
following
table would
help
practitioners
to choose appropriate drugs for use in
pregnancy.
It has been prepared from the booklet "Medicines in
pregnancy"by
the
"Australian Drug Evaluation Committee" (1989). Let us
quote
from the "introduction
*
of this booklet.
The Australian catagorisation of risk associated
with
the
use
of
pharmaceutical
drugs in pregnancy was
developed
from
systems used in Sweden and the USA.
The categorisation has taken into account all known
harmful
effects
of
the
drugs
on the developing
baby
regardless of
mechanisms,
including the potential to cause the birth
defects,
the
potential to cause unwanted pharmacological
effects
around
the time of birth ( effects which may or may not be
reversible)
and
the
potential
to
cause the cancer
in
later
life.
The
catagorisation applies
only to
reccomended therapeutic
doses
in women in the reproductive age group.
The Australian
catagories.
catagorisation consists
of
five
separate
Catagory A
:
Drug which have been taken
by
large
number
of
pregnant women and women of child bearing age without an increase
in
the
frequency of malformations or other direct or
indirect
harmful effects on the fetus having been observed.
Catagory B
:
Drugs which have been taken
by only
a
limited
number of pregnent women and women of child bearing age withoput
an
increase in the freqency of the malformation or other
direct
or
indirect
harmful
effects on the
human
fetus
having
been
observed,
As experience of effects of drugs in this catagory in humuns
is
limited, results of toxicological studies to date
(including
reproduction
studies in animals) are indicated by allocation
to
one of three subgroups.
Group Bl
: Studies in animals * have not shown evidence
increased occurence of fetal damage.
of
an
Group B2 : Studies in animals * are inadequete and may be lacking
but available data show no evidence of an increased occurence of
fetal damage.
Group B3
:
Studies
in animals * have
shown
evidence of
an
increased occurance of fetal damage, the significance of which is
considered uncertain in humans.
effects
Catagory C : Drugs which owing to their pharmacologicl
have caused or may be suspected of causing harmful effects in the
causing
malformations.
These
human
fetus
or
neonate without
consulted
effects may be reversible. Accompanying text should be
for further details.
Catagory D :
Drugs which have caused an
increased
incidence
of
human fetal malformations or irreversible damage. These drugs may
also
have
adverse pharmacological effects.
Accompanying
text
should be consulted for furthe details.
Catagory
X
:
Drugs
that have such
a
high
risk of
causing
permanent
damage
to the fetus that they should not be
used
in
pregnency or when there is a posobility of pregnency.
SAFETY STATUS OF COMMONLY USED DRUGS IN PREGNANCY
No Name of drug
Possible adverse effects
Safety status and
on pregnancy/foetus/neonate recommendations
Category
1 OPIOD ANALGESICS
Morphine, Pethidine
Pentazocine,
Dextropropoxyphene
Respiratory depression
in newborn when given
2-3 hours before delivary
use with specific
precautions
C
2 Codeine
—
can be safely used
A
3 NSAID
Aspirin,Ibuprofen,
Phenylbutazone
Indomethacin
Diclofenac
Piroxicam
closure of foetal ductus
arteriosus.Given at term
may prolong labour and
delay parturition
Not to be used in
late pregnancy
C
can be safely used
A
Use if must
Overall risky
teratogenicity is
far outweighed by the
dangers to mother
and foetus of
uncontrolled
convulsions
Use when necessary
D
Paracetamol
4 ANTICONVULSANT
Phenobarbitone
Phenytoin-Na
Ethosuccimide
carbamazepine
5 ANTIEMETICS
Phenothiazines
Others
Meclozine,Cyclozine
Metelopramide
craniofacial abnormality
mental and growth
def/iciancies, oral
clefts.cardiac
abnormalities
malformations in rats
High doses in late pregnancyNot to be used in
cause prolonged
late pregnancy
extrapyramidal disturbances
in the new born
-
B3
C
can be used safely
A
----------------
can be safely used
A
Nephrotoxic and ototoxic
to the foetus
Strictly avoided
D
8 CEPHALOSPORINS
—
can be safely used
A
9 PENICILLINS
—
can be safely used
A
> 6 ANTIHISTAMINICS
Clorpheniramine
Diphenhydramine
7 AMINOGLYCO^DES
Gentamycin
Neomycin,Kanamycin
Penicillins,Ampi
Amoxy,Cloxa.
--
No Name of drug
Possible adverse effects
Safety status and
Category
10 Nalidixic acid
—
can be safely used
A
11 SULFAS
When given in last
trimaster may cause
kernicterus in babies
not to be used in
last trimester
C
12 SULPHONES
Dapsone
No adverse action on
human foetus so far
use if necessary
B2
13 TETRACYCLINE
When given in '2nd,'3rd
trimaster,hypoplasia of
enamel and discolouration
of teeth of the newborn
may occur
strictly avoided
C
14 ANTIMAL^RIALS
Chloroquins etc.
Neurogenic interferance
with hearing balance;but
risk of malaria far
outweighs this risk
use when diagnosis
is certain
D
can be safely used
A
Bleeding due to
hypoprothrombinaemia in
neonates and mothers
Vit. K to be given
in late pregnancy and
to newborn infants
C
Grey-baby syndrome in the
newborn
avoided at term
C
can be safely used
A
use when necessary
if used folic acid
supplementation
be used
B2
B3
17 ANTI-ASTHAMATICS
Theophylline
derivatives
Adrenaline
Salbutamol
can be safely used
A
18 ANTI-CHOLINERGIC
Atropine,Belladona
Hyoscine
can be used safely
A
19 Digoxine and
other cardiac
glycosides
-can be used safely
A
to be given when is
must in late
pregnancy and
delivery
C
15 ANTI_T.B.
INH, Ethambutol
Rifampicin
16 OTHER ANTIBIOTICS
Cloramphenicol
Clinda,Linco,
Erythromycin
Metronidazale
Trimethoprim
BETA-BLOCKERS
Inderal,Ciplar etc
No malformations in humans
High doses give rise to
birth defects typical of
folic acid antagonism
May cause bradicardia
in foetus and newborn
__________
No Name of drug
Possible adverse effects
Safety status and
Category
20 Ca-CHANNEL BLOCKERS
Nifedipine
Verapami1
Foetal hypoxia with
maternal hypotention
should be avoided
unless a must
C
21 DIURETICS
Thiazides and
others
May cause electrolyte
disturbances in foetus,
neonatal thrombocytopenia
only be given on
sound indication and
at lowest effective
dose
C
22 ANTACIDS
—
can be used safely
A
23 H2-Blockers
Ranitidine
No adverse effect on
human foetus
may be used when
necessary
B
—
—
Nasal discharge, lethargy
poor feeding in neonate
can be used safely
can be used safely
use when a must
A
A
C
can be used safely
A
24 ANTIHYPERTENSIVES
Guanithidine
Methyl dopa
Reserpine
25 LAXATIVES
Bisacodyl dioctyl-Na
Sulphosuccinate
26 ANTI-HELMENTIC
27 HAEMOPOIETICS
Iron
Folic Acid
28 CORTICOSTEROIDS
B3
No adverse effect on
human foetus
can be used safely
A
Malformations in animals,
short term treatment
C
Possibility of adrenal
cortex supression in fetus
after long term treatment
may be given when
indicated
29 PROGESTAGENS
High doses can cause mascu- should not be used
-linization of female fetus
D
30 ORAL-ANTI DIABETICS
Chlorpropamide,
Tolbutamide,
G1ibenclamide , etc.
Metphormin
Phenphormin, etc.
Sulfonyl ureas may cause
hypo-glycaemia in fetus
Birth defects in animal
studies
Metphormin may cause fetal
lactic acidosis
C
be avoided, insulin
be used instead
No Name of drug
31 HYPNOTICS
Barbiturates
Benzodiazepins
Diazepam and
analogues
Possible adverse effects
Safety status and
Category
Prolonged use can resultin
hypotension, depressed
respiration, hypothermia in
new born
continuous use be
avoided
C
as above
continuous use be
avoided
C
High doses in late pregnane}r use when essential
may cause prolonged
extrapyramidal symptoms
in new borns
C
may cause birth
defects
Use only on sound
indication
C
33 VACCINES
Typhoid,Cholera
BCG,Hepatitis B
Use when necessary
B2
Tetanus toxoid
Can be safely used
A
32 ANTIPSYCHOTICS
Phenothiazines
Chlorpromazines
Promazine
Trifluoperazine
Tricyclic anti
depressants
Imipramine and
analogues
The table is prepared from from the booklet" Median Pregnancy"prepared
by Australian Drug
Evaluation Committee 1989.
EDITION
EIGHTH
' ■■ v .' ' T
.
■'
■
«•
Injectable
Drugs
by Lawrence A. Trissei
\o°
(>C
LAWRENCE A. TR1SSEL, F.A.S.H.P., the author of the Handbook on Injectable Drugs,
is Director, Drug Delivery and Stability Research, Division of Pharmacy, University of
Texas, M, D. Anderson Cancer Center, Houston.
,
Mr. Trissei was assisted in the preparation of the eighth edition of the Handbook by the
following individuals:
MICHAEL C. ALLWOOD, Ph.D., Professor of Clinical Pharmaceutics and Director,
Pharmacy Academic Practice Unit, Universit)’ of Derby, Derby, United Kingdom.
DANIEL P. HAAS, Assistant Director, Department of Pharmacy, The Ohio State Uni
versity Medical Center, and Clinical Instructor, The Ohio State University College of
Pharmacy.
KAREN NAQUIN HALE, Clinical Specialist, Investigational Drug Service, Depart
ment of Pharmacy, The Ohio State University Medical Center, and Clinical Assistant
Professor, The Ohio State University College of Pharmacy.
Correspondence to the author should be sent in care of the publisher, American Society of
Hospital Pharmacists, 7272 Wisconsin Avenue, Bethesda, MD 20814.
The information presented herein reflects the opinions of the authorfs) and reviewer(s). It
should not be interpreted as official policy of ASHP or as an endorsement of any product(s).
Drug information is constantly evolving because of ongoing research and clinical experi
ence, and it is often subject to interpretation and the uniqueness of a clinical situation. The
author and ASHP have made every effort to ensure the accuracy and completeness of the
information presented in this book. However, the reader is advised that the publisher,
author, contributors, editors, and reviewers cannot be responsible for the continued cur
rency of the information, for any errors or omissions, and for any consequences arising
therefrom.
Produced by the American Society of Hospital Pharmacists’ Special Projects Division.
Cover design: Hector L. Coronado.
©1994, American Society of Hospital Pharmacists, Inc. All rights reserved.
No part of this publication may be reproduced or transmitted in any form or by any means,
electronic or mechanical, including photocopying, microfilming, and recording, or by any
information storage and retrieval system, without written permission from the American
Society of Hospital Pharmacists.
*ASHP is a service mark of the American Society of Hospital Pharmacists, Inc.; registered
in the U.S. Patent and Trademark Office.
ISBN: 1-879907^42-9
CONTENTS
Preface
VII
How to Use the Handbook....................................................
IX
Drug Stability and Compatibility Issues in Drug Delivery
XIII
Commercial Drug Monographs
1
Drugs Available Outside United States
1063
Investigational Drugs
1095
Intravenous Infusion Solutions
1107
Appendix I: Parenteral Nutrition Solution Formulas
1118
Appendix II: ASHP Technical Assistance Bulletin on Quality Assurance
for Pharmacy-Prepared Sterile Products
1128
References
1140
Index.................................................. ....................................................... 1169
Preface/VII
PREFACE
The Handbook on injectable Drugs has evolved considerably
from its initial conception in 1975. Over the years, numerous
changes, additions, restructurings, and format enhancements, as
well as a vastly increased volume of information, have led to an
eighth edition that is more thorough and complete than ever.
Nearly 1200 pages of information are presented on 272 commer
cially available drugs plus investigational drugs and infusion
solutions. Eighteen new monographs on commercially available
drugs are presented:
Aldesleukin
Bupivacaine HC1
Calcitriol
Diltiazem HC1
Filgrastim
Gallium nitrate
Indomethacin sodium trihydrate
lohexol
lopamidol
Ketorolac tromethamine
Melphalan HC1
Milrinone lactate
Ofloxacin
Paclitaxel
Piperacillin sodium-tazobactam sodium
Rifampin
Streptozocin
Teniposide
In addition, a section on parenteral drugs available commer
cially outside the United States has been updated and expanded.
Seven new drugs, each having considerable published informa
tion on its stability and/or compatibility, are included:
Aclarubicin HC1
Amsacrine
Cefsulodin sodium
Clonazepam
Cyclizine lactate
Diethanolamine fusidate
Vindesine sulfate
All previously existing information has been completely up
dated. An additional 188 references were utilized to prepare the
eighth edition, bringing the total to 1709.
The Handbook on Injectable Drugs has roots back in the
innovations of the 1950s and 1960s with the landmark work of
Bogash,1 Kirkland et al.,2 and Williams and Morovec? Yet it
remains a work of contemporary interest. This eighth edition
incorporates almost 200 pages of new information. Even with all
of the changes, the intent is unchanged from the first edition many
years ago: to organize and summarize in a concise, standardized
format the results of the primary research in parenteral drug
stability and compatibility.
Note of A pprcciation
I want to express my gratitude to Ms. Karen Hale, Mr. Daniel
Haas, and Dr. Michael Allwood. Again for this edition, these
friends as well as colleagues ably assisted me in completing this
difficult and extraordinarily time-consuming project Their con
tinued interest and extensive help in making the Handbook fl
better reference are greatly appreciated.
Similarly, the editorial talents of Ms. Carmen Huddleston, Ms.
Linda Sekino, and Ms. Kathy Brock of First DataBank greatly
facilit ited the revision process. Their invaluable assistance con
tributed significandy to improving the Handbook, uid I am
indebted to them for their efforts.
Of course, the extensive contributions of Ms. Shelly Elliott,
Ms. Johnna Hershey, and Mr. Michael Soares of the Special
Projects staff of the American Society of Hospital Pharmacists are
especially appreciated. I want to extend to them my deep thanks
for making the revision process bo± possible and pleasant.
My continuing thanks go to those users of the Handbook who
make valuable suggestions for its improvement and to the numer
ous drug companies that supply information on their products.
Finally, my deepest thanks must go, once again, to my family
who continues to endure and endeavors to understand my devo
tion to the Handbook. My love and gratitude go to them for their
support and forbearance, which make it possible for me to
undertake the demanding challenge the Handbook represents, fl
References
1.
2.
3.
Bogash RC: Compatibilities and incompatibilities of some parenteral medication. Bull Am Soc Hosp Pharm 72:445—448 (July-Aug)
1955.
Kirkland WD, Jones RW, Ellis JR, et al.: Compatibility studies of
parenteral admixtures, Am J Hosp Pharm 78:694-699 (Dec) 1961.
Willians JT and Morovec DF: Intravenous therapy, Clissold
Putlishing, Hammond, Indiana, 1967.
LAT
April 1994
How to Use the Handbook/IX
HOW TO USE THE HANDBOOK
Organization of the Handbook
The Handbook on Injectable Drugs has been organized as a
collection of monographs on each of 272 commercially available
drugs. In addition, information on 42 investigational drugs and 16
drugs available outside the United States has been included. A
section on the composition and characteristics of commercially
available intravenous infusion solutions is presented at the end of
the book. The monographs on the commercial drugs are arranged
alphabetically by nonproprietary name. The names of the drugs
follow the style of USAN and the USP Dictionary of Drug Names,
1993 edition. Also included are some of the trade names and
manufacturers of the drug products; this listing is not necessarily
comprehensive and should not be considered an endorsement of
P-ny product or manufacturer.
All of the information included in the Handbook is referenced
so that those who wish to study the original sources may find them.
In addition, the American Hospital Formulary Service Classifica
tion System numbers have been included to facilitate the location
of therapeutic information on the drugs.
The monographs have been divided into the subheadings
described below:
Products—lists many of the sizes, strengths, volumes, and
forms in which the drug is supplied, along with other components
of the formulation. Instructions for constitution (when applicable)
are included in this section.
The products cited do not necessarily constitute a comprehen
sive list of all available products. Rather, some common represen
tative products are described. Furthermore, dosage forms, sizes.
and container configurations of parenteral products may undergo
significant changes during the lifespan of this edition of the
Handbook.
Following the product descriptions, the pH of the drug prod
ucts, the osmotic value(s) of the drug and/or dilutions (when
available), and other miscellaneous product information such as
the sodium content and definition of units are presented.
Dosage—provides administration information first, followed
by dosage information. The administration information includes
route(s), rates of infusion (when applicable), and other related
administration details. The recommended adult and then pediat
ric doses of the drug are presented. Finally, a notation is included
when dosage reduction for renal and/or hepatic impairment is
needed.
The dosage and administration information is derived primar
ily from the product's official labeling and the American Hospital
Formulary Service. This information is, of necessity, a conden
sation of the available information from these sources. The
intention is to provide the reader with a convenient and readily
available resource for quickly verifying proper and appropriate
doses and dosage ranges of injectable drugs. This information is
insufficient for prescribing. For that purpose, the reader should
refer to the official labeling and more therapeutically comprehen
sive references such as the American Hospital Formulary Service.
Stability—describes the drug's stability and storage require
ments, if any. In addition, pH effects, the effects of freezing and
exposure to light, and the sorption and filtration characteristics of
the drug are presented.
Compatibility Information—tabulates the results of pub
lished reports from primary reference sources of compatibility
testing of the subject drug with infusion solutions and the other
drugs. The various citations are listed alphabetically by solution
or drug name; the information is completely cross-referenced
among the monographs.
Four types of tables are utilized to present the available
information, depending on the kind of test being reported. The
first type is for information on the compatibility of a drug in
various infusion solutions and is depicted in Table 1. The second
type of table presents information on two or more drugs in
intravenous solutions and is shown in Table 2. The third type of
table is used for tests of two or more drugs in syringes and is shown
in Table 3. The fourth table format is used for reports of simulated
or actual injection into Y-sites of administration sets and is showrf
in Table 4.
Many published articles, especially older ones, do not include
all of the information necessary to complete the tables. However,
the tables have been completed as fully as possible from the
original articles.
Additional Compatibility Information—provides addition
al information and discussions of compatibility presented in
narrative form.
Other Information—contains any relevant auxiliary infor
mation concerning the drug which does not fall into the previous
categories.
Ths Listing of Concentration
Th: concentrations of all admixtures in intravenous solutions
in the tables have been indicated in terms of concentration per liter
to facilitate comparison of the various studies. In some cases, this
may result in amounts of the drug that are greater or lesser than
those normally administered (as when the recommended dose is
tested in 100 ml of vehicle), but the listings do accurately reflect
the actual concentrations tested, expressed in standardized terms.
For studies involving syringes, the amounts actually used are
indicated The volumes are also listed if indicated in the original
article.
For studies of actual or simulated Y-site injection of drugs, the
concentrations used are cited. Note that this table is designed with
the assumption of a 1:1 mixture of the subject drug and infusion
solution or admixture. For citations reporting other than a 1:1
mixture, the actual amounts tested are specifically noted.
Designating Compatibility or Incompatibility
Each citation in the Compatibility Information tables has been
X/How to Use the Handbook
Table 1.
Solution Compatibility
Monograph drug name
1
Solution
|
(1)
1.
2.
3.
4.
5.
6.
7.
(2)
M/r
| CondL j
Remarks
(3)
(4)
(5)
[
Rr!
| CH
(6)
(7)
Solution in which the test was conducted.
Manufacturer of the solution.
Manufacturer of the drug about which the monograph is written.
Concentration of the drug about which the monograph is written.
Description of the results of the test.
Reference to the original source of the information.
Designation of the compatibility (C) or incompatibility (I) of the test result according to conventional guidelines.
Table 2.
Additive Compatibility
Monograph drug name
Drug
M/r
CondL
Mfr
CondL
Test
Soln
Remarks
R'f
CH
(1)
(2)
(3)
(4)
(5)
(6)
(7)
(8)
(9)
/-d
CH
(7)
(8)
1. Test drug.
2. Manufacturer of the test drug.
3. Concentration of the test drug.
4. Manufacturer of the drug about which the monograph is written.
5. Concentration of the drug about which the monograph is written.
6. Infusion solution in which the test was conducted.
7. Description of the results of the test.
8. Reference to the original source of the information.
9. Designation of the compatibility (C) or incompatibib'ty (I) of the test result according to conventional guidelines.
Table 3.
Drugs in Syringe Compatibility
Monograph drug name
Drug (in syringe)
Mfr
Amt
(1)
(2)
(3)
1
Mfr
(4)
1
Amt
I
(5)
Remarks
1
(6)
1. Test drug.
2. Manufacturer of the test drug.
3. Actual amount of the test drug.
4. Manufacturer of the drug about which the monograph is written.
5. Actual amount of the drug about which the monograph is written.
6. Description of the results of the test.
7. Reference to the original source of the information.
8. Designation of the compatibility (C) or incompatibility (I) of the test result according to conventional guidelines.
u
*
Table 4.
Y-Site Injection Compatibility (1:1 Mixture)
Monograph drug name
Drug
(1)
1
Mfr
(2)
1
Cone
1 Af/r
Cone
Remarks
(3)
(4)
(5)
(6)
1. Test drug.
2. Manufacturer of the test drug.
3. Concentration of the test drug.
4. Manufacturer of the drug about which the monograph is written.
5. Concentration of the drug about which the monograph is written.
6. Description of the results of the test.
7. Reference to the original source of the information.
8. Designation of the compatibility (C) or incompatibility (1) of the test result according to conventional guidelines.
|
R'f
CH
(7)
(8)
How to Use the Handbook/XI
designated as being a determination of compatibility (C) or
incompatibility (I) according to specific guidelines. The citation
is designated compatible when the results of the original article
indicated one or more of the following criteria:
1.
2.
3.
Physical compatibility (no visible sign of incompatibility).
Stability of the components for at least 24 hours in an
admixture under the specified conditions (decomposition of
10% or less).
Stability of the components for the entire test period, al
though in some cases it was less than 24 hours (time periods
less than 24 hours have been noted).
The citation is designated as incompatible when the results of
the original article indicated one or more of the following criteria:
1.
2.
Physical incompatibility (haze, precipitate, color change,
etc.).
Greater than 10% decomposition of one or more components
in an admixture in 24 hours or less under the specified
conditions (time periods less than 24 hours have been noted).
Although these criteria have become the conventional defini
tions of compatibility and incompatibility, the reader should
recognize that the criteria may need to be tempered with profes
sional judgment Inflexible adherence to the compatibility desig
nations should be avoided. Instead, they should be used as aids in
the exercising of professional judgment.
Therapeutic incompatibilities or other drug interactions are
not within the scope of the Handbook and have not been included.
To gather the bulk of the published compatibility and stability
information, a literature search is performed on the International
Pharmaceutical Abstracts database. By using key terms (e.g.,
stability), a listing of candidate articles for inclusion in the
Handbook is generated. From this list, truly relevant articles are
selected and summarized. As a supplement to this automated
literature searching, the references of each article selected for
inclusion are also reviewed, and any publications not included
previously are obtained. Although this labor-intensive approach
yields a very high percentage of the relevant articles published in
the world’s literature, it is not 100% inclusive. Occasionally,
users of the Handbook call my attention to articles that were
overlooked. I am grateful to these readers and encourage anyone
who finds such an article to contact me.
Limitations of the Literature
The literature on drug-drug and drug-vehicle compatibility
has many contradictions. With the exception of a study indicating
physical compatibility and another indicating chemical decom
position of the same admixture, such conflicting information has
been included. The conflicting information will be readily appar
ent to the reader because of the content of the Remarks as well as
the C and I designations following each citation. Many factors
influence the compatibility and stability of drugs, and absolute
statements are often difficult or impossible to make. Differences
in buffering systems, preservatives, vehicles, temperatures, con
centrations, and order of mixing may all play a role. By reviewing
a variety of reports, the practitioner is better able to exercise
professional judgment with regard to the compatibility of the
admixture. If only one reference is used, valuable alternatives
may be overlooked or marginal compatibility conditions may not
be recognized.
Further, it should be noted that many of the citations designated
incompatible are not absolute. While a particular admixture may
incur more than 10% decomposition within 24 hours, the combi
nation may be useful for a shorter time period. The concept of
“utility time” or the time to 10% decomposition may be useful in
these cases. Unfortunately, such information is often not avail
able. Included in the Remarks columns of the tables are the
amount of decomposition, the time period involved, and the
temperature at which the study was conducted when this informa
tion is available.
Another limitation is that much of the work done has evaluated
only “physical" compatibility. While a finding of precipitation,
haze, or other visually observable effect may be a definite
incompatibility, the lack of such changes does not rule out
chemical deterioration. In many cases, drugs originally listed as
compatible because of their lack of a visual change were later
shown to undergo chemical decomposition. (As previously noted,
such physical compatibility citations have not been included in
the Handbook.) The reader must always bear this possibility in
mind when physical compatibility is the only information avail
able. Similarly, the determination of chemical stability does not
rule out the presence of unacceptable levels of subvisual physical
phenomena such as particles and turbidity.
And, finally, contemporary practitioners have come to expect
that the analytical methods used in reports on the chemical
stability of drugs will be validated stability-indicating methods.
However, many early studies usbd methods that were not demon
strated to be stability indicating.
Solution Abbreviations
AA
Amino acids (percentage specified)
D
Dextrose solution (percentage unspecified)
D5LR
Dextrose 5% in Ringer’s injection, lactated
D5R
Dextrose 5% in Ringer’s injection
D-S
Dextrose-saline combinations
D2.516S Dextrose 2.5% in sodium chloride 0.45%
D2.5S
Dextrose 2.5% in sodium chloride 0.9%
D514S
Dextrose 5% in sodium chloride 0.225%
D515S
Dextrose 5% in sodium chloride 0.45%
D5S
Dextrose 5% in sodium chloride 0.9%
DIOS
Dextrose 10% in sodium chloride 0.9%
D5W
Dextrose 5% in water
D10W
Dextrose 10% in water
DXN-S Dextran 6% in sodium chloride 0.9%
IDCM
lonosol DCM
IG
lonosol G
XIl/How to Use the Handbook
IM
IP
IS
LR
NM
NR
NS
PH
R
S
SL
TPN
W
Isolyte M
Isolyte P
Invert sugar
Ringer’s injection, lactated
Normosol M
Normosol R
Sodium chloride 0.9%
Protein hydrolysate
Ringer’s injection
Saline solution (percentage unspecified)
Sodium lactate V6 M
Total parenteral nutrition solution
Sterile water for injection
Manufacturer and Compendium Abbreviations
AB
ACC
AD
AH
AHP
Abbott
American Critical Care
Adria
Allen & Hanburys
Ascot Hospital
Pharmaceuticals
AMG Amgen
AMR American Regent
ANT Antigen
Asta-Pbarma
AP
AQ
American Quinine
AR
Armour
ARC American Red Cross
AS
Arnar-Stone
ASC Ascot
AST Astra
AT
Alpha Therapeutic
AW Asta Werke
AY
Ayerst
BA
Baxter
BAY Bayer
BC
Bencard
BE
Beecham
BEL R. Bellon
BI
Boehringer Ingelheim
BK
Berck
BN
Breon
BP
British Pharmacopoeia
*
BPC British Pharmaceutical
*
Codex
BR
Bristol
BRN Braun
BT
Boots
BV
Ben Venue
BW
Burroughs Wellcome
BX
Berlex
BY
Bayer
CA
Calmic
Carlo Erba
CE
CET
CH
CI
CL
CN
CO
CR
CU
DB
DCC
DI
DIA
DM
DU
EA
EN
ES
EV
EX
FA
FC
FI
FRE
FUJ
GEM
GEN
GG
GL
HC
HO
HR
HY
ICI
IMM
IMS
Cetus
Lab. Choay Soci<
Anonyme
Ciba
Clintec
Connaught
Cole
Critikon
Cutter
David Bull
Laboratories
Dupont Critical
Care
Dista
Diamant
Dome
DuPont
Eaton
Endo
Elkins-Sinn
Evans
Essex
Farmitalia
Frosst & Cic
Fisons
Fresenius
Fujisawa
Geneva-Mars am
Genentech
Geigy
Glaxo
Hillcross
Hoechst-Roussel
Homer
Hyland
ICI
Pharmaceutical
Immunex
IMS Ltd.
Intra
IN
IV
Ives
Invenex
IX
Janssen
JN
KA
Kabi
Knoll
KN
Kabi Pharmacia
KP
Kabi-Vitrum
KV
Kyowa
KY
Lagap
LA
Lederle
LE
LEM Lemmon
LEO Leo Laboratories
LI
Lilly
Lyphomed
LY
Labaz Laboratories
LZ
Mallinckrodt
MA
May & Baker
MB
ME
Merck
McGaw
MG
Miles
MI
Mead Johnson
MJ
McNeil
MN
MMD Marion Merrell Dow
MRD Merrill-Dow
MRN Merrill-National
MSD Merck Sharp & Dohme
MY
Maney
NA
National
NCI National Cancer
Institute
NE
Norwich-Eaton
NF
National Formulary
*
Nordic
NO
NOV Novo
ON
Orion
OR
Organon
ORT Ortho
PD
Parke-Davis
PE
Pentagone
PF
Pfizer
PFM Pfrimmer
PH
Pharmacia
PHX Phoenix
PO
Poulenc
PR
Pasadena
Research
PX
Pharmax
Quad
QU
RB
Robins
RC
Roche
RI
Riker
RKC Reckitt-Colman
ROR Rorer
RP
Rhone-Poulenc
RR
Roerig
Roussel
RS
RU
Rugby
Schering
SC
SCN Schein
SE
Searle
SKB , Smith Kline
Beecham
SKF Smith Kline &
French
Smith
SM
Smith +. Nephew
SN
SoloPak
SO
SQ
Squibb
Sterilab
ST
STR Sterling
STS Stcris
STU Stuart
SV
Savage
SX
Sabex
Syntcx
SY
Sandoz
SZ
Teva
TE
Tillotts
TL
Torigian
TO
Travenol
TR
Upjohn
UP
USP United States
*
Pharmacopeia
1
USV USV
Pharmaceutical
Vitarine
VI
Vitrum
VT
Winthrop-Breon
WB
WC Wamer-Chilcott
WED Weddel
Winthrop
WI
Warner Lambert
WL
WY Wyeth
'While reference to a compendium does not indicate the specific
manufacturer of a product, it does help to indicate the formulation that
was used in the test.
452/Fludarabine Phosph ate
every 28 days. Safety and efficacy of fludarabine phosphate in chil
dren have not been established (2; 4).
The dosage may need to be reduced in geriatric patients and
patients with impaired renal or bone marrow function (2; 4).
FLUDARABINE PHOSPHATE
AHFS 10:00
Berlex
Fludara
Products— Fludarabine phosphate (Berlex) is supplied as a lyo
philized product in 6-ml vials containing 50 mg of drug with man
nitol 50 mg and sodium hydroxide for pH adjustment. Constitute
with 2 ml of sterile water for injection to yield a 25-mg/ml con
centration (2).
pH— From 7.2 to 8.2 (2).
Stability— Intact vials should be stored under refrigeration (2). The
manufacturer recommends use of the constituted solution within
eight hours because it does not contain an antibacterial preservative.
Nevertheless, the drug is chemically stable in solution, exhibiting
less than 2% decomposition in 16 days when stored at room tem
perature and exposed to normal laboratory light (234).
Osmolality— Fludarabine phosphate 25 mg/ml in sterile water for in
pH Effects— Fludarabine phosphate is chemically stable in aqueous
solution at pH 4.5 to 8. The pH of optimum stability is approxi
mately 7.6 (234).
jection has an osmolality of 352 mOsm/kg (1689).
Dosage— Fludarabine phosphate is administered by intravenous in
fusion over 30 minutes in 100 or 125 ml of dextrose 5% in water
or sodium chloride 0.9% (2; 4). The drug also has been adminis
tered by rapid intravenous injection and continuous infusion (4).
The usual adult dose is 25 mg/m3 daily for five consecutive days
Sorption— Fludarabine phosphate 0.04 mg/ml in dextrose 5% in wa
ter or sodium chloride 0.9% was equally stable in either glass or
PVC containers, exhibiting no loss due to sorption during 48 hours
at room temperature or under refrigeration (234).
Compatibility Information
Y-Site Injection Compatibility (1:1 Mixture)
Fludarabine phosphate
Drug
J
Mfr
j
Cone
1
Mfr
1
Cone
1
Remarks
|
«<■/
| Cll
Acyclovir sodium
BW
7 mg/ml"
BX
1 mg/ml"
Darker color visible with high intensity
light within 4 hr
1439
I
Allopurinol sodium
BW
3 mg/mlb
BX
1 mg/mlb
Physically compatible with no change in
measured turbidity or increase in parti
cle content in 4 hr at 22 °C under flu
orescent light
1686
c
Amikacin sulfate
BR
5 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Aminophylline
ES
2.5 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Amphotericin B
SQ
0.6 mg/ml"
BX
1 mg/ml"
Small amount of particulate matter devel
ops in 4 hr at room temperature
1439
I
Ampicillin sodium
BR
20 mg/mlb
BX
1 mg/ml’
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Ampicillin sodium-sulbactam
sodium
RR
20 +
10 mg/mlb
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Amsacrine
NCI
1 mg/ml"
BX
1 mg/ml’
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Aztreonam
SQ
40 mg/ml"
BX
1 mg/ml’
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Bleomycin sulfate
BR
1 unit/mlb
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Butorphanol tartrate
BR
0.04 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Carboplatin
BR
5 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Carmustine
BR
1.5 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Fludarabine Phosph at e/453
Y-Site Injection Compatibility (1:1 Mixture) (Cont.)
Fludarabine phosphate
Drug
Mfr
|
|
Cone
|
|
Cone
|
Remarks
|
«<■/
| CH
Cefazolin sodium
LEM
20 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
C
Cefepime HC1
BR
20 mg/ml"
BX
1 mg/ml"
Physically compatible with no change in
measured turbidity or increase in parti
cle content in 4 hr at 22 °C under flu
orescent light
1689
C
Cefoperazone sodium
RR
40 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Cefotaxime sodium
HO
20 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Cefotetan disodium
STU
20 mg/ml"
BX
1 mg/m!"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Ceftazidime (sodium carbonate)
GL
40 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c 1
Ceftizoxime sodium
SKF
20 mg/mla
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Ceftriaxone sodium
RC
20 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Cefuroxime sodium
GL
30 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Chlorpromazine HCI
ES
2 mg/ml"
BX
1 mg/ml"
Initial light haze intensifies within 30
min
1439
I
Cimetidine HCI
SKF
12 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Cisplatin
BR
1 mg/ml
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescenf light
1439
c
Clindamycin phosphate
LY
10 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Cyclophosphamide
MJ
10 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Cytarabine
UP
50 mg/ml
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c ’
Dacarbazine
Ml
4 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Dactinomycin
MSD
0.01 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Daunorubicin HCI
WY
2 mg/ml"
BX
1 mg/ml"
Slight haze, visible with high intensity
light, forms within 4 hr at room tem
perature
1439
I
Dexamethasone sodium
phosphate
MSD
1 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Diphenhydramine HCI
WY
2 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Doxorubicin HCI
CET
2 mg/ml
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
454/Fludarabine Phosphate
y-Site Injection Compatibility (1:1 Mixture) (Cont.)
Fludarabinc phosphate
Mfr
|
j
j
/?<•/
| CH
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
1 mg/ml4
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
BX
1 mg/ml4
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
2 mg/ml"
BX
1 mg/ml4
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
AMG
30 p.g/ml"
BX
1 mg/ml"
Physically compatible with no change in
measured turbidity or increase in parti
cle content in 4 hr at 22 °C under flu
orescent light
1687
c
^loxuridine
RC
3 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Fluconazole
RR
2 mg/ml
BX
1 mg/ml"
Physically compatible for 4 hr al room
temperature under fluorescent light
1439
c
Fluorouracil
LY
16 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Furosemide
AB
3 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Drug
Doxycycline hyclate
Droperidol
Cone
1 Mfr
Cone
BX
1 mg/ml"
0.4 mg/ml"
BX
BR
0.4 mg/ml4
Famotidine
MSD
Filgrastim
ES
1 mg/ml"
JA
Etoposide
|
Remarks
Ganciclovir sodium
SY
20 mg/ml"
BX
1 mg/ml"
Darker color forms within 4 hr
1439
Gentamicin sulfate
ES
5 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
I
c
Haloperidol lactate
MN
0.2 mg/ml3
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Heparin sodium
SO.
WY
40. 100..
1000 units/
ml4
BX
1 mg/ml"
Physically compatible for 4 hr at room ,
temperature under fluorescent light
1439
c
Hydrocortisone sodium
k phosphate
MSD
I mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Hydrocortisone sodium
succinate
UP
1 mg/ml
*
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Hydromorphone HC1
KN
0.5 mg/ml4
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Hydroxyzine HC1
Wl
4 mg/ml"
BX
1 mg/ml"
Slight haze, visible with high intensity
light, forms immediately
1439
1
Ifosfamide
MJ
25 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Imipenem-cilastatin sodium
MSD
5 mg/mlb
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Lorazepam
WY
0.1 mg/ml
*
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Magnesium sulfate
so
100 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Mannitol
BA
150 mg/ml
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Fludarabine Phosphate/455
Y-Sile Injection Compatibility (1:1 Mixture) (Cont.)
Fludarabine phosphate
Drug
Mfr
|
|
Cone
1
1
Cone
|
Remarks
j
«<■/
j cn
1439
c
Mechlorethamine HCI
MSD
1 mg/ml
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
Melphalan HCI
BW
0.1 mg/mlb
BX
1 mg/mlb
Physically compatible with no change in
measured turbidity or increase in parti
cle content in 3 hr at 22 °C under flu
orescent light
1557
c
Meperidine HCI
W1
4 mg/ml“
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Mesna
BR
10 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Methotrexate sodium
CET
15 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Methylprednisolone sodium
succinate
UP
5 mg/ml’
BX
1 mg/mlJ
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
C j
Metoclopramide HCI
DU
5 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Mezlocillin sodium
Ml
40 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Miconazole
JA
3.5 mg/ml
*
BX
1 mg/ml
*
Light haze, greater than for miconazole
alone, forms immediately
1439
I
Minocycline HCI
LE
0.2 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Mitoxantrone HCI
LE
0.5 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Morphine sulfate
WI
1 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Multivitamins
ROR
0.01 ml/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Nalbuphine HCI
DU
10 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Netilmicin sulfate
SC
5 mg/ml”
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c1
Ondansetron HCI
GL
0.5 mg/ml
*
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Pentostatin
NCI
0.4 mg/mlb
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Piperacillin sodium
LE '■
40 mg/ml
*
BX
1 mg/ml”
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Piperacillin sodium-tazobactam
sodium
LE
40 mg/ml
*
BX
1 mg/ml”
Physically compatible with no change in
measured turbidity or increase in parti
cle content in 4 hr at 22 °C under flu
orescent light
1688
c
Potassium chloride
AB
0.1 mEq/ml”
BX
1 mg/ml
*
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Prochlorperazine edisylate
WY
0.5 mg/ml
*
BX
1 mg/ml
*
Slight haze forms within 30 min
1439
I
456/Fludarabine Phosphate
y~Sile Injection Compatibility (1:1 Mixture) (Cont.)
Fludarabine phosphate
j”
/?<•/
| CT
Promethazine HC1
WY
2 mg/ml‘
BX
1 mg/ml’
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
C
Ranitidine HC1
GL
2 mg/ml
*
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Sodium bicarbonate
AB
1 mEq/ml
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Tetracycline HC1
LE
2.5 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Ticarcillin disodium
BE
30 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Ticarcillin disodium-clavulanate
potassium
BE
31 mg/ml"
BX
.1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Tobramycin sulfate
LI
5 mg/ml"
BX
1 mg/mla
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Trimethoprim-sulfamethoxazole
ES
0.8 + 4 mg/ BX
ml’
1 mg/ml’
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Vancomycin HC1
LI
10 mg/ml"
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Vinblastine sulfate
LY
0.12 mg/ml
BX
I mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Vincristine sulfate
LY
1 mg/ml
BX
1 mg/ml"
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Vinorelbine tartrate
BW
1 mg/mlb
BX
1 mg/mlb
Physically compatible with no change in
measured turbidity or increase in parti
cle content in 4 hr at 22 °C under flu
orescent light
1558
c
Zidovudine
BW
4 mg/ml"
BX
I mg/ml’
Physically compatible for 4 hr at room
temperature under fluorescent light
1439
c
Drug
Mfr
|
|
Cone
|
Mfr
1
Cone
Remarks
“Tested in dextrose 5% in water.
bTested in sodium chloride 0.9%.
Additional Compatibility Information
The manufacturer recommends diluting the dose in 100 to 125 ml
of dextrose 5% in water or sodium chloride 0.9% (2). At a concen
tration of 1 mg/ml in these solutions, less than 3% decomposition
occurred in 16 days at room temperature with exposure to normal
laboiatory light. At a concentration of 0.04 mg/ml in dextrose 5% in
water or sodium chloride 0.9%, little or no loss occurred in 48 hours
al room temperature or under refrigeration (234).
£>t-
Taisia
SATURDAY,MAY 15,1993;. 13
Dr Zafrullah
Chowdhury, who
has earned world
renown for giving
a
people-oriented
drug policy, talks
to Bharati
Sadashivam
The man with lhe.1
• right prescription}
“Keep drug formulations re
stricted to essential drugs, control
prices and start consumer educa
tion and awareness,” is Dr Zafrullah Chowdhury's message to In
dian drug policy-makers.
As the man whose pioneering
efforts in people-oriented health
programmes have made Bangla
desh a uniquely successful exam
ple of rational drug policies, Dr
Chowdhury is eminently qualified
to give this piece of advice. What's
more, he has, almost single-hand
edly, helped his poor and tiny
untry achieve what its giant
:ighbour has failed to do: by imementing in spirit India’s Hathi
committee recommendations of
1974 to regulate the drug market.
f
Bangladesh's National Drug
Policy of 1982, formulated by Dr
Chowdhury, has ended the mono
poly cartel of multi-national phar
maceutical corporations, forced
them to put health before profits,
transferred production to local
companies, brought down prices
while increasing the volume of
business and improved the quality
of medicines.
His efforts earned him the Magsaysay Award in 1984 and the Al
ternative Nobel last year, much
admiration and encouragement
from scientists the world over and opposition and opprobrium
from the drug and doctor lobbies
at home.
"Over the last ten years, the
price of every commodity in Ban
gladesh has gone up, except drugs.
Drug prices have remained low
despite the taka dropping from 18
to the dollar to 40 and drugs being
taxed now, unlike in 1982,” says
Dr Chowdhury’, who was in Bombav recently to interview doctors
"n an effort to start an tntraSAARCexchange programme.
Just one figure points to the tell
ing contrast between the drug si
tuations in India and Bangladesh.
India has over 60,000 drug formu
lations, ranging from unnecessary
to useless, of which more than
two-thirds are irrational multi-in
gredient combinations. Banglade
sh's total is 250 (the WHO lists a
total of 270 drugs as being enough
to treat all the world's ailments),
most of which are generic drugs.
“The Hathi committee had the
right prescription for India. It is a
pity that your government threw it
away because of pressure from the
drug lobby,” says Dr Chowdhury,
It is especially unfortunate, he
adds, that India is one of the
world's worst examples of irra
tional drug policies despite the In
dian Patent Act of 1970 which has
helped the indigenous drug indus
try grow from Rs 10 crore in 1974
to Rs 4,300 crore today.
The Indian Patent Act, which
protects process and not product
patents, was an inspiring factor for
both Bangladesh and Sri Lanka in
the '70s. But, under US pressure,
Sri Lanka abandoned its unique
drug policy based on price control
and competition between MNCs
which saw prices fall over seven
years.
Determined to avoid the pitfalls
in India and Sri Lanka which led to
the failure of people-oriented poli
cies, Dr Chowdhury made tight
regulation of the eight MNCs op
erating in Bangladesh a key ele
ment of his strategy. He had the
strong support of the then presi
dent, Gen. H.M.Ershad who, un
like his neighbourhood counter
parts. withstood pressure from the
highest quarters in the US urging
him to allow the MNCs a free hand
and remove price controls.
"Most Third World countries
draw up a list of essential drugs for
the public sector, allowing the rest
to be imported. We said that what
cannot be produced locally cannot
be produced by the MNCs and that
no drug outside the list of 250 can
be produced or imported."
The Bangladesh drug policy
barred the MNCs from producing
high-priced drugs, like antacids,
vitamins and syrups, to enable lo
cal companies enter this market
segment. It made them compete
with one another, which helped
slash prices and improve quality.
And it put an end to the cost-cut
ting methods they employed to
maximise profits with minimum
investment -such as using local
small-scale factories to manufac
ture drugs, or producing injection
drugs and getting a local company
to supply the water.
All this predictably raised a
howl of protest from the MNCs,
many of which threatened to
leave. “But none have left. In fact,
two more have come in," says Dr
Chowdhury.
1981.
11
Along
with
q the
‘demythification’ of MNCs,< Dr
Chowdhury’s singular succesi lies
in his demystification of health and
medical procedures. The Gotoshasthaya Kendra, acharitable.Jrust
devoted to public health set Op by
him just outside Dhaka, cover
*;
ten
areasof Bangladesh. It hasm^dc it
a point to educate and involvt^ wo
men, whose role in development is
crucial in a Muslim and agricultur
al society, says Dr Chowdhuqji.
Women have been taughj to
take blood pressure, give Ejec
tions, even perform tubectotaies.
The results have been dramatic:
the infant mortality rate in ttfeas
covered by the Kendra is 65 I i',000
(Bangladesh national average
120-140), maternal mortality-irate
1-2 (6.9), birth rate 1.5 (2.4).}
The Gonoshasthaya Kendra.has
also made consumer education a
priority. One of its effective meth
ods is to place ads in newspapers,
as conspicuously as those by phar
maceutical companies, question
ing or clarifying their claims.t“A
Most developing countries hesi drug is like any other commodity.
tate to criticise the functioning of
But while you make your owrgdeMNCs, he says, because they are ■
cision when you buy clothes or
thought to bring in valuable for food, your doctor decides skhat
eign investment. "But these claims
drugs you buy, and he is most of
must be examined. In 1989, the
ten tutored not by medical text
MNCs’ total investment in Ban
books but by drug companies.
gladesh was 381.86 million takas,
while their profits were 972.88 mil That’s why consumers have to be
informed.'1
lion takas. In 1981, Pfizer invested
11.4 million takas and took out 200
There are still a few failures
million takas.”
dogging Bangladesh's enormous
An important reason for quality success in rational medicine -Hike
control of drugs in Bangladesh is bad prescriptions by doetprs.
that most of them are single-ingre There is also the problem of ban
ned drugs being smuggled in from
dient or generic products -a Hathi
committee recommendation - India. “You complain about Ban
which enables faster testing, he gladeshis living illegally in yoqr ci
says. Only 8 per cent of the drugs ties. But they contribute to tour
in the market today are sub-stan GDP. while your illegal drug? af
fect our health!”
dard, as against 35 per cent in
eally needed
If one goes
lies say, the
year new
promising
am colds to
any of them
drugs, and
waste of re
cce a pleth■es.
□rid I lealth
is been entf developing
d number
provide a
Medicines tor
~
_z
’.•HO has a
;."s found that
level 10 to 15
tediate needs,
40 drugs can
>f complaints,
e about 100
ger hr
als
the essential
aiends are no
can be nianutheir generic
1 names. The
illectual prop
chemicals and
result of ’
ants will make
tore expensive
But the fact
ned remedies
ity of ailments
tor in reducing
•
o mal^^lb
available is to
«eneric, as op
s'and the need
e and sale of
ial drugs. In a
t that “all the
imiting the hst —
.'vantages than
- health- *l 1S.
? is less risk of
and mistakes;
ii<rributine the
,re<crmers, dis-
eliects and
enerie or inter-V name
the producer s
mpediments to a WHO programme
brand name. It points out that “a
simple name linked to the active in
gredient is easily recognisable; it also
makes for greater safety in prescribing,
dispensing and administering. Most of
e essential drugs are no longer under
patent and can be manufactured freely
under the;r generic names?”
Various consumer groups and non
governmental organisations have also
stressed the need to reduce the number
of inessential drugs and regulate the
pharmaceuf’ :al industry in developing
countries. Panos, a London-based
group, has described the pharmaceuti
cal market in the developing world as a
“strange combination of too many and
too few drugs”? It adds that “the
wrong drugs proliferate — those that
have little or no efficacy, poor safety
records, are expensive and divert at
tention from useful therapies. At the
same time, drugs that can meet public
health needs effectively, safely and at
an affordable price are often hard to
find.”
Consumer and public interest groups
are also sceptical about the value of
many of the new drugs that are coming
into the market. According to Health
Action International, a network of
public interest groups, as many as
seven out of every 10 new products of
fered “little or no therapeutic gain
over existing products.” It also report
ed that more than four in five cough
and cold products contained ineffective
ingredients, and more than two out of
five vitamin preparations contained
non-essential or ineffective ingre
dients.”
Various reports.and resolutions of
the WHO have urged poorer countries
to adopt national drug policies geared.
to the production and marketing of a
basket of essential drugs. This has
aroused stiff opposition from the pharmaceuticu! industry, which argues that
promotion of generic names and. re
striction of d:ug use will affect their
ability to develop new drugs. Panos, in
a briefing paper, stated that the phar
maceutical industry has consistently
opposed the implementation of the
Frontline, June 17, 1994
line. June >’• 1994
policy. Officially, the industry has not
opposed the essential drugs pro
gramme provided it is limited to the
public sector in developing countries.
But, given the retreat of the state and
the growing importance given to the
private sector in health care even
in developing countries, this would
seriously weaken the concept of an
essential drugs programme.
Consumer and public
interest groups are
sceptical about the
value of many of the
new drugs coming into
the market.
The WHO, in a report to its recent
ly-concluded annual meeting in Gene
va, has expressed itself strongly in fa
vour of firm state intervention. “Gov
ernment regulation of the pharma
ceutical market is essential for appro
priate drug use,” the report stated. It
stated that it was “essential that the
state defines the objectives of rational
use and develops a policy for the bene
fit of public health and the patient
rather than relying totally on free
choice and the exchange between con
sumers and providers, which fails to
ensure universal coverage or equal ac
cess to even the most essential drugs or
their rational use.”
But the majority of governments are
unwilling to take the strong regulatory
steps necessary to implement an essen
tial drugs programme. Every two
years, the World Health Assembly, the
annual meeting of WHO member
countries, discusses the programme
and passes a resolution calling for its
strengthening. This year was no excep
tion. The resolution urged the mem
bers to “commit themselves to the de
velopment and implementation or na
tional drug policies to improve equi
table access to essential drugs of good
quality at affordable cost and to inten
sify efforts to promote the rational use
of drugs.”
But only a few countries follow an
essential drugs policy. Bangladesh, in
1982, was one of the first countries to
develop such a policy. Panos estimates
that in 10 years, Bangladesh had saved
$600 million in health care, and the
proportion of substandard drugs had
fallen from 36 to 9 per cent, while local
production increased from 35 to more
than 60 per cent. However, with
changes in the government and greater
liberalisation of the economy, Panos
has reported that inessential drugs such
as vitamin syrups have begun to ap
pear on the market.
Nigeria also passed sweeping legisla
tion in 1989 banning the import, sale
or manufacture of any drug which was
not on a list of 400 drugs, and making
it compulsory for drugs to be sold un
der their generic names.
More than 113 countries are report
ed to have, adopted model lists of
drugs, but despite this a WHO report
acknowledges that a lot remains to be
done. ‘‘Access to essential drugs re
mains limited and inequitable in many
countries, despite much effort. Struc
tural weakness of the public drug sec
tor continues to handicap the function
ing of tjie health system.”
Thus more than a decade after its
launching, the idea of an essential
drugs programme is widely acknowl
edged as desirable, but few countries
seem to have had the administrative
ability or political will to put it into
operation. One of the reasons for this
is the influence wielded by multi
nationals. The WHO refers to this,
though obliquely: “There is a global
imbalance in the pharmaceutical sector:
a strong supply side influences con
sumption in the wrong way when the
demand side consists of often poorlyinformed prescribers and public. This
is particularly true in the developing
countries, where the administration of
ten has limited resources and negotiat
ing power. Such an imbalance contrib
utes greatly to the difficulty of imple
menting rational drug policies.” H
4S
)
Jr?
J
-jJ^
■> - <zde,s,
■
’
. ■ >
.^7—
ffT"''^'’'"
/—
0
t
,T----’i p^----'-^
czjr>-^^><7’<jLvx?-^
^>^117
tiy^J .
^jT^f
K
r)
(ffl BvocUctSS;
CM
/?(/''?-
&ioaw^_
n^Aly
fe> &>
<^A-'E>JL«-^ ‘M
- 6 6 , /c=>
en-e^JEji aja /?So'S/ . dLe- (^feO’-S cJLso otoa fcocf
-.^Zecl
e^X'u.^o.CSj
I 2 iro
&-&. -^epCuK-Cu^ 'SJ J-b^ySAcQfy
/^?2
^o&aLT
cf
, p> ,jsCxc0
-r^
j-ICj.itt
Ax S. Cf '-^ f 'v<>-\ \'>^__
*T~X^fc.v.o»
J” A/ LO-o,.
£)C
H^'eubeX
S^ CC’-^xl'
1Q /
Cs-^
\_Ci_v >' /vO-'ltX
o p k • • Vo.
C cr>->n rrv-'—>_k_>-£^
t A|e.,_o
uvaJtELiJ
<p-s
lS.i-l_<O_l
,
=6- ~T^
bet
dp j'-tz<_o.
— I/O Ofb.
I^S'j
^L^-LclA f^l&J^^J!-c^y.
I 3
/?
flu^dbxiu-e- ^©’-n . ^.xa^-A
■^pOtu<i l’-u=.l£J Gis2-S.^j\. • ^-
J5oc->.C-B Au-xst’J'-
“Ssx.s.'Cch<te/ Zcax
S^ptpJAZ^ .
A-V^Lo.^LL{ jwcxjJaGtE^fe
-o£ &J^-C<sJ\ c^a-j^C
O-CzxfJiil'^p ,
HeixtCk CjSL.’^e_- - ce-k.<£J)x
i_»a-O-jJ-
l '^ ^o
"H
t&od f
t/ooo2
£plxsz4/^c_Q
^.uj '^e^^Cc Q^-U
&-2> <21 —
Jcwuusa -A_£j_ ( 7 £’ X ,
^V'C'V'JLc?_.t> t-c_ .
|' V '|L&J
K-J
JxjE-Ij.U.I'-
\J Ml /) /
<g_p
cnAOvTfcS-
~^)\' «-va_vc_\ <rx c.o-v^p-^c.Le_iA_2ixLy-<_
C'cl h--—5. -i Cc^ —. y/ <-pX<, o Qt^^. ZtaT' ct’qumxaa^—.
A.L'JSa CxaJl’<_<iu_?
, cj^-rCC^o—co_
zw.C?_j^Iz\
° l^--c^L vtA o5icyx_x_^ c e?»-v>_p><-'>-Aj3
o^-o p^-rv^J-e-o1 ■
'rK>i^i bD^hJic/
c£x^
A-uJ>
^c^-LAj-eJ)
i s •? g-
K< Q., c\^-- ■s.e
J
<3l<-
01 ItCT
^sjpxAucJ1
S'-
0-0
—Lvo.;=’.•'
,
^'-'^‘jp--<~^C
)
ctGs
2->i>lQ_
<-’A
<.QC I'
V)--' 'z^ACej-/</~'^2_l<J r \\
A|O~ £\aj^a_S__
PRINCIPLES OF IRRATIONAL DRUG THERAPY
Michael A. Vance
William R. Millington
Drugs are extensively used in medicine when they are unlikely to produce a
benefit to the patient. In most instances this does no apparent harm to the patient
but sometimes (for example, the extensive use of thorotrast) the results are tragic.
Even when the patient is not injured, overuse of medicines is an undesirable and
money-wasting behavioral pattern. Several factors relating to the social process of
drug use w hich encourage overprescribing arc discussed and the Principles of Irrational
Drug Therapy are derived. These principles are presented as negative role models for
the use of medicines in developing countries.
A drug is irrationally used if it is employed when there is little likelihood that it will
have a beneficial effect or when the anticipated benefit is not worth the potential
harm or cost of the drug. The basic contention of this article is that drugs are routinely
overused in the practice of medicine (1, 2). Contributing to excessive drug use are
subtle pressures to use medicines which are independent of any specific therapeutic
action of the drug. This paper outlines several of these non-pharmacologic factors,
which generally operate on a subconscious level.
NON-PHARMACOLOGIC FACTORS THAT ENCOURAGE DRUG USE
Drugs are Seductive
Drugs appear more effective than they really are. A drug is likely to be given credit
for a cure in which it played no part if the patient improves as a result of the natural
course of the disease. Both the patient and especially the physician (“Oh, thank you
Doctor") receive incentive to use the drug repeatedly as long as the drug appears occa
sionally effective and does no apparent harm.
There is also the placebo effect in which case the act of taking medicine causes
improvement in the patient regardless of any curative agent the medicine may contain.
An apparent example of the placebo effect is the marketing success of a propoxyphene
(Darvon). Numerous double-blind studies have documented that propoxyphene is at
best a weak analgesic (3). Yet as little as 11 years ago a propoxyphene-containing
preparation was the largest selling prescription drug in the United States and many
Part of the materia! in this article was presented by M.A.V. at the Primero Coloquio Gentifico
en Gencias Medicas Nicaraguerue-Norte-americano in Managua, Nicaragua in November, 1983.
International Journal of Health Services. Volume 16. Number 3,1986
O19S6. Baywood Publlshlni Co., inc.
355
Principles of Irrational Drug Therapy ' 35’ .
35b
Vance and Millington
propoxyphcne-contaming drugs continue to be big sellers today (4). The explanation
for the widespread use of these essentially inactive compounds is that pain responds
well to placebo. These drugs would therefore be almost as effective if they contained
milk sugar instead of propoxyphene. Unfortunately propoxyphene is not as inocuous
as sugar, it has been implicated in 1.000-2.000 overdose deaths per year (5).
There are many additional examples of popular drugs of questionable utility (6).
Sleeping medications are used by millions of people on a regular or semiregular basis
although they are effective as sleep aids only when used for brief periods and despite
the fact that regular users have an unexplained increase in mortality (7). A possible
cause of drug overuse involves cimetidine, a staggeringly popular and expensive
medication used to accelerate the healing of ulcers. Moerman has demonstrated that
the published studies, which often are cited to document the efficacy of the drug, indi
cate that when properly administered to ulcer patients a placebo is at least as effective
as cimetidine and is certainly less toxic (8).
It is unfortunate that the placebo effect is frequently under-valued. To many, a
favorable response to a placebo is suggestive of mental instability. However, virtually
everyone responds to placebos. This is reason to be grateful-not ashamed-because it
indicates that the human body is capable of readjusting itself without depending upon
exogenous chemicals.
Drags Are An Easy Way Out
If a person becomes ill because of poor living or working conditions it is much
easier to administer a drug than to address the underlying issues of social injustice. In
some cases this may be a valid short-term approach. Thus, for example, the use of an
anti-infective drug may be appropriate if limited resources preclude improvement of
' public sanitation. However, this practice is less justifiable when drugs are used to con
trol behavior such as when physicians load patients with haloperidol to keep them
from disrupting ward routine or give housewives diazepam to coerce them into
The dangers of thalidomide and DES were discovered only because the drug-induced
diseases were very severe and very rare in the unexposed population. In light of the
high level of drug use by pregnant women (10), it is probable that some portion of
commonly occurring birth defects are the result of preventable exposure to medicines
Recent knowledge about DES further highlights the threat of delayed toxicities. Il ap
pears that mothers who were given DES are now, 20 or more years later, at an in
creased risk of developing breast cancer (11. 12). This is especially regretable because
the drug was useless for its intended purpose in the first place (13).
As a generalization it is reasonable to conclude that drug toxicity is underrated.
However, it is important to realize that in some instances side effects are improperly
attributed to drugs (14, 15).
Drug Toxicity Information May be Intentionally Suppressed
When Seligweiss announced that unhygienic practices of physicians led to deadly
childbirth fever he was persecuted by the medical profession. Such pressure to protect
physicians and the medical establishment are still operant today (16).
In 1980 the diuretic drug triciynafen (Selacryn) was withdrawn from the U.S. mar
ket because it causes liver and kidney damage (17). One physician was interviewed
after a patient for whom he prescribed the drug died of liver toxicity (18). He ex
pressed surprise that the manufacturer had continued to promote tricrynafen after it
had learned of drug-related deaths. There was no reason to be surprised. Withholding
information on life-threatening side effects has occurred repeatedly over the years and
continues today (19, 20). The only reasonable conclusion is that it is a standard oper
ating procedure for drug manufacturers to suppress reports on the toxicity of their
products as long as they can get away with it.
Advertising Promotes Irrational Drug Use
adapting to an unwanted life situation.
Drug Toxicity is Often Underestimated
By nature, many toxic effects of drugs are hidden. If a drug-induced disease is com
mon in the population receiving the drug, the relationship between the drug and the
disease will be obscured. For instance, the use of estrogens by post-menopausal women
may be associated with an increased risk of breast cancer (9). Yet, despite millions of
patient years experience, there is no clear consensus as to whether these drugs cause
breast cancer because the background rate of this disease is high.
In some cases serious toxic reactions to drugs do not develop until after drug
therapy has been discontinued. This also hampers identification of the drug-related
nature of the disease. Examples of delayed toxicity include aplastic anemia associated
with chloramphenicol, retinal damage associated with chloroquine, and liver damage
associated
halothane.
Lastly, with
toxicities
may occur in the offspring of patients such as was the case with
thalidomide-induced phocomelia and diethylstilbesterol (DES)-induced vaginal cancer.
It is estimated that selling costs represent about 25 percent of the total expenditures
of the large drug companies (21,22). This is a huge sum and, as with all advertising.
drug advertising is designed to create an image of the product that will maximize its
consumption. That a significant amount of advertising is aimed at encouraging irra
tional drug use has been suggested (22) and is indeed obvious when one peruses the
advertising pages of almost any medical journal. It appears that such advertising does
succeed in producing inappropriate drug therapy (23) although this is disputed (24).
There is no way of knowing how many people have been needlessly killed by aplastic
anemia caused by misuse of the antibiotic chloramphenicol (Chloromycetin)-but the
number is undoubtedly in the thousands. In the United States the surges in popularity
of the drug-and in the inevitable deaths associated with its use-are directly related to
increased promotion of the drug by its manufacturer, Parke Davis (25, 26).
While doctors are aware that printed propaganda and visits by company-paid drug
promoters are advertising, they may not believe that industry support of medical edu
cation and the physicians’ privileged lifestyle arc just that too. One physician, who
35o
Principles of Irrational Drug Therapy
Vance and Millington
was in a position to know, was Dale Console, a former Medical Director of Squibb
Pharmaceuticals who said (27):
It seems impossible lo connnre my medical brethren that drug company execu
tives and delail men are either shreud salesmen or shrewd businessmen, never phil
anthropists. They make investments, not gifts.
Physicians Arc Often Unaware of the High Cost
of Drugs, or Worse Yet. May Not Even Care (28)
The cost of some drugs, especially antineoplastics and new antibiotics, is astronom
ical. For example, a week of therapy for one patient with 12 grams a day of cephamandole could cost the pharmacy 500 dollars for the drug alone (29). Moreover, the
growth of third-party coverage for drug purchases has led to a decrease in incentive for
health care providers and consumers to behave responsibly in regard to excessive drug
expenditures. When external controls are brought to bear on drug prescribers, such as
restricting the indications for which expensive antibiotics may be used, considerable
monetary savings can be achieved without loss of therapeutic benefit (30).
Education is Very Pro-drug
Pharmacology courses in pharmacy, nursing, and medical schools are taught by per
sons whose vocation is the study of drugs. Their identity exists, in part, due to the fact
that they are drug experts and their livelihood depends upon the continued use of
drugs in medicine. It is to be expected, therefore, that they would approach almost
every problem in medicine with the question, “What drug should be used?”
instead told that they didn't need to take medicine As Oliver Wendell Holmes said
100 years ago, "Another part of the blame (apart from that which falls upon the phys
ician) rests upon the public itself, which insists upon being poisoned” (32). How much
more fitting this statement must be today in a population brought up on television
commercials which insist that such phenomena as everyday headaches and irregularity
constitute normality and that the solution to the problem of eating and drinking too
much-as well as virtually every discomfort-is to take a pill.
There Is Overt As Well As Subtle Pressure To Take Medicines
Consider the occasional patient who escapes the early socialization toward liberal
drug use. He or she presents themself to the medical profession as someone reluctant
to take drugs; in other words as a compliance problem. The second line of socializa
tion springs into action when physicians, nurses,- and pharmacists employ various
strategies to coerce the patient into adopting the correct attitude toward drug treat
ment—that is, the attitude of physicians, nurses, and pharmacists. So sensitive is the
medical community to deviation on this matter that a leading journal published an
article entitled “Diagnosis and management of patient noncompliance” which sug-.
gested that patient reluctance to follow doctors’ orders be viewed as if it were a dis
ease (33). This attitude is curious, to say the least, given the long list of crippling and
killing drugs which have been pushed upon unprotesting victims. This ever-growing
list includes, but is not limited to, thorium dioxide (34, 35), chloramphenicol (36),
DES (13), MER-29 (19), and thalidomide (37). An intravenous preparation of vitamin
E, which is apparently responsible for numerous neonatal deaths, is one of the newest
additions (38).
The Social Side Effects of Drugs Are Not Fully Appreciated
A product of our highly industrialized society is alienation. Ritualistic drug inges
tion to escape the pain of alienation legitimizes the pain, diminishes our ability to deal
with life's problems and denies the healing power of our body. The phenomenon of
social iatrogenesis is developed in the work of Illich (31).
The Suffering Caused by Drug Reactions Is Not Fully Appreciated
Expectedly patients, who are usually ignorant of the toxic potential of the drugs
they are given, do not appreciate the misery caused by serious reactions until they ex
perience them. Physicians who time and again see people who have been devastated by
drug toxicity (“the acute leukemia secondary to chemotherapy in room 1" or the
“exfoliative dermatitis after antibiotics in room 2") are often unaware or unwilling to
be aware that these persons are suffering because to do so would bring into focus some
painful questions about indiscriminate drug use.
Table 1
Principles of irrational drug therapy
1.
2.
Double-blind studies are informative but not as useful as your own clinical experi
ence.
3.
Stay on the cutting edge of medicine; always choose new and exciting drug treat
ments in preference to mundane, extensively used therapies.
4.
The best source of information on the side effects of drugs is your professional sales
representative.
5.
If you have never encountered a toxicity it probably doesn't exist. (Examples:
Aplastic anemia and chloramphenicol and cancer and thorotrast).
6.
Choose what drug to use on the basis of which manufacturer gives you the best
gifts.
7.
People who do not comply with prescribed drug treatment regimens are contempt
ible wierdos.
Patients Share Wish Physicians rhe Same Unhealthy Attitudes Towards Drugs
Physicians are aware that many or most of their patients arrive with the expectation
that they are going to receive a prescription and would be dissatisfied if they were
No discomfort is so trivial that it does not warrant drug treatment.
360
Principles of Irrational Drug Therapy / 361
Vance and Millington
CONCLUSIONS'
Brockcwbank, V. C. et al. Drug prescribing during pregnancy: a controlled study of Tennessee .
Medicaid recipients Amer J. Obstet. Gynecol 132: 235-244. 1978.
Clark, L C.. and Portier. K. M. Diethyls’.iibesterol and the risk of cancer. Aew Eng. J. McJ.
300. 262-263. 1979.
12.
Bcral. V., and Colwell. L. Randomised trial of high doses of stilbesterol and ethisterone in
pregnancy, long-term follow up of mothers. Brit. J Med 281. 1098-1 101.1980.
13.
Brackbill. Y., and Berendes, H. W. Dangers of diethylstilbesterol. review of a 1953 paper
Lancet 2; 520, 1978.
14.
Karch. 1- E., et al Adverse drug reactions: a matter of opinion. Clin. Phsrmac. Ther. 19:
489-492. 1976.
15.
Lasagna. L. The halcion story: trial by media. Lancet 1: 815-816. 1980.
16.
Crompton. D. O. Medical ethics and hospital acquired disease. lancet 2: 146.1978.
17.
Anon Ticrynafen recalled. F.D.A. Bulletin 10(1): 3-4, 1980.
18.
The Bad Drug. Sixty Minutes,C.B.S. Television. February 8. 1981.
19.
Mintz, M. By Prescription Only. Beacon Press. Boston, 1966.
20.
Anon. T.D.A. claims Lilly knew of deaths (Washington Post Service). Salt Lake City Tribune.
December 4, J 982.
21. U.S. Task Force on Prescription Drugs. The Drug Makers and Drug Distributors. U.S. Govern
ment Printing Office, Washington. DC, 1968.-22.
Silverman. M.. and Lee, P. Pills. Profits and Politics. University of California Press. Berkeley,
California, 1974.
23.
Avorn.J., Chen, M., and Hartley, R. Scientific versus commercial sources of influence on pre
scribing behavior of physicians. Amer. J. Med. 73: 4-8,1977.
24.
Smith, M. C. Drug product advertising and prescribing. Amer. J. Hosp. Pharm. 34: ]208-1224,
1977.
25.
Subcommittee on Monopoly, Select Committee on Small Business (U.S. Senate). Part 6.
pp. 2421-2517. 1968.
26.
Anon. The peculiar success of chloromycetm. Consumer Reports (October): 616-619,1970.
27.
Console, D. Subcommittee on Monopoly, Select Committee on Small Business (U.S. Senate).
Part 2.1969.
28.
Zelino, R. N., and Gagnon, J. P. The effect of drug price information on physician prescribing
patterns. Drug Intell. din. Pharm. 13: 156-159.1979.
29.
Anon. Drug Topics Red Book. Medical Economics, Oradell. New Jersey, 1983.
30.
Britton, H. L., Schwinghaumer, T. L.. and Romano, M. J. Cost containment through restric
tions of cephalosporins. Amer. J. Hosp. Pharm. 38: 1897-1900. 1981.
31. lllich, I. Medical Nemesis: The Expropiation of Health. Random House. New York. 1976.
32.
Sartwell, P. E. Iatrogenic disease: An epidemiologic perspective. Ink J. Health Ser. 4: 89-93.
10.
11.
These are not just hypothetical constructs of problems that might happen.
Tragedies have already occurred because these factors have not been recognized
in the past. American physicians persisted in the use of thorium dioxide for many
years in spite of warnings that the drug was radioactive and in spite of the fact that
it was banned in other countries (33, 34). DES was used in spite of a well controlled
study demonstrating its inefficacy (13). Its supporters, ignoring the fact that many
women with high-risk pregnancies have safe deliveries and healthy babies without
medication, believed that DES was effective because they had observed (“in my
clinical experience”) that some women did well while taking the drug. And in the
case of chloramphenicol some prescribers apparently believed that the drug did not
cause aplastic anemia simply because the drug company told them so. It is clear
that the Principles of Irrational Drug Therapy (Table 1) have been.widely adhered
to in the past.
We recognized that many experts do not agree that drugs are overused in medi
cine (39, 40) but we find their arguments unconvincing. We also realize that the
present overview dealt primarily with North American experiences. However, excessive
drug usage is likely a universal phenomenon. Il is of particular importance to de
veloping countries where multinational drug companies display greater irresponsibility
promoting drugs (41-44) and a larger proportion of inadequate health care monies
is spent on drugs (42). In addition to knowingly exporting dangerous drugs, multi
national pharmaceutical companies have collected excessive payments on drugs sold
to developing countries (44, 45). Developing countries should be aware that along with
the importation of medical technology they receive indoctrination with prevailing
medical attitudes, one of which is an unhealthy reliance upon ritualistic drug inges
tion. Rational drug use can be achieved only when it is widely appreciated that the
use of drugs in medicine is a social process that is under the control of a number
of forces, only one of which is the desire to better health care by reasoned pharma
cologic intervention.
REFERENCES
Simmons, H. E-. and Stolley, P. D. This is medical progress? J.A.M^A. 227: 1023-1028,
1974.
Finland, M. Emergence of antibiotic resistance in hospitals. Rev. Infect. Dis. 1: 4-21,
1979.
3.
Miller, R. R. Propoxyphene: a review.Xmer. J. Hosp. Pharm. 34: 414-423, 1977.
4.
Anon. Top 200 drugs. Pharmacy Times (April): 35-41,1974.
5.
Anon. Fatalities due to propoxyphene. F.D.A. Bulletin 9(1): 2, 1979.
6.
Wolfe, S. M., and Coley, C. M. Pills That Don't Work. Farrar, Strauss, and Giroux Publishers.
New York. 1981.
7.
Kripke, D. Why we need a tax on sleeping pills. South. Med. J. 76: 632-636, 1983.
8.
Moerman. D. E. Placebo effect in the treatment of ulcer disease. Med. Anthropol. Quart.
14(4): 19.1983.
9.
Brinton. L. A. et aL Menopausal estrogen use and risk of breast cancer. Cancer 47: 2517-2522,
1981.
1.
2.
Gillum, R., and Barsky, A. Diagnosis and management of patient noncompliance. J.A.M.A.
228: 1563-1567, 1974.
DaMotta, L. C., da Silva Horta, J., and Tavares, N. J. Prospective epidemiologic study of thorotrast exposed patients in Portugal. Environ. Res. 18: 152-172. 1979.
35.
Van Kaick, G. L, Lieberman, D., and Lorenz, D. Recent results of the German thorotrast
study. Health Phys. 44(Suppl. 1): 299-306.1983.
36.
Best, W. R. Chloramphenicol-associated blood dyscrasias. J.A.M.A. 201: 181-188.1967.
37.
Tabssig, H. B. The evils of camouflage as illustrated by thalidomide. New Eng. J. Med. 269:
92-94,1972.
38.
Williams. B. A. F.D.A. made *wrong *decision on sale of vitamin E drug. St. Petersburg Times.
May 5,1984 (Associated Press).
39.
Rickels,K. Are benZodiazepinesoverused and abused? Br.J. Qin. Pharmac. 11: 815-835,1983.
40.
Morgan. J. P. The politicsof medication. In Controversies in Therapeutics, edited by L. Lasagna.
W. B. Saunders, Philadelphia, 1980.
41. Norris, R. Pills. Pesticides and Profits: The International Trade in Toxic Substances. North
River Press. New York, 1982.
42. Yudkin, J. S, The economics of pharmaceutical supply in Tanzania. Int. J. Health Serv. 10:
455-471. 1980.
43. Ledogar, R. J. Hungry for Profits: U.S Food and Drug Multinationals in Latin America.
IDOC/North America, New York. 1975.
44. Glucksberg. J., and Singer. J. The multinational drug companies and Zaire: their adverse effect
on cost and availability of essential drugs. Ink J. Health Serv. 12: 381-387, 198245. Lernoux. P. Cry of the People. Doubleday and Company. Garden City, New York. 1980.
33.
34.
T7£-i ■
Table 1. Diagnostics.
1.
A 32 year old woman,
a childless divorcee attended the
hospital asking for treatment for 'mitral valve prolapse1 (MVP)
which was causing her severe chest pain.
On clinical examina
tion,
she was found to be normal.
She then showed a newspaper
article on MVP in which, she had underlined all the symptoms that
tallied with that of hers.
She wanted tests including echo scan
as advised in the article.
They were done and turned out to be
normal.
Then she said "You doctors do not know how to diagnose
the disease, I know I have MVP". She showed a newsletter on a new
cardiologist
in town and asked "he seems good - shall I consult
him?"
[Copy of the newsletter is enclosed],
(For discussion:
Psychological problems manifesting as diseases,
power of printed
messages, can doctors and hospitals advertise?)
2.
A 70 year old man,
a rich farm land owner had pain of upper
abdomen for 12 hours.
"Heart problem" had been predicted by an
astro-palmist one year ago.
So he consulted a heart specialist
for opinion.
On clinical examination,
he was normal.
However,
ECG showed minor changes and he was advised further consultation
at a corporate hospital in Madras.
There he was put on 24 hour
ECG recording, in addition to other tests like X-rays, echo scan,
blood tests etc.
A computerised exercise ECG was done.
All
these were normal.
He was sent back home but his pain worsened
despite medicines for heart.
On the fourth day,
he became
moribund and was taken to a teaching hospital.
General surgeons
diagnosed perforated peptic ulcer with shock.
He died one hour
later.
(For discussion: Danger of lateral entry into health care
system, blind belief in predictions by astrologers etc.)
3.
A 48 year old university professor has severe head ache in
the evenings for one week - apparently related to a stressful
situation.
Past history of similar episodes present for many
years since student days.
His friend had died of brain cancer
six weeks ago.
So he wants to rule out brain cancer and asks for
a C.T.
scan.
(For discussion: How do lay people get the idea
that C.T. scan rules out brain cancer? Is such faith justified?)
4.
A 47 year old statistician had a proven peptic ulcer and was
on repeated courses of medicine over four years.
The pain
shifted to right side after recent treatment.
Some friends sug
gested liver disease.
He got a physician's advice.
After an
ultrasound scan and blood test, "fatty liver” was diagnosed.
The
patient was obese and was advised weight reduction.
He got two
more scans repeated at two other centers.
One reported "four
gall stones likely", and the other reported "irregular gall blad
On this,
he became
der wall - cancer cannot be excluded".
depressed,
anxious,
miserable and did not know what to do.
He
was not willing for any surgical option but wanted cancer to be
ruled out.
He consulted at least ten different doctors in three
1
weeks'
time before returning to the personal physician.
(For
discussion:
burden of diagnostic uncertainty - can it be passed
on to a patient in the name of consumer empowerment?
Problem of
doctor shopping, is there a need for a personal physician?)
5.
Shocked by the news of some innocent brides contracting HIV
(virus causing AIDS) from their husbands after marriage,
a sug
gestion was made by a group of senior citizens to enforce compul
sory HIV testing of all prospective grooms before marriage.
As
suming HIV positivity of 1:25000 of general population in South
India,
what are the consequences and the feasibility of taking
such a step?
(Hints: ELISA test does not miss a HIV positive
specimen, but gives false positivity of about 4%.
Cost per test
is Rs.60.
Western Blot,
the confirmatory test costs about
Rs.200).
d, 3
.L
(COPY OF NEWSLETTER - NAMES CHANGED TO PRESERVE CONFIDENTIALITY)
Dear Coi1eagues/Investors/Friend,
CUREALL CARDIAC CENTRE (CCC) with its unrelenting enthusiasm
to extend health care
facilities,
now proudly
introduces ,the
Department of Cardiology, headed by Dr. Irudayanathan,
a unique,
invasive and non-invasive
consultant Cardiologist of special
calibre.
Dr. Irudayanathan,
a qualified DM Cardiologist,
knows much
more
than what his
stethoscope can do for him,
can read ECG
beyond the trace,
can interpret the stress system and the Holter
with accuracy and can extract more details from the Colour Dop
pler beyond its potential.
As you can see,
even his name shows
that: lie is l>nrn to care for the heart
and
to master all
Car<liologic.il problems.
Dr.
Irudayanathan,
the
first
recipient of the Fellowship
award from the Department of Cardiology,
Edward George Medical
College,
Bangalore,
after having worked in different centres in
1 ndia for nearly a decade, lias gained enormous experience and ac
quired vast knowledge by travelling across the world.
His visits
to Massachusettes - United States,
Edinburgh United Kingdom,
Melbourne - Australia,
Paris etc.
have helped him to master his
I ix hniques in Bal loon Valvuloplasty, Atrial Septostomy, Pacemaker
implant.il ion,
Coronary angiography and PTCA (PERCUTANEOUS TRANS
LUMINAL CORONARY ANGIOPLASTY).
Ho bad hands-on training in in
vasive Cardiology at TH IRU VAI. LUVAR
INSTITUTE OF CARDIOLOGY,
MADRAS, TAMILNADU.
Being son of the soil, his care to the patients of Tamilnadu
Is extraordinary.
His personal.attention is such that he praqtJ^-_
rally lives with every single patient in the hospital which makes
the recovery faster.
Such a person is, needless to say, will be
.in asset to every heart patient and of course to CCC hospitals
too.
With the rich experience of Dr.
Irudayanathan,
coupled
with most modern high tech cardiac equipments,
we should be able
to provide the best possible service.
State-of-the-art equipments,
affordable costs,
comfortable
slay,
excellent nursing service,
competent and popular experts,
proper administration and symbiotic growth are a few characteris
tics of CCC hospitals.
Please visit and appreciate
THE DIFFERENCE OF CCC HOSPITALS
for unmatched health care.
MANAGING DIRECTOR
5.
(a) A 15 year old girl with one day fever of 102 degrees and
body ache, vomited twice.
On consultation,
the physician diag
nosed viral
fever and ordered tests to rule out malaria and
typhoid.
Parents wants their only child to be cured without
wasting time.
She was given Ciprofloxacin and anti-vomiting
drugs with vitamins and drugs for fever.
The problem persisted
and on the third day,
they consulted gastroenterologist. He did
an endoscopy (Cost: Rs.1000) and ruled out any serious problems
in the stomach.
He gave two drugs for vomiting and brain tonic
for h£r nervous weakness.
The child recovered on the seventh
day.
(b)
A domestic servant took her 15 year old son to a
primary health centre with similar complaints as
(a).
Viral
fever was diagnosed and paracetamol was given to control fever
and body ache.
The mother demanded an i.v.
drip or atleast an
injection to cure her only surviving son.
She was scolded and
sent out for creating disturbance. On the way back,
she entered
a retail pharmacy and asked the small boy on night duty to give
some strong medicine for fever.
The boy sold her a 'fever set’
which contained two tablets each of antibiotic,
anti-allergic
drug,
steroid and paracetamol.
(For discussion:
Socio-cultural
factors and communication gaps that cause irrational therapy.
Unregulated drug sale in retail shops)
5
Table.2
Macro level drug issues
1.
All bad drugs are to be removed by regulatory bodies and
good
usage
of
drugs to be promoted by education
(Ivan
Dharamsjah).
Do you agree with this?
2.
Please go through the statistics of drug sale at retail
level
in South India highlighting sale by means other than
through doctors' prescriptions.
What is your comment on this?
3.
About 70,000 formulations are on sale in India at a
when free market economy is being embraced by the country.
is the likely effect of unbridled market forces on the
scene? What should be done to curb any adverse influences?
time
What
drug
4.
"Our attitudes towards medicine are shaped by the society in
which we live - with all
its irrationality.
To strive for
rationality may be a grand long term goal".
This was stated by
Mark Nichter in the Australian Workshop on wise use of medicine.
Can you promote prudent use of medicine in a society like India?
If so, how?
5.
"The hand that prescribes is nothing but an extension of the
marketing arm of the drug industry".
Crores of rupees spent on
medical promotion seems to justify this statement.
It is a fact
that the only continuing education received by practising doctors
especially in rural areas is through
detailmen striving to
promote their products. Suggest ways and means by which unbiased
information,
communication,
education can be disseminated to
professionals who need them most.
3
Table.3
Micro level issues on therapy
1.
A few small blood banks in Germany were found to cut corners
in testing blood and blood products for HIV contamination.
This
serious offence is being investigated in Germany.
The media
played up this scandal
during October-November 1993 meriting a
cover story on news magazines like Time.
On 14th November,
a
young German got
injured in a road traffic accident and was
bleeding severely due to abdominal
injuries.
In spite of
repeated pleas to accept blood transfusion as a life saving pro
cedure, the young man totally refused to accept "AIDS blood".
He
died next day of continued bleeding.
(For discussion: Media hype
and scare mongering.
Information for education or for nihilism?)
2.
A 55 year old man with diabetes,
high BP and anginal
chest
pain was taking the following drugs: 3 types of anti-diabetic
tablets,
six types of medicines for BP and heart and two
medicines for preventing blood clot,
vitamins and sleeping pills
plus pain killer for headache!
When asked how so many drugs were
prescribed, he showed prescriptions from three different doctors.
(For discussion: Family doctor concept. Why is it fading?)
3.
A 60 years old ex-Bharatanatyam dancer,
160 cms tall and
weighing 87 kgs with osteoarthritis (degenerative joint disease)
of both knees came to consult her 25th doctor in eight years.
She said
"I have tried all pain killers - no use.
Tried Ayurvedha, Siddha, Unani, Homeopathy, Naturopathy, Acupuncture,
Mag
netotherapy,
Pyramid therapy.
Crystal therapy. Gem therapy etc.
All of them work for 1-3 weeks but not longer than that.
Please
advise me on what to do".
When advised to reduce body weight by
25 kgs over two years by strict diet and exercise,
she said "I
cannot even walk without pain,
how can you expect me to do exer
cise and diet?".
The next doctor (26th) suggested experimental
interferon therapy which will cost Rs.25000/- per month.
Unknown to public,
the area manager promoting interferon in
India tells doctors: If you can make a quick study of 10 patients
on
interferon therapy,
we can sponsor you as an Indian Delegate
to a Conference in Germany early next year.
(For discussion:
Consumer's inability to modify life style,
relief in chronic degenerative diseases - care or cure? Indirect
pressure on doctors to use experimental therapy.
Who should bell
the cat - the dancer in this case?)
4.
A diabetic difficult to control
saw the effects of mag
netised water highlighted in a TV program.
Thereafter,
he
stopped all drugs and changed over to magnetised water therapy.
He was admitted in coma two weeks later with blood sugar level of
564 mg% (normal is about 100 mg%).
(For discussion:
Consumer's
freedom to be foolish - who are responsible,
how to inform and
educate in a prudent manner?)
TABLE.1
NUTRITION
Case 1.
At the time of discharge,
every mother from a maternity
hospital is routinely advised to give her newborn the following:
Water between milk feeds
Bonnisan 1/2 tsp once a day (Herbal appetiser)
Liv 52, 5 drops twice a day (about 1£T herbal ingredients)
Vitamin C drops 5- drops once a day
Multivitamin drops- 5 drops once a day
Case 2.
A three month old child had watery motion (4 times) and
vomiting (2 times) in one day.
The child was regularly getting
water in a bottle in between breast feeds and was also being
given gripe water.
The mother was medically advised to stop
breast feeds and switch over to formula feeds.
In addition,
child was put on streptomagma (antibiotic),
pectokab (a bowel
binder) and loperamide
(an antimotility drug).
Loperamide has
been incriminated in many infant deaths in Pakistan & India due
to dilatation and paralysis of the gut ( a serious side effect).
Case 3.
A seven month old infant was exclusively breast fed till 6
months of age and then was put on home based cereal pulse mix
alongwith continued breast feeds.
He developed fever and cough
for 2 days and was taken to a Paediatrician.
Child was
prescribed:
Syrup Amoxycillin (antibiotic) 1 tsp 3 times/day x 4 days
Syrup Protussa (cough syrup) - 1/2 tsp 3 times/day x 4 days
Vit C drops - 5 twice daily
Cerelac infant food
In spite of mother's explanation of home made cereal pulse
mix, she was advised to give a formula weaning food.
Case 4.
A six year old boy, the only child, was brought to a govern
ment hospital by his mother (poor S.E.
status,
her husband died
in an accident and she was given employment on compassionate
grounds).
He had loss of appetite,
cough and fever for 3 days.
He was malnourished weighing 15 Kg. On examination, he was found
to have signs of mild chest respiratory infection (without in
creased respiratory rate and chest retraction). The hospital had
cotrimoxazole,
penicillin tablets and injections, vitamin A
preparation, cough syrups. Blood tests (TLC, DLC) and chest x-ray
were ordered and the mother was advised to buy the following
medicines outside:
1
Tab Ceptalexin Becadexamin cap
Cough Syrup Ped 3
Syrup Elcarim
Entamezole
3
1
1
1
1
daily
daily
tsp x thrice daily
tsp x thrice daily
thrice daily
Case 5.
A two year old child weighing 12 Kg. was brought for loss of
appetite of two months duration.
On examination,
child was ac
tive and energetic and there was no abnormal finding.
Child was
advised
Syrup Bonnisan Syrup Ciplactin
Syrup Mulmin
-
1 tsp x tds
1 tsp x bd
1 tsp x tds
(zinc multivitamin drops)
IMMUNISATION
A prestigious hospital has given repeated advertisements in
dailies and periodicals about the need for vaccination against
Japanese B Encephalitis,
a viral induced brain fever which often
affects children and adults of poor socio-economic status in
specific areas of Tamilnadu,
Karnataka and Andhra Pradesh. _ The
advertisements outline the gravity of the condition and creates a
sort of fright or panic in the minds of the readers who are often
from middle class and rich strata of society where this condition
usually does not occur.
This disease is caused by a virus trans
mitted from pigs or herons to man by field mosquito bites.
The
vaccine to prevent is an imported one and two vaccines should be
given to prevent the disease and they must be given much earlier
to be effective.
It needs to be repeated once in two or three
years if the effectiveness has to be maintained.
(Discuss the relevance and ethics of such advertisements
from medical,
consumer and media points of view and give your
comments and recommendations in the plenary session regarding
similar situations which may be appropriately or inappropriately
highlighted in the media)
GROUP TASK - TABLE.2
A.
(CHECK-LIST)
DISCUSS AMONG YOUR GROUP THE ROLE AND RESPONSIBILITIES OF:
a.
b.
c.
d.
the medical professionals,
the industry,
the media,
and
the consumer beneficiaries.
1.
in the implementation and practice of rational drug therapy
and in the use of essential drugs for common childhood ail
ments .
2.
in the provision of adequate, relevant,
correct and factual
informations to the professionals and consumers regarding
childhood diseases and drugs (health educational, communica
tion and advertisement materials and media reports).
3.
in the implementation and monitoring of ethical
advertisement policies and practices.
B.
IDENTIFY THE EXISTING PROBLEMS.
C.
SUBMIT IN THE PLENARY SESSION SOLUTIONS, RECOMMENDATIONS AND
AN APPROPRIATE PLAN OF ACTION.
The common
sion are:
1.
2.
3.
promotional
childhood problems to be covered in the discus
diarrhoeal disorders
respiratory (chest infections, primary complex)
mental illness.
Enclosed: 3 situations (brief case reports).
3
I.
An eight month old child of a casual labourer with two loose
motions since morning was given an antibacterial agent (nalidixic
acid),
a stool binding agent (pectokab),- antispasmodic and an
timotility drugs (loperamide and diphenoxylate) and antivomiting
agent (metaclopromide).
Child continued to have 3 to 4 loose mo
tions for the next two days and the mother was advised to stop
breast milk and other dietary cereal food and was put on an ar
tificial lactose free commercial formula food.
Child was given
this formula by bottle (lactonyl) and child became progressively
drowsy and the child was also given injection gentamicin (an an
tibiotic with potential kidney damaging side effect).
The child
developed abdominal distension and was referred to this hospital
where within 12 hours the child died.
Before admission,
the
father had already spent Rs.500/- towards the medical expenses.
POINTS TO BE DISCUSSED ARE:
1.
Role and need of antibacterial
agents and antibiotics in
diarrhoea;
its harmful
and undesirable effects when routinely
prescribed (advised for control of loose motions).
2.
The dangers of stopping breast milk.
3.
The need for introduction of commercial lactose free artifi
cial formula.
4.
The use of bottle feeds and its role in causation
rhoeal episodes.
of
diar
5.
Hazards and irrelevance of use of antimotility and antispas
modic drugs sold in the market.
6.
7.
The promotional and advertisement aspects of such agents.
Means to be adopted to educate the public.
II.
A two year old child weighing 12 kg.
was brought for recur
rent episodes of cold and cough,
each episode lasting for 2-4
days.
Each episode was treated with costly antibiotics for 5-7
days and cough and cold medicines,
vitamin C drops
and
paracetamol
(for fever).
The child's father had allergic
problems of the skin.
There was no family history of tuber
culosis.
Child had received BCG immunisation immediately after
birth.
Child was started on isoniazid,
antituberculous drug for
primary complex.
Even after 3 months, the child continued to get
the same episodes as frequently as before.
(DISCUSS WITH YOUR
MEDICAL COLLEAGUES AND OFFER APPROPRIATE SOLUTIONS TO
THE
PROBLEM).
III. A four year old only male child not sitting and walking from
birth with mental
retardation and small head was given costly
brain tonics for the last 3 years without any advise regarding
physiotherapy and prognosis.
Monthly costs worked out to about
Rs.600/-.
There was no apparent benefit.
Then the parents (low
middle class) went to a teaching hospital for advice.
4
Subject: Fw: Medication Recall
Date: Mon, 4 Feb 2002 17:32:08 +0530
From: "Parveen Sikanci’ <parveen@vwebsol.com>
To: "Aditva" <aditva®vwebsol.com>, "Dr. Ravi Narayan" <sochara@vsnl.com>,
"Dr. Sylvan Rego" <syivanrcgo@yahoo.com>, "Dr. Subba Rao" <nikan@vsni.com>,
"sanjiv lewin" <lewin@vsnl.com>
a.
A.ilergy
ol Cold
Count
then at 800-5^8-3708
if you know of anyone
DO
PASS ALONG
ttp: / /www. zeta,gov/caer/arug/inropage/ppa/aeiauit.n cm>
1'0 ALL ON
(t,
Tel ' 3379016
DRUG ACTION FORUM, KARNATAKA
CLINIC APARNA, 1st Main. 4th Cross. Yeswanthpur, Bangalore -560022.
I. <$• cJW /
Date:------------
Ref:
Cka-b 'Y\£.
Ta/^k
•
P (kb 1 ‘ 4-
l-|exd2fk/
f-T’Tu^ cv\
A c C'ff k
Se s
4
F A\jQ/M_CR(5
PcCR-v
Svkf'Tc^e
560^
rbcc^<Xu'\cj
Z}nt-\€
I
Pc(A
3 O
l
Dooo'')
A
OJ.
k Ati \j rACC G
D I'
CXixc^
ntAoV- e &
a
'fdCO w rr\ a r*
c<cctc
G
c.7\ S
'(k\<T.GC-4 ■
> \€GCSSft c/
cj' cks2/\ d
p-m-
'Y'&jl d
pN
Bvd
'bu^p
U^cACj
p>(tc^,
di
cw
.
dccU^e^J-
J.
Hops.
(a5c_
No Cbxa.
I-Vk-Cj
Pob-Cj
dcxfi-
Go^ i'<£j2^rcrt-czr>
l/^AL
<Xo
P^-S'Pmv.
c<
■) o U
ofc^ <■ £ fcuz^> i <^\ ru
c^
£r\hs)s _Ccnw
<^&Cc\ pns-rd
bi'p
my
Pao pL
O
■ Hope.
pbf
Ut?oCp
bo
C\
d^YA Y"e.c-^j fs> cPwp
'
r\4~e^ 20V?i^
z 'pme
“Hv<zi
cb<
7) g.
d'.SLv.bn
p
Pm,
‘S^i'v
*( *>
■(orvpco -! a <d
Vga.
a
Pvp-
'fbJCo )
P ’ 'c /
^"pp1 cd,V/G
C<
cd
be
cccbcke </<j ■
bVaojc
pedke
cmpecbs ■
f~j ^cJUcLxj
£
ci^
DN
Pkc^ .
ycrwi ?
Sbme^dyy
■3-b ^^bfz~<JbAz)di G 2-2-^j
,
3A
A cP’ (C C\y\
l<C^\Yyc4^C\
Ct ^va
£\/c?LVlM^
A-
LiCy
Ka rn a t aka
~~~
FctzZ
CO N? E NTS
o^c$~
J_ rJ T (7_ © <<u_cA-c ovzv
h'V
. D/J-Ug Po Ipry
/T
'D^UCj
Pot/Cy
^SSB^TiAg
Supply
T-
PoR ^AiznAMM
Uit-
A
!
© irons’
9(Z.OCO &c
Patio (Nal
.Dqu^
f
N~
'
1
°v
I7
pc-kca
A N N £x * 0 (2-
/
W \jCj
\- o f2-A T) o f\!
\^^j)e L
A- Nm; 7<.(J A.& T_
o-ki
Cou(T$p
Short
iP/y7i c’iMal
C’Auyu.se;
3
A^N&At>l2E
So MM A^y
0 riOAJ
c Vi A fir
A N N 5 y (J (2.
QS Pl?^&AZ(5<
ANN&AOPt
Cy(20p MA ^^PAc-TOPJ fN^
(3 T H E. P-
J^SUgS
P^ACTlCtJ
pcH2_ 6-(9<A
'-Ok AAT/Oaj
^Cxjocvi Ng
krp-^a/av1-^
g bo a
kJHo k 6^U
tu
(ft
j
g
'PvizvJ .-<- 5?k<-4
p-VO b)
O|_
%X2
^y>a^d<^
[^j\ jv\o^t
Drv^S O^J
p^o,i^e.^
Sc?^°
^.corx^t-c
q pj?
r\ J f
p <2^\
Cbtrcz-v^- '
Lr
be^JLXx
°p
ctj>
"Vo
.
o U
mzgcxig
4-u?
uy\
Av«.
C^rwcpj
boc^Ut
be
t)-
pe^
ghc-^rbe^
CC/\ rxeGAn Cioyy
-N
favx&'Arone
Cao
t)U-<4
cbvgp
St^ppp
'P^C’VH nrxc^C^Go ’
c>u4S(<^
pfo 'J i'd2_G—c(
* Tk.
r*
CUM/3
Y^mJ.
^-fen $
a Cex <jp> c
p bcMi
Q^c-
Hcoig
p -^?
b u. cj rre^ cz~l—
oj.
AVxGtvx
pv e-3<A t pVccnrA
a^_
bz. kappf
^.o
n^f"
y Rrezoc^ ;pfrco
e^p^yo,
-fo -f^
-P
'l
0
b
y
Gl Vc<
.a p G? i Q
VeXocp • S
pe.a pk
Y<2 cc^kv- 5 e-d
tCc^Ota
• A-s
U)Q_
3
s
2
ou^
6ov\A.
VxJHy
(^xgpjr’le—
^
*
GsrxS^^pP'
$
Pouoy
a
P1
X^^exv^.
f^\ A?
kcx>r AYAaCcx^-c^Gx) y
pro c^czctTo^
1Ar_c_ rj
3
C^'J(\V\G2^
[
U-
'n
okW> po&Mr , W
a
/vY
-q^
KdVt^
PC~^G
p^-.bw
VCKAAjH
Me^e,
„
*'^
b
'"'
po Wh ,
s°c'^ }^h_o •
•
Gw\0cP
in
h\'
S Ho ^J2.cL
G t"\ Gc£vje_ct
r<%4
5 Deotc^Lt&e.ck
L'
'tiA
'/Co
L.
3
p
Tb
M-
Tb
'cao'tc
Cor\t
Th t&ns i + o>
rs
oc^d
h') Py
vqJ^v<l
4^2.
:<uy
;s
kcLcJLb-x
'b^.
0=3 M .
"it-e
pvot/e^
^SeotvcA
a
by
S^C=r\d
<T
yy
Iq^cLs
Lo^je^x
Co^sh
Cpc^2-L kj
V do
„ dlKh'! Wccxzx
>v^c^ Fcv^
P'/e.-)ol i
j
hv^
'<rY\^e
c^o
S
C^^nT-tfee
SHJ^-cV
^cnns'-p-ele-v<J
PxJbc
t ^UC^CzyO?~(C
Jra.
3
Stv^ck
bd_
wH<
N^
fcSL
^Wa
J-oU-p
/Le -o/4 Ji.
“$e(g cr e d
ci
,0-
vt
Q^.c\
>\/
| ode—
^e / v> cp
pYDp2<Vc^
pubVrC
d~U?
5
v
c<bc>u^t
^Pp^7
Vao<
',
TLe
(oc^c
4t4n
CcCOGax’
SU^ UM.
-j
s,
be_
Sc^C>S |tk
-p
-fev\c&2zvtu^>
p-t e c^txzJlX tp;
3-pVc
4
C4) p [tco4-r<
•^\C1. k\ Cf
VJ |4"D
Y cX^i4?' l-v j-y
he
'yG.p
Tk
P
p^'o&a ct"
Y
o'cxzk^o
^u,
7
)<x/
•TiO/X
*^tYov^Ut)^+w
U'-’
pK?ce_c^<^
Ph&'-YYYY^
P-^C^-U
fCj
he
<SSv\i2z>
S biJ'-J 'I
t>L dA.;ccvne-4
TLp
S vzp.4 <
%
EJ>/1
jjl CZ ctAO c(
15
Ujs e.
LJ'U
4
4Mjl
pR^y
you
_by
(^
mCvd"
(^ J\J(2^
c<^op/-;^
c(i
a.
i
f RBp 2
d&veJLop
uta^i’zJv'’.
rwf
be
t\
b/
acccrr-pck^^cX
YY^dfCt^od
p^cl^c^
Oyjp^pyK^G
f^/Lvn-^^
+u ^^'+y
St^fe Stco^w .
C,he^c(
S-Rn-xaJtf^
Sbt zxcCc^> (Ly
bei
C^<^ lcJn^>
bc^c d
CX-Jve£_c\
c^
f <A c C e^r>; P) Cl
i<
4
R
z Pi loi
|K v-xJLpa^ce^J z
lA«e^
o-cc^y: bi
Ck^"TLm
\° J
jpb
f Cvi
SPjJM
I '"-^A YTM^t f Cf^s
A
‘^c’
^>e
c\
(>b Cfc-f S
iKJe«-o^ LeStfe^ i~°
lX
t'V'^z'^A,
|T“
Sh.Ov'-fbzA
"/Ka<
d l/CvtTp^G
-DooPci s
Hjcxa,
cCi L^-^p fax'
'W^e.
Cv^v
"Mm
iX
?JL!L
I C-'vJ'bl CblW
Ca^AS
dc^s
>
TT-G-Q
'Y£'->V$ 4c< vaj
C^xtlnc^
OTM-^
P lc^c~x ajz^S
I"X
pvO^jQ^oyXLCx)
K
<XU 0
Vx-j
S Pa o —L (X
'
U(Gl
''Mm s^-3
V^CMW
--Spar^-tq
'fw.
Gv/ntS
bm? cA
,
cJUQH^^rvfixx
TV^
X) rj-c>
Slcra
1-la-YxUi
-h?
ev^ucctk
Sho-W
p^Xg(^c£oz5Xc
P ovfc> Cv'c-
cUc^
E--C^. C<_ ccct t c\^x
fe-ve^z>
<A/\
'—Y'l
S p j <__x X_
c\d~^cJJ^.
h o ^JL eV
U.
“ h
ta i S IjzcLdlr v~(
be-^M -
SiUcJ^-^ fC^ «
r^p^bU
A
fp^^xr
^C-j
PuJb [< G
dsM j-tf
p^Lvc
-------- e^Tv^s
------ftt-t—^Sz^c-r^
bo^<^
^v1
Lp
p^ct^HXAy
ciH E5S£v<h'U
]&K c^<_
a
ShoJU
^-J-C-^lcSVs >bO<2-r4
SeM.
ts
S/^<te^zcH
dliS^u^ge-
-h
x e^,uA g \ 4 e- ' nv0-
p u~b 1/ C p^SVxnA^t'^
h p' 'b^'
o
Vo^lcdiAp
'P'le.t'A: q-o.
^W3~K/S^
' ^VuL
Uf-/O
•
fesCA^-cJi-
cL|
■it
4<>
^&v6?n
Hc^G-
pc-vA rv^
A"
pV^^rloC^/
," c
S't^fb S>'\~' ^~v<^ >
I'-'F mcfcu^
cs
C^iY^A
TU
KiC^p
k^Jr
i 4 fS
C^q^firX.
crjr\
c^
' nfr e.^ e-
4ve
'TH.^'Ci^rS/v\S
^
*
/fUAefu^c
SkjJU
"TU
cfi^u^-
Sh^JU
< GcJ
Co?t
o|_
TV I"
^/YtHiC
Lfi-PrTCA
o^ecl
tee.
^tec 4
fy p
0"^
b^.
F>c^f^
cv\
cUi/Jjp
O^Ca
lJCJ£'''i
p 11 G2-)
(Jca/+
te-|
pr<vY\CApQ
cSUppk'Cn
S b\ O uJ c<
IV SPJvJA
T.V'SPj-XV
I'A >^2-^i~
F^v\(j2
'Kq
b«_ OrcU.afec( V
b<
rrycJJL^
cd~yF
b)€ c^v^i i"C
.
rko_ Cp9v4 L^b^JlA
cC<U^
. jp?
&Y\o^<^
kv<
'H-e.
lec^/-
'R<L_
bc^Uf-
/&ve^
pi f CQ
ck
Tke-
’
kcvvG
ote^j '
r^J;
p^
pol><y
Y&UtSe o{
e,n^o$e<
DVOct<<(Aj
CM
CWcUd £Z&)\ U.
(^.d-WvL^
•
d<uy\c<^
%
PcxUc^t/
S> W
^VdL'/e^5 «
T\
HxiL^ccC^- r
(AjZiC
S4
J, rxi^-cr^M AT | cr^ £ HOV L D
*2-,
A
fl H C C-^Ji
CD''
I-) O
flAVL CcUl
fl
bro He
R
I
g
Pc^-Q^J- j
T~1-j2. s^-p -7
<^/0L~\
|^Ovn°^\'c^
3
SuMM/jAy
4-crigyx/
i\){-|c2 ks S e%zAcx_i
dk. i^j-^
c?j-»C>v~p q
Wp^A
kssc^vxH"cJ
Dvi^
J >nn plp-tv-o-t'
*
~S
-
k foe
CL<£eJpk-^
H-C-z SeccYA^^--j
t^LL
IP^p, >-&X
(TLzd
S-J)L
Lrtf
"fo (r? Sic~G pr>3_£^o| "f<i
-n^ettci^e k
&
<xct<’pkJt
bs
-H
^c7
LO^Ic^ 5
Ph C Do of-Cr 5
VCw< OT^A
eP L
'D-jiaC;
4-
€-v^g^
cxArCcx^
pR-dl,
C^CA^^k-ve-,
he^dfr^At Q^
A r-AA "hh_
1^1 Vk^
Cm
Pt'oCCAxy?
■>' 6- ^y-uve.. krOr^'j
‘5pZCcJ~-)t £_^
A
^>=ofc«-J
"H-
RR
CH t
dhd^<.
-S
l$
Se.c&n&.c^ Co^j> ^-~T-e^~^-o^
(^\
-|o
2^w>
£ Sf&v^f fcX 3?/'
6/>
W A- <3
'Lssc
7
!(■ i n ctad^
P? ed-ry'
M^n<A^<J2- cWy
<^pe^.cc/;.
I— c^qJSx^
p->c/~^;y
<^J
Yeoicjff <ztaZ
TClhe^ JSSaeo
Ms dU-Cc-k'''!M
(TO’, }-ctf ; v^j
Or^+-
JDi"5
■7000,^
p,
c^C^JQ^
Sl\/\ v I L{ O\ n O’
G
A-P
Or
. Tackling Drugs to Build a Better Britain
http://www.officiaI-documcnts.co.Uk/dociIment/cm39/3945/3945.h
I
Tackling Drugs
to Build a
Better Britain
The Government's Ten-Year Strategy
for Tackling Drugs Misuse
Presented to Parliament by
the President ofthe Council
by Command of Her Majesty, April 1998
Contents
A Personal Statement from the Prime Minister
The Government's Ten-Year Strategy for Tackling Prues
The Government's Anti-Drugs Strategy: Outline
Rcpoit ol The UK Anti-Drugs Coordin.nor - Introduction
The Drugs Problem: Where We .Are Now
The I nderlv ing Principles of The Strategy
Aims:
Young People - To Help Young People Resist Drug Misuse in Order to
Achieve Their Full Potential in Society
(ii) Communities - To Protect our Communities from Drug-Related
Anti-Social and Criminal Behaviour
(i)
Treatment - To Enable People With Drug Problems to Overcome them and
Live Healthy and Crime-free Lives
(iv) Availability - To Stifle the Availability of Illegal Drugs on our Streets
(iii)
Resourcing and Managing the Work
Previous
1 of I
j
13/05/98 11:1
http://www.official-docunicnts.co.uk/docunienl/cin39/3945/stateinnt.ht
Tackling Drugs to Build a Better Britain
A Personal Statement from the Prime Minister
Cm 3945
A Personal Statement from the Prime Minister
10 DOWNING STREET
LONDON SW1A2AA
The Prime Minister
This government was elected on a promise of change. A promise to create a new and
modem Britain for the 21st century. That is what we pledged to do. And we are
delivering.
Step by step that change is happening and Britain is becoming a better place to live
in. But it could be so much better if we could break once and for all the vicious cycle
of drugs and crime which wrecks lives and threatens communities.
The fight against drugs should be part of a wider range of policies to renew our
communities and ensure decent opportunities are available to all.
We are tackling inequalities through the largest ever programme to get people off
benefit and into work and a series of reforms in the welfare state, education, health,
criminal justice and the economy.
But that is not enough. I am determined to tackle the drugs problem. That is why 1
appointed Keith Hellawell as the first ever UK Anti-Drugs Coordinator to put
together a comprehensive strategy, coming at the problem afresh.
This strategy is an important step forward in developing a cooperative approach. But
the fight is not just for the Government. It is for teachers, parents, community groups,
those working in the field and everyone who cares about the future of our society.
We owe it to our children to come up with a truly imaginative solution and create the
better Britain they deserve.
Tony Blair
H'e welcome your comments on this site.
I Of 1
Prepared 27 April 1998
5/13/98 11.07 A
Tackling Drugs to Build a Better Britain
Cm 3945
http://www.official-documcnts.co.uk/document/cm39/3945/strategy.ht
The Government's Ten-Year Strategy for Tackling Drugs
The Government's Ten-Year Strategy for Tackling
Drugs
Ann Taylor
John Prescott
Gordon Brown
Robin Cook
Jack Straw
David Blunkett
Donald Dewar
Frank Dobson
Mo Mowlam
Ron Davies
The Problem
Drugs are a very serious problem in the UK. No one has any illusions about that.
Illegal drugs are now more widely available than ever before and children are
increasingly exposed to them. Drugs are a threat to health, a threat on the streets and
a serious threat to communities because of drug-related crime.
Some progress has been made. The last Government's strategy for England "Tackling
Drugs Together" was an important step in the right direction. It has been
implemented with some success. For the first time, Drug Action Teams set up
partnerships to tackle the problem. We will build on that valuable work. But a fresh
long-term approach is now needed.
Vision
There are no easy answers. To really make a difference in tackling drugs, goals must
be long term. Our new vision is to create a healthy and confident society,
increasingly free from the harm caused by the misuse of drugs. Our approach
combines firm enforcement with prevention.
Drug problems do not occur in isolation. They are often tied in with other social
problems. The Government is tackling inequalities through the largest ever
programme to get people off benefit and into work and a series of reforms in the
welfare state, education, health, criminal justice and the economy. And a new Social
Exclusion Unit is looking at many of the problems often associated with drug taking.
The Government will promote action against drugs that makes substantial progress
over the long term. Action will be concentrated in areas of greatest need and risk. All
drugs are harmful and enforcement against all illegal substances will continue. And
we will focus on those that cause the greatest damage, including heroin and cocaine.
Partnership is the key to the new approach, building on the good work that has
already been done. This strategy is based on an extensive review by the UK
Anti-Drugs Coordinator, Keith Hellawell and his Deputy, Mike Trace. They analysed
all the available evidence and together consulted over'2,000 people and
organisations.
The strategy has four elements:
Young People - to help young people resist drug misuse in order to achieve their full
1 of3
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.official-docuinents.co.uk/docuinent/cm39/3945/stratcgy.ht
potential in society;
Communities - to protect our communities from drug-related anti-social and
criminal behaviour;
Treatment - to enable people with drug problems to overcome them and live healthy
and crime-free lives;
Availability' - to stifle the availability of illegal drugs on our streets.
This is a framework for designing and implementing policies to tackle drugs. It is
just the beginning of a long-term strategy.
In the first year of the strategy, clear, consistent and rigorous targets will be set to
help achieve our aims. The performance of the Government and its agencies
therefore will be readily measurable against these targets. And the UK Anti-Drugs
Coordinator will publish an annual report to check progress.
Partnership
Because of the complexity of the problem, partnership really is essential at every
level. At government level, the work will be led by the Cabinet Sub-Committee on
Drug Misuse chaired by Ann Taylor and by other groups chaired by Keith Hellawell
and his Deputy Mike Trace.
These will bring together key players in the field from the statutory, voluntary and
private sectors and others with an interest. They will work closely with the local
partnerships set up by Drug Action Teams. The Drug Action Teams are the critical
link in the chain, ensuring that this strategy is translated into concrete action. To
assist in that, detailed guidance notes are being issued to those working in the field
putting this strategy into practice.
Resources
In central and local government alone, well over £1 billion a year is spent on tackling
the drugs problem. And yet the number of addicts is going up and availability and
drug-related crime are on the increase. We need to improve the efficiency and
coordination of anti-drugs work. And eventually, we hope to achieve better results. If
we invest wisely now, there is a real chance of breaking the cycle of drugs and crime
which wrecks lives and threatens communities. Along with the obvious benefits of
creating a healthier society, there could also be significant savings through big
reductions in crime and health risks.
To achieve that, all government departments have committed themselves to the
principles guiding the allocation of resources described in Keith Ilellawell’s report.
There will be a progressive shift away from reactive expenditure, dealing with the
consequences of drug misuse, to positive investment in helping prevent them ever
arising. The Coordinator's report takes into account work currently being done on the
comprehensive spending review of drugs-related spending which will be completed
later this year. And for the first time, a proportion of assets seized from drug barons
will be channelled back into anti-drug programmes to help those who have suffered
at their hands and on whose misfortune they have prospered. The Government is
considering how this can best be achieved. More details of these considerations will
be issued later this year.
The Way Ahead
2 of3
5/13/98 I 1:08 A
' Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/document/cm39/3945/stratcgyJit
The strategy is a challenging work programme to which all relevant agencies will
need to respond. Work must be properly coordinated. The Government will make
clear what it expects from its key agencies with an interest - police forces and
authorities, probation committees, prison establishments, health authorities, local
authorities (including Directors of Education and Social Services), HM Customs and
Excise, the National Crime Squad and the National Criminal Intelligence Service.
Similarly, with Drug Action Teams.
Although the strategy focuses mainly on England, it is relevant to Scotland, Wales
and Northern Ireland and it highlights our international responsibilities. We will
make sure it gets the widest circulation. And our international effort remains vitally
important, working with our European and other partners, to stem the flow of illegal
drugs into the UK.
The legal framework provided by the Misuse of Drugs Act 1971 and other legislation
provides some of the tools needed to crack down on the availability of drugs and
reduce the misery they cause. But enforcement alone will never be enough. We need
to ensure that young people have all the information they need to make informed
decisions about drugs; that we follow up tough words with decisive action; and that
there really is proper partnership to tackle the problem. If we can make our vision a
reality, we have the chance to make Britain a better place. This new strategy presents
a real opportunity to do that.
li'e welcome your comments on th is site.
3 of 3
Prepared 27 April 1998
5/13/98 11:08 A
http://www.oftkial-docuincnts.co.uk/document/cm39/3945/outline.lit
Tackling Drugs to Build a Better Britain
The Government's Anti-Drugs Strategy: Outline
Cm 3945
The Government's Anti-Drugs Strategy: Outline
VHJon -a^eatthy-and confident- .
sodety.lncreaslngty.tree-fromthe
Mtm caused tootjr.cltUtns-by-themisuse cd-dnigii
; Policy co wettjre to-worK,-sodal •
exdu si co jt cut h ■j ust I ce ,-p ubl Io h Mi I hz
community safety;.edu.olloft/locai
democracy 4
1
T
Alm ’.tobeipyoung people-<
resirf drug rricusc to order-toadilere Ihetr-fun potentlal-lmsociety 4.
'•
Aimi.MO «M W0 peopte-xith;
.drug prctie ere tooverccmothemand-lrve hcolthyvid■ . crime-free llvaid'
Alm- toproud our
communities from t4 •
dry g-relatedanH-sodolMd
: criminal (xhewlourf
;Xin Most'll le-thiavaibbility.
ibf-lllegat drugs oa oursUceU.
Adbri'ty;-pertQrm3nc« indicators and targets; fcsoarch and hforrrollon<evaluaUcr>, ■adjustments and updating!.
tv art though 8
Nations ocpnisationSM'ith adregsremil-committcd-lo '
: pultlng-the.vlsfonandalms. ,
Into practice L. ■
■
. Central GcMrnmenl as-eftaolef-Md^^cocrdlnatoGMiol$tera: UK Aritl-Orugs Cocrdinatcr-aod Dcpwty;UKADCU, Departments and Ager>des;Stralrjlo
'
Steedng.Croupand-StrategySupportfiroupaX'
Local organ isatlcnswrlha dcugseJ
remit-cocrrrutted topulling-the y v doo and aims Int o practice-1 .
tool prug-Actlofv-Tearm,\rofWngcolaboratrr ely-and-wiUi. local*^
network
Prlvale-scctoc-YOlufiUry.
sector agendas; media 4.
PrfrdteMdor.-Yoiuntary sector,.
media,-common iies;-pafenl$,you ngpeople!.
Departmental expenditure eet-b-Une with objectives; CAIt-wrthin a
framework- sei -cwt-ty-thcCom pcehensive-Sptnding-Rt'rirw;-additionalrewjrcealhrcughrhatlonaVreglonai and locW-portnerahlpel
Mortfoiodl>yj
i
Cocrdlfw»to^tAnriuai-RrportandPton-of-AdJcn;-DAT-r»pcrl» to- Coordinator,
lfitfi/l4wrag«ncJw'-p»rfonronclnionltoclr>9,'-ln4ep4ntfioi-
Previous^
JF? welcome your comments on this site.
1 Of 1
Prepared 27 April 1998
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
Cm 3945
http://www.ofTicial-documents.co.uk/document/cm39/3945/ad-intro.lit
Report of The UK Anti-Drugs Coordinator - Introduction
Report of The UK Anti-Drugs Coordinator
Introduction
I share the Government's vision for the future - a healthy and confident society
increasingly free from the harm caused by the misuse of drugs.
To achieve this we must all combine to:
. address the social issues which contribute to young people, in particular,
becoming attracted to drug taking;
. bolster and support those who wish to help and guide them;
• provide sufficient services to treat those who have drugs problems;
• concentrate our international and law enforcement effort on those who
produce, process, distribute and sell them;
. develop a criminal justice system which deals effectively both with those who
appear before it for greed and for need.
The focus of this document is on illegal drugs as determined by the Misuse of Drugs
Act 1971. However it is clear to me that legally obtainable substances such as
alcohol, tobacco, solvents and prescribed drugs used without medical control have
close links with illegal drugs problems and should therefore be addressed, as
appropriate, within the strategy.
Drug misuse in the late 1990s poses many problems for our society. Research
suggests that there are all kinds of reasons for misuse; that key factors include
unemployment, low self esteem, educational failure, boredom and physical,
psychological or family problems. Even where the cause relates more to
experimentation or enjoyment, or to a shift from alcohol or tobacco, the fact is that
overtly mind-altering substances have greater pull than other activities. And many
people misuse drugs because they don't have the opportunity to lead fulfilling lives.
The consequences of drug activity include serious and organised crime; wide-spread
acquisitive crime for drug addicts funding their habit; violence generated by drug
intoxication and dealers; and hidden social problems - in homes and schools, on the
roads and in the workplace.
The social, economic, psychological, crime and health-related costs are formidable.
The latest Government-funded research suggests that annual costs arising from the
most serious drug misusers alone are well over £4 billion.
Significant health risks are associated with drugs - the more evidence that becomes
available about the risks of, for example, cannabis and ecstasy, the more discredited
the notion that any of the substances currently controlled under the 1971 Act are
harmless.
But there are many misconceptions. All young people do not take drugs; all drug
takers are not addicts; all drugs do not kill; all drug takers do not commit crime;
illegal drugs are not the unique preserve of people from particular social or ethnic
backgrounds.
1 of 3
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www,official-documents. co.uk/docuinent/cin39/3945/ad-intro. hi
The majority of people in this country do not nor have ever taken an illegal
substance; and the majority of those who have are experimenters or casual users. A
majority of illegal drug users do so for so-called "recreational purposes". By far the
minority of illegal drug users - between 100,000 and 200,000 peoplel - become
addicts.'It is this group which causes the greatest problem for society and themselves.
They are responsible for a substantial amount of crime; many are victims of abuse
from drug dealers and pimps; they are often disruptive and make disproportionate
demands on law enforcement, medical, counselling and social services. The response
to this group has so far been patchy. Although individuals and agencies.are working
very hard within their own area, they are trying to achieve progress against
inconsistencies within the operation of the criminal justice system; inadequate
treatment and prescribing facilities; haphazard funding arrangements which have a
bias towards reacting rather than preventing; and a paucity of timely and consistent
information. It is crucial that we learn from the past and adopt a consistent approach
in the future.
I believe that the four aims of helping young people, protecting communities,
enabling those with problems to overcome them and stifling availability of drugs will
allow us all to channel our efforts towards significant 'improvements over time. I
believe that over the next ten years we should be looking to achieve significant
reductions in young people's drug use and drug-related offending; an increase in the
participation of problem drug misusers in treatment programmes;and reductions in
the availability of drugs. In our progress towards these aims it is essential that we
monitor the effectiveness of our individual and collective activities in an objective
way. We need also to set about achieving our corporate and single agency targets on
an annual basis and monitoring our progress in reaching them. Much work will need
to be done within the next twelve months to develop these targets in relation to the
activities outlined in each section of this report.
A
The focus of this first report is on England, but I would expect all other parts of the
UK to reflect on the implications of this strategy for them and report back on relevant
developments by February 1999.
By March 1999:
• all agencies should realign their priorities, resources and operational focus in
line with this White Paper and produce their forward plan;
• all agencies should develop corporate and individual performance targets and
measures;
* national, local, private and voluntary sector funding should be realigned in
support of the plan;
. I will publish my first Annual Report and Plan of Action Against Drugs.
This process will be repeated every year. It will be influenced by experience,
research, evaluation, changes in patterns of drug misuse, successes and failures at
national, corporate and individual level. Every three years, we need to have a
systematic and comprehensive appraisal of the strategy's impact based on
independent evaluations, and adjust the way forward accordingly. The importance of
rigorous evaluation cannot be overstated.
In tackling the drugs problem, we must now shift our emphasis from reacting to the
consequences of drug misuse to tackling its root causes. This should be reflected in
Government financial programmes. The challenge is to protect the young and
vulnerable, offer alternatives to the disaffected, stop those who flout the "rules, and
arrest and imprison those who profit from the drugs trade.
There are a great many talented and committed people working in the field. 1 want to
see them really working together. I want them to be free from obstacles which stop
them doing that effectively now. Action against drugs should be at the heart of
government policy. Working together we can make an impact in schools, colleges,
universities, on the streets, in the workplace and in our homes. There is now a unique
opportunity to invest in the future. We must not squander it.
Keith Hellawell
a
W
Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/docunicnt/cm39/3945/problem.ht
Cm 3945
The Drugs Problem: Where We Are Now
The Drugs Problem: Where We Are Now
"Tackling Drugs Together", published in May 1995, was the first genuinely strategic
response in England to the complexities of the drugs problem. It had cross-Party
support and has been successful in sustaining a coordinated approach to a difficult
issue. The fact that all 88 of the tasks required in that White Paper have been
completed indicates good progress. It remains one of the best and most influential
strategies for effective action against drugs. But in building on its success, we need to
recognise its weaknesses:
• it focused on structures rather than results, with the general public
insufficiently engaged as a consequence;
. it treated drug misuse largely in isolation from other social and environmental
factors;
• it advocated partnership without making sufficient structural and fiscal changes
to support it;
• it was too short-term and did not bring together common research, information
and performance bases.
Alongside "Tackling Drugs Together", there have been other important
developments:
. A strategic review of international drugs activity - with a clear overall
commitment of all the law enforcement, intelligence and diplomatic agencies
to reduce the flow of illicit drugs to the UK.
• Strengthened links between a wide range of national agencies, working
together to achieve collaborative goals on drug prevention/education and
enforcement - an approach which has been confirmed by recent reports from
the statutory Inspectorates on the Police. Probation, Prisons, Education and
Social Services.
. Increased collaboration on resources between the statutory, private and
voluntary sectors - for example, the £2 million drugs Challenge Fund in 1996/7
and 1997/8 respectively has generated a total of over £2.5 million resources
from those sectors.
. The creation and development of Drug Action Teams and their Reference
Groups which has been very encouraging, with substantially greater cohesion
of effort and sharing of resources amongst health and local authorities,
criminal justice agencies and other key players, agreed action plans and better
prioritisation of local needs.
. Community initiatives which have generated a diverse range of projects,
clearly highlighting that local people are best placed to tackle local drugs
problems. Evidence of this has been disseminated, in particular by the Home
Office Drugs Prevention Initiative.
Significant progress too has been made in Scotland, Wales and Northern Ireland:
• in Scotland, the 1994 strategy "Drugs in Scotland: meeting the challenge" has
1 of2
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/dociinieiit/cni39/3945/probleni.lit
been implemented, along with the development of the Scotland Against Drugs
campaign and a Scottish drugs Challenge Fund. The emphasis has been on an
integrated approach to service provision, the development of a national
information base and strong partnership links with the private and voluntary
sectors;
. in Wales, a drug and alcohol strategy "Forward Together" was launched in
1996. The Welsh Drug and Alcohol Unit oversees the strategy, and is
committed to developing a national prevention campaign, action on treatment
and rehabilitation, and guidance for those involved in combatting drug and
alcohol misuse;
. in Northern Ireland, the Central Coordinating Group for Action Against
Drugs was established in 1995 to oversee coherent efforts against drug misuse
within a clearly defined policy statement. The key action areas are education
and prevention, treatment and rehabilitation, law enforcement, information and
research - including a major publicity campaign - and monitoring and
evaluation.
The scale of the problem
Despite this progress, the drugs problem remains formidable. For example:
. record levels of drug seizures reveal the increasing threat of a widening range
of trafficking routes to the UK, against a background of expanding global
production;
. offenders dealt with under the Misuse of Drug Act 1971 are up from 86,000 in
1994 to 95,000 in 1996;
• 48% of 16-24 year olds questioned in 1996 had ever used illegal drugs
compared with 45% in 1994 (and 18% had used in the last month, compared
with 17% in 1994);
• the number of drug misusers attending services was 24,879 in the six month
period ending September 1996, 48% higher than the equivalent period three
years earlier;
. the number of deaths in the UK attributable to the misuse of drugs has risen
from 1,399 in 1993 to 1,805 in 1995.
In addition, more localised trends - particularly the increasing availability and use of
cheap, smokeable heroin - suggest growing exposure and consumption by
increasingly younger people.
' Contents
* . • Next
T
H'e welcome your comments on this site.
2 of 2
-J
Prepared 27 April 1998
5/13/98 I 1:08 A
Taikling Drugs to Build a Better Britain
http://www.official-documents.co.uk/document/cm39/3945/prncpls;hi
Cm 3945
The Underlying Principles of The Strategy
The Underlying Principles of The Strategy
Integration. Drug problems do not occur in isolation. They are often tied in with
other social problems. The Government is tackling inequalities through the
largest-ever programme to get people off benefit and into work and a series of
reforms in the welfare state, education, health, criminal justice and the economy. And
a new Social Exclusion Unit is looking at many of the problems often associated with
drug taking such as school exclusions, truancy, rough sleeping and poor housing. It is
important to remember these connections, and that key results in other areas of
activity, such as general take-up rates for further and higher education and
employment, relate clearly to the development of this strategy.
Evidence. Drug misuse can be a highly-charged subject. Learning about an illicit
activity can be difficult but our strategy must be based on accurate, independent
research, approached in a level-headed, analytical fashion.
Joint Action. Partnership is not an end in itself, and can be an excuse for blurring
responsibilities and inactivity. But the evidence is that joint action - if managed
effectively - has a far greater impact on the complex drugs problem than disparate
activities.
Consistency of Action. While activities must relate to local circumstances and
priorities, drugs misuse is a national problem requiring fairness and consistency in
our response.
Effective Communication. We need to be clear and consistent in the messages we
send to young people and to society D in particular, the importance of reinforcing at
every opportunity that drug-taking can be harmful.
Accountability. Through the Coordinator's Annual Report and Plan of Action
Against Drugs, we can dispassionately and objectively track progress. The structures,
resources and performance mechanisms set out in this report exist solely for that
purpose, so that we can be sure our achievements are real. A special focus will be
given to the four key objectives identified below - one for each aim.
«- Next '®-
We welcome your comments on th is site.
1 of 1
Prepared 27 April 1998
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.ofricial-docuinents.co.uk/docutnent/cni39/3945/aim-l .ht
Cm 3945
Aim i
Aim (i): Young People - To Help Young People Resist
Drug Misuse in Order to Achieve Their Full Potential in
Society
Young people, and those responsible for them, need to be prepared both to resist
drugs and, as necessary, to handle drug-related problems. Information, skills and
support need to be provided in ways which are sensitive to age and circumstances,
and particular efforts need to be made to reach and help those groups at high risk of
developing very serious problems. Prevention should start early, with broad
life-skills approaches at primary school, and built on over time with appropriate
programmes for young people as they grow older via youth work, peer approaches,
training and wider community support. The aim is for approaches to be better
integrated nationally and locally.
Key objective
Reduce proportion of people under 25 reporting use of illegal drugs in the last month
and previous year.
Drugs and young people: the facts
We now know a great deal about the relationship between drugs and young people.
Many never take drugs at all, many who do experiment grow out of it quickly, but a
small hardcore develop very serious problems. In particular:
• drugs misuse is most common amongst people in their teens and early
twenties, but the average age of first drug use is becoming younger;2
• almost half of young people are likely to take drugs at some time in their lives,
but only about one-fifth will become regular misusers, (ie at least once a
month), with a tiny minority of that group taking drugs on a daily basis; 2
. most young people who take drugs do so out of curiosity, boredom, or peer
pressure - and continue misusing drugs through a combination of factors
ranging from enjoyment to physical and psychological dependency;
. cannabis is easily the most commonly-used drug amongst the young, followed
by amphetamines, poppers, LSD and ecstasy2 - while there are some
identifiable groups such as cannabis users , dance drug users and addicts, the
trend is towards more indiscriminate use, based on price and availability;
. there is a very strong correlation between the use of illegal drugs and the use of
volatile substances, tobacco and alcohol amongst young people;
. there is increasingly strong evidence that the earlier a young person starts
taking drugs, the greater the chance that he or she will develop serious drugs
problems over time;
. for early to mid-teenagers, there are strong links between drugs problems,
exclusion or truancy from school, break-up of the family, and initiation into
criminal activity;
1 of3
5/13/98 11:08 A
. Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/document/cni39/3945/aim-l.ht
• for older teenagers and people in their twenties, there are strong links between
drugs problems and unemployment, homelessness, prostitution and other
features of social exclusion;
. whatever other influences affect young people, the role of parents throughout
this process is crucial.
Programme of action
All activity supported by this stategy will:
• inform young people, parents, and those who advise/work with them about the
risks and consequences of drug misuse, linked to other substances - including
alcohol, tobacco and solvents - where appropriate;
. teach young people from the age of five upwards - both in and out of formal
education settings - the skills needed to resist pressure to misuse drugs,
including a more integrated approach to Personal Social and Health Education
in schools, and with particular reference to the forthcoming 1998 DfEE
guidance;
. help make the misuse of drugs less culturally acceptable to young people,
including the use of effective and targeted national and local publicity and
information;
• promote healthy lifestyles and positive activities not involving drugs and other
substance misuse;
.
• ensure that the groups of young people most at risk of developing serious
drugs problems receive appropriate and specific interventions;
• ensure that young people from all backgrounds, whatever their culture, gender
or race, have access to appropriate programmes:
. build on and disseminate good practice in identifying what works best in
prevention and education activity.
Assessment
Performance indicators for each of these activities will be introduced to monitor
achievement and specific targets set for agencies against the following objectives:
. reduce proportion of people under 25 reporting use of illegal drugs in the last
month and previous year - Key Objective;
• increase levels of knowledge of 5-16 year olds about risks and consequences of
drug misuse;
• delay age of first use of illegal drugs;
. reduce exclusions from schools arising from drug-related incidents;
• reduce the number of people under 25 using heroin;
• increase access to information and services for vulnerable groups - including
school excludees, truants, looked after children, young offenders, young
homeless and children of drug-misusing parents.
5/13/98 11:08 A
2 of 3
/3,
Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/document/cm39/3945/aim-l.ht
Research and Information
To support these objectives we will make use of the best available sources of
information and plan as a priority to commission additional research as follows:
. comprehensive surveys of young people (age 5 upwards) and drugs misuse;
• qualitative studies of patterns of misuse of regular young users;
• long-term evaluations of effectiveness of prevention and education
programmes;
• qualitative and long-term assessment of impact on drug misuse of wider social
factors;
• operational summary of effective prevention and education.
ZDrug Misuse Declared in 1996: Key Results from the British Crime Survey" - Ramsy H an Spiller J,
Home Office Research Findings 56 (1997)
ll'e welcome your comments on this site.
of3
Prepared 27 April 1998
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/documcnt/cm39/3945/aim-2.hi
Cm 3945
Aim ii
Aim (ii): Communities - To protect our Communities
from Drug-Related Anti-Social and Criminal Behaviour
Helping drug-misusing offenders to tackle their drug problems and become better
integrated into society has a significant impact on levels of crime. Local partnerships
can work successfully to tackle local drug problems, and to improve the quality of
life for communities.
Key objective
Reduce levels of repeat offending amongst drug misusing offenders.
Drugs and the communities: the facts
Drugs and crime are of concern to all communities, particularly drug possession,
manufacture and trafficking, the involvement of criminal syndicates in the drugs
trade, the acquisitive crime committed by drug misusing offenders to feed their
habits, and the anti-social behaviour and feeling of menace that the drug culture
generates within neighbourhoods. It is very clear that effective enforcement under the
1971 Act remains vital to minimising the availability of drugs and the threats to the
community that the drug culture carries in its wake. The criminal justice system
operates with considerable discretion within this framework but we must guard
against this resulting in inconsistencies. The growing clarity of the relationship
between drugs and crime has highlighted that:
• many police forces estimate that around half of all recorded crime has some
drug related element to it, whether in terms of individual consumption or
supply of drugs, or the consequent impact of it on criminal behaviour;
. a small number of people are responsible for huge numbers of crimes - 664
addicts surveyed committed 70,000 offences over a three month period;!
• latest indications from a random sample of suspected offenders arrested by the
police suggest that over 600/0 of arrestees have traces of illegal drugs in their
urine;!
• emerging evidence suggests that effective and targeted treatment for drug
misusing offenders can have a major impact on reducing subsequent
offending;3
• the general costs to the criminal justice system of drug-related crime are, at a
very conservative estimate, at least £1 billion every' year;!
• community safety partnerships - which target specific drugs problems in the
community - such as disrupting visible markets, drugs in pubs and clubs, drugs
in the workplace and drugs and driving - have great potential where the
approach taken is locally based, properly resourced, consistently delivered and
long-term.
Programme of Action
1 of3
5/13/98 11:08 A
hltp://www.oll'icial-docuincnts.co.uk/docuiuenl/cin39/3lAI5/niin-2,ltt
Tackling Drugs to Build a Better Britain
AU activity supported by this strategy will:
, develop sustained and collaborative treatment for those committing
drug-related crime - including support for the piloting of Drug Treatment and
Testing Orders, promotion of Caution Plus schemes (according to Home
Office and ACPO guidelines) and associated projects within existing
legislation, ensuring that their lessons are spread and implemented as widely as
possible;
. target police resources on the detection of drug-related crime and refer
offenders where appropriate;
. provide visible deterrence and public reassurance through the consistent
punishment of drug dealers and suppliers, and the disruption of their markets;
. ensure community support in achieving a consistent application of the drugs
laws, including compatibility in dealing with low level possession offences
amongst different prosecution agencies;
. energise and involve local communities through collaborative responses to
local drug problems - with imaginative use of existing and planned community
safety/estate action/drug network partnerships - so that positive outcomes,
focused on the drugs and the people that cause most damage and danger, are
achieved;
• increase take-up rate of further education and employment by former addicted
criminals through welfare to work, New Deal and other means;
. tackle drugs in clubs in line with recent Home Office guidance;
• implement drugs in the workplace initiatives in line with Health and Safety
Executive guidance for employers;
• enhance detection and underline the social unacceptability of driving while
influenced by drugs.
Assessment
Performance indicators for each of these activities will be introduced to monitor
achievement and specific targets set for agencies against the following objectives:
. reduce levels of repeat offending amongst drug misusing offenders - Key
Objective;
. increase the number of offenders referred to and entering treatment
programmes as a result of arrest referral schemes, the court process and
post-sentencing provision;
• reduce levels of crime committed to pay for drug misuse;
• ieduce drugs market places that are of particular concern to local communities;
. reduce levels of drug-related absenteeism/dismissals from work;
* facto”6 nUm^erS
road deaths and injuries where drugs are a contributory
Research and Information
2 of 3
5/13/98 I 1:08 A
Tackling Drugs to Build a Better Britain
http://www.official-documents.co.Uk/document/cm39/3945/aim-2:ht
To support these objectives we will make use of the best available sources of
information and plan as a priority to commission additional research as follows:
• long-term evaluations of community safety programmes within high risk
communities;
• further assessment of cost-effective treatment in the criminal justice system;
• practices that have led to sustained reductions in drug-related crime and
community fear; and
studies into the links between drug misuse and absenteeism, and between drugs
and road deaths.
3"National Treatment Outcom Research Study. Summary of the Project, the clients and preliminary
findings" - Gossop M. NTORS (1996)
T'Drug Testing Arrestees, Home Office Research Finding", No 70 - Bennett T. (1998)
^Preliminary Results from Drugs Comprehensive Spending Review.
'-Contents
We welcome your comments on this site.
3 of 3
Prepared 27 April 1998
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.ofncial-documenls.co.uk/docunienl/cm39/3945/tiiin-3.ht
Aim (iii): Treatment - To Enable People With Drug
Problems to Overcome them and Live Healthy and
Crime-free Lives
Many of those with the most serious drugs problems have a range of other problems,
including lack of housing or employment. We will ensure that specific, appropriate
and timely help is provided to those with drug problems and that their needs are
recognised and addressed by wider Government programmes.
Key objective
Increase participation of problem drug misusers, including prisoners, in drug
treatment programmes which have a positive impact on health and crime.
Drug treatment: the facts
There is growing evidence that treatment works. In particular, harm reduction work
over the last 15 years has had a major impact on the rate of HIV and other
drug-related infections. And rehabilitation programmes have shown real gains in
crime reduction. The rate of demand for treatment services amongst seriously
dependent drug misusers shows no sign of abating, and the supply of effective
treatment services is failing to match that demand. In particular:
. the number of addicts has risen steadily - there were 38,000 people notified in
England as drug addicts in 1996, compared with 22,000 in 1992;£
• the total number of seriously problematic drug misusers in this country is
estimated to be between 100,000 and 200,000, many of whom do not seek or
cannot get access to effective services;?
. the scope, accessibility and effectiveness of available treatments are
inconsistent between localities and generally insufficient. There is considerable
insecurity about funding and disparity in provision. Consequently, there is
rarely immediate access for a drug misuser to a treatment programme - given
the urgency of the needs of most drug misusers, this is unacceptable. The
Department of Health report “The Task Force to Review Services for Drug
Misusers" (1996) points a clear way forward for developing effective treatment
provision in this country - as does the Health Advisory Service report on
“Children and Young People - Substance Misuse Services" (1996) with respect
to services to adolescents. The challenge is to put the recommendations of
these two reports firmly into practice;
• the most significant health risks for this group beyond drug dependency are
HIV, hepatitis B and C, and a wide range of psychiatric and psychological
problems. Drug related deaths - proportionately rare but probably
under-reported - are increasing. Injecting, however, appears to be continuing
its fall, with only 2 in 5 addicts now admitting ever injecting;!!
°
. there is increasing evidence of the links between health problems of individual
drug misusers and public health concerns - notably mental health problems.
l of3
5/13/98 11:08 A
lacking Drugs to Build a Better Britain
littp://www.official-documents.co.uk/documcnt/cm39/3945/aim-3. hl
alcohol abuse and tobacco use, and social exclusion.
Programme of Action
All activity supported by this strategy will:
• ensure all problem drug misusers - irrespective of age, gender, race and drug
with which they have a problem - have proper access to support from
appropriate services - including primary care - when needed, providing specific
support services for young people, ethnic minorities, women and their babies;
. provide problem drug misusers with accurate information, advice and practical
help to avoid infections and other health problems related to their misuse;
• support problem drug misusers in reviewing and changing their behaviour
towards more positive lifestyles - linking up where appropriate with
accommodation, education and employment services;
. provide an integrated, effective and efficient response to people with drugs and
mental health problems;
• ensure that prescription of substitute medications (eg methadone) in particular
and dispensing of clinical services in general (including prescribed legal drugs)
are in line with forthcoming Department of Health clinical guidelines;
• improve the range and quality of treatment services provision specifically for
the under 25s, in line with Standing Conference on Drug Abuse guidance;
. ensure that throughcare and aftercare arrangements for drug misusing prisoners
are coherent, focused and linked to community provision;
• develop collaborative, coherent, accessible and cost-effective service provision
through Drug Action Teams.
Assessment
Performance indicators for each of these activities will be introduced to monitor
achievement and specific targets set for agencies against the following objectives:
• increase participation of problem drug misusers, including prisoners, in drug
treatment programmes which have a positive impact on health and crime - Key
Objective;
• increase the proportion of problem drug misusers in contact with drugs
services;
• reduce the proportion of drug misusers who inject, and the proportion of those
sharing injecting equipment over previous three months;
• reduce numbers of drug-related deaths;
• reduce numbers of drug misusers being denied immediate access to appropriate
treatment.
Research and Information
To support these objectives we will make use of the best available sources of
information and plan as a priority to commission additional research as follows:
2 of 3
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.official-docunients.co.uk/docuiiient/cni39/39.l5/aim-3.lit
• the clinical and social care of people with drugs and mental health problems;
. the cost-effectiveness of current treatment and care options;
. the effectiveness of treatment interventions for young people;
. the lessons from the Advisory Council on the Misuse of Drugs study of
drug-related deaths;
. the links between recreational drug misuse (including cannabis) and later
health problems;
• the treatment of stimulant drug dependency.
^Statistics of Drug Addicts Notified to the Home Office, United Kingdom, 1996 - Corkcry JM (1997)
Z"Arrest Referral - Emerging lessons from research" - Edmunds M et al( 1998)
SDrug Misuse Statistics for six months ending September 1996 - Department of Health (1998)
I I'e welcome your comments on this site.
3 of 3
Prepared 2 7 April 1998
5/13/98 11:08 A
Tackling Drugs to Build a Better Britain
http://www.ofTicial-documents.co.uk/document/cm39/3945/aim-4.hl
Cm 3945
Aim iv
Aim (iv): Availability - To stifle the Availability of
Illegal Drugs on our Streets
Constant vigilance is needed to tackle availability where it matters most, close to
home. It is crucial to gain a better understanding of which activities have the most
impact on local availability and to pursue them, improving partnership between
agencies along the way.
Key objective
Reduce access to drugs amongst 5-16 year olds.
The drugs trade: the facts
The drugs trade is an international multi-billion pound industry. A 1997 report by the
UN Drug Control Programme estimates that the industry's turnover amounts to about
8% of total international trade, approximately the same as textiles, oil, gas or world
tourism. The threat is ever present and growing. And, however impressive the
enforcement activity in general, there have been no signs of street level availability
reducing over recent years. The facts are:
• the routes into the UK for heroin and cocaine have become increasingly
complex, but remain primarily, for heroin, the Golden Crescent through
Turkey and the Balkan route and, for cocaine, South America and the
Caribbean - over half of all seizures arrive in the UK via other EU countries;
. the routes for synthetic drugs have been characterised by heavy ecstasy
production in the Netherlands and increasing flows of manufactured drugs
from Eastern Europe;
. the UK is primarily an importer of drugs. Domestic production, although
limited, is increasing.
• proven cases of internal corruption within enforcement agencies are few, but
the threat is real and requires constant vigilance;
• the impact on street level availability of activity against supplies is difficult to
assess and the price of drugs within the UK has generally shown a stable or
downward trend. However, there is a marked difference between the price of
drugs here and in source and transit countries - for example, heroin is sold at
£850 per kg in Pakistan, £7,000 in Turkey, £15,300 in the Netherlands and
£24,000 in the UK, which then translates into £72,000 on our streets. There is
therefore evidence to suggest that effective enforcement is a factor in pushing
up those prices;
. the direct impact of enforcement on short term availability is difficult to
establish. There is, however, Home Office research evidence which suggests
that focused and coordinated activity on local drug markets can make a
significant and sustained impact on availability, reducing supplies, pushing
prices up and reducing the threat of exposure of young people to drugs;
• the drugs trade also includes significant quantities of drugs which have been
5/13/98 11:09 A
1 of3
2-(
Tackling Drugs to Build a Better Britain
http://www.official-docuincnts.co.iik/dociiinent/cin39/39 ‘l5/aiin-4.lit
legally manufactured and then "leaked" on to the illicit market, primarily via
the prescription system.
Programme of Action
All activity supported by this strategy will:
• reduce the acreage of drug crops produced and the amounts processed; control
the illicit supply of chemicals and materials used in production and
manufacture of drugs; and control the movement of drugs from producer to
processing countries;
* raise the commitment and effectiveness of interdiction efforts in countries
which pose a threat of drug supplies to the UK;
• reduce the amount of drugs coming to and crossing the UK borders through
seizures and by dismantling or disrupting trafficking organisations;
• reduce the growth, manufacture and distribution of drugs within the UK,
preventing them from reaching local dealers through seizures and by
dismantling or disrupting internal networks;
• target money launderers and increase the amount of assets confiscated and
recovered from drug activities;
. reduce levels of street dealing and the availability of drugs.in communities;
• reduce the availability of drugs within prisons;
• ensure full cooperation and collaboration, at every level, amongst the
enforcement and intelligence agencies, with the focus clearly on tackling
activity which causes the most damage to local communities
The respective roles and responsibilities of the police and HM Customs and Excise
are well defined. Within that framework, the creation of the National Crime Squad as
of 1st April 1998 will enhance the effectiveness of the police service. During
1998/99 we shall look at how the objectives of the various agencies engaged in
stifling availability can be further coordinated to secure increased effectiveness.
Assessment
Performance indicators for each of these activities will be introduced to monitor
achievement and specific targets set for agencies against the following objectives:
£
. reduce access to drugs amongst 5-16 year olds - Key Objective;
. increase the effectiveness of the overseas diplomatic and operational effort;
. increase the value of illegal drugs seized and/or prevented from entering or
distributed within the UK;
. increase the number of trafficking groups disrupted or dismantled;
. increase the numbers of offenders dealt with for supply offences;
. increase the amount of assets identified, and the proportion confiscated and
recovered from drug trafficking and money laundering;
• reduce prisoner access to drugs.
2 of 3
5/13/9S I 1:09 A
Tackling Drugs to Build a Belter Britain
http://www.official-documents.co.uk/documcnt/cm39/3945/aim-4.ht
Research and Information
To support these objectives we will make use of the best available sources of
information and plan as a priority to commission additional research as follows:
• harness all the information gathering agencies, both within our control and
those with whom we have influence, to produce a common data model which
has strategic as well as operational benefits;
• establish the quantity, quality and type of drugs reaching our streets; its place
of origin, distribution network and means of transport; and the most effective
methods of intervention at each stage of the process;
• establish the quantity and type of precursor chemical manufactured, its place of
origin’, its destination and its route of passage;
• establish an objective base for the level of assets and money associated with
the drug industry mapping the agencies and individual concerned;
• establish the relationship between street level prices, availability and demand.
c'K'T.u: -) C • 'ST)
We welcome your comments on this site.
3 of3
Prepared 27 April 199S
5/13/98 11:09 A
Tackling Drugs to Build a Better Britain
llltp://www.t> fncial-docunients.co.uk/docuiiient/cin39/39-l:'(resource. lit
Cm 39-15
Resourcing and Managing the Work
Resourcing and Managing the Work
For the strategy to be effective, clarity about the delivery mechanisms - the
structures, resources, responsibilities, accountability and basis for audit and
evaluation - is essential.
UK Coordination
Genuine collaboration across Government is the driving force behind this strategy.
The role of individual departments, agencies and the voluntary and private sectors is
to contribute to the overall vision and aims, in addition to their own specific tasks.
The Cabinet sub-Committee on Drug Misuse - known as HS(D) - will be the
Ministerial body responsible for ensuring that this occurs.
The UK Anti-Drugs Coordinator and his Deputy report to HS(D). Their role on
behalf of Ministers is to provide the day-to-day leadership and focus on
implementing and developing the Government's strategy. The Coordinator will, in
particular, scrutinise rigorously the performance of departments and agencies individually and collectively - against the actions, objectives and performance
indicators set out in this report; and produce a National Anti-Drugs Plan for
implementation in each succeeding year. Departments will continue to be responsible
for their own policies and resources, and accountable to their Ministers accordingly.
But the Coordinator's responsibility to the Government for the production of his
Annual Report and Plan, means that progress across the board will be coordinated
and open to scrutiny.
To aid his role, the Coordinator will chair a new body named the UK Anti-Drugs
Strategic Steering Group, which will meet regularly to help the Coordinator assess
overall progress in implementing the strategy, including its resources; consider
relevant developments in the rest of the UK and internationally; and plan to account
for progress and the way forward via the Coordinator's Annual Report and Plan.
Representation on the Strategic Steering Group will include senior officials from
within Government, and individuals from independent bodies, professional drug
agencies, local government, business and Drug Action Teams.
The Deputy UK Anti-Drugs Coordinator will, in turn, lake forward the key elements
of this White Paper through four newly formed Strategy Support Groups - one group
for each aim of the strategy, each group meeting regularly. The key tasks of these
groups will be to monitor progress against each aim; assess the need for further
support in its implementation; consider emerging training, research and information
needs; and monitor resource implications. These groups will report back to the
Steering Group.
The Coordinator’s and Deputy's roles can only be effective through collaboration and
involvement of a wide range of supportive groups and individuals. To this end they
will have support from the UK Anti-Drugs Coordination Unit (previously known as
the Central Drugs Coordination Unit), a Unit in the Privy Council Office, reporting
to the President of the Council, whose funding arrangements will be put on a
long-term basis. The UKADCU's role will be to support the monitoring and effective
implementation of this strategy. To fulfil this role, the UKADCU will work very
closely with Departments, Drug Action Teams and individual agencies to develop a
comprehensive network of resources and support mechanisms geared towards the
I of7
5/I3/9S 11:09 A
• , Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/document/cm39/3945/resourcc.hi
strategy's implementation.
Resources
Government expenditure in tackling drug misuse is considerable but poorly
coordinated. As a result of the work on drug-related spending carried out for the
Comprehensive Spending Review, we know that totalGovernment expenditure for
1997/98 was in the region of £1.4 billion. This big increase in estimated expenditure
- compared to £500 million in 1993/94 - relates primarily to a more realistic
assessment of the drugs related proportion of generic ■
police/prison/probation/education/health activity. We estimate that 62% of this total
is currently spent on enforcement related work, much of it reactive and not
drugs-specific (eg police, court, probation and prisions) and therefore, not
straightforwardly transferable to preventative programmes; 13% on treatment; 12%
on prevention and education; and 13% on international supply reduction. No more
than a third of that total expenditure is currently spent on preventing drug misuse (as
opposed to coping with the consequences of the problem). Minimum estimated costs
of the social problems generated by severely dependent drug misusers alone are in
the region of £3-4 billion annually.
Existing resource provision is ad hoc rather than strategic; allocation mechanisms are
largely historically driven; the pattern of the delivery of resources to local anti-drugs
projects is complicated and random; efforts to realise substantial confiscated assets
from drug-related activity have not previously been successful; and there has been a
lack of clear coordination between objectives, resources and outcomes. In moving
forward, it is clear that the Government's resources must be linked to this strategy.
An announcement on funding from 1999/2000 will be made later in the year,
following the outcome of the Government's Comprehensive Spending Review.
Reforms will be guided by the following principles:
• drug-related expenditure should over time shift away from reacting to the
consequences of the drugs problem and towards positive investment in
preventing and targeting it;
• the bulk of targeted resources should be spent on collaborative projects which
tackle high priority groups - in particular vulnerable young people,
drug-related offenders and problem drug misusers;
• resources for drug-specific activities should receive priority within health
authorities budgets, and on the basis of partnership work wherever appropriate.
Health authorities should be required to deliver this strategy through the NHS
Priorities and Planning Guidance. The development of the new NHS and
Public Health White Papers should be used to ensure that health authorities
give adequate provision to meeting the aims of the strategy through central
guidance. Health authorities will be expected to include anti-drugs measures in
their Health Improvement Programme;
• an element should be identified within health authorities' drug allocation for
developing specific young people's services. This should enable health
authorities to develop services in line with Department of Health guidance;
• funding for the purchase of community care services for drug misusers should
be given adequate priority by local authorities. The Department of Health
should take steps to ensure that this money is used for drug-specific
partnership work, with mechanisms put in place to ensure that current
expenditure on drug misusers from local authority community care funding is
protected;
5/13/98 11:09 A
2 of 7
2 <?
Tackling Drugs to Build a Better Britain
http://www.official-documents.co.uk/docuinent/cni39/3945/resource.lu
. police forces should aim to direct resources from within their budgets to
drugs-speciftc partnership work, with explicit priority given to this work in
Police Authority Annual Policing plans and the national key policing
objectives, set by the Home Secretary and performance indicators and targets
aligned explicitly to the new strategy;
• the Prison Service should aim to direct resources from within their budget to
drugs-speciftc partnership work, including treatment provision, with explicit
priority given to this work in the Prison Service business plan, and
performance indicators and targets aligned explicitly to the new strategy;
. probation services should aim to direct resources from within their budgets to
drugs-speciftc partnership work, with explicit priority given to this work in
local plans and the national key probation objectives, and performance
indicators and targets aligned explicitly to the new strategy;
. local education authorities should include clear policy statements on drugs
education, and any performance indicators and targets aligned to the new
strategy, within their behaviour support plans. An LEA's anti-drugs strategy
will also be reflected in its education development plan where this emerges as
a priority;
• HM Customs and Excise should maintain their commitment to funding
drug-related activity - and ensure that partnership work is reaffirmed strongly
in their management plans, with performance indicators and targets aligned
explicitly to the new strategy;
. the National Criminal Intelligence Service should ensure that partnership
work is reaffirmed strongly in their service plan, and to consider in
consultation with the Coordinator the development of objectives with
performance indicators and targets aligned explicitly to the new strategy;
• the National Crime Squad should ensure that partnership work is reaffirmed
strongly in their service plan, and to consider in consultation with the
Coordinator the development of objectives with performance indicators
aligned explicitly to the new strategy;
• Drug Action Teams should be the principal mechanism by which agencies
will develop the resource partnerships outlined above, and will assess regularly
whether the spending plans and projected outcomes of all agencies represented
on them are aligned explicitly to the new strategy;
• the value for money of Government and other anti-drugs expenditure against
outcomes should be monitored at national level via the UK Strategic Steering
Group and Strategy Support Groups and locally via the Drug Action Teams;
and
. securing partnership funding should be given high priority at every level, led
by the national partnership between Government and Business in the
Community;
For the first time, a proportion of assets seized from drug barons will be channelled
back into anti-drugs programmes to help those who have suffered at their hands and
on whose misfortune they have prospered. The Government is considering how this
can best be achieved. More details of these considerations will be issued later this
year.
The efficient and effective delivery of the strategy's objectives will, of course,
determine the specific resources required over time, and resource provision will
accordingly be regularly reviewed in the Coordinator's Annual Report and Plan of
3 of7
5/13/98 I 1:09 A
lacklmg Drugs to Build a Better Britain
http://www.officiaI-documents.co.ul</documeiit/cm39/3945/rcsource.hi
Action Against Drug Misuse.
Regional Coordination and Delivery of Strategy
Drug Action Teams, supported by their Reference Groups, have worked well in most
parts of the country in forging partnerships against drugs amongst the key local
agencies. The time is right to step up a gear in relation to this partnership activity, so
that a sharper focus is brought to bear on implementing this strategy. This should link
up where necessary with other local partnership initiatives on welfare-to-work,
health, education, housing, community safety, youth justice, local democracy and
social exclusion. Links with these other partnerships will develop over time, but will
not diminish the importance of the work against drugs at local and regional level, via
Drug Action Teams. The strategic requirements set out below reinforce both the need
for a continuing focus on local drugs problems and ensuring that other social
partnerships contribute to that work.
Al! Drug Action Teams in England are to agree corporate plans annually with the UK
Anti-Drugs Coordinator by the end of each calendar year. Templates will be provided
by UKADCU. These plans will feed into the Annual Report and Plan and include:
• an assessment of current progress against the new strategy;
B
. an analysis of existing local resources upon which each DAT has influence
both within its own organisations and jointly targeted;
• proposals for allocating those resources to match the priority aims and actions
set out in this strategy;
. specific outcome measures against all relevant areas under the aims set out in
this strategy - including services for vulnerable young people, criminal
justice/treatment; rehabilitation of problem drug misusers and disruption of
local drug markets;
• proposals for short, medium and longer-term targets against those measures in
line with the national targets to be developed;
• agreement with all other Drug Action Teams within their metropolitan or shire
county area on the basis of a corporate and strategic overview to the plans
individual DATs have drawn up. This is to ensure strategic coherence to the
plans across each county, a genuinely senior level of strategic input from the
key players, and consonance with the development of other relevant shire and
metropolitan county partnerships. Where appropriate, DATs will wish to liaise
with relevant regional tiers of government. This overview will be the most
important part of the plan in enabling the Coordinator to take stock of
progress. Those DATs which currently do not operate on a shire or
metropolitan county level will have a more complex process to go through than
the 26 DATs currently operating on those lines. The focus of our support will
therefore be on the remaining 80 DATs.
These plans will deliver greater consistency and provide the basis for attracting
additional resources - including some drugs-specific funding from central
Government, Lottery funding and partnership money from the private and voluntary
sectors - and will be assessed on that basis. The Government and the Coordinators
will be engaging directly with Drug Action Teams across England to ensure that the
planning process is as clear and unbureaucratic as possible.
Drug Action Teams must develop as the mechanism for ensuring local resource
collaboration in line with this strategy. Their corporate plans will provide the
benchmark for distributing resources from 1999/2000 onwards - further guidance to
5/13/98 11:09 A
4 of 7
2 7
Tackling Drugs to Build a Better Britain
http://www.official-docunients.co.uk/docuineni/cin39/3945/resouicc.lit
DATs will be provided later this year taking forward this challenging remit. This will
include more information about the future of centrally provided development
funding.
This funding has helped DATs in providing essential local coordination. Most DATs
have demonstrated best value in using this resource through an identifiable
coordinator, working closely to the DAT Chair, and with a clear role and set of
requirements. This coordination role must include coherent representation to the
DAT of the views and expertise available from local communities. The Chair of each
Drug Action Team will continue to have overall responsibility for the formulation
and Implementation of corporate plans. Clearly that responsibility, which also entails
some accountability to the Coordinator, can only be discharged by individuals with
considerable authority and influence within their DAT area. The personal qualities of
any individual Chair are far more significant than the agency from which they come.
Representation on DATs - beyond the core agencies of health authorities,
education, social services, police, prisons and probation - will continue to be a local
matter, with the exception that all DATs should include senior representatives from
local authority housing. They should also liaise more closely with the Crown
Prosecution Service, key sentencers, the Employment Service, the voluntary sector.
Training and Enterprise Councils and Chambers of Commerce. DATs must also
actively engage their elected members and Members of Parliament, to ensure that
there is no "democratic deficit" to their activity. Developing the representation and
function of Drug Reference Groups and other networks in support of the agreed plans
of the Drug Action Teams will be a local matter, but will need to ensure effective
community involvement, consultation networks and clarity of responsibilities for
implementation.
V
Drug Action Teams or their equivalents in Scotland, Wales and Northern Ireland are
invited to consider their own development in the light of this strategy, as part of the
overall response to the Coordinator by February 1999.
Partnerships
Action against drugs problems cannot be undertaken effectively by any single
agency. The performance of all statutory agencies, accountable to central
Government Departments, will be scrutinised to assess their progress in forging
effective, enduring and practical partnerships with other agencies. The following are
being developed as a priority:
. The FCO's Special Representative's international coordination committee
will continue under the Chairmanship of the Special Representative to ensure
the strongest possible links with our European partners to give continuing
effect to the leading role of the UK in the fight against drugs established during
our Presidency of the EU from January to June 1998. The UK will also take a ~
visible lead in international coordinated efforts against drugs, through the UN
and other mechanisms, where that has a direct contribution to make to this
strategy's vision. Our resources will be made available accordingly;
W
• statutory Inspectorates - each HM Inspectorate will continue to have direct
responsibility lor monitoring the impact of drugs policies for which their
agencies are responsible. The importance of collaborative working across and
beyond the Inspectorates is recognised by all of them. A multi-disciplinary
review process - involving representatives from HM Inspectorate of
Constabulary, HM Inspectorate of Prisons, HM.I Probation, OFSTED and the
Social Services Inspectorate - will be established by December 1998. The
importance of monitoring health authorities in this context will need further
examination;
>of7
5/13/9S 11:09 A
Tackliiig Drugs to Build a Better Britain
http://www.of Ticial-documents. co.uk/docunicnt/cni39/3945/resourcc.ht
• national programme delivery - the role of Government is to facilitate and
enable this strategy's implementation through leadership and resource
provision. In areas such as publicity, spreading of best practice, project
programmes, information collation, and specialist guidance, there is already
expertise and experience among a number of organisations, funded by
Government or others. In view of its valuable contribution to date, it is planned
that there should be some successor arrangements to the Home Office Drugs
Prevention Initiative after its current programme ends in March 1999, which
will support this strategy and promote community-based drugs prevention
across England. Other bodies with a role to play include the Standing
Conference on Drug Abuse, the Institute for the Study of Drug Dependence,
Alcohol Concern, the Substance Misuse Advisory Service, the Local
Government Drugs Forum and the Health Education Authority. To avoid
unnecessary duplication of effort, any work the Government commissions in
support of the vision, aims and actions set out in this strategy - contracted to
one or more of these agencies - will only be provided on the basis of clear
partnership agreements;
• Advisory Council on the Misuse of Drugs - the ACMD has the statutory
responsibility to advise Government on the continuing operation of the Misuse
of Drugs Act 1971, and to any changes to the law necessary in the light of
emerging evidence. The Council will continue to exercise that vital function.
In addition, the Council has produced many extremely valuable reports on
specific issues - most recently on drugs and the environment which will be
published soon. Its composition and focus of work need to be harnessed as
closely as possible to the thrust of this long-term strategy and to the work of
the Coordinator, and its future work priorities will evolve in that context;
• private sector - the private sector plays a vital foie at national, regional and
local level in working to combat drug misuse. Many businesses now recognise
the commercial benefits and ethical imperatives of involvement in this work.
Some - such as BT. Boots, Proctor and Gamble. Marks & Spencer, Royal and
Sun Alliance, McDonald's, Lloyds TSB - have already contributed significant
resources and commitment to this work. Business in the Community is driving
forward a major strategy programme to engage the private sector as
systematically as possible - especially through initiatives aimed at young
people;
• voluntary' sector - much of the energy and innovation in tackling drug misuse.
as well as professional and cost-effective delivery, comes from the voluntary
sector. We are determined to maximise the contributions that this sector can
make set against this strategy. The UK Anti-Drugs Coordinator will convene
an annual national stocktake of voluntary sector providers, in concert with the
Standing Conference on Drug Abuse, to ensure that their interests and
contributions to the developing strategy are fully developed and properly used,
and that best practice is being implemented;
. the media - responsible and informed coverage of drugs stories can make an
important contribution to the strategy's vision. We will engage extensively
with national, regional and local media to try' to ensure a good level of
informed debate, analysis and coverage;
• parents/young peoplc/communities - drugs impact on all of us, our lives,
worries and aspirations. We will consult and engage with people in schools,
clubs,'at parents meetings, with users, at community events and in all locations
where there is real concern and real commitment to addressing it.
6 of 7
5/13/98 11:09 A
Tackling Dinas to Build a Better Britain
htlp://www.official-documents.co.uk/docuinent/cin39/39-l5/resource.lit
Audit and Evaluation
Objective and rigorous assessment of the effectiveness of implementing this strategy
will be a central feature of its development, and necessary adjustments will be made
as a consequence. The key components of this process will be as follows:
. the Coordinator's Annual Report and Plan of Action Against Drug Misuse
which will be published every Spring, based on the strategic framework set out
here, together with data on progress and proposals for future priorities;
. annual reports from Drug Action Teams in England made to the Coordinator these will be submitted as part of the corporate planning process at the end of
each calendar year. Results and best practice will be incorporated into the
Coordinator's Annual Report and Plan;
-
■
. the statutory Inspectorates - regular thematic and multi-disciplinary reviews
will be published by these bodies;
. quality indicators for the core statutory agencies - these will reflect the fact that
the quantitative indicators to be set out need harnessing to more qualitative
assessments of progress, which will form part of the DAT reporting process at
local level and of an overview from the Coordinator's Annual Report and Plan;
. research and information - this will be regularly assessed against each of the
strategy's four aims by the four strategy support groups, as an integral part of
the implementation process. They will consult a wide range of external bodies
as necessary, and report collectively to the Strategic Steering Group;
W
• independent strategic evaluation - over the longer term, we will all need to be
satisfied that the implementation of this strategy is achieving the most effective
results possible. The National Audit Office and the Audit Commission will be
engaged in discussions about what might be undertaken over the next decade
to fulfil this remit;
. consultations - the continual process of "listening and learning" which the
Coordinator and his Deputy have undertaken from day one, will form a more
informal, but essential, part of evaluating the strategy. They will continue this
consultation for the rest of their appointments, so that progress on the ground where it really matters - can be properly assessed.
I Ke welcome your comments on this site.
7 of 7
Prepared 27 April 1998
5/13 98 11:09 A
Laws that protect
Various laws exist for ,he protection ofpublic health. But a lack of knowledge or a neglect of
their provisions ■ ften results in drug induced ill health. Dr S.G. KA BRA describes
some of the (Xfjes that suffer due to a neglect or a non implementation of the
law arid the efforts made to bring breaches before law courts.
here are several laws, the |,iovi- this purpose.”
sons of which are meant to tegulate health care facilities for the benefit Taking into account specific provi
,f the public. Indifference to or ne sions, Section 3 of the Act states:
glect cf these legal provisions en
genders a tacit nexus between oftund- "Subject to the provisions of this Act, no
ers and the authorities. It is therefore person shall take part in the publication
necessary to identify these legal pro of any advertisement referring to any
visions to create awareness and to drug in terms which suggest or are cal
evolve a strategy to ensure that the culated to lead to the use of that drug
authorises entrusted with the enforce for:
ment cf these provisions do in fa^t do
so. Enumerated below are several jaws a) promoting miscarriage in women or
with a direct bearing on public health.
prevention of conception in women;
or
. b) the maintenance or improvement of
Drugs and Magic Remedies
the capacity of human beings for
(Objectionable Advertisement)
sexual pleasure; or-.
Act,1954
c) the correction of menstrual disorder
• in women; or
Implement of objects and reasons :
■d) the diagnosis, cure, mitigation, treat
"In recent years there has bean a
ment or prevention of any disease,
•eat increase in the number of objec
disorder or condition specified in the
tionable advertisements in newspapers
*'or
Schedule,
any other disease,
or magazines or otherwise relating to
disorder or condition (by whatsoever
alleged cures of venereal diseases,
name called) which may be specified
sexual stimulants and alleged cures for
in the rules made under this Act.
diseases and conditions peculiar to
women. These advertisements tend to
(* The Schedule appended to the Act
cause the ignorant and the unwaly to
lists 54 diseases, disorders and con
resort to self-medication with haijiful
ditions which cannot be advertised.)
drugs and appliances or to resqq to
quacks who indulge in such advertise Section 4 of the Act states :
ments for treatments which cause g. eat
harm. It s necessary in the public inter Subject to the provisions of this Act. no
est to put a stop to such undesirable ad person shall take any part in the publica
vertisements. This bill is intended for tion of any advertisement relating to a
drug if the advertisement contains mat
ter which : a) directly or indirectly gives
a false impression regarding the true
character of the drug; or b) makes a
false claim for the drug; or c) is other
wise false or misleading.
No person carrying on or purporting to
carry on the profession of administering
magic remedies shall take any part in
the publication of any advertisement
referring to any magic remedy which
directly or indirectly claims to be effica
cious for any of the purposes in Section
3. Under Section 9A of this Act, an of
fence punishable under this Act Is a
cognizable one.
A test case
Offending advertisements are a very
common feature in the print media in
India. To invoke the provisions of this
Act, we initiated a test case in a magis
trate’s court in Ajmer against the then
Editor and Publisher of The Hindustan
Times, Delhi (Khushwant Singh and Dr
Hans Raj respectively) for an advertise
ment by Dr Sablok which appeared in
the newspaper. The case was regis
tered only after letters written to the
editor, drawing attention to the provi
sions of the Act went unheeded, the
advertisements appearing unchecked.
Though the case was ultimately dis
missed through default, it did succeed
in ensuring that all three defendants
December 1990
HEALTH for the Millions
21
appear in court whenever required
through the execution of a bond and
surety. The case also succeeded in
establishing the following :
The offence is cognisable. Any court
in whose jurisdiction a newspapei or
magazine is sold or circulated has
jurisdiction in the case if the offence
is deemed to be committed locally
and the cause of action local
* The editor and publisher along tyith
the advertizer are all equally liably to
offence.
^forts at implementation
After my deputation to SDM Hospital,
Jaipur, I wrote letters to the Director,
Health Services, Inspector General of
Police and Health Secretary of Rajast
han, drawing their attention to the provi
sions of the law and its breach. There
was no response. Marudhar Mridul. a
■'
HEALTH for the Million:,
leading lawyer of Rajasthan, agreed to
file a writ petition which was decided on
September 1989. The Hon'ble Mr. Jus
tice SN Bhargava issued a directive to
the Inspector General of Police, Rajast
han, to establish a special cell to moni
tor such advertisements in the print
media and initiate prompt action
against the offenders. Some cases
have been registered by the police.
Some of the newspapers have stopped
carrying such advertisements. Much
still remains to be done to fully get the
court's order Implemented.
tion of its provisions throughout the
country.
Despite its existence, precious little has
been done to implement its provisions.
A case in point is drug induced blind
ness. Eye drops and ointments with
steroid content are widely used for aller
gic conjunctivitis.,Due to prolonged use
of eye drops, I have known several
cases turn blind through drug induced
glaucoma and cataract. Though every
text book of medicine and pharmacol
ogy mentions that steroids should not
be used for prolonged periods, no
warning to this effect is written on prepa
Drugs and Cosmetics Act
rations. The implications are specially
This Act provides for the control and ominous when one considers the fact
regulation of safe production, distribu that self medication is a very common
tion and sale of drugs and cosmetics. phenomena. Even well meaning par
Powers to enforce the provisions of the ents regularly administer eye drops to
Act are vested in the State Drugs Con children, oblivious of the dangers; The
trollers whose activities are coordi six year old son of a compounder first
nated by the Drug Controller of India put me on the trail which led me to
who in turn ensures the uniform applica compile over 18 cases of blindness in
December 1990
was issued by the Drugs Controller state government machinery exists to
against the prolonged use of sterold- ensure that these safety provisions are
containlng eye drops. Partially Imple followed. The result: no x-ray units fol
mented, the court order has not been low them. With commercialisation of
Letters were written to apprise the Diug followed In true spirit.
diagnostic x-rays and their rapid prolif
Controllers of Rajasthan and Indi^i of
eration, there is grave danger to the
the cases in point. Articles were written Banned and bannable drugs
population. After having written to all
in the lay press, giving case histories of
authorities bringing to their notice the
the patients to highlight the dangeiij of According to a writ petition filed under mandatory provisions and having failed
steroids in eye medicines. One sgch the Drugs and Cosmetics Act, the deci to persuade them to fulfill their responsi
article which appeared in Rajasthan sions of the Drugs Consultative Com bilities under the Act, a writ petition has
Patrika, a Jaipur daily, attracted thy at mittee and the Drugs Technical Advi been filed in the High Court with notices
tention of the local government, A sory Board, the highest technical bod issued to'the central and concerned
committee of experts was appointed to ies under the Act, once accepted and State government
investigate the facts and to submit tfieir communicated by the government, are
report.
5
binding on all health authorities and The Indian Medical Council Act and
government doctors. A drug that has the Medical Degrees Act
The committee recommended that all been declared harmful or irrational by
steroid eye preparations should cat i y a the technical bodies cannot be pur Provisions of these two Acts have been
warning that the medicine’s prolonged chased or prescribed by any govern invoked to prevent advertisements and
use may lead to blindness due to cata- ment authority. This Is irrespective of unethical practices, professional mis
ct, glaucoma or fungal infection, [he the fact that government orders prohib conduct and the use of unrecognised or
viate government forwarded the -fec- iting manufacture and sale of the drug fake degrees by doctors. The State
ommendations to the State Drugs Con might have been stayed by a court. Pro Medical Council must be made to do its
troller, who in turn, instead of acting hibiting the manufacture and sale of a duty to regulate and supervise the pro
under the provisions of the law, Jor- drug and directing all government fessional conduct of the doctors regis
warded it to the Drugs Controller of doctors not to prescribe a drug found tered with it and to ensure ethical stan
India. The Central Drugs Controller re to be harmful are two different conse- dards of medical practice.
turned it to the State Drugs Controller, quence^that flow from the decisions of
agreeing with the recommendation^ of the two technical bodies.
The.Insecticides Act.
the Committee. The State Drugs Con
troller still did not act. Even the report of An interesting observation made by the The provisions of this Act have been
the Committee was not made publtj,.
court during the hearing was that a stay invoked to prevent the availability of the
order by one High Court is not automati deadly pesticide, aluminium phosphide,
A writ petition was then filed in the F iigh cally binding on the other High court. in the open market. Numerous articles
Court on 20th January 1989. Hottble Evidence of banned drugs still being have been written to bring to light a large
Mr. Justice Mahendra Bhushan Sharma purchased, prescribed and reimbursed number of deaths that result every year
and Mr. Justice LS. Israni directed the by health authorities was produced from aluminium phosphide. All the con
Drugs Controller of Rajasthan to ensure before the court. The case is still pend cerned authorities have been warned.
■ printing of the necessary warning on ing before it.
Questions have been raised and an
all steroid-containing eye preparations.
swered In parliament. Though there are
Their lordships quoted etttensively the Atomic Energy Act, 1962
widespread assertions on the illegality
specific rules under which the State
of open market sale of aluminium
Drugs Controller had the power to Im The Atomic Energy Regulation Board phosphide, nothing has been done to
plement the provisions so as to allay constituted by the Central Government prevent it. A writ petition, it is felt, should
any impression to the contrary.
under the provisions of the Act have now be filed to prevent thousands of
codified the mandatory safety provi deaths due to this deadly pesticide. A
Though a number of-steroid prepara sions for diagnostic x-ray units. The
tions now carry a warning, many sti,i do safety code details the mandatory - Dr S.G. Kabra is a Professor ofA natomy, a trained
not. Despite a large number of cases measures necessary to prevent unnec surgeon, a medicaljournalist who has also done law
brought to his notice, no public warjilng essary exposure to radiation. Yet no and written extensively on medical - legal issues.
one year due to prolonged use of: ieroid - containing eye drops. None .,ad
been warned.
t
December 1990
HEALTH for the Millions
23
CONSUMER ACTION
WHAT YOU CAN DO
1. Stop using banned a<_.J hazardous drugs. Stop using useless and
irrational drugs.
j
Wheneyer you are prescribed a drug, ask your doctor politely what
side effects may occur, how long you should continue taking the drug
and what are the expected benefits. Know your rights as a patient.
3. Encourage the use of traditional home remedies, instead
of expensive «nd unnecessary drugs for trivial problems.
4.
Refuse to take a drug if it's
expiry date is over, or if it is
discoloured and if there are
suspended particles in it.
December 1990
HEALTH for the Millions
33
§. If given a'very long prescription, fiqd out which
ere the most essential drugs for your
*heafth
prob
lems and which can be avoided. (Studies have
shown that many patients can buy only the first one
or two drugs listed on long prescriptions).
6. Ensure that anyone prescribed antibiotics or put
on long term treatment, as for TB or leprosy, takes
medicine regularly and for the required length of
time to avoid emergence of drug resistance.
34
HEALTH for the Millions
December 1990
FORUM
XII SUN DAY, DECEMBER 25,1994
FTER a long wait of eight
years the New Drug Policy
(NDP) has been announced,
the objective of which is to create
'conditions of adequate availability
of medicines of good quality at rea
sonable prices'.
While the objectives are laudable.
one doubts whether these would be
achieved in the light of the earlier
experience and the contents of the
NDP.
For, what we have as a drug pol
icy is basically a pricing and pro
duction policy where the dominant
force is the “profit motive'. It is a
policy which is heavily oriented
towards the benefit of , the
multinationals. It attempts to ad
dress many cf the problems facing
the drug industry and not the avail
ability of cheap and good quality
medicare to the public.
From the consumers point of
view any drug policy should not
only ensure good quality of medi
cines at reasonable prices but also
eliminate irrational, useless and
hazardous drugs.
In addition, an ideal drug policy
should provide a list of graded es
sential and priority list of drugs in
keeping with the actual health
needs of the people. But the NDP
does not seem to answer to any of
these requirements.
For the past many years, the
objective of drug policies has been
hovering around the same prin
ciples of price, quality and easy
availability. For instance the SI.
Bhatia Committee (1953) laid em
phasis on quality and recoin maid
ed centralisation of drug regulatory
set up in the country. The Borkar
Committee did the same a few
years later.
During 1974 the Jaisuklal Hath!
Committee not only recommended
strengthening
quality
control
measures, but also nationalisation
of multinational drug companies,
establishment of a National Drug
Authority, elimination of irrational
drug combinations etc., While these
recommendations were put to prac
tice in the neighbouring Bangla
desh. it was not implemented in In
dia.
Even the successive Drug Policy
statements of 1978, 1982 and 1986
had similar objectives. These state
ments aimed to ensure that drugs
are available in abundance to meet
the health needs of our people, to
make drugs available at reasonable
prices, to keep a careful watch on
the quality and malpractice etc..
But none of these objectives have
been achieved India is a signatory
t\. the .Alma Ata of bringing health
A
DECCAN & HERALD
New Drug Policy has many loopholes...
to all by AD 2000. Only a miracle
can bring about this in another five
years.
One of the objectives of the NDP
is to control prices. But bow does
it propose to do? By decontrolling
more dn.ig7 The NDP states that “it
has been decided to keep the drugs
having an annual turnover cf Rs.
400 lakh or more under price con
trol. In effect drugs, the turnover
of which is below Rs. 4 crore will
be out of price control
As a result of this decision, the
number cf drugs under price con
trol will get reduced to 73 from the
present 142 and the span of control
to about 50 per cent from the pres
ent 70 per cent
Decontrolling half of the present
drugs un der control would defin itely mean , rise in prices. As such it
would defeat one of the objectives
of the NDP. The policy further
states that the government would
keep a dose watch on the price
movement cf drugs not _i the list
and reclamp price control, if necess
ary.
But the earlier efforts in this
direction have not been encourag
ing Drugs came under price control
for the first time in 1962. The Drugs
(Display of Price) Ords’ 1962 and
the Drugs (Control of Price) Order
1963 were promuhfated under the
Defence of India Act, freezing prices
of medicines as of April 1, 1963.
The Drugs Price Control Ords'
(DPCO) 1970 was issued under the
Esssitial Commodities Act 1955 to
bring down prices cf 17 essential
bulk drugs and their combinations.
The DPCO 1979 and 1987 was also
issued with the same objective
Despite price control mechanism,
prices cf drugs have increased
steadily. And many of the drug in
dustries have been pulled up by the
courts to pay back the excess
amount collected on price control
led drugs.
Following the Supreme Court
verdict against over-pricing by drug
companies the government is to
realise Rs, 270 crore from the indus
try The available figures indicate
that the actual recoveries is not
more than Rs. 1382 crore up to 1992.
However in reality, pnces of all
categories cf drugs have increased
by almost 50 per cent The prices cf
cardiac and hypertension drugs
hare increased by 40 per cent Simi
larly. prices of anu-TB drugs like
Rifampicin have gone up by 40 per
cent in the last two vears Several
From the consumer point of view any drug policy should not only ensure good
quality of medicines at reasonable prices but also eliminate irrational, useless
and hazardous drugs. In addition, an ideal drug policy should provide a
graded, essential and priority list of drugs in keeping with the actual health
needs of the people. But the NDP does not seem to answer any of these
requirements, writes Y G muralidharan
However, simultaneously efforts
were not made to ensure produc
tion of these price-controlled es
sential drugs and check prolifer
ation of non-essential drugs. The
NDP states that the DPCO will be
issued in “three months time".
This was in September 1994. The
DPCO is yet to be announced. The
time lag has given enough oppor
tunity to the interest groups to
step up their lobbying efforts at
New Delhi, to be out of the list
It is fortunate that the NDP has
a provision for setting up an auth
ority for price fixation. This is a
welcome move. The NDP states
that the government would set up
an independent body of experts to
be called the Pharmaceutical Pric
ing Authority (NPPA) to do the
work of price fixation. In addition
it will also oversee the enforce
ment of the provisions of the
DPCO. The degree of autonomy of
this proposed authority is to be
watched.
For the past few years drug
manufacturers have been trying to
pressurise the government to con
cede its demand for decontrol of
production and pricing. The drug
industry has been claiming that
its turnover and profit have suf
fered due to controls. And the NDP
has favoured the industry. But in
reality, the sales and profits of
drug companies have increased
over the last few years. The half
yearly results (up to March 1994)
of drug industry shows that sales
has gone up by 32 per cent and
profit by 84 per cent
essential drugs are not available in
the market
Even after the DPCO cf 1987 was
issu ed prices of drugs has shown
an upward trend. Though the gov
ernment intends to monitor price
rise, one cannot be optimistic about
it Way back in 1978, the Lovraj
Committee was set up to investigate
the allegation cf large profits cf
foreign companies, suggested that
the effect of DPCO (1979) on profit
ability cf the drug industry should
be assessed periodically So far no
attempt has been made to monitor
prices and profits.
The NDP states that prices would
be kept in check by forces of market
com petition'. One need not be an
economist to understand the econ
omics of drug industry
The Indian drug industry has all
the problems associated with an
oligopolistic industry dominated by
a few private firms and an industry
dominated by foreign companies Le
MNCs.
As such, market is a poor mech
anism for regulation of prices of
drugs. Production and price control
measures are very much essential
to ensure drugs at low prices
Secondly, the market for drugs is
not determined by consumers but
by pharmaceutical companies, de
tail men (medical representatives)
and doctors. Unlike all other com
modities in the market, in case of
drugs, the consumer has no say
over the choice of the commodity
he purchases. He goes entirely by
the doctor's prescription.
The very fact that the concept of
‘turnover’ has been taken as basis
to determine drugs which are to be
brought under price control is itself
an indication that the NDP is trade
oriented.
Although medicinal products con
stitute essential tools for health
care, it is observed that drug polic
ies are often directed towards in
dustrial and trade development h
is precisely for this distorted object
ive, that the drug policy is formu
lated by the Ministry of Chemicals
and Fertilisers and not by the Min
istry of Health.
This is the first time that we have
a policy which determines the list
of drugs under price control on tte
basis of turnover. In the DPCO 1976,
essentially was the basis for
categorisation of drugs. The Kelkar
Committee list of drugs for DPCO
1987 also used essentiality as basis.
This concept of essential drugs find
no mention in the NDP
According to the Health Action
International (HAD an essential
drug is one which meet real medi
cal needs, has sufficient therapeutic
value, be acceptably safe arid offer
satisfactory value for tial drugs are
those that satisfy the health care
needs cf the majority of the popula
tion.
Some efforts have been made in
the past to prepare a list of essential
drugs with the main objective of
price control. The Committee on Es
sential Drugs (1967) listed 17 drugs.
The Hathi Committee gave 104
drugs as essential
The Drug Policy of 1978 prepared
37 bulk drugs grouped in Category
I and n which are highly essential
and life saving The Steering Com
mittee of NDPDC shifted from the
essential drug list and prepared pri
ority list cf 95 drugs.
Another set back to consumers
is the provision in the NDP to
bring companies with foreign
equity up to 51 per cent on par
with wholly Indian companies.
The NDP states that automatic ap
proval would be given for foreign
technology agreements, as per the
Industrial Policy for all products
except those produced by the use
of recombinant DNA technology'
Since the government aims to re
vise the drug policy "so as to bring
it in consonance with the Indus
trial Policy 1991 and the present
EXIM policy" allowing foreign
companies is no surprise.
ested in the financial health of the
companies and not in health of
consumers. Secondly, they are not
interested in producing essential
bulk drugs, but in multiplying
unnecessary medicines, tonics and
syrups. The recommendations of
the Bhore Committee, Sokhey
Committee, Mudaliar Committee
and the Hathi Committee have
warned the exploitation of the con
sumers in our country by the
MNC’s. Again these MNC’s utilise
developing countries including In
dia, as dumping grounds for sub
standard and discarded drugs
which have been banned in the
country of origin.
Due to extensive price decon
trol. liberal licencing and free ac
cess to multinationals, the drug
market will go unregulated. This
will lead to economic drain of
crores of rupees on non-essential
drugs. As long as the industry is
free to produce what it likes, it is
almost impossible for the cus
tomers to get rational drugs. Back
ed by vast promotional network,
the MNC’s are capable of distort
ing the genuine marketing infor
mation and pushing the people to
consumer irrational drugs. Nonessentials like tonics, vitamins,
health drinks, digestive enzymes,
sex
stimulants
and
cough
expectorants will increase as
against essential drugs to combat
TB, Malaria etc.,
A welcome feature of the NDP
is that it provides for setting up
of a National Drug Authority
(NDA) to ensure quality control
and rational use of medicines. The
NDA to be set up by an Act of Par
liament would also prepare and
publish national formulary and
also the formularies relevant to
various levels (like district hospi
tals, community centres. PHC
etc.,) for the guidance of con
sumers as well as doctors. One
hopes that drug information,
which is almost absent in the
country would be soon available to
consumers.
The establishment of more zonal
and sub-zonal offices under the
Central Drug Standards Control
Organisations as well as addition
al regional drug testing laborator
ies is a welcome move. If the qual
ity of drugs is not up to the mark,
it is also because of insufficient
manpower, and other facilities.
Allowing foreign companies (al The NDP needs to be reviewed be
ready we have in surplus) to oper fore implementation so that the
ate without restrictions would hit welfare of the consumers will get
the welfare of the consumers. It is priority and not the industry as it
well known that MNCs are inter is now.
VI SUNDAY. OCTOBER 9,1994
FORUM
The big question on drugs — healers or killers?
Sub-standard drugs, contaminated intravenous (IV) fluids and infected blood have been taking their toll of innocent lives quite
regularly. It is strange that medicines and drugs which are meant to cure patients are killing them, says Y G MURALIDHARAN
ESPITE differences of opinion
with regard to the quantum of
sub-standard and spurious
drugs, the fact remains that the coun
try’s drug market is not all that dean
and safe. Though sub-standard drugs
have been in the market for a long
time, it caught the attention of the pub
lic after the J J Hospital tragedy of
1966, in which 14 patients died due to
contaminated glycerol. The findings cf
the Justice Lentin Commission which
went into the causes cf the tragedy are
too known well to be repeated.
Over the years a number of studies
have established that a substantial
number of drugs sold in the market are
either sub-standard or are not up to the
mark. Thirty years ago the Drugs
Equipment Standard Committee found
that one out of every five (20 per cent)
drugs are either substandard or spuri
ous. In 1986-87, over 26000 drugs drawn
by drug inspectors of various states re
vealed that nearly 4000 samples were
of low quality.
The Joint Council of Pharmacists of
Delhi alleged that as many as 16 per
cent of indigenously produced drugs
could be sub-standard. However none
of these figures are palatable, to the
Drugs Control officials or the FDA. The
reason, apart from others, lie in the
concept of substandard or spurious
drugs.
The definition Of substandard drugs
is wide and includes all drugs which
do not meet the prescribed standards
like improper colouration in tablets
and chipped tablets. However, from the
common man's point of view, substan
dard drugs are those which do not con
form to the standards as specified by
the Drugs and Cosmetics Act 1940
While sub-standard drugs can be
manufactured by licensed manufactur
ers, spurious drugs are those which
may be manufactured and sold by
unlicensed manufacturers. Stated in
simple words spurious drugs are those
which are (a) manufactured without li
cense (b) manufactured/ sold without
testing (c) the content of active ingredient is lesser than that mentioned on
the label (d) drugs sold on the basis of
false laboratory analysis report Many
drugs available in the market will fit
into one of these definitions.
Patients have been put into great dif
ficulty by contaminated eye solutions
and IV fluids. It is feared that hundreds
of elderly people may have turned com
pletely blind because of a contaminated
eye solution used during cataract sur
D
gery. It has now come to light that a
batch of 20000 vials of the Balance Salt
Solution (BSS) sold in 1992 contained a
chemical preservative that causes the
cornea to turn opaque
In another case, at least five persons
lost their eye sight due to administra
tion of contaminated solution after eye
surgery in a private hospital at Kochi.
When complaints of eye sore, blurred
vision etc., came in, tests were conduct
ed which showed that Irgasol, used
intraoccularly had fungus called
Aspergillus which infected the eye
leading to loss of vision.
Perhaps more than drugs and medi
cines, it is contaminated IV fluids that
has had sent patients into unnecessary
trouble. If Bombay leads in spurious
drugs. New Delhi has the dubious dis
tinction of more cases of contaminated
IV fluids.
During 1989, life saving IV fluids re
portedly claimed seven lives in Delhi
of which two were in the Safdarjung
Hospital In the same year, at the All
India Institute of Medical Sciences, a
highly contaminated bottle of IV fluid
was found by a doctor just before it was
to be injected. The CBI registered a
case against the Drug Controller of
Delhi and a pharmaceutical firm of
Coimbatore which had supplied con
taminated bottles of IV glucose to a
Delhi based dealer.
A study conducted in 1989 by the
Voluntary Health Association of India,
came out with several unpleasant facts.
As per medical norms, IV fluid should
be manufactured in sterile, automatic
units with no physical contact. But the
study found that due to lack of con
tamination test units, in several states,
the fluid is taken to other places, which
may lead to contamination.
Again, the temperature limit for
these fluids (maximum 35 degrees
celcius) is also often ignored even dur
ing summer months. The study has
pointed out that since many storage de
pots lack adequate air conditioning fa
cilities, the solution expires much be
fore the scheduled date.
With Ayurvedic and Homeopathic
medicines gaining popularity, there
are reports of selling sub-stindard or
adulterated traditional drugs. It was re
ported that in the Delhi liquor tragedy
of November 91, in which 175 people
died, liquor was sold under an
Ayurvedic label Such labels are used
because traditional medicines can be
sold by anybody and can also avoid Ex
cise Duty.
When the Centre received many com
plaints of sellers misusing Ayurvedic
labels for liquor, the Health Ministry
set up a commltte under Prof. Nam
Joshi which suggested that Ayurvedic
drugs which contain alcohol should be
in small 30 ml bottles, so that it should
not be possible to consume them in
large quantities. It also suggested that
no color should be added to drugs so
that consumers should know by the
transparency that they contain alcohol.
Unethical business practices does not
end here. There are also cases of fake
syringes, saline etc., being sold as
‘sterilised' and ‘non-toxlc’. With the
spread of AIDS, disposable syringes is
now mandatory. But these disposed
syringes are collected by unscrupulous
scrap dealers and are sold with labels
of reputed pharmaceutical companies.
In one case the West Bengal police
found that one seller had sold contami
nated syringes worth Rs.12 lakh to the
Burdwan District Hospital They also
seized lables which said that the syr
inges were gamma ray sterilised, while
there is no gamma ray machine In the
whole of Eastern India.
Innocent consumers have been taken
for a ride by scrap dealers who sell
drugs by recycling rejected and expired
capsules, tablets etc., discarded by the
multinational pharmaceutical compan
ies. According to the guidelines issued
by the Drugs Control authorities, the
manufacturer is expected to grind pills.
crash bottles, shred lables and foil
wrappers before any of the rejected ma
terial is handed over to the scrap
dealer. But very rarely the manufac
turer follow these guidelines. Other
wise how could Bombay's 'Dawa Bazar’
be a centre for fake drug business? In
a massive raid, the Bombay drug in
spectors seized 5.75 lakhs of recycled
capsules of which 3.75 lakhs were in
tended to be life saving drugs.
A recycling trade in drugs exist be
cause of faulty systems of waste
destruction, allowing rejects to be
smuggled out of the factories instead
of being destroyed. Drugs which expire
are supposed to be returned by the dis
tributors to the manufacturer in time.
It is here the scrap dealers play their
trick. Drugs are smuggled out of
gowdons and sold to unsuspecting con
sumers.
In India we have the Drugs and Cos
metics Act 1940, which provides for the
Government to control the manufac
ture of drugs and cosmetics. The Act
also lays down principles of fixation of
prices of drugs. In addition to this, the
Drugs Control Act 1950, The Drugs and
Magic Remedies (Objectionable Adver
tisement) Act 1956, Drugs Price Control
Rules have been framed to protect the
health of the consumers. Yet con
sumers interest is in jeopardy many a
time.
The existence of sub-standard drugs
may be attributed to several factors.
Firstly, there is no organised effort
equal to that of the turnover, to check
and
ensure
the
quality
of
pharmaceuticals. At present, testing fa
cilities are available only in Bangalore.
Calcutta, Ghaziabad and Kasaull.
As a result, these centres are overbur
dened and are unable to check required
lot of samples.
To overcome this problem partly, the
Drug Rules (1977) was amended accord
ing to which every drug manufacturing
unit, big or small should set up an 'in
house' laboratory for testing drugs.
While this is a right step in right direc
tion, it has its pitfalls. While multina
tional companies obliged without any
effect on their sales, small units had
their own problems. Secondly, the Gov
ernment health schemes like CGHS,
ESI etc., which are the largest purchas
ers of drugs (around Rs.30 crore) have
few testing facilities. The inadequate
number of drug inspectors is another
reason for unchecked growth of spuri
ous drug sales. It is estimated that just
five per cent of drugs are subjected to
quality tests. The Hath! Committee
recommended that proper check could
be maintained if there was one drug
inspector for every 25 manufacturing
units and one inspector for every 100
sales outlets. However, even now not
even one-fourth of the required inspec
tors are available. There are nearly
20000 manufacturing units and two
lakh sales outlets in the country with
680 to 700 drug inspectors. This figure
is grossly inadequate even as per the
recommendations of the task force set
up in 1990-91 which suggested 2690 drug
inspectors. As such the first step to en
sure quality is to enhance manpower.
Secondly, steps are to be taken to im
plement the rules and regulations un
der the Good Manufacturing Practices
(GMP) which India as a member state
has agreed to. The practices as laid
down in the GMP are designed to en
sure that the drugs received by the con
sumers have been subjected to strin
gent control from the begining to the
end of the manufacturing cycle involv
ing the operations of processing, com
pounding, formulating, filing, packag
ing and labelling.
Again the responsibility of the drug
company does not end with the manu
facturing of a drug. The manufacturer
has to take care that the drug is stored
under prescribed appropriate storing
conditions in the factory warehouse
and the same has to be followed by the
dealer and the chemist who is the last
point before the drug is passed on the
consumer.
Ultimately it is the duty of the con
sumer to be careful while buying the
medicines.
ALL INDIA DRUG ACTION NETWORK
C-14 COMMUNITY CENTRE S. D. A. NEW DELHI 110016
RATIONAL DRUG POLICY - STATEMENT
All India Drug Action Network (AIDAN), is a forum, and
coordinating body of organizations, and individuals
all over the country working towards the adoption and
implementation of a people oriented Rational Drug Policy
in India as a part of a Peoples Health Policy. It sets out
the following outline for the Drug Policy :
Health
Policy
and
drugs
T’
drugs
f
Present
situation
. f’
Majority of the Indians suffer from the diseases of
poverty and ignorance, i.e. communicable diseases,
diseases due to undernutrition etc. Most of these illnesses
are preventable and curable. In addition, distorted pattern
of industrialisation and urbanisation has led to the deve
lopment of so called diseases of industrialisation. What
we need most is adequate nutrition, adequate and safe
water, universal sanitation, development without damaging
environmental balance and primary medical service,
available to all.
Although drugs constitute only a small part of the overall
health care, they are
most urgent, essential and
hence a priority need in the country where incidence
of death and disability from diseases is high. So long
the basic elements of health care are not made available
universally, medical care will continue to be the priority
service to reduce death and disability and in this context,
drugs understandably assume a vital and priority role.
The fact that drugs can save life and relieve sufferings
has been exploited by the drug industry, which is oriented
mainly to profit making, to push all sorts of irrational
druqs onto the consumers. The druq industry and the
medical establishment has created a very drug-dependant
health culture which eclipses the much-needed sustainable
solutions to the real health problems. Doctors and non
doctors alike are made to believe that drugs are "cure all"_
-:2:-
for all ills. Health is still regarded as basically an indivi
dual or personal responsibility and not a product of
social factors.
It is also believed that freedom from diseases could be
obtained by better and better and more and more drugs.
Such a belief among educated and illiterate alike, has
led
to a universal craze for drugs and
this DRUG
CULTURE has come to dominate the society. In this
situation it is not surprising that drugs provide an oppor
tunity for unlimited profit-making by the drug industry,
since hardly any consumer asks for the necessity, utility, 0)
rationality,
price-justifiability and harmful effects
of a drug. It is not even asked whether a substance sqld
as Drug is actually a Drug at all. As a result, about 60%
of the drugs in the market are unscientific or harmful
or substandard; a large number of these are not actually
drugs; many drugs are consumed by those who do not
need it; people die or are disabled from the effects of
harmful drugs; drugs are sold at fantastically high prices;
and most serious of all life saving and essential drugs
are not available to the majority that need them most.
Even 38 years after independence, multinational corpo
rations continue to dominate the drug industry in India.
Further, the majority of their production consists of
drug formulations and not bulk drugs. Though, according
to UNIDO, India has the capacity to be self sufficient
in bulk drugs, we still import 40% of our bulk-drug
requirement.
Objectives
of the
Rational
drug
policy
We feel that the Rational Drug Policy objectives should
include the following
A.
ASSESSING THE DRUG-NEEDS
1)
To identify the drug needs in consonance with
the , health needs of the people, particularly
those required for primary health care; to
prepare a graded essential and priority list of
drugs for different levels of health expertise
inkeeping with actual health needs of the people.
2)
To eliminate
drugs.
irrational,
useless and
hazardous
-:3:~
B.
C.
PRODUCTION, PRICE AND QUALITY CONTROL
1)
To make all drugs available at low prices to the
people, particularly the essential- & priority drugs.
2)
To ensure quality control of all drugs.
DRUG DISTRIBUTION
To establish a national corporation for the distri
bution of drugs; retailing of drugs through fair
price shops and government's health infrastru
ctures.
D.
E.
DRUG INFORMATION AND ETHICAL MARKETING
1)
To ensure a drug information system for health
personnel and consumers.
2)
To ensure ethical marketing.
3)
To abolish brand names and introduce generic
names for all drugs.
SELF - RELIANCE
1) To
develop
self
reliance
in
drug
technology.
2) To foster and encourage the growth of the Indian
Sector and to provide a leadership role to the
public sector.
3)
F.
To aim at quick self sufficiency in the output of
drugs with a view to reducing the quantum of
imports.
RESEARCH AND DEVELOPMENT
To promote research and development for selfreliance and in accordance with the needs of
the Indian people.
G.
LEGISLATION AND ADMINISTRATION
1) To provide comprehensive drug legislation
and administrative support to deal effectively
with and implement all the above aims and
objectives.
-:4:2) To ensure smooth Centre-State relations and
inter-departmental coordination for effective
and relevant drug production, drug control and
drug supply.
H.
HUMANPOWER DEVELOPMENT
To fulfill the needs of the above Rational Drug
Policy, different type of technical personnel
(e.g. druggists, paramedics, etc.) need to be
adequately and appropriately trained in adequate
numbers.
A.
A
ASSESSING THE DRUG NEEDS
1.
Identification of Drug needs and Prioritized Essential Drug List
i)
The National Drug Formulary should be revised and compiled
by an expert multi-disciplinary committee with suitable repre
sentation from all the sections of health professionals. This
committee should draw up the essential priority drug list,
keeping the following criteria in mind -
* Medico-social justification should act as a primary
criterion keeping in mind - efficacy, safety, cost, ease of
administration, potential for misuse, indigenous production.
* Priority for production has to be given to the drugs
required for diseases causing greater mortality (death),
greater morbidity (illness), severe sequelae (after effects).
*
Drugs used in National Programmes e.g. TB, leprosy,
malaria, blindness, goitre control, and immunisation
programmes should get priority.
This list should be revised periodically.
ii)
Selection of the essential and priority drugs would be followed
by preparation of graded drug list for different categories of
health personnel and health institutions. These lists should
form the basic guidelines for bulk purchase procurement and
requisition stocking and dispensing.
An appropriate authority (see section G2) should continuously
assess drug needs and drug production and monitor capacity
utilisation in the industry, drug utilisation patterns, health
needs, changing pattern of diseases, drug requirements, new
information on old drugs, introduction of new drugs, efficacy
of the existing policy of production, distribution and use of
drugs.
2.
Withdrawal of hazardous, irrational and therapeutically useless
drugs.
i)
All the drugs in the market should be scrutinised to assess
their rationality on the basis of standard text books of medicine
and pharmacology. All drugs which are not recommended
in these text books should be banned. Those drugs which have
life-threatening or serious side-effects and for which equally
effective alternatives are available should be banned immedia
tely. The rest of these drugs should disappear from the market
within one year.
ii)
No fixed dose combination forms should be allowed to be
manufactured if an alternative single ingredient drug is available
for the purpose, which is therapeutically equivalent and more
cost effective.
iii)
Drug Legislation should be modified to ensure that no stay
order is granted in cases pertaining to banning hazardous
drugs in the interest of public health.
B.
B
PRODUCTION, PRICE AND QUALITY CONTROL
1.
Production and Price Controls
i)
The priority drug list should be a part of much larger essential
drug list based on WHO recommendations as zwell as those
of our own National Drugs and Therapeutics Authority. In
this essential drug list, life saving drugs and drugs for primary
health care shall be put as category I termed as priority drug
list and the rest of the list shall be put in category II.
ii)
The production of essential drug formulations shall be a minimum
75% of total formulation turnover of each manufacturer now
and shall be brought up to 90% in five years. The priority
drugs shall constitute 60% of the above essential drugs and
shall be raised to 80% of the essential druos in the next 5
years. The above production quota should include all dosage
forms of essential and priority druqs.
-:6:-
B
iii)
All companies having equity above 26% shall be identified
as foreign companies (as per RBI definition).
iv)
All foreign companies shall produce bulk as to formulation
ratio of 1:5. For other companies the ratio shall be 1:10.
v)
A mechanism should be evolved to provide incentive to those
companies which produce more than the required quota of
essential/priority drugs and deterrent punishment to those
companies which produce less than the required quota as
given above.
vi)
The priority drugs should be made available at low prices.
If required, they may even be subsidized. Before any major
revision in the pricing policy is done, as a policy there should
be an independent study to assess the cost, profitability as
well as availability and price from the point of view of consu
mers. Profit-making should not be the sole basis of the drug
industry. All taxes from priority drugs should be abolished
to reduce the prices of such drugs.
vii)
The trade commission shall be fixed at 20%. However, this
is the total commission which will be paid from the principal
manufacturer to the distributors and the intermediaries. While
the markup under the head of trade commission will be increa
sed, the markup under the head of sales promotion will be
decreased for essential and priority drugs.
viii)
All drugs including nutritional supplements, except that produced
by small scale sector, shall be under price control.
ix)
The small scale sector can be free from price and production
controls. However, the small scale sector will be defined
as those companies whose turnover is less than 20 lakhs and
not linked to large scale and organised sector units through
ownership, financial participation or marketing arrangements.
2.
Proper Drug Registration and Monitoring
Registration
1.
All pharmaceutical products, both ethical drugs and over-thecounter (OTC) preparations offered for sale should be duly
registered by a competent authority.
2.
Commercially sold indigenous medicines should also be registered
and pharmaceutical products which are not registered should
not be allowed to be marketed.
3.
Pharmaceutical manufacturers and traders must provide the
registration authority with a list of all countries in which the
specific product has not been accepted for registration.
4.
Pharmaceutical manufacturers and traders should inform the
registration authority if a pharmaceutical product already
registered in the country has been removed from the register
of any other country together with the reason for its removal.
5.
Pharmaceutical manufacturers and traders, when applying for
registration of a product, must be made to undertake that
subsequent to the product's registration, they will provide
the registration authority and consumers with all new informa
tions they receive about its effects, adverse reactions and
interactions.
6.
Central Drug Control authorities should have an up-to-date
information about the various drug formulations in the market,
their combinations, their date of licensing, drug information
being given with them by the producers and the latest inter
national medical views on the products.
7.
Drugs which have been banned from sale after being marketed
for some time in one country must not be submitted for clinical
trial or marketing in India. The onus of proving why such
a non-essential drug should be introduced or allowed to continue
in the market should be with the manufacturers.
8.
Whenever a new drug is tested on healthy human subjects
or on patients, the clinical trial must be authorised and moni
tored by a local "Ethical Committee" and must be carried
out only with the full informed consent of the people and
patients concerned.
Medical Audit System
It should be introduced to review the medical costs, the prescription
practices, patient complaints of negligence or financial exploitation
and drug misuse. At least minimal medical/clinical record keeping
should be made mandatory. Medical audit systems should be intro
duced in a systematic manner.
-:8:Physicians and pharmacists should be answerable to Rational Thera
peutics Committee of Experts. This could be appointed by Medical
Council or any other academic neutral body. Medical experts involved
in primary, secondary and tertiary medical care, chemists and
consumer organisations should be represented.
C.
DRUG DISTRIBUTION
1)
A National Corporation for distribution of drugs and pharma
ceuticals to retail drug outlets, hospitals and dispensaries
should be established.
ii)
National Drugs and Therapeutics Authority (see section G2)
(or its sub-committee) should look into the drug needs of
the peripheral health units to identify the bottle-necks and
deal with them as a priority and ensure timely drug supply.
iii)
This corporation should look into
-
requirement estimation of various drugs and their dosage
forms;
-
purchasing effective, safe and quality drugs at most
reasonable costs through bulk purchase and other purchase
procedures;
-
operating an efficient inventory and stock control system;
-
developing an efficient workable system, where drug
needs of the peripheral institutions can be a gauged
and timely drug supplies ensured.
iv)
Adequate drug distribution through the Government's health
service infrastructure should be ensured. Essential drugs in
adequate quantities and at subsidised rates should be available
at PHCs, and their sub-centres.
v)
Quality essential drugs should be made available from Govern
ment fair-price pharmacy shops. These could be handed over
to PHCs and sub-centres.
vi)
Education and relevant material on good pharmacy management
as produced by WHO should be made available to pharmacy
management system.
-:9:-
D
D
vii)
Trained and qualified pharmacists should dispense drugs.
D.
DRUG INFORMATION AND ETHICAL MARKETING
1.
Drug Information
i)
It should be the statutory duty of the drug control authorities
to inform health personnel and consumers of the WHO's concept
of essential drugs, India's graded essential drug lists, drug
policies and their rationale regarding banning of drugs. Rational
drug policy as a topic should be included in medical and para
medical education.
ii)
Names of the brands banned for manufacture and sales should
be widely publicized in medical journals, magazines, national
newspapers, giving briefly the explanation and rationale of
the ban.
2.
Ethical Marketing
i)
All sales promotion material including package inserts, medical
data sheets by the drug units should be screened by a permanent
National Drug Information body, which will be part of the
National Drugs and Therapeutics Authority. This body should
be responsible for screening as well as ensuring availability
of unbiased drug information to the health personnel and
consumers.
ii)
Use of audio-visuals for sales promotion on drugs to doctors
in absence of a printed copy (to be kept with the doctor),
of the claims made, should not be allowed.
iii)
All drug promotional literature should contain balanced and
verified scientific information about indication, contra-indications
side effects and drug interaction and antidotes.
iv)
Inadeguate and inaccurate information in medical promotional
literature or package insert or worse still of the total commi
ssion of the package insert (as is the trend at present) should
be considered a punishable offence.
v)
Seminars, scientific sessions held by drug companies to present
mainly industry sponsored research studies should be closely
monitored and if heed, be restricted as it is associated with
presentation usually only'' of favourable results and tend to
create a sense of obligation in the minds of certain medical
personnel towards drug companies for sponsoring .their research.
-:10:-
vi)
Sponsoring of National Conventions of professional medical
and academic societies by drug industry should be discouraged
since consumers have to ultimately indirectly foot the bill
and such sponsorship inevitably introduces bias in favour of
the company and its products. The health ministry should
take up the responsibility for making funds available for such
seminars.
vii)
Advertisement of tonics and food supplements should not
be allowed in the lay-press. OTC sales advertisements making
false or misleading or inaccurate claims should be banned.
Authorities should ensure that adequate consumer caution
is provided to the consumer in regional languages.
viii)
Labelling should be clear. International non-proprietory names
(generic names) should be used. Consumer caution should
be in regional languages.
For food supplements, nutrients, tonics in the consumer caution
in regional languages it should be added that "This is not
a substitute for normal food" and message given pictorially
wherever possible.
D
ix)
"The International Code for Ethical Marketing" as drafted by
the Health Action International should be adopted by India.
3.
Drug Nomenclature
International non-proprietary names should be used for sales, labelling
and prescription writing. This being so because of several advantages:
i)
Generic drug names are used in under-graduate/postgraduate
medical and pharmaceutical education.
ii)
Generic names are used in medical
medical journals and WHO publications.
iii)
All purchases of medicines from international
international markets are based on generic names.
iv)
Use of generic names also ensure production, sale and dispensing
of more rational single ingredient drugs.
v)
Generic name assures clarity by giving information of the
class of drug and thus avoiding confusion arising out of many
dissimilar brand names of one drug.
/
text
books,
scientific
tenders
and
vi)
Drugs of equal quality are usually cheaper when purchased
by their non-proprietary names than when bought using brand
names.
vii)
Use of non-proprietary names is a valuable aid to memory
as health workers have to learn and remember each drug
by one name only.
1.
Technological self-reliance
i)
In view of the high importance of achieving the goal of selfreliance in the drug sector, it is imperative that all technology
transfer agreements are made in accordance with the United
Nations Council for Trade and Development draft code.
ii)
Protective mechanisms should be evolved for process that
are being developed in the national laboratories so that techno
logy being developed indigenously does not get aborted as
it has happened in the recent past in case of processes deve
loped at NCL and Central Drug Research Institute.
iii)
While encouraging in house R&D activity through fiscal incen
tives, mechanism should be evolved that the R&D effort
undertaken by different firms is in accordance with the priority
drug needs of the Indian people.
E.
E
SELF - RELIANCE
2.
Encouragement to Indian Sector
i)
Make priority drugs, already produced in the country from
basic stage by the public sector and wholly Indian companies,
a reserved category for which companies holding foreign equity
more than 26% should not be allowed any fresh license.
ii)
Stipulate a strict time limit of five years for all
foreign
companies to start production from basic stage for the existing
already licensed production capacities.
' iii)
Ensure implementation of the time limit of two years stipu
lated for foreign companies to undertake production from
the basic stage for fresh license.
E
iv)
No Carry on Business license or production over the licensed
capacity should be allowed for MRTP, FERA and ex-FERA
companies.
v)
Loan licenses being used by the small scale sector units linked
through ownership, financial participation and/or marketing
arrangements should be cancelled.
3.
Reduction of Imports
i)
The canalisation of all imports snould be streamlined. Open
general licence system should be abolished. There should be
raw material pool in each State to ensure proper pricing and
availability of raw materials.
ii)
Import and excise duties should be fixed in such a way that
the landed cost of imported raw materials and bulk drugs
should not be lower than that of indigenous raw materials
and bulk drug production.
F.
RESEARCH AND DEVELOPMENT
i)
Priorities in research should be guided by the health needs
of the people in India. Drugs required in diseases causing
greater mortality, morbidity, serious sequelae should get
priority. Vaccines should get priority over other drugs.
ii)
Even 38 years after the cessation of British Colonial Rule
in India, research on non-allopathic drugs continues to get
step-motherly treatment. Hence research on these drugs should
be encouraged. None of these drugs, however, should be allowed
to be produced on commercial scale unless their efficacy
and safety has been proved through scientific research.
iii)
Research policy on drugs should be reviewed every ten years
to respond to changing pattern of diseases in India.
iv)
All medical research on human beings must be statutorily
required to conform to the 1975 Helsinki (Mark II) Declaration.
All research proposal must be approved by a central authority
before research is started. This should be strictly adhered
to in case of contraceptive research also.
The present policy of giving priority to research on hormonal
contraceptives rather than to barrier methods must be reversed.
-:13:-
G.
G
1.
DRUGS LEGISLATION AND ADMINISTRATION
Drug legislation should provide for the following:
a system of registration of all medical products (including
traditional medicines)
enforcement of good manufacturing practice
full control of labelling and advertisement
-
control of prices of finished drugs and therapeutic raw
materials
prescription control of toxic/poisonous and habit forming
drugs
summary trial for violations against the drug policy by
manufacturers and traders in special drug courts
heavy penalties including confiscation of equipments and
properties for the manufacture and/or selling of spurious
and sub-standard drugs.
The legislation should be reviewed, regularly modified and
updated in the interest of the public and they should not
become bottlenecks for implementation of the national drug
policy.
q
*
2.
National Drug and Therapeutics Authority
i)
The greatest need of the moment is greater public accounta
bility and a greater social control over pharmaceutical industry.
For this, setting up an independent machinery such as a National
Drug and Therapeutics Authority is imperative, which can
scrutinize all the drugs currently marketed in India on an
ongoing basis and be held responsible for the nature of drugs
in the market. This permanent body should have representatives
with medical, pharmacy and management expertise. Repre
sentation being from :
1) drug and health authorities from states
2) Ministry of Chemicals and Fertilzers and Ministry of Finance
3)
medical professional and medical academic bodies
4)
consumer groups and NGOs involved in health work
-:14s5)
Trade Unions related to drug industry
6)
chemists and druggists.
The Government should establish National Drug Authorities
(NDA) at the State level also. The Drug Controllers should
be accountable to NDAs.
ii)
The recommendations of the National Drugs and Therapeutics
Authority should be binding on the drug industry.
iii)
Appropriate powers be delegated to Central Drug Controller
and State Drug Control Authorities for the proper implemen
tation of the recommendations of the Drug and Therapeutics
Authority.
iv)
Relationship of NDA with centre and state drug and health
authorities should be clearly defined. Its constitution, function
ing and powers should be aimed at proper implementation
of National Drug Policy. Suitable drug ' legislation support
should be given to this authority so that its decisions aTe.
not unnecessarily challenged in the court.
v)
Drugs should be dealt with by this NDA rather than by Ministry
of Chemicals and Fertilizers, to give greater emphasis to
the therapeutic relevance rather than industrial profits and
Government's revenue.
H.
HUMAN POWER DEVELOPMENT
Not merely medical and pharmacology related manpower development
is required, but also development of drug managers, drug inspectors,
quality control technicians, researchers and scientists willing to
do R and D in areas of grater concern to the health of our people.
The training and development should include training of legal personnel
who will be dealing with Food and Drug Courts.
Exposure and training of policy makers to other dimension of drug
issues as experienced by consumers and health personnel in the
field is also relevant.
Drug control mechanism has to be developed in keeping with the
growth of our drug industry and be proportionate to our drug prod
uction and sales.
(V
THE ALL INDIA DRUG ACTION NETWORK (AIDAN)
COORDINATION COMMITTEE CONSISTS OF
(1)
Arogya Dakshata Mandal, Pune.
(2)
Catholic Hospital Association of India, Delhi.
(3)
Consumer Education & Research Centre, Ahmedabad.
(4)
Consumer Guidance Society of India, Bombay.
(5)
Drug Action Forum West Bengal, Calcutta.
(6)
Delhi Science Forum, Delhi.
(7)
Kerala Sashtra Sahitya Parishad, Kerala.
(8)
Locost, Baroda.
(9)
Lok Vigyan Sangathana, Bombay.
(10)
Medico Friends Circle, Pune.
(11)
Voluntary Health Association of India, Delhi.
AIDAN Coordinator
DR. MIRA SHIVA
c/o VHAI
C-14 Community Centre
S.D.A. New Delhi 110 016.
All India
©ryg Aetffen !rfeffw©rk
-ABDAN .
OUR DEMANDS
*
availability of essential and life saving drugs (i.e. adequate
*
withdrawal of hazardous and irrational drugs
*
availability of unbiased drug information to health personnel
and consumers (including updating our National Drug Formu
lary), and provision of therapeutic guidelines as in British
National Formulary; provision for consumer caution in
regional languages for problem drugs
*
adequate quality control and drug control so that every
production and streamlined distribution to peripheral areas).
fifth drug in the market is not sub-standard as in at present
according to Government's own figures
*
drug legislation reform to prevent drug companies from
misusing legalistic loopholes against the people.
Printed at JS Bros, A30/1 Naralna Indi. Area Phase-I
New Delhi 110 028
COMMENT
~~'T~
~
—
7■
MEDICINE
,-g-.,
r~
Drugged policy
Senseless, it lets people die of dangerous pills
•pwERSISTENT fever dogged N.
! py1 Narasimhan, managing director
£> of Crystal Cab Pvt Ltd., Banga
lore. Doctors put him on an oral
'Ultragin'course for five days. On the
sixth day, however, his condition took
a turn for the worse and he developed
purpuric rashes. Eventually, he had
i^^e shifted to the intensive care
terns vary in different countries, each
country has to choose the drugs it
needs most.
The Jayasukhlal Hathi committee
appointed by the government in 1975
reviewed the overall medications!
needs of India, and recommended
guidelines for its future drug policies.
The report pointed out that thefndian
pharmaceutical industry'was capable
of manufacturing all the essentia!
the manufacturers reduce expendi
ture on promotion of brand names
and cut the drug prices. Among the
other recommendations were prior
ity production of 116 essentia! drugs,
elimination of irrational drug combi
nations and improved quality control.
Most of the recommendations
have not yet been implemented in
India. But the report did not go waste.
It inspired the drug policy of
The massive doses of Ultragin, an
analgin-based antipyretic.
had induced a life-threaten
ing condition known as
‘thrombocytopenic
purpura'. The drug, banned
in several countries, had se
verely affected Narasimhan's
bone marrow and caused the
platelet count to fall drasti
cally. Timely medical inter
vention saved his life but
many others may not be so
lucky.
For, India, which has no
rational policy, is a dumping
ground for many banned
drugs.
Take the case of
Clioquinol,
an
antidiarrhoeal that has partially
blinded many Japanese.
fiifaa-Geigy withdrew the
T^Jg from Japan in 1976 after the victims went to court Fighting a tough battle. Members of the Community Health Centre, Bangalore,
and banned it in 1986. Yet it who advocate a rational drug policy
is still prescribed in India.
The story of estrogen-progester- drugs needed by the country and that Bangladesh, which banned many un
one drugs used for pregnancy tests is the multinational companies were essential and hazardous drugs. There
not very different. Safety to the un- hindering the growth of the Indian are under 3,500 drug formulations in
Bangladesh today while India has
' born child cannot be ensured and drug industry.
the users face an increased risk of
The committee recommended the nearly 70,000. In Norway and Sweden,
clotting and stroke. However, India nationalisation of the multinational there are hardly 3,000 formulations
banned them only in 1988, seven drug companies and use of generic representing about 300 essential
years after the WHO issued a warning. names instead of brand names. Use drugs.
According to Dr Shirdi Prasad
The Drug Controller of India had, of generic names, it said, would make
Tekur of Community Health
in fact, called for a ban on
Cell of Bangalore, “Every fifth
them in 1982, but two com
drug tested in India is sub
panies—Unichem in Bombay
standard; yet half of the drugs
and Organon in Calcutta—
A few drugs which are banned in other coun
in India are sold without prewent to court and obtained a
tries, but still manufactured and sold in India:
scription." India’s drug
stay order. Drug companies
Analgin and Analgin combinations. (Ultragin,
policy, he says, is a mere
invariably go to court when
pricing policy.
Baralgan, Buscopan, Oxalgin, Novalgin, etc.)
ever a ban is announced.
The doctors who demand
Clioquinal, Hydroxyquinoline, Vioform, etc. (antiThe fact is that the world
a rational drug policy point
can do without thousands of
diarrhoeals)
_
.
out that India produces only
Phenyl Butazone and Oxyphe'n'butazone.
drugs in the market. All it
a third of anti-TB drugs it
(Bestophen, Butalgin, Butaproxyvon, Esgipyrin,
needs to treat the diseases is
requires; the country has half
just 250 drugs, according to
Reducin, Suganril, Zolandin, etc.)
the world's TB patients. Be
the WHO. Since disease pat
?
L
Banned but available
48 .
THE WEEK ■ SEPT. 3. 1995
came. Now we have reached a stage
where we can’t cope with more,"
elaborates Birinder.
She changes the potted plants in
every establishment every week. The
flower arrangements are done either
every other day or twice a week de
pending on the client's needs. ‘‘But
Mondays are busiest days as every
one wants to start the week with a
new flower arrangement. Over a
thousand pots are rotated every
week, and a very large number of
flower arrangements aredone by us.”
With her home
garden and farm not
enough to meet the
demand she started
buying flowers from
outside. ‘‘I buy the
flowers from grow
ers in Chail. Dochi.
Shimla and other
parts of Himachal,”
shesays. Among her
suppliers is an army
officer-turnedflower grower from
Fatehgarh Sahib dis
trict of Punjab.
constantly goads them to improve
the quality of pots.
THE business
has clearly grown.
“In fact.we have
reached saturation
point. I started with
less than a thousand
rupees, now the investment is about
Rs 60,000 to 70.000 a month. Where 1
had one gardener, I have almost 50
employees now, and an outlet at a
hotel here. But all these things hap
pened so gradually, step by step,
that it is difficult to quantify the incomeand expenditure, turnover, net
profit and so on. Also, it being an
agricultural activity meant no income
tax.”
Happiest with Birinder's business
are perhaps the potters of Mani Majra
village in Chandigarh. They owe their
newfound prosperity to her as she
keeps designing pots for them, and
AT a glance, her tightly
centralised venture is more in the
class of a small shop rather than an
institutionalised business, but
Birinder is emphatic that she cannot
grow more. “1 don't even take orders
for flower arrangements and pot ro
tations in Panchkula or Mohali (both
about 5 km from the city periph
ery),” she points out. Nor does she
try out new strains and varieties
sought
to
be
popularised
by
Hower growers col
laborating with
counterparts in
Holland, Israel, etc.
“I do them the tradi
tional way, stick to
our own varieties
with the philosophy
of
maximum
utilisation of inputs.
These are the best
suited to our cli
matic conditions,"
says she.
Her work in
volves the whole
day, the whole year
with seed sowing
beginning in Sep
tember, and going
on up to January.
The new year begins with planting of
seedlings, and growing the flowers,
picking of seeds in April, drying and
packing them. Then the time for
summer seedlings begins, and before
that is over, it is time for chrysan
themums.
There is no lean period for her.
“For me being in the garden is holi
daying, so I don't need to go out
anywhere." Nor does she read books
on gardening and flowers, for the
garden and flowers directly teach
her more than books, she believes.
The judge at the rose festival may
or may not acknowledge it, but it is
■ Maintain quality: Her winning
flower arrangements remain
unbeaten in Le Corbusier’s city. In
fact, she acquired many of her
clients when people who had seen
her work passed on details to
others by word of mouth. In a way
her quality ensured free advertise
ments for her products.
■ Expand gradually: Her business
has grown slowly but surely. Do
not rush into expansion without
checking whether the market can
take your production.
Goodwill: The prosperity of
many small businessmen like the
flower grower in Fatehgarh and
the potters in Mani Mara is linked
to her venture. A very important
asset in any business.
START YOUR OWN
BUSINESS
INFORMATION on the
various types of loans is
continued from the previous
column. We had mentioned
how entrepreneurs could raise
funds for their equity and
venture capital, working capital
and loans against the
borrower's assets.
We give below other
sources which small-scale
industries can tap to raise
I funds:
S
j S Hire-purchase: This loan is
J usually given when the SSI unit
j wants to purchase plant or
equipment. Source: Financial
institutions, National Small
Industries Corporation, State
Small Industries Corporations.
Some private finance compa
nies too have entered the field
now. Terms: The machinery
bought with the loan is gener
ally hypothecated to the
institution which has advanced
the loan. The interest is
charged at a flat rate over the
duration of the loan. In certain
cases borrowers are required
to furnish collateral security.
□ Leasing finance: If an
entrepreneur wants to lease
some equipment or the plant
itself, he can approach banks,
financial institutions or leasing
companies for leasing loans.
The amount and the duration of
the loans are based on the
economic life of the machinery.
The interest rate is usually
higher than the short and
medium term loans but
payments are fully deductible
from pre-tax income.
(To be continued)
generally believed in this city that a
number of those determined to walk
away with prizes in fact buy the plants
and flowers at Birinder’s nursery and
pass them off as the flowers of their
efforts. Her businessman husband
does not even know the name of one
flower from another, but her children
have taken keen interest. They too
have been entering the rose festival,
though the hobby-turned-business
is exclusively Birinder’s.
—VIJAYA PUSHKARNA
THE WEEK ■ SEPT. 3.1995
47
sides, drugs like streptomy
cin which are needed for the
treatment of TB are mar
keted in unnecessary and
hazardous combinations.
For the last two years,
theSupremeCourthas been
hearing a public interest
litigation which, the medical
fraternity hopes, will lead to
the weeding out of hazard
ous drugs and to a more ra
tional use of drugs. Dr
Sridhar of Community
Health Cell has already
laughed a programme to
ei^^ite people about haz
ardous, banned
and
bannable drugs.
The Indian myopia is
clear from the fact that the
government has clubbed
drugs and pharmaceutical
products with industrial An auth antic source ;c-r information on prescriptive drugs in India. P.V.V.
of UMS (left) depends on information from trade journals
products, it is no surprise Krishnan, c
then that the minister of
chemicals and fertilisers—not the drugs and helps doctors avoid pre interactions and adverse reactions.
health minister—announced the new scribing irrational combinations. Dr “CIMS gets its information from the
drug policy on September 15 last year. Francis also wants the government to pharmaceutical industry and trade
If the Hathi committee had sought provide a medical auditing system to magazines. It keeps track of the inter
nationalisation of multinational com monitor over prescribing, costly national drug scene through the
British pharmaceutical manual,
panies, the new drug policy promised prescribing and wrong prescribing.
Currently, the doctors rely on the Scrib," says P.V.V. Krishnan, director
automatic clearance for any new
of
Biogard.
tri-annual
Current
Index
of
Medical
company with 51 per cent foreign
Noting that there are 20,000 phar
equity. The plight of Indian compa Specialities (CIMS), published by the
nies will worsen when GATT laws and Bangalore-based Biogard Medical maceutical units in India, producing
the Dunkel draft replace the Indian Services, for information on drugs, nearly 70,000 formulations,” DrTekur
Patent Law of 1970. Since Dunkel draft their formulations, brand names, says that the drug controlling and
inspecting apparatus is grossly inad
stipulates product patent, Indian prices and contraindications.
It recently introduced a column equate. Drugs banned in India are
c^M>anies which have developed ine^Bhsive drugs under the process ‘Alert Index' that offers data on drug sold over the counter by unscrupu
lous pharmacists, claims
patents will have to close
another doctor. Anand
shop.
Rajashekar, drug controller
Recently, Eli Lilly of the
of Karnataka, says that
US and Novo of Denmark
hardly any such case canie
obtained the ‘product
COMPONENTS of a rational drug policy pre
to the notice of drug con
patent’ for insulin. This
pared by the All-lndia Drug Action Network and
trollers last year. “The drug
means Indian companies
Voluntary Health Association of India.
control act (1940) has been
which know how to make
■ Drug availablfity/production in consonance with
quite stringent," he says.
insulin will not be allowed to
health needs of the people.
Many doctors do not
make it. Naturally the price
■ Elimination of irrational, useless and hazardous
agree. In the absence of a
of insulin will increase.
drugs.
rational
drug policy in the
The medical fraternity,
new liberalised and com
■ Low cost drugs in adequate quantities particu
too, can do with better
petitive
era, they fear it
larly essential/priority drugs.
awareness. That is why
would be easier for medical
■ Adequate quality control and drug control.
doctors like C.M. Francis,
horrors
like
the thalidomide
■ Availability of unbiased drug information and
coordinator of the Commu
tragedy to recur. Taken by
ethical marketing of drugs.
nity Health Cell, Bangalore,
pregnant
women,
thalido
■ Drug legislation reform.
feel the need for a national
mide
caused
birth
formulary modelled on the
■ Generic prescribing.
deformities
in
10,000
chil
British National Formulary
■ Technological self-reliance.
dren during the early six
published by the British
■ increase drug availability through fair price
ties
in
West
Germany.
Irra
Medical Assciation and the
shops and government health infrastructure.
tional use of drugs cannot
Pharmaceutical Society of
■ Training of health personnel in rational thera
but
give
birth
to
such
medi
Great Britain. Updated ev
peutics and rational drug policy.
cal holocausts.
ery six months, it gives a
—DR VEENA BHARATHI
range of costs for rational
Requ$re<$, a new policy
THE WEEK ■ SEPT. 3. 1995
49
BUSINESS SCAN
CORPORATE PROFILE
INDUSTRY
Th® ‘green’ rubber
MARCHING ON
■ Indian industry is marching
ahead, going by the trends in the
month of March. The index of
industrial production went up by
as much as 11.7 per cent for the
month—the highest monthly
growth seen since May 1990.
The fiscal year 1994-95 ended
with industrial production
growing by 8.4 per cent as against
the 5.6 per cent growth in the
previous year, says the July
review of the Indian economy
published by the Centre for
Monitoring Indian Economy
Private Limited. During 1994-95,
the biggest growth was witnessed
in the manufacturing sector
which grew by 8.8 per cent. Power
generation which grew by 8.5 per
cent was followed by the mining
and quarrying segment with a 6.3
per cent growth.
When viewed from the use
based classification of industries,
the capital goods industry
contributed more than 50 percent
to the growth in the overall
industrial sector during 1994-95.
Meanwhile, the overall
foodgrains production is
expected to bearound 191 million
tonnes during 1995-96, showing a
nominal increase of 0.7 per cent
over and above the 4 per cent
increase recorded in 1994-95.
A Malaysian-born Indian chemist has answers
to the tyre mountains
HE "Canadian fire" lasted for 12
years: Virginia fire earned its
notoriety in 1993; there was an
other tyre mountain fire in Australia.
These are the tiring problems en
countered by environmentalists to
day. India, ten years from now, will
have tyre mountains too.
B.C Shekar, a Malaysian Indian,
nick-named the'rubber ambassador'.
has an answer to this mountainous
problem. He has developed a
reactant called De Link, using which
rubber with 75 per cent of its orignal
properties can be reclaimed from
T
cycled give raw material in plenty
and the cost efficient source is en
sured," says Shekar.
The De Link process begins with
the removal of metal, fibre and non
rubber parts from the scrap tyres.
The tyres are then treated wajia
mixt ure of sulphur and organic d^pe
degradents in a high temperature
reactor. The resultant polymer
resembles a miniature fish net and
the De Link reactant is used to break
it down. This it does by breaking up
the sulphur cross links without
affecting the main rubber chain. The
COMPUTERS
A TIE-UP
IS Informix, the world leader in
parallel processing database
technology, and Netscape have
signed a world-wide web
agreement. The Informix data
baseserverswill now be available
in the Netscape Internet Appli
cations (TM) family of turnkey
solutions. NetscapeCommunications is a giant in open software
for electronic commerce on the
Internet.
“Through this agreement, we
can bring the parallel processing
power of online dynamic server
and the simplicity of Informix-Se
to that essential group of users
who are laying the foundations
for electronic commerce on the
Internet," says Govind Nangrani,
Informix general manager.
Informix had opened its India
business office and software
development centre for product
development in Bombay in July.
’ so
Innovative. The De Link plant. (Inset) Shekar
tyre crumbs.
Efforts are
on to link the
De Link reac
tant to the
whole rubber
world across the continents. Shekar.
heading the STI Corp Sdn Bhd,
headquartered in Kuala Lumpur.
plans to go in for joint ventures
globally to put the process to
optimum use. He is eying the growing
Indian market to widen the product's
scope. Already companies have been
set up in the US, Asia and Australia.
Shekar has undone what the US
Goodyear had done with the
invention of sulphur vulcanisation.
"Burning tyre is environmently haz
ardous. Discarded tyres when re
THE WEEK ■ SEPT.3. 1095
end product obtained contains 75
per cent of natural rubber that can
be reused for vulcanisation.
The Ramon Magsaysay award
winner has been lauded by premier
R&D institutions and top scientists
for his pioneering work. A top
polymer scientist. Sir Geoffery Allen.
has termed Shekar's work as
innovative. Shekar had hit upon this
idea at a seminar in Ottawa. Canada.
where the Russian scientist Vitaly
Kormer talked about a method of
reclaiming rubber using a toxic
chemical.
This ‘rubber man', being an
authority on natural rubber, is flex
ible enough to stretch his vast ex
—R. KESAVA IWALLIA in Kuala Lumpur
- Media
 RF_DR_1_PART_1_SUDHA.pdf
RF_DR_1_PART_1_SUDHA.pdf
Position: 929 (13 views)